- AGA Journals
- AGA University
- AGA Research Foundation
- AGA Community
- AGA Job Board
- Create Account


Clinical Guidance
Our clinical guidelines and updates help you make the best evidence-based decisions for your patients.
- Library AGA’s guidelines, practice updates and care pathways in one place.
- Guideline Toolkits Comprehensive resources for managing diseases – Crohn’s disease now available.

Journals & Publications
Latest research and ideas from the GI field.
- Gastroenterology The premier journal in GI.
- Clinical Gastroenterology and Hepatology (CGH) The go-to resource in clinical GI.
- Cellular and Molecular Gastroenterology and Hepatology (CMGH) Impactful digestive biology research.
- Techniques and Innovations in Gastrointestinal Endoscopy (TIGE) Cutting-edge advances in GI endoscopy.
- Gastro Hep Advances Open access GI and hepatology journal.
- GI & Hepatology News AGA’s official newspaper.
- The New Gastroenterologist Insights for fellows and early career GIs.

Meetings & Learning
Earn CME, MOC and improve your skills.
- AGA University Your hub for the best in GI education – AGA Postgraduate Course, Tech Summit and more.
- Digestive Disease Week® The most prestigious GI meeting.
- Crohn's & Colitis Congress® The premier meeting on IBD.
- Maintenance of Certification Resources for maintaining certification.
- DDSEP® The leading self-assessment tool for GI.
- Inside Scope Podcast An AGA podcast with bite-sized education.

More than 16,000 professionals worldwide call AGA their professional home.
- Join AGA Join our diverse mix of professionals.
- Renew Membership Continue to receive exclusive benefits and discounts.
- Benefits Unrivaled by any other GI organization.
- Membership Directory Contact other AGA members.
- Recognition Awards We honor our esteemed members.
- Initiatives & Programs Advancing the science and practice of GI.
- Get Involved with AGA Help us achieve a world free from digestive diseases.
- Advocacy & AGA PAC Advancing public policies that support gastroenterology.

Practice Resources
Tools to maximize efficiency and help you deliver high-quality care.
- Practice Tools Cutting-edge resources to improve your patient care.
- New Technology & Techniques The latest innovations in GI.
- Quality & Performance Measures Support to meet reporting requirements.
- Reimbursement Tools to understand policies and advocate for reimbursement.
- GI Patient Center By specialists, for patients.

Research & Awards
Funding opportunities and other initiatives advancing discovery.
- Research Awards More than $2 million in annual research funding.
- Registries & Studies Data to support new techs and treatments.
- Gut Microbiome One of GI’s most promising areas of research.
- AGA Research Foundation Funding the future of gastroenterology.

Fellows & Early Career
Resources designed for early career gastroenterologists.
- Resources Resources for every stage of your career.
- Fellowship Match Information for programs and candidates.
- AGA GTE® The first training exam for GI programs and fellows.
- Mentoring Connect with prospective mentors.
- Job Board Find your next opportunity.
GERD and Refractory GERD: A Case Based Approach
Review of treatments GERD:
Download the session audio:
Download the PowerPoint presentation:

4930 Del Ray Avenue, Bethesda, MD 20814 301-654-2055
Connect with aga.
© American Gastroenterological Association

- Privacy Overview
- Strictly Necessary Cookies
- Cookie Policy
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
More information about our Cookie Policy
Gastroesophageal Reflux Disease (GERD)
Sep 25, 2014
620 likes | 1.71k Views
Gastroesophageal Reflux Disease (GERD). Dr. Kairu S. M. GERD - Definitions. Gastro-oesophageal reflux disease (GORD): Abnormal reflux of gastric juice (acid and bile) into the oesophagus leading to symptoms Pathological reflux ranges from simple to erosive to Barrett’s
Share Presentation
- reflux disease
- gastric pressure
- pathological reflux
- chronic ppi therapy hypergastrinemia

Presentation Transcript
Gastroesophageal Reflux Disease (GERD) Dr. Kairu S. M.
GERD - Definitions Gastro-oesophageal reflux disease (GORD): Abnormal reflux of gastric juice (acid and bile) into the oesophagus leading to symptoms Pathological reflux ranges from simple to erosive to Barrett’s Non-erosive reflux disease (NERD): Reflux disease in which erosion does not occur Heartburn: Burning retrosternal pain radiating upward due to exposure of the oesophagus to acid Oesophagitis: Endoscopically demonstrated damage to the oesophageal mucosa
Prevalence. • Increased prevalence last 10 years. • Accompanied increase in adenocarcinoma lower esophagus. • Obesity associated with increased GERD.
Anti Reflux Mechanism(ARM) • This has both:- (1) Anatomical. (2) Functional.
Anatomical. • The lower esophageal sphincter (LES) at the OG junction consists of tonically contracted smooth muscle at approx. 8-20 mmHg above the gastric pressure. • The outside (extrinsic) compression at the OG junction from the crural diaphragm. • Sharp angle- entry of esophagus into stomach (angle of His).
TLESR (Transient Lower Esophageal Sphincter Relaxations) • A normal phenomenon in healthy individuals. • Dominant mechanism of pathological reflux. • Too frequent TLESRs. • Too prolonged TLESRs.
Functional. • Esophageal peristalsis that serves to clear luminal contents into the stomach. • Secretion and swallowing of saliva to neutralize the acid and enhance clearance. • Prompt Gastric emptying.
bile reflux Pathophysiology of GERD salivary HCO3 Impaired mucosal defence oesophageal clearance of acid (lying flat, alcohol, coffee) Impaired LOS (smoking, fat, alcohol) – transient LOS relaxations – basal tone Hiatus hernia acid output (smoking, coffee) H+ Pepsin Bile and pancreatic enzymes intragastric pressure(obesity, lying flat) gastric emptying (fat)
Heartburn and Regurgitation are the two cardinal symptoms of GERD. • Others:- (1) Dysphagia-due to peptic stricture or peristaltic dysfunction. (2) Chest pain (NCCP). (3) Water brash. (4) Globus Sensation. (5) Odynophagia.
Extra Esophageal Manifestations. • Asthma. • Microaspiration. • Vagal reflex activation. • Laryngitis. • Complications of GERD. • Bleeding. • Stricture. • Barrets esophagus adenocarcinoma
Role of Endoscopy in GERD. • Confirm diagnosis of GERD -erosions/ulcerations. • Diagnose endoscopy-negative reflux. • Exclude other causes of esophagitis/ odynophagia e.g.Candida, Herpes Simplex. • Diagnose complications of chronic GERD e.g Barrets esophagus, stricture, adenocarcinoma.
1.Savary-Miller classification. • Solitary erythematous /erosions covering one mucosal fold. • Solitary erythematous /erosion covering more than one mucosal folds but not circumferential. • Circumferential erythematous / erosions. • Complications • Ulcers. • Strictures. • Barrett’s esophagus.
Modes of Treatment • Proton Pump Inhibitors • Longer acting PPI’s. • Adverse events/effects of PPIs. • Potassium –competitive acid blockers (PCABs) • Motility agents. • GABA agonists • Endoscopic therapy • Full-thickness plication
The Step up Approach. PPI LOW DOSE PB. H2RA +PROKINETIC. H2RA OTC ANTACIDS + LIFESTYLE ADVICE.
The Step Down Approach. • PPI LOW DOSE PB. H2RA +PROKINETIC. H2RA+LIFESTYLE ADVICE. OTC ANTACIDS.
Long Term Therapy. • Many patients, GERD a chronic relapsing problem because the underlying motor abnormalities persist. • PPI’s. • Majority of patients require PPI even in low doses. • Occasional patients may require high doses (double dose of PPI to control symptoms.) • Nocturnal acid breakthrough.
Surgery in GERD Nissan Fundoplication • 40-50% have required medical treatment after surgery. • High failure rate. • Mortality – operatordependent. • Morbidity / complications: ~ 10% dysphagia requiring repeated esophageal dilatation.
Potential Risks of Chronic PPI Therapy • Hypergastrinemia, carcinoids • Gastritis, intestinal metaplasia, gastric cancer • Achlorhydria and loss of gastric sterility • Increased enteric infections, C, difficile. • N-nitrosamine and carcinogen risk • Community =acquired pneumonia • Safety during pregnancy /lactation • Drug interactions.
Potential Risks of Chronic PPI Therapy Hypergastrinemia, carcinoids • RATS • Elevated gastrin • ECL cell hyperplasia • ECL cell carcinoid tumors • HUMANS • Elevated gastrin • ECL cell hyperplasia • NO CARCINOID TUMORS Species specific problem (rat) Up to 8 year continuous use in patients (as of 2000)
Potential Risks of Chronic PPI TherapyAchlorhydria, N-nitrosamine generation The RISK The REALITY • Increased UGI bacteria has been detected in PPI takers. • N-nitrosamine formation is also catalyzed by acid. • Achlorhydria permits growth of bacteria that can convert nitrates to nitrites to N- nitrosamine (carcinogen) Data on PPI use and increased gastric N-nitrosamine remain uncertain and the cancer risk is speculative
Potential Risks of Chronic PPI Therapy Achlorhydria, enteric infection The RISK The REALITY • Achlorhydria disables the gastric barrier to ingested pathogens • Case-control study: Small increase in enteric infections with PPIs for 2 months. • Relative risk 1.6 (Cl 1.0-2.4) • PPPI use is independent risk of C. difficile diarrhea in antibiotic users. • PPI use OR 2.1 (Cl 1.2-3.5) • ≥3 AB OR 2.1 (Cl 1.3-3.4) • Medical ward OR 4.1 (Cl 2.3-7.3) Only occasional cases of enteric infections in patients taking PPI’s have been reported. Garcia Rodriguez LA et al. Epidemiol 1997:8:571-4, Dial S et al CMAJ 2004: 171: 33-8
Potential Risks of Chronic PPI TherapyCommunity –acquired pneumonia The RISK The REALITY • Case-control Dutch primary case database 1/1/95-12/31/2002. • 364,683 Individuals • 5551 1st Pneumonias • PPI user risk 0.60/100 pt yrs • Nested case control analysis to reduce confounding effects of indication • Non-PPI user risk 0.60/100 pt yrs Adjusted OR all 1.27 (Cl 1.06-1.54) • Adjusted OR PPI 1.73 (Cl 1.33-2.25) • Gastric colonization followed by reflux and aspiration of gastric contents results in pneumonia Association does not prove causation PPI takers are also more likely to smoke, drink, be obese, have GERD, and ?? (note how OR 4.08 dwindled to 1.73) Laheji RJ et al. JAMA 2004: 292: 1955-60
Potential Risks of Chronic PPI Therapy Safety during pregnancy/lactation The RISK The REALITY • Omeprazole crosses placenta, category C; Other PPI’s category B • controlled human studies no risk. • animal studies or, adverse fetal. • no adequate studies or, adverse fetal effects in animals at some dose. • evidence of fetal risk: benefit > risk • Evidence of fetal risk: benefit < risk • 1992-2001 prospective controlled evaluation of PPI gestational exposures • Omeprazole: 247 births 3.6% major anomalies. • Lansoprazole: 50 births, 3.9% MA • Pantoprazole: 48 births, 2.1% MA • Controls: 787 births, 3.8%MA European Network of Teratology Information Services…the PPI’s do not represent a major teratogenic risk in humans Diav-Citrin O et al, Aliment Pharmacol Ther 2005: 21: 269-75
PPI’s: Adverse Events/Effects • Clopidogrel • Prospective studies of platelet aggregation. • Retrospepctive studies of clinical outcomes. • Randomized, double-blind trail of PPI vs placebo among clopidogrel users. • No difference in cardiac events, mortality • Significant reduction in GI events with PPI
GABA – β AgonistBaclofen • Baclofen 40mg • Reduced TLESR’s in patients with GERD • Reduced esophageal acid exposure • Limitations • CNS side-effects mainly drowsiness. • Short half-life. Van Herwaarden et al. Aliment Phar,acol Ther 2002
New motility agent (GABA β Agonist)Lesogaberan • Lesogaberan – a peripheral acting GABA β agonist. • Study showed 35% ↓ in TLESR. • A potential agent for treatment of GERD as co-therapy.
Summary • PPI’s remain the standard treatment for GERD. • Well established to be very safe. • Prevalence of GERD increasing with increase in lower esophageal adenocarcinoma. • New motility drugs in development – Lesogaberan.
- More by User
Gastroesophageal Reflux Disease Drug Pipeline Analysis 2016
The GERD Therapeutics Market is Forecast to Show Decline Until 2016
651 views • 4 slides
Gastroesophageal Reflux Disease
Gastroesophageal Reflux Disease. Howard J. McGowan, Maj, USAF, MC. Objectives. Definition of GERD Epidemiology of GERD Pathophysiology of GERD Clinical Manisfestations Diagnostic Evaluation Treatment Complications. Definition. American College of Gastroenterology (ACG)
2.37k views • 38 slides
Gastroesophageal reflux disease
Gastroesophageal reflux disease. Dr. Navin Kumar Assistant Professor. GERD. Defined as troublesome symptoms or complications that result from the reflux of gastric contents into the esophagus or beyond into the oral cavity or lung . Troublesome is defined by consensus as
1.39k views • 33 slides
Gastroesophageal reflux GER AND Gastroesophageal reflux diseaseGERD
. GERD :most common esophageal disorder in children.GER :retrograde movement of gastric contents.Physiological reflux: regurgitation in normal infant.GERD: pathological reflux in children more frequent or persistent produce esophagitis or esophageal symptoms respiratory complications failure
469 views • 11 slides
Gastroesophageal Reflux Disease. Scott Stolte, Pharm.D. Shenandoah University. Overview of GERD. Definition Symptoms or mucosal damage produced by the abnormal reflux of gastric contents into the esophagus Classic symptom is frequent and persistent heartburn
1.1k views • 48 slides
GastroEsophageal Reflux Disease (GERD)
GastroEsophageal Reflux Disease (GERD). Marijo Čukelj Mentor: A. Žmegač Horvat. Definition. prolonged reflux of hydrochloric acid and pepsin in esophagus, oral cavity and respiratory system chronic and relapsing condition
495 views • 13 slides
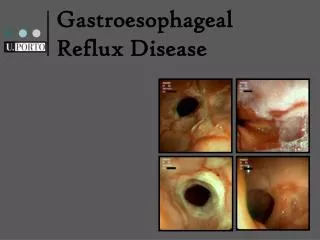
Gastroesophageal Reflux Disease. “a prevalent and chronic condition in which reflux of the stomach contents into the oesophagus causes a range of troublesome symptoms (including heartburn, acid regurgitation and epigastric pain) and complications”. Gastroesophageal Reflux Disease (GERD).
869 views • 15 slides
Gastroesophageal Reflux Disease (GERD) . By: Joe Hollis & Spencer Poprawski. Table of Contents . Overview of GERD (definition of the disorder) Signs and Symptoms (diagnosis) Treatment of GERD Risk Factors Tests Video . Overview of GERD .
658 views • 11 slides
Gastroesophageal Reflux Disease in Infants
Gastroesophageal Reflux Disease in Infants. GERD is a very common and usually benign physiological event in infants.
1.25k views • 79 slides
GASTROESOPHAGEAL REFLUX DISEASE (GERD)
GASTROESOPHAGEAL REFLUX DISEASE (GERD). Ahmed A. Elberry, MD. Anatomy of the stomach:. Incidence:. GERD is the most common GIT disorder (over 1.0 million out patient visits to physicians every year!)
3.46k views • 25 slides
Gastroesophageal Reflux Disease (GERD). * Definition : inflammation of the lower part of the esophagus due to abnormal reflux of gastric contents into the esophagus Often chronic and relapsing.
649 views • 22 slides
Gastroesophageal Reflux Disease (G.E.R.D.)
Gastroesophageal Reflux Disease (G.E.R.D.). Rory Loveland Paramedic class ’08-’09. What is GERD. Loosening of the lower esophageal sphincter (LES). Allows gastric acid to splash into the esophagus. Refluxed stomach acid touches the lining of the esophagus causing a burning sensation.
519 views • 13 slides
Gastroesophageal Reflux Disease (GERD). Presented by: Rachel Lang April 15, 2003 ASC 823 C. GERD. Often called reflux It is the recurring backflow of acid from the stomach into the esophagus. FACTS. According to the U.S. Department of Health and Human Services :
577 views • 15 slides
gastroesophageal reflux disease GERD
gastroesophageal reflux disease GERD. Department of gastroenterology, 1 st hospital of jilin university Tongyu Tang. Definition. American College of Gastroenterology (ACG)
2.71k views • 32 slides
309 views • 15 slides

Gastroesophageal reflux disease: from surgeon’s perspective
F Chow Queen Mary Hospital, University of Hong Kong. Joint Hospital Surgical Grand Round 16 July, 2016. Gastroesophageal reflux disease: from surgeon’s perspective. Gastro-esophageal reflux disease (GERD).
1.39k views • 37 slides
Gastroesophageal Reflux Disease (GERD) Devices Market
Gastroesophageal Reflux Disease (GERD) Devices Market: Introduction of Advanced Diagnostic Devices for GERD Treatment to Create Substantial Revenue Generation Opportunities: Global Industry Analysis 2013-2017 & Opportunity Assessment 2018-2028
113 views • 10 slides

Gastroesophageal Reflux Disease | Best Cancer Surgeon in Bangalore
Best Cancer Surgeon in Bangalore | Dr Prabhu talks all about GERD, its symptoms, diagnosis and the treatment options available, To know more visit: http://cancerandbariatricsurgeon.com/blog/gerd/
37 views • 1 slides

GERD | Gastroesophageal Reflux Disease Treatment in Bangalore
Gastroesophageal Reflux Disease Treatment in Bangalore | Dr Prabhu talks about the symptoms of GERD in infants. If you think your baby might have GERD do not delay and call your doctor right away. To know more visit: http://cancerandbariatricsurgeon.com/blog/gerd/
48 views • 1 slides
- Cell Biology
Case Study: Gastroesophageal Reflux Disease
Related documents

Add this document to collection(s)
You can add this document to your study collection(s)
Add this document to saved
You can add this document to your saved list
Suggest us how to improve StudyLib
(For complaints, use another form )
Input it if you want to receive answer
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

11 templates
28 templates

holy spirit
36 templates

islamic history
memorial day
12 templates

165 templates
Gastroesophageal Reflux Clinical Case
Gastroesophageal reflux clinical case presentation, free google slides theme and powerpoint template.
Clinical cases help medicine students understand better the symptoms, treatment and development of a disease. They’re also very valued in the international scientific community, as they foster communication between professionals so they can learn new techniques and practises. This clinical case is focused on Gastroesophageal reflux disease (GERD). What symptomatology does it have? What treatments are now available and how are they applied? These slides have all the resources you need for explaining medical concepts in a visual and clear way!

Features of this template
- 100% editable and easy to modify
- 27 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.
Premium template
Unlock this template and gain unlimited access

We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 34: Gastroesophageal Reflux Disease: A Burning Question Level II
Brian A. Hemstreet
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Learning objectives, patient presentation.
- CLINICAL PEARL
- Full Chapter
- Supplementary Content
Instructors can request access to the Casebook Instructor's Guide on AccessPharmacy. Email User Services ( [email protected] ) for more information.
After completing this case study, the reader should be able to:
Describe the clinical presentation of gastroesophageal reflux disease (GERD), including typical, atypical, and alarm symptoms.
Discuss appropriate diagnostic approaches for GERD, including when patients should be referred for further diagnostic evaluation.
Recommend appropriate nonpharmacologic and pharmacologic measures for treating GERD.
Develop a treatment plan for a patient with GERD, including both nonpharmacologic and pharmacologic measures and monitoring for efficacy and toxicity of selected drug regimens.
Outline a patient education plan for proper use of drug therapy for GERD.
Chief Complaint
“I’m having a lot of heartburn. These pills I have been using have helped a little but it’s still keeping me up at night.”
Janet Swigel is a 68-year-old woman who presents to the GI clinic with complaints of heartburn four to five times a week over the past 5 months. She also reports some regurgitation after meals that is often accompanied by an acidic taste in her mouth. She states that her symptoms are worse at night, particularly when she goes to bed. She finds that her heartburn worsens and she coughs a lot at night, which keeps her awake. She has had difficulty sleeping over this time period and feels fatigued during the day. She reports no difficulty swallowing food or liquids. She has tried OTC Prevacid 24HR once daily for the past 3 weeks. This has reduced the frequency of her symptoms to 3–4 days per week, but they are still bothering her.
Atrial fibrillation × 12 years
Asthma × 10 years
Type 2 DM × 5 years
HTN × 10 years
Patient is married with three children. She is a retired school bus driver. She drinks one to two glasses of wine 4–5 days per week. She does not use tobacco. She has commercial prescription drug insurance.
Father died of pneumonia at age 75; mother died at age 68 of gastric cancer
Diltiazem CD 120 mg PO once daily
Hydrochlorothiazide 25 mg PO once daily
Metformin 500 mg PO twice daily
Aspirin 81 mg PO daily
Fluticasone/salmeterol DPI 100 mcg/50 mcg one inhalation twice daily
Peanuts (hives)
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

- Barry R. Katz, M.D.
- Raaj K. Popli, M.D.
- Sanjay K. Reddy, M.D.
- Harry H. Shephard, M.D.
- Jorge A. Zapatier, M.D.
- Robert A. Shultz, D.O., FACOI
- Hanna R. Agard, MSN, APRN
- Jeanine Febres, MSN, APRN-C
- Naomi Ringer, APRN
- Accepted Insurances
- Patient Portal
Case Study: Self Diagnosis, Denial and Danger With GERD
In a previous blog, we introduced you to GERD patient, Elena , our DDC Orlando case study. She continued to endure worsening heartburn and acid reflux for years. Yet she had barely mentioned her self-diagnosed GERD problem to her doctor. She tried to shrug it off as indigestion, dyspepsia and just a bad stomach.
Here at DDC Orlando, in Dr. Sanjay Reddy’s words, “Not all GERD is just dyspepsia.” As we continue Elena’s case study over several more blogs, you will see that not every case of GERD simply signifies indigestion. Likewise, no case should be self-diagnosed because of a magazine article or a friend’s story.
Case Study: Patient faces Denial, Takes the First Steps

Case Study in GERD shows a dangerous tendency to self-diagnose.
It is true that most patients with GERD can be successfully treated with medications and lifestyle changes. However, self-diagnosis of GERD can be medically dangerous because the symptoms of GERD can indicate more serious digestive problems.
In a recent interview, DDC Orlando’s Dr. Sanjay Reddy stated, “Chronic heartburn and acid reflux can mean more than “just” GERD. Gastro Esophageal Reflux Disease itself can be the body’s way of sending alarm signals to indicate more serious problems.” This is exactly the reason your primary doctor might refer you to Digestive Disease Consultants of Orlando. With a careful examination, case history and state-of-the-art testing, we can interpret the alarm signals from your body. We need to know if your GERD symptoms are just dyspepsia, like most patients. Or if we should investigate more serious possibilities.
Perhaps, like our case study, Elena, you do not know about all the other possibilities such as Barrett’s Esophagus or the beginnings of esophageal cancer. In the mind and experience of a patient, the symptoms of those diseases might seem like a straight-forward case of GERD.
At DDC Orlando, when patients exhibit GERD symptoms, doctors work to discern and monitor your risk of a condition that can result in cancer without proper treatment. GERD is not always simply dyspepsia. In the words of experts, “It is essential for individuals who suffer persistent heartburn or other chronic and recurrent symptoms of GERD to seek an accurate diagnosis , to work with their physician, and to receive the most effective treatment available.”
Case Study: Elena’s Denial and Excuses for Avoiding Diagnosis

Doctor explains GERD to DDC Orlando Patient
Toughness: Her parents raised her to be strong. Years of conditioning to be tough had taught her to grin and bear it. So she developed a high tolerance for pain when her throat burned or her chest ached. She avoided the doctor and months stretched into years. Like many people who deal daily with acid reflux, she blamed it on dyspepsia.
She was in denial that there could be anything more severe than indigestion interrupting her life. She refused to let GERD take more than a few moments of her time. This mind-set worked for a while, but as in many case studies, symptoms grew very severe. Finally, it became obvious to Elena that the over-the-counter antacids did not have the power to treat her illness.
Timidity: Elena could not be considered an introverted person. However, she had a deep-seated shyness about discussing bodily functions. Even admitting her diarrhea embarrassed her. Additionally, her friends had told her horror stories about the type of testing her condition might require. ( Rest assured, DDC Orlando will be addressing that issue in the near future. )
Case Study: Elena and the Lifestyle Changes—Her Baby-Steps
After a few more attacks l ike the one at her Birthday dinner , our case study patient’s family became concerned. Elena’s husband hugged her as he said, “Three trips to the emergency room in two months? Hon, something’s wrong. I took the liberty of making you an appointment. Keep it or change it, but you can’t go on like this.”
She kept the appointment with her primary care doctor. Based on her description of her reflux and heartburn symptoms, he diagnosed GERD. He immediately suggested life-style and dietary changes. (She thought, “Tell me something I don’t know. I’ve already started changing my life. I know some of my triggers . I am keeping a food diary.)
He also wrote prescriptions for stronger medications than over-the-counter antacids and booked her for a re-check in six weeks. She smiled weakly when the doctor gave her several brochures about GERD lifestyle changes. Our case study dreaded trying to lose her extra 38 pounds of body weight.
Case Study Quiz: Find the Anti-GERD Lifestyle Changes in Elena’s Story Below!
We challenge you to find the lifestyle changes woven into the following case-study scenario:
Elena drove home slowly and fought sadness because now GERD was a real medical diagnosis . As she picked up her prescriptions at the pharmacy, she hated the idea of depending on her new pills to control it. Then she desperately wanted a cigarette, but she had quit two weeks ago because she knew they were a trigger. They literally hurt her throat and chest. She smiled grimly. A good strong cup of coffee would improve her mood, she thought. But it wasn’t worth the choking hot lava in the throat, the reflux. Caffeine was another one of the first triggers she discovered . She had not had a cup in three weeks, since her last trip to the emergency room.
Case Study Scenario: GERD vs. Family life
Upon her return home, Elena’s 6-year-old daughter Ashleigh met her at the door,
“Mommy, Mommy, Daddy turned your bed into a slide,” she shrilled.
We re-join patient Elena’s story of her diagnosis of GERD. To enrich your understanding, we suggest you read or review the introduction of her case study in our one of our previous blogs. Before the dramatic episode on her birthday , which resulted in an emergency room visit, Elena had never seriously discussed her chronic heartburn and reflux with her primary physician. Her knowledge of the condition came from conversations with friends and a few magazine articles.
Case Study: The Patient’s Top Three Excuses for Avoiding a Discussion of GERD
Time: Elena is a busy mom of three with her own part-time real estate job. Our case study patient, Elena, had a hectic life and a full schedule. She declared, “I just don’t have time to go see the doctor every time I have a belly ache or heartburn.”

Case Study Patient With GERD finds hope with family support.
Elena could see the head of the bed had been raised on pretty polished wooden blocks. Our case study patient started to smile. Her husband, still holding an electric drill from his bed-tilting project, strode into the room and hugged her.
14-year-old Lisa popped her head around the kitchen doorway, “Hi, Mom! I made Baked Parmesan Chicken Breasts for dinner. You’ll love them. They’re crispy even without skin!” Elena’s 9-year-old son, Mike chimed in, “And Dad made me eat the rest of those cookies so you wouldn’t be tempted !” Elena laughed, hugged, and stopped feeling sad. “Yeah,” added Mike, as if to explain the cookies, “We read all about Gerdie on the Internet.” … And that is how our DDC Orlando GERD case study patient named her condition!
Please join us at this blog next week for all the answers to the above case study quiz . You’ll find out more about Elena’s lifestyle changes. Also, learn why, six weeks after diet, medication and lifestyle changes, she ended up in the emergency room again with GERD symptoms.

Case Studies
CR, a 44-year-old man, comes to the pharmacy looking for a remedy for his heartburn. He reports that his heartburn has been bothering him for the past few weeks, and he complains of an acidic taste in his mouth and a burning feeling in his throat about twice a week. CR does not complain of any other related symptoms, such as pain when swallowing. CR has a box of omeprazole (Prilosec) in his hand. He asks if it would be the best product to help alleviate his symptoms.
As the pharmacist, how would you respond?
EF is a 30-year-old woman who comes to the pharmacy with dry, demarcated lesions in linear streaks, with some vesicles, on her hands, arms, and face. She says she was gardening yesterday for a few hours and must have touched poison ivy. EF says she tried to hide it with makeup to go to work this morning, but it only made it worse. She exclaims, “I cannot stand the itching anymore.” Upon questioning, you find out that she has had similar lesions before, but they were less extensive and not as bothersome. EF asks if there is pharmacy product that could help. She has no significant medical history and is not taking any prescription or OTC medications.
As the pharmacist, what would you recommend?
Case 1: Based on his reported symptoms, CR likely suffers from mild/ episodic gastroesophageal reflux disease (GERD), so he is a candidate for self-treatment. OTC proton pump inhibitors (PPIs) such as omeprazole, lansoprazole, and esomeprazole are appropriate for self-treatment of GERD for up to 14 days. However, before you recommend these products, you should educate CR that OTC omeprazole, lansoprazole, and esomeprazole are not intended for immediate relief of heartburn. These drugs have a slow onset but a long duration of action, and CR may have to take one of these drugs for 1 to 4 days before he feels better. CR should be cautioned to speak to his doctor if his symptoms do not resolve after 2 weeks or his heartburn worsens.
Alternatively, CR could try a histamine2 (H2)-receptor antagonist such as ranitidine, cimetidine, famotidine, or nizatidine. H2-receptor antagonists have a different mechanism of action than PPIs and provide relief of heartburn more quickly than PPIs. H2-receptor antagonists can be taken prophylactically before meals to prevent GERD.
CR might also consider taking an antacid, including calcium carbonate, sodium bicarbonate, magnesium hydroxide/aluminum hydroxide, or bismuth subsalicylate. These agents have the fastest onset of action, but they provide only symptomatic relief of heartburn and have the shortest duration of action.
Case 2: Allergic contact dermatitis is an inflammatory skin reaction to a foreign substance, such as urushiol in the sap of the poison ivy plant. Sensitized patients can develop clinical symptoms such as erythema, intense itching, and formation of plaques and vesicles within 4 to 96 hours after exposure to an allergen.
EF appears to have severe contact dermatitis. She is not a candidate for self-treatment because of the facial involvement of her dermatitis and the presence of vesicles and intense itching. If left untreated, allergic contact dermatitis resolves within 1 to 3 weeks; however, it can cause significant discomfort. EF should be referred to her primary care provider to obtain a prescription for an oral corticosteroid, such as prednisone to decrease itching, and perhaps a high-potency topical corticosteroid such as clobetasol propionate 0.05% cream, which is generally not applied to the face. A 21-day course of oral prednisone (starting at 1 mg/kg/day and tapered over 3 weeks) is appropriate and can significantly reduce symptoms, including itching.
EF should be told to keep the area clean and to avoid scratching and using makeup, as they can irritate the skin. In addition, nonpharmacologic treatments, including the application of cold compresses, can be recommended. EF might try using astringents such as aluminum acetate (Burrow’s solution) or calamine to reduce inflammation and promote drying, and healing of the lesions.
Read the answers
function showAnswer() {document.getElementById("answer").style.display = 'block';document.getElementById("link").style.display = 'none';}
Dr. Coleman is professor of pharmacy practice, as well as codirector and methods chief at Hartford Hospital Evidence-Based Practice Center, at the University of Connecticut School of Pharmacy.

Commercializing CRISPR/Cas9 Therapy: FDA Approval of Exa-Cel Marks Milestone in Treatment Development

It’s Crunch Time for Cash Flow and Closures. What’s on the Other Side?

Hello, Generation Z: Welcome to Provider Status

Considering Financial Perspectives With Gene Therapy Breakthroughs

Pharmacist Shares Screenshot of a Patient’s Prescription, Which Results in Termination

OPC Summer 2024: Connecting Oncology Pharmacists With Cutting-Edge Insights and Opportunities to Collaborate
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


- Nutrition counsellor
- Food Allergy
- gastroenterology
- Heptologist In Delhi
- Liver transplant
- Case Study on Gastroesophageal Reflux in Middle-Aged Woman
Patient: Female, 52
Final diagnosis: Gastroesophageal Reflux
Gastroesophageal Reflux signs and Symptoms: burning pain in the chest that usually occurs after eating and worsens when lying down.
Speciality: Gastroenterology
Causes, symptoms, and treatment of Gastroesophageal Reflux
Gastroesophageal reflux disease (GERD) affects as many middle-aged women as males. It might manifest as heartburn, regurgitation, dysphagia, or chest discomfort. We examined the severity of symptoms in women is significantly more than in men and may contribute to earlier disease recognition and different disease management.
Gastroesophageal Reflux Case Study
A 52-year-old woman was referred to gastroenterology practice for a history of gastroesophageal reflux disease. The patient claims to have had heartburn symptoms for at least five years. Her symptoms responded to over-the-counter medications such as antacid tablets and liquids, but they grew so frequent that she sought medical attention from her primary care physician.
Later, she reported minor acid reflux at least twice a week. She does not have any other chronic medical issues and does not use any other drugs. Her social background includes severe alcohol usage for 20 years, which she discontinued after being diagnosed with liver illness four years ago. There is no family history of gastrointestinal cancer in her family.
Gastroesophageal Reflux Causes
Gastroesophageal reflux disease, often known as GERD, is a digestive illness that affects the muscular ring between your oesophagus and stomach. The lower esophageal sphincter is the term given to this ring (LES). You may have heartburn or acid indigestion if you have it. Doctors believe that some people develop it as a result of a disease known as hiatal hernia. In most situations, GERD symptoms can be alleviated via dietary and lifestyle modifications. However, some people may require taking medication or going under surgery.
Dysphagia, nausea or vomiting, blood in her stool, or accidental weight loss were all symptoms she encountered. Most people can control their GERD symptoms with simple lifestyle modifications and over-the-counter medicines. However, she may require more potent medication or surgery to cure her problems. Because the patient has a history of alcoholism, she is particularly sensitive to this condition.
Gastroesophageal Reflux Age Range
We observed that the usual age group with GERD symptoms is primarily middle-aged women, i.e. (age range 36 to 55).
Gastroesophageal Reflux symptoms
Heartburn is the most common symptom of GERD. (GERD) occurs when stomach acid regularly rushes back into the tube that links your mouth and stomach (oesophagus). Acid reflux (backwash) can irritate the esophageal lining. Many people experience acid reflux on a regular basis.
Common signs and symptoms of GERD include:
- A burning sensation in your chest (heartburn), usually after eating, which could be worse during the night
- Difficulty swallowing
- Regurgitation of food or sour liquid
- Throat lump sensation
Night-time acid reflux, one might also experience:
- Chronic cough
- New or worsening asthma
- Disrupted sleep
Gastroesophageal reflux risk factors include:
- Bulging the top of the stomach up into the diaphragm
- Connective tissue disorders, such as scleroderma
- Delayed stomach emptying
Gastroesophageal Reflux Symptoms and Treatment
Lying down is one of the home treatments for GERD. According to most researchers, the optimal height of bed head elevation is at least 6-8 inches (15-20 centimetres). This height has been shown in studies to reduce acid reflux when lying down. In reality, the higher the height, the better.
Gastroesophageal reflux management
GERD therapy aims to reduce the quantity of reflux or decrease the damage to the oesophagus lining affected by the refluxed materials.
Over the counter or prescription, medicine recommendations work to address Gastroesophageal reflux causes and symptoms.
- Antacids: These medications can help neutralize the acid in the oesophagus and stomach, therefore alleviating heartburn. Non-prescription antacids give brief or partial relief for many people. Some people benefit from an antacid coupled with a foamy agent. These chemicals, according to researchers, form a foam barrier on top of the stomach, preventing acid reflux.
- H2 blockers: For persistent reflux and heartburn, the doctor may prescribe medicines to decrease stomach acid. H2 blockers, which assist in inhibiting acid production in the stomach, are among these medications. Cimetidine (Tagamet), famotidine (Pepcid), and nizatidine are models of H2 blockers.
- Proton pump inhibitors (PPIs): Often known as acid pumps, medications that reduce stomach acid production by blocking a protein. Dexlansoprazole (Dexilant), esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec), omeprazole/sodium bicarbonate (Zegerid), pantoprazole (Protonix), and rabeprazole are all proton pump inhibitors (Aciphex).
- Prokinetics: In rare circumstances, these medicines assist your stomach empty faster, resulting in less acid being left behind. They may also aid in the treatment of symptoms such as bloating, nausea, and vomiting. Domperidone and metoclopramide are two samples of prokinetics (Clopra, Maxolon, Metozolv, Reglan). Many individuals are unable to take them, and those who can only do so for a short time.
In this case, she was initially given an H2 blocker, which proved ineffective, so she was put on proton pump inhibitor treatment for a while. She presently takes 20mg of omeprazole daily, which she finds beneficial, although she does have heartburn if she skips a dosage. The patient can now comfortably swallow meals and liquids and shows no indications of vomiting or nausea. The patient is constantly monitored and encouraged to make certain dietary and lifestyle modifications. She is recommended to abstain totally from alcohol and cigarettes.
Routine check-ups and proper treatments can help patients with Gastroesophageal Reflux cure. Suppose you are experiencing any symptoms mentioned above. In that case, you can follow the Gastroesophageal reflux care plan by getting in touch with the online gastroenterologist doctor . You can talk to the gastroenterologist and consult gastroenterologist online free. Services are available in different cities, consult her as a gastroenterologist, the best doctor in Patna for the stomach , best female gynaecologist in Jhansi , gastro surgeon in Delhi , liver cirrhosis specialist doctor in India, NCR gastro liver clinic Gurgaon, max hospital liver specialist, the gastro & liver clinic Patna Bihar and best physician in Jammu city .
1. Can GERD affect my heart?
GERD and the associated heartburn have nothing to do with heart or heart disease even though the burning chest in pain seems like a pain in the heart.
2. Are there symptoms other than heartburn for GERD?
Other symptoms include regurgitation of acid up in the throat, bitter taste in the mouth, persistent dry cough, and wheezing among others.
3. Why doesn’t the acid harm the stomach?
The stomach has a thick lining that protects it from damage by acid. The oesophagus does not have this lining.
Privacy Preference Center
Privacy preferences, nutrition counselling.
Nutrition counseling is the assessment of an individual’s dietary intake after which, they are helped set achievable goals and taught various ways of maintaining these goals. The nutrition counselor provides information, educational materials, support and follow-up care to help an individual make and maintain the needed dietary changes for problems like obesity.
Obesity/ Food allergy
I assist people dealing with weight-related health problems by evaluating the health risks and help in obesity management. I also help patients manage various food allergies.
As a hepatologist, I specialize in the treatment of liver disorders, pancreas, gallbladder, hepatitis C, jaundice and the biliary tree. I also see patients suffering from pancreatitis, liver cancers alcoholic cirrhosis and drug induced liver disease(DILI), which has affected the liver.
Gastroenterology
As a gastroenterologist, my primary focus is the overall health of the digestive system. I treat everything from acid reflux to ulcers, IBS, IBD: Crohns disease and ulcerative colitis, and colon cancer.
Endoscopy is a nonsurgical procedure to examine a person’s digestive tract. It is carried out with an endoscope, a flexible tube with a light and camera attached to it so that the doctor can see pictures of the digestive tract on a color TV monitor.
Medical Gastroenterology
Gastroenterology is a specialty that evaluates the entire alimentary tract from the mouth to anus and involves studying the diseases of the pancreas.
Liver Transplant Services
A liver transplant is a surgical procedure that removes a patient’s non-functioning liver and replaces it with a healthy liver from a deceased donor or a portion of healthy liver from a living donor. It is reserved as a treatment option for people who have significant complications due to end-stage chronic liver disease or in case of sudden failure of a previously healthy liver.
Disclaimer » Advertising
- HealthyChildren.org
Study Design and Setting
Survey development and administration, study population, statistical analysis.
Respondent Characteristics
Case Scenarios and Likelihood to Consider ARP
General attitudes and reported-practice about arp, conclusions, acknowledgments, antireflux procedures in children with neurologic impairment: a national survey of physician perspectives.
FUNDING : This study is supported by the University of Calgary and the Alberta Children’s Hospital Research Institute. These organizations had no role in study design, study conduct, writing or publication.
CONFLICT OF INTEREST DISCLOSURES: None of the authors have any conflict of interest related to this study.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Tammie Dewan , Vishal Avinashi , Paul Beaudry , Marie-Joëlle Doré-Bergeron , Nathalie Gaucher , Kate Nelson; Antireflux Procedures in Children With Neurologic Impairment: A National Survey of Physician Perspectives. Hosp Pediatr 2024; e2023007643. https://doi.org/10.1542/hpeds.2023-007643
Download citation file:
- Ris (Zotero)
- Reference Manager
Decision-making about antireflux procedures (ARPs) to treat gastroesophageal reflux disease in children with neurologic impairment and gastrostomy tubes is challenging and likely influenced by physicians’ experience and perspectives. This study will explore physician attitudes about ARPs and determine if there are relationships to clinical practice and personal characteristics.
This is a national observational cross-sectional study that used an electronic questionnaire addressing reported practice, attitudes regarding the ARPs, and responses to clinical vignettes. Participants were physicians in Canadian tertiary-care pediatric settings. Descriptive statistics were used to analyze physician attitudes. Multivariable logistic regression modeling was used to determine associations between physician and practice characteristics and likelihood to consider ARP.
Eighty three respondents represented 12 institutions, with a majority from general or complex care pediatrics. There was a wide disparity between likelihood to consider ARP in each clinical scenario. Likelihood to consider ARP ranged from to 19% to 78% depending on the scenario. Two scenarios were equally split in whether the respondent would offer an ARP. None of the demographic characteristics were significantly associated with likelihood to consider ARP. Often, gastrojejunostomy tubes alone were considered (56% to 68%).
There is considerable variability in physician attitudes toward and recommendations regarding ARPs to treat gastroesophageal reflux disease. We did not find a significant association with clinical experience or location of practice. More research is needed to define indications and outcomes for ARPs. This is a scenario where shared decision-making, bringing together physician and family knowledge and expertise, is likely the best course of action.
Gastroesophageal reflux disease (GERD) is an important comorbidity for children with neurologic impairment (NI), affecting up to 75%. 1 , 2 GERD refers to the passage of gastric contents into the esophagus leading to troublesome symptoms and/or complications. 3 GERD can impair nutrition, contribute to lung disease through secondary aspiration, and cause significant pain. 4 , 5 – 8 The diagnosis of GERD in children with NI is complicated by their frequent inability to self-report symptoms, lack of a gold standard diagnostic test, and variable definitions across the literature. 3 , 9 In addition, GERD symptoms frequently overlap with those of other conditions in this population, such as intestinal dysmotility, feeding intolerance, and visceral hyperalgesia. 10 For the purposes of this study, symptoms such as vomiting, aspiration, and pain will be described as “GERD symptoms,” acknowledging that there may be other conditions contributing to the clinical presentation. This is consistent with real-world practice wherein physicians are often managing this cluster of symptoms without a discrete and confirmed diagnosis.
In cases of refractory GERD, guidelines recommend consideration of antireflux procedures (ARPs) - such as fundoplication and postpyloric feeding through gastrojejunostomy tubes (GJTs). 3 , 9 However, these guidelines are difficult to apply to children with NI and gastrostomy feeds considering their comorbidities, fragility, and frequent communication impairments. Further, evidence for ARPs is weak with no clinical trials comparing ARP to medical therapy or comparing GJT to fundoplication. Observational data are conflicting in terms of the impact of ARPs on lung disease 2 , 11 – 13 and which ARP is superior at improving symptoms and mitigating complications of GERD. 14 Further, adverse events with ARPs are more common in children with NI, including major complications such as intussusception with GJTs and wrap migration or failure with fundoplication. 15
Given the lack of evidence regarding ARPs, decision-making is challenging. There are no targeted tools or algorithms to support clinical decision-making regarding the use of ARPs in children with NI and gastrostomy. In making decisions, physicians are influenced by their own attitudes about different treatment options, organizational culture and constraints, and demographic and clinical characteristics of the child and family. 15 , 16 A deeper understanding of these perspectives is needed to design and implement much-needed prospective studies and clinical trials. This study will specifically explore physician attitudes and reported practice regarding the ARP treatment options (fundoplication and GJTs) for GERD in children with NI and gastrostomy tubes in association with salient physician characteristics such as professional location and years of practice.
We conducted a cross-sectional electronic survey study of physicians who practice at tertiary-care pediatric hospitals in Canada between November 2021 and February 2022. The design and administration of the survey followed guidelines developed by Burns et al. 17 This study was approved by the Conjoint Health Research Ethics Board at our institution.
The survey was codeveloped by a pediatric surgeon, a pediatric gastroenterologist, a pediatric emergency medicine/palliative care physician, and complex care/hospitalist physicians based on clinical experience and review of existing literature. This multispecialty team determined the survey topics, question stems (including clinical scenarios), and the response options for each question. The survey contained 3 sections: (1) participant demographics; (2) general questions about ARPs (diagnostic tests, potential risks and harms, perceived barriers); and (3) case-based questions designed to imitate “real world” clinical practice ( Fig 1 ). Following a clinical vignette, respondents were asked to report their likelihood to consider an ARP and what treatments or interventions they would attempt before an ARP (full questionnaire in Supplemental Fig 5 ). The vignettes corresponded broadly to the following clinical scenarios: (1) severe aspiration events (“Severe Asp”); (2) moderate aspiration events (“Mod Asp”); (3) failure to thrive because of vomiting or GERD (“FTT”); and (4) pain possibly secondary to GERD (“Pain”). A 4-point Likert scale was used with space for written comments after each question.

Clinical scenarios and likelihood to consider ARP.
This instrument was pilot tested in 5 cognitive interviews with relevant pediatric specialists and subspecialists for content validity, question clarity, item interpretation, and item redundancy. Revisions were made after each interview. After the fifth interview, no further modifications were required. This survey was also reviewed by an expert in survey design. A final survey was created consisting of 8 demographic questions, 7 general ARP questions, and 4 clinical scenarios with 6 questions each. The survey was translated into French by a member of our research team with both French and English language proficiency.
Qualtrics software was used to administer the survey, collect, and store data. Invitations to participate were distributed by e-mail to all members of the relevant divisions at the 14 pediatric hospitals across Canada. Pediatric surgeons were recruited by e-mail invitation through the Canadian Association of Pediatric Surgeons. Potential participants were contacted using Dillman’s tailored design method for mixed-mode surveys. 18 The introductory e-mail contained a link where the recipient could indicate their eligibility and express interest. A survey link was sent directly to each individual respondent to allow for tracking of response rates. A total of 3 reminders were sent at 1-week intervals. An implied consent form was presented before the survey.
Respondents were physicians who practice at tertiary-care pediatric hospitals in Canada and represent 1 of the following subspecialty groups: hospital or general pediatricians, complex care pediatricians, pediatric gastroenterologists, and pediatric surgeons. These subspecialties were chosen as those most likely to be involved in decision-making regarding the management of GERD in this complex population of children. The study is limited to tertiary care hospitals as these sites typically have access to ARPs. Additional eligibility criteria included the respondent having treated a child with GERD, NI, and enteral feeding in the past year and having the ability to respond in either English or French.
Descriptive statistics were calculated, including means with SD and interquartile ranges for continuous variables, and count with proportions for categorical variables. The primary outcome variable of likelihood to consider an ARP was coded as 2 categories (consider and do not consider) and physician characteristics were coded as years in practice (<10, 11–20, ≥30), subspecialty (hospital pediatrics or complex care, gastroenterology, surgery) and location of practice (province).
Bivariable association between potential predictor variables and likelihood to consider an ARP in each clinical scenario were determined using χ-square tests. In bivariable analyses, a significant level of 0.3 was used for variable selections. Any variable with P value < .3 was planned to be included in the multivariable models (although no associations reached this threshold). Multivariable logistic regression modeling was, therefore, conducted including all variables because of their clinical importance to determine if there were any independent effects on the primary outcome of physician consideration of ARP. Multiple imputation technique was used in a sensitivity analysis to account for any missing or incomplete information obtained from the surveys.
A total of 119 physicians indicated eligibility via the invitation link. Of those, 83 provided at least partial responses giving a response rate of 70%. Full responses were available for 76. Table 1 presents respondent characteristics. The majority of respondents represented hospital pediatrics, complex care, and/or general pediatrics, whereas 15% ( n = 15) of respondents identified as gastroenterologists and 5% ( n = 4) as pediatric surgeons. There was representation in this sample from every province with a tertiary care pediatric hospital and a total of 12 institutions.
A summary of the clinical scenarios and likelihood to consider ARP is shown in Fig 1 . Two of the scenarios (#1 – Severe Asp and #4 - Pain) were equally split with approximately half of respondents indicating that they were very or somewhat likely to consider ARP ( n = 45, 56% for scenario 1 and n = 44, 57% for scenario 4), whereas the other half were somewhat or very unlikely to consider. Respondents were less likely to consider ARPs for scenario 2 (Mod Asp), wherein only 19% ( n = 15) of them would consider this intervention. Scenario 3 (FTT) was most favored for ARP with 78% ( n = 60) of respondents indicating they were very or somewhat likely to consider. When asked which ARP they are likely to present as an option (fundoplication or GJT), most respondents would offer GJT only (22% to 49%), whereas very few would offer only fundoplication (4% to 8%) ( Supplemental Table 3 ). On bivariable analysis, none of the potential predictor variables studied were significantly associated with the respondents’ likelihood to consider an ARP in any of the clinical scenarios ( Supplemental Table 4 ). Multivariable logistic regression was performed including all variables (because of suspected clinical importance) with a cutoff of statistical significance at P < .05. This likewise did not reveal any independent predictors of physician likelihood to consider ARP in any clinical scenario. There were missing responses in 7 surveys (8%), but sensitivity analysis suggested this does not significantly impact our results (Supplemental Information).
There were no respondents who indicated they would proceed immediately to ARP in any scenario, instead suggesting a wide range of diagnostic investigations or treatments to be considered before ( Table 2 ). The most common intervention was feeding changes (including changing rate or volumes or switching to continuous feeding) with 49% to 90% of respondents choosing this option. Prokinetics were also commonly trialed, particularly in scenarios 1, 3, and 4 (73%, 86%, and 78% respectively). Some respondents would trial baclofen (13% to 32%), NJ tube feeds (23% to 52%), formula changes (38% to 76%), or blenderized diets (24% to 54%). Depending on the scenario, up to half of respondents (19% to 54%) also indicated they would attempt to treat a comorbid condition, most commonly sialorrhea.
Treatments and Interventions Before ARP
Scenario 1 ( n = 80), scenario 2 ( n = 78), scenario 3 ( n = 77), scenario 4 ( n = 77).
Including medications (new or increased doses), subspecialist consultation (respirology, gastroenterology), additional investigations (sialogram, upper gastrointestinal series, gastric emptying scan, videofluoroscopic feeding study, bedside feeding assessment, immunodeficiency workup, metabolic testing, pH probe, impedance study, endoscopy), chest physio or airway clearance or cough assist, constipation treatment.
In terms of diagnostic testing before ARP, over half of respondents would order an upper gastrointestinal series for either GJT ( n = 53, 64%) or fundoplication ( n = 57, 69%). About one third would complete a gastric emptying scan ( n = 30, 35% for GJT; n = 37, 45% for fundoplication) and progressively smaller numbers would request impedance studies ( n = 16, 19% for GJT; n = 35, 42% for fundoplication), fluoroscopic evaluation of feeding and swallowing or videofluoroscopic feeding study ( n = 30, 36% for GJT; n = 21, 25% for fundoplication) or pH probes ( n = 12, 14% for GJT; n = 24, 29% for fundoplication) ( Supplemental Fig 4 ). Aside from feeding and swallowing studies, all other diagnostic tests were more commonly ordered before fundoplication compared with GJT.
Respondents were asked about the perceived risks associated with fundoplication. Most were concerned the procedure would be ineffective ( n = 60, 72% moderately or very concerned) or cause worsening GERD symptoms ( n = 67, 81% moderately or very concerned) ( Fig 2 ). For GJT, the highest levels of concern were regarding the need for continuous feeding ( n = 62, 75% moderately or very concerned), need for emergent GJT changes ( n = 60, 72% moderately or very concerned), and major late complications such as intussusception ( n = 52, 63% moderately or very concerned) ( Fig 3 ).

Concern for risks and harms of fundoplication.

Concern for risks and harms of GJT.
The majority of respondents indicated that it was very easy or somewhat easy ( n = 57, 77%) to access GJT although one-quarter had difficulty accessing this procedure. Only half reported that it was very or somewhat easy ( n = 39, 51%) to access fundoplication at their institution. Most respondents (70%) were concerned about the ability of patients or families to access tertiary care sites for either routine or emergent GJT care.
This study provided a broad overview of the opinions and reported-practice of tertiary-care based physicians across Canada with respect to the use of ARPs among children with NI and gastrostomy tubes. A substantial majority of respondents were pediatricians practicing in hospital medicine or complex care, corresponding to the higher numbers of these specialists in Canada. Our results, thereby, predominantly reflect the perspectives of this group. We discovered considerable practice variability with no clear relationship to subspecialty, experience, or location of practice, although we may not have achieved sufficient power to detect these differences. Some responses reflected issues with access to ARPs because of a variety of geographic barriers (distribution of population) and resource limitations (surgeon or radiologist availability), which likely also impact physician practice. The scenario considered most amenable to ARP was scenario 3 (FTT), which is consistent with available guidelines recommending ARP for refractory GERD symptoms and failure of intragastric feeds. 3 , 16 Even still, nearly one-quarter of respondents would not offer an ARP in this scenario, raising questions about guideline awareness and adherence. The scenario that had the lowest likelihood of ARP was scenario 2 (Mod Asp), which presented a child with chronic lung disease and infrequent episodes of aspiration pneumonia. Interestingly, scenarios 1 (Severe Asp) and 4 (Pain) were evenly split in in terms of likelihood to consider ARP. To some degree, this variability may reflect the lack of evidence available to guide clinical decision-making, which is an established contributor to practice variability. 17 No randomized controlled trials have established the effectiveness of GJT or fundoplication compared with nonsurgical management in children with NI and gastrostomy feeds. Observational studies have mainly conducted head-to-head comparison of GJT and fundoplication, 14 , 18 including a meta-analysis (2015) finding no difference in mortality or frequency of pneumonia. 19 Interestingly, most physicians did not consider ARPs to be second-line treatment, instead suggesting many other interventions they would attempt before ARP. For instance, many would trial prokinetics before ARP even though existing guidelines do not recommend prokinetic agents for treatment of GERD (except in severe refractory cases). 3 , 9
Respondents rated high levels of comfort with ARPs even though their reported practice varied considerably. We hypothesized that practices were often concordant within an institution and/or subspecialty but varied between them. Internally consistent practices could result in higher levels of physician comfort even with a lack of evidence. However, this association was not confirmed in our results. Other research suggests a dissociation between physician-reported comfort and clinical decision-making. 20 , 21 It would thereby be possible to have comfort even if decision-making was not optimal or evidence-based. We cannot exclude the possibility that some variation could be because of different interpretations of the clinical scenarios. However, our results are supported by prior studies that report similar degrees of practice variation in the treatment of GERD. A large cross-sectional study in the United States revealed that the odds of undergoing an ARP in the southwest were twice that of the northeast, even after adjusting for age, case-mix, and case-volume. 22 Another study by Goldin et al reported changing rates of ARPs in relation to common procedures, such as appendectomies, at 36 children’s hospitals in the United States between 2001 and 2006. The overall decline in ARPs was unequally distributed with institutional rates that ranged from 40 fewer per year to 10 greater per year in comparison with 2001. 11 A national survey of pediatric surgeons also found that about 80% of them required an upper gastrointestinal series before ARP and only 13% required a pH probe, similar to the proportions in our study. 23
Existing evidence cannot determine who would benefit from an ARP, particularly in children with NI and other complex needs. There is a need for future research including large prospective, comparative studies that can determine crucial outcomes, such as impact on respiratory morbidity and GERD symptoms. Another area that is under-explored is the impact of ARP on child and family quality of life. One small prospective study suggested improvement with fundoplication in the short term. 24 Another interview study with parents whose child had undergone ARP better reflected the complexity of these scenarios, highlighting how feeding tolerance, caregiving requirements, continuous feeding, and changes in health care utilization could also mediate the impact of these procedures on quality of life. 25 It is also concerning that physicians may be under-appreciating and, thereby, under-treating GERD symptoms, particularly in scenario 4 (Pain). Existing evidence suggests that pain and other distressing symptoms are often overlooked in children with NI and other complex conditions, 26 – 28 whereas physicians may be more comfortable making decisions in the face of “objective” evidence, such as episodes of aspiration pneumonia or growth failure (as in scenarios 1 and 3).
Even as we strive to build a stronger evidence base informing the use of ARPs, the clinical issues and dilemmas persist. The complexity of these children’s care and the nonspecific nature of these symptoms alongside social and logistical variables complicates the development of guidelines and standardization on the use of ARPs. Intentional shared decision-making (SDM) is a valuable approach that could acknowledge the limitations of current evidence and allow for patient and parent values, goals, and preferences to be emphasized and incorporated. 29 One framework suggests that for medical decisions where there is more than 1 reasonable option without a clearly favorable benefit to burden ratio, an in-depth exploration of family preferences can ensure that child and parent values align with the chosen option. 30 Children with medical complexity (including NI) are less likely to be engaged in SDM, 31 , 32 potentially because of the difficulty predicting outcomes in the setting of multiple comorbidities. However, these parents appreciate the complexity of these decisions and highly value their own involvement. 32 Uncertainties in the decision for ARP and the child’s course should be acknowledged, which can further facilitate parents’ participation and comfort. 32
Although 70% of individuals indicating eligibility were included, this study enrolled a relatively small sample skewed largely toward pediatric hospital medicine and complex care physicians, limiting generalizability to other subspecialties. These nuanced and complex clinical scenarios are difficult to describe in a brief vignette. The diagnosis of GERD may not have been obvious, but vignettes were intentionally designed to reflect “real world” scenarios where formal diagnostic testing is seldom used. The survey underwent a structured, iterative process of development, including cognitive interviewing but not formal clinical sensibility testing, which would have strengthened our findings. The style of the questions may have inhibited respondents from communicating more details about their perspectives, although there was space for written comments after each question. The distribution of responses, with some scenarios having more positive responses for ARP, suggests that the questions could discriminate different practice styles. However, it remains possible that some of the variation in responses is related to different interpretations of the clinical scenarios. Other treatment options for GERD were not addressed in this study (such as surgical jejunostomy tube) as they are infrequently used in Canada. No concerns about this omission were raised in the cognitive interviews.
With the lack of evidence regarding the impact of ARPs on clinical and patient-centered outcomes, considerable variability exists in physician perspectives and reported practice. Strengthening the evidence base with prospective studies should be prioritized. As with many complex medical decisions, SDM would acknowledge the limitations in our knowledge and best incorporate patient and family preferences, values, and goals when approaching decisions about ARP.
We thank Dr Brent Hagel, Dr Tamara Simon, Dr Marialena Mouzaki, and Dr Sarah Lai for their assistance in developing and testing the questionnaire; and the contributions of our survey respondents.
The first draft of this manuscript was written by Dr Dewan. This study was presented as a poster presentation at the American Academy of Cerebral Palsy and Developmental Medicine conference in 2023. There are no prior publications or other submissions with any overlapping information, including studies and patients.
Competing Interests
Supplementary data.
Advertising Disclaimer »
Citing articles via
Email alerts.
Affiliations
- Editorial Board
- Editorial Policies
- Pediatrics On Call
- Online ISSN 2154-1671
- Print ISSN 2154-1663
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account

IMAGES
VIDEO
COMMENTS
A CASE PRESENTATION ON GERD ( GASTROESOPHAGEAL REFLUX DISEASE) This document presents a case study of a 60-year-old male patient admitted to the hospital with abdominal discomfort for 10 days and a history of bronchial asthma and GERD. Examination findings and investigation reports are provided. The patient is assessed and diagnosed with ...
Gastroesophageal reflux disease ( GERD) 1. CASE PRESENTATION ON GASTRO OESOPHAGEAL REFLUX DISEASE Submitted by : B.RAJU Pharm D 2 year 19HF1T0005 Submitted to : Dr. SRIDEVI mam. 3. 4. Clinical symptoms • Gastric ulcer pain • Dyspepsia • Nausea • Vomiting • Heart burn Diagnosis I. UPPER ENDOSCOPY : it examines the inside of oesophagus ...
This document discusses gastroesophageal reflux disease (GERD). It begins by defining GERD as a condition caused by stomach contents refluxing into the esophagus and causing troublesome symptoms or complications. It then discusses the pathophysiology of GERD, noting that the lower esophageal sphincter normally acts as a barrier but can become ...
Gastroesophageal reflux disease (GERD) is a chronic gastrointestinal disorder characterized by the regurgitation of gastric contents into the esophagus. It is one of the most commonly diagnosed digestive disorders in the US with a prevalence of 20%, resulting in a significant economic burden in direct and indirect costs and adversely affects the quality of life[1][2]. GERD is caused by ...
Registries & Studies Data to support new techs and treatments. Gut Microbiome One of GI's most promising areas of research. ... GERD and Refractory GERD: A Case Based Approach. Outline PPI-unresponsive GERD Review of treatments GERD: Download the session audio: MP3 File.
Gastroesophageal Reflux Disease (GERD). ... enteric infection The RISK The REALITY • Achlorhydria disables the gastric barrier to ingested pathogens • Case-control study: Small increase in enteric infections with PPIs for 2 months. • Relative risk 1.6 (Cl 1.0-2.4) • PPPI use is independent risk of C. difficile diarrhea in antibiotic ...
GERD case study. A case study assignment that outlines GERD. Course. Nursing Medical Surgical Care of Adults 1 (NURS 323) 165 Documents. Students shared 165 documents in this course. University California State University San Marcos. Academic year: 2019/2020. Uploaded by: Kayla Chapman. California State University San Marcos.
Abstract. Gastroesophageal reflux disease (GERD) is the most prevalent gastrointestinal disorder in the United States, and leads to substantial morbidity, though associated mortality is rare. The prevalence of GERD symptoms appeared to increase until 1999. Risk factors for complications of GERD include advanced age, male sex, white race ...
CASE STUDY - CHAPTER 41 UPPER GI PROBLEMS. Gastroesophageal Reflux Disease. Patient Profile C. is a 49-year-old male who goes to the health care provider because he is experiencing heartburn more frequently and it is keeping him awake at night. He had asthma as a child. He is currently taking Mylanta as needed for heartburn.
Case Study #1: Case 7 (GERD) Answer the following questions: 1. How is acid produced and controlled within the gastrointestinal tract? Gastric acid secretion contains three phases: the cephalic phase, the gastric phase, and the intestinal phase. The cephalic phase occurs when there is the anticipation. of eating food thus sending signals to the ...
Nurse Max works in a primary care office and is caring for Anuja, a 54-year-old woman with a history of gastroesophageal reflux disease, or GERD, who's being seen for a three-month follow-up appointment. After settling Anuja in her room, Nurse Max goes through the steps of the Clinical Judgment Measurement Model to make clinical decisions about ...
Clinical cases help medicine students understand better the symptoms, treatment and development of a disease. They're also very valued in the international scientific community, as they foster communication between professionals so they can learn new techniques and practises. This clinical case is focused on Gastroesophageal reflux disease ...
After completing this case study, the reader should be able to: Describe the clinical presentation of gastroesophageal reflux disease (GERD), including typical, atypical, and alarm symptoms. Discuss appropriate diagnostic approaches for GERD, including when patients should be referred for further diagnostic evaluation.
The Problem. In the United States, GERD is a frequent disorder, affecting 10-20% of the population on a regular basis. 1 Barrett's esophagus (BE) is a metaplastic change of the normal esophageal mucosa, in which the normal squamous epithelium of the esophagus is transformed into columnar epithelium with goblet cells in response to chronic inflammation from reflux of acidic gastric contents.
6 Patrick L. Gastroesophageal Reflux Disease (GERD): A Review of Conventional and Alternative Treatments. Alternative Med - icine Review 2011; 16(2): 18. 7 Ersin NK, Önçag Ö, Tümgör G, Aydogdu S, Hilmioglu S. Oral and Dental Manifestations of Gastroesophageal Reflux Disease in Children: A Preliminary Study. Pediatric Dentistry 2006; 28(3): 6.
Case Study Quiz: Find the Anti-GERD Lifestyle Changes in Elena's Story Below! We challenge you to find the lifestyle changes woven into the following case-study scenario: Elena drove home slowly and fought sadness because now GERD was a real medical diagnosis. As she picked up her prescriptions at the pharmacy, she hated the idea of depending ...
Sign in. Access personal subscriptions, purchases, paired institutional or society access and free tools such as email alerts and saved searches.
Case 1: Based on his reported symptoms, CR likely suffers from mild/ episodic gastroesophageal reflux disease (GERD), so he is a candidate for self-treatment. OTC proton pump inhibitors (PPIs) such as omeprazole, lansoprazole, and esomeprazole are appropriate for self-treatment of GERD for up to 14 days.
Gastroesophageal Reflux Case Study. A 52-year-old woman was referred to gastroenterology practice for a history of gastroesophageal reflux disease. The patient claims to have had heartburn symptoms for at least five years. Her symptoms responded to over-the-counter medications such as antacid tablets and liquids, but they grew so frequent that ...
OBJECTIVE:. Decision-making about antireflux procedures (ARPs) to treat gastroesophageal reflux disease in children with neurologic impairment and gastrostomy tubes is challenging and likely influenced by physicians' experience and perspectives. This study will explore physician attitudes about ARPs and determine if there are relationships to clinical practice and personal characteristics ...