Featured Topics
Featured series.
A series of random questions answered by Harvard experts.

Explore the Gazette
Read the latest.

How do you read organization’s silence over rise of Nazism?

Got milk? Does it give you problems?

Cancer risk, wine preference, and your genes
Studies show that about 9 percent of the population and nearly 28 percent of high school students are e-cigarette users.
Diego Cervo/iStock by Getty Images
Restricted airways, scarred lung tissue found among vapers
MGH News and Public Affairs
Small study looks at chronic e-cigarette users, seeing partial improvement once they stop
Chronic use of e-cigarettes, commonly known as vaping, can result in small airway obstruction and asthma-like symptoms, according to researchers at Harvard-affiliated Massachusetts General Hospital.
More like this

Teen vaping rising fast, research says

Survey of oncologists finds knowledge gap on medical marijuana
Chemical flavorings found in e-cigarettes linked to respiratory disease
In the first study to microscopically evaluate the pulmonary tissue of e-cigarette users for chronic disease, the team found in a small sample of patients fibrosis and damage in the small airways, similar to the chemical inhalation damage to the lungs typically seen in soldiers returning from overseas conflicts who had inhaled mustard or similar types of noxious gases. The study was published in New England Journal of Medicine Evidence .
“All four individuals we studied had injury localized to the same anatomic location within the lung, manifesting as small airway-centered fibrosis with constrictive bronchiolitis, which was attributed to vaping after thorough clinical evaluations excluded other possible causes,” says lead author Lida Hariri, an associate professor of pathology at Harvard Medical School and a pathologist and physician investigator at MGH. “We also observed that when patients ceased vaping, they had a partial reversal of the condition over one to four years, though not complete due to residual scarring in the lung tissue.”
A huge increase in vaping, particularly among young adults and adolescents, has occurred in the United States, with studies showing about 9 percent of the population and nearly 28 percent of high school students are e-cigarette users. Unlike cigarette smoking, however, the long-term health risks of chronic vaping are largely unknown.
In order to determine the underlying pathophysiology of vaping-related symptoms, the MGH team examined a cohort of four patients, each with a three- to eight-year history of e-cigarette use and chronic lung disease. All patients underwent detailed clinical evaluation, including pulmonary function tests, high resolution chest imaging, and surgical lung biopsy. Constrictive bronchiolitis, or narrowing of the small airways due to fibrosis within the bronchiolar wall, was observed in each patient. So was significant overexpression of MUC5AC, a gel-forming protein in the mucus layer of the airway that has been seen in airway cell and sputum samples of individuals who vape. In addition, three of the four patients had evidence of mild emphysema consistent with their former combustible cigarette smoking history, though researchers concluded this was distinct from the findings of constrictive bronchiolitis seen in the patient cohort.
Because the same type of lung damage was observed in all patients, as well as partial improvement in symptoms after e-cigarette usage was stopped, researchers concluded that vaping was the most likely cause after thorough evaluation and exclusion of other possible causes. “Our investigation shows that chronic pathological abnormalities can occur in vaping exposure,” says senior author David Christiani, a professor of medicine at HMS and a physician investigator at Mass General Research Institute. “Physicians need to be informed by scientific evidence when advising patients about the potential harm of long-term vaping, and this work adds to a growing body of toxicological evidence that nicotine vaping exposures can harm the lung.”
A hopeful sign from the study was that three of the four patients showed improvements in their pulmonary function tests and high-resolution computed tomography (HRCT) chest imaging after they ceased vaping. “While there is growing evidence to show that vaping is a risky behavior with potential long-term health consequences for users,” says Hariri, “our research also suggests that quitting can be beneficial and help to reverse some of the disease.”
The study was funded by the National Institutes of Health.
Share this article
You might like.
Medical historians look to cultural context, work of peer publications in wrestling with case of New England Journal of Medicine

Biomolecular archaeologist looks at why most of world’s population has trouble digesting beverage that helped shape civilization

Biologist separates reality of science from the claims of profiling firms
Epic science inside a cubic millimeter of brain
Researchers publish largest-ever dataset of neural connections
Finding right mix on campus speech policies
Legal, political scholars discuss balancing personal safety, constitutional rights, academic freedom amid roiling protests, cultural shifts
Good genes are nice, but joy is better
Harvard study, almost 80 years old, has proved that embracing community helps us live longer, and be happier
Advertisement
How bad is vaping for your health? We’re finally getting answers
As more of us take up vaping and concerns rise about the long-term effects, we now have enough data to get a grip on the health impact – and how it compares to smoking
By Graham Lawton
6 December 2023

Klaus Kremmerz
AS THE old joke goes, when I read about the dangers of smoking, I gave up reading. If you are a vaper, you might feel like you want to stop reading now. Don’t: you need to know this.
I am a vaper. Like many others, I used to smoke and switched to vaping for health reasons. I plan to quit completely, but I haven’t managed it yet. I am sure vaping is better for me than smoking, but I am also sure it is worse than not vaping. I cough in the morning and feel massively addicted to the nicotine. I don’t even really know what I am inhaling. I worry that it will be hard to quit, that I am causing long-term damage to my body and that by vaping, I am susceptible to slipping back down the slope to cigarettes. I also have the same worries for the teenagers I see coming out of school and immediately enveloping themselves in sweet-smelling clouds.
Is CBD a wonder drug or waste of money? Here's what the evidence says
As vaping has increased throughout the Western world, these fears have been repeated often. Part of last month’s King’s Speech in the UK focused on new legislation aiming to create a smoke-free generation in part by cracking down on youth vaping. Worldwide, there have been calls for tougher regulation and more investigation into vaping’s health effects as increasing numbers of children admit to taking up the habit.
But there hasn’t been a huge amount to say on whether fears over health effects are well-founded – until recently. Now, vaping…
Sign up to our weekly newsletter
Receive a weekly dose of discovery in your inbox! We'll also keep you up to date with New Scientist events and special offers.
To continue reading, subscribe today with our introductory offers
No commitment, cancel anytime*
Offer ends 2nd of July 2024.
*Cancel anytime within 14 days of payment to receive a refund on unserved issues.
Inclusive of applicable taxes (VAT)
Existing subscribers
More from New Scientist
Explore the latest news, articles and features
Cannabis vaping liquids contain lead and other toxic metals
Subscriber-only
Why does the UK want to ban disposable vapes and when will it happen?
Patchwork vaping regulation can show the way to a smoke-free world, vaping vs edibles: how does the way we use cannabis alter its effects, popular articles.
Trending New Scientist articles
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Impact of vaping on...
Impact of vaping on respiratory health
Linked editorial.
Protecting children from harms of vaping
- Related content
- Peer review
- Andrea Jonas , clinical assistant professor
- Division of Pulmonary, Allergy, and Critical Care, Department of Medicine, Stanford University, Stanford, CA, USA
- Correspondence to A Jonas andreajonas{at}stanford.edu
Widespread uptake of vaping has signaled a sea change in the future of nicotine consumption. Vaping has grown in popularity over the past decade, in part propelled by innovations in vape pen design and nicotine flavoring. Teens and young adults have seen the biggest uptake in use of vape pens, which have superseded conventional cigarettes as the preferred modality of nicotine consumption. Relatively little is known, however, about the potential effects of chronic vaping on the respiratory system. Further, the role of vaping as a tool of smoking cessation and tobacco harm reduction remains controversial. The 2019 E-cigarette or Vaping Use-Associated Lung Injury (EVALI) outbreak highlighted the potential harms of vaping, and the consequences of long term use remain unknown. Here, we review the growing body of literature investigating the impacts of vaping on respiratory health. We review the clinical manifestations of vaping related lung injury, including the EVALI outbreak, as well as the effects of chronic vaping on respiratory health and covid-19 outcomes. We conclude that vaping is not without risk, and that further investigation is required to establish clear public policy guidance and regulation.
Abbreviations
BAL bronchoalveolar lavage
CBD cannabidiol
CDC Centers for Disease Control and Prevention
DLCO diffusing capacity of the lung for carbon monoxide
EMR electronic medical record
END electronic nicotine delivery systems
EVALI E-cigarette or Vaping product Use-Associated Lung Injury
LLM lipid laden macrophages
THC tetrahydrocannabinol
V/Q ventilation perfusion
Introduction
The introduction of vape pens to international markets in the mid 2000s signaled a sea change in the future of nicotine consumption. Long the mainstay of nicotine use, conventional cigarette smoking was on the decline for decades in the US, 1 2 largely owing to generational shifts in attitudes toward smoking. 3 With the advent of vape pens, trends in nicotine use have reversed, and the past two decades have seen a steady uptake of vaping among young, never smokers. 4 5 6 Vaping is now the preferred modality of nicotine consumption among young people, 7 and 2020 surveys indicate that one in five US high school students currently vape. 8 These trends are reflected internationally, where the prevalence of vape products has grown in both China and the UK. 9 Relatively little is known, however, regarding the health consequences of chronic vape pen use. 10 11 Although vaping was initially heralded as a safer alternative to cigarette smoking, 12 13 the toxic substances found in vape aerosols have raised new questions about the long term safety of vaping. 14 15 16 17 The 2019 E-cigarette or Vaping product Use-Associated Lung Injury (EVALI) outbreak, ultimately linked to vitamin E acetate in THC vapes, raised further concerns about the health effects of vaping, 18 19 20 and has led to increased scientific interest in the health consequences of chronic vaping. This review summarizes the history and epidemiology of vaping, and the clinical manifestations and proposed pathophysiology of lung injury caused by vaping. The public health consequences of widespread vaping remain to be seen and are compounded by young users of vape pens later transitioning to combustible cigarettes. 4 21 22 Deepened scientific understanding and public awareness of the potential harms of vaping are imperative to confront the challenges posed by a new generation of nicotine users.
Sources and selection criteria
We searched PubMed and Ovid Medline databases for the terms “vape”, “vaping”, “e-cigarette”, “electronic cigarette”, “electronic nicotine delivery”, “electronic nicotine device”, “END”, “EVALI”, “lung injury, diagnosis, management, and treatment” to find articles published between January 2000 and December 2021. We also identified references from the Centers for Disease Control and Prevention (CDC) website, as well as relevant review articles and public policy resources. Prioritization was given to peer reviewed articles written in English in moderate-to-high impact journals, consensus statements, guidelines, and included randomized controlled trials, systematic reviews, meta-analyses, and case series. We excluded publications that had a qualitative research design, or for which a conflict of interest in funding could be identified, as defined by any funding source or consulting fee from nicotine manufacturers or distributors. Search terms were chosen to generate a broad selection of literature that reflected historic and current understanding of the effects of vaping on respiratory health.
The origins of vaping
Vaping achieved widespread popularity over the past decade, but its origins date back almost a century and are summarized in figure 1 . The first known patent for an “electric vaporizer” was granted in 1930, intended for aerosolizing medicinal compounds. 23 Subsequent patents and prototypes never made it to market, 24 and it wasn’t until 1979 that the first vape pen was commercialized. Dubbed the “Favor” cigarette, the device was heralded as a smokeless alternative to cigarettes and led to the term “vaping” being coined to differentiate the “new age” method of nicotine consumption from conventional, combustible cigarettes. 25 “Favor” cigarettes did not achieve widespread appeal, in part because of the bitter taste of the aerosolized freebase nicotine; however, the term vaping persisted and would go on to be used by the myriad products that have since been developed.

Timeline of vape pen invention to widespread use (1970s-2020)
- Download figure
- Open in new tab
- Download powerpoint
The forerunner of the modern vape pen was developed in Beijing in 2003 and later introduced to US markets around 2006. 26 27 Around this time, the future Juul Laboratories founders developed the precursor of the current Juul vape pen while they were students at the Stanford Byers-Center for Biodesign. 28 Their model included disposable cartridges of flavored nicotine solution (pods) that could be inserted into the vape pen, which itself resembled a USB flash drive. Key to their work was the chemical alteration of freebase nicotine to a benzoate nicotine salt. 29 The lower pH of the nicotine salt resulted in an aerosolized nicotine product that lacked a bitter taste, 30 and enabled manufacturers to expand the range of flavored vape products. 31 Juul Laboratories was founded a decade later and quickly rose to dominate the US market, 32 accounting for an estimated 13-59% of the vape products used among teens by 2020. 6 8 Part of the Juul vape pen’s appeal stems from its discreet design, as well as its ability to deliver nicotine with an efficiency matching that of conventional cigarettes. 33 34 Subsequent generations of vape pens have included innovations such as the tank system, which allowed users to select from the wide range of different vape solutions on the market, rather than the relatively limited selection available in traditional pod based systems. Further customizations include the ability to select different vape pen components such as atomizers, heating coils, and fluid wicks, allowing users to calibrate the way in which the vape aerosol is produced. Tobacco companies have taken note of the shifting demographics of nicotine users, as evidenced in 2018 by Altria’s $12.8bn investment in Juul Laboratories. 35
Vaping terminology
At present, vaping serves as an umbrella term that describes multiple modalities of aerosolized nicotine consumption. Vape pens are alternatively called e-cigarettes, electronic nicotine delivery systems (END), e-cigars, and e-hookahs. Additional vernacular terms have emerged to describe both the various vape pen devices (eg, tank, mod, dab pen), vape solution (eg, e-liquid, vape juice), as well as the act of vaping (eg, ripping, juuling, puffing, hitting). 36 A conventional vape pen is a battery operated handheld device that contains a storage chamber for the vape solution and an internal element for generating the characteristic vape aerosol. Multiple generations of vape pens have entered the market, including single use, disposable varieties, as well as reusable models that have either a refillable fluid reservoir or a disposable cartridge for the vape solution. Aerosol generation entails a heating coil that atomizes the vape solution, and it is increasingly popular for devices to include advanced settings that allow users to adjust features of the aerosolized nicotine delivery. 37 38 Various devices allow for coil temperatures ranging from 110 °C to over 1000 °C, creating a wide range of conditions for thermal degradation of the vape solution itself. 39 40
The sheer number of vape solutions on the market poses a challenge in understanding the impact of vaping on respiratory health. The spectrum of vape solutions available encompasses thousands of varieties of flavors, additives, and nicotine concentrations. 41 Most vape solutions contain an active ingredient, commonly nicotine 42 ; however, alternative agents include tetrahydrocannabinol (THC) or cannabidiol (CBD). Vape solutions are typically composed of a combination of a flavorant, nicotine, and a carrier, commonly propylene glycol or vegetable glycerin, that generates the characteristic smoke appearance of vape aerosols. Some 450 brands of vape now offer more than 8000 flavors, 41 a figure that nearly doubled over a three year period. 43 Such tremendous variety does not account for third party sellers who offer users the option to customize a vape solution blend. Addition of marijuana based products such as THC or CBD requires the use of an oil based vape solution carrier to allow for extraction of the psychoactive elements. Despite THC vaping use in nearly 9% of high schoolers, 44 THC vape solutions are subject to minimal market regulation. Finally, a related modality of THC consumption is termed dabbing, and describes the process of inhaling aerosolized THC wax concentrate.
Epidemiology of vaping
Since the early 2000s, vaping has grown in popularity in the US and elsewhere. 8 45 Most of the 68 million vape pen users are concentrated in China, the US, and Europe. 46 Uptake among young people has been particularly pronounced, and in the US vaping has overtaken cigarettes as the most common modality of nicotine consumption among adolescents and young adults. 47 Studies estimate that 20% of US high school students are regular vape pen users, 6 48 in contrast to the 5% of adults who use vape products. 2 Teen uptake of vaping has been driven in part by a perception of vaping as a safer alternative to cigarettes, 49 50 as well as marketing strategies that target adolescents. 33 Teen use of vape pens is further driven by the low financial cost of initiation, with “starter kits” costing less than $25, 51 as well as easy access through peer sales and inconsistent age verification at in-person and online retailers. 52 After sustained growth in use over the 2010s, recent survey data from 2020 suggest that the number of vape pen users has leveled off among teens, perhaps in part owing to increased perceived risk of vaping after the EVALI outbreak. 8 53 The public health implications of teen vaping are compounded by the prevalence of vaping among never smokers (defined as having smoked fewer than 100 lifetime cigarettes), 54 and subsequent uptake of cigarette smoking among vaping teens. 4 55 Similarly, half of adults who currently vape have never used cigarettes, 2 and concern remains that vaping serves as a gateway to conventional cigarette use, 56 57 although these results have been disputed. 58 59 Despite regulation limiting the sale of flavored vape products, 60 a 2020 survey found that high school students were still predominantly using fruit, mint, menthol, and dessert flavored vape solutions. 48 While most data available surround the use of nicotine-containing vape products, a recent meta-analysis showed growing prevalence of adolescents using cannabis-containing products as well. 61
Vaping as harm reduction
Despite facing ongoing questions about safety, vaping has emerged as a potential tool for harm reduction among cigarette smokers. 12 27 An NHS report determined that vaping nicotine is “around 95% less harmful than cigarettes,” 62 leading to the development of programs that promote vaping as a tool of risk reduction among current smokers. A 2020 Cochrane review found that vaping nicotine assisted with smoking cessation over placebo 63 and recent work found increased rates of cigarette abstinence (18% v 9.9%) among those switching to vaping compared with conventional nicotine replacement (eg, gum, patch, lozenge). 64 US CDC guidance suggests that vaping nicotine may benefit current adult smokers who are able to achieve complete cigarette cessation by switching to vaping. 65 66
The public health benefit of vaping for smoking cessation is counterbalanced by vaping uptake among never smokers, 2 54 and questions surrounding the safety of chronic vaping. 10 11 Controversy surrounding the NHS claim of vaping as 95% safer than cigarettes has emerged, 67 68 and multiple leading health organizations have concluded that vaping is harmful. 42 69 Studies have demonstrated airborne particulate matter in the proximity of active vapers, 70 and concern remains that secondhand exposure to vaped aerosols may cause adverse effects, complicating the notion of vaping as a net gain for public health. 71 72 Uncertainty about the potential chronic consequences of vaping combined with vaping uptake among never smokers has complicated attempts to generate clear policy guidance. 73 74 Further, many smokers may exhibit “dual use” of conventional cigarettes and vape pens simultaneously, further complicating efforts to understand the impact of vape exposure on respiratory health, and the role vape use may play in smoking cessation. 12 We are unable to know with certainty the extent of nicotine uptake among young people that would have been seen in the absence of vaping availability, and it remains possible that some young vape pen users may have started on conventional cigarettes regardless. That said, declining nicotine use over the past several decades would argue that many young vape pen users would have never had nicotine uptake had vape pens not been introduced. 1 2 It remains an open question whether public health measures encouraging vaping for nicotine cessation will benefit current smokers enough to offset the impact of vaping uptake among young, never smokers. 75
Vaping lung injury—clinical presentations
Vaping related lung injury: 2012-19.
The potential health effects of vape pen use are varied and centered on injury to the airways and lung parenchyma. Before the 2019 EVALI outbreak, the medical literature detailed case reports of sporadic vaping related acute lung injury. The first known case was reported in 2012, when a patient presented with cough, diffuse ground glass opacities, and lipid laden macrophages (LLM) on bronchoalveolar lavage (BAL) return in the context of vape pen use. 76 Over the following seven years, an additional 15 cases of vaping related acute lung injury were reported in the literature. These cases included a wide range of diffuse parenchymal lung disease without any clear unifying features, and included cases of eosinophilic pneumonia, 77 78 79 hypersensitivity pneumonitis, 80 organizing pneumonia, 81 82 diffuse alveolar hemorrhage, 83 84 and giant cell foreign body reaction. 85 Although parenchymal lung injury predominated the cases reported, additional cases detailed episodes of status asthmaticus 86 and pneumothoraces 87 attributed to vaping. Non-respiratory vape pen injury has also been described, including cases of nicotine toxicity from vape solution ingestion, 88 89 and injuries sustained owing to vape pen device explosions. 90
The 2019 EVALI outbreak
In the summer of 2019 the EVALI outbreak led to 2807 cases of idiopathic acute lung injury in predominantly young, healthy individuals, which resulted in 68 deaths. 19 91 Epidemiological work to uncover the cause of the outbreak identified an association with vaping, particularly the use of THC-containing products, among affected individuals. CDC criteria for EVALI ( box 1 ) included individuals presenting with respiratory symptoms who had pulmonary infiltrates on imaging in the context of having vaped or dabbed within 90 days of symptom onset, without an alternative identifiable cause. 92 93 After peaking in September 2019, EVALI case numbers steadily declined, 91 likely owing to identification of a link with vaping, and subsequent removal of offending agents from circulation. Regardless, sporadic cases continue to be reported, and a high index of suspicion is required to differentiate EVALI from covid-19 pneumonia. 94 95 A strong association emerged between EVALI cases and the presence of vitamin E acetate in the BAL return of affected individuals 96 ; however, no definitive causal link has been established. Interestingly, the EVALI outbreak was nearly entirely contained within the US with the exception of several dozen cases, at least one of which was caused by an imported US product. 97 98 99 The pattern of cases and lung injury is most suggestive of a vape solution contaminant that was introduced into the distribution pipeline in US markets, leading to a geographically contained pattern of lung injury among users. CDC case criteria for EVALI may have obscured a potential link between viral pneumonia and EVALI, and cases may have been under-recognized following the onset of the covid-19 pandemic.
CDC criteria for establishing EVALI diagnosis
Cdc lung injury surveillance, primary case definitions, confirmed case.
Vape use* in 90 days prior to symptom onset; and
Pulmonary infiltrate on chest radiograph or ground glass opacities on chest computed tomography (CT) scan; and
Absence of pulmonary infection on initial investigation†; and
Absence of alternative plausible diagnosis (eg, cardiac, rheumatological, or neoplastic process).
Probable case
Pulmonary infiltrate on chest radiograph or ground glass opacities on chest CT; and
Infection has been identified; however is not thought to represent the sole cause of lung injury OR minimum criteria** to exclude infection have not been performed but infection is not thought to be the sole cause of lung injury
*Use of e-cigarette, vape pen, or dabbing.
†Minimum criteria for absence of pulmonary infection: negative respiratory viral panel, negative influenza testing (if supported by local epidemiological data), and all other clinically indicated infectious respiratory disease testing is negative.
EVALI—clinical, radiographic, and pathologic features
In the right clinical context, diagnosis of EVALI includes identification of characteristic radiographic and pathologic features. EVALI patients largely fit a pattern of diffuse, acute lung injury in the context of vape pen exposure. A systematic review of 200 reported cases of EVALI showed that those affected were predominantly men in their teens to early 30s, and most (80%) had been using THC-containing products. 100 Presentations included predominantly respiratory (95%), constitutional (87%), and gastrointestinal symptoms (73%). Radiological studies mostly featured diffuse ground glass opacities bilaterally. Of 92 cases that underwent BAL, alveolar fluid samples were most commonly neutrophil predominant, and 81% were additionally positive for LLM on Oil Red O staining. Lung biopsy was not required to achieve the diagnosis; however, of 33 cases that underwent tissue biopsy, common features included organizing pneumonia, inflammation, foamy macrophages, and fibrinous exudates.
EVALI—outcomes
Most patients with EVALI recovered, and prognosis was generally favorable. A systematic review of identified cases found that most patients with confirmed disease required admission to hospital (94%), and a quarter were intubated. 100 Mortality among EVALI patients was low, with estimates around 2-3% across multiple studies. 101 102 103 Mortality was associated with age over 35 and underlying asthma, cardiac disease, or mental health conditions. 103 Notably, the cohorts studied only included patients who presented for medical care, and the samples are likely biased toward a more symptomatic population. It is likely that many individuals experiencing mild symptoms of EVALI did not present for medical care, and would have self-discontinued vaping following extensive media coverage of the outbreak at that time. Although most EVALI survivors recovered well, case series of some individuals show persistent radiographic abnormalities 101 and sustained reductions in DLCO. 104 105 Pulmonary function evaluation of EVALI survivors showed normalization in FEV 1 /FVC on spirometry in some, 106 while others had more variable outcomes. 105 107 108
Vaping induced lung injury—pathophysiology
The causes underlying vaping related acute lung injury remain interesting to clinicians, scientists, and public health officials; multiple mechanisms of injury have been proposed and are summarized in figure 2 . 31 109 110 Despite increased scientific interest in vaping related lung injury following the EVALI outbreak, the pool of data from which to draw meaningful conclusions is limited because of small scale human studies and ongoing conflicts due to tobacco industry funding. 111 Further, insufficient time has elapsed since widespread vaping uptake, and available studies reflect the effects of vaping on lung health over a maximum 10-15 year timespan. The longitudinal effects of vaping may take decades to fully manifest and ongoing prospective work is required to better understand the impacts of vaping on respiratory health.

Schematic illustrating pathophysiology of vaping lung injury
Pro-inflammatory vape aerosol effects
While multiple pathophysiological pathways have been proposed for vaping related lung injury, they all center on the vape aerosol itself as the conduit of lung inflammation. Vape aerosols have been found to harbor a number of toxic substances, including thermal degradation products of the various vape solution components. 112 Mass spectrometry analysis of vape aerosols has identified a variety of oxidative and pro-inflammatory substances including benzene, acrolein, volatile organic compounds, and propylene oxide. 16 17 Vaping additionally leads to airway deposition of ultrafine particles, 14 113 as well as the heavy metals manganese and zinc which are emitted from the vaping coils. 15 114 Fourth generation vape pens allow for high wattage aerosol generation, which can cause airway epithelial injury and tissue hypoxia, 115 116 as well as formaldehyde exposure similar to that of cigarette smoke. 117 Common carrier solutions such as propylene glycol have been associated with increased airway hyper-reactivity among vape pen users, 31 118 119 and have been associated with chronic respiratory conditions among theater workers exposed to aerosolized propylene glycol used in the generation of artificial fog. 120 Nicotine salts used in pod based vape pen solutions, including Juul, have been found to penetrate the cell membrane and have cytotoxic effects. 121
The myriad available vape pen flavors correlate with an expansive list of chemical compounds with potential adverse respiratory effects. Flavorants have come under increased scrutiny in recent years and have been found to contribute to the majority of aldehyde production during vape aerosol production. 122 Compounds such as cinnamaldehyde, 123 124 2,5-dimethylpyrazine (chocolate flavoring), 125 and 2,3-pentanedione 126 are common flavor additives and have been found to contribute to airway inflammation and altered immunological responses. The flavorant diacetyl garnered particular attention after it was identified on mass spectrometry in most vape solutions tested. 127 Diacetyl is most widely associated with an outbreak of diacetyl associated bronchiolitis obliterans (“popcorn lung”) among workers at a microwave popcorn plant in 2002. 128 Identification of diacetyl in vape solutions raises the possibility of development of a similar pattern of bronchiolitis obliterans among individuals who have chronic vape aerosol exposure to diacetyl-containing vape solutions. 129
Studies of vape aerosols have suggested multiple pro-inflammatory effects on the respiratory system. This includes increased airway resistance, 130 impaired response to infection, 131 and impaired mucociliary clearance. 132 Vape aerosols have further been found to induce oxidative stress in lung epithelial cells, 133 and to both induce DNA damage and impair DNA repair, consistent with a potential carcinogenic effect. 134 Mice chronically exposed to vape aerosols developed increased airway hyper-reactivity and parenchymal changes consistent with chronic obstructive pulmonary disease. 135 Human studies have been more limited, but reveal increased airway edema and friability among vape pen users, as well as altered gene transcription and decreased innate immunity. 136 137 138 Upregulation of neutrophil elastase and matrix metalloproteases among vape users suggests increased proteolysis, potentially putting those patients at risk of chronic respiratory conditions. 139
THC-containing products
Of particular interest during the 2019 EVALI outbreak was the high prevalence of THC use among EVALI cases, 19 raising questions about a novel mechanism of lung injury specific to THC-containing vape solutions. These solutions differ from conventional nicotine based products because of the need for a carrier capable of emulsifying the lipid based THC component. In this context, additional vape solution ingredients rose to attention as potential culprits—namely, THC itself, which has been found to degrade to methacrolein and benzene, 140 as well as vitamin E acetate which was found to be a common oil based diluent. 141
Vitamin E acetate has garnered increasing attention as a potential culprit in the pathophysiology of the EVALI outbreak. Vitamin E acetate was found in 94% of BAL samples collected from EVALI patients, compared with none identified in unaffected vape pen users. 96 Thermal degradation of vitamin E acetate under conditions similar to those in THC vape pens has shown production of ketene, alkene, and benzene, which may mediate epithelial lung injury when inhaled. 39 Previous work had found that vitamin E acetate impairs pulmonary surfactant function, 142 and subsequent studies have shown a dose dependent adverse effect on lung parenchyma by vitamin E acetate, including toxicity to type II pneumocytes, and increased inflammatory cytokines. 143 Mice exposed to aerosols containing vitamin E acetate developed LLM and increased alveolar protein content, suggesting epithelial injury. 140 143
The pathophysiological insult underlying vaping related lung injury may be multitudinous, including potentially compound effects from multiple ingredients comprising a vape aerosol. The heterogeneity of available vape solutions on the market further complicates efforts to pinpoint particular elements of the vape aerosol that may be pathogenic, as no two users are likely to be exposed to the same combination of vape solution products. Further, vape users may be exposed to vape solutions containing terpenes, medium chain triglycerides, or coconut oil, the effects of which on respiratory epithelium remain under investigation. 144
Lipid laden macrophages
Lipid laden alveolar macrophages have risen to prominence as potential markers of vaping related lung injury. Alveolar macrophages describe a scavenger white blood cell responsible for clearing alveolar spaces of particulate matter and modulating the inflammatory response in the lung parenchyma. 145 LLM describe alveolar macrophages that have phagocytosed fat containing deposits, as seen on Oil Red O staining, and have been described in a wide variety of pulmonary conditions, including aspiration, lipoid pneumonia, organizing pneumonia, and medication induced pneumonitis. 146 147 During the EVALI outbreak, LLM were identified in the alveolar spaces of affected patients, both in the BAL fluid and on both transbronchial and surgical lung biopsies. 148 149 Of 52 EVALI cases reported in the literature who underwent BAL, LLM were identified in over 80%. 19 100 101 148 149 150 151 152 153 Accordingly, attention turned to LLM as not only a potential marker of lung injury in EVALI, but as a possible contributor to lung inflammation itself. This concern was compounded by the frequent reported use of oil based THC vape products among EVALI patients, raising the possibility of lipid deposits in the alveolus resulting from inhalation of THC-containing vape aerosols. 154 The combination of LLM, acute lung injury, and inhalational exposure to an oil based substance raised the concern for exogenous lipoid pneumonia. 152 153 However, further evaluation of the radiographic and histopathologic findings failed to identify cardinal features that would support a diagnosis of exogenous lipoid pneumonia—namely, low attenuation areas on CT imaging and foreign body giant cells on histopathology. 155 156 However, differences in the particle size and distribution between vape aerosol exposure and traditional causes of lipoid pneumonia (ie, aspiration of a large volume of an oil-containing substance), could reasonably lead to differences in radiographic appearance, although this would not account for the lack of characteristic histopathologic features on biopsy that would support a diagnosis of lipoid pneumonia.
Recent work suggests that LLM reflect a non-specific marker of vaping, rather than a marker of lung injury. One study found that LLM were not unique to EVALI and could be identified in healthy vape pen users, as well as conventional cigarette smokers, but not in never smokers. 157 Interestingly, this work showed increased cytokines IL-4 and IL-10 among healthy vape users, suggesting that cigarette and vape pen use are associated with a pro-inflammatory state in the lung. 157 An alternative theory supports LLM presence reflecting macrophage clearance of intra-alveolar cell debris rather than exogenous lipid exposure. 149 150 Such a pattern would be in keeping with the role of alveolar macrophages as modulating the inflammatory response in the lung parenchyma. 158 Taken together, available data would support LLM serving as a non-specific marker of vape product use, rather than playing a direct role in vaping related lung injury pathogenesis. 102
Clinical aspects
A high index of suspicion is required in establishing a diagnosis of vaping related lung injury, and a general approach is summarized in figure 3 . Clinicians may consider the diagnosis when faced with a patient with new respiratory symptoms in the context of vape pen use, without an alternative cause to account for their symptoms. Suspicion should be especially high if respiratory complaints are coupled with constitutional and gastrointestinal symptoms. Patients may present with non-specific markers indicative of an ongoing inflammatory process: fevers, leukocytosis, elevated C reactive protein, or elevated erythrocyte sedimentation rate. 19

Flowchart outlining the procedure for diagnosing a vaping related lung injury
Vaping related lung injury is a diagnosis of exclusion. Chest imaging via radiograph or CT may identify a variety of patterns, although diffuse ground glass opacities remain the most common radiographic finding. Generally, patients with an abnormal chest radiograph should undergo a chest CT for further evaluation of possible vaping related lung injury.
Exclusion of infectious causes is recommended. Testing should include evaluation for bacterial and viral causes of pneumonia, as deemed appropriate by clinical judgment and epidemiological data. Exclusion of common viral causes of pneumonia is imperative, particularly influenza and SARS-CoV-2. Bronchoscopy with BAL should be considered on a case-by-case basis for those with more severe disease and may be helpful to identify patients with vaping mediated eosinophilic lung injury. Further, lung biopsy may be beneficial to exclude alternative causes of lung injury in severe cases. 92
No definitive therapy has been identified for the treatment of vaping related lung injury, and data are limited to case reports and public health guidance on the topic. Management includes supportive care and strong consideration for systemic corticosteroids for severe cases of vaping related lung injury. CDC guidance encourages consideration of systemic corticosteroids for patients requiring admission to hospital, or those with higher risk factors for adverse outcomes, including age over 50, immunosuppressed status, or underlying cardiopulmonary disease. 100 Further, given case reports of vaping mediated acute eosinophilic pneumonia, steroids should be implemented in those patients who have undergone a confirmatory BAL. 77 79
Additional therapeutic options include empiric antibiotics and/or antivirals, depending on the clinical scenario. For patients requiring admission to hospital, prompt subspecialty consultation with a pulmonologist can help guide management. Outpatient follow-up with chest imaging and spirometry is recommended, as well as referral to a pulmonologist. Counseling regarding vaping cessation is also a core component in the post-discharge care for this patient population. Interventions specific to vaping cessation remain under investigation; however, literature supports the use of behavioral counseling and/or pharmacotherapy to support nicotine cessation efforts. 66
Health outcomes among vape pen users
Health outcomes among chronic vape pen users remains an open question. To date, no large scale prospective cohort studies exist that can establish a causal link between vape use and adverse respiratory outcomes. One small scale prospective cohort study did not identify any spirometric or radiographic changes among vape pen users over a 3.5 year period. 159 Given that vaping remains a relatively novel phenomenon, many users will have a less than 10 “pack year” history of vape pen use, arguably too brief an exposure period to reflect the potential harmful nature of chronic vaping. Studies encompassing a longer period of observation of vape pen users have not yet taken place, although advances in electronic medical record (EMR) data collection on vaping habits make such work within reach.
Current understanding of the health effects of vaping is largely limited to case reports of acute lung injury, and health surveys drawing associations between vaping exposure and patient reported outcomes. Within these limitations, however, early work suggests a correlation between vape pen use and poorer cardiopulmonary outcomes. Survey studies of teens who regularly vape found increased frequencies of respiratory symptoms, including productive cough, that were independent of smoking status. 160 161 These findings were corroborated in a survey series identifying more severe asthma symptoms and more days of school missed owing to asthma among vape pen users, regardless of cigarette smoking status. 162 163 164 Studies among adults have shown a similar pattern, with increased prevalence of chronic respiratory conditions (ie, asthma or chronic obstructive pulmonary disease) among vape pen users, 165 166 and higher risk of myocardial infarction and stroke, but lower risk of diabetes. 167
The effects of vaping on lung function as determined by spirometric studies are more varied. Reported studies have assessed lung function after a brief exposure to vape aerosols, varying from 5-60 minutes in duration, and no longer term observational cohort studies exist. While some studies have shown increased airway resistance after vaping exposure, 130 168 169 others have shown no change in lung function. 137 170 171 The cumulative exposure of habitual vape pen users to vape aerosols is much longer than the period evaluated in these studies, and the impact of vaping on longer term respiratory heath remains to be seen. Recent work evaluating ventilation-perfusion matching among chronic vapers compared with healthy controls found increased ventilation-perfusion mismatch, despite normal spirometry in both groups. 172 Such work reinforces the notion that changes in spirometry are a feature of more advanced airways disease, and early studies, although inconsistent, may foreshadow future respiratory impairment in chronic vapers.
Covid-19 and vaping
The covid-19 pandemic brought renewed attention to the potential health impacts of vaping. Studies investigating the role of vaping in covid-19 prevalence and outcomes have been limited by the small size of the populations studied and results have been inconsistent. Early work noted a geographic association in the US between vaping prevalence and covid-19 cases, 173 and a subsequent survey study found that a covid-19 diagnosis was five times more likely among teens who had ever vaped. 174 In contrast, a UK survey study found no association between vaping status and covid-19 infection rates, although captured a much smaller population of vape pen users. 175 Reports of nicotine use upregulating the angiotensin converting enzyme 2 (ACE-2) receptor, 176 which serves as the binding site for SARS-CoV-2 entry, raised the possibility of increased susceptibility to covid-19 among chronic nicotine vape pen users. 177 178 Further, vape use associated with sharing devices and frequent touching of the mouth and face were posited as potential confounders contributing to increased prevalence of covid-19 in this population. 179
Covid-19 outcomes among chronic vape pen users remain an open question. While smoking has been associated with progression to more severe infections, 180 181 no investigation has been performed to date among vaping cohorts. The young average age of chronic vape pen users may prove a protective factor, as risk of severe covid-19 infection has been shown to increase with age. 182 Regardless, a prudent recommendation remains to abstain from vaping to mitigate risk of progression to severe covid-19 infection. 183
Increased awareness of respiratory health brought about by covid-19 and EVALI is galvanizing the changing patterns in vape pen use. 184 Survey studies have consistently shown trends toward decreasing use among adolescents and young adults. 174 185 186 In one study, up to two thirds of participants endorsed decreasing or quitting vaping owing to a combination of factors including difficulty purchasing vape products during the pandemic, concerns about vaping effects on lung health, and difficulty concealing vape use while living with family. 174 Such results are reflected in nationwide trends that show halting growth in vaping use among high school students. 8 These trends are encouraging in that public health interventions countering nicotine use among teens may be meeting some measure of success.
Clinical impact—collecting and recording a vaping history
Vaping history in electronic medical records.
Efforts to prevent, diagnose, and treat vaping related lung injury begin with the ability of our healthcare system to identify vape users. Since vaping related lung injury remains a diagnosis of exclusion, clinicians must have a high index of suspicion when confronted with idiopathic lung injury in a patient with vaping exposure. Unlike cigarette use, vape pen use is not built into most EMR systems, and is not included in meaningful use criteria for EMRs. 187 Retrospective analysis of outpatient visits showed that a vaping history was collected in less than 0.1% of patients in 2015, 188 although this number has been increasing. 189 190 In part augmented by EMR frameworks that prompt collection of data on vaping history, more recent estimates indicate that a vaping history is being collected in up to 6% of patients. 191 Compared with the widespread use of vaping, particularly among adolescent and young adult populations, this number remains low. Considering generational trends in nicotine use, vaping will likely eventually overcome cigarettes as the most common mode of nicotine use, raising the importance of collecting a vaping related history. Further, EMR integration of vaping history is imperative to allow for retrospective, large scale analyses of vape exposure on longitudinal health outcomes at a population level.
Practical considerations—gathering a vaping history
As vaping becomes more common, the clinician’s ability to accurately collect a vaping history and identify patients who may benefit from nicotine cessation programs becomes more important. Reassuringly, gathering a vaping history is not dissimilar to asking about smoking and use of other tobacco products, and is summarized in box 2 . Collecting a vaping history is of particular importance for providers caring for adolescents and young adults who are among the highest risk demographics for vape pen use. Adolescents and young adults may be reluctant to share their vaping history, particularly if they are using THC-containing or CBD-containing vape solutions. Familiarity with vernacular terms to describe vaping, assuming a non-judgmental approach, and asking parents or guardians to step away during history taking will help to break down these barriers. 192
Practical guide to collecting a vaping history
Ask with empathy.
Young adults may be reluctant to share history of vaping use. Familiarity with vaping terminology, asking in a non-judgmental manner, and asking in a confidential space may help.
Ask what they are vaping
Vape products— vape pens commonly contain nicotine or an alternative active ingredient, such as THC or CBD. Providers may also inquire about flavorants, or other vape solution additives, that their patient is consuming, particularly if vaping related lung injury is suspected.
Source— ask where they source their product from. Sources may include commercially available products, third party distributors, or friends or local contacts.
Ask how they are vaping
Device— What style of device are they using?
Frequency— How many times a day do they use their vape pen (with frequent use considered >5 times a day)? Alternatively, providers may inquire how long it takes to deplete a vape solution cartridge (with use of one or more pods a day considered heavy use).
Nicotine concentration— For individuals consuming nicotine-containing products, clinicians may inquire about concentration and frequency of use, as this may allow for development of a nicotine replacement therapy plan.
Ask about other inhaled products
Clinicians should ask patients who vape about use of other inhaled products, particularly cigarettes. Further, clinicians may ask about use of water pipes, heat-not-burn devices, THC-containing products, or dabbing.
The following provides a practical guide on considerations when collecting a vaping history. Of note, collecting a partial history is preferable to no history at all, and simply recording whether a patient is vaping or not adds valuable information to the medical record.
Vape use— age at time of vaping onset and frequency of vape pen use. Vape pen use >5 times a day would be considered frequent. Alternatively, clinicians may inquire how long it takes to deplete a vape solution pod (use of one or more pods a day would be considered heavy use), or how frequently users are refilling their vape pens for refillable models.
Vape products— given significant variation in vape solutions available on the market, and variable risk profiles of the multitude of additives, inquiring as to which products a patient is using may add useful information. Further, clinicians may inquire about use of nicotine versus THC-containing vape solutions, and whether said products are commercially available or are customized by third party sellers.
Concurrent smoking— simultaneous use of multiple inhaled products is common among vape users, including concurrent use of conventional cigarettes, water pipes, heat-not-burn devices, and THC-containing or CBD-containing products. Among those using marijuana products, gathering a history regarding the type of product use, the device, and the modality of aerosol generation may be warranted. Gathering such detailed information may be challenging in the face of rapidly evolving product availability and changing popular terminology. Lastly, clinicians may wish to inquire about “dabbing”—the practice of inhaling heated butane hash oil, a concentrated THC wax—which may also be associated with lung injury. 193
Future directions
Our understanding of the effects of vaping on respiratory health is in its early stages and multiple trials are under way. Future work requires enhanced understanding of the effects of vape aerosols on lung biology, such as ongoing investigations into biomarkers of oxidative stress and inflammation among vape users (clinicaltrials.gov NCT03823885 ). Additional studies seek to elucidate the relation between vape aerosol exposure and cardiopulmonary outcomes among vape pen users ( NCT03863509 , NCT05199480 ), while an ongoing prospective cohort study will allow for longitudinal assessment of airway reactivity and spirometric changes among chronic vape pen users ( NCT04395274 ).
Public health and policy interventions are vital in supporting both our understanding of vaping on respiratory health and curbing the vaping epidemic among teens. Ongoing, large scale randomized controlled studies seek to assess the impact of the FDA’s “The Real Cost” advertisement campaign for vaping prevention ( NCT04836455 ) and another trial is assessing the impact of a vaping prevention curriculum among adolescents ( NCT04843501 ). Current trials are seeking to understand the potential for various therapies as tools for vaping cessation, including nicotine patches ( NCT04974580 ), varenicline ( NCT04602494 ), and text message intervention ( NCT04919590 ).
Finally, evaluation of vaping as a potential tool for harm reduction among current cigarette smokers is undergoing further evaluation ( NCT03235505 ), which will add to the body of work and eventually lead to clear policy guidance.
Several guidelines on the management of vaping related lung injury have been published and are summarized in table 1 . 194 195 196 Given the relatively small number of cases, the fact that vaping related lung injury remains a newer clinical entity, and the lack of clinical trials on the topic, guideline recommendations reflect best practices and expert opinion. Further, published guidelines focus on the diagnosis and management of EVALI, and no guidelines exist to date for the management of vaping related lung injury more generally.
Summary of clinical guidelines
- View inline
Conclusions
Vaping has grown in popularity internationally over the past decade, in part propelled by innovations in vape pen design and nicotine flavoring. Teens and young adults have seen the biggest uptake in use of vape pens, which have superseded conventional cigarettes as the preferred modality of nicotine consumption. Despite their widespread popularity, relatively little is known about the potential effects of chronic vaping on the respiratory system, and a growing body of literature supports the notion that vaping is not without risk. The 2019 EVALI outbreak highlighted the potential harms of vaping, and the consequences of long term use remain unknown.
Discussions regarding the potential harms of vaping are reminiscent of scientific debates about the health effects of cigarette use in the 1940s. Interesting parallels persist, including the fact that only a minority of conventional cigarette users develop acute lung injury, yet the health impact of sustained, longitudinal cigarette use is unquestioned. The true impact of vaping on respiratory health will manifest over the coming decades, but in the interval a prudent and time tested recommendation remains to abstain from consumption of inhaled nicotine and other products.
Questions for future research
How does chronic vape aerosol exposure affect respiratory health?
Does use of vape pens affect respiratory physiology (airway resistance, V/Q matching, etc) in those with underlying lung disease?
What is the role for vape pen use in promoting smoking cessation?
What is the significance of pulmonary alveolar macrophages in the pathophysiology of vaping related lung injury?
Are particular populations more susceptible to vaping related lung injury (ie, by sex, demographic, underlying comorbidity, or age)?
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: AJ conceived of, researched, and wrote the piece. She is the guarantor.
Competing interests: I have read and understood the BMJ policy on declaration of interests and declare the following interests: AJ receives consulting fees from DawnLight, Inc for work unrelated to this piece.
Patient involvement: No patients were directly involved in the creation of this article.
Provenance and peer review: Commissioned; externally peer reviewed.
- ↵ US Department of Health and Human Services. The health consequences of smoking—50 years of progress: a report of the Surgeon General. 2014. doi: 10.1037/e510072014-001 .
- Cornelius ME ,
- Loretan CG ,
- Marshall TR
- Fetterman JL ,
- Benjamin EJ ,
- Barrington-Trimis JL ,
- Leventhal AM ,
- Cullen KA ,
- Gentzke AS ,
- Sawdey MD ,
- ↵ Centers for Disease Control and Prevention. Surgeon General’s Advisory on E-cigarette Use Among Youth. 2018. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/surgeon-general-advisory/index.html
- Leventhal A ,
- Johnston L ,
- O’Malley PM ,
- Patrick ME ,
- Barrington-Trimis J
- ↵ Foundation for a Smoke-Free World https://www.smokefreeworld.org/published_reports/
- Kaisar MA ,
- Calfee CS ,
- Matthay MA ,
- ↵ Royal College of Physicians (London) & Tobacco Advisory Group. Nicotine without smoke: tobacco harm reduction: a report. 2016. https://www.rcplondon.ac.uk/projects/outputs/nicotine-without-smoke-tobacco-harm-reduction
- ↵ National Academies of Sciences, Engineering, and Medicine. Public health consequences of e-cigarettes. 2018. doi: 10.17226/24952 OpenUrl CrossRef
- Manigrasso M ,
- Buonanno G ,
- Stabile L ,
- Agnihotri R
- LeBouf RF ,
- Koutrakis P ,
- Christiani DC
- Perrine CG ,
- Pickens CM ,
- Boehmer TK ,
- Lung Injury Response Epidemiology/Surveillance Group
- Layden JE ,
- Esposito S ,
- Spindle TR ,
- Eissenberg T ,
- Kendler KS ,
- McCabe SE ,
- ↵ Joseph R. Electric vaporizer. 1930.
- ↵ Gilbert HA. Smokeless non-tobacco cigarette. 1965.
- ↵ An Interview With A 1970’s Vaping Pioneer. Ashtray Blog. 2015 . https://www.ecigarettedirect.co.uk/ashtray-blog/2014/06/favor-cigarette-interview-dr-norman-jacobson.html (2014).
- Benowitz N ,
- ↵ National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, & Committee on the Review of the Health Effects of Electronic Nicotine Delivery Systems. Public Health Consequences of E-Cigarettes . (National Academies Press (US), 2018).
- ↵ Tolentino J. The Promise of Vaping and the Rise of Juul. The New Yorker . 2018 https://www.newyorker.com/magazine/2018/05/14/the-promise-of-vaping-and-the-rise-of-juul
- ↵ Bowen A, Xing C. Nicotine salt formulations for aerosol devices and methods thereof. 2014.
- Madden DR ,
- McConnell R ,
- Gammon DG ,
- Marynak KL ,
- ↵ Jackler RK, Chau C, Getachew BD, et al. JUUL Advertising Over its First Three Years on the Market. Stanford Research into the Impact of Tobacco Advertising, Stanford University School of Medicine. 2019. https://tobacco-img.stanford.edu/wp-content/uploads/2021/07/21231836/JUUL_Marketing_Stanford.pdf
- Prochaska JJ ,
- ↵ Richtel M, Kaplan S. Juul May Get Billions in Deal With One of World’s Largest Tobacco Companies. The New York Times . 2018.
- ↵ Truth Initiative. Vaping Lingo Dictionary: A guide to popular terms and devices. 2020. https://truthinitiative.org/research-resources/emerging-tobacco-products/vaping-lingo-dictionary
- Williams M ,
- Pepper JK ,
- MacMonegle AJ ,
- Nonnemaker JM
- ↵ The Physics of Vaporization. Jupiter Research. 2020. https://www.jupiterresearch.com/physics-of-vaporization/
- Bonnevie E ,
- ↵ National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. 2016. https://www.ncbi.nlm.nih.gov/books/NBK538680/
- Trivers KF ,
- Phillips E ,
- Stefanac S ,
- Sandner I ,
- Grabovac I ,
- ↵ Knowledge-Action-Change. Burning Issues: The Global State of Tobacco Harm Reduction 2020. 2020. https://gsthr.org/resources/item/burning-issues-global-state-tobacco-harm-reduction-2020
- Creamer MR ,
- Park-Lee E ,
- Gorukanti A ,
- Delucchi K ,
- Fisher-Travis R ,
- Halpern-Felsher B
- Amrock SM ,
- ↵ Buy JUUL Products | Shop All JUULpods, JUUL Devices, and Accessories | JUUL. https://www.juul.com/shop
- Schiff SJ ,
- Kechter A ,
- Simpson KA ,
- Ceasar RC ,
- Braymiller JL ,
- Barrington-Trimis JL
- Moustafa AF ,
- Rodriguez D ,
- Audrain-McGovern J
- Berhane K ,
- Stjepanović D ,
- Hitchman SC ,
- Bakolis I ,
- Plurphanswat N
- Warner KE ,
- Cummings KM ,
- ↵ FDA finalizes enforcement policy on unauthorized flavored cartridge-based e-cigarettes that appeal to children, including fruit and mint. FDA . 2020 . https://www.fda.gov/news-events/press-announcements/fda-finalizes-enforcement-policy-unauthorized-flavored-cartridge-based-e-cigarettes-appeal-children
- ↵ Henderson, E. E-cigarettes: an evidence update. 113.
- Hartmann-Boyce J ,
- McRobbie H ,
- Lindson N ,
- Phillips-Waller A ,
- ↵ Centers for Disease Control and Prevention. Electronic Cigarettes. 2020. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/index.htm l
- Patnode CD ,
- Henderson JT ,
- Thompson JH ,
- Senger CA ,
- Fortmann SP ,
- Whitlock EP
- Kmietowicz Z
- ↵ World Health Organization. E-cigarettes are harmful to health. 2020. https://www.who.int/news/item/05-02-2020-e-cigarettes-are-harmful-to-health
- Lachireddy K ,
- Sleiman M ,
- Montesinos VN ,
- Kalkhoran S ,
- Filion KB ,
- Kimmelman J ,
- Eisenberg MJ
- McCauley L ,
- Aoshiba K ,
- Nakamura H ,
- Wiggins A ,
- Hudspath C ,
- Kisling A ,
- Hostler DC ,
- Sommerfeld CG ,
- Weiner DJ ,
- Mantilla RD ,
- Darnell RT ,
- Khateeb F ,
- Agustin M ,
- Yamamoto M ,
- Cabrera F ,
- ↵ Long. Diffuse Alveolar Hemorrhage Due to Electronic Cigarette Use | A54. CRITICAL CARE CASE REPORTS: ACUTE HYPOXEMIC RESPIRATORY FAILURE/ARDS. https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2016.193.1_MeetingAbstracts.A1862
- Ring Madsen L ,
- Vinther Krarup NH ,
- Bergmann TK ,
- Bradford LE ,
- Rebuli ME ,
- Jaspers I ,
- Clement KC ,
- Loughlin CE
- Bonilla A ,
- Alamro SM ,
- Bassett RA ,
- Osterhoudt K ,
- Slaughter J ,
- ↵ Health CO. on S. and. Smoking and Tobacco Use; Electronic Cigarettes. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html (2019).
- ↵ For State, Local, Territorial, and Tribal Health Departments | Electronic Cigarettes | Smoking & Tobacco Use | CDC. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease/health-departments/index.html (2019).
- ↵ 2019 Lung Injury Surveillance Primary Case Definitions. 2.
- Callahan SJ ,
- Collingridge DS ,
- Armatas C ,
- Heinzerling A ,
- Blount BC ,
- Karwowski MP ,
- Shields PG ,
- Lung Injury Response Laboratory Working Group
- ↵ Government of Canada. Vaping-associated lung illness. 2020. https://www.canada.ca/en/public-health/services/diseases/vaping-pulmonary-illness.html (2020).
- Marlière C ,
- De Greef J ,
- Casanova GS ,
- Blagev DP ,
- Guidry DW ,
- Grissom CK ,
- Werner AK ,
- Koumans EH ,
- Chatham-Stephens K ,
- Lung Injury Response Mortality Working Group
- Tsirilakis K ,
- Yenduri NJS ,
- Guillerman RP ,
- Anderson B ,
- Serajeddini H ,
- Knipping D ,
- Brasky TM ,
- Pisinger C ,
- Godtfredsen N ,
- Jensen RP ,
- Pankow JF ,
- Strongin RM ,
- Lechasseur A ,
- Altmejd S ,
- Turgeon N ,
- Goessler W ,
- Chaumont M ,
- van de Borne P ,
- Bernard A ,
- Kosmider L ,
- Sobczak A ,
- Aldridge K ,
- Afshar-Mohajer N ,
- Koehler K ,
- Varughese S ,
- Teschke K ,
- van Netten C ,
- Beyazcicek O ,
- Onyenwoke RU ,
- Khlystov A ,
- Samburova V
- Lavrich KS ,
- van Heusden CA ,
- Lazarowski ER ,
- Carson JL ,
- Pawlak EA ,
- Lackey JT ,
- Sherwood CL ,
- O’Sullivan M ,
- Vallarino J ,
- Flanigan SS ,
- LeBlanc M ,
- Kullman G ,
- Simoes EJ ,
- Wambui DW ,
- Vardavas CI ,
- Anagnostopoulos N ,
- Kougias M ,
- Evangelopoulou V ,
- Connolly GN ,
- Behrakis PK
- Sussan TE ,
- Gajghate S ,
- Thimmulappa RK ,
- Hossain E ,
- Perveen Z ,
- Lerner CA ,
- Sundar IK ,
- Garcia-Arcos I ,
- Geraghty P ,
- Baumlin N ,
- Coakley RC ,
- Mascenik T ,
- Staudt MR ,
- Hollmann C ,
- Radicioni G ,
- Coakley RD ,
- Kalathil SG ,
- Bogner PN ,
- Goniewicz ML ,
- Thanavala YM
- Massey JB ,
- Matsumoto S ,
- Traber MG ,
- Ranpara A ,
- Stefaniak AB ,
- Williams K ,
- Fernandez E ,
- Basset-Léobon C ,
- Lacoste-Collin L ,
- Courtade-Saïdi M
- Boland JM ,
- Maddock SD ,
- Cirulis MM ,
- Tazelaar HD ,
- Mukhopadhyay S ,
- Dammert P ,
- Kalininskiy A ,
- Davidson K ,
- Brancato A ,
- Heetderks P ,
- Dicpinigaitis PV ,
- Trachuk P ,
- Suhrland MJ
- Khilnani GC
- Simmons A ,
- Freudenheim JL ,
- Hussell T ,
- Cibella F ,
- Caponnetto P ,
- Schweitzer RJ ,
- Williams RJ ,
- Vindhyal MR ,
- Munguti C ,
- Vindhyal S ,
- Lappas AS ,
- Tzortzi AS ,
- Konstantinidi EM ,
- Antoniewicz L ,
- Brynedal A ,
- Lundbäck M ,
- Ferrari M ,
- Boulay MÈ ,
- Boulet LP ,
- Morissette MC
- Kizhakke Puliyakote AS ,
- Elliott AR ,
- Anderson KM ,
- Crotty Alexander LE ,
- Jackson SE ,
- McAlinden KD ,
- McKelvey K ,
- Patanavanich R ,
- NVSS - Provisional Death Counts for COVID-19 - Executive Summary
- Sokolovsky AW ,
- Hertel AW ,
- Micalizzi L ,
- Klemperer EM ,
- Peasley-Miklus C ,
- Villanti AC
- Henricks WH
- Young-Wolff KC ,
- Klebaner D ,
- Mowery DL ,
- Don’t Forget to Ask
- Stephens D ,
- Siegel DA ,
- Jatlaoui TC ,
- Lung Injury Response Clinical Working Group ,
- Ramalingam SS ,
- Schuurmans MM
Jump to navigation
- Bahasa Indonesia
- Bahasa Malaysia

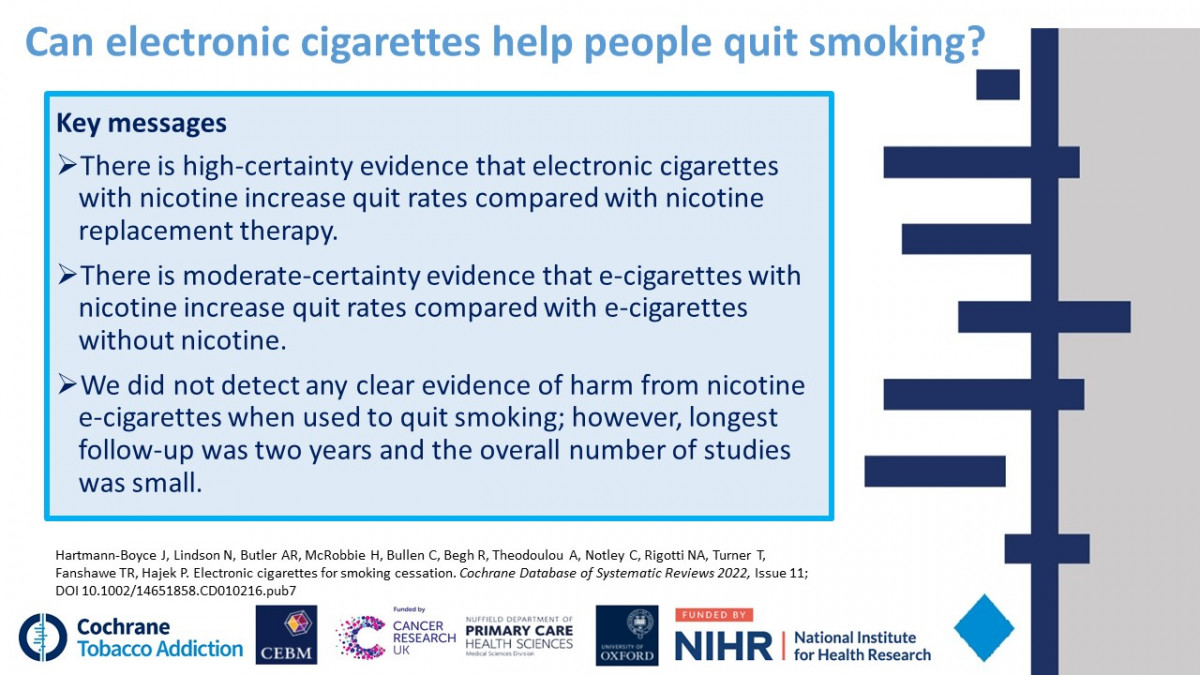
Latest Cochrane Review finds high certainty evidence that nicotine e-cigarettes are more effective than traditional nicotine-replacement therapy (NRT) in helping people quit smoking

A Cochrane review has found the strongest evidence yet that e-cigarettes, also known as ‘vapes’, help people to quit smoking better than traditional nicotine replacement therapies, such as patches and chewing gums.
New evidence published today in the Cochrane Library finds high certainty evidence that people are more likely to stop smoking for at least six months using nicotine e-cigarettes, or ‘vapes’, than using nicotine replacement therapies, such as patches and gums. Evidence also suggested that nicotine e-cigarettes led to higher quit rates than e-cigarettes without nicotine, or no stop smoking intervention, but less data contributed to these analyses. The updated Cochrane review includes 78 studies in over 22,000 participants – an addition of 22 studies since the last update in 2021.
Smoking is a significant global health problem. According to the World Health Organisation (WHO), in 2020, 22.3% of the global population used tobacco, despite it killing up to half of its users. Stopping smoking reduces the risk of lung cancer, heart attacks and many other diseases. Though most people who smoke want to quit, many find it difficult to do so permanently. Nicotine patches and gum are safe, effective and widely used methods to help individuals quit.
E-cigarettes heat liquids with nicotine and flavourings, allowing users to ‘vape’ nicotine instead of smoking. Data from the review showed that i f six in 100 people quit by using nicotine replacement therapy, eight to twelve would quit by using electronic cigarettes containing nicotine. This means an additional two to six people in 100 could potentially quit smoking with nicotine containing electronic cigarettes.
Dr Jamie Hartmann-Boyce, Associate Professor at the University of Oxford, Editor of the Cochrane Tobacco Addiction Group, and an author of the new publication, said:
“Electronic cigarettes have generated a lot of misunderstanding in both the public health community and the popular press since their introduction over a decade ago. These misunderstandings discourage some people from using e-cigarettes as a stop smoking tool. Fortunately, more and more evidence is emerging and provides further clarity. With support from Cancer Research UK, we search for new evidence every month as part of a living systematic review. We identify and combine the strongest evidence from the most reliable scientific studies currently available. For the first time, this has given us high-certainty evidence that e-cigarettes are even more effective at helping people to quit smoking than traditional nicotine replacement therapies, like patches or gums.”
In studies comparing nicotine e-cigarettes to nicotine replacement treatment, significant side effects were rare. In the short-to-medium term (up to two years), nicotine e-cigarettes most typically caused throat or mouth irritation, headache, cough, and feeling nauseous. However, these effects appeared to diminish over time.
Dr Nicola Lindson, University Research Lecturer at the University of Oxford, Cochrane Tobacco Addiction Group’s Managing Editor, and author of the publication said:
“ E-cigarettes do not burn tobacco; and as such they do not expose users to the same complex mix of chemicals that cause diseases in people smoking conventional cigarettes. E-cigarettes are not risk free, and shouldn’t be used by people who don’t smoke or aren’t at risk of smoking. However, evidence shows that nicotine e-cigarettes carry only a small fraction of the risk of smoking. In our review, we did not find evidence of substantial harms caused by nicotine containing electronic cigarettes when used to quit smoking. However, due to the small number of studies and lack of data on long-term nicotine-containing electronic cigarette usage – usage over more than two years – questions remain about long-term effects.”
The researchers conclude that more evidence, particularly about the effects of newer e-cigarettes with better nicotine delivery than earlier ones, is needed to assist more people quit smoking. Longer-term data is also needed.
Michelle Mitchell, chief executive at Cancer Research UK, said:
“We welcome this report which adds to a growing body of evidence showing that e-cigarettes are an effective smoking cessation tool. We strongly discourage those who have never smoked from using e-cigarettes, especially young people. This is because they are a relatively new product and we don’t yet know the long term health effects. While the long term effects of vaping are still unknown, the harmful effects of smoking are indisputable – smoking causes around 55,000 cancer deaths in the UK every year. Cancer Research UK supports balanced evidence-based regulation on e-cigarettes from UK governments which maximises their potential to help people stop smoking, whilst minimising the risk of uptake among others.”
- Read the full Cochrane review and plain language summary
- Learn more about Cochrane Tobacco Addition Group
- Science Media Centre: Expert reaction to cochrane review on electronic cigarettes for smoking cessation

Hartmann-Boyce J, Lindson N, Butler AR, McRobbie H, Bullen C, Begh R, Theodoulou A, Notley C, Rigotti NA, Turner T, Fanshawe TR, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database of Systematic Reviews 2022, Issue 11. Art. No.: CD010216. DOI: 10.1002/14651858.CD010216.pub7
This work was supported by Cancer Research UK [A ref. A29845]
To speak to a team member about this project please contact Dr. Hartmann-Boyce, [email protected] or Dr. Lindson, [email protected] .
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
News Release
Wednesday, October 26, 2022
NIH-funded studies show damaging effects of vaping, smoking on blood vessels
Combining e-cigarettes with regular cigarettes may increase health risks.

Long-term use of electronic cigarettes, or vaping products, can significantly impair the function of the body’s blood vessels, increasing the risk for cardiovascular disease. Additionally, the use of both e-cigarettes and regular cigarettes may cause an even greater risk than the use of either of these products alone. These findings come from two new studies supported by the National Heart, Lung, and Blood Institute (NHLBI), part of the National Institutes of Health (NIH).
The findings, which appear today in the journal Arteriosclerosis, Thrombosis, and Vascular Biology , add to growing evidence that long-term use of e-cigarettes can harm a person’s health. Researchers have known for years that tobacco smoking can cause damage to blood vessels. However, the effects of e-cigarettes on cardiovascular health have been poorly understood. The two new studies – one on humans, the other on rats – aimed to change that.
“In our human study, we found that chronic e-cigarettes users had impaired blood vessel function, which may put them at increased risk for heart disease,” said Matthew L. Springer, Ph.D., a professor of medicine in the Division of Cardiology at the University of California in San Francisco, and leader of both studies. “It indicates that chronic users of e-cigarettes may experience a risk of vascular disease similar to that of chronic smokers.”
In this first study, Springer and his colleagues collected blood samples from a group of 120 volunteers that included those with long-term e-cigarette use, long-term cigarette smoking, and those who didn't use. The researchers defined long-term e-cigarette use as more than five times/week for more than three months and defined long-term cigarette use as smoking more than five cigarettes per day.
They then exposed each of the blood samples to cultured human blood vessel (endothelial) cells in the laboratory and measured the release of nitric oxide, a chemical marker used to evaluate proper functioning of endothelial cells. They also tested cell permeability, the ability of molecules to pass through a layer of cells to the other side. Too much permeability makes vessels leaky, which impairs function and increases the risk for cardiovascular disease.
The researchers found that blood from participants who used e-cigarettes and those who smoked caused a significantly greater decrease in nitric oxide production by the blood vessel cells than the blood of nonusers. Notably, the researchers found that blood from those who used e-cigarettes also caused more permeability in the blood vessel cells than the blood from both those who smoked cigarettes and nonusers. Blood from those that used e-cigarettes also caused a greater release of hydrogen peroxide by the blood vessel cells than the blood of the nonusers. Each of these three factors can contribute to impairment of blood vessel function in people who use e-cigarettes, the researchers said.
In addition, Springer and his team discovered that e-cigarettes had harmful cardiovascular effects in ways that were different from those caused by tobacco smoke. Specifically, they found that blood from people who smoked cigarettes had higher levels of certain circulating biomarkers of cardiovascular risks, and the blood people who used e-cigarettes had elevated levels of other circulating biomarkers of cardiovascular risks.
“These findings suggest that using the two products together, as many people do, could increase their health risks compared to using them individually,” Springer said. “We had not expected to see that.”
In the second study, the researchers tried to find out if there were specific components of cigarette smoke or e-cigarette vapor that were responsible for blood vessel damage. In studies using rats, they exposed the animals to various substances found in tobacco smoke or e-cigarettes. These included nicotine, menthol (a cigarette additive), the gases acrolein and acetaldehyde (two chemicals found in both tobacco smoke and e-cigarette vapors), and inert carbon nanoparticles to represent the particle-like nature of smoke and e-cigarette vapor.
Using special arterial flow measurements, the researchers demonstrated that blood vessel damage does not appear to be caused by a specific component of cigarette smoke or e-cigarette vapor. Instead, they said, it appears to be caused by airway irritation that triggers biological signals in the vagus nerve that somehow leads to blood vessel damage, possibly through an inflammatory process. The vagus is a long nerve extending from the brain that connects the airway to the rest of the nervous system and plays a key role in heart rate, breathing, and other functions. The researchers showed that detaching the nerve in rats prevented blood vessel damage caused by tobacco smoke, demonstrating its key role in this process.
“We were surprised to find that there was not a single component that you could remove to stop the damaging effect of smoke or vapors on the blood vessels,” Springer said. “As long as there’s an irritant in the airway, blood vessel function may be impaired.”
The finding has implications for efforts to regulate tobacco products and e-cigarettes, as it underscores how difficult it is to pinpoint any one ingredient in them that is responsible for blood vessel damage. “What I like to tell people is this: Just breathe clean air and avoid using these products,” Springer said.
Lisa Postow, Ph.D., an NHLBI program officer in NHLBI’s Division of Lung Diseases, agreed that the study results “provide further evidence that exposure to e-cigarettes could lead to harmful cardiovascular health effects.” She added that more data is needed to fully understand the health effects of e-cigarettes. The NIH and others are continuing to explore this area.
Research reported in the e-cigarette study was funded by NHLBI grants U54HL147127, P50HL120163, and R01HL120062 and the U.S. Food and Drug Administration Center for Tobacco Products (FDA CTP); and grant P50CA180890 from the National Cancer Institute at the NIH and FDA CTP. Research reported in the cigarette smoke/-vagal nerve study was supported by NHLBI grants R01HL120062 and U54HL147127 and FDA CTP and grant P50CA180890 from the National Cancer Institute at the NIH and FDA CTP. For additional funding details, please see the full journal articles.
About the National Heart, Lung, and Blood Institute (NHLBI): NHLBI is the global leader in conducting and supporting research in heart, lung, and blood diseases and sleep disorders that advances scientific knowledge, improves public health, and saves lives. For more information, visit www.nhlbi.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
Chronic e-cigarette use impairs endothelial function on the physiological and cellular levels. Arteriosclerosis, Thrombosis, and Vascular Biology. DOI: 10.1161/ATVBAHA.121.317749
Impairment of Endothelial Function by Cigarette Smoke is not Caused by a Specific Smoke Constituent, but by Vagal Input from the Airway. Arteriosclerosis, Thrombosis, and Vascular Biology. DOI: 10.1161/ATVBAHA.122.318051
Connect with Us
- More Social Media from NIH

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- News and Events
- < Back To All News
New study links vaping to increased respiratory symptoms in young adults

Young people who use electronic cigarettes or vape report increased respiratory symptoms, including wheezing and shortness of breath, compared to those who don’t use e-cigarettes, according to a new study. The use of electronic cigarettes has increased in recent years among adolescents and young adults. Use of these products produces aerosols that contain volatile chemicals, including flavorings and oxidant metals with known lung toxicity. Detailed studies of the association of e-cigarette use with respiratory symptoms have been limited.
In the study, researchers evaluated the associations of e-cigarette use with self-reported respiratory symptoms in a group of over 2,000 U.S. teens during a series of annual surveys across a 4-year time span. The participants were part of the Southern California Children’s Health Study between 2014 and 2018. The odds of wheezing among the participants were 81% more likely among those who used e-cigarettes in the past 30 days than among those who never vaped. Similarly, the odds of bronchitis-like symptoms were twice as likely in users, while those of shortness of breath were 78% more likely after adjusting for age, sex, race, and other factors. The findings remained statistically significant even after further adjustment for concurrent use of cigarettes and cannabis and secondhand exposure to e-cigarettes, cigarettes, and/or cannabis.
Published in journal Thorax , the study was funded in part by the NHLBI.
Media Coverage
- E-Cigarette Use Tied to Respiratory Symptoms in Young Adults
- Study links lung conditions to young people who vape
- Vaping Doubles Risk of Lung Problems in Teens: Study
- Vaping can take a toll on respiratory health of teens
- Vaping linked to bronchitic symptoms, shortness of breath in young people
Latest Cochrane Review finds high certainty evidence that nicotine e-cigarettes are more effective than traditional nicotine-replacement therapy (NRT) in helping people quit smoking
17 November 2022
Research led by the University of Oxford, and funded by Cancer Research UK, has found the strongest evidence yet that e-cigarettes, also known as ‘vapes’, help people to quit smoking better than traditional nicotine replacement therapies, such as patches and chewing gums.
New evidence published today in the Cochrane Library finds high certainty evidence that people are more likely to stop smoking for at least six months using nicotine e-cigarettes, or ‘vapes’, than using nicotine replacement therapies, such as patches and gums. Evidence also suggested that nicotine e-cigarettes led to higher quit rates than e-cigarettes without nicotine, or no stop smoking intervention, but less data contributed to these analyses. The updated Cochrane review includes 78 studies in over 22,000 participants – an addition of 22 studies since the last update in 2021.
Smoking is a significant global health problem. According to the World Health Organisation (WHO), in 2020, 22.3% of the global population used tobacco, despite it killing up to half of its users. Stopping smoking reduces the risk of lung cancer, heart attacks and many other diseases. Though most people who smoke want to quit, many find it difficult to do so permanently. Nicotine patches and gum are safe, effective and widely used methods to help individuals quit.
E-cigarettes heat liquids with nicotine and flavourings, allowing users to ‘vape’ nicotine instead of smoking. Data from the review showed that if six in 100 people quit by using nicotine replacement therapy, eight to twelve would quit by using electronic cigarettes containing nicotine. This means an additional two to six people in 100 could potentially quit smoking with nicotine containing electronic cigarettes.
Dr Jamie Hartmann-Boyce, Associate Professor at the University of Oxford, Editor of the Cochrane Tobacco Addiction Group, and an author of the new publication, said: “Electronic cigarettes have generated a lot of misunderstanding in both the public health community and the popular press since their introduction over a decade ago. These misunderstandings discourage some people from using e-cigarettes as a stop smoking tool. Fortunately, more and more evidence is emerging and provides further clarity. With support from Cancer Research UK, we search for new evidence every month as part of a living systematic review. We identify and combine the strongest evidence from the most reliable scientific studies currently available.
For the first time, this has given us high-certainty evidence that e-cigarettes are even more effective at helping people to quit smoking than traditional nicotine replacement therapies, like patches or gums.”
In studies comparing nicotine e-cigarettes to nicotine replacement treatment, significant side effects were rare. In the short-to-medium term (up to two years), nicotine e-cigarettes most typically caused throat or mouth irritation, headache, cough, and feeling nauseous. However, these effects appeared to diminish over time.
Dr Nicola Lindson, University Research Lecturer at the University of Oxford, Cochrane Tobacco Addiction Group’s Managing Editor, and author of the publication said: “E-cigarettes do not burn tobacco; and as such they do not expose users to the same complex mix of chemicals that cause diseases in people smoking conventional cigarettes. E-cigarettes are not risk free, and shouldn’t be used by people who don’t smoke or aren’t at risk of smoking. However, evidence shows that nicotine e-cigarettes carry only a small fraction of the risk of smoking. In our review, we did not find evidence of substantial harms caused by nicotine containing electronic cigarettes when used to quit smoking. However, due to the small number of studies and lack of data on long-term nicotine-containing electronic cigarette usage – usage over more than two years – questions remain about long-term effects.”
The researchers conclude that more evidence, particularly about the effects of newer e-cigarettes with better nicotine delivery than earlier ones, is needed to assist more people quit smoking. Longer-term data is also needed.
Michelle Mitchell, chief executive at Cancer Research UK, said: “We welcome this report which adds to a growing body of evidence showing that e-cigarettes are an effective smoking cessation tool. We strongly discourage those who have never smoked from using e-cigarettes, especially young people. This is because they are a relatively new product and we don’t yet know the long term health effects.“
“While the long term effects of vaping are still unknown, the harmful effects of smoking are indisputable – smoking causes around 55,000 cancer deaths in the UK every year. Cancer Research UK supports balanced evidence-based regulation on e-cigarettes from UK governments which maximises their potential to help people stop smoking, whilst minimising the risk of uptake among others.”
This work was supported by Cancer Research UK [A ref. A29845]
Notes to Editors:
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010216.pub7/full
doi: 10.1002/14651858.CD010216.pub7 Lead authors: Associate Professor at the Nuffield Department of Primary Care Health Sciences, University of Oxford and Editor of the Cochrane Tobacco Addiction Group, Dr Jamie Hartmann-Boyce and Senior Researcher at the Nuffield Department of Primary Care Health Sciences, University of Oxford and Managing Editor of the Cochrane Tobacco Addiction Group, Dr Nicola Lindson.
To speak to a team member about this project please contact Dr. Hartmann-Boyce, [email protected] or Dr. Lindson, [email protected] .
About Cochrane Cochrane is a global independent network of researchers, professionals, patients, carers, and people interested in health. Cochrane produces reviews which study all the best available evidence generated through research and make it easier to inform decisions about health. These are called systematic reviews. Cochrane is a not-for profit organization with collaborators from more than 130 countries working together to produce credible, accessible health information that is free from commercial sponsorship and other conflicts of interest. Our work is recognized as representing an international gold standard for high-quality, trusted information. Find out more at cochrane.org
The University of Oxford Oxford University has been placed number 1 in the Times Higher Education World University Rankings for the seventh year running, and 2 in the QS World Rankings 2022. At the heart of this success is our ground-breaking research and innovation. Oxford is world-famous for research excellence and home to some of the most talented people from across the globe. Our work helps the lives of millions, solving real-world problems through a huge network of partnerships and collaborations. The breadth and interdisciplinary nature of our research sparks imaginative and inventive insights and solutions. Through its research commercialisation arm, Oxford University Innovation, Oxford is the highest university patent filer in the UK and is ranked first in the UK for university spinouts, having created more than 200 new companies since 1988. Over a third of these companies have been created in the past three years. The university is a catalyst for prosperity in Oxfordshire and the United Kingdom, contributing £15.7 billion to the UK economy in 2018/19, and supports more than 28,000 full time jobs.
Oxford University’s Medical Sciences Division : The Medical Sciences Division is an internationally recognised centre of excellence for biomedical and clinical research and teaching and is the largest of the four academic divisions within the University. Over 5000 academics, researchers, NHS clinicians and GPs, and administrative staff, 1500 graduate and 1600 undergraduate students, together contribute to our extensive and exemplary research, teaching, and clinical portfolios. We aim to be the best university biomedical institution in Europe and amongst the best five biomedical institutions in the world and have been ranked number one for the last twelve years in the Times Higher Education World University Rankings for clinical, pre-clinical and health sciences - the only non-North American institution to be top-ranked by THE in any subject discipline.
Within the division, the Nuffield Department of Primary Care Health Sciences has been one of the world’s most important primary care centres for over 20 years; leading world-class research and training to rethink the way healthcare is delivered in general practice and other primary care settings. The department’s main research focus is on the prevention, early diagnosis, and management of common illness, bringing together academics from many diverse backgrounds to work together to produce benefits for the NHS, for populations and for patients. www.phc.ox.ac.uk .
DISCOVER MORE
- Support Oxford's research
- Partner with Oxford on research
- Study at Oxford
- Research jobs at Oxford
You can view all news or browse by category
- Open access
- Published: 18 May 2021
An updated overview of e-cigarette impact on human health
- Patrice Marques ORCID: orcid.org/0000-0003-0465-1727 1 , 2 ,
- Laura Piqueras ORCID: orcid.org/0000-0001-8010-5168 1 , 2 , 3 &
- Maria-Jesus Sanz ORCID: orcid.org/0000-0002-8885-294X 1 , 2 , 3
Respiratory Research volume 22 , Article number: 151 ( 2021 ) Cite this article
395k Accesses
129 Citations
358 Altmetric
Metrics details
The electronic cigarette ( e-cigarette ), for many considered as a safe alternative to conventional cigarettes, has revolutionised the tobacco industry in the last decades. In e-cigarettes , tobacco combustion is replaced by e-liquid heating, leading some manufacturers to propose that e-cigarettes have less harmful respiratory effects than tobacco consumption. Other innovative features such as the adjustment of nicotine content and the choice of pleasant flavours have won over many users. Nevertheless, the safety of e-cigarette consumption and its potential as a smoking cessation method remain controversial due to limited evidence. Moreover, it has been reported that the heating process itself can lead to the formation of new decomposition compounds of questionable toxicity. Numerous in vivo and in vitro studies have been performed to better understand the impact of these new inhalable compounds on human health. Results of toxicological analyses suggest that e-cigarettes can be safer than conventional cigarettes, although harmful effects from short-term e-cigarette use have been described. Worryingly, the potential long-term effects of e-cigarette consumption have been scarcely investigated. In this review, we take stock of the main findings in this field and their consequences for human health including coronavirus disease 2019 (COVID-19).
Electronic nicotine dispensing systems (ENDS), commonly known as electronic cigarettes or e-cigarettes , have been popularly considered a less harmful alternative to conventional cigarette smoking since they first appeared on the market more than a decade ago. E-cigarettes are electronic devices, essentially consisting of a cartridge, filled with an e-liquid, a heating element/atomiser necessary to heat the e-liquid to create a vapour that can be inhaled through a mouthpiece, and a rechargeable battery (Fig. 1 ) [ 1 , 2 ]. Both the electronic devices and the different e-liquids are easily available in shops or online stores.
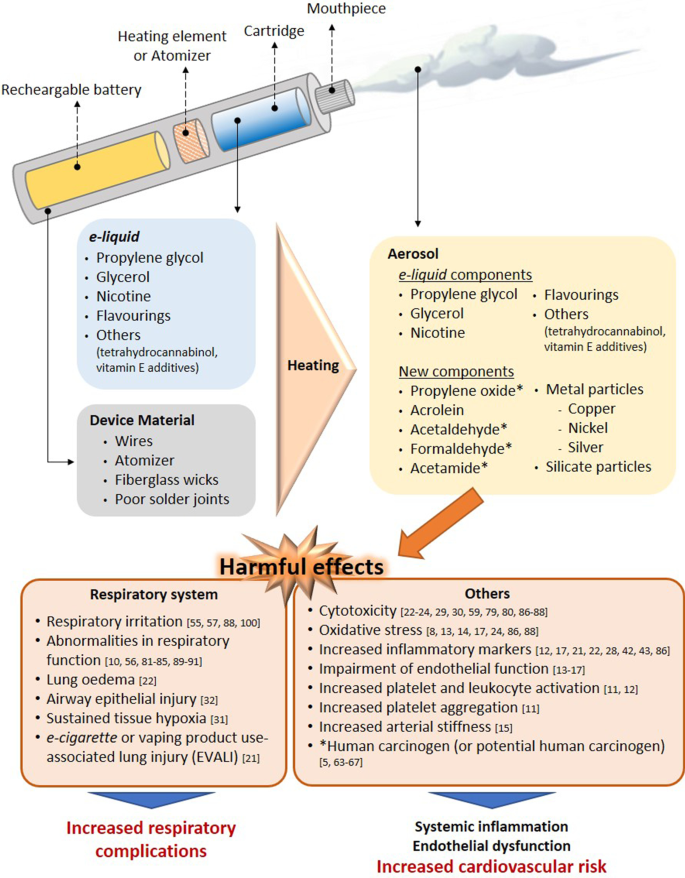
Effect of the heating process on aerosol composition. Main harmful effects documented. Several compounds detected in e-cigarette aerosols are not present in e-liquid s and the device material also seems to contribute to the presence of metal and silicate particles in the aerosols. The heating conditions especially on humectants, flavourings and the low-quality material used have been identified as the generator of the new compounds in aerosols. Some compounds generated from humectants (propylene glycol and glycerol) and flavourings, have been associated with clear airways impact, inflammation, impairment of cardiovascular function and toxicity. In addition, some of them are carcinogens or potential carcinogens
The e-liquid typically contains humectants and flavourings, with or without nicotine; once vapourised by the atomiser, the aerosol (vapour) provides a sensation similar to tobacco smoking, but purportedly without harmful effects [ 3 ]. However, it has been reported that the heating process can lead to the generation of new decomposition compounds that may be hazardous [ 4 , 5 ]. The levels of nicotine, which is the key addictive component of tobacco, can also vary between the commercially available e-liquids, and even nicotine-free options are available. For this particular reason, e-cigarettes are often viewed as a smoking cessation tool, given that those with nicotine can prevent smoking craving, yet this idea has not been fully demonstrated [ 2 , 6 , 7 ].
Because e-cigarettes are combustion-free, and because most of the damaging and well-known effects of tobacco are derived from this reaction, there is a common and widely spread assumption that e-cigarette consumption or “vaping” is safer than conventional cigarette smoking. However, are they risk-free? Is there sufficient toxicological data on all the components employed in e-liquids ? Do we really know the composition of the inhaled vapour during the heating process and its impact on health? Can e-cigarettes be used to curb tobacco use? Do their consumption impact on coronavirus disease 2019 (COVID-19)? In the present review, we have attempted to clarify these questions based on the existing scientific literature, and we have compiled new insights related with the toxicity derived from the use of these devices.
Effect of e-cigarette vapour versus conventional cigarette exposure: in vivo and in vitro effects
Numerous studies have been performed to evaluate the safety/toxicity of e-cigarette use both in vivo and in in vitro cell culture.
One of the first studies in humans involved the analysis of 9 volunteers that consumed e-cigarettes , with or without nicotine, in a ventilated room for 2 h [ 8 ]. Pollutants in indoor air, exhaled nitric oxide (NO) and urinary metabolite profiles were analysed. The results of this acute experiment revealed that e-cigarettes are not emission-free, and ultrafine particles formed from propylene glycol (PG) could be detected in the lungs. The study also suggested that the presence of nicotine in e-cigarettes increased the levels of NO exhaled from consumers and provoked marked airway inflammation; however, no differences were found in the levels of exhaled carbon monoxide (CO), an oxidative stress marker, before and after e-cigarette consumption [ 8 ]. A more recent human study detected significantly higher levels of metabolites of hazardous compounds including benzene, ethylene oxide, acrylonitrile, acrolein and acrylamide in the urine of adolescent dual users ( e-cigarettes and conventional tobacco consumers) than in adolescent e-cigarette -only users (Table 1 ) [ 9 ]. Moreover, the urine levels of metabolites of acrylonitrile, acrolein, propylene oxide, acrylamide and crotonaldehyde, all of which are detrimental for human health, were significantly higher in e-cigarette -only users than in non-smoker controls, reaching up to twice the registered values of those from non-smoker subjects (Table 1 ) [ 9 ]. In line with these observations, dysregulation of lung homeostasis has been documented in non-smokers subjected to acute inhalation of e-cigarette aerosols [ 10 ].
Little is known about the effect of vaping on the immune system. Interestingly, both traditional and e-cigarette consumption by non-smokers was found to provoke short-term effects on platelet function, increasing platelet activation (levels of soluble CD40 ligand and the adhesion molecule P-selectin) and platelet aggregation, although to a lesser extent with e-cigarettes [ 11 ]. As found with platelets, the exposure of neutrophils to e-cigarette aerosol resulted in increased CD11b and CD66b expression being both markers of neutrophil activation [ 12 ]. Additionally, increased oxidative stress, vascular endothelial damage, impaired endothelial function, and changes in vascular tone have all been reported in different human studies on vaping [ 13 , 14 , 15 , 16 , 17 ]. In this context, it is widely accepted that platelet and leukocyte activation as well as endothelial dysfunction are associated with atherogenesis and cardiovascular morbidity [ 18 , 19 ]. In line with these observations the potential association of daily e-cigarettes consumption and the increased risk of myocardial infarction remains controversial but benefits may occur when switching from tobacco to chronic e-cigarette use in blood pressure regulation, endothelial function and vascular stiffness (reviewed in [ 20 ]). Nevertheless, whether or not e-cigarette vaping has cardiovascular consequences requires further investigation.
More recently, in August 2019, the US Centers for Disease Control and Prevention (CDC) declared an outbreak of the e-cigarette or vaping product use-associated lung injury (EVALI) which caused several deaths in young population (reviewed in [ 20 ]). Indeed, computed tomography (CT scan) revealed local inflammation that impaired gas exchange caused by aerosolised oils from e-cigarettes [ 21 ]. However, most of the reported cases of lung injury were associated with use of e-cigarettes for tetrahydrocannabinol (THC) consumption as well as vitamin E additives [ 20 ] and not necessarily attributable to other e-cigarette components.
On the other hand, in a comparative study of mice subjected to either lab air, e-cigarette aerosol or cigarette smoke (CS) for 3 days (6 h-exposure per day), those exposed to e-cigarette aerosols showed significant increases in interleukin (IL)-6 but normal lung parenchyma with no evidence of apoptotic activity or elevations in IL-1β or tumour necrosis factor-α (TNFα) [ 22 ]. By contrast, animals exposed to CS showed lung inflammatory cell infiltration and elevations in inflammatory marker expression such as IL-6, IL-1β and TNFα [ 22 ]. Beyond airway disease, exposure to aerosols from e-liquids with or without nicotine has also been also associated with neurotoxicity in an early-life murine model [ 23 ].
Results from in vitro studies are in general agreement with the limited number of in vivo studies. For example, in an analysis using primary human umbilical vein endothelial cells (HUVEC) exposed to 11 commercially-available vapours, 5 were found to be acutely cytotoxic, and only 3 of those contained nicotine [ 24 ]. In addition, 5 of the 11 vapours tested (including 4 that were cytotoxic) reduced HUVEC proliferation and one of them increased the production of intracellular reactive oxygen species (ROS) [ 24 ]. Three of the most cytotoxic vapours—with effects similar to those of conventional high-nicotine CS extracts—also caused comparable morphological changes [ 24 ]. Endothelial cell migration is an important mechanism of vascular repair than can be disrupted in smokers due to endothelial dysfunction [ 25 , 26 ]. In a comparative study of CS and e-cigarette aerosols, Taylor et al . found that exposure of HUVEC to e-cigarette aqueous extracts for 20 h did not affect migration in a scratch wound assay [ 27 ], whereas equivalent cells exposed to CS extract showed a significant inhibition in migration that was concentration dependent [ 27 ].
In cultured human airway epithelial cells, both e-cigarette aerosol and CS extract induced IL-8/CXCL8 (neutrophil chemoattractant) release [ 28 ]. In contrast, while CS extract reduced epithelial barrier integrity (determined by the translocation of dextran from the apical to the basolateral side of the cell layer), e-cigarette aerosol did not, suggesting that only CS extract negatively affected host defence [ 28 ]. Moreover, Higham et al . also found that e-cigarette aerosol caused IL-8/CXCL8 and matrix metallopeptidase 9 (MMP-9) release together with enhanced activity of elastase from neutrophils [ 12 ] which might facilitate neutrophil migration to the site of inflammation [ 12 ].
In a comparative study, repeated exposure of human gingival fibroblasts to CS condensate or to nicotine-rich or nicotine-free e-vapour condensates led to alterations in morphology, suppression of proliferation and induction of apoptosis, with changes in all three parameters greater in cells exposed to CS condensate [ 29 ]. Likewise, both e-cigarette aerosol and CS extract increased cell death in adenocarcinomic human alveolar basal epithelial cells (A549 cells), and again the effect was more damaging with CS extract than with e-cigarette aerosol (detrimental effects found at 2 mg/mL of CS extract vs. 64 mg/mL of e-cigarette extract) [ 22 ], which is in agreement with another study examining battery output voltage and cytotoxicity [ 30 ].
All this evidence would suggest that e-cigarettes are potentially less harmful than conventional cigarettes (Fig. 2 ) [ 11 , 14 , 22 , 24 , 27 , 28 , 29 ]. Importantly, however, most of these studies have investigated only short-term effects [ 10 , 14 , 15 , 22 , 27 , 28 , 29 , 31 , 32 ], and the long-term effects of e-cigarette consumption on human health are still unclear and require further study.
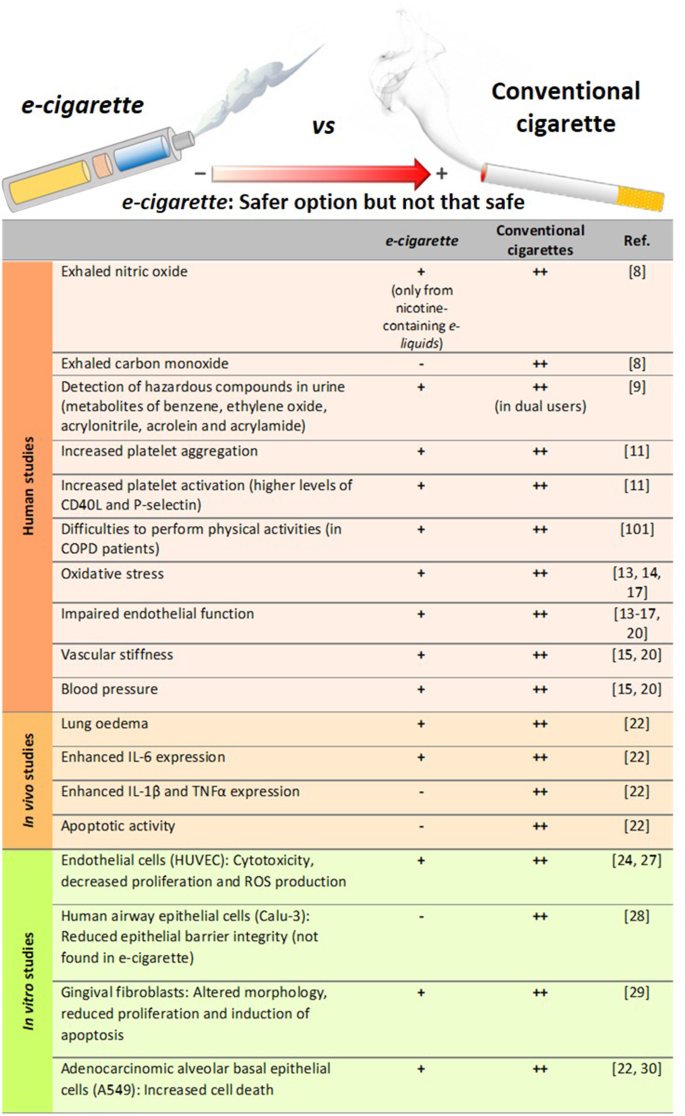
Comparison of the degree of harmful effects documented from e-cigarette and conventional cigarette consumption. Human studies, in vivo mice exposure and in vitro studies. All of these effects from e-cigarettes were documented to be lower than those exerted by conventional cigarettes, which may suggest that e-cigarette consumption could be a safer option than conventional tobacco smoking but not a clear safe choice
Consequences of nicotine content
Beyond flavour, one of the major issues in the e-liquid market is the range of nicotine content available. Depending on the manufacturer, the concentration of this alkaloid can be presented as low , medium or high , or expressed as mg/mL or as a percentage (% v/v). The concentrations range from 0 (0%, nicotine-free option) to 20 mg/mL (2.0%)—the maximum nicotine threshold according to directive 2014/40/EU of the European Parliament and the European Union Council [ 33 , 34 ]. Despite this normative, however, some commercial e-liquids have nicotine concentrations close to 54 mg/mL [ 35 ], much higher than the limits established by the European Union.
The mislabelling of nicotine content in e-liquids has been previously addressed [ 8 , 34 ]. For instance, gas chromatography with a flame ionisation detector (GC-FID) revealed inconsistencies in the nicotine content with respect to the manufacturer´s declaration (average of 22 ± 0.8 mg/mL vs. 18 mg/mL) [ 8 ], which equates to a content ~ 22% higher than that indicated in the product label. Of note, several studies have detected nicotine in those e-liquids labelled as nicotine-free [ 5 , 35 , 36 ]. One study detected the presence of nicotine (0.11–6.90 mg/mL) in 5 of 23 nicotine-free labelled e-liquids by nuclear magnetic resonance spectroscopy [ 35 ], and another study found nicotine (average 8.9 mg/mL) in 13.6% (17/125) of the nicotine-free e-liquids as analysed by high performance liquid chromatography (HPLC) [ 36 ]. Among the 17 samples tested in this latter study 14 were identified to be counterfeit or suspected counterfeit. A third study detected nicotine in 7 of 10 nicotine-free refills, although the concentrations were lower than those identified in the previous analyses (0.1–15 µg/mL) [ 5 ]. Not only is there evidence of mislabelling of nicotine content among refills labelled as nicotine-free, but there also seems to be a history of poor labelling accuracy in nicotine-containing e-liquids [ 37 , 38 ].
A comparison of the serum levels of nicotine from e-cigarette or conventional cigarette consumption has been recently reported [ 39 ]. Participants took one vape from an e-cigarette , with at least 12 mg/mL of nicotine, or inhaled a conventional cigarette, every 20 s for 10 min. Blood samples were collected 1, 2, 4, 6, 8, 10, 12 and 15 min after the first puff, and nicotine serum levels were measured by liquid chromatography-mass spectrometry (LC–MS). The results revealed higher serum levels of nicotine in the conventional CS group than in the e-cigarette group (25.9 ± 16.7 ng/mL vs. 11.5 ± 9.8 ng/mL). However, e-cigarettes containing 20 mg/mL of nicotine are more equivalent to normal cigarettes, based on the delivery of approximately 1 mg of nicotine every 5 min [ 40 ].
In this line, a study compared the acute impact of CS vs. e-cigarette vaping with equivalent nicotine content in healthy smokers and non-smokers. Both increased markers of oxidative stress and decreased NO bioavailability, flow-mediated dilation, and vitamin E levels showing no significant differences between tobacco and e-cigarette exposure (reviewed in [ 20 ]). Inasmuch, short-term e-cigarette use in healthy smokers resulted in marked impairment of endothelial function and an increase in arterial stiffness (reviewed in [ 20 ]). Similar effects on endothelial dysfunction and arterial stiffness were found in animals when they were exposed to e-cigarette vapor either for several days or chronically (reviewed in [ 20 ]). In contrast, other studies found acute microvascular endothelial dysfunction, increased oxidative stress and arterial stiffness in smokers after exposure to e-cigarettes with nicotine, but not after e-cigarettes without nicotine (reviewed in [ 20 ]). In women smokers, a study found a significant difference in stiffness after smoking just one tobacco cigarette, but not after use of e-cigarettes (reviewed in [ 20 ]).
It is well known that nicotine is extremely addictive and has a multitude of harmful effects. Nicotine has significant biologic activity and adversely affects several physiological systems including the cardiovascular, respiratory, immunological and reproductive systems, and can also compromise lung and kidney function [ 41 ]. Recently, a sub-chronic whole-body exposure of e-liquid (2 h/day, 5 days/week, 30 days) containing PG alone or PG with nicotine (25 mg/mL) to wild type (WT) animals or knockout (KO) mice in α7 nicotinic acetylcholine receptor (nAChRα7-KO) revealed a partly nAChRα7-dependent lung inflammation [ 42 ]. While sub-chronic exposure to PG/nicotine promote nAChRα7-dependent increased levels of different cytokines and chemokines in the bronchoalveolar lavage fluid (BALF) such as IL-1α, IL-2, IL-9, interferon γ (IFNγ), granulocyte-macrophage colony-stimulating factor (GM-CSF), monocyte chemoattractant protein-1 (MCP-1/CCL2) and regulated on activation, normal T cell expressed and secreted (RANTES/CCL5), the enhanced levels of IL-1β, IL-5 and TNFα were nAChRα7 independent. In general, most of the cytokines detected in BALF were significantly increased in WT mice exposed to PG with nicotine compared to PG alone or air control [ 42 ]. Some of these effects were found to be through nicotine activation of NF-κB signalling albeit in females but not in males. In addition, PG with nicotine caused increased macrophage and CD4 + /CD8 + T-lymphocytes cell counts in BALF compared to air control, but these effects were ameliorated when animals were sub-chronically exposed to PG alone [ 42 ].
Of note, another study indicated that although RANTES/CCL5 and CCR1 mRNA were upregulated in flavour/nicotine-containing e-cigarette users, vaping flavour and nicotine-less e-cigarettes did not significantly dysregulate cytokine and inflammasome activation [ 43 ].
In addition to its toxicological effects on foetus development, nicotine can disrupt brain development in adolescents and young adults [ 44 , 45 , 46 ]. Several studies have also suggested that nicotine is potentially carcinogenic (reviewed in [ 41 ]), but more work is needed to prove its carcinogenicity independently of the combustion products of tobacco [ 47 ]. In this latter regard, no differences were encountered in the frequency of tumour appearance in rats subjected to long-term (2 years) inhalation of nicotine when compared with control rats [ 48 ]. Despite the lack of carcinogenicity evidence, it has been reported that nicotine promotes tumour cell survival by decreasing apoptosis and increasing proliferation [ 49 ], indicating that it may work as a “tumour enhancer”. In a very recent study, chronic administration of nicotine to mice (1 mg/kg every 3 days for a 60-day period) enhanced brain metastasis by skewing the polarity of M2 microglia, which increases metastatic tumour growth [ 50 ]. Assuming that a conventional cigarette contains 0.172–1.702 mg of nicotine [ 51 ], the daily nicotine dose administered to these animals corresponds to 40–400 cigarettes for a 70 kg-adult, which is a dose of an extremely heavy smoker. We would argue that further studies with chronic administration of low doses of nicotine are required to clearly evaluate its impact on carcinogenicity.
In the aforementioned study exposing human gingival fibroblasts to CS condensate or to nicotine-rich or nicotine-free e-vapour condensates [ 29 ], the detrimental effects were greater in cells exposed to nicotine-rich condensate than to nicotine-free condensate, suggesting that the possible injurious effects of nicotine should be considered when purchasing e-refills . It is also noteworthy that among the 3 most cytotoxic vapours for HUVEC evaluated in the Putzhammer et al . study, 2 were nicotine-free, which suggests that nicotine is not the only hazardous component in e-cigarettes [ 24 ] .
The lethal dose of nicotine for an adult is estimated at 30–60 mg [ 52 ]. Given that nicotine easily diffuses from the dermis to the bloodstream, acute nicotine exposure by e-liquid spilling (5 mL of a 20 mg/mL nicotine-containing refill is equivalent to 100 mg of nicotine) can easily be toxic or even deadly [ 8 ]. Thus, devices with rechargeable refills are another issue of concern with e-cigarettes , especially when e-liquids are not sold in child-safe containers, increasing the risk of spilling, swallowing or breathing.
These data overall indicate that the harmful effects of nicotine should not be underestimated. Despite the established regulations, some inaccuracies in nicotine content labelling remain in different brands of e-liquids . Consequently, stricter regulation and a higher quality control in the e-liquid industry are required.
Effect of humectants and their heating-related products
In this particular aspect, again the composition of the e-liquid varies significantly among different commercial brands [ 4 , 35 ]. The most common and major components of e-liquids are PG or 1,2-propanediol, and glycerol or glycerine (propane-1,2,3-triol). Both types of compounds are used as humectants to prevent the e-liquid from drying out [ 2 , 53 ] and are classified by the Food and Drug Administration (FDA) as “Generally Recognised as Safe” [ 54 ]. In fact, they are widely used as alimentary and pharmaceutical products [ 2 ]. In an analysis of 54 commercially available e-liquids , PG and glycerol were detected in almost all samples at concentrations ranging from 0.4% to 98% (average 57%) and from 0.3% to 95% (average 37%), respectively [ 35 ].
With regards to toxicity, little is known about the effects of humectants when they are heated and chronically inhaled. Studies have indicated that PG can induce respiratory irritation and increase the probability of asthma development [ 55 , 56 ], and both PG and glycerol from e-cigarettes might reach concentrations sufficiently high to potentially cause irritation of the airways [ 57 ]. Indeed, the latter study established that one e-cigarette puff results in a PG exposure of 430–603 mg/m 3 , which is higher than the levels reported to cause airway irritation (average 309 mg/m 3 ) based on a human study [ 55 ]. The same study established that one e-cigarette puff results in a glycerol exposure of 348–495 mg/m 3 [ 57 ], which is close to the levels reported to cause airway irritation in rats (662 mg/m 3 ) [ 58 ].
Airway epithelial injury induced by acute vaping of PG and glycerol aerosols (50:50 vol/vol), with or without nicotine, has been reported in two randomised clinical trials in young tobacco smokers [ 32 ]. In vitro, aerosols from glycerol only-containing refills showed cytotoxicity in A549 and human embryonic stem cells, even at a low battery output voltage [ 59 ]. PG was also found to affect early neurodevelopment in a zebrafish model [ 60 ]. Another important issue is that, under heating conditions PG can produce acetaldehyde or formaldehyde (119.2 or 143.7 ng/puff at 20 W, respectively, on average), while glycerol can also generate acrolein (53.0, 1000.0 or 5.9 ng/puff at 20 W, respectively, on average), all carbonyls with a well-documented toxicity [ 61 ]. Although, assuming 15 puffs per e-cigarette unit, carbonyls produced by PG or glycerol heating would be below the maximum levels found in a conventional cigarette combustion (Table 2 ) [ 51 , 62 ]. Nevertheless, further studies are required to properly test the deleterious effects of all these compounds at physiological doses resembling those to which individuals are chronically exposed.
Although PG and glycerol are the major components of e-liquids other components have been detected. When the aerosols of 4 commercially available e-liquids chosen from a top 10 list of “ Best E-Cigarettes of 2014” , were analysed by gas chromatography-mass spectrometry (GC–MS) after heating, numerous compounds were detected, with nearly half of them not previously identified [ 4 ], thus suggesting that the heating process per se generates new compounds of unknown consequence. Of note, the analysis identified formaldehyde, acetaldehyde and acrolein [ 4 ], 3 carbonyl compounds with known high toxicity [ 63 , 64 , 65 , 66 , 67 ]. While no information was given regarding formaldehyde and acetaldehyde concentrations, the authors calculated that one puff could result in an acrolein exposure of 0.003–0.015 μg/mL [ 4 ]. Assuming 40 mL per puff and 15 puffs per e-cigarette unit (according to several manufacturers) [ 4 ], each e-cigarette unit would generate approximately 1.8–9 μg of acrolein, which is less than the levels of acrolein emitted by a conventional tobacco cigarette (18.3–98.2 μg) [ 51 ]. However, given that e-cigarette units of vaping are not well established, users may puff intermittently throughout the whole day. Thus, assuming 400 to 500 puffs per cartridge, users could be exposed to up to 300 μg of acrolein.
In a similar study, acrolein was found in 11 of 12 aerosols tested, with a similar content range (approximately 0.07–4.19 μg per e-cigarette unit) [ 68 ]. In the same study, both formaldehyde and acetaldehyde were detected in all of the aerosols tested, with contents of 0.2–5.61 μg and 0.11–1.36 μg, respectively, per e-cigarette unit [ 68 ]. It is important to point out that the levels of these toxic products in e-cigarette aerosols are significantly lower than those found in CS: 9 times lower for formaldehyde, 450 times lower for acetaldehyde and 15 times lower for acrolein (Table 2 ) [ 62 , 68 ].
Other compounds that have been detected in aerosols include acetamide, a potential human carcinogen [ 5 ], and some aldehydes [ 69 ], although their levels were minimal. Interestingly, the existence of harmful concentrations of diethylene glycol, a known cytotoxic agent, in e-liquid aerosols is contentious with some studies detecting its presence [ 4 , 68 , 70 , 71 , 72 ], and others finding low subtoxic concentrations [ 73 , 74 ]. Similar observations were reported for the content ethylene glycol. In this regard, either it was detected at concentrations that did not exceed the authorised limit [ 73 ], or it was absent from the aerosols produced [ 4 , 71 , 72 ]. Only one study revealed its presence at high concentration in a very low number of samples [ 5 ]. Nevertheless, its presence above 1 mg/g is not allowed by the FDA [ 73 ]. Figure 1 lists the main compounds detected in aerosols derived from humectant heating and their potential damaging effects. It would seem that future studies should analyse the possible toxic effects of humectants and related products at concentrations similar to those that e-cigarette vapers are exposed to reach conclusive results.
Impact of flavouring compounds
The range of e-liquid flavours available to consumers is extensive and is used to attract both current smokers and new e-cigarette users, which is a growing public health concern [ 6 ]. In fact, over 5 million middle- and high-school students were current users of e-cigarettes in 2019 [ 75 ], and appealing flavours have been identified as the primary reason for e-cigarette consumption in 81% of young users [ 76 ]. Since 2016, the FDA regulates the flavours used in the e-cigarette market and has recently published an enforcement policy on unauthorised flavours, including fruit and mint flavours, which are more appealing to young users [ 77 ]. However, the long-term effects of all flavour chemicals used by this industry (which are more than 15,000) remain unknown and they are not usually included in the product label [ 78 ]. Furthermore, there is no safety guarantee since they may harbour potential toxic or irritating properties [ 5 ].
With regards to the multitude of available flavours, some have demonstrated cytotoxicity [ 59 , 79 ]. Bahl et al. evaluated the toxicity of 36 different e-liquids and 29 different flavours on human embryonic stem cells, mouse neural stem cells and human pulmonary fibroblasts using a metabolic activity assay. In general, those e-liquids that were bubblegum-, butterscotch- and caramel-flavoured did not show any overt cytotoxicity even at the highest dose tested. By contrast, those e-liquids with Freedom Smoke Menthol Arctic and Global Smoke Caramel flavours had marked cytotoxic effects on pulmonary fibroblasts and those with Cinnamon Ceylon flavour were the most cytotoxic in all cell lines [ 79 ]. A further study from the same group [ 80 ] revealed that high cytotoxicity is a recurrent feature of cinnamon-flavoured e-liquids. In this line, results from GC–MS and HPLC analyses indicated that cinnamaldehyde (CAD) and 2-methoxycinnamaldehyde, but not dipropylene glycol or vanillin, were mainly responsible for the high cytotoxicity of cinnamon-flavoured e-liquids [ 80 ]. Other flavouring-related compounds that are associated with respiratory complications [ 81 , 82 , 83 ], such as diacetyl, 2,3-pentanedione or acetoin, were found in 47 out of 51 aerosols of flavoured e-liquids tested [ 84 ] . Allen et al . calculated an average of 239 μg of diacetyl per cartridge [ 84 ]. Assuming again 400 puffs per cartridge and 40 mL per puff, is it is possible to estimate an average of 0.015 ppm of diacetyl per puff, which could compromise normal lung function in the long-term [ 85 ].
The cytotoxic and pro-inflammatory effects of different e-cigarette flavouring chemicals were also tested on two human monocytic cell lines—mono mac 6 (MM6) and U937 [ 86 ]. Among the flavouring chemicals tested, CAD was found to be the most toxic and O-vanillin and pentanedione also showed significant cytotoxicity; by contrast, acetoin, diacetyl, maltol, and coumarin did not show any toxicity at the concentrations assayed (10–1000 µM). Of interest, a higher toxicity was evident when combinations of different flavours or mixed equal proportions of e-liquids from 10 differently flavoured e-liquids were tested, suggesting that vaping a single flavour is less toxic than inhaling mixed flavours [ 86 ]. Also, all the tested flavours produced significant levels of ROS in a cell-free ROS production assay. Finally, diacetyl, pentanedione, O-vanillin, maltol, coumarin, and CAD induced significant IL-8 secretion from MM6 and U937 monocytes [ 86 ]. It should be borne in mind, however, that the concentrations assayed were in the supra-physiological range and it is likely that, once inhaled, these concentrations are not reached in the airway space. Indeed, one of the limitations of the study was that human cells are not exposed to e-liquids per se, but rather to the aerosols where the concentrations are lower [ 86 ]. In this line, the maximum concentration tested (1000 µM) would correspond to approximately 80 to 150 ppm, which is far higher than the levels found in aerosols of some of these compounds [ 84 ]. Moreover, on a day-to-day basis, lungs of e-cigarette users are not constantly exposed to these chemicals for 24 h at these concentrations. Similar limitations were found when five of seven flavourings were found to cause cytotoxicity in human bronchial epithelial cells [ 87 ].
Recently, a commonly commercialized crème brûlée -flavoured aerosol was found to contain high concentrations of benzoic acid (86.9 μg/puff), a well-established respiratory irritant [ 88 ]. When human lung epithelial cells (BEAS-2B and H292) were exposed to this aerosol for 1 h, a marked cytotoxicity was observed in BEAS-2B but not in H292 cells, 24 h later. However, increased ROS production was registered in H292 cells [ 88 ].
Therefore, to fully understand the effects of these compounds, it is relevant the cell cultures selected for performing these assays, as well as the use of in vivo models that mimic the real-life situation of chronic e-cigarette vapers to clarify their impact on human health.
The e-cigarette device
While the bulk of studies related to the impact of e-cigarette use on human health has focused on the e-liquid components and the resulting aerosols produced after heating, a few studies have addressed the material of the electronic device and its potential consequences—specifically, the potential presence of metals such as copper, nickel or silver particles in e-liquids and aerosols originating from the filaments and wires and the atomiser [ 89 , 90 , 91 ].
Other important components in the aerosols include silicate particles from the fiberglass wicks or silicone [ 89 , 90 , 91 ]. Many of these products are known to cause abnormalities in respiratory function and respiratory diseases [ 89 , 90 , 91 ], but more in-depth studies are required. Interestingly, the battery output voltage also seems to have an impact on the cytotoxicity of the aerosol vapours, with e-liquids from a higher battery output voltage showing more toxicity to A549 cells [ 30 ].
A recent study compared the acute effects of e-cigarette vapor (with PG/vegetable glycerine plus tobacco flavouring but without nicotine) generated from stainless‐steel atomizer (SS) heating element or from a nickel‐chromium alloy (NC) [ 92 ]. Some rats received a single e-cigarette exposure for 2 h from a NC heating element (60 or 70 W); other rats received a similar exposure of e-cigarette vapor using a SS heating element for the same period of time (60 or 70 W) and, a final group of animals were exposed for 2 h to air. Neither the air‐exposed rats nor those exposed to e-cigarette vapor using SS heating elements developed respiratory distress. In contrast, 80% of the rats exposed to e-cigarette vapor using NC heating units developed clinical acute respiratory distress when a 70‐W power setting was employed. Thus, suggesting that operating units at higher than recommended settings can cause adverse effects. Nevertheless, there is no doubt that the deleterious effects of battery output voltage are not comparable to those exerted by CS extracts [ 30 ] (Figs. 1 and 2 ).
E-cigarettes as a smoking cessation tool
CS contains a large number of substances—about 7000 different constituents in total, with sizes ranging from atoms to particulate matter, and with many hundreds likely responsible for the harmful effects of this habit [ 93 ]. Given that tobacco is being substituted in great part by e-cigarettes with different chemical compositions, manufacturers claim that e -cigarette will not cause lung diseases such as lung cancer, chronic obstructive pulmonary disease, or cardiovascular disorders often associated with conventional cigarette consumption [ 3 , 94 ]. However, the World Health Organisation suggests that e-cigarettes cannot be considered as a viable method to quit smoking, due to a lack of evidence [ 7 , 95 ]. Indeed, the results of studies addressing the use of e-cigarettes as a smoking cessation tool remain controversial [ 96 , 97 , 98 , 99 , 100 ]. Moreover, both FDA and CDC are actively investigating the incidence of severe respiratory symptoms associated with the use of vaping products [ 77 ]. Because many e-liquids contain nicotine, which is well known for its powerful addictive properties [ 41 ], e-cigarette users can easily switch to conventional cigarette smoking, avoiding smoking cessation. Nevertheless, the possibility of vaping nicotine-free e-cigarettes has led to the branding of these devices as smoking cessation tools [ 2 , 6 , 7 ].
In a recently published randomised trial of 886 subjects who were willing to quit smoking [ 100 ], the abstinence rate was found to be twice as high in the e-cigarette group than in the nicotine-replacement group (18.0% vs. 9.9%) after 1 year. Of note, the abstinence rate found in the nicotine-replacement group was lower than what is usually expected with this therapy. Nevertheless, the incidence of throat and mouth irritation was higher in the e-cigarette group than in the nicotine-replacement group (65.3% vs. 51.2%, respectively). Also, the participant adherence to the treatment after 1-year abstinence was significantly higher in the e-cigarette group (80%) than in nicotine-replacement products group (9%) [ 100 ].
On the other hand, it is estimated that COPD could become the third leading cause of death in 2030 [ 101 ]. Given that COPD is generally associated with smoking habits (approximately 15 to 20% of smokers develop COPD) [ 101 ], smoking cessation is imperative among COPD smokers. Published data revealed a clear reduction of conventional cigarette consumption in COPD smokers that switched to e-cigarettes [ 101 ]. Indeed, a significant reduction in exacerbations was observed and, consequently, the ability to perform physical activities was improved when data was compared with those non-vapers COPD smokers. Nevertheless, a longer follow-up of these COPD patients is required to find out whether they have quitted conventional smoking or even vaping, since the final goal under these circumstances is to quit both habits.
Based on the current literature, it seems that several factors have led to the success of e-cigarette use as a smoking cessation tool. First, some e-cigarette flavours positively affect smoking cessation outcomes among smokers [ 102 ]. Second, e-cigarettes have been described to improve smoking cessation rate only among highly-dependent smokers and not among conventional smokers, suggesting that the individual degree of nicotine dependence plays an important role in this process [ 97 ]. Third, the general belief of their relative harmfulness to consumers' health compared with conventional combustible tobacco [ 103 ]. And finally, the exposure to point-of-sale marketing of e-cigarette has also been identified to affect the smoking cessation success [ 96 ].
Implication of e-cigarette consumption in COVID-19 time
Different reports have pointed out that smokers and vapers are more vulnerable to SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2) infections or more prone to adverse outcomes if they suffer COVID-19 [ 104 ]. However, while a systematic review indicated that cigarette smoking is probably associated with enhanced damage from COVID-19, a meta-analysis did not, yet the latter had several limitations due to the small sample sizes [ 105 ].
Interestingly, most of these reports linking COVID-19 harmful effects with smoking or vaping, are based on their capability of increasing the expression of angiotensin-converting enzyme 2 (ACE2) in the lung. It is well known that ACE2 is the gate for SARS-CoV-2 entrance to the airways [ 106 ] and it is mainly expressed in type 2 alveolar epithelial cells and alveolar macrophages [ 107 ]. To date, most of the studies in this field indicate that current smokers have higher expression of ACE2 in the airways (reviewed by [ 108 ]) than healthy non-smokers [ 109 , 110 ]. However, while a recent report indicated that e-cigarette vaping also caused nicotine-dependent ACE2 up-regulation [ 42 ], others have revealed that neither acute inhalation of e-cigarette vapour nor e-cigarette users had increased lung ACE2 expression regardless nicotine presence in the e-liquid [ 43 , 110 ].
In regard to these contentions, current knowledge suggests that increased ACE2 expression is not necessarily linked to enhanced susceptibility to SARS-CoV-2 infection and adverse outcome. Indeed, elderly population express lower levels of ACE2 than young people and SARS-CoV-2/ACE2 interaction further decreases ACE2 expression. In fact, most of the deaths provoked by COVID-19 took place in people over 60 years old of age [ 111 ]. Therefore, it is plausible that the increased susceptibility to disease progression and the subsequent fatal outcome in this population is related to poor angiotensin 1-7 (Ang-1-7) generation, the main peptide generated by ACE2, and probably to their inaccessibility to its anti-inflammatory effects. Furthermore, it seems that all the efforts towards increasing ACE2 expression may result in a better resolution of the pneumonic process associated to this pandemic disease.
Nevertheless, additional complications associated to COVID-19 are increased thrombotic events and cytokine storm. In the lungs, e-cigarette consumption has been correlated to toxicity, oxidative stress, and inflammatory response [ 32 , 112 ]. More recently, a study revealed that while the use of nicotine/flavour-containing e-cigarettes led to significant cytokine dysregulation and potential inflammasome activation, none of these effects were detected in non-flavoured and non-nicotine-containing e-cigarettes [ 43 ]. Therefore, taken together these observations, e-cigarette use may still be a potent risk factor for severe COVID-19 development depending on the flavour and nicotine content.
In summary, it seems that either smoking or nicotine vaping may adversely impact on COVID-19 outcome. However, additional follow up studies are required in COVID-19 pandemic to clarify the effect of e-cigarette use on lung and cardiovascular complications derived from SARS-CoV-2 infection.
Conclusions
The harmful effects of CS and their deleterious consequences are both well recognised and widely investigated. However, and based on the studies carried out so far, it seems that e-cigarette consumption is less toxic than tobacco smoking. This does not necessarily mean, however, that e-cigarettes are free from hazardous effects. Indeed, studies investigating their long-term effects on human health are urgently required. In this regard, the main additional studies needed in this field are summarized in Table 3 .
The composition of e-liquids requires stricter regulation, as they can be easily bought online and many incidences of mislabelling have been detected, which can seriously affect consumers’ health. Beyond their unknown long-term effects on human health, the extended list of appealing flavours available seems to attract new “never-smokers”, which is especially worrying among young users. Additionally, there is still a lack of evidence of e-cigarette consumption as a smoking cessation method. Indeed, e-cigarettes containing nicotine may relieve the craving for smoking, but not the conventional cigarette smoking habit.
Interestingly, there is a strong difference of opinion on e-cigarettes between countries. Whereas countries such as Brazil, Uruguay and India have banned the sale of e-cigarettes , others such as the United Kingdom support this device to quit smoking. The increasing number of adolescent users and reported deaths in the United States prompted the government to ban the sale of flavoured e-cigarettes in 2020. The difference in opinion worldwide may be due to different restrictions imposed. For example, while no more than 20 ng/mL of nicotine is allowed in the EU, e-liquids with 59 mg/dL are currently available in the United States. Nevertheless, despite the national restrictions, users can easily access foreign or even counterfeit products online.
In regard to COVID-19 pandemic, the actual literature suggests that nicotine vaping may display adverse outcomes. Therefore, follow up studies are necessary to clarify the impact of e-cigarette consumption on human health in SARS-CoV-2 infection.
In conclusion, e-cigarettes could be a good alternative to conventional tobacco cigarettes, with less side effects; however, a stricter sale control, a proper regulation of the industry including flavour restriction, as well as further toxicological studies, including their chronic effects, are warranted.
Availability of data and materials
Not applicable.
Abbreviations
Angiotensin-converting enzyme 2
Angiotensin 1-7
Bronchoalveolar lavage fluid
Cinnamaldehyde
US Centers for Disease Control and Prevention
Carbon monoxide
Chronic obstructive pulmonary disease
Coronavirus disease 2019
Cigarette smoke
Electronic nicotine dispensing systems
e-cigarette or vaping product use-associated lung injury
Food and Drug Administration
Gas chromatography with a flame ionisation detector
Gas chromatography-mass spectrometry
Granulocyte–macrophage colony-stimulating factor
High performance liquid chromatography
Human umbilical vein endothelial cells
Interleukin
Interferon γ
Liquid chromatography-mass spectrometry
Monocyte chemoattractant protein-1
Matrix metallopeptidase 9
α7 Nicotinic acetylcholine receptor
Nickel‐chromium alloy
Nitric oxide
Propylene glycol
Regulated on activation, normal T cell expressed and secreted
Reactive oxygen species
Severe acute respiratory syndrome coronavirus 2
Stainless‐steel atomizer
Tetrahydrocannabinol
Tumour necrosis factor-α
Hiemstra PS, Bals R. Basic science of electronic cigarettes: assessment in cell culture and in vivo models. Respir Res. 2016;17(1):127.
Article PubMed PubMed Central CAS Google Scholar
Bertholon JF, Becquemin MH, Annesi-Maesano I, Dautzenberg B. Electronic cigarettes: a short review. Respiration. 2013;86(5):433–8.
Article CAS PubMed Google Scholar
Rowell TR, Tarran R. Will chronic e-cigarette use cause lung disease? Am J Physiol Lung Cell Mol Physiol. 2015;309(12):L1398–409.
Article CAS PubMed PubMed Central Google Scholar
Herrington JS, Myers C. Electronic cigarette solutions and resultant aerosol profiles. J Chromatogr A. 2015;1418:192–9.
Hutzler C, Paschke M, Kruschinski S, Henkler F, Hahn J, Luch A. Chemical hazards present in liquids and vapors of electronic cigarettes. Arch Toxicol. 2014;88(7):1295–308.
Pokhrel P, Herzog TA, Muranaka N, Fagan P. Young adult e-cigarette users’ reasons for liking and not liking e-cigarettes: a qualitative study. Psychol Health. 2015;30(12):1450–69.
Article PubMed PubMed Central Google Scholar
Harrell PT, Simmons VN, Correa JB, Padhya TA, Brandon TH. Electronic nicotine delivery systems (“e-cigarettes”): review of safety and smoking cessation efficacy. Otolaryngol Head Neck Surg. 2014;151(3):381–93.
Schober W, Szendrei K, Matzen W, Osiander-Fuchs H, Heitmann D, Schettgen T, et al. Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. Int J Hyg Environ Health. 2014;217(6):628–37.
Rubinstein ML, Delucchi K, Benowitz NL, Ramo DE. Adolescent exposure to toxic volatile organic chemicals from E-cigarettes. Pediatrics. 2018;141(4):e20173557.
Article PubMed Google Scholar
Staudt MR, Salit J, Kaner RJ, Hollmann C, Crystal RG. Altered lung biology of healthy never smokers following acute inhalation of E-cigarettes. Respir Res. 2018;19(1):78.
Nocella C, Biondi-Zoccai G, Sciarretta S, Peruzzi M, Pagano F, Loffredo L, et al. Impact of tobacco versus electronic cigarette smoking on platelet function. Am J Cardiol. 2018;122(9):1477–81.
Higham A, Rattray NJW, Dewhurst JA, Trivedi DK, Fowler SJ, Goodacre R, et al. Electronic cigarette exposure triggers neutrophil inflammatory responses. Respir Res. 2016;17(1):56.
Antoniewicz L, Bosson JA, Kuhl J, Abdel-Halim SM, Kiessling A, Mobarrez F, et al. Electronic cigarettes increase endothelial progenitor cells in the blood of healthy volunteers. Atherosclerosis. 2016;255:179–85.
Carnevale R, Sciarretta S, Violi F, Nocella C, Loffredo L, Perri L, et al. Acute impact of tobacco vs electronic cigarette smoking on oxidative stress and vascular function. Chest. 2016;150(3):606–12.
Vlachopoulos C, Ioakeimidis N, Abdelrasoul M, Terentes-Printzios D, Georgakopoulos C, Pietri P, et al. Electronic cigarette smoking increases aortic stiffness and blood pressure in young smokers. J Am Coll Cardiol. 2016;67(23):2802–3.
Franzen KF, Willig J, Cayo Talavera S, Meusel M, Sayk F, Reppel M, et al. E-cigarettes and cigarettes worsen peripheral and central hemodynamics as well as arterial stiffness: a randomized, double-blinded pilot study. Vasc Med. 2018;23(5):419–25.
Caporale A, Langham MC, Guo W, Johncola A, Chatterjee S, Wehrli FW. Acute effects of electronic cigarette aerosol inhalation on vascular function detected at quantitative MRI. Radiology. 2019;293(1):97–106.
von Hundelshausen P, Schmitt MM. Platelets and their chemokines in atherosclerosis-clinical applications. Front Physiol. 2014;5:294.
Google Scholar
Landmesser U, Hornig B, Drexler H. Endothelial function: a critical determinant in atherosclerosis? Circulation. 2004;109(21 Suppl 1):Ii27-33.
PubMed Google Scholar
Münzel T, Hahad O, Kuntic M, Keaney JF, Deanfield JE, Daiber A. Effects of tobacco cigarettes, e-cigarettes, and waterpipe smoking on endothelial function and clinical outcomes. Eur Heart J. 2020;41:4057–70.
Javelle E. Electronic cigarette and vaping should be discouraged during the new coronavirus SARS-CoV-2 pandemic. Arch Toxicol. 2020;94(6):2261–2.
Husari A, Shihadeh A, Talih S, Hashem Y, El Sabban M, Zaatari G. Acute exposure to electronic and combustible cigarette aerosols: effects in an animal model and in human alveolar cells. Nicotine Tob Res. 2016;18(5):613–9.
Zelikoff JT, Parmalee NL, Corbett K, Gordon T, Klein CB, Aschner M. Microglia activation and gene expression alteration of neurotrophins in the hippocampus following early-life exposure to E-cigarette aerosols in a murine model. Toxicol Sci. 2018;162(1):276–86.
Putzhammer R, Doppler C, Jakschitz T, Heinz K, Forste J, Danzl K, et al. Vapours of US and EU market leader electronic cigarette brands and liquids are cytotoxic for human vascular endothelial cells. PLoS One. 2016;11(6):e0157337.
Bernhard D, Pfister G, Huck CW, Kind M, Salvenmoser W, Bonn GK, et al. Disruption of vascular endothelial homeostasis by tobacco smoke: impact on atherosclerosis. Faseb J. 2003;17(15):2302–4.
Newby DE, Wright RA, Labinjoh C, Ludlam CA, Fox KA, Boon NA, et al. Endothelial dysfunction, impaired endogenous fibrinolysis, and cigarette smoking: a mechanism for arterial thrombosis and myocardial infarction. Circulation. 1999;99(11):1411–5.
Taylor M, Jaunky T, Hewitt K, Breheny D, Lowe F, Fearon IM, et al. A comparative assessment of e-cigarette aerosols and cigarette smoke on in vitro endothelial cell migration. Toxicol Lett. 2017;277:123–8.
Herr C, Tsitouras K, Niederstraßer J, Backes C, Beisswenger C, Dong L, et al. Cigarette smoke and electronic cigarettes differentially activate bronchial epithelial cells. Respir Res. 2020;21(1):67.
Alanazi H, Park HJ, Chakir J, Semlali A, Rouabhia M. Comparative study of the effects of cigarette smoke and electronic cigarettes on human gingival fibroblast proliferation, migration and apoptosis. Food Chem Toxicol. 2018;118:390–8.
Otreba M, Kosmider L. E-cigarettes: voltage- and concentration-dependent loss in human lung adenocarcinoma viability. J Appl Toxicol. 2018;38(8):1135–43.
Chaumont M, Bernard A, Pochet S, Melot C, El Khattabi C, Reye F, et al. High-wattage E-cigarettes induce tissue hypoxia and lower airway injury: a randomized clinical trial. Am J Respir Crit Care Med. 2018;198(1):123–6.
Chaumont M, van de Borne P, Bernard A, Van Muylem A, Deprez G, Ullmo J, et al. Fourth generation e-cigarette vaping induces transient lung inflammation and gas exchange disturbances: results from two randomized clinical trials. Am J Physiol Lung Cell Mol Physiol. 2019;316(5):L705–19.
European Parliament and the council of the European Union. Directive 2014/40/EU. 2014 (updated April 29, 2014). https://ec.europa.eu/health//sites/health/files/tobacco/docs/dir_201440_en.pdf . Accessed 17 April 2020.
Cameron JM, Howell DN, White JR, Andrenyak DM, Layton ME, Roll JM. Variable and potentially fatal amounts of nicotine in e-cigarette nicotine solutions. Tob Control. 2014;23(1):77–8.
Hahn J, Monakhova YB, Hengen J, Kohl-Himmelseher M, Schussler J, Hahn H, et al. Electronic cigarettes: overview of chemical composition and exposure estimation. Tob Induc Dis. 2014;12(1):23.
Omaiye EE, Cordova I, Davis B, Talbot P. Counterfeit electronic cigarette products with mislabeled nicotine concentrations. Tob Regul Sci. 2017;3(3):347–57.
Buettner-Schmidt K, Miller DR, Balasubramanian N. Electronic cigarette refill liquids: child-resistant packaging, nicotine content, and sales to minors. J Pediatr Nurs. 2016;31(4):373–9.
Jackson R, Huskey M, Brown S. Labelling accuracy in low nicotine e-cigarette liquids from a sampling of US manufacturers. Int J Pharm Pract. 2019;28(3):290–4.
Yingst JM, Foulds J, Veldheer S, Hrabovsky S, Trushin N, Eissenberg TT, et al. Nicotine absorption during electronic cigarette use among regular users. PLoS One. 2019;14(7):e0220300.
Farsalinos KE, Romagna G, Tsiapras D, Kyrzopoulos S, Voudris V. Evaluation of electronic cigarette use (vaping) topography and estimation of liquid consumption: implications for research protocol standards definition and for public health authorities’ regulation. Int J Environ Res Public Health. 2013;10(6):2500–14.
Mishra A, Chaturvedi P, Datta S, Sinukumar S, Joshi P, Garg A. Harmful effects of nicotine. Indian J Med Paediatr Oncol. 2015;36(1):24–31.
Wang Q, Sundar IK, Li D, Lucas JH, Muthumalage T, McDonough SR, et al. E-cigarette-induced pulmonary inflammation and dysregulated repair are mediated by nAChR α7 receptor: role of nAChR α7 in SARS-CoV-2 Covid-19 ACE2 receptor regulation. Respir Res. 2020;21(1):154.
Lee AC, Chakladar J, Li WT, Chen C, Chang EY, Wang-Rodriguez J, et al. Tobacco, but not nicotine and flavor-less electronic cigarettes, induces ACE2 and immune dysregulation. Int J Mol Sci. 2020;21(15):5513.
Article CAS PubMed Central Google Scholar
England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA. Nicotine and the developing human: a neglected element in the electronic cigarette debate. Am J Prev Med. 2015;49(2):286–93.
Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain. J Physiol. 2015;593(16):3397–412.
Holbrook BD. The effects of nicotine on human fetal development. Birth Defects Res C Embryo Today. 2016;108(2):181–92.
Sanner T, Grimsrud TK. Nicotine: carcinogenicity and effects on response to cancer treatment—a review. Front Oncol. 2015;5:196.
Waldum HL, Nilsen OG, Nilsen T, Rørvik H, Syversen V, Sanvik AK, et al. Long-term effects of inhaled nicotine. Life Sci. 1996;58(16):1339–46.
Cucina A, Dinicola S, Coluccia P, Proietti S, D’Anselmi F, Pasqualato A, et al. Nicotine stimulates proliferation and inhibits apoptosis in colon cancer cell lines through activation of survival pathways. J Surg Res. 2012;178(1):233–41.
Wu SY, Xing F, Sharma S, Wu K, Tyagi A, Liu Y, et al. Nicotine promotes brain metastasis by polarizing microglia and suppressing innate immune function. J Exp Med. 2020;217(8):e20191131.
Roemer E, Stabbert R, Rustemeier K, Veltel DJ, Meisgen TJ, Reininghaus W, et al. Chemical composition, cytotoxicity and mutagenicity of smoke from US commercial and reference cigarettes smoked under two sets of machine smoking conditions. Toxicology. 2004;195(1):31–52.
Mayer B. How much nicotine kills a human? Tracing back the generally accepted lethal dose to dubious self-experiments in the nineteenth century. Arch Toxicol. 2014;88(1):5–7.
Brown CJ, Cheng JM. Electronic cigarettes: product characterisation and design considerations. Tob Control. 2014;23(Suppl 2):ii4-10.
Food and Drug Administration. SCOGS (Select Committee on GRAS Substances). 2019 (updated April 29, 2019). https://www.accessdata.fda.gov/scripts/fdcc/index.cfm?set=SCOGS&sort=Sortsubstance&order=ASC&startrow=251&type=basic&search= . Accessed 14 April 2020.
Wieslander G, Norback D, Lindgren T. Experimental exposure to propylene glycol mist in aviation emergency training: acute ocular and respiratory effects. Occup Environ Med. 2001;58(10):649–55.
Choi H, Schmidbauer N, Sundell J, Hasselgren M, Spengler J, Bornehag CG. Common household chemicals and the allergy risks in pre-school age children. PLoS One. 2010;5(10):e13423.
Kienhuis AS, Soeteman-Hernandez LG, Bos PMJ, Cremers HWJM, Klerx WN, Talhout R. Potential harmful health effects of inhaling nicotine-free shisha-pen vapor: a chemical risk assessment of the main components propylene glycol and glycerol. Tob Induc Dis. 2015;13(1):15.
Renne RA, Wehner AP, Greenspan BJ, Deford HS, Ragan HA, Westerberg RB, et al. 2-Week and 13-week inhalation studies of aerosolized glycerol in rats. Inhal Toxicol. 1992;4(2):95–111.
Article CAS Google Scholar
Behar R, Wang Y, Talbot P. Comparing the cytotoxicity of electronic cigarette fluids, aerosols and solvents. Tob Control. 2018;27(3):325.
Massarsky A, Abdel A, Glazer L, Levin ED, Di Giulio RT. Neurobehavioral effects of 1,2-propanediol in zebrafish (Danio rerio). Neurotoxicology. 2018;65:111–24.
Geiss O, Bianchi I, Barrero-Moreno J. Correlation of volatile carbonyl yields emitted by e-cigarettes with the temperature of the heating coil and the perceived sensorial quality of the generated vapours. Int J Hyg Environ Health. 2016;219(3):268–77.
Counts ME, Morton MJ, Laffoon SW, Cox RH, Lipowicz PJ. Smoke composition and predicting relationships for international commercial cigarettes smoked with three machine-smoking conditions. Regul Toxicol Pharmacol. 2005;41(3):185–227.
Agency for Toxic Substances & Disease Registry. Toxicological Profile for Formaldehyde. 2019 (updated September 26, 2019). https://www.atsdr.cdc.gov/ToxProfiles/tp.asp?id=220&tid=39 . Accessed 9 April 2020.
Agency for Toxic Substances & Disease Registry. Toxicological Profile for Acrolein. 2019 (updated September 26, 2019). https://www.atsdr.cdc.gov/toxprofiles/TP.asp?id=557&tid=102 . Accessed 9 April 2020
Moghe A, Ghare S, Lamoreau B, Mohammad M, Barve S, McClain C, et al. Molecular mechanisms of acrolein toxicity: relevance to human disease. Toxicol Sci. 2015;143(2):242–55.
Seitz HK, Stickel F. Acetaldehyde as an underestimated risk factor for cancer development: role of genetics in ethanol metabolism. Genes Nutr. 2010;5(2):121–8.
Faroon O, Roney N, Taylor J, Ashizawa A, Lumpkin MH, Plewak DJ. Acrolein health effects. Toxicol Ind Health. 2008;24(7):447–90.
Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133–9.
Farsalinos KE, Voudris V. Do flavouring compounds contribute to aldehyde emissions in e-cigarettes? Food Chem Toxicol. 2018;115:212–7.
Kavvalakis MP, Stivaktakis PD, Tzatzarakis MN, Kouretas D, Liesivuori J, Alegakis AK, et al. Multicomponent analysis of replacement liquids of electronic cigarettes using chromatographic techniques. J Anal Toxicol. 2015;39(4):262–9.
Etter JF, Zather E, Svensson S. Analysis of refill liquids for electronic cigarettes. Addiction. 2013;108(9):1671–9.
Etter JF, Bugey A. E-cigarette liquids: constancy of content across batches and accuracy of labeling. Addict Behav. 2017;73:137–43.
Varlet V, Farsalinos K, Augsburger M, Thomas A, Etter JF. Toxicity assessment of refill liquids for electronic cigarettes. Int J Environ Res Public Health. 2015;12(5):4796–815.
McAuley TR, Hopke PK, Zhao J, Babaian S. Comparison of the effects of e-cigarette vapor and cigarette smoke on indoor air quality. Inhal Toxicol. 2012;24(12):850–7.
Cullen KA, Gentzke AS, Sawdey MD, Chang JT, Anic GM, Wang TW, et al. e-Cigarette use among youth in the United States, 2019. JAMA. 2019;322(21):2095–103.
Villanti AC, Johnson AL, Ambrose BK, Cummings KM, Stanton CA, Rose SW, et al. Flavored tobacco product use in youth and adults: findings from the first wave of the PATH Study (2013–2014). Am J Prev Med. 2017;53(2):139–51.
Food and Drug Administration. Vaporizers, E-Cigarettes, and other Electronic Nicotine Delivery Systems (ENDS) 2020 (updated April 13, 2020). https://www.fda.gov/tobacco-products/products-ingredients-components/vaporizers-e-cigarettes-and-other-electronic-nicotine-delivery-systems-ends . Accessed 15 April 2020
Omaiye EE, McWhirter KJ, Luo W, Tierney PA, Pankow JF, Talbot P. High concentrations of flavor chemicals are present in electronic cigarette refill fluids. Sci Rep. 2019;9(1):2468.
Bahl V, Lin S, Xu N, Davis B, Wang YH, Talbot P. Comparison of electronic cigarette refill fluid cytotoxicity using embryonic and adult models. Reprod Toxicol. 2012;34(4):529–37.
Behar R, Davis B, Wang Y, Bahl V, Lin S, Talbot P. Identification of toxicants in cinnamon-flavored electronic cigarette refill fluids. Toxicol In Vitro. 2014;28(2):198–208.
Morgan DL, Flake GP, Kirby PJ, Palmer SM. Respiratory toxicity of diacetyl in C57BL/6 mice. Toxicol Sci. 2008;103(1):169–80.
Hubbs AF, Cumpston AM, Goldsmith WT, Battelli LA, Kashon ML, Jackson MC, et al. Respiratory and olfactory cytotoxicity of inhaled 2,3-pentanedione in Sprague-Dawley rats. Am J Pathol. 2012;181(3):829–44.
Vas CA, Porter A, Mcadam K. Acetoin is a precursor to diacetyl in e-cigarette liquids. Food Chem Toxicol. 2019;133:110727.
Allen JG, Flanigan SS, LeBlanc M, Vallarino J, MacNaughton P, Stewart JH, et al. Flavoring chemicals in E-cigarettes: diacetyl, 2,3-pentanedione, and acetoin in a sample of 51 products, including fruit-, candy-, and cocktail-flavored E-cigarettes. Environ Health Perspect. 2016;124(6):733–9.
Park RM, Gilbert SJ. Pulmonary impairment and risk assessment in a diacetyl-exposed population: microwave popcorn workers. J Occup Environ Med. 2018;60(6):496–506.
Muthumalage T, Prinz M, Ansah KO, Gerloff J, Sundar IK, Rahman I. Inflammatory and oxidative responses induced by exposure to commonly used e-cigarette flavoring chemicals and flavored e-liquids without nicotine. Front Physiol. 2017;8:1130.
Sherwood CL, Boitano S. Airway epithelial cell exposure to distinct e-cigarette liquid flavorings reveals toxicity thresholds and activation of CFTR by the chocolate flavoring 2,5-dimethypyrazine. Respir Res. 2016;17(1):57.
Pinkston R, Zaman H, Hossain E, Penn AL, Noël A. Cell-specific toxicity of short-term JUUL aerosol exposure to human bronchial epithelial cells and murine macrophages exposed at the air–liquid interface. Respir Res. 2020;21(1):269.
Williams M, Villarreal A, Bozhilov K, Lin S, Talbot P. Metal and silicate particles including nanoparticles are present in electronic cigarette cartomizer fluid and aerosol. PLoS One. 2013;8(3):e57987.
Mikheev VB, Brinkman MC, Granville CA, Gordon SM, Clark PI. Real-time measurement of electronic cigarette aerosol size distribution and metals content analysis. Nicotine Tob Res. 2016;18(9):1895–902.
Williams M, Bozhilov K, Ghai S, Talbot P. Elements including metals in the atomizer and aerosol of disposable electronic cigarettes and electronic hookahs. PLoS One. 2017;12(4):e0175430.
Kleinman MT, Arechavala RJ, Herman D, Shi J, Hasen I, Ting A, et al. E-cigarette or vaping product use-associated lung injury produced in an animal model from electronic cigarette vapor exposure without tetrahydrocannabinol or vitamin E oil. J Am Heart Assoc. 2020;9(18):e017368.
Patnode CD, Henderson JT, Thompson JH, Senger CA, Fortmann SP, Whitlock EP. Behavioral counseling and pharmacotherapy interventions for tobacco cessation in adults, including pregnant women: a review of reviews for the U.S. preventive services task force. Ann Intern Med. 2015;163(8):608–21.
Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34(3):509–15.
Bansal V, Kim K-H. Review on quantitation methods for hazardous pollutants released by e-cigarette (EC) smoking. Trends Analyt Chem. 2016;78:120–33.
Mantey DS, Pasch KE, Loukas A, Perry CL. Exposure to point-of-sale marketing of cigarettes and E-cigarettes as predictors of smoking cessation behaviors. Nicotine Tob Res. 2019;21(2):212–9.
Selya AS, Dierker L, Rose JS, Hedeker D, Mermelstein RJ. The role of nicotine dependence in E-cigarettes’ potential for smoking reduction. Nicotine Tob Res. 2018;20(10):1272–7.
Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4(2):116–28.
Levy DT, Yuan Z, Luo Y, Abrams DB. The relationship of e-cigarette use to cigarette quit attempts and cessation: insights from a large, nationally representative U.S. survey. Nicotine Tob Res. 2017;20(8):931–9.
Article PubMed Central Google Scholar
Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, et al. A randomized trial of E-cigarettes versus nicotine-replacement therapy. N Engl J Med. 2019;380(7):629–37.
Polosa R, Morjaria JB, Caponnetto P, Prosperini U, Russo C, Pennisi A, et al. Evidence for harm reduction in COPD smokers who switch to electronic cigarettes. Respir Res. 2016;17(1):166.
Litt MD, Duffy V, Oncken C. Cigarette smoking and electronic cigarette vaping patterns as a function of e-cigarette flavourings. Tob Control. 2016;25(Suppl 2):ii67–72.
Palmer AM, Brandon TH. How do electronic cigarettes affect cravings to smoke or vape? Parsing the influences of nicotine and expectancies using the balanced-placebo design. J Consult Clin Psychol. 2018;86(5):486–91.
Majmundar A, Allem JP, Cruz TB, Unger JB. Public health concerns and unsubstantiated claims at the intersection of vaping and COVID-19. Nicotine Tob Res. 2020;22(9):1667–8.
Berlin I, Thomas D, Le Faou A-L, Cornuz J. COVID-19 and smoking. Nicotine Tob Res. 2020;22(9):1650–2.
Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh C-L, Abiona O, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–3.
Wang K, Gheblawi M, Oudit GY. Angiotensin Converting Enzyme 2: A Double-Edged Sword. Circulation. 2020;142(5):426–8.
Sharma P, Zeki AA. Does vaping increase susceptibility to COVID-19? Am J Respir Crit Care Med. 2020;202(7):1055–6.
Brake SJ, Barnsley K, Lu W, McAlinden KD, Eapen MS, Sohal SS. Smoking upregulates angiotensin-converting enzyme-2 receptor: a potential adhesion site for novel coronavirus SARS-CoV-2 (Covid-19). J Clin Med. 2020;9(3):841.
Zhang H, Rostamim MR, Leopold PL, Mezey JG, O’Beirne SL, Strulovici-Barel Y, et al. Reply to sharma and zeki: does vaping increase susceptibility to COVID-19? Am J Respir Crit Care Med. 2020;202(7):1056–7.
Cheng H, Wang Y, Wang GQ. Organ-protective effect of angiotensin-converting enzyme 2 and its effect on the prognosis of COVID-19. J Med Virol. 2020;92(7):726–30.
Lerner CA, Sundar IK, Yao H, Gerloff J, Ossip DJ, McIntosh S, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS ONE. 2015;10(2):e0116732.
Download references
Acknowledgements
The authors gratefully acknowledge Dr. Cruz González, Pulmonologist at University Clinic Hospital of Valencia (Valencia, Spain) for her thoughtful suggestions and support.
This work was supported by the Spanish Ministry of Science and Innovation [Grant Number SAF2017-89714-R]; Carlos III Health Institute [Grant Numbers PIE15/00013, PI18/00209]; Generalitat Valenciana [Grant Number PROMETEO/2019/032, Gent T CDEI-04/20-A and AICO/2019/250], and the European Regional Development Fund.
Author information
Authors and affiliations.
Department of Pharmacology, Faculty of Medicine, University of Valencia, Avda. Blasco Ibañez 15, 46010, Valencia, Spain
Patrice Marques, Laura Piqueras & Maria-Jesus Sanz
Institute of Health Research INCLIVA, University Clinic Hospital of Valencia, Valencia, Spain
CIBERDEM-Spanish Biomedical Research Centre in Diabetes and Associated Metabolic Disorders, ISCIII, Av. Monforte de Lemos 3-5, 28029, Madrid, Spain
Laura Piqueras & Maria-Jesus Sanz
You can also search for this author in PubMed Google Scholar
Contributions
All authors discussed and agreed to the scope of the manuscript and contributed to the development of the manuscript at all stages. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Maria-Jesus Sanz .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors of the manuscript declare no conflicts of interest and take sole responsibility for the writing and content of the manuscript. None of the authors have been involved in legal or regulatory matters related to the contents of this paper.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Marques, P., Piqueras, L. & Sanz, MJ. An updated overview of e-cigarette impact on human health. Respir Res 22 , 151 (2021). https://doi.org/10.1186/s12931-021-01737-5
Download citation
Received : 22 October 2020
Accepted : 03 May 2021
Published : 18 May 2021
DOI : https://doi.org/10.1186/s12931-021-01737-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Electronic cigarette
- E-cigarette
- Flavourings
- Smoking cessation tool
Respiratory Research
ISSN: 1465-993X
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 08 May 2024
Forecasting vaping health risks through neural network model prediction of flavour pyrolysis reactions
- Akihiro Kishimoto 1 ,
- Dan Wu 2 &
- Donal F. O’Shea 2
Scientific Reports volume 14 , Article number: 9591 ( 2024 ) Cite this article
9103 Accesses
1444 Altmetric
Metrics details
- Cheminformatics
- Public health
Vaping involves the heating of chemical solutions (e-liquids) to high temperatures prior to lung inhalation. A risk exists that these chemicals undergo thermal decomposition to new chemical entities, the composition and health implications of which are largely unknown. To address this concern, a graph-convolutional neural network (NN) model was used to predict pyrolysis reactivity of 180 e-liquid chemical flavours. The output of this supervised machine learning approach was a dataset of probability ranked pyrolysis transformations and their associated 7307 products. To refine this dataset, the molecular weight of each NN predicted product was automatically correlated with experimental mass spectrometry (MS) fragmentation data for each flavour chemical. This blending of deep learning methods with experimental MS data identified 1169 molecular weight matches that prioritized these compounds for further analysis. The average number of discrete matches per flavour between NN predictions and MS fragmentation was 6.4 with 92.8% of flavours having at least one match. Globally harmonized system classifications for NN/MS matches were extracted from PubChem, revealing that 127 acute toxic, 153 health hazard and 225 irritant classifications were predicted. This approach may reveal the longer-term health risks of vaping in advance of clinical diseases emerging in the general population.
Similar content being viewed by others

Augmenting large language models with chemistry tools

Predicting equilibrium distributions for molecular systems with deep learning

Physics-informed machine learning
Introduction.
The delivery of nicotine to the lungs through the inhalation of tobacco smoke has been practiced by mankind for centuries with devastating impacts on public health 1 . Relatively recently, vaping of e-liquids has emerged as a modern variant of this ancient practice. In their original construction, the constituents of e-liquids contained only four chemical entities, nicotine, propane-1,2-diol, propane-1,2,3-triol and water, with the goal of providing a less hazardous means of nicotine delivery than tobacco leaf 2 . Their use as an aid for tobacco smoking cessation has evolved as a cornerstone of some national public health policies, though others have restricted or prohibited their use 3 .
Soon after their first commercialization in the mid 2000’s, the number of chemical entities used in vaping e-liquids dramatically increased as an array of flavours were added. Currently, at least 180 discrete chemicals are known to be in use in e-liquids, blended in various amounts to produce a specific flavour branded product 4 . A European based study identified a mean and range of 6 (±) 4 chemical flavours used per specific e-liquid product, whereas a comparable US study found a range of 22 to 47 chemical flavours per e-liquid 5 , 6 . In both studies it was found that the total flavour chemical concentration in the majority of e-liquids exceeded that of nicotine. Furthermore, several studies have shown that flavoured e-liquids are linked to a lowering of the vaping age demographic 7 . Their appeal to non-smoking teenagers and young adults has led to a divergence of opinion on their use as an aid for tobacco smoking cessation in the established smoking population 8 . Concerns are growing that vaping in younger generations jeopardizes the decline in nicotine use and also risks the emergence of future vaping induced diseases 9 . Yet, while the strongly polarized debates about the pros and cons of vaping are ongoing, the implications for long-term effects on public health, morbidity and mortality are simply unknown 10 , 11 , 12 , 13 . While the health risks from exposure to the carcinogenic chemicals in tobacco smoke are known, it can take decades of accumulative damage before clinical manifestation of disease occurs.
Intuitively for vaping, it would be reasonable to anticipate that lung exposure to a large number of chemical entities can only increase health risks. In 2019, the potential for vaping health risks became apparent when cases of acute lung injury emerged attributable to tetrahydrocannabinol vaping products. E-cigarette or vaping use-associated lung injury (EVALI) statistics from the CDC document 2807 hospitalizations and 68 deaths over one year in the United States. A single chemical additive, vitamin E acetate (VEA), has been strongly linked to the outbreak that ended once its use stopped 14 . Our previous research showed that the action of pyrolysis heating within a vaping device could transform VEA into more than ten different substances including the highly toxic gas ketene which could account for the severe lung injuries 15 . While the chemicals used for nicotine vaping are different from tetrahydrocannabinol products 16 , 17 , the number of chemicals is considerably higher. Prolonged exposure to these chemicals and their pyrolysis products makes it plausible that we are standing at the starting line of a new wave of chronic diseases that will only emerge in 15 to 20 years from now.
The chemicals used as e-liquid flavours are not specifically developed for vaping and are adopted from the food industry 18 . Much like VEA, which is also widely used in foodstuffs and cosmetics, these compounds have a good safety record for these specific uses. However, it was not envisaged that they would be used in a significantly different manner that involves heating to high temperatures with inhalation into the lungs. Remarkably, there are a myriad of different vaping devices whose operating temperature ranges are often unknowingly determined by user preferences. Studies have measured typical temperatures ranging from 100 to 400 °C depending upon factors such as power, heating coil materials, puff size and e-liquid quantity, with dry coil temperature measured above 1000 °C 19 , 20 . Pyrolysis decomposition of flavours at these temperatures could produce large numbers of unknown secondary chemical entities, thereby hugely amplifying the health risks from each flavour. In contrast to tobacco smoking, combustion products are minor in vaping so were not included in this initial study.
As hundreds of chemicals are used in tens of thousands of commercial e-liquid products, the experimental analysis of all their vaping induced chemistries and associated products could take decades of research. In this study, a holistic research strategy employing artificial intelligence (AI) was adopted to simultaneously investigate all flavours in e-liquids. AI is increasingly being used to perform chemistry tasks such as retrosynthetic route planning, the prediction of reaction outcomes and the acceleration of drug discovery 21 , 22 , 23 . Currently, a unique opportunity exists to exploit AI to anticipate vaping risks in advance of their public health impact, which may take years to emerge.
Overview of 180 e-liquid flavour chemicals
While the exact number of flavour chemicals in current worldwide e-liquid use is unclear, 180 representative chemicals known to be used as flavourings in e-liquids were chosen for this study based on literature reports 4 , 5 , 6 , 18 . Structural inspection of the chemical functional groups within the 180 flavours revealed 66 esters, 46 ketones/aldehydes, 27 alcohols/acetals, 26 aromatics/heterocycles/carbocycles and 15 carboxylic acids/amides, clearly indicating the potential for a wide range of pyrolysis reactions (Supplementary Table S1 ). Flavour structural diversity was analyzed by comparing their molecular weight, hydrogen bond donors/acceptors, topological polar surface area, number of rotatable bonds, and octanol–water partition coefficient properties 24 . A 3D visualization of the chemical space reflecting these six properties shows that compounds are clustered in a similar area, indicating moderate diversity with 85.5% of the variance accounted for by molecular weight, surface area and number of rotatable bonds (Fig. 1 A, red circles, Supplementary Dataset S1 ). Their mean molecular weight was 146.2 signifying a relative volatile set of molecules (Fig. 1 B, red distribution profile).
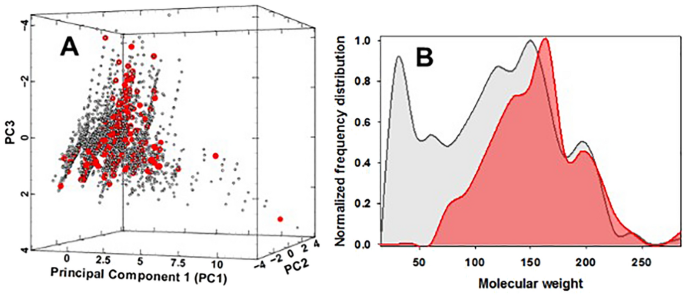
Chemistry diversity analysis of 180 flavour chemicals and their predicted pyrolysis products. ( A ) 3D representation of the chemical space occupied by 180 e-liquid compounds (red circles) and their discrete 4524 NN predicted pyrolysis products (grey circles). Principal component (PC) scale refers to normalized projections of the six molecular properties. ( B ) Molecular weight distribution of 180 e-liquid compounds (red distribution profile) and their discrete 4524 NN predicted pyrolysis products (grey distribution profile).
Workflow for e-liquid flavour risk identification and classification
All 180 flavours were subjected to a common workflow that blended NN pyrolysis prediction with experimental electron-impact mass spectrometry (EI-MS) data. An overview of each stage is shown in Fig. 2 , which started with transcribing the 180 chemical structures into their simplified molecular-input line-entry system (SMILES) format. A graph-convolutional neural network model was used to predict pyrolysis chemical transformations and their associated products for each flavour. Experimental MS data containing the molecular ion, associated fragmentation masses and their relative abundances were sourced for each flavour. As both pyrolysis reactions and MS fragmentations involved energy induced bond breaking; a correlation between both was anticipated. Using specifically written script, the molecular weight of each NN predicted product from each flavour was correlated against the MS fragmentation masses for that flavour. A data subset was formed containing NN-reactions with a predicted product which matched a MS fragmentation mass. Next, the GHS classification was identified for each NN/MS matched product. A second NN was used to predict activation energies (AE) for reactions producing products with the most significant health implications. Data collation generated an enumerated list of NN predicted products, MS matched products and their associated GHS hazard classification for each of the 180 flavours (Fig. 2 ). Each step was automated and could accept new compound inputs as required.
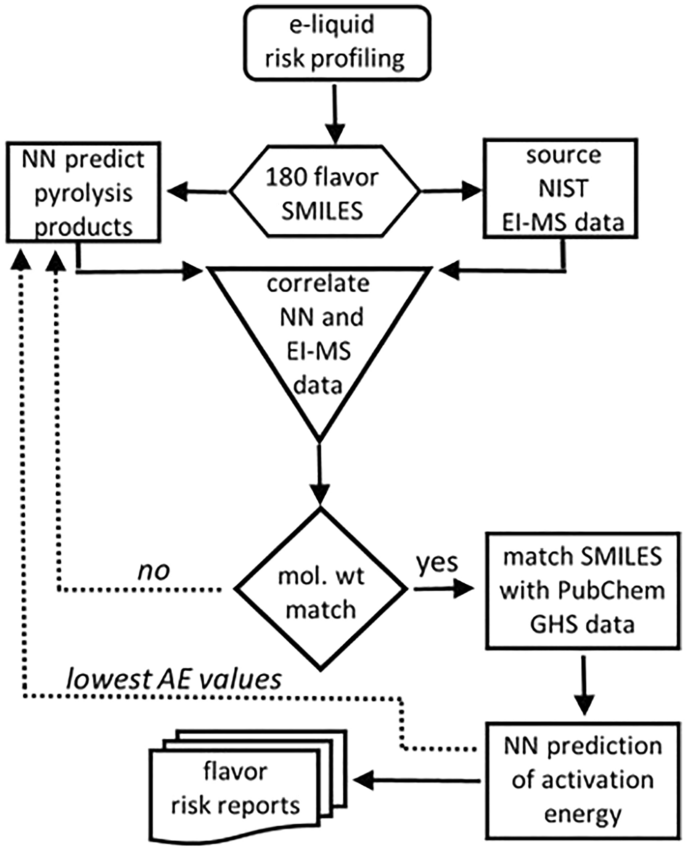
Workflow chart for the pyrolysis risk identification of vaping e-liquid components (solid arrows). Dashed arrows indicate future scope for an informative feedback into NN pyrolysis predictor.
Graph-convolutional neural network model for pyrolysis products prediction
To date, reaction prediction methods have primarily focused on synthetic transformations in which at least two reactants generate a product and a byproduct under varying experimental conditions 25 , 26 , 27 . Pyrolysis reactions differ in that a single reactant produces an array of lower molecular weight products by different transformation pathways with heat being the driving force of the reactions (Fig. 3 ).
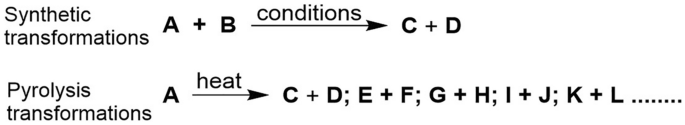
Synthetic and pyrolysis transformations.
It was found that the previously described Weisfeiler–Lehman neural network (W–L NN) model suited our requirements as it operates by prediction of reaction centers based on bond changes for every pair of atoms in a molecule 26 . As a graph convolutional network, it can predict unimolecular pyrolysis transformations without any training data specific to pyrolysis reactions. Supervised learning of the W–L NN was achieved using US patent literature as a source of data, with pyrolysis predictions based on a training set of 354,937 reactions 26 , 28 , 29 . For this study, only first phase pyrolysis products were considered with further pyrolysis of initial pyrolysis products not included. All reactions that included flavour molecules were removed from the training data to ensure that no characteristics of these flavour molecules were leaked before their pyrolysis predictions were performed. Prevention of such data leakage allows the performance assessment of the trained W–L NN model without bias, even if a new flavour molecule is passed to the trained model. As designed, the W–L NN architecture embedded the inherent computations in the W–L graph kernel to learn atomic representations. This starts by converting chemical SMILES (notation to describe a chemical structure that can be understood by computer software) to attributed graph representations of molecules. For example, the SMILES for flavour 2,3-pentanedione being CCC(=O)C(=O)C converts to a labelled form of atoms 1 to 7 as shown in Fig. 4 A,B. Each atom representation was computed by including contributions from adjacent atoms such as atom 3 with atom 2, 4, and 5. Specifically, each atom was initialized with a feature vector f atom indicating its key properties such as atomic number, connectivity, valence, formal charge, and aromaticity. Representation of the bond order (number of chemical bonds between a pair of atoms) and connectivity of each bond was through the feature vectors f bond (Fig. 4 C). Local feature vectors were calculated for each atom based on its representation and those of other atoms directly bonded to it. Next, global atom features were produced for each atom to account for the influence of atoms not directly bonded to it. Finally, a combination of local and global feature vectors was used to predict the likelihood of bond changes for each pair of atoms (Fig. 4 D).
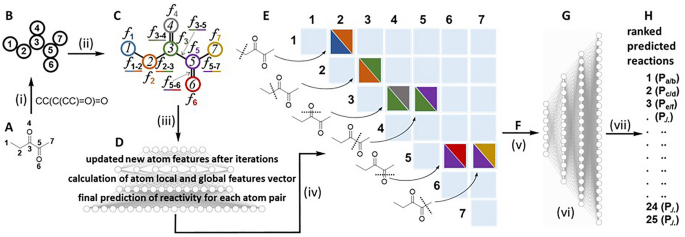
W–L neural network for predicting bond changes between every pair of atoms in 2,3-pentandione. (i) Molecular SMILES converted to attributed graph. (ii) Atom descriptors generated by incorporating information from neighboring atoms. (iii) Updated new atom features after iterations, calculation of atom local and global features vector and final prediction of reactivity for each pair of atoms. (iv) Calculated scores for each likelihood bond change by W–L neural network. (v) Potential products enumerated after removal of those failing chemical valence rules. (vi): W–L difference network model for ranking pyrolysis reactions enumerated based on the most probable bond changes. (vii) Predicted pyrolysis reactions ranked from 1 to 25 and their associated products (P).
In the representative input example of 2,3-pentandione, all atom pairs were “tested” to identify high probability bond breaking positions (Fig. 4 E). Up to 16 likely bond-breaking positions were identified to enumerate their possible pyrolysis transformations and associate output products. Up to five simultaneous chemically feasible bond changes per pyrolysis reaction were allowed. Any predicted products that did not comply with chemical valence rules (correct number of bonds from each atom) were removed (Fig. 4 F). Next, a W–L difference network (W–L DN) generated a probability score for each predicted pyrolysis transformation based on the differences in atom representations between the products and the original molecule (Fig. 4 G). The W–L DN then selected and ranked the twenty-five most likely transformations based on their probability scores (Fig. 4 H). Analysis of the NN output of 4500 pyrolysis predictions for the 180 flavours showed 7307 products (Supplementary Dataset S2 ). When duplicate products from the same flavour are not included, the total number was 4524. The average number of discrete products per flavour was 25.1 with a greater number predicted for compounds of larger molecular size and complexity. The top 20 predicted pyrolysis products (excluding duplicates arising from the same flavour) included alkanes, alkene, alcohols, aldehydes, acids, and aromatics, as shown in Table 1 .
Structural diversity of the 4524 predicted products was determined using the same molecular parameters used for the 180 flavours (23). The 3D chemical space visualization showed the NN-predicted pyrolysis products clustered in a similar space as their originating flavours (Fig. 1 A, grey circles, Supplementary Dataset S1 ). The expected difference was a significant shift to lower molecular weight compounds, with a mean molecular weight of 111.7 indicating the production of highly volatile organic compounds (Fig. 1 B, grey distribution profile).
Sourcing experimental EI-MS data for each e-liquid flavour
Mass spectrometry fragmentation identifies intramolecular bond breaking positions that occur as a result of molecular interaction with the applied energy from the instrument source. As pyrolysis is a heat induced bond breaking process, a correlation between both can exist 30 . Experimental EI-MS mass data was retrieved, using Python script, from the online National Institute of Standards and Technology (NIST) database for each of the 180 e-liquid flavours 31 , 32 . Data obtained included the molecular weight of all fragmentations from the parent ion and their relative abundance. Representative flavour examples for 2,3-pentandione, linalool, 2-acetyl pyridine and α-methylbenzyl acetate in Fig. 5 , show their MS fragmentation patterns and corresponding molecular weights. Specifically for 2,3-pentandione, the series of fragmentation masses (% relative abundance) of 100 (11), 57 (32), 43 (100), 42 (12), 29 (60), 27 (25) and 15 (14) can be seen which correspond to the molecular ion and the most likely bond breaking positions of the molecule (Fig. 5 ). In this way, the MS fragmentation data for each e-liquid component can act as a minable dataset to identify molecular weight alignments with the products from the NN predicted pyrolysis reactions. A 5% relative abundance threshold for each mass peak was applied to the MS data to eliminate the possibility of instrument noise or isotope contributions. The average number of mass fragmentation peaks per e-liquid component was 16.5 with the maximum at 54 and the minimum at 2. As expected, larger molecular weight compounds typically have more fragmentation mass peaks than those of lower weight.
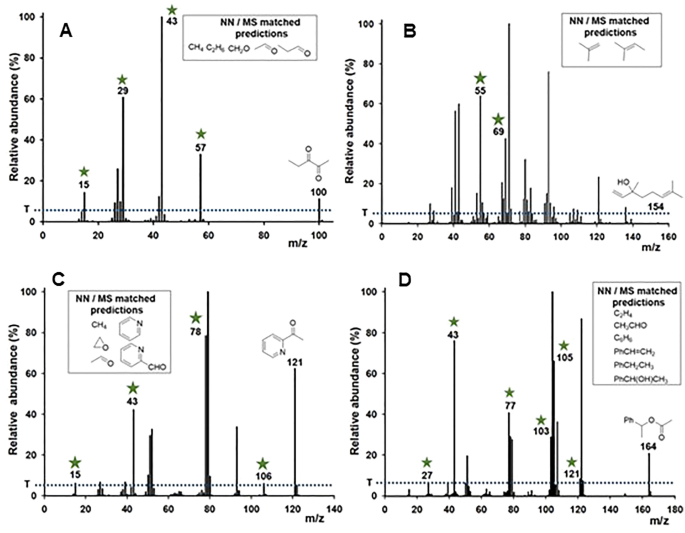
Representative flavour EI-MS data of ( A ) 2,3-pentandione; ( B ) linalool; ( C ) 2-acetyl pyridine; ( D ) α-methylbenzyl acetate from the NIST database. Threshold (T) set at 5% relative abundance indicated by blue dotted line. Green asterisk indicates the molecular weight matches with W–L NN predicted products. Insets show structures of NN-predicted products that are molecular weight matched with an MS fragmentation.
Amalgamation of W–L NN and EI-MS data
Next, automated amalgamation of in silico NN with experimental MS data was carried out 32 . The goal of merging these two information sources was to identify the most likely pyrolysis products for each flavour, from which their health risks could be assigned. Correlation of molecular weights of NN predicted products with their experimental MS fragmentation masses identified 1169 discrete matches between the two datasets (not counting repeat matches for a flavour) (Supplementary Dataset S2 ). The average number of NN/MS matches per flavour was 6.4 with 92.8% having at least one match and 86% having more than one match. Examples of specific NN/MS matches are shown in Fig. 5 for four structurally different flavours. Green asterisks indicate the molecular weight matches in the mass spectral data with W–L NN predicted products and the insets show structures of the matched compounds. It is noteworthy that this data amalgamation was successful for a wide variety of different molecular structures and functional groups.
Encouragingly, plotting the number of MS matches against the NN rank position for each predicted product shows a clear bias towards higher rank positions, with the highest NN-rank 1 accounting for 8.7% of all matches (Fig. 6 , rank 1). Comparison of the cumulative number of matches for the top (1–5) and bottom (21–25) rank positions show that the higher positions accounted for 29% of all matches whereas the lower ranks accounted for only 15% (Fig. 6 ). These correlations indicate that NN predicted products could be substantiated through experimental MS fragmentations and that in future work MS data could be used in a hybrid supervised and reinforcement learning model. The non-matched W–L NN predicted products were not used further in this work but may serve as an informative feedback allowing future refinement of the NN pyrolysis predictor (Fig. 2 , dashed arrow).
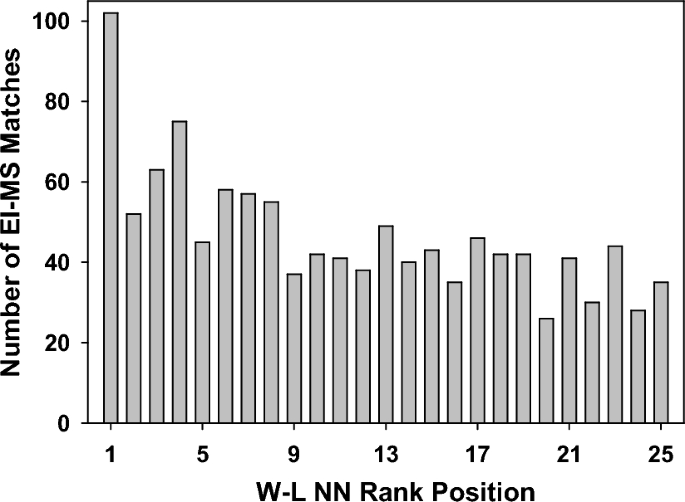
Comparative plot of W–L NN rank position from 1 to 25 for predicted products matched with experimental EI-MS data.
Examining the most commonly matched compounds it was encouraging to find that a broad distribution of molecular classes was matched (saturated, unsaturated and aromatic hydrocarbons, aliphatic alcohols and carboxylic acids) (Table 2 ). Seventeen of the top twenty W–L NN predicted products (Table 1 ) were also in the top 20 matched compounds, further increasing confidence in the NN/MS matched predictions. Next, the health risk of each NN/MS matched product was identified.
Acquisition of risk assessment data for W–L NN and EI-MS matched products
Using specifically written Python script, the GHS classifications for each NN/MS matched product was obtained from the open-source PubChem database 32 , 33 . The script used the SMILES string of each compound as a query keyword to identify matching URLs within the site. Within each URL, the hazard statements in the GHS classification section were downloaded in JSON format. Three different classification categories were used to build each flavour risk profile (i) acute toxic; (ii) health hazard; or (iii) irritant. In addition, a category (iv) was used to group compounds not classified as either (i), (ii) or (iii) but that may have other hazard warnings, and category (v) was compounds for which a search query did not produce a result, indicating they were not in the database (Supplementary Dataset S3 ). The GHS classifications of acute toxic (127 compounds), health hazard (153 compounds) and irritant (225 compounds) accounted for 11%, 13% and 19% of classifications attributed to the dataset respectively (Fig. 7 A). Only 49% of products were not included in the categories (i) to (iii) and 8% had no classification information available. Mining classification data specifically for inhalation health hazards revealed further insights into their health risks with a representative selection of these results for a structurally diverse set of the functional compounds shown in Fig. 7 B (Supplementary Dataset S3 ). It is noteworthy that while some similarities to compounds produced by tobacco smoke exist (e.g. formaldehyde, ethylene oxide, aromatic amines), many others differ such as α,β-unsaturated carbonyl compounds (aldehydes, ketones, esters), heterocycles and phenols. This is due to the diverse chemical makeup of the individual vaping flavours, which differ from the natural products found within tobacco leaf. This indicates that, while related, vaping biomarkers and their clinical disease manifestations could differ significantly from those of tobacco smoking 34 . Furthermore, vaping biomarkers are likely to differ based on commercial e-liquid product, as the spectrum of pyrolysis products differ for each chemical flavour 35 .
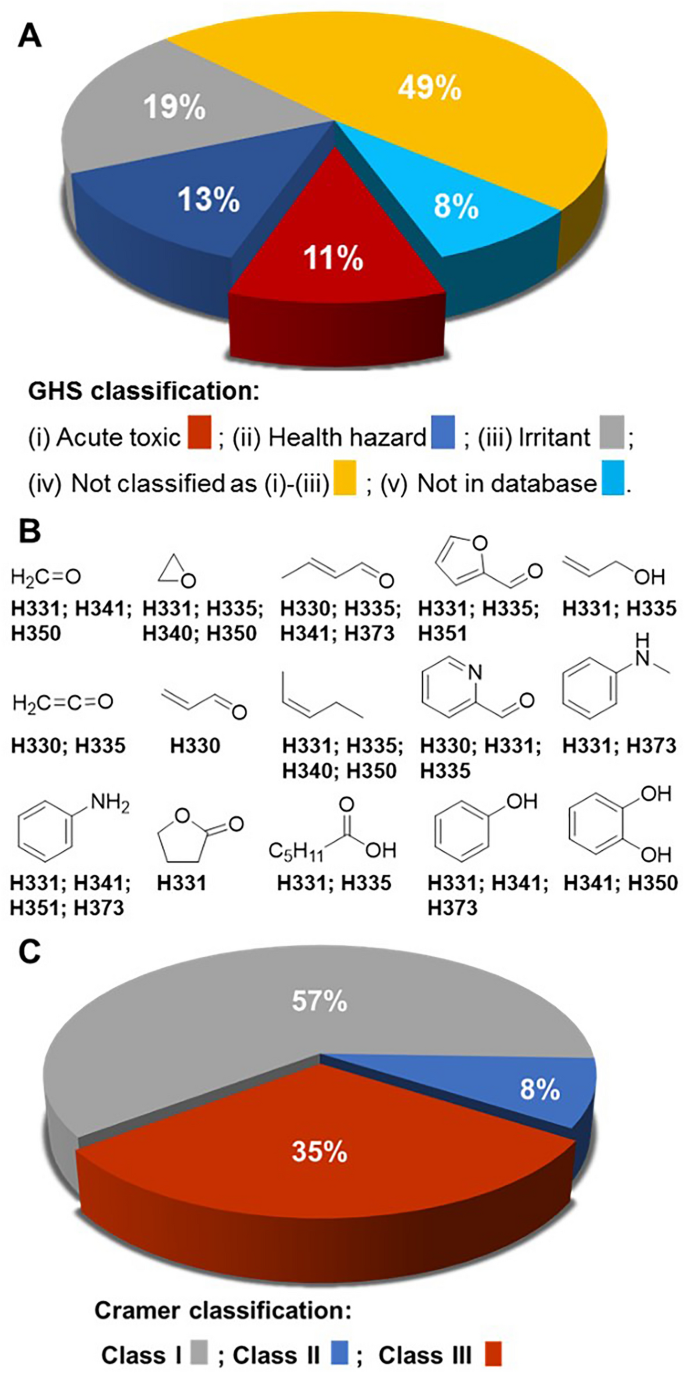
( A ) Distribution of globally harmonized system classifications of W–L NN/MS matched products (for compounds with more than one classification only the most serious classification is included). ( B ) Representative examples of the structure for W–L NN/MS predicted compounds with acute toxic GHS classification and their specific inhalation hazard warning. GHS hazard statements: H330 fatal if inhaled; H331 toxic if inhaled; H335 may cause respiratory irritation; H340 may cause genetic defects; H341 suspected of causing genetic defects; H350 may cause cancer; H373 causes damage to organs through prolonged or repeated exposure. ( C ) Distribution of Cramer classifications of W–L NN/MS matched products.
Additionally, NN/MS matched products were grouped using the three Cramer classes (Supplementary Dataset S4 ) 36 . Cramer classification is a commonly used predictive approach for classifying chemicals on the basis of their expected level of oral toxicity. Cramer Class III, which represents the most severe potential toxic hazard, accounted for 35% of these compounds with Class II (moderate risk) and Class I (low risk) accounting for 8 and 57% respectively (Fig. 7 C). It was noteworthy that many of the more commonly used flavour chemicals (e.g. cis -3-hexenol, isoamyl acetate, benzaldehyde, ethyl hexanoate, cinnamaldehyde, benzyl acetate, hexyl acetate) had one or more predicted products identified as Class III. Across all 180 flavours, the most common Cramer III classifications were for benzene, ketene and ethylene oxide predicted by 16, 10 and 8 different flavours respectively (Supplementary Dataset S4 ).
W–L NN prediction of pyrolysis activation energies
The activation energy (AE) of a chemical reaction is the minimum energy required for a reaction to proceed. With respect to vaping, AEs are an excellent means of obtaining a first approximation of the thermal conditions required for pyrolysis to occur. Yet, determination of AEs is experimentally very laborious and computationally expensive, as it requires quantum chemical calculations. As such, the use of NN methods to obtain quantitative values for flavour pyrolysis reactions would be of significant value. To address this goal, a recently reported directed message passing neural network (D-MPNN) for AE predictions has been employed 37 , 38 . D-MPNN is a graph convolutional neural network, similar to that used for pyrolysis predictions described earlier, though it should be noted that other NN methods have been employed for AE predictions 39 , 40 . The training data used consisted of published gas phase energy activation data of 16,264 transformations determined by quantum chemistry calculations using B97-D3/def2-mSVP theory following the exclusion of flavour compounds to prevent data leakage of the test set 38 . AEs for 482 NN predicted reactions were determined. The reactions were chosen to reflect different transformation types and reactions that generated products classified as high health risk were prioritized (Supplementary Dataset S5 ). The outcome gave a wide range of AE values from 45 to 121 kcal/mol indicating that comparisons could be made between different degradation pathways for each flavour.
Fruit flavoured products are the most popular commercial brands for the younger vaping demographic so warrant particular attention. These compounds commonly have an ester functional group which are known to undergo thermal decomposition by different elimination and free radical β-scission reactions, both of which are plausible under vaping conditions 41 , 42 . To illustrate use of AE values, ten acetate esters with substituent containing β-hydrogens were selected for comparative data analysis (Fig. 8 ). Previously reported experimental and computational studies have mostly focused on the simplest derivatives such as ethyl acetate with others as of yet unstudied 42 , 43 , 44 , 45 . These results show that three different elimination pathways are possible to generate either acetic acid and substituted alkenes (pathway A); ketene with substituted alcohols (pathway B); or C–O cleavage resulting in the formation of two carbonyls (pathway C) 42 . Analysis of the NN predicted reactions for each of these acetates showed that these transformation pathways were common to all. Comparison of the D-MPNN derived AE values for these reactions showed that pathway A consistently predicted the lowest energy requirement for most of the acetates (Fig. 8 , table). The identification of pathway A as most favorable is consistent with literature reports and thus identifies inhalation of acetic acid and substituted alkenes as the likely health hazards 46 . It is noteworthy that of the ten different alkenes producible via AE favored pathway A, eight are GHS classified as either irritant or health hazard (ethene, hexene, 1,3-hexadiene, 2-methylpropene, 3-methyl-1-butene, 2-methyl-1-butene, 3,7-dimethylocta-1,6-diene, styrene). Additionally, it is important to recognize that due to the complex reacting conditions within a vaping device, pyrolysis would not be expected to follow a single pathway 47 . In the case of acetates, products could also occur via free radical β-scission reactions as vaping conditions have been shown to promote radical type reactions 48 , 49 .
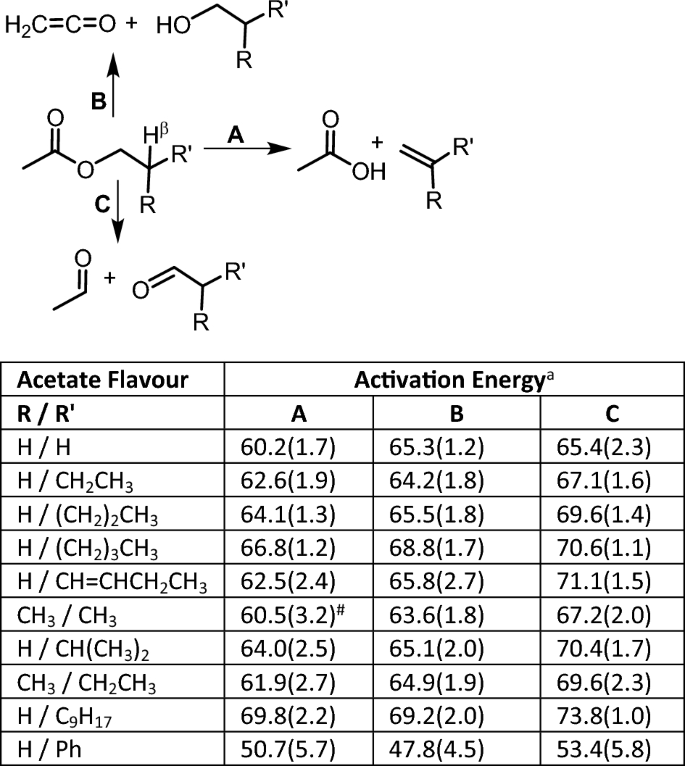
D-MPNN derived activation energies applied to three different NN predicted pyrolysis pathways of acetate fruit flavours (ethyl acetate, butyl acetate, amyl acetate, hexyl acetate, cis -3-hexenyl acetate, isobutyl acetate, isoamyl acetate, 2-methylbutyl acetate, citronellyl acetate, 2-phenylethyl acetate). a kcal/mol, # not predicted by NN.
While these AE values are, as yet, a first approximation, taking no account of the conditions under which reactions are taking place, their importance will grow as the accuracy in predicting these values improves. It could be envisaged that they play a future role in reinforcement learning models in conjunction with MS fragmentation data (Fig. 2 , dashed arrows).
E-Liquid flavour reports
Collation of all data generated an output for each of the 180 flavours with an enumerated list of NN predicted reactions and their associated products, EI-MS matched products identified and their associated GHS hazard classifications (Supplementary Datasets S2 , S3 ). Taken together, these constitute a minable reference source that encompasses the complex and interconnected facets of vaping with the potential to be refined and adapted in the future.
The e-liquid marketplace is vast and growing, driven by increased investment by tobacco companies into vaping products 50 . The original source of flavours in e-liquids stems from food flavouring compounds so it could be anticipated that the number of compounds being used will increase over time 4 , 5 , 6 . Since their inception, an incorrect assumption has grown that the flavour ingredients used in e-liquids are designated “generally recognized as safe” (GRAS) under health regulations. However, this GRAS status only relates to human consumption via ingestion (compatible with their use in foodstuffs) and not inhalation following thermal activation 18 . While the health concerns for lung exposure to the flavours themselves are serious, what is even more concerning is the array of thermal degradation products which they generate as a consequence of their heating immediately prior to inhalation 51 . The vast majority of these degradation products remain unknown as do their health consequences from long-term exposure. From a public health perspective, the use of flavours in e-liquids can be viewed as a double-edged sword. The role for vaping flavours is cited as a support for smoking cessation for those already addicted to nicotine tobacco products, but the same flavours are the main attractant for a non-smoking younger demographic 8 , 52 .
Experimental research into the heat-induced breakdown of organic compounds has its origins in the early twentieth century with the seminal work of Hurd and others 53 . Such research was conducted to gain fundamental scientific insights into the nature of chemical bond dissociations and formations. Vaping devices can be considered as crude versions of a laboratory pyrolysis apparatus 54 . Both are designed to rapidly heat organic molecules to high temperatures, although when using an experimental apparatus the products are safely trapped, quantified and characterized whereas in vaping they are drawn into the lungs. A laboratory pyrolysis apparatus has rigorous control over temperature, is made from materials to limit radical formation and is used to study test molecules individually. In contrast, a vaping device has poor temperature control, is constructed using metal materials that induce radical reactions and simultaneously heats an array of chemical entities in an e-liquid. By its nature, experimental pyrolysis chemistry is highly complex, but within vaping this complexity is magnified due to e-liquid, device and user variabilities making it a daunting task to map all possible chemical outcomes from a vaping “experiment”.
To date, experimental studies on the thermal decomposition products from vaping flavours have focused on detecting and quantifying volatile carbonyls (VC) as they have known negative health implications 55 , 56 , 57 , 58 , 59 , 60 . Several research teams have conclusively shown that VCs such as formaldehyde, acetalaldehyde and propanaldehyde are produced in concerning quantities as a result of the vaping decomposition of flavours. The quantity of aldehydes produced is proportional to the specific commercial brands, flavour and nicotine quantity in the e-liquid, the vaping device power, and users’ puff topography 61 , 62 , 63 , 64 . Establishing which flavours produced which VCs is challenging, as the e-liquids tested were comprised of mixtures of several flavour chemicals, propane-1,2-diol, propane-1,2,3-triol (which also produce aldehydes) and nicotine. Mining our dataset allows mapping of VC producers back to specific flavour chemicals while also identifying the other chemicals co-produced with these VCs. For example, the results for acetaldehyde revealed over forty flavours as having the potential to produce it with co-products including heterocycles, aromatics, aldehydes, alkenes and alkanes (Fig. 9 , Supplementary Dataset S6 ). Sources were mostly fruit, candy and dessert flavoured products containing ester, ketone, di-ketone, aldehyde and carboxylic acid functional groups. Cross-referencing this list with the most commonly used fruit and candy flavours 4 , 5 , 6 implicates ethyl acetate, ethyl butyrate, ethyl 2-methylbutryate and 2,3-pentanedione as the more common sources of pyrolysis produced acetaldehyde. The rapid identification of chemicals of concern is an advantageous feature of this dataset which could be of assistance in focusing experimental work to confirm their generation which could in turn inform regulatory agencies.
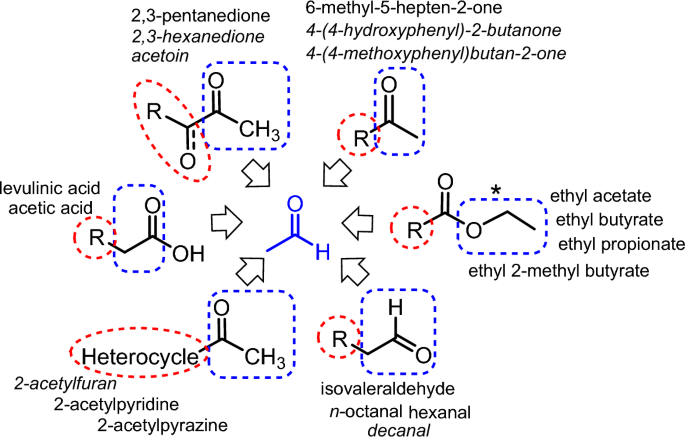
Map showing structural classes of e-liquid flavour chemicals identified as having the potential to produce acetaldehyde (blue box) with a representative selection of co-products (red circle) and the names of the chemical flavours from which they could be produced (see Supplementary Dataset S6 ). *For ethyl esters the prediction of CH 3 CH 2 O˙ (blue box) indicates the first step in formation of acetaldehyde 47 .
Reflecting on the limitations of this study, it is important to identify areas that warrant further development. In this initial iteration of our AI-vape forecast, only the first phase of pyrolysis products has been explored. It would be expected that some pyrolysis products would themselves undergo further pyrolysis reactions and that intermolecular reactions between pyrolysis products could occur 65 . The framework we have put in place lends itself to building a second layer of prediction using the predicted products described in this work as new starting points. Generation of combustion products has not been included in this study as they are considered minor to pyrolysis products, though ambient oxygen reactions could be investigated by inclusion of O 2 as a reagent in the NN predictions 66 . The cross correlation of predicted pyrolysis products with experimental MS fragmentation data does not distinguish between different structural isomers with the same molecular weights, though in the future more elaborate MS experiments may do so if needed. A limitation of the NN-predictions is the current size of the training sets, though it is anticipated that these will continue to grow in the near future. Additionally, improvements in NN ranking of reaction predictions could be guided by predicted AEs acting as an informative feedback loop (Fig. 2 , dashed arrows). A merit of the scientific approach adopted in this work is its openness to continual refinement as chemistry related NNs evolve and that it can serve as a benchmark for other AI methods to achieve similar aims. We hope that this work motivates further research in these areas.
The aerosols produced by e-cigarette vaping contain immensely complex uncharacterized mixtures of pyrolysis products, the health implications of which are, as yet, mostly unidentified. In advance of health effects of vaping becoming apparent in the general population, AI can be exploited to give guidance to the public, policy makers and health care professionals. It was envisaged that this could be achieved through a strategy that utilizes a combination of innovative NN prediction of pyrolysis transformations and freely accessible experimental EI-MS data to construct an in silico dataset of pyrolysis products from e-liquid chemical flavours. Screening of predicted pyrolysis products against databases of chemical hazard classifications identified those of highest health risk, allowing individual flavour risk profiles to be constructed. Results show that relatively low molecular weight volatile compounds can be produced of which 24% are categorized as either acute toxic or health hazard using the GHS classification system. Collated flavour risk reports may act as an informative public health resource and assist experimental vaping research. Results show that while similarities do exist with conventional tobacco smoking, a significantly different profile of hazardous compounds emerges from vaping. As such, using tobacco smoking as the sole comparison for gauging vaping health risks is likely to give a false sense of security, especially for younger non-tobacco smokers. Regulations could be employed such that attempts to remedy nicotine addictions of older tobacco smokers does not risk the transferal of new health issues to younger generations. A protective balance needs to be struck for both cohorts rather than pitching one against the other. AI methods appear ideally suited to address the complex and multifaceted health concerns that vaping raises. As vaping is a new and unprecedented stress to the human body, with the ability to generate pyrolysis products more toxic that their parent compounds, it seems prudent to strictly limit the number of chemical entities in e-liquids.
Diversity analysis of flavours and WL-NN predicted pyrolysis products
Chemical diversity analysis was carried out using PUMA 1.0 ( http://132.248.103.152:3838/PUMA/ ) 24 . The SMILES structure of 180 flavours and 4524 NN predicted products (duplicate predicted products from the same flavour removed) were used as inputs. This platform computed six molecular properties of pharmaceutical relevance including molecular weight (MW), hydrogen bond donors (nHBDon), hydrogen bond acceptors (nHBAcc), topological polar surface area (TopoPSA), number of rotatable bonds (nRotB), and the octanol–water partition coefficient (ALogP). Then six principal components (PCs) were computed based on these molecular properties. The 3D representation of the chemical space was plotted by using Veusz 3.3.1 software using the three PCs that contributed the most proportion of the variance.
WL–NN pyrolysis reaction predictions
Supervised learning of Weisfeiler–Lehman network was achieved utilizing the US patent literature as a source of data. The starting dataset which consists of 409,035 reactions is available at: https://github.com/connorcoley/rexgen_direct/tree/master/rexgen_direct/data/ 26 . All reactions within the training data that included a flavour molecule were removed to prevent the trained W–L network from data leakage of the test set. In total, a training set of 354,937 reactions was used, on which the pyrolysis predictions were based. The Python script to remove flavour molecules from the original dataset is available at https://github.com/IBM/pyrolysis-prediction . SMILES of the 180 flavour chemicals were used as inputs for the W–L NN using the published protocols. The computational training and prediction were run using a machine with eight CPU cores (Intel Xeon E5-2690 at 2.60 GHz), one GPU (Tesla V100) and 60 GB memory. The number of iterations to train the W–L network and W-LDN was set to 140,000 mini-batches of size 20 and 1,000,000 mini-batches of a single reaction and its candidate outcomes, respectively. Accuracy of prediction tasks was determined using 40,000 test examples 26 (not in the training set) which gave 0.924 for the model to identify reaction mode when the top 25 predictions are considered and 0.9341 for ranking reactions when the top 5 predictions are considered. The total training time was 2.5 days to train both models (reaction centre and ranking) for reaction prediction. Results from 4500 pyrolysis predictions for 180 flavours gave 7307 products of which 4524 were discrete products (when duplicate products from the same flavour are not included). Average reaction prediction times were 40 ms per reaction for reaction core identification and 127 ms per reaction for ranking.
Experimental EI-MS data retrieval
Using specifically written script available at https://github.com/IBM/pyrolysis-prediction , the SMILES representations for each flavour were converted to their corresponding InChIKey and the EI-mass spectra data associated with each InChIKey was extracted from the online NIST database at https://webbook.nist.gov/chemistry/ 31 . EI-mass data including fragmentation molecular weights and relative abundance were retrieved in JCAMP format. The data for each flavour was checked manually to ensure that the correct data had been acquired for each flavour and errors corrected. Data for some flavours (2-ethyl-3-methyl pyrazine, 2-methoxy-3-methylpyrazine, acetoin, α-damascone, benzaldehyde propylene glycol acetal, benzyl alcohol, β-damascenone, cedrol, citral, ethyl lactate, ethyl vanillin propylene glycol acetal, γ-dodecalactone, γ-octalactone, menthone, neral, propenyl guaethol, tabanone, thio-menthone, trans-2-hexenylacetate, vanillin propylene glycol acetal) were either not available in the NIST database or not accessible and data was manually extracted from the NIST or from Spectrabase ( https://spectrabase.com/ ).
Correlation of EI-MS fragmentation molecular weights with W–L NN predicted products
Using specifically written script available at https://github.com/IBM/pyrolysis-prediction , the molecular weight of each W–L NN predicted product was calculated using the Descriptors.ExactMolWt method in RDKit. The value of 1 was subtracted from that weight, followed by a rounding to the nearest whole number. NN predictions with the same molecular weight as the flavour molecular ion were not included. The values obtained for each product were correlated with the EI-mass spectrum fragmentation mass data for the relevant flavour molecule available in JCAMP format. Correlation results identified 1169 discrete matches between NN predicted products with EI-MS fragmentations.
GHS classification data retrieval and cramer classifications
Using specifically written script available at https://github.com/IBM/pyrolysis-prediction , a NN/MS matched product represented as SMILES was converted to its InChIKey and all compounds matching the InChIKey in the PubChem database ( https://pubchem.ncbi.nlm.nih.gov/ ) were retrieved. For each compound identifier, the script retrieved the hazard keywords in the pictographs that appeared in the GHS Classification subsection. Specific inhalation hazards were searched and compiled manually. Cramer classifications were obtained by using compound SMILES inputs into the available prediction software 36 . Results of GHS classifications identified 127 NN/MS matched product predictions as acute toxic, 153 as health hazard, 225 as irritant, 566 as neither acute, health hazard nor irritant and 95 were not identified in the database.

Mapping reactions for activation energy predictions
The SMILES of reactant and NN-predicted products were used as inputs for the automated mapping algorithm available at http://mapper.grzybowskigroup.pl/marvinjs/ 67 . The full atoms reaction maps were completed by using the “map the drawing” command after adding explicit hydrogen atoms.
D-MPNN pyrolysis activation energy predictions
The original training dataset for activation energy prediction consisting of 16,365 reactions is available at https://zenodo.org/record/3715478#.Yich5BPP2Wj 37 , 38 . To prevent from data leakage of the test set, reactions involving the 180 flavour chemicals were removed using specific Python script available at https://github.com/IBM/pyrolysis-prediction . The resulting dataset consisted of default hyper-parameters and the b97d3 theory data consisting of 16,264 reactions. Accuracy for AE predictions was determined by performing a tenfold cross validation to train the model with the data split into 85% training, 5% validation and 10% test data 38 . The performance/accuracy metric for the AE is the rooted mean square error defined as \(\sqrt {\frac{1}{N}\backslash_{i = 1}^{N} \left( {y_{i} - z_{i} } \right)^{2} }\) where N is the number of examples, y i is an AE value in the i-th example, and z i is a predicted AE value in the i-the example. The average accuracy for AE prediction was determined as the root mean square error (RMSE) which was 7.53 mol −1 with standard deviation of 0.74 mol −1 . The average AE value calculated by the 10 models was used to predict AE for pyrolysis with standard deviations included.
Data availability
All data are available in the main text, Supplementary Information or GitHub ( https://github.com/IBM/pyrolysis-prediction ). Raw data files are available from the corresponding author upon request.
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Google Scholar
Sapru, S. et al. E-cigarettes use in the United States: Reasons for use, perceptions, and effects on health. BMC Public Health 20 , 1518 (2020).
Article PubMed PubMed Central Google Scholar
Fairchild, A., Healton, C., Curran, J., Abrams, D. & Bayer, R. Evidence, alarm, and the debate over e-cigarettes. Science 366 , 1318 (2019).
Article ADS CAS PubMed Google Scholar
Krüsemann, E. J. Z. et al. Comprehensive overview of common e-liquid ingredients and how they can be used to predict an e-liquid’s flavour category. Tob. Control 30 , 185–191 (2021).
Article PubMed Google Scholar
Omaiye, E. E. et al. High concentrations of flavour chemicals are present in electronic cigarette refill fluids. Sci. Rep. 9 , 2468 (2019).
Article ADS PubMed PubMed Central Google Scholar
Krüsemann, E. J. Z. et al. GC-MS analysis of e-cigarette refill flavoring solutions: A comparison of composition between flavor categories. J. Pharm. Biomed. Anal. 118 , 113364 (2020).
Article Google Scholar
Miech, R., Johnston, L., O’Malley, P. M., Bachman, J. G. & Patrick, M. E. Trends in adolescent vaping, 2017–2019. N. Engl. J. Med. 381 , 15 (2019).
Yoong, S. L. et al. Prevalence of electronic nicotine delivery systems and electronic non-nicotine delivery systems in children and adolescents: A systematic review and meta-analysis. Lancet Public Health 6 , e661–e673 (2021).
Kelesidis, T. et al. Association of 1 vaping session with cellular oxidative stress in otherwise healthy young people with no history of smoking or vaping: A randomized clinical crossover trial. JAMA Pediatr. 175 , 1174–1176 (2021).
Marques, P., Piqueras, L. & Sanz, M.-J. An updated overview of e-cigarette impact on human health. Respir. Res. 22 , 151 (2021).
Article CAS PubMed PubMed Central Google Scholar
Tsai, M. C., Byun, M. K., Shin, J. & Crotty Alexander, L. E. Effects of e-cigarettes and vaping devices on cardiac and pulmonary physiology. J. Physiol. 598 , 5039 (2020).
Article CAS PubMed Google Scholar
Abouassali, O. et al. In vitro and in vivo cardiac toxicity of flavored electronic nicotine delivery systems. Am. J. Physiol. Heart Circ. Physiol. 320 , H133 (2021).
Chaumont, X. M. et al. Fourth generation e-cigarette vaping induces transient lung inflammation and gas exchange disturbances: Results from two randomized clinical trials. Am. J. Physiol. Lung Cell Mol. Physiol. 316 , 705–719 (2019).
Blount, B. C. et al. Lung injury response laboratory working group, vitamin E acetate in bronchoalveolar-lavage fluid associated with EVALI. N. Engl. J. Med. 382 , 697 (2020).
Wu, D. & O’Shea, D. F. Potential for release of pulmonary toxic ketene from vaping pyrolysis of vitamin E acetate. PNAS 117 , 6349 (2020).
Article ADS CAS PubMed PubMed Central Google Scholar
Lynch, J. et al. Simultaneous temperature measurements and aerosol collection during vaping for the analysis of Δ 9 -tetrahydrocannabinol and vitamin E acetate mixtures in ceramic coil style cartridges. Front. Chem. 9 , 734793 (2021).
Attfield, K. R. et al. Potential of ethenone (Ketene) to contribute to electronic cigarette, or vaping, product use-associated lung injury. Am. J. Respir. Crit. Care Med. 202 , 1187–1189 (2020).
Hallagan, J. The Safety Assessment and Regulatory Authority to Use Flavor: Focus on e-cigarettes . https://www.femaflavour.org/node/24344 .
Chen, W. et al. Measurement of heating coil temperature for e-cigarettes with a “topcoil” clearomizer. PLoS ONE 13 , e0195925 (2018).
Geiss, O., Bianchi, I. & Barrero-Moreno, J. Correlation of volatile carbonyl yields emitted by e-cigarettes with the temperature of the heating coil and the perceived sensorial quality of the generated vapours. Int. J. Hyg. Environ. Health 219 , 268 (2016).
Keith, J. A. et al. Combining machine learning and computational chemistry for predictive insights into chemical systems. Chem. Rev. 121 , 9816 (2021).
Ayres, L. B., Gomez, F. J. V., Linton, J. R., Silva, M. F. & Garcia, C. D. Taking the leap between analytical chemistry and artificial intelligence. Anal. Chim. Acta 1161 , 338403 (2021).
Baum, Z. J. et al. Artificial intelligence in chemistry: Current trends and future directions. J. Chem. Inf. Model. 61 , 3197 (2021).
González-Medina, M. & Medina-Franco, J. L. Platform for unified molecular analysis: PUMA. J. Chem. Inf. Model 57 , 1735 (2017).
Schwaller, P. et al. Molecular transformer: A model for uncertainty-calibrated chemical reaction prediction. ACS Cent. Sci. 5 , 1572 (2019).
Coley, C. W. et al. A graph-convolutional neural network model for the prediction of chemical reactivity. Chem. Sci. 10 , 370 (2019).
Jin, W., Coley, C., Barzilay, R. & Jaakkola, T. Predicting organic reaction outcomes with Weisfeiler–Lehman network. NeurIPS 30 , 2604 (2017).
Lowe, D. M. Patent Reaction Extractor . https://github.com/dan2097/patent-reaction-extraction .
Lowe, D. M. Extraction of Chemical Structures and Reactions from the Literature (Doctoral Thesis) . https://doi.org/10.17863/CAM.16293 (2012).
Cao, L. et al. MolDiscovery: Learning mass spectrometry fragmentation of small molecules. Nat. Commun. 12 , 3718 (2021).
NIST Chemistry WebBook. Standard Reference Database Number 69 . https://webbook.nist.gov/chemistry/ .
Source Codes for Retrieval of Flavour EI-MS Data; Molecular Weight Correlation of W-L NN Predicted Products and EI-MS Fragmentations and Retrieval of GHS Classifications . https://github.com/IBM/pyrolysis-prediction .
PubChem is an Open Chemistry Database at the National Institutes of Health (NIH) . https://pubchem.ncbi.nlm.nih.gov/ .
Wilson, N. et al. Improving on estimates of the potential relative harm to health from using modern ENDS (vaping) compared to tobacco smoking. BMC Public Health 21 , 2038 (2021).
Singh, K. P. et al. Systemic biomarkers in electronic cigarette users: Implications for noninvasive assessment of vaping associated pulmonary injuries. ERJ Open Res. 5 , 00182 (2019).
Toxtree v3.1.0. Toxtree—Toxic Hazard Estimation by Decision Tree Approach . http://toxtree.sourceforge.net .
Grambow, C. A., Pattanaik, L. & Green, W. H. Deep learning of activation energies. J. Phys. Chem. Lett. 11 , 2992 (2020).
Grambow, C. A., Pattanaik, L. & Green, W. H. Reactants, products, and transition states of elementary chemical reactions based on quantum chemistry. Sci. Data 7 , 137 (2020).
Lewis-Atwell, T., Townsend, P. A. & Grayson, M. N. Machine learning activation energies of chemical reactions. WIREs Comput. Mol. Sci. 12 , e1593 (2022).
Article CAS Google Scholar
Raza, A. et al. A machine learning approach for predicting defluorination of pe rand polyfluoroalkyl substances (PFAS) for their efficient treatment and removal. Environ. Sci. Technol. Lett. 6 , 624 (2019).
Hurd, C. D. & Blunck, F. H. The pyrolysis of esters. J. Am. Chem. Soc. 60 , 2419 (1938).
Vargas, D. C., Salazar, S., Mora, J. R., Van Geem, K. M. & Streitwieser, D. A. Experimental and theoretical study of the thermal decomposition of ethyl acetate during fast pyrolysis. Chem. Eng. Res. Des. 157 , 153 (2020).
Porterfield, J. P. et al. Thermal decomposition of potential ester biofuels. Part I: Methyl acetate and methyl butanoate. J. Phys. Chem. A 121 , 4658–4677 (2017).
Guo, T. et al. Real-time analysis of intermediate products from non-thermal plasma degradation of ethyl acetate in air using PTR-MS: Performance evaluation and mechanism study. Chemosphere 264 , 128430 (2021).
Wang, Q.-D. Theoretical studies on the hydrogen abstraction reactions of methyl esters with HO2 radical and the following β-scission reactions. J. Phys. Org. Chem. 30 , e3668 (2017).
Article ADS Google Scholar
Sutton, R. & Harr, W. E. Optimum temperatures in pyrolysis gas chromatography. Can. J. Chem. 46 , 2623 (1968).
Sun, W. et al. Experimental and modelling efforts towards a better understanding of the high-temperature combustion kinetics of C 3 –C 5 ethyl esters. Comb. Flame 185 , 173 (2017).
Goel, R. et al. Highly reactive free radicals in electronic cigarette aerosols. Chem. Res. Toxicol. 28 , 1675 (2015).
Son, Y. et al. Hydroxyl radicals in e-cigarette vapor and e-vapor oxidative potentials under different vaping patterns. Chem. Res. Toxicol. 32 , 1087 (2019).
Mathers, A., Hawkins, B. & Lee, K. Transnational tobacco companies and new nicotine delivery systems. Am. J. Public Health 109 , 227 (2019).
Hua, M. et al. Identification of cytotoxic flavour chemicals in top-selling electronic cigarette refill fluids. Sci. Rep. 9 , 2782 (2019).
Hartmann-Boyce, J. et al. Electronic cigarettes for smoking cessation. Cochrane Database of Syst. Rev. 9 , CD010216 (2021).
Hurd, C. D. The Pyrolysis of Carbon Compounds (Chemical Catalog Company, 1929).
Wentrup, C. Flash vacuum pyrolysis: Techniques and reactions. Angew. Chem. Int. Ed. 56 , 14808 (2017).
Chen, J. Y., Canchola, A. & Lin, Y.-H. Carbonyl composition and electrophilicity in vaping emissions of flavoured and unflavored e-liquids. Toxics 9 , 345 (2021).
Son, Y., Bhattarai, C., Samburova, V. & Khlystov, A. Carbonyls and carbon monoxide emissions from electronic cigarettes affected by device type and use patterns. Int. J. Environ. Res. Public Health 17 , 2767 (2020).
Gillman, I. G., Pennington, A. S. C., Humphries, K. E. & Oldham, M. J. Determining the impact of flavored e-liquids on aldehyde production during vaping. Reg. Toxicol. Pharmacol. 112 , 104588 (2020).
Kosmider, L. et al. Daily exposure to formaldehyde and acetaldehyde and potential health risk associated with use of high and low nicotine e-liquid concentrations. Sci. Rep. 10 , 6546 (2020).
Khlystov, A. & Samburova, V. Flavouring compounds dominate toxic aldehyde production during e-cigarette vaping. Environ. Sci. Technol. 50 , 13080 (2016).
Samburova, V. et al. Aldehydes in exhaled breath during e-cigarette vaping: Pilot study results. Toxics 6 , 46 (2018).
Paul Jensen, R., Luo, W., Pankow, J. F., Strongin, R. M. & Peyton, D. H. Hidden formaldehyde in e-cigarette aerosols. N. Engl. J. Med. 372 , 392 (2015).
Jensen, R. P., Strongin, R. M. & Peyton, D. H. Solvent chemistry in the electronic cigarette reaction vessel. Sci. Rep. 7 , 42549 (2017).
Wang, P. et al. A device-independent evaluation of carbonyl emissions from heated electronic cigarette solvents. PLoS ONE 12 , e0169811 (2017).
Li, Y. et al. Impact of e-liquid composition, coil temperature, and puff topography on the aerosol chemistry of electronic cigarettes. Chem. Res. Toxicol. 34 , 1640 (2021).
Narimani, M., Adams, J. & da Silva, G. Toxic chemical formation during vaping of ethyl ester flavour additives: A chemical kinetic modeling study. Chem. Res. Toxicol. 35 , 522 (2022).
Jaegers, N. R., Hu, W., Weber, T. J. & Hu, J. Z. Low-temperature (< 200 °C) degradation of electronic nicotine delivery system liquids generates toxic aldehydes. Sci. Rep. 11 , 7800 (2021).
Jaworski, W. et al. Automatic mapping of atoms across both simple and complex chemical reactions. Nat. Commun. 10 , 1434 (2019).
Download references
Acknowledgements
D.W. acknowledges the Synthesis and Solid State Pharmaceutical Centre (SSPC) and Science foundation Ireland for funding support, Grant Number 12/RC/2275_P2.
Author information
Authors and affiliations.
IBM Research - Tokyo, Shin-Kawasaki, Japan
Akihiro Kishimoto
Department of Chemistry, Royal College of Surgeons in Ireland (RCSI), Dublin 2, Ireland
Dan Wu & Donal F. O’Shea
You can also search for this author in PubMed Google Scholar
Contributions
D.F.O. designed research; A.K. and D.W. performed research; D.F.O., A.K. and D.W. analyzed data; D.F.O., A.K. and D.W. wrote the paper.
Corresponding authors
Correspondence to Dan Wu or Donal F. O’Shea .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Kishimoto, A., Wu, D. & O’Shea, D.F. Forecasting vaping health risks through neural network model prediction of flavour pyrolysis reactions. Sci Rep 14 , 9591 (2024). https://doi.org/10.1038/s41598-024-59619-x
Download citation
Received : 23 August 2023
Accepted : 11 April 2024
Published : 08 May 2024
DOI : https://doi.org/10.1038/s41598-024-59619-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- All Publications
- Priorities Magazine Spring 2018
- The Next Plague and How Science Will Stop It
- Priorities Magazine Winter 2018
- Priorities Magazine Fall 2017
- Little Black Book of Junk Science
- Priorities Magazine Winter 2017
- Should You Worry About Artificial Flavors Or Colors?
- Should You Worry About Artificial Sweeteners?
- Summer Health and Safety Tips
- How Toxic Terrorists Scare You With Science Terms
- Adult Immunization: The Need for Enhanced Utilization
- Should You Worry About Salt?
- Priorities Magazine Spring 2016
- IARC Diesel Exhaust & Lung Cancer: An Analysis
- Teflon and Human Health: Do the Charges Stick?
- Helping Smokers Quit: The Science Behind Tobacco Harm Reduction
- Irradiated Foods
- Foods Are Not Cigarettes: Why Tobacco Lawsuits Are Not a Model for Obesity Lawsuits
- The Prevention and Treatment of Osteoporosis: A Review
- Are "Low Dose" Health Effects of Chemicals Real?
- The Effects of Nicotine on Human Health
- Traditional Holiday Dinner Replete with Natural Carcinogens - Even Organic Thanksgiving Dinners
- A Primer On Dental Care: Quality and Quackery
- Nuclear Energy and Health And the Benefits of Low-Dose Radiation Hormesis
- Priorities in Caring for Your Children: A Primer for Parents
- Endocrine Disrupters: A Scientific Perspective
- Good Stories, Bad Science: A Guide for Journalists to the Health Claims of "Consumer Activist" Groups
- A Comparison of the Health Effects of Alcohol Consumption and Tobacco Use in America
- Moderate Alcohol Consumption and Health
- Irradiated Foods Fifth Edition
- Media/Contact
- Write For Us
Health Risks Of Vaping: Let's Stick To The Science And Speculate Less
Related articles.
Despite increasing evidence that vaping is safer than smoking, uncertainty surrounds the long-term effects of electronic cigarette use. Many in the tobacco control field have used the lack of data to speculate about these unknown risks. Here's a better way to deal with the uncertainty.

A growing body of evidence gathered over the last 15 years has shown that using an electronic cigarette ("vaping") is probably far safer than smoking and likely to help smokers quit their deadly habit forever. Certain segments of the public health establishment have reacted oddly to these results—they've ignored them and treated vaping as a serious threat. The American Heart Association, for example, has even called for e-cigarettes to be taxed and regulated as stringently as tobacco products are. [1]
Fortunately, this view doesn't seem to be as predominant as it once was; we're beginning to see more physicians, scientists, and public health organizations make statements based on the available science instead of what they think the evidence might show one day.
Consider this May 24 review article published in Prescriber : E-cigarettes: informing the conversation with patients by Anna Kate Barton. The author, a clinical research fellow at the University of Edinburgh in the UK, helpfully outlined the history, anatomy, and science of e-cigarettes with the aim of helping doctors more knowledgeably discuss vaping with their patients. Compared to the typical news report about vaping —"Vaping is not better than smoking, and it still causes long-term lung damage"—Barton's article illustrated how we should talk about scientific issues when the evidence surrounding them is evolving. Let's consider a few examples.
Smoking cessation
What does the current evidence say about vaping and smoking cessation? ACSH has previously reported that vaping very likely helps smokers quit cigarettes, and maybe even nicotine , for good. Citing some of the same literature we have, Barton reached a similar conclusion about smoking cessation. While acknowledging the limitations of these studies ( discussed here ), she explained:
Patients using e-cigarettes also often report greater satisfaction and greater reduction in smoking than those using nicotine patches, and e-cigarettes are regarded as the most popular form of smoking cessation aid with smokers wishing to quit. Current position statements and the existing evidence base advocate their combination with stop smoking counseling, the most effective smoking cessation tool.
This comes down to a concept known as “ harm reduction .” Ideally, people would never take up smoking. But since they do, the goal should be to help them mitigate the risks when abstinence isn't feasible. More experts are beginning to embrace this approach in order to enhance smoking cessation campaigns, as Barton noted:
E-cigarettes as aids to smoking cessation are advocated by several organizations including Public Health England. This is based on the principle of risk-reduction – simply, e-cigarettes provide nicotine in a much safer form that traditional cigarettes. Although neither are entirely risk-free, e-cigarettes are generally accepted to confer less risk to both the user and passive smokers than traditional cigarettes.
Health risks of vaping
After contrasting the overall risk of vaping with smoking, Barton added that some preliminary studies have indeed associated e-cigarette use with various negative outcomes. For example, an onslaught of headlines in mid-2019 warned the public about an outbreak of “e-cigarette or vaping product use-associated lung injury” (EVALI). Under-reported at the time was the fact that the injury-causing devices were typically purchased illegally and contained THC or certain dangerous additives, which made them far more harmful than the nicotine-containing devices adult customers can legally purchase in licensed vape shops in the US and UK. Surveying the literature nearly two years later, we get a better sense of the problem:
Interestingly, 82% [of EVALI cases] reported use of THC-containing [vape] products. Vitamin E acetate is sometimes added as a condensing agent in e-liquid, particularly in those containing THC, and this has been associated with EVALI. As such, the CDC discourages use of THC-containing [vape products], particularly those sourced informally from family or friends.
The point, then, is that proper regulation and vigilance by individual users can minimize these types of injuries. The UK, where vaping has proven to be a similarly popular smoking cessation approach, “has not thus far experienced a similar epidemic of EVALI as the USA,” Barton added, though she mentioned two severe cases that apparently weren't related to THC or Vitamin E acetate .
About those long-term effects
Opponents of vaping often point to the dearth of research on its chronic health effects as a first line of criticism. This is a fair enough point, but I hasten to add that it cuts both ways. If we don't know the long-term effects of vaping, we don't know the long-term effects of vaping. “At present,” Barton observed in reference to chronic lung disease, “we can only reflect on potential consequences of 10–15 years of widespread e-cigarette use.”
But that's often not what tobacco control advocates do. “The long-term risks of exclusive use of e-cigarettes are not fully known,” The American Cancer Society claims, “but evidence is accumulating that e-cigarette use has negative effects on the cardiovascular system and lungs. Without immediate measures to stop epidemic use of these products, the long-term adverse health effects will increase.” Retired University of California, San Francisco tobacco researcher Stanton Glantz has even suggested that e-cig users would “be better off just smoking.”
The impulse to reject anything tobacco-related is understandable. But we have to stick with the data we have, which suggests vaping is far safer than smoking, and wait for the long-term results to come in. What we can't do is minimize the existing evidence while simultaneously making statements about the future. Uncertainty is acceptable when we don't have enough evidence, as Barton wrote:
It seems unlikely that e-cigarettes will be without pathological consequences within the human lung and elsewhere, though when we will be able to prove or disprove this is less clear … Regular monitoring of suspected adverse events arising from e-cigarettes … will aid recognition of new complications in [the] future, though it is unlikely we will appreciate the full picture of any long-term harms until well into this century.
[1] The FDA classifies e-cigarettes as tobacco products, but this designation makes little sense. According to Nicotine and Tobacco Research , "If all products containing nicotine derived from tobacco were labeled as 'tobacco products' internationally, then nicotine-replacement therapies would be classified as tobacco products, which they are clearly not."
View the discussion thread.

By Cameron English
Director of Bioscience
Cameron English is a writer, editor and co-host of the Science Facts and Fallacies Podcast. Before joining ACSH, he was managing editor at the Genetic Literacy Project.
Latest from Cameron English :
Together we are beating cancer
- Cancer types
- Breast cancer
- Bowel cancer
- Lung cancer
- Prostate cancer
- Cancers in general
- Clinical trials
- Causes of cancer
- Coping with cancer
- Managing symptoms and side effects
- Mental health and cancer
- Money and travel
- Death and dying
- Cancer Chat forum
- Health Professionals
- Cancer Statistics
- Cancer Screening
- Learning and Support
- NICE suspected cancer referral guidelines
- Make a donation
- By cancer type
- Leave a legacy gift
- Donate in Memory
- Find an event
- Race for Life
- Charity runs
- Charity walks
- Search events
- Relay for Life
- Volunteer in our shops
- Help at an event
- Help us raise money
- Campaign for us
- Do your own fundraising
- Fundraising ideas
- Get a fundraising pack
- Return fundraising money
- Fundraise by cancer type
- Set up a Cancer Research UK Giving Page
- Find a shop or superstore
- Become a partner
- Cancer Research UK for Children & Young People
- Our Play Your Part campaign
- Brain tumours
- Skin cancer
- All cancer types
- By cancer topic
- New treatments
- Cancer biology
- Cancer drugs
- All cancer subjects
- All locations
- By Researcher
- Professor Duncan Baird
- Professor Fran Balkwill
- Professor Andrew Biankin
- See all researchers
- Our achievements timeline
- Our research strategy
- Involving animals in research
- Research opportunities
- For discovery researchers
- For clinical researchers
- For population researchers
- In drug discovery & development
- In early detection & diagnosis
- For students & postdocs
- Our funding schemes
- Career Development Fellowship
- Discovery Programme Awards
- Clinical Trial Award
- Biology to Prevention Award
- View all schemes and deadlines
- Applying for funding
- Start your application online
- How to make a successful applicant
- Funding committees
- Successful applicant case studies
- How we deliver research
- Our research infrastructure
- Events and conferences
- Our research partnerships
- Facts & figures about our funding
- Develop your research career
- Recently funded awards
- Manage your research grant
- Notify us of new publications
- Find a shop
- Volunteer in a shop
- Donate goods to a shop
- Our superstores
- Shop online
- Wedding favours
- Cancer Care
- Flower Shop
- Our eBay store
- Shoes and boots
- Bags and purses
- We beat cancer
- We fundraise
- We develop policy
- Our global role
- Our organisation
- Our strategy
- Our Trustees
- CEO and Executive Board
- How we spend your money
- Early careers
- Your development
Cancer News
- For Researchers
- For Supporters
- Press office
- Publications
- Update your contact preferences
- About cancer
- Get involved
- Our research
- Funding for researchers
The latest news, analysis and opinion from Cancer Research UK
- Science & Technology
- Health & Medicine
- Personal Stories
- Policy & Insight
- Charity News
- Health & Medicine
Can vaping cause changes in our cells?
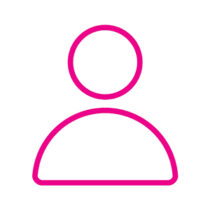
20 March 2024
You may have seen recent media coverage of a study that looked at changes in different types of cells from people who smoked and people who vaped. In this article, we take a closer look at what the researchers did, what they found and what the results of the study could mean.
Does this study show that vaping causes cancer?
No. The type of change that this study looked at is different from changes to a cell’s DNA sequence (mutations) . This study shows that some changes were there but not what they might be doing. So, we don’t have enough information yet to understand what these findings mean in terms of any potential health effects.
E-cigarettes haven’t been around for long enough for us to know what their longer-term health effects could be . So, vaping isn’t risk-free and children and people who have never smoked shouldn’t vape. But research overall still finds that legal vaping is far less harmful than smoking and can help people who smoke to stop.
What did the researchers do?
The researchers looked at chemical ‘marks’ that add information to the genetic code in our DNA. This is called epigenetics. It’s a bit like highlighting or adding notes to a page in a book – the words themselves don’t change, but we read them differently. The epigenetic marks affect how our cells ‘read’ the instructions in their genes.
Epigenetic changes ‘turn on’ or ‘turn off’ genes. They’re a way for cells to respond to what’s happening around them by following the instructions from the right gene(s). Epigenetic changes can be temporary and reverse when they’re no longer needed, whereas genetic mutations in our DNA tend to be permanent.
In this study, the researchers looked into a type of epigenetic change called methylation, i n which a small molecule (made up of one carbon atom and three hydrogen atoms, a ‘methyl group’) gets attached to some of the building blocks of DNA. In particular, they focused on methylation in different types of cells in people who smoked but also looked at it in a small number of people who vaped and another small group of people who used smokeless tobacco.
What did the study find?
The study found methylation changes in cells taken from people who smoked, including cheek (which are directly exposed to smoke), cervical (which aren’t) and blood cells. The kind of changes seen varied depending on the type of cell. As mentioned above, epigenetic changes can be temporary, enabling cells to respond to their environment and then stop when the response is no longer needed. The researchers found variation in methylation patterns depending on how long someone had smoked for, and some changes were only seen in samples from people who currently smoked and not in people who had stopped smoking.
The researchers also compared methylation changes in cell DNA samples from people who vaped with those from people who smoked. They found some similarities between the kinds of changes seen in people who vaped and people who smoked.
What does it mean?
This research is at an early stage, so we don’t have enough information yet to understand what the findings mean. For example, the study looked at some changes that were seen in cell DNA samples, not how the cells with those changes were behaving compared to cells without the changes.
When two things occur together, it could mean that:
- one is causing the other;
- they could also be there by chance; or
- they could both be caused by a third factor that we don’t know yet.
So, the epigenetic changes could be part of our cells’ response to cigarette smoke or e-cigarette vapour, they could be unrelated or they could be caused by something else that was affecting both the study participants who smoked and the participants who vaped.
There were also some limitations to what the study was able to do, for example, participants who vaped may have smoked in the past, so we can’t be completely sure that the changes seen weren’t caused by previous smoking.
Should I stop vaping?
If you used to smoke and are vaping to help you to stay off tobacco, the most important thing is not to go back to smoking. So, if you’re thinking of stopping vaping, make sure you only do so if you think you won’t start smoking again. If you think there’s a risk that you’ll smoke if you stop vaping, talk to your free local stop smoking service, GP or pharmacist for advice on stopping vaping or switching to an alternative stop smoking tool.
Because vaping isn’t risk free, it’s important that children and people who have never smoked don’t start to vape. By contrast, however, decades of research have proven the harmful effects of smoking, which kills one person every five minutes in the UK. Research so far has found that e-cigarettes are far less harmful than smoking and can help people to stop. So, if you smoke and want to stop , e-cigarettes are an option.
What could epigenetics research mean in the future?
Epigenetics is an interesting area of research and we look forward to seeing what future studies can tell us about cancer and how it develops.
What are the UK governments doing about smoking and vaping?
In October 2023, the UK Government announced plans to create the first ever smokefree generation by raising the age of sale of tobacco as well as action to tackle youth vaping . Today, those plans are being introduced in Parliament as the Tobacco and Vapes Bill.
Under the Bill, anyone born on or after 1 January 2009 will never legally be able to be sold tobacco.
As an individual who once believed in the promise of vaping as a safer alternative to smoking, I embarked on a journey that ultimately led me to a profound realization: prioritizing my health over convenience was paramount.
It’s undeniable that traditional tobacco products wreak havoc on our bodies, causing irreversible damage to our lungs and increasing the risk of life-threatening diseases like cancer. In my quest for a healthier alternative, I turned to vaping, hoping to break free from the chains of tobacco addiction.
However, my experience with vaping proved to be far from the panacea I had envisioned. Despite its touted benefits, vaping failed to satisfy my cravings and instead left me feeling depleted and unwell. Dehydration, coupled with a lack of essential nutrients from improper eating habits, took its toll on my body, manifesting in alarming symptoms such as liver pain and debilitating fatigue.
Concerned for my well-being, I sought medical advice and underwent a liver scan, revealing unsettling fatty deposits in my liver—a stark reminder of the detrimental effects of vaping on my health. Faced with this sobering reality, I made a conscious decision to reclaim control of my life and pursue a healthier lifestyle.
Quitting vaping marked the beginning of a remarkable transformation. Freed from the shackles of addiction, I experienced a newfound sense of vitality and vigor. The burden of liver pain lifted, replaced by an abundance of energy and vitality that I had long forgotten.
Today, I stand as living testimony to the power of resilience and determination in overcoming adversity. By embracing the simple pleasures of life and relinquishing the harmful habits that once held me captive, I have unlocked a world of boundless possibilities.
To those who may find themselves ensnared by the allure of vaping or any other harmful habit, I implore you to heed this cautionary tale. Embrace the gift of life with gratitude and reverence, for it is a precious treasure to be cherished and nurtured.
In closing, let us remember that true fulfillment lies not in succumbing to the temptations of vice, but in embracing the purity of existence and breathing the air as nature intended. As I bask in the radiance of newfound health and vitality, I invite you to join me on this transformative journey towards a brighter, healthier future.
Yours in health and healing,
I think until there is solid proof that vaping is as bad as cigarettes then people should stop putting fake news on the internet. Smoking contains over 7000 toxins, including tar that they use on the roads , vaping has about 5 substances in and is actually around 95% safer than smoking . My Dr adviced me to switch to vaping to quit the cancer sticks , which I did , my breathing has improved loads and my horrid,rattly smokers cough I had for years had gone , I no longer get out of breath just walking up the stairs. I agree if people have never smoked then they shouldn’t just start vaping and kids shouldn’t do it either . But my Dr said the nail thing in vapes is nicotine, which is not harmful at all , it’s just addictive. We breath in toxins every time we leave the house , with all the car fumes and pollution that’s in the air . The reason the government don’t want people quitting smoking and start vaping is because there’s millions weeks millions of pounds to be made in smoking and killing millions of people a year . There is no money to be made in the vaping . What’s more important, people’s health or money … The government are the most untrustworthy ,lying snakes on the planet. And until there is concrete proof people should vape to quit the cancer sticks.
Every way of smoking, including vaping, is, in my layman understanding, a huge cancer risk. After all, you inhale smoke with plenty of dangerous ingredients that go right up your brain, down your throat and also down your lungs and no one could ever convince me that this is healthy or free of any cancer danger. There are other articles on this (great) website, which clearly explain that the greatest dangers of developing cancer are drinking alcohol and smoking. Luckily, I have never smoked anything in my entire life and I have no interest in starting this, in fact I am very disgusted if someone on the streets is smoking and I have to pass by or even walk behind that person, which makes me holding my breath until I got away, yet, from my observation while walking the streets, when somebody is vaping the clouds are way thicker and the smell seems to go way farther than the smell of burning tobacco. To me, those are clearly warning signs that vaping may even be far more dangerous, also when it comes to cancer development, than smoking cigarettes, although I highly advise to stay away from any kind of smoking anyway. And I would not be surprised if later studies will finally figure out that vaping is indeed coming with a far greater risk than smoking cigarettes, although, again, my layman advise is to just stay away from smoking anything, no matter what it is.
WOAH! This shared a lot of info about how bad vaping is!
Cancer research has a responsibility to protect the public, not the Corporations pushing Vapes on the population under the guise of “safer than cigarettes”. This is akin to saying there is no evidence that walking across the motorway with a blindfold on is unsafe because there is no evidence to suggest you would get run over (as no one has carried out a real study to confirm or deny this)
This nanny state will not stop me vaping it saved me from smoking and your never stop children smoking just like cannabis
Nobody has ever asked my husband about his vaping – e-cigarette use despite having lung cancer🙀 what is going on?
Methyl is not a molecule (the closest molecule to it is methane). It is usually called a group (or, maybe, a moiety).
Tell us what you think
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Read our comment policy .
Highlighted content
An animal's guide to staying safe in the sun, hpv vaccine slashes cervical cancer rates across society, the ‘mystery’ culprit causing kidney cancer worldwide, proteins in blood could give cancer warning seven years earlier, are ultra-processed foods linked to cancer, following cupid’s arrow: a new blood test to find cancer of unknown primary, making cancer screening work for you, that cancer conversation podcast - one to one with dr anisha patel, related topics.
- Research and trials
- Cancer controversies
- Epigenetics
- Cancer in the news
- Help & Support
Where There’s Smoke: New Research Publication Lights Fire about Dangers of Vaping
by Stacey Sturner | January 12, 2023
- E-Cigarettes
The American Journal of Preventive Medicine recently published a new paper, titled “ Cigarette-E-cigarette Transitions and Respiratory Symptom Development ,” which assessed the respiratory health effects of 16 tobacco product transitions, including from non-use to e-cigarette use.
Funded in part by the American Lung Association, the study suggests e-cigarette initiation among nonusers and subsequent cigarette smoking may cause significant lung health impacts. These results reinforce the urgency for robust e-cigarette regulations, as well as demonstrate that additional research is needed to better determine the specific harms of e-cigarettes.
“The topline finding that e-cigarette initiation among nonusers is associated with increased respiratory morbidity is an important point to emphasize given continued high rates of e-cigarette usage among youth and young adult never smokers in the U.S.,” stated Andrew Stokes, PhD , assistant professor of global health at the Boston University School of Public Health and senior author of the paper. “It adds to our body of scientific evidence urgently calling for the public health intervention in support of more stringent regulatory e-cigarette standards.”
Dr. Stokes was a 2020-2022 recipient of the Lung Association’s Public Policy Research Award, which aims to empower scientists who are impacting lung health. In February 2022, he likewise served as senior author of a paper published in the American Journal of Respiratory and Critical Care Medicine , revealing young adults who use e-cigarettes are more likely to develop respiratory issues within one year of vaping.
The latest study, like the one published in February, used data from the Food and Drug Administration’s (FDA) Population Assessment of Tobacco and Health (PATH) cohort, a longitudinal study tracking changes in tobacco use over time among participants. Among 33,231 observations from 13,528 unique participants, the study authors found that nonusers who started e-cigarette use had 62% greater rate of wheezing.
Albert Rizzo, MD, Chief Medical Officer of the Lung Association, added, “Anything that can be done to help curb the e-cigarette epidemic is an important step forward. This research further amplifies our organization’s warning against e-cigarette use due to the resulting health ramifications. It’s a mission-critical public policy initiative, now and always.”
“What is exceedingly clear is that e-cigarette initiation among nonusers is associated with increased respiratory morbidity,” continued Dr. Stokes. “We’re just starting to scratch the surface in our systematic identification of behavioral patterns most closely tied to respiratory events.”
The Lung Association has called on the FDA to end the sale of all flavored tobacco products, including flavored e-cigarettes. Flavors attract youth and the high levels of nicotine found in many e-cigarettes quickly hook kids. States including California and Massachusetts, as well as Washington, D.C. and multiple other cities have passed legislation to end the sale of flavored tobacco products in their states.
In addition, the Lung Association has called on federal officials to do more to ensure youth who are addicted to vaping and other tobacco products have resources to help them end their addiction.
To learn more about e-cigarette risks or a list of proven-effective cessation programs available to help youth and adults quit all tobacco products for good, please visit: Lung.org/quit-smoking .
Related Blogs
“i almost died”: a vaping horror story.
May 8, 2024
Keeping Your Pets Safe from Nicotine Poisoning
July 24, 2023
January 12, 2023
Blog last updated: August 25, 2023
A Breath of Fresh Air in Your Inbox
Join over 700,000 people who receive the latest news about lung health, including research, lung disease, air quality, quitting tobacco, inspiring stories and more!
You will now receive email updates from the American Lung Association.
Make a Donation
Your tax-deductible donation funds lung disease and lung cancer research, new treatments, lung health education, and more.
Become a Lung Health Insider
Thank you! You will now receive email updates from the American Lung Association.
Select Your Location
Select your location to view local American Lung Association events and news near you.
Change Language
Lung helpline.
Talk to our lung health experts at the American Lung Association. Our service is free and we are here to help you.
1-800-LUNG-USA
(1-800-586-4872)

RESOURCES INFORMATION LIBRARY
Research, data & articles.
This resource is collection of the best and latest research on vaping and other reduced-harm products, medical journal articles, as well as journalistic pieces organized by topic that contain valuable data, information, and perspectives on tobacco harm reduction, vaping, and safer nicotine products.
Our intention is update this resource with additional sources as they become available, so please check back often.
Jump to Topic…
Science // Smoking Cessation Science // Harm Reduction Science // Health Effects Science // Flavors Science // Youth Usage Science // Smokeless Tobacco Science // Regulatory Effects News // Smoking Cessation News // Harm Reduction News // COVID-19 News // EVALI News // Youth Usage News // Social Justice News // Taxes News // Tobacco Control
Highlighted Resources
These resources are some of the highest rated, latest research on vaping.
Balancing Consideration of the Risks and Benefits of E-Cigarettes
Nicotine without smoke: tobacco harm reduction, electronic cigarettes for smoking cessation, a randomized trial of e-cigarettes versus nicotine-replacement therapy, educational videos, recommended videos, what vaping did.

Vaping: what people are getting wrong | The Economist

Vaping: a more balanced message | Michigan Public Health
Why bans of low-risk nicotine alternatives to smoking in lmic's will do more harm than good, vaping demystified.

The E-Cigarette Summit 2019, London | Ethan Nadelman Presentation

Why Health Groups Lie About Vaping

Vaporized: U.K. Government Promotes Vaping As Smoking Cessation Tool | CNBC Prime

Marc Slis, Vape Shop Owner - Michigan Testimony
Recommended reading.

Stop Smoking Start Vaping
Dr. Colin Mendelsohn

Velvet Glove, Iron Fist
Christopher Snowden

The Rediscovery of Tobacco
Jacob Grier

The Cigarette Century
Allan M. Brandt

The Cigarette
Sarah Milov

Cigarette Wars
Cassandra Tate

Sander L. Gilman & Zhou Xun

Cigarettes Are Sublime
Richard Klein

For Smokers Only

Ashes to Ashes
Richard Kluger

Say Why To Drugs
Dr. Suzi Gage
Scientific Research / Articles
Smoking cessation, harm reduction, health effects, youth usage, smokeless tobacco, regulatory effects, news media / blog articles, social justice, tobacco control.
This site uses functional cookies and external scripts to improve your experience.
Privacy settings
Privacy Settings
This site uses functional cookies and external scripts to improve your experience. Which cookies and scripts are used and how they impact your visit is specified on the left. You may change your settings at any time. Your choices will not impact your visit.
NOTE: These settings will only apply to the browser and device you are currently using.
Google Analytics
By continuing to browse or by clicking ‘Accept’, you agree to the storing of cookies on your device to enhance your site experience and for analytical purposes.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
July 17, 2023
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Current evidence identifies health risks of e-cigarette use, long-term research needed
by American Heart Association

Research increasingly reveals health risks of e-cigarette use, and more studies are needed about the long-term impact e-cigarettes may have on the heart and lungs, according to a new scientific statement from the American Heart Association published in the journal Circulation .
The statement, "Cardiopulmonary Impact of Electronic Cigarettes and Vaping Products," details the latest usage data and trends, identifies current health impacts, highlights existing basic and clinical scientific evidence surrounding e-cigarettes and recommends research priorities to further understand the short- and long-term health effects of e-cigarette use.
Vaping products, also known as e-cigarettes, are battery-operated systems that heat a liquid solution, or e-liquid, to create an aerosol that is inhaled into the lungs. Most e-liquid formulations deliver nicotine, which has been established as having negative health effects as well as strong addictive properties.
The products may also contain other substances, most commonly tetrahydrocannabinol (THC), the psychoactive element of cannabis, as well as methamphetamine, methadone or vitamins. The liquids also include humectants (hygroscopic carriers such as propylene glycol and vegetable glycerol) that act as solvents and create a water aerosol or vapor, flavoring agents, cooling agents such as menthol and sweeteners, in addition to metals from the heating coil and other chemicals.
"E-cigarettes deliver numerous substances into the body that are potentially harmful, including chemicals and other compounds that are likely not known to or understood by the user. There is research indicating that nicotine-containing e-cigarettes are associated with acute changes in several hemodynamic measures, including increases in blood pressure and heart rate ," said the volunteer chair of the scientific statement writing committee Jason J. Rose, M.D., M.B.A., an associate professor of medicine at the University of Maryland School of Medicine in Baltimore.
"There has also been research indicating that even when nicotine is not present, ingredients in e-cigarettes, particularly flavoring agents, independently carry risks associated with heart and lung diseases in animals. Negative effects of e-cigarettes have been shown through in vitro studies and in studies of individuals exposed to chemicals in commercially available products."
The writing committee points to the significance of the clinical diagnosis of "E-cigarette, or Vaping, product use Associated Lung Injury" (EVALI). EVALI was first recognized as a condition by the U.S. Centers for Disease Control and Prevention in 2019, when approximately 2,800 hospitalizations occurred among e-cigarette users in less than a year. This is cited in the statement as one example that emphasizes the lack of knowledge surrounding the risks of e-cigarettes and their ingredients.
In the case of the EVALI hospitalizations, vitamin E acetate has been implicated as the ingredient likely causing illness. This substance is used as a thickening agent in some e-cigarette liquids.
Studies gauging the specific impact e-cigarettes have on heart attacks and strokes are limited. Much research on e-cigarette use has been conducted in people who have also used or were currently using traditional cigarettes. Additionally, large survey studies have focused on younger adults who have a low occurrence of heart attacks and strokes. The writing committee says longer-term studies of e-cigarettes users of all ages are needed, including among people who already have cardiovascular disease.
One recent analysis of the adult Population Assessment of Tobacco and Health (PATH) study found a statistically significant association between former or current e-cigarette use at the time participants enrolled in the study and the development of incident respiratory disease (chronic obstructive pulmonary disease/COPD, chronic bronchitis, emphysema or asthma) within the next two years. The PATH Study, an ongoing study that started in 2013, is one of the first large tobacco research efforts undertaken by the National Institutes of Health and the U.S. Food and Drug Administration.
Additional studies cited in the statement indicate a rapid increase since 2010 in the number of people who had ever used e-cigarettes or were currently using the devices, and most of those users were current or former traditional cigarette smokers. In addition, by 2016, data from the Behavioral Risk Factor Surveillance System indicated about 1.2 million adults in the U.S. who had never smoked combustible cigarettes before were currently using e-cigarettes.
The writing committee noted that e-cigarettes are reported to be the most commonly used tobacco product among youth, particularly high school and middle school students. The statement cites data showing that almost three out of four young people using e-cigarettes exclusively report using flavored e-cigarette products. This high rate of use by youth makes it critical to assess the short- and long-term health effects of these products, according to the statement.
"Young people often become attracted to the flavors available in these products and can develop nicotine dependence from e-cigarette use. There is significant concern about young people assuming e-cigarettes are not harmful because they are widely available and marketed to an age group that includes many people who have never used any tobacco products," Rose said.
"The long-term risks of using e-cigarettes are unknown, but if the risks of chronic use are like combustible cigarettes, or even if the risks are reduced but still present, we may not observe them for decades. What is equally concerning is that studies show that some youth who use e-cigarettes go on to use other tobacco products, and there is also a correlation between e-cigarette use and substance use disorders."
Given the established, high health risks of smoking combustible cigarettes, e-cigarette products have been evaluated as smoking cessation tools. The writing committee examined the limited research in this area and concluded that any benefits e-cigarettes may offer to help people stop smoking or stop using tobacco products needs to be clearly balanced alongside the products' known and unknown potential health risks, including the known risk of long-term dependence on these products.
"E-cigarette companies have suggested that their products are a way to quit smoking traditional cigarettes. There is no strong evidence to support this beyond any short-term benefit. The lack of long-term scientific safety data on e-cigarette use, along with the potential for the addiction to e-cigarette products seen among youth, are among the reasons the American Heart Association does not recommend e-cigarette use for cessation efforts," said Rose Marie Robertson, M.D., FAHA, the Association's deputy chief science and medical officer and co-director of the Association's Tobacco Center of Regulatory Science.
"It's also important to note that e-cigarette products are not approved by the U.S. Food and Drug Administration (FDA) for tobacco cessation. The Association recommends a combination of multiple-episode cessation counseling accompanied by personalized nicotine replacement therapy with FDA-approved doses and formulations, as well as medications to help control cravings, to help people who smoke combustible cigarettes with cessation. And all of this needs to be undertaken with the understanding that quitting often takes many tries, and any failures should be seen as just episodes to learn from on the road to finally beating a powerful addiction for good."
The scientific statement writing committee emphasizes a critical need for additional knowledge and research, specifically:
- Future research should focus on gaining knowledge about serious and potentially long-term effects of e-cigarettes on the heart, blood vessels and lungs.
- Studies are needed that include patients with pre-existing cardiopulmonary disease, such as coronary artery disease or chronic obstructive pulmonary disease , to evaluate and compare outcomes among e-cigarette users in comparison to traditional smokers, and those who use e-cigarettes along with traditional cigarettes (referred to as dual users) and nonsmokers.
- More in-depth research is needed about the common chemical ingredients in e-cigarettes and the effects they independently have on pulmonary and cardiac health.
- Clinical studies are needed to study the risks and potential benefits of e-cigarettes as alternatives to traditional combustible cigarettes.
- Since the long-term health impact of e-cigarettes may take decades to emerge, more molecular and laboratory studies are needed in the interim to help determine the biological implications of e-cigarette use .
"Because e-cigarettes and other vaping systems have only been in the U.S. for about 15 years, we do not yet have enough information on their long-term health effects, so we must rely on shorter term studies, molecular experiments and research in animals to try to assess the true risk of using e-cigarettes," Jason Rose added. "It is necessary for us to expand this type of research since the adoption of e-cigarettes has grown exponentially, especially in young people, many of whom may have never used combustible cigarettes."
Explore further
Feedback to editors

New analysis estimates the effects of race-neutral lung function testing on patients, hospitals, and beyond
12 hours ago

World-first trial shows benefits of finding and treating undiagnosed asthma and COPD
15 hours ago

Acetaminophen shows promise in warding off acute respiratory distress syndrome, organ injury in patients with sepsis
18 hours ago

Modular communicative leadless ICD found to be safe and exceeds performance expectations
May 18, 2024

Creativity and humor shown to promote well-being in older adults via similar mechanisms

Sweet taste receptor affects how glucose is handled metabolically by humans

Better medical record-keeping needed to fight antibiotic overuse, studies suggest

Repeat COVID-19 vaccinations elicit antibodies that neutralize variants, other viruses

A long-term ketogenic diet accumulates aged cells in normal tissues, new study shows
May 17, 2024

Gut bacteria enhance cancer immunotherapy in mouse study
Related stories.

Few adult smokers and non-smokers think e-cigarettes have lower levels of harmful chemicals than cigarettes, finds study
May 23, 2023

Most e-cigarette users want to quit, study finds
May 21, 2019

AMA calls for greater electronic cigarette regulation
Aug 7, 2018

No health benefits among adults who used both e-cigarettes and traditional cigarettes
May 6, 2022

Are 'vaping' and 'e-cigarettes' the same, and should all these products be avoided?
Nov 29, 2019
E-cigarette users experience vascular damage similar to that of smokers of combustible cigarettes
Apr 29, 2020
Recommended for you

Link between e-cigarette use and early age of asthma onset in US adults discovered

Global life expectancy projected to increase by nearly 5 years by 2050 despite various threats
May 16, 2024

Number of people experiencing poor health, early death from metabolism-related risk factors has increased since 2000

Men at greater risk of major health effects of diabetes than women, study suggests

Likelihood of kids and young people smoking and vaping linked to social media use
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Resources for healthcare professionals
Latest Research
What is Prevalence of Youth Tobacco Use

What is the Prevalence of Youth Tobacco Use?
Read Time: 36 Seconds
1 in 5 high schoolers self-reported that they currently use or have used an e-cigarette/vape product in the past 30 days. 1 in 20 middle schoolers reported the same.
More than 8 out of 10 young people who currently vape report using flavored e-cigarettes.
There has been a notable increase in the use of disposable e-cigarettes. A few examples include Puff Bar, Cali Bar, EonSmoke Stik Pod and Stig Pod.
Click here for more at the FDA website
CDC's 2020 National Youth Tobacco Survey (NYTS)
CDC’s 2019 Youth Risk Behavior Survey (YRBS)
CDC's State Tobacco Activities Tracking and Evaluation (STATE) System
National Data for E-Cig Use Among Youth

What is the Prevalence of Youth Cannabis Use?
Read Time: 45 Seconds
Past-Year Marijuana Vaping
The percentage of teens who vaped marijuana in the past 12 months remained stable between 2019 and 2020.
Daily or Near-Daily Marijuana Vaping Decreased Significantly Among 10th Graders
The percentage of respondents who vaped marijuana daily or almost daily decreased significantly among 10th graders.
Marijuana Use Remains Steady
Since 2018, both past-year and daily marijuana use remained nearly the same across all age groups.
Click here for more at the NIDA website
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Health Effects of Cigarette Smoking
- Secondhand Smoke
- E-cigarettes (Vapes)
- Menthol Tobacco Products
- Morbidity and Mortality Weekly Reports (MMWR)
- About Surveys
- Other Tobacco Products
- Smoking and Tobacco Use Features
- Patient Care Settings and Smoking Cessation
- Patient Care
- Funding Opportunity Announcements
- State and Community Work
- National and State Tobacco Control Program
- Multimedia and Tools
- Tobacco - Health Equity
- Tobacco - Surgeon General's Reports
- State Tobacco Activities Tracking and Evaluation (STATE) System
- Global Tobacco Control
Health Effects of Vaping
At a glance.
Learn more about the health effects of vaping.
- No tobacco products, including e-cigarettes, are safe.
- Most e-cigarettes contain nicotine, which is highly addictive and is a health danger for pregnant people, developing fetuses, and youth. 1
- Aerosol from e-cigarettes can also contain harmful and potentially harmful substances. These include cancer-causing chemicals and tiny particles that can be inhaled deep into lungs. 1
- E-cigarettes should not be used by youth, young adults, or people who are pregnant. E-cigarettes may have the potential to benefit adults who smoke and are not pregnant if used as a complete substitute for all smoked tobacco products. 2 3 4
- Scientists still have a lot to learn about the short- and long-term health effects of using e-cigarettes.
Most e-cigarettes, or vapes, contain nicotine, which has known adverse health effects. 1
- Nicotine is highly addictive. 1
- Nicotine is toxic to developing fetuses and is a health danger for pregnant people. 1
- Acute nicotine exposure can be toxic. Children and adults have been poisoned by swallowing, breathing, or absorbing vaping liquid through their skin or eyes. More than 80% of calls to U.S. poison control centers for e-cigarettes are for children less than 5 years old. 5
Nicotine poses unique dangers to youth because their brains are still developing.
- Nicotine can harm brain development which continues until about age 25. 1
- Youth can start showing signs of nicotine addiction quickly, sometimes before the start of regular or daily use. 1
- Using nicotine during adolescence can harm the parts of the brain that control attention, learning, mood, and impulse control. 1
- Adolescents who use nicotine may be at increased risk for future addiction to other drugs. 1 6
- Youth who vape may also be more likely to smoke cigarettes in the future. 7 8 9 10 11 12
Other potential harms of e-cigarettes
E-cigarette aerosol can contain substances that can be harmful or potentially harmful to the body. These include: 1
- Nicotine, a highly addictive chemical that can harm adolescent brain development
- Cancer-causing chemicals
- Heavy metals such as nickel, tin, and lead
- Tiny particles that can be inhaled deep into the lungs
- Volatile organic compounds
- Flavorings such as diacetyl, a chemical linked to a serious lung disease. Some flavorings used in e-cigarettes may be safe to eat but not to inhale because the lungs process substances differently than the gut.
E-cigarette aerosol generally contains fewer harmful chemicals than the deadly mix of 7,000 chemicals in smoke from cigarettes. 7 13 14 However, this does not make e-cigarettes safe. Scientists are still learning about the immediate and long-term health effects of using e-cigarettes.
Dual use refers to the use of both e-cigarettes and regular cigarettes. Dual use is not an effective way to safeguard health. It may result in greater exposure to toxins and worse respiratory health outcomes than using either product alone. 2 3 4 15
Some people who use e-cigarettes have experienced seizures. Most reports to the Food and Drug Administration (FDA ) have involved youth or young adults. 16 17
E-cigarettes can cause unintended injuries. Defective e-cigarette batteries have caused fires and explosions, some of which have resulted in serious injuries. Most explosions happened when the batteries were being charged.
Anyone can report health or safety issues with tobacco products, including e-cigarettes, through the FDA Safety Reporting Portal .
Health effects of vaping for pregnant people
The use of any tobacco product, including e-cigarettes, is not safe during pregnancy. 1 14 Scientists are still learning about the health effects of vaping on pregnancy and pregnancy outcomes. Here's what we know now:
- Most e-cigarettes, or vapes, contain nicotine—the addictive substance in cigarettes, cigars, and other tobacco products. 18
- Nicotine is a health danger for pregnant people and is toxic to developing fetuses. 1 14
- Nicotine can damage a fetus's developing brain and lungs. 13
- E-cigarette use during pregnancy has been associated with low birth weight and pre-term birth. 19 20
Nicotine addiction and withdrawal
Nicotine is the main addictive substance in tobacco products, including e-cigarettes. With repeated use, a person's brain gets used to having nicotine. This can make them think they need nicotine just to feel okay. This is part of nicotine addiction.
Signs of nicotine addiction include craving nicotine, being unable to stop using it, and developing a tolerance (needing to use more to feel the same). Nicotine addiction can also affect relationships with family and friends and performance in school, at work, or other activities.
When someone addicted to nicotine stops using it, their body and brain have to adjust. This can result in temporary symptoms of nicotine withdrawal which may include:
- Feeling irritable, jumpy, restless, or anxious
- Feeling sad or down
- Having trouble sleeping
- Having a hard time concentrating
- Feeling hungry
- Craving nicotine
Withdrawal symptoms fade over time as the brain gets used to not having nicotine.
Nicotine addiction and mental health
Nicotine addiction can harm mental health and be a source of stress. 21 22 23 24 More research is needed to understand the connection between vaping and mental health, but studies show people who quit smoking cigarettes experience: 25
- Lower levels of anxiety, depression, and stress
- Improved positive mood and quality of life
Mental health is a growing concern among youth. 26 27 Youth vaping and cigarette use are associated with mental health symptoms such as depression. 22 28
The most common reason middle and high school students give for currently using e-cigarettes is, "I am feeling anxious, stressed, or depressed." 29 Nicotine addiction or withdrawal can contribute to these feelings or make them worse. Youth may use tobacco products to relieve their symptoms, which can lead to a cycle of nicotine addiction.
- U.S. Department of Health and Human Services. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General . Centers for Disease Control and Prevention; 2016. Accessed Feb 14, 2024.
- Goniewicz ML, Smith DM, Edwards KC, et al. Comparison of nicotine and toxicant exposure in users of electronic cigarettes and combustible cigarettes . JAMA Netw Open. 2018;1(8):e185937.
- Reddy KP, Schwamm E, Kalkhoran S, et al. Respiratory symptom incidence among people using electronic cigarettes, combustible tobacco, or both . Am J Respir Crit Care Med. 2021;204(2):231–234.
- Smith DM, Christensen C, van Bemmel D, et al. Exposure to nicotine and toxicants among dual users of tobacco cigarettes and e-cigarettes: Population Assessment of Tobacco and Health (PATH) Study, 2013-2014 . Nicotine Tob Res. 2021;23(5):790–797.
- Tashakkori NA, Rostron BL, Christensen CH, Cullen KA. Notes from the field: e-cigarette–associated cases reported to poison centers — United States, April 1, 2022–March 31, 2023 . MMWR Morb Mortal Wkly Rep. 2023;72:694–695.
- Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain . J Physiol. 2015;593(16):3397–3412.
- National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes . The National Academies Press; 2018.
- Barrington-Trimis JL, Kong G, Leventhal AM, et al. E-cigarette use and subsequent smoking frequency among adolescents . Pediatrics. 2018;142(6):e20180486.
- Barrington-Trimis JL, Urman R, Berhane K, et al. E-cigarettes and future cigarette use . Pediatrics. 2016;138(1):e20160379.
- Bunnell RE, Agaku IT, Arrazola RA, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011-2013 . Nicotine Tob Res. 2015;17(2):228–235.
- Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis . JAMA Pediatr. 2017;171(8):788–797.
- Sun R, Méndez D, Warner KE. Association of electronic cigarette use by U.S. adolescents with subsequent persistent cigarette smoking . JAMA Netw Open. 2023;6(3):e234885.
- U.S. Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease . Centers for Disease Control and Prevention; 2010. Accessed Feb 13, 2024.
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General . Centers for Disease Control and Prevention; 2014. Accessed Feb 12, 2024.
- Mukerjee R, Hirschtick JL, LZ Arciniega, et al. ENDS, cigarettes, and respiratory illness: longitudinal associations among U.S. youth . AJPM. Published online Dec 2023.
- Faulcon LM, Rudy S, Limpert J, Wang B, Murphy I. Adverse experience reports of seizures in youth and young adult electronic nicotine delivery systems users . J Adolesc Health . 2020;66(1):15–17.
- U.S. Food and Drug Administration. E-cigarette: Safety Communication - Related to Seizures Reported Following E-cigarette Use, Particularly in Youth and Young Adults . U.S. Department of Health and Human Services; 2019. Accessed Feb 14, 2024.
- Marynak KL, Gammon DG, Rogers T, et al. Sales of nicotine-containing electronic cigarette products: United States, 2015 . Am J Public Health . 2017;107(5):702-705.
- Regan AK, Bombard JM, O'Hegarty MM, Smith RA, Tong VT. Adverse birth outcomes associated with prepregnancy and prenatal electronic cigarette use . Obstet Gynecol. 2021;138(1):85–94.
- Regan AK, Pereira G. Patterns of combustible and electronic cigarette use during pregnancy and associated pregnancy outcomes . Sci Rep. 2021;11(1):13508.
- Kutlu MG, Parikh V, Gould TJ. Nicotine addiction and psychiatric disorders . Int Rev Neurobiol. 2015;124:171–208.
- Obisesan OH, Mirbolouk M, Osei AD, et al. Association between e-cigarette use and depression in the Behavioral Risk Factor Surveillance System, 2016-2017 . JAMA Netw Open. 2019;2(12):e1916800.
- Prochaska JJ, Das S, Young-Wolff KC. Smoking, mental illness, and public health . Annu Rev Public Health. 2017;38:165–185.
- Wootton RE, Richmond RC, Stuijfzand BG, et al. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a Mendelian randomisation study . Psychol Med. 2020;50(14):2435–2443.
- Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis . BMJ. 2014;348:g1151.
- Centers for Disease Control and Prevention. Youth Risk Behavior Survey Data Summary & Trends Report: 2011–2021 . U.S. Department of Health and Human Services; 2023. Accessed Dec 15, 2023.
- U.S. Department of Health and Human Services. Protecting Youth Mental Health: The U.S. Surgeon General's Advisory . Office of the Surgeon General; 2021. Accessed Jan 5, 2024.
- Lechner WV, Janssen T, Kahler CW, Audrain-McGovern J, Leventhal AM. Bi-directional associations of electronic and combustible cigarette use onset patterns with depressive symptoms in adolescents . Prev Med. 2017;96:73–78.
- Gentzke AS, Wang TW, Cornelius M, et al. Tobacco product use and associated factors among middle and high school students—National Youth Tobacco Survey, United States, 2021 . MMWR Surveill Summ. 2022;71(No. SS-5):1–29.
Smoking and Tobacco Use
Commercial tobacco use is the leading cause of preventable disease, disability, and death in the United States.
For Everyone
Health care providers, public health.
- International edition
- Australia edition
- Europe edition

Chemicals in vapes could be highly toxic when heated, research finds
AI analysis of 180 vape flavours finds that products contain 127 ‘acutely toxic’ chemicals, 153 ‘health hazards’ and 225 ‘irritants’
Chemicals used to produce vapes could be acutely toxic when heated and inhaled, according to research .
Vaping devices heat the liquid flavouring to high temperatures to form an aerosol that is then inhaled. They contain chemicals including vegetable glycerin, propylene glycol, nicotine and flavourings, blended in various amounts.
Previous experiments have shown that some fruit-flavoured vapes – such as strawberry, melon and blueberry – produce dangerous compounds called volatile carbonyls due to this heating process.
These compounds are known to have health implications for chronic obstructive pulmonary disease (COPD), cardiovascular disease and cancers.
With so many chemicals used in tens of thousands of different vape products, conducting experiments to test every brand and flavour for toxicity could take decades of research.
Instead, the study used AI to analyse the chemical composition of 180 vape flavours and simulate how they decompose when heated. The research, published in Scientific Reports , predicted that vapes produce 127 “acutely toxic” chemicals, 153 “health hazards” and 225 “irritants”.
Nearly every flavour put through the AI predictor showed at least one product that was classified as a health hazard, with many predicting several. The toxins were associated with vapes containing no nicotine, as well as those with.
The research team at RCSI University of Medicine and Health Sciences, Dublin , conclude there is a “potential public health threat facing the 4.5 million vapers in the UK” and an urgent need for “enhanced restrictions” on flavours and regulations that are reflective of the health risks of vaping, especially for young people.
In January, the government announced that it would ban disposable vapes and restrict sweet and fruity flavours . Lead author Donal O’Shea, professor of chemistry at RCSI, said that the UK government should go further and remove all flavours from vapes.
It is crucial to understand the impact of flavoured vapes on health “before it’s too late”, he added.
“It is plausible that we are on the cusp of a new wave of chronic diseases that will emerge 15 to 20 years from now due to these exposures.”
Given the popularity of flavoured vapes among non-smoking teenagers and young adults, understanding the long-term effects of these products on public health, morbidity and mortality is crucial, the study concludes.
“Without comprehensive regulation, as we try to treat the nicotine addictions of older tobacco smokers, there is a substantial risk of transferring new health issues to younger generations.”
Responding to the findings, a Department of Health and Social Care spokesperson said: “The health advice is clear – if you don’t smoke, don’t vape and children should never vape.
“That’s why we are banning disposable vapes and our tobacco and vapes bill includes powers to limit flavours, packaging and displays of vapes to reduce the appeal to children.
“It is clear that flavours like cotton candy and cherry cola are deliberately being targeted at children, not adult smokers trying to quit, which is completely unacceptable. That is why we are taking decisive action and will be restricting vape flavours.”
Prof Sanjay Agrawal, the Royal College of Physicians’ special adviser on tobacco, said that while vaping can be a very effective way to break the addiction to tobacco, it should only be used for this purpose.
“Vaping is not risk-free, so those who don’t smoke, including children and young people, should not vape either,” he said.
John Dunne, director general at the trade body the UK Vaping Industry Association, said: “The science on vaping is very clear, it is the most effective way for smokers to quit and is at least 95% less harmful than smoking. Every chemical used in vaping e-liquid in the UK is stringently tested, including analysing chemicals when heated, and is only approved for use by the UK government if it is deemed safe.”
Most viewed

IMAGES
VIDEO
COMMENTS
The new scientific statement, "Cardiopulmonary Impact of Electronic Cigarettes and Vaping Products," details the latest usage data and trends, identifies current health impacts, highlights existing basic and clinical scientific evidence surrounding e-cigarettes and recommends research priorities to further understand the short- and long ...
Chronic use of e-cigarettes, commonly known as vaping, can result in small airway obstruction and asthma-like symptoms, according to researchers at Harvard-affiliated Massachusetts General Hospital. In the first study to microscopically evaluate the pulmonary tissue of e-cigarette users for chronic disease, the team found in a small sample of ...
29 September 2022. Vaping substantially less harmful than smoking, largest review of its kind finds. New research from the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King's College London has found that the use of vaping products rather than smoking leads to a substantial reduction in exposure to toxicants that promote cancer, lung disease and cardiovascular disease.
NIH-funded studies show damaging effects of vaping, smoking on blood vessels. October 26, 2022, 2:00 PM EDT. Combining e-cigarettes with regular cigarettes may increase health risks. Long-term use of electronic cigarettes, or vaping products, can significantly impair the function of the body's blood vessels, increasing the risk for ...
Health. How bad is vaping for your health? We're finally getting answers. As more of us take up vaping and concerns rise about the long-term effects, we now have enough data to get a grip on the ...
Further research is required to elucidate the short- and long-term consequences of vaping to determine whether e-cigarettes are truly a "safer" alternative to traditional cigarettes for ...
The origins of vaping. Vaping achieved widespread popularity over the past decade, but its origins date back almost a century and are summarized in figure 1.The first known patent for an "electric vaporizer" was granted in 1930, intended for aerosolizing medicinal compounds.23 Subsequent patents and prototypes never made it to market,24 and it wasn't until 1979 that the first vape pen ...
The scientific statement from the American Heart Association, published Monday in the journal Circulation, highlights the latest usage data and scientific evidence showing health effects of e-cigarette use, also called vaping. It also recommends research priorities to better understand how these products may affect people's health over time.
While the long term effects of vaping are still unknown, the harmful effects of smoking are indisputable - smoking causes around 55,000 cancer deaths in the UK every year. Cancer Research UK supports balanced evidence-based regulation on e-cigarettes from UK governments which maximises their potential to help people stop smoking, whilst ...
Gloved hands of lab technician conducts research on electronic cigarettes, or e-cigs, and vaping pens, inside a laboratory environment. CDC/ Von Roebuck Long-term use of electronic cigarettes, or vaping products, can significantly impair the function of the body's blood vessels, increasing the risk for cardiovascular disease.
August 15, 2023. Young people who use electronic cigarettes or vape report increased respiratory symptoms, including wheezing and shortness of breath, compared to those who don't use e-cigarettes, according to a new study. The use of electronic cigarettes has increased in recent years among adolescents and young adults.
With support from Cancer Research UK, we search for new evidence every month as part of a living systematic review. We identify and combine the strongest evidence from the most reliable scientific studies currently available. ... "While the long term effects of vaping are still unknown, the harmful effects of smoking are indisputable ...
Little is known about the effect of vaping on the immune system. Interestingly, both traditional and e-cigarette consumption by non-smokers was found to provoke short-term effects on platelet function, increasing platelet activation (levels of soluble CD40 ligand and the adhesion molecule P-selectin) and platelet aggregation, although to a lesser extent with e-cigarettes [].
B.A. King and OthersN Engl J Med 2020; 382:689-691. Interventions aimed at curbing two related U.S. epidemics connected with vaping — an outbreak of lung injuries and a continued surge in use by ...
Shields is one of few researchers who has already probed human lungs for e-cigarettes' effects. Last month, his group published a paper in Cancer Prevention Research that compared 15 healthy volunteers who used e-cigarettes without nicotine for 4 weeks with 15 people who never smoked or vaped. (He did the study before concerns about acute lung ...
Two new analyses from research comparing cardiovascular function in people who vape, people who smoke and people who did not use any nicotine found significant negative health impacts among participants after vaping and smoking combustible cigarettes. In one report, people who used e-cigarettes and people who smoked combustible cigarettes had ...
Vaping involves the heating of chemical solutions (e-liquids) to high temperatures prior to lung inhalation. A risk exists that these chemicals undergo thermal decomposition to new chemical ...
The epidemic of teen vaping [1-3] and the outbreak of vaping-related lung injuries and deaths in the U.S. [4] underscore the urgent need to systematically regulate electronic cigarette manufacturing, marketing, and distribution. However, development of plausible and effective vaping regulations and most importantly, their enforcement are likely to present unique challenges to countries ...
A growing body of evidence gathered over the last 15 years has shown that using an electronic cigarette ("vaping") is probably far safer than smoking and likely to help smokers quit their deadly habit forever. Certain segments of the public health establishment have reacted oddly to these results—they've ignored them and treated vaping as a serious threat.
A study released today from the U.S. Food and Drug Administration and the U.S. Centers for Disease Control and Prevention (CDC) found that 2.55 million U.S. middle and high school students reported current (past 30-day) e-cigarette use in 2022, which includes 14.1% of high school students and 3.3% of middle school students.
So, vaping isn't risk-free and children and people who have never smoked shouldn't vape. But research overall still finds that legal vaping is far less harmful than smoking and can help people who smoke to stop. What did the researchers do? The researchers looked at chemical 'marks' that add information to the genetic code in our DNA.
In addition, the Lung Association has called on federal officials to do more to ensure youth who are addicted to vaping and other tobacco products have resources to help them end their addiction. ... New Research Publication Lights Fire about Dangers of Vaping. January 12, 2023. Blog last updated: August 25, 2023.
This resource is collection of the best and latest research on vaping and other reduced-harm products, medical journal articles, as well as journalistic pieces organized by topic that contain valuable data, information, and perspectives on tobacco harm reduction, vaping, and safer nicotine products. Our intention is update this resource with ...
Research increasingly reveals health risks of e-cigarette use, and more studies are needed about the long-term impact e-cigarettes may have on the heart and lungs, according to a new scientific ...
1 in 5 high schoolers self-reported that they currently use or have used an e-cigarette/vape product in the past 30 days. 1 in 20 middle schoolers reported the same. More than 8 out of 10 young people who currently vape report using flavored e-cigarettes. There has been a notable increase in the use of disposable e-cigarettes.
Vaping also is strongly linked with a serious medical condition that damages the lungs due to the vitamin E acetate, an additive used in tetrahydrocannabinol-containing e-cigarettes. In 2022, 6% of adults in the U.S. reported current vaping device use. Widespread use by adults has raised concerns about EVP use among adolescents.
Mental health is a growing concern among youth. 26 27 Youth vaping and cigarette use are associated with mental health symptoms such as depression. 22 28. The most common reason middle and high school students give for currently using e-cigarettes is, "I am feeling anxious, stressed, or depressed."
The research team at RCSI University of Medicine and Health Sciences, Dublin, conclude there is a "potential public health threat facing the 4.5 million vapers in the UK" and an urgent need ...
Kids and young adults who use social media for seven or more hours per day have double the risk of taking up vaping or smoking or both, new research shows. Health News // 15 hours ago.
The emergence of future cancers and cardiovascular problems is "almost a certainty" from long-term exposure to vapes, according to a Professor of Chemistry at Royal College of Surgeons Ireland.