

Dementia Case Study Essay – 3500 words
HEALTH ISSUES FOR OLDER ADULTS.
The Case Study
Previous History: Social
The case study chosen is that of a 74 year old male patient with a history of challenging health issues. John (an assumed name in order to protect the patients identity in accordance with the Code of Professional Conduct as per the Nursing & Midwifery Council, 2006) has been happily married for 54 years and does not have any children. He does belong to a large extended family – he has twelve siblings. He has spent his working life as a plumber. He has been a sociable person enjoying the company of friends and family. Before admission to the Dementia ward he was living with his wife in their family home. His wife is finding it increasingly difficult to deal with John’s behaviour and condition as recently he has become significantly cognitively impaired. On admission, John was clean and tidy and it was obvious that his wife takes very good care of him despite the considerable effort that is required by her. During his stay on the ward John did receive regular visitors and his family and friends showed a great deal of affection for him.
Previous History: Medical
On admission it was noted that John has a long history of ill health.
His main conditions are:
Multi-Infarct Dementia: “MID is a common cause of memory loss in the elderly. MID is caused by multiple strokes (disruption of blood flow to the brain). Disruption of blood flow leads to damaged brain tissue.” (NINDS). This was diagnosed three months ago after John exhibited trademark symptoms such as short term memory loss, confusion, shuffling feet. He also started losing bladder and bowel control. MID is usually found within the 60 – 74 year age group, more often in men than women. A MRI scan showed up this condition.
Cardiac Diverticulitis: a rare congenital heart malformation
Aortic Aneurysm
Hypertension
These conditions cause John great pain and distress. He is currently being administered several pain relieving medications – Morphine, Sevradol, Diclofenic and paracetamol. He also received medication for the hypertension.
John was told 15 months ago that the prognosis for the treatment of his Aortic Aneurysm was not good and it was anticipated that his life expectancy was six months.
The severity of the pain experienced by John results in very aggressive physical and verbal behaviour. This aggression is very difficult for his loved ones to deal with.
He was admitted to the dementia ward for a six week assessment with a view to providing suitable pain relief which could then lessen his challenging behaviour to an extent.
Care assessment
On admission to the ward, John was attended by psychiatric staff who carried out an evaluation on John’s memory. This is known as a Mini Mental State Examination. The MMSE indicates the importance of cognitive stimulation therapy that can be consistently offered to the patient. (Weavers (2007, p.1) (see Appendix 1). The MMSE is a series of questions and tests designed to establish whether a drug treatment would be appropriate. NHS guidelines state that the patient should score 12 points or more out of a maximum of 30 points to be considered for medication. The tests cover orientation to time, registration, naming and reading skills. (Alzheimer’s Society information sheet 436).
John was also assessed in terms of diet and sleep.
The Discomfort Scale-Dementia of the Alzheimers’s Type (DS-DAT) was carried out with John. DS-DAT measures discomfort in elderly patients with dementia who are losing cognitive capacity and communication skills and are increasingly reliant on nursing staff. It was originally conceived to measure discomfort but it can be used to assess pain.
Assessment on John revealed that when he is in pain he is prone to be more aggressive. Staff worked with him to find strategies he could use to alleviate the pain. He received psychological assistance from the Pain Management Specialists. According to research on care of the elderly pain assessment is always an important aspect of what is done to take care of patients with dementia. The pain manifestation in John’s case has been a concern for everyone involved in his care. This is supported by Smith (2005) who says that it is important for healthcare providers to make correct assessment in the treatment of elderly people. There are many deterrents to making correct assessment. The fact that our culture looks at dementia as a disease that is only in the mind and that people with dementia do not experience pain can create a problem because often doctors may not see symptoms as belonging to dementia. Also, as patients begin to lose the ability to understand their internal states, they cannot identify easily “sensations, feelings and experiences” (Smith 2005 p.2). This will also lead to a time when they may not be able to verbalise what they are feeling. When the condition gets to this stage it is important to take care of the comfort needs of the individual. Many healthcare providers assess this by means of a Comfort Checklist. Smith (2005) was able to show professionals that there are several assessment tools that can be used to assess pain levels in patients with dementia.
Kaasalainen (2007) presents another idea of how to assess the pain of patients with dementia by using behaviour observation methods. This literature supports that pain is “underestimated and undertreated” in the older population. Assessment then becomes even more important.
Early pain assessment is important because the patient may start to lose the cognitive ability to let their discomforts be known. A system of behavioural observation would be useful. In order for this to be accurate a system of criteria for behaviour indicators can be set. Some indicators include “rapid blinking and other facial expressions, agitation or aggression, crying or moaning, becoming withdrawn and guarding the body part “
(Kaasalainen, 2007 p.7).
When John starts getting aggressive it can be an indication that he is in pain. “ It is important to find out how patients with dementia communicate about their pain and to determine relevant background information about their pain needs.” McClean (2000) cited in Cunningham (2006) p.5. In order that a full assessment could be made of John and his pain communication and management, he was allocated a nurse to be with him all of the time to achieve an accurate record.
The Discomfort Scale for Patients with Dementia of the Alzheimer’s Type (DS-DAT) previously referred to has been challenged by Kaasalainen (2007). Some of the challenges she stated include:
“ * some of the items measured may be due to other situations and not only dementia.
· the way the tools are scored can be difficult and therefore not easy to use in the clinical setting
· most of the new tools (and other DS-DAT) are in preliminary stages and need more testing
· there is lack of consensus on how pain should be assessed with older adults so verbal reports continue to be used in most situations.
· The concept of discomfort may be due to other facts like infection, hunger, depression or anxiety which means that behavioural observations cannot be the sole basis for giving medication.” (Kaasalainen, 2007 p.8)
Gloth (2001) presented information about pain management in older adults. He stated that it is difficult to make sure that older patients are getting enough medication to manage their pain adequately. Most older patients have at least one chronic condition and take multiple medications which make it harder to tell what they require. For some healthcare providers it becomes more frustrating to make sure the pain is managed properly. Gloth (2001 p.188).
It is important to understand when giving medication that drugs have a different reaction in older adults that they have in younger patients. This must be taken into account when prescribing. When pain is managed well an individual will have ‘secondary gain’ whereby he will feel better and it will help family members stay and visit longer. All of this will help the patient manage his pain. (Gloth 2001 p.189). Gloth (2001) also suggests that clinicians use a variety of methods for pain management including no interventions and alternative therapies where possible.
In the ward the environment is kept as quiet as possible as it is policy not to administer neuroleptic drugs unless really necessary. Pharmacological treatment options are recommended only if behaviour poses an immediate risk to the individual or to others Weaver (2007), McShane et al (1997) cited in Narzarko (2007 p.118) states that researchers have found that people with dementia who are treated with neuroleptic drugs deteriorate more quickly than those who are not treated with such drugs.
Besides having his own individual nursing care, John is offered activities to help him stay as active as possible. It was reported in Jacques et al (2000 p.366) “offering patients the appropriate activity, i.e. Games, exercise, sitting and chatting can reduce boredom and agitation. John responds well to this individual attention and it does have a settling effect. During his working life, John was always working with his hands so he is keen to participate in games and exercise. He does try to engage in social contact with other patients but unfortunately this interaction has not been reciprocated so it has caused him upset and frustration and after a few attempts he now only talks with the nurse caring for him. His physical activity is also hindered by his pain.
John has lost a lot of weight recently so he has been seen regularly by the dietitian who is ensuring that he is eating a healthy nutritional diet. He does have a good appetite.
John’s sleep pattern has been erratic the last several months. “Many people with dementia are restless at night and find it difficult to sleep. Dementia can affect people’s body clocks so that they might get up during the night, get dressed or even go outside. Ensure that the person has enough exercise during the day and that they use the toilet before bed.(Alzheimer’s information sheet 525). John was gently reminded that it was night-time and that he should go back to sleep. A sleep diary was also kept to record the level of restlessness.
There are two types of carers involved in looking after John – those who work within the clinical setting and those family members who must care for a chronically ill family member. The family member is predominately John’s wife.
Rasin and Kautz (2007) carried out a study that focused on caregivers in assisted living facilities. The National Centre for Assisted Living (NCAL) estimates that “42% to 50% of residents in assisted living facilities have dementia and 34% of them exhibit behavioural symptoms of dementia at least once a week.” NCAL (2006) cited in Rasin and Kautz (2007 p.2). They found that caregiver training was different depending on the state in which the individual lived and many were not formally trained to work with dementia patients – instead they received training either on the job or through life experience. The study used focus groups for data collection. Carers said that there were two types of knowledge that caregivers had that were effective in dealing with dementia patients: behavior centred knowledge – knowing recommended approaches to use with specific behavioural symptoms of dementia and person centred knowledge – knowing the residents well enough that they could look beyond the behaviour of the person (Rasin and Kautz. 2007 p.33-34).
They felt that the person centred knowledge was the strongest and most effective in caring for a person with dementia. From this study they made several recommendations for nursing:
· get to know the resident so you can determine what might be causing the disruptive behaviour.
· Giving individualised care for the residents can increase their quality of life.
· Caregivers should be taught how to incorporate patients life stories into their treatment plans to help them understand why the behaviour is being exhibited.
· Caregivers who understand and use person centred knowledge need to be acknowledged (Rasin and Kautz p.36).
A person centred approach was used in John’s treatment. He was encouraged to talk about his past and his wife was able to provide a lot of useful details which allowed John to be seen and treated as a ‘whole person’. It did also allow staff to make sense of some of the behaviour displayed by John.
Hepburn et al (2007) researched another way of effectively educating family members. They looked at a transportable psycho-education program geared towards helping to reduce caregivers stress. Several programs are spotlighted in this article. What they found was that a one to one behaviour management program given by home support team help to reduce the burden on caregivers and help to reduce depression. This program combined education with counselling. With the knowledge given to families, it was possible to delay the hospitalisation of the patient with dementia. (Hepburn et al, p.31-35)
Most caregivers are women, at least partly because it is a role that all women are expected to play in most societies. Doress-Wortens (1994) researched the effects of caregivers’ stress on women who already had multiple roles. They found that the stress in certain types of care giving situations were higher than others – e.g. when the caregiver involved personal care or dealing with a family member with dementia, they tended to experience more stress. A family member who was physically frail and needed minimal help was less stressful. John’s wife stress levels decreased with experience of looking after him – this information was apparent from reading of previous case notes. From this study it was apparent that women handle many different situations and they need coping strategies when they add the care of an ill family member to the set of tasks they perform.
Evaluation:
It is important to evaluate John’s care plan with regard to establishing the best possible attention for him. This has been done with reference to the National Institute for Health and Clinical Excellences (2006). According to NICHE (2006) there were 700,000 cases of dementia in the United Kingdom and there are approximately a million caregivers for them. As a result of these figures NICHE provided recommendations for those dealing with patients who have dementia.
NICHE Recommendation 1 : A coordinated and integrated approach between health and social care to treat and care for patients with dementia and carers.
John’s care : John has received the care of a specialist team who are trained to coordinate the day to day assessment and management of his condition. This comprised doctors, nurses, psychiatric team. Each professional provides guidance and support both for John and his family. His wife receives education and assistance with techniques on how to handle his aggression at home. Because she is his main carer at home, she has been given details of support groups where she will be able to get additional advice.
NICHE Recommendation 2 : The needs of carers should be assessed and support should be offered as part of the overall plan.
John’s care : It is important for staff from the dementia ward to offer support and help John’s wife deal with his physical and verbally aggressive behaviour. Caplan, G.A. Et al (2006) states that families need to be given clear information about the disease trajectory , complications of dementia and limited treatment available.
John and his wife have been married for 54 years and have no children. The emotions of the medical prognosis need to be dealt with. Schulz et al (2003) cited in Ouldred and Bryant (2008) has found that the progression of dementia confronts families with difficult decisions and they need to be supported through this difficult period. It is important to receive pre-bereavement counselling which can lead to better adjustment post-bereavement. Bright (2008) researched the quality of elderly care of those who have dementia as they move into end of life situations. He pointed out that palliative care is not as developed for dementia as it is for cancer so levels of care will vary between different geographical regions.
It is difficult for John’s wife to deal with the stress that comes from living with a man she has known for so many years as his life deteriorates. She has been advised where to gain support where needed. Support groups can bring enormous relief and help to deal with some of the challenges of the caring role.
NICHE Recommendation 3 : Memory assessment should be given to all patients with dementia.
John’ care : The Pain Management Team kept close observations using the Abbey Rating Scale and weekly evaluations on John were used to get his pain under control (see attachment 2). Wood (2002) states that the nurse’s role in pain management is vital, therefore, nurses should be fully educated and trained to recognise when patients are in pain.
NICHE Recommendation 4: People with dementia should not be denied services they need because of their age.
John’s care : The dementia ward is staffed by healthcare workers who are trained to work with patients with dementia and there is an understanding of what is required in each situation. This works on the person centred approach. Staff work with John on a regular basis and many get to know him well. The staff can see when he is getting anxious and angry and can intervene as appropriate. As stated by Fitzpatrick and Roberts (2004) healthcare professionals caring for older people require a range of core skills and knowledge, with explicit attention to the principles of patient and family-centred care, promoting autonomy, dignity and respect, along with good communication skills.
In conclusion, there has been a positive outcome after John’s assessment on the dementia ward. Aggressive outbursts are less frequent and this makes a better quality of time for John with his wife, family and friends. He still tries hard to be independent.

Alzheimer’s Society Information sheet 436, 525. Available to download from:
hhtp:/www.alzheimers.org.uk
Bright, L. (2005). Palliative care for people with dementia. Management Matters Available to download from
http:// . [28 March2008}
Bephage, G. (2005). Quality sleep in older people: the nursing care role. British Journal of Nursing. Vol. 14 (4) pp.205-210
Bephage, G. (2007). Care approaches to sleeplessness & dementia. Nursing & Residential Care. Vol. 9 (12) pp. 571-573.
Caplan, G.A., Meller, A., Squires, B., Chan, S., Willet, W. (2006). Advance care planning and hospital in the nursing home. Age Ageing. Vol. 35 (6) pp. 581-585.
Chambers, M. & Conner, S.L. (2002). User-friendly technology to help family carers cope. Journal of Advanced Nursing . Vol. 40 (5) pp. 568-577.
Cook, A.K., Niven, C.A., Downs, M.G. (1999). Assessing the pain of people with cognitive impairment. International Journal of Geriatric Psychiatry . Vol. 14 (6) pp.421-425.
Cunningham, C. (2006). Managing pain in patients with dementia in hospital. Nursing Standard. Vol. 20 (46) pp.54-59
Doress-Wortes, P.B. (1994). Adding elder care to women’s multiple roles: a critical review of the caregiver stress and multiple roles literatures. Journal of Research . Vol. 31. pp.1-6.
Fitzpatrick, J.M. & Roberts, J.D. (2004). Challenges for care homes: Education and training of healthcare assistants. British Journal of Nursing . Vol. 13 (21) pp.1258-1260
Gloth, F.M. (2001). Pain management in older adults: prevention and treatment. Journal of the American Geriatric Society. Vol. 49 (2) pp.188-199.
Jaques, A. Jackson, G.A. (2000) Understanding Dementia 3 rd ed Churchill, Livingstone, London. pp.235-269, p. 336
Hepburn, K. Lewis, M. Tomatore, J. Sherman, C.W. & Bremner, K.L. (2007). The savvy caregivers program: The demonstrated effectiveness of a transportable dementia caregiver psycho education program. Journal of Gerontological Nursing. (2007)
Vol. 33 pp. 30-37.
Kaasalainen, S. (2007) Pain assessment in older adults with dementia: Using behavioural observation methods in clinical practice. Journal of gerontological Nursing Vol. 33 (6) pp. 6-10
Lewis, M.M. & Trzinski,A. (2006). Counselling older adults with dementia who are dealing with death: Innovative interventions for practitioners. Death Studies . Vol .30 (8)npp. 777-787
National Institute for health and Clinical Excellence (NHS) and Social Care Institute for Excellent (SCIE) (2006) NICE SCIE guidelines to improve care of people with dementia. Available to download from http://www.nice.org.uk/nice/media/pdf/2006-052 [Assessed 13/03/08]
National Institute of Neurological Disorders and Stroke NINDS Multi-Infarct Dementia Information Page. Available to download from http:/wwwninds.nih.gov/disorders
Nazarko, L. (2007). Behaviour that challenges: types and treatment. British Journal Of Healthcare Assistants . Vol. 1 (3) pp116-119
Ouldred, E. & Bryant, C. (2008). Dementia Care. Part 3: end-of-life care for people with advanced dementia. British Journal of Nursing. Vol. 17 (5) pp. 308-314
Rasin,J & Kautz, D. (2007). Knowing the resident with dementia: Perspectives of assisted living facility caregivers. Journal of Gerontological Nursing. Vol. 33 (9) pp.30-36.
SA Carers. (2005). Understanding the role of the family carers in healthcare. Available to download from http://www.carers-sa.asn.au/pdf_files . [Assessed 15/03/08]
Scottish Intercollegiate Guidelines Network (2006) Guideline 86: Management of Patients With Dementia. Edinburgh, SIGN.
Smith, M. (2005). Pain assessment in nonverbal older adults with advanced dementia. Perspectives in Psychiatric Care. Vol 41 Available to download from http://www.questia.com
Stokes, G. (2000). Challenging Behaviour In Dementia. A Person Centred Approach. Oxon Winslow-press Ltd. pp.206
Weaver, D. (2007). Behavioural Changes: Dementia & Its interventions. Nursing & Residential Care. Vol. 9 (8) pp. 375-377
Woods, S. (20020. Nursing care & implications for nursing. Nursing Times. Vol. 98 (40) pp. 39-42
Bibliography
Abbey, J. (2004).The Abbey pain scale: a 1-minute numerical indicator for people with end-stage dementia. International Journal of Palliative Nursing. Vol.10 (1) pp6-13
DeWaters, T. & Popovich, J. (2003). An evaluation of clinical tools to measure pain in older people with cognitive impairment. British Journal of Community Nursing. Vol. 8 (5) pp226-234
Dingwall, L. (2007). Medication issues for nursing older people (part 1). Nursing Older People. Vol. 19 (1) pp25-35
Evers, C. (2008). Positive dementia care: taking perspective. Nursing & Residential Care. Vol. 10 (4) pp184-187
Hobson, P. (2008). Understanding dementia: developing person-centred communication. British Journal of Healthcare Assistants. Vol. 2 (4) pp162-164
Kirkwood, T. Dementia Reconsidered: A person comes first. (2004). Open University Press U.K.

- Advanced Life Support
- Endocrinology
- Gastroenterology
- Infectious disease
- Intensive care
- Palliative Care
- Respiratory
- Rheumatology
- Haematology
- Endocrine surgery
- General surgery
- Neurosurgery
- Ophthalmology
- Plastic surgery
- Vascular surgery
- Abdo examination
- Cardio examination
- Neurolo examination
- Resp examination
- Rheum examination
- Vasc exacmination
- Other examinations
- Clinical Cases
- Communication skills
- Prescribing

Dementia case study with questions and answers

Dementia case study with questions and answers
Common dementia exam questions for medical finals, OSCEs and MRCP PACES
The case below illustrates the key features in the assessment of a patient with dementia or undiagnosed memory decline. It works through history, examination and investigations – click on the plus symbols to see the answers to each question
Part 1: Mavis
- Mavis is an 84-year old lady, referred to you in the memory clinic for assessment of memory impairment. She attends in the company of her son and daughter-in-law.
- On the pre-clinic questionnaire her son has reported a severe deterioration in all aspects of her cognition over the past 12 months.
- The patient herself acknowledges that there have been memory problems, but feels it is just her short term memory that is an issue.
Question 1.
- To begin the history, start broadly. Build rapport and establish both the patient’s view on memory impairment (if any) and the family’s (or other collateral history).
- Patient’s (and collateral) view of memory decline
- Biographical history
- Objective view of memory decline (e.g. knowledge of current affairs)
- Impact of memory decline on day-to-day living and hobbies
- Social history, including safety and driving
- General medical history (especially medications)
- See below for details on these…
Question 2.
- Is it for everything or are specific details missed out/glossed over?
- Try to pin down specific details (e.g. names of people/places).
- At what time in chronological order do things start to get hazy?
Question 3.
- If under 12 years this will lead to additional point being awarded on some cognitive tests
- Ask about long term memories, e.g. wedding day or different jobs
- Then move on to more recent memories, e.g. last holiday
Question 4.
- If your patient watches the news/read newspapers on a regular basis, ask them to recount the headlines from the past few days.
- Be sure to look for specifics to prevent your patient masking memory deficiencies with broad statements. For example: “The government are incompetent, aren’t they?!” should be clarified by pinning down exactly why they are incompetent, for example: “Jeremy Hunt”.
- If they like to read, can they recall plotlines from current books or items from magazines?
- If they watch TV, can they recount recent plot lines from soaps, or formats of quiz shows?
Question 5.
- Ask about hobbies and other daily activities, and whether or not these have declined recently.
- If your patient no longer participates in a particular hobby, find out why: is it as a result of a physical impairment (e.g. arthritis making cooking difficult), or as the result of a loss of interest/ability to complete tasks (e.g. no longer able to complete crosswords/puzzles).
- Once you have a good idea of the memory decline itself, begin to ask about other features. Including a social and general medical history.
Question 6.
- Review their social history and current set-up, and also subjective assessments from both patient and family over whether or not the current arrangements are safe and sustainable as they are.
- Previous and ongoing alcohol intake
- Smoking history
- Still driving (and if so, how safe that is considered to be from collateral history)
- Who else is at home
- Any package of care
- Upstairs/downstairs living
- Meal arrangements (and whether weight is being sustained).
- Of all these issues, that of driving is perhaps one of the most important, as any ultimate diagnosis of dementia must be informed (by law) to both the DVLA and also the patient’s insurers. If you feel they are still safe to drive despite the diagnosis, you may be asked to provide a report to the DVLA to support this viewpoint.
Now perform a more generalised history, to include past medical history and – more importantly – a drug history.
Question 7.
- Oxybutynin, commonly used in primary care for overactive bladder (anticholinergic side effects)
- Also see how the medications are given (e.g. Dossett box)
- Are lots of full packets found around the house?
Part 2: The History
On taking a history you have found:
- Mavis was able to give a moderately detailed biographical history, but struggled with details extending as far back as the location of her wedding, and also her main jobs throughout her life.
- After prompting from her family, she was able to supply more information, but it was not always entirely accurate.
- Her main hobby was knitting, and it was noted that she had been able to successfully knit a bobble hat for her great-grand child as recently as last month, although it had taken her considerably longer to complete than it might have done a few years previously, and it was a comparatively basic design compared to what she has been able to create previously.
- She has a few children living in the area, who would frequently pop in with shopping, but there had been times when they arrived to find that she was packed and in her coat, stating that she was “just getting ready to go home again”.
- She had been helping occasionally with the school run, but then a couple of weekends ago she had called up one of her sons – just before she was due to drive over for Sunday lunch – and said that she could not remember how to drive to his house.
- Ever since then, they had confiscated her keys to make sure she couldn’t drive. Although she liked to read the paper every day, she could not recall any recent major news events. Before proceeding to examine her, you note that the GP referral letter has stated that her dementia screen investigations have been completed.
Question 8.
- Raised WCC suggests infection as a cause of acute confusion
- Uraemia and other electrolyte disturbances can cause a persistent confusion.
- Again, to help rule out acute infection/inflammatory conditions
- Liver failure can cause hyperammonaemia, which can cause a persistent confusion.
- Hyper- or hypothyroidism can cause confusion.
- B12 deficiency is an easily missed and reversible cause of dementia.
- This looks for space occupying lesions/hydrocephalus which may cause confusion.
- This can also help to determine the degree of any vascular component of an ultimately diagnosed dementia.
Part 3: Examination
- With the exception of age-related involutional changes on the CT head (noted to have minimal white matter changes/small vessel disease), all the dementia screen bloods are reassuring.
- You next decide to perform a physical examination of Mavis.
Question 9.
- Important physical findings that are of particular relevance to dementia, are looking for other diseases that may have an effect on cognition.
- To look for evidence of stroke – unlikely in this case given the CT head
- Gait (shuffling) and limb movements (tremor, rigidity, bradykinesia)
- Affect is also important here and may also point to underlying depression
- Pay attention to vertical gaze palsy, as in the context of Parkinsonism this may represent a Parkinson plus condition (e.g. progressive supranuclear palsy).
- It is also useful to look at observations including blood pressure (may be overmedicated and at risk of falls from syncope) and postural blood pressure (again, may indicate overmedication but is also associated with Parkinson plus syndromes e.g. MSA)
Part 4: Cognitive Testing
- On examination she is alert and well, mobilising independently around the clinic waiting room area. A neurological examination was normal throughout, and there were no other major pathologies found on a general examination.
- You now proceed to cognitive testing:
Question 10.
- Click here for details on the MOCA
- Click here for details on the MMSE
- Click here for details on the CLOX test
Part 5: Diagnosis
- Mavis scores 14/30 on a MOCA, losing marks throughout multiple domains of cognition.
Question 11.
- Given the progressive nature of symptoms described by the family, the impairment over multiple domains on cognitive testing, and the impact on daily living that this is starting to have (e.g. packing and getting ready to leave her own home, mistakenly believing she is somewhere else), coupled with the results from her dementia screen, this is most likely an Alzheimer’s type dementia .
Question 12.
- You should proceed by establishing whether or not Mavis would like to be given a formal diagnosis, and if so, explain the above.
- You should review her lying and standing BP and ECG, and – if these give no contraindications – suggest a trial of treatment with an acetylcholinesterase inhibitor, such as donepezil.
- It is important to note the potential side effects – the most distressing of which are related to issues of incontinence.
- If available, put her in touch with support groups
- Given the history of forgetting routes before even getting into the care, advise the patient that she should stop driving and that they need to inform the DVLA of this (for now, we will skip over the depravation of liberty issues that the premature confiscation of keys performed by the family has caused…)
- The GP should be informed of the new diagnosis, and if there are concerns over safety, review by social services for potential support should be arranged.
- Follow-up is advisable over the next few months to see whether the trial of treatment has been beneficial, and whether side effects have been well-tolerated.
Now click here to learn more about dementia
Perfect revision for medical students, finals, osces and mrcp paces, …or click here to learn about the diagnosis and management of delirium.

Case study 3: Joan
Download the Full Case Study for Joan PDF file (58KB)
Download the Vignette for Joan PDF file (49KB)
Name: Joan O’Leary
Gender: Female
Ethnicity: White Irish
Religion: Catholic
Disability: dementia with Lewy Bodies
First language: English
Family: estranged and in Ireland
Location: village in South West
Joan lives in a house in a small village. She has lived there for 28 years. She has two dogs and 11 chickens. Joan has always been quite private but is well known in her village. She goes to the nearby town on the bus to church, visits the local shop and community café, and goes away frequently. Joan goes for a long walk with her dogs each day. Joan hadn’t been to her GP for 6 years.
The café owner, Margaret, was worried about Joan. Joan has appeared very forgetful and disorientated. She has been seen in the village wearing her slippers and her neighbours have seen her out late at night with her dogs. Margaret went to Joan’s house and wasn’t allowed in but thought there was quite a strong smell.
Margaret phoned the GP in the village who went round to Joan’s house and persuaded her to have some tests. She has been diagnosed with moderate dementia with Lewy Bodies.
The GP phoned social services and you go out to do an assessment.
Download the Ecogram for Joan PDF file (48KB)
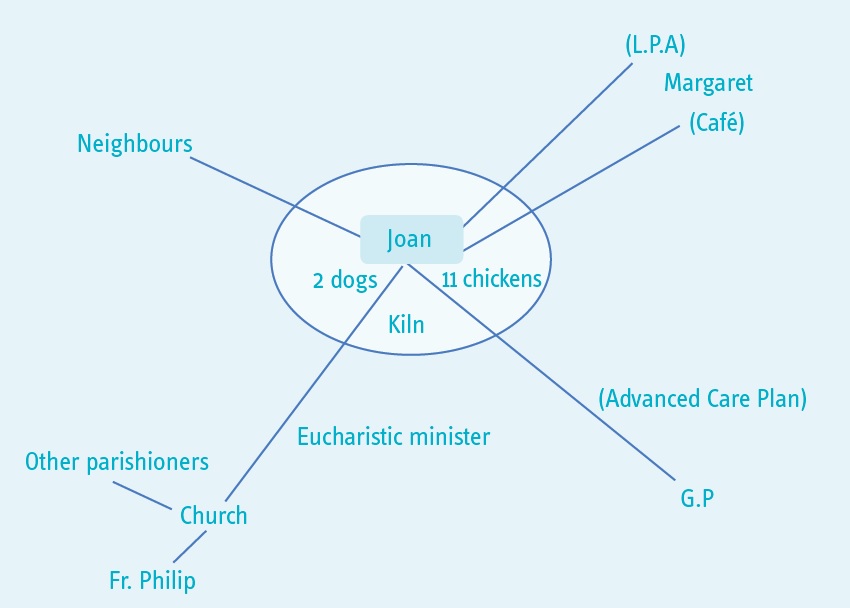
You told me that you didn’t really want to have an assessment. I explained that your GP had asked me to talk to you about what is happening for you at the moment because you have been diagnosed with dementia. You agreed to the assessment but you don’t want to have lots of information about you written down. These are the main things that you were happy for me to know.
At the moment you have capacity to make decisions about whether to have support or not. In the future you may find it more difficult to make decisions or not be able to make a particular decision. We talked about you arranging a lasting power of attorney and also doing an advanced care plan.
What’s important to you?
You said that you are quite a private person. You have two dogs and 11 chickens. You like to walk the dogs, go to the café and go to church in Lyme Regis. You take eggs to the café for Margaret (the owner) to sell.
You are a talented artist and have a small pottery shed and kiln in the garden.
You like to plan trips to different local areas and travel using the bus.
Your family is in Ireland and you haven’t seen them for many years. Your Catholic faith is important to you. You are a Eucharistic minister and you take holy communion to parishioners who can’t get to church.
What’s happening for you at the moment?
Your GP asked me to come and see you because you have been diagnosed with moderate dementia with Lewy Bodies.
You told me that you understand this is similar to Parkinson’s disease. You have noticed that your muscles have been aching and that you are not sleeping well.
The GP explained to me that you might find that you are unsteady at times or have tremors, and you might have some hallucinations, as these are common with this kind of dementia.
Margaret told me that you have been into the village wearing your slippers and that your neighbours have noticed you being out late at night which you agreed is unusual for you. However, you also told me that what you do is your own business. We talked about the risks that are attached to you going out late or not wearing appropriate clothing. You told me that you don’t think it is a problem, as you have always walked a lot and always find your way home. Also you said that you have the dogs with you when you are out and they know their way home. You already used reminders around the house so you said you would put a reminder on the front door to check your coat and shoes.
We talked about how you were managing day to day. You told me that you think you are managing well. However you haven’t been able to put the rubbish out or to clean out the chickens. You also have not been able to clean the bathroom. This is because you sometimes feel dizzy and your arms ache.
What is the impact on you?
You are concerned that people, like me, might start interfering with your life because of your illness.
What would you like to happen in the future?
You said that you want to continue to live in your home, looking after your animals, and doing the things that you currently do. We talked about what you think will happen and you said that you knew you will become less well. If you did need help in the future, you would like to arrange this yourself. We talked about having a personal assistant in the future.
How might we achieve this?
We talked about the importance of you having the right support in the future. You agreed that I could share this assessment with Margaret and your GP so that if you are not well enough to ask for advice or assistance in the future, they can ring the council. You will discuss a lasting power of attorney for finances, and health and care for Margaret. And you will do an advanced care plan with your GP. You will also talk to your GP about any medical support that might be available now, for example memory clinic and help with sleeping.
We also called your Parish Priest, Father Philip, and let him know that you have been diagnosed with dementia. He will ask a parishioner to give you a lift to church if you aren’t able to go on the bus.
You agreed to some help with keeping the animals and putting the rubbish out. Margaret and you will make an advert to put in the café window.
What strengths and support networks do you have to help you?
You said you are a very independent person. You have managed your home and finances for many years. You are managing well despite your illness and have strategies in place for things you might forget. You are active and have wide interests and talents. You also earn money through selling eggs. You contribute to the community through the parish. You are familiar with your local area and are used to travelling around.
You have a good relationship with Margaret, with your parish priest and with your GP. They are all willing and able to offer support.
Social care assessor conclusion
You have recently been diagnosed with dementia. This is starting to have an impact on your life and because of the nature of the illness the impact will increase as time goes on.
You have a lot of strengths to draw on and a good support network. You want to remain independent and, although there are some concerns about how you are managing, these are currently relatively minor and you have identified how to minimise them.
It is important that you plan ahead so that you remain in control of what happens and so that you can continue to achieve what matters to you for as long as possible.
Eligibility decision
You are not currently eligible for care and support under the Care Act 2014 because you can currently manage all day to day activities, apart from needing some help with maintaining your home. However, we have done a care and support plan that says what you will do to get help with the house and to plan for the future.
What’s happening next
See care and support plan .
Download the care and support plan document PDF file (178KB)

- Equal opportunities
- Complaints procedure
- Terms and conditions
- Privacy policy
- Cookie policy
- Accessibility

A sample case study: Mrs Brown
On this page, social work report, social work report: background, social work report: social history, social work report: current function, social work report: the current risks, social work report: attempts to trial least restrictive options, social work report: recommendation, medical report, medical report: background information, medical report: financial and legal affairs, medical report: general living circumstances.
This is a fictitious case that has been designed for educative purposes.
Mrs Beryl Brown URN102030 20 Hume Road, Melbourne, 3000 DOB: 01/11/33
Date of application: 20 August 2019
Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke, which has left her with moderate weakness in her left arm and leg. A diagnosis of vascular dementia was also made, which is overlaid on a pre-existing diagnosis of Alzheimer’s disease (2016). Please refer to the attached medical report for further details.
I understand that Mrs Brown has been residing in her own home, a two-story terrace house in Melbourne, for almost 60 years. She has lived alone since her husband died two years ago following a cardiac arrest. She has two daughters. The youngest daughter Jean has lived with her for the past year, after she lost her job. The eldest daughter Catherine lives on the Gold Coast with her family. Mrs Brown is a retired school teacher and she and both daughters describe her as a very private woman who has never enjoyed having visitors in her home. Mrs Brown took much encouragement to accept cleaning and shopping assistance once a week after her most recent admission; however, she does not agree to increase service provision. Jean has Enduring Power of Attorney (EPOA) paperwork that indicates that Mrs Brown appointed her under an EPOA two years ago. She does not appear to have appointed a medical treatment decision maker or any other decision-supporter.
I also understand from conversations with her daughters that Jean and Mrs Brown have always been very close and that there is a history of long-standing conflict between Catherine and Jean. This was exacerbated by the death of their father. Both daughters state they understand the impact of the stroke on their mother’s physical and cognitive functioning, but they do not agree on a discharge destination. Mrs Brown lacks insight into her care needs and says she will be fine once she gets back into her own home. Repeated attempts to discuss options with all parties in the same room have not resulted in a decision that is agreeable to all parties.
Mrs Brown has a history of Alzheimer’s disease; type II diabetes – insulin dependent; hypertension; high cholesterol and osteoarthritis. She has had two recent admissions to hospital for a urinary tract infection and a fall in the context of low blood sugars. She is currently requiring one to two people to assist her into and out of bed and one person with managing tasks associated with post-toilet hygiene. She can walk slowly for short distances with a four-wheel frame with one person to supervise. She benefits from prompting to use her frame; she needs someone to cut her food and to set her up to eat and drink regularly and to manage her medication routine. She requires one person to assist her to manage her insulin twice daily.
The team believe that Mrs Brown’s capacity for functional improvement has plateaued in the last ten days. They recommend that it is in her best interests to be discharged to a residential care setting due to her need for one to two people to provide assistance with the core tasks associated with daily living. Mrs Brown is adamant that she wants to return home to live with Jean who she states can look after her. Jean, who has a history of chronic back pain, has required several admissions to hospital over the past five years, and states she wants to be able to care for her mother at home. Jean states she is reluctant to agree to extra services as her mother would not want this. Her sister Catherine is concerned that Jean has not been coping and states that given this is the third admission to hospital in a period of few months, believes it is now time for her mother to enter residential care. Catherine states that she is very opposed to her mother being discharged home.
Mrs Brown is at high risk of experiencing falls. She has reduced awareness of the left side of her body and her ability to plan and process information has been affected by her stroke. She is now requiring one to two people to assist with all her tasks of daily living and she lacks insight into these deficits. Mrs Brown is also at risk of further significant functional decline which may exacerbate Jean’s back pain. Jean has stated she is very worried about where she will live if her mother is to enter residential care.
We have convened two family meetings with Mrs Brown, both her daughters and several members of the multi-disciplinary team. The outcome of the first meeting saw all parties agree for the ward to provide personalised carer training to Jean with the aim of trialling a discharge home. During this training Jean reported significant pain when transferring her mother from the bed and stated she would prefer to leave her mother in bed until she was well enough to get out with less support.
The team provided education to both Jean and Catherine about the progressive impact of their mother’s multiple conditions on her functioning. The occupational therapist completed a home visit and recommended that the downstairs shower be modified so that a commode can be placed in it safely and the existing dining room be converted into a bedroom for Mrs Brown. Mrs Brown stated she would not pay for these modifications and Jean stated she did not wish to go against her mother’s wishes. The team encouraged Mrs Brown to consider developing a back-up plan and explore residential care options close to her home so that Jean could visit often if the discharge home failed. Mrs Brown and Jean refused to consent to proceed with an Aged Care Assessment that would enable Catherine to waitlist her mother’s name at suitable aged care facilities. We proceeded with organising a trial overnight visit. Unfortunately, this visit was not successful as Jean and Catherine, who remained in Melbourne to provide assistance, found it very difficult to provide care without the use of an accessible bathroom. Mrs Brown remains adamant that she will remain at home. The team is continuing to work with the family to maximise Mrs Brown’s independence, but they believe that it is unlikely this will improve. I have spent time with Jean to explore her adjustment to the situation, and provided her with information on community support services and residential care services. I have provided her with information on the Transition Care Program which can assist families to work through all the logistics. I have provided her with more information on where she could access further counselling to explore her concerns. I have sought advice on the process and legislative requirements from the Office of the Public Advocate’s Advice Service. I discussed this process with the treating team and we decided that it was time to lodge an application for guardianship to VCAT.
The treating team believe they have exhausted all least restrictive alternatives and that a guardianship order is required to make a decision on Mrs Brown’s discharge destination and access to services. The team recommend that the Public Advocate be appointed as Mrs Brown’s guardian of last resort. We believe that this is the most suitable arrangement as her daughters are not in agreement about what is in their mother’s best interests. We also believe that there is a potential conflict of interest as Jean has expressed significant concern that her mother’s relocation to residential care will have an impact on her own living arrangements.
Mrs Brown’s medical history includes Alzheimer’s disease; type II diabetes; hypertension; high cholesterol and osteoarthritis. She was admitted to Hume Hospital on 3 March 2019 following a stroke that resulted in moderate left arm and leg weakness. This admission was the third hospital admission in the past year. Other admissions have been for a urinary tract infection, and a fall in the context hypoglycaemia (low blood sugars), both of which were complicated by episodes of delirium.
She was transferred to the subacute site under my care, a week post her admission, for slow-stream rehabilitation, cognitive assessment and discharge planning.
Mrs Brown was diagnosed with Alzheimer’s disease by Dr Joanne Winters, Geriatrician, in April 2016. At that time, Mrs Brown scored 21/30 on the Standardised Mini-Mental State Examination (SMMSE). During this admission, Mrs Brown scored 15/30. I have undertaken cognitive assessment and agree with the diagnosis; further cognitive decline has occurred in the context of the recent stroke. There are global cognitive deficits, but primarily affecting memory, attention and executive function (planning, problem solving, mental flexibility and abstract reasoning). The most recent CT-Brain scan shows generalised atrophy along with evidence of the new stroke affecting the right frontal lobe. My assessments suggest moderate to severe mixed Alzheimer’s and vascular dementia.
While able to recall some key aspects of her financial affairs, including the general monetary value of her pension and regular expenses, Mrs Brown was unable to account for recent expenditure (for repairs to her home) or provide an estimate of its value, and had difficulty describing her investments. In addition, I consider that she would be unable to make complex financial decisions due to her level of cognitive impairment. Accordingly, I am of the view that Mrs Brown now lacks capacity to make financial decisions.
Mrs Brown states that she previously made an Enduring Power of Attorney (EPOA) but could no longer recall aspects of the EPOA, such as when it would commence and the nature of the attorney’s powers. Moreover, she confused the EPOA with her will. Her understanding of these matters did not improve with education, and therefore I consider that she no longer has capacity to execute or revoke an EPOA.
Mrs Brown acknowledges that she needs some assistance but lacks insight into the type of assistance that she requires, apart from home help for cleaning and shopping. She does not appreciate her risk of falling. She is unable to get in and out of bed without at least one person assisting her. She frequently forgets to use her gait aid when mobilising and is not able to describe how she would seek help in the event of falling. She is not able to identify or describe how she would manage her blood sugar levels, and this has not improved with education. Accordingly, I consider that she lacks capacity to make decisions about accommodation arrangements and services.
Mrs Brown does not agree with the treating team’s recommendation to move into residential care and maintains her preference to return home. This is in spite of a failed overnight trial at home with both her daughters assisting her. Unfortunately, she was unable to get out of bed to get to the toilet and required two people to assist her to do so in the morning. In light of these matters, and in the context of family disagreement regarding the matter, the team recommends that the Office of the Public Advocate be appointed as a guardian of last resort.
Reviewed 22 July 2022
- Hospitals & health services
- Public hospitals in Victoria
- Patient care
- Ambulance and patient transport
- Non-emergency patient transport
- Non-emergency patient transport review
- NEPT legislation and clinical practice protocols
- Non-emergency patient transport licensing
- NEPT licensing fees
- NEPT services information and guidance
- First Aid Services
- First aid licences
- First aid services information and guidance
- First aid service fees
- Victorian State Trauma System
- Acute medicine
- Emergency care
- Surgical services
- Better at Home
- Critical care
- Hospital in the Home
- Virtual care (Telehealth)
- Perinatal and reproductive services
- Rehabilitation and complex care
- Renal health
- Renal services in Victoria
- Funding for renal services
- Different approaches to haemodialysis
- Specialist clinics
- Access to non-admitted services
- Minimum referral information
- Communication toolkit
- Integrated care
- HealthLinks: Chronic Care
- Community Health Integrated Program (CHIP) guidelines
- Service coordination in Victoria
- Victorian integrated care online resources
- Specialist clinics programs
- Specialist clinics reform
- Specialty diagnostics, therapeutics and programs
- Older people in hospital
- End of life and palliative care in Victoria
- Voluntary assisted dying
- Quality, safety and service improvement
- Planned surgery recovery and reform program
- Digital Health
- Roadmap and Maturity Model
- Standards and guidelines
- Policies and frameworks
- Health Information Sharing Legislation Reform
- My Health Record
- Public hospital accreditation in Victoria
- Credentialing for senior medical staff in Victoria
- Clinical risk management
- Preventing infections in health services
- Healthy choices
- Victorian Perinatal Data Collection
- Rural health
- Improving Access to Primary Care in Rural and Remote Areas Initiative
- Rural x-ray services
- Rural health regions and locations
- Rural and regional medical director role
- Victorian Patient Transport Assistance Scheme
- Rural and isolated practice registered nurses
- Urgent care in regional and rural Victoria
- Private health service establishments
- Private hospitals
- Day procedure centres
- Mobile health services
- Fees for private health service establishments in Victoria
- Design resources for private health service establishments
- Professional standards in private health service establishments
- Legislation updates for private health service establishments
- Complaints about private health service establishments
- Cosmetic procedures
- Guideline for providers of liposuction
- Private hospital funding agreement
- Boards and governance
- About health service boards in Victoria
- Information and education
- Education resources for boards
- Sector leadership
- Data, reporting and analytics
- Health data standards and systems
- Funding, performance and accountability
- Statements of Priorities
- Performance monitoring framework
- Integrity governance framework and assessment tool
- Pricing and funding framework
- Patient fees and charges
- Fees and charges for admitted patients
- Non-admitted patients - fees and charges
- Other services
- Planning and infrastructure
- Sustainability in Healthcare
- Medical equipment asset management framework
- Health system design, service and infrastructure planning
- Complementary service and locality planning
- Primary & community health
- Primary care
- Community pharmacist pilot
- EOI - Victorian Community Pharmacist Statewide Pilot
- Victorian Community Pharmacist Statewide Pilot – Resources for pharmacists
- Emergency Response Planning Tool
- Working with general practice
- Victorian Supercare Pharmacies
- NURSE-ON-CALL
- Priority Primary Care Centres
- Local Public Health Units
- Community health
- Community health services
- Community health pride
- Registration and governance of community health centres
- Community Health Directory
- Community Health Program in Victoria
- Community health population groups
- Dental health
- Access to public dental care services
- Victoria's public dental care fees
- Victoria's public dental care waiting list
- Dental health for SRS residents
- Dental health program reporting
- Smile Squad school dental program
- Maternal and Child Health Service
- Nursery Equipment Program
- Maternal and Child Health Service Framework
- Maternal and Child Health Service resources
- Child Development Information System
- Early parenting centres
- Maternal Child and Health Reporting, Funding and Data
- Baby bundle
- Sleep and settling
- Maternal and Child Health Workforce professional development
- Aboriginal Maternal and Child Health
- Public Dental and Community Health Program funding model review
- Public health
- Women's Health and Wellbeing Program
- Inquiry into Women's Pain
- Inquiry into Women's Pain submissions
- Support groups and programs
- About the program
- Victorian Women's Health Advisory Council
- Cemeteries and crematoria
- Cemetery trust member appointments
- Cemetery search
- Cemeteries and crematoria complaints
- Exhumations
- Governance and finance
- Cemetery grants
- Interments and memorials
- Land and development
- Legislation governing Victorian cemeteries and crematoria
- Cemeteries and crematoria publications
- Repatriations
- Rights of interment
- Medicines and Poisons Regulation
- Patient Schedule 8 treatment permits
- Schedule 8 MDMA and Schedule 8 psilocybine
- Schedule 9 permits for clinical trials
- Documents and forms to print or download
- Legislation and Approvals
- Frequently Asked Questions - Medicines and Poisons Regulation
- Health practitioners
- Licences and permits to possess (& possibly supply) scheduled substances
- Medicinal cannabis
- Pharmacotherapy (opioid replacement therapy)
- Recent updates
- Environmental health
- Improving childhood asthma management in Melbourne's inner west
- Climate and weather, and public health
- Environmental health in the community
- Environmental health in the home
- Environmental health professionals
- Face masks for environmental hazards
- Human health risk assessments
- Lead and human health
- Per- and poly-fluoroalkyl substances (PFAS)
- Pesticide use and pest control
- Food safety
- Information for community groups selling food to raise funds
- Food businesses
- Food safety information for consumers
- Food regulation in Victoria
- Food safety library
- Food allergens
- Introducing Standard 3.2.2A: Food safety management tools
- Immunisation
- Respiratory syncytial virus (RSV) immunisation
- Seasonal influenza vaccine
- Immunisation schedule and vaccine eligibility criteria
- Ordering vaccine
- Immunisers in Victoria
- Immunisation provider information
- Cold chain management
- Adverse events following immunisation reporting
- Vaccine error management
- Vaccination for infants and children
- Vaccination for adolescents
- Vaccination program for adults
- Vaccination for special-risk groups
- Immunisation resources order form
- Victorian coverage rates for Victoria
- Infectious diseases guidelines & advice
- Infection control guidelines
- Disease information and advice
- Advice to the cruise industry: reporting infections
- Notifiable infectious diseases, conditions and micro-organisms
- Notification procedures for infectious diseases
- Infectious diseases surveillance in Victoria
- Germicidal ultraviolet light
- Protecting patient privacy in Victoria
- Population health systems
- Evidence and evaluation
- Health promotion
- Health status of Victorians
- Municipal public health and wellbeing planning
- Population screening
- Cancer screening
- Conditions not screened
- Improving outcomes in under-screened groups
- Infant hearing screening
- Newborn bloodspot screening
- Prenatal screening
- Screening registers
- Preventive health
- Type 2 diabetes and cardiovascular disease prevention
- Eye health promotion
- Injury prevention
- Healthy eating
- Oral health promotion
- Physical activity
- Sexual health
- Sex worker health
- Decriminalisation of sex work
- Automatic mutual recognition
- Domestic smoke detectors
- Lasers, IPL and LED devices for cosmetic treatments and beauty therapy
- Victoria's regulatory framework for radiation
- Radiation newsletter
- Tobacco reforms
- Tobacco reform legislation and regulations
- E-cigarettes and vaping
- Quitting smoking and vaping
- Smoke-free and vape-free areas
- Building entrances
- Children's indoor play centres
- Public hospitals and health centres
- Children's recreational areas
- Playground equipment
- Skate parks
- Swimming pools
- Under-age sporting events
- Enclosed workplaces
- Government buildings
- Learning environments
- Outdoor dining
- Outdoor drinking areas
- Patrolled beaches
- Train platforms and bus and tram shelters
- Under-age music or dance events
- Tobacco and e-cigarette retailers
- Making a report or complaint
- Resources and factsheets
- Alternative water supplies
- Aquatic facilities
- Blue-green algae (cyanobacteria)
- Drinking water in Victoria
- Legionella risk management
- Private drinking water
- Recreational water use and possible health risks
- Water fluoridation
- Chief Health Officer
- About the Chief Health Officer
- Chief Health Officer publications
- Health alerts and advisories
- Mental health
- Mental Health and Wellbeing Act 2022
- Mental Health and Wellbeing Act 2022 Handbook
- Community information
- Mental Health and Wellbeing Act 2022 in your language
- About Victoria's mental health services
- Area-based services
- Statewide and specialist mental health services
- Mental Health Community Support Services
- Support and intervention services
- Language services - when to use them
- Access to mental health services across areas
- Transport for people in mental health services
- Practice and service quality
- Medical Treatment Planning and Decisions Act
- Service quality
- Specialist responses
- Mental health and wellbeing reform
- Reform activity updates
- Priority areas
- Latest news
- Working with consumers and carers
- Consumer and carer engagement
- Consumer and Carer Experience Surveys
- Family support and crisis plans
- Consumer and carer financial support
- Supporting children whose parents have a mental illness
- Supporting parents with a mental illness
- Prevention and promotion
- Early intervention in mental illness
- Mental health promotion in Victoria
- Suicide prevention in Victoria
- Priorities and transformation
- Supporting the social and emotional wellbeing of Aboriginal and Torres Strait Islander Victorians
- National mental health strategy
- Rights and advocacy
- Making a complaint about a mental health service
- Chief Psychiatrist
- About the Chief Psychiatrist
- Principles in the Mental Health and Wellbeing Act and the Chief Psychiatrist's guidelines
- Obligations under the Mental Health and Wellbeing Act 2022
- Reporting a failure to comply with the Mental Health and Wellbeing Act 2022
- Governance and committees
- Reporting obligations for clinical mental health and wellbeing services
- Mental health and wellbeing support
- Making a complaint and seeking advocacy
- Second psychiatric opinion and process of review by Chief Psychiatrist
- Office of the Chief Psychiatrist's reform activities and news
- Oversight of forensic mental health and wellbeing services
- Resources and reports
- Chief psychiatrist guidelines
- Chief Mental Health Nurse
- About Victoria's Chief Mental Health Nurse
- Best practice
- Reducing restrictive interventions
- Research and reporting
- Mental health performance reports
- Reporting requirements and business rules for clinical mental health services
- Alcohol & drugs
- Alcohol and other drug treatment services
- Overview of Victoria's alcohol and drug treatment system
- Pathways into alcohol and other drugs treatment
- Prevention and harm reduction
- Medically supervised injecting room
- Victoria's Take-Home Naloxone Program
- Community-based AOD treatment services in Victoria
- Residential treatment services
- Mildura statewide alcohol and drug residential treatment service
- Drug rehabilitation plan
- Hospital-based services
- Forensic services
- Pharmacotherapy treatment
- Services for Aboriginal people
- Services for young people
- Statewide and specialist services
- Compulsory treatment
- Family and peer support
- Public intoxication reform
- New public intoxication response services
- Policy, research and legislation
- Alcohol and drug research and data
- Legislation governing alcohol and other drug treatment
- Alcohol and other drug service standards and guidelines
- Alcohol and other drug client charter and resources
- Alcohol and other drug treatment principles
- Service quality and accreditation
- Alcohol and other drug program guidelines
- Maintenance pharmacotherapy
- Specialist Family Violence Advisor capacity building program in mental health and alcohol and other drug services - Victoria
- Alcohol and other drug workforce
- Learning and development
- Alcohol and other drug workforce Minimum Qualification Strategy
- Workforce data and planning
- Funding and reporting for alcohol and other drug services
- Funding of alcohol and other drugs services in Victoria
- Reporting requirements and business rules for alcohol and other drug services
- Drug alerts
- 25C-NBOMe and 4-FA sold as '2C-B'
- Novel stimulants sold as MDMA, cocaine or speed
- Protonitazene sold as ketamine
- High potency benzodiazepine tablets
- MDMA adulterated with PMMA
- 25B-NBOH sold as powdered 'LSD'
- Green 'UPS' pills containing N-ethylpentylone (no MDMA)
- N-ethylpentylone in cocaine
- Ageing & aged care
- Supporting independent living
- Low cost accommodation support programs
- Personal Alert Victoria
- Dementia services
- Victorian Aids and Equipment Program
- Residential aged care services
- Public sector residential aged care services
- Safety and quality in public sector residential aged care
- Physical and social environments
- Emergency preparedness in residential aged care services
- My Aged Care assessment services
- Home and Community Care Program for Younger People
- HACC data reporting
- HACC PYP fees policy and schedule of fees
- Wellbeing and participation
- Age-friendly Victoria
- Healthy ageing
- Seniors participation
- Dementia-friendly environments
- Designing for people with dementia
- Maintaining personal identity
- Personal enjoyment
- Interior design
- Dining areas, kitchens and eating
- Bedrooms and privacy
- Gardens and outdoor spaces
- Assistive technology
- Staff education and support
- Strategies, checklists and tools
- Our Strategic Plan 2023-27
- Our organisation
- Our secretary
- Leadership charter
- Our services
- Our vision and values
- Specialist offices
- Senior officers in health
- Human Research Ethics Committee (HREC)
- Gifts, benefits and hospitality policy
- Information Asset Register
- Health legislation
- Health legislation overview
- Health Complaints legislation
- Health Records Act
- Human Tissue Act 1982
- Public Health and Wellbeing Act 2008
- Voluntary Assisted Dying Act
- Victoria's pandemic management framework
- Independent Pandemic Management Advisory Committee
- Pandemic Order Register
- Our ministers
- Our role in emergencies
- State Health Emergency Response Arrangements
- Emergency type
- Department's responsibilities in emergencies
- Health services’ responsibilities in emergencies
- Aboriginal employment
- Current vacancies
- Employment programs for students and graduates
- Rise program
- Inclusion and diversity at the Department of Health
- Health workforce
- Working in health
- Information sharing and MARAM
- Child Safe Standards
- Regulatory functions
- Reviews of decisions
- Victorian Public Healthcare Awards
- Aboriginal healthcare workers
- Mental health workforce
- Lived and living experience workforces
- Engaging with lived and living experience workforces
- Our workforce, our future
- Nursing and midwifery
- Free nursing and midwifery study
- Additional funding for nursing and midwifery positions
- Becoming a nurse or midwife
- Undergraduate nursing and midwifery scholarships
- Undergraduate student employment programs
- Nursing and midwifery graduates
- Nursing and midwifery graduate sign-on bonus
- Working as a nurse or midwife
- Enrolled nurse to registered nurse transition scholarships
- Support for new nurse practitioners
- Postgraduate scholarships for nurses and midwives
- Nurse practitioners
- Returning to nursing or midwifery
- Refresher pathway for nurses and midwives
- Re-entry pathway scholarships for nurses and midwives
- Nursing and midwifery - legislation and regulation
- Nursing and midwifery program - health sector
- Allied health workforce
- Education and training
- Enterprise agreements
- Worker health and wellbeing
- Working with us
- Grants and programs
- Freedom of Information
- Part II - Information Statements
- Procurement policies
- Protective markings
- Health and medical research
- Sponsorship application information
- Publications
- Annual reports
- Fact sheets
- Strategies, plans and charters
- Policies, standards and guidelines
- Research and reports
- Forms and templates
- Communities
- Designing for Diversity
- Vulnerable children
- Vulnerable children - responsibilities of health professionals
- Identifying and responding to children at risk
- Pathway to good health for children in care
- Older people
- Aboriginal health
- Improving health for Victorians from culturally and linguistically diverse backgrounds
- Asylum seeker and refugee health in Victoria
- News and media hub
- Media releases
- Health alerts
- Feedback and complaints
- Make a payment
- Fees, charges and penalties subject to automatic indexation
- Our campaigns
Share this page
- Facebook , opens a new window
- X (formerly Twitter) , opens a new window
- LinkedIn , opens a new window
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Gridley K, Brooks J, Birks Y, et al. Improving care for people with dementia: development and initial feasibility study for evaluation of life story work in dementia care. Southampton (UK): NIHR Journals Library; 2016 Aug. (Health Services and Delivery Research, No. 4.23.)

Improving care for people with dementia: development and initial feasibility study for evaluation of life story work in dementia care.
Chapter 10 discussion and conclusions.
- Discussion of findings
Stage 1: literature review and qualitative work
- Both elements of stage 1 showed that LSW is not simple conceptually, nor is it easy to pin down its potential benefits. Personal, temporal and organisational challenges may prevent positive outcomes being achieved, and an individually tailored approach is essential to ensuring maximum benefit for different people at different times.
- The different models of LSW identified in the review and the theories of change that emerged echoed the different purposes of LSW identified in the qualitative work. Is LSW mainly about people preserving their own memories or is it to help staff learn about the person they are working with? Is its aim to improve QoL by reaffirming identity, or by personalising care and responding better to behaviour that challenges?
- We saw these tensions played out in care settings in the survey and in the feasibility study, where the focus was on LSW as a tool for care and for managing behaviour. This does not necessarily make LSW in those settings any less valuable, but it may narrow the scope for benefit. It also raises the question of whether or not the potential personal benefits might be better achieved earlier in the dementia journey, when people with dementia themselves may have more control over the process and final product.
- The experiences of people with dementia, family carers and professionals about good practice in LSW were consistent with messages from the literature review and, together, suggested a set of learning points for good practice (see Conclusions ).
Stage 2: surveys
The survey of services suggests that LSW has spread relatively widely, particularly in hospital assessment settings, albeit to a lesser extent in care homes.
We found wide variation between different services in the type of LSW they did, and in its overall objectives, including involvement of the person with dementia, whether it was past or forward looking and how it was used in the care setting. We saw throughout that these differences may reflect the different places on the dementia care pathway at which the services were located. Settings with an assessment and care planning focus tended to produce life story products that were less dynamic and sometimes designed specifically to capture information to pass on to other care settings. Care homes were more likely to be capturing information to inform everyday care and interactions with the person with dementia.
Across the board, however, the actual use of the life story product was not as common as might be hoped for. Doing LSW is one thing; using it to inform and improve care is clearly another.
The service survey emphasised the role of carers in doing LSW, and the survey of carers gave further detail. Although carers played an important part in services’ LSW, they were unlikely to be trained to do it beforehand. Carers were likely to report heavy involvement and, in some cases, had led the LSW. Again, however, the actual use of the life story by care staff, and even by the person with dementia and carers, was lower than might be expected.
Different models of LSW in the carers’ accounts echoed those found in the review, the qualitative work and the services survey, suggesting again two different types and uses of LSW.
Stage 2: feasibility study process
Our overall conclusion from this stage is that formal evaluation of LSW would be possible only with substantial staffing. Enabling people with dementia (and, to some extent, their family carers) to participate in a meaningful way meant that we used essentially qualitative methods to collect quantitative data. Working with people with dementia requires patience, and there will always be a high risk that data cannot be collected on a given day.
However, working in care homes and hospital wards is, of itself, labour intensive and runs the risk of ‘wasted’ researcher time. Contacting family members and other consultees relies on the goodwill of staff, and carers themselves often have busy/stressful lives and other priorities. Embedding researchers in the care settings is probably the best way to deal with these types of problems.
Staff turnover and the differing priorities of care settings also mean that the best-laid plans for data collection can fail. Continuity in management commitment to the intervention itself and to the research is clearly an issue, as others have also found. 140
Overall, our work means that we now have a clear idea of the challenges and benefits of attempting to establish evaluation of this complex intervention in care settings that are themselves complex and often complicated.
Stage 2: feasibility study outcomes
Even after successful recruitment of people to the study, gathering data was challenging. Completion rates for outcome measures were mixed, being best overall for family carers in care homes and worst for people with dementia in hospital wards. Completion of measures by staff in care homes was particularly disappointing, given the commitment of the care home provider to the study.
However, we learned much of use for future research.
First, we observed fatigue effects, both immediate (for people with dementia) and over time (for staff and carers). To deal with the first issue, future research should randomise the order in which measures are presented to people with dementia. To deal with the second issue, two follow-up points after baseline, rather than three, might be better. We saw a considerable reduction in completion in all groups at 6 months after baseline. A shorter follow-up period would certainly have benefits in relation to the participation of people with dementia and carers. However, we think that follow-up for staff should be at longer intervals. This would allow for the ‘bedding in’ of the intervention into the culture of the care setting but also help to avoid any learning of the ‘right’ answers caused by repeating measurement at short intervals.
Completion was not always a function of capacity for people with dementia. Local or embedded research teams could be more flexible in response to the priorities of the care settings and needs of residents or patients, and allow data to be gathered at a time and pace to suit both.
We felt strongly that the QoL measures both missed and were influenced by ‘in-the-moment’ benefits for people with dementia. Different methods – whether qualitative (such as observation, photovoice or video ethnography) or quantitative (such as measurement of QoL ‘in the moment’ with subsequent aggregation) – are needed to catch these more fleeting benefits. Exploring and developing different methods is essential for any future research if it is properly to include the views of people with dementia themselves, rather than those of their proxies. Our observations also have implications for the way in which QoL measures are used with people with dementia in care settings, where many different activities may take place across each day and week.
The measures also missed how LSW was used, in particular the use of LSW for de-escalation of behaviour that challenges in hospital settings. Formal observational techniques at selected times of the day, in care homes and hospitals, would be useful for future research, but have substantial resource implications.
We did observe some change in our outcome measures from baseline to follow-up and these were significant for staff attitudes towards dementia in care homes, for self-reported QoL (using DEMQOL) for people with dementia in care homes between baseline and final follow-up, and for the experiences of carers.
The first change we think could be an effect of LSW, as we saw evidence of it in both measures of staff attitudes. Whether the change was due to the training associated with implementing LSW or to LSW itself is not clear. Neither is it clear whether the change can be maintained over time or whether it alters staff behaviour. However, we believe that this apparent effect is worth exploring in future research.
The second effect was measured only for the 12 people with dementia able to complete DEMQOL; they may thus have been less cognitively impaired than others in the study. However, the pattern was consistent over time (QoL improved further at each follow-up) and was also evident when we reran the analysis for only those who completed DEMQOL at all three follow-up points.
We saw deterioration in carers’ experience scores in the care homes and an improvement in the hospital setting. We are not sure that either effect is related to LSW. People with dementia in the care homes were often approaching the end of the dementia journey, as we saw from the number of deaths in our sample. It is perhaps unsurprising that carers were less able to engage in their usual activities, and so on, as time passed. For carers of people in hospital, by contrast, it was often the case that the person with dementia had been admitted in a crisis, but, during his or her stay, was stabilised and assessed and had his or her future care planned (in some cases meaning admission to long-term-care). Again, we can understand why carers might feel that restrictions in their lives might have lightened somewhat. These findings, however, do suggest that the CES is a good candidate measure for any future research looking at the experiences of carers of people with dementia.
Stage 2: collecting resource-use data
Staff collected resource-use data from care homes either alone or in conjunction with researchers. Data collection forms were filled out more consistently and completely if researchers were involved. Hospital staff collected data from hospital wards and this was equally time-consuming. In a full evaluation, either researchers would need to gain ethical approval and consent from study participants to extract data from their care/medical notes, or care home/ward staff would need to be appropriately trained in collecting the data and their time for doing so would have to be ring-fenced.
Reporting some data, for example on antipsychotic prescribing, was simple for the care homes, as their systems were already set up to run these queries. In the hospital intervention wards, the only way to provide an indication of the volume of prescribing was through the total cost per drug over a specified time period. In a full evaluation, this may be a useful reporting method for a ward-level intervention.
Stage 2: resource-use outcomes
The cost of delivering the LSW training in care homes ranged from £950 to £1581; these costs would change if different staff members attended training sessions. The average cost (based on salary only) of creating and using LSW products for a resident in the care homes was £37.42 spread over a 16-week period. These costs included staff working in conjunction with residents as well as working alone, making it difficult to categorise which were additional costs and which were part of routine care. If we assume all costs are additional, resource implications would be relatively small at an individual resident level but could be substantial if extrapolated to all residents.
Life story work was a part of routine care in the hospital intervention wards, so there were no initial training costs. The average cost (salary only) of creating and using LSW products was £68.21 per patient over a 3-week period. The more intensive activity here may be due to staff attempting to complete life story products before patients are discharged, or to OTTI staff having dedicated time for this activity.
The intention had been to calculate the monetary value of, and the potential savings from, the NHS and other resources, including prescribing. However, given the small number of data, we did not calculate these costs, as they would not be robust and might be misleading.
However, the main drivers of costs are usually the services used most frequently or that have the highest costs per use.
The most frequently used services in care homes were visits to the care home by the GP and the district nurse. Care home staff accompanied residents to these consultations on at least 25% of occasions, which would add to overall costs if this took staff away from other valuable duties. Visits by the GP showed some reduction at follow-up compared with baseline, but visits by the district nurse did not.
The resources with the highest monetary values per use were an inpatient stay on a general medical ward, an accident and emergency (A&E) attendance by ambulance, an outpatient appointment and a GP visit to a care home. Because of their relatively high costs, these events are more likely to affect total costs than, for example, visits to the care home by professionals allied to medicine. As an example, four residents taken to A&E by ambulance in the 3 months prior to baseline would have cost £920, plus the value of the time for care home staff to accompany them on two of these occasions. During the follow-up period, two residents attended A&E by ambulance with no accompanying staff, at a cost of £460. Over a larger number of residents in a full evaluation, any differences in the costs of this type of activity might be substantial.
In a full evaluation, then, the priority should be on collecting data on high-cost or high-volume services such as hospital inpatient admissions, outpatient attendances, A&E attendances, and visits to care homes by GPs and district nurses. The number of times care home staff accompany residents to such appointments should also be recorded, as these may have opportunity costs.
The use of prescribed medication for anxiety and depression by participants in the care homes was small, with no recorded PRNs. Care-home-wide data on antipsychotic prescribing were provided by two homes. In one, prescribing of antipsychotic medication was low; in the other (the SCH) 12 residents were prescribed antipsychotics, all but one on a continuous basis. Overall, however, for study participants in these care homes, the use of antipsychotic or other drugs was not a big driver of costs.
Owing to the small numbers of participants in the hospital settings, it is not possible to judge from individual patient data how extensively antipsychotic drugs were used. However, ward-level data suggest antipsychotic prescribing costs up to £1350 per ward over 6 months.
Some drugs might drive overall costs but the majority, especially those available in generalist form, are not expensive, even on an ongoing basis, in comparison with other costs such as A&E attendances or GP consultations. In a full evaluation, the daily costs of the most expensive drugs or the ones most likely to be affected by LSW would need to be calculated for each participant. From this study, these are amisulpride, quetiapine, venlafaxine and aripiprazole.
Each result shows little on its own, as we would expect from small numbers, but taken as a whole there is the suggestion of a decrease in service use and adverse events. Although these data were never intended to be robust enough to demonstrate change, they do suggest a possible reduction in service use and an indication of the main drivers of costs that might be collected in a full evaluation.
Stage 2: participants’ experiences of life story work as part of the research project
Carers, in particular, were unsure of the benefits of LSW for their relatives with dementia, particularly when the dementia had progressed and the person could no longer even recognise people in photographs. This sometimes led to carers’ reluctance to get involved in the LSW, feeling that it would have no effect. However, people with dementia in the study appeared to enjoy looking at their life story books, and staff were more certain that there was a positive effect, particularly in terms of facilitating interactions with both visiting family members and staff (particularly temporary staff), as well as encouraging staff to get to know the person. This suggests indirect benefits to LSW for the person with dementia, however far the dementia has progressed.
Staff were positive about collecting life story information, and many described how this was ‘already’ done, whether through use of a template on admission to the care setting or through the course of everyday interactions with the person. There was some scepticism about the need for a physical life story product, particularly as these were considered time-consuming to make. When products were made, staff usually led the process, often with some family involvement through, for example, providing photographs or stories. However, lack of time was a barrier, and some staff described how they spent time outside work making products. LSW was considered easier when one person or a small team took responsibility for it; where this had been implemented in sites, all staff members were encouraged to collect information, but did not have responsibility for making a product. This person or team could also take the lead in encouraging family members to be involved.
Although some aspects of LSW can be beneficial for people with dementia, it is unclear whether this is attributable to the presence of a physical life story product, or the act of spending time with someone, learning about their life. This may, of course, occur without LSW, but LSW can be a mechanism for this, and a physical life story product can have further benefits in facilitating interactions and therefore enhancing relationships with family members and staff.
- Strengths and limitations
There are two main strengths to our work.
The first strength was the use of a mixed-methods design, which allowed us to identify strong commonalities across the existing literature about LSW and carry out new qualitative exploration and preliminary outcome assessment. This enabled us to identify hypothesised routes to efficacy for LSW and then to explore these in a small outcome study. The qualitative work produced in-depth understanding; the literature review allowed us to develop models of LSW and theories of change; the survey generated insights into the practice of LSW nationally; the feasibility study was completed despite substantial challenges to process and progress; we observed some effects; and we were able to ascribe costs and possible savings to LSW. We thus generated new knowledge about LSW itself while improving understanding about how to approach the next stage of evaluation.
The second strength was the involvement of people with dementia, family carers, organisations that advocate for the rights of both, and care providers. Their involvement was not only as participants but also as influential advisors at all stages of the work. This strengthened our research practice and our understanding about the benefits and challenges of being involved in research for people with dementia and their carers. This understanding is invaluable for planning our own future research and also, we hope, that of others.
The two main limitations of the research are what we were not able to do.
We had planned to use the literature review to estimate the size of outcomes achieved in LSW, but there was insufficient evidence to allow this.
We had also hoped to do some Markov chain modelling to inform decisions about whether or not to carry out future evaluation. Five main factors militated against this:
- There was a dearth of outcome data in the existing literature.
- There were very low levels of data return for people with dementia in the hospital settings.
- The only detected effect for people with dementia (and only in care homes) was for a very small proportion of respondents, and they were probably not typical residents.
- There were question marks about implementation of LSW in both hospital and care home settings.
- The largest effect observed related to attitudes to dementia for staff in care homes, not for people with dementia.
Given these issues, we did not feel that modelling would provide a secure basis for future research.
- Conclusions
Life story work has spread widely in health settings in England (although less so in social care settings), but our work has shown that what it is, how it is done and the outcomes it achieves vary substantially.
There are two predominant models of LSW.
First, there is LSW that is led by the person with dementia, usually at a relatively early stage of the dementia journey, and which serves to reinforce a sense of identity and support pride in the life led to date. This sort of LSW may be carried out over a long period and generate detailed and substantial life story products. This work is often narrative or at least biographical.
The second model, found more often in care settings (and thus at a later stage of the dementia journey), is less likely to involve the person with dementia (although there is no reason why it should not) and more likely to involve family carers. Although it is also about telling the story of a person’s life, it is more often directed to aspects of and contents about a person’s life that might aid communication with and increase staff understanding about the person. It may also be used to calm or soothe the person with dementia. This type of LSW is, thus, almost entirely care-focused, although there is no reason why a ‘type 1’ life story should not inform a ‘type 2′ life story.
The feasibility element of our project was more about the second type of LSW and found some evidence that it might improve care home staff attitudes about dementia, although it is not clear whether this change comes from the LSW training or from doing LSW itself. Care homes are important in the later stages of the dementia journey and the challenges of delivering person-centred care in these settings are widely acknowledged. We therefore feel that future LSW evaluative research could profitably focus on staff attitudes and whether or not changed attitudes lead to changed care practices. Overall, it does not seem to be expensive to implement this type of LSW, and there are some hints of areas of resource-use savings. Taken together, these suggest an agenda for future evaluation and one that can be carefully informed by the rich learning that came from our feasibility work.
Implications for health care
Stage 1 of our work was based on in-depth qualitative research and a systematic review of the literature. Although this work could not point to definite outcomes from LSW, it did find consistent messages about good practice in doing LSW. The survey of health and social care services showed that not all services follow these practices. We have, therefore, drawn together good practice learning points which are summarised below, and we will disseminate these widely to health and social care audiences.
Good practice learning points for life story work
- Whether someone wants to take part in LSW is an individual thing. It should not be assumed that a person necessarily wants to make or share a life story and no one should be pushed into doing so.
- A person’s life story is never finished and LSW needs to reflect this. To avoid setting people ‘in stone’, ensure that life story documents can be added to and updated.
- LSW can be emotional and may raise sensitive issues. Some people will value the opportunity to talk about these issues, but staff require training to handle this and should not be expected to do so without support.
- A person with dementia may have very different views from others about what their life story is for. Respect the person’s wishes about what goes into the life story and who will see it, now and in the future. If they do not have capacity to express their views, consult someone who knows them well.
- Staff should consider making and sharing their own life stories. How does this feel? Who would they share them with?
- Beginning the process early will enable people with dementia to take a more active role in producing their life story and communicate how they would like it to be used in the future. However, it is never too late to use LSW to improve care for a person and invoke a ‘nice feeling’.
- Outcomes for better care will only come about if care staff take (and, indeed, are granted) the time to absorb life story information and the flexibility to use this to inform and improve the care they provide.
- Short summaries might be useful for busy staff, helping them to achieve better care, but they cannot replace a life story owned, shared and added to by a person with dementia him- or herself.
- The process of collecting life story information enables staff to connect and build relationships with people with dementia and their families. However, in order to have wider benefits it is also important to produce something that can be used and enjoyed by others.
Stage 2 was intentionally exploratory. Although we did observe effects in this stage of the work, particularly in relation to staff attitudes in care homes, it is clearly not right at this stage to draw out implications for health and social care providers.
- Recommendations for research
The main point of stage 2 was to learn whether or not formal evaluation of LSW is possible and we have outlined above some of the detailed learning about how such evaluation might be designed and carried out. We will not repeat that detail here but confine ourselves to the larger research needs that have emerged. In order of priority, there is a need for:
- Formal evaluation of LSW as a method of changing staff attitudes about dementia, and particularly in care homes. This should compare LSW, as such, against more general training input about dementia.
- Qualitative research that explores the motivation and ‘emotional intelligence’ of care staff, recognising that delivering person-centred care for people with dementia requires particular qualities of both.
- Methodological development in assessing QoL for people with dementia ‘in the moment’. Existing measures of QoL do not capture the temporary pleasure that LSW (and other interventions) may give to people with dementia, even if the interventions do not have an effect that is measurable with existing instruments. The additive effect of episodes of temporary pleasure may well be worth having, but without ways of measuring it we will never be able to tell. Given the predominance of QoL measurement in health economics, and thereby its influencing on commissioning, we believe that this type of development is essential to the future of good-quality care for people with dementia. Such development would need to be multidisciplinary, involving cognitive psychologists and health economists as well as health service researchers.
Included under terms of UK Non-commercial Government License .
- Cite this Page Gridley K, Brooks J, Birks Y, et al. Improving care for people with dementia: development and initial feasibility study for evaluation of life story work in dementia care. Southampton (UK): NIHR Journals Library; 2016 Aug. (Health Services and Delivery Research, No. 4.23.) Chapter 10, Discussion and conclusions.
- PDF version of this title (60M)
In this Page
Other titles in this collection.
- Health Services and Delivery Research
Recent Activity
- Discussion and conclusions - Improving care for people with dementia: developmen... Discussion and conclusions - Improving care for people with dementia: development and initial feasibility study for evaluation of life story work in dementia care
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient Case Study
Description of a clinical condition.
This paper will discuss a case study of Loretta, a 72-year-old Australian diagnosed with dementia, describing a woman’s clinical condition by using ICF terminology and structure and outlining the measures which need to be imposed for providing her with effective interventions and enhancing the professionalism of the involved exercise physician.
Body structures and functions
Loretta is a 72-year-old Australian citizen living in Melbourne who is diagnosed with dementia. The pathological neurofibrillary changes in her central nervous system caused the structural impairments and had a devastating impact upon her cognitive functions, including the impaired memory and semantic processes which in their turn affected Loretta’s communicative abilities. The conversational difficulties in Loretta were caused by the decline of the mental processes essential to the communicative functions, including the functions of recognition and usage of language signs. The impairments of declarative memory resulted in communication difficulties, repetitive questions, and word-finding problems.
Activities and participation
The impaired cognitive abilities in Loretta significantly reduced her skills of learning applying knowledge and communicating with others. The communicative difficulties limited Loretta’s participation in the community and social life and threatened her interpersonal interactions and relationships. It made Loretta passive and uninvolved in domestic and community life.
Environment and contextual factors
Loretta’s communication disability can be regarded as the outcome of her ineffective interaction with her environment. She lacked interpersonal support because her husband and children perceived her clinical cognition as the loss of self. Having problems communicating with large groups of people and strangers, Loretta isolated herself and rejected any contacts.
Intervention project
An effective treatment program for Loretta’s condition requires developing multi-component interventions with special emphasis put upon physical training, psychosocial and emotional support through educating the family caregivers and involving the community in the treatment of patients with dementia. This approach would allow considering the body structures along with the environmental factors for providing complex treatment for the patient diagnosed with dementia.
Taking into account the fact that elderly individuals with dementia are under the threat of decline in their physical functioning, it can be stated that the physical training component is significant for developing an effective intervention program for Loretta. The multi-component physical training interventions, including the exercises intended to enhance the patient’s endurance, strength and balance have proven to be effective for improving the participants’ physical functioning, regardless of the stage of disease (Blankevoort, van Heuvelen, Boersma, Luning, and Scherder, 2010, p. 393; Flicker, Liu-Ambrose, & Kramer, 2011, p. 466). Moreover, the best intervention outcomes can be received from the programs with the largest training volume.
Due to the significant impact of environmental factors upon the condition of patients diagnosed with dementia, their passivity and segregation from the rest of the community, educating their relatives and community members and encouraging them to provide the patients with psychosocial support is of paramount importance for receiving a positive outcome from the intervention program. Burton (2010) pointed out the importance of creating dementia-friendly neighborhoods instead of focusing on the internal environment of dementia care homes. Taking into account the fact that conversational difficulties caused by cognitive impairments traditionally result in the patient’s passivity, understanding, and support of the surrounding people are critical in terms of palliative care. Another influential factor is the people’s misconceptions concerning the patients with dementia, their communicative needs, and abilities. These stereotypes need to be overcome through educational measures.
Three characteristics of professionalism
The three characteristics of professionalism that are essential for conducting the above-discussed intervention program successfully include the skills of an exercise physiologist to develop an appropriate training program for every individual patient, inter-professional collaboration, and addressing exercise as medicine clearly understanding its role in a complex intervention program.
Recognizing the significant impact that physical exercises can have upon the patient’s condition, an exercise physiologist has to make the right prescription for each person (Boone, 2011). Thus, Loretta’s physical functioning at the moment when the prescription is made needs to be taken into consideration for developing an appropriate multi-component physical intervention project.
With the current tendencies of professionalization in the exercise physiology domain, exercise physiologists need to gain a clear understanding of their role in the overall system of modern healthcare services. It would allow them to convince the patients with dementia and their relatives of the importance of appropriate physical training for the palliative care of patients with dementia, Due to the fact that dementia interventions require a complex approach and a combination of measures, it can be stated that inter-professional collaboration is critical for developing effective projects. Thus, exercise physiologists should realize the importance of their role in developing the intervention programs without understating the importance of inter-professional collaboration with other specialists.
The role of another professional
As it has been stated above, the recognition of the role of other professionals is significant for improving the outcomes of the intervention projects. Thus, the role of social workers and nurses in the implementation of an effective intervention project is as important as the role of exercise physicians (Perry, Draskovic, Lucassen, Vernooij-Dassen, van Achterberg, & Olde Rickert, 2011; Stevens, Lancer, Smith, & McGee, 2009 ). In that regard, their successful teamwork, information exchange, and recognition of the fact that the interventions need to be multi-component are essential to the quality of the provided services. To develop a specific training program for Loretta, an exercise physician will need to consider the impact of other interventions to make the components complementary.
Two strategies for making the practice person-centered
Taking into account the fact that the conversational difficulties in individuals diagnosed with dementia predetermine their passivity and segregation from the community, the person-centered approach is the most appropriate strategy for creating more comfortable conditions for individuals with dementia. The two strategies of person-centered care include looking at the world from the point of view of a patient diagnosed with dementia and creating a positive social environment for them.
There is evidence that person-centered strategies have a positive impact on the intervention outcomes (Kontos, Mitchell, & Baloon, 2010; Robinson, Bamford, Briel, Spencer, & Whitty, 2010). Empathy is critical for effective care for Loretta and other patients diagnosed with dementia. Looking at the surrounding world and community through the patients’ eyes would enhance understanding of the underlying problems and processes. Regarding the strategy aimed at creating a positive social environment, it should be noted that the community involvement and recognition of the problem of dementia in elderly people is critical for arriving at an appropriate resolution.
Two strategies for professional development
The two strategies which can be implemented for the professional development of an exercise physician include an evidence-based approach to professional practice and enhancing one’s knowledge in the related disciplines. Implementing the results of the recent research in professional practice can be beneficial for improving the outcomes and increasing one’s professional level. As to the importance of acquiring knowledge on the related professional domains, it would allow enhancing the effectiveness of the teamwork and improving the patients’ outcomes from the complex interventions in general.
In general, it can be concluded that interventions for Loretta diagnosed with dementia should comprise several components, including those of physical training educational and social work, and effective inter-professional work is required for improving the patient’s outcomes.
Blankevoort, C., van Heuvelen, M., Boersma, F., Luning, H., and Scherder, E. (2010). Review of effects of physical activity on strength, balance, mobility and ADL performance in elderly subjects with Dementia. Dementia and Geriatric Cognitive Disorders , 30(5), 392-402.
Boone, T. (2011). Contemporary exercise physiology: The big picture. Professionalization of Exercises Physiology Online, 14(3), 1-17. Web.
Burton, E. (2010). Designing dementia-friendly neighborhoods: Helping people with dementia to get out and about. Journal of Integrated Care , 18(6), 11-18.
Flicker, L., Liu-Ambrose, T. & Kramer, A. (2011). Why so negative about preventing cognitive decline and dementia? The jury has already come to the verdict for physical activity and smoking cessation. British Journal of Sports Medicine , 45(6), 465-467.
Kontos, P., Mitchell, G., & Baloon. B. (2010). Using drama to improve person-centered dementia care. International Journal of Older People Nursing, 5(2), 159-168.
Perry, M., Draskovic, I., Lucassen, P., Vernooij-Dassen, M., van Achterberg, T & Olde Rickert, M. (2011). Effects of educational interventions on primary dementia care: A systematic review. International Journal of Geriatric Psychiatry , 26(1), 1-11.
Robinson, L., Bamford, C., Briel, R., Spencer, J., & Whitty, P. (2010). Improving patient-centered care for people with dementia in medical encounters: An educational intervention for old age psychiatrists. International Psychogeriatrics , 22(1), 129-138.
Stevens, A., Lancer, K., Smith, E., & McGee, R. (2009). Engaging communities in evidence-based interventions for dementia caregivers. Family & Community Health , 32(1), S83-S92.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, March 31). Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient. https://ivypanda.com/essays/inter-professional-health-case-study/
"Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient." IvyPanda , 31 Mar. 2022, ivypanda.com/essays/inter-professional-health-case-study/.
IvyPanda . (2022) 'Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient'. 31 March.
IvyPanda . 2022. "Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient." March 31, 2022. https://ivypanda.com/essays/inter-professional-health-case-study/.
1. IvyPanda . "Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient." March 31, 2022. https://ivypanda.com/essays/inter-professional-health-case-study/.
Bibliography
IvyPanda . "Inter-Professional Healthcare Collaboration: 72-Year-Old Dementia Patient." March 31, 2022. https://ivypanda.com/essays/inter-professional-health-case-study/.
- The Person-Centered Care in Nursing
- Interprofessional Collaboration in Healthcare
- Childhood Obesity: Review and Recommendations
- Nursing Interventions and Hemoglobin Levels
- Patient Compliance to Health Care Recommendations
- Health Research and Educational Trust
- Pre-Operative Education and Postoperative Pain
- Evidence Based Medicine
Managing Challenging Behaviour. A Dementia Case Study
Essay, 2018, 11 pages, grade: 78.00, leonard kahungu (author).
Abstract or Introduction
The human behaviour, whether good, bad, or unusual, exhibits the expression of emotional needs and feelings. It is a form of communication, which is presented in innumerable ways. Nevertheless, these behaviours may at times be considered abnormal when the fall short of social expectations. This is exemplified by the loss of memory, concentration and the inability to reason or make rational decisions are some of the socially and clinically significant behaviours in people with dementia. Restless, disturbing behaviours that hinder the creativity, skills along with the coping resources of the caregiver is commonly known as challenging behaviours. A person diagnosed with dementia may display agitation and aggressive behaviours in reaction to various external and internal stimuli. These features are mirrored on Mr. Holt’s case scenario. The details obtained indicates that the patient was initially fine and considered a model patient, until his behaviours drastically deteriorated and made it difficult for the caregivers to administer standard procedures and treatments. This illustrates the significance of understanding the concepts of challenging behaviours is paramount in behaviour therapies, especially in dementia management.
- No comments yet.
Similar texts

Urban Management Studies in the Urban Regeneration Context
Factors Affecting Safety Behaviours of Construction Workers in Malaysia
Issues & Challenges of Quality Management faced by MSMEs

Managing and Working across Cultures - Eastern Europe Challenges for Manager...
Challenges in Innovation Management
Harvard Business Case Borealis
Challenges in management and leadership
Creative Accounting, the Enron Case and its impact on Corporate Governance


The Challenge to Manage Variety. A Current Evaluation of Diversity Managemen...
Fixed Assets Management. A Study of Kesoram Cement
Effect of Sales Promotion Activities on Consumer Buying Behaviour. A Case Stu...
Optimierung des Vertriebsprozesses bei der Dental Y AG. Eine vertriebliche Ca...

Marketing Case Study: Canadian Jet

Assessing Smallholder Farmers’ Perceptions to Climatic Factors Affecting Maiz...
The Business Case of Diversity - Siemens AG

The CSH Program. Die modellhafte Idee der Case Study Houses (1945 - 1966 Kali...
Strategic Decision Making - A Case Study Review
Case Study: A Study On Causes Of Stress In The Public Banks Of The Jodhpur City
The Facebook acquisition of Instagram. A Case Study
Upload papers
Your term paper / thesis:
- Publication as eBook and book - High royalties for the sales - Completely free - with ISBN - It only takes five minutes - Every paper finds readers
Publish now - it's free
- New Zealand
- [email protected]
- +974-55545283
- +353-858275584
Case Study of a Patient Dementia
Introduction
A nurse associate is responsible to provide adequate medical care to the dementia patients so that they get optimal well-being. This essay highlights the case of a dementia patient who is suffering from health issues due to sleep disorders, hallucinations and short-term memory loss. Dementia is the deterioration of the cortex region of the brain and cause abnormalities in the sensorimotor cortical regions. In order to maintain the patient's confidentialit y , the patient is named as Mrs. X as per NMC (2018). The responsibilities of a nurse associate are outlined sharply that helps a dementia patient to lead an independent and healthy life with the ability to overcome or face barriers and challenges. Hence, through the implementation of adequate medical care and effective social services, a dementia patient can be encouraged to feel motivated to live a healthy life.
Mrs. X is an eighty-four years old woman. She lives with husband and two daughters. Her professional career states that, she used to be a lawyer and enjoyed writing and reading books. Five years ago, she was diagnosed with vascular dementia. Due to this, she faces short-term memory loss, anxiety, depression, and loss of appetite. Mrs. X was suffering from reduced mobility as dementia has significant impact mobility at later stage of her life. The dementia report of 2014 stated, "more than 79.3% of people having dementia feel depressed and anxious” (T O'Brien and Thomas, 2015, pp. 1698). According to the dementia report of 2014, around 34% of all kinds of dementia are expected to occur due to vascular dysfunction. Mrs. X was diagnosed with delirium and that delirium is considered as a co-factor or early detection agent for dementia (Dewing and Dijk, 2016, pp. 107).
PHYSICAL AND PSYCHOSOCIAL HEALTH ISSUES "Any of several psychological illnesses, generally characterized by loss of a person's general brain, behavioural, or behavioural performance, and induced by biological or social reasons," is how The WHO describes mental illness. Although mental disorders can be a physical ailment, this is not always the case, unlike with conditions such as diabetes. Doctors can do tests to check for specific disease signs in the plasma, such as blood sugar and Glycosylated haemoglobin levels, in conditions like hypertension. Mental diseases can also be brought on by physical issues. Diagnoses for mental health conditions frequently rely more on the patient conveying their sensations and background than for illnesses like hypertension. If a patient has clinical depression, the primary care doctor may recommend medications. They can also perform tests to verify sure disease is not solely mental rather than biological in origin. A doctor could overlook a medical diagnosis that could be the root of a mental health issue if long-term health treatments are not provided together. All of the above basic information should be included in a mental health case study essay.
List Of Top Assignment Services Provided By BestAssignmentExperts.Com
When Mrs. X was admitted to a hospital having extreme urinary tract infection and severe agitation, delirium was diagnosed, as proven by the 4AT screening tool. Due to the disturbed sleep patterns, she used to feel agitated and anxious, which brought a feeling of apprehension and fear. This had a significant impact on the emotional, mental and psychological well-being of Mrs. X. As stated by Alzheimer’s society (2018), dementia is a progressive and long-term condition that destroys the brain cells of the patient. It leads to memory loss and the symptoms are seen to get worse with emerging time (Livingston et al . 2017, pp. 504). Through the development of an effective therapeutic approach, a healthy relationship was built with Mrs. X. Thus, the rationale behind the essay is to evaluate the usual causes of delirium that has affected the well-being of Mrs. X. As Mrs. X faced abnormal drowsiness due to delirium, she showed less eagerness in her interview.
The case study of Mrs. X revealed the adversities of Dementia like anxiety, short-term memory loss, and its potential impact on the well-being of the patient (Jönsson et al . 2019, pp. 3). Additionally, anxiety and depression have made her secluded from all other social activities. She used to remain confused between the time and place. Due to excessive disruption in the brain functioning, Mrs. X faced communication difficulties. Besides this, Mrs. X also faced reduced mobility. The medical reports of Mrs. X suggest that the progression of vascular dementia has a significant impact on the swallowing function of Mrs. X. Furthermore, this caused severe dehydration and additional weight loss. Thus, Mrs. X was provided with nursing aid so that she can take her regular nutritional intake by getting adequate nutrition support (Kontos et al. 2017, pp. 183).
The extreme impact of dementia caused Mrs. X to have communication difficulties. Therefore, use of simple words, low voice tone and utilization of verbal cues helped her to decode the information (Fazio et al. 2018, pp. S11). The nurses were given the responsibility to monitor the crucial signs of hourly-basis. This is because due to short-term memory loss or frequent drowsiness, the patients’ skip their medicines. Additionally, she was treated with antibiotics to prevent additional health issues besides dementia (Latham and Brooker 2017, pp. 504). In this regard, diagnostic tests and screening methodologies can help diagnose people with dementia for early detection (Alzheimer's society, 2018). A nurse must be responsible to support a dementia patient with adequate care. In the case of Mrs. X, the nurse was provided the task to aid Mrs. X with reassurance and empathy. This has also helped her to reduce fears and anxieties. Additionally, the role of the nurse was to promote her autonomy. The code of practice was maintained throughout the treatment phase of Mrs. X so that it can emphasize the best interest to generate effective decisions about the care of patients. A calm environment was given to Mrs. X so that she gets a peaceful sleep by avoiding noise (Corey 2017, pp. 575). Additionally, a pressure mattress was given to Mrs. X so that she can avoid pressure sores. Moreover, the integrity of the pressure skin was maintained in Mrs. X, as she was vulnerable to excessive illness due to poor nutritional intake. The role of the nurse was to carry out a urine dip stick to identify UTIs. Effective communication was done with Mrs. X so that the nurse can understand her problem effectively. Moreover, the nurse performed an effective role in maintaining the well-being of Mrs. X through continuous monitoring and hourly observations of her vital signs. This will help the physicians to monitor her health progress. Furthermore, the tasks of the nurse were to check her well-being to make sure that Mrs. X remained well-nourished, hydrated and sufficiently oxygenated, so that episodes of delirium were reduced. Additionally, the nurse associate was provided the responsibility to record fluid and food balance charts. Assessment of nutritional dietary intake acts to be an efficient intervention in dementia patients because lack of coordination between neurons affects their senses of hunger (Jones et al . 2016, pp. 280). Furthermore, the nurse associate assisted the dieticians with the regular monitoring reports so that an accurate nutritional balance is developed and the nurse associate can provide on-time nutritional content to Mrs. X. As Mrs. X was suffering from malnutrition (as evident from case study), it was necessary to monitor her diet charts to keep her healthy. Besides all these, the nurse associate was given the responsibility to monitor MUST (Malnutrition Universal Screening Tool) and Waterloo scale, and care plan was evaluated weekly. In comparison to this, intervention is a necessary element that will support the meal choices, drinking and eating habits of people suffering from dementia (Surr et al . 2016, pp. 145).
Several assisted activities were provided to Mrs. X so that she can lead her daily live independently. Numerous new symptoms restlessness, moaning, etc. came into effect due to the severe impact of delirium (Latham and Brooker 2017, pp. 506). This was difficult for Mrs. X and her family to cope with the situation. Personal centered care plan and discharge planning were designed based on the medical background and history. The alignment with effective medical care, provision of care package was formulated that supports Mrs. X’s daily activities at her home. Occupational therapists and physiotherapists encouraged Mrs. X’s behavior so that she becomes independent to carry out her daily exercises and other activities. This enhanced her confidence and she started to carry out her daily activities of living independently. Additionally, NHS England (2012) outlined the significance of supporting patients to re-gain their independence. A MTD (Multidisciplinary team) involved Mrs. X to plan her care and to highlight the importance of efficient delirium management. Additionally, health care promotional events have proven to be helpful for both Mrs. X and her husband to deal with a happy and healthy life. Thus, it helped to raise awareness regarding dehydration and UTIs. Mrs. X was able to eat and drink efficiently, which improved her nutrition intake. Mr. X was involved in numerous therapeutic activities and enjoyed listening to her favorite music. This enhanced her stimulation to live life happily, thereby reducing depression. Social services evaluated the potential needs for Mrs. X and numerous local authorities collaborated to meet the demands of her emotional, social and financial needs to promote independnce. The voluntary services that were provided to Mrs. X made her feel listened to and valued by other individuals. Hence, it had a positive impact on her mental health and well-being.
This essay has explored dementia and the impact of a UTI on dementia patients and the competency of the nurse associates to carry out their responsibilities efficiently. From the study, it is evident that Mrs. X is suffering from dementia for the past five years. Due to this, she has faced hallucination, memory loss, and other health issues. In this phase, a nurse associate must develop effective communication with a dementia patient so that she can express her needs through verbal cues, simple words and other means of communication. Thus, the importance of nurse associates to impose effective strategies will help a dementia patient to lead a happy, independent healthy life.
Alzheimer's society (2018) Dementia UK: The full report. London: Alzheimer’s Society
Corey, T, (2017). Genetic and environment factor associated with delirium severity in older adults with dementia: International journal of Geriatrics psychiatry. Vol. 32(5), pp,574-581.
Dewing, J. and Dijk, S., (2016). What is the current state of care for older people with dementia in general hospitals? A literature review. Dementia , 15 (1), pp.106-124.
Fazio, S., Pace, D., Flinner, J. and Kallmyer, B., (2018). The fundamentals of person-centered care for individuals with dementia. The Gerontologist , 58 (suppl_1), pp. S10-S19.
T O'Brien, J. and Thomas, A., 2015. Vascular dementia. The Lancet , 386 (10004), pp.1698-1706.
Jones, L., Candy, B., Davis, S., Elliott, M., Gola, A., Harrington, J., Kupeli, N., Lord, K., Moore, K., Scott, S. and Vickerstaff, V., (2016). Development of a model for integrated care at the end of life in advanced dementia: a whole systems UK-wide approach. Palliative medicine , 30 (3), pp.279-295.
Jönsson, K.E., Ornstein, K., Christensen, J. and Eriksson, J., (2019), June. A reminder system for independence in dementia care: a case study in an assisted living facility. In Proceedings of the 12th ACM International Conference on PErvasive Technologies Related to Assistive Environments (pp. 176-185). ACM.
Kontos, P., Miller, K.L. and Kontos, A.P., (2017). Relational citizenship: supporting embodied selfhood and relationality in dementia care. Sociology of Health & Illness , 39 (2), pp.182-198.
Latham, I. and Brooker, D., (2017). Reducing anti-psychotic prescribing for care home residents with dementia. Nurse Prescribing , 15 (10), pp.504-511.
Livingston, G., Sommerlad, A., Orgeta, V., Costafreda, S.G., Huntley, J., Ames, D., Ballard, C., Banerjee, S., Burns, A., Cohen-Mansfield, J. and Cooper, C., (2017). Dementia prevention, intervention, and care. The Lancet , 390 (10113), pp.2673-2734.
NHS England (2012). 6Cs of Nursing Standards. British Medical Journal. Accessed December 2011, Vol. 343.
Nursing and Midwifery Council (NMC, 2018). The Code. London: Nursing and Midwifery Council.
Surr, C.A., Smith, S.J., Crossland, J. and Robins, J., 2016. Impact of a person-centred dementia care training programme on hospital staff attitudes, role efficacy and perceptions of caring for people with dementia: A repeated measures study. International journal of nursing studies , 53 , pp.144-151.
List Of Biology Assignment Services Provided By BestAssignmentExperts.Com
No need to pay extra.
Turnitin Report
Proofreading and Editing
Consultation with Expert
Live Session 1-on-1
Quality Check
- Let's Proceed
New Special Offer
Get 25% Off
Our services.
- Academic Writing Help
- Marketing Assignment Help
- Computer Assignment Help
- Essay Types
- Case Study Help
- Management Assignment Help
- Academic Assignment Help
- Assignment Help
- Other Services
Enter Your Detail
Word count: 2000, share your reviews.

IN A HURRY?
GET A CALLBACK.
Adverse childhood experiences and risk of late-life dementia: a systematic review and meta-analysis
- Open access
- Published: 08 May 2024
Cite this article
You have full access to this open access article

- Moaz Elsayed Abouelmagd ORCID: orcid.org/0000-0002-0511-2429 1 ,
- Maickel AbdelMeseh ORCID: orcid.org/0000-0002-4703-4203 2 na1 ,
- Amr Elrosasy ORCID: orcid.org/0000-0002-5592-3908 1 ,
- Hatem Abdelmoneim Eldeeb ORCID: orcid.org/0000-0001-6270-3180 3 &
- Yehia Nabil ORCID: orcid.org/0000-0002-1349-2978 4
335 Accesses
1 Altmetric
Explore all metrics
Adverse childhood experiences (ACEs) refer to distressing events before age 18 that can lead to potential mental and physical health consequences. This systematic review and meta-analysis aimed to examine the association between ACEs and the risk of dementia in elderly adults who experienced ACEs during childhood, addressing the existing inconsistencies and methodological variations.
A comprehensive search strategy was employed across key databases (PubMed, Web of Science, Scopus, and Embase) to identify relevant articles. Our primary outcome was ACEs-dementia risk, and our secondary outcome was mild cognitive impairment risk. A quality assessment was conducted using the Newcastle–Ottawa Quality Assessment Scale and GRADE. A random-effects model was utilized to calculate pooled odds ratios (ORs) and 95% confidence intervals (CIs). Subgroup analyses were performed to explore potential sources of heterogeneity and assess the reliability of the results.
Out of 1,376 screened papers, nine studies were included. The studies consisted of two case-control, one prospective cohort, and six retrospective cohort studies conducted in the UK, France, USA, China, and Spain. Five studies were of good methodological quality according to the NOS. according to the GRADE, all outcomes were classified as very low or low quality of evidence. A significant association was observed between ACEs and dementia risk (OR = 1.35; 95% CI 1.20, 1.52; P = 0.00001) and mild cognitive impairment risk (OR = 1.28; 95% CI 0.63, 2.62; P = 0.49). A meta-analysis by type of adversity revealed significant results for the maltreatment subgroup(OR = 1.30; 95% CI 0.07-1.58; P = 0.007; I² = 0%). Subgroup analysis based on the dementia definition revealed no between-subgroup difference ( P = 0.71) between tool-based and register/criteria-based subgroups. No possibility of Publication bias was observed upon inspection of the funnel plot.
Adverse childhood experiences may be associated with an increased risk of dementia. However, caution is warranted in interpreting these results due to the limited number of studies. Larger high-quality studies investigating the association between ACEs and dementia risk are needed to confirm the reliability of our results.
Similar content being viewed by others
Traumatic life events and risk for dementia: a systematic review and meta-analysis
The association between adverse childhood experiences and common mental disorders and suicidality: an umbrella review of systematic reviews and meta-analyses

Evidence for Revising the Adverse Childhood Experiences Screening Tool: a Scoping Review
Avoid common mistakes on your manuscript.
Introduction
Adverse childhood experiences (ACEs) encompass a range of stressful and traumatic events that have significant implications for the health of adolescents and adults. Globally, approximately one billion children aged between two and seventeen years are estimated to have experienced such violence at least once, with rates of 58% in North America and 42% in Europe [ 1 , 2 ]. These experiences include various forms of abuse (physical and emotional), neglect (physical and emotional), household dysfunction (such as substance misuse, incarceration, chronic depression or mental illness, domestic violence, and disrupted family structure), and exposure to bullying and community violence [ 3 ].
Dementia, a neurodegenerative disease characterized by cognitive decline, represents a major global health concern. In 2015 alone, 47 million individuals were affected, with projections indicating that this number will triple by 2050 [ 4 ]. Dementia has been associated with structural and functional alterations in brain regions involved in cognition, including the hippocampus and prefrontal cortex, the same areas affected by childhood stress. These findings suggest that early life adversities may serve as risk factors for the development of dementia and cognitive impairment later in life [ 5 , 6 ].
Stress and trauma have been linked to an increased risk of developing dementia. A recent meta-analysis (MA) revealed that the risk of dementia in individuals with posttraumatic stress disorder is 1.61–1.99 times greater than the risk in people without this disorder [ 7 ]. Childhood represents a crucial period in human development during which neurological connections are established. Any events occurring during this time can have long-lasting effects on health outcomes. A recent study has shown that ACEs are linked to an increased need for specialized healthcare, such as prescription medication, special therapies, and additional support services [ 8 ].
Although the exact connection between psychological trauma and dementia is not yet fully understood, proposed mechanisms suggest that neurobiological activity may be altered, stress-related pathways may be affected, cognitive stimulation may be reduced, and shared genetic vulnerabilities may play a role [ 7 ]. Furthermore, ACEs may impact dementia risk by influencing other associated risk factors. A recent study revealed that ACEs were positively correlated with increased dementia risk factors, including lower educational attainment, limited social contact, smoking, and clinical depression [ 9 ].
While previous systematic reviews have provided valuable qualitative insights into the relationship between ACEs and cognitive functions and Alzheimer’s disease in late life [ 10 , 11 ], there is currently a lack of MA studies specifically examining the association between ACEs and the risk of developing dementia. Our systematic review and meta-analysis aims to fill this gap and provide a more comprehensive understanding of how ACEs impact the likelihood of developing dementia in late life.
In this study, we followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and the Cochrane Handbook of Systematic Review and Meta-analysis. We registered the detailed protocol of this MA on open science framework (OSF) with the following DOI: https://doi.org/10.17605/OSF.IO/6EBDZ .
Search strategy
A comprehensive search was conducted across major electronic databases (PubMed, Web of Science, Scopus, and Embase) for relevant keywords from conception through the 15th of December 2023.
For example, the PubMed search strategy used was as follows: ((childhood OR Child OR children OR “early life”) AND (Maltreatment OR adversity OR violence OR Trauma OR “Adverse childhood” OR neglect OR ACEs OR abuse OR stress) AND (Alzheimer OR dementia OR cognitive decline OR MCI) AND (observational OR COHORT OR CASE-CONTROL OR “case-control” OR RCT OR TRIAL OR register). Additionally, the references of the included studies were screened for potential articles to include.
Study selection
To select the most relevant studies for this research, the titles and abstracts of the retrieved records from the search strategy were imported into Rayyan [ 12 ], an online platform for screening studies in systematic reviews. Duplicate records were eliminated, and two authors independently screened all abstracts. Conflicts were resolved by the first author. Subsequently, eligible studies underwent a full-text screening phase based on predefined inclusion and exclusion criteria.
Inclusion criteria
English-language studies published in peer-reviewed journals.
Participants experienced adverse childhood experiences (ACEs) before the age of 18, including violence, abuse, neglect, witnessing violence in the home, family member’s death, living in an unstable house with substance use/mentally ill/incarcerated parents, traumatic experiences, etc.
Participants aged > 60 at follow-up.
Dementia or cognitive impairment was defined using validated diagnostic criteria, tools, or medical records.
The studies included sufficient data, such as odds ratios (ORs), risk ratios (RRs), hazard ratios (HRs), or data for calculation.
Longitudinal study design (case-control or cohort).
A healthy control group was included.
Exclusion criteria
Studies that focused on head trauma, childhood diseases, or physical injury that may lead to dementia or mild cognitive impairment (MCI).
Studies on high-risk medical populations (e.g., diabetes, hypertension).
The full texts of the studies were unavailable after contacting the corresponding author.
Data extraction
Two authors extracted relevant data from the included studies into a data extraction Google Sheet. The extracted data for each study included the study ID, study design, country, baseline characteristics, sociodemographic characteristics, measurement tools for cognition and early-life adversity, number of participants, length of follow-up, adjustment factors, outcomes, and key findings.
Methodological quality assessment
We used the Newcastle–Ottawa Quality Assessment Scale (NOS) to assess the quality of the studies. The NOS consists of eight questions. This scale evaluates three parameters of quality (selection, comparability, and outcome) and includes specific items that vary slightly for case-control and cohort studies. Each item on the scale can receive a maximum score of 1 point, except for comparability, which can be adjusted to the specific topic of interest, and a maximum score of 2 points, with the highest overall score being 9 [ 13 ]. To convert the NOS to fit the standards set by the Agency for Healthcare Research and Quality—good, fair, and poor—the following thresholds are applied [ 14 ]:
Good quality: 3 or 4 stars in the selection domain 1 or 2 stars in the comparability domain AND 2 or 3 stars in the outcome/exposure domain.
Fair quality: 2 stars in the selection domain 1 or 2 stars in the comparability domain AND 2 or 3 stars in the outcome/exposure domain.
Poor quality: 0 or 1 star in the selection domain; 0 stars in the comparability domain; and 0 or 1 star in the outcome/exposure domain.
Additionally, the GRADE approach was applied to rate the overall quality of evidence and strength of recommendations for each outcome of interest. This approach considers factors such as risk of bias, inconsistency, indirectness, imprecision, and publication bias. The confidence in the estimates is categorized as high, moderate, low, or very low [ 15 ].
Statistical analysis
The primary outcome of interest was the odds of dementia in ACEs-exposed elderly individuals with 2 or more ACEs, and the secondary outcome was the odds of MCI in ACEs-exposed elderly individuals. The effect sizes of the included studies were expressed as odds ratios (ORs), risk ratios (RRs), or hazard ratios (HRs). If multiple outcomes were reported, the outcomes with the best diagnostic criteria, highest number of cases, and best adjustment were chosen. An OR of 1 indicates no association, an OR between 0 and 1 indicates a negative relationship and an OR greater than 1 indicates a positive relationship, indicating that early-life adversity is associated with a greater risk of dementia/MCI.
Heterogeneity between studies was assessed visually using forest plots and the I² test. I² values less than 50% indicated insignificant heterogeneity, while values ≥ 50% indicated substantial heterogeneity. A random-effects model (DerSimonian‒Laird) was used to calculate the pooled OR and 95% confidence interval (CI) to account for within- and between-study heterogeneity originating from different effect sizes and/or ACE measurement tools. Sensitivity and subgroup analyses were performed to investigate potential sources of heterogeneity and to test the stability of the results. Subgroup analyses were also conducted for primary outcomes based on the type of adversity, definition of dementia, and quality of evidence if there were at least 2 studies for each subgroup.
Publication Bias
Funnel plots of the primary MA model were visually examined to assess potential publication bias. The uneven distribution of studies around the pooled effect estimate suggested the possibility of publication bias. Additionally, Egger’s test was used.
Search results and characteristics of the included studies
We retrieved 1376 papers through a literature search; 327 of these were duplicates, and we ultimately included nine studies [ 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ] that presented data from 283,108 participants in the MA (see Fig. 1 ; Table 1 ). We included two case-control studies [ 21 , 23 ], one prospective cohort study [ 19 ], and six retrospective cohort studies [ 16 , 17 , 18 , 20 , 22 , 24 ]. The studies included data from various countries, such as the UK, France, the USA, China, and Spain. The detailed characteristics of the included studies are shown in (Table 1 . )
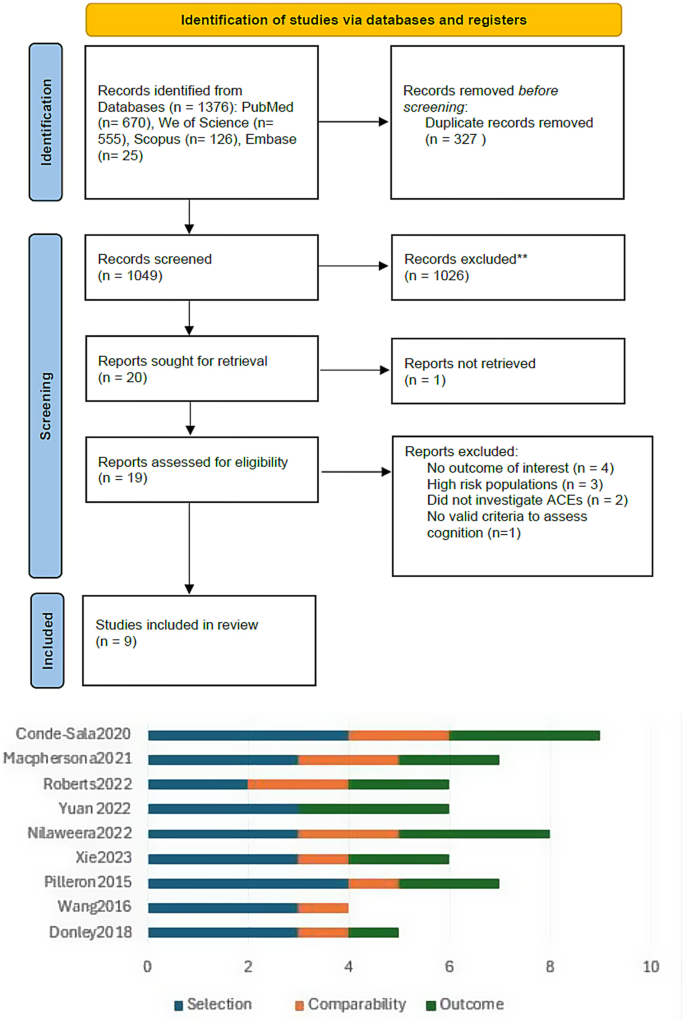
upward is the PRISMA flow diagram showing the details of the study selection process. Downward is the quality assessment summary of the included studies according to the Newcastle-Ottawa Quality Assessment Scale
Quality assessment of the included studies
Among the cohort and case-control studies, six were classified as having good or fair methodological quality [ 16 , 17 , 19 , 20 , 21 , 24 ] (see Fig. 1 ; Table 1 ). These studies exhibited strong adherence to methodological principles and minimal risk of bias, while the remaining studies were categorized as poor quality [ 18 , 22 , 23 ]. According to the GRADE system, all the included outcomes yielded very low-quality evidence. The details and explanations are clarified in Table 2 .
Risk of dementia and MCI
Seven studies were included in the dementia risk analysis [ 16 , 17 , 18 , 19 , 20 , 22 , 24 ], and 2 studies were included in the MCI analysis [ 23 , 24 ]. All the studies examined ACEs as a cumulative score of 2 or more ACEs through questionnaires containing several domains. However, one study was excluded from this analysis because it measured only 1 adverse event—parents’ death—to avoid heterogeneity [ 21 ]. The definition of dementia or MCI was based on screening tools [diagnosis by a neurologist or registers using International Classification-of-diseases Version 8 (ICD-8)]. The results showed that exposure to ACEs was associated with dementia risk (OR = 1.38; 95% CI 1.25–1.52); P < 0.00001), with no significant heterogeneity (I2 = 0%). However, there was no significant difference in the risk of developing MCI (OR = 1.28; 95% CI 0.63–2.62); P = 0.49), and there was moderate heterogeneity (I² = 51%, P = 0.15) (Fig. 2 ) .
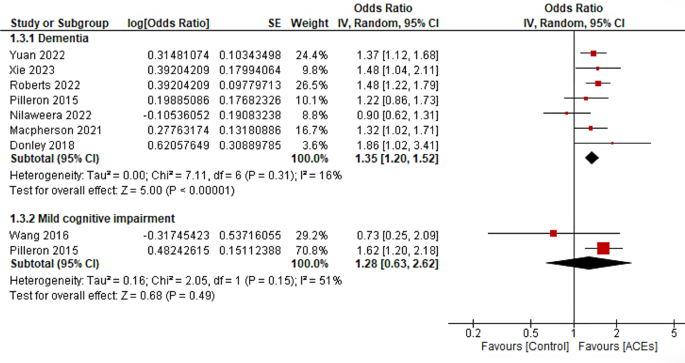
Forrest plot of the association between ACEs and risk of Dementia and Mild cognitive impairment
Publication bias
Inspection of the funnel plot of dementia risk outcome didn’t reveal significant asymmetry and the results of Egger’s test were not significant ( P = 0.473). (Fig. 3 )
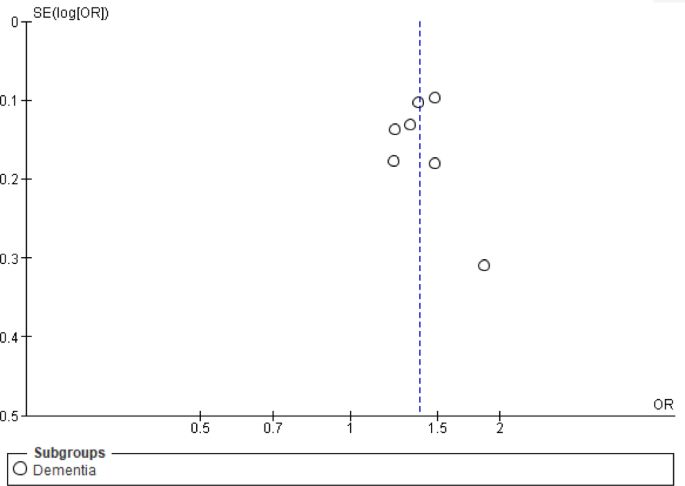
Publication bias of the association between ACEs and dementia risk
Risk of dementia based on type of adversity
Six studies reported specific types of childhood adversity, especially childhood maltreatment and the death of a parent. Childhood maltreatment showed a slight significant association with the risk of dementia (OR = 1.30; 95% CI 0.07-1.58; P = 0.007; I² = 0%), while the death of a parent showed no significant association (OR = 1.15; 95% CI 0.76–1.73; P = 0.002; I² = 84%). The test of subgroup differences was not significant (0.58). Heterogeneity was resolved in the second subgroup after excluding Conde-Sala 2020 in the second subgroup [ 23 ] (supplementary material Fig. 1 , Fig. 2 ).
Risk of dementia based on the definition of dementia
Seven studies were included in the subgroup analysis based on the definition of dementia. Three studies defined dementia through registries and diagnostic criteria, while 4 studies defined dementia based on cutoff points of screening tools. The tool-based subgroup exhibited a significant association between ACEs and dementia (OR = 1.41; 95% CI 1.25–1.60; P < 0.00001; I² = 0%), but the register-based subgroup did not exhibit a significant difference (OR = 1.30; 95% CI 0.86–1.97; P = 0.49; I² = 42%). No significant heterogeneity was found in either subgroup analysis, and the test for subgroup differences was not significant (P = 0.71). (supplementary material Fig. 3 )
Risk of dementia based on the quality of the included studies
Seven studies were included in the subgroup analysis based on the quality of the studies: 5 were of good or fair quality, and 2 were of low quality. The associations between ACEs and the risk of dementia were significant in both the good/fair subgroup (OR = 1.31; 95% CI 1.11–1.53; P < 0.0010; I² = 33%) and the low subgroup (OR = 1.41; 95% CI 1.17–1.71; P = 0.0004; I² = 0%). The test of subgroup differences was not significant (P = 0.74), and no significant heterogeneity was found within the subgroups (supplementary material Fig. 4 ).
Recent research predicts that the prevention of ACEs is associated with depression, stroke, coronary heart disease, diabetes, and obesity [ 25 , 26 ]. Our MA aimed to investigate the association between ACEs and the risk of developing dementia and MCI in adulthood. We found a significant relationship between exposure to ACEs and an increased risk of dementia. Subgroup analyses were also conducted to explore specific adverse events, diagnostic criteria, and study quality.
In terms of specific childhood adversities, our findings showed that childhood maltreatment was slightly significantly associated with increased dementia risk, while the death of a parent was not. However, these results are limited by the low number of included studies in each of these analyses and should be interpreted with caution. Regarding diagnostic criteria, individuals diagnosed based on tools showed a significant association, while those diagnosed based on registers did not. When considering study quality, both acceptable and low-quality studies demonstrated a significant association with the risk of dementia. Although most of the studies in our analysis adjusted their results for more than 3 factors, there may be other confounding factors that drive the relationship between traumatic experiences and dementia, which were not adequately accounted for in the analyzed studies.
Three studies [ 16 , 17 , 19 ] in our primary analysis of dementia reported outcomes as cumulative ACEs score > 3 experiences. While three of them reported significant results, Nilaweera et al. [ 17 ]. did not. This study was of good quality and used the largest questionnaire of 25 items for adversity. The absence of findings is mostly due to selection bias, as authors included only participants older than 65 years at baseline who were followed up for 14 years. This may have induced selection bias, as participants who had dementia were excluded during the selection stage.
Pilleron et al. [ 24 ]. also did not find significant results for dementia but did find significant results for MCI. This may be attributed to the limited number and types of adversities asked about in their questionnaire. This questionnaire included five life events before the age of 16 (death of a parent, divorce of parents, growing up with one parent, different guardians, and extreme poverty); these five life events are substantially different from the other measurement tools used in our primary MA, where most studies included questions about emotional, physical and/or sexual abuse.
Yuan et al . reported an independent relationship between ‘Child abuse’ and a higher risk of cognitive impairment in elderly Chinese people, which our pooled analysis confirmed. Conde-Sala et al . reported an increased risk of dementia associated with early parental death. However, our MA did not find a significant relationship between maltreatment or parental death and an increasing risk of dementia.
Various methods were employed to measure ACEs in the studies included in our analysis. Some studies utilized structured questionnaires to assess cumulative ACEs, while others relied on self-reports focusing on specific ACEs. Several studies have used validated questionnaires to assess several ACEs. One study [ 20 ] used the Childhood Trauma Screener (CTS) [ 27 ], two studies [ 17 , 23 ] used modified versions of the Childhood Trauma Questionnaire (CTQ) [ 28 , 29 ], and two studies [ 18 , 19 ] used the Adverse Childhood Experiences International Questionnaire (ACE-IQ) [ 30 ] or a modified version of it. However, some studies have used simple questions to assess several ACEs [ 16 , 22 , 24 ] or a record to define the death of parents in childhood [ 21 ].
Cumulative scores ACE methods such as ACE-IQ and CTQ, involve summing the number of ACEs reported by each individual. Although these cumulative scores do not capture the severity of the experiences, they are widely accepted and favored in ACE research due to their greater predictive power compared to single-item scores [ 31 , 32 ]. The ACE-IQ is currently the standard tool for measuring ACEs in clinical research [ 30 ]. Accordingly, our primary analysis included studies using cumulative or composite scores, and a secondary analysis was conducted based on specific ACEs, which were reported to be significant only for child maltreatment. It is worth noting that the number and categories of ACE items varied across studies, which may be accounted for by the ACEs dose-response effect [ 33 , 34 ].
The majority of the evidence in this study comes from retrospective studies, which should be considered when interpreting the results. Retrospective studies have reported discrepancies when compared to prospective studies on ACEs [ 35 ]. In our included studies, ACE data were mostly obtained through subjective measures, such as self-reports. It is crucial to acknowledge that subjective measures of ACEs may introduce recall bias, as individuals may have difficulties remembering or may choose not to report past ACEs. Previous research has indicated a moderate correlation between subjective measures and objective measures, such as records or registries [ 36 ]. Nonetheless, this highlights the significance of the subjective nature of each child’s experience with traumatic events and its potential long-term effects.
Previous studies highlighted the possible association between ACEs and late-life cognition. Corney et al. [ 10 ]. suggested a link between ACEs and Alzheimer’s disease, although their study included only two studies and focused solely on Alzheimer’s disease. Patel et al. [ 11 ] conducted a systematic review of cross-sectional and cohort studies on the association between ACEs and late-life cognitive impairment. While their qualitative synthesis provided valuable insights, they did not explore the association between ACEs and dementia risk. In this study, we aimed to build upon previous research by conducting a quantitative synthesis with a rigorous methodology, focusing on the association between ACEs and dementia risk. Our analysis included cohort and case-control studies, incorporating six studies that were not included in the latest systematic review [ 11 ].
Strengths and limitations
Our study represents the first systematic review and MA examining the association between ACEs and the risk of late-life dementia. We adhered to the PRISMA guidelines for systematic reviews, ensuring a comprehensive and rigorous approach. The strengths of our study include the use of a robust methodology: we implemented strict inclusion and exclusion criteria to focus specifically on ACEs and dementia risk. We utilized the adjusted Newcastle–Ottawa Scale and GRADE criteria to assess the quality of the evidence. However, it is important to acknowledge the potential for human bias at any stage of the study.
This MA has certain limitations that should be acknowledged. First, the retrospective observational study designs utilized in the included studies did not establish causal relationships but rather indicated associations. However, given the nature of our study, this design was the most practical and suitable approach. Second, the number of included studies and the number of events may limit the generalizability of our results. Third, the incorporation of different measurement tools for ACEs and dementia may have introduced heterogeneity. However, we addressed this by employing a random-effects model in our MA and specifically included studies that utilized composite scores for ACEs in our primary analysis. Additionally, we conducted a subgroup analysis to explore different potential sources of heterogeneity. Fourth, the quality of evidence assessed using the GRADE approach was determined to be very low for all outcomes, underscoring the importance of additional high-quality studies to strengthen the overall evidence base. Fifth, the grey literature was not thoroughly explored which may increase the possibility of publication bias. Last, it is worth noting that our study included only publications in English, which may have resulted in the exclusion of relevant studies published in other languages.
Recommendations for future studies
Future studies should consider (1) conducting larger high-quality controlled case‒controls or retrospective cohort studies; (2) using validated cumulative ACEs score measurement tools such as the Adverse Childhood Experiences International Questionnaire and reporting data on specific adversities whenever applicable; (3) incorporating both subjective and objective ACE measurements to overcome reporting bias; (4) preferring the use of diagnostic criteria for dementia over screening tools for identifying dementia cases; and (5) including diverse representative populations from different races, education, and socioeconomic statuses.
In conclusion, the findings of this systematic review and meta-analysis suggest that ACEs may be associated with an increased risk of dementia in elderly adults. However, it is important to exercise caution when interpreting these results due to the limited number of studies and the very low quality of evidence provided by the grading system. These findings underscore the importance of recognizing early-life adversities in assessing dementia risk. However, additional high-quality longitudinal studies are needed to support our findings. ACEs have already been linked to many negative health and developmental outcomes. Understanding the association between ACEs and dementia risk has crucial clinical implications. Healthcare professionals should be attentive to children with a history of ACEs and should implement early interventions and support systems to mitigate the long-term consequences for cognitive health. Tailored strategies for individuals with specific adversities or diagnosed through certain criteria may enhance preventive measures.
To our knowledge, this is the first attempt to quantify and analyze studies on the association between ACEs and dementia risk.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. Guarantor: Moaz Elsayed
Abbreviations
Adverse Childhood experiences
Mild Cognitive Impairment
Hazard ratio
Newcastle-Ottawa Quality Assessment Scale
confidence interval
Meta-Analysis
Stressful Life experiences
International Classification of Diseases
The Mini-Mental State Examination
Montreal Cognitive Assessment
Community Screening Interview for Dementia
Hillis S, Mercy J, Amobi A, Kress H (2016) Global prevalence of past-year violence against children: a systematic review and minimum estimates. Pediatrics 137(3):e20154079. https://doi.org/10.1542/peds.2015-4079
Article PubMed Google Scholar
Bellis MA, Hughes K, Ford K, Rodriguez GR, Sethi D, Passmore J (2019) Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health 4:e517–e28
Article PubMed PubMed Central Google Scholar
Lorenc T, Lester S, Sutcliffe K et al (2020) Interventions to support people exposed to adverse childhood experiences: a systematic review of systematic reviews. BMC Public Health 20:657. https://doi.org/10.1186/s12889-020-08789-0
Alzheimer’s Disease International (2024) World Alzheimer Report 2015: the Global Impact of Dementia. An Analyses of Prevalence, incidence, Cost and Trends. https://www.alz.co.uk/research/WorldAlzheimerReport2015.pdf . Accessed February 20
Lupien SJ, McEwen BS, Gunnar MR, Heim C (2009) Effects of stress throughout the lifespan on the brain, behavior, and cognition. Nat Rev Neurosci 10(6):434–445
Article CAS PubMed Google Scholar
Richards M, Wadsworth ME (2004) Long-term effects of early adversity on cognitive function. Arch Dis Child 89(10):922–927
Article CAS PubMed PubMed Central Google Scholar
Günak MM, Billings J, Carratu E, Marchant NL, Favarato G, Orgeta V (2020) Post-traumatic stress disorder as a risk factor for dementia: systematic review and meta-analysis. Br J Psychiatry: J Mental Sci 217(5):600–608. https://doi.org/10.1192/bjp.2020.150
Article Google Scholar
Webster EM (2022) The impact of adverse childhood experiences on health and development in young children. Global Pediatr Health 9:1–11. https://doi.org/10.1177/2333794X221078708
Widom CS, Do HH, Lynch KS, Manly JJ (2023) Childhood maltreatment and dementia risk factors in midlife: a prospective investigation. Curr Alzheimer Res Published Online Dec 28. https://doi.org/10.2174/0115672050281539231222071355
Corney KB, West EC, Quirk SE, Pasco JA, Stuart AL, Manavi BA, Kavanagh BE, Williams LJ (2022) The relationship between adverse childhood experiences and Alzheimer’s Disease: a systematic review. Front Aging Neurosci 14:831378. https://doi.org/10.3389/fnagi.2022.831378 PMID: 35601624; PMCID: PMC9115103
Patel P, Oremus M (2023) The Association between adverse childhood experiences and late-life cognition: a systematic review of cross-sectional and case-control studies. Gerontologist 63(6):1087–1103. https://doi.org/10.1093/geront/gnac041
Mourad Ouzzani H, Hammady Z, Fedorowicz, Ahmed Elmagarmid (2016) Rayyan — a web and mobile app for systematic reviews. Syst Reviews 5:210. https://doi.org/10.1186/s13643-016-0384-4
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2012) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Retrieved from http://wwwohrica/programs/clinicalepidemi
Viswanathan M, Ansari MT, Berkman ND, Chang S, Hartling L, McPheeters LM (2012) Assessing the risk of bias of individual studies in systematic reviews of health care interventions. Agency for Healthcare Research and Quality Methods Guide for Comparative Effectiveness Reviews. March 2012. AHRQ Publication No. 12-EHC047-EF. Retrieved from https://effectivehealthcare.ahrq.gov/
Schünemann HJ, Higgins JPT, Vist GE, Glasziou P, Akl EA, Skoetz N, Guyatt GH (2022) Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, www.training.cochrane.org/handbook
Xie Z, Li M, Sun H et al (2023) Childhood, adulthood, and cumulative traumatic experiences experienced from childhood to adulthood and dementia risk: a population-based cohort study. J Public Health (Berl). https://doi.org/10.1007/s10389-023-02140-8
Nilaweera D, Freak-Poli R, Gurvich C, Ritchie K, Chaudieu I, Ancelin ML, Ryan J (2022) The association between adverse childhood experiences and later-life cognitive function and dementia risk. J Affect Disord 304:128–132. https://doi.org/10.1016/j.jad.2022.02.062
Yuan M, Qin F, Xu C, Fang Y (2022) Heterogeneous adverse childhood experiences and cognitive function in an elderly Chinese population: a cohort study. BMJ open 12(6):e060477. https://doi.org/10.1136/bmjopen-2021-060477
Roberts AL, Zafonte R, Chibnik LB, Baggish A, Taylor H, Baker J, Whittington AJ, Weisskopf MG (2022) Association of Adverse Childhood Experiences with Poor Neuropsychiatric Health and Dementia among former Professional US Football players. JAMA Netw open 5(3):e223299. https://doi.org/10.1001/jamanetworkopen.2022.3299
Macpherson JM, Gray SR, Ip P, McCallum M, Hanlon P, Welsh P, Chan KL, Mair FS, Celis-Morales C, Minnis H, Pell JP, Ho FK (2021) Child maltreatment and incident mental disorders in middle and older ages: a retrospective UK Biobank cohort study. Lancet Reg Health Eur 11:100224. https://doi.org/10.1016/j.lanepe.2021.100224 PMID: 34917999; PMCID: PMC8642708
Conde-Sala JL, Garre-Olmo J (2020) Early parental death and psychosocial risk factors for dementia: a case-control study in Europe. Int J Geriatr Psychiatry 35(9):1051–1059. https://doi.org/10.1002/gps.5328
Donley GAR, Lönnroos E, Tuomainen TP, Kauhanen J (2018) Association of childhood stress with late-life dementia and Alzheimer’s disease: the KIHD study. Eur J Pub Health 28(6):1069–1073. https://doi.org/10.1093/eurpub/cky134
Wang L, Yang L, Yu L, Song M, Zhao X, Gao Y, Han K, An C, Xu S, Wang X (2016) Childhood physical neglect promotes development of mild cognitive impairment in old age - a case-control study. Psychiatry Res 242:13–18. https://doi.org/10.1016/j.psychres.2016.04.090
Pilleron S, Guerchet M, Ndamba-Bandzouzi B, Mbelesso P, Dartigues JF, Preux PM, Clément JP (2015) Association between Stressful Life experiences and Cognitive disorders in Central Africa: results from the EPIDEMCA Program. Neuroepidemiology 44(2):99–107. https://doi.org/10.1159/000375462
Merrick MT, Ford DC, Ports KA et al (2019) Vital signs: estimated proportion of adult health problems attributable to adverse childhood experiences and implications for Prevention – 25 states, 2015–2017. MMWR Morb Mortal Wkly Rep 68(44):999–1005 Published 2019 Nov 8. https://doi.org/10.15585/mmwr.mm6844e1
Trivedi GY, Pillai N, Trivedi RG (2021) Adverse Childhood Experiences & Mental Health - the urgent need for public health intervention in India. J Prev Med Hyg 62(3):E728–E735. https://doi.org/10.15167/2421-4248/jpmh2021.62.3.1785 PMID: 34909501; PMCID: PMC8639107
Glaesmer H, Schulz A, Häuser W, Freyberger HJ, Brähler E, Grabe HJ (2013) Der Childhood Trauma Screener (CTS) - Entwicklung und Validierung von Schwellenwerten zur Klassifikation [The childhood trauma screener (CTS) - development and validation of cut-off-scores for classificatory diagnostics] [published correction appears in Psychiatr Prax. ;40(4):e1]. Psychiatr Prax. 2013;40(4):220–226. https://doi.org/10.1055/s-0033-1343116
Bernstein DP, Stein JA, Newcomb MD et al (2003) Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl 27(2):169–190. https://doi.org/10.1016/s0145-2134(02)00541-0
Liebschutz JM, Buchanan-Howland K, Chen CA et al (2018) Childhood trauma questionnaire (CTQ) correlations with prospective violence assessment in a longitudinal cohort. Psychol Assess 30(6):841–845. https://doi.org/10.1037/pas0000549
Emily M, Zarse MR, Neff R, Yoder L, Hulvershorn, Joanna E, Chambers & R. Andrew Chambers | Udo Schumacher (reviewing editor) (2019) the adverse childhood experiences questionnaire: two decades of research on childhood trauma as a primary cause of adult mental illness, addiction, and medical diseases. Cogent Med, 6:1, https://doi.org/10.1080/2331205X.2019.1581447
Hardt J, Rutter M (2004) Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry 45(2):260–273. https://doi.org/10.1111/j.1469-7610.2004.00218.x
Webster EM (2022) The impact of adverse childhood experiences on Health and Development in Young Children. Global Pediatr Health 9. https://doi.org/10.1177/2333794X221078708
Merrick MT, Ports KA, Ford DC, Afifi TO, Gershoff ET, Grogan-Kaylor A (2017) Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse Negl 69:10–19. https://doi.org/10.1016/j.chiabu.2017.03.016
Tan M, Mao P (2023) Type and dose-response effect of adverse childhood experiences in predicting depression: a systematic review and meta-analysis. Child Abuse Negl 139:106091. https://doi.org/10.1016/j.chiabu.2023.106091
Baldwin JR, Reuben A, Newbury JB, Danese A (2019) Agreement between prospective and retrospective measures of Childhood Maltreatment: a systematic review and Meta-analysis. JAMA Psychiatry 76(6):584–593. https://doi.org/10.1001/jamapsychiatry.2019.0097
Francis ER, Tsaligopoulou A, Stock SE, Pingault JB, Baldwin JR (2023) Subjective and objective experiences of childhood adversity: a meta-analysis of their agreement and relationships with psychopathology. J Child Psychol Psychiatry 64(8):1185–1199. https://doi.org/10.1111/jcpp.13803
Download references
Acknowledgements
No acknowledgments.
There was no funding for this paper.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Amr Elrosasy and Hatem Abdelmoneim Eldeeb contributed equally to this work.
Authors and Affiliations
Faculty of Medicine, Cairo University, Cairo, Egypt
Moaz Elsayed Abouelmagd & Amr Elrosasy
Faculty of Medicine, Alexandria University, Alexandria, Egypt
Maickel AbdelMeseh
Faculty of Medicine, Alazhar University, Cairo, Egypt
Hatem Abdelmoneim Eldeeb
Faculty of Medicine, Zagazig University, Zagazig, Egypt
Yehia Nabil
You can also search for this author in PubMed Google Scholar
Contributions
Study Conceptualization and design: Moaz Elsayed. Protocol design: Moaz Elsayed, Amr Elrosasy. Abstract screening on Rayyan, Full-text screening, and study selection: Maickel AbdelMeseh, Yehia Nabil, Moaz Elsayed. Data extraction, and Quality assessment: All authors. Data analysis: Amr Elrosasy. Writing: Moaz Elsayed , Maickel AbdelMeseh, , Amr Elrosasy, Hatem Abdelmoneim Eldeeb. Figures and Tables: Moaz Elsayed, Hatem Abdelmoneim Eldeeb, Yehia Nabil, . Proofreading and Revision: Moaz Elsayed, Maickel AbdelMeseh, , Amr Elrosasy.
Corresponding author
Correspondence to Moaz Elsayed Abouelmagd .
Ethics declarations
Informed consent, ethical approval.
and Ethical approval were not sought for this paper because it included no direct interaction with human participants.
Conflict of interest
The authors declare that they have no conflicts of interest.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Abouelmagd, M.E., AbdelMeseh, M., Elrosasy, A. et al. Adverse childhood experiences and risk of late-life dementia: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol (2024). https://doi.org/10.1007/s00127-024-02676-4
Download citation
Received : 10 January 2024
Accepted : 17 April 2024
Published : 08 May 2024
DOI : https://doi.org/10.1007/s00127-024-02676-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adverse childhood experiences
- Cognitive impairment
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
CASE PRESENTATION. A 55-year-old right-handed woman presented with a 3-year history of cognitive changes. Early symptoms included mild forgetfulness—for example, forgetting where she left her purse or failing to remember to retrieve a take-out order her family placed—and word-finding difficulties.
Early onset Alzheimer disease (EOAD) is a neurodegenerative dementing disorder that is relatively rare (<1% of all Alzheimer cases). Various genetic mutations of the presenilin 1 (PSEN1) and presenilin 2 (PSEN2) as well as the amyloid precursor protein (APP) gene have been implicated.Mutations of PSEN1 and PSEN2 alter γ-secretase enzyme that cleaves APP resulting in increase in the relative ...
These three case studies help you to consider different situations that people with dementia face. They are: Raj, a 52 year old with a job and family, who has early onset dementia. Bob and Edith, an older married couple who both have dementia and are struggling to cope, along with their family. Joan, an older woman, who lives alone and has just ...
One study adopted 18F-florbetaben PET imaging in Down syndrome patients, suggesting potential role of amyloid imaging in identifying population at risk of dementia. 17 Similar study was conducted on patients with Down syndrome, but with 18F-florbetapir tracer. 18 An attempt to differentiate Down Syndrome pathology from AD has also been made ...
Rasin and Kautz (2007) carried out a study that focused on caregivers in assisted living facilities. The National Centre for Assisted Living (NCAL) estimates that "42% to 50% of residents in assisted living facilities have dementia and 34% of them exhibit behavioural symptoms of dementia at least once a week.".
Case Studies in Dementia - March 2021. A 62-year-old right-handed lady presented at initial consultation with an 18 months history of slowly progressive short-term memory problems and personality change.
Case Study. Download the Full Case Study for Bob and Edith PDF file (64KB) Vignette - Bob. Download the Vignette for Bob PDF file (56KB) Name: Robert (Bob) Woodgate. ... Edith was diagnosed with vascular dementia a few months ago when Gary became concerned about her mixing up household tasks, for example putting shopping in the oven. ...
Part 1: Mavis. Mavis is an 84-year old lady, referred to you in the memory clinic for assessment of memory impairment. She attends in the company of her son and daughter-in-law. On the pre-clinic questionnaire her son has reported a severe deterioration in all aspects of her cognition over the past 12 months.
Psychiatry and Clinical Psychology , Neurology and Clinical Neuroscience , Medicine , Psychiatry. Series: Case Studies in Neurology. 68.99 (GBP) Digital access for individuals. (PDF download and/or read online) Add to cart. Export citation. Buy a print copy.
Case Study. Download the Full Case Study for Joan PDF file (58KB) Vignette. Download the Vignette for Joan PDF file (49KB) Name: Joan O'Leary. Gender: Female. ... She has been diagnosed with moderate dementia with Lewy Bodies. The GP phoned social services and you go out to do an assessment. Ecogram. Download the Ecogram for Joan PDF file ...
Social work report: Background. Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke ...
For carers of people in hospital, by contrast, it was often the case that the person with dementia had been admitted in a crisis, but, during his or her stay, was stabilised and assessed and had his or her future care planned (in some cases meaning admission to long-term-care). Again, we can understand why carers might feel that restrictions in ...
Dementia Case Study Essay. After reading the case study about John and Lydia, it appears that the individual's heath is declining. Lydia and John home seems to be showing early signs of dementia, due to their memory declining. According to Broderick and Blewitt (2015) said that "Dementia is a syndrome that affects multiple functional ...
Check out Smart'n, the exclusive platform for nursing students, for more case study types. It offers over 2,500 NCLEX practice questionsand 60+ hours of NGN-NCLEX-style nursing case studies, helping you track progress and become a more confident registered nurse. Start your journey to NCLEX success with Smart'n. Understanding dementia.
The prevalence and study of dementia increased as the lifespan of humans extended. In the late 1800s, with advancements in medicine and the ability to look inside the brain, the medical community realized that diseases could cause this deterioration. The most common dementia was named, in 1910, after Alois Alzheimer, a German psychiatrist.
This paper will discuss a case study of Loretta, a 72-year-old Australian diagnosed with dementia, describing a woman's clinical condition by using ICF terminology and structure and outlining the measures which need to be imposed for providing her with effective interventions and enhancing the professionalism of the involved exercise physician.
Case Analysis And Problems With Dementia Nursing Essay. Dementia is a progressive and irreversible decline in mental function1. Lewy Body Dementia (DLB) is a form of degenerative dementia characterised by the presence of "Lewy Bodies" which are clumps of alpha-synuclein and ubiquitin protein in neurons2. These are only detectable in post ...
Dementia Case Study Essay. Decent Essays. 950 Words. 4 Pages. Open Document. As of 2010, an estimated 5.1 million Americans were affected by Alzheimer's Dementia and related Dementias (Hebert et al., 2003). Dementia is a syndrome that results in decline of memory and at least one other cognitive ability, significant enough to interfere with ...
Donepezil hydrochloride/Aricept 10 mg once daily at bedtime: is a reversible inhibitor of acetylcholinesterase.They are for the adjunctive treatment of moderate Alzheimer's disease. Like all other medication donepezil has its side effects which are nausea,vomiting,anorexia,diarrhoea,insomnia,dizziness and agitation just to mention a few.
Essay for assignment case study: my patient mrs. diagnosed with dementia has an advance directive of do not resuscitate (dnr). dnr is type of legal order from. ... Dementia case study - Essay for assignment. University: Northern Virginia Community College. Course: Bio ethics (227) 5 Documents. Students shared 5 documents in this course.
A Dementia Case Study Course LRPM Grade 78.00 Author Leonard Kahungu (Author) Year 2018 Pages 11 Catalog Number V428637 ISBN (eBook) 9783668745131 ISBN (Book) 9783668745148 File size 479 KB ... Upload papers. Your term paper / thesis: - Publication as eBook and book - High royalties for the sales - Completely free - with ISBN
Case Study of a Patient Dementia. Introduction. A nurse associate is responsible to provide adequate medical care to the dementia patients so that they get optimal well-being. This essay highlights the case of a dementia patient who is suffering from health issues due to sleep disorders, hallucinations and short-term memory loss. ...
The End- of- Life Decision Making case study presents a problem where a public guardian has been appointed for Ms. Long, and is seeing her for the first time to compose an assessment, and make several determinations. One of those determinations is whether Ms. Long is terminally ill. Upon seeing her, the guardian takes note of the facts.
Out of 1,376 screened papers, nine studies were included. The studies consisted of two case-control, one prospective cohort, and six retrospective cohort studies conducted in the UK, France, USA, China, and Spain. ... Early parental death and psychosocial risk factors for dementia: a case-control study in Europe. Int J Geriatr Psychiatry 35(9 ...
DOI: 10.1016/j.jad.2024.05.031 Corpus ID: 269662129; Association between gabapentin use and risk of dementia in adults with chronic pain: A nested case-control study. @article{Tsai2024AssociationBG, title={Association between gabapentin use and risk of dementia in adults with chronic pain: A nested case-control study.}, author={Sheng-En Tsai and Shun-Fa Yang and Yu-Hsun Wang and Chao-Bin Yeh ...