July 24, 2023


Emory’s Gavegnano Group demonstrates ability to remove key barrier to an HIV cure.
The results of a novel study presented by Emory researchers during the International AIDS Society (IAS) Conference in Brisbane, Australia, have revealed exciting findings in the pursuit of an HIV cure. The study, led by Monica Reece, a PhD candidate in Emory’s Microbiology and Genetics Program, and directed by Christina Gavegnano, PhD, demonstrates the potential of Jak inhibitors, specifically ruxolitinib, to significantly decay the viral reservoir in people with HIV, offering a novel pathway toward long-term remission or a cure.
The HIV viral reservoir, essentially a small number of immune cells containing dormant virus integrated into the genomes of individuals who have suppressed viral replication with HIV treatment, has posed a major impediment to achieving an HIV cure. These cells are completely undetectable by the immune system because the virus is dormant. But as soon as treatment stops, the virus reactivates.
“The barrier to an HIV cure is that the virus hides inside the DNA of cells,” says Gavegnano, director of the Gavegnano Drug Discovery Program and senior author on the study. “The brass ring is an agent that can eliminate these‘reservoir cells,’ which would ultimately eliminate HIV from a person’s body.”
While Gavegnano and her Emory colleagues have shown that Jak inhibitors (Janus kinase inhibitors) could reverse the immune dysfunction caused by HIV since their discovery in 2010, questions about their impact on the HIV reservoir and the exact mechanism contributing to the immunologic improvements have remained unanswered, until now.
The data presented at IAS represented secondary results from a Phase 2a clinical trial centered on investigating ruxolitinib’s effects on viral reservoirs in people with HIV during a five-week regimen, specifically in a subset of individuals with high viral reservoir levels at baseline.
The study measured integrated proviral DNA, which is the genetic material of a virus as incorporated into, and able to replicate with, the genome of a host cell, and examined changes in total, intact only, and defective proviral DNA copies over time. Based on a linear model of decay, the researchers estimated an astonishing 99.99% clearance of the peripheral HIV-1 reservoir in less than three years. These data provide optimism for the use of Jak inhibitors as a backbone for cure-based eradication strategies in the battle against HIV.
Reece, lead author of the study says, “These data suggest that our Jak inhibitors can not only reverse the immune dysfunction that prevents HIV-1 cure, but also significantly decay the reservoir in people living with HIV. Collectively our trial demonstrates a mechanism by which ruxolitinib, or other Jak inhibitors such as baricitinib, also extensively studied by our group, decay the reservoir, which underscores potential for cure-based therapies.”
The profound impact of Ruxolitinib treatment was not limited to reservoir reduction. The study also shed light on several significant biomarkers that were altered by the drug primarily related to:
- Immune activation: Ruxolitinib exhibited the potential to modulate immune activation, which is crucial in controlling viral replication and maintaining immune health in individuals with HIV.
- Cell survival: Ruxolitinib demonstrated the ability to impact cell survival, influencing the lifespan of reservoir cells and potentially limiting viral reservoir longevity.
- Immune dysregulation: The study identified ruxolitinib’s impact on immune dysregulation, offering hope for mitigating the chronic inflammation and immune dysfunction often observed in individuals with HIV.
It is important to note that the study focused on the peripheral viral reservoir and may not fully represent the entire viral reservoir within the body, including sanctuary sites where HIV can persist despite treatment.
Regardless, the findings from Emory University’s study offer hope and renewed enthusiasm for efforts to unravel the complexities of HIV persistence and ultimately find a cure.
“These data are valuable because they show that Jak inhibitors can contribute to a long-term cure strategy for HIV, but they can also be used to slow the inflammatory process caused by other infectious diseases,” says Vincent Marconi, MD, professor of medicine and global health at Emory University School of Medicine.
Marconi, who led the initial phase 2a trial, has already been investigating the efficacy of Jak inhibitors, like ruxolitinib and baricitinib, in patients with acute COVID and now long COVID. He continues, “using an anti-inflammatory drug to treat the effects of a virus could be revolutionary.”
In addition to the data presented by Reece and Gavegnano, another presentation at IAS has shown how ruxolitinib administered to a patient following a stem cell transplant led to an undetectable viral load 20 months after stopping antiretroviral therapy, highlighting the different mechanisms in which these class of drugs could be valuable in HIV care and treatment.
Further research and clinical trials will be needed to fully understand the effects of Jak inhibitor use in HIV and other immune-suppressing conditions. Emory researchers have an extensive history of working with Jak inhibitors. Gavegnano and researcher Raymond Schinazi are listed on the issued patents as sole inventors, and they, alongside their co-investigators, have built a roadmap for tackling a variety of immunosuppressive viruses with these drugs.
Gavegnano emphasizes, “The safety and efficacy outcomes we observed in this study provide a strong foundation for further research on cure-based interventions containing a Jak inhibitor, and we hope to bring this therapy one step closer to helping people living with HIV.”
- News Releases
- School of Medicine
- School of Medicine's Department of Medicine
- Woodruff Health Sciences Center
- Graduate School
- Infectious Diseases
- Global Health
- Health Sciences Research
- GDBBS Program
- GDBBS: Microbiology and Molecular Genetics
Recent News
Download emory news photo.
By downloading Emory news media, you agree to the following terms of use:
Creative Commons Attribution-NoDerivatives 4.0 International Public License
By exercising the Licensed Rights (defined below), You accept and agree to be bound by the terms and conditions of this Creative Commons Attribution-NoDerivatives 4.0 International Public License ("Public License"). To the extent this Public License may be interpreted as a contract, You are granted the Licensed Rights in consideration of Your acceptance of these terms and conditions, and the Licensor grants You such rights in consideration of benefits the Licensor receives from making the Licensed Material available under these terms and conditions.
Section 1 – Definitions.
- Adapted Material means material subject to Copyright and Similar Rights that is derived from or based upon the Licensed Material and in which the Licensed Material is translated, altered, arranged, transformed, or otherwise modified in a manner requiring permission under the Copyright and Similar Rights held by the Licensor. For purposes of this Public License, where the Licensed Material is a musical work, performance, or sound recording, Adapted Material is always produced where the Licensed Material is synched in timed relation with a moving image.
- Copyright and Similar Rights means copyright and/or similar rights closely related to copyright including, without limitation, performance, broadcast, sound recording, and Sui Generis Database Rights, without regard to how the rights are labeled or categorized. For purposes of this Public License, the rights specified in Section 2(b)(1)-(2) are not Copyright and Similar Rights.
- Effective Technological Measures means those measures that, in the absence of proper authority, may not be circumvented under laws fulfilling obligations under Article 11 of the WIPO Copyright Treaty adopted on December 20, 1996, and/or similar international agreements.
- Exceptions and Limitations means fair use, fair dealing, and/or any other exception or limitation to Copyright and Similar Rights that applies to Your use of the Licensed Material.
- Licensed Material means the artistic or literary work, database, or other material to which the Licensor applied this Public License.
- Licensed Rights means the rights granted to You subject to the terms and conditions of this Public License, which are limited to all Copyright and Similar Rights that apply to Your use of the Licensed Material and that the Licensor has authority to license.
- Licensor means the individual(s) or entity(ies) granting rights under this Public License.
- Share means to provide material to the public by any means or process that requires permission under the Licensed Rights, such as reproduction, public display, public performance, distribution, dissemination, communication, or importation, and to make material available to the public including in ways that members of the public may access the material from a place and at a time individually chosen by them.
- Sui Generis Database Rights means rights other than copyright resulting from Directive 96/9/EC of the European Parliament and of the Council of 11 March 1996 on the legal protection of databases, as amended and/or succeeded, as well as other essentially equivalent rights anywhere in the world.
- You means the individual or entity exercising the Licensed Rights under this Public License. Your has a corresponding meaning.
Section 2 – Scope.
- reproduce and Share the Licensed Material, in whole or in part; and
- produce and reproduce, but not Share, Adapted Material.
- Exceptions and Limitations . For the avoidance of doubt, where Exceptions and Limitations apply to Your use, this Public License does not apply, and You do not need to comply with its terms and conditions.
- Term . The term of this Public License is specified in Section 6(a) .
- Media and formats; technical modifications allowed . The Licensor authorizes You to exercise the Licensed Rights in all media and formats whether now known or hereafter created, and to make technical modifications necessary to do so. The Licensor waives and/or agrees not to assert any right or authority to forbid You from making technical modifications necessary to exercise the Licensed Rights, including technical modifications necessary to circumvent Effective Technological Measures. For purposes of this Public License, simply making modifications authorized by this Section 2(a)(4) never produces Adapted Material.
- Offer from the Licensor – Licensed Material . Every recipient of the Licensed Material automatically receives an offer from the Licensor to exercise the Licensed Rights under the terms and conditions of this Public License.
- No downstream restrictions . You may not offer or impose any additional or different terms or conditions on, or apply any Effective Technological Measures to, the Licensed Material if doing so restricts exercise of the Licensed Rights by any recipient of the Licensed Material.
- No endorsement . Nothing in this Public License constitutes or may be construed as permission to assert or imply that You are, or that Your use of the Licensed Material is, connected with, or sponsored, endorsed, or granted official status by, the Licensor or others designated to receive attribution as provided in Section 3(a)(1)(A)(i) .
Other rights .
- Moral rights, such as the right of integrity, are not licensed under this Public License, nor are publicity, privacy, and/or other similar personality rights; however, to the extent possible, the Licensor waives and/or agrees not to assert any such rights held by the Licensor to the limited extent necessary to allow You to exercise the Licensed Rights, but not otherwise.
- Patent and trademark rights are not licensed under this Public License.
- To the extent possible, the Licensor waives any right to collect royalties from You for the exercise of the Licensed Rights, whether directly or through a collecting society under any voluntary or waivable statutory or compulsory licensing scheme. In all other cases the Licensor expressly reserves any right to collect such royalties.
Section 3 – License Conditions.
Your exercise of the Licensed Rights is expressly made subject to the following conditions.
Attribution .
If You Share the Licensed Material, You must:
- identification of the creator(s) of the Licensed Material and any others designated to receive attribution, in any reasonable manner requested by the Licensor (including by pseudonym if designated);
- a copyright notice;
- a notice that refers to this Public License;
- a notice that refers to the disclaimer of warranties;
- a URI or hyperlink to the Licensed Material to the extent reasonably practicable;
- indicate if You modified the Licensed Material and retain an indication of any previous modifications; and
- indicate the Licensed Material is licensed under this Public License, and include the text of, or the URI or hyperlink to, this Public License.
- You may satisfy the conditions in Section 3(a)(1) in any reasonable manner based on the medium, means, and context in which You Share the Licensed Material. For example, it may be reasonable to satisfy the conditions by providing a URI or hyperlink to a resource that includes the required information.
- If requested by the Licensor, You must remove any of the information required by Section 3(a)(1)(A) to the extent reasonably practicable.
Section 4 – Sui Generis Database Rights.
Where the Licensed Rights include Sui Generis Database Rights that apply to Your use of the Licensed Material:
- for the avoidance of doubt, Section 2(a)(1) grants You the right to extract, reuse, reproduce, and Share all or a substantial portion of the contents of the database, provided You do not Share Adapted Material;
- if You include all or a substantial portion of the database contents in a database in which You have Sui Generis Database Rights, then the database in which You have Sui Generis Database Rights (but not its individual contents) is Adapted Material; and
- You must comply with the conditions in Section 3(a) if You Share all or a substantial portion of the contents of the database.
Section 5 – Disclaimer of Warranties and Limitation of Liability.
- Unless otherwise separately undertaken by the Licensor, to the extent possible, the Licensor offers the Licensed Material as-is and as-available, and makes no representations or warranties of any kind concerning the Licensed Material, whether express, implied, statutory, or other. This includes, without limitation, warranties of title, merchantability, fitness for a particular purpose, non-infringement, absence of latent or other defects, accuracy, or the presence or absence of errors, whether or not known or discoverable. Where disclaimers of warranties are not allowed in full or in part, this disclaimer may not apply to You.
- To the extent possible, in no event will the Licensor be liable to You on any legal theory (including, without limitation, negligence) or otherwise for any direct, special, indirect, incidental, consequential, punitive, exemplary, or other losses, costs, expenses, or damages arising out of this Public License or use of the Licensed Material, even if the Licensor has been advised of the possibility of such losses, costs, expenses, or damages. Where a limitation of liability is not allowed in full or in part, this limitation may not apply to You.
- The disclaimer of warranties and limitation of liability provided above shall be interpreted in a manner that, to the extent possible, most closely approximates an absolute disclaimer and waiver of all liability.
Section 6 – Term and Termination.
- This Public License applies for the term of the Copyright and Similar Rights licensed here. However, if You fail to comply with this Public License, then Your rights under this Public License terminate automatically.
Where Your right to use the Licensed Material has terminated under Section 6(a) , it reinstates:
- automatically as of the date the violation is cured, provided it is cured within 30 days of Your discovery of the violation; or
- upon express reinstatement by the Licensor.
- For the avoidance of doubt, the Licensor may also offer the Licensed Material under separate terms or conditions or stop distributing the Licensed Material at any time; however, doing so will not terminate this Public License.
- Sections 1 , 5 , 6 , 7 , and 8 survive termination of this Public License.
Section 7 – Other Terms and Conditions.
- The Licensor shall not be bound by any additional or different terms or conditions communicated by You unless expressly agreed.
- Any arrangements, understandings, or agreements regarding the Licensed Material not stated herein are separate from and independent of the terms and conditions of this Public License.
Section 8 – Interpretation.
- For the avoidance of doubt, this Public License does not, and shall not be interpreted to, reduce, limit, restrict, or impose conditions on any use of the Licensed Material that could lawfully be made without permission under this Public License.
- To the extent possible, if any provision of this Public License is deemed unenforceable, it shall be automatically reformed to the minimum extent necessary to make it enforceable. If the provision cannot be reformed, it shall be severed from this Public License without affecting the enforceability of the remaining terms and conditions.
- No term or condition of this Public License will be waived and no failure to comply consented to unless expressly agreed to by the Licensor.
- Nothing in this Public License constitutes or may be interpreted as a limitation upon, or waiver of, any privileges and immunities that apply to the Licensor or You, including from the legal processes of any jurisdiction or authority.
Creative Commons is not a party to its public licenses. Notwithstanding, Creative Commons may elect to apply one of its public licenses to material it publishes and in those instances will be considered the “Licensor.” The text of the Creative Commons public licenses is dedicated to the public domain under the CC0 Public Domain Dedication . Except for the limited purpose of indicating that material is shared under a Creative Commons public license or as otherwise permitted by the Creative Commons policies published at creativecommons.org/policies , Creative Commons does not authorize the use of the trademark “Creative Commons” or any other trademark or logo of Creative Commons without its prior written consent including, without limitation, in connection with any unauthorized modifications to any of its public licenses or any other arrangements, understandings, or agreements concerning use of licensed material. For the avoidance of doubt, this paragraph does not form part of the public licenses.

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Office of AIDS Research
- HIV Policy and Research
- Research Priorities
- NIH Strategic Plan for HIV and HIV-Related Research
- NIH HIV Research Budget
- NIH HIV Research Priority Areas
- Reduce the Incidence of HIV
- Develop Next-Generation HIV Therapies
Research Toward HIV Cure
- Address HIV-Associated Comorbidities, Coinfections, & Complications
- Cross-Cutting Areas

Viral latency and sanctuaries
Latent HIV reservoirs—small amounts of HIV that persist in people taking ART—present a significant challenge to finding a cure for HIV. Latent reservoirs remain in people with HIV when HIV becomes part of the body’s DNA in infected cells. Additionally, reservoirs of HIV can be found in certain “sanctuary” sites in the body that allow the virus to hide and be protected from both the immune system and ART. To cure HIV, the NIH supports studies to develop novel approaches and treatments that target these HIV reservoirs.
Sustained viral remission and viral eradication

Current science suggests that the path to an HIV cure involves first achieving sustained viral remission without ART. This is called sustained ART-free viral remission or a functional cure. For sustained ART-free viral remission, infectious virus must remain undetectable by sensitive testing methods for a long time without treatment. One research aim will be to prolong the time between treatments to be measured eventually not in weeks, but in months or even years. The NIH supports research into treatments leading to sustained ART-free viral remission . New cure-inducing treatments must be as safe, effective, and available for widespread use as are current-day ART regimens.
Viral eradication—eliminating the virus entirely—is the more challenging, longer-term goal.
Research Strategies
The NIH supports research to better understand how the HIV reservoir forms, persists, and reactivates, as well as investigations to develop new cure treatment strategies targeting HIV reservoirs.
A range of biomarkers and techniques, including single-cell and imaging technologies, are being studied to determine how to identify and describe the HIV reservoir. These techniques also are being used to better understand mechanisms of viral reactivation from latently infected cells.
Experimental treatments in development include therapeutic vaccines, genetically engineered immune cells that are resistant to HIV infection, drugs that reactivate latent HIV to make the virus visible to the immune system, cure-inducing immunotherapies, and interventions to permanently silence HIV in infected cells.
The search for an HIV cure involves important behavioral and social processes that complement the domains of biomedicine. BSSR in HIV cure research is focused on important aspects such as: counseling and support interventions to address the psychosocial needs and concerns of study participants related to analytical treatment interruptions (ATIs); risk reduction in the course of ATI study participation; motivation, acceptability, and decision‐making processes of potential study participants; how cure affects the identity and social position of people with HIV; and the scalability of a proven cure strategy in the context of further advances in HIV prevention and treatment.

The NIH is leveraging resources toward an HIV cure through several public-private partnerships. NIH small business awards enable companies to help foster a diverse pipeline of experimental treatments in development. The combined support of government, industry, and nongovernmental foundations is fostering the expansion of a talented scientific workforce dedicated to advancing HIV cure research.
OAR scientist Dr. Paul Sato coordinates Research Toward an HIV Cure .
This page last reviewed on September 8, 2022
- China Mainland
- Saudi Arabia
- Türkiye
- United Arab Emirates
- South Africa
- Australia and New Zealand
- Belgium and Luxembourg
- Czech Republic & Slovakia
- Netherlands
- Poland & The Baltics
- Switzerland
- United Kingdom
Press Releases
June 04, 2024
MEDIA UPDATE: Gilead Sciences Advances Enrollment in Collaborative Studies to Assess Twice-Yearly HIV Prevention Option for Both Cisgender Women in the U.S. and People Who Inject Drugs in the U.S.
– The studies, conducted in partnership with the U.S. National Institutes of Health and the HIV Prevention Trials Network, are evaluating the potential of lenacapavir as a twice-yearly prevention option for people who could benefit from pre-exposure prophylaxis (PrEP) –
FOSTER CITY, Calif. – Gilead Sciences, Inc. (Nasdaq: GILD) today announced the company is advancing enrollment in two groundbreaking collaborative studies to evaluate the tolerability of an investigational long-acting HIV prevention option in groups of people in the United States who are disproportionately affected by HIV but who are often underrepresented in HIV clinical trials.
The Phase 2 studies, PURPOSE 3 (HPTN-102, NCT06101329 ) and PURPOSE 4 (HPTN-103, NCT06101342 ), are part of Gilead’s PURPOSE program. The PURPOSE program, which also includes two ongoing Phase 3 clinical trials, is assessing the potential of twice-yearly subcutaneous injections of lenacapavir to help a diverse range of people around the world who could benefit from HIV-
1 pre-exposure prophylaxis (PrEP). PURPOSE 3/HPTN-102 is enrolling cisgender women in the U.S. who are disproportionately affected by HIV, with a focus on Black women and other women of color. PURPOSE 4/HPTN-103 is enrolling people in the U.S. who inject drugs.
The studies, sponsored and funded by Gilead, are being implemented through the HIV Prevention Trials Network (HPTN). HPTN is supported by grants from the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH), with scientific collaboration on this study and others from the National Institute on Drug Abuse (NIDA) as well as co-funding from NIDA and other NIH institutes.
“HIV prevention is only effective when people are able to access and adhere to the prevention methods that fit within their lives, and a twice-yearly subcutaneous injectable could be an important option for some people for whom existing PrEP modalities—for varying reasons—are not feasible. Gilead is proud to partner with NIH, HPTN and members of communities across the U.S. on these important studies, recognizing that lenacapavir for PrEP, if deemed safe and effective, could potentially help more people, in more populations, prevent HIV,” said Jared Baeten, MD, PhD, Vice President, HIV Clinical Development, Gilead Sciences . “These collaborations are a vital part of Gilead’s vision and commitment to developing innovative, person-centric options that help contribute to our goal of ending the HIV epidemic for everyone, everywhere—including helping the U.S. move closer toward achieving the goals of the Ending the HIV Epidemic in the U.S. initiative.”
According to the U.S. Centers for Disease Control and Prevention (CDC) , 18% (6,666) of new HIV diagnoses in the U.S. in 2021 were among cisgender women. More than half (54%) of those diagnoses were among Black/African American women, and 18% were among Hispanic/Latina women. PrEP uptake among women in the U.S. has so far lagged behind uptake among men: According to preliminary CDC data , only 15% of women in the U.S. who could benefit from PrEP were prescribed it in 2022, compared with 41% of men who could benefit from PrEP.
“Ending the HIV epidemic means ending it for everyone—including and especially women, who are often underrepresented in HIV research and clinical trials and whose need for new HIV prevention options is critical. This is particularly true for women of color, who bear a disproportionate burden of new HIV infections and who often face structural barriers that can inhibit uptake and adherence to available PrEP methods,” said PURPOSE 3/HPTN-102 protocol chair Shobha Swaminathan, MD, Professor of Medicine and Director of HIV Services at Rutgers New Jersey Medical School. “This collaborative study is an important milestone in HIV prevention research and, if the results are positive, could help provide an additional PrEP option to a number of women across the U.S. that may fit into their lifestyles.”
PURPOSE 3/HPTN-102 was also led by protocol co-chair Ada Adimora, MD, MPH, the Sarah Graham Kenan Distinguished Professor of Medicine at the University of North Carolina School of Medicine and Professor of Epidemiology at the UNC Gillings School of Global Public Health. Dr. Adimora passed away on January 1, 2024. “Dr. Adimora dedicated her life to shining a light on the societal barriers facing many people—especially women of color—who are affected by HIV, as well as helping them overcome those barriers to help them live healthier lives,” said Myron “Mike” Cohen, MD, Co-Principal Investigator of the HPTN and the Director of the UNC Institute for Global Health and Infectious Diseases. “PURPOSE 3/HPTN-102 is already an important part of her legacy.”
The first participants in PURPOSE 3/HPTN-102 were enrolled at a site at the University of California San Diego led by Jill Blumenthal, MD, an Associate Professor of Medicine at UCSD and also a principal investigator for Gilead’s pivotal PURPOSE 2 clinical trial, which is assessing the potential of lenacapavir for PrEP among cisgender men who have sex with men, transgender men, transgender women and gender non-binary individuals who have sex with partners assigned male at birth in seven countries around the world. “If our collective goal is to end the HIV epidemic for everyone, everywhere, we need to include as many different populations in HIV prevention studies as possible,” Blumenthal said. “The diversity of locations and populations is a hallmark of Gilead’s PURPOSE program, and I’m thrilled that Gilead is now able to include cisgender women and people who inject drugs in the U.S. in its PURPOSE 3/HPTN-102 and PURPOSE 4/HPTN-103 trials.”
In addition to focusing on cisgender women, reaching people who inject drugs will be critical to ending the HIV epidemic. According to CDC data , more than 2,500 people who inject drugs were diagnosed with HIV in 2021, comprising about 7% of total diagnoses in the U.S. Among this group, PrEP uptake has been severely limited: A July 2022 JAMA Network Open study showed that, between 2010-2019, fewer than 1 in 500 people who inject drugs had pharmacy claims for PrEP.
“The vast majority of people in the U.S. who inject drugs are not taking advantage of current PrEP options, signaling that we must identify more appropriate HIV prevention solutions for them,” said PURPOSE 4/HPTN-103 investigator Sally Hodder, MD, Director of the West Virginia Clinical & Translational Science Institute at West Virginia University. “PURPOSE 4 is the first trial to evaluate a long-acting PrEP modality in this disenfranchised and commonly overlooked population. Findings from this trial could be critical to advancing the Ending the HIV Epidemic in the U.S. initiative.”
About Gilead’s PURPOSE program
PURPOSE 3/HPTN-102 and PURPOSE 4/HPTN-103 are part of Gilead’s PURPOSE program, which is assessing the potential of lenacapavir to help a diverse range of people around the world who could benefit from PrEP. The pivotal trials for the PURPOSE program are PURPOSE 1 and 2. The use of lenacapavir for HIV prevention is investigational and the safety and efficacy of lenacapavir for this use have not been established.
PURPOSE 1 ( NCT04994509 ) is evaluating lenacapavir for PrEP and emtricitabine/tenofovir alafenamide (F/TAF) for PrEP in cisgender adolescent girls and young women ages 16-25 in South Africa and Uganda. This pivotal registrational trial completed full enrollment in late 2023, and results are expected in the second half of 2024.
PURPOSE 2 ( NCT04925752 ) is assessing lenacapavir for PrEP among cisgender men who have sex with men, transgender men, transgender women and gender non-binary individuals who have sex with partners assigned male at birth in Argentina, Brazil, Mexico, Peru, South Africa, Thailand and the U.S. This pivotal registrational trial completed enrollment in late 2023, and results are expected in late 2024/early 2025.
PURPOSE 5 will assess the persistence—defined as consistent and continuous use—of lenacapavir compared with emtricitabine/ tenofovir disoproxil fumarate (F/TDF) in people who may benefit from PrEP and who are not currently taking PrEP in France and the United Kingdom. Enrollment will begin in 2024.
Additional information about the PURPOSE program can be found at www.purposestudies.com .
About Gilead
Gilead Sciences, Inc. is a biopharmaceutical company that has pursued and achieved breakthroughs in medicine for more than three decades, with the goal of creating a healthier world for all people. The company is committed to advancing innovative medicines to prevent and treat life-threatening diseases, including HIV, viral hepatitis, COVID-19, and cancer. Gilead operates in more than 35 countries worldwide, with headquarters in Foster City, California.
About Gilead HIV
For more than 35 years, Gilead has been a leading innovator in the field of HIV, driving advances in treatment, prevention and cure research. Gilead researchers have developed 12 HIV medications , including the first single-tablet regimen to treat HIV, the first antiretroviral for pre-exposure prophylaxis (PrEP) to help reduce new HIV infections, and the first long-acting injectable HIV treatment medication administered twice-yearly. Our advances in medical research have helped to transform HIV into a treatable, preventable, chronic condition for millions of people.
Gilead is committed to continued scientific innovation to provide solutions for the evolving needs of people affected by HIV around the world. Through partnerships , collaborations and charitable giving, the company also aims to improve education, expand access and address barriers to care, with the goal of ending the HIV epidemic for everyone, everywhere. Gilead was recognized as the number one philanthropic funder of HIV-related programs in a report released by Funders Concerned About AIDS.
Learn more about Gilead’s unique collaborations worldwide and the work to help end the global HIV epidemic.
Forward-Looking Statements
This press release includes forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995 that are subject to risks, uncertainties and other factors, including Gilead’s ability to initiate, progress and complete clinical trials in the anticipated timelines or at all, and the possibility of unfavorable results from ongoing and additional clinical trials, including those involving lenacapavir (such as PURPOSE 3 and PURPOSE 4); the possibility that Gilead may make a strategic decision to discontinue development of lenacapavir for indications currently under evaluation and, as a result, lenacapavir may never be successfully commercialized for such indications; and any assumptions underlying any of the foregoing. These and other risks, uncertainties and factors are described in detail in Gilead’s Quarterly Report on Form 10-Q for the quarter ended March 31, 2024, as filed with the U.S. Securities and Exchange Commission. These risks, uncertainties and other factors could cause actual results to differ materially from those referred to in the forward-looking statements. All statements other than statements of historical fact are statements that could be deemed forward-looking statements. The reader is cautioned that any such forward-looking statements are not guarantees of future performance and involve risks and uncertainties, and is cautioned not to place undue reliance on these forward-looking statements. All forward-looking statements are based on information currently available to Gilead, and Gilead assumes no obligation and disclaims any intent to update any such forward-looking statements.
Gilead and the Gilead logo are trademarks of Gilead Sciences, Inc. or its related companies. For more information about Gilead, please visit the company’s website at www.gilead.com.
Jacquie Ross, Investors
Meaghan Smith, Media
Intersititial body copy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

A Review of Recent HIV Prevention Interventions and Future Considerations for Nursing Science
Author Contributions
As our knowledge of HIV evolved over the decades, so have the approaches taken to prevent its transmission. Public health scholars and practitioners have engaged in four key strategies for HIV prevention: behavioral-, technological-, biomedical-, and structural/community-level interventions. We reviewed recent literature in these areas to provide an overview of current advances in HIV prevention science in the United States. Building on classical approaches, current HIV prevention models leverage intimate partners, families, social media, emerging technologies, medication therapy, and policy modifications to effect change. Although much progress has been made, additional work is needed to achieve the national goal of ending the HIV epidemic by 2030. Nurses are in a prime position to advance HIV prevention science in partnership with transdisciplinary experts from other fields (e.g., psychology, informatics, and social work). Future considerations for nursing science include leveraging transdisciplinary collaborations and consider social and structural challenges for individual-level interventions.
Approximately 1.2 million people in the United States are currently living with HIV, and an estimated 14% are infected, yet unaware of their status ( Office of Infectious Disease and HIV/AIDS Policy, 2020 ). HIV and AIDS continue to have a disproportionate impact on certain populations, including youth—gay, bisexual, and other men who have sex with men (MSM)—racial and ethnic minorities, people who inject drugs, and residents of highly affected geographic regions such as the Southeastern United States ( Aral et al., 2020 ; Hill et al., 2018 ; Lanier & Sutton, 2013 ). Ending the HIV epidemic requires increasing engagement along the HIV prevention and care continua ( Kay et al., 2016 ; McNairy & El-Sadr, 2014 ). Early and repeat HIV testing are recommended strategies for early entry into HIV care and improved HIV-related outcomes ( DiNenno et al., 2017 ). Late and infrequent HIV testing may result in receiving an initial HIV diagnosis late in the disease trajectory, and individuals unaware they are living with HIV may be more likely to transmit HIV to others. It is essential for people living with HIV (PLWH) to receive a timely diagnosis so that they can begin combination antiretroviral therapy with the goal of achieving an undetectable viral load, a key HIV prevention strategy ( Cohen et al., 2016 ). To improve linkage and retention along the prevention and care continua, researchers have developed HIV prevention interventions in four key areas: behavioral-, technological-, biomedical-, and structural/community-level interventions.
Behavioral interventions are approaches that promote protective or risk-reduction behavior in individuals and social groups via informational, motivational, skill-building, and community-normative strategies ( Coates et al., 2008 ). HIV-specific examples include, but are not limited to, interventions promoting abstinence, condom use, sex communication, condom negotiation, HIV testing, reduction in number of sexual partners, stigma reduction, and use of clean needles among people who inject drugs. Behavioral interventions target various HIV risk behavior mediators and moderators, including symptoms of mental illness and emotion regulation ( Brawner et al., 2019 ), attitudes, beliefs, subjective norms, intentions ( Fishbein & Ajzen, 1975 ), and self-efficacy ( Bandura, 2001 ). The effectiveness of behavior-change interventions in reducing risk for HIV during the early stages of the HIV pandemic demonstrated the importance and utility of this approach ( Bekker et al., 2012 ). Classic approaches to behavioral interventions established in the early 1990s and 2000s paved the way for future research to build on, replicate, adapt, tailor, and disseminate a multitude of programs to meet the needs of various populations, such as women ( Jemmott et al., 2007 ; Wingood et al., 2004 ), MSM ( Crosby et al., 2009 ), and adolescents ( DiClemente et al., 2009 ; Jemmott et al, 1992 , 1998 , 1999 , 2010 ; Villarruel et al., 2007 ). To extend the reach of behavioral interventions, in recent years, researchers have begun leveraging technologies to promote protective and risk reduction behaviors.
The rapid expansion of the internet, mobile, and social computing technologies (e.g., text messaging, e-mail, chat, mobile phones, social media, video games, and geospatial networking applications) has provided new strategies for engaging populations who may be harder to reach through traditional venue-based HIV prevention interventions. Electronic health (eHealth) and mobile health (mHealth) have become especially popular for the delivery of technology-enabled HIV prevention interventions among populations reporting high technology ownership and use ( Barry et al., 2018 ; Conserve et al., 2016 ; Duarte et al., 2019 ; Henny et al., 2018; Hightow-Weidman & Bauermeister, 2020 ; Jongbloed et al., 2015 ; Maloney et al., 2020 ; Nadarzynski et al., 2017 ). In recent years, gamification, serious games, and virtual reality have been used in HIV prevention interventions to deliver highly engaged content and bolster interactions/behaviors in and outside of planned interventions ( Enah et al., 2013 ; Hightow-Weidman et al., 2017 , 2018 ; Liran et al., 2019 ; Muessig et al., 2015 , 2018 ). The potential role that technologies can play in increasing the scale of HIV prevention interventions, including those that aim to increase the adoption of biomedical HIV prevention methods, add to the appeal of these strategies ( Hightow-Weidman et al., 2020 ; Horvath et al., 2020 ; Maloney et al., 2020 ; Marcus et al., 2019 ; Muessig et al., 2015 ; Ramos et al., 2019 ; Threats & Bond 2021 ).
Efficacious biomedical advancements in HIV prevention, such as treatment as prevention (TasP) and pre-exposure prophylaxis (PrEP), remain underutilized because of structural barriers and social determinants of health ( Cahill et al., 2017 ; Jaiswal et al., 2018 ; Kuhns et al., 2019 ). TasP, postexposure prophylaxis (PEP), PrEP, and pharmacologic therapy for substance abuse treatment have proven to be effective for reducing the transmission of HIV and minimizing the risk of new HIV infection ( Coffin et al., 2015 ; El-Bassel & Strathdee, 2015 ; Hosek, Green, et al., 2013 ; Page et al., 2015 ; Springer et al., 2018 ). Although biomedical prevention methods such as PEP and TasP are highly effective, we explicitly focus on PrEP because of its status as the premiere user-controlled HIV prevention medication regimen and its ability to be taken without disclosure to sexual partner(s).
In addition to behavioral, technological, and biomedical strategies that help to mitigate risk at the individual-, structural-, and community-levels, additional intervention strategies are needed to address broader social and structural factors that contribute to inequitable geobehavioral vulnerability to HIV ( Brawner, 2014 ). Such HIV prevention interventions target contextual factors (e.g., social, political–economic, policy–legal, and cultural factors) that influence transmission of and infection with HIV ( Blankenship et al., 2015 ), with an effect that diffuses out to members of key populations. Where individual-level interventions are designed to change individual beliefs, norms, and behaviors, community-level interventions aim to change the social environment (e.g., community-level norms and collective self-efficacy) and behaviors of entire populations ( Underwood et al., 2014 ). Structural- and community-level interventions are crucial to a comprehensive HIV prevention plan because they are designed to target macrolevel contextual factors (e.g., concentrated disadvantage in neighborhoods, syringe exchange policies, community-level stigma, and limited PrEP accessibility) that shape individual risk or hamper adoption of risk reduction strategies and therapeutics ( Allen et al., 2016 ; Colarossi et al., 2016 ; Gamble et al., 2017 ; Hoth et al., 2019 ; Kerr et al., 2015 ). Researchers in this space have successfully partnered with churches to decrease stigma and increase HIV testing ( Berkley-Patton et al., 2016 ; Payne-Foster et al., 2018 ), expand access to screening and prevention resources and change provider behavior ( Bagchi, 2020 ; Bernstein et al., 2017 ; Wood et al., 2018 ), and increase HIV testing in correctional facilities ( Belenko et al., 2017 ).
In this review of the literature, we explore the evolution of HIV prevention science over the past 5 years, presenting an overview of recent advances in the United States. We focused on four intervention categories—behavioral-, technological-, biomedical- (PrEP), and structural-/community-level—given the advancement of HIV prevention approaches over time. The findings highlight areas where nurses and others can advance the science of strategies to reach the national goal of ending the HIV epidemic by 2030 ( Fauci et al., 2019 ).
In our review of recent randomized controlled trials testing the efficacy of condom use and/or abstinence interventions, most targeted vulnerable populations included MSM ( Arnold et al., 2019 ; Crosby et al., 2018 ; Rhodes et al., 2017 ), adolescents ( Donenberg et al., 2018 ; Houck et al., 2016 ; Peskin et al., 2019 ), and adolescent/caregiver dyads ( Hadley et al., 2016 ; Jemmott et al., 2019 , 2020 ). Other interventions targeted incarcerated women ( Fogel et al., 2015 ) and illicit drug users ( Tobin et al., 2017 ). Many interventions were delivered in a health care or school setting, where multiple 60- to 120-min group sessions were presented. However, some interventions used a variation of frequencies and durations, such as a single 60-min one-to-one session ( Crosby et al., 2018 ) or multiple 4-hour group sessions ( Rhodes et al., 2017 ). One intervention allowed participants to attend one or two independent learning sessions, totaling 3 hours ( Hadley et al., 2016 ). About half of the reviewed studies tested the efficacy of new interventions, whereas the other half adapted previously established behavioral interventions. Crosby et al. (2018) , Fogel et al. (2015) , and Hadley et al. (2016) each adapted a different sexual health intervention. Conversely, Donenberg et al. (2018) adapted an intervention from a combination of three evidence-based programs. Instead of adapting an intervention, Peskin et al. (2019) replicated an evidence-based intervention. All interventions, except one ( Rhodes et al., 2017 ), were delivered in English.
Although several behavioral interventions led to significant increases in condom use and/or abstinence, compared with control conditions, others found no indication of intervention efficacy. For instance, Hadley et al. (2016) reported no significant group by time differences for condom use at the 3-month follow-up. These findings may be the result of delayed effects, as seen in the Fogel et al. (2015) intervention where significant group differences in condom use occurred at the 6-month follow-up, but not at the 3-month follow-up. Conversely, neither Arnold et al. (2019) nor Donenberg et al. (2018) found significant group by time differences in condom use at or beyond the 6-month follow-up, and Peskin et al. (2019) did not find differences in sexual initiation at the 24-month follow-up. These findings show that longer follow-up periods do not always have better results compared with short (i.e., 3 months) follow-up periods.
Among efficacious behavioral interventions, there was a single-session skill-building condom buffet activity ( Crosby et al., 2018 ) and multisession programs focusing on the costs and benefits of behavior change ( Fogel et al., 2015 ), emotion regulation ( Houck et al., 2016 ), cultural values ( Rhodes et al., 2017 ), environmental stressors ( Tobin et al., 2017 ), mother–son communication ( Jemmott et al., 2019 ), and scripture- and nonscripture-based abstinence ( Jemmott et al., 2020 ). Each was rooted in theoretical foundations, including those of the Theory of Planned Behavior, Social Cognitive Theory, cognitive behavioral techniques, and the AIDS Risk Reduction Model ( Azjen, 1991 ; Bandura, 1991 ; Catania et al., 1990 ). The Jemmott et al. (2019) intervention was unique in that intervention outcomes were assessed for both mothers and their sons, although the intervention was only implemented among the mothers. All other studies reported the findings of interventions that were implemented among the same participants for which outcomes were assessed.
We unexpectedly identified a nearly equal number of efficacious and nonefficacious behavioral interventions. Many studies reported increases in constructs leading to behavior change, such as self-efficacy, intentions, and attitudes, but did not find changes in actual condom use or abstinence behaviors ( Arnold et al., 2019 ; Donenberg et al., 2018 ; Hadley et al., 2016 ; Peskin et al., 2019 ). Interventions that were effective in increasing condom use and/or abstinence varied in characteristics, showing that single-session and multisession, short- and long-duration, newly created and adapted interventions can be efficacious.
Of the four interventions adapted from existing evidence-based programs, two were efficacious ( Crosby et al., 2018 ; Fogel et al., 2015 ). These interventions adapted the Focus on the Future ( Crosby et al., 2009 ) and Sexual Awareness for Everyone ( Shain et al., 1999 ) interventions. Adaptation has been long supported as an effective way to bring evidence-based interventions to new target populations and is often preferred over the creation of new interventions ( McKleroy et al., 2006 ; Solomon et al., 2006 ). However, with only half of the adapted interventions showing increased condom use among participants, it is critical that interventionists pay close attention to fidelity, proper use of theoretical foundations, and inclusion of core components during intervention adaptation and replication to maintain efficacy of the original intervention.
In accordance with previous research, the identified studies indicate the need to move away from interventions addressing a single behavior to those focusing on a combination of behavioral, biomedical, and structural approaches ( Belgrave & Abrams, 2016 ; Kurth et al., 2011 ) and those using popular technologically advanced delivery methods.
Technological Interventions
Most of the technological intervention literature we reviewed reported on studies that were at lower levels of the hierarchy of evidence ( Melnyk & Fineout-Overholt, 2011 ). Specifically, there was an imbalance in studies favoring more formative qualitative work or pilot studies compared with fewer studies reporting on randomized control trials or meta-analysis. Many studies reporting on randomized control trials also did not report on HIV-related outcomes but focused on content, protocols, or feasibility aspects of the randomized control trials. As a result, most studies reviewed were cross-sectional descriptive studies or qualitative descriptive studies using data collection strategies such as focus groups, interviews expert panels, surveys, and mixed methods ( Rodríguez Vargas et al., 2019 ; Velloza et al., 2019 ). Many of these formative studies ( Bauermeister et al., 2019 ; Cordova et al., 2018 ; Do et al., 2018 ; Enah et al., 2019 ; Erguera et al., 2019 ; Maloney et al., 2020 ; Sullivan et al., 2017 ) focused on the appeal, usability, acceptability, and feasibility of using mHealth and eHealth HIV prevention intervention across the continuum from primary prevention to disease management.
Reviewed studies show that technological interventions in HIV prevention have been studied in various target populations. These target populations include youth and young adults ( Cordova et al., 2018 ; Do et al., 2018 ; Erguera et al., 2019 ), MSM ( Alarcón Gutiérrez et al., 2018 ; Fan et al., 2020 ; Holloway et al., 2017 ), incarcerated women ( Kuo et al., 2019 ), couples ( Mitchell, 2015 ; Velloza et al., 2019 ), adults in drug recovery ( Liang et al., 2018 ), and PLWH ( Bauermeister et al., 2018 ; Schnall et al., 2019 ). These interventions vary in the technological innovations used, duration, language, format of delivery, and target outcomes.
The technology-enabled intervention studies reviewed used varying strategies to target different areas along the continuum of HIV prevention and care. In HIV testing, the focus was on synching home test results with phone counseling support ( Wray et al., 2017 ) and ordering, scheduling, and reminders associated with testing kits (e.g., Sullivan et al., 2017 ). Some studies focused on education using interactive web-based games and social media platforms ( Bauermeister et al., 2019 ; Bond & Ramos, 2019 ; Cordova et al., 2018 ; Gabarron & Wynn, 2016 ), behavioral change interventions ( Danielsonetal.,2014 ),or linkage to care and care support ( Bauermeister et al., 2018 ) targeting people who are living without HIV. Other studies focused on similar points along the care and prevention continuum targeting PLWH ( Maloney et al., 2020 ). Studies reviewed also focused on a wide range of interventions such as provision of information, self-assessments, adherence reminders, delivery of prevention information, referrals, and service from providers ( Boni et al., 2018 ; De Boni et al., 2018 ; Maloney et al., 2020 ). A number of studies included text messaging for health education, reminders, and assessments ( Dietrich et al., 2018 ; Njuguna et al., 2016 ; Ware et al., 2016 ), whereas others focused on primary behavioral preventions such as drug use ( Cordova et al., 2018 ) and engagement in care and disease management for PLWH ( Fan et al., 2020 ; Jongbloed et al., 2015 ). Reviewed studies targeting both persons living with and without HIV also used various technological-based approaches, such as interactive web-based content ( Bauermeister et al., 2019 ), smartphone geolocators near gay venues reinforcing safer sex practices ( Besoain et al., 2015 ), immersive adventure games ( Enah et al., 2019 ), and use of eye tracking technologies to monitor use ( Cho et al., 2018 , 2019 ).
Eight studies reviewed were narrative, scoping, and systematic reviews of the use and efficacy of technology-based interventions ( Bailey et al., 2015 ; Duarte et al., 2019 ; Gabarron & Wynn, 2016 ; Henny et al., 2018; Jongbloed et al., 2015 ; Maloney et al., 2020 ; Nadarzynski et al., 2017 ; Niakan et al., 2017 ). Scoping reviews of earlier digital STI prevention interventions revealed moderate effects on sexual health knowledge, small effect of behavior change, and no significant changes in biological outcomes ( Bailey et al., 2015 ; Gabarron & Wynn, 2016 ). These reviews examined studies that incorporated interventions using various designs, content, formats, target populations, and quality of content. Taken together, these reviews suggest that more research is needed to identify or develop components that can promote changes in biological outcomes. The most recent systematic review ( Maloney et al., 2020 ) found a wealth of published literature on technology-based interventions. However, findings from this systematic review suggest that most of the studies focus on educational and behavior change interventions, whereas relatively few focused on linkage to and retention in HIV prevention and care and adherence to HIV medicines, especially PrEP.
The drug combination of tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC), widely known by its brand name Truvada, used as oral PrEP in preventing HIV infections for MSM in the United States, is a well-documented, effective prevention strategy ( Grant et al., 2010 ; Mayer et al., 2020 ). However, many communities impacted by HIV are underrepresented in research trials in the United States, including transgender populations, cisgender women, and people who inject drugs. Most of the research in these groups has occurred internationally and has not had as strong an impact on HIV incidence as that of the MSM ( Baeten et al., 2012 ; Kibengo et al., 2013 ; MacLachlan & Cowie, 2015 ; Marrazzo et al., 2015 ; Martin et al., 2017 ; Mutua et al., 2012 ; Peterson et al., 2007 ; Thigpen et al., 2012 ; Van Damme et al., 2012 ).
Despite Black MSM bearing a disproportionate burden of HIV infection in comparison to MSM of other ethnicities, they are underrepresented in PrEP studies ( Hess et al., 2017 ). Most PrEP clinical trials, open-label studies, and observational studies included less than 10% Black MSM. ( Grant et al., 2010 ; Mayer et al., 2020 ). The few studies that included higher proportions of Black MSM had small numbers, including three community studies by Chan (49%, n = 109), Project PrEPare-ATN 082 (53%, n = 31), Project PrEPare-ATN 110 (47%, n = 93), and Project PrEPare-ATN 113 (29%, n = 23; Hosek et al., 2017 ; Hosek, Siberry, et al., 2013 ). Moreover, there are study gaps in sex, and the number of studies on high-risk cisgender women and transgender women is significantly smaller compared with MSM ( Kamitani et al., 2019 )
In 2019, the U.S. Food and Drug Administration (FDA) approved tenofovir alafenamide/emtricitabine (TAF/FTC), widely known as Descovy, as the first alternative medication for PrEP for MSM and transfeminine communities (FDA, 2019). TAF/FTC was shown to be noninferior to TDF/FTC. The side-effect profiles differ in that TDF/FTC has increases in renal and bone toxicities and TAF/FTC has increases in weight and lipids ( Mayer et al., 2020 ). TAF/FTC was not studied in other communities and did not gain an FDA indication for cisgender women and transmasculine communities. Some studies have found a potential link between the use of estradiol for gender-affirming care and lower tenofovir levels in the blood ( Hiransuthikul et al., 2019 ; Shieh et al., 2019 ; Yager & Anderson, 2020 ).There have been smaller studies to verify this interaction, but reported controlling for confounding variables was difficult. Further research is needed to understand whether there is effect on the efficacy of TDF and how this may impact nondaily dosing strategies.
Currently, daily oral PrEP is the only antiretroviral medication recommended for the prevention of HIV through sexual contact and drug injection use among people without HIV by the U.S. Centers for Disease Control and Prevention (CDC; U.S. Centers for Disease Control and Prevention & U.S. Public Health Service, 2018 ). In 2015, Molina et al. (2015) published a placebo-controlled trial of an “On-Demand” or 2-1-1 dosing strategy for MSM and transfeminine communities where 2 TDF/FTC pills would be taken 2 to 24 hr before sex, followed by 1 pill every 24 hr while sex continues, and ending 2 doses after the last sex act. This study found high efficacy and acceptability with an 86% reduction in HIV incidence relative to placebo on an intention to treat basis; no one acquired HIV while using 2-1-1 dosing of this nondaily dosing strategy. Furthermore, additional prospective open-label studies also showed no HIV acquisition among study participants ( Hojilla et al., 2020 ; Siguier et al., 2019 ). Despite the lack of endorsement by the CDC, many local Departments of Public Health support PrEP 2-1-1 as a way to make PrEP more attainable for the MSM community ( Los Angeles County Department of Public Health, 2019 ; New York City Department of Health and Mental Hygiene, 2019 ; San Francisco Department of Public Health, 2019 ).
Although effective, researchers and primary care providers note the need to simplify current PrEP delivery models. The CDC recommends a follow-up visit every 3 months while on PrEP, which can often be challenging for individuals to attend visits and pay laboratory costs ( U.S. Centers for Disease Control and Prevention & U.S. Public Health Service, 2018 ). A new model of care that leverages mHealth (e.g., mobile and social computing technologies) to increase initiation, retention, and adherence to PrEP, such as electronic PrEP (ePrEP), has been introduced and found to be acceptable and effective among PrEP users ( Siegler et al., 2020 ). PrEPmate is one such multicomponent mHealth intervention that uses short-message service (SMS) and youth-tailored interactive online content to enhance PrEP adherence among at-risk young MSM ( Liu et al., 2019 ). Currently, it is the only PrEP study identified as an Evidence-Based Intervention by the CDC Prevention Research Synthesis project ( CDC, 2020 ). Siegler et al. implemented the PrEP at Home Study among 50 young Black MSM in a rural area. In the study, 42% of participants received PrEP via the ePrEP system, whereas 93% preferred to use ePrEP over standard provider visit and 67% were more likely to remain on PrEP if ePrEP were available ( Siegler et al., 2019 ).
Future biomedical HIV prevention modalities such as long-acting injectable agents have the potential to prevent HIV acquisition without relying on adherence to a daily or 2-1-1 oral dosing regimen. In MSM and transfeminine communities, an injectable form of cabotegravir given intramuscularly every 2 months had an estimated 66% lower incidence of HIV, compared with daily TDF/FTC ( Landovitz, 2020 ). Additional cabotegravir studies in cisgender women are being conducted under HPTN 084 to evaluate safety and efficacy (the LIFE Study; HIV Prevention Trials Network, 2020 ). The dapivirine (DAP) vaginal ring, for use by cis-women as a flexible silicone ring that continuously releases the antiretroviral HIV drug DAP in the vagina as a long-acting option for HIV prevention is another biomedical HIV prevention modality being studied ( Psomas et al., 2017 ). A phase 2a trial of a 25-mg DAP vaginal ring has been shown to be safe and acceptable among U.S. adolescents ages 15–17 ( Psomas et al., 2017 ). The DAP vaginal ring has been approved by the European Medicines Agency for women older than 25 years, and further studies are ongoing for women ages 15–25 years in the United States ( National Institutes of Health, 2020 ).
Although there are clear benefits to the aforementioned intervention strategies, structural- and community-level interventions are distinctly different, given their focus on macrolevel factors that influence risk versus individual beliefs and behaviors. This is imperative because in many highly affected demographics (e.g., Black women and young racial and ethnic minority MSM), broader social and structural factors drive HIV risk more than individual behavior ( Bauermeister et al., 2017 ; Brawner, 2014 ). With this wider focus, changes are seen in factors such as social diffusion of safer sex messages and comfort with being gay ( Eke et al., 2019 ), better viral suppression and continuity in care ( El-Sadr et al., 2017 ; Towe et al., 2019 ; Wohl et al., 2017 ), and increased HIV testing in populations that may not have otherwise been tested ( Belenko et al., 2017 ; Berkley-Patton et al., 2019 ; Frye et al., 2019 ).
Addressing structural barriers can reduce viral load, prevent HIV infection, and increase HIV testing. In homeless populations, researchers used a rapid rehousing intervention to place participants in stable housing faster (3 months earlier than usual service clients), doubling the likelihood of achieving or maintaining viral suppression ( Towe et al., 2019 ), and worked through primary care providers in Veterans Affairs to increase PrEP access ( Gregg et al., 2020 ). Community-level interventions that used financial incentives reduced viral load and decreased self-reported stimulant use among sexual minority men who use methamphetamine ( Carrico et al., 2016 ) and increased viral suppression and continuity in care in HIV-positive patients ( El-Sadr et al., 2017 ). The latter intervention, however, did not demonstrate an effect on increasing linkage to care.
Health care access remains a concern, and novel strategies can be used to get services to those in need. Pharmacies have also been promising locations for HIV prevention work. Persons who inject drugs were more likely to report always using a sterile syringe than not when they were connected to pharmacies that received in-depth harm reduction training and provided additional services (i.e., HIV prevention/medical/social service referrals and syringe disposal containers; Lewis et al., 2015 ). Providing a PEP informational video and direct pharmacy access to PEP also increased PEP knowledge and willingness; however, this did not translate to more PEP requests ( Lewis et al., 2020 ).
In correctional facilities, researchers have used strategies such as referral to care within 5 days after release, medication text reminders, and local change teams with external coaching to maintain viral suppression post-release and increase HIV testing among inmates ( Belenko et al., 2017 ; Wohl et al., 2017 ). High fidelity to the required institutional changes needed to improve HIV services was also noted ( Pankow et al., 2017 ). With the detrimental effects of mass incarceration, including disparate HIV outcomes while incarcerated and post-release, correctional settings are prime targets for future structural intervention work.
Success is tied to meeting people where they are—engaging them through existing programs, organizations, and institutions they are already connected to. Congregation-level interventions have demonstrated success in doubling HIV testing rates and reducing HIV stigma ( Berkley-Patton et al., 2019 ; Derose et al., 2016 ; Payne-Foster et al., 2018 ); however, effects on HIV stigma varied across studies. The studies demonstrating an effect on HIV stigma only achieved this at the individual—not congregation—level ( Payne-Foster et al., 2018 ), and in Latino—but not African American—churches ( Derose et al., 2016 ). Key to these interventions was the inclusion of multilevel activities (e.g., ministry group activities, HIV testing events during services, and pastors delivered sermons on HIV-related topics) and flexibility to accommodate church schedules and levels of comfort with covering different topics. Churches were not the only setting where addressing HIV stigma beyond the individual-level was a challenge. In a community-level intervention on HIV stigma, homophobia, and HIV testing, researchers used workshops, space-based events, and bus shelter ads in a high HIV prevalence area but did not have an effect on HIV stigma or homophobia ( Frye et al., 2019 ). They did, however, increase HIV testing by 350%.
Individuals within key systems and communities can also be pivotal to share HIV-related information and increase access to services. Integration of lay health advisors (“Navegantes”) into existing social networks (i.e., recreational soccer teams) among Hispanic/Latino men led to twice the likelihood of reporting consistent condom use in the past 30 days and HIV testing at the 18-month follow-up ( Rhodes, Leichliter, et al., 2016 ). A year after the intervention ended, 2 years after their training, 84% of the Navegantes (16 of 19) continued to conduct 9 of the 10 primary health promotion activities (e.g., talking about sexual health, describing where to get condoms, and showing segments of the intervention DVD; Sun et al., 2015 ). Furthermore, using a popular opinion leader model targeting alcohol-using social networks, researchers demonstrated a decline in composite sexual risk (e.g., having sex while high or with a partner who is high and exchanging sex for drugs or money) and an increase in HIV knowledge ( Theall et al., 2015 ). An intervention developed for college students and those in the surrounding area integrated HIV testing and education, mental health, and substance abuse services and referrals and noted a preliminary effect on social norms and sexual health messages on campus ( Ali et al., 2017 ).
Culturally situated marketing and other media approaches reach a broader audience to effect change. Successful social marketing campaigns to promote HIV testing should be performed in a way that enhances well-being (rather than fear-based messages), does not represent the target community in stigmatizing ways, and acknowledges barriers to HIV testing (e.g., stigma; Colarossi et al., 2016 ). One study evaluated a city-level, culturally-tailored media intervention combined with an individual risk reduction curriculum in comparison to no city-level media and a general health curriculum ( Kerr et al., 2015 ). Study findings suggested that all media-exposed participants had greater HIV-related knowledge at 6 months, and those who received the media intervention and risk reduction content had lower stigma scores at 3 and 12 months. A community-level intervention designed to decrease HIV risk among young MSM via persuasive media communication and peer-led networking outreach reduced anal sex risk among participants who reported binge drinking and/or marijuana use; the effect was not sustained for those who used other drugs ( Lauby et al., 2017 ). Another community mobilization intervention (e.g., publicity, groups, and outreach) addressed psychosocial factors at individual, interpersonal, social, and structural levels and documented an increase in HIV testing and a reduction in condom-less sex (although not sustained at 6 months; Shelley et al., 2017 ).
Interventions targeting providers and care delivery increase risk screening, HIV testing, timely linkage to care, and PrEP access for eligible individuals. Similar to the ways lay health workers are activated internationally, Health Promotion Advocates were employed in pediatric emergency departments to survey patients (e.g., health risks, stresses, and needs; Bernstein et al., 2017 ). Positive screens triggered critical resources (e.g., brief conversation on risks and needs and treatment as indicated), and, as a result, the intervention extended emergency services beyond the scope of the presenting complaint, engaging more than 800 youth in critical services such as mental health treatment and HIV testing. By pairing intensive medical case management with formalized relationships with local health departments and resources and addressing structural barriers (e.g., ability to access HIV prevention, testing, and medical care), researchers were able to decrease the average number of days to link to care and maintain the decline over a 6-year period ( Miller et al., 2019 ). Ninety percent of those linked to care had an initial medical visit in 42 or fewer days postdiagnosis. The integration of PrEP referrals into STI partner services led to 54% of PrEP eligible men accepting a PrEP referral and a 2.5-fold increase in PrEP use after partner services among MSM ( Katz et al., 2019 ).
Another group had health professional students (e.g., medicine and pharmacy) provide education about PrEP to public health providers, contributing to an increase in PrEP prescriptions, including for PrEP-eligible at-risk groups who previously were not given prescriptions ( Bunting et al., 2020 ). An underway pilot targets training primary care providers to better understand historical influences of structural factors, assess structural vulnerability among patients, create a more integrated system of care (e.g., opioid use and HIV risk) and empathy and nonjudgement in patient interactions ( Bagchi, 2020 ). There is strong precedent for this, given that significant effects were noted in creating affirming environments for sexual and sex minority youth, including improvements in providers’ and staff’s knowledge and attitudes, clinical practices, individual practices, and perceived environmental friendliness/safety ( Jadwin-Cakmak et al., 2020 ).
Policy changes can hinder or advance HIV prevention efforts, and modeling is an effective strategy to project outcomes and identify targeted prevention strategies. In an examination of Washington, DC’s buffer zone policy—prohibition of syringe exchange program operations within 1,000 feet of schools—researchers found that adherence to this 1,000 Foot Rule reduced syringe exchange program operational space by more than 50% a year ( Allen et al., 2016 ). These restrictions on the amount of legal syringe exchange program operational space have a significant impact on service delivery among injection drug users, which in turn affects HIV transmission through syringe sharing ( Allen et al., 2016 ). Analysis of a natural policy intervention indicated that removing a ban that prohibited the use of federal funds for syringe exchange programs potentially averted 120 HIV cases ( Ruiz et al., 2016 ).
In examining which prevention approach would achieve the greatest impact on HIV transmission, in light of available resources, study findings suggested that targeted testing by venue is more cost effective than routine emergency department testing ($31,507 vs. $59,435, respectively; Holtgrave et al., 2016 ). Modeling of interventions in 6 cities indicated that HIV incidence could be reduced by up to 50% by 2030, with cost savings of $95,416 per quality-adjusted life-year, by implementing combinations of evidence-based interventions (e.g., medication for opioid use disorder, HIV testing, ART initiation, and retention; Nosyk et al., 2020 ). Of note, nurse-initiated rapid testing was included in the optimal combination that produced that greatest health benefit while remaining cost effective across all cities. An ongoing microenterprise RCT will determine the effects of multiple strategies (e.g., weekly text on job openings, educational sessions on HIV prevention, and $11,000 start-up grant) on sexual risk behaviors, employment, and HIV preventive behaviors among economically vulnerable African American young adults ( Mayo-Wilson et al., 2019 ); a paucity of reviewed studies focus in this area. A comparable holistic health demonstration project, which engaged young Black MSM, successfully achieved viral suppression, connected participants to employment opportunities, and addressed housing discrimination ( Brewer et al., 2019 ).
Discussion and Future Considerations for Nursing Science
This review of current HIV prevention interventions provides a substantial contribution to the literature by synthesizing literature on four key areas of HIV prevention science. Nursing focuses on holistic care, assessing, diagnosing, and treating all areas that influence individual and population health. As we consider where and how to develop these programs, research indicates that more people may receive HIV prevention interventions in community-based clinics than in primary care or acute care settings ( Levy et al., 2016 ). Future nursing research should aim to address the needs of underserved populations who may benefit from robust HIV prevention strategies as outlined in this discussion section.
As we continue to generate knowledge about the multidimensional nature of HIV risk, especially for marginalized and vulnerable populations, there are increasing opportunities to learn from and use previous research to design multilevel and combination intervention strategies to better overcome barriers to HIV prevention ( Brawner, 2014 ; Frew et al., 2016 ). As suggested by the identified behavioral intervention studies, classic and current prevention programs have used useful strategies, but there remains room for improvement. These studies advance the science of HIV prevention, which helps fill gaps in the current literature and offer valuable insights that can contribute toward advancing the plan of Ending the HIV Epidemic ( U.S. Department of Health and Human Services, 2019 ; Treston, 2019 ).
As behavioral interventions continue to be created, replicated, and adapted, researchers should focus on implementing and testing these interventions in real-life settings. Implementation science strategies include planning, education, finance, restructuring, quality management, and policy strategies ( Powell et al., 2012 ). These strategies include various aspects of collecting data from stakeholders and community members, assessing setting readiness, determining realistic dosing, and assessing intervention acceptability and feasibility among target populations. The translation of science from research settings to real-life settings is imperative in the sustainability of efficacious behavioral interventions.
Technological
Although there is a plethora of technological-based HIV interventions with many in the pipeline, gaps persist in the current literature. There is a lack of precise knowledge regarding the content components of these interventions that are associated with improving clinical outcomes ( Dillingham et al., 2018 ; Ramos, 2017 ). There is also limited knowledge of optimal delivery approaches for these types of digital HIV interventions ( Côté et al., 2015 ; Schnall et al., 2015 ). In addition, there is a dearth of studies evaluating the efficacy, effectiveness, and cost effectiveness of using emerging technologies in HIV prevention interventions, such as gaming, gamification, social media, and virtual interventions ( Garett et al., 2016 ; Kemp & Velloza, 2018 ; LeGrand et al., 2018 ). Furthermore, there is a lack of resource-sharing platforms that would allow for new research to build on impactful elements of technology-based HIV prevention interventions without recreation of these components. Making these components available in an open platform would substantially reduce time and costs of developing new technological interventions and prevent wasteful use of resources on elements that do lead to desired outcomes.
In all, because technology continues to evolve and potential users of these interventions gain more access and complex skills in the use of other applications in everyday life, the demand for more user-centric HIV prevention interventions will likely continue to grow. Current interventions will need to be updated to maintain relevance, and new interventions will need to be designed to be adaptable to continuing technological advances. Policymakers have a role to play in allowing for governmental sharable databases of impactful interventions so that limited resources can be used to design predictably effective components of technological interventions leading to better health outcomes.
The nurse plays a vital role in HIV prevention and PrEP care ( O’Byrne et al., 2014 ). The University of California, San Francisco School of Nursing, recently developed and validated a set of entry-level nurse practioner competencies to provide culturally appropriate comprehensive HIV care ( Portillo et al., 2016 ). Similar programs should be implemented to train nurses and further the delivery of nursing-led biomedical HIV interventions. Magnet is a nurse-led clinic in San Francisco that has successfully leveraged expanded scopes of practice to allow for nurses to practice to the full extent of their licensure and allow for the rapid expansion of PrEP services to the community ( Holjilla et al., 2018 ). Such a unique and successful community-based PrEP delivery intervention led to the development and implementation of pharmacist-led PrEP clinics ( Havens et al., 2019 ; Lopez et al., 2020 ; Tung et al., 2018 ). More community-based, nursing-led biomedical HIV interventions are needed. Furthermore, future research should explore the efficacy of biomedical HIV prevention among transmasculine and cis-women populations, especially those of color who are underrepresented in existing research efforts ( Bond & Gunn, 2016 ; Chandler et al., 2020 ; Deutsch et al., 2015 ; Golub et al., 2019 ; Rowniak et al., 2017 ; Willie et al., 2017 ). Community-based nursing-led HIV interventions may be opportune for reaching these populations.
Structural and Community
Most HIV prevention structural- and community-level interventions still focus on developing countries, with less attention in the United States ( Adimora & Auerbach, 2010 ). However, with several communities facing limited resources, large percentages of individuals living below the federal poverty level and high HIV incidence and prevalence rates, it is time to expand these international success stories to domestic work (e.g., microfinance, credit programs, and comprehensive sexual health education). There is also a paucity of these interventions targeted to women and youth. Relative to the other reviewed strategies, very few nurses are engaged in structural-/community-level interventions. If successful, the in-progress microenterprise RCT by Mayo-Wilson et al. (2019) has the potential to serve as a blueprint for integrating multiple structural approaches that have demonstrated effectiveness abroad into U.S. contexts. The work by Werb et al. (2016) can also transform approaches to structural approaches to prevent injection drug initiation—given nursing’s focus on prevention, initiation of, and/or partnership in such work could be pivotal.
An approach to consider moving forward is applying the multiphase optimization strategy (MOST) to HIV prevention strategies ( Collins et al., 2016 ). MOST uses randomized experimentation to assess the individual performance of each intervention component. This rigorous process, based on a priori optimization criteria (e.g., cost and time), identifies whether aspects of an intervention component (e.g., presence, absence, and setting) have an impact on the performance of other components. Ultimately, this knowledge is used to engineer an intervention that is effective, efficient, and readily scalable. Multilevel interventions that target more than one level can lead to the most sustainable behavior change and can be delivered in venues known to be associated with HIV risk (e.g., bars and nightclubs; Pitpitan & Kalichman, 2016 ). An ongoing study on neighborhood contexts (e.g., poverty, HIV prevalence, and access to care) and network characteristics (e.g., size and frequency of communication) among Black MSM in the deep south will generate rich data to inform interventions for this key demographic ( Duncan et al., 2019 ). There also remains a need for explicit research with transgender populations—versus only including them in other samples—to fill gaps and meet unique needs ( Mayer et al., 2016 ).
Nursing Advancements
Nurse scientists around the globe are contributing to the development of interventions along the care continuum. Jemmott et al. have created numerous behavioral interventions over the past 30 years, which have been adapted for use in new settings and with different populations ( Advancing Health Equity: ETR, 2019 ). Behavioral interventions have been implemented using technology. Nursing exemplars in technology include the development of an immersive adventure game for African American adolescents ( Enah et al., 2019 ; Enahet al., 2015). In a series of studies in the primary prevention end of the prevention and care continuum, Enah et al. studied relevant content and design elements, evaluated an existing web-based game for relevance, developed and qualitatively studied acceptability of an individually tailored adventure game, and evaluated the potential efficacy of the game among African American adolescents ( Enah et al., 2019 ; Enah, Piper & Moneyham, 2015 ). At the care end of the continuum, Schnall et al. adapted an existing intervention for MSM ( Schnall et al., 2016 ), addressing co-morbidities for PLWH using multimodal techniques ( Schnall et al., 2019 ).
Flores developed a novel sex communication video series to support parent–child communication for gay, bisexual, and queer male adolescents ( Flores et al., 2020 ). Nurses have also collaborated on telehealth interventions to identify barriers to HIV care access and adherence and address mental health, substance use, and other issues among youth and young adults living with HIV ( Wootton et al., 2019 ). Other researchers piloted HIV/STI prevention content curated from online resources (e.g., YouTube and public and private websites) and found that youth who received links to publicly accessible online prevention content had a significant improvement in HIV self-efficacy and a significant reduction in unprotected vaginal or anal sex ( Whiteley et al., 2018 ). Nurses can partner with public health experts, computer scientists, and others to leverage these resources for population health improvement because new technologies continue to emerge ( Rhodes, McCoy, et al., 2016 ; Stevens et al., 2017 ; Stevens et al., 2020 ). Nurses, including members of the Association of Nurses in AIDS Care, have also been instrumental in the All of Us Research Program, a National Institutes of Health initiative aiming to enroll one million people across the United States to increase accessibility to data on individual variability in factors including genetics, lifestyle, and socioeconomic determinants of health to speed up medical breakthroughs ( National Institutes of Health, 2020 ).
As experts in community-engaged HIV research, partnerships that are committed to engaging key communities will lead to the development of interventions—across levels—to help achieve national goals of ending the HIV epidemic by 2030 ( Fauci et al., 2019 ). Health departments, academia, and community partners can also collaborate on policy modeling to improve resource allocation and better address HIV prevention priority setting ( Holtgrave et al., 2016 ). Investigators have also called for legal reform to address state-level structural stigma (index including density of same-sex couples and state laws protecting sexual minorities) experienced by MSM, given linkages between decreased state-level stigma and reduced condomless anal intercourse and increased PEP and/or PrEP use ( Oldenburg et al., 2015 ). Geographic information systems mapping can also be used to identify areas of greatest need and allocate necessary resources ( Brawner et al., 2017 ; Brawner, Reason, Goodman, Schensul, & Guthrie, 2015 ; Eberhart et al., 2015 ).
Recommendations to Further Advance HIV Prevention Intervention Science
Based on the literature reviewed and gaps identified, we offer three recommendations to further advance HIV prevention intervention science. First, nurses should leverage transdisciplinary partnerships to lead the development and testing of comprehensive interventions. For example, nurses could develop and test a nurse-delivered intervention model that engages pharmacists for PrEP access, psychologists and social workers for mental health treatment, librarians and health communication scholars for improving health literacy, and health informaticists to program the content for virtual delivery. Second, nurse researchers are at the cutting edge of knowledge generation in multiple fields, including HIV science (as evidenced by this review), and should be highly sought after for research collaboration accordingly. Although nursing is one of the most trusted professions, nurses are often overlooked when researchers in other disciplines search for collaborators with advanced methodological skill sets, content-specific expertise, or additional perceived benefits to their research teams. Finally, regardless of the intervention type (e.g., behavioral and biomedical), future intervention work must account for social and structural challenges experienced by the intended intervention recipients (e.g., racism, homelessness, and concentrated poverty in neighborhoods). This could include activities such as adding social service linkages to research protocols (e.g., providing participants with information on stable housing programs) or implementing structural interventions to improve neighborhood conditions (e.g., hiring community members to green vacant lots).
Nurses have made tremendous strides in behavioral interventions; however, representation in biomedical-, technological-, and structural-/community-level interventions is limited. We believe this hinders possible advancements in HIV prevention science, given the uniqueness a nursing lens contributes to research endeavors. We encourage nurses to expand the scope of their intervention work, and for individuals working in fields of HIV prevention where nurses are underrepresented, to seek out nursing collaborators. Together, these transdisciplinary teams can curb the epidemic and achieve an AIDS-free generation.
Key Considerations
- Nurses should leverage transdisciplinary partnerships to lead the development and testing of comprehensive interventions.
- Future intervention work must account for social and structural challenges experienced by the intended intervention recipients.
- Nurse researchers should be used for their advanced methodological skill sets and expertise in HIV prevention science.
Disclosures
The authors report no real or perceived vested interests related to this article that could be construed as a conflict of interest.
- Adimora AA, & Auerbach JD (2010). Structural interventions for HIV prevention in the United States . Journal of Acquired Immune Deficiency Syndromes , 55 ( Suppl 2 ), S132–S135. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Advancing Health Equity: ETR. (2019). Be Proud! Be Responsible! An Evidence-Based Intervention to Empower Youth to Reduce Their Risk of HIV . Retrieved from https://www.etr.org/ebi/programs/be-proud-be-responsible/
- Alarcón Gutiérrez M, Fernández Quevedo M, Martín Valle S, Jacques-Aviñó C, Díez David E, Caylà JA, & García de Olalla P (2018). Acceptability and effectiveness of using mobile applications to promote HIV and other STI testing among men who have sex with men in Barcelona , Spain. Sexually Transmitted Infections , 94 ( 6 ), 443–448. 10.1136/sextrans-2017-053348 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ali S, Al Rawwad T, Leal RM, Wilson MI, Mancillas A, Keo-Meier B, & Torres LR (2017). SMART cougars: Development and feasibility of a campus-based HIV prevention intervention . Journal of Health Care for the Poor and Underserved , 28 ( 2 ), 81–99. [ PubMed ] [ Google Scholar ]
- Allen ST, Ruiz MS, & Jones J (2016). Quantifying syringe exchange program operational space in the District of Columbia . AIDS and Behavior , 20 ( 12 ), 2933–2940. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aral SO, O’Leary A, & Baker C (2020). Sexually transmitted infections and HIV in the southern United States: An overview . Sexually Transmitted Diseases , 33 ( 7 ), S1–S5. doi: 10.1097/01.olq.0000223249.04456.76 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Arnold EA, Kegeles SM, Pollack LM, Neilands TB, Cornwell SM, Stewart WR, Benjamin M, Weeks J, Lockett G, Smith CD, & Operario D (2019). A randomized controlled trial to reduce HIV-related risk in African American men who have sex with men and women: The Bruthas project . Prevention Science , 20 ( 1 ), 115–125. 10.1007/s11121-018-0965-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Azjen I (1991). The theory of planned behavior . Organizational Behavior and Human Decision Processes , 50 ( 2 ), 179–211. [ Google Scholar ]
- Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, Tappero JW, Bukusi EA, Cohen CR, Katabira E, Ronald A, Tumwesigye E, Were E, Fife KH, Kiarie J, Farquhar C, John-Stewart G, Kakia A, Odoyo J, Mucunguzi A, … & Celum C. (2012). Antiretroviral prophylaxis for HIV prevention in heterosexual men and women . New England Journal of Medicine , 367 ( 5 ), 399–410. 10.1056/NEJMoa1108524 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bagchi AD (2020). A structural competency curriculum for primary care providers to address the opioid use disorder, HIV, and hepatitis C syndemic . Frontiers in Public Health , 8 , 210. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bailey J, Mann S, Wayal S, Hunter R, Free C, Abraham C, & Murray E (2015). Sexual health promotion for young people delivered via digital media: A scoping review . 10.3310/phr03130 (Public Health Research) [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bandura A (1991). Social cognitive theory of self-regulation . Organizational behavior and human decision processes , 50 ( 2 ), 248–287. [ Google Scholar ]
- Bandura A (2001). Social cognitive theory: An agentic perspective . Annual Review of Psychology , 52 ( 1 ), 1–26. 10.1146/annurev.psych.52.1.1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barry MC, Threats M, Blackburn NA, LeGrand S, Dong W, Pulley DV, Sallabank G, Harper GW, Hightow-Weidman LB, Bauermeister JA, & Muessig KE (2018). “Stay strong! Keep ya head up! Move on! It gets better!!!!”: Resilience processes in the healthMpowerment online intervention of young black gay, bisexual and other men who have sex with men . AIDS Care , 30 ( Suppl 5 ), S27–S38. 10.1080/09540121.2018.1510106 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bauermeister JA, Connochie D, Eaton L, Demers M, & Stephenson R (2017). Geospatial indicators of space and place: A review of multilevel studies of HIV prevention and care outcomes among young men who have sex with men in the United States . The Journal of Sex Research , 54 ( 4–5 ), 446–464. 10.1080/00224499.2016.1271862 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bauermeister JA, Golinkoff JM, Horvath KJ, Hightow-Weidman LB, Sullivan PS, & Stephenson R (2018). A multilevel tailored web app-based intervention for linking young men who have sex with men to quality care (get connected): Protocol for a randomized controlled trial . Journal of Medical Internet Research , 20 ( 8 ), 77. 10.2196/10444 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bauermeister JA, Tingler RC, Demers M, Connochie D, Gillard G, Shaver J, Chavanduka T, & Harper GW (2019). Acceptability and preliminary efficacy of an online HIV prevention intervention for single young men who have sex with men seeking partners online: The myDEx Project . AIDS and Behavior , 23 ( 11 ), 3064–3077. 10.1007/s10461-019-02426-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bekker L-G, Beyrer C, & Quinn TC (2012). Behavioral and biomedical combination strategies for HIV prevention . Cold Spring Harbor Perspectives in Medicine , 2 ( 8 ), a007435. 10.1101/cshperspect.a007435 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Belenko S, Visher C, Pearson F, Swan H, Pich M, O’Connell D, Dembo R, Frisman L, Hamilton L, & Willett J (2017). Efficacy of structured organizational change intervention on HIV testing in correctional facilities . AIDS Education and Prevention , 29 ( 3 ), 241–255. [ PubMed ] [ Google Scholar ]
- Belgrave FZ, & Abrams JA (2016). Reducing disparities and achieving equity in African American women’s health . American Psychologist , 71 ( 8 ), 723–733. 10.1037/amp0000081 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Berkley-Patton J, Thompson CB, Moore E, Hawes S, Simon S, Goggin K, Martinez D, Berman M, & Booker A (2016). An HIV testing intervention in African American churches: Pilot study findings . Annals of Behavioral Medicine , 50 ( 3 ), 480–485. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berkley-Patton JY, Thompson CB, Moore E, Hawes S, Berman M, Allsworth J, Williams E, Wainright C, Bradley-Ewing A, Bauer AG, Catley D, & Goggin K (2019). Feasibility and outcomes of an HIV testing intervention in African American churches . AIDS and Behavior , 23 ( 1 ), 76–90. 10.1007/s10461-018-2240-0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bernstein J, Dorfman D, Lunstead J, Topp D, Mamata H, Jaffer S, & Bernstein E (2017). Reaching adolescents for prevention: The role of pediatric emergency department health promotion advocates . Pediatric Emergency Care , 33 ( 4 ), 223–229. [ PubMed ] [ Google Scholar ]
- Besoain F, Perez-Navarro A, Cayl JA, Avi CJ, & de Olalla P. G. a. (2015). Prevention of sexually transmitted infections using mobile devices and ubiquitous computing [Report] . International Journal of Health Geographics . 10.1186/s12942-015-0010-z [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blankenship KM, Reinhard E, Sherman SG, & El-Bassel N (2015). Structural interventions for HIV prevention among women who use drugs: A global perspective . JAIDS Journal of Acquired Immune Deficiency Syndromes , 69 , S140–S145. 10.1097/qai.0000000000000638 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bond KT, & Gunn AJ (2016). Perceived advantages and disadvantages of using pre-exposure prophylaxis (PrEP) among sexually active Black women: An exploratory study . Journal of Black Sexuality and Relationships , 3 ( 1 ), 1–24. 10.1353/bsr.2016.0019 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bond KT, & Ramos SR (2019). Utilization of an animated electronic health video to increase knowledge of post- and pre-exposure prophylaxis for HIV among African American women: Nationwide cross-sectional survey . JMIR Formative Research , 3 ( 2 ), e9995. 10.2196/formative.9995 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Boni RB, Lentini N, Santelli C, Barbosa A, Cruz M, Bingham T, Cota V, Correa RG, Veloso VG, & Grinsztejn B (2018). Self-testing, communication and information technology to promote HIV diagnosis among young gay and other men who have sex with men (MSM) in Brazil . Journal of the International AIDS Society , 21 ( Suppl 5 ), e25116. 10.1002/jia2.25116 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brawner BM (2014). A multilevel understanding of HIV/AIDS disease burden among African American women . Journal of Obstetric, Gynecologic, and Neonatal Nursing , 43 ( 5 ), 633–643. 10.1111/1552-6909.12481 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brawner BM, Abboud S, Reason J, Wingood G, & Jemmott LS (2019). The development of an innovative, theory-driven, psychoeducational HIV/STI prevention intervention for heterosexually active black adolescents with mental illnesses . Vulnerable Children and Youth Studies , 14 ( 2 ), 151–165. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brawner BM, Guthrie B, Stevens R, Taylor L, Eberhart M, & Schensul JJ (2017). Place still matters: Racial/ethnic and geographic disparities in HIV transmission and disease burden . Journal of Urban Health , 94 , 716–729. 10.1007/s11524-017-0198-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brawner BM, Reason JL, Goodman BA, Schensul JJ, & Guthrie B (2015). Multilevel drivers of human immunodeficiency virus/acquired immune deficiency syndrome among Black Philadelphians: Exploration using community ethnography and geographic information systems . Nursing Research , 64 ( 2 ), 100–110. 10.1097/NNR.0000000000000076 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brewer R, Daunis C, Ebaady S, Wilton L, Chrestman S, Mukherjee S, Moore M, Corrigan R, & Schneider J (2019). Implementation of a socio-structural demonstration project to improve HIV outcomes among young Black men in the deep south . Journal of Racial and Ethnic Health Disparities , 6 ( 4 ), 775–789. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bunting SR, Saqueton R, & Batteson TJ (2020). Using a student-led, community-specific training module to increase PrEP uptake amongst at-risk populations: Results from an exploratory pilot implementation . AIDS Care - Psychological and Socio-Medical Aspects of AIDS/HIV , 32 ( 5 ), 546–550. [ PubMed ] [ Google Scholar ]
- Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, & Mayer KH (2017). Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in black compared to white gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts . AIDS Care , 29 ( 11 ), 1351–1358. 10.1080/09540121.2017.1300633 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carrico AW, Jain J, Discepola MV, Olem D, Andrews R, Woods WJ, Neilands TB, Shoptaw S, Gómez W, Dilworth SE, & Moskowitz JT (2016). A community-engaged randomized controlled trial of an integrative intervention with HIV-positive, methamphetamine-using men who have sex with men . BMC Public Health , 16 , 673. 10.1186/s12889-016-3325-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Catania JA, Kegeles SM, & Coates TJ (1990). Towards an understanding of risk behavior: An AIDS risk reduction model (ARRM) . Health Education Quarterly , 17 ( 1 ), 53–72. 10.1177/109019819001700107 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Centers for Disease Control and Prevention. (2020). Compendium of evidence-based interventions and best practices for HIV prevention . Retrieved from: https://www.cdc.gov/hiv/research/interventionresearch/compendium/index.html
- Chandler R, Hull S, Ross H, Guillaume D, Paul S, Dera N, & Hernandez N (2020). The pre-exposure prophylaxis (PrEP) consciousness of black college women and the perceived hesitancy of public health institutions to curtail HIV in black women . BMC Public Health , 20 ( 1 ), 1172. 10.1186/s12889-020-09248-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cho H, Powell D, Pichon A, Kuhns LM, Garofalo R, & Schnall R (2019). Eye-tracking retrospective think-aloud as a novel approach for a usability evaluation . International Journal of Medical Informatics , 129 , 366–373. 10.1016/j.ijmedinf.2019.07.010 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cho H, Powell D, Pichon A, Thai J, Bruce J, Kuhns LM, Garofalo R, & Schnall R (2018). A mobile health intervention for HIV prevention among racially and ethnically diverse young men: Usability evaluation . JMIR Mhealth Uhealth , 6 ( 9 ), e11450. 10.2196/11450 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coates TJ, Richter L, & Caceres C (2008). Behavioural strategies to reduce HIV transmission: How to make them work better . Lancet , 372 ( 9639 ), 669–684. 10.1016/S0140-6736(08)60886-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coffin PO, Rowe C, & Santos GM (2015). Novel interventions to prevent HIV and HCV among persons who inject drugs . Current HIV/AIDS Reports , 12 ( 1 ), 145–163. 10.1007/s11904-014-0248-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Hakim JG, Kumwenda J, Grinsztejn B, Pilotto JHS, Godbole SV, Chariyalertsak S, Santos BR, Mayer KH, Hoffman IF, Eshleman SH, Piwowar-Manning E, Cottle L, Zhang XC, Makhema J, … & Fleming TR (2016). Antiretroviral therapy for the prevention of HIV-1 transmission . New England Journal of Medicine , 375 ( 9 ), 830–839. 10.1056/NEJMoa1600693 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Colarossi LG, Hazel DS, Collier KL, Desouza S, & Pappas L (2016). Research with Latina and Black women for an HIV prevention campaign . Social Marketing Quarterly , 22 ( 3 ), 236–252. [ Google Scholar ]
- Collins LM, Kugler KC, & Gwadz MV (2016). Optimization of multicomponent behavioral and biobehavioral interventions for the prevention and treatment of HIV/AIDS . AIDS and Behavior , 20 ( 1 ), 197–214. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Conserve DF, Jennings L, Aguiar C, Shin G, Handler L, & Maman S (2016). Systematic review of mobile health behavioural interventions to improve uptake of HIV testing for vulnerable and key populations . Journal of Telemedicine and Telecare , 23 ( 2 ), 347–359. 10.1177/1357633X16639186 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cordova D, Alers-Rojas F, Lua FM, Bauermeister J, Nurenberg R, Ovadje L, Fessler K, Delva J, Salas-Wright CP, & Council YL (2018). The usability and acceptability of an adolescent mHealth HIV/STI and drug abuse preventive intervention in primary care . Behavioral Medicine , 44 ( 1 ), 36–47. 10.1080/08964289.2016.1189396 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Côté J, Rouleau G, Ramirez-Garcia P, & Bourbonnais A (2015). Virtual nursing intervention adjunctive to conventional care: The experience of persons living with HIV . JMIR Research Protocols , 4 ( 4 ), e124. 10.2196/resprot.4158 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crosby RA, Mena L, & Smith RV (2018). Promoting positive condom use experiences among young black MSM: A randomized controlled trial of a brief, clinic-based intervention . Health Education Research , 33 ( 3 ), 197–204. 10.1093/her/cyy010 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crosby R, DiClemente RJ, Charnigo R, Snow G, & Troutman A (2009). A brief, clinic-based, safer sex intervention for heterosexual African American men newly diagnosed with an STD: A randomized controlled trial . American Journal of Public Health , 99 ( Suppl 1 ), S96–S103. 10.2105/AJPH.2007.123893 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Danielson CK, McCauley JL, Gros KS, Jones AM, Barr SC, Borkman AL, Bryant BG, & Ruggiero KJ (2014). SiHLEWeb.com: Development and usability testing of an evidence-based HIV prevention website for female African-American adolescents . Health Informatics Journal , 22 ( 2 ), 194–208. 10.1177/1460458214544048 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- De Boni RB, Lentini N, Santelli AC, Barbosa A Jr., Cruz M, Bingham T, Cota V, Correa RG, Veloso VG, & Grinsztejn B (2018). Self-testing, communication and information technology to promote HIV diagnosis among young gay and other men who have sex with men (MSM) in Brazil . Journal of the International AIDS Society , 21 ( Suppl 5 ), e25116. 10.1002/jia2.25116 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Derose KP, Griffin BA, Kanouse DE, Bogart LM, Williams MV, Haas AC, Flórez KR, Collins DO, Hawes-Dawson J, Mata MA, Oden CW, & Stucky BD (2016). Effects of a pilot church-based intervention to reduce HIV stigma and promote HIV testing among African Americans and Latinos . AIDS and Behavior , 20 ( 8 ), 1692–1705. 10.1007/s10461-015-1280-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Deutsch MB, Glidden DV, Sevelius J, Keatley J, McMahan V, Guanira J, Kallas EG, Chariyalertsak S, & Grant RM (2015). HIV pre-exposure prophylaxis in transgender women: A subgroup analysis of the iPrEx trial . The Lancet HIV , 2 ( 12 ), e512–e519. 10.1016/S2352-3018(15)00206-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- DiClemente RJ, Wingood GM, Rose ES, Sales JM, Lang DL, Caliendo AM, Hardin JW, & Crosby RA (2009). Efficacy of sexually transmitted disease/human immunodeficiency virus sexual risk-reduction intervention for African American adolescent females seeking sexual health services: A randomized controlled trial . Archives of Pediatrics & Adolescent Medicine , 163 ( 12 ), 1112–1121. 10.1001/archpediatrics.2009.205 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dietrich JJ, Lazarus E, Andrasik M, Hornschuh S, Otwombe K, Morgan C, & Isaacs AJ (2018). Mobile phone questionnaires for sexual risk data collection among young women in Soweto, South Africa . AIDS and Behavior , 7 , 2312. 10.1007/s10461-018-2080-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dillingham R, Ingersoll K, Flickinger TE, Waldman AL, Grabowski M, Laurence C, Wispelwey E, Reynolds G, Conaway M, & Cohn WF (2018). PositiveLinks: A mobile health intervention for retention in HIV care and clinical outcomes with 12-month follow-up . AIDS Patient Care and STDs , 32 ( 6 ), 241–250. 10.1089/apc.2017.0303 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- DiNenno EA, Prejean J, Irwin K, Delaney KP, Bowles K, Martin T, Tailor A, Dumitru G, Mullins MM, Hutchinson AB, & Lansky A (2017). Recommendations for HIV screening of gay, bisexual, and other men who have sex with men—United States, 2017 . MMWR. Morbidity and Mortality Weekly Report , 66 ( 31 ), 830–832. 10.15585/mmwr.mm6631a3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Do TTT, Le MD, Van Nguyen T, Tran BX, Le HT, Nguyen HD, Nguyen LH, Nguyen CT, Tran TD, Latkin CA, Ho RCM, & Zhang MWB (2018). Receptiveness and preferences of health-related smartphone applications among Vietnamese youth and young adults . BMC Public Health , 18 ( 1 ), 764. 10.1186/s12889-018-5641-0 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Donenberg G, Emerson E, & Kendall AD (2018). HIV-risk reduction intervention for juvenile offenders on probation: The PHAT Life group randomized controlled trial . Health Psychology , 37 ( 4 ), 364–374. 10.1037/hea0000582 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Duarte G, Vanegas J, Bravo G, Rada G, & Pantoja T (2019). Effectiveness of digital interventions based on mobile phones for the prevention of sexually transmitted infections: A systematic review protocol . Medwave , 19 ( 2 ), e7605. 10.5867/medwave.2019.02.7605 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Duncan DT, Hickson DA, Goedel WC, Callander D, Brooks B, Chen YT, Hanson H, Eavou R, Khanna AS, Chaix B, Regan SD, Wheeler DP, Mayer KH, Safren SA, Melvin SC, Draper C, Magee-Jackson V, Brewer R, Schneider JA, on behalf of the, N., & Network Cohort Study, T. (2019). The social context of HIV prevention and care among black men who have sex with men in three U.S. cities: The neighborhoods and networks (N2) cohort study . International Journal of Environmental Research and Public Health , 16 ( 11 ), e1922. 10.3390/ijerph16111922 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eberhart MG, Yehia BR, Hillier A, Voytek CD, Fiore DJ, Blank M, Frank I, Metzger DS, & Brady KA (2015). Individual and community factors associated with geographic clusters of poor HIV care retention and poor viral suppression . Journal of Acquired Immune Deficiency Syndromes , 69 , S37–S43. 10.1097/QAI.0000000000000587 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eke AN, Johnson WD, O’Leary A, Rebchook GM, Huebner DM, Peterson JL, & Kegeles SM (2019). Effect of a community-level HIV prevention intervention on psychosocial determinants of HIV risk behaviors among young Black men who have sex with men (YBMSM) . AIDS and Behavior , 23 ( 9 ), 2361–2374. [ PubMed ] [ Google Scholar ]
- El-Bassel N, & Strathdee SA (2015). Women who use or inject drugs: An action agenda for women-specific, multilevel, and combination HIV prevention and research . Journal of Acquired Immune Deficiency Syndromes , 69 ( Suppl 2 ), S182–S190. 10.1097/QAI.0000000000000628 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- El-Sadr WM, Donnell D, Beauchamp G, Hall HI, Torian LV, Zingman B, Lum G, Kharfen M, Elion R, Leider J, Gordin FM, Elharrar V, Burns D, Zerbe A, Gamble T, & Branson B (2017). Financial incentives for linkage to care and viral suppression among HIV-positive patients: A randomized clinical trial (HPTN 065) . JAMA Internal Medicine , 177 ( 8 ), 1083–1092. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Enah C, Lambert C, Gakumo CA, Daniel M, & Wehby PS (2019). Working with potential users to develop an HIV/STI prevention video game for rural adolescents . Clinical HIV and AIDS Journal , 2 ( 1 ), 108. [ Google Scholar ]
- Enah C, Moneyham L, Vance DE, & Childs G (2013). Digital gaming for HIV prevention with young adolescents . The Journal of the Association of Nurses in AIDS Care: JANAC , 24 ( 1 ), 71–80. 10.1016/j.jana.2012.03.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Enah C, Piper K, & Moneyham L (2015). Qualitative evaluation of the relevance and acceptability of a web-based HIV prevention game for rural adolescents . Journal of pediatric nursing , 30 ( 2 ), 321–328. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Erguera XA, Johnson MO, Neilands TB, Ruel T, Berrean B, Thomas S, & Saberi P (2019). WYZ: A pilot study protocol for designing and developing a mobile health application for engagement in HIV care and medication adherence in youth and young adults living with HIV . BMJ Open , 9 ( 5 ), e030473. 10.1136/bmjopen-2019-030473 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fan X, She R, Liu C, Zhong H, Lau JTF, Hao C, Li J, Hao Y, Li L, & Gu J (2020). Evaluation of smartphone APP-based case-management services among antiretroviral treatment-naive HIV-positive men who have sex with men: A randomized controlled trial protocol . BMC Public Health , 20 ( 1 ), 1–13. 10.1186/s12889-020-8171-5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fauci AS, Redfield RR, Sigounas G, Weahkee MD, & Giroir BP (2019). Ending the HIV epidemic: A plan for the United States . Journal of the American Medical Association , 321 ( 9 ), 844–845. [ PubMed ] [ Google Scholar ]
- Fishbein M, & Ajzen I (1975). Belief, attitude, intention and behavior: An introduction to theory and research . Addison-Wesley. [ Google Scholar ]
- Flores DD, Rosario AA, Bond KT, Villarruel AM, & Bauermeister JA (2020). Parents ASSIST (Advancing Supportive and Sexuality-Inclusive Sex Talks): Iterative development of a sex communication video series for parents of gay, bisexual, and queer male adolescents . Journal of Family Nursing , 26 ( 2 ), 90–101. 10.1177/1074840719897905 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fogel CI, Crandell JL, Neevel AM, Parker SD, Carry M, White BL, Fasula AM, Herbst JH, & Gelaude DJ (2015). Efficacy of an adapted HIV and sexually transmitted infection prevention intervention for incarcerated women: A randomized controlled trial . American Journal of Public Health , 105 ( 4 ), 802–809. 10.2105/AJPH.2014.302105 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frew PM, Parker K, Vo L, Haley D, O’Leary A, Diallo DD, Golin CE, Kuo I, Soto-Torres L, Wang J, Adimora AA, Randall LA, del Rio C, Hodder S, & the, H. I. V. P. T. N. S. T (2016). Socioecological factors influencing women’s HIV risk in the United States: Qualitative findings from the women’s HIV SeroIncidence study (HPTN 064) . BMC Public Health , 16 ( 1 ), 803. 10.1186/s12889-016-3364-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frye V, Paige MQ, Gordon S, Matthews D, Musgrave G, Greene E, Kornegay M, Farhat D, Smith PH, Usher D, Phelan JC, Koblin BA, & Taylor-Akutagawa V (2019). Impact of a community-level intervention on HIV stigma, homophobia and HIV testing in New York City: Results from project CHHANGE . Stigma and Health , 4 ( 1 ), 72–81. 10.1037/sah0000109 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gabarron E, & Wynn R (2016). Use of social media for sexual health promotion: A scoping review . Global Health Action , 9 ( 1 ), 32193. 10.3402/gha.v9.32193 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gamble T, Branson B, Donnell D, Hall HI, King G, Cutler B, Hader S, Burns D, Leider J, Wood AF, Volpp KG, Buchacz K, & El-Sadr WM (2017). Design of the HPTN 065 (TLC-Plus) study: A study to evaluate the feasibility of an enhanced test, link-to-care, plus treat approach for HIV prevention in the United States . Clinical Trials , 14 ( 4 ), 322–332. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gardner EM, McLees MP, Steiner JF, Del Rio C, & Burman WJ (2011). The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection . Clinical Infectious Diseases , 52 ( 6 ), 793–800. 10.1093/cid/ciq243 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Garett R, Smith J, & Young SD (2016). A review of social media technologies across the global HIV care continuum . Current Opinion in Psychology , 9 , 56–66. 10.1016/j.copsyc.2015.10.024 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Golub SA, Fikslin RA, Starbuck L, & Klein A (2019). High rates of PrEP eligibility but low rates of PrEP access among a national sample of transmasculine individuals . Journal of Acquired Immune Deficiency Syndromes , 82 ( 1 ), e1–e7. https://journals.lww.com/jaids/Fulltext/2019/09010/High_Rates_of_PrEP_Eligibility_but_Low_Rates_of.6.aspx [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, Goicochea P, Casapía M, Guanira-Carranza JV, Ramirez-Cardich ME, Montoya-Herrera O, Fernández T,Veloso VG, Buchbinder SP, Chariyalertsak S, Schechter M, Bekker L-G, Mayer KH, Kallás EG, Amico KR, … & Glidden DV (2010). Preexposure chemoprophylaxis for HIV prevention in men who have sex with men . New England Journal of Medicine , 363 ( 27 ), 2587–2599. 10.1056/NEJMoa1011205 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gregg E, Linn C, Nace E, Gelberg L, Cowan B, & Fulcher JA (2020). Implementation of HIV preexposure prophylaxis in a homeless primary care setting at the Veterans Affairs . Journal of Primary Care & Community Health , 11 , 2510132720908370. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hadley W, Brown LK, Barker D, Warren J, Weddington P, Fortune T, & Juzang I (2016). Work It Out Together: Preliminary efficacy of a parent and adolescent DVD and workbook intervention on adolescent sexual and substance use attitudes and parenting behaviors . AIDS and Behavior , 20 ( 9 ), 1961–1972. 10.1007/s10461-016-1418-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Havens JP, Scarsi KK, Sayles H, Klepser DG, Swindells S, & Bares SH (2019). Acceptability and feasibility of a pharmacist-led human immunodeficiency virus pre-exposure prophylaxis program in the Midwestern United States . Open Forum Infectious Diseases , 6 ( 10 ), ofz365. 10.1093/ofid/ofz365 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Henny KD, Wilkes AL, McDonald CM, Denson DJ, & Neumann MS (2018a). A Rapid Review of eHealth Interventions Addressing the Continuum of HIV Care (2007–2017) . AIDS and Behavior , 22 ( 1 ), 43–63. 10.1007/s10461-017-1923-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hess KL, Hu X, Lansky A, Mermin J, & Hall HI (2017). Lifetime risk of a diagnosis of HIV infection in the United States . Annals of Epidemiology , 27 ( 4 ), 238–243. 10.1016/j.annepidem.2017.02.003 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hightow-Weidman LB, & Bauermeister JA (2020). Engagement in mHealth behavioral interventions for HIV prevention and care: Making sense of the metrics . MHealth , 6 , 7. 10.21037/mhealth.2019.10.01 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hightow-Weidman LB, Muessig KE, Bauermeister JA, LeGrand S, & Fiellin LE (2017). The future of digital games for HIV prevention and care . Current Opinion in HIV and AIDS , 12 ( 5 ), 501–507. 10.1097/COH.0000000000000399 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hightow-Weidman L, Muessig K, Claude K, Roberts J, Zlotorzynska M, & Sanchez T (2020). Maximizing digital interventions for youth in the midst of Covid-19: Lessons from the adolescent trials network for HIV interventions . AIDS and Behavior , 24 ( 8 ), 2239–2243. 10.1007/s10461-020-02870-w [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hightow-Weidman L, Muessig K, Knudtson K, Srivatsa M, Lawrence E, LeGrand S, Hotten A, & Hosek S (2018). A gamified smartphone app to support engagement in care and medication adherence for HIV-positive young men who have sex with men (AllyQuest): Development and pilot study . JMIR Public Health and Surveillance , 4 ( 2 ), e34. 10.2196/publichealth.8923 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hill MJ, Holt M, Hanscom B, Wang Z, Cardenas-Turanzas M,& Latkin C (2018). Gender and race as correlates of high risk sex behaviors among injection drug users at risk for HIV enrolled in the HPTN 037 study . Drug and Alcohol Dependence , 183 , 267–274. 10.1016/j.drugalcdep.2017.11.018 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hiransuthikul A, Janamnuaysook R, Himmad K, Kerr SJ, Thammajaruk N, Pankam T, Phanjaroen K, Mills S, Vannakit R, Phanuphak P, & Phanuphak N (2019). Drug-drug interactions between feminizing hormone therapy and pre-exposure prophylaxis among transgender women: The iFACT study . Journal of the International AIDS Society , 22 ( 7 ), e25338. 10.1002/jia2.25338 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- HIV Prevention Trials Network. (2020). A phase 3 double blind safety and efficacy study of long-acting injectable cabotegravir compared to daily oral TDF/FTC for pre-exposure prophylaxis in HIV-uninfected women . Retrieved from https://www.hptn.org/research/studies/hptn084
- Hojilla JC, Marcus JL, Silverberg MJ, Hare CB, Herbers R, Hurley L, Satre DD, & Volk JE (2020). Early adopters of event-driven human immunodeficiency virus pre-exposure prophylaxis in a large healthcare system in San Francisco . Clinical Infectious Diseases , 71 ( 10 ), 2710–2712. 10.1093/cid/ciaa474 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hojilla JC, Vlahov D, Crouch PC, Dawson-Rose C, Freeborn K, & Carrico A (2018). HIV pre-exposure prophylaxis (PrEP) uptake and retention among men who have sex with men in a community-based sexual health clinic . AIDS and Behavior , 22 ( 4 ), 1096–1099. 10.1007/s10461-017-2009-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Holloway IW, Winder TJ, Lea CH III, Tan D, Boyd D, & Novak D (2017). Technology use and preferences for mobile phone-based HIV prevention and treatment among Black young men who have sex with men: Exploratory research . JMIR mHealth and uHealth , 5 ( 4 ), e46. 10.2196/mhealth.6436 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Holtgrave DR, Maulsby C, Kim JJ, Cassidy-Stewart H, & Hauck H (2016). Using resource allocation modeling to inform HIV prevention priority setting for Baltimore-Towson, Maryland . Progress in Community Health Partnerships: Research, Education, and Action , 10 ( 1 ), 133–139. [ PubMed ] [ Google Scholar ]
- Horvath KJ, Walker T, Mireles L, Bauermeister JA, Hightow-Weidman L, & Stephenson R (2020). A systematic review of technology-assisted HIV testing interventions . Current HIV/AIDS Reports , 17 ( 4 ), 269–280. 10.1007/s11904-020-00506-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hosek SG, Green KR, Siberry G, Lally M, Balthazar C, Serrano PA, Kapogiannis B, & The Adolescent Medicine Trials Network for, H. I. V. A. I. (2013). Integrating behavioral HIV interventions into biomedical prevention trials with youth: Lessons from Chicago’s Project PrEPare . Journal of HIV/AIDS & Social Services , 12 ( 3–4 ), 333–348. 10.1080/15381501.2013.773575 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hosek SG, Rudy B, Landovitz R, Kapogiannis B, Siberry G, Rutledge B, Liu N, Brothers J, Mulligan K, Zimet G, Lally M, Mayer KH, Anderson P, Kiser J, Rooney JF, Wilson CM, & Adolescent Trials Network for, H. I. (2017). An HIV preexposure prophylaxis demonstration project and safety study for young MSM . Journal of Acquired Immune Deficiency Syndromes , 74 ( 1 ), 21–29. 10.1097/QAI.0000000000001179 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hosek SG, Siberry G, Bell M, Lally M, Kapogiannis B, Green K, Fernandez MI, Rutledge B, Martinez J, Garofalo R, Wilson CM, & Adolescent Trials Network for, H. I. (2013). The acceptability and feasibility of an HIV preexposure prophylaxis (PrEP) trial with young men who have sex with men . Journal of Acquired Immune Deficiency Syndromes , 62 ( 4 ), 447–456. 10.1097/QAI.0b013e3182801081 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hoth AB, Shafer C, Dillon DB, Mayer R, Walton G, & Ohl ME (2019). Iowa TelePrEP: A public-health-partnered telehealth model for human immunodeficiency virus preexposure prophylaxis delivery in a rural state . Sexually Transmitted Diseases , 46 ( 8 ), 507–512. [ PubMed ] [ Google Scholar ]
- Houck CD, Hadley W, Barker D, Brown LK, Hancock E, & Almy B (2016). An emotion regulation intervention to reduce risk behaviors among at-risk early adolescents . Prevention Science , 17 ( 1 ), 71–82. 10.1007/s11121-015-0597-0 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jadwin-Cakmak L, Bauermeister JA, Cutler JM, Loveluck J, Kazaleh Sirdenis T, Fessler KB, Popoff EE, Benton A, Pomerantz NF, Gotts Atkins SL, Springer T, & Harper GW (2020). The Health Access Initiative: A training and technical assistance program to improve health care for sexual and gender minority youth . Journal of Adolescent Health , 67 ( 1 ), 115–122. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jaiswal J, Griffin M, Singer SN, Greene RE, Acosta ILZ, Kaudeyr SK, Kapadia F, & Halkitis PN (2018). Structural barriers to pre-exposure prophylaxis use among young sexual minority men: The P18 cohort study . Current HIV Research , 16 ( 3 ), 237–249. 10.2174/1570162X16666180730144455 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jemmott JB III, Jemmott LS, & Fong GT (1992). Reductions in HIV risk-associated sexual behaviors among black male adolescents: Effects of an AIDS prevention intervention . American Journal of Public Health , 82 ( 3 ), 372–377. 10.2105/AJPH.82.3.372 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jemmott JB III, Jemmott LS, & Fong GT (1998). Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: A randomized controlled trial . JAMA , 279 ( 19 ), 1529–1536. 10.1001/jama.279.19.1529 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jemmott JB III, Jemmott LS, & Fong GT (2010). Efficacy of a theory-based abstinence-only intervention over 24 months: A randomized controlled trial with young adolescents . Archives of Pediatrics & Adolescent Medicine , 164 ( 2 ), 152–159. 10.1001/archpediatrics.2009.267 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jemmott JB III, Jemmott LS, Fong GT, & McCaffree K (1999). Reducing HIV risk-associated sexual behavior among African American adolescents: Testing the generality of intervention effects . American Journal of Community Psychology , 27 ( 2 ), 161–187. 10.1007/BF02503158 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jemmott LS, Jemmott JB III, Chittamuru D, & Icard LD (2019). Effects of a sexual HIV risk reduction intervention for African American mothers and their adolescent sons: A randomized controlled trial . Journal of Adolescent Health , 65 ( 5 ), 643–650. 10.1016/j.jadohealth.2019.05.017 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jemmott LS, Jemmott JB III, Icard LD, & Hsu J (2020). Effects of church-based parent–child abstinence-only interventions on adolescents’ sexual behaviors . Journal of Adolescent Health , 66 ( 1 ), 107–114. 10.1016/j.jadohealth.2019.07.021 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jemmott LS, Jemmott JB III, & O’Leary A (2007). Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary care settings . American Journal of Public Health , 97 ( 6 ), 1034–1040. 10.2105/AJPH.2003.020271 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jongbloed K, Parmar S, Kop M, Spittal PM, & Lester RT (2015). Recent evidence for emerging digital technologies to support global HIV engagement in care . Current HIV/AIDS Reports , 12 ( 4 ), 451–461. 10.1007/s11904-015-0291-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kamitani E, Mizuno Y, Wichser M, Adegbite AH, DeLuca JB, & Higa DH (2019). Mapping the study characteristics and topics of HIV pre-exposure prophylaxis research literature: A scoping review . AIDS Education and Prevention , 31 ( 6 ), 505–522. 10.1521/aeap.2019.31.6.505 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Katz DA, Dombrowski JC, Barry M, Spellman D, Bell TR, & Golden MR (2019). STD partner services to monitor and promote HIV pre-exposure prophylaxis use among men who have sex with men . Journal of Acquired Immune Deficiency Syndromes , 80 ( 5 ), 533–541. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kay ES, Batey DS, & Mugavero MJ (2016). The HIV treatment cascade and care continuum: Updates, goals, and recommendations for the future . AIDS Research and Therapy , 13 , 35. 10.1186/s12981-016-0120-0 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kemp CG, & Velloza J (2018). Implementation of eHealth interventions across the HIV care cascade: A review of recent research . Current HIV/AIDS Reports , 15 ( 6 ), 403–413. 10.1007/s11904-018-0415-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kerr JC, Valois RF, Diclemente RJ, Carey MP, Stanton B, Romer D, Fletcher F, Farber N, Brown LK, Vanable PA, Salazar LF, Juzang I, & Fortune T (2015). The effects of a mass media HIV-risk reduction strategy on HIV-related stigma and knowledge among African American adolescents . AIDS Patient Care and STDs , 29 ( 3 ), 150–156. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kibengo FM, Ruzagira E, Katende D, Bwanika AN, Bahemuka U, Haberer JE, Bangsberg DR, Barin B, Rooney JF, Mark D, Chetty P, Fast P, Kamali A, & Priddy FH (2013). Safety, adherence and acceptability of intermittent tenofovir/emtricitabine as HIV pre-exposure prophylaxis (PrEP) among HIV-uninfected Ugandan volunteers living in HIV-serodiscordant relationships: A randomized, clinical trial . PLoS One , 8 ( 9 ), e74314. 10.1371/journal.pone.0074314 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kuhns LM, Hotton AL, Perloff J, Paul J, Parker C, Muldoon AL, Johnson AK, & Garofalo R (2019). Evaluation of translife care: An intervention to address social determinants of engagement in HIV care among transgender women of color . AIDS and Behavior . 10.1007/s10461-019-02548-y [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kuo CC, Rosen RK, Zlotnick C, Wechsberg WM, Peabody M, & Johnson JE (2019). Sexual health prevention for incarcerated women: Eroticising safe sex during re-entry to the community . Journal of Family Planning & Reproductive Health Care , 45 ( 1 ), 17–22. 10.1136/bmjsrh-2017-200024 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kurth AE, Celum C, Baeten JM, Vermund SH, & Wasserheit JN (2011). Combination HIV prevention: Significance, challenges, and opportunities . Current HIV/AIDS Reports , 8 ( 1 ), 62–72. 10.1007/s11904-010-0063-3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Landovitz RJ., Donnell D, Clement M, Hanscom H, Cottle L, Coelho L, et al. (2020). HPTN083 interim results: Pre-exposure prophylaxis (PrEP) containing long-acting injectable cabotegravir (CAB-LA) is safe and highly effective for cisgender men and transgender women who have sex with men (MSM,TGW) . IAS Conference, San Francisco . 2020. [ Google Scholar ]
- Lanier Y, & Sutton MY (2013). Reframing the context of preventive health care services and prevention of HIV and other sexually transmitted infections for young men: New opportunities to reduce racial/ethnic sexual health disparities . American Journal of Public Health , 103 ( 2 ), 262–269. 10.2105/AJPH.2012.300921 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lauby J, Zhu L, Milnamow M, Batson H, Bond L, Curran-Groome W, & Carson L (2017). Get real: Evaluation of a community level HIV prevention intervention for young MSM who engage in episodic substance use . AIDS Education and Prevention , 29 ( 3 ), 191–204. [ PubMed ] [ Google Scholar ]
- LeGrand S, Knudtson K, Benkeser D, Muessig K, McGee A, Sullivan PS, & Hightow-Weidman L (2018). Testing the efficacy of a social networking gamification app to improve pre-exposure prophylaxis adherence (P3: Prepared, Protected, emPowered): Protocol for a randomized controlled trial . JMIR Research Protocols , 7 ( 12 ), e10448. 10.2196/10448 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levy ME, Watson CC, Glick SN, Kuo I, Wilton L, Brewer RA, Fields SD, Criss V, & Magnus M (2016). Receipt of HIV prevention interventions is more common in community-based clinics than in primary care or acute care settings for Black men who have sex with men in the District of Columbia . AIDS Care - Psychological and Socio-Medical Aspects of AIDS/HIV , 28 ( 5 ), 660–664. 10.1080/09540121.2015.1120266 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lewis CF, Lekas HM, Rivera A, Williams SZ, Crawford ND, Pérez-Figueroa RE, Joseph AM, & Amesty S (2020). Pharmacy PEP access intervention among persons who use drugs in New York City: iPEPcare Study—Rethinking biomedical HIV prevention strategies . AIDS and Behavior , 24 ( 7 ), 2101–2111. [ PubMed ] [ Google Scholar ]
- Lewis CF, Rivera AV, Crawford ND, DeCuir J, & Amesty S (2015). Pharmacy-randomized intervention delivering HIV prevention services during the syringe sale to people who inject drugs in New York City . Drug and Alcohol Dependence , 153 , 72–77. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Liang D, Han H, Du J, Zhao M, & Hser Y-I (2018). A pilot study of a smartphone application supporting recovery from drug addiction . Journal of Substance Abuse Treatment , 88 , 51–58. 10.1016/j.jsat.2018.02.006 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liran O, Dasher R, & Kaeochinda K (2019). Using virtual reality to improve antiretroviral therapy adherence in the treatment of HIV: Open-label repeated measure study . Interactive Journal of Medical Research , 8 ( 2 ), e13698. 10.2196/13698 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu AY, Vittinghoff E, von Felten P, Rivet Amico K, Anderson PL, Lester R, Andrew E, Estes I, Serrano P, Brothers J, Buchbinder S, Hosek S, & Fuchs JD (2019). Randomized controlled trial of a mobile health intervention to promote retention and adherence to preexposure prophylaxis among young people at risk for human immunodeficiency virus: The EPIC study . Clinical Infectious Diseases , 68 ( 12 ), 2010–2017. 10.1093/cid/ciy810 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lopez MI, Cocohoba J, Cohen SE, Trainor N, Levy MM, & Dong BJ (2020). Implementation of pre-exposure prophylaxis at a community pharmacy through a collaborative practice agreement with San Francisco Department of Public Health . Journal of the American Pharmacists Association: JAPHA , 60 ( 1 ), 138–144. 10.1016/j.japh.2019.06.021 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Los Angeles County Department of Public Health. (2019). What’s new in HIV PrEP? 2-1-1 dosing and FDA advisory panel recommendation new drug for PrEP . Retrieved February 9, 2021 from. http://rx.ph.lacounty.gov/RxHIV211PrEP0919 .
- MacLachlan JH, & Cowie BC (2015). Hepatitis B virus epidemiology . Cold Spring Harbor Perspectives in Medicine , 5 ( 5 ), a021410. 10.1101/cshperspect.a021410 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Maloney KM, Bratcher A, Wilkerson R, & Sullivan PS (2020). Electronic and other new media technology interventions for HIV care and prevention: A systematic review . Journal of the International AIDS Society Electronic Resource , 23 ( 1 ), e25439. 10.1002/jia2.25439 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Marcus JL, Hurley LB, Krakower DS, Alexeeff S, Silverberg MJ, & Volk JE (2019). Use of electronic health record data and machine learning to identify candidates for HIV pre-exposure prophylaxis: A modelling study . The Lancet HIV , 6 ( 10 ), e688–e695. 10.1016/S2352-3018(19)30137-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Marrazzo JM, Ramjee G, Richardson BA, Gomez K, Mgodi N, Nair G, Palanee T, Nakabiito C, van der Straten A, Noguchi L, Hendrix CW, Dai JY, Ganesh S, Mkhize B, Taljaard M, Parikh UM, Piper J, Mâsse B, Grossman C, Rooney J, … & Chirenje ZM (2015). Tenofovir-based preexposure prophylaxis for HIV infection among African Women . New England Journal of Medicine , 372 ( 6 ), 509–518. 10.1056/NEJMoa1402269 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Martin M, Vanichseni S, Suntharasamai P, Sangkum U, Mock PA, Chaipung B, Worrajittanon D, Leethochawalit M, Chiamwongpaet S, Kittimunkong S, Gvetadze RJ, McNicholl JM, Paxton LA, Curlin ME, Holtz TH, Samandari T, & Choopanya K (2017). Factors associated with the uptake of and adherence to HIV pre-exposure prophylaxis in people who have injected drugs: An observational, open-label extension of the Bangkok Tenofovir Study . The Lancet HIV , 4 ( 2 ), e59–e66. 10.1016/S2352-3018(16)30207-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mayer KH, Grinsztejn B, & El-Sadr WM (2016). Transgender people and HIV prevention: What we know and what we need to know, a call to action . Journal of Acquired Immune Deficiency Syndromes , 72 , S207–S209. 10.1097/QAI.0000000000001086 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mayer KH, Molina JM, Thompson MA, Anderson PL, Mounzer KC, De Wet JJ, DeJesus E, Jessen H, Grant RM, Ruane PJ, Wong P, Ebrahimi R, Zhong L, Mathias A, Callebaut C, Collins SE, Das M, McCallister S, Brainard DM, Brinson C, …& Hare CB (2020). Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): Primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial . Lancet , 396 ( 10246 ), 239–254. 10.1016/S0140-6736(20)31065-5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mayo-Wilson LJ, Glass NE, Ssewamala FM, Linnemayr S, Coleman J, Timbo F, Johnson MW, Davoust M, Labrique A, Yenokyan G, Dodge B, & Latkin C (2019). Microenterprise intervention to reduce sexual risk behaviors and increase employment and HIV preventive practices in economically-vulnerable African-American young adults (EMERGE): Protocol for a feasibility randomized clinical trial . Trials Electronic Resource , 20 ( 1 ), 439. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McKleroy VS, Galbraith JS, Cummings B, Jones P, Harshbarger C, Collins C, Gelaude D, Carey JW, & Team A (2006). Adapting evidence–based behavioral interventions for new settings and target populations . AIDS Education and Prevention , 18 ( Suppl ), 59–73. 10.1521/aeap.2006.18.supp.59 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McNairy ML, & El-Sadr WM (2014). A paradigm shift: Focus on the HIV prevention continuum . Clinical Infectious Diseases , 59 ( Suppl 1 ), S12–S15. 10.1093/cid/ciu251 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Melnyk BM, & Fineout-Overholt E (2011). Evidence-based practice in nursing & healthcare: A guide to best practice . Lippincott Williams & Wilkins. [ Google Scholar ]
- Miller RL, Chiaramonte D, Strzyzykowski T, Sharma D, Anderson-Carpenter K, & Fortenberry JD (2019). Improving timely linkage to care among newly diagnosed HIV-infected youth: Results of SMILE . Journal of Urban Health , 96 ( 6 ), 845–855. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mitchell JW (2015). The use of technology to advance HIV prevention for couples . Current HIV/AIDS Reports , 12 ( 4 ), 516–522. 10.1007/s11904-015-0290-8 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Molina J-M, Capitant C, Spire B, Pialoux G, Cotte L, Charreau I, Tremblay C, Le Gall J-M, Cua E, Pasquet A, Raffi F, Pintado C, Chidiac C, Chas J, Charbonneau P, Delaugerre C, Suzan-Monti M, Loze B, Fonsart J, Peytavin G, …, & Delfraissy J-F (2015). On-demand preexposure prophylaxis in men at high risk for HIV-1 infection . New England Journal of Medicine , 373 ( 23 ), 2237–2246. 10.1056/NEJMoa1506273 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Muessig KE, Knudtson KA, Soni K, Larsen MA, Traum D, Dong W, Conserve DF, Leuski A, Artstein R, & Hightow-Weidman LB (2018). “I didn’t tell you sooner because I didn’t know how to handle it myself.” Developing a virtual reality program to support HIV-status disclosure decisions . Digital Culture & Education , 10 , 22–48. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Muessig KE, Nekkanti M, Bauermeister J, Bull S, & Hightow-Weidman LB (2015). A systematic review of recent smartphone, Internet and Web 2.0 interventions to address the HIV continuum of care . Current HIV/AIDS Reports , 12 ( 1 ), 173–190. 10.1007/s11904-014-0239-3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mutua G, Sanders E, Mugo P, Anzala O, Haberer JE, Bangsberg D, Barin B, Rooney JF, Mark D, Chetty P, Fast P, & Priddy FH (2012). Safety and adherence to intermittent pre-exposure prophylaxis (PrEP) for HIV-1 in African men who have sex with men and female sex workers . PLoS One , 7 ( 4 ), e33103. 10.1371/journal.pone.0033103 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nadarzynski T, Morrison L, Bayley J, & Llewellyn C (2017). The role of digital interventions in sexual health . Sexually Transmitted Infections , 93 ( 4 ), 234–235. 10.1136/sextrans-2016-052926 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Institutes of Health. (2020). All of us research program . www.joinallofus.org/
- New York City Department of Health and Mental Hygiene. (2019). “On-Demand” dosing for PrEP: guidance for medical providers . Retrieved from https://www1.nyc.gov/assets/doh/downloads/pdf/ah/prep-on-demand-dosing-guidance.pdf .
- Niakan S, Mehraeen E, Noori T, & Gozali E (2017). Web and mobile based HIV prevention and intervention programs pros and cons: A review . Studies in Health Technology and Informatics , 236 , 319–327. https://umasslowell.idm.oclc.org/login?url5http://search.ebscohost.com/login.aspx?direct5true&db5cmedm&AN528508813&site5eds-live [ PubMed ] [ Google Scholar ]
- Njuguna N, Ngure K, Mugo N, Sambu C, Sianyo C, Gakuo S, Irungu E, Baeten J, & Heffron R (2016). The effect of human immunodeficiency virus prevention and reproductive health text messages on human immunodeficiency virus testing among young women in Rural Kenya: A pilot study . Sexually Transmitted Diseases , 43 ( 6 ), 353–359. 10.1097/OLQ.0000000000000450 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nosyk B, Zang X, Krebs E, Enns B, Min JE, Behrends CN, del Rio C, Dombrowski JC, Feaster DJ, Golden M, Marshall BDL, Mehta SH, Metsch LR, Pandya A, Schackman BR, Shoptaw S, Strathdee SA, Gebo KA, Kirk G, Montaner J, & Localized, H. I. V. M. S. G. (2020). Ending the HIV epidemic in the USA: An economic modelling study in six cities . The Lancet HIV , 7 ( 7 ), e491–e503. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- O’Byrne P, Macpherson P, Roy M, & Kitson C (2014). Overviewing a nurse-led, community-based HIV PEP program: Applying the extant literature in frontline practice . Public Health Nursing , 32 ( 3 ), 256–265. 10.1111/phn.12123 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Office of Infectious Disease and HIV/AIDS Policy. (2020). About ending the HIV epidemic: Plan for America . HIV.gov. Retrieved August 16, from https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview [ Google Scholar ]
- Oldenburg CE, Perez-Brumer AG, Hatzenbuehler ML, Krakower D, Novak DS, Mimiaga MJ, & Mayer KH (2015). State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States . AIDS , 29 ( 7 ), 837–845. 10.1097/QAD.0000000000000622 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Page K, Tsui J, Maher L, Choopanya K, Vanichseni S, Mock PA, Celum C, & Martin M (2015). Biomedical HIV prevention including pre-exposure prophylaxis and opiate agonist therapy for women who inject drugs: State of research and future directions . Journal of Acquired Immune Deficiency Syndromes , 69 ( Suppl 2 ), S169–S175. 10.1097/QAI.0000000000000641 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pankow J, Willett J, Yang Y, Swan H, Dembo R, Burdon WM, Patterson Y, Pearson FS, Belenko S, & Frisman LK (2017). Evaluating fidelity to a modified NIATx process improvement strategy for improving HIV services in correctional facilities . The Journal of Behavioral Health Services & Research , 45 ( 2 ), 187–203. https://link.springer.com/content/pdf/10.1007/s11414-017-9551-1.pdf [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Payne-Foster P, Bradley ELP, Aduloju-Ajijola N, Yang X, Gaul Z, Parton J, Sutton MY, & Gaskins S (2018). Testing our FAITHH: HIV stigma and knowledge after a faith-based HIV stigma reduction intervention in the Rural South . AIDS Care , 30 ( 2 ), 232–239. https://www.tandfonline.com/doi/pdf/10.1080/09540121.2017.1371664?needAccess5true [ PubMed ] [ Google Scholar ]
- Peskin MF, Coyle KK, Anderson PM, Laris BA, Glassman JR, Franks HM, Thiel MA, Potter SC, Unti T, Edwards S, Johnson-Baker K, Cuccaro PM, Diamond P, Markham CM, Shegog R, Baumler ER, Gabay EK, & Emery ST (2019). Replication of it’s your game… Keep it real! In Southeast Texas . The Journal of Primary Prevention , 40 ( 3 ), 297–323. 10.1007/s10935-019-00549-0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peterson L, Taylor D, Roddy R, Belai G, Phillips P, Nanda K, Grant R, Clarke EEK, Doh AS, Ridzon R, Jaffe HS, & Cates W (2007). Tenofovir disoproxil fumarate for prevention of HIV infection in women: A phase 2, double-blind, randomized, placebo-controlled trial . PLoS Clinical Trials , 2 ( 5 ), e27. 10.1371/journal.pctr.0020027 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pitpitan EV, & Kalichman SC (2016). Reducing HIV risks in the places where people drink: Prevention interventions in alcohol venues . AIDS and Behavior , 20 , 119–133. 10.1007/s10461-015-1116-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Portillo CJ, Stringari-Murray S, Fox CB, Monasterio E, & Rose CD (2016). The HIV primary care workforce of tomorrow: The UCSF integrated HIV/AIDS primary care capacity nurse practitioner program . Journal of the Association of Nurses in AIDS Care , 27 ( 3 ), 214–222. https://journals.lww.com/janac/Fulltext/2016/05000/The_HIV_Primary_Care_Workforce_of_Tomorrow__The.3.aspx [ PubMed ] [ Google Scholar ]
- Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, Glass JE, & York JL (2012). A compilation of strategies for implementing clinical innovations in health and mental health . Medical Care Research and Review , 69 ( 2 ), 123–157. 10.1177/1077558711430690 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Psomas CK, Barber TJ, Rutsaert S, & Kinloch-de Loës S (2017). Highlights from the 9th IAS Conference on HIV Science, 23–26 July 2017, Paris, France . Journal of Virus Eradication , 3 ( 4 ), 242–249. https://pubmed.ncbi.nlm.nih.gov/29057090 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ramos SR (2017). User-centered design, experience, and usability of an electronic consent user interface to facilitate informed decision-making in an HIV clinic . Computers, Informatics, Nursing: CIN , 35 ( 11 ), 556–564. 10.1097/CIN.0000000000000356 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ramos SR, Warren R, Shedlin M, Melkus G, Kershaw T, & Vorderstrasse A (2019). A framework for using ehealth interventions to overcome medical mistrust among sexual minority men of color living with chronic conditions . Behavioral Medicine , 45 ( 2 ), 166–176. 10.1080/08964289.2019.1570074 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rhodes SD, Alonzo J, Mann L, Song EY, Tanner AE, Arellano JE, Rodriguez-Celedon R, Garcia M, Freeman A, Reboussin BA, & Painter TM (2017). Small-group randomized controlled trial to increase condom use and HIV testing among Hispanic/Latino gay, bisexual, and other men who have sex with men . American Journal of Public Health , 107 ( 6 ), 969–976. 10.2105/AJPH.2017.303814 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rhodes SD, Leichliter JS, Sun CJ, & Bloom FR (2016). The HoMBReS and HoMBReS Por un Cambio interventions to reduce HIV disparities among immigrant Hispanic/Latino men . MMWR Supplements , 65 ( 1 ), 51–56. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rhodes SD, McCoy TP, Tanner AE, Stowers J, Bachmann LH, Nguyen AL, & Ross MW (2016). Using social media to increase HIV testing among gay and bisexual men, other men who have sex with men, and transgender persons: Outcomes from a randomized community trial . Clinical Infectious Diseases , 62 ( 11 ), 1450–1453. 10.1093/cid/ciw127 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rodríguez Vargas B, Sánchez-Rubio Ferrández J, Garrido Fuentes J, Velayos R, Morillo Verdugo R, Sala Piñol F, Onteniente González A, & Rodríguez Sagrado MÁ (2019). Usability and acceptability of a comprehensive HIV and other sexually transmitted infections prevention app . Journal of Medical Systems , 43 ( 6 ), 175. 10.1007/s10916-019-1323-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rowniak S, Ong-Flaherty C, Selix N, & Kowell N (2017). Attitudes, beliefs, and barriers to PrEP among trans men . AIDS Education and Prevention , 29 ( 4 ), 302–314. http://dx.doi.org/101521aeap2017294302 [ PubMed ] [ Google Scholar ]
- Ruiz MS, O’Rourke A, & Allen ST (2016). Impact evaluation of a policy intervention for HIV prevention in Washington, DC . AIDS and Behavior , 20 ( 1 ), 22–28. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- San Francisco Department of Public Health. (2019). San Francisco Department of Public Health (SFDPH) statement on non-daily (2-1-1) emtricitabine/tenofovir dosing for PrEP . Retrieved from http://www.gettingtozerosf.org/wp-content/uploads/2018/11/HIVUpdate_02122019_v2.pdf
- Schnall R, Bakken S, Rojas M, Travers J, & Carballo-Dieguez A (2015). mHealth technology as a persuasive tool for treatment, care and management of persons living with HIV . AIDS and Behavior , 19 ( 2 ), 81–89. 10.1007/s10461-014-0984-8 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schnall R, Rojas M, Bakken S, Brown W, Carballo-Dieguez A, Carry M, … & Travers J (2016). A user-centered model for designing consumer mobile health (mHealth) applications (apps) . Journal of biomedical informatics , 60 , 243–251. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schnall R, Liu J, Mohr DC, Bakken S, Hirshfield S, Siegel K, Stonbraker S, Cho H, Iribarren S, & Voss J (2019). Multi-modal methodology for adapting digital health tools to new populations: Adaptation of the video information provider (VIP) for persons living with HIV with HIV-associated non-AIDS (HANA) conditions . Studies in Health Technology and Informatics , 264 , 1347–1351. 10.3233/SHTI190446 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shain RN, Piper JM, Newton ER, Perdue ST, Ramos R, Champion JD, & Guerra FA (1999). A randomized, controlled trial of a behavioral intervention to prevent sexually transmitted disease among minority women . New England Journal of Medicine , 340 ( 2 ), 93–100. 10.1056/NEJM199901143400203 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shelley G, Williams W, Uhl G, Hoyte T, Eke A, Wright C, Rebchook G, Pollack L, Bell K, Wang Y, Cheng Q, & Kegeles SM (2017). An evaluation of Mpowerment on individual-level HIV risk behavior, testing, and psychosocial factors among young MSM of color: The monitoring and evaluation of MP (MEM) project . AIDS Education and Prevention , 29 ( 1 ), 24–37. [ PubMed ] [ Google Scholar ]
- Shieh E, Marzinke MA, Fuchs EJ, Hamlin A, Bakshi R, Aung W, Breakey J, Poteat T, Brown T, Bumpus NN, & Hendrix CW (2019). Transgender women on oral HIV pre-exposure prophylaxis have significantly lower tenofovir and emtricitabine concentrations when also taking oestrogen when compared to cisgender men . Journal of the International AIDS Society , 22 ( 11 ), e25405. 10.1002/jia2.25405 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Siegler AJ, Brock JB, Hurt CB, Ahlschlager L, Dominguez K, Kelley CF, & Mena LA (2019). An electronic pre-exposure prophylaxis initiation and maintenance home care system for nonurban young men who have sex with men: Protocol for a randomized controlled trial . JMIR Research Protocols , 8 ( 6 ), e13982. 10.2196/13982 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Siegler AJ, Steehler K, Sales JM, & Krakower DS (2020). A review of HIV pre-exposure prophylaxis streamlining strategies . Current HIV/AIDS Reports , 17 , 643–653. 10.1007/s11904-020-00528-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Siguier M, Mera R, Pialoux G, Ohayon M, Cotte L, Valin N, Ghosn J, Cua E, Pintado C, Chas J, Barriere G, Durand F, & Molina JM (2019). First year of pre-exposure prophylaxis implementation in France with daily or on-demand tenofovir disoproxil fumarate/emtricitabine . Journal of Antimicrobial Chemotherapy , 74 ( 9 ), 2752–2758. 10.1093/jac/dkz220 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Solomon J, Card JJ, & Malow RM (2006). Adapting efficacious interventions: Advancing translational research in HIV prevention . Evaluation & the Health Professions , 29 ( 2 ), 162–194. 10.1177/0163278706287344 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Springer SA, Di Paola A, Azar MM, Barbour R, Biondi BE, Desabrais M, Lincoln T, Skiest DJ, & Altice FL (2018). Extended-release naltrexone improves viral suppression among incarcerated persons living with HIV with opioid use disorders transitioning to the community: Results of a double-blind, placebo-controlled randomized trial . Journal of Acquired Immune Deficiency Syndromes , 78 ( 1 ), 43–53. 10.1097/QAI.0000000000001634 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stevens RC, Brawner BM, Kranzler E, Giorgi S, Lazarus E, Abera M, Huang S, & Ungar L (2020). Exploring substance use tweets of youth in the United States: Mixed methods study . JMIR Public Health Surveillance , 6 ( 1 ), e16191. 10.2196/16191 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stevens R, Gilliard-Matthews S, Dunaev J, Todhunter-Reid A, Brawner B, & Stewart J (2017). Social media use and sexual risk reduction behavior among minority youth: Seeking safe sex information . Nursing Research , 66 ( 5 ), 368–377. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sullivan PS, Driggers R, Stekler JD, Siegler A, Goldenberg T, McDougal SJ, Caucutt J, Jones J, & Stephenson R (2017). Usability and acceptability of a mobile comprehensive HIV prevention app for men who have sex with men: A pilot study . JMIR mHealth and uHealth , 5 ( 3 ), e26. 10.2196/mhealth.7199 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sun CJ, Mann L, Eng E, Downs M, & Rhodes SD (2015). Once a navegante, always a navegante: Latino men sustain their roles as lay health advisors to promote general and sexual health to their social network . AIDS Education and Prevention , 27 ( 5 ), 465–473. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Theall KP, Fleckman J, & Jacobs M (2015). Impact of a community popular opinion leader intervention among African American adults in a southeastern united states community . AIDS Education and Prevention , 27 ( 3 ), 275–288. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, Henderson FL, Pathak SR, Soud FA, Chillag KL, Mutanhaurwa R, Chirwa LI, Kasonde M, Abebe D, Buliva E, Gvetadze RJ, Johnson S, Sukalac T, Thomas VT, Hart C, … & Brooks JT (2012). Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana . New England Journal of Medicine , 367 ( 5 ), 423–434. 10.1056/NEJMoa1110711 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Threats M & Bond K (2021). HIV information acquisition and use among young Black men who have sex with men who use the internet: a mixed methods study . Journal of Medical Internet Research , 23 ( 5 ), e22986. https://pubmed.ncbi.nlm.nih.gov/33960953 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tobin K, Davey-Rothwell MA, Nonyane BAS, Knowlton A, Wissow L, & Latkin CA (2017). RCT of an integrated CBT-HIV intervention on depressive symptoms and HIV risk . PLoS One , 12 ( 12 ), e0187180. 10.1371/journal.pone.0187180 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Towe VL, Wiewel EW, Zhong Y, Linnemayr S, Johnson R, & Rojas J (2019). A randomized controlled trial of a rapid re-housing intervention for homeless persons living with HIV/AIDS: Impact on housing and HIV medical outcomes . AIDS and Behavior , 23 ( 9 ), 2315–2325. 10.1007/s10461-019-02461-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Treston C (2019). Ending the HIV epidemic: A plan for America—Nurses needed . Journal of the Association of Nurses in AIDS Care , 30 ( 3 ), 379–380. 10.1097/JNC.0000000000000091 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tung EL, Thomas A, Eichner A, & Shalit P (2018). Implementation of a community pharmacy-based pre-exposure prophylaxis service: A novel model for pre-exposure prophylaxis care . Sexual Health , 15 ( 6 ), 556–561. 10.1071/sh18084 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Underwood C, Hendrickson Z, Van Lith LM, Lengwe Kunda JE, & Mallalieu EC (2014). Role of community-level factors across the treatment cascade: A critical review . Journal of Acquired Immune Deficiency Syndromes , 66 , S311–S318. 10.1097/qai.0000000000000234 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- U.S. Centers for Disease Control and Prevention, & U.S. Public Health Service. (2018). Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: A clinical practice guideline . https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf
- U.S. Department of Health and Human Services. (2019). Ending the HIV epidemic: a plan for America . Retrieved from: https://www.cdc.gov/endhiv/docs/ending-HIV-epidemic-overview-508.pdf
- U.S. Food & Drug Administration. (2019, October 3). FDA approves second drug to prevention HIV infection as part of ongoing efforts to end the HIV epidemic . Retrieved August 3, from https://www.fda.gov/news-events/press-announcements/fda-approves-second-drug-prevent-hiv-infection-part-ongoing-efforts-end-hiv-epidemic
- Van Damme L, Corneli A, Ahmed K, Agot K, Lombaard J, Kapiga S, Malahleha M, Owino F, Manongi R, Onyango J, Temu L, Monedi MC, Mak’Oketch P, Makanda M, Reblin I, Makatu SE, Saylor L, Kiernan H, Kirkendale S, Wong C, … & Taylor D (2012). Preexposure prophylaxis for HIV infection among African women . New England Journal of Medicine , 367 ( 5 ), 411–422. 10.1056/NEJMoa1202614 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Velloza J, Ngure K, Kiptinness C, Quame-Amaglo J, Thuo N, Dew K, Kimani M, Gakuo S, Unger JA, Kolko B, Baeten JM, Celum C, Mugo N, & Heffron R (2019). A clinic-based tablet application to support safer conception among HIV serodiscordant couples in Kenya: Feasibility and acceptability study . MHealth , 5 , 4. 10.21037/mhealth.2019.01.04 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Villarruel AM, Jemmott JB, Jemmott LS, & Ronis DL (2007). Predicting condom use among sexually experienced Latino adolescents . Western Journal of Nursing Research , 29 ( 6 ), 724–738. 10.1177/0193945907303102 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ware NC, Pisarski EE, Tam M, Wyatt MA, Atukunda E, Musiimenta A, Bangsberg DR, & Haberer JE (2016). The Meanings in the messages: How SMS reminders and real-time adherence monitoring improve antiretroviral therapy adherence in rural Uganda . AIDS , 30 ( 8 ), 1287–1293. 10.1097/QAD.0000000000001035 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Werb D, Garfein R, Kerr T, Davidson P, Roux P, Jauffret-Roustide M, Auriacombe M, Small W, & Strathdee SA (2016). A socio-structural approach to preventing injection drug use initiation: Rationale for the PRIMER study . Harm Reduction Journal , 13 ( 1 ), 25. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Whiteley LB, Brown LK, Curtis V, Ryoo HJ, & Beausoleil N (2018). Publicly available internet content as a HIV/STI prevention intervention for urban youth . Journal of Primary Prevention , 39 ( 4 ), 361–370. 10.1007/s10935-018-0514-y [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Willie T, Kershaw T, Campbell JC, & Alexander KA (2017). Intimate partner violence and PrEP acceptability among low-income, young Black women: Exploring the mediating role of reproductive coercion . AIDS and Behavior , 21 ( 8 ), 2261–2269. 10.1007/s10461-017-1767-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wingood GM, DiClemente RJ, Mikhail I, Lang DL, McCree DH, Davies SL, Hardin JW, Hook EW, & Saag M (2004). A randomized controlled trial to reduce HIV transmission risk behaviors and sexually transmitted diseases among women living with HIV: The WiLLOW Program . Journal of Acquired Immune Deficiency Syndromes , 37 ( Suppl 2 ), S58–S67. 10.1097/01.qai.0000140603.57478.a9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wohl DA, Golin CE, Knight K, Gould M, Carda-Auten J, Groves JS, Napravnik S, Cole SR, White BL, Fogel C, Rosen DL, Mugavaro MJ, Pence BW, & Flynn PM (2017). Randomized controlled trial of an intervention to maintain suppression of HIV viremia after prison release: The imPACT Trial . Journal of Acquired Immune Deficiency Syndromes , 75 ( 1 ), 81–90. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5443668/pdf/nihms853764.pdf [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wood BR, Mann MS, Martinez-Paz N, Unruh KT, Annese M, Spach DH, Scott JD, & Stekler JD (2018). Project ECHO: Telementoring to educate and support prescribing of HIV pre-exposure prophylaxis by community medical providers . Sexual Health , 15 ( 6 ), 601–605. [ PubMed ] [ Google Scholar ]
- Wootton AR, Legnitto DA, Gruber VA, Dawson-Rose C, Neilands TB, Johnson MO, & Saberi P (2019). Telehealth and texting intervention to improve HIV care engagement, mental health and substance use outcomes in youth living with HIV: A pilot feasibility and acceptability study protocol . BMJ Open , 9 ( 7 ), e028522. 10.1136/bmjopen-2018-028522 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wray T, Chan PA, Simpanen E, & Operario D (2017). eTEST: Developing a smart home HIV testing kit that enables active, real-time follow-up and referral after testing . JMIR mHealth and uHealth , 5 ( 5 ), e62. 10.2196/mhealth.6491 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yager JL, & Anderson PL (2020). Pharmacology and drug interactions with HIV PrEP in transgender persons receiving gender affirming hormone therapy . Expert Opinion on Drug Metabolism & Toxicology , 16 ( 6 ), 463–474. 10.1080/17425255.2020.1752662 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
Media Advisory
Tuesday, June 4, 2024
U.S. clinical trials begin for twice-yearly HIV prevention injection
Studies will focus on priority populations underrepresented in HIV clinical research.

Two clinical trials have launched to examine a novel long-acting form of HIV pre-exposure prophylaxis (PrEP) in cisgender women and people who inject drugs. The mid-stage studies will assess the safety, acceptability, and pharmacokinetics (how a drug moves through the body) of lenacapavir, an antiretroviral drug administered by injection every six months. The studies are sponsored and funded by Gilead Sciences, Inc., and implemented through the HIV Prevention Trails Network (HPTN). The HPTN is supported by grants from the National Institutes of Health’s (NIH) National Institute of Allergy and Infectious Diseases (NIAID), with scientific collaboration on this study and others from the National Institute on Drug Abuse (NIDA) as well as co-funding from NIDA and other NIH institutes.
Lenacapavir is already approved by the Food and Drug Administration for HIV treatment, in combination with other antiretroviral therapy, of heavily treatment-experienced individuals, whose HIV infections cannot be successfully treated with other available treatments due to resistance, intolerance, or safety considerations with other drugs and developed multidrug resistance. Lenacapavir is the first of a class of drugs called capsid inhibitors to be FDA-approved for treating HIV infection. It is the first long-acting injectable to be offered with administration just once every six months. Cisgender women—people who self-identify as female and were assigned female sex at birth—and people who inject drugs accounted for 18% and 7% of new HIV diagnoses in the United States in 2021, respectively. Both population groups have been underrepresented in HIV clinical studies, as have transgender people, pregnant people and U.S. communities of color. Both trials complement ongoing large efficacy studies and are intended to provide insights on how these two priority populations experience lenacapavir-based HIV PrEP.
The studies will take place at HPTN sites in the United States and enroll people who might benefit from taking PrEP. The first trial will enroll cisgender women, with a focus on making enrollment accessible to women who self-identify as Black and/or Latina. The second trial will enroll a diverse group of people who inject drugs. In both studies, participants will be randomly assigned to receive either injectable lenacapavir or an FDA-approved PrEP formulation consisting of oral tenofovir disoproxil fumarate and emtricitabine. Participants’ health will be monitored closely throughout the study. Participants will provide laboratory samples and give qualitative feedback on their experience taking each form of PrEP.
The studies will add important clinical data to a global manufacturer-led clinical development program for lenacapavir as HIV PrEP. NIH is supporting the implementation of these two studies through its clinical trials networks to help ensure the meaningful inclusion of diverse and representative populations in clinical research, so that everyone can contribute to scientific progress and benefit from its applications.
For more information about these trials, please visit ClinicalTrials.gov study identifiers NCT06101329 and NCT06101342 .
Sheryl Zwerski, D.N.P., director of the Prevention Sciences Program in NIAID’s Division of AIDS, is available to discuss these studies.
NIAID conducts and supports research—at NIH, throughout the United States, and worldwide—to study the causes of infectious and immune-mediated diseases, and to develop better means of preventing, diagnosing and treating these illnesses. News releases, fact sheets and other NIAID-related materials are available on the NIAID website .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
Connect with Us
- More Social Media from NIH
- What Are HIV and AIDS?
- How Is HIV Transmitted?
- Who Is at Risk for HIV?
- Symptoms of HIV
- U.S. Statistics
- Impact on Racial and Ethnic Minorities
- Global Statistics
- HIV and AIDS Timeline
- In Memoriam
- Supporting Someone Living with HIV
- Standing Up to Stigma
- Getting Involved
- HIV Treatment as Prevention
- Pre-exposure Prophylaxis (PrEP)
- Post-exposure Prophylaxis (PEP)
- Preventing Sexual Transmission of HIV
- Alcohol and HIV Risk
- Substance Use and HIV Risk
- Preventing Perinatal Transmission of HIV
- HIV Vaccines
- Long-acting HIV Prevention Tools
- Microbicides
- Who Should Get Tested?
- HIV Testing Locations
- HIV Testing Overview
- Understanding Your HIV Test Results
- Living with HIV
- Talking About Your HIV Status
- Locate an HIV Care Provider
- Types of Providers
- Take Charge of Your Care
- What to Expect at Your First HIV Care Visit
- Making Care Work for You
- Seeing Your Health Care Provider
- HIV Lab Tests and Results
- Returning to Care
- HIV Treatment Overview
- Viral Suppression and Undetectable Viral Load
- Taking Your HIV Medicine as Prescribed
- Tips on Taking Your HIV Medicine as Prescribed
- Paying for HIV Care and Treatment
- Other Health Issues of Special Concern for People Living with HIV
- Alcohol and Drug Use
- Coronavirus (COVID-19) and People with HIV
- Hepatitis B & C
- Vaccines and People with HIV
- Flu and People with HIV
- Mental Health
- Mpox and People with HIV
- Opportunistic Infections
- Sexually Transmitted Infections
- Syphilis and People with HIV
- HIV and Women's Health Issues
- Aging with HIV
- Emergencies and Disasters and HIV
- Employment and Health
- Exercise and Physical Activity
- Food Safety and Nutrition
- Housing and Health
- Traveling Outside the U.S.
- Civil Rights
- Workplace Rights
- Limits on Confidentiality
- National HIV/AIDS Strategy (2022-2025)
- Implementing the National HIV/AIDS Strategy
- Prior National HIV/AIDS Strategies (2010-2021)
- Key Strategies
- Priority Jurisdictions
- HHS Agencies Involved
- Learn More About EHE
- Ready, Set, PrEP
- Ready, Set, PrEP Pharmacies
- Ready, Set, PrEP Resources
- AHEAD: America’s HIV Epidemic Analysis Dashboard
- HIV Prevention Activities
- HIV Testing Activities
- HIV Care and Treatment Activities
- HIV Research Activities
- Activities Combating HIV Stigma and Discrimination
- The Affordable Care Act and HIV/AIDS
- HIV Care Continuum
- Syringe Services Programs
- Finding Federal Funding for HIV Programs
- Fund Activities
- The Fund in Action
- About PACHA
- Members & Staff
- Subcommittees
- Prior PACHA Meetings and Recommendations
- I Am a Work of Art Campaign
- Awareness Campaigns
- Global HIV/AIDS Overview
- U.S. Government Global HIV/AIDS Activities
- U.S. Government Global-Domestic Bidirectional HIV Work
- Global HIV/AIDS Organizations
- National Black HIV/AIDS Awareness Day February 7
- HIV Is Not A Crime Awareness Day February 28
- National Women and Girls HIV/AIDS Awareness Day March 10
- National Native HIV/AIDS Awareness Day March 20
- National Youth HIV & AIDS Awareness Day April 10
- HIV Vaccine Awareness Day May 18
- National Asian & Pacific Islander HIV/AIDS Awareness Day May 19
- HIV Long-Term Survivors Awareness Day June 5
- National HIV Testing Day June 27
- Zero HIV Stigma July 21
- Southern HIV/AIDS Awareness Day August 20
- National Faith HIV/AIDS Awareness Day August 27
- National African Immigrant and Refugee HIV/AIDS and Hepatitis Awareness Day September 9
- National HIV/AIDS and Aging Awareness Day September 18
- National Gay Men's HIV/AIDS Awareness Day September 27
- National Latinx AIDS Awareness Day October 15
- World AIDS Day December 1
- Event Planning Guide
- U.S. Conference on HIV/AIDS (USCHA)
- National Ryan White Conference on HIV Care & Treatment
- AIDS 2020 (23rd International AIDS Conference Virtual)
Want to stay abreast of changes in prevention, care, treatment or research or other public health arenas that affect our collective response to the HIV epidemic? Or are you new to this field?
HIV.gov curates learning opportunities for you, and the people you serve and collaborate with.
Stay up to date with the webinars, Twitter chats, conferences and more in this section.
CDC Publishes New HIV Surveillance Reports
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email

Cross-Posted from: CDC
Today, the Centers for Disease Control and Prevention (CDC) published three new HIV surveillance reports:
- Estimated HIV Incidence and Prevalence in the United States, 2018-2022 ;
- Monitoring Selected National HIV Prevention and Care Objectives by Using HIV Surveillance Data, United States and 6 Territories and Freely Associated States, 2022; and
- Diagnoses, Deaths, and Prevalence of HIV in the United States and 6 Territories and Freely Associated States, 2022.
All data are also available on NCHHSTP AtlasPlus . These data can assist HIV prevention partners in focusing prevention efforts, allocating resources, monitoring trends, and determining gaps and successes in HIV prevention.
Estimated HIV Incidence and Prevalence * : Key Findings
The new HIV incidence estimates show that national prevention efforts are continuing to move in the right direction overall, although substantial disparities exist. The estimated number of new HIV infections in 2022 (31,800) decreased 12% compared with 2018 (36,200), driven by a 30% decrease among young people aged 13 - 24 years. Increases in preexposure prophylaxis prescriptions, viral suppression and HIV testing likely contributed to the decline. Data also show significant declines geographically, with estimated new HIV infections decreasing 16% in the South in 2022 compared with 2018. In 2022, HIV incidence in Ending the HIV Epidemic (EHE) (phase I) jurisdictions decreased 21% among persons aged ≥ 13 years, compared with the 2017 EHE baseline year. There were no increases in HIV incidence for any populations in 2022 compared with 2018.
Although data demonstrate continued progress in HIV prevention, longstanding social and economic factors continue to contribute to health inequities—particularly among Black/African American (hereafter referred to as Black) persons and Hispanic/Latino persons. Among women overall, in 2022, 47% (2,800) of estimated new HIV infections were among Black women. New HIV infections attributed to male-to-male sexual contact (MMSC) accounted for 67% (21,400) of estimated new infections. New HIV infections among gay, bisexual, and other men who have sex with men (MSM) were about 16% lower among Black men in 2022 (7,400) compared with 2018 (8,800) and 20% lower among White men in 2022 (4,400) compared with 2018 (5,500). Although the number of new HIV infections remained about the same among Hispanic/Latino MSM (8,200 in 2018 and 8,300 in 2022), due to the declines among other groups, Hispanic/Latino men accounted for 39% of estimated new HIV infections among gay, bisexual, and other MSM in 2022.
It is estimated that 1.2 million persons in the United States were living with diagnosed and undiagnosed HIV at the end of 2022. More people with HIV were aware of their status in 2022 than in 2018, with a slight increase from 86% to 87%. Knowledge of HIV status increased among persons aged 13 - 24 years, Asian persons, Black persons, Hispanic/Latino persons, persons in the South, and among males with infections attributed to MMSC. Knowledge of HIV status decreased among persons aged 35-44 years (84% in 2022 compared with 86% in 2018).
Monitoring Report: PrEP Coverage
This CDC Monitoring Report does not include data on PrEP coverage. CDC has paused PrEP coverage reporting for one year to address a formula error that affects a subset of race/ethnicity data, update overall PrEP coverage estimates using newly available data sets, and determine the best way to present PrEP coverage. CDC believes this update will yield greater precision and a more complete picture of the PrEP coverage landscape in the United States.
Earlier this year a formula error was found in the calculation used to determine the number of people with indications for PrEP by race/ethnicity. This only affects the PrEP coverage estimates for two groups – White persons and persons of other races/ethnicities – and does not affect the overall PrEP coverage estimate or estimates by sex or by age group. It does, however, affect all years of PrEP coverage data (2017-2022). CDC does not expect general trends in disparities to change, but magnitudes of certain disparities are expected to shift (i.e., current PrEP coverage estimates for White persons are likely an overestimate).
Furthermore, in March 2024, data were made available to CDC that can improve the representativeness of the number of persons prescribed PrEP in the United States. In the coming months, CDC also expects to have updates to the data sets used to estimate the number of persons with indications for PrEP. Pausing PrEP coverage reporting for the next year will allow CDC to update all PrEP coverage estimates (2017-2022) using newly available data sets, rather than simply correcting the formula error using current data sources.
CDC plans to resume PrEP coverage reporting in the next Monitoring Report , currently scheduled for publication in June 2025. Until updated estimates are published, CDC advises against citing specific PrEP coverage data points and instead recommends referencing general trends and disparities.
Monitoring Report: Key Findings
Among persons who received diagnoses of HIV infection during 2022, 82% were linked to care within one month of diagnosis. Asian persons had the highest percentage of linkage to care within one month (88%), and Native Hawaiian/other Pacific Islander persons (74%), American Indian/Alaska Native persons (78%), Black persons (78%), and women (80%) had the lowest percentages. Among persons with diagnosed HIV and alive at year-end 2022, 65% were virally suppressed at the most recent viral load test. The lowest percentages of viral suppression were among Black persons (61%) and women overall (64%). Despite overall progress in eliminating perinatally acquired HIV, in 2022, the rate of perinatally acquired HIV among Black persons was 5 times the overall annual rate of 1.1 per 100,000 live births. To meet national HIV goals and ensure that all persons with diagnosed HIV receive high quality care and treatment, prevention efforts must address the drivers of social inequities and other barriers to care that cause and exacerbate health disparities.
HIV Diagnoses ** : Key Findings
In 2022, in the United States and 6 territories and freely associated states, there were 38,043 HIV diagnoses, more than half of which (52%) occurred among people living in the South. Compared to 2018, in 2022, the number of HIV diagnoses among gay, bisexual, and other MSM overall (67%) and the number of HIV diagnoses among Black gay, bisexual, and other MSM (35% of MSM) remained stable. White persons accounted for almost half (47%) of all HIV diagnoses attributed to injection drug use. Notably, compared with 2018, in 2022, HIV diagnoses increased among transgender women (25% increase), Hispanic/Latino gay, bisexual, and other MSM (22% increase), Hispanic/Latino persons overall (17% increase), and males who inject drugs (7% increase). HIV diagnoses decreased among persons aged 13–24 years (14% decrease) and Black women (10% decrease). Although Black women accounted for only 9% of HIV diagnoses overall in 2022, among cisgender women, Black women accounted for 50% of HIV diagnoses and, among transgender women, Black women accounted for 41% of HIV diagnoses. Finally, HIV diagnosis data show that the rate of HIV-related deaths declined 25%, highlighting the effectiveness of early diagnosis and linking people with diagnosed HIV to quality care and treatment.
Overall, data from these reports demonstrate that expanding the reach of HIV testing, PrEP, and treatment have been effective – but our reach must extend even further, and progress must be faster, to achieve our national goal of ending new HIV infections in the United States. This requires sharpening our collective focus on efforts that address inequities and their drivers, including racism and other social and structural determinants of health, and ensuring that whole person approaches to HIV prevention, care, and treatment are brought to scale and equitably reach all people who need them to stay healthy.
Thank you for your continued support for HIV prevention in the United States.
/Robyn Fanfair/
Robyn Neblett Fanfair, MD, MPH Captain, USPHS Director Division of HIV Prevention National Center for HIV, Viral Hepatitis, STD, and TB Prevention Centers for Disease Control and Prevention www.cdc.gov/hiv
/Jonathan Mermin/
Jonathan Mermin, MD, MPH Rear Admiral, USPHS ( retired ) Director National Center for HIV, Viral Hepatitis, STD, and TB Prevention Centers for Disease Control and Prevention Stay connected @DrMerminCDC Exit Disclaimer and Connections
* HIV estimates for years 2020, 2021, and 2022 should be interpreted with caution due to adjustments made to the CD4-based depletion model to account for the impact of COVID-19 on HIV testing and diagnosis in the United States. Please see the Technical Notes section of this report for additional information.
** In 2022, reporting of HIV diagnoses was 5% higher than in 2021. Based on pre-pandemic data, an increase in diagnoses of 2-3% is expected each year. As the COVID-19 pandemic lasted beyond 2020, readers should consider the potential influence of these pandemic effects on U.S. public health systems when interpreting data HIV data for years 2021–2022.
Related HIV.gov Blogs
- CDC Centers for Disease Control & Prevention
- Surveillance Public health surveillance
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 29, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Proof-of-concept study pioneers new brain imaging technique through a transparent skull implant
by Keck School of Medicine of USC
In the first study of its kind, researchers from the Keck School of Medicine of USC and the California Institute of Technology (Caltech) designed and implanted a transparent window in the skull of a patient, then used functional ultrasound imaging (fUSI) to collect high-resolution brain imaging data through the window.
Their preliminary findings , published in Science Translational Medicine , suggest that this sensitive, non-invasive approach could open new avenues for patient monitoring and clinical research , as well as broader studies of how the brain functions.
"This is the first time anyone had applied functional ultrasound imaging through a skull replacement in an awake, behaving human performing a task," said Charles Liu, MD, Ph.D., a professor of clinical neurological surgery, urology and surgery at the Keck School of Medicine and director of the USC Neurorestoration Center.
"The ability to extract this type of information noninvasively through a window is pretty significant, particularly since many of the patients who require skull repair have or will develop neurological disabilities. In addition, 'windows' can be surgically implanted in patients with intact skulls if functional information can help with diagnosis and treatment."
The research participant, 39-year-old Jared Hager, sustained a traumatic brain injury (TBI) from a skateboarding accident in 2019. During emergency surgery , half of Hager's skull was removed to relieve pressure on his brain, leaving part of his brain covered only with skin and connective tissue. Because of the pandemic, he had to wait more than two years to have his skull restored with a prosthesis.
During that time, Hager volunteered for earlier research conducted by Liu, Jonathan Russin, MD, associate surgical director of the USC Neurorestoration Center, and another Caltech team on a new type of brain imaging called fPACT.
The experimental technique had been done on soft tissue, but could only be tested on the brain in patients like Hager who were missing a part of their skull. When the time came for implanting the prosthesis, Hager again volunteered to team up with Liu and his colleagues, who designed a custom skull implant to study the utility of fUSI—which cannot be done through the skull or a traditional implant—while repairing Hager's injury.
Before the reconstructive surgery, the research team tested and optimized fUSI parameters for brain imaging, using both a phantom (a scientific device designed to test medical imaging equipment) and animal models. They then collected fUSI data from Hager while he completed several tasks, both before his surgery and after the clear implant was installed, finding that the window offered an effective way to measure brain activity.
Functional brain imaging, which collects data on brain activity by measuring changes in blood flow or electrical impulses, can offer key insights about how the brain works, both in healthy people and those with neurological conditions.
But current methods, such as functional magnetic resonance imaging (fMRI) and intracranial electroencephalography (EEG) leave many questions unanswered. Challenges include low resolution, a lack of portability or the need for invasive brain surgery. fUSI may eventually offer a sensitive and precise alternative.
"If we can extract functional information through a patient's skull implant, that could allow us to provide treatment more safely and proactively," including to TBI patients who suffer from epilepsy, dementia, or psychiatric problems, Liu said.
A new frontier for brain imaging
As a foundation for the present study, Liu has collaborated for years with Mikhail Shapiro, Ph.D. and Richard Andersen, Ph.D., of Caltech, to develop specialized ultrasound sequences that can measure brain function, as well as to optimize brain-computer interface technology, which transcribes signals from the brain to operate an external device.
With these pieces in place, Liu and his colleagues tested several transparent skull implants on rats, finding that a thin window made from polymethyl methacrylate (PMMA)—which resembles plexiglass—yielded the clearest imaging results. They then collaborated with a neurotechnology company, Longeviti Neuro Solutions, to build a custom implant for Hager.
Before surgery, the researchers collected fUSI data while Hager did two activities: solving a "connect-the-dots" puzzle on a computer monitor and playing melodies on his guitar. After the implant was installed, they collected data on the same tasks, then compared the results to determine whether fUSI could provide accurate and useful imaging data.
"The fidelity of course decreased, but importantly, our research showed that it's still high enough to be useful," Liu said. "And unlike other brain-computer interface platforms, which require electrodes to be implanted in the brain, this has far less barriers to adoption."
fUSI may offer finer resolution than fMRI and unlike intracranial EEG, it does not require electrodes to be implanted inside the brain. It is also less expensive than those methods and could provide some clinical advantages for patients over non-transparent skull implants, said Russin, who is also an associate professor of neurological surgery at the Keck School of Medicine and director of cerebrovascular surgery at Keck Hospital of USC.
"One of the big problems when we do these surgeries is that a blood clot can form underneath the implant, but having a clear window gives us an easy way to monitor that," he said.
Refining functional ultrasound technology
In addition to better monitoring of patients, the new technique could offer population-level insights about TBI and other neurological conditions. It could also allow scientists to collect data on the healthy brain and learn more about how it controls cognitive, sensory, motor and autonomic functions.
"What our findings show is that we can extract useful functional information with this method," Liu said. "The next step is: What specific functional information do we want, and what can we use it for?"
Until the new technologies undergo clinical trials, fUSI and the clear implant are experimental. In the meantime, the research team is working to improve their fUSI protocols to further enhance image resolution . Future research should also build on this early proof-of-concept study by testing more participants to better establish the link between fUSI data and specific brain functions, the researchers said.
"Jared is an amazing guy," said Liu, who is continuing to collaborate with the study participant on refining new technologies, including laser spectroscopy, which measures blood flow in the brain. "His contributions have really helped us explore new frontiers that we hope can ultimately help many other patients."
Explore further
Feedback to editors

Study uncovers how cancer stem cells spread and resist treatment
8 minutes ago

Novel AI method could improve tissue, tumor analysis and advance treatment of disease
9 minutes ago

'Artificial lymph node' used to treat cancer in mice
53 minutes ago

Mouth-based touchpad enables people living with paralysis to interact with computers

Clinical study shows zebrafish avatars of cancer patients have high predictive power

People feel more connected to 'tweezer-like' bionic hands in virtual reality, study shows

Clinical trial investigates using electronic alerts to help control blood pressure


Engineered bacteria deliver chemotherapy directly to tumors
2 hours ago

The body's own lipids affect mental disorders: Can specific inhibitors help?

New study challenges 'pop psychology' myths about habits
3 hours ago
Related Stories

Doctors can now watch spinal cord activity during surgery
Mar 7, 2024

New approach to brain imaging leaves skulls intact in mice
Sep 5, 2022

Musk's Neuralink says issue in brain implant fixed
May 9, 2024

Musk says patient moves cursor with brain implant
Feb 21, 2024

Ultrasound enables less-invasive brain-machine interfaces
Nov 30, 2023

Neuralink shows quadriplegic playing chess with brain implant
Mar 21, 2024
Recommended for you

Study shows orexin neurons can track how fast blood glucose changes
4 hours ago

Smart hydrogel injected into intracranial fluid can measure changes in temperature, pH or pressure

New study redefines how antidepressants aid in treating major depressive disorder
21 hours ago

Brain imaging study shows how THC in cannabis disrupts brain activity and may cause cognitive impairment
23 hours ago
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
HIV infections articles from across Nature Portfolio
HIV infections (human immunodeficiency virus infections) include the spectrum of infections caused by the virus HIV that range from asymptomatic seropositivity to acquired immunodeficiency syndrome (AIDS)-related complex (ARC) and AIDS.
Latest Research and Reviews
Sustained aviraemia despite anti-retroviral therapy non-adherence in male children following in utero hiv transmission.
After early initiation of anti-retroviral therapy in infants infected with HIV-1 in utero, some children sustain undetectable virus levels, despite treatment interruption, and which associated with distinct features of the transmitted virus.
- Nomonde Bengu
- Gabriela Cromhout
- Philip Goulder
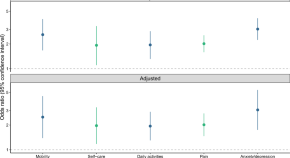
Associations between HIV stigma and health-related quality-of-life among people living with HIV: cross-sectional analysis of data from HPTN 071 (PopART)
- Katherine Davis
- Wafaa el-Sadr
Vaccination induces broadly neutralizing antibody precursors to HIV gp41
Schief and colleagues show that germline-targeting epitope scaffolds can elicit responses from rare broadly neutralizing antibody precursor B cells with predefined binding specificities and genetic features.
- Torben Schiffner
- William R. Schief
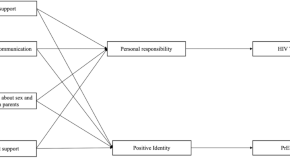
The importance of developmental assets in HIV prevention behaviors among young black men who have sex with men (MSM)
- Donte T. Boyd
- Orlando O. Harris
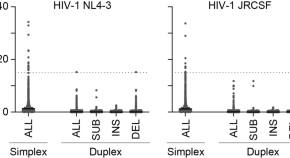
Population-based nanopore sequencing of the HIV-1 pangenome to identify drug resistance mutations
- Hirotaka Ode
- Masakazu Matsuda
- Yasumasa Iwatani
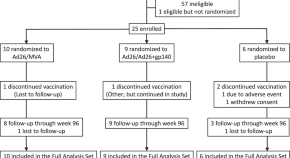
Immunogenicity of 2 therapeutic mosaic HIV-1 vaccine strategies in individuals with HIV-1 on antiretroviral therapy
- Kathryn E. Stephenson
- Dan H. Barouch
News and Comment
Combination treatment for immune-mediated HIV remission
In rhesus macaques, treatment with an IL-15 superagonist and broad neutralizing antibodies led to durable suppression of viremia after discontinuation of antiretroviral therapy.
- Karen O’Leary
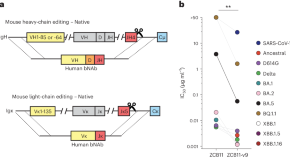
Affinity maturation of CRISPR-engineered B cell receptors in vivo
CRISPR–Cas12a was used to directly replace mouse antibody variable chain genes with human versions in primary B cells. The edited cells underwent affinity maturation in vivo, improving the potency of HIV-1 and SARS-CoV-2 neutralizing antibodies without loss of bioavailability. Affinity maturation of edited cells also enables new vaccine models and adaptive B cell therapies.
CARD8 kills CD4 + T cells in response to HIV entry
- Alexandra Flemming
Blockbuster obesity drug leads to better health in people with HIV
Semaglutide reduces weight and fat accumulation associated with the antiretroviral regimen that keeps HIV at bay.
- Mariana Lenharo
Why have T cell-inducing vaccines for HIV failed so far?
The failure of T cell-targeted vaccines for HIV in clinical trials is likely due to impaired degranulation of low-avidity CD8 + T cells in the context of low levels of antigen presentation.
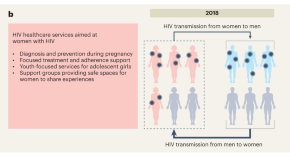
Close the gender gap in Africa’s HIV epidemic
Improving HIV interventions for men could reduce HIV acquisition in women, close the growing gender gap in HIV infections and further reduce HIV incidence in African countries.
- Bryan Tegomoh
- Boghuma K. Titanji
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES
VIDEO
COMMENTS
An international team of researchers led by Eric Arts, professor at the Schulich School of Medicine & Dentistry, and Jamie Mann, senior lecturer at the University of Bristol (U.K.), has brought us ...
Regardless, the findings from Emory University's study offer hope and renewed enthusiasm for efforts to unravel the complexities of HIV persistence and ultimately find a cure. "These data are valuable because they show that Jak inhibitors can contribute to a long-term cure strategy for HIV, but they can also be used to slow the inflammatory ...
Young people, aged 15-24, account for around 27% of new HIV infections globally. ... Underfunding cannabis research hampers sensible policymaking and boosts the black market.
The likelihood of discontinuing the assigned regimen due to adverse events or experiencing unsuppressed HIV was 10% among people taking long-acting ART compared to 26% among those taking daily ART. These findings were statistically significant. Dr. Dieffenbach observed that these results may support expanding the use of long-acting ART among a ...
An effective and scalable cure strategy is a top priority for the HIV research field; this Review discusses recent advances, knowledge gaps, and priority research areas for the next 5 years.
FOSTER CITY, Calif.--(BUSINESS WIRE)-- Gilead Sciences, Inc. (Nasdaq: GILD) today announced the presentation of key data highlighting the breadth of its innovative HIV treatment research pipeline. The latest results explore clinical outcomes from a study evaluating an investigational combination regimen of bictegravir and lenacapavir, new findings from a study evaluating the investigational ...
The findings, published in Science ... Compared with people infected with other HIV strains, those infected with the new variant had up to 5.5 times more virus in their blood, and their CD4 T ...
What. In a presentation today at AIDS 2022, the 24 th International AIDS Conference in Montreal, scientists with the National Institute of Allergy and Infectious Diseases' (NIAID) Vaccine Research Center (VRC) and their collaborators described how their use of cutting-edge technology revealed new insights into cellular reservoirs of HIV and what those observations could mean for the next ...
Using a combination of cutting-edge immunologic technologies, researchers have successfully stimulated animals' immune systems to induce rare precursor B cells of a class of HIV broadly neutralizing antibodies (bNAbs). The findings, published today in Nature Immunology, are an encouraging, incremental step in developing a preventive HIV vaccine.
Findings from the HIV cure research program include results from three studies evaluating strategies to maintain virologic control in the absence of ART. Results from the Phase 2a TITAN trial show that dual treatment with the broadly neutralizing HIV antibodies (bNAbs; 3BNC117 and 10-1074) led to a significant delay in viral rebound.
Investing in research to find a cure for HIV is focused on two broad aims: sustained viral remission and, in the longer term, viral eradication. Viral latency and sanctuaries. Latent HIV reservoirs—small amounts of HIV that persist in people taking ART—present a significant challenge to finding a cure for HIV. Latent reservoirs remain in ...
These findings will help the researchers with future clinical trials aiming to eliminate the HIV-1 reservoirs. Research for curing HIV is at an infant stage but a promising one. Scientists are working on two broad types of HIV cures—a functional cure and a sterilising one.
CROI Research Highlights Affirm Strength of New HIV Discoveries. Submitted by Jessica_Wheeler_SCG on Tue, 03/26/2024 - 15:32. In her first blog as Acting OAR Director, Diana Finzi, Ph.D., discusses groundbreaking HIV research findings and perspectives from community members at the 2024 Conference on Retroviruses and Opportunistic Infections (CROI).
At the National Institutes of Health, the HIV/AIDS research effort is led by the National Institute of Allergy and Infectious Diseases (NIAID). A vast network of NIAID-supported scientists, located on the NIH campus in Bethesda, Maryland, and at research centers around the globe, are exploring new ways to prevent and treat HIV infection, as ...
"PURPOSE 4 is the first trial to evaluate a long-acting PrEP modality in this disenfranchised and commonly overlooked population. Findings from this trial could be critical to advancing the Ending the HIV Epidemic in the U.S. initiative." About Gilead's PURPOSE program
Approximately 1.2 million people in the United States are currently living with HIV, and an estimated 14% are infected, yet unaware of their status (Office of Infectious Disease and HIV/AIDS Policy, 2020).HIV and AIDS continue to have a disproportionate impact on certain populations, including youth—gay, bisexual, and other men who have sex with men (MSM)—racial and ethnic minorities ...
Studies will focus on priority populations underrepresented in HIV clinical research. Studies will focus on priority populations underrepresented in HIV clinical research. ... self-identify as female and were assigned female sex at birth—and people who inject drugs accounted for 18% and 7% of new HIV diagnoses in the United States in 2021 ...
As the 23rd International AIDS Conference (AIDS 2020: Virtual) drew to a close yesterday, HIV.gov shared a final interview with Carl Dieffenbach, Ph.D., director of the Division of AIDS at NIH's National Institute of Allergy and Infectious Diseases (NIAID), about more of the week's important HIV research developments.
It is estimated that 1.2 million persons in the United States were living with diagnosed and undiagnosed HIV at the end of 2022. More people with HIV were aware of their status in 2022 than in 2018, with a slight increase from 86% to 87%. Knowledge of HIV status increased among persons aged 13 - 24 years, Asian persons, Black persons, Hispanic ...
The 2024 Conference on Retroviruses and Opportunistic Infections (CROI), held in Denver, Colorado, provided an opportunity for global exchange of research findings and community voices on HIV and other infectious diseases.While I have attended CROI many times over the years it was particularly exciting to see the renewed energy and focus on HIV. There were still talks focusing on Covid but ...
HIV capsid inhibitors represent a potential new class of antiretrovirals with high in vitro potency and very slow metabolic clearance leading to a prolonged half-life in in-vivo preclinical models ...
The CDC said it saw HIV infections among those age 13 to 24 drop by 34%, while annual HIV infections dropped from to 6,100 in 2021 from 9,300 in 2017 in that age group. More information
The findings were recently ... The company is currently testing the platform in a human clinical trial for HIV. Their initial research focused on using the platform as an HIV T cell vaccine ...
An HIV drug that suppresses the activity of the CCR5 receptor—a collection of proteins on the surface of certain immune cells—was associated with better renal function in kidney transplant recipients with HIV compared to people who took a placebo in a randomized trial. According to the authors, these findings warrant further exploration of the benefit of CCR5 antagonists in all kidney ...
Weight loss is followed by a reduction in several organ sizes, including the heart, pancreas and kidneys." (This paper led by researchers in New York, reports that, in participants who lost 11 percent of body weight, heart mass decreased by 26 percent and the kidneys by 19 percent.) And it is important to note that the metabolic rate of ...
Their preliminary findings, published in Science Translational Medicine, suggest that this sensitive, non-invasive approach could open new avenues for patient monitoring and clinical research, as ...
Findings could help guide public health resources to prevent unwanted pregnancy, sexually transmitted infections. ... a new study led by UC San Francisco found. ... sexually transmitted illnesses, including HIV infections, having unplanned pregnancies and becoming depressed, research shows. This is the first known study to look at how children ...
Blockbuster obesity drug leads to better health in people with HIV. Semaglutide reduces weight and fat accumulation associated with the antiretroviral regimen that keeps HIV at bay. Mariana ...