Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

Research disruption during PhD studies and its impact on mental health: Implications for research and university policy
Contributed equally to this work with: Maria Aristeidou, Angela Aristidou
Roles Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Institute for Educational Technology, The Open University, Milton Keynes, Buckinghamshire, United Kingdom
Roles Conceptualization, Investigation, Resources, Writing – original draft, Writing – review & editing
Affiliation UCL School of Management, London, United Kingdom
- Maria Aristeidou,
- Angela Aristidou

- Published: October 18, 2023
- https://doi.org/10.1371/journal.pone.0291555
- Reader Comments
Research policy observers are increasingly concerned about the impact of the disruption caused by the Covid-19 pandemic on university research. Yet we know little about the effect of this disruption, specifically on PhD students, their mental health, and their research progress. This study drew from survey responses of UK PhD students during the Covid-19 pandemic. We explored evidence of depression and coping behaviour (N = 1780) , and assessed factors relating to demographics, PhD characteristics, Covid-19-associated personal circumstances, and significant life events that could explain PhD student depression during the research disruption (N = 1433) . The majority of the study population (86%) reported a negative effect on their research progress during the pandemic. Results based on eight mental health symptoms (PHQ-8) showed that three in four PhD students experienced significant depression. Live-in children and lack of funding were among the most significant factors associated with developing depression. Engaging in approach coping behaviours (i.e., those alleviating the problem directly) related to lower levels of depression. By assessing the impact of research disruption on the UK PhD researcher community, our findings indicate policies to manage short-term risks but also build resilience in academic communities against current and future disruptions.
Citation: Aristeidou M, Aristidou A (2023) Research disruption during PhD studies and its impact on mental health: Implications for research and university policy. PLoS ONE 18(10): e0291555. https://doi.org/10.1371/journal.pone.0291555
Editor: Yadeta Alemayehu, Mettu University, ETHIOPIA
Received: January 23, 2023; Accepted: August 31, 2023; Published: October 18, 2023
Copyright: © 2023 Aristeidou, Aristidou. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The raw dataset on PhD students' patient health questionnaire scale and coping mechanisms is available from the Open Research Data Online (ORDO) database: https://doi.org/10.21954/ou.rd.22794203 .
Funding: This work was supported by the Institute of Educational Technology at The Open University (MA) and the University College London (UCL) School of Management (AA). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The abrupt outbreak in January 2020 and the global proliferation of a novel virus (Covid-19) has created a crisis for many sectors, including the international higher education (HE) sector [ 1 ] that continues during the ‘post-pandemic’ period. A point of particular alarm for HE leaders, policy observers, and governments is the disruption to the typical flow and pace of university research activity. While research related to Covid-19 is still in overdrive, other research was slowed or stopped due to worldwide physical distancing measures to contain the virus’ spread (e.g., sudden campus and laboratory closures, mobility restrictions, stay-at-home orders) [ 2 ]. The resulting ‘drop in research work’ is suggested to have a detrimental impact on the HE sector on the ‘research and innovation pipeline’ [ 3 ], and on ‘research capacity, innovation and research impact’ [ 4 ].
As research and university policies internationally are being (re)shaped at a rapid pace in efforts to meet the challenge of university research disruption [ 5 ], we contribute to academic and policy conversations by examining the effect of the research disruption on the mental health of PhD students. A considerable body of research acknowledges the role of PhD students in the innovation process, in knowledge creation and diffusion (e.g., [ 6 ]) and further posits that the period of one’s PhD program is key to early career success and research productivity (e.g., [ 7 ]). These outcomes, which matter to research policy, have been linked to PhD student mental health [ 8 – 10 ]. In those times of relative stability, research had additionally demonstrated the higher prevalence of mental health issues amongst the PhD student population across research disciplines, as compared to other students within academia [ 9 ] and the general population [ 9 , 11 , 12 ]. In the period since Covid-19 disrupted our social and economic lives, depression levels in the general population have been exacerbated globally [ 13 , 14 ]. These trends suggested that the already high prevalence of poor mental health in PhD students is likely to be further exacerbated during the pandemic. Indeed, as reported in early studies on research students’ experience of the Covid-19 pandemic (e.g., [ 15 ]) and the post-pandemic period (e.g., [ 16 ]) the impact on students’ mental wellbeing has been significant, with students suggesting a number of support measures at institutional and national level.
Ignoring, at this critical moment, the increased likelihood of poor mental health in PhD students may jeopardize research capacity and HE competitiveness for years to come. Therefore, there is a pressing need to identify–within the PhD student population–those whose mental health is more affected by the research disruption, so that policies and assistance can be timelier and more targeted. Additionally, by understanding more clearly the factors that may contribute to poor mental health, and their interrelationships (presented in Methods), policymakers and HE leaders may be better placed to tackle, and ultimately overcome, this and future research disruptions.
Motivated by the current lack of an empirical basis for insights into PhD students’ mental health during the pandemic-induced disruption, we collected survey data contemporaneously during July 2020. Our 1780 survey respondents are PhD students in 94 UK Universities, across the natural and social sciences and across PhD stages. Our study has three objectives: first, to explore mental health prevalence (depression) and coping behaviour in a large-scale representative sample of PhD students in the UK (O1); second, to evaluate the relationships among mental health prevalence and coping behaviour (O2); third, to identify factors that increase the likelihood of poor PhD student mental health during the period of research disruption (O3). Our study extends previous research on mental health in the HE sector by considering the dynamics of severe disruption, as opposed to the dynamics of relative stability, on PhD students’ mental health, performance satisfaction, and coping behaviours.
Background and literature review
Uk phd students’ mental health in times of disruption.
In the UK, there are approximately 100,000 postgraduate students completing doctoral research [ 17 ]. Since 2018, significant government funding has been targeted at developing insights into supporting UK PhD students’ mental health [ 18 ]. Still, with the exception of Byrom et al. [ 11 ], published research on PhD students’ mental health in the UK exhibits the same limitations as the international research: It reflects discipline- or institution-related specificity (e.g., [ 19 ]) or utilizes samples of early career researchers in general (e.g., [ 20 ]).
Early findings on postgraduate research students’ wellbeing during the pandemic showed that only a small proportion of them are in good mental health wellbeing (28%) while the rest demonstrate possible or probable depression or anxiety [ 15 ]. Goldstone and Zhang [ 15 ] further highlight the differences among student groups with, for example, students with disabilities or caring responsibilities or female students having lower levels of mental wellbeing. The post-pandemic findings have been more promising, as only about one in four students were at risk of experiencing mental health issues [ 16 ].
In response to the Covid-19 research disruption, substantive actions have been taken by the HE sector and the UK Government to disseminate approaches deployed by UK universities to support student mental health (e.g., [ 18 ]) and to update mental health frameworks for UK universities (e.g., [ 4 ]), but so far, mitigation activities have been targeting mental health for UK university students broadly, not UK PhD students specifically.
Overcoming the paucity of evidence on UK PhD students’ mental health during the pandemic is a crucial first step to drawing strong conclusions on the prevalence and determinants of mental health issues and ways to mitigate them specific to the PhD population. For example, policy recommendations by UK postgraduate respondents during the pandemic [ 15 ] focused mainly on financial support, such as extensions to their funded period of study and tuition and visa fee support (including waivers to fees). To develop an overarching framework specific to the Objectives of our study, we synthesize insights from the international literature on PhD student mental health conducted in the period before the research disruption.
International research on PhD student mental health in times of relative stability
In the international literature examining mental health specifically for PhD students (see the systematic review in [ 21 ], the issue of mental health for PhD students is acknowledged to be multidimensional and complex [ 10 ]. In this growing research area, some address mental health as an aspect of the broader ‘health’ of the PhD students (e.g., [ 22 ]), some focus on psychological distress [ 23 ], while others take depression as a specific manifestation of distress [ 9 , 24 ]. The latter is particularly interesting because depression within the PhD population in these studies is often assessed with standardised questionnaires (e.g., PHQ, see below) that allow for developing comparative insights. It is also the approach adopted by the only global survey of PhD students’ mental health by Evans et al. [ 12 ], showing that 39% of PhD students report moderate-to-severe depression, significantly more than the general population.
Literature on PhD student’s mental health determinants in times of relative stability
Past literature on PhD students’ mental health offers insights into the determinants of PhD students’ mental health in times of stability, which may help understand the relationships we want to examine between PhD mental health, performance satisfaction and coping in times of research disruption.
First, past studies evidence the influence of PhD students’ personal lives on poor mental health. PhD students with children or with partners are less likely to have or develop psychological distress [ 9 ]. The normalcy of family roles is a much-needed antidote to the known pressures of a PhD program [ 25 ] and might even protect against mental health problems [ 22 , 26 ]. Other aspects of PhD students’ personal lives, such as significant life events (e.g., severe problems in personal relationships or severe illness of the student or someone close to them), have been linked to dissatisfaction with their research progress [ 24 ]. Research progress is defined as students’ perception of their progress in the completion of their degree [ 27 ] and is linked to their mental health. Dissatisfaction is tied to negative outcomes, such as attrition and delay [ 28 ], but also to lower productivity and mental health problems, such as worry, anxiety, exhaustion, and stress [ 29 ]. Related to this, Levecque and colleagues [ 9 ] observed that PhD students expressing a high interest in an academic career are in better mental health than those with no or little interest in remaining in academia.
Second, gender was the key personal factor that emerged as a determinant for mental health in past studies: PhD students who self-identify as female report greater clinical [ 9 , 30 ] and non-clinical problems with their mental health [ 23 , 31 ]. This is explained through the additional pressure women report on their professional and personal lives [ 23 ].
Third, past studies argue that each PhD phase presents PhD students with specific sets of challenges and should thus be explored discreetly in relation to mental health [ 32 ]. Still, the evidence on the link between the PhD phase (or the year of study as a proxy for the PhD phase) and mental health is inconclusive. Barry et al.’s [ 33 ] survey reports no connection between the PhD phase and depression levels in an Australian PhD population. However, Levecque et al. [ 9 ] report high degrees of depression in the early PhD stage of students in Belgium, and a global survey of PhD students across countries and disciplines shows that depression likelihood increases as the PhD program progresses [ 32 ].
Fourth, past research offers strong evidence that financial concerns impact PhD students’ mental health negatively. In a study by El-Ghoroury et al. [ 34 ], 63.9% of PhD students cited debt or financial issues as a cause for poor wellbeing and cited financial constraints as the major barrier to improving their wellness (through social interactions, outside-PhD activities, etc). Even uncertainty about funding was shown to predict poor mental health [ 9 ]. To this end, Geven et al. [ 35 ] explored packages of reforms in a pre-pandemic graduate school programme, including an extension of the grant period, and indicated that such policies can increase students’ completion rates to up to 20%.
Finally, age is not shown to be associated with mental health [ 9 ], but numerous studies found that having children, particularly for female PhD students and in Science-Technology-Engineering-Maths (STEM) disciplines [ 36 ], consistently corresponds with heightened stress [ 37 ]. However, a specific examination of the relationship between children and mental health indicates that PhD students with one or more children in the household showed significantly lower odds of having or developing a common psychiatric disorder [ 9 ]. Further, parenting and, in particular, motherhood during doctorate studies contribute to the development of students’ coping mechanisms that allows them to succeed in a balance in both worlds [ 38 ].
Past research insights into PhD mental health and coping
Past research explored how PhD students may “cope” with stressors and thus mitigate poor mental health [ 39 ]. Studies identify the importance of social interactions (e.g., [ 22 ]); balancing life demands (e.g., [ 16 ]), reaching out for social support (e.g., [ 40 ]) sometimes through peer relationships (e.g., [ 10 , 39 ]); and ‘planning’ (e.g., [ 22 ]); As invaluable as these insights are, drawing comparisons between these findings is difficult because often the identification of coping styles or strategies was not the focus of these studies, making it difficult to draw fine-grained conclusions as to their effect on PhD students’ mental health.
There is, however, a long tradition of research on coping for physiological wellbeing that provides standardised measures for individuals’ coping and their link to mental health [ 41 ]. The most widely used measurement instrument in the literature reviewed is the COPE Inventory, which allows researchers to assess how people cope in a variety of stressful situations, including in HE for students [ 42 – 44 ], making it particularly relevant to the context and sample under investigation in our study of PhD students. Additionally, COPE allows for the identification of consistent ways of coping, which provides predictive validity across a range of situations. Predictive validity is desired when examining the role of coping in relation to mental health. Indeed, multiple studies have linked the COPE measurement to mental health outcomes (e.g., [ 45 , 46 ]), including depression [ 43 ], which is a focus of our study.
Data and methods
Participants.
For the current study, we recruited participants that were active PhD students from March to July 2020 at any stage of their research to take part in an online survey. The survey ran between the 31st of July and the 23rd of August 2020, with the aim of capturing the potential impact of the Covid-19 disruption during the first lockdown on their research progress and mental health. The use of online surveys to assess the scope of mental health problems is particularly appropriate during the Covid-19 outbreak [ 47 ]. The current study has been reviewed by, and received a favourable opinion, from The Open University Human Research Ethics Committee (reference number: HREC/3605/Aristeidou), http://www.open.ac.uk/research/ethics/ . For the recruitment of a diverse audience, we followed a snowball sampling method, forwarding our invitation to PhD student groups in a number of UK-based universities, but also exploited the reach of PhD social media channels and online PhD groups, and we invited academics and respondents to recruit other participants. Vouchers were provided as an incentive for participation to the first 300 respondents. Before completing the survey, the respondents were provided with an online information sheet and were asked to provide their written consent through a digital consent form. They reported their email addresses to be identifiable and contactable for validation, consent issues, potential withdrawal, and incentive processing. The dataset was anonymized on the 30th of August 2020, prior to initiating data analysis.
Exclusion criteria included survey respondents who ‘straight-lined’ (chose the same answer option repeatedly), gave inconsistent responses to similar questions, or did not use their institution emails (rendering them unidentifiable). Finally, there were 1790 PhD students in the study from 94 different HE institutions across all four UK nations (England, Scotland, Northern Ireland and Wales). The majority of the study population (86%) reported that their research progress had been impacted in a negative way. The dataset [ 48 ] included 44.4% male and 55.4% female participants, while the doctoral students in the UK consist of 51% male and 49% female students [ 17 ]. Weighting adjustments were made to correct the sample representativeness. The majority of the survey respondents were 25–34 years old (80.4%), with live-in children (71%). Most respondents (86.7%) were conducting their PhDs full-time, and almost two-thirds (64.4%) were funded by a research council or a charitable body in the UK. At the time of the survey, a large proportion of the survey respondents were in the ‘executing’ phase of their research (i.e., data collection/analysis). Finally, a natural science-related PhD was being pursued by slightly over two-thirds of the respondents (68.8%). According to data sourced from HESA [ 17 ], the likelihood of individuals embarking on a research postgraduate degree at a younger age (such as 18–20) appears to be relatively low. This is evident from the fact that only 90–130 students within this age group register for such programs each year. More details on the demographics and characteristics of the sample can be found in Table 1 and below.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0291555.t001
Variables and instruments
Brief cope inventory (bci)..
The BCI [ 49 ] is a 28-item self-report questionnaire designed to measure effective and ineffective ways to cope with a stressful life event, and it is the abbreviated version of the original 60-item COPE inventory developed by [ 42 ]. The BCI has a 4-point Likert scale with options on each item ranging from 0 (I usually do not do this at all) to 3 (I usually do this a lot). Coping in this study is categorised in two overarching coping behaviours, as per Eisenberg et al. [ 50 ]: (a) the approach behaviours that attempt to reduce stress by alleviating the problem directly, which include 12 items related to active coping, positive reframing, planning, acceptance, seeking emotional support, and seeking informational support; and (b) the avoidant coping behaviours that attempt to reduce stress by distancing oneself from the problem, which include 12 items related to denial, substance use, venting, behavioural disengagement, self-distraction, and self-blame. Items that belong to neither overarching behaviour are coping related to humour and religion. These were included in the overall coping score but excluded from the analysis based on the two overarching behaviours. A higher score indicates frequent use of that coping behaviour. Cronbach’s alpha for the BCI was .88. Further, both the approach and avoidant scales have shown very good internal consistency in this sample, with Cronbach’s alpha equal to 0.83 and 0.80, respectively.
Patient health questionnaire eight-item depression scale (PHQ-8).
PHQ-8 [ 57 ] is an eight-item version of the Patient Health Questionnaire (PHQ-9). PHQ is a popular measure for assessing depression and is frequently used for PhD mental health (e.g., [ 12 , 51 ]), making it an ideal choice for our study. PHQ-9 has been validated as both a diagnostic and severity measure [ 52 , 53 ] in population-based settings [ 54 ] and self-administered modes [ 55 , 56 ], and it was recently used in a global survey of PhD students’ depression prevalence [ 12 ]. PHQ-8 omits the ninth question that assesses suicidal or self-injurious thoughts, and it was deemed more appropriate for our research because researchers in web-based interviews/surveys are unable to provide adequate interventions remotely. The PHQ-8 items employ a 4-point Likert scale with options on each item ranging from 0 (not at all) to 3 (nearly every day). Then, the scores are summed to give a total score between 0 and 24 points, where 0–4 represent no significant depressive symptoms, 5–9 mild depressive symptoms, 10–13 moderate, 15–19 moderately severe, and 20–24 severe [ 55 ]. Evidence from a large-scale validation study [ 57 ] indicates that a PHQ-8 score ≥ 10 represents clinically significant depression. In this study, Cronbach’s alpha for the PHQ-8 was 0.71, indicating a good internal consistency.
Performance satisfaction.
Performance satisfaction is an 8-item self-report scale designed to measure the students’ self-perceived progress in their PhD research, their confidence in being able to finish on time, and their satisfaction. The scale was successfully used in a PhD student well-being study at the university of Groningen [ 24 ] prior to the Covid-19 pandemic. The performance satisfaction 5-point Likert scale responses range from 1 (completely disagree) to 5 (completely agree). The score for each respondent equals the mean score of the 8-item responses. A reliability analysis was carried out on the performance satisfaction scale. Cronbach’s alpha showed the scale to reach acceptable reliability, α = 0.86.
Significant life events Significant Life events is a questionnaire designed to capture whether PhD students had experienced any significant life events in the 12 months prior to the survey. This was successfully used in studying PhD students’ mental health at the university of Groningen [ 24 ] prior to the Covid-19 pandemic research disruption. Events include the death of someone close, severe problems in personal relationships, financial problems, severe illness of oneself or someone close, being in the process of buying a house, getting married, expecting a child, none of these events, and prefer not to say. Significant life events were used as an incident control variable in this study.
Statistical analyses
SPSS (Version 25) was used for statistical analysis. In the first phase, descriptive statistics were used to describe the PHQ-8 Depression and coping behaviours of the sample and the distribution of these three variables among demographics, PhD characteristics, and Covid-19-related circumstances (O1). We used a weighting adjustment for gender to correct the survey representativeness for descriptive analysis; females were given a ‘corrective’ weight of 0.88 and males of 1.15.
In relation to O2, Spearman rank correlations were used to examine the degree of association between all of the 28 coping behaviours and PHQ-8 Depression scores. This finding contributed to our understanding of how individual coping behaviours could relate to lower or higher depressive symptoms.
To assess whether the behaviours significant to our study (i.e., those with a negative or the strongest positive PHQ-8 Depression association) were used more frequently by students of a particular demographic group (O2), we used independent-samples t-test and ANOVA. Before assessing the relationship between our variables, outliers, and groups with a sample size smaller than 15 for each group were removed from the tests (e.g., Gender = other; Funding = partially funded; Likelihood in HE = already employed in academia).
In relation to O3, a binary logistic regression analysis was performed to examine whether Covid-19-related circumstances explain significant depression in PhD students, while controlling for demographics, PhD characteristics, and external incidents. Prior to performing the regression analysis, PHQ-8 Depression score outliers, as well as groups with fewer than 10 events per variable (e.g., gender = other; age = 55–64; Impact reason = mental health), were detected and excluded from the dataset. The dichotomous dependent variable was calculated based on PHQ-8 Depression scores smaller than 10 for non-significant depression, and equal or larger than 10 for significant depression. Associations between Depression in PhD students and the independent variables in our dependency model were estimated using odds ratios (ORs) as produced by the logistic regression procedure in SPSS (Version 25). The ORs were used to explain the strength of the presence or absence of significant depression. Wald tests were used to assess the significance of each predictor. A test of the full model against a constant only model was statistically significant, indicating that the predictors as a set reliably distinguished between PhD students who are having or developing significant depression and those who are not ( Χ 2 (25) = 405.258, p < . 001 ). A Nagelkerke R 2 of .798 indicated a good to substantial relationship between prediction and grouping (68% of variance explained by the proposed model in completion rates). Table 2 presents response percentages about the categorical variables entered in the model, including the two dependent variables (significant depression and non-significant depression).
https://doi.org/10.1371/journal.pone.0291555.t002
Exploring depression prevalence and coping behaviours
The average PHQ-8 Depression score was 10.13 ( SD = 3.23) on a scale of 0–24 (weighted cases). Importantly, this highlights that the majority of survey respondents are facing moderate depression symptoms ( Fig 1 ). The PHQ-8 item with the highest score, in a range of 0–4, was ‘having trouble to concentrate on things, such as reading the newspaper or watching television’ ( M = 1.45; SD = 0.84), and the item with the lowest score was ‘moving or speaking so slowly that other people could have noticed; or the opposite–being so fidgety or restless that have been moving around a lot more than usual’ ( M = 1.10; SD = 0.75). Of the study population, 75% self-reported significant depression (moderate, moderately severe, or severe major).
https://doi.org/10.1371/journal.pone.0291555.g001
The coping behaviours that the majority of PhD students used in a medium or large amount to overcome the Covid-19 disruption were “accepting the reality of the fact that it has happened” (84%), followed by “thinking hard about what steps to make” (76%) ( Fig 2 ). Both are approaching coping behaviours. Other coping behaviours used to a great extent were “praying or meditating” (73%) , “blaming myself for things that happened” (avoidant) (71%) , and “expressing my negative feelings” (avoidant) (69%). On the other hand, coping behaviours that were used the least were all avoidant ones: “giving up attempting to cope” ( 13%) , “refusing to believe that it has happened” (15%) , “using alcohol or other drugs to make myself feel better” (17%) , and “giving up trying to deal with it” (17%) . Overall, approach coping behaviours were used to a greater extent ( M = 26.43, SD = 5.15) than avoidant coping behaviours ( M = 23.97, SD = 4.90).
https://doi.org/10.1371/journal.pone.0291555.g002
The Spearman correlations between coping behaviours and PHQ-8 scores ( Table 3 ), which included outliers, suggested that only two items have significant negative (very weak) associations with depression: Item 15, “getting comfort and understanding from someone” ( r s (1780) = -.107, p < .01); and Item 7, “taking action to try to make the situation better” ( r s (1762) = -.077, p < .01). The majority of the coping behaviours had a significant positive relationship with higher scores in depressive symptoms. The coping behaviours with the largest effect and a moderate to strong association were Item 13, “criticizing myself” ( r s (1762) = .452, p < .01), followed by Item 11 “using alcohol or other drugs to help me go through it” ( r s (1762) = .387, p < .01).
https://doi.org/10.1371/journal.pone.0291555.t003
Table 4 shows the relationship among approach and avoidant coping behaviours, and demographics. Our analyses indicated that both approach and avoidant coping behaviours had been significantly used to a greater extent by the female over male PhD students, by students without a live-in partner than those with a live-in partner, and by those without live-in children than those with live-in children. There is no evidence that the students of a particular age group were using avoidant coping more than those of another age group. However, students aged 25–34 were using approach coping behaviours less than other groups, and those aged 45–54 more ( Table 5 ).
https://doi.org/10.1371/journal.pone.0291555.t004
https://doi.org/10.1371/journal.pone.0291555.t005
Our analyses indicated that female PhD students, who had significantly lower PHQ-8 Depression scores, were using Table 3 ‘s Items 15 ( t [1778] = 14.61, p < .001) and Item 7 ( t [480] = 15.11, p < .001) significantly more than male students. Also, those without live-in partners were getting comfort and understanding from someone to a significantly greater extent than those without ( t [702] = 20.09, p < .001). PhD students without live-in children were taking action to try to make the situation better significantly more than those who have them ( t [894] = 25.21, p < .001).
Predictors of depression and relative influence
Covid-19-related circumstances (receiving an extension, impact reasons, and impact results), performance satisfaction, and coping behaviours (approach and avoidant) were entered together as predictors of depression. Demographics (gender, age, live-in partner, and live-in children), PhD characteristics (discipline, PhD phase, PhD mode, funding, interest in HE, and likelihood in HE) and external incidents were used as control variables. Table 6 reports the findings of the analyses.
https://doi.org/10.1371/journal.pone.0291555.t006
Prediction success overall was 95.3% (83.1% for not significant depression and 98.0% for significant depression). The Wald criterion demonstrated that not having an extension ( p = .014), having caring responsibilities ( p < .001), and using approach ( p < .001) or avoidant ( p < .001) coping behaviours made significant contributions to prediction. The OR value indicated that in the case that PhD students were not receiving an extension amid the Covid-19 disruption, or they did not know whether they were receiving one yet, they were 5.4 times more likely to experience significant depression. For the impact reason, our findings showed that–compared to those who experienced personal illness–PhD students who had caring responsibilities (e.g., childcare or other) showed slightly lower depressive symptoms (OR = 0.10). The OR for approach and avoidant coping behaviours were 0.13 and 43.73, respectively. This finding indicates that when approach coping is raised by one unit (e.g., +1 to the score), we see evidence for better mental health, while when avoidant coping is raised by one unit, a PhD student is very likely (44 times) to experience significant depression.
Turning to our control variables, PhD students with children in the household and with live-in partners showed significantly higher odds (about 14 and 7 times more, respectively) of having or developing depressive symptoms than those without. The latter can be explained by the fact that 88% of the participants with live-in partners also reported having live-in children. Also, male students were slightly more likely than female students to experience significant depression (with a borderline p-value), but this might be explained by the significantly increased use of coping approaches by female students. This gender-related finding that shows nearly no difference between the two categories slightly differs from Goldstone and Zhang’s model [ 15 ] which highlights a difference between female and male participants’ mental wellbeing. This difference can be explained by the fact that the research instruments used in the two studies were different, as well as the survey period.
Some PhD characteristics that made significant contributions to prediction were the discipline of PhD studies and the interest of students to remain in academia after finishing their PhD projects. The risk of experiencing significant depression in PhD students in social sciences (OR = 9.68) was lower than in students conducting a PhD in natural sciences. In contrast to findings by Levecque et al. [ 9 ], we observed that PhD students expressing a high interest in an academic career were 3.5 times more likely to develop depressive symptoms than those with no or only little interest in remaining in academia. Further, those considering having a high likelihood of remaining in academia were slightly more depressed (OR = 3.73), as well as those who were in the executing phase of their PhD research (OR = 3.33). No differences between funded and self-funded students were detected. Finally, the OR for the external incident variable was 6.13, indicating that for each incident unit (e.g., one more incident), we see evidence for depressive symptoms that are six times worse.
Our study contributes new empirical data and new insights needed to develop knowledge on the effect of university research disruption on the PhD student population. In turn, new knowledge may provide the evidence base for university and research policy.
Exploring mental health and coping behaviours
Our first contribution is to provide empirical estimates for the performance satisfaction, prevalence of mental health problems, and coping behaviours of PhD students during the pandemic-induced research disruption, on the basis of representative data across disciplines and across universities in the UK.
Our findings show that most UK PhD students across universities and disciplines report that their research progress has been affected negatively (86%). By contrast, in pre-pandemic periods, 79% of UK PhD students across Universities and disciplines had indicated excellent research progress [ 11 ]. This shift within the same population is important to reveal because of its potential implications for PhDs’ careers and university research capacity and innovation, as we know that dissatisfaction about the PhD trajectory is tied to negative outcomes such as attrition and delay [ 24 , 28 ], but also to lower productivity [ 58 ].
We found that during the period of severe research disruption caused by the Covid-19 pandemic, 75% of the UK students surveyed from 94 universities and across disciplines self-reported in the moderate-severe range for depression. This is at least three times more compared to the reported prevalence of depression among the general population internationally during the Covid-19 outbreak (16–28%, [ 59 ]). Our findings are also in line with findings in Goldstone and Zhang’s study [ 15 ] on UK postgraduate students’ mental wellbeing during the pandemic, in which 72% of the surveyed students were found to demonstrate possible or probable depression or anxiety.
By adopting widely used standardised questionnaires, our findings provide an accessible benchmark for the comparison with studies that took place among PhD student populations in periods of HE stability (pre-2020), thereby providing the empirical basis to accurately estimate the issue of poor mental health among PhD students during a period of research disruption. Using the same questionnaire as in our survey (PHQ-9) and drawing on a sample of PhD students from multiple universities and across research disciplines, a pre-pandemic global survey reported that 39% of PhD students scored in the moderate-severe range for depression [ 12 ]. Pre-pandemic national surveys of PhD students across institutions and disciplines report similar rates of depression, between 32% (in Belgium, Levecque et al. [ 9 ] and 38% (in the Netherlands, Van der Weijden et al. [ 60 ]. In a pre-pandemic (2018–2019) survey of UK PhD students across 48 universities and disciplines, only 25% reported levels that would indicate probable depression or anxiety [ 11 ]. These comparisons indicate that the prevalence of depression among the UK PhD student population of our study during the pandemic-induced period of research disruption is two-to-three times more than that which was reported in periods of stability for the UK PhD student population, for PhD student populations of other countries, and the global PhD population.
Our findings on PhD students’ mental health and PhD students’ coping advance past literature [ 22 , 23 , 34 ] in two significant ways. First, by using a highly reliable coping measure (COPE), we are able to demonstrate the relationship between coping styles and mental health outcomes in PhD students in a way that allows for comparisons and to build further research in this area. Second, we identify specific coping behaviours amongst the UK PhD students that are associated with lower depression scores and some that have a negative association with depression (i.e., getting comfort and understanding from someone and taking action to try to make the situation better ). Both are ‘coping approach’ behaviours (i.e., attempts to reduce stress by alleviating the problem directly; [ 50 ]). Studies using COPE in other populations have also linked coping-approach behaviours to fewer symptoms of psychological distress [ 45 ], more physical and psychological well-being at work [ 46 ], and an absence of anxiety and depression [ 61 ].
Factors explaining PhD students’ depression
Our second contribution is to explain–within the UK PhD population–whose mental health is more affected by the pandemic-induced research disruption. We find that several factors have a significant impact on PhD students to have or develop mental health issues during a period of research disruption.
Consistent with past research on PhD students’ mental health, our findings reveal the significant influence of their personal lives on poor mental health. The relationships we observed during a period of research disruption, however, differ from those suggested in studies conducted in periods of stability (e.g., [ 9 , 22 , 25 , 26 , 62 ]). We found that PhD students with live-in children or with a live-in partner and PhDs with caring responsibilities are more likely to have or develop significant depression compared to those without. This difference can be explained by the closure of schools that resulted in parents home-schooling their children, a greater demand for devices and the internet in households, and parents going through emotional hardship [ 63 ]. We additionally find six times worse depressive symptoms for each ‘external life incident’ (e.g., childbirth, moving home) that occurred in the PhD students’ lives. A larger number of external incidents were found to be associated with students with live-in partners and students with live-in children, which may explain these as reinforcing negative effects. These new insights explain that–although most of these realities in PhD students’ personal lives existed besides the research disruption—when combined with the research disruption, their mental health can spiral downward.
Our findings also address the role of structural PhD characteristics (PhD discipline and PhD phase) in predicting whether a student might present mental health issues in times of research disruption. We find that in a period of research disruption, the risk of significant depression is higher in the execution phase of the PhD compared to the beginning or extension phases, contrary to Levecque and colleagues’ findings [ 9 ]. Because there is very limited research on the PhD stage and mental health, our findings contribute insights to a broader community of scholars who advocate for the further study of the challenges in each PhD stage discreetly (e.g., [ 32 ]). Furthermore, we find that the risk of experiencing significant depression in PhD students in social sciences was lower than students conducting a PhD in natural sciences. Our survey respondents offered explanations on the role of PhD discipline in mental health during the pandemic in the open text responses. These converge on the fact that natural sciences often require being physically in a laboratory, which is probably unfeasible when university facilities are closed.
In tune with past research on finances and mental health in PhD students [ 9 , 64 ], we found those without funded extensions are more likely to have or develop significant depression (moderate, moderately severe, and severe) compared to those with them. We reveal the size of this association (about 5.5 times more) and link PhD funding extensions to standardized assessments of depression prevalence, thus uniquely providing new evidence for policy scholars.
Implications for research and higher education policy
Our findings show an alarming increase in self-reported depression levels among the UK PhD student population. The long-term mental health impact of Covid-19 may take years to become fully apparent, and managing this impact requires concerted effort not just from the healthcare system at large [ 59 ] but also from the HE sector specifically. With mental illness a cause for PhD student attrition, loss of research capacity and productivity, data from our survey should prompt consideration of immediate intervention strategies.
For research and education policy scholars, our findings contribute directly to the development of evidence-based research and university policies on support for targeted groups of PhD students in times of disruption. Specifically, our findings show that institutional and funder support should not only be in the form of PhD-funded extensions–which are nevertheless shown in our study and other studies (e.g., [ 15 ]) to be very significant. But also, in the form of providing expedited alternatives to the changes evoked by the pandemic for PhD students, such as new and adjusted policies that explicitly consider those PhDs with caring responsibilities, since 77% of our respondents reported that childcare and other caring responsibilities are the reason for dissatisfaction with their PhD progress. If not, the Covid-19 research disruption could erase decades of progress towards equality in academia [ 65 ].
Our main contribution is that we offer insights into how to mitigate mental health consequences for PhD students in times of research disruption. Individual-driven coping behaviours are suggested to be of equal importance to those promoted by the PhD students’ institutions [ 66 ]. In this study, approach coping behaviours were found to associate with lower depression levels, which may eventually contribute to PhD completion. The importance of developing coping mechanisms has also been highlighted in pre-pandemic studies, with, for instance, mothers finding ways to combine academic work and family responsibilities and succeed in both roles [ 38 ]. Still, institutions may play a crucial role in offering training for PhD students on coping and wellbeing through, for instance, a virtual platform to comply with social distancing policies. Such efforts may include mental health support and coping behaviour guidance, so that students are guided on how to successfully deal with disruptions (for example, to avoid avoidant coping behaviours that may lead them to higher levels of depression). Pre-pandemic reforms have previously shown that a well-structured programme and well-timed financial support can facilitate and uphold PhD completion, alongside student efforts [ 35 ]. As the future generation of academics, PhD students would be better equipped to handle the current and future disruptions and better cope with other disruptions in their academic journeys.
Limitations and implications for further research
Although our study has gone some way towards enhancing our understanding of Covid-19-related effects on UK PhD students’ mental health, it is plausible that a number of limitations could have influenced the results obtained. First, while our research attracted a representative number of students from different age groups, PhD modes, phases and funding, there was a very strong presence of students in natural sciences [ 17 ]. Second, as this was a cross-sectional study, we did not follow the UK PhD population longitudinally, and we may not offer insights into the trajectory of the relationships we articulate in our findings. Nevertheless, our adoption of standardized questionnaires allows for a platform for comparisons with past and future research efforts. Third, findings in this survey are based on self-report and may be subject to unconscious biases (e.g., PhD students assessing themselves or the situation inaccurately). Fifth, the research undertaken employed the PHQ-8 with a specific emphasis on assessing aspects related to depression. It is important to acknowledge that while these questionnaires offer valuable insights into depression, they may not comprehensively encompass the broader spectrum of general mental health. Therefore, the findings of the study should be interpreted within the context of its targeted focus on depression, recognizing the potential existence of other dimensions of mental health that were not directly addressed within this research framework. Finally, despite the high percentage of prediction in our findings (80%), additional factors may likely explain variabilities in our study outcomes, such as leadership factors or supervision styles in the 94 UK Universities whose PhD students participated in our survey.
As our study strongly demonstrates, juxtaposing findings from studies conducted during periods of relative HE stability with those conducted during periods of disruption is a fruitful approach for advancing research and university policy. By identifying which insights that would have been invaluable during periods of stability are less so during a period of disruption, scholars can provide significant advancements to existing research and new insights for policy, research and HE leadership.
Conclusions
Our study extends previous research on mental health in the HE sector by considering the dynamics of a severe disruption as opposed to the dynamics of relative stability in PhD mental health and coping behaviours. Drawing on our insights into these interrelationships, we suggest extensions to the literature on PhD students’ mental health, research and university policy. With our findings, HE leaders and policymakers may be better placed to tackle and ultimately overcome this and future research disruptions.
Acknowledgments
The authors would like to thank all the PhD students who committed time for taking part in this study and their responses informed the writing of this paper.
- View Article
- Google Scholar
- 3. O’Malley B. 180 congressmen support call for US$26bn research support. University World News [Internet]. 2020 [cited 2023 Jan 15]; Available from: https://www.universityworldnews.com/post.php?story=20200502080814674
- PubMed/NCBI
- 39. Drake KL. Psychology Graduate Student Well-being: The Relationship between Stress, Coping, and Health Outcomes. University of Cincinnati; 2010.
- 40. Pychyl T. Personal projects, subjective well-being and the lives of doctoral students. | CURVE [Internet]. Carleton University; 1995 [cited 2023 Jan 15]. Available from: https://curve.carleton.ca/d330c15c-eeaa-459c-afea-4bf841b7daa0
- 48. Aristeidou M, Aristidou A. PhDMentalHealth_UKDataset [Internet]. The Open University; 2023 [cited 2023 May 10]. Available from: https://ordo.open.ac.uk/articles/dataset/PhDMentalHealth_UKDataset/22794203/0 .
- 65. Malisch JL, Harris BN, Sherrer SM, Lewis KA, Shepherd SL, McCarthy PC, et al. Opinion: In the wake of COVID-19, academia needs new solutions to ensure gender equity [Internet]. Vol. 117, Proceedings of the National Academy of Sciences of the United States of America. National Academy of Sciences; 2020 Jul [cited 2023 Jan 15]. Available from: https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2010636117/-/DCSupplemental .

Managing While and Post-PhD Depression And Anxiety: PhD Student Survival Guide
Embarking on a PhD journey can be as challenging mentally as it is academically. With rising concerns about depression among PhD students, it’s essential to proactively address this issue. How to you manage, and combat depression during and after your PhD journey?
In this post, we explore the practical strategies to combat depression while pursuing doctoral studies.
From engaging in enriching activities outside academia to finding supportive networks, we describe a variety of approaches to help maintain mental well-being, ensuring that the journey towards academic excellence doesn’t come at the cost of your mental health.
How To Manage While and Post-Phd Depression
Why phd students are more likely to experience depression than other students.
The journey of a PhD student is often romanticised as one of intellectual rigour and eventual triumph.
However, beneath this veneer lies a stark reality: PhD students are notably more susceptible to experiencing depression and anxiety.
This can be unfortunately, quite normal in many PhD students’ journey, for several reasons:
Grinding Away, Alone
Imagine being a graduate student, where your day-to-day life is deeply entrenched in research activities. The pressure to consistently produce results and maintain productivity can be overwhelming.
For many, this translates into long hours of isolation, chipping away at one’s sense of wellbeing. The lack of social support, coupled with the solitary nature of research, often leads to feelings of isolation.
Mentors Not Helping Much
The relationship with a mentor can significantly affect depression levels among doctoral researchers. An overly critical mentor or one lacking in supportive guidance can exacerbate feelings of imposter syndrome.
Students often find themselves questioning their capabilities, feeling like they don’t belong in their research areas despite their achievements.
Nature Of Research Itself
Another critical factor is the nature of the research itself. Students in life sciences, for example, may deal with additional stressors unique to their field.
Specific aspects of research, such as the unpredictability of experiments or the ethical dilemmas inherent in some studies, can further contribute to anxiety and depression among PhD students.
Competition Within Grad School
Grad school’s competitive environment also plays a role. PhD students are constantly comparing their progress with peers, which can lead to a mental health crisis if they perceive themselves as falling behind.

This sense of constant competition, coupled with the fear of failure and the stigma around mental health, makes many hesitant to seek help for anxiety or depression.
How To Know If You Are Suffering From Depression While Studying PhD?
If there is one thing about depression, you often do not realise it creeping in. The unique pressures of grad school can subtly transform normal stress into something more insidious.
As a PhD student in academia, you’re often expected to maintain high productivity and engage deeply in your research activities. However, this intense focus can lead to isolation, a key factor contributing to depression and anxiety among doctoral students.
Changes in Emotional And Mental State
You might start noticing changes in your emotional and mental state. Feelings of imposter syndrome, where you constantly doubt your abilities despite evident successes, become frequent.
This is especially true in competitive environments like the Ivy League universities, where the bar is set high. These feelings are often exacerbated by the lack of positive reinforcement from mentors, making you feel like you don’t quite belong, no matter how hard you work.
Lack Of Pleasure From Previously Enjoyable Activities
In doctoral programs, the stressor of overwork is common, but when it leads to a consistent lack of interest or pleasure in activities you once enjoyed, it’s a red flag. This decline in enjoyment extends beyond one’s research and can pervade all aspects of life.
The high rates of depression among PhD students are alarming, yet many continue to suffer in silence, afraid to ask for help or reveal their depression due to the stigma associated with mental health issues in academia.
Losing Social Connections
Another sign is the deterioration of social connections. Graduate student mental health is significantly affected by social support and isolation.

You may find yourself withdrawing from friends and activities, preferring the solitude that ironically feeds into your sense of isolation.
Changes In Appetite And Weight
Changes in appetite and weight can be a significant indicator of depression. As they navigate the demanding PhD study, students might experience fluctuations in their eating habits.
Some may find themselves overeating as a coping mechanism, leading to weight gain. Others might lose their appetite altogether, resulting in noticeable weight loss.
These changes are not just about food; they reflect deeper emotional and mental states.
Such shifts in appetite and weight, especially if sudden or severe, warrant attention as they may signal underlying depression, a common issue in the high-stress environment of PhD studies.
Unhealthy Coping Mechanisms
PhD students grappling with depression often feel immense pressure to excel academically while battling isolation and imposter syndrome. Lacking adequate mental health support, some turn to unhealthy coping mechanisms like substance abuse. These may include:
- Overeating,
- And many more.
These provide temporary relief from overwhelming stress and emotional turmoil. However, such methods can exacerbate their mental health issues, creating a vicious cycle of dependency and further detachment from healthier coping strategies and support systems.
It’s essential for PhD students experiencing depression to recognise these signs and seek professional help. Resources like the National Suicide Prevention Lifeline are very helpful in this regard.
Suicidal Thoughts Or Attempts

Suicidal thoughts or attempts may sound extreme, but they can happen in PhD studies. This is because of the high-pressure environment of PhD studies.
Doctoral students, often grappling with intense academic demands, social isolation, and imposter syndrome, can be susceptible to severe mental health crises.
When the burden becomes unbearable, some may experience thoughts of self-harm or suicide as a way to escape their distress. These thoughts are a stark indicator of deep psychological distress and should never be ignored.
It’s crucial for academic institutions and support networks to provide robust mental health resources and create an environment where students feel safe to seek help and discuss their struggles openly.
How To Prevent From Depression During And After Ph.D?
A PhD student’s experience is often marked by high rates of depression, a concern echoed in studies from universities like the University of California and Arizona State University. If you are embarking on a PhD journey, make sure you are aware of the issue, and develop strategies to cope with the stress, so you do not end up with depression.
Engage With Activities Outside Academia
One effective strategy is engaging in activities outside academia. Diverse interests serve as a lifeline, breaking the monotony and stress of grad school. Some activities you can consider include:
- Social gatherings.
These activities provide a crucial balance. For instance, some students highlighted the positive impact of adopting a pet, which not only offered companionship but also a reason to step outside and engage with the world.
Seek A Supportive Mentor
The role of a supportive mentor cannot be overstated. A mentor who adopts a ‘yes and’ approach rather than being overly critical can significantly boost a doctoral researcher’s morale.
This positive reinforcement fosters a healthier research environment, essential for good mental health.
Stay Active Physically
Physical exercise is another key element. Regular exercise has been shown to help cope with symptoms of moderate to severe depression. It’s a natural stress reliever, improving mood and enhancing overall wellbeing. Any physical workout can work here, including:
- Brisk walking
- Swimming, or
- Gym sessions.
Seek Positive Environment
Importantly, the graduate program environment plays a critical role. Creating a community where students feel comfortable to reveal their depression or seek help is vital.
Whether it’s through formal support groups or informal peer networks, building a sense of belonging and understanding can mitigate feelings of isolation and imposter syndrome.
This may be important, especially in the earlier stage when you look and apply to universities study PhD . When possible, talk to past students and see how are the environment, and how supportive the university is.
Choose the right university with the right support ensures you keep depression at bay, and graduate on time too.
Remember You Have The Power
Lastly, acknowledging the power of choice is empowering. Understanding that continuing with a PhD is a choice, not an obligation. If things become too bad, there is always an option to seek a deferment, pause. You can also quit your studies too.

Work on fixing your mental state, and recover from depression first, before deciding again if you want to take on Ph.D studies again. There is no point continuing to push yourself, only to expose yourself to self-harm, and even suicide.
Wrapping Up: PhD Does Not Need To Ruin You
Combating depression during PhD studies requires a holistic approach. Engaging in diverse activities, seeking supportive mentors, staying physically active, choosing positive environments, and recognising one’s power to make choices are all crucial.
These strategies collectively contribute to a healthier mental state, reducing the risk of depression. Remember, prioritising your mental well-being is just as important as academic success. This helps to ensure you having a more fulfilling and sustainable journey through your PhD studies.

Dr Andrew Stapleton has a Masters and PhD in Chemistry from the UK and Australia. He has many years of research experience and has worked as a Postdoctoral Fellow and Associate at a number of Universities. Although having secured funding for his own research, he left academia to help others with his YouTube channel all about the inner workings of academia and how to make it work for you.
Thank you for visiting Academia Insider.
We are here to help you navigate Academia as painlessly as possible. We are supported by our readers and by visiting you are helping us earn a small amount through ads and affiliate revenue - Thank you!

2024 © Academia Insider


The Savvy Scientist
Experiences of a London PhD student and beyond
PhD Burnout: Managing Energy, Stress, Anxiety & Your Mental Health

PhDs are renowned for being stressful and when you add a global pandemic into the mix it’s no surprise that many students are struggling with their mental health. Unfortunately this can often lead to PhD fatigue which may eventually lead to burnout.
In this post we’ll explore what academic burnout is and how it comes about, then discuss some tips I picked up for managing mental health during my own PhD.
Please note that I am by no means an expert in this area. I’ve worked in seven different labs before, during and after my PhD so I have a fair idea of research stress but even so, I don’t have all the answers.
If you’re feeling burnt out or depressed and finding the pressure too much, please reach out to friends and family or give the Samaritans a call to talk things through.
Note – This post, and its follow on about maintaining PhD motivation were inspired by a reader who asked for recommendations on dealing with PhD fatigue. I love hearing from all of you, so if you have any ideas for topics which you, or others, could find useful please do let me know either in the comments section below or by getting in contact . Or just pop me a message to say hi. 🙂
This post is part of my PhD mindset series, you can check out the full series below:
- PhD Burnout: Managing Energy, Stress, Anxiety & Your Mental Health (this part!)
- PhD Motivation: How to Stay Driven From Cover Letter to Completion
- How to Stop Procrastinating and Start Studying
What is PhD Burnout?
Whenever I’ve gone anywhere near social media relating to PhDs I see overwhelmed PhD students who are some combination of overwhelmed, de-energised or depressed.
Specifically I often see Americans talking about the importance of talking through their PhD difficulties with a therapist, which I find a little alarming. It’s great to seek help but even better to avoid the need in the first place.
Sadly, none of this is unusual. As this survey shows, depression is common for PhD students and of note: at higher levels than for working professionals.
All of these feelings can be connected to academic burnout.
The World Health Organisation classifies burnout as a syndrome with symptoms of:
– Feelings of energy depletion or exhaustion; – Increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job; – Reduced professional efficacy. Symptoms of burnout as classified by the WHO. Source .
This often leads to students falling completely out of love with the topic they decided to spend years of their life researching!
The pandemic has added extra pressures and constraints which can make it even more difficult to have a well balanced and positive PhD experience. Therefore it is more important than ever to take care of yourself, so that not only can you continue to make progress in your project but also ensure you stay healthy.
What are the Stages of Burnout?
Psychologists Herbert Freudenberger and Gail North developed a 12 stage model of burnout. The following graphic by The Present Psychologist does a great job at conveying each of these.

I don’t know about you, but I can personally identify with several of the stages and it’s scary to see how they can potentially lead down a path to complete mental and physical burnout. I also think it’s interesting that neglecting needs (stage 3) happens so early on. If you check in with yourself regularly you can hopefully halt your burnout journey at that point.
PhDs can be tough but burnout isn’t an inevitability. Here are a few suggestions for how you can look after your mental health and avoid academic burnout.
Overcoming PhD Burnout
Manage your energy levels, maintaining energy levels day to day.
- Eat well and eat regularly. Try to avoid nutritionless high sugar foods which can play havoc with your energy levels. Instead aim for low GI food . Maybe I’m just getting old but I really do recommend eating some fruit and veg. My favourite book of 2021, How Not to Die: Discover the Foods Scientifically Proven to Prevent and Reduce Disease , is well worth a read. Not a fan of veggies? Either disguise them or at least eat some fruit such as apples and bananas. Sliced apple with some peanut butter is a delicious and nutritious low GI snack. Check out my series of posts on cooking nutritious meals on a budget.
- Get enough sleep. It doesn’t take PhD-level research to realise that you need to rest properly if you want to avoid becoming exhausted! How much sleep someone needs to feel well-rested varies person to person, so I won’t prescribe that you get a specific amount, but 6-9 hours is the range typically recommended. Personally, I take getting enough sleep very seriously and try to get a minimum of 8 hours.
A side note on caffeine consumption: Do PhD students need caffeine to survive?
In a word, no!
Although a culture of caffeine consumption goes hand in hand with intense work, PhD students certainly don’t need caffeine to survive. How do I know? I didn’t have any at all during my own PhD. In fact, I wrote a whole post about it .
By all means consume as much caffeine as you want, just know that it doesn’t have to be a prerequisite for successfully completing a PhD.
Maintaining energy throughout your whole PhD
- Pace yourself. As I mention later in the post I strongly recommend treating your PhD like a normal full-time job. This means only working 40 hours per week, Monday to Friday. Doing so could help realign your stress, anxiety and depression levels with comparatively less-depressed professional workers . There will of course be times when this isn’t possible and you’ll need to work longer hours to make a certain deadline. But working long hours should not be the norm. It’s good to try and balance the workload as best you can across the whole of your PhD. For instance, I often encourage people to start writing papers earlier than they think as these can later become chapters in your thesis. It’s things like this that can help you avoid excess stress in your final year.
- Take time off to recharge. All work and no play makes for an exhausted PhD student! Make the most of opportunities to get involved with extracurricular activities (often at a discount!). I wrote a whole post about making the most of opportunities during your PhD . PhD students should have time for a social life, again I’ve written about that . Also give yourself permission to take time-off day to day for self care, whether that’s to go for a walk in nature, meet friends or binge-watch a show on Netflix. Even within a single working day I often find I’m far more efficient when I break up my work into chunks and allow myself to take time off in-between. This is also a good way to avoid procrastination!
Reduce Stress and Anxiety
During your PhD there will inevitably be times of stress. Your experiments may not be going as planned, deadlines may be coming up fast or you may find yourself pushed too far outside of your comfort zone. But if you manage your response well you’ll hopefully be able to avoid PhD burnout. I’ll say it again: stress does not need to lead to burnout!
Everyone is unique in terms of what works for them so I’d recommend writing down a list of what you find helpful when you feel stressed, anxious or sad and then you can refer to it when you next experience that feeling.
I’ve created a mental health reminders print-out to refer to when times get tough. It’s available now in the resources library (subscribe for free to get the password!).

Below are a few general suggestions to avoid PhD burnout which work for me and you may find helpful.
- Exercise. When you’re feeling down it can be tough to motivate yourself to go and exercise but I always feel much better for it afterwards. When we exercise it helps our body to adapt at dealing with stress, so getting into a good habit can work wonders for both your mental and physical health. Why not see if your uni has any unusual sports or activities you could try? I tried scuba diving and surfing while at Imperial! But remember, exercise doesn’t need to be difficult. It could just involve going for a walk around the block at lunch or taking the stairs rather than the lift.
- Cook / Bake. I appreciate that for many people cooking can be anything but relaxing, so if you don’t enjoy the pressure of cooking an actual meal perhaps give baking a go. Personally I really enjoy putting a podcast on and making food. Pinterest and Youtube can be great visual places to find new recipes.
- Let your mind relax. Switching off is a skill and I’ve found meditation a great way to help clear my mind. It’s amazing how noticeably different I can feel afterwards, having not previously been aware of how many thoughts were buzzing around! Yoga can also be another good way to relax and be present in the moment. My partner and I have been working our way through 30 Days of Yoga with Adriene on Youtube and I’d recommend it as a good way to ease yourself in. As well as being great for your mind, yoga also ticks the box for exercise!
- Read a book. I’ve previously written about the benefits of reading fiction * and I still believe it’s one of the best ways to relax. Reading allows you to immerse yourself in a different world and it’s a great way to entertain yourself during a commute.
* Wondering how I got something published in Science ? Read my guide here .
Talk It Through
- Meet with your supervisor. Don’t suffer in silence, if you’re finding yourself struggling or burned out raise this with your supervisor and they should be able to work with you to find ways to reduce the pressure. This may involve you taking some time off, delegating some of your workload, suggesting an alternative course of action or signposting you to services your university offers.
Also remember that facing PhD-related challenges can be common. I wrote a whole post about mine in case you want to cheer yourself up! We can’t control everything we encounter, but we can control our response.
A free self-care checklist is also now available in the resources library , providing ideas to stay healthy and avoid PhD burnout.

Top Tips for Avoiding PhD Burnout
On top of everything we’ve covered in the sections above, here are a few overarching tips which I think could help you to avoid PhD burnout:
- Work sensible hours . You shouldn’t feel under pressure from your supervisor or anyone else to be pulling crazy hours on a regular basis. Even if you adore your project it isn’t healthy to be forfeiting other aspects of your life such as food, sleep and friends. As a starting point I suggest treating your PhD as a 9-5 job. About a year into my PhD I shared how many hours I was working .
- Reduce your use of social media. If you feel like social media could be having a negative impact on your mental health, why not try having a break from it?
- Do things outside of your PhD . Bonus points if this includes spending time outdoors, getting exercise or spending time with friends. Basically, make sure the PhD isn’t the only thing occupying both your mental and physical ife.
- Regularly check in on how you’re feeling. If you wait until you’re truly burnt out before seeking help, it is likely to take you a long time to recover and you may even feel that dropping out is your only option. While that can be a completely valid choice I would strongly suggest to check in with yourself on a regular basis and speak to someone early on (be that your supervisor, or a friend or family member) if you find yourself struggling.
I really hope that this post has been useful for you. Nothing is more important than your mental health and PhD burnout can really disrupt that. If you’ve got any comments or suggestions which you think other PhD scholars could find useful please feel free to share them in the comments section below.
You can subscribe for more content here:
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Reddit (Opens in new window)
Related Posts

How to Master Data Management in Research
25th April 2024 27th April 2024

Thesis Title: Examples and Suggestions from a PhD Grad
23rd February 2024 23rd February 2024

How to Stay Healthy as a Student
25th January 2024 25th January 2024
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Notify me of follow-up comments by email.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Privacy Overview
PhD students’ mental health is poor and the pandemic made it worse – but there are coping strategies that can help
Senior Lecturer in Technology Enhanced Learning, The Open University
Assistant Professor in Strategy and Entrepreneurship, UCL
Disclosure statement
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
University College London and The Open University provide funding as founding partners of The Conversation UK.
View all partners
A pre-pandemic study on PhD students’ mental health showed that they often struggle with such issues. Financial insecurity and feelings of isolation can be among the factors affecting students’ wellbeing.
The pandemic made the situation worse. We carried out research that looked into the impact of the pandemic on PhD students, surveying 1,780 students in summer 2020. We asked them about their mental health, the methods they used to cope and their satisfaction with their progress in their doctoral study.
Unsurprisingly, the lockdown in summer 2020 affected the ability to study for many. We found that 86% of the UK PhD students we surveyed reported a negative impact on their research progress.
But, alarmingly, 75% reported experiencing moderate to severe depression. This is a rate significantly higher than that observed in the general population and pre-pandemic PhD student cohorts .
Risk of depression
Our findings suggested an increased risk of depression among those in the research-heavy stage of their PhD – for example during data collection or laboratory experiments. This was in contrast to those in the initial stages, or who were nearing the end of their PhD and writing up their research. The data collection stage was more likely to have been disrupted by the pandemic.
Our research also showed that PhD students with caring responsibilities faced a greatly increased risk of depression. In our our study , we found that PhD students with childcare responsibilities were 14 times more likely to develop depressive symptoms than PhD students without children.
This does align with findings on people in the general UK population with childcare responsibilities during the pandemic. Adults with childcare responsibilities were 1.4 times more likely to develop depression or anxiety compared to their counterparts without children or childcare duties.
It was also interesting to find that PhD students facing the disruption caused by the pandemic who did not receive an extension – extra financial support and time beyond the expected funding period – or were uncertain about whether they would receive an extension at the time of our study, were 5.4 times more likely to experience significant depression.
Our research also used a questionnaire designed to measure effective and ineffective ways to cope with stressful life events. We used this to look at which coping skills – strategies to deal with challenges and difficult situations — used by PhD students were associated with lower depression levels. These “good” strategies included “getting comfort and understanding from someone” and “taking action to try to make the situation better”.

Interestingly, female PhD students, who were slightly less likely than men to experience significant depression, showed a greater tendency to use good coping approaches compared to their counterparts. Specifically, they favoured the above two coping strategies that are associated with lower levels of depression.
On the other hand, certain coping strategies were associated with higher depression levels. Prominent among these were self-critical tendencies and the use of substances like alcohol or drugs to cope with challenging situations.
A supportive environment
Creating a supportive environment is not solely the responsibility of individual students or academic advisors. Universities and funding bodies must play a proactive role in mitigating the challenges faced by PhD students.
By taking proactive steps, universities could create a more supportive environment for their students and help to ensure their success.
Training in coping skills could be extremely beneficial for PhD students. For instance, the University of Cambridge includes this training as part of its building resilience course .
A focus on good strategies or positive reframing – focusing on positive aspects and potential opportunities – could be crucial. Additionally, encouraging PhD students to seek emotional support may also help reduce the risk of depression.
Another example is the establishment of PhD wellbeing support groups , an intervention funded by the Office for Students and Research England Catalyst Fund .
Groups like this serve as a platform for productive discussions and meaningful interactions among students, facilitated by the presence of a dedicated mental health advisor.
Our research showed how much financial insecurity and caring responsibilities had an effect on mental health. More practical examples of a supportive environment offered by universities could include funded extensions to PhD study and the availability of flexible childcare options.
By creating supportive environments, universities can invest in the success and wellbeing of the next generation of researchers.
- Higher education
- Mental health
- Coping strategies
- PhD students
- Give me perspective

Compliance Lead

Lecturer / Senior Lecturer - Marketing

Assistant Editor - 1 year cadetship

Executive Dean, Faculty of Health

Lecturer/Senior Lecturer, Earth System Science (School of Science)

Alarming Increase of Depression and Anxiety Among the PhD and Post-doctoral Researchers
PhD and post-doctoral researchers are feeling exhausted, overworked, and are worried about their future. If this is how you are feeling, you are not alone. The stress and pressure of academic life can be relentless, leading to depression and anxiety. Disturbingly, it is becoming common for young researchers to battle with mental health issues. This is especially prevalent in life sciences and engineering. Why is this happening?
Why are Researchers Struggling?
The American author Zig Ziglar summed up what people thrive on well: “ Research indicates that employees have three prime needs: Interesting work, recognition for doing a good job, and being let in on things that are going on in the company.”
Researchers tend to be passionate and enthusiastic about their work. They want to make a meaningful contribution to their field. Therefore, the above quote describes them well. The factors that contribute to stress and lead to anxiety and depression are listed below. It comes as no surprise that researchers, by nature, try too hard and fall victim to these stresses .
- Extended hours: As you know, academia comes with a considerable amount of responsibility. As you progress up the academic ladder, your responsibilities increase. You must balance teaching, admin, and research. You spend evenings and weekends working to keep up.
- Mentorship Relationship : Many researchers feel unsupported by their PIs. Some PIs expect a lot from their researchers, or PIs themselves are overwhelmed and therefore unable to offer the required
- Future: Uncertainty about your career prospects for the future can be frustrating and worrying.
- Financial uncertainty: Often, in academia, researchers are underpaid and funds are available for short time periods, leading to financial insecurity.
- Frequent evaluation: The constant reports to faculty and funders put extra pressure on researchers.
- Competitive atmosphere: Resources are scarce. Therefore, the competition for funding is enormous. Postdocs and PhDs are under more pressure to be productive.
- Management style: Researchers are at higher risk of mental health issues if their lab culture is bureaucratic. People are happier when they are part of the decision process, especially at D. and postdoc level where one expects to run with a project.
- Mental wellbeing of University staff: Emotional and physical exhaustion among the PIs, negatively impact the students under them.
Stress intensifies as things become urgent towards the end of your project. Your submission deadlines are looming, and your funds are coming to an end. It can be overwhelming to complete a project as well as plan your future at the same time.
Signs that your mental health is in trouble include:
- Disrupted sleep
- Cognitive impairment
- Mood changes
- Working long hours at night
- Emotional outbursts
- Eating disorders
Mental Wellbeing Studies
The stats are high. Research on the mental health of Ph.D. students showed that 32 % are likely to develop depression. A 2016 survey found that 41 % of PhDs and postdocs were anxious, and 39 % were depressed. This is not new news, in 2013 and 2014, similar studies found that about one-third of postdocs were struggling with their mental health.
Mentors can Help
If you are a PI or a supervisor, you understand first-hand the pressures that your researchers are under. Here are some tips to help your students :
- This is a great prevention strategy. Mentors should be aware of their student’s mental health and educate them about the risks and signs of anxiety and depression.
- Training: Mentors could benefit from training on this subject so that they can identify a student who is struggling and assist them.
- Career Advice: Future employment opportunities are worrying Therefore, mentors should inform students of the low prospects of securing an academic position. Furthermore, they should advise them to research alternative career paths as possible options at the start of their project. It becomes too stressful to find employment when your deadline is approaching.
- Compassionate and kind leadership: Listen to your students and put yourself in their shoes.
- Be inspirational to your researchers. This will help create a happy team.
Keep Your Mind Healthy
We all know what we should be doing to keep physically and mentally healthy . Let me remind you.
- Get enough sleep.
- Exercise regularly, relieve stress.
- Eat healthy food.
- Connect with friends and family.
- Get professional help to resolve stress and anxiety.
- Make time for things you enjoy.
Get Help – Speak Out
It is time to get help if you start thinking about harming yourself, you feel overwhelmed about things that you usually cope with, you rely on drugs or alcohol to feel better, you still feel down even if something good happens, you are unsure why you are feeling down or you struggle with daily tasks.
If you are struggling, consult your healthcare practitioner or University counseling program. Chances are you are one of many academics suffering from a mild mental disorder. When researchers do eventually get help, they wonder why they waited so long. It is amazing to know how much better you will function with your daily tasks.
Remember, there is life outside the lab!
Academia can be a rewarding career. You just need to know what you are in for, manage your stress and remember your life outside the lab. Most of all, understand that you are not alone, a lot of researchers are feeling the same, but possibly not talking about it. Postdocs who have spoken up about their struggles have had many responses from researchers in similar situations. If everyone who struggled with mental health issues spoke up, we would realize how prevalent it is. This would go a long way toward fighting the stigma associated with mental health struggles.
Have you noticed that you or your colleagues are struggling with mental wellbeing? Help us fight the stigma by speaking out in the comments section below.
Rate this article Cancel Reply
Your email address will not be published.

Enago Academy's Most Popular Articles

- Reporting Research
Choosing the Right Analytical Approach: Thematic analysis vs. content analysis for data interpretation
In research, choosing the right approach to understand data is crucial for deriving meaningful insights.…

Comparing Cross Sectional and Longitudinal Studies: 5 steps for choosing the right approach
The process of choosing the right research design can put ourselves at the crossroads of…

- Career Corner
Unlocking the Power of Networking in Academic Conferences
Embarking on your first academic conference experience? Fear not, we got you covered! Academic conferences…

Research Recommendations – Guiding policy-makers for evidence-based decision making
Research recommendations play a crucial role in guiding scholars and researchers toward fruitful avenues of…

- AI in Academia
Disclosing the Use of Generative AI: Best practices for authors in manuscript preparation
The rapid proliferation of generative and other AI-based tools in research writing has ignited an…
Intersectionality in Academia: Dealing with diverse perspectives
Meritocracy and Diversity in Science: Increasing inclusivity in STEM education
Avoiding the AI Trap: Pitfalls of relying on ChatGPT for PhD applications

Sign-up to read more
Subscribe for free to get unrestricted access to all our resources on research writing and academic publishing including:
- 2000+ blog articles
- 50+ Webinars
- 10+ Expert podcasts
- 50+ Infographics
- 10+ Checklists
- Research Guides
We hate spam too. We promise to protect your privacy and never spam you.
- Commitment to Diversity
- Current Center Members
- Former Center Members
- Current Openings
- Anxiety and Traumatic Stress Disorders Laboratory
- Laboratory for Affective and Translational Neuroscience
- Motivated Learning & Memory Laboratory
Treatment and Etiology of Depression in Youth Laboratory
- McLean Conte Center for the Neurobiology of Approach-Avoidance Decision Making
- Collaborators
- Publications
- Latest News
- Active Studies
- How To Help

Director: Isabelle M. Rosso, PhD. The Anxiety and Traumatic Stress Disorders Laboratory conducts research on the neurobiological basis of posttraumatic stress disorder (PTSD) and anxiety disorders, which may help inform diagnosis and lead to new treatment development for these...

Director: Diego A. Pizzagalli, PhD. Using a multi-modal approach spanning different levels of analyses (e.g., environment, genes, brain, behavior), lab members are working towards a better understanding of the causes, consequences, and pathophysiology of depression. One of...

Director: Daniel G. Dillon, PhD. The Motivated Learning & Memory Lab uses methods from cognitive and affective neuroscience to provide new insight into psychiatric illness. We are focused on understanding how depression affects long-term memory and reinforcement learning. Our ultimate goal is to generate new targets for prevention and treatment interventions.

Director: Christian A. Webb, PhD. Lab Website: https://WebbsLab.com The Treatment and Etiology of Depression in Youth (TEDY) Laboratory uses a multimodal approach (EEG, fMRI, ecological momentary assessment, passive smartphone sensor data, laboratory-based experiments, and...
- About The Center

The Center for Depression, Anxiety and Stress Research embraces a multi-disciplinary approach to improve our understanding of the psychological, environmental, and neurobiological factors associated with affective disorders. Depression, anxiety and related disorders are major public health problems. In the United States, one out of every five people will develop depression or an anxiety disorder in […]
Director’s Message

Diego A Pizzagalli, Ph.D. is Director of the Center for Depression, Anxiety and Stress Research, and a Professor of Psychiatry at Harvard Medical School.

Individually and collaboratively, the four labs in the Center for Depression, Anxiety and Stress Research maintain a robust and diverse research agenda. Here you’ll find descriptions of current research topics in each lab.
There are no upcoming events.
Dr. Diego Pizzagalli received the Neuropsychopharmacology Editor’s Award for a Review (NEAR)
Kevin Clancy awarded a Joseph & Susan Gatto Foundation Award for his project entitled “Phenomenological and mechanistic properties of trauma-related intrusive memories and their roles in maladaptive coping behaviors”.
- Hormones, depression and the brain , males and females, ages 18 to 25
- Depression treatment for adolescents ages 12 to 18, with a parent
- The effects of stress on learning , adults with current or past depression
- Brain activity during cognition , healthy adults ages 18 to 45
- Avoiding adolescent depression , ages 12 to 18 with a parent
- Healthy adults , all studies, ages 18 to 45
- Treatment and Etiology of Depression in Youth
- News & Events
- Participate
Designed by Elegant Themes | Powered by WordPress

Dr. Meghan Keely McMackin
Psychologist , phd (she, her), my practice at a glance.
3108 Mount Pleasant Street Northwest Suite 4
Washington, DC 20010
1350 Connecticut Avenue Northwest
Washington, DC 20036
- Individual Sessions $230
- Pay by American Express, Cash, Check, Discover, Mastercard, Visa
- Out of Network
Qualifications
- Verified by Psychology Today Licensed by State of Virginia / 0810007920 Dr. Meghan Keely McMackin License state differs from primary location state.
- In Practice for 3 Years
- Attended University of Wisconsin - Madison , PhD in Educational Psychology , Graduated 2020
Specialties and Expertise
Top specialties.
- Obsessive-Compulsive (OCD)
- Coping Skills
- Impulse Control Disorders
- Life Coaching
- Life Transitions
- Mood Disorders
- Peer Relationships
- Relationship Issues
- School Issues
- Self Esteem
- Trauma and PTSD
Endorsement

Client Focus
Participants, treatment approach, types of therapy.
- Acceptance and Commitment (ACT)
- Cognitive Behavioral (CBT)
- Exposure Response Prevention (ERP)
- Motivational Interviewing
- Trauma Focused
Primary Location
Additional location, nearby areas.
- Washington, DC
- District Of Columbia
Neighborhoods
- Dupont Circle
- Mount Pleasant
A Systematic Review of Grief and Depression in Adults
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
Although grief is a normal response to loss, it is a complex and multidimensional process that can involve a wide range of distressing symptoms and significantly affect an individual’s functioning. People respond to death in diverse ways, both adaptively and maladaptively, and these reactions are highly personalized. During this time, bereaved individuals engage in tasks such as accepting the reality of the loss, managing emotional distress, adjusting to life without the deceased, and eventually letting go of the emotional attachment to the person who has died.

- This systematic review synthesized findings on depression and grief in adults, aiming to identify specificities of depression in grief and whether grief varies based on the type of loss.
- Factors like gender, education level, socioeconomic status, age of the deceased, cause of death, and time since loss significantly affect grief outcomes and the development of depression.
- The research, while enlightening, has limitations, such as the inability to isolate depression from other grief symptoms in some studies and variation in the types of losses examined.
- Understanding the relationship between grief and depression is universally relevant, as most people will experience the loss of a loved one and may be at risk for negative mental health outcomes.
Grief is a profound life experience that can lead to complications like depression for bereaved individuals. Depressive symptoms place a heavy burden on societal resources (Moreira et al., 2023).
Previous research has shown significant overlap between grief and depression in terms of symptoms, characteristics, family history, and response to medication (Kendler et al., 2008; Lamb et al., 2010; Zisook & Kendler, 2007; Zisook et al., 2001, 2007).
Increasing evidence indicates losing a loved one can lead to prolonged grief disorder and depressive symptoms/syndromes (Bonanno et al., 2007; Prigerson et al., 2009; Shear et al., 2011).
This systematic review aimed to synthesize findings on depression and grief to identify specificities of depression in grief and factors influencing grief outcomes.
Understanding the distinctions between grief and depression has important implications for the mental and physical health of bereaved individuals.
This systematic review followed PRISMA guidelines. Studies were identified through searching EBSCO, PubMed, and Web of Science databases.
- Search terms included variations of “depression,” “grief,” “bereavement,” and “mourning.”
- Inclusion criteria were having a grief sample and depression measures.
- Exclusion criteria included case studies, theoretical essays, reviews, instrument validations, not examining grief and depression, non-bereaved samples, and low study quality.
41 studies published between 1939-2021 were included. Two independent reviewers selected studies with almost perfect agreement (Cohen’s κ = .86). Study quality was assessed with the Quantitative Research Assessment Tool.
The search equation used variations of the key terms in the databases:
- EBSCO: TI (depress* OR mood disorder) AND TI (mourn* OR grief OR bereave* OR death OR loss)
- PubMed: (depress [Title] OR mood disorder[Title]) AND (mourn [Title] OR grief[Title] OR bereave* OR death[Title] OR loss)
- Web of Science: TI=(depress* OR mood disorder) AND TI=(mourn* OR grief OR bereave* OR death OR loss)
Studies can be grouped into two categories based on time of loss, namely grief during pregnancy or grief of a close relative
- After spontaneous abortion, women experienced more grief and depressive symptoms than their male partners. Childless women and those with infertility had higher grief.
- After miscarriage, 26.6% of women who met grief criteria also had depressive episodes.
- Grief symptoms decreased over a year after pregnancy loss, but depressive symptoms increased around 6 months for women who experienced sudden losses.
- Negative cognitions predicted grief 16-19 months after a perinatal death. Having more children was associated with less depression.
Early Childhood
- Infant death was associated with increased depression and psychosis-like experiences in mothers.
- 34% of caregivers had clinically significant depressive symptoms 3 months after losing a loved one.
Childhood/Adolescence
- 30% of bereaved parents had depression 5 years after a child’s cancer death vs. 14% of parents whose child survived. Mothers had more depression than fathers.
- Parental grief was predicted more by couple-level factors while depression was predicted more by individual factors. Traumatic child deaths led to more parental grief.
Adults/Elderly
- In gay men who lost a friend to AIDS, grief and depression were distinct. Depression was predicted by negative affect, health concerns, and loneliness. Grief was predicted by number of AIDS losses.
- 16% met criteria for complicated grief (CG) 1-2 years after losing a friend/relative. Relationship depth predicted CG while dependence predicted depression.
- Pre-loss grief, being a partner, and low education predicted post-loss CG and depression in caregivers.
- Violent deaths led to more depression, especially in females. CG and depression decreased over time after loss. More years since loss was associated with less depression in elders.
This review provides insights into the complex relationship between grief and depression after different types of losses.
While there is overlap, they emerge as distinct responses – certain factors uniquely predict grief (e.g., relationship depth, couple-level factors), while others uniquely predict depression (e.g., personal vulnerabilities, less time since loss).
Gender, education level, socioeconomic status, age of the deceased, cause of death, and time since loss are significant factors that influence grief outcomes and the development of depression following bereavement.
Research has shown that women often experience more intense grief and depressive symptoms compared to men, particularly in cases of miscarriage or child loss. Lower levels of education and socioeconomic status have been associated with a higher risk of complicated grief and difficulty coping with loss.
The age of the deceased also plays a role, with the loss of a child or younger individual often leading to more severe grief reactions compared to the loss of an older person.
Sudden, traumatic, or violent causes of death, such as accidents, homicide, or suicide, can result in more complicated grief and depression compared to losses due to natural causes or prolonged illness.
Finally, the time elapsed since the loss is a significant factor, as grief and depressive symptoms tend to decrease over time as individuals adjust to their new reality.
However, for some, grief may remain intense and prolonged, leading to complicated grief or persistent depression. Understanding these factors can help identify individuals at higher risk for adverse grief outcomes and inform targeted interventions.
Future research could further examine how the predictors of grief and depression vary depending on kinship to the deceased and expand to include more diverse causes of death.
- Followed PRISMA guidelines for systematic reviews
- Broad search of multiple databases
- Rigorous inclusion/exclusion criteria
- Independent reviewer selection of studies with high inter-rater reliability
- Assessed study quality with a standardized tool
- Examined grief and depression in response to various types of losses across the lifespan
Limitations
- Some included studies could not statistically isolate depression from other grief symptoms
- High variability in the types of losses and kinship of bereaved individuals across studies
- Conclusions may be limited by the demographics of study samples and countries where research was conducted
- Cross-sectional and retrospective designs of some studies prevent causal conclusions
Clinical Implications
The results have significant real-world implications, especially for clinical practice.
Understanding risk factors for intense, prolonged grief and depression can help practitioners identify bereaved clients who may need more support.
For example, those with prior depression/mental health issues, traumatic losses, or fewer coping resources may be more vulnerable.
Screening for complicated grief (CG) is important since it is underpinned more by interpersonal factors and may not respond to depression treatments.
Distinguishing between grief and depression is important for intervention and treatment, as grief is a normal response while depression may be more likely in individuals with certain vulnerabilities. However, some individuals with vulnerabilities may have a decreased ability to grieve.
The findings also suggest value in dyadic and family interventions since couple/family dynamics can influence grief. Gender differences imply the potential benefits of tailoring treatments.
Broadly, the review underscores the need to recognize the long-term impacts of bereavement, as grief and depressive symptoms can persist for years. Societal resources should be allocated to make bereavement support accessible.
More public education on the range of normal grief responses may help destigmatize the grief experience.
Primary reference
Moreira, D., Azeredo, A., Moreira, D. S., Fávero, M., & Sousa-Gomes, V. (2022). Why Does Grief Hurt?. European Psychologist, 28 (1), 35–52. https://doi.org/10.1027/1016-9040/a000490
Other references
Bonanno, G. A., Neria, Y., Mancini, A., Coifman, K. G., Litz, B., & Insel, B. (2007). Is there more to complicated grief than depression and posttraumatic stress disorder? A test of incremental validity. Journal of Abnormal Psychology, 116 (2), 342–351. https://doi.org/10.1037/0021-843x.116.2.342
Kendler, K. S., Myers, J., & Zisook, S. (2008). Does bereavement-related major depression differ from major depression associated with other stressful life events? American Journal of Psychiatry, 165 (11), 1449-1455. https://doi.org/10.1176/appi.ajp.2008.07111757
Lamb, K., Pies, R., & Zisook, S. (2010). The bereavement exclusion for the diagnosis of major depression: To be or not to be. Psychiatry, 7 (7), 19-25.
Moreira, D., Azeredo, A., Moreira, D.S., Fávero, M., & Sousa-Gomes, V. (2023). Why does grief hurt? A systematic review of grief and depression in adults. European Psychologist, 28 (1), 35-52. https://doi.org/10.1027/1016-9040/a000490
Prigerson, H. G., Horowitz, M. J., Jacobs, S. C., Parkes, C. M., Aslan, M., Goodkin, K., Raphael, B., Marwit, S. J., Wortman, C., Neimeyer, R. A., Bonanno, G. A., Block, S. D., Kissane, D., Boelen, P., Maercker, A., Litz, B. T., Johnson, J. G., First, M. B., & Maciejewski, P. K. (2009). Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Medicine, 6 (8), Article e1000121. https://doi.org/10.1371/journal.pmed.1000121
Shear, M. K., Simon, N., Wall, M., Zisook, S., Neimeyer, R., Duan, N., Reynolds, C., Lebowitz, B., Sung, S., Ghesquiere, A., Gorscak, B., Clayton, P., Ito, M., Nakajima, S., Konishi, T., Melhem, N., Meert, K., Schiff, M., O’Connor, M., … Keshaviah, A. (2011). Complicated grief and related bereavement issues for DSM-5. Depression and Anxiety, 28 (2), 103–117. https://doi.org/10.1002/da.20780
Zisook, S., & Kendler, K. S. (2007). Is bereavement-related depression different than non-bereavement-related depression?. Psychological Medicine, 37 (6), 779-794. https://doi.org/10.1017/S0033291707009865
Zisook, S., Shuchter, S. R., Pedrelli, P., Sable, J., & Deaciuc, S. C. (2001). Bupropion sustained release for bereavement: Results of an open trial. Journal of Clinical Psychiatry, 62 (4), 227-230. https://doi.org/10.4088/jcp.v62n0403
Zisook, S., Shear, K., & Kendler, K. S. (2007). Validity of the bereavement exclusion criterion for the diagnosis of major depressive episode. World Psychiatry, 6 (2), 102-107.
Keep Learning
- What factors do you think might influence how an individual responds to and copes with the death of a loved one? How could cultural background play a role?
- This review found some gender differences in grief and depression. Why do you think men and women may respond differently to loss? What are the implications for providing support?
- Imagine someone close to you experienced a significant loss one year ago. Based on the findings, what signs might indicate they are struggling with complicated grief and could benefit from professional help?
- The results suggest grief and depression are distinct but overlapping responses. How would you explain the difference between grief and depression to a friend who recently lost a loved one?
- Many of the studies used self-report measures of grief and depression symptoms. What are the strengths and limitations of this type of data? What other methods could provide useful insights?
- No single theory can fully explain the range of grief responses. What are some different theoretical perspectives on the grieving process? How could integrating them help us better understand the complexity of coping with loss?
Related Articles

Clinical Psychology
A Study Of Social Anxiety And Perceived Social Support

Psychological Impact Of Health Misinformation: A Systematic Review

Sleep Loss and Emotion: A Systematic Review and Meta-Analysis

Family History Of Autism And ADHD Vary With Recruitment Approach And SES

Measuring And Validating Autistic Burnout

Anxiety in Early Adolescents During the Covid-19 Pandemic
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Trends in U.S. Depression Prevalence From 2015 to 2020: The Widening Treatment Gap
Renee d. goodwin.
1 Department of Epidemiology and Biostatistics, Graduate School of Public Health and Health Policy, City University of New York, New York, New York
2 Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, New York
Lisa C. Dierker
3 Psychology Department, Wesleyan University, Middletown, Connecticut
Sandro Galea
4 Boston University School of Public Health, Boston, Massachusetts
Christina W. Hoven
5 New York State Psychiatric Institute, New York, New York
6 Department of Psychiatry, College of Physicians and Surgeons, Columbia University, New York, New York
Andrea H. Weinberger
7 Ferkauf Graduate School of Psychology, Yeshiva University, Bronx, New York
8 Department of Epidemiology & Population Health, Albert Einstein College of Medicine, Bronx, New York
Associated Data
Introduction.
Major depression is a common and potentially lethal condition. Early data suggest that the population-level burden of depression has been exacerbated by the COVID-19 pandemic. Prepandemic estimates of depression prevalence are required to quantify and comprehensively address the pandemic's impact on mental health in the U.S.
Data were drawn from the 2015–2020 National Survey on Drug Use and Health, a nationally representative study of U.S. individuals aged ≥12 years. The prevalence of past-year depression and help seeking for depression were estimated from 2015 to 2019, and time trends were tested with Poisson regression with robust SEs. Point estimates were calculated for 2020 and not included in statistical trend analyses because of differences in data collection procedures.
In 2020, 9.2% (SE=0.31) of Americans aged ≥12 years experienced a past-year major depressive episode. Depression was more common among young adults aged 18–25 years (17.2%, SE=0.78), followed closely by adolescents aged 12–17 years (16.9%, SE=0.84). Depression increased most rapidly among adolescents and young adults and increased among nearly all sex, racial/ethnic, income, and education groups. Depression prevalence did not change among adults aged ≥35 years, and the prevalence of help seeking remained consistently low across the study period.

Conclusions
From 2015 to 2019, there were widespread increases in depression without commensurate increases in treatment, and in 2020, past 12‒month depression was prevalent among nearly 1 in 10 Americans and almost 1 in 5 adolescents and young adults. Decisive action involving a multipronged public health campaign that includes evidence-based prevention and intervention to address this ongoing mental health crisis is urgently needed.
INTRODUCTION
Major depression is the most common mental disorder in the U.S. 1 and is the strongest risk factor for suicide behavior. 2 , 3 , 4 Previous findings show increases in depression in the U.S. population from 6.6% in 2005 to 7.3% in 2015, 5 consistent with other data. 6 The most rapid increases from 2005 to 2015 were observed among adolescents and those at the highest and lowest income levels. For race/ethnicity and sex, trends were generally equivalent with increases across all groups. 6 Early reports in 2020 and forward suggest that the coronavirus 2019 (COVID-19) pandemic has contributed to a worsening mental health crisis in the U.S., 7 , 8 , 9 , 10 especially among adolescents and young adults. 4 Obtaining accurate prepandemic national estimates is critical to eventually quantifying and adequately addressing the mental health impact of the pandemic.
Most individuals with depression remain untreated or undertreated. 11 , 12 , 13 Although substantial progress has been made in evidence-supported pharmacologic and psychotherapeutic treatments for depression over the past several decades, 13 , 14 commensurate and comprehensive implementation of and access to affordable high-quality mental health care has not occurred.
Moreover, substantive sociodemographic differences in help seeking and receipt of treatment for depression persist. For instance, individuals with higher SES and/or insurance coverage (versus those with lower SES and/or without insurance) are more likely to access and receive depression treatment, more likely to engage more extensively in treatment, and less likely to discontinue medication treatment for depression. 15 , 16 , 17 , 18 Over the past 2 decades, policy changes (e.g., the 2008 Mental Health Parity and Addiction Equity Act) that increased coverage of mental health and addiction treatment services and efforts to reduce the stigma associated with mental disorders (e.g., celebrity disclosures 19 , 20 ) should theoretically have resulted in increases in help seeking and receipt of treatment.
This study estimated the prevalence of past 12‒month major depression among U.S. individuals aged ≥12 years in each year from 2015 to 2020. The study then estimated changes in the prevalence of depression from 2015 to 2019 overall and by sociodemographic characteristics. Finally, the study investigated the prevalence of help seeking, including receipt of pharmacologic treatment for depression, among individuals with past-year depression from 2015 to 2019 and in 2020, overall and by sociodemographic characteristics.
Study Sample
Data were drawn from the National Survey on Drug Use and Health (NSDUH). The NSDUH provides annual cross-sectional national data on substance use and mental health in the U.S. and is described elsewhere. 21 A multistage area probability sample for each of the 50 states and the District of Columbia was conducted to represent the male and female civilian non-institutionalized population of the U.S. aged ≥12 years. Datasets from each year included in this analysis (2015–2019) were pooled, adding a variable for the survey year. Estimates for 2020 were added but not in the statistical analysis of trends because methods used in 2020 differed because of the COVID-19 pandemic, making these incomparable statistically with previous estimates. Person-level analysis sampling weights were computed to control for individual-level nonresponse and were adjusted to ensure consistency with population estimates obtained from the U.S. Census Bureau. A new weight was created by dividing the original weight by the number of data sets combined. For this study, analyses were restricted to those who responded to questions about past-year depression at the time of the interview (98.4%), resulting in a total analytic sample of N=278,176 (mean per survey year=55,635; range=55,132–56,292) from 2015 to 2019 and n =32,893 for 2020. The study was exempt from IRB review.
Questions to assess major depressive episodes (MDEs) were based on DSM-IV criteria, and separate depression modules were administrated to adults versus youth aged 12–17 years. Depression modules were adapted from the National Comorbidity Survey-Replication 22 for adult respondents (aged ≥18 years) and from the National Comorbidity Survey-Adolescent 23 for adolescent respondents (aged 12–17 years). Both adult and adolescent respondents were classified as having had a lifetime MDE on the basis of reporting ≥5 of 9 symptoms for MDE, including either depressed mood or loss of interest or pleasure in daily activities, during the same 2-week period in their lifetime. Respondents with lifetime MDE were further classified as having past-year MDE if they met the criteria for a lifetime MDE and reported feeling depressed or having lost interest or pleasure in daily activities as well as other symptoms for at least 2 weeks during the past 12 months. The past-year MDE variable for this study was created by combining the adolescent and adult variables.
Past-year help seeking for depression was assessed by 2 questions. Respondents were asked whether they had seen or talked to a medical doctor (MD) or other professional about their MDE symptoms in the past 12 months and whether they had received prescription medication for their MDE symptoms in the past 12 months.
Statistical Analysis
First, the prevalence of past-year depression and associated SEs for each survey year were calculated. Time trends in the prevalence of past-year depression from 2015 to 2019 were tested using Poisson regression, with continuous year as the predictor for the linear time trend. These analyses were conducted twice: first with no covariates (unadjusted) and then while adjusting for age, race/ethnicity, sex, marital status, income, and education.
Second, the prevalence of past-year depression and associated SEs for each survey year and sociodemographic subgroup were calculated. Time trends from 2015 to 2019 in the prevalence of past-year depression by sociodemographic subgroup were tested using Poisson regression, with continuous year as the predictor for the linear time trend. These analyses were conducted twice: first with no covariates (unadjusted) and then while adjusting for the sociodemographic characteristics other than the stratified variable.
Third, the sample was restricted to those meeting the criteria for past-year MDE, and the prevalence of help seeking and associated SEs were calculated for each survey year. Time trends from 2015 to 2019 in the prevalence of speaking with an MD or other professional about MDE symptoms and receiving a prescription medication for MDE symptoms in the past 12 months were tested in separate Poisson regression models, with continuous year as the predictor for the linear time trend. These analyses were conducted twice: first with no covariates (unadjusted) and then while adjusting for age, race/ethnicity, sex, marital status, income, and education. These analyses were also repeated stratifying by the same sociodemogrpahic variables.
All analyses were conducted in 2021–2022 with SAS (version 9.4) and used appropriate sample weights to correct for differences in the probability of selection and were adjusted for survey design effects to obtain accurate SEs. RRs with robust SEs were calculated for the effects within each model.
The prevalence of past-year depression increased from 7.3% (SE=0.15) in 2015 to 8.6% (SE=0.18) in 2019 ( Figure 1 ), and this monotonic increase from 2015 to 2019 remained after adjusting for sociodemographic characteristics. The prevalence of past-year depression in 2020 was 9.2% (SE=0.31).

Prevalence of past-year depression in the U.S., 2015 to 2020.
*Statistical significance at p <0.05.
Stratifying the population by age, the highest prevalences of depression across time were found among adolescents (aged 12–17 years) and young adults (aged 18–25 years). Increases in depression from 2015 to 2019 were observed among those aged 12–17 years (2015: 12.7% [SE=0.40] to 2019: 15.8% [SE=0.34] and 2020: 16.9% [SE=0.84]), 18–25 years (2015: 10.3% [SE=0.31] to 2019: 15.5% [SE=0.41] and 2020: 17.2% [SE=0.78]), and 26–34 years (2015: 7.5% [SE=0.31] to 2019: 10.9% [SE=0.52] and 2020: 9.9% [SE=0.65]) ( Figure 2 ). These trends remained relatively unchanged after adjusting for sociodemographic characteristics. No increases in depression were observed among those aged 35–49 years or aged ≥50 years in unadjusted models.

Prevalence of past-year depression in the U.S., 2015 to 2020, by age group.
Stratifying the population by race/ethnicity, the prevalence of depression among non-Hispanic White individuals exceeded that among all other racial/ethnic groups. An increase in depression from 2015 to 2019 was observed among those in each racial/ethnic subgroup (2015: 8.0% [SE=0.18] to 2019: 9.2% [SE=0.24] and 2020: 10.1% [SE=0.40] for non-Hispanic White; 2015: 5.4% [SE=0.34] to 2019: 6.6% [SE=0.40] and 2020: 6.9% [SE=0.83] for non-Hispanic Black; 2015: 6.0% [SE=0.31] to 2019: 8.22% [SE=0.44] and 2020: 7.9% [SE=0.59] for Hispanic; and 2015: 6.9% [SE=0.60] to 2019: 8.0% [SE=0.57] and 2020: 8.1% [SE=0.59] for additional races/ethnicities) ( Figure 3 ). Increases remained after adjusting for sociodemographic characteristics.

Prevalence of past-year depression in the U.S., 2015 to 2020, by race/ethnicity.
The prevalence of depression was consistently higher for women than for men. Depression increased from 2015 to 2019 among both men (2015: 4.7% [SE=0.16] to 2019: 6.3% [SE=0.21] and 2020: 6.4% [SE=0.32]) and women (2015: 9.7% [SE=0.24] to 2019: 10.8% [SE=0.26] and 2020: 11.8% [SE=0.44]) ( Appendix Figure 1 , available online). Increases remained after adjusting for sociodemographic characteristics.
Stratifying by marital status, the prevalence of depression was highest among adults who were not currently nor previously married. In unadjusted models there was an increase in depression from 2015 to 2019 for those who had not been married (2015: 10.1% [SE=0.23] to 2019: 13.7% [SE=0.34] and 2020: 14.2% [SE=0.51) ( Appendix Figure 2 , available online]). This finding remained after adjusting for other sociodemographic characteristics. No increases in depression were found among married individuals or those who were widowed, divorced, or separated in unadjusted or adjusted models.
Considering income, the highest prevalence of depression was evident among those with the lowest household income, whereas those with the highest household income exhibited the lowest prevalence of depression. There was an increase in depression from 2015 to 2019 for those in each income group (2015: 10.1% [SE=0.37] to 2019: 12.1% [SE=0.54] and 2020: 11.6% [SE=0.73] for <$20,000; 2015: 7.2% [SE=0.29] to 2019: 9.1% [SE=0.35] and 2020: 10.2% [SE=0.67] for $20,000 to $49,999; 2015: 7.5% [SE=0.42] to 2019: 8.7% [SE=0.43] and 2020: 9.3% [SE=0.80] for $50,000–$74,999; and 2015: 5.8% [SE=0.24] to 2019: 6.9% [SE=0.21] and 2020: 7.5% [SE=0.43] for ≥$75,000) ( Appendix Figure 3 , available online]). These associations remained after adjusting for sociodemographic characteristics.
Considering education, the prevalence of depression was higher among those with some college education than among all other education subgroups. The prevalence of depression increased from 2015 to 2019 among those who were high-school graduates (2015: 6.2% [SE=0.28] to 2019: 7.1% [SE=0.35] and 2020: 7.5% [SE=0.60]), those with some college education (2015: 8.9% [SE=0.37] to 2019: 10.4% [SE=0.35] and 2020: 7.6% [SE=0.48]), and those with a college or graduate degree (2015: 5.6% [SE=0.28] to 2019: 6.9% [SE=0.33] and 2020: 7.6% [SE=0.47]) ( Appendix Figure 4 , available online]). These associations remained after adjusting for sociodemographic characteristics. There was no change in the prevalence of depression from 2015 to 2019 among those without a high-school diploma in unadjusted or adjusted analyses.
Overall, the prevalence of (1) seeing or talking to an MD or other professional about symptoms of MDE and (2) receiving a prescription medication for MDE symptoms did not change from 2015 to 2019 among those with past-year depression ( Figure 4 ).

Prevalence of past-year depression and talking with a medical professional and medication prescription among those with past-year depression in the U.S. from 2015 to 2020.
Stratifying the population by age, modest increases in both talking to an MD or other professional (2015: 42.4% [SE=1.47] to 2019: 47.4% [SE=1.28] and 2020: 51.7% [SE=1.94]) and receiving a prescription medication for symptoms of depression (2015: 30.0% [SE=1.45] to 2019: 31.8% [SE=1.08] and 2020: 38.7% [SE=1.64]) were observed only among young adults aged 18 to 25 years ( Appendix Figures 5 and 6 , available online). These results were evident in both unadjusted and adjusted models. Among adolescents ages 12 to 17 years, there was no change in the prevalence of receiving prescription medication in either unadjusted or adjusted models, but in the model adjusted for other sociodemographic variables, an increase in talking to an MD or other professional was observed between 2015 and 2019 (2015: 36.0% [SE=1.29] to 2019: 39.7% [SE=1.55] and 2020: 40.1% [SE=2.48]). This increase was also modest, and most adolescents with depression neither told a healthcare professional about depression symptoms nor received pharmacologic treatment from 2015 through 2020. No change in the prevalence of help seeking was found in the age groups of ≥26 years.
Stratifying the population by sex, modest increases in help seeking and receiving a prescription medication for symptoms of depression from 2015 to 2019 were observed among females (2015: 60.2% [SE=1.12] to 2019: 62.4% [SE=1.21] and 2020: 61.2% [SE=1.95] for talking to an MD or other professional; 2015: 47.9% [SE=1.46] to 2019: 48.9% [SE=1.11] and 2020: 48.0% [SE=2.20] for receiving a prescription medication) but only within the adjusted models and were not observed among males either in unadjusted or adjusted models ( Appendix Figure 7 , available online). Stratifying by race/ethnicity, marital status, education, and income did not reveal subgroup differences in talking to an MD/other professional or receiving prescription medication for depression.
This study updates the depression prevalence estimates for the U.S. general population through the year 2020 and confirms increases in depression from 2015 to 2019, reflecting an escalating public health crisis in the U.S. even before the onset of the pandemic. Depression increased among those aged younger than 35 years, among those who never married (after adjusting for age), and among those with at least a high-school diploma. Across sex, income, and racial/ethnic subgroups, increases were generally equivalent. It should also be noted that the prevalence of depression did not decline in any sociodemographic subgroup during this period. In 2020, past-year depression was common among nearly 1 of 10 Americans overall, and the depression prevalence approached 20% among adolescents and young adults.
The percentage of those with depression in the overall population who reported speaking with a medical professional about or receiving medication for depression did not change appreciably from 2015 to 2019 and remained low, below 6%. Depression prevalence from 2015 to 2019 increased most rapidly among young adults aged 18–25 years (consistent with recent evidence on anxiety 24 ), and in 2020, the depression prevalence was approximately 17% among adolescents aged 12–17 years, although fewer than half of those with depression spoke with a health professional or received prescription medication. This gap in treatment is consistent with and extends findings from earlier studies. 25 , 26 Help seeking did not increase for any group by race/ethnicity, income, marital status, or education. The net effect of these trends suggests an escalating public health crisis and that parity and public-service announcement efforts have been unsuccessful in achieving equity in depression treatment. The elevated level and concentration of untreated depression among adolescents and young adults are especially problematic because untreated depression early in life is predictive of a more intractable course and increased risk of subsequent additional mental health problems. 27 , 28 The short- and long-term impact of the pandemic on depression are not yet clear, but these estimates are a start toward quantifying the consequences.
Although the NSDUH does not provide information about specific depression treatments received, in the context of extant evidence about mental health care in the U.S., these results suggest that undertreatment of depression may be widespread even among the proportion who sought help. Severe shortages of psychiatrists—particularly child and adolescent psychiatrists—exist in many U.S. states and are concentrated in lower SES and racial/ethnic minority communities. For instance, reports indicate that there are 30 psychiatrists per 100,000 people in Massachusetts versus 5.3 per 100,000 in Idaho. 29 Psychiatrists are more likely to practice in counties with higher average income and a proportion of adults with extensive formal education. 29 Therefore, although cost-effective, evidence-supported treatments for depression exist, they may still be difficult to access in community healthcare settings and, as such, remain inaccessible for most Americans who could benefit from them. 26 Greater investment in testing the effectiveness of evidence-based treatments in the community and making them as widely available and affordable as possible through trained healthcare professionals is needed. Pediatricians and primary care providers are a potential key to addressing the treatment gap because they are more likely to be involved in the delivery of mental health care than specialists. Unfortunately, with few exceptions, such as the work of REACH, 30 which offers a training program in patient-centered mental health in pediatric primary care to increase clinician comfort with addressing pediatric mental health problems, there is very little training for pediatricians or primary care physicians in the diagnosis or treatment of common mental health conditions. Collaborative care and integrated care models have also shown promise and could be implemented more widely. 31 , 32 , 33 Beyond lack of training for physicians, a purely clinical approach is not likely feasible because of inadequate number of providers, inadequate access, and ongoing stigma associated with help seeking. Community- and school-based programs that educate gatekeepers are another low-cost, evidence-based approach that could be expanded. 34 , 35 , 36
Limitations
Limitations of this study must be considered. Observed increases in the prevalence of depression may be because of greater reporting. Yet, it is not immediately clear why reporting would increase more dramatically in certain groups than in others. Furthermore, there were no available data on the depth of engagement when talking with a health care professional about depressive symptoms or the suitability of specific pharmacologic treatments. It is also possible that help seeking for other mental health problems such as anxiety, which is highly overlapping with depression in terms of concurrent diagnoses and treatments, could impact estimates of depression prevalence and/or treatment. In addition, combining racial/ethnic categories to conduct the analyses with adequate sample sizes may have obscured the differences in depression prevalence and depression treatment between groups. 15 , 37
CONCLUSIONS
These U.S. national data reveal a clear increase in depression and, critically, in untreated depression. Depression is the strongest risk factor for suicide behavior, and these patterns demand immediate action, especially for adolescents and young adults, at both the clinical and public health levels. Expanding evidence-based campaigns that promote early intervention, prevention, and education about depression are needed now.
ACKNOWLEDGMENTS
No financial disclosures were reported by the authors of this paper.
CRediT AUTHOR STATEMENT
Renee D. Goodwin: Conceptualization, Investigation, Methodology, Project administration, Writing – original draft. Lisa C. Dierker: Data curation, Formal analysis, Investigation, Methodology, Software, Visualization. Sandro Galea: Investigation, Methodology, Visualization. Christina W. Hoven: Investigation, Writing – review and editing. Melody Wu: Investigation, Visualization, Writing – review and editing. Andrea H. Weinberger: Investigation, Writing – review and editing.
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2022.05.014 .
Appendix. SUPPLEMENTAL MATERIAL
- Open access
- Published: 16 May 2024
Procrastination, depression and anxiety symptoms in university students: a three-wave longitudinal study on the mediating role of perceived stress
- Anna Jochmann 1 ,
- Burkhard Gusy 1 ,
- Tino Lesener 1 &
- Christine Wolter 1
BMC Psychology volume 12 , Article number: 276 ( 2024 ) Cite this article
83 Accesses
Metrics details
It is generally assumed that procrastination leads to negative consequences. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. Therefore, the aim of our study was to examine the harmful consequences of procrastination on students’ stress and mental health. We selected the procrastination-health model as our theoretical foundation and tried to evaluate the model’s assumption that trait procrastination leads to (chronic) disease via (chronic) stress in a temporal perspective. We chose depression and anxiety symptoms as indicators for (chronic) disease and hypothesized that procrastination leads to perceived stress over time, that perceived stress leads to depression and anxiety symptoms over time, and that procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress.
To examine these relationships properly, we collected longitudinal data from 392 university students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models.
Procrastination did lead to depression and anxiety symptoms over time. However, perceived stress was not a mediator of this effect. Procrastination did not lead to perceived stress over time, nor did perceived stress lead to depression and anxiety symptoms over time.
Conclusions
We could not confirm that trait procrastination leads to (chronic) disease via (chronic) stress, as assumed in the procrastination-health model. Nonetheless, our study demonstrated that procrastination can have a detrimental effect on mental health. Further health outcomes and possible mediators should be explored in future studies.
Peer Review reports
Introduction
“Due tomorrow? Do tomorrow.”, might be said by someone who has a tendency to postpone tasks until the last minute. But can we enjoy today knowing about the unfinished task and tomorrow’s deadline? Or do we feel guilty for postponing a task yet again? Do we get stressed out because we have little time left to complete it? Almost everyone has procrastinated at some point when it came to completing unpleasant tasks, such as mowing the lawn, doing the taxes, or preparing for exams. Some tend to procrastinate more frequently and in all areas of life, while others are less inclined to do so. Procrastination is common across a wide range of nationalities, as well as socioeconomic and educational backgrounds [ 1 ]. Over the last fifteen years, there has been a massive increase in research on procrastination [ 2 ]. Oftentimes, research focuses on better understanding the phenomenon of procrastination and finding out why someone procrastinates in order to be able to intervene. Similarly, the internet is filled with self-help guides that promise a way to overcome procrastination. But why do people seek help for their procrastination? Until now, not much research has been conducted on the negative consequences procrastination could have on health and well-being. Therefore, in the following article we examine the effect of procrastination on mental health over time and stress as a possible facilitator of this relationship on the basis of the procrastination-health model by Sirois et al. [ 3 ].
Procrastination and its negative consequences
Procrastination can be defined as the tendency to voluntarily and irrationally delay intended activities despite expecting negative consequences as a result of the delay [ 4 , 5 ]. It has been observed in a variety of groups across the lifespan, such as students, teachers, and workers [ 1 ]. For example, some students tend to regularly delay preparing for exams and writing essays until the last minute, even if this results in time pressure or lower grades. Procrastination must be distinguished from strategic delay [ 4 , 6 ]. Delaying a task is considered strategic when other tasks are more important or when more resources are needed before the task can be completed. While strategic delay is viewed as functional and adaptive, procrastination is classified as dysfunctional. Procrastination is predominantly viewed as the result of a self-regulatory failure [ 7 ]. It can be understood as a trait, that is, as a cross-situational and time-stable behavioral disposition [ 8 ]. Thus, it is assumed that procrastinators chronically delay tasks that they experience as unpleasant or difficult [ 9 ]. Approximately 20 to 30% of adults have been found to procrastinate chronically [ 10 , 11 , 12 ]. Prevalence estimates for students are similar [ 13 ]. It is believed that students do not procrastinate more often than other groups. However, it is easy to examine procrastination in students because working on study tasks requires a high degree of self-organization and time management [ 14 ].
It is generally assumed that procrastination leads to negative consequences [ 4 ]. Negative consequences are even part of the definition of procrastination. Research indicates that procrastination is linked to lower academic performance [ 15 ], health impairment (e.g., stress [ 16 ], physical symptoms [ 17 ], depression and anxiety symptoms [ 18 ]), and poor health-related behavior (e.g., heavier alcohol consumption [ 19 ]). However, most studies targeting consequences of procrastination are cross-sectional [ 4 ]. For that reason, it often remains unclear whether an examined outcome is a consequence or an antecedent of procrastination, or whether a reciprocal relationship between procrastination and the examined outcome can be assumed. Additionally, regarding negative consequences of procrastination on health, it is still largely unknown by which mechanisms they are mediated. Uncovering such mediators would be helpful in developing interventions that can prevent negative health consequences of procrastination.
The procrastination-health model
The first and only model that exclusively focuses on the effect of procrastination on health and the mediators of this effect is the procrastination-health model [ 3 , 9 , 17 ]. Sirois [ 9 ] postulates three pathways: An immediate effect of trait procrastination on (chronic) disease and two mediated pathways (see Fig. 1 ).
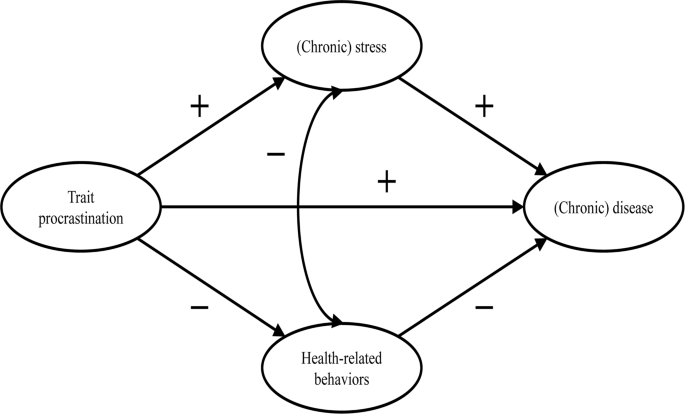
Adopted from the procrastination-health model by Sirois [ 9 ]
The immediate effect is not further explained. Research suggests that procrastination creates negative feelings, such as shame, guilt, regret, and anger [ 20 , 21 , 22 ]. The described feelings could have a detrimental effect on mental health [ 23 , 24 , 25 ].
The first mediated pathway leads from trait procrastination to (chronic) disease via (chronic) stress. Sirois [ 9 ] assumes that procrastination creates stress because procrastinators are constantly aware of the fact that they still have many tasks to complete. Stress activates the hypothalamic-pituitary-adrenocortical (HPA) system, increases autonomic nervous system arousal, and weakens the immune system, which in turn contributes to the development of diseases. Sirois [ 9 ] distinguishes between short-term and long-term effects of procrastination on health mediated by stress. She believes that, in the short term, single incidents of procrastination cause acute stress, which leads to acute health problems, such as infections or headaches. In the long term, chronic procrastination, as you would expect with trait procrastination, causes chronic stress, which leads to chronic diseases over time. There is some evidence in support of the stress-related pathway, particularly regarding short-term effects [ 3 , 17 , 26 , 27 , 28 ]. However, as we mentioned above, most of these studies are cross-sectional. Therefore, the causal direction of these effects remains unclear. To our knowledge, long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress have not yet been investigated.
The second mediated pathway leads from trait procrastination to (chronic) disease via poor health-related behavior. According to Sirois [ 9 ], procrastinators form lower intentions to carry out health-promoting behavior or to refrain from health-damaging behavior because they have a low self-efficacy of being able to care for their own health. In addition, they lack the far-sighted view that the effects of health-related behavior only become apparent in the long term. For the same reason, Sirois [ 9 ] believes that there are no short-term, but only long-term effects of procrastination on health mediated by poor health-related behavior. For example, an unhealthy diet leads to diabetes over time. The findings of studies examining the behavioral pathway are inconclusive [ 3 , 17 , 26 , 28 ]. Furthermore, since most of these studies are cross-sectional, they are not suitable for uncovering long-term effects of trait procrastination on (chronic) disease mediated by poor health-related behavior.
In summary, previous research on the two mediated pathways of the procrastination-health model mainly found support for the role of (chronic) stress in the relationship between trait procrastination and (chronic) disease. However, only short-term effects have been investigated so far. Moreover, longitudinal studies are needed to be able to assess the causal direction of the relationship between trait procrastination, (chronic) stress, and (chronic) disease. Consequently, our study is the first to examine long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, using a longitudinal design. (Chronic) disease could be measured by a variety of different indicators (e.g., physical symptoms, diabetes, or coronary heart disease). We choose depression and anxiety symptoms as indicators for (chronic) disease because they signal mental health complaints before they manifest as (chronic) diseases. Additionally, depression and anxiety symptoms are two of the most common mental health complaints among students [ 29 , 30 ] and procrastination has been shown to be a significant predictor of depression and anxiety symptoms [ 18 , 31 , 32 , 33 , 34 ]. Until now, the stress-related pathway of the procrastination-health model with depression and anxiety symptoms as the health outcome has only been analyzed in one cross-sectional study that confirmed the predictions of the model [ 35 ].
The aim of our study is to evaluate some of the key assumptions of the procrastination-health model, particularly the relationships between trait procrastination, (chronic) stress, and (chronic) disease over time, surveyed in the following analysis using depression and anxiety symptoms.
In line with the key assumptions of the procrastination-health model, we postulate (see Fig. 2 ):
Procrastination leads to perceived stress over time.
Perceived stress leads to depression and anxiety symptoms over time.
Procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress.
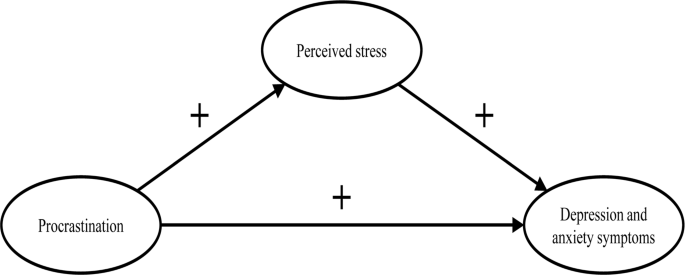
The section of the procrastination-health model we examined
Materials and methods
Our study was part of a health monitoring at a large German university Footnote 1 . Ethical approval for our study was granted by the Ethics Committee of the university’s Department of Education and Psychology. We collected the initial data in 2019. Two occasions followed, each at an interval of six months. In January 2019, we sent out 33,267 invitations to student e-mail addresses. Before beginning the survey, students provided their written informed consent to participate in our study. 3,420 students took part at the first occasion (T1; 10% response rate). Of these, 862 participated at the second (T2) and 392 at the third occasion (T3). In order to test whether dropout was selective, we compared sociodemographic and study specific characteristics (age, gender, academic semester, number of assessments/exams) as well as behavior and health-related variables (procrastination, perceived stress, depression and anxiety symptoms) between the participants of the first wave ( n = 3,420) and those who participated three times ( n = 392). Results from independent-samples t-tests and chi-square analysis showed no significant differences regarding sociodemographic and study specific characteristics (see Additional file 1: Table S1 and S2 ). Regarding behavior and health-related variables, independent-samples t-tests revealed a significant difference in procrastination between the two groups ( t (3,409) = 2.08, p < .05). The mean score of procrastination was lower in the group that participated in all three waves.
The mean age of the longitudinal respondents was 24.1 years ( SD = 5.5 years), the youngest participants were 17 years old, the oldest one was 59 years old. The majority of participants was female (74.0%), 7 participants identified neither as male nor as female (1.8%). The respondents were on average enrolled in the third year of studying ( M = 3.9; SD = 2.3). On average, the students worked about 31.2 h ( SD = 14.1) per week for their studies, and an additional 8.5 h ( SD = 8.5) for their (part-time) jobs. The average income was €851 ( SD = 406), and 4.9% of the students had at least one child. The students were mostly enrolled in philosophy and humanities (16.5%), education and psychology (15.8%), biology, chemistry, and pharmacy (12.5%), political and social sciences (10.6%), veterinary medicine (8.9%), and mathematics and computer science (7.7%).
We only used established and well evaluated instruments for our analyses.
- Procrastination
We adopted the short form of the Procrastination Questionnaire for Students (PFS-4) [ 36 ] to measure procrastination. The PFS-4 assesses procrastination at university as a largely stable behavioral disposition across situations, that is, as a trait. The questionnaire consists of four items (e.g., I put off starting tasks until the last moment.). Each item was rated on a 5-point scale ((almost) never = 1 to (almost) always = 5) for the last two weeks. All items were averaged, with higher scores indicating a greater tendency to procrastinate. The PFS-4 has been proven to be reliable and valid, showing very high correlations with other established trait procrastination scales, for example, with the German short form of the General Procrastination Scale [ 37 , 38 ]. We also proved the scale to be one-dimensional in a factor analysis, with a Cronbach’s alpha of 0.90.
Perceived stress
The Heidelberger Stress Index (HEI-STRESS) [ 39 ] is a three-item measure of current perceived stress due to studying as well as in life in general. For the first item, respondents enter a number between 0 (not stressed at all) and 100 (completely stressed) to indicate how stressed their studies have made them feel over the last four weeks. For the second and third item, respondents rate on a 5-point scale how often they feel “stressed and tense” and as how stressful they would describe their life at the moment. We transformed the second and third item to match the range of the first item before we averaged all items into a single score with higher values indicating greater perceived stress. We proved the scale to be one-dimensional and Cronbach’s alpha for our study was 0.86.
Depression and anxiety symptoms
We used the Patient Health Questionnaire-4 (PHQ-4) [ 40 ], a short form of the Patient Health Questionnaire [ 41 ] with four items, to measure depression and anxiety symptoms. The PHQ-4 contains two items from the Patient Health Questionnaire-2 (PHQ-2) [ 42 ] and the Generalized Anxiety Disorder Scale-2 (GAD-2) [ 43 ], respectively. It is a well-established screening scale designed to assess the core criteria of major depressive disorder (PHQ-2) and generalized anxiety disorder (GAD-2) according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). However, it was shown that the GAD-2 is also appropriate for screening other anxiety disorders. According to Kroenke et al. [ 40 ], the PHQ-4 can be used to assess a person’s symptom burden and impairment. We asked the participants to rate how often they have been bothered over the last two weeks by problems, such as “Little interest or pleasure in doing things”. Response options were 0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day. Calculated as the sum of the four items, the total scores range from 0 to 12 with higher scores indicating more frequent depression and anxiety symptoms. The total scores can be categorized as none-to-minimal (0–2), mild (3–5), moderate (6–8), and severe (9–12) depression and anxiety symptoms. The PHQ-4 was shown to be reliable and valid [ 40 , 44 , 45 ]. We also proved the scale to be one-dimensional in a factor analysis, with a Cronbach’s alpha of 0.86.
Data analysis
To test our hypotheses, we performed structural equation modelling (SEM) using R (Version 4.1.1) with the package lavaan. All items were standardized ( M = 0, SD = 1). Due to the non-normality of some study variables and a sufficiently large sample size of N near to 400 [ 46 ], we used robust maximum likelihood estimation (MLR) for all model estimations. As recommended by Hu and Bentler [ 47 ], we assessed the models’ goodness of fit by chi-square test statistic, root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), Tucker-Lewis index (TLI), and comparative fit index (CFI). A non-significant chi-square indicates good model fit. Since chi-square is sensitive to sample size, we also evaluated fit indices less sensitive to the number of observations. RMSEA and SRMR values of 0.05 or lower as well as TLI and CFI values of 0.97 or higher indicate good model fit. RMSEA values of 0.08 or lower, SRMR values of 0.10 or lower, as well as TLI and CFI values of 0.95 or higher indicate acceptable model fit [ 48 , 49 ]. First, we conducted confirmatory factor analysis for the first occasion, defining three factors that correspond to the measures of procrastination, perceived stress, and depression and anxiety symptoms. Next, we tested for measurements invariance over time and specified the measurement model, before testing our hypotheses.
Measurement invariance over time
To test for measurement invariance over time, we defined one latent variable for each of the three occasions, corresponding to the measures of procrastination, perceived stress, and depression and anxiety symptoms, respectively. As recommended by Geiser and colleagues [ 50 ], the links between indicators and factors (i.e., factor loadings and intercepts) should be equal over measurement occasions; therefore, we added indicator specific factors. A first and least stringent step of testing measurement invariance is configural invariance (M CI ). It was examined whether the included constructs (procrastination, perceived stress, depression and anxiety symptoms) have the same pattern of free and fixed loadings over time. This means that the assignment of the indicators to the three latent factors over time is supported by the underlying data. If configural invariance was supported, restrictions for the next step of testing measurement invariance (metric or weak invariance; M MI ) were added. This means that each item contributes to the latent construct to a similar degree over time. Metric invariance was tested by constraining the factor loadings of the constructs over time. The next step of testing measurement invariance (scalar or strong invariance; M SI ) consisted of checking whether mean differences in the latent construct capture all mean differences in the shared variance of the items. Scalar invariance was tested by constraining the item intercepts over time. The constraints applied in the metric invariance model were retained [ 51 ]. For the last step of testing measurement invariance (residual or strict invariance; M RI ), the residual variables were also set equal over time. If residual invariance is supported, differences in the observed variables can exclusively be attributed to differences in the variances of the latent variables.
We used the Satorra-Bentler chi-square difference test to evaluate the superiority of a more stringent model [ 52 ]. We assumed the model with the largest number of invariance restrictions – which still has an acceptable fit and no substantial deterioration of the chi-square value – to be the final model [ 53 ]. Following previous recommendations, we considered a decrease in CFI of 0.01 and an increase in RMSEA of 0.015 as unacceptable to establish measurement invariance [ 54 ]. If a more stringent model had a significant worse chi-square value, but the model fit was still acceptable and the deterioration in model fit fell within the change criteria recommended for CFI and RMSEA values, we still considered the more stringent model to be superior.
Hypotheses testing
As recommended by Dormann et al. [ 55 ], we applied autoregressive time-lagged panel models to test our hypotheses. In the first step, we specified a model (M 0 ) that only included the stabilities of the three variables (procrastination, perceived stress, depression and anxiety symptoms) over time. In the next step (M 1 ), we added the time-lagged effects from procrastination (T1) to perceived stress (T2) and from procrastination (T2) to perceived stress (T3) as well as from perceived stress (T1) to depression and anxiety symptoms (T2) and from perceived stress (T2) to depression and anxiety symptoms (T3). Additionally, we included a direct path from procrastination (T1) to depression and anxiety symptoms (T3). If this path becomes significant, we can assume a partial mediation [ 55 ]. Otherwise, we can assume a full mediation. We compared these nested models using the Satorra-Bentler chi-square difference test and the Akaike information criterion (AIC). The chi-square difference value should either be non-significant, indicating that the proposed model including our hypotheses (M 1 ) does not have a significant worse model fit than the model including only stabilities (M 0 ), or, if significant, it should be in the direction that M 1 fits the data better than M 0 . Regarding the AIC, M 1 should have a lower value than M 0 .
Table 1 displays the means, standard deviations, internal consistencies (Cronbach’s alpha), and stabilities (correlations) of all study variables. The alpha values of procrastination, perceived stress, and depression and anxiety symptoms are classified as good (> 0.80) [ 56 ]. The correlation matrix of the manifest variables used for the analyses can be found in the Additional file 1: Table S3 .
We observed the highest test-retest reliabilities for procrastination ( r ≥ .74). The test-retest reliabilities for depression and anxiety symptoms ( r ≥ .64) and for perceived stress ( r ≥ .54) were a bit lower (see Table 1 ). The pattern of correlations shows a medium to large but positive relationship between procrastination and depression and anxiety symptoms [ 57 , 58 ]. The association between procrastination and perceived stress was small, the one between perceived stress and depression and anxiety symptoms very large (see Table 1 ).
Confirmatory factor analysis showed an acceptable to good fit (x 2 (41) = 118.618, p < .001; SRMR = 0.042; RMSEA = 0.071; TLI = 0.95; CFI = 0.97). When testing for measurement invariance over time for each construct, the residual invariance models with indicator specific factors provided good fit to the data (M RI ; see Table 2 ), suggesting that differences in the observed variables can exclusively be attributed to differences of the latent variables. We then specified and tested the measurement model of the latent constructs prior to model testing based on the items of procrastination, perceived stress, and depression and anxiety symptoms. The measurement model fitted the data well (M M ; see Table 3 ). All items loaded solidly on their respective factors (0.791 ≤ β ≤ 0.987; p < .001).
To test our hypotheses, we analyzed the two models described in the methods section.
The fit of the stability model (M 0 ) was acceptable (see Table 3 ). Procrastination was stable over time, with stabilities above 0.82. The stabilities of perceived stress as well as depression and anxiety symptoms were somewhat lower, ranging from 0.559 (T1 -> T2) to 0.696 (T2 -> T3) for perceived stress and from 0.713 (T2 -> T3) to 0.770 (T1 -> T2) for depression and anxiety symptoms, respectively.
The autoregressive mediation model (M 1 ) fitted the data significantly better than M 0 . The direct path from procrastination (T1) to depression and anxiety symptoms (T3) was significant (β = 0.16; p < .001), however, none of the mediated paths (from procrastination (T1) to perceived stress (T2) and from perceived stress (T2) to depression and anxiety symptoms (T3)) proved to be substantial. Also, the time-lagged paths from perceived stress (T1) to depression and anxiety symptoms (T2) and from procrastination (T2) to perceived stress (T3) were not substantial either (see Fig. 3 ).
To examine whether the hypothesized effects would occur over a one-year period rather than a six-months period, we specified an additional model with paths from procrastination (T1) to perceived stress (T3) and from perceived stress (T1) to depression and anxiety symptoms (T3), also including the stabilities of the three constructs as in the stability model M 0 . The model showed an acceptable fit (χ 2 (486) = 831.281, p < .001; RMSEA = 0.048; SRMR = 0.091; TLI = 0.95; CFI = 0.95), but neither of the two paths were significant.
Therefore, our hypotheses, that procrastination leads to perceived stress over time (H1) and that perceived stress leads to depression and anxiety symptoms over time (H2) must be rejected. We could only partially confirm our third hypothesis, that procrastination leads to depression and anxiety over time, mediated by perceived stress (H3), since procrastination did lead to depression and anxiety symptoms over time. However, this effect was not mediated by perceived stress.
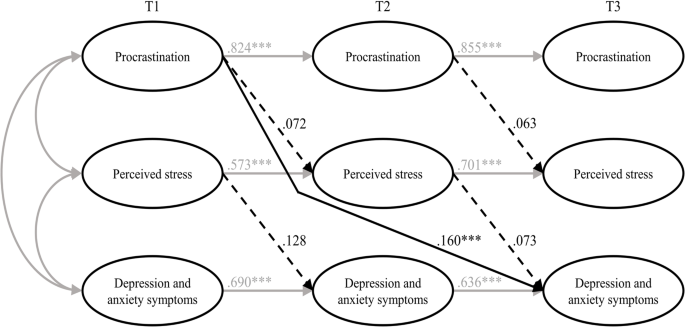
Results of the estimated model including all hypotheses (M 1 ). Note Non-significant paths are dotted. T1 = time 1; T2 = time 2; T3 = time 3. *** p < .001
To sum up, we tried to examine the harmful consequences of procrastination on students’ stress and mental health. Hence, we selected the procrastination-health model by Sirois [ 9 ] as a theoretical foundation and tried to evaluate some of its key assumptions in a temporal perspective. The author assumes that trait procrastination leads to (chronic) disease via (chronic) stress. We chose depression and anxiety symptoms as indicators for (chronic) disease and postulated, in line with the key assumptions of the procrastination-health model, that procrastination leads to perceived stress over time (H1), that perceived stress leads to depression and anxiety symptoms over time (H2), and that procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress (H3). To examine these relationships properly, we collected longitudinal data from students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models. Our first and second hypotheses had to be rejected: Procrastination did not lead to perceived stress over time, and perceived stress did not lead to depression and anxiety symptoms over time. However, procrastination did lead to depression and anxiety symptoms over time – which is in line with our third hypothesis – but perceived stress was not a mediator of this effect. Therefore, we could only partially confirm our third hypothesis.
Our results contradict previous studies on the stress-related pathway of the procrastination-health model, which consistently found support for the role of (chronic) stress in the relationship between trait procrastination and (chronic) disease. Since most of these studies were cross-sectional, though, the causal direction of these effects remained uncertain. There are two longitudinal studies that confirm the stress-related pathway of the procrastination-health model [ 27 , 28 ], but both studies examined short-term effects (≤ 3 months), whereas we focused on more long-term effects. Therefore, the divergent findings may indicate that there are short-term, but no long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress.
Our results especially raise the question whether trait procrastination leads to (chronic) stress in the long term. Looking at previous longitudinal studies on the effect of procrastination on stress, the following stands out: At shorter study periods of two weeks [ 27 ] and four weeks [ 28 ], the effect of procrastination on stress appears to be present. At longer study periods of seven weeks [ 59 ], three months [ 28 ], six months, and twelve months, as in our study, the effect of procrastination on stress does not appear to be present. There is one longitudinal study in which procrastination was a significant predictor of stress symptoms nine months later [ 34 ]. The results of this study should be interpreted with caution, though, because the outbreak of the COVID-19 pandemic fell within the study period, which could have contributed to increased stress symptoms [ 60 ]. Unfortunately, Johansson et al. [ 34 ] did not report whether average stress symptoms increased during their study. In one of the two studies conducted by Fincham and May [ 59 ], the COVID-19 pandemic outbreak also fell within their seven-week study period. However, they reported that in their study, average stress symptoms did not increase from baseline to follow-up. Taken together, the findings suggest that procrastination can cause acute stress in the short term, for example during times when many tasks need to be completed, such as at the end of a semester, but that procrastination does not lead to chronic stress over time. It seems possible that students are able to recover during the semester from the stress their procrastination caused at the end of the previous semester. Because of their procrastination, they may also have more time to engage in relaxing activities, which could further mitigate the effect of procrastination on stress. Our conclusions are supported by an early and well-known longitudinal study by Tice and Baumeister [ 61 ], which compared procrastinating and non-procrastinating students with regard to their health. They found that procrastinators experienced less stress than their non-procrastinating peers at the beginning of the semester, but more at the end of the semester. Additionally, our conclusions are in line with an interview study in which university students were asked about the consequences of their procrastination [ 62 ]. The students reported that, due to their procrastination, they experience high levels of stress during periods with heavy workloads (e.g., before deadlines or exams). However, the stress does not last, instead, it is relieved immediately after these periods.
Even though research indicates, in line with the assumptions of the procrastination-health model, that stress is a risk factor for physical and mental disorders [ 63 , 64 , 65 , 66 ], perceived stress did not have a significant effect on depression and anxiety symptoms in our study. The relationship between stress and mental health is complex, as people respond to stress in many different ways. While some develop stress-related mental disorders, others experience mild psychological symptoms or no symptoms at all [ 67 ]. This can be explained with the help of vulnerability-stress models. According to vulnerability-stress models, mental illnesses emerge from an interaction of vulnerabilities (e.g., genetic factors, difficult family backgrounds, or weak coping abilities) and stress (e.g., minor or major life events or daily hassles) [ 68 , 69 ]. The stress perceived by the students in our sample may not be sufficient enough on its own, without the presence of other risk factors, to cause depression and anxiety symptoms. However, since we did not assess individual vulnerability and stress factors in our study, these considerations are mere speculation.
In our study, procrastination led to depression and anxiety symptoms over time, which is consistent with the procrastination-health model as well as previous cross-sectional and longitudinal evidence [ 18 , 21 , 31 , 32 , 33 , 34 ]. However, it is still unclear by which mechanisms this effect is mediated, as perceived stress did not prove to be a substantial mediator in our study. One possible mechanism would be that procrastination impairs affective well-being [ 70 ] and creates negative feelings, such as shame, guilt, regret, and anger [ 20 , 21 , 22 , 62 , 71 ], which in turn could lead to depression and anxiety symptoms [ 23 , 24 , 25 ]. Other potential mediators of the relationship between procrastination and depression and anxiety symptoms emerge from the behavioral pathway of the procrastination-health model, suggesting that poor health-related behaviors mediate the effect of trait procrastination on (chronic) disease. Although evidence for this is still scarce, the results of one cross-sectional study, for example, indicate that poor sleep quality might mediate the effect of procrastination on depression and anxiety symptoms [ 35 ].
In summary, we found that procrastination leads to depression and anxiety symptoms over time and that perceived stress is not a mediator of this effect. We could not show that procrastination leads to perceived stress over time, nor that perceived stress leads to depression and anxiety symptoms over time. For the most part, the relationships between procrastination, perceived stress, and depression and anxiety symptoms did not match the relationships between trait procrastination, (chronic) stress, and (chronic) disease as assumed in the procrastination-health model. Explanations for this could be that procrastination might only lead to perceived stress in the short term, for example, during preparations for end-of-semester exams, and that perceived stress may not be sufficient enough on its own, without the presence of other risk factors, to cause depression and anxiety symptoms. In conclusion, we could not confirm long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, as assumed for the stress-related pathway of the procrastination-health model.
Limitations and suggestions for future research
In our study, we tried to draw causal conclusions about the harmful consequences of procrastination on students’ stress and mental health. However, since procrastination is a trait that cannot be manipulated experimentally, we have conducted an observational rather than an experimental study, which makes causal inferences more difficult. Nonetheless, a major strength of our study is that we used a longitudinal design with three waves. This made it possible to draw conclusions about the causal direction of the effects, as in hardly any other study targeting consequences of procrastination on health before [ 4 , 28 , 55 ]. Therefore, we strongly recommend using a similar longitudinal design in future studies on the procrastination-health model or on consequences of procrastination on health in general.
We chose a time lag of six months between each of the three measurement occasions to examine long-term effects of procrastination on depression and anxiety symptoms mediated by perceived stress. However, more than six months may be necessary for the hypothesized effects to occur [ 72 ]. The fact that the temporal stabilities of the examined constructs were moderate or high (0.559 ≤ β ≤ 0.854) [ 73 , 74 ] also suggests that the time lags may have been too short. The larger the time lag, the lower the temporal stabilities, as shown for depression and anxiety symptoms, for example [ 75 ]. High temporal stabilities make it more difficult to detect an effect that actually exists [ 76 ]. Nonetheless, Dormann and Griffin [ 77 ] recommend using shorter time lags of less than one year, even with high stabilities, because of other influential factors, such as unmeasured third variables. Therefore, our time lags of six months seem appropriate.
It should be discussed, though, whether it is possible to detect long-term effects of the stress-related pathway of the procrastination-health model within a total study period of one year. Sirois [ 9 ] distinguishes between short-term and long-term effects of procrastination on health mediated by stress, but does not address how long it might take for long-term effects to occur or when effects can be considered long-term instead of short-term. The fact that an effect of procrastination on stress is evident at shorter study periods of four weeks or less but in most cases not at longer study periods of seven weeks or more, as we mentioned earlier, could indicate that short-term effects occur within the time frame of one to three months, considering the entire stress-related pathway. Hence, it seems appropriate to assume that we have examined rather long-term effects, given our study period of six and twelve months. Nevertheless, it would be beneficial to use varying study periods in future studies, in order to be able to determine when effects can be considered long-term.
Concerning long-term effects of the stress-related pathway, Sirois [ 9 ] assumes that chronic procrastination causes chronic stress, which leads to chronic diseases over time. The term “chronic stress” refers to prolonged stress episodes associated with permanent tension. The instrument we used captures perceived stress over the last four weeks. Even though the perceived stress of the students in our sample was relatively stable (0.559 ≤ β ≤ 0.696), we do not know how much fluctuation occurred between each of the three occasions. However, there is some evidence suggesting that perceived stress is strongly associated with chronic stress [ 78 ]. Thus, it seems acceptable that we used perceived stress as an indicator for chronic stress in our study. For future studies, we still suggest the use of an instrument that can more accurately reflect chronic stress, for example, the Trier Inventory for Chronic Stress (TICS) [ 79 ].
It is also possible that the occasions were inconveniently chosen, as they all took place in a critical academic period near the end of the semester, just before the examination period began. We chose a similar period in the semester for each occasion for the sake of comparability. However, it is possible that, during this preparation periods, stress levels peaked and procrastinators procrastinated less because they had to catch up after delaying their work. This could have introduced bias to the data. Therefore, in future studies, investigation periods should be chosen that are closer to the beginning or in the middle of a semester.
Furthermore, Sirois [ 9 ] did not really explain her understanding of “chronic disease”. However, it seems clear that physical illnesses, such as diabetes or cardiovascular diseases, are meant. Depression and anxiety symptoms, which we chose as indicators for chronic disease, represent mental health complaints that do not have to be at the level of a major depressive disorder or an anxiety disorder, in terms of their quantity, intensity, or duration [ 40 ]. But they can be viewed as precursors to a major depressive disorder or an anxiety disorder. Therefore, given our study period of one year, it seems appropriate to use depression and anxiety symptoms as indicators for chronic disease. At longer study periods, we would expect these mental health complaints to manifest as mental disorders. Moreover, the procrastination-health model was originally designed to be applied to physical diseases [ 3 ]. Perhaps, the model assumptions are more applicable to physical diseases than to mental disorders. By applying parts of the model to mental health complaints, we have taken an important step towards finding out whether the model is applicable to mental disorders as well. Future studies should examine additional long-term health outcomes, both physical and psychological. This would help to determine whether trait procrastination has varying effects on different diseases over time. Furthermore, we suggest including individual vulnerability and stress factors in future studies in order to be able to analyze the effect of (chronic) stress on (chronic) diseases in a more differentiated way.
Regarding our sample, 3,420 students took part at the first occasion, but only 392 participated three times, which results in a dropout rate of 88.5%. At the second and third occasion, invitation e-mails were only sent to participants who had indicated at the previous occasion that they would be willing to participate in a repeat survey and provided their e-mail address. This is probably one of the main reasons for our high dropout rate. Other reasons could be that the students did not receive any incentives for participating in our study and that some may have graduated between the occasions. Selective dropout analysis revealed that the mean score of procrastination was lower in the group that participated in all three waves ( n = 392) compared to the group that participated in the first wave ( n = 3,420). One reason for this could be that those who have a higher tendency to procrastinate were more likely to procrastinate on filling out our survey at the second and third occasion. The findings of our dropout analysis should be kept in mind when interpreting our results, as lower levels of procrastination may have eliminated an effect on perceived stress or on depression and anxiety symptoms. Additionally, across all age groups in population-representative samples, the student age group reports having the best subjective health [ 80 ]. Therefore, it is possible that they are more resilient to stress and experience less impairment of well-being than other age groups. Hence, we recommend that future studies focus on other age groups as well.
It is generally assumed that procrastination leads to lower academic performance, health impairment, and poor health-related behavior. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. In consequence, the aim of our study was to examine the effect of procrastination on mental health over time and stress as a possible facilitator of this relationship. We selected the procrastination-health model as a theoretical foundation and used the stress-related pathway of the model, assuming that trait procrastination leads to (chronic) disease via (chronic) stress. We chose depression and anxiety symptoms as indicators for (chronic) disease and collected longitudinal data from students at three occasions over a one-year period. This allowed us to draw conclusions about the causal direction of the effects, as in hardly any other study examining consequences of procrastination on (mental) health before. Our results indicate that procrastination leads to depression and anxiety symptoms over time and that perceived stress is not a mediator of this effect. We could not show that procrastination leads to perceived stress over time, nor that perceived stress leads to depression and anxiety symptoms over time. Explanations for this could be that procrastination might only lead to perceived stress in the short term, for example, during preparations for end-of-semester exams, and that perceived stress may not be sufficient on its own, that is, without the presence of other risk factors, to cause depression and anxiety symptoms. Overall, we could not confirm long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, as assumed for the stress-related pathway of the procrastination-health model. Our study emphasizes the importance of identifying the consequences procrastination can have on health and well-being and determining by which mechanisms they are mediated. Only then will it be possible to develop interventions that can prevent negative health consequences of procrastination. Further health outcomes and possible mediators should be explored in future studies, using a similar longitudinal design.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
University Health Report at Freie Universität Berlin.
Abbreviations
Comparative fit index
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
Generalized Anxiety Disorder Scale-2
Heidelberger Stress Index
Hypothalamic-pituitary-adrenocortical
Robust maximum likelihood estimation
Short form of the Procrastination Questionnaire for Students
Patient Health Questionnaire-2
Patient Health Questionnaire-4
Root mean square error of approximation
Structural equation modeling
Standardized root mean square residual
Tucker-Lewis index
Lu D, He Y, Tan Y, Gender S, Status. Cultural differences, Education, family size and procrastination: a sociodemographic Meta-analysis. Front Psychol. 2021. https://doi.org/10.3389/fpsyg.2021.719425 .
Article PubMed PubMed Central Google Scholar
Yan B, Zhang X. What research has been conducted on Procrastination? Evidence from a systematical bibliometric analysis. Front Psychol. 2022. https://doi.org/10.3389/fpsyg.2022.809044 .
Sirois FM, Melia-Gordon ML, Pychyl TA. I’ll look after my health, later: an investigation of procrastination and health. Pers Individ Dif. 2003;35:1167–84. https://doi.org/10.1016/S0191-8869(02)00326-4 .
Article Google Scholar
Grunschel C. Akademische Prokrastination: Eine qualitative und quantitative Untersuchung von Gründen und Konsequenzen [Unpublished doctoral dissertation]: Universität Bielefeld; 2013.
Steel P. The Nature of Procrastination: a Meta-Analytic and Theoretical Review of Quintessential Self-Regulatory failure. Psychol Bull. 2007;133:65–94. https://doi.org/10.1037/0033-2909.133.1.65 .
Article PubMed Google Scholar
Corkin DM, Yu SL, Lindt SF. Comparing active delay and procrastination from a self-regulated learning perspective. Learn Individ Differ. 2011;21:602–6. https://doi.org/10.1016/j.lindif.2011.07.005 .
Balkis M, Duru E. Procrastination, self-regulation failure, academic life satisfaction, and affective well-being: underregulation or misregulation form. Eur J Psychol Educ. 2016;31:439–59. https://doi.org/10.1007/s10212-015-0266-5 .
Schulz N. Procrastination und Planung – Eine Untersuchung zum Einfluss von Aufschiebeverhalten und Depressivität auf unterschiedliche Planungskompetenzen [Doctoral dissertation]: Westfälische Wilhelms-Universität Münster; 2007.
Sirois FM. Procrastination, stress, and Chronic Health conditions: a temporal perspective. In: Sirois FM, Pychyl TA, editors. Procrastination, Health, and well-being. London: Academic; 2016. pp. 67–92. https://doi.org/10.1016/B978-0-12-802862-9.00004-9 .
Harriott J, Ferrari JR. Prevalence of procrastination among samples of adults. Psychol Rep. 1996;78:611–6. https://doi.org/10.2466/pr0.1996.78.2.611 .
Ferrari JR, O’Callaghan J, Newbegin I. Prevalence of Procrastination in the United States, United Kingdom, and Australia: Arousal and Avoidance delays among adults. N Am J Psychol. 2005;7:1–6.
Google Scholar
Ferrari JR, Díaz-Morales JF, O’Callaghan J, Díaz K, Argumedo D. Frequent behavioral Delay tendencies by adults. J Cross Cult Psychol. 2007;38:458–64. https://doi.org/10.1177/0022022107302314 .
Day V, Mensink D, O’Sullivan M. Patterns of academic procrastination. JCRL. 2000;30:120–34. https://doi.org/10.1080/10790195.2000.10850090 .
Höcker A, Engberding M, Rist F, Prokrastination. Ein Manual Zur Behandlung Des Pathologischen Aufschiebens. 2nd ed. Göttingen: Hogrefe; 2017.
Kim KR, Seo EH. The relationship between procrastination and academic performance: a meta-analysis. Pers Individ Dif. 2015;82:26–33. https://doi.org/10.1016/j.paid.2015.02.038 .
Khalid A, Zhang Q, Wang W, Ghaffari AS, Pan F. The relationship between procrastination, perceived stress, saliva alpha-amylase level and parenting styles in Chinese first year medical students. Psychol Res Behav Manag. 2019;12:489–98. https://doi.org/10.2147/PRBM.S207430 .
Sirois FM. I’ll look after my health, later: a replication and extension of the procrastination–health model with community-dwelling adults. Pers Individ Dif. 2007;43:15–26. https://doi.org/10.1016/j.paid.2006.11.003 .
Reinecke L, Meier A, Aufenanger S, Beutel ME, Dreier M, Quiring O, et al. Permanently online and permanently procrastinating? The mediating role of internet use for the effects of trait procrastination on psychological health and well-being. New Media Soc. 2018;20:862–80. https://doi.org/10.1177/1461444816675437 .
Westgate EC, Wormington SV, Oleson KC, Lindgren KP. Productive procrastination: academic procrastination style predicts academic and alcohol outcomes. J Appl Soc Psychol. 2017;47:124–35. https://doi.org/10.1111/jasp.12417 .
Feyzi Behnagh R, Ferrari JR. Exploring 40 years on affective correlates to procrastination: a literature review of situational and dispositional types. Curr Psychol. 2022;41:1097–111. https://doi.org/10.1007/s12144-021-02653-z .
Rahimi S, Hall NC, Sticca F. Understanding academic procrastination: a longitudinal analysis of procrastination and emotions in undergraduate and graduate students. Motiv Emot. 2023. https://doi.org/10.1007/s11031-023-10010-9 .
Patrzek J, Grunschel C, Fries S. Academic procrastination: the perspective of University counsellors. Int J Adv Counselling. 2012;34:185–201. https://doi.org/10.1007/s10447-012-9150-z .
Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J Abnorm Psychol. 1988;97:346–53. https://doi.org/10.1037//0021-843x.97.3.346 .
Cândea D-M, Szentagotai-Tătar A. Shame-proneness, guilt-proneness and anxiety symptoms: a meta-analysis. J Anxiety Disord. 2018;58:78–106. https://doi.org/10.1016/j.janxdis.2018.07.005 .
Young CM, Neighbors C, DiBello AM, Traylor ZK, Tomkins M. Shame and guilt-proneness as mediators of associations between General Causality orientations and depressive symptoms. J Soc Clin Psychol. 2016;35:357–70. https://doi.org/10.1521/jscp.2016.35.5.357 .
Stead R, Shanahan MJ, Neufeld RW. I’ll go to therapy, eventually: Procrastination, stress and mental health. Pers Individ Dif. 2010;49:175–80. https://doi.org/10.1016/j.paid.2010.03.028 .
Dow NM. Procrastination, stress, and sleep in tertiary students [Master’s thesis]: University of Canterbury; 2018.
Sirois FM, Stride CB, Pychyl TA. Procrastination and health: a longitudinal test of the roles of stress and health behaviours. Br J Health Psychol. 2023. https://doi.org/10.1111/bjhp.12658 .
Hofmann F-H, Sperth M, Holm-Hadulla RM. Psychische Belastungen Und Probleme Studierender. Psychotherapeut. 2017;62:395–402. https://doi.org/10.1007/s00278-017-0224-6 .
Liu CH, Stevens C, Wong SHM, Yasui M, Chen JA. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: implications for addressing disparities in service use. Depress Anxiety. 2019;36:8–17. https://doi.org/10.1002/da.22830 .
Aftab S, Klibert J, Holtzman N, Qadeer K, Aftab S. Schemas mediate the Link between Procrastination and Depression: results from the United States and Pakistan. J Rat-Emo Cognitive-Behav Ther. 2017;35:329–45. https://doi.org/10.1007/s10942-017-0263-5 .
Flett AL, Haghbin M, Pychyl TA. Procrastination and depression from a cognitive perspective: an exploration of the associations among Procrastinatory Automatic thoughts, rumination, and Mindfulness. J Rat-Emo Cognitive-Behav Ther. 2016;34:169–86. https://doi.org/10.1007/s10942-016-0235-1 .
Saddler CD, Sacks LA. Multidimensional perfectionism and academic procrastination: relationships with Depression in University students. Psychol Rep. 1993;73:863–71. https://doi.org/10.1177/00332941930733pt123 .
Johansson F, Rozental A, Edlund K, Côté P, Sundberg T, Onell C, et al. Associations between procrastination and subsequent Health outcomes among University students in Sweden. JAMA Netw Open. 2023. https://doi.org/10.1001/jamanetworkopen.2022.49346 .
Gusy B, Jochmann A, Lesener T, Wolter C, Blaszcyk W. „Get it done – schadet Aufschieben Der Gesundheit? Präv Gesundheitsf. 2023;18:228–33. https://doi.org/10.1007/s11553-022-00950-4 .
Glöckner-Rist A, Engberding M, Höcker A, Rist F. Prokrastinationsfragebogen für Studierende (PFS): Zusammenstellung sozialwissenschaftlicher items und Skalen. ZIS - GESIS Leibniz Institute for the Social Sciences; 2014.
Klingsieck KB, Fries S. Allgemeine Prokrastination: Entwicklung Und Validierung Einer Deutschsprachigen Kurzskala Der General Procrastination Scale (Lay, 1986). Diagnostica. 2012;58:182–93. https://doi.org/10.1026/0012-1924/a000060 .
Lay CH. At last, my research article on procrastination. J Res Pers. 1986;20:474–95. https://doi.org/10.1016/0092-6566(86)90127-3 .
Schmidt LI, Obergfell J. Zwangsjacke Bachelor?! Stressempfinden Und Gesundheit Studierender: Der Einfluss Von Anforderungen Und Entscheidungsfreiräumen Bei Bachelor- Und Diplomstudierenden Nach Karaseks Demand-Control-Modell. Saarbrücken: VDM Verlag Dr. Müller; 2011.
Kroenke K, Spitzer RL, Williams JB, Löwe B. An Ultra-brief Screening Scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–21. https://doi.org/10.1016/S0033-3182(09)70864-3 .
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA. 1999;282:1737–44. https://doi.org/10.1001/jama.282.18.1737 .
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item Depression Screener. Med Care. 2003;41:1284–92.
Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in Primary Care: prevalence, impairment, Comorbidity, and detection. Ann Intern Med. 2007;146:317–25. https://doi.org/10.7326/0003-4819-146-5-200703060-00004 .
Khubchandani J, Brey R, Kotecki J, Kleinfelder J, Anderson J. The Psychometric properties of PHQ-4 depression and anxiety screening scale among College Students. Arch Psychiatr Nurs. 2016;30:457–62. https://doi.org/10.1016/j.apnu.2016.01.014 .
Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disorders. 2010;122:86–95. https://doi.org/10.1016/j.jad.2009.06.019 .
Boomsma A, Hoogland JJ. The robustness of LISREL modeling revisited. In: Cudeck R, Du Toit S, Sörbom D, editors. Structural equation modeling: Present and Future: a festschrift in honor of Karl Jöreskog. Lincolnwood: Scientific Software International; 2001. pp. 139–68.
Hu L, Bentler PM. Fit indices in Covariance structure modeling: sensitivity to Underparameterized Model Misspecification. Psychol Methods. 1998;3:424–53. https://doi.org/10.1037/1082-989X.3.4.424 .
Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: test of significance and descriptive goodness-of-fit measures. MPR. 2003;8:23–74.
Hu L, Bentler PM. Cutoff criteria for fit indexes in Covariance structure analysis: conventional criteria Versus New Alternatives. Struct Equ Model. 1999;6:1–55. https://doi.org/10.1080/10705519909540118 .
Geiser C, Eid M, Nussbeck FW, Courvoisier DS, Cole DA. Analyzing true change in Longitudinal Multitrait-Multimethod studies: application of a Multimethod Change Model to Depression and anxiety in children. Dev Psychol. 2010;46:29–45. https://doi.org/10.1037/a0017888 .
Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. 2016;41:71–90. https://doi.org/10.1016/j.dr.2016.06.004 .
Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–14. https://doi.org/10.1007/BF02296192 .
Geiser C. Datenanalyse Mit Mplus: Eine Anwendungsorientierte Einführung. Wiesbaden: VS Verlag für Sozialwissenschaften; 2010.
Book Google Scholar
Chen F, Curran PJ, Bollen KA, Kirby J, Paxton P. An empirical evaluation of the use of fixed cutoff points in RMSEA Test Statistic in Structural equation models. Sociol Methods Res. 2008;36:462–94. https://doi.org/10.1177/0049124108314720 .
Dormann C, Zapf D, Perels F. Quer- und Längsschnittstudien in der Arbeitspsychologie [Cross-sectional and longitudinal studies in occupational psychology.]. In: Kleinbeck U, Schmidt K-H,Enzyklopädie der Psychologie [Encyclopedia of psychology]:, Themenbereich D, Serie III, Band 1, Arbeitspsychologie [Subject Area, Series D. III, Volume 1, Industrial Psychology]. Göttingen: Hogrefe Verlag; 2010. pp. 923–1001.
Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994.
Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Pers Indiv Differ. 2016;102:74–8. https://doi.org/10.1016/j.paid.2016.06.069 .
Funder DC, Ozer DJ. Evaluating effect size in Psychological Research: sense and nonsense. Adv Methods Practices Psychol Sci. 2019;2:156–68. https://doi.org/10.1177/2515245919847202 .
Fincham FD, May RW. My stress led me to procrastinate: temporal relations between perceived stress and academic procrastination. Coll Stud J. 2021;55:413–21.
Daniali H, Martinussen M, Flaten MA. A Global Meta-Analysis of Depression, anxiety, and stress before and during COVID-19. Health Psychol. 2023;42:124–38. https://doi.org/10.1037/hea0001259 .
Tice DM, Baumeister RF. Longitudinal study of procrastination, performance, stress, and Health: the costs and benefits of Dawdling. Psychol Sci. 1997;8:454–8. https://doi.org/10.1111/j.1467-9280.1997.tb00460.x .
Schraw G, Wadkins T, Olafson L. Doing the things we do: a grounded theory of academic procrastination. J Educ Psychol. 2007;99:12–25. https://doi.org/10.1037/0022-0663.99.1.12 .
Slavich GM. Life Stress and Health: a review of conceptual issues and recent findings. Teach Psychol. 2016;43:346–55. https://doi.org/10.1177/0098628316662768 .
Phillips AC, Carroll D, Der G. Negative life events and symptoms of depression and anxiety: stress causation and/or stress generation. Anxiety Stress Coping. 2015;28:357–71. https://doi.org/10.1080/10615806.2015.1005078 .
Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. https://doi.org/10.1146/annurev.clinpsy.1.102803.143938 .
Blazer D, Hughes D, George LK. Stressful life events and the onset of a generalized anxiety syndrome. Am J Psychiatry. 1987;144:1178–83. https://doi.org/10.1176/ajp.144.9.1178 .
Southwick SM, Charney DS. The Science of Resilience: implications for the Prevention and Treatment of Depression. Science. 2012;338:79–82. https://doi.org/10.1126/science.1222942 .
Ingram RE, Luxton DD. Vulnerability-stress models. In: Hankin BL, Abela JR, editors. Development of psychopathology: a vulnerability-stress perspective. Thousand Oaks: Sage; 2005. pp. 32–46.
Chapter Google Scholar
Maercker A. Modelle Der Klinischen Psychologie. In: Petermann F, Maercker A, Lutz W, Stangier U, editors. Klinische psychologie – Grundlagen. Göttingen: Hogrefe; 2018. pp. 13–31.
Krause K, Freund AM. Delay or procrastination – a comparison of self-report and behavioral measures of procrastination and their impact on affective well-being. Pers Individ Dif. 2014;63:75–80. https://doi.org/10.1016/j.paid.2014.01.050 .
Grunschel C, Patrzek J, Fries S. Exploring reasons and consequences of academic procrastination: an interview study. Eur J Psychol Educ. 2013;28:841–61. https://doi.org/10.1007/s10212-012-0143-4 .
Dwyer JH. Statistical models for the social and behavioral sciences. New York: Oxford University Press; 1983.
Cohen JA, Power Primer. Psychol Bull. 1992;112:155–9. https://doi.org/10.1037//0033-2909.112.1.155 .
Ferguson CJ. An effect size primer: a Guide for clinicians and Researchers. Prof Psychol Res Pr. 2009;40:532–8. https://doi.org/10.1037/a0015808 .
Hinz A, Berth H, Kittel J, Singer S. Die zeitliche Stabilität (Test-Retest-Reliabilität) Von Angst Und Depressivität Bei Patienten Und in Der Allgemeinbevölkerung. Z Med Psychol. 2011;20:24–31. https://doi.org/10.3233/ZMP-2010-2012 .
Adachi P, Willoughby T. Interpreting effect sizes when controlling for stability effects in longitudinal autoregressive models: implications for psychological science. Eur J Dev Psychol. 2015;12:116–28. https://doi.org/10.1080/17405629.2014.963549 .
Dormann C, Griffin M. Optimal time lags in Panel studies. Psychol Methods. 2015;20:489–505. https://doi.org/10.1037/met0000041 .
Weckesser LJ, Dietz F, Schmidt K, Grass J, Kirschbaum C, Miller R. The psychometric properties and temporal dynamics of subjective stress, retrospectively assessed by different informants and questionnaires, and hair cortisol concentrations. Sci Rep. 2019. https://doi.org/10.1038/s41598-018-37526-2 .
Schulz P, Schlotz W, Becker P. TICS: Trierer Inventar Zum chronischen stress. Göttingen: Hogrefe; 2004.
Heidemann C, Scheidt-Nave C, Beyer A-K, Baumert J, Thamm R, Maier B, et al. Health situation of adults in Germany - results for selected indicators from GEDA 2019/2020-EHIS. J Health Monit. 2021;6:3–25. https://doi.org/10.25646/8459 .
Download references
Acknowledgements
Not applicable.
Open Access Funding provided by Freie Universität Berlin.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Division of Prevention and Psychosocial Health Research, Department of Education and Psychology, Freie Universität Berlin, Habelschwerdter Allee 45, 14195, Berlin, Germany
Anna Jochmann, Burkhard Gusy, Tino Lesener & Christine Wolter
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: A.J., B.G., T.L.; methodology: B.G., A.J.; validation: B.G.; formal analysis: A.J., B.G.; investigation: C.W., T.L., B.G.; data curation: C.W., T.L., B.G.; writing–original draft preparation: A.J., B.G.; writing–review and editing: A.J., T.L., B.G., C.W.; visualization: A.J., B.G.; supervision: B.G., T.L.; project administration: C.W., T.L., B.G.; All authors contributed to the article and approved the submitted version.
Corresponding authors
Correspondence to Anna Jochmann or Burkhard Gusy .
Ethics declarations
Ethics approval and consent to participate.
This study was performed in line with the principles of the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Department of Education and Psychology, Freie Universität Berlin. All methods were carried out in accordance with relevant guidelines and regulations. The participants provided their written informed consent to participate in this study.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Selective dropout analysis and correlation matrix of the manifest variables
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jochmann, A., Gusy, B., Lesener, T. et al. Procrastination, depression and anxiety symptoms in university students: a three-wave longitudinal study on the mediating role of perceived stress. BMC Psychol 12 , 276 (2024). https://doi.org/10.1186/s40359-024-01761-2
Download citation
Received : 25 May 2023
Accepted : 02 May 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s40359-024-01761-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Student health
- Longitudinal study
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]

Why Are College Students So Depressed?
It may not always feel like the best four years of your life
Depression is one of the most common mental health conditions and affects people of all ages, including college students. It impacts thoughts, feelings, and behaviors and is characterized by persistent sadness and loss of interest in once-enjoyable activities.
This condition is prevalent on college campuses, affecting an estimated 53% of students at some point.
"College students are a vulnerable population who are faced with a range of new and often wonderful—yet sometimes stressful—experiences," explains Randall Dwenger, MD , the chief medical officer at Mountainside Treatment Center. He also notes that people who have a predisposition to depression typically start to display symptoms during their early 20s.
Depression can take a toll on many aspects of a young person's life, including academic performance, social life, and physical health. It can also increase their risk of substance abuse and co-occurring mental health conditions.
For this reason, it is crucial to recognize the signs of depression in college students and provide tools, resources, and support that can help.
At a Glance
College students are faced with multiple stressors like living on their own for the first time, meeting new people, and taking a rigorous course load. All of these changes happen at one time and cause major stress.
Any symptoms—both mild and severe—can affect college students' performance and mental health.
Fortunately, help is available and schools have also stepped in to address mental health concerns.
Symptoms of Depression in College Students
"Even mild symptoms may significantly interfere with academic and social functioning," explains Amy Mezulis, PhD , a licensed clinical psychologist and chief clinical officer of Joon. She also notes that it can lead to symptoms such as trouble concentrating, fatigue , and low energy, which can make it tough for students to keep up with academic work.
"Some students may experience frustration with themselves at not being able to keep up with the challenges of living independently: balancing academics, social life, and tasks of daily living. These frustrations turned inward may present as depression."
Randall Dwenger, MD
Symptoms of depression that college students may experience include:
- Feeling sad, low, or "empty"
- Loss of interest in previously enjoyed activities
- Difficulty concentrating and making decisions
- Missing class
- Poor grades
- Not having the motivation to finish assignments
- Poor self-care and personal hygiene
- Using drugs or alcohol to cope with difficult emotions
- Irritability or restlessness
- Guilt, helplessness, or hopelessness
- Lack of energy or fatigue
- Feelings of worthlessness
- Reduced physical activity
- Changes in sleep habits and appetite
- Thoughts of self-harm or suicide
If you are having suicidal thoughts, contact the National Suicide Prevention Lifeline at 988 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
For more mental health resources, see our National Helpline Database .
Unfortunately, it isn’t easy to predict which students will excel and which will struggle with all the changes and challenges that college brings.
“Some students may experience frustration with themselves at not being able to keep up with the challenges of living independently: balancing academics, social life, and tasks of daily living. These frustrations turned inward may present as depression,” Dr. Dwenger says.
In one study that involved interviewing college students about their experiences, students suggested that depression affected many academic areas, including their effort, ability to focus, and time management.
Struggling with motivation and falling behind on academic work were common themes.
"[Depression] can definitely be a drain on focus because if I’m having a particularly bad episode, it’s hard to do anything at all," one student explained.
For some students, falling behind in classes can make depression feel even worse. "Once you start falling behind, then the depression kicks in, it will make me think less of myself for that. Then it’s even harder to catch up. As the things pile up, it gets more difficult to pull myself out of [the depression]," another student told researchers.
What Percentage of College Students Experience Depression?
Depression rates among U.S. college students are at an all-time high and growing. According to one internet-based survey, 44% reported that they currently have symptoms of depression, and 15% said they had considered suicide in the past year.
A 2022 study published in the Journal of Affective Disorders examined data from the national Healthy Minds study between the years 2013 and 2021. The researchers found that there has been a steady, consistent decline in the mental health of college students throughout the United States, amounting to a 135% increase in depression over the course of those eight years.
Between 2013 and 2021, the number of college students who met the diagnostic criteria for one or more mental disorders doubled.
Such numbers are sobering, but the survey also found some positive indicators; more students are participating in therapy, and fewer are turning to alcohol to cope with their mental health problems. Unfortunately, the increasing rates of depression may also be outpacing the resources that are available to treat it.
And while the COVID-19 pandemic was associated with significant increases in rates of depression, the survey data shows that these increases are part of a larger trend and not simply attributable to a singular pandemic-era dip in mental well-being.
For students to get the help they need, researchers, public health experts, and academic institutions need to learn more about why students are struggling with depression. By identifying the factors that play a role, they can offer better interventions and develop prevention programs to combat depression in college students.
What Really Causes Depression in College Students?
Leaving home for the first time can be an exciting but also challenging time for many students. It can be a time of self-discovery and personal growth, but it can also be stressful, anxiety-provoking, and isolating for many.
The following are just some of the common factors that can play a role in the onset of depression among college-age students.
Transitions and Adjustments
"The transition to college can be a big change, both academically and socially," explains Laura Erickson-Schroth, MD , chief medical officer of The Jed Foundation (JED). Going to college often means leaving behind social connections and support and starting over in a new environment.
For most students, college is their first experience living away from home. Moving out, adjusting to a new environment, and forging new social connections can contribute to stress that can play a part in causing depression, Dr. Erickson-Schroth says.
Students are also dealing with a lot of pressure to perform well. This stress can affect well-being and contribute to feelings of inadequacy and helplessness.
Relationships and Social Pressures
Students also face the pressure of fitting in with their peers in a new setting. They may feel disconnected from their old friends and struggle to form new friendships in an unfamiliar environment. This lack of social support may contribute to depression.
The college years can also be a time to forge new relationships with friends and romantic partners, but this can also be a source of conflict and strife. Arguments with roommates, losing touch with old friends, and problems in romantic relationships can sometimes leave college students feeling distressed.
Financial Stress
Paying for school and managing living expenses can create additional pressures. College is the first time many young people have had to deal with this type of financial pressure, and it can create feelings of stress that can play a part in the onset of depression.
Dr. Erickson-Schroth notes that students from lower-income households experience more financial stress, including struggles related to finding stable housing, food, and healthcare.
Surveys suggest that three out of every five college students face some type of insecurity related to essential needs.
Social activities and academic demands can contribute to poor sleep habits. Depression and sleep have a bidirectional relationship. Irregular or poor sleep habits are linked to the onset of depression, but depression can make sleeping more difficult. Sleep disturbances are also associated with an increased risk of suicidal ideation.
Research has also found that 82% of college students who experience suicidal thinking also experience sleep disturbances.
Substance Use
Some students may experiment with alcohol and drugs in college, in some cases as a way to cope with negative emotions and stress. Unfortunately, such substance use is also associated with increased depressive symptoms.
Other Hurdles
Dr. Erickson-Schroth notes that some young adults face additional challenges that can make them more susceptible to depression.
"Youth of color who attend college at predominantly white institutions (PWIs) often experience microaggressions and have trouble finding spaces where they feel they can be themselves," she explains.
Research also suggests that LGBTQIA+ students, financially insecure students, and lower-division students have a higher risk of experiencing more severe depression.
Generational Challenges
The COVID-19 pandemic also played a role in fueling struggles that many college students have experienced over the past few years. Dr. Dwenger notes that the social disruptions caused by the pandemic left many students struggling without the tools, resources, and coping skills they needed to navigate what is already a tricky period in most people's lives.
"Many experienced a sort of “whiplash” in adjusting back to in-person learning and resuming social interactions," he explains.
Unique global concerns facing today's generation of college students can also contribute to depression. This can include environmental worries, climate anxiety , political turmoil, social justice issues, and other concerns.
Impact of Depression on Academic and Personal Life
The high rates of depression among college students negatively affect physical health, mental well-being, academic success, and interpersonal relationships . These effects can be distressing and far-reaching. They can also potentially interfere with a student's long-term academic and professional goals.
One of the most immediate effects of depression in college students is its effect on academic performance, attendance, and participation. Depression makes it harder to concentrate, reduces motivation to learn, and even makes it hard for students to attend class sessions.
The toll on a student's academic life can be severe. It can lead to poor test performance and bad grades, which even jeopardize a student's ability to graduate and, for those depending on academic scholarships, impair their ability to keep their form of financial support.
Declining grades and poor feedback from instructors can worsen the feelings of hopelessness and inadequacy that many students are already struggling with.
Life Outside of School
Depression also makes it more challenging for students to enjoy many of the experiences that are often associated with college. Extracurricular activities, social events, and hobbies that they used to enjoy lose their appeal. This often means that they stop participating in these activities altogether.
Because social withdrawal is another common symptom of depression, making important connections and getting the social support they need becomes even more of a challenge. As a result, a student with depression may feel disconnected from their friends, roommates, family members, and college community.
Related: How Depression Affects Relationships for Young People
Physical Health
Depression can also affect a college student's physical health. When people are depressed, they also experience increases in stress hormones such as adrenaline and cortisol .
This stress response is associated with a variety of health effects, including impaired immunity. Periods of prolonged stress associated with depression can also elevate the risk of health problems such as autoimmune conditions, cardiovascular disease, high blood pressure, and gastrointestinal disorders.
It is also common for people with depression to experience a variety of physical symptoms, including back pain, stomach upset, reduced psychomotor activity, and joint pain.
Coping With Depression in College
If you are a college student struggling with depression, there are a few things that you can do that may help make it easier to cope.
Make a Plan
Dr. Erickson-Schroth suggests proactive plans for how you'll take care of your mental health before college begins.
"Make a list of some of the potential challenges you may face. This could include finding community, adjusting to living in a new place away from family and friends, keeping up with a different level of academic work, or getting the right amount of good nutrition, exercise, and sleep," she explains.
Once you have a list, brainstorm some ways you'll tackle these challenges. This can include checking out resources your school might offer and leaning on tactics that have worked for you in the past.
Try Behavioral Activation
Dr. Mezulis says that one of the best ways to manage depression is to use a strategy known as behavioral activation . It involves scheduling activities that help promote a positive mood and well-being, even if you might not necessarily feel in the mood.
This includes scheduling things like social events, exercise, and even daily tasks like doing your laundry and homework. Start by taking stock of some of your daily habits and look for ways to schedule activities that will support your emotional well-being:
- Make it a habit to go to bed and wake up at the same time each day
- Eat a balanced diet
- Utilize relaxation techniques to cope with stress
- Start a mindfulness or meditation practice
- Get regular physical activity
- Seek support from family, friends, professors, advisors, and others
Treatments for Depression in College Students
While there are many strategies you can use on your own to improve your mental health and ability to cope, it is important to seek professional help if your symptoms have lasted longer than two weeks and/or are making it difficult to function in your daily life. Treatment options can include on- or off-campus options.
Talking to a mental health professional at your school's counseling center or student health services can be a great place to start. They can provide further options about mental health services that are available on-campus or refer you to off-campus providers.
Your doctor or therapist may recommend a few different options to treat your depression. Because depression is complex and influenced by a number of factors, research suggests that a combination of therapy and medication is often the most effective treatment approach.
During talk therapy , you can discuss the challenges you are facing with a professional. Your therapist can help you gain insights, improve relationships, and develop new coping skills.
There are different types of therapy that can help, including cognitive-behavioral therapy (CBT) , which focuses on changing negative thoughts; interpersonal therapy (IPT) , which focuses on improving relationships; and dialectical behavior therapy (DBT) , which improves thoughts, emotions, and relationships.
There are also medications that can help people find relief from symptoms of depression. Antidepressants that are commonly prescribed include Prozac (fluoxetine), Paxil (paroxetine), Zoloft (sertraline), Celexa (citalopram), and Lexapro (escitalopram).
Some antidepressants carry a black box warning of an increased risk of suicide in young people under the age of 25. This risk tends to be highest when treatment is first initiated, so young people should be monitored for signs of increased suicidal thinking or behavior while taking antidepressant medication.
Resources for Professional Help
Dr. Dwenger recommends reaching out for professional support sooner rather than later. "Don’t try to hide it when you find yourself falling behind or missing commitments. All colleges have Student Services that include mental health services, academic guidance, and many resources both on campus and off," he suggests.
While all colleges offer different services, you might be able to access mental health services at the following locations:
- Student Support Services : Offers a range of services for academic and personal development and may provide counseling services
- Counseling Center : Provides counseling services to students experiencing mental health concerns
- Student Health Center : Offers a variety of health services to students, including mental health care
- Psychology Clinic : Provides psychological services to students and community members
Some colleges and universities may also offer teletherapy services. Other places to turn if you are experiencing depression include your resident advisor (RA), academic advisor, a trusted professor, or campus helpline.
While colleges and universities offer resources to combat depression, evidence suggests that around 60% of students are unaware of these options.
How Schools Can Help
Dr. Erickson-Schroth says every college should have a comprehensive plan designed to address aspects of student mental health. Such plans should include strategies that make student mental health a priority:
- Ways to promote social connections: Strategies for promoting social connections include improving student coping skills, identifying students at risk, providing mental health and crisis support, and encouraging help-seeking
- Staff mental health training: Training can help higher education faculty feel empowered, informed, and knowledgeable when it comes to helping students with mental health problems
- Peer training programs: These can be particularly helpful since students are more likely to turn to their peers instead of other adults.
- Community-building spaces: These can help students build connections, including LGBTQIA+ centers and clubs for students of color.
Colleges and universities must offer comprehensive support for students experiencing depression. Recognizing the signs of this condition can allow students to better access resources that can help support their well-being and recovery.
Schools can help by promoting depression awareness and working to combat the stigma that might prevent students from seeking help.
Frequently Asked Questions
What is the leading cause of depression in college students?
While depression does not have a single cause, stress is a common factor that plays a major role in causing depression in college students. Coping with many different new challenges, including moving away from home, juggling new responsibilities, dealing with roommates, and adjusting to all of these transitions, can be stressful for many people.
Is depression considered a disability in college?
Students who have mental health conditions such as depression may experience interruptions in their life that make it difficult to manage their normal daily needs and achieve their educational goals. If you have been diagnosed with depression or another psychiatric illness, you can request that your school make reasonable accommodations. Such accommodations may include more time to complete assignments or additional time on exams.
Read Next: 7 Tips for College Students With ADHD
Read the original article on Verywell Mind .

- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Have I Fallen Out of Love or Am I Depressed?
Or what to consider when you've lost some interest in your partner
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Verywell Mind / Getty
Am I Falling Out of Love…or Is it a Sign of Depression?
- Do People Fall Out of Love When They're Depressed?
- Can Depression Make You Think You're Not in Love?
Overlapping Symptoms
Is depression a reason to end a relationship, seeking professional help, self-reflection and communication, coping strategies.
Every relationship has a natural ebb and flow, but if you're stuck in what feels like an endless low point, you might wonder, "Am I falling out of love , or am I depressed?" The answer to that question can sometimes be much more complicated than expected.
"People often fall out of love when they are depressed because they no longer feel connected to themselves and their partner," says licensed therapist Abbey Sangmeister, MSEd, LPC, ACS . "Depression creates a fog around us that does not allow us to see or feel clearly, which can cause us to feel that no one loves us, we feel or don’t have the energy to love and give, or feel overall numb and disconnected."
Your love life and your emotions are intricately interconnected, which is why it's sometimes challenging to tell whether you're experiencing changes in how you feel about your partner or if it might be something more serious like depression.
Plus, depression can affect your life and relationships in complex ways. Problems in your romantic relationships can sometimes be a source of deep sadness or even feelings of depression. So how can you tell if what you are feeling means you're no longer in love or if it's a symptom of depression (or a combination of the two)?
Understanding the difference between the two is vital, not only for the health of your relationship but for your own mental health. After all, the sooner you recognize the signs of depression, the sooner you can get help and find relief.
At a Glance
Falling out of love with someone can be a painful, heartbreaking experience. Feeling depressed can also affect how you feel about your relationships since it causes symptoms like loss of interest, sadness, irritability, and social withdrawal. Keep reading to get advice from experts on why falling out of love can be mistaken for depression, and whether depression is ever a reason to walk away from a relationship.
So, what does falling out of love actually feel like? Psychologists have introduced various frameworks to help define and categorize love . One of the best-known theories is Robert Sternberg's triangular theory of love , which conceptualizes love as having three main components: passion, intimacy, and commitment.
When you think about what it feels like to "fall out of love," what you might actually be describing is the loss of passion. It's the gradual decline in the intense feelings of excitement, attraction, and physical chemistry that are the hallmarks of the early stages of a relationship .
It's normal for those feelings to lessen over time and the other two components of Sternberg's theory, intimacy and commitment, to take center stage. However, it’s a more serious sign when all three of these elements start to disappear.
Common signs that you might be falling out of love include:
- Not enjoying spending time with your partner
- Feeling irritated by your partner's presence, quirks, and habits
- Losing interest in what's going on in your partner's life
- Not feeling attracted to them anymore
- Not sharing details of your life or talking about how you are feeling
- Feeling happier when you are not with them
- Thinking about being alone or with someone else
Here's where it gets complicated— symptoms of depression can contribute to some of these feelings. You might feel irritated with your partner because, well, you just feel more irritated in general lately. Or you might not want to spend time with them because being around other people takes more energy than you can give right now.
"People who are depressed can fall out of love like anyone else. Depression may not directly cause someone to fall out of love, but depression is complex and can impact thinking, mood, self-esteem, energy, desire, and more," explains Susan Trotter, PhD , a relationship expert and coach. Trotter also notes that this often results in more conflict, fewer shared activities, less intimacy, and greater isolation.
Susan Trotter, PhD
When these things are occurring, they can, of course, affect how we feel about someone and they can change how we interact in and approach a relationship. This can subsequently lead someone to fall out of love–or at least think and feel like they have fallen out of love.
Figuring out what's really going on means you'll need to take a closer look at how you're feeling and decide whether it represents a change in how you view your relationship or a change in the state of your mental health. In either case, figuring out the cause can help you better decide how to tackle the problem, whether that means seeing a couples therapist, seeking treatment for depression, or breaking up with your partner.
Do People Fall Out of Love When They're Depressed?
Depression might not be the reason why you fall out of love with someone, but it can play a major part in how you feel about yourself, your partner, and your relationship.
Depression can impact many different areas of your life, including how you feel about others, your emotions, and your relationships. After all, it’s hard to feel connected with other people (your partner included) when you’re feeling isolated, sad, and hopeless.
It can also be challenging to feel many of the emotions that normally happen in a happy, healthy relationship , like joy, excitement, and anticipation. It might not necessarily mean the relationship has changed, but how you feel about it may have shifted, making it much harder to appreciate the good things.
Social withdrawal is another common symptom of depression. When you are depressed, you may find yourself pulling away from your partner. This makes it tough to maintain feelings of intimacy and closeness.
Because you feel less connected to your partner, it's easy to see why this might seem a lot like falling out of love.
Depression doesn't always cause a person to fall out of love, but the way it manifests can create problems in a relationship. You might feel more irritable and short-tempered around your partner. You might not feel like doing things you used to enjoy, so you might turn down opportunities to spend time together.
How your partner responds to these symptoms can also damage your relationship. They might interpret your reactions as rejection or start to behave in ways that undermine the closeness that you once shared.
However, it's important to remember that depression and love are complex. Your own experience of depression is unique, and how it affects your relationship can depend on a wide variety of factors. Depression can make you feel like you're falling out of love, but communicating your needs, seeing support, and getting professional help can help you navigate these challenges without jeopardizing your relationship.
Can Depression Make You Think You're Not in Love?
Unfortunately, depression can make you believe a lot of things that aren’t really true. It might tell you that you deserve to be miserable or that you don’t deserve to be loved. It might even make you think that you aren’t really in love at all.
According to therapist and coach Christina Granahan, LICSW , the symptoms of depression, particularly the numbing and sense of isolation that accompanies depression, can cause people to lose touch with feelings of love and connection with their partner. "Depression makes us think a lot of things that aren’t necessarily true. It can make us feel alone, like we don’t belong, like we’re unloved, or a victim of someone else," she notes.
Some characteristics of depression that might make you think you aren’t really in love at all include:
A Loss of Interest
A loss of interest in things that you used to enjoy or that used to be important to you is one of the hallmark symptoms of depression. Such disinterest is common when you find yourself drifting away from your partner. So if you find yourself losing interest in spending time with your partner, it’s normal to wonder if the root of this sudden loss of interest says more about your state of mind or the state of your relationship.
Changes in How You See Yourself
Depression also contributes to issues with poor self-esteem and feelings of worthlessness. You might find yourself wondering what your partner sees in you. Or you might start to think that you don't deserve their attention. You might even feel like you are burdening them. To cope, you might push them away or even try to convince yourself that you aren't in love with them at all.
Negative Thinking
Depression also leads to distorted, negative thoughts that can make symptoms worse and exacerbate issues in your relationship. Small things that used to not bother you suddenly start to seem much worse than they really are.
You might find yourself misinterpreting your partner's actions, jumping to conclusions , or engaging in all-or-nothing thinking . Such thoughts ultimately undermine your connection and may cause you to think that you aren't in love with your partner like you were before.
Reduced Libido
Depression can significantly impact things like energy levels and libido, but changes in your relationship can have a similar effect. The social withdrawal that often accompanies depression can lead to a lower desire for physical closeness with your partner. If your partner doesn’t understand how this might be a sign of depression, they might interpret this as a loss of interest in the relationship as well.
Even more confusing is the fact that depression and falling out of love can share some remarkably similar symptoms. Common feelings you might experience with both include:
- Sadness or emptiness
- Emotional numbness
- Losing interest in spending time together
- Having a hard time concentrating
- Sleep disturbances
- Feelings of guilt or anger
- Feelings of hopelessness and helplessness
Researchers have even found that the emotions people experience at the end of a relationship are very similar to clinical depression. So it's no wonder that feeling depressed can make you think you're relationship might be on the rocks (and vice versa).
Symptoms are more persistent
Symptoms affect many areas of life
Loss of interest in many activities
Feelings may come and go
Symptoms are focused specifically on your partner
Loss of interest in your relationship but not in other enjoyable activities
Sangmeister notes that leaving a relationship may be the right choice if your partner is contributing to feelings of depression. Before doing so, however, she suggests talking to a licensed mental health professional. This can help clarify your decision, explore ways to work on the relationship, and make clear decisions that are right for your life and well-being.
"It is important to distinguish whether your mental health–and in this case, depression–is making you want to end a relationship or if you are struggling because of the relationship," Trotter says. Ending it may be your best option if you're struggling because of the relationship. But if it's your depression causing these feelings, it's important to dig deeper into your feelings and symptoms.
"Ending a good relationship could be self-sabotaging and self-destructive if it’s actually a good relationship, and there are many things you can do to stabilize your depression, such as therapy, medication, groups, and more," Trotter explains.
If you do decide to end a relationship, it's important to remember that breaking up can also trigger additional feelings of depression and grief. Both experiences are connected to painful life events—including the end of important relationships in your life.
It's normal to experience things like sadness, loneliness , and emotional distress when a relationship is over. You'll need to go through a period of adjustment where you allow yourself to process the experience and take steps to heal. Having social support is important, but you should also reach out to a mental health professional if you are experiencing symptoms of depression or prolonged grief following a breakup.
If you are experiencing symptoms of depression, it's important to talk to a licensed mental health professional. They can help you better understand your emotional experience, including whether it is really depression–or a sign that your relationship is in trouble.
"If depression is significantly impacting you and your relationship, the first step is to seek treatment, which might include therapy and medication to help alleviate symptoms and help you create better strategies for managing your depression," Trotter suggests.
A therapist can evaluate your symptoms and give you perspective on the emotional states you are experiencing. Therapy can also help you understand how depression might be affecting your connection with your partner.
In addition to treating depression, couples therapy can also be beneficial. By working with a therapist, your partner can learn more about what you are experiencing, and you can strengthen your connection, build greater intimacy , and resolve conflicts more effectively.
If you’re struggling to tell if you’re actually falling out of love or if you might be depressed, it’s important to reflect on your thoughts, emotions, and experiences. As you engage in this self-reflection, ask yourself the following questions:
- Do you feel like you and your partner don't share the same emotional connection you once had?
- Are you avoiding spending time with your partner because your differences seem too great to overcome?
- Have you stopped planning your future together?
- Have you stopped caring about the things that matter to your partner?
- Do the unique traits and behaviors that used to seem cute, quirky, and charming suddenly seem like red flags or deal-breakers ?
- Do you feel happier when you are alone than when you are together?
If you answered yes to many of these questions, there's a good chance that your feelings for your partner have changed. This doesn't mean that you aren't also dealing with symptoms of depression, but it does indicate that it might be time to evaluate your relationship and think about what steps you want to take next.
If you answered no to many or most of these questions, it might be because your recent moods and feelings are linked to symptoms of depression more than a sudden shift in how you feel about your partner.
In either case, communication is critical. Talk to your partner about what’s going on with you emotionally so you can make a plan for your next steps. This might include finding ways to rebuild your connection by spending more time together and talking more often. It might involve you seeking professional treatment for your depression. If the relationship is worth holding on to, it may also mean talking to a couples therapist.
If you’re struggling with your love life or experiencing symptoms of depression (or both), finding ways to cope with these challenges is essential.
With good treatment, effective communication, and motivation, couples can enjoy a happy and healthy relationship even when one of the partners has depression.
Relationships change over time, and it isn't uncommon for people to lose romantic feelings and experience breakups. The key is knowing how to handle these feelings, knowing when it's worth it to try to salvage a relationship, and when to move on.
- Communicate: Discussing what you’re experiencing with your partner is an important first step. "It is also important for you to talk with your partner about what you’re experiencing so that they can better understand it," Trotter says.
- Care for yourself : Make sure that you are doing things to support your emotional well-being. " Self-care is critically important and taking even small steps to improve connection and intimacy will also help to alleviate the overwhelming feeling of disconnection," Trotter suggests. Even taking small daily steps like eating balanced meals, getting plenty of rest, and treating yourself kindly can help you feel better and gain more perspective on your situation.
- Reconnect : If you’ve decided to try to fall back in love, start taking steps toward rebuilding your connection with your partner. Remind yourself of their good qualities, take time to appreciate them, and start spending more time together.
- Consider couples therapy : Talking to a relationship professional can also help. "Working to improve healthy communication is also important, and couples therapy may be an effective way to help you with that," says Trotter.
Keep in Mind
If you're worried that you've fallen out of love, it can be hard to decode what you're experiencing if you suspect you might also be depressed. Are you depressed because of the relationship, or are symptoms of depression affecting your relationship in negative ways?
It's important to work with a mental health professional to sort out your feelings, build a greater awareness of what you are experiencing, and make the right decision about how to cope, Granahan suggests.
She also says getting help and support to deal with depression is what matters most. "Some of us might need to stay in a healthy, life-giving relationship as part of the healing. Enlist the help of trusted allies–including professionals–to help you make these decisions if you aren't sure, but healing comes first."
Sorokowski P, Sorokowska A, Karwowski M, et al. Universality of the triangular theory of love: Adaptation and psychometric properties of the triangular love scale in 25 countries . The Journal of Sex Research . 2021;58(1):106-115. doi:10.1080/00224499.2020.1787318
Sheets VL. Passion for life: Self-expansion and passionate love across the life span . Journal of Social and Personal Relationships . 2014;31(7):958-974. doi:10.1177/0265407513515618
Sharabi LL, Delaney AL, Knobloch LK. In their own words: How clinical depression affects romantic relationships . Journal of Social and Personal Relationships . 2016;33(4):421-448. doi:10.1177/0265407515578820
National Institute of Mental Health. Depression .
Verhallen AM, Renken RJ, Marsman JC, Ter Horst GJ. Romantic relationship breakup: An experimental model to study effects of stress on depression (-like) symptoms . PLoS ONE . 2019;14(5):e0217320. doi:10.1371/journal.pone.0217320
Field T. Romantic breakup distress, betrayal and heartbreak: A review . Int J Behav Res Psychol . 2017;5(2):217-225. doi:10.19070/2332-3000-1700038
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 22 December 2022
Doctoral researchers’ mental health and PhD training satisfaction during the German COVID-19 lockdown: results from an international research sample
- Sandra Naumann ORCID: orcid.org/0000-0001-8992-2930 1 , 2 na1 ,
- Magdalena Matyjek ORCID: orcid.org/0000-0003-4546-6480 1 , 2 na1 ,
- Katharina Bögl 1 , 2 na1 &
- Isabel Dziobek 1 , 2
Scientific Reports volume 12 , Article number: 22176 ( 2022 ) Cite this article
3782 Accesses
7 Citations
22 Altmetric
Metrics details
- Health policy
- Population screening
- Risk factors
Academia has been facing a mental health crisis particularly affecting early career researchers (ECRs). Moreover, the COVID-19 pandemic posed an unprecedented burden on the mental health of many individuals. Therefore, we cross-sectionally investigated how doctoral researchers (N = 222) evaluate their mental health status and satisfaction with their PhD training before and during the pandemic. As compared to self-reported, retrospective evaluations about the pre-pandemic state, we found decreased satisfaction with PhD training and overall well-being. The whole sample exhibited high levels of personal and work-related burnout, a fifth indicated clinically meaningful levels of depressive symptoms and almost 25% experienced severe loneliness. When exploring predictors of depression, anxiety, and burnout, we identified low satisfaction with PhD training as the most prominent predictor for poor mental health, suggesting a link between the doctoral work and their mental health status. Females vs. males and doctoral researchers in individual doctorate vs. structured PhD programs reported higher symptoms of burnout. Our study replicates previous findings of poor mental health in doctoral researchers and indicates further decreases of mental wellbeing under the influence of the pandemic. Systematic adjustments in academia are required to improve the mental health of ECRs.
Similar content being viewed by others

Academic burnout among master and doctoral students during the COVID-19 pandemic
Association between mental health and duty hours of postgraduate residents in Japan: a nationwide cross-sectional study
Burnout increased among university students during the covid-19 pandemic: a systematic review and meta-analysis, introduction.
Although many academics indicate to love research and to experience fulfilment from various tasks which belong to their profession 1 , mounting evidence suggests that working in academia might contribute to mental health problems 2 , 3 . Early career researchers (ECRs), i.e., doctoral and early postdoctoral researchers, have been found to be at risk for mental disorders with prevalence rates up to 24% for depression and 17% for anxiety 4 . These levels are up to three times higher as compared to the prevalences in the general population 5 , 6 . Consequently, it has been suggested that academia faces a “mental health crisis” 2 , sparking a discussion of its causes and possible remedies.
Among the main stressors for ECRs are the unpredictable length of the PhD training, financial instability, and high competitiveness for subsequent academic jobs 4 . Further, the prevailing ‘publish or perish’ culture pressures academics to put quantity over quality in their scientific work 7 , increasing stress and work dissatisfaction. Poorer work-life balance and higher conflict between work responsibilities are also linked to higher burnout rates in ECRs 8 . Other, not directly work-related, factors such as feelings of loneliness 5 also have been shown to negatively affect their mental health.
With the onset of the COVID-19 pandemic, mental health worsened in the general population with elevated levels of depression, anxiety, and feelings of loneliness 9 , 10 . First studies indicate that ECRs' mental health was also negatively affected 10 . Pandemic-related changes imposed additional major stressors on ECRs 11 : Empirical work, which involved interactions with participants, had to be terminated for longer periods of time causing unforeseeable delays in PhD projects 12 . Social distancing forced researchers to stay at home, isolated from their support networks of colleagues. This might have been especially challenging for first year doctoral researchers and international doctoral researchers, who were disconnected from previous social networks and had limited chances to establish new ones after their relocation. For ECRs with children and family care duties, personal responsibilities increased as kindergarten and eldercare facilities closed, which had a disproportionate impact on female scientists 13 .
Taken together, the pandemic accumulated many additional problems on ECRs 11 who were shown to be already at high risk for developing mental health problems due to the pressure and working conditions in the academic system 2 , 3 , 4 . So far, specific research on the impact of the COVID-19 pandemic on ECRs’ mental health is scarce, however, and mostly limited to anecdotal evidence 14 . Therefore, we assessed the mental health status of a defined group of ECRs, particularly doctoral researchers, under the consideration of pandemic influences. Data were collected in Berlin, a central German research hub with numerous international research institutions. Given the international science context, we assumed that our results would be informative beyond national borders.
Firstly, we sought to assess the current mental health of doctoral researchers including existing clinical diagnoses of mental disorders, acute symptoms of common mental problems (i.e., depression, anxiety, burnout, loneliness), and support structures (e.g., strength of social network, individual coping strategies). In accordance with the literature 3 , 4 , we expected to find elevated rates for depression and anxiety symptoms in our sample. Secondly, we aimed to examine the effects of the COVID-19 pandemic on doctoral researchers’ mental health and satisfaction with the PhD training. During data collection (January and February 2021), the pandemic status had been officially declared for almost a year in Germany (starting in March 2020). By then, two waves of infection had been observed and a strict lockdown had been imposed on the public for almost two months, with restrictions on public life still effective at the time of data collection. We assumed that, given the additional stressors implied on research by the pandemic, satisfaction would decrease for various PhD-related aspects when comparing ratings of pre-pandemic times with the current, in-pandemic, situation. Further, we expected that many aspects related to the PhD training would contribute more to mental health problems in the pandemic, compared to how much they did before its onset. Thirdly, in an exploratory analysis, we investigated potential predictors of doctoral researchers’ depression, anxiety, and burnout symptoms. Given the exploratory nature of this procedure, hypotheses were more tentative: We assumed that higher PhD training satisfaction and integration into a structured graduate program would be associated with lower symptom scores.
Mental health status
Standardized questionnaires concerning mental health.
Table 1 includes an overview of the results for BSI, CBI, and De Jong Gierveld Loneliness Scale scores. Regarding the BSI, 21% of the sample exceeded the threshold for depression and 4% for anxiety. Means of the CBI subscales for personal burnout and work-related burnout were 49 and 47, the mean score in the CBI total scale was 48 (including only the personal and work-related burnout subscales). Both subscale scores were substantially higher than the means in the validation sample 15 . Regarding loneliness, 24% of the sample indicated to be severely or very severely lonely (scores 9 or higher).
Mental disorder manifestation, mental health problems, and expectations related to the PhD training
Participants were asked whether they had been diagnosed with a mental disorder before or after the start of their PhD training. As depicted in Fig. 1 , 16% of the respondents indicated that they received a mental disorder diagnosis before they started their PhD training. From this group, 49% stated that they were diagnosed with an additional mental disorder after the start of their doctorate. A majority of 84% indicated that they were not diagnosed with a mental disorder before. From this group, 13% indicated that they got diagnosed with a mental disorder after they started their PhD training. In total, 27% of doctoral researchers reported at least one clinically diagnosed mental disorder before or after the start of their PhD training.
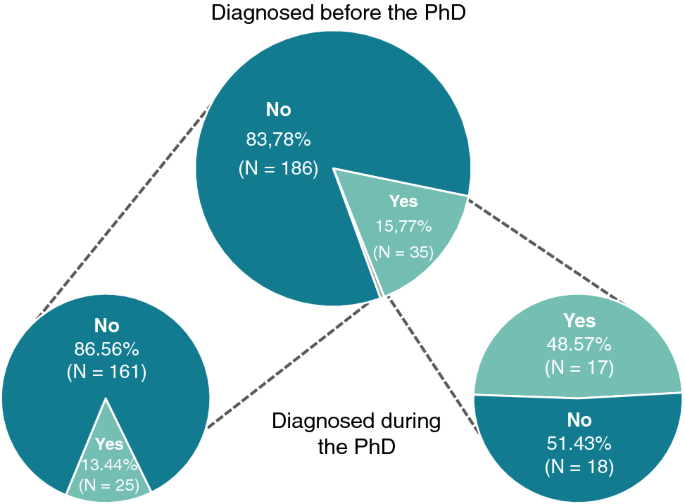
Diagnosis of a mental disorder. The top chart shows proportions of participants diagnosed with a mental disorder or not prior to the beginning of the PhD training (1 person preferred not to answer this question; in grey). Separately for those who answered yes and no, bottom charts show proportions of participants further diagnosed and not diagnosed with a mental disorder during their PhD training. Please note: One person preferred not to answer.
As shown in Fig. 2 , the majority of doctoral researchers stated that their current mental health problems were at least partially related to their PhD training (51%), whereas only 17% reported to have no mental health problems. 62% of the responders indicated that their PhD training is a little or much worse than they imagined before they started it (see Fig. 3 ).
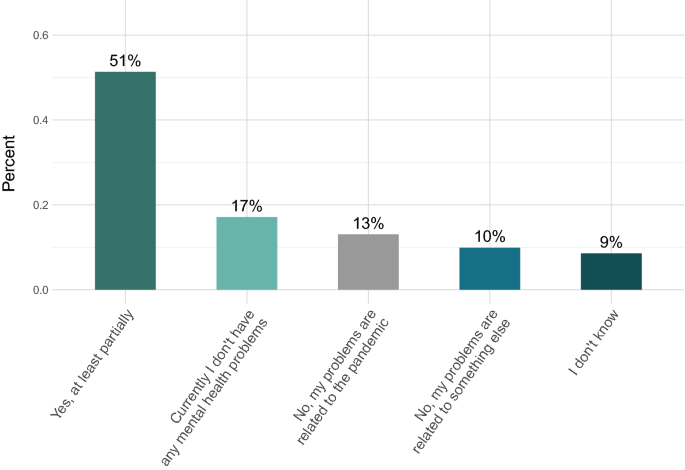
Mental health problems in relation to the PhD training. Participants were asked whether they think that their current mental health problems are related to their PhD training.
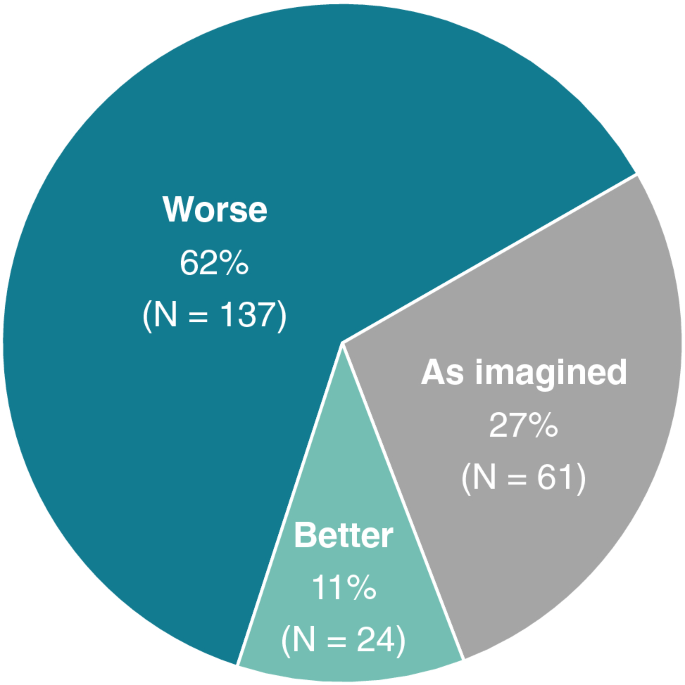
Expectations of the PhD training. Participants were asked whether their PhD training is how they had imagined it, better, or worse. Answers including “slightly” and “much” for both “worse” and “better” were collapsed.
Support structures
Only 16% of respondents expressed no interest in receiving psychological support. In contrast, 40% of doctoral researchers endorsed the answer “Yes, I would like it (or I am receiving some)” and 39% “Yes, I would like it, but I don’t need it now”. The forms of support rated as of most interest were psychotherapy in person (62%), psychological counselling (52%), and psychotherapy online (40%). Further, respondents stated that the coping strategies they use the most comprise social engagements (indicated by 85%) and recreational activities (78%; multiple answers were possible). To further delineate the role of social engagements, we asked participants to rate the strength of their overall social network ( M = 73; SD = 23) and the strength of their social network in Berlin ( M = 53; SD = 31). Further information on the forms of support as well as coping strategies are provided in the supplementary material (see the HTML file on the OSF page).
Changes in PhD training satisfaction and mental health during the pandemic
As shown in Fig. 4 , 43% of the respondents indicated that they were satisfied with their PhD training before the pandemic started, whereas only 32% stated that they were satisfied with it currently, in pandemic times. Evaluating the pre-pandemic situation, 38% of the sample indicated that they were dissatisfied, which increased to 46% after the start of the pandemic. Regarding the perceived change in wellbeing before and in the pandemic (see Fig. 5 ), 76% indicated that their mental wellbeing worsened during the pandemic.
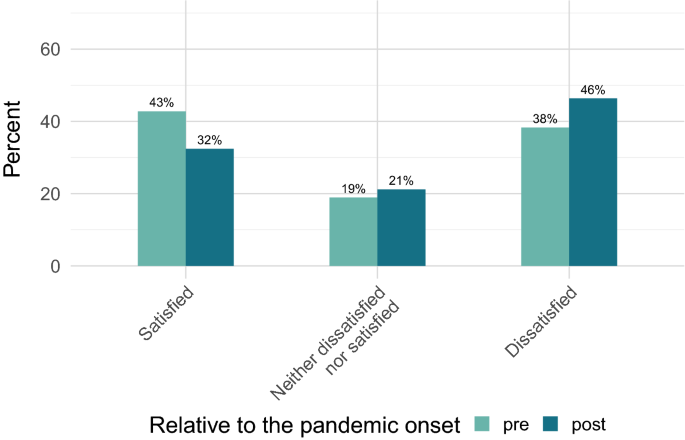
Overall satisfaction with the PhD training before and during the pandemic. Answers including “very” and “somewhat” for both “satisfied” and “dissatisfied” were collapsed.
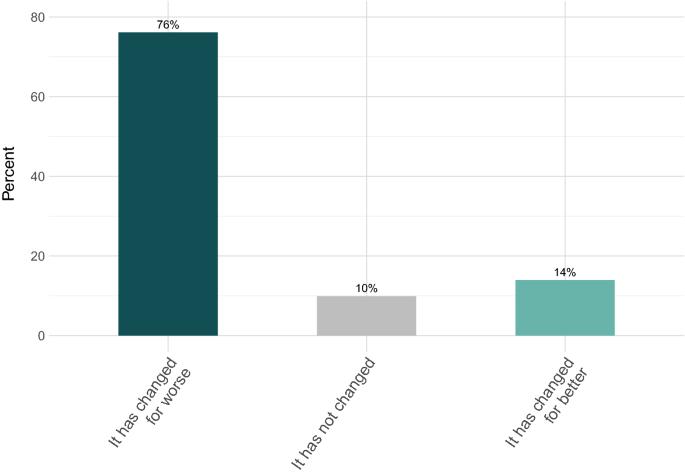
Mental wellbeing in the pandemic relative to pre-pandemic. Answers including “significantly” and “slightly” for both “worse” and “better” were collapsed.
As shown in Fig. 6 A, respondents evaluated their satisfaction with PhD-related aspects generally lower after than before the onset of the pandemic. Pre-pandemic, doctoral researchers were descriptively most satisfied with their research topic, working conditions, and holidays (all items rated at around 75%). We found the lowest satisfaction ratings for career perspectives, work-life balance, and academic results (the lowest at 50%). In pandemic times, research topic, salary, and holidays were rated highest (highest averaged rating at 68%); work-life balance, career perspectives, and work environment were rated the lowest (the lowest at 43%). We found significant decreases in the pandemic in self-rated satisfaction from workload, work environment, working conditions, work-life balance, supervision, research topic, career perspectives, and holidays, (all ps < 0.01). The satisfaction from academic results and salary did not change significantly during the pandemic.
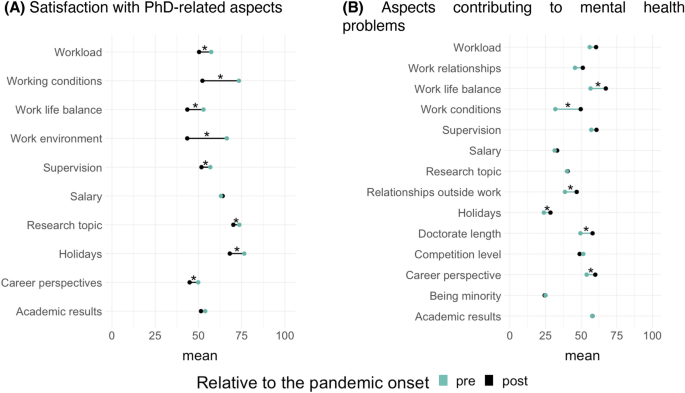
Average ratings of satisfaction with PhD-related aspects and of aspects contributing to mental health problems pre- and post-pandemic onset. The asterisks mark items for which t-tests reached statistical significance ( p < 0.05, uncorrected).
Participants also rated how these aforementioned aspects contributed to their mental health problems before and after the beginning of the pandemic (see Fig. 6 B). Descriptively, the aspects that contributed most to mental health issues pre-pandemic were academic results, supervision, work-life balance, and workload. In pandemic times, the major contributor was work-life balance, followed by workload, supervision, and career perspectives. We observed significant increases for the ratings of career perspectives ( p = 0.002), work-life balance ( p < 0.001), relationships outside of work ( p = 0.003), and holidays ( p = 0.043), indicating that in the pandemic these factors played a larger negative role for the mental health of doctoral researchers. Other aspects did not change during the pandemic (See OSF page for exact t-values).
Predictive value of PhD training variables for mental health problems
Figure 7 shows the effect sizes (Cohen’s partial f ) for the terms selected in the stepwise selection process for models predicting the depression, anxiety, and (work-related) burnout scores. Table 2 summarizes the models’ statistics and directions of the effects. Gender was significant in all models: While males tended to show higher values for anxiety and depression, being female was predictive of higher burnout scores. Years into PhD training was not significantly related to any outcome variable. PhD type (individual doctorate vs. structured program) was only predictive of burnout scores, with higher levels of burnout for the PhD researchers pursuing an individual doctorate compared to being in a structured program. Years spent in Germany, although showing significant main effects in all models, did not survive corrections for multiple comparisons. The diagnosis of a mental disorder (acquired before or during the PhD) was consistently predictive of all three mental health problems (i.e., higher scores of depression, anxiety, and burnout). Lower scores of depression and anxiety were predicted by strength of the overall social network, while higher self-efficacy was linked to lower burnout scores. The overall current satisfaction with the PhD training predicted lower scores for mental health problems in all models. In terms of PhD-related aspects, those of the ratings which reached significance were all linked to lower scores of mental health problems. In burnout, these predictors were: supervision, work-life balance, and holidays; in anxiety: work-life balance and career perspectives; in depression: work-life balance, career perspectives, and holidays.
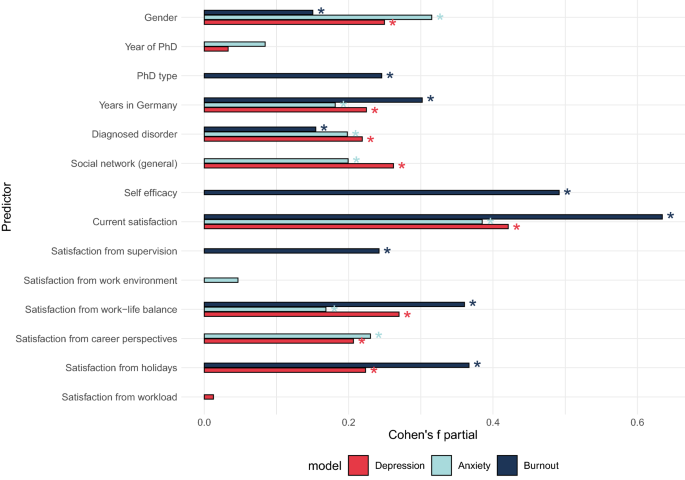
Effect sizes (Cohen’s partial f ) in the exploratory models of depression, anxiety, and burnout. The asterisks mark predictors for which the main effects reached statistical significance ( p < 0.05).
We examined different self-report measures capturing the mental health status of doctoral researchers of the wider Berlin area. Self-report ratings implied increased levels of depression, burnout, and loneliness, which further exacerbated under the pandemic influence. Critically, these problems were linked to the PhD training.
Under the magnifying glass: doctoral researchers’ mental health status
Firstly, we investigated the mental health status of doctoral researchers regarding pre-existing clinical and subclinical manifestations. In line with previous research 2 , 3 , 4 , our participants displayed severe mental health problems. One quarter of the sample indicated to have at least one diagnosed mental disorder. Doctoral researchers with a pre-existing diagnosis more often developed an additional mental disorder during the years of their PhD training and the context of the COVID-19 pandemic. Thus our data suggests that negative mental health impacts seem to be magnified particularly for ECRs with pre-existing vulnerabilities. Comparable to previous findings, one fifth crossed the cut-off for clinically relevant depressive symptoms 16 . These numbers are higher than the depression prevalence in the general German population before (7.7% 6 ) and during the pandemic (14.3% 17 ). However, some studies which were conducted outside of Germany reported similarly elevated levels of depression in the general population within this time period 18 . Therefore, the increased depression levels in our sample might not just be attributable to the academic training but to the high mental burden caused by the pandemic itself. We also detected higher scores of burnout as compared to the general population 15 , paralleling recent findings presenting a three-fold increase of burnout in ECRs 11 . Alarmingly, the majority of the sample reporting mental health problems indicated that they were related to their PhD training. Moreover, most of our sample reported their PhD training experience to be worse than expected and that they would be interested in receiving psychological support.
Various PhD training-related aspects may underlie the reported mental health problems: Firstly, pursuing a doctorate constitutes a time of professional and personal growth 19 . ECRs need to master complex theoretical frameworks, develop expertise in research methodologies and make an original contribution to their field 20 . Additionally, establishing boundaries between work and other areas of life is challenging: Academics assume that pervasive commitment and profound concentration on the research subject are expected 21 . Increased workload may cause a neglect of physical health or personal relationships, leading to work-life imbalances 22 . Lastly, research facility structures which do not buffer the psychological and emotional costs of the PhD training may contribute to a deterioration of ECRs’ mental health 23 .
Changes in satisfaction with the PhD training during the COVID-19 pandemic
Secondly, we aimed to unravel potential changes in satisfaction with the PhD training under the influence of the pandemic (which started about a year before this survey). We compared respondents' retrospective evaluation of their satisfaction before the pandemic with their current satisfaction. Almost all ratings significantly dropped during the pandemic with the largest decreases for working conditions and work environment. The German government introduced regulations to enforce social distancing to contain the COVID-19 virus, which also led to the closing of research facilities. Thus, a likely explanation for our results is that the disrupted or discontinued work on doctoral projects increased uncertainty and dissatisfaction with the PhD training 24 . Additionally, the workload and time spent on work might have increased significantly during the pandemic 25 , which corroborates the reported levels of increased work-related burnout in our survey.
There were no changes in satisfaction regarding doctoral researchers’ salaries during the pandemic. In contrast to the general German population, ECRs were not affected by Germany-wide short-time working measures (i.e., temporary reduction in normal working hours and thus reduction in salary). Further, at the time of the survey, the first pandemic-related extensions of PhD contracts and scholarships were granted. However, given that many empirical projects were on hold, the time until completion of the PhD training might prolong beyond the period of the granted extensions, which could increase the burden of financial insecurity in the long run. Although this hypothesis cannot be tested with the current data, it should be considered in future studies.
Likewise, we did not detect significant changes in satisfaction with academic results before and during the pandemic. It is possible that because some aspects of academic life (i.e., attending conferences) were limited, doctoral researchers had more resources to focus on output related to their PhD projects. In that vein, research indicated that the number of journal paper submissions increased during the pandemic 26 . Notably, our sample consisted of doctoral researchers which were at least three months into their PhD training in mostly empirical scientific fields. Given that they had already collected data for PhD-project related publications, they might have rated their academic results not to be significantly impacted by the pandemic.
Greater satisfaction with the PhD training in general, and with work-life balance in particular, were important resilience factors for all depression, anxiety, and burnout. This finding is in line with previous studies, which indicated that higher job satisfaction was associated with lower prevalence rates of depression and burnout in the general population 27 . Other studies highlighted that employees, who are satisfied with their work, can transfer positive feelings to non-work related contexts, resulting in a positive relationship between job and life satisfaction 28 , as well as psychological and social wellbeing 27 . Thus, maintaining ECRs’ satisfaction with their PhD training seems to be an essential mechanism to prevent mental health problems.
Further, our data showed that decreased satisfaction with PhD supervision is linked to burnout. Although we have no detailed information on the nature of the supervision quality, support from supervisors and other members of the research facilities have previously been reported to be critical to doctoral researchers’ persistence and scientific outcomes 29 . Research showed that the quantity and quality of meetings with supervisors can impact ECRs’ satisfaction 30 . Quality supervision can be characterized as involving precise and timely feedback, frequent meetings that include open discussion about roles and responsibilities, a supportive and collegial relationship, and encouragement to maintain the flow of work throughout the PhD training 31 . One driver of supervision dissatisfaction could arise from misaligned interests of ECRs and their supervisors: While the latter might be more inclined to tune their interest towards the scientific community as a whole, they might lose sight of ECR’s individual needs 32 .
In addition, we found that satisfaction with career perspectives is an important predictor of anxiety and burnout. It was recently argued that being optimistic about career prospects might help to decrease levels of depression and anxiety about the future 33 . However, long- and short-term academic career perspectives are uncertain, which may degrade academia to an “alternative career” path. Missing career outlooks, in or outside of academia, amplify the mental burden of ECRs, leading to the levels of anxiety and burnout 34 . This factor might be even more pronounced in countries of the Global South, where—compared to the Global North—levels of inequality and labour informality are higher and research funding is more limited 35 .
Within our analysis, the strength of doctoral researchers' social network emerged as an important resilience factor for depression and anxiety. Indeed, there is substantial evidence that individuals with richer networks of active social relationships tend to be more satisfied and happier with their lives 36 . However, due to the demands of their PhD training, ECRs often report declines in social interactions 37 . Lack of social support has also been found to correspond with lower wellbeing and a higher prevalence of mental illness in ECRs 38 . Similarly, in the current study ECRs who pursued an individual doctorate were more likely to suffer from burnout than their peers in structured graduate programs. Within a structured PhD program, doctoral researchers are integrated in a framework with peers from the start of the training, whereas individual doctorates require ERCs to build their own scientific community.
Another resilience factor identified in our data was self-efficacy, with higher levels being linked to lower burnout scores. Self-efficacy is an important motivational factor for identity development of ECRs 39 , especially when it comes to the confidence in successfully performing research tasks 40 . It has been found to be significantly correlated with interest in research and the production of scholarly publications 41 . Conversely, ECRs with low levels of self-efficacy may be more likely to engage in self-handicapping (e.g., procrastination) to avoid being perceived as incompetent 42 .
Finally, men in our sample showed higher levels of depression and anxiety symptoms than women. This finding is at odds with the literature, where women have been reported to suffer more often from mental health problems than men both in the general population 6 and ECR samples 2 . Although this finding is difficult to interpret, previous research showed that men have lower participation rates in voluntary surveys 43 and engage more rarely in help-seeking behavior 44 . Thus, it seems possible that the data reflect the effects of our convenience sample: Men may have participated in our survey because they experienced mental health problems, which resulted in increased clinical symptoms in this group. Further, although our male participants reported higher levels of depression and anxiety, female participants reported higher burnout scores. As shown in previous studies during the pandemic, women were more likely to engage in housework, care and family 13 , which relates to physical and psychological fatigue and exhaustion 15 , but less so to depression.
Call to action
Our sample of doctoral researchers reported profound PhD training-related mental health problems, which worsened during the COVID-19 pandemic. Currently, mostly single researchers or initiatives founded by ECRs (e.g., German ECR initiatives like N 2 , Scholar Minds) devote their mission to reduce harmful work conditions and the stigmatization of mental health matters in academia. However, sustainable preventive and interventional solutions aiming to improve ECRs’ mental health should be prioritized and addressed on different systemic levels, such as academic institutions and political initiatives, to ensure a healthy and supportive work environment. Combining our findings with recent literature, we have identified several factors to improve conditions for ECRs. These factors are not exclusively tied to improving the situation regarding the COVID-19 pandemic but relate to more general aspects of ECRs’ mental health:
Institutional mental health support
Firstly, psychological burden could be alleviated if the institutional culture of a research facility was more welcoming, inclusive, and understanding of ECRs’ backgrounds 20 . To this end, an open discourse about mental health problems is needed, which would also help to increase personal and public de-stigmatization of mental health problems still being present in academia 45 .
Secondly, institution-based psychological counseling should be the standard at every research institution for prevention and interventional needs. Especially for international ECRs who are not familiar with the local health care system, institution-based counselling could be a first low-level opportunity to de-escalate arising mental health problems. Although some counselling opportunities are already in place, ECRs are often unaware of their existence (e.g., no advertisement of services; information difficult to access 46 ). In addition, psychological counselling opportunities do not seem to be specifically tailored to doctoral researchers’ needs, but are rather similar to those designed for undergraduate students 47 . Thus, institutions would need to provide easily accessible PhD training-tailored psychological counselling.
Work-life balance
Working overtime and disregarding holidays is still part of the academic culture 48 . With an average of more than 46 h of work per week 16 , doctoral researchers contribute to the normalization of this culture, likely neglecting their work-life balance. When employed part time, doctoral researchers have been shown to work even more over-time hours than postdoctoral researchers (difference of up to 7 h per week 48 ). Irrespective of the type of working contract, the implicit rule to work overtime should be discouraged by employers and supervisors. Additionally, workshops on self- and time management provided by research institutions can strengthen ECRs’ ability to deal with the stressful demands of academia.
Quality of supervision
Mentoring contracts between ECRs and supervisors could help to set expectations for both parties. This procedure is already in place at many research facilities, however, it is yet to become a common practice. Further, improving supervision quality should be incentivized by research facilities. Whereas ratings of teaching are already a part of applications for professorships, a similar quantification for supervision skills could maintain supervision quality over the course of the PhD training. Integrated evaluations by doctoral researchers could both incentivize senior academics to monitor their quality of supervision and offer tangible rewards for their efforts.
Providing career perspectives and transferable skills
Even though staying in academia is still viewed as the most desirable career path for ECRs 49 , only a small percentage can continue to work in academia after the completion of their PhD training 50 . The creation of more permanent positions on a post-doctoral level is an important political challenge. In Germany, 98% of employees under 35 years of age are working on limited contracts in academia. Thanks to public attention on precarious working conditions in academia initiated by the German grass-root movement “#ichbinHanna” ( https://ichbinhanna.wordpress.com ) , first political consequences that will lead to the creation of more tenure track positions, have been taken. Furthermore, opportunities to continue a career outside of science should be considered more strongly. Although many structured PhD programs have started to integrate educational content on alternative career paths, more room should be given for concrete opportunities to develop new skills as, for example, in the form of internships or role plays 51 . As skills acquired during the PhD training can successfully be transferred to careers outside of academia 34 , these real-life experiences might decrease anxiety regarding future job perspectives.
Growing social networks
Research facilities play a major role in socializing ECRs 51 which is why an important task constitutes the establishment of sustainable ECR networks in research facilities to grow sustainable social networks to discuss science matters and work-related challenges. Some graduate schools already provide induction days and buddy programs (e.g., connecting doctoral researchers across different PhD cohorts) to facilitate ECRs’ future academic career. In addition, regular check-ins with members of the research facility could help to identify and solve problems with settling into the research institution and its social network structure.
Moreover, within- and between-institutional networks have the potential to help ECRs to shape their career paths. Some graduate schools are already providing alumni talks to connect ECRs with graduates from various career fields. This approach not only helps to expand the professional network, but also sharpens the view of which career options may be available after the doctorate and how to target these options early on.
Fostering self-efficacy
To maintain self-efficacy, the PhD training should entail tasks that are challenging, but achievable within the specific conditions of the doctoral project. Quite often, there is a mismatch in expectation between ECRs and research facilities 52 , likely arising from insufficient information at the admission stage regarding roles and responsibilities 53 . This parallels our finding that the majority of ECRs rated their PhD training experience markedly below their expectations. Thus, ECRs need to understand what explicit and implicit requirements are present toward the completion of their PhD training. One opportunity to enable clear expectation management is to offer an orientation day in graduate schools where potential doctoral candidates have the opportunity to receive information from administrative members, but also ECRs who are in different stages of their PhD training to provide testimonials.
Limitations
Due to different potential biases in our sample, we acknowledge that our data might not be representative of the whole population of interest. As we might have mainly reached doctoral researchers, who are interested in or even affected by mental health problems, we recognize that this procedure may have created a sampling bias. Further, the nature of the survey questions might have created a demand characteristics bias, potentially leading to elevated levels of reported burden. However, we think that the extent of these biases is comparable to other studies investigating mental health using self-report questionnaires. We also detected a gender response bias: We had more female responders even though we targeted mainly research fields related to neuroscience with a slightly men-dominated gender distribution 16 . BSI scores of our sample were rather low for overall anxiety, but rather high for the subscale phobic anxiety (56%). The latter subscale includes items that might have changed in weighting in pandemic times (e.g., “being in large crowds”), leading to increased scores. We also acknowledge that doctoral researchers’ retrospective assessment of their wellbeing might have led to biased judgements of aspects before the pandemic.
In addition to this limitation, we captured the history of mental illness more broadly (e.g., having contact with psychiatry/psychology or being previously diagnosed with a mental disorder), but did not ask for the specific diagnosis. Thus, our data does not allow for the exploration of the relationship between the mental health indexes and one or another mental disorder in-depth. We recognize that this could be especially important as we observed that a prior diagnosis was the main predictor of several dependent variables. Further, we did not assess the direct impact of the pandemic on the participants (e.g., being infected or having lost relatives or colleagues due to the pandemic). However, we asked participants if they experienced any event within two weeks prior to participation which would render their answers unrepresentative for a longer time perspective and excluded the respective data. We believe that losing a loved one or experiencing high stress due to a COVID-19 infection would have been captured in this response.
On a global scale, our survey focused on German doctoral researchers, with a certain focus on international students within the field of neuroscience, which may be generalizable to countries of similar funding opportunities and research culture. However, limited assumptions should be made about ECRs’ mental health in countries with diverging research conditions (e.g., of the Global South 35 ).
Our findings extend the ongoing debate about the mental health crisis in academia: Doctoral researchers’ self-reports showed increased levels of depression, burnout, and loneliness and further decreased mental wellbeing under the influence of the pandemic. Importantly, self-reported mental health problems were strongly linked to the PhD training, which emphasizes the need to improve academic work culture. Initiatives founded by ECRs have sought to actively reduce harmful work conditions and the stigmatization of mental health problems in academia. However, long-term change also demands top-down solutions. We thus call research institutions to action to create PhD training conditions that target the factors we identified and bring about sustainable systemic changes for academia.
Materials and methods
Participants.
We sought to target early career researchers pursuing their doctorate at research facilities in Berlin and the greater Berlin area to investigate the status of their mental health and potential COVID-19 related mental health changes via an online survey. The cross-sectional study was approved by the ethics committee of the Faculty of Psychology of the Humboldt-Universität zu Berlin and was conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent. Participants had the option to take part in a raffle to win 25 Euro. In total, 335 doctoral researchers completed the survey. As we aimed to compare the perceived mental health and satisfaction with PhD training of doctoral researchers before and after the start of the COVID-19 pandemic, we excluded participants who did not start their PhD training at least three months prior to the beginning of the pandemic (March 2020 in Germany; n = 75). Additionally, we excluded participants who indicated that they experienced an important life event which could have influenced their mental health significantly in the last two weeks (n = 38). In the remaining sample of 222 participants, the age ranged from 24 to 52 years ( M = 29.8; SD = 3.4). Gender, nationality, years into the PhD training, and type of the PhD program are summarised in Table 3 . Type of PhD program refers to structured programs (as often provided by graduate schools) vs. individual doctoral projects. They differ in characteristics, which are potentially important for doctoral researchers’ wellbeing, especially in the pandemic. For example, doctoral researchers in structured programs are often organized in cohorts or years, which facilitates the growth of a professional peer network.
Data were collected cross-sectionally between January and February 2021 with an online survey administered via the SoSci Survey platform ( www.soscisurvey.de ) and further processed in R ver. 4.0.2. The R code including data, analysis code and a HTML file with all procedures rendered in accessible form, are available at an OSF repository ( https://osf.io/q5w4g/ ). The survey consisted of standardized measures of mental health and self-developed questions regarding changes in satisfaction before and during the pandemic in relation to PhD-specific aspects.
Standardized measures of mental health
We included three standardized questionnaires to assess participants’ mental health state. For all these questionnaires, higher scores relate to greater significance of the measured mental health problem. We used the Brief Symptom Inventory (BSI 54 ), which has 53 items to assess nine mental health symptom dimensions: somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Participants were asked to choose how much a described problem bothered them in the last week (e.g., “Nervousness or shakiness inside”, scale: “Not at all”, “A little bit”, “Moderately”, ”Quite a bit”, and “Extremely”). For each dimension, raw scores were transformed into t-scores to relate the results to the general population. In reference to the BSI manual 54 , we considered t-scores equal to or larger than1 SD (t-score = 60) as clinically relevant.
The Copenhagen Burnout Inventory (CBI 15 ) was used to measure personal and work-related burnout (the third CBI scale, namely client-related burnout, was omitted in our survey as the work of doctoral researchers is rarely concerned with clients). In 13 questions, participants were asked how often they experienced described problems in the last weeks (e.g., “How often do you feel tired?”, scale: “Never/Almost never”, ”Seldom”, ”Sometimes”, ”Often”, “Always”) or how intense these problematic experiences were (“To a very low degree”, ”To a low degree”, ”Somewhat”, ”To a high degree”, ”To a very high degree”). For scoring, each answer is assigned a numerical value from 0 for “Never/almost never” or “To a very low degree” to 100 for “Always” or “To a very high degree”. The score is calculated as the mean of all items.
Further, we used the De Jong Gierveld Loneliness Scale (11-item version 55 ) to measure social and emotional loneliness. Participants were asked to indicate how often they experienced different situations (e.g., “There is always someone I can talk to about my day-to-day problems”, scale: “None of the time”, “Rarely”, “Some of the time”, “Often”, “All the time”). Maximum total score is 11 (one per item), which combines six items from the emotional subscale and five items from the social subscale.
Self-developed questions on mental health and satisfaction with PhD training under consideration of the pandemic
In order to assess participants’ perceived mental health and satisfaction in relation to their PhD training, we created questions specifically targeting these topics considering the context of the pandemic situation. We based wording and content of the questions on other surveys targeting ECRs’ mental health, such as the survey of the N 2 network 16 and the annual Nature survey 3 . We subsequently adapted the questions to capture the influence of the pandemic.
Besides demographic questions and PhD specifics (e.g., years into PhD training), we collected information on existing and past clinical mental health diagnosis, expectations regarding the PhD training before its start, potential support structures, and changes in satisfaction with PhD-specific aspects (e.g., supervision) caused by the pandemic. We thus asked our participants to evaluate these aspects retrospectively for the times before the pandemic as well as the current in-pandemic situation. The results reported here include a subset of all questions administered in the survey; the full list can be found in the OSF repository ( https://osf.io/q5w4g/ ).
Statistical analyses
To conceive the actual mental health state of our participants, we used descriptive statistics for the standardized questionnaires. Therefore, we computed the mean and standard deviation of the BSI, CBI, and De Jong Gierveld Loneliness Scale scores to compare these values with existing literature. For the self-developed questions on mental health of doctoral researchers and ratings of satisfaction with PhD training, we calculated percentages per response category. We then performed two exploratory statistical analyses: The first analysis aimed to investigate whether there was a change in retrospective pre-pandemic and current in-pandemic ratings of PhD-related satisfaction aspects and items contributing to mental health issues. We performed two-tailed dependent t-tests for all related items. The second analysis aimed to investigate potential predictors of three mental health aspects: depression, anxiety, and burnout. We chose these aspects because they are most frequently considered in the context of the mental health of ECRs 2 , 3 , 4 . To this goal, we built three multiple regression models with the BSI depression t-scores, the BSI anxiety t-scores, and the CBI work-related burnout scores as dependent variables. To control for mental health issues potentially unrelated to the PhD, we included prior clinical diagnosis of a mental disorder (pre- or since the beginning of the PhD) as a control variable in all models. We expected that the three mental health aspects would be related to years into the PhD training, overall satisfaction with the PhD training, being a member of a graduate program, and gender, but we were also interested in the contribution of other factors. Therefore, we entered all suitable survey questions (see column “Predictor” within the HTML file on the OSF page) as potential predictors in the models, and conducted a stepwise selection of the best model with the bidirectional step() function (stats package). This procedure allows for iterative adding and removing predictors based on the model’s fit estimated with the Akaike Information Criterion (AIC). The predictors in the selected models are chosen based on their statistical significance for explaining variance. Due to few data points in the following categories, we excluded participants who (1) did not identify as a woman or a man (n = 9), (2), did not indicate being part of a structured or individual PhD program (n = 14), and (3) chose not to provide information about whether they were diagnosed with a mental disorder (n = 1). This procedure resulted in a sample size of 198 participants for this exploratory analysis. Responses to the question “How long have you been living in Germany?” were binned into three categories: 0–3 years, 4 + years, and native. Due to the design of the survey (participants could not proceed without giving a response for each item concerned for analysis), there was no missing data.
It should be noted that stepwise regression is a discouraged method for hypothesis testing and should be interpreted with caution in data exploration. The reason for this is that it may produce narrow confidence intervals, high t statistics and low p values 56 . However, when treated with caution, it could generate valuable insights about the relationships in the dataset and produce ideas for future hypothesis testing studies. Further, because stepwise regression is less effective with more explanatory variables 56 , we did not include interaction terms in our exploratory models. Finally, because the p values in stepwise regression are not accurate and should not be interpreted as they would in a hypothesis-testing, theory-driven analysis, we do not correct for multiple comparisons, as there is no straightforward method to do so and no apparent benefit for the interpretability of the results. With all this in mind, in the current study, we do not encourage other researchers to use the reported statistics as true effect sizes in the population, but rather to consider this procedure as an exploratory tool for building insights about our data and generating future hypotheses in theory-driven studies.
The stepwise selection procedure confirmed that prior diagnosis explained significant portions of variance in all models. Hence, other predictors explained additional variance in the data suggesting that PhD-related aspects may have a somewhat additive (to clinical diagnoses) influence on mental health problems. We also explored models without prior diagnosis as a predictor, which showed a similar pattern of results as the full models presented below (see point 6.2 in the HTML file in the repository). The selected models were checked for regression assumptions (normality, linearity, multicollinearity (with Variance Inflation Factors), homoscedasticity), which were met for all models (details for each model are reported in the HTML file). The significance level for all the tests was set to 0.05. However, it should be noted that these analyses are data-driven and thus any statistical significance should be considered with care. To estimate the main effects in the analyses (across levels of multiple categorical predictors), we conducted a type-II analysis of variance using the model parameters.
Ethics approval
The study protocol was reviewed and approved by the ethics committee of the Department of Psychology at Humboldt-Universität zu Berlin. The study was conducted in accordance with the Declaration of Helsinki.
Data availability
Data and code that support the findings of this study are openly available at the OSF repository: https://osf.io/q5w4g/ .
Christian, K., Johnstone, C., Larkins, J. A., Wright, W. & Doran, M. R. A survey of early career researchers in Australia. Elife 10 , 1–19. https://doi.org/10.7554/ELIFE.60613 (2021).
Article Google Scholar
Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T. & Vanderford, N. L. Evidence for a mental health crisis in graduate education. Nat. Biotechnol. 36 (3), 282–284. https://doi.org/10.1038/nbt.4089 (2018).
Article CAS PubMed Google Scholar
Woolston, C. PhD poll reveals fear and joy, contentment and anguish. Nature 575 , 403–406 (2019).
Article ADS CAS PubMed Google Scholar
Satinsky, E. N. et al. Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students. Sci. Rep. 11 (1), 1–12. https://doi.org/10.1038/s41598-021-93687-7 (2021).
Article ADS CAS Google Scholar
Barreira, P., Basilico, M., Bolotnyy, V. Graduate Student Mental Health: Lessons from American Economics Departments. Working Paper. (2020). https://scholar.harvard.edu/bolotnyy/publications/graduate-student-mental-health-lessons-american-economics-departments .
Jacobi, F. et al. Mental disorders in the general population. Study on the health of adults in Germany and the additional module mental health (DEGS1-MH). Nervenarzt 85 (1), 77–87. https://doi.org/10.1007/s00115-013-3961-y (2014).
Rawat, S. & Meena, S. Publish or perish: Where are we heading?. J. Res. Med. Sci. 19 (2), 87–89 (2014).
PubMed PubMed Central Google Scholar
Kusurkar, R. A. et al. Burnout and engagement among PhD students in medicine: The BEeP study. Perspect. Med. Educ. 10 (2), 110–117 (2021).
Article PubMed Google Scholar
Killgore, W., Cloonan, S. A., Taylor, E. C. & Dailey, N. S. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res. 290 , 113117. https://doi.org/10.1016/j.psychres.2020.113117 (2020).
Article CAS PubMed PubMed Central Google Scholar
Torales, J., O’Higgins, M., Castaldelli-Maia, J. M. & Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 66 (4), 317–320. https://doi.org/10.1177/0020764020915212 (2020).
Harrop, C., Bal, V., Carpenter, K. & Halladay, A. A lost generation? The impact of the COVID-19 pandemic on early career ASD researchers. Autism Res. 14 (6), 1078–1087. https://doi.org/10.1002/aur.2503 (2021).
Article PubMed PubMed Central Google Scholar
Byrom, N. The challenges of lockdown for early-career researchers. Elife 9 , 1–3. https://doi.org/10.7554/ELIFE.59634 (2020).
Humphries, B. A. et al. Overstretched and overlooked: Solving challenges faced by early-career investigators after the pandemic. Trends Cancer 7 (10), 879–882. https://doi.org/10.1016/j.trecan.2021.07.005 (2021).
Mattijssen, L. M. S., Bergmans, J. E., van der Weijden, I. C. M. & Teelken, J. C. In the eye of the storm: The mental health situation of PhD candidates. Perspect. Med. Educ. 10 (2), 71–72. https://doi.org/10.1007/s40037-020-00639-4 (2021).
Kristensen, T. S., Borritz, M., Villadsen, E. & Christensen, K. B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work Stress. 19 (3), 192–207. https://doi.org/10.1080/02678370500297720 (2005).
PhDnet Survey Group. PhDNet Survey Report 2019 (2020).
Bäuerle, A. et al. Mental health burden of the COVID-19 outbreak in Germany: Predictors of mental health impairment. J. Prim. Care Community Health https://doi.org/10.1177/2150132720953682 (2020).
Salari, N. et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 16 (1), 1–11. https://doi.org/10.1186/s12992-020-00589-w (2020).
Manathunga, C. Early warning signs in postgraduate research education: A different approach to ensuring timely completions. Teach. High. Educ. 10 (2), 219–232. https://doi.org/10.1080/1356251042000337963 (2005).
Ryan, T., Baik, C. & Larcombe, W. How can universities better support the mental wellbeing of higher degree research students? A study of students’ suggestions. High. Educ. Res. Dev. https://doi.org/10.1080/07294360.2021.1874886 (2021).
Ylijoki, O.-H. Boundary-work between work and life in the high-speed university. Stud. High. Educ. 38 (2), 242–255. https://doi.org/10.1080/03075079.2011.577524 (2013).
Rizzolo, S., DeForest, A. R., DeCino, D. A., Strear, M. & Landram, S. Graduate student perceptions and experiences of professional development activities. J. Career Dev. 43 (3), 195–210. https://doi.org/10.1177/0894845315587967 (2016).
Sverdlik, A., Hall, C. & N., McAlpine, L. & Hubbard, K.,. The PhD experience: A review of the factors influencing doctoral students’ completion, achievement, and well-being. Int. J. Dr. Stud. 13 , 361–388. https://doi.org/10.28945/4113 (2018).
Safeguard research in the time of COVID-19. Nat. Med. 26 , 443 (2020). https://doi.org/10.1038/s41591-020-0852-1 .
Xiao, Y., Becerik-Gerber, B., Lucas, G. & Roll, S. C. Impacts of working from home during COVID-19 pandemic on physical and mental well-being of office workstation users. J. Occup. Environ. Med. 63 (3), 181–190. https://doi.org/10.1097/JOM.0000000000002097 (2021).
Else, H. How a torrent of COVID science changed research publishing—In seven charts. Nature 588 (7839), 553. https://doi.org/10.1038/d41586-020-03564-y (2020).
Capone, V. & Petrillo, G. Mental health in teachers: Relationships with job satisfaction, efficacy beliefs, burnout and depression. Curr. Psychol. 39 (5), 1757–1766. https://doi.org/10.1007/s12144-018-9878-7 (2020).
Tadić, M., Bakker, A. B. & Oerlemans, W. G. M. Work happiness among 781 teachers: A day reconstruction study on the role of self-concordance. J. Sch. Psychol. 51 (6), 735–750. https://doi.org/10.1016/j.jsp.2013.07.002 (2013).
Posselt, J. Normalizing struggle: Dimensions of faculty support for doctoral students and implications for persistence and well-being. J. High. Educ. 89 (6), 988–1013. https://doi.org/10.1080/00221546.2018.1449080 (2018).
Heath, T. A quantitative analysis of PhD students’ views of supervision. High. Educ. Res. Dev. 21 (1), 41–53. https://doi.org/10.1080/07294360220124648 (2002).
Latona, K. & Browne, M. Factors Associated with Completion of Research Higher Degrees (Higher Education Division, Department of Education, Training and Youth Affairs, Canberra, Australia, 2001).
Schneijderberg, C. Supervision practices of doctoral education and training. Stud. High. Educ. 46 (7), 1285–1295. https://doi.org/10.1080/03075079.2019.1689384 (2021).
Charles, S. T., Karnaze, M. M. & Leslie, F. M. Positive factors related to graduate student mental health. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1841207 (2021).
Sinche, M. et al. An evidence-based evaluation of transferrable skills and job satisfaction for science PhDs. PLoS ONE 12 (9), 771. https://doi.org/10.1371/journal.pone.0185023 (2017).
Article CAS Google Scholar
Reidpath, D. D. & Allotey, P. The problem of “trickle-down science” from the Global North to the Global South. BMJ Glob. Health 4 (4), e001719. https://doi.org/10.1136/bmjgh-2019-001719 (2019).
Amati, V., Meggiolaro, S., Rivellini, G. & Zaccarin, S. Social relations and life satisfaction: The role of friends. Genus 74 (1), 7. https://doi.org/10.1186/s41118-018-0032-z (2018).
Longfield, A., Romas, J. & Irwin, J. The self-worth, physical and social activities of graduate students: A qualitative study. Coll. Stud. J. 40 (2), 282–292 (2006).
Google Scholar
Levecque, K., Anseel, F., de Beuckelaer, A., van der Heyden, J. & Gisle, L. Work organization and mental health problems in PhD students. Res. Policy 46 (4), 868–879. https://doi.org/10.1016/j.respol.2017.02.008 (2017).
Virtanen, V., Taina, J. & Pyhältö, K. What disengages doctoral students in the biological and environmental sciences from their doctoral studies?. Stud. Contin. Educ. 39 (1), 71–86. https://doi.org/10.1080/0158037X.2016.1250737 (2017).
Forester, M., Kahn, J. H. & Hesson-McInnis, M. S. Factor structures of three measures of research self-efficacy. J. Career Assess. 12 (1), 3–16. https://doi.org/10.1177/1069072703257719 (2004).
Lambie, G. W. & Vaccaro, N. Doctoral counselor education students’ levels of research self-efficacy, perceptions of the research training environment, and interest in research. Couns. Educ. Superv. 50 (4), 243–258. https://doi.org/10.1002/j.1556-6978.2011.tb00122.x (2011).
Schwinger, M. & Stiensmeier-Pelster, J. Prevention of self-handicapping—The protective function of mastery goals. Learn. Individ. Differ. 21 (6), 699–709. https://doi.org/10.1016/j.lindif.2011.09.004 (2011).
Cheung, K. L., Ten Klooster, P. M., Smit, C., De Vries, H. & Pieterse, M. E. The impact of non-response bias due to sampling in public health studies: A comparison of voluntary versus mandatory recruitment in a Dutch national survey on adolescent health. BMC Public Health 17 (1), 1–10. https://doi.org/10.1186/s12889-017-4189-8 (2017).
Seidler, Z. E., Dawes, A. J., Rice, S. M., Oliffe, J. L. & Dhillon, H. M. The role of masculinity in men’s help-seeking for depression: A systematic review. Clin. Psychol. Rev. 49 , 106–118. https://doi.org/10.1016/j.cpr.2016.09.002 (2016).
Wada, M. et al. University students’ perspectives on mental illness stigma. Ment. Health Prev. 14 , 200159. https://doi.org/10.1016/j.mph.2019.200159 (2019).
Waight, E. & Giordano, A. Doctoral students’ access to non-academic support for mental health. J. High. Educ. Policy Manag. 40 (4), 390–412. https://doi.org/10.1080/1360080X.2018.1478613 (2018).
Mackie, S. A. & Bates, G. W. Contribution of the doctoral education environment to PhD candidates’ mental health problems: A scoping review. High. Educ. Res. Dev. 38 (3), 565–578. https://doi.org/10.1080/07294360.2018.1556620 (2019).
Frei, I. & Grund, C. Antecedents of overtime work: The case of junior academics. German J. Hum. Resource Manag. 34 (4), 371–397. https://doi.org/10.1177/2397002220903247 (2020).
St. Clair, R. et al. The “new normal”: Adapting doctoral trainee career preparation for broad career paths in science. PLoS ONE 12 , e0177035. https://doi.org/10.1371/journal.pone.0177035 (2017).
Seo, G., Ahn, J., Huang, W.-H., Makela, J. P. & Yeo, H. T. Pursuing careers inside or outside academia? Factors associated with doctoral students’ career decision making. J. Career Dev. 48 (6), 957–972. https://doi.org/10.1177/0894845320907968 (2021).
O’Meara, K. et al. By design: How departments influence graduate student agency in career advancement. Int. J. Dr. Stud. 9 , 155–179. https://doi.org/10.28945/2048 (2014).
Holbrook, A. et al. PhD candidate expectations: Exploring mismatch with experience. Int. J. Dr. Stud. 9 , 329–346 (2014).
Gardner, S. K. Student and faculty attributions of attrition in high and low-completing doctoral programs in the United States. High. Educ. 58 (1), 97–112. https://doi.org/10.1007/s10734-008-9184-7 (2009).
Derogatis, L. R. BSI Brief Symptom Inventory: Administration, Scoring, and Procedures Manual 4th edn. (National Computer Systems, 1993).
de Jong-Gierveld, J. & Kamphuls, F. The development of a rasch-type loneliness scale. Appl. Psychol. Meas. 9 (3), 289–299. https://doi.org/10.1177/014662168500900307 (1985).
Smith, G. Step away from stepwise. J. Big Data. https://doi.org/10.1186/s40537-018-0143-6 (2018).
Download references
Acknowledgements
We would like to thank all members of Scholar Minds for their support in conceptualizing this survey project. Scholar Minds is a Berlin-based initiative of PhD candidates concerned with mental health in academia ( www.scholar-minds.net ; Berlin, Germany) which was, together with other PhD researchers, co-founded by S.N., M.M., K.B.
Open Access funding enabled and organized by Projekt DEAL. This study was supported by funding from the Berlin School of Mind and Brain, Humboldt-Universität zu Berlin and Stiftung der Deutschen Wirtschaft (sdw). We acknowledge support by the Open Access Publication Fund of Humboldt-Universität zu Berlin and the German Research Foundation (DFG)—337619223/RTG2386.
Author information
These authors contributed equally: Sandra Naumann, Magdalena Matyjek and Katharina Bögl.
Authors and Affiliations
Berlin School of Mind and Brain, Humboldt-Universität zu Berlin, Berlin, Germany
Sandra Naumann, Magdalena Matyjek, Katharina Bögl & Isabel Dziobek
Department of Psychology, Institute of Life Sciences, Humboldt-Universität zu Berlin, Berlin, Germany
You can also search for this author in PubMed Google Scholar
Contributions
S.N., M.M. and K.B. were involved in the survey design, data collection, and interpretation of the data. M.M. conducted the statistical analysis S.N., M.M., K.B. and I.D. drafted and reviewed the manuscript.
Corresponding author
Correspondence to Sandra Naumann .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Naumann, S., Matyjek, M., Bögl, K. et al. Doctoral researchers’ mental health and PhD training satisfaction during the German COVID-19 lockdown: results from an international research sample. Sci Rep 12 , 22176 (2022). https://doi.org/10.1038/s41598-022-26601-4
Download citation
Received : 17 March 2022
Accepted : 16 December 2022
Published : 22 December 2022
DOI : https://doi.org/10.1038/s41598-022-26601-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Strukturen, ziele und bedürfnisse der early career scientists am deutschen zentrum für psychische gesundheit.
- Simone C. Behrens
- Isabel Brandhorst
Der Nervenarzt (2024)
- Diego Andrade
- Icaro J. S. Ribeiro
- Orsolya Máté
Scientific Reports (2023)
Burnout dynamic among Ukrainian academic staff during the war
- Natalia Tsybuliak
- Yana Suchikova
- Olha Hurenko
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Depression in Persons With Epilepsy: Lessons From Case Review
Affiliations.
- 1 From the Department of Psychiatry and Behavioral Health, George Washington University School of Medicine and Health Sciences, Washington, DC.
- 2 Asher Center for the Study and Treatment of Depressive Disorders, Department of Psychiatry and Behavioral Sciences, Northwestern University Feinberg School of Medicine, Chicago, IL.
- 3 Developing Brain Institute, Children's National Hospital, Washington, DC.
- PMID: 38684049
- DOI: 10.1097/JCP.0000000000001848
Background: Major depressive disorder is highly prevalent among persons with epilepsy (PWEs). Between 30% and 50% of PWEs suffer from depression. Many factors contribute to this prevalence, including the psychosocial impact of the diagnosis, restrictions on driving and certain types of work, and adverse effects associated with antiseizure medications. Without proper treatment, depressed PWEs have increased risks for suicide, strained relationships, lowered seizure control, and impairment in functioning. Our objective was to use the existing literature and insights from our experience in treating depression and anxiety in PWEs within an academic mood disorders center. We aimed to provide practical guidance for health care professionals who treat depression in this population.
Methods: Persons with epilepsy and depression were identified by their treating psychiatrists. Their electronic health records were reviewed and compiled for this report, with a total of 12 included in this review. Records were reviewed regarding antiseizure medications, psychotropic medications, light therapy, psychotherapy, other interventions, and treatment response.
Results: Based on our review of literature, as well as review of cases of individuals with epilepsy and comorbid psychiatric conditions, we recommend a step-wise evidence-based approach of optimizing psychiatric medication doses, augmenting with additional medication and/or implementing nonpharmacological interventions such as light therapy and psychotherapy.
Conclusions: In PWEs, improvement in depression, other psychiatric symptoms, and function are the goals of drug and nondrug interventions. Depression care has the potential to significantly improve the quality of life of PWEs and reduce both morbidity and mortality.
Copyright © 2024 Wolters Kluwer Health, Inc. All rights reserved.
Publication types
- Case Reports
- Anticonvulsants / adverse effects
- Anticonvulsants / therapeutic use
- Antidepressive Agents / therapeutic use
- Comorbidity
- Depressive Disorder, Major / drug therapy
- Depressive Disorder, Major / epidemiology
- Depressive Disorder, Major / therapy
- Epilepsy* / drug therapy
- Middle Aged
- Psychotherapy / methods
- Anticonvulsants
- Antidepressive Agents

IMAGES
VIDEO
COMMENTS
When a 2018 study revealed that Ph.D. students suffer from depression at rates far higher than the general population, it sparked a landslide of concern about graduate student mental health, with some calling it a mental health crisis.The study highlighted a need to understand what aspects of graduate school affect depression, says Katelyn Cooper, an assistant professor at Arizona State ...
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety. The ...
Anxiety and depression among graduate students seems to be on the rise. Systemic change is needed to halt an ongoing crisis. Anxiety and depression in graduate students is worsening.
However, few studies have examined how graduate school specifically affects depression. In this qualitative interview study of 50 life sciences PhD students from 28 institutions, we examined how research and teaching affect depression in PhD students and how depression in turn affects students' experiences teaching and researching.
PhD and master's students worldwide report rates of depression and anxiety that are six times higher than those in the general public (T. M. Evans et al. Nature Biotech. 36, 282-284; 2018).The ...
In all, 16 studies reported the prevalence of depression among a total of 23,469 Ph.D. students (Fig. 2; range, 10-47%).Of these, the most widely used depression scales were the PHQ-9 (9 studies ...
Associations between Depression in PhD students and the independent variables in our dependency model were estimated using odds ratios (ORs) as produced by the logistic regression procedure in SPSS (Version 25). The ORs were used to explain the strength of the presence or absence of significant depression. Wald tests were used to assess the ...
Second, we were only able to aggregate depression prevalence across 16 studies and anxiety prevalence across nine studies (the majority of which were conducted in the U.S.) - far fewer than the 183 studies included in a meta-analysis of depression prevalence among medical students 30 and the 54 studies included in a meta-analysis of resident ...
A PhD student's experience is often marked by high rates of depression, a concern echoed in studies from universities like the University of California and Arizona State University. If you are embarking on a PhD journey, make sure you are aware of the issue, and develop strategies to cope with the stress, so you do not end up with depression.
Graduate students are more than six times as likely to experience depression compared with the general population. However, few studies have examined how graduate school specifically affects depression. In this qualitative interview study of 50 life sciences PhD students from 28 institutions, we exa …
Approximately one-third of Ph.D. students are at risk of having or developing a common psychiatric disorder like depression, a recent study reports. Although these results come from a small sample—3659 students at universities in Flanders, Belgium, 90% of whom were studying the sciences and social sciences—they are nonetheless an important addition to the growing literature about the ...
In an international sample of Masters' and PhD students, 39% of respondents indicated moderate to severe depression, and 41% moderate to severe anxiety scores (Evans et al., 2018). In comparison, the Centers for Disease Control and Prevention (CDC) estimate that approximately 16% of adults in the United States experience anxiety, and ...
Levesque et al found that 33.33% of doctoral students experienced a common psychiatric disorder (GHQ12), such as depression. A PhD candidate was 2.4 times more likely to develop psychiatric health problems than someone in the general population with a bachelor's degree. 3 Bernstein reported that 42% of PhD students in science and 48% of PhD ...
Sadly, none of this is unusual. As this survey shows, depression is common for PhD students and of note: at higher levels than for working professionals. All of these feelings can be connected to academic burnout. The World Health Organisation classifies burnout as a syndrome with symptoms of: - Feelings of energy depletion or exhaustion;
2. Feeling hopeless, guilty, and worthless. Although at some point, many PhD students and postdocs will be made to feel like they are worthless, if this becomes a regular occurrence, it is time to take note. This may be combined with a feeling of guilt and worthlessness. It is important to remember your value as a PhD.
Interestingly, female PhD students, who were slightly less likely than men to experience significant depression, showed a greater tendency to use good coping approaches compared to their counterparts.
Credit: Getty. PhD students in the United Kingdom are more likely than other educated members of the general public to report symptoms of depression or anxiety, according to a survey.
Mental Illness is on the Rise Among the Ph.D. and Post-doctoral Researchers Researcher's life is ridden with lows and highs throughout the doctoral studies. Work-life balance, financial issues and funding opportunities, high expectations, peer pressure, lack of career opportunities, and relationship with the mentor contribute to anxiety, depression, burn-out, chronic fatigue among the ...
Tip #3: Managing sleep, food, & physical health. Every mental health strategy advice will tell you to sleep well, exercise, and eat healthy. That level of advice is often useless. Depression and anxiety tends to push people towards physical extremes, but everyone presents differently.
The Center for Depression, Anxiety and Stress Research embraces a multi-disciplinary approach to improve our understanding of the psychological, environmental, and neurobiological factors associated with affective disorders. Depression, anxiety and related disorders are major public health problems. In the United States, one out of every five ...
Depression is a mood disorder that prevents individuals from leading a normal life at work, socially, or within their family. Seligman (1973) referred to. ... Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the ...
Dr. Meghan Keely McMackin, Psychologist, Washington, DC, 20010, (571) 290-2452, I specialize in treating anxiety and OCD and co-occurring problems, including ADHD and depression.
This systematic review synthesized findings on depression and grief in adults, aiming to identify specificities of depression in grief and whether grief varies based on the type of loss. ... Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer ...
A synthesis of articles published through 2019 yielded a pooled estimate of "clinically significant symptoms of depression" in 24% of PhD students (across 16 studies covering 23,469 students ...
Major depression is the most common mental disorder in the U.S. 1 and is the strongest risk factor for suicide behavior.2, 3, 4 Previous findings show increases in depression in the U.S. population from 6.6% in 2005 to 7.3% in 2015, 5 consistent with other data. 6 The most rapid increases from 2005 to 2015 were observed among adolescents and ...
Background It is generally assumed that procrastination leads to negative consequences. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. Therefore, the aim of our study was to examine the harmful consequences of procrastination on students' stress and mental health. We selected the procrastination ...
Reviewed by David Susman, PhD. Depression is one of the most common mental health conditions and affects people of all ages, including college students. It impacts thoughts, feelings, and ...
"People who are depressed can fall out of love like anyone else. Depression may not directly cause someone to fall out of love, but depression is complex and can impact thinking, mood, self-esteem, energy, desire, and more," explains Susan Trotter, PhD, a relationship expert and coach.Trotter also notes that this often results in more conflict, fewer shared activities, less intimacy, and ...
When exploring predictors of depression, anxiety, and burnout, we identified low satisfaction with PhD training as the most prominent predictor for poor mental health, suggesting a link between ...
Abstract. Background: Major depressive disorder is highly prevalent among persons with epilepsy (PWEs). Between 30% and 50% of PWEs suffer from depression. Many factors contribute to this prevalence, including the psychosocial impact of the diagnosis, restrictions on driving and certain types of work, and adverse effects associated with ...