Advanced Mental Health Nursing Assessment, Formulation and Decision-Making
- First Online: 07 November 2022

Cite this chapter

- Diana Polhuis 4 &
- Annmarie Grealish 5
1449 Accesses
This chapter aims to provide an understanding of advanced clinical assessment skills in mental health practice that considers the interface between physical and mental health, comorbidities, complexities and environmental and social factors. Advanced mental health assessment and decision-making require intuitive and analytic clinical reasoning, critical thinking, professional knowledge and shared decision-making. It also requires the integration of nursing knowledge, with knowledge from other fields (medicine, psychology, sociology, pharmacology). In addition, a comprehensive assessment needs to be underpinned by the principles of recovery, trauma-informed care and a strengths-based approach. Therefore, it stands to reason that these concepts will be incorporated in this chapter by focusing on the knowledge and skills required to build an account of why and how problems arise, developing collaborative formulation and goal settings, whilst managing the challenges and pitfalls of the essential part of the therapeutic process.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Trauma-Informed Care: Progressive Mental Health Care for the Twenty-First Century
Care planning for consumers on community treatment orders: an integrative literature review.

Optimising outcomes for complex trauma survivors: assessing the motivators, barriers and enablers for implementing trauma informed practice within a multidisciplinary health setting
Herdman TH, Kamitsuru S, Lopes CT. NANDA international nursing diagnoses: definitions and classifications, 2021–2023. 12th ed. New York: Thieme Medical Publishers; 2021.
Google Scholar
Tanner CA. Thinking like a nurse: a research-based model of clinical judgement in nursing. J Nurs Educ. 2006;45(6):204–11. https://doi.org/10.3928/01484834-20060601-04 .
Article PubMed Google Scholar
Schober M. Introduction to advanced nursing practice: an international focus. Switzerland: Springer International Publishing; 2016.
Book Google Scholar
Boeving W. HEE Over Herstel, Empowerment en Ervaringsdeskundigheid in de psychiatrie [phd dissertation]. Maastricht: University of Maastricht; 2017. https://www.trimbos.nl/wp-content/uploads/sites/31/2021/09/af1550-hee.pdf .
Department of Health. Strengths-based social work practice with adults: roundtable report United Kingdom: Department of Health; 2017.
Shields-Zeeman L, Petrea I, Smit F, Hipple Walters B, Dedovic J, Rojnic Kuzman M, Nakov V, Nica R, Novotni A, Roth C, Tomcuk A, Wijnen BFM, Wensing M. Towards community-based and recovery-oriented care for severe mental disorders in Southern and Eastern Europe: aims and design of a multi-country implementation and evaluation study (RECOVER-E). Int J Ment Health Syst. 2020;14:30. https://doi.org/10.1186/s13033-020-00361-y . eCollection 2020.
Article PubMed PubMed Central Google Scholar
Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry. 2011;199(6):445–52. https://doi.org/10.1192/bjp.bp.110.083733 .
Fox J. The contribution of experiential wisdom to the development of the mental health professional discourse. Schizophr Bull. 2017;43(3):481–5. https://doi.org/10.1093/schbul/sbv082 .
Isobel S, Wilson A, Gill K, Howe D. ‘What would a trauma-informed mental health service look like?’ Perspectives of people who access services. Int J Ment Health Nurs. 2021;30(2):495–505. https://doi.org/10.1111/inm.12813 . Epub 2020 Nov 21.
Reeves E. A synthesis of the literature on trauma-informed care. Issues Ment Health Nurs. 2015;36(9):698–709. https://doi.org/10.3109/01612840.2015.1025319 .
Rapp CA, Sullivan WP. The strengths model: birth to toddlerhood. Adv Soc Work. 2014;15(1):129–42. https://doi.org/10.18060/16643 .
Article Google Scholar
Price A, Ahuja L, Bramwell C, Briscoe S, Shaw L, Nunns M, et al. Research evidence on different strengths-based approaches within adult social work: a systematic review. Southampton: NIHR Health Services and Delivery Research Topic Report; 2020. https://doi.org/10.3310/hsdr-tr-130867 .
Wand T, Acret L, D’Abrew N. Introducing solution-focussed brief therapy to mental health nurses across a local health district in Australia. Int J Ment Health Nurs. 2018;27(2):774–82. https://doi.org/10.1111/inm.12364 . Epub 2017 Jun 23.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersly P, et al. Shared decision-making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–7. https://doi.org/10.1007/s11606-012-2077-6 .
Fisher A, Mills K, Teesson M, Marel C. Shared decision-making among people with problematic alcohol/other drug us and co-occurring mental health conditions: a systematic review. Drug Alcohol Rev. 2021;40:307–24. https://doi.org/10.1111/dar.13149 .
Shared decision-making in mental health care. Practice, research, and future directions, SAMHSA. 2011. https://store.samhsa.gov/sites/default/files/d7/priv/sma09-4371.pdf . Accessed 19 Oct 2021.
Alguera-Lara V, Dowsey MM, Ride J, Kinder S, Castle D. Shared decision making in mental health: the importance for current clinical practice. Australas Psychiatry. 2017;25(6):578–82. https://doi.org/10.1177/1039856217734711 .
Pohar Manhas K, Olson K, Churchill K, Vohra S, Wasylak T. Experiences of shared decision-making in community rehabilitation: a focused ethnography. BMC Health Serv Res. 2020;20:329. https://doi.org/10.1186/s12913-020-05223-4 .
Huang C, Plummer V, Lam L, Cross W. Perceptions of shared decision-making in severe mental illness: an integrative review. J Psychiatr Ment Health Nurs. 2020;27:103–27. https://doi.org/10.1111/jpm.12558 .
Article CAS PubMed Google Scholar
Menear M, Dugas M, Careau E, Chouinard MC, Dogba MJ, Gagnon MP, et al. Strategies for engaging patients and families in collaborative care programs for depression and anxiety disorders: a systematic review. J Affect Disord. 2020;263:528–39. https://doi.org/10.1016/j.jad.2019.11.008 .
Haines A, Perkins E, Evans EA, McCabe R. Multidisciplinary team functioning and decision making within forensic mental health. Ment Health Rev (Brighton). 2018;23(3):185–96. https://doi.org/10.1108/MHRJ-01-2018-0001 .
Marks J, Foster R, Gibson SL, Simpson A, Rinaldi M, Repper J, Worner J, Patel S, Lucock M, Ussher M, White S, Goldsmith L, Barlow S, Gillard S. Development of a peer support intervention to improve the experience and outcomes of discharge from inpatient mental health care: the role of experiential knowledge in a coproduced approach. BMC Res Notes. 2021;14(1):320. https://doi.org/10.1186/s13104-021-05735-0 .
Williamson P. A 4-step model of relationship-centered communication. In: Suchman A, Sluyter D, Williamson P, editors. Leading change in healthcare: transforming organizations using complexity, positive psychology and relationship centered care. Oxford: Radcliffe Publishing; 2011.
Argyle M. Bodily communication. 2nd ed. Madison: International Universities Press; 1988.
Egan G. The skilled helper: a systematic approach to effective helping. Brooks/Cole: Pacific Grove; 1975.
Sunderland M, Batterham P, Calear A, Carragher N. Self-report scales for common mental disorders: an overview of current and emerging methods. In: Sellbom M, Suhr J, editors. The Cambridge handbook of clinical assessment and diagnosis (Cambridge handbooks in psychology). Cambridge: Cambridge University Press; 2019. p. 263–77. https://doi.org/10.1017/9781108235433.019 .
Chapter Google Scholar
Kingsley C, Patel S. Patient-reported outcome measures and patient-reported experience measures. BJA Educ. 2017;17(4):137–44. https://doi.org/10.1093/bjaed/mkw060 .
Shoman Y, Majery N, Otelea M, Lambreghts C, Canu IG. How to identify the most suitable questionnaires and rating scales for your research and clinical practice? Int J Clin Pract. 2021;00:e14895. https://doi.org/10.1111/ijcp.14895 .
Priebe S, Huxley P, Knight S, Evans S. Application and results of the Manchester short assessment of quality of life (MANSA). Int J Soc Psychiatry. 1999;45(1):7–12. https://doi.org/10.1177/002076409904500102 .
Gordon M. Manual of nursing diagnosis. 13th ed. Burlington: Jones & Bartlett Learning; 2014.
Rookhuizen ED, Stringer B, Huising MS, de Ruijter E, van Meijel B. Prescribing psychotropic medication by the nurse practitioner in mental health care: an explorative study (article in Dutch). Tijdschr Psychiatr. 2017;59(4):229–233.
Earl EA, Taylor J, Peet M, Grant G. Nurse prescribing in specialist mental health (part 1): the views and experiences of practising and non-practising nurse prescribers and service users. J Psychiatr Ment Health Nurs. 2011;18(3):189–97. https://doi.org/10.1111/j.1365-2850.2010.01672.x .
Earl EA, Taylor J, Peet M, Grant G. Nurse prescribing in specialist mental health (part 2): the views and experiences of psychiatrists and health professionals. J Psychiatr Ment Health Nurs. 2011;18(4):281–7. https://doi.org/10.1111/j.1365-2850.2009.01517.x .
Moorhead S, Swanson E, Johnson M, Maas M. Nursing outcome classification (NOC). 6th ed. St. Louis: Mosby/Elsevier; 2018.
Butcher HK, Bulechek GM, Dochterman JM, Wagner CM. Nursing interventions classification (NIC). 7th ed. St. Louis: Mosby/Elsevier; 2019.
Koekkoek B, van Meijel B, Perquin A, Hutschemeakers G. Decision-making on (dis)continuation of long-term treatment in mental health services is an interpersonal negotiation rather than an objective process: qualitative study. BMC Psychiatry. 2019;19:92. https://doi.org/10.1186/s12888-019-2072-0 .
Article CAS PubMed PubMed Central Google Scholar
Ameel M, Leino H, Kontio R, van Achterberg T, Junttila K. Using the nursing interventions classification to identify nursing interventions in free-text nursing documentation in adult psychiatric outpatient care setting. J Clin Nurs. 2020;29(17–18):3435–44. https://doi.org/10.1111/jocn.15382 .
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Buckley MR. Back to basics: using the DSM-5 to benefit clients. The Professional Counselor. 2014;4(3):159–65. https://doi.org/10.15241/mrb.4.3.159 .
Gaebel W, Stricker J, Riesbeck M, Zielasek J, Kerst A, et.al. Accuracy of diagnostic classification and clinical utility assessment of ICD-11 compared to ICD-10 in 10 mental disorders: findings from a web-based field study. Eur Arch Psychiatry Clin Neurosci 2020; 270(3): 281–289. https://doi.org/10.1007/s00406-019-01076-z .
Van Os J, Delespaul P, Wigman J, Myin-Germeys I, Wichers M. Beyond DSM and ICD: introducing “precision diagnosis” for psychiatry using momentary assessment technology. World Psychiatry. 2013;12(2):113–7. https://doi.org/10.1002/wps.20046 .
WHO. International Classification of Functioning, Disability and Health (ICF) [Internet]. https://www.who.int/classifications/international-classification-of-functioning-disability-and-health . Accessed 2 Feb 2021.
Lundälv J, Törnbom M, Larsson P, Sunnerhagen KS. Awareness and the arguments for and against the international classification of functioning, disability and health among representatives of disability organisations. Int J Environ Res Public Health. 2015;12(3):3293–300. https://doi.org/10.3390/ijerph120303293 .
Macneil CA, Hasty MK, Conus P, Berk M. Is diagnosis enough to guide interventions in mental health? Using case formulation in clinical practice. BMC Med. 2012;10(111):1–3. https://doi.org/10.1186/1741-7015-10-111 .
Restifo S. An empirical categorization of psychosocial factors for clinical case formulation and treatment planning. Aust Psychiatry. 2010;18(3):210–3. https://doi.org/10.3109/10398561003681335 . PMID: 20367292.
Weerasekera P. Formulation: a multiperspective model. Can J Psychiatry. 1993;38(5):351–8. https://doi.org/10.1177/070674379303800513 . PMID: 8348476.
Harder K, Munro I, Woodhouse A. Diagnostic systems used in clinical assessment. In: Edward K, Munro I, Welch A, Cross W, editors. Mental health nursing: dimensions of praxis. 3rd ed. Oxford: Oxford University Press; 2018. p. 23–53.
Redhead S, Johnstone L, Nightingale J. Clients’ experiences of formulation in cognitive behaviour therapy. Psychol Psychother. 2015;88(4):453–67. https://doi.org/10.1111/papt.12054 .
Richards DA, Richards A, Barkham M, Cahill J, Williams C. PHASE: a ‘health technology’ approach to psychological treatment in primary mental health care. Primary Health Care Res Dev. 2002;3(3):159–68. https://doi.org/10.1191/1463423602pc103oa .
Crowe MC, Carlyle D, Farmar R. Clinical formulation for mental health nursing practice. J Psychiatr Ment Health Nurs. 2008;15(10):800–7. https://doi.org/10.1111/j.1365-2850.2008.01307.x .
Chen SL, Hsu HY, Chang CF, Lin ECL. An exploration of the correlates of nurse practitioners’ clinical decision-making abilities. J Clin Nurs. 2016;25(7–8):1016–24. https://doi.org/10.1111/jocn.13136 .
Lee DSK, Lim Abdullah K, Subramanian P, Bachmann RT, Ong SL. An integrated review of the correlation between critical thinking ability and clinical decision-making in nursing. J Clin Nurs. 2017;26:4065–79. https://doi.org/10.1111/jocn.13901 .
Hammond KR, Hamm RM, Grassia J, Pearson T. Direct comparison of the efficacy of intuitive and analytical cognition in expert judgment. IEEE Trans Syst Man Cybern. 1987;17(5):753–70. https://doi.org/10.1109/TSMC.1987.6499282 .
Dhami MK, Mumpower JL, Kenneth R. Hammond’s contributions on the study of judgment and decision making. Judgm Decis Mak. 2018;13(1):1–22.
van Graan AC, Williams MJS, Koen MP. Professional nurses’ understanding of clinical judgement: a contextual inquiry. Health SA Gesondheid. 2016;21:280–93. https://doi.org/10.1016/j.hsag.2016.04.001 .
Shapiro F. The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: addressing the psychological and physical symptoms stemming from adverse life experiences. Perm J. 2014;18(1):71–7. https://doi.org/10.7812/TPP/13-098 .
Peeters N, van Passel B, Krans J. The effectiveness of schema therapy for patients with anxiety disorders, OCD, or PTSD: a systematic review and research agenda. Br J Clin Psychol. 2021:1–19. https://doi.org/10.1111/bjc.12324 .
Download references
Author information
Authors and affiliations.
GGZ-VS University of Applied Science, Utrecht, the Netherlands
Diana Polhuis
University of Limerick, Limerick, Ireland
Annmarie Grealish
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
School of Nursing and Midwifery, Trinity College Dublin, Dublin, Ireland
Agnes Higgins
School of Social Services and Health Care, Tampere University of Applied Sciences, Tampere, Finland
Nina Kilkku
School of Health Sciences, University of Akureyri, Akureyri, Iceland
Gisli Kort Kristofersson
Rights and permissions
Reprints and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Polhuis, D., Grealish, A. (2022). Advanced Mental Health Nursing Assessment, Formulation and Decision-Making. In: Higgins, A., Kilkku, N., Kort Kristofersson, G. (eds) Advanced Practice in Mental Health Nursing. Springer, Cham. https://doi.org/10.1007/978-3-031-05536-2_5
Download citation
DOI : https://doi.org/10.1007/978-3-031-05536-2_5
Published : 07 November 2022
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-05535-5
Online ISBN : 978-3-031-05536-2
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Research article
- Open access
- Published: 16 April 2019
Recovery-focused mental health care planning and co-ordination in acute inpatient mental health settings: a cross national comparative mixed methods study
- Michael Coffey ORCID: orcid.org/0000-0002-0380-4704 1 ,
- Ben Hannigan 2 ,
- Sally Barlow 3 ,
- Martin Cartwright 4 ,
- Rachel Cohen 5 ,
- Alison Faulkner 6 ,
- Aled Jones 2 &
- Alan Simpson 3 , 7
BMC Psychiatry volume 19 , Article number: 115 ( 2019 ) Cite this article
45 Citations
52 Altmetric
Metrics details
Involving mental health service users in planning and reviewing their care can help personalised care focused on recovery, with the aim of developing goals specific to the individual and designed to maximise achievements and social integration. We aimed to ascertain the views of service users, carers and staff in acute inpatient wards on factors that facilitated or acted as barriers to collaborative, recovery-focused care.
A cross-national comparative mixed-methods study involving 19 mental health wards in six service provider sites in England and Wales. This included a survey using established standardised measures of service users ( n = 301) and staff ( n = 290) and embedded case studies involving interviews with staff, service users and carers ( n = 76). Quantitative and qualitative data were analysed within and across sites using descriptive and inferential statistics, and framework method.
For service users, when recovery-oriented focus was high, the quality of care was rated highly, as was the quality of therapeutic relationships. For staff, there was a moderate correlation between recovery orientation and quality of therapeutic relationships, with considerable variability. Staff members rated the quality of therapeutic relationships higher than service users did. Staff accounts of routine collaboration contrasted with a more mixed picture in service user accounts. Definitions and understandings of recovery varied, as did views of hospital care in promoting recovery. Managing risk was a central issue for staff, and service users were aware of measures taken to keep them safe, although their involvement in discussions was less apparent.
Conclusions
There is positive practice within acute inpatient wards, with evidence of commitment to safe, respectful, compassionate care. Recovery ideas were evident but there remained ambivalence on their relevance to inpatient care. Service users were aware of efforts taken to keep them safe, but despite measures described by staff, they did not feel routinely involved in care planning or risk management decisions. Research on increasing therapeutic contact time, shared decision making in risk assessment and using recovery focused tools could further promote personalised and recovery-focused care planning.
This paper arises from a larger study published by National Institute for Health Research (Simpson A, et al, Health Serv Deliv Res 5(26), 2017).
Peer Review reports
Improving the treatment and care of people with mental illness is amongst key priorities for health and social care in both England and Wales [ 1 ]. However, despite the shift to community-based models of care, considerable resources are still spent on acute inpatient beds: as much as £585million in 2009–10 [ 2 ].
In England in 2016–17, 101,589 people in contact with mental health and learning disability services spent time in hospital, with an estimated 45,864 people detained under the Mental Health Act (MHA) 1983 [ 3 ]. In Wales, 8723 admissions to hospital for mental illness took place in 2016–17, with 1776 of these taking place using sections of the MHA 1983 [ 4 ]. This volume of admissions requires considerable planning and coordination to ensure effective care is delivered consistently.
Health care is a devolved responsibility in the UK meaning that the context and delivery of mental health care is diverging between countries, providing a rich geographical comparison for research. In England the care programme approach (CPA), and in Wales care and treatment plans (CTPs), oblige providers to: comprehensively assess health/social care needs and risks; develop a written care plan; allocate a care co-ordinator; and regularly review care. CPA/CTP processes are now also expected to reflect a philosophy of recovery and to promote personalised care [ 5 , 6 ]. These similarities between CPA and CTP mask an important difference too however. CPA in England is central guidance while CTP in Wales is legislative and places legal obligations on health boards and local authorities. CTP in Wales uniquely has an associated code of practice, stipulating for example that only specifically qualified workers (e.g. registered mental health nurses, occupational therapists and clinical psychologists) can act as care co-ordinators [ 7 ].
The concept of recovery in mental health was initially developed by service users and refers to “a way of living a satisfying, hopeful, and contributing life even with limitations caused by illness,” while developing new purpose or meaning [ 8 ]. (p527) The importance of addressing personal recovery, alongside more conventional ideas of clinical recovery [ 9 ] is now supported in guidance for all key professions [ 10 , 11 , 12 , 13 ]. To this has been added the idea of personalisation. This aims to see people and their families taking more control over their support and treatment options, alongside new levels of partnership and collaboration between service users (or citizens) and professionals [ 14 ]. (p3) Recovery and personalisation in combination mean tailoring support to fit the specific needs of the individual and enabling social integration through greater involvement of local communities [ 15 ].
The CPA/CTP are central to modern mental health care [ 16 ] yet there are few studies that explicitly explore the practices of care planning and coordination in community services and even fewer focusing on inpatient care planning [ 17 ]. A relatively rare example of the former is the recently completed COCAPP study [ 18 , 19 ]. In the UK national quality statements include the requirement that service users can jointly develop a care plan with mental health professionals, are given a copy with an agreed date to review it, and are routinely involved in shared decision-making [ 20 ]. National policies [ 1 , 6 ] outline expectations of recovery and involvement in decisions about treatment. This holds true for both informal and detained inpatients, with a requirement that reasonable adjustments are made where necessary to ensure that people are supported to live as full and socially participative lives as possible [ 21 ]. However, national quality reviews reveal limited evidence of service users’ views being listened to, with concerns being raised that control and containment are prioritised over treatment and support [ 21 ].
Earlier national reviews across both nations found that service users remained largely mystified by the care planning and review process itself, with significant proportions not understanding their care plans, not receiving written copies of their plan and often not feeling involved in the writing of care plans and setting of goals [ 22 , 23 ]. Clearly, there are significant problems with inpatient care planning with the Care Quality Commission (CQC) noting “significant gap between the realities observed in practice and the ambitions of the national mental health policy” [ 21 ]. (p5) The House of Commons Health Committee [ 24 ] subsequently reported widespread concerns about delays in care planning and an imbalance between a focus on risk rather than recovery.
Previously, the Healthcare Commission [ 25 ] measured performance on 554 wards across 69 NHS Trusts providing mental health acute inpatient services. They found that almost two-fifths of trusts (39%) scored weak on involving service users and carers; 50% of care plans sampled did not record the service user’s views; and nearly a third of care records (30%) did not record whether or not the service user had a carer. A third of all care records sampled (33%) showed that community care coordinators provided input into the service users’ care review meetings only “some or none of the time”.
The aim of this study was to identify factors that facilitate or hinder recovery-focused personalised care planning and coordination in acute inpatient mental health settings. As an exploratory study guided by the Medical Research Council (MRC) [ 26 ] Complex Interventions Framework we aimed to generate empirical data, new theoretical knowledge and greater understanding of the complex relationships between collaborative care planning, recovery and personalisation.
We conducted a cross-national comparative study of recovery-focused care planning and coordination in inpatient mental healthcare settings, employing a concurrent transformative mixed methods approach with embedded case studies [ 27 ]. A full account of our methods is provided elsewhere [ 28 ].
In summary, our study was informed by systems ideas emphasising connections between macro, meso and micro levels of organisation [ 29 ]. Cross-national comparative research involves “comparisons of political and economic systems …and social structures” [ 30 ] (p93) where “one or more units in two or more societies, cultures or countries are compared in respect of the same concepts and concerning the systematic analysis of phenomena, usually with the intention of explaining them and generalising from them” [ 31 ]. (p1–2) In this study, devolved government and the emergence of similar but distinct health policy, legislation and service development in England and Wales provided the macro-level national context.
A case study method [ 32 ] allows the exploration of a particular phenomenon within dynamic contexts where multiple influencing variables are difficult to isolate [ 33 ]. It allows consideration of historical and social contexts [ 34 ] and is especially useful in explaining real-life links that are potentially too complex for survey or experimental approaches [ 35 ]. The definitions of the case studies were predetermined [ 36 ], focusing on selected NHS Trust/Health Boards. Data collection at this meso-level included identifying local policy and service developments alongside empirical investigations of care planning and inpatient care, recovery, personalisation, therapeutic relationships and empowerment, employing mixed quantitative and qualitative methods. This design is represented in Fig. 1 .
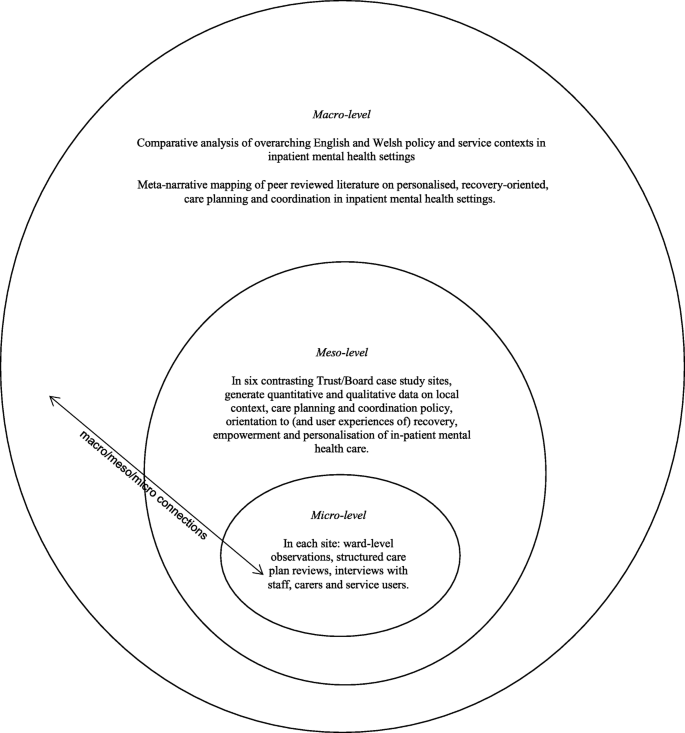
Diagram illustrating embedded case study design and integration of care planning and coordination in acute inpatient mental health settings
We selected six case study sites to match our earlier community study [ 18 ] so that comparisons and connections between community and inpatient services could be drawn [ 32 ]. These consisted of four NHS Trusts in England and two Local Health Boards in Wales that are commissioned to provide inpatient mental health services. In total 19 acute wards were selected for data collection. These sites reflected a mix of rural, urban and inner city settings in which routine inpatient care is provided to people with complex and enduring mental health problems. In each site, a single acute inpatient ward was chosen for further in-depth investigation and up to six service users, six multidisciplinary staff and four informal carers were sampled as embedded micro-level case studies [ 27 ]. Inclusion criteria for wards included that these were providing acute mental health care admissions facilities to the local adult population and had an established ward manager/team leader in post. Inclusion criteria for service user participants included that they were currently admitted to the in-patient facility, had been on the ward for a minimum of 7 days, 18 years or older, with a history of severe mental illness and able to provide informed consent. Staff inclusion criteria were staff working on inpatient wards involved in care planning or review. Full inclusion and exclusion criteria are provided elsewhere [ 28 ].
Sample size calculations
For the survey, an a priori sample size calculation was conducted using the G*Power software (version 3.1) [ 37 ]. The estimated sample size for service users was calculated for the global effect of a one-way multivariate analysis of variance (MANOVA) with six groups (sites), 17 outcomes (Recovery Self-Assessment Scale total (+ 5 sub-scales), Scale To Assess the Therapeutic Relationship total (+ 3 sub-scales), Empowerment Scale total (+ 5 sub-scales) and the Views of Inpatient Care Scale total), an α level of 0.05, power of 0.8 and a small effect size (f 2 = 0.029). This calculation suggested that a total of 276 service user participants was required.
We anticipated that with non-response and incomplete measures we would need to oversample, we therefore decided to recruit 300 service users ( n = 50 per Trust/Health Board) and 300 inpatient staff ( n = 50 per site). We anticipated that we would not achieve this sample size for informal carers and therefore aimed to recruit 150 informal carers ( n = 25 per Trust/Health Board). This was because not every service user would have a carer, therefore analysis for the informal carers would be underpowered (estimated power was 0.44). The data for the informal carers was therefore anticipated to be exploratory.
Sample size calculations for qualitative interviews were based on previous research with similar populations by the co-investigators and others. Calculations were based on understanding of the practicalities and time commitments of recruiting and interviewing participants and analysing in-depth qualitative data; and the numbers required to feel confident that the findings would be transferable to other similar settings.
Instrumentation
The data collection measures reported in this paper are;
The Recovery Self-Assessment Scale (RSA) [ 38 ]: a 36-item scale measuring the extent of recovery-oriented practices. The scale addresses the domains of life goals, involvement, treatment options, choice and individually tailored services. Acceptable internal consistency of the RSA with Cronbach’s alpha has previously been demonstrated [ 18 ]. It was completed by service users, carers and ward staff. In the current study Cronbach’s alpha for the Total RSA scale for service users was 0.98 ( N = 103) and for staff was 0.95 ( N = 186); Life Goals subscale, for service users was 0.93 ( N = 179) and for staff was 0.86 ( N = 246); Involvement subscale, for service users 0.91 ( N = 163) and for staff was 0.85 ( N = 225); Diversity of Treatment options subscale, for service users was 0.81 ( N = 172) and for staff was 0.77 (N = 225); Choice subscale, for service users was 0.81 ( N = 217) and for staff was 0.68 ( N = 254) and Individually Tailored Services subscale for service users was 0.85 ( N = 159) and for staff was 0.71 ( N = 253).
The patient and clinician versions of the Scale To Assess the Therapeutic Relationship (STAR-P and STAR-C) [ 39 ]: a 12-item scale assessing therapeutic relationships. A total STAR score is obtained by summing individual items. The subscales measure positive collaborations (possible scores 0–24), positive clinician input (possible score 0–12) and non-supportive clinician input in the patient version and emotional difficulties in the staff version (possible score 0–12). It was completed by service users and ward staff. Cronbach’s alpha for the total STAR-P scale for service users was 0.89 ( N = 264) and for staff was 0.81 ( N = 263); Positive Collaboration subscale, for service users was 0.92 ( N = 279) and for staff was 0.81 ( N = 269); Positive clinician input subscale, for service users was 0.72 ( N = 282) and for staff was 0.56 ( N = 268); and Non-Supportive clinician input subscale, for service users was 0.67 ( N = 284) and for staff was 0.63 ( N = 273).
The Empowerment Scale (ES) [ 40 ]: a 28-item questionnaire with five subscales: self-esteem, power, community activism, optimism and righteous anger. A total empowerment score is obtained by summing individual items and dividing them by the number of items. Subscale values can also be provided for ‘self-esteem-self-efficacy’, ‘power-powerlessness’, community activism and autonomy’, ‘optimism and control over the future’ and ‘righteous anger’. This scale was completed by service users. Cronbach’s alpha for the total Empowerment scale for service users was 0.82 ( N = 255); Self-esteem-self-efficacy subscale, 0.91 ( N = 272); Power-Powerlessness subscale 0.56 ( N = 271); Community activism and autonomy subscale, 0.58 ( N = 276); Optimism and control, 0.70 ( N = 275) and Righteous anger, 0.40 ( N = 281).
The Views of Inpatient Care Scale (VOICE) [ 41 ]: a 19-item patient-reported outcome measure of perceptions of acute mental health care that includes questions on involvement in care planning and ward round discussions. VOICE total score was obtained by summing individual item scores, possible total scores range from 19 to 114. The higher the total score for the VOICE the more negative the perception of the quality of care on the ward. It was completed by service users.
We further investigated internal consistency using alternative approaches, mean item-total correlations and Spearman-Brown prediction values (see Additional file 1 ). These additional analyses suggested that all subscales had acceptable internal consistency, although two subscales of the Empowerment Scale would merit further psychometric development.
We additionally conducted semi-structured interviews with ward staff, service users and carers. Interview schedules were based on our previous study and refined in consultation with our Scientific Steering Committee and Lived Experience Advisory Group (LEAG) and drawing on relevant literature. The aim of all interviews was to explore participants’ views and experiences of care planning and co-ordination, safety and risk, recovery and personalisation, and the context within which these operated. Care plan reviews and observations of ward rounds were also conducted but are not reported in this paper. In some cases participants on the case study sites completed surveys and research interviews but this was not a requirement of the study and the majority chose to participate in one part of the study only.
Research ethics
The study received NHS Research Ethics approval from the NRES Committee NRES Committee London – Fulham (Ref: 13/LO/2062) on 29th December 2014.
Considerable attention was given to ensuring the welfare of service user, carer and other participants and of the researchers. This included providing opportunities to pause or withdraw from interviews, assurances of anonymity and confidentiality and responding to concerns for people’s welfare.
Public and patient involvement (PPI) and study oversight
The study was developed and designed with full involvement of co-investigator and independent service user researcher (AF) and in consultation with SUGAR (Service User and Carer Group Advising on Research [ 42 ]). In addition, a Lived Experience Advisory Group (LEAG) met every 4/6 months during the study, consisting of seven service users and one carer with direct experience of inpatient mental health care.
The 12-member independently chaired Scientific Steering Committee (SSC) consisted of representatives with a clinical or research background from each of the participating NHS Trusts/Health Boards, as well as independent academics. One service user and one carer member also represented the LEAG.
Three Service User Researcher Assistants (SURAs)/Service User Project Assistants (SUPAs) were employed to recruit participants and conduct research interviews. All received training and ongoing support throughout the study.
Suitable local wards meeting inclusion criteria were identified with the assistance of local NHS Trust/Health Board principal investigators. Ward managers were approached by a researcher who explained the study, responded to any queries and invited them to participate. No service declined to take part. We sought approval to participate from two or three wards in each area and one of the three wards was then selected for in-depth case study of care planning including interviews. Each site was given a pseudonym to help maintain anonymity of participants. French names were chosen to avoid any accidental connection with English or Welsh sites or regions. The site names are:
All managers and ward staff involved in care planning or care plan review received written and verbal information about the study and were invited to participate in the survey (target n = 50 per Trust/Health Board).
Staff from participating wards were asked to identify service users who had been on that ward for a minimum of seven days, and who in their view potentially had the capacity to participate in the study. The service user was provided with written and verbal information by a researcher, who then ensured the person was able to provide informed consent to participate. Each participant was then given a survey pack to complete, with assistance if required. A thank you gift of £10 was given to service user participants on completion of the survey pack.
Ward staff were asked to give carer survey packs to carers (family members and friends) visiting service users on the ward (target n = 25 per Trust/Health Board). The packs included an information sheet and a Freepost return envelope. Researchers working on the ward also approached carers to invite them to participate by completing measures.
Semi-structured interviews
Key personnel (registered nurses, ward managers, occupational therapists, psychologists and psychiatrists) were identified using purposive sampling to reflect meso and micro level functions. They were invited to participate in research interviews for the in-depth case study (target n = 6 per case study ward; total n = 36). Micro-level refers to the level at which face-to-face care is organised, provided and received. For our purposes meso-level refers to management functions that enable or structure micro-level work. Staff were given written materials describing the purpose of the study including the option to decline or withdraw at any time. Informed consent procedures were followed.
Service users approaching discharge were invited to participate in an interview about their experiences of care planning and jointly review their care plan (target n = 6 per case study ward; total n = 36). Informed consent procedures were followed. A thank you gift of £10 was given to service user participants on completion of the research interview.
Service users were asked to identify a carer (if applicable) to take part in an interview (target n = 4 per case study ward; total n = 24). Carers were contacted by telephone or when visiting, in the presence of the service user if possible. Informed consent procedures were followed.
Data management and analysis
Qualitative and quantitative data in each of the sites were considered on a within-group basis prior to a cross-case analysis aimed at identifying common themes and divergences. The between-group analysis of the quantitative data compared service users and staff across sites on key markers of the service user experience (recovery-oriented care, therapeutic relationship and empowerment). The quantitative analyses were conducted alongside the qualitative analyses in a convergent parallel design that facilitates the integration of mixed methods data [ 27 ]. Large scale survey data provides a broad picture while the interview data offers more micro detail. This is a pragmatic approach to mixed method research that can generate a more complete understanding of complex phenomena or processes. Quantitative and qualitative data analyses were conducted independently and subsequently synthesised to generate understanding of the links across micro, meso and macro levels than either approach could achieve alone.
Quantitative data
Data from the questionnaires were entered into SPSS version 21 [ 43 ] and distribution of the data assessed for normality using descriptive quantitative measures of skewness and kurtosis. There were few deviations from normality (2 of 27 scale outcomes exceeded the conservative criteria of +/− 1), one was small in the extent of deviation (within +/− 2) however one scale displayed larger deviation of skewness (Emotional differences subscale, Staff outcome on the STAR-C).
A missing value analysis was completed for the 27 scale outcomes. Moderate to high levels of missing data, not missing at random, were identified on a small number of items (mean level of missing data across the 27 scales/subscales was 20%, range from 6 to 55%). The service user version of the RSA questionnaire in particular had a moderate amount of missing data. Mean replacement was used to avoid unnecessary loss of cases from the analysis. The mean of the available items for the scale and participant were used for replacement of the missing values on the scale. A series of sensitivity analyses were conducted to determine what effect mean replacement would have in the primary analyses at different levels of replacement ranging from 20 to 50% replacement. Utilising a 50% mean replacement had no substantive changes in the key statistical parameters ( p -values and associated effect sizes) and the inferences drawn, therefore it was deemed appropriate to maximise the number of cases included in the analyses.
Descriptive statistics were calculated for the four measures (VOICE, RSA, STAR and ES). Where appropriate these scores were compared against reference values (VOICE, STAR and ES) or to the participant groups (RSA). Several unadjusted one-way Analysis of Variance (ANOVA) were conducted to compare differences between the six sites on the RSA, STAR, ES and VOICE measures. Subsequent Tukey post hoc tests were conducted to ascertain which measures differed between which locations. A series of one-way analysis of covariance (ANCOVA) were completed to adjust the analyses for potential confounders. The demographic variables that were chosen for service users were: age; gender; ethnicity and living status. Three care-related variables were chosen for service users: previous admissions; time in mental health services and time on the ward. The demographic variables that were chosen for staff were: age, gender, ethnicity, personal experience of mental illness and family experience of mental illness. Two clinical variables were also chosen: time working in mental health services and time working on the ward. The criteria for adjusted analysis between the ANOVA and ANCOVA were the p -value from the omnibus test, the adjusted means and the p-value from the post-hoc test. If the p-value from the omnibus test for the ANCOVAs were not substantively different from the ANOVAs then no further post –hoc analyses were completed. A series of independent t-tests were completed to determine if there were differences between service users and staff on the outcome measures.
Correlations of the service user data were completed to identify if there was a relationship between the scores on the outcome measures used. Six Pearson’s correlations were conducted to identify if there were relationships between the mean total scores for the measures RSA and VOICE; RSA and STAR-P; RSA and ES; STAR-P and ES; STAR-P and VOICE and VOICE and ES for all service user participants and by individual site. Cohen’s [ 44 ] effect sizes were used to describe the data (Small, r = 0.10, medium r = 0.30 and large r = 0.50). A Pearson correlation was also completed for staff on the mean total scores for the RSA and STAR-C.
For all the ANOVA and ANCOVA analysis the statistical significance level was set at a level of 0.05. To account for multiple comparisons for the t-tests the significance threshold was raised to 0.005 to accommodate for the number of tests applied ( n = 10).
Qualitative data
All digital interview recordings were professionally transcribed and checked against original recordings for accuracy and identifying information redacted, before being imported into QSR International’s NVivo10 qualitative data analysis software [ 45 ] for analysis using Framework method [ 46 , 47 ]. The Framework matrix used was developed a priori from the interview schedules, with sections focusing on organisational background and developments, care planning, recovery, personalisation, safety and risk, and recommendations for improvement. Each matrix section also had an ‘other’ column for the inclusion of data-led emergent categories. Once all charting was completed, second-level summarising was undertaken to further précis data and to identify commonalities and differences.
Data collection across the six sites is summarised in Table 1 and consisted of n = 301 service users (target was 300), n = 290 members of staff (target was 300), n = 28 carers (target 150) completing survey measures.
We completed 31 research interviews with staff (target was 36), 36 with service users (target was 36); and nine with carers (target was 24).
Cross-site analyses will be presented for the four service user questionnaires (VOICE, RSA, STAR-P and ES) followed by a cross-site analysis of the two staff questionnaires (RSA and STAR-C).
Service users
To explore cross-site differences one-way ANOVAs of all total score and subscales were conducted and revealed that there were no global differences across the sites for any of the four measures. Table 2 shows the mean item scores, alongside the parameters of significance for service user participants.
For staff, one-way ANOVAs were conducted for the mean RSA and STAR-C total scores and the subscales (Table 3 ). There was a significant difference between the research sites in the mean RSA total score (F 5, 279) = 6.35, p < 0.001, η 2 = 0.32) and the mean total score for the STAR-C (F 5, 273) = 3.02, p = 0.011, η 2 = 0.23). There were also significant differences found in all of the mean item subscale scores of the RSA and the positive collaboration subscale for the STAR-C. Table 3 shows summary scores for staff.
When using Artois and Champagne as reference sites (the sites with the lowest scores) Provence and Dauphine sites scored significantly higher for the mean RSA total score indicating more recovery focused care (see Fig. 2 ). This scale measures some important perceptions that may have a significant effect on patient outcomes and concordance to care and collaboration with service users. Subsequent Tukey post-hoc tests revealed that staff in Artois (3.36, s.d. = 0.59) score significantly lower than Provence (3.76, s.d. = 0.56, p = 0.009, CI.95–0.73, − 0.07, Cohen’s d = 0.69) and Dauphine (3.74, s.d. = 0.53, p = 0.009, CI.95–0.70, − 0.06, Cohen’s d = 0.68). Staff in Champagne (3.21, s.d. = 0.46) score significantly lower than Provence ( p < 0.001, CI.95–0.92, − 0.19, Cohen’s d = 1.07) and Dauphine ( p < 0.001, CI.95–0.88, − 0.19, Cohen’s d = 1.07).
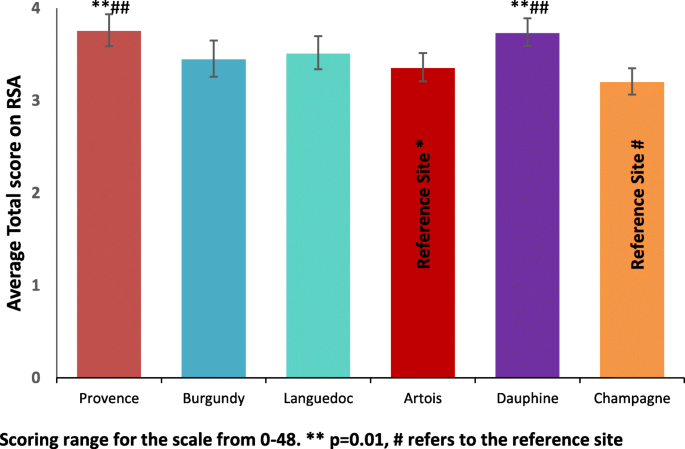
Mean Total RSA score for staff +_95% CI
STAR-C questionnaire
There were no significant differences in the staff responses across sites for the Positive Clinician Input subscale (F (5,272) = 1.53, p = 0.182, η 2 = 0.16) and the Emotional Difficulties subscale (F (5,270) = 1.91, p = 0.092, η 2 = 0.16) There were however significant differences found between sites for the Positive Collaboration subscale (F (5, 274) = 2.42, p = 0.036, η 2 = 0.20) and the STAR-C Total score (F (5, 273) = 3.02, p = 0.011, η 2 = 0.23).
STAR-C positive collaboration
Burgundy performs significantly better for the mean Positive collaboration subscale score than Artois (see Fig. 3 ). This scale measures some important perceptions around rapport and shared understanding of goals focused on mutual openness and trust. Subsequent Tukey post-hoc tests revealed that staff in Artois (17.17, s.d. = 2.65) score significantly lower on the subscale than Burgundy (18.86, s.d. = 2.57, p = 0.019, CI.95–3.20, − 0.18, Cohen’s d = 0.65). There were no significant differences between all of the other sites on this subscale.
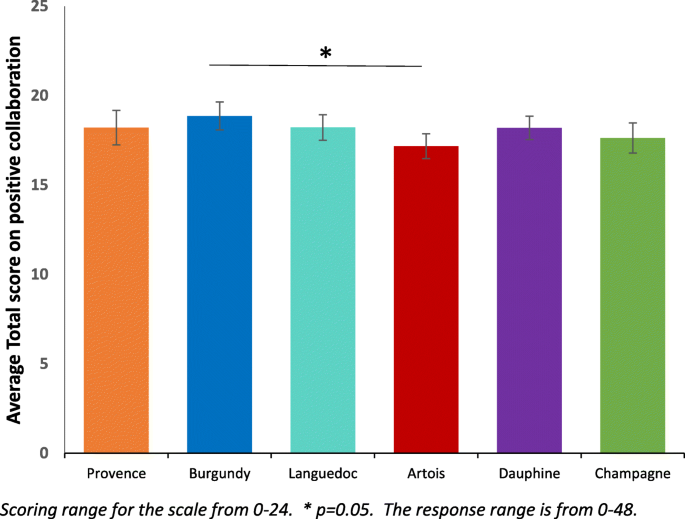
Mean Positive Collaboration subscale score for staff ±95% CI
STAR-C Total
Burgundy performs significantly better for the mean positive collaboration subscale score than Artois (see Fig. 4 ). This scale measures some important perceptions that may have a significant effect on patient outcomes and concordance to care and collaboration with service users. Subsequent Tukey post-hoc tests revealed that staff in Artois (36.08, s.d. = 4.18) score significantly lower on the subscale than Burgundy (39.33, s.d. = 4.31, p = 0.011, CI.95–5.76, − 0.75, Cohen’s d = 0.77). There were no significant differences between all of the other sites on total score.
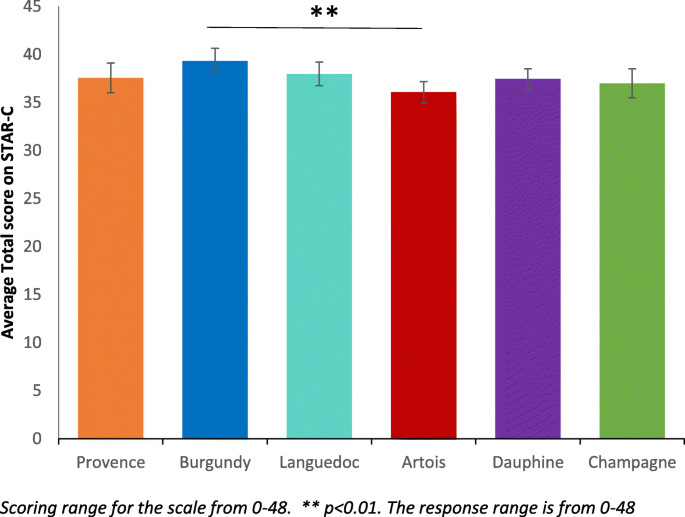
Mean STAR-C Total score for staff ±95% CI
Correlations between outcome measures
Pearson’s correlations were used for the service user survey scores to determine if there were associations between responses on the four scales. Table 4 shows that there is a strong negative correlation between the RSA and VOICE ( r = −.70, n = 285, p < 0.001). This shows that there is an inverse association between the recovery-oriented focus and the negative perception of quality of care amongst service users meaning when recovery-oriented focus was high the quality of care was viewed highly. There is also a positive correlation between the RSA and the STAR-P ( r = .61, n = 282, p < 0.001), indicating an association between the recovery-oriented focus and ratings of the quality of therapeutic relationships amongst service users. There is also a strong negative correlation between the STAR-P and VOICE scale ( r = −.64, n = 294, p < 0.001). There is also an inverse association between the quality of therapeutic relationships and the negative perception of quality of care meaning that when therapeutic relationships are scored highly the perception of quality of care is also scored highly. There are negligible relationships between the RSA and ES; STAR-P and ES and the VOICE and ES.
A Pearson’s correlation was completed at the global level with all participants to determine if there were associations for staff scores between the responses on the two questionnaire scales. This correlation were completed using pairwise deletion. There is a small to moderate correlation between the RSA and STAR-C ( r = −.28, n = 279 p < 0.001).
When comparing the correlation between the RSA and STAR-C (see Table 5 ) there is a considerable amount of variability across sites. There is a large correlation in Burgundy ( r = 0.50, n = 43, p = 0.001). There are moderate or small to moderate correlations in Artois ( r = 0.28, n = 56, p = 0.034), Languedoc ( r = 0.35, n = 47, p = 0.015) and Provence ( r = 0.28, n = 56, p = 0.034). Only small correlations were found in Champagne ( r = 0.16, n = 41, p = 0.331) and Dauphine ( r = 0.35, n = 50, p = 0.015).
Across all of the six research sites staff score significantly higher than service users on the scale to assess therapeutic relationships. In Burgundy and Dauphine the same pattern is present across all of the subscales. Positive clinician input was scored higher by staff than service users across the six sites (see Table 2 ).
Qualitative findings
Table 1 summarises the characteristics of each of the six meso-level case study sites and the types and quantity of data generated in each. Illustrative quotations used below are labelled with the initial of the site pseudonym; then ST, SU, or CA for staff, service user or carer; and their unique number, e.g. B-ST-001 (Burgundy-Staff-001).
Care planning and coordination
Staff across sites talked of the importance of collaborative care planning. Many also spoke of the value of plans being kept up-to-date with service users actively involved, and of plans being used as a way of collecting multidisciplinary contributions and of helping manage transitions between hospital and community. For example,
“[B]ringing a person’s care all together really, so it’s like a standard to work around, that it’s all centred around the patient’s care, so everything works for them in the best way, I think.” (L-ST-103)
However, staff, service user and carer interviews all revealed gaps between shared aspirations and realities, even where service users drew attention to receiving good quality care. Staff accounts of routine collaboration with service users in care planning contrasted with service user accounts which pointed to lack of involvement. In all sites some service users report that they were not involved in the planning of their care, were unaware of the content of their care plans or had not received copies, or did not feel a sense of care plan ownership. For example,
“There isn’t a treatment plan. There’s no treatment, there’s just containment. Walking to the shop to get a newspaper isn’t treatment. There’s no therapy here.” (C-SU-103)
Staff sometimes spoke of service users’ unwillingness or inability to collaborate in care planning, or of the barriers to collaborating brought about by the introduction of electronic records. Lack of a shared language was cited as a barrier in one inner city site (Dauphine). Staff in Burgundy said how the all-Wales CTP template was not well-suited to the short-term nature of acute hospital care with some domains (e.g., housing) emerging as higher priority than others.
“I think I struggle with the principles [of CTP] and how that fits perhaps into the ward – the confusion that still exists is very much present in terms of the fundamentals of it.” (B-ST-102)
Coherence and continuity in care across hospital and community interfaces were identified as important by many of those taking part, and examples of detailed and collaborative discharge planning involving staff and service users were given. Innovations were also described, such as ‘interim discharge summaries’. However, rapidly arranged discharges caused some concern with little time then available for considered planning, one service user recalled being ‘pulled in out of the blue’ to be told ‘right, you can go’ (P-SU-102).
Two types of care plan review were described: formal, typically weekly, multidisciplinary meetings chaired invariably by consultant psychiatrists and daily handovers where care on a more immediate basis was reviewed by staff. Formal ward rounds were described as key events by staff and as places where progress and plans could be reviewed in a multidisciplinary context. Service user views and experiences of these differed, within and across sites. For some they were helpful, serving as opportunities for catching up with psychiatrists and the whole multidisciplinary team.
“Sometimes you’ve got a load of people in there and you sort of feel a bit like you’re on stage, you know like the spotlight’s on you, sort of thing. But yeah. I’ve had problems with ward rounds but more recently things have been OK, I’ve been able to sort of express myself more.” (P-SU-104)
Some service users also described the opportunity to plan and prepare for formal ward round participation. Others spoke of limited time to fully consider their needs, of excessive jargon being used and of inflexibility over ward round scheduling.
Safety and risk
Assessing and managing risk were customarily seen by staff as central parts of the work of planning and providing care so that risk assessments were described as proliferating so much they were “ coming out of your eyeballs” (P-ST-101). Formal ward round-based review meetings were named as a place for risks to be discussed although not necessarily in the presence of service users. Some staff also talked of the particular issues surrounding risk and decision-making in the care of service users who were detained. Risks mentioned by staff included those to self and others, with some also noting the dangers of over-estimating risks and the importance of attending to strengths and of positive risk-taking.
“ if you let the risk rule over the actual care plan then you’re never going to get anywhere .” (L-ST-102)
Most service users talked of their safety being considered and attended to, sometimes giving specific examples of this in action (e.g., through removal of objects and the use of observations), even though risk assessments and management plans were often not actively discussed with them. Others did, however, talk of feeling unsafe in hospital and of asking for more staff.
Definitions and understandings of recovery varied amongst staff, service users and carers, as did views of the role of hospitals in promoting this. Participants, in many cases, were also aware of the disparate meanings of ‘recovery’. Some staff (e.g., in Artois) viewed recovery as problematic in the inpatient context, saying that this raised expectations or was too poorly understood to help effective care planning.
“ I think it’s about being realistic as well. … certainly it’s about fostering hope, looking for things as well, and working towards those things, but in an acute ward where people can’t … leave [the ward] ” (A-ST-106)
In Languedoc, antipathy to the idea of recovery was reported by some staff who challenged both its meaning and utility. Most service users said that hospital had helped (e.g., to stabilise medication), though some complained of having been largely left to their own devices or subjected to containment. The use of tools to aid recovery (e.g., Recovery Star) were occasionally mentioned (e.g., in Burgundy), but in most cases these were either not deployed or were described as being more suitable beyond the acute hospital care context. Service users and carers revealed a range of views around recovery, from the cure of symptoms, to the prospects of life without medication, to the idea of coming to terms with difficulties.
“getting rid of the voices and what I see. That’s my recovery” (P-SU-101).
- Personalisation
The term ‘personalisation’ was not a familiar one, with few revealing knowledge of personal budgets, “ It doesn’t mean anything, it just sounds like a made-up word .” (L-SU-102).
In all settings there was recognition of the idea that care and services should be oriented to the individual. Whilst some staff talked of inpatient care as being person-centred there was also widespread recognition of the challenges to this (e.g., tensions between different approaches to providing care, the fact that staff only get to know people as patients, and the relative (un)availability of resources). Within and across sites there were differences in service user views and experiences of individually tailored care. Some were clear that hospital had been pivotal in their care, “ without this place it would be the end of me ” (C-SU-105). Others were equally clear that their care had not been personalised, or talked of their care at home being more personalised. Carers gave positive accounts of care provided although most remained uncertain about the term personalisation,
“ I guess personalisation means the way her treatment was personalised for her and I guess it was, because everyone is different and everyone needs different help, but I don’t really know what you mean.” (P-CA-101)
The aim of this study was to identify factors that facilitate or hinder recovery-focused personalised care planning and coordination in acute inpatient mental health settings. The intention was to generate new theoretical knowledge and greater understanding of the complex relationships between collaborative care planning, recovery and personalisation.
Comparison and consideration of our survey results and interview data across sites provides some reason for optimism concerning the overall quality of mental health inpatient care but also indicators of areas where greater attention may be required.
We found no global differences across the six sites on the service user measures. The VOICE measure [ 41 ] examined service users’ perceptions of inpatient care and found marginally lower scores than the reference value [42]. However, the mean scores in all six research sites in this study were lower (so more positive) than those reported in a recently published study which examined different inpatient service models over a period from 2008 to 2010 [ 48 ]. We found that service users leaned towards a positive perception of the wards but there was wide variation within sites, suggesting a mix of views. These results converge with our research interview data showing service users being largely positive about their care, acknowledging being treated with dignity, respect and compassion. This was irrespective of legal status. Those carers interviewed also spoke positively about care provided and attitudes of staff.
Staff spoke of the challenges of collaborating on care planning with service users in severe mental distress or lacking insight and this is likely to include those formally detained. However, despite specific questions related to the legal status of services users, this was not explicitly identified as an issue perhaps reflecting the now high proportion of inpatients legally detained.
On ratings of the quality of therapeutic relationships, across all six sites staff consistently rated these relationships significantly more positively than did service users. The STAR-P measure used was initially designed for rating the one-to-one relationships that service users have with care coordinators in community teams [ 15 ] so it may be that, despite having a ‘named nurse’, the more dispersed nature of relationships with a number of ward staff over days and weeks, across shifts and 24-h care weaken any rating. Inpatient care also includes the greater likelihood of restrictions, limitations, rules and regulations necessary to provide a safe environment [ 49 ]. First- or second-hand experience of coercion and containment are also likely to be more prevalent in an inpatient setting [ 50 ]. Nevertheless, the need for further investigation to identify how positive relationships can be mutually achieved is indicated.
There was a strong perception across sites that staff were aware of policy drives to provide a greater focus on recovery, to provide respectful, compassionate and dignified care. Most staff articulated clear values and understandings reflecting core components of the focus on recovery as well as other initiatives that have been promoted in an attempt to improve inpatient services, such as the Royal College of Psychiatrists’ Accreditation for Inpatient Mental Health Services (AIMS) [ 51 ], Bright charity’s Star Wards [ 52 ] and most recently, the mental health nurse-led evidence-based intervention, SafeWards [ 53 ].
Staff participants suggested that severity of illness and/or lack of insight sometimes means that collaborative care planning is difficult to achieve, that there was often insufficient time to devote to this task, or that some service users were unwilling or unable to collaborate on care planning. Staff found it difficult to discuss care with service users especially where there was a mismatch in goals and expectations and limited advice on what a good care plan looks like or on how to identify achievable goals. Some of these barriers such as staff views on severity of illness have been found in other studies and highlighted in systematic reviews of barriers to involvement [ 54 ] and the consistency of this finding across our study sites can be read in a number of ways. First, it is undoubtedly the case that some people admitted to inpatient services are in severe distress and the process of discussing and negotiating a care plan in those first few days is unlikely to be a priority for them.
A second reading is that mental health professionals despite their claimed interest and support of involvement actually struggle to put this idea into practice and may need some guidance to achieve the aspiration of true collaboration. A possible contributor here was highlighted by both service users and staff and this relates to inflexible documentation and information technology on inpatient wards. In tandem these two elements prevent service users and staff writing care plans together as staff have to leave to type up a care plan once discussed, service users feel removed from the process and unable to alter the document which can often be presented to them without adequate explanation.
Services are also pressured to meet organisational demands and staff may simply not prioritise collaboration with service users. Service users report that time with staff is highly valued but for the most part was a limited resource. Time is an important and taken for granted feature of social life; it is used by individuals to impose order, understand and handle discontinuities [ 55 , 56 ]. A universal expectation reported by staff and service users in this current study was that individual one to one time would provide the means for problem resolution, help establish rapport and trust and ultimately engender a sense of collaboration towards preferred goals. However, time was a scarce resource and organisational schedules were reported to quickly over-ride those of the service user and their primary nurse.
Interprofessional ward rounds were of critical importance to service users and staff alike as the site for discussion, planning and review. Service users and staff may experience the timetabling of ward rounds differently, for example there may be diverse perceptions of scheduling delays or contradictory understandings of what happened [ 57 ]. For service users in our study ward rounds involved anxious hours waiting to be called, followed by sometimes short but overwhelming or intimidating experiences in the meeting itself [ 58 ]. It was noted that few service users were adequately prepared on what to expect. Some told us they had expected to meet only the doctor but found themselves shown into a room full of unfamiliar faces, others felt that their contributions were not valued or that they had been poorly treated. For people who are already distressed and anxious about their treatment or future outcomes it seems ward rounds handled poorly can worsen their sense of efficacy and discourage attempts to achieve involvement.
Both staff and service users said that reviewing care plans in ward rounds would help mark progress towards agreed goals. This finding from our research interviews aligns with our quantitative survey showing that participants rated highly the recovery language used by staff and the regular monitoring of progress towards recovery goals. Additionally, the information needs of service users could be better met by helping them prepare for ward rounds, including determining expectations and the agenda. In addition it was suggested to us that service users be given summaries of ward round outcomes.
Recovery, therapeutic relationships and care planning
The focus of recovery for many service users was around medication and symptom suppression (perhaps reflecting the primary focus of inpatient care) indicating a more ‘clinical’ as opposed to a ‘personal’ concept of recovery [ 9 ]. In some sites, there was greater ambivalence around the suitability or relevance of ‘recovery’ in inpatient care, particularly where people are very unwell. There may be tensions with working in recovery-focused ways when people are formally detained. It is possible however that this is the very time where a recovery-focused approach would be most powerful.
Our data on recovery shows convergence between results from standardised measures and findings from qualitative research interviews. Across five of the six sites service user participants rated highly the use of recovery language from workers and services alongside their perspective that workers believe that people can recover and participate in their own life choices. Service users also rated highly that there is regular monitoring of progress towards their recovery goals. Workers rated these items highly too suggesting that notions of recovery and therapeutic optimism were supported. Qualitative data indicate staff recognised the complex and individual nature of recovery. For example some staff saw a more recent orientation towards recovery focused care as representing the shift from previous authoritarian and prescriptive asylum based care to more collaborative models that encourage patient and family involvement.
There was a strong association amongst service users between their perceptions of recovery-oriented care and their perception of the quality of care on the ward. Likewise there were close correlations between the therapeutic relationships and the perception of quality of care. These findings were robust and consistent across all research sites. Whilst it is not possible to determine which factor might be influencing which, it does suggest an important interrelationship between service users’ subjective valuing of their relationships with staff, the quality of inpatient care and the recovery-focus of the service.
Across all sites staff consistently scored practices as more recovery-oriented than did service users. Our interviews, however, revealed ambivalence and a range of staff perspectives on recovery in line with previous research [ 59 ]. The concern that recovery creates ‘unrealistic’ expectations can perhaps be read as anxiety about what services have to offer to achieve this desired outcome. It may be that participants are simply acknowledging that recovery opportunities are hindered in settings where insufficient space is afforded to wider structural and social issues that give rise to and maintain mental distress. All participants appear to recognise the non-linear complex nature of recovery but place the emphasis differently.
One site that scored recovery highly, Dauphine, had made local attempts to introduce innovations such as service user-focused ‘This is Me’ care plans and short summary ‘management plans’, but these are in addition to standard documents and care plans, adding to workload. Interestingly, in Wales service user participants recognized that their goals were being monitored on a regular basis. This was appreciated to a lesser extent in England with just one site scoring this highly which may be a positive indication of the use of the structured care and treatment plan (CTP) approach in Wales.
Risk and safety remain key concerns for mental health workers [ 60 ] and issues around safety and risk are reported to be central to inpatient work for staff. In the mental health system more widely risk is constructed as an unwanted outcome arising from the actions or behaviours of individuals with mental health problems. In this sense risk is seen to emanate from the person who is seen as the chief agent of unwanted harmful behaviours. Harm does occur of course and mental health services appear to be chiefly concerned with harms from the person to themselves or others. For example, there are approximately 5500 suicides each year in the UK, 30% of which are known to mental health services [ 61 , 62 , 63 ]. Risk of suicide in the transition from inpatient care is now firmly established [ 64 ] and there is some suggestion that this risk has been transferred from inpatient to crisis resolution and home treatment services [ 65 , 66 ]. Harm to others is a much rarer event but nevertheless is likely to have significant negative consequences for the victim, the individual with mental health problems and their family, and the wider system including individual workers such that risk averse practice is common [ 67 ]. The pressure to ensure safety and avoid blame appears to be omnipresent in mental health services.
Coherence and continuity in care across hospital and community interfaces is known to be important in delivering safe, supportive mental health care [ 68 ] and were identified as important by many of those taking part in this study, with examples of detailed and collaborative discharge planning involving staff and service users given. Innovations were also described, such as ‘interim discharge summaries’. However, participants also reported rapidly arranged discharges with little time for discussion or planning. Decisions on movement through phases of inpatient treatment will in part depend on the presenting symptomatology of the person, an assessment of their risk status, their needs for treatment and an assessment of their post discharge needs such as accommodation [ 69 ].
Staff acknowledged tensions around sensitive discussions and especially with people detained. Workers openly acknowledged that this was to avoid difficult conversations but others seemed less aware that in denying service users access to knowledge about their risk that they are effectively excluding people from participation in decisions about their care [ 70 ]. Previously we have noted that workers position risk assessment as legitimate work despite limitations in the predictive power of these judgements as one way of gaining normative certainty [ 71 ].
Here, unlike in the community study [ 18 , 71 ], service users seemed to be more aware of their safety being considered and managed in that they understood why certain items were removed or restrictions were imposed. Some service users spoke of not feeling safe on wards as reported in previous studies [ 72 , 73 ] and this needs to be considered in ongoing discussions and policy developments on safe staffing [ 74 ]. It remained a curious finding that while workers saw risk assessment as central to their efforts that they appear to largely exclude the service user from meaningful discussions about these.
Drawing on the evidence presented here, personalisation is not widely recognized as a concept and not actively used in inpatient services by staff or service users, although there was wide discussion amongst staff of aiming to provide personal care or a personalised approach to care.
Staff spoke about some of the constraints and challenges in trying to work in a personalised way and these included a lack of resources, short ward stays, service users being formally detained, disagreements, risk behaviours, limited capacity, and a primary focus on medical treatment. It was recognised that to enable personalised care, it was necessary to have the time to get to know people as individuals and to provide some element of continuous care. Too often this was difficult to achieve in inpatient settings. Staff in the Welsh sites thought that the format of the CTP process and care plan was supportive of working in a personalised way and helped service users and staff get to know each other better.
Some service users were clear that their care was very personalized and that staff had considered their unique needs with several good examples provided. Others felt that inpatient care was more routine and standard for all and that individually tailored care was less possible in hospital, especially when people are detained. However, it was notable that some wards and staff were able to provide care in a more personalised way and support should continue to be given to achieve this everywhere. Personalisation is an integral component of a recovery-focused approach to mental health care and needs to be promoted and supported as such [ 75 ].
Strengths and limitations
Achieving our target numbers for each grouping on the survey was challenging. Service user numbers were achieved but fell just short for staff. To achieve our target recruitment figures we approached all eligible participants meaning that our sample was not randomly selected. Despite considerable efforts we were unable to recruit sufficient numbers of carers. Researchers in the field reported how few carers visit wards, often preferring to meet service users elsewhere. The difficulties of involving carers in studies of inpatient mental health services has been reported elsewhere [ 76 ] and poses a particular challenge for researchers keen to include the views of family members and friends.
Due to the nature of the survey it is not possible to make comparisons between responders and non-responders as we had no access to data for non-participants. There was a moderate level of missing data for the RSA scale completed by service users, possibly due to some of the difficult language used and the community focus of the measure. As a consequence, more detailed analysis of covariations within the data was restricted by lack of power.
The interview data is rich and the framework method provided a time-consuming but structured and visible method of organising, analysing and comparing that data within and across sites. We believe the framework method and detailed presentation of results supports the transferability of these findings to other similar services. The involvement of service users and carers throughout the study as researchers and advisors has also provided added value to the study through additional viewpoints and interpretations.
The findings of this cross-national, multi-site mixed methods study suggests positive practice is taking place within acute inpatient wards with evidence of a widespread commitment amongst staff to provide safe, respectful, compassionate care with strong values underpinning practice. Whilst ideas of recovery were evident amongst staff there was some uncertainty and discrepancy about the relevance of recovery ideals to inpatient care or the ability of people experiencing high levels of distress to engage in recovery-focused approaches. However, service users saw inpatient admissions as a necessary stage in stabilising their mental state, with medication an important component, and often appreciated the efforts that were made to keep them safe and to help them take the next tentative steps on their recovery. They also rate highly staff using recovery-focused language and values. Many spoke of care being personalised with examples given of staff being very responsive and considerate to particular needs or concerns. Carers often similarly described positive views of patient care. However, whilst service users valued the relationships they have with staff on the wards, they do not rate these as highly as staff. As discussed earlier, this is perhaps not surprising given all the tensions and anxieties associated with an inpatient stay, but this perhaps can best be summarised as ‘doing well, but could do better’.
Staff were clearly able to articulate the care planning processes and documentation required of them and described some of their frustrations with lengthy, unwieldy forms and at times distancing computerised systems that required more time in front of monitors than in conversation with service users. Most staff also spoke of their understanding and efforts to involve service users, and carers and families where possible, in the care planning process. However, most service users did not really appreciate the written care plan as an integral or important part of their experience and many did not have copies or could not find them. The majority of service users did not feel they had been genuinely involved in the process. Unfortunately, in relation to service users receiving sufficient time with nursing staff and being involved in planning their care, very little progress appears to have made since the report of the Healthcare Commission of nearly a decade ago [ 25 ].
Issues of risk and safety are ever-present in mental health services and it was clear that this was central to the work of staff, whilst they displayed an awareness of the sensitivities and challenges involved. Service users, and carers, were often aware of efforts being made by staff to keep them safe. However, involvement of service users in discussions about personal risk factors and safety is challenging and requires greater training and support to encourage staff to develop the skills and confidence to undertake such sensitive and important work with confidence.
Abbreviations
Analysis of Covariance
Analysis of Variance
Care Programme Approach
Care Quality Commission
Care and Treatment Planning
Empowerment Scale
Lived Experience Advisory Group
Multivariate Analysis
Multidisciplinary Team
Medical Research Council
National Health Service
National Research Ethics Service
Recovery Self-Assessment
Scientific Steering Committee
Scale to Assess the Therapeutic Relationship – Clinician version
Scale to Assess the Therapeutic Relationship – Patient version
Service User and Carer Group Advising on Research
Service User Project Assistants
Service User Researcher Assistants
United Kingdom
Views of Inpatient Care Scale
HM Government. No health without mental health: a cross-government mental health outcomes strategy for people of all ages. London: HM Government; 2011.
Google Scholar
Naylor C, Bell A. Mental health and the productivity challenge. Improving quality and value for money. London: Kings Fund; 2010.
Health and Social Care Information Centre: Mental Health Bulletin, 2016–17 Annual Report. Leeds: Health and Social Care Information Centre; 2017.
Statistics for Wales. Admission of patients to mental health facilities in Wales, 2016–17. Cardiff: Welsh Government; 2018.
Department of Health. Refocusing the care Programme approach: policy and positive practice guidance. London: Department of Health; 2008.
Welsh Government. Together for mental health: a strategy for mental health and wellbeing in Wales. Cardiff: Welsh Government; 2012.
Welsh Government. Code of practice to parts 2 and 3 of the mental health (Wales) measure 2010. In. Cardiff: Welsh Government; 2012.
Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal. 1993;16(4):11–23.
Article Google Scholar
Slade M. Personal recovery from mental illness: a guide for mental health professionals. Cambridge: Cambridge University Press; 2009.
Book Google Scholar
British Psychological Society: Understanding Mental Illness: Recent advances in understanding mental illness and psychotic experiences. In . Leicester: British Psychological Society; 2000.
COT. Recovering Ordinary Lives. London: College of Occupational Therapists; 2006.
CNO/DH. From values to action: The Chief Nursing Officer's review of mental health nursing. London: Department of Health; 2007.
RCPsych. Fair Deal for Mental Health. London: Royal College of Psychiatrists; 2008.
Duffy S. Personalisation in mental health. Sheffield: Centre for Welfare Reform; 2010.
Shepherd G, Boardman J, Rinaldi M, Roberts G. Supporting recovery in mental health services: quality and outcomes. London: Implementing Recovery Through Organisational Change; 2014.
Coffey M, Hannigan B, Simpson A. Care planning and coordination: Imperfect solutions in a complex world. J. Psychiatr. Ment. Health Nurs. 2017;24(6):333–4.
Article PubMed Google Scholar
Jones A, Hannigan B, Coffey M, Simpson A. Traditions of research into community mental health care planning and care coordination: a meta narrative review. PloSOne. 2018;13(6):e0198427.
Article CAS Google Scholar
Simpson A, Hannigan B, Coffey M, Barlow S, Cohen R, Jones A, Všetečková J, Faulkner A, Thornton A, Cartwright M. Recovery-focused care planning and coordination in England and Wales: a cross-national mixed methods comparative case study. BMC Psychiatry. 2016;16(1):1–18.
Simpson A, Hannigan B, Coffey M, Jones A, Barlow S, Cohen R, Všetečková J, Faulkner A: Cross-national comparative mixed-methods case study of recovery-focused mental health care planning and co-ordination: Collaborative Care Planning Project (COCAPP). Health Serv Deliv Res 2016, 4(5).
NICE: NICE Guidance on improving the experience of care for people using adult NHS mental health services. NICE; 2011.
CQC: Monitoring the Mental Health Act in 2011/12. Newcastle-Upon-Tyne: Care Quality Commission; 2013.
CQC: Community mental health services survey 2011. Newcastle-Upon-Tyne: Care Quality Commission; 2011.
WAO. Adult mental health services: follow up report. Cardiff: Wales Audit Office; 2011.
House of Commons Health Committee: Post-legislative scrutiny of the Mental Health Act 2007: HC584, First Report of Session 2013–14, vol. HC584. London: The Stationery Office Limited; 2013.
Healthcare Commission. The pathway to recovery. A review of NHS acute inpatient mental health services. London: Healthcare Commission; 2008.
MRC. Developing and evaluating complex interventions. London: Medical Research Council; 2008.
Creswell J. Research design: qualitative, quantitative and mixed methods approaches. London: Sage; 2009.
Simpson A, Coffey M, Hannigan B, Barlow S, Cohen R, Jones A, Faulkner A, Thornton A, Všetečková J, et al. Cross-national mixed-methods comparative case study of recovery-focused mental health care planning and co-ordination in acute inpatient mental health settings (COCAPP-A). Health Serv Deliv Rese. 2017;5(26).
Byrne DS. Complexity theory and the social sciences: an introduction. London: Routledge; 1998.
Kohn M. Cross-National Research in Sociology. Newbury Park: Sage; 1993.
Hantrais L, Mangen S. cross-National Research Methods in the social sciences. London: Pinter; 1996.
Stake RE. The art of case study research. London: Sage; 1995.
Fitzgerald L. Case studies as a research tool. Quality in health care: QHC. 1999;8(2):75.
Article CAS PubMed PubMed Central Google Scholar
Platt J. Case study in American methodological thought. Curr Sociol. 1992;40(1):17–48.
Yin RK. Case study: design and methods. Newbury Park: Sage Publications; 1994.
Robson C. Real world research: a resource for social scientists and practitioners-researchers. Oxford: Blackwell; 1993.
Faul F, Erdfelder E, Lang AG, Buchner A. G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91.
O'Connell M, Tondora J, Croog G, Evans A, Davidson L. From rhetoric to routine: assessing perceptions of recovery-oriented practices in a state mental health and addiction system. Psychiatric Rehabilitation Journal. 2005;28(4):378.
Mcguire-Snieckus R, McCabe R, Catty J, Hansson L, Priebe S. A new scale to assess the therapeutic relationship in community mental health care: STAR. Psychol Med. 2007;37(1):85–95.
Rogers ES, Chamberlin J, Ellison ML, Crean T. A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatr Serv. 1997;48(8):1042–7.
Article CAS PubMed Google Scholar
Evans J, Rose D, Flach C, Csipke E, Glossop H, McCrone P, Craig T, Wykes T. VOICE: developing a new measure of service users' perceptions of inpatient care, using a participatory methodology. J Ment Health. 2012;21(1):57–71.
Article PubMed PubMed Central Google Scholar
Simpson A, Barlow S, Cox L, Jones J. SUGAR : adding SUGAR: collaborating with service users and carers in mental health nursing research. J Psychosoc Nurs Health Serv. 2014;52(1):22–30.
IBM Corp: IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp; Released 2012.
Cohen J. A power primer. Psychol Bull. 1992;112(1):155–9.
QSR International Pty Ltd. NVivo qualitative data analysis software; version 10. Doncaster: QSR International Pty Ltd; 2012.
Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative research practice: a guide for social science students and researchers. London: Sage; 2013.
Ritchie J, Spencer L. The analysis of qualitative data: an approach to analysis for applied social policy research. In: Bryman A, RG B, editors. Analyzing qualitative data. London: Routledge; 1993.
Csipke E, Williams P, Rose D, Koeser L, McCrone P, Wykes T, Craig T. Following the Francis report: investigating patient experience of mental health in-patient care. Br J Psychiatry. 2016;209(1):35-39.
Bowers L, Simpson A, Alexander J, Hackney D, Nijman H, Grange A, Warren J. The nature and purpose of acute psychiatric wards: the Tompkins acute Ward study. J Ment Health. 2005;14(6):625–35.
Whittington R, Bowers L, Nolan P, Simpson A, Neil L. Approval ratings of inpatient coercive interventions in a national sample of mental health service users and staff in England. Psychiatr Serv. 2009;60(6):792–8.
Cresswell J, Beavon M. Accreditation for inpatient mental health services (AIMS): standards for inpatient wards-working-age adults. London: Royal College of Psychiatrists; 2010.
Star Wards’ 75 Ideas. http://www.starwards.org.uk/ . Accessed 5 Apr 2019.
Bowers L, James K, Quirk A, Simpson A, SUGAR, Stewart D, Hodsoll J. Reducing conflict and containment rates on acute psychiatric wards: the Safewards cluster randomised controlled trial. Int J Nurs Stud. 2015;52:1412–22.
Storm M, Davidson L. Inpatients’ and providers’ experiences with user involvement in inpatient care. Psychiatry Q. 2010;81:111–25.
Roth JA. Timetables: structuring the passage of time in hospital treatment and other careers. Bobbs-Merrill: Indianapolis; 1963.
Coffey M. Time and its uses in accounts of conditional discharge in forensic psychiatry. Sociology of Health and Illness. 2013;35(8):1181–95.
Klitzman R. "patient-time", "doctor-time", and "institution-time": perceptions and definitions of time among doctors who become patients. Patient Educ Couns. 2007;66(2):147–55.
White R, Karim B. Patients’ views of the ward round: a survey. Psychiatrist. 2005;29(6):207–9.
Aston V, Coffey M. Recovery: what mental health nurses and service users say about the concept of recovery. J Psychiatr Ment Health Nurs. 2012;19(3):257–63.
Dixon J. Balancing risk and recovery in mental health: an analysis of the way in which policy objectives around risk and recovery affect professional practice in England. In: Chamberlain M, editor. Medicine, Power, and Discourse. London: Taylor & Francis; 2015.
Cavanagh B, Ibrahim S, Roscoe A, Bickley H, While D, Windfuhr K, Appleby L, Kapur N. The timing of general population and patient suicide in England, 1997–2012. J Affect Disord. 2016;197:175–81.
Coope C, Gunnell D, Hollingworth W, Hawton K, Kapur N, Fearn V, Wells C, Metcalfe C. Suicide and the 2008 economic recession: who is most at risk? Trends in suicide rates in England and Wales 2001–2011. Soc Sci Med. 2014;117:76–85.
National Confidential Inquiry into homicide and suicide by people with mental illness: annual report: England, Northern Ireland, Scotland and Wales July 2015 . . Manchester: University of Manchester; 2015.
Meehan J, Kapur N, Hunt IM, Turnbull P, Robinson J, Bickley H, Parsons R, Flynn S, Burns J, Amos T. Suicide in mental health in-patients and within 3 months of discharge. Br J Psychiatry. 2006;188(2):129–34.
Johnson S. Crisis resolution and home treatment teams: an evolving model. Adv Psychiatr Treat. 2013;19(2):115–23.
Hunt IM, Rahman MS, While D, Windfuhr K, Shaw J, Appleby L, Kapur N. Safety of patients under the care of crisis resolution home treatment services in England: a retrospective analysis of suicide trends from 2003 to 2011. Lancet Psychiatry. 2014;1(2):135–41.
Coffey M. A risk worth taking? Value differences and alternative risk constructions in accounts given by patients and their community workers following conditional discharge from forensic mental health services. Health Risk and Society. 2012;14(5):465–82.
Weaver N, Coffey M, Hewitt J. Concepts, models and measurement of continuity of care in mental health services: a systematic appraisal of the literature. J Psychiatr Ment Health Nurs. 2017;24(6):431–50.
Bowers L, Chaplin R, Quirk A, Lelliott P. A conceptual model of the aims and functions of acute inpatient psychiatry. J Ment Health. 2009;18(4):316–25.
Fricker M. Epistemic injustice: power and the ethics of knowing. Oxford: Oxford University Press; 2007.
Coffey M, Cohen R, Faulkner A, Hannigan B, Simpson A, Barlow S. Ordinary risks and accepted fictions: how contrasting and competing priorities work in risk assessment and mental health care planning. Health Expect. 2017;20(3):471–83.
Jones J, Nolan P, Bowers L, Simpson A, Whittington R, Hackney D, Bhui K. Psychiatric wards: places of safety? J Psychiatr Ment Health Nurs. 2010;17(2):124–30.
Quirk A, Lelliott P, Seale C. Service users’ strategies for managing risk in the volatile environment of an acute psychiatric ward. Soc Sci Med. 2004;59(12):2573–83.
NHS Improvement accused of 'dismantling' NICE safe staffing work. https://www.hsj.co.uk/workforce/exclusive-nhs-improvement-accused-of-dismantling-nice-safe-staffing-work/7005462.article . Accessed 5 Apr 2019.
Alakeson V, Perkins R. Recovery, personalisation and personal budgets. London: Centre for Mental Health; 2012.
Nolan F: An evaluation of protected engagement time on staff and patient outcomes in acute mental health inpatient wards: implications for mental health nursing and research . In: Network for Psychiatric Nursing Research . University of Warwick; 2013.
Download references
Acknowledgements
All members of the Lived Experience Advisory Group, the Study Steering Group, the service user researchers and research staff who ensured the success of the study.
The project reported in this article was commissioned and funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research Programme (HS&DR 13/10/75). The NIHR had no role in the design of the study and collection, analysis, and interpretation of data or in writing of the manuscript. The views and opinions expressed here are those of the authors and do not necessarily reflect those of the HS&DR programme, NIHR, the National Health Service (NHS) or the Department of Health and Social Care.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
Department of Public Health, Policy and Social Sciences, Swansea University, Singleton Park, Swansea, SA2 8PP, UK
Michael Coffey
School of Healthcare Sciences, Cardiff University, Cardiff, CF24 0AB, UK
Ben Hannigan & Aled Jones
Centre for Mental Health Research, School of Health Sciences, City, University of London, Northampton, Square, EC1V 0HB, UK
Sally Barlow & Alan Simpson
Centre for Health Services Research, School of Health Sciences, City, University of London, Square, EC1V 0HB, Northampton, UK
Martin Cartwright
Centre for Academic Mental Health, Bristol Medical School, University of Bristol, Oakfield House, Oakfield Grove, Clifton, Bristol, BS8 2BN, UK
Rachel Cohen
Independent Service User Researcher Consultant, London, UK
Alison Faulkner
East London NHS Foundation Trust, 9 Alie St, London, E1 8DE, UK
Alan Simpson
You can also search for this author in PubMed Google Scholar
Contributions
MCo contributed to the design of the study, data collection, analysis, interpretation, write-up and final edit of the paper. BH contributed to the design of the study, data collection, analysis, interpretation, and write-up of the paper. SB contributed to data collection, led on quantitative analysis, contributed to qualitative analysis, interpretation, and write-up of the paper. MCa advised and contributed to statistical analysis and write-up of the paper. RC contributed to data collection, qualitative analysis, interpretation, and write-up of the paper. AF contributed to the design of the study, data collection, analysis, interpretation, and write-up of the paper. AJ led on the literature review and contributed to interpretation and write-up of the paper. AS contributed to the design of the study, analysis, interpretation and write-up of the paper. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Michael Coffey .
Ethics declarations
Ethics approval and consent to participate.
The study received NHS Research Ethics approval from the NRES Committee NRES Committee London – Fulham (Ref: 13/LO/2062) on 29th December 2014. All participants provided written informed consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Reliability Assessment.docx showing additional reliability checks for the internal consistency of the scales and subscales. (DOCX 23 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Coffey, M., Hannigan, B., Barlow, S. et al. Recovery-focused mental health care planning and co-ordination in acute inpatient mental health settings: a cross national comparative mixed methods study. BMC Psychiatry 19 , 115 (2019). https://doi.org/10.1186/s12888-019-2094-7
Download citation
Received : 12 June 2018
Accepted : 27 March 2019
Published : 16 April 2019
DOI : https://doi.org/10.1186/s12888-019-2094-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Care planning
- Inpatient care
- Therapeutic relationships
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Brooker D. Person-centred dementia care.London: Jessica Kingsley; 2007
What is a nursing intervention: a beginner's guide. 2019. https://tinyurl.com/mh2mwhb6 (accessed 1 November 2021)
Butterworth C. How to achieve a person-centred writing style in care plans. Nurs Older People. 2012; 24:(8)21-26 https://doi.org/10.7748/nop2012.10.24.8.21.c9310
Centre for Policy on Ageing. The effectiveness of care pathways in health and social care. 2014. https://tinyurl.com/3t835kfd (accessed 1 November 2021)
Clinical and service integration. The route to improved outcomes. 2010. https://tinyurl.com/whb87xd6 (accessed 1 November 2021)
Department of Health. Refocusing the Care Programme Approach. Policy and positive practice guidance. 2008. https://tinyurl.com/anyrzhy6 (accessed 3 November 2021)
Department of Health. Personalised care planning: improving care for people with Long term conditions. 2011. https://tinyurl.com/uc3u3tkh (accessed 1 November 2021)
Department of Health. Care planning in the treatment of long term conditions: final report of the CAPITOL Project. 2013a. https://tinyurl.com/7399vphc
Department of Health. Mental health payment by results guidance 2013-2014. 2013b. https://tinyurl.com/9zyfmy87 (accessed 1 November 2021)
Dimond B. Exploring the legal status of healthcare documentation in the UK. Br J Nurs. 2005; 14:(9)517-518 https://doi.org/10.12968/bjon.2005.14.9.18078
Foundations of nursing practice: making the difference, 2nd edn. In: Hogston R, Simpson PM (eds). London: Palgrave Macmillan; 2002
Kozier B, Erb G, Berman A, Snyder S, Lake R, Harvey S. Fundamentals of nursing: concepts, process and practice, 8th edn. Harlow: Pearson Education; 2008
Leach M. Clinical decision making in complementary & alternative medicine.Chatswood (NSW, Australia): Elsevier; 2010
Lloyd M. A practical guide to care planning in health and social care.Maidenhead: Open University Press; 2010
Matthews E. Nursing care planning made incredibly easy!.Philadelphia (PA): Lippincott Williams and Wilkins; 2010
Monitor. Delivering better integrated care: A summary of what delivering better integrated care means and how Monitor is supporting the sector. 2015. https://tinyurl.com/825k8kd6 (accessed 1 November 2021)
NHS website. NHS launches accredited suppliers for electronic patient records. 2019. https://tinyurl.com/4fzs4up5 (accessed 1 November 2021)
National Institute for Clinical Excellence. What to expect during assessment and care planning. 2021. https://tinyurl.com/63hm5vvp (accessed 1 November 2021)
NHS England. Personalised care and support planning handbook: the journey to person-centred care: Core information. 2016a. https://tinyurl.com/9fyrtw45 (accessed 1 November 2021)
NHS England. Mental health clustering booklet v5.0 (2016/17). 2016b. https://tinyurl.com/7p6dfnry (accessed 1 November 2021)
NurseChoice. Nursing smart goals: how to set smart goals for Nursing. 2018. https://tinyurl.com/s292baez (accessed 1 November 2021)
Nursing and Midwifery Council. Future nurse: standards of proficiency for registered nurses. 2018a. http://tinyurl.com/yddpadva (accessed 1 November 2021)
Nursing and Midwifery Council. The code: professional standards of practice and behaviour for nurses, midwives and nursing associates. 2018b. https://tinyurl.com/gozgmtm (accessed 1 November 2021)
Nursing and Midwifery Council. Keep records of all evidence and decisions. 2021. https://tinyurl.com/4pcabhms (accessed 1 November 2021)
Revello K, Fields W. An educational intervention to increase nurse adherence in eliciting patient daily goals. Rehabil Nurs. 2015; 40:(5)320-326 https://doi.org/10.1002/rnj.201
Royal College of Nursing. RCN factsheet on nurse prescribing in the UK. 2014. https://tinyurl.com/hkndnbhv (accessed 3 November 2021)
Nursing process. 2021. https://www.ncbi.nlm.nih.gov/books/NBK499937 (accessed 1 November 2021)
Wing JK, Beevor AS, Curtis RH, Park SGB, Hadden J, Burns A. Health of the Nation Outcome Scales (HoNOS). Br J Psychiatry. 1998; 172:(1)11-18 https://doi.org/10.1192/bjp.172.1.11
World Health Organization. Integrated care models: an overview. 2016. https://tinyurl.com/6encn9a5 (accessed 1 November 2021)
Yeomans D. Clustering in mental health payment by results: a critical summary for the clinician. Adv Psychiatr Treat. 2014; 20:(4)227-234 https://doi.org/10.1192/apt.bp.113.011320
Assessing the patient's needs and planning effective care
Benjamin Ajibade
Senior Lecturer, Mental Health Nursing, Northumbria University
View articles · Email Benjamin

Nurses have an essential role to play in the assessment and planning of patient care. This is emphasised in the Nursing and Midwifery Council's 2018Future Nurse proficiency standards. In this article, the author discusses the importance of person-centred care in assessing needs and highlights the need for all nursing interventions to be evidence based. The topics covered include assessing people's needs, care planning, stages of care planning, benefits of care planning, models of care, care pathways, and care clustering in mental health care. The article also highlights the significance of record-keeping.
The central role of nurses in assessing patient needs and planning care is one of the core areas emphasised in Future Nurse, the Nursing and Midwifery Council's (NMC) (2018a) nursing proficiency standards. The document categorises ‘assessing needs and planning care’ as the third of seven areas of proficiency, which are grouped into ‘platforms’. Future Nurse emphasises that the delivery of person-centred care and evidence-based nursing interventions are vital components for effective patient assessment and care planning. The standards further highlight that the nurse should understand the need to assess each patient's capacity to make their own decisions and to allow them the opportunity to give and withdraw consent.
An assessment is a form of a dialogue between client and practitioner, in which they discuss the needs of the former to promote their wellbeing and what they expect to happen in their daily life ( National Institute for Health and Care Excellence (NICE), 2021 ). Nursing assessment involves collecting data from the patient and analysing the information to identify the patient's needs, which are sometimes described as problems.
The process of planning care employs different strategies to resolve the needs identified as part of an assessment. Ideally, this will include the selection of appropriate evidence-based nursing interventions. When planning care, the patient's needs and wishes should be prioritised, and the individual must be involved in the decision-making process to ensure a person-centred approach. The planned care must take into account the patient's conditions, personal attributes and choices. It is worth noting that the principles of care planning are transferable between hospital, home and care home settings.
Section 2 of the NMC Code highlights the importance of partnership working with patients to ensure the delivery of effective high-quality care and of involving them in their care, which includes empowering patients by enabling them to make their own decisions ( NMC, 2018b ). The patient should be viewed holistically, with importance placed on the physical, psychological, social and spiritual aspects of the person's life, which are inextricable.
The intrinsic factors of a patient's condition will often affect their concordance with the advice and treatment offered. Consequently, it is important to understand the reasons for non-concordance and to tailor treatments/recommendations to each individual, which will improve the quality of care delivered.
Brooker (2007) developed the acronym VIPS to address some of the confusion surrounding what should or should not be perceived as person-centred care. VIPS stresses the following:
- V is a value base that affirms the value of each human being, irrespective of age and cognitive ability. This is the foundation for individualised care
- I is individualised care that considers the individual's distinctiveness and holistic needs
- P is about seeing the world from the patient's perspective, to ensure that the health professional takes the patient's point of view into account when providing care
- S is about maintaining a social environment that supports the patient's psychological needs, including their mental, emotional and spiritual needs.
Health professionals should endeavour to involve the patient in decision-making and enable them to make choices as much as possible, using a range of approaches to achieve this ( Lloyd, 2010 ). Unless proven otherwise, a nurse must assume that a patient has the capacity to make their own decisions, in line with the Mental Capacity Act 2005.
The following draws on the author's experience in mental health nursing but can be applied to other areas of nursing care.
Care planning
Planning care is essential in the delivery of appropriate nursing care. Following assessment of a patient's needs, the next stage is to ‘plan care’ to address the actual and potential problems that have been identified. This helps to prioritise the client's needs and assists in setting person-centred goals. Planned care will change as a patient's needs change and as the nurse and/or other health professionals identify new needs. Care planning assists professionals to communicate information about the patient's care to others ( Department of Health (DH), 2013a ; NICE, 2021 ), to facilitate continuity of care. Communication may be predominantly verbal, but it will also always involve documentation in a variety of formats, including computer-based, handwritten or preprinted care plans.
It is essential for nurses to consider their consultation style when developing a care plan in order to reduce the risk of paternalism when communicating with the patient and discussing their needs. Collaborative consultation encourages patients to participate in their care and improves rapport, while a paternalistic approach will generally minimise an individual's part in, and responsibility for, their own care needs and may compromise care outcomes and concordance ( Leach, 2010 ). A collaborative/partnership consultation style facilitates a person-centred approach by the practitioners and involves the patient in their care. Such an approach can include asking questions such as: ‘We have different types of treatment approaches that could be considered, what are your preferences?’ This is in contrast to a paternalistic consultation style with the health professional announcing any decisions with a statement such as: ‘I am going to prescribe a certain treatment for you.’
When drawing up a care plan with a patient the nurse should take into account a number of considerations ( Box 1 ).
Box 1.Nursing considerations
- The patient should know the reason for the assessment
- The assessment should be flexible and adaptable to the needs of the individual
- The patient must be fully involved and their dignity, independence, and interests should be paramount
- The patient can have someone with them, if preferred
- Appropriate language and terminologies should be used throughout the consultation
- The diversity of the individual client, their beliefs, values, culture and their circumstances must be considered
- It is essential to consider the patient's gender, sexuality, ethnicity, disability and religion as part of the assessment
- Be open to listening to the patient's personal history and life story
- The entire family's needs should be considered, inclusive of the patient and their carers: remember the importance of providing holistic care
- Cost-effectiveness should also be taken into account
Sources: Department of Health, 2011; National Institute for Health and Care Excellence, 2021

Stages of care planning
Care planning has been described as the third stage of the nursing process ( NMC, 2018a ; Toney-Butler and Thayer, 2021 ). It includes assessing the patient's needs, identifying the problem(s), setting goals, developing evidence-based interventions and evaluating outcomes ( Matthews, 2010 ). This will require the health professional to apply high-level critical thinking, decision-making and problem-solving skills. It is important to note that a care plan can be prescriptive: it is devised after a patient has been assessed through the prescription of nursing actions ( Hogston and Simpson, 2002 ) or through collaborative working involving the multidisciplinary team.
In some situations there will be differences between what the nurse sees as a priority in terms of the patient's needs and what the patient wants. An example of this would be a patient with mental health problems who may be at high risk of self-harm, who may need to be put on intermittent 15-minute observation. In such cases, a patient would be deemed as not having capacity to make decisions and the nurse will need to use their clinical judgement to prescribe the best treatment option. The care plan can still be agreed in conjunction with the patient once the nurse has explained the reasons for the interventions and acknowledged in the care plan that this is not the patient's preferred choice.
In situations where the patient has capacity to make decisions, the care plan should be agreed in collaboration with the service user ( NHS England, 2016a ).
Identifying needs
As part of the care planning process, the nurse will identify a patient's needs/problems and propose a set of interventions to address them in order of priority, ensuring that everything is in agreement with the patient. To ensure that appropriate goals are set, a patient's needs will be classified as high, intermediate and low.
Each goal provides an indication as to the expected outcome, along with the proposed interventions required to meet the patient's problems/needs, all of which must be patient centred. It is important, in collaboration with the patient, to set both short-term, achievable goals and longer-term goals that may take days, weeks or months to accomplish. One way nurses can ensure this is to apply the SMART goal-setting approach to ensure that the goals are ( Revello and Fields, 2015 ; NurseChoice, 2018 ):
- M easurable
- A chievable
- T imely (within a defined time frame).
Interventions
Interventions are nursing actions/procedures or treatments built on clinical judgement and knowledge, performed to meet the needs of patients. The actions should be evidence based and indicate who will carry them out, when and how often ( Hogston and Simpson, 2002 ). The scheduled interventions will have been agreed with the patient with the aim of improving their health condition, and each subsequent action should strive to meet the goals set at the previous stage. Brooks (2019) outlined three types of intervention:
- Those independently initiated by nurses
- Those that are dependent on a physician or other health professionals
- Those that are interdependent, that is, those rely on the experience, skills and knowledge of multiple professionals.
Independent nursing interventions are planned and actioned by nurses autonomously ( NMC, 2018a ), and these actions do not require the nurse to have direction from another health professional. When actioning interventions dependent on other health professionals, the nurses must determine the appropriateness of any directions from other health professionals before carrying them out because the nurse remains accountable for the actions, for example, the administration of prescribed medication ( NMC, 2018a ). Due to developments in the nursing profession, some advanced nurse practitioners can now prescribe interventions, eg prescription of medication can be done by nurse independent prescribers or nurse supplementary prescribers ( Royal College of Nursing, 2014 ). Interdependent interventions are usually recorded in collaborative care plans reviewed in multidisciplinary (MDT) meetings and must be agreed by all parties involved. Both the goals and interventions must be communicated in a timely manner to all those involved in the patient's care.
This is the stage when a planned intervention is evaluated to assess whether or not it has been achieved. This can be an ongoing process, and the care plan should document the frequency and time frame for evaluating the intervention. If the initial goal becomes unachievable, the nurse will be required to reassess the patient's needs, and review and revise the interventions.
Benefits of care planning
The DH (2011) highlighted that the aim of care planning is to improve the quality of care and outcomes by respecting individual wishes and enabling patients to acknowledge the ownership of their condition and ensuring they have the ability to influence the outcomes. Health professionals should engage individuals in decision-making and facilitate them to take control of their health by agreeing common goals to improve outcomes. This will have additional benefits for both the patient and health services as it should reduce the number of GP appointments and emergency admissions the patient may require. Promoting self-management of long-term conditions can also help slow progression of illness.
Care planning empowers patients to care for themselves when they are self-managing their health and when they may have difficulty accessing a health professional. This became evident during the pandemic, with patients often having to go for extended periods between appointments with their health professionals. Care planning has really come into its own in community care in the past few years, which became evident during the pandemic—particularly in the field of mental health—because it leads to better patient concordance with treatment and other care needs without the need for constant input by health professionals. This benefits both health professionals and the NHS: it increases job satisfaction, brings efficiency savings and improves the quality of patient care ( DH, 2011 ).
Model of care
Models of care are used to deliver best practice in health care. An integrated services care model is multifaceted and enables the co-ordination of care by different health and social care professionals to meet individual patient needs. It encompasses patient-centred care and enables care staff across different providers to reduce duplication, confusion, delay and gaps in services ( Monitor, 2015 ). In the modern NHS, this is the preferred model of care.
The care plan is an integral part of this model because it enables the creation of shared care plans that map different care processes. It becomes a point of reference for various providers involved in the care of the patients, ensuring the co-ordination of care across services ( Curry and Ham, 2010 ; World Health Organization, 2016 ).
Care pathways
Care pathways, which are also known as critical pathways, clinical pathways, integrated care pathways, care paths and care maps, are used to describe a specific patient journey that dictates the care to be provided or process to be followed for a patient's particular condition or needs. An evidence-based care process is established for specific conditions by considering expert opinion that takes into account the evidence to recommend interventions that have been shown to achieve better health outcomes cost-effectively ( Centre for Policy on Ageing, 2014 ).
Care pathways are often developed at local level and have been shown to be efficacious at meeting local needs. They are also known to improve cross-setting collaborations. Clinical pathways are aimed at providing effective health care appropriate for the patient group of conditions, thereby reducing hospital stays, leading to cost-effective health care ( Kozier et al, 2008 ).
Care clusters
Care clustering is a needs assessment tool that is used to rate a patient's care need against specific scales:
‘A cluster is a global description of a group of people with similar characteristics as identified from a holistic assessment and then rated using the Mental Health Clustering Tool (MHCT).’
NHS England, 2016b
This framework is used to plan and organise mental health services, including the care and support provided to individuals based on their illness and individual needs. One of the care clustering tools used in the NHS is the Health of the Nations Outcome Scales (HoNOS) ( Wing et al, 1998 ; Yeomans, 2014 ; NHS England, 2016b ).
Mental health services were brought under the scope of Payment by Results (PbR) in the NHS in 2012-2013.
‘Payment by Results (PbR) is the transparent rules-based payment system in England under which commissioners pay healthcare providers for each patient seen or treated, taking into account the complexity of the patient's healthcare needs.’
Consequently, as part of the care planning process, nurses need to take into account the cost-effectiveness of any interventions in order to consider how much funding is likely to be available for an initial completion of assessments, during scheduled reassessment and at any subsequent reassessment after a significant change in the patient's needs.
Box 2.Importance of complying with guidelines when undertaking assessment and planning care
- You must be compliant with the Nursing and Midwifery Council (2018b ; 2021 ) guidelines for record and record-keeping
- Adhere to the employing local organisation's policy on record-keeping, eg local trust policy
- Follow the NHS trust Care Programme Approach (CPA) policy ( Department of Health, 2008 )
- Collaborate with all those involved in a patient's care planning process
Importance of record-keeping
Accurate record-keeping is essential in the assessment of needs and planning care. This complies with the NMC (2018b) which states that record-keeping is fundamental to nursing practice, emphasising that records must be accurate and precise.
Health professionals should be aware of the need for legal accountability when documenting care in a written record because such records could be used in any legal proceedings ( Dimond, 2005 ). A record refers to not only a patient's record, but encompasses all records related to an individual nurse's range of practice. It is important to include the person being cared for in the record-keeping process, who should be asked to sign the plan of care, if they have capacity to do so ( NMC, 2021 ).
It is good practice to make an entry in the care documentation if a service user is unable to sign or agree to their planned care and state the reason for this ( Butterworth, 2012 ). In addition to paper-based records, care plans can be entered into the electronic health/patient record system used in the practitioner's service ( NHS website, 2019 ).
Best practice in writing care plans
There are some critical factors to consider when writing a focused person-centred care plan. One of these is to clearly document in detail the needs of the patient and to use the patient's language whenever possible, for example: ‘Mr D likes to dress smart every morning, but has been finding it difficult to make the choice of clothing to wear.’ An example of a poor way to record the same issue might be: ‘Mr D is unable to dress by himself’ and the aim is ‘Mr D will appear to dress smartly’.
The documented goal/aim of the care plan should be determined by applying the SMART acronym. It is therefore vital to ensure that the aim is specific by focusing on issues that can be measured, with goals that are achievable and realistic. It is also important to suggest and record a time frame within which a patient's short-term and long-term goals could be achieved. In relations to Mr D's clothing, a daily time frame might be appropriate. To come to an agreement over this issue, Mr D might be asked: ‘Mr D, would you like to be able to make your own choice of clothes to wear every day with the support of staff?’ The projected daily goal would then be recorded as part of the care plan documentation.
An intervention must specify how a goal/aim will be achieved, including who will be responsible for implementing each task. This could be the staff nurse on duty, team nurse, team leader, the nurse in charge and/or the patient (please put the patient's name). Evaluation should be carried out regularly and documented, and should conform with the proposed time frame outlined as part of the suggested intervention. Evaluations should be undertaken whenever actions are performed in accordance with each proposed intervention, and details of the progress of the patient's problem/needs documented.
In conclusion, the article has discussed the importance of assessing patients' needs, emphasising person-centred care using the VIPS acronym devised by Brooker (2007) . It has stressed the notion for all nursing interventions to be evidence based. The stages of care planning were discussed, and the application of the SMART goal-setting approach was highlighted. Record-keeping is an integral part of care planning in the communication of patient's care and progress. The benefits of care planning in improving quality of care and outcomes, respecting individual wishes, thereby empowering the patient was recognised.
LEARNING OUTCOMES
- Nurses must ensure that assessment of patient needs and care planning are always focused on the person
- All nursing interventions must be evidence based
- The goals set out in a patient's care plan must be achievable and measurable, and should include time frames within which both short- and long-term goals can be achieved
- Record-keeping is a vital component of care planning and is part of communicating aspects of a patient's care, and their progress towards their goals, with other health professionals involved in their care
CPD reflective questions
- In the context of a patient's health, what should you aim to do when care planning?
- Who should you involve in the care planning and why? Should the patient have a copy of the care plan?
- Is it acceptable to destroy care plans or other records?
- When should care plans be reviewed?
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier Sponsored Documents
Effective nurse–patient relationships in mental health care: A systematic review of interventions to improve the therapeutic alliance
Samantha hartley.
a Division of Psychology and Mental Health, School of Health Sciences, Faculty of Biology, Medicine and Health, Manchester Academic Health Sciences Centre, University of Manchester, Manchester M139PL, United Kingdom
b Pennine Care NHS Foundation Trust, Ashton-under-Lyne OL6 7SR, United Kingdom
Jessica Raphael
Karina lovell.
c Division of Nursing, Midwifery and Social Work, Faculty of Biology, Medicine and Health, University of Manchester, Manchester M139PL, United Kingdom
Katherine Berry
Therapeutic alliance is a core part of the nursing role and key to the attainment of positive outcomes for people utilising mental health care services. However, these relationships are sometimes difficult to develop and sustain, and nursing staff would arguably benefit from evidence-based support to foster more positive relationships.
We aimed to collate and critique papers reporting on interventions targeted at improving the nurse–patient therapeutic alliance in mental health care settings.
Systematic literature review.
Data sources
The online databases of Excerpta Medica database (Embase), PsycINFO, Medical Literature Analysis and Retrieval System Online (MEDLINE) and Cumulative Index of Nursing and Allied Health Literature (CINAHL) were searched, eligible full text paper references lists reviewed for additional works and a forward citation search conducted.
Review methods
Original journal articles in English language were included where they reported on interventions targeting the nurse–patient therapeutic relationship and included a measure of alliance. Data were extracted using a pre-determined extraction form and inter-rater reliability evaluations were conducted. Information pertaining to design, participants, interventions and findings was collated. The papers were subject to quality assessment.
Relatively few eligible papers ( n = 8) were identified, highlighting the limitations of the evidence base in this area. A range of interventions were tested, drawing on diverse theoretical and procedural underpinnings. Only half of the studies reported statistically significant results and were largely weak in methodological quality.
Conclusions
The evidence base for methods to support nursing staff to develop and maintain good therapeutic relationships is poor, despite this being a key aspect of the nursing role and a major contributor to positive outcomes for service users. We reflect on why this might be and make specific recommendations for the development of a stronger evidence base, with the hope that this paper serves as a catalyst for a renewed research agenda into interventions that support good therapeutic relationships that serve both staff and patients.
What is already known about the topic?
- • The therapeutic relationship between nursing staff and patients in mental health care is key to positive outcomes.
- • Therapeutic alliance is a multi-faceted concept that is valued by patients while being difficult for staff to develop.
What this paper adds
- • Interventions targeting the therapeutic alliance were identified; including training, psychological formulation, reflective groups, consultation and shared activity.
- • The review showed that none of these is as yet confirmed effective and that the methodological quality of the evidence base at present is predominantly poor.
1. Introduction
Nursing staff are the core of the caring profession and central to their role is the development of effective relationships with the individuals they support ( Hoeve et al., 2014 ; Zugai et al., 2015 ). In the United Kingdom, engaging meaningfully with patients (rather than ‘doing to’) runs through the principles of the nursing profession ( Royal College of Nursing, 2010 ); while in the United States, the interpersonal relationship is seen as foundational to a person-centred, recovery-oriented approach within mental health nursing ( Kane, 2015 ). Internationally, the alliance features heavily in the remit of European and Australasian nursing associations, who highlight the need for human connection and the ability to demonstrate effective therapeutic relationships ( Australian College of Mental Health Nurses, 2018 ; World Health Organisation, 2003 ).
The nursing relationship has been conceptualised as ‘a significant therapeutic interpersonal process [that] functions co‐operatively with other human processes that make health possible for individuals and communities’ ( Peplau, 1988 , p. 16). This therapeutic alliance—the relationship connecting professional and service user—is between one human and another, with a uniqueness of each dyad ( Forchuk, 1995 ), which therefore requires renewed efforts at each new pairing. Nurses see the development of the alliance as requiring a convergence of interpersonal professional skills with personal life experience ( Scanlon, 2006 ) and clients view it as life-sustaining in its ability to foster collaboration and a sense of being understood ( O'Brien, 2001 ). The concept has recently enjoyed a renewed focus, with an emphasis on consumer-models that encourage personal recovery assisted by therapeutic alliance ( Zugai et al., 2015 ).
Therapeutic alliance has the greatest impact on treatment outcomes for those with mental health difficulties, over and above the specific mode or model of intervention that is provided ( Duncan et al., 2010 ; Martin et al., 2000 ; Messer and Wampold, 2002 ; Priebe and McCabe, 2006 ; Wampold, 2001 ). Emerging initially within the psychoanalytic discipline and later generalised to multiple therapeutic contexts, the concept of alliance has been defined as an agreement on goals, tasks and a therapeutic bond between therapist and client ( Bordin, 1979 ). The phenomena can be measured using various tools from both the perspective of the professional and service user, with important differences between the two ( Bachelor and Salamé, 2000 ; Fitzpatrick et al., 2005 ). In an age of increasingly remote therapeutic interactions, the alliance and concomitants of it are still seen as intrinsic to change, whether therapy is facilitated by phone ( Mulligan et al., 2014 ), online dialogue ( Cook and Doyle, 2002 ) or even fully-automated chat-bot ( Fitzpatrick et al., 2017 ).
Traditionally, research has focused on understanding and improving the alliance between therapist and client; as part of one-to-one, psychotherapeutic interventions ( Lambert and Barley, 2001 ; Martin et al., 2000 ). In contrast to these direct therapy roles, there are also staff members who adopt a care coordination role or act as a key worker; assessing, engaging and organising care with individuals ( Burns, 2004 ; Simpson, 2005 ; Thurston, 2003 ). All of these roles inevitably involve the building and maintenance of an effective alliance and therefore research has shifted to include definitions and exploration of the relationship as built within these guises ( Farrelly et al., 2014 ; Kirsh and Tate, 2006 ), where it remains correlated with outcomes ( Cruz and Pincus, 2002 ; Howgego et al., 2003 ) and is developed in a range of settings.
As part of secondary care community services, nursing staff coordinate care and deliver brief therapies, which despite (or possibly because of) their short-term nature require the adept building of alliance. People supported by secondary care services are those experiencing severe mental health difficulties, often in the context of challenging relational and social circumstances. Here, nurses strive to develop mutuality, reciprocity, synchrony, and sense of belonging with their clients ( Spiers and Wood, 2010 ) and clients value being known and related to as a person rather than service-recipient ( Shattell et al., 2007 ), requiring a skilful use of the self ( O'Brien, 2000 ). Service users value therapeutic relationships with care coordinators in community settings, and view these as central to recovery; over and above the role of specific care plans ( Simpson et al., 2016 ). These complex processes are rendered difficult for staff members by burnout, struggles building engagement with patients and ineffective team-working ( Koekkoek et al., 2011 ; Singh, 2000 ), with the nature of organisational structures and roles limiting the care that nurses can provide ( Simpson, 2005 ).
The therapeutic role of nursing staff in mental health care is especially pertinent in settings such as inpatient wards, where patients interact with nurses for the largest proportion of time and the relationship with them is cited as key to therapeutic progression ( Hopkins et al., 2009 ; McAndrew et al., 2014 ), with a perceived interplay between therapeutic relationships and the quality of care ( Coffey et al., 2019 ) . Engagement in these challenging contexts requires a balance of approaches, the development of personalised understanding and use of the self to facilitate recovery-oriented growth of the patient ( McAllister et al., 2019 ). However, how these specific competencies can be developed is not fully elucidated in the literature or supported by service structures. The alliance can be impeded by individual and organisational factors that leave it unseen and stifled in practice ( Pazargadi et al., 2015 ), with nurses left to negotiate contradictory and challenging relational minefields ( Cleary et al., 2012 ).
Despite the potential value and best efforts, attempts to develop strong nursing alliance in mental health care can be hampered by challenging settings where its development is impeded ( McAndrew et al., 2014 ). Moreover, interactions between nursing staff and patients are often not supported or guided by the psychological theory of relationships; there is a substantial theory-practice gap ( Cameron et al., 2005 ) that might leave both staff and service users vulnerable to relational difficulties and the consequent impact on wellbeing and outcomes. It seems that services, patients and staff place value on the therapeutic alliance, its core attributes have been explored and conceptualised, and yet theoretically-driven, evidenced systems that support its development and maintenance are lacking. With this deficiency in targeted support, staff members increasingly report feeling burnt-out as a result of managing complex and emotionally difficult relationships ( Holmqvist, and Jeanneau, 2006 ; Nathan et al., 2007 ). This could lead to compassion sometimes waning when it is needed most ( Lombardo, and Eyre, 2011 ; Ray et al., 2013 ) and staff retention proving extremely difficult, with subsequent strategic priorities to improve this in both the United Kingdom and internationally ( Andrews, and Wan, 2009 ; European Commission, 2014 ; NHS, 2019 ; Parliament of Australia, 2002 ).
There has been some tentative progress in supporting effective relationships, with indications that clinical supervision can protect against staff burnout ( Edwards et al., 2006 ) and psychologically-informed case discussions can enhance positive feelings towards service users and reduce staff self-blame ( Berry et al., 2009 ). Team-based training to develop staff skills using psychological models can even improve patient engagement with the service ( Caruso et al., 2013 ). However, there is no comprehensive, critical summary of interventions that have specifically targeted the element of treatment that we know is essential; the therapeutic alliance, for the group who potentially has the capacity and context to deliver compassionate, caring relationships; nurses.
In conducting this review, we systematically collated and critiqued studies reporting on interventions targeting the therapeutic relationship between nursing staff and service users in mental health settings. We aimed to answer some key questions; what intervention methods have been tested, in what clinical contexts and with which groups, what outcome measures were utilised, what effects were demonstrated and what was the quality of the methods used.
3.1. Protocol and registration
The review protocol was pre-registered and is available online within the international prospective register of systematic reviews (PROSPERO) under the registration number CRD42018111022.
3.2. Criteria for inclusion
Papers were considered eligible for inclusion if they: were published as an original, peer-reviewed journal article; written in English; included an intervention aimed to improve the therapeutic relationship between nursing staff and user/s of psychiatric or mental health services; included analysis of the impact of the intervention utilising a standardised measure of alliance. The review includes studies from any mental health service context (such as community, inpatient), client groups of any age, with any mental health diagnosis or need and interventions targeted at the relationship with either qualified or non-qualified nursing staff. Where the staff group incorporated other disciplines, these findings were still eligible if that included nurses in the overall sample.
3.3. Search methods
The current review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines ( Moher et al., 2009 ). Search terms were generated through review of empirical and opinion pieces regarding alliance and systematic review papers of alliance (for example, Elvins, and Green, 2008 ; Flückiger et al., 2012 ; Horvath, and Luborsky, 1993 ; Priebe, and McCabe, 2006 ; Zaitsoff et al., 2015 ), scoping literature searches and consultation with experts in the field. A systematic search of Excerpta Medica database (Embase), PsycINFO, Medical Literature Analysis and Retrieval System Online (MEDLINE) and Cumulative Index of Nursing and Allied Health Literature (CINAHL) databases was conducted on 05/07/18 and then updated on 04/04/19 using the following search strings: (nurse* OR nursing OR staff) AND (alliance OR relationship*) AND (mental OR psychiatry*) AND (improve* OR interven* OR change OR support). The reference lists of eligible papers were also consulted for any additional studies and a forward citation search undertaken.
3.4. Data collection and analysis
All potentially eligible records were imported into Endnote reference management software package (Version 8) and duplicate references identified and deleted. One reviewer screened titles and abstracts for relevance, using the inclusion criteria set out above and alongside regular discussion with the research team. Another independent reviewer blindly assessed 50% (randomly selected) of the full texts against the inclusion criteria demonstrating 88% agreement, with any remaining disagreements resolved through discussion with the project team, resulting in full agreement. Data extraction was guided by a pre-specified data extraction sheet detailing key features of the study: sample, setting, design, intervention, outcome measure, analysis, effect size, limitations. Authors were contacted where effect size data was not available in the original paper. The review used a narrative synthesis approach, whereby an attempt was made to go beyond a description of the studies to explore relationships within and between them ( Popay et al., 2006 ).
3.5. Assessment of methodological quality
In order to evaluate the methodological rigour of the studies included and therefore to inform the critical synthesis of the findings produced and subsequent recommendations, the papers were assessed using a standardised quality tool. There is a distinct lack of assessment tools that fulfil both the need to be demonstrably reliable and valid and also appropriate for use with a range of study designs. Based on a previous review of quality assessment tools ( Deeks et al., 2003 ), the Effective Public Health Practice Project tool ( Effective Public Health Practice Project, 1998 ) was selected as one that could offer valid ( Thomas et al., 2004 ), reliable ( Armijo-Olivo et al., 2012 ) and flexible appraisal of varying study designs. All of the eligible papers were assessed for quality by the first author and blind second-rated, with 86% agreement demonstrated. Initial ratings from the first author were reviewed collaboratively with the second rater and a decision was made to retain these scores.
4.1. Flow of records
The flow of records through the review process can be seen in Fig. 1 , in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines ( Moher et al., 2009 ). The search resulted in a total of eight papers which met inclusion criteria. These are summarised in Table 1 .

Flow of records
Summary of papers and quality ratings.
4.2. Methodological quality
Table 1 provides the overall quality rating for each paper, based on the constituent ratings of the Effective Public Health Practice Project tool and its guideline procedure. Full details of the ratings are available from the first author. As is evident, six of the eight studies were rated as weak methodologically. Berry et al. (2016) was the only study that met ‘strong’ design criteria, while Moreno-Poyato et al. (2018) was deemed moderate. The studies were predominantly down-rated due to lack of randomised designs, blinding, confounder control and full reporting of retention information.
4.3. Participant and settings
The eligible papers included interventions delivered in a range of settings (inpatient and community services, acute, rehabilitation), in a number of different countries (United Kingdom, Australia, Sweden, Spain, Netherlands) for individuals with a range of conditions under the umbrella of severe mental health problems, including psychosis and difficulties associated with a diagnosis of personality disorder. As per the inclusion criteria, all studies targeted the relationship between mental health nursing staff and service users, although there were a range of additional criteria. The range of settings and participants is reflective of the variety of roles and services within which the therapeutic alliance is fostered.
4.4. Interventions
The interventions varied in scope, focus and theoretical underpinning. Berry et al. (2012 , 2016 ) drew on psychological formulation (allied mainly to a cognitive behavioural model) to foster understanding of drivers for patients’ behaviour and clinical presentation within staff group workshops. Carpenter et al. (2007) offered group training in psycho-social interventions that included focus on specific models and also core values of therapeutic engagement. Kellett et al. (2019) utilised a consultancy model provided to pairs of staff members and service users, with cognitive analytic therapy as the underlying approach. Molin et al. (2018) focused on the structure of ward timetables, creating space for time spent together between nursing staff and patients, providing opportunity for joint activities and meaningful engagement. The authors involved staff on each ward in the precise implementation structure to provide a good fit to routine ward activities and preferences. Moreno-Poyato et al. (2018) utilised a participatory action research approach whereby the nurses involved in the study generated intervention elements in a bid to reach best practice, which ultimately involved daily interactions with individual patients, reflective groups for staff and study of scientific texts as selected by staff. Stringer et al. (2015) adopted a broad-based collaborative care programme that consisted of elements including understanding (via timeline work), structural changes (teams, treatment plans), specific interventions (problem solving) and psycho-education. The primary focus of Byrne and Deane's (2011) intervention was to improve medication adherence, with the alliance targeted as a mediating variable, involving modifying clinician beliefs about non-adherent patients that can pose barriers to the relationship and support for adherence.
4.5. Outcome measurement
The majority of the studies ( Berry et al., 2012 , 2016 ; Byrne and Deane, 2011 ; Kellett et al., 2019 ; Moreno-Poyato et al., 2018 ) utilised the Working Alliance Inventory (WAI; Horvath and Greenberg, 1989 ) as the primary alliance outcome, reflecting its prominence in the literature, although only Berry et al. (2016) and Kellett et al. (2019) used both the patient- and clinician-rated version, with the rest opting for the latter only. Others ( Molin et al., 2018 ; Stringer et al., 2015 ) used the Caring Professional Scale ( Swanson, 2000 ), as rated by service users and the scale to asses therapeutic relationships (STAR; McGuire-Snieckus et al., 2007 ), respectively. Carpenter et al. (2007) relied on a non-validated but user-defined outcome scale ( Barnes et al., 2000 ), which included numerous items relevant to the alliance; including involvement, listening and understanding.
Four of the eight included studies reported no statistically significant difference as a result of the intervention in terms of assessed therapeutic alliance ( Berry et al., 2012 , 2016 ; Molin et al., 2018 ; Stringer et al., 2015 ). Molin et al. (2018) did not provide data to facilitate a more nuanced interpretation. Berry et al. (2016) findings are intriguing as staff-rated alliance was better for the control than intervention group (similar to Berry et al., 2012 ), whereas client-rated alliance delivered a large effect size in favour of the intervention, which was presumably then diluted by a more rigorous analysis method in their strongly rated study. Stringer et al. (2015) showed a small effect in favour of the intervention group at nine months, although crucially, both groups declined in reported alliance through the course of the intervention period, leaving the findings difficult to interpret and confounded by a weak study design.
Carpenter et al. (2007) did not report longitudinal statistical improvement but did find a difference between the intervention and control groups in terms of user-rated involvement with staff, although sufficient data was not available to comment on the size of this effect and the weak study quality rating detracts from the significance. Byrne and Deane (2011) reported a statistically significant change in Working Alliance Inventory scores between baseline and six months following the alliance intervention with a medium effect size, although no improvement at 12 month follow-up and concerns raised by the weak study quality rating. Moreno-Poyato et al. (2018) demonstrated a significant difference in post-intervention alliance scores between the active and comparison group, with a median difference of 7 scale points, and large effect size. This study was one of only two in the review to score better than a weak rating in terms of quality assessment, placing more weight on the potential effectiveness of their collaboratively developed intervention. Kellett et al. (2019) demonstrated statistically significant change and a large effect size improvement for client-rated alliance in their case series study, but not for staff-rated alliance or for their larger ( n = 12 staff-client pairings) pre-post service evaluation. The weak study rating also means that these findings should be interpreted with caution, despite the encouraging ratings from service-user perspectives.
5. Discussion
We set out to collate and synthesise information pertaining to interventions that aim to support effective therapeutic alliance between nursing staff and users of mental health services, which has been shown to be central to positive outcomes in both psychotherapy and broader engagement contexts ( Cruz and Pincus, 2002 ; Duncan et al., 2010 ; Howgego et al., 2003 ; Martin et al., 2000 ; Messer and Wampold, 2002 ; Priebe and McCabe, 2006 ). The central finding of note, in the authors’ view, is the dearth of studies in this area. It seems surprising that an element of care that is so intrinsic to both patient progress and clinician role does not have a robust evidence base on which to draw in order to provide effective foundations for its development and maintenance. It might be that this has emerged from an assumption of alliance building and maintenance as an implicit ability rather than a skill to be honed and scaffolded, or of the difficulty in addressing a complex issue with a readily-evaluated design.
The evaluated interventions adopted a range of methods, including psychosocial approaches ( Berry et al., 2012 , 2016 ; Carpenter et al., 2007 ; Kellett et al., 2019 ), those targeting specific clinician attitudes ( Byrne and Deane, 2011 ) and those derived from action research, where the intervention content was collaboratively developed with staff in an attempt to bridge the gap between current and best practice ( Moreno-Poyato et al., 2018 ). The lack of a coherent, shared theoretical underpinning might contribute to the deficiency of robust research and consistent evidence base. The interventions largely consisted of group-based programmes, whereas the relationship that is predominantly measured is a dyadic one between one nurse and one service user; this discrepancy might be contributing to lack of consistent positive change. Kellett et al. (2019) did demonstrate change when the dyadic relationship was specifically targeted and measured as such in the context of a dynamic consultation approach rather than workshop-based training. It is also not entirely clear what level of public (staff and/ or service user) involvement there was in the development of the intervention packages, which might have enhanced the feasibility, acceptability and ultimately, impact ( Brett et al., 2014 ).
Data gathered by the current review do not permit recommendations in terms of effective interventions and their theoretical underpinnings. The evolution of the concept of the therapeutic alliance, from one of dyadic and confined psychotherapeutic engagement to one that often spans relationships within complex team structures, with multiple professionals at once and in varying roles outside of the narrow remit of formal therapy no doubt contribute to the difficulty in developing interventions that are sufficiently targeted yet appropriately flexible. Given the nuanced conceptualisation of the core elements of therapeutic relationships between different settings ( Cleary et al., 2012 ; McAllister et al., 2019 ; O'Brien, 2000 ; Pazargadi et al., 2015 ; Shattell et al., 2007 ; Spiers and Wood, 2010 ), it might be that the development of an alliance intervention needs to draw from both theoretical understanding, alongside setting-based contextual needs, which will need to be explored and supported in situ.
As the methodological quality assessment indicates, the studies were predominantly under-controlled, with a lack of randomised designs and matched comparison groups or controls. This limits conclusions that can be drawn even from those studies where positive outcomes were identified. The relatively small samples sizes might also have limited statistical power to detect differences, and those studies that showed promise in terms of effect sizes will need to be replicated with more adequate samples and appropriate statistical control. Few studies checked the validity of their intervention with any kind of fidelity tool ( Santacroce et al., 2004 ). It is therefore also possible that negative outcomes were due to a dilution of or divergence from the intervention protocol, rather than necessarily an intrinsic limitation of the active elements. The lack of statistical control also highlights difficulties central to the issue of intervention design and evaluation in this field. As the alliance is conceptualised as a reciprocally developed, genuine human connection, then how can this be reliably supported and measured between different pairs of individuals, where the goals, needs and definition of the relationship will be inherently idiosyncratic? The current review therefore also points to the need for a range of evaluation methods, alongside the development of controlled trials, which can adequately capture the key elements of the alliance both in terms of supporting its development and evaluating its progress.
Most studies chose to measure outcome using the working alliance inventory. Although fairly ubiquitous, this might be somewhat problematic. The Working Alliance Inventory is a tool designed for use in the context of therapy that does not fully converge with the nature of a nurse–patient relationship, which might often be more accurately conceptualised as a therapeutic key worker role, where therapeutic conversations might be had in the context of a broader care-coordination or care-planning role ( Burns, 2004 ; Simpson, 2005 ; Thurston, 2003 ). Thus, the relationship of interest and its quality might not be accurately evaluated by the use of Working Alliance Inventory. In terms of the source of the ratings, two studies that reported mixed findings ( Kellett et al., 2019 ; Berry et al., 2016 ) demonstrated larger effect sizes for the client perspective as compared to the staff member. This underscores the importance of considering multiple sources but also the need to elaborate on the best method for determining good relational outcomes, especially since client-rated alliance is the better predictor of therapeutic progress ( Bachelor, 1991 ; Fitzpatrick et al., 2005 )
5.1. Strengths and limitations of the review
We aimed to provide a comprehensive and critical summary of current evidence pertaining to intervention to support nursing staff in their therapeutic relationships with people utilising mental health services. The systematic, thorough nature of the review offers a contribution to an important area of literature hitherto unreported. The small sample of studies is reflective of the field as it stands while also limiting the utility of the review and it will be important to repeat the process as the evidence based develops, incorporating more nuanced analysis of the findings and methods and robust meta-analysis or meta-synthesis, where the nature of the interventions delivered and their qualitative impact could be more fully explored. Our decision to include both qualified and non-qualified staff interventions, and to include studies whose sample include nurses alongside other staff groups was pragmatic in nature to ensure any relevant intervention was highlighted, particularly in a limited evidence base. However, future work might wish to consider how to delineate samples more precisely and thus provide evidence best-suited to the target discipline. This review has focused on interventions that specifically target the therapeutic alliance as a core aspect of effective mental health care. It is acknowledged that the alliance is part of the approach of other modality-specific therapies, such as cognitive behavioural therapy, dialectical behaviour therapy or cognitive analytic therapy ( Bennettet al., 2006 ; Bedics et al., 2015 ; Gilbert, and Leahy, 2007 ). Therefore, synthesising findings from modality-specific intervention research, where the alliance might be evaluated as a mechanism of change, with the current, more focused conceptualisation might be warranted.
5.2. Clinical implications and recommendations for future work
The nature of the evidence base as it stands renders it difficult to make clear clinical recommendations in terms of how nursing staff should be best supported to develop and maintain effective therapeutic relationships with the individuals they work with in the settings they operate. There is some indication that interventions targeting clinician attitudes and reflective capacity, relational understanding and dynamic interactions might be helpful, although further work is needed. There is also a relative absence of service user and clinical staff involvement in the development of the reported interventions, which might limit their acceptability and feasibility. This paper, therefore, should serve as an impetus to develop a clear trajectory of research endeavours that build on the current findings and creates a more robust body of work incorporating the following key elements: i) intervention based on strong theoretical underpinnings and service user and clinician involvement; ii) methodologically sound studies; iii) assessment of fidelity to the intervention model; iv) targeting and evaluation of the alliance aligned with its conceptualisation as a dyadic, mutual, professional relationship outside the specific bounds of psychotherapy.
Conflict of interest
Dr Samantha Hartley is funded by a National Institute for Health Research (NIHR) Integrated Clinical Academic Clinical Lectureship for this research project. This paper presents independent research funded by the National Institute for Health Research (NIHR). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.

NurseStudy.Net
Nursing Education Site
Mental Health Nursing Diagnosis and Nursing Care Plan
Last updated on April 30th, 2023 at 12:00 am
Mental Health Nursing Care Plans Diagnosis and Interventions
Mental Health Nursing NCLEX Review and Nursing Care Plans
The history of mental illness, developments in treatment, recent concerns in mental health, and the responsibilities of the mental health nurse will all be discussed in this article to provide more ideas about mental health nursing.
Visualizing what it would be like or what nurses do in the field of mental health is a bit challenging, as it is often unfamiliar or strange. Working as a mental health nurse, despite the hurdles, can be a rewarding vocation.
Mental Health
Mental health is a state of emotional, psychological, and social well-being. There is no one-size-fits-all description of mental health, but in general, an individual’s actions and behaviors can tell a lot about his or her mental state.
Every culture of a society has a significant influence on its ideas and values, which has an impact on how mental health is defined. Satisfying interpersonal relationships, effective behavior and coping with the normal stresses of life, positive self-concept, and emotional stability are all indicators of mental health, as it affects how we think, feel, and act.
From childhood and adolescence through maturity, mental health is crucial at all stages of life. Some commonly ignore it, but mental health is an integral part of health.
World Health Organization (WHO) defines health as “ a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity .” absolutely, there is no health without mental health.
It is imperative to keep in mind that a person’s mental health can fluctuate over a wide range of circumstances. At any one time, an individual’s level of mental health can be affected by a number of social, interpersonal, psychological/biological factors.
- Social/cultural or environmental aspects comprise a sense of community, access to essential resources, intolerance of violence, support of diversity among individuals, environmental mastery, and a positive yet realistic outlook on life.
- Interpersonal. Effective communication, the ability to help others, intimacy, and a balance of separateness and connectivity are all interpersonal or relationship aspects affecting mental health.
- Biological/Psychological. People are more susceptible to mental health issues because of diverse psychological and personality traits, while genetic variables are also a part of biological factors. A person’s biological makeup, autonomy and independence, self-esteem, and capacity for growth are all part of the biological aspects of mental health. This aspect further includes vitality, ability to find meaning in life, emotional resilience or toughness, sense of belonging, reality orientation, and coping or stress management abilities.
Mental Illness
Poor mental health and mental illness are not the same things, despite the fact that they are frequently used interchangeably. A person’s mental health can deteriorate without being diagnosed with a mental illness.
A person with a mental illness, on the other hand, can have moments of physical, mental, and social well-being.
According to the American Psychiatric Association (APA, 2000), mental disorder is “ a clinically significant behavioral or psychological syndrome or pattern that occurs in an individual and is associated with current distress or a significantly increased risk of death, pain, disability, or a significant loss of freedom “.
Mental illness is one of the most common health issues in the United States, according to the Center for Disease Control and Prevention (CDC). However, over half of those who suffer from mental illness do not seek treatment for their conditions.
People frequently avoid or delay obtaining treatment because they are afraid of being discriminated against or losing their employment and livelihoods. Because persons with mental illnesses are still stigmatized, prejudiced, and discriminated against by some.
There is no sole reason for mental illness. The likelihood of mental illness can be influenced by a variety of circumstances, including:
- Trauma or a history of abuse as examples of early negative life events (child abuse, sexual assault, witnessing violence, etc.)
- Other continuous (chronic) medical conditions, such as cancer , diabetes , or stroke
- Biological and chemical imbalances in the brain
- Drugs or alcohol use
- Experiencing feelings of solitude or seclusion
Diagnostic and Statistical Manual of Mental Disorders
The American Psychiatric Association (APA) published the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR). It is widely used by healthcare providers, particularly mental health professionals.
Mental disorders are described in the DSM-IV-TR, featuring precise diagnostic criteria for each based on relevant clinical experience and extensive research. It serves three main purposes:
- To enable the use of standardized terminology and nomenclature for all mental health professionals.
- To distinguish diagnoses apart from each other by identifying particular traits or symptoms.
- To aid in the identification of mental illnesses’ underlying causes
Multiaxial classification in the DSM-IV-TR allows the mental health professionals to identify all of the aspects that contribute to a person’s condition by assessing multiple axes, or domains of information.
- Axis I. Except for mental retardation and personality disorders, Axis I is used to provide information on all major psychiatric disorders. Mood disorders, anxiety disorders, and eating disorders were among the conditions that were classified.
- Axis II. It is used to outline mental retardation and personality disorders, as well as major maladaptive personality traits and defense mechanisms. Some of the conditions of personality disorders include antisocial and histrionic personality disorders. While mental retardation, which has now been referred to as intellectual disability, is characterized by intellectual impairment and deficits in other areas such as self-care and interpersonal skills.
- Axis III. It is used to record current medical conditions that may be significant to understanding or managing a person’s mental illness. These medical conditions influence or worsen Axis I and Axis II disorders. Examples include HIV/AIDS and brain injuries, among others.
- Axis IV. This axis took into account any social or environmental issues that could affect Axis I or Axis II disorders. Unemployment, relocation, divorce, or the death of a loved one are all examples of these situations.
- Axis V. It is where the physicians use Global Assessment of Functioning (GAF) scale from 0 to 100 and give their impression of the client’s overall level of functioning. A greater understanding of how the other four axes interacted and the impact on the individual’s life may be gained from this assessment.
History of Treating Mental Illness
Any illness, according to ancient belief, signaled the gods’ disapproval and was considered as retribution for sins and transgression, therefore persons with mental illnesses were considered as either divine or demonic, depending on how they behaved.
Later, Aristotle attempted to link mental and physical disorders and created his theory that mental disorders were caused by imbalances in happiness, tranquility, rage, and sadness. Bloodletting, starvation, and purging were then used as a treatment to restore balance.
All diseases were blamed on demons again in early Christian times, and the mentally sick were considered as possessed, so priests execute exorcism to expel bad spirits.
During the Renaissance period in England and neighboring European countries, people with mental illness were distinguished from criminals; those thought harmless were permitted to roam the countryside and/or live in rural communities, while the more “dangerous lunatics” were imprisoned, chained, and starved to death.
The poor history of mental illness treatment continued as the Hospital of St. Mary of Bethlehem was officially declared an infirmary for the insane, the first of its kind in 1547. The visitors were privileged to watch and mock the mentally sick, who were treated as animals rather than humans, for a corresponding fee.
The time when mental illness was more understood and treated came in the 1970s. Asylum was formed as a safe haven or shelter for persons who had been lashed, abused, or starved solely because they were mentally ill in institutions. A crusade to improve mental health treatment was started, which then resulted in the opening of 32 state-run hospitals in England, where patients could seek sanctuary.
In the 1850s, Sigmund Freud and other Psychiatrists began the period of scientific study and treatment of mental illnesses. Because of these men, the study of psychiatry, as well as the diagnosis and treatment of mental illness, officially began.
The development of psychotropic medicines or pharmaceuticals used to treat mental disorders marked a significant step forward in the treatment of mental illness around 1950. More pharmacologic interventions were introduced over the next ten years.
Mental Health Nursing
Mental health nursing is a specialized branch of nursing that focuses on the treatment of individuals who have a mental illness to help them recover and live a better life.
It necessitates a wide range of interventions, psychological, and neurobiological skills. In addition to the assessment, diagnosis, care, and treatment of mental health and substance use disorders, it focuses on enhancing well-being through prevention and education.
Mental Health Nurses work in a variety of setting and provide comprehensive care to individuals, families, groups, and societies.
They build strong therapeutic relationships with people of all ages, learning about their lives and issues to make a positive impact on their lives.
Mental Health Nurses also have a deep understanding of mental health disorders and how to assess, diagnose, and treat them to provide specialized care. They usually collaborate with other healthcare professionals to ensure that the patient’s clinical outcomes are as effective as possible.
Mental Health Nursing Diagnosis
Mental health nursing care plan 1.
Impaired Verbal Communication
Nursing Diagnosis: Impaired Verbal Communication secondary to schizophrenia as evidenced by difficulty communicating thoughts verbally, struggle in identifying and maintaining the regular communication pattern, and disorganized thinking.
Desired Outcomes:
- The patient will articulate his or her thoughts and feelings in a rational, logical, and goal-oriented manner.
- The patient will be trained in one or two diversionary techniques to help manage anxiety and improve the ability to think clearly and talk more sensibly.
Mental Health Nursing Care Plan 2
Impaired Social Interaction
Nursing Diagnosis: Impaired Social Interaction secondary to major depressive disorder as evidenced by verbalized discomfort in social situations, avoiding interaction with others, and lacking eye contact.
Desired Outcome: Within one month, the patient will be able to recognize feelings that result in poor social interactions and exhibit improvement in resuming relationships with friends and family members.
Mental Health Nursing Care Plan 3
Disturbed Sensory Perception (Auditory/Visual)
Nursing Diagnosis: Disturbed Sensory Perception related to neurologic/biochemical changes and psychological stress as evidenced by frequent blinking of the eyes, auditory distortions, inappropriate responses, and hallucinations.
Desired Outcome: The patient will demonstrate techniques to refrain from responding to hallucinations and identify at least two stressful events that trigger them.
Mental Health Nursing Care Plan 4
Ineffective Coping
Nursing Diagnosis: Ineffective coping secondary to anxiety and panic disorders as evidenced by an inability to meet basic needs and role expectations, inadequate problem solving, and ritualistic behavior.
Desired Outcome: The patient will demonstrate the ability to cope effectively and how to maintain anxiety at a manageable level.
Mental Health Nursing Care Plan 5
Interrupted Family Processes
Nursing Diagnosis: Interrupted Family Processes secondary to Bipolar Disorder as evidenced by changes in communication patterns, the crisis in the family, and changes in participation in decision making and problem-solving.
Desired Outcome: The family members and/or significant others will demonstrate awareness of what bipolar disorder is, how it is treated, and the importance of medication and treatment adherence.
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care . St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2017). Nursing care plans: Diagnoses, interventions, & outcomes . St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care . St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination . St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines, policies, and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes.
This information is intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.
Anna Curran. RN, BSN, PHN
Leave a Comment Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .


- Clinical articles
- CPD articles
- CPD Quizzes
- Practice question
- Expert advice
- Career advice
- Revalidation
- Cancer Nursing Practice
- Emergency Nurse
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Jobs Fairs
- RCNi events calendar
- CPD webinars on-demand
Assessment and Care Planning in Mental Health Nursing
Posted 25 may 2016.

Supporting older adults who misuse alcohol
Nurse wins tribunal case after losing shifts for raising concerns, a culturally competent compassionate approach to support veterans with alcohol issues, characteristics and outcomes of people in suicidal crisis at two emergency departments, 5 most read articles, are you micromanaged, or empowered in a team with a shared vision, protected time for clinical supervision: which nurses will benefit from new rules, dnacpr tragedy will prey on the consciences of nurses involved, but they are all of us, help for overseas nurses struggling to get on the register, ‘we need to get comfortable talking about racism in the nhs’, other rcni websites.
- RCNi Learning
- RCNi Nursing Careers and Jobs Fairs
- RCNi Nursing Jobs
- RCNi Portfolio

IMAGES
VIDEO
COMMENTS
Whilst the focus is on assessment and care planning; knowledge and skills on a range of essential areas are present in this text. It is an essential handbook for key mental health nursing skills. Case studies are presented with clarity, and Nick Wrycraft is clearly committed to nurses learning from service users, which is essential for values ...
Psychiatric-mental health nursing is, "The nursing practice specialty committed to promoting mental health through the assessment, diagnosis, and treatment of behavioral problems, mental disorders, and comorbid conditions across the life span. Psychiatric-mental health nursing intervention is an art and a science, employing a purposeful use of self and a wide range of nursing, psychosocial ...
Phillip Barker, (2004, p6) says that it was suggested by most psychologists that a definition relevant to psychiatric and mental health nursing should focus on estimation of character or person's worth and what they may become. An assessment is very important because it provides the scientific basis for a complete care plan.
I am going to discuss the assessment and development of the care plan of the service user. The essay will also consist of a brief biography of the patient's contributing factors towards her present mental health circumstances. The relevant culturally sensitive engagement and assessment skills used by the nurse in their relationships with the ...
Nick Wrycraft. McGraw-Hill Education (UK), Sep 16, 2015 - Medical - 232 pages. Assessment of mental health problems is a challenging area of practice that covers a range of symptoms and behaviours - and involves building a trust relationship with service users while also using specialist skills. Using a values-based approach focused on ...
Abstract. Nurses have an essential role to play in the assessment and planning of patient care. This is emphasised in the Nursing and Midwifery Council's 2018 Future Nurse proficiency standards. In this article, the author discusses the importance of person-centred care in assessing needs and highlights the need for all nursing interventions to ...
Books. Assessment and Care Planning in Mental Health Nursing. Nick Wrycraft. McGraw-Hill Education, 2015 - Medical - 192 pages. Assessment of mental health problems is a challenging area of practice that covers a range of symptoms and behaviours - and involves building a trust relationship with service users while also using specialist skills.
Advanced mental health assessment and decision-making require intuitive and analytic clinical reasoning, critical thinking, professional knowledge and shared decision-making. It also requires the integration of nursing knowledge, with knowledge from other fields (medicine, psychology, sociology, pharmacology).
SECTION 1. Initiating relationships with service users and conducting assessments. 1 Assessment in mental health. 2 Communication and interpersonal skills in assessment. 3 Engaging with the service user in assessment. 4 Risk assessment. 5 Care planning. 6 Partnership working. 7 Interventions.
Background Involving mental health service users in planning and reviewing their care can help personalised care focused on recovery, with the aim of developing goals specific to the individual and designed to maximise achievements and social integration. We aimed to ascertain the views of service users, carers and staff in acute inpatient wards on factors that facilitated or acted as barriers ...
Assessment is essential because the health care professionals need to know the physical, social, psychological, and cultural aspect of the patient's life Wolters et al. (2008). An assessment is done to obtain information to create a detailed history about the patient, and to distinguish problems and to create a nursing diagnosis along with a ...
This book offers an informative resource for new students in the field of mental health nursing practice. There is a good introduction to the care planning process in section one, with a heavy emphasis on assessment, exploring communication skills and engaging the service user, noting how assessment guides the nursing process as a whole.
Planning care is essential in the delivery of appropriate nursing care. Following assessment of a patient's needs, the next stage is to 'plan care' to address the actual and potential problems that have been identified. This helps to prioritise the client's needs and assists in setting person-centred goals. Planned care will change as a patient's needs change and as the nurse and/or other ...
The therapeutic role of nursing staff in mental health care is especially pertinent in settings such as inpatient wards, where patients interact with nurses for the largest proportion of time and the relationship with them is cited as key to therapeutic progression (Hopkins et al., 2009; McAndrew et al., 2014), with a perceived interplay ...
Introduction In this essay I will outline, discuss and analyse the assessment and planning of care of a service user which I encountered during my placement in an acute adult inpatient mental health ward. This is an assessment inpatient service which provides support for service users with functional and organic mental illnesses. The life history of the service user will be explained, and this ...
Mental health nursing is a specialized branch of nursing that focuses on the treatment of individuals who have a mental illness to help them recover and live a better life. It necessitates a wide range of interventions, psychological, and neurobiological skills. In addition to the assessment, diagnosis, care, and treatment of mental health and ...
Application of the holistic approach can be seen in the Biopsychosocial model used today in psychiatric and mental health nursing. The interdependent domains, biological (physical functioning), psychological (thoughts feelings and, behavior), and social (influence from family and communities) all come together with each having its own knowledge and treatment focus for the patient (source pg. 70).
This book is an informative resource for new students in the field of mental health nursing practice. In section one there is a useful introduction to the care planning process, with an emphasis on assessment, exploring communication skills, engaging with service users and noting how assessment guides the nursing process as a whole.
Introduction. This report will focus on the assessment and care planning for an individual using the mental health services. Evidence based approach will be deploy in order to be able to record, review and monitor the progress of the service user. Evidence-based practice is a structured and systematic approach to using research based knowledge ...
Introduction In this essay, I will outline, discuss and analyze the assessment and planning of care of a service user which I encountered during my placement in an acute adult inpatient mental health ward. This is an assessment inpatient service that provides support for service users with functional and organic mental illnesses. The life history of the service user will be explained, and this ...
this is a care plan and then written essay as part of an assignment. the careplan is about violet a uni patient made for the assignment. it goes through all ... Violet does not understand how nutriion and diet are important to maintain her healthy physical and mental state. ... J. and Kelley, J. (2003). Health assessment in nursing. Ageuk.org ...
Introduction In this essay I will outline, discuss and analyse the assessment and planning of care of a service user which I encountered during my placement in an acute adult inpatient mental health ward. This is an assessment inpatient service which provides support for service users with functional and organic mental illnesses. The life history of the service user will be explained, and this ...