- Patient Care & Health Information
- Diseases & Conditions
Syphilis is an infection caused by bacteria. Most often, it spreads through sexual contact. The disease starts as a sore that's often painless and typically appears on the genitals, rectum or mouth. Syphilis spreads from person to person through direct contact with these sores. It also can be passed to a baby during pregnancy and childbirth and sometimes through breastfeeding.
After the infection happens, syphilis bacteria can stay in the body for many years without causing symptoms. But the infection can become active again. Without treatment, syphilis can damage the heart, brain or other organs. It can become life-threatening.
Early syphilis can be cured, sometimes with a single shot of medicine called penicillin. That's why it's key to get a health care checkup as soon as you notice any symptoms of syphilis. All pregnant people should get tested for syphilis at their first prenatal checkup too.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition

- Primary syphilis
Primary syphilis causes painless sores (chancres) on the genitals, rectum, tongue or lips. The disease can be present with the appearance of a single chancre (shown here on a penis) or many.
Syphilis develops in stages. The symptoms vary with each stage. But the stages may overlap. And the symptoms don't always happen in the same order. You may be infected with syphilis bacteria without noticing any symptoms for years.
The first symptom of syphilis is a small sore called a chancre (SHANG-kur). The sore is often painless. It appears at the spot where the bacteria entered your body. Most people with syphilis develop only one chancre. Some people get more than one.
The chancre often forms about three weeks after you come in contact with syphilis bacteria. Many people who have syphilis don't notice the chancre. That's because it's usually painless. It also may be hidden within the vagina or rectum. The chancre heals on its own within 3 to 6 weeks.
Secondary syphilis
You may get a rash while the first chancre heals or a few weeks after it heals.
A rash caused by syphilis:
- Often is not itchy.
- May look rough, red or reddish-brown.
- Might be so faint that it's hard to see.
The rash often starts on the trunk of the body. That includes the chest, stomach area, pelvis and back. In time, it also could appear on the limbs, the palms of the hands and the soles of the feet.
Along with the rash, you may have symptoms such as:
- Wartlike sores in the mouth or genital area.
- Muscle aches.
- Sore throat.
- Tiredness, also called fatigue.
- Weight loss.
- Swollen lymph nodes.
Symptoms of secondary syphilis may go away on their own. But without treatment, they could come and go for months or years.
Latent syphilis
If you aren't treated for syphilis, the disease moves from the secondary stage to the latent stage. This also is called the hidden stage because you have no symptoms. The latent stage can last for years. Your symptoms may never come back. But without treatment, the disease might lead to major health problems, also called complications.
Tertiary syphilis
After the latent stage, up to 30% to 40% of people with syphilis who don't get treatment have complications known as tertiary syphilis. Another name for it is late syphilis.
The disease may damage the:
- Blood vessels.
- Bones and joints.
These problems may happen many years after the original, untreated infection.
Syphilis that spreads
At any stage, untreated syphilis can affect the brain, spinal cord, eyes and other body parts. This can cause serious or life-threatening health problems.
Congenital syphilis
Pregnant people who have syphilis can pass the disease to their babies. Unborn babies can become infected through the organ that provides nutrients and oxygen in the womb, called the placenta. Infection also can happen during birth.
Newborns with congenital syphilis might have no symptoms. But without fast treatment, some babies might get:
- Sores and rashes on the skin.
- A type of discolored skin and eyes, called jaundice.
- Not enough red blood cells, called anemia.
- Swollen spleen and liver.
- Sneezing or stuffed, drippy nose, called rhinitis.
- Bone changes.
Later symptoms may include deafness, teeth problems and saddle nose, a condition in which the bridge of the nose collapses.
Babies with syphilis also can be born too early. They may die in the womb before birth. Or they could die after birth.
When to see a doctor
Call a member of your health care team if you or your child has any symptoms of syphilis. These could include any unusual discharge, a sore or a rash, especially in the groin area.
Also get tested for syphilis if you:
- Have had sexual contact with someone who might have the disease.
- Have another sexually transmitted disease such as HIV .
- Are pregnant.
- Regularly have sex with more than one partner.
- Have unprotected sex, meaning sex without a condom.
- Mayo Clinic Minute: Signs and symptoms of syphilis
Vivien Williams: Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum. Dr. Stacey Rizza, an infectious diseases specialist at Mayo Clinic, says syphilis affects men and women and can present in various stages.
Stacey Rizza, M.D.: Primary syphilis causes an ulcer, and this sometimes isn't noticed because it's painless and can be inside the vagina or on the cervix…after a few weeks, two months, they can get secondary syphilis, which is a rash.
Vivien Williams: It may then progress to latent stage syphilis and, finally, the most serious stage: tertiary. Pregnant women are not immune to syphilis. Congenital syphilis can lead to miscarriage, stillbirth or infant deaths. That's why all pregnant women should be screened. Syphilis is preventable and treatable. As for prevention, Dr. Rizza recommends barrier protection during sex.
Dr. Rizza: And that's during oral sex, anal sex, vaginal sex — using condoms, dental dams and any other barrier protection.
Vivien Williams: For the Mayo Clinic News Network, I'm Vivien Williams.
More Information
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
The cause of syphilis is a bacterium called Treponema pallidum. The most common way syphilis spreads is through contact with an infected person's sore during vaginal, oral or anal sex.
The bacteria enter the body through minor cuts or scrapes in the skin or in the moist inner lining of some body parts.
Syphilis is contagious during its primary and secondary stages. Sometimes it's also contagious in the early latent period, which happens within a year of getting infected.
Less often, syphilis can spread by kissing or touching an active sore on the lips, tongue, mouth, breasts or genitals. It also can be passed to babies during pregnancy and childbirth and sometimes through breastfeeding.
Syphilis can't be spread through casual contact with objects that an infected person has touched.
So you can't catch it by using the same toilet, bathtub, clothing, eating utensils, doorknobs, swimming pools or hot tubs.
Once cured, syphilis doesn't come back on its own. But you can become infected again if you have contact with someone's syphilis sore.
Risk factors
The risk of catching syphilis is higher if you:
- Have unprotected sex.
- Have sex with more than one partner.
- Live with HIV , the virus that causes AIDS if untreated.
The chances of getting syphilis also are higher for men who have sex with men. The higher risk may be linked, in part, with less access to health care and less use of condoms among this group. Another risk factor for some people in this group includes recent sex with partners found through social media apps.
Complications
Without treatment, syphilis can lead to damage throughout the body. Syphilis also raises the risk of HIV infection and can cause problems during pregnancy. Treatment can help prevent damage. But it can't repair or reverse damage that's already happened.
Small bumps or tumors
Rarely in the late stage of syphilis, bumps called gummas can form on the skin, bones, liver or any other organ. Most often, gummas go away after treatment with medicine called antibiotics.
Neurological problems
Syphilis can cause many problems with the brain, its covering or the spinal cord. These issues include:
- Meningitis, a disease that inflames the protective layers of tissue around the brain and spinal cord.
- Confusion, personality changes or trouble focusing.
- Symptoms that mimic dementia, such as loss of memory, judgment and decision-making skills.
- Not being able to move certain body parts, called paralysis.
- Trouble getting or keeping an erection, called erectile dysfunction.
- Bladder problems.
Eye problems
Disease that spreads to the eye is called ocular syphilis. It can cause:
- Eye pain or redness.
- Vision changes.
Ear problems
Disease that spreads to the ear is called otosyphilis. Symptoms can include:
- Hearing loss.
- Ringing in the ears, called tinnitus.
- Feeling like you or the world around you is spinning, called vertigo.
Heart and blood vessel problems
These may include bulging and swelling of the aorta — the body's major artery — and other blood vessels. Syphilis also may damage heart valves.
HIV infection
Syphilis sores on the genitals raise the risk of catching or spreading HIV through sex. A syphilis sore can bleed easily. This provides an easy way for HIV to enter the bloodstream during sex.
Pregnancy and childbirth complications
If you're pregnant, you could pass syphilis to your unborn baby. Congenital syphilis greatly raises the risk of miscarriage, stillbirth or your newborn's death within a few days after birth.
There is no vaccine for syphilis. To help prevent the spread of syphilis, follow these tips:
- Have safe sex or no sex. The only certain way to avoid contact with syphilis bacteria is not to have sex. This is called abstinence. If a person is sexually active, safer sex means a long-term relationship in which you and your partner have sex only with each other, and neither of you is infected. Before you have sex with someone new, you should both get tested for syphilis and other sexually transmitted infections (STIs).
- Use a latex condom. Condoms can lower your risk of getting or spreading syphilis. But condoms work only if they cover an infected person's syphilis sores. Other types of birth control do not lower your risk of syphilis.
- Be careful with alcohol and stay away from street drugs. Drinking too much alcohol or taking drugs can get in the way of your judgment. Either can lead to unsafe sex.
- Do not douche. It can remove some of the healthy bacteria that's usually in the vagina. And that might raise your risk of getting STIs .
- Breastfeed with caution. Syphilis can pass from a parent to a baby during breastfeeding if sores are on one or both breasts. This can happen when the baby or pumping equipment touches a sore. To keep that from happening, pump or hand-express breastmilk from the breast with sores. Do so until the sores heal. If your pump touches a sore, get rid of the milk you just pumped.
Partner notification and preventive treatment
If tests show that you have syphilis, your sex partners need to know so that they can get tested. This includes your current partners and any others you've had over the last three months to 1 year. If they're infected, they can then get treatment.
After you learn you have syphilis, your local health department may contact you. A department employee talks with you about private ways to let your partners know that they've been exposed to syphilis. You can ask the department to do this for you without revealing your identity to your partners.
Or you can contact your partners along with a department employee or simply tell your partners yourself. This free service is called partner notification. It can help limit the spread of syphilis. The practice also steers those at risk toward counseling and the right treatment.
And since you can get syphilis more than once, partner notification lowers your risk of getting infected again.
Screening tests for pregnant people
You can be infected with syphilis and not know it. And the disease can have deadly effects on unborn babies. For this reason, health officials recommend that all pregnant people be tested for the disease.
- Syphilis — CDC detailed fact sheet. Centers for Disease Control and Prevention. https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm. Accessed April 27, 2023.
- Sexually transmitted infections treatment guidelines, 2021: Syphilis. Centers for Disease Control and Prevention. https://www.cdc.gov/std/treatment-guidelines/syphilis.htm. Accessed April 27, 2023.
- Hicks CB, et al. Syphilis: epidemiology, pathophysiology, and clinical manifestations in patients without HIV. https://www.uptodate.com/contents/search. Accessed April 27, 2023.
- Syphilis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/sexually-transmitted-diseases-stds/syphilis. Accessed April 27, 2023.
- Hicks CB, et al. Syphilis: Treatment and monitoring. https://www.uptodate.com/contents/search. Accessed April 27, 2023.
- Hicks CB, et al. Syphilis: Screening and diagnostic testing. https://www.uptodate.com/contents/search. Accessed April 27, 2023.
- Syphilis — CDC basic fact sheet. Centers for Disease Control and Prevention. https://www.cdc.gov/std/syphilis/stdfact-syphilis.htm. Accessed April 27, 2023.
- Loscalzo J, et al., eds. Syphilis. In: Harrison's Principles of Internal Medicine. 21st ed. McGraw Hill; 2022. https://accessmedicine.mhmedical.com. Accessed July 14, 2019.
- AskMayoExpert. Syphilis (adult). Mayo Clinic; 2021.
- Sexually transmitted infections. Office on Women's Health. http://womenshealth.gov/publications/our-publications/fact-sheet/sexually-transmitted-infections.html. Accessed April 27, 2023.
- Tosh PK (expert opinion). Mayo Clinic. May 1, 2023.
- Cáceres CF, et al. Syphilis in men who have sex with men: advancing research and human rights. The Lancet Global Health. 2021; doi:10.1016/S2214-109X(21)00269-2.
- How can partner services programs help me and my patients? Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/clinicians/screening/partner-notification.html. Accessed April 28, 2023.
- Penicillin allergy FAQ. American Academy of Allergy, Asthma & Immunology. https://www.aaaai.org/tools-for-the-public/conditions-library/allergies/penicillin-allergy-faq. Accessed April 28, 2023.
- Just diagnosed? Next steps after testing positive for gonorrhea or chlamydia. Centers for Disease Control and Prevention. https://www.cdc.gov/std/prevention/NextSteps-GonorrheaOrChlamydia.htm. Accessed May 1, 2023.
News from Mayo Clinic
- Newborns diagnosed with syphilis at alarming rates Feb. 19, 2024, 03:30 p.m. CDT
- Mayo Clinic Minute: Syphilis surge is cause for concern Feb. 03, 2024, 12:00 p.m. CDT
- Syphilis: A rising community presence Aug. 01, 2022, 04:30 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
● In the late 19 th century, a Norwegian physician described the evolution of infection in more than 1400 patients with primary and secondary syphilis. Because he believed that the available therapies at the time were highly toxic and of little benefit, patients received no treatment [ 1 ].
● Additional data were collected from a study of 382 adults with syphilis who underwent autopsies between 1917 and 1941 [ 2 ]. This compilation provided pathologic confirmation of the late manifestations of syphilis.
● Finally, the Tuskegee study conducted between 1932 and 1972 collected data on 431 Black men whose syphilis was untreated [ 3 ]. This project was initiated prior to the availability of effective therapy for syphilis, but it profoundly violated ethical standards by not providing study participants with treatment proven to be effective once it became available. Moreover, the study participants were not given sufficient information about the study to provide informed consent. These ethical concerns significantly impacted clinical research by engendering distrust between investigators and potential study participants that persists to this day; efforts to address these concerns have led to major reforms in clinical research standards and requirements.
The epidemiology, pathogenesis, and clinical manifestations of syphilis will be reviewed here. Discussions of the diagnosis and treatment of syphilis, as well as syphilis in special populations, are found elsewhere:
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Related content
- Peer review
This article has a correction. Please see:
- Syphilis - July 19, 2019
- Patrick O'Byrne , associate professor, nurse practitioner 1 2 ,
- Paul MacPherson , infectious disease specialist 3
- 1 School of Nursing, University of Ottawa, Ottawa, Ontario K1H 8M5, Canada
- 2 Sexual Health Clinic, Ottawa Public Health, Ottawa, Ontario K1N 5P9
- 3 Division of Infectious Diseases, Ottawa Hospital General Campus, Ottawa, Ontario
- Correspondence to: P O'Byrne patrick.obyrne{at}uottawa.ca
What you need to know
Incidence rates of syphilis have increased substantially around the world, mostly affecting men who have sex with men and people infected with HIV
Have a high index of suspicion for syphilis in any sexually active patient with genital lesions or rashes
Primary syphilis classically presents as a single, painless, indurated genital ulcer (chancre), but this presentation is only 31% sensitive; lesions can be painful, multiple, and extra-genital
Diagnosis is usually based on serology, using a combination of treponemal and non-treponemal tests. Syphilis remains sensitive to benzathine penicillin G
Staging syphilis is important because it is the basis of management (treatment, expected treatment response, follow-up periods, and partner follow-up)
Patients with syphilis should be screened for HIV, gonorrhoea, and chlamydia
Caused by the bacteria Treponema pallidum , 1 2 syphilis is transmitted through direct (usually sexual) contact with infected mucosal lesions. Other bodily fluids are also infectious when patients are bacteraemic. With infectivity up to 10-30% per sexual contact or 60% per relationship, 3 syphilis rates have risen 300% since 2000 in many Western countries. 4 5 6 7 While most infections involve men who have sex with men, infections among people with opposite sex partners also occur. 4 5 6 7 In addition to increasing rates, syphilis can cause early complications such as irreversible loss of vision, so awareness of the infection is important for primary care clinicians. 8 9 10
What symptoms should alert me to this diagnosis?
While syphilis causes protean symptoms ( box 1 ), the diagnosis should be considered in any sexually active patient with genital lesions or with rashes. 16 17 18
Symptoms of syphilis by stage of infection (see fig 1 )
Symptoms appear 10-90 days (mean 21 days) after exposure
Main symptom is a <2 cm chancre:
Progresses from a macule to papule to ulcer over 7 days
Painless, solitary, indurated, clean base (98% specific, 31% sensitive)
On glans, corona, labia, fourchette, or perineum
A third are extragenital in men who have sex with men and in women
Localised painless adenopathy
Symptoms appear 2 weeks to 6 months (mean 2-12 weeks) after exposure. Can be concurrent with, or up to 8 weeks after, chancre
Rash—Diffuse, symmetric, on trunk (often subtle or atypical)
Mucus lesions, condylomata lata
Patchy alopecia (4-11%)
Fever, headaches, generalised painless adenopathy
Neurologic symptoms—Cranial nerve palsies (II,VIII), eye redness or pain, meningitis, changes to mental status or memory
No symptoms
In early latent stage (<12 months* or <24 months† after exposure) 25% of subjects relapse to secondary syphilis (90% of these in first year, 94% within 2 years)
In late latent stage (>12* or 24† months after exposure), no relapse and not infectious
1-46 years after exposure
Neurologic—paresis, tabes dorsalis
Cardiovascular—aortitis
Gummatous—necrotic granulomatous lesions
*According to US, 11 UK, 12 and Canadian 13 guidelines
†According to World Health Organization 14 and European 15 guidelines
Primary syphilis— Patients with primary syphilis ( fig 1 ) have a chancre at the site of inoculation—classically a solitary, painless, indurated, non-exudative ulcer ( fig 2 ). 17 19 While often on the glans, corona, labia, fourchette, or perineum, it may occur in the mouth ( fig 3 ), rectum, or vagina. 17 Chancres can be inconspicuous ( fig 4 ) and resolve in 3-10 weeks, possibly explaining why 60% of patients do not recall this lesion. Chancres may be multiple, painful, or atypical due to coinfection with other bacteria or herpesvirus. 20 Depending on inoculum size, chancres appear 10-90 days after exposure (mean 21 days). 17 Localised painless adenopathy may occur. 17

Stages of syphilis
- Download figure
- Open in new tab
- Download powerpoint

Chancre (sore) on penis due to syphilis

Syphilis in the mouth

Inconspicuous syphilitic chancre on penis
Secondary syphilis— Secondary syphilis is a manifestation of bacterial dissemination and classically presents as a diffuse, symmetric, copper, maculopapular, possibly pruritic rash of any morphology except vesicular ( fig 5 ). 17 20 21 A rash on the palms or soles is common (11-70%, fig 6 ). Mucus lesions ( fig 7 ), patchy alopecia, fever, headaches, and generalised painless adenopathy may also occur. 17 18 19 20 21 Early neurosyphilis develops in 25-60% of people ( box 1 ). 9 17 18 19 20 21 22 Secondary symptoms appear 2-24 weeks after infection, concurrently with or up to eight weeks after chancres, and disappear spontaneously after several weeks with or without marking. 17 19

Rash associated with secondary syphilis

Secondary syphilis on palms of hands

Condylomata lata in secondary syphilis
Latent syphilis— Syphilis then becomes latent, although symptoms of secondary syphilis recur in 25% of people, mostly (90%) within one year of acquiring the infection. 17 Latent syphilis has early and late stages. 17 Early latent disease includes the period of potential symptom relapse, classified by the WHO 14 and European 15 guidelines as <2 years since inoculation and as <1 year by US, 11 UK, 12 and Canadian 13 guidelines. As symptom relapse indicates bacterial replication, early latent disease can be infectious. Late latent syphilis occurs >1-2 years after acquisition and is non-infectious (see fig 1 ).
Tertiary syphilis— Without treatment, 14-40% of people with syphilis progress to tertiary disease—irreversible damage to any organ—within 1-46 years. The damage is primarily neurologic, cardiovascular, or gummatous (necrotic granulomatous lesions pathognomonic of tertiary syphilis). 2 17
Which diagnostic test should be done ( table 1 )?
Diagnostic tests for syphilis 23 24 25
- View inline
Treponema pallidum may be visualised from lesions using dark field microscopy, direct fluorescent antibody testing, or polymerase chain reaction. 11 12 13 14 15 Because these tests are not widely available, diagnosis predominantly relies on serology. 17 26 27 While serologic tests and laboratory algorithms vary, testing usually begins with a screening treponemal test, such as an enzyme or chemiluminescence immunoassay (EIA or CLIA) to detect treponemal antibodies. A positive screening test should be followed by a confirmatory treponemal test, typically the T pallidum particle agglutination (TPPA). If both tests are positive, infection with syphilis is confirmed. Thereafter, the rapid plasma reagin (RPR) test (a quantitative non-treponemal test) should be used to measure disease activity and to track response to treatment (although 15-41% of patients remain reactive even after successful treatment). 28
Test timing
Screening treponemal tests (EIA or CLIA) usually become reactive first, often within two weeks of the chancre. However, patients with negative results who have syphilis-like symptoms or who report a high risk contact should be re-tested after a further two to four weeks. 13
The RPR test may remain non-reactive for up to four weeks after the chancre, so it is often negative in primary syphilis, but it is 98-100% sensitive in secondary syphilis. However, because the RPR is a test of non-specific tissue damage, it may be positive for reasons other than syphilis. 15
In the absence of treatment, a negative non-treponemal test three months after potential exposure effectively rules out a new syphilis infection.
Note that treponemal tests cannot distinguish active from treated infections and generally remain positive for life (see table 2 ).
Interpretation of results from diagnostic tests for syphilis
Staging of syphilis
Staging of syphilis cannot be done based on laboratory results alone, and requires history and examination. Primary and secondary syphilis are symptomatic; early and late latent syphilis are generally asymptomatic. Careful examination to identify any symptoms not noticed by the patient is important and should include thorough anogenital and dermatologic inspection. 21
The staging criteria for early latent syphilis are given in box 2 . Asymptomatic patients with positive serology who do not fulfil the criteria of early latent syphilis could be staged as latent syphilis or as having syphilis of unknown duration.
Staging criteria for early latent syphilis 11 12 13 14 15
Patients with early latent syphilis are asymptomatic, with one of the following:
New positive serology with a documented negative test within previous 12* or 24† months
≥4-fold increase in the RPR titre relative to a previous test done within 12* or 24† months
Unequivocal symptoms of primary or secondary syphilis within the previous 12* or 24† months
Only one possible exposure, which occurred within previous 12* or 24† months
What should I do with inconclusive results?
Generally, inconclusive results arise in early infection or from waning antibody levels in late infection. The most common combinations are:
A positive RPR with negative treponemal screening (EIA/CLIA) and confirmatory tests (TPPA) suggests the RPR result is a false positive
A positive screen (EIA/CLIA) with negative confirmatory test (TPPA) and negative RPR is likely a false positive but could indicate early infection
A positive screen (EIA/CLIA) with indeterminant confirmatory test (TPPA) and negative RPR could represent waning antibody levels after a previous, treated infection or a new infection.
When results are inconclusive, clinicians should inquire about previous syphilis infection and treatment, and, if early syphilis is possible, retest in two to four weeks. 13 If results are unchanged, interpretation is based on history—consider the possibility of late untreated infection, treated infection, or non-venereal treponemal disease in adults from endemic countries in South and Central America, South-East Asia, and Africa.
What are the recommended treatment options? ( box 3 )
Recommended treatments for syphilis, primary, secondary, and early latent disease.
First line treatment
Benzathine penicillin G 2.4×10 6 units, single intramuscular dose*†
Doxycycline 100 mg, taken orally twice daily for 14 days*†
Alternate treatments
Ceftriaxone 1 g, intravenous or intramuscular once daily for 10 days*
Procaine penicillin G 1.2×10 6 units, intramuscular once daily for 10 days†
Azithromycin 2 g, single oral dose†
Late latent disease
Benzathine penicillin G 2.4×10 6 units, intramuscular dose once weekly for 3 weeks*†
Doxycycline 100 mg, taken orally twice daily for 28 days*†
Procaine penicillin G 1.2×10 6 units, intramuscular once daily for 14-21 days†
†According to WHO, 14 UK, 12 and European 15 guidelines
For primary, secondary, and early latent syphilis, in the absence of neurologic findings, first-line treatment is benzathine penicillin G (BPG) 2.4×10 6 units as a single intramuscular injection. Late latent syphilis is treated with the same dose of BPG weekly for three weeks with no more than 14 days between doses (no more than 7 days for pregnant women). 11 12 13 14 15 Additional BPG doses do not improve treatment outcomes for patients with early syphilis, 28 29 30 although some guidelines suggest pregnant women with early syphilis can receive up to two doses. 13 BPG has not been evaluated in controlled trials, but remains the first-line treatment because it is long acting (so covering the long dividing time of T pallidum ) and because penicillin-resistant syphilis has not been documented in 60 years of the drug’s use. 28 30 31
Non-pregnant patients who are allergic to penicillin can be given doxycycline 100 mg by mouth twice daily for two weeks for primary, secondary, and early latent syphilis, or for four weeks for late latent syphilis, 11 12 13 14 15 although doxycycline, compared with BPG, may yield more treatment failures (defined according to the CDC as a fourfold or higher increase in RPR titre). 28 30 31 There is no alternative treatment to BPG for pregnant women.
Counsel patients about the possibility of Jarish-Herxheimer reactions, which start two to four hours after treatment and usually resolve within 24 hours. Symptoms include fever and systemic symptoms (such as chills, rigors, myalgias, arthralgias) with worsening rash or chancre. 17 While UK guidelines 12 state prednisolone can be used for symptom management, other guidelines 11 13 14 15 recommend only over-the-counter antipyretics.
What about follow-up?
Because syphilis has no test-of-cure, conversion to a non-reactive RPR is the best evidence of successful treatment. 28 Patients should be tested at the start of treatment and monitored at six and 12 months. No clinical data guide interpretation of RPR titres after treatment, and guidelines are based on expert opinion. See table 3 for recommendations from European, UK, US, Canadian, and WHO guidelines. 11 12 13 14 15
Recommendations for assessment of treatment of syphilis
When should I consider evaluation of cerebrospinal fluid?
Indications for lumbar puncture and evaluation of cerebrospinal fluid (CSF) include neurologic symptoms or tertiary disease ( table 3 ). 11 12 13 14 15 CSF evaluation can also be considered for the 10-20% of patients with earlier disease who do not achieve a fourfold decline in RPR titres by 6-12 months after treatment. 11 12 13 14 15
Because BPG poorly penetrates CSF, 11 neurosyphilis should be treated with aqueous penicillin G, 4×10 6 units intravenously every 4 hours for 10-14 days. If neurosyphilis is ruled out, optimal management is unclear. 11 Clinicians may monitor the RPR titre until it is low or non-reactive, or repeat the treatment for early or late latent syphilis. 11 Factors limiting post-treatment RPR declines in the absence of neurosyphilis include prior infection, longer duration of infection, older age, HIV co-infection, and low pre-treatment titres. 11 12 14 15
Referral to secondary care may be necessary for patients requiring CSF evaluation and should be considered for those with uncertain diagnoses or poor response to treatment.
Are there specific considerations for patients with HIV?
Syphilis and HIV infection often co-exist. 32 33 Patients with syphilis should be screened for HIV and, if negative, offered pre-exposure prophylaxis. 32 33 34 They should also be screened for gonorrhoea and chlamydia. HIV-positive patients have additional indications for CSF evaluation (see table 3 ). Otherwise, diagnosis and treatment are unchanged. 31 35 36 37
How should I manage contact tracing?
Contacts (people who have had sex with a person diagnosed with infectious (early) syphilis) within 90 days should receive treatment with one dose of BPG even if their serology results are is negative; asymptomatic contacts who had sex with an infected person more than 90 days ago could defer treatment until their serology results are available, but only if follow-up is assured. Discussions about contact tracing should be non-stigmatising and sensitive to patients’ concerns about confidentiality. Explain that contact tracing has important benefits for the individual concerned and their contacts. It helps to limit ongoing transmission of a serious infection and prevent re-infection. Patients need help and support to notify contacts confidentially.
How this article was created
This article was created based on a review of international guidelines, expert opinion (local public health unit, STI clinic, and infectious disease department), and through a review of Medline and CINAHL, using the search term “syphilis.” We also undertook a manual review of the reference lists of identified articles.
Education into practice
Do you consider syphilis as a differential diagnosis of genital lesions and rashes among sexually active patients?
How would you approach a conversation about contact tracing with a young man, recently diagnosed?
How patients were involved in this article
We reviewed the contents of this material with Max Ottawa, a local “community-based organisation that focuses on maximising the health and wellness of gay, bisexual, Two-spirit, queer, and other guys who are into guys, both cis and trans.”
Acknowledgments
PO’B holds a research chair in public health and HIV prevention from the Ontario HIV Treatment Network.
Competing interests: We have read and understood the BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Holmes KK ,
- Sparling PF ,
- Lukehard SA
- LaFond RE ,
- Lukehart SA
- Stoltey JE ,
- ↵ Centers of Disease Control and Prevention (CDC). Sexually transmitted disease surveillance 2017–Syphilis. https://www.cdc.gov/std/stats17/syphilis.htm .
- Choudhri Y ,
- ↵ European Centre for Disease Control and Prevention. Syphilis–Annual epidemiologic report for 2016. https://ecdc.europa.eu/en/publications-data/syphilis-annual-epidemiological-report-2016 .
- Golden MR ,
- Nyatsanza F ,
- ↵ Centers of Disease Control and Prevention. 2015 sexually transmitted diseases treatment guidelines–Syphilis. https://www.cdc.gov/std/tg2015/syphilis.htm .
- Kingston M ,
- Higgins S ,
- Members of the Syphilis guidelines revision group 2015
- ↵ Public Health Agency of Canada. Canadian guidelines on sexually transmitted infections: management and treatment of specific infections–syphilis. https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/sexually-transmitted-infections/canadian-guidelines-sexually-transmitted-infections-27.html .
- ↵ World Health Organization. WHO guidelines for the treatment of Treponema pallidum (syphilis). https://www.who.int/reproductivehealth/publications/rtis/syphilis-treatment-guidelines/en/ .
- ↵ Janier M, Hegyi V, Dupin N, et al. 2014 European guideline on the management of syphilis. https://www.iusti.org/regions/europe/pdf/2014/2014SyphilisguidelineEuropean.pdf .
- Swartz MN ,
- Musher DM ,
- Romanowski B
- Ballard RC ,
- Moreland AA
- ↵ Cherneskie T. An update and review of the diagnosis and management of syphilis. https://www.nycptc.org/x/Syphilis_Module_Online.pdf .
- Baughn RE ,
- Oliver SE ,
- ↵ Cantor A, Nelson HD, Daeges M, Pappas M. Screening for syphilis in nonpregnant adolescents and adults: systematic review to update the 2004 US Preventive Services Task Force recommendation. Evidence Synthesis No 136. Agency for Healthcare Research and Quality, 2016. https://www.ncbi.nlm.nih.gov/books/NBK368467/pdf/Bookshelf_NBK368467.pdf .
- Fakile YF ,
- Wheeler HL ,
- Agarwal S ,
- Morshed MG ,
- Levett PN ,
- Fonseca K ,
- Tsang RSW ,
- Clement ME ,
- Pathela P ,
- Braunstein SL ,
- Shepard C ,
- Schillinger JA
- Solomon MM ,
- Glidden DV ,
- iPrEx Study Team
- Biomedical HIV Prevention Working Group of the CIHR Canadian HIV Trials Network
- Larsen SA ,
- Clement MJ ,
- Bacchetti P ,
- Yinnon AM ,
- Coury-Doniger P ,
- Reichman RC

STD Clinical Slides
The STD Clinical Slides depict clinical manifestations of sexually transmitted diseases and may include laboratory images of the organisms. The first option under each disease below, “View or download in Microsoft PowerPoint” is a ready to use PowerPoint 97 slide show with captions for each photograph. The second option under each disease below “Download graphics only”, includes separate files for each photograph without captions. These files could be used to create slide shows or documents.
- View or download in Microsoft PowerPoint (ppt) format ppt icon (146KB)
- View or download in Microsoft PowerPoint (ppt) format ppt icon (172KB)
- View or download in Microsoft PowerPoint (ppt) format ppt icon (278KB)
- View or download in Microsoft PowerPoint (ppt) format ppt icon (174KB)
- View or download in Microsoft PowerPoint (ppt) format ppt icon (218KB)
- View or download in Microsoft PowerPoint (ppt) format ppt icon (124KB)
- View or download in Microsoft PowerPoint (ppt) format ppt icon (242KB)
- View or download in Microsoft PowerPoint (ppt) format ppt icon (622KB)
For Public Health Professionals
- STD on Twitter
- STD on Facebook
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Achieve Mastery of Medical Concepts
Study for medical school and boards with lecturio.
USMLE Step 1 | USMLE Step 2 | COMLEX Level 1 | COMLEX Level 2 | ENARM | NEET
Syphilis (Clinical)
Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis is a bacterial infection caused by the spirochete Spirochete Treponema is a gram-negative, microaerophilic spirochete. Owing to its very thin structure, it is not easily seen on Gram stain, but can be visualized using dark-field microscopy. This spirochete contains endoflagella, which allow for a characteristic corkscrew movement. Treponema Treponema pallidum Treponema pallidum The causative agent of venereal and non-venereal syphilis as well as yaws. Treponema subspecies pallidum (T. pallidum) , which is usually spread through sexual contact. Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Primary syphilis Primary Syphilis Syphilis begins with a chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis , a painless ulcer on the genitals. Progression to secondary syphilis Secondary Syphilis Syphilis manifests as a generalized maculopapular Maculopapular Dermatologic Examination rash Rash Rocky Mountain Spotted Fever , which includes the palms and soles. The development of tertiary syphilis Tertiary Syphilis Syphilis can cause severe neurologic ( neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis ), cardiovascular, and/or gummatous disease. The diagnosis is through both treponemal and nontreponemal testing. Penicillin Penicillin Rheumatic Fever G is the antibiotic of choice. The duration of management varies based on the stage of the disease.
Last updated: Mar 4, 2024
Clinical Presentation
Differential diagnosis.
Share this concept:
Epidemiology [3,11,12]
- Worldwide annual new cases: approximately 6.3 million
- Worldwide case rate: 17‒18 per 100,000
- Highest prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency in the WHO Western Pacific region: 93 cases per 100,000
- Second highest prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency in WHO African region: 47 cases per 100,000
- WHO Americas region: 34 cases per 100,000 population
- Incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency in the United States is rising.
- Men > women, particularly in men who have sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria with men (MSM)
- Most common age group: 20–29 years old
- Increased prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency in minorities
- Note: Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis increases the rate of HIV HIV Anti-HIV Drugs acquisition by 2‒5 times.
- Treponema pallidum Treponema pallidum The causative agent of venereal and non-venereal syphilis as well as yaws. Treponema subsp. pallidum (T. pallidum)
- Gram-negative spirochete Spirochete Treponema is a gram-negative, microaerophilic spirochete. Owing to its very thin structure, it is not easily seen on Gram stain, but can be visualized using dark-field microscopy. This spirochete contains endoflagella, which allow for a characteristic corkscrew movement. Treponema (spiral-shaped)
- Human to human: T. pallidum has very limited ability to survive outside the body.
- Bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology may enter through genital, anorectal, or oral sites.
- Transmission rate: Approximately ⅓ of sexual contacts develop the disease.
- Via direct contact during primary or secondary syphilis Secondary Syphilis Syphilis with a syphilitic sore, mucous patch Patch Nonpalpable lesion > 1 cm in diameter Generalized and Localized Rashes , condyloma Condyloma Sexually transmitted form of anogenital warty growth caused by the human papillomaviruses. Male Genitourinary Examination latum, or rash Rash Rocky Mountain Spotted Fever
- Sharing needles with an infected person
- Bacterial entry into the fetus through the placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity
- Transmission rate: 60%‒80% from an infected mother to a fetus
- Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with a sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria partner with primary, secondary, or early latent syphilis Latent syphilis The stage of syphilis that occurs following the primary (chancre) and secondary stages. The patient is asymptomatic at the latent stage but remains seropositive for the spirochete. Syphilis
- Sexually active MSM
- People living with HIV HIV Anti-HIV Drugs
- Unprotected sexual contact
- Multiple sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria partners
- Work in the sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria trade
- History of incarceration Incarceration Inguinal Canal: Anatomy and Hernias
- Men < 29 years of age
- Late or no prenatal care Prenatal care Prenatal care is a systematic and periodic assessment of pregnant women during gestation to assure the best health outcome for the mother and her fetus. Prenatal care prevents and identifies maternal and fetal problems that adversely affect the pregnancy outcome. Prenatal Care
- Maternal drug use
- Inadequate treatment of syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis during pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care
Pathophysiology [11‒13]
- Allows tissue invasion
- Facilitates dissemination
- Able to move in thick substances (e.g., connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology )
- Assists with dissemination
- Protective coating
- Comes from the host
- Prevents phagocytosis Phagocytosis The engulfing and degradation of microorganisms; other cells that are dead, dying, or pathogenic; and foreign particles by phagocytic cells (phagocytes). Innate Immunity: Phagocytes and Antigen Presentation and immune recognition Immune Recognition Yaws, Bejel, and Pinta
- T. pallidum adheres to skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions or mucosal membranes → hyaluronidase Hyaluronidase Bacteroides production → tissue invasion
- The organism coats itself in the host’s fibronectin Fibronectin Glycoproteins found on the surfaces of cells, particularly in fibrillar structures. The proteins are lost or reduced when these cells undergo viral or chemical transformation. They are highly susceptible to proteolysis and are substrates for activated blood coagulation factor VIII. The forms present in plasma are called cold-insoluble globulins. Connective Tissue: Histology → prevents recognition and phagocytosis Phagocytosis The engulfing and degradation of microorganisms; other cells that are dead, dying, or pathogenic; and foreign particles by phagocytic cells (phagocytes). Innate Immunity: Phagocytes and Antigen Presentation by the immune system Immune system The body’s defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs → development of the chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis (initial ulcerative lesion)
- Eventual local immune control → resolution of chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis
- During the primary period, some spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema move into local lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy .
- Spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema multiply and disseminate through the bloodstream → invade other organs and tissues
- Host immune-inflammatory response → systemic clinical manifestations
Related videos
Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis is a multistage disease. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship can present at any stage, and infected individuals may not exhibit symptoms for years.
Primary syphilis Primary Syphilis Syphilis [1,3,5,11‒13,15]
- Initial: localized infection
- Incubation Incubation The amount time between exposure to an infectious agent and becoming symptomatic. Rabies Virus period is approximately 10–90 days (average, 3 weeks).
- Symptoms may go unnoticed.
- Begins as a firm, red papule Papule Elevated lesion Generalized and Localized Rashes
- Becomes a firm ulcer (typically 1‒2 cm in diameter) with raised, indurated borders
- Posterior pharynx Pharynx The pharynx is a component of the digestive system that lies posterior to the nasal cavity, oral cavity, and larynx. The pharynx can be divided into the oropharynx, nasopharynx, and laryngopharynx. Pharyngeal muscles play an integral role in vital processes such as breathing, swallowing, and speaking. Pharynx: Anatomy
- Lips Lips The lips are the soft and movable most external parts of the oral cavity. The blood supply of the lips originates from the external carotid artery, and the innervation is through cranial nerves. Lips and Tongue: Anatomy
- Heals spontaneously in 3–6 weeks (regardless of treatment)
- Note: Because these lesions are painless , and often occur in areas that are hard to see, the patient may not notice them.
- Palpable, rubbery lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy
- Usually inguinal

Primary, painless chancre of syphilis ( T. pallidum infection)
Secondary syphilis Secondary Syphilis Syphilis [1,3,5,11‒13,15]
- Systemic disease that develops 2–12 weeks after the primary infection Primary infection Herpes Simplex Virus 1 and 2
- Lasts 4–8 weeks
- Fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever
- Malaise Malaise Tick-borne Encephalitis Virus
- Myalgias Myalgias Painful sensation in the muscles. Tick-borne Encephalitis Virus
- Anorexia Anorexia The lack or loss of appetite accompanied by an aversion to food and the inability to eat. It is the defining characteristic of the disorder anorexia nervosa. Anorexia Nervosa
- Weight loss Weight loss Decrease in existing body weight. Bariatric Surgery
- Nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics
- Tender (may be very mild)
- Affected nodes usually are in the axillary, cervical, inguinal, and femoral regions.
- Nonpruritic
- Macular, papular, or nodular
- Scaly or smooth
- Red, reddish-brown, or copper Copper A heavy metal trace element with the atomic symbol cu, atomic number 29, and atomic weight 63. 55. Trace Elements color
- Involves the trunk, extremities, palms, and soles
- White erosions Erosions Corneal Abrasions, Erosion, and Ulcers
- May be seen in the mouth (buccal or lingual mucosa) or genital regions
- Grayish-white color
- Wart-like lesions
- Mostly seen around the anus and vagina Vagina The vagina is the female genital canal, extending from the vulva externally to the cervix uteri internally. The structures have sexual, reproductive, and urinary functions and a rich blood supply, mainly arising from the internal iliac artery. Vagina, Vulva, and Pelvic Floor: Anatomy (near the location of the primary chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis , in warm, moist areas)
- More severe, ulcerating skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions
- Seen in immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship (e.g., HIV HIV Anti-HIV Drugs )
- Alopecia Alopecia Alopecia is the loss of hair in areas anywhere on the body where hair normally grows. Alopecia may be defined as scarring or non-scarring, localized or diffuse, congenital or acquired, reversible or permanent, or confined to the scalp or universal; however, alopecia is usually classified using the 1st 3 factors. Alopecia (hair loss): can be in a diffuse or a “moth-eaten” pattern
- GI infiltration and/or ulcerations
- Proctitis Proctitis Inflammation of the mucous membrane of the rectum, the distal end of the large intestine. Chronic Granulomatous Disease
- Periostitis Periostitis Inflammation of the periosteum. The condition is generally chronic, and is marked by tenderness and swelling of the bone and an aching pain. Acute periostitis is due to infection, is characterized by diffuse suppuration, severe pain, and constitutional symptoms, and usually results in necrosis. Reactive Arthritis
- Synovitis Synovitis Inflammation of the synovial membrane. Rheumatoid Arthritis
- Nephrotic syndrome Nephrotic syndrome Nephrotic syndrome is characterized by severe proteinuria, hypoalbuminemia, and peripheral edema. In contrast, the nephritic syndromes present with hematuria, variable loss of renal function, and hypertension, although there is sometimes overlap of > 1 glomerular disease in the same individual. Nephrotic Syndrome
- Acute nephritis
- Renal failure Renal failure Conditions in which the kidneys perform below the normal level in the ability to remove wastes, concentrate urine, and maintain electrolyte balance; blood pressure; and calcium metabolism. Renal insufficiency can be classified by the degree of kidney damage (as measured by the level of proteinuria) and reduction in glomerular filtration rate. Crush Syndrome
- Keratitis Keratitis Inflammation of the cornea. Herpes Simplex Virus 1 and 2
- Anterior uveitis Uveitis Uveitis is the inflammation of the uvea, the pigmented middle layer of the eye, which comprises the iris, ciliary body, and choroid. The condition is categorized based on the site of disease; anterior uveitis is the most common. Diseases of the Uvea
- Posterior uveitis Posterior Uveitis Diseases of the Uvea
- Optic neuritis Optic neuritis Inflammation of the optic nerve. Commonly associated conditions include autoimmune disorders such as multiple sclerosis, infections, and granulomatous diseases. Clinical features include retro-orbital pain that is aggravated by eye movement, loss of color vision, and contrast sensitivity that may progress to severe visual loss, an afferent pupillary defect (Marcus-Gunn pupil), and in some instances optic disc hyperemia and swelling. Inflammation may occur in the portion of the nerve within the globe (neuropapillitis or anterior optic neuritis) or the portion behind the globe (retrobulbar neuritis or posterior optic neuritis). Cranial Nerve Palsies
- Hearing loss Hearing loss Hearing loss, also known as hearing impairment, is any degree of impairment in the ability to apprehend sound as determined by audiometry to be below normal hearing thresholds. Clinical presentation may occur at birth or as a gradual loss of hearing with age, including a short-term or sudden loss at any point. Hearing Loss
- Tinnitus Tinnitus A nonspecific symptom of hearing disorder characterized by the sensation of buzzing, ringing, clicking, pulsations, and other noises in the ear. Objective tinnitus refers to noises generated from within the ear or adjacent structures that can be heard by other individuals. The term subjective tinnitus is used when the sound is audible only to the affected individual. Tinnitus may occur as a manifestation of cochlear diseases; vestibulocochlear nerve diseases; intracranial hypertension; craniocerebral trauma; and other conditions. Cranial Nerve Palsies
- Vertigo Vertigo Vertigo is defined as the perceived sensation of rotational motion while remaining still. A very common complaint in primary care and the ER, vertigo is more frequently experienced by women and its prevalence increases with age. Vertigo is classified into peripheral or central based on its etiology. Vertigo

Diffuse cutaneous lesions on the palms of a patient with secondary syphilis

Generalized maculopapular rash on the trunk of a patient with secondary syphilis

Condyloma lata in a patient with secondary syphilis
Latent syphilis Latent syphilis The stage of syphilis that occurs following the primary (chancre) and secondary stages. The patient is asymptomatic at the latent stage but remains seropositive for the spirochete. Syphilis [1,3,5,11‒13,15]
- Period between secondary and tertiary syphilis Tertiary Syphilis Syphilis during which the disease lays dormant
- Positive serologic test with no visible signs or symptoms
- Early: < 1‒2 years after initial infection
- Late: > 1‒2 years after initial infection
- May last months to years (often decades)
- The disease can resolve, relapse Relapse Relapsing Fever with skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions /mucosal lesions (i.e., recurrent secondary disease), or progress to tertiary syphilis Tertiary Syphilis Syphilis .
Tertiary syphilis Tertiary Syphilis Syphilis [1,3,5,10‒15]
- Seen in 33% of untreated cases
- Occurs 1–30 years after the initial infection
- Headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess
- Nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia
- Neck stiffness Neck Stiffness Meningitis
- Photophobia Photophobia Abnormal sensitivity to light. This may occur as a manifestation of eye diseases; migraine; subarachnoid hemorrhage; meningitis; and other disorders. Photophobia may also occur in association with depression and other mental disorders. Migraine Headache
- Focal neurologic deficits Neurologic Deficits High-Risk Headaches
- Cranial nerve deficits
- Seizures Seizures A seizure is abnormal electrical activity of the neurons in the cerebral cortex that can manifest in numerous ways depending on the region of the brain affected. Seizures consist of a sudden imbalance that occurs between the excitatory and inhibitory signals in cortical neurons, creating a net excitation. The 2 major classes of seizures are focal and generalized. Seizures
- Endarteritis → stroke
- Meningomyelitis → spastic weakness, paresthesia, muscular atrophy Atrophy Decrease in the size of a cell, tissue, organ, or multiple organs, associated with a variety of pathological conditions such as abnormal cellular changes, ischemia, malnutrition, or hormonal changes. Cellular Adaptation
- Chronic progressive meningoencephalitis Meningoencephalitis Encephalitis → cerebral atrophy Cerebral Atrophy Subdural Hemorrhage
- Mood disturbances
- Psychiatric disease (e.g., depression, mania Mania A state of elevated excitement with over-activity sometimes accompanied with psychotic symptoms (e.g., psychomotor agitation, inflated self esteem and flight of ideas). It is often associated with mental disorders (e.g., cyclothymic disorder; and bipolar diseases). Bipolar Disorder , psychosis)
- Memory Memory Complex mental function having four distinct phases: (1) memorizing or learning, (2) retention, (3) recall, and (4) recognition. Clinically, it is usually subdivided into immediate, recent, and remote memory. Psychiatric Assessment impairment
- Dysarthria Dysarthria Disorders of speech articulation caused by imperfect coordination of pharynx, larynx, tongue, or face muscles. This may result from cranial nerve diseases; neuromuscular diseases; cerebellar diseases; basal ganglia diseases; brain stem diseases; or diseases of the corticobulbar tracts. The cortical language centers are intact in this condition. Wilson Disease
- Pupillary abnormalities can occur but are rare.
- Demyelination Demyelination Multiple Sclerosis of the dorsal columns Dorsal Columns Posterior Cord Syndrome and the dorsal roots
- Ataxia Ataxia Impairment of the ability to perform smoothly coordinated voluntary movements. This condition may affect the limbs, trunk, eyes, pharynx, larynx, and other structures. Ataxia may result from impaired sensory or motor function. Sensory ataxia may result from posterior column injury or peripheral nerve diseases. Motor ataxia may be associated with cerebellar diseases; cerebral cortex diseases; thalamic diseases; basal ganglia diseases; injury to the red nucleus; and other conditions. Ataxia-telangiectasia
- Stabbing (“lightning-like”) pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways in the back and legs
- Loss of vibratory sense and proprioception Proprioception Sensory functions that transduce stimuli received by proprioceptive receptors in joints, tendons, muscles, and the inner ear into neural impulses to be transmitted to the central nervous system. Proprioception provides sense of stationary positions and movements of one’s body parts, and is important in maintaining kinesthesia and postural balance. Neurological Examination
- Loss of reflexes
- Paresthesia
- Charcot joints
- Urine retention and incontinence
- Argyll Robertson pupils (pupils accommodate but do not react to light)
- A consequence of vasculitis Vasculitis Inflammation of any one of the blood vessels, including the arteries; veins; and rest of the vasculature system in the body. Systemic Lupus Erythematosus in the vasa vasorum Vasa vasorum Nutrient blood vessels which supply the walls of large arteries or veins. Arteries: Histology
- Aortitis Aortitis Inflammation of the wall of the aorta. Ankylosing Spondylitis
- Aortic aneurysm Aortic aneurysm An abnormal balloon- or sac-like dilatation in the wall of aorta. Thoracic Aortic Aneurysms and aortic root dilation Aortic root dilation Aortic Regurgitation → aortic regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD)
- Coronary artery Coronary Artery Truncus Arteriosus narrowing
- Soft, solitary, granulomatous lesions with central necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage
- Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables in size
- Destructive (leaves scars)
- Occurs on skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions , bones, or organs
- Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types involvement may cause deep, boring pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways (worse at night).

A gumma on the palate of a patient with tertiary syphilis
Screening Screening Preoperative Care [7]
Screening Screening Preoperative Care asymptomatic individuals every 3‒12 months is recommended in individuals at high risk for disease. These individuals include:
- Individuals with a sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria partner with early syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis
- Individuals with HIV HIV Anti-HIV Drugs
- Multiple partners
- Sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria without condoms Condoms A sheath that is worn over the penis during sexual behavior in order to prevent pregnancy or spread of sexually transmitted disease. Nonhormonal Contraception
- Sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria with individuals with other sexually transmitted infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease ( STIs STIs Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) )
- Commercial sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria work
Pregnant patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship :
- All should be screened at the initial patient encounter.
- Individuals at high risk should have repeat screening Screening Preoperative Care at 28‒32 weeks of gestation and again at delivery.
General approach [2‒5]
It is difficult to diagnose syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis . However, specific labs and the correlation Correlation Determination of whether or not two variables are correlated. This means to study whether an increase or decrease in one variable corresponds to an increase or decrease in the other variable. Causality, Validity, and Reliability of history and examination results can lead to a diagnosis.
- Treponemal tests (TTs): detect antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions specific for T. pallidum
- Nontreponemal tests (NTTs): detect antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions against anticardiolipin, lecithin Lecithin A complex mixture of phospholipids; glycolipids; and triglycerides; with substantial amounts of phosphatidylcholines; phosphatidylethanolamines; and phosphatidylinositols, which are sometimes loosely termed as 1, 2-diacyl-3-phosphocholines. Lecithin is a component of the cell membrane and commercially extracted from soybeans and egg yolk. The emulsifying and surfactant properties are useful in food additives and for forming organogels (gels). Fatty Acids and Lipids , and cholesterol Cholesterol The principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils. Cholesterol Metabolism , which are released from damaged host cells
- Confirming the diagnosis typically requires a positive result on both treponemal and nontreponemal tests.
- Screening Screening Preoperative Care test (1st): NTT
- Confirmatory test (2nd): TT
- Screening Screening Preoperative Care test (1st): TT
- Confirmatory test (2nd): NTT
- Will result in more false positives than the traditional approach
- Those with very early disease
- The 15%‒25% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with late or latent syphilis Latent syphilis The stage of syphilis that occurs following the primary (chancre) and secondary stages. The patient is asymptomatic at the latent stage but remains seropositive for the spirochete. Syphilis whose NTTs become nonreactive over time
- Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship should also be tested for other STIs STIs Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) .
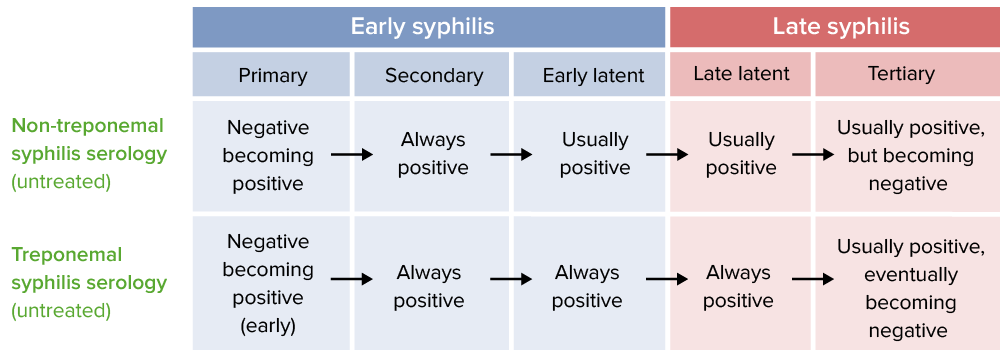
Reactivity of serological tests by stage of syphilis
Nontreponemal testing [5]
- Tests are sensitive but not specific.
- Detects IgG IgG The major immunoglobulin isotype class in normal human serum. There are several isotype subclasses of igg, for example, igg1, igg2a, and igg2b. Hypersensitivity Pneumonitis or IgM IgM A class of immunoglobulin bearing mu chains (immunoglobulin mu-chains). Igm can fix complement. The name comes from its high molecular weight and originally being called a macroglobulin. Immunoglobulins: Types and Functions antilipid antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions
- Takes 1‒4 weeks after chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis appears to become reactive → will miss early-phase primary syphilis Primary Syphilis Syphilis
- May become nonreactive ( false negative False negative An FN test result indicates a person does not have the disease when, in fact, they do. Epidemiological Values of Diagnostic Tests ) in late neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis (especially tabes dorsalis Tabes dorsalis Parenchymatous neurosyphilis marked by slowly progressive degeneration of the posterior columns, posterior roots, and ganglia of the spinal cord. The condition tends to present 15 to 20 years after the initial infection and is characterized by lightning-like pains in the lower extremities, urinary incontinence; ataxia; severely impaired position and vibratory sense, abnormal gait, optic atrophy; Argyll-Robertson pupils, hypotonia, hyperreflexia, and trophic joint degeneration. Syphilis )
- Rapid plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products reagin ( RPR RPR Treponema ) test: 1st choice
- Best initial test for CSF analysis CSF analysis Meningitis
- Test of choice for neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis
- Toluidine red unheated serum test ( TRUST Trust Confidence in or reliance on a person or thing. Conflict of Interest ): used less frequently [16,17]
- Qualitative (reactive or nonreactive)
- Tests provide titer levels.
- Results are used to follow titers → monitor treatment response
- Pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care
- Viral infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease
- Rheumatic fever Rheumatic fever Acute rheumatic fever (ARF) is an autoimmune inflammatory process that usually follows Streptococcal pharyngitis. Acute rheumatic fever usually occurs 2-4 weeks after an untreated infection and affects the heart, skin, joints, and nervous system. Rheumatic Fever
- Systemic lupus erythematosus Systemic lupus erythematosus Systemic lupus erythematosus (SLE) is a chronic autoimmune, inflammatory condition that causes immune-complex deposition in organs, resulting in systemic manifestations. Women, particularly those of African American descent, are more commonly affected. Systemic Lupus Erythematosus
Treponemal testing [5,17]
- Tests that detect antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions to Treponema Treponema Treponema is a gram-negative, microaerophilic spirochete. Owing to its very thin structure, it is not easily seen on Gram stain, but can be visualized using dark-field microscopy. This spirochete contains endoflagella, which allow for a characteristic corkscrew movement. Treponema antigens
- Even after treatment, treponemal antibody titers are positive for life.
- Reported as “reactive” or “nonreactive”
- Does not distinguish between an active and a prior, treated infection
- Typically, becomes positive 5‒15 days after appearance of the chancre Chancre The primary sore of syphilis, a painless indurated, eroded papule, occurring at the site of entry of the infection. Syphilis
- Can be done on CSF to evaluate for neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis
- Less specific than the CSF-VDRL test
- Expensive, time-consuming, and difficult to read
- Microhemagglutination assay for T. pallidum ( MHA-TP MHA-TP Treponema ); in Europe: T. pallidum haemagglutination test (TPHA)
- T. pallidum particle agglutination test ( TPPA TPPA Syphilis )
- T. pallidum enzyme immunoassay Enzyme immunoassay HIV Infection and AIDS ( TP-EIA TP-EIA Syphilis )
- Chemiluminescence immunoassay Chemiluminescence Immunoassay Syphilis ( CIA CIA Syphilis )
- Prior treated syphilis: In a patient with a history of prior treated syphilis; the patient will require no further treatment (unless there is a reexposure).
- Untreated syphilis: Those without a history of treatment for syphilis require treatment. Unless there is medical history indicating a recent infection, previously untreated patients should be treated as having syphilis of unknown duration or late latent syphilis. [1]
- False positive treponemal test: can be seen in African immigrants with exposure to endemic treponematoses (e.g., yaws, pinta).
Direct methods [5]
Definitive tests using obtained specimens (such as exudates from mucosal lesions). However, use is limited since the tests are not routinely available.
- A microscopy technique illuminating specimens against a dark background.
- Motile spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema are seen.
- Must be performed immediately after specimen collection
- Sensitivity is < 50% (high false negative False negative An FN test result indicates a person does not have the disease when, in fact, they do. Epidemiological Values of Diagnostic Tests rate).
- Direct fluorescent antibody Direct Fluorescent Antibody A form of fluorescent antibody technique utilizing a fluorochrome conjugated to an antibody, which is added directly to a tissue or cell suspension for the detection of a specific antigen. Congenital TORCH Infections (DFA) testing
- Recommended over darkfield microscopy if using direct methods
- Low sensitivity in blood
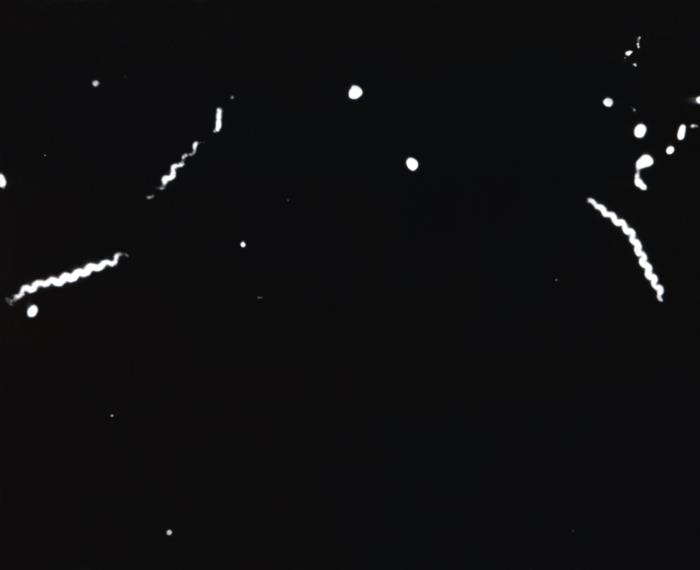
Darkfield microscopy of T. pallidum : Corkscrew-shaped bacteria are seen.
CSF assessment [2,5,6]
- Tests are better at excluding neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis rather than diagnosing it.
- TT (TPHA, MHA-TP MHA-TP Treponema , or TPPA TPPA Syphilis )
- NTT (preferably VDRL VDRL Treponema , owing to its better sensitivity than RPR RPR Treponema in CSF)
- Total protein Total protein Liver Function Tests
- Number of mononuclear cells or WBCs
- Neurologic, ocular, and/or otic/auricular findings
- Tertiary syphilis Tertiary Syphilis Syphilis
- Treatment failure in any stage
- Have RPR RPR Treponema or VDRL VDRL Treponema titers ≥ 1:32
- Have a CD4+ count ≤ 350/ mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma 3
- Have detectable plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products HIV RNA HIV RNA HIV Infection and AIDS
- Are not on antiretroviral therapy Antiretroviral therapy Antiretroviral therapy (ART) targets the replication cycle of the human immunodeficiency virus (HIV) and is classified based on the viral enzyme or mechanism that is inhibited. The goal of therapy is to suppress viral replication to reach the outcome of undetected viral load. Anti-HIV Drugs
- Consider in follow-up of late syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship treated with alternative regimens (e.g., doxycycline)
General management for syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis [2–6,9]
- Bactericidal Bactericidal Penicillins levels should be maintained for 7‒10 days (longer with late syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis ).
- Long-acting penicillin Penicillin Rheumatic Fever G benzathine is the treatment of choice.
- Typical dose: 2.4 million units (provides treponemicidal levels for up to 21 days)
- Offer HIV HIV Anti-HIV Drugs preexposure prophylaxis Prophylaxis Cephalosporins to those who test negative.
- In geographic areas with high prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of HIV HIV Anti-HIV Drugs , offer preexposure prophylaxis Prophylaxis Cephalosporins and retest for HIV HIV Anti-HIV Drugs in 3 months (if initial result is negative).
- Screening Screening Preoperative Care for other STIs STIs Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs)
- Offer vaccination Vaccination Vaccination is the administration of a substance to induce the immune system to develop protection against a disease. Unlike passive immunization, which involves the administration of pre-performed antibodies, active immunization constitutes the administration of a vaccine to stimulate the body to produce its own antibodies. Vaccination for hepatitis B Hepatitis B Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Most individuals with acute HBV infection are asymptomatic or have mild, self-limiting symptoms. Chronic infection can be asymptomatic or create hepatic inflammation, leading to liver cirrhosis and hepatocellular carcinoma (HCC). Hepatitis B Virus , if appropriate.
- Full neurologic exam
- CSF assessment
- Cranial nerve exam
- Ocular slit-lamp exam
- Ophthalmologic exam
- CSF assessment is recommended by some expert guidelines.
- Presumptively treat all partners from the past 90 days.
- Secondary syphilis Secondary Syphilis Syphilis : Test all partners from within the past 6 months; treat based on results.
- Early latent syphilis Latent syphilis The stage of syphilis that occurs following the primary (chancre) and secondary stages. The patient is asymptomatic at the latent stage but remains seropositive for the spirochete. Syphilis : Test all partners from within the past 12 months; treat based on results.
- Test all partners from the past 1 year; treat based on results.
- Test all long-term sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria partners; treat based on results.
- All lesions are healed (if present).
- 2 weeks after completion of treatment
- Individuals with HIV HIV Anti-HIV Drugs are monitored more frequently.
- Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with late syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis should also be tested at 24 months.
- Consider CSF assessment.
- Compare titers to initial baseline levels to assess treatment response.
- < 4-fold decrease in NTT titers lasting 6‒12 months after treatment
- Persistent low antibody titers ≤ 4 at 1–2 years after treatment
Early syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis management
For primary, secondary, or early latent syphilis Latent syphilis The stage of syphilis that occurs following the primary (chancre) and secondary stages. The patient is asymptomatic at the latent stage but remains seropositive for the spirochete. Syphilis , the following antibiotics can be used:
- Penicillin Penicillin Rheumatic Fever G benzathine 2.4 million units IM once
- If penicillin Penicillin Rheumatic Fever G benzathine is not available: procaine Procaine A local anesthetic of the ester type that has a slow onset and a short duration of action. It is mainly used for infiltration anesthesia, peripheral nerve block, and spinal block. Local Anesthetics penicillin Penicillin Rheumatic Fever 600,000 units IM daily for 10‒14 days
- Includes pregnant patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship and those with HIV HIV Anti-HIV Drugs
- For individuals with penicillin Penicillin Rheumatic Fever allergies Allergies A medical specialty concerned with the hypersensitivity of the individual to foreign substances and protection from the resultant infection or disorder. Selective IgA Deficiency , consider desensitization and/or skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions testing prior to starting an alternative agent.
- Doxycycline (best-studied alternative) 100 mg by mouth twice a day for 14 days
- Ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins 1 g IM or IV once daily for 10‒14 days
- Tetracycline Tetracycline A naphthacene antibiotic that inhibits amino Acyl tRNA binding during protein synthesis. Drug-Induced Liver Injury 500 mg by mouth 4 times daily for 14 days
- Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins 3 g + probenecid Probenecid The prototypical uricosuric agent. It inhibits the renal excretion of organic anions and reduces tubular reabsorption of urate. Probenecid has also been used to treat patients with renal impairment, and, because it reduces the renal tubular excretion of other drugs, has been used as an adjunct to antibacterial therapy. Gout Drugs 500 mg twice daily for 14 days
- Azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides (should be considered only as a last resort owing to resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing ): 2 g by mouth once
- Erythromycin Erythromycin A bacteriostatic antibiotic macrolide produced by streptomyces erythreus. Erythromycin a is considered its major active component. In sensitive organisms, it inhibits protein synthesis by binding to 50s ribosomal subunits. This binding process inhibits peptidyl transferase activity and interferes with translocation of amino acids during translation and assembly of proteins. Macrolides and Ketolides (a possibility per the WHO, but not recommended by US, UK, or European guidelines): 500 mg 4 times daily for 14 days
- Azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides and erythromycin Erythromycin A bacteriostatic antibiotic macrolide produced by streptomyces erythreus. Erythromycin a is considered its major active component. In sensitive organisms, it inhibits protein synthesis by binding to 50s ribosomal subunits. This binding process inhibits peptidyl transferase activity and interferes with translocation of amino acids during translation and assembly of proteins. Macrolides and Ketolides do not cross the placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity well, so they are poor choices in pregnant women.
- Doxycycline is teratogenic and is contraindicated.
Late syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis management [2,5,6,9]
For late-latent syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis , tertiary syphilis Tertiary Syphilis Syphilis , or syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis of unknown duration, the following regimen is used:
- Penicillin Penicillin Rheumatic Fever G benzathine 2.4 million units IM once per week for 3 weeks (i.e., on days 1, 8, and 15)
- If penicillin Penicillin Rheumatic Fever G benzathine is not available: procaine Procaine A local anesthetic of the ester type that has a slow onset and a short duration of action. It is mainly used for infiltration anesthesia, peripheral nerve block, and spinal block. Local Anesthetics penicillin Penicillin Rheumatic Fever 600,000–1.2 million units IM once daily for 17‒21 days
- Doxycycline 100 mg by mouth twice daily for 21‒30 days
- Ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins 2 g IV or IM daily for 10‒14 days
Neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis [2,5,6,9,10,14]
- Invasion of T. pallidum into the CSF is common in primary and secondary syphilis Secondary Syphilis Syphilis , but the clinical significance of this is unclear.
- Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with ocular and/or otologic findings should be treated for neurosyphilis Neurosyphilis Infections of the central nervous system caused by treponema pallidum which present with a variety of clinical syndromes. The initial phase of infection usually causes a mild or asymptomatic meningeal reaction. The meningovascular form may present acutely as brain infarction. The infection may also remain subclinical for several years. Late syndromes include general paresis; tabes dorsalis; meningeal syphilis; syphilitic optic atrophy; and spinal syphilis. General paresis is characterized by progressive dementia; dysarthria; tremor; myoclonus; seizures; and argyll-robertson pupils. Syphilis regardless of CSF findings.
- 3‒4 million units IV every 4 hours OR
- Continuous infusion
- Procaine Procaine A local anesthetic of the ester type that has a slow onset and a short duration of action. It is mainly used for infiltration anesthesia, peripheral nerve block, and spinal block. Local Anesthetics penicillin Penicillin Rheumatic Fever G 2.4 million units IM once daily for 10‒14 days PLUS
- Probenecid Probenecid The prototypical uricosuric agent. It inhibits the renal excretion of organic anions and reduces tubular reabsorption of urate. Probenecid has also been used to treat patients with renal impairment, and, because it reduces the renal tubular excretion of other drugs, has been used as an adjunct to antibacterial therapy. Gout Drugs 500 mg by mouth 4 times daily for 10‒14 days
- Alternative regimen: ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins 2 g IV once daily for 10‒14 days
- Serial neurologic examinations every 6 months
- Consider CSF assessment (especially if treated with an alternative regimen).
Jarisch–Herxheimer reaction Jarisch–Herxheimer Reaction Syphilis [9]
- Caused by an immune response to the antigens released by dying spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema
- Rigors Rigors Fever
- Rise in temperature
- Increased respiratory rate Respiratory rate The number of times an organism breathes with the lungs (respiration) per unit time, usually per minute. Pulmonary Examination
- Hypotension Hypotension Hypotension is defined as low blood pressure, specifically Hypotension
- Occurs within 24 hours
- Resolves within 12–24 hours
- Seen in 10%–35% of cases
- Antipyretics (e.g., acetaminophen Acetaminophen Acetaminophen is an over-the-counter nonopioid analgesic and antipyretic medication and the most commonly used analgesic worldwide. Despite the widespread use of acetaminophen, its mechanism of action is not entirely understood. Acetaminophen , aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) , ibuprofen Ibuprofen A nonsteroidal anti-inflammatory agent with analgesic properties used in the treatment of rheumatism and arthritis. Nonsteroidal Antiinflammatory Drugs (NSAIDs) )
- IV fluids IV fluids Intravenous fluids are one of the most common interventions administered in medicine to approximate physiologic bodily fluids. Intravenous fluids are divided into 2 categories: crystalloid and colloid solutions. Intravenous fluids have a wide variety of indications, including intravascular volume expansion, electrolyte manipulation, and maintenance fluids. Intravenous Fluids
- Chancroid Chancroid Chancroid is a highly transmissible STD caused by Haemophilus ducreyi. The disease presents with painful ulcer(s) on the genital tract (termed chancroid or “soft chancre”). Up to 50% of patients will develop painful inguinal lymphadenopathy. Chancroid : STI STI Sexually transmitted infections (STIs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) caused by Haemophilus ducreyi Haemophilus ducreyi A species of Haemophilus that appears to be the pathogen or causative agent of the sexually transmitted disease, chancroid. Haemophilus . Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship develop painful, necrotizing genital ulcers and inguinal lymphadenopathy Inguinal Lymphadenopathy Lymphadenopathy . Diagnosis is usually clinical, but PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) and cultures can help to confirm. Management is with macrolide antibiotics.
- Donovanosis Donovanosis Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis : STI STI Sexually transmitted infections (STIs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) caused by Klebsiella Klebsiella Klebsiella are encapsulated gram-negative, lactose-fermenting bacilli. They form pink colonies on MacConkey agar due to lactose fermentation. The main virulence factor is a polysaccharide capsule. Klebsiella pneumoniae is the most important pathogenic species. Klebsiella granulomatis . Donovanosis Donovanosis Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis is also known as granuloma inguinale Granuloma inguinale Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis . The progressive, nodular genital lesions can form into painless ulcerations and cause tissue damage. Lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy is uncommon. Diagnosis is confirmed with microscopic findings of Donovan bodies Donovan Bodies Donovanosis from the lesion. Management involves antibiotics, such as macrolides Macrolides Macrolides and ketolides are antibiotics that inhibit bacterial protein synthesis by binding to the 50S ribosomal subunit and blocking transpeptidation. These antibiotics have a broad spectrum of antimicrobial activity but are best known for their coverage of atypical microorganisms. Macrolides and Ketolides , tetracyclines Tetracyclines Tetracyclines are a class of broad-spectrum antibiotics indicated for a wide variety of bacterial infections. These medications bind the 30S ribosomal subunit to inhibit protein synthesis of bacteria. Tetracyclines cover gram-positive and gram-negative organisms, as well as atypical bacteria such as chlamydia, mycoplasma, spirochetes, and even protozoa. Tetracyclines , and trimethoprim-sulfamethoxazole.
- Lymphogranuloma venereum Lymphogranuloma venereum Subacute inflammation of the inguinal lymph glands caused by certain immunotypes of Chlamydia trachomatis. It is a sexually transmitted disease in the U.S. But is more widespread in developing countries. It is distinguished from granuloma venereum, which is caused by calymmatobacterium granulomatis. Chlamydial Infections : STI STI Sexually transmitted infections (STIs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) caused by 3 strains of Chlamydia trachomatis Chlamydia trachomatis Type species of Chlamydia causing a variety of ocular and urogenital diseases. Chlamydia . Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may have a small, transient, painless genital ulcer followed by lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy ( bubo Bubo Yersinia pestis/Plague ). Diagnosis is clinical, though PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) testing can help with confirmation. Management involves tetracyclines Tetracyclines Tetracyclines are a class of broad-spectrum antibiotics indicated for a wide variety of bacterial infections. These medications bind the 30S ribosomal subunit to inhibit protein synthesis of bacteria. Tetracyclines cover gram-positive and gram-negative organisms, as well as atypical bacteria such as chlamydia, mycoplasma, spirochetes, and even protozoa. Tetracyclines or erythromycin Erythromycin A bacteriostatic antibiotic macrolide produced by streptomyces erythreus. Erythromycin a is considered its major active component. In sensitive organisms, it inhibits protein synthesis by binding to 50s ribosomal subunits. This binding process inhibits peptidyl transferase activity and interferes with translocation of amino acids during translation and assembly of proteins. Macrolides and Ketolides .
- Genital herpes Genital Herpes Genital herpes infections are common sexually transmitted infections caused by herpes simplex virus (HSV) type 1 or 2. Primary infection often presents with systemic, prodromal symptoms followed by clusters of painful, fluid-filled vesicles on an erythematous base, dysuria, and painful lymphadenopathy. Labial and Genital Herpes : a common STI STI Sexually transmitted infections (STIs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) caused by HSV HSV Herpes simplex virus (HSV) is a double-stranded DNA virus belonging to the family Herpesviridae. Herpes simplex virus commonly causes recurrent infections involving the skin and mucosal surfaces, including the mouth, lips, eyes, and genitals. Herpes Simplex Virus 1 and 2 type 1 Type 1 Spinal Muscular Atrophy or 2. Prodromal symptoms often precede clusters of painful, fluid-filled vesicles Vesicles Female Genitourinary Examination on an erythematous base, which eventually form ulcers that can coalesce. Lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy , dysuria Dysuria Painful urination. It is often associated with infections of the lower urinary tract. Urinary tract infections (UTIs) , and severe neuralgia can occur. The diagnosis is generally clinical but confirmed with PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) and serologic testing. Management includes antiviral Antiviral Antivirals for Hepatitis B therapy.
- Genital warts Warts Benign epidermal proliferations or tumors; some are viral in origin. Female Genitourinary Examination (also called condylomata acuminata Condylomata Acuminata Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts) ): a human papillomavirus Human papillomavirus Human papillomavirus (HPV) is a nonenveloped, circular, double-stranded DNA virus belonging to the Papillomaviridae family. Humans are the only reservoir, and transmission occurs through close skin-to-skin or sexual contact. Human papillomaviruses infect basal epithelial cells and can affect cell-regulatory proteins to result in cell proliferation. Papillomavirus (HPV) ( HPV HPV Human papillomavirus (HPV) is a nonenveloped, circular, double-stranded DNA virus belonging to the Papillomaviridae family. Humans are the only reservoir, and transmission occurs through close skin-to-skin or sexual contact. Human papillomaviruses infect basal epithelial cells and can affect cell-regulatory proteins to result in cell proliferation. Papillomavirus (HPV) ) infection causing a range of mucocutaneous findings, including broad-based smooth or velvety papules or rough verrucous or fungating plaques, in the anogenital region. The diagnosis is clinical. Management may include cytodestructive therapy ( podophyllotoxin Podophyllotoxin A lignan (lignans) found in podophyllin resin from the roots of podophyllum plants. It is a potent spindle poison, toxic if taken internally, and has been used as a cathartic. It is very irritating to skin and mucous membranes, has keratolytic actions, has been used to treat warts and keratoses, and may have antineoplastic properties, as do some of its congeners and derivatives. Molluscum Contagiosum ), immune-mediated therapy ( imiquimod Imiquimod A topically-applied aminoquinoline immune modulator that induces interferon production. It is used in the treatment of external genital and perianal warts, superficial carcinoma, basal cell; and actinic keratosis. Hypertrophic and Keloid Scars ), or surgical therapy.
Practical application in the clinic (checklist for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship presenting with a genital ulcer): [4]
- Take a careful medical and sexual history.
- Examination of the genital, anal, and oral areas
- Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis ( PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) from lesion and serologic TT and/or NTT)
- Herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology ( nucleic acid amplification Nucleic acid amplification Laboratory techniques that involve the in-vitro synthesis of many copies of DNA or RNA from one original template. Septic Arthritis test (NAAT) from lesion)
- Consider other ulcerative diseases, including lymphogranuloma venereum Lymphogranuloma venereum Subacute inflammation of the inguinal lymph glands caused by certain immunotypes of Chlamydia trachomatis. It is a sexually transmitted disease in the U.S. But is more widespread in developing countries. It is distinguished from granuloma venereum, which is caused by calymmatobacterium granulomatis. Chlamydial Infections , chancroid Chancroid Chancroid is a highly transmissible STD caused by Haemophilus ducreyi. The disease presents with painful ulcer(s) on the genital tract (termed chancroid or “soft chancre”). Up to 50% of patients will develop painful inguinal lymphadenopathy. Chancroid , and donovanosis Donovanosis Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis .
- Provide same-day treatment for syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis and/or HSV HSV Herpes simplex virus (HSV) is a double-stranded DNA virus belonging to the family Herpesviridae. Herpes simplex virus commonly causes recurrent infections involving the skin and mucosal surfaces, including the mouth, lips, eyes, and genitals. Herpes Simplex Virus 1 and 2 based on history, point-of-care testing, and clinical findings.
- Screen for other STIs STIs Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs) .
- Address safe sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria , abstinence during and after treatment, and partner treatment.
- Adjust management based on test results when they become available.
- Centers for Disease Control and Prevention. (2021). Sexually transmitted infections treatment guidelines, 2021: syphilis. Retrieved August 8, 2022, from https://www.cdc.gov/std/treatment-guidelines/syphilis.htm
- Centers for Disease Control and Prevention. (2022). Syphilis—CDC detailed fact sheet. Retrieved August 8, 2022, from https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm
- World Health Organization. (2016). WHO guidelines for the treatment of Treponema pallidum (syphilis). Retrieved August 8, 2022, from https://www.who.int/publications/i/item/9789241549714
- World Health Organization. (2021). Guidelines for the management of symptomatic sexually transmitted infections. Retrieved August 8, 2022, from https://www.who.int/publications/i/item/9789240024168
- Janier, M., Unemo, M., Dupin, N., et al. (2020). 2020 European guideline on the management of syphilis. https://onlinelibrary.wiley.com/doi/full/10.1111/jdv.16946
- Kingston, M., French, P., Higgins, S., et al. (2015). UK national guidelines on the management of syphilis 2015. International Journal of STD & AIDS. https://journals.sagepub.com/doi/10.1177/0956462415624059?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
- US Preventive Services Task Force. (2022). Recommendation statement: screening for syphilis infection in nonpregnant adults and adolescents. Retrieved November 30, 2022, from https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/syphilis-infection-nonpregnant-adults-adolescents-screening
- Hicks, C., Clement, M. (2020). Syphilis: screening and diagnostic testing. UpToDate. Retrieved January 18, 2021, from https://www.uptodate.com/contents/syphilis-screening-and-diagnostic-testing
- Hicks, C., Clement, M. (2020). Syphilis: treatment and monitoring. UpToDate. Retrieved January 18, 2021, from https://www.uptodate.com/contents/syphilis-treatment-and-monitoring
- Marra, C. (2020). Neurosyphilis. UpToDate. Retrieved January 18, 2021, from https://www.uptodate.com/contents/neurosyphilis
- Hicks, C., Clement, M. (2020). Syphilis: epidemiology, pathophysiology, and clinical manifestations in patients without HIV. UpToDate. Retrieved January 18, 2021, from https://www.uptodate.com/contents/syphilis-epidemiology-pathophysiology-and-clinical-manifestations-in-patients-without-hiv
- Chandrasekar, P. H. (2017). Syphilis. Medscape. Retrieved February 19, 2021, from https://emedicine.medscape.com/article/229461-overview
- Tudor, M. E., Al Aboud, A. M., Gossman, W. G. (2020). Syphilis. StatPearls. Retrieved February 19, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK534780/
- Ha, T., Taki, P., and Dubensky, L. (2020). Neurosyphilis. StatPearls. Retrieved February 19, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK540979/
- Morris, S. R. (2020). Syphilis. MSD Manual Professional Version. Retrieved February 19, 2021, from https://www.msdmanuals.com/professional/infectious-diseases/sexually-transmitted-diseases-stds/syphilis
- Gu, W. M., Yang, Y., Wang, Q. Z., Pan, B. S., Guo, W., Wu, L., Hu, W. Z., Yang, S., Song, B. B., Zhang, C. Y. (2013). Comparing the performance of traditional non-treponemal tests on syphilis and non-syphilis serum samples. International Journal of STD & AIDS, 24(12), 919–925. https://doi.org/10.1177/0956462413491399
- Henao-Martínez, A. F., Johnson, S. C. (2014). Diagnostic tests for syphilis: new tests and new algorithms. Neurology Clinical Practice, 4(2), 114–122. https://doi.org/10.1212/01.CPJ.0000435752.17621.48
Study with Lecturio for
Medical School
Nursing School
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
Create your free account or log in to continue reading!
Sign up now and get free access to Lecturio with concept pages, medical videos, and questions for your medical education.
Log in to your account
User Reviews
Get Premium to test your knowledge
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.
Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.
Clinical presentation and serological diagnosis of syphilis reinfection in men living with HIV: a retrospective cohort study
Affiliations.
- 1 Department of Dermatology, University Hospital Zurich, University of Zurich, Zurich, Switzerland.
- 2 Division of Infectious Diseases and Hospital Epidemiology, University Hospital Zurich, Zurich, Switzerland.
- 3 Department of Public Health, University of Zurich, Zurich, Switzerland.
- 4 Department of Dermatology, University Hospital Zurich, University of Zurich, Zurich, Switzerland [email protected].
- PMID: 34475233
- DOI: 10.1136/sextrans-2020-054923
Objectives: Studies on the characteristics of syphilis reinfection are scarce despite increasing numbers and proportions of cases. We aimed to gain insights into the clinical and serological presentation of reinfected men living with HIV and to evaluate diagnostic criteria for syphilis reinfection.
Methods: We conducted a retrospective cohort study of 259 HIV-positive men diagnosed with syphilis between January 1999 and September 2015 at the University Hospital Zurich. We compared patients with a single syphilis infection (n = 109) to patients with reinfections (n = 150).
Results: The two groups matched in age, sexual orientation and numbers of other STIs. Reinfected patients more often presented with latent syphilis than patients with a single syphilis episode (41.9% vs 8.9%; p<0.001). Although generally high venereal diseases research laboratory (VDRL) or rapid plasma reagin (RPR) titres (median 1:32) were seen in reinfected patients, 19.4% had titres ≤1:8. Treponema pallidum passive particle agglutination (TPPA) titres were significantly higher (1:81 840 vs 1:10 240; p<0.001), while IgM values were significantly lower (1.27 vs 3.5; p<0.001) in syphilis reinfections than in first infections. The TPPA increased ≥fourfold in >92.3% of reinfected patients.
Conclusions: Our data highlight the paramount importance of regularly screening patients at risk as syphilis reinfections in men living with HIV are more likely to be latent infections, that is, without symptoms. As non-treponemal tests might be biologically false-positive (up to a titre of 1:8) due to various conditions, a ≥fourfold increase of the TPPA might be considered as optional criterion for the diagnosis of syphilis reinfections. This could be especially valuable for diagnosing reinfected latent stage patients.
Keywords: diagnosis; diagnostic techniques and procedures; serology; syphilis.
© Author(s) (or their employer(s)) 2022. No commercial re-use. See rights and permissions. Published by BMJ.
- HIV Infections* / complications
- Reinfection
- Retrospective Studies
- Syphilis Serodiagnosis
- Syphilis* / complications
- Syphilis* / diagnosis
- Syphilis* / epidemiology
- Treponema pallidum
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 98, Issue 5
- Clinical presentation and serological diagnosis of syphilis reinfection in men living with HIV: a retrospective cohort study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Ksenia Mischler-Gornostaeva 1 ,
- Martin Glatz 1 ,
- Jan Fehr 2 , 3 ,
- http://orcid.org/0000-0002-1154-2281 Philipp Peter Bosshard 1
- 1 Department of Dermatology , University Hospital Zurich, University of Zurich , Zurich , Switzerland
- 2 Division of Infectious Diseases and Hospital Epidemiology , University Hospital Zurich , Zurich , Switzerland
- 3 Department of Public Health , University of Zurich , Zurich , Switzerland
- Correspondence to Dr Philipp Peter Bosshard, Department of Dermatology, University Hospital Zurich, Zurich, Switzerland; philipp.bosshard{at}usz.ch
Objectives Studies on the characteristics of syphilis reinfection are scarce despite increasing numbers and proportions of cases. We aimed to gain insights into the clinical and serological presentation of reinfected men living with HIV and to evaluate diagnostic criteria for syphilis reinfection.
Methods We conducted a retrospective cohort study of 259 HIV-positive men diagnosed with syphilis between January 1999 and September 2015 at the University Hospital Zurich. We compared patients with a single syphilis infection (n = 109) to patients with reinfections (n = 150).
Results The two groups matched in age, sexual orientation and numbers of other STIs. Reinfected patients more often presented with latent syphilis than patients with a single syphilis episode (41.9% vs 8.9%; p<0.001). Although generally high venereal diseases research laboratory (VDRL) or rapid plasma reagin (RPR) titres (median 1:32) were seen in reinfected patients, 19.4% had titres ≤1:8. Treponema pallidum passive particle agglutination (TPPA) titres were significantly higher (1:81 840 vs 1:10 240; p<0.001), while IgM values were significantly lower (1.27 vs 3.5; p<0.001) in syphilis reinfections than in first infections. The TPPA increased ≥fourfold in >92.3% of reinfected patients.
Conclusions Our data highlight the paramount importance of regularly screening patients at risk as syphilis reinfections in men living with HIV are more likely to be latent infections, that is, without symptoms. As non-treponemal tests might be biologically false-positive (up to a titre of 1:8) due to various conditions, a ≥fourfold increase of the TPPA might be considered as optional criterion for the diagnosis of syphilis reinfections. This could be especially valuable for diagnosing reinfected latent stage patients.
- diagnostic techniques and procedures
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. Not applicable.
https://doi.org/10.1136/sextrans-2020-054923
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Syphilis is a STI caused by the spirochete Treponema pallidum subsp. pallidum . It is often associated with other STIs and can facilitate the transmission of the HIV. 1 We are currently witnessing a global epidemic. A study by WHO estimated 20 million prevalent cases of syphilis worldwide in 2016. 2 In EU/EAA countries, despite a decline in 2004–2009, the subsequent resurgence of syphilis since 2010 resulted in 33 193 cases in 2017, with an incidence of 7.1 cases per 100 000 population. Data on transmission category in 2017 showed 77% of cases being reported in men who have sex with men (MSM). 3
Likewise, the rate of syphilis reinfections, that is, of multiple consecutive syphilis episodes in a particular individual, increases. For example, the proportion of reinfections of all syphilis cases increased from 0.2% to 5.1% in Florida, USA, between 2000 and 2008 and from 9% to 19% in Sydney, Australia, between 2006 and 2011. 4 5 Up to 61% of syphilis cases in STI clinics can be attributed to reinfections, with particularly high rates among MSM. 6 7
For the serological diagnosis of syphilis, treponemal tests (TTs) such as the Treponema pallidum passive particle agglutination (TPPA) test, chemiluminescent immunoassay (CLIA) or enzyme immunoassay (EIA) and non-treponemal tests (NTTs) such as the venereal diseases research laboratory (VDRL) or the rapid plasma reagin (RPR) test are used. 8 It is generally accepted that an increase in ≥2 dilution steps (fourfold) in a NTT suggests reinfection. 8 9 However, NTT make use of a cardiolipin–cholesterin–lecithin–antigen complex and are as thus non-specific. They might be positive (also termed biological false-positive) due to various medical conditions other than syphilis such as myocardial infarction, autoimmune disease, malignancies and infections such as hepatitis, HIV infection and other viral infections. 8 This is of importance, as 42% of MSM with syphilis are HIV positive. 10 Up to 14% of NTT positive sera of HIV patients might be false positive. 11–13 False-positive titres are often ≤1:8, although rarely higher titres are found. 14 Thus, it might be difficult to diagnose a reinfection based on the NTT titre alone when the titre is 1:4, 1:8 or rarely higher, especially in HIV-coinfected patients.
In the presented study, we focus on syphilis reinfection and its serological diagnosis. We retrospectively analysed syphilis cases in men living with HIV from 1999 to 2015 in the Zurich area and aimed to: (1) analyse the clinical and demographic characteristics of reinfected patients, (2) compare the test results of VDRL/RPR, TPPA and IgM-EIA of reinfected patients to the results of patients with first syphilis episode and (3) investigate the significance of serological tests to diagnose reinfections.
In this retrospective cohort study, we reviewed all patients with syphilis seen at the University Hospital of Zurich between January 1999 and September 2015. Inclusion criteria were: (1) male, (2) HIV coinfected, (3) serologically confirmed syphilis, (4) all three tests performed, that is, VDRL/RPR, TPPA, and IgM-EIA, (5) previous syphilis serology that documented whether patients had syphilis in the past (now being reinfected) or whether they had no previous infection (now having the first syphilis episode), (6) comprehensive documentation of patient metadata and clinical symptoms, (7) consisting documentation of clinical symptoms and final diagnosis and (8) antibiotic therapy not started more than 2 weeks prior to serum collection. Serological diagnosis was done in accordance with current guidelines. 8 9 A syphilis reinfection, in particular, was defined as increase by ≥2 dilution steps (≥fourfold) of VDRL/RPR. Additionally, two cases were defined as having a reinfection based on a positive PCR result from the ulcer although the VDRL/RPR was not increased by ≥2 dilution steps. 15 The following patient metadata were assessed: age, sexual orientation and diagnosis of other STI in history. HIV positivity was defined as being positive at any visit during the study period.
Patients with positive serology and (1) ulcers in anogenital or oropharyngeal region and without concomitant maculopapular exanthema were considered to have the primary stage; (2) maculopapular exanthema or other presentations that are typical in the secondary stage such as condylomata lata, angina specifica and ocular involvement, respectively, were considered to have secondary syphilis; and (3) no symptoms were classified as having latent syphilis.
Syphilis episodes
Each syphilis episode was categorised based on patient charts and results of previous syphilis serology in first syphilis episodes, second syphilis episodes (eg, first reinfection), third syphilis episode (eg, second reinfection) and ≥fourth syphilis episode (eg, ≥third reinfection).
Serological tests
As NTT, the VDRL (Dade Behring, Düdingen, Germany) was used until the year 2010; thereafter, sera were tested by the RPR (Biomérieux SA, Marcy-l’Etoile, France). For TT, we used the TPPA (Fujirebio Inc, Tokyo, Japan) and an IgM-EIA (Euroimmun AG, Lübeck, Germany). All tests were done according to manufacturers’ instructions from the same serum sample. We considered borderline or equivocal results, that is, TPPA titre 1:80 indeterminate (n = 2), RPR/VDRL titre 1:1 (n = 1) and IgM-EIA Index 0.8–1.1 (n = 33) as positive for statistical analysis. All tests were performed in all cases with active syphilis disease (n=344). Additionally, previous serologies (pretitres) were available in all cases: in these previous serologies, the TPPA had been performed in 340/344 cases, the VDRL/RPR in 293/344 and the IgM-EIA in 137/344 cases.
Data analysis
We performed descriptive and inferential statistical analyses using GraphPad Prism V.8.00 (GraphPad Software, La Jolla, California, USA). Normal distributions for continuous metadata were tested with Kolmogorov-Smirnov tests and Q–Q plots. These parameters were treated non-parametric and presented as median and IQR for descriptive statistics. For inferential statistics, we analysed continuous parameters by the Mann-Whitney test and non-continuous parameters by Fisher’s exact test. Statistical significance for all tests was ascribed to a two-sided alpha level of the adjusted p values <0.05.
Patient characteristics
During the study period from January 1999 to September 2015, 520 patients were diagnosed with syphilis ( online supplemental figure 1 ). Two-hundred sixty-one (50.2%) did not fulfil the inclusion criteria, resulting in 259 HIV-positive men included in this study. The median age was 38 years (IQR 33–44). The median CD4 cell count/mm 3 was 450 (IQR 352–615). Two hundred and twenty-seven (87.6%) patients declared to be MSM, and 150 (57.9%) had additional STIs during the study period and/or in their medical history. One hundred and nine (42.1%) patients had a single syphilis episode, while 150 (57.9%) patients had syphilis reinfections, which was defined as increase by ≥2 dilution steps (≥fourfold) of VDRL/RPR. The two groups were comparable in age, sexual orientation and rate of other STI coinfections, except that reinfected patients more often had chlamydia infections ( table 1 ). Of 150 reinfected patients, 107 (71.3%) had one reinfection, 32 (21.3%) had two reinfections and 11 (7.3%) had three or more reinfections during the study period.
Supplemental material
- View inline
Patient characteristics of patients with one syphilis infection versus reinfected patients
Clinical stage of patients with the first syphilis infection versus patients with reinfections
The 259 patients included had 344 syphilis episodes during the study period. Of these, 158 (45.9%) were first syphilis infections, that is, of patients with only one episode and of patients with their first of several episodes, and 186 (54.1%) were syphilis reinfection episodes. Reinfected patients were more frequently diagnosed without symptoms, that is, being in a latent syphilis stage than patients who were diagnosed with their first syphilis episode (78/186 (41.9%) vs 14/158 (8.9%); p<0.001) but less often with symptoms of secondary stage syphilis (69/186 (37.1%) vs 98/158 (62%); p<0.001) ( figure 1 ). The proportion of primary syphilis cases was comparable in both groups, that is, 39/186 (21%) in the reinfection group vs 46/158 (29.1%) in the first episode group. Within the latent syphilis cases, a majority (65/92, 70.7%) were early latent, whereas the other 27 (29.3%) cases could not be definitely assigned as early or late latent.
- Download figure
- Open in new tab
- Download powerpoint
Number of cases (%) found for each syphilis stage according to first, second, third and fourth syphilis episode.
Differences in serology of patients with the first syphilis infection versus patients with reinfections
TPPA titres were significantly lower during first syphilis episodes than during syphilis reinfections for each disease stage (p<0.01) and vice versa for IgM values (p<0.05) ( figure 2 and online supplemental table 1 ). In primary stage patients who had their first syphilis episode, the VDRL/RPR was significantly lower as compared with reinfected patients with primary syphilis symptoms (median 1:4 vs 1:16; p<0.001) and was even negative in 17/46 (37%) of them. These cases were diagnosed based on a positive TPPA and IgM-EIA and the clinical symptoms. Overall in reinfected patients, the VDRL/RPR was median 1:32, being, however, ≤1:8 in 36/186 (19.4 %) of cases.
Syphilis serology (median and IQR) in patients with the first syphilis infection and patients with reinfections. Stars indicate significant differences in the median titre or test value between first infection and reinfection: *p<0.05, **p<0.01 and ***p<0.001.
Next, we investigated the increase of serological test results (titre and EIA-index) of each individual case by comparing values from the new diagnosed episode to the prior values from the last visit. The median time interval in between was 227 days (IQR 122–370). The changes of VDRL/RPR, TPPA and IgM are shown in figure 3 and online supplemental table 2 ; the VDRL/RPR increased median 4–5 dilution steps irrespective of whether it was a first infection or a reinfection, except in first episode primary stage cases, which were often diagnosed with a low positive or negative VDRL/RPR. The TPPA increased median 4–9 dilution steps across all stages. In particular for reinfections, the TPPA titre increase was ≥2 dilution steps for 92.4% of cases. The IgM-EIA considerably increased only in patients who had a first syphilis infection diagnosed as primary or secondary stage while in patients with their first episode diagnosed in latent stage and in all reinfected patients, IgM-values on average were elevated only minimally.
Change of serological values (median and IQR) from the last serum before diagnosis (pretitre) to the values of the serum at diagnosis in patients with the first syphilis infection and patients with reinfections. Stars indicate significant differences in the median titre increase or test value increase between first infection and reinfection: *p<0.05, **p<0.01, ***p<0.001.
This study describes 150 HIV-coinfected male patients with syphilis reinfections and compares their clinical and serological data with those of 109 HIV-coinfected male patients with a single syphilis episode. Previous studies on syphilis reinfections described between 32 and 643 patients with reinfections from North America, South America, Asia and Australia, while data from Europe are scarce. For example, Courjon and colleagues 16 described clinical characteristics of only 12 patients with syphilis reinfections among a HIV cohort in France. Kenyon and colleagues 7 provided epidemiologic data on 170 patients with syphilis reinfections but clinically characterised only 10 individuals with five or more reinfection episodes. Our study provides a comprehensive epidemiological, clinical and serological description of patients with syphilis reinfections from Zurich.
One aim of our study was to depict clinical and demographic characteristics. As all patients belonged to the male HIV cohort at our centre, they were regularly (once per year) scheduled for medical appointments including STI screening. Overall, a majority were MSM (87.6%). Patients who were infected for the first time with T. pallidum and reinfected patients did not differ significantly, except that reinfected patients had more chlamydia infections. Similar data have been found in previous studies from other regions, where 20%–100% of individuals with reinfections were HIV positive and MSM and besides HIV also had chlamydia infections or gonorrhoea. 4 5 16–21
We found more syphilis reinfections diagnosed in the latent stage than in the primary or secondary stage what is in line with previous reports. 5 16 22 The proportion of latent stage syphilis patients increased with each reinfection from 8.9% in those who only had a single syphilis episode, to 37% in those who had one reinfection, to more than 50% in those who had two or more reinfections. It also has been shown that reinfected patients might present with less pronounced symptoms than during their first episodes. 16 The high proportion of less symptomatic or even asymptomatic patients may owe to several reasons. First, patients with reinfections have an altered immune response against T. pallidum with lower IL-10 levels reflecting a weaker inflammatory response. 22–24 Second, patients with treated syphilis are followed up until the VDRL/RPR titre drops fourfold or becomes negative. This is usually done at 3, 6 and 12 months after treatment in our clinic. Therefore, the chance to detect a next latent syphilis episode might be higher in patients who once had syphilis. Third, MSM might miss typical symptoms, for example, anal ulcers. This elucidates that a clinical diagnosis of syphilis reinfections often is impaired and that some patients might not even be aware of having a reinfection thus supporting the practice of regular STI screening in high-risk patients.
A second aim of our study was to analyse the serological test results and compare them among reinfected patients and patients with a first syphilis episode. TPPA titres were higher, while IgM values were lower in reinfections as compared with first syphilis episodes. For the non-treponemal VDRL/RPR, we would like to emphasise two points. First, the test had a very low sensitivity (63%) in first syphilis episodes diagnosed during primary stage. Thus, if only the non-treponemal VDRL/RPR is being used as screening test, the diagnosis relies on clinical evaluation alone and is not confirmed in these cases. This substantiates the previous suggestion of our group to use TTs such as the TPPA in combination with an IgM-EIA as primary screening tests in case of suspected primary stage syphilis. 25 26 Second, although generally high VDRL/RPR titres were seen in reinfected patients, 19.4% of them had titres ≤1:8. Even more, two reinfections were diagnosed by PCR without fourfold VDRL/RPR increase. This is in line with a previous study on 88 patients with syphilis reinfections, where the RPR did not increase ≥2 dilution steps compared with a prevalue in >10% of reinfections. 21
The third aim of our study was to investigate the significance of serological tests to diagnose syphilis reinfections. In our patients, TPPA titres increased median 4–9 dilution steps with each syphilis episode. Only in 7.7% of reinfected cases, the TPPA did not increase ≥2 dilution steps. It has to be noted, however, that TPPA titres might increase alone for several dilutions steps without evidence for reinfection. 27 The IgM-EIA kinetics in syphilis reinfections were heterogeneous. While in some cases the IgM became highly positive, 43.6% among all reinfections were negative or equivocal. This is in stark contrast to the high sensitivity (90%–95%) of the IgM-EIA in first syphilis infections found here and in previous studies of our group. 25 26 It might be speculated that repeated contact with treponemal antigens during reinfections elicit a less intense IgM response. Hence, in contrast to the TPPA, the IgM-EIA seems to have limited value for the diagnosis of reinfections.
Guidelines from the USA and Europe currently suggest a ≥fourfold increase of a NTT such as the VDRL or RPR for the diagnosis of a syphilis reinfection. 8 9 This recommendation is based on the rationale that a difference of ±1 dilution step might be attributed to a test-to-test variation, whereas a difference of ≥2 dilution steps reflects a biological true change. Patients with a ≥4-fold increase of a NTT titre thus qualify for treatment. However, owing to the possibility of false-positive NTT up to a titre of 1:8 (or rarely even higher), 11–14 there might be some degree of uncertainty when in asymptomatic cases the NTT increases from, for example, 1:1 to 1:4 or from 1:2 to 1:8. These cases are treated according to the guidelines, yet, in our opinion, definite proof of reinfection is not provided with the NTT (≤1:8) alone in asymptomatic patients. We suggest considering a TPPA titre increase by ≥2 dilution steps as optional additional criterion for the diagnosis of syphilis reinfections especially in patients without symptoms. When the criterion is fulfilled, it strengthens the diagnosis of syphilis reinfection in asymptomatic patients. We observed 13 asymptomatic cases, which were diagnosed having latent syphilis reinfection based on a fourfold increase of NTT where the titre, however, was ≤1:8. In 11 of them, the TPPA also increased ≥2 dilution steps, thus strengthening the syphilis diagnosis.
Our study has limitations: (1) only data from HIV-positive men were analysed. The results are thus not generalisable to HIV-negative patients. (2) Despite careful retrospective analysis of patient charts, we cannot exclude that some patients did not report previous syphilis episodes, thus the true number of reinfections might be higher. (3) In reinfected patients without symptoms, that is, latent syphilis, it is difficult to ascertain whether it was a reinfection or a relapse due to treatment failure. However, 77% of reinfected patients that were diagnosed as having latent stage syphilis had residual antibodies in the preceding control hence documenting successful therapy of a previous syphilis episode.
A significant high portion of reinfected patients is diagnosed during the latent, symptom-free stage of syphilis, a circumstance that supports the practice of regular STI screening in HIV patients. TPPA titres were higher, and IgM-EIA values were lower during syphilis reinfections than during first infections. We suggest considering an increase of the TPPA by ≥2 dilution steps (≥fourfold) as optional criterion for the diagnosis of syphilis reinfections especially when the patient does not have any symptoms.
Key messages
HIV patients with syphilis reinfection more often presented with latent syphilis than those with a single syphilis episode.
Venereal diseases research laboratory/rapid plasma reagin titres generally were high in reinfected patients; however, 19% had titres ≤1:8.
Treponema pallidum passive particle agglutination (TPPA) titres were significantly higher, while IgM values were significantly lower in syphilis reinfections than in first infections
A ≥fourfold increase of the TPPA titre might be considered as optional criterion for the diagnosis of syphilis reinfections.
Ethics statements
Patient consent for publication.
Not required.
Ethics approval
The study was approved by the ethics committee of Zurich, Switzerland under the number 2016-01518.
Acknowledgments
We would like to thank all physicians of the University Hospital of Zurich who examined the patients and documented the cases and all technicians who performed the serological tests.
- Jarzebowski W ,
- Dupin N , et al
- Vander Hoorn S ,
- Korenromp E , et al
- European Centre for Disease Prevention and Control
- Botham SJ ,
- Ressler K-A ,
- Maywood P , et al
- Brewer TH ,
- Peterman TA ,
- Florence E , et al
- Workowski KA ,
- Bolan GA , Centers for Disease Control and Prevention
- Centers for Disease Control and Prevention
- Kittler H ,
- Hein U , et al
- Moore RD , et al
- Rompalo AM ,
- Cannon RO ,
- Quinn TC , et al
- Sparling PF
- Juricevic N ,
- Altwegg M , et al
- Courjon J ,
- Hubiche T ,
- Almeida VCde ,
- Donalisio MR ,
- Ding Y , et al
- Roberts CP , et al
- Kohn R , et al
- Ogilvie GS ,
- Taylor DL ,
- Moniruzzaman A , et al
- Tsoumanis A ,
- Osbak K , et al
- Morgan CA ,
- Lukehart SA ,
- Van Voorhis WC
- Bosshard PP
- Knaute DF ,
- Lautenschlager S , et al
- Bosshard PP ,
- Knaute DF , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
Handling editor Jo Gibbs
Contributors JF and PPB contributed to the study concept and design. KM-G and PPB contributed to the acquisition of clinical and laboratory data. PPB has done the statistical analysis. MG and PPB interpreted the data. KM-G, MG and PPB contributed to initial manuscript drafting. MG, JF and PPB were responsible for revisions for intellectual content. All authors approved the final version to be published and agree to be accountable for all aspects of the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:

IMAGES
VIDEO
COMMENTS
Tertiary (late) syphilis is slowly progressive and may affect any organ. The disease is generally not thought to be infectious at this stage. Manifestations may include the following: Impaired balance, paresthesias, incontinence, and impotence. Focal neurologic findings, including sensorineural hearing and vision loss.
Syphilis is a systemic bacterial infection caused by the spirochete Treponema pallidum. Due to its many protean clinical manifestations, it has been named the "great imitator and mimicker." The origin of syphilis has been controversial and under great debate, and many theories have been postulated regarding this.
The rash often starts on the trunk of the body. That includes the chest, stomach area, pelvis and back. In time, it also could appear on the limbs, the palms of the hands and the soles of the feet. Along with the rash, you may have symptoms such as: Wartlike sores in the mouth or genital area. Hair loss.
Tertiary syphilis is rare and develops in a subset of untreated syphilis infections. It can appear 10-30 years after a person gets the infection, and it can be fatal. Tertiary syphilis can affect multiple organ systems, including the: ... a population-level analysis of New York City men. Clinical Infectious Diseases 2015;61:281-287. 7.
Syphilis is an infection caused by the bacterium Treponema pallidum. Most new cases of syphilis are sexually acquired. The clinical manifestations depend upon the stage of disease. Studies performed in the preantibiotic era permit a relatively complete understanding of the natural history of untreated syphilis.
Introduction. Syphilis is caused by the bacterium Treponema pallidum subspecies pallidum. 1 This motile, gram-negative spirochete can be transmitted both sexually and from mother to child, and can invade virtually any organ or structure in the human body. The disease, which should be considered systemic throughout, is characterised by overlapping clinical stages and a relapsing and remitting ...
Some studies suggest that infection with HIV may affect the clinical presentation of syphilis, as atypical or multiple genital lesions are more apparent, and accelerated progression of syphilis may be seen in people with advanced immunosuppression. 16,17,19-22 Primary or secondary syphilis also may cause a transient decrease in CD4 T lymphocyte ...
If you are pregnant and have syphilis, you can give the infection to your unborn baby. Having syphilis can lead to a low-birth-weight-baby. It can make it more likely you will deliver your baby too early or stillborn (a baby born dead). To protect your baby, you should receive syphilis testing at least once during your pregnancy. Receive ...
Latent syphilis—Syphilis then becomes latent, although symptoms of secondary syphilis recur in 25% of people, mostly (90%) within one year of acquiring the infection.17 Latent syphilis has early and late stages.17 Early latent disease includes the period of potential symptom relapse, classified by the WHO14 and European15 guidelines as <2 years since inoculation and as <1 year by US,11 UK,12 ...
Syphilis coinfection with human immunodeficiency virus is emphasized because it is increasingly common in the United States and affects the initial presentation, disease course, diagnosis, and treatment of syphilis. Of particular consequence is the effect of human immunodeficiency virus on the clinical diagnosis, prevalence, and course of ...
Diagnosis and treatment of syphilis are challenging because of its variable clinical presentation and course and the lack of definitive tests of cure after treatment. This review of the most recent literature on the epidemiology, clinical manifestations, current diagnosis, and treatment of syphilis is focused toward clinicians who treat patients with this disease. Syphilis coinfection with ...
Introduction. Syphilis is caused by the bacterium Treponema pallidum subspecies pallidum. 1 This motile, gram-negative spirochete can be transmitted both sexually and from mother to child, and can invade virtually any organ or structure in the human body. The disease, which should be considered systemic throughout, is characterised by overlapping clinical stages and a relapsing and remitting ...
Moreover, HIV infection may modulate the clinical presentation and the clinical and serologic response to syphilis treatment [3,4,5,6]. In 2017, the annual rate of primary and secondary syphilis in the United States was 11% higher than in 2016: more than 60% of infected individuals were MSM, of whom 46% were people living with HIV infection ...
by positive syphilis serology with no clinical manifestations. Latent syphilis is often divided into two phases: early latent syphilis is defined as infection for less than two years while late latent syphilis is the presence of the disease for two years or more. Sexual transmission typically occurs during primary, secondary or early latent ...
The STD Clinical Slides depict clinical manifestations of sexually transmitted diseases and may include laboratory images of the organisms. The first option under each disease below, "View or download in Microsoft PowerPoint" is a ready to use PowerPoint 97 slide show with captions for each photograph. The second option under each disease ...
Clinical Presentation. Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis is a multistage disease. Patients Patients Individuals participating in the health care system for the purpose of ...
Syphilis is a multisystem infection caused by the spirochete Treponema pallidum. ... The clinical presentation varies and is determined by the structures involved and duration of infection. The absence of gold-standard tests and the broad clinical features contribute to difficulties in diagnosis. The laboratory diagnosis of neurosyphilis ...
The clinical presentation of syphilis does not differ between pregnant and nonpregnant women. Primary syphilis is characterized by one or more indurated chancres at the site of inoculation, which ...
We aimed to gain insights into the clinical and serological presentation of reinfected men living with HIV and to evaluate diagnostic criteria for syphilis reinfection. Methods: We conducted a retrospective cohort study of 259 HIV-positive men diagnosed with syphilis between January 1999 and September 2015 at the University Hospital Zurich.
1.2.3. Clinical Presentation. The natural history of syphilis is characterized by the cyclical alternation of symptomatic and asymptomatic periods. The first year after infection is the early stage of syphilis, which is divided into primary, secondary, and transient stages.
Objectives Studies on the characteristics of syphilis reinfection are scarce despite increasing numbers and proportions of cases. We aimed to gain insights into the clinical and serological presentation of reinfected men living with HIV and to evaluate diagnostic criteria for syphilis reinfection. Methods We conducted a retrospective cohort study of 259 HIV-positive men diagnosed with syphilis ...
syphilis, the clinical manifestations of syphilis are similar to those observed in people without HIV. Some studies suggest that infection with HIV may affect the clinical presentation of syphilis, as atypical or multiple genital lesions are more apparent, and accelerated progression of syphilis may be seen in people with advanced ...
Tami Conn introduced the next presentation under the same agenda item is Dr. Roshanda Clemons. Dr. Roshanda Clemons gives a presentation on Congenital Syphilis, a sentinel event. Dr. Clemons presents an overview of syphilis, congenital syphilis, neurosyphilis, and ocular syphilis symptoms, risk factors, stages, clinical presentation, effects on
Coinfection is dangerous because HIV infection may modulate the clinical presentation and the serologic response to syphilis treatment . PLWH with a syphilis infection seem to have a higher risk of developing neurosyphilis and mount an abnormal serological response [8,9]. Many diagnostic and therapeutic challenges remain, as there are currently ...