How to build a better health system: 8 expert essays

We need to focus on keeping people healthy, not just treating them when they're sick Image: REUTERS/Rupak De Chowdhuri

.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Global Future Council on Health and Healthcare
Introduction
By Francesca Colombo , Head, Health Division, Organisation for Economic Co-operation and Development (OECD) and Helen E. Clark , Prime Minister of New Zealand (1999-2008), The Helen Clark Foundation
Our healthy future cannot be achieved without putting the health and wellbeing of populations at the centre of public policy.
Ill health worsens an individual’s economic prospects throughout the lifecycle. For young infants and children, ill health affects their capacity to acumulate human capital; for adults, ill health lowers quality of life and labour market outcomes, and disadvantage compounds over the course of a lifetime.
And, yet, with all the robust evidence available that good health is beneficial to economies and societies, it is striking to see how health systems across the globe struggled to maximise the health of populations even before the COVID-19 pandemic – a crisis that has further exposed the stresses and weaknesses of our health systems. These must be addressed to make populations healthier and more resilient to future shocks.
Each one of us, at least once in our lives, is likely to have been frustrated with care that was inflexible, impersonal and bureaucratic. At the system level, these individual experiences add up to poor safety, poor care coordination and inefficiencies – costing millions of lives and enormous expense to societies.
This state of affairs contributes to slowing down the progress towards achieving the sustainable development goals to which all societies, regardless of their level of economic development, have committed.
Many of the conditions that can make change possible are in place. For example, ample evidence exists that investing in public health and primary prevention delivers significant health and economic dividends. Likewise, digital technology has made many services and products across different sectors safe, fast and seamless. There is no reason why, with the right policies, this should not happen in health systems as well. Think, for example, of the opportunities to bring high quality and specialised care to previously underserved populations. COVID-19 has accelerated the development and use of digital health technologies. There are opportunities to further nurture their use to improve public health and disease surveillance, clinical care, research and innovation.
To encourage reform towards health systems that are more resilient, better centred around what people need and sustainable over time, the Global Future Council on Health and Health Care has developed a series of stories illustrating why change must happen, and why this is eminently possible today. While the COVID-19 crisis is severally challenging health systems today, our healthy future is – with the right investments – within reach.
1. Five changes for sustainable health systems that put people first
The COVID-19 crisis has affected more than 188 countries and regions worldwide, causing large-scale loss of life and severe human suffering. The crisis poses a major threat to the global economy, with drops in activity, employment, and consumption worse than those seen during the 2008 financial crisis . COVID-19 has also exposed weaknesses in our health systems that must be addressed. How?
For a start, greater investment in population health would make people, particularly vulnerable population groups, more resilient to health risks. The health and socio-economic consequences of the virus are felt more acutely among disadvantaged populations, stretching a social fabric already challenged by high levels of inequalities. The crisis demonstrates the consequences of poor investment in addressing wider social determinants of health, including poverty, low education and unhealthy lifestyles. Despite much talk of the importance of health promotion, even across the richer OECD countries barely 3% of total health spending is devoted to prevention . Building resilience for populations also requires a greater focus on solidarity and redistribution in social protection systems to address underlying structural inequalities and poverty.
Beyond creating greater resilience in populations, health systems must be strengthened.
High-quality universal health coverage (UHC) is paramount. High levels of household out-of-pocket payments for health goods and services deter people from seeking early diagnosis and treatment at the very moment they need it most. Facing the COVID-19 crisis, many countries have strengthened access to health care, including coverage for diagnostic testing. Yet others do not have strong UHC arrangements. The pandemic reinforced the importance of commitments made in international fora, such as the 2019 High-Level Meeting on Universal Health Coverage , that well-functioning health systems require a deliberate focus on high-quality UHC. Such systems protect people from health threats, impoverishing health spending, and unexpected surges in demand for care.
Second, primary and elder care must be reinforced. COVID-19 presents a double threat for people with chronic conditions. Not only are they at greater risk of severe complications and death due to COVID-19; but also the crisis creates unintended health harm if they forgo usual care, whether because of disruption in services, fear of infections, or worries about burdening the health system. Strong primary health care maintains care continuity for these groups. With some 94% of deaths caused by COVID-19 among people aged over 60 in high-income countries, the elder care sector is also particularly vulnerable, calling for efforts to enhance control of infections, support and protect care workers and better coordinate medical and social care for frail elderly.
Third, the crisis demonstrates the importance of equipping health systems with both reserve capacity and agility. There is an historic underinvestment in the health workforce, with estimated global shortages of 18 million health professionals worldwide , mostly in low- and middle-income countries. Beyond sheer numbers, rigid health labour markets make it difficult to respond rapidly to demand and supply shocks. One way to address this is by creating a “reserve army” of health professionals that can be quickly mobilised. Some countries have allowed medical students in their last year of training to start working immediately, fast-tracked licenses and provided exceptional training. Others have mobilised pharmacists and care assistants. Storing a reserve capacity of supplies such as personal protection equipment, and maintaining care beds that can be quickly transformed into critical care beds, is similarly important.
Fourth, stronger health data systems are needed. The crisis has accelerated innovative digital solutions and uses of digital data, smartphone applications to monitor quarantine, robotic devices, and artificial intelligence to track the virus and predict where it may appear next. Access to telemedicine has been made easier. Yet more can be done to leverage standardised national electronic health records to extract routine data for real-time disease surveillance, clinical trials, and health system management. Barriers to full deployment of telemedicine, the lack of real-time data, of interoperable clinical record data, of data linkage capability and sharing within health and with other sectors remain to be addressed.
Fifth, an effective vaccine and successful vaccination of populations around the globe will provide the only real exit strategy. Success is not guaranteed and there are many policy issues yet to be resolved. International cooperation is vital. Multilateral commitments to pay for successful candidates would give manufacturers certainty so that they can scale production and have vaccine doses ready as quickly as possible following marketing authorisation, but could also help ensure that vaccines go first to where they are most effective in ending the pandemic. Whilst leaders face political pressure to put the health of their citizens first, it is more effective to allocate vaccines based on need. More support is needed for multilateral access mechanisms that contain licensing commitments and ensure that intellectual property is no barrier to access, commitments to technology transfer for local production, and allocation of scarce doses based on need.
The pandemic offers huge opportunities to learn lessons for health system preparedness and resilience. Greater focus on anticipating responses, solidarity within and across countries, agility in managing responses, and renewed efforts for collaborative actions will be a better normal for the future.
OECD Economic Outlook 2020 , Volume 2020 Issue 1, No. 107, OECD Publishing, Paris
OECD Employment Outlook 2020 : Worker Security and the COVID-19 Crisis, OECD Publishing, Paris
OECD Health at a Glance 2019, OECD Publishing, Paris
https://www.un.org/pga/73/wp-content/uploads/sites/53/2019/07/FINAL-draft-UHC-Political-Declaration.pdf
OECD (2020), Who Cares? Attracting and Retaining Care Workers for the Elderly, OECD Health Policy Studies, OECD Publishing, Paris
Working for Health and Growth: investing in the health workforce . Report of the High-Level Commission on Health Employment and Economic Growth, Geneva.
Colombo F., Oderkirk J., Slawomirski L. (2020) Health Information Systems, Electronic Medical Records, and Big Data in Global Healthcare: Progress and Challenges in OECD Countries . In: Haring R., Kickbusch I., Ganten D., Moeti M. (eds) Handbook of Global Health. Springer, Cham.
2. Improving population health and building healthy societies in times of COVID-19
By Helena Legido-Quigley , Associate Professor, London School of Hygiene and Tropical Medicine
The COVID-19 pandemic has been a stark reminder of the fragility of population health worldwide; at time of writing, more than 1 million people have died from the disease. The pandemic has already made evident that those suffering most from COVID-19 belong to disadvantaged populations and marginalised communities. Deep-rooted inequalities have contributed adversely to the health status of different populations within and between countries. Besides the direct and indirect health impacts of COVID-19 and the decimation of health systems, restrictions on population movement and lockdowns introduced to combat the pandemic are expected to have economic and social consequences on an unprecedented scale .
Population health – and addressing the consequences of COVID-19 – is about improving the physical and mental health outcomes and wellbeing of populations locally, regionally and nationally, while reducing health inequalities.¹ Moreover, there is an increasing recognition that societal and environmental factors, such as climate change and food insecurity, can also influence population health outcomes.
The experiences of Maria, David, and Ruben – as told by Spanish public broadcaster RTVE – exemplify the real challenges that people living in densely populated urban areas have faced when being exposed to COVID-19.¹
Maria is a Mexican migrant who has just returned from Connecticut to the Bronx. Her partner Jorge died in Connecticut from COVID-19. She now has no income and is looking for an apartment for herself and her three children. When Jorge became ill, she took him to the hospital, but they would not admit him and he was sent away to be cared for by Maria at home with their children. When an ambulance eventually took him to hospital, it was too late. He died that same night, alone in hospital. She thinks he had diabetes, but he was never diagnosed. They only had enough income to pay the basic bills. Maria is depressed, she is alone, but she knows she must carry on for her children. Her 10-year old child says that if he could help her, he would work. After three months, she finds an apartment.
David works as a hairdresser and takes an overcrowded train every day from Leganés to Chamberi in the centre of Madrid. He lives in a small flat in San Nicasio, one of the poorest working-class areas of Madrid with one of the largest ageing populations in Spain. The apartments are very small, making it difficult to be in confinement, and all of David’s neighbours know somebody who has been a victim of COVID-19. His father was also a hairdresser. David's father was not feeling well; he was taken to hospital by ambulance, and he died three days later. David was not able to say goodbye to his father. Unemployment has increased in that area; small local shops are losing their customers, and many more people are expecting to lose their jobs.
Ruben lives in Iztapalapa in Mexico City with three children, a daughter-in-law and five grandchildren. Their small apartment has few amenities, and no running water during the evening. At three o’clock every morning, he walks 45 minutes with his mobile stall to sell fruit juices near the hospital. His daily earnings keep the family. He goes to the central market to buy fruit, taking a packed dirty bus. He thinks the city's central market was contaminated at the beginning of the pandemic, but it could not be closed as it is the main source of food in the country. He has no health insurance, and he knows that as a diabetic he is at risk, but medication for his condition is too expensive. He has no alternative but to go to work every day: "We die of hunger or we die of COVID."
These real stories highlight the issues that must be addressed to reduce persistent health inequalities and achieve health outcomes focusing on population health. The examples of Maria, David and Ruben show the terrible outcomes COVID-19 has had for people living in poverty and social deprivation, older people, and those with co-morbidities and/or pre-existing health conditions. All three live in densely populated urban areas with poor housing, and have to travel long distances in overcrowded transport. Maria’s loss of income has had consequences for her housing security and access to healthcare and health insurance, which will most likely lead to worse health conditions for her and her children. Furthermore, all three experienced high levels of stress, which is magnified in the cases of Maria and David who were unable to be present when their loved ones died.
The COVID-19 pandemic has made it evident that to improve the health of the population and build healthy societies, there is a need to shift the focus from illness to health and wellness in order to address the social, political and commercial determinants of health; to promote healthy behaviours and lifestyles; and to foster universal health coverage.² Citizens all over the world are demanding that health systems be strengthened and for governments to protect the most vulnerable. A better future could be possible with leadership that is able to carefully consider the long-term health, economic and social policies that are needed.
In order to design and implement population health-friendly policies, there are three prerequisites. First, there is a need to improve understanding of the factors that influence health inequalities and the interconnections between the economic, social and health impacts. Second, broader policies should be considered not only within the health sector, but also in other sectors such as education, employment, transport and infrastructure, agriculture, water and sanitation. Third, the proposed policies need to be designed through involving the community, addressing the health of vulnerable groups, and fostering inter-sectoral action and partnerships.
Finally, within the UN's Agenda 2030 , Sustainable Development Goal (SDG) 3 sets out a forward-looking strategy for health whose main goal is to attain healthier lives and wellbeing. The 17 interdependent SDGs offer an opportunity to contribute to healthier, fairer and more equitable societies from which both communities and the environment can benefit.
The stories of Maria, David and Ruben are real stories featured in the Documentary: The impact of COVID19 in urban outskirts, Directed by Jose A Guardiola. Available here. Permission has been granted to narrate these stories.
Buck, D., Baylis, A., Dougall, D. and Robertson, R. (2018). A vision for population health: Towards a healthier future . [online] London: The King's Fund. [Accessed 20 Sept. 2020]
Wilton Park. (2020). Healthy societies, healthy populations (WP1734). Wiston House, Steyning. Retrieved from https://www.wiltonpark.org.uk/event/wp1734/ Cohen B. E. (2006). Population health as a framework for public health practice: a Canadian perspective. American journal of public health , 96 (9), 1574–1576.
3. Imagine a 'well-care' system that invests in keeping people healthy
By Maliha Hashmi , Executive Director, Health and Well-Being and Biotech, NEOM, and Jan Kimpen , Global Chief Medical Officer, Philips
Imagine a patient named Emily. Emily is aged 32 and I’m her doctor.
Emily was 65lb (29kg) above her ideal body weight, pre-diabetic and had high cholesterol. My initial visit with Emily was taken up with counselling on lifestyle changes, mainly diet and exercise; typical advice from one’s doctor in a time-pressured 15-minute visit. I had no other additional resources, incentives or systems to support me or Emily to help her turn her lifestyle around.
I saw Emily eight months later, not in my office, but in the hospital emergency room. Her husband accompanied her – she was vomiting, very weak and confused. She was admitted to the intensive care unit, connected to an insulin drip to lower her blood sugar, and diagnosed with type 2 diabetes. I talked to Emily then, emphasizing that the new medications for diabetes would only control the sugars, but she still had time to reverse things if she changed her lifestyle. She received further counselling from a nutritionist.
Over the years, Emily continued to gain weight, necessitating higher doses of her diabetes medication. More emergency room visits for high blood sugars ensued, she developed infections of her skin and feet, and ultimately, she developed kidney disease because of the uncontrolled diabetes. Ten years after I met Emily, she is 78lb (35kg) above her ideal body weight; she is blind and cannot feel her feet due to nerve damage from the high blood sugars; and she will soon need dialysis for her failing kidneys. Emily’s deteriorating health has carried a high financial cost both for herself and the healthcare system. We have prevented her from dying and extended her life with our interventions, but each interaction with the medical system has come at significant cost – and those costs will only rise. But we have also failed Emily by allowing her diabetes to progress. We know how to prevent this, but neither the right investments nor incentives are in place.
Emily could have been a real patient of mine. Her sad story will be familiar to all doctors caring for chronically ill patients. Unfortunately, patients like Emily are neglected by health systems across the world today. The burden of chronic disease is increasing at alarming rates. Across the OECD nearly 33% of those over 15 years live with one or more chronic condition, rising to 60% for over-65s. Approximately 50% of chronic disease deaths are attributed to cardiovascular disease (CVD). In the coming decades, obesity, will claim 92 million lives in the OECD while obesity-related diseases will cut life expectancy by three years by 2050.
These diseases can be largely prevented by primary prevention, an approach that emphasizes vaccinations, lifestyle behaviour modification and the regulation of unhealthy substances. Preventative interventions have been efficacious. For obesity, countries have effectively employed public awareness campaigns, health professionals training, and encouragement of dietary change (for example, limits on unhealthy foods, taxes and nutrition labelling).⁴,⁵ Other interventions, such as workplace health-promotion programmes, while showing some promise, still need to demonstrate their efficacy.

The COVID-19 crisis provides the ultimate incentive to double down on the prevention of chronic disease. Most people dying from COVID-19 have one or more chronic disease, including obesity, CVD, diabetes or respiratory problems – diseases that are preventable with a healthy lifestyle. COVID-19 has highlighted structural weaknesses in our health systems such as the neglect of prevention and primary care.
While the utility of primary prevention is understood and supported by a growing evidence base, its implementation has been thwarted by chronic underinvestment, indicating a lack of societal and governmental prioritization. On average, OECD countries only invest 2.8% of health spending on public health and prevention. The underlying drivers include decreased allocation to prevention research, lack of awareness in populations, the belief that long-run prevention may be more costly than treatment, and a lack of commitment by and incentives for healthcare professionals. Furthermore, public health is often viewed in a silo separate from the overall health system rather than a foundational component.
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
Fee-for-service models that remunerate physicians based on the number of sick patients they see, regardless the quality and outcome, dominate healthcare systems worldwide. Primary prevention mandates a payment system that reimburses healthcare professionals and patients for preventive actions. Ministries of health and governmental leaders need to challenge skepticism around preventive interventions, realign incentives towards preventive actions and those that promote healthy choices by people. Primary prevention will eventually reduce the burden of chronic diseases on the healthcare system.
As I reflect back on Emily and her life, I wonder what our healthcare system could have done differently. What if our healthcare system was a well-care system instead of a sick-care system? Imagine a different scenario: Emily, a 32 year old pre-diabetic, had access to a nutritionist, an exercise coach or health coach and nurse who followed her closely at the time of her first visit with me. Imagine if Emily joined group exercise classes, learned where to find healthy foods and how to cook them, and had access to spaces in which to exercise and be active. Imagine Emily being better educated about her diabetes and empowered in her healthcare and staying healthy. In reality, it is much more complicated than this, but if our healthcare systems began to incentivize and invest in prevention and even rewarded Emily for weight loss and healthy behavioural changes, the outcome might have been different. Imagine Emily losing weight and continuing to be an active and contributing member of society. Imagine if we invested in keeping people healthy rather than waiting for people to get sick, and then treating them. Imagine a well-care system.
Anderson, G. (2011). Responding to the growing cost and prevalence of people with multiple chronic conditions . Retrieved from OECD.
Institute for Health Metrics and Evaluation. GBD Data Visualizations. Retrieved here.
OECD (2019), The Heavy Burden of Obesity: The Economics of Prevention, OECD Health Policy Studies, OECD Publishing, Paris.
OECD. (2017). Obesity Update . Retrieved here.
Malik, V. S., Willett, W. C., & Hu, F. B. (2013). Global obesity: trends, risk factors and policy implications. Nature Reviews Endocrinology , 9 (1), 13-27.
Lang, J., Cluff, L., Payne, J., Matson-Koffman, D., & Hampton, J. (2017). The centers for disease control and prevention: findings from the national healthy worksite program. Journal of occupational and environmental medicine , 59 (7), 631.
Gmeinder, M., Morgan, D., & Mueller, M. (2017). How much do OECD countries spend on prevention? Retrieved from OECD.
Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198.
Richardson, A. K. (2012). Investing in public health: barriers and possible solutions. Journal of Public Health , 34 (3), 322-327.
Yong, P. L., Saunders, R. S., & Olsen, L. (2010). Missed Prevention Opportunities The healthcare imperative: lowering costs and improving outcomes: workshop series summary (Vol. 852): National Academies Press Washington, DC.
OECD. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Retrieved here .
McDaid, D., F. Sassi and S. Merkur (Eds.) (2015a), “Promoting Health, Preventing Disease: The Economic Case ”, Open University Press, New York.
OECD. (2019). The Heavy Burden of Obesity: The Economics of Prevention. Retrieved from OECD.
4. Why e arly detection and diagnosis is critical
By Paul Murray , Head of Life and Health Products, Swiss Re, and André Goy , Chairman and Executive Director & Chief of Lymphoma, John Theurer Cancer Center, Hackensack University Medical Center
Although healthcare systems around the world follow a common and simple principle and goal – that is, access to affordable high-quality healthcare – they vary significantly, and it is becoming increasingly costly to provide this access, due to ageing populations, the increasing burden of chronic diseases and the price of new innovations.
Governments are challenged by how best to provide care to their populations and make their systems sustainable. Neither universal health, single payer systems, hybrid systems, nor the variety of systems used throughout the US have yet provided a solution. However, systems that are ranked higher in numerous studies, such as a 2017 report by the Commonwealth Fund , typically include strong prevention care and early-detection programmes. This alone does not guarantee a good outcome as measured by either high or healthy life expectancy. But there should be no doubt that prevention and early detection can contribute to a more sustainable system by reducing the risk of serious diseases or disorders, and that investing in and operationalizing earlier detection and diagnosis of key conditions can lead to better patient outcomes and lower long-term costs.
To discuss early detection in a constructive manner it makes sense to describe its activities and scope. Early detection includes pre-symptomatic screening and treatment immediately or shortly after first symptoms are diagnosed. Programmes may include searching for a specific disease (for example, HIV/AIDS or breast cancer), or be more ubiquitous. Prevention, which is not the focus of this blog, can be interpreted as any activities undertaken to avoid diseases, such as information programmes, education, immunization or health monitoring.
Expenditures for prevention and early detection vary by country and typically range between 1-5% of total health expenditures.¹ During the 2008 global financial crisis, many countries reduced preventive spending. In the past few years, however, a number of countries have introduced reforms to strengthen and promote prevention and early detection. Possibly the most prominent example in recent years was the introduction of the Affordable Care Act in the US, which placed a special focus on providing a wide range of preventive and screening services. It lists 63 distinct services that must be covered without any copayment, co-insurance or having to pay a deductible.

Whilst logic dictates that investment in early detection should be encouraged, there are a few hurdles and challenges that need to be overcome and considered. We set out a few key criteria and requirements for an efficient early detection program:
1. Accessibility The healthcare system needs to provide access to a balanced distribution of physicians, both geographically (such as accessibility in rural areas), and by specialty. Patients should be able to access the system promptly without excessive waiting times for diagnoses or elective treatments. This helps mitigate conditions or diseases that are already quite advanced or have been incubating for months or even years before a clinical diagnosis. Access to physicians varies significantly across the globe from below one to more than 60 physicians per 10,000 people.² One important innovation for mitigating access deficiencies is telehealth. This should give individuals easier access to health-related services, not only in cases of sickness but also to supplement primary care.
2. Early symptoms and initial diagnosis Inaccurate or delayed initial diagnoses present a risk to the health of patients, can lead to inappropriate or unnecessary testing and treatment, and represents a significant share of total health expenditures. A medical second opinion service, especially for serious medical diagnoses, which can occur remotely, can help improve healthcare outcomes. Moreover, studies show that early and correct diagnosis opens up a greater range of curative treatment options and can reduce costs (e.g. for colon cancer, stage-four treatment costs are a multiple of stage-one treatment costs).³
3. New technology New early detection technologies can improve the ability to identify symptoms and diseases early: i. Advances in medical monitoring devices and wearable health technology, such as ECG and blood pressure monitors and biosensors, enable patients to take control of their own health and physical condition. This is an important trend that is expected to positively contribute to early detection, for example in atrial fibrillation and Alzheimers’ disease. ii. Diagnostic tools, using new biomarkers such as liquid biopsies or volatile organic compounds, together with the implementation of machine learning, can play an increasing role in areas such as oncology or infectious diseases.⁴
4. Regulation and Intervention Government regulation and intervention will be necessary to set ranges of normality, to prohibit or discourage overdiagnosis and to reduce incentives for providers to overtreat patients or to follow patients' inappropriate requests. In some countries, such as the US, there has been some success through capitation models and value-based care. Governments might also need to intervene to de-risk the innovation paradigm, such that private providers of capital feel able to invest more in the development of new detection technologies, in addition to proven business models in novel therapeutics.
OECD Health Working Papers No. 101 "How much do OECD countries spend on prevention" , 2017
World Health Organization; Global Health Observatory (GHO) data; https://www.who.int/gho/health_workforce/physicians_density/en/
Saving lives, averting costs; A report for Cancer Research UK, by Incisive Health, September 2014
Liquid Biopsy: Market Drivers And Obstacles; by Divyaa Ravishankar, Frost & Sullivan, January 21, 2019
Liquid Biopsies Become Cheap and Easy with New Microfluidic Device; February 26, 2019
How America’s 5 Top Hospitals are Using Machine Learning Today; by Kumba Sennaar, February 19, 2019
5. The business case for private investment in healthcare for all
Pascal Fröhlicher, Primary Care Innovation Scholar, Harvard Medical School, and Ian Wijaya, Managing Director in Lazard’s Global Healthcare Group
Faith, a mother of two, has just lost another customer. Some households where she is employed to clean, in a small town in South Africa, have little understanding of her medical needs. As a type 2 diabetes patient, this Zimbabwean woman visits the public clinic regularly, sometimes on short notice. At her last visit, after spending hours in a queue, she was finally told that the doctor could not see her. To avoid losing another day of work, she went to the local general practitioner to get her script, paying more than three daily wages for consultation and medication. Sadly, this fictional person reflects a reality for many people in middle-income countries.
Achieving universal health coverage by 2030, a key UN Sustainable Development Goal (SDG), is at risk. The World Bank has identified a $176 billion funding gap , increasing every year due to the growing needs of an ageing population, with the health burden shifting towards non-communicable diseases (NCDs), now the major cause of death in emerging markets . Traditional sources of healthcare funding struggle to increase budgets sufficiently to cover this gap and only about 4% of private health care investments focus on diseases that primarily affect low- and middle-income countries.
In middle-income countries, private investors often focus on extending established businesses, including developing private hospital capacity, targeting consumers already benefiting from quality healthcare. As a result, an insufficient amount of private capital is invested in strengthening healthcare systems for everyone.

Why is this the case? We discussed with senior health executives investing in Lower and Middle Income Countries (LMIC) and the following reasons emerged:
- Small market size . Scaling innovations in healthcare requires dealing with country-specific regulatory frameworks and competing interest groups, resulting in high market entry cost.
- Talent . Several LMICs are losing nurses and doctors but also business and finance professionals to European and North American markets due to the lack of local opportunities and a significant difference in salaries.
- Untested business models with relatively low gross margins. Providing healthcare requires innovative business models where consumers’ willingness to pay often needs to be demonstrated over a significant period of time. Additionally, relatively low gross margins drive the need for scale to leverage administrative costs, which increases risk.
- Government Relations. The main buyer of health-related products and services is government; yet the relationship between public and private sectors often lacks trust, creating barriers to successful collaboration. Add to that significant political risk, as contracts can be cancelled by incoming administrations after elections. Many countries also lack comprehensive technology strategies to successfully manage technological innovation.
- Complexity of donor funding. A significant portion of healthcare is funded by private donors, whose priorities might not always be congruent with the health priorities of the government.
Notwithstanding these barriers, healthcare, specifically in middle-income settings, could present an attractive value proposition for private investors:
- Economic growth rates . A growing middle class is expanding the potential market for healthcare products and services.
- Alignment of incentives . A high ratio of out-of-pocket payments for healthcare services is often associated with low quality. However, innovative business models can turn out of pocket payments into the basis for a customer-centric value proposition, as the provider is required to compete for a share of disposable income.
- Emergence of National Health Insurance Schemes . South Africa, Ghana, Nigeria and others are building national health insurance schemes, increasing a population’s ability to fund healthcare services and products .
- Increased prevalence of NCDs. Given the increasing incidence of chronic diseases and the potential of using technology to address these diseases, new business opportunities for private investment exist.
Based on the context above, several areas in healthcare delivery can present compelling opportunities for private companies.
- Aggregation of existing players.
- Leveraging primary care infrastructure. Retail companies can leverage their real estate, infrastructure and supply chains to deploy primary care services at greater scale than is currently the case.
- Telemedicine . Telecommunications providers can leverage their existing infrastructure and customer base to provide payment mechanisms and telehealth services at scale. As seen during the COVID-19 pandemic, investment in telemedicine can ensure that patients receive timely and continuous care in spite of restrictions and lockdowns.
- Cost effective diagnostics . Diagnostic tools operated by frontline workers and combined with the expertise of specialists can provide timely and efficient care.
To fully realize these opportunities, government must incentivise innovation, provide clear regulatory frameworks and, most importantly, ensure that health priorities are adequately addressed.
Venture capital and private equity firms as well as large international corporations can identify the most commercially viable solutions and scale them into new markets. The ubiquity of NCDs and the requirement to reduce costs globally provides innovators with the opportunity to scale their tested solutions from LMICs to higher income environments.
Successful investment exits in LMICs and other private sector success stories will attract more private capital. Governments that enable and support private investment in their healthcare systems would, with appropriate governance and guidance, generate benefits to their populations and economies. The economic value of healthy populations has been proven repeatedly , and in the face of COVID-19, private sector investment can promote innovation and the development of responsible, sustainable solutions.
Faith – the diabetic mother we introduced at the beginning of this article - could keep her client. As a stable patient, she could measure her glucose level at home and enter the results in an app on her phone, part of her monthly diabetes programme with the company that runs the health centre. She visits the nurse-led facility at the local taxi stand on her way to work when her app suggests it. The nurse in charge of the centre treats Faith efficiently, and, if necessary, communicates with a primary care physician or even a specialist through the telemedicine functionality of her electronic health system.
Improving LMIC health systems is not only a business opportunity, but a moral imperative for public and private leaders. With the appropriate technology and political will, this can become a reality.
6. How could COVID-19 change the way we pay for health services?
John E. Ataguba, Associate Professor and Director, University of Cape Town and Matthew Guilford, Co-Founder and Chief Executive Officer, Common Health
The emergence of the new severe acute respiratory syndrome coronavirus (SARS-Cov-2), causing the coronavirus disease 2019 (COVID-19), has challenged both developing and developed countries.
Countries have approached the management of infections differently. Many people are curious to understand their health system’s performance on COVID-19, both at the national level and compared to international peers. Alongside limited resources for health, many developing countries may have weak health systems that can make it challenging to respond adequately to the pandemic.
Even before COVID-19, high rates of out-of-pocket spending on health meant that every year, 800 million people faced catastrophic healthcare costs ,100 million families were pushed into poverty, and millions more simply avoided care for critical conditions because they could not afford to pay for it.
The pandemic and its economic fallout have caused household incomes to decline at the same time as healthcare risks are rising. In some countries with insurance schemes, and especially for private health insurance, the following questions have arisen: How large is the co-payment for a COVID-19 test? If my doctor’s office is closed, will the telemedicine consultation be covered by my insurance? Will my coronavirus care be paid for regardless of how I contracted the virus? These and other doubts can prevent people from seeking medical care in some countries.
In Nigeria, like many other countries in Africa, the government bears the costs associated with testing and treating COVID-19 irrespective of the individual’s insurance status. In the public health sector, where COVID-19 cases are treated, health workers are paid monthly salaries while budgets are allocated to health facilities for other services. Hospitals continue to receive budget allocations to finance all health services including the management and treatment of COVID-19. That implies that funds allocated to address other health needs are reduced and that in turn could affect the availability and quality of health services.
Although health workers providing care for COVID-19 patients in isolation and treatment centres in Nigeria are paid salaries that are augmented with a special incentive package, the degree of impact on the quality improvement of services remains unclear. The traditional and historical allocation of budgets does not always address the needs of the whole population and could result in poor health services and under-provision of health services for COVID-19 patients.
In some countries, the reliance on out-of-pocket funding is hardly better for private providers, who encounter brand risks, operational difficulties, and – in extreme cases – the risk of creating “debtor prisons” as they seek to collect payment from patients. Ironically, despite the huge demand for medical services to diagnose and treat COVID-19, large healthcare institutions and individual healthcare practitioners alike are facing financial distress.
Dependence on a steady stream of fee-for-service payments for outpatient consultations and elective procedures is leading to pay cuts for doctors in India , forfeited Eid bonuses for nurses in Indonesia , and hospital bankruptcies in the United States . In a recent McKinsey & Company survey, 77% of physicians reported that their business would suffer in 2020 , and 46% were concerned about their practice surviving the coronavirus pandemic.
COVID-19 is exposing how fee-for-service, historical budget allocation and out-of-pocket financing methods can hinder the performance of the health system. Some providers and health systems that deployed “value-based” models prior to the pandemic have reported that these approaches have improved financial resilience during COVID-19 and may support better results for patients. Nevertheless, these types of innovations do not represent the dominant payment model in any country.
How health service providers are paid has implications for whether service users can get needed health services in a timely fashion, and at an appropriate quality and an affordable cost. By shifting from fee-for-service reimbursements to fixed "capitation" and performance-based payments, these models incentivize providers to improve quality and coordination while also guaranteeing a baseline income level, even during times of disruption.
Health service providers could be paid either in the form of salaries, a fee for services they provide, by capitation (whether adjusted or straightforward), through global budgets, or by using a case-based payment system (for example, the diagnostics-related groups), among others. Because there are different incentives to consider when adopting any of the methods, they could be combined to achieve a specific goal. For example, in some countries, health workers are paid salaries , and some specific services are paid on a fee-for-service basis.
Ideally, health services could be purchased strategically , incorporating aspects of provider performance in transferring funds to providers and accounting for the health needs of the population they serve.
In this regard, strategic purchasing for health has been advocated and should be highlighted as crucial with the emergence of the COVID-19 pandemic. There is a need to ensure value in the way health providers are paid, inter alia to increase efficiency, ensure equity, and improve access to needed health services. Value-based payment methods, although not new in many countries, provide an avenue to encourage long-term value for money, better quality, and strategic purchasing for health, helping to build a healthier, more resilient world.
7. L essons in integrated care from the COVID-19 pandemic
Sarah Ziegler, Postdoctoral Researcher, Department of Epidemiology and Biostatistics, University of Zurich, and Ninie Wang, Founder & CEO, Pinetree Care Group.
Since the start of the COVID-19 pandemic, people suffering non-communicable diseases (NCDs) have been at higher risk of becoming severely ill or dying. In Italy, 96.2% of people who died of COVID-19 lived with two or more chronic conditions.
Beyond the pandemic, cardiovascular disease, cancer, respiratory disease and diabetes are the leading burden of disease, with 41 million annual deaths. People with multimorbidity - a number of different conditions - often experience difficulties in accessing timely and coordinated healthcare, made worse when health systems are busy fighting against the pandemic.
Here is what happened in China with Lee, aged 62, who has been living with Chronic Obstructive Pulmonary Disease (COPD) for the past five years.
Before the pandemic, Lee’s care manager coordinated a multi-disciplinary team of physicians, nurses, pulmonary rehabilitation therapists, psychologists and social workers to put together a personalized care plan for her. Following the care plan, Lee stopped smoking and paid special attention to her diet, sleep and physical exercises, as well as sticking to her medication and follow-up visits. She participated in a weekly community-based physical activity program to meet other COPD patients, including short walks and exchange experiences. A mobile care team supported her with weekly cleaning and grocery shopping.
Together with her family, Lee had follow-up visits to ensure her care plan reflected her recovery and to modify the plan if needed. These integrated care services brought pieces of care together, centered around Lee’s needs, and provided a continuum of care that helped keep Lee in the community with a good quality of life for as long as possible.
Since the COVID-19 outbreak, such NCD services have been disrupted by lockdowns, the cancellation of elective care and the fear of visiting care service . These factors particularly affected people living with NCDs like Lee. As such, Lee was not able to follow her care plan anymore. The mobile care team was unable to visit her weekly as they were deployed to provide COVID-19 relief. Lee couldn’t participate in her community-based program, follow up on her daily activities, or see her family or psychologists. This negatively affected Lee’s COPD management and led to poor management of her physical activity and healthy diet.
The pandemic highlights the need for a flexible and reliable integrated care system to enable healthcare delivery to all people no matter where they live, uzilizing approaches such as telemedicine and effective triaging to overcome care disruptions.
Lee’s care manager created short videos to assist her family through each step of her care and called daily to check in on the implementation of the plan and answer questions. Lee received tele-consultations, and was invited to the weekly webcast series that supported COPD patient communities. When her uncle passed away because of pneumonia complications from COVID-19 in early April, Lee’s care manager arranged a palliative care provider to support the family through the difficult time of bereavement and provided food and supplies during quarantine. Lee could even continue with her physical activity program with an online training coach. There were a total of 38 exercise videos for strengthening and stretching arms, legs and trunk, which she could complete at different levels of difficulty and with different numbers of repetitions.
Lee’s case demonstrates that early detection, prevention, and management of NCDs play a crucial role in a global pandemic response. It shows how we need to shift away from health systems designed around single diseases towards health systems designed for the multidimensional needs of individuals. As part of the pandemic responses, addressing and managing risks related to NCDs and prevention of their complications are critical to improve outcomes for vulnerable people like Lee.
How to design and deliver successful integrated care
The challenge for the successful transformation of healthcare is to tailor care system-wide to population needs. A 2016 WHO Framework on integrated people-centered health services developed a set of five general strategies for countries to progress towards people-centered and sustainable health systems, calling for a fundamental transformation not only in the way health services are delivered, but also in the way they are financed and managed . These strategies call for countries to:
- Engage and empower people / communities: an integrated care system must mobilize everyone to work together using all available resources, especially when continuity of essential health and community services for NCDs are at risk of being undermined.
- Strengthen governance and accountability, so that integration emphasizes rather than weakens leadership in every part of the system, and ensure that NCDs are included in national COVID-19 plans and future essential health services.
- Reorient the model of care to put the needs and perspectives of each person / family at the center of care planning and outcome measurement, rather than institutions.
- Coordinate services within and across sectors, for example, integrate inter-disciplinary medical care with social care, addressing wider socio-economic, environmental and behavioral determinants of health.
- Create an enabling environment, with clear objectives, supportive financing, regulations and insurance coverage for integrated care, including the development and use of systemic digital health care solutions.
Whether due to an unexpected pandemic or a gradual increase in the burden of NCDs, each person could face many health threats across the life-course.
Only systems that dynamically assess each person’s complex health needs and address them through a timely, well-coordinated and tailored mix of health and social care services will be able to deliver desired health outcomes over the longer term, ensuring an uninterrupted good quality of life for Lee and many others like her.
- Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY) 2020;12: 6049–57.
- WHO. Noncommunicable diseases in emergencies. Geneva: World Health Organization, 2016.
- WHO. COVID-19 significantly impacts health services for noncommunicable diseases. June 2020.
- Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicalbe diseases in the COVID-19 response. The Lancet. 2020. 395:1678-1680
- WHO. Framework on integrated people-centred health services. Geneva: World Health Organization, 2016.
8 . Why access to healthcare alone will not save lives
Donald Berwick, President Emeritus and Senior Fellow, Institute for Healthcare Improvement; Nicola Bedlington, Special Adviser, European Patient Forum; and David Duong, Director, Program in Global Primary Care and Social Change, Harvard Medical School.
Joyce lies next to 10 other women in bare single beds in the post-partum recovery room at a rural hospital in Uganda. Just an hour ago, Joyce gave birth to a healthy baby boy. She is now struggling with abdominal pain. A nurse walks by, and Joyce tries to call out, but the nurse was too busy to attend to her; she was the only nurse looking after 20 patients.
Another hour passes, and Joyce is shaking and sweating profusely. Joyce’s husband runs into the corridor to find a nurse to come and evaluate her. The nurse notices Joyce’s critical condition - a high fever and a low blood pressure - and she quickly calls the doctor. The medical team rushes Joyce to the intensive care unit. Joyce has a very severe blood stream infection. It takes another hour before antibiotics are started - too late. Joyce dies, leaving behind a newborn son and a husband. Joyce, like many before her, falls victim to a pervasive global threat: poor quality of care.
Adopted by United Nations (UN) in 2015, the Sustainable Development Goals (SDG) are a universal call to action to end poverty, protect the planet and ensure that all enjoy peace and prosperity by 2030. SDG 3 aims to ensure healthy lives and promote wellbeing for all. The 2019 UN General Assembly High Level Meeting on Universal Health Coverage (UHC) reaffirmed the need for the highest level of political commitment to health care for all.
However, progress towards UHC, often measured in terms of access, not outcomes, does not guarantee better health, as we can see from Joyce’s tragedy. This is also evident with the COVID-19 response. The rapidly evolving nature of the COVID-19 pandemic has highlighted long-term structural inefficiencies and inequities in health systems and societies trying to mitigate the contagion and loss of life.
Systems are straining under significant pressure to ensure standards of care for both COVID-19 patients and other patients that run the risk of not receiving timely and appropriate care. Although poor quality of care has been a long-standing issue, it is imperative now more than ever that systems implement high-quality services as part of their efforts toward UHC.
Poor quality healthcare remains a challenge for countries at all levels of economic development: 10% of hospitalized patients acquire an infection during their hospitalization in low-and-middle income countries (LMIC), whereas 7% do in high-income countries. Poor quality healthcare disproportionally affects the poor and those in LMICs. Of the approximately 8.6 million deaths per year in 137 LMICs, 3.6 million are people who did not access the health system, whereas 5 million are people who sought and had access to services but received poor-quality care.
Joyce’s story is all too familiar; poor quality of care results in deaths from treatable diseases and conditions. Although the causes of death are often multifactorial, deaths and increased morbidity from treatable conditions are often a reflection of defects in the quality of care.
The large number of deaths and avoidable complications are also accompanied by substantial economic costs. In 2015 alone, 130 LMICs faced US $6 trillion in economic losses. Although there is concern that implementing quality measures may be a costly endeavor, it is clear that the economic toll associated with a lack of quality of care is far more troublesome and further stunts the socio-economic development of LMICs, made apparent with the COVID-19 pandemic.
Poor-quality care not only leads to adverse outcomes in terms of high morbidity and mortality, but it also impacts patient experience and patient confidence in health systems. Less than one-quarter of people in LMICs and approximately half of people in high-income countries believe that their health systems work well.
A lack of application and availability of evidenced-based guidelines is one key driver of poor-quality care. The rapidly changing landscape of medical knowledge and guidelines requires healthcare workers to have immediate access to current clinical resources. Despite our "information age", health providers are not accessing clinical guidelines or do not have access to the latest practical, lifesaving information.
Getting information to health workers in the places where it is most needed is a delivery challenge. Indeed, adherence to clinical practice guidelines in eight LMICs was below 50%, and in OECD countries, despite being a part of national guidelines, 19-53% of women aged 50-69 years did not receive mammography screening.4 The evidence in LMICs and HICs suggest that application of evidence-based guidelines lead to reduction in mortality and improved health outcomes.
Equally, the failure to change and continually improve the processes in health systems that support the workforce takes a high toll on quality of care. During the initial wave of the COVID-19 pandemic, countries such as Taiwan, Hong Kong, Singapore and Vietnam, which adapted and improved their health systems after the SARS and H1N1 outbreaks, were able to rapidly mobilize a large-scale quarantine and contact tracing strategy, supported with effective and coordinated mass communication.
These countries not only mitigated the economic and mortality damage, but also prevented their health systems and workforce from enduring extreme burden and inability to maintain critical medical supplies. In all nations, investing in healthcare organizations to enable them to become true “learning health care systems,” aiming at continual quality improvement, would yield major population health and health system gains.
The COVID-19 pandemic underscores the importance for health systems to be learning systems. Once the dust settles, we need to focus, collectively, on learning from this experience and adapting our health systems to be more resilient for the next one. This implies a need for commitment to and investment in global health cooperation, improvement in health care leadership, and change management.
With strong political and financial commitment to UHC, and its demonstrable effect in addressing crises such as COVID-19, for the first time, the world has a viable chance of UHC becoming a reality. However, without an equally strong political, managerial, and financial commitment to continually improving, high-quality health services, UHC will remain an empty promise.
1. United Nations General Assembly. Political declaration of the high-level meeting on universal health coverage. New York, NY2019.
2. Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J. Health equity in England: the Marmot review 10 years on. Institute of Health Equity;2020.
3. National Academies of Sciences, Engineering, and Medicine: Committee on Improving the Quality of Health Care Globally. Crossing the global quality chasm: Improving health care worldwide. Washington, DC: National Academies Press;2018.
4. World Health Organization, Organization for Economic Co-operation and Development, World Bank Group. Delivering quality health services: a global imperative for universal health coverage. World Health Organization; 2018.
5. Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health. 2018;6(11):e1196-e1252.
6. Ricci-Cabello I, Violán C, Foguet-Boreu Q, Mounce LT, Valderas JM. Impact of multi-morbidity on quality of healthcare and its implications for health policy, research and clinical practice. A scoping review. European Journal of General Practice. 2015;21(3):192-202.
7. Valtis YK, Rosenberg J, Bhandari S, et al. Evidence-based medicine for all: what we can learn from a programme providing free access to an online clinical resource to health workers in resource-limited settings. BMJ global health. 2016;1(1).
8. Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America . Washington, DC: National Academies Press 2012.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
13.1 Sociological Perspectives on Health and Health Care
Learning objective.
- List the assumptions of the functionalist, conflict, and symbolic interactionist perspectives on health and medicine.
Before discussing these perspectives, we must first define three key concepts—health, medicine, and health care—that lie at the heart of their explanations and of this chapter’s discussion. Health refers to the extent of a person’s physical, mental, and social well-being. As this definition suggests, health is a multidimensional concept. Although the three dimensions of health just listed often affect each other, it is possible for someone to be in good physical health and poor mental health, or vice versa. Medicine refers to the social institution that seeks to prevent, diagnose, and treat illness and to promote health in its various dimensions. This social institution in the United States is vast, to put it mildly, and involves more than 11 million people (physicians, nurses, dentists, therapists, medical records technicians, and many other occupations). Finally, health care refers to the provision of medical services to prevent, diagnose, and treat health problems.
With these definitions in mind, we now turn to sociological explanations of health and health care. As usual, the major sociological perspectives that we have discussed throughout this book offer different types of explanations, but together they provide us with a more comprehensive understanding than any one approach can do by itself. Table 13.1 “Theory Snapshot” summarizes what they say.
Table 13.1 Theory Snapshot
The Functionalist Approach
As conceived by Talcott Parsons (1951), the functionalist perspective emphasizes that good health and effective medical care are essential for a society’s ability to function. Ill health impairs our ability to perform our roles in society, and if too many people are unhealthy, society’s functioning and stability suffer. This was especially true for premature death, said Parsons, because it prevents individuals from fully carrying out all their social roles and thus represents a “poor return” to society for the various costs of pregnancy, birth, child care, and socialization of the individual who ends up dying early. Poor medical care is likewise dysfunctional for society, as people who are ill face greater difficulty in becoming healthy and people who are healthy are more likely to become ill.
For a person to be considered legitimately sick, said Parsons, several expectations must be met. He referred to these expectations as the sick role . First, sick people should not be perceived as having caused their own health problem. If we eat high-fat food, become obese, and have a heart attack, we evoke less sympathy than if we had practiced good nutrition and maintained a proper weight. If someone is driving drunk and smashes into a tree, there is much less sympathy than if the driver had been sober and skidded off the road in icy weather.
Second, sick people must want to get well. If they do not want to get well or, worse yet, are perceived as faking their illness or malingering after becoming healthier, they are no longer considered legitimately ill by the people who know them or, more generally, by society itself.
Third, sick people are expected to have their illness confirmed by a physician or other health-care professional and to follow the professional’s instructions in order to become well. If a sick person fails to do so, she or he again loses the right to perform the sick role.

Talcott Parsons wrote that for a person to be perceived as legitimately ill, several expectations, called the sick role, must be met. These expectations include the perception that the person did not cause her or his own health problem.
Nathalie Babineau-Griffith – grand-maman’s blanket – CC BY-NC-ND 2.0.
If all these expectations are met, said Parsons, sick people are treated as sick by their family, their friends, and other people they know, and they become exempt from their normal obligations to all these people. Sometimes they are even told to stay in bed when they want to remain active.
Physicians also have a role to perform, said Parsons. First and foremost, they have to diagnose the person’s illness, decide how to treat it, and help the person become well. To do so, they need the cooperation of the patient, who must answer the physician’s questions accurately and follow the physician’s instructions. Parsons thus viewed the physician-patient relationship as hierarchical: the physician gives the orders (or, more accurately, provides advice and instructions), and the patient follows them.
Parsons was certainly right in emphasizing the importance of individuals’ good health for society’s health, but his perspective has been criticized for several reasons. First, his idea of the sick role applies more to acute (short-term) illness than to chronic (long-term) illness. Although much of his discussion implies a person temporarily enters a sick role and leaves it soon after following adequate medical care, people with chronic illnesses can be locked into a sick role for a very long time or even permanently. Second, Parsons’s discussion ignores the fact, mentioned earlier, that our social backgrounds affect the likelihood of becoming ill and the quality of medical care we receive. Third, Parsons wrote approvingly of the hierarchy implicit in the physician-patient relationship. Many experts say today that patients need to reduce this hierarchy by asking more questions of their physicians and by taking a more active role in maintaining their health. To the extent that physicians do not always provide the best medical care, the hierarchy that Parsons favored is at least partly to blame.
The Conflict Approach
The conflict approach emphasizes inequality in the quality of health and of health-care delivery (Weitz, 2013). As noted earlier, the quality of health and health care differs greatly around the world and within the United States. Society’s inequities along social class, race and ethnicity, and gender lines are reproduced in our health and health care. People from disadvantaged social backgrounds are more likely to become ill, and once they do become ill, inadequate health care makes it more difficult for them to become well. As we will see, the evidence of disparities in health and health care is vast and dramatic.
The conflict approach also critiques efforts by physicians over the decades to control the practice of medicine and to define various social problems as medical ones. Physicians’ motivation for doing so has been both good and bad. On the good side, they have believed they are the most qualified professionals to diagnose problems and to treat people who have these problems. On the negative side, they have also recognized that their financial status will improve if they succeed in characterizing social problems as medical problems and in monopolizing the treatment of these problems. Once these problems become “medicalized,” their possible social roots and thus potential solutions are neglected.
Several examples illustrate conflict theory’s criticism. Alternative medicine is becoming increasingly popular, but so has criticism of it by the medical establishment. Physicians may honestly feel that medical alternatives are inadequate, ineffective, or even dangerous, but they also recognize that the use of these alternatives is financially harmful to their own practices. Eating disorders also illustrate conflict theory’s criticism. Many of the women and girls who have eating disorders receive help from a physician, a psychiatrist, a psychologist, or another health-care professional. Although this care is often very helpful, the definition of eating disorders as a medical problem nonetheless provides a good source of income for the professionals who treat it and obscures its cultural roots in society’s standard of beauty for women (Whitehead & Kurz, 2008).
Obstetrical care provides another example. In most of human history, midwives or their equivalent were the people who helped pregnant women deliver their babies. In the nineteenth century, physicians claimed they were better trained than midwives and won legislation giving them authority to deliver babies. They may have honestly felt that midwives were inadequately trained, but they also fully recognized that obstetrical care would be quite lucrative (Ehrenreich & English, 2005).
According to conflict theory, physicians have often sought to define various social problems as medical problems. An example is the development of the diagnosis of ADHD, or attention deficit/hyperactivity disorder.
birgerking – What I Really Do… ADD/ADHD – CC BY 2.0.
In a final example, many hyperactive children are now diagnosed with ADHD, or attention deficit/hyperactivity disorder. A generation or more ago, they would have been considered merely as overly active. After Ritalin, a drug that reduces hyperactivity, was developed, their behavior came to be considered a medical problem and the ADHD diagnosis was increasingly applied, and tens of thousands of children went to physicians’ offices and were given Ritalin or similar drugs. The definition of their behavior as a medical problem was very lucrative for physicians and for the company that developed Ritalin, and it also obscured the possible roots of their behavior in inadequate parenting, stultifying schools, or even gender socialization, as most hyperactive kids are boys (Conrad, 2008; Rao & Seaton, 2010).
Critics say the conflict approach’s assessment of health and medicine is overly harsh and its criticism of physicians’ motivation far too cynical. Scientific medicine has greatly improved the health of people around the world. Although physicians are certainly motivated, as many people are, by economic considerations, their efforts to extend their scope into previously nonmedical areas also stem from honest beliefs that people’s health and lives will improve if these efforts succeed. Certainly there is some truth in this criticism of the conflict approach, but the evidence of inequality in health and medicine and of the negative aspects of the medical establishment’s motivation for extending its reach remains compelling.
The Symbolic Interactionist Approach
The symbolic interactionist approach emphasizes that health and illness are social constructions . This means that various physical and mental conditions have little or no objective reality but instead are considered healthy or ill conditions only if they are defined as such by a society and its members (Buckser, 2009; Lorber & Moore, 2002). The ADHD example just discussed also illustrates symbolic interactionist theory’s concerns, as a behavior that was not previously considered an illness came to be defined as one after the development of Ritalin. In another example first discussed in Chapter 7 “Alcohol and Other Drugs” , in the late 1800s opium use was quite common in the United States, as opium derivatives were included in all sorts of over-the-counter products. Opium use was considered neither a major health nor legal problem. That changed by the end of the century, as prejudice against Chinese Americans led to the banning of the opium dens (similar to today’s bars) they frequented, and calls for the banning of opium led to federal legislation early in the twentieth century that banned most opium products except by prescription (Musto, 2002).
In a more current example, an attempt to redefine obesity is now under way in the United States. Obesity is a known health risk, but a “fat pride” or “fat acceptance” movement composed mainly of heavy individuals is arguing that obesity’s health risks are exaggerated and calling attention to society’s discrimination against overweight people. Although such discrimination is certainly unfortunate, critics say the movement is going too far in trying to minimize obesity’s risks (Diamond, 2011).
The symbolic interactionist approach has also provided important studies of the interaction between patients and health-care professionals. Consciously or not, physicians “manage the situation” to display their authority and medical knowledge. Patients usually have to wait a long time for the physician to show up, and the physician is often in a white lab coat; the physician is also often addressed as “Doctor,” while patients are often called by their first name. Physicians typically use complex medical terms to describe a patient’s illness instead of the more simple terms used by laypeople and the patients themselves.
Management of the situation is perhaps especially important during a gynecological exam, as first discussed in Chapter 12 “Work and the Economy” . When the physician is a man, this situation is fraught with potential embarrassment and uneasiness because a man is examining and touching a woman’s genital area. Under these circumstances, the physician must act in a purely professional manner. He must indicate no personal interest in the woman’s body and must instead treat the exam no differently from any other type of exam. To further “desex” the situation and reduce any potential uneasiness, a female nurse is often present during the exam.
Critics fault the symbolic interactionist approach for implying that no illnesses have objective reality. Many serious health conditions do exist and put people at risk for their health regardless of what they or their society thinks. Critics also say the approach neglects the effects of social inequality for health and illness. Despite these possible faults, the symbolic interactionist approach reminds us that health and illness do have a subjective as well as an objective reality.
Key Takeaways
- A sociological understanding emphasizes the influence of people’s social backgrounds on the quality of their health and health care. A society’s culture and social structure also affect health and health care.
- The functionalist approach emphasizes that good health and effective health care are essential for a society’s ability to function, and it views the physician-patient relationship as hierarchical.
- The conflict approach emphasizes inequality in the quality of health and in the quality of health care.
- The interactionist approach emphasizes that health and illness are social constructions; physical and mental conditions have little or no objective reality but instead are considered healthy or ill conditions only if they are defined as such by a society and its members.
For Your Review
- Which approach—functionalist, conflict, or symbolic interactionist—do you most favor regarding how you understand health and health care? Explain your answer.
- Think of the last time you visited a physician or another health-care professional. In what ways did this person come across as an authority figure possessing medical knowledge? In formulating your answer, think about the person’s clothing, body position and body language, and other aspects of nonverbal communication.
Buckser, A. (2009). Institutions, agency, and illness in the making of Tourette syndrome. Human Organization, 68 (3), 293–306.
Conrad, P. (2008). The medicalization of society: On the transformation of human conditions into treatable disorders . Baltimore, MD: Johns Hopkins University Press.
Diamond, A. (2011). Acceptance of fat as the norm is a cause for concern. Nursing Standard, 25 (38), 28–28.
Lorber, J., & Moore, L. J. (2002). Gender and the social construction of illness (2nd ed.). Lanham, MD: Rowman & Littlefield.
Musto, D. F. (Ed.). (2002). Drugs in America: A documentary history . New York, NY: New York University Press.
Parsons, T. (1951). The social system . New York, NY: Free Press.
Rao, A., & Seaton, M. (2010). The way of boys: Promoting the social and emotional development of young boys . New York, NY: Harper Paperbacks.
Weitz, R. (2013). The sociology of health, illness, and health care: A critical approach (6th ed.). Thousand Oaks, CA: Wadsworth.
Whitehead, K., & Kurz, T. (2008). Saints, sinners and standards of femininity: Discursive constructions of anorexia nervosa and obesity in women’s magazines. Journal of Gender Studies, 17 , 345–358.
Social Problems Copyright © 2015 by University of Minnesota is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
- Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
- Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring
Health and Human Society, Essay Example
Pages: 2
Words: 532
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
Contrary to what one may perceive, the wealthier nations may not be healthier at all time. The efforts towards health improvements may be overridden by conflict as well as inequalities. Not The same way that some individuals are healthier compared to others applies to societies and this is not attributed to their potentials in affording proper nutrition as well as better health care. Researchers have focused their attention on health determinants and analyzed issues past the risk factors associated with diseases to come to light of the underlying forces that account for extended patterns in the disparities notable in health status. They have adopted diverse sources of insight in this regard such as the working age, birth primate models involving society and health, ethnographies, social influences on brain function and development as well as elderly cohorts. These facilitates for a better understanding of the health of an entire population and its relationship with economic as well as social conditions.
The wealth, history as well as institutional and social arrangements in the human societies can be associated with sturdy influence on psychosocial as well as material environments that the members of that particular society experience. An individual in the course of development encounters these conditions in the course of interaction with the civic, the intimate, as well as the broader physical as well as socioeconomic environment. The environment is responsible for shaping the human biology as well as setting health prospects throughout the life course of the person. This can at first be manifested in form of a latent effect at early stages of development with such factors as nurturance, genetic endowment as well as infant nutrition having significant effects in the later life of the individual regardless of the intervening experiences.
Pathway effect has also been suggested in other research studies that reflect health as being determined by the conditions of living which are closely linked to socioeconomic careers of the well-travelled individuals coupled with cumulative effect through youth, maturity as well as oldage that are associated with the resources of an individual, the level of resilience, vulnerabilities and injuries.
The influences are generally exhibited through the phenomenon of socioeconomic gradient with respect to the health of an individual. The average status of health of all the members in a particular society increases in a step by step fashion with the ascendance of an individual from the low point to the top of the social ladder. This ascendance is based on factors such as the level of education, type of occupation as well as income. This gradient can hardly be explained through reverse causality in the selection of health. The people who are involved in population health are interested in understanding the process of the gradient generation within the societal processes as well as the cause of the steep slope in as far as some societies are concerned as compared to others.
This research has contributed significantly in the generation of discrete as well as robust observations that can lead successfully to the identification of the issue in discussion which entails the important determinants that explain the health status of different people in the human societies.
Stuck with your Essay?
Get in touch with one of our experts for instant help!
Turning Adversity Into Creative Growth, Essay Example
The Need for Pretend Play in Child Development, Essay Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Pages: 1
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Pages: 4
Words: 999
The Term “Social Construction of Reality”, Essay Example
Words: 371
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.

- IMF at a Glance
- Surveillance
- Capacity Development
- IMF Factsheets List
- IMF Members
- IMF Financial Statements
- IMF Senior Officials
- IMF in History
- Archives of the IMF
- Job Opportunities
- Climate Change
- Fiscal Policies
- Income Inequality
Flagship Publications
Other publications.
- World Economic Outlook
- Global Financial Stability Report
- Fiscal Monitor
- External Sector Report
- Staff Discussion Notes
- Working Papers
- IMF Research Perspectives
- Economic Review
- Global Housing Watch
- Commodity Prices
- Commodities Data Portal
- IMF Researchers
- Annual Research Conference
- Other IMF Events
IMF reports and publications by country
Regional offices.
- IMF Resident Representative Offices
- IMF Regional Reports
- IMF and Europe
- IMF Members' Quotas and Voting Power, and Board of Governors
- IMF Regional Office for Asia and the Pacific
- IMF Capacity Development Office in Thailand (CDOT)
- IMF Regional Office in Central America, Panama, and the Dominican Republic
- Eastern Caribbean Currency Union (ECCU)
- IMF Europe Office in Paris and Brussels
- IMF Office in the Pacific Islands
- How We Work
- IMF Training
- Digital Training Catalog
- Online Learning
- Our Partners
- Country Stories
- Technical Assistance Reports
- High-Level Summary Technical Assistance Reports
- Strategy and Policies
For Journalists
- Country Focus
- Chart of the Week
- Communiqués
- Mission Concluding Statements
- Press Releases
- Statements at Donor Meetings
- Transcripts
- Views & Commentaries
- Article IV Consultations
- Financial Sector Assessment Program (FSAP)
- Seminars, Conferences, & Other Events
- E-mail Notification
Press Center
The IMF Press Center is a password-protected site for working journalists.
- Login or Register
- Information of interest
- About the IMF
- Conferences
- Press briefings
- Special Features
- Middle East and Central Asia
- Economic Outlook
- Annual and spring meetings
- Most Recent
- Most Popular
- IMF Finances
- Additional Data Sources
- World Economic Outlook Databases
- Climate Change Indicators Dashboard
- IMF eLibrary-Data
- International Financial Statistics
- G20 Data Gaps Initiative
- Public Sector Debt Statistics Online Centralized Database
- Currency Composition of Official Foreign Exchange Reserves
- Financial Access Survey
- Government Finance Statistics
- Publications Advanced Search
- IMF eLibrary
- IMF Bookstore
- Publications Newsletter
- Essential Reading Guides
- Regional Economic Reports
- Country Reports
- Departmental Papers
- Policy Papers
- Selected Issues Papers
- All Staff Notes Series
- Analytical Notes
- Fintech Notes
- How-To Notes
- Staff Climate Notes

Reflections on a healthy society
December 2021
Download PDF
Michelle Bachelet

Leave no one behind is not just a mantra, it is a necessity. The pandemic has exposed and exacerbated inequalities within and between states and demonstrated the huge costs to people and prosperity of leaving those gaps unaddressed. Yet, due in significant part to short-sighted vaccine policies, we are faced with deepening economic hardship in the developing world, while richer countries welcome signs of an economic recovery.
To recover better, we need an economy that puts human beings and rights at the center of economic policy. One that invests in health, social protection, and other human rights to curb inequalities and discrimination; embraces progressive taxation, labor rights, and decent work; and promotes meaningful public participation and civic spaces.
This human-rights-based approach to the economy is an essential lever to relaunch and accelerate our path toward realizing the United Nations 2030 Agenda for Sustainable Development.
MICHELLE BACHELET is the United Nations high commissioner for human rights.
Jeffrey Sachs
The basic lessons of happiness are these: society (and therefore government policies) should attend to people’s economic needs, physical health, mental health, social connections, sense of purpose, and confidence in government. The pandemic has threatened almost every dimension of well-being and indeed has fostered rising anxieties, clinical depression, social isolation, and in many places, a loss of confidence in government.
We need more government outlays in response to the pandemic and its aftermath, but this poses two challenges: first, poor countries cannot afford to increase the provision of public services, so they urgently need access to incremental financing and debt relief on adequate terms. Second, governments need much more professionalism and competence than many (perhaps most) have displayed in response to the pandemic during the past two years.
Aristotle wrote two books as a pair: Nicomachean Ethics and Politics. Nicomachean Ethics is mainly about personal virtues and the household and friends, while Politics is about civic life, public education, and sociality at the scale of the polis (the city-state). Virtuous citizens lead to a virtuous state, while a virtuous state (and government) promotes virtues in the population. And the virtues—wisdom, justice, moderation, honesty—are all supportive of a good life.
JEFFREY SACHS is the director of the Center for Sustainable Development at Columbia University.
K. K. Shailaja

The worst crisis of the century has underscored the need to reassess existing health systems and formulate an effective and socially equitable strategy to combat health crises in the future. It is imperative that governments continue to strengthen their public health systems and augment the capacity to treat more infections. Protecting the physical and mental health of frontline workers should be given priority. At times of crisis, it is equally vital to galvanize the trust of the community through engagement and transparency in dissemination of information. The right to health and protection of human rights in providing care should be upheld for one and all. An inclusive response to the pandemic must be aligned with the United Nations 2030 Agenda for Sustainable Development in order to ensure that no one is left behind.
The emergence and reemergence of new and old diseases and the public health aftereffects of natural disasters are unavoidable. Health policymakers should monitor and maintain a well-functioning disease surveillance system informed by the application of principles of epidemiology to help reduce the impact of future diseases and outbreaks. This proactive approach should be further complemented by preventive health care services, along with health workforce education and training in disease surveillance and public health actions. An integrated and collaborative One Health method needs to be promoted to share scientific and research data to tackle emerging challenges in global health and to attain optimal health for people, animals, and our environment.
K. K. SHAILAJA is the former health minister of Kerala, India.
Christian Happi
The world was not prepared to respond to the emergence of a new and deadly pathogen. With pathogens, we need to start playing offense and stop playing defense. Preventive measures must be put in place to ensure the health and wellness of citizens. This will require crucial investments in novel genomic tools and technologies for surveillance and real-time data capture and sharing.
Fortunately, we have seen the establishment of new health and wellness initiatives by private philanthropies, governments, and global health organizations, especially in the field of public health and outbreak preparedness. Examples of these initiatives include the World Health Organization’s Hub for Pandemic and Epidemic Intelligence and an early warning system program called SENTINEL that is being co-led by the African Center of Excellence for Genomics of Infectious Disease at Nigeria’s Redeemer’s University and the Broad Institute of Harvard and MIT.
The pandemic has also highlighted the importance of investing in basic and translational scientific research on infectious diseases, especially in Africa. Most pandemic-potential pathogens are found in Africa, which means that the continent could lead the world in the development of countermeasures and tools for preventing, detecting, and responding to outbreaks. But this has not been an investment priority for African leaders. As an example, if African countries had previously invested in vaccine research and development, they would not be waiting for vaccine donations.
Many countries on the continent also lack the local production capacity for biotechnology and the manufacture of medical supplies, drugs, and vaccines. This makes the continent vulnerable. Thankfully, we are seeing a renewed urgency toward investments in these sectors.
CHRISTIAN HAPPI is a professor of molecular biology and genomics and the director of the African Center of Excellence for Genomics of Infectious Diseases.

The pandemic has added to global inequalities—in 2020, it pushed 124 million more people into poverty—and revealed the topsy-turvy nature of an economy that undervalues its most essential workers while massively rewarding its financial elite. It has also shown how environmental misuse is implicated in lifestyle illness and the spread of pandemic disease. At the same time, the lockdown experience shed light on the benefits to health and well-being of adopting slower-paced and less acquisitive ways of living, and it allowed more citizenly feeling to come into play.
If there is a lesson to be learned here, it is that our collective health and well-being can be secured only through correcting the huge disparities of wealth and eco-privilege of the current world order. The more affluent nations must now promote a green renaissance founded upon an alternative politics of prosperity. There is an opportunity here to advance beyond a way of living that is not just bad for the planet and ourselves, but also in many respects self-denying and overly fixated on work and moneymaking at the expense of the enjoyment that comes with having more time, doing more things for oneself, traveling more slowly, and consuming less stuff.
Nations whose environmental footprint grossly exceeds the planet’s carrying capacity can no longer be aspirational models for the rest of the world. A cultural revolution along these lines will be comparable to the forms of social transformation and personal epiphany brought about through the feminist, anti-racist, and anti-colonial movements of recent history. It will not be easy to mount and will be fiercely opposed by those currently in power. But the gains it promises will be immense, and without them, the future is bleak for us all.
KATE SOPER is emeritus professor of philosophy at London Metropolitan University and author of Post-Growth Living: For an Alternative Hedonism.
María del Rocío Sáenz Madrigal

I am a doctor by training but served for four years in government as the minister of health for Costa Rica—the first woman to do so. Those years in government gave me a 360-degree view of how the health sector and public policy intersect. After I finished my term as minister and took some leave, I was called back to serve as the executive president of the Costa Rican Social Security Fund. That allowed me to see the health system from a different perspective. Serving in those positions fundamentally shaped my view that while regulation and the provision of services are extremely important, we cannot forget the role of people, populations, and the communities we serve. They must be at the center of decision-making.
I think there are three lessons the pandemic has taught us. The first is that it has deepened preexisting gaps—access gaps, income gaps, inequality gaps. These are all very evident. The second, which is related, is that you cannot have a sufficient response without greater equity. Equity not only in terms of health outcomes, but equity in how policies are designed and implemented. The third, which I think is extremely important, is the role of community and of primary health care—strengthening the services that are close to the population. Countries with stronger primary care health systems and greater penetration at the community level have without a doubt shown greater resilience during the pandemic.
MARÍA DEL ROCÍO SÁENZ MADRIGAL is a professor of health promotion at the University of Costa Rica.
Opinions expressed in articles and other materials are those of the authors; they do not necessarily reflect IMF policy.
You might also like
- Distribution Matters
- Financing Future Health Systems
- Life Post-COVID-19
- Overhauling Health Systems
Latest Issues
December 2023
September 2023

The Crucial Role of Healthcare in Society
This essay is about the importance of healthcare and its broad impact on society. It highlights how healthcare prevents and treats diseases, manages chronic conditions, and promotes overall well-being. Healthcare’s role in economic stability is emphasized, noting that a healthy population contributes to productivity and growth. The essay also discusses social equity, stressing that access to quality healthcare should be a right for all, helping to reduce disparities. It underscores the significance of healthcare in public health and safety, especially during pandemics, and the importance of mental health services. Additionally, the essay notes how healthcare drives innovation and research, leading to medical advancements.
How it works
Healthcare emerges as a foundational element of human existence, serving as a bedrock for individual wellness and societal progress. Its significance transcends the immediate imperative of addressing maladies or injuries; healthcare stands as a linchpin for fostering a robust populace, bolstering economic resilience, and upholding communal parity. Unraveling the essence of healthcare’s indispensability entails grasping its multifaceted influence on individuals and collectives alike.
At its essence, healthcare assumes paramount importance in averting and combating maladies. Routine medical screenings, inoculations, and health education constitute pivotal facets of a healthcare paradigm geared toward preempting ailments before they escalate.
Timely detection and management of diseases hold the potential to substantially curtail morbidity and mortality rates, thereby augmenting the overall well-being of communities. Notably, widespread immunization initiatives have vanquished or contained afflictions like smallpox and polio, underscoring the efficacy of proactive healthcare measures.
Beyond the purview of disease mitigation and management, healthcare assumes a pivotal mantle in addressing chronic ailments. With rising life expectancies, the prevalence of chronic maladies such as diabetes, cardiovascular ailments, and hypertension surges. Apt management of these conditions through pharmacotherapy, lifestyle modifications, and periodic surveillance stands poised to significantly enhance individuals’ quality of life while alleviating strains on healthcare infrastructures. In the absence of adequate healthcare provision, multitudes would endure needless suffering from ailments amenable to therapeutic intervention or preventive measures.
Moreover, healthcare serves as a linchpin for economic stability and advancement. A hale and hearty populace breeds heightened productivity, thereby propelling economic prosperity. Optimal health equips individuals to discharge their professional obligations with enhanced efficacy, curbing absenteeism and bolstering contributions to societal endeavors. Conversely, compromised health precipitates substantial economic ramifications, including productivity losses, spiraling healthcare outlays, and familial financial distress. Ergo, investments in healthcare transcend altruism, assuming the guise of strategic economic imperatives. Nations endowed with robust healthcare architectures invariably exhibit resilient economies, buoyed by citizenry empowered to unleash their full potential in the labor milieu.
Social equity constitutes yet another pivotal facet underpinning healthcare’s significance. Access to quality healthcare ought to be enshrined as an inalienable entitlement rather than a prerogative of privilege. Disparities in healthcare accessibility and outcomes possess the potential to exacerbate socioeconomic cleavages. Historically marginalized cohorts frequently encounter impediments to healthcare access, ranging from pecuniary constraints to logistical hurdles and discriminatory practices. Addressing these chasms through inclusive healthcare policies furnishes all individuals with the opportunity to pursue optimal health, irrespective of their socioeconomic strata. Equitable healthcare access, by leveling the playing field, bequeaths all denizens the opportunity to lead wholesome, productive lives.
Furthermore, healthcare stands as an arbiter of public health and safety. The scourge of epidemics and pandemics, epitomized by the COVID-19 pandemic, underscores the imperatives of a robust healthcare infrastructure adept at navigating public health exigencies. A resilient healthcare apparatus adept at managing and mitigating infectious disease dissemination stands as a bulwark shielding populace at large. Public health imperatives encompassing sanitation initiatives, vaccination drives, and health literacy campaigns assume salience in preserving communal health and staving off widespread health exigencies.
The psychological and emotional welfare of individuals constitutes yet another arena where healthcare exerts a transformative influence. Mental health services represent an indispensable facet of a comprehensive healthcare mosaic. Maladies such as depression, anxiety, and assorted psychiatric afflictions exact a profound toll on individuals’ well-being and functional capacities. Unfettered access to mental health provisions, spanning counseling, psychotherapy, and psychiatric interventions, undergirds individuals in attaining emotional equipoise and fortitude. The acknowledgment and redressal of mental health exigencies assume commensurate importance vis-à-vis their physical counterparts, thereby fortifying societal well-being holistically.
Additionally, healthcare catalyzes innovation and inquiry, propelling medical science to fresh frontiers. Unceasing endeavors in healthcare research and development yield novel therapeutics, technologies, and methodologies heralding superior patient outcomes. Pioneering strides in medical intervention beget lifesaving treatments and elevate life quality for innumerable individuals. A robust healthcare fabric buttresses ongoing research endeavors, guaranteeing the perpetuation of medical advancement in tackling nascent health quandaries.
In sum, healthcare stands as an indispensable linchpin for nurturing wholesome, thriving, and equitable societies. Its ramifications traverse individual health, economic robustness, societal equity, communal safety, and scientific ingenuity. By channeling resources into healthcare, societies invest in communal well-being and fortify the bedrock of their future trajectories. The vouchsafing of unfettered access to quality healthcare assumes not merely a moral prerogative but also a pragmatic necessity for fostering flourishing, resilient global milieus.
Cite this page
The Crucial Role of Healthcare in Society. (2024, May 21). Retrieved from https://papersowl.com/examples/the-crucial-role-of-healthcare-in-society/
"The Crucial Role of Healthcare in Society." PapersOwl.com , 21 May 2024, https://papersowl.com/examples/the-crucial-role-of-healthcare-in-society/
PapersOwl.com. (2024). The Crucial Role of Healthcare in Society . [Online]. Available at: https://papersowl.com/examples/the-crucial-role-of-healthcare-in-society/ [Accessed: 24 May. 2024]
"The Crucial Role of Healthcare in Society." PapersOwl.com, May 21, 2024. Accessed May 24, 2024. https://papersowl.com/examples/the-crucial-role-of-healthcare-in-society/
"The Crucial Role of Healthcare in Society," PapersOwl.com , 21-May-2024. [Online]. Available: https://papersowl.com/examples/the-crucial-role-of-healthcare-in-society/. [Accessed: 24-May-2024]
PapersOwl.com. (2024). The Crucial Role of Healthcare in Society . [Online]. Available at: https://papersowl.com/examples/the-crucial-role-of-healthcare-in-society/ [Accessed: 24-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
- HEAS Home div.mega__menu -->
- Why Health and Society?
- Learning Outcomes
- Minor Requirements
- Course Offerings
- Research Opportunities
- Ellen Carol Barreto Research Fellowship
- The Bioethics Hub at LMU
- The Center for Service & Action
- Upcoming Events
- Program Newsletters
- Contact div.mega__menu -->

What is Health and Society?
Health and illness are central aspects of human experience that are deeply shaped by cultural, political, and economic conditions. Health and Society is a cutting-edge area of interdisciplinary scholarship that examines the social drivers behind historic and contemporary patterns in health and disease. Scholars in the field take a critical approach to studying how societies define what it means to be healthy or sick, why some groups suffer disproportionate burdens of disease and premature death, how culture shapes the delivery of health care, and how individuals experience illness in their everyday lives. The curriculum of the Health and Society minor employs a variety of disciplinary lenses to examine these areas, providing students with the ability to critically engage with and formulate solutions to some of today’s most pressing health problems.
What Do Health and Society Minors Do?
The highly interdisciplinary curriculum is designed to equip students to pursue thoughtful and ethically engaged careers in medicine, public health, health policy, health advocacy, and related fields. Students take five courses beginning with Introduction to Health and Society. This course introduces students to important conceptual frameworks in Health and Society and prepares them for interdisciplinary coursework. Students select the remaining four courses based on their interests from a list of approved courses offered through departments and programs including Bioethics, Biology, Health and Human Sciences, History, Film and Television Studies, Psychology, Sociology, and Women and Gender Studies.
Is This Minor Right for You?
If you are interested in people and how health is shaped by culture and the organization of society, then Health and Society might be the right minor for you. The minor is especially well suited to “prehealth” students who are interested in broadening their knowledge and deepening their skillset before pursuing medical school or other health sciences degrees. It is equally appropriate for students in the liberal arts seeking preparation for careers in public health, health policy, and health advocacy.
Our goal is for students to be transformed by the curriculum through developing new skills and a new awareness of the connections between the physical and social foundations of health. Health and Society students gain key competencies in how social forces (e.g., culture, policies, racism, and class structures) shape health, in specific historic and current efforts to improve the health of populations, and in how to gather and analyze information related to health topics. They also gain the ability to engage in rigorous and thoughtful interdisciplinary scholarship.
The following topics are addressed in the minor:
- Health disparities and health justice
- History of medicine and disease
- Healthcare financing and organization
- Media representations of the body, health, and disease
- Gender and health
- Health advocacy and community organizing
- Ethical principles that shape clinical practices
- Cultural constructions of health and illness
- Individual experiences of health and illness
- Patient-provider communication
- Interventions aimed at reducing suffering and disease
About Our Faculty
Our faculty members come from a variety of disciplinary backgrounds, but share the scholarly goal of situating health, disease, and the body in social, cultural, and historic contexts. We seek to promote research and/or creative activities that advance our understanding of the ways in which social forces shape health and disease. All of the faculty participating in the minor are engaged scholars with active research agendas on a variety of topics related to health and disease. Our faculty publish their findings in a range of venues and frequently present their research at conferences and invited talks in their areas of expertise.
About Our Students and Graduates
Students minoring in Health and Society come from a variety of disciplines across the university but are bound by a shared interest in approaching health and disease through an innovative and interdisciplinary lens. Our students strive to live “lives of meaning and purpose” and express a deep curiosity about the under-appreciated social drivers of health and disease. Many of our students seek to apply the skills they gain through the Health and Society minor to careers in medicine, nursing, public health, health policy, law, health advocacy, and other related fields.
Representative Courses
Courses that fulfill the Health and Society Minor include the following:
- Epidemics and Infectious Diseases
- Introduction to Bioethics
- Communication and Healthcare
- Public Health
- Science, Nature & Society in the West
- Health and Disease in American Culture
- Poverty and Community Resilience
- Science, Medicine, and Media
- Sociology of Health and Illness
- Sociology of Aging
- Health and Social Justice
- Drugs and Society
- Community Psychology
- Women, Health, Bodies, and Sexualities
- Health Services for Marginalized Populations
More Resources
- St. Joseph Health
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Lippincott Open Access
Practice Full Report
Promoting health and well-being in healthy people 2030, associated data.
Supplemental Digital Content is Available in the Text.
Healthy People 2030 describes a vision and offers benchmarks that can be used to track progress toward the goal of all people in the United States achieving their full potential for health and well-being across the life span. This vision can be realized through evidence-based interventions and policies that address the economic, physical, and social environments in which people live, learn, work, and play. Securing health and well-being for all will benefit society as a whole. Gaining such benefits requires eliminating health disparities, achieving health equity, attaining health literacy, and strengthening the physical, social, and economic environments. Implementation of Healthy People 2030 will by strengthened by engaging users from many sectors and ensuring the effective use and alignment of resources. Promoting the nation's health and well-being is a shared responsibility—at the national, state, territorial, tribal, and community levels. It requires involving the public, private, and not-for-profit sectors.
Healthy People provides science-based national objectives with 10-year targets for improving the health of the nation. Healthy People 2030—the fifth edition of the Healthy People initiative—describes a vision and offers benchmarks that can be used to track progress toward the goal of helping all people in the United States achieve their full potential for health and well-being across the life span. Healthy People 2030 expresses an expanded focus on health and well-being and an understanding that health and well-being for all people is a shared responsibility. This vision can be achieved through evidence-based interventions and policies that address the economic, physical, and social environments in which people are born, live, learn, work, play, worship, and age. High-quality data that are accurate, timely, and accessible are required to record and report on progress 1 over the course of the decade and to direct interventions to populations that are most likely to benefit from them.
Healthy People sets the federal agenda for the nation's health, guides its direction and allocation of resources, informs federal data collection and programmatic activities, and provides a model for promoting health and well-being at the state and local levels. The initiative's emphasis on promoting health and well-being signals to the nation that it is time to work across sectors to achieve health equity. This decade Healthy People 2030 is a resource for all sectors.
As part of the development of Healthy People 2030, the US Department of Health and Human Services (HHS) sought guidance from the Secretary's Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2030 (Secretary's Advisory Committee), a federal advisory committee composed of nonfederal, independent subject matter experts. The Secretary's Advisory Committee presented recommendations to the HHS Secretary for developing and implementing the objectives for 2030. The Secretary's Advisory Committee convened regularly between December 2016 and September 2019, with meetings open to the public.
Health promotion has been a cornerstone of the Healthy People initiative since its inception in 1979. The Secretary's Advisory Committee recommended that the focus of Healthy People 2030 expand beyond health promotion to the broader purpose of promoting “health and well-being.” The process that has been called health promotion no longer focuses on health alone, but now leads to health and well-being for individuals in addition to society as a whole. This offers a chance to balance the needs of individuals and society. Society is defined as “a voluntary association of individuals for common ends.” 2 Health and well-being are elements among the common ends that motivate us, as individuals, to act for the good of all. In return for participating in society, individuals expect fair and just opportunities to be as healthy and well as possible. This article provides insights into defining health and well-being, promoting health and well-being, fostering user collaboration to improve health and well-being, and measuring health and well-being, in addition to implications for policy and practice.
The Secretary's Advisory Committee produced 2 detailed briefs that offered guidance for promoting health and well-being. Secretary's Advisory Committee members, joined by additional subject matter experts, developed these 2 briefs. The original documents are available on the HealthyPeople.gov Web site. 3 , 4
Defining Health and Well-being
Healthy People 2030 refers to health and well-being in every aspect of the framework, including the vision, mission, foundational principles, plan of action, and overarching goals. 5 The expanded role for health and well-being in Healthy People 2030 was supported by the Secretary's Advisory Committee's recommendations and its definition of health and well-being as how people think, feel, and function—at a personal and social level—and how they evaluate their lives as a whole. 6 How people think, feel, and function affects their beliefs about whether their lives have meaning and purpose 7 , 8 (Table (Table1). 1 ). This definition recognizes the multilevel nature of health and well-being. It acknowledges that social structures, such as families, neighborhoods, communities, organizations, institutions, policies, economies, societies, cultures, and physical environments, strongly influence health and well-being. Such influence is reciprocal between individual, social, and societal health and well-being. *
The terms “health” and “well-being” describe separate but related states; health influences well-being and, conversely, well-being affects health. 9 Health incorporates both physical and mental conditions; it implies fitness under changing circumstances, such as degradation of the physical, social, or economic environments, and must be safeguarded against threats from illness, injury, or death. Safety, as a result, is an important determinant of health. Well-being is both a determinant and an outcome of health. 10 It encompasses objective and subjective elements and reflects many aspects of life and states of being. These include physical and mental, as well as emotional, social, financial, occupational, intellectual, and spiritual, elements. 11 The terms apply to individuals as well as to groups of people (eg, families, communities) and environments (eg, physical, social, economic).
The World Health Organization defines health promotion as:
The process of enabling people to increase control over, and to improve, their health. 12 Health promotion ... covers a wide range of social and environmental interventions that are designed to benefit and protect individual people's health and quality of life by addressing and preventing the root causes of ill health, not just focusing on treatment and cure. 12
The World Health Organization identifies 3 key elements for health promotion: good governance for health; health literacy; and healthy cities. Adding the concept of well-being to this definition emphasizes that promotion of health and well-being takes place across different environments and users.
Promoting Health and Well-being
The concept of promoting health and well-being at both personal and systems levels has evolved over history, starting with ancient and classical civilizations. 13 Policy strategies for promoting health have been proposed since the 1970s. 14 More than 3 decades ago, the Ottawa Charter for Health Promotion described health as a “resource for everyday life, not the objective of living.” It noted that prerequisites for health include “peace, shelter, education, food, income, a stable ecosystem, sustainable resources, social justice, and equity.” 15 This guidance remains relevant today. Promoting well-being requires engaging an expanded and diverse array of users, disciplines, and sectors that extend beyond public health, such as mental health, housing, childcare/education, business, and aging.
Interventions to promote health and well-being occur at the individual, site-specific community, and societal levels. They address economic, social, and physical environmental and political factors (“determinants of health”) that influence health and well-being. Promoting health and well-being is critical because determinants of health—the physical, social, and economic circumstances in which people are born, live, learn, work, play, worship, and age—have disparate effects on vulnerable populations. These factors interact to affect people disproportionately based on race and class. All sectors are needed to remedy such disparities and achieve health equity.
At the individual level, interventions to promote health and well-being might focus on health behaviors, employment, housing, food security, or childcare. These interventions also would apply to the community level since they target settings where people spend their time, including home, school, work, or places where they socialize such as community centers and parks. These interventions can address designs of the built environment for ease of access and to ensure safety. The Robert Wood Johnson Foundation's Culture of Health initiative is one such national model. The Foundation defines a culture of health as one in which “good health and well-being flourish across geographic, demographic, and social sectors; fostering healthy equitable communities guides public and private decision making; and everyone has the opportunity to make choices that lead to healthy lifestyles.” 16
The concept of promoting health and well-being has evolved over the decades (Figure). Health and well-being operate on more than 1 level. Broader conditions shape individual experiences of health and well-being, and organized efforts can influence those conditions. Social structures, such as families, neighborhoods and communities, and policies, economies, and cultures also play important roles. 17 – 21

How the Concept of Health Promotion Has Evolved Over Decades of Healthy People
Engaging users from many sectors and ensuring the effective use and alignment of resources will strengthen implementation of Healthy People 2030. To promote health and well-being for all people and foster equity and social justice, socioecological factors and determinants of health must be addressed at all levels. A dynamic mix of resources will be needed for long-term improvements to livability (eg, stable housing, healthy food, clean air, education, living wage jobs) and for urgent needs (eg, acute care for illness or injury, food assistance, shelter, addiction treatment, disaster relief). Such resources will need to address a more diverse range of factors than in the past.
All too often, communities and institutions function in a reactive and responsive mode, deferring or delaying long-term investments. This way of functioning generates persistent needs for urgent services, along with pressure to maintain them. Collaborative decision-making across sectors can optimize the positive impact of resources and reduce the number of crises that happen in the first place. Identifying evidence-based programs to promote health and well-being among users can serve common interests, help users expand their thinking about solutions, and set priorities for limited time, money, and other scarce resources.
Multisectoral Collaborations to Improve Health and Well-being
Achieving population-level improvements in the coming decade will require users working at all levels to function across sectors and establish or participate in multisectoral collaborations. Such efforts can improve outcomes—not only in the health sector but also in nonpublic health or health care sectors, such as education, economics, the environment, and social cohesion. Collaboration among various users groups can benefit all partners by creating win-win solutions that recognize the interrelatedness of population health status with factors that lie outside the health care and public health systems.
Achieving optimal health and well-being requires efforts that include partners from different sectors, who operate at multiple levels (eg, state, local, community) and address the circumstances of people's lives. † Such efforts could span the behavioral, psychosocial, socioeconomic, cultural, and political circumstances of the population. No single actor has sole ownership of, accountability for, or capacity to sustain the health and well-being of an entire population. 22 – 24 The 10 “causes of the causes” of poor health comprise psychological influences (eg, social gradient, stress, and social exclusion), as well as elements of community infrastructure, such as food and transportation. 25 Thus, success depends on strengthening the capacity of communities to cocreate their own futures. 26
The COVID-19 pandemic is a case study of the reciprocal, complex relationships between the health of individuals and the health of society as a whole, as well as the resulting unintended consequences. An individual's decision not to wear a mask at a grocery store or other indoor gathering place can result in the virus' spread to other people who are present. Defining some workers as essential and required to work, such as those who work in grocery stores, transportation, health care, and in other occupations that require interaction with the public, increases the risk of infection for many low-wage earners. When essential workers are compensated with low wages, lack of financial viability creates challenges to their overall health and well-being. When health insurance is tied to employment and unemployment is soaring, unemployed people often delay seeking care. When older adults stay in isolation to avoid the possibility of infection, they can experience loneliness, depression, and mental health issues. When schools are closed and children stay at home, those who lack Internet connectivity are at risk of falling behind in their schoolwork. Those who receive free school lunches may go hungry.
To help local health departments identify strategies for promoting population health and well-being and addressing determinants of health, the National Association of County and City Health Officials (NACCHO) identified 9 domains of determinants, 27 as well as data sources for each (Table (Table2). 2 ). Healthy People users at the state and tribal levels may find NACCHO's domains and data sources useful for identifying and acting upon opportunities to improve and monitor measures of health and well-being. These include indicators that are important to the success of other sectors, such as high school graduation, crime reduction, and economic prosperity.
Measuring Health and Well-being
Monitoring and documenting changes to the population's health and well-being will require the use of new data sources and types of measures. The way people evaluate their own lives as a whole is one indicator of health and well-being. Yet, systems that are outside of an individual's control shape the exposures, choices, and services that people experience. An important distinction exists between individuals' subjective ratings of their own health and well-being and the objective conditions that surround and support people as they strive to improve their health and well-being.
Measures of progress that go beyond those specific to public health and health care settings will require tapping into existing data sources across other domains and sectors. For example, data used by agricultural extension offices, planning departments at all levels, schools, businesses, parks and recreation agencies, transportation systems, the Bureau of the Census, aging services, and the financial sector, among others, can inform health and well-being. Data partnerships between public health, health care settings, and other sectors can often benefit collaborators by providing a much richer source of information for each partner as well as for the entire partnership. 28
Healthy People 2020 used functional measures, including Healthy Life Expectancy, ‡ Summary Mortality and Population Health, § and Disparities, as global health measures for assessing progress. Earlier iterations of Healthy People used life expectancy and other measures. ∥ Holistic evaluations of health and well-being status of individuals, communities, and systems require broad measures, such as life satisfaction or social cohesion. 29 – 33 Assessing progress toward improved health and well-being must consider health disparities, health literacy, multisectoral policies, and determinants of health and well-being.
Realizing the potential of Healthy People 2030 will require accurate data from credible sources at all levels, with a renewed emphasis on local action. There are barriers to generating high-quality data (eg, funding, staffing, technology). Healthy People supports local action by providing guidance for consistent data collection methods and measures, as well as examples of best practices and innovations. A data partnership infrastructure and network focused on Healthy People objectives could address and respond to new developments in data sources and data analytics. For example, a data partnership could expand the availability of locally relevant data, stimulate access to new data sources to measure determinants of health and health equity, and enable linkage of geographic and demographic data in presentation formats for Healthy People users.
Partners would be able to share data, methods, and analyses and access guidance on data developments relevant to all 3 Healthy People objective types—core, developmental, and research. A data partnership infrastructure and network that links national, tribal, state, territorial, and local data through partnerships and collaborations could enhance the nation's capacity to identify and record the achievement of Healthy People objectives and overarching goals.
Healthy People 2030 continues the Healthy People initiative's tradition of serving as a catalyst for action by expanding the focus of health promotion to promoting health and well-being (see Supplemental Digital Content file, available at http://links.lww.com/JPHMP/A716 ). This emphasizes the need to shift from a disease-specific orientation to more upstream policy efforts. Healthy People 2030 offers data, objectives, and tools for creating well-being and a healthier nation. Realizing the potential of Healthy People 2030 will require the active involvement of a variety of public and private institutions and organizations, including national, tribal, state, territorial, and local health departments. Health departments at all levels can contribute to this work by engaging multiple sectors in the implementation and monitoring of objectives.
Discussions within the public health community, and between public health and other sectors, around defining health and well-being offer opportunities to engage partners that historically have not been involved in Healthy People. Engaging new partners in the Healthy People initiative will require those who traditionally have led the initiative to understand what those partners need to succeed, communicate how new partners' goals complement those of Healthy People, and convey how engaging with Healthy People can benefit the new partners. For example, partnering to improve high school graduation rates benefits the education and public health sectors, as well as the financial sector and potentially the criminal justice system. Accomplishing that goal might involve engaging with the telecommunications sector to support students' access to affordable Internet service. By engaging in such partnerships, everyone would become more familiar with the goals of other sectors and discover more win-win opportunities.
In their health improvement plans, public health departments at all levels should think broadly about which partners from other sectors could help them advance health and well-being goals, while considering what public health can offer those sectors in achieving their own goals. For example, in Maryland, each county has been charged with having a local health improvement coalition that brings together key users to achieve locally identified needs for health and well-being and to eliminate health disparities. Organizations and individuals often need to see value for investing their time and resources before they agree to participate. Involving partners early allows them to be part of identifying issues and finding solutions.
Open access data portals at the state level are proliferating and can inform decision makers as well as the public. These data portals and related data dashboards provide community leaders and residents with current geographically tracked data and tools that support assessments and linkages to evidence-based interventions. These data initiatives offer yet another opportunity for partners to convene and develop collaborative programs for their respective populations.
One of Healthy People 2030's foundational principles is that “the health and well-being of all people and communities are essential to a thriving, equitable society.” Achieving health and well-being for all will benefit society as a whole. Achieving such benefits requires eliminating health disparities, achieving health equity, attaining health literacy, and strengthening the physical, social, and economic environments. Promoting the nation's health and well-being is a shared responsibility—at the national, state, territorial, tribal, and community levels. By enlisting the involvement of the public, private, and not-for-profit sectors in efforts to promote the health and well-being of our populations, we will improve the health of the nation and the achievement of Healthy People 2030's targets.
Implications for Policy & Practice
- Across the field of public health, the focus on health promotion should be expanded to include health and well-being.
- No one sector has the ability, responsibility, or needed expertise to promote health and well-being for all. Multisectoral approaches are needed to address the social, economic, and physical determinants of health and well-being.
- It will be critical to identify common data sources and indicators that can be used to measure and evaluate trends in health and well-being.
Supplementary Material
* Other definitions exist of the terms “health” and “well-being,” respectively. This is the definition proposed for Healthy People 2030, and it considers “health and well-being” as a single term.
† In the coming decade, Healthy People 2030 will highlight innovative and successful state- and local-level efforts through HealthyPeople.gov, webinars, and other channels.
‡ Healthy Life Expectancy (HLE) includes the following: HLE free from activity limitations at birth/age 65 years; HLE free from disability at birth/age 65 years; HLE in good or better health at birth/age 65 years.
§ Summary Mortality and Population Health includes the following: life expectancy at birth/age 65 years; any activity limitation at birth/age 65 years; any disability at birth/age 65 years; percentage in fair or poor health at birth/age 65 years.
∥ Healthy People 2010 used Life Expectancy, Healthy Life Expectancy, and Disparities. Healthy People 2000 used Years of Healthy Life; Disparities; and Clinical Preventive Services.
This article is based on 2 briefs that were prepared by the Secretary's Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2030 and are available online at HealthyPeople.gov . The authors acknowledge and thank the following contributors to these original briefs: Tom Kottke, MD, MSPH; Bobby Milstein, PhD, MPH; Rebecca Rossom, MD, MSCR; Matt Stiefel, MPA, MS; and Elaine Auld, MPH, MCHES.
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's Web site ( http://www.JPHMP.com ).
Essay on Health for Students and Children
500+ words essay on health.
Essay on Health: Health was earlier said to be the ability of the body functioning well. However, as time evolved, the definition of health also evolved. It cannot be stressed enough that health is the primary thing after which everything else follows. When you maintain good health , everything else falls into place.

Similarly, maintaining good health is dependent on a lot of factors. It ranges from the air you breathe to the type of people you choose to spend your time with. Health has a lot of components that carry equal importance. If even one of them is missing, a person cannot be completely healthy.
Constituents of Good Health
First, we have our physical health. This means being fit physically and in the absence of any kind of disease or illness . When you have good physical health, you will have a longer life span. One may maintain their physical health by having a balanced diet . Do not miss out on the essential nutrients; take each of them in appropriate quantities.
Secondly, you must exercise daily. It may be for ten minutes only but never miss it. It will help your body maintain physical fitness. Moreover, do not consume junk food all the time. Do not smoke or drink as it has serious harmful consequences. Lastly, try to take adequate sleep regularly instead of using your phone.
Next, we talk about our mental health . Mental health refers to the psychological and emotional well-being of a person. The mental health of a person impacts their feelings and way of handling situations. We must maintain our mental health by being positive and meditating.
Subsequently, social health and cognitive health are equally important for the overall well-being of a person. A person can maintain their social health when they effectively communicate well with others. Moreover, when a person us friendly and attends social gatherings, he will definitely have good social health. Similarly, our cognitive health refers to performing mental processes effectively. To do that well, one must always eat healthily and play brain games like Chess, puzzles and more to sharpen the brain.
Get the huge list of more than 500 Essay Topics and Ideas
Physical Health Alone is Not Everything
There is this stigma that surrounds mental health. People do not take mental illnesses seriously. To be completely fit, one must also be mentally fit. When people completely discredit mental illnesses, it creates a negative impact.
For instance, you never tell a person with cancer to get over it and that it’s all in their head in comparison to someone dealing with depression . Similarly, we should treat mental health the same as physical health.
Parents always take care of their children’s physical needs. They feed them with nutritious foods and always dress up their wounds immediately. However, they fail to notice the deteriorating mental health of their child. Mostly so, because they do not give it that much importance. It is due to a lack of awareness amongst people. Even amongst adults, you never know what a person is going through mentally.
Thus, we need to be able to recognize the signs of mental illnesses . A laughing person does not equal a happy person. We must not consider mental illnesses as a taboo and give it the attention it deserves to save people’s lives.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

- Content Guidelines
- Privacy Policy
Receive your Favorite Topics right in your Inbox.
Essay on sociology and health (the best one) | sociology.
ADVERTISEMENTS:
Sociology and Health Essay – This is one of the best essays on ‘Sociology and Health’ especially written for school and college students.
Essay on Sociology and Health
Essay Contents:
- Essay on Social Deviance
ADVERTISEMENTS: (adsbygoogle = window.adsbygoogle || []).push({}); 1. Essay on Introduction to Sociology and Health:
Man is a gregarious animal, he likes to live in society and each individual influences the others and also the environment. Sociology—the science of society, or science of social processes, or the behaviour of men in groups—studies the interaction of its type that seems to result from contact between human individuals.
Medicine and Social Sciences are concerned in their own special way with human behavior. It seeks illness behavior of people which has intervention in community health, clinical medicine and epidemiology.
(A) Epidemiology:
Disease is studied in relationship to such factors like social status, income, occupation, housing, overcrowding, social customs, habits and behavior.
(B) Community Medicine:
Health care services and community health programme are having strong bearing with belief, custom, tradition, attitude, knowledge and practices, e.g., social barriers in acceptance of Universal Immunisation Programme, Family Planning, improvement of sanitation and dietary patterns.
(C) Clinical Medicine:
Illness behaviour is studied under medical sociology, psychophysiological stress reactions are involved in cases of rheumatic arthritis, ulceration, hypertension, constipation, peptic ulcer, angina and diabetes. It also includes doctor-patient relationship, patient care management, hospital organisation and cultural practices.
2. Essay on the Types of Social Sciences:
a. Economics:
It deals with human relationship in production, scarce resources, services and allocation of money for the programme.
b. Political Science:
It is concerned with the study of the system of laws and institutions.
c. Sociology:
It deals with the study of Human relationships and Human behavior for a better understanding of patterns of human life.
d. Social Psychology:
It deals with psychology of individuals living in human society or groups. It includes opinion, attitudes, general motivation and basis of perception.
e. Anthropology:
It is study of the physical, social and cultural history of man.
(a) Physical anthropology.
(b) Social anthropology.
(c) Cultural anthropology.
(d) Medical anthropology.
3. Essay on Social Organization :
The groups of people needed for different purposes known as social organization:
This is the basic unit of the society. It is a group of biologically related individuals living together and eating from a common kitchen.
2. Religion and Caste:
Religion and caste are forms of social organization which govern groups of people by certain rules and sanctions related to endogamy, food taboos, ritual purity etc.
3. Temporary Social Groups :
It is aggregate of human beings with a common focus of attention. It automatically goes out when common focus of attention disappears, e.g. viewers of cricket match.
It is aggregation of people in positive action usually motivated by joy or anger and having a leader and a symbol in the shape of slogan. Mob is more emotional than a crowd.
(iii) Herd:
It is also aggregation of people with a leader but no strong emotional motivation. Here all focus to the directions of the leader and to the goal at hand and certain amount of social interaction plays in it, e.g. tourist with guide.
(iv) Audience:
It is also group of people with the least amount of inter-stimulation between individuals but having the common interest in the performer on the stage.
4. Permanent Social Groups :
It consist of number of families, group attached to an area from which it draws its substances by gathering, hunting and fishing etc.
(ii) Village:
Collection of people permanently settled in a locality with their homes and cultural equipment’s. There are farming, non-farming, industrial and suburban villages.
(iii) Tribe:
By fission a group of bands is formed into a large unit which the sociologists term a tribe.
(iv) Towns & Cities:
It is relatively large, dense and permanent settlement of socially heterogeneous individuals when population exceeds more than 1 lac known as city.
(v) Metropolitan:
Big, dense and permanent settlement of heterogeneous persons of more that 10 lac population known as metropolitan.
(vi) State:
It is an ecological Social Group based on territory. It is more stabilized of heterogeneous groups of people.
5. Government and Political Organization :
(i) Democracy:
‘Government by the people of the people for the people’, e.g., India, USA.
(ii) Autocracy:
Ruler is absolute in power, e.g. Jordan.
(iii) Monarchy:
Head of State is Monarch, e.g., UK.
(iv) Socialistic:
Production is owned and controlled by state, e.g., China and Cuba.
(v) Oligarchy:
The country is ruled by a family group, e.g., Thailand, Saudi Arabia.
4. Essay on Family and Its Types :
The family is a primary unit in all societies. It is a group of biologically related individuals living together and eating from a common kitchen. Household members are not blood-related, e.g., servants. Family is representative of biological unit, social unit, cultural unit, epidemiological unit and unit for providing social services.
Types of Families:
a. Nuclear Families or Elementary Families:
It includes married couples and their children where children are regarded as dependents. They occupy same dwelling house.
b. New Families :
It is applied to those under 10 year duration and consist of parents and children.
c. Joint Families or Extended Families :
It consists of a number of married couples and their children who live together in the same household.
All the men are related by blood and women of household are their wives, unmarried girls and widows of the family kinsmen.
All the property held in common and a common family purse.
All the authority is vested in the senior male member of the family.
d. Three Generation Family :
When couple lives with parents and the couple have their children—hence three generations living together.
5. Essay on Cultural Factors Effecting Health :
Transmission of behaviour by learning from one generation to another is called culture. Talor defines “culture is that complex whole which included knowledge, belief, art, morals, law, custom and other capabilities acquired by man as a member of society”.
a. Customs :
It arose from the impelling force of need which lead to efforts and certain course of action thus habits, routine and skills were developed and were practiced by the entire group. The way then turned into customs and became phenomenon of mass population.
b. Folkways :
Ways of acting which are common to a society on a group and which are handed down from one generation to another are known as folkways.
Mores are common ways of acting which are regarded as proper and right than folkways. When man is walking on the left side of road accompanying a woman is a folkway but a man marrying a woman after he has seduced her is a more.
Common mores customs are recognised by Sovereignty/Government are known as law.
e. Tradition :
When knowledge as part of culture is handed down orally from generation to generation and practiced in the group of people it is known as tradition.
f. Belief :
It is customary faith and confidence and practiced by the group of people as truth, e.g.. People believe in supernatural powers of some kind.
g. Religion:
It is characterised by a belief in and an emotional attitude towards some super-natural being.
h. Superstition:
Formal mode of behaviour and faith in supernatural power and act accordingly without arguments.
6. Essay on Causation and Prevention of Diseases:
a. Causation of Disease:
(i) Breach of Taboo :
Venereal diseases are believed by some due to illicit sexual intercourse with a woman of low caste or woman during menses.
(ii) Past Sins :
Leprosy is caused by sins.
(iii) Evil Eye :
Children are very much susceptible from evil eye.
(iv) Wrath of Gods and Goddesses :
Smallpox and chickenpox known as Bari Mata & Chhoti Mata—Pujas are made for them.
(v) Ghost Intrusion :
Hysteria and epilepsy are sought due to ghost or spirit.
(vi) Impure Blood :
Boils and scabies are considered due to impure blood.
b. Food Habits :
(i) Vegetarianism and Non-Vegetarianism :
Jain and Higher Caste traditional Hindus do not eat meat and eggs. Muslims do not eat pork. Non-Veg. Hindus do not eat cow-meat.
(ii) Cold Food and Hot Food :
Curd, Radish considered Cold food can cause cold, coryza and rhinitis. Jaggery, Eggs, Cashew nuts and dates are considered hot food; can cause bleeding through nose and skin rashes.
(iii) Papaya is not Eaten by Pregnant Lady:
It is considered that Papaya initiates pregnant abortion.
c. Environmental Sanitation :
(i) More than 95% people in rural areas are habituated for open area defecation.
(ii) Disposal of wastes is done nearby residence causing insect nuisance.
(iii) Rural houses are kutehan and damp, ill- lighted and ill-ventilated.
d. Personal Hygiene :
(i) Indian is very particular for using of twig of Neem for oral hygiene.
(ii) Bathing:
Few groups of society are very particular in bathing.
(iii) Smoking:
Smoking is very common in Indian communities. It includes bidis, Hubble-bubble, cigarette and cigar.
(iv) People in rural area moving bare feet causing hookworm infestation.
7. Essay on Social Classification—Need for Constant Updating:
Socio-economic status influences the health of individuals and also the utilization of available health facilities. Of several available parameters, such as income, occupation, education, religion, caste, place of residence etc., the per capita monthly income has been the basis of the Prasad’s Social Classifications which is most commonly used in Indian studies.
With inflationary trends of the economy this classification needs constant revision. An attempt has been made to link it with the all India Consumer Pride Index (AICP) and a modified classification has been proposed with a built-in provision of its updating from time to time to keep it relevant and useful.
8. Essay on Social Elastification: Consumer Price Index (CPI):
Social scientists the world over have considered occupation as the most important determinant of the level of social standing of an individual in society. The classification of the British Registrar General, which has been tried in Indian studies too, is based on occupation.
Prasad’s Classification was further modified in 1968(3) and 1970 is based on per capita monthly income. Kuppuswamy’s (1976) classification takes into account all the three characteristics (occupation, income and education) but its utility is restricted in urban population only.
So far Prasad’s classifications have been quite effective in their task. But with the passage of time and inflationary trends of the economy, the original income limits set in these classifications have become substantially low and impractical. In order to solve this problem, what was needed was an hypothetical value of CIP in relation of 1960-61 so that the original classification can still be used with necessary modifications.
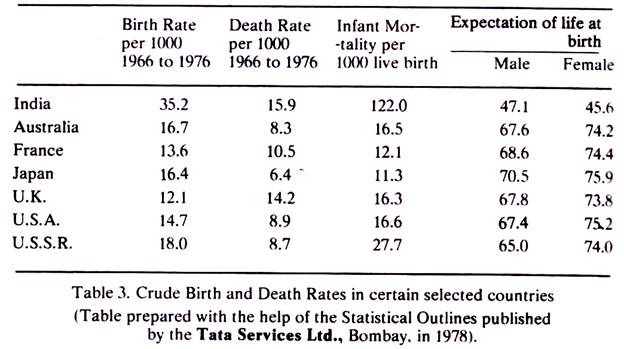
By deriving a multiplication factor of 4.93 which transforms current values of CPI (base year 1981-82) into a hypothetical value of CPI in relation to the base year 1960-61.
Therefore, the multiplication factor will be:
= Value of CPI x 4.93/100
The next step is to multiply the income limits with this factor and round them off to the nearest ten rupees. Income limits thus obtained, are for more practical and realistic. For example, to compute a social classification for March 1991, the multiplication factor will be
= 588 x 4.93/100
…. 28.99 or 29
588 = AICPI for March 2007 (8)
Prefer give for Jan. 2009
The proposed classification for this period is given in above table. It can be derived for any period by referring AICPI (All India Consumer Price Index) of same period.
9. Essay on Social Sciences Dealing with Human Behaviour:
a. Sociology:
i. Deals with the study of society, social interactions and social institutions and organisations.
ii. Its related social sciences are history, political sciences, economics and geography.
iii. Benefits significantly from cultural anthropology and social psychology studies the behaviour of individuals in social groups.
iv. Analyses social processes determining group behaviour.
b. Anthropology:
i. Deals with the study of the primitive man.
ii. Its branches are physical anthropology, social anthropology, cultural anthropology and medical anthropology.
iii. Cultural anthropology provides an in-depth understanding of human culture right from priimitive times.
iv. Traces the origin, growth and development of human culture and behaviour from historical roots.
c. Psychology:
i. Deals with the study of the human mind.
ii. Its branches are social psychology educational psychology, industrial psychology, clinical psychology and child psychology.
iii. Social psychology deals with collective behaviour of individuals.
iv. Analyses mental processes determining the behaviour of individuals.
10. Essay on Social Constraints:
a. Poverty and Destitution:
i. Problem Statement:
Poverty is a relative condition opposed to richness. It denotes poor economic status in relation to others. Destitution is a state of abject poverty, a state of extreme deprivation.
ii. Problem Outcome:
Poverty-striken families are condemned to poor housing, insanitary surrounding, underfeeding, undernutrition, illiteracy and ignorance. Destitute families are not even able to obtain minimum quantity or food for survival. Poverty and destitution are associated with high morbidity, high mortality and high fertility rates.
iii. Problem Management:
Poverty can be managed by people-friendly government by introducing a balanced national development based on distributive justice with preferential consideration for the poorest of the poor.
Poverty alleviation, employment generation, vocation-oriented education and family planning are quite useful approaches.
b. Illiteracy and Ignorance:
A person is considered illiterate if he cannot read and wirte. Ignorance is a wider concept, which can affect literate as well as illiterate individuals.
Ignorance and illiteracy contribute significantly to morbidity, mortality and population overgrowth. Ignorance and illiteracy of people make them resist public health measures, refuse education and avoid health care facilities available to them.
Only education can eliminate illiteracy and ignorance. Non-formal education, basic compulsory education and vocation oriented education are useful approaches. Relevant legislation and motivation can play a supportive role.
c. Migration and Environmental Crisis:
Population migration may be rural-urban or rural-rural; both forms lead to environmental crisis.
Migration results in environmental insanitation and environmental degradation which threaten the health and well-being of the local population, but migrants are the worst sufferers. Besides suffering from environmental diseases they are also exposed to traffic hazards and sexual evils of various kinds.
Can be managed through programmes that can generate employment opportunities for the agricultural labourers and marginal farmers. Public awareness programmes on the undesirable consequences of environmental insanitation and environmental degeneration can prepare the ground.
d. Industrialisation and Urbanisation:
Industrialisation provides the necessary basis for socioeconomic development all over the world. It generates huge demand for man-power necessitating migration of young population from rural areas which accelerate the pace of urbanisation.
Reckless industrialisation increases the magnitude of public health problems through environmental and migration of pollution. Industrial workers as well as the local population are exposed to industrial and environmental diseases and also to social evils of multiple kinds’ origination from migrant workers.
Can be managed by enactment of laws and their enforcement to guide the growth and development of industries on scientific lines and to prevent environmental pollution. Health education and public awareness on ill effect of industrialisation and slum proliferation can facilitate the legal effort.
11. Essay on Compartments of Social Environment:
i. Differentiating Features of Socio-Cultural Environment:
a. Represented by- Cultural milieu of people and their way of life
b. Reflected in- Traits mores, fashions and folkways of people.
c. Positive Impact- A healthy socio-cultural environment to promote community health through healthy belief, customs and traditions.
d. Negative Impact- An unhealthy socio-cultural environment undermines community health through unhealthy beliefs, customs and traditions.
ii. Differentiating Features of Socio-Economic Environment:
a. Represented by- Economic milieu of people and their quality of life.
b. Reflected in- National income, family income, standard of living and social class.
c. Positive impact- A healthy socio-economic environment can promote community health through better standard of life and greater access to health and health care.
d. Negative impact- An unhealthy socioeconomic environment can undermine community health by denying basic necessities of life and health care facilities.
iii. Differentiating Features of Socio-Political Environment:
a. Represented by- Political milieu of people and their political system.
b. Reflected in- Structure, functioning and performance of the government
c . Positive Impact- A healthy socio-political environment created by a performing goverment can promote community health by paying due attention to health, education and social welfare.
d. Negative Impact- An unhealthy socio-political environment and a non-performing government can promote poverty, destitution and ill-health.
iv. Differentiating Features of Socio-Ethical Environment:
a. Represented by – Ethical milieu of people and their religious and moral roots.
b. Reflected in- Religious beliefs, moral values and community perceptions.
c. Positive Impact- A healthy socio-ethical environment can promote community health and welfare by organising social defence against social evils.
d. Negative Impact- An unhealthy socio-ethical environment can promote antisocial activities like casteism, sectarianism and social evils of various kinds.
12. Essay on Social Deviance:
a. Drug Abuse:
When a drug is taken for non-medical purpose, especially in a dosage or frequency that exceeds the pharmacological norms, it amounts to drug abuse.
Drug abusers pass through the stages of induction, continuation and addiction. They undergo personality changes associated with physical, mental and psychological manifestation, which undermines their health. They eventually succumb to complications of addiction.
Drug abuse can be prevented by health education and public awareness programmes, timely intervention in susceptible individuals and rehabilitation of the drug addicts.
b. Juvenile:
Juvenile delinquency is a behaviour disorder of deviant adolescents. Its spectrum extends from misbehaviour to assault and includes robbery and heinous crimes. There are several types of delinquents.
Sociological delinquents carry approval of their community. They assault in groups and maintain close links with their community. Psychopathic delinquents are indifferent to human sufferings that they cause. Neurotic delinquents are isolated and depressed and surrender to law enforcing agencies quite readily.
Preventive measures include education of parents for responsible parenting, timely intervention for appropriate counselling and rehabilitation of delinquent children.
c. Suicide:
Suicide is usually committed by those who are unable to face stress owing to their poor coping competence. The suiciders generally suffer from poor self-image, consider themselves as a burden on society, and eventually commit suicide, believing it to be the only face-saving mechanism of escape.
The nature of suicide outcome is extremely variable. It depends on the extent of social, emotional and economical void caused by the deceased individuals.
Suicide attempts can be prevented by timely intervention, appropriate counselling and rehabilitation of suicide-prone individuals. Legislation can serve as a deterrent.

Related Articles:
- Rural Health Services in India
- Essay on Indian Society: Top 3 Essays | Sociology
- Essay on Sociology: Top 6 Essays on Sociology
- Essay on Equality | Sociology
Upload and Share Your Article:
- Description *
- Author Name *
- Author Email Id. (required) *
- File Drop files here or
- Name This field is for validation purposes and should be left unchanged.
Essay , Health , Sociology , Sociology and Health
Upload Your Knowledge on Sociology:
Privacy overview.
- Essay Editor
Dentists, How They Can Help in Society Report
1. introduction.
People are becoming increasingly aware of the interconnectedness of our lives and of the role of each individual in contributing to the well-being of society. This is particularly the case in the professions that deal with the citizens of the country, the most personal of which is health care, especially that of general practitioners who are responsible for total patient health. The profession of dentistry, which is concerned with the care of the oral cavity in which diseases frequently affect the rest of the body, is played out in relatively intimate terms with the patient. The present report considers the unique unholy crossroads of education, research, health care, and business on which dentistry is premised and discusses ways in which the field can move forward. There is no comprehensive current report showing the future needs of dental education. There is limited or no comprehensive data on trends and projections for the various aspects of dentistry and its interface with the medical field and overall health. How, why, and in what form are they interacting and which patterns are they developing? Although some lay people believe that dentistry is an esoteric activity standing by itself and, therefore, not connected to the health and well-being of persons, the opposite is true. The body is completely interconnected, and the interdigitations of maintaining the health of various organ systems are well recognized. In short, the health of the oral cavity is linked to the health of the entire body.
1.1. Background and Significance
The history of dentistry suggests that physicians were concerned with the oral health of individuals as early as the first century A.D. Aulus Cornelius Celsus, a physician living in the first century A.D., wrote the first comprehensive book on medicine, "De Medicina". This widely recognized work clearly emphasizes the importance of teeth for general health. Since then, some medical problems related to oral health were transferred to dental practitioners. Edward White, who is widely recognized as the first regular dentist in the American colonies, came from England in 1683 to establish his home and practice in Boston. Although recognized as an operative dentist, Edward White was also commissioned into the Royal Province of Massachusetts to practice all branches of general medicine in the colony. It is worth noting that those surgical-dental interactions practicing within a general surgery context continued in the 19th century to become more defined in the opening academic dental schools and the subsequent development of the dental profession. This is simply because many of the medical schools during these early periods included dental subjects in the dental curriculum.
2. Dental Health and Overall Well-being
Dental caries is an infectious disease that is caused by bacteria and it invites pain and other sequelae when the degree of development advances. The need for implementation of national policies to preserve the oral condition of children, including approaches for dental caries, has been pointed out. Tooth loss might give rise to difficulty in eating, reduced nutritional intake, altered food selection, and impaired deglutition, which in turn might lead to systemic diseases. Several other reports indicated a relationship between oral diseases and general health. Such claims have attracted widespread attention because through this mechanism, oral health has been thought to be related to a variety of systemic diseases involving diabetes, pneumonia, cardiovascular diseases, and adverse pregnancy outcomes. Aims: To provide a comprehensive report on the overall well-being-related services provided by dentists from the public health perspective. Materials and Methods: A data search was performed for the items: 'dental treatment and disease prevention'. The data analysis was carried out with a focus on the relationship of dentists within the community, and attention was paid to their supporting roles in connection with the establishment, realization, and dissemination of policies around them. Results and Conclusion: By identifying the activities of dentists with the public health perspective, the aim is to disseminate their roles and usefulness to the public. Through the study of local supportive policies alongside national policies, it becomes possible to understand the relationships among the variety of approaches and their connections.
2.1. The Impact of Oral Health on General Health
Oral and general health are inextricably intermingled - oral health care is a vital part of maintaining general health. The mouth is very much a multifunctional organ, with local, systemic, psychological, infectious, and neoplastic attributes that relate to the general body. In fact, the health of the oral cavity mirrors overall health and well-being. Some of the most conspicuous associations are found in the following: 1. Diet The thought processes that participate in the decisions made about food and in the act of eating involve many different parts of the brain working together to control voluntary functions. More and more, this oral-brain connection in eating behavior has gained attention in the field of neurobiology. Teeth, as tools designed for breaking down food; the tongue, crucial for creating a bolus; and saliva, the buffer, lubricant, and cleansing fluid for the bolus; together play essential roles during the selection, mastication, and ingestion of food. Accomplishing voluntary oral functions properly and efficiently is sincerely appreciated and cherished after the loss of dentition. Proper oral health care, which results in successful mastication, is crucial for good nutrition. The development of the dentition and proper oral health care are necessary to enhance the general well-being of neonates, infants, children, and adolescents. With correct attention to diet and an understanding of the many facets of nutrition, dentists are able to help with a number of conditions, from healthy eating habits and associated activities to promoting dietary means of avoiding or lessening obesity, diabetes, and other chronic conditions related to diet. 2. Communicative ability Promoting oral health care which ensures the preservation of natural dentition and keeps structure and function in an aesthetically satisfying condition is an essential contribution to furthering a sense of wholeness and self-esteem, since the face and oral cavity are undeniably important to personal appearance. It is generally believed that occlusal anomalies are linked to a reduced ability to masticate, swallow, and deliver nourishment. 3. Positioning in society Proper oral care promotes the perception of wellness, which improves the appearance and can inspire great confidence in relationships at home and in the community. This can help social, educational, and professional development.
3. Preventive Care and Education
As in many other dental surveys, the authors emphasize more heavily the importance of prevention and maintenance of oral health than restorative prosthodontics. Dental instruction should be directed to assist the student to establish in the patient a proclivity for prevention of dental disease and preservation of health. There can be little question as to the import of this concept. Those engaged in teaching could well pay more attention to student ideology and encouragement of students in preventive care through stable reinforcement of existing concepts. This could serve as the basis for encouragement of the development of more precise concepts with respect to the proper role of the dentist and his stewardship to the community. Many authors have classified drugs, food habits, heredity, oral habits, tooth defects, and oral infection as a recognized list of predisposing and inducing factors. The relative importance of these factors, which remain to be personalized in the patient, is known. It is generally accepted by those engaged in group education, as well as by individual practitioners, that the prevention of disease is the responsibility for both spheres. Some have elected for the other extreme and would place it entirely in the one or in the other sphere. Those in a position to educate others have a moral obligation to help them recognize that there is a meeting place. Preventive dentistry should result with some ease from a philosophical approach to the patient. Its practice should be fostered. Not only should patients be educated as to the causes, progression, and sequelae of caries and periodontal disease, they should also be aided by instructing them how to prevent dental and oral disease.
3.1. Promoting Oral Hygiene Practices
One of the main roles of dentists in the community is to promote oral health through educating individuals and communities. Oral disease has unfortunately been prevalent worldwide. This significant problem is due to, inter alia, low support for oral diseases in addition to limited access to oral health care which influences the long-term well-being of the individuals as most parts of the population stay underserved. Remarkably, 15-20% of the global population are compelled to suffer the adverse periodontal conditions due to inadequate dental coverage for many individuals. To fully prevent these diseases, many preventive and educational programs and practices should be conducted not only by medical teams but also by dental teams. Due to the frequent use of public health professionals to assist in changing individual and community behaviors or attitudes, dental professionals in countries with such facilities can utilize their positions to assist state and non-state actors on relatively seamless and routine bases. Confident professionals can lead these tasks in close cooperation with other professionals from agriculture, education, and other relevant areas. Dental professionals can be supported to fulfill these tasks at maximum potential if they are trained accordingly in professional curriculums and have the determination to perform according to this training.
4. Treatment and Intervention
Dentistry is based on biomedical knowledge. It is absolutely essential for dental practitioners to provide accurate advice and medical intervention based on a sound scientific and evidence base. Ensuring that education and training programs are based on a foundation of comprehensive academic knowledge and a sound base of scientific research will contribute to the progression and development of dental practice and promote a healthy practice environment leading to safer and more secure treatments. Therefore, it can be said that a dentist is a wearer of two 'hats' - the first is the "humanitarian hat", and the other is the "minister/beautician hat". Complete information is required to prevent relapse. Intervention and prevention are central to dentistry. We should always take a proactive approach to apply necessary measures to minimize the need for intervention. In particular, a considerable quantity of individualized measures that require comprehensive knowledge and experience are needed to prevent acknowledgement of insufficiently complete patient information can lead to relapse. The present situation in which dentistry has become business-oriented in many respects (a tendency to emphasize effectiveness and efficiency above all), revealing many blind spots increasing the risk need for rapid treatment and corresponding price hold downs can hinder supportive conferences and advice to eliminate said blind spots. Treatment that does not sufficiently serve the patient's welfare and happiness, even under these conditions, is meaningless. Efforts to protect the patient's survival and health are vitally important works for society. If we forget the essence of dentistry, society will lose confidence in and hesitate to call on dental services, and unscrupulous business models will sprout like bamboo in a warm and moist environment.
4.1. Common Dental Procedures
This section will discuss some of the common dental procedures and their specific benefits to you as an individual. Keep in mind that these are general descriptions of treatments. Your dentist will explain the specific treatment plan and its expected results to you. The first six treatments discussed in this section (i.e., preventive care, X-rays, fillings, dental cleaning/root planing, oral cancer examination, and extractions) are general preventive procedures that can be performed to help maintain good oral hygiene. The following nine treatments discussed are different options to replace missing teeth including dentures, bridges, and implants. Periodontal or gum surgery procedures are outlined in the next category. The next seven procedures involve adjusting or correcting your bite and tooth structure including crowns, bridges, or implants. Finally, root canals and other dental procedures are discussed in the last section. In general, the choice of treating a dental problem can often be the difference between saving a tooth and losing a tooth.
5. Community Outreach and Public Health Initiatives
This chapter addresses the role of dentists in activities that promote community life, such as volunteerism and outreach programs. Specifically, the chapters in this section examine definitions, types of programs, models and frameworks for community outreach, and the participating providers. Each chapter addresses the setting - in which dentists in the community participate - by looking at participatory and non-participatory groups, influential attendees, participation rates and user groups, and motivating factors for volunteer participation. Each chapter also identifies and describes the types of outreach programs that dentists participate in. Characteristics include the program's sponsorship (e.g., formal or informal), client location and duration, timing, origins (e.g., local, national, international), goals, participating providers, and other relevant details. This chapter looks at a specialized type of community-based outreach: public health dentistry. Jobs in this field can include work in public health fields such as local, state, and federal health departments, health programs, and Indian Health Services. This area of dentistry often emphasizes reaching those who are most in need, such as poor people or members of different underserved communities. In PDSA, health professionals go out into the community, either in rural areas or related to local health programs. These providers receive support from state, regional, and national specialists. Specially equipped vehicles known as "mobile teams" travel long distances to places such as nursing homes, schools, and community organizations. Naval Health Program recipients are treated in a similar way. Finally, support programs may include group dental health activities by various organizations.
5.1. Partnerships with Schools and Nonprofit Organizations
Given the above challenges and the opportunities for partnerships between schools and dental professionals, Jetton and colleagues conducted an exploratory investigation aimed at identifying procedures for establishing partnerships between dental schools and local schools whose students lack access to dental care. In addition, the authors sought to determine the needs of the students and the level of interest among dental schools in providing care for them in their schools or on other local sites. The procedures entailed contacting the schools to ascertain if there was an interest in partnerships that would provide clinical exposure and dental care for their students. If they were interested, the types, quality, and quantity of care that the local school was interested in providing and the possible benefits of such a relationship were discussed. Because of the exploratory intent of the investigation, the data collection was qualitative. The results indicate that when dental schools are made aware of the services that school partnerships can provide, the schools are more than willing to provide necessary care. This exploration is a good beginning for dental schools to develop relationships with local schools whose students do not typically have access to dental care. Another intriguing opportunity occurred in the Pacific Northwest in 2010, when a community-based teaching clinic conducted rotavirus immunizations on a non-outbreak day for 10 children in a clinical setting when their siblings were seen for dental care. In a carefully conducted study, the team administered the immunizations, discussing rotavirus with the families as an educational and service opportunity since the dental team's assignment was to educate children and families. Together, these studies indicate a culturally competent approach that expands the typical range of incorporated behaviors for dental professionals - underscoring the broad paradigm that characterizes today's residency model.
Related articles
Most satisfying experience related to community service.
1. Introduction During the past decade, a vast amount of research literature has emerged about the benefits of changing college experiences. Much of this research has examined how college can promote cognitive development, sometimes focusing on how unique community-related opportunities could be designed. It has also begun to model the complex psychological development that is associated with the revolutionary changes of emerging adulthood. What can colleges do to maximize the potential for pro ...
Classroom Dynamics and Its Effect on Learning
1. Introduction The primary goal of education is learning, a goal that is influenced by a variety of factors encompassing human cognitive processes. These factors can be classified into pedagogical and psychological, the former residing in the field of instructional training, while the latter lies within the realm of cognitive psychology. Explaining the success or failure in learning is an essential issue for both disciplines. This explanation may be more successful if a combination of their fi ...
The Development of Present Skills for the Future
1. Introduction The objective of this special issue is to deepen our understanding of how to develop the skills needed for the global workforce in the 21st century. The 21st century-specific skills were first emphasized by the U.S. National Research Council, who identified six key areas: cognitive skills, interpersonal skills, intrapersonal skills, adaptability, communication, and learning in formal and informal methods. These skills are necessary not only for all people but also for developmen ...
In the Basement of the Ivory Tower
1. Introduction A critical examination of higher education in the 21st century can hardly overlook neoliberalism and managerialism, the hallmarks of the contemporary architecture of the economic and social order. Higher education systems are becoming increasingly wrapped up with the needs of an advanced capitalism, and that acquires diverse but coherent forms and guises, including sensitization to competition, focus on efficiency and performance, and a specific attention to market needs. This r ...
Teaching Profession
1. Introduction Teaching has long been considered the mother of all professions. Society has looked to the bearer of knowledge as one responsible for the preparation of the future caretakers of that society. As the evolution of the teaching professional has occurred over time, there have been many interpretations and expectations, but most have agreed that the teaching profession is a public office with a moral and knowledge base charged with the responsibility for the world's most important ci ...
Watching TV Makes Us Smarter
1. Introduction Television is a relatively new medium of commercial communication that requires specific research. The growth of its ability in the postwar period and its pervasive impact make this a matter of broad concern. The excitement of the new information, communication, learning, and entertainment media is balanced by a range of concerns: that it affects the development of childhood relations and thus becomes an agent of socialization; that it initiates, affirms, and shapes distinctions ...
Communication Process during the Interview
1. Introduction to Interview Communication An interview is an effective way to determine how well a candidate matches the needs of a job and how well they will fit the organization. Clearly, this is important to both the job seeker and the employer. The selection of employees is probably the most significant responsibility a manager has, yet many are never formally trained in conducting effective and efficient interviews. The ability to communicate effectively and efficiently does not appear au ...
Empowerment of Students for Their Motivation
1. Introduction At present, in our country, there is an important demand for changing the paradigm when the teaching-learning process at the university is also renovated. The previous traditional model was seen from an intermediate level with the needs of society and the students. Besides, the university was seen as a calm institution focused more on the academy with minor connection with the society and its own members. The teachers, in turn, had greater leisure and possibility for authority i ...
- Entertainment
- Environment
- Information Science and Technology
- Social Issues
Home Essay Samples Food Fast Food
Cause and Effect of Fast Food: the Impact on Health and Society
Table of contents, causes of fast food consumption, effects on physical well-being, cultural and societal impact, economic considerations, promoting healthier lifestyles, conclusion: balancing convenience and health.
- Ludwig, D. S., Peterson, K. E., & Gortmaker, S. L. (2001). Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. The Lancet, 357(9255), 505-508.
- Malik, V. S., Pan, A., Willett, W. C., & Hu, F. B. (2013). Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. The American Journal of Clinical Nutrition, 98(4), 1084-1102.
- Story, M., Kaphingst, K. M., Robinson-O'Brien, R., & Glanz, K. (2008). Creating healthy food and eating environments: policy and environmental approaches. Annual Review of Public Health, 29, 253-272.
- Stuckler, D., McKee, M., Ebrahim, S., & Basu, S. (2012). Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLOS Medicine, 9(6), e1001235.
- World Health Organization. (2016). Report of the Commission on Ending Childhood Obesity. WHO Press.
*minimum deadline
Cite this Essay
To export a reference to this article please select a referencing style below

- Genetically Modified Food
Related Essays
Need writing help?
You can always rely on us no matter what type of paper you need
*No hidden charges
100% Unique Essays
Absolutely Confidential
Money Back Guarantee
By clicking “Send Essay”, you agree to our Terms of service and Privacy statement. We will occasionally send you account related emails
You can also get a UNIQUE essay on this or any other topic
Thank you! We’ll contact you as soon as possible.

39 Facts About Khimki
Written by Sharlene Kight
Modified & Updated: 19 May 2024
Reviewed by Sherman Smith
- Russian History Facts

Khimki, located in the Moscow Oblast region of Russia, is a vibrant city with a rich history and a promising future. Known for its strategic location near Moscow and its close proximity to major transportation routes, Khimki has become a hub for economic and cultural development. With a population of over 200,000 people, the city is bustling with activity and offers a wide range of amenities and attractions for visitors and residents alike. In this article, we will explore 39 fascinating facts about Khimki, delving into its history, landmarks, industries, and unique characteristics that make it a standout destination in the region. So, buckle up and get ready to discover the wonders of Khimki!
Key Takeaways:
- Khimki, a city near Moscow, offers a blend of history, nature, and culture. From the Khimki Reservoir to vibrant nightlife, it’s a charming destination for all types of travelers.
- With its warm community and diverse attractions, Khimki is a convenient and captivating getaway from the bustling city center of Moscow. Whether you’re a nature lover or a sports enthusiast, there’s something for everyone to enjoy.
Khimki is situated just 19 kilometers northwest of Moscow, making it a convenient getaway from the bustling city center.
Khimki’s close proximity to Moscow allows visitors to explore both the cosmopolitan offerings of the capital and the peaceful charm of the suburban landscape.
The city is home to the picturesque Khimki Reservoir, a stunning artificial lake spread across an area of 27 square kilometers.
The Khimki Reservoir serves as a popular recreational spot, offering opportunities for boating, fishing , and picnicking amidst breathtaking natural surroundings.
Khimki was officially founded in 1939 as an industrial settlement, primarily focused on timber and chemical production.
Over the years, Khimki has transformed into a thriving city with a diverse economy and a flourishing business sector.
The Khimki Forest, also known as the Moscow Forest, is one of the largest green areas near the city, covering approximately 3,500 hectares.
This expansive forest provides a peaceful escape from the urban landscape, featuring winding trails, lush vegetation, and diverse wildlife.
Khimki has a rich cultural scene, boasting numerous theaters, art galleries, and cultural centers that showcase both local and international talent.
Art lovers will be delighted by the variety of exhibitions, performances, and concerts available throughout the year.
The city’s transportation infrastructure is well-developed, with a modern network of roads, railways, and an international airport.
Getting to and around Khimki is convenient, ensuring seamless travel experiences for visitors.
Khimki is famous for its football team, FC Khimki, which competes in the Russian Football National League.
Sports enthusiasts can catch an exciting match and cheer on the local team, immersing themselves in the fervor of the game .
The Khimki City Museum offers a captivating journey through the history and heritage of the region, from ancient times to the present day.
Visitors can explore archaeological artifacts , learn about important historical events, and gain insights into the city’s evolution.
The Church of St. George the Victorious is a prominent religious landmark in Khimki, known for its stunning architecture and serene ambiance.
It serves as a place of worship and a symbol of spiritual unity for the local community.
Khimki is well-regarded for its educational institutions, including universities, colleges, and schools that offer quality education across various fields of study.
Students from all over Russia come to Khimki to pursue their academic aspirations.
The Khimki Central Market is a bustling hub of activity, where locals and visitors can find an array of fresh produce, local delicacies, and unique souvenirs.
Exploring the market is an immersive experience that awakens the senses and provides glimpses into the local culinary scene.
The Lianozovsky Park, located in the heart of Khimki, is a serene green oasis with picturesque landscapes, tranquil ponds, and charming walking paths.
Visitors can take a leisurely stroll, have a picnic, or simply relax amidst the beauty of nature.
Khimki is known for its thriving industrial sector, with numerous factories and manufacturing plants contributing to the city’s economic growth.
These industries play a crucial role in providing employment opportunities for the local population .
The 39km-long Moscow Canal passes through the outskirts of Khimki, connecting the city with the Moscow River and providing a scenic waterway.
Boat rides along the canal offer a unique perspective of Khimki’s landscape and highlight the importance of water transportation.
The Khimki Railway Station serves as a major transportation hub, connecting the city with various destinations across Russia and neighboring countries.
It plays a vital role in facilitating trade, tourism, and commuter travel.
The Khimki Plaza shopping mall is a popular retail destination in the city, offering a wide range of stores, eateries, and entertainment options.
Shoppers can indulge in a day of retail therapy and explore the latest fashion trends.
Khimki has a vibrant nightlife scene, with numerous bars, clubs, and entertainment venues offering a lively atmosphere for nocturnal adventures.
Whether you’re looking for a sophisticated cocktail lounge or a high-energy dance floor, Khimki has options to suit all tastes.
The Khimki City Park is a beloved recreational spot, featuring beautifully landscaped gardens, playgrounds, and sports facilities.
Families can enjoy quality time together, and nature enthusiasts can revel in the beauty of the park’s flora and fauna.
Khimki has a strong sense of community, with various local events and festivals that bring residents together to celebrate their cultural heritage.
Attending these festivities allows visitors to immerse themselves in the traditions and customs of Khimki.
The Sheremetyevo International Airport, located near Khimki, is one of the busiest airports in Russia, connecting the city with numerous international destinations.
Travelers can easily access Khimki from around the world, making it a gateway to the wonders of Russia.
The famous Moscow Metro extends into Khimki, providing seamless connectivity to Moscow’s metro system and making commuting efficient and convenient.
This integration offers visitors the opportunity to explore both Khimki and Moscow with ease.
Khimki has a growing technology sector, with various IT companies and startups establishing their presence in the city.
The city’s focus on technological advancements and innovation contributes to its ongoing economic development.
The Khimki History and Art Museum is a treasure trove of historical artifacts, artworks, and exhibitions that showcase the city’s cultural heritage and artistic achievements.
It provides visitors with a deeper understanding of Khimki’s past and its place in the broader historical context.
The Khimki Business Park is a modern business district that hosts various national and international companies, attracting investment and fostering economic growth.
The business park serves as a hub for innovation, entrepreneurship, and collaboration.
Khimki is home to the Otkritie Arena, a renowned sports stadium that hosts various sporting events, including football matches and athletic competitions.
Sports enthusiasts can relish the electrifying atmosphere and witness the skills of both local and international athletes.
The Khimki City Library is a valuable resource for knowledge seekers, offering an extensive collection of books and educational materials.
Visitors can explore literary treasures and engage in intellectual pursuits within the walls of this cultural institution.
Khimki boasts a diverse culinary scene, with restaurants and eateries serving a wide array of cuisines, ranging from traditional Russian delicacies to international flavors.
Food enthusiasts can embark on a gastronomic journey that tantalizes their taste buds and satisfies their cravings.
The Khimki Youth Theater is a platform for young talent, showcasing innovative performances that push the boundaries of artistic expression.
Attending a theatrical production here provides a unique glimpse into the emerging theater scene of Khimki.
For adrenaline junkies, Khimki offers various adventure sports and outdoor activities, such as rock climbing, hiking, and zip-lining.
These thrilling experiences allow visitors to embrace their adventurous spirit and create lasting memories.
The Khimki City Stadium is a sporting arena that hosts local and regional events, bringing the community together in the spirit of competition.
Cheering on athletes and teams in this vibrant stadium creates an atmosphere of camaraderie and excitement.
Khimki has a strong commitment to environmental sustainability, with initiatives aimed at preserving the natural beauty of the region and promoting eco-friendly practices.
Visitors can appreciate Khimki’s efforts in creating a greener and more sustainable future.
The Khimki Concert Hall is a cultural landmark that hosts a wide variety of musical performances, from classical symphonies to contemporary concerts.
Audience members can revel in the power of music and witness exceptional talent on stage.
Khimki is home to several beautiful parks and gardens, offering tranquil spaces for relaxation, exercise, and leisurely walks.
Nature enthusiasts will be delighted by the abundance of green spaces dotted throughout the city.
The Khimki History and Architectural Museum-Preserve is a captivating institution that showcases the city’s architectural heritage and highlights its role in Russian history.
Exploring the museum-preserve allows visitors to step back in time and appreciate the architectural marvels of Khimki.
Khimki has a vibrant street art scene, with colorful murals and graffiti adorning the walls of buildings, adding an artistic flair to the city’s urban landscape.
Art enthusiasts can embark on a street art tour and marvel at the creativity and talent displayed by local artists.
The Khimki Concert and Exhibition Center is a versatile venue that hosts a wide range of events, including concerts, exhibitions, conferences, and trade shows.
Attending an event at this multifunctional center offers opportunities for networking and cultural enrichment .
Khimki has a strong tradition of folk arts and crafts, with local artisans creating intricate handmade products that showcase the region’s cultural heritage.
Exploring the local markets and shops allows visitors to purchase unique souvenirs and support the local craft community.
The Khimki Sports Palace is a hub of sporting activities, housing facilities for various indoor sports such as ice hockey, volleyball, and basketball.
Sports enthusiasts can watch thrilling matches or participate in their favorite sports in this state-of-the-art arena.
Khimki has a warm and welcoming community, known for its hospitality and friendly demeanor towards visitors.
Interacting with the locals provides a glimpse into the genuine warmth and charm that defines the city.
Embark on an unforgettable journey through the enchanting city of Khimki and discover the hidden gems that make this destination truly remarkable. Whether you’re intrigued by its history, captivated by its natural beauty, or enthralled by its cultural offerings, Khimki has something to captivate every traveler.
In conclusion, Khimki is a fascinating city with a rich history, vibrant culture , and numerous attractions. From its stunning natural landscapes to its impressive architectural landmarks, Khimki offers something for every visitor. Whether you’re interested in exploring the city’s historical sites, enjoying outdoor activities, or indulging in its delicious cuisine, Khimki has it all. With its convenient location near Moscow and its excellent transportation network, Khimki is a perfect destination for both locals and tourists alike. So, plan your visit to Khimki and immerse yourself in the charm and beauty of this wonderful city.
1. What is the population of Khimki?
Khimki has a population of approximately 207,425 people.
2. What is the weather like in Khimki?
Khimki experiences a typical continental climate with hot summers and cold winters. The average temperature in summer ranges from 20°C to 30°C, while in winter , it can drop to -10°C or even lower.
3. Are there any famous landmarks in Khimki?
Yes , Khimki is home to several notable landmarks, including the Khimki Reservoir, Khimki Cathedral, and the Memorial Complex “To the Warriors of the Khimki Front.
4. How can I reach Khimki from Moscow?
Khimki is conveniently located near Moscow, and you can easily reach it by taking a train, bus, or taxi. The journey usually takes around 30 minutes, depending on the mode of transportation and traffic conditions.
5. What are some popular outdoor activities in Khimki?
Khimki offers a variety of outdoor activities, such as hiking, cycling , and boating. You can explore the beautiful forests and parks surrounding the city or indulge in water sports on the Khimki Reservoir.
6. Are there any shopping malls in Khimki?
Yes, Khimki is known for its modern shopping malls, including Mega Khimki, Grand Canyon , and Aviapark. These malls offer a wide range of shops, entertainment facilities, and dining options.
Khimki's allure extends beyond its 39 fascinating facts. Sports enthusiasts can explore the captivating history of Arena Khimki , home to thrilling matches and unforgettable moments. Football fans won't want to miss the intriguing facts about FC Khimki , a club with a rich legacy and passionate supporters. Delving into these additional topics will enrich your understanding of Khimki's vibrant sports culture and the pride its residents take in their beloved teams.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
Share this Fact:
Khimki, Moscow Oblast, Russia Weather
Get more from weather.com for free
Khimki, Moscow Oblast, Russia
Khimki, moscow oblast, russia forecast, weather today in khimki, moscow oblast, russia, latest news.

Health & Activities
Seasonal allergies and pollen count forecast.
Tree pollen is high in your area
Today's Activities Forecast NEW
Pleasant conditions for the rest of the day will be great for outdoor activities.
Weather in your inbox
Your local forecast, plus daily trivia, stunning photos and our meteorologists’ top picks. All in one place, every weekday morning.
By signing up, you're opting in to receive the Morning Brief email newsletter. To manage your data, visit Data Rights . Terms of Use | Privacy Policy
Air Quality Index
Air quality is acceptable; however, for some pollutants there may be a moderate health concern for a very small number of people who are unusually sensitive to air pollution.
Your Privacy
We collect data from your device to personalize your product experience and the ads you see. We may use or share your data with our data vendors. We may also use or disclose your precise geolocation data to specific data vendors to provide our products and services. This data is considered sensitive personal information under CPRA. Please refer to the CPRA Notice in our Privacy Policy to learn more.
Do Not Sell or Share My Personal Information
You opted out

IMAGES
VIDEO
COMMENTS
Health benefits aside, increasing investment in primary prevention presents a strong economic imperative. For example, obesity contributes to the treatment costs of many other diseases: 70% of diabetes costs, 23% for CVD and 9% for cancers. Economic losses further extend to absenteeism and decreased productivity.
Table 18.1 "Theory Snapshot" summarizes what they say. Good health and effective medical care are essential for the smooth functioning of society. Patients must perform the "sick role" in order to be perceived as legitimately ill and to be exempt from their normal obligations.
Simply, sociology is the study of human society and social problems. Sociology is the scientific study of social relations, institutions, and society (Smelser 1994) . In addition, sociology can be defined as the scientific study of the dynamics of society and their intricate connection to patterns of behaviour.
Table 13.1 "Theory Snapshot" summarizes what they say. Good health and effective medical care are essential for the smooth functioning of society. Patients must perform the "sick role" in order to be perceived as legitimately ill and to be exempt from their normal obligations.
In 2020, a virus that thrived on chronic disease and inequality became the great revealer. COVID-19 revealed the fragility of civilisations built on social injustices, short-term policies, and a dangerous disregard for the environment. The need to become more resilient to crises of all kinds is almost universally agreed on. But to construct that resilience, a philosophical change in how we ...
Health and Human Society, Essay Example. Pages: 2. Words: 532. Essay. Hire a Writer for Custom Essay. Use 10% Off Discount: "custom10" in 1 Click 👇. HIRE A WRITER! You are free to use it as an inspiration or a source for your own work. Contrary to what one may perceive, the wealthier nations may not be healthier at all time.
The COVID-19 pandemic makes the importance of health and wellbeing clear. The pandemic's implications for societies are far reaching. Yet the response to this pandemic and the creation and promotion of health and wellbeing require action beyond the health sector—and beyond the usual ways of working in global health. Governments are not adequately tackling inequality, ongoing economic crises ...
Jeffrey Sachs. The basic lessons of happiness are these: society (and therefore government policies) should attend to people's economic needs, physical health, mental health, social connections, sense of purpose, and confidence in government. The pandemic has threatened almost every dimension of well-being and indeed has fostered rising ...
This essay is about the importance of healthcare and its broad impact on society. It highlights how healthcare prevents and treats diseases, manages chronic conditions, and promotes overall well-being. Healthcare's role in economic stability is emphasized, noting that a healthy population contributes to productivity and growth.
The Society and Population Health Reader, Volume I. Google Scholar; 14. For papers on methodological and data problems, see Section 2 of The Society and Population Health Reader, Volume I. Perhaps ...
Health and illness are central aspects of human experience that are deeply shaped by cultural, political, and economic conditions. Health and Society is a cutting-edge area of interdisciplinary scholarship that examines the social drivers behind historic and contemporary patterns in health and disease. Scholars in the field take a critical ...
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
Defining Health and Well-being. Healthy People 2030 refers to health and well-being in every aspect of the framework, including the vision, mission, foundational principles, plan of action, and overarching goals.5 The expanded role for health and well-being in Healthy People 2030 was supported by the Secretary's Advisory Committee's recommendations and its definition of health and well-being ...
Finally, comparative analyses allow testing of the fundamental hypothesis that variation in sociality affects health and fitness outcomes by contrasting solitary and group-living species while taking potential other variables, such as shared phylogenetic history, into account, provided sufficient data on the same health or fitness variables are ...
Health And Illnesses Defined By Society Sociology Essay. Health is the general condition of a person in all aspects of life. It can be seen as the level of functional and or metabolic efficiency of an organism, often implicitly human. According to World Health Organization (WHO), health is 'a state of complete physical, mental, and social ...
500+ Words Essay on Environment and Human Health. The environment is all that surrounds us. It can be a living or a non-living thing. It includes many forces that are physical, chemical and other natural forces. These living things live in their environment. They consistently react with it and adapt themselves according to the conditions in ...
500+ Words Essay on Health. Essay on Health: Health was earlier said to be the ability of the body functioning well. However, as time evolved, the definition of health also evolved. It cannot be stressed enough that health is the primary thing after which everything else follows. When you maintain good health, everything else falls into place.
1. Essay on Introduction to Sociology and Health: Man is a gregarious animal, he likes to live in society and each individual influences the others and also the environment. Sociology—the science of society, or science of social processes, or the behaviour of men in groups—studies the interaction of its type that seems to result from ...
1. Introduction People are becoming increasingly aware of the interconnectedness of our lives and of the role of each individual in contributing to the well-being of society. This is particularly the case in the professions that deal with the citizens of the country, the most personal of which is health care, especially that of general practitioners who are responsible for total patient health ...
30 Postmodern Perspective towards Human Health and Illness. Postmodernity refers to changes in capitalist society over the past 30 years. Broadly. these are the decline of the industrial sector ...
Fast food, a convenient and readily available option, has significant effects on individuals' health and the broader society. This cause and effect essay delves into the reasons why people consume fast food and examines its far-reaching consequences on physical well-being, cultural practices, and the economy.
With the continuous acceleration of urbanization, air pollution has become an increasingly serious threat to public health. Strengthening the detection and control of pollutants has become a focal point in current society. In light of the increasing amount of literature in the field of air pollution control with every passing year, numerous reviews have been compiled; however, only a limited ...
Yevgeniya Chirikova is leader of the movement for the protection of Khimki forest. The plan to construct a section of the new Moscow-St.Petersburg motorway through the legally-protected Khimki ...
39 Facts About Khimki. Khimki, located in the Moscow Oblast region of Russia, is a vibrant city with a rich history and a promising future. Known for its strategic location near Moscow and its close proximity to major transportation routes, Khimki has become a hub for economic and cultural development. With a population of over 200,000 people ...
Khimki, Russia. Khimki, city and centre of a rayon (sector), Moscow oblast (region), western Russia. It lies along the Moscow-St. Petersburg railway northwest of the capital. Incorporated in 1939, Khimki grew from a small nucleus of summer cottages ( dachi ). It is now an important industrial centre, with engineering, tile, and glass concerns.
Today's and tonight's Khimki, Moscow Oblast, Russia weather forecast, weather conditions and Doppler radar from The Weather Channel and Weather.com