- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
- Introduction
- Conclusions
- Article Information
Error bars represent 95% CIs. GAS indicates gender-affirming surgery.
Percentages are based on the number of procedures divided by number of patients; thus, as some patients underwent multiple procedures the total may be greater than 100%. Error bars represent 95% CIs.
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Wright JD , Chen L , Suzuki Y , Matsuo K , Hershman DL. National Estimates of Gender-Affirming Surgery in the US. JAMA Netw Open. 2023;6(8):e2330348. doi:10.1001/jamanetworkopen.2023.30348
Manage citations:
© 2024
- Permissions
National Estimates of Gender-Affirming Surgery in the US
- 1 Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, New York, New York
- 2 Department of Obstetrics and Gynecology, University of Southern California, Los Angeles
Question What are the temporal trends in gender-affirming surgery (GAS) in the US?
Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Meaning These findings suggest that there will be a greater need for clinicians knowledgeable in the care of transgender individuals with the requisite expertise to perform gender-affirming procedures.
Importance While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, Setting, and Participants This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main Outcome Measures Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and Relevance Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
Gender dysphoria is characterized as an incongruence between an individual’s experienced or expressed gender and the gender that was assigned at birth. 1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS). 2 GAS encompasses a variety of procedures that align an individual patient’s gender identity with their physical appearance. 2 - 4
While numerous surgical interventions can be considered GAS, the procedures have been broadly classified as breast and chest surgical procedures, facial and cosmetic interventions, and genital reconstructive surgery. 2 , 4 Prior studies 2 - 7 have shown that GAS is associated with improved quality of life, high rates of satisfaction, and a reduction in gender dysphoria. Furthermore, some studies have reported that GAS is associated with decreased depression and anxiety. 8 Lastly, the procedures appear to be associated with acceptable morbidity and reasonable rates of perioperative complications. 2 , 4
Given the benefits of GAS, the performance of GAS in the US has increased over time. 9 The increase in GAS is likely due in part to federal and state laws requiring coverage of transition-related care, although actual insurance coverage of specific procedures is variable. 10 , 11 While prior work has shown that the use of inpatient GAS has increased, national estimates of inpatient and outpatient GAS are lacking. 9 This is important as many GAS procedures occur in ambulatory settings. We performed a population-based analysis to examine trends in GAS in the US and explored the temporal trends in the types of GAS performed across age groups.
To capture both inpatient and outpatient surgical procedures, we used data from the Nationwide Ambulatory Surgery Sample (NASS) and the National Inpatient Sample (NIS). NASS is an ambulatory surgery database and captures major ambulatory surgical procedures at nearly 2800 hospital-owned facilities from up to 35 states, approximating a 63% to 67% stratified sample of hospital-owned facilities. NIS comprehensively captures approximately 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP), covering more than 97% of the US population. Both NIS and NASS contain weights that can be used to produce US population estimates. 12 , 13 Informed consent was waived because data sources contain deidentified data, and the study was deemed exempt by the Columbia University institutional review board. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We selected patients of all ages with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) diagnosis codes for gender identity disorder or transsexualism ( ICD-10 F64) or a personal history of sex reassignment ( ICD-10 Z87.890) from 2016 to 2020 (eTable in Supplement 1 ). We first examined all hospital (NIS) and ambulatory surgical (NASS) encounters for patients with these codes and then analyzed encounters for GAS within this cohort. GAS was identified using ICD-10 procedure codes and Common Procedural Terminology codes and classified as breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures. 2 , 4 Breast and chest surgical procedures encompassed breast reconstruction, mammoplasty and mastopexy, or nipple reconstruction. Genital reconstructive procedures included any surgical intervention of the male or female genital tract. Other facial and cosmetic procedures included cosmetic facial procedures and other cosmetic procedures including hair removal or transplantation, liposuction, and collagen injections (eTable in Supplement 1 ). Patients might have undergone procedures from multiple different surgical groups. We measured the total number of procedures and the distribution of procedures within each procedural group.
Within the data sets, sex was based on patient self-report. The sex of patients in NIS who underwent inpatient surgery was classified as either male, female, missing, or inconsistent. The inconsistent classification denoted patients who underwent a procedure that was not consistent with the sex recorded on their medical record. Similar to prior analyses, patients in NIS with a sex variable not compatible with the procedure performed were classified as having undergone genital reconstructive surgery (GAS not otherwise specified). 9
Clinical variables in the analysis included patient clinical and demographic factors and hospital characteristics. Demographic characteristics included age at the time of surgery (12 to 18 years, 19 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, 61 to 70 years, and older than 70 years), year of the procedure (2016-2020), and primary insurance coverage (private, Medicare, Medicaid, self-pay, and other). Race and ethnicity were only reported in NIS and were classified as White, Black, Hispanic and other. Race and ethnicity were considered in this study because prior studies have shown an association between race and GAS. The income status captured national quartiles of median household income based of a patient’s zip code and was recorded as less than 25% (low), 26% to 50% (medium-low), 51% to 75% (medium-high), and 76% or more (high). The Elixhauser Comorbidity Index was estimated for each patient based on the codes for common medical comorbidities and weighted for a final score. 14 Patients were classified as 0, 1, 2, or 3 or more. We separately reported coding for HIV and AIDS; substance abuse, including alcohol and drug abuse; and recorded mental health diagnoses, including depression and psychoses. Hospital characteristics included a composite of teaching status and location (rural, urban teaching, and urban nonteaching) and hospital region (Northeast, Midwest, South, and West). Hospital bed sizes were classified as small, medium, and large. The cutoffs were less than 100 (small), 100 to 299 (medium), and 300 or more (large) short-term acute care beds of the facilities from NASS and were varied based on region, urban-rural designation, and teaching status of the hospital from NIS. 8 Patients with missing data were classified as the unknown group and were included in the analysis.
National estimates of the number of GAS procedures among all hospital encounters for patients with gender identity disorder were derived using discharge or encounter weight provided by the databases. 15 The clinical and demographic characteristics of the patients undergoing GAS were reported descriptively. The number of encounters for gender identity disorder, the percentage of GAS procedures among those encounters, and the absolute number of each procedure performed over time were estimated. The difference by age group was examined and tested using Rao-Scott χ 2 test. All hypothesis tests were 2-sided, and P < .05 was considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
A total of 48 019 patients who underwent GAS were identified ( Table 1 ). Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged 12 to 18 years. Private insurance coverage was most common in 29 064 patients (60.5%), while 12 127 (25.3%) were Medicaid recipients. Depression was reported in 7192 patients (15.0%). Most patients (42 467 [88.4%]) were treated at urban, teaching hospitals, and there was a disproportionate number of patients in the West (22 037 [45.9%]) and Northeast (12 396 [25.8%]). Within the cohort, 31 668 patients (65.9%) underwent 1 procedure while 13 415 (27.9%) underwent 2 procedures, and the remainder underwent multiple procedures concurrently ( Table 1 ).
The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. Among encounters with a billing code for gender identity disorder, there was a consistent rise in the percentage that were for GAS from 4552 (32.9%) in 2016 to 13 011 (37.1%) in 2019, followed by a decline to 12 818 (33.3%) in 2020 ( Figure 1 and eFigure in Supplement 1 ). Among patients undergoing ambulatory surgical procedures, 37 394 (80.3%) of the surgical procedures included gender-affirming surgical procedures. For those with hospital admissions with gender identity disorder, 10 625 (11.8%) of admissions were for GAS.
Breast and chest procedures were most common and were performed for 27 187 patients (56.6%). Genital reconstruction was performed for 16 872 patients (35.1%), and other facial and cosmetic procedures for 6669 patients (13.9%) ( Table 2 ). The most common individual procedure was breast reconstruction in 21 244 (44.2%), while the most common genital reconstructive procedure was hysterectomy (4489 [9.3%]), followed by orchiectomy (3425 [7.1%]), and vaginoplasty (3381 [7.0%]). Among patients who underwent other facial and cosmetic procedures, liposuction (2945 [6.1%]) was most common, followed by rhinoplasty (2446 [5.1%]) and facial feminizing surgery and chin augmentation (1874 [3.9%]).
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020 ( Figure 1 ). Similar trends were noted for breast and chest surgical procedures as well as genital surgery, while the rate of other facial and cosmetic procedures increased consistently from 2016 to 2020. The distribution of the individual procedures performed in each class were largely similar across the years of analysis ( Table 3 ).
When stratified by age, patients 19 to 30 years had the greatest number of procedures, 25 099 ( Figure 2 ). There were 10 476 procedures performed in those aged 31 to 40 years and 4359 in those aged 41 to 50 years. Among patients younger than 19 years, 3678 GAS procedures were performed. GAS was less common in those cohorts older than 50 years. Overall, the greatest number of breast and chest surgical procedures, genital surgical procedures, and facial and other cosmetic surgical procedures were performed in patients aged 19 to 30 years.
When stratified by the type of procedure performed, breast and chest procedures made up the greatest percentage of the surgical interventions in younger patients while genital surgical procedures were greater in older patients ( Figure 2 ). Additionally, 3215 patients (87.4%) aged 12 to 18 years underwent GAS and had breast or chest procedures. This decreased to 16 067 patients (64.0%) in those aged 19 to 30 years, 4918 (46.9%) in those aged 31 to 40 years, and 1650 (37.9%) in patients aged 41 to 50 years ( P < .001). In contrast, 405 patients (11.0%) aged 12 to 18 years underwent genital surgery. The percentage of patients who underwent genital surgery rose sequentially to 4423 (42.2%) in those aged 31 to 40 years, 1546 (52.3%) in those aged 51 to 60 years, and 742 (58.4%) in those aged 61 to 70 years ( P < .001). The percentage of patients who underwent facial and other cosmetic surgical procedures rose with age from 9.5% in those aged 12 to 18 years to 20.6% in those aged 51 to 60 years, then gradually declined ( P < .001). Figure 2 displays the absolute number of procedure classes performed by year stratified by age. The greatest magnitude of the decline in 2020 was in younger patients and for breast and chest procedures.
These findings suggest that the number of GAS procedures performed in the US has increased dramatically, nearly tripling from 2016 to 2019. Breast and chest surgery is the most common class of procedure performed while patients are most likely to undergo surgery between the ages of 19 and 30 years. The number of genital surgical procedures performed increased with increasing age.
Consistent with prior studies, we identified a remarkable increase in the number of GAS procedures performed over time. 9 , 16 A prior study examining national estimates of inpatient GAS procedures noted that the absolute number of procedures performed nearly doubled between 2000 to 2005 and from 2006 to 2011. In our analysis, the number of GAS procedures nearly tripled from 2016 to 2020. 9 , 17 Not unexpectedly, a large number of the procedures we captured were performed in the ambulatory setting, highlighting the need to capture both inpatient and outpatient procedures when analyzing data on trends. Like many prior studies, we noted a decrease in the number of procedures performed in 2020, likely reflective of the COVID-19 pandemic. 18 However, the decline in the number of procedures performed between 2019 and 2020 was relatively modest, particularly as these procedures are largely elective.
Analysis of procedure-specific trends by age revealed a number of important findings. First, GAS procedures were most common in patients aged 19 to 30 years. This is in line with prior work that demonstrated that most patients first experience gender dysphoria at a young age, with approximately three-quarters of patients reporting gender dysphoria by age 7 years. These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments. 19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent GAS, even in the highest volume years. GAS in adolescents has been the focus of intense debate and led to legislative initiatives to limit access to these procedures in adolescents in several states. 20 , 21
Second, there was a marked difference in the distribution of procedures in the different age groups. Breast and chest procedures were more common in younger patients, while genital surgery was more frequent in older individuals. In our cohort of individuals aged 19 to 30 years, breast and chest procedures were twice as common as genital procedures. Genital surgery gradually increased with advancing age, and these procedures became the most common in patients older than 40 years. A prior study of patients with commercial insurance who underwent GAS noted that the mean age for mastectomy was 28 years, significantly lower than for hysterectomy at age 31 years, vaginoplasty at age 40 years, and orchiectomy at age 37 years. 16 These trends likely reflect the increased complexity of genital surgery compared with breast and chest surgery as well as the definitive nature of removal of the reproductive organs.
This study has limitations. First, there may be under-capture of both transgender individuals and GAS procedures. In both data sets analyzed, gender is based on self-report. NIS specifically makes notation of procedures that are considered inconsistent with a patient’s reported gender (eg, a male patient who underwent oophorectomy). Similar to prior work, we assumed that patients with a code for gender identity disorder or transsexualism along with a surgical procedure classified as inconsistent underwent GAS. 9 Second, we captured procedures commonly reported as GAS procedures; however, it is possible that some of these procedures were performed for other underlying indications or diseases rather than solely for gender affirmation. Third, our trends showed a significant increase in procedures through 2019, with a decline in 2020. The decline in services in 2020 is likely related to COVID-19 service alterations. Additionally, while we comprehensively captured inpatient and ambulatory surgical procedures in large, nationwide data sets, undoubtedly, a small number of procedures were performed in other settings; thus, our estimates may underrepresent the actual number of procedures performed each year in the US.
These data have important implications in providing an understanding of the use of services that can help inform care for transgender populations. The rapid rise in the performance of GAS suggests that there will be a greater need for clinicians knowledgeable in the care of transgender individuals and with the requisite expertise to perform GAS procedures. However, numerous reports have described the political considerations and challenges in the delivery of transgender care. 22 Despite many medical societies recognizing the necessity of gender-affirming care, several states have enacted legislation or policies that restrict gender-affirming care and services, particularly in adolescence. 20 , 21 These regulations are barriers for patients who seek gender-affirming care and provide legal and ethical challenges for clinicians. As the use of GAS increases, delivering equitable gender-affirming care in this complex landscape will remain a public health challenge.
Accepted for Publication: July 15, 2023.
Published: August 23, 2023. doi:10.1001/jamanetworkopen.2023.30348
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Wright JD et al. JAMA Network Open .
Corresponding Author: Jason D. Wright, MD, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, 161 Fort Washington Ave, 4th Floor, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Wright had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Wright, Chen.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Wright.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Wright, Chen.
Administrative, technical, or material support: Wright, Suzuki.
Conflict of Interest Disclosures: Dr Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Elective surgeries were postponed during the coronavirus outbreak. But my gender-affirming surgery isn't optional — it's lifesaving.
- I'm a reporter for Business Insider who is male and nonbinary. I was worried that my upcoming gender-affirming surgery will be canceled because of the coronavirus outbreak.
- In March, Governor Cuomo called on health systems to stop performing elective procedures in New York state because hospitals are overwhelmed with patients.
- My gender-affirming surgery is considered "elective." However, if my surgery is postponed, it will have a severe impact on my mental and physical health.
- Visit Business Insider's homepage for more stories .

Sign up here to receive updates on all things Gender at Work.
[EDITOR'S NOTE: When this story was originally published in March, elective surgeries had been canceled. As part of New York's statewide reopening plan, Gov. Andrew Cuomo has allowed elective surgeries to resume in New York City, according to New York Post ]
I took the subway two weeks ago to one of the few transgender healthcare centers in New York City to retrieve my last psychological letter for gender-affirming surgery.
Yet, when I arrived at the center in Manhattan, the psychiatrist wasn't there. I was told she was adhering to the state's mandates and began social distancing.
Outside the office, it was a ghost town.
The streets that are normally filled with halal trucks and people selling knockoff purses were nearly empty. And then there was me: a guy who left his house and essentially risked coming in contact with coronavirus for no reason.
This was one of the last letters I need for Medicaid to begin approving my gender-affirming procedure — more simply known as bottom surgery. Without these letters, my health insurance will not deem the surgery "medically necessary." And as a result, I will not be able to afford it.
This happened soon after the US Surgeon General requested that health systems consider pausing elective surgeries . Last week, New York Governor Andrew Cuomo ordered that medical centers pause elective surgeries . What's more, a staff member at the health center warned me that because of the outbreak my surgery could be postponed.
I am not alone: Transgender and nonbinary people face many barriers when it comes to finding access to gender-affirming healthcare. In 2015, the US Transgender Survey found that one-third of trans and nonbinary people face discrimination at the doctor's office. Their findings also show that 33% of trans people postponed medical care because of the cost.
On the other hand, research shows gender confirmation surgeries improve the overall mental health and wellbeing of trans and nonbinary people .
Related stories
For many people, when they hear "elective surgery" they assume cosmetic surgeries. I've waited nearly a year for SRS and now the growing coronavirus pandemic is threatening to take it away.
Trans and nonbinary people face barriers in healthcare
I am scheduled to have bottom surgery or metoidioplasty in July 2020, but because of the delay in elective procedures, it's likely that my pre-op appointment and surgery will be rescheduled. Before then I've had to go through a number of psychological evaluations to be deemed "sane" for the procedure.
According to national trans health guidelines from WPATH (The World Professional Association of Transgender Health), trans and nonbinary patients who want bottom surgery must have gender dysphoria, have their mental illnesses under control, receive hormone replacement therapy for a year, and live consistently as their gender (whether male, female, or nonbinary). Also, you need letters from a doctor, psychiatrist, and counselor that prove this procedure is medically necessary.
Not only do we face strict requirements for treatment, but this system is backlogged with patients. Last September, I called Mount Sinai's Transgender Health Clinic, was put on a waitlist, and then scheduled for my first appointment in November.
At the appointment, I didn't make the weight requirement. All transgender and nonbinary patients are required to have a BMI of 33. At the time, my BMI was closer to 34. Business Insider has previously reported that BMI is an outdated system that doesn't measure body fat. According to health experts, physicians can yield a more accurate result of your health by measuring your waist circumference .
Yet, the facility did not allow me to schedule surgery until I lost the weight. I lost 10 pounds through a crash diet. Hours before I graduated from the Craig Newmark School of Journalism, I weighed in at Mount Sinai's Transgender Health Clinic. Then, I had my first consultation with the doctor in January.
I also faced bias from mental health counselors who could write a letter. The first therapist I went to for a letter for bottom surgery told me she didn't feel comfortable advocating for me to get surgery. So, I had to look elsewhere. And my former psychiatrist who is covered under Medicaid calls me "Mrs." at every appointment, despite knowing I am male. Therefore, receiving a letter from him was not an option. Now, social distancing has delayed me even further. To this day, I have not received a letter.
The surgery isn't elective — it's lifesaving
In August of 2018, a doctor officially diagnosed me with gender dysphoria, the debilitating distress I feel because of a disconnect between my brain and how the world perceives my body. Since then, I've received treatment through hormone replacement therapy or injecting my stomach every week with testosterone. This has relieved a lot of my symptoms, such as depression and anxiety.
Much of my dysphoria comes from not feeling socially included in male spaces. On a day-to-day basis, this means finding another bathroom at work because there are no open stalls. At a former internship and graduate school, this meant people intentionally calling me by my dead pronouns and grouping me in with "women" or "ladies."
It's only recently that I've started to be read as male in public (for example, grocery store cashiers calling me sir, people on the street calling me brother and guy). While this is a relief, it's also scary. I avoid public gyms because I fear the potential violence and stigma I'll face in the men's locker. Receiving this surgery as soon as possible will allow me to avoid potential violence and live my life safely.
Now, I am waiting for a call from my surgeon's office on whether or not my surgery and pre-op appointment will be rescheduled or canceled. Bottom surgery is one of the final steps I'm taking in my gender transition. Most of my legal documents are male. My mail is addressed to "Mr. Tatyana Bellamy-Walker" and I have an "M" on my driver's license, social security records, and birth certificate.
And although transgender people are banned from the US military, I managed to be registered into the US Selective Service System, a military draft system for all males under the age of 26.
Yet, somehow, the pandemic is becoming my latest obstacle to participating in public life.
This story was originally published on March 30, 2020.
Watch: What it's like to be a 'deathcare' worker collecting bodies during the coronavirus pandemic
- Main content
- For Journalists
- News Releases
- Latest Releases
- News Release
Age restriction lifted for gender-affirming surgery in new international guidelines
'Will result in the need for parental consent before doctors would likely perform surgeries'
Media Information
- Release Date: September 16, 2022
Media Contacts
Kristin Samuelson
- (847) 491-4888
- Email Kristin
- Expert can speak to transgender peoples’ right to bodily autonomy, how guidelines affect insurance coverage, how the U.S. gender regulations compare to other countries, more
CHICAGO --- The World Professional Association for Transgender Health (WPATH) today today announced its updated Standards of Care and Ethical Guidelines for health professionals. Among the updates is a new suggestion to lift the age restriction for youth seeking gender-affirming surgical treatment, in comparison to previous suggestion of surgery at 17 or older.
Alithia Zamantakis (she/her), a member of the Institute of Sexual & Gender Minority Health at Northwestern University Feinberg School of Medicine, is available to speak to media about the new guidelines. Contact Kristin Samuelson at [email protected] to schedule an interview.
“Lifting the age restriction will greatly increase access to care for transgender adolescents, but will also result in the need for parental consent for surgeries before doctors would likely perform them,” said Zamantakis, a postdoctoral fellow at Northwestern, who has researched trans youth and resilience. “Additionally, changes in age restriction are not likely to change much in practice in states like Alabama, Arkansas, Texas and Arizona, where gender-affirming care for youth is currently banned.”
Zamantakis also can speak about transgender peoples’ right to bodily autonomy, how guidelines affect insurance coverage and how U.S. gender regulations compare to other countries.
Guidelines are thorough but WPATH ‘still has work to do’
“The systematic reviews conducted as part of the development of the standards of care are fantastic syntheses of the literature on gender-affirming care that should inform doctors' work,” Zamantakis said. “They are used by numerous providers and insurance companies to determine who gets access to care and who does not.
“However, WPATH still has work to do to ensure its standards of care are representative of the needs and experiences of all non-cisgender people and that the standards of care are used to ensure that individuals receive adequate care rather than to gatekeep who gets access to care. WPATH largely has been run by white and/or cisgender individuals. It has only had three transgender presidents thus far, with Marci Bower soon to be the second trans woman president.
“Future iterations of the standards of care must include more stakeholders per committee, greater representation of transgender experts and stakeholders of color, and greater representation of experts and stakeholders outside the U.S.”
Transgender individuals’ right to bodily autonomy
“WPATH does not recommend prior hormone replacement therapy or ‘presenting’ as one's gender for a certain period of time for surgery for nonbinary people, yet it still does for transgender women and men,” Zamantakis said. “The reality is that neither should be requirements for accessing care for people of any gender.
“The recommendation of requiring documentation of persistent gender incongruence is meant to prevent regret. However, it's important to ask who ultimately has the authority to determine whether individuals have the right to make decisions about their bodily autonomy that they may or may not regret? Cisgender women undergo breast augmentation regularly, which is not an entirely reversible procedure, yet they are not required to have proof of documented incongruence. It is assumed that if they regret the surgery, they will learn to cope with the regret or will have an additional surgery. Transgender individuals also deserve the right to bodily autonomy and ultimately to regret the decisions they make if they later do not align with how they experience themselves.”
- Reconstructive Procedures
Gender Confirmation Surgeries Transgender-Specific Facial, Top and Bottom Procedures
What surgical options are available to transgender and gender non-conforming patients? Gender confirmation surgeries, also known as gender affirmation surgeries, are performed by a multispecialty team that typically includes board-certified plastic surgeons. The goal is to give transgender individuals the physical appearance and functional abilities of the gender they know themselves to be. Listed below are many of the available procedures for transwomen (MTF) and transmen (FTM) to aid in their journey.
Facial Feminization Surgery
Transfeminine top surgery, transfeminine bottom surgery, facial masculinization surgery, transmasculine top surgery, transmasculine bottom surgery, on the blog.

Facial feminization surgery is a combination of procedures designed to soften the facial features and feminize the face. There are many procedures that are available to feminize the face.
- Facial feminization surgery improves gender dysphoria in trans women Josef Hadeed, MD, FACS
- The impact of COVID-19 on gender dysphoria patients Cristiane Ueno, MD
On The Vlog

Facial feminization surgery is always tailored to the individual, but as ASPS member Justine Lee, MD, PhD, explains there are general characteristics such as hairline, brow bones, cheeks and jawline that many patients note and plastic surgeons plan for.
- Gender Affirmation Top Surgery with Dr. Julie Hansen
Find Your Surgeon
Patient care center, before & after photos.

Video Gallery
3d animations, patient safety.
It’s time to stop describing lifesaving health care as “elective”
Labels like “nonessential” are getting in the way of urgent treatments and surgeries. There’s a better way.
by Andréa Becker

Emily Lipstein lived with 10 years of debilitating, unexplained chronic pain before she finally received a diagnosis — endometriosis — and was scheduled for excision surgery . But when the pandemic hit, her surgery was deemed nonessential and indefinitely postponed.
“It felt like everything I’d been looking forward to with my health just evaporated into thin air,” Lipstein told Vox. In the months she waited for a rescheduled surgery, she had to pay for an extra MRI scan and experienced mental health issues, for which she was prescribed antidepressants.
Around the start of the Covid-19 pandemic in March 2020, the US federal government told health providers to postpone elective surgeries and “nonessential” medical procedures. These cancellations and delays, which affected everything from hip replacements to cataract surgeries to colonoscopies, were meant to conserve health care resources and minimize exposure to Covid-19. More than 100 hospitals have again resorted to this strategy in recent months because of the delta surge .
For the thousands of people across the country who were and are awaiting important medical care, these indefinite cancellations have been devastating. Experts and patients told Vox that the perceived importance of a given procedure is largely up to interpretation — as well as the whims of local politics.
“The term ‘elective care’ can be misleading,” said Joseph Sakran, a trauma surgeon at Johns Hopkins Hospital who performs both elective and emergency surgeries. Many people may assume that elective surgeries are unnecessary or cosmetic, but doctors use the word to describe pretty much any procedure that can be scheduled in advance . When officials hit pause on huge swaths of the medical system, some patients are forced to “prolong their suffering,” Sakran said.
The term “nonessential” often devalues care for women, LGBTQ people, and the chronically ill, said Virginia Kuulei Berndt, a medical sociologist and professor at Texas A&M University. “Some illnesses are prioritized less than others, and their corresponding treatments are deemed less urgent,” she said.
As a medical sociologist, I research how the binary system of “lifesaving” versus “elective” care is used and abused, and how these categories worsen social inequalities. The current system is supposed to help doctors triage, helping patients in dire need come to the front of the line. But labels have big consequences in health care: They can deem a condition worthy of medical treatment, drastically affect the support insurance companies will offer, and even stigmatize entire identities.
While we continue to hear calls to halt nonessential care, it’s a critical moment to ask: Who decides what counts as essential health care? And what happens when your care is deemed unnecessary? It’s time to move from a binary choice to a model with more tiers, which would capture quality of life and mental health and codify devalued forms of health care as nonnegotiable.
Labels like “nonessential” and “elective” can be inaccurate and misleading
Data shows that more than 90 percent of US surgeries are considered elective or nonessential. Collectively, they bring the nation’s health care system between $48 billion and $64 billion of revenue per year. This is why so many hospital systems struggled financially in the early days of the pandemic: While beds filled with Covid-19 patients, many profitable services ground to a halt.
Yet the definition of essential care has varied not only by health care provider, insurance company, and hospital system, but also by the state, city, or town that a person happens to live in. Some conditions are clearly emergencies, such as a rupturing appendix. But “nonessential” does not necessarily mean something purely cosmetic like a rhinoplasty or tummy tuck. During the pandemic, Sakran said, he has had to postpone surgeries to repair hernias that impede people from comfortably eating or walking.
The logistical difficulty of defining essential care has been “an ongoing challenge for insurance companies,” said Jesse Ehrenfeld, a physician and LGBTQ health advocate who chairs the American Medical Association board of trustees. It “leads to a lot of individual decision-making happening that is inconsistent.”
“The term ‘nonessential’ often devalues care for women, LGBTQ people, and the chronically ill”
Without a widely accepted definition, the focus tends to be on risk of immediate death, while other facets of health aren’t factored into the necessity equation. In some cases, providers, insurance companies, and government agencies have latitude to decide whether a procedure is essential based on cultural beliefs or political agendas.
Insurance companies also ask patients and providers to prove the necessity of a procedure or medication, using a controversial bureaucratic process called prior authorization . Designed as a cost-control tool, this approach adds 16 hours to the work week of the average US physician, according to a study conducted by the American Medical Association. The administrative hassle and wait times can lead to patients giving up on getting the care they need.
Existing categories are failing women, LGBTQ people, and the chronically ill
In the US, access to high-quality care already depends too much on a person’s social status and ability to pay — and when certain care can be deemed nonessential, these gaps in access grow wider.
Leigh Senderowicz, a health demographer at the University of Wisconsin Madison, describes the ambiguity around essential care as “a fissure” that allows groups “to pursue whatever existing agenda they have.” Abortion is one prominent example, said Senderowicz, whose team has researched reproductive autonomy during the pandemic .
While some groups have used the pandemic as a reason to restrict abortion, others pushed for increased access through telemedicine appointments for medication abortion . These groups used the same word to demand very different health policies.
I first grasped the problem with the words “elective” and “nonessential” during research interviews with over 100 hysterectomy patients. Hysterectomy, or the surgical removal of the uterus, is the most common gynecological surgery outside of pregnancy-related issues in the United States. While around 10 percent of hysterectomies are performed to treat cancer and may be classified as emergencies, the overwhelming majority are classified as elective procedures, whether they’re gender-affirming care for trans patients or aim to manage a chronic reproductive illness.
While hysterectomy doesn’t immediately prevent death in these cases, timely access to this surgery can have a vast impact on a patient’s quality of life, mental health, and ability to attend work or school. The reason these procedures are deemed elective is not that they aren’t urgently needed, but that the underlying condition will not immediately kill them. The words “elective” and “nonessential” create additional obstacles when insurance companies reject claims or a hospital blocks a physician from providing a hysterectomy.
- Americans are dying because no hospital will take them
Jordan, a Massachusetts resident who asked to be identified by a pseudonym to protect her privacy, has experienced debilitating chronic pain and bleeding since she was a teenager due to adenomyosis , an illness that impacts the lining of the uterus. Her adenomyosis led her to drop out of college and move in with her parents, and she spends most days managing her symptoms. After years of seeking diagnosis and relief, she found a physician who finally presented a viable solution: hysterectomy.
Then the hospital intervened, Jordan told me, on the grounds that it was an unnecessary sterilization procedure. “The hospital does not see it as medically necessary, despite my surgeon specifically telling them that it was for quality-of-life purposes,” she said. “No, it won’t kill me, it’s a benign disease, but I might kill myself because I have it. And still, they denied it.”
Her doctor even suggested she leave the state, Jordan said, despite its reputation for progressive policies and leading medical care, because hysterectomies are more commonly performed in other regions, such as the South. Many patients won’t have the money or means to travel between states.
Gender-affirming care for trans people is also “viewed by some as unnecessary or low-priority, [resulting] in inequities becoming even more pronounced,” said Jesse Ehrenfeld. For a population that’s already affected by a shortage of specialists and big gaps in research, the nonessential label is an additional obstacle to what Ehrenfeld and other public health experts view as lifesaving care.
Ash, an agender person in Pennsylvania who requested a pseudonym to protect their privacy, for years wanted a hysterectomy to affirm their gender, but said that many doctors deemed it an unnecessary procedure that wouldn’t be covered by insurance. A doctor who finally agreed to the surgery, they added, said it would be easier to get it approved if it was classified as treatment for endometriosis, rather than as part of trans health care.
“He told me, ‘Listen, we’re gonna fill out the paperwork to say ... that you probably have endometriosis,” Ash said, paraphrasing the doctor. “This is what we have to do for insurance.” Their insurance company seemed to classify their hysterectomy as elective or cosmetic, Ash said, and coverage for the procedure seemed to depend on finding a doctor who would misrepresent the reason for the surgery.
When the meaning of a procedure varies so drastically by location and physician, and leads patients and doctors to lie to insurance companies, we should consider overhauling the system.
A new system could classify medical care by its urgency, whether or not it’s an emergency
The current way of defining essential health care is failing many patients. While the current designation is either/or — based on whether a patient is immediately at risk of death — our actual experience of health has many shades and subtleties. Doctors and health officials need to consider the impact of medical care on a person’s quality of life, mental health, and ability to work, as well as the impact on families and communities.
The best alternative to the binary system is a tiered framework, which would group different types of care based on varying degrees of urgency. For example, health systems could adopt three tiers: emergency, intermediate urgency, and routine. In this model, emergencies would still describe risks of imminent death or severe harm — such as a heart attack — and routine cases would refer to primary care, preventative screenings, and genuinely cosmetic procedures.
It’s the middle tier that has the greatest potential to improve and even save lives. This tier includes acute cases that aren’t life-threatening but require attention within 24 hours, such as a broken bone or a wound that needs stitches. But the medical care I’ve described in this article, from trans health care to abortion, also has intermediate urgency: It may increase mortality risk, reduce quality of life, or negatively impact mental health.
While a condition like chronic pain might not pose immediate mortality risk, the daily toll can have detrimental impact on one’s mental health and ability to function across all areas of life and work. In the case of trans patients, there is substantial evidence that access to gender-affirming care, including access to hormone replacement therapy, can save lives by improving mental health and by reducing suicide rates . Research also shows that when people can’t access abortion, their financial, physical, and mental health suffer. These elements of health, in addition to immediate risk of death, are considered in a tiered system of urgency.

This additional category would make it harder for local officials to make sweeping decisions that postpone or cancel a wide range of needed care. A tiered model would work best with proper oversight by public health experts and clear guidance about each type of care, to prevent the devaluation of historically sidelined care as “low urgency” or “routine.”
Without such standardization, Ehrenfeld said, legislative bodies can restrict access to care and put physicians in a bind — making it difficult for them to “act in the best interest of their patients and follow the evidence-based guidelines.” Any system that fails to define what kind of care is nonnegotiable leaves open the possibility of discrimination against stigmatized patients.
The pandemic has laid bare many gaps in the American approach to public health. Some have widened in the past year and a half. But now that we’ve seen the massive impact of delayed and canceled care, we have a big opportunity to fix a longstanding problem. We should change the way we categorize and prioritize different types of health care, and move toward a more holistic understanding of health and well-being.
Kuulei Berndt aptly summarized the problem before us. It’s fixable, as long as we have the will to solve it. “Nonessential does not mean it doesn’t need to happen,” she said. “Elective does not mean superfluous.”
Andréa Becker is a medical sociologist, researcher, and writer. She is a PhD candidate at the CUNY Graduate Center in New York and teaches sociology of health at Lehman College.
Most Popular
Why are whole-body deodorants suddenly everywhere, if trump wins, what would hold him back, take a mental break with the newest vox crossword, what the death of iran’s president could mean for its future, the known unknowns about ozempic, explained, today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
More in Politics

Biden promised to defeat authoritarianism. Reality got in the way.

Blood, flames, and horror movies: The evocative imagery of King Charles’s portrait

Why the US built a pier to get aid into Gaza

The controversy over Gaza’s death toll, explained

Bridgerton’s third season is more diverse — and even shallower — than ever


The misleading, wasteful way we measure gas mileage, explained

The Republican Party's man inside the Supreme Court

Why Trump's running mate could be the most important VP pick of our time

Rent control for child care?

Introducing Vox’s next chapter
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
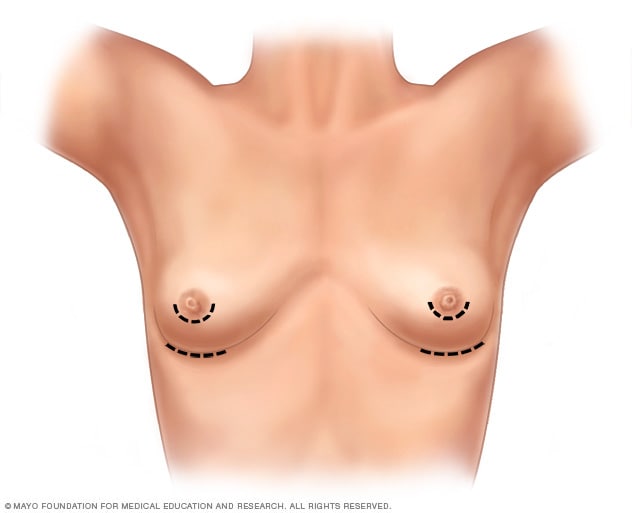
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
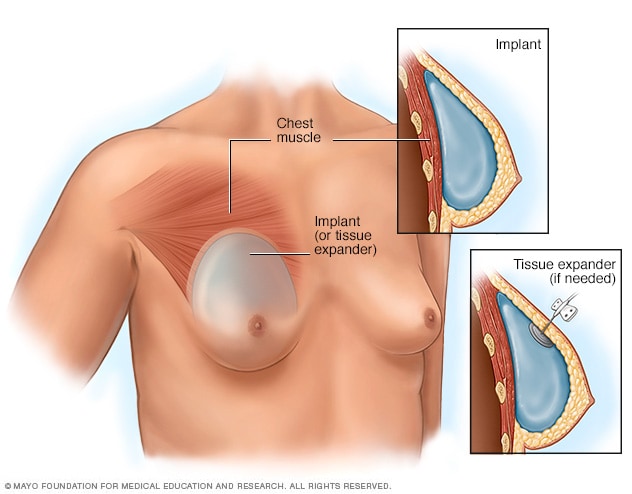
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
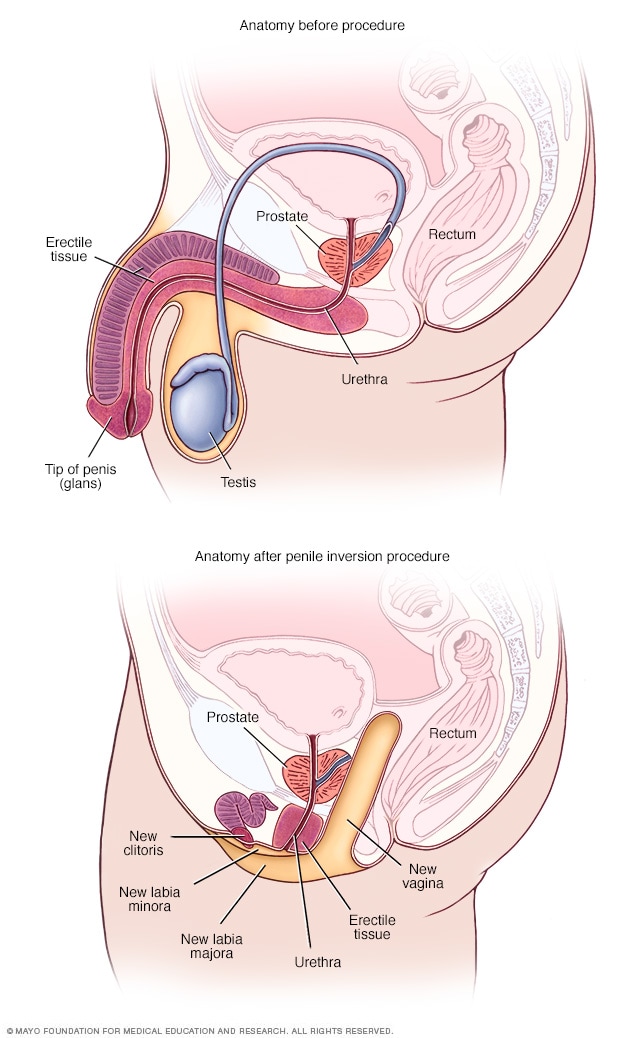
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
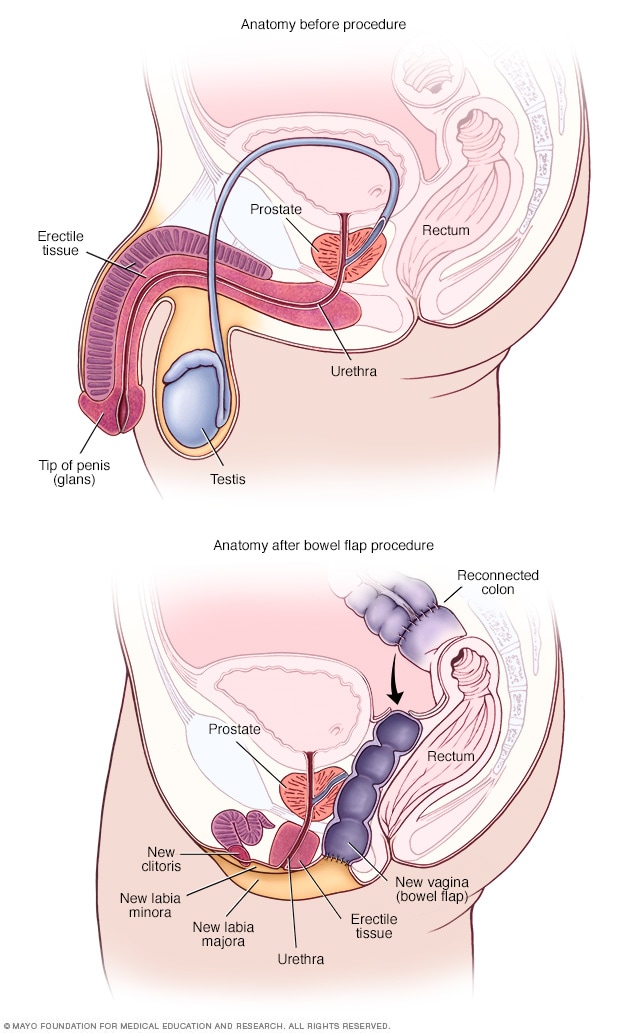
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

Free Associations Podcast 146: The Effects of Early Cessation of Oxytocin

SPH Convocation Season 2024
Transgender healthcare “is not cosmetic or elective. it is essential” ..

Transgender Healthcare “Is Not Cosmetic or Elective. It is Essential”
Alums Gray Babbs and Dani Brooks and MPH student Madeline Stump are working to understand the health experiences of transgender adults in Massachusetts seeking long-term hair removal services to inform policy and address insurance gaps.
Mallory bersi.
Long-term hair removal is an important part of many transgender individuals’ transition journey, as it alleviates dysphoria and is a requisite for some gender-affirming surgeries. However, even when gender-affirming hair removal is covered by insurance, the usual providers of this care—electrologists and aestheticians—are not considered medical providers and thus cannot bill insurance. This roadblock greatly limits access to care.
With funding from an Impact Grant from the Activist Lab at the School of Public Health, alums Gray Babbs (SPH’21) and Dani Brooks (SPH’21) and second-year MPH student Madeline Stump are working with the Massachusetts Transgender Health Coalition to gather survey data on the health experiences of transgender adults in Massachusetts seeking hair removal services to inform policy and address these insurance gaps.
The project has gone through several iterations since its conception in March 2020, initially focusing on characterizing rates of uninsurance and underinsurance among transgender individuals across the Commonwealth. After conversations with the Coalition suggesting that a survey was not the ideal research tool for these questions, Babbs, Brooks, Stump, and alum Meghan Walsh (SPH’21), who is no longer involved in the project, conducted several key informant interviews to better understand the issues that the transgender community in Massachusetts faces regarding health insurance. The team and Coalition ultimately decided to narrow their focus on access to gender-affirming hair removal services.
“Through conversations with practitioners and advocates, we have heard that around less than one-percent of insured transgender people who seek out these services actually get them covered by their insurance. That is not accounting for those people who are uninsured,” says Babbs. “We have to do better.”
Additionally, in preparing for the project, the team found that published literature around access to hair removal for transgender individuals was severely lacking.
“I was only able to find two articles on the topic,” says Stump. “So often, if the research being done on transgender healthcare doesn’t go beyond HIV prevalence, surgery, or hormonal care, it doesn’t exist in the literature.”
To begin to address some of these research gaps, Babbs, Brooks, and Stump hope to publish an in-depth analysis of their survey findings to influence policy change and make a meaningful impact on transgender individuals across the Commonwealth and beyond.
“The great thing about the Impact Grant program is that we have had the opportunity to connect with people who are at the forefront of policy change for trans populations,” says Babbs, who recently spoke about barriers to electrolysis access with the Massachusetts Association of Electrologists. “It has been a learning experience to figure out how to brave this path between being researchers and affecting real policy change as public health practitioners.”
“This is the kind of work that really can make a meaningful difference in people’s lives,” says Brooks. “Even small policy changes can make a huge impact, and it is incredibly exciting to be able to give a voice to the trans folks who are actively dealing with these barriers to care.”
Stump also emphasizes that having the opportunity to play a role in expanding access to healthcare for transgender individuals through this project is especially meaningful to her and the rest of the team because it plays into dispelling a larger narrative around transgender care. “It is not cosmetic or elective; it is essential and necessary,” she says.
From writing their Impact Grant application to now, over a year and a half later, the team has worked closely with the Activist Lab to bring their project to life. This consistent support from the Activist Lab team, Brooks says, has been tremendous in helping them think through some of the logistical challenges of the project and navigate research roadblocks along the way, especially over the course of the COVID-19 pandemic.
The funding provided by the Impact Grant has also allowed Babbs, Brooks, and Stump to directly compensate survey participants, which is something that they strongly believe in.
“It is important to compensate people for their time, but in our case especially, since we are asking questions that are very personal to their experiences. We are asking them to do a lot of emotional work,” says Brooks. “I don’t think that this project would exist without the Activist Lab’s support in this way.”
Among the many people who have been involved in the project and supported it along the way, including SPH faculty members Sarah Gordon , assistant professor of health law, policy & management, and Allegra Gordon , assistant professor of community health sciences, Babbs highlights that the Activist Lab team has served as a core guiding resource for them throughout. “They have created an amazing platform for us to explore our ideas and achieve our goals. They have truly been the gravity that has made this a real project for us rather than just an ambition,” he says.
Read more about the Impact Grant program at SPH here . If you are interested in learning more or getting involved in the gender-affirming hair removal project, you can contact Gray Babbs at [email protected] .
Explore Related Topics:
- access to care
- activist lab
- health insurance
- transgender health
- underinsurance
- Share this story
- 1 Comments Add
Mallory Bersi is the managing editor of Public Health Post at the School of Public Health. Profile
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.
There is 1 comment on Transgender Healthcare “Is Not Cosmetic or Elective. It is Essential”
Great work and a great article!
Post a comment. Cancel reply
Your email address will not be published. Required fields are marked *
Connection denied by Geolocation Setting.
Reason: Blocked country: Russia
The connection was denied because this country is blocked in the Geolocation settings.
Please contact your administrator for assistance.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Should Gender Reassignment Surgery be Publicly Funded?
Johann j. go.
Worcester College, University of Oxford, Walton Street, Oxford, Oxfordshire, OX1 2HB UK
Transgender people have among the highest rates of suicide attempts of any group in society, driven strongly by the perception that they do not belong in the sex of their physical body. Gender reassignment surgery (GRS) is a procedure that can change the transgender person’s physical body to accord with their gender identity. The procedure raises important ethical and distributive justice concerns, given the controversy of whether it is a cosmetic or medical procedure and the economic costs associated with performing the procedure. This paper argues that there is a strong case for funding GRS as a matter of clinical necessity and justice. This paper will be divided in four key sections: First, the state of transgender health will be outlined, including the role of GRS and common objections to it. Second, a number of common objections to GRS will be analysed at the outset and shown to be unconvincing. Third, a constructive argument will be advanced, arguing that publicly funded GRS is clinically necessary, cost-effective, and demanded by principles of justice. Fourth, the paper will briefly discuss moralistic biases and why we demand a higher burden of justification for funding GRS compared with other analogous procedures.
Introduction
Healthcare rationing is inevitable. There are finite health resources for an almost infinite number of health needs. Given this reality, this paper analyses whether gender reassignment surgery (GRS) should be funded using our finite health budget and, if so, on what grounds. The issue of publicly funding gender reassignment surgery is fraught with immense difficulty, with complex ethical issues arising from clinical, policy, and economic considerations. The purpose of this paper is to argue that healthcare systems should publicly fund GRS and, where it is already funded, should make it more accessible to patients. The paper serves as additional affirmation for those jurisdictions who already fund GRS, showing that their policies are in line with their ethical and clinical obligations. Transgender persons are those whose physical or assigned sex does not accord with their gender identity (American Psychiatric Association [APA] 2013 ). According to the Diagnostic and Statistical Manual of Mental Disorders (DSM), transgender persons generally suffer from gender dysphoria (GD), which is the clinical distress associated with not fitting in their physical sex (APA 2013 ). I will hereinafter use the terms GD and transgender interchangeably. Across virtually all measures of physical and mental health, transgender persons have poorer outcomes than their non-transgender counterparts (Reisner et al. 2016 ). Compared to non-transgender people, transgender persons have higher rates of drug and alcohol abuse, HIV seroprevalence, diabetes, suicide ideation, and suicide attempts (Reisner et al. 2016 ). There is evidence to suggest that as many as 50 per cent of transgender youth experience suicide ideation and as many as 32 per cent have attempted suicide (Clements-Nolle, Marx, and Katz 2006 ; Grossman and D‘Augelli 2011 ). The primary contributor to these poor health outcomes is the transgender person’s strong psychological dissatisfaction with the fact that their physical sex does not correspond to their gender identity (Grossman and D‘Augelli 2011 ).
Gender reassignment surgery is promoted by the world’s leading medical authority on the issue, the World Professional Association for Transgender Health (WPATH), as an effective potential treatment for those whose GD meet specific clinical criteria (WPATH 2011 ). The clinical rationale for GRS is to alleviate the severe psychological angst the transgender person experiences as a result of their gender identity not aligning with their physical sex. Gender reassignment surgery can reduce or eliminate the psychological distress and is strongly associated with the prevention of suicide which might otherwise be attempted (Clements-Nolle et al. 2006 ; Grossman and D’Augelli 2011 ). It is currently offered in the United Kingdom in a limited capacity, with 457 operations performed in the last financial year (NHS, e-mail message to author, May 22, 2018). 1 In New Zealand, a very small number of operations are offered each year subject to very strict conditions, though the waiting list is significant due to a lack of willing surgeons to perform the procedure (Ministry of Health 2012 , 2017 ).
The Problem of GRS Funding
The philosophical literature on GRS is extremely limited, with scant publications focusing on the ethics of publicly funding the procedure. While a range of ethical issues surround the funding of GRS, space constraints necessitate the setting of some parameters for this discussion. First, this paper is concerned only with the funding of gender reassignment surgery in jurisdictions with a state-funded universal healthcare system. It is not concerned with the issue of individual patients having the right to access privately funded GRS. Second, I will assume that those seeking GRS are of legal adult age, competent, and seeking the treatment voluntarily. Third, I will not undertake an analysis of whether or not GD should even be classified as a health issue or not. Arguments in other fields such as sociology have sought to remove GD as a clinical pathology and to instead treat it as a variation of the norm (Ault and Bryzuzy 2009 ). This issue is beyond the scope of this paper, but it should be noted that if GD is removed as a diagnosable clinical condition, it may have implications for transgender persons’ health-based claim to GRS and may therefore affect their ability to draw on the arguments I intend to present. I will instead take the approach of the DSM-5, which classifies GD as a diagnosable mental health condition.
The proposal for publicly funding GRS is, not surprisingly, often met with controversy and strident objections. There are three primary objections to publicly funding GRS: First, GRS may be opposed on the grounds that it is supposedly a cosmetic or enhancement procedure rather than a medical one (NHS 2018 ). Second, those who oppose GRS may advance the claim that it is not cost-effective and that the conditions of scarcity and opportunity costs do not support its funding. Third, a slippery slope argument may be advanced to oppose the public funding of GRS. This argument suggests that if we fund GRS, we will inexorably have to fund other procedures such as elective cosmetic surgery or race-alteration surgery. I demonstrate that these arguments are faulty and unconvincing.
The first objection is what we may call the cosmetic objection. This objection argues that GRS is a cosmetic procedure rather than a clinically necessary one and that we should therefore not fund it. Consider the basic argument structure below:
- P1GRS is a cosmetic procedure.
- P2The state should not publicly fund cosmetic procedures.
- CTherefore, the state should not publicly fund GRS.
The problem with this argument is that it is not clear that Premise 1 or Premise 2 are as defensible as they may initially appear. First, Premise 1 is not altogether convincing, given that GRS is a clinically indicated procedure supported by medical evidence and experts to treat a recognized medical condition (APA 2013 ; WPATH 2011 ). It may involve cosmetic procedures on one level, but it is clearly not solely a cosmetic procedure. The objection therefore sets up a false dichotomy between clinical and cosmetic procedures. Second, even if Premise 1 is granted, it is not clear that Premise 2 can be defended. Some cosmetic procedures may be medically warranted for the attainment of an adequate state of mental and physical health, thus falling under the purview of the healthcare system, and thereby refuting Premise 2. Many public health systems, for example, fully fund breast reconstruction surgery for women who have undergone a mastectomy. This is a cosmetic procedure performed on the grounds that it will improve the patient’s mental well-being. Gender reassignment surgery, even if it involves cosmetic procedures, is done for this same reason. Cosmetic and clinical procedures, therefore, often intersect. Gender reassignment surgery is one such circumstance, given its rationale for promoting the mental and physical health of those with diagnosed GD.
The second objection is based on health resource scarcity and the opportunity costs of funding GRS. Information I obtained from the United Kingdom National Health Service (NHS) via a Freedom of Information Request identifies the average cost of one male-to-female GRS at £10,369 (NHS, e-mail message to author, May 22, 2018). 2 A GRS procedure for a female-to-male, which is far more complex, is an average of £31,780 (NHS, e-mail message to author, May 22, 2018). The majority of GRS performed are for male-to-female assignment, with a total cost to the NHS of £3,525,460 in the financial year of 2016/2017 (NHS, e-mail message to author, May 22, 2018). Using these funds for GRS, it is argued, means unjustifiably depriving other patients of other essential healthcare.
The resource scarcity argument is not convincing. First, GRS can itself be life-saving, and therefore analogous in this way to other essential healthcare services such as intensive care and emergency surgeries that cost more than a single GRS procedure. Without GRS, statistics suggest up to 32 per cent of transgender persons will attempt to commit suicide (Clements-Nolle, Marx, and Katz 2006 ; Grossman and D’Augelli 2011 ; Reisner et al. 2016 ). In purely economic terms, the cost of one death from suicide is identified by some sources at £1.7 million (NHS, 2017a ). It may well transpire, therefore, that a cost–benefit or cost–utility analysis would support funding GRS based on the benefits of saving lives, reducing the economic burden on mental health services, and losing fewer years of productive life to suicide.
Second, as far as medical procedures cost the NHS, this is fairly high, though it is comparable to other procedures which are routinely funded, highlighting the issue of consistency. For example, a lung transplant operation costs the NHS £40,076.32 per patient in the financial year 2016/2017 (NHS 2017b ). A case of complex tuberculosis costs the NHS £21,598.34 (NHS 2017b ). Treatment in an intensive care bed costs £1,932 per night, with a significant portion of patients requiring multiple days of care (NHS 2013 , 2017c ). Gender reassignment surgery fits within these parameters, given its life-saving and economic benefit, and so consistency demands that we either include it as part of the schedule of publicly funded procedures or identify a morally relevant difference. No such morally relevant difference stands up to critical scrutiny, as I shall later demonstrate.
The third objection to GRS is a slippery slope argument, claiming that if we fund GRS it will lead inexorably to the funding of numerous other procedures. For example, we may have to fund surgery for people who demand rhinoplasty. This objection can be responded to, again, through the principles of consistency. I am willing to accept the implications of this objection if, and only if, the rhinoplasty-seeking person experiences the same adverse health effects as the GD-sufferer. If rhinoplasty will prevent a severely anxious and insecure person from committing suicide, then it seems prima facie justified to publicly fund the procedure. However, the standards required to even be a candidate for GRS are very stringent, and similar standards should apply to the hypothetical life-saving rhinoplasty procedure. The patient must have a genuine and identifiable risk of self-harm and have made an autonomous request, there must be no other viable alternative treatments, and rhinoplasty should have been subjected to the two-level funding evaluation process I shall outline.
A related strand is around race appearance alteration surgery, for example, whether funding GRS means the state would also need to fund a dark-skinned person wanting to make her skin fairer on the basis of the mental distress she feels by being dark-skinned. Unlike GRS, race-based surgery may have morally important third-party effects, such as implicitly making others with dark-skin feel devalued or increasing racial stigma. Changing social attitudes is also the preferred approach since the insecurity stems almost purely from racism in society. While transgender people may be stigmatized in society, the primary effect of GD is the internal turmoil experienced independently of society’s discriminatory attitudes. Even if we removed transgender discrimination in society altogether, the GRS-seeking person would still suffer from the internal psychological distress of not belonging in their physical sex (APA 2013 ; WPATH 2011 ). The same does not seem to apply for racism. If we removed racist attitudes from society altogether, it is not clear that the dark-skinned person would continue to experience any distress from their skin colour. 3
The Constructive Argument for GRS
Having shown that the common objections against publicly funding GRS do not succeed, I now turn to a constructive argument in favour of such a policy. My constructive argument is to develop a two-level account with which to justify the public funding of GRS. This approach can also serve as a general framework for evaluating other issues of distributive justice in healthcare and is, in fact, likely already used in various jurisdictions around the world in some form or another. The first level of evaluating whether to fund GRS is to first ascertain whether the condition it intends to treat (i.e. GD) fits the criteria of a health issue and, if so, would the treatment (i.e. GRS) enable the person to improve their health. The second level of evaluation is to consider other morally relevant factors, such as opportunity costs of funding the treatment, third party effects, availability of qualified personnel, existence of alternatives, relative utility, and its impact on justice and health equity. The first-level requirement, namely that GD fits the definition of a health issue and that GRS improves health, is therefore a necessary but not sufficient condition for funding. The second level determines ultimately whether or not to fund GRS, given that the first level evaluation has been satisfied, based upon a series of further ethical considerations.
The First Level of Evaluation
The first stage of the constructive argument is to determine whether or not GRS is a clinically-indicated procedure for a medical condition, based on some definition of health. The definition of health we adopt has profound implications for the two-level approach, since it is the definition that primarily determines whether or not GRS should even be advanced to the second-level for consideration of public funding. At the same time, the definition of health we adopt has implications not only for GRS but for other health conditions more widely. Whatever definition we espouse, we must therefore be prepared to accept its implications and the demands of consistency.
Consider, for example, the World Health Organization’s (WHO) definition of health: “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (WHO 1948 , 1–2). If a health system is given the duty of promoting health, as indeed is generally the case, then it follows that its responsibilities under a WHO definition will be very broad indeed. On the other hand, Daniel Callahan rejects the WHO concept of health in favour of a purely physical account, where health is merely a state of physical well-being (Callahan 1973 ). One implication of Callahan’s account is that mental health conditions would not fall within the purview of health, and so a health system would have no obligations to provide any mental health services.
Both the WHO and Callahan accounts have implications that few of us would likely be willing to accept. With the WHO account, it may transpire that the health system ought to fund or provide a great number of services on the basis that it would promote a person’s complete physical, mental, and social well-being. For example, it may have to provide lonely rural farmers with sex workers to satisfy their social well-being and buy car fanatics Ferraris to promote complete mental well-being. With Callahan’s account of health, the state has no duty to provide care for those suffering from severe clinical depression, hallucinations, post-traumatic stress disorder, or any other mental illness regardless of its impact. I suspect few of us would be willing to accept the implications of either of these accounts.
Accordingly, I will present a basic definition of health that is pragmatic, likely to be widely accepted, has plausible implications, and is already in use by most healthcare systems. Space constraints will not allow me to defend or develop this account in any detail, but it will be sufficient to support my present argument. I propose that health is a state of physical and mental well-being. To be healthy is to be in an adequate but not necessarily complete nor perfect state of physical and mental health. My basic definition is distinct from Callahan’s account, though not drastically so. The definition does not expand the concept of health to include social and spiritual well-being and can therefore accommodate Callahan’s concerns about the “tyranny of health” where nearly every negative experience ends up being subsumed within the domain of health. The definition also does not give health a utopic or unrealistic goal of complete well-being, unlike the WHO’s definition, which Callahan is rightly critical of. However, my account can capture the problem of mental illness as a domain of health, which accords with most clinicians’ and laypeople’s considered judgements about health. It is also how most health systems and funders today view the nature of health and the role of clinicians.
The basic definition of health I propose is sufficientarian rather than “perfectionist” in nature; it strives to reach a certain threshold rather than some absolute standard. The state has no obligation to promote complete health in all its citizens. A further clarification should also be made. A condition that fits my basic definition of health does not necessarily mean that the state ought therefore to publicly fund the associated treatments. The role of the definition of health is to clarify and delineate which conditions fit within the purview of the healthcare system. There may be other morally relevant considerations, such as opportunity costs, third party effects, availability of qualified personnel, and existence of reliable clinical evidence. However, these considerations should be addressed in the second-level evaluation after understanding the health condition itself. In general, a condition that falls within the purview of the definition of health should at least be given consideration for public funding.
A consistency or derivative argument for the funding of GRS can then be advanced on the basis of this definition of health. First, given the profound effects of GD on mental and physical health, in accordance with our definition, it is a health issue that falls under the purview of the health system. Second, given that we fund a raft of other analogous health conditions on the basis of clinical necessity, for example, depression, anxiety, and other conditions which affect a person’s mental health, consistency demands that we also fund GRS unless we can highlight the presence of morally relevant differences. This argument can, of course, be rebutted by using consistency to argue that we should not fund any of the above treatments for depression or anxiety. However, this would diverge with most reasonable persons’ considered judgement that diagnosable mental health conditions should generally fall within the purview of health. The argument could also be rebutted on the basis of faulty analogy, either on the grounds that GD is not analogous to other mental health conditions or that the treatment for those conditions is not analogous to GRS. This argument, however, is not convincing. The conditions are analogous in that they fit our basic definition of health and are diagnosable conditions with a set of accepted guidelines (APA 2013 ). The treatments are analogous in that they are clinically necessary and are based on an attempt to enable a person to improve towards or reach an adequate state of physical and mental health (WPATH 2011 ).
The claim I am advancing, then, is that what matters for our first level of evaluation is not the specific condition nor the treatment itself, but rather the effect of the condition on the person’s state of physical or mental health and the ability for the treatment to help the person attain an adequate state of physical or mental health. This approach means the first-level evaluation is condition-blind . It does not matter what specific condition it is as long as it fits our definition of health. Gender dysphoria passes the criteria required in the first-level analysis. Gender dysphoria is a recognized and diagnosable condition, which affects a person’s health per our definition. Gender reassignment surgery, as a course of treatment, is supported by the clinical evidence and is effective for restoring a person to the threshold of physical and mental health or at least greatly improving the transgender person’s health (Wierck, Caenege, and Elaut 2011 ; WPATH 2011 ).
The Second Level of Evaluation
Once the first-level evaluation is completed, namely that the condition (GD) be one that fits our definition of health, we turn to the second-level evaluation to analyse other relevant factors regarding public funding. A number of relevant considerations should be taken into account. One important consideration for publicly funding GRS is the wider distributive justice impact as a result of using scarce health resources. These may include considerations of efficiency, relative utility, and opportunity costs. As already pointed out in my rejoinder to the cost-effectiveness objection to funding GRS, the claims of the critics do not stack up empirically. On the face of it, the economic impact of publicly funding GRS seems favourable (NHS 2017a , 2017b ).
Opportunity costs are important considerations in any issue involving health resource allocation, given our finite health budget (Bognar and Hirose 2014 ; Daniels 2008 ). The £10,369 to fund one male-to-female GRS could be used for an alternative need, such as funding a certain number of immunizations or a health promotion programme. There must therefore be strong grounds for funding GRS over another procedure. The case for publicly funding GRS is strong, given its potential to be a life-saving procedure and provide immense benefit to the GD patient (APA 2013 ; WPATH 2011 ).
Identifying and ethically reasoning about opportunity costs is complex, however, as we cannot be certain that cutting funding from one area will mean it going into another area of essential health need. The £10,369 could, for example, be used to install a new car park for the hospital manager or fund a hospital corporate function instead. Opportunity cost is an important consideration to acknowledge as a general principle of distributive justice in healthcare, but it cannot be the sole justification for declining funding unless the treatment is exceedingly expensive such that it would very clearly deprive other patients’ access to an even more important health service. It is not clear that GRS fits this criterion, and so we may not rely solely upon its opportunity costs to deny public funding.
Considerations of justice and health equity are morally relevant in deciding to fund GRS. If a particular procedure has especially high benefits for a marginalized or disadvantaged group, we may have extra grounds for supporting it. This could be defended on a number of different grounds including prioritarian distributive justice, whereby we ought to morally give priority to the worst-off; on utilitarian grounds, whereby the principle of diminishing marginal utility posits that the gain in utility is greater for those who are worse off; or on Rawlsian maximin reasoning (Parfit 1997 ; Rawls 1999 ). Transgender persons remain one of the most discriminated-against people in society, as well as experiencing poorer physical and mental health than their non-transgender counterparts (Clements-Nolle, Marx, and Katz 2006 ; Grossman and D’Augelli 2011 ; Reisner et al. 2016 ). Gender reassignment surgery improves the mental and physical health of a disadvantaged group, and we may therefore have an increased obligation to publicly fund the treatment on prioritarian, Rawlsian, or utilitarian grounds.
Other considerations at the second-level include the availability of qualified medical and support personnel and the availability of viable alternative treatments. Most developed countries have qualified GRS surgeons, often qualified as plastic surgeons. In the event that no qualified medical personnel are available to perform the procedure, the primary obligation becomes recruiting a workforce that is able to perform GRS. It is not an appropriate response to refuse to publicly fund GRS solely on the basis of the state of the workforce, in the same way that if no qualified clinicians are available to treat schizophrenia, the answer is to recruit such personnel rather than using it as a reason to not treat schizophrenics. As for the existence of viable alternative treatments, WPATH does not actually recommend GRS as a first-line course of treatment for those with GD. In fact, there are strict sets of guidelines for clinicians to follow (WPATH 2011). Gender reassignment surgery is therefore the appropriate treatment for certain people, given that there are no viable alternative treatments available for their GD.
One consideration that may worry policymakers is around consumer behaviour and increased demand for GRS services if it becomes fully funded. A number of responses can be offered to address this concern. First, GD is a recognized condition with diagnostic criteria in the DSM and strict treatment protocols outlined in the WPATH document (APA 2013 ; WPATH 2011 ). This fact alone limits the number of those who can make a legitimate claim on the healthcare system to fund their GRS procedure. Second, if the number of people seeking GRS increases as a result of public funding, this will likely be due to more people being able to access a service they needed all along. In such cases, existing clinical need is the driving factor. It is unlikely that people will suddenly “decide” they want to change their gender identity simply because the state now subsidizes GRS. Even if people make decisions on a whim, the criteria in the DSM and WPATH guidelines can respond by declining GRS as an appropriate avenue of treatment. Considerations about inducing demand therefore do not withstand critical scrutiny, and the constructive argument in favour of publicly funding GRS is not affected.
GRS and Moralistic Bias
The constructive argument in favour of public funding GRS, then, can be summarized as follows: First, GD is a recognized clinical condition with diagnosable criteria. It passes the first stage of evaluation, namely that the condition we are treating be one that falls within the purview of the health per our sufficientarian definition (APA 2013 ; WPATH 2011 ). Second, GRS is an effective and evidence-based procedure with clear guidelines, and one that is clinically indicated for the treatment of GD (WPATH 2011 ). Third, considerations of other morally relevant factors do not damage the constructive case to publicly fund GRS. Gender reassignment surgery is cost-effective, and the opportunity costs are worth incurring given its strong potential to be a life-saving procedure (Clements-Nolle, Marx, and Katz 2006 ; Grossman and D’Augelli 2011 ; NHS 2017a ; WPATH 2011). There are strong justice-based considerations grounded in prioritarian, utilitarian, or Rawlsian theory to fund GRS, given that transgender people are one of the most disadvantaged groups in society (Reisner et al. 2016 ). Qualified medical personnel are available to carry out the procedure, and there are no other alternative treatments in the subset of GD patients for whom GRS is clinically indicated (APA 2013 ; WPATH, 2011 ).
The constructive argument I have presented in favour of publicly funding GRS may strike some as surprisingly straightforward. However, the fact that people place such a high burden on having to justify an evidence-based, potentially life-saving medical procedure for a medically recognized condition shows that other biases may be at play. These “moralistic biases” refer to existing views and intuitions people may have about GRS and transgender and gender identity issues in general. If there were a pill that could alleviate a person’s severe psychological distress and prevent them from committing suicide at a one-off cost of £10,369, I suspect the burden of justification to fund it would be significantly less than what is demanded for GRS. The fact that we do not place such a high burden of justification for even more expensive life-saving procedures such as transplants, intensive care, and emergency department treatment shows that there are other intuitions at play in the GRS funding debate.
One of these other intuitions could be an implicit bias against altering the human body in any way (NHS 2018 ). However, altering the human body is often an essential part of medical procedures—appendectomy for the treatment of appendicitis, amputation of a limb with gangrene, or even breast reduction surgery to alleviate weight for those with back problems. These critics would very likely not object to these procedures. The intuition, then, cannot merely be about objecting to altering the body. The biases people have against GRS is probably that they do not see it as a real, medical condition that warrants clinical intervention. Given the large body of medical and scientific evidence about GD and GRS, the burden of proof now rests with those who are attempting to oppose the clinical consensus (APA 2013 ; Ministry of Health 2012 ; NHS 2017a , 2018 ; WPATH, 2011 ). In the absence of a cogent rebuttal of the clinical consensus, we should treat GRS as merely another clinical procedure for a recognized condition.
Another subset of those who oppose the public funding of GRS could be those influenced by conservative or religious views about the rights of transgender people (NHS 2018 ; Schwartz and Lindley 2009 ). In a secular, liberal state, this would arguably be problematic (Raz 1986 ). Decisions about which medical procedures to fund should be informed by clinical evidence, economic analysis, and sound ethical reasoning. If we allow religious views to dictate which clinical procedures to provide, we may find a host of services being opposed, including contraception and sexual health services. Regardless, my constructive argument does not necessarily depend on subscribing to the transgender rights movement. The argument is driven primarily by the notions of clinical necessity, as well as reasoning in an ethically consistent manner given that we fund other analogous life-saving procedures.
Not all opponents of publicly funding GRS are influenced by so-called moralistic biases. The vast majority of people who oppose GRS, I suspect, are simply unaware of the facts surrounding GD and GRS. This is not necessarily through any fault of their own, as the issue is seldom discussed in social or political circles. The lack of awareness of the empirical evidence leads critics of GRS to resort to knee-jerk intuitions, often informed through biases, social attitudes, the media, and prevailing norms. However, once we acknowledge that GD is a recognized clinical condition and that GRS is a cost-effective evidence-based surgical procedure to treat it, it becomes very difficult to continue opposing public funding.
This paper has argued that the state should publicly fund GRS. First, I have argued that initial objections to the state funding GRS do not withstand critical scrutiny. Second, I have gone on to propose a constructive argument, based on the principles of clinical necessity, cost-effectiveness, justice, and ethical consistency. Given that the procedure is analogous to numerous other cost-effective, evidence-based, life-saving procedures we fund routinely, there is a strong argument for publicly funding GRS. Third, I considered a number of further important factors and objections. None of the objections against publicly funding GRS hold, and several considerations lend further support to my constructive case. Once we overcome our initial biases and moralistic intuitions about GD and GRS, and instead treat it as we would any other condition and medical procedure, the positive case for publicly funding GRS becomes very hard to deny.
1 Data from Freedom of Information Request. Received from the NHS via email on May 22, 2018.
2 Information obtained through a Freedom of Information Request. Information received 22 May 2018
3 In our non-ideal real world, I will deliberately leave open the question of whether such race-alteration surgeries should be funded if the dark-skinned person is at very serious risk of suicide, as the lesser of two evils.
- American Psychological Association . Diagnostic and statistical manual of mental disorders . 5. Washington: American Psychological Association; 2013. [ Google Scholar ]
- Ault A, Bryzuzy S. Removing gender identity disorder from the diagnostic and statistical manual of mental disorders: A call for action. Social Work. 2009; 54 (2):187–189. doi: 10.1093/sw/54.2.187. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bognar G, Hirose I. The ethics of health care rationing: An introduction . London: Routledge; 2014. [ Google Scholar ]
- Callahan D. The WHO definition of “health.” Hastings Centre Report. 1973; 1 (3):77–87. doi: 10.2307/3527467. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Clements-Nolle K, Marx R, Katz M. Attempted suicide among transgender persons: The influence of gender-based discrimination and victimization. Journal of Homosexuality. 2006; 51 (3):53–69. doi: 10.1300/J082v51n03_04. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Daniels N. Just health: Meeting health needs fairly . Cambridge: Cambridge University Press; 2008. [ Google Scholar ]
- Grossman AH, D’Augelli AR. Transgender youth and life-threatening behaviors. Suicide and Life Threatening Behavior. 2011; 37 (5):527–537. doi: 10.1521/suli.2007.37.5.527. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ministry of Health . Gender reassignment surgery for trans people within New Zealand: Good practice guide for health professionals . Wellington: Ministry of Health; 2012. [ Google Scholar ]
- Ministry of Health. 2017. Delivering health services to transgender people. Retrieved from https://www.health.govt.nz/our-work/preventative-health-wellness/delivering-health-services-transgender-people . Accessed May 4, 2018.
- NHS . Together for health: A delivery plan for the critically ill . Wales: NHS Wales; 2013. [ Google Scholar ]
- ———. 2017a. Clinical commissioning policy: Gender identity services. United Kingdom: NHS England.
- ———. 2017b. Reference cost collection: National schedule of reference costs, 2016–2017. United Kingdom: NHS Improvement.
- ———. 2017c. Hospital adult critical care activity. Newport, U.K.: NHS Digital.
- ———. 2018. Analysis of public consultation on proposed service specifications for specialised gender identity services for adults. Edinburgh: NHS England and NHS Scotland.
- Parfit D. Equality and priority. Ratio. 1997; 10 (3):202–221. doi: 10.1111/1467-9329.00041. [ CrossRef ] [ Google Scholar ]
- Rawls, J. 1999. A theory of justice: Revised edition . Massachusetts: Harvard University Press.
- Raz J. The morality of freedom . Oxford: Oxford University Press; 1986. [ Google Scholar ]
- Reisner SL, Poteat T, Keatley J, et al. Global health burden and needs of transgender populations: A review. Lancet. 2016; 388 (10042):412–436. doi: 10.1016/S0140-6736(16)00684-X. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwartz JP, Lindley LD. Religious fundamentalism and attachment: Prediction of homophobia. The International Journal for the Psychology of Religion. 2009; 15 (2):145–157. doi: 10.1207/s15327582ijpr1502_3. [ CrossRef ] [ Google Scholar ]
- Wierck K, Van Caenegem E, Elaut E, et al. Quality of life and sexual health after sex reassignment surgery in transsexual men. Journal of Sexual Medicine. 2011; 8 (12):3379–3388. doi: 10.1111/j.1743-6109.2011.02348.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization . Constitution of the World Health Organization . Geneva: World Health Organization; 1948. [ Google Scholar ]
- World Professional Association for Transgender Health. 2011. Standards of care for the health of transsexual, transgender, and gender nonconforming people, 7th version . World Professional Association for Transgender Health.
Bias of InfoWars
- Balanced News
- Story of the Week
- News Curation Principles
- Newsletters
- Balanced Search
People Who Undergo Gender-Reassignment Surgery Have a 12x Increased Risk of Suicide

People who undergo gender-reassignment surgery have a 12x increased risk of attempting to commit suicide, according to a new study, as well as suffering other mental-health problems like PTSD and self-harm. The study, published in the journal Cureus, clearly shows that undergoing gender-reassignment, where the patient’s genitals are surgically rearranged and they also embark on a regimen of hormonal therapy, carries significant, potentially deadly, risks. The researchers note, “There is ongoing controversy surrounding the benefits of gender-affirmation surgery on mental health.” Their aim was to explore the risk of “adverse...
Related Coverage

AllSides Picks

May 20th, 2024

Malayna J. Bizier
May 17th, 2024

AllSides Staff
May 16th, 2024
More News about General News from the Left , Center and Right
From the left, from the center, from the right.

Life in Taiwan is rowdy and proud, never mind China’s threats

TAIPEI, Taiwan — Taiwan lives in the shadow of its much larger, more powerful and aggressive neighbor — one that never hesitates to remind it exactly how much larger and powerful it is.
The threat of China permeates much of political life in this island democracy, and right now it looms large. On Monday, Taiwan inaugurates its fifth democratically elected president, who won the top job in January: Lai Ching-te , the vice president under Tsai Ing-wen.
Chinese leaders in Beijing have long refused to deal with Lai because of his past position on Taiwanese independence: He was once a scrappy advocate for Taiwanese independence, although he is now a key proponent of the Democratic Progressive Party’s (DPP) efforts to maintain peace with Beijing while repelling its aggression.
The Chinese Communist Party in Beijing claims Taiwan as its own territory, even though it’s never ruled the island, and says it will take Taiwan by military force if necessary. It is expected to ramp up intimidation as Lai takes office.
But beyond the geopolitical tensions, a vibrant democratic society of 23 million people has blossomed — a development that irks Beijing beyond measure because it clearly shows that democracy and Chinese culture are in fact highly compatible.

Here in Taiwan, just 100 miles across the sea from China, seemingly competing influences come together. Taipei, the capital, buzzes with an energy both chaotic and orderly as 2.6 million people go about their lives.
It’s a cacophony of motorcycles, karaoke, day markets and night markets — life in perpetual motion.
As the day begins, elderly residents perform tai chi in the city’s many parks or visit wet markets. At the other end of the day, tourists and young people saunter through shopping districts and night markets, sometimes spilling out of karaoke bars in the early-morning hours.

In between, people eat lunch at outdoor tables and zip around on scooters, the preferred mode of transport for half of Taiwan’s adults. Other commuters crowd into the city’s extensive subway system.
Modern skyscrapers and sprawling apartment complexes abut temples that are neighborhood gathering places, especially during raucous election seasons. Shaking off its colonial and authoritarian past, its elections feel like weeks-long street parties. It was the first place in Asia to legalize same-sex marriage and has an energetic drag season. And Taiwan loves its baseball with a passion that makes the scene at Yankee Stadium look sleepy.

A love of ‘frozen garlic’
Much of this is done in a distinctly Taiwanese way, which is often to say: cute.
That even extends to the presidential office. Few embody Taiwan’s affection for cuteness better than its outgoing president Tsai, who fills her social media with photos of her adopted cats and dogs, and even donned cat ears for public events. Even at serious military parades, one can see floats depicting F-16 fighter jets as adorable, bubbly planes soaring above cheerful cartoon clouds.
Visitors marvel at the polite orderliness of residents used to picking up after themselves: During a campaign rally ahead of the presidential election in January, the main boulevard in front of the president’s office was packed with thousands of people. Within half an hour after the event, all the plastic stools were stacked neatly to the side and the ground cleared of litter.

Taiwan’s presidential election campaigns are quite a spectacle: a mix between a nationwide pop concert and a street party, complete with dancers and cheerleaders. People grow hoarse shouting “dong suan” — Taiwanese for “get elected” — which also sounds like the term “frozen garlic” in Mandarin. It feels like everyone from young parents with kids to elderly residents is on the street lobbying for their preferred candidate for the four weeks of the election campaign.
At one concert held to stir up support for young DPP candidates vying for the legislature, former parliamentarian and current metalhead Freddy Lim performed with the Buddhist death metal band Dharma.

Ahead of the January election, candidates such as Hsieh Tzu-han, running for the DPP in Taichung, cruised neighborhoods, strapped onto the back of pickup trucks, blasting slogans and music from loudspeakers. The streets were emblazoned with huge posters exhorting residents to support a multitude of candidates.
Taiwan’s democracy is a young but vibrant one. It held its first full election in 1992, five years after martial law was lifted. Today, Taiwanese citizens are known for being dedicated voters, with many expats flying home to cast their ballots. This year, voter turnout was 72 percent.

Rainbow pioneer
Taiwan has long been seen as a leader on lesbian, gay, bisexual and transgender rights, considered one of the most progressive, LGBTQ-friendly places in Asia. School textbooks extol equality, and gays and lesbians serve openly in the military.
Taiwanese often attribute the relatively tolerant atmosphere to the island’s cultural mix, which has been shaped by Indigenous groups, Dutch and Japanese colonizers, and folk practices carried across the Taiwan Strait from the Chinese mainland.

Taipei hosts the region’s largest gay pride parade. Last year more than 176,000 people attended, including then-vice president Lai.
After legalizing same-sex marriage in 2019, Taiwan last year gave same-sex couples the right to adopt children. But LGBTQ+ advocates say their work is not over. Same-sex couples are still barred from accessing reproductive technology like in vitro fertilization, and trans rights are still lagging. To change one’s gender legally, residents must show proof that they have undergone gender reassignment surgery.

Temples at the center
Temples are the cornerstone of Taiwanese society, with more than 12,000 across the country dedicated to Taoist, Buddhist or Confucian religious rites — or a mix of all three.
People leave flowers, fruit and other gifts for their local gods. Older residents can be seen smoking and chatting with friends, and students sometimes use the temple spaces as study spots. Two major festivals honoring the seafaring goddess Mazu attract millions of residents each year.

Temples feature heavily in Taiwanese politics too. They are key campaign stops for candidates and then become polling booths.
They are also places where the old and new come together. Nymphia Wind, a Taiwanese American drag queen who won the latest season of “RuPaul’s Drag Race,” held a show at a temple.

Few pastimes embody Taiwan’s hybrid identity as much as baseball. Japan, which colonized Taiwan for 50 years starting in 1895, introduced the American sport.
As China pushed Taiwan from the international stage, Taiwan’s leaders poured money into the sport as a way to forge a national identity.

Between the late 1960s and 1990s, Taiwan dominated the Little League World Series, winning 17 times, and several Taiwanese players have played in Major League Baseball.
Today, baseball is a national obsession. Watching a game in Taiwan today involves nonstop cheering, dancing and singing — by performers as well as the crowd. Being in the stands is a serious workout for many, with crowds bringing batons, horns, drums and even their own microphones and amplifiers as they try to make maximum noise for their team.

Status: It’s complicated
Taiwan, which is officially called the Republic of China (as opposed to the People’s Republic of China across the strait), exists in a kind of diplomatic gray zone. It has its own government, passport and currency and, despite Beijing’s claims otherwise, has enjoyed de facto sovereignty for the past 75 years. Still, it does not have a formal seat at the United Nations, and only 12 nations formally recognize it as a country — and that number has diminished as Beijing methodically picks off Taipei’s remaining diplomatic allies.
Today, allegiance to the Republic of China is complicated. Taiwan’s citizens lived through four decades of martial law in a one-party state led by the Kuomintang, whose members fled to Taiwan after losing mainland China to the Communists in 1949. That time of political repression under the KMT was known as the “White Terror.”

In recent years, Chinese leader Xi Jinping, who has linked unification with Taiwan as key to his dream of national “rejuvenation,” has escalated military activity around Taiwan. According to Xi, it is “inevitable” that Taiwan will become part of China.
That has created a constant sense of foreboding about a conflict that could kick off another world war involving the world’s two largest militaries — China and the United States — and potentially American regional allies including Japan, South Korea and the Philippines too.
These photos of everyday life on the island show what would be lost if China’s threats became reality.
About this story
Photography by An Rong Xu. Story by Lily Kuo. Vic Chiang in Taipei contributed to this report. Story editing by Jennifer Samuel and Anna Fifield. Copy editing by Vanessa Larson. Design and development by Andrew Braford and Jake Crump. Design editing by Joe Moore.

IMAGES
VIDEO
COMMENTS
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Insurance coverage for gender affirmation surgery is often based on WPATH guidelines. Learn more about insurance coverage, restrictions, and denials. ... Outdated terms like "sex reassignment" or "sex change" should not be used. ... (Part A and Part B) will cover gender-affirmation surgery when it is considered medically necessary. Prior to ...
Gender-affirming surgery was, at first, seen as a cosmetic or elective surgery, but research shows that the surgery is an effective treatment for people who have gender dysphoria.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender. A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery. The term "transexual" was previously used by the medical community to describe people ...
While numerous surgical interventions can be considered GAS, ... particularly as these procedures are largely elective. Analysis of procedure-specific trends by age revealed a number of important findings. ... Lellé JD, et al. Male-to-female sex reassignment surgery using the combined technique leads to increased quality of life in a ...
Gender reassignment surgery may also be referred to as gender-affirming or gender-confirmation ... A. Gender Reassignment Surgery (GRS) may be considered medically necessary when ALL the following criteria are met: 1. The member is at least 18 years of age, and 2. The member has been diagnosed with gender identity disorder, and
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Strategy. Elective surgeries were postponed during the coronavirus outbreak. But my gender-affirming surgery isn't optional — it's lifesaving. Tat Bellamy Walker. Jun 11, 2020, 6:10 AM PDT. Mr ...
The World Professional Association for Transgender Health (WPATH) today announced its updated Standards of Care and Ethical Guidelines for health professionals. Among the updates is a new suggestion to lift the age restriction for youth seeking gender-affirming surgical treatment, in comparison to previous suggestion of surgery at 17 or older.
The new diagnosis was intended to clear hurdles to gender-affirming treatment, including surgical procedures. But some contend that it inappropriately pathologizes transgender identity by ...
Gender confirmation surgeries, also known as gender affirmation surgeries, are performed by a multispecialty team that typically includes board-certified plastic surgeons. The goal is to give transgender individuals the physical appearance and functional abilities of the gender they know themselves to be. Listed below are many of the available ...
Data shows that more than 90 percent of US surgeries are considered elective or nonessential. Collectively, they bring the nation's health care system between $48 billion and $64 billion of ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Gender confirmation (also called sex reassignment) with hormones, mental therapy, and surgical transition, has been shown to relieve symptoms of gender dysphoria and to provide patients with a regained socialization in their true gender, as opposed to their gender assigned at birth. 3, 4. As a society and more specifically as a scientific ...
A trans person can choose from multiple procedures to make their appearance match their self-identified gender identity. Doctors refer to this as gender "affirmation" surgery. Trans people might ...
transgender health. Transgender Healthcare "Is Not Cosmetic or Elective. It is Essential". Alums Gray Babbs and Dani Brooks and MPH student Madeline Stump are working to understand the health experiences of transgender adults in Massachusetts seeking long-term hair removal services to inform policy and address insurance gaps. October 7 ...
Introduction. Gender dysphoria is characterized as an incongruence between an individual's experienced or expressed gender and the gender that was assigned at birth. 1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS). 2 GAS encompasses a variety of procedures that align an individual patient's gender ...
Plastic Surgery Resident; Face the Case; Keynotes Podcast; ... whereas more elective surgeries might be considered cosmetic and imputable to the patient. This dichotomy might not be as clearly defined in the reality of various situations that the plastic surgeon deals with. ... Gender confirmation (also called sex reassignment) with hormones ...
The 2016 decision memo was based on an original review of the research by a six-member team that included three medical doctors and a Ph.D. Conclusion. The burden of proof must rest on those who claim that gender reassignment surgery is "medically necessary." The 2016 CMS Decision Memo strongly suggests that the evidence is lacking to make this ...
The issue of publicly funding gender reassignment surgery is fraught with immense difficulty, with complex ethical issues arising from clinical, policy, and economic considerations. The purpose of this paper is to argue that healthcare systems should publicly fund GRS and, where it is already funded, should make it more accessible to patients.
surgeries (36). Procedures that are considered part of gender affirming treatments, namely any type of breast augmentation or prosthesis, as well as any reproductive organ surgery, are excluded from ... New South Wales Health's elective surgery policy ( 37) designates 'gender reassignment surgery' as "discretionary", without also ...
Some people in the legal community believe that a transgender worker could take FMLA leave for gender reassignment surgery as long as the worker's doctor says that the surgery is necessary to alleviate the worker's depression. Because depression is considered a serious health condition, its treatment is protected under the FMLA.
From The Right. People who undergo gender-reassignment surgery have a 12x increased risk of attempting to commit suicide, according to a new study, as well as suffering other mental-health problems like PTSD and self-harm. The study, published in the journal Cureus, clearly shows that undergoing gender-reassignment, where the patient's ...
To change one's gender legally, residents must show proof that they have undergone gender reassignment surgery. Story continues below advertisement Advertisement