Personal Nursing Philosophy, Values and Beliefs Essay
Introduction, my personal philosophy, why i am in school, works cited.
A personal philosophy can be defined as a set of beliefs, attitudes, concepts, and convictions that guide an individual’s way of living and doing things, personally and professionally. Many people consider the creation of personal philosophy as an elementary exercise that serves only to fulfill the requirements of certain academic endeavors. However, it is an indispensable component of proper life because it allows people to make better choices that are based on personal values and beliefs.
Moreover, it gives their life purpose because they act and behave in ways that aim to achieve certain desired outcomes. As a nursing major, my personal philosophy is based on my inclination to help people alleviate suffering and improve the quality of their lives. It is my duty to apply my knowledge and skills to prevent and manage illnesses so as to improve the physical, psychological, and spiritual well-being of patients.
My personal philosophy is founded on certain beliefs and values that guide my decision-making and that inspire me to engage in a meaningful contribution in my career as a nurse. My beliefs and values influence the choices I make every day. Therefore, it is important for me to identify them, clarify their influence, and live them daily. These values include honesty, responsibility, compassion, lifelong learning, and kindness.
Nursing is not only a career, but a calling that requires the possession of integrity, knowledge, and compassion (Kim 54). My personal philosophy postulates that I have a responsibility to use my knowledge and abilities to help people alleviate their suffering by providing safe and holistic patient-centered care regardless of their race, ethnicity, gender, religion, or sexual orientation. It is my responsibility to meet my needs and those of my patients by being honest, kind, and compassionate. Moreover, it is my obligation as a nurse to create a healthy environment that will promote a speedy recovery and improve the physical and psychological well-being of patients. I am committed to lifelong learning because that is the best approach to improving the quality of my life and progressing in my career.
I am a passionate and spiritual human being who is committed to using physical, mental, and spiritual capabilities to live a meaningful life through service in the nursing profession. I am a product of my beliefs, ideas, and values that have been acquired through life experiences and the acquisition of knowledge. Spirituality is an important component that enhances an individual’s kindness and compassion (Smith and Parker 83). Important components of self-identity include world view, self-esteem, personality attributes, physical attributes, and knowledge of one’s skills (Masters 95). Self-identity is an important aspect of building a strong character. I chose to pursue a career in nursing owing to my attributes that include compassion and commitment to alleviate physical suffering.
My goals are to graduate with a bachelor’s degree in nursing, maintain a lifelong learning habit, and help people to prevent and manage diseases through the application of skills and knowledge obtained in school. In addition, I want to become a nurse practitioner and researcher so that I can make meaningful contributions to society. After graduation, I intend to pursue a Master of Science in Nursing (MSN) degree and go into advanced nursing practice. I believe that pursuing a master’s degree in nursing will empower me to make significant contributions to society by becoming an advanced nursing practitioner (Hood 65). In addition, it will equip me with advanced research skills that will be useful in my commitment to lifelong learning.
I am in school to acquire the necessary knowledge that is required for advanced nursing practice. The nursing program’s courses, extracurricular activities, and personal as well as professional interactions and networks will equip me with the skills necessary for success in life. The main goal of attending school is to develop proper attitudes and competencies, as well as improving skills in human interactions, problem-solving, and decision-making (Smith and Parker 35).
The core skills, values, and attitudes of nursing can be obtained only by enrolling in an appropriate nursing program (Schober 62). One of my goals is to maintain a lifelong habit of learning. In that regard, attending school will enhance my creativity and research skills, which are necessary for lifelong learning. I am also in school to enhance my communication skills. Effective communication is an important skill to possess in nursing because it enhances the provision of quality health care (Smith and Parker 48).
My personal philosophy is applicable to all aspects of my personal and professional endeavors. It is based on values that include integrity, kindness, responsibility, compassion, and lifelong learning. My major goal is to pursue a Master of Science in Nursing (MSN) degree after completing my undergraduate degree. I want to go into advanced nursing practice because it will offer me the opportunity to contribute to society in a meaningful way. The knowledge and skills that I will acquire in school will be necessary for the attainment of personal and professional goals.
Hood, Lucy. Leddy and Pepper’s Conceptual Bases of Professional Nursing . Lippincott Williams & Wilkins, 2013.
Kim, Hesook Suzie. Essence of Nursing Practice: Philosophy and Perspective . Springer Publishing Company, 2015.
Masters, Kathleen. Role Development in Professional Nursing Practice . 4 th ed., Jones & Bartlett Publishers, 2015.
Schober, Madrean. Strategic Planning for Advanced Nursing Practice . Springer International Publishing, 2017.
Smith, Marlaine C., and Marilyn Parker. Nursing Theories and Nursing Practice . F. A. Davis, 2015.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, May 18). Personal Nursing Philosophy, Values and Beliefs. https://ivypanda.com/essays/personal-nursing-philosophy-values-and-beliefs/
"Personal Nursing Philosophy, Values and Beliefs." IvyPanda , 18 May 2021, ivypanda.com/essays/personal-nursing-philosophy-values-and-beliefs/.
IvyPanda . (2021) 'Personal Nursing Philosophy, Values and Beliefs'. 18 May.
IvyPanda . 2021. "Personal Nursing Philosophy, Values and Beliefs." May 18, 2021. https://ivypanda.com/essays/personal-nursing-philosophy-values-and-beliefs/.
1. IvyPanda . "Personal Nursing Philosophy, Values and Beliefs." May 18, 2021. https://ivypanda.com/essays/personal-nursing-philosophy-values-and-beliefs/.
Bibliography
IvyPanda . "Personal Nursing Philosophy, Values and Beliefs." May 18, 2021. https://ivypanda.com/essays/personal-nursing-philosophy-values-and-beliefs/.
- Lifelong Learning in Bedside Nursing
- Heutagogy and Lifelong Learning
- Lifelong Learning is Necessarily Essential to Globalization
- Collaborative Success Plan in Nursing
- Effect of a Multi-Level Intervention on Nurse
- Leadership Roles and Management Functions in Nursing
- Nursing Practice: Notes from Personal Journal
- Ethical Issues in Nursing Education and Practice

Top 25 Professional Nursing Values + Why They're Important

If you are a nurse seeking to find ways to boost your career and your relationships, the best way to start is by developing strong professional nursing values. Maybe you are wondering, “What are the top professional nursing values?” or “How do I learn about professional nursing values?” If that sounds like you, this article is for you. As you continue reading, you will find 25 top professional nursing values and why they are important to successful nursing.
What Exactly Are Professional Nursing Values?
7 main reasons why professional values are important in nursing, what are the top professional nursing values, 1. trustworthiness, what is it:, why is it important in nursing:, 2. accountability, 3. compassion, 4. integrity, 5. value diversity, 6. curiosity, 7. autonomy, 8. positive self-esteem, 10. professionalism, 11. desire for excellence, 12. altruism, 13. ingenuity, 14. respect for human dignity, 15. ethical, 16. advocacy, 17. precision, 18. loyalty, 19. cultural humility, 20. dedicated to learning, 21. selflessness, 22. supports social justice, 23. sympathy, 24. professional competency, 25. commitment to nursing, my final thoughts.

Nursing Values and Beliefs: Influence on Nursing Profession
The essay focuses on how values and beliefs shape the nursing profession. It will examine the core principles such as compassion, advocacy, ethics, and lifelong learning that underpin nursing practice. The piece will discuss how these values are essential in patient care, influencing decision-making and the nurse-patient relationship. The overview will also explore the evolving nature of these values in response to changes in healthcare systems and societal expectations. Also at PapersOwl you can find more free essay examples related to Cognition.
How it works
Anyone that has ever worked in the healthcare field knows that caring for individuals in their most vulnerable state is a very rewarding yet difficult job to do. Throughout this paper, I will be discussing my personal philosophy of nursing and all the factors that affect it. My self-concept, my values, and how I believe culture influences my philosophy of nursing will also be addressed throughout this paper. I will later discuss a professional and official nursing theory, framework, or model that reflects and support my personal philosophy.
I will then be applying my philosophy of nursing into how I currently apply it in my practice as a Registered Nurse.
My personal philosophy of nursing is definitely influenced by my own beliefs, convictions, and experiences that I have had all throughout my life. Growing up, my mom was also very sick. Being in and out of hospitals with her constantly allowed me to see the true power of honorable nursing. I learned very quickly that I wanted to be a nurse so that I could be a glimpse of hope to my patients’ families. I believe that one of the most important aspects of my philosophy is being your patient’s advocate. During a general hospital stay, there are so many different interdisciplinary providers that are going to be involved in your patient’s care that want all different things. As a nurse, it is important to be able to be the voice for your patient and advocate for their desires, all while respecting the advice coming from the other providers. Although advocacy has not also been recognized as a rightful duty of a nurse, the American Nurse Association that advocacy is now a major component of high-quality practice (ANA, n.d.).
Another major aspect of my philosophy of nursing is to continue refreshing my skills and knowledge by keeping up to date with current evidence-based practice. I have met and worked with lots of nurses who are known as “old-school” and refuse to refine their skills based on current practices. This is not only an issue of pride but a safety concern as well. I believe in order to provide the most efficient care, we must know what new breakthroughs are taking place.
I believe in complete honesty with my patients, and integrity must be upheld in and outside of my patient’s rooms, all while standing true to my own personal spiritual and ethical values and beliefs.
- 0.1 Self-concept
- 0.3 Culture
- 0.4 Nursing Model and Framework
- 0.5 Application into Practice
- 1 Conclusion
Self-concept
In order to be an honest, trustworthy, and respected nurse, I must be honest with myself. Not many of us enjoy discussing our strengths, weaknesses, shortcomings, or gaps in knowledge, but all of these things affect our philosophy of nursing and how we practice. As I develop into an experienced nurse, I hope that the things I view as my strengths help me in areas of nursing. I have extreme control and calamity in stressful situations allowing me to take control of codes, think clearly, and not allow fear to overcome during these stressful times. Although I see compassion as both a strength and a weakness, I feel as though it has benefited me more than hurt me. I also have very strong communication skills. Thanks to my extensive experience in customer service, I have developed dependable communication skills in all different types of situations. In addition to the previously listed strengths, I strangely enjoy critical thinking! I am also curious to learn how cause and effect have played in any situation.
Some weaknesses of mine include overly empathizing with people and being able to be manipulated. Even though I believe a necessary value to uphold in nursing is compassion and empathy, I tend to grow attached to my long-term patients, and some people see that as an opportunity to take advantage of me. Ever since I started nursing, I have struggled with believing in myself and giving myself the self-encouragement and confidence needed. My weakness and fears go hand in hand. I am fearful of making a fatal error in my patient care and fearful I am not going to catch a critical mistake on my end or anyone’s end, for that matter.
I view Cardiology as a major gap in knowledge. Although I know the basics and have educated myself on the most common disease process, I have always struggled with this complex system. This gap in my knowledge influences my self-concept negatively. I see Cardiology as a weakness for me, and it causes me to doubt my ability to care for complex diseases within the cardiac system.
My self-concept influences my philosophy of nursing in a few ways. As I stated above, my strengths include self-control and calamity, compassion, empathy, and communication skills. Being an advocate for patients is very hard to do without compassion, empathy, or communication skills. In times of need, our patients rely on us to be their voice when they cannot speak. Also, in order for my patients to trust me and be able to view me as an honest nurse, I must be willing to communicate with them on any and every level they need.
My values originate from my childhood, what I was taught to believe in as a child, and have developed over time as I have blossomed into my adult life. Although most of my values reflect my philosophy of nursing, some beliefs do conflict with my nursing practice. I work in the NICU, so none of my patients have a voice to speak for themselves. Advocacy is a constant conflict between the nurses, parents, and doctors caring for a particular newborn. There are many doctors who assume a god complex, and there have been times when the parents have stated that they do not wish for any “extraordinary measures” taken, but the doctors fail to abide. I believe in complete honesty as a core value in and out of practice, so that reflects in my philosophy, forcing me to be honest with my patients. I believe in doing my best in all things, not for my own gain, so keeping up my skills, doing my own research, and practicing underneath the most current evidenced-based practice supports that value of mine.
My decision-making process is influenced by the ICN Code of Ethics for Nurses. According to the ICN Code of Ethics, we have four responsibilities as caretakers. “to promote health, to prevent illness, to restore health and to alleviate suffering…” (ICN, 2012). In order to uphold these values, I must be responsible for thoroughly assessing my patients, educating them on their available options honestly, promoting their active decision-making in their own care, and treating them free of judgments and presumptions.
Being culturally diverse in my nursing care means that I will care for and treat all my patients equally, regardless of their cultural or spiritual beliefs, convictions, and limitations. I have a belief set spiritually that I follow in my everyday life. I would be lying if I said that I don’t struggle with bringing that into my nursing practice. Being a nurse, I will come into contact with all different types of cultures, some that I just simply do not understand, but it is important to become culturally competent so that ethnocentrism does not occur. Ethnocentrism is a thought process that can occur that compares other cultures to our own while believing that ours is superior (Barger, 2017). Having this mindset in practice will cause confusion and conflict.
Nursing Model and Framework
A popular nursing model that goes hand-in-hand with my philosophy of nursing is Kolcaba’s Theory of Comfort. Developed in the 90s, this theory focuses on promoting and advocating for comfort in our patients. Some key characteristics of the model include ease, relief, and transcendence in our patients. The theory is that if the needs of the patients are met and if the patient is satisfied by our care health-wise, they will feel more at ease and feel relief. Our job as nurses, according to this model, is to assess and be aware of what our patient’s needs are, develop appropriate nursing care plans, and then reassess later for how the patient’s comforts are (Petiprin, 2016.) Kolcaba’s model relates to my philosophy of nursing because I stated above how important advocacy is to me. The only way to promote accurate advocacy is to thoroughly assess my patient and promote their needs and wants. Along with implementing the most appropriate care, I must communicate with them to find out their comfort levels, desires, and how they would like to proceed with their care which reflects Kolcaba’s model of assessing the patient’s comfort.
Application into Practice
My personal philosophy of nursing is translated into practice every day as I treat patients. Patient advocacy, honest communication, and my belief in keeping up with current breakthroughs are the key elements in my philosophy. With that being said, I have and will continue to treat my patients equally, advocating for their care regardless of my opinion and the conflict that it could cause, communicating their diagnosis and treatment options to them honestly, and not relying on my knowledge only in clinical care but instead, keeping up with new evidence-based practices.
It is hard to balance business and patient care, but it definitely is possible. Our goal clinically is to provide the best ethically sound, patient-centered care that we possibly can as healthcare provider, but it is hard to do so without considering the business aspect of healthcare. There are many current trends that are affecting quality care. One trend in specific is the lack of access to care that some individuals have. Private medical insurance costs are through the roof, and according to AFSCME, about 29 million people with private health insurance are at a very high risk of financial disaster if they were to endure a serious illness or injury (AFSCME, 2018.). These are real problems, and people who are without proper health insurance or fearful of what their financial situation would be if they were diagnosed fail to get the care they need because of the cost.
This paper gave me the opportunity to share what I view as important. It allowed me to share my philosophy of nursing and the key elements that have influenced how I view nursing. My self-concept, values, and cultural beliefs help influence my philosophy of nursing, along with researching different types of nursing models. I was able to describe how I put my philosophy into action in my everyday clinical practice.
Cite this page
Nursing Values and Beliefs: Influence on Nursing Profession. (2023, Jun 19). Retrieved from https://papersowl.com/examples/nursing-values-and-beliefs-influence-on-nursing-profession/
"Nursing Values and Beliefs: Influence on Nursing Profession." PapersOwl.com , 19 Jun 2023, https://papersowl.com/examples/nursing-values-and-beliefs-influence-on-nursing-profession/
PapersOwl.com. (2023). Nursing Values and Beliefs: Influence on Nursing Profession . [Online]. Available at: https://papersowl.com/examples/nursing-values-and-beliefs-influence-on-nursing-profession/ [Accessed: 18 May. 2024]
"Nursing Values and Beliefs: Influence on Nursing Profession." PapersOwl.com, Jun 19, 2023. Accessed May 18, 2024. https://papersowl.com/examples/nursing-values-and-beliefs-influence-on-nursing-profession/
"Nursing Values and Beliefs: Influence on Nursing Profession," PapersOwl.com , 19-Jun-2023. [Online]. Available: https://papersowl.com/examples/nursing-values-and-beliefs-influence-on-nursing-profession/. [Accessed: 18-May-2024]
PapersOwl.com. (2023). Nursing Values and Beliefs: Influence on Nursing Profession . [Online]. Available at: https://papersowl.com/examples/nursing-values-and-beliefs-influence-on-nursing-profession/ [Accessed: 18-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
- Toggle navigation
Carolann Mclawrence's ePortfolio
A city tech openlab eportfolio.

Personal Statement of Beliefs/Philosophy about Nursing
My philosophy is one which I will stand by for the duration of my nursing profession. This philosophy is based on providing competent, empathetic, compassionate and optimal holistic care to the best of my ability. This philosophy stems from the values and beliefs instilled in me during my early childhood. These values and beliefs are accompanied by trustworthiness, respect, compassion, and that is what drove me to this profession and is currently driving me as I continue to provide care to my patients, family and the community.
It is my belief that in order to keep in stride with what my philosophy is education will have to play a very significant role. Continued education about issues related to patient care is very important. Through extensive research a wealth of information is found, this information can be transposed to the knowledge I already have, can greatly enhance my skills, therefore allowing me to be better able to provide optimal quality care.
I believe that the cultural beliefs, ethnic background and sexual orientation of patients and families should be respected and I am confident in my ability to continue my profession without showing any form of discrimination. I vow to uphold the ethical codes of the American Nurses Association and Joint Commission Standards by providing safe care, privacy and confidentiality and protecting the patient’s rights. I strive to be an educator, an advocate and a promoter of disease awareness, good health practices, and a supporter of strong family values within the community and the world. I believe that nursing is more than just a career, it is a privilege taken upon by persons who are passionate about using their knowledge and skills to help those who are unable to help themselves.
The OpenLab at City Tech: A place to learn, work, and share
The OpenLab is an open-source, digital platform designed to support teaching and learning at City Tech (New York City College of Technology), and to promote student and faculty engagement in the intellectual and social life of the college community.

New York City College of Technology | City University of New York
Accessibility
Our goal is to make the OpenLab accessible for all users.
Learn more about accessibility on the OpenLab
Creative Commons
- - Attribution
- - NonCommercial
- - ShareAlike

© New York City College of Technology | City University of New York

How to Write a Nursing Reflective Essay (Guide for Nurse Students)

If you are a nursing or medicine student, you are aware that you will come across or have already come across assignments requiring you to write a nursing reflection essay. At first, such a task always appears challenging, but given the understanding of the steps, things flat out, and you can write reflective essays and get better grades.
Reflective practice is highly encouraged in nursing. Reflection entails making sense of situations, events, actions, and phenomena in the workplace.
As a nursing student, you will be asked to write a reflective essay on your clinical placement, practicum, shadowing experience, shadow health DCE activities, personal nursing philosophy, why you want to become a nurse, nursing program, ethical dilemma, knowledge, skills, and abilities, systems, and processes.
The easiest way to complete the reflective essay assignment is by first determining what reflective writing entails, its significance, its steps, and some of the best tips that form the core of this ultimate guide.
Basics of Reflective Writing in Nursing
Reflective writing is an analytical writing practice where the writer describes a real or imaginary event, scene, phenomenon, occurrence, or memory, including their takeaway. It entails the critical analysis of an experience, including recording how it has impacted you and what you intend to do with the new knowledge or how to act when such an occurrence recurs.
As you document the encounter, you can use first-person pronouns and write subjectively and objectively. This means that you can decide to either use personal experiences alone or support these experiences using citations from scholarly sources.
When writing a reflective essay in nursing, you must recount the events and give critical detail of how the events shaped your knowledge acquisition. Reflection helps nursing students develop skills in self-directed learning, which is directly associated with high motivation and improved quality of care .
In most cases, reflection occurs on what went well and what went wrong. It could be a successful operation, a thank you note from a patient, a patient who regained their health faster, or a new nursing care plan that worked. However, it can also be about adverse events such as death, postoperative complications, death of an infant at birth, dissatisfied patient, medical error, or a failed procedure.
As a nursing student, when you learn to reflect on situations, you grow to become a professional nurse who diligently does their noble duty.
When writing a reflective essay, you begin by setting the scene (explaining what, where, how, and who-the situation), detailing how you felt (emotional state), why it happened (making sense of the situation), critical review and development of insights, a note on what was learned, and strategies to address future recurrence.
Your professor may ask you to write a nursing reflective paper about various topics in your course or your experience working in a group, how you solved a problem, a healthcare issue, or clinical practice. Consider the following example of a reflective statement in nursing; in my clinical practices, I realized I focused more on the technical aspects but failed to explain what it was doing to improve their health. I would like to understand more about listening to patience and their concerns to better care for them.
As you will notice later, these reflective stages are structured into different reflective models and frameworks that we will explore in-depth. So, with the understanding of what comprises reflective writing and its importance in nursing, let's now get solid on the structure.
Related Reading:
- Philosophy of Nursing Example.
- Ideas and topics for nursing capstone or project papers
- How to write a SOAP note paper
- Top nursing debate topics
- Nursing Theories and Theorists.
Structure of a Reflective Essay in Nursing
A reflective essay is an analytical writing piece describing and evaluating encounters or experiences. When asked to write one, you should know that an excellent reflective essay consists of different parts, just like a typical academic essay. It comprises the cover or title page, introduction, body paragraphs, conclusions, and a references page.
The title page contains information about the assignment. If you are writing the reflective essay in APA, include these on the title page:
- Title of the reflective essay
- Course code and name
- Instructors name
- Name of your institution
- Date of submission
When writing in Harvard format, the title or the cover page will consist of the following:
- Title of the essay in title case and the page number (upper right margin),
- Title of the essay in CAPS,
- Name of class or course,
- Name of the instructor,
- Name of your school,
- City and state where your school is located and,
- The date of submission.
Introduction
The introduction begins with an attention grabber or a hook sentence to attract readers' attention. It should then explain the essay's purpose and signpost the ideas that will come later in the essay. The introduction also has a thesis statement at the end of the paragraph- the last sentence. The thesis is concise, clear, and relatable and should reflect your position.
Body Paragraphs
The body paragraphs of a reflective essay can be three or more, depending on the length of the essay. Essentially, the body comprises 80% of the total word count.
The first paragraph is where you describe the situation, including the events, why they occurred, how they occurred, and those involved.
The second paragraph entails your personal feelings or reaction to the situation and how it made you feel.
The third paragraph can include making sense of the situation. You have to think about why things happened the way they did. You should also critically review and develop insights based on the situation. Finally, think of the factors that could have influenced the situation.
The next paragraph should explain how the event or situation will change your practice, approach, decisions, perspective, or perception. This is where you evaluate the experience by detailing the knowledge and skills you took from the experience.
The last body paragraph should entail a critical reflection on the learning opportunities. First, describe the situation and what it made you learn. Next, elaborate on how you intend to make yourself better poised to address such situations.
Mostly, you should structure the body of your essay as per the preferred nursing reflective model.
After everything else falls into place, you need to summarize the information you presented in the essay. Then, finally, restate your thesis and have a call to action to bring a sense of closure to your readers.
Steps for Writing a Nursing Reflection Essay � The Guide
When assigned to write a reflective essay for your nursing class, here are the surefire steps to get you to success.
Read the instructions
The first step after receiving an assignment is to begin reading the instructions. as you read, note what your instructor or professor expects in the paper you will submit for marking.
Reading instructions helps you to get informed on the scope of the paper, word count, number of references and pages, and the formatting style to use.
Besides, you also get to plan your paper with the deadline highlighted in the instructions.
You need to get a conducive environment where you can start writing.
The first step of writing is to brainstorm about situations during your clinical hours when you were shadowing a Nurse Practitioner or one you have read about.
Assess whether the situation or scenario you have thought, encountered, or chosen can help you write a reflective essay that meets the requirements.
Research and Plan
After choosing a scenario, the next step is researching the best reflective model.
You can use your class text, the instructions, the college library, course readings, and online nursing journals to get articles and resources with information about specific reflective models.
Select the best reflective model and take notes on the steps it entails.
As you research, write down notes on how to address your paper based on your selected framework or model of reflection . Additionally, research nursing journal articles with information you can use when critically analyzing a situation.
Plan how you will handle the paper as well. For instance, as you research, develop a thesis statement that grounds your entire paper, then draft an outline on how to develop the thesis.
Write an Outline
Outlining is a crucial aspect of writing. It helps you envision how you will meet the objective of writing a reflective essay. As an essential part of the essay writing process, outlining helps create a good flow of ideas and can come in handy in helping you overcome writer's block. Your outline should comprise the following:
- The hook or attention grabber
- Thesis statement
- Main points of each body paragraph (topic sentence, evidence, examples, illustrations, etc.)
- Conclusion (restated thesis and call-to-action)
With the outline done, you should take a break and resume writing your first draft of the nursing reflection essay. Writing with an outline helps avoid mistakes and also helps you write faster.
Describe the Experience
Once you have identified the relevant experience, begin describing it chronologically.
Describe the experience that prompted you to consider nursing your ideal career goal. Think of this experience's key elements, such as the setting, patient demographics, and significant events that impacted you.
Show how these events changed your perspective on life. Ensure you are as descriptive as possible to paint a clear picture for readers.
Consider the following questions to come up with a good description:
- What happened?
- Was there someone involved? If yes, what part did they play?
- Where did the event take place?
- What actions did you take?
Set the context of this experience by giving relevant background information. Ensure you are objective and pay attention to the facts.
Provide a Reflection
Talk about your feelings and thoughts concerning the particular experience you went through. You have to be honest and open up about your initial expectations and challenges you faced at each stage of the experience. The following questions can help you come up with a good reflection:
- What was I trying to achieve?
- What prompted me to act the way I did?
- Are there any consequences for my actions? If yes, what are they?
- How did I feel about this event as it was happening?
- How did those around me react to it?
- How do I know how those around me felt about it?
Analyze the Experience
Description of an experience is essential, but so is analysis. You have to move beyond the surface and give a critical analysis of your experience.
State your actions, and your overall experience will give insights into your experience. Think of how the experience has impacted your actions, feelings, and thoughts.
Give an Evaluation
Evaluate the skills and knowledge you got from the experience. Show how you can apply these skills and knowledge in your nursing practice. Also, state the actions and interventions you took during the nursing experience.
State whether you achieved the desired outcome and if there are any specific areas that you need to improve on.
Talk about how you built or improved skills like communication, teamwork, and critical thinking.
As you evaluate the experience, identify what you believe to be your strengths and weaknesses in the nursing experience. What have you learned from the experience? State the areas where you excelled and what abilities contributed to your success.
Talk about how those you were with during the clinical experience complimented you. Similarly, acknowledge your weaknesses.
What kind of mistakes did you make, and how did you improve them? Talk about the tasks that drain you most during the experience.
Illustrate Learning
Demonstrate elements of deeper thought and reflection levels. This is a great point to include nursing theories in your reflection essay to support analysis of your experience.
Relate your experiences to the theoretical frameworks you were taught in class. This is effective learning and will demonstrate your ability to apply knowledge to real-life nursing situations.
Doing this will also show that you can effectively deduce different things from observations made during the reflection process.
Ensure you also demonstrate a change in perspective, as this will prove that you learned something from the experience.
Write Your Conclusion
Conclude by summarizing your points and highlighting the lessons learned.
The lessons you reached as part of your reflection should support your overall conclusion.
Also, restate your thesis statement.
Come Up with an Action Plan
Now that you have learned from your reflection develop an action plan for future nursing practice.
This part should contain all the details you have learned and actions needed to improve when faced with a similar situation. Consider the following questions:
- What would I change if faced with a similar situation?
- How can I develop the necessary skills needed to face this situation?
- How can I act differently in a similar situation?
Ensure you identify areas to improve and set realistic goals to enhance your nursing skills. Discuss how you intend to seek additional education, training, or mentorship to address your shortcomings.
Finally, end the essay with a happy note so readers know you learned something from the experiences.
Proofread, Edit, and Polish
After doing your first draft, take a break to relax and get out of the writing mood - it helps you to become objective.
You can then resume reading out loud to yourself, make necessary tweaks, and ensure that every part you include meets the rubric requirements.
Edit for grammar, punctuation, tenses, voice, spelling, and use of language. You should also proofread the essay to adhere to the style, organization, and presentation requirements.
Ensure that all the in-text citations are accounted for in the reference list and are up-to-date. You are good to go when you have an essay that meets all the instructions.
Finally, you can submit the paper for grading.
Writing is not everyone's cup of tea. For that reason, you can hire a nursing reflection essay writer from our website to assist you in crafting a top-grade paper. In addition, we have nursing writers whose forte is writing various nursing papers.
Choosing the suitable Reflective Model or Framework
As you can see above, many reflective models are used for your reflective essay. We have not exhaustively listed and expounded on all of them. Other reflective models and frameworks you can also consider when writing a reflective essay in nursing include:
- Bouds Reflective Model
- Brookfield Reflective Model
- Pender's Health Promotion Model
- Roper Logan and Tierney Model
- Driscoll Reflective Model
- The Johari window model
Note that most nursing instructors will often suggest the models they prefer for you to use in your essay.
For example, in most nursing reflective essays. Whichever the case, readily available information expands on each model to make it easier to write a reflection essay on a specific aspect of nursing education or practice.
Read the assignment rubric and instructions to understand the specific model. If it is unclear, ask for clarification from your instructor early enough.
Tips for Writing a Good Nursing Reflective Essay
As you try to figure out how to write a nursing reflective essay, keep the following tips in mind.
Choose the Right Topic
If the instructions from your professors involve choosing a topic for the reflective essay, you must select one that is meaningful to you.
This will ensure you can easily write and easily develop relevant elements about the topic. Therefore, take time to pick a topic that you find interesting.
As you write, ensure you stay on topic, whether sharing a one-off event or a recurrent story.
Use the Right Tone
A reflective essay is more personal, unlike other types of academic essays. This means you don't need a strict or formal tone.
Since this is about your experiences, use personal pronouns such as I and Me.
Be Vulnerable
You must be extremely vulnerable to learn how to write a reflective essay in nursing.
Be open about your thoughts, feelings, and beliefs about something you went through that sparked an interest in nursing.
It's okay to share mistakes or things you did wrong that eventually led you to this career path.
Choose the Right Focus
A reflection essay is all about narrating your experience during the nursing experience.
While including other people in your experience is okay, please let them not be the center of your reflection.
This is your essay, so you should be the focus of attention.
Keep it Brief
A good nursing reflection essay should be between 300 and 800 consciously written words. Because of this length, you must only write relevant information about your reflection. Refrain from lengthy reflections, as they make it difficult to pass your points across.
Convey Your Information Wisely
Even though a nursing reflection essay is about your personal experiences, it doesn't mean you should reveal everything about yourself. Ask yourself whether something is appropriate before including it in your paper.
Mistakes to Avoid When Writing a Reflection Essay in Nursing
A good reflection essay involves reflecting on your nursing studies and practices throughout school and career to demonstrate your competence. For this reason, there are certain mistakes you should be aware of when writing an essay.
Not including a Personal Story
Like food tastes bland without salt, so does a reflection essay without a personal story. At the center of a reflection essay is You. This means the essay should focus on your personal story that led you to want a nursing career. A lot of times, students miss out on this instead of talking about their story. You need more than just the personal qualities you think will be a great fit for the nursing program; you must also share a story that shows how well you contributed to nursing care.
Failing to Share Your Experience
You will lose points when you fail to include nursing-related experiences in your reflection essay. Mentioning that you want to be a nurse is great, but failing to show specific events that led to the desire will cost you a great point.
Plagiarizing Your Essay
Plagiarism is a serious academic offense because it is considered taking other people's ideas and using them as your own without crediting the author. So, provide relevant citations and references for any ideas that aren't your own. Also, an AI will not write your essay as a human writer would.
Related Readings:
- How to write a student nurse resume with no experience.
- PICOT examples and guides
Sample of a Nursing Reflective Essay
The following is a sample of a nursing Reflective essay using Gibb's Model of Reflection. Use this sample to guide you when writing your own.
Introduction Communication is an important element in healthcare practice as it determines patient satisfaction and treatment outcomes. This essay will focus on reflecting on an experience I went through with a 40-year-old diabetic patient who also had a foot infected with an ulcer. When I approached the patient to sign the consent form, I noticed that he wasn't happy because of the news given to him about his health. I concluded that there must be a communication dilemma. I will reflect on the experience using Gibb's Model of Reflection. Using this model, I will identify and discuss the actions taken to resolve the issue. Description This incident happened a few months ago when I was working as a wound nurse in a Methodist hospital in my hometown. I was part of a care team handling the case of a 40-year-old male patient with diabetes and an infected diabetic foot ulcer. After careful examination, a team comprising various specialists concluded that his leg needed amputation below the knee. After making this decision, the team left, and I was asked to give the patient a consent form to sign. When I came back from retrieving the form, I noticed the patient looked sorrowful because of the news given to him. Feelings As soon as I saw the patient, I knew what he was going through. He perceived the situation to be irreparable, but I wasn't sure whether to console the patient or not. I was powerless and couldn't imagine what he was going through. At the same time, I was startled that the team left without showing any compassion. They could have handled the situation more delicately. I, on the other hand, could have relayed the information better. I wasn't sure whether my approach would be acceptable or appropriate. Evaluation I always go back to that particular situation and wonder whether I could have acted better. The situation helped me better understand the importance of good communication in patient care, particularly in therapeutic care. Before the incident, I didn't acknowledge the role of nurses play in caring for patient's emotional needs. I realized nurses must show compassion and console patients in their low moments. Analysis Most healthcare professionals do not know how to deliver bad news to patients. They find the process extremely challenging and always feel psychologically unprepared. This has a negative impact on patients and could lead to bad health outcomes. Furthermore, how information is relayed could impact a patient's adherence to treatment. Because of these effects, multiple protocols and approaches were developed to help with communicating bad news to patients. One of the approaches that was proposed is emotion-centered. This proposes that a healthcare provider acknowledges how sad the patient is and builds a professional relationship based on empathy and sympathy. Action Plan I now understand the essence of communicating bad news with compassion. The experience allowed me to look closely at different aspects of my professional development that needed more improvement. Thus, I plan to be more empathetic and speak up in support of patient's emotional and psychological well-being, especially when presented with traumatic news about their health. Additionally, I now understand I am not powerless when dealing with a sorrowful patient. I believe I have learned from my experience, and I'm not able to communicate well with patients any more. Conclusion The experience allowed me to value good communication in nursing and the need to incorporate it into daily nurse-patient interaction. Nurses must learn how to deliver bad news and manage patient's sorrow. This has been and will continue to be my biggest priority in patient care. References Street Jr, R. L., Makoul, G., Arora, N. K., & Epstein, R. M. (2009). How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient education and counselling, 74(3), 295-301. Buckman, R. (1992). Breaking bad news: why is it still so difficult? BMJ: British Medical Journal, 304(6842), 886. Ptacek, J. T., & Eberhardt, T. L. (1996). Breaking bad news: a review of the literature. The Journal of the American Medical Association, 276(6), 496-502.
Writing is not everyone's cup of tea. For that reason, you can hire a nursing reflection essay writer from NurseMyGrade to assist you in crafting a top-grade paper. In addition, we have nursing writers whose forte is writing various nursing papers. Just place an order , and we will get back to you ASAP.
Struggling with
Related Articles
Nursing Capstone Paper for BSN, MSN, and DNP Students

AMA Citation and Formatting Style for Medical Paper
Application of Kohlberg Heinz Dilemma in Nursing Practice
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Healthcare (Basel)

Spirituality and Religious Diversity in Nursing: A Scoping Review
Carla murgia.
1 Department of Biomedicine and Prevention, University of Rome Tor Vergata, 00133 Rome, Italy
Ippolito Notarnicola
2 Centre of Excellence for Nursing Scholarship, OPI, 00133 Rome, Italy
Rosario Caruso
3 Health Professions Research and Development Unit, IRCCS Policlinico San Donato, 20097 Milano, Italy
4 Department of Biomedical Sciences for Health, University of Milan, 20122 Milan, Italy

Maddalena De Maria
Gennaro rocco, alessandro stievano.
5 Department of Experimental and Clinical Medicine, University of Messina, 98125 Messina, Italy
Spirituality is a common theme in the field of healthcare research. This study aimed to examine nurses’ perceptions of spirituality in the context of the religious diversity of patients in pluri-religious settings. We performed a scoping review following the methodology on studies conducted between 2010 and 2020. We searched the following databases: CINAHL Plus, PubMed, and PsycINFO. For the identification of grey literature, the OpenGrey database was used. In total, 789 articles were reviewed. Of these, 16 met predetermined inclusion criteria. Two main overarching themes emerged from our inductive analysis: (a) the intertwining of spirituality and spiritual care in diverse religious landscapes and (b) obstacles impeding the inclusion of spiritual care in pluri-religious settings. According to our results, nurses consider that spirituality is interconnected with spiritual care for individuals from different religious backgrounds. Interpretations of spirituality in nursing practice vary widely, with spirituality and religiosity often shaped and influenced by culture and the experience of the professionals. Nurses attribute various meanings to spiritual care, most of which center on respecting personal, interpersonal, and relational aspects of religious and cultural beliefs and practices. Lack of education and specific skills, insufficient time, role ambiguity, and different religious beliefs were identified as hurdles to spiritual care. A poor work environment, a lack of patient privacy, including personal space, and a lack of compassion were also reported as deterrents to spiritual healing. More knowledge and training on different religions and spirituality are required to meet patients’ spiritual needs to better overcome these hurdles.
1. Introduction
Spirituality is a common theme in healthcare research and on healthcare professionals worldwide, and it constitutes one of the six quality of life domains in the World Health Organization Quality of Life Instrument (World Health Organization, 2012) [ 1 ]. Spiritual diversity is widespread due to the existence of pluri-religious societies worldwide. Consequently, nurses commonly care for patients from diverse religious backgrounds. According to the literature, people with and without religious convictions report the need for and benefits of spiritual support in healthcare [ 2 , 3 , 4 ]. Growing attention to spiritual aspects of care exists even within highly secular societal environments [ 5 ]. Worldwide, nurses’ interest in spiritual care is increasing [ 6 , 7 ].
Many studies have shown that nurses consistently recognize the importance of spiritual comfort and value the fundamentals of a holistic approach without any religious and cultural distinction [ 8 , 9 ]. Modern professional nursing arose in a Christian-based values environment and was imbued with religiously derived principles from its beginnings. However, according to the ethical codes of professional organizations and official statements of the International Council of Nurses (2021), holistic nursing must respond to all patients’ spiritual needs, irrespective of their religious beliefs [ 10 ]. Nursing spirituality has been at the heart of nursing theory and research for over 30 years. In this framework, the literature reveals that nurses have examined different spiritual perspectives. Stephenson and Hebeshy [ 11 ] pointed out that spiritual care should be incorporated into care plans and that nurses need updated knowledge and training on different forms of spirituality [ 12 , 13 , 14 ]. Other research found that the effectiveness of nursing care depended on nurses’ awareness of and sensitivity to the spiritual needs of their patients [ 15 ].
In the contemporary literature, there are three main approaches to spirituality: religious, secular, and holistic [ 16 ]. Spirituality is often viewed in broad terms, in which it is defined by the individual and is not necessarily connected to organized religion [ 17 , 18 ]. Worldwide, there is a concerted effort for spiritual assistance and spiritual support to be an integral part of the role of the nurse [ 19 , 20 ]. In clinical nursing practice, it is frequently unclear how to engage patients in spiritual care, especially in complex health systems and societies characterized by secularism and religious pluralism [ 12 , 14 , 21 ]. Although the role of spiritual care in palliative care and oncology is well recognized, less is known about its role in other areas of nursing, where spirituality and spiritual care are often neglected or absent [ 5 ]. Nurses do not consistently integrate patients’ spiritual needs into their daily practice, either because they do not have the time to explore patients’ spiritual demands or because they perceive they lack the skills to provide their patients with spiritual support. In the cultural context of this review, Catholic or Protestant priests or pastors and chaplains or spiritual care providers [ 22 ] are the only institutional figures in healthcare settings (hospitals and clinics) that provide spiritual support to patients [ 12 , 14 , 23 , 24 ]. However, other professionals also provide spiritual assistance and services, although their involvement may be minor or not recognized. These include nurses [ 5 , 23 , 25 ], rehabilitation health professionals [ 26 ], psychologists, and physicians [ 27 ].
Thus far, most studies on spirituality have been conducted in Western countries among homogeneous samples from predominantly Judeo–Christian cultures [ 5 , 28 , 29 ]. There is a need for studies on spirituality in the healthcare setting, especially nursing, in Asian countries [ 6 , 30 ] and in diverse ethnocultural and practice contexts [ 5 ]. The primary aim of this scoping review was to examine studies that focused on the sensitivity of nurses to issues pertaining to spirituality and religious diversity in nursing in Western and non-Western contexts.
2. Materials and Methods
2.1. design.
This study adopted the methodology of Arksey and O’Malley [ 31 ] for scoping reviews, one of the first methodological frameworks to shape this research synthesis. A scoping review is an evidence-based methodology that systematically maps vast bodies of emerging, complex, and extensive evidence (quantitative and qualitative or mixed) to broadly identify data sources and literature gaps [ 31 , 32 ]. For clarity, the Arksey and O’Malley method [ 31 ], in conjunction with that of Colquhoun et al. [ 33 ], was used. The six-stage methodological structure applied was as follows:
Stage 1: Identification of the research question.
Stage 2: Identification of studies relevant to the research question.
Stage 3: Selection of studies for inclusion in the review.
Stage 4: Charting of information and data in the included studies.
Stage 5: Collection, summary, and reporting of the results.
Stage 6: Stakeholder consultation (optional).
2.2. Identification of the Research Question
Our research question aimed to examine what was known about nurses’ sensitivity and understanding of spirituality in the context of patients’ religious diversity in pluri-religious settings. The “population, concept, and context” (PCC) framework has been adopted as per the indication of Arksey and O’Malley [ 31 ] to define the research question. In our framework, the population was composed of nurses, the concept was the nurses’ views of spirituality, and the context encompassed all healthcare settings but palliative care.
2.3. Identification of Studies Relevant to the Research Question
To shed light on nurses’ understanding of patients’ spirituality, we conducted a literature search of three electronic databases: CINAHL Plus, PubMed, and PsycINFO. The keywords utilized in the literature search included “spirituality”, “diversity religion”, and “nursing”. Boolean operators were employed as conjunctions to merge these keywords in the search [ 31 ]. The exact search string used in the search of CINAHL Plus was used to identify grey literature in the OpenGrey database.
All materials were managed via Zotero software, and identical references were eliminated. Three reviewers (CM, IN, and AS) then conducted an iterative two-step screening process of the articles, reviewing first the titles and abstracts and then the full texts, if deemed suitable for further examination. Throughout the process, any disagreement in terms of article selection was resolved by discussion.
2.4. Selection of Studies for Inclusion in the Review
This scoping review included papers of different designs (qualitative and quantitative primary research, secondary research, editorials, and commentaries) considering their purpose, which had to be consistent with mapping nurses’ views of spirituality for patients. The extracted data from the included papers were organized considering the aim, design, participants, and context.
2.5. Eligibility and Selection Process
Eligible studies were empirical publications that fit the following criteria: (a) qualitative, quantitative, and mixed methodologies; primary and secondary studies; (b) studies written in English and published between 2010 and 2020 to include the most recent research on the topic, as a literature review including papers until 2010 is available [ 34 ]; (c) studies with abstracts and full texts, with a focus on religious diversity in nursing care; (d) studies performed in various care settings (hospitals and homes) but not palliative care environments; and (e) studies where nurses were the main surveyed population, followed by patients, caregivers, and other healthcare workers. Studies focusing on palliative care settings were excluded because much of the current nursing spirituality literature focuses on these backgrounds rather than on other types of care settings (e.g., acute care). All studies without abstracts and not written in English were also excluded. Reviews and other types of studies, such as commentaries or analyses of concepts, provided background knowledge of the research problem, and these were read for valuable insights that involved religious diversity but were not included.
2.6. Charting of Information and Data in the Included Studies
Following a literature search, in total, 787 articles were initially selected. The process for item selection is outlined in Figure 1 . Reporting was compliant with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews Checklist (PRISMA-ScR) [ 35 ]. PRISMA-ScR contains 20 fundamental reporting requirements and two discretionary requirements to include when conducting a scoping study. The publications retrieved described how nurses defined spirituality as interconnected with spiritual care in the context of religious diversity. After meticulously reading all the included research, the synthesis and interpretation of data were performed, and finally, the results were obtained [ 31 ].

Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews Checklist (PRISMA-ScR) flow diagram.
2.7. Collection, Summary, and Reporting of the Results
Although a quality assessment of studies included in a scoping review is not mandatory, we conducted a preliminary assessment of the quality of the included papers using the Critical Appraisal Skills Program checklist [ 36 ]. Our aim in doing so was to provide a preliminary background on the included materials that sustained the discussion among authors regarding the evaluation of the studies retrieved. Two of the authors performed this preliminary assessment independently. When they reached a consensus on evaluating the included papers, their evaluations were shared with the entire group of authors. The salient characteristics of the studies were organized as follows: summary of the authors, study location, year, context, study design, number of participants, purpose, analysis, and results.
In line with the purpose of our review, we included studies that focused on the sensitivity of nurses to spiritual needs in Western and non-Western contexts. The data extrapolated from the selected articles were coded using an inductive content analysis [ 37 ], extracting significant elements from the information retrieved. Verbatim transcriptions were read and reread to acquire a general sense of the content. Checking the content gathered by the research team members enabled the identification of key concepts. These key concepts were discussed, processed, and reconceptualized into categories describing the sensitivity of nurses regarding spirituality and religious diversity in nursing in Western and non-Western contexts. In this final phase, the categories were divided into two main overarching themes (abductive approach) [ 38 ]: (a) the intertwining of spirituality and spiritual care in diverse religious landscapes, and (b) obstacles impeding the inclusion of spiritual care in pluri-religious settings.
3.1. Characteristics of the Included Studies
The reviewed studies were retrieved from those published in Western (e.g., Australia, Canada, UK, and U.S.) and non-Western countries (i.e., Asia and the Middle East). Our results are based on 16 studies, 8 quantitative and 8 qualitative. The studies were published between 2010 and 2020 in the following countries: Canada ( n = 4), Turkey ( n = 2), the U.S. ( n = 2), Australia ( n = 1), Jordan ( n = 1), Korea ( n = 1), Iran ( n = 1), Malaysia ( n = 1), Saudi Arabia ( n = 1), Singapore ( n = 1), and the UK ( n = 1). Together, these investigations represented a sample of 3723 participants who comprised nurses, caregivers, other healthcare practitioners, and recipients of care (i.e., patients). The nurses worked in different care settings in various countries ( Table 1 ).
Summary of the included studies.
In most of the studies conducted in Western countries, the participants were predominantly Christian nurses. Some of the studies on spirituality mentioned other religions, such as Buddhism and Hinduism [ 13 ]. Islam was rarely cited [ 13 ]. As reported in Table 1 , the included studies assessed nurses’ perceptions of spirituality and spiritual care in association with socio-demographic characteristics [ 6 , 7 , 8 , 13 , 39 , 40 , 41 , 42 , 43 ], various hospital settings [ 6 , 7 , 12 , 22 , 41 , 42 , 43 , 44 ], acute care [ 6 , 24 , 37 , 44 ], home care [ 45 ], and their involvement in spiritual care practices [ 6 , 7 , 13 , 22 , 24 , 40 , 42 , 44 , 45 ]. Many of the studies used validated tools to explore the spiritual observations of the nurses [ 7 , 13 , 29 , 43 ].
Heterogeneous samples of nurses from different ethnic and religious backgrounds considered spirituality from different points of view [ 6 , 7 , 12 , 13 , 22 , 24 , 41 , 45 , 46 , 47 ]. Nurses, caregivers, patients, family members, administrators, and other practitioners were included in only three qualitative investigations [ 22 , 39 , 45 ]. In one 4-year study, religious diversity was considered through the concept of shared sacred space [ 39 ]. Four studies explored perceptions of spirituality in a sample of nurses with the same religious affiliation [ 5 , 40 , 42 , 48 ]. These studies focused on nurses from Arab cultural and religious backgrounds [ 5 , 40 , 42 , 48 ]. Only one study provided nursing skills development guidelines to help non-Muslim nurses in Saudi Arabia understand the needs and preferences of Muslim patients [ 11 ].
Based on the findings of most of the studies, nurses consider spirituality to be pivotal in nursing [ 6 , 7 , 8 , 13 , 22 , 24 , 28 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 ] and attribute various meanings to spirituality and spiritual care, most of which are centered on their religious beliefs [ 6 , 7 , 8 , 13 , 22 , 24 , 28 , 39 , 40 , 41 , 42 , 43 , 45 , 46 ]. However, there was some confusion regarding the meanings of spirituality and spiritual care [ 6 , 7 , 12 ].
Generally, spiritual care was influenced by the individual’s religious identity [ 7 , 12 , 22 , 28 , 45 ], the specific healthcare organization [ 7 , 12 , 24 , 28 , 39 , 42 , 44 ], and the reference environment [ 6 , 7 , 8 , 12 , 22 , 39 , 42 , 45 ]. There seemed to be broad agreement that spirituality and spiritual care education had to be integrated into university teaching programs and continuing education [ 41 , 43 , 44 ]. For example, concerning the healthcare setting, the results indicated that the workplace, such as the type of structure, religious or nondenominational [ 7 ], or private or governmental [ 40 ], influenced nurses’ practices concerning spirituality and spiritual care. Healthcare organizations that operated within economic constraints created barriers to spiritual care provision [ 22 , 39 ]. Several obstacles to the practice of spiritual assistance emerged, the main one being time constraints [ 6 , 12 , 22 , 24 , 39 , 41 , 42 , 44 , 45 ], followed by a shortage of personnel, fear of crossing professional boundaries, fear of proselytism [ 22 , 24 , 28 , 45 ], and difficulty in recognizing spiritual needs when spiritual beliefs differed from those of the care provider (nurse/healthcare institution) [ 41 , 44 ]. However, most surveyed nurses in all clinical areas provided spiritual assistance as a personal creed and as part of their clinical practice. Elements of spiritual care included a range of behaviors, such as sitting with patients in silence, praying with them, and respecting privacy [ 7 , 13 , 22 , 24 , 39 , 41 , 42 ]; listening, giving, and receiving comfort; or communicating with the healthcare chaplain or spiritual assistant, regardless of the religion of the patient or affiliation with particular religious bodies. [ 6 , 22 , 24 , 39 , 42 , 44 ].
3.2. Intertwining of Spirituality and Spiritual Care in Diverse Religious Landscapes
Spirituality has long been part of nursing and represents an essential value for nurses, patients, and their families. Spirituality is intertwined with spiritual care, which can enhance health outcomes [ 6 ] and is part of a holistic approach to medicine [ 39 , 41 , 46 , 47 ]. Spirituality is manifested uniquely in each individual and among different religions or spiritual groups (e.g., Buddhism, Christianity, Hinduism, Islam, Judaism, and others). Spirituality is considered an essential aspect of life in all world cultures; it is a dimension of the person that nurses in Western, Middle Eastern, and Asian countries respect [ 8 , 48 ].
Cumulative evidence points to a positive contribution of spirituality to the health and well-being of the individual, family, and community [ 18 , 47 , 49 , 50 ], and spirituality plays a significant role in stressful work circumstances [ 51 ]. Nevertheless, nurses’ interpretations of spirituality in nursing practice vary widely [ 4 , 47 ]. Spirituality is an umbrella term covering an extensive array of personal meanings, interpretations, and associations [ 28 ]. Nurses likened spirituality to a unifying “force” that enables patients to seek peace, meaning, and resolution in life during periods of healing from illnesses [ 52 ].
In many societal contexts, spirituality is interpreted as religion [ 6 , 40 ]. Spirituality is often understood as the antithesis of religiosity [ 45 ]. Today, the dominant forms of spirituality are Eastern or Western [ 53 , 54 ]. However, the two forms overlap and have points in common [ 21 , 55 ]. Spirituality is primarily influenced by religion, culture, societal pluralism, history, and personal perspectives [ 18 , 38 , 47 , 48 , 56 , 57 ]. Nevertheless, there is little clarity and consensus on spirituality’s meaning [ 18 , 38 , 47 ]. One definition of spirituality contends that spirituality is a dynamic and intrinsic aspect of humanity through which persons seek ultimate meaning, purpose, and transcendence, and experience relationships to self, family, others, community, society, nature, and the significant or sacred. Spirituality is expressed through beliefs, values, traditions, and practices [ 18 , 58 ].
Religious diversity is a term used to indicate the existence of many religious traditions in a multiethnic, multicultural society. Our secular society, which is becoming progressively more globalized, is characterized by increased spiritual diversity. Such diversity is growing in many communities, with immigrants contributing significantly to this diversification [ 22 , 39 , 45 , 50 , 54 , 59 ]. The religious landscape in the Western world differs from that in other parts. In the West, membership of (Christian) religious organizations or groups has remained stable or decreased. For example, church membership in the United States decreased from 67% in 1996 to 32% in 2015 [ 58 ]. However, religion remains a potent force in Canada, although no officially recognized state religion exists. In fact, the influence of Christianity (both Protestantism and Catholicism) remains strong at the societal level [ 22 , 59 ]. In Europe, the leading Christian religions, particularly Catholicism, Orthodoxy, and Protestantism, are the most widespread. As of 2018, about 70% of the European population identified as Christian in some form [ 60 ]. Nevertheless, in the U.S., the population, both Christian and unaffiliated, is noticeably more religious than their European counterparts [ 18 , 61 ].
Beyond a single institutional religion (Christianity) in Western countries and the European continent, religious diversity reflects growth in new spiritualties, with different spiritual expressions in many societal contexts, especially among people who identify as “spiritual but not religious” [ 14 , 18 , 22 , 39 ]. The division between religion and spirituality is more difficult to perceive in the Middle East. Furthermore, in the Middle East, nonreligious terminology is uncommon [ 48 ], and spirituality is inseparable from religion, as it derives from the Holy Quran [ 8 ]. Confucianism, Buddhism, and Daoism do not qualify as religions because they are not organized and formal [ 30 ].
From a Middle Eastern religious perspective, there is no distinction between spirituality and religion [ 8 , 40 , 42 ]. It is part of the culture and beliefs of the Middle East to pray several times a day, even during working hours. For most Muslims, religiosity pervades all aspects of their daily lives, including their working lives [ 13 , 48 ]. Spirituality in a Middle Eastern context is crucial and is founded on respect for Islamic religious beliefs and the values of persons [ 7 , 40 , 42 , 48 ]. Islamic spirituality is regarded in terms of the relationship with Allah [ 7 , 11 ]. Of the studies included in this review, one study, that of Stephenson and Hebeshy [ 11 ], provided brief guidelines on the principles and practices of Islam to help non-Muslim nurses in Saudi Arabia understand the needs and preferences of Muslim patients. In terms of spiritual care and religion, many nurses, who identified with the Islamic religion and prayed at work every day, attributed the utmost importance to patients’ religious needs, considering the fulfilment of these needs an ethical obligation and commitment. Weathers [ 48 ] compared perspectives on spiritualism in the Middle East to those in the West. Similar results were reported in studies conducted in Turkey [ 43 , 46 ], Jordan [ 9 ], and Iran [ 42 ]. The separation of spirituality from religion in Western thinking is recent and is the result of sociological disengagement from religious organizations. In this framework, to ponder spirituality as a residual religion rather than as some universal entity or substance is essential to comprehend all human beings everywhere. Places such as Saudi Arabia, where such societal disengagement has not occurred, do not require a separate category.
Nurses are occasionally unaware of these sociological aspects and sometimes consider patients as belonging to one faith, especially in Western countries where Christianity predominates, now and then silently influencing care with its creeds. Practicing deep listening and encouraging patients to discuss spiritual or existential issues, sharing prayers or songs [ 47 , 52 ], referring patients to a chaplain or a spiritual leader [ 30 ], and using religious texts for Muslims [ 42 ] can strengthen the nurse/patient relationship and provide spiritual comfort to patients. However, religious diversity and secular issues may give rise to conflict among care providers regarding the appropriateness of praying [ 52 ].
As mentioned, nurses sometimes do not have the sociological background to comprehend the different nuances of religious diversity fully. However, according to them, spiritual care involved empathic discourse, and empathy was regarded as a personal and profound form of expression associated with spirituality [ 7 ]. Canadian ethnographic studies highlighted the roles of religion and spirituality. These studies included diverse populations in terms of ethnic, religious, and spiritual affiliations (Christian, Sikh, none, Muslim/Islamic, atheist, Hindu, Greek Orthodox, and others); care settings (medicine and nephrology); and organizational settings (community hospitals, home care, and hospices) [ 22 , 45 ].
Spirituality and spiritual care have been interpreted as mutually beneficial. Spiritual care could take the form of preparing a patient to attend their temple [ 45 ] (p. 20). Respect for others and privacy, dignity, and support for the culture and beliefs of individual patients, together with compassion, kindness, and joy, are the cardinal principles of care interpreted as spiritual [ 13 , 14 , 39 ]. For example, a healthcare practitioner can show respect for a patient during a home visit by recognizing religious differences via the presence of symbols and signs (e.g., home altars featuring Hindu statuettes, Buddha icons, or crucifixes). These are crucial factors that are not usually achieved in hospitals.
The role of nurses in managing religious diversity is multifaceted. In-home caregivers and health workers may come from a variety of religious or nonreligious backgrounds (agnostics and atheists) and hold spiritual beliefs or not. This was evident in one homecare patient’s comment: “the world comes to my home” [ 45 ] (p. 15). Here, the patient was referring to Filipino migrant workers. As clear in various studies, individuals in need of care, whether home care or hospitalization, attach great significance to having their emotional (e.g., kindness, humor, and friendship) and spiritual needs met [ 22 , 41 ].
In previous research, Reimer-Kirkham [ 14 ] conducted a critical analysis of religion, politics, nursing, and healthcare and demonstrated the role of religion and spirituality in health institutions and how health institutions were committed to respecting different forms of religion. Importantly, Reimer-Kirkham [ 14 ] reflected on how spirituality related to religiosity in different social contexts and how it was identified and addressed by health professionals and nurses. Reimer-Kirkham et al. [ 39 , 45 ] focused on studies in which religious and ethnic diversity received equal attention from healthcare managers, caregivers, and care recipients. They examined the negotiation of the dynamics of religious, spiritual, and ethnic plurality in hospital and home health services and analyzed how social, economic, and political contexts and gender shaped these dynamics. Religion and spirituality intersected with class relationships, creating tension and marginalization rather than connection [ 22 ]. However, in other settings, there was an intimate exchange between the patients and health professionals who explored the complexity of diversity in homecare [ 39 , 45 ]. Reimer-Kirkham et al. [ 45 ] stated that what united the interviewees was their shared religious identity, which led to comfort and connection. The “religion taboo” seemed to disappear [ 45 ]. The nurse became the guardian of care [ 12 ] and the provider of emotional support [ 22 ].
A Korean [ 24 ] and a Singaporean [ 7 ] study selected a heterogeneous sample of respondents for consistency with diversity. The Korean research considered the religious diversity of nurses with different opinions, perspectives, and experiences as inclusion criteria to ensure homogeneity within groups and heterogeneity and effective communication among groups. Clinical practice and religion strongly exerted influence on spiritual healing [ 24 ]. Always in the context of religious diversity, Cooper et al. [ 47 ] explored the social and power characteristics underlying nurses’ communication. The participants were a group of 20 nurses, with 14 nurses employed in a private religious hospital managed by a religious body and 6 nurses employed in a nondenominational hospital. The sample comprised Christian and Islamic nurses and those without religious affiliations. The nurses worked in different settings, had different years of experience, and had diverse socio-demographic, cultural, and religious backgrounds. The selection of a sample with these characteristics allowed for a broader vision of how nurses conceptualized spirituality based on religious differences. The first critical discourse that emerged from the interviews was personal religious belief, followed by other beliefs and faiths [ 7 ].
Instruments to Measure Spirituality
Chew et al. [ 7 ] used Tiew and Creedy’s Spiritual Care-Giving Scale (SCGS) [ 62 ] to explore possible associations between the personal and professional characteristics of nurses and their perceptions and experiences of spirituality and spiritual care in an acute-care hospital in Singapore, a multicultural and pluri-religious city-state. Their findings showed that nurses expressed positive perceptions about spirituality and spiritual care, making themselves available to provide spiritual care through an interprofessional collaborative approach involving other nurses, clergy (e.g., chaplains), and leaders of other religious groups, thereby enabling a broader, more inclusive perspective. However, nurses were often unclear on the meaning of spiritual care. The high participation rate (76%) and the diversity of the multiethnic (Indian, Chinese, Malaysian, and others) and pluri-religious (Christian/Catholic, Islamic, Hindu, and other affiliations) sample constitute strengths of their study. In the study by Chew et al. [ 7 ], the SCGS scores were statistically significantly associated with three variables: the area of clinical practice, religion, and the perception of the spiritual self.
In line with the study by Chew et al. [ 7 ], Atharim et al. [ 13 ] reported that nurses in Malaysia navigate a society characterized by religious diversity. Official religions recorded in Malaysia in 1965 included Islamism (61.3%), Buddhism (19.8%), Hinduism (6.3%), Christianity (9.2%), and atheism (0.8%), with followers of the indigenous faith recorded more recently [ 7 , 13 , 45 ]. Atarhim et al. [ 13 ] used the Spirituality and Spiritual Healing Rating Scale (SSCRS), translated into Malay and applied it in a Malaysian professional context. They obtained similar results to those of studies in other countries, such as in Turkey by Akgün Şahin and Ozdemir [ 43 ]. Their study provides preliminary information on spirituality and spiritual care from the nurses’ perspectives. More than 90% of the respondents were Muslim, and the remainder identified as Buddhist, Christian, and Hindu. Although the nurses provided spiritual care because this is required in line with their religious beliefs and societal norms, they pondered whether spiritual care could be provided to nonreligious individuals, such as atheists and agnostics [ 13 ]. In the study, higher education, marital status, older age, more years of work experience, longer working hours, medical department work, and spiritual care training were positively associated with higher SSCRS scores [ 13 ].
3.3. Obstacles Impeding the Inclusion of Spiritual Care in Pluri-Religious Settings
Lack of education in the area of spiritual care and skills specific to this field of care [ 28 , 43 ], insufficient time, role ambiguity [ 12 , 13 , 22 , 24 , 42 , 43 , 44 ], economic constraints [ 22 , 59 ], and different religious beliefs of nurses [ 27 ] were identified as the main hurdles to spiritual care. Another significant barrier to the provision of spiritual care arose from the absence of a shared definition of spirituality between providers and patients, contributing to embarrassment and confusion about what spirituality and nurses’ spiritual care practices comprised. Furthermore, it was not clear how spiritual care differed from nursing in general [ 11 ]. In addition, busy and noisy work environments and insensitivity to compassion due to space constraints [ 55 ] were reported as deterrents to spiritual healing [ 24 , 39 ]. Other barriers revolved around ethical aspects of spiritual care [ 23 ] or making patients feel uncomfortable about spiritual care [ 22 , 24 , 55 ]. In addition, the difficulty in distinguishing spiritual care from proselytism [ 24 , 55 ], the fear of criticism from others [ 6 ], and the lack of a registration system for preferences regarding spirituality [ 24 ] were cited as obstacles to the provision of spiritual care. These factors were considered possible hindrances that created doubt or confusion among nurses and patients regarding spiritual care choices. Most nurses cited the need for more education and training on the spiritual aspects of care delivered to different ethnic groups [ 24 ]. Education is needed to enhance nurses’ awareness of religious and spiritual diversity and to enable them to meet the spiritual needs of their patients [ 6 , 41 ].
At the same time, spirituality has to be addressed within the nursing curricula, ensuring that the practice of spiritual care is not neglected [ 6 , 13 , 46 ]. Regarding the inclusion of spirituality at a practical level in care, three categories emerged: personal influences, organizational influences, and social influences.
3.3.1. Personal Influences
The findings of several studies suggested that definitions of spirituality and spiritual care were expressed according to the nurses’ beliefs [ 39 , 41 , 44 ]. Although this finding was robust among participants of Christian origin, for Muslims, there was no distinction between religion and spirituality, with spirituality an inherent part of daily life. All aspects of their daily lives were guided by faith and rituals [ 11 , 42 ]. Discourse on personal religious beliefs molded spirituality. Nurses were influenced by their religious attitudes or by the religious perspectives of their family, even for those who were not religious. Talking about spirituality meant using religious terms. For example, spirituality often coincides with personal religion. Consequently, nurses viewed their religion as a guide and a motivation, thus influencing the spiritual care they provided [ 28 , 44 ]. Another influencing factor was conceptual ambiguity, consequently making it a conditioning or a marginalizing factor among nurses [ 24 , 55 ].
3.3.2. Organizational Influences
Nurses’ attitudes to caring strongly influenced limiting or making possible the practice of spiritual care. The type of organizational structure (religious or nondenominational) affected nurses’ attitudes to spiritual care provision, university training, and the work environment. Despite its influence and relevance, Reimer-Kirkham et al. [ 45 ] concluded that religion was like the “elephant on the table” because it was stated that it was not a nursing competence. A similar conclusion was reached in the study by Janzen et al. [ 12 ], in which, in a temporal context of diversity, spirituality was recognized as precious, but it was added that “for spirituality it would have been necessary to spend a little more time, to make an extra effort, but this did not happen because it was airy-fairy. Therefore, pushing it under the carpet was easier to avoid offending anyone” [ 12 ] (p. 256). In this situation, nurses preferred not to be involved in spiritual care. Sometimes, spirituality was considered not to be a nursing competence.
Lack of institutional support, time, and sufficient staff to provide comprehensive care and a heavy workload were frequent problems that hindered spiritual care [ 40 , 41 ]. The professional boundaries between nurses and chaplains in healthcare settings constituted another hindrance. Blurring boundaries regarding roles could lead to conflict among healthcare professionals [ 23 , 41 ]. Nurses considered the risk of proselytism another potential barrier to the provision of spiritual care [ 24 , 28 , 41 , 55 ].
To conclude, in the narratives of the nurses working in private and religious healthcare settings regarding spiritual care provision, nondenominational public hospitals were more guided by the local culture and the values of openness [ 12 ].
3.3.3. Social Influences
From a critical analysis of 20 interviews at two hospitals by Cooper et al. [ 8 ], one nondenominational public and one private religious hospital, social characteristics and implicit religious power emerged, consequently affecting spiritual assistance and the nurse–patient relationship. In terms of religious diversity, recognizing spirituality as an integral part of the person is a goal of health services. Understanding the social context and how social and cultural–religious factors intertwine, for example, socioeconomic status with environmental factors, can enable nurses to identify factors impeding or facilitating the development of spiritual skills and improving these skills [ 12 , 39 , 45 ].
Over the past century, secularism has permeated healthcare provision. This might be due to religious diversity or a lack of religious conviction among the people healthcare organizations serve. In this environment, some respondents expressed fear of providing spiritual care [ 28 , 39 ]. In globalized health systems, nurses often consider caring for multifaith patients problematic and uncertain.
4. Discussion
This scoping review aimed to identify and summarize nurses’ perceptions of spirituality in the context of the religious diversity of patients in Western and non-Western settings. Sixteen articles met the preset inclusion criteria and were retrieved and analyzed in depth. The results revealed that research on spirituality and health has been predominantly conducted in Western countries on the Christian religion. In Middle Eastern countries, research has focused exclusively on the Islamic religion. This analysis indicated that nurses generally consider spirituality interconnected with spiritual care and the fundamentals of nursing. It also showed that the importance of spirituality in nursing is recognized in professional standards worldwide [ 10 , 19 , 63 ].
According to some studies, patients find comfort in rituals, prayers, conversations with supernatural entities, and the diligent attention healthcare professionals provide [ 12 , 22 ]. This support, through respect for religion, has been considered engrossing, as spirituality and religiosity are often shaped and influenced by culture [ 18 ] and the experience of the care provider [ 17 ]. Providing person-centered spiritual care is an essential dimension of dignified care in multicultural settings. This review shows that nurses attributed various meanings to spirituality and spiritual care, mostly centered on respecting personal, interpersonal, and relational aspects of religious and cultural beliefs and practices. Thus, the nurses adopted a personal position based on their identity and responded to the challenge of integrating spiritual assistance into a spiritually diverse landscape according to their personal, organizational, and social positions, which were also shaped by their education, age, years of clinical experience, and workplace environment [ 12 , 21 , 22 , 47 ].
In a multifaith society, recognizing spirituality as an integral part of the person and a fundamental goal of health services is vital to comprehend the factors hindering or facilitating the provision of spiritual care [ 14 ]. This is particularly true in Western healthcare settings attempting to provide spiritual assistance to patients from various cultural backgrounds. For example, most research in the U.S. defines spirituality according to Christian principles, and there is a lack of information regarding other faiths’ spirituality [ 11 ].
In Western and Middle Eastern countries, health organizations are (historically) rooted in a specific religious tradition. In some of these countries, aides known as holy assistants from the same religious background as the patient provide spiritual care. However, religious diversity must be considered when caring for patients from various cultures and religions. Reconceptualizing the meaning of spirituality in healthcare settings and pluri-religious societies is an ongoing challenge [ 14 , 19 , 60 ]. Through this scoping study, a continuum that extends from resistance and avoidance at one end to deep commitment and responsible pluralism at the other was identified, corresponding to different attitudes among nurses to spiritual care provision, mirroring those of a secular society [ 12 ].
At the practical level of care provision, the disconnect between the perceived importance of spiritual care and poor provision of care is explained by several barriers identified by nurses [ 12 , 14 , 39 , 53 ]. From the nurses’ perspectives, numerous and distinct factors can hamper the provision of spiritual care, all of which deserve deep reflection. According to Reimer-Kirkham [ 14 ], there must be full awareness regarding the concept of spirituality to allow it to be applied and utilized correctly in the discipline of nursing. There are also practical obstacles to the application of spiritual care, such as a lack of institutional and organizational support, a lack of adequate training, and a Christian-centered approach to care in Western healthcare settings, where priests or chaplains provide spiritual care, regardless of the religious beliefs of the patient [ 22 , 43 ]. In these settings, spiritual care provision by non-Christian figures is notably absent [ 57 ]. The aforementioned poses a challenge to nurses and could provoke resistance to spiritual care provision, as such care is not one of their competencies. Nurses may also fear misunderstanding the concept of diversity or influencing care recipients with personal beliefs [ 13 , 21 , 63 ]. The following provides an example of the problems that can arise when religious diversity and personal beliefs are not respected/understood. Hindu family members, on the death of their mother, asked for respect in the management of mourning according to Hindu rites. Instead of contacting a representative of the Hindu religion, as requested by the patient’s family, the nurse called on the services of a Roman Catholic priest [ 18 ].
In some cases, patients’ religious and spiritual beliefs may be vital in decisions relating to their health [ 22 , 54 ]. Knowledge of the principles underlying such beliefs is necessary to provide adequate patient-centered care. A trust-based relationship between healthcare professionals and patients is essential to realizing spiritual care. Trust is necessary to help patients and their families to use their resources in the healing or grieving process, irrespective of their personal or professional beliefs or traditions and those of the healthcare organizations [ 8 , 59 ].
The findings of this review indicate that most of the participants received no training related to spiritual care and felt insufficiently trained, despite recent attention on the spiritual dimensions of nursing [ 13 ]. To overcome this problem, more comprehensive training on different religions and spirituality is needed to improve nurses’ knowledge in these areas and better meet patients’ spiritual needs [ 13 , 26 , 39 , 45 ]. Nurses need to be aware of individual differences and expand their ability to relate to patients of different cultures, faiths, and colleagues. Achieving these goals requires in-depth advanced skills and lifelong learning [ 18 ].
In conclusion, nurses need to be aware of patients’ beliefs to ensure that they provide care that is culturally, religiously, and appropriately for the individual care recipient [ 8 , 18 , 22 ]. Nurses must speak and listen to patients without prejudice and provide personalized and impartial care with the utmost compassion and sensitivity. Knowledge of the basic tenets of these cultures is a prerequisite to helping patients utilize their internal resources in the healing process, irrespective of the nurse’s personal beliefs.
5. Limitations
This review included only studies published in English between 2010 and 2020, and it does no justice to the complexity of spirituality and religious diversity in nursing expressed by manuscripts written in other languages. Moreover, it was difficult to delineate clear boundaries among the concepts of religion, spirituality, and spiritual care practices because they are strongly intertwined. Some details that refer to a specific term could have been blurred during the analysis. Moreover, this review did not explore spirituality as residual religion in detail. In this regard, more search terms could have been used to elicit additional studies, especially in grey databases, to achieve a more precise overview of the topic. Furthermore, although we searched a number of well-known health databases, we omitted some sociological and religious studies’ databases. Nevertheless, the qualitative and quantitative papers included in this scoping review allowed for a better understanding of the topic.
6. Conclusions and Relevance for Clinical Practice
As revealed in this scoping review, the concept of spirituality is interrelated with spiritual care, and it is an essential and complex concept that has not reached full maturity in the perception of religious diversity in nursing. This review demonstrates that integrating spiritual care into healthcare in a highly pluralized and spiritually diverse landscape is challenging and that there is no single way to address this issue. There are different points of view on integrating spiritual care in healthcare [ 21 ]. In this respect, it is necessary for the future to adopt an eclectic approach. Such an approach is critical if the definition of spirituality and the provision of spiritual care is to be inclusive and embrace diversity within society [ 29 ].
This review highlights significant challenges and concerns regarding the provision of spiritual care in the nursing profession. These challenges also include severe hospital understaffing, difficult work conditions, and stress and burn-out, which can further hinder spiritual care provision. The knowledge gained from this review may be helpful for nurses to reflect on their position in addressing the spiritual needs of an increasingly diverse patient population in clinical practice. All nurses need to be fully aware of and know the different ways to express spirituality and spiritual care. Through better training in world religions, possibly via postgraduate courses, nursing educators can help to foster continuing education on the topic. Lastly, for hospital managers and policymakers to make informed, bias-free decisions on organizing or implementing spiritual care in healthcare settings, fostering excellence in the provision of spiritual care and nurses’ training in this area should be a priority [ 64 ].
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, C.M. and A.S.; methodology, I.N. and R.C.; formal analysis C.M., M.D.M. and G.R.; data curation, C.M., I.N., R.C., G.R. and M.D.M.; writing—original draft preparation C.M. and A.S.; writing—review and editing C.M., I.N., R.C., G.R., M.D.M. and A.S.; visualization C.M., I.N., R.C., G.R., M.D.M. and A.S.; supervision C.M. and A.S.; project administration C.M., I.N., R.C., G.R., M.D.M. and A.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Open access
- Published: 14 May 2024
Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study
- Jocelyn Schroeder 1 ,
- Barbara Pesut 1 , 2 ,
- Lise Olsen 2 ,
- Nelly D. Oelke 2 &
- Helen Sharp 2
BMC Nursing volume 23 , Article number: 326 ( 2024 ) Cite this article
31 Accesses
Metrics details
Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Canada’s legislation is the first to permit Nurse Practitioners (NP) to serve as independent MAiD assessors and providers. Registered Nurses’ (RN) also have important roles in MAiD that include MAiD care coordination; client and family teaching and support, MAiD procedural quality; healthcare provider and public education; and bereavement care for family. Nurses have a right under the law to conscientious objection to participating in MAiD. Therefore, it is essential to prepare nurses in their entry-level education for the practice implications and moral complexities inherent in this practice. Knowing what nursing students think about MAiD is a critical first step. Therefore, the purpose of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context.
The design was a mixed-method, modified e-Delphi method that entailed item generation from the literature, item refinement through a 2 round survey of an expert faculty panel, and item validation through a cognitive focus group interview with nursing students. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
During phase 1, a 56-item survey was developed from existing literature that included demographic items and items designed to measure experience with death and dying (including MAiD), education and preparation, attitudes and beliefs, influences on those beliefs, and anticipated future involvement. During phase 2, an expert faculty panel reviewed, modified, and prioritized the items yielding 51 items. During phase 3, a sample of nursing students further evaluated and modified the language in the survey to aid readability and comprehension. The final survey consists of 45 items including 4 case studies.
Systematic evaluation of knowledge-to-date coupled with stakeholder perspectives supports robust survey design. This study yielded a survey to assess nursing students’ attitudes toward MAiD in a Canadian context.
The survey is appropriate for use in education and research to measure knowledge and attitudes about MAiD among nurse trainees and can be a helpful step in preparing nursing students for entry-level practice.
Peer Review reports
Medical Assistance in Dying (MAiD) is permitted under an amendment to Canada’s Criminal Code which was passed in 2016 [ 1 ]. MAiD is defined in the legislation as both self-administered and clinician-administered medication for the purpose of causing death. In the 2016 Bill C-14 legislation one of the eligibility criteria was that an applicant for MAiD must have a reasonably foreseeable natural death although this term was not defined. It was left to the clinical judgement of MAiD assessors and providers to determine the time frame that constitutes reasonably foreseeable [ 2 ]. However, in 2021 under Bill C-7, the eligibility criteria for MAiD were changed to allow individuals with irreversible medical conditions, declining health, and suffering, but whose natural death was not reasonably foreseeable, to receive MAiD [ 3 ]. This population of MAiD applicants are referred to as Track 2 MAiD (those whose natural death is foreseeable are referred to as Track 1). Track 2 applicants are subject to additional safeguards under the 2021 C-7 legislation.
Three additional proposed changes to the legislation have been extensively studied by Canadian Expert Panels (Council of Canadian Academics [CCA]) [ 4 , 5 , 6 ] First, under the legislation that defines Track 2, individuals with mental disease as their sole underlying medical condition may apply for MAiD, but implementation of this practice is embargoed until March 2027 [ 4 ]. Second, there is consideration of allowing MAiD to be implemented through advanced consent. This would make it possible for persons living with dementia to receive MAID after they have lost the capacity to consent to the procedure [ 5 ]. Third, there is consideration of extending MAiD to mature minors. A mature minor is defined as “a person under the age of majority…and who has the capacity to understand and appreciate the nature and consequences of a decision” ([ 6 ] p. 5). In summary, since the legalization of MAiD in 2016 the eligibility criteria and safeguards have evolved significantly with consequent implications for nurses and nursing care. Further, the number of Canadians who access MAiD shows steady increases since 2016 [ 7 ] and it is expected that these increases will continue in the foreseeable future.
Nurses have been integral to MAiD care in the Canadian context. While other countries such as Belgium and the Netherlands also permit euthanasia, Canada is the first country to allow Nurse Practitioners (Registered Nurses with additional preparation typically achieved at the graduate level) to act independently as assessors and providers of MAiD [ 1 ]. Although the role of Registered Nurses (RNs) in MAiD is not defined in federal legislation, it has been addressed at the provincial/territorial-level with variability in scope of practice by region [ 8 , 9 ]. For example, there are differences with respect to the obligation of the nurse to provide information to patients about MAiD, and to the degree that nurses are expected to ensure that patient eligibility criteria and safeguards are met prior to their participation [ 10 ]. Studies conducted in the Canadian context indicate that RNs perform essential roles in MAiD care coordination; client and family teaching and support; MAiD procedural quality; healthcare provider and public education; and bereavement care for family [ 9 , 11 ]. Nurse practitioners and RNs are integral to a robust MAiD care system in Canada and hence need to be well-prepared for their role [ 12 ].
Previous studies have found that end of life care, and MAiD specifically, raise complex moral and ethical issues for nurses [ 13 , 14 , 15 , 16 ]. The knowledge, attitudes, and beliefs of nurses are important across practice settings because nurses have consistent, ongoing, and direct contact with patients who experience chronic or life-limiting health conditions. Canadian studies exploring nurses’ moral and ethical decision-making in relation to MAiD reveal that although some nurses are clear in their support for, or opposition to, MAiD, others are unclear on what they believe to be good and right [ 14 ]. Empirical findings suggest that nurses go through a period of moral sense-making that is often informed by their family, peers, and initial experiences with MAID [ 17 , 18 ]. Canadian legislation and policy specifies that nurses are not required to participate in MAiD and may recuse themselves as conscientious objectors with appropriate steps to ensure ongoing and safe care of patients [ 1 , 19 ]. However, with so many nurses having to reflect on and make sense of their moral position, it is essential that they are given adequate time and preparation to make an informed and thoughtful decision before they participate in a MAID death [ 20 , 21 ].
It is well established that nursing students receive inconsistent exposure to end of life care issues [ 22 ] and little or no training related to MAiD [ 23 ]. Without such education and reflection time in pre-entry nursing preparation, nurses are at significant risk for moral harm. An important first step in providing this preparation is to be able to assess the knowledge, values, and beliefs of nursing students regarding MAID and end of life care. As demand for MAiD increases along with the complexities of MAiD, it is critical to understand the knowledge, attitudes, and likelihood of engagement with MAiD among nursing students as a baseline upon which to build curriculum and as a means to track these variables over time.
Aim, design, and setting
The aim of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context. We sought to explore both their willingness to be involved in the registered nursing role and in the nurse practitioner role should they chose to prepare themselves to that level of education. The design was a mixed-method, modified e-Delphi method that entailed item generation, item refinement through an expert faculty panel [ 24 , 25 , 26 ], and initial item validation through a cognitive focus group interview with nursing students [ 27 ]. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
Participants
A panel of 10 faculty from the two nursing education programs were recruited for Phase 2 of the e-Delphi. To be included, faculty were required to have a minimum of three years of experience in nurse education, be employed as nursing faculty, and self-identify as having experience with MAiD. A convenience sample of 5 fourth-year nursing students were recruited to participate in Phase 3. Students had to be in good standing in the nursing program and be willing to share their experiences of the survey in an online group interview format.
The modified e-Delphi was conducted in 3 phases: Phase 1 entailed item generation through literature and existing survey review. Phase 2 entailed item refinement through a faculty expert panel review with focus on content validity, prioritization, and revision of item wording [ 25 ]. Phase 3 entailed an assessment of face validity through focus group-based cognitive interview with nursing students.
Phase I. Item generation through literature review
The goal of phase 1 was to develop a bank of survey items that would represent the variables of interest and which could be provided to expert faculty in Phase 2. Initial survey items were generated through a literature review of similar surveys designed to assess knowledge and attitudes toward MAiD/euthanasia in healthcare providers; Canadian empirical studies on nurses’ roles and/or experiences with MAiD; and legislative and expert panel documents that outlined proposed changes to the legislative eligibility criteria and safeguards. The literature review was conducted in three online databases: CINAHL, PsycINFO, and Medline. Key words for the search included nurses , nursing students , medical students , NPs, MAiD , euthanasia , assisted death , and end-of-life care . Only articles written in English were reviewed. The legalization and legislation of MAiD is new in many countries; therefore, studies that were greater than twenty years old were excluded, no further exclusion criteria set for country.
Items from surveys designed to measure similar variables in other health care providers and geographic contexts were placed in a table and similar items were collated and revised into a single item. Then key variables were identified from the empirical literature on nurses and MAiD in Canada and checked against the items derived from the surveys to ensure that each of the key variables were represented. For example, conscientious objection has figured prominently in the Canadian literature, but there were few items that assessed knowledge of conscientious objection in other surveys and so items were added [ 15 , 21 , 28 , 29 ]. Finally, four case studies were added to the survey to address the anticipated changes to the Canadian legislation. The case studies were based upon the inclusion of mature minors, advanced consent, and mental disorder as the sole underlying medical condition. The intention was to assess nurses’ beliefs and comfort with these potential legislative changes.
Phase 2. Item refinement through expert panel review
The goal of phase 2 was to refine and prioritize the proposed survey items identified in phase 1 using a modified e-Delphi approach to achieve consensus among an expert panel [ 26 ]. Items from phase 1 were presented to an expert faculty panel using a Qualtrics (Provo, UT) online survey. Panel members were asked to review each item to determine if it should be: included, excluded or adapted for the survey. When adapted was selected faculty experts were asked to provide rationale and suggestions for adaptation through the use of an open text box. Items that reached a level of 75% consensus for either inclusion or adaptation were retained [ 25 , 26 ]. New items were categorized and added, and a revised survey was presented to the panel of experts in round 2. Panel members were again asked to review items, including new items, to determine if it should be: included, excluded, or adapted for the survey. Round 2 of the modified e-Delphi approach also included an item prioritization activity, where participants were then asked to rate the importance of each item, based on a 5-point Likert scale (low to high importance), which De Vaus [ 30 ] states is helpful for increasing the reliability of responses. Items that reached a 75% consensus on inclusion were then considered in relation to the importance it was given by the expert panel. Quantitative data were managed using SPSS (IBM Corp).
Phase 3. Face validity through cognitive interviews with nursing students
The goal of phase 3 was to obtain initial face validity of the proposed survey using a sample of nursing student informants. More specifically, student participants were asked to discuss how items were interpreted, to identify confusing wording or other problematic construction of items, and to provide feedback about the survey as a whole including readability and organization [ 31 , 32 , 33 ]. The focus group was held online and audio recorded. A semi-structured interview guide was developed for this study that focused on clarity, meaning, order and wording of questions; emotions evoked by the questions; and overall survey cohesion and length was used to obtain data (see Supplementary Material 2 for the interview guide). A prompt to “think aloud” was used to limit interviewer-imposed bias and encourage participants to describe their thoughts and response to a given item as they reviewed survey items [ 27 ]. Where needed, verbal probes such as “could you expand on that” were used to encourage participants to expand on their responses [ 27 ]. Student participants’ feedback was collated verbatim and presented to the research team where potential survey modifications were negotiated and finalized among team members. Conventional content analysis [ 34 ] of focus group data was conducted to identify key themes that emerged through discussion with students. Themes were derived from the data by grouping common responses and then using those common responses to modify survey items.
Ten nursing faculty participated in the expert panel. Eight of the 10 faculty self-identified as female. No faculty panel members reported conscientious objector status and ninety percent reported general agreement with MAiD with one respondent who indicated their view as “unsure.” Six of the 10 faculty experts had 16 years of experience or more working as a nurse educator.
Five nursing students participated in the cognitive interview focus group. The duration of the focus group was 2.5 h. All participants identified that they were born in Canada, self-identified as female (one preferred not to say) and reported having received some instruction about MAiD as part of their nursing curriculum. See Tables 1 and 2 for the demographic descriptors of the study sample. Study results will be reported in accordance with the study phases. See Fig. 1 for an overview of the results from each phase.
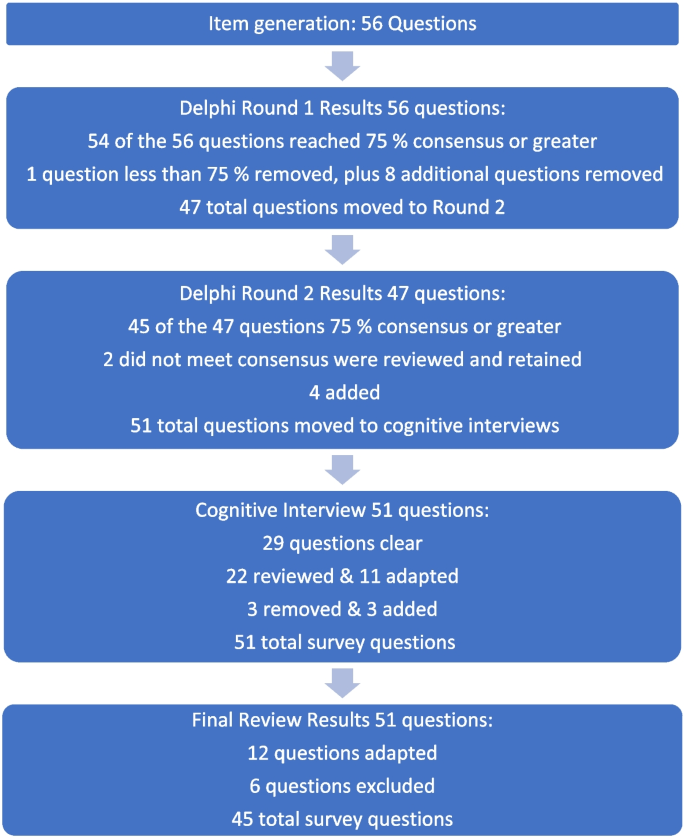
Fig. 1 Overview of survey development findings
Phase 1: survey item generation
Review of the literature identified that no existing survey was available for use with nursing students in the Canadian context. However, an analysis of themes across qualitative and quantitative studies of physicians, medical students, nurses, and nursing students provided sufficient data to develop a preliminary set of items suitable for adaptation to a population of nursing students.
Four major themes and factors that influence knowledge, attitudes, and beliefs about MAiD were evident from the literature: (i) endogenous or individual factors such as age, gender, personally held values, religion, religiosity, and/or spirituality [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ], (ii) experience with death and dying in personal and/or professional life [ 35 , 40 , 41 , 43 , 44 , 45 ], (iii) training including curricular instruction about clinical role, scope of practice, or the law [ 23 , 36 , 39 ], and (iv) exogenous or social factors such as the influence of key leaders, colleagues, friends and/or family, professional and licensure organizations, support within professional settings, and/or engagement in MAiD in an interdisciplinary team context [ 9 , 35 , 46 ].
Studies of nursing students also suggest overlap across these categories. For example, value for patient autonomy [ 23 ] and the moral complexity of decision-making [ 37 ] are important factors that contribute to attitudes about MAiD and may stem from a blend of personally held values coupled with curricular content, professional training and norms, and clinical exposure. For example, students report that participation in end of life care allows for personal growth, shifts in perception, and opportunities to build therapeutic relationships with their clients [ 44 , 47 , 48 ].
Preliminary items generated from the literature resulted in 56 questions from 11 published sources (See Table 3 ). These items were constructed across four main categories: (i) socio-demographic questions; (ii) end of life care questions; (iii) knowledge about MAiD; or (iv) comfort and willingness to participate in MAiD. Knowledge questions were refined to reflect current MAiD legislation, policies, and regulatory frameworks. Falconer [ 39 ] and Freeman [ 45 ] studies were foundational sources for item selection. Additionally, four case studies were written to reflect the most recent anticipated changes to MAiD legislation and all used the same open-ended core questions to address respondents’ perspectives about the patient’s right to make the decision, comfort in assisting a physician or NP to administer MAiD in that scenario, and hypothesized comfort about serving as a primary provider if qualified as an NP in future. Response options for the survey were also constructed during this stage and included: open text, categorical, yes/no , and Likert scales.
Phase 2: faculty expert panel review
Of the 56 items presented to the faculty panel, 54 questions reached 75% consensus. However, based upon the qualitative responses 9 items were removed largely because they were felt to be repetitive. Items that generated the most controversy were related to measuring religion and spirituality in the Canadian context, defining end of life care when there is no agreed upon time frames (e.g., last days, months, or years), and predicting willingness to be involved in a future events – thus predicting their future selves. Phase 2, round 1 resulted in an initial set of 47 items which were then presented back to the faculty panel in round 2.
Of the 47 initial questions presented to the panel in round 2, 45 reached a level of consensus of 75% or greater, and 34 of these questions reached a level of 100% consensus [ 27 ] of which all participants chose to include without any adaptations) For each question, level of importance was determined based on a 5-point Likert scale (1 = very unimportant, 2 = somewhat unimportant, 3 = neutral, 4 = somewhat important, and 5 = very important). Figure 2 provides an overview of the level of importance assigned to each item.
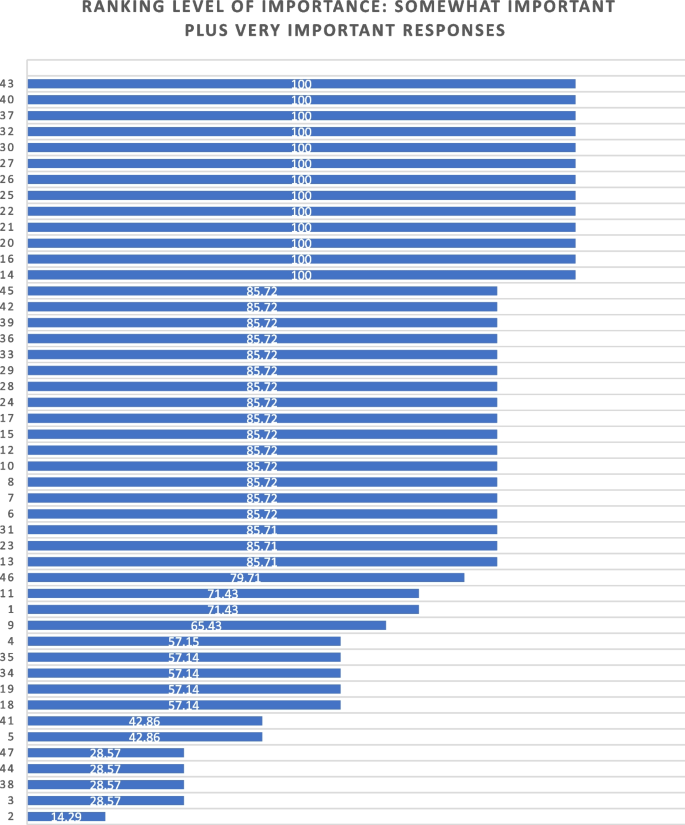
Ranking level of importance for survey items
After round 2, a careful analysis of participant comments and level of importance was completed by the research team. While the main method of survey item development came from participants’ response to the first round of Delphi consensus ratings, level of importance was used to assist in the decision of whether to keep or modify questions that created controversy, or that rated lower in the include/exclude/adapt portion of the Delphi. Survey items that rated low in level of importance included questions about future roles, sex and gender, and religion/spirituality. After deliberation by the research committee, these questions were retained in the survey based upon the importance of these variables in the scientific literature.
Of the 47 questions remaining from Phase 2, round 2, four were revised. In addition, the two questions that did not meet the 75% cut off level for consensus were reviewed by the research team. The first question reviewed was What is your comfort level with providing a MAiD death in the future if you were a qualified NP ? Based on a review of participant comments, it was decided to retain this question for the cognitive interviews with students in the final phase of testing. The second question asked about impacts on respondents’ views of MAiD and was changed from one item with 4 subcategories into 4 separate items, resulting in a final total of 51 items for phase 3. The revised survey was then brought forward to the cognitive interviews with student participants in Phase 3. (see Supplementary Material 1 for a complete description of item modification during round 2).
Phase 3. Outcomes of cognitive interview focus group
Of the 51 items reviewed by student participants, 29 were identified as clear with little or no discussion. Participant comments for the remaining 22 questions were noted and verified against the audio recording. Following content analysis of the comments, four key themes emerged through the student discussion: unclear or ambiguous wording; difficult to answer questions; need for additional response options; and emotional response evoked by questions. An example of unclear or ambiguous wording was a request for clarity in the use of the word “sufficient” in the context of assessing an item that read “My nursing education has provided sufficient content about the nursing role in MAiD.” “Sufficient” was viewed as subjective and “laden with…complexity that distracted me from the question.” The group recommended rewording the item to read “My nursing education has provided enough content for me to care for a patient considering or requesting MAiD.”
An example of having difficulty answering questions related to limited knowledge related to terms used in the legislation such as such as safeguards , mature minor , eligibility criteria , and conscientious objection. Students were unclear about what these words meant relative to the legislation and indicated that this lack of clarity would hamper appropriate responses to the survey. To ensure that respondents are able to answer relevant questions, student participants recommended that the final survey include explanation of key terms such as mature minor and conscientious objection and an overview of current legislation.
Response options were also a point of discussion. Participants noted a lack of distinction between response options of unsure and unable to say . Additionally, scaling of attitudes was noted as important since perspectives about MAiD are dynamic and not dichotomous “agree or disagree” responses. Although the faculty expert panel recommended the integration of the demographic variables of religious and/or spiritual remain as a single item, the student group stated a preference to have religion and spirituality appear as separate items. The student focus group also took issue with separate items for the variables of sex and gender, specifically that non-binary respondents might feel othered or “outed” particularly when asked to identify their sex. These variables had been created based upon best practices in health research but students did not feel they were appropriate in this context [ 49 ]. Finally, students agreed with the faculty expert panel in terms of the complexity of projecting their future involvement as a Nurse Practitioner. One participant stated: “I certainly had to like, whoa, whoa, whoa. Now let me finish this degree first, please.” Another stated, “I'm still imagining myself, my future career as an RN.”
Finally, student participants acknowledged the array of emotions that some of the items produced for them. For example, one student described positive feelings when interacting with the survey. “Brought me a little bit of feeling of joy. Like it reminded me that this is the last piece of independence that people grab on to.” Another participant, described the freedom that the idea of an advance request gave her. “The advance request gives the most comfort for me, just with early onset Alzheimer’s and knowing what it can do.” But other participants described less positive feelings. For example, the mature minor case study yielded a comment: “This whole scenario just made my heart hurt with the idea of a child requesting that.”
Based on the data gathered from the cognitive interview focus group of nursing students, revisions were made to 11 closed-ended questions (see Table 4 ) and 3 items were excluded. In the four case studies, the open-ended question related to a respondents’ hypothesized actions in a future role as NP were removed. The final survey consists of 45 items including 4 case studies (see Supplementary Material 3 ).
The aim of this study was to develop and validate a survey that can be used to track the growth of knowledge about MAiD among nursing students over time, inform training programs about curricular needs, and evaluate attitudes and willingness to participate in MAiD at time-points during training or across nursing programs over time.
The faculty expert panel and student participants in the cognitive interview focus group identified a need to establish core knowledge of the terminology and legislative rules related to MAiD. For example, within the cognitive interview group of student participants, several acknowledged lack of clear understanding of specific terms such as “conscientious objector” and “safeguards.” Participants acknowledged discomfort with the uncertainty of not knowing and their inclination to look up these terms to assist with answering the questions. This survey can be administered to nursing or pre-nursing students at any phase of their training within a program or across training programs. However, in doing so it is important to acknowledge that their baseline knowledge of MAiD will vary. A response option of “not sure” is important and provides a means for respondents to convey uncertainty. If this survey is used to inform curricular needs, respondents should be given explicit instructions not to conduct online searches to inform their responses, but rather to provide an honest appraisal of their current knowledge and these instructions are included in the survey (see Supplementary Material 3 ).
Some provincial regulatory bodies have established core competencies for entry-level nurses that include MAiD. For example, the BC College of Nurses and Midwives (BCCNM) requires “knowledge about ethical, legal, and regulatory implications of medical assistance in dying (MAiD) when providing nursing care.” (10 p. 6) However, across Canada curricular content and coverage related to end of life care and MAiD is variable [ 23 ]. Given the dynamic nature of the legislation that includes portions of the law that are embargoed until 2024, it is important to ensure that respondents are guided by current and accurate information. As the law changes, nursing curricula, and public attitudes continue to evolve, inclusion of core knowledge and content is essential and relevant for investigators to be able to interpret the portions of the survey focused on attitudes and beliefs about MAiD. Content knowledge portions of the survey may need to be modified over time as legislation and training change and to meet the specific purposes of the investigator.
Given the sensitive nature of the topic, it is strongly recommended that surveys be conducted anonymously and that students be provided with an opportunity to discuss their responses to the survey. A majority of feedback from both the expert panel of faculty and from student participants related to the wording and inclusion of demographic variables, in particular religion, religiosity, gender identity, and sex assigned at birth. These and other demographic variables have the potential to be highly identifying in small samples. In any instance in which the survey could be expected to yield demographic group sizes less than 5, users should eliminate the demographic variables from the survey. For example, the profession of nursing is highly dominated by females with over 90% of nurses who identify as female [ 50 ]. Thus, a survey within a single class of students or even across classes in a single institution is likely to yield a small number of male respondents and/or respondents who report a difference between sex assigned at birth and gender identity. When variables that serve to identify respondents are included, respondents are less likely to complete or submit the survey, to obscure their responses so as not to be identifiable, or to be influenced by social desirability bias in their responses rather than to convey their attitudes accurately [ 51 ]. Further, small samples do not allow for conclusive analyses or interpretation of apparent group differences. Although these variables are often included in surveys, such demographics should be included only when anonymity can be sustained. In small and/or known samples, highly identifying variables should be omitted.
There are several limitations associated with the development of this survey. The expert panel was comprised of faculty who teach nursing students and are knowledgeable about MAiD and curricular content, however none identified as a conscientious objector to MAiD. Ideally, our expert panel would have included one or more conscientious objectors to MAiD to provide a broader perspective. Review by practitioners who participate in MAiD, those who are neutral or undecided, and practitioners who are conscientious objectors would ensure broad applicability of the survey. This study included one student cognitive interview focus group with 5 self-selected participants. All student participants had held discussions about end of life care with at least one patient, 4 of 5 participants had worked with a patient who requested MAiD, and one had been present for a MAiD death. It is not clear that these participants are representative of nursing students demographically or by experience with end of life care. It is possible that the students who elected to participate hold perspectives and reflections on patient care and MAiD that differ from students with little or no exposure to end of life care and/or MAiD. However, previous studies find that most nursing students have been involved with end of life care including meaningful discussions about patients’ preferences and care needs during their education [ 40 , 44 , 47 , 48 , 52 ]. Data collection with additional student focus groups with students early in their training and drawn from other training contexts would contribute to further validation of survey items.
Future studies should incorporate pilot testing with small sample of nursing students followed by a larger cross-program sample to allow evaluation of the psychometric properties of specific items and further refinement of the survey tool. Consistent with literature about the importance of leadership in the context of MAiD [ 12 , 53 , 54 ], a study of faculty knowledge, beliefs, and attitudes toward MAiD would provide context for understanding student perspectives within and across programs. Additional research is also needed to understand the timing and content coverage of MAiD across Canadian nurse training programs’ curricula.
The implementation of MAiD is complex and requires understanding of the perspectives of multiple stakeholders. Within the field of nursing this includes clinical providers, educators, and students who will deliver clinical care. A survey to assess nursing students’ attitudes toward and willingness to participate in MAiD in the Canadian context is timely, due to the legislation enacted in 2016 and subsequent modifications to the law in 2021 with portions of the law to be enacted in 2027. Further development of this survey could be undertaken to allow for use in settings with practicing nurses or to allow longitudinal follow up with students as they enter practice. As the Canadian landscape changes, ongoing assessment of the perspectives and needs of health professionals and students in the health professions is needed to inform policy makers, leaders in practice, curricular needs, and to monitor changes in attitudes and practice patterns over time.
Availability of data and materials
The datasets used and/or analysed during the current study are not publicly available due to small sample sizes, but are available from the corresponding author on reasonable request.
Abbreviations
British Columbia College of Nurses and Midwives
Medical assistance in dying
Nurse practitioner
Registered nurse
University of British Columbia Okanagan
Nicol J, Tiedemann M. Legislative Summary: Bill C-14: An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying). Available from: https://lop.parl.ca/staticfiles/PublicWebsite/Home/ResearchPublications/LegislativeSummaries/PDF/42-1/c14-e.pdf .
Downie J, Scallion K. Foreseeably unclear. The meaning of the “reasonably foreseeable” criterion for access to medical assistance in dying in Canada. Dalhousie Law J. 2018;41(1):23–57.
Nicol J, Tiedeman M. Legislative summary of Bill C-7: an act to amend the criminal code (medical assistance in dying). Ottawa: Government of Canada; 2021.
Google Scholar
Council of Canadian Academies. The state of knowledge on medical assistance in dying where a mental disorder is the sole underlying medical condition. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-Where-a-Mental-Disorder-is-the-Sole-Underlying-Medical-Condition.pdf .
Council of Canadian Academies. The state of knowledge on advance requests for medical assistance in dying. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2019/02/The-State-of-Knowledge-on-Advance-Requests-for-Medical-Assistance-in-Dying.pdf .
Council of Canadian Academies. The state of knowledge on medical assistance in dying for mature minors. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-for-Mature-Minors.pdf .
Health Canada. Third annual report on medical assistance in dying in Canada 2021. Ottawa; 2022. [cited 2023 Oct 23]. Available from: https://www.canada.ca/en/health-canada/services/medical-assistance-dying/annual-report-2021.html .
Banner D, Schiller CJ, Freeman S. Medical assistance in dying: a political issue for nurses and nursing in Canada. Nurs Philos. 2019;20(4): e12281.
Article PubMed Google Scholar
Pesut B, Thorne S, Stager ML, Schiller CJ, Penney C, Hoffman C, et al. Medical assistance in dying: a review of Canadian nursing regulatory documents. Policy Polit Nurs Pract. 2019;20(3):113–30.
Article PubMed PubMed Central Google Scholar
College of Registered Nurses of British Columbia. Scope of practice for registered nurses [Internet]. Vancouver; 2018. Available from: https://www.bccnm.ca/Documents/standards_practice/rn/RN_ScopeofPractice.pdf .
Pesut B, Thorne S, Schiller C, Greig M, Roussel J, Tishelman C. Constructing good nursing practice for medical assistance in dying in Canada: an interpretive descriptive study. Global Qual Nurs Res. 2020;7:2333393620938686. https://doi.org/10.1177/2333393620938686 .
Article Google Scholar
Pesut B, Thorne S, Schiller CJ, Greig M, Roussel J. The rocks and hard places of MAiD: a qualitative study of nursing practice in the context of legislated assisted death. BMC Nurs. 2020;19:12. https://doi.org/10.1186/s12912-020-0404-5 .
Pesut B, Greig M, Thorne S, Burgess M, Storch JL, Tishelman C, et al. Nursing and euthanasia: a narrative review of the nursing ethics literature. Nurs Ethics. 2020;27(1):152–67.
Pesut B, Thorne S, Storch J, Chambaere K, Greig M, Burgess M. Riding an elephant: a qualitative study of nurses’ moral journeys in the context of Medical Assistance in Dying (MAiD). Journal Clin Nurs. 2020;29(19–20):3870–81.
Lamb C, Babenko-Mould Y, Evans M, Wong CA, Kirkwood KW. Conscientious objection and nurses: results of an interpretive phenomenological study. Nurs Ethics. 2018;26(5):1337–49.
Wright DK, Chan LS, Fishman JR, Macdonald ME. “Reflection and soul searching:” Negotiating nursing identity at the fault lines of palliative care and medical assistance in dying. Social Sci & Med. 2021;289: 114366.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;54(4):511–20.
Bruce A, Beuthin R. Medically assisted dying in Canada: "Beautiful Death" is transforming nurses' experiences of suffering. The Canadian J Nurs Res | Revue Canadienne de Recherche en Sci Infirmieres. 2020;52(4):268–77. https://doi.org/10.1177/0844562119856234 .
Canadian Nurses Association. Code of ethics for registered nurses. Ottawa; 2017. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-ethics .
Canadian Nurses Association. National nursing framework on Medical Assistance in Dying in Canada. Ottawa: 2017. Available from: https://www.virtualhospice.ca/Assets/cna-national-nursing-framework-on-maidEng_20170216155827.pdf .
Pesut B, Thorne S, Greig M. Shades of gray: conscientious objection in medical assistance in dying. Nursing Inq. 2020;27(1): e12308.
Durojaiye A, Ryan R, Doody O. Student nurse education and preparation for palliative care: a scoping review. PLoS ONE. 2023. https://doi.org/10.1371/journal.pone.0286678 .
McMechan C, Bruce A, Beuthin R. Canadian nursing students’ experiences with medical assistance in dying | Les expériences d’étudiantes en sciences infirmières au regard de l’aide médicale à mourir. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2019;5(1). https://doi.org/10.17483/2368-6669.1179 .
Adler M, Ziglio E. Gazing into the oracle. The Delphi method and its application to social policy and public health. London: Jessica Kingsley Publishers; 1996
Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53(2):205–12.
Keeney S, Hasson F, McKenna H. The Delphi technique in nursing and health research. 1st ed. City: Wiley; 2011.
Willis GB. Cognitive interviewing: a tool for improving questionnaire design. 1st ed. Thousand Oaks, Calif: Sage; 2005. ISBN: 9780761928041
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood EW. Conscience, conscientious objection, and nursing: a concept analysis. Nurs Ethics. 2017;26(1):37–49.
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood K. Nurses’ use of conscientious objection and the implications of conscience. J Adv Nurs. 2018;75(3):594–602.
de Vaus D. Surveys in social research. 6th ed. Abingdon, Oxon: Routledge; 2014.
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: A primer. Front Public Health. 2018;6:149. https://doi.org/10.3389/fpubh.2018.00149 .
Puchta C, Potter J. Focus group practice. 1st ed. London: Sage; 2004.
Book Google Scholar
Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. 5th ed. Oxford: Oxford University Press; 2015.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Adesina O, DeBellis A, Zannettino L. Third-year Australian nursing students’ attitudes, experiences, knowledge, and education concerning end-of-life care. Int J of Palliative Nurs. 2014;20(8):395–401.
Bator EX, Philpott B, Costa AP. This moral coil: a cross-sectional survey of Canadian medical student attitudes toward medical assistance in dying. BMC Med Ethics. 2017;18(1):58.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;53(4):511–20.
Brown J, Goodridge D, Thorpe L, Crizzle A. What is right for me, is not necessarily right for you: the endogenous factors influencing nonparticipation in medical assistance in dying. Qual Health Res. 2021;31(10):1786–1800.
Falconer J, Couture F, Demir KK, Lang M, Shefman Z, Woo M. Perceptions and intentions toward medical assistance in dying among Canadian medical students. BMC Med Ethics. 2019;20(1):22.
Green G, Reicher S, Herman M, Raspaolo A, Spero T, Blau A. Attitudes toward euthanasia—dual view: Nursing students and nurses. Death Stud. 2022;46(1):124–31.
Hosseinzadeh K, Rafiei H. Nursing student attitudes toward euthanasia: a cross-sectional study. Nurs Ethics. 2019;26(2):496–503.
Ozcelik H, Tekir O, Samancioglu S, Fadiloglu C, Ozkara E. Nursing students’ approaches toward euthanasia. Omega (Westport). 2014;69(1):93–103.
Canning SE, Drew C. Canadian nursing students’ understanding, and comfort levels related to medical assistance in dying. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2022;8(2). https://doi.org/10.17483/2368-6669.1326 .
Edo-Gual M, Tomás-Sábado J, Bardallo-Porras D, Monforte-Royo C. The impact of death and dying on nursing students: an explanatory model. J Clin Nurs. 2014;23(23–24):3501–12.
Freeman LA, Pfaff KA, Kopchek L, Liebman J. Investigating palliative care nurse attitudes towards medical assistance in dying: an exploratory cross-sectional study. J Adv Nurs. 2020;76(2):535–45.
Brown J, Goodridge D, Thorpe L, Crizzle A. “I am okay with it, but I am not going to do it:” the exogenous factors influencing non-participation in medical assistance in dying. Qual Health Res. 2021;31(12):2274–89.
Dimoula M, Kotronoulas G, Katsaragakis S, Christou M, Sgourou S, Patiraki E. Undergraduate nursing students’ knowledge about palliative care and attitudes towards end-of-life care: A three-cohort, cross-sectional survey. Nurs Educ Today. 2019;74:7–14.
Matchim Y, Raetong P. Thai nursing students’ experiences of caring for patients at the end of life: a phenomenological study. Int J Palliative Nurs. 2018;24(5):220–9.
Canadian Institute for Health Research. Sex and gender in health research [Internet]. Ottawa: CIHR; 2021 [cited 2023 Oct 23]. Available from: https://cihr-irsc.gc.ca/e/50833.html .
Canadian Nurses’ Association. Nursing statistics. Ottawa: CNA; 2023 [cited 2023 Oct 23]. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-statistics .
Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025–47. https://doi.org/10.1007/s11135-011-9640-9 .
Ferri P, Di Lorenzo R, Stifani S, Morotti E, Vagnini M, Jiménez Herrera MF, et al. Nursing student attitudes toward dying patient care: a European multicenter cross-sectional study. Acta Bio Medica Atenei Parmensis. 2021;92(S2): e2021018.
PubMed PubMed Central Google Scholar
Beuthin R, Bruce A. Medical assistance in dying (MAiD): Ten things leaders need to know. Nurs Leadership. 2018;31(4):74–81.
Thiele T, Dunsford J. Nurse leaders’ role in medical assistance in dying: a relational ethics approach. Nurs Ethics. 2019;26(4):993–9.
Download references
Acknowledgements
We would like to acknowledge the faculty and students who generously contributed their time to this work.
JS received a student traineeship through the Principal Research Chairs program at the University of British Columbia Okanagan.
Author information
Authors and affiliations.
School of Health and Human Services, Selkirk College, Castlegar, BC, Canada
Jocelyn Schroeder & Barbara Pesut
School of Nursing, University of British Columbia Okanagan, Kelowna, BC, Canada
Barbara Pesut, Lise Olsen, Nelly D. Oelke & Helen Sharp
You can also search for this author in PubMed Google Scholar
Contributions
JS made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. JS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. BP made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. BP has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. LO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. LO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. NDO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. NDO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. HS made substantial contributions to drafting and substantively revising the work. HS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Authors’ information
JS conducted this study as part of their graduate requirements in the School of Nursing, University of British Columbia Okanagan.
Corresponding author
Correspondence to Barbara Pesut .
Ethics declarations
Ethics approval and consent to participate.
The research was approved by the Selkirk College Research Ethics Board (REB) ID # 2021–011 and the University of British Columbia Behavioral Research Ethics Board ID # H21-01181.
All participants provided written and informed consent through approved consent processes. Research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schroeder, J., Pesut, B., Olsen, L. et al. Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study. BMC Nurs 23 , 326 (2024). https://doi.org/10.1186/s12912-024-01984-z
Download citation
Received : 24 October 2023
Accepted : 28 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12912-024-01984-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical assistance in dying (MAiD)
- End of life care
- Student nurses
- Nursing education
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Jump to navigation
CALL FOR SUBMISSIONS: NEPCA 2024's Philosophy, Belief, and Pop Culture Area
The 2024 Northeast Popular Culture Association (NEPCA) will host its annual conference this fall as a hybrid conference from Thursday, October 3 – Saturday, October 5. Virtual sessions will take place on Thursday evening and Friday morning via Zoom, and in-person sessions will take place on Friday evening and Saturday morning at Nichols College, Dudley, Massachusetts.
We are excited to be back together again face-to-face and to continue providing a virtual option for access and affordability. We are looking forward to another engaging and rewarding conference for new and seasoned members alike. We are seeking proposals for panels and presentations for this year’s conference, including proposals for the Philosophy, Belief, and Pop Culture Area.
Philosophy questions general and fundamental concepts of our world and reality, such as reason, values, language, knowledge, existence, and the mind, body and soul. It functions as one of our oldest means of studying, understanding, and explaining, and prominent practitioners feature across time and cultures (e.g., Plato, Nietzsche, Confucius, Laozi, Ibn Rushd, Ptahhotep, Adi Shankara, Anthony William Amo, Nezahualcoyotl, etc.). This area welcomes proposals from all academic and methodological perspectives that either use philosophic principles to engage with/analyze examples of pop culture or explore depictions of philosophy within pop culture. Some specific potential topics include but are not limited to:
- The portrayal of philosophy, belief systems, religions, and mythologies across any medium (e.g., literature, film, television, comics/graphic novels, poetry, anime and manga, video games, tabletop role-playing games, etc.)
- The depiction of historic philosophers and religious leaders in pop culture and media
- The evolution of philosophical principles, belief systems, religions, and mythologies in pop culture and media
- The application of philosophic principles and religious teachings in American politics and news media
- The development of new philosophical principles, belief systems, religions, and mythologies through fiction
NEPCA’s call-for-papers will be open until June 15 by 11:59p.m. (EST). You can submit your proposal here - https://nepca.blog/2024-conference-page/
- Share full article
Advertisement
Supported by
Guest Essay
The View Within Israel Turns Bleak

By Megan K. Stack
Ms. Stack is a contributing Opinion writer who has reported from the Middle East.
It was the pictures of Palestinians swimming and sunning at a Gaza beach that rubbed Yehuda Shlezinger, an Israeli journalist, the wrong way. Stylish in round red glasses and a faint scruff of beard, Mr. Shlezinger unloaded his revulsion at the “disturbing” pictures while appearing on Israel’s Channel 12.
“These people there deserve death, a hard death, an agonizing death, and instead we see them enjoying on the beach and having fun,” complained Mr. Shlezinger, the religious affairs correspondent for the widely circulated right-wing Israel Hayom newspaper. “We should have seen a lot more revenge there,” Mr. Shlezinger unrepentantly added. “A lot more rivers of Gazans’ blood.”
It would be nice to think that Mr. Shlezinger is a fringe figure or that Israelis would be shocked by his bloody fantasies. But he’s not, and many wouldn’t be.
Israel has hardened, and the signs of it are in plain view. Dehumanizing language and promises of annihilation from military and political leaders. Polls that found wide support for the policies that have wreaked devastation and starvation in Gaza. Selfies of Israeli soldiers preening proudly in bomb-crushed Palestinian neighborhoods. A crackdown on even mild forms of dissent among Israelis.
The Israeli left — the factions that criticize the occupation of Palestinian lands and favor negotiations and peace instead — is now a withered stump of a once-vigorous movement. In recent years, the attitudes of many Israelis toward the “Palestinian problem” have ranged largely from detached fatigue to the hard-line belief that driving Palestinians off their land and into submission is God’s work.
This bleak ideological landscape emerged slowly and then, on Oct. 7, all at once.
The massacre and kidnappings of that day, predictably, brought a public thirst for revenge. But in truth, by the time Hamas killers rampaged through the kibbutzim — in a bitter twist, home to some of the holdout peaceniks — many Israelis had long since come to regard Palestinians as a threat best locked away. America’s romantic mythology and wishful thinking about Israel encourage a tendency to see Prime Minister Benjamin Netanyahu as the main cause of the ruthlessness in Gaza, where Israel has killed more than 35,000 people. The unpopular, scandal-ridden premier makes a convincing ogre in an oversimplified story.
But Israel’s slaughter in Gaza, the creeping famine, the wholesale destruction of neighborhoods — this, polling suggests, is the war the Israeli public wanted. A January survey found that 94 percent of Jewish Israelis said the force being used against Gaza was appropriate or even insufficient. In February, a poll found that most Jewish Israelis opposed food and medicine getting into Gaza. It was not Mr. Netanyahu alone but also his war cabinet members (including Benny Gantz, often invoked as the moderate alternative to Mr. Netanyahu) who unanimously rejected a Hamas deal to free Israeli hostages and, instead, began an assault on the city of Rafah, overflowing with displaced civilians.
“It’s so much easier to put everything on Netanyahu, because then you feel so good about yourself and Netanyahu is the darkness,” said Gideon Levy, an Israeli journalist who has documented Israel’s military occupation for decades. “But the darkness is everywhere.”
Like most political evolutions, the toughening of Israel is partly explained by generational change — Israeli children whose earliest memories are woven through with suicide bombings have now matured into adulthood. The rightward creep could be long-lasting because of demographics, with modern Orthodox and ultra-Orthodox Jews (who disproportionately vote with the right) consistently having more babies than their secular compatriots.
Most crucially, many Israelis emerged from the second intifada with a jaundiced view of negotiations and, more broadly, Palestinians, who were derided as unable to make peace. This logic conveniently erased Israel’s own role in sabotaging the peace process through land seizures and settlement expansion. But something broader had taken hold — a quality that Israelis described to me as a numb, disassociated denial around the entire topic of Palestinians.
“The issues of settlements or relations with Palestinians were off the table for years,” Tamar Hermann told me. “The status quo was OK for Israelis.”
Ms. Hermann, a senior research fellow at the Israel Democracy Institute, is one of the country’s most respected experts on Israeli public opinion. In recent years, she said, Palestinians hardly caught the attention of Israeli Jews. She and her colleagues periodically made lists of issues and asked respondents to rank them in order of importance. It didn’t matter how many choices the pollsters presented, she said — resolving the Israeli-Palestinian conflict came in last in almost all measurements.
“It was totally ignored,” she said.
The psychological barrier between Israelis and Palestinians was hardened when Israel built the snaking West Bank barrier, which helped to forestall attacks on Israelis toward the end of the second intifada — the five-year Palestinian uprising that erupted in 2000, killing about 1,000 Israelis and roughly three times as many Palestinians. The wall helped keep West Bank suicide bombers from penetrating Israel and piled extra misery on ever-more-constrained Palestinian civilians, many of whom refer to it as the apartheid wall.
Many Israelis, Ms. Hermann told me, are at a loss when asked to identify the border where Israel ends and the West Bank begins. Her research from 2016 found that only a small percentage of Israelis knew for sure that the Green Line was the border delineated by the 1949 Armistice. The question of whether this border should even be depicted on Israeli school maps has been a heated topic of debate within Israel; with a rueful laugh, Ms. Hermann described many of the classroom maps as “from the river to the sea.”
Such ignorance is a luxury exclusive to Israelis. Palestinians make it their business to know exactly where the border between Israel and the West Bank lies, which checkpoints are open on a given day, which roads they may and may not use. These are not abstract ideas; they dictate the daily movements of Palestinians, and confusing them could be fatal.
Israel’s uneasy detachment turned to rage on Oct. 7.
A handful of songs with lyrics calling for the annihilation of a dehumanized enemy have been circulated in Israel these past months, including “Launch,” a hip-hop glorification of the military promising “from kisses to guns, until Gaza is erased” and suggesting that the West Bank city of Jenin is under the “plague of the firstborn,” a reference to the biblical story in which God smites the eldest sons of Egypt. The smash hit “ Harbu Darbu ,” addressed to “you sons of Amalek,” promises “another X on the rifle, ’cause every dog will get what’s coming to him.”
“There is no forgiveness for swarms of rats,” another song goes . “They will die in their rat holes.”
Israeli shops hawk trendy products like a bumper sticker that reads, “Finish them,” and a pendant cut into the shape of Israel, with East Jerusalem, the West Bank and Gaza seamlessly attached.
Israeli protesters have repeatedly taken to the streets in anguish over the hostages held in Gaza and rage at Mr. Netanyahu (who faced intense domestic opposition long before Oct. 7) for failing to save them. But the demonstrations should not be conflated with international calls to protect civilians in Gaza. Many Israelis want a cease-fire to free the hostages, followed by the ouster of Mr. Netanyahu — but the protests do not reflect a groundswell of sympathy for Palestinians or a popular desire to rethink the status quo ante of occupation and long-silenced peace talks.
If anything, with the world’s attention fixed on Gaza, Israel’s far-right government has intensified the domination of Palestinians. The single largest Israeli land grab in more than 30 years happened in March , when Finance Minister Bezalel Smotrich announced the state seizure of 10 square kilometers of the West Bank. The land takeovers are accompanied by a bloody campaign of terror , with an ever-less-distinguishable mix of soldiers and settlers killing at least 460 Palestinians in the West Bank since Oct. 7, the Palestinian health ministry says.
Meanwhile, inside Israel, the police have handed out guns to civilians and set up de facto militias in the name of self-defense. But questions about whom these newly armed groups are meant to defend, and from whom, have created a creeping unease.
The weapons have gone not only to West Bank settlements or towns adjacent to Palestinian territories and Lebanon but also to communities set deep in Israel’s interior, particularly places that are home to a mix of Arab and Jewish residents . An analysis published in January by the newspaper Haaretz found that while the national security ministry wouldn’t disclose which communities got gun licenses or the criteria used to decide, Arab communities — even those on Israel’s frontier — did not seem to be eligible.
The guns sent a chill through Palestinian citizens of Israel, who have often been invoked in defense of the state. Look, Israel’s advocates often say, Arabs live more freely in Israel than anywhere else in the Middle East.
Hassan Jabareen, a prominent Palestinian lawyer who founded Adalah, Israel’s main legal center for Arab rights, told me that many Arab citizens of Israel — who constitute one-fifth of the population — live in fear.
Israel’s attacks on Gaza have in the past provoked community protests, riots and clashes among Arabs and Jews in Israel. After Oct. 7, though, the message was clear: Stay quiet.
“The police left no doubt that we were enemies of the state,” Mr. Jabareen said, “when they started arming the Jewish citizens of Israel and called Jewish citizens to come to the station and take your arms to defend yourself from your Palestinian neighbor.”
Diana Buttu, a Palestinian lawyer who lives with her family in the Israeli city of Haifa, told me that these past months have been thick with unease. She has long imagined herself as a living holdover from the once-thriving Arab population that was largely displaced from what is now Israel. A “remnant,” she calls herself, who for years moved through Israel feeling invisible.
Now the sense of invisibility has melted. Both Ms. Buttu and Mr. Jabareen said that the current atmosphere in Israel had drawn closer and sharpened in their minds the mass displacement known in Arabic as the nakba, or catastrophe, as if history might yet loop back. Mr. Netanyahu evoked the same era when he referred to Israel’s current onslaught as “Israel’s second war of independence.”
“They didn’t see us,” Ms. Buttu said. “We were the ghosts; we were just there. And now it’s like, ‘Wow, they’re here.’ There is an interest in trying to get rid of Palestinians. We’re on the rhetorical front lines.”
Long before this current storm of violence, Mr. Netanyahu’s far-right government had worked to strengthen Jewish supremacy. The 2018 “nation-state law” codified the right to national self-determination as “unique to the Jewish people,” removed Arabic as an official language and established “Jewish settlement as a national value” that the government must support. Palestinian members of the Knesset famously shredded copies of the bill in Parliament and yelled, “Apartheid,” but it passed all the same.
In 2022, Israel reauthorized its controversial family unification law, largely barring Palestinians who marry Israeli citizens from receiving legal status — or living with their spouses in Israel — if they are from the West Bank or Gaza. The law also applies to people from the “enemy states” of Lebanon, Syria and Iraq (homes to Palestinian refugee communities), as well as Iran.
With legal disadvantages and social pressures mounting, Palestinian citizens of Israel have started to look abroad for support. Mr. Jabareen told me that his organization is preparing an application to the United Nations to request international legal protections for Palestinians inside Israel. In March a Palestinian citizen of Israel was granted asylum in Britain after arguing that returning would very likely expose him to persecution because of his political views and activism for Palestinian rights and Israel’s “apartheid system of racial control of its Jewish citizens over its Palestinian citizens.”
Another stark sign of Israel’s hardening is the hundreds of Israelis — mostly Arabs, but some Jews, too — who have been arrested, fired or otherwise punished for statements or actions regarded as endangering national security or undermining Israel’s war efforts. Even a social media post expressing concern for Palestinians in Gaza is enough to draw police scrutiny.
Nadera Shalhoub-Kevorkian, a scholar who lectures at Hebrew University of Jerusalem and Queen Mary University of London, said on a podcast that Zionism should be abolished, that Israel may be lying about the extent of sexual assault that took place on Oct. 7 and that Israelis were “criminals” who “cannot kill and not be afraid, so they better be afraid.” Israeli police responded in April by jailing Ms. Shalhoub-Kevorkian overnight and asking a judge to keep her locked up while they investigated her on suspicion of incitement. The judge decided to release her but acknowledged that she “may have crossed the line from free expression to incitement.”
For nearly two decades — starting with the quieting of the second intifada and ending calamitously on Oct. 7 — Israel was remarkably successful at insulating itself from the violence of the occupation. Rockets fired from Gaza periodically rained down on Israeli cities, but since 2011 , Israel’s Iron Dome defense system has intercepted most of them. The mathematics of death heavily favored Israel: From 2008 until Oct. 7, more than 6,000 Palestinians were killed in what the United Nations calls “the context of occupation and conflict”; during that time, more than 300 Israelis were killed.
Human rights organizations — including Israeli groups — wrote elaborate reports explaining why Israel is an apartheid state. That was embarrassing for Israel, but nothing really came of it. The economy flourished. Once-hostile Arab states showed themselves willing to sign accords with Israel after just a little performative pestering about the Palestinians.
Those years gave Israelis a taste of what may be the Jewish state’s most elusive dream — a world in which there simply did not exist a Palestinian problem.
Daniel Levy, a former Israeli negotiator who is now president of the U.S./Middle East Project think tank, describes “the level of hubris and arrogance that built up over the years.” Those who warned of the immorality or strategic folly of occupying Palestinian territories “were dismissed,” he said, “like, ‘Just get over it.’”
If U.S. officials understand the state of Israeli politics, it doesn’t show. Biden administration officials keep talking about a Palestinian state. But the land earmarked for a state has been steadily covered in illegal Israeli settlements, and Israel itself has seldom stood so unabashedly opposed to Palestinian sovereignty.
There’s a reason Mr. Netanyahu keeps reminding everyone that he’s spent his career undermining Palestinian statehood: It’s a selling point. Mr. Gantz, who is more popular than Mr. Netanyahu and is often mentioned as a likely successor, is a centrist by Israeli standards — but he, too, has pushed back against international calls for a Palestinian state.
Daniel Levy describes the current divide among major Israeli politicians this way: Some believe in “managing the apartheid in a way that gives Palestinians more freedom — that’s [Yair] Lapid and maybe Gantz on some days,” while hard-liners like Mr. Smotrich and Security Minister Itamar Ben Gvir “are really about getting rid of the Palestinians. Eradication. Displacement.”
The carnage and cruelty suffered by Israelis on Oct. 7 should have driven home the futility of sealing themselves off from Palestinians while subjecting them to daily humiliations and violence. As long as Palestinians are trapped under violent military occupation, deprived of basic rights and told that they must accept their lot as inherently lower beings, Israelis will live under the threat of uprisings, reprisals and terrorism. There is no wall thick enough to suppress forever a people who have nothing to lose.
Israelis did not, by and large, take that lesson. Now apathy has been replaced by vengeance.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Megan K. Stack is a contributing Opinion writer and author. She has been a correspondent in China, Russia, Egypt, Israel, Afghanistan and the U.S.-Mexico border area. Her first book, a narrative account of the post-Sept. 11 wars, was a finalist for the National Book Award in nonfiction. @ Megankstack

IMAGES
VIDEO
COMMENTS
These values include honesty, responsibility, compassion, lifelong learning, and kindness. Nursing is not only a career, but a calling that requires the possession of integrity, knowledge, and compassion (Kim 54). My personal philosophy postulates that I have a responsibility to use my knowledge and abilities to help people alleviate their ...
1. A personal nursing philosophy serves as a guideline to help nurses live by standards they have set for themselves. 2. Having a personal philosophy of nursing can improve how you interact with patients, their loved ones, and your peers. 3. Personal nursing philosophies help guide ethical, competent, evidence-based, and science-driven nursing ...
The top 25 professional nursing values listed below are some of the most important values nurses can learn, develop, and continue to cultivate throughout their careers. 1. Trustworthiness. What is it: Trustworthiness is one of the most essential nursing values. Trustworthiness encompasses traits such as reliability, competence, and honesty.
There are four fundamental patterns of knowing in nursing: empirical knowing, ethical knowing, personal knowing, and aesthetic knowing (Carper, 2009). White (2009) has added sociopolitical knowing as a fifth pattern. My nursing practice, both in the clinical and education arenas, is primarily driven by empirical ways of knowing.
A personal nursing philosophy statement is a statement that shows a nurse's values, ethics, and beliefs about patient care and nursing in general. In other words, it is a statement that clarifies a nurse's thoughts, ideas, and principles regarding patient care and nursing. ... Inspirational nursing topics for nursing papers. How to write a ...
Nurses begin to develop a professional identity in nursing school by embracing the core values of nursing and through engagement with student peers, nursing faculty, and patients. Students integrate critical thinking and clinical reasoning with these core values as they begin to think, feel, and perform like a nurse.
A philosophy of nursing is a statement that outlines a nurse's values, ethics, and beliefs, as well as their motivation for being part of the profession. It covers a nurse's perspective regarding their education, practice, and patient care ethics. A philosophy of nursing helps you identify the beliefs and theories that shape the choices you ...
Articulating a philosophy statement is an intellectual activity that requires careful thought, because values need to be identified, clarified, and prioritized. Once these values are identified, putting them together into a short, cohesive statement is a challenging process ( Chitty, 2001 ).
However, in several areas, influences of social, cultural, and economical status and religious beliefs on values result in a different definition of these values. This study revealed that based on humanistic nature of nursing, common values in nursing protect human dignity and respect to the patients.
Values are recognised as important within nursing (Rassin, 2008), and recent policy initiatives to recruit nursing staff based on their values underlines the centrality of values for the profession (NHS England, 2012).All Registered Nurses (RNs) possess values that will influence their attitudes, behaviours and emotions.
The essay focuses on how values and beliefs shape the nursing profession. It will examine the core principles such as compassion, advocacy, ethics, and lifelong learning that underpin nursing practice. The piece will discuss how these values are essential in patient care, influencing decision-making and the nurse-patient relationship.
Introduction. Values are goals and beliefs that establish a behavior and provide a basis for decision making [].In a profession, values are standards for action that are preferred by experts and professional groups and establish frameworks for evaluating behavior [].Nursing is a profession rooted in professional ethics and ethical values, and nursing performance is based on such values.
With holistic care, nurses focus on the mind, body, and spirit. Not only does nursing deal with caring for the individual, but also education is a large part of nursing. To me, the second concept of nursing, Get Access. Free Essay: Philosophy of Nursing Everyone's values and beliefs about the profession of nursing are all different.
A number of papers implied that philosophy was a powerful way to gain "freedom" from knowledge as traditionally understood. ... knowledgeably access the complexity of nursing or as a strategy to move beyond classical knowledge structures to ground nursing in individual or community beliefs and values, which are different depending on the ...
This philosophy is based on providing competent, empathetic, compassionate and optimal holistic care to the best of my ability. This philosophy stems from the values and beliefs instilled in me during my early childhood. These values and beliefs are accompanied by trustworthiness, respect, compassion, and that is what drove me to this ...
The hook or attention grabber. Thesis statement. Main points of each body paragraph (topic sentence, evidence, examples, illustrations, etc.) Conclusion (restated thesis and call-to-action) With the outline done, you should take a break and resume writing your first draft of the nursing reflection essay.
The Five Professional Values Of Altruism In Nursing. 1386 Words | 6 Pages. Every nursing, in order to consider the profession must have an understanding of at least three of the five professional values, in my opinion. These values consist of altruism, autonomy, human dignity, integrity and social justice (Taylor 96).
Briefly introduce your topic after the hook. This may involve presenting your essay's key theme or focus, such as a particular experience, challenge, or aspiration related to nursing. Then, present Your Thesis Statement. It outlines your essay's main idea or argument in one or two sentences.
16 values in nursing. The following list includes some values important to the nursing community: 1. Human dignity. One of the most important values of nursing is to respect the dignity of their patients. This means treating patients with kindness and thoughtfulness as you provide care, and remembering to consider their emotions about the ...
Spirituality is a common theme in the field of healthcare research. This study aimed to examine nurses' perceptions of spirituality in the context of the religious diversity of patients in pluri-religious settings. We performed a scoping review following the methodology on studies conducted between 2010 and 2020.
This concept makes up my personal philosophy of nursing and it is the main doctrine of the field of nursing. I as the nursing student view health as a dynamic state of being along a health-illness continuum. It is affected by health beliefs and health behaviors. Health is holistic, encompassing physical, physiological, emotional, spiritual, and ...
Therefore, the purpose of this study was to develop a survey to measure nursing students' knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context. The design was a mixed-method, modified e-Delphi method that entailed item generation from the literature, item refinement through a 2 round ...
Read the latest articles of International Journal of Nursing Studies at ScienceDirect.com, Elsevier's leading platform of peer-reviewed scholarly literature. Skip to main content. ... Reviews and Discussion papers. select article Combined healthy lifestyle behaviours and incident dementia: A systematic review and dose-response meta-analysis ...
The portrayal of philosophy, belief systems, religions, and mythologies across any medium (e.g., literature, film, television, comics/graphic novels, poetry, anime and manga, video games, tabletop role-playing games, etc.) The depiction of historic philosophers and religious leaders in pop culture and media
Nursing officer question papers will help applicants to identify which topics are relevant from an exam point of view. Get the direct link to the previous paper PDF on this page.
This bleak ideological landscape emerged slowly and then, on Oct. 7, all at once. The massacre and kidnappings of that day, predictably, brought a public thirst for revenge.