Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 November 2021

A study of awareness on HIV/AIDS among adolescents: A Longitudinal Study on UDAYA data
- Shobhit Srivastava ORCID: orcid.org/0000-0002-7138-4916 1 ,
- Shekhar Chauhan ORCID: orcid.org/0000-0002-6926-7649 2 ,
- Ratna Patel ORCID: orcid.org/0000-0002-5371-7369 3 &
- Pradeep Kumar ORCID: orcid.org/0000-0003-4259-820X 1
Scientific Reports volume 11 , Article number: 22841 ( 2021 ) Cite this article
10k Accesses
7 Citations
11 Altmetric
Metrics details
- Health care
- Health services
- Public health
Acquired Immunodeficiency Syndrome caused by Human Immunodeficiency Virus (HIV) poses a severe challenge to healthcare and is a significant public health issue worldwide. This study intends to examine the change in the awareness level of HIV among adolescents. Furthermore, this study examined the factors associated with the change in awareness level on HIV-related information among adolescents over the period. Data used for this study were drawn from Understanding the lives of adolescents and young adults, a longitudinal survey on adolescents aged 10–19 in Bihar and Uttar Pradesh. The present study utilized a sample of 4421 and 7587 unmarried adolescent boys and girls, respectively aged 10–19 years in wave-1 and wave-2. Descriptive analysis and t-test and proportion test were done to observe changes in certain selected variables from wave-1 (2015–2016) to wave-2 (2018–2019). Moreover, random effect regression analysis was used to estimate the association of change in HIV awareness among unmarried adolescents with household and individual factors. The percentage of adolescent boys who had awareness regarding HIV increased from 38.6% in wave-1 to 59.9% in wave-2. Among adolescent girls, the percentage increased from 30.2 to 39.1% between wave-1 & wave-2. With the increase in age and years of schooling, the HIV awareness increased among adolescent boys ([Coef: 0.05; p < 0.01] and [Coef: 0.04; p < 0.01]) and girls ([Coef: 0.03; p < 0.01] and [Coef: 0.04; p < 0.01]), respectively. The adolescent boys [Coef: 0.06; p < 0.05] and girls [Coef: 0.03; p < 0.05] who had any mass media exposure were more likely to have an awareness of HIV. Adolescent boys' paid work status was inversely associated with HIV awareness [Coef: − 0.01; p < 0.10]. Use of internet among adolescent boys [Coef: 0.18; p < 0.01] and girls [Coef: 0.14; p < 0.01] was positively associated with HIV awareness with reference to their counterparts. There is a need to intensify efforts in ensuring that information regarding HIV should reach vulnerable sub-groups, as outlined in this study. It is important to mobilize the available resources to target the less educated and poor adolescents, focusing on rural adolescents.
Similar content being viewed by others

Predictors of never testing for HIV among sexually active individuals aged 15–56 years in Rwanda
Awareness and use of HIV pre-exposure prophylaxis and factors associated with awareness among MSM in Beijing, China

Identification of adolescent girls and young women for targeted HIV prevention: a new risk scoring tool in KwaZulu Natal, South Africa
Introduction.
Acquired Immunodeficiency Syndrome (AIDS) caused by Human Immunodeficiency Virus (HIV) poses a severe challenge to healthcare and is a significant public health issue worldwide. So far, HIV has claimed almost 33 million lives; however, off lately, increasing access to HIV prevention, diagnosis, treatment, and care has enabled people living with HIV to lead a long and healthy life 1 . By the end of 2019, an estimated 38 million people were living with HIV 1 . More so, new infections fell by 39 percent, and HIV-related deaths fell by almost 51 percent between 2000 and 2019 1 . Despite all the positive news related to HIV, the success story is not the same everywhere; HIV varies between region, country, and population, where not everyone is able to access HIV testing and treatment and care 1 . HIV/AIDS holds back economic growth by destroying human capital by predominantly affecting adolescents and young adults 2 .
There are nearly 1.2 billion adolescents (10–19 years) worldwide, which constitute 18 percent of the world’s population, and in some countries, adolescents make up as much as one-fourth of the population 3 . In India, adolescents comprise more than one-fifth (21.8%) of the total population 4 . Despite a decline projection for the adolescent population in India 5 , there is a critical need to hold adolescents as adolescence is characterized as a period when peer victimization/pressure on psychosocial development is noteworthy 6 . Peer victimization/pressure is further linked to risky sexual behaviours among adolescents 7 , 8 . A higher proportion of low literacy in the Indian population leads to a low level of awareness of HIV/AIDS 9 . Furthermore, the awareness of HIV among adolescents is quite alarming 10 , 11 , 12 .
Unfortunately, there is a shortage of evidence on what predicts awareness of HIV among adolescents. Almost all the research in India is based on beliefs, attitudes, and awareness of HIV among adolescents 2 , 12 . However, few other studies worldwide have examined mass media as a strong predictor of HIV awareness among adolescents 13 . Mass media is an effective channel to increase an individuals’ knowledge about sexual health and improve understanding of facilities related to HIV prevention 14 , 15 . Various studies have outlined other factors associated with the increasing awareness of HIV among adolescents, including; age 16 , 17 , 18 , occupation 18 , education 16 , 17 , 18 , 19 , sex 16 , place of residence 16 , marital status 16 , and household wealth index 16 .
Several community-based studies have examined awareness of HIV among Indian adolescents 2 , 10 , 12 , 20 , 21 , 22 . However, studies investigating awareness of HIV among adolescents in a larger sample size remained elusive to date, courtesy of the unavailability of relevant data. Furthermore, no study in India had ever examined awareness of HIV among adolescents utilizing information on longitudinal data. To the author’s best knowledge, this is the first study in the Indian context with a large sample size that examines awareness of HIV among adolescents and combines information from a longitudinal survey. Therefore, this study intends to examine the change in the awareness level of HIV among adolescents. Furthermore, this study examined the factors associated with a change in awareness level on HIV-related information among adolescents over the period.
Data and methods
Data used for this study were drawn from Understanding the lives of adolescents and young adults (UDAYA), a longitudinal survey on adolescents aged 10–19 in Bihar and Uttar Pradesh 23 . The first wave was conducted in 2015–2016, and the follow-up survey was conducted after three years in 2018–2019 23 . The survey provides the estimates for state and the sample of unmarried boys and girls aged 10–19 and married girls aged 15–19. The study adopted a systematic, multi-stage stratified sampling design to draw sample areas independently for rural and urban areas. 150 primary sampling units (PSUs)—villages in rural areas and census wards in urban areas—were selected in each state, using the 2011 census list of villages and wards as the sampling frame. In each primary sampling unit (PSU), households to be interviewed were selected by systematic sampling. More details about the study design and sampling procedure have been published elsewhere 23 . Written consent was obtained from the respondents in both waves. In wave 1 (2015–2016), 20,594 adolescents were interviewed using the structured questionnaire with a response rate of 92%.
Moreover, in wave 2 (2018–2019), the study interviewed the participants who were successfully interviewed in 2015–2016 and who consented to be re-interviewed 23 . Of the 20,594 eligible for the re-interview, the survey re-interviewed 4567 boys and 12,251 girls (married and unmarried). After excluding the respondents who gave an inconsistent response to age and education at the follow-up survey (3%), the final follow-up sample covered 4428 boys and 11,864 girls with the follow-up rate of 74% for boys and 81% for girls. The effective sample size for the present study was 4421 unmarried adolescent boys aged 10–19 years in wave-1 and wave-2. Additionally, 7587 unmarried adolescent girls aged 10–19 years were interviewed in wave-1 and wave-2 23 . The cases whose follow-up was lost were excluded from the sample to strongly balance the dataset and set it for longitudinal analysis using xtset command in STATA 15. The survey questionnaire is available at https://dataverse.harvard.edu/file.xhtml?fileId=4163718&version=2.0 & https://dataverse.harvard.edu/file.xhtml?fileId=4163720&version=2.0 .
Outcome variable
HIV awareness was the outcome variable for this study, which is dichotomous. The question was asked to the adolescents ‘Have you heard of HIV/AIDS?’ The response was recorded as yes and no.
Exposure variables
The predictors for this study were selected based on previous literature. These were age (10–19 years at wave 1, continuous variable), schooling (continuous), any mass media exposure (no and yes), paid work in the last 12 months (no and yes), internet use (no and yes), wealth index (poorest, poorer, middle, richer, and richest), religion (Hindu and Non-Hindu), caste (Scheduled Caste/Scheduled Tribe, Other Backward Class, and others), place of residence (urban and rural), and states (Uttar Pradesh and Bihar).
Exposure to mass media (how often they read newspapers, listened to the radio, and watched television; responses on the frequencies were: almost every day, at least once a week, at least once a month, rarely or not at all; adolescents were considered to have any exposure to mass media if they had exposure to any of these sources and as having no exposure if they responded with ‘not at all’ for all three sources of media) 24 . Household wealth index based on ownership of selected durable goods and amenities with possible scores ranging from 0 to 57; households were then divided into quintiles, with the first quintile representing households of the poorest wealth status and the fifth quintile representing households with the wealthiest status 25 .
Statistical analysis
Descriptive analysis was done to observe the characteristics of unmarried adolescent boys and girls at wave-1 (2015–2016). In addition, the changes in certain selected variables were observed from wave-1 (2015–2016) to wave-2 (2018–2019), and the significance was tested using t-test and proportion test 26 , 27 . Moreover, random effect regression analysis 28 , 29 was used to estimate the association of change in HIV awareness among unmarried adolescents with household factors and individual factors. The random effect model has a specific benefit for the present paper's analysis: its ability to estimate the effect of any variable that does not vary within clusters, which holds for household variables, e.g., wealth status, which is assumed to be constant for wave-1 and wave-2 30 .
Table 1 represents the socio-economic profile of adolescent boys and girls. The estimates are from the baseline dataset, and it was assumed that none of the household characteristics changed over time among adolescent boys and girls.
Figure 1 represents the change in HIV awareness among adolescent boys and girls. The percentage of adolescent boys who had awareness regarding HIV increased from 38.6% in wave-1 to 59.9% in wave-2. Among adolescent girls, the percentage increased from 30.2% in wave-1 to 39.1% in wave-2.
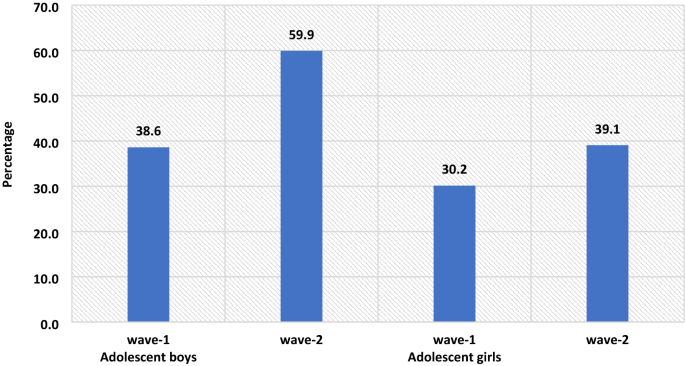
The percenate of HIV awareness among adolescent boys and girls, wave-1 (2015–2016) and wave-2 (2018–2019).
Table 2 represents the summary statistics for explanatory variables used in the analysis of UDAYA wave-1 and wave-2. The exposure to mass media is almost universal for adolescent boys, while for adolescent girls, it increases to 93% in wave-2 from 89.8% in wave-1. About 35.3% of adolescent boys were engaged in paid work during wave-1, whereas in wave-II, the share dropped to 33.5%, while in the case of adolescent girls, the estimates are almost unchanged. In wave-1, about 27.8% of adolescent boys were using the internet, while in wave-2, there is a steep increase of nearly 46.2%. Similarly, in adolescent girls, the use of the internet increased from 7.6% in wave-1 to 39.3% in wave-2.
Table 3 represents the estimates from random effects for awareness of HIV among adolescent boys and girls. It was found that with the increases in age and years of schooling the HIV awareness increased among adolescent boys ([Coef: 0.05; p < 0.01] and [Coef: 0.04; p < 0.01]) and girls ([Coef: 0.03; p < 0.01] and [Coef: 0.04; p < 0.01]), respectively. The adolescent boys [Coef: 0.06; p < 0.05] and girls [Coef: 0.03; p < 0.05] who had any mass media exposure were more likely to have an awareness of HIV in comparison to those who had no exposure to mass media. Adolescent boys' paid work status was inversely associated with HIV awareness about adolescent boys who did not do paid work [Coef: − 0.01; p < 0.10]. Use of the internet among adolescent boys [Coef: 0.18; p < 0.01] and girls [Coef: 0.14; p < 0.01] was positively associated with HIV awareness in reference to their counterparts.
The awareness regarding HIV increases with the increase in household wealth index among both adolescent boys and girls. The adolescent girls from the non-Hindu household had a lower likelihood to be aware of HIV in reference to adolescent girls from Hindu households [Coef: − 0.09; p < 0.01]. Adolescent girls from non-SC/ST households had a higher likelihood of being aware of HIV in reference to adolescent girls from other caste households [Coef: 0.04; p < 0.01]. Adolescent boys [Coef: − 0.03; p < 0.01] and girls [Coef: − 0.09; p < 0.01] from a rural place of residence had a lower likelihood to be aware about HIV in reference to those from the urban place of residence. Adolescent boys [Coef: 0.04; p < 0.01] and girls [Coef: 0.02; p < 0.01] from Bihar had a higher likelihood to be aware about HIV in reference to those from Uttar Pradesh.
This is the first study of its kind to address awareness of HIV among adolescents utilizing longitudinal data in two indian states. Our study demonstrated that the awareness of HIV has increased over the period; however, it was more prominent among adolescent boys than in adolescent girls. Overall, the knowledge on HIV was relatively low, even during wave-II. Almost three-fifths (59.9%) of the boys and two-fifths (39.1%) of the girls were aware of HIV. The prevalence of awareness on HIV among adolescents in this study was lower than almost all of the community-based studies conducted in India 10 , 11 , 22 . A study conducted in slums in Delhi has found almost similar prevalence (40% compared to 39.1% during wave-II in this study) of awareness of HIV among adolescent girls 31 . The difference in prevalence could be attributed to the difference in methodology, study population, and study area.
The study found that the awareness of HIV among adolescent boys has increased from 38.6 percent in wave-I to 59.9 percent in wave-II; similarly, only 30.2 percent of the girls had an awareness of HIV during wave-I, which had increased to 39.1 percent. Several previous studies corroborated the finding and noticed a higher prevalence of awareness on HIV among adolescent boys than in adolescent girls 16 , 32 , 33 , 34 . However, a study conducted in a different setting noticed a higher awareness among girls than in boys 35 . Also, a study in the Indian context failed to notice any statistical differences in HIV knowledge between boys and girls 18 . Gender seems to be one of the significant determinants of comprehensive knowledge of HIV among adolescents. There is a wide gap in educational attainment among male and female adolescents, which could be attributed to lower awareness of HIV among girls in this study. Higher peer victimization among adolescent boys could be another reason for higher awareness of HIV among them 36 . Also, cultural double standards placed on males and females that encourage males to discuss HIV/AIDS and related sexual matters more openly and discourage or even restrict females from discussing sexual-related issues could be another pertinent factor of higher awareness among male adolescents 33 . Behavioural interventions among girls could be an effective way to improving knowledge HIV related information, as seen in previous study 37 . Furthermore, strengthening school-community accountability for girls' education would augment school retention among girls and deliver HIV awareness to girls 38 .
Similar to other studies 2 , 10 , 17 , 18 , 39 , 40 , 41 , age was another significant determinant observed in this study. Increasing age could be attributed to higher education which could explain better awareness with increasing age. As in other studies 18 , 39 , 41 , 42 , 43 , 44 , 45 , 46 , education was noted as a significant driver of awareness of HIV among adolescents in this study. Higher education might be associated with increased probability of mass media and internet exposure leading to higher awareness of HIV among adolescents. A study noted that school is one of the important factors in raising the awareness of HIV among adolescents, which could be linked to higher awareness among those with higher education 47 , 48 . Also, schooling provides adolescents an opportunity to improve their social capital, leading to increased awareness of HIV.
Following previous studies 18 , 40 , 46 , the current study also outlines a higher awareness among urban adolescents than their rural counterparts. One plausible reason for lower awareness among adolescents in rural areas could be limited access to HIV prevention information 16 . Moreover, rural–urban differences in awareness of HIV could also be due to differences in schooling, exposure to mass media, and wealth 44 , 45 . The household's wealth status was also noted as a significant predictor of awareness of HIV among adolescents. Corroborating with previous findings 16 , 33 , 42 , 49 , this study reported a higher awareness among adolescents from richer households than their counterparts from poor households. This could be because wealthier families can afford mass-media items like televisions and radios for their children, which, in turn, improves awareness of HIV among adolescents 33 .
Exposure to mass media and internet access were also significant predictors of higher awareness of HIV among adolescents. This finding agrees with several previous research, and almost all the research found a positive relationship between mass-media exposure and awareness of HIV among adolescents 10 . Mass media addresses such topics more openly and in a way that could attract adolescents’ attention is the plausible reason for higher awareness of HIV among those having access to mass media and the internet 33 . Improving mass media and internet usage, specifically among rural and uneducated masses, would bring required changes. Integrating sexual education into school curricula would be an important means of imparting awareness on HIV among adolescents; however, this is debatable as to which standard to include the required sexual education in the Indian schooling system. Glick (2009) thinks that the syllabus on sexual education might be included during secondary schooling 44 . Another study in the Indian context confirms the need for sex education for adolescents 50 , 51 .
Limitations and strengths of the study
The study has several limitations. At first, the awareness of HIV was measured with one question only. Given that no study has examined awareness of HIV among adolescents using longitudinal data, this limitation is not a concern. Second, the study findings cannot be generalized to the whole Indian population as the study was conducted in only two states of India. However, the two states selected in this study (Uttar Pradesh and Bihar) constitute almost one-fourth of India’s total population. Thirdly, the estimates were provided separately for boys and girls and could not be presented combined. However, the data is designed to provide estimates separately for girls and boys. The data had information on unmarried boys and girls and married girls; however, data did not collect information on married boys. Fourthly, the study estimates might have been affected by the recall bias. Since HIV is a sensitive topic, the possibility of respondents modifying their responses could not be ruled out. Hawthorne effect, respondents, modifying aspect of their behaviour in response, has a role to play in HIV related study 52 . Despite several limitations, the study has specific strengths too. This is the first study examining awareness of HIV among adolescent boys and girls utilizing longitudinal data. The study was conducted with a large sample size as several previous studies were conducted in a community setting with a minimal sample size 10 , 12 , 18 , 20 , 53 .
The study noted a higher awareness among adolescent boys than in adolescent girls. Specific predictors of high awareness were also noted in the study, including; higher age, higher education, exposure to mass media, internet use, household wealth, and urban residence. Based on the study findings, this study has specific suggestions to improve awareness of HIV among adolescents. There is a need to intensify efforts in ensuring that information regarding HIV should reach vulnerable sub-groups as outlined in this study. It is important to mobilize the available resources to target the less educated and poor adolescents, focusing on rural adolescents. Investment in education will help, but it would be a long-term solution; therefore, public information campaigns could be more useful in the short term.
WHO. HIV/AIDS . https://www.who.int/news-room/fact-sheets/detail/hiv-aids (2020).
Singh, A. & Jain, S. Awareness of HIV/AIDS among school adolescents in Banaskantha district of Gujarat. Health Popul.: Perspect. Issues 32 , 59–65 (2009).
Google Scholar
WHO & UNICEF. adolescents Health: The Missing Population in Universal Health Coverage . 1–31 https://www.google.com/search?q=adolescents+population+WHO+report&rlz=1C1CHBF_enIN904IN904&oq=adolescents+population+WHO+report&aqs=chrome..69i57.7888j1j7&sourceid=chrome&ie=UTF-8 (2018).
Chauhan, S. & Arokiasamy, P. India’s demographic dividend: state-wise perspective. J. Soc. Econ. Dev. 20 , 1–23 (2018).
Tiwari, A. K., Singh, B. P. & Patel, V. Population projection of India: an application of dynamic demographic projection model. JCR 7 , 547–555 (2020).
Troop-Gordon, W. Peer victimization in adolescence: the nature, progression, and consequences of being bullied within a developmental context. J. Adolesc. 55 , 116–128 (2017).
PubMed Google Scholar
Dermody, S. S., Friedman, M., Chisolm, D. J., Burton, C. M. & Marshal, M. P. Elevated risky sexual behaviors among sexual minority girls: indirect risk pathways through peer victimization and heavy drinking. J. Interpers. Violence 35 , 2236–2253 (2020).
Lee, R. L. T., Loke, A. Y., Hung, T. T. M. & Sobel, H. A systematic review on identifying risk factors associated with early sexual debut and coerced sex among adolescents and young people in communities. J. Clin. Nurs. 27 , 478–501 (2018).
Gurram, S. & Bollampalli, B. A study on awareness of human immunodeficiency virus among adolescent girls in urban and rural field practice areas of Osmania Medical College, Hyderabad, Telangana, India. (2020).
Jain, R., Anand, P., Dhyani, A. & Bansal, D. Knowledge and awareness regarding menstruation and HIV/AIDS among schoolgoing adolescent girls. J. Fam. Med. Prim Care 6 , 47–51 (2017).
Kawale, S., Sharma, V., Thaware, P. & Mohankar, A. A study to assess awareness about HIV/AIDS among rural population of central India. Int. J. Commun. Med. Public Health 5 , 373–376 (2017).
Lal, P., Nath, A., Badhan, S. & Ingle, G. K. A study of awareness about HIV/AIDS among senior secondary school Children of Delhi. Indian J. Commun. Med. 33 , 190–192 (2008).
CAS Google Scholar
Bago, J.-L. & Lompo, M. L. Exploring the linkage between exposure to mass media and HIV awareness among adolescents in Uganda. Sex. Reprod. Healthcare 21 , 1–8 (2019).
McCombie, S., Hornik, R. C. & Anarfi, J. K. Effects of a mass media campaign to prevent AIDS among young people in Ghana . Public Health Commun. 163–178 (Routledge, 2002). https://doi.org/10.4324/9781410603029-17 .
Sano, Y. et al. Exploring the linkage between exposure to mass media and HIV testing among married women and men in Ghana. AIDS Care 28 , 684–688 (2016).
Oginni, A. B., Adebajo, S. B. & Ahonsi, B. A. Trends and determinants of comprehensive knowledge of HIV among adolescents and young adults in Nigeria: 2003–2013. Afr. J. Reprod. Health 21 , 26–34 (2017).
Rahman, M. M., Kabir, M. & Shahidullah, M. Adolescent knowledge and awareness about AIDS/HIV and factors affecting them in Bangladesh. J. Ayub. Med. Coll. Abbottabad 21 , 3–6 (2009).
Yadav, S. B., Makwana, N. R., Vadera, B. N., Dhaduk, K. M. & Gandha, K. M. Awareness of HIV/AIDS among rural youth in India: a community based cross-sectional study. J. Infect. Dev. Countries 5 , 711–716 (2011).
Alhasawi, A. et al. Assessing HIV/AIDS knowledge, awareness, and attitudes among senior high school students in Kuwait. MPP 28 , 470–476 (2019).
Chakrovarty, A. et al. A study of awareness on HIV/AIDS among higher secondary school students in Central Kolkata. Indian J. Commun. Med. 32 , 228 (2007).
Katoch, D. K. S. & Kumar, A. HIV/AIDS awareness among students of tribal and non-tribal area of Himachal Pradesh. J. Educ. 5 , 1–9 (2017).
Shinde, M., Trivedi, A., Shinde, A. & Mishra, S. A study of awareness regarding HIV/AIDS among secondary school students. Int. J. Commun. Med. Public Health https://doi.org/10.18203/2394-6040.ijcmph20161611 (2016).
Article Google Scholar
Council, P. UDAYA, adolescent survey, Bihar and Uttar Pradesh, 2015–16. Harvard Dataverse https://doi.org/10.7910/DVN/RRXQNT (2018).
Kumar, P. & Dhillon, P. Household- and community-level determinants of low-risk Caesarean deliveries among women in India. J. Biosoc. Sci. 53 , 55–70 (2021).
Patel, S. K., Santhya, K. G. & Haberland, N. What shapes gender attitudes among adolescent girls and boys? Evidence from the UDAYA Longitudinal Study in India. PLoS ONE 16 , e0248766 (2021).
CAS PubMed PubMed Central Google Scholar
Fan, C., Wang, L. & Wei, L. Comparing two tests for two rates. Am. Stat. 71 , 275–281 (2017).
MathSciNet Google Scholar
Kim, T. K. T test as a parametric statistic. Korean J. Anesthesiol. 68 , 540–546 (2015).
PubMed PubMed Central Google Scholar
Bell, A., Fairbrother, M. & Jones, K. Fixed and random effects models: making an informed choice. Qual. Quant. 53 , 1051–1074 (2019).
Jarrett, R., Farewell, V. & Herzberg, A. Random effects models for complex designs. Stat. Methods Med. Res. 29 , 3695–3706 (2020).
MathSciNet CAS PubMed PubMed Central Google Scholar
Neuhaus, J. M. & Kalbfleisch, J. D. Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics 54 , 638–645 (1998).
CAS PubMed MATH Google Scholar
Kaur, G. Factors influencing HIV awareness amongst adolescent women: a study of slums in Delhi. Demogr. India 47 , 100–111 (2018).
Alene, G. D., Wheeler, J. G. & Grosskurth, H. Adolescent reproductive health and awareness of HIV among rural high school students, North Western Ethiopia. AIDS Care 16 , 57–68 (2004).
CAS PubMed Google Scholar
Oljira, L., Berhane, Y. & Worku, A. Assessment of comprehensive HIV/AIDS knowledge level among in-school adolescents in eastern Ethiopia. J. Int. AIDS Soc. 16 , 17349 (2013).
Samkange-Zeeb, F. N., Spallek, L. & Zeeb, H. Awareness and knowledge of sexually transmitted diseases (STDs) among school-going adolescents in Europe: a systematic review of published literature. BMC Public Health 11 , 727 (2011).
Laguna, E. P. Knowledge of HIV/AIDS and unsafe sex practices among Filipino youth. in 15 (PAA, 2004).
Teitelman, A. M. et al. Partner violence, power, and gender differences in South African adolescents’ HIV/sexually transmitted infections risk behaviors. Health Psychol. 35 , 751–760 (2016).
Oberth, G. et al. Effectiveness of the Sista2Sista programme in improving HIV and other sexual and reproductive health outcomes among vulnerable adolescent girls and young women in Zimbabwe. Afr. J. AIDS Res. 20 , 158–164 (2021).
DeSoto, J. et al. Using school-based early warning systems as a social and behavioral approach for HIV prevention among adolescent girls. Preventing HIV Among Young People in Southern and Eastern Africa 280 (2020).
Ochako, R., Ulwodi, D., Njagi, P., Kimetu, S. & Onyango, A. Trends and determinants of Comprehensive HIV and AIDS knowledge among urban young women in Kenya. AIDS Res. Ther. 8 , 11 (2011).
Peltzer, K. & Supa, P. HIV/AIDS knowledge and sexual behavior among junior secondary school students in South Africa. J. Soc. Sci. 1 , 1–8 (2005).
Shweta, C., Mundkur, S. & Chaitanya, V. Knowledge and beliefs about HIV/AIDS among adolescents. WebMed Cent. 2 , 1–9 (2011).
Anwar, M., Sulaiman, S. A. S., Ahmadi, K. & Khan, T. M. Awareness of school students on sexually transmitted infections (STIs) and their sexual behavior: a cross-sectional study conducted in Pulau Pinang, Malaysia. BMC Public Health 10 , 47 (2010).
Cicciò, L. & Sera, D. Assessing the knowledge and behavior towards HIV/AIDS among youth in Northern Uganda: a cross-sectional survey. Giornale Italiano di Medicina Tropicale 15 , 29–34 (2010).
Glick, P., Randriamamonjy, J. & Sahn, D. E. Determinants of HIV knowledge and condom use among women in madagascar: an analysis using matched household and community data. Afr. Dev. Rev. 21 , 147–179 (2009).
Rahman, M. Determinants of knowledge and awareness about AIDS: Urban-rural differentials in Bangladesh. JPHE 1 , 014–021 (2009).
Siziya, S., Muula, A. S. & Rudatsikira, E. HIV and AIDS-related knowledge among women in Iraq. BMC. Res. Notes 1 , 123 (2008).
Gao, X. et al. Effectiveness of school-based education on HIV/AIDS knowledge, attitude, and behavior among secondary school students in Wuhan, China. PLoS ONE 7 , e44881 (2012).
ADS CAS PubMed PubMed Central Google Scholar
Kotecha, P. V. et al. Reproductive health awareness among urban school going adolescents in Vadodara city. Indian J. Psychiatry 54 , 344–348 (2012).
Dimbuene, T. Z. & Defo, K. B. Fostering accurate HIV/AIDS knowledge among unmarried youths in Cameroon: do family environment and peers matter?. BMC Public Health 11 , 348 (2011).
Kumar, R. et al. Knowledge attitude and perception of sex education among school going adolescents in Ambala District, Haryana, India: a cross-sectional study. J. Clin. Diagn. Res. 11 , LC01–LC04 (2017).
ADS PubMed PubMed Central Google Scholar
Tripathi, N. & Sekher, T. V. Youth in India ready for sex education? Emerging evidence from national surveys. PLoS ONE 8 , e71584 (2013).
Rosenberg, M. et al. Evidence for sample selection effect and Hawthorne effect in behavioural HIV prevention trial among young women in a rural South African community. BMJ Open 8 , e019167 (2018).
Gupta, P., Anjum, F., Bhardwaj, P., Srivastav, J. & Zaidi, Z. H. Knowledge about HIV/AIDS among secondary school students. N. Am. J. Med. Sci. 5 , 119–123 (2013).
Download references
This paper was written using data collected as part of Population Council’s UDAYA study, which is funded by the Bill and Melinda Gates Foundation and the David and Lucile Packard Foundation. No additional funds were received for the preparation of the paper.
Author information
Authors and affiliations.
Ph.D. Research Scholar, Department of Survey Research & Data Analytics, International Institute for Population Sciences, Mumbai, India
Shobhit Srivastava & Pradeep Kumar
Ph.D. Research Scholar, Department of Family and Generations, International Institute for Population Sciences, Mumbai, India
Shekhar Chauhan
Ph.D. Research Scholar, Department of Public Health and Mortality Studies, International Institute for Population Sciences, Mumbai, India
Ratna Patel
You can also search for this author in PubMed Google Scholar
Contributions
Conception and design of the study: S.S. and P.K.; analysis and/or interpretation of data: P.K. and S.S.; drafting the manuscript: S.C., and R.P.; reading and approving the manuscript: S.S., P.K., S.C. and R.P.
Corresponding author
Correspondence to Pradeep Kumar .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Srivastava, S., Chauhan, S., Patel, R. et al. A study of awareness on HIV/AIDS among adolescents: A Longitudinal Study on UDAYA data. Sci Rep 11 , 22841 (2021). https://doi.org/10.1038/s41598-021-02090-9
Download citation
Received : 05 June 2021
Accepted : 29 September 2021
Published : 24 November 2021
DOI : https://doi.org/10.1038/s41598-021-02090-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 07 December 2021
The lived experience of HIV-infected patients in the face of a positive diagnosis of the disease: a phenomenological study
- Behzad Imani ORCID: orcid.org/0000-0002-1544-8196 1 ,
- Shirdel Zandi 2 ,
- Salman khazaei 3 &
- Mohamad Mirzaei 4
AIDS Research and Therapy volume 18 , Article number: 95 ( 2021 ) Cite this article
7523 Accesses
3 Citations
3 Altmetric
Metrics details
AIDS as a human crisis may lead to devastating psychological trauma and stress for patients. Therefore, it is necessary to study different aspects of their lives for better support and care. Accordingly, this study aimed to explain the lived experience of HIV-infected patients in the face of a positive diagnosis of the disease.
This qualitative study is a descriptive phenomenological study. Sampling was done purposefully and participants were selected based on the inclusion and exclusion criteria. Data collection was conducted, using semi-structured interviews. Data analysis was performed using Colaizzi’s method.
12 AIDS patients participated in this study. As a result of data analysis, 5 main themes and 12 sub-themes were identified, which include : emotional shock (loathing, motivation of social isolation), the fear of the consequences (fear of the death, fear of loneliness, fear of disgrace), the feeling of the guilt (feeling of regret, feeling guilty, feeling of conscience-stricken), the discouragement (suicidal ideation, disappointment), and the escape from reality (denial, trying to hide).
The results of this study showed that patients will experience unpleasant phenomenon in the face of the positive diagnosis of the disease and will be subjected to severe psychological pressures that require attention and support of medical and laboratory centers.
Patients will experience severe psychological stress in the face of a positive diagnosis of HIV.
Patients who are diagnosed with HIV are prone to make a blunder and dreadful decisions.
AIDS patients need emotional and informational support when they receive a positive diagnosis.
As a piece of bad news, presenting the positive diagnosis of HIV required the psychic preparation of the patient
Introduction
HIV/AIDS pandemic is one of the most important economic, social, and human health problems in many countries of the world, whose, extent and dimensions are unfortunately ever-increasing [ 1 ]. In such circumstances, this phenomenon should be considered as a crisis, which seriously affects all aspects of the existence and life of patients and even the health of society [ 2 ]. Diagnosing and contracting HIV/AIDS puts a person in a vague and difficult situation. Patients suffer not only from the physical effects of the disease, but also from the disgraceful consequences of the disease. HIV/AIDS is usually associated with avoidable behaviors that are not socially acceptable, such as unhealthy sexual, relations and drug abuse: So the patients are usually held guilty for their illness [ 3 ]. On the other hand, the issue of disease stigma in the community is the cause of rejection and isolation of these patients, and in health care centers is a major obstacle to providing services to these patients [ 4 ]. Studies show that HIV/AIDS stigma has a completely negative effect on the quality of life of these patients [ 5 ]. Criminal attitudes towards these patients and disappointing behavior by family, community, and medical staff cause blame and discrimination in patients [ 6 ]. HIV/AIDS stigma is prevalent among diseases, making concealment a major problem in this behavioral disease. The stigma comes in two forms: a negative inner feeling and a negative feeling that other people in the community have towards the patient [ 7 ]. The findings of a study that conducted in Iran indicated that increasing HIV/AIDS-related stigma decreases quality of life of people living with HIV/AIDS [ 8 ]. Robert Beckman has defined bad news as “any news that seriously and unpleasantly affects persons’ attitudes toward their future”. He considers the impact of counseling on moderating a person’s feeling of being important [ 9 ]. Therefore, being infected by HIV / AIDS due to the stigma can be bad news, which will lead to unpleasant emotional reactions [ 10 ]. Studies that have examined the lives of these patients have shown that these patients will experience mental and living problems throughout their lives. These studies highlight the need for age-specific programming to increase HIV knowledge and coping, increase screening, and improve long-term planning [ 11 , 12 ].
A prerequisite for any successful planning and intervention for people living with HIV/AIDS is approaching them and conducting in-depth interviews in order to discover their feelings, attitudes; their views on themselves, their illness, and others; and finally, their motivation to follow up and the participation in interventions [ 13 ]. Accordingly, the present study aimed to explain the lived experience of HIV-infected patients in the face of a positive diagnosis of the disease, since the better understanding of the phenomena leads to the smoother ways to help and care for these patients.
Study setting
In this study, a qualitative method of descriptive phenomenology was used to discover and interpret the lived experience of HIV-positive patients, when they face a positive diagnosis of the disease. The philosophical strengths underlying descriptive phenomenology afford a deeper understanding of the phenomenon being studied [ 14 ]. Husserl’s four steps of descriptive phenomenology were employed: bracketing, intuiting, analyzing and interpreting [ 15 ].
Participants and sampling
Sampling was done purposefully and participants were selected based on inclusion criteria. In this purposeful sampling, participants were selected among those patients who had sufficient knowledge about this phenomenon. The sample size was not determined at the beginning of the study, instead, it continued until no new idea emerged and data-saturated. Participants were selected from patients who were admitted to the Shohala Behavioral Diseases Counseling Center in Hamadan-Iran. The center has been set up to conduct tests, consultations, medical and dental services, and to distribute medicines among the patients. Additional inclusion criteria for selecting a participant are: having a positive diagnosis experience at the center, Ability to recall events and mental thoughts in the face of the first positive diagnosis of the disease, having psychological and mental stability, having a favorable clinical condition, willingness to work with the research team, and the possibility of re-access for the second interview if needed. Exclusion criteria were unwillingness to participate in the study and inability of verbal communication in Persian language.
Data collection
The interviews began with a non-structured question (tell us about your experience with a positive diagnosis) and continued with semi-structured questions. Each interview lasted 35–70 min and was conducted in two sessions if necessary. All interviews were conducted by the main investigator (ShZ) that who has experience in qualitative research and interviewing. The interview was recorded and then written down with permission of the participant.
Data analysis
The descriptive Colaizzi method was used to analyses the collected data [ 16 ]. This method consists of seven steps: (1) collecting the participants’ descriptions, (2) understanding the meanings in depth, (3) extracting important sentences, (4) conceptualizing important themes, (5) categorizing the concepts and topics, (6) constructing comprehensive descriptions of the issues examined, and (7) validating the data following the four criteria set out by Lincoln and Guba.
Trustworthiness criteria were used to validate the research, due to the fact that importance of data and findings validity in qualitative research [ 17 ]. This study was based on four criteria of Lincoln and Guba: credibility, transferability, dependability, and conformability [ 18 ]. For data credibility, prolong engagement and follow-up observations, as well as samplings with maximum variability were used. For dependability of the data, the researchers were divided into two groups and the research was conducted as two separate studies. At the same time, another researcher with the most familiarity and ability in conducting qualitative research, supervised the study as an external observer. Concerning the conformability, the researchers tried not to influence their own opinions in the coding process. Moreover, the codes were readout by the participants as well as two researcher colleagues with the help of an independent researcher and expert familiar with qualitative research. Transferability of data was confirmed by offering a comprehensive description of the subject, participants, data collection, and data analysis.
Ethical considerations (ethical approval)
The present study was registered with the ethics code IR.UMSHA.REC.1398.1000 in Hamadan University of Medical Sciences. The purpose of the study was explained and all participants’ consents were obtained at first step. All participants were assured that the information obtained would remain confidential and no personal information would be disclosed. Participants were also told that there was no need to provide any personal information to the interviewer, including name, surname, phone number and address. To gain more trust, interviews were conducted by a person who was not resident of Hamadan and was not a native of the region, this case was also reported to the participants.
Twelve HIV-infected participated in this study. The mean age of the participants was 36.41 ± 4.12 years. 58.33% of the participants were male and 41.66% were married. Of these, 2 were illiterate, 2 had elementary diploma, 6 had high school diploma and 2 had academic education. Six of them were unemployed, 5 were self-employed and 1 was an official employee. These people had been infected by this disease for 6.08 ± 2.71 years, in average (Table 1 ).
Analysis of the HIV-infected patients’ experiences of facing the positive diagnosis of the disease by descriptive phenomenology revealed five main themes: emotional shock, the fear of the consequences, the feeling of the guilt, the discouragement, and the escape from reality (Table 2 ).
Emotional shock
Emotional shock is one of the unpleasant events that these patients have experienced after facing a positive diagnosis of the disease. This experience has manifested in loathing and motivation of social isolation.
These patients stated that after facing a positive diagnosis of the disease, they developed a strong inner feeling of hatred towards the source of infection. The patients feel hatred, since they hold the carrier as responsible for their infection. “…After realizing I was affected, I felt very upset with my husband, I did not want to see him again, because it made me miserable, I even decided to divorce ….”(P3).
Motivation of social isolation
The experiences of these patients showed that after facing the incident, they have suffered an internal failure that has caused them to try to distance from other people. These patients have become isolated, withdrawing from the community and sometimes even from their families. “…After this incident, I decided to live alone forever and stay away from all my family members. I made a good excuse and broke up our engagement…” (P7).
Fear of the consequences
Fear of the consequences is one of the unpleasant experiences that these patients will face, as soon as they receive a positive diagnosis of the disease. Based on experiences, these patients feel fear of loneliness, death, and disgrace as soon as they hear the positive diagnosis.
Fear of the death
The patients said that as soon as they got the positive test results, they thought that the disease was incurable and would end their lives soon. “…When I found I had AIDS, I was very upset and moved like a dead man because I was really afraid that at any moment this disease might kill me and I would die …” (P1).
Fear of loneliness
The participants stated that one of the feelings that they experienced as soon as they received a positive diagnosis of the disease was the fear of being alone. They stated that at that moment, the thought of being excluded from society and losing their intimacy with them was very disturbing. “…The thought that I could no longer have a family and had to stay single forever bothered me a lot, it was terrifying to me when I thought that society could no longer accept me as a normal person …” (P10).
Fear of disgrace
One of the feelings that these patients experienced when faced the positive diagnosis of the disease was the fear of disgrace. They suffer from the perception that the spread of news of the illness hurts the attitudes of those around them and causes them to be discredited. “…It was very annoying for me when I thought I would no longer be seen as a member of my family, I felt I would no longer have a reputation and everyone would think badly of me …” (P2).
Feeling of the guilt
From other experiences of these patients in facing the positive diagnosis of the disease is feeling guilty. This feeling appears in patients as feeling of regret, guilty and remorse.
Feeling of regret
These patients stated that they felt remorse for their lifestyle and actions as soon as they heard the positive diagnosis of the disease, because they thought that if they had lived healthier, they would not have been infected. “…After realizing this disease, I was very sorry for my past, because I really did not have a healthy life. I made a series of mistakes that caused me to get caught. At that moment, I just regretted why I had this disaster …” (P11).
Feeling guilty
The experience of these patients has shown that after receiving a positive diagnosis of the disease, they consider themselves guilty and complain about themselves. These patients condemn their lifestyle and sometimes even consider themselves deserving of the disease and think that it is a ransom that they have paid back. “…after getting the disease, I realized that I was paying the ransom because I was hundred percent guilty, I was the one who caused this situation with a series of bad deeds, and now I have to be punished …” (P5).
Feeling of conscience-stricken
One of the experiences that these patients reported is the pangs of conscience. These patients stated that after receiving a positive diagnosis of the disease, the thought that as a carrier they might have contaminated those around them was very unpleasant and greatly affected their psyche. “…after getting the disease. It was shocked and I was just crazy about the fact that if my wife and children had taken this disease from me, what would I do, I made them hapless … and this as very annoying for me …” (P8).
Discouragement
Discouragement is an unpleasant experience that patients experienced after receiving a positive HIV test results. Discouragement in these patients appears in the suicidal ideation and disappointment.
Suicidal ideation
The patients stated that they were so upset with the positive diagnosis of the illness and they immediately thought they could not live with the fact and the best thing to do was to end their own lives. “…The news was so bad for me that I immediately thought that if the test result was correct and I had AIDS, I would have to kill myself and end this wretch life, oh, I had a lot of problem and the thought of having to wait for a gradual death was horrible to me …” (P12).
Disappointment
The experience of these patients shows that a positive diagnosis of the disease for these patients leads to a destructive feeling of disappointment. So that they are completely discouraged from their lives. These patients think that their dreams and goals are vanished and that they have reached the end and everything is over. “…It was a horrible experience, so at that moment I felt my life was over, I had to prepare myself for a gradual death, I was at marriage ages when I thought I could no longer get married, I saw life as meaningless …” (P7).
Escape from reality
The lived experience of these patients shows that after receiving a positive diagnosis of the disease, they found that this fact was difficult to accept and somehow tried to escape from the reality. This experience has been in the form of denial and trying to hide from others.
One of the experiences of these patients in dealing with the positive test result of this disease has been to deny it. In this way, patients believed that the test result was wrong or that the result belonged to someone else. For this reason, the patients referred to other laboratories after receiving the first positive diagnosis of the disease. “…After the lab told me this and found out what the disease really was, I was really shocked and said it was impossible, it was definitely wrong and it is not true … I could not believe it at all, because I was a professional athlete and this could not happen to me. So I immediately went to a bigger city and there I went to a few laboratories for further tests …” (P6).
Trying to hide
These patients stated that after receiving the first positive diagnosis of the disease, they thought that no one should notice their disease and should remain anonymous as much as possible. “…I immediately decided that no one in my city should know that I got this disease and the news should not be spread anywhere, so I discard my phone number through which our city laboratory communicated with me and I came here to do a re-examination and go to the doctor, and after all these years, I always come here again for an examination …” (P4).
In this qualitative study, we attempted to discover lived experience of HIV-infected patients in the face of a positive diagnosis of the disease. Therefore, a descriptive phenomenological method was applied. As a result of this study, based on the experiences of the HIV-infected patients, the five main themes of emotional shock, fear of the consequences, feelings of guilt, discouragement and, escape from reality were obtained.
In this study, it was shown that the confrontation of these patients with the positive diagnosis of the disease causes them to experience a severe emotional shock. In this regard, Yangyang Qiu et al. [ 19 ] argued that anxiety and depression are very common among HIV-infected patients who have recently been diagnosed with the disease. The experience of the participants has shown that this emotional shock appears in the form of loathing and the motivation of social isolation. In fact, in these patients, the feeling of the loathing is an emotional response to the primary carrier that has infected them. The study of Imani et al. [ 20 ] have shown that decrease emotional intelligence in an environment where there is an HIV carrier, other people hate him/her, because they see him/her as a risk factor for their infection. The experience of the participants has also shown that receiving a positive diagnosis will motivate social isolation in these patients. Various studies have revealed that one of the consequences of AIDS/HIV that patients will suffer from, is social isolation [ 21 , 22 ].
Another experience of the participants, according to this study is fear of the consequences. This phenomenon appears in these patients as fear of the death, fear of loneliness, and fear of disgrace. Due to the nature of the disease, these patients feel an inner fear of premature death, as soon as they receive a positive diagnosis. In this regard, the study of Audrey K Miller et al. [ 23 ] showed that death anxiety in AIDS patients is a psychological complication. the participants have stated that they are very afraid of being alone after receiving a positive diagnosis, which is a natural feeling according to Keith Cherry and David H. Smith [ 24 ]; because these patients will mainly experience some degree of loneliness. HIV-infected patients also experienced a fear of disgrace, which will go back to the nature of the disease and people’s insight; but they should be aware that, as Newman Amy states, AIDS/ HIV is a disease, not a scandal [ 25 ].
Another experience of the participants in dealing with the positive diagnosis of the disease is guilt feeling. The patients will experience feelings of regret, the feeling guilty and feeling of the conscience-stricken. The experience of the participants shows that they regret their past. Earlier studies have also revealed that regret for the past is a common phenomenon among the patients living with HIV [ 26 , 27 , 28 ]. HIV-infected feel guilty while facing the positive diagnosis of the disease and consider themselves the main culprit of the situation. They often play a direct role in their infection, and their past lifestyle for sure [ 29 ]. Our study also found that these patients feel the conscience-stricken after a positive diagnosis, because they suspect that they may have infected people around them. This disease can be easily transmitted from the carrier to others if the health protocols are not followed [ 30 , 31 , 32 ].
Another experience of HIV-infected in dealing with the receiving a positive diagnosis of the disease is discouragement. These patients are disappointed and sometimes decide to suicide. Based on the lived experience of HIV-infected, it was found that receiving a positive diagnosis of the disease, will discourage them from life and patients will be disappointed in many aspects of life. Studies have shown that AIDS/HIV, as a crisis, will greatly reduce the patients' life expectancy and that they will continue to live in despair [ 33 ]. Studies also stated that they considered suicide as a solution to relieve stress when receiving a positive diagnosis. In this regard, various studies have emphasized that among the AIDS/HIV patients, loss of self-esteem and severe stress have led to high suicide rates [ 34 , 35 , 36 ].
According to the patients, trying to escape from reality is another phenomenon that they will experience. This phenomenon will occur in patients as denial and trying to hide the disease from others. Based on the lived experience of these patients, it was found that after facing a positive diagnosis, HIV-infected tend to deny that they are infected. In this regard, various studies have shown that AIDS/HIV patients in different stages of the disease and their lives try to deny it in different ways [ 37 , 38 , 39 ]. The HIV-infected also stated that at the beginning of the positive diagnosis of the disease, did not want others to know, so they wanted to hide themselves from others in any way possible. In this regard, Emilie Henry et al. [ 40 ] have shown that a high percentage of the patients living with AIDS/HIV have tried that others do not notice that they are ill.
One of the strengths of this study is the methodology of the study, because in this study, an attempt has been made to use descriptive phenomenology to explain the lived experience of HIV-infected patients when faced with a positive diagnosis of this disease. In fact, in this study, patients' experience of this particular situation was identified, and with careful analysis, the experiences of these people became codes and concepts, each of which can be a bridge that keeps the path of modern knowledge open to help these patients. One of the limitations of this study is the generalizability of the findings because patients’ experiences in different societies that have cultural, religious, subsistence, and economic differences can be different.
The results of this study showed that patients will experience unpleasant experiences in the face of receiving a positive diagnosis of the HIV. Patients’ unpleasant experiences at that moment include emotional shock, fear of the consequences, feeling guilty, discouragement and escape from reality. Therefore, medical and laboratory centers must pay attention to the patients' lived experience, and try to support the patients through education, counseling and other support programs to minimize the psychological trauma caused by the disease.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding authors through reasonable request.
Acknowledgements
The authors would like to express their gratitude to the Hamadan Health Network, the Hamadan Shohada Behavioral Diseases Counseling Center, and the participants who helped us in this study.
The study was funded by Vice-chancellor for Research and Technology, Hamadan University of Medical Sciences (No. 9812209934).
Author information
Authors and affiliations.
Department of Operating Room, School of Paramedicine, Hamadan University of Medical Sciences, Hamadan, Iran
Behzad Imani
Department of Operating Room, Student Research Committee, Hamadan University of Medical Sciences, Hamadan, Iran
Shirdel Zandi
Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran
Salman khazaei
Department of Epidemiology, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
Mohamad Mirzaei
You can also search for this author in PubMed Google Scholar
Contributions
BI designed the study, collected the data, and provide the first draft of manuscript. ShZ designed the study and revised the manuscript. SKh participated in design of the study, the data collection, and revised the manuscript. MM participated in design of the study and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Shirdel Zandi .
Ethics declarations
Ethics approval and consent to participate.
This study is the result of a student project that has been registered in Hamadan University of Medical Sciences of Iran with the ethical code IR.UMSHA.REC.1398.1000.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Imani, B., Zandi, S., khazaei, S. et al. The lived experience of HIV-infected patients in the face of a positive diagnosis of the disease: a phenomenological study. AIDS Res Ther 18 , 95 (2021). https://doi.org/10.1186/s12981-021-00421-4
Download citation
Received : 15 July 2021
Accepted : 26 November 2021
Published : 07 December 2021
DOI : https://doi.org/10.1186/s12981-021-00421-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lived experience
- Phenomenological study
AIDS Research and Therapy
ISSN: 1742-6405
- Submission enquiries: [email protected]
- Español (Spanish)
HIV Overview
Hiv and aids clinical trials.
- A clinical trial is a research study in which people volunteer to help find answers to specific health questions. HIV and AIDS clinical trials help researchers find better ways to prevent, detect, or treat HIV and AIDS.
- Examples of HIV and AIDS clinical trials underway include studies of new HIV medicines, studies of vaccines to prevent or treat HIV, and studies of medicines to treat infections related to HIV and AIDS such as opportunistic infections .
- The details on the benefits and possible risks of participating in an HIV and AIDS clinical trial are explained to volunteers before they decide whether to participate in a study, through a process called an informed consent .
- Use the search feature on ClinicalTrials.gov to find HIV and AIDS studies looking for volunteer participants. Some HIV and AIDS clinical trials enroll only people who have HIV. Other studies enroll people who do not have HIV.
What is a clinical trial?
A clinical trial is a research study in which people volunteer to help find answers to specific health questions. These studies are conducted according to a plan, called a protocol, which include—
- New medicines or new combinations of medicines.
- New medical devices or surgical procedures.
- New, different ways to use an approved, existing medicine or device.
- New ways to change behaviors to improve health.
Clinical trials are conducted in several phases to determine whether new medical studies are safe and effective in people. Results from a Phase 1 Trial , Phase 2 Trial , and Phase 3 Trial are used to determine whether a new drug should be approved by the U.S. Food and Drug Administration for sale in the United States. Once a new drug is approved, researchers continue to track its safety in a Phase 4 Trial .
Interventional trial and observational trial are two main types of clinical trials:
- An interventional study tests (or tries out) an intervention—a potential drug or treatment, medical device, or procedure—in people. Interventional studies are often prospective and are specifically tailored to evaluate the direct effects of new drugs or treatments on disease.
- An observational study does not test potential treatments. Instead, researchers observe participants on their current treatment plan and track health outcomes. Observational studies (also called epidemiologic studies) are mostly retrospective .
What is an HIV and AIDS clinical trial?
HIV and AIDS clinical trials help researchers find better ways to prevent, detect, or treat HIV and AIDS. Every HIV medicine was first studied through clinical trials.
Examples of HIV and AIDS clinical trials include—
- studies of new medicines to prevent or treat HIV and AIDS.
- studies of vaccines to prevent or treat HIV.
- studies of medicines to treat infections related to HIV and AIDS, such as opportunistic infections.
Can anyone participate in an HIV and AIDS clinical trial?
Participation in a clinical trial depends on the study. Some HIV and AIDS clinical trials enroll only people who have HIV. Other studies include people who do not have HIV.
Participation in an HIV and AIDS clinical trial may also depend on other factors, such as age, gender, pregnancy, HIV treatment history, or other medical conditions.
What are the benefits of participating in an HIV and AIDS clinical trial?
Many people participate in HIV and AIDS clinical trials because they want to contribute to HIV and AIDS research. They may have HIV or know someone who has HIV.
People with HIV who participate in an HIV and AIDS clinical trial may benefit from new HIV medicines before they are widely available. HIV medicines being studied in clinical trials are called investigational drugs . To learn more, read the HIVinfo What is an Investigational HIV Drug? fact sheet.
Another benefit of participating in an HIV and AIDS clinical trial is that participants can receive regular and careful medical care from a research team that includes doctors and other health professionals. Often the medicines and medical care are free of charge.
Sometimes people get paid for participating in a clinical trial. For example, they may receive money or a gift card. They may be reimbursed for the cost of meals or transportation.
Are HIV and AIDS clinical trials safe?
Researchers try to make HIV and AIDS clinical trials as safe as possible. However, volunteering to participate in a study testing an experimental treatment for HIV can involve risks of varying degrees. Most volunteers do not experience serious side effects; however, potential side effects that may be serious or even life-threatening can occur from the treatment being studied.
Before enrolling in a clinical trial, potential volunteers learn about the study in a process called informed consent . The process includes an explanation of the possible risks and benefits of participating in the study.
The FDA believes that obtaining a research participant's written informed consent is only part of the process. Once enrolled in a study, people continue to receive information about the study through the informed consent process.
If a person decides to participate in an HIV and AIDS clinical trial, will their personal information be shared?
The privacy of study volunteers is very important to everyone involved in an HIV and AIDS clinical trial. The informed consent process includes an explanation of how a study volunteer’s personal information is protected.
How can one find an HIV and AIDS clinical trial looking for volunteer participants?
There are several ways to find an HIV and AIDS clinical trial searching for volunteer participants.
Use the find a case study search feature ClinicalTrials.gov to find HIV and AIDS studies looking for volunteer participants.
- Call a Clinicalinfo health information specialist at 1-800-448-0440 or email [email protected]
- Join ResearchMatch , which is a free, secure online tool that makes it easier for the public to become involved in clinical trials.
This fact sheet is based on information from the following sources:
From the National Institutes of Health (NIH):
- NIH Clinical Research Trials and You: The Basics
From the National Library of Medicine:
- Learn About Clinical Studies
From the Food and Drug Administration:
- Clinical Trials: What Patients Need to Know
- Informed Consent for Clinical Trials
Also see the HIV Source collection of HIV links and resources.
- Open access
- Published: 27 March 2023
A case study of HIV/AIDS services from community-based organizations during COVID-19 lockdown in China
- Jennifer Z.H. Bouey 1 , 2 ,
- Jing Han 3 ,
- Yuxuan Liu 1 ,
- Myriam Vuckovic 1 ,
- Keren Zhu 2 ,
- Kai Zhou 4 &
BMC Health Services Research volume 23 , Article number: 288 ( 2023 ) Cite this article
2062 Accesses
2 Citations
8 Altmetric
Metrics details
Introduction
People living with HIV (PLHIV) relied on community-based organizations (CBOs) in accessing HIV care and support during the COVID-19 pandemic in China. However, little is known about the impact of, and challenges faced by Chinese CBOs supporting PLHIV during lockdowns.
A survey and interview study was conducted among 29 CBOs serving PLHIV in China between November 10 and November 23, 2020. Participants were asked to complete a 20-minute online survey on their routine operations, organizational capacity building, service provided, and challenges during the pandemic. A focus group interview was conducted with CBOs after the survey to gather CBOs’ policy recommendations. Survey data analysis was conducted using STATA 17.0 while qualitative data was examined using thematic analysis.
HIV-focused CBOs in China serve diverse clients including PLHIV, HIV high-risk groups, and the public. The scope of services provided is broad, ranging from HIV testing to peer support. All CBOs surveyed maintained their services during the pandemic, many by switching to online or hybrid mode. Many CBOs reported adding new clients and services, such as mailing medications. The top challenges faced by CBOs included service reduction due to staff shortage, lack of PPE for staff, and lack of operational funding during COVID-19 lockdowns in 2020. CBOs considered the ability to better network with other CBOs and other sectors (e.g., clinics, governments), a standard emergency response guideline, and ready strategies to help PLHIV build resilience to be critical for future emergency preparation.
Chinese CBOs serving vulnerable populations affected by HIV/AIDS are instrumental in building resilience in their communities during the COVID-19 pandemic, and they can play significant roles in providing uninterrupted services during emergencies by mobilizing resources, creating new services and operation methods, and utilizing existing networks. Chinese CBOs’ experiences, challenges, and their policy recommendations can inform policy makers on how to support future CBO capacity building to bridge service gaps during crises and reduce health inequalities in China and globally.
Peer Review reports
The COVID-19 pandemic is a defining catastrophic public health event of our lifetimes.In China, the COVID-19 pandemic started with a national lockdown in 2020. After two years of conservative intervention focusing on mass testing and quarantine, COVID-19 came back in 2022 and caused millions of infections and an overwhelming death toll, which put a significant strain on China’s healthcare system and paralyzed the economic engine. How do Chinese community organizations support vulnerable populations such as HIV/AIDS patients during such disasters? What policy changes do the Chinese CBOs hope to see? Our case study strives to answer these questions.
China was the first country to encounter the novel coronavirus disease and to implement a strict, large-scale lockdown between January 23, 2020, and April 2020 to contain the virus [ 1 , 2 ]. Most of the 31 provinces in China declared the highest Emergency Level on January 23rd of 2020, enabling local governments to employ social policing mechanisms to enforce quarantine and to close public events with crowd gatherings across the country. Most highways and public transportation were shut down (January 23- February 7) [ 2 ]. All businesses and recreational facilities were closed, except for medical emergency rooms, grocery stores, and keyinfrastructure-related economic activities. In rural areas, many villages stalled traffic and set up entrance checks, whereas urban residential communities required residents to prove their residence to use the weekly grocery shopping quota [ 3 ]. After the outbreak peaked in mid-February, many prefecture-level cities switched from the stringentshutdown to semi-lockdown for another month [ 4 ]. Wuhan, the capital of Hubei province and the origin of the outbreak, experienced the longest lockdown from January 21 to April 7, 2020 [ 5 ]. COVID-19 and the stringent intervention had a profound impact on the lives of the Chinese people during this initial period of the COVID-19 pandemic [ 6 , 7 ].
China is also home to 1.05 million people living with HIV (PLHIV) who needed long-term antiviral medical treatment and care in 2020 [ 8 ]. The central government provides PLHIVs access to free antiretroviral therapy (ART) and free voluntary counseling and testing since 2003 [ 9 ]. In 2016, the new “Treatment for All’’ policy removed the requirement of low CD4 levels as a treatment qualifier. By 2020, about 978,138 PLHIV had gained access to ART, covering 92.9% of all PLHIV in China [ 8 ]. Despite this progress and updated policies, various structural, psychological, and behavioral barriers to ART adherence persist [ 10 ]. Barriers including patients’ concerns for side effects and “pill burden,” lack of effective communication between patients and health care providers, low patient self-efficacy of ART, competing priorities for patients, and depression and stigma associated with HIV [ 11 , 12 ]. Like many Community-Based Organizations (CBO) serving vulnerable populations globally, Chinese CBOs play critical roles in helping PLHIV to improve their access to HIV screening, treatment and care, and reduce stigma, especially among men who have sex with men (MSM) [ 13 , 14 , 15 , 16 ]. In China, there are two main types of CBOs providing services to PLHIV: those independently registered with the state/provincial or local government of Civil Affairs as a non-profit organization, and those affiliated with health clinics and local public health offices without an independent registry [ 17 ]. Both types of CBOs rely on government public health agencies for funding.
COVID-19 has led to unprecedented stress on health and public health systems and has intensified disruptions in HIV prevention, testing, and HIV care continuum services worldwide [ 18 ]. China is not an exception. A Chinese provincial study based on the HIV registration system found a 49% drop in HIV testing rates and a 37% drop in new HIV diagnoses during the first months of COVID-19. In addition, only half of the 475 newly diagnosed HIV patients underwent CD4 count testing and 28.6% did not receive routine linkage to care in the same time period [ 19 ].
Around the world,PLHIV and high-risk populations rely on CBOs for their rich local knowledge, operational flexibility, and direct contact to people in need, to provide humanitarian aid during a crisis [ 20 ]. Facing challenges due to quarantine requirements and transportation service requirements, CBOs in many countries responded by moving their services online and utilizing technology-driven solutions to promote access to HIV counseling, testing, and treatment [ 21 ]. Global [ 22 , 23 ] and China-specific [ 24 ] studies have shown that CBOs promoting community connectedness among MSM resulted in higher HIV testing rates during COIVD-19. However, CBOs themselves are not immune to the negative impact of COVID-19. Preliminary studies in the U.S. have found that the COVID-19 pandemic presents multifaceted challenges to CBOs providing HIV services, including but not limited to structural inequality, resources shortages, and disruption to patient-centered services provision [ 25 , 26 ].
Clearly, more in-depth studies among CBOs are necessary to understand COVID-19’s impact among CBOs serving PLHIV in China. Although several studies in China highlighted the challenges to PLHIV [ 19 , 27 , 28 , 29 ] and healthcare workers [ 30 , 31 ], few looked at the implications for Chinese CBOs during the lockdowns. Only one stakeholder study published in English included 17 CBO workers in the interviews and found that CBOs could assist HIV care among PLHIV in multiple ways during COVID-19 [ 13 ].
In this study, a team of CBO leaders, clinicians, and public health researchers try to answer the following questions using data collected from a mixed-method study (survey and focus group): What challenges did PLHIV face during the first pandemic lockdown in China? What were the challenges to the CBOs and how did they cope? What innovation came out of the crisis? What gaps in CBOs’ capacity were revealed and how to build better preparedness for future emergencies? The study provides critical information on how best to prepare and utilize community organization services on HIV care during a public health emergency or a disaster.
Study design and participants
The study research team included HIV specialists of a large infectious disease hospital in Beijing, their affiliated and long-term CBO partner “Home of Red Ribbon (HRR),” staff of the Joint United Nations Programme on HIV/AIDS (UNAIDS) Beijing office, and global health researchers from Georgetown University and the RAND Corporation, an American think tank that develops solutions to public policy challenges. HRR was founded in 1999 to serve local PLHIV. In 2019, HRR founded the “Beijing Red Ribbon Alliance,” a national platform with 60 + CBO members serving PLHIV. In this study, CBO participants were recruited by HRR from the Alliance. They come from all seven geographic regions of China and were considered reliable information sources based on previous collaborations with HRR. Organizations participating in the study had to meet the following criteria: (a) established Chinese CBOs providing HIV prevention and treatment services; (b) delivered services from January 20, 2020, to April 29, 2020; and (c) would like to provide informed consent for the study. Among survey invitations to 32 qualified CBOs, 29 CBOs responded. Three CBOs have multiple branch offices that completed the survey, yielding a 90% response rate.
Data collection
Both qualitative and quantitative data on service provision and needs during the COVID-19 pandemic were collected from the participating CBOs. A 20-minute online survey with both closed- and open-ended questions was first disseminated and collected between November 10 and November 23, 2020, and a virtual focus group interview was conducted on November 13, 2020. In addition to the survey data, detailed notes from the focus group interview were used for theme analysis. All data collection followed the principles of confidentiality and voluntary participation. There were no consequences if a participant withdrew from the study. The study protocol was approved by the Ditan Hospital Internal Research Board (IRB number: KY2020-019).
The online survey questionnaire was designed by the research team staff from Beijing Ditan Hospital with HRR. A Chinese online survey platform “Wen-Juan-Xing’’ was used to host the survey, which was then disseminated to the invited participants through the social media app WeChat. The CBO organizations that completed the online survey received RMB 800 (approximately USD 125) for their participation. The questionnaire contained nineteen close-ended multiple-choice questions and eleven open-ended short-answer questions to cover the following three domains:
CBO routine operational characteristics
questions obtained information on the CBO’s location of operation, operational years, registration status, number of full-time and part-time staff and volunteers, presence of PLHIV among staff and volunteers, CBO’s social media platform usage, target client populations and routine services provided.
Service provision during COVID-19
questions included CBO’s operational modes during COVID-19, presence of operation interruptions during the pandemic, CBO’s target client populations during the pandemic, types of services requested and provided during the pandemic. The survey also asked about the ways clients contacted CBOs during the COVID-19 lockdown.
If CBOs reported unresolved requests or an interruption in service provision during COVID-19 lockdowns, they were asked to provide follow-up information on the types of such requests in open-ended short answers, whether service provision had resumed, and whether there was staff loss. Finally, the CBOs were asked to rate their satisfaction on their collaborations with government agencies and other CBOs during the pandemic.
Needs and organizational capacity building
questions started with a description of the CBO’s operational advantages and challenges during COVID-19, including short answers on CBOs’ most urgent needs, the relative advantages of their organizations compared to other CBOs, and whether their services were better recognized and expanded during COVID-19. They also estimated whether COVID-19 was helpful or not, in terms of future prospects of the organization.
Focus group interview
While the survey focused on the challenges CBOs faced during the lockdown, a focus group interview was set up to help researchers contextualize the findings of the survey and to collect policy recommendations to support CBOs’ work in future outbreaks. All 29 survey participants were invited to the focus group interviews and eighteen CBOs (62%) participated through Tencent Meeting (an online meeting platform in China) after they completed the survey. The focus group interview was led by a Ditan Hospital HIV specialist and an HRR staff following a semi-structured question guide. The semi-structured question guide was developed to capture the following themes: (a) what services delivery challenges they encountered during COVID-19 in 2020; (b) which special groups of patients (e.g., elderly, people with disability etc.) came to their service during the COVID-19 lockdown; (c) what innovation and lessons they have learned from providing services for PLHIV during the COVID-19 pandemic; and (d) what policy recommendations do they have to enhance CBOs’ service delivery in future pandemics.The online focus group interview lasted two hours until data saturation was achieved. Detailed field notes were used for data analyses.
Data analysis
Online survey data was collected and managed through the online service platform Wen-Juan-Xing and analyzed using STATA 17.0 [ 32 ]. We first provided descriptive statistics to summarize the characteristics of the CBOs operations, services, and clients during COVID-19 with multiple choice questions. We then used thematic analysis to analyze and explore potential themes of the open-ended questions. Two independent researchers followed the analytic process recommended for thematic analysis [ 33 ]: (a) familiarizing themselves with the data; (b) generating-e initial themes and codes; (c) coding the open-ended answers according to the themes; (d) discussing the differences, obtaining consensus, and finalizing the name of the themes; and (e) producing the report for the results section. The same approach was used to summarize additional themes from the notes of the focus group interview. Quotations were used to highlight the findings. Both survey and focus group scripts were analyzed in Chinese and translated to English for the report. Back translations were used to check for translation accuracy.
Characteristics of CBOs
29 CBOs participated in the study and their characteristics aree summarized in Table 1 . More than half (55.2%) were registered with the Chinese government as a civil organization, while 13 CBOs (44.8%) were affiliated with hospitals or the local public health agencies. More than one third of the CBOs (41.4%) in the study were located in the North or Northeast Region of China, about another third (34.5%) were from Eastern or Southern China, and seven (24.1%) CBOs were from West China. Number of staff was another measurement of the operation scale: 41.4% (n = 12) of CBOs reported more than 50 staff, while only two (6.9%) reported having less than 10 staff (Table 1 ). 69.0% of CBOs employed PLHIV, and all organizations reported having PLHIV among their volunteers.
CBOs’ new services during the COVID-19 lockdown
Even before COVID-19, Chinese CBOs often served a diverse client population. In our study, the majority (96.4%) of CBOs reported providing services to MSM, 80% catered to PLHIV, 60.7% provided services to adolescents at risk, and others facilitated services to migrants (28.6%), female commercial sex workers (25%), substance users (7.1%), children affected and orphaned by AIDS (14.3%), and the general public (25%) before the COVID-19 pandemic (Table 2 ). During COVID-19 lockdowns, almost all CBOs reported providing new services to non-local clients seeking HIV related services when they could not go back to their routine medical services (n = 28, 96.6%), and to their regular clients who got stranded in other cities (n = 26, 89.7%), in addition to their regular local clients. These new services were requested through various channels, including peer referrals, online platforms and group chats, hospitals and clinics, and through CBOs’ pre-pandemic services.
The scope of CBO services also changed during the COVID-19 lockdown period. While most CBOs reported continued provision of regular services, they had to add services unique to the lock-down period, including mailing ART medicines and post-exposure prophylaxis (PEP), supporting family notification of PLHIV’s HIV status, and peer support (Table 2 ).
Not only did the service requests intensify during the COVID-19 lockdown, but many CBOs also had to switch their on-site services to phone- and online-based when the travel restrictions hit. All participating CBOs reported using one or more new platforms such as WeChat, TikTok, etc. for services during this period (Table 2 ). Meanwhile, most CBOs still maintained on-site services except for five who stopped providing in-person services.
To cope with the challenges brought by the pandemic, many CBOs turned to innovative communication strategies and digital technology to secure medicine supplies. One CBO said: “There are 10 internet volunteers to promote online, and 5 volunteers to make appointments for testing, so that you can ensure access to various HIV supplies via the internet without having to come to the office.” (Medium CBO, 5–9 yrs of operation, independent, large city in the West). Six CBOs also attributed human-centered care and respect for PLHIV, their rapport with marginalized clients, and their ability to operate at the grass-roots level as key factors in their success. As one CBO put it: “Government agencies work according to rules and regulations, while friends of the community work more on the basis of their enthusiasm and human feelings for the community.” (Large CBO,10–14 yrs of operation, independent, small city in the Northeast/North).
Challenges and coping strategies during COVID-19
While many CBOs successfully carried out services for PLHIV, challenges still mounted during the unexpected lockdowns. In the survey, most CBOs (90%) reported unmet needs from their clients during the pandemic, especially on access to ART (41%), referral to health care (24%), and HIV testing and confirmation (21%). About a third of CBOs reported that their services were disrupted by the pandemic, particularly their in-person services (31.0%). Among the services most impacted were in-person HIV testing (27.6%), in-person counseling (10.3%), in-person volunteering (3.4%) and outreach (3.4%). After the lockdown, all CBOs resumed their services. However, 33.3% of organizations reported losing staff.
When asked about the top three challenges during the COVID-19 lockdown, 18 CBOs identified limited service provision modes as their main challenge, followed by shortage of personal protective equipment (PPE) for staff (51.7%), lack of funding (37.9%), staff shortages and loss of staff and volunteers (17.2%), limited or slow HIV testing services (10.3%), lack of support from other sectors and society at large (3.4%), limited medical resources (3.4%), and hard to obtain and deliver medication (13.8%). CBOs also mentioned short-term funding shortfalls, weak Wi-Fi, and inaccessibility of office space as challenges.
One additional challenge CBOs reported was the lack of mail courier services, especially in remote areas and to college students who live on locked-down campuses. One CBO observed: “Some patients stop taking their medication when they can’t even get to the courier company in places where transportation is inconvenient.” (Medium CBO, 5–9 yrs of operation, civil governance registered, medium city in the West). Another said: “It is difficult to give medication to students because the school is very strict, no deliveries to campus for 8 months, and security checks to enter school, risking exposure of privacy.” (Medium CBO, 5–9 yrs of operation, independent, small city in the West).
Another common challenge was associated with HIV testing and confirmation tests: “There has been no opportunity to confirm and then start treatment for infected persons with positive initial screening due to the lockdown and home isolation…. Someone tested positive in July and it took three months to confirm.” (Medium CBO, 5–9 yrs of operation, independent, small city in the West).
Finally, several CBOs mentioned that they could not meet clients’ needs in gaining peer support, resolving financial issues and how to navigate other barriers.
An important coping strategy among the CBOs was building collaboration with various government agencies, including local CDC (86.2%), hospitals (86.2%), the Ministry of Public Security (10.3%), and local government organizations or other agencies (10.3%). On a scale from 0 to 10, most organizations were very satisfied with their collaborations during the pandemic (24 CBOs > 8), four CBOs were somewhat satisfied (ratings of 5–7), and only one CBO was completely unsatisfied (rating of 0). Almost 80% of CBOs reported collaborations with other non-governmental organizations, mostly with similar organizations in the same region (e.g., provincial and municipal sister agencies). Such collaboration helped relieve shortages of service, medicine, and PPEs.
CBO’s sustainability and capacity building needs
When asked about the top three areas of needs, 15 CBOs named funding and personnel as their top need (51.72%). Other top needs included technical assistance, supplies, organizational capacity building, and collaboration among CBOs and with other sectors. While the second and third needs varied, organizational capacity building was mentioned seven times (24.14%), demonstrating its significance for the CBOs. Only two CBOs did not report any external needs.
Many organizations felt that the capacity needed during the pandemic were better coordination and communication skills (27.6%), flexibility (20.7%), and good service provision (13.8%). Six CBOs also emphasized that the ability to provide online consultation and telemedicine services were useful skills during a pandemic. A large network and emergency response training were also desirable capacities reported by the CBOs.
Despite the many challenges faced by the participating CBOs and their clients during the COVID-19 pandemic, most of the CBOs felt that they had gained popularity during the pandemic, and many mentioned thank-you-notes from their clients. They were also able to build a larger network with requests from other organizations (34.5%), received media coverage (20.7%), and additional project funding (31.0%) during the pandemic. About half of the CBOs considered the COVID-19 pandemic beneficial to their organization’s development.
Policy recommendations from the CBOs
The focus group interview helped confirm capacity-building needs. More importantly participating CBOs also offered the following recommendations during the focus group discussion, which expand on the needs expressed in the survey. We summarized the policy recommendations in the following:
Create regional CBO service alliance networks : “Alliances can be formed between community organizations, and a directory of information on local drug assistance, etc., can be produced and sent to patients so that they can refer to the directory for targeted help.” (Large CBO, 5–9 yrs of operation, independent, mega city in the Northeast/North).
Strengthen multisectoral cooperation between CBOs, hospitals, the CDC, community level government and community health centers from different regions: “… the local CDC alone may not be able to get the job done. There is a need for the creation of a network of emergency support services in the event of an emergency.” (Large CBO, 14 yrs + of operation, civil governance registered, large city in the Northeast/North).
Develop standardized emergency response operational manuals/guidelines (including recruitment). One CBO talked about preparing both CBOs and their clients by establishing guidelines: “There should be guidelines for patients, but also for community organizations, including what community organizations can do, how to do it, how to do risk assessment (e.g. group lending, mutual aid lending), and what are the channels for obtaining supplies; for patients, it is a manual for self-management of infected persons in case of emergency.” (Large CBO, 14 yrs + of operation, civil governance registered, large city in the Northeast/North).
Support PLHIV community resilience building . Many CBOs discussed ways to build resilience among PLHIV during emergencies, including on ART: “Infected people need to be better guided and educated about treatment adherence.” (Small CBO, 5–9 yrs of operation, independent, medium city in the East/South).
Optimize medicine access during a crisis . CBOs identified access to medicine as the top challenge during COVID-19 and the necessity of flexible policy on longer-term prescriptions: “It would be better for the infected to be prepared when something like this happens again, and to have peace of mind, if they are advised by the agency that dispenses the drugs.” (Large CBO,5–9 yrs of operation, independent, medium city in the East/South).
Build a larger volunteer pool to offset staff shortage during a crisis : “Policies are needed to involve volunteers in the fight against the pandemic and AIDS.” (Medium CBO, 5–9 yrs of operation, independent, small city in the West).
COVID-19 posed unprecedented challenges to global health and reversed decades of hard-earned progress on health [ 34 ]. Our study was one of the first to survey and interview frontline CBO staff that serve PLHIV around China in the first year of the pandemic. The CBOs in our study varied in their operational size and their affiliations status with the CDC and clinics. While some work in urban centers with advanced economic development, others are located in rural districts. In both the survey and the focus group interview, the common themes were the challenges they faced unexpectedly when COVID-19 hit and how the strict lockdown added to their service scope and forced them to change service methodology. Our survey findings add to the growing literature on resilience of communities during a natural disaster and highlight the importance of networking, digital platforms, and operational flexibility among grass-root community organizations. The focus group interview with the CBOs further explained the mechanisms of coping and provided a much-needed reflection on the need for capability building for future pandemics or disasters.
Our study found that CBOs serving people living with HIV in China often had at least 5–10 years of experience working with local PLHIV and generally have good working knowledge and close collaborations with local public health agencies and medical institutions. This type of three-in-one network has proven to improve performance metrics on disease testing and detections among high-risk populations [ 35 ]. The community organizations also serve a diverse population, including PLHIV as well as people at higher risk for HIV, such as MSM and female sex workers, and routinely carry out services including health promotion, peer support, and treatment coordination. Many CBOs have volunteers from the local PLHIV or high-risk population, which enables them to conduct targeted outreach and build trust with their clients. This finding validates a community resilience theory [ 36 ] that named four primary sets of adaptive capacities as critical to community resilience: social capital, economic development, information and communication, and community competence. The social capital, community competency, and communication skills of the CBOs have helped the organizations to achieve high efficiency in HIV control with flexible working venues and low operating costs.
During emergencies, to build collective resilience, communities must create organizational linkages, boost and protect social supports, and plan for not having a plan – which requires flexibility, decision-making skills, and trusted sources of information that function in the face of unknowns [ 36 ]. Our study found that CBOs that can provide PLHIV with wider organizational connections and mobilize social support through flexible operation plans, had a pivotal role in building community resilience during COVID-19. For example, despite the fact that the National Center for AIDS/STD Control and Prevention of China’s CDC issued a special policy to facilitate ART treatment continuity among PLHIV at the early stage of the COVID-19 pandemic [ 37 ], travel restrictions under the COVID-19 lockdown still had a significant impact on PLHIV’s access to and the CBO’s ability to provide services, such as ART, testing, and other medical care [ 13 ]. Since the lockdown happened at Chinese New Year, a time when internal migration is at its peak and a large population visits their family away from where they work, many PLHIV found themselves stuck in places away from their routine care. Many who had to quarantine with their parents found themselves having to forgo privacy and to disclose to their parents and families for the first time that they needed HIV care [ 27 , 38 ]. Meanwhile, most of the local staff at public health stations were redeployed to respond to COVID-19. CBOs found significant workload increase with new clients stranded in their location in need of HIV care, new demands to coordinate HIV treatment continuity and testing, and additional requests on peer support in this time of crisis. In response, many CBOs had to make quick decisions to switch their service online and to seek new connections with fellow organizations and new government agencies– with varying success as our survey showed. Similar to our study’s findings, a 2020 China AIDS Fund for NGOs and UNAIDS’s CBO survey found that 87% of community organizations set up their own hotlines and implemented flexible working hours for volunteers during the COVID-19 epidemic from February to April 2020, to provide AIDS-related services. Nearly half added express mailing services for delivery of HIV self-testing kits and medicine to their services [ 39 ].
The same UNAIDS survey revealed that some CBOs encountered difficulties in HIV/AIDS services during the peak of the pandemic during February and March of 2020. The main reasons for the service interruption were urban traffic control (86%) and CDC staff who were unable to support AIDS prevention work (51%) because of their participation in the prevention and control of the COVID-19 epidemic. By the end of April 2020, about 53% of community organizations had fully restored their services, and 42% had restored some services [ 39 ]. Our findings are in line with the scenario described in the UNAIDS report and found the most critical challenges to the CBOs to be a lack of funding, limited service provision methods, shortage of staff and PPE, limited medical resources, testing and medication delivery capacities, and lack of support and understanding from society at large. All these factors contributed to CBOs’ service disruption, in addition to the reasons identified by the UNAIDS survey.
Paton (2000) defined community resilience as the capacity to bounce back and use physical and economic resources effectively to aid recovery following exposure to hazards [ 40 ]. In an earlier report for UNAIDS, we found that as a vulnerable population, PLHIV faced unique challenges during the unexpected COVID-19 lockdowns [ 41 ]. However, they had better resiliency resources – the CBOs that had already served their community before the pandemic – compared to other vulnerable populations, such as migrant workers and people with disabilities in China [ 41 ]. To build stronger resilience in the face of future disaster situations, the CBOs in our study offered multiple suggestions that we can summarize into four recommendations: First, enhance CBOs network building both horizontally and vertically: horizontally among CBOs with similar missions across different geographic areas so that when PLHIV travel, they can rely on the network for the continuation of support; vertically between CBOs and multiple hierarchies of government and healthcare facilities for resource coordination. Such collaborations should be included in government-level emergency response plans and policies to ensure the continuation of support for PLHIVs.
Secondly, funding agencies should consider supporting CBOs’ capacity building in communication and technology upgrades so that CBOs can expand their digital direct service platforms and mobilize resources during a crisis.
Thirdly, CBOs should consider strengthening their volunteer base and building a workforce reserve for their community-based services to prepare for staff shortages during emergencies. CBOs can mobilize these local talents from various groups. One way is to empower PLHIV to become peer supporters/volunteers during emergencies. Their presence in an emergency response would benefit the utilization of community-based services, and reduce PLHIV’s unease to disclose their status and seek help. Another way to engage more talents to grassroot community governance is to provide CBO-based internships for college students and professional training institutes (e.g., to students of public health, medicine, sociology, or other related fields). Efforts should also be made to cultivate professional talent serving grassroot communities, adjust policies and incentive mechanisms, and encourage more experts to provide intellectual support for community governance. Encouraging the public to participate in grassroots social governance can also help empower community members and generate increased cohesion and community resilience.
Finally, the CBOs’ capacity building should include a community-level emergency response plan. Education on disaster prevention and mitigation at the community level should be strengthened, and communities with excellent emergency response and disaster relief operations should be promoted as models, so their experiences can be shared. Bureaucratically and institutionally, the division of labor in emergency response and community governance should be further clarified, and community staff should receive training in emergency planning and response, to provide speedy and efficient public service when faced with future uncertainties and emergencies.
The findings of this study should be viewed in the context of several limitations. First, the study survey was cross-sectional. Therefore, causal inference could not be established, and the results can only reflect the situation of CBOs during a certain period during the pandemic. Second, the study only analyzed 29 responses from different CBOs and their operational branches, utilizing the connections of HRR. The limited number of participants and the recruitment method may have led to biased results, as the selected CBOs might not be representative of the population. Third, all information in the study was self-reported by one manager of each CBO, thus is subject to risk of bias.
Risks and vulnerabilities induced by pandemics and other natural hazards and disasters are on the rise globally. Some emergencies, such as COVID-19, have severe and widespread destructive impacts on health, the economy, social development, and global supply chains. In this context, community resilience to disasters is critical for government hazard mitigation and recovery planning [ 36 , 42 ]. Our case study showed that CBOs serving a highly stigmatized and vulnerable population before the crisis were instrumental in building resilience in the community. They were able to quickly mobilize resources, set up new business platforms/models, and expand their network to meet unprecedented challenges. They also identified key areas for capacity building for future crisis preparedness. Their experience and reflections may help governments, communities, and international organizations when considering how to reduce health inequity and how to serve those who need long-term healthcare during an unexpected natural or manmade crisis.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Molefi M, Tlhakanelo JT, Phologolo T, Hamda SG, Masupe T, Tsima B, et al. The impact of China’s Lockdown Policy on the incidence of COVID-19: an interrupted Time Series Analysis. Biomed Res Int. 2021;2021:9498029.
Article PubMed PubMed Central Google Scholar
Full, Text. Fighting COVID-19: China in Action [Internet]. [cited 2022 Apr 12]. Available from: http://www.scio.gov.cn/zfbps/32832/Document/1681809/1681809.htm
Ren X. Pandemic and lockdown: a territorial approach to COVID-19 in China, Italy and the United States. Eurasian Geogr Econ. 2020 Sep;61(2):423–34.
Leung K, Wu JT, Liu D, Leung GM. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. The Lancet. 2020 Apr25;395(10233):1382–93.
Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of Public Health Interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020 May;19(19):1915–23.
Jia P, Liu L, Xie X, Yuan C, Chen H, Guo B et al. Changes in dietary patterns among youths in China during COVID-19 epidemic: The COVID-19 impact on lifestyle change survey (COINLICS). Appetite. 2021 Mar 1;158:105015.
Ren X, Huang W, Pan H, Huang T, Wang X, Ma Y. Mental Health during the Covid-19 outbreak in China: a Meta-analysis. Psychiatr Q. 2020 Dec;91(4):1033–45.
He N. Research Progress in the Epidemiology of HIV/AIDS in China.China CDC Wkly. 2021 Nov26;3(48):1022–30.
Wu Z, Chen J, Scott SR, McGoogan JM. History of the HIV Epidemic in China. Curr HIV/AIDS Rep. 2019;16(6):458–66.
Zhou G, Li X, Qiao S, Zhou Y, Shen Z. Psychological and behavioral barriers to ART adherence among PLWH in China: role of self-efficacy. AIDS Care. 2017 Dec;29(12):1533–7.
Zhou G, Li X, Qiao S, Shen Z, Zhou Y. Influence of Side Effects on ART Adherence Among PLWH in China: The Moderator Role of ART-Related Knowledge. AIDS Behav. 2018 Mar 1;22(3):961–70.
Chen W-T, Shiu C, Yang JP, Chuang P, Zhang L, Bao M, et al. A structural equation model of patient-healthcare provider relationships and HIV-infected patient outcomes in chinese populations. AIDS Care. 2018 Mar;30(3):383–90.
Sun Y, Zhan Y, Li H, Yuan T, Gao Y, Liang B, et al. Stakeholder efforts to mitigate antiretroviral therapy interruption among people living with HIV during the COVID-19 pandemic in China: a qualitative study. J Int AIDS Soc. 2021 Sep;24(9):e25781.
Yan H, Zhang M, Zhao J, Huan X, Ding J, Wu S, et al. The increased effectiveness of HIV preventive intervention among men who have sex with men and of follow-up care for people living with HIV after “task-shifting” to community-based organizations: a “cash on service delivery” model in China. PLoS ONE. 2014;9(7):e103146.
Tao J, Li M, Qian H-Z, Wang L-J, Zhang Z, Ding H-F, et al. Home-based HIV testing for men who have sex with men in China: a novel community-based partnership to complement government programs. PLoS ONE. 2014;9(7):e102812.
Cheng W, Cai Y, Tang W, Zhong F, Meng G, Gu J et al. Providing HIV-related services in China for men who have sex with men. Bull World Health Organ. 2016 Mar 1;94(3):222–7.
Liu L, Wang D, Qin X, Hu Z, Chen R. The impact of social capital on civil society organizations delivering voluntary counseling and testing HIV/AIDS service: a cross-sectional study in China.Biosci Trends. 2020 Jul17;14(3):182–91.
Ogunbodede OT, Zablotska-Manos I, Lewis DA. Potential and demonstrated impacts of the COVID-19 pandemic on sexually transmissible infections.Curr Opin Infect Dis. 2021 Feb1;34(1):56–61.
Shi L, Tang W, Hu H, Qiu T, Marley G, Liu X et al. The impact of COVID-19 pandemic on HIV care continuum in Jiangsu, China. BMC Infect Dis. 2021 Aug 7;21(1):768.
Han J, Su Y, Zhou Z, Wang K, Yu Y, Huang H, et al. Analysis of antiretroviral medicine availability to people living with HIV from different designated medical institutions during the COVID-19 pandemic. Chin J AIDS STD. 2020;26(07):698–700.
Google Scholar
Harsono D, Deng Y, Chung S, Barakat LA, Friedland G, Meyer JP et al. Experiences with Telemedicine for HIV Care During the COVID-19 Pandemic: A Mixed-Methods Study. AIDS Behav. 2022.
Painter TM, Song EY, Mullins MM, Mann-Jackson L, Alonzo J, Reboussin BA, et al. Social support and other factors associated with HIV testing by Hispanic/Latino gay, bisexual, and other men who have sex with men in the U.S. South. AIDS Behav. 2019 Oct;23(Suppl 3):251–65.
Grover E, Grosso A, Ketende S, Kennedy C, Fonner V, Adams D, et al. Social cohesion, social participation and HIV testing among men who have sex with men in Swaziland. AIDS Care. 2016;28(6):795–804.
Article PubMed Google Scholar
Lyu H, Zhou Y, Dai W, Zhen S, Huang S, Zhou L, et al. Solidarity and HIV Testing willingness during the COVID-19 epidemic: a Study among Men who have sex with men in China. Front Public Health. 2021 Dec;9:9:752965.
Pinto RM, Park S. COVID-19 pandemic disrupts HIV Continuum of Care and Prevention: implications for research and practice concerning community-based Organizations and Frontline Providers. AIDS Behav. 2020;24(9):2486–9.
Robillard AG, Julious CH, Smallwood SW, Douglas M, Gaddist BW, Singleton T. Structural inequities, HIV Community-Based Organizations, and the end of the HIV Epidemic. Am J Public Health. 2022 Mar;112(3):417–25.
Sun Y, Li H, Luo G, Meng X, Guo W, Fitzpatrick T, et al. Antiretroviral treatment interruption among people living with HIV during COVID-19 outbreak in China: a nationwide cross-sectional study. J Int AIDS Soc. 2020 Nov;23(11):e25637.
Sun S, Hou J, Chen Y, Lu Y, Brown L, Operario D. Challenges to HIV Care and Psychological Health during the COVID-19 pandemic among people living with HIV in China. AIDS Behav. 2020 Oct;24(10):2764–5.
Booton RD, Fu G, MacGregor L, Li J, Ong JJ, Tucker JD et al. The impact of disruptions due to COVID-19 on HIV transmission and control among men who have sex with men in China. J Int AIDS Soc. 2021 Apr 6;24(4):e25697.
Yang X, Zeng C, Tam CC, Qiao S, Li X, Shen Z et al. HIV Service Interruptions During the COVID-19 Pandemic in China: The Role of COVID-19 Challenges and Institutional Response from Healthcare Professional’s Perspective. AIDS Behav. 2021 Oct 6
Qiao S, Yang X, Sun S, Li X, Mi T, Zhou Y, et al. Challenges to HIV service delivery and the impacts on patient care during COVID-19: perspective of HIV care providers in Guangxi, China. AIDS Care. 2021 May;33(5):559–65.
StataCorp. Stata Statistical Software: Release 17. College Station. TX: StataCorp LLC; 2021.
Nowell LS, Norris JM, White DE, Moules NJ. Thematic Analysis: Striving to Meet the Trustworthiness Criteria. International Journal of Qualitative Methods. 2017 Dec 1;16(1):1609406917733847.
Fenner R, Cernev T. The implications of the Covid-19 pandemic for delivering the Sustainable Development Goals. Futures. 2021 Apr;128:102726.
Zhang D, Lu H, Zhuang M, Wu G, Yan H, Xu J et al. Enhancing HIV Testing and Treatment among Men Who Have Sex with Men in China: A Pilot Model with Two-Rapid Tests, Single Blood Draw Session, and Intensified Case Management in Six Cities in 2013. PLoS One. 2016 Dec 1;11(12):e0166812.
Norris FH, Stevens SP, Pfefferbaum B, Wyche KF, Pfefferbaum RL. Community Resilience as a Metaphor, Theory, Set of Capacities, and Strategy for Disaster Readiness. Am J Community Psychol. 2008;41(1–2):127–50.
National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention. Notice on guaranteeing the free HIV antiretroviral treatment drugs supply for stranded people living with HIV - Notice - Chongqing Network for HIV/AIDS Communication and Education [Internet]. [cited 2022 Apr 12]. Available from: http://www.cqaidsw.com/index php?m=content&c=index&a=show&catid=58&id=4389
Mi T, Li X, Zhou G, Qiao S, Shen Z, Zhou Y. HIV Disclosure to Family Members and Medication Adherence: role of social support and self-efficacy. AIDS Behav. 2020 Jan;24(1):45–54.
UNAIDS. Research | The impact of the COVID-19 pandemic on CBOs. ’ HIV prevention and treatment services [Internet]. WeChat. [cited 2022 Apr 12]. Available from: http://mp.weixin.qq.com/s?__biz=MzA3OTgxODkwNA==&mid=2649756780&idx=1&sn=99f89e502150e931386347ca2d2948d0&chksm=87a90d9bb0de848db8760a36e4e2358d150f1e9081f6a4eb6ccb6f554accba23b749251584e0#rd
Paton D. Emergency planning: integrating community development, community resilience and hazard mitigation. J Am Soc Prof Emerg Managers. 2000 Jan;1:7:109–18.
Guo W, Wen H L, Bai H, Liu J, Wei X N, Zhou K, Sande A. Quick community survey on the impact of COVID-19 outbreak for the healthcare of people living with HIV. Chinese J Epidemiol. 2020 May;41(5):662–666.
Rose A. Defining and measuring economic resilience to disasters. Disaster Prevention and Management: An International Journal. 2004 Jan 1;13(4):307–14.
Download references
Acknowledgements
Thanks to all community organizations serving HIV patients and people who are at high risk for HIV in China, who participated in the survey and focus group discussion. Special thanks to the House of Red Ribbon that coordinated interviews and focus groups, and to UNAIDS China Office for providing support on information and data analysis.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Department of Global Health, School of Health, Georgetown University, 3700 Reservoir Road NW, Washington, DC, 20057, USA
Jennifer Z.H. Bouey, Yuxuan Liu & Myriam Vuckovic
RAND Corporation, Santa Monica, CA, USA
Jennifer Z.H. Bouey & Keren Zhu
Ditan Infectious Disease Hospital, Beijing, China
UNAIDS China, Beijing, China
Home of Red Ribbon, Beijing, China
You can also search for this author in PubMed Google Scholar
Contributions
Jing Han, Jennifer Bouey designed the study and manuscript, Jing Han and Ye Su. collected data, Yuxuan Liu, Myriam Vuckovic conducted data analysis, Jennifer Bouey, Yuxuan Liu, Myriam Vuckovic drafted the manuscript., Keren Zhu and Kai Zhou participated in drafting and editing.
Corresponding author
Correspondence to Jennifer Z.H. Bouey .
Ethics declarations
Ethical approval.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Ditan Hospital Internal Research Board (IRB number: KY2020-019).
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Not applicable.
Competing interests
The authors have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bouey, J.Z., Han, J., Liu, Y. et al. A case study of HIV/AIDS services from community-based organizations during COVID-19 lockdown in China. BMC Health Serv Res 23 , 288 (2023). https://doi.org/10.1186/s12913-023-09271-4
Download citation
Received : 02 August 2022
Accepted : 10 March 2023
Published : 27 March 2023
DOI : https://doi.org/10.1186/s12913-023-09271-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- HIV/AIDS care
- Community-based Organizations
- Telemedicine
- Community capacity building
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- High-Impact Prevention
- Case Studies
- National Center for HIV, Viral Hepatitis, STD, and Tuberculosis Prevention
HIV Screening and Testing
What to know.
HIV testing and screening are important first steps in diagnosing infection. Diagnosing HIV infection early is cost-effective and saves the public money on direct medical costs. Expanding HIV testing saves lives and prevents others from getting infected.

The benefits of HIV screening and testing
In 2015, approximately 39,000 persons received a new HIV (human immunodeficiency virus) infection diagnosis. HIV testing is the vital first step for HIV care and effective prevention. These persons had been living undiagnosed with HIV but now know their status and have the opportunity to receive life-saving treatment.
HIV diagnosis also greatly reduces the risk of transmitting the virus to others. Persons without HIV learn about effective tools for reducing their risk of getting infected.
Cost-effectiveness of HIV screening and testing
Initial studies reported voluntary HIV screening to be cost-effective in health care settings where undiagnosed HIV infection is less than ≥0.1% 1 2 . It was also reported to be more cost-effective than many established screening programs for chronic disease (e.g., hypertension, colon cancer, and breast cancer). 2 3 Treatment costs are lowered as well because treatment can begin before severe immunologic compromise occurs.
A more recent study reported HIV testing in clinical settings is cost-saving. This study focused on a model with consistent, standardized methods of evaluating the costs and effects of established and emerging HIV prevention strategies. 4
The unit cost of testing was adjusted by the positivity rate of persons tested (0.6%). This was based on reports of HIV testing from CDC-funded sites to find a cost per new diagnosis. It found that the cost per case of HIV prevented by testing in a clinical setting was less than the lifetime treatment cost per HIV case.
Effectiveness of expanded testing in the United States
CDC-funded testing programs in the U.S. are substantial. They led to approximately one-third of all new HIV diagnoses in 2013.
From 2007 to 2010, CDC-funded Expanded Testing Initiative sites provided more than 2.8 million HIV tests. These tests resulted in approximately 18,000 new HIV diagnoses and saved $1.2 billion in direct medical costs. 4 For every $1.00 spent on HIV testing, CDC saved the general public $2.00 on direct medical costs.
As more people receive an HIV infection diagnosis, the percentage of people who are unaware of their infection decreases. In 2006, 19% of persons with HIV were unaware of their infection. In 2014, this decreased to 15%. 5 Some of the biggest improvements were among young gay and bisexual males between the ages of 13-24. 6 This group was previously at the highest risk of HIV infection.
- Walensky RP, Weinstein MC, Kimmel AD, et al. Routine human immunodeficiency virus testing: an economic evaluation of current guidelines. Am J Med 2005;118:292–300.
- Paltiel AD, Weinstein MC, Kimmel AD, et al. Expanded screening for HIV in the United States—an analysis of cost-effectiveness. N Engl J Med 2005;352:586–95.
- Sanders GD, Bayoumi AM, Sundaram V, et al. Cost-effectiveness of screening for HIV in the era of highly active antiretroviral therapy. N Engl J Med 2005;352:570–85.
- Lin F, Farnham PG, Shrestha RK, Mermin J, Sansom SL. Cost effectiveness of HIV prevention interventions in the U.S. Am J Prev Med 2016; 50:699–708.
- Satcher Johnson A, Song R, Hall HI. State-level estimates of HIV incidence, prevalence, and undiagnosed infections [Abstract 899]. Presented at the Conference on Retroviruses and Opportunistic Infections, Seattle, Washington, February 13–16, 2017.
- Singh S, Song R, Satcher Johnson A, McCray E, Hall HI. HIV incidence, prevalence and undiagnosed infections in men who have sex with men [Abstract 30]. Presented at the Conference on Retroviruses and Opportunistic Infections, Seattle, Washington, February 13–16, 2017.
- Krueger A, Dietz P, Van Handel M, Belcher L, Johnson AS. Estimates of CDC-funded and national HIV diagnoses: a comparison by demographic and HIV-related factors. AIDS Behav 2016;20:2961–5.
High-Impact Prevention is a cost-effective, proven, scalable public health approach that prevents new infections, saves life-years, and reduces disparities.
- Research article
- Open access
- Published: 18 March 2022
Experiences of new diagnoses among HIV-positive persons: implications for public health
- Adobea Yaa Owusu ORCID: orcid.org/0000-0003-2223-7896 1
BMC Public Health volume 22 , Article number: 538 ( 2022 ) Cite this article
2866 Accesses
4 Citations
Metrics details
Ready acceptance of experiences of new diagnoses among HIV-positive persons is a known personal and public health safety-net. Its beneficial effects include prompt commencement and sustenance of HIV-positive treatment and care, better management of transmission risk, and disclosure of the HIV-positive status to significant others. Yet, no known study has explored this topic in Ghana; despite Ghana’s generalised HIV/AIDS infection rate. Existing studies have illuminated the effects of such reactions on affected significant others; not the infected.
This paper studied qualitatively the experiences of new diagnoses among 26 persons living with HIV/AIDS. Sample selection was random, from two hospitals in a district in Ghana heavily affected by HIV/AIDS. The paper applied the Hopelessness Theory of Depression.
As expected, the vast majority of respondents experienced the new diagnoses of their HIV-positive infection with a myriad of negative psychosocial reactions, including thoughts of committing suicide. Yet, few of them received the news with resignation. For the vast majority of respondents, having comorbidities from AIDS prior to the diagnosis primarily shaped their initial reactions to their diagnosis. The respondents’ transitioning to self-acceptance of their HIV-positive status was mostly facilitated by receiving counselling from healthcare workers.
Conclusions
Although the new HIV-positive diagnosis was immobilising to most respondents, the trauma faded, paving the way for beneficial public health actions. The results imply the critical need for continuous education on HIV/AIDS by public health advocates, using mass media, particularly, TV. Healthcare workers in VCTs should empathise with persons who experience new diagnoses of their HIV-positive status.
Peer Review reports
News of a newly-diagnosed HIV-positive status has the tendency to lead to negative psychosocial outcomes for persons living with HIV/AIDS (PLWHAs) [ 1 , 2 , 3 ]. In this paper, the concept of newly-diagnosed refers to the first time a respondent was informed of his/her HIV-positive status. Implications of this operational definition are discussed later on in the paper. Humans depict cognitive, emotional, and motivational deficits on hearing bad news and experiencing what is deemed uncontrollable events [ 4 ]. This is very likely to apply to PLWHAs particularly, when confronted with the news of being HIV-positive for the first time. Particularly, PLWHAs are known to mostly experience neurocognitive disorders associated with the infection [ 5 ], and often experience common mental disorders [ 6 , 7 ]. This is especially the case when PLWHAs fairly expect or self-perceive negative social reactions such as spousal abuse, dismissal from employment, stigma and discrimination, among others [ 8 ]. Peterson and Seligman ([ 4 ], p. 347) christened these series of responses on such occasions as “learned helplessness phenomenon.”
There are numerous news reports of persons who have committed suicide shortly after an HIV-positive diagnosis. This includes even the case of a female physician from the Eket local government area of Akwa Ibom, Nigeria [ 9 ]. Previous researchers note that after the initial diagnosis of a disease believed to be life-threatening, and particularly incurable, patients are known to experience an immediate descent into several distressing psychological and emotional states of mind [ 1 , 2 , 10 ]. These range from disbelief to denial to being utterly scared and shocked. Some even think that their life is not worth living anymore and imagine that indeed, the disease has already taken a final toll on them [ 2 , 3 ]. This brings to the fore the need to study the reactions of PLWHAs right after their initial diagnosis. Research and programme interventions on adaptation to a new HIV diagnosis provide personal and public health safety-nets and are thus needed [ 2 , 11 ]. Such research and interventions are helpful in educating newly-diagnosed PLWHAs on HIV [ 1 , 10 ] and promoting their health [ 1 , 8 , 12 ].
Acceptance of the news of an HIV-positive diagnosis is critical for several reasons [ 2 ]. Engagement in and sustenance of HIV treatment and care [ 1 , 2 ], viral load (VL), CD4 counts [ 2 , 13 ], and transmission risk [ 2 , 11 , 14 ] are affected by the reaction to the news of diagnosis. Reactions also affect perceptions of stigma and disclosure activity [ 2 , 11 ]. Conversely, difficulties with accepting diagnosed HIV-positive status has serious potential negative consequences for individuals and the general public [ 15 , 16 ]. From the angle of healthcare practitioners, better handling of new diagnosis of an HIV-positive status and related disclosure could greatly buffer the psychosocial and mental health of the newly-diagnosed PLWHAs, and help facilitate healthcare seeking and retention. These include the management of less traumatised disclosure, reduction of self-stigmatisation, and better management of romantic and family relationships [ 2 , 14 ]. Others are the reduction of viral transmission [ 14 , 17 ], and improvement in general public health and well-being of populations [ 1 , 14 ]. Knowing the experiences of new diagnoses among HIV-positive persons is, therefore, likely to facilitate successful linkage and retention of such persons in healthcare for HIV [ 1 , 2 ]. This is critical and is also known to be a significant gap in the HIV care continuum in some parts of the world, even the U.S. with all its known medical advancement [ 11 ].
Based on previous related literature, this paper primarily examines qualitatively the experiences of new diagnoses of 26 Ghanaian PLWHAs to the first news of their HIV-positive status. Second, it attempts to untangle the situations surrounding these experiences to determine what might have influenced such reactions. Third, the paper delineates the processes that particularly helped the PLWHAs transition from negative psychological reactions to showing positive reactions and seeking HIV treatment. Fourth, it adds to the core literature on managing experiences of new diagnoses of an HIV-positive status, and illuminates their importance to public health. It is hoped that this paper will facilitate a better acceptance of an HIV-positive sense of self which is known to aid PLWHAs to accept, adjust, and more effectively cope with their diagnosis. This will aid them to better manage the complexities of living with the infection [ 2 , 18 ]. This paper specifies the knowledge to Ghana and more importantly, Ghana’s most HIV/AIDS-affected district [ 19 , 20 ]. A thorough search on the experiences of PLWHAs’ new diagnoses in Ghana yielded no known results despite the fact that Ghana has a generalised HIV/AIDS epidemic: more than 1% of the residents have the infection [ 21 ]. This paper aims to fill that gap.
Immediate reactions to news of HIV positive status in Africa
The literature on the immediate reactions to the initial diagnosis of HIV-positive status is also sparse, and a majority of what research there is comes from South Africa. Such findings overwhelmingly corroborate each other: immediately after being diagnosed HIV-positive, PLWHAs studied depict deep negative emotions. Visser et al. [ 22 ] studied the phenomenon in South Africa, using a semi-structured interview of 293 pregnant women who were undergoing HIV test during antenatal care. On hearing the news, those who tested positive were shocked, and got frightened that they would be abandoned and discriminated against.
Fabianova [ 23 ] undertook a longitudinal study in Nairobi, Kenya, on the psychosocial aspects of being PLWHA. When the respondents who visited VCTs were first informed of their HIV-positive status, 89% of them felt sad due to their HIV-positive status, 60% had feelings of fear and anxiety, 30% felt angry, 25% felt distressed, and 15% cried. Additional psychosocial behaviours exhibited by the respondents included grief, guilt, hopelessness, helplessness, anger, disbelief, self-blame or blamed others, and aggression towards a counsellor. Their sadness was mostly in reference to close relatives who had died of AIDS. Their fears related mostly to the loss of their social position. Other fears surrounded loss of life, ambition, sexual relations, independence, physical performance, and financial stability [ 23 ]. While Fabianova [ 23 ] observed from the extant literature that suicide is a common reaction for persons who are first informed of their HIV/AIDS status, her study found that less than 1% of participants attempted suicide on hearing of their confirmed HIV-positive status. Most of Fabianova’s ([ 23 ], p. 201) respondents already considered themselves to be “walking corpses” and even visualised their funeral and grave.
Fabianova [ 23 ] enumerated several explanatory factors that unpacked her respondents’ reactions to their initial diagnoses of being HIV-positive. These included gender, level of preparedness of a client in the pre-testing session, and type of sexual relationship(s) they were in. Others included levels of general knowledge of HIV/AIDS, and HIV/AIDS-related stigma in their community. Fabianova ([ 23 ], p. 199) discovered that males responded to the initial HIV/AIDS diagnosis with anger, disbelief, and aggression. The females cried, got shocked, “swallowed big lumps of air, saliva subconsciously, shook both their hands in refusal and blame [sic] the others almost immediately.”
Other key explanatory factors for Fabianova’s ([ 23 ], p. 199) respondents’ immediate reactions included concerns about “lack of immediate elaborate support structures”, extent of level of awareness about HIV/AIDS, level of HIV/AIDS-related stigma, availability of antiretroviral therapy (ART), and support groups to enable them move on with their lives. Feelings of guilt for the infection were explained by whether the individual felt his/her lifestyle exposed him/her to it, and type of sexual involvement they were engaged in. They felt guilty that they would infect a spouse if they were married. If they were in an unstable/non-married relationship, they did not feel guilty, and shared the blame with the casual sexual partner. Sixty-two percent blamed their partners or the environment with the excuse that they stayed loyal to their partners. Fabianova’s ([ 23 ], p. 200) respondents who tested on their own volition did so based on their own or a partner’s “failure”, poor health or “accidental happening”, or work commitments.
The theoretical framework adopted for this paper, the Hopelessness Theory of Depression, is grounded on depression. Depression is currently one of the five leading causes of the disease burden internationally, except in sub-Saharan Africa (SSA) [ 24 ]. Researchers note that depressive disorders and other common mental health disorders (CMDs--depression, anxiety and somatization) were critically linked to the Millennium Development Goals, particularly gender equity, poverty, HIV/AIDS, and maternal and child health [ 24 , 25 ]. Importantly, depression is the most diagnosed psychiatric disorder among PLWHAs. Depression also serves as a risk factor for the progression of HIV/AIDS. In African settings, a growing appreciation of an important link between CMDs and HIV/AIDS has been established [ 7 , 23 ] as well. HIV has unleashed “a significant strain” on mental health in Africa ([ 24 ], p. 61; [ 26 ]). The huge burden of HIV/AIDS in SSA accounts for 16% of depression in the sub-region [ 24 ]. Alternatively, a neurobiological association exists between HIV and CMDs: “the HIV virus has quite specific detrimental effects on neuronal function” ([ 24 ], pp. 61 & 65). Evidence-based reports in African settings and other developing nations (studies conducted in Sao Paulo, Bangkok, Kinshasa, Nairobi, and Ethiopia), found both more symptoms and a higher prevalence of depression among symptomatic PLWHAs than among non-symptomatic or HIV-negative persons [ 24 ].
Theoretical framework: the hopelessness theory of depression
The Hopelessness Theory of Depression is applied to this paper. It is a diathesis-stress theory which posits that organisms express some form of cognitive and emotional deficits after experiencing a bad event. The theory argues that three depressogenic inferential styles serve as risk factors of depression [ 27 , 28 ]. These are the tendency to attribute a bad event to a global or stable cause; the tendency to perceive bad events as having many disastrous consequences; and the propensity to view oneself as flawed or inefficient [ 28 , 29 ]. Making negative inference upsurges the possibility of hopelessness while feeling hopeless makes depression inevitable. With this explanation, the theory assumes hopelessness as a critical underlying factor to depression. Adding to the causal explanation, Seligman [ 30 ] stated that the symptoms, cure and prevention of a bad event also model depression. In societies like Ghana, where HIV is associated with nonconformity to societal expectations and/or sexual promiscuity, PLWHAs may be more exposed to adverse emotional and cognitive symptoms after receiving an HIV-positive report.
The application of the thesis of the Hopelessness Theory of Depression to HIV-positive populations in SSA is not new. Govender and Schlebusch’s [ 31 ] study in Kwa-Zulu Natal, South Africa, applied Beck’s Hopelessness Scale and Beck’s Depression Inventory [ 32 ] to their assessment of the correlation between depression, hopelessness, and suicidal thoughts in PLWHAs. Schlebusch and Govender [ 33 ] used the same inventories to study PLWHAs in a University-affiliated hospital in South Africa. Primarily, they studied the prevalence of risk of suicidal ideation in PLWHAs immediately after their first diagnosis. Kylmä et al. [ 34 ] also studied the full gamut/dynamics of the concept of hope (hope, despair, hopelessness) among PLWHAs. Their study yielded information on how PLWHAs’ perceptions of hope could facilitate their clinical care. The Hopelessness Theory of Depression is applied to the discussion of the findings.
Study setting and cultural context of LMKM
The LMKM, the catchment area for the study, is situated in the Eastern Region of Ghana. The region, one of ten at the time of data collection, had 2,633,154 residents by Ghana’s last Population and Housing census of 2010, making it the third most-populated region. The Eastern Region is mostly semi-urban [ 35 ]. The LMKM, one of 26 administrative municipalities/districts in the Eastern Region by the time of data collection, covers 12.4% of the region, with total land mass of 304.4 km 2 . The 2010 Population and Housing Census recorded 89,246 residents of the Municipality comprising 46.5% males and 53.5% females. Christians were 92.8%; other religious groups include Muslims and traditionalists [ 36 ]. The indigenes are ethnic Dangmes and speak Krobo. They are a patrilineal descent group, which means they inherit property through their father’s lineage.
Sampling and data collection
This study used a “descriptive, multiple case study approach” ([ 2 ], p. 2; [ 37 ]). This method generates interviewees’ in-depth descriptions of their situations, views and realities regarding issues. This provides deep insights of their actions and choices [ 38 ]. In this study, the pool of cases of the individual respondents is considered a “multiple case study approach” ([ 2 , p. 2; 37 ]). Additionally, the findings from the study municipality forms a case study. As Kutnick et al. [ 2 ] note, case studies are exceptionally useful in eliciting contextual situations, when they are important to a particular study. Examples are cultural, social and structural impediments (such as stigma, and fear) to post-diagnosis HIV care [ 37 ].
This paper analysed data from 26 (13 each from two hospitals studied) out of 38 PLWHAs interviewed qualitatively through personal interviews from June to July 2015. The data used for this study formed part of a large data set from a project which primarily studied the linkages between housing conditions and the reported health status of PLWHAs (see [ 39 , 40 , 41 , 42 ]). The implications of recruiting individuals further away from their diagnosis for this paper are addressed in the section on limitations. The interviews were conducted with the aid of a pretested semi-structured question guide. Table 1 has the key questions asked. Some of these key questions in Table 1 were probing questions that emanated from the main/initial interview guide, because it is open ended, as is the norm with data collection tools for qualitative studies. The initial sample of 38 comprised both males and females who were selected using random sampling [ 2 ] as part of a research project which primarily studied the nexus between the health status of PLWHAs in the LMKM and their housing conditions.
The project comprised both qualitative and quantitative data collection. The qualitative interview guide has been submitted as Additional file 1 . First, the study district, LMKM, was conveniently selected based on its lead, by the time of developing the project proposal, in having persons with HIV/AIDS in Ghana, due to which the government had focused on strengthening healthcare institutions and personnel in the district for the fight against HIV/AIDS. Second, two out of three health facilities in the study district were also conveniently selected—a government and quasi-government hospitals. These had been specially equipped by the Government since 2002, to manage HIV/AIDS cases, thus conveniently leaving out the other government hospital [ 39 , 40 , 41 , 42 ]. Respondents had come to HIV/AIDS Voluntary Counseling and Testing (VCT) Centres in the two hospitals--St. Martins de Porres Hospital in Agormanya and Atua Government Hospital in Atua, near Agormanya, for care. Third, respondents were initially selected conveniently for having been medically diagnosed of being HIV-positive prior to the study, after which they had to verbally self-confirm their status to the PIs of the study.
Interviewing took place in these VCTs. The VCTs operated only on weekdays. For each day during the weekdays, based on prior reconnaissance survey, 40 respondents were targeted for both qualitative and quantitative interviews from the daily list of attendees in each hospital. One-third of these were selected randomly and interviewed. If there were less than 40 people in a day, half of them were randomly selected for interviews. For each day fewer than one-fourth of our initial sample were males, we increased the chances of having males in the sample, by including every fourth male from the initial list of persons who did not make it to the list from which final sampling was done [see [ 20 , 40 , 42 ]. This is justified based on a preponderance of female PLWHAs in the study district [ 20 , 40 , 42 ], Ghana, and also, sub-Sahara Africa generally [ 40 , 42 , 43 , 44 ]. Respondents were given unique codes to prevent being re-interviewed during the course of the study. Five male and female graduate student interviewers were assigned to each study hospital, including one qualitative interviewer.
Qualitative or otherwise, a respondent got randomly selected for an interview when a prior interview had ended, beginning with a random start from the list of assigned codes, till the selected list was exhausted in a day. Similar sampling arrangements were made for each VCT used. The random selection of the respondents was necessary to spread their selection over the designated one month of study, for purposes of having a variety of cases/stories over the study period, for richer analysis. Out of the estimated average of about 40 PLWHAs who would visit each VCT per day, it was necessary to randomly select some and leave others out, to facilitate spreading respondent selection over time as said already. Additionally, it was expedient to randomly distribute the respondents between the qualitative study and survey data collection approaches for the larger project, to avoid possible biases in the responses from these two approaches.
Respondents were males and females, 18 years or older, and confirmed their HIV-positive status to the principal investigators (PIs). The interviewing time for a respondent in the qualitative study ranged between 35 and 50 min. The language used for the interview was left to the respondent’s choice between Krobo, the indigenous language in the LMKM, Twi, the indigenous language spoken the most in Ghana, and English, Ghana’s official language due to its colonial past. With prior permission from the respondents, the interviews were audio recorded.
This paper uses the qualitative data from the project. The original sample of 38 for the initial qualitative data was primarily informed by previous literature on the need to reach saturation in qualitative interviews [ 20 , 42 , 45 , 46 ] which was achieved subjectively after interviewing about 10 respondents in each of the two study sites [ 20 ]. Although thematic saturation is usually achieved with 30 qualitative participants [ 20 , 45 , 46 ], 10 respondents gave us thematic saturation at each VCT, because they were quite homogenous [ 20 ]. Previous studies [ 20 , 38 , 42 , 45 , 47 ] have defined thematic saturation as recurrence or repetitiveness of responses from qualitative respondents. Despite reaching saturation with a combined 20 respondents from both VCT centres, we continued interviewing up to 38 of them to meet an initial objective of spreading respondent selection over a month [ 40 , 42 ], with the hope of having some variety of responses due to the case study nature. The sample of 26 for this paper were selected from the 38 because the rest did not respond to the primary question on how they experienced the new diagnoses of their HIV-positive status (see [ 2 ]).
Ethical clearance and data quality approaches
Ethical clearance was sought from the Ethical Committee for Humanities at the University of Ghana, Legon ( ECH 017/14–15 ) , and the Ethical Review Board of the Memorial University at St. Johns, Newfoundland, Canada. Permissions were also sought from the Ethical Review Committee of the Ghana Health Service (GHS-ERC: 02/11/14) for using institutions under its jurisdiction for the study, as well as from the Eastern Regional Directorate of the Ghana Health Service. The District Health Management Directorate of the LMKM and the administrators of the study hospitals responded to the written permissions with verbal permissions to undertake the study. The respondents were informed of the objectives of the study, assured of confidentiality, and their informed consent was sought. They were also informed that their participation was voluntary and they would not be penalised if they opted to turn down the interview at any time during the process.
One person declined to be interviewed, citing time constraints. No identifiable markers were used for the respondents (see [ 20 , 39 , 40 , 42 ]).
Data analysis
The data were transcribed verbatim, and reviewed by the author and team of transcribers to ensure accuracy. The adequacy of translation from the local languages to English was ascertained by holding several meetings between the author and the transcribers to interrogate the correct translations forth and back till a mutual agreement was reached on the correct translations.
Based on the deductive approach, the data analysis was done focusing on the objectives of the study [ 40 ]. Qualitative thematic content analysis, which enables interrogating narratives from all cases studied for a combined result [ 20 , 40 , 42 , 48 ], guided generating themes and subthemes for this paper. In this paper, the qualitative thematic content analysis used also qualifies to be called a discourse or conversation analysis [ 49 , 50 ]. It used a qualitative thematic coding [ 50 , 51 ] of the different interviews/conversations with the respondents and observed the three key features of qualitative content analysis described by Schreier [ 50 ]. These are reducing the data, systematically analysing them, and applying flexibility in the analysis. The systematic analysis meant carefully examining every single aspect of the transcribed data and systematically describing their meaning [ 50 , 52 ], as well as comparing and relating different parts of the data to one another [ 50 ]. NVivo version 11 professional software [ 53 ] was used to identify themes and sub-themes relevant to the objectives of the study and other relevant information. Again, back and forth meetings were held between the author and the team of two coding assistants, who coded the data independently, to mutually agree on their meaning and context.
These repeated processes of reviewing the data enhance intercoder reliability subjectively and improve the credibility/validity and reliability of qualitative data [ 40 , 42 , 54 ].
Based on previous research [ 2 , 11 , 34 ] respondents’ experiences of the new diagnoses of their HIV-positive status were adjudged as negative if the respondent either expressed shock, disbelief, worry, fear/panic, felt the HIV infection would kill him/her, or immediately contemplated suicide. Respondents’ experiences of their new diagnoses were classified as resigned acceptance if they readily accepted the new diagnoses and/or showed some optimism instantly that they could survive the infection. Finally, their experiences of the new diagnoses were considered resigned neutral when the respondent indicated he/she showed no emotion upon receiving the first news of his/her HIV-positive status (Fig. 1 & Table 2 ).
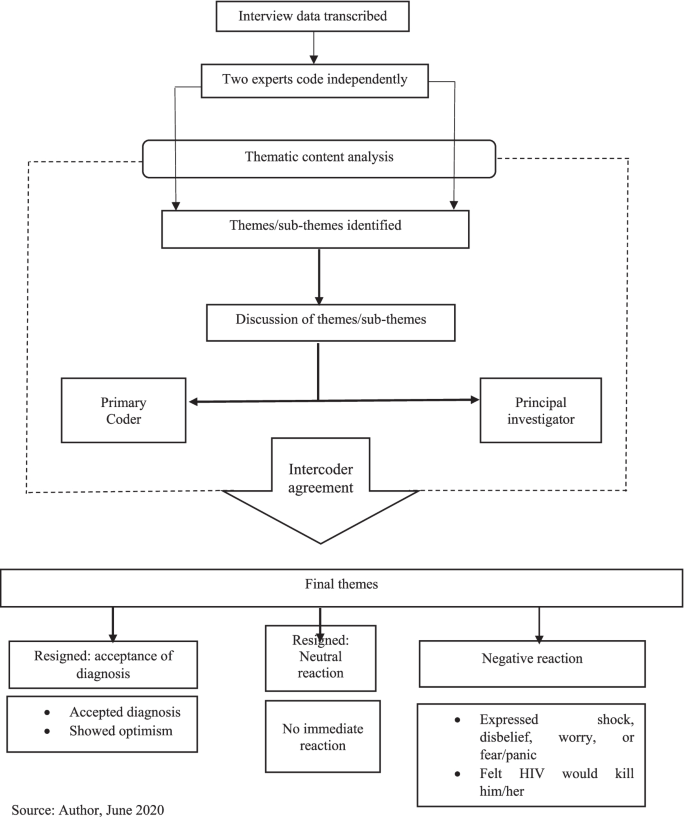
Data analysis workflow
Reflexivity
Reflexively, the author’s cultural and theoretical population health orientation admittedly had some influence on aspects of the research process, although these were minimal. These included the choice of the title. Being fully aware of the extent of stigmatisation culturally associated with HIV/AIDS in Ghana [ 20 , 40 , 42 ], the PIs of the project from which data for this paper emanates were curious about how respondents would experience the new diagnoses with the infection.
Nevertheless, given the author’s extensive training in the dogma and ethics of scientific research, particularly regarding the need for value-neutrality and objectivity [ 54 ], the author’s cultural and theoretical backgrounds did not otherwise influence the data analysis and interpretation. This was applicable to most of the research process as well.
Socio-demographic characteristics of respondents
The respondents’ ages ranged from 25 to 68 years old. They were mostly females (80.77%, n = 21), primarily indigenous Dangmes (84.62%, n = 22), and generally had low socio-economic status. Also, they were mostly single (separated/widowed after cohabiting/never married/widowed), and they had been officially diagnosed HIV-positive for a range of six months to 12 years (Table 3 ).
Thematic findings
Experiences of new diagnoses of hiv/aids.
Table 2 summarises the experiences of new diagnoses among the respondents, upon hearing of their HIV seropositive status. There were negative and resigned reactions. Verbatim responses are identified with the type of hospital the respondent used: government or quasi-government.
Negative reactions
The data showed that the vast majority of the respondents seemed to have been very hard hit and traumatised by the news of HIV-positive test result, and expressed very negative sentiments. For these, the experiences of new diagnoses ranged from disbelief, to being very disturbed. Few mentioned the thought of killing themselves, incessant crying, and feeling that they would die from AIDS. Other reactions included being very frustrated, very surprised, very frightened, deep shock, deep worry, being heartbroken/devastated, self-blame, and avoiding going to hospital till conversion to AIDS (Table 2 ):
“ It was very hard for me when I first heard it; in fact, I cried and cried.” ( Government hospital).
“In fact I was very frustrated. I even decided to take poison so that I will die before the sickness [HIV] becomes worse.” (Government hospital).
“I was very surprised and shocked when I was first told I had this disease. It was very heart-breaking.” (Government hospital).
Resigned reactions
On the contrary, few respondents showed resignation towards the bad news. These comprised three who readily accepted the diagnosis and two who seemed neutral to it. From their responses, respondents who accepted their diagnosis seemed to have readily and consciously accepted/embraced the diagnosis of HIV-positive and encoded it rather smoothly as part of their identity.
“When I was told I was not perturbed because I knew people who were also taking the drug” [ARVs]. (Quasi-government hospital).
The very few respondents who seemed to have been neutral to their new diagnosis of HIV/AIDS seemed to have continued with their lives seamlessly on the spare of the moment they received the news, and did not take a break to react to the news of being HIV-positive.
“I was ill for long time so when I was told about it I only continued to take medications.” (Government hospital) .
Further analysis indicated that these experiences of the new diagnoses were influenced by certain background situations. These are discussed in the next section.
Factors influencing experiences of the new diagnoses
For the very few respondents whose new diagnoses experiences were neutral, being ill for a long time before the HIV-positive diagnosis, and accepting that sickness is inevitable and could happen anytime, were what influenced their experiences of the new HIV-positive diagnoses:
“ … as for sickness, it’s sickness; you have less control over sickness, so I didn’t really do anything.” (Quasi-government hospital).
Two of the few respondents who readily accepted their new diagnosed HIV-positive status said they experienced persistent comorbidities from the HIV infection. Resultantly, they voluntarily went to the VCTs to test for their HIV status:
“I started falling sick and strange rashes kept appearing on my skin, so when I took it to the hospital, I was told it was the virus.” (Government hospital).
“I frequently fell sick … and it was not getting better so I came to the hospital myself … I came (willingly) to them to be tested when I realised I have changed. So they were even happy I walked to them myself to be tested.” (Quasi-government hospital).
Including two multiple responses, the vast majority who responded negatively to the experiences of new diagnoses of HIV-positive status, mentioned four main situations that informed their experiences of the new diagnoses. Mostly, they suffered comorbidities from their infection.
“For about seven months I was not feeling well. It even got to a point I lost consciousness. All forms of tests were ran on me … but they could not find exactly what was wrong...My boss advised me … so I went to the hospital for the test and the nurses said I was HIV-positive.” (Government hospital).
Next, nearly half of the respondents who reacted negatively said a spouse/partner was HIV-positive and thus knew they had contracted the infection from them, and/or due to that, health personnel tested them also for the infection. Importantly, half of these PLWHAs did not know their partners’ HIV status prior to respondent’s diagnosis.
“ I was staying with my husband by then but he died so it was after he died that the doctors realised that it was this disease he died of … afterwards I was tested and diagnosed with this disease.” (Government hospital).
Similar to those who readily embraced their diagnosis, a few of those whose new diagnoses experiences were negative were tested voluntarily based on their sexual partner’s infection. Likewise, several participants whose new diagnoses experiences were triggered by the onset of comorbidities said they voluntarily went for the testing. Additionally, for a slim minority of the latter, their conviction to go for the VCT was based on mass media (often television) announcements and discussions on the signs and symptoms of HIV/AIDS.
“Already I suspected that my husband had all the symptoms that are discussed on TV and radio about this disease. He fell sick often and also coughed most of the time.” (Government hospital).
“Even though I wasn’t falling sick, I came to be tested willingly after they announced everybody should get tested … .” (Government hospital).
“… I used to fall sick frequently and that was when a lot of noise and adverts were made about this disease on television and radio...I went to the St. Martin’s hospital and told the doctors about my situation and he asked me go for an HIV test and that was when I got to know I had this disease.” (Quasi-government hospital ).
Finally, few (including two who gave multiple responses—primarily that a spouse/partner was HIV-positive) mentioned that they got tested when they were pregnant.
“I was about to give birth to my second born … my husband is also HIV-positive.” (Government hospital ).
“I was diagnosed when I was pregnant when my second born and I visited the hospital … Yes, [my husband is HIV-positive].” (Government hospital).
Factors that facilitated transitioning to accept HIV-positive self
For the few respondents who showed resignation towards the experiences of their new HIV-positive diagnoses, there was no need for transitioning to accepting an HIV-positive self. Two of these respondents who readily embraced the new HIV-positive diagnoses said they already knew persons who were HIV-positive and were taking antiretroviral medications (ARVs):
“I realised I was not the only victim; many people are also victims …” (Quasi-government hospital ).
Two others said they already had comorbidities from AIDS and started treatment right after diagnoses:
“ I was ill for a long time so when I was told about it I only continued to take medications.”
(Government hospital ).
Another participant thought sickness is inevitable and thus did not need to worry about such diagnosis.
Nearly one-third of the respondents whose experiences of the new HIV-positive diagnoses were negative gave no response regarding what influenced their transitioning to accepting their new HIV-positive diagnoses. They mostly felt uncomfortable/reluctant talking about it. The rest mentioned what facilitated their transitioning more spontaneously and/or more readily after some amount of probing. The vast majority of the rest who experienced negative reactions said the most important help with their transitioning was counselling from health workers who encouraged them to initiate and continue treatment, with the assurance that if they did so, they would survive the infection.
“… After I came here [VCT] and was advised and encouraged to see something to live for, I have been okay. They [health personnel] have been very friendly and encouraging. In fact, they have helped me a lot .” (Government hospital).
“ They [health personnel] counsel us and tell us the fact that we have this virus does not mean our world has come to an end.” (Government hospital).
“… After being put on medication, going through counselling and tests, and being told what to do, I was hopeful that if you adhered to the medication you could live long.” ( Quasi-government hospital).
For one of these, her mother-in-law was the main person who empathised with her:
“I was really worried and disturbed but the encouragement and advice from the nurses and my mother-in-law … has helped me. After I told her [mother-in-law] I had been diagnosed … she brought me here [VCT] to introduce me [to a nurse] , so she has been helpful.” (Government hospital).
The second main issue that facilitated the transitioning for few of the respondents was their awareness of the current medical advancement in the treatment of HIV infection, due to which “you would live long” ( Quasi-government hospital) despite the infection:
“… because they have drugs to treat it, I was OK. Provided it will not cut short my life span I am happy.” ( Quasi-government hospital).
“In the olden days when there were no drugs you thought you would die … after being told, so you become afraid, but now we know there are drugs available so if you are able to take your drugs you don’t have any problem.” ( Quasi-government hospital).
Three respondents alluded to accepting medical diagnoses, facing reality, and living by Biblical principles as facilitating their acceptance of their new diagnoses.
“ I accepted it because you can’t deny what a doctor says” ( Quasi-government hospital).
“I was disturbed but I thought to myself that it had already happened ” ( Quasi-government hospital) .
“I didn’t kill myself because I am a Christian and the Bible speaks against that. I forgot about everything and decided to keep coming for the medications and now by the grace of God I have lived for over twelve years .” ( Government hospital).
There was, however, a lone-voice who said she had still not settled down to the reality of being HIV-positive after having been diagnosed three years prior and seeking treatment for one-year post diagnosis. Thus, she has not been consistent in getting treatment and is already feed up with seeking treatment:
“It seemed to be untrue. From time to time I stopped taking the medication … I am fed up with coming to seek treatment. I have been treating the sickness for over a year but the symptoms recur after I see the doctor.” ( Quasi-government hospital).
This lone-voice mentioned having severe comorbidities which were probably due to starting healthcare for HIV two years after diagnosis. She also mentioned experiencing extreme discrimination and ostracisation both at home and in public, which no doubt, are linked to her comorbidities.
This section discusses the findings of the study, with a bearing on the tenets of the Hopelessness Theory of Depression. Fear has been associated with HIV since its discovery in the 1980s. Fear is mostly fueled by misconceptions associated with the virus which is mostly linked to death and stigmatisation [ 55 ]. Grounded on fear of death and a feeling of helplessness, a wide range of reactions are exhibited upon diagnosis or disclosure of an individual’s HIV-positive status. Although these reactions are both from the individual in question and significant others of this individual, the literature has mostly focused on the reactions of the persons affiliated with these individuals after disclosure [ 56 , 57 ]. Indeed, very few studies explore the individual’s reactions upon diagnosis or testing positive for the virus [ 55 , 58 ]. Based on this drawback and the known public health significance of such immediate reactions to HIV-positive diagnosis, this paper examined the experiences of new diagnoses of Ghanaian PLWHAs after hearing the “bad news.”
Importantly, a critical examination of differences between participants from each of the two hospitals studied shows that 11 respondents from the government hospital had negative reactions to the new experience of their HIV/AIDS diagnosis while ten in the quasi-government hospital did so. On the other hand, the experiences of two respondents from the quasi-government hospital was adjudged as “Resigned: accepted diagnosis” while one participant from the government hospital showed a ‘Resigned: accepted diagnosis.” There were no other differences in the participants’ reactions between the two study sites (Table 2 ). Rather, the difference between the respondents basically stemmed from the influences on their experiences of the new HIV-positive diagnoses discussed earlier (Table 2 ), which did not have a relationship with the particular hospital they received healthcare from. While previous researchers have articulated the lack of major differences in the findings from the respondents used for the qualitative study in the project [ 39 , 41 ], they have further clarified that the respondents’ similar socio-bio-demographic background is mostly responsible for the lack of major differences in the findings [ 20 , 39 , 41 ].
The findings from this study have corroborated those of previous authors that receiving the news of newly-diagnosed HIV-positive status is often met with reactions that are “complex and multi-faceted” ([ 2 ], p. 12). Additionally, the findings that respondents had varied responses and a myriad of experiences to the new diagnoses of their HIV-positive status is in line with reports from several studies (example: [ 2 , 58 ]). Most of the initial reactions of respondents in this study were very traumatising and discouraging. These included a few who contemplated suicide upon hearing the news; supporting Fabianova’s [ 23 ] findings in Nairobi.
Similar to previous research [ 55 , 58 ], findings from this study indicate that though negative emotional and psychological reactions may occur upon learning of an HIV-positive status, respondents may also resign themselves to their fate—to accept or numb their feelings about the new disclosure of their HIV+ diagnoses. Likewise, this study found that respondents who were already exposed to HIV/AIDS needed no transitioning to self-acceptance of their HIV-positive status. This corroborates previous findings [ 55 ]. Nearly all the respondents settled down later, after experiencing the new diagnoses, initiated and continued with their healthcare for HIV/AIDS. This affirms previous assertions that such initial feelings regarding information on a newly-diagnosed HIV-positive status mostly fade away eventually [ 3 , 23 ].
Again, the paper corroborates previous findings and highlights the buffering role of healthcare providers in moderating the experiences of new diagnoses of HIV-positive persons [ 1 , 11 ]: the vast majority of the respondents who adapted to their HIV-positive status attributed it to counselling and support from healthcare personnel. This role of the healthcare workers in aiding respondents’ transition to accepting their HIV-positive selves affirms the documented importance of social support in ameliorating the otherwise negative effects of experiencing a health trauma [ 23 , 59 ]. Research has identified HIV counsellors’ or health providers’ choice of words and emotions as crucial in determining peoples’ reaction to the initial diagnosis of HIV infection [ 55 , 58 ]. When these emotions were hopeful and assuaging, patients were more likely to be calm and comforted, and vice versa [ 58 ].
The findings of this study underscore the fact that PLWHAs who experience new HIV-positive diagnosis will need to receive such interventions early [ 12 ]. These interventions are needed to give them hope in life to abate extreme psychosocial trauma that can be associated with experiences of new HIV-positive status [ 11 , 60 ]. Per the findings of this paper, such interventions should include educating PLWHAs experiencing new HIV-positive diagnosis that new medical advances for HIV-positive infection make it possible for PLWHAs experiencing new HIV-positive diagnosis to lead normal lives and live long, if they seek early treatment and adhere to prescribed healthcare.
A fair number of the respondents mentioned being infected by their spouses/partners who were alive or deceased (also see [ 40 ]), implying that they probably were not using condoms and other modes to prevent HIV transmission from their sexual partners. This finding is not unlikely considering that Owusu [ 42 ] found that the PLWHAs studied were hardly using any form of protection against HIV with their sexual partners, whether in stable or unstable relationships. Two respondents were exceptions--they used condoms, but inconsistently [ 40 ]. Furthermore, Owusu [ 40 ] found that the unmarried or non-co-habiting PLWHAs had not disclosed their HIV-positive status to their sexual partners, with the exception of one respondent. PLWHAs who fail to disclose their status to their partners may have been living in a state of denial and or may fear/have feared the ramifications of disclosing their status. They may thus refuse to disclose as a way of attenuating the anticipated effect of disclosing, as previous authors have attested to [ 12 , 15 , 23 ].
Additionally, findings from this paper illuminate the importance of voluntary counseling and testing. Majority of the respondents mentioned having had comorbidities before they tested for their HIV-positive status. Other researchers have indicated that anticipated reaction influences decisions on voluntary testing for HIV [ 55 , 58 ]. Previous research clearly notes potential barriers to voluntary testing for HIV in Ghana. These include the fear of stigma, discrimination and abuse, and possible dissolution of romantic relationships associated with being a PLWHA. Importantly, there is fear of the perception that an HIV-positive diagnosis is a death warrant [ 16 , 61 ]. Antenatal-linked VCT is a policy strategy in Ghana for HIV control through a nationwide integration of VCT and antenatal care [ 62 ]. However, clients may disagree to it.
The findings from this paper mostly tally with the Hopelessness Theory of Depression’s core proposition; the respondents overwhelmingly perceived the experiences of their new HIV-positive status as translating into unwelcome consequences and negative inferences, as did respondents in other SSA settings [ 12 , 23 ]. This plausibly led to depression and feelings of hopelessness among them. Also, this perspective may have underlain the self-blame by a few of them for being HIV-positive [ 28 , 29 ]. Furthermore, this paper confirms the Hopelessness Theory of Depression’s propositions that underlying perceived bad situations and experiences which are attributed to internal factors lead to depression. Conversely, those ascribed to presumed external factors/influences give comfort/are reassuring [ 4 ]. In this study, the experiences of new HIV-positive diagnoses were mostly negative for respondents with internal factors such as having comorbidities and having a spouse/partner with HIV/AIDS.
In consonance with Peterson’s and Seligman’s [ 4 ] Hopelessness Theory of Depression’s propositions, respondents of this study said that external factors motivated them to take commendable actions such as going for VCT. These included the influence of health education through mass media, counselling by healthcare practitioners, and information regarding modern medical advancements which can help PLWHAs live without comorbidities, and possibly survive the infection. Furthermore, these factors facilitated their adaptation to their HIV-positive selves.
Nevertheless, this paper does not substantiate Peterson and Seligman’s [ 4 ] Hopelessness Theory of Depression fully. Contrary to their proposition, in this study, fewer respondents mentioned that a series of external factors such as knowing someone who has HIV/AIDS, and being given a near-mandatory HIV test at an antenatal clinic were what influenced their negative reactions. Conversely, other internal factors such as having comorbidities and having an HIV-positive romantic partner influenced few of the respondents to positively adapt to their HIV-positive diagnoses. In this study, therefore, the clear diathesis of external factors giving psychosocial comfort and internal factors unleashing mental discomfort in response to hearing the often unwelcome first news of being HIV-positive was not fully supported. This was also true of Assen et al.’s [ 12 ] study in Ethiopia.
Hence, this paper corroborates Govender and Schlebusch’s [ 31 ] synthesis of the Hopelessness Theory of Depression. These authors emphasise that the numerous internal and external challenges that face PLWHAs such as discrimination, stigmatisation, abuse, financial, marital, and healthcare challenges, among others, may [also combine to] have connotations for the loss of control over one’s life, fear of the future, and feeling of helplessness. As well, they may underlie the negative inferences which exacerbate the feeling of hopelessness and increase the likelihood of depressive symptoms stemming from experiencing new diagnosis of HIV/AIDS.
This paper adds to the knowledge on the personal and public health effects of experiencing new HIV-positive diagnosis. Particularly, it highlights the commendable public health effects of receiving new diagnosis for HIV-positive status and illuminates the role of social support in seeking and continuing healthcare for the diagnosis. Also, it attests to the role of healthcare workers and behaviour change communication, using mass media, in fighting the menace of HIV/AIDS. Furthermore, as articulated above, this paper did not fully support the conclusions of Peterson’s and Seligman’s [ 4 ] Hopelessness Theory of Depression’s framework. Rather, the paper contributes additional information to it in the form of an anti-thesis. Additionally, unlike Fabianova’s [ 23 ] study in Nairobi, this study did not find that the respondents acted with aggression towards counsellors who first broke the news of their HIV-positive status to them.
More importantly, this paper has navigated new frontiers in the body of knowledge in its thematic area of study. First, contrary to Fabianova’s [ 23 ] findings that some of her respondents attempted suicide, non-of the respondents in this study mentioned having attempted to take their lives, although a few of them revealed they had suicidal ideation. This may be due to the fewer respondents this study engaged as well as its cross-sectional design, compared to Fabianova’s [ 23 ] respondents, and the longitudinal approach to her study. Second, this study has newly articulated outstanding information on factors which facilitate PLWHAs’ transitioning to accepting and settling down to their experiences of new HIV-positive status. Third, unlike previous literature, this study has uniquely found that having comorbidities from HIV/AIDS was the primary reason that influenced the respondents to voluntarily test for their HIV-positive status. The uniqueness of this finding may be linked to the awareness that VCT of HIV/AIDS status is very rare in Ghana [ 63 , 64 ].
Limitations
The qualitative nature of this study better facilitates unearthing the complexities associated with experiences of new diagnoses among HIV-positive persons and learning about the adaptation process [ 2 ]. Also, the repeated data analyses this paper employed strengthens its reliability and validity. However, when interpreting these findings, some limitations should be considered. With HIV-positive status being a very sensitive issue, and highly stigmatised in Ghana [ 16 , 65 , 66 ], social desirability of responses may have influenced the findings [ 2 ]. Being a retrospective study, recall bias may also affect the reliability of the responses [ 2 , 20 ]. This is with particular reference to the time lapse between the moment a respondent was newly-diagnosed with HIV/AIDS, as operationalised above, and the time of the study. Recruiting individuals further away from their diagnosis is a limitation; it could lead to recall bias. Furthermore, the study is cross-sectional and does not permit inference of causality [ 67 ]. Additionally, being a qualitative study with a fairly small sample size, the findings are not generalisable to non-respondents in the LMKM and also, Ghana as a whole [ 67 ].
Omona ([ 68 ], p. 181) posits that although random sampling is rare in qualitative studies, they are not out of place as they facilitate sampling the “desired number of individuals …” from a generated sampling frame, which he asserts improves the credibility of the sample (also see [ 69 ], p. 28). Yet, as hinted previously in this paper, random sampling in qualitative studies could pose some limitations. A careful search of the literature does not specify such limitations. However, the author guesstimates that random sampling in qualitative studies may rob the data of the quality of focusing on some key persons/texts of interest to the study which convenience sampling will provide. Lastly, based on the primary focus of the project, this paper did not undertake a diagnostic assessment for depression among the respondents. The paper is thus unable to ascertain if depression contributed to experiences of the new diagnoses of HIV-positive status among the PLWHAs studied.
Evidence elsewhere suggests that upon receiving the initial news of an HIV-positive diagnosis, most people have strong psychosocial reactions [ 23 , 55 , 70 ]. Such reactions are also known to have very critical public health implication [ 1 , 2 , 14 ]. Yet little research has focused on the initial reactions of newly-diagnosed PLWHAs in SSA, particularly Ghana. Neither has the implications of their reactions for personal and public health been extensively studied [ 2 , 11 ]]. This makes this study of the experiences of new HIV-positive diagnoses very timely. The personal and public health implications of one’s experience of new diagnosis of HIV-positive status is critically important for Ghana, which has a generalised HIV-positive infection [ 21 ].
Consistent with the literature, the vast majority of the respondents became extremely traumatised and immobilised when they experienced new diagnoses of their HIV-positive status. A few, however, more readily resigned to their HIV-positive identity. Regardless of their experiences of new diagnoses of HIV/AIDS, having comorbidities prior to diagnosis influenced their experiences the most. This was followed by having/having had a spouse/partner especially, and/or knowing someone who was HIV-positive, prior to their diagnoses. Next, respondents mentioned being influenced by health education through mass media, TV particularly, on signs and symptoms of HIV/AIDS. Importantly, health education, counselling, reassurance and empathy from healthcare workers provided hope. Furthermore, these facilitated their transitioning to settling down to self-acceptance of an HIV-positive status and continuing with healthcare. Finally, this paper concludes that to a large extent, the findings are applicable to the tenets of the Hopelessness Theory of Depression used as a framework for this study. Consequently, this paper found hopelessness as an important driving force to negative reactions towards one’s experience of his/her new HIV-positive diagnosis.
Conclusions from this paper have several public health significances. It highlights the continuous need for and strengthening of behaviour change communication on HIV/AIDS by the Ghana AIDS Commission and Ghana Health Service. This should emphasise its signs and symptoms, the need to seek early treatment, and adherence to prescribed ARVs. Strengthening the use of mass media, small groups, schools, churches/mosques and person-to-person channels in such endeavours is important. HIV/AIDS-related health promotion and education should also continue to emphasise prevention, but importantly, state that once infected, HIV/AIDS can be controlled; the infected person can live without comorbidities and need not succumb to the infection. Stakeholders should work harder towards educating residents in the LMKM, and for that matter, Ghanaians generally, about voluntary testing of HIV status. Most of the respondents in this study mentioned having had comorbidities from HIV/AIDS prior to their new diagnoses. Onset of comorbidities for HIV/AIDS prior to diagnosis and treatment can make the treatment expensive; it can also diminish the chances of surviving the infection severely [ 71 , 72 ].
Given the high rates of HIV/AIDS in the study district and Region, the health education should also emphasise the need for persons whose sexual partners are HIV-positive—particularly those who show signs and symptoms of the infection, and all who engage in at-risk sex, to practice safer sex. Finally, the paper recommends increased social support and empathy for PLWHAs in LMKM particularly and in Ghana generally, from family, friends, neighbors, community leaders, healthcare professionals, and organised groups such as members of their religious affiliation, if any [ 20 , 40 , 42 ]. This study has unearthed social support as a critical moderating element in the transitioning of PLWHAs to integrating their HIV-positive self-concept, initiating, and adhering to prescribed healthcare. Families, social groups, and healthcare professionals should empathise with PLWHAs.
Availability of data and materials
The datasets used and/or analysed during this study are available from the author on reasonable request. The key questions for the study have been provided in the paper, in Table 1 . The complete question guide used to collect the data has also been provided online as Additional file 1 .
Abbreviations
Acquired immune deficiency syndrome
Anti-retroviral therapy
Antiretroviral medications
Common mental health disorders
Ethics Committee on Humanities
Ethical Review Committee
Ghana AIDS Commission
Ghana Health Service
Ghana Statistical Service
Human immunodeficiency virus
Lower Manya Krobo Municipality
Principal Investigator
Persons living with HIV/AIDS
Research Assistants
Sub-Saharan Africa
University of California San Francisco
Voluntary counselling and testing
Chu C, Selwyn PA. Diagnosis and initial management of acute HIV infection. Am Fam Physician. 2010;81(10):1239–44.
PubMed Google Scholar
Kutnick AH, Gwadz MV, Cleland CM, Leonard NR, Freeman R, Ritchie AS, et al. It’s a process: reactions to HIV diagnosis and engagement in HIV care among high-risk heterosexuals. Front Public Health. 2017;10(5):100. https://doi.org/10.3389/fpubh.2017.00100 .
Article Google Scholar
University of California San Franscisco. Coping with HIV/AIDS: Mental Health. HIV in Site Project: the UCSF Center for HIV Information. 2018. http://hivinsite.ucsf.edu/insite?page=pb-daily-mental . Accessed 2 May 2018.
Google Scholar
Peterson C, Seligman ME. Causal explanations as a risk factor for depression: theory and evidence. Psychol Rev. 1984;91(3):347. https://doi.org/10.1037/0033-295X.91.3.347 .
Article CAS PubMed Google Scholar
Alford K, Banerjee S, Nixon E, O’Brien C, Pounds O, Butler A, et al. Assessment and management of HIV-associated cognitive impairment: experience from a multidisciplinary memory service for people living with HIV. Brain Sci. 2019;9(2):37. https://doi.org/10.3390/brainsci9020037 .
Article PubMed Central Google Scholar
Stein DJ, Seedat S, Emsley RA, Olley BO. HIV/AIDS in Africa—a role for the mental health practitioner? S Afr J Psychiatry. 2005;95(3):167–8.
Rivera-Rivera Y, García Y, Toro V, Cappas N, López P, Yamamura Y, et al. Depression correlates with increased plasma levels of inflammatory cytokines and a dysregulated oxidant/antioxidant balance in HIV-1-infected subjects undergoing antiretroviral therapy. J Clin Cell Immunol. 2014;5(6). https://doi.org/10.4172/2155-9899.1000276 .
Wanyenze RK, Kamya MR, Fatch R, Mayanja-Kizza H, Baveewo S, Sawires S, et al. Missed opportunities for HIV testing and late-stage diagnosis among HIV-infected patients in Uganda. PLoS One. 2011;6(7). https://doi.org/10.1371/journal.pone.0021794 .
Nairaland Forum. A female doctor commits suicide after testing positive to HIV. 2011. http://www.nairaland.com/720421/female-doctor-commits-suicide-after . Accessed 25 May 2018.
Hosek SG, Lemos D, Harper GW, Telander K. Evaluating the acceptability and feasibility of project ACCEPT: An intervention for youth newly diagnosed with HIV. AIDS Educ Prev. 2011;23(2):128–44. https://doi.org/10.1521/aeap.2011.23.2.128 .
Article PubMed PubMed Central Google Scholar
Moitra E, Chan PA, Stein MD. Open trial of an acceptance-based behavior therapy intervention to engage newly diagnosed HIV patients in care: rationale and evidence of feasibility and acceptability. Behav Modif. 2015;39(5):670–90. https://doi.org/10.1177/0145445515590977 .
Assen A, Molla F, Wondimu A, Abrha S, Melkam W, Tadesse E, et al. Late presentation for diagnosis of HIV infection among HIV positive patients in South Tigray zone, Ethiopia. BMC Public Health. 2016;16(1):558. https://doi.org/10.1186/s12889-016-3263-y .
Dodd PJ, Garnett GP, Hallett TB. Examining the promise of HIV elimination by ‘test and treat’ in hyper-endemic settings. AIDS (London, England). 2010;24(5):729–35. https://doi.org/10.1097/QAD.0b013e32833433fe .
Pettifor A, MacPhail C, Corneli A, Sibeko J, Kamanga G, Rosenberg N, et al. NIAID center for HIV/AIDS vaccine immunology. Continued high risk sexual behavior following diagnosis with acute HIV infection in South Africa and Malawi: implications for prevention. AIDS Behav. 2011;15(6):1243–50. https://doi.org/10.1007/s10461-010-9839-0 .
Skinner D, Mfecane S. Stigma, discrimination and the implications for people living with HIV/AIDS in South Africa. SAHARA J. 2004;1(3):157–64.
Article CAS Google Scholar
Koka E, Ahorlu CK, Agyeman DK. Social death through HIV and AIDS stigmatization and discrimination in Ghana: a case study of the central regional hospital, Cape Coast, Ghana. Advanc Appl Sociol. 2013;3(06):231–6.
Miller WC, Rosenberg NE, Rutstein SE, Powers KA. The role of acute and early HIV infection in the sexual transmission of HIV. Curr Opin HIV AIDS. 2010;5(4):277–82. https://doi.org/10.1097/COH.0b013e32833a0d3a .
Gwadz M, de Guzman R, Freeman R, Kutnick A, Silverman E, Leonard NR, et al. Exploring how substance use impedes engagement along the HIV care continuum: a qualitative study. Front Public Health. 2016;4:62. https://doi.org/10.3389/fpubh.2016.00062 .
Lund R, Agyei-Mensah S. Queens as mothers: the role of the traditional safety net of care and support for HIV/AIDS orphans and vulnerable children in Ghana. Geo J. 2008;71(2–3):93–106. https://doi.org/10.1007/s10708-008-9145-9 .
Owusu AY, Laar A. Managing HIV-positive sero-status in Ghana’s most HIV concentrated district: self-perceived explanations and theoretical discourse. Afr J AIDS Res. 2018;17(1):82–90. https://doi.org/10.2989/16085906.2017.1419268 .
Article PubMed Google Scholar
GAC. Summary of the 2016 sentinel survey report. Accra: GAC; 2017. http://www.ghanaids.gov.gh/gac1/aids_info.php . Accessed 10 Jan 2018
Visser MJ, Makin JD, Vandormael A, Sikkema KJ, Forsyth BW. HIV/AIDS stigma in a south African community. AIDS Care. 2009;21(2):197–206.
Fabianova L. Psychosocial aspects of people living with HIV/AIDS. In Social and psychological aspects of HIV/AIDS and their ramifications 2011. IntechOpen. doi: https://doi.org/10.5772/21148 . https://www.intechopen.com/books/social-and-psychological-aspects-of-hiv-aids-and-their-ramifications/psychosocial-aspects-of-people-living-with-hiv-aids . Accessed 14 Oct 2019.
Patel V, Stein DJ. Common mental disorders in sub-Saharan Africa: the triad of depression, anxiety and somatization. In: Akyeampong E, Hill A, Kleinman A, editors. The culture of mental illness and psychiatric practice in Africa. Bloomington: Indiana University Press; 2015. p. 50–72. http://www.jstor.org/stable/j.ctt16gz69f.6 . Accessed 26 Jun 2019.
Miranda JJ, Patel V. Achieving the Millennium Development Goals: does mental health play a role? PLoS Med. 2005;2(10):e291.
Collins PY, Holman AR, Freeman MC, Patel V. What is the relevance of mental health to HIV/AIDS care and treatment programs in developing countries? A systematic review. AIDS (London, England). 2006;20(12):1571–82.
Abela JR. The hopelessness theory of depression: a test of the diathesis–stress and causal mediation components in third and seventh grade children. J Abnorm Child Psychol. 2001;29(3):241–54.
Abela JR, Payne AV. A test of the integration of the hopelessness and self-esteem theories of depression in schoolchildren. Cogn Ther Res. 2003;27(5):519–35. https://doi.org/10.1023/A:1026303020478 .
Waszczuk MA, Coulson AE, Gregory AM, Eley TC. A longitudinal twin and sibling study of the hopelessness theory of depression in adolescence and young adulthood. Psychol Med. 2016;46(9):1935–49. https://doi.org/10.1017/S0033291716000489 .
Seligman ME. Helplessness. On depression, development and death. San Francisco: Freeman; 1975.
Govender RD, Schlebusch L. Hopelessness, depression and suicidal ideation in HIV-positive persons. S Afr J Psychiatry. 2012;18(1):16–21. https://doi.org/10.4102/sajpsychiatry.v18i1.302 .
Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42(6):861 52. GSS. Population and Housing census 2010. Final results. Accra: GSS.2012.
Schlebusch L, Govender RD. Elevated risk of suicidal ideation in HIV-positive persons. Depress Res Treat. 2015;2015. https://doi.org/10.1155/2015/609172 .
Kylmä J, Vehviläinen-Julkunen K, Lähdevirta J. Hope, despair and hopelessness in living with HIV/AIDS: a grounded theory study. J Adv Nurs. 2001;33(6):764–75. https://doi.org/10.1046/j.1365-2648.2001.01712.x .
GSS. Population and Housing census 2010. Final results. Accra: GSS; 2012.
GSS. Population and Housing Report: District Analytical Report 2010, Lower Manya Krobo Municipal. 2014. http://www.statsghana.gov.gh/docfiles/2010_District_Report/Eastern/LOWER%20 MANYA%20KROBO.pdf. Accessed 14 Jul 2019.
Yin RK. Case study research: design and methods. Thousand Oaks, SAGE 2013;14(1):69–71.
Baxter P, Jack S. Qualitative case study methodology: study design and implementation for novice researchers. Qual Rep. 2008;13(4):544–59.
Tenkorang EY, Owusu AY, Laar AK. Housing and health outcomes of persons living with HIV/AIDS (PLWHAs) in the lower Manya Krobo district, Ghana. J Health Care Poor Underserved. 2017;28(1):191–215. https://doi.org/10.1353/hpu.2017.0017 .
Owusu AY. A gendered analysis of living with HIV/aids in the eastern region of Ghana. BMC Public Health. 2020;20:751. https://doi.org/10.1186/s12889-020-08702-9 .
Tenkorang EY, Owusu AY, Laar AK, Yeboah EH. Housing, psychosocial and adherence counseling among HIV+ persons in Ghana. Health Promot Int. 2019;34(2):204–14. https://doi.org/10.1093/heapro/dax072 .
Owusu AY. Social contexts of living with HIV/AIDS in the eastern region of Ghana. Istanbul Univ J Sociol. 2019;39(2):425–54. https://doi.org/10.26650/SJ.2019.39.2.0109 .
NACP. HIV sentinel survey report. Accra: Ghana Health Service/Ministry of Health; 2018. p. 2019.
Owusu, A. Y. Gender, Adolescents, and Achieving Sustainable Development Goals in Ghana. In A. Williams & I. Luginaah (Eds.). Gender Matters Globally: Geography, Health and Sustainability (Chapter 4). Routledge. Forthcoming. ISBNS: Hardback: 9780367743901; Ebook: 9780367743918; Future paperback: 9780367743925.
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82.
Mason M. Sample size and saturation in PhD studies using qualitative interviews. In Forum qualitative Sozialforschung/Forum: qualitative social research 2010;11(3).
Sedziafa AP, Tenkorang EY, Owusu AY. “… he always slaps me on my ears”: the health consequences of intimate partner violence among a group of patrilineal women in Ghana. Culture Health Sexual. 2016;18(12):1379–92. https://doi.org/10.1080/13691058.2016.1187291 .
Lieblich A, Tuval-Mashiach R, Zilber T. Narrative research: reading, analysis, and interpretation, vol. 27: Thousand Oaks, Sage; 1998.
Book Google Scholar
Krippendorff K. Content analysis: an introduction to its methodology. Thousand Oaks: Sage; 2004.
Schreier M. Qualitative content analysis in practice. Thousand Oaks: Sage; 2012.
Boyatzis RE. Transforming qualitative information: thematic analysis and code development. Thousand Oaks: Sage; 1998.
Mayring P. Qualitative content analysis. Forum Qualitative Sozialforschung/ Forum. Qual Soc Res. 2000;1(2):20. https://doi.org/10.17169/fqs-1.2.1089 https://www.qualitative-research.net/index.php/fqs/article/view/1089 . Accessed 20 Apr 2021.
QSR International. NVivo professional version 11. Boston: QSR International; 2015.
Babbie ER. The practice of social research. 13th ed. Scarborough: Wadsworth/Cengage Learning; 2013.
Anderson M, Elam G, Gerver S, Solarin I, Fenton K, Easterbrook P. “It took a piece of me”: initial responses to a positive HIV diagnosis by Caribbean people in the UK. AIDS Care. 2010;22(12):1493–8. https://doi.org/10.1080/09540121.2010.482125 .
Greeff M, Phetlhu R, Makoae LN, Dlamini PS, Holzemer WL, Naidoo JR, et al. Disclosure of HIV status: experiences and perceptions of persons living with HIV/AIDS and nurses involved in their care in Africa. Qual Health Res. 2008;18(3):311–24. https://doi.org/10.1177/1049732307311118 .
Simbayi LC, Kalichman SC, Strebel A, Cloete A, Henda N, Mqeketo A. Disclosure of HIV status to sex partners and sexual risk behaviours among HIV-positive men and women, Cape Town, South Africa. Sex Transm Infect. 2007;83(1):29–34.
Hult JR, Maurer SA, Moskowitz JT. “I'm sorry, you're positive”: a qualitative study of individual experiences of testing positive for HIV. AIDS Care. 2009;21(2):185–8. https://doi.org/10.1080/09540120802017602 .
de-Graft Aikins A. Mental illness and destitution in Ghana: A Social-psychological perspective. In: Akyeampong E, Hill AG, Kleinman AM, editors. The Culture of Mental Illness and Psychiatric Practice in Africa. Bloomington: Indiana university press; 2015. p. 112–43. http://www.jstor.org/stable/j.ctt16gz69f.6 Accessed 26 Jun 2019.
Baumgartner LM, David KN. Accepting being poz: the incorporation of the HIV identity into the self. Qual Health Res. 2009;19(12):1730–43. https://doi.org/10.1177/1049732309352907 .
NAP+, GAC and UNAIDS. Persons living with HIV Stigma Index Study, Ghana. Accra: NAP+, GAC and UNAIDS; 2014. http://www.stigmaindex.org/sites/default/files/reports/GHANA%20Stigma%20Index%20report%202014.pdf . Accessed 4 Apr 2016. Revised report
Baiden F, Baiden R, Williams J, Akweongo P, Clerk C, Debpuur C, et al. Review of antenatal-linked voluntary counseling and HIV testing in sub-Saharan Africa: lessons and options for Ghana. Ghana Med J. 2005;39(1):8–13. https://doi.org/10.4314/gmj.v39i1.35974 .
Article CAS PubMed PubMed Central Google Scholar
Gadegbeku C, Saka R, Mensah B. Attitude of the Youth towards Voluntary Counselling and Testing (VCT) of HIV/AIDS in Accra, Ghana. J Biol Agri Healthcare. 2013;3(11):133 www.iiste.org .
Oppong AK. HIV/AIDS knowledge and uptake of HIV counselling and testing among undergraduate private university students in Accra, Ghana. Reprod Health. 2013;10:17. https://doi.org/10.1186/1742-4755-10-17 .
Tenkorang EY, Owusu AY. Examining HIV-related stigma and discrimination in Ghana: what are the major contributors? Sex Health. 2013;10(3):253–62. https://doi.org/10.1071/SH12153 .
Dapaah JM, Spronk R. When the clinic becomes a home. Successful VCT and ART services in a stressful environment. J Soc Aspects HIV/AIDS. 2016;13(1):142–51. https://doi.org/10.1080/17290376 .
Badaru UM, Ogwumike OO, Adeniyi AF, Nelson EE. Determinants of caregiving burden and quality of life of informal caregivers of African stroke survivors: literature review. Int J Disabil Human Dev. 2017;16(3):249–58. https://doi.org/10.1515/ijdhd-2016-0041 .
Omona J. Sampling in qualitative research: improving the quality of research outcomes in higher education. Makerere J Higher Educ. 2013;4(2):169–85. https://doi.org/10.4314/majohe.v4i2.4 .
Miles M, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2nd ed. Thousand oaks: Sage; 1994.
Peirce A. The emotional impact of an HIV diagnosis. 2017. https://www.everydayhealth.com/hiv-aids/hiv-diagnosis-emotional-impact.aspx . Accessed 2 May 2018.
GAC. National HIV & AIDS Strategic Plan 2016-2020. 2016. http://www.ghanaids.gov.gh/gac1/pubs/COMPREHENSIVE%20NSP%202016-2020.pdf . Accessed 17 May 2020.
Owusu AY, Asante KT. Current HIV/AIDS status, access to antiretroviral treatment, and HIV related stigma in Ghana. Policy Brief. 2020. Accra: ISSER.
Download references
Acknowledgements
Professor Eric Y. Tenkorang of the Department of Sociology, Memorial University of Newfoundland and Labrador in Canada, was the PI for the project and participated in the data collection. Professor Tenkorang also principally solicited for the funds for this study from the IDRC. The Author is grateful to him. Dr. Kofi Takyi Asante of ISSER, University of Ghana, Legon, is also acknowledged for proofreading an earlier version of this paper.
Funding for data collection for this research was provided by the International Development Research Centre (IDRC), through the Canadian-African Research Grant. Matching grants were provided by the Department of Sociology, Memorial University of Newfoundland and Labrador, Canada. IDRC and the Memorial University played no role in the design of the study, data collection, analysis, and interpretation, as well as the writing of the manuscript.
Author information
Authors and affiliations.
Institute of Statistical, Social and Economic Research (ISSER), University of Ghana, P. O. Box LG 74, Legon, Ghana
Adobea Yaa Owusu
You can also search for this author in PubMed Google Scholar
Contributions
AYO contributed to conceptualising the study and served as a co-Principal Investigator (co-PI). AYO mostly focused on the qualitative aspect of the project from which the data for this paper emanates. AYO also developed the in-depth interview guide, helped to liaise with technical staff of the Ghana Health Service and Ghana AIDS Commission for explanations to some HIV/AIDS technical and policy-related issues in Ghana. Furthermore, AYO led in the acquisition of ethical clearance from the University of Ghana. Additionally, AYO co-supervised field staff during the data collection, and handled the quality control, and analysis of the qualitative data. AYO wrote and finalised this paper single-handedly. Since this paper is sole-authored, the final version of the manuscript does not require the approval of any other person prior to being submitted and published.
Author’s information
AYO is an Associate Professor at the Institute of Statistical, Social and Economic Research, College of Humanities, University of Ghana, Legon, Ghana. AYO is a Medical Sociologist, Public Health, and behavioural health specialist.
Corresponding author
Correspondence to Adobea Yaa Owusu .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval were sought from the following: 1) Ethical Review Board of the Memorial University at St. Johns, Newfoundland, Canada, 2) the Ethics Committee for Humanities at the University of Ghana, Legon (ECH 017/14–15), and 3) the Ghana Health Service’s Ethical Review Board (GHS-ERC: 02/11/14). The Protocol Submission form which was filled to seek ethical permission from the Ghana-based ethical committees included five options for types of consent to be sought from the respondents, under the section on “consent process”, with instructions to “circle all that applies.” We chose all of "written”, “oral”, “English language”, and "local language” options. These were approved by the ethics committees, as part of the general approval we received. The need to approve non-written consent as well as the use of the local languages is informed by the fact that not everyone in the study’s catchment area, which is applicable to the rest of Ghana, can read and write. Respondents who consented to participate in the study by writing had to append their signature or initials to a written form provided by the Ethical Committee for Humanities at the University of Ghana. Field enumerators recorded verbal consent on the said form for respondents who could not read and write. Permission to conduct the study were also received from 1) the Ghana Health Service’s Eastern Regional Directorate, 2) The LMKM Directorate of the Ghana Health Service, and 3) the Administrators of the Atua Government, and St. Martins De Pores hospitals. Each participant gave a written or verbal informed consent to participate before they were interviewed.
Consent for publication
Not applicable.
Competing interests
The author declares that there are no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Qualitative/Indepth Interview Guide. Housing and Health Needs of Persons Living with HIV/AIDS Project. Open-ended qualitative indepth interview guide with sections A to G and ending with demographic/background data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Owusu, A.Y. Experiences of new diagnoses among HIV-positive persons: implications for public health. BMC Public Health 22 , 538 (2022). https://doi.org/10.1186/s12889-022-12809-6
Download citation
Received : 04 July 2020
Accepted : 21 February 2022
Published : 18 March 2022
DOI : https://doi.org/10.1186/s12889-022-12809-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Comorbidities
- Psychosocial outcomes
- Qualitative research
- Experiences of new HIV-positive diagnoses
- Hopelessness theory of depression
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Study highlights need for cell-type-specific therapies in treatment of HIV
R esearchers from the University of Illinois have demonstrated the importance of cell-type-specific targeting in the treatment of HIV. Their study, published in the Proceedings of the National Academy of Sciences , is one of the first to examine the differential or cell-type specific effects of HIV latency modulation on myeloid cells, a type of immune cell made in bone marrow.
A major barrier to eliminating HIV infection is how to manage latency, or the period in which an infected cell is dormant and unable to produce virus. Latent HIV cells congregate throughout the body in pockets known as reservoirs. Latent reservoirs are problematic because they can start producing virus at any time.
Complete eradication of the disease would require removal of all latent cells from the body or permanent resistance to activation stimuli. But reactivation can be triggered by numerous factors, including cues that direct the differentiation of myeloid cells.
For years, HIV cure research has centered around two approaches, known as "shock and kill" and "block and lock." The former works in tandem with antiretroviral therapy to activate latently infected cells and deplete them through apoptosis, or programmed cell death, while the latter forces infected cells into a deep latent state from which they cannot spontaneously reactivate.
Research around these techniques has historically focused on a type of white blood cell called a T-cell, which is the main target of HIV infection. But latent reservoirs are composed of more than just T-cells; in fact, they contain dozens of diverse cell types, each with their own unique HIV gene expression patterns.
"There is a huge amount of heterogeneity in cells, even within the same lineage," said Collin Kieffer, an assistant professor of microbiology and an author on the paper. "The variability of response within these reservoirs increases with each new cell type."
Alexandra Blanco, a Ph.D. student in Kieffer's lab, wanted to study cell types that had been overlooked in conventional HIV research. Concentrating on myeloid cells, she created a clonal library containing 70 populations of latently infected monocytes. Blanco then analyzed the clonal populations and their responses to activation. The responses varied significantly, highlighting a large degree of heterogeneity within a single cell type.
This observation prompted a new question: Do different cell types exhibit different responses to HIV latency treatment? Indeed, their study results showed that certain HIV latency therapeutics can promote latency in T-cells and monocytes, while reversing latency in macrophages.
"Not all cells in the body are the same," Kieffer said. "So it makes sense that not all HIV-infected cells would react to the virus in the same way."
Their paper highlights the need for future HIV treatments to consider all types of cells and the ways each cell might respond to potential therapies.
Their findings build upon the research of Roy Dar, a former Illinois professor of bioengineering whose lab studied heterogeneity in HIV gene expression.
"He started this, and we picked it up and moved it to its current state," Kieffer said. "So collaboration really built the foundation for these results. It's evolved into a new direction for our lab, and one we're really excited about."
An additional and unexpected finding from Blanco's analysis revealed changes to cell size and shape in response to infection, suggesting that HIV can alter cell morphology. Blanco's next goal is to identify the biological mechanisms behind these phenotypic changes.
Kieffer and members of his lab also look forward to reproducing their results—which were mostly conducted on a cell line—in primary cells. Replicating the results in a more human-like model would enhance the study's clinical relevancy, Kieffer explained.
"We'd like to conduct larger screens in T-cells, monocytes, and macrophages to identify potential drugs that could work across all these cell types," Blanco said. "We might be able to find even more molecules that don't behave in a cell-type-specific manner."
More information: Alexandra Blanco et al, Monocyte to macrophage differentiation and changes in cellular redox homeostasis promote cell type-specific HIV latency reactivation, Proceedings of the National Academy of Sciences (2024). DOI: 10.1073/pnas.2313823121
Provided by University of Illinois at Urbana-Champaign

The Effect of HIV on the Association of Hyperglycaemia and Active Tuberculosis in Zambia, a Case–Control Study
- Research Article
- Open access
- Published: 07 May 2024
Cite this article
You have full access to this open access article

- Sarah Lou Bailey ORCID: orcid.org/0000-0002-8425-3472 1 , 2 ,
- Sian Floyd 1 ,
- Maina Cheeba-Lengwe 2 ,
- Kwitaka Maluzi 2 ,
- Kasanda Chiwele-Kangololo 2 ,
- Deborah Kaluba-Milimo 2 ,
- Modupe Amofa-Sekyi 2 ,
- John S. Yudkin 3 ,
- Peter Godfrey-Faussett 1 &
- Helen Ayles 1 , 2
184 Accesses
Explore all metrics
To determine if HIV modifies the association between hyperglycaemia and active tuberculosis in Lusaka, Zambia.
A case–control study among newly—diagnosed adult tuberculosis cases and population controls in three areas of Lusaka. Hyperglycaemia is determined by random blood glucose (RBG) concentration measured at the time of recruitment; active tuberculosis disease by clinical diagnosis, and HIV status by serological result. Multivariable logistic regression is used to explore the primary association and effect modification by HIV.
The prevalence of RBG concentration ≥ 11.1 mmol/L among 3843 tuberculosis cases was 1.4% and among 6977 controls was 1.5%. Overall, the adjusted odds ratio of active tuberculosis was 1.60 (95% CI 0.91–2.82) comparing those with RBG concentration ≥ 11.1– < 11.1 mmol/L. The corresponding adjusted odds ratio among those with and without HIV was 5.47 (95% CI 1.29–23.21) and 1.17 (95% CI 0.61–2.27) respectively; p -value for effect modification by HIV = 0.042. On subgroup analysis, the adjusted odds ratio of smear/Xpert-positive tuberculosis was 2.97 (95% CI 1.49–5.90) comparing RBG concentration ≥ 11.1– < 11.1 mmol/L.
Conclusions
Overall, no evidence of association between hyperglycaemia and active tuberculosis was found, though among those with HIV and/or smear/Xpert-positive tuberculosis there was evidence of association. Differentiation of hyperglycaemia caused by diabetes mellitus and stress-induced hyperglycaemia secondary to tuberculosis infection is important for a better understanding of these findings.
Similar content being viewed by others
The association of hyperglycaemia with prevalent tuberculosis: a population-based cross-sectional study.
The association of glycemic level and prevalence of tuberculosis: a meta-analysis
Tuberculosis and diabetes mellitus comorbidity in an adult Ugandan population
Avoid common mistakes on your manuscript.
1 Introduction
HIV and hyperglycaemia are independently associated with an increased risk of active tuberculosis (TB) [ 1 , 2 ]. However, the dual effect of HIV and hyperglycaemia on the risk of developing TB disease is unclear. A systematic review [ 3 ] identified two prior studies investigating the effect of HIV on the association between hyperglycaemia or diabetes mellitus (DM) and tuberculosis [ 4 , 5 ]. Another systematic review [ 6 ] identified a further two studies that stratified their estimates by HIV status [ 7 , 8 ], and we identified one additional study that has investigated these associations [ 9 ]. The findings differed for each study depending on the analysis strategy and the method used to measure glycaemia.
Global guidelines exist for the care and control of co-existing diabetes mellitus and tuberculosis, but these were developed using evidence from studies largely based in low HIV prevalence settings [ 2 , 10 , 11 ]. If HIV does modify the association, this could lead to a different overall association in areas of high HIV prevalence. Understanding this could allow location-specific guidelines to be developed and implemented, to optimise the care and control of DM and TB.
This study aims to determine whether HIV modifies the association between hyperglycaemia and active TB in Lusaka, Zambia.
2.1 Study Design and Setting
This unmatched case–control study took place among adults in three urban communities in Lusaka, Zambia. Each community has a high incidence of TB and a high prevalence of HIV. The exposure of interest was hyperglycaemia and the outcome was diagnosed active TB disease.
Consecutive newly—diagnosed TB cases who had not yet started TB treatment or were within 2 days of starting TB treatment were recruited from National TB Programme government clinics between September 2013 and September 2015. A TB case was defined as any person presenting to a TB clinic with a clinical diagnosis of TB (pulmonary or extra-pulmonary) with or without microbiological confirmation of TB and prescribed a full course of antitubercular chemotherapy [ 12 ]. This is the definition used in the study clinics—use of this aimed to facilitate translation of results to the clinical setting. At the time of data collection the study clinics were using sputum smear, Xpert MTB/RIF or both to diagnose TB, depending on the availability of reagents and equipment. Exclusion criteria for cases were age < 18 years, commenced TB treatment > 2 days prior to recruitment or inability to give consent due to disability/incapacitation. All eligible cases were identified in the TB clinic and invited to participate during a routine clinic attendance.
2.3 Controls
Unmatched controls were recruited between January and December 2010 as part of a cross-sectional survey that measured prevalent TB for a large cluster randomised trial (the ZAMSTAR trial) [ 13 , 14 ]. They were sampled randomly from all adults living in the catchment areas of the clinics, using a 2-stage cluster sampling technique within each community. Exclusion criteria for controls were age < 18 years, refusal to submit a respiratory sample, diagnosed TB at the time of the survey (culture positive sputum for Mycobacterium tuberculosis ), currently on treatment for TB at the time of the survey (self-report), inability to give consent due to disability/incapacitation or any persons living in institutional settings. All eligible controls were recruited in their homes.
2.4 Data Collection
Glycaemia was determined by random capillary blood glucose (RBG) sampling measured at the time of recruitment. An Optium Xceed point-of-care glucometer was used for controls and an Accu-Chek Aviva point-of-care glucometer was used for cases. Manufacture of the former had been discontinued between the start of data collection for controls and cases so the Aviva was identified as being a similar and well-performing option instead. The time of last oral intake (excluding water) was recorded. RBG concentration was measured during daylight hours and throughout the year. Research staff were trained on the use of the glucometers and were required to undergo proficiency testing. Standardised control solution was used for performance checks on test strips and meters. The validity of glucose measurement was assessed for the Aviva glucometer, giving an intraclass correlation of 0.996 (95% CI 0.991–0.999) for intra-operator variability and 0.983 (95% CI 0.954–0.995) for inter-operator variability. All research assistants contributed to this assessment, using known normoglycaemic volunteers and a standard hyperglycaemic specimen. For intra-operator variability each research assistant repeated the test 5 consecutive times on 13 subjects/specimens. For inter-operator variability research assistants each performed the test on a single subject/specimen in the same place at the same time for 7 subjects/specimens.
For a stratified subset of cases, fasting blood glucose (FBG) concentration was measured within 3 days of commencement of TB treatment and again 3 months later, to indicate if the hyperglycaemia was transient or persistent.
HIV was measured using point-of-care rapid blood-based kits. Determine™ HIV-1/2 was used as the first line test and if positive Uni-Gold™ HIV was used as a confirmatory test. Self-reported use of antiretroviral therapy (ART) was recorded for individuals who were already known to be infected with HIV.
Participants who tested positive for HIV or were identified to have abnormal blood glucose were referred to local healthcare facilities for management.
In order to adjust for potential confounding factors, a structured questionnaire was used to obtain information on age, sex, smoking history, household socio-economic position and education level. Height, weight and waist circumference were measured using standardised methods.
Data were electronically entered directly onto personal digital assistants by research assistants at the time of data collection, using pre-programmed questionnaires and result sheets with error and range checks. All data were downloaded into a SQL (structured query language) database and exported into Stata.
All questions, measurement tools (HIV testing kits but not glucometers) and test standard operating procedures were identical for cases and controls.
Each participant was required to give written informed consent. Ethics approval was granted from the London School of Hygiene and Tropical Medicine Ethics Committee and the University of Zambia Biomedical Research Ethics Committee.
2.6 Statistical Analysis
The study sample size was calculated to give sufficient power for determination of effect modification by HIV. Principal components analysis was used to create a measure of household socio-economic position. Hyperglycaemia was initially examined with RBG concentration as an ordered categorical variable. We then used the RBG cut-off 11.1 mmol/L to explore hyperglycaemia as a binary variable.
Unadjusted and adjusted odds ratios of the association between hyperglycaemia and active TB were estimated using logistic regression analysis. Interaction terms were used to assess for effect modification by HIV, adjusting for variables considered a priori as potential confounding factors.
Restriction of the outcome definition separately to sputum smear-positive or Xpert MTB/RIF positive tuberculosis, smear-negative and Xpert MTB/RIF negative pulmonary TB, and extrapulmonary TB were identified a priori for sub-group analyses, as was exploration of the impact of ART use on HIV as an effect modifier.
Potential bias was assessed using chi-squared tests of association of glycaemia with time of last oral intake before measurement and time of day of measurement of RBG concentration, each comparing cases to controls. Intra- and inter-operator variability were assessed for absolute agreement using a one-way and a two-way random-effects model respectively [ 15 ].
There were 3909 eligible TB cases identified, of whom 3843 (98.3%) consented to participate. There were 11,271 adults randomly selected from the three study communities and enrolled in the ZAMSTAR survey, of whom 6977 (61.9%) were eligible to be control participants for this study (Fig. 1 ).
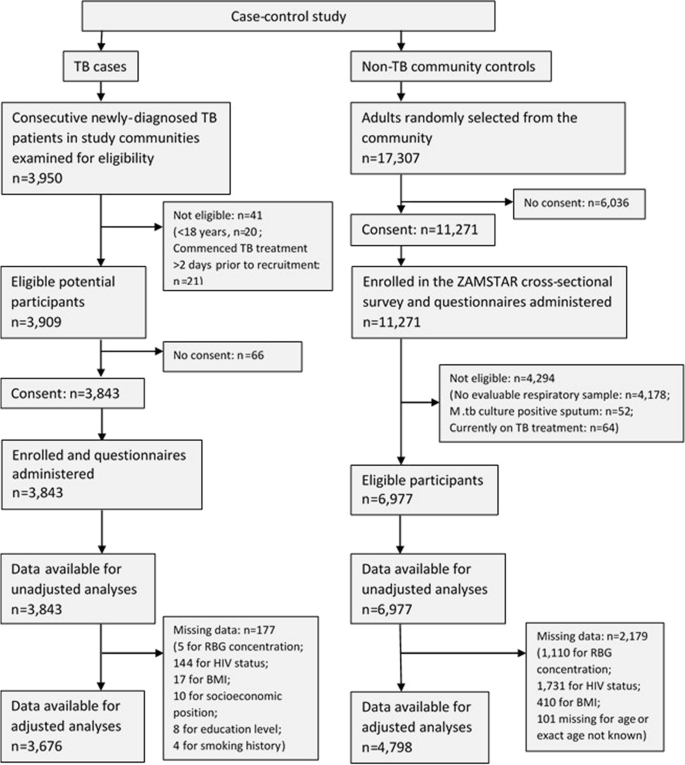
Number and flow of cases and controls
The characteristics of participants are shown in Table 1 . Among cases and controls 1.4% and 1.5% respectively had a RBG concentration ≥ 11.1 mmol/L (Table 1 ). 65% of cases and 18% of controls were living with HIV.
Comparing participants with RBG ≥ 11.1 mmol/L to those with RBG < 11.1 mmol/L, the unadjusted odds ratio of TB was 0.91 (95% CI 0.65–1.28). When analysed with RBG concentration as an ordered categorical variable, there was evidence of an association between hyperglycaemia and tuberculosis, but there was strong evidence that the association did not follow a linear trend. We therefore did not examine the association with RBG concentration as a continuous variable. On unadjusted analysis there was no evidence to suggest that the odds of TB for the effect of hyperglycaemia differed between individuals infected and uninfected with HIV (Table 1 ).
The adjusted odds of TB was 1.60 times higher in those with RBG ≥ 11.1 mmol/L compared to those with RBG < 11.1 mmol/L (95% CI 0.91–2.82), adjusting for the effect of age, gender, education, socioeconomic position, body mass index, smoking history and community. As a categorical variable there remained strong evidence of a non-linear association. Among individuals with HIV, the adjusted odds of TB was 5.47 times higher in those with RBG ≥ 11.1 mmol/L compared to those with RBG < 11.1 mmol/L (95% CI 1.29–23.21). Among individuals without HIV, the adjusted odds of TB was 1.17 times higher for the same comparison (95% CI 0.61–2.27). The p -value for interaction was 0.042. The main confounding factors were age, sex and body mass index.
When the analysis was restricted to separate TB categories, there was evidence of association between hyperglycaemia and sputum smear/Xpert-positive tuberculosis, and this association was stronger in individuals infected than uninfected with HIV ( p -value for interaction = 0.028, Table 2 ).
Among individuals infected with HIV, 36.7% of cases and 21.2% of controls were taking ART. There was evidence of association between hyperglycaemia and active tuberculosis among individuals who were HIV-positive and not currently taking ART, but not among individuals who were HIV-positive and taking ART (Table 3 ).
FBG concentration was measured in 232 participants with TB at baseline and 3 months later. Nine participants had hyperglycaemia at baseline (FBG ≥ 7.0 mmol/L) and 4 (44.4%) of these had persistent hyperglycaemia 3 months later. Three (75%) participants with persistent hyperglycaemia were uninfected with HIV. Four (80%) participants with transient hyperglycaemia were infected with HIV.
Participants reported the time of last oral intake prior to measurement of RBG concentration to be a mean of 4.9 h (standard deviation 4.6 h). There was no evidence of a difference in time (< or ≥ 6 h) of last oral intake between participants with RBG < and ≥ 11.1 mmol/L ( p = 0.815), nor between individuals with and without TB ( p = 0.793). There was no evidence of a difference in the time (hour) of measurement between participants with RBG < and ≥ 11.1 mmol/L ( p = 0.832).
4 Discussion
In this case–control study in Lusaka, Zambia, we found no evidence of association between hyperglycaemia and active tuberculosis, except for when TB was restricted to individuals with smear/Xpert-positive pulmonary TB. There was evidence of effect modification by HIV for the association between hyperglycaemia and active TB. When adjusted for confounding factors, the association was stronger among individuals infected with HIV than among uninfected individuals.
When analysed as an ordered categorical variable with pre-defined categories, there was evidence of a non-linear association between hyperglycaemia and tuberculosis in our study population, as individuals with RBG concentration 7.0–8.9 mmol/L had a lower odds of TB than individuals with lower or higher RBG concentration ( p < 0.001). This was an unexpected finding and may be due to chance as there is no biological reason to explain this pattern.
Although our primary association findings are not in keeping with the findings of the most recent systematic review, which reported a pooled odds ratio of 2.77 for the association between hyperglycaemia and tuberculosis in Africa [ 6 ], they do mirror the findings of some studies in nearby communities in Guinea-Bissau [ 16 ], South Africa [ 9 ] and Tanzania [ 5 ]. Boillat-Blanco et al. in Tanzania found a positive association between hyperglycaemia and tuberculosis at the time of TB treatment initiation, but the association disappeared when measurement of diabetes was repeated 5 months after TB treatment initiation, suggesting that the initial positive association was due to an increase in stress-induced hyperglycaemia among TB cases secondary to acute TB infection rather than due to DM [ 5 ].
Our findings of a stronger association among HIV infected than uninfected individuals are in keeping with Oni’s findings [ 9 ] and could suggest that HIV and hyperglycaemia work synergistically to increase an individual’s risk of TB. Another possible explanation is an increase in stress-induced hyperglycaemia among newly—diagnosed TB cases, as seen in Boillat-Blanco’s study [ 5 ]. It is plausible that the most unwell newly diagnosed TB cases, and therefore the most likely to have stress-induced hyperglycaemia, could be found among individuals with HIV and smear/Xpert-positive pulmonary TB.
This study used a single RBG concentration to measure hyperglycaemia. This method is simple, quick, and minimises participant inconvenience, so is ideal for use in large community-based studies. However, use of this method is also a limitation of the study as it is not as sensitive for diabetes diagnosis as other glycaemia measures. We chose to go ahead with using this method because all other methods would have been challenging to perform on a large scale in the community and could have led to selection bias if considered to be unacceptable to healthy control participants. An alternative could have been the use of a clinic-based control population as a proxy to community controls, but this too could have led to selection bias. Assessing shifts in proportions of glucose concentration between cases and controls in addition to using a binary cut-off definition of hyperglycaemia has limited potential misclassification error that could exist with the use of this less sensitive measurement.
Our assessment of intra- and inter-operator variability suggests that measurement of point-of-care RBG among cases in this study was consistent and valid. We explored the possibility of also undertaking laboratory validation of glucose measurements but this was not possible in our setting, as point-of-care glucose measurement is the principal method for measuring glycaemia in the community and centrally. The laboratory alternatives were therefore not equipped to offer a reliable benchmark. This lack of laboratory validation of glucose measurements is a limitation of our study. Finding a solution to this challenge in our setting would be valuable for future similar studies.
The temporal space between recruitment of controls and cases is another potential source of bias and limitation of our study, though the study communities have relatively stable populations and to our knowledge there were no major changes in the prevalence of hyperglycaemia, diabetes or HIV, or the incidence of TB during the study period. Any potential change in use of ART is unlikely to have had a major impact on hyperglycaemia, as protease inhibitors—which are associated with the development of glucose disorders [ 17 ]—are not included among first-line ART regimes in Zambia [ 18 ]. This is supported by exploration of the impact of ART on the associations studied. Any bias introduced by the recruitment gap is therefore likely to have been, at the most, minimal. However, an unforeseen consequence of the gap was the discontinuation of the initial glucometer model used for control participants. It was therefore necessary to use a different model for case participants. We chose a similar model to minimise any potential variability between models and so any difference in measurement of glycaemia is likely to be small rather than large.
Complete data were unavailable for analysis for a substantial proportion of control participants, reasons for which are discussed elsewhere [ 8 , 19 , 20 ]. This has resulted in reduced study power but is unlikely to have introduced bias to our study results.
Control participants are representative of the general population and case participants are representative of TB cases in each community. The findings from this study are therefore generalizable to the study communities and likely also to communities elsewhere in sub-Saharan Africa with similar high incidence of TB and high prevalence of HIV.
5 Conclusions
Overall, no evidence of association between hyperglycaemia and active tuberculosis was found in this study population, though among those with HIV and those with smear/Xpert-positive pulmonary TB there was evidence of an association. Differentiation of hyperglycaemia caused by diabetes mellitus and stress-induced hyperglycaemia secondary to tuberculosis infection is important to understand these data further. Future similar studies should aim to minimise the potential sources of bias that we have identified in our study.
Availability of Data and Materials
The dataset generated and analysed during the current study is not publicly available because it could be possible to identify individuals from the dataset despite the dataset being anonymised.
Abbreviations
Antiretroviral therapy
Confidence interval
- Diabetes mellitus
Fasting blood glucose
Human immunodeficiency virus
Random blood glucose
Structured query language
- Tuberculosis
Aaron L, et al. Tuberculosis in HIV-infected patients: a comprehensive review. Clin Microbiol Infect. 2004;10(5):388–98.
Article CAS PubMed Google Scholar
Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLoS Med. 2008;5(7):e152.
Article PubMed PubMed Central Google Scholar
Bailey SL, Ayles H. Association between diabetes mellitus and active tuberculosis in Africa and the effect of HIV. Trop Med Int Health. 2017;22(3):261–8.
Article CAS PubMed PubMed Central Google Scholar
Faurholt-Jepsen D, et al. Diabetes is a risk factor for pulmonary tuberculosis: a case-control study from Mwanza, Tanzania. PLoS ONE. 2011;6(8):e24215.
Boillat-Blanco N, et al. Transient hyperglycemia in patients with tuberculosis in tanzania: implications for diabetes screening algorithms. J Infect Dis. 2016;213(7):1163–72.
Obels I, et al. Tuberculosis risk among people with diabetes mellitus in Sub-Saharan Africa: a systematic review. Trop Med Int Health. 2022;27(4):369–86.
Kubjane M, et al. Tuberculosis, human immunodeficiency virus, and the association with transient hyperglycemia in Periurban South Africa. Clin Infect Dis. 2020;71(4):1080–8.
Article PubMed Google Scholar
Bailey SL, et al. The association of hyperglycaemia with prevalent tuberculosis: a population-based cross-sectional study. BMC Infect Dis. 2016;16(1):733.
Oni T, et al. Trilateral overlap of tuberculosis, diabetes and HIV-1 in a high-burden African setting: implications for TB control. Eur Respir J. 2017;50(1):1.
Article Google Scholar
Jeon CY, et al. Bi-directional screening for tuberculosis and diabetes: a systematic review. Trop Med Int Health. 2010;15(11):1300–14.
WHO & IUTLD. Collaborative framework for care and control of tuberculosis and diabetes. Geneva: World Health Organization; 2011.
Google Scholar
World Health Organization, Treatment of tuberculosis: guidelines . 4th ed. 2010, Geneva, Switzerland: World Health Organization.
Ayles HM, et al. ZAMSTAR, The Zambia South Africa TB and HIV reduction study: design of a 2 × 2 factorial community randomized trial. Trials. 2008;9:63.
Ayles H, et al. Effect of household and community interventions on the burden of tuberculosis in southern Africa: the ZAMSTAR community-randomised trial. Lancet. 2013;2013:1.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–63.
Haraldsdottir TL, et al. Diabetes mellitus prevalence in tuberculosis patients and the background population in Guinea-Bissau: a disease burden study from the capital Bissau. Trans R Soc Trop Med Hyg. 2015;109(6):400–7.
Larson R, et al. Disorders of glucose metabolism in the context of human immunodeficiency virus infection. J Am Acad Nurse Pract. 2006;18(3):92–103.
Republic of Zambia Ministry of Health, Zambia Consolidated Guidelines for Treatment and Prevention of HIV Infection . 2014, The Government of Zambia: Lusaka, Zambia.
Ayles H, et al. Effect of household and community interventions on the burden of tuberculosis in southern Africa: the ZAMSTAR community-randomised trial. Lancet. 2013;382(9899):1183–94.
Bailey SL, et al. Diabetes mellitus in Zambia and the Western Cape province of South Africa: prevalence, risk factors, diagnosis and management. Diabetes Res Clin Pract. 2016;118:1–11.
Download references
Acknowledgements
We thank all the members of all study teams who contributed to data collection. We thank the Zambian Ministry of Health, the Zambian National TB Programme, the Lusaka District Medical Officer and all health facility staff for allowing us to work in the TB clinics. The work presented in this paper contributed to SLB’s Ph.D. work, the thesis for which can be accessed via an open access repository ( https://researchonline.lshtm.ac.uk/id/eprint/4646636/ ).
SLB was supported by a Wellcome Trust Clinical Ph.D. Fellowship (100141/Z/12/Z), and this study was funded by the fellowship. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the Wellcome Trust.
Author information
Authors and affiliations.
LSHTM TB Centre and Department of Clinical Research, London School of Hygiene and Tropical Medicine, London, UK
Sarah Lou Bailey, Sian Floyd, Peter Godfrey-Faussett & Helen Ayles
Zambart, Lusaka, Zambia
Sarah Lou Bailey, Maina Cheeba-Lengwe, Kwitaka Maluzi, Kasanda Chiwele-Kangololo, Deborah Kaluba-Milimo, Modupe Amofa-Sekyi & Helen Ayles
Division of Medicine, University College London, London, UK
John S. Yudkin
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to initial study concept and study design. SLB and HA oversaw participant recruitment and data collection. SLB performed the data analysis. SLB wrote initial drafts and all authors contributed to final editing of the paper.
Corresponding author
Correspondence to Sarah Lou Bailey .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Consent for Publication
Not applicable.
Ethics Approval and Consent to Participate
Each participant was required to give written informed consent. Ethics approval was granted from the London School of Hygiene and Tropical Medicine Ethics Committee (Ref. 6368) and the University of Zambia Biomedical Research Ethics Committee (Ref. 007-04-13).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Bailey, S.L., Floyd, S., Cheeba-Lengwe, M. et al. The Effect of HIV on the Association of Hyperglycaemia and Active Tuberculosis in Zambia, a Case–Control Study. J Epidemiol Glob Health (2024). https://doi.org/10.1007/s44197-024-00236-2
Download citation
Received : 17 October 2022
Accepted : 22 April 2024
Published : 07 May 2024
DOI : https://doi.org/10.1007/s44197-024-00236-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hyperglycaemia
- Epidemiology
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Experiences and Attitudes of People with HIV/AIDS: A Systematic Review of Qualitative Studies
Tomás arias-colmenero.
1 Guadalajara Hospital, 19002 Guadalajara, Spain; se.neaju.der@30000cat
Mª Ángeles Pérez-Morente
2 Faculty of Health Sciences, University of Jaén, 23071 Jaén, Spain
Antonio Jesús Ramos-Morcillo
3 Department of Nursing, Faculty of Nursing, University of Murcia, 30100 Espinardo, Spain; se.mu@somarja (A.J.R.-M.); se.mu@afazuram (M.R.-M.)
Concepción Capilla-Díaz
4 Faculty of Health Sciences, University of Granada, 51001 Ceuta, Spain; se.rgu@dcihcnoc (C.C.-D.); se.rgu@oseuhrasec (C.H.-M.)
María Ruzafa-Martínez
César hueso-montoro, associated data.
The aim of this article was to explore the experiences and attitudes of people with HIV/AIDS. A systematic review of qualitative studies was carried out. Twenty-seven articles were included, with sample sizes ranging from 3 to 78. Articles from North America, South America, Central America, Europe, and Africa were included. Five topics emerged from the synthesis: feelings about the diagnosis of HIV/AIDS; stigma and HIV/AIDS; changes in sexual behavior after becoming infected; living with the virus; and pregnancy and motherhood in seropositive women. The moment of diagnosis is of vital importance for these people due to feelings such as disappointment, sadness, fear, despair, lack of awareness, and pain. Social support is highly valued among these people and is linked to an improvement in these peoples’ quality of life. Different kinds of stigma accompany people with HIV/AIDS throughout their life, like social stigma, self-stigma, and health professionals’ stigma. Seropositive women who decide to become mothers can feel frustration because they cannot breastfeed. Spirituality helps some people to deal with the fact of being a virus or disease carrier.
1. Introduction
HIV is one of the main problems with regard to public health, with greater representation in developing countries [ 1 ]. The most affected region is Africa, where almost two thirds of new HIV infections can be found [ 2 ]. Worldwide, amongst the population with HIV, 54% of adults and 43% of children are currently being treated with antiretroviral therapy, with the global coverage of these medications for pregnant women or for women who are breastfeeding being approximately 75%.
Being seropositive or having the disease tends to occur in several stages, among which are: the stage of diagnosis, where the person is normally in shock; and the stage of acceptance (positive adaptation) or denial (negative adaptation) [ 3 ]. From the beginning of the disease, when it was labelled the so-called “gay-syndrome”, it was characterized by a huge burden of discrimination [ 4 ]. This stigma is a negative element that limits the individual’s adaptation to the disease/seropositivity, as well as complicating the management and treatment of the disease; it also creates difficulties in the relationship with the population in general, and with health care professionals [ 5 ].
Currently, there are global proposals, such as the well-known 90–90–90, the Joint United Nations Program on HIV/AIDS [ 6 ], whose aims include raising awareness of the HIV/AIDS epidemic. This proposal, through an ambitious project, suggests that, by 2020, 90% of seropositive people must be diagnosed in the world, 90% of them must be treated, and 90% of them must be free of viral load. It also suggests that different governments and policies join forces to control the disease. In this sense, this research aims to explore the disease from the individual’s own perspective and, therefore, to contribute to making the daily life of people who suffer from it visible.
The purpose of this review was to explore the experiences and attitudes of people with HIV/AIDS. We consider that knowledge-based outcomes from this study can help improve decision-making on health strategies to cope with HIV, and also guide future research on the topic.
2. Materials and Methods
A systematic review of qualitative studies was developed. Our research included studies published in Spanish, Portuguese and English. We selected original articles oriented to qualitative methodologies, whose interest of study was to explore the perspective of people with HIV/AIDS. Studies regarding a pediatric population or focused on adolescence were excluded. We intended to show a broad view regarding the phenomenon under study, which incorporated works from a wide geographical context. That is why different search sources and databases were used, such as CINAHL, PubMed, Lilacs, Cuiden and Google Scholar. In the same way, descriptors from MESH, CINAHL/MeSH, Subject Headings and DeCS (for the Spanish Language) were employed, in addition to non-standardized terms. The English terms that we used were: Human Immunodeficiency Virus, HIV, AIDS, qualitative research or studies; whereas the Spanish terms were: VIH, SIDA, cualitativo. The search was conducted from January to March 2019, including publications until 2018. The oldest article included in the review was published in 2004.
Search. Different search strings were designed with thematic, main, and free descriptors for the different databases. For instance, we used the following search string for the PubMed database: <(HIV[mj] OR Human Immunodeficiency Virus*[tiab] OR Human T Cell Lymphotropic Virus Type III[tiab] OR Human T Cell Leukemia Virus Type III[tiab] OR Lymphadenopathy Associated Virus*[tiab] OR Lymphadenopathy-Associated Viruses[tiab] OR Human T Lymphotropic Virus Type III[tiab] OR AIDS Virus*[tiab] OR Acquired Immunodeficiency Syndrome Virus[tiab]) AND (qualitative research[mh])>. Supplementary File 1 shows the different search strings employed in each data source.
Initially, duplicate studies were excluded and after that, a screening process took place based on: (1) title; (2) abstract; and (3) the full text. The discrepancies regarding article selection were solved by consensus. Finally, the articles’ methodological quality was evaluated. Hence, 27 articles remained in this review. Figure 1 shows the flowchart.

Flow chart of study inclusion and exclusion.
Critical Evaluation. The articles which we considered to be relevant after reading the full text were evaluated via peer review. An evaluation of these articles’ methodological quality was conducted through the CASPe program for qualitative research [ 7 ]. The items included in this guide are “present”, “doubtful” and “not on record”. Therefore, some eligibility criteria were proposed; first, that one of the elimination items does not have “not on record” (1, 2, 3), and also that the rest of the items do not have four or more “doubtful” or “not on record” (4, 5, 6, 7, 8, 9). Item number 10 was not evaluated because it does not focus on the applicability of this research in concrete situations, which exceeds the discoveries’ methodological evaluation and evaluation of relevance. The results of this phase are shown in Supplementary File 2 .
Despite the fact that 26 articles passed the quality evaluation according to the proposed criteria, we decided to include an article that did not pass it because of the relevance of its results in relation to the aim of the research. On this matter, regarding the syntheses procedures of qualitative studies was followed, which suggests giving priority to the discoveries’ quality in the article selection [ 8 ]. Hence, the final number of articles included in the systematic review was 27.
Data Extraction. Relevant data (author/s; participants’ country, number and other features: man or woman -mothers or pregnant-; type of research; qualitative approach chosen in the research and field where it was developed, understanding “Hospital” as any hospital field and “Community” as any association, advice or monitoring clinic or health center) were extracted by the main author of this review and verified by the rest of the authors.
Data Analysis. After repeated reading of the articles, we carried out the narrative synthesis. It consisted of joining the information by means of common topics, creating in this way different categories and subcategories when necessary. The results are presented here, taking the identified topics as the core idea, describing the main discoveries of the different studies in an integrated manner and incorporating, in some discoveries, direct quote of the studies’ informant participants to show evidence of their narratives.
This research is consistent with the guide “Enhancing Transparency in Reporting the Synthesis of Qualitative Research” [ 9 ] with the purpose of giving uniformity to the publications of qualitative synthesis studies.
Of the 27 studies that met inclusion criteria, sample sizes ranged from 3 to 78, with participants coming from Canada, Ireland, Spain, Kenya, Malawi, Ghana, Ethiopia, South Africa, Brazil, Chile, Peru and Mexico. Moreover, 63% of the participants came from the community field, whereas 27% belonged to the hospital one. All of the articles used the interview in different forms, and, furthermore, only two of them used focus groups among their methods of data collection ( Table 1 ).
Summary of studies included in the review and narrative synthesis.
Source: own elaboration.
Five topics emerged after the narrative synthesis: feelings about the diagnosis of HIV/AIDS; stigma and HIV/AIDS; changes in sexual behavior after becoming infected; living with the virus; pregnancy and motherhood in seropositive women ( Table 2 ).
Categories identified in each study.
Note: We opted to unify the references by mentioning the first and the second author, if there were two authors. From three authors or more, the first is mentioned and we add “et al.” for the rest. Note 1: “✓” = Article included in the category. Source: own elaboration.
3.1. Feelings about the Diagnosis of HIV/AIDS
This category was identified in 33.33% of the articles, which includes the feelings that the study participants experienced after the diagnosis of HIV/AIDS, as well as the different attitudes that they took to face the situation. The feelings we can highlight are disappointment, sadness, fear, despair, lack of awareness, and pain. In some cases, these emotions lead to depression, or they might intensify it. Hence, feelings of frustration might appear as well due to not achieving the targets that the subjects have set in their life [ 16 ].
After the diagnosis of HIV/AIDS, it was highlighted that people were afraid of being alone, because the lack of awareness about it causes social exclusion toward the people infected. The acceptance of the diagnosis is difficult; however, it depends on the cultural and social traits of the person. In some cases, people opt for submission to the diagnosis and its consequences or to conformism.
In some cases, they accept that the risky practices they have made in their life have resulted in the fact that they are carriers of the virus and they accept their mistake. One participant of the research by Carrasco et al. [ 15 ] expresses it in this way: “...when I was informed that I suffered from HIV, I felt an extremely huge sorrow, an extremely huge helplessness, but, at the same time, I was very calm because I admitted and accepted the mistake that I had made when I did not take care of myself...”. However, it should be noted that there are many ways in which a person could become infected (transmitted from a HIV+ mother during birth, blood transfusion), so it does not follow that each person infected did something wrong, made a mistake. Furthermore, even people felt that they were a mistake, it seems unlikely that every one of them would get to a stage where they all “accept their mistake”.
Many women discover their HIV status (seropositive) in prenatal care or when the children they have had get sick. This leads to an intensification of all of the feelings previously described and, above them, the fear of transmission to their children, in cases where they are pregnant.
After the diagnosis, we can notice in the articles’ results that the advice on and treatment of HIV/AIDS helped participants to accept their situation, avoiding in this way feelings of hopelessness or exclusion. Moreover, they helped to increase their responsibility in regard to self-care, which guarantees longevity and the fact of trying to lead a normal life.
3.2. Stigma and HIV/AIDS
This category was identified in 44.44% of the articles, which was, in turn, divided in three subcategories: social stigma, self-stigma and health professionals’ stigma.
3.2.1. Social Stigma
Social stigma is linked to family stigma; that is, the feeling of prejudice against people with HIV/AIDS which, in many cases, results in the social exclusion of the people who suffer from it. Social stigma is a common issue that people infected with the virus suffer, although it is more highlighted in developing countries. For instance, in these countries, women do not undergo a diagnostic test for fear of being judged by people. Therefore, they have to go to other villages to undergo the test because they are afraid of being isolated from the community. Another characteristic of these countries is that women are the ones who undergo these tests, so that men can blame them (even if they are the main carriers) when they are HIV-positive. Seropositive people are still labelled and judged every day, being treated as promiscuous, homosexual or less honorable, which is linked in many cases to the virus being transmitted through sexual contact.
HIV-positive people or people with AIDS make new circles with infected people because they feel free of any judgement. This results in the fact that these people close old social or family circles and they do not divulge the diagnosis. Stigma causes a serologic silence as a means of protection, as well as to avoid discrimination and prejudice. When the serological status is revealed to close people or to relatives, people infected with HIV feel liberated and, generally, accepted. Nevertheless, there are some families that prefer this news to be kept in the privacy of their home to avoid being judged by close people, such as their neighbors. This family acceptance has an influence on the increase in the quality of life, acceptance of the virus/disease and better adherence to antiretroviral therapy in HIV-positive people. In the case of homosexual people with the virus, they frequently suffer the so-called “double stigma”: one because of their sexual orientation, and another because of being seropositive.
3.2.2. Self-Stigma
Most HIV-positive people or people with AIDS, besides suffering discrimination and prejudice by others, also suffer these feelings toward themselves. The fear of transmitting the disease to their relatives or to people in their environment is a common feeling in these people. They even go so far as to take exaggerated hygiene measures or to use different pieces of cutlery to the rest of the family.
They also experience feelings of guilt and embarrassment, as well as the belief that the disease is a divine punishment because of their risky behavior some time ago. In the research by Peñarrieta de Córdova et al. [ 31 ], one participant stated that: “...every bad act leads to a bad consequence... It is the price that I am paying because of everything that I have done...”. The feeling of being useless, not respectable to society, and undesirable to other people causes social isolation and the retirement of social circles.
3.2.3. Health Professionals’ Stigma
Some seropositive people take the views of the health professionals who treat them as a reference point because of all the knowledge which they have concerning health. That is why some of these professionals’ practices or attitudes can make people with the virus internalize the discriminatory behaviors that some professionals carry out.
In some cases, the fact that health professionals take additional measures as extra-safety precautions during procedures, when they provide clinical care and treatment, is mentioned. This is obvious from the clinical safety point of view; however, participants might misunderstand it in terms of stigma.
Although the patients reveal that they felt more singled out and judged by these professionals in the past, they still sometimes perceive it in their clinical care. Other results make reference to the opposite. Health professionals support and reinforce people with HIV/AIDS, which leads to a better adherence to the therapy and to the fact that these professionals become people with whom they can relieve their feelings. This support is more emphasized and necessary when people know they are carriers, because of the psychological impact that this entails.
3.3. Changes in Sexual Behavior after Becoming Infected
This issue is addressed in 37% of the articles included in this review, so that the main changes, measures and attitudes regarding the sexual behaviors of people with HIV/AIDS are presented. Feelings of anxiety when talking about this matter, insecurity, fears caused by the possible refusal of the others when becoming intimate, decrease in desire and sexual appetite, and apathy and lack of interest are common among seropositive people regarding their sexual lives.
It was highlighted that sexual pleasure and intimacy became affected after diagnosis of HIV/AIDS due to fear of transmitting the virus, guiltiness, and lack of freedom. In the majority of them, a change of behavior after the diagnosis prevails concerning the use of a condom. The goal of its use is to prevent the transmission to their sexual partners or to avoid repeated exposure to the virus. The use of a condom is a limitation for many seropositive people, maybe because of the loss of feeling or freedom of choice as they are “forced” to use them (as a preventive measure). This fact makes the adaptation of the individual to live with HIV difficult.
In some cases, practices like sexual abstinence for fear of infection are reported. Other people deny accepting their seropositivity and they prefer to give up on sex, which even leads to the person’s isolation on several occasions. In the research by Freitas et al. [ 20 ], one of the participants expressed: “I cannot be cured, so I stopped going out, I stopped dating, I isolated myself”.
Among these individuals, there is an inability to look for sexual partners with whom they can enjoy life. This is due to the fear of rejection after revealing their serological status, which causes anxiety and constant concern on this matter. On the other hand, the ideal of romantic love and confidence that exists among steady partners (those who are serodiscordant, that is, one of the individuals is carrier of the virus and the other is not) makes them feel less vulnerable to infection themselves, and they forget about the prevention measures.
In developing countries, as can be seen in the study carried out by Sikweyiya et al. [ 32 ], men feel a loss of masculinity when they find out about the diagnosis, because they have to use a condom (which is one of the reasons why it is hardly used in these countries) and because they have to reduce the number of their sexual partners (polygamy). Another feeling expressed by men is sadness, which is linked to the impossibility to perpetuate their family name and, therefore, this results in a sense of castration.
Another relevant issue consists of who is in charge of taking care of the prevention means or of accepting unsafe sexual behaviors. As the reviewed studies present, this responsibility can be understood in three different ways. On the one hand, the responsibility lies with the seropositive person, who has the “duty” to protect the others and to take care of themselves. This is the ethical and correct option. On the other hand, the responsibility is shared, that is, both people must decide whether to take precautions or not to avoid risks. Finally, many people defend the idea that the responsibility of looking after and protecting oneself is individual, as is indicated in one of the participants’ statement that appears in the research by Fernández-Dávila et al. [ 17 ]: “The boy took it off from me (the condom). I didn’t say anything. Because this depends on him. I do not think it was necessary that he said any word to me...”.
Finally, in spite of understanding concepts like safe sex and preventive measures, condoms are still not used as they should to avoid new infections. As Juárez and Pozo [ 25 ] specified in their research, people who are in antiretroviral therapy, despite the fact that the possibilities of infecting the rest have only diminished, feel invulnerable. This makes them relax and employ risky behaviors in their sexual practices.
3.4. Living with the Virus
This category was identified in 44.44% of the articles, where the confrontation strategies that people with HIV/AIDS apply in their lives are principally addressed. According to many of the participants of the studies, being seropositive, or a carrier of the disease, means that they increase their self-care, fight for their lives and love other people more in order to receive the necessary support.
To overcome the diagnosis with the desire to continue living requires that people with HIV/AIDS make changes in their lifestyles voluntarily and with the full conviction that they are necessary actions to lead a “normal” life. Understanding how the disease functions and what it involves is fundamental for the participants of the different studies reviewed. What helps to put bad practices aside is to focus on healthy habits such as maintaining a positive attitude, moderate physical exercise, a healthy diet and trying to have an active social life. This helps to avoid depression, loneliness, isolation and hopelessness.
Among the responsibilities that being seropositive entails, we can include taking medication (antiretrovirals), which help these people to retain their wellbeing as the age. Like Juárez and Pozo [ 25 ] mentioned in their research, participants who took medication noticed some improvement in their quality of life. That is why adherence to the therapy and good monitoring is important for them. In Oliveira’s article [ 30 ], one of the participants states: “It is a responsibility, because you must take that medication, you must have medical monitoring and you must be careful because you can develop some other diseases”.
In developing countries, men who are infected by the virus believe that the search for social support to cope with HIV disease or with being HIV-seropositive is a sign of weakness. Nevertheless, some others express that, after being diagnosed, they had to change their life a lot and to adapt themselves to this new situation. Having to take medication made them feel prisoners and it made the acceptance and adaptation to life with HIV/AIDS difficult.
Social support is valued highly among these people. The desire to have more social relationships in their lives is expressed, because this helps them to overcome the negative situation linked with the virus. Their close family and friends are an essential source of support, helping them to make their everyday life more bearable and to make their adaptation positive. Most seropositive people learn to give more value to life, family and friends, as they already know that they are fundamental pillars of support, just like one participant states in the research by Braga et al. [ 13 ]: “In this case, it happens that you give more value to life”. Some others, however, avoid speaking about the disease/seropositivity and the feelings that it entails with people close to them, omitting in this way the problem and showing some maladjustment.
Finally, another way in which participants attempt to confront the diagnosis and to live with the virus is to get close to religion, which emerges as an emotional support. Faith in some superior being fills these people with motivation, relief, self-improvement and strength. They ask for courage through prayer to not to fall into depression. In Neves and Gir researched [ 29 ], one participant declares: “I devoted myself to God’s hands, he is going to give me the answer”. However, other people in De la Cruz et al. [ 16 ] described that God punished them for something wrong that they had done in spite of being faithful believers, which creates some uncertainty in them.
3.5. Pregnancy and Motherhood in Seropositive Women
This category was identified in 37.03% of the articles. It includes comments of seropositive women, some of them being mothers, some others pregnant, and some others with the intention of having offspring. Several issues, such as the causes of becoming pregnant, breastfeeding, and the feelings they experience regarding pregnancy with their condition of seropositivity, are addressed.
Among the different reasons that women have for continuing with their pregnancy, as most of them are not planned, we found a need to satisfy their spouses or count on their support. On occasion, family is another kind of support that helps them to continue. Nevertheless, some other times they advise them not to continue with the pregnancy to focus on their own health, because of their condition. Some ecclesiastic communities support these women and encourage them during the motherhood process. Lastly, the most important cause in this category is their own feelings and the availability of antiretrovirals. Some women who are diagnosed before pregnancy tend to be more negative about pregnancy due to the concern about vertical transmission.
Many seropositive women should be conscious of the right to motherhood, because they have the same rights as any other women. Many participants of the studies included in the review are aware of this. However, some others, in spite of knowing this, prefer to refrain from motherhood for fear of transmitting the virus, even if it is desired. Regarding breastfeeding, we found distinguishable comments among women who are treated with antiretrovirals and who decide to breastfeed, either by choice or because of the social pressure, and women who, with regret, avoid breastfeeding for the baby’s benefit.
With respect to the first group, in many countries, especially in developing ones, it should be noted that breastfeeding is a cultural norm which continues through generations. Women who are virus carriers live with the difficulty of motherhood in these communities, as Acheampong et al. [ 10 ] described, and they normally suffer and feel pressured when they breastfeed the baby. Among the feelings that they experience, we can highlight the fear and dread of transmitting the virus to their children through their milk, anxiety because of the uncertainty of knowing if their children are contaminated or not by drinking their milk, and the feeling of guilt when they contract HIV because the responsibility is theirs alone. Hope for the use of antiretrovirals and the effect that these have when they reduce the burden to almost imperceptible levels have also been shown.
In the second group, we find mothers who present feelings of failure, sorrow, helplessness or suffering. One participant of the study by Sousa and Gimeniz [ 33 ] points out: “It was my dream to have a child and to see him nurse... When he was crying, I could breastfeed him and see how he stopped crying”. For the majority, breastfeeding was a symbol of motherhood.
Because of the fact that these women are recommended not to breastfeed, to reduce the virus transmission to their children, the people around them have many prejudices when they see them feeding their children with infant formula. This means that these women do not reveal their diagnosis for fear of rejection, either of themselves or of their children in the future, having to lie on several occasions, as one participant explains in the article by Linder et al. [ 26 ]: “When people ask me if I don’t breastfeed, I say that I have an inverted nipple and, although it is true, it is an excuse as well...”. Many of them stated that the information they received from health care providers about why they must not breastfeed was very superficial.
Finally, motherhood is perceived as a support in their lives, giving seropositive women a reason to continue living eagerly. They have hope of seeing their children grow up and this is a positive factor in the face of the disease/seropositivity. These mothers usually overprotect their children in order to avoid suffering and rejection from people, as was described by Spindola et al. [ 34 ] in their research. Motherhood is a positive factor with respect to the adherence to antiretroviral therapy as well, because the possibility of their children growing up healthily encourages mothers to follow health recommendations.
4. Discussion
Systematic reviews of qualitative studies provide a broad view of the experiences of people facing health problems. This research focused on analyzing the experiences and attitudes of people who live with HIV/AIDS, based on a wide review that includes works from several countries, with representation in North America, South America, Central America, Europe and Africa. The analysis allowed us to identify the common elements regarding the feelings when facing the seropositivity/disease diagnosis, the stigma, sexual behaviors, and motherhood, which consolidates the work’s international relevance. This review updates the discoveries which were already generated in previous works of similar characteristics, although they were published more than 10 years ago [ 37 , 38 ]. On the other hand, the publication of systematic reviews in this field has progressed in recent years [ 39 , 40 , 41 , 42 , 43 ]; however, the ones that include qualitative research as a source of results or that focus on very specific aspects are scarce. This strengthens the review that is presented in this work, as it is based on qualitative studies, helping topics which were not treated before to emerge.
Based on our results, we can highlight the stigma that people who are carriers of HIV suffer. Three types of stigma (social stigma, self-stigma and health professionals’ stigma) were relevant in the results. In accordance with the research by Sandelowski et al. [ 38 ], in their metasynthesis, although they focus on the female population, one of the problems of revealing the diagnosis to other people is the prejudices that exist toward seropositive people. On the one hand, when they reveal it, they feel relief and their relationships now provide authenticity. On the other hand, it can also be a reason for social isolation because of the non-acceptance of the others. Barroso et al. [ 37 ], in their metasynthesis, supported the results obtained in the research about social relationships, as these are a foothold to better adapt to the virus or to the disease. On the other hand, Villa et al. [ 40 ] confirmed in their literature review that the psychological aspects of seropositive people are reinforced by the social support they receive, which helps their adherence to the therapy and improves their quality of life. This last idea was also shown by Tavera [ 41 ] in her systematic review.
Regarding adherence to the therapy, in one review, Puigventós et al. [ 39 ] stated that, in general, people with HIV/AIDS adapted well to the therapy. In the cases in which they do not adhere, the reasons might be that they are social outcasts (stigma), that they are minors, or the lack of motivation, among others. In the results obtained, we observed that, for instance, motherhood is a positive factor (apart from social support) in better adherence to the therapy, reducing in this way the possibility of vertical transmission to the baby. Concerning this last matter, guides for HIV/AIDS management have been published [ 42 , 44 ] which are particularly interesting regarding the approach to motherhood, including recommendations which result in a reduction of vertical transmission.
Among the ways to adapt to the disease/seropositivity, we found in the results of this research that religion or the practice of healthy habits favored its normalization in their lives. This is in line with the proposals suggested by other studies [ 37 , 41 ], which claim that spirituality helps some people to confront HIV/AIDS. In addition, it is stated that understanding the disease makes the adaptation favorable as well, as it helps them to carry out positive strategies, such as physical exercise, changes in their diet or safe sexual behaviors. Benito [ 43 ], in his systematic review, explained that physical exercise in people with HIV/AIDS makes them gain weight and is favorable to their psychological wellbeing.
Based on the results obtained, we suggest the further exploration of themes like the experiences of pregnant women or of mothers and their sexual behaviors in future research, as the fact that some HIV carriers adapt to their situation and some others deny it, despite knowing the risks, can be underlined. Likewise, new research on the moment of diagnosis would be enriching, as it is a crucial moment because of the great psychological impact that it entails.
This review is not exempt from limitations. First, even though the sources used for the studies’ search are pertinent, they might not give an account of all of the relevant studies for the objective of this research. To compensate for this limitation, it should be pointed out that the database and the base of resources used are specific to the Health Sciences area (the area in which this research is circumscribed), so that they are widely known and relevant sources in this area. Although no exclusion criteria was applied on a geographical basis, there are regions such as Asia that are not represented in this review, which may be of interest in future research. In this regard, it would also be interesting in future research to locate studies published in languages other than those included in this review.
On the other hand, an excessive number of duplicate documents were avoided, which could have happened with the use of other databases that might have a high degree of overlap with the ones used in this review. Another limitation of this review involves the synthesis procedure. We opted for a classic procedure of narrative synthesis, which limits the descriptive and explanatory ability of the studied phenomenon. It would be relevant to progress toward metasynthesis procedures in future research and, in this regard, the discoveries of this review might be the base on which this future research can be oriented.
Finally, it would be interesting to specifically include in future research an analysis that could differentiate the findings of the studies analyzed based on various factors. For example, how people feel about being diagnosed is likely to be qualitatively different when there are few options compared to when people can live long lives with effective treatment. It is important to note how the country of origin is related to such feelings, as those in under-developed countries may have less access to treatment, which could impact their feelings about the diagnosis.
5. Conclusions
Most of the people who are carriers of the virus have common feelings when they are informed about their seropositivity. Among them, we found disappointment, sadness, fear, despair, lack of awareness and pain. Sometimes, the diagnosis might lead to depression and social isolation. Social culture and environment are determining factors regarding the acceptance of the diagnosis. Intimacy and sexual pleasure are affected after the disclosure of the diagnosis; some seropositive people feel a decrease of their sexual appetite and, in general, there are changes in their sexual behaviors (e.g. use of condoms). In other cases, they opt for abstinence or, on the contrary, for risky practices, despite knowing their consequences.
In the case of pregnant women, many of them find out about the diagnosis when they get pregnant. Some others decide to have children in spite of being carriers and the causes that drive them to do this might be the satisfaction of being mothers or the need to satisfy their partners. Being mothers is a positive factor to fight HIV/AIDS, because it gives them the strength to continue and see how their children grow up. Furthermore, breastfeeding generates distinguishable comments between the ones who desire it and find themselves forced to breastfeed because of the social pressure, for whom the use of antiretrovirals relieves their fears in the face of transmission danger, and the ones who opt for not breastfeeding, showing an evident helplessness.
The fact of being seropositive implies a high degree of stigma, as the prejudices against people with HIV/AIDS are evident. Some people lean on their intimate social circle to confront the disease or seropositivity. Religious practices are a positive factor in which they take refuge as well.
Practical Implications
In the moment of diagnosis, the approach of healthcare providers is of vital importance, because of the impact that the news about being carriers causes on people. Thus, enough support and advice must be offered to these people to avoid future isolation and for appropriate therapeutic adherence. In the same way, correct health education is key to avoiding risk behaviors. It is relevant, from the social environment, to ensure the inclusion of these people in society, avoiding social exclusion.
Regarding pregnant women, an early diagnosis of HIV status makes it possible to adopt measures that drastically reduce the risk of mother-to-child transmission. The information provided about the risk of breastfeeding babies must be complete. The fact that these mothers fully assimilate the information before they make a decision must be checked, avoiding uncertainty, sadness or feelings of helplessness.
Finally, the COCHRANE collaboration recognizes that “evidence from qualitative studies that explore the experience of those involved in providing and receiving interventions, and studies evaluating factors that shape the implementation of interventions, have an important role in ensuring that systematic reviews are of maximum value to policy, practice and consumer decision-making” [ 45 ]. Therefore, this review offers an understanding of the perceptions and feelings of people with HIV/AIDS, and thus it can help to improve the implementation of interventions focused on people and guide public health policies or the development of protocols and clinical practice guidelines, which are in tune with the UNAIDS proposal worldwide [ 6 ].
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/17/2/639/s1 , Table S1: Search strategy in the databases; Table S2: Results after the methodological evaluation CASPe.
Author Contributions
Conceptualization, T.A.-C., M.Á.P.-M., and C.H.-M.; methodology, T.A.-C., M.Á.P.-M., A.J.R.-M., C.C.-D., M.R.-M., and C.H.-M.; Supervision, M.Á.P.-M., and C.H.-M.; writing—original draft, T.A.-C., M.Á.P.-M., and C.H.-M., writing—review and editing, T.A.-C., M.Á.P.-M., A.J.R.-M., C.C.-D., M.R.-M., and C.H.-M. All authors have read and agreed to the published version of the manuscript.
This review received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.

IMAGES
VIDEO
COMMENTS
A 35-year-old HIV-positive man was admitted to our hospital with intermittent fever for several months (Figure 1) and chronic diarrhea. He was diagnosed HIV-positive 4 years earlier and had subsequently developed several AIDS-defining diseases such as Pneumocystis carinii pneumonia and CMV retinitis. Three months before admission the patient began complaining of watery diarrhea and recurrent ...
In a 2014 study, the standardized incidence ratio for non-Hodgkin's lymphoma in persons with HIV as compared with the general U.S. population was 11.5. 24 However, although rates of diffuse ...
An estimated 1 in 2 Black men who have sex with men in the United States will become infected with HIV over a lifetime. 1 Among the nearly 50,000 adolescents and young adults (13 to 24 years of ...
Based on this case study and literature review, it is evident that co-infection presents typical clinical, diagnostic, and therapeutic features, and can be observed in the prognosis of the disease. Therefore, prospective studies are required to clarify gaps such as the efficacy of secondary prophylaxis and need for clinical and laboratory ...
One study found that the overall rate of infections up to four months after the insertion of an intrauterine device was the same among HIV-negative women as among HIV-positive women. 29 Therefore ...
Case study methods involve an in-depth, longitudinal (over a long period of time) examination of a single instance or event, a case. This case study is about Anamika (name changed), a 35-year-old female who is an empowered HIV-positive and presently works as Community Co-ordinator at an anti-retroviral treatment (ART) centre.
A medically and socially complex patient with HIV is presented as the initial case study that leads to identification of barriers and needs on individual, community, and public policy levels. This is an active-learning resource that includes both small- and large-group discussion driven by self-directed learners using the provided resources.
The worst-case scenario could be that the gains of HIV control could be reversed, precipitating a loss of confidence, funding reductions, and increased incidence and mortality. ... We are the change—an innovative community-based response to address self-stigma: a pilot study focusing on people living with HIV in Zimbabwe. PLoS One. 2019; 14 ...
A study conducted in slums in Delhi has found almost similar prevalence (40% compared to 39.1% during wave-II in this study) of awareness of HIV among adolescent girls 31. The difference in ...
AIDS as a human crisis may lead to devastating psychological trauma and stress for patients. Therefore, it is necessary to study different aspects of their lives for better support and care. Accordingly, this study aimed to explain the lived experience of HIV-infected patients in the face of a positive diagnosis of the disease. This qualitative study is a descriptive phenomenological study.
A clinical trial is a research study in which people volunteer to help find answers to specific health questions. HIV and AIDS clinical trials help researchers find better ways to prevent, detect, or treat HIV and AIDS. Examples of HIV and AIDS clinical trials underway include studies of new HIV medicines, studies of vaccines to prevent or treat HIV, and studies of medicines to treat ...
Introduction People living with HIV (PLHIV) relied on community-based organizations (CBOs) in accessing HIV care and support during the COVID-19 pandemic in China. However, little is known about the impact of, and challenges faced by Chinese CBOs supporting PLHIV during lockdowns. Methods A survey and interview study was conducted among 29 CBOs serving PLHIV in China between November 10 and ...
Cost-effectiveness of HIV screening and testing. Initial studies reported voluntary HIV screening to be cost-effective in health care settings where undiagnosed HIV infection is less than ≥0.1% 1 2.It was also reported to be more cost-effective than many established screening programs for chronic disease (e.g., hypertension, colon cancer, and breast cancer). 2 3 Treatment costs are lowered ...
We did a matched, nested case-control study among adult men at high risk of HIV infection between Jan 1, 2016, and June 30, 2020, using data from the French national health data system. Men who were newly diagnosed with HIV infection up to Dec 31, 2020, were individually matched with up to five controls for age, socioeconomic status, place of ...
Numerous studies have led to the conclusion that a once-daily, single-pill PrEP regimen is 99% effective in preventing sexual acquisition of HIV infection by an at-risk uninfected person.
In 2020, over 30,600 people received an HIV diagnosis in the United States, and 20,758 cases were due to male-to-male sexual contact; data for 2020 should be interpreted with caution due to the impact of the COVID-19 pandemic on access to HIV testing, care-related services, and case surveillance activities.
Abstract. This case study demonstrates a 36-year-old ex-intravenous drug user (IVDU) who had been initially tested positive for human immunodeficiency virus (HIV) twice using Enzyme Immunoassay (EIA) method (Particle agglutination, PA done), but a year later he was tested HIV-negative. The patient was asymptomatic for HIV and T helper cells ...
In this retrospective case-control study, people with HIV from Washington University in St Louis, MO, USA, and people without HIV identified through community organisations or the Research Participant Registry were clinically characterised and underwent 3-Tesla T 1-weighted MRI between Dec 3, 2008, and Oct 4, 2022.Exclusion criteria were established by a combination of self-reports and medical ...
Clinical Case Studies Active Resources; Archived Resources; Events; Resources: 23. ... The National HIV Curriculum (NHC) provides free, up-to-date content for clinicians to learn about HIV diagnosis, treatment, and prevention. The 37 les... Type. Curricula. Publication Date. 09/05/2023.
Human immunodeficiency virus (HIV) is an infection that attacks the body's immune system. Acquired immunodeficiency syndrome (AIDS) is the most advanced stage of the disease. HIV targets the body's white blood cells, weakening the immune system. This makes it easier to get sick with diseases like tuberculosis, infections and some cancers.
Management of Newly Diagnosed HIV Infection. Author: Scott M. Hammer, M.D. Author Info & Affiliations. Published October 20, 2005. N Engl J Med 2005;353: 1702 - 1710. DOI: 10.1056/NEJMcp051203 ...
Ready acceptance of experiences of new diagnoses among HIV-positive persons is a known personal and public health safety-net. Its beneficial effects include prompt commencement and sustenance of HIV-positive treatment and care, better management of transmission risk, and disclosure of the HIV-positive status to significant others. Yet, no known study has explored this topic in Ghana; despite ...
Their study, published in the Proceedings of the National Academy of Sciences, is one of the first to examine the differential or cell-type specific effects of HIV latency modulation on myeloid ...
Case study 3: Reluctance to take antiretroviral therapy; Case study 4: A child with uncertain treatment history and extensive drug resistance; Case study 5: Unrecognised transmitted resistance; Case study 6: A case of persistent low-level viraemia; Case study 7: A young black African woman presenting for HIV testing
Advances in anti-retroviral therapy (ART) have decreased mortality rates and subsequently led to a rise in the number of HIV-positive people living longer. The housing experiences of this new population of interest—older adults (50 years and older) living with HIV—are under-researched. Understanding the housing experiences and unmet needs of older people with HIV can better provide ...
Objectives To determine if HIV modifies the association between hyperglycaemia and active tuberculosis in Lusaka, Zambia. Methods A case-control study among newly—diagnosed adult tuberculosis cases and population controls in three areas of Lusaka. Hyperglycaemia is determined by random blood glucose (RBG) concentration measured at the time of recruitment; active tuberculosis disease by ...
Abstract. The aim of this article was to explore the experiences and attitudes of people with HIV/AIDS. A systematic review of qualitative studies was carried out. Twenty-seven articles were included, with sample sizes ranging from 3 to 78. Articles from North America, South America, Central America, Europe, and Africa were included.