- Open access
- Published: 27 May 2020

How to use and assess qualitative research methods
- Loraine Busetto ORCID: orcid.org/0000-0002-9228-7875 1 ,
- Wolfgang Wick 1 , 2 &
- Christoph Gumbinger 1
Neurological Research and Practice volume 2 , Article number: 14 ( 2020 ) Cite this article
729k Accesses
294 Citations
84 Altmetric
Metrics details
This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions, and focussing on intervention improvement. The most common methods of data collection are document study, (non-) participant observations, semi-structured interviews and focus groups. For data analysis, field-notes and audio-recordings are transcribed into protocols and transcripts, and coded using qualitative data management software. Criteria such as checklists, reflexivity, sampling strategies, piloting, co-coding, member-checking and stakeholder involvement can be used to enhance and assess the quality of the research conducted. Using qualitative in addition to quantitative designs will equip us with better tools to address a greater range of research problems, and to fill in blind spots in current neurological research and practice.
The aim of this paper is to provide an overview of qualitative research methods, including hands-on information on how they can be used, reported and assessed. This article is intended for beginning qualitative researchers in the health sciences as well as experienced quantitative researchers who wish to broaden their understanding of qualitative research.
What is qualitative research?
Qualitative research is defined as “the study of the nature of phenomena”, including “their quality, different manifestations, the context in which they appear or the perspectives from which they can be perceived” , but excluding “their range, frequency and place in an objectively determined chain of cause and effect” [ 1 ]. This formal definition can be complemented with a more pragmatic rule of thumb: qualitative research generally includes data in form of words rather than numbers [ 2 ].
Why conduct qualitative research?
Because some research questions cannot be answered using (only) quantitative methods. For example, one Australian study addressed the issue of why patients from Aboriginal communities often present late or not at all to specialist services offered by tertiary care hospitals. Using qualitative interviews with patients and staff, it found one of the most significant access barriers to be transportation problems, including some towns and communities simply not having a bus service to the hospital [ 3 ]. A quantitative study could have measured the number of patients over time or even looked at possible explanatory factors – but only those previously known or suspected to be of relevance. To discover reasons for observed patterns, especially the invisible or surprising ones, qualitative designs are needed.
While qualitative research is common in other fields, it is still relatively underrepresented in health services research. The latter field is more traditionally rooted in the evidence-based-medicine paradigm, as seen in " research that involves testing the effectiveness of various strategies to achieve changes in clinical practice, preferably applying randomised controlled trial study designs (...) " [ 4 ]. This focus on quantitative research and specifically randomised controlled trials (RCT) is visible in the idea of a hierarchy of research evidence which assumes that some research designs are objectively better than others, and that choosing a "lesser" design is only acceptable when the better ones are not practically or ethically feasible [ 5 , 6 ]. Others, however, argue that an objective hierarchy does not exist, and that, instead, the research design and methods should be chosen to fit the specific research question at hand – "questions before methods" [ 2 , 7 , 8 , 9 ]. This means that even when an RCT is possible, some research problems require a different design that is better suited to addressing them. Arguing in JAMA, Berwick uses the example of rapid response teams in hospitals, which he describes as " a complex, multicomponent intervention – essentially a process of social change" susceptible to a range of different context factors including leadership or organisation history. According to him, "[in] such complex terrain, the RCT is an impoverished way to learn. Critics who use it as a truth standard in this context are incorrect" [ 8 ] . Instead of limiting oneself to RCTs, Berwick recommends embracing a wider range of methods , including qualitative ones, which for "these specific applications, (...) are not compromises in learning how to improve; they are superior" [ 8 ].
Research problems that can be approached particularly well using qualitative methods include assessing complex multi-component interventions or systems (of change), addressing questions beyond “what works”, towards “what works for whom when, how and why”, and focussing on intervention improvement rather than accreditation [ 7 , 9 , 10 , 11 , 12 ]. Using qualitative methods can also help shed light on the “softer” side of medical treatment. For example, while quantitative trials can measure the costs and benefits of neuro-oncological treatment in terms of survival rates or adverse effects, qualitative research can help provide a better understanding of patient or caregiver stress, visibility of illness or out-of-pocket expenses.
How to conduct qualitative research?
Given that qualitative research is characterised by flexibility, openness and responsivity to context, the steps of data collection and analysis are not as separate and consecutive as they tend to be in quantitative research [ 13 , 14 ]. As Fossey puts it : “sampling, data collection, analysis and interpretation are related to each other in a cyclical (iterative) manner, rather than following one after another in a stepwise approach” [ 15 ]. The researcher can make educated decisions with regard to the choice of method, how they are implemented, and to which and how many units they are applied [ 13 ]. As shown in Fig. 1 , this can involve several back-and-forth steps between data collection and analysis where new insights and experiences can lead to adaption and expansion of the original plan. Some insights may also necessitate a revision of the research question and/or the research design as a whole. The process ends when saturation is achieved, i.e. when no relevant new information can be found (see also below: sampling and saturation). For reasons of transparency, it is essential for all decisions as well as the underlying reasoning to be well-documented.
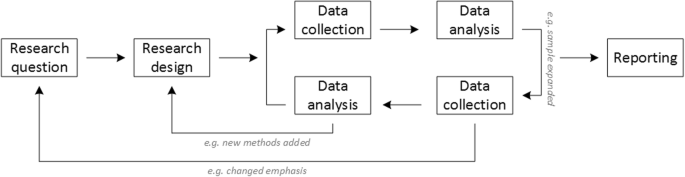
Iterative research process
While it is not always explicitly addressed, qualitative methods reflect a different underlying research paradigm than quantitative research (e.g. constructivism or interpretivism as opposed to positivism). The choice of methods can be based on the respective underlying substantive theory or theoretical framework used by the researcher [ 2 ].
Data collection
The methods of qualitative data collection most commonly used in health research are document study, observations, semi-structured interviews and focus groups [ 1 , 14 , 16 , 17 ].
Document study
Document study (also called document analysis) refers to the review by the researcher of written materials [ 14 ]. These can include personal and non-personal documents such as archives, annual reports, guidelines, policy documents, diaries or letters.
Observations
Observations are particularly useful to gain insights into a certain setting and actual behaviour – as opposed to reported behaviour or opinions [ 13 ]. Qualitative observations can be either participant or non-participant in nature. In participant observations, the observer is part of the observed setting, for example a nurse working in an intensive care unit [ 18 ]. In non-participant observations, the observer is “on the outside looking in”, i.e. present in but not part of the situation, trying not to influence the setting by their presence. Observations can be planned (e.g. for 3 h during the day or night shift) or ad hoc (e.g. as soon as a stroke patient arrives at the emergency room). During the observation, the observer takes notes on everything or certain pre-determined parts of what is happening around them, for example focusing on physician-patient interactions or communication between different professional groups. Written notes can be taken during or after the observations, depending on feasibility (which is usually lower during participant observations) and acceptability (e.g. when the observer is perceived to be judging the observed). Afterwards, these field notes are transcribed into observation protocols. If more than one observer was involved, field notes are taken independently, but notes can be consolidated into one protocol after discussions. Advantages of conducting observations include minimising the distance between the researcher and the researched, the potential discovery of topics that the researcher did not realise were relevant and gaining deeper insights into the real-world dimensions of the research problem at hand [ 18 ].
Semi-structured interviews
Hijmans & Kuyper describe qualitative interviews as “an exchange with an informal character, a conversation with a goal” [ 19 ]. Interviews are used to gain insights into a person’s subjective experiences, opinions and motivations – as opposed to facts or behaviours [ 13 ]. Interviews can be distinguished by the degree to which they are structured (i.e. a questionnaire), open (e.g. free conversation or autobiographical interviews) or semi-structured [ 2 , 13 ]. Semi-structured interviews are characterized by open-ended questions and the use of an interview guide (or topic guide/list) in which the broad areas of interest, sometimes including sub-questions, are defined [ 19 ]. The pre-defined topics in the interview guide can be derived from the literature, previous research or a preliminary method of data collection, e.g. document study or observations. The topic list is usually adapted and improved at the start of the data collection process as the interviewer learns more about the field [ 20 ]. Across interviews the focus on the different (blocks of) questions may differ and some questions may be skipped altogether (e.g. if the interviewee is not able or willing to answer the questions or for concerns about the total length of the interview) [ 20 ]. Qualitative interviews are usually not conducted in written format as it impedes on the interactive component of the method [ 20 ]. In comparison to written surveys, qualitative interviews have the advantage of being interactive and allowing for unexpected topics to emerge and to be taken up by the researcher. This can also help overcome a provider or researcher-centred bias often found in written surveys, which by nature, can only measure what is already known or expected to be of relevance to the researcher. Interviews can be audio- or video-taped; but sometimes it is only feasible or acceptable for the interviewer to take written notes [ 14 , 16 , 20 ].
Focus groups
Focus groups are group interviews to explore participants’ expertise and experiences, including explorations of how and why people behave in certain ways [ 1 ]. Focus groups usually consist of 6–8 people and are led by an experienced moderator following a topic guide or “script” [ 21 ]. They can involve an observer who takes note of the non-verbal aspects of the situation, possibly using an observation guide [ 21 ]. Depending on researchers’ and participants’ preferences, the discussions can be audio- or video-taped and transcribed afterwards [ 21 ]. Focus groups are useful for bringing together homogeneous (to a lesser extent heterogeneous) groups of participants with relevant expertise and experience on a given topic on which they can share detailed information [ 21 ]. Focus groups are a relatively easy, fast and inexpensive method to gain access to information on interactions in a given group, i.e. “the sharing and comparing” among participants [ 21 ]. Disadvantages include less control over the process and a lesser extent to which each individual may participate. Moreover, focus group moderators need experience, as do those tasked with the analysis of the resulting data. Focus groups can be less appropriate for discussing sensitive topics that participants might be reluctant to disclose in a group setting [ 13 ]. Moreover, attention must be paid to the emergence of “groupthink” as well as possible power dynamics within the group, e.g. when patients are awed or intimidated by health professionals.
Choosing the “right” method
As explained above, the school of thought underlying qualitative research assumes no objective hierarchy of evidence and methods. This means that each choice of single or combined methods has to be based on the research question that needs to be answered and a critical assessment with regard to whether or to what extent the chosen method can accomplish this – i.e. the “fit” between question and method [ 14 ]. It is necessary for these decisions to be documented when they are being made, and to be critically discussed when reporting methods and results.
Let us assume that our research aim is to examine the (clinical) processes around acute endovascular treatment (EVT), from the patient’s arrival at the emergency room to recanalization, with the aim to identify possible causes for delay and/or other causes for sub-optimal treatment outcome. As a first step, we could conduct a document study of the relevant standard operating procedures (SOPs) for this phase of care – are they up-to-date and in line with current guidelines? Do they contain any mistakes, irregularities or uncertainties that could cause delays or other problems? Regardless of the answers to these questions, the results have to be interpreted based on what they are: a written outline of what care processes in this hospital should look like. If we want to know what they actually look like in practice, we can conduct observations of the processes described in the SOPs. These results can (and should) be analysed in themselves, but also in comparison to the results of the document analysis, especially as regards relevant discrepancies. Do the SOPs outline specific tests for which no equipment can be observed or tasks to be performed by specialized nurses who are not present during the observation? It might also be possible that the written SOP is outdated, but the actual care provided is in line with current best practice. In order to find out why these discrepancies exist, it can be useful to conduct interviews. Are the physicians simply not aware of the SOPs (because their existence is limited to the hospital’s intranet) or do they actively disagree with them or does the infrastructure make it impossible to provide the care as described? Another rationale for adding interviews is that some situations (or all of their possible variations for different patient groups or the day, night or weekend shift) cannot practically or ethically be observed. In this case, it is possible to ask those involved to report on their actions – being aware that this is not the same as the actual observation. A senior physician’s or hospital manager’s description of certain situations might differ from a nurse’s or junior physician’s one, maybe because they intentionally misrepresent facts or maybe because different aspects of the process are visible or important to them. In some cases, it can also be relevant to consider to whom the interviewee is disclosing this information – someone they trust, someone they are otherwise not connected to, or someone they suspect or are aware of being in a potentially “dangerous” power relationship to them. Lastly, a focus group could be conducted with representatives of the relevant professional groups to explore how and why exactly they provide care around EVT. The discussion might reveal discrepancies (between SOPs and actual care or between different physicians) and motivations to the researchers as well as to the focus group members that they might not have been aware of themselves. For the focus group to deliver relevant information, attention has to be paid to its composition and conduct, for example, to make sure that all participants feel safe to disclose sensitive or potentially problematic information or that the discussion is not dominated by (senior) physicians only. The resulting combination of data collection methods is shown in Fig. 2 .
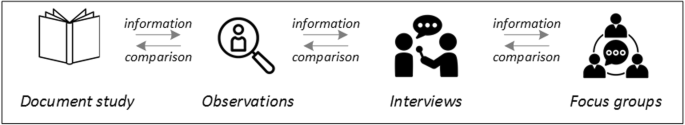
Possible combination of data collection methods
Attributions for icons: “Book” by Serhii Smirnov, “Interview” by Adrien Coquet, FR, “Magnifying Glass” by anggun, ID, “Business communication” by Vectors Market; all from the Noun Project
The combination of multiple data source as described for this example can be referred to as “triangulation”, in which multiple measurements are carried out from different angles to achieve a more comprehensive understanding of the phenomenon under study [ 22 , 23 ].
Data analysis
To analyse the data collected through observations, interviews and focus groups these need to be transcribed into protocols and transcripts (see Fig. 3 ). Interviews and focus groups can be transcribed verbatim , with or without annotations for behaviour (e.g. laughing, crying, pausing) and with or without phonetic transcription of dialects and filler words, depending on what is expected or known to be relevant for the analysis. In the next step, the protocols and transcripts are coded , that is, marked (or tagged, labelled) with one or more short descriptors of the content of a sentence or paragraph [ 2 , 15 , 23 ]. Jansen describes coding as “connecting the raw data with “theoretical” terms” [ 20 ]. In a more practical sense, coding makes raw data sortable. This makes it possible to extract and examine all segments describing, say, a tele-neurology consultation from multiple data sources (e.g. SOPs, emergency room observations, staff and patient interview). In a process of synthesis and abstraction, the codes are then grouped, summarised and/or categorised [ 15 , 20 ]. The end product of the coding or analysis process is a descriptive theory of the behavioural pattern under investigation [ 20 ]. The coding process is performed using qualitative data management software, the most common ones being InVivo, MaxQDA and Atlas.ti. It should be noted that these are data management tools which support the analysis performed by the researcher(s) [ 14 ].
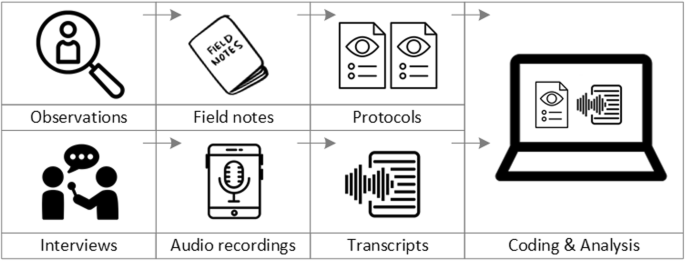
From data collection to data analysis
Attributions for icons: see Fig. 2 , also “Speech to text” by Trevor Dsouza, “Field Notes” by Mike O’Brien, US, “Voice Record” by ProSymbols, US, “Inspection” by Made, AU, and “Cloud” by Graphic Tigers; all from the Noun Project
How to report qualitative research?
Protocols of qualitative research can be published separately and in advance of the study results. However, the aim is not the same as in RCT protocols, i.e. to pre-define and set in stone the research questions and primary or secondary endpoints. Rather, it is a way to describe the research methods in detail, which might not be possible in the results paper given journals’ word limits. Qualitative research papers are usually longer than their quantitative counterparts to allow for deep understanding and so-called “thick description”. In the methods section, the focus is on transparency of the methods used, including why, how and by whom they were implemented in the specific study setting, so as to enable a discussion of whether and how this may have influenced data collection, analysis and interpretation. The results section usually starts with a paragraph outlining the main findings, followed by more detailed descriptions of, for example, the commonalities, discrepancies or exceptions per category [ 20 ]. Here it is important to support main findings by relevant quotations, which may add information, context, emphasis or real-life examples [ 20 , 23 ]. It is subject to debate in the field whether it is relevant to state the exact number or percentage of respondents supporting a certain statement (e.g. “Five interviewees expressed negative feelings towards XYZ”) [ 21 ].
How to combine qualitative with quantitative research?
Qualitative methods can be combined with other methods in multi- or mixed methods designs, which “[employ] two or more different methods [ …] within the same study or research program rather than confining the research to one single method” [ 24 ]. Reasons for combining methods can be diverse, including triangulation for corroboration of findings, complementarity for illustration and clarification of results, expansion to extend the breadth and range of the study, explanation of (unexpected) results generated with one method with the help of another, or offsetting the weakness of one method with the strength of another [ 1 , 17 , 24 , 25 , 26 ]. The resulting designs can be classified according to when, why and how the different quantitative and/or qualitative data strands are combined. The three most common types of mixed method designs are the convergent parallel design , the explanatory sequential design and the exploratory sequential design. The designs with examples are shown in Fig. 4 .
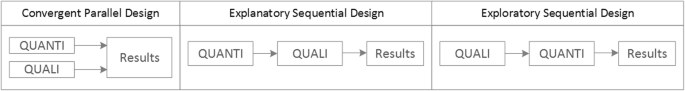
Three common mixed methods designs
In the convergent parallel design, a qualitative study is conducted in parallel to and independently of a quantitative study, and the results of both studies are compared and combined at the stage of interpretation of results. Using the above example of EVT provision, this could entail setting up a quantitative EVT registry to measure process times and patient outcomes in parallel to conducting the qualitative research outlined above, and then comparing results. Amongst other things, this would make it possible to assess whether interview respondents’ subjective impressions of patients receiving good care match modified Rankin Scores at follow-up, or whether observed delays in care provision are exceptions or the rule when compared to door-to-needle times as documented in the registry. In the explanatory sequential design, a quantitative study is carried out first, followed by a qualitative study to help explain the results from the quantitative study. This would be an appropriate design if the registry alone had revealed relevant delays in door-to-needle times and the qualitative study would be used to understand where and why these occurred, and how they could be improved. In the exploratory design, the qualitative study is carried out first and its results help informing and building the quantitative study in the next step [ 26 ]. If the qualitative study around EVT provision had shown a high level of dissatisfaction among the staff members involved, a quantitative questionnaire investigating staff satisfaction could be set up in the next step, informed by the qualitative study on which topics dissatisfaction had been expressed. Amongst other things, the questionnaire design would make it possible to widen the reach of the research to more respondents from different (types of) hospitals, regions, countries or settings, and to conduct sub-group analyses for different professional groups.
How to assess qualitative research?
A variety of assessment criteria and lists have been developed for qualitative research, ranging in their focus and comprehensiveness [ 14 , 17 , 27 ]. However, none of these has been elevated to the “gold standard” in the field. In the following, we therefore focus on a set of commonly used assessment criteria that, from a practical standpoint, a researcher can look for when assessing a qualitative research report or paper.
Assessors should check the authors’ use of and adherence to the relevant reporting checklists (e.g. Standards for Reporting Qualitative Research (SRQR)) to make sure all items that are relevant for this type of research are addressed [ 23 , 28 ]. Discussions of quantitative measures in addition to or instead of these qualitative measures can be a sign of lower quality of the research (paper). Providing and adhering to a checklist for qualitative research contributes to an important quality criterion for qualitative research, namely transparency [ 15 , 17 , 23 ].
Reflexivity
While methodological transparency and complete reporting is relevant for all types of research, some additional criteria must be taken into account for qualitative research. This includes what is called reflexivity, i.e. sensitivity to the relationship between the researcher and the researched, including how contact was established and maintained, or the background and experience of the researcher(s) involved in data collection and analysis. Depending on the research question and population to be researched this can be limited to professional experience, but it may also include gender, age or ethnicity [ 17 , 27 ]. These details are relevant because in qualitative research, as opposed to quantitative research, the researcher as a person cannot be isolated from the research process [ 23 ]. It may influence the conversation when an interviewed patient speaks to an interviewer who is a physician, or when an interviewee is asked to discuss a gynaecological procedure with a male interviewer, and therefore the reader must be made aware of these details [ 19 ].
Sampling and saturation
The aim of qualitative sampling is for all variants of the objects of observation that are deemed relevant for the study to be present in the sample “ to see the issue and its meanings from as many angles as possible” [ 1 , 16 , 19 , 20 , 27 ] , and to ensure “information-richness [ 15 ]. An iterative sampling approach is advised, in which data collection (e.g. five interviews) is followed by data analysis, followed by more data collection to find variants that are lacking in the current sample. This process continues until no new (relevant) information can be found and further sampling becomes redundant – which is called saturation [ 1 , 15 ] . In other words: qualitative data collection finds its end point not a priori , but when the research team determines that saturation has been reached [ 29 , 30 ].
This is also the reason why most qualitative studies use deliberate instead of random sampling strategies. This is generally referred to as “ purposive sampling” , in which researchers pre-define which types of participants or cases they need to include so as to cover all variations that are expected to be of relevance, based on the literature, previous experience or theory (i.e. theoretical sampling) [ 14 , 20 ]. Other types of purposive sampling include (but are not limited to) maximum variation sampling, critical case sampling or extreme or deviant case sampling [ 2 ]. In the above EVT example, a purposive sample could include all relevant professional groups and/or all relevant stakeholders (patients, relatives) and/or all relevant times of observation (day, night and weekend shift).
Assessors of qualitative research should check whether the considerations underlying the sampling strategy were sound and whether or how researchers tried to adapt and improve their strategies in stepwise or cyclical approaches between data collection and analysis to achieve saturation [ 14 ].
Good qualitative research is iterative in nature, i.e. it goes back and forth between data collection and analysis, revising and improving the approach where necessary. One example of this are pilot interviews, where different aspects of the interview (especially the interview guide, but also, for example, the site of the interview or whether the interview can be audio-recorded) are tested with a small number of respondents, evaluated and revised [ 19 ]. In doing so, the interviewer learns which wording or types of questions work best, or which is the best length of an interview with patients who have trouble concentrating for an extended time. Of course, the same reasoning applies to observations or focus groups which can also be piloted.
Ideally, coding should be performed by at least two researchers, especially at the beginning of the coding process when a common approach must be defined, including the establishment of a useful coding list (or tree), and when a common meaning of individual codes must be established [ 23 ]. An initial sub-set or all transcripts can be coded independently by the coders and then compared and consolidated after regular discussions in the research team. This is to make sure that codes are applied consistently to the research data.
Member checking
Member checking, also called respondent validation , refers to the practice of checking back with study respondents to see if the research is in line with their views [ 14 , 27 ]. This can happen after data collection or analysis or when first results are available [ 23 ]. For example, interviewees can be provided with (summaries of) their transcripts and asked whether they believe this to be a complete representation of their views or whether they would like to clarify or elaborate on their responses [ 17 ]. Respondents’ feedback on these issues then becomes part of the data collection and analysis [ 27 ].
Stakeholder involvement
In those niches where qualitative approaches have been able to evolve and grow, a new trend has seen the inclusion of patients and their representatives not only as study participants (i.e. “members”, see above) but as consultants to and active participants in the broader research process [ 31 , 32 , 33 ]. The underlying assumption is that patients and other stakeholders hold unique perspectives and experiences that add value beyond their own single story, making the research more relevant and beneficial to researchers, study participants and (future) patients alike [ 34 , 35 ]. Using the example of patients on or nearing dialysis, a recent scoping review found that 80% of clinical research did not address the top 10 research priorities identified by patients and caregivers [ 32 , 36 ]. In this sense, the involvement of the relevant stakeholders, especially patients and relatives, is increasingly being seen as a quality indicator in and of itself.
How not to assess qualitative research
The above overview does not include certain items that are routine in assessments of quantitative research. What follows is a non-exhaustive, non-representative, experience-based list of the quantitative criteria often applied to the assessment of qualitative research, as well as an explanation of the limited usefulness of these endeavours.
Protocol adherence
Given the openness and flexibility of qualitative research, it should not be assessed by how well it adheres to pre-determined and fixed strategies – in other words: its rigidity. Instead, the assessor should look for signs of adaptation and refinement based on lessons learned from earlier steps in the research process.
Sample size
For the reasons explained above, qualitative research does not require specific sample sizes, nor does it require that the sample size be determined a priori [ 1 , 14 , 27 , 37 , 38 , 39 ]. Sample size can only be a useful quality indicator when related to the research purpose, the chosen methodology and the composition of the sample, i.e. who was included and why.
Randomisation
While some authors argue that randomisation can be used in qualitative research, this is not commonly the case, as neither its feasibility nor its necessity or usefulness has been convincingly established for qualitative research [ 13 , 27 ]. Relevant disadvantages include the negative impact of a too large sample size as well as the possibility (or probability) of selecting “ quiet, uncooperative or inarticulate individuals ” [ 17 ]. Qualitative studies do not use control groups, either.
Interrater reliability, variability and other “objectivity checks”
The concept of “interrater reliability” is sometimes used in qualitative research to assess to which extent the coding approach overlaps between the two co-coders. However, it is not clear what this measure tells us about the quality of the analysis [ 23 ]. This means that these scores can be included in qualitative research reports, preferably with some additional information on what the score means for the analysis, but it is not a requirement. Relatedly, it is not relevant for the quality or “objectivity” of qualitative research to separate those who recruited the study participants and collected and analysed the data. Experiences even show that it might be better to have the same person or team perform all of these tasks [ 20 ]. First, when researchers introduce themselves during recruitment this can enhance trust when the interview takes place days or weeks later with the same researcher. Second, when the audio-recording is transcribed for analysis, the researcher conducting the interviews will usually remember the interviewee and the specific interview situation during data analysis. This might be helpful in providing additional context information for interpretation of data, e.g. on whether something might have been meant as a joke [ 18 ].
Not being quantitative research
Being qualitative research instead of quantitative research should not be used as an assessment criterion if it is used irrespectively of the research problem at hand. Similarly, qualitative research should not be required to be combined with quantitative research per se – unless mixed methods research is judged as inherently better than single-method research. In this case, the same criterion should be applied for quantitative studies without a qualitative component.
The main take-away points of this paper are summarised in Table 1 . We aimed to show that, if conducted well, qualitative research can answer specific research questions that cannot to be adequately answered using (only) quantitative designs. Seeing qualitative and quantitative methods as equal will help us become more aware and critical of the “fit” between the research problem and our chosen methods: I can conduct an RCT to determine the reasons for transportation delays of acute stroke patients – but should I? It also provides us with a greater range of tools to tackle a greater range of research problems more appropriately and successfully, filling in the blind spots on one half of the methodological spectrum to better address the whole complexity of neurological research and practice.
Availability of data and materials
Not applicable.
Abbreviations
Endovascular treatment
Randomised Controlled Trial
Standard Operating Procedure
Standards for Reporting Qualitative Research
Philipsen, H., & Vernooij-Dassen, M. (2007). Kwalitatief onderzoek: nuttig, onmisbaar en uitdagend. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Qualitative research: useful, indispensable and challenging. In: Qualitative research: Practical methods for medical practice (pp. 5–12). Houten: Bohn Stafleu van Loghum.
Chapter Google Scholar
Punch, K. F. (2013). Introduction to social research: Quantitative and qualitative approaches . London: Sage.
Kelly, J., Dwyer, J., Willis, E., & Pekarsky, B. (2014). Travelling to the city for hospital care: Access factors in country aboriginal patient journeys. Australian Journal of Rural Health, 22 (3), 109–113.
Article Google Scholar
Nilsen, P., Ståhl, C., Roback, K., & Cairney, P. (2013). Never the twain shall meet? - a comparison of implementation science and policy implementation research. Implementation Science, 8 (1), 1–12.
Howick J, Chalmers I, Glasziou, P., Greenhalgh, T., Heneghan, C., Liberati, A., Moschetti, I., Phillips, B., & Thornton, H. (2011). The 2011 Oxford CEBM evidence levels of evidence (introductory document) . Oxford Center for Evidence Based Medicine. https://www.cebm.net/2011/06/2011-oxford-cebm-levels-evidence-introductory-document/ .
Eakin, J. M. (2016). Educating critical qualitative health researchers in the land of the randomized controlled trial. Qualitative Inquiry, 22 (2), 107–118.
May, A., & Mathijssen, J. (2015). Alternatieven voor RCT bij de evaluatie van effectiviteit van interventies!? Eindrapportage. In Alternatives for RCTs in the evaluation of effectiveness of interventions!? Final report .
Google Scholar
Berwick, D. M. (2008). The science of improvement. Journal of the American Medical Association, 299 (10), 1182–1184.
Article CAS Google Scholar
Christ, T. W. (2014). Scientific-based research and randomized controlled trials, the “gold” standard? Alternative paradigms and mixed methodologies. Qualitative Inquiry, 20 (1), 72–80.
Lamont, T., Barber, N., Jd, P., Fulop, N., Garfield-Birkbeck, S., Lilford, R., Mear, L., Raine, R., & Fitzpatrick, R. (2016). New approaches to evaluating complex health and care systems. BMJ, 352:i154.
Drabble, S. J., & O’Cathain, A. (2015). Moving from Randomized Controlled Trials to Mixed Methods Intervention Evaluation. In S. Hesse-Biber & R. B. Johnson (Eds.), The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry (pp. 406–425). London: Oxford University Press.
Chambers, D. A., Glasgow, R. E., & Stange, K. C. (2013). The dynamic sustainability framework: Addressing the paradox of sustainment amid ongoing change. Implementation Science : IS, 8 , 117.
Hak, T. (2007). Waarnemingsmethoden in kwalitatief onderzoek. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Observation methods in qualitative research] (pp. 13–25). Houten: Bohn Stafleu van Loghum.
Russell, C. K., & Gregory, D. M. (2003). Evaluation of qualitative research studies. Evidence Based Nursing, 6 (2), 36–40.
Fossey, E., Harvey, C., McDermott, F., & Davidson, L. (2002). Understanding and evaluating qualitative research. Australian and New Zealand Journal of Psychiatry, 36 , 717–732.
Yanow, D. (2000). Conducting interpretive policy analysis (Vol. 47). Thousand Oaks: Sage University Papers Series on Qualitative Research Methods.
Shenton, A. K. (2004). Strategies for ensuring trustworthiness in qualitative research projects. Education for Information, 22 , 63–75.
van der Geest, S. (2006). Participeren in ziekte en zorg: meer over kwalitatief onderzoek. Huisarts en Wetenschap, 49 (4), 283–287.
Hijmans, E., & Kuyper, M. (2007). Het halfopen interview als onderzoeksmethode. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [The half-open interview as research method (pp. 43–51). Houten: Bohn Stafleu van Loghum.
Jansen, H. (2007). Systematiek en toepassing van de kwalitatieve survey. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Systematics and implementation of the qualitative survey (pp. 27–41). Houten: Bohn Stafleu van Loghum.
Pv, R., & Peremans, L. (2007). Exploreren met focusgroepgesprekken: de ‘stem’ van de groep onder de loep. In L. PLBJ & H. TCo (Eds.), Kwalitatief onderzoek: Praktische methoden voor de medische praktijk . [Exploring with focus group conversations: the “voice” of the group under the magnifying glass (pp. 53–64). Houten: Bohn Stafleu van Loghum.
Carter, N., Bryant-Lukosius, D., DiCenso, A., Blythe, J., & Neville, A. J. (2014). The use of triangulation in qualitative research. Oncology Nursing Forum, 41 (5), 545–547.
Boeije H: Analyseren in kwalitatief onderzoek: Denken en doen, [Analysis in qualitative research: Thinking and doing] vol. Den Haag Boom Lemma uitgevers; 2012.
Hunter, A., & Brewer, J. (2015). Designing Multimethod Research. In S. Hesse-Biber & R. B. Johnson (Eds.), The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry (pp. 185–205). London: Oxford University Press.
Archibald, M. M., Radil, A. I., Zhang, X., & Hanson, W. E. (2015). Current mixed methods practices in qualitative research: A content analysis of leading journals. International Journal of Qualitative Methods, 14 (2), 5–33.
Creswell, J. W., & Plano Clark, V. L. (2011). Choosing a Mixed Methods Design. In Designing and Conducting Mixed Methods Research . Thousand Oaks: SAGE Publications.
Mays, N., & Pope, C. (2000). Assessing quality in qualitative research. BMJ, 320 (7226), 50–52.
O'Brien, B. C., Harris, I. B., Beckman, T. J., Reed, D. A., & Cook, D. A. (2014). Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine : Journal of the Association of American Medical Colleges, 89 (9), 1245–1251.
Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality and Quantity, 52 (4), 1893–1907.
Moser, A., & Korstjens, I. (2018). Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. European Journal of General Practice, 24 (1), 9–18.
Marlett, N., Shklarov, S., Marshall, D., Santana, M. J., & Wasylak, T. (2015). Building new roles and relationships in research: A model of patient engagement research. Quality of Life Research : an international journal of quality of life aspects of treatment, care and rehabilitation, 24 (5), 1057–1067.
Demian, M. N., Lam, N. N., Mac-Way, F., Sapir-Pichhadze, R., & Fernandez, N. (2017). Opportunities for engaging patients in kidney research. Canadian Journal of Kidney Health and Disease, 4 , 2054358117703070–2054358117703070.
Noyes, J., McLaughlin, L., Morgan, K., Roberts, A., Stephens, M., Bourne, J., Houlston, M., Houlston, J., Thomas, S., Rhys, R. G., et al. (2019). Designing a co-productive study to overcome known methodological challenges in organ donation research with bereaved family members. Health Expectations . 22(4):824–35.
Piil, K., Jarden, M., & Pii, K. H. (2019). Research agenda for life-threatening cancer. European Journal Cancer Care (Engl), 28 (1), e12935.
Hofmann, D., Ibrahim, F., Rose, D., Scott, D. L., Cope, A., Wykes, T., & Lempp, H. (2015). Expectations of new treatment in rheumatoid arthritis: Developing a patient-generated questionnaire. Health Expectations : an international journal of public participation in health care and health policy, 18 (5), 995–1008.
Jun, M., Manns, B., Laupacis, A., Manns, L., Rehal, B., Crowe, S., & Hemmelgarn, B. R. (2015). Assessing the extent to which current clinical research is consistent with patient priorities: A scoping review using a case study in patients on or nearing dialysis. Canadian Journal of Kidney Health and Disease, 2 , 35.
Elsie Baker, S., & Edwards, R. (2012). How many qualitative interviews is enough? In National Centre for Research Methods Review Paper . National Centre for Research Methods. http://eprints.ncrm.ac.uk/2273/4/how_many_interviews.pdf .
Sandelowski, M. (1995). Sample size in qualitative research. Research in Nursing & Health, 18 (2), 179–183.
Sim, J., Saunders, B., Waterfield, J., & Kingstone, T. (2018). Can sample size in qualitative research be determined a priori? International Journal of Social Research Methodology, 21 (5), 619–634.
Download references
Acknowledgements
no external funding.
Author information
Authors and affiliations.
Department of Neurology, Heidelberg University Hospital, Im Neuenheimer Feld 400, 69120, Heidelberg, Germany
Loraine Busetto, Wolfgang Wick & Christoph Gumbinger
Clinical Cooperation Unit Neuro-Oncology, German Cancer Research Center, Heidelberg, Germany
Wolfgang Wick
You can also search for this author in PubMed Google Scholar
Contributions
LB drafted the manuscript; WW and CG revised the manuscript; all authors approved the final versions.
Corresponding author
Correspondence to Loraine Busetto .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Busetto, L., Wick, W. & Gumbinger, C. How to use and assess qualitative research methods. Neurol. Res. Pract. 2 , 14 (2020). https://doi.org/10.1186/s42466-020-00059-z
Download citation
Received : 30 January 2020
Accepted : 22 April 2020
Published : 27 May 2020
DOI : https://doi.org/10.1186/s42466-020-00059-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative research
- Mixed methods
- Quality assessment
Neurological Research and Practice
ISSN: 2524-3489
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

Research Methodologies: Research Instruments
- Research Methodology Basics
- Research Instruments
- Types of Research Methodologies
Header Image

Types of Research Instruments
A research instrument is a tool you will use to help you collect, measure and analyze the data you use as part of your research. The choice of research instrument will usually be yours to make as the researcher and will be whichever best suits your methodology.
There are many different research instruments you can use in collecting data for your research:
- Interviews (either as a group or one-on-one). You can carry out interviews in many different ways. For example, your interview can be structured, semi-structured, or unstructured. The difference between them is how formal the set of questions is that is asked of the interviewee. In a group interview, you may choose to ask the interviewees to give you their opinions or perceptions on certain topics.
- Surveys (online or in-person). In survey research, you are posing questions in which you ask for a response from the person taking the survey. You may wish to have either free-answer questions such as essay style questions, or you may wish to use closed questions such as multiple choice. You may even wish to make the survey a mixture of both.
- Focus Groups. Similar to the group interview above, you may wish to ask a focus group to discuss a particular topic or opinion while you make a note of the answers given.
- Observations. This is a good research instrument to use if you are looking into human behaviors. Different ways of researching this include studying the spontaneous behavior of participants in their everyday life, or something more structured. A structured observation is research conducted at a set time and place where researchers observe behavior as planned and agreed upon with participants.
These are the most common ways of carrying out research, but it is really dependent on your needs as a researcher and what approach you think is best to take. It is also possible to combine a number of research instruments if this is necessary and appropriate in answering your research problem.
Data Collection
How to Collect Data for Your Research This article covers different ways of collecting data in preparation for writing a thesis.
- << Previous: Research Methodology Basics
- Next: Types of Research Methodologies >>
- Last Updated: Sep 27, 2022 12:28 PM
- URL: https://paperpile.libguides.com/research-methodologies
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- QuestionPro

- Solutions Industries Gaming Automotive Sports and events Education Government Travel & Hospitality Financial Services Healthcare Cannabis Technology Use Case NPS+ Communities Audience Contactless surveys Mobile LivePolls Member Experience GDPR Positive People Science 360 Feedback Surveys
- Resources Blog eBooks Survey Templates Case Studies Training Help center
Home Market Research
Qualitative Research Methods: Types, Analysis + Examples

Qualitative research is based on the disciplines of social sciences like psychology, sociology, and anthropology. Therefore, the qualitative research methods allow for in-depth and further probing and questioning of respondents based on their responses. The interviewer/researcher also tries to understand their motivation and feelings. Understanding how your audience makes decisions can help derive conclusions in market research.
What is qualitative research?
Qualitative research is defined as a market research method that focuses on obtaining data through open-ended and conversational communication .
This method is about “what” people think and “why” they think so. For example, consider a convenience store looking to improve its patronage. A systematic observation concludes that more men are visiting this store. One good method to determine why women were not visiting the store is conducting an in-depth interview method with potential customers.
For example, after successfully interviewing female customers and visiting nearby stores and malls, the researchers selected participants through random sampling . As a result, it was discovered that the store didn’t have enough items for women.
So fewer women were visiting the store, which was understood only by personally interacting with them and understanding why they didn’t visit the store because there were more male products than female ones.
Gather research insights
Types of qualitative research methods with examples
Qualitative research methods are designed in a manner that helps reveal the behavior and perception of a target audience with reference to a particular topic. There are different types of qualitative research methods, such as in-depth interviews, focus groups, ethnographic research, content analysis, and case study research that are usually used.
The results of qualitative methods are more descriptive, and the inferences can be drawn quite easily from the obtained data .
Qualitative research methods originated in the social and behavioral research sciences. Today, our world is more complicated, and it is difficult to understand what people think and perceive. Online research methods make it easier to understand that as it is a more communicative and descriptive analysis .
The following are the qualitative research methods that are frequently used. Also, read about qualitative research examples :
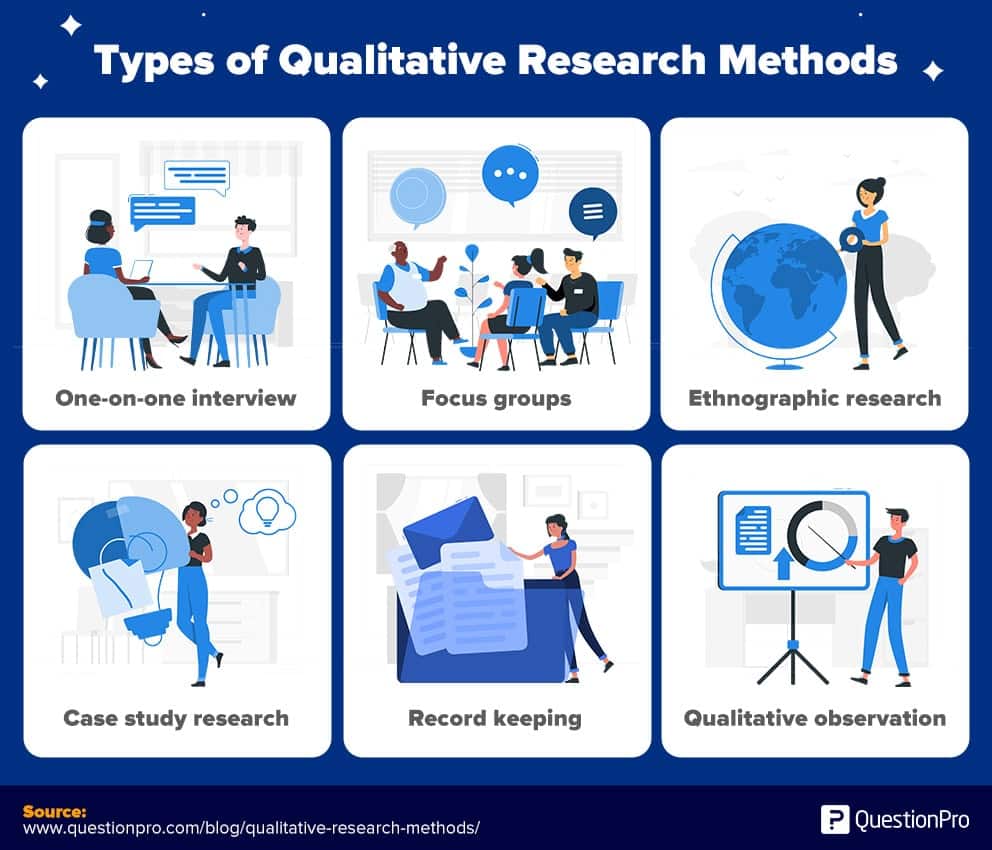
1. One-on-one interview
Conducting in-depth interviews is one of the most common qualitative research methods. It is a personal interview that is carried out with one respondent at a time. This is purely a conversational method and invites opportunities to get details in depth from the respondent.
One of the advantages of this method is that it provides a great opportunity to gather precise data about what people believe and their motivations . If the researcher is well experienced, asking the right questions can help him/her collect meaningful data. If they should need more information, the researchers should ask such follow-up questions that will help them collect more information.
These interviews can be performed face-to-face or on the phone and usually can last between half an hour to two hours or even more. When the in-depth interview is conducted face to face, it gives a better opportunity to read the respondents’ body language and match the responses.
2. Focus groups
A focus group is also a commonly used qualitative research method used in data collection. A focus group usually includes a limited number of respondents (6-10) from within your target market.
The main aim of the focus group is to find answers to the “why, ” “what,” and “how” questions. One advantage of focus groups is you don’t necessarily need to interact with the group in person. Nowadays, focus groups can be sent an online survey on various devices, and responses can be collected at the click of a button.
Focus groups are an expensive method as compared to other online qualitative research methods. Typically, they are used to explain complex processes. This method is very useful for market research on new products and testing new concepts.
3. Ethnographic research
Ethnographic research is the most in-depth observational research method that studies people in their naturally occurring environment.
This method requires the researchers to adapt to the target audiences’ environments, which could be anywhere from an organization to a city or any remote location. Here, geographical constraints can be an issue while collecting data.
This research design aims to understand the cultures, challenges, motivations, and settings that occur. Instead of relying on interviews and discussions, you experience the natural settings firsthand.
This type of research method can last from a few days to a few years, as it involves in-depth observation and collecting data on those grounds. It’s a challenging and time-consuming method and solely depends on the researcher’s expertise to analyze, observe, and infer the data.
4. Case study research
T he case study method has evolved over the past few years and developed into a valuable quality research method. As the name suggests, it is used for explaining an organization or an entity.
This type of research method is used within a number of areas like education, social sciences, and similar. This method may look difficult to operate; however , it is one of the simplest ways of conducting research as it involves a deep dive and thorough understanding of the data collection methods and inferring the data.
5. Record keeping
This method makes use of the already existing reliable documents and similar sources of information as the data source. This data can be used in new research. This is similar to going to a library. There, one can go over books and other reference material to collect relevant data that can likely be used in the research.
6. Process of observation
Qualitative Observation is a process of research that uses subjective methodologies to gather systematic information or data. Since the focus on qualitative observation is the research process of using subjective methodologies to gather information or data. Qualitative observation is primarily used to equate quality differences.
Qualitative observation deals with the 5 major sensory organs and their functioning – sight, smell, touch, taste, and hearing. This doesn’t involve measurements or numbers but instead characteristics.
Explore Insightfully Contextual Inquiry in Qualitative Research
Qualitative research: data collection and analysis
A. qualitative data collection.
Qualitative data collection allows collecting data that is non-numeric and helps us to explore how decisions are made and provide us with detailed insight. For reaching such conclusions the data that is collected should be holistic, rich, and nuanced and findings to emerge through careful analysis.
- Whatever method a researcher chooses for collecting qualitative data, one aspect is very clear the process will generate a large amount of data. In addition to the variety of methods available, there are also different methods of collecting and recording the data.
For example, if the qualitative data is collected through a focus group or one-to-one discussion, there will be handwritten notes or video recorded tapes. If there are recording they should be transcribed and before the process of data analysis can begin.
- As a rough guide, it can take a seasoned researcher 8-10 hours to transcribe the recordings of an interview, which can generate roughly 20-30 pages of dialogues. Many researchers also like to maintain separate folders to maintain the recording collected from the different focus group. This helps them compartmentalize the data collected.
- In case there are running notes taken, which are also known as field notes, they are helpful in maintaining comments, environmental contexts, environmental analysis , nonverbal cues etc. These filed notes are helpful and can be compared while transcribing audio recorded data. Such notes are usually informal but should be secured in a similar manner as the video recordings or the audio tapes.
B. Qualitative data analysis
Qualitative data analysis such as notes, videos, audio recordings images, and text documents. One of the most used methods for qualitative data analysis is text analysis.
Text analysis is a data analysis method that is distinctly different from all other qualitative research methods, where researchers analyze the social life of the participants in the research study and decode the words, actions, etc.
There are images also that are used in this research study and the researchers analyze the context in which the images are used and draw inferences from them. In the last decade, text analysis through what is shared on social media platforms has gained supreme popularity.
Characteristics of qualitative research methods
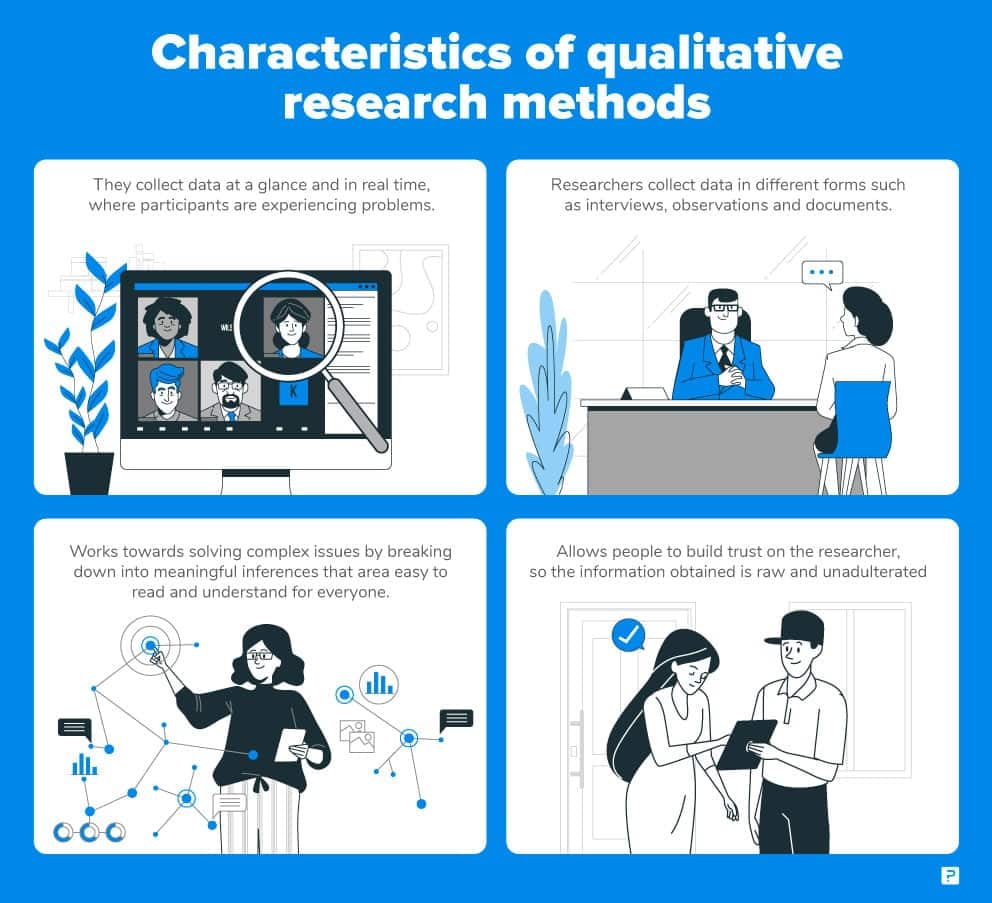
- Qualitative research methods usually collect data at the sight, where the participants are experiencing issues or research problems . These are real-time data and rarely bring the participants out of the geographic locations to collect information.
- Qualitative researchers typically gather multiple forms of data, such as interviews, observations, and documents, rather than rely on a single data source .
- This type of research method works towards solving complex issues by breaking down into meaningful inferences, that is easily readable and understood by all.
- Since it’s a more communicative method, people can build their trust on the researcher and the information thus obtained is raw and unadulterated.
Qualitative research method case study
Let’s take the example of a bookstore owner who is looking for ways to improve their sales and customer outreach. An online community of members who were loyal patrons of the bookstore were interviewed and related questions were asked and the questions were answered by them.
At the end of the interview, it was realized that most of the books in the stores were suitable for adults and there were not enough options for children or teenagers.
By conducting this qualitative research the bookstore owner realized what the shortcomings were and what were the feelings of the readers. Through this research now the bookstore owner can now keep books for different age categories and can improve his sales and customer outreach.
Such qualitative research method examples can serve as the basis to indulge in further quantitative research , which provides remedies.
When to use qualitative research
Researchers make use of qualitative research techniques when they need to capture accurate, in-depth insights. It is very useful to capture “factual data”. Here are some examples of when to use qualitative research.
- Developing a new product or generating an idea.
- Studying your product/brand or service to strengthen your marketing strategy.
- To understand your strengths and weaknesses.
- Understanding purchase behavior.
- To study the reactions of your audience to marketing campaigns and other communications.
- Exploring market demographics, segments, and customer care groups.
- Gathering perception data of a brand, company, or product.
LEARN ABOUT: Steps in Qualitative Research
Qualitative research methods vs quantitative research methods
The basic differences between qualitative research methods and quantitative research methods are simple and straightforward. They differ in:
- Their analytical objectives
- Types of questions asked
- Types of data collection instruments
- Forms of data they produce
- Degree of flexibility
LEARN MORE ABOUR OUR SOFTWARE FREE TRIAL
MORE LIKE THIS
Data Information vs Insight: Essential differences
May 14, 2024
Pricing Analytics Software: Optimize Your Pricing Strategy
May 13, 2024

Relationship Marketing: What It Is, Examples & Top 7 Benefits
May 8, 2024
The Best Email Survey Tool to Boost Your Feedback Game
May 7, 2024
Other categories
- Academic Research
- Artificial Intelligence
- Assessments
- Brand Awareness
- Case Studies
- Communities
- Consumer Insights
- Customer effort score
- Customer Engagement
- Customer Experience
- Customer Loyalty
- Customer Research
- Customer Satisfaction
- Employee Benefits
- Employee Engagement
- Employee Retention
- Friday Five
- General Data Protection Regulation
- Insights Hub
- Life@QuestionPro
- Market Research
- Mobile diaries
- Mobile Surveys
- New Features
- Online Communities
- Question Types
- Questionnaire
- QuestionPro Products
- Release Notes
- Research Tools and Apps
- Revenue at Risk
- Survey Templates
- Training Tips
- Uncategorized
- Video Learning Series
- What’s Coming Up
- Workforce Intelligence
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 05 October 2018
Interviews and focus groups in qualitative research: an update for the digital age
- P. Gill 1 &
- J. Baillie 2
British Dental Journal volume 225 , pages 668–672 ( 2018 ) Cite this article
27k Accesses
48 Citations
20 Altmetric
Metrics details
Highlights that qualitative research is used increasingly in dentistry. Interviews and focus groups remain the most common qualitative methods of data collection.
Suggests the advent of digital technologies has transformed how qualitative research can now be undertaken.
Suggests interviews and focus groups can offer significant, meaningful insight into participants' experiences, beliefs and perspectives, which can help to inform developments in dental practice.
Qualitative research is used increasingly in dentistry, due to its potential to provide meaningful, in-depth insights into participants' experiences, perspectives, beliefs and behaviours. These insights can subsequently help to inform developments in dental practice and further related research. The most common methods of data collection used in qualitative research are interviews and focus groups. While these are primarily conducted face-to-face, the ongoing evolution of digital technologies, such as video chat and online forums, has further transformed these methods of data collection. This paper therefore discusses interviews and focus groups in detail, outlines how they can be used in practice, how digital technologies can further inform the data collection process, and what these methods can offer dentistry.
You have full access to this article via your institution.
Similar content being viewed by others

Interviews in the social sciences

Professionalism in dentistry: deconstructing common terminology
A review of technical and quality assessment considerations of audio-visual and web-conferencing focus groups in qualitative health research, introduction.
Traditionally, research in dentistry has primarily been quantitative in nature. 1 However, in recent years, there has been a growing interest in qualitative research within the profession, due to its potential to further inform developments in practice, policy, education and training. Consequently, in 2008, the British Dental Journal (BDJ) published a four paper qualitative research series, 2 , 3 , 4 , 5 to help increase awareness and understanding of this particular methodological approach.
Since the papers were originally published, two scoping reviews have demonstrated the ongoing proliferation in the use of qualitative research within the field of oral healthcare. 1 , 6 To date, the original four paper series continue to be well cited and two of the main papers remain widely accessed among the BDJ readership. 2 , 3 The potential value of well-conducted qualitative research to evidence-based practice is now also widely recognised by service providers, policy makers, funding bodies and those who commission, support and use healthcare research.
Besides increasing standalone use, qualitative methods are now also routinely incorporated into larger mixed method study designs, such as clinical trials, as they can offer additional, meaningful insights into complex problems that simply could not be provided by quantitative methods alone. Qualitative methods can also be used to further facilitate in-depth understanding of important aspects of clinical trial processes, such as recruitment. For example, Ellis et al . investigated why edentulous older patients, dissatisfied with conventional dentures, decline implant treatment, despite its established efficacy, and frequently refuse to participate in related randomised clinical trials, even when financial constraints are removed. 7 Through the use of focus groups in Canada and the UK, the authors found that fears of pain and potential complications, along with perceived embarrassment, exacerbated by age, are common reasons why older patients typically refuse dental implants. 7
The last decade has also seen further developments in qualitative research, due to the ongoing evolution of digital technologies. These developments have transformed how researchers can access and share information, communicate and collaborate, recruit and engage participants, collect and analyse data and disseminate and translate research findings. 8 Where appropriate, such technologies are therefore capable of extending and enhancing how qualitative research is undertaken. 9 For example, it is now possible to collect qualitative data via instant messaging, email or online/video chat, using appropriate online platforms.
These innovative approaches to research are therefore cost-effective, convenient, reduce geographical constraints and are often useful for accessing 'hard to reach' participants (for example, those who are immobile or socially isolated). 8 , 9 However, digital technologies are still relatively new and constantly evolving and therefore present a variety of pragmatic and methodological challenges. Furthermore, given their very nature, their use in many qualitative studies and/or with certain participant groups may be inappropriate and should therefore always be carefully considered. While it is beyond the scope of this paper to provide a detailed explication regarding the use of digital technologies in qualitative research, insight is provided into how such technologies can be used to facilitate the data collection process in interviews and focus groups.
In light of such developments, it is perhaps therefore timely to update the main paper 3 of the original BDJ series. As with the previous publications, this paper has been purposely written in an accessible style, to enhance readability, particularly for those who are new to qualitative research. While the focus remains on the most common qualitative methods of data collection – interviews and focus groups – appropriate revisions have been made to provide a novel perspective, and should therefore be helpful to those who would like to know more about qualitative research. This paper specifically focuses on undertaking qualitative research with adult participants only.
Overview of qualitative research
Qualitative research is an approach that focuses on people and their experiences, behaviours and opinions. 10 , 11 The qualitative researcher seeks to answer questions of 'how' and 'why', providing detailed insight and understanding, 11 which quantitative methods cannot reach. 12 Within qualitative research, there are distinct methodologies influencing how the researcher approaches the research question, data collection and data analysis. 13 For example, phenomenological studies focus on the lived experience of individuals, explored through their description of the phenomenon. Ethnographic studies explore the culture of a group and typically involve the use of multiple methods to uncover the issues. 14
While methodology is the 'thinking tool', the methods are the 'doing tools'; 13 the ways in which data are collected and analysed. There are multiple qualitative data collection methods, including interviews, focus groups, observations, documentary analysis, participant diaries, photography and videography. Two of the most commonly used qualitative methods are interviews and focus groups, which are explored in this article. The data generated through these methods can be analysed in one of many ways, according to the methodological approach chosen. A common approach is thematic data analysis, involving the identification of themes and subthemes across the data set. Further information on approaches to qualitative data analysis has been discussed elsewhere. 1
Qualitative research is an evolving and adaptable approach, used by different disciplines for different purposes. Traditionally, qualitative data, specifically interviews, focus groups and observations, have been collected face-to-face with participants. In more recent years, digital technologies have contributed to the ongoing evolution of qualitative research. Digital technologies offer researchers different ways of recruiting participants and collecting data, and offer participants opportunities to be involved in research that is not necessarily face-to-face.
Research interviews are a fundamental qualitative research method 15 and are utilised across methodological approaches. Interviews enable the researcher to learn in depth about the perspectives, experiences, beliefs and motivations of the participant. 3 , 16 Examples include, exploring patients' perspectives of fear/anxiety triggers in dental treatment, 17 patients' experiences of oral health and diabetes, 18 and dental students' motivations for their choice of career. 19
Interviews may be structured, semi-structured or unstructured, 3 according to the purpose of the study, with less structured interviews facilitating a more in depth and flexible interviewing approach. 20 Structured interviews are similar to verbal questionnaires and are used if the researcher requires clarification on a topic; however they produce less in-depth data about a participant's experience. 3 Unstructured interviews may be used when little is known about a topic and involves the researcher asking an opening question; 3 the participant then leads the discussion. 20 Semi-structured interviews are commonly used in healthcare research, enabling the researcher to ask predetermined questions, 20 while ensuring the participant discusses issues they feel are important.
Interviews can be undertaken face-to-face or using digital methods when the researcher and participant are in different locations. Audio-recording the interview, with the consent of the participant, is essential for all interviews regardless of the medium as it enables accurate transcription; the process of turning the audio file into a word-for-word transcript. This transcript is the data, which the researcher then analyses according to the chosen approach.
Types of interview
Qualitative studies often utilise one-to-one, face-to-face interviews with research participants. This involves arranging a mutually convenient time and place to meet the participant, signing a consent form and audio-recording the interview. However, digital technologies have expanded the potential for interviews in research, enabling individuals to participate in qualitative research regardless of location.
Telephone interviews can be a useful alternative to face-to-face interviews and are commonly used in qualitative research. They enable participants from different geographical areas to participate and may be less onerous for participants than meeting a researcher in person. 15 A qualitative study explored patients' perspectives of dental implants and utilised telephone interviews due to the quality of the data that could be yielded. 21 The researcher needs to consider how they will audio record the interview, which can be facilitated by purchasing a recorder that connects directly to the telephone. One potential disadvantage of telephone interviews is the inability of the interviewer and researcher to see each other. This is resolved using software for audio and video calls online – such as Skype – to conduct interviews with participants in qualitative studies. Advantages of this approach include being able to see the participant if video calls are used, enabling observation of non-verbal communication, and the software can be free to use. However, participants are required to have a device and internet connection, as well as being computer literate, potentially limiting who can participate in the study. One qualitative study explored the role of dental hygienists in reducing oral health disparities in Canada. 22 The researcher conducted interviews using Skype, which enabled dental hygienists from across Canada to be interviewed within the research budget, accommodating the participants' schedules. 22
A less commonly used approach to qualitative interviews is the use of social virtual worlds. A qualitative study accessed a social virtual world – Second Life – to explore the health literacy skills of individuals who use social virtual worlds to access health information. 23 The researcher created an avatar and interview room, and undertook interviews with participants using voice and text methods. 23 This approach to recruitment and data collection enables individuals from diverse geographical locations to participate, while remaining anonymous if they wish. Furthermore, for interviews conducted using text methods, transcription of the interview is not required as the researcher can save the written conversation with the participant, with the participant's consent. However, the researcher and participant need to be familiar with how the social virtual world works to engage in an interview this way.
Conducting an interview
Ensuring informed consent before any interview is a fundamental aspect of the research process. Participants in research must be afforded autonomy and respect; consent should be informed and voluntary. 24 Individuals should have the opportunity to read an information sheet about the study, ask questions, understand how their data will be stored and used, and know that they are free to withdraw at any point without reprisal. The qualitative researcher should take written consent before undertaking the interview. In a face-to-face interview, this is straightforward: the researcher and participant both sign copies of the consent form, keeping one each. However, this approach is less straightforward when the researcher and participant do not meet in person. A recent protocol paper outlined an approach for taking consent for telephone interviews, which involved: audio recording the participant agreeing to each point on the consent form; the researcher signing the consent form and keeping a copy; and posting a copy to the participant. 25 This process could be replicated in other interview studies using digital methods.
There are advantages and disadvantages of using face-to-face and digital methods for research interviews. Ultimately, for both approaches, the quality of the interview is determined by the researcher. 16 Appropriate training and preparation are thus required. Healthcare professionals can use their interpersonal communication skills when undertaking a research interview, particularly questioning, listening and conversing. 3 However, the purpose of an interview is to gain information about the study topic, 26 rather than offering help and advice. 3 The researcher therefore needs to listen attentively to participants, enabling them to describe their experience without interruption. 3 The use of active listening skills also help to facilitate the interview. 14 Spradley outlined elements and strategies for research interviews, 27 which are a useful guide for qualitative researchers:
Greeting and explaining the project/interview
Asking descriptive (broad), structural (explore response to descriptive) and contrast (difference between) questions
Asymmetry between the researcher and participant talking
Expressing interest and cultural ignorance
Repeating, restating and incorporating the participant's words when asking questions
Creating hypothetical situations
Asking friendly questions
Knowing when to leave.
For semi-structured interviews, a topic guide (also called an interview schedule) is used to guide the content of the interview – an example of a topic guide is outlined in Box 1 . The topic guide, usually based on the research questions, existing literature and, for healthcare professionals, their clinical experience, is developed by the research team. The topic guide should include open ended questions that elicit in-depth information, and offer participants the opportunity to talk about issues important to them. This is vital in qualitative research where the researcher is interested in exploring the experiences and perspectives of participants. It can be useful for qualitative researchers to pilot the topic guide with the first participants, 10 to ensure the questions are relevant and understandable, and amending the questions if required.
Regardless of the medium of interview, the researcher must consider the setting of the interview. For face-to-face interviews, this could be in the participant's home, in an office or another mutually convenient location. A quiet location is preferable to promote confidentiality, enable the researcher and participant to concentrate on the conversation, and to facilitate accurate audio-recording of the interview. For interviews using digital methods the same principles apply: a quiet, private space where the researcher and participant feel comfortable and confident to participate in an interview.
Box 1: Example of a topic guide
Study focus: Parents' experiences of brushing their child's (aged 0–5) teeth
1. Can you tell me about your experience of cleaning your child's teeth?
How old was your child when you started cleaning their teeth?
Why did you start cleaning their teeth at that point?
How often do you brush their teeth?
What do you use to brush their teeth and why?
2. Could you explain how you find cleaning your child's teeth?
Do you find anything difficult?
What makes cleaning their teeth easier for you?
3. How has your experience of cleaning your child's teeth changed over time?
Has it become easier or harder?
Have you changed how often and how you clean their teeth? If so, why?
4. Could you describe how your child finds having their teeth cleaned?
What do they enjoy about having their teeth cleaned?
Is there anything they find upsetting about having their teeth cleaned?
5. Where do you look for information/advice about cleaning your child's teeth?
What did your health visitor tell you about cleaning your child's teeth? (If anything)
What has the dentist told you about caring for your child's teeth? (If visited)
Have any family members given you advice about how to clean your child's teeth? If so, what did they tell you? Did you follow their advice?
6. Is there anything else you would like to discuss about this?
Focus groups
A focus group is a moderated group discussion on a pre-defined topic, for research purposes. 28 , 29 While not aligned to a particular qualitative methodology (for example, grounded theory or phenomenology) as such, focus groups are used increasingly in healthcare research, as they are useful for exploring collective perspectives, attitudes, behaviours and experiences. Consequently, they can yield rich, in-depth data and illuminate agreement and inconsistencies 28 within and, where appropriate, between groups. Examples include public perceptions of dental implants and subsequent impact on help-seeking and decision making, 30 and general dental practitioners' views on patient safety in dentistry. 31
Focus groups can be used alone or in conjunction with other methods, such as interviews or observations, and can therefore help to confirm, extend or enrich understanding and provide alternative insights. 28 The social interaction between participants often results in lively discussion and can therefore facilitate the collection of rich, meaningful data. However, they are complex to organise and manage, due to the number of participants, and may also be inappropriate for exploring particularly sensitive issues that many participants may feel uncomfortable about discussing in a group environment.
Focus groups are primarily undertaken face-to-face but can now also be undertaken online, using appropriate technologies such as email, bulletin boards, online research communities, chat rooms, discussion forums, social media and video conferencing. 32 Using such technologies, data collection can also be synchronous (for example, online discussions in 'real time') or, unlike traditional face-to-face focus groups, asynchronous (for example, online/email discussions in 'non-real time'). While many of the fundamental principles of focus group research are the same, regardless of how they are conducted, a number of subtle nuances are associated with the online medium. 32 Some of which are discussed further in the following sections.
Focus group considerations
Some key considerations associated with face-to-face focus groups are: how many participants are required; should participants within each group know each other (or not) and how many focus groups are needed within a single study? These issues are much debated and there is no definitive answer. However, the number of focus groups required will largely depend on the topic area, the depth and breadth of data needed, the desired level of participation required 29 and the necessity (or not) for data saturation.
The optimum group size is around six to eight participants (excluding researchers) but can work effectively with between three and 14 participants. 3 If the group is too small, it may limit discussion, but if it is too large, it may become disorganised and difficult to manage. It is, however, prudent to over-recruit for a focus group by approximately two to three participants, to allow for potential non-attenders. For many researchers, particularly novice researchers, group size may also be informed by pragmatic considerations, such as the type of study, resources available and moderator experience. 28 Similar size and mix considerations exist for online focus groups. Typically, synchronous online focus groups will have around three to eight participants but, as the discussion does not happen simultaneously, asynchronous groups may have as many as 10–30 participants. 33
The topic area and potential group interaction should guide group composition considerations. Pre-existing groups, where participants know each other (for example, work colleagues) may be easier to recruit, have shared experiences and may enjoy a familiarity, which facilitates discussion and/or the ability to challenge each other courteously. 3 However, if there is a potential power imbalance within the group or if existing group norms and hierarchies may adversely affect the ability of participants to speak freely, then 'stranger groups' (that is, where participants do not already know each other) may be more appropriate. 34 , 35
Focus group management
Face-to-face focus groups should normally be conducted by two researchers; a moderator and an observer. 28 The moderator facilitates group discussion, while the observer typically monitors group dynamics, behaviours, non-verbal cues, seating arrangements and speaking order, which is essential for transcription and analysis. The same principles of informed consent, as discussed in the interview section, also apply to focus groups, regardless of medium. However, the consent process for online discussions will probably be managed somewhat differently. For example, while an appropriate participant information leaflet (and consent form) would still be required, the process is likely to be managed electronically (for example, via email) and would need to specifically address issues relating to technology (for example, anonymity and use, storage and access to online data). 32
The venue in which a face to face focus group is conducted should be of a suitable size, private, quiet, free from distractions and in a collectively convenient location. It should also be conducted at a time appropriate for participants, 28 as this is likely to promote attendance. As with interviews, the same ethical considerations apply (as discussed earlier). However, online focus groups may present additional ethical challenges associated with issues such as informed consent, appropriate access and secure data storage. Further guidance can be found elsewhere. 8 , 32
Before the focus group commences, the researchers should establish rapport with participants, as this will help to put them at ease and result in a more meaningful discussion. Consequently, researchers should introduce themselves, provide further clarity about the study and how the process will work in practice and outline the 'ground rules'. Ground rules are designed to assist, not hinder, group discussion and typically include: 3 , 28 , 29
Discussions within the group are confidential to the group
Only one person can speak at a time
All participants should have sufficient opportunity to contribute
There should be no unnecessary interruptions while someone is speaking
Everyone can be expected to be listened to and their views respected
Challenging contrary opinions is appropriate, but ridiculing is not.
Moderating a focus group requires considered management and good interpersonal skills to help guide the discussion and, where appropriate, keep it sufficiently focused. Avoid, therefore, participating, leading, expressing personal opinions or correcting participants' knowledge 3 , 28 as this may bias the process. A relaxed, interested demeanour will also help participants to feel comfortable and promote candid discourse. Moderators should also prevent the discussion being dominated by any one person, ensure differences of opinions are discussed fairly and, if required, encourage reticent participants to contribute. 3 Asking open questions, reflecting on significant issues, inviting further debate, probing responses accordingly, and seeking further clarification, as and where appropriate, will help to obtain sufficient depth and insight into the topic area.
Moderating online focus groups requires comparable skills, particularly if the discussion is synchronous, as the discussion may be dominated by those who can type proficiently. 36 It is therefore important that sufficient time and respect is accorded to those who may not be able to type as quickly. Asynchronous discussions are usually less problematic in this respect, as interactions are less instant. However, moderating an asynchronous discussion presents additional challenges, particularly if participants are geographically dispersed, as they may be online at different times. Consequently, the moderator will not always be present and the discussion may therefore need to occur over several days, which can be difficult to manage and facilitate and invariably requires considerable flexibility. 32 It is also worth recognising that establishing rapport with participants via online medium is often more challenging than via face-to-face and may therefore require additional time, skills, effort and consideration.
As with research interviews, focus groups should be guided by an appropriate interview schedule, as discussed earlier in the paper. For example, the schedule will usually be informed by the review of the literature and study aims, and will merely provide a topic guide to help inform subsequent discussions. To provide a verbatim account of the discussion, focus groups must be recorded, using an audio-recorder with a good quality multi-directional microphone. While videotaping is possible, some participants may find it obtrusive, 3 which may adversely affect group dynamics. The use (or not) of a video recorder, should therefore be carefully considered.
At the end of the focus group, a few minutes should be spent rounding up and reflecting on the discussion. 28 Depending on the topic area, it is possible that some participants may have revealed deeply personal issues and may therefore require further help and support, such as a constructive debrief or possibly even referral on to a relevant third party. It is also possible that some participants may feel that the discussion did not adequately reflect their views and, consequently, may no longer wish to be associated with the study. 28 Such occurrences are likely to be uncommon, but should they arise, it is important to further discuss any concerns and, if appropriate, offer them the opportunity to withdraw (including any data relating to them) from the study. Immediately after the discussion, researchers should compile notes regarding thoughts and ideas about the focus group, which can assist with data analysis and, if appropriate, any further data collection.
Qualitative research is increasingly being utilised within dental research to explore the experiences, perspectives, motivations and beliefs of participants. The contributions of qualitative research to evidence-based practice are increasingly being recognised, both as standalone research and as part of larger mixed-method studies, including clinical trials. Interviews and focus groups remain commonly used data collection methods in qualitative research, and with the advent of digital technologies, their utilisation continues to evolve. However, digital methods of qualitative data collection present additional methodological, ethical and practical considerations, but also potentially offer considerable flexibility to participants and researchers. Consequently, regardless of format, qualitative methods have significant potential to inform important areas of dental practice, policy and further related research.
Gussy M, Dickson-Swift V, Adams J . A scoping review of qualitative research in peer-reviewed dental publications. Int J Dent Hygiene 2013; 11 : 174–179.
Article Google Scholar
Burnard P, Gill P, Stewart K, Treasure E, Chadwick B . Analysing and presenting qualitative data. Br Dent J 2008; 204 : 429–432.
Gill P, Stewart K, Treasure E, Chadwick B . Methods of data collection in qualitative research: interviews and focus groups. Br Dent J 2008; 204 : 291–295.
Gill P, Stewart K, Treasure E, Chadwick B . Conducting qualitative interviews with school children in dental research. Br Dent J 2008; 204 : 371–374.
Stewart K, Gill P, Chadwick B, Treasure E . Qualitative research in dentistry. Br Dent J 2008; 204 : 235–239.
Masood M, Thaliath E, Bower E, Newton J . An appraisal of the quality of published qualitative dental research. Community Dent Oral Epidemiol 2011; 39 : 193–203.
Ellis J, Levine A, Bedos C et al. Refusal of implant supported mandibular overdentures by elderly patients. Gerodontology 2011; 28 : 62–68.
Macfarlane S, Bucknall T . Digital Technologies in Research. In Gerrish K, Lathlean J (editors) The Research Process in Nursing . 7th edition. pp. 71–86. Oxford: Wiley Blackwell; 2015.
Google Scholar
Lee R, Fielding N, Blank G . Online Research Methods in the Social Sciences: An Editorial Introduction. In Fielding N, Lee R, Blank G (editors) The Sage Handbook of Online Research Methods . pp. 3–16. London: Sage Publications; 2016.
Creswell J . Qualitative inquiry and research design: Choosing among five designs . Thousand Oaks, CA: Sage, 1998.
Guest G, Namey E, Mitchell M . Qualitative research: Defining and designing In Guest G, Namey E, Mitchell M (editors) Collecting Qualitative Data: A Field Manual For Applied Research . pp. 1–40. London: Sage Publications, 2013.
Chapter Google Scholar
Pope C, Mays N . Qualitative research: Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ 1995; 311 : 42–45.
Giddings L, Grant B . A Trojan Horse for positivism? A critique of mixed methods research. Adv Nurs Sci 2007; 30 : 52–60.
Hammersley M, Atkinson P . Ethnography: Principles in Practice . London: Routledge, 1995.
Oltmann S . Qualitative interviews: A methodological discussion of the interviewer and respondent contexts Forum Qualitative Sozialforschung/Forum: Qualitative Social Research. 2016; 17 : Art. 15.
Patton M . Qualitative Research and Evaluation Methods . Thousand Oaks, CA: Sage, 2002.
Wang M, Vinall-Collier K, Csikar J, Douglas G . A qualitative study of patients' views of techniques to reduce dental anxiety. J Dent 2017; 66 : 45–51.
Lindenmeyer A, Bowyer V, Roscoe J, Dale J, Sutcliffe P . Oral health awareness and care preferences in patients with diabetes: a qualitative study. Fam Pract 2013; 30 : 113–118.
Gallagher J, Clarke W, Wilson N . Understanding the motivation: a qualitative study of dental students' choice of professional career. Eur J Dent Educ 2008; 12 : 89–98.
Tod A . Interviewing. In Gerrish K, Lacey A (editors) The Research Process in Nursing . Oxford: Blackwell Publishing, 2006.
Grey E, Harcourt D, O'Sullivan D, Buchanan H, Kipatrick N . A qualitative study of patients' motivations and expectations for dental implants. Br Dent J 2013; 214 : 10.1038/sj.bdj.2012.1178.
Farmer J, Peressini S, Lawrence H . Exploring the role of the dental hygienist in reducing oral health disparities in Canada: A qualitative study. Int J Dent Hygiene 2017; 10.1111/idh.12276.
McElhinney E, Cheater F, Kidd L . Undertaking qualitative health research in social virtual worlds. J Adv Nurs 2013; 70 : 1267–1275.
Health Research Authority. UK Policy Framework for Health and Social Care Research. Available at https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/uk-policy-framework-health-social-care-research/ (accessed September 2017).
Baillie J, Gill P, Courtenay P . Knowledge, understanding and experiences of peritonitis among patients, and their families, undertaking peritoneal dialysis: A mixed methods study protocol. J Adv Nurs 2017; 10.1111/jan.13400.
Kvale S . Interviews . Thousand Oaks (CA): Sage, 1996.
Spradley J . The Ethnographic Interview . New York: Holt, Rinehart and Winston, 1979.
Goodman C, Evans C . Focus Groups. In Gerrish K, Lathlean J (editors) The Research Process in Nursing . pp. 401–412. Oxford: Wiley Blackwell, 2015.
Shaha M, Wenzell J, Hill E . Planning and conducting focus group research with nurses. Nurse Res 2011; 18 : 77–87.
Wang G, Gao X, Edward C . Public perception of dental implants: a qualitative study. J Dent 2015; 43 : 798–805.
Bailey E . Contemporary views of dental practitioners' on patient safety. Br Dent J 2015; 219 : 535–540.
Abrams K, Gaiser T . Online Focus Groups. In Field N, Lee R, Blank G (editors) The Sage Handbook of Online Research Methods . pp. 435–450. London: Sage Publications, 2016.
Poynter R . The Handbook of Online and Social Media Research . West Sussex: John Wiley & Sons, 2010.
Kevern J, Webb C . Focus groups as a tool for critical social research in nurse education. Nurse Educ Today 2001; 21 : 323–333.
Kitzinger J, Barbour R . Introduction: The Challenge and Promise of Focus Groups. In Barbour R S K J (editor) Developing Focus Group Research . pp. 1–20. London: Sage Publications, 1999.
Krueger R, Casey M . Focus Groups: A Practical Guide for Applied Research. 4th ed. Thousand Oaks, California: SAGE; 2009.
Download references
Author information
Authors and affiliations.
Senior Lecturer (Adult Nursing), School of Healthcare Sciences, Cardiff University,
Lecturer (Adult Nursing) and RCBC Wales Postdoctoral Research Fellow, School of Healthcare Sciences, Cardiff University,
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to P. Gill .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Gill, P., Baillie, J. Interviews and focus groups in qualitative research: an update for the digital age. Br Dent J 225 , 668–672 (2018). https://doi.org/10.1038/sj.bdj.2018.815
Download citation
Accepted : 02 July 2018
Published : 05 October 2018
Issue Date : 12 October 2018
DOI : https://doi.org/10.1038/sj.bdj.2018.815
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Translating brand reputation into equity from the stakeholder’s theory: an approach to value creation based on consumer’s perception & interactions.
- Olukorede Adewole
International Journal of Corporate Social Responsibility (2024)
Perceptions and beliefs of community gatekeepers about genomic risk information in African cleft research
- Abimbola M. Oladayo
- Oluwakemi Odukoya
- Azeez Butali
BMC Public Health (2024)
Assessment of women’s needs, wishes and preferences regarding interprofessional guidance on nutrition in pregnancy – a qualitative study
- Merle Ebinghaus
- Caroline Johanna Agricola
- Birgit-Christiane Zyriax
BMC Pregnancy and Childbirth (2024)
‘Baby mamas’ in Urban Ghana: an exploratory qualitative study on the factors influencing serial fathering among men in Accra, Ghana
- Rosemond Akpene Hiadzi
- Jemima Akweley Agyeman
- Godwin Banafo Akrong
Reproductive Health (2023)
Revolutionising dental technologies: a qualitative study on dental technicians’ perceptions of Artificial intelligence integration
- Galvin Sim Siang Lin
- Yook Shiang Ng
- Kah Hoay Chua
BMC Oral Health (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Grad Med Educ
- v.7(4); 2015 Dec
Choosing a Qualitative Research Approach
Associated data.
Editor's Note: The online version of this article contains a list of further reading resources and the authors' professional information .
The Challenge
Educators often pose questions about qualitative research. For example, a program director might say: “I collect data from my residents about their learning experiences in a new longitudinal clinical rotation. If I want to know about their learning experiences, should I use qualitative methods? I have been told that there are many approaches from which to choose. Someone suggested that I use grounded theory, but how do I know this is the best approach? Are there others?”
What Is Known
Qualitative research is the systematic inquiry into social phenomena in natural settings. These phenomena can include, but are not limited to, how people experience aspects of their lives, how individuals and/or groups behave, how organizations function, and how interactions shape relationships. In qualitative research, the researcher is the main data collection instrument. The researcher examines why events occur, what happens, and what those events mean to the participants studied. 1 , 2
Qualitative research starts from a fundamentally different set of beliefs—or paradigms—than those that underpin quantitative research. Quantitative research is based on positivist beliefs that there is a singular reality that can be discovered with the appropriate experimental methods. Post-positivist researchers agree with the positivist paradigm, but believe that environmental and individual differences, such as the learning culture or the learners' capacity to learn, influence this reality, and that these differences are important. Constructivist researchers believe that there is no single reality, but that the researcher elicits participants' views of reality. 3 Qualitative research generally draws on post-positivist or constructivist beliefs.
Qualitative scholars develop their work from these beliefs—usually post-positivist or constructivist—using different approaches to conduct their research. In this Rip Out, we describe 3 different qualitative research approaches commonly used in medical education: grounded theory, ethnography, and phenomenology. Each acts as a pivotal frame that shapes the research question(s), the method(s) of data collection, and how data are analyzed. 4 , 5
Choosing a Qualitative Approach
Before engaging in any qualitative study, consider how your views about what is possible to study will affect your approach. Then select an appropriate approach within which to work. Alignment between the belief system underpinning the research approach, the research question, and the research approach itself is a prerequisite for rigorous qualitative research. To enhance the understanding of how different approaches frame qualitative research, we use this introductory challenge as an illustrative example.
The clinic rotation in a program director's training program was recently redesigned as a longitudinal clinical experience. Resident satisfaction with this rotation improved significantly following implementation of the new longitudinal experience. The program director wants to understand how the changes made in the clinic rotation translated into changes in learning experiences for the residents.
Qualitative research can support this program director's efforts. Qualitative research focuses on the events that transpire and on outcomes of those events from the perspectives of those involved. In this case, the program director can use qualitative research to understand the impact of the new clinic rotation on the learning experiences of residents. The next step is to decide which approach to use as a frame for the study.
The table lists the purpose of 3 commonly used approaches to frame qualitative research. For each frame, we provide an example of a research question that could direct the study and delineate what outcomes might be gained by using that particular approach.
Methodology Overview

How You Can Start TODAY
- 1 Examine the foundations of the existing literature: As part of the literature review, make note of what is known about the topic and which approaches have been used in prior studies. A decision should be made to determine the extent to which the new study is exploratory and the extent to which findings will advance what is already known about the topic.
- 2 Find a qualitatively skilled collaborator: If you are interested in doing qualitative research, you should consult with a qualitative expert. Be prepared to talk to the qualitative scholar about what you would like to study and why . Furthermore, be ready to describe the literature to date on the topic (remember, you are asking for this person's expertise regarding qualitative approaches—he or she won't necessarily have content expertise). Qualitative research must be designed and conducted with rigor (rigor will be discussed in Rip Out No. 8 of this series). Input from a qualitative expert will ensure that rigor is employed from the study's inception.
- 3 Consider the approach: With a literature review completed and a qualitatively skilled collaborator secured, it is time to decide which approach would be best suited to answering the research question. Questions to consider when weighing approaches might include the following:
- • Will my findings contribute to the creation of a theoretical model to better understand the area of study? ( grounded theory )
- • Will I need to spend an extended amount of time trying to understand the culture and process of a particular group of learners in their natural context? ( ethnography )
- • Is there a particular phenomenon I want to better understand/describe? ( phenomenology )
What You Can Do LONG TERM
- 1 Develop your qualitative research knowledge and skills : A basic qualitative research textbook is a valuable investment to learn about qualitative research (further reading is provided as online supplemental material). A novice qualitative researcher will also benefit from participating in a massive online open course or a mini-course (often offered by professional organizations or conferences) that provides an introduction to qualitative research. Most of all, collaborating with a qualitative researcher can provide the support necessary to design, execute, and report on the study.
- 2 Undertake a pilot study: After learning about qualitative methodology, the next best way to gain expertise in qualitative research is to try it in a small scale pilot study with the support of a qualitative expert. Such application provides an appreciation for the thought processes that go into designing a study, analyzing the data, and reporting on the findings. Alternatively, if you have the opportunity to work on a study led by a qualitative expert, take it! The experience will provide invaluable opportunities for learning how to engage in qualitative research.
Supplementary Material
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Uniformed Services University of the Health Sciences, the Department of the Navy, the Department of Defense, or the US government.
References and Resources for Further Reading
- Open access
- Published: 16 May 2024
Integrating qualitative research within a clinical trials unit: developing strategies and understanding their implementation in contexts
- Jeremy Segrott ORCID: orcid.org/0000-0001-6215-0870 1 ,
- Sue Channon 2 ,
- Amy Lloyd 4 ,
- Eleni Glarou 2 , 3 ,
- Josie Henley 5 ,
- Jacqueline Hughes 2 ,
- Nina Jacob 2 ,
- Sarah Milosevic 2 ,
- Yvonne Moriarty 2 ,
- Bethan Pell 6 ,
- Mike Robling 2 ,
- Heather Strange 2 ,
- Julia Townson 2 ,
- Qualitative Research Group &
- Lucy Brookes-Howell 2
Trials volume 25 , Article number: 323 ( 2024 ) Cite this article
Metrics details
Background/aims
The value of using qualitative methods within clinical trials is widely recognised. How qualitative research is integrated within trials units to achieve this is less clear. This paper describes the process through which qualitative research has been integrated within Cardiff University’s Centre for Trials Research (CTR) in Wales, UK. We highlight facilitators of, and challenges to, integration.
We held group discussions on the work of the Qualitative Research Group (QRG) within CTR. The content of these discussions, materials for a presentation in CTR, and documents relating to the development of the QRG were interpreted at a workshop attended by group members. Normalisation Process Theory (NPT) was used to structure analysis. A writing group prepared a document for input from members of CTR, forming the basis of this paper.
Actions to integrate qualitative research comprised: its inclusion in Centre strategies; formation of a QRG with dedicated funding/roles; embedding of qualitative research within operating systems; capacity building/training; monitoring opportunities to include qualitative methods in studies; maximising the quality of qualitative research and developing methodological innovation. Facilitators of these actions included: the influence of the broader methodological landscape within trial/study design and its promotion of the value of qualitative research; and close physical proximity of CTR qualitative staff/students allowing sharing of methodological approaches. Introduction of innovative qualitative methods generated interest among other staff groups. Challenges included: pressure to under-resource qualitative components of research, preference for a statistical stance historically in some research areas and funding structures, and difficulties faced by qualitative researchers carving out individual academic profiles when working across trials/studies.

Conclusions
Given that CTUs are pivotal to the design and conduct of RCTs and related study types across multiple disciplines, integrating qualitative research into trials units is crucial if its contribution is to be fully realised. We have made explicit one trials unit’s experience of embedding qualitative research and present this to open dialogue on ways to operationalise and optimise qualitative research in trials. NPT provides a valuable framework with which to theorise these processes, including the importance of sense-making and legitimisation when introducing new practices within organisations.
Peer Review reports
The value of using qualitative methods within randomised control trials (RCTs) is widely recognised [ 1 , 2 , 3 ]. Qualitative research generates important evidence on factors affecting trial recruitment/retention [ 4 ] and implementation, aiding interpretation of quantitative data [ 5 ]. Though RCTs have traditionally been viewed as sitting within a positivist paradigm, recent methodological innovations have developed new trial designs that draw explicitly on both quantitative and qualitative methods. For instance, in the field of complex public health interventions, realist RCTs seek to understand the mechanisms through which interventions generate hypothesised impacts, and how interactions across different implementation contexts form part of these mechanisms. Proponents of realist RCTs—which integrate experimental and realist paradigms—highlight the importance of using quantitative and qualitative methods to fully realise these aims and to generate an understanding of intervention mechanisms and how context shapes them [ 6 ].
A need for guidance on how to conduct good quality qualitative research is being addressed, particularly in relation to feasibility studies for RCTs [ 7 ] and process evaluations embedded within trials of complex interventions [ 5 ]. There is also guidance on the conduct of qualitative research within trials at different points in the research cycle, including development, conduct and reporting [ 8 , 9 ].
A high proportion of trials are based within or involve clinical trials units (CTUs). In the UK the UKCRC Registered CTU Network describes them as:
… specialist units which have been set up with a specific remit to design, conduct, analyse and publish clinical trials and other well-designed studies. They have the capability to provide specialist expert statistical, epidemiological, and other methodological advice and coordination to undertake successful clinical trials. In addition, most CTUs will have expertise in the coordination of trials involving investigational medicinal products which must be conducted in compliance with the UK Regulations governing the conduct of clinical trials resulting from the EU Directive for Clinical Trials.
Thus, CTUs provide the specialist methodological expertise needed for the conduct of trials, and in the case of trials of investigational medicinal products, their involvement may be mandated to ensure compliance with relevant regulations. As the definition above suggests, CTUs also conduct and support other types of study apart from RCTs, providing a range of methodological and subject-based expertise.
However, despite their central role in the conduct and design of trials, (and other evaluation designs) little has been written about how CTUs have integrated qualitative work within their organisation at a time when such methods are, as stated above, now recognised as an important aspect of RCTs and evaluation studies more generally. This is a significant gap, since integration at the organisational level arguably shapes how qualitative research is integrated within individual studies, and thus it is valuable to understand how CTUs have approached the task. There are different ways of involving qualitative work in trials units, such as partnering with other departments (e.g. social science) or employing qualitative researchers directly. Qualitative research can be imagined and configured in different ways—as a method that generates data to inform future trial and intervention design, as an embedded component within an RCT or other evaluation type, or as a parallel strand of research focusing on lived experiences of illness, for instance. Understanding how trials units have integrated qualitative research is valuable, as it can shed light on which strategies show promise, and in which contexts, and how qualitative research is positioned within the field of trials research, foregrounding the value of qualitative research. However, although much has been written about its use within trials, few accounts exist of how trials units have integrated qualitative research within their systems and structures.
This paper discusses the process of embedding qualitative research within the work of one CTU—Cardiff University’s Centre for Trials Research (CTR). It highlights facilitators of this process and identifies challenges to integration. We use the Normalisation Process Theory (NPT) as a framework to structure our experience and approach. The key gap addressed by this paper is the implementation of strategies to integrate qualitative research (a relatively newly adopted set of practices and processes) within CTU systems and structures. We acknowledge from the outset that there are multiple ways of approaching this task. What follows therefore is not a set of recommendations for a preferred or best way to integrate qualitative research, as this will comprise diverse actions according to specific contexts. Rather, we examine the processes through which integration occurred in our own setting and highlight the potential value of these insights for others engaged in the work of promoting qualitative research within trials units.
Background to the integration of qualitative research within CTR
The CTR was formed in 2015 [ 10 ]. It brought together three existing trials units at Cardiff University: the South East Wales Trials Unit, the Wales Cancer Trials Unit, and the Haematology Clinical Trials Unit. From its inception, the CTR had a stated aim of developing a programme of qualitative research and integrating it within trials and other studies. In the sections below, we map these approaches onto the framework offered by Normalisation Process Theory to understand the processes through which they helped achieve embedding and integration of qualitative research.
CTR’s aims (including those relating to the development of qualitative research) were included within its strategy documents and communicated to others through infrastructure funding applications, annual reports and its website. A Qualitative Research Group (QRG), which had previously existed within the South East Wales Trials Unit, with dedicated funding for methodological specialists and group lead academics, was a key mechanism through which the development of a qualitative portfolio was put into action. Integration of qualitative research within Centre systems and processes occurred through the inclusion of qualitative research in study adoption processes and representation on committees. The CTR’s study portfolio provided a basis to track qualitative methods in new and existing studies, identify opportunities to embed qualitative methods within recently adopted studies (at the funding application stage) and to manage staff resources. Capacity building and training were an important focus of the QRG’s work, including training courses, mentoring, creation of an academic network open to university staff and practitioners working in the field of healthcare, presentations at CTR staff meetings and securing of PhD studentships. Standard operating procedures and methodological guidance on the design and conduct of qualitative research (e.g. templates for developing analysis plans) aimed to create a shared understanding of how to undertake high-quality research, and a means to monitor the implementation of rigorous approaches. As the QRG expanded its expertise it sought to develop innovative approaches, including the use of visual [ 11 ] and ethnographic methods [ 12 ].
Understanding implementation—Normalisation Process Theory (NPT)
Normalisation Process Theory (NPT) provides a model with which to understand the implementation of new sets of practices and their normalisation within organisational settings. The term ‘normalisation’ refers to how new practices become routinised (part of the everyday work of an organisation) through embedding and integration [ 13 , 14 ]. NPT defines implementation as ‘the social organisation of work’ and is concerned with the social processes that take place as new practices are introduced. Embedding involves ‘making practices routine elements of everyday life’ within an organisation. Integration takes the form of ‘sustaining embedded practices in social contexts’, and how these processes lead to the practices becoming (or not becoming) ‘normal and routine’ [ 14 ]. NPT is concerned with the factors which promote or ‘inhibit’ attempts to embed and integrate the operationalisation of new practices [ 13 , 14 , 15 ].
Embedding new practices is therefore achieved through implementation—which takes the form of interactions in specific contexts. Implementation is operationalised through four ‘generative mechanisms’— coherence , cognitive participation , collective action and reflexive monitoring [ 14 ]. Each mechanism is characterised by components comprising immediate and organisational work, with actions of individuals and organisations (or groups of individuals) interdependent. The mechanisms operate partly through forms of investment (i.e. meaning, commitment, effort, and comprehension) [ 14 ].
Coherence refers to how individuals/groups make sense of, and give meaning to, new practices. Sense-making concerns the coherence of a practice—whether it ‘holds together’, and its differentiation from existing activities [ 15 ]. Communal and individual specification involve understanding new practices and their potential benefits for oneself or an organisation. Individuals consider what new practices mean for them in terms of tasks and responsibilities ( internalisation ) [ 14 ].
NPT frames the second mechanism, cognitive participation , as the building of a ‘community of practice’. For a new practice to be initiated, individuals and groups within an organisation must commit to it [ 14 , 15 ]. Cognitive participation occurs through enrolment —how people relate to the new practice; legitimation —the belief that it is right for them to be involved; and activation —defining which actions are necessary to sustain the practice and their involvement [ 14 ]. Making the new practices work may require changes to roles (new responsibilities, altered procedures) and reconfiguring how colleagues work together (changed relationships).
Third, Collective Action refers to ‘the operational work that people do to enact a set of practices’ [ 14 ]. Individuals engage with the new practices ( interactional workability ) reshaping how members of an organisation interact with each other, through creation of new roles and expectations ( relational interaction ) [ 15 ]. Skill set workability concerns how the work of implementing a new set of practices is distributed and the necessary roles and skillsets defined [ 14 ]. Contextual integration draws attention to the incorporation of a practice within social contexts, and the potential for aspects of these contexts, such as systems and procedures, to be modified as a result [ 15 ].
Reflexive monitoring is the final implementation mechanism. Collective and individual appraisal evaluate the value of a set of practices, which depends on the collection of information—formally and informally ( systematisation ). Appraisal may lead to reconfiguration in which procedures of the practice are redefined or reshaped [ 14 , 15 ].
We sought to map the following: (1) the strategies used to embed qualitative research within the Centre, (2) key facilitators, and (3) barriers to their implementation. Through focused group discussions during the monthly meetings of the CTR QRG and in discussion with the CTR senior management team throughout 2019–2020 we identified nine types of documents (22 individual documents in total) produced within the CTR which had relevant information about the integration of qualitative research within its work (Table 1 ). The QRG had an ‘open door’ policy to membership and welcomed all staff/students with an interest in qualitative research. It included researchers who were employed specifically to undertake qualitative research and other staff with a range of study roles, including trial managers, statisticians, and data managers. There was also diversity in terms of career stage, including PhD students, mid-career researchers and members of the Centre’s Executive team. Membership was therefore largely self-selected, and comprised of individuals with a role related to, or an interest in, embedding qualitative research within trials. However, the group brought together diverse methodological perspectives and was not solely comprised of methodological ‘champions’ whose job it was to promote the development of qualitative research within the centre. Thus whilst the group (and by extension, the authors of this paper) had a shared appreciation of the value of qualitative research within a trials centre, they also brought varied methodological perspectives and ways of engaging with it.
All members of the QRG ( n = 26) were invited to take part in a face-to-face, day-long workshop in February 2019 on ‘How to optimise and operationalise qualitative research in trials: reflections on CTR structure’. The workshop was attended by 12 members of staff and PhD students, including members of the QRG and the CTR’s senior management team. Recruitment to the workshop was therefore inclusive, and to some extent opportunistic, but all members of the QRG were able to contribute to discussions during regular monthly group meetings and the drafting of the current paper.
The aim of the workshop was to bring together information from the documents in Table 1 to generate discussion around the key strategies (and their component activities) that had been adopted to integrate qualitative research into CTR, as well as barriers to, and facilitators of, their implementation. The agenda for the workshop involved four key areas: development and history of the CTR model; mapping the current model within CTR; discussing the structure of other CTUs; and exploring the advantages and disadvantages of the CTR model.
During the workshop, we discussed the use of NPT to conceptualise how qualitative research had been embedded within CTR’s systems and practices. The group produced spider diagrams to map strategies and actions on to the four key domains (or ‘generative mechanisms’ of NPT) summarised above, to aid the understanding of how they had functioned, and the utility of NPT as a framework. This is summarised in Table 2 .
Detailed notes were made during the workshop. A core writing group then used these notes and the documents in Table 1 to develop a draft of the current paper. This was circulated to all members of the CTR QRG ( n = 26) and stored within a central repository accessible to them to allow involvement and incorporate the views of those who were not able to attend the workshop. This draft was again presented for comments in the monthly CTR QRG meeting in February 2021 attended by n = 10. The Standards for QUality Improvement Reporting Excellence 2.0 (SQUIRE) guidelines were used to inform the structure and content of the paper (see supplementary material) [ 16 ].
In the following sections, we describe the strategies CTR adopted to integrate qualitative research. These are mapped against NPT’s four generative mechanisms to explore the processes through which the strategies promoted integration, and facilitators of and barriers to their implementation. A summary of the strategies and their functioning in terms of the generative mechanisms is provided in Table 2 .
Coherence—making sense of qualitative research
In CTR, many of the actions taken to build a portfolio of qualitative research were aimed at enabling colleagues, and external actors, to make sense of this set of methodologies. Centre-level strategies and grant applications for infrastructure funding highlighted the value of qualitative research, the added benefits it would bring, and positioned it as a legitimate set of practices alongside existing methods. For example, a 2014 application for renewal of trials unit infrastructure funding stated:
We are currently in the process of undertaking […] restructuring for our qualitative research team and are planning similar for trial management next year. The aim of this restructuring is to establish greater hierarchical management and opportunities for staff development and also provide a structure that can accommodate continuing growth.
Within the CTR, various forms of communication on the development of qualitative research were designed to enable staff and students to make sense of it, and to think through its potential value for them, and ways in which they might engage with it. These included presentations at staff meetings, informal meetings between project teams and the qualitative group lead, and the visibility of qualitative research on the public-facing Centre website and Centre committees and systems. For instance, qualitative methods were included (and framed as a distinct set of practices) within study adoption forms and committee agendas. Information for colleagues described how qualitative methods could be incorporated within funding applications for RCTs and other evaluation studies to generate new insights into questions research teams were already keen to answer, such as influences on intervention implementation fidelity. Where externally based chief investigators approached the Centre to be involved in new grant applications, the existence of the qualitative team and group lead enabled the inclusion of qualitative research to be actively promoted at an early stage, and such opportunities were highlighted in the Centre’s brochure for new collaborators. Monthly qualitative research network meetings—advertised across CTR and to external research collaborators, were also designed to create a shared understanding of qualitative research methods and their utility within trials and other study types (e.g. intervention development, feasibility studies, and observational studies). Training events (discussed in more detail below) also aided sense-making.
Several factors facilitated the promotion of qualitative research as a distinctive and valuable entity. Among these was the influence of the broader methodological landscape within trial design which was promoting the value of qualitative research, such as guidance on the evaluation of complex interventions by the Medical Research Council [ 17 ], and the growing emphasis placed on process evaluations within trials (with qualitative methods important in understanding participant experience and influences on implementation) [ 5 ]. The attention given to lived experience (both through process evaluations and the move to embed public involvement in trials) helped to frame qualitative research within the Centre as something that was appropriate, legitimate, and of value. Recognition by research funders of the value of qualitative research within studies was also helpful in normalising and legitimising its adoption within grant applications.
The inclusion of qualitative methods within influential methodological guidance helped CTR researchers to develop a ‘shared language’ around these methods, and a way that a common understanding of the role of qualitative research could be generated. One barrier to such sense-making work was the varying extent to which staff and teams had existing knowledge or experience of qualitative research. This varied across methodological and subject groups within the Centre and reflected the history of the individual trials units which had merged to form the Centre.
Cognitive participation—legitimising qualitative research
Senior CTR leaders promoted the value and legitimacy of qualitative research. Its inclusion in centre strategies, infrastructure funding applications, and in public-facing materials (e.g. website, investigator brochures), signalled that it was appropriate for individuals to conduct qualitative research within their roles, or to support others in doing so. Legitimisation also took place through informal channels, such as senior leadership support for qualitative research methods in staff meetings and participation in QRG seminars. Continued development of the QRG (with dedicated infrastructure funding) provided a visible identity and equivalence with other methodological groups (e.g. trial managers, statisticians).
Staff were asked to engage with qualitative research in two main ways. First, there was an expansion in the number of staff for whom qualitative research formed part of their formal role and responsibilities. One of the three trials units that merged to form CTR brought with it a qualitative team comprising methodological specialists and a group lead. CTR continued the expansion of this group with the creation of new roles and an enlarged nucleus of researchers for whom qualitative research was the sole focus of their work. In part, this was linked to the successful award of projects that included a large qualitative component, and that were coordinated by CTR (see Table 3 which describes the PUMA study).
Members of the QRG were encouraged to develop their own research ideas and to gain experience as principal investigators, and group seminars were used to explore new ideas and provide peer support. This was communicated through line management, appraisal, and informal peer interaction. Boundaries were not strictly demarcated (i.e. staff located outside the qualitative team were already using qualitative methods), but the new team became a central focus for developing a growing programme of work.
Second, individuals and studies were called upon to engage in new ways with qualitative research, and with the qualitative team. A key goal for the Centre was that groups developing new research ideas should give more consideration in general to the potential value and inclusion of qualitative research within their funding applications. Specifically, they were asked to do this by thinking about qualitative research at an early point in their application’s development (rather than ‘bolting it on’ after other elements had been designed) and to draw upon the expertise and input of the qualitative team. An example was the inclusion of questions on qualitative methods within the Centre’s study adoption form and representation from the qualitative team at the committee which reviewed new adoption requests. Where adoption requests indicated the inclusion of qualitative methods, colleagues were encouraged to liaise with the qualitative team, facilitating the integration of its expertise from an early stage. Qualitative seminars offered an informal and supportive space in which researchers could share initial ideas and refine their methodological approach. The benefits of this included the provision of sufficient time for methodological specialists to be involved in the design of the proposed qualitative component and ensuring adequate costings had been drawn up. At study adoption group meetings, scrutiny of new proposals included consideration of whether new research proposals might be strengthened through the use of qualitative methods where these had not initially been included. Meetings of the QRG—which reviewed the Centre’s portfolio of new studies and gathered intelligence on new ideas—also helped to identify, early on, opportunities to integrate qualitative methods. Communication across teams was useful in identifying new research ideas and embedding qualitative researchers within emerging study development groups.
Actions to promote greater use of qualitative methods in funding applications fed through into a growing number of studies with a qualitative component. This helped to increase the visibility and legitimacy of qualitative methods within the Centre. For example, the PUMA study [ 12 ], which brought together a large multidisciplinary team to develop and evaluate a Paediatric early warning system, drew heavily on qualitative methods, with the qualitative research located within the QRG. The project introduced an extensive network of collaborators and clinical colleagues to qualitative methods and how they could be used during intervention development and the generation of case studies. Further information about the PUMA study is provided in Table 3 .
Increasing the legitimacy of qualitative work across an extensive network of staff, students and collaborators was a complex process. Set within the continuing dominance of quantitative methods with clinical trials, there were variations in the extent to which clinicians and other collaborators embraced the value of qualitative methods. Research funding schemes, which often continued to emphasise the quantitative element of randomised controlled trials, inevitably fed through into the focus of new research proposals. Staff and external collaborators were sometimes uncertain about the added value that qualitative methods would bring to their trials. Across the CTR there were variations in the speed at which qualitative research methods gained legitimacy, partly based on disciplinary traditions and their influences. For instance, population health trials, often located within non-health settings such as schools or community settings, frequently involved collaboration with social scientists who brought with them experience in qualitative methods. Methodological guidance in this field, such as MRC guidance on process evaluations, highlighted the value of qualitative methods and alternatives to the positivist paradigm, such as the value of realist RCTs. In other, more clinical areas, positivist paradigms had greater dominance. Established practices and methodological traditions across different funders also influenced the ease of obtaining funding to include qualitative research within studies. For drugs trials (CTIMPs), the influence of regulatory frameworks on study design, data collection and the allocation of staff resources may have played a role. Over time, teams gained repeated experience of embedding qualitative research (and researchers) within their work and took this learning with them to subsequent studies. For example, the senior clinician quoted within the PUMA case study (Table 3 below) described how they had gained an appreciation of the rigour of qualitative research and an understanding of its language. Through these repeated interactions, embedding of qualitative research within studies started to become the norm rather than the exception.
Collective action—operationalising qualitative research
Collective action concerns the operationalisation of new practices within organisations—the allocation and management of the work, how individuals interact with each other, and the work itself. In CTR the formation of a Qualitative Research Group helped to allocate and organise the work of building a portfolio of studies. Researchers across the Centre were called upon to interact with qualitative research in new ways. Presentations at staff meetings and the inclusion of qualitative research methods in portfolio study adoption forms were examples of this ( interactive workability ). It was operationalised by encouraging study teams to liaise with the qualitative research lead. Development of standard operating procedures, templates for costing qualitative research and methodological guidance (e.g. on analysis plans) also helped encourage researchers to interact with these methods in new ways. For some qualitative researchers who had been trained in the social sciences, working within a trials unit meant that they needed to interact in new and sometimes unfamiliar ways with standard operating procedures, risk assessments, and other trial-based systems. Thus, training needs and capacity-building efforts were multidirectional.
Whereas there had been a tendency for qualitative research to be ‘bolted on’ to proposals for RCTs, the systems described above were designed to embed thinking about the value and design of the qualitative component from the outset. They were also intended to integrate members of the qualitative team with trial teams from an early stage to promote effective integration of qualitative methods within larger trials and build relationships over time.
Standard Operating Procedures (SOPs), formal and informal training, and interaction between the qualitative team and other researchers increased the relational workability of qualitative methods within the Centre—the confidence individuals felt in including these methods within their studies, and their accountability for doing so. For instance, study adoption forms prompted researchers to interact routinely with the qualitative team at an early stage, whilst guidance on costing grants provided clear expectations about the resources needed to deliver a proposed set of qualitative data collection.
Formation of the Qualitative Research Group—comprised of methodological specialists, created new roles and skillsets ( skill set workability ). Research teams were encouraged to draw on these when writing funding applications for projects that included a qualitative component. Capacity-building initiatives were used to increase the number of researchers with the skills needed to undertake qualitative research, and for these individuals to develop their expertise over time. This was achieved through formal training courses, academic seminars, mentoring from experienced colleagues, and informal knowledge exchange. Links with external collaborators and centres engaged in building qualitative research supported these efforts. Within the Centre, the co-location of qualitative researchers with other methodological and trial teams facilitated knowledge exchange and building of collaborative relationships, whilst grouping of the qualitative team within a dedicated office space supported a collective identity and opportunities for informal peer support.
Some aspects of the context in which qualitative research was being developed created challenges to operationalisation. Dependence on project grants to fund qualitative methodologists meant that there was a continuing need to write further grant applications whilst limiting the amount of time available to do so. Similarly, researchers within the team whose role was funded largely by specific research projects could sometimes find it hard to create sufficient time to develop their personal methodological interests. However, the cultivation of a methodologically varied portfolio of work enabled members of the team to build significant expertise in different approaches (e.g. ethnography, discourse analysis) that connected individual studies.
Reflexive monitoring—evaluating the impact of qualitative research
Inclusion of questions/fields relating to qualitative research within the Centre’s study portfolio database was a key way in which information was collected ( systematisation ). It captured numbers of funding applications and funded studies, research design, and income generation. Alongside this database, a qualitative resource planner spreadsheet was used to link individual members of the qualitative team with projects and facilitate resource planning, further reinforcing the core responsibilities and roles of qualitative researchers within CTR. As with all staff in the Centre, members of the qualitative team were placed on ongoing rather than fixed-term contracts, reflecting their core role within CTR. Planning and strategy meetings used the database and resource planner to assess the integration of qualitative research within Centre research, identify opportunities for increasing involvement, and manage staff recruitment and sustainability of researcher posts. Academic meetings and day-to-day interaction fulfilled informal appraisal of the development of the group, and its position within the Centre. Individual appraisal was also important, with members of the qualitative team given opportunities to shape their role, reflect on progress, identify training needs, and further develop their skillset, particularly through line management systems.
These forms of systematisation and appraisal were used to reconfigure the development of qualitative research and its integration within the Centre. For example, group strategies considered how to achieve long-term integration of qualitative research from its initial embedding through further promoting the belief that it formed a core part of the Centre’s business. The visibility and legitimacy of qualitative research were promoted through initiatives such as greater prominence on the Centre’s website. Ongoing review of the qualitative portfolio and discussion at academic meetings enabled the identification of areas where increased capacity would be helpful, both for qualitative staff, and more broadly within the Centre. This prompted the qualitative group to develop an introductory course to qualitative methods open to all Centre staff and PhD students, aimed at increasing understanding and awareness. As the qualitative team built its expertise and experience it also sought to develop new and innovative approaches to conducting qualitative research. This included the use of visual and diary-based methods [ 11 ] and the adoption of ethnography to evaluate system-level clinical interventions [ 12 ]. Restrictions on conventional face-to-face qualitative data collection due to the COVID-19 pandemic prompted rapid adoption of virtual/online methods for interviews, observation, and use of new internet platforms such as Padlet—a form of digital note board.
In this paper, we have described the work undertaken by one CTU to integrate qualitative research within its studies and organisational culture. The parallel efforts of many trials units to achieve these goals arguably come at an opportune time. The traditional designs of RCTs have been challenged and re-imagined by the increasing influence of realist evaluation [ 6 , 18 ] and the widespread acceptance that trials need to understand implementation and intervention theory as well as assess outcomes [ 17 ]. Hence the widespread adoption of embedded mixed methods process evaluations within RCTs. These broad shifts in methodological orthodoxies, the production of high-profile methodological guidance, and the expectations of research funders all create fertile ground for the continued expansion of qualitative methods within trials units. However, whilst much has been written about the importance of developing qualitative research and the possible approaches to integrating qualitative and quantitative methods within studies, much less has been published on how to operationalise this within trials units. Filling this lacuna is important. Our paper highlights how the integration of a new set of practices within an organisation can become embedded as part of its ‘normal’ everyday work whilst also shaping the practices being integrated. In the case of CTR, it could be argued that the integration of qualitative research helped shape how this work was done (e.g. systems to assess progress and innovation).
In our trials unit, the presence of a dedicated research group of methodological specialists was a key action that helped realise the development of a portfolio of qualitative research and was perhaps the most visible evidence of a commitment to do so. However, our experience demonstrates that to fully realise the goal of developing qualitative research, much work focuses on the interaction between this ‘new’ set of methods and the organisation into which it is introduced. Whilst the team of methodological specialists was tasked with, and ‘able’ to do the work, the ‘work’ itself needed to be integrated and embedded within the existing system. Thus, alongside the creation of a team and methodological capacity, promoting the legitimacy of qualitative research was important to communicate to others that it was both a distinctive and different entity, yet similar and equivalent to more established groups and practices (e.g. trial management, statistics, data management). The framing of qualitative research within strategies, the messages given out by senior leaders (formally and informally) and the general visibility of qualitative research within the system all helped to achieve this.
Normalisation Process Theory draws our attention to the concepts of embedding (making a new practice routine, normal within an organisation) and integration —the long-term sustaining of these processes. An important process through which embedding took place in our centre concerned the creation of messages and systems that called upon individuals and research teams to interact with qualitative research. Research teams were encouraged to think about qualitative research and consider its potential value for their studies. Critically, they were asked to do so at specific points, and in particular ways. Early consideration of qualitative methods to maximise and optimise their inclusion within studies was emphasised, with timely input from the qualitative team. Study adoption systems, centre-level processes for managing financial and human resources, creation of a qualitative resource planner, and awareness raising among staff, helped to reinforce this. These processes of embedding and integration were complex and they varied in intensity and speed across different areas of the Centre’s work. In part this depended on existing research traditions, the extent of prior experience of working with qualitative researchers and methods, and the priorities of subject areas and funders. Centre-wide systems, sometimes linked to CTR’s operation as a CTU, also helped to legitimise and embed qualitative research, lending it equivalence with other research activity. For example, like all CTUs, CTR was required to conform with the principles of Good Clinical Practice, necessitating the creation of a quality management system, operationalised through standard operating procedures for all areas of its work. Qualitative research was included, and became embedded, within these systems, with SOPs produced to guide activities such as qualitative analysis.
NPT provides a helpful way of understanding how trials units might integrate qualitative research within their work. It highlights how new practices interact with existing organisational systems and the work needed to promote effective interaction. That is, alongside the creation of a team or programme of qualitative research, much of the work concerns how members of an organisation understand it, engage with it, and create systems to sustain it. Embedding a new set of practices may be just as important as the quality or characteristics of the practices themselves. High-quality qualitative research is of little value if it is not recognised and drawn upon within new studies for instance. NPT also offers a helpful lens with which to understand how integration and embedding occur, and the mechanisms through which they operate. For example, promoting the legitimacy of a new set of practices, or creating systems that embed it, can help sustain these practices by creating an organisational ambition and encouraging (or requiring) individuals to interact with them in certain ways, redefining their roles accordingly. NPT highlights the ways in which integration of new practices involves bi-directional exchanges with the organisation’s existing practices, with each having the potential to re-shape the other as interaction takes place. For instance, in CTR, qualitative researchers needed to integrate and apply their methods within the quality management and other systems of a CTU, such as the formalisation of key processes within standard operating procedures, something less likely to occur outside trials units. Equally, project teams (including those led by externally based chief investigators) increased the integration of qualitative methods within their overall study design, providing opportunities for new insights on intervention theory, implementation and the experiences of practitioners and participants.
We note two aspects of the normalisation processes within CTR that are slightly less well conceptualised by NPT. The first concerns the emphasis within coherence on identifying the distinctiveness of new practices, and how they differ from existing activities. Whilst differentiation was an important aspect of the integration of qualitative research in CTR, such integration could be seen as operating partly through processes of de-differentiation, or at least equivalence. That is, part of the integration of qualitative research was to see it as similar in terms of rigour, coherence, and importance to other forms of research within the Centre. To be viewed as similar, or at least comparable to existing practices, was to be legitimised.
Second, whilst NPT focuses mainly on the interaction between a new set of practices and the organisational context into which it is introduced, our own experience of introducing qualitative research into a trials unit was shaped by broader organisational and methodological contexts. For example, the increasing emphasis placed upon understanding implementation processes and the experiences of research participants in the field of clinical trials (e.g. by funders), created an environment conducive to the development of qualitative research methods within our Centre. Attempts to integrate qualitative research within studies were also cross-organisational, given that many of the studies managed within the CTR drew together multi-institutional teams. This provided important opportunities to integrate qualitative research within a portfolio of studies that extended beyond CTR and build a network of collaborators who increasingly included qualitative methods within their funding proposals. The work of growing and integrating qualitative research within a trials unit is an ongoing one in which ever-shifting macro-level influences can help or hinder, and where the organisations within which we work are never static in terms of barriers and facilitators.
The importance of utilising qualitative methods within RCTs is now widely recognised. Increased emphasis on the evaluation of complex interventions, the influence of realist methods directing greater attention to complexity and the widespread adoption of mixed methods process evaluations are key drivers of this shift. The inclusion of qualitative methods within individual trials is important and previous research has explored approaches to their incorporation and some of the challenges encountered. Our paper highlights that the integration of qualitative methods at the organisational level of the CTU can shape how they are taken up by individual trials. Within CTR, it can be argued that qualitative research achieved high levels of integration, as conceptualised by Normalisation Process Theory. Thus, qualitative research became recognised as a coherent and valuable set of practices, secured legitimisation as an appropriate focus of individual and organisational activity and benefitted from forms of collective action which operationalised these organisational processes. Crucially, the routinisation of qualitative research appeared to be sustained, something which NPT suggests helps define integration (as opposed to initial embedding). However, our analysis suggested that the degree of integration varied by trial area. This variation reflected a complex mix of factors including disciplinary traditions, methodological guidance, existing (un)familiarity with qualitative research, and the influence of regulatory frameworks for certain clinical trials.
NPT provides a valuable framework with which to understand how these processes of embedding and integration occur. Our use of NPT draws attention to the importance of sense-making and legitimisation as important steps in introducing a new set of practices within the work of an organisation. Integration also depends, across each mechanism of NPT, on the building of effective relationships, which allow individuals and teams to work together in new ways. By reflecting on our experiences and the decisions taken within CTR we have made explicit one such process for embedding qualitative research within a trials unit, whilst acknowledging that approaches may differ across trials units. Mindful of this fact, and the focus of the current paper on one trials unit’s experience, we do not propose a set of recommendations for others who are working to achieve similar goals. Rather, we offer three overarching reflections (framed by NPT) which may act as a useful starting point for trials units (and other infrastructures) seeking to promote the adoption of qualitative research.
First, whilst research organisations such as trials units are highly heterogenous, processes of embedding and integration, which we have foregrounded in this paper, are likely to be important across different contexts in sustaining the use of qualitative research. Second, developing a plan for the integration of qualitative research will benefit from mapping out the characteristics of the extant system. For example, it is valuable to know how familiar staff are with qualitative research and any variations across teams within an organisation. Thirdly, NPT frames integration as a process of implementation which operates through key generative mechanisms— coherence , cognitive participation , collective action and reflexive monitoring . These mechanisms can help guide understanding of which actions help achieve embedding and integration. Importantly, they span multiple aspects of how organisations, and the individuals within them, work. The ways in which people make sense of a new set of practices ( coherence ), their commitment towards it ( cognitive participation ), how it is operationalised ( collective action ) and the evaluation of its introduction ( reflexive monitoring ) are all important. Thus, for example, qualitative research, even when well organised and operationalised within an organisation, is unlikely to be sustained if appreciation of its value is limited, or people are not committed to it.
We present our experience of engaging with the processes described above to open dialogue with other trials units on ways to operationalise and optimise qualitative research in trials. Understanding how best to integrate qualitative research within these settings may help to fully realise the significant contribution which it makes the design and conduct of trials.
Availability of data and materials
Some documents cited in this paper are either freely available from the Centre for Trials Research website or can be requested from the author for correspondence.
O’Cathain A, Thomas KJ, Drabble SJ, Rudolph A, Hewison J. What can qualitative research do for randomised controlled trials? A systematic mapping review. BMJ Open. 2013;3(6):e002889.
Article PubMed PubMed Central Google Scholar
O’Cathain A, Thomas KJ, Drabble SJ, Rudolph A, Goode J, Hewison J. Maximising the value of combining qualitative research and randomised controlled trials in health research: the QUAlitative Research in Trials (QUART) study – a mixed methods study. Health Technol Assess. 2014;18(38):1–197.
Clement C, Edwards SL, Rapport F, Russell IT, Hutchings HA. Exploring qualitative methods reported in registered trials and their yields (EQUITY): systematic review. Trials. 2018;19(1):589.
Hennessy M, Hunter A, Healy P, Galvin S, Houghton C. Improving trial recruitment processes: how qualitative methodologies can be used to address the top 10 research priorities identified within the PRioRiTy study. Trials. 2018;19:584.
Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350(mar19 6):h1258.
Bonell C, Fletcher A, Morton M, Lorenc T, Moore L. Realist randomised controlled trials: a new approach to evaluating complex public health interventions. Soc Sci Med. 2012;75(12):2299–306.
Article PubMed Google Scholar
O’Cathain A, Hoddinott P, Lewin S, Thomas KJ, Young B, Adamson J, et al. Maximising the impact of qualitative research in feasibility studies for randomised controlled trials: guidance for researchers. Pilot Feasibility Stud. 2015;1:32.
Cooper C, O’Cathain A, Hind D, Adamson J, Lawton J, Baird W. Conducting qualitative research within Clinical Trials Units: avoiding potential pitfalls. Contemp Clin Trials. 2014;38(2):338–43.
Rapport F, Storey M, Porter A, Snooks H, Jones K, Peconi J, et al. Qualitative research within trials: developing a standard operating procedure for a clinical trials unit. Trials. 2013;14:54.
Cardiff University. Centre for Trials Research. Available from: https://www.cardiff.ac.uk/centre-for-trials-research . Accessed 10 May 2024.
Pell B, Williams D, Phillips R, Sanders J, Edwards A, Choy E, et al. Using visual timelines in telephone interviews: reflections and lessons learned from the star family study. Int J Qual Methods. 2020;19:160940692091367.
Thomas-Jones E, Lloyd A, Roland D, Sefton G, Tume L, Hood K, et al. A prospective, mixed-methods, before and after study to identify the evidence base for the core components of an effective Paediatric Early Warning System and the development of an implementation package containing those core recommendations for use in th. BMC Pediatr. 2018;18:244.
May C, Finch T, Mair F, Ballini L, Dowrick C, Eccles M, et al. Understanding the implementation of complex interventions in health care: the normalization process model. BMC Health Serv Res. 2007;7:148.
May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology. 2009;43(3):535–54.
Article Google Scholar
May CR, Mair F, Finch T, Macfarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci. 2009;4:29.
Ogrinc G, Davies L, Goodman D, Batalden PB, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. BMJ Quality and Safety. 2016;25:986-92.
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655.
Jamal F, Fletcher A, Shackleton N, Elbourne D, Viner R, Bonell C. The three stages of building and testing mid-level theories in a realist RCT: a theoretical and methodological case-example. Trials. 2015;16(1):466.
Download references
Acknowledgements
Members of the Centre for Trials Research (CTR) Qualitative Research Group were collaborating authors: C Drew (Senior Research Fellow—Senior Trial Manager, Brain Health and Mental Wellbeing Division), D Gillespie (Director, Infection, Inflammation and Immunity Trials, Principal Research Fellow), R Hale (now Research Associate, School of Social Sciences, Cardiff University), J Latchem-Hastings (now Lecturer and Postdoctoral Fellow, School of Healthcare Sciences, Cardiff University), R Milton (Research Associate—Trial Manager), B Pell (now PhD student, DECIPHer Centre, Cardiff University), H Prout (Research Associate—Qualitative), V Shepherd (Senior Research Fellow), K Smallman (Research Associate), H Stanton (Research Associate—Senior Data Manager). Thanks are due to Kerry Hood and Aimee Grant for their involvement in developing processes and systems for qualitative research within CTR.
No specific grant was received to support the writing of this paper.
Author information
Authors and affiliations.
Centre for Trials Research, DECIPHer Centre, Cardiff University, Neuadd Meirionnydd, Heath Park, Cardiff, CF14 4YS, UK
Jeremy Segrott
Centre for Trials Research, Cardiff University, Neuadd Meirionnydd, Heath Park, Cardiff, CF14 4YS, UK
Sue Channon, Eleni Glarou, Jacqueline Hughes, Nina Jacob, Sarah Milosevic, Yvonne Moriarty, Mike Robling, Heather Strange, Julia Townson & Lucy Brookes-Howell
Division of Population Medicine, School of Medicine, Cardiff University, Neuadd Meirionnydd, Heath Park, Cardiff, CF14 4YS, UK
Eleni Glarou
Wales Centre for Public Policy, Cardiff University, Sbarc I Spark, Maindy Road, Cardiff, CF24 4HQ, UK
School of Social Sciences, Cardiff University, King Edward VII Avenue, Cardiff, CF10 3WA, UK
Josie Henley
DECIPHer Centre, School of Social Sciences, Cardiff University, Sbarc I Spark, Maindy Road, Cardiff, CF24 4HQ, UK
Bethan Pell
You can also search for this author in PubMed Google Scholar
Qualitative Research Group
- , D. Gillespie
- , J. Latchem-Hastings
- , R. Milton
- , V. Shepherd
- , K. Smallman
- & H. Stanton
Contributions
JS contributed to the design of the work and interpretation of data and was responsible for leading the drafting and revision of the paper. SC contributed to the design of the work, the acquisition of data and the drafting and revision of the paper. AL contributed to the design of the work, the acquisition of data and the drafting and revision of the paper. EG contributed to a critical review of the manuscript and provided additional relevant references. JH provided feedback on initial drafts of the paper and contributed to subsequent revisions. JHu provided feedback on initial drafts of the paper and contributed to subsequent revisions. NG provided feedback on initial drafts of the paper and contributed to subsequent revisions. SM was involved in the acquisition and analysis of data and provided a critical review of the manuscript. YM was involved in the acquisition and analysis of data and provided a critical review of the manuscript. MR was involved in the interpretation of data and critical review and revision of the paper. HS contributed to the conception and design of the work, the acquisition and analysis of data, and the revision of the manuscript. JT provided feedback on initial drafts of the paper and contributed to subsequent revisions. LB-H made a substantial contribution to the design and conception of the work, led the acquisition and analysis of data, and contributed to the drafting and revision of the paper.
Corresponding author
Correspondence to Jeremy Segrott .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was not sought as no personal or identifiable data was collected.
Consent for publication
Competing interests.
All authors are or were members of staff or students in the Centre for Trials Research. JS is an associate editor of Trials .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Segrott, J., Channon, S., Lloyd, A. et al. Integrating qualitative research within a clinical trials unit: developing strategies and understanding their implementation in contexts. Trials 25 , 323 (2024). https://doi.org/10.1186/s13063-024-08124-7
Download citation
Received : 20 October 2023
Accepted : 17 April 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s13063-024-08124-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative research
- Qualitative methods
- Trials units
- Normalisation Process Theory
- Randomised controlled trials
ISSN: 1745-6215
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

No products in the cart.
What is Qualitative Data Analysis Software (QDA Software)?

Qualitative Data Analysis Software (QDA software) allows researchers to organize, analyze and visualize their data, finding the patterns in qualitative data or unstructured data: interviews, surveys, field notes, videos, audio files, images, journal articles interviews, web content etc.
Quantitative vs. Qualitative Data Analysis
What is the difference between quantitative and qualitative data analysis. As the name implies, quantitative data analysis has to do with numbers. For example, any time you are doing statistical analysis, you are doing quantitative data analysis. Some examples of quantitative data analysis software are SPSS, STATA, SAS, and Lumivero’s own powerful statistics software, XLSTAT .
In contrast, qualitative analysis "helps you understand people’s perceptions and experiences by systematically coding and analyzing the data", as described in Qualitative vs Quantitative Research 101 . It tends to deal more with words than numbers. It can be useful when working with a lot of rich and deep data and when you aren’t trying to test something very specific. Some examples of qualitative data analysis software are MAXQDA, ATLAS.ti, Quirkos, and Lumivero’s NVivo, the leading tool for qualitative data analysis .
When would you use each one? Well, qualitative data analysis is often used for exploratory research or developing a theory, whereas quantitative is better if you want to test a hypothesis, find averages, and determine relationships between variables. With quantitative research you often want a large sample size to get relevant statistics. In contrast, qualitative research, because so much data in the form of text is involved, can have much smaller sample sizes and still yield valuable insights.
Of course, it’s not always so cut and dry, and many researchers end up taking a «mixed methods» approach, meaning that they combine both types of research. In this case they might use a combination of both types of software programs.
Learn how some qualitative researchers use QDA software for text analysis in the on-demand webinar Twenty-Five Qualitative Researchers Share How-To's for Data Analysis .

How is Qualitative Data Analysis Software Used for Research?
Qualitative Data Analysis Software works with any qualitative research methodology used by a researcher For example, software for qualitative data analysis can be used by a social scientist wanting to develop new concepts or theories may take a ‘grounded theory’ approach. Or a researcher looking for ways to improve health policy or program design might use ‘evaluation methods’. QDA software analysis tools don't favor a particular methodology — they're designed to facilitate common qualitative techniques no matter what method you use.
NVivo can help you to manage, explore and find patterns in your data and conduct thematic and sentiment analysis, but it cannot replace your analytical expertise.
Qualitative Research as an Iterative Process
Handling qualitative and mixed methods data is not usually a step-by-step process. Instead, it tends to be an iterative process where you explore, code, reflect, memo, code some more, query and so on. For example, this picture shows a path you might take to investigate an interesting theme using QDA software, like NVivo, to analyze data:

How Do I Choose the Best Approach for My Research Project with QDA Software?
Every research project is unique — the way you organize and analyze the material depends on your methodology, data and research design.
Here are some example scenarios for handling different types of research projects in QDA software — these are just suggestions to get you up and running.
A study with interviews exploring stakeholder perception of a community arts program
Your files consist of unstructured interview documents. You would set up a case for each interview participant, then code to codes and cases. You could then explore your data with simple queries or charts and use memos to record your discoveries.

A study exploring community perceptions about climate change using autocoding with AI
Your files consist of structured, consistently formatted interviews (where each participant is asked the same set of questions). With AI, you could autocode the interviews and set up cases for each participant. Then code themes to query and visualize your data.

A literature review on adolescent depression
Your files consist of journal articles, books and web pages. You would classify your files before coding and querying them; and then you could critique each file in a memo. With Citavi integration in NVivo, you can import your Citavi references into NVivo.

A social media study of the language used by members of an online community
Your files consist of Facebook data captured with NCapture. You would import it as a dataset ready to code and query. Use memos to record your insights.

A quick analysis of a local government budget survey
Your file is a large dataset of survey responses. You would import it using the Survey Import Wizard, which prepares your data for analysis. As part of the import, choose to run automated insights with AI to identify and code to themes and sentiment so that you can quickly review results and report broad findings.

Ways to Get Started with Your Project with Qualitative Analysis Software
Since projects (and researchers) are unique there is no one 'best practice' approach to organizing and analyzing your data but there are some useful strategies to help you get up and running:
- Start now - don't wait until you have collected all the data. Import your research design, grant application or thesis proposal.
- Make a project journa l and state your research questions and record your goals. Why are you doing the project? What is it about? What do you expect to find and why?
- Make a mind map for your preliminary ideas. Show the relationships or patterns you expect to find in your data based on prior experience or preliminary reading.
- Import your interviews, field notes, focus groups —organize these files into folders for easy access.
- Set up an initial code structure based on your early reading and ideas—you could run a Word Frequency query over your data to tease out the common themes for creating your code structure.
- Set up cases for the people, places or other cases in your project.
- Explore your material and code themes as they emerge in your data mining —creating memos and describing your discoveries and interpretations.
- To protect your work, get in the habit of making regular back-ups.
QDA Analysis Tools Help You Work Toward Outcomes that are Robust and Transparent
Using QDA software to organize and analyze your data also increases the 'transparency' of your research outcomes—for example, you can:
- Demonstrate the evolution of your ideas in memos and maps.
- Document your early preconceptions and biases (in a memo or map) and demonstrate how these have been acknowledged and tested.
- Easily find illustrative quotes.
- Always return to the original context of your coded material.
- Save and revisit the queries and visualizations that helped you to arrive at your conclusions.
QDA software, like NVivo, can demonstrate the credibility of your findings in the following ways:
- If you used NVivo for your literature review, run a query or create a chart to demonstrate how your findings compare with the views of other authors.
- Was an issue or theme reported by more than one participant? Run a Matrix Coding query to see how many participants talked about a theme.
- Were multiple methods used to collect the data (interviews, observations, surveys)—and are the findings supported across these text data and video data files? Run a Matrix Coding query to see how often a theme is reported across all your files.

- If multiple researchers analyzed the material — were their findings consistent? Use coding stripes (or filter the contents in a code) to see how various team members have coded the material and run a Coding Comparison query to assess the level of agreement.

QDA Software Integrations
Many qualitative analysis software options have integration with other software to enhance your research process. NVivo integrates or can be used with the following software:
- NVivo Transcription to save you time and jump start your qualitative data analysis. Learn how in the on-demand webinar Transcription – Go Beyond the Words .
- Reference management software, like Lumivero’s Citavi, for reference management and writing. By combining Citavi and NVivo, you can create complicated searches for certain keywords, terms, and categories and make advanced search syntax, like wildcards, boolean operators, and regular expressions. This integration allows you to take your analyses beyond reference management by developing a central location to collect references and thoughts, analyze literature, and connect empirical data.
- Statistical software, like Lumivero’s XLSTAT , SPSS, or STATA to export your queries from NVivo to run statistical analysis
- Qualtrics, SurveyMonkey to import your survey results into NVivo to start analyzing.
Make Choosing QDA Software Easy — Try NVivo Today!
It's tough choosing QDA software! Test out NVivo, the most cited qualitative data analysis tool, by requesting a free 14-day trial of NVivo to start improving your qualitative and mixed methods research today.
Recent Articles
- Open access
- Published: 11 May 2024
Nursing students’ stressors and coping strategies during their first clinical training: a qualitative study in the United Arab Emirates
- Jacqueline Maria Dias 1 ,
- Muhammad Arsyad Subu 1 ,
- Nabeel Al-Yateem 1 ,
- Fatma Refaat Ahmed 1 ,
- Syed Azizur Rahman 1 , 2 ,
- Mini Sara Abraham 1 ,
- Sareh Mirza Forootan 1 ,
- Farzaneh Ahmad Sarkhosh 1 &
- Fatemeh Javanbakh 1
BMC Nursing volume 23 , Article number: 322 ( 2024 ) Cite this article
257 Accesses
Metrics details
Understanding the stressors and coping strategies of nursing students in their first clinical training is important for improving student performance, helping students develop a professional identity and problem-solving skills, and improving the clinical teaching aspects of the curriculum in nursing programmes. While previous research have examined nurses’ sources of stress and coping styles in the Arab region, there is limited understanding of these stressors and coping strategies of nursing students within the UAE context thereby, highlighting the novelty and significance of the study.
A qualitative study was conducted using semi-structured interviews. Overall 30 students who were undergoing their first clinical placement in Year 2 at the University of Sharjah between May and June 2022 were recruited. All interviews were recorded and transcribed verbatim and analyzed for themes.
During their first clinical training, nursing students are exposed to stress from different sources, including the clinical environment, unfriendly clinical tutors, feelings of disconnection, multiple expectations of clinical staff and patients, and gaps between the curriculum of theory classes and labatories skills and students’ clinical experiences. We extracted three main themes that described students’ stress and use of coping strategies during clinical training: (1) managing expectations; (2) theory-practice gap; and (3) learning to cope. Learning to cope, included two subthemes: positive coping strategies and negative coping strategies.
Conclusions
This qualitative study sheds light from the students viewpoint about the intricate interplay between managing expectations, theory practice gap and learning to cope. Therefore, it is imperative for nursing faculty, clinical agencies and curriculum planners to ensure maximum learning in the clinical by recognizing the significance of the stressors encountered and help students develop positive coping strategies to manage the clinical stressors encountered. Further research is required look at the perspective of clinical stressors from clinical tutors who supervise students during their first clinical practicum.
Peer Review reports
Nursing education programmes aim to provide students with high-quality clinical learning experiences to ensure that nurses can provide safe, direct care to patients [ 1 ]. The nursing baccalaureate programme at the University of Sharjah is a four year program with 137 credits. The programmes has both theoretical and clinical components withs nine clinical courses spread over the four years The first clinical practicum which forms the basis of the study takes place in year 2 semester 2.
Clinical practice experience is an indispensable component of nursing education and links what students learn in the classroom and in skills laboratories to real-life clinical settings [ 2 , 3 , 4 ]. However, a gap exists between theory and practice as the curriculum in the classroom differs from nursing students’ experiences in the clinical nursing practicum [ 5 ]. Clinical nursing training places (or practicums, as they are commonly referred to), provide students with the necessary experiences to ensure that they become proficient in the delivery of patient care [ 6 ]. The clinical practicum takes place in an environment that combines numerous structural, psychological, emotional and organizational elements that influence student learning [ 7 ] and may affect the development of professional nursing competencies, such as compassion, communication and professional identity [ 8 ]. While clinical training is a major component of nursing education curricula, stress related to clinical training is common among students [ 9 ]. Furthermore, the nursing literature indicates that the first exposure to clinical learning is one of the most stressful experiences during undergraduate studies [ 8 , 10 ]. Thus, the clinical component of nursing education is considered more stressful than the theoretical component. Students often view clinical learning, where most learning takes place, as an unsupportive environment [ 11 ]. In addition, they note strained relationships between themselves and clinical preceptors and perceive that the negative attitudes of clinical staff produce stress [ 12 ].
The effects of stress on nursing students often involve a sense of uncertainty, uneasiness, or anxiety. The literature is replete with evidence that nursing students experience a variety of stressors during their clinical practicum, beginning with the first clinical rotation. Nursing is a complex profession that requires continuous interaction with a variety of individuals in a high-stress environment. Stress during clinical learning can have multiple negative consequences, including low academic achievement, elevated levels of burnout, and diminished personal well-being [ 13 , 14 ]. In addition, both theoretical and practical research has demonstrated that increased, continual exposure to stress leads to cognitive deficits, inability to concentrate, lack of memory or recall, misinterpretation of speech, and decreased learning capacity [ 15 ]. Furthermore, stress has been identified as a cause of attrition among nursing students [ 16 ].
Most sources of stress have been categorized as academic, clinical or personal. Each person copes with stress differently [ 17 ], and utilizes deliberate, planned, and psychological efforts to manage stressful demands [ 18 ]. Coping mechanisms are commonly termed adaptation strategies or coping skills. Labrague et al. [ 19 ] noted that students used critical coping strategies to handle stress and suggested that problem solving was the most common coping or adaptation mechanism used by nursing students. Nursing students’ coping strategies affect their physical and psychological well-being and the quality of nursing care they offer. Therefore, identifying the coping strategies that students use to manage stressors is important for early intervention [ 20 ].
Studies on nursing students’ coping strategies have been conducted in various countries. For example, Israeli nursing students were found to adopt a range of coping mechanisms, including talking to friends, engaging in sports, avoiding stress and sadness/misery, and consuming alcohol [ 21 ]. Other studies have examined stress levels among medical students in the Arab region. Chaabane et al. [ 15 ], conducted a systematic review of sudies in Arab countries, including Saudi Arabia, Egypt, Jordan, Iraq, Pakistan, Oman, Palestine and Bahrain, and reported that stress during clinical practicums was prevalent, although it could not be determined whether this was limited to the initial clinical course or occurred throughout clinical training. Stressors highlighted during the clinical period in the systematic review included assignments and workload during clinical practice, a feeling that the requirements of clinical practice exceeded students’ physical and emotional endurance and that their involvement in patient care was limited due to lack of experience. Furthermore, stress can have a direct effect on clinical performance, leading to mental disorders. Tung et al. [ 22 ], reported that the prevalence of depression among nursing students in Arab countries is 28%, which is almost six times greater than the rest of the world [ 22 ]. On the other hand, Saifan et al. [ 5 ], explored the theory-practice gap in the United Arab Emirates and found that clinical stressors could be decreased by preparing students better for clinical education with qualified clinical faculty and supportive preceptors.
The purpose of this study was to identify the stressors experienced by undergraduate nursing students in the United Arab Emirates during their first clinical training and the basic adaptation approaches or coping strategies they used. Recognizing or understanding different coping processes can inform the implementation of corrective measures when students experience clinical stress. The findings of this study may provide valuable information for nursing programmes, nurse educators, and clinical administrators to establish adaptive strategies to reduce stress among students going clinical practicums, particularly stressors from their first clinical training in different healthcare settings.
A qualitative approach was adopted to understand clinical stressors and coping strategies from the perspective of nurses’ lived experience. Qualitative content analysis was employed to obtain rich and detailed information from our qualitative data. Qualitative approaches seek to understand the phenomenon under study from the perspectives of individuals with lived experience [ 23 ]. Qualitative content analysis is an interpretive technique that examines the similarities and differences between and within different areas of text while focusing on the subject [ 24 ]. It is used to examine communication patterns in a repeatable and systematic way [ 25 ] and yields rich and detailed information on the topic under investigation [ 23 ]. It is a method of systematically coding and categorizing information and comprises a process of comprehending, interpreting, and conceptualizing the key meanings from qualitative data [ 26 ].
Setting and participants
This study was conducted after the clinical rotations ended in April 2022, between May and June in the nursing programme at the College of Health Sciences, University of Sharjah, in the United Arab Emirates. The study population comprised undergraduate nursing students who were undergoing their first clinical training and were recruited using purposive sampling. The inclusion criteria for this study were second-year nursing students in the first semester of clinical training who could speak English, were willing to participate in this research, and had no previous clinical work experience. The final sample consisted of 30 students.
Research instrument
The research instrument was a semi structured interview guide. The interview questions were based on an in-depth review of related literature. An intensive search included key words in Google Scholar, PubMed like the terms “nursing clinical stressors”, “nursing students”, and “coping mechanisms”. Once the questions were created, they were validated by two other faculty members who had relevant experience in mental health. A pilot test was conducted with five students and based on their feedback the following research questions, which were addressed in the study.
How would you describe your clinical experiences during your first clinical rotations?
In what ways did you find the first clinical rotation to be stressful?
What factors hindered your clinical training?
How did you cope with the stressors you encountered in clinical training?
Which strategies helped you cope with the clinical stressors you encountered?
Data collection
Semi-structured interviews were chosen as the method for data collection. Semi structured interviews are a well-established approach for gathering data in qualitative research and allow participants to discuss their views, experiences, attitudes, and beliefs in a positive environment [ 27 ]. This approach allows for flexibility in questioning thereby ensuring that key topics related to clinical learning stressors and coping strategies would be explored. Participants were given the opportunity to express their views, experiences, attitudes, and beliefs in a positive environment, encouraging open communication. These semi structured interviews were conducted by one member of the research team (MAS) who had a mental health background, and another member of the research team who attended the interviews as an observer (JMD). Neither of these researchers were involved in teaching the students during their clinical practicum, which helped to minimize bias. The interviews took place at the University of Sharjah, specifically in building M23, providing a familiar and comfortable environment for the participant. Before the interviews were all students who agreed to participate were provided with an explanation of the study’s purpose. The time and location of each interview were arranged. Before the interviews were conducted, all students who provided consent to participate received an explanation of the purpose of the study, and the time and place of each interview were arranged to accommodate the participants’ schedules and preferences. The interviews were conducted after the clinical rotation had ended in April, and after the final grades had been submitted to the coordinator. The timings of the interviews included the month of May and June which ensured that participants have completed their practicum experience and could reflect on the stressors more comprehensively. The interviews were audio-recorded with the participants’ consent, and each interview lasted 25–40 min. The data were collected until saturation was reached for 30 students. Memos and field notes were also recorded as part of the data collection process. These additional data allowed for triangulation to improve the credibility of the interpretations of the data [ 28 ]. Memos included the interviewers’ thoughts and interpretations about the interviews, the research process (including questions and gaps), and the analytic progress used for the research. Field notes were used to record the interviewers’ observations and reflections on the data. These additional data collection methods were important to guide the researchers in the interpretation of the data on the participants’ feelings, perspectives, experiences, attitudes, and beliefs. Finally, member checking was performed to ensure conformability.
Data analysis
The study used the content analysis method proposed by Graneheim and Lundman [ 24 ]. According to Graneheim and Lundman [ 24 ], content analysis is an interpretive technique that examines the similarities and differences between distinct parts of a text. This method allows researchers to determine exact theoretical and operational definitions of words, phrases, and symbols by elucidating their constituent properties [ 29 ]. First, we read the interview transcripts several times to reach an overall understanding of the data. All verbatim transcripts were read several times and discussed among all authors. We merged and used line-by-line coding of words, sentences, and paragraphs relevant to each other in terms of both the content and context of stressors and coping mechanisms. Next, we used data reduction to assess the relationships among themes using tables and diagrams to indicate conceptual patterns. Content related to stress encountered by students was extracted from the transcripts. In a separate document, we integrated and categorized all words and sentences that were related to each other in terms of both content and context. We analyzed all codes and units of meaning and compared them for similarities and differences in the context of this study. Furthermore, the emerging findings were discussed with other members of the researcher team. The final abstractions of meaningful subthemes into themes were discussed and agreed upon by the entire research team. This process resulted in the extraction of three main themes in addition to two subthemes related to stress and coping strategies.
Ethical considerations
The University of Sharjah Research Ethics Committee provided approval to conduct this study (Reference Number: REC 19-12-03-01-S). Before each interview, the goal and study procedures were explained to each participant, and written informed consent was obtained. The participants were informed that participation in the study was voluntary and that they could withdraw from the study at any time. In the event they wanted to withdraw from the study, all information related to the participant would be removed. No participant withdrew from the study. Furthermore, they were informed that their clinical practicum grade would not be affected by their participation in this study. We chose interview locations in Building M23that were private and quiet to ensure that the participants felt at ease and confident in verbalizing their opinions. No participant was paid directly for involvement in this study. In addition, participants were assured that their data would remain anonymous and confidential. Confidentiality means that the information provided by participants was kept private with restrictions on how and when data can be shared with others. The participants were informed that their information would not be duplicated or disseminated without their permission. Anonymity refers to the act of keeping people anonymous with respect to their participation in a research endeavor. No personal identifiers were used in this study, and each participant was assigned a random alpha-numeric code (e.g., P1 for participant 1). All digitally recorded interviews were downloaded to a secure computer protected by the principal investigator with a password. The researchers were the only people with access to the interview material (recordings and transcripts). All sensitive information and materials were kept secure in the principal researcher’s office at the University of Sharjah. The data will be maintained for five years after the study is completed, after which the material will be destroyed (the transcripts will be shredded, and the tapes will be demagnetized).
In total, 30 nursing students who were enrolled in the nursing programme at the Department of Nursing, College of Health Sciences, University of Sharjah, and who were undergoing their first clinical practicum participated in the study. Demographically, 80% ( n = 24) were females and 20% ( n = 6) were male participants. The majority (83%) of study participants ranged in age from 18 to 22 years. 20% ( n = 6) were UAE nationals, 53% ( n = 16) were from Gulf Cooperation Council countries, while 20% ( n = 6) hailed from Africa and 7% ( n = 2) were of South Asian descent. 67% of the respondents lived with their families while 33% lived in the hostel. (Table 1 )
Following the content analysis, we identified three main themes: (1) managing expectations, (2) theory-practice gap and 3)learning to cope. Learning to cope had two subthemes: positive coping strategies and negative coping strategies. An account of each theme is presented along with supporting excerpts for the identified themes. The identified themes provide valuable insight into the stressors encountered by students during their first clinical practicum. These themes will lead to targeted interventions and supportive mechanisms that can be built into the clinical training curriculum to support students during clinical practice.
Theme 1: managing expectations
In our examination of the stressors experienced by nursing students during their first clinical practicum and the coping strategies they employed, we identified the first theme as managing expectations.
The students encountered expectations from various parties, such as clinical staff, patients and patients’ relatives which they had to navigate. They attempted to fulfil their expectations as they progressed through training, which presented a source of stress. The students noted that the hospital staff and patients expected them to know how to perform a variety of tasks upon request, which made the students feel stressed and out of place if they did not know how to perform these tasks. Some participants noted that other nurses in the clinical unit did not allow them to participate in nursing procedures, which was considered an enormous impediment to clinical learning, as noted in the excerpt below:
“…Sometimes the nurses… They will not allow us to do some procedures or things during clinical. And sometimes the patients themselves don’t allow us to do procedures” (P5).
Some of the students noted that they felt they did not belong and felt like foreigners in the clinical unit. Excerpts from the students are presented in the following quotes;
“The clinical environment is so stressful. I don’t feel like I belong. There is too little time to build a rapport with hospital staff or the patient” (P22).
“… you ask the hospital staff for some guidance or the location of equipment, and they tell us to ask our clinical tutor …but she is not around … what should I do? It appears like we do not belong, and the sooner the shift is over, the better” (P18).
“The staff are unfriendly and expect too much from us students… I feel like I don’t belong, or I am wasting their (the hospital staff’s) time. I want to ask questions, but they have loads to do” (P26).
Other students were concerned about potential failure when working with patients during clinical training, which impacted their confidence. They were particularly afraid of failure when performing any clinical procedures.
“At the beginning, I was afraid to do procedures. I thought that maybe the patient would be hurt and that I would not be successful in doing it. I have low self-confidence in doing procedures” (P13).
The call bell rings, and I am told to answer Room No. XXX. The patient wants help to go to the toilet, but she has two IV lines. I don’t know how to transport the patient… should I take her on the wheelchair? My eyes glance around the room for a wheelchair. I am so confused …I tell the patient I will inform the sister at the nursing station. The relative in the room glares at me angrily … “you better hurry up”…Oh, I feel like I don’t belong, as I am not able to help the patient… how will I face the same patient again?” (P12).
Another major stressor mentioned in the narratives was related to communication and interactions with patients who spoke another language, so it was difficult to communicate.
“There was a challenge with my communication with the patients. Sometimes I have communication barriers because they (the patients) are of other nationalities. I had an experience with a patient [who was] Indian, and he couldn’t speak my language. I did not understand his language” (P9).
Thus, a variety of expectations from patients, relatives, hospital staff, and preceptors acted as sources of stress for students during their clinical training.
Theme 2: theory-practice gap
Theory-practice gaps have been identified in previous studies. In our study, there was complete dissonance between theory and actual clinical practice. The clinical procedures or practices nursing students were expected to perform differed from the theory they had covered in their university classes and skills lab. This was described as a theory–practice gap and often resulted in stress and confusion.
“For example …the procedures in the hospital are different. They are different from what we learned or from theory on campus. Or… the preceptors have different techniques than what we learned on campus. So, I was stress[ed] and confused about it” (P11).
Furthermore, some students reported that they did not feel that they received adequate briefing before going to clinical training. A related source of stress was overload because of the volume of clinical coursework and assignments in addition to clinical expectations. Additionally, the students reported that a lack of time and time management were major sources of stress in their first clinical training and impacted their ability to complete the required paperwork and assignments:
“…There is not enough time…also, time management at the hospital…for example, we start at seven a.m., and the handover takes 1 hour to finish. They (the nurses at the hospital) are very slow…They start with bed making and morning care like at 9.45 a.m. Then, we must fill [out] our assessment tool and the NCP (nursing care plan) at 10 a.m. So, 15 only minutes before going to our break. We (the students) cannot manage this time. This condition makes me and my friends very stressed out. -I cannot do my paperwork or assignments; no time, right?” (P10).
“Stressful. There is a lot of work to do in clinical. My experiences are not really good with this course. We have a lot of things to do, so many assignments and clinical procedures to complete” (P16).
The participants noted that the amount of required coursework and number of assignments also presented a challenge during their first clinical training and especially affected their opportunity to learn.
“I need to read the file, know about my patient’s condition and pathophysiology and the rationale for the medications the patient is receiving…These are big stressors for my learning. I think about assignments often. Like, we are just focusing on so many assignments and papers. We need to submit assessments and care plans for clinical cases. We focus our time to complete and finish the papers rather than doing the real clinical procedures, so we lose [the] chance to learn” (P25).
Another participant commented in a similar vein that there was not enough time to perform tasks related to clinical requirements during clinical placement.
“…there is a challenge because we do not have enough time. Always no time for us to submit papers, to complete assessment tools, and some nurses, they don’t help us. I think we need more time to get more experiences and do more procedures, reduce the paperwork that we have to submit. These are challenges …” (P14).
There were expectations that the students should be able to carry out their nursing duties without becoming ill or adversely affected. In addition, many students reported that the clinical environment was completely different from the skills laboratory at the college. Exposure to the clinical setting added to the theory-practice gap, and in some instances, the students fell ill.
One student made the following comment:
“I was assisting a doctor with a dressing, and the sight and smell from the oozing wound was too much for me. I was nauseated. As soon as the dressing was done, I ran to the bathroom and threw up. I asked myself… how will I survive the next 3 years of nursing?” (P14).
Theme 3: learning to cope
The study participants indicated that they used coping mechanisms (both positive and negative) to adapt to and manage the stressors in their first clinical practicum. Important strategies that were reportedly used to cope with stress were time management, good preparation for clinical practice, and positive thinking as well as engaging in physical activity and self-motivation.
“Time management. Yes, it is important. I was encouraging myself. I used time management and prepared myself before going to the clinical site. Also, eating good food like cereal…it helps me very much in the clinic” (P28).
“Oh yeah, for sure positive thinking. In the hospital, I always think positively. Then, after coming home, I get [to] rest and think about positive things that I can do. So, I will think something good [about] these things, and then I will be relieved of stress” (P21).
Other strategies commonly reported by the participants were managing their breathing (e.g., taking deep breaths, breathing slowly), taking breaks to relax, and talking with friends about the problems they encountered.
“I prefer to take deep breaths and breathe slowly and to have a cup of coffee and to talk to my friends about the case or the clinical preceptor and what made me sad so I will feel more relaxed” (P16).
“Maybe I will take my break so I feel relaxed and feel better. After clinical training, I go directly home and take a long shower, going over the day. I will not think about anything bad that happened that day. I just try to think about good things so that I forget the stress” (P27).
“Yes, my first clinical training was not easy. It was difficult and made me stressed out…. I felt that it was a very difficult time for me. I thought about leaving nursing” (P7).
I was not able to offer my prayers. For me, this was distressing because as a Muslim, I pray regularly. Now, my prayer time is pushed to the end of the shift” (P11).
“When I feel stress, I talk to my friends about the case and what made me stressed. Then I will feel more relaxed” (P26).
Self-support or self-motivation through positive self-talk was also used by the students to cope with stress.
“Yes, it is difficult in the first clinical training. When I am stress[ed], I go to the bathroom and stand in the front of the mirror; I talk to myself, and I say, “You can do it,” “you are a great student.” I motivate myself: “You can do it”… Then, I just take breaths slowly several times. This is better than shouting or crying because it makes me tired” (P11).
Other participants used physical activity to manage their stress.
“How do I cope with my stress? Actually, when I get stressed, I will go for a walk on campus” (P4).
“At home, I will go to my room and close the door and start doing my exercises. After that, I feel the negative energy goes out, then I start to calm down… and begin my clinical assignments” (P21).
Both positive and negative coping strategies were utilized by the students. Some participants described using negative coping strategies when they encountered stress during their clinical practice. These negative coping strategies included becoming irritable and angry, eating too much food, drinking too much coffee, and smoking cigarettes.
“…Negative adaptation? Maybe coping. If I am stressed, I get so angry easily. I am irritable all day also…It is negative energy, right? Then, at home, I am also angry. After that, it is good to be alone to think about my problems” (P12).
“Yeah, if I…feel stress or depressed, I will eat a lot of food. Yeah, ineffective, like I will be eating a lot, drinking coffee. Like I said, effective, like I will prepare myself and do breathing, ineffective, I will eat a lot of snacks in between my free time. This is the bad side” (P16).
“…During the first clinical practice? Yes, it was a difficult experience for us…not only me. When stressed, during a break at the hospital, I will drink two or three cups of coffee… Also, I smoke cigarettes… A lot. I can drink six cups [of coffee] a day when I am stressed. After drinking coffee, I feel more relaxed, I finish everything (food) in the refrigerator or whatever I have in the pantry, like chocolates, chips, etc” (P23).
These supporting excerpts for each theme and the analysis offers valuable insights into the specific stressors faced by nursing students during their first clinical practicum. These insights will form the basis for the development of targeted interventions and supportive mechanisms within the clinical training curriculum to better support students’ adjustment and well-being during clinical practice.
Our study identified the stressors students encounter in their first clinical practicum and the coping strategies, both positive and negative, that they employed. Although this study emphasizes the importance of clinical training to prepare nursing students to practice as nurses, it also demonstrates the correlation between stressors and coping strategies.The content analysis of the first theme, managing expectations, paves the way for clinical agencies to realize that the students of today will be the nurses of tomorrow. It is important to provide a welcoming environment where students can develop their identities and learn effectively. Additionally, clinical staff should foster an environment of individualized learning while also assisting students in gaining confidence and competence in their repertoire of nursing skills, including critical thinking, problem solving and communication skills [ 8 , 15 , 19 , 30 ]. Another challenge encountered by the students in our study was that they were prevented from participating in clinical procedures by some nurses or patients. This finding is consistent with previous studies reporting that key challenges for students in clinical learning include a lack of clinical support and poor attitudes among clinical staff and instructors [ 31 ]. Clinical staff with positive attitudes have a positive impact on students’ learning in clinical settings [ 32 ]. The presence, supervision, and guidance of clinical instructors and the assistance of clinical staff are essential motivating components in the clinical learning process and offer positive reinforcement [ 30 , 33 , 34 ]. Conversely, an unsupportive learning environment combined with unwelcoming clinical staff and a lack of sense of belonging negatively impact students’ clinical learning [ 35 ].
The sources of stress identified in this study were consistent with common sources of stress in clinical training reported in previous studies, including the attitudes of some staff, students’ status in their clinical placement and educational factors. Nursing students’ inexperience in the clinical setting and lack of social and emotional experience also resulted in stress and psychological difficulties [ 36 ]. Bhurtun et al. [ 33 ] noted that nursing staff are a major source of stress for students because the students feel like they are constantly being watched and evaluated.
We also found that students were concerned about potential failure when working with patients during their clinical training. Their fear of failure when performing clinical procedures may be attributable to low self-confidence. Previous studies have noted that students were concerned about injuring patients, being blamed or chastised, and failing examinations [ 37 , 38 ]. This was described as feeling “powerless” in a previous study [ 7 , 12 ]. In addition, patients’ attitudes towards “rejecting” nursing students or patients’ refusal of their help were sources of stress among the students in our study and affected their self-confidence. Self-confidence and a sense of belonging are important for nurses’ personal and professional identity, and low self-confidence is a problem for nursing students in clinical learning [ 8 , 39 , 40 ]. Our findings are consistent with a previous study that reported that a lack of self-confidence was a primary source of worry and anxiety for nursing students and affected their communication and intention to leave nursing [ 41 ].
In the second theme, our study suggests that students encounter a theory-practice gap in clinical settings, which creates confusion and presents an additional stressors. Theoretical and clinical training are complementary elements of nursing education [ 40 ], and this combination enables students to gain the knowledge, skills, and attitudes necessary to provide nursing care. This is consistent with the findings of a previous study that reported that inconsistencies between theoretical knowledge and practical experience presented a primary obstacle to the learning process in the clinical context [ 42 ], causing students to lose confidence and become anxious [ 43 ]. Additionally, the second theme, the theory-practice gap, authenticates Safian et al.’s [ 5 ] study of the theory-practice gap that exists United Arab Emirates among nursing students as well as the need for more supportive clinical faculty and the extension of clinical hours. The need for better time availability and time management to complete clinical tasks were also reported by the students in the study. Students indicated that they had insufficient time to complete clinical activities because of the volume of coursework and assignments. Our findings support those of Chaabane et al. [ 15 ]. A study conducted in Saudi Arabia [ 44 ] found that assignments and workload were among the greatest sources of stress for students in clinical settings. Effective time management skills have been linked to academic achievement, stress reduction, increased creativity [ 45 ], and student satisfaction [ 46 ]. Our findings are also consistent with previous studies that reported that a common source of stress among first-year students was the increased classroom workload [ 19 , 47 ]. As clinical assignments and workloads are major stressors for nursing students, it is important to promote activities to help them manage these assignments [ 48 ].
Another major challenge reported by the participants was related to communicating and interacting with other nurses and patients. The UAE nursing workforce and population are largely expatriate and diverse and have different cultural and linguistic backgrounds. Therefore, student nurses encounter difficulty in communication [ 49 ]. This cultural diversity that students encounter in communication with patients during clinical training needs to be addressed by curriculum planners through the offering of language courses and courses on cultural diversity [ 50 ].
Regarding the third and final theme, nursing students in clinical training are unable to avoid stressors and must learn to cope with or adapt to them. Previous research has reported a link between stressors and the coping mechanisms used by nursing students [ 51 , 52 , 53 ]. In particular, the inability to manage stress influences nurses’ performance, physical and mental health, attitude, and role satisfaction [ 54 ]. One such study suggested that nursing students commonly use problem-focused (dealing with the problem), emotion-focused (regulating emotion), and dysfunctional (e.g., venting emotions) stress coping mechanisms to alleviate stress during clinical training [ 15 ]. Labrague et al. [ 51 ] highlighted that nursing students use both active and passive coping techniques to manage stress. The pattern of clinical stress has been observed in several countries worldwide. The current study found that first-year students experienced stress during their first clinical training [ 35 , 41 , 55 ]. The stressors they encountered impacted their overall health and disrupted their clinical learning. Chaabane et al. [ 15 ] reported moderate and high stress levels among nursing students in Bahrain, Egypt, Iraq, Jordan, Oman, Pakistan, Palestine, Saudi Arabia, and Sudan. Another study from Bahrain reported that all nursing students experienced moderate to severe stress in their first clinical placement [ 56 ]. Similarly, nursing students in Spain experienced a moderate level of stress, and this stress was significantly correlated with anxiety [ 30 ]. Therefore, it is imperative that pastoral systems at the university address students’ stress and mental health so that it does not affect their clinical performance. Faculty need to utilize evidence-based interventions to support students so that anxiety-producing situations and attrition are minimized.
In our study, students reported a variety of positive and negative coping mechanisms and strategies they used when they experienced stress during their clinical practice. Positive coping strategies included time management, positive thinking, self-support/motivation, breathing, taking breaks, talking with friends, and physical activity. These findings are consistent with those of a previous study in which healthy coping mechanisms used by students included effective time management, social support, positive reappraisal, and participation in leisure activities [ 57 ]. Our study found that relaxing and talking with friends were stress management strategies commonly used by students. Communication with friends to cope with stress may be considered social support. A previous study also reported that people seek social support to cope with stress [ 58 ]. Some students in our study used physical activity to cope with stress, consistent with the findings of previous research. Stretching exercises can be used to counteract the poor posture and positioning associated with stress and to assist in reducing physical tension. Promoting such exercise among nursing students may assist them in coping with stress in their clinical training [ 59 ].
Our study also showed that when students felt stressed, some adopted negative coping strategies, such as showing anger/irritability, engaging in unhealthy eating habits (e.g., consumption of too much food or coffee), or smoking cigarettes. Previous studies have reported that high levels of perceived stress affect eating habits [ 60 ] and are linked to poor diet quality, increased snacking, and low fruit intake [ 61 ]. Stress in clinical settings has also been linked to sleep problems, substance misuse, and high-risk behaviors’ and plays a major role in student’s decision to continue in their programme.
Implications of the study
The implications of the study results can be grouped at multiple levels including; clinical, educational, and organizational level. A comprehensive approach to addressing the stressors encountered by nursing students during their clinical practicum can be overcome by offering some practical strategies to address the stressors faced by nursing students during their clinical practicum. By integrating study findings into curriculum planning, mentorship programs, and organizational support structures, a supportive and nurturing environment that enhances students’ learning, resilience, and overall success can be envisioned.
Clinical level
Introducing simulation in the skills lab with standardized patients and the use of moulage to demonstrate wounds, ostomies, and purulent dressings enhances students’ practical skills and prepares them for real-world clinical scenarios. Organizing orientation days at clinical facilities helps familiarize students with the clinical environment, identify potential stressors, and introduce interventions to enhance professionalism, social skills, and coping abilities Furthermore, creating a WhatsApp group facilitates communication and collaboration among hospital staff, clinical tutors, nursing faculty, and students, enabling immediate support and problem-solving for clinical situations as they arise, Moreover, involving chief nursing officers of clinical facilities in the Nursing Advisory Group at the Department of Nursing promotes collaboration between academia and clinical practice, ensuring alignment between educational objectives and the needs of the clinical setting [ 62 ].
Educational level
Sharing study findings at conferences (we presented the results of this study at Sigma Theta Tau International in July 2023 in Abu Dhabi, UAE) and journal clubs disseminates knowledge and best practices among educators and clinicians, promoting awareness and implementation of measures to improve students’ learning experiences. Additionally we hold mentorship training sessions annually in January and so we shared with the clinical mentors and preceptors the findings of this study so that they proactively they are equipped with strategies to support students’ coping with stressors during clinical placements.
Organizational level
At the organizational we relooked at the available student support structures, including counseling, faculty advising, and career advice, throughout the nursing program emphasizing the importance of holistic support for students’ well-being and academic success as well as retention in the nursing program. Also, offering language courses as electives recognizes the value of communication skills in nursing practice and provides opportunities for personal and professional development.
For first-year nursing students, clinical stressors are inevitable and must be given proper attention. Recognizing nursing students’ perspectives on the challenges and stressors experienced in clinical training is the first step in overcoming these challenges. In nursing schools, providing an optimal clinical environment as well as increasing supervision and evaluation of students’ practices should be emphasized. Our findings demonstrate that first-year nursing students are exposed to a variety of different stressors. Identifying the stressors, pressures, and obstacles that first-year students encounter in the clinical setting can assist nursing educators in resolving these issues and can contribute to students’ professional development and survival to allow them to remain in the profession. To overcome stressors, students frequently employ problem-solving approaches or coping mechanisms. The majority of nursing students report stress at different levels and use a variety of positive and negative coping techniques to manage stress.
The present results may not be generalizable to other nursing institutions because this study used a purposive sample along with a qualitative approach and was limited to one university in the Middle East. Furthermore, the students self-reported their stress and its causes, which may have introduced reporting bias. The students may also have over or underreported stress or coping mechanisms because of fear of repercussions or personal reasons, even though the confidentiality of their data was ensured. Further studies are needed to evaluate student stressors and coping now that measures have been introduced to support students. Time will tell if these strategies are being used effectively by both students and clinical personnel or if they need to be readdressed. Finally, we need to explore the perceptions of clinical faculty towards supervising students in their first clinical practicum so that clinical stressors can be handled effectively.
Data availability
The data sets are available with the corresponding author upon reasonable request.
Almarwani AM. The effect of integrating a nursing licensure examination preparation course into a nursing program curriculum: a quasi-experimental study. Saudi J Health Sci. 2022;11:184–9.
Article Google Scholar
Horntvedt MT, Nordsteien A, Fermann T, Severinsson E. Strategies for teaching evidence-based practice in nursing education: a thematic literature review. BMC Med Educ. 2018;18:172.
Article PubMed PubMed Central Google Scholar
Larsson M, Sundler AJ, Blomberg K, Bisholt B. The clinical learning environment during clinical practice in postgraduate district nursing students’ education: a cross-sectional study. Nurs Open. 2023;10:879–88.
Article PubMed Google Scholar
Sellberg M, Palmgren PJ, Möller R. A cross-sectional study of clinical learning environments across four undergraduate programs using the undergraduate clinical education environment measure. BMC Med Educ. 2021;21:258.
Saifan A, Devadas B, Mekkawi M, Amoor H, Matizha P, James J, et al. Managing the theory-practice gap in nursing education and practice: hearing the voices of nursing students in the United Arab Emirates. J Nurs Manag. 2021;29:1869–79.
Flott EA, Linden L. The clinical learning environment in nursing education: a concept analysis. J Adv Nurs. 2016;72:501–13.
Kalyani MN, Jamshidi N, Molazem Z, Torabizadeh C, Sharif F. How do nursing students experience the clinical learning environment and respond to their experiences? A qualitative study. BMJ Open. 2019;9:e028052.
Mahasneh D, Shoqirat N, Alsaraireh A, Singh C, Thorpe L. From learning on mannequins to practicing on patients: nursing students’ first-time experience of clinical placement in Jordan. SAGE Open Nurs. 2021;7:23779608211004298.
PubMed PubMed Central Google Scholar
Stubin C. Clinical stress among undergraduate nursing students: perceptions of clinical nursing faculty. Int J Nurs Educ Scholarsh. 2020;17:20190111.
Ahmed WAM. Anxiety and related symptoms among critical care nurses in Albaha, Kingdom of Saudi Arabia. AIMS Med Sci. 2015;2:303–9.
Alhassan. Duke Phillips. 2024.
Ekstedt M, Lindblad M, Löfmark A. Nursing students’ perception of the clinical learning environment and supervision in relation to two different supervision models - a comparative cross-sectional study. BMC Nurs. 2019;18:49.
Bradshaw C, Murphy Tighe S, Doody O. Midwifery students’ experiences of their clinical internship: a qualitative descriptive study. Nurse Educ Today. 2018;68:213–7.
McCarthy B, Trace A, O’Donovan M, O’Regan P, Brady-Nevin C, O’Shea M, et al. Coping with stressful events: a pre-post-test of a psycho-educational intervention for undergraduate nursing and midwifery students. Nurse Educ Today. 2018;61:273–80.
Chaabane S, Chaabna K, Bhagat S, Abraham A, Doraiswamy S, Mamtani R, et al. Perceived stress, stressors, and coping strategies among nursing students in the Middle East and North Africa: an overview of systematic reviews. Syst Rev. 2021;10:136.
Pines EW, Rauschhuber ML, Norgan GH, Cook JD, Canchola L, Richardson C, et al. Stress resiliency, psychological empowerment and conflict management styles among baccalaureate nursing students. J Adv Nurs. 2012;68:1482–93.
Lazarus RS. Coping theory and research: past, present, and future. Psychosom Med. 1993;55:234–47.
Article CAS PubMed Google Scholar
Boyd MA. Essentials of psychiatric nursing. Philadelphia, PA: Wolters Kluwer; 2017.
Google Scholar
Labrague LJ, McEnroe-Petitte DM, Gloe D, Thomas L, Papathanasiou IV, Tsaras K. A literature review on stress and coping strategies in nursing students. J Ment Health. 2017;26:471–80.
Ni C, Lo D, Liu X, Ma J, Xu S, Li L. Chinese female nursing students’ coping strategies, self-esteem and related factors in different years of school. J Nurs Educ Pract. 2012;2:33–41.
Jan LK, Popescu L. Israel’s nursing students’ stress sources and coping strategies during their first clinical experience in hospital wards-a qualitative research. Soc Work Rev / Rev Asistenta Soc. 2014;13:163–88.
Tung YJ, Lo KKH, Ho RCM, Tam WSW. Prevalence of depression among nursing students: a systematic review and meta-analysis. Nurse Educ Today. 2018;63:119–29.
Speziale HS, Streubert HJ, Carpenter DR. Qualitative research in nursing: advancing the humanistic imperative. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–12.
Bryman A. Integrating quantitative and qualitative research: how is it done? Qual Res. 2006;6:97–113.
Holloway I, Wheeler S. Qualitative research in nursing and healthcare. New York, NY: Wiley; 2013.
Richards L, Morse J. A user’s guide to qualitative methods. London, UK: Sage; 2007.
Lincoln Y, Guba EG. The SAGE handbook of qualitative research. Newbury Park, CA: SAGE Publications Inc; 2017.
Park S, Park KS. Family stigma: a concept analysis. Asian Nurs Res. 2014;8:165–71.
Onieva-Zafra MD, Fernández-Muñoz JJ, Fernández-Martínez E, García-Sánchez FJ, Abreu-Sánchez A, Parra-Fernández ML. Anxiety, perceived stress and coping strategies in nursing students: a cross-sectional, correlational, descriptive study. BMC Med Educ. 2020;20:370.
Albloushi M, Ferguson L, Stamler L, Bassendowski S, Hellsten L, Kent-Wilkinson A. Saudi female nursing students experiences of sense of belonging in the clinical settings: a qualitative study. Nurse Educ Pract. 2019;35:69–74.
Arkan B, Ordin Y, Yılmaz D. Undergraduate nursing students’ experience related to their clinical learning environment and factors affecting to their clinical learning process. Nurse Educ Pract. 2018;29:127–32.
Bhurtun HD, Azimirad M, Saaranen T, Turunen H. Stress and coping among nursing students during clinical training: an integrative review. J Nurs Educ. 2019;58:266–72.
Jamshidi N, Molazem Z, Sharif F, Torabizadeh C, Kalyani MN. The challenges of nursing students in the clinical learning environment: a qualitative study. ScientificWorldJournal. 2016;2016:1846178.
Porter SL. First year nursing students’ perceptions of stress and resilience during their initial clinical placement and the introduction of a stress management app: a mixed methods approach. A thesis submitted in partial fulfilment of the requirements of Edinburgh Napier University, for the award of Doctor of Philosophy. 2019. https://www.napier.ac.uk/~/media/worktribe/output-2086663/first-year-nursing-students-perceptions-of-stress-and-resilience-during-their-initial.pdf
Panda S, Dash M, John J, Rath K, Debata A, Swain D, et al. Challenges faced by student nurses and midwives in clinical learning environment - A systematic review and meta-synthesis. Nurse Educ Today. 2021;101:104875.
Ahmadi G, Shahriari M, Keyvanara M, Kohan S. Midwifery students’ experiences of learning clinical skills in Iran: a qualitative study. Int J Med Educ. 2018;9:64–71.
Harrison-White K, Owens J. Nurse link lecturers’ perceptions of the challenges facing student nurses in clinical learning environments: a qualitative study. Nurse Educ Pract. 2018;32:78–83.
Grobecker PA. A sense of belonging and perceived stress among baccalaureate nursing students in clinical placements. Nurse Educ Today. 2016;36:178–83.
Msiska G, Kamanga M, Chilemba E, Msosa A, Munkhondya TE. Sources of stress among undergraduate nursing students during clinical practice: a Malawian perspective. Open J Nurs. 2019;9:1.
Joolaee S, Amiri SRJ, Farahani MA, Varaei S. Iranian nursing students’ preparedness for clinical training: a qualitative study. Nurse Educ Today. 2015;35:e13–7.
Günay U, Kılınç G. The transfer of theoretical knowledge to clinical practice by nursing students and the difficulties they experience: a qualitative study. Nurse Educ Today. 2018;65:81–6.
Farzi S, Shahriari M, Farzi S. Exploring the challenges of clinical education in nursing and strategies to improve it: a qualitative study. J Educ Health Promot. 2018;7:115.
Hamaideh SH, Al-Omari H, Al-Modallal H. Nursing students’ perceived stress and coping behaviors in clinical training in Saudi Arabia. J Ment Health. 2017;26:197–203.
Yaghoobi A, Mohagheghi H, Zade MY, Ganji K, Olfatii N. The effect of time management training on test anxiety and academic achievement motivation among high school students. J Sch Psychol. 2014;3:131–44.
Kebriaei A, Bidgoli MS, Saeedi A. Relationship between use of time management skills and satisfaction with spending time among students of Zahedan University of Medical Sciences. J Med Educ Dev. 2014;6:79–88.
Chen YW, Hung CH. Predictors of Taiwanese baccalaureate nursing students’ physio-psycho-social responses during clinical practicum. Nurse Educ Today. 2014;34:73–7.
Ab Latif R, Mat Nor MZ. Stressors and coping strategies during clinical practice among diploma nursing students. Malays J Med Sci. 2019;26:88–98.
Al-Yateem N, Almarzouqi A, Dias JM, Saifan A, Timmins F. Nursing in the United Arab Emirates: current challenges and opportunities. J Nurs Manag. 2021;29:109–12.
Baraz-Pordanjani S, Memarian R, Vanaki Z. Damaged professional identity as a barrier to Iranian nursing students’ clinical learning: a qualitative study. J Clin Nurs Midwifery. 2014;3:1–15.
Labrague LJ, McEnroe-Petitte DM, Papathanasiou IV, Edet OB, Tsaras K, Leocadio MC, et al. Stress and coping strategies among nursing students: an international study. J Ment Health. 2018;27:402–8.
Madian AAEM, Abdelaziz MM, Ahmed HAE. Level of stress and coping strategies among nursing students at Damanhour University, Egypt. Am J Nurs Res. 2019;7:684–96.
Wu CS, Rong JR, Huang MZ. Factors associated with perceived stress of clinical practice among associate degree nursing students in Taiwan. BMC Nurs. 2021;20:89.
Zhao FF, Lei XL, He W, Gu YH, Li DW. The study of perceived stress, coping strategy and self-efficacy of Chinese undergraduate nursing students in clinical practice. Int J Nurs Pract. 2015;21:401–9.
Bektaş H, Terkes N, Özer Z. Stress and ways of coping among first year nursing students: a Turkish perspective. J Hum Sci. 2018;15:319–30.
John B, Al-Sawad M. Perceived stress in clinical areas and emotional intelligence among baccalaureate nursing students. J Indian Acad Appl Psychol. 2015;41:76–85.
Mapfumo JS, Chitsiko N, Chireshe R. Teaching practice generated stressors and coping mechanisms among student teachers in Zimbabwe. S Afr J Educ. 2012;32:155–66.
Timmins F, Corroon AM, Byrne G, Mooney B. The challenge of contemporary nurse education programmes. Perceived stressors of nursing students: mental health and related lifestyle issues. J Psychiatr Ment Health Nurs. 2011;18:758–66.
Hegberg NJ, Tone EB. Physical activity and stress resilience: considering those at-risk for developing mental health problems. Ment Health Phys Act. 2015;8:1–7.
Shudifat RM, Al-Husban RY. Perceived sources of stress among first-year nursing students in Jordan. J Psychosoc Nurs Ment Health Serv. 2015;53:37–43.
El Ansari W, Adetunji H, Oskrochi R. Food and mental health: relationship between food and perceived stress and depressive symptoms among university students in the United Kingdom. Cent Eur J Public Health. 2014;22:90–7.
Dias JM, Aderibigbe SA, Abraham MS. Undergraduate nursing students’ mentoring experiences in the clinical practicum: the United Arab Emirates (UAE) perspective. J Nurs Manag. 2022;30:4304–13.
Download references
Acknowledgements
The authors are grateful to all second year nursing students who voluntarily participated in the study.
No funding was received. Not applicable.
Author information
Authors and affiliations.
Department of Nursing, College of Health Sciences, University of Sharjah, POBox, Sharjah, 272272, UAE
Jacqueline Maria Dias, Muhammad Arsyad Subu, Nabeel Al-Yateem, Fatma Refaat Ahmed, Syed Azizur Rahman, Mini Sara Abraham, Sareh Mirza Forootan, Farzaneh Ahmad Sarkhosh & Fatemeh Javanbakh
Health Care Management, College of Health Sciences, University of Sharjah, Sharjah, United Arab Emirates
Syed Azizur Rahman
You can also search for this author in PubMed Google Scholar
Contributions
JMD conceptualized the idea and designed the methodology, formal analysis, writing original draft and project supervision and mentoring. MAS prepared the methodology and conducted the qualitative interviews and analyzed the methodology and writing of original draft and project supervision. NY, FRA, SAR, MSA writing review and revising the draft. SMF, FAS, FJ worked with MAS on the formal analysis and prepared the first draft.All authors reviewed the final manuscipt of the article.
Corresponding author
Correspondence to Jacqueline Maria Dias .
Ethics declarations
Ethics approval and consent to participate.
The Research Ethics Committee (REC) under) the Office of the Vice Chancellor for Research and Graduate Studies UOS approved this study (REC 19-12-03-01-S). Additionally, a written consent was obtained from all participants and the process followed the recommended policies and guidelines of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
Dr Fatma Refaat Ahmed is an editorial board member in BMC Nursing. Other authors do not have any conflict of interest
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dias, J.M., Subu, M.A., Al-Yateem, N. et al. Nursing students’ stressors and coping strategies during their first clinical training: a qualitative study in the United Arab Emirates. BMC Nurs 23 , 322 (2024). https://doi.org/10.1186/s12912-024-01962-5
Download citation
Received : 06 January 2024
Accepted : 22 April 2024
Published : 11 May 2024
DOI : https://doi.org/10.1186/s12912-024-01962-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical practicums
- Coping strategies
- Nursing students
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 15.5.2024 in Vol 26 (2024)
Rapport Building in Written Crisis Services: Qualitative Content Analysis
Authors of this article:

Original Paper
- Laura Schwab-Reese 1 , BSc, MA, PhD ;
- Caitlyn Short 1 , BSc, MPH ;
- Larel Jacobs 2 , MEd, MSc ;
- Michelle Fingerman 2 , MSc
1 Department of Public Health, Purdue University, West Lafayette, IN, United States
2 Childhelp, Scottsdale, AZ, United States
Corresponding Author:
Laura Schwab-Reese, BSc, MA, PhD
Department of Public Health
Purdue University
West Lafayette, IN, 47907
United States
Phone: 1 765 496 6723
Email: [email protected]
Background: Building therapeutic relationships and social presence are challenging in digital services and maybe even more difficult in written services. Despite these difficulties, in-person care may not be feasible or accessible in all situations.
Objective: This study aims to categorize crisis counselors’ efforts to build rapport in written conversations by using deidentified conversation transcripts from the text and chat arms of the National Child Abuse Hotline. Using these categories, we identify the common characteristics of successful conversations. We defined success as conversations where help-seekers reported the hotline was a good way to seek help and that they were a lot more hopeful, a lot more informed, a lot more prepared to address the situation, and experiencing less stress, as reported by help-seekers.
Methods: The sample consisted of transcripts from 314 purposely selected conversations from of the 1153 text and chat conversations during July 2020. Hotline users answered a preconversation survey (ie, demographics) and a postconversation survey (ie, their perceptions of the conversation). We used qualitative content analysis to process the conversations.
Results: Active listening skills, including asking questions, paraphrasing, reflecting feelings, and interpreting situations, were commonly used by counselors. Validation, unconditional positive regard, and evaluation-based language, such as praise and apologies, were also often used. Compared with less successful conversations, successful conversations tended to include fewer statements that attend to the emotional dynamics. There were qualitative differences in how the counselors applied these approaches. Generally, crisis counselors in positive conversations tended to be more specific and tailor their comments to the situation.
Conclusions: Building therapeutic relationships and social presence are essential to digital interventions involving mental health professionals. Prior research demonstrates that they can be challenging to develop in written conversations. Our work demonstrates characteristics associated with successful conversations that could be adopted in other written help-seeking interventions.
Introduction
Since the 1990s, mental health providers have explored how to support clients via internet-based communication [ 1 ]. Prior work suggests that young people may be particularly interested in these approaches, as digital communication feels more private and emotionally safe [ 2 ]. However, internet-based communication, particularly written communication, may have significant barriers for providers and clients, including the inability to express emotion and challenges in communicating clearly [ 2 ]. Currently, there is limited evidence on how to overcome these communication issues in counseling settings [ 3 ]. Understanding how to do so may help telehealth providers build stronger therapeutic relationships, thus improving the help-seeking process. Further, this understanding may help agencies improve services and training for providers.
Technology-Based Mental Health Interventions
Technology-based (ie, telehealth) mental health services may not be as effective as in-person services. One recent meta-analysis suggests that videoconferencing-based therapeutic relationships may be inferior to those developed during in-person therapy [ 4 ]. However, there may be times when in-person care is not accessible or feasible. Nearly half of people in the United States live in a mental health shortage area, and there are areas with less than 2 psychiatrists per 100,000 residents [ 5 , 6 ]. As a result, increasing access to mental health care may depend on telehealth approaches. Within telehealth studies, interventions retaining elements of human contact are more effective than entirely computer-based interventions [ 7 , 8 ].
Two critical aspects of the helping relationship, therapeutic relationship and social presence, may be challenged when engaging digitally. A therapeutic relationship based on mutual trust, respect, empathy, and positive regard is essential in counseling [ 9 ]. Hundreds of studies have confirmed the importance of this collaborative relationship [ 10 ]. For most help-seekers, confidence in the provider, including perceptions of empathy and expertise, is key to developing a strong relationship [ 11 - 13 ].
Social presence [ 14 ], the sense of connecting and being with another, is another element that may be compromised during digital communication. Social presence may also be defined as the degree to which the other person feels “real” [ 15 ]. Although it is a natural element of face-to-face counseling, telehealth providers may have to be intentional in building a social presence. When conversing with unknown entities through written technology, it is common to question whether the other person is a human or a bot [ 16 ], in part because people are not reliably able to differentiate between the two [ 17 ]. Some prior work suggests that social presence is an important aspect of digital helping relationships because it assists in building therapeutic partnerships, professional bonds, and open communication [ 18 , 19 ].
Much of the literature on telehealth counseling focuses on verbal communication via videoconferencing or phone [ 20 ]. Few studies examine written mental health counseling services, and there is reason to believe that spoken and written communication are substantially different. In a recent review of the digital therapeutic relationship, Bantjes and Slabbert [ 20 ] suggest practical strategies for establishing rapport in digital spaces, such as maintaining eye contact, having high-speed internet to avoid lags, and attending to lighting and microphone placement. These strategies improve the audio and visual cues, which are not applicable to written communication.
Written Interventions
The literature on written counseling is limited [ 21 , 22 ]. In the 1990s, a small group of mental health providers offered therapy via email [ 23 ]. This early work identified several possible strengths and limitations. It was helpful for clients to write about their feelings, and the anonymity of email allowed them to share more openly. This asynchronous approach also increased many individuals’ sense of control, as they could choose when and where to engage with the therapist. Conversely, building a relationship and understanding nuances could be difficult without the usual social cues [ 23 ]. Two more recent literature reviews support many of the impressions formed by the early adopters, although most of the studies had very small sample sizes [ 22 , 24 ].
Written interventions may be challenging for the provider and patient, and both experience similar challenges. One randomized controlled trial of a chat-based cognitive behavioral therapy demonstrated reduced depression symptoms after 10 sessions [ 25 ]. In a parallel qualitative study, participants reported mixed perceptions of the experience [ 26 ]. Some reported feeling more able to share openly and process because of the anonymous platform. Others felt it was challenging to develop a relationship and express complex feelings and thoughts via writing [ 26 ]. Another study assessed differences between email-based cognitive behavioral therapy and unguided treatment. The email and unguided programs had better outcomes than the wait-list control group for some, but not all, outcomes [ 27 , 28 ]. Other studies, with and without in-person or telephone comparison groups, showed similarly mixed results [ 29 , 30 ]. In one unpublished dissertation, counselors who provided email services reported feeling substantial anxiety due to uncertainty, limited sensory information, and concerns about misunderstanding clients’ intentions [ 31 ]. The lack of visual, verbal, and social cues was particularly challenging [ 31 ]. They often focused more on the tasks and transactional aspects of helping to manage these uncertain dynamics [ 31 ]. Many also talked about needing much more time than usual to build the therapeutic relationship, although it did eventually happen for most [ 31 ].
Beyond mental health counseling, some recent work has examined written communication for brief counseling and advocacy [ 3 , 32 , 33 ]. Overall, privacy, autonomy, control, anonymity, and accessibility are seen as benefits of written services [ 34 - 36 ]. Building social presence and connection is an important aspect of the experience [ 34 ]. Often this professional connection builds over time, but because the help-seeker and crisis counselor or advocate do not have an ongoing relationship, it may be particularly difficult to communicate adequately and build a relationship [ 2 , 30 , 37 , 38 ]. Correctly understanding sarcasm, humor, and other nuanced language is particularly challenging in these brief interventions [ 3 , 39 ]. Like mental health counseling, the impact of written crisis and advocacy services is unclear in the current literature and may depend on geographical location, counselor training, and the help-seekers’ situations [ 33 , 40 - 46 ].
Study Purpose
Overall, establishing a human connection based on a strong therapeutic relationship and social presence will likely result in more effective, acceptable interventions. Providing crisis services is complex, and the confines of written communication create additional challenges. Rapport-building is particularly difficult, and mistakes may cause the help-seeker to feel worse [ 47 ]. However, there are not yet best practices for building rapport in these conversations, as existing approaches to rapport-building often depend on verbal and nonverbal cues [ 48 ]. As part of a larger study focused on building best practices for written hotlines, we worked with a child maltreatment-focused text or chat hotline. This analysis aims to categorize crisis counselors’ efforts to build rapport and convey active listening in written conversations. Using these categories, we identified characteristics associated with successful conversations, as reported by help-seekers. This work provides an important foundation for how to build therapeutic relationships in written mental health and hotline services.
Data Source
The data for this study are from the PACTECH (Prevent Abuse of Children Text and Chat Hotline), the text and chat arm of the Childhelp National Child Abuse Hotline [ 49 ]. Since 1982, Childhelp has offered 24/7 phone-based hotline services focused on support and resources related to child maltreatment. In 2018, the hotline expanded to include text and chat capabilities. Crisis counselors are employees rather than volunteers. Most are master-level professionals with specialized training in hotline services and child maltreatment. After conducting a quantitative pilot evaluation for 2 years, hotline leadership partnered with the lead author to use qualitative and mixed method approaches to identify best practices for services. As part of the data sharing agreement, the lead author and her research team received access to deidentified transcripts and metadata from conversations that were purposefully selected to represent a wide range of experiences and perceived outcomes.
Ethical Considerations
The Purdue University Institutional Review Board approved the research protocol (IRB-2020-965). The service terms and conditions disclosed that data may be shared with researchers. As a secondary data analysis of deidentified data, additional consent from participants was not required by the Institutional Review Board. The contract teams from Purdue University and Childhelp negotiated the terms of the data sharing agreement, including data security and access. As a result of the data sharing agreement, the data may not be released publicly.
The sample consists of 314 purposely selected conversations out of the 1153 text and chat conversations during July 2020. In addition to maintaining the written transcript of the conversation for 60 days, Childhelp collects preconversation and postconversation surveys from the help-seekers. The preconversation surveys focus on help-seeker characteristics (ie, age, gender, state of residence, and referral source), while the postconversation survey focuses on their perceptions of the conversation (eg, do they feel more hopeful, less stressed, and more prepared). We used maximum variation sampling to capture diverse help-seekers and outcomes, although not necessarily in the proportions present in the overall data [ 50 ]. This approach is particularly useful when looking for diverse perspectives, as was the case for our study. We sampled based on the preconversation and postconversation surveys. In our sample, 297 (94.6%) help-seekers answered at least 1 presurvey question, and 263 (83.8%) answered at least 1 postconversation survey question. First, we selected conversations where help-seekers reported that they were satisfied, unsatisfied, or mixed. We also included some conversations without surveys to reduce survey response bias. Then, we reviewed the demographic characteristics of the selected conversations to ensure help-seekers of different ages, races or ethnicities, and genders were included in the sample. For example, most help-seekers are girls, so there were relatively few conversations with boys in our initial sample. We added additional conversations with boys to ensure the results were not only relevant to girls.
We analyzed and reported the findings from all 314 conversations. When reporting quotes, however, we were particularly interested in the 45 conversations where help-seekers reported in the postconversation survey that the hotline was a good way to seek help and that they were a lot more hopeful, a lot more informed, a lot more prepared to address the situation, and experiencing less stress. Except when specifically referencing less successful conversations, all example quotes come from these conversations, as they represent those most successful from the help-seekers’ perspectives. All quotes are reported verbatim from the conversations, including any errors.
We used qualitative content analysis to process the conversations. We used both inductive and deductive processes to develop the codes. The first draft of the coding frame was based on our work with child maltreatment–related conversations within the Crisis Text Line [ 51 - 53 ]. Then, we revised the framework based on the content of the conversations.
Our development process followed the adaptation of grounded theory described by Schreier [ 54 ]. The lead author and her graduate research assistant reviewed all the conversations. During a second review of the conversations, we took notes on commonalities within the conversations, emphasizing material not captured in the first draft of the codebook. As we refined the codebook, all team members met weekly to discuss emerging materials and define and develop codes. After completing the framework and definitions, we coded 30 conversations and met to compare the code applications. We discussed differences in coding and refined the framework with the entire team. Then, we coded 30 additional conversations and assessed the coder agreement. After the second round of pilot coding, we reached 95% agreement on the codes and moved to code the full data set. In sum, we had 127 codes in the codebook, which were applied 22,326 times. After coding all the conversations, we reviewed the materials within each code. This process followed the segmentation process described by Schreier [ 54 ], where coded materials are decontextualized and reviewed to identify commonalities and themes. Through this process, we also assessed whether we met saturation, which occurs when all categories have been identified in the data set. Schrier’s [ 54 ] definition of qualitative content analysis saturation is different from other forms of qualitative methods. In other forms of qualitative analysis, saturation refers to the point at which reviewing additional material does not provide new information. We informally assessed this type of saturation by examining whether all codes were used if we considered only half of the sample. We found that all codes were used when we reviewed 2 different randomly selected split samples, which suggests that few new insights would be gained if we added additional conversations to our sample. After conducting these checks, we categorized the conversations by the outcomes and focused on similarities and differences across the groups.
For this analysis, we focused on the codes related to rapport building and active listening conversations. There were two main types of approaches used by crisis counselors: (1) counseling approaches and (2) evaluation-based language. Active listening skills, otherwise known as attending skills, are how counselors build connections with clients, express empathy, and convey that they are listening [ 48 ]. These skills may be defined slightly differently; asking questions, paraphrasing, reflecting feelings, and interpreting or summarizing the situation are generally recognized skills. We added validation [ 55 ] and unconditional positive regard [ 56 ], which are also commonly incorporated into helping relationships. Evaluation-based language, such as praise and apologies, is commonly used by adults when talking with children [ 57 ]. These statements differ from other approaches because the counselor’s evaluation of the situation is included.
We also examined how these approaches differed between the help-seekers most satisfied with the conversation (ie, answered all after-conversation survey questions as “Yes”) and those who were least satisfied with the conversation. We intended to define the least satisfied as those who answered all the after-conversation survey questions as “No.” However, only 4 people fit that criterion, so we included all help-seekers who answered most of the questions negatively.
Research Team
The research team included the lead author, a graduate research assistant, and 2 collaborators at Childhelp. The lead author is a family violence prevention researcher with a PhD in public health and an MA in counseling. She has experience conducting qualitative analyses of written hotline transcripts. The graduate research assistant was a master of public health student and had worked on the lead author’s research team for 3 years. She had experience with qualitative child maltreatment research. The Childhelp collaborators have substantial experience in hotline counseling and leadership. One has an MS in counseling psychology. The second has an MS in family and human development and an MEd in guidance counseling.
Help-Seeker Characteristics
Overall, our sample of help-seekers was generally similar to Childhelp’s overall text and chat users ( Table 1 ) [ 58 , 59 ]. Help-seekers tended to be female, young, and seeking help for themselves. Overall, they were generally at least a little more hopeful, informed, and prepared to deal with the situation after the conversation ( Table 2 ).
a Includes children who were distressed but did not necessarily describe events consistent with maltreatment.
a Do you feel more positive or hopeful after this chat/text session?
b Did you get the information you needed from this chat or text session?
c Do you feel better prepared to deal with the situation after this chat or text session?
d Do you feel less stress after the chat or text session?
e Was using chat or text a good way for you to get help?
Active Listening Skills
Paraphrasing information and feelings.
When paraphrasing (387 times across 170 conversations), the crisis counselor repeated what was said by the help-seeker in a way that honed the focus of the conversation. Often, it included the most important words shared by the help-seeker, along with a shortened, clarified version of the essential information or feelings. For example, when seeking to understand the situation, a crisis counselor said, “It does not sound like she is able to listen to your needs and wants at this time.” At other times, the crisis counselor wanted to convey that they have been listening. Saying, “...you mentioned that they are screaming at him and from what you have said it sounds like they might be being really aggressive with him” demonstrated that they have been paying attention to the information shared.
Sometimes, the crisis counselors reflected the feelings shared by the help-seeker, saying things like, “That sounds like it can be frustrating from what you shared,” “it sounds very overwhelming and scary,” or “I can see how stressful this is.” In these situations, the crisis counselor was often distilling the feelings to support the help-seeker in identifying what is most bothering them about the situation or what feeling is driving their response to the situation. Once the help-seeker recognized the most troubling aspect of the situation, they were often more able to brainstorm ways to address it with the crisis counselor.
Interpretation
Interpreting the situation was also common (236 times across 125 conversations). Often, help-seekers were confused or had ambivalent thoughts about the situation. In these cases, they usually struggled to identify the next steps or reduce their emotional activation. By interpreting the situation, the crisis counselors offered a coherent overview of the situation and a different perspective. In most active listening skills, crisis counselors stayed quite close to the information provided by the help-seeker (eg, paraphrasing or reflecting what was said). When interpreting the situation, crisis counselors often included their perspectives on the situation with the intent of supporting the help-seeker to see themes or new ideas. For example, one help-seeker shared that their caregivers regularly say hurtful things about their gender identity and sexual orientation, scream and yell, and tell the help-seeker that they are a disappointment. In response, the crisis counselor said, “Sounds like it would be very hard to be happy living with people who treat you like that.” Although the help-seeker had not overtly shared about their unhappiness, this interpretation led to the help-seeker sharing about active suicidal ideation.
Open Questions
Open questions (208 across 124 conversations) served multiple purposes. At the beginning of the conversations, they invited the help-seeker to share about the experience. For example, “Could you tell me what’s going on?” or “What’s making you feel unsafe?” was used to begin the conversation in a nonthreatening way. As the conversation moved to explore the issues, open questions could elicit specific details (eg, “What’s happened since then?” and “What does that mean?”) or focus attention on feelings (eg, “How does it make you feel when your mom lashes out?” and “How are you feeling about all this happening?”).
Other Common Counseling Approaches
Validation was the most used approach to active listening (647 times across 226 conversations), and it took many forms depending on the situation. Throughout the conversations, it was used to affirm the help-seeker, their feelings, and their thoughts. For example, one counselor said, “It can be hard living in a house where you don’t feel supported and respected.” In this situation, the help-seeker had a difficult relationship with a father, who regularly called the help-seeker “overdramatic or a crybaby.” By validating the difficulty of feeling unsupported, the crisis counselor communicated that the help-seeker and their feelings were important.
In other instances, the crisis counselor validated the help-seeker’s perspectives about what was or was not appropriate behavior within families. In one instance, a help-seeker shared concerns about an older sibling’s treatment of an infant. The brother was rough with the infant and burned the infant with hot milk. In response, the crisis counselor said, “I can see why you would be concerned for the baby’s safety.” In doing so, the crisis counselor communicated that the help-seeker’s feelings were valid but without confirming that the infant was being maltreated. The crisis counselor had not seen evidence of the situation, so they could not accurately validate whether the infant was being maltreated. Simple phrases, such as “I hear you. This is difficult,” “That must be really hard for you,” and “It’s okay to feel stressed that is normal,” also validated the help-seeker and their perspectives.
Unconditional Positive Regard
Unconditional positive regard (102 times across 66 conversations) occurred when crisis counselors provided basic acceptance and support of the help-seeker, regardless of their behavior or things that have been done to them. Unconditional positive regard primarily focused on the abuse experience. It was common for counselors to say things like, “No one deserves to be abused” or “No one deserves to be treated like that.” These statements were often particularly well received by help-seekers, like this example:
You don’t deserve to be emotionally abused. It’s not o.k. [Counselor]
Thank you for saying that. You are the first person ive ever talked about this personally with. [Help-seeker]
Evaluation-Based Language
Evaluation-based language involved a judgment by the crisis counselor about whether an aspect of the help-seekers’ experiences was good (eg, behavior worthy of praise) or bad (eg, an apology for something that happened to the help-seeker). Evaluation and judgment are generally not a part of helping relationships [ 48 , 60 , 61 ] but are quite common when adults speak with children [ 57 , 62 ]. Although these approaches are not generally part of counseling relationships, there is nothing inherently wrong with using them intentionally.
Praise (268 times across 145 conversations) occurred when the crisis counselor conveyed that they approved of the help-seekers or their behavior. Sometimes, praise focused on the behaviors occurring during the conversations, like “Thank you for sharing with me” and “I’m glad you reached out today.” At other times, the praise centered on behaviors that they would do in the future, such as “Yes, I believe you’re doing the right thing by calling)” and “I think that will be a good move for you.”
Apologies (372 times across 213 conversations) tended to focus on the help-seeker’s situation or issues with the hotline. Apologies for the hotline were usually about a technical difficulty (eg, “sorry, our system is not working well”). Apologies about the help-seeker’s situation could be very broad, such as “I’m so sorry to hear about all of this” and “I’m so sorry that you’re having to go through this.” Apologies could also be specific to the situation, like “I am sorry to hear Mom yelled at you yesterday too.”
Differences Between Successful and Less Successful Conversations
There were some differences in active listening skills, other counseling skills, and evaluation-based language between successful and less successful conversations. Although the sample of successful and less successful conversations was too small for formal statistical analysis, some commonalities emerged. First, although conversations were approximately the same length, less successful conversations tended to have more statements that attended to rapport building. Second, there were also differences in how the counselors applied these approaches. Unlike the preceding sections, this section includes quotes from both successful and less successful conversations.
Overall, counselors in less successful conversations tended to be vague or to directly repeat what was said by the help-seeker. These differences were particularly apparent when counselors were paraphrasing, asking open questions, or apologizing. For example, paraphrasing in less successful conversations tended to be either very vague (eg, “It sounds like you are being hurt already”) or very specific (eg, “I am hearing you have some future plans to get a job and earn your own money...”). In the last example, the help-seeker used the same phrasing in their previous statement. Conversely, successful conversations tended to be specific without direct repetition (eg, “Sounds like they are something to help you cope”). Similarly, less successful conversations tended to include open questions that were either broad (eg, “What’s happening?”) or focused on clarifying how the crisis counselor could help (eg, “How are you hoping that I can help?”). Some successful conversations also included questions clarifying how the crisis counselor could help, but it was more common to ask more specific questions, like “What is it that you would like to vent about?” and “What are their thoughts on CPS involvement?” Finally, crisis counselors used generally vague apologies about the situation in less successful conversations. Saying things like “I am so sorry this happened to you” or “I’m sorry to hear that” was common. Although some successful conversations also included these types of apologies, it was more common to pair the apology with a specific reason, such as “I’m so sorry that you have been experiencing this for so long” or “I am sorry to hear Mama is sick.”
Principal Results
Overall, our study suggests that it is possible to build therapeutic relationships via a text and chat hotline with individuals seeking child maltreatment–related information and support. Approximately 15% (n=45) of our sample reported that the hotline was a good way to seek help and that they were a lot more hopeful, a lot more informed, a lot more prepared to address the situation, and experiencing less stress. However, our sample was intentionally selected to represent a wide range of help-seeker perceptions, so this does not indicate that 15% of the hotline’s help-seekers felt this way. Based on the 2022 Childhelp data report, about 85% of help-seekers reported getting the information they needed, 80% of help-seekers reported feeling more hopeful after the conversation, and 75% reported feeling better prepared to deal with the situation [ 59 ]. These percentages suggest that the hotline provides a well-received service.
Generally, counselors built rapport through active listening skills, other counseling techniques, and evaluation-based language (ie, apologies, praise). Through active listening skills and other counseling techniques, counselors often expressed that they were listening, wanted to understand the help-seekers, and cared for them. They expressed their approval or disapproval of the help-seekers and aspects of their experiences through evaluation-based language. Although there is nothing inherently wrong with using apologies and praise, they tend to be avoided in many therapeutic approaches. Praise may undermine intrinsic motivation (ie, internal drive) and reduce engagement in the process [ 63 - 65 ]. Further, these types of evaluation-based language are rooted in control, as they are given based on something that another individual (ie, the crisis counselor) deems desirable [ 63 ]. As a result, the help-seeker might seek praise by giving answers that they believe the crisis counselor wants to receive instead of accurate answers, which may reduce the benefit of the conversation. However, praise and compliments may be a quick way to build encouraging feelings [ 66 ]. As it is challenging to build relationships via writing, praise may be one way to build a relationship quickly. Additional research into the impact of evaluation-based language is necessary to understand its role in written crisis counseling.
There were some differences between successful and less successful conversations. Surprisingly, less successful conversations tended to include more attending language than successful conversations. However, there were differences in the ways that crisis counselors apply these techniques. Overall, the crisis counselors in successful conversations tended to be more specific and tailor their responses to the help-seekers. Possibly, counselors who gave tailored responses built rapport more quickly; thus, fewer attending statements were required. If this is the case, they could move to problem-solving more quickly, which may also contribute to help-seekers’ perceptions that they were more prepared to address the situation and were more informed. These tailored responses may increase help-seekers’ perceptions that the crisis counselor is invested in the conversation. Several help-seekers explicitly asked if they were speaking with a bot in this sample. Having tailored responses may increase crisis counselors’ social presence and reduce help-seekers’ concerns about whether they are “real.” As organizations consider using large language models and chatbots in these types of services, careful attention should be given to help-seekers’ perceptions about the service and its appropriateness for the audience. As the National Eating Disorders Association learned when its wellness chatbot began providing diet information, large language models trained on outside data may not be a good fit for conversations with help-seekers [ 67 ].
Limitations
Our work has several limitations, including some inherent to secondary data analysis. First, we could not speak with the help-seekers or the counselors about the conversations. Although we were able to identify similarities across well-received conversations, it is possible that other aspects of the conversations contributed to help-seekers’ perceptions. Second, we do not know how these conversations shaped long-term outcomes. Moreover, it is difficult to follow up with help-seekers, as evidenced by the 6% response rate to a 2-week follow-up survey conducted by the National Domestic Violence Hotline [ 68 ]. Further, many of the help-seekers in this sample indicated that it is unsafe to speak aloud about their experiences, so qualitative data collection with this sample would likely have an even lower response rate. It would be more feasible to speak with counselors about their experiences, but their perspectives may be disconnected from those of the help-seekers. Despite this limitation, we incorporated the help-seekers’ perspectives through the postconversation survey, which is more than is usually possible in secondary data analysis.
Our work may not generalize to conversations unrelated to child maltreatment. As a child maltreatment–specific hotline, all conversations included elements of child maltreatment. Conversations about other topics may require other approaches. However, our results are consistent with prior work on building rapport in other forms of counseling [ 48 , 55 , 56 ], so it is reasonable to expect these findings would translate to written conversations about other topics.
Comparison With Prior Work
To the best of our knowledge, there is no other work examining specific ways to build a therapeutic relationship in written mental health counseling or crisis counseling. However, the ways that crisis counselors attended to the dynamics of the conversations were generally like those found in in-person counseling [ 48 , 55 , 56 ].
Telehealth approaches to counseling may be particularly important for young people experiencing maltreatment. Other formal resources, such as law enforcement, schools, and child protection systems, often fail to respond adequately [ 53 , 69 , 70 ]. Further, internet-based approaches, particularly written approaches, are highly acceptable to young people experiencing maltreatment [ 69 ]. In our sample and past research, children shared that they could not call resources because an audible conversation would cause parents to know they were seeking help. In work conducted with Crisis Text Line, it was common for young people sharing child maltreatment to report that the abuse escalated when parents discovered their attempts to seek help. Written, anonymous communication that is available 24/7 may be a safer way for these young people to seek help. Thus, written communication may be particularly important for children in unsafe homes.
There is also limited evidence on how to respond when young people share maltreatment experiences. Regardless of the ability to impact or end the maltreatment, individuals who receive a child maltreatment disclosure need to receive an appropriate, supportive response [ 71 - 74 ]. Supportive responses encourage the young person experiencing maltreatment to reframe their experience, which substantially reduces the likelihood of poor outcomes otherwise associated with maltreatment [ 75 ]. Conversely, unsupportive experiences often have long-lasting consequences [ 74 , 76 ]. Receiving a hurtful or unsupportive response increases the likelihood that the young person will experience more significant physical and mental health issues [ 74 , 76 , 77 ]. Unfortunately, many young people receive unsupportive responses to their disclosures [ 53 , 70 ]. Often, they report that others, particularly adults, do not believe them and are unwilling to help [ 70 , 78 ]. These experiences reduce their willingness to seek help or share their experiences in the future [ 70 ]. Our work suggests that responding to these disclosures adequately in written conversations is possible.
Our work also contributes to a small body of literature on using text and chat hotlines to provide services to people experiencing violence more generally. Michigan State University added chat services to its existing sexual assault support and advocacy hotline. Their evaluation was consistent with many of the benefits and limitations of other forms of written counseling, including challenges with nuance, misunderstanding written language, and communicating empathy [ 3 ]. However, the format also gave help-seekers a greater sense of control [ 3 ]. Another study focused on agencies providing digital violence-related support and advocacy services [ 32 ]. This work also emphasized the importance of clear communication and building rapport, although help-seeker perceptions of these factors were not assessed [ 32 ].
Conclusions
Building therapeutic relationships and social presence are important components of digital interventions involving mental health professionals. Prior research suggests that they can be challenging to develop in written conversations. Our work demonstrates characteristics of conversations associated with greater satisfaction among help-seekers. These findings may be adopted by other organizations building mental health or support interventions that include written communication. However, additional research is needed to identify how to train providers to adopt these strategies while also tailoring their approach to the help-seeker. Further, our findings may inform future work with large language models, including how large language models could contribute to these interventions. However, future research is needed to understand how help-seekers would interface with these methods and to ensure that the models consistently convey appropriate, supportive information.
Acknowledgments
This project was supported by the Children’s Bureau (CB) and Administration for Children and Families (ACF) of the US Department of Health and Human Services (HHS) as part of a financial assistance award in the amount of US $6,000,000 that was 100% funded by the CB and ACF of the HHS. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, the CB and ACF of the HHS or the US government. For more information, please visit administrative and national policy requirements.
Conflicts of Interest
None declared.
- Murphy LJ, Mitchell DL. When writing helps to heal: e-mail as therapy. Br J Guid Counc. 1998;26(1):21-32. [ CrossRef ]
- King R, Bambling M, Lloyd C, Gomurra R, Smith S, Reid W, et al. Online counselling: the motives and experiences of young people who choose the internet instead of face to face or telephone counselling. Couns Psychother Res. 2006;6(3):169-174. [ CrossRef ]
- Moylan CA, Carlson ML, Campbell R, Fedewa T. "It's hard to show empathy in a text": developing a web-based sexual assault hotline in a college setting. J Interpers Violence. 2022;37(17-18):NP16037-NP16059. [ CrossRef ] [ Medline ]
- Norwood C, Moghaddam NG, Malins S, Sabin-Farrell R. Working alliance and outcome effectiveness in videoconferencing psychotherapy: a systematic review and noninferiority meta-analysis. Clin Psychol Psychother. 2018;25(6):797-808. [ CrossRef ] [ Medline ]
- Cheng N, Mohiuddin S. Addressing the nationwide shortage of child and adolescent psychiatrists: determining factors that influence the decision for psychiatry residents to pursue child and adolescent psychiatry training. Acad Psychiatry. 2022;46(1):18-24. [ CrossRef ] [ Medline ]
- Morales DA, Barksdale CL, Beckel-Mitchener AC. A call to action to address rural mental health disparities. J Clin Transl Sci. 2020;4(5):463-467. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev. 2012;32(4):329-342. [ CrossRef ] [ Medline ]
- Spek V, Cuijpers P, Nyklícek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med. 2007;37(3):319-328. [ CrossRef ] [ Medline ]
- Torous J, Hsin H. Empowering the digital therapeutic relationship: virtual clinics for digital health interventions. NPJ Digit Med. 2018;1:16. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Karver MS, Handelsman JB, Fields S, Bickman L. Meta-analysis of therapeutic relationship variables in youth and family therapy: the evidence for different relationship variables in the child and adolescent treatment outcome literature. Clin Psychol Rev. 2006;26(1):50-65. [ CrossRef ] [ Medline ]
- Finsrud I, Nissen-Lie HA, Vrabel K, Høstmælingen A, Wampold BE, Ulvenes PG. It's the therapist and the treatment: the structure of common therapeutic relationship factors. Psychother Res. 2022;32(2):139-150. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Elliott R, Bohart AC, Watson JC, Murphy D. Therapist empathy and client outcome: an updated meta-analysis. Psychotherapy (Chic). 2018;55(4):399-410. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nienhuis JB, Owen J, Valentine JC, Black SW, Halford TC, Parazak SE, et al. Therapeutic alliance, empathy, and genuineness in individual adult psychotherapy: a meta-analytic review. Psychother Res. 2018;28(4):593-605. [ CrossRef ] [ Medline ]
- Short J, Williams E, Christie B. The Social Psychology of Telecommunications. Hoboken, NJ. Jon Wiley & Sons; 1976.
- Gunawardena CN. Social presence theory and implications for interaction and collaborative learning in computer conferences. Int J Educ Telecommun. 1995;1(2):147-166. [ FREE Full text ]
- Batish R. Voicebot and Chatbot Design: Flexible Conversational Interfaces with Amazon Alexa, Google Home, and Facebook Messenger. Birmingham, UK. Packt Publishing Ltd; 2018.
- Warwick K, Shah H. The importance of a human viewpoint on computer natural language capabilities: a turing test perspective. AI Soc. 2016;31(2):207-221. [ CrossRef ]
- Lopez A. An investigation of the use of internet based resources in support of the therapeutic alliance. Clin Soc Work J. 2014;43(2):189-200. [ CrossRef ]
- Holmes C, Foster V. A preliminary comparison study of online and face-to-face counseling: client perceptions of three factors. J Technol Hum Serv. 2012;30(1):14-31. [ CrossRef ]
- Bantjes J, Slabbert P. The digital therapeutic relationship: retaining humanity in the digital age. In: Stein DJ, Fineberg NA, Chamberlain SR, editors. Mental Health in a Digital World. Amsterdam. Elsevier; 2022;223-237.
- Berger T. The therapeutic alliance in internet interventions: a narrative review and suggestions for future research. Psychother Res. 2017;27(5):511-524. [ CrossRef ] [ Medline ]
- Richards D, Viganó N. Online counseling: a narrative and critical review of the literature. J Clin Psychol. 2013;69(9):994-1011. [ CrossRef ] [ Medline ]
- Chechele PJ, Stofle G. Individual therapy online via email and internet relay chat. In: Anthony K, editor. Technology in Counselling and Psychotherapy: A Practitioner's Guide. London. Palgrave Macmillan; 2003;39-58.
- Stoll J, Müller JA, Trachsel M. Ethical issues in online psychotherapy: a narrative review. Front Psychiatry. 2019;10:993. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kessler D, Lewis G, Kaur S, Wiles N, King M, Weich S, et al. Therapist-delivered internet psychotherapy for depression in primary care: a randomised controlled trial. Lancet. 2009;374(9690):628-634. [ CrossRef ] [ Medline ]
- Beattie A, Shaw A, Kaur S, Kessler D. Primary-care patients' expectations and experiences of online cognitive behavioural therapy for depression: a qualitative study. Health Expect. 2009;12(1):45-59. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Vernmark K, Lenndin J, Bjärehed J, Carlsson M, Karlsson J, Oberg J, et al. Internet administered guided self-help versus individualized e-mail therapy: a randomized trial of two versions of CBT for major depression. Behav Res Ther. 2010;48(5):368-376. [ CrossRef ] [ Medline ]
- Andersson G, Paxling B, Roch-Norlund P, Östman G, Norgren A, Almlöv J, et al. Internet-based psychodynamic versus cognitive behavioral guided self-help for generalized anxiety disorder: a randomized controlled trial. Psychother Psychosom. 2012;81(6):344-355. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dowling M, Rickwood D. Investigating individual online synchronous chat counselling processes and treatment outcomes for young people. Adv Ment Health. 2015;12(3):216-224. [ CrossRef ]
- King R, Bambling M, Reid W, Thomas I. Telephone and online counselling for young people: a naturalistic comparison of session outcome, session impact and therapeutic alliance. Couns Psychother Res. 2006;6(3):175-181. [ CrossRef ]
- Francis-Smith C. Email counselling and the therapeutic relationship: a grounded theory analysis of therapists' experiences [dissertation]. University of the West of England. 2014. URL: https://uwe-repository.worktribe.com/index.php/preview/806312/Thesis%20amended%20for%20repository.pdf [accessed 2024-04-17]
- Wood L, Hairston D, Schrag RV, Clark E, Parra-Cardona R, Temple JR. Creating a digital trauma informed space: chat and text advocacy for survivors of violence. J Interpers Violence. 2022;37(19-20):NP18960-NP18987. [ CrossRef ] [ Medline ]
- Gould MS, Chowdhury S, Lake AM, Galfalvy H, Kleinman M, Kuchuk M, et al. National suicide prevention lifeline crisis chat interventions: evaluation of chatters' perceptions of effectiveness. Suicide Life Threat Behav. 2021;51(6):1126-1137. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gibson K, Cartwright C. Young people's experiences of mobile phone text counselling: balancing connection and control. Child Youth Serv Rev. 2014;43:96-104. [ CrossRef ]
- Evans WP, Davidson L, Sicafuse L. Someone to listen: increasing youth help-seeking behavior through a text-based crisis line for youth. J Community Psychol. 2013;41(4):471-487. [ CrossRef ]
- Predmore Z, Ramchand R, Ayer L, Kotzias V, Engel C, Ebener P, et al. Expanding suicide crisis services to text and chat. Crisis. 2017;38(4):255-260. [ CrossRef ] [ Medline ]
- Chardon L, Bagraith KS, King RJ. Counseling activity in single-session online counseling with adolescents: an adherence study. Psychother Res. 2011;21(5):583-592. [ CrossRef ] [ Medline ]
- Bambling M, King R, Reid W, Wegner K. Online counselling: the experience of counsellors providing synchronous single-session counselling to young people. Couns Psychother Res. 2008;8(2):110-116. [ CrossRef ]
- Rodda SN, Lubman DI, Cheetham A, Dowling NA, Jackson AC. Single session web-based counselling: a thematic analysis of content from the perspective of the client. Br J Guid Counc. 2015;43(1):117-130. [ CrossRef ]
- Fukkink RG, Hermanns JMA. Children's experiences with chat support and telephone support. J Child Psychol Psychiatry. 2009;50(6):759-766. [ CrossRef ] [ Medline ]
- Fukkink R, Hermanns J. Counseling children at a helpline: chatting or calling? Am J Community Psychol. 2009;37(8):939-948. [ CrossRef ]
- Sindahl TN, van Dolen W. Texting at a child helpline: how text volume, session length and duration, response latency, and waiting time are associated with counseling impact. Cyberpsychol Behav Soc Netw. 2020;23(4):210-217. [ FREE Full text ] [ CrossRef ] [ Medline ]
- van Dolen W, Weinberg CB. Child helplines: how social support and controllability influence service quality and well-being. J Serv Mark. 2017;31(4/5):385-396. [ CrossRef ]
- van Dolen W, Weinberg CB. An empirical investigation of factors affecting perceived quality and well-being of children using an online child helpline. Int J Environ Res Public Health. 2019;16(12):2193. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Navarro P, Bambling M, Sheffield J, Edirippulige S. Exploring young people's perceptions of the effectiveness of text-based online counseling: mixed methods pilot study. JMIR Ment Health. 2019;6(7):e13152. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Thompson LK, Sugg MM, Runkle JR. Adolescents in crisis: a geographic exploration of help-seeking behavior using data from crisis text line. Soc Sci Med. 2018;215:69-79. [ CrossRef ] [ Medline ]
- Fildes D, Williams K, Bradford S, Grootemaat P, Kobel C, Gordon R. Implementation of a pilot SMS-based crisis support service in Australia. Crisis. 2022;43(1):46-52. [ CrossRef ] [ Medline ]
- Ivey AE, Packard NG, Ivey MB. Basic Attending Skills. San Diego, CA. Cognella; 2018.
- The Childhelp National Child Abuse Hotline. Childhelp. 2020. URL: https://www.childhelp.org/hotline/ [accessed 2024-04-17]
- Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42(5):533-544. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cash SJ, Murfree L, Schwab-Reese L. "I'm here to listen and want you to know I am a mandated reporter": understanding how text message-based crisis counselors facilitate child maltreatment disclosures. Child Abuse Negl. 2020;102:104414. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Schwab-Reese L, Kanuri N, Cash S. Child maltreatment disclosure to a text messaging-based crisis service: content analysis. JMIR Mhealth Uhealth. 2019;7(3):e11306. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Schwab-Reese LM, Cash SJ, Lambert NJ, Lansford JE. "They aren't going to do jack shit": text-based crisis service users' perceptions of seeking child maltreatment-related support from formal systems. J Interpers Violence. 2022;37(19-20):NP19066-NP19083. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Schreier M. Qualitative Content Analysis in Practice. Thousand Oaks, CA. Sage; 2012.
- Linehan MM. Validation and psychotherapy. In: Bohart AC, Greenberg LS, editors. Empathy Reconsidered: New Directions in Psychotherapy. Washington, DC. American Psychological Association; 1997;353-392.
- Wilkins P. Unconditional positive regard reconsidered. Br J Guid Counc. 2010;28(1):23-36. [ CrossRef ]
- Brummelman E, Crocker J, Bushman BJ. The praise paradox: when and why praise backfires in children with low self-esteem. Child Dev Perspect. 2016;10(2):111-115. [ CrossRef ]
- Wolfersteig W, Moreland D, Diaz M, Gotlieb E. Prevent Abuse of Children Text and Chat Hotline (PACTECH) project: semi-annual data report. Childhelp. Scottsdale, Arizona.; 2022. URL: https://www.childhelphotline.org/wp-content/uploads/2022/05/PACTECH-Data-Report-April-2022.pdf [accessed 2024-04-17]
- Hotline impact report. Childhelp. 2022. URL: https://www.childhelphotline.org/wp-content/uploads/2022/10/Hotline-Impact-Report-FY22.pdf [accessed 2024-04-17]
- Nicholas A, Pirkis J, Reavley N. What responses do people at risk of suicide find most helpful and unhelpful from professionals and non-professionals? J Ment Health. 2022;31(4):496-505. [ CrossRef ] [ Medline ]
- Rogers CR. A Way of Being. Boston, MA. Houghton Mifflin Harcourt; 1980.
- Brummelman E, Nelemans SA, Thomaes S, de Castro BO. When parents' praise inflates, children's self-esteem deflates. Child Dev. 2017;88(6):1799-1809. [ CrossRef ] [ Medline ]
- Kelsey J. The negative impact of rewards and ineffective praise on student motivation. ESSAI. 2011;8(1):24. [ FREE Full text ]
- Kakinuma K, Nishiguti F, Sonoda K, Tajiri H, Tanaka A. The negative effect of ability-focused praise on the "praiser's" intrinsic motivation: face-to-face interaction. Front Psychol. 2020;11:562081. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pellecchia M, Nuske HJ, Straiton D, Hassrick ME, Gulsrud A, Iadarola S, et al. Strategies to engage underrepresented parents in child intervention services: a review of effectiveness and co-occurring use. J Child Fam Stud. 2018;27(10):3141-3154. [ CrossRef ]
- Landrum RE, Gurung RA, Nolan SA, McCarthy MA, Dunn DS. Everyday Applications of Psychological Science: Hacks to Happiness and Health. Milton Park, UK. Routledge; 2022.
- McCarthy L. A wellness chatbot is offline after its 'harmful' focus on weight loss. The New York Times. 2023. URL: https://www.nytimes.com/2023/06/08/us/ai-chatbot-tessa-eating-disorders-association.html [accessed 2024-04-17]
- McDonnell K, Nagaraj N, Fuerst M. Short-term outcomes following contact with the national domestic violence hotline and loveisrespect. U.S. Department of Health & Human Services. 2020. URL: https://www.acf.hhs.gov/opre/report/short-term-outcomes-following-contact-national-domestic-violence-hotline-and [accessed 2024-04-17]
- Al-Eissa MA. Utilization of child helpline (CHL) among adolescents in Saudi Arabia: results from a national survey. Child Fam Soc Work. 2019;24(1):84-89. [ CrossRef ]
- Tucker S. Listening and believing: an examination of young people's perceptions of why they are not believed by professionals when they report abuse and neglect. Child Soc. 2011;25(6):458-469. [ CrossRef ]
- Collin-Vézina D, De La Sablonnière-Griffin M, Palmer AM, Milne L. A preliminary mapping of individual, relational, and social factors that impede disclosure of childhood sexual abuse. Child Abuse Negl. 2015;43:123-134. [ CrossRef ] [ Medline ]
- Goodman-Brown TB, Edelstein RS, Goodman GS, Jones DPH, Gordon DS. Why children tell: a model of children's disclosure of sexual abuse. Child Abuse Negl. 2003;27(5):525-540. [ CrossRef ] [ Medline ]
- Jensen TK, Gulbrandsen W, Mossige S, Reichelt S, Tjersland OA. Reporting possible sexual abuse: a qualitative study on children's perspectives and the context for disclosure. Child Abuse Negl. 2005;29(12):1395-1413. [ CrossRef ] [ Medline ]
- Palmer SE, Brown RA, Rae-Grant NI, Loughlin MJ. Responding to children's disclosure of familial abuse: what survivors tell us. Child Welfare. 1999;78(2):259-282. [ Medline ]
- Briere J, Jordan CE. Violence against women: outcome complexity and implications for assessment and treatment. J Interpers Violence. 2004;19(11):1252-1276. [ CrossRef ] [ Medline ]
- Arata CM. To tell or not to tell: current functioning of child sexual abuse survivors who disclosed their victimization. Child Maltreatment. 1998;3(1):63-71. [ CrossRef ]
- Palo AD, Gilbert BO. The relationship between perceptions of response to disclosure of childhood sexual abuse and later outcomes. J Child Sex Abus. 2015;24(5):445-463. [ CrossRef ] [ Medline ]
- Cossar J, Belderson P, Brandon M. Recognition, telling and getting help with abuse and neglect: young people's perspectives. Child Youth Serv Rev. 2019;106:104469. [ CrossRef ]
Edited by T de Azevedo Cardoso; submitted 19.08.22; peer-reviewed by K Zhang, V Franzoni, B Li, Z Aghaei; comments to author 28.03.23; revised version received 21.08.23; accepted 26.03.24; published 15.05.24.
©Laura Schwab-Reese, Caitlyn Short, Larel Jacobs, Michelle Fingerman. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 15.05.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Cornell Chronicle
- Architecture & Design
- Arts & Humanities
- Business, Economics & Entrepreneurship
- Computing & Information Sciences
- Energy, Environment & Sustainability
- Food & Agriculture
- Global Reach
- Health, Nutrition & Medicine
- Law, Government & Public Policy
- Life Sciences & Veterinary Medicine
- Physical Sciences & Engineering
- Social & Behavioral Sciences
- Coronavirus
- News & Events
- Public Engagement
- New York City
- Photos of the Week
- Big Red Sports
- Freedom of Expression
- Student Life
- University Statements
Around Cornell
- All Stories
- In the News
- Expert Quotes
- Cornellians

News directly from Cornell's colleges and centers
BTPI will research relationship between Bitcoin and financial freedom
By giles morris cornell jeb e. brooks school of public policy.
The Brooks School Tech Policy Institute (BTPI) has announced a $1M project to study financial freedom in countries with authoritarian governments. Led by BTPI Director Sarah Kreps , John L. Wetherill Professor in the Department of Government in the College of Arts & Sciences and the Cornell Jeb E. Brooks School of Public Policy, the research will employ quantitative and qualitative approaches to understanding the use of Bitcoin and stablecoins by individuals around the world.
“If you live in a place where the government silences its critics by threatening their assets or where you cannot trust the local banking system, you understand the importance of financial freedom to democracy,” said Kreps. “We want to study how people in these countries are using Bitcoin and stablecoins in the pursuit of their financial security.”

BTPI Director Dr. Sarah Kreps
The innovative approach to purpose-driven research is designed to build a framework for the creation of a Bitcoin and stablecoins adoption index that would map and analyze uptake globally. Supported by funding from Human Rights Foundation– a nonpartisan, nonprofit organization that promotes and protects human rights globally, with a focus on closed societies– and the Reynolds Foundation– a family foundation dedicated to supporting medical and spinal cord research and treatment, education, and democracy and freedom– the project is scheduled to kick off in July 2024 and conclude in 2026.
Reynolds Foundation president and CEO Dr. Álvaro Salas Castro MPA '14 explained the multimodal and collaborative nature of the inquiry would lead to wider access to knowledge at a critical moment in global policy.
"The Tech Policy Institute at Cornell University's Brooks School of Public Policy stands as a crucial center for investigating the intricate relationship between emerging technology and global politics. Through a dedicated focus on critical issues such as artificial intelligence, cybersecurity, and digital privacy regulations, the Institute's interdisciplinary research aims to shed light on the complexities of our rapidly evolving technological landscape," said Dr. Salas Castro. "As Bitcoin adoption continues to exert influence over the global economic system, the Institute's steadfast commitment to fostering collaboration among scholars, policymakers, and industry leaders aligns seamlessly with the Reynolds Foundation's vision to support a network of knowledge-sharing that harnesses this technology for societal benefit."
According to Professor Kreps, the project will focus on about 12 countries, including India, Nigeria, El Salvador, Indonesia, and Turkey, and investigate Bitcoin and stablecoin uptake. Kreps and her research team will partner with a major global research firm to develop and deliver surveys to 1,000 participants in each country that query not just adoption behaviors on the basis of demographic within each country but also perceptions and attitudes toward these digital currencies. A research team that includes undergraduate students will then conduct interviews to dig deeper into the basis for use.
According to HRF chief strategy officer Alex Gladstein, the combination of survey data and qualitative research in countries where relatively little is known about the use of Bitcoin and stablecoins represents a new approach to creating a baseline of understanding about their potential to enhance financial freedom around the world.
"Bitcoin continues to grow into a bigger part of the global economic system. Today we have nation-state adoption, widespread mining operations on all continents, spot Exchange Traded Funds (ETFs) trading in the United States, and recent all-time-highs in price. The Human Rights Foundation has also observed that human rights groups and nonprofits are adopting Bitcoin in order to challenge financial repression from authoritarian regimes," said Gladstein. "This research under Professor Kreps will illuminate exactly who out there in the world is using Bitcoin and dollar-substitute stable coins, and why."
The goals of the financial freedom research project include:
- Increasing shared understanding of the factors driving cryptocurrency adoption, usage patterns, and the broader implications for financial inclusion and technological innovation.
- Assessing the ability of policymakers, industry stakeholders, and community organizations to make informed decisions regarding regulatory frameworks, product development, and educational initiatives related to cryptocurrencies.
- Expanding access to financial services and economic opportunities for individuals who are underserved or excluded by traditional banking systems.
- Raising public awareness and understanding of cryptocurrency technology, its potential benefits, risks, and implications for individuals and society.
“Researchers have posited a number of different reasons why citizens in these countries might use crypto and our research will probe these mechanisms of uptake to understand motivations and goals and whether these vary depending on region or type of government,” said Kreps.
Giles Morris is assistant dean for communications in the Cornell Jeb E. Brooks School of Public Policy.
Media Contact
Media relations office.
Get Cornell news delivered right to your inbox.
You might also like

Gallery Heading
Correction to: Motives of Therapists for Using Routine Outcome Monitoring (ROM) and How it is Used by Them in Clinical Practice: Two Qualitative Studies
- Open access
- Published: 16 May 2024
Cite this article
You have full access to this open access article

- Shaghayegh Azizian Kia 1 ,
- Lisette Wittkampf 1 ,
- Jacobine van Lankeren 1 &
- Pauline Janse 1 , 2
The Original Article was published on 08 April 2024
Avoid common mistakes on your manuscript.
Correction to: Administration and Policy in Mental Health and Mental Health Services Research
https://doi.org/10.1007/s10488-024-01374-2
In this article, the author Dr. Azizian Kia given name “Shaghayegh” was incorrectly written as “Sharaya”.
That is, Sharaya Azizian Kia should be Shaghayegh Azizian Kia.
The original article has been corrected.
Author information
Authors and affiliations.
Pro Persona Research, Wolfheze, The Netherlands
Shaghayegh Azizian Kia, Lisette Wittkampf, Jacobine van Lankeren & Pauline Janse
Behavioural Science Institute, Radboud University, Nijmegen, The Netherlands
Pauline Janse
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Pauline Janse .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The online version of the original article can be found at https://doi.org/10.1007/s10488-024-01374-2 .
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Azizian Kia, S., Wittkampf, L., van Lankeren, J. et al. Correction to: Motives of Therapists for Using Routine Outcome Monitoring (ROM) and How it is Used by Them in Clinical Practice: Two Qualitative Studies. Adm Policy Ment Health (2024). https://doi.org/10.1007/s10488-024-01383-1
Download citation
Published : 16 May 2024
DOI : https://doi.org/10.1007/s10488-024-01383-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
[email protected], 0246502881. Abstract. Deciding on the appropriate data collection instrument to use in capturing the needed. data to address a research problem as a novice qualitative ...
Qualitative research involves collecting and analyzing non-numerical data (e.g., text, video, or audio) to understand concepts, opinions, or experiences. It can be used to gather in-depth insights into a problem or generate new ideas for research. Qualitative research is the opposite of quantitative research, which involves collecting and ...
While many books and articles guide various qualitative research methods and analyses, there is currently no concise resource that explains and differentiates among the most common qualitative approaches. We believe novice qualitative researchers, students planning the design of a qualitative study or taking an introductory qualitative research course, and faculty teaching such courses can ...
Advisor Consultation Checklist Use the checklist below to ensure that you consulted with your advisor during the key steps in the process of selecting and describing your research instruments. 1. _____ Read this checklist. 2. _____ Made an appointment for our first meeting to discuss the instrument selection. 3.
Qualitative research is used to gain insights into people's feelings and thoughts, which may provide the basis for a future stand-alone qualitative study or may help researchers to map out survey instruments for use in a quantitative study. It is also possible to use different types of research in the same study, an approach known as "mixed ...
Abstract. This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions ...
Qualitative Research. Qualitative research is a type of research methodology that focuses on exploring and understanding people's beliefs, attitudes, behaviors, and experiences through the collection and analysis of non-numerical data. It seeks to answer research questions through the examination of subjective data, such as interviews, focus ...
in research design and data collection methods and instruments. WHAT IS QUALITATIVE RESEARCH? There are about as many definitions of qualitative research as there are books on the ... authors, the defining criterion is the type of data generated and/or used. In short, qualitative research involves collecting and/or working with text, images, or ...
Introduction to Qualitative Research Methodology. Karina Kielmann Fabian Cataldo Janet Seeley. 2. Karina Kielmann Senior Lecturer in International Health Institute for International Health & Development Queen Margaret University Edinburgh, Scotland EH21 6UU Email: [email protected]. Karina Kielmann is a medical anthropologist who has been ...
Qualitative research Footnote 1 —research that primarily or exclusively uses non-numerical data—is one of the most commonly used types of research and methodology in the social sciences. Unfortunately, qualitative research is commonly misunderstood. It is often considered "easy to do" (thus anyone can do it with no training), an "anything goes approach" (lacks rigor, validity and ...
The greatest strength of the qualitative research approach lies in the richness and depth of the healthcare exploration and description it makes. In health research, these methods are considered as the most humanistic and person-centered way of discovering and uncovering thoughts and actions of human beings. Table 1.
Fundamental Criteria: General Research Quality. Various researchers have put forward criteria for evaluating qualitative research, which have been summarized in Table 3.Also, the criteria outlined in Table 4 effectively deliver the various approaches to evaluate and assess the quality of qualitative work. The entries in Table 4 are based on Tracy's "Eight big‐tent criteria for excellent ...
Quality assessment. This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component ...
debates, narratives and interviews, questionnaires and surveys. 1. Introduction. This chapter sets out various methods for gathering important data on the language uses of participants in a research project. These methods imply interaction between students, teachers and researchers. They are used in the design of research projects based on ...
First, research instruments are designed by the researcher because a qualitative researcher cannot use instruments designed by previous researchers . The qualitative researcher must design different tools and instruments used in collecting data from the different sources mentioned earlier in this chapter.
A research instrument is a tool you will use to help you collect, measure and analyze the data you use as part of your research. The choice of research instrument will usually be yours to make as the researcher and will be whichever best suits your methodology. There are many different research instruments you can use in collecting data for ...
A focus group is also a commonly used qualitative research method used in data collection. A focus group usually includes a limited number of respondents (6-10) from within your target market. ... Data collection Instrument: Use semi-structured methods such as in-depth interviews, focus groups, and participant observation:
What is a Research Instrument? A Research Instrument is a tool used to collect, measure, and analyze data related to your research interests. These tools are most commonly used in health sciences, social sciences, and education to assess patients, clients, students, teachers, staff, etc. A research instrument can include interviews, tests,
The most common methods of data collection used in qualitative research are interviews and focus groups. While these are primarily conducted face-to-face, the ongoing evolution of digital ...
Qualitative research was historically employed in fields such as sociology, history, and anthropology. 2 Miles and Huberman 2 said that qualitative data "are a source of well-grounded, rich descriptions and explanations of processes in identifiable local contexts. With qualitative data one can preserve chronological flow, see precisely which ...
When collecting and analyzing data, quantitative research deals with numbers and statistics, while qualitative research deals with words and meanings. Both are important for gaining different kinds of knowledge. Quantitative research. Quantitative research is expressed in numbers and graphs. It is used to test or confirm theories and assumptions.
In qualitative research, the researcher is the main data collection instrument. The researcher examines why events occur, what happens, and what those events mean to the participants studied. 1, 2. ... The table lists the purpose of 3 commonly used approaches to frame qualitative research. For each frame, we provide an example of a research ...
conducting: quantitative, qualitative, or mixed-method (i.e. research alignments). Types ... For this reason, the main research instrument used . in the aforementio ned study was the questionnaire
The value of using qualitative methods within clinical trials is widely recognised. How qualitative research is integrated within trials units to achieve this is less clear. This paper describes the process through which qualitative research has been integrated within Cardiff University's Centre for Trials Research (CTR) in Wales, UK. We highlight facilitators of, and challenges to, integration.
Qualitative Data Analysis Software works with any qualitative research methodology used by a researcher For example, software for qualitative data analysis can be used by a social scientist wanting to develop new concepts or theories may take a 'grounded theory' approach. Or a researcher looking for ways to improve health policy or program ...
Research instrument. The research instrument was a semi structured interview guide. The interview questions were based on an in-depth review of related literature. ... Semi structured interviews are a well-established approach for gathering data in qualitative research and allow participants to discuss their views, experiences, attitudes, ...
We used qualitative content analysis to process the conversations. Results: Active listening skills, including asking questions, paraphrasing, reflecting feelings, and interpreting situations, were commonly used by counselors. Validation, unconditional positive regard, and evaluation-based language, such as praise and apologies, were also often ...
The Brooks School Tech Policy Institute (BTPI) has announced a $1M project to study financial freedom in countries with authoritarian governments. Led by BTPI Director Sarah Kreps, the research will employ quantitative and qualitative approaches to understanding the use of Bitcoin and stablecoins by individuals around the world.
Administration and Policy in Mental Health and Mental Health Services Research - Skip to main content. Account. Menu. Find a journal Publish with us Track your research ... Two Qualitative Studies. Correction; Open access; Published: 16 May 2024 (2024) Cite this article; Download PDF. You have full access to this open access article.