

Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
- Theresa Cerulli, MD
- Tina Matthews-Hayes, DNP, FNP, PMHNP
Custom Around the Practice Video Series
Experts in psychiatry review the case of a 27-year-old woman who presents for evaluation of a complex depressive disorder.

EP: 1 . Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
Ep: 2 . clinical significance of bipolar disorder, ep: 3 . clinical impressions from patient case #1, ep: 4 . diagnosis of bipolar disorder, ep: 5 . treatment options for bipolar disorder, ep: 6 . patient case #2: 47-year-old man with treatment resistant depression (trd), ep: 7 . patient case #2 continued: novel second-generation antipsychotics, ep: 8 . role of telemedicine in bipolar disorder.
Michael E. Thase, MD : Hello and welcome to this Psychiatric Times™ Around the Practice , “Identification and Management of Bipolar Disorder. ”I’m Michael Thase, professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Joining me today are: Dr Gustavo Alva, the medical director of ATP Clinical Research in Costa Mesa, California; Dr Theresa Cerulli, the medical director of Cerulli and Associates in North Andover, Massachusetts; and Dr Tina Matthew-Hayes, a dual-certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.
Today we are going to highlight challenges with identifying bipolar disorder, discuss strategies for optimizing treatment, comment on telehealth utilization, and walk through 2 interesting patient cases. We’ll also involve our audience by using several polling questions, and these results will be shared after the program.
Without further ado, welcome and let’s begin. Here’s our first polling question. What percentage of your patients with bipolar disorder have 1 or more co-occurring psychiatric condition? a. 10%, b. 10%-30%, c. 30%-50%, d. 50%-70%, or e. more than 70%.
Now, here’s our second polling question. What percentage of your referred patients with bipolar disorder were initially misdiagnosed? Would you say a. less than 10%, b. 10%-30%, c. 30%-50%, d. more than 50%, up to 70%, or e. greater than 70%.
We’re going to go ahead to patient case No. 1. This is a 27-year-old woman who’s presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode. It began back in the fall, and she described the episode as occurring right “out of the blue.” Further discussion revealed, however, that she had talked with several confidantes about her problems and that she realized she had been disappointed and frustrated for being passed over unfairly for a promotion at work. She had also been saddened by the unusually early death of her favorite aunt.
Now, our patient has a past history of ADHD [attention-deficit/hyperactivity disorder], which was recognized when she was in middle school and for which she took methylphenidate for adolescence and much of her young adult life. As she was wrapping up with college, she decided that this medication sometimes disrupted her sleep and gave her an irritable edge, and decided that she might be better off not taking it. Her medical history was unremarkable. She is taking escitalopram at the time of our initial evaluation, and the dose was just reduced by her PCP [primary care physician]from 20 mg to 10 mg because she subjectively thought the medicine might actually be making her worse.
On the day of her first visit, we get a PHQ-9 [9-item Patient Health Questionnaire]. The score is 16, which is in the moderate depression range. She filled out the MDQ [Mood Disorder Questionnaire] and scored a whopping 10, which is not the highest possible score but it is higher than 95% of people who take this inventory.
At the time of our interview, our patient tells us that her No. 1 symptom is her low mood and her ease to tears. In fact, she was tearful during the interview. She also reports that her normal trouble concentrating, attributable to the ADHD, is actually substantially worse. Additionally, in contrast to her usual diet, she has a tendency to overeat and may have gained as much as 5 kg over the last 4 months. She reports an irregular sleep cycle and tends to have periods of hypersomnolence, especially on the weekends, and then days on end where she might sleep only 4 hours a night despite feeling tired.
Upon examination, her mood is positively reactive, and by that I mean she can lift her spirits in conversation, show some preserved sense of humor, and does not appear as severely depressed as she subjectively describes. Furthermore, she would say that in contrast to other times in her life when she’s been depressed, that she’s actually had no loss of libido, and in fact her libido might even be somewhat increased. Over the last month or so, she’s had several uncharacteristic casual hook-ups.
So the differential diagnosis for this patient included major depressive disorder, recurrent unipolar with mixed features, versus bipolar II disorder, with an antecedent history of ADHD. I think the high MDQ score and recurrent threshold level of mixed symptoms within a diagnosable depressive episode certainly increase the chances that this patient’s illness should be thought of on the bipolar spectrum. Of course, this formulation is strengthened by the fact that she has an early age of onset of recurrent depression, that her current episode, despite having mixed features, has reverse vegetative features as well. We also have the observation that antidepressant therapy has seemed to make her condition worse, not better.
Transcript Edited for Clarity
Dr. Thase is a professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Dr. Alva is the medical director of ATP Clinical Research in Costa Mesa, California.
Dr. Cerulli is the medical director of Cerulli and Associates in Andover, Massachusetts.
Dr. Tina Matthew-Hayes is a dual certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.

An Update on Early Intervention in Psychotic Disorders

Blue Light, Depression, and Bipolar Disorder

The 2024 APA Annual Meeting: Sunday, May 5

Four Myths About Lamotrigine

The Week in Review: April 1-5

FDA Approves Fanapt for Mixed, Manic Episodes Associated With Bipolar I Disorder
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 07 July 2021
Assessment of suicide attempt and death in bipolar affective disorder: a combined clinical and genetic approach
- Eric T. Monson ORCID: orcid.org/0000-0002-8552-8300 1 ,
- Andrey A. Shabalin 1 ,
- Anna R. Docherty 1 ,
- Emily DiBlasi 1 ,
- Amanda V. Bakian ORCID: orcid.org/0000-0001-6805-1160 1 , 2 ,
- Qingqin S. Li ORCID: orcid.org/0000-0003-4182-4535 3 ,
- Douglas Gray 1 , 4 ,
- Brooks Keeshin 1 , 5 ,
- Sheila E. Crowell 1 , 6 , 7 ,
- Niamh Mullins ORCID: orcid.org/0000-0001-8021-839X 8 , 9 ,
- Virginia L. Willour 10 &
- Hilary Coon ORCID: orcid.org/0000-0002-8877-5446 1 , 11 , 12
Translational Psychiatry volume 11 , Article number: 379 ( 2021 ) Cite this article
16k Accesses
9 Citations
72 Altmetric
Metrics details
- Bipolar disorder
- Comparative genomics
Bipolar disorder (BP) suicide death rates are 10–30 times greater than the general population, likely arising from environmental and genetic risk factors. Though suicidal behavior in BP has been investigated, studies have not addressed combined clinical and genetic factors specific to suicide death. To address this gap, a large, harmonized BP cohort was assessed to identify clinical risk factors for suicide death and attempt which then directed testing of underlying polygenic risks. 5901 individuals of European ancestry were assessed: 353 individuals with BP and 2498 without BP who died from suicide (BPS and NBPS, respectively) from a population-derived sample along with a volunteer-derived sample of 799 individuals with BP and a history of suicide attempt (BPSA), 824 individuals with BP and no prior attempts (BPNSA), and 1427 individuals without several common psychiatric illnesses per self-report (C). Clinical and subsequent directed genetic analyses utilized multivariable logistic models accounting for critical covariates and multiple testing. There was overrepresentation of diagnosis of PTSD (OR = 4.9, 95%CI: 3.1–7.6) in BPS versus BPSA, driven by female subjects. PRS assessments showed elevations in BPS including PTSD (OR = 1.3, 95%CI:1.1–1.5, versus C), female-derived ADHD (OR = 1.2, 95%CI:1.1–1.4, versus C), and male insomnia (OR = 1.4, 95%CI: 1.1–1.7, versus BPSA). The results provide support from genetic and clinical standpoints for dysregulated traumatic response particularly increasing risk of suicide death among individuals with BP of Northern European ancestry. Such findings may direct more aggressive treatment and prevention of trauma sequelae within at-risk bipolar individuals.
Similar content being viewed by others
Dissecting clinical heterogeneity of bipolar disorder using multiple polygenic risk scores
Key subphenotypes of bipolar disorder are differentially associated with polygenic liabilities for bipolar disorder, schizophrenia, and major depressive disorder

Clinical and genetic validity of quantitative bipolarity
Introduction.
Suicidal behavior, which can be defined in many ways, is here defined as behaviors that include suicide attempt and death by suicide [ 1 ]. Prior suicide attempt is consistently one of the strongest predictors of eventual death by suicide [ 2 , 3 ]. However, the vast majority of individuals that attempt suicide will not die by suicide. Only ~2.8% of individuals with at least one prior suicide attempt die by suicide [ 4 ]. Despite this, existing research on suicidal behavior primarily focuses on the evaluation of suicide attempt under the assumption that attempt acts as an adequate proxy for suicide death. Distinguishing factors important to suicide attempt versus suicide death will be crucial to the implementation of effective interventions to those most likely to die.
Patients with bipolar disorder (BP) have high rates of suicide attempt (30–50%) and death (15–20%) [ 5 , 6 , 7 ]. The rates for attempt and death are approximately twice those seen for major depression [ 5 , 8 ] and the rate of death is greater than in any disorder except schizophrenia [ 9 ]. These features suggest potential elevation of biological risk of suicide specific to BP. For this study, we leveraged the largest cohort of population-ascertained suicide decedents available, representing over 7000 individuals collected over two decades in the state of Utah [ 10 ]. The majority of these subjects have genetic data available via array genotyping. Electronic health records (EHRs) of these subjects allowed for the identification of 353 individuals with BP who died by suicide. In addition to this unique sample, we utilized a large array-genotyped NIMH Genetics Initiative sample ( N = 3050) including individuals with diagnosed BP, with and without a history of suicide attempt, and a comparison group that was screened for several common psychiatric illnesses via self-report [ 11 , 12 , 13 , 14 ]. Together, these cohorts allowed a comprehensive study of clinical and hypothesis-driven genetic risk factors for suicide death in bipolar disorder and allowed for differentiation of risk factors between attempt and death.
Materials and methods
Sample selection.
Two distinct sample sets were utilized. The first was composed of >7000 population-ascertained individuals who died from suicide from the Utah Suicide Genetics Research Study (USGRS). These samples were collected through a collaboration with the Utah Medical Examiner’s office and have been securely linked to electronic health record (EHR) information via the Utah Population Database (UPDB), a statewide data resource of demographic and health information ( https://healthcare.utah.edu/huntsmancancerinstitute/research/updb ). Because the study design involved analysis of EHR followed by hypothesis-driven analyses of polygenic risk, a subset of 2851 suicide deaths with screened genome-wide genotyping data and who were linked to existing EHR data (see supplementary methods) were retained. Inpatient and ambulatory EHRs were obtained from Utah providers covering approximately 85% of the state, though they may not represent all health records for each individual. After EHR linking, identifying data were stripped before providing data to the research team; suicide cases were referenced by anonymous IDs. The individuals selected for this study had at least one prior diagnostic code for bipolar disorder (specifically bipolar I or bipolar NOS). EHR were also screened for schizophrenia diagnoses and these Individuals were removed from the BP group to increase the probability of diagnostic homogeneity. All individuals excluded from diagnosis in the BP suicide death group were also excluded from the non-BP suicide deaths to ensure that no known BP diagnoses (including diagnoses of cyclothymia, manic depressive disorder, and bipolar II) would be present within the non-BP suicide death group. A total of 353 individuals with BP who died from suicide (referred to as “BPS”) and 2498 individuals without a diagnosis of BP who died from suicide (referred to as “NBPS”) from Utah were included in the analyses. This sample represents the single largest known genotyped sample of BP suicide deaths and, in a post-hoc evaluation of power, was predicted to have 80% power to identify a clinical diagnostic difference between suicide death and comparison groups with an odds ratio of 1.7 as calculated via the UCSF online sample size calculator [ 15 ].
The second set of individuals was composed of a pre-existing de-identified genotyped dataset derived from the NIMH genetics initiative bipolar GWAS [ 11 , 12 , 13 , 16 ] with a history of bipolar I or schizoaffective, bipolar type diagnoses as determined by formal evaluation and best-estimate diagnosis meeting criteria from the DSM-IIIR [ 17 ] or DSM-IV [ 18 ]. These individuals were selected for having complete clinical information from interview evaluation (individuals with missing information were excluded from this study). It is noted that interviews did not systematically evaluate for all included diagnoses, and that information from collected medical records and family informants that were used to support diagnoses were not available for all subjects (see Supplementary materials for more specific details of collected subject data). Individuals with a diagnosis of bipolar disorder and a history one or more suicide attempts ( N = 799, referred to as “BPSA”) and individuals with a diagnosis of BP and no history of prior suicide attempt ( N = 824, referred to as “BPNSA”) were selected for inclusion in the study with diagnostic and historical data being obtained via the Diagnostic Interview for Genetic Studies (DIGS v4) [ 19 ]. A comparison group of individuals who were screened for several common psychiatric disorders via self-report [ 14 ] were also included ( N = 1427, referred to as “C”). Briefly, screened illnesses excluded at the time of sample construction included major depression, psychosis, and bipolar disorder [ 12 ]. This sample has been described elsewhere (including acquisition and quality control efforts), noting that informed consent and appropriate IRB approval for all involved subjects was obtained in the original studies [ 11 , 12 , 13 , 14 ].
Utah suicide decedent DNAs were extracted from whole blood, and were genotyped using the Illumina Infinium PsychArray ( https://www.illumina.com/products/by-type/microarray-kits/infinium-psycharray.html ) as described elsewhere [ 10 ]. DNAs from the NIMH BP and control populations were extracted from lymphoblastoid cell lines maintained at the NIMH DNA Repository (Infinite biologics, Rutgers RUCDR, https://www.rucdr.org/ ), and were genotyped using the Affymetrix Genome-Wide Human SNP Array 6.0 ( https://www.thermofisher.com/us/en/home/life-science/microarray-analysis/affymetrix.html ) and processed as previously described [ 12 , 16 , 20 ,]. Shared high-quality called variants from both platforms were combined and imputed via the Michigan Imputation Server [ 21 ] to a total of 7 437 997 high quality imputed variants. Extensive quality control steps, including assessment for ancestry and relatedness, were utilized to prepare this sample for analysis (see Supplementary methods ). Due to sensitivity of polygenic risk scores to ancestry effects, this study focused only on individuals of >90% European ancestry.
Analysis of sample characteristics
Statistical evaluation of the distribution of sex, age, education level, and clinical categories across all comparison groups were evaluated by chi-square (sex, education, clinical categories) or ANOVA (age).
Analyses of clinical data
Five clinical diagnostic categories were constructed from available diagnoses based on consensus of M.D./Ph.D.-level clinicians (E.M., B.K., A.D.) for all subjects with full details within the Supplementary methods and Supplementary Table S1 . Briefly, these categories represented non-traumatic anxiety disorders, behavioral disorders, personality disorders, eating disorders, and PTSD. The primary clinical analysis compared BPS, BPSA, and BPNSA within these categories.
All clinical categories were also secondarily evaluated to determine if observed effects were specific to BPS. NBPS were compared with BPS for these assessments.
All clinical analyses utilized logistic multivariable regression in R [ 22 ] accounting for age, sex, and education level. All variables were derived from single, independent measures for each subject. It was also noted that BPS had considerably more clinical diagnoses, on average, than NBPS, necessitating the inclusion of a clinical diagnosis count covariate within analyses comparing these groups. Effect size estimates were calculated via adjusted odds ratio from each model. Correction for multiple testing of 15 primary and 30 sex-specific clinical analyses utilized the Benjamini–Hochberg method with a false discovery rate of 0.05.
Analyses of genetic data
PRS calculations of several phenotypes, selected via significant clinical analysis results, were generated from 9 GWAS datasets (19 PRS total). Summary GWAS data arose from meta-analyses with publicly available summary statistics for ADHD [ 23 , 24 ], anxiety [ 25 ], insomnia [ 26 ], PTSD [ 27 ], suicide attempt [ 28 ], and neuroticism [ 29 ]. Many of these sets included summary statistics for population subsets, including male- and female-only analyses, referred to here as “sex-derived” sets, which were also analyzed. Suicide death PRS was calculated from the USGRS suicide death GWAS using a cross-validation approach described elsewhere [ 10 ]. Suicide attempt in bipolar disorder PRS were calculated from published Psychiatric Genomic Consortium data [ 28 ] with all overlapping study subjects removed. PRS calculations were conducted using PRSice 2.0 [ 30 ] with a p -value threshold of 1.0 as described in the Supplemental note. All PRS were standardized to Z-scores prior to statistical analysis.
Pairwise comparisons of BPS, BPSA, BPNSA, and C utilized multivariable logistic regression models in R [ 22 ], accounting for age, sex, and the first 10 principal components to control for residual ancestry effects. As with the clinical variables and covariates, all variables were obtained from independent measures without duplication. PRS measures were evaluated to have similar variance across groups during assessment and as visualized in plots. Effect size estimates were calculated by adjusted odds ratio from each model. Correction for multiple testing of 114 primary and 204 sex-specific PRS analyses utilized Benjamini–Hochberg calculations with a false discovery rate of 0.05.
Sample evaluation
Sample demographics, including frequency of comorbid diagnoses within the defined clinical categories and statistical evaluation of the distribution across the groups for each demographic are outlined in Table 1 . It is noted that the groups varied from one another significantly, but particularly striking differences can be appreciated in the sex distribution of each group. These differences are consistent with expectations that more males than females die from suicide, and more females than males attempt suicide [ 31 ]. However, it is notable that the excess of male deaths was significantly lower in BPS when compared to NBPS (62.0% of BPS being male versus 79.5% of NBPS being male, OR = 0.42, 95%CI = 0.33–0.53; X 2 = 54.1, P = 1.9 × 10 –13 ).
Clinical analyses of BPS, BPSA, and BPNSA
Complete results can be viewed within Supplementary Tables S2 and S3 with odds ratios and confidence intervals displayed in Fig. 1 . All results are corrected for multiple testing and covariates. BPS versus BPSA showed overrepresentation for diagnoses of PTSD (OR = 4.9, 95%CI = 3.1–7.6; P = 6.0 × 10 −11 ), personality disorders (OR = 4.6, 95%CI = 3.0–7.0; P = 2.2 × 10 −11 ; noting the caveat discussed in the limitations), and non-traumatic anxiety disorders (OR = 2.0, 95%CI = 1.4–2.8; P = 1.3 × 10 −4 ). Eating disorder diagnoses were significantly reduced within BPS versus BPSA (OR = 0.2, 95%CI = 0.1–0.4; P = 2.2 × 10 −6 ). No comparisons were significant between BPSA and BPNSA.
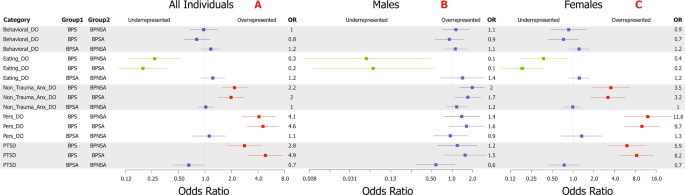
Forest plot distribution of corrected odds ratios of the primary clinical category comparisons (with 95% confidence interval represented by whiskers) within all individuals ( A ), males ( B ), and females ( C ). Labeling of comparison groups is as follows: BPS = individuals with bipolar disorder who died by suicide, BPSA = individuals with bipolar disorder who have a history of one or more suicide attempts, and BPNSA = individuals with bipolar disorder who have no history of a suicide attempt. Significant results are colored with overrepresentation shown in red and underrepresentation in green. Non-significant results are shown in blue. Results were corrected for multiple testing via the Benjamini–Hochberg method with an FDR of 0.05 for a total of 15 tests in the primary analysis ( A ) and 30 in the sex-specific analyses ( B , C ) and for critical covariates.
Secondary sex-specific results are shown in Fig. 1 B and C . Females strongly drove overrepresentations of PTSD (OR = 8.2, 95%CI = 4.7–14.4; P = 3.4 × 10 −11 ), personality disorder (OR = 9.7, 95%CI = 5.5–17.4; P = 4.5 × 10 −13 ), and non-traumatic anxiety disorder (OR = 3.2, 95%CI = 1.7–5.7; P = 6.1 × 10 −4 ) in BPS versus BPSA. Females also drove the reduced rate of eating disorder diagnoses in BPS versus BPSA (OR = 0.2, 95%CI = 0.1–0.4; P = 1.1 × 10 −5 ). Though male BPS versus male BPSA showed nominal overrepresentation of non-traumatic anxiety disorders, personality disorders, and PTSD, none of these results survived correction for multiple testing.
Clinical analysis of BPS versus NBPS
Comparisons are shown in Fig. 2 with complete results in Supplementary Tables S4 and S5 . Even after correction for medical record completeness and years of education, BPS were elevated versus NBPS for all comorbid psychiatric diagnoses, including within sex-specific analyses (except for the male eating disorders comparison). The strongest elevations were noted within personality disorders (OR = 3.6, 95%CI = 2.6–5.1; P = 9.1 × 10 −13 ) and behavioral disorders (OR = 3.1, 95%CI = 2.3–4.3; P = 1.3 × 10 −11 ). In addition, findings show similar effect sizes within the sex-specific comparisons (Fig. 2 B and C ), regardless of sex, though all diagnoses were seen at higher frequencies within females, both within the BPS and NBPS.
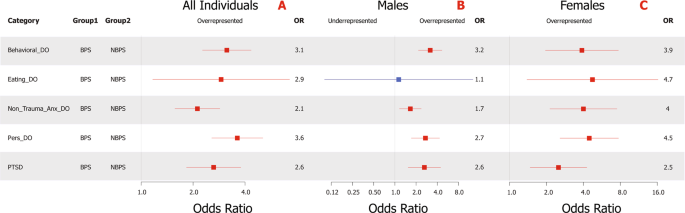
Forest plot distribution of corrected odds ratios of the suicide-only clinical category comparisons (with 95% confidence interval represented by whiskers) within all subjects ( A ), male subjects ( B ), and female subjects ( C ). Labeling of comparison groups is as follows: BPS = individuals with bipolar disorder who died by suicide and NBPS = individuals without a diagnosis of bipolar disorder who died from suicide. Significant results are colored with overrepresentation shown in red and underrepresentation in green. Non-significant results are shown in blue. Results were corrected for multiple testing via the Benjamini–Hochberg method with an FDR of 0.05 for a total of 5 tests in the primary analysis ( A ) and 10 in the sex-specific analyses ( B , C ) and for critical covariates.
Genetic risk analysis across BPS, BPSA, BPNSA, and C
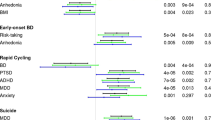
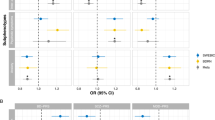
See Figs. 3 and 4 with full results in Supplementary Tables S6 and S7 .
Suicide attempt in MDD and BP and suicide death PRS.
Suicide death PRS (Fig. 3A ) was elevated in BPS versus BPSA (OR = 1.6, 95%CI = 1.4–1.9; P = 7.8 × 10 −10 ). Suicide attempt in BP PRS (Fig. 3B ) showed elevations in BPS versus BPNSA (OR = 1.5, 95%CI = 1.3–1.8; P = 1.9 × 10 −6 ) and BPSA versus BPNSA (OR = 1.5, 95%CI = 1.3–1.6; P = 1.1 × 10 −11 ). Suicide attempt in BP was also reduced in BPNSA versus C (OR = 0.7, 95%CI = 0.7–0.8; P = 4.2 × 10 −8 ). PRS for suicide attempt within major depressive disorder (Fig. 3C ) was elevated in BPS compared with all comparison groups, including versus BPSA (OR = 1.3, 95%CI = 1.1–1.6; P = 1.8 × 10 −2 ).
Anxiety, and neuroticism PRS.
Anxiety (Fig. 3D ; OR = 1.2, 95%CI = 1.1–1.3, P = 1.8 × 10 −2 ) and neuroticism (worry subcluster, not shown; OR = 1.2, 95%CI = 1.1–1.3, P = 6.0 × 10 −3 ) showed elevated PRS in BPSA versus C. Notably, PRS for anxiety and neuroticism also showed either significant or nominal elevation in BPS, BPSA, and BPNSA versus C, and ad-hoc comparisons of BPS, BPSA, and BPNSA combined into a single comparison group versus C showed P = 5.6 × 10 –5 for anxiety and 3.8 × 10 −4 for neuroticism.
PTSD and behavioral PRS.
The PTSD GWAS published summary statistics for males, females, and all subjects [ 27 ]. All-subject (not shown; OR = 1.3, 95%CI = 1.1–1.5, P = 7.8 × 10 −3 ) and male-derived PTSD PRS (Fig. 4A ; OR = 1.3, 95%CI = 1.1–1.5, P = 8.0 × 10 −3 ) were elevated within BPS versus C. Female-derived PTSD PRS (Fig. 4B ), however, was elevated in both BPSA versus C (OR = 1.2, 95%CI = 1.1–1.3, P = 3.6 × 10 −3 ) and BPS versus C (OR = 1.2, 95%CI = 1.1–1.4, P = 2.5 × 10 −2 ). None of these comparisons remained significant in sex-specific analyses, but effect sizes were similar.
Female-derived ADHD PRS (Fig. 4C ) was elevated within BPS versus C (OR = 1.2, 95%CI = 1.1–1.4, P = 2.0 × 10 −2 ).
Sex-specific PRS.
Sex-specific PRS analyses (Supplementary Table S7 ) generally reproduced findings with similar effect sizes in both sexes, but often did not survive correction for multiple testing in the setting of smaller comparison groups. One new finding was identified, however: male-specific polygenic risk for insomnia (daytime napping subgroup, Fig. 4D ) was elevated in BPS versus BPSA with OR = 1.4, 95%CI = 1.1–1.7, P = 4.3 × 10 −2 .
BPS versus NBPS PRS.
PRS analyses of BPS versus NBPS (Supplementary Tables S8 – S9 ) showed no significant differences between groups, including within sex-specific analyses.
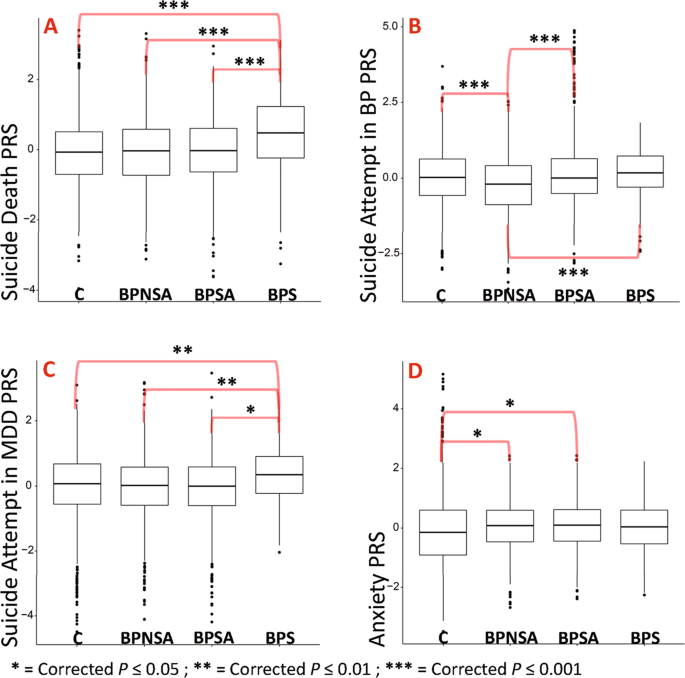
Box plot representations of the top findings from polygenic risk score association testing. Each plot represents comparison group ( x -axis) versus standardized polygenic risk score for the given phenotype ( y -axis). A Suicide death PRS. B Suicide attempt in bipolar disorder PRS. C Suicide attempt in MDD PRS. D Anxiety PRS. Comparison group definitions: BPS = individuals with bipolar disorder who died by suicide, BPSA = individuals with bipolar disorder who have a history of one or more suicide attempts, BPNSA = individuals with bipolar disorder who have no history of a suicide attempt, and C = comparison individuals without several common psychiatric illnesses per self-report [ 14 ]. Selected results shown; all displayed results have been corrected for multiple testing (Benjamini–Hochberg method with FDR of 0.05 correcting for 114 tests for all displayed results) and account for critical covariates. All shown results arose from evaluating all subjects (male and female).
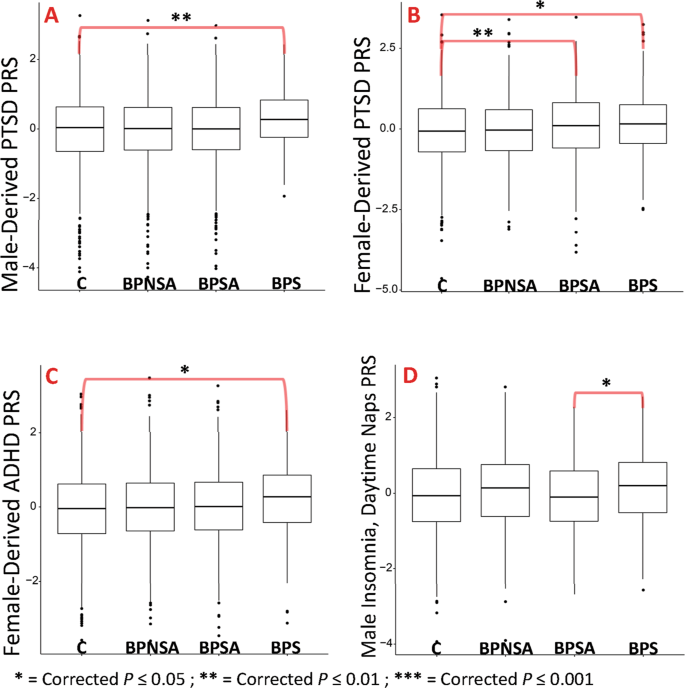
Box plot representations of the top findings from polygenic risk score association testing. Each plot represents comparison group ( x -axis) versus standardized polygenic risk score for the given phenotype ( y -axis). A Male-derived PTSD PRS. B Female-derived PTSD PRS. C Female-derived ADHD PRS. D Male only (sex-specific) insomnia (daytime napping subgroup) PRS. Comparison group definitions: BPS = individuals with bipolar disorder who died by suicide, BPSA = individuals with bipolar disorder who have a history of one or more suicide attempts, BPNSA = individuals with bipolar disorder who have no history of a suicide attempt, and C = comparison individuals without several common psychiatric illnesses per self-report [ 14 ]. Selected results shown; all displayed results have been corrected for multiple testing (Benjamini–Hochberg method with FDR of 0.05 correcting for 114 tests for A – C and 204 tests for D ) and account for critical covariates. Note that sex-derived refers to PRS calculated based on weighted results from the given sex in the original GWAS. All results were evaluated from all (male and female) subjects in the current study with the exception of D , which was an evaluation of only males.
Suicide attempt is often used as a proxy for suicide death and, as such, frequently serves as the primary phenotype within studies of suicide. Suicide attempts and deaths, however, are separate groups that overlap. The unique resource of the USGRS dataset allowed more thorough exploration of suicide death within BP, identifying several potentially important clinical and genetic associations that may aid in identifying and differentiating those at highest risk for suicide attempt and death.
The role of trauma and its enduring effects in suicidal behavior
This study is the first, to our knowledge, to identify combined clinical and genetic evidence of factors that may distinguish risk for suicide death from attempt in BP. Specifically, PTSD and personality disorder diagnoses were strongly elevated in BPS versus BPSA. In addition, clinically informed genetic analyses identified elevated polygenic risk for PTSD in BPS. Trauma, and subsequent response, is a common factor in these findings. A history of trauma is required for PTSD [ 32 ] and is correlated with a more severe course [ 33 ] with an increased risk for suicidal behavior in BP [ 34 , 35 ]. Trauma is also frequently present in personality disorders [ 32 ] which are associated with suicidal behavior [ 36 ] and often comorbid with PTSD [ 37 ].
Such findings may also provide unifying support for the role of stress response pathways such as the hypothalamic pituitary axis (HPA) [ 38 ]. Prior evidence suggests that genetic disruption of the HPA-axis may interact with trauma/severe stress exposure to increase risk for suicide attempt [ 39 ]. This study provides novel evidence that traumatic disruption may increase risk of death from suicide. Indeed, recent evidence has arisen that early-life traumatic exposure in the setting of elevated polygenic risk for BP is significantly correlated with an increase in suicide attempts [ 40 ]. Taken together, the clinical and genetic findings of this study support the long-standing stress-diathesis model for suicidal behavior in BP [ 41 ], and specifically extend those findings to risk for suicide death.
Data from this study also demonstrate potentially important sex-related differences, with trauma-related diagnoses being driven by female BPS. In contrast, males and female BPS demonstrate relatively equal effects within polygenic risk for PTSD. This suggests potential differences in care seeking or clinical presentation in males that may not lead to the same diagnoses. BPS also showed elevated male- and female-derived PTSD PRS, but BPSA was only significantly associated with the female-derived PTSD PRS. This may indicate that genetic loci that interact with certain types of trauma, such as military trauma exposures identified within males of the PTSD GWAS [ 27 ], may be more closely associated with suicide death risk than attempt.
Finally, the clinical evaluation of BPS versus NBPS showed a striking overrepresentation of comorbid diagnoses, particularly trauma-associated diagnoses, but polygenic risk comparison yielded no significant findings. It is possible that genetic liability among BPS and NBPS is similar, but patients diagnosed with BP may receive additional clinical evaluation leading to identification of comorbid diagnoses such as PTSD.
Other potential risk factors
The clinically directed genetic analyses generated novel correlations of ADHD and insomnia polygenic risk in BPS versus C. ADHD diagnosis was also overrepresented in BPS versus NBPS. ADHD has been shown to be correlated with suicidal behavior [ 42 ] and may increase risk when comorbid with BP [ 43 ]. Together, ADHD and BP could be theorized to increase risk for “impulsive aggression”, a potentially important risk factor for suicidal behavior [ 44 ]. Insomnia has also been correlated with increased suicide behavior risk [ 45 ] and may be an important predictive factor for the presence of comorbid disease, such as PTSD [ 46 ]. It is notable that in comparing BPS to NBPS, 44.8% versus 18.3% of females and 28.4% versus 13.2% of males had a concurrent diagnosis of insomnia, respectively. This suggests that female BPS are more frequently diagnosed with insomnia despite a male-driven genetic finding, which may indicate sex-specific differences in diagnosis or care seeking.
Limitations
This study had several limitations. Among these is modest sample size, though the assessed sample of BPS is the largest known sample of its kind. Also, replication is currently not possible as no comparable BPS sample is currently known to exist. Though not the focus of this study, efforts are also underway to collect larger BPSA and BPNSA samples with clinical data to allow more effective comparisons of these groups.
The use of two distinct cohorts introduced several potential limitations. Different genotyping arrays led to a limited number of overlapping variants, somewhat limiting the efficacy of imputation and PRS calculation. In addition, population ascertainment differed substantially: a general population sample (USGRS) versus an assembled research sample (NIMH), both with strengths but potentially biased comparisons. For example, the USGRS samples were not evaluated with a comprehensive diagnostic interview, potentially missing important comorbidities and weakening current associations. It must also be noted that diagnoses within a population sample arise only through individuals seeking clinical encounters and are less likely to represent every diagnosis an individual might have. This leads to a high likelihood that individuals with undiagnosed BP may be present within NBPS, potentially weakening comparisons between these groups. Conversely, the NIMH sample represents voluntary cohorts that may not adequately reflect the general population, but who were rigorously assessed by multiple providers via a consistent, extensive questionnaire to provide best estimate diagnoses. Despite this rigorous evaluation, however, all potentially relevant comorbidities, and particularly the personality disorders other than antisocial personality disorder, were not systematically evaluated as part of the core questionnaire, being identified through family informant, medical records, and early life trauma evaluation which were not available for all subjects. Indeed, it was noted that <1% of BP individuals within the NIMH cohort were diagnosed with borderline personality disorder, though a recent meta-analysis of the frequency of comorbid borderline personality disorder in bipolar disorder predicted an average of 21.6% [ 47 ], suggesting that many diagnoses may have been missed in this cohort. Finally, the evaluation of only Northern European subjects limits the generalizability of this study and was necessitated by a limited number of samples from other ethnicities. Ongoing efforts to collect a larger, more diverse, and cohesive sample are underway. Despite these inherent challenges, however, it is notable that the comparison of such datasets is necessitated by the relative rarity of these phenotypes (particularly suicide death) and is supported by evidence of a convergent finding within clinical and genetic data evaluations of prior trauma as a potential factor in suicide death risk in BP, illustrating the potential power of this complimentary approach.
This study represents the first large-scale evaluation of suicide death in BP to utilize a combined clinical and genetic approach. In identifying converging evidence of factors specifically associated with suicide death, particularly prior trauma and its associated phenotypes, this study provides potentially tractable targets for future evaluation and indicates the need to specifically collect and evaluate individuals who have died from suicide to best characterize risk factors for this preventable outcome. Findings may serve to improve current screening measures for suicide death risk and, ultimately, help reduce death by suicide.
Turecki G, Brent DA, Gunnell D, O'Connor RC, Oquendo MA, Pirkis J, et al. Suicide and suicide risk. Nat Rev Dis Primers. 2019;5:74. https://doi.org/10.1038/s41572-019-0121-0.
Article PubMed Google Scholar
Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry. 2002;181:193–9. https://doi.org/10.1192/bjp.181.3.193.
Bostwick JM, Pabbati C, Geske JR, McKean AJ. Suicide attempt as a risk factor for completed suicide: even more lethal than we knew. Am J Psychiatry. 2016;173:1094–100. https://doi.org/10.1176/appi.ajp.2016.15070854.
Article PubMed PubMed Central Google Scholar
Hawton K, Fagg J. Suicide, and other causes of death, following attempted suicide. Br J Psychiatry. 1988;152:359–66. https://doi.org/10.1192/bjp.152.3.359.
Article CAS PubMed Google Scholar
Valtonen H, Suominen K, Mantere O, Leppämäki S, Arvilommi P, Isometsä ET. Suicidal ideation and attempts in bipolar I and II disorders. J Clin Psychiatry. 2005;66:1456–62.
Article Google Scholar
Gonda X, Pompili M, Serafini G, Montebovi F, Campi S, Dome P, et al. Suicidal behavior in bipolar disorder: epidemiology, characteristics and major risk factors. J Affect Disord. 2012;143:16–26. https://doi.org/10.1016/j.jad.2012.04.041.
Miller JN, Black DW. Bipolar disorder and suicide: a review. Curr Psychiatry Rep. 2020;22:6. https://doi.org/10.1007/s11920-020-1130-0.
Chen YW, Dilsaver SC. Lifetime rates of suicide attempts among subjects with bipolar and unipolar disorders relative to subjects with other Axis I disorders. Biol. psychiatry. 1996;39:896–9. https://doi.org/10.1016/0006-3223(95)00295-2.
Yeh HH, Westphal J, Hu Y, Peterson EL, Williams LK, Prabhakar D, et al. Diagnosed mental health conditions and risk of suicide mortality. Psychiatr. Serv. 2019;70:750–7. https://doi.org/10.1176/appi.ps.201800346.
Docherty AR, Shabalin AA, DiBlasi E, Monson E, Mullins N, Adkins DE, et al. Genome-wide association study of suicide death and polygenic prediction of clinical antecedents. Am J Psychiatry. 2020;177:917–27. https://doi.org/10.1176/appi.ajp.2020.19101025.
Genomic survey of bipolar illness in the NIMH genetics initiative pedigrees: a preliminary report. Am J Med. Genet. 1997;74:227–37.
Smith EN, Bloss CS, Badner JA, Barrett T, Belmonte PL, Berrettini W, et al. Genome-wide association study of bipolar disorder in European American and African American individuals. Mol Psychiatry. 2009;14:755–63. https://doi.org/10.1038/mp.2009.43.
Article CAS PubMed PubMed Central Google Scholar
McMahon FJ, Akula N, Schulze TG, Muglia P, Tozzi F, Detera-Wadleigh SD, et al. Meta-analysis of genome-wide association data identifies a risk locus for major mood disorders on 3p21.1. Nat Genet. 2010;42:128–31. https://doi.org/10.1038/ng.523.
Sanders AR, Levinson DF, Duan J, Dennis JM, Li R, Kendler KS, et al. The Internet-based MGS2 control sample: self report of mental illness. Am. J. psychiatry. 2010;167:854–65. https://doi.org/10.1176/appi.ajp.2010.09071050.
Kohn MA, S. J. Sample Size Calculators , 2021, https://sample-size.net/sample-size-proportions/ .
Willour VL, Seifuddin F, Mahon PB, Jancic D, Pirooznia M, Steele J, et al. A genome-wide association study of attempted suicide. Mol Psychiatry. 2012;17:433–44. https://doi.org/10.1038/mp.2011.4.
American Psychiatric Association. Desk reference to the diagnostic criteria from DSM-III . American Psychiatric Association; 1982.
American Psychiatric Association. Diagnostic criteria from DSM-IV . The Association; 1994.
Nurnberger JI Jr, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, et al. Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH Genetics Initiative. Arch Gen Psychiatry. 1994;51:849–59. discussion 863-844.
Smith EN, Koller DL, Panganiban C, Szelinger S, Zhang P, Badner JA, et al. Genome-wide association of bipolar disorder suggests an enrichment of replicable associations in regions near genes. PLoS Genet. 2011;7:e1002134. https://doi.org/10.1371/journal.pgen.1002134.
Das S, Forer L, Schönherr S, Sidore C, Locke AE, Kwong A, et al. Next-generation genotype imputation service and methods. Nat Genet. 2016;48:1284–7. https://doi.org/10.1038/ng.3656.
R: A Language and Environment for Statisitcal Computing (R Foundation for Statistical Computing, Vienna, Austria, 2020).
Martin J, Walters RK, Demontis D, Mattheisen M, Lee SH, Robinson E, et al. A genetic investigation of sex bias in the prevalence of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2018;83:1044–53. https://doi.org/10.1016/j.biopsych.2017.11.026.
Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E, et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat Genet. 2019;51:63–75. https://doi.org/10.1038/s41588-018-0269-7.
Otowa T, Hek K, Lee M, Byrne EM, Mirza SS, Nivard MG, et al. Meta-analysis of genome-wide association studies of anxiety disorders. Mol. Psychiatry. 2016;21:1391–9. https://doi.org/10.1038/mp.2015.197.
Jansen PR, Watanabe K, Stringer S, Skene N, Bryois J, Hammerschlag AR, et al. Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways. Nat. Genet. 2019;51:394–403. https://doi.org/10.1038/s41588-018-0333-3.
Nievergelt CM, Maihofer AX, Klengel T, Atkinson EG, Chen CY, Choi KW, et al. International meta-analysis of PTSD genome-wide association studies identifies sex- and ancestry-specific genetic risk loci. Nat Commun. 2019;10:4558. https://doi.org/10.1038/s41467-019-12576-w.
Mullins N, Bigdeli TB, Børglum AD, Coleman J, Demontis D, Mehta D, et al. GWAS of suicide attempt in psychiatric disorders and association with major depression polygenic risk scores. Am J Psychiatry. 2019;176:651–60. https://doi.org/10.1176/appi.ajp.2019.18080957.
Nagel M, Jansen PR, Stringer S, Watanabe K, de Leeuw CA, Bryois J, et al. Meta-analysis of genome-wide association studies for neuroticism in 449,484 individuals identifies novel genetic loci and pathways. Nat Genet. 2018;50:920–7. https://doi.org/10.1038/s41588-018-0151-7.
Euesden J, Lewis CM, O’Reilly PF. PRSice: polygenic risk score software. Bioinformatics. 2015;31:1466–8. https://doi.org/10.1093/bioinformatics/btu848.
Schrijvers DL, Bollen J, Sabbe BG. The gender paradox in suicidal behavior and its impact on the suicidal process. J Affect Disord. 2012;138:19–26. https://doi.org/10.1016/j.jad.2011.03.050.
American Psychiatric Association. & American Psychiatric Association. DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5 . 5th edn, American Psychiatric Association, 2013.
Etain B, Aas M, Andreassen OA, Lorentzen S, Dieset I, Gard S, et al. Childhood trauma is associated with severe clinical characteristics of bipolar disorders. J Clin Psychiatry. 2013;74:991–8. https://doi.org/10.4088/JCP.13m08353.
Schaffer A, Isometsä ET, Azorin JM, Cassidy F, Goldstein T, Rihmer Z, et al. A review of factors associated with greater likelihood of suicide attempts and suicide deaths in bipolar disorder: Part II of a report of the International Society for Bipolar Disorders Task Force on Suicide in Bipolar Disorder. Aust N Z J Psychiatry. 2015;49:1006–20. https://doi.org/10.1177/0004867415594428.
Park, YM, Shekhtman, T, Kelsoe, JR. Effect of the Type and Number of Adverse Childhood Experiences and the Timing of Adverse Experiences on Clinical Outcomes in Individuals with Bipolar Disorder. Brain Sci. 2020;10: https://doi.org/10.3390/brainsci10050254 .
Hawton, K & Heeringen, K v. The International Handbook of Suicide and Attempted Suicide . Wiley; 2000.
Jowett S, Karatzias T, Albert I. Multiple and interpersonal trauma are risk factors for both post-traumatic stress disorder and borderline personality disorder: a systematic review on the traumatic backgrounds and clinical characteristics of comorbid post-traumatic stress disorder/borderline personality disorder groups versus single-disorder groups. Psychol Psychother. 2020;93:621–38. https://doi.org/10.1111/papt.12248.
Jokinen J, Nordstrom P. HPA axis hyperactivity and attempted suicide in young adult mood disorder inpatients. J Affect Disord. 2009;116:117–20. https://doi.org/10.1016/j.jad.2008.10.015.
Guillaume S, Perroud N, Jollant F, Jaussent I, Olié E, Malafosse A, et al. HPA axis genes may modulate the effect of childhood adversities on decision-making in suicide attempters. J Psychiatr Res. 2013;47:259–65. https://doi.org/10.1016/j.jpsychires.2012.10.014.
Wilcox HC, Fullerton JM, Glowinski AL, Benke K, Kamali M, Hulvershorn LA, et al. Traumatic stress interacts with bipolar disorder genetic risk to increase risk for suicide attempts. J Am Acad Child Adolesc. Psychiatry. 2017;56:1073–80. https://doi.org/10.1016/j.jaac.2017.09.428.
van Heeringen K, Mann JJ. The neurobiology of suicide. Lancet Psychiatry. 2014;1:63–72. https://doi.org/10.1016/S2215-0366(14)70220-2.
Furczyk K, Thome J. Adult ADHD and suicide. Atten Defic Hyperact Disord. 2014;6:153–8. https://doi.org/10.1007/s12402-014-0150-1.
Lan WH, Bai YM, Hsu JW, Huang KL, Su TP, Li CT, et al. Comorbidity of ADHD and suicide attempts among adolescents and young adults with bipolar disorder: a nationwide longitudinal study. J Affect Disord. 2015;176:171–5. https://doi.org/10.1016/j.jad.2015.02.007.
Brent DA, Mann JJ. Family genetic studies, suicide, and suicidal behavior. Am J Med Genet Part C, Semin Med Genet. 2005;133C:13–24. https://doi.org/10.1002/ajmg.c.30042.
McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Curr Psychiatry Rep. 2013;15:389. https://doi.org/10.1007/s11920-013-0389-9.
Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. J Clin Psychol. 2011;67:1240–58. https://doi.org/10.1002/jclp.20845.
Fornaro M, Orsolini L, Marini S, De Berardis D, Perna G, Valchera A, et al. The prevalence and predictors of bipolar and borderline personality disorders comorbidity: Systematic review and meta-analysis. J Affect Disord. 2016;195:105–18. https://doi.org/10.1016/j.jad.2016.01.040.
Download references
Acknowledgements
This study was supported by the American Foundation of Suicide Prevention (AFSP) BSG-1-005-18 (VW and HC); the National Institute of Mental Health, R01MH122412 (HC), R01MH123489 (HC), R01MH123619 (AD), the Clark Tanner Foundation (HC and EM), and the Utah Division of Substance Abuse and Mental Health (HC). Processing of Utah suicide samples was done with assistance from the GCRC M01-RR025764 from the National Center for Research Resources. Genotyping of these samples was done with support from Janssen Research & Development, LLC to the University of Utah. We thank the University of Utah psychiatry residency research track for their support. Partial support for all datasets within the Utah Population Database was provided by the University of Utah Huntsman Cancer Institute. We thank the staff of the Utah Office of the Medical Examiner for their work in making the collection of samples from suicide deaths possible. Please see the Supplementary materials and methods for full NIMH sample acknowledgement.
Author information
Authors and affiliations.
Department of Psychiatry & Huntsman Mental Health Institute, University of Utah, Salt Lake City, UT, USA
Eric T. Monson, Andrey A. Shabalin, Anna R. Docherty, Emily DiBlasi, Amanda V. Bakian, Douglas Gray, Brooks Keeshin, Sheila E. Crowell & Hilary Coon
Department of Family and Preventative Medicine, Division of Public Health, University of Utah, Salt Lake City, UT, USA
Amanda V. Bakian
Neuroscience Therapeutic Area, Janssen Research and Development, Titusville, NJ, USA
Qingqin S. Li
VISN 19 Rocky Mountain MIRECC, George E. Wahlen VA Medical Center, Salt Lake City, UT, USA
Douglas Gray
Department of Pediatrics, University of Utah, Salt Lake City, UT, USA
Brooks Keeshin
Department of Psychology, University of Utah, Salt Lake City, UT, USA
Sheila E. Crowell
Department of Obstetrics and Gynecology, University of Utah, Salt Lake City, UT, USA
Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York City, NY, USA
Niamh Mullins
Department of Genetics and Genomic Sciences, Icahn School of Medicine at Mount Sinai, New York City, NY, USA
Department of Psychiatry, University of Iowa, Iowa City, IA, USA
Virginia L. Willour
Department of Biomedical Informatics, University of Utah, Salt Lake City, UT, USA
Hilary Coon
Division of Genetic Epidemiology, University of Utah, Salt Lake City, UT, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Eric T. Monson .
Ethics declarations
Competing interests.
Dr. Qingqin Li is an investigator at Janssen Research, LLC. No other conflicts of interest or financial disclosures are reported by any of the other authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Online supplement, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Monson, E.T., Shabalin, A.A., Docherty, A.R. et al. Assessment of suicide attempt and death in bipolar affective disorder: a combined clinical and genetic approach. Transl Psychiatry 11 , 379 (2021). https://doi.org/10.1038/s41398-021-01500-w
Download citation
Received : 01 February 2021
Revised : 18 June 2021
Accepted : 23 June 2021
Published : 07 July 2021
DOI : https://doi.org/10.1038/s41398-021-01500-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Integrating summary information from many external studies with population heterogeneity and a study of covid-19 pandemic impact on mental health of people with bipolar disorder.
- Peisong Han
- Melvin G. McInnis
Statistics in Biosciences (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Allkins S Perinatal mental health support in the UK. Br J Midwifery. 2023; 31:(9) https://doi.org/10.12968/bjom.2023.31.9.485
Bergink V, Rasgon N, Wisner K Postpartum psychosis: madness, mania, and melancholia in motherhood. Am J Psychiatry. 2016; 173:(12)1179-1188 https://doi.org/10.1176/appi.ajp.2016.16040454
Huang YC, Chen HH, Yeh ML, Chung YC Case studies combined with or without concept maps improve critical thinking in hospital-based nurses: a randomized-controlled trial. Int J Nurs Stud. 2012; 49:(6)747-754 https://doi.org/10.1016/j.ijnurstu.2012.01.008
Saving lives, improving mothers' care: core report: lessons learned to inform maternity care from the UK and Ireland confidential enquiries into maternal deaths and morbidity 2018–20. 2022. https//www.npeu.ox.ac.uk/assets/downloads/mbrrace-uk/reports/maternal-report-2022/MBRRACE-UK_Maternal_MAIN_Report_2022_v10.pdf
McAllister-Williams RH, Baldwin DS, Cantwell R British association for psychopharmacology consensus guidance on the use of psychotropic medication preconception, in pregnancy and postpartum. J Psychopharmacol. 2017; 31:(5)519-552 https://doi.org/10.1177/0269881117699361
Munk-Olsen T, Lui X, Viktorin A Maternal and infant outcomes associated with Lithium use in pregnancy: an international collaborative meta-analysis of six cohort studies. Lancet Psychiatry. 2018; 5:(8)644-645 https://doi.org/10.1016/S2215-0366(18)30180-9
National Institute for Health and Care Excellence. Bipolar disorder: assessment and management. 2020. https//www.nice.org.uk/guidance/cg185/chapter/Introduction
National Mental Health Division. Specialist perinatal mental health services; a model of care for Ireland. 2017. https//www.hse.ie/eng/services/list/4/mental-healthservices/specialist-perinatal-mental-health
NHS. Pan-London perinatal mental health networks pre-birth planning: best practice toolkit for perinatal mental health services. 2019. https//www.transformationpartnersinhealthandcare.nhs.uk/wp-content/uploads/2019/01/Pre-birth-planning-guidance-for-Perinatal-Mental-Health-Networks.pdf
Noonan M, Doody O, Jomeen J, Galvin R Midwives' perceptions and experiences of caring for women who experience perinatal mental health problems: an integrative review. Midwifery. 2017; 45:56-71 https://doi.org/10.1016/j.midw.2016.12.010
O'Hare MF, Manning E, O'Herlihy CCork: Hackett Retrographics; 2015
Peirson L, Ciliska D, Dobbins M, Mowat D Building capacity for evidence informed decision making in public health: a case study of organizational change. BMC Public Health. 2012; 12:(1) https://doi.org/10.1186/1471-2458-12-137
Ritter PS, Marx C, Bauer M, Lepold K, Pfennig A The role of disturbed sleep in the early recognition of bipolar disorder: a systematic review. Bipolar Disorders. 2011; 13:(3)227-237 https://doi.org/10.1111/j.1399-5618.2011.00917.x
Rosso G, Umberto GA, Di Salvo G Lithium prophylaxis during pregnancy and the postpartum period in women with lithium-responsive bipolar I disorder. Arch Womens Mental Health. 2016; 19:(2)429-432 https://doi.org/10.1007/s00737-016-0601-0
Spinelli MG Postpartum psychosis: detection of risk and management. Am J Psychiatry. 2009; 166:(4)405-408 https://doi.org/10.1176/appi.ajp.2008.08121899
Wesseloo R, Kamperman AM, Munk-Olsen T, Pop VJM, Kushner SA, Bergink V Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry. 2016; 173:(2)117-127 https://doi.org/10.1176/appi.ajp.2015.15010124
Kathleen's journey: improving mental health outcomes for women with bipolar affective disorder
Pauline Walsh
Health Service Executive, Ireland
View articles · Email Pauline
Margaret Graham
Department of Nursing and Midwifery, University of Limerick
View articles
Mas Mahady Mohamad
Health Service Executive, Ireland; School of Medicine, University of Limerick

For most women, pregnancy and the postpartum period are times of great joy and expectation. However, for women with a diagnosis of bipolar affective disorder, there is an exceptionally high risk of deterioration in their mental health. There is the real possibility of developing postpartum psychosis, possibly requiring acute psychiatric admission and being separated from their baby. This can have devastating consequences for a woman, her baby, the family and society. Multiple services/disciplines across primary, secondary and tertiary care settings need to work together to enhance outcomes for these women. In Ireland, a relatively new collaborative way of working is emerging, as specialist perinatal mental health teams are developed. This case review aims to illustrate the complexities of and potential in collaborative team working to support a woman with a pre-existing a mental health disorder, and her family, during pregnancy. This was done through a specialist perinatal mental health teams collaboration co-ordinated by a clinical nurse specialist.
The British Journal of Midwifery's September editorial, ‘perinatal mental health support in the UK’ ( Allkins, 2023 ), highlighted the need to support women with mental health problems during pregnancy. This article focuses on a collaborative approach to supporting a woman with a pre-existing mental health condition.
The development of perinatal mental health services in Ireland is guided by their counterparts internationally, particularly in the NHS. The National Institute for Health and Care Excellence ( NICE, 2020 ) stated that the population risk for bipolar affective disorder is approximately 1%. Nevertheless, for women who have a diagnosis of bipolar affective disorder, there can be significant impact on both the individual and their family. The condition is characterised by periods of depression and periods of hypomania or mania; in some instances there can be features of both depression and mania during the one episode. Common symptoms associated with these mood changes are listed in Table 1 .
Source: NICE, 2020
A systematic review by Wesseloo et al (2016) established that for women with a diagnosis of bipolar affective disorder, there was a relapse risk for 1 in 3 women in the postpartum period. These women were more likely to require inpatient psychiatric admission than women with any other psychiatric diagnosis, including schizophrenia. Ireland has no mother and baby unit ( National Mental Health Division, 2017 ). Therefore, unfortunately, for women with bipolar affective disorder who require inpatient treatment, there is a possibility that they may be admitted to a general adult psychiatry ward, most likely without their baby.
Women with bipolar affective disorder are at increased risk of developing postpartum psychosis, a severe and potentially life-threatening condition for both mother and baby. Approximately 5% of women affected by postpartum psychosis end their life by suicide and 4% commit infanticide ( Spinelli, 2009 ). As a result of the severity of postpartum psychosis and the increased risk to the life of the mother and her baby, all healthcare professionals need to be aware of the symptoms of the condition, in order to identify women who are more at risk of developing it. An estimated 134 women in Ireland experience postpartum psychosis each year, although it is thought this number under-represents the true incidence rates, because of challenges around how diagnoses are reported and recorded in different areas. ( National Mental Health Division, 2017 ).
Interdisciplinary working in perinatal mental health
Given the statistics related to women with bipolar affective disorder, promoting interdisciplinary mental health services is critical across the perinatal period ( Knight et al, 2022 ). The specialist perinatal mental health services, and specifically the clinical nurse specialist, have key roles and responsibilities in the care of women with bipolar affective disorder, which often require them to provide and co-ordinate shared care. The clinical nurse specialist's responsibilities include patient focus, patient advocacy, education and training. The principles of care for pregnant women with bipolar affective disorder include co-ordination across services, with clear responsibilities for each distinct time period outlined ( NICE, 2020 ).
As registered advanced nurse practitioners are introduced to perinatal mental health services in Ireland, it is anticipated that leading and co-ordinating episodes of care for such vulnerable women falls in the remit of registered advanced nurse practitioner. Clinical case reviews have proved valuable in nursing; researchers such as Huang et al (2012) found that they can inform nurses’ decision-making skills during episodes of complex care. Raising midwives’ awareness of risk factors and presentations for mental illness enhances confidence when caring for these women (Noonan et al, 2018). This approach requires healthcare professionals to work in close collaboration and is illustrated though Kathleen's journey, organised around a clinical case study framework ( Box 1 ). Permission was sought from the women involved in this case review, and ‘Kathleen’ is a pseudonym.
Box 1.Case and backgroundKathleen (pseudonym) is a 33-year-old woman, recently married and in her first pregnancy. She lives with her husband and parents, and works 30 hours/week in the family business. She has a diagnosis of bipolar affective disorder, type 1, since the age of 19 years. She has experienced depressive episodes, which featured significant and life-threatening self-harm episodes. During other episodes of depression, she has experienced psychotic symptoms. She has experienced several episodes of hypomania and one episode of mania. Kathleen has been hospitalised for her safety on eight occasions, with one of these admissions being on an involuntary basis. The duration of the admissions ranged from 2 weeks to 4 months. Her last admission was 7 years ago. In the past 7 years, she has remained stable on a pharmacological regime, including lithium 1000mg/day. She planned a pregnancy with her husband but did not discuss this with her adult mental health team and was not offered the pre-conception assessment service from the local specialist perinatal mental health team. Physically, her pregnancy was uncomplicated until approximately 28/40 weeks, when she developed gestational diabetes, which was managed with diet and lifestyle moderations.
Kathleen's journey demonstrating interdisciplinary working
Prior to becoming pregnant, Kathleen was actively engaged with a community mental health team, with attendance every 3 months for review and monitoring of lithium plasma levels. She had not been offered or requested any preconception mental health assessment. When Kathleen became pregnant (discovered at 5/40 weeks) and informed her community mental health team, they immediately linked with the specialist perinatal mental health team to arrange an urgent pharmacological regime review.
Midwifery and obstetric care was under the consultant obstetrician who leads care for women with severe and enduring mental illness. A joint clinic is run with the specialist perinatal mental health team and Kathleen attended both clinics within 3 days of initial contact.
Kathleen was initially assessed by the perinatal consultant psychiatrist and a full history was taken. Specific attention was given to her prescription of lithium (1000 mg/day). This was a long-term prescription since her acute episodes of mania and depression. Once stabilised on this medication 7 years ago, with good quality of life, she experienced no readmissions or relapses, returned to work, started a relationship and became pregnant. However, some studies have associated lithium with a slight increase in birth defects, most commonly cardiac defects, so careful consideration of this medication was needed. Munk-Olsen et al (2018) reported no association between lithium and birth defects. Pharmacological decisions during pregnancy are guided by the British Association for Psychopharmacology's ( McAllister-Williams et al, 2017 ) consensus guidance on the use of psychotropic medication preconception, in pregnancy and postpartum. These guidelines highlight the need to balance the risks to the fetus versus the potential risks/benefits of the medication for the mother, and to consider the risks associated with relapse or untreated perinatal mental illness ( Table 2 ). It was decided that reducing Kathleen's lithium dose could potentially lead to relapse and the risk factors associated with managing an acute episode while pregnant were considered.
Adapted from: McAllister-Williams et al (2017)
Kathleen was advised that her lithium levels would be reviewed or monitored monthly for the first and second trimester, as plasma levels tend to decrease from as early as 6/40 weeks, which could potentially result in sub-therapeutic plasma levels, most likely requiring an increase in lithium ( Rosso et al, 2016 ). At this stage, Kathleen was referred to the clinical nurse specialist in the specialist perinatal mental health team, with the expectation of developing a therapeutic alliance and commencing engagement regarding the pre-birth planning meeting. It was expected that they would work together to develop plans to maintain mental stability, and provide early intervention if any deterioration occurred in mental state during the pregnancy and postpartum periods. Available parenting supports in the local community were explored, and it was decided that the appropriate referrals would be made later in the pregnancy.
Pre-birth planning meeting
A pre-birth planning meeting is a valuable mechanism, bringing together key healthcare professionals with women and their families to plan care for the remainder of pregnancy, hospital admission and the postpartum period ( NHS, 2019 ). Pre-birth planning meetings generally occur around 32/40 weeks and a copy of the minutes from this meeting is kept by all professionals involved. A copy was also held by Kathleen, in her case.
The clinical nurse specialist facilitated Kathleen to outline her mental health history, her early warning signs of relapse and the supports she had available to her. Kathleen's self-efficacy was encouraged and supported to facilitate her to tell her story and be an active participant in her plan of care. The meeting included Kathleen and her husband, the clinical nurse specialist, perinatal consultant psychiatrist and the registrar from the specialist perinatal mental health team. The community mental health nurse, who was familiar with Kathleen and engaged in her care, attended on behalf of the community mental health team. Both the consultant obstetrician and registrar attended, as well as midwives from the antenatal clinic, and the antenatal, labour and postnatal wards. Kathleen's GP and public health nurse were also in attendance. The meeting therefore included professionals across primary, secondary and tertiary services, encompassing obstetrics, mental health and public health services.
This meeting followed the format outlined by the NHS (2019) pre-birth planning: best practice toolkit for perinatal mental health services. One major early warning sign and potential trigger for deterioration of Kathleen's mental state was reduced or disturbed sleep. Kathleen described a relapse pattern where she may be overstimulated, and have difficulty initiating sleep and falling into a deep sleep. This would have a negative impact on her mood and could potentially be a prodrome for a manic episode ( Ritter et al, 2011 ). The risk of postpartum deterioration was discussed in terms of the potential risks to herself and the baby, as well as risks from others to Kathleen. She had a significant history of deliberate self-harm via a potentially lethal method, as well as risks associated with her character, as when she was manic, she behaved in a way that was not in keeping with her personality.
Kathleen's strengths and protective factors were outlined, which included her concordance with the pharmacological regime, the 7-year period of being mentally stable and her engagement with both the specialist perinatal mental health team and community mental health team. Kathleen lived with her husband and parents, who were all supportive towards her in terms of her emotional and physical wellbeing.
The specifics of Kathleen's care for each stage of pregnancy and postpartum were discussed, and key care commitments were made ( Table 3 ).
As is often true for complex cases, some aspects could not be predicted. Kathleen was diagnosed with gestational diabetes, which was well controlled. However, around 38/40 weeks, her blood sugars became harder to regulate. Baby size for gestational age was large and the decision was taken to plan induction. When it began, a lithium level revealed her plasma level was climbing to potentially toxic levels. This necessitated an abrupt withdrawal of lithium while Kathleen was in labour,, with commencement of intravenous fluids to increase hydration and reduce the potential for toxicity. To counter the abrupt withdrawal of lithium, a low dose of an anti-psychotic, Olanzapine, was prescribed.
Kathleen delivered a healthy baby boy 16 hours after induction began and while she did miss some sleep, the Olanzapine aided sleep the following night. Lithium was recommenced on day 1 postpartum, at the pre-pregnancy dose of 1000mg/day with daily lithium level monitoring. Kathleen was facilitated with a quiet single room with less stimulation, her baby was fed overnight, and she was facilitated with increased visiting from her husband and daily reviews by both the obstetric and specialist perinatal mental health team. Her baby was reviewed by the neonatology team, who reported the baby as healthy and well. Kathleen was discharged on day 6 postpartum and was mentally well and stable, having not experiencing any fluctuations in mood.
During each day of admission, the specialist perinatal mental health team liaised with, and provided guidance and support to, midwives on the wards. These midwives were well placed to observe subtle changes in mental state and were informed of what symptoms to look for and the potential impact of any changes to mental state. This specific protected time between the specialist perinatal mental health team and ward midwives facilitated collaboration between the different disciplines, enabling a sharing of knowledge and experience.
Kathleen's outcome was what every mother hopes for; she left the hospital with both herself and her baby healthy and happy. She continues to be mentally well, now 18 weeks’ postpartum. Given the high risk of relapse and the significant potential for a postpartum psychosis, she attributes this outcome to the ‘safety net’ provided by the professionals involved. In this case, individual members of the team worked well together. Different mental health teams provided shared care in a way that was not familiar to them. The obstetric and mental health teams worked side by side, developing and adjusting care plans as required, providing robust care to Kathleen. Midwives in the hospital, and community services engaged with each other, developing new relationships and respect for each other's roles and practices. Community colleagues, such as the public health nurse and GP, engaged with the specialist perinatal mental health, community mental health and obstetric teams in a way that was not familiar to them. All interdisciplinary professionals working in their own fields came together for a common goal, to give Kathleen the best chance to avoid relapse. Kathleen and her family did not experience the trauma of a postpartum relapse.
Conclusions
Pregnancy and the postpartum period are a special time for a woman's life. Women who have enduring severe mental health issues, such as bipolar affective disorder, require support during such a vulnerable time. Women with bipolar affective disorder have the potential to become seriously mentally ill, with possibly devastating consequences for women, babies, families and society in general. As professionals, it is our responsibility to develop our services and respond to meet the needs of these women. This case review demonstrates that when services collaborate, outcomes for vulnerable perinatal women are improved. Discussing Kathleen's journey illustrates the clinical and organisational collaboration with women and their partners during this high-risk time. The case review strives to promote discussion of the complexities surrounding the perinatal health needs and support for women and their families.
‘My baby is 18 weeks old now. I am mentally well and stable. Having all the right mental health and obstetric supports in place supported me to become the mother I hoped and dreamed I would be’ Kathleen
Education and support for midwives is essential in continuing to promote quality care with women with complex needs. It is critical to increase knowledge of the mental healthcare needs of this vulnerable cohort of women among midwives and obstetricians, and similarly for mental health practitioners to increase their understanding of pregnancy and its potential impacts on a woman's mental health.
- When services are open to new ways of working, great work can be done for the benefit of women.
- Pre-birth planning meetings are an essential means of bringing many services together to form a strong safety net for vulnerable populations of women, such as those with bipolar affective disorder.
- Most professionals in healthcare have a goal to achieve good outcomes for patients; bringing together like-minded professionals for the benefit of the patient is a positive experience for all involved.
CPD reflective questions
- Is engaging in this way of team working a new concept?
- What would you foresee these challenges to working in this way?
- What are the potential benefits of working in this way?
- Could you envision working in this way within your healthcare setting?
- How do you think Kathleen felt at the pre-birth planning meeting? In terms of discussing her mental health history and planning for the future?
- Open access
- Published: 15 May 2024
The clinical significance of emotional urgency in bipolar disorder: a scoping review
- Wen Lin Teh 1 , 2 ,
- Sheng Yeow Si 3 ,
- Jianlin Liu 1 ,
- Mythily Subramaniam 1 &
- Roger Ho 2 , 4
BMC Psychology volume 12 , Article number: 273 ( 2024 ) Cite this article
179 Accesses
Metrics details
Emotional urgency, defined as a trait concept of emotion-based impulsivity, is at least moderately associated with general psychopathology. However, its clinical significance and associations with clinically relevant features of bipolar disorder remain unclear. This scoping review aims address this gap by determining the extent of evidence in this niche scope of study.
Evidence of between-group differences of positive and negative urgency, its associations with mood severity, and all peripheral associations related to illness and psychosocial outcomes were synthesized based on PRISMA checklists and guidelines for scoping reviews (PRISMA-ScR).
Electronic databases were searched for articles published between January 2001 and January 2024. A total of 1013 entries were gathered, and a total of 10 articles were included in the final selection after the removal of duplicates and ineligible articles.
Differences in urgency scores between bipolar disorder and healthy controls were large (Cohen’s d ranged from 1.77 to 2.20). Negative urgency was at least moderately associated with overall trauma, emotional abuse, neglect, suicide ideation, neuroticism, and irritable/cyclothymic temperament, whereas positive urgency was at least moderately associated with various aspects of aggression and quality of life. Positive but not negative urgency was associated with quality of life in bipolar disorder.
Large between-group differences found for emotional urgency in bipolar disorder imply large clinical significance. Emotional urgency was associated with worse clinical features and outcomes. Given the high clinical heterogeneity of the disorder, emotional urgency may be an important phenotype indicative of greater disorder severity.
Peer Review reports
Introduction
Bipolar disorder (BD), which encompasses primarily bipolar I and II disorders, is a subcategory of mood disorders that is characterized by episodes of mania and depression causing significant dysfunction. A diagnosis of bipolar II disorder requires at least one depressive episode and a hypomanic episode, whereas a diagnosis of bipolar I requires only a manic episode [ 1 , 2 ], though, research has shown that that the majority of individuals with bipolar I (94.2%) do report having experienced at least one depressive episode [ 3 ]. High mortality, disease burden, poor psychosocial functioning, and well-being, are several adverse outcomes associated with bipolar disorders [ 4 , 5 , 6 , 7 ].
Impulsivity is a core putative feature of bipolar disorders [ 8 , 9 ] that becomes elevated during mania [ 10 ]. Impulsivity is typically conceptualized as the tendency to make rash decisions or responses that lead to undesirable consequences [ 11 , 12 ]. The inability to inhibit undesired actions can adversely impact various aspects of functioning due to a disregard for future consequences in favour of immediate rewards [ 13 , 14 , 15 ]. Generally, trait (i.e., a predisposition toward rash actions) and behavioural facets (i.e., the lack of inhibition of ongoing actions, such as delay of gratification or response inhibition) of impulsivity are heightened in bipolar disorders [ 16 , 17 , 18 ]. According to meta-analytic studies, behavioural aspects are significantly impaired with medium effect sizes (Hedge’s g estimates ranging from 0.41 to 0.51; [ 18 , 19 ]), whereas trait aspects, such as motor, cognitive, and non-planning impulsivity, commonly measured by the Barratt’s Impulsivity Scale (BIS), are significantly elevated in bipolar disorders [ 17 , 20 ]. In addition, trait impulsivity has been associated with disorder onset [ 21 ], and certain sub-features have been linked prospectively to illness severity [ 22 ].
One facet of impulsivity that has gained popularity in recent decades is emotional urgency, defined as a trait-tendency to react impulsively amidst strong emotions. Emotional urgency represents a combination of the two dimensions (negative and positive urgency) of the UPPS-P Impulsive Behaviour scale (Urgency, Perseverance, Premeditation, Sensation Seeking, and Positive Urgency), which is an updated version of the original UPPS scale that features a total of five trait impulsivity dimensions: (lack of) premeditation, (lack of) perseverance, sensation seeking, negative and positive urgency [ 23 ]. Negative and positive urgency are referred to as trait tendencies of rash action amidst negative and positive emotions respectively—the latter dimension [ 24 ] is the most recent dimension incorporated into the UPPS-P, and it is also the least studied. Unlike other UPPS-P facets that are operationalized separately from emotionality, emotional urgency represents a unique aspect of impulsivity that ties rash decision making with intense positive and negative emotions [ 25 , 26 ].
Each of the final five dimensions of the UPPS corresponds to a facet of the five-factor model of personality. For instance, negative urgency clusters closely with the personality trait factor neuroticism [ 12 ]. However, theories of emotional urgency have since moved beyond personality concepts due to a growth of neuroscience based research in cognition and emotion [ 27 ]. Emotional urgency is thus linked to impaired executive control and positively associated with maladaptive behaviours. Negative urgency has been associated with a neurocognitive vulnerability arising from reduced neurochemical activity or dysfunction in key neural areas of the ventromedial pre-frontal cortex and orbitofrontal cortex, which results in less efficacious regulatory control over pathological impulses (i.e., addictive impulses) from the basal ganglia and extended amygdala, and emotional arousal from sensory and visceromotor circuitries within the orbitofrontal cortex [ 28 , 29 , 30 ]. In an experimental study among non-clinical college students, it was found that only positive urgency (and not other facets of the UPPS-P) significantly and uniquely predicted risk-taking and increased alcohol consumption after a positive mood induction [ 31 ]. After facing (experimentally induced) social rejection, individuals with average to high levels of negative urgency were more likely than those with low levels to show increased impulsivity (i.e., failing to inhibit a prepotent response; [ 32 ]). In both experiments, non-emotional facets of impulsivity failed to achieve similar results as urgency, suggesting their relative smaller roles. Emotional urgency has been an important predictor of substance misuse (Smith and Cyders, 2016), gambling [ 33 ], drinking problems [ 34 ]. However, one may argue that based on conventional effect size cut-off criteria, the effect sizes are small ( r =.23 for nicotine severity for instance; [ 35 ]).
Personality constructs typically do not yield large effect sizes — a medium effect size of .29, for instance, corresponds to the 75th percentile of all personality correlations; less than 3% of all personality correlations documented are large ( r ≥.50; [ 36 ]). Thus, at the 75th percentile, personality constructs with correlations of r ≥.29 are considered to have large practical significance. A meta-analysis of 115 studies ( N = 40,432) found that emotional urgency had the greatest effect on general psychopathology (a medium effect, r =.34) whereas non-emotional aspects of impulsivity only had a small effect ( r ranging from .08 to .14). More crucially, the meta-analysis found large effects on depression ( r =.45) and borderline personality disorder ( r =.58), implying that negative urgency has greater relevance in disorders of negative mood dysregulation [ 37 ].
While a large repertoire of existing research has been dedicated to the study of general impulsivity in bipolar disorders, most have not examined emotional urgency. It is unclear if there is sufficient empirical evidence for its clinical significance. Systematic reviews published thus far have synthesized important work in non-emotional constructs of impulsivity [ 18 , 20 ], impulsivity constructs in relation to addictions and substance misuse [ 26 , 29 , 30 , 38 , 39 , 40 , 41 ], problematic eating and related disorders [ 26 , 42 , 43 ], aggression [ 44 ], self-injurious behaviours [ 45 ], psychosis with comorbid substance use [ 46 ], and general psychopathology [ 37 ]. However, to the best of knowledge, there have been no attempts to synthesize existing empirical evidence of positive and negative urgency in relation to important clinical and psychosocial factors in bipolar disorders.
Prevailing research shows that emotional urgency is more closely associated with psychopathology and externalizing behaviours (i.e., behaviours directed outwards or rule-breaking behaviours), such as outward aggression, gambling, substance use, than the remaining facets of the UPPS. Unlike the other facets, negative urgency is positively correlated with internalizing behaviours (i.e., behaviours that are inflicted inwards toward the self) with medium to large effect sizes, such as non-suicidal self-injurious behaviours (NSSI; d = 0.56 to 0.59, a medium effect size; [ 45 , 47 ] and binge-eating (d = 0.64, a medium effect size; [ 42 ]. Emotional urgency underlies many forms of behavioural addictions [ 48 , 49 ], risk-taking behaviours [ 18 ], and to a lesser extent, suicidality [ 50 ]. Furthermore, mood instability, irritability, depression, and mania, are part of spectrums of emotionality that, when heightened, can nudge individuals to engage in maladaptive behaviours [ 34 , 37 , 42 , 45 , 51 ]. While the association between negative emotions and maladaptive behaviours is well known and accepted in psychopathology, few studies have investigated the role of emotional urgency in this relationship. Finally, where mania is the primary mood state of concern, support for the association between emotional urgency and mania remains unclear.
Considering the existing gaps in research on emotional urgency in bipolar disorders, we conducted a scoping review to answer a fundamental question, “what is the clinical significance and clinically relevant correlates of emotional urgency in bipolar disorder?” This approach was adopted to determine the extent of evidence in a niche area of study before proceeding with a systematic review approach. Thus, this review aims to, firstly, determine the extent of emotional urgency’s clinical relevance by qualitatively summarizing prevailing research that reported between-group differences of emotional urgency scores (i.e. bipolar disorder vs. healthy controls, and/or vs. other clinical populations) and associations between emotional urgency and bipolar disorders (i.e. both categorical diagnosis and continuous symptom measures); and secondly, summarize clinically relevant associations between emotional urgency and all aspects relevant to illness (e.g., aetiological factors and clinical outcomes, psychiatric comorbidities), psychosocial outcomes (e.g., functioning or quality of life), and maladaptive behaviours (e.g., suicidality, self-harm) in individuals with bipolar disorders.
The protocol was published in the International Prospective Register of Systematic Reviews (PROSPERO) on 2nd July 2021 (Reg no.: CRD42021258230) in preparation for a systematic review. However, a systematic synthesis of data did not materialize due to the small number of studies found. The quality of reporting and conduct of this scoping review is based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklists and guidelines for scoping reviews (PRISMA-ScR; [ 52 , 53 ]).
Inclusion criteria
(1) Articles that investigated emotion-related impulsivity, emotional urgency, positive urgency, or negative urgency in bipolar disorders, its association (if any) with psychiatric comorbidities (i.e., anxiety disorders), and/or maladaptive behaviours (e.g., suicidality, self-harm); (2) work that had reported the use of at least one of the positive or negative urgency subscale of the UPPS/UPPS-P/PUM; (3) studies that had recruited adults who either met the Diagnostic Statistical Manual of Mental Disorders (DSM-IV or DSM-5) criteria for bipolar disorder or were recruited from a clinical setting; (4) peer-reviewed journal articles published between January 2001 and January 2024; and (5) written in the English language.
Exclusion criteria
Conference abstracts, commentaries, editorials, reviews, meta-analyses, dissertations, qualitative studies, and case-series.
Identification and selection of studies
Electronic databases, such as MEDLINE (PubMed), PsychINFO, Web of Science, and Embase, were searched to identify eligible articles published between January 2001 and January 2024. This comprised an initial search of articles between January 2001 and May 2023, and a secondary search conducted in February 2024 for articles published between June 2023 and January 2024, using the search syntax: (Bipolar, Mani* or cyclothymi* or manic-depressi* or hypomani*) AND (positive urgency or negative urgency or emotion* impuls* or emotion* urgency).
Study selection
The primary reviewer (WLT) and a second reviewer (SYS) independently screened article titles and abstracts to determine study inclusion. Any discrepancies were resolved through consensus discussions; if consensus could not be reached, senior authors (JLL, MS, RCH) were consulted. Both the primary reviewer (WLT) and a second reviewer (SYS) further screened the articles independently based on full texts obtained and extracted the data.

Data extraction and analysis
General information related to study characteristics including study design, recruitment setting, and sample size were extracted from each study. Emotional urgency and mood severity measures, clinical outcomes, group differences between bipolar disorders and various comparison groups (e.g., healthy controls), statistical associations between emotional urgency and bipolar disorder diagnosis (categorical), and mood symptoms were extracted to address the primary aim of the review. Any additional statistical associations between emotional urgency and illness (e.g., aetiological factors, clinical or recovery outcomes, psychiatric comorbidities), well-being (e.g., functioning or quality of life), or maladaptive behaviours (e.g., suicidality, self-harm) in individuals with bipolar disorders were extracted to address the secondary aim of the review. Given the small number of articles, an overall qualitative synthesis was deemed appropriate.
The initial search yielded 999 entries. A total of 10 entries were included in the qualitative synthesis after the removal of 295 duplicates, 680 ineligible records (i.e., review articles, articles unrelated to emotional urgency and/or bipolar disorders) at the first screening at the abstract and title level, and 14 ineligible records after the second assessment at the full-text level (Bøen et al., 2015; Johnson et al., 2019, 2017; Johnson and Carver, 2016; Kwapil et al., 2000; Muhtadie et al., 2014; Quilty et al., 2010; Reich et al., 2019; Shakeel et al., 2019; Victor et al., 2011). An additional 14 entries were extracted from an additional search of publications between June 2023 and January 2024. However, none of the 14 additional entries were included for the following reasons: duplicates (5 entries), ineligible records (8 entries), and potential bias stemming from potential conflict of interest (1 entry is first author’s article). See Fig. 1 for the flowchart.
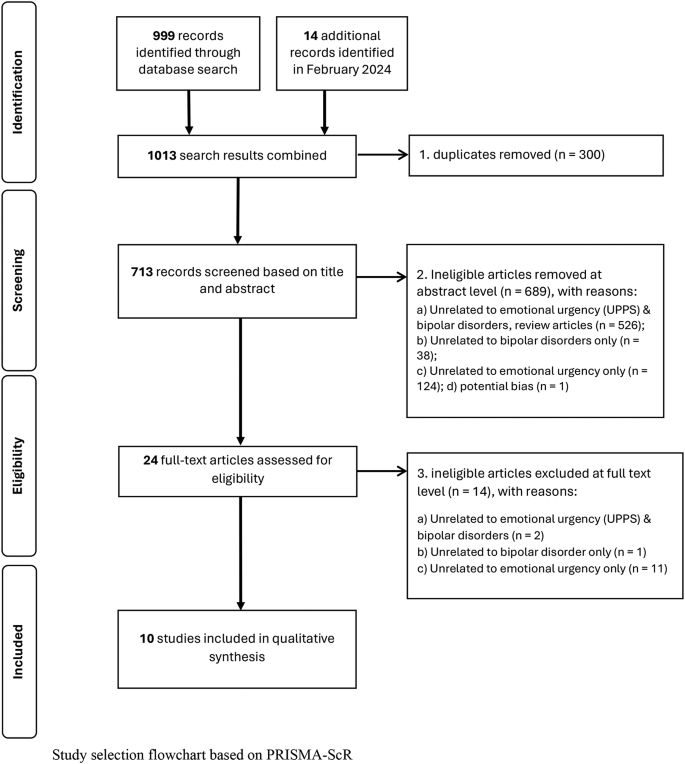
Flowchart for study selection flowchart based on PRISMA-ScR
Overview of included studies
In all 10 studies reviewed, clinical protocols (e.g., Structured Clinical Interview for DSM-IV) were used to assess participants’ diagnoses of bipolar disorder. Most studies reported a female majority. Only one study had explicitly indicated that participants were in the remission stage [ 54 ]. Seven out of ten of studies were conducted in the United States and the remaining three were conducted in Canada or Norway. All studies reviewed had relied on convenience sampling. Two studies [ 55 , 56 ] had drawn data from a larger study [ 57 ] and may have overlapping datasets. Finally, most studies had investigated either positive or negative urgency; only three out of ten studies examined both dimensions in the same report. Three studies had used the original UPPS which comprises four factors of impulsivity by Whiteside and Lynam (2001), two studies had utilized the UPPS-Positive scale (UPPS-P) which comprises five factors of impulsivity (an additional factor of positive urgency), and five studies had adopted the Positive Urgency Measure (PUM) scale by Cyders et al. (2007). The UPPS-P, which contains components of the original UPPS and PUM, has been validated in psychiatric populations [ 58 ]. The total number of participants with bipolar disorders across all studies was 451. Sample sizes ranged from 19 to 145 participants, and study samples were composed of adult and young adult patients. Tables 1 and 2 summarizes between-group differences of emotional urgency scores and associations between emotional urgency and clinical/psychosocial outcomes respectively.
Bipolar disorder vs. healthy controls
Five out of ten studies compared emotional urgency scores between bipolar disorders and healthy controls [ 54 , 59 , 60 , 61 , 62 ]. In these studies, healthy controls were commonly individuals who were assessed in structured interviews to have no psychiatric illness; only one study had used matched controls [ 60 ]. Overall, the results overwhelmingly suggest that individuals with bipolar disorders consistently report substantially high tendencies of impulsivity during intense positive and negative mood. All five studies found significant between-group differences of negative urgency with large effect sizes (partial eta-square = 0.23 [ 61 ]; calculated Cohen’s d = 2.20 [ 59 ]; calculated Cohen’s d = 1.40 [ 62 ]), and positive urgency (partial eta-square = 0.32 [ 61 ]; calculated Cohen’s d = 1.82 [ 54 ]; calculated Cohen’s d = 1.86 [ 60 ]; and calculated Cohen’s d = 1.77 [ 62 ]).
Bipolar disorders vs. other comparison groups
Four out of ten studies compared differences in emotional urgency scores between bipolar disorder and various other groups—each study’s comparison group comprising of individuals with other psychiatric illnesses or clinical attributes [ 59 , 62 , 63 , 64 ]. Overall, negative urgency was not endorsed significantly differently within mood disorders. One study reported no significant group differences in negative urgency between bipolar disorder and depressive disorder [ 63 ]. Additionally, no group differences were reported between individuals with bipolar disorders with severe depressive symptoms than those without [ 59 ]. None of the studies reviewed had investigated between-group differences in positive urgency.
Individuals with borderline personality disorder endorsed significantly greater negative urgency than individuals with bipolar disorders [ 59 ]. Another study found between-group differences that were borderline significant in positive urgency between gambling disorder ( n = 31) and bipolar disorder ( n = 19, p =.05; [ 62 ]; Individuals with gambling disorder endorsed lower levels of positive urgency than individuals with bipolar disorder. Within the context of suicidality, individuals with bipolar disorders and with a history of attempt ( n = 12) did not differ significantly in negative or positive urgency scores than those without any history of attempt ( n = 18, p =.06 to.07; [ 64 ]) but alike the aforementioned study [ 62 ], the lack of significance (or borderline significance) could be due to a lack of statistical power.
Association between emotional urgency and mood severity
None of the three studies that had examined the link between depression severity and negative urgency found support for its association [ 55 , 59 , 61 ]. Positive urgency too was not significantly associated with mania/hypomania severity in two studies [ 61 , 65 ]. On the other hand, one study found a positive correlation between positive urgency and depression severity [ 54 ] which corroborated findings of another study which reported that higher positive urgency was associated with higher frequency of Major Depressive Disorder (MDD) episodes [ 55 ]. Though it had been noted in a previous study that emotional urgency was positively associated with having a history of bipolar disorder, i.e., r =.30 and.50 for negative and positive urgency respectively [ 61 ], prevailing empirical evidence, on the other hand, shows a lack of a linear association with depressive/mania/hypomania severity.
Association with psychiatric comorbidity and maladaptive behaviours
A total of four studies reported the association between emotional urgency and psychiatric comorbid conditions or maladaptive behaviours [ 54 , 55 , 61 , 63 ]. Negative urgency was positively related to anxiety, impulse control (e.g., kleptomania, pathological gambling), and substance use disorders, with b ranging from 0.20 to 0.34 in one study [ 61 ], and with r ranging from .27 to .37 in another [ 55 ]. Two out of three studies [ 54 , 55 , 61 ] that had examined the association between positive urgency and comorbid conditions found a significant positive correlation with substance use disorders only, ranging from r = .22 to .34 [ 55 , 65 ].
Three distinct types of maladaptive behaviours—problem gambling, suicidality, and self-harm behaviours—were investigated separately in two studies [ 55 , 63 ]. Negative urgency was not associated with self-report problem gambling [ 63 ]. Positive and negative urgency were independently and positively associated with suicide ideation, r = .20 and .50 respectively. Positive urgency was positively associated with suicide attempt and self-harm, r = .20 respectively [ 55 ]. However, after accounting for sociodemographic and clinical covariates, only negative urgency had a significant positive influence on self-harm and suicidality [ 55 ].
Association with personality, aggression, trauma
Four studies investigated trait-like constructs of temperament, aggression, and childhood trauma history [ 54 , 55 , 59 , 66 ] among those with bipolar disorder. Greater scores in negative urgency was associated with higher neuroticism ( b = 0.30), and extraversion ( b = 0.160) traits, but was associated with lower agreeableness ( b = − 0.32) and conscientiousness ( b = − 0.22888) aspects of personality [ 66 ]. The study further noted that negative urgency predicted cyclothymic/irritable temperament—a combined characteristic of mood and negative affect reactivity during negative life episodes ( b = 0.40; [ 66 ]). Next, negative urgency was highly associated with all aspects of childhood trauma, such as emotional abuse, physical and emotional neglect, r estimates with a medium-high effect, ranging from 0.48 to 0.69. However, there was no significant relationship between trauma history and emotional urgency [ 55 ]. The strongest association was found for emotional neglect [ 59 ]. In the context of aggression and dominance, positive urgency was significantly associated with anger, hostility, physical and verbal aggression, r ranging from 0.38 to 0.51 [ 54 ].
Association with quality of life and functioning
Quality of life and functioning were operationalized by two widely used validated scales: the quality of life in bipolar disorder (QOL-BD) scale by Michalak et al. (2010) and the global assessment of functioning (GAF) scale, respectively. Positive urgency was negatively correlated with quality of life ( r = -.50; [ 56 ]), negatively associated with overall functioning, (β = -0.40 to -0.45), and had accounted for a significant amount of variance (14–24%) of overall quality of life or functioning scores [ 56 , 61 ].
A scoping review was conducted to exploratorily determine the extent of available evidence of the clinically significance of emotional urgency in BD. Overall, there is support for the clinical relevancy of emotional urgency in the extant literature. Across studies, individuals with bipolar disorders consistently endorsed higher levels of emotional urgency than healthy individuals. There is moreover a high percentage of statistical variance of quality of life and functioning scores that are explained by emotional urgency, which supports its relevance to clinical recovery. There is, however, a lack of consistent evidence for the association between negative urgency and mania or depression severity. Finally, existing data suggests that emotional urgency is not endorsed any differently across mood disorders, providing preliminary support for its transdiagnostic nature.
Empirical evidence based on community data found significant associations between emotional urgency and mania or depression risk/severity [ 67 , 68 ], but this was not strongly evident in clinical samples. This could imply that, like other non-emotion-based trait pathways of impulsivity, heightened emotional urgency is a stable trait of bipolar disorder regardless of illness phases or mood state. However, important limitations have to be noted and addressed, such as the lack of sufficiently powered studies to detect associations [ 59 , 61 ] and the lack of an account of disorder heterogeneity. Within mania, the types of mood experience can vary greatly, ranging from euphoria to dysphoric emotions [ 69 ]. Certain manic features, such as irritability, may be more associated with negative urgency than other features [ 66 ]. Similarly, the predominant polarity of the illness (e.g., individuals who experience primarily manic/hypomanic or depressive episodes or no predominant polarity); [ 70 , 71 , 72 ] have shown to influence impulsivity levels. Only two out of four studies had accounted for illness phases [ 54 , 61 ] and no studies reviewed had considered the role of clinical relevant moderators, such as predominant polarity or mixed mood states [ 73 ]. Future research could parse emotional urgency by mood features rather than in broad general dimensions of hedonic mood and severity to further delineate the role of emotional urgency.
The relationship between emotional urgency and maladaptive behaviours varied widely between studies. In general, this review found preliminary support for a positive association with aggression, and hostility constructs, childhood trauma, and suicide ideation which corroborates past research [ 24 , 34 , 65 , 74 , 75 ]. Associations with medium to large effect sizes were found for anger and hostility constructs of aggression, major forms of childhood trauma, and suicide ideation (see Tables 1 and 2 for a clearer summary). Positive but not negative urgency was associated with self-harm and suicide attempt [ 47 , 76 , 77 ] which was an unexpected finding. This could be explained by the understanding that different facets of suicidality may be differentially linked to impulsivity [ 78 , 79 ]. In certain contexts, emotional urgency may act as an amplifier [ 78 , 79 ] or be moderated by other constructs of suicidality [ 69 ].
Limitations
Several important limitations must be considered before concrete conclusions can be made. Most crucially, as the aim of this scoping review was to descriptively summarize results of existing studies, it does not allow for drawing conclusions beyond integrated findings. Secondly, due to the limitations of a scoping review, the quality of studies remains to be assessed by future systematic reviews. Thirdly, most studies were designed to detect group differences but not associations— the latter investigation was often not part of the main study design focus, and thus, the outcomes of this review were significantly hampered by the lack of adequately powered studies. As most studies reviewed had investigated negative or positive urgency alone (i.e., studies that had utilized the UPPS or PUM, but not the updated version of UPPS-P, which contained both negative and positive urgency dimensions), this review is unable to ascertain which dimension played a more significant role in bipolar disorders. As a result of these limitations, a greater volume of basic research using diverse cultural samples is needed to validate and generalize the findings of this review and expand knowledge on emotion-based impulsivity in bipolar disorders (See Table 2 ).
Future directions, clinical implications, and conclusion
Emotional urgency is a promising concept of trait impulsivity due to its profoundly large clinical significance in psychopathology. Similarly, large effect sizes were found in this scoping review extending support for future research in bipolar disorder. At this juncture, more basic science studies with adequate statistical power must be conducted to thoroughly elucidate its role in mood dysfunction. While it is premature to draw any real clinical implications, a consolidation of existing work can inform future directions pertaining to its role in bipolar disorders and disorders of mood dysfunction in general.
One important characteristic of trait concepts is its inherent nature, and thus, incorporating emotional urgency into clinical interventions may pose a challenge due to its resistance to change. However, recent work does suggest that negative urgency can impede therapeutic success if left unaddressed [ 80 , 81 , 82 ], and further evidence does show that negative urgency can be significantly reduced by existing psychological interventions, such as dialectic behavioural therapy and cognitive behavioural therapy [ 83 , 84 ].
Finally, the gathered evidence suggests that there may be great value in investigating the role of emotional urgency in the context of a theoretical framework—to elucidate its role as an indirect or conditional variable within conceptual models. Parsing emotional urgency and mood states in the context of cognition and emotional dysregulation in mood disorders [ 28 , 32 , 85 , 86 , 87 ] for instance, could further ascertain the role of emotional urgency in complex maladaptive behaviours.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
Barratt’s Impulsivity Scale
Bipolar Disorder(s)
Diagnostic Statistical Manual of Mental Disorders
the Global Assessment of Functioning scale
Major Depressive Disorder
Non-suicidal Self-Injurious behaviours
Positive Urgency Measure
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklists and guidelines for Scoping Reviews
the International Prospective Register of Systematic Reviews
the Quality of Life in Bipolar Disorder scale
Urgency, Perseverance, Premeditation, Sensation Seeking, and Positive Urgency
American Psychiatric Association, Association D. AP. Diagnostic and statistical manual of mental disorders: DSM-5. American psychiatric association Washington, DC; 2013.
American Psychiatric Association, Association A. AP. Diagnostic and statistical manual of mental disorders: DSM-IV. American psychiatric association Washington, DC; 1994.
Karanti A, Kardell M, Joas E, Runeson B, Pålsson E, Landén M. Characteristics of bipolar I and II disorder: a study of 8766 individuals. Bipolar Disord. 2020;22(4):392–400.
Article PubMed Google Scholar
Bonnín CM, Reinares M, Martínez-Arán A, Jiménez E, Sánchez-Moreno J, Solé B, et al. Improving functioning, quality of life, and well-being in patients with bipolar disorder. Int J Neuropsychopharmacol. 2019;22(8):467–77.
PubMed PubMed Central Google Scholar
He H, Hu C, Ren Z, Bai L, Gao F, Lyu J. Trends in the incidence and DALYs of bipolar disorder at global, regional, and national levels: results from the global burden of Disease Study 2017. J Psychiatr Res. 2020;125:96–105.
Kessing LV, Vradi E, Andersen PK. Life expectancy in bipolar disorder. Bipolar Disord. 2015;17(5):543–8.
Laursen TM. Life expectancy among persons with schizophrenia or bipolar affective disorder. Schizophr Res. 2011;131(1–3):101–4.
Dervic K, Garcia-Amador M, Sudol K, Freed P, Brent DA, Mann J, et al. Bipolar I and II versus unipolar depression: clinical differences and impulsivity/aggression traits. Eur Psychiatry. 2015;30(1):106–13.
Strakowski SM, Fleck DE, DelBello MP, Adler CM, Shear PK, Kotwal R, Arndt S. Impulsivity across the course of bipolar disorder. Bipolar Disord. 2010;12(3):285–97.
Article PubMed PubMed Central Google Scholar
Swann AC, Pazzaglia P, Nicholls A, Dougherty DM, Moeller FG. Impulsivity and phase of illness in bipolar disorder. J Affect Disord. 2003;73(1–2):105–11.
Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001;158(11):1783–93.
Whiteside SP, Lynam DR. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Pers Indiv Differ. 2001;30(4):669–89.
Article Google Scholar
Devlin HC, Johnson SL, Gruber J. Feeling good and taking a chance? Associations of hypomania risk with cognitive and behavioral risk taking. Cogn Therapy Res. 2015;39:473–9.
Drakopoulos J, Sparding T, Clements C, Pålsson E, Landén M. Executive functioning but not IQ or illness severity predicts occupational status in bipolar disorder. Int J Bipolar Disorders. 2020;8(1):1–9.
O’Donnell LA, Deldin PJ, Grogan-Kaylor A, McInnis MG, Weintraub J, Ryan KA, Himle JA. Depression and executive functioning deficits predict poor occupational functioning in a large longitudinal sample with bipolar disorder. J Affect Disord. 2017;215:135–42.
Faedda GL, Serra G, Marangoni C, Salvatore P, Sani G, Vázquez GH, et al. Clinical risk factors for bipolar disorders: a systematic review of prospective studies. J Affect Disord. 2014;168:314–21.
Najt P, Perez J, Sanches M, Peluso M, Glahn D, Soares JC. Impulsivity and bipolar disorder. Eur Neuropsychopharmacol. 2007;17(5):313–20.
Ramírez-Martín A, Ramos-Martín J, Mayoral-Cleries F, Moreno-Küstner B, Guzman-Parra J. Impulsivity, decision-making and risk-taking behaviour in bipolar disorder: a systematic review and meta-analysis. Psychol Med. 2020;50(13):2141–53.
Wright L, Lipszyc J, Dupuis A, Thayapararajah SW, Schachar R. Response inhibition and psychopathology: a meta-analysis of go/no-go task performance. J Abnorm Psychol. 2014;123(2):429.
Saddichha S, Schuetz C. Is impulsivity in remitted bipolar disorder a stable trait? A meta-analytic review. Compr Psychiatr. 2014;55(7):1479–84.
Alloy LB, Urošević S, Abramson LY, Jager-Hyman S, Nusslock R, Whitehouse WG, Hogan M. Progression along the bipolar spectrum: a longitudinal study of predictors of conversion from bipolar spectrum conditions to bipolar I and II disorders. J Abnorm Psychol. 2012;121(1):16.
Rote J, Dingelstadt A-M-L, Aigner A, Bauer M, Fiebig J, König B, et al. Impulsivity predicts illness severity in long-term course of bipolar disorder: a prospective approach. Australian New Z J Psychiatry. 2018;52(9):876–86.
Lynam DR, Smith GT, Whiteside SP, Cyders MA. The UPPS-P: Assessing five personality pathways to impulsive behavior. West Lafayette, IN: Purdue University. 2006;10.
Cyders MA, Smith GT. Mood-based rash action and its components: positive and negative urgency. Pers Indiv Differ. 2007;43(4):839–50.
Cyders MA, Coskunpinar A, VanderVeen JD. Urgency: A common transdiagnostic endophenotype for maladaptive risk taking. 2016.
Cyders MA, Smith GT. Emotion-based dispositions to rash action: positive and negative urgency. Psychol Bull. 2008;134(6):807.
Phillips ML, Ladouceur CD, Drevets WC. A neural model of voluntary and automatic emotion regulation: implications for understanding the pathophysiology and neurodevelopment of bipolar disorder. Mol Psychiatry. 2008;13(9):833–57.
Johnson SL, Elliott MV, Carver CS. Impulsive responses to positive and negative emotions: parallel neurocognitive correlates and their implications. Biol Psychiatry. 2020;87(4):338–49.
Um M, Whitt ZT, Revilla R, Hunton T, Cyders MA. Shared neural correlates underlying addictive disorders and negative urgency. Brain Sci. 2019;9(2):36.
Zorrilla EP, Koob GF. Impulsivity derived from the dark side: neurocircuits that contribute to negative urgency. Front Behav Neurosci. 2019;13:136.
Cyders MA, Zapolski TC, Combs JL, Settles RF, Fillmore MT, Smith GT. Experimental effect of positive urgency on negative outcomes from risk taking and on increased alcohol consumption. Psychol Addict Behav. 2010;24(3):367.
Chester DS, Lynam DR, Milich R, DeWall CN. Social rejection magnifies impulsive behavior among individuals with greater negative urgency: an experimental test of urgency theory. J Exp Psychol Gen. 2017;146(7):962.
Cyders MA, Smith GT. Clarifying the role of personality dispositions in risk for increased gambling behavior. Pers Indiv Differ. 2008;45(6):503–8.
Coskunpinar A, Dir AL, Cyders MA. Multidimensionality in impulsivity and alcohol use: a meta-analysis using the UPPS model of impulsivity. Alcoholism: Clin Experimental Res. 2013;37(9):1441–50.
Kale D, Stautz K, Cooper A. Impulsivity related personality traits and cigarette smoking in adults: a meta-analysis using the UPPS-P model of impulsivity and reward sensitivity. Drug Alcohol Depend. 2018;185:149–67.
Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Pers Indiv Differ. 2016;102:74–8.
Berg JM, Latzman RD, Bliwise NG, Lilienfeld SO. Parsing the heterogeneity of impulsivity: a meta-analytic review of the behavioral implications of the UPPS for psychopathology. Psychol Assess. 2015;27(4):1129.
Atkinson EA, Ortiz AM, Smith GT. Affective risk for problem drinking: reciprocal influences among negative urgency, affective lability, and rumination. Curr Drug Res Reviews Formerly: Curr Drug Abuse Reviews. 2020;12(1):42–51.
Herman AM, Duka T. Facets of impulsivity and alcohol use: what role do emotions play? Neurosci Biobehavioral Reviews. 2019;106:202–16.
Maxwell AL, Gardiner E, Loxton NJ. Investigating the relationship between reward sensitivity, impulsivity, and food addiction: a systematic review. Eur Eat Disorders Rev. 2020;28(4):368–84.
Smith GT, Cyders MA. Integrating affect and impulsivity: the role of positive and negative urgency in substance use risk. Drug Alcohol Depend. 2016;163:S3–12.
Culbert KM, Lavender JM, Crosby RD, Wonderlich SA, Engel SG, Peterson CB, et al. Associations between negative affect and binge/purge behaviors in women with anorexia nervosa: considering the role of negative urgency. Compr Psychiatr. 2016;66:104–12.
Pearson CM, Riley EN, Davis HA, Smith GT. Research Review: two pathways toward impulsive action: an integrative risk model for bulimic behavior in youth. J Child Psychol Psychiatry. 2014;55(8):852–64.
Mancke F, Herpertz SC, Bertsch K. Correlates of aggression in personality disorders: an update. Curr Psychiatry Rep. 2018;20:1–14.
Hamza CA, Willoughby T, Heffer T. Impulsivity and nonsuicidal self-injury: a review and meta-analysis. Clin Psychol Rev. 2015;38:13–24.
Oh H, Jang S-K, Lee H-S, Lee E-B, Choi K-H. Personality traits in individuals with the dual diagnosis of psychosis and Substance Use disorders: a Comprehensive Review and Meta-Analysis. J Dual Diagnosis. 2021;17(1):34–51.
Peckham AD, Jordan H, Silverman A, Steele SJ, Björgvinsson T, Beard C. From urges to action: negative urgency and nonsuicidal self-injury in an acute transdiagnostic sample. Archives of suicide research; 2019.
Di Nicola M, Tedeschi D, Mazza M, Martinotti G, Harnic D, Catalano V, et al. Behavioural addictions in bipolar disorder patients: role of impulsivity and personality dimensions. J Affect Disord. 2010;125(1–3):82–8.
Varo C, Murru A, Salagre E, Jiménez E, Solé B, Montejo L, et al. Behavioral addictions in bipolar disorders: a systematic review. Eur Neuropsychopharmacol. 2019;29(1):76–97.
Watkins HB, Meyer TD. Is there an empirical link between impulsivity and suicidality in bipolar disorders? A review of the current literature and the potential psychological implications of the relationship. Bipolar Disord. 2013;15(5):542–58.
Halcomb M, Argyriou E, Cyders MA. Integrating preclinical and clinical models of negative urgency. Front Psychiatry. 2019;10:324.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Peters MD, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synthesis. 2020;18(10):2119–26.
Johnson SL, Carver CS. Emotion-relevant impulsivity predicts sustained anger and aggression after remission in bipolar I disorder. J Affect Disord. 2016;189:169–75.
Johnson SL, Carver CS, Tharp JA. Suicidality in bipolar disorder: the role of emotion-triggered impulsivity. Suicide Life‐Threatening Behav. 2017;47(2):177–92.
Victor SE, Johnson SL, Gotlib IH. Quality of life and impulsivity in bipolar disorder. Bipolar Disord. 2011;13(3):303–9.
Muhtadie L, Johnson SL. Threat sensitivity in bipolar disorder. J Abnorm Psychol. 2015;124(1):93.
Dugré JR, Giguére C-É, Percie du Sert O, Potvin S, Dumais A, Signature C. The psychometric properties of a short UPPS-P impulsive behavior scale among psychiatric patients evaluated in an emergency setting. Front Psychiatry. 2019;10:139.
Bøen E, Hummelen B, Elvsåshagen T, Boye B, Andersson S, Karterud S, Malt UF. Different impulsivity profiles in borderline personality disorder and bipolar II disorder. J Affect Disord. 2015;170:104–11.
Johnson SL, Mehta H, Ketter TA, Gotlib IH, Knutson B. Neural responses to monetary incentives in bipolar disorder. NeuroImage: Clin. 2019;24:102018.
Muhtadie L, Johnson SL, Carver CS, Gotlib IH, Ketter TA. A profile approach to impulsivity in bipolar disorder: the key role of strong emotions. Acta Psychiatrica Scandinavica. 2014;129(2):100–8.
Shakeel MK, Hodgins DC, Goghari VM. A comparison of self-reported impulsivity in gambling disorder and bipolar disorder. J Gambl Stud. 2019;35:339–50.
Quilty LC, Mehra P, Toneatto T, Bagby M. Impulsivity and pathological gambling across depressive versus bipolar disorders. Int Gambl Stud. 2010;10(1):81–90.
Reich R, Gilbert A, Clari R, Burdick KE, Szeszko PR. A preliminary investigation of impulsivity, aggression and white matter in patients with bipolar disorder and a suicide attempt history. J Affect Disord. 2019;247:88–96.
Johnson SL, Tharp JA, Peckham AD, Sanchez AH, Carver CS. Positive urgency is related to difficulty inhibiting prepotent responses. Emotion. 2016;16(5):750.
Kwapil TR, DeGeorge D, Walsh MA, Burgin CJ, Silvia PJ, Barrantes-Vidal N. Affective temperaments: unique constructs or dimensions of normal personality by another name? J Affect Disord. 2013;151(3):882–90.
Giovanelli A, Hoerger M, Johnson SL, Gruber J. Impulsive responses to positive mood and reward are related to mania risk. Cognition Emot. 2013;27(6):1091–104.
King KM, Halvorson MA, Kuehn KS, Feil MC, Lengua LJ. Cross-study, cross-method associations between negative urgency and internalizing symptoms. Assessment. 2022;29(3):572–82.
Martino DJ, Valerio MP, Parker G. The structure of mania: an overview of factorial analysis studies. Eur Psychiatry. 2020;63(1):e10.
Ekinci O, Albayrak Y, Ekinci AE, Caykoylu A. Relationship of trait impulsivity with clinical presentation in euthymic bipolar disorder patients. Psychiatry Res. 2011;190(2–3):259–64.
Pallaskorpi S, Suominen K, Rosenström T, Mantere O, Arvilommi P, Valtonen H, et al. Predominant polarity in bipolar I and II disorders: a five-year follow-up study. J Affect Disord. 2019;246:806–13.
Popovic D, Torrent C, Goikolea J, Cruz N, Sánchez-Moreno J, González‐Pinto A, Vieta E. Clinical implications of predominant polarity and the polarity index in bipolar disorder: a naturalistic study. Acta Psychiatrica Scandinavica. 2014;129(5):366–74.
Jaggers JA, Gruber J. Mixed mood states and emotion-related urgency in bipolar spectrum disorders: a call for greater investigation. Int J Bipolar Disorders. 2020;8(1):12.
Bresin K. Impulsivity and aggression: a meta-analysis using the UPPS model of impulsivity. Aggress Violent Beh. 2019;48:124–40.
Kim JH, Choi JY. Influence of childhood trauma and post-traumatic stress symptoms on impulsivity: focusing on differences according to the dimensions of impulsivity. Eur J Psychotraumatology. 2020;11(1):1796276.
Lynam DR, Miller JD, Miller DJ, Bornovalova MA, Lejuez CW. Testing the relations between impulsivity-related traits, suicidality, and nonsuicidal self-injury: a test of the incremental validity of the UPPS model. Personality Disorders: Theory Res Treat. 2011;2(2):151.
Riley EN, Combs JL, Jordan CE, Smith GT. Negative urgency and lack of perseverance: identification of differential pathways of onset and maintenance risk in the longitudinal prediction of nonsuicidal self-injury. Behav Ther. 2015;46(4):439–48.
Anestis MD, Bagge CL, Tull MT, Joiner TE. Clarifying the role of emotion dysregulation in the interpersonal-psychological theory of suicidal behavior in an undergraduate sample. J Psychiatr Res. 2011;45(5):603–11.
Cole AB, Littlefield AK, Gauthier JM, Bagge CL. Impulsivity facets and perceived likelihood of future suicide attempt among patients who recently attempted suicide. J Affect Disord. 2019;257:195–9.
Heinz AJ, Bui L, Thomas KM, Blonigen DM. Distinct facets of impulsivity exhibit differential associations with substance use disorder treatment processes: a cross-sectional and prospective investigation among military veterans. J Subst Abuse Treat. 2015;55:21–8.
Hershberger AR, Um M, Cyders MA. The relationship between the UPPS-P impulsive personality traits and substance use psychotherapy outcomes: a meta-analysis. Drug Alcohol Depend. 2017;178:408–16.
Um M, Cyders MA. Positive emotion-based impulsivity as a. transdiagnostic endophenotype: Oxford University Press; 2019.
Google Scholar
Axelrod SR, Perepletchikova F, Holtzman K, Sinha R. Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. Am J Drug Alcohol Abus. 2011;37(1):37–42.
Zapolski TC, Smith GT. Pilot study: implementing a brief DBT skills program in schools to reduce health risk behaviors among early adolescents. J School Nurs. 2017;33(3):198–204.
Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30(2):217–37.
Fossati A, Gratz KL, Maffei C, Borroni S. Impulsivity dimensions, emotion dysregulation, and borderline personality disorder features among Italian nonclinical adolescents. Borderline Personality Disorder Emot Dysregulation. 2014;1(1):1–11.
Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26:41–54.
Download references
Acknowledgements
Not applicable.
This research is supported by the Singapore National Medical Research Council (NMRC) Research Training Fellowship (RTF) grant (Grant No.: MOH-RTF22jul-0011).
Author information
Authors and affiliations.
Institute of Mental Health, 10 Buangkok View, Buangkok Green, Medical Park, Singapore, S539747, Singapore
Wen Lin Teh, Jianlin Liu & Mythily Subramaniam
Yong Loo Lin School of Medicine, National University of Singapore, 21 Lower Kent Ridge Rd, Singapore, S119077, Singapore
Wen Lin Teh & Roger Ho
MOH Holdings, 1 Maritime Square, #11-25, Singapore, S099253, Singapore
Sheng Yeow Si
Institute of Health Innovation and Technology (iHealthtech), National University of Singapore, 14 Medical Dr, #14-01 MD6, Singapore, S117599, Singapore
You can also search for this author in PubMed Google Scholar
Contributions
The first and co-author Wen Lin Teh and Sheng Yeow Si independently screened article titles and abstracts to determine study inclusion. Wen Lin Teh synthesized the results and drafted the first draft of the manuscript. Jianlin Liu, Mythily Subramaniam, and Roger Ho reviewed the manuscript and provided guidance and intellectual input.
Corresponding author
Correspondence to Wen Lin Teh .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Teh, W.L., Si, S.Y., Liu, J. et al. The clinical significance of emotional urgency in bipolar disorder: a scoping review. BMC Psychol 12 , 273 (2024). https://doi.org/10.1186/s40359-024-01700-1
Download citation
Received : 09 February 2024
Accepted : 02 April 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s40359-024-01700-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emotion-based impulsivity
- Emotional urgency
- Bipolar disorder
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]

- Bipolar Disorder
A Hidden Struggle People Living With Bipolar Disorder Face
Can you trust your happiness.
Posted May 19, 2024 | Reviewed by Jessica Schrader
- What Is Bipolar Disorder?
- Find a therapist to treat bipolar disorder
- A common difficulty for people with bipolar disorder is trusting one's happiness.
- The euphoria of mania can sometimes be mistaken for joy and vice versa.
- Recognizing one's unique warning signs and triggers can help.
As a psychotherapist, one of the most engaging groups of people I have gotten to meet are people diagnosed with bipolar disorder . The pain of the illness can be immense, with serious, sometimes life-threatening depressions and equally dangerous manias. Yet, it is also linked with creativity (Santosa et al., 2007) both during mood episodes and times of wellness.
The exuberance and intense fight for recovery I have seen in individuals with bipolar disorder is fierce.
Yet, there is an insidious challenge. Bipolar disorder is unique in its ability to corrupt the positive. In bipolar disorder, manic or hypomanic "highs" mimic in ways many of the joys of flow and happiness . There is a signature feeling of euphoria, enhanced productivity , and ability to create, which accompanies the destructive irritability, sleeplessness , and impulsivity of mania .
Fear and memories of manic highs can leave one in a state of distrust in the territories of happiness. Is a glowing, spirited day something to celebrate or a sign of mania? This can encourage vigilance, which presents a barrier to enjoying life.
While there is no "surefire" way of distinguishing between an oncoming mania and a good mood, what follows are three questions that might help one in the process.
1. Are you doing things that go against your values?
If you are a person who enjoys spontaneity and find yourself in a park flying a kite, you might wonder, "Is this normal?" The answer is likely "yes." While flying a kite suggests curiosity and happiness, it doesn't hurt anyone or necessarily indicate mania. However, if you are leaving work to go fly a kite without returning, or if you are spending a significant amount of money such that you won't be able to meet your responsibilities later in the week, those are more clues of mania.
2. Are you getting enough sleep?
Sleeplessness is common, even in people without mood disorders. Still, sleep issues are a powerful trigger for mood episodes as well as an indicator of mania. If you are getting less than your usual amount of sleep and not missing, mania could be the reason.
3. Is there something superficial about this?
Elation blossoms at certain times and events, such as on your wedding day. Still, if you are met with a "high" mood that has a superficial quality to it and is not linked up with any joyful events in your life, it may be something to monitor.
Difficulty trusting one's happiness is a difficulty for many living with bipolar disorder. Understanding one's unique triggers and warning signs can help one to rebuild trust in their experiences and their ability to distinguish between happiness and mania.
To find a therapist, please visit the Psychology Today Therapy Directory .
Santosa, C. M., Strong, C. M., Nowakowska, C., Wang, P. W., Rennicke, C. M., & Ketter, T. A. (2007). Enhanced creativity in bipolar disorder patients: A controlled study. Journal of affective disorders , 100 (1-3), 31-39.

Jennifer Gerlach, LCSW, is a psychotherapist based in Southern Illinois who specializes in psychosis, mood disorders, and young adult mental health.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry
Comorbid Bipolar and Alcohol Use Disorder—A Therapeutic Challenge
Heinz grunze.
1 Psychiatrie Schwäbisch Hall, Schwäbisch Hall, Germany
2 Paracelsus Medical University Nuremberg, Nuremberg, Germany
Martin Schaefer
3 Klinik für Psychiatrie, Psychotherapie, Psychosomatik, und Suchtmedizin, Evang. Kliniken Essen-Mitte, Essen, Germany
4 Klinik für Psychiatrie und Psychotherapie, Campus Charité Mitte, Charité Universitätsmedizin Berlin, Berlin, Germany
Harald Scherk
5 Vitos Klinikum Riedstadt, Riedstadt, Germany
Christoph Born
Ulrich w. preuss.
6 Vitos Klinik Psychiatrie und Psychotherapie, Herborn, Germany
7 Klinik für Psychiatrie, Psychotherapie, und Psychosomatik, Martin-Luther-Universität Halle-Wittenberg, Halle, Germany
Comorbidity rates in Bipolar disorder rank highest among major mental disorders, especially comorbid substance use. Besides cannabis, alcohol is the most frequent substance of abuse as it is societally accepted and can be purchased and consumed legally. Estimates for lifetime comorbidity of bipolar disorder and alcohol use disorder are substantial and in the range of 40–70%, both for Bipolar I and II disorder, and with male preponderance. Alcohol use disorder and bipolarity significantly influence each other's severity and prognosis with a more complicated course of both disorders. Modern treatment concepts acknowledge the interplay between these disorders using an integrated therapy approach where both disorders are tackled in the same setting by a multi-professional team. Motivational interviewing, cognitive behavioral and socio- therapies incorporating the family and social environment are cornerstones in psychotherapy whereas the accompanying pharmacological treatment aims to reduce craving and to optimize mood stability. Adding valproate to lithium may reduce alcohol consumption whereas studies with antipsychotics or naltrexone and acamprosate did not affect mood fluctuations or drinking patterns. In summary, there is a continuous need for more research in order to develop evidence-based approaches for integrated treatment of this frequent comorbidity.
Epidemiology of Bipolar Disorder and Substance Use Disorder
Both bipolar affective disorder (BD) and substance use disorder (SUD) are wide-spread in the general population. Most epidemiological and treatment studies were conducted according to DSM-IV or ICD-10 criteria that distinguishes between substance abuse and dependence as diagnostic entities on its own. Depending on the diagnostic system (ICD or DSM) used and subject sample studied, bipolar affective disorder (BD) in the general population has a lifetime prevalence between 1.3 and 4.5% ( 1 ). The World Health Organization World Mental Health Survey Initiative ( 2 ) conducted across eleven countries reported a 4.8% lifetime prevalence of all manifestations of bipolarity, including subthreshold and spectrum disorder.
Looking at specific countries, a representative survey applying the Composite International Diagnostic Interview [CIDI ( 3 )] for ICD 10 and DSM-IV criteria reports a 1-year prevalence rate of 1% for BD -I and 0.6% for BD-II disorder for Germany ( 4 ). The same study reports on a 1-year prevalence of 5.7% for substance abuse (except nicotine) according to DSM-IV criteria. Three percent fulfilled criteria for alcohol dependence and 1.8% for abuse ( 4 ). In a prior survey, looking at lifetime prevalence rate, the same group reports on similar numbers for BD, and 9.9 and 8.5% for alcohol abuse and dependence, respectively ( 5 ). These numbers are in a similar range as in other European countries; while prevalence rates from the US are much higher, both for BD and substance abuse/dependence ( 6 ). Whereas numbers for legal substances, e.g., alcohol, are considered as relatively robust and reproducible, many cases of illicit drug use remain undetected in patients with BD. Cannabis is likely to be second after alcohol as substance of abuse in BD patients, affecting approximately one quarter of bipolar patients ( 7 ).
Whereas, the incidence of BD across countries and cultures is within a similar range, reported rates for AUD differ considerably due to cultural and religious diversity. For example, a representative household survey in Iran found a 12-month prevalence of alcohol use disorders of 1% according to DSM-IV criteria and 1.3% according to DSM-5, with higher prevalence rates in urban vs. rural areas ( 8 ). For comparison, a recent US household survey reports a 12-month prevalence of DSM-5 AUD of 13.9% ( 9 ).
SUD comorbidity is not exclusive to adult bipolar patients but starts early in life. Pediatric onset BD rarely occurs in the absence of comorbid conditions, and the co-occurrence of additional disorders complicates both the accurate diagnosis of BD and its treatment. Manifestation of BD in children and adolescents is not as infrequent as previously assumed, with rates of bipolar spectrum disorder reaching an estimated 4%, especially in US samples ( 10 ).
In the meantime, DSM-5 ( 11 ) abolished the distinction between substance use, abuse and dependency by defining threshold numbers of criteria for different grades of severity of substance use. Of the 11 criteria, 2–3 should be fulfilled to diagnose mild alcohol use disorder (AUD) ( 12 ). Also, BD criteria experienced some adaptions with yet speculative consequences for epidemiological figures. Whereas, criteria for a manic episode were tightened ( 13 , 14 ) preceding substance use per se is no more an exclusion criterion for a genuine BD diagnosis as long as the mental alterations exceed well the physiological effect of the substance. This may change figures of future epidemiological studies on SUD and BD comorbidity to some degree.
Both disorders follow a chronic course and considerably impair social functioning and quality of life ( 15 – 17 ), general health and ultimately life expectancy ( 18 – 20 ). Antecedent SUD has been associated with earlier age of onset of BD ( 21 ) and a greater need of hospitalization at onset of BD ( 22 ). In addition, both disorders have a significantly increased rate of suicides and suicide attempts with an added risk in case of coexistence of both disorders ( 23 – 25 ).
Comorbidity of Bipolar Affective Disorders in Alcohol Use Disorder Patients
Among mental health disorders, BD has probably the highest risk of having a second, comorbid DSM -IV axis I disorder ( 26 ). Epidemiological data from the US report life-time prevalence rates of up to 90% for comorbidities in BD ( 6 ), with 62.3% for AUD (39.1% for DSM-IV alcohol abuse and 23.2% for alcohol dependency) followed by cannabis (46%), cocaine (24%) and opioids (8.5%) ( 27 ). The already cited WHO census across 11 countries showed a mean SUD life time comorbidity with BD of 36.6% with a large variation between countries ( 2 ). A meta-analysis including nine national surveys conducted between 1990 and 2015 revealed a mean prevalence of 24% for AUD and of 33% for any SUD except nicotine ( 28 ). Analyzing SUD and bipolar comorbidity in clinical settings, the same group reports the highest prevalence for AUD (42%) followed by cannabis use (20%) and any other illicit drug use (17%) ( 21 ). Cannabis ranking second after AUD has also been confirmed in other studies ( 7 , 27 , 29 ). Similar rates of SUD were also reported in the Systematic Treatment Enhancement Program Bipolar Disorders (STEP BD) study including 3,750 Bipolar I or II patients ( 30 ).
Our own study in BD patients recruited from the Stanley Foundation Bipolar Network (SFBN) outpatient clinic with more comprehensive care found life-time SUD in 42% and AUD in 33% of BD patients ( 31 ). Secondary analysis of this data examined the gender-specific relationships between AUD and BD. In line with epidemiological catchment area studies ( 26 ), absolute numbers of AUD in males with BD were higher (49 vs. 29%), however, the relative risk of suffering from AUD was significantly greater for women with BD [odds ratio (OR) = 7.35] than for men (OR = 2.77) in relation to the general population ( 32 ). Among other factors such has higher rates of depression, previous trauma might play a role for the higher OR in female BD patients; additional analysis in a larger sample of SFBN patients revealed that bipolar women with AUD had also a significantly higher rate of post-traumatic stress disorder (PTSD) than those without AUD ( 33 ).
The risk of developing comorbid SUD is obviously much higher in BD than in Major Depressive Disorder (MDD) suggesting that depressive mood is not the main driver of comorbidity in BD, but other factors imminent to BD, such as personality, early onset and impaired functionality, might play a decisive role. The OR for developing a SUD has been estimated 1.8 in patients with a lifetime MDD and 6.9 for those with a lifetime BD-I, compared with the general population ( 34 ), and prevalence rates for SUD are ~25–50% higher in BD-I than BD-II patients ( 26 , 35 ). The latter appears to be mainly driven by illicit drugs (OR 7.46 in BD-I and 3.30 in BD-II) ( 28 ). For AUD, however, a recent meta-analysis of 22 studies showed no difference between BD-I (OR 3.78) and BD-II (OR 3.81) ( 28 ). A recent catchment area study in Northeast England found a 40% lifetime comorbidity between BD II and AUD, surprisingly with little difference between female (38%) and male (43%) subjects ( 36 ).
As mentioned, there is a wide variation of prevalence rates for BD-SUD comorbidity across countries ( 2 ) with higher rates in the US than in other industrialized countries. Analyzing the SFBN sample of the two German centers revealed a life-time prevalence of 17.8% for AUD only—compared to 33% in the whole SFBN which included four US and three European centers (two in Germany, one in the Netherlands). The transatlantic difference for illicit drug use might be even higher, as SUD other than AUD was only present in 8.5% of the German SFBN sample ( 37 ). The higher SUD comorbidity rates in the US might directly relate to the poorer prognosis and higher treatment resistance in the SFBN US compared to the European sample ( 38 ).
Less data has been generated for the rate of BD in samples of AUD patients. Not only that BD pre-disposes for SUD, also the opposite is true: According to the already cited meta-analysis by Hunt and colleagues, people with an AUD were 4.1 times on greater risk of having a BD compared to those without an AUD ( 21 ). The US- National Comorbidity Survey ( 39 ) found that 6.5% of males and 10.6% of females with alcohol dependency had also suffered from at least one manic episode. As a limitation, this survey did not differentiate between manic episodes which preceded SUD, those which followed SUD and those which were possibly induced by substance use. In addition, it is fair to assume that there is a substantial dark figure as symptoms of BD are often masked by SUD. Recognizing an underlying BD in SUD patients, however, is essential to tailor adequate treatment plans.
Is There a Shared Etiology Between BD and Aud?
Family studies indicate that AUD and affective disorders, especially BD have a shared genetic pre-disposition. Examining the family history of bipolar patients participating in the SFBN we observed that, among others, AUD not only in parents ( 40 ), but also grandparents of a bipolar patient is associated with a more severe course of BD and poor prognosis ( 41 ). Temperament traits, prevalent in BD and AUD and genetically determined such as sensation seeking behavior may play a decisive role across illness boundaries ( 42 , 43 ). Candidate genes include a shared polymorphism of the aldehyde hydrogenase and alcohol dehydrogenase ( 44 ), a Ser23Cys (rs6318) polymorphism of the 5HT2C gene (in female bipolar patients) ( 45 ) and a VAL-158-MET polymorphism of the cathechol-o-methyltransferase (COMT) ( 46 ) impacting on the monoamine metabolism. However, recent GWAS finding pointed out that the correlation between genetic alterations and psychiatric disorders is not simple; the genetic connection of substance use and psychiatric disorders is rather highly pleiotropic and involves shared neurodevelopmental path, neurotransmission, and intracellular trafficking ( 47 ).
Diagnosis of AUD in Bipolar Patients
Symptoms of AUD and SUD may often obscure an underlying diagnosis of BD, and frequently result in a long delay before a BD diagnosis has been established by careful clinical observation. Brown et al. reported rates of SUDs in patients with BD ranging from 14 to 65% in treatment settings ( 48 ) but only a minority has received a correct diagnosis so far. Given the high incidence of psychiatric comorbidities in AUD, the German S3 Guideline recommend in every patient with AUD to carefully screen for psychiatric comorbidities after completing treatment of acute intoxication or withdrawal ( 49 ).
Uncovering AUD in people with BD appears less problematic. A recent systematic review on comorbidity of BD and AUD ( 50 ) recommends the use of the Alcohol use disorder Identification Test [AUDIT, ( 51 , 52 )] to detect heavy and frequent alcohol use, and AUDIT appears to be also sensitive in patients with comorbid mental health disorders. The AUDIT is also recommended to screen comorbid individuals by several evidence- based guidelines, e.g., the German S3-Guidelines on AUD ( 49 , 53 ).
Consequences of Comorbidity
The detrimental impact of substance use and BD has been well-established, both for the individual and for society ( 54 , 55 ). Numerous investigations demonstrated that comorbid AUD influences the clinical course of BDs unfavorably [for a review, see ( 50 )]. Especially in younger people BD as well as SUD results in severe and lasting impairment and a loss of healthy years lived ( 56 , 57 ). BD and SUD are afflicted with high rates of suicide attempts and suicide that are even topped in case of coexistence of both disorders ( 24 ). A Brazilian study reports of at least one suicide attempt in 68% of BD patients with AUD compared to 35% in BD without AUD, with virtually no difference between BD patients with DSM-IV alcohol abuse and dependence ( 23 ).
Gender differences have a significant influence on treatment outcomes in BD ( 58 ) but not as much on outcomes in alcohol dependence ( 59 ). AUD also facilitates additional comorbidities in BD patients such as anxiety disorders in female patients ( 33 ) and has a detrimental effect on the course of BD in general with an earlier onset ( 28 ), delayed recovery from episodes, more frequent mood switches, rapid cycling, mixed states, more severe depression and suicidal ideation ( 30 , 32 , 60 ) and lower adherence to treatment ( 61 ). Especially a history of verbal abuse and rates of social phobia and depression are higher in female than male BD patients with AUD ( 32 ). Whereas, AUD in female BD patients fosters rather self-destructive consequences, males appear more likely to externalize anger and impulsivity, and stand out by a history of criminal actions ( 62 ). Specific numbers for AUD and BD are not available, but for affective disorders (AD) in general and SUD, criminal behavior has been observed twice as frequent in AD with SUD compared to AD without ( 63 ).
The relationship between BD and AUD is bidirectional. In younger patients, it appears that alcohol use and bipolar symptoms are more likely to increase or decrease in unison ( 64 ). Depression increases alcohol craving in BD patients with AUD. An exploratory sub-analysis ( 65 ) examined the impact of depressive symptoms on craving and drinking behavior in 30 comorbid patients participating in a 8-week, placebo-controlled relapse prevention study (acamprosate vs. placebo). The analyzed subgroup of bipolar patients was well-stabilized on different mood stabilizers (antipsychotics, antiepileptics, or lithium). Severity of depression correlated significantly with craving and drinking behavior 1 week later.
However, also the reverse is true ( 66 ), the pattern and frequency of AUD can foster new episodes of BD, both mania and depression ( 67 , 68 ); increasing severity of AUD predicts occurrence of a new major depressive episode (MDE) ( 69 ). Co-occuring BD has a detrimental impact on subjects with AUD. The Collaborative Study on the Genetics of Alcoholism is a family pedigree investigation that enrolled treatment-seeking alcohol-dependent probands who met the DSM-IV criteria for alcohol dependence ( 70 ). Of the 228 Bipolar probands, 75.4% (74% in bipolar I patients and 77% in bipolar II patients) fulfilled criteria for DSM-IV life time alcohol dependence. Comparing 5-year prospective data of BP-I and -II probands with and without alcohol dependence confirmed ( 71 ), in line with previous retrospective studies ( 60 ), a more severe course of BD in comorbid bipolar I individuals, whereas bipolar II individuals were less severely impaired by comorbid alcohol use.
The sequence of onset of each respective disorder might be of importance for early detection and possibly treatment of persons on risk. In a study by Frank et al., substance use preceded in 60% but succeeded in 7% the first manic episode which favors SUD and AUD as a trigger for BD. In one third of cases the temporal sequence remained unclear ( 72 ). Analysis of data from the National Comorbidity Survey Replication study revealed that SUD starting in adolescence leads to an ~3-fold increased odds of subsequent mood disorders, especially BD ( 73 ). The fact that juvenile-onset BD is a risk factor for SUD was also replicated in other studies ( 74 , 75 ). Other studies, however, are in support of BD as the primary disorder followed by SUD and/or AUD. Preisig et al. ( 76 ) concluded from their study on familial relationship between mood disorders and alcoholism that BD tends to precede AUD. Comparing retrospectively three samples of bipolar patients (group 1: BD without AUD and SUD, group 2: onset of BD precedes AUD and SUD, and group 3: onset of a SUD precedes BD), Feinman and colleagues found that subjects in the second group showed a significantly earlier onset of affective symptoms than those in the other two groups, also suggesting that BD is a breeding ground for AUD or SUD ( 77 ). Whether SUD or AUD onset prior to BD results in a more or less severe course of BD is still a matter of discussion. The study of Feinman and Dunner found higher rates of suicide attempts in their group 3 (SUD prior to BD), whereas Winokur et al. report on a milder course of BD in those with prior onset of SUD ( 78 ). The relationship between SUD or AUD and BD is probably not just bidirectional but more complex with several confounding variables. McElroy et al. ( 79 ), for example, retrospectively showed an association between early onset BD, mixed symptoms, psychiatric comorbidity and SUD. Thus, early detection of both BD and being on risk for SUD is essential to avoid disastrous outcomes ( 10 ), but further prospective research of the complex relationship in larger samples is still needed.
Treatment Strategies in Comorbid BD and AUD—General Principles of Treatment
This chapter deals with the intermediate and long-term treatment of comorbid BD and AUD. We do not recap acute treatments for detoxification or delirium on one side, and mania or severe depression on the other side. These acute treatments are symptom-orientated, rarely different in comorbid vs. non-comorbid patients and depend on the predominant symptomatology (affective vs. addictive) that needs attention first. For intermediate and long-term treatment, the dogma persisted for a long time that AUD needs to be treated first and sufficiently before attention should be paid to the mental health disorder. Today, strategies that promote concomitant therapy of dual disorders are the established treatment of choice ( 80 ) and recommended in major guidelines ( 81 ). However, treatment adherence and compliance remain a challenge in this special group, since medications are often not taken as prescribed ( 61 ) and psychotherapy appointments are often missed. Studies support that the most important predictor of non-adherence in BD is comorbid alcohol and/or drug abuse ( 82 , 83 ). Thus, effective psychosocial ( 84 ), psychoeducational ( 85 , 86 ) or psychotherapeutic ( 87 , 88 ) intervention for AUD and BD can also positively impact on medication adherence and, by this, ameliorate the course especially of BD ( 84 ).
Successful treatment of comorbid BD and AUD is a time-consuming process. Except from few specialized long-term inpatient settings for comorbid patients ( 89 ) the emphasis of all treatment concepts is on outpatient settings as behavioral changes and building up resilience is a long process in both disorders. As relapses and recurrences are rather the rule than the exception, regular outpatient contacts, emergency numbers to call in case of an imminent relapse and a timely and easy access to inpatient treatment for either one of the disorders are crucial. The German S3 Guidelines for AUD recommend that both disorders, BD and AUD, should be treated in one setting and by the same therapeutic team ( 49 , 81 ). If not feasible, a close coordination of therapies, e.g., by means of a case manager, should be established.
Psychotherapy
The evidence base for suitable psychotherapies in comorbid BD and AUD remains poor. The German S3 Guidelines for AUD ( 49 ) recommends cognitive behavioral therapy (CBT) as the best evidenced modality whereas there is no recommendation for other psychotherapies due to insufficient data.
This recommendation is, by large, based on the CBT studies conducted by Farren et al. In a prospective cohort study, 232 comorbid patients with alcohol dependence and an affective disorder (among whom 102 were individuals with BDs), received inpatient treatment with cognitive behavioral therapy for 4 weeks ( 90 ). The program also included psychoeducation on both disorders. At 6-month follow-up both groups (depressive and bipolar patients) showed a significant reduction of alcohol consumption, but no difference was found between patients with unipolar and bipolar disorder. At 5-year follow-up, there was still a significant long-term benefit, particularly in those who engaged in post-discharge supportive therapy. Early abstinence predicted later abstinence, and a significant number of those who reduced their drinking by 6 months also achieved complete abstinence after 5 years ( 91 ).
Other guidelines, e.g., the Canadian Network for Mood and Anxiety Treatments (CANMAT) do not recommend CBT but rather the integrated group therapy (IGT) developed by Weiss and colleagues which includes CBT and psychoeducation components. IGT has been studied in a pilot study ( 92 ) and 2 separate RCTs ( 93 , 94 ) comparing it with either group drug counseling or no treatment. This manualized program with 20 weekly group sessions demonstrated effectiveness both for the prevention of alcohol and bipolar relapses ( 93 ) even at 8-month follow-up. IGT topics are identification of triggers preceding substance use, refusing drugs and alcohol, coping with BD without abusing substances, medication adherence, relationships with friends and family members, self-help group participation, weighing the pros and cons of recovery, and recognizing the warning signs of relapse, among other topics ( 95 ). A slimmed version with twelve sessions, developed by the same group, also demonstrated effectiveness ( 94 ).
The evidence for Assertive community treatment (AST) that has been examined in two RCTs is inconclusive, with one study showing a reduction of alcohol use, the other not when compared to standard clinical case management. Both studies included also patients with other major mental health disorders, such as MDD and schizophrenia; thus, both do not supply information exclusively about changes in the course of BD ( 96 , 97 ). Only a follow-up evaluation of the first study after 3 years specifically reports about 51 patients with BD and comorbid SUD, stating that taking part in the AST program has also improved quality of life (QoL) and diverse functionality measures ( 98 ).
For contingency management and motivational therapy in comorbid BD and SUD, only low-level evidence exists, e.g., non-randomized, prospective studies, case series or retrospective studies. In the CANMAT guidelines they are only recommended as second-choice in situations where first choice treatments are not indicated or cannot be used, or when first-choice treatments have not worked ( 89 ).
In adolescents with comorbid BD and SUD, inclusion of the family appears crucial. Family-focused treatment (FFT) with psychoeducation is recommended and effective ( 99 ).
In summary, only few psychotherapeutic interventions have been studied in a randomized study design and mostly only by one research group. The most recent Cochrane review on psychotherapies of mental illness and comorbid SUDs examined 41 RCTs and concluded that it was impossible to rule in favor of any specific psychosocial treatment, because of a large array of methodological differences and difficulties impeding data pooling as well as interpretation ( 100 ).
E-Mental Health Approaches
Not only in times of pandemics, but for the sake of high visibility, easy access and cost-effectiveness digital media are increasingly on the rise in health care, and have been used for screening and supplementing psychotherapy in affective disorders comorbid with AUD during recent years ( 101 ). For unipolar depression, efficacy for depressive symptoms as well as drinking behavior (cumulative duration of abstinence) was reported in a study comparing SMS twice daily ( n = 26) vs. control condition (14-day “thank you” —SMS, n = 28). After 3 months of study completion, both Beck Depression Inventory scores and cumulative abstinence were significantly improved in the experimental group ( 102 ); however, the effect did not last ( 103 ). A subsequent, slightly larger study ( n = 95) included comorbid patients both with unipolar and bipolar depression. Unfortunately, numbers and outcomes are not reported separately for unipolar and BD subjects. The study found a significant reduction in depression scores ( p = 0.02) and perceived stress scores ( p < 0.01) 3 months after completing a 30-day rehabilitation program in the intervention group. The intervention group- again receiving twice daily supportive text messages- also showed a significantly greater reduction in units per drinking day from baseline to 6 months after completion of the rehabilitation program. treatment point compared to the control group with a medium effect size ( P = 0.03). At follow up 6 months after stopping text messaging (12 months after completion of the rehabilitation program) group differences in drinking or mood measures had vanished, again suggesting that the effect of text messaging was transient but not lasting.
The use or digital media and “blended care” is likely to increase in the future across treatment settings and will facilitate diagnosis and treatment of mental disorders including comorbid conditions. It's usefulness in BD patients comorbid with AUD, however, still needs to be further investigated.
Pharmacological Options
Besides psychotherapy an individually tailored pharmacotherapy is essential in almost all BD patients with comorbid AUD. For BD, pharmacotherapy is an essential component to stabilize mood and prevent recurrences, whereas its role for treating AUD beyond controlling acute withdrawal symptoms is less clear. Randomized controlled studies in BD traditionally exclude patient with concurrent SUD. Thus, the evidence for choosing a mood stabilizer in BD with comorbid AUD is rather weak; strictly speaking, high levels evidence consists of altogether three placebo-controlled studies in this patient group ( 104 – 106 ). To make any suggestion (not even recommendations) about best available treatments we therefore rely on additional low-level evidence from open or retrospective studies and expert opinion.
In general, treatment-refractory patients are over-represented in the group of BD patients with comorbid SUD ( 107 ). As with most treatments, concurrent SUD including AUD is thus a predictor for inferior response to lithium. However, as shown in adolescents, achieving more mood stability with lithium can result in lower levels of alcohol or drug consumption ( 108 ). Positive effects of lithium on SUD apart from indirect effects via mood stabilization could not be substantiated so far ( 109 ).
Anticonvulsants, namely valproate, carbamazepine and lamotrigine, had been first line alternatives in BD to lithium for a long time. An open pilot study with valproate by Brady and colleagues in 1995 suggested a reduction of drinking days in parallel to a reduction of manic and depressive symptoms ( 110 ). Subsequently, Brady and colleagues conducted a 12-week, double-blind, placebo-controlled trial ( 105 ) in a small group of BD patients with comorbid AUD ( n = 29). In this study, the valproate group had a significantly smaller percentage of subjects who relapsed to heavy drinking, but otherwise there were no significant differences in other alcohol-related outcomes. As far as BD symptomatology was concerned, there was only a significantly greater decrease in irritability. In the following, Salloum and colleagues conducted a 24-week, double-blind, placebo- controlled study with a slightly greater number of patients ( n = 59). Valproate failed to demonstrate improvement in mood stabilization. The number of heavy drinking days, number of drinks per heavy drinking day, and serum biomarker levels of alcohol use in the valproate-treated group, however, were significantly reduced compared to the placebo group ( 106 ). Finally, the study by Kemp and colleagues in rapid-cycling (RC) BD patients with comorbid SUD (alcohol, cannabis or cocaine) consisted of an open label stabilization (up to 24 weeks) with all patients receiving lithium plus valproate, follow by a 6-month double- blind phase with randomization of stabilized patients to either lithium alone or lithium plus valproate. The study failed to demonstrate any effect of valproate on mood- related parameters ( 104 ). As far as AUD is concerned, the authors reported that of the 19 subjects with AUD, 58% no longer met criteria for active abuse or had entered into early full remission while in the open-label phase. Due to the very small number of subjects entering the double-blind phase ( n = 31, corresponding to 21% of the original sample), there are no reliable data whether adding valproate to lithium is superior to lithium monotherapy, neither for mood-nor alcohol related outcomes.
For lamotrigine, only open-label evidence exists. In this small study ( n = 28), lamotrigine improved mood symptoms, as well as decreased craving for alcohol and decreased carbohydrate deficient transferrin over 12 weeks ( 111 ). Unfortunately, so far, no confirmative controlled studies in BD + AUD with lamotrigine have been conducted ( 112 ). The only placebo-controlled study with lamotrigine in BD comorbid with SUD (cocaine) was negative across mood and substance related outcomes ( 113 ).
Carbamazepine has been traditionally used in acute alcohol withdrawal to reduce the risk of seizures and ameliorate physical symptoms. However, there are no reliable data whether it is of any usefulness in the long-term treatment of BD + AUD. Carbamazepine is metabolized by the liver and can, by itself, induce an increase in liver transaminases (ALAT, ASAT, γGT) and, in rare cases, cause liver failure. Thus, its use might put active alcohol users on risk.
A controlled study with topiramate in BD + AUD failed due to slow recruitment ( 114 ).
Atypical antipsychotics (aAP) have increasingly become a treatment of choice in BD. There was some expectation that their dopamine-stabilizing effects might also lead to a reduction of craving; however, a meta-analysis of the use of aAP as a group in primary AUD without comorbidities could not find any effects on drinking behavior or craving ( 115 ). The only exception was aripiprazole which reduced significantly number of drinks and heavy drinking days in one study ( 116 ).
Retrospective data suggested that, similar to aripiprazole ( 117 ), quetiapine might relieve alcohol graving in patients with BD and concomitant cocaine use ( 118 ). Subsequently, the same group conducted a double-blind, placebo-controlled study ( 119 ) in patients with BD + AUD. At the time of the study, 82% of subjects were in a depressive state. Quetiapine add-on to treatment as usual (TAU) had no effect on any alcohol-related outcomes, but produced a faster and significantly greater decrease of depressive symptoms. This finding is of note as many antidepressant treatment modalities are less effective in BD patients with comorbid AUD. The lack of efficacy of quetiapine against AUD was also confirmed in another placebo- controlled study ( 120 ). No controlled data for other aAP or antidepressants have, so far, been generated (see Table 1 ).
Randomized controlled studies on pharmacological treatments of comorbid BD and AUD.
The table illustrates the results of a systematic PubMed search on January 15, 2021, covering the years 1970–2020, using the following MeSH terms: alcohol abuse or alcohol dependence or alcohol use disorder and bipolar disorder or mania or manic depression and Randomized Controlled Trial. We also checked the literature lists of major textbooks on bipolar disorder for additional references .
AUD, Alcohol use disorder; BD, Bipolar disorder; DB, double-blind; HRSD, Hamilton Rating scale for Depression; PLC, Placebo; RC, Rapid cycling; RCT, randomized controlled trial; TAU, Treatment as usual .
Limited data exist on the effect of anti-craving medication in AUD with comorbid BD. Results of an open study suggested a reduction of both craving and stabilization of mood with naltrexone in patients with BD + AUD ( 125 ). However, improvement of mood was not confirmed in a double-blind study with naltrexone add-on to cognitive behavioral therapy, and there was only a trend toward less alcohol consumption ( 121 ). Similar disappointing results have been reported from a controlled study with acamprosate in BD + AUD ( 122 ).
A recent experimental approach used ondansetron. Ondansetron is a 5-HT 3 receptor antagonist used to prevent nausea and vomiting caused by chemo- or radiation therapy. A controlled study suggested a reduction of alcohol consumption with ondansetron ( 126 ). However, in a randomized, double-blind, placebo-controlled trial in outpatients with BD and early onset AUD ( 124 ) no reduction of alcohol use measures were observed; but interestingly, ondansetron led to an improvement of depressive symptomatology measured with the Hamilton Depression rating scale [HDRS ( 127 )].
Table 1 supplies an overview of double-blind, randomized pharmacological studies for comorbid bipolar affective and AUDs, based on a systematic PubMed search.
In BD, comorbid SUD and especially AUD are rather the rule than the exception. Pharmacological and integrated psychotherapeutic approaches that give equal weight to both disorders, while still scarce, are recommended. CBT and IGT have the best, but still insufficient evidence- base as psychosocial treatments. Figure 1 depicts a proposed therapy algorithm based on the evidence presented in this article. Supportive pharmacotherapy should be mainly centered around BD, with mood stabilizer, e.g., lithium and valproate, still the treatment of choice. However, there is clearly more research needed to develop reliable treatment algorithms for comorbid BD and AUD.

Proposed treatment and support algorithm for patients with comorbid AUD and BD. aAP, atypical antipsychotics; AC, Anticonvulsants; AD, Antidepressants; AST, Assertive community treatment; AUD, Alcohol use disorder; BD, Bipolar Disorder; BZD, benzodiazepines; CBT, Cognitive behavioral therapy; ECT, Electroconvulsive therapy; EMH, E-Mental Health; FFT, Family-focused therapy; IGT, Integrated group therapy; MS, Mood stabilizer.
Author Contributions
All authors designed the work, conducted the necessary literature search, drafted the manuscript, provide approval for publication, and agree to be accountable for all aspects of the work.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Cerebrospinal fluid synaptic biomarker changes in bipolar disorder - A longitudinal case-control study
Affiliations.
- 1 Copenhagen Affective Disorder Research Center (CADIC), Psychiatric Center Copenhagen, Department Rigshospitalet, Copenhagen, Denmark; Department of Clinical Medicine, University of Copenhagen, Denmark. Electronic address: [email protected].
- 2 Danish Dementia Research Center, Rigshospitalet, University of Copenhagen, Copenhagen, Denmark.
- 3 Institute of Neuroscience and Physiology, Department of Psychiatry and Neurochemistry, the Sahlgrenska Academy at the University of Gothenburg, Mölndal, Sweden.
- 4 Institute of Neuroscience and Physiology, Department of Psychiatry and Neurochemistry, the Sahlgrenska Academy at the University of Gothenburg, Mölndal, Sweden; Clinical Neurochemistry Laboratory, Sahlgrenska University Hospital, Mölndal, Sweden.
- 5 Institute of Neuroscience and Physiology, Department of Psychiatry and Neurochemistry, the Sahlgrenska Academy at the University of Gothenburg, Mölndal, Sweden; Clinical Neurochemistry Laboratory, Sahlgrenska University Hospital, Mölndal, Sweden; Department of Neurodegenerative Disease, University College London, Queen Square, London, United Kingdom; UK Dementia Research Institute University College London, London, United Kingdom; Hong Kong Center for Neurodegenerative Diseases, Hong Kong, China; Wisconsin Alzheimer's Disease Research Center, University of Wisconsin School of Medicine and Public Health, University of Wisconsin-Madison, Madison, WI, USA.
- 6 Institute of Neuroscience and Physiology, Department of Psychiatry and Neurochemistry, the Sahlgrenska Academy at the University of Gothenburg, Mölndal, Sweden; Clinical Neurochemistry Laboratory, Sahlgrenska University Hospital, Mölndal, Sweden; Paris Brain Institute, ICM, Pitié-Salpêtrière Hospital, Sorbonne University, Paris, France; Neurodegenerative Disorder Research Center, Division of Life Sciences and Medicine, and Department of Neurology, Institute on Aging and Brain Disorders, University of Science and Technology of China and First Affiliated Hospital of USTC, Hefei, PR China.
- 7 Section of Biostatistics, Department of Public Health, University of Copenhagen, Denmark.
- 8 Danish Dementia Research Center, Rigshospitalet, University of Copenhagen, Copenhagen, Denmark; Department of Clinical Medicine, University of Copenhagen, Denmark.
- 9 Copenhagen Affective Disorder Research Center (CADIC), Psychiatric Center Copenhagen, Department Rigshospitalet, Copenhagen, Denmark; Department of Clinical Medicine, University of Copenhagen, Denmark.
- PMID: 38723679
- DOI: 10.1016/j.jad.2024.05.034
Background: This exploratory study investigated cerebrospinal fluid (CSF) synaptic protein biomarkers in bipolar disorder (BD), aiming to highlight the neurobiological basis of the disorder. With shared cognitive impairment features between BD and Alzheimer's disease, and considering increased dementia risk in BD patients, the study explores potential connections.
Methods: Fifty-nine well-characterized patients with BD and thirty-seven healthy control individuals were examined and followed for one year. Synaptic proteins encompassing neuronal pentraxins (NPTX)1, NPTX2, and NPTX-receptor, 14-3-3 protein family epsilon, and zeta/delta, activating protein-2 complex subunit beta, synucleins beta-synuclein and gamma-synuclein, complexin-2, phosphatidylethanolamine-binding protein 1, rab GDP dissociation inhibitor alpha, and syntaxins 1B and 7 were measured in CSF using a microflow liquid chromatography-mass spectrometric multiple reaction monitoring set-up. Biomarker levels were compared between BD and HC and in BD before, during, and after mood episodes.
Results: The synaptic proteins revealed no statistically significant differences between BD and HC, neither at baseline, one-year follow-up, or in terms of changes from baseline to follow-up. Moreover, the CSF synaptic protein levels in patients with BD were unaltered compared to baseline when they stabilized in euthymia following an affective episode and at one-year follow-up.
Limitation: It is uncertain what the CSF biomarker concentrations reflect since we yet do not know the mechanisms of release of these proteins, and we are uncertain of what increased or decreased levels reflect.
Conclusion: This first-ever investigation of a panel of CSF protein biomarkers of synaptic dysfunction in patients with BD and HC individuals found no statistically significant differences cross-sectionally or longitudinally.
Keywords: Biomarkers; Bipolar disorder; Case-control; Cerebrospinal fluid; Longitudinal; Synaptic dysfunction.
Copyright © 2024 The Authors. Published by Elsevier B.V. All rights reserved.

IMAGES
VIDEO
COMMENTS
We're going to go ahead to patient case No. 1. This is a 27-year-old woman who's presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode.
Case Report on Bipolar Affective Disorder: Mania with Psychotic Symptoms Kounassegarane Deepika AbstrAct Bipolar affective disorder (BPAD) is a major psychiatric disorder all around the world, which is mainly characterized by frequent and recurrent episodes of mania, hypomania, and depression. A majority of complete etiology or pathogenesis of ...
CASE STUDY Gary (bipolar disorder) Case Study Details. Gary is a 19-year-old who withdrew from college after experiencing a manic episode during which he was brought to the attention of the Campus Police ("I took the responsibility to pull multiple fire alarms in my dorm to ensure that they worked, given the life or death nature of fires"). ...
Case Study Details. Sarah is a 42-year-old married woman who has a long history of both depressive and hypomanic episodes. Across the years she has been variable diagnoses as having major depression, borderline personality disorder, and most recently, bipolar disorder. Review of symptoms indicates that she indeed have multiple episodes of ...
1.5.1. Definition of bipolar disorders. Bipolar disorder is an episodic, potentially life-long, disabling disorder that can be difficult to diagnose. Need to. improve recognition, reduce sub ...
As in our case, the majority of individuals who ultimately develop bipolar disorder report a depressive episode first , but the later age of onset of manic symptoms and temporal relationship to TBI lends credence to the TBI's primary role in the development of manic symptoms. In the case presented here, the patient exhibited a combination of ...
The current study is a case report involving three Japanese patients with bipolar II disorder, who started CBT during the depressive phase after a hypomanic episode was stabilized by pharmacotherapy. All patients experienced excessively positive thinking one week apart and were able to choose behaviors that would stabilize bipolar mood by ...
INTRODUCTION. Bipolar affective disorder (BAD) is a complex, severe, disabling, recurrent, and multifactorial psychiatric illness that affects approximately 1% of the world's population.[] Contrary to the classical teaching about its episodic course, in reality, several patients with BAD do not reach full interepisodic remission and continue to have residual subsyndromal symptomatology ...
Abstract. Bipolar disorder (formerly called manic-depressive illness or manic depression) is a mental disorder that causes unusual shifts in mood, energy, activity levels, concentration, and the ...
Bipolar disorder (BP) suicide death rates are 10-30 times greater than the general population, likely arising from environmental and genetic risk factors. Though suicidal behavior in BP has been ...
The article, A case study on bipolar affective disorder, current episode without psychotic symptoms (ICD F 31.1), is a reco rd of original research effort, we therefore declare.
sing mania since medical management is different based on its etiology. Herein, we report a case of a manic episode in a middle-aged female with a prolonged history of BD who received a recent diagnosis of MS 1 year ago. Patient Concerns: A 56-year-old female presented with an episode of mania and psychosis while receiving a phenobarbital taper for chronic lorazepam use. She had a prolonged ...
In a replication of an earlier published study, case notes of 75 elderly in-patients with bipolar affective disorder were examined. Few of the patients had experienced a manic episode before the age of 40. Mean age of onset of affective disorder was 46 years, and first manic episode at 60 years.
Klinefelter syndrome (KS) is the most common sex chromosomal disorder with an estimated prevalence of 1 in 500-1000. Increased incidences of anxiety, depression, substance abuse, psychotic and behavioral disorders, and sexual disorders have been reported in patients with KS. The aim of this case stu …
The article, A case study on bipolar affective disorder, current episode without psychotic symptoms (ICD F 31.1), is a record of original research effort, we therefore declare. We attest to the work's originality and the absence of any instances of plagiarism across the whole manuscript.
Given the statistics related to women with bipolar affective disorder, promoting interdisciplinary mental health services is critical across the perinatal period (Knight et al, 2022). The specialist perinatal mental health services, and specifically the clinical nurse specialist, have key roles and responsibilities in the care of women with bipolar affective disorder, which often require them ...
Bipolar disorder vs. healthy controls. Five out of ten studies compared emotional urgency scores between bipolar disorders and healthy controls [54, 59,60,61,62].In these studies, healthy controls were commonly individuals who were assessed in structured interviews to have no psychiatric illness; only one study had used matched controls [].Overall, the results overwhelmingly suggest that ...
Early-onset Bipolar Disorder. Studies have shown that bipolar disorder usually begins with an index episode of depression: positive family history (Pavuluri, Birmaher, & Naylor, 2005), clinical severity, psychotic symptoms, and psychomotor retardation are well documented predictors of bipolarity.Approximately 20% of youths with a first major depressive episode will develop a manic episode.
Bipolar affective disorder (BPAD) is a chronic mental disorder, characterised by mood swings, alternating between depression and manic or hypomanic episodes. ... In the presented case study of a male patient, thanks to the introduction of the ketogenic diet, full remission of the disease was achieved, doses of lamotrigine were reduced and ...
In bipolar disorder, manic or hypomanic "highs" mimic in ways many of the joys of flow and happiness. There is a signature feeling of euphoria, enhanced productivity, and ability to create, which ...
In a replication of an earlier published study, case notes of 75 elderly in-patients with bipolar affective disorder were examined. Few of the patients had experienced a manic episode before the age of 40. Mean age of onset of affective disorder was 46 years, and first manic episode at 60 years. Cerebral insults before the first manic attacks ...
The role of expressed emotions (EEs) in relapse is poorly understood in bipolar affective disorder (BPAD). Understanding the association between EE and relapse will be useful in predicting further relapse and improving the prognosis. The present study was conducted with the objectives of assessing the relationship between EEs of caregivers and relapse of the illness in patients with BPAD on ...
The findings underline that there appear to be central regions involved in BD that are observed in all mood states, however, there appear to be underlying mechanisms of cognitive dysfunction that may vary across different mood states in BD. Background Bipolar disorder (BD) is a severe psychiatric disorder characterized by changes in mood that alternate between (hypo) mania or depression and ...
Deepika, K. (2019). conducted a study on a case report on bipolar affective disorder: Mania with psychotic symptoms. The study adopted the method of a case study which aims to find the key characteristics and implications of mania with psychotic symptoms. Akdemir, D., & Gokler, B. (2017) conducted a study on
Comorbidity of Bipolar Affective Disorders in Alcohol Use Disorder Patients. Among mental health disorders, BD has probably the highest risk of having a second, comorbid DSM -IV axis I disorder ().Epidemiological data from the US report life-time prevalence rates of up to 90% for comorbidities in BD (), with 62.3% for AUD (39.1% for DSM-IV alcohol abuse and 23.2% for alcohol dependency ...
Bipolar Affective disorder (BPAD) is one of the world's ten most disabling conditions, earlier known as manic depressive psychosis (MDP) is a major psychiatric disorder
Building on a separate study on affective lability in people with schizophrenia and bipolar disorder, the researchers explored the feature as a possible target for psychiatric treatment. They also ...
Background: This exploratory study investigated cerebrospinal fluid (CSF) synaptic protein biomarkers in bipolar disorder (BD), aiming to highlight the neurobiological basis of the disorder. With shared cognitive impairment features between BD and Alzheimer's disease, and considering increased dementia risk in BD patients, the study explores potential connections.