Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials
Affiliations.
- 1 Keele University, School of Psychology, Keele, UK. Electronic address: [email protected].
- 2 Department of Psychology, The University of Sheffield, UK.
- 3 School of Health and Related Research (ScHARR), The University of Sheffield, UK.
- 4 Clinical Psychology Unit, Department of Psychology, The University of Sheffield, UK.
- PMID: 34607184
- PMCID: PMC8651630
- DOI: 10.1016/j.smrv.2021.101556
The extent to which sleep is causally related to mental health is unclear. One way to test the causal link is to evaluate the extent to which interventions that improve sleep quality also improve mental health. We conducted a meta-analysis of randomised controlled trials that reported the effects of an intervention that improved sleep on composite mental health, as well as on seven specific mental health difficulties. 65 trials comprising 72 interventions and N = 8608 participants were included. Improving sleep led to a significant medium-sized effect on composite mental health (g+ = -0.53), depression (g+ = -0.63), anxiety (g+ = -0.51), and rumination (g+ = -0.49), as well as significant small-to-medium sized effects on stress (g+ = -0.42), and finally small significant effects on positive psychosis symptoms (g+ = -0.26). We also found a dose response relationship, in that greater improvements in sleep quality led to greater improvements in mental health. Our findings suggest that sleep is causally related to the experience of mental health difficulties. Future research might consider how interventions that improve sleep could be incorporated into mental health services, as well as the mechanisms of action that explain how sleep exerts an effect on mental health.
Keywords: Anxiety; CBTi; Causal inference; Depression; Insomnia; Mental health; Meta-analysis; Psychosis; Sleep; Stress.
Copyright © 2021 The Authors. Published by Elsevier Ltd.. All rights reserved.

Publication types
- Meta-Analysis
- Research Support, Non-U.S. Gov't
- Mental Health*
- Psychotic Disorders*
- Randomized Controlled Trials as Topic
- Sleep Quality
Grants and funding
- PB-PG- 0817-20027/DH_/Department of Health/United Kingdom
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 20 April 2021
Association of sleep duration in middle and old age with incidence of dementia
- Séverine Sabia ORCID: orcid.org/0000-0003-3109-9720 1 , 2 ,
- Aurore Fayosse ORCID: orcid.org/0000-0003-2646-9408 1 ,
- Julien Dumurgier 1 , 3 ,
- Vincent T. van Hees 4 ,
- Claire Paquet 3 ,
- Andrew Sommerlad 5 , 6 ,
- Mika Kivimäki ORCID: orcid.org/0000-0002-4699-5627 2 , 7 ,
- Aline Dugravot 1 &
- Archana Singh-Manoux ORCID: orcid.org/0000-0002-1244-5037 1 , 2
Nature Communications volume 12 , Article number: 2289 ( 2021 ) Cite this article
137k Accesses
246 Citations
3664 Altmetric
Metrics details
- Epidemiology
- Risk factors
Sleep dysregulation is a feature of dementia but it remains unclear whether sleep duration prior to old age is associated with dementia incidence. Using data from 7959 participants of the Whitehall II study, we examined the association between sleep duration and incidence of dementia (521 diagnosed cases) using a 25-year follow-up. Here we report higher dementia risk associated with a sleep duration of six hours or less at age 50 and 60, compared with a normal (7 h) sleep duration, although this was imprecisely estimated for sleep duration at age 70 (hazard ratios (HR) 1.22 (95% confidence interval 1.01–1.48), 1.37 (1.10–1.72), and 1.24 (0.98–1.57), respectively). Persistent short sleep duration at age 50, 60, and 70 compared to persistent normal sleep duration was also associated with a 30% increased dementia risk independently of sociodemographic, behavioural, cardiometabolic, and mental health factors. These findings suggest that short sleep duration in midlife is associated with an increased risk of late-onset dementia.
Similar content being viewed by others
Poorer sleep impairs brain health at midlife

Associations between self-reported sleep characteristics and incident mild cognitive impairment: The Heinz Nixdorf Recall Cohort Study
Polygenic predisposition, sleep duration, and depression: evidence from a prospective population-based cohort
Introduction.
Changes in sleep patterns are common in persons with Alzheimer’s disease and other dementias 1 , 2 . These changes are believed to result from sleep–wake cycle dysregulation due to pathophysiological processes in dementia, particularly those affecting the hypothalamus and the brainstem 3 . Besides sleep disturbance, there is growing interest in the association between sleep duration and dementia 1 , 2 , 4 , 5 . Observational studies show both short and long sleep duration to be associated with the increased risk of cognitive decline and dementia 1 , 4 . Some studies also report change in sleep duration in older adults to be associated with the risk of dementia 1 , 6 , 7 , 8 .
Much of the evidence on the association between sleep duration and dementia comes from studies with a follow-up of <10 years. As most dementias are characterized by pathophysiological changes over 20 years or more 9 , 10 , studies with a long follow-up are needed to provide an insight into the association between sleep duration and subsequent dementia. Among studies with a follow-up of 10 years or longer 7 , 11 , 12 , 13 , 14 , 15 , many are based on participants aged 65 years and older at baseline 7 , 13 , 14 , 15 , not allowing the examination of the importance of sleep characteristics earlier in the lifecourse. The number of dementia cases in the short and long sleep groups in these studies is often small 7 , 11 , 12 , 13 , leading to imprecise associations due to limited statistical power. Whether the patterns of change in sleep duration leading up to old age is associated with incidence of dementia is also unclear. In addition, the role of mental health in the association of sleep duration with dementia merits consideration 16 , 17 as mental health disorders are associated with both sleep duration 18 and cognitive health 19 .
In this work, we use data from the Whitehall II cohort study spanning 30 years to examine the association of sleep duration at age 50, 60, and 70 with incident dementia, and to investigate whether patterns of change in sleep duration over this period were associated with dementia. In our analyses, we examine whether mental disorders in midlife affects the association of sleep duration with dementia. Given potential bias in self-reported measures of sleep duration, we examine the association between objectively assessed sleep duration and risk of dementia in a sub-sample 20 of the study. We find that short sleep duration in midlife is associated with the higher risk of dementia later in life, independently of sociodemographic, behavioural, cardiometabolic, and mental health factors.
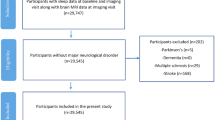
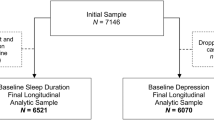
Among the 10,308 persons recruited to the study in 1985–1988, 7959 had data on sleep duration and covariates when they were 50 years (mean age at clinical assessment = 50.6 years, standard deviation (SD) = 2.6 years; flow chart in Fig. 1 ). Among these participants, 521 developed dementia over a mean follow-up period of 24.6 (SD = 7.0) years, the follow-up being 25.7 (SD = 5.1) years in dementia cases and 24.6 (SD = 7.1) years in non-cases. Figure 1 also shows the construction of the analytic sample for sleep duration at age 60 and 70. Cumulative hazards of dementia as a function of sleep duration at age 50, 60, and 70 are presented in Supplementary Fig. 1 , and show that most cases of dementia were diagnosed after the age of 70 years. Mean age at diagnosis was 77.1 (SD = 5.6; range = 53.4–87.6) years.
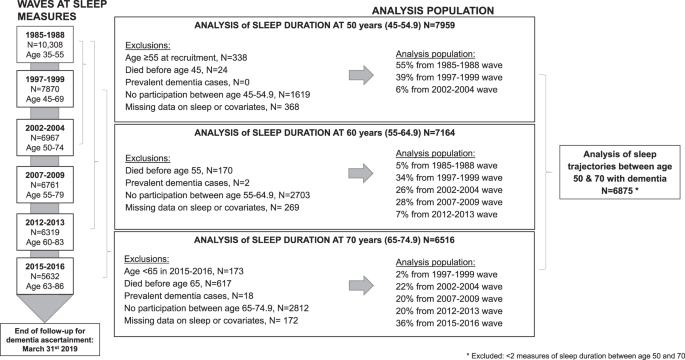
This figure represents the sample selection for the analysis of sleep duration at age 50, 60, and 70, as well as for the analysis of sleep trajectories.
Characteristics of study participants at age 50 are presented in Table 1 . Participants with sleep duration of 7 h per night, labelled as normal sleep duration, were more likely to be men (69.1% compared to 67.1% and 61.5% in short (≤6 h) and long (≥8 h) sleepers, respectively), white (91.5% compared to 89.6 and 86.3%), married (77.9% compared to 72.9 and 75.6%), and to have better cardiometabolic and mental health profile. Characteristics of study participants at age 60 and 70 are shown in Supplementary Table 1 . As there was no evidence of systematic sex differences (interaction of sex with sleep duration variables, all P > 0.31), the analyses were conducted combining men and women and adjusted for sex.
Association of sleep duration with dementia
Table 2 presents the association of sleep duration at age 50, 60, and 70 with incident dementia over a mean follow-up of 24.6 (SD = 7.0), 14.8 (SD = 5.9), and 7.5 (SD = 4.7) years, respectively. The lowest dementia incidence per 1000 person-years was observed among those who slept 7 h per night, irrespective of the age at which sleep duration was measured. In analysis adjusted for sociodemographic factors, short sleep duration was associated with the higher risk of incident dementia at all ages (all P < 0.02). Further adjustment for health behaviours and cardiometabolic and mental health factors attenuated associations, but there remained an association for short sleep at 50 (hazard ratio (HR) = 1.22, 95% confidence interval (CI) = 1.01–1.48) and 60 years (HR = 1.37, 95% CI = 1.10–1.72). There was no clear evidence of an association between long sleep duration and incident dementia.
A total of 6875 participants were alive, free of dementia at age 70, and had at least two out of the three measures of sleep duration at age 50, 60, and 70. Among them, 426 had incident dementia over a mean follow-up period of 7.4 (SD = 4.7) years. Using these data on sleep duration, six trajectories were identified and labelled as: persistent short sleep, persistent normal sleep, persistent long sleep, change from short to normal sleep, change from normal to long sleep, and change from normal to short sleep (Table 3 ). Persistent short sleep duration was associated with an increased risk of dementia (HR = 1.30, 95% CI = 1.00–1.69) compared to those with persistent normal sleep duration (Table 4 ). There was also a signal of higher risk in participants with persistent long sleep and those who reported short sleep at least once, but the associations did not reach statistical significance. Analyses restricted to participants without a history of mental illness before age 65 years (Table 5 ) showed associations of sleep duration and change in sleep duration with subsequent dementia to be similar to that in the main analyses.
Data on accelerometer-assessed sleep duration collected in 2012–2013 were available on 4267 participants. Data were excluded due to absence of sleep log ( n = 140), technical problem ( n = 175), significant non-wear ( n = 23), and missing covariates ( n = 41) leading to a total of 3888 participants included in the analysis, among whom 111 developed dementia over a mean 6.4-year follow-up period. Characteristics of this analytical sample are presented in Supplementary Table 2 . The Pearson’s correlation between questionnaire and accelerometer-assessed measures of sleep duration in 2012–2013 was 0.41 ( P < 0.001). The association between accelerometer-assessed sleep duration, modelled as a continuous variable, and dementia is shown in Fig. 2 . Compared to 7 h of sleep, sleep duration <6 h per night was associated with the higher risk of dementia, whereas sleep duration >8 h per night was not associated with risk of dementia (Fig. 2a , Source data ), the estimates for long sleep duration were further attenuated when missing data were taken into account (Fig. 2b , Source data ). The analysis of these data using tertiles, with the second tertile as the reference (6 h 14 min–7 h per night), showed sleep duration in the first tertile (1 h 16 min–6 h 13 min) to be associated with an increased risk of dementia (HR = 1.63, 95% CI = 1.04–2.57), while there was no association with dementia in the highest tertile (7 h 1 min–10 h 6 min), Table 6 .
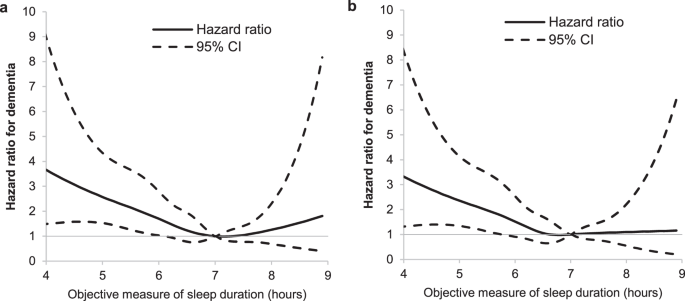
a The hazard ratio for dementia (black plain line) with the corresponding 95% confidence interval (black dotted line) as a function of sleep duration from a Cox regression adjusted for age (timescale), sex, ethnicity, education, marital status, alcohol consumption, physical activity, smoking status, fruit and vegetable consumption, BMI, hypertension, diabetes, cardiovascular disease, GHQ depression, and CNS medications ( Source data ). b The hazard ratio for dementia (black plain line) with the corresponding 95% confidence interval (black dotted line) as a function of sleep duration from a Cox regression using inverse-probability weighting to account for missing data and adjusted for age (timescale), sex, ethnicity, education, marital status, alcohol consumption, physical activity, smoking status, fruit and vegetable consumption, BMI, hypertension, diabetes, cardiovascular disease, GHQ depression, and CNS medications ( Source data ).
Sensitivity analysis
Participants who could not be included in the analyses due to missing data ( N = 1987) were older at recruitment to the study in 1985–1988 (45.4 vs 41.5 years, P < 0.001), and more likely to develop dementia over the follow-up (6.6% vs 4.0%, P < 0.001), although no differences were observed in relation to sex ( P = 0.81) or sleep duration ( P = 0.65) categories. Analyses using inverse-probability weighting to account for missing data led to results that were consistent with those in the main analysis, as well as the accelerometer sub-study (Table 7 ).
Adding apolipoprotein E (APOE) ε4 as a covariate in the analysis did not alter observed associations between sleep duration at age 50, 60, and 70 and risk of dementia (Supplementary Table 3 ). Use of dementia without history of cardiovascular disease as a proxy for Alzheimer’s disease type of dementia ( N cases = 404, 77.5% of the 521 all cause dementia cases) yielded results similar to those in the main analysis although the estimates were imprecise due to smaller numbers in analysis (Supplementary Table 4 ).
This longitudinal study of nearly 8000 participants with repeat data on sleep duration and a long follow-up for dementia suggests short sleep duration in midlife to be associated with the increased risk of incident dementia. This finding was confirmed in analysis using sleep duration measured by an accelerometer. Measurement of sleep duration at age 50, 60, and 70 years along with change in sleep duration over this period provides consistent results for increased risk of dementia in those with short sleep. A further key finding is that the association between short sleep duration and dementia is not attributable to mental health.
Two recent meta-analyses suggest a U-shaped association between sleep duration and incident dementia, with lower risk in people sleeping 7 h per night, and greater risk among those with shorter sleep and also among those with longer sleep duration 4 , 5 . The studies included in these meta-analyses had a follow-up duration ranging from 3 to 23 years, but most studies had a follow-up of <10 years 4 , 5 . Dementia at older ages is characterized by a long preclinical period 9 , 20 , and studies with a follow-up of 10 years are likely to be subject to reverse causation bias, whereby the putative risk factor is affected by the disease process in dementia.
Some studies 11 , 12 , 13 , 14 , 15 are noteworthy because of their long follow-up. In the Kuopio Ischaemic Heart Disease study on 2386 men aged 42–62 years at assessment of sleep duration, there was no association between sleep duration (categorized as ≤6.5, 7–8, and ≥8.5 h) and incidence of dementia over a 22-year mean follow-up 12 . On the other hand, a U-shaped association between sleep duration and dementia was observed in three studies, where the mean age at sleep duration assessment varied between 50 and 73 years, and follow-up between 15 and 23 years 11 , 13 , 14 . In the Framingham Heart study, long ( N = 96) but not short ( N = 209) sleep duration at mean age 72 years was associated with dementia over a 10-year follow-up 7 . In a large-scale Swedish cohort of 28,775 individuals aged 65 years and older, the association between long sleep duration and dementia over a 13-year follow-up was completely attenuated after cases occurring in the first 5 years of follow-up were excluded from the analysis, highlighting the role of reverse causation bias 15 . All these studies use a wide age range at baseline for assessment of sleep duration and it is likely that the older participants, those most likely to be diagnosed with dementia over the follow-up, are already subject to preclinical changes that characterize dementia. This long preclinical period of dementia makes it less amenable to research using gold-standard approaches, such as randomized controlled trials. Observation studies are not ideally suited for causal inference, but careful analysis that considers time between exposure and outcome can be helpful in determining changes over time in the nature of the association between the exposure of interest and dementia.
In the present study, we used an innovative approach consisting of extracting data on sleep duration at age 50, 60, and 70 in order to remove the uncertainty in estimations caused by inclusion of a wide age range at the start of the follow-up. The pattern of associations in relation to short sleep duration and dementia was similar at age 50, 60, and 70, even though sleep duration at age 70 was not associated with dementia after adjustment for health-related factors. Analysis of trajectories of sleep duration using data from sleep duration at age 50, 60, and 70 showed persistent short sleep duration to be associated with an increased risk of dementia. Depression and mood disorders in general are related to changes in sleep and thought to play an important part in the association of sleep duration with dementia 8 . In the present study, adjustment for depressive symptoms and central nervous system (CNS) drugs, as well as analysis undertaken among those without a history of mental disorders did not show mental health to explain the association. Our results are consistent with a recent Mendelian randomization study, where sleep-related phenotypes were found not to be related to mental disorder 17 . Results in our study were robust to adjustments for a wide range of covariates, including cardiovascular disease 16 , suggesting a consistent association between short sleep duration in midlife and incident dementia.
There is evidence of a bidirectional association between sleep dysfunction and pathophysiological changes in dementia 21 , 22 , highlighting the need for a longer time frame in studies. The results for short sleep duration seen in our study is likely to involve several processes 1 , including neuroinflammation 23 , atherosclerosis 24 , alpha-synucleinopathies (dementia with Lewy bodies and Parkinson disease dementia) 25 , and impaired amyloid-β clearance 26 , possibly due to impaired glymphatic function 27 . Experimental studies support a detrimental effect of sleep deprivation on cognitive performance 28 and β-amyloid (Aβ) clearance 29 , 30 , 31 . Amyloid plaque build-up contributes to poor sleep in older adults through its direct impact on sleep–wake regulator brain regions 21 , 22 . There is also some evidence of an association of Aβ accumulation with disruption of the circadian rhythm and sleep pattern in cognitively normal adults 32 . Much of the research on mechanisms focusses on sleep disturbance rather than sleep duration, particularly in relation to the years leading up to dementia diagnosis. The mechanisms linking short sleep duration to dementia may be similar 1 , 33 , but a better understanding of how sleep features (duration, disturbance, sleep apnoea, and sleep–wake regulation) over the adult lifecourse shape risk of dementia at older ages is required to identify windows of opportunity for therapeutic interventions to reduce the risk or delay the progression of dementia and its subtypes.
In contrast to some previous studies 7 , 11 , 14 , 15 , we did not find strong evidence to support the hypothesis that long sleep duration is associated with dementia. As in most previous studies 7 , 11 , 12 , 13 , the number of long sleepers in our study was small and did not allow a robust estimation of the association with long sleep duration. Two large-scale studies based on individuals with a mean age of 72 years, followed for 12 and 14 years reported sleep duration >9 h to be associated with the increased risk of dementia 14 , 15 . Given the age of these individuals at the start of follow-up, more data on long sleepers in midlife and old age are needed to draw conclusions on the importance of long sleep duration for dementia.
Strengths of the present study include repeat measures of sleep duration and a long follow-up for dementia allowing the examination of age at assessment of sleep duration, and change therein to provide insight into the nature of the association between sleep duration and dementia. Use of an objective measure of sleep duration confirmed the main findings that were based on self-reported sleep duration. We also undertook sensitivity analysis using inverse-probability weighting to take missing data into account, and results from these analyses were in accordance with the main findings.
Assessment of dementia cases via electronic health records is not ideal but has some advantages. It allows ascertainment of dementia status in all participants and not only those who agree to continue to participate in multiple waves of data collection over time. However, this method may misclassify some dementia cases, particularly milder cases of dementia 34 , although the misclassification is likely to be independent from measures of sleep duration. Data on dementia type were incomplete in the records and our use of a proxy measure of Alzheimer’s disease dementia may not be precise despite the proportion of cases being in accordance with that in the general population 10 . The observational nature of the study cannot preclude residual confounding despite our adjustment for a large set of covariates. A further limitation is that Whitehall II study participants were all in employment at recruitment and are healthier than the general population, both in terms of risk factor profiles and incidence of disease. However, the association between risk factors and disease of interest is not necessarily affected 35 . A previous study showed that the association between cardiovascular risk factors and risk of CVD in the Whitehall II study was similar to that in general population studies 36 .
There is a widely acknowledged association between sleep and cognitive function 1 , primarily due to the role of sleep in learning and memory, synaptic plasticity, and waste clearance from the brain 1 , 37 , 38 . Whether sleep parameters also affect late-life dementia remains the subject of debate. While incipient dementia is known to affect sleep–wake cycles 1 , 2 , 7 , the extent to which sleep duration over the adult lifecourse is associated with late-onset dementia is unclear because most studies have not explicitly considered age at assessment of sleep duration or the length of follow-up. Our approach pays attention to both these aspects along with inclusion of a wide array of covariates to show that short sleep duration in midlife is associated with an increased risk of dementia. Public health messages to encourage good sleep hygiene 39 may be particularly important for people at a higher risk of dementia.
Study population
The Whitehall II study is a cohort study that was established among 10,308 British civil servants (33.1% women, age range 35–55) in 1985–1988 (ref. 40 ). Since baseline, follow-up clinical data collection waves have taken place every 4–5 years with each wave lasting ~2 years, with the last wave conducted in 2015–2016. In addition to clinical examinations in the study, data over the follow-up are obtained via linkage to electronic health records of the UK National Health Service (NHS) for participants recruited to the study. The NHS provides most of the health care in the country, including in- and out-patient care, and record linkage is undertaken using a unique NHS identifier held by all UK residents. Data from linked records were updated on an annual basis, until 31st March 2019. Written, informed consent from participants was obtained at each contact. Research ethics approvals were renewed at each wave; the most recent approval was obtained from the University College London Hospital Committee on the Ethics of Human Research (reference number 85/0938).
Sleep duration
Sleep duration was assessed by questionnaire in 1985–1988, 1997–1999, 2002–2004, 2007–2009, 2012–2013, and 2015–2016 using the question ‘how many hours of sleep do you have on an average weeknight?’. Response categories were 5 h or less, 6, 7, 8, and 9 h or more. We extracted sleep duration at age 50, 60, and 70 for each participant across the data waves, allowing a ±5-year margin for each age category. In order to allow sufficient number of dementia cases in each sleep category, we pooled categories of sleep duration as follows: short (≤6 h per night), normal (7 h per night), and long (≥8 h per night) 41 .
Trajectories of change in sleep duration between age 50 and 70 were defined using group-based trajectory modelling using the traj-command in Stata 42 . Groups were chosen according to model fit statistics (Bayesian Information Criterion values and average posterior probabilities) and meaningful interpretation 43 . The sleep duration categories in the construction of trajectories were the same as in the main analyses, and were based on participants who were alive and free of dementia at age 70 with at least two out of three measures of sleep duration at age 50, 60, and 70.
The accelerometer substudy was undertaken in 2012–2013 (ref. 44 ) on study participants who either attended the central London research clinic or were seen at home in those living in the South-Eastern regions of England. These participants were asked to wear a wrist-worn accelerometer, the GENEActiv (Activinsights Ltd, Kimbolton, UK), during nine consecutive days over 24 h. Sleep duration was estimated using a validated algorithm guided by a sleep log and implemented in R (version 3.6.3) package GGIR version 2.0-1 (ref. 45 ); data from the first and last nights were removed leading to data over 7 nights 45 . Usual daily sleep duration was estimated as the mean of sleep duration over the 7 nights and for those with <7 days of measurement, weighted average of sleep duration was calculated according to week days and weekend days 46 . Accelerometer-assessed sleep duration was categorized into tertiles rather than categories used for self-reported sleep as only 167 (six dementia cases) participants had accelerometer-assessed sleep duration of 8 h or more. Study participants were between 60 and 83 years in this sub-study, a one-off addition to the main data collection. Therefore, age-specific analysis as in the self-reported measure of sleep duration was not possible with the accelerometer data.
Dementia cases were ascertained by linkage to three national registers (the national hospital episode statistics (HES) database, the Mental Health Services Data Set, and the mortality register) up to the 31st of March 2019 using the unique National Health Service (NHS) identification number. Dementia cases were identified based on ICD-10 codes F00-F03, F05.1, G30, and G31. The NHS provides most of the health care, including out- and in-patient care. The sensitivity and specificity of dementia in the NHS HES data is 78.0 and 92.0% (ref. 34 ). The sensitivity in our study is likely to be higher as we also used data from the Mental Health Services Data Set, a national database that contains information on dementia for persons in contact with mental health services in hospitals, out-patient clinics, and the community 47 . The first record of dementia diagnosis in any of the three registers was used as date of dementia in the analysis.
Sociodemographic variables included age, sex, ethnicity (white and non-white), education (lower primary school or less, lower secondary school, higher secondary school diploma, and university), and marital status (married or cohabiting, and other). Health behaviours included cigarette smoking status (never smoker, ex-smoker, and current smoker), alcohol consumption in the previous week (no alcohol in the previous week, 1–14 units per week, and >14 units per week), time spent in moderate and vigorous physical activity, and frequency of fruits and vegetables consumption (less than daily, once a day, and twice or more a day).
Health-related variables included measures of cardiometabolic risk factors and mental health. Cardiometabolic factors were hypertension (systolic ≥140 or diastolic ≥90 mmHg or use of antihypertensive medication), diabetes mellitus (determined by fasting glucose ≥7.0 mmol/L, reported doctor-diagnosed diabetes, use of diabetes medication, or hospital record), body mass index (BMI, categorized as <20, 20–24.9, 25–29.9, and ≥30 kg/m²) based on height and weight assessment at the clinical examination using standard clinical protocols, and cardiovascular disease (including coronary heart disease and stroke identified using linkage to national hospital records). Mental health factors included current depressive symptomatology defined by the four-item depression subscale of the General Health Questionnaire 48 , and self-reported use of CNS medication (anti-depressant, antipsychotic, hypnotic, anxiolytic, or Parkinson medications).
History of mental disorders before age 65 was assessed based on self-reported use of anti-depressants or linkage to national hospital records and mental health registry based on ICD codes F06, F07, F09, F20–48, and F60–69 (excluding F65 and F66).
Statistical analysis
Four sets of analyses were undertaken, described below (Fig. 1 for flow chart). All analyses were performed using Cox regression with age as the timescale to model the associations with incident dementia. Participants were included into the analysis if they had data on sleep duration and covariates assessed at the age of interest allowing a ±5-year margin and were free of dementia at this date. Data were censored at date of record of dementia, death, or March 31st 2019, whichever came first. The proportional hazard assumption was verified using Schoenfeld residuals. Analyses were first adjusted for sociodemographic factors, then additionally for health behaviours, and finally for health-related factors.
We first examined the association between sleep duration at age 50, 60, and 70, in separate models, and incident dementia. For these analyses, age of entry was the age at clinical assessment closest to the age of interest from which the sleep duration measure and covariates were drawn.
We examined the association of trajectories of sleep duration, to reflect changes between the age of 50 and 70, with incident dementia with age of entry and covariates drawn from when participants were 70 years.
In order to assess the role of mental disorders in the association of sleep duration with dementia, we repeated the previous analyses, excluding participants with mental disorders before the age of 65. Mental disorders diagnosed after age 65 were not excluded as they could be features of the preclinical period of dementia 49 .
The final analyses examined the association between objectively assessed sleep duration and incident dementia. Participants were followed from the age at accelerometer assessment, and covariates were drawn from the same wave of data collection. To examine the shape of the association between accelerometer-assessed sleep duration, measured in rich detail, and incidence of dementia we used restricted cubic spline regressions with Harrell knots 50 , Stata command xblc 51 , with 7 h as the reference. Then, in further analyses tertiles of accelerometer-assessed sleep duration were used.
We undertook a series of additional/sensitivity analysis. One, we repeated the main analyses using inverse-probability weighting to account for missing data 52 . This involved first calculating the probability of being included in the analytical sample using logistic regression that included demographic, socioeconomic, behavioural factors, as well as sleep duration at recruitment, morbidities including dementia and mortality over follow-up, and stepwise-selected interactions between covariates. The inverse of these probabilities were used as weights in Cox regression. Two, in a sub-sample of participants with data on APOE genotype, we repeated the main analyses with APOE ε4 (1 or 2, vs 0) as a covariate in the analysis. Three, in order to examine whether observed results apply to dementia due Alzheimer’s disease, we repeated the analyses using a proxy definition of this outcome. This consisted of defining Alzheimer’s disease dementia as dementia cases free of cardiovascular disease (stroke or myocardial infarction) 53 over the follow-up. Analyses 2 and 3 were exploratory and due to smaller numbers in analysis the direction of results rather than statistical significance should be given more importance. All analyses were performed using STATA version 16.1 (StataCorp). A two-sided P value ≤ 0.05 was considered statistically significant. STROBE statement is available in the online Supplement.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Data used for analyses comprise data assessed at study clinical examinations in 1985–1988, 1997–1999, 2002–2004, 2007–2009, 2012–2013, and 2015–2016. In addition to clinical examinations in the study, data over the follow-up were obtained via linkage to electronic health records of the UK National Health services for participants recruited to the study, including hospital episode statistics databased, Mental Health Services Data Set, and the mortality register. Data from linked records were updated on an annual basis, until 31st March 2019. Following NHS Digital guidelines, these data are available for sharing with the scientific community either through the study specific data sharing https://www.ucl.ac.uk/epidemiology-health-care/research/epidemiology-and-public-health/research/whitehall-ii/data-sharing or using the Dementias platform UK https://www.dementiasplatform.uk/for-researchers/data-portal-getting-started-with-cohort-data . Source data are provided with this paper.
Code availability
Code for statistical analysis is provided in https://doi.org/10.5281/zenodo.4572438 .
Yaffe, K., Falvey, C. M. & Hoang, T. Connections between sleep and cognition in older adults. Lancet Neurol. 13 , 1017–1028 (2014).
Article PubMed Google Scholar
Kent B. A., Feldman H. H. & Nygaard H. B. Sleep and its Regulation: An Emerging Pathogenic and Treatment Frontier in Alzheimer’s disease. Prog Neurobiol , 101902 (2020).
Zhong, G., Naismith, S. L., Rogers, N. L. & Lewis, S. J. Sleep-wake disturbances in common neurodegenerative diseases: a closer look at selected aspects of the neural circuitry. J. Neurol. Sci. 307 , 9–14 (2011).
Liang, Y., Qu, L. B. & Liu, H. Non-linear associations between sleep duration and the risks of mild cognitive impairment/dementia and cognitive decline: a dose-response meta-analysis of observational studies. Aging Clin. Exp. Res 31 , 309–320 (2019).
Fan, L., Xu, W., Cai, Y., Hu, Y. & Wu, C. Sleep Duration and the Risk of Dementia: A Systematic Review and Meta-analysis of Prospective Cohort Studies. J. Am. Med Dir. Assoc. 20 , 1480–1487 e1485 (2019).
Lu Y., Sugawara Y., Zhang S., Tomata Y. & Tsuji I. Changes in sleep duration and the risk of incident dementia in the elderly Japanese: the Ohsaki Cohort 2006 Study. Sleep 41 (2018).
Westwood, A. J. et al. Prolonged sleep duration as a marker of early neurodegeneration predicting incident dementia. Neurology 88 , 1172–1179 (2017).
Article PubMed PubMed Central Google Scholar
Hahn, E. A., Wang, H. X., Andel, R. & Fratiglioni, L. A change in sleep pattern may predict Alzheimer disease. Am. J. Geriatr. Psychiatry 22 , 1262–1271 (2014).
Jack, C. R. Jr. et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 12 , 207–216 (2013).
Article CAS PubMed PubMed Central Google Scholar
Alzheimer’s association report. 2020 Alzheimer’s disease facts and figures. Alzheimers Dement 16 , 391–460 (2020).
Article Google Scholar
Virta, J. J. et al. Midlife sleep characteristics associated with late life cognitive function. Sleep 36 , 1533–1541, 1541A (2013).
Luojus, M. K. et al. Self-reported sleep disturbance and incidence of dementia in ageing men. J. Epidemiol. Community Health 71 , 329–335 (2017).
Lutsey, P. L. et al. Sleep characteristics and risk of dementia and Alzheimer’s disease: The Atherosclerosis Risk in Communities Study. Alzheimers Dement 14 , 157–166 (2018).
Bokenberger, K. et al. Association Between Sleep Characteristics and Incident Dementia Accounting for Baseline Cognitive Status: A Prospective Population-Based Study. J. Gerontol. A Biol. Sci. Med Sci. 72 , 134–139 (2017).
Larsson, S. C. & Wolk, A. The Role of Lifestyle Factors and Sleep Duration for Late-Onset Dementia: A Cohort Study. J. Alzheimers Dis. 66 , 579–586 (2018).
Livingston, G. et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396 , 413–446 (2020).
Huang J., Zuber V., Matthews P. M., Elliott P., Tzoulaki J. & Dehghan A. Sleep, major depressive disorder and Alzheimer’s disease: A Mendelian randomisation study. Neurology (2020).
Abad, V. C. & Guilleminault, C. Sleep and psychiatry. Dialogues Clin. Neurosci. 7 , 291–303 (2005).
Ownby, R. L., Crocco, E., Acevedo, A., John, V. & Loewenstein, D. Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch. Gen. Psychiatry 63 , 530–538 (2006).
Silverberg, N., Elliott, C., Ryan, L., Masliah, E. & Hodes, R. NIA commentary on the NIA-AA Research Framework: Towards a biological definition of Alzheimer’s disease. Alzheimers Dement 14 , 576–578 (2018).
Ju, Y. E., Lucey, B. P. & Holtzman, D. M. Sleep and Alzheimer disease pathology–a bidirectional relationship. Nat. Rev. Neurol. 10 , 115–119 (2014).
Article CAS PubMed Google Scholar
Musiek, E. S., Xiong, D. D. & Holtzman, D. M. Sleep circadian rhythms, and the pathogenesis of Alzheimer disease. Exp. Mol. Med 47 , e148 (2015).
Zhu, B. et al. Sleep disturbance induces neuroinflammation and impairment of learning and memory. Neurobiol. Dis. 48 , 348–355 (2012).
McAlpine, C. S. et al. Sleep modulates haematopoiesis and protects against atherosclerosis. Nature 566 , 383–387 (2019).
Article CAS PubMed PubMed Central ADS Google Scholar
Stang, C. D. et al. Timeline of Rapid Eye Movement Sleep Behavior Disorder in Overt Alpha-Synucleinopathies. Ann. Neurol. 89 , 293–303 (2021).
Spira, A. P. et al. Self-reported sleep and beta-amyloid deposition in community-dwelling older adults. JAMA Neurol. 70 , 1537–1543 (2013).
PubMed PubMed Central Google Scholar
Reeves, B. C. et al. Glymphatic System Impairment in Alzheimer’s Disease and Idiopathic Normal Pressure Hydrocephalus. Trends Mol. Med 26 , 285–295 (2020).
Goel, N., Rao, H., Durmer, J. S. & Dinges, D. F. Neurocognitive consequences of sleep deprivation. Semin Neurol. 29 , 320–339 (2009).
Ooms, S. et al. Effect of 1 night of total sleep deprivation on cerebrospinal fluid beta-amyloid 42 in healthy middle-aged men: a randomized clinical trial. JAMA Neurol. 71 , 971–977 (2014).
Benedict, C., Blennow, K., Zetterberg, H. & Cedernaes, J. Effects of acute sleep loss on diurnal plasma dynamics of CNS health biomarkers in young men. Neurology 94 , e1181–e1189 (2020).
Shokri-Kojori, E. et al. beta-Amyloid accumulation in the human brain after one night of sleep deprivation. Proc. Natl Acad. Sci. USA 115 , 4483–4488 (2018).
Musiek, E. S. et al. Circadian Rest-Activity Pattern Changes in Aging and Preclinical Alzheimer Disease. JAMA Neurol. 75 , 582–590 (2018).
Shi, L. et al. Sleep disturbances increase the risk of dementia: A systematic review and meta-analysis. Sleep. Med Rev. 40 , 4–16 (2018).
Sommerlad, A. et al. Accuracy of general hospital dementia diagnoses in England: Sensitivity, specificity, and predictors of diagnostic accuracy 2008-2016. Alzheimers Dement 14 , 933–943 (2018).
Rothman, K. J., Gallacher, J. E. & Hatch, E. E. Why representativeness should be avoided. Int J. Epidemiol. 42 , 1012–1014 (2013).
Batty, G. D. et al. Generalizability of occupational cohort study findings. Epidemiology 25 , 932–933 (2014).
Xie, L. et al. Sleep drives metabolite clearance from the adult brain. Science 342 , 373–377 (2013).
Article CAS PubMed ADS Google Scholar
Cirelli C. & Tononi G. The Sleeping Brain. Cerebrum 2017 (2017).
Stepanski, E. J. & Wyatt, J. K. Use of sleep hygiene in the treatment of insomnia. Sleep. Med Rev. 7 , 215–225 (2003).
Marmot, M. G. et al. Health inequalities among British civil servants: the Whitehall II study. Lancet 337 , 1387–1393 (1991).
Chen, J. C. et al. Sleep duration, cognitive decline, and dementia risk in older women. Alzheimers Dement 12 , 21–33 (2016).
Jones, B. L. & Nagin, D. S. A Note on a Stata Plugin for Estimating Group-based Trajectory Models. Sociological Methods Res. 42 , 608–613 (2013).
Article MathSciNet Google Scholar
Nagin, D. S. & Odgers, C. L. Group-based trajectory modeling in clinical research. Annu Rev. Clin. Psychol. 6 , 109–138 (2010).
Sabia, S. et al. Association between questionnaire- and accelerometer-assessed physical activity: the role of sociodemographic factors. Am. J. Epidemiol. 179 , 781–790 (2014).
van Hees, V. T. et al. A Novel, Open Access Method to Assess Sleep Duration Using a Wrist-Worn Accelerometer. PLoS One 10 , e0142533 (2015).
Article PubMed PubMed Central CAS Google Scholar
Jones, S. E. et al. Genetic studies of accelerometer-based sleep measures yield new insights into human sleep behaviour. Nat. Commun. 10 , 1585 (2019).
Article PubMed PubMed Central ADS CAS Google Scholar
Wilkinson, T. et al. Identifying dementia cases with routinely collected health data: A systematic review. Alzheimers Dement 14 , 1038–1051 (2018).
Goldberg, D. P. & Hillier, V. F. A scaled version of the General Health Questionnaire. Psychol. Med 9 , 139–145 (1979).
Singh-Manoux, A. et al. Trajectories of Depressive Symptoms Before Diagnosis of Dementia: A 28-Year Follow-up Study. JAMA Psychiatry 74 , 712–718 (2017).
Harrell F. E. Jr. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis . Springer (2001).
Orsini, N. & Greenland, S. A procedure to tabulate and plot results after flexible modeling of a quantitative covariate. Stata J. 11 , 1–29 (2011).
Weuve, J. et al. Accounting for bias due to selective attrition: the example of smoking and cognitive decline. Epidemiology 23 , 119–128 (2012).
Akbaraly, T. N. et al. Association of Midlife Diet With Subsequent Risk for Dementia. JAMA 321 , 957–968 (2019).
Download references
Acknowledgements
The Whitehall II study is supported by grants from the National Institute on Aging, NIH (R01AG056477, RF1AG062553); the Wellcome Trust (221854/Z/20/Z); the UK Medical Research Council (R024227, S011676); and the British Heart Foundation (RG/16/11/32334). In addition, M.K. was supported by grants from NordForsk (70521, the Nordic Research Programme on Health and Welfare), the Academy of Finland (311492, 329202), and Helsinki Institute of Life Science (H970). A.S. is funded by the UCL/Wellcome Trust Institutional Strategic Support Fund (204841/Z/16/Z) and by the University College London Hospitals’ (UCLH) National Institute for Health Research (NIHR) Biomedical Research Centre (BRC). S.S. is supported by the French National Research Agency (ANR-19-CE36-0004-01).
Author information
Authors and affiliations.
Université de Paris, Inserm U1153, Epidemiology of Ageing and Neurodegenerative diseases, Paris, France
Séverine Sabia, Aurore Fayosse, Julien Dumurgier, Aline Dugravot & Archana Singh-Manoux
Department of Epidemiology and Public Health, University College London, London, UK
Séverine Sabia, Mika Kivimäki & Archana Singh-Manoux
Université de Paris, Inserm U1144, Cognitive Neurology Center, GHU APHP Nord Lariboisière – Fernand Widal Hospital, Paris, France
Julien Dumurgier & Claire Paquet
Accelting, Andorrastraat 13, Almere, The Netherlands
Vincent T. van Hees
Division of Psychiatry, University College London, London, UK
Andrew Sommerlad
Camden and Islington NHS Foundation Trust, London, UK
Clinicum, University of Helsinki, Helsinki, Finland
Mika Kivimäki
You can also search for this author in PubMed Google Scholar
Contributions
S.S. and A.S.-M. developed the hypothesis and study design. S.S., A.F. and A.D. performed statistical analysis. S.S. wrote first and successive drafts of the manuscript. S.S., A.F., J.D., V.T.v.H., C.P., A.S., M.K., A.D. and A.S.-M. contributed to interpretation of data, and critical revision of the manuscript for important intellectual content. A.S.-M. and M.K. obtained funding.
Corresponding author
Correspondence to Séverine Sabia .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Peer review information Nature Communications thanks Christian Benedict and the other, anonymous reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, peer review file, reporting summary, source data, source data, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Sabia, S., Fayosse, A., Dumurgier, J. et al. Association of sleep duration in middle and old age with incidence of dementia. Nat Commun 12 , 2289 (2021). https://doi.org/10.1038/s41467-021-22354-2
Download citation
Received : 21 October 2020
Accepted : 09 March 2021
Published : 20 April 2021
DOI : https://doi.org/10.1038/s41467-021-22354-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Epilepsy and epileptiform activity in late-onset alzheimer disease: clinical and pathophysiological advances, gaps and conundrums.
- Anita Kamondi
- Madeleine Grigg-Damberger
- Andras Attila Horvath
Nature Reviews Neurology (2024)
Link between insomnia, cognitive impairment and stroke
- Keisuke Suzuki
Sleep and Biological Rhythms (2024)
Role of sleep in neurodegeneration: the consensus report of the 5th Think Tank World Sleep Forum
- Luigi Ferini-Strambi
- Claudio Liguori
- Claudio Bassetti
Neurological Sciences (2024)
Progress on early diagnosing Alzheimer’s disease
- Murad Al-Nusaif
Frontiers of Medicine (2024)
Association between sleep problems and multimorbidity patterns in older adults
- Stefany Cristina Claudino Idalino
- Jaquelini Betta Canever
- Núbia Carelli Pereira de Avelar
BMC Public Health (2023)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Advertisement
Supported by
Personal Health
The Health Toll of Poor Sleep
Finding that slumber sweet spot can be helpful for fending off a range of mental and bodily ills.
- Share full article

By Jane E. Brody
Sleep — both its quantity and its quality — is one of the most frequently discussed health topics. How often have you told a friend or relative, “I’m exhausted, I was up half the night”?
Surveys have found that more than a third of American adults are unable to consistently get a good night’s sleep , with millions having trouble falling asleep or staying asleep. And the pandemic seems to have only made things worse , even for those who were previously “good” sleepers.
Remote work gave many people more hours in the day for personal use, but at the same time turned the workday into a 24/7 endeavor, with emails, texts and Zoom calls occurring at odd and often unpredictable times.
Working parents who lacked child care options or had to help young children with online schoolwork during the day may have resorted to late night or early morning hours to get their own work done with minimal interruptions. They essentially became shift workers with erratic sleep schedules. Others lost sleep pondering whether their jobs were worth the stress and how they might reshape their working lives going forward.
And for countless thousands, the death of a loved one from Covid-19 has resulted in long-lasting difficulty falling asleep and staying asleep long enough to feel rested. A study from 2019 by researchers at Northwestern Medicine and Rice University found that grieving spouses who reported sleeping poorly had high levels of chronic, body-wide inflammation, which can increase their susceptibility to heart disease and cancer.
Poor sleep takes a toll on mind and body
Persistent fatigue may be the main complaint of sleep-deprived people. But beneath the surface, growing evidence indicates that disrupted or insufficient sleep can have widespread damaging effects on their physical and mental health. Sleep deprivation increases the risk of developing heart disease, high blood pressure, stroke and Type 2 diabetes. It muddies clear thinking, depletes energy, increases irritability and dampens one’s sex drive.
Even those who sleep soundly but for fewer than the commonly recommended seven or eight hours a night, may not be as medically well off with short sleep cycles as they think.
For example, a major study suggests that middle-aged people who are chronically short on shut-eye face an increased risk of developing dementia in their later years. The study, published last spring in the journal Nature Communications, followed nearly 8,000 50-year-olds in Britain for about 25 years. Compared with those who averaged seven hours of sleep a night, the study participants who slept six hours or less on weeknights were 30 percent more likely to be diagnosed with dementia nearly three decades later.
There is a sleep sweet spot
Those who sleep significantly more than seven hours a night, however, are not necessarily spared sleep-related health risks. For optimal health, there seems to be a sweet spot of six to eight hours of nightly sleep. A six-year study of more than a million adults ages 30 to 102 by researchers at the University of California, San Diego, and the American Cancer Society revealed a U-shaped curve, with the highest mortality rates among those who slept more than eight hours or less than four hours a night.
In the Nurses’ Health Study that followed 71,617 women for a decade , those who slept eight hours a night had the lowest risk of developing heart disease. But in another study that followed 84,794 nurses for up to 24 years, those who slept nine or more hours a night were twice as likely to develop Parkinson’s disease as those who averaged six hours or less.
Still, many more people, both lay and professional, worry more about too little sleep than an excess of shut-eye, and with good reason. Sleep-deprived people have more accidents and are more likely to fall asleep at inappropriate times, like at a play or concert or, most seriously, while driving.
Drowsy driving slows reaction time as much as drunken driving does. According to the National Highway Traffic Safety Administration, fatigue results in 100,000 auto crashes and 1,550 automotive deaths a year in the United States. Several automakers, including Subaru, Audi, Mercedes and Volvo, now offer drowsiness detection systems that monitor a car’s movements, such as lane deviations, and alert sleepy drivers to take a break.
Sleep deprivation was a factor in some of the biggest environmental disasters in recent decades, including the 1979 nuclear accident at Three Mile Island, the 1986 nuclear meltdown at Chernobyl and the 1989 Exxon Valdez oil spill in Alaska.
How we sleep may affect how we eat
Although you might expect the opposite, several studies have shown that short sleepers tend to weigh more than those who sleep for longer periods, even though people expend more calories while awake than asleep. A study of 990 working adults in rural Iowa found that the less sleep they got on weeknights, the higher their body mass index tended to be.
A Canadian study of 240 children who ranged in age from 8 to 17 showed it was not helpful to try to make up for short weeknights by sleeping longer on the weekend. Fluctuating hours of sleep can affect appetite-regulating hormones in ways that prompt people to eat when they’re not hungry and eat past the point of satiation. The Wisconsin Sleep Cohort Study found that short sleepers had low levels of the appetite-suppressing hormone leptin, and higher levels of the hormone ghrelin, which signals people to eat more.
Furthermore, an attempt to make up for lost sleep on the weekend has been associated with eating in the absence of hunger or in response to fatigue, as well as being unduly tempted by the sight or smell of food. I can attest to a common tendency to eat more — especially snacks of questionable nutritional value — when staying up past what should have been a reasonable bedtime.
Fostering a good night’s sleep
Experts offer a variety of tips for getting a better night’s sleep. Among them:
Avoid all sources of caffeine in the late afternoon and evening, as well as a big heavy meal close to bedtime.
Practice good sleep hygiene. Go to bed and get up at about the same time each day.
Do not use alcohol to help you unwind. Try a warm bath or meditation.
Reading before bed is great, as long as it’s not on a computer or tablet that emits sleep-inhibiting light.
If outside light impedes sleep, install light-blocking shades or curtains or use a sleep mask. If noise is a problem, use earplugs or a white-noise machine.
Consider cognitive behavioral therapy, which challenges underlying thoughts or behaviors that may be keeping you up at night.
Jane Brody is the Personal Health columnist, a position she has held since 1976. She has written more than a dozen books including the best sellers “Jane Brody’s Nutrition Book” and “Jane Brody’s Good Food Book.” More about Jane E. Brody

‘Sleeping on it’ really does help and four other recent sleep research breakthroughs
Marie Skłodowska-Curie Senior Research Fellow, University of York
Disclosure statement
Dan Denis receives funding from the European Union's Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No 101028886.
University of York provides funding as a member of The Conversation UK.
View all partners
Twenty-six years. That is roughly how much of our lives are spent asleep. Scientists have been trying to explain why we spend so much time sleeping since at least the ancient Greeks , but pinning down the exact functions of sleep has proven to be difficult.
During the past decade, there has been a surge of interest from researchers in the nature and function of sleep. New experimental models coupled with advances in technology and analytical techniques are giving us a deeper look inside the sleeping brain. Here are some of the biggest recent breakthroughs in the science of sleep.
1. We know more about lucid dreaming
No longer on the fringes, the neuroscientific study of dreaming has now become mainstream.
US researchers in a 2017 study woke their participants up at regular intervals during the night and asked them what was going through their minds prior to the alarm call. Sometimes participants couldn’t recall any dreaming. The study team then looked at what was happening in the participant’s brain moments before waking.
Participants’ recall of dream content was associated with increased activity in the posterior hot zone, an area of the brain closely linked to conscious awareness . Researchers could predict the presence or absence of dream experiences by monitoring this zone in real time.
Another exciting development in the study of dreams is research into lucid dreams, in which you are aware that you are dreaming. A 2021 study established two-way communication between a dreamer and a researcher. In this experiment, participants signalled to the researcher that they were dreaming by moving their eyes in a pre-agreed pattern.
The researcher read out maths problems (what is eight minus six?). The dreamer could respond to this question with eye movements. The dreamers were accurate, indicating they had access to high level cognitive functions. The researchers used polysomnography , which monitors bodily functions such as breathing and brain activity during sleep, to confirm that participants were asleep.
These discoveries have dream researchers excited about the future of “interactive dreaming”, such as practising a skill or solving a problem in our dreams.
Read more: As we dream, we can listen in on the waking world – podcast
2. Our brain replays memories while we sleep
This year marks the centenary of the first demonstration that sleep improves our memory . However, a 2023 review of recent research has shown that memories formed during the day get reactivated while we are sleeping. Researchers discovered this using machine learning techniques to “decode” the contents of the sleeping brain.
A 2021 study found that training algorithms to distinguish between different memories while awake makes it possible to see the same neural patterns re-emerge in the sleeping brain. A different study, also in 2021, found that the more times these patterns re-emerge during sleep, the bigger the benefit to memory.
In other approaches, scientists have been able to reactivate certain memories by replaying sounds associated with the memory in question while the participant was asleep. A 2020 meta-analysis of 91 experiments found that when participants’ memory was tested after sleep they remembered more of the stimuli whose sounds were played back during sleep, compared with control stimuli whose sounds were not replayed.

Research has also shown that sleep strengthens memory for the most important aspects of an experience, restructures our memories to form more cohesive narratives and helps us come up with solutions to problems we are stuck on. Science is showing that sleeping on it really does help.
3. Sleep keeps our minds healthy
We all know that a lack of sleep makes us feel bad. Laboratory sleep deprivation studies, where researchers keep willing participants awake throughout the night, have been combined with functional MRI brain scans to paint a detailed picture of the sleep-deprived brain. These studies have shown that a lack of sleep severely disrupts the connectivity between different brain networks. These changes include a breakdown of connectivity between brain regions responsible for cognitive control , and an amplification of those involved in threat and emotional processing .
The consequence of this is that the sleep-deprived brain is worse at learning new information , poorer at regulating emotions , and unable to suppress intrusive thoughts . Sleep loss may even make you less likely to help other people . These findings may explain why poor sleep quality is so ubiquitous in poor mental health .
4. Sleep protects us against neurodegenerative diseases
Although we naturally sleep less as we age , mounting evidence suggests that sleep problems earlier in life increase the risk of dementia.
The build-up of β-amyloid, a metabolic waste product , is one of the mechanisms underlying Alzheimer’s disease. Recently, it has become apparent that deep, undisturbed sleep is good for flushing these toxins out of the brain. Sleep deprivation increases the the rate of build-up of β-amyloid in parts of the brain involved in memory, such as the hippocampus . A longitudinal study published in 2020 found that sleep problems were associated with a higher rate of β-amyloid accumulation at a follow-up four years later . In a different study, published in 2022, sleep parameters forecasted the rate of cognitive decline in participants over the following two years.
5. We can engineer sleep
The good news is that research is developing treatments to get a better night’s sleep and boost its benefits.
For example, the European Sleep Research Society and the American Academy of Sleep Medicine recommend cognitive behavioural therapy for insomnia (CBT-I). CBT-I works by identifying thoughts, feelings and behaviour that contribute to insomnia, which can then be modified to help promote sleep.
In 2022, a CBT-I app became the first digital therapy recommended by England’s National Institute for Health and Care Excellence for treatment on the NHS.
These interventions can improve other aspects of our lives as well. A 2021 meta-analysis of 65 clinical trials found that improving sleep via CBT-I reduced symptoms of depression, anxiety, rumination and stress.
- Neuroscience
- Sleep deprivation
- Lucid dream

Head of School, School of Arts & Social Sciences, Monash University Malaysia

Chief Operating Officer (COO)

Clinical Teaching Fellow

Data Manager

Director, Social Policy
A monthly newsletter from the National Institutes of Health, part of the U.S. Department of Health and Human Services
Search form
Print this issue
Good Sleep for Good Health
Get the Rest You Need

Sometimes, the pace of modern life barely gives you time to stop and rest. It can make getting a good night’s sleep on a regular basis seem like a dream.
But sleep is as important for good health as diet and exercise. Good sleep improves your brain performance, mood, and health.
Not getting enough quality sleep regularly raises the risk of many diseases and disorders. These range from heart disease and stroke to obesity and dementia.
There’s more to good sleep than just the hours spent in bed, says Dr. Marishka Brown, a sleep expert at NIH. “Healthy sleep encompasses three major things,” she explains. “One is how much sleep you get. Another is sleep quality—that you get uninterrupted and refreshing sleep. The last is a consistent sleep schedule.”
People who work the night shift or irregular schedules may find getting quality sleep extra challenging. And times of great stress—like the current pandemic—can disrupt our normal sleep routines. But there are many things you can do to improve your sleep.
Sleep for Repair
Why do we need to sleep? People often think that sleep is just “down time,” when a tired brain gets to rest, says Dr. Maiken Nedergaard, who studies sleep at the University of Rochester.
“But that’s wrong,” she says. While you sleep, your brain is working. For example, sleep helps prepare your brain to learn, remember, and create.
Nedergaard and her colleagues discovered that the brain has a drainage system that removes toxins during sleep.
“When we sleep, the brain totally changes function,” she explains. “It becomes almost like a kidney, removing waste from the system.”
Her team found in mice that the drainage system removes some of the proteins linked with Alzheimer’s disease. These toxins were removed twice as fast from the brain during sleep.
Everything from blood vessels to the immune system The system that protects your body from invading viruses, bacteria, and other microscopic threats. uses sleep as a time for repair, says Dr. Kenneth Wright, Jr., a sleep researcher at the University of Colorado.
“There are certain repair processes that occur in the body mostly, or most effectively, during sleep,” he explains. “If you don’t get enough sleep, those processes are going to be disturbed.”
Sleep Myths and Truths
How much sleep you need changes with age. Experts recommend school-age children get at least nine hours a night and teens get between eight and 10. Most adults need at least seven hours or more of sleep each night.
There are many misunderstandings about sleep. One is that adults need less sleep as they get older. This isn’t true. Older adults still need the same amount. But sleep quality can get worse as you age. Older adults are also more likely to take medications that interfere with sleep.
Another sleep myth is that you can “catch up” on your days off. Researchers are finding that this largely isn’t the case.
“If you have one bad night’s sleep and take a nap, or sleep longer the next night, that can benefit you,” says Wright. “But if you have a week’s worth of getting too little sleep, the weekend isn’t sufficient for you to catch up. That’s not a healthy behavior.”
In a recent study, Wright and his team looked at people with consistently deficient sleep. They compared them to sleep-deprived people who got to sleep in on the weekend.
Both groups of people gained weight with lack of sleep. Their bodies’ ability to control blood sugar levels also got worse. The weekend catch-up sleep didn’t help.
On the flip side, more sleep isn’t always better, says Brown. For adults, “if you’re sleeping more than nine hours a night and you still don’t feel refreshed, there may be some underlying medical issue,” she explains.
Sleep Disorders
Some people have conditions that prevent them from getting enough quality sleep, no matter how hard they try. These problems are called sleep disorders.
The most common sleep disorder is insomnia. “Insomnia is when you have repeated difficulty getting to sleep and/or staying asleep,” says Brown. This happens despite having the time to sleep and a proper sleep environment. It can make you feel tired or unrested during the day.
Insomnia can be short-term, where people struggle to sleep for a few weeks or months. “Quite a few more people have been experiencing this during the pandemic,” Brown says. Long-term insomnia lasts for three months or longer.
Sleep apnea is another common sleep disorder. In sleep apnea, the upper airway becomes blocked during sleep. This reduces or stops airflow, which wakes people up during the night. The condition can be dangerous. If untreated, it may lead to other health problems.
If you regularly have problems sleeping, talk with your health care provider. They may have you keep a sleep diary to track your sleep for several weeks. They can also run tests, including sleep studies. These look for sleep disorders.
Getting Better Sleep
If you’re having trouble sleeping, hearing how important it is may be frustrating. But simple things can improve your odds of a good night’s sleep. See the Wise Choices box for tips to sleep better every day.
Treatments are available for many common sleep disorders. Cognitive behavioral therapy can help many people with insomnia get better sleep. Medications can also help some people.
Many people with sleep apnea benefit from using a device called a CPAP machine. These machines keep the airway open so that you can breathe. Other treatments can include special mouthguards and lifestyle changes.
For everyone, “as best you can, try to make sleep a priority,” Brown says. “Sleep is not a throwaway thing—it’s a biological necessity.”
Related Stories

Beyond Basic Blood Tests

Mindfulness Training Can Promote Healthy Choices

Yoga for Health: A New e-Book

Addressing Childhood Bullying
NIH Office of Communications and Public Liaison Building 31, Room 5B52 Bethesda, MD 20892-2094 [email protected] Tel: 301-451-8224
Editor: Harrison Wein, Ph.D. Managing Editor: Tianna Hicklin, Ph.D. Illustrator: Alan Defibaugh
Attention Editors: Reprint our articles and illustrations in your own publication. Our material is not copyrighted. Please acknowledge NIH News in Health as the source and send us a copy.
For more consumer health news and information, visit health.nih.gov .
For wellness toolkits, visit www.nih.gov/wellnesstoolkits .
- Search by keyword
- Search by citation
Page 1 of 2
Central sleep apnea in chronic heart failure with hypoxemia - treatment efficacy and hemodynamic effects of three different treatment modalities: a case report
The optimal treatment for central sleep apnea (CSA) depends on the underlying pathophysiology and should consider the potential for hemodynamic impairment when using positive airway pressure devices. While the...
- View Full Text
Gender-specific associations between sleep quality, sleep duration and cognitive functioning among older Indians: findings from WHO-SAGE study
Sleep is an essential component of human health and well-being, playing a crucial role in several cognitive processes, including attention, memory, and executive function. In this study, we aimed to examine th...
Disruption of sleep by one night of in-home polysomnographic recording: a longitudinal actigraphy study of patients with chronic musculoskeletal pain and pain-free controls
Patients with chronic pain frequently have comorbid sleep disturbances. Since improvement of sleep may alleviate both sleep problems and to some extent pain, sleep studies in this group becomes relevant. Polys...
Sex-specific prevalence and correlates of possible undiagnosed obstructive sleep apnea in rural Canada
Obstructive Sleep Apnea (OSA) has been under-investigated in rural communities, particularly through a sex/gender lens. The purpose of this study was to examine the prevalence and correlates of OSA risk among ...
A preliminary study of factors influencing the occurrence of post-arousal hypersynchrony
Post-arousal hypersynchrony (PAH) is a continuous delta wave occurring after arousal. We hypothesized that PAH would decrease with age because PAH is affected by sleep pressure, which decreases with age.
Evaluation of psychometric properties of sleep quality questionnaire among medical students of Guilan University of Medical Sciences
Since evaluating sleep quality among students is of great importance and is one of the challenges facing the health field regarding this group, we were determined to conduct this study to evaluate the psychome...
Didge you sleep: a feasibility study of didgeridoo training for obstructive sleep apnea
Intolerance of positive airway pressure therapy for obstructive sleep apnea is common. Upper airway muscle therapies show promise as alternative treatments. The didgeridoo, which is a musical instrument, can b...
Synthesizing the risk of morbidities and lifestyle factors on insomnia symptoms among middle-aged and older adult persons in India
Most of the time increasing age and improper lifestyle enhance the burgeoning health challenge for middle-aged and older adult persons. In this way, the present study seeks to know the association of morbidity...
Associations between circadian, sleep, and mood disturbances in Uruguayan dance students
Current evidence supports associations between circadian, sleep, and mood disturbances. However, it is still debated to what extent different chronobiological and mood variables act independently or in synergy...
Anthropometric screening approach for obstructive sleep apnea in Japanese men: development and validation of the ABC scale
The existing screening tools for the detection of moderate and severe obstructive sleep apnea (OSA) are tailored to Western individuals. The aim of this study was to formulate and validate a simple anthropomet...
Comparison of the clinical and electrophysiological characteristics between type 1 and type 2 narcolepsy: a cross-sectional study
Narcolepsy is a chronic brain disease characterized by excessive sleepiness and classified into two types based on the presence of cataplexy or reduced level of cerebrospinal fluid orexin-A (hypocretine-1): na...
The effect of nutrition and physical activity on sleep quality among adults: a scoping review
Sleep quality and its effects have become a public concern over the last few years. While the prevalence of sleep disorders was increasing, several studies have linked diet and physical activity as a cause of ...
Understanding daytime functioning in insomnia: responder and correlation analyses in patients treated with daridorexant
Improving daytime functioning is a key treatment goal for patients with insomnia disorder. In a phase 3 study, using the Insomnia Daytime Symptoms and Impacts Questionnaire (IDSIQ), daridorexant 50 mg signific...
Hyperactivity in patients with narcolepsy and idiopathic hypersomnia: an exploratory study
Patients with either Idiopathic Hypersomnia or Narcolepsy demonstrate excessive daytime somnolence (EDS) with resultant inattention mimicking Attention Deficit Hyperactivity Disorder (ADHD). Patients with ADHD...
Gender differences in obstructive sleep apnea with comorbid treatment-resistant depression
A bidirectional relationship between major depression and obstructive sleep apnea (OSA) has been established, suggesting the possibility of overlapping and compounding disease processes. Depression, however, w...
Impairment in sleep health in young adults with chronic pain: a modifiable risk factor
Impairments in sleep health are associated with the development or worsening of chronic pain. Further, chronic pain can cause sleep health disruption by impacting sleep onset, sleep maintenance, sleep quality,...
Sleep as a vital sign
Sleep is causally linked to the maintenance of every major physiological body system and disturbed sleep contributes to myriad diseases. The problem is, however, is that patients do not consistently, nor spont...
Clinical application of headache impact test (HIT)-6 and epworth sleepiness scale (ESS) for sleep apnea headache
Sleep apnea headache is a major symptom accompanying obstructive sleep apnea (OSA), but relatively little evidence has been reported on the magnitude of its negative effects on patients or the evaluation of th...
From good sleep to health and to quality of life – a path analysis of determinants of sleep quality of working adults in Abu Dhabi
Sleep quality has significant impacts on many aspects of quality of life. Therefore, identifying the association of sleep quality with that quality of life domains could lead to deeper insights for social poli...
Lingering impacts on sleep following the Daylight Savings Time transition in the Project Baseline Health Study
The “spring forward” change to Daylight Savings Time (DST) has been epidemiologically linked with numerous health and safety risks in the days following the transition, but direct measures of sleep are infrequ...
The relationship between perinatal circadian rhythm and postnatal depression: an overview, hypothesis, and recommendations for practice
Postnatal depression (PND) is an important public health problem with far-reaching consequences for mothers, families, and society. Current treatment approaches tend to focus on the depressive symptoms of the ...
Sleep quality and associated factors among type 2 Dm patients and non-Dm individuals in Bahir Dar governmental hospitals: comparative cross-sectional study
Multiple factors may contribute to sleep disruption among individuals with type 2 diabetes mellites. Sleep disruption among individuals with type 2 diabetes mellites is frequently associated with long-term dam...
Prevalence and associated factors of sleep deprivation among Haramaya University students, Ethiopia, 2021: cross-sectional study
Sleep deprivation is the lack of sleep that is associated with an increased risk of cardiovascular illness, diabetes, obesity, cognitive impairment, vehicle accidents, and workplace accidents, as well as being...
Chinese translation and validation of the adolescent sleep wake scale
Inadequate sleep is a problem for teens world-wide. Identifying the biological and cultural factors that underlie this phenomenon is dependent on tools that can accurately query sleep-related behaviors. While ...
Poor sleep quality and associated factors among pregnant women on antenatal care follow up at Nekemte Referral Hospital and Wollega University Hospital, Nekemte, Ethiopia, 2019: a cross-sectional study
Sleep disturbances are common in women, especially during pregnancy. This can result in emotional and psychological consequences for pregnant women, and it could lead to some serious complications for both mot...
Correction: Measurement properties of the minimal insomnia symptom scale (MISS) in adolescents
The original article was published in Sleep Science and Practice 2022 6 :5
The prevalence of obstructive sleep apnea in patients with type 2 diabetes: a systematic review and meta-analysis
Obstructive Sleep Apnea (OSA) is one of the diseases related to diabetes. Considering the varying prevalence of OSA in patients with type 2 diabetes in different parts of the world, in order to aggregate the r...
Measurement properties of the minimal insomnia symptom scale (MISS) in adolescents
The Minimal Insomnia Symptom Scale (MISS) is a three-item screening instrument that has been found to be psychometrically sound and capable of screening for insomnia among adults and older people. This study a...
The Correction to this article has been published in Sleep Science and Practice 2022 6 :8
In-office communication about excessive daytime sleepiness associated with treated obstructive sleep apnea: insights from an ethnographic study of physician-patient visits
Excessive daytime sleepiness (EDS), a primary symptom of obstructive sleep apnea (OSA), negatively affects functioning and quality of life (QoL). EDS can persist despite primary airway therapy, and often remai...
Effects of mattress support on sleeping position and low-back pain
To determine the efficacy of decreasing spinal curvature – when sleeping laterally – in reducing low-back pain (LBP) and improving sleep quality in people with chronic LBP. Secondly, to investigate whether sle...
Quantitative effects of head rotation angle on apnea hypopnea index in positional obstructive sleep apnea – a preliminary case series
Quantify the effects of head rotation and head incline on obstructive sleep apnea (OSA) severity.
Objectively-measured sleep patterns and cardiometabolic health in a rural South African setting: a cross sectional analysis
To investigate the relationship between objectively-measured, free-living sleep patterns, and cardiometabolic health, in a rural South African health and demographic surveillance site.
Obstructive sleep apnea and associated factors among hypertensive patients attending a tertiary cardiac center in Tanzania: a comparative cross-sectional study
There is mounting evidence for a reciprocal yet bidirectional association between sleep-disordered breathing and hypertension. Obstructive sleep apnea (OSA), a common cause of systemic hypertension is an indep...
Correlations between sleep disturbance and brain cortical morphometry in healthy children
While the importance of adequate sleep duration to normal brain development is well known, more studies are needed to characterize how undiagnosed sleep disturbance other than suboptimal sleep duration may imp...
Sleep apnea and unilateral upper and lower extremity allodynia as a result of a large thoracic disc herniation: a case report
Clinically significant disc herniations in the thoracic spine are rare accounting for approximately 1% of all disc herniations. In patients with significant spinal cord compression, presenting symptoms typical...
Human blood serum proteome changes after 6 hours of sleep deprivation at night
The aim of this study was to discover significantly changed proteins in human blood serum after loss of 6 h sleep at night. Furthermore, to reveal affected biological process- and molecular function categories...
Palmitoylethanolamide for sleep disturbance. A double-blind, randomised, placebo-controlled interventional study
Sleep is essential for wellbeing, yet sleep disturbance is a common problem linked to a wide range of health conditions. Palmitoylethanolamide (PEA) is an endogenous fatty acid amide proposed to promote better...

Sleep during infancy, inhibitory control and working memory in toddlers: findings from the FinnBrain cohort study
Sleep difficulties are associated with impaired executive functions (EFs) in school-aged children. However, much less is known about how sleep during infancy relates to EF in infants and toddlers. The aim of t...
Revisiting level II sleep studies in the era of COVID-19: a theoretical economic decision model in patients with suspected obstructive sleep apnea
The recent pandemic has made it more challenging to assess patients with suspected obstructive sleep apnea (OSA) with in laboratory polysomnography (PSG) due to concerns of patient and staff safety. The purpos...
Case report: fast reversal of malignant obesity hypoventilation syndrome after noninvasive ventilation and pulmonary rehabilitation
Malignant obesity hypoventilation syndrome (MOHS) is described as a subtype condition of OHS, characterized by extreme obesity, obese-related hypoventilation, and multiorgan dysfunction. Because of low awarene...
Energy cost of walking and functional aerobic capacity during moderate intensity exercise in adults with obstructive sleep apnea: a cross-sectional study
Autonomic dysregulation associated with obstructive sleep apnea (OSA) may limit cardiopulmonary responses to exercise, which, in turn, may impair functional aerobic capacity (FAC) and walking economy. We aimed...
Self-administered electroencephalography-based sleep assessment: compliance and perceived feasibility in children and adults
Sleep is a crucial part of our lives and insufficient sleep has been linked to several health disorders in both children and adults. However, most studies are based on single night laboratory polysomnography, ...
Magnitude and correlates of sleep quality among undergraduate medical students in Ethiopia: cross –sectional study
Poor quality of sleep has a negative effect on academic performance of medical students. Quantity and quality of sleep in addition to average sleep time are strongly linked with students’ learning abilities, p...
Correction to: Transcranial magnetic stimulation therapeutic applications on sleep and insomnia: a review
An amendment to this paper has been published and can be accessed via the original article.
The original article was published in Sleep Science and Practice 2021 5 :3
Transcranial magnetic stimulation therapeutic applications on sleep and insomnia: a review
Repetitive transcranial magnetic stimulation (rTMS) is a neuromodulatory technique approved by the US Food and Drug Administration for use in treatment-resistant major depressive disorder. It works by generati...
The Correction to this article has been published in Sleep Science and Practice 2021 5 :6
Changes in insomnia as a risk factor for the incidence and persistence of anxiety and depression: a longitudinal community study
The aim of this investigation was to examine the longitudinal association between change in insomnia status and the development of anxiety and depression in the general population.
Association between cardiometabolic health and objectively-measured, free-living sleep parameters: a pilot study in a rural African setting
To investigate the relationship between objectively-measured, free-living sleep quantity and quality, and cardiometabolic health, in a rural African setting in 139 adults (≥40 years, female: n = 99, male: n = 40)...
Quality of sleep and associated factors among people living with HIV/AIDS on follow up at Ethiopian Zewditu memorial hospital, 2018
Sleep disturbance is a common complaint in people living with HIV/AIDS. Despite the influence of sleep disturbance on treatment adherence, quality of life, work productivity, risk of chronic illness, it remain...
Cardiac function and cognitive function in patients with obstructive sleep apnea
This study was designed to evaluate echocardiographic findings in patients with obstructive sleep apnea (OSA) with cognitive impairment and compare it with the control group.
An automatic estimation of the rest-interval for MotionWatch8© using uniaxial movement and lux data
Poor sleep is linked with chronic conditions common in older adults, including diabetes, heart disease, and dementia. Valid and reliable field methods to objectively measure sleep are thus greatly needed to ex...
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Sign up for article alerts and news from this journal
Annual Journal Metrics
2023 Speed 23 days submission to first editorial decision for all manuscripts (Median) 135 days submission to accept (Median)
2023 Usage 195,913 downloads 89 Altmetric mentions
Sleep Science and Practice
ISSN: 2398-2683
- General enquiries: [email protected]
- Search Menu
- Sign in through your institution
- Advance Articles
- Supplements
- Editor's Choice
Virtual Issues
- Virtual Roundtables
- Abstract Supplements
- Basic Science
- Circadian Disorders
- Cognitive, Affective and Behavioral Neuroscience of Sleep
- Neurological Disorders
- Sleep Across the Lifespan
- Sleep and Metabolism
- Sleep Disordered Breathing
- Sleep Health and Safety
- Author Guidelines
- Instructions for Reviewers
- Submission Site
- Open Access Options
- Additional Resources
- Self-Archiving Policy
- Why publish with this journal?
- About SLEEP
- Editorial Board
- Dispatch Dates
- Permissions
- Advertising & Corporate Services
- Journals Career Network
- Reprints and ePrints
- Sponsored Supplements
- Journals on Oxford Academic
- Books on Oxford Academic

Latest Articles
Oup neuro hub: neurocritical care.
In the second collection of OUP’s Neuro Hub, we’ve organized more than 70 book chapters, journal articles, and entries from our reference products on neurocritical care.
Start reading

Email alerts
Register to receive email alerts as soon as new content from SLEEP is published online.

Explore curated collections of influential articles on sleep and trauma exposure, narcolepsy, insomnia, and REM Sleep Behavior Disorder.

Abstract supplements
Click here for an archive of previous abstract supplements.

Read and Publish deals
Authors interested in publishing in SLEEP may be able to publish their paper Open Access using funds available through their institution’s agreement with OUP.
Find out if your institution is participating

SRS Membership
Join more than 1,300 other sleep researchers in discovering the professional benefits of the Sleep Research Society (SRS) membership.
More details

SRS Podcast
The SRS Podcast discusses the latest findings in sleep and circadian research, with an emphasis on research published in SLEEP and SLEEP Advances . Join us the first Tuesday of every month for new episodes!

Contact the society
Email [email protected] for any inquiries about the Sleep Research Society (SRS).

SRS Virtual Seminar Series
Join the SRS Virtual Seminar Series as trainees and early career investigators deliver professional talks to an audience of peers and colleagues.
Related Titles

- Recommend to Your Librarian
- Advertising and Corporate Services
Affiliations
- Online ISSN 1550-9109
- Print ISSN 0161-8105
- Copyright © 2024 Sleep Research Society
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Join [MO_SAML_FORM] --> Join [MO_SAML_FORM] -->
- Bylaws & Policies
- Advocacy Updates
- Sleep Research Network
- Permanent Standard Time
- Strategic Plan
- Leadership Nominations Procedure
- Our Foundation
- Categories & Benefits
- Application
- Member Directory
- 2024 Trainee Symposia Series
- Sleep Europe 2024
- SLEEP Advances
- Learning Center
- SRS Podcasts
- Public Education Papers
- White Papers
- Public Datasets
- Grant Repository
- Course Syllabi
- Traditional Courses
- Online Courses
- Laboratory Directory
- Historical Papers
- 2020 Trainee Symposia Series
- 2021 Trainee Symposia Series
- Annual Meeting
- Funding Information
- Employer Control Panel
- NIH Grant Reviewer Training Program
- Trainee Opportunities
- Virtual Seminar Series
- Distinguished Scientist Award
- Outstanding Scientific Achievement Award
- Mary A. Carskadon Outstanding Educator Award
- Public Service Award
- Rising Star Award
- Outstanding Early Investigator Award
- SRSF Career Development Award
- SRSF Focused Research Award
- SRSF Small Research Grant Program
- SRSF Mentored Collaboration Grant
- Conference Awards
- SRS Diversity Membership Initiative and Award
- SRS Dependent Care & Accessibility Scholarship
- SRS Infographic Contest
- Career Development Award
- Focused Research Award
- Small Research Grant
- SRSF Conference Scholarships
- Mentored Collaboration Grant
- Donor Recognition
- Funding Our Future Scientists Campaign
- Corporate Opportunities
Advance Articles for November 2021
Neural mechanisms that promote food consumption following sleep loss and social stress: An fMRI study in adolescent girls with overweight/obesity Chad D Jensen, Kelsey K Zaugg, Nathan M Muncy, Whitney D Allen, Robyn Blackburn, Kara M Duraccio, Kimberly A Barnett, C Brock Kirwan, Johanna M Jarcho
High-throughput visual assessment of sleep stages in mice using machine learning Brian Geuther, Mandy Chen, Raymond J Galante, Owen Han, Jie Lian, Joshy George, Allan I Pack, Vivek Kumar
Associations of sleep measures with neural activations accompanying fear conditioning and extinction learning and memory in trauma-exposed individuals Jeehye Seo, Katelyn I Oliver, Carolina Daffre, Kylie N Moore, Samuel Gazecki, Natasha B Lasko, Mohammed R Milad, Edward F Pace-Schott
Share This Story, Choose Your Platform!
Related posts.

Sleep Research Society position statement supports adoption of permanent standard time
Newest Articles in SLEEP Advances: April 22, 2022

Editor’s Choice Articles for April 2022

Advance Articles for April 2022
Call for Papers: War, Trauma & Sleep
- Patient Care & Health Information
- Diseases & Conditions
- Sleep apnea
Sleep apnea is a potentially serious sleep disorder in which breathing repeatedly stops and starts. If you snore loudly and feel tired even after a full night's sleep, you might have sleep apnea.
The main types of sleep apnea are:
- Obstructive sleep apnea (OSA), which is the more common form that occurs when throat muscles relax and block the flow of air into the lungs
- Central sleep apnea (CSA) , which occurs when the brain doesn't send proper signals to the muscles that control breathing
- Treatment-emergent central sleep apnea , also known as complex sleep apnea, which happens when someone has OSA — diagnosed with a sleep study — that converts to CSA when receiving therapy for OSA
If you think you might have sleep apnea, see your health care provider. Treatment can ease your symptoms and might help prevent heart problems and other complications.
Products & Services
- A Book: Future Care
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Mayo Clinic Store — Solutions for a Healthier Living
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Sleep Apnea Products from Mayo Clinic Store
The symptoms of obstructive and central sleep apneas overlap, sometimes making it difficult to determine which type you have. The most common symptoms of obstructive and central sleep apneas include:
- Loud snoring.
- Episodes in which you stop breathing during sleep — which would be reported by another person.
- Gasping for air during sleep.
- Awakening with a dry mouth.
- Morning headache.
- Difficulty staying asleep, known as insomnia.
- Excessive daytime sleepiness, known as hypersomnia.
- Difficulty paying attention while awake.
- Irritability.
When to see a doctor
Loud snoring can indicate a potentially serious problem, but not everyone who has sleep apnea snores. Talk to your health care provider if you have symptoms of sleep apnea. Ask your provider about any sleep problem that leaves you fatigued, sleepy and irritable.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Obstructive sleep apnea
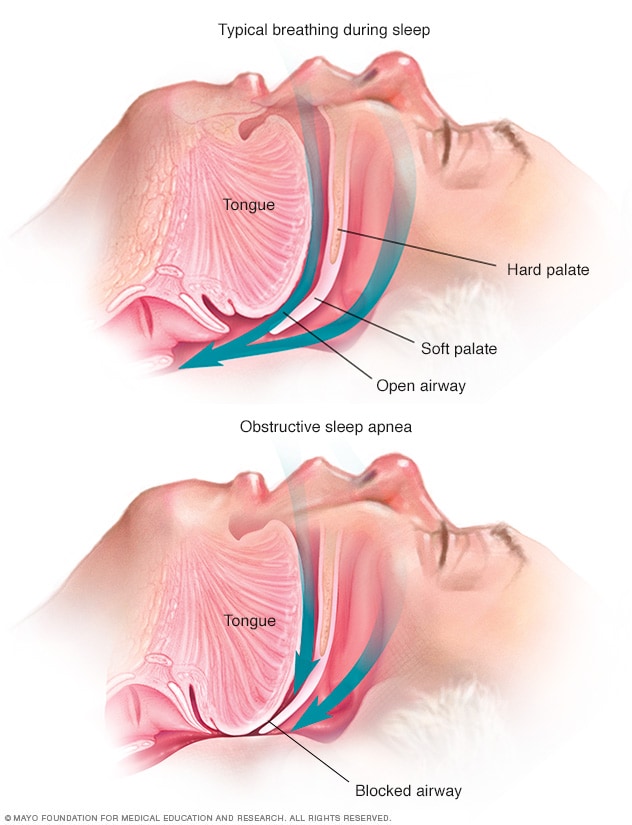
Obstructive sleep apnea occurs when the muscles that support the soft tissues in your throat, such as your tongue and soft palate, temporarily relax. When these muscles relax, your airway is narrowed or closed, and breathing is momentarily cut off.
This type of sleep apnea happens when the muscles in the back of the throat relax. These muscles support the soft palate, the triangular piece of tissue hanging from the soft palate called the uvula, the tonsils, the side walls of the throat and the tongue.
When the muscles relax, your airway narrows or closes as you breathe in. You can't get enough air, which can lower the oxygen level in your blood. Your brain senses that you can't breathe, and briefly wakes you so that you can reopen your airway. This awakening is usually so brief that you don't remember it.
You might snort, choke or gasp. This pattern can repeat itself 5 to 30 times or more each hour, all night. This makes it hard to reach the deep, restful phases of sleep.
Central sleep apnea
This less common form of sleep apnea occurs when your brain fails to send signals to your breathing muscles. This means that you make no effort to breathe for a short period. You might awaken with shortness of breath or have a difficult time getting to sleep or staying asleep.
Risk factors
Sleep apnea can affect anyone, even children. But certain factors increase your risk.
Factors that increase the risk of this form of sleep apnea include:
- Excess weight. Obesity greatly increases the risk of OSA . Fat deposits around your upper airway can obstruct your breathing.
- Neck circumference. People with thicker necks might have narrower airways.
- A narrowed airway. You might have inherited a narrow throat. Tonsils or adenoids also can enlarge and block the airway, particularly in children.
- Being male. Men are 2 to 3 times more likely to have sleep apnea than are women. However, women increase their risk if they're overweight or if they've gone through menopause.
- Being older. Sleep apnea occurs significantly more often in older adults.
- Family history. Having family members with sleep apnea might increase your risk.
- Use of alcohol, sedatives or tranquilizers. These substances relax the muscles in your throat, which can worsen obstructive sleep apnea.
- Smoking. Smokers are three times more likely to have obstructive sleep apnea than are people who've never smoked. Smoking can increase the amount of inflammation and fluid retention in the upper airway.
- Nasal congestion. If you have trouble breathing through your nose — whether from an anatomical problem or allergies — you're more likely to develop obstructive sleep apnea.
- Medical conditions. Congestive heart failure, high blood pressure and type 2 diabetes are some of the conditions that may increase the risk of obstructive sleep apnea. Polycystic ovary syndrome, hormonal disorders, prior stroke and chronic lung diseases such as asthma also can increase risk.
Risk factors for this form of sleep apnea include:
- Being older. Middle-aged and older people have a higher risk of central sleep apnea.
- Being male. Central sleep apnea is more common in men than it is in women.
- Heart disorders. Having congestive heart failure increases the risk.
- Using narcotic pain medicines. Opioid medicines, especially long-acting ones such as methadone, increase the risk of central sleep apnea.
- Stroke. Having had a stroke increases the risk of central sleep apnea.
Complications
Sleep apnea is a serious medical condition. Complications of OSA can include:
Daytime fatigue. The repeated awakenings associated with sleep apnea make typical, restorative sleep impossible, in turn making severe daytime drowsiness, fatigue and irritability likely.
You might have trouble concentrating and find yourself falling asleep at work, while watching TV or even when driving. People with sleep apnea have an increased risk of motor vehicle and workplace accidents.
You might also feel quick-tempered, moody or depressed. Children and adolescents with sleep apnea might perform poorly in school or have behavior problems.
High blood pressure or heart problems. Sudden drops in blood oxygen levels that occur during OSA increase blood pressure and strain the cardiovascular system. Having OSA increases your risk of high blood pressure, also known as hypertension.
OSA might also increase your risk of recurrent heart attack, stroke and irregular heartbeats, such as atrial fibrillation. If you have heart disease, multiple episodes of low blood oxygen (hypoxia or hypoxemia) can lead to sudden death from an irregular heartbeat.
- Type 2 diabetes. Having sleep apnea increases your risk of developing insulin resistance and type 2 diabetes.
- Metabolic syndrome. This disorder, which includes high blood pressure, abnormal cholesterol levels, high blood sugar and an increased waist circumference, is linked to a higher risk of heart disease.
Complications with medicines and surgery. Obstructive sleep apnea is also a concern with certain medicines and general anesthesia. People with sleep apnea might be more likely to have complications after major surgery because they're prone to breathing problems, especially when sedated and lying on their backs.
Before you have surgery, tell your doctor about your sleep apnea and how it's being treated.
- Liver problems. People with sleep apnea are more likely to have irregular results on liver function tests, and their livers are more likely to show signs of scarring, known as nonalcoholic fatty liver disease.
- Sleep-deprived partners. Loud snoring can keep anyone who sleeps nearby from getting good rest. It's common for a partner to have to go to another room, or even to another floor of the house, to be able to sleep.
Complications of CSA can include:
Fatigue. The repeated awakening associated with sleep apnea makes typical, restorative sleep impossible. People with central sleep apnea often have severe fatigue, daytime drowsiness and irritability.
You might have difficulty concentrating and find yourself falling asleep at work, while watching television or even while driving.
Cardiovascular problems. Sudden drops in blood oxygen levels that occur during central sleep apnea can adversely affect heart health.
If there's underlying heart disease, these repeated multiple episodes of low blood oxygen — known as hypoxia or hypoxemia — worsen prognosis and increase the risk of irregular heart rhythms.
- Kline LR. Clinical presentation and diagnosis of obstructive sleep apnea in adults. https://www.uptodate.com/contents/search. Accessed June 28, 2022.
- Selim BJ, et al. The association of nocturnal cardiac arrhythmias and sleep-disordered breathing: The DREAM study. Journal of Clinical Sleep Medicine. 2016; doi:10.5664/jcsm.5880.
- Jameson JL, et al., eds. Sleep apnea. In: Harrison's Principles of Internal Medicine. 21st ed. McGraw-Hill; 2022. https://accessmedicine.mhmedical.com. Accessed June 28, 2022.
- Sleep apnea. National Heart, Lung, and Blood Institute. http://www.nhlbi.nih.gov/health/health-topics/topics/sleepapnea/. Accessed June 28, 2022.
- Badr MS. Central sleep apnea: Risk factors, clinical presentation, and diagnosis. https://www.uptodate.com/contents/search. Accessed June 28, 2022.
- Kryger MH, et al. Management of obstructive sleep apnea in adults. https://www.uptodate.com/contents/search. Accessed June 28, 2022.
- Aurora RN, et al. Practice parameters for the surgical modification of the upper airway for obstructive sleep apnea in adults. Sleep. 2010; doi:10.1093/sleep/33.10.1408.
- Amali A, et al. A comparison of uvulopalatopharyngoplasty and modified radiofrequency tissue ablation in mild to moderate obstructive sleep apnea: A randomized clinical trial. Journal of Clinical Sleep Medicine. 2017; doi:10.5664/jcsm.6730.
- Parthasarathy S. Treatment-emergent central sleep apnea. https://www.uptodate.com/contents/search. Accessed June 29, 2022.
- Mehra R. Sleep apnea and the heart. Cleveland Clinic Journal of Medicine. 2019; doi:10.3949/ccjm.86.s1.03.
- Badr MS. Central sleep apnea: Treatment. https://www.uptodate.com/contents/search. Accessed July 1, 2022.
- Olson EJ (expert opinion). Mayo Clinic. June 30, 2022.
- Continuous positive airway pressure (CPAP)
- CPAP machines: Tips for avoiding 10 common problems
- CPAP: How it works
- Which CPAP masks are best for you?
Associated Procedures
- Endoscopic sleeve gastroplasty
- Polysomnography (sleep study)
- Septoplasty
- Tonsillectomy
- Tracheostomy
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
June 2, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
written by researcher(s)
'Sleeping on it' really does help and four other recent sleep research breakthroughs
by Dan Denis, The Conversation

Twenty-six years. That is roughly how much of our lives are spent asleep. Scientists have been trying to explain why we spend so much time sleeping since at least the ancient Greeks , but pinning down the exact functions of sleep has proven to be difficult.
During the past decade, there has been a surge of interest from researchers in the nature and function of sleep. New experimental models coupled with advances in technology and analytical techniques are giving us a deeper look inside the sleeping brain. Here are some of the biggest recent breakthroughs in the science of sleep.
1. We know more about lucid dreaming
No longer on the fringes, the neuroscientific study of dreaming has now become mainstream.
US researchers in a 2017 study woke their participants up at regular intervals during the night and asked them what was going through their minds prior to the alarm call. Sometimes participants couldn't recall any dreaming. The study team then looked at what was happening in the participant's brain moments before waking.
Participants' recall of dream content was associated with increased activity in the posterior hot zone, an area of the brain closely linked to conscious awareness . Researchers could predict the presence or absence of dream experiences by monitoring this zone in real time.
Another exciting development in the study of dreams is research into lucid dreams, in which you are aware that you are dreaming. A 2021 study established two-way communication between a dreamer and a researcher. In this experiment, participants signaled to the researcher that they were dreaming by moving their eyes in a pre-agreed pattern.
The researcher read out math problems (what is eight minus six?). The dreamer could respond to this question with eye movements. The dreamers were accurate, indicating they had access to high level cognitive functions. The researchers used polysomnography , which monitors bodily functions such as breathing and brain activity during sleep, to confirm that participants were asleep.
These discoveries have dream researchers excited about the future of "interactive dreaming", such as practicing a skill or solving a problem in our dreams.
2. Our brain replays memories while we sleep
This year marks the centenary of the first demonstration that sleep improves our memory . However, a 2023 review of recent research has shown that memories formed during the day get reactivated while we are sleeping. Researchers discovered this using machine learning techniques to "decode" the contents of the sleeping brain.
A 2021 study found that training algorithms to distinguish between different memories while awake makes it possible to see the same neural patterns re-emerge in the sleeping brain. A different study, also in 2021, found that the more times these patterns re-emerge during sleep, the bigger the benefit to memory .
In other approaches, scientists have been able to reactivate certain memories by replaying sounds associated with the memory in question while the participant was asleep. A 2020 meta-analysis of 91 experiments found that when participants' memory was tested after sleep they remembered more of the stimuli whose sounds were played back during sleep, compared with control stimuli whose sounds were not replayed.
Research has also shown that sleep strengthens memory for the most important aspects of an experience, restructures our memories to form more cohesive narratives and helps us come up with solutions to problems we are stuck on. Science is showing that sleeping on it really does help.
3. Sleep keeps our minds healthy
We all know that a lack of sleep makes us feel bad. Laboratory sleep deprivation studies, where researchers keep willing participants awake throughout the night, have been combined with functional MRI brain scans to paint a detailed picture of the sleep-deprived brain. These studies have shown that a lack of sleep severely disrupts the connectivity between different brain networks. These changes include a breakdown of connectivity between brain regions responsible for cognitive control , and an amplification of those involved in threat and emotional processing .
The consequence of this is that the sleep-deprived brain is worse at learning new information , poorer at regulating emotions , and unable to suppress intrusive thoughts . Sleep loss may even make you less likely to help other people . These findings may explain why poor sleep quality is so ubiquitous in poor mental health .
4. Sleep protects us against neurodegenerative diseases
Although we naturally sleep less as we age , mounting evidence suggests that sleep problems earlier in life increase the risk of dementia.
The build-up of β-amyloid, a metabolic waste product , is one of the mechanisms underlying Alzheimer's disease. Recently, it has become apparent that deep, undisturbed sleep is good for flushing these toxins out of the brain. Sleep deprivation increases the rate of build-up of β-amyloid in parts of the brain involved in memory, such as the hippocampus . A longitudinal study published in 2020 found that sleep problems were associated with a higher rate of β-amyloid accumulation at a follow-up four years later . In a different study, published in 2022, sleep parameters forecasted the rate of cognitive decline in participants over the following two years.
5. We can engineer sleep
The good news is that research is developing treatments to get a better night's sleep and boost its benefits.
For example, the European Sleep Research Society and the American Academy of Sleep Medicine recommend cognitive behavioral therapy for insomnia (CBT-I). CBT-I works by identifying thoughts, feelings and behavior that contribute to insomnia, which can then be modified to help promote sleep.
In 2022, a CBT-I app became the first digital therapy recommended by England's National Institute for Health and Care Excellence for treatment on the NHS.
These interventions can improve other aspects of our lives as well. A 2021 meta-analysis of 65 clinical trials found that improving sleep via CBT-I reduced symptoms of depression, anxiety, rumination and stress.
Explore further
Feedback to editors

Metabolic parameters found to be similar in children born via frozen versus fresh embryo transfer, research shows
10 hours ago

Researchers identify key differences in inner workings of immune cells

Researchers detail molecular pathway that impacts pancreatic cancer progression and treatment response

Epstein-Barr virus and brain cross-reactivity: Possible mechanism for multiple sclerosis detected

Precision laser surgery cuts focal epileptic seizure spread
11 hours ago

Researchers find flavor restrictions affect tobacco buyers differently depending on socioeconomic status

Younger children are more commonly diagnosed with ADHD than their older classmates, says new study

Researchers say AI blood test provides a reliable way to identify lung cancer

New combination therapy shows promise for bladder cancer patients unresponsive to standard treatment

What toilet paper and game shows can teach us about the spread of epidemics
Related stories.

Breathing patterns during sleep found to impact memory processes
Dec 18, 2023

The science of dreams and nightmares: What is going on in our brains while we're sleeping?
Sep 8, 2023

Sleep and Alzheimer's disease connection
Oct 17, 2017

The dreaming brain tunes out the outside world
May 15, 2020

Sleeping sheep may offer clues to human brain disease
Mar 2, 2020

Study shows an association between sleep apnea and brain volume
May 31, 2023
Recommended for you

Could ultra-processed foods be associated with your insomnia?
May 30, 2024

The mind after midnight: Study shows disrupted sleep increases risk for suicide and homicide
May 29, 2024

The light or the content? What we know about screens and sleep disruption
May 28, 2024

Eating more fruits and vegetables may lead to optimal sleep duration
May 27, 2024

Social media-related nightmares: Study explores links between social media use, mental health and sleep quality
May 20, 2024

Research links sleep apnea severity during REM stage to verbal memory decline
May 14, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Better sleep is linked with lower loneliness levels
The relationship between sleep and loneliness is stronger in younger adults.
A new study to be presented at the SLEEP 2024 annual meeting found that better sleep health was associated with lower levels of loneliness, and this association was stronger among younger adults.
Results indicate that better sleep health was associated with significantly lower total loneliness, emotional loneliness and social loneliness. While better sleep health was associated with lower total and emotional loneliness across ages, this association was stronger for younger adults. However, age did not moderate the association between sleep health and social loneliness.
"Loneliness is an urgent public health crisis, and there is a pressing need for providers to better understand and treat it," said lead author and principal investigator Joseph Dzierzewski, who has a doctorate in clinical psychology and is vice president of research at the National Sleep Foundation in Washington, D.C. "Our results highlight the important role that sleep plays in understanding loneliness across the adult lifespan. Perhaps efforts to improve sleep health could have a beneficial effect on loneliness, especially for young people."
According to the American Academy of Sleep Medicine, sleep is essential to health. The AASM and the Sleep Research Society recommend that adults should sleep seven hours per night on a regular basis to promote optimal health, productivity and daytime alertness.
The study involved 2,297 adults with a mean age of 44 years; 51% were male. Participants completed an online sleep health questionnaire and loneliness scale. The researchers analyzed the results using correlation and linear regression analyses along with moderation analyses.
In 2023 an advisory from the U.S. surgeon general warned about a public health crisis of loneliness, isolation, and lack of connection. It noted that even before the onset of the COVID-19 pandemic, approximately half of U.S. adults reported experiencing measurable levels of loneliness.
According to the authors, efforts and programs that aim to reduce loneliness should include an emphasis on promoting sleep health, especially in younger adults.
"Why younger adults might experience more sleep-related benefits to loneliness than older adults is unknown and intriguing -- certainly worth further investigation," Dzierzewski said.
The research abstract was published recently in an online supplement of the journal Sleep and will be presented Monday, June 3, during SLEEP 2024 in Houston. SLEEP is the annual meeting of the Associated Professional Sleep Societies, a joint venture of the American Academy of Sleep Medicine and the Sleep Research Society.
- Sleep Disorders
- Obstructive Sleep Apnea
- Mental Health
- Disorders and Syndromes
- Child Development
- Child Psychology
- Sleep deprivation
- Circadian rhythm sleep disorder
- Night terror
- Yoga (alternative medicine)
- Sleep disorder
- Delayed sleep phase syndrome
- Rapid eye movement
Story Source:
Materials provided by American Academy of Sleep Medicine . Note: Content may be edited for style and length.
Journal Reference :
- Spencer Nielson, Julia Boyle, Joseph Dzierzewski. 0746 Rested and Connected: An Exploration of Sleep Health and Loneliness Across the Adult Lifespan . SLEEP , 2024; 47 (Supplement_1): A319 DOI: 10.1093/sleep/zsae067.0746
Cite This Page :
Explore More
- Marine Cyanobacteria Can Communicate
- 'Tweezer-Like' Bionic Tools Feel Right
- Odd Planet-Forming Disks Around Low-Mass Stars
- Toward Blood Stem Cell Self-Renewal
- Restored Hearing and Speech in Kids Born Deaf
- Babies and AI Both Learn Key Foundation Models
- Myelination May Drive Drug Addiction
- Freshwater On Earth 4 Billion Years Ago
- Extended Battle: 3,500-Year-Old Mycenaean Armor
- Oral Insulin Drops: Relief for Diabetes Patients
Trending Topics
Strange & offbeat.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.43(12); 2018 Dec
The Extraordinary Importance of Sleep
New sleep deprivation studies confirm the relationship between inadequate sleep and a wide range of disorders, such as hypertension, obesity and type-2 diabetes, cardiovascular disease, impaired immune functioning, and more.
In the inaugural issue of the Journal of Clinical Sleep Medicine (2005), a feature article 1 traced early milestones in the developing field of sleep medicine, which slowly emerged from the older field of sleep research during the 1970s and 1980s. Sleep medicine, the article noted, was closely linked with and made possible by the discovery of electrical activity in the brain. The examination of electroencephalogram (EEG) patterns that occur during sleep led to the classification of stages of sleep, which in turn created an important foundation for probing human sleep, discerning abnormalities, and discovering significant relationships between sleep and health. By 2005, scientists and clinicians had not only identified and clearly defined a large number of sleep disorders but had discovered that many of them were highly prevalent.
The pace of research and discovery has only accelerated since 2005, and the number of peer-reviewed sleep journals has more than tripled. Today, researchers are more deeply probing the cellular and subcellular effects of disrupted sleep, as well as the effects of sleep deprivation on metabolism, hormone regulation, and gene expression. Newer studies are strengthening known and suspected relationships between inadequate sleep and a wide range of disorders, including hypertension, 2 obesity and type-2 diabetes, 3 impaired immune functioning, 4 cardiovascular disease and arrhythmias, 5 , 6 mood disorders, 7 neurodegeneration and dementia, 8 , 9 and even loneliness. 10
Research findings continue to underscore early concerns about public safety that were first raised when major industrial disasters such as the Exxon Valdez oil spill were linked to inadequate sleep. 11 Related research sponsored by major organizations, including the U.S. Department of Transportation, the U.S. Department of Defense, the National Institutes of Health, and the National Aeronautics and Space Administration (NASA), has helped to inspire national initiatives aimed at improving public safety and health. However, despite the astounding acceleration in research during the past few decades, inadequate sleep due to sleep disorders, work schedules, and chaotic lifestyles continues to threaten both health and safety.
“Pushing against the wave of accelerated growth in the field has been a shoreline of indifference,” says David F. Dinges, PhD, Professor and Chief of the Division of Sleep and Chronobiology in the Department of Psychiatry at the University of Pennsylvania Perelman School of Medicine. “Modern industrial pressures to use time 24 hours a day have led to shiftwork and a world in which virtually everything—law Susan L. Worley is a freelance medical writer who resides in Pennsylvania. enforcement, airports and all kinds of transportation, industrial operations, and hospitals—operates 24/7. People have come to value time so much that sleep is often regarded as an annoying interference, a wasteful state that you enter into when you do not have enough willpower to work harder and longer.”

David F. Dinges, PhD
It has become increasingly clear, however, that no matter how hectic our lives may be, we can no longer afford to ignore what research is telling us about the importance of sleep for our safety and mental and physical well-being.
Impact on Attention, Cognition, and Mood
While scientists are still working to identify and clarify all of the functions of sleep, 12 decades of studies—many of which have used the method of disrupting sleep and examining the consequences—have confirmed that sleep is necessary for our healthy functioning and even survival.
“We know for sure that sleep serves multiple functions,” says Dr. Dinges. “Nature tends to be very parsimonious in that it often uses a single system or biology in multiple ways to optimize the functioning of an organism. We know, for example, that sleep is critical for waking cognition—that is, for the ability to think clearly, to be vigilant and alert, and sustain attention. We also know that memories are consolidated during sleep, and that sleep serves a key role in emotional regulation.”
Studies conducted by Dr. Dinges and other scientists have shown that cognitive performance and vigilant attention begin to decline fairly quickly after more than 16 hours of continuous wakefulness, and that sleep deficits from partial sleep deprivation can accumulate over time, resulting in a steady deterioration in alertness. The widely used psychomotor vigilance test (PVT), a simple neurocognitive test developed by Dr. Dinges and colleagues that assesses an individual’s ability to sustain attention and respond to signals in a timely manner, has proven to be an exceptionally sensitive tool for capturing dose–response effects of sleep loss on neurobehavioral functioning. 13 The PVT also reliably detects sleep deficits caused by disrupted or fragmented sleep, and/or poorly timed sleep, which is important because a growing body of evidence suggests that the continuity and timing (or circadian alignment) of sleep may be as important as the total amount of time spent sleeping.
“We know that sleep is much more restorative of waking functions and health when it is consolidated and not fragmented,” explains Dr. Dinges. “That is, when sleep goes through the appropriate physiological sequences of non-REM (rapid eye movement) and REM states at night, and occurs when human sleep is temporally programmed by our circadian clock to occur. Such consolidated sleep is typically of a longer duration and better sleep quality than sleep taken at other times of the day, such as that which occurs with nightshift work, jet lag, and other conditions of circadian misalignment.”
Dr. Dinges and his colleagues have found that people whose daily sleep duration is inadequate, or repeatedly disrupted (e.g., by obstructive sleep apnea, restless legs syndrome, pain or stress, or shiftwork or jet lag), often are not aware of their accumulating sleep deficits or the toll that these deficits can take on their waking cognitive functions, including their performance, working memory, cognitive speed, and accuracy. Inadequate sleep also can take a toll on psychological well-being, significantly affecting our emotional and psychosocial interpretation of events and exacerbating our stress levels. Studies have indicated that changes in mood may be due in part to the effects of sleep deprivation on the processing of emotional memory—in other words, our tendency to select and remember negative memories after inadequate sleep. 14
In one study conducted by Dr. Dinges and colleagues, participants’ mood was observed after they were confronted with “high” and “low” performance demands, following varying degrees of sleep deprivation. 15
“To our surprise, those who were sleep-deprived responded to low stressors in much the same way that people without any sleep deprivation tended to respond to high stressors,” said Dr. Dinges. “In other words, we tend to become much more sensitive emotionally and socially when we are sleep-deprived. That is what I like to call the ‘who was at my desk or who touched my coffee cup?’ phenomenon. I think we all have experienced having an extreme reaction or a very negative emotional response to a mild stressor when we have not had enough sleep.”
Aiming for the Sweet Spot
How much sleep is enough? After decades of investigation, it appears that scientists have gathered enough evidence to begin to answer that question. 16
“When duration of sleep drops below seven hours, and especially when it starts to move toward six and half hours or less, a number of different disorders begin to increase in prevalence,” says Dr. Dinges. “Most experts would agree that there is a kind of sweet spot that most people should aim for, and for the average healthy adult that zone is ideally somewhere between 7 and 7 and a half hours. That is what the consensus evaluations of more than a thousand scientific articles have yielded—the consensus of evaluations conducted by the AASM (American Academy of Sleep Medicine) and Sleep Research Society jointly.”
Numerous large U.S. surveys—beginning with a 1982 survey by the American Cancer Society—have been used to estimate the number of hours that most people spend sleeping. Many surveys have identified a worrisome prevalence of “short” sleepers (people who sleep 6 hours or less) among respondents, and a general trend toward decreasing sleep duration between 1975 and 2006. More recently, however, an analysis of the American Time Use Survey (ATUS), spearheaded by Mathias Basner, MD, PhD, at the University of Pennsylvania 17 , has suggested that there may be cause for optimism.
“The analysis shows that there is a slight but steady increase in sleep time that stretches back to about 2003 or 2004,” says Dr. Dinges. “We think this increase, which is modest—at most a minute or two more per year—is due in part to the development of the field of sleep medicine, and public and scientific reports in the media about sleep loss contributing to accidents and catastrophes, and so forth. Ever so slowly, the message that it is important not to get sleep deprived, and to get help if you have a sleep disorder, has begun to penetrate to the public.”
The analysis notes that one sign of greater interest in sleep on the part of the public has been a significant increase in Google searches containing the word “sleep” since 2004. Data from the ATUS also suggest that over time, people have been willing to trade some of their daily activities in exchange for more sleep. It is important to note, says Dr. Dinges, that self-reports of time spent sleeping are not always accurate—they can be off by a half an hour or more, usually with people tending to estimate that they slept more than they did. He also notes that there is still a fairly large population sleeping 6 hours or less.
“Although there are signs that sleep time is increasing, it is not happening at nearly the dramatic rate that most experts would like to see,” says Dr. Dinges. “This is especially true for vulnerable populations. There is concern about school start times and bus times affecting the sleep of children and adolescents, and about extracurricular activities at the end of the school day sometimes leading to a delay in bed times for teenagers. All of this is an ongoing, evolving picture, with more research results coming out all the time, and with consequent changes in recommendations, to make sure that at least our most vulnerable populations are getting adequate sleep.”
Interindividual Differences in Vulnerability to Sleep Loss
While it is well established that the effects of sleep loss accumulate over time, with repeated exposure to inadequate, fragmented, or disrupted sleep, the degree to which individuals demonstrate adverse effects of inadequate sleep can vary considerably. 18
“We have learned that there are astonishingly mysterious phenotypes, or trait-like differences, in how vulnerable people are to sleep loss,” says Dr. Dinges. “This is still a relatively new area of research, and it has only been in the past few years that scientists have begun to replicate early findings regarding these phenotypic differences in vulnerability to the negative neurobehavioral effects of sleep loss. The interindividual differences that have been observed so far raise some extremely provocative scientific questions. We may find that there is something in waking biology that can substitute for, or somehow reduce, the impact of sleep loss on waking functioning, but thus far there is no evidence as to what that might be.”
Differences among individuals exist with regard to both the effects of sleep loss and the ability to recover from the effects of sleep loss. Differences in performance also have been shown to be task-dependent, suggesting that people who are vulnerable to the effects of sleep loss in one or more cognitive or neurobehavioral domains may be resistant to the effects of sleep loss in others. To better understand interindividual variability, scientists are investigating possible genetic mechanisms that may underlie complex interactions between circadian and sleep homeostatic systems—the systems that affect our drive for sleep as well as our alertness and performance during waking hours. A current goal is to discover biomarkers that may help predict individual performance after varying degrees of sleep loss. 19 And one hope is that biomarkers—ideally in the form of a simple “roadside” test such as a breathalyzer—may eventually be used to detect sleep loss-related impairment in drivers or in individuals responsible for operating sophisticated equipment or machinery. To date, no viable candidates have been found.
Investigators also are shedding light on the role that age may play in resilience to sleep loss. The results of one recent study indicate that younger adults are more vulnerable to the adverse effects of chronic sleep loss and recurring circadian disruption than older adults. 20 Although the neurobiological basis for these age-related differences is not yet understood, such findings may help to inform new approaches to the prevention of drowsy driving and related motor-vehicle accidents among young drivers.
Dr. Dinges emphasizes that findings regarding interindividual differences in response to sleep loss and in recovery from sleep loss should not diminish the message that adequate sleep is critical for everyone.
“Research has shown us that sleep is not an optional activity,” says Dr. Dinges. “There is no question that sleep is fundamentally conserved across species and across lifespans, and that any effort to eliminate it has been unsuccessful. We must plan our lives in the time domain with a serious consideration for sleep—planning when to sleep, ensuring that we get adequate sleep, and making sure that our sleep is not disturbed by disorders or diseases, whether or not they are sleep-related.”
Addressing Sleep Disorders
As connections between sleep disruption and both disease and mortality have become more firmly established, accurate and efficient diagnosis and management of sleep disorders (see Table 1 ) have become increasingly critical. Recent directions in the field of sleep medicine include a move toward patient-centered care, greater collaboration between specialists and primary care physicians, and the incorporation of new tools—including home-based diagnostic tests and novel electronic questionnaires—in the effort to create a comprehensive yet more personalized approach to assessment and treatment.
ICSD-3 Major Diagnostic Sections *
A chief goal is to improve the diagnosis of sleep disorders. Although approximately 70 million people in the U.S. have at least one sleep disorder, experts estimate that up to 80% of sleep disorders may go undetected or undiagnosed. One major challenge that clinicians face during the initial assessment of people with sleep disorders is the process of identifying and sorting out comorbidities. Untangling the causes and effects in bidirectional comorbidities can be particularly difficult. For example, insomnia—by far the most common sleep disorder—often is complicated by the presence of another sleep disorder, such as sleep apnea or restless legs syndrome.
“Some experts have even suggested that all cases of insomnia coexist with, or are caused by, another sleep disorder, most commonly sleep apnea,” says Clete A. Kushida, MD, PhD, Professor of Psychiatry and Behavioral Sciences at Stanford, and Division Chief and Medical Director of Stanford Sleep Medicine. “I’m not sure I would go quite that far, but certainly bidirectional comorbidities among individuals who experience sleep disorders are common. For example, pain syndromes—including back pain and limb pain, especially among older patients—are common comorbidities in patients with insomnia. Mood disorders also frequently occur in patients who experience insomnia.”
Comorbidities can complicate treatment and often require sleep specialists to collaborate with not only primary care physicians but also specialists in other therapeutic areas.
“If, for example, a person with insomnia also has been diagnosed with depression by a psychiatrist,” says Dr. Kushida, “our goal is to work hand in hand with the psychiatrist to find the right medication. There are both sedating and alerting antidepressants, and a patient may need to try one medication for a couple of weeks to months, slowly increasing the dose to a therapeutic level, until the effect on both the depression and the patient’s sleep can be determined. For some individuals, an alerting antidepressant can cause poor sleep, which in turn can exacerbate the depression. The process of achieving the right dose of the right medication can be complex, and benefits from a collaboration between specialists.”
Undetected obstructive sleep apnea (OSA) in patients with chronic pain, or other serious illnesses, can result in potentially dangerous comorbidities. Opioids, for example, are known to have adverse effects on respiration, and can lead to central sleep apnea (CSA)—shallow and irregular or interrupted breathing and sustained hypoventilation—a potentially lethal condition that can intensify the consequences of OSA. These risks underscore the need to improve methods for identifying and properly diagnosing the estimated 23.5 million U.S. adults with OSA. Public education and advocacy efforts are already helping to improve detection—in part by helping to address misconceptions about OSA.
“One of the biggest misconceptions is that only people who are significantly overweight experience sleep apnea,” says Dr. Kushida. “In fact, only up to 67% of people who have OSA are overweight, the rest are of normal weight. OSA also can be caused by craniofacial dysmorphism, or a defect of the airway that occurs during development. A narrow airway caused by deficient growth of the craniofacial skeleton, particularly the jaws, can become narrower and more prone to collapse with age, leading to sleep apnea.”
Treating Insomnia: The Value of Cognitive Behavioral Therapy
Insomnia, the most prevalent sleep disorder, affects approximately one third of all adults and is the most common condition that family and primary-care physicians encounter. According to the International Classification of Sleep Disorders (ICSD-3), chronic insomnia is the inability to attain sufficient sleep (despite adequate opportunity) for at least three nights per week for three months or longer, with negative daytime consequences. For most people, the disorder is transient, but for approximately 10% to 15% of those who experience insomnia (around 30 million people) it becomes chronic. Although pharmacologic treatments for insomnia ( Table 2 ) can be effective, most experts now recommend against the long-term use of pharmacotherapy.
Selected Pharmaceutical Treatments for Insomnia 21 , 27
“If a person has been diagnosed with chronic insomnia, the only treatment that has been shown to have long-term benefit is cognitive behavioral therapy, “says Dr. Kushida. “Medications really should be considered short-term treatments, because patients tend to develop dependence on, or tolerance to, hypnotic drugs. In our clinic, we commonly see that, over time, medications stop having an effect, and that means that patients may try higher doses of a medication, or keep switching to different medications. So, medications are a temporary solution—they just put a Band-Aid on the problem of insomnia, whereas cognitive behavioral therapy targets one of the pathways toward success.”
Cognitive behavioral therapy (CBT), which involves techniques that work in part by reducing cognitive and somatic arousal, is estimated to be effective in approximately 70% to 80% of people who experience chronic insomnia. Dr. Kushida notes that while drugs can sometimes be useful in the treatment of acute insomnia, they become problematic after acute insomnia transitions to chronic insomnia.
“A person might be an OK sleeper for several years, and then suddenly experience a traumatic event, such as the loss of a job, a divorce, or the death of a loved one, resulting in very poor sleep,” says Dr. Kushida. “Down the road, that person might obtain a better job, overcome grief, or find a new relationship, but continue to experience insomnia. We think in some cases the transition from acute insomnia to chronic insomnia occurs because the behavioral event triggers something in the person’s physiology that may lead to long-term changes. Once they are in a chronic insomnia phase, we tell patients that CBT is the only truly effective intervention.”
If a patient is already taking hypnotics, Dr. Kushida says that he will gradually wean the patient off medications while introducing CBT. He notes that often it is necessary for sleep specialists to manage the expectations of chronic sufferers.

Clete A. Kushida, MD, PhD
“We sometimes have to let patients with chronic insomnia know that we may never get them back to where they were when they had optimal sleep,” Dr. Kushida explains. “The behavioral methods we use work well, and usually we can get patients to the point where the insomnia is having less of an impact on their quality of life. Our inability to completely restore the patient’s ability to sleep well may partly be explained by as yet unidentified changes in his or her neurophysiology or neurochemistry. Some patients with chronic insomnia can begin to sleep normally again, but for the vast majority, we aim to make insomnia less of a burden on a patient’s daily life.”
Improving Clinical Research
In the field of sleep medicine, as in many other therapeutic areas, future directions in clinical trial research will place an emphasis on patient engagement and patient-centered outcomes.
“Perhaps the most important aim these days when developing and implementing any type of large-scale clinical research study is to incorporate the patient’s perspective,” says Dr. Kushida, who is currently analyzing the results of a comparative effectiveness sleep study sponsored by the Patient-Centered Outcomes Research Institute (PCORI). 22 The study, designed and conducted by a team at Stanford, introduced a new model of patient-centered, coordinated care and tested it against conventional outpatient treatment for sleep disorders.
“The patient’s perspective is so invaluable in guiding the success of a study that ideally it should be incorporated right at the inception of a research question or idea,” says Dr. Kushida. “When you are designing an especially complicated trial, for example, it is easy to incorporate a lot of tests and measures without being aware of the burden these can place on the participants. It’s critical to learn from patients whether they are overwhelmed by the number of tests, or whether travel time or the amount of time they need to take off from work may be impractical.”
Other efforts to improve clinical research include those focused on correcting for and/or eliminating several confounding variables that tend to plague sleep research. The surprising power of the placebo effect, 23 the related disconnect between objective and subjective evaluations of sleep loss and recovery from sleep loss, variable adherence to treatments, and, more recently, deceptive practices among clinical trial participants, are a few examples.
The placebo effect, which refers to any outcome that may be attributable to the expectations of clinical trial participants rather than to the drug or device being tested, can be especially problematic in experimental protocols that involve self-reports of sleep quality.
“Clinical trials involving patients with disorders such as insomnia or RLS that rely solely on subjective measures, or ratings of severity based on patient report, are particularly vulnerable to the placebo effect,” says Dr. Kushida. “It has been demonstrated that when these patients believe that they are receiving the study drug or device the likelihood of their experiencing a positive effect can increase significantly. There have been efforts to develop or introduce new objective endpoints in these studies, which may help with this problem.”
Achieving the right balance of subjective and objective measures of sleep is an important goal in both research and clinical practice. The current gold standard for objective assessment of sleep is polysomnography (PSG), which includes electrophysiological recordings of brain activity (EEG), muscle activity (EMG), and eye movements (EOG). A valuable, non-invasive method for determining sleep continuity and sleep architecture, PSG has been an indispensable objective endpoint in clinical trials, but it is expensive and not always practical. Novel approaches to objective measurement, including actigraphy, which may be used to help minimize recall bias and complement subjective measures of sleep (e.g., sleep logs or diaries), still have drawbacks. 24
“The problem with wearable devices right now,” says Dr. Kushida, “is that they tend to overestimate sleep, sometimes by as much as an hour. They also are not yet capable of accurately detecting different stages of sleep, such as non-REM and REM sleep. Because of our proximity to Silicon Valley, our laboratory tests a lot of these new devices, and often by the time we have finished testing one prototype, new ones have emerged. The product cycles are rapid, and the companies keep incorporating newer and newer technology. So, down the road, within about five to ten years, I think these devices will likely estimate sleep and detect sleep stages with precision.”
Also, objective tools are needed for addressing problems with adherence to treatment. One important current aim is to detect and correct for non-obvious factors that result in failure to adhere to treatment, whether unintended or deliberate, to ensure that trial outcomes accurately reflect the efficacy of a drug, medical device, or behavioral intervention. 25 A related problem is deliberate deception by trial participants. As part of a National Heart, Lung, and Blood Institute (NHLBI)-supported study focused on detecting and correcting for adherence problems, Dr. Kushida and colleagues began to explore the prevalence of deceptive practices among clinical trial participants. 26
“We found that deception among clinical trial participants is pretty common and that there is quite a range of deceptive practices, “says Dr. Kushida. “They include underreported drug holidays, fabrication or withholding of medical histories, pill dumping, exaggerated symptoms, and falsification of current health status. It’s important that we find a way to address these deceptive practices because both the integrity of research data and the safety of participants are at risk.”
Dr. Kushida adds that newer tools, such as electronic monitoring of pill dispensing and statistical predictive adherence models, may uncover and remedy pressing problems related to adherence and deceptive practices. “It already takes about 12 years for a new drug to be approved, and about three to five years for a new device to be approved. When deceptive practices are discovered too late, it can lead to the invalidation of research findings and further delays in approving much-needed treatments.”
Enhancing clinical research in the field will require a cooperative, international effort focused on advancing knowledge about sleep, circadian rhythms, and sleep disorders worldwide. During Dr. Kushida’s tenure as inaugural president of the World Sleep Society (WSS), he led an initiative to create international sleep fellowships to prepare physicians and scientists from various countries for future leadership roles in basic and/or clinical sleep research. He also oversaw the development of an International Sleep Research Network, designed to help sleep scientists and clinicians find collaborators with similar clinical/research interests. As the WSS continues to offer new services and expand its programs, it will be with an awareness of the needs of disadvantaged populations and the importance of access to appropriate treatment.
“One initiative of the WSS involves reviewing current published guidelines in various countries, to determine whether they meet international standards,” says Dr. Kushida. “Many guidelines are region-specific and list only medications approved in specific countries or regions. As we review the guidelines, we endorse them with caveats; we may note that particular treatments for insomnia are recommended, and when these are not available we recommend acceptable substitutes. The goal is to ensure that specialists can use practice guidelines in whichever country they practice sleep medicine, and that patients are receiving the best possible treatment available.”

COMMENTS
Advances in sleep research in 2021 have brought about clinical developments for the next decade. Additionally, sleep telemedicine services have expanded rapidly, driven by the COVID-19 pandemic, to best serve patients with sleep disorders.1 Here, we will explore some of the most impactful clinical studies from this field in 2021.
INTRODUCTION. Sleep is vital for health and well-being in children, adolescents, and adults. 1-3 Healthy sleep is important for cognitive functioning, mood, mental health, and cardiovascular, cerebrovascular, and metabolic health. 4 Adequate quantity and quality of sleep also play a role in reducing the risk of accidents and injuries caused by sleepiness and fatigue, including workplace ...
Evidence on the relationship between sleep and mental health. The association between sleep and mental health is well documented [9,13,, , , , , [23]∗].For example, people with insomnia are 10 and 17 times more likely than those without insomnia to experience clinically significant levels of depression and anxiety, respectively [].Furthermore, a meta-analysis of 21 longitudinal studies ...
Advances in sleep research in 2021 have brought about clinical developments for the next decade. Additionally, sleep telemedicine services have expanded rapidly, driven by the COVID-19 pandemic, to best serve patients with sleep disorders. 1 Here, we will explore some of the most impactful clinical studies from this field in 2021. Progress has been made in evaluating the relationship between ...
Sleep articles from across Nature Portfolio. Sleep is a state characterized by a reduced responsiveness to sensory stimuli, suppressed locomotor activity and rapid reversibility to wakefulness. It ...
1. Introduction. Sleep loss has a negative effect on multiple neurobehavioral functions, such as psychomotor vigilance performance (cognitive), daytime sleepiness, and affect (Franzen et al., 2011; Van Dongen et al., 2003).Degradation of vigilance following sleep deprivation is one of the most robust alterations in healthy young adults aged 18-30 years (Lim & Dinges, 2010).
The extent to which sleep is causally related to mental health is unclear. One way to test the causal link is to evaluate the extent to which interventions that improve sleep quality also improve mental health. ... Sleep Med Rev. 2021 Dec:60:101556. doi: 10.1016/j.smrv.2021.101556. Epub 2021 Sep 23. ... Future research might consider how ...
Much of the research on mechanisms focusses on sleep disturbance rather than sleep duration, particularly in relation to the years leading up to dementia diagnosis. ... Neurol. 89, 293-303 (2021 ...
Advances in sleep research in 2021 have brought about clinical developments for the next decade. Additionally, sleep telemedicine services have expanded rapidly, driven by the COVID-19 pandemic, to best serve patients with sleep disorders.1 Here, we will explore some of the most impactful clinical studies from this field in 2021.
Decades of work have shown that sleep contains distinct neural dynamics linked to cognition, such as slow waves in neural activity that appear in non-rapid eye movement (NREM) sleep ().More recent discoveries have shown that sleep is also a heightened state for waste removal from the brain (5, 6).Metabolic waste products are transported out of brain tissue via the interstitial fluid (ISF ...
The Journal of Sleep Research, owned by the European Sleep Research Society, is an international journal dedicated to basic and clinical sleep research. reflecting the progress in this rapidly expanding field, promoting the exchange of ideas between scientists at a global level. Detailed Author Guidelines with valued input and quick decision ...
Decades of research have linked chronic sleep deprivation to an increased risk for obesity, heart disease, Type 2 diabetes, and problems with immune function (" Sleep and Sleep Disorders ," Centers for Disease Control and Prevention). Sleeping more or less than recommended—typically 7 to 9 hours a night—is a significant predictor of ...
FULL STORY. All it takes is three consecutive nights of sleep loss to cause your mental and physical well-being to greatly deteriorate. A new study published in Annals of Behavioral Medicine ...
Published Dec. 6, 2021 Updated Dec. 13, 2021. Leer en español. ... Sleep deprivation was a factor in some of the biggest environmental disasters in recent decades, including the 1979 nuclear ...
2. Our brain replays memories while we sleep. This year marks the centenary of the first demonstration that sleep improves our memory. However, a 2023 review of recent research has shown that ...
The latest news, features, original research, and expert advice to help you sleep better. Updated May 3, 2024. 46% of People with Below-Average Sleep Quality Rate Their Mental Health As Poor. A new SleepFoundation.org survey shows a strong link between sleep quality and mental health: when one suffers, the other does as well.
It can make getting a good night's sleep on a regular basis seem like a dream. But sleep is as important for good health as diet and exercise. Good sleep improves your brain performance, mood, and health. Not getting enough quality sleep regularly raises the risk of many diseases and disorders. These range from heart disease and stroke to ...
This study was designed to evaluate echocardiographic findings in patients with obstructive sleep apnea (OSA) with cognitive impairment and compare it with the control group. Ensieh Vahedi, Arezoo Khosravi, Rahman Alizadian and Taleb Badri. Sleep Science and Practice 2021 5 :1.
Below are two lists that highlight noteworthy studies published in 2021 in the Journal of Clinical Sleep Medicine. The first list includes the 10 articles with the highest Altmetric scores. ... case reports and commentaries applicable to the clinical diagnosis and treatment of sleep disorders. Read more sleep research on the website of the ...
Chia-Luen Leu and others. Restless legs syndrome (RLS) is a neurological disorder characterized by uncomfortable or unpleasant sensations in the legs during rest periods. To relieve these sensations, patients move their legs, causing sleep disruption. While the pathogenesis of RLS has yet to be resolved, there is a strong ...
A few empirical studies have shown that sleep helps extract statistical regularities (1-3), solve problems (4, 5), or reorganize associative memories in a way that promotes creativity (6-8).Although the role of sleep in creative problem-solving is oft cited in the sleep literature (9, 10), supporting evidence is unexpectedly scarce when compared to other cognitive functions like memory ...
Chao et al. (2021) [126] CBTi: WLC: Depression: HADS-D: 32: 39: ... the timing of sleep is particularly important in circadian rhythm disorders and daytime sleepiness is a key outcome in sleep apnoea research. Future research might consider examining the effect of improving specific sleep disorders on mental health by conceptualising ...
Polysomnographic recordings were performed on the patients with sleep bruxism sleeping in the low Fowler's (15°-30°) or supine position (n = 11), and with methazolamide or placebo treatment (100 mg, 3-4 hr before bedtime, P.O., n = 9), and changes in sleep variables and heart rate variance during sleep in the low Fowler's position or with ...
Advance Articles for November 2021 Neural mechanisms that promote food consumption following sleep loss and social stress: An fMRI study in adolescent girls with overweight/obesity Chad D Jensen, Kelsey K Zaugg, Nathan M Muncy, Whitney D Allen, Robyn Blackburn, Kara M Duraccio, Kimberly A Barnett, C Brock Kirwan, Johanna M Jarcho
Research has also shown that sleep strengthens memory for the most important aspects of an experience, restructures our memories to form more cohesive narratives and helps us come up with solutions to problems we are stuck on. Science is showing that sleeping on it really does help. 3. Sleep keeps our minds healthy.
You might also feel quick-tempered, moody or depressed. Children and adolescents with sleep apnea might perform poorly in school or have behavior problems. High blood pressure or heart problems. Sudden drops in blood oxygen levels that occur during OSA increase blood pressure and strain the cardiovascular system.
SLEEP is the annual meeting of the Associated Professional Sleep Societies, a joint venture of the AASM and the Sleep Research Society. RELATED TOPICS. ... Aug. 18, 2021 — Children and ...
2. Our brain replays memories while we sleep. This year marks the centenary of the first demonstration that sleep improves our memory. However, a 2023 review of recent research has shown that ...
A new study to be presented at the SLEEP 2024 annual meeting found that better sleep health was associated with lower levels of loneliness, and this association was stronger among younger adults ...
In the inaugural issue of the Journal of Clinical Sleep Medicine (2005), a feature article 1 traced early milestones in the developing field of sleep medicine, which slowly emerged from the older field of sleep research during the 1970s and 1980s. Sleep medicine, the article noted, was closely linked with and made possible by the discovery of electrical activity in the brain.