Key EBP Nursing Topics: Enhancing Patient Results through Evidence-Based Practice
This article was written in collaboration with Christine T. and ChatGPT, our little helper developed by OpenAI.

Evidence-based practice (EBP) is the use of the best available evidence to inform clinical decision-making in nursing. EBP has become increasingly popular in nursing practice because it ensures that patient care is based on the most current and relevant research. In this article, we will discuss the latest evidence-based practice nursing research topics, how to choose them, and where to find EBP project ideas.

What is Evidence-Based Practice Nursing?
EBP nursing involves a cyclical process of asking clinical questions, seeking the best available evidence, critically evaluating that evidence, and then integrating it with the patient’s clinical experience and values to make informed decisions. By following this process, nurses can provide the best care for their patients and ensure that their practice is informed by the latest research.
One of the key components of EBP nursing is the critical appraisal of research evidence. Nurses must be able to evaluate the quality of studies, including study design, sample size, and statistical analysis. This requires an understanding of research methodology and the ability to apply critical thinking skills to evaluate research evidence.
EBP nursing also involves the use of clinical practice guidelines and protocols, which are evidence-based guidelines for clinical practice. These guidelines have been developed by expert groups and are based on the best available evidence. By following these guidelines, nurses can ensure that their practice is in line with the latest research and can provide the best possible care for their patients.
Finally, EBP nursing involves continuous professional development and a commitment to lifelong learning. Nurses must keep abreast of the latest research and clinical practice guidelines to ensure that their practice is informed by the latest research. This requires a commitment to ongoing learning and professional development, including attending conferences, reading scholarly articles, and participating in continuing education programs.
You can also learn more about evidence-based practice in nursing to gain a deeper understanding of the definition, stages, benefits, and challenges of implementing it.
Medical Studies Overwhelming?
Delegate Your Nursing Papers to the Pros!
Get 15% Discount
+ Plagiarism Report for FREE
How to Choose Evidence-Based Practice Nursing Research Topics
Choosing a science-based topic for nursing practice can be a daunting task, especially if you are new to the field. Here are some tips to help you choose a relevant and interesting EBP topic:
- Look for controversial or debated issues
Look for areas of nursing practice that are controversial or have conflicting evidence. These topics often have the potential to generate innovative and effective research.
- Consider ethical issues
Consider topics related to ethical issues in nursing practice. For example, bereavement care, informed consent , and patient privacy are all ethical issues that can be explored in an EBP project.
- Explore interdisciplinary topics
Nursing practice often involves collaboration with other health professionals such as physicians, social workers, and occupational therapists. Consider interdisciplinary topics that may be useful from a nursing perspective.
- Consider local or regional issues
Consider topics that are relevant to your local or regional healthcare facility. These topics may be relevant to your practice and have a greater impact on patient outcomes in your community.
- Check out the latest research
Review recent research in your area of interest to identify gaps in the literature or areas where further research is needed. This can help you develop a research question that is relevant and innovative.
With these tips in mind, you can expand your options for EBP nursing research topics and find a topic that fits your interests and goals. Remember that patient outcomes should be at the forefront of your research and choose a topic that has the potential to improve treatment and patient outcomes.
Where to Get EBP Project Ideas
There are several sources that nurses can use to get EBP project ideas. These sources are diverse and can provide valuable inspiration for research topics. By exploring these sources, nurses can find research questions that align with their interests and that address gaps in the literature. These include:
- Clinical Practice Guidelines
Look for clinical practice guidelines developed by professional organizations or healthcare institutions. These guidelines provide evidence-based guidelines for clinical practice and can help identify areas where further research is needed.
- Research databases
Explore research databases such as PubMed, CINAHL, and the Cochrane Library to find the latest studies and systematic reviews. These databases can help you identify gaps in the literature and areas where further research is needed.
- Clinical Experts
Consult with clinical experts in your practice area. These experts may have insights into areas where further research is needed or may provide guidance on areas of practice that may benefit from an EBP project.
- Quality Improvement Projects
Review quality improvement projects that have been implemented in your healthcare facility. These projects may identify areas where further research is needed or identify gaps in the literature that could be addressed in an EBP project.
- Patient and family feedback
Consider patient and family feedback to identify areas where further research is needed. Patients and families can provide valuable information about areas of nursing practice that can be improved or that could benefit from further research.
Remember, when searching for ideas for EBP nursing research projects, it is important to consider the potential impact on patient care and outcomes. Select a topic that has the potential to improve patient outcomes and consider the feasibility of the project in terms of time, resources, and access to data. By choosing a topic that matches your interests and goals and is feasible at your institution, you can conduct a meaningful and productive EBP research project in nursing.
Nursing EBP Topics You Can Use in Your Essay
Here are some of the latest evidence-based practice nursing research topics that you can use in your essay or explore further in your own research:
- The impact of telehealth on patient outcomes in primary care
- The use of music therapy to manage pain in post-operative patients
- The effectiveness of mindfulness-based stress reduction in reducing stress and anxiety in healthcare workers
- Combating health care-associated infections: a community-based approach
- The impact of nurse-led discharge education on readmission rates for heart failure patients
- The use of simulation in nursing education to improve patient safety
- The effectiveness of early mobilization in preventing post-operative complications
- The use of aromatherapy to manage agitation in patients with dementia
- The impact of nurse-patient communication on patient satisfaction and outcomes
- The effectiveness of peer support in improving diabetes self-management
- The impact of cultural competence training on patient outcomes in diverse healthcare settings
- The use of animal-assisted therapy in managing anxiety and depression in patients with chronic illnesses
- The effectiveness of nurse-led smoking cessation interventions in promoting smoking cessation among hospitalized patients
- Importance of literature review in evidence-based research
- The impact of nurse-led care transitions on hospital readmission rates for older adults
- The effectiveness of nurse-led weight management interventions in reducing obesity rates among children and adolescents
- The impact of medication reconciliation on medication errors and adverse drug events
- The use of mindfulness-based interventions to manage chronic pain in older adults
- The effectiveness of nurse-led interventions in reducing hospital-acquired infections
- The impact of patient-centered care on patient satisfaction and outcomes
- The use of art therapy to manage anxiety in pediatric patients undergoing medical procedures
- Pediatric oncology: working towards better treatment through evidence-based research
- The effectiveness of nurse-led interventions in improving medication adherence among patients with chronic illnesses
- The impact of team-based care on patient outcomes in primary care settings
- The use of music therapy to improve sleep quality in hospitalized patients
- The effectiveness of nurse-led interventions in reducing falls in older adults
- The impact of nurse-led care on maternal and infant outcomes in low-resource settings
- The use of acupressure to manage chemotherapy-induced nausea and vomiting
- The effectiveness of nurse-led interventions in promoting breastfeeding initiation and duration
- The impact of nurse-led palliative care interventions on end-of-life care in hospice settings
- The use of hypnotherapy to manage pain in labor and delivery
- The effectiveness of nurse-led interventions in reducing hospital length of stay for surgical patients
- The impact of nurse-led transitional care interventions on readmission rates for heart failure patients
- The use of massage therapy to manage pain in hospitalized patients
- The effectiveness of nurse-led interventions in promoting physical activity among adults with chronic illnesses
- The impact of technology-based interventions on patient outcomes in mental health settings
- The use of mind-body interventions to manage chronic pain in patients with fibromyalgia
- Optimizing the clarifying diagnosis of stomach cancer
- The effectiveness of nurse-led interventions in reducing medication errors in pediatric patients
- The impact of nurse-led interventions on patient outcomes in long-term care settings
- The use of aromatherapy to manage anxiety in patients undergoing cardiac catheterization
- The effectiveness of nurse-led interventions in improving glycemic control in patients with diabetes
- The impact of nurse-led interventions on patient outcomes in emergency department settings
- The use of relaxation techniques to manage anxiety in patients with cancer
- The effectiveness of nurse-led interventions in improving self-management skills among patients with heart failure
- The impact of nurse-led interventions on patient outcomes in critical care settings
- The use of yoga to manage symptoms in patients with multiple sclerosis
- The effectiveness of nurse-led interventions in promoting medication safety in community settings
- The impact of nurse-led interventions on patient outcomes in home healthcare settings
- The role of family involvement in the rehabilitation of stroke patients
- Assessing the effectiveness of virtual reality in pain management
- The impact of pet therapy on mental well-being in elderly patients
- Exploring the benefits of intermittent fasting on diabetic patients
- The efficacy of acupuncture in managing chronic pain in cancer patients
- Effect of laughter therapy on stress levels among healthcare professionals
- The influence of a plant-based diet on cardiovascular health
- Analyzing the outcomes of nurse-led cognitive behavioral therapy sessions for insomnia patients
- The role of yoga and meditation in managing hypertension
- Exploring the benefits of hydrotherapy in post-operative orthopedic patients
- The impact of digital health applications on patient adherence to medications
- Assessing the outcomes of art therapy in pediatric patients with chronic illnesses
- The role of nutrition education in managing obesity in pediatric patients
- Exploring the effects of nature walks on mental well-being in patients with depression
- The impact of continuous glucose monitoring systems on glycemic control in diabetic patients
The Importance of Incorporating EBP in Nursing Education
Evidence-based practice is not just a tool for seasoned nurses; it’s a foundational skill that should be integrated early into nursing education. By doing so, students learn the mechanics of nursing and the rationale behind various interventions grounded in scientific research.
- Bridging Theory and Practice:
Introducing EBP in the curriculum helps students bridge the gap between theoretical knowledge and clinical practice. They learn how to perform a task and why it’s done a particular way.
- Critical Thinking:
EBP promotes critical thinking. By regularly reviewing and appraising research, students develop the ability to discern the quality and applicability of studies. This skill is invaluable in a rapidly evolving field like healthcare.
- Lifelong Learning:
EBP instills a culture of continuous learning. It encourages nurses to regularly seek out the most recent research findings and adapt their practices accordingly.
- Improved Patient Outcomes:
At the heart of EBP is the goal of enhanced patient care. We ensure patients receive the most effective, up-to-date care by teaching students to base their practices on evidence.
- Professional Development:
Familiarity with EBP makes it easier for nurses to contribute to professional discussions, attend conferences, and conduct research. It elevates their professional stature and opens doors to new opportunities.
To truly prepare nursing students for the challenges of modern healthcare, it’s essential to make EBP a core part of their education.
In summary, evidence-based practice nursing is an essential component of providing quality patient care. As a nurse, it is important to stay up to date on the latest research in the field and incorporate evidence-based practices into your daily work. Choosing a research topic that aligns with your interests and addresses a gap in the literature can lead to valuable contributions to the field of nursing.
When it comes to finding EBP project ideas, there are many sources available, including professional organizations, academic journals, and healthcare conferences. By collaborating with colleagues and seeking feedback from mentors, you can refine your research question and design a study that is rigorous and relevant.
The nursing evidence-based practice topics listed above provide a starting point for further exploration and investigation. By studying the effectiveness of various nursing interventions and techniques, we can continue to improve patient outcomes and deliver better care. Ultimately, evidence-based practice nursing is about using the best available research to inform our decisions and provide the highest quality care possible to our patients.
📎 Related Articles
1. Top Nursing Research Topics for Students and Professionals 2. Nursing Debate Topics: The Importance of Discussing and Debating Nursing Issues 3. Mental Health Nursing Research Topics: Inspiring Ideas for Students 4. Top Nursing Argumentative Essay Topics: Engage in Thought-Provoking Debates 5. Top Nursing Topics for Discussion: Engaging Conversations for Healthcare Professionals 6. Exploring Controversial Issues in Nursing: Key Topics and Examples 7. Pediatric Nursing Research Topics for Students: A Comprehensive Guide
Table of content
Crafted with Care:
Nursing Essays!
Precision, Passion, & Professionalism in Every Page.

Presentations made painless
- Get Premium
103 Evidence Based Practice Essay Topic Ideas & Examples
Inside This Article
Evidence-based practice (EBP) is a crucial component of modern healthcare, as it involves using the best available evidence to make informed clinical decisions. In order to promote the use of EBP in the healthcare field, it is important for students and professionals to have a thorough understanding of the concept and its applications. One effective way to do this is through writing essays on EBP topics.
To help you get started, here are 103 evidence-based practice essay topic ideas and examples:
- The importance of evidence-based practice in healthcare
- The history and evolution of evidence-based practice
- The barriers to implementing evidence-based practice in healthcare settings
- The role of research in evidence-based practice
- The impact of evidence-based practice on patient outcomes
- The ethical considerations of evidence-based practice
- The role of healthcare providers in promoting evidence-based practice
- The benefits of evidence-based practice for healthcare organizations
- The challenges of integrating evidence-based practice into clinical practice
- The relationship between evidence-based practice and patient-centered care
- The role of technology in supporting evidence-based practice
- The impact of evidence-based practice on healthcare costs
- The role of evidence-based practice in improving healthcare quality
- The importance of evidence-based practice in preventing medical errors
- The role of evidence-based practice in reducing healthcare disparities
- The impact of evidence-based practice on healthcare policy
- The relationship between evidence-based practice and clinical guidelines
- The role of evidence-based practice in nursing practice
- The benefits of evidence-based practice for patients
- The role of evidence-based practice in mental health treatment
- The impact of evidence-based practice on chronic disease management
- The role of evidence-based practice in improving medication adherence
- The relationship between evidence-based practice and shared decision making
- The role of evidence-based practice in health education
- The impact of evidence-based practice on public health initiatives
- The benefits of evidence-based practice for healthcare professionals
- The challenges of conducting evidence-based practice research
- The role of evidence-based practice in improving healthcare communication
- The impact of evidence-based practice on healthcare disparities
- The relationship between evidence-based practice and health literacy
- The role of evidence-based practice in healthcare leadership
- The benefits of evidence-based practice for healthcare systems
- The challenges of implementing evidence-based practice in rural healthcare settings
- The role of evidence-based practice in emergency medicine
- The impact of evidence-based practice on healthcare decision making
- The relationship between evidence-based practice and healthcare innovation
- The role of evidence-based practice in improving healthcare outcomes
- The benefits of evidence-based practice for healthcare payers
- The challenges of using evidence-based practice in pediatric healthcare
- The role of evidence-based practice in improving healthcare access
- The impact of evidence-based practice on healthcare equity
- The relationship between evidence-based practice and health policy
- The role of evidence-based practice in healthcare quality improvement
- The benefits of evidence-based practice for healthcare administrators
- The challenges of implementing evidence-based practice in long-term care settings
- The role of evidence-based practice in improving healthcare efficiency
- The impact of evidence-based practice on healthcare regulation
- The relationship between evidence-based practice and healthcare ethics
- The role of evidence-based practice in healthcare communication
- The benefits of evidence-based practice for healthcare educators
- The challenges of using evidence-based practice in mental health settings
- The role of evidence-based practice in improving healthcare teamwork
- The impact of evidence-based practice on healthcare leadership
- The relationship between evidence-based practice and healthcare technology
- The role of evidence-based practice in healthcare decision making
- The benefits of evidence-based practice for healthcare researchers
- The challenges of implementing evidence-based practice in primary care settings
- The role of evidence-based practice in improving healthcare collaboration
- The impact of evidence-based practice on healthcare training
- The relationship between evidence-based practice and healthcare culture
- The role of evidence-based practice in healthcare advocacy
- The benefits of evidence-based practice for healthcare policymakers
- The challenges of using evidence-based practice in community healthcare settings
- The role of evidence-based practice in improving healthcare coordination
- The impact of evidence-based practice on healthcare information sharing
- The relationship between evidence-based practice and healthcare decision support
- The role of evidence-based practice in healthcare quality assurance
- The benefits of evidence-based practice for healthcare informatics
- The challenges of implementing evidence-based practice in global healthcare settings
- The role of evidence-based practice in improving healthcare transparency
- The impact of evidence-based practice on healthcare workforce development
- The relationship between evidence-based practice and healthcare financing
Want to create a presentation now?
Instantly Create A Deck
Let PitchGrade do this for me
Hassle Free
We will create your text and designs for you. Sit back and relax while we do the work.
Explore More Content
- Privacy Policy
- Terms of Service
© 2023 Pitchgrade

Best Evidence-Based Practice (EBP) Nursing Research Topics and Ideas

We have already explored as much as there is regarding evidence-based nursing in our comprehensive EBP paper-writing guide . A time comes in your nursing school journey, either at basic (ADN, LPN, or BSN) or advanced levels (MSN, DNP, or PhD), when you are required to select a suitable evidence-based practice nursing research topic, research, and write an evidence-based nursing paper, report, or white paper. The process for selecting the topic is more or less the same as when selecting a nursing dissertation topic or topic for a nursing capstone .
You have to go through the instructions, consider an area of nursing specialization that interests you, do some thorough research, reading, and analysis, come up with a few topics, and eliminate and remain with the most suitable topic for your EBP nursing paper. You can locate good EBP project ideas from course materials (readings, handouts, PPTs, and class notes), online blogs and websites (like NurseMyGrade), nursing textbooks, nursing journals and articles, and other online resources.
General, Current, and Latest Evidence-Based Nursing Topics
- Effects of evidence-based practice on the quality and safety of patients
- Attitudes and readiness for Evidence-Based Nursing Practice among newly hired nurses
- Engaging advanced practice nurses in evidence-based practice through an e-monitoring program
- Effectiveness of EBP practice guidelines in preventing adverse events in clinical settings
- The attitudes of nurses toward adhering to clinical guidelines regarding the management of various conditions
- Prevention of deep vein thrombosis (DVT) among surgical patients
- Effectiveness of warming interventions for women undergoing Cesarean Section
- Strategies for managing second-stage labor
- Effects of gum chewing and early mobilization on intestinal mobility after cesarean birth
- Therapeutic use of music in maternity wards post-cesarean section
- Strategies for preparing women for unplanned Cesarean birth
- Effectiveness of hydrotherapy during labor
- Strategies to implement skin-to-skin contact in the OR following Cesarean birth
- Benefits of the EBP Organizational culture and readiness scale
- Transferability, reach, and impact of the EBP Questionnaire
- Barriers and facilitators influencing the implementation of EBP in clinical settings
- Challenges to implementing EBP in healthcare systems
- The beliefs and competencies of medical-surgery nurses on EBP
- Effects of EBP courses on MSN and DNP students' attitudes and beliefs on EBP
- The impacts of gamification on EBP training among nursing students
- Strategies to promote evidence-based nursing practice among nursing students
- The link between knowledge of EBP and nurse job satisfaction
- Impacts of nursing ethics on evidence-based practice
- Strategies to address the implementation gap between practice, research, and knowledge in nursing
- Using social media to promote the dissemination of evidence-based practice
- Strategies for implementing and translating evidence-based practice
- Benefits of frequently training nursing staff on evidence-based practice
- Role of evidence-based practice in modeling professional nursing practice
- Strategies for enhancing utility and understanding of evidence-based practice during undergraduate nursing education
- Knowledge, attitude, beliefs, and use of evidence-based practice among registered pediatric nurses
- Improving the readiness of evidence-based practice in critical care units
- Strategies for improving evidence-based practice among registered nurses (RNs)
- Best strategies for assessing compliance to EBP guidelines for VAP prevention among ICU nurses
- Impacts of EBP guidelines on clinical decision-making
- Challenges in communicating research evidence and translating it to practice
- Effectiveness of SBAR Tool Implementation to advanced communication and collaboration in clinical settings
- Knowledge of EBP and the confidence of newly recruited nurses
- Role of evidence-based practice guidelines in maintaining competence among mental health nurses
- Impacts of teaching advanced evidence-based practice research in doctoral nursing programs
Evidence-Based Topics for Anesthesia
- Primary concerns in the process of extubation in the anesthesia settings
- Perceptions and attitudes of anesthesia professionals on digital anesthesia information management system
- Benefits of nurse anesthetist perioperative dialog
- Causes of high attrition rates and turnover among nurse anesthetists
- Perceptions and attitudes of nurses on automatic dispensing cabinets
- Strategies for translating evidence-based research into anesthesia practice
- Addressing challenges associated with anesthesia in clinical settings
- Causes and solutions to anesthesia-associated mortality and morbidity
- An evidence-based approach to airway management via anesthesia administration
- Attitudes, knowledge, skills, and use of anesthesia teams toward EBP practice in clinical settings
- Why anesthetists are hesitant to implement ERAS guidelines
Related read: How to complete Shadow Health Assessments .
Cardiovascular and Respiratory Evidence-Based Topics
- Improving the quality of cardiovascular care through evidence-based practice
- Addressing social determinants of health as a means of addressing cardiovascular diseases
- Effects of listening to music during cardiac rehabilitation on clinical outcomes
- Effectiveness of physical activity on cardiovascular health
- Role of physical therapists in the management of venous thromboembolism
- Effectiveness of aerobic exercise training in improving aerobic capacity after heart transplant
- Impacts of guarding on the outcomes of the 6-minute walk test
- Role of Mitsungumin 53 in cardiovascular diseases (CVD)
- Effects of autophagy on the cardiovascular system
- The ethics of using embryonic stem cells in cardiovascular research
- Use of telehealth in early detection of anxiety and depression in post-coronary patients
- Effectiveness of indoor allergen reduction in the management of asthma
- Non-invasive technologies for diagnosing coronary artery disease in women
- Impacts of smoking on the lungs of a fetus
- Strategies to address obstructive sleep apnea and cardiovascular disease
- The link between consuming fatty animal meat and cardiovascular health
- Benefits of prone positioning for patients with ARDS
- Response of COPD to prophylactic antibiotics
- Evidence-based nursing strategies for the prevention of contrast-induced acute kidney injury
- Impacts of home monitoring on COPD patients
Complementary and Alternative Medicine Evidence-Based Topics
- The link between probiotics use and diarrhea
- The effectiveness of vitamin C in the prevention of complex regional pain syndrome following wrist fractures
- The link between using essential oils and hypertension
- Effectiveness of cranberry products for the treatment of UTIs
- Effectiveness of botulism toxin in the treatment of restless legs syndrome
- Using therapeutic honey in tropical wound management
- Impacts of scalp cooling on alopecia among cancer patients
- Effects of spiritual beliefs on type 2 diabetes mellitus patients
- Effects of aromatherapy in the management of depression and anxiety
- Non-pharmacologic interventions for treatment-resistant depression among adolescents
Nursing Ethics Evidence-Based Topics
- Effects of abandonment on nursing staff shortage
- Effects of negligence on patient outcomes
- AI ethics awareness, attitudes, and beliefs, and the behavioral intentions of nursing students
- Attitudes and perspectives of nursing faculty on noncompliance with ethics in nursing academic environments
- Application of Nightingale's professionalism among student nurses
- Influence of nursing ethics on clinical decision-making
- Perceptions and awareness of student nurses on social justice in the healthcare system
- Benefits of increased ethical competency of nurses in clinical settings
- Ethical problems of clinical nursing practice
- Factors influencing professionalism in nursing among Registered Nurses
- Information literacy and ethical decision-making among nurses
- The link between clinical dishonesty and perceived clinical stress among nursing students
- Strategies to help nurses handle compassion fatigue
- Ethical perspectives of evidence-based practice
- Influence of laws and Legislation on evidence-based practice
- Moral distress among Registered Nurses
- Barriers and facilitators of addressing nursing research ethics
- Role of nursing ethics in the implementation of evidence-based practice
Family Practice Evidence-Based Topics
- The significance of genetic counseling in diabetes prevention
- Challenges for contraception for women with diabetes
- Management of autism in children
- Diagnosis, treatment, and management of psoriasis
- Using a gluten-free diet to improve outcomes in patients with psoriasis
- The link between psoriasis and cardiovascular diseases
- Impacts of nutritional counseling on the BMI of patients
- Using Metformin over Sulfonylurea for initial treatment of gestational diabetes
- Best ways to diagnose menopause in perimenopausal women
- Dinoprostone vs. vaginal misoprostol in labor induction: which is better?
- Effectiveness of using narcotics to treat patients with chronic daily headaches
- Vitamins and cognitive decline in Alzheimer's disease
- The link between regular family dinners and obesity in adolescent patients
- Is the Mediterranean diet better for bone health?
- Benefits of self-managed diabetes programs
- Is acupuncture effective in the treatment of allergic rhinitis?
- The link between antibiotic use and acute sinusitis
- Effectiveness of Flu vaccine on prevention of community-acquired pneumonia
- The link between male obesity and infertility
- Lower back pains and NSAIDS
- Seasonal Nasal Irrigation and Seasonal Allergic Reactions: Best management strategies
- Effectiveness of abortive treatment for acute migraine
- Effectiveness of combination treatment for hepatitis C
- Benefits of tailored education for melanoma management
- Genetic testing and obesity
- Treatment and management of atopic dermatitis
Nursing Forensics Evidence-Based Topics
- Strategies to document injuries from domestic violence abuse by forensic nurses
- Perceptions of forensic nurses on victim counseling before post-domestic violence cases
- Stress management and coping strategies in prison settings
- Mental health as a risk factor for sexual assault
- Barriers and challenges to implementing remote sexual assault nurse examiner programs
- Limit setting and de-escalation in forensic mental health units
- The risk factors for domestic minor sex trafficking in the USA
- Benefits of sexual assault nurse examiners practicing trauma-informed care
- Ethical issues involved during forensic nursing investigations
- Strategies for preparing victims of sexual assault to be witnesses in courts of law
- Role of forensic nurses in combating human and sexual trafficking
- The link between sexual assault and suicide
- Strategies to handle compassion fatigue among forensic nurses
- Strategies for emergency contraception administration among the SANE and non-SANE medical providers
- Strategies forensic nurses use to resolve difficulties in supporting offenders with mental health disorders
- Role of forensic nurses in addressing challenges for children in foster care
- Forensic nursing interventions for patients with personality disorders
- Application of telehealth among sexual assault forensic examiners
- Strategies for handling children facing maltreatment from parents
- Interprofessional collaboration to optimize trauma-informed care
- Role of pediatric forensics in clinical settings
- Role of forensic nurses in abortion investigations
- Steps and evidence-based methods for screening children for neglect or abuse
- Strategies for solving burnout among forensic nurses
- Role of forensic nurses in death investigations
- Attitudes of Sexual Assault Nurse Examiners (SANE) toward sexual assault victims
- Methods for promoting resilience, competence, and quality of life of Sexual Assault Nurse Examiners
- Role of correctional nurses in advocating for pregnant women's rights in prison
- An evidence-based approach to suicide risk assessment following sexual assault
Gastroenterology Evidence-Based Topics
- The use of probiotics to treat and manage irritable bowel syndrome (IBS)
- Using behavioral therapy adjunct to drug therapy in the management of urinary incontinence
- Pharmacological strategies for the management of Crohn's disease
- Complementary alternative medicine approaches to the management of Gastroesophageal Reflux Disease (GERD)
- Intermittent fasting among obese women and the management of pylori
- Homemade solutions for constipation among pregnant women
Geriatrics or Long-Term Care Evidence-Based Topics
- The effectiveness of the North Dakota Association of director of Nursing Administration (NADONA) /Long-Term Care standards of Practice in managing long-term care facilities
- Strategies to encourage elderly people to age in place
- Methods to improve drug adherence among elderly patients with Alzheimer's disease
- Methods for managing polypharmacy among elderly adults
- Design strategies to address falls for patients aging in place
- Use of technology to address the challenges of elderly adults who choose to age in place
- Benefits of music therapy for patients with Multiple Sclerosis
- Strategies for addressing pressure ulcers among the elderly
- Benefits of teaching self-care practices to elderly patients with long-term in-dwelling catheter
- Using stories to entertain and give hope to elderly patients in long-term care facilities
- Multifactorial approach towards management of falls in long-term care facilities
Hospital-Acquired Infections Evidence-Based Topics
- Effectiveness of hand hygiene in reducing hospital-acquired infections
- Strategies to prevent blood contamination and infection during transfusion
- The value of Central Line-Associated Bloodstream Infection Bundle Compliance in preventing CLABSI
- Impacts of implementing central nervous catheter bundle in reducing central line-associated bloodstream infections (CLABSI)
- The knowledge and attitudes of nurses on evidence-based guidelines for the prevention of surgical site infections
- Benefits of governments supporting nursing homes in infection management
- How effective are leadership rounds in reducing healthcare-associated infections?
- Knowledge, beliefs, and attitude of newly graduated nurses on infection prevention and control
- Evidence-based strategies to prevent ventilator-associated pneumonia
- Perceptions of NICU nurses regarding measures to prevent HAIs
- The role of chlorhexidine gluconate bathing in preventing HAIs
- Importance of communication networks in the management of infections in ICUs
- Strategies to reduce catheter-associated urinary tract infections (CAUTIs)
- The perspectives and experiences of patients on HAIs
- Nurse-led quality improvement interventions to reduce hospital-acquired infections in the NICU
- Using a multimodal approach to institute hand hygiene
- The correlation between hospital length of stay and acquiring infections
- Evidence-based strategies to prevent nosocomial infections in clinical settings
- Value of e-learning for preventing healthcare-associated infections
- Impacts of nurse burnout and shortage on HAIs
- Core components of an infection prevention and control program for a nursing home
- Leadership skills of the APRNs and prevention of HAIs
- The motivations of healthcare workers to reduce HAIs
- Hand hygiene knowledge and beliefs among newly recruited nurses
- Impacts of hospital design on HAIs
- Overcrowding in the ER and hospital-acquired infections
- Effects of training on nurses' knowledge and skills in indwelling urinary catheters in preventing CAUTIs
- Low rates of Influenza vaccination among nurses and HAIs
- Role of environmental cleaning in the control of HAIs
- Green cleaning and HAIs
- Compliance with Chlorhexidine wipes to prevent Hospital-acquired infections
- The knowledge of nurses of the WHO Five Moments of Hand hygiene and HAIs in the Operating rooms
Nursing Education Evidence-Based Topics
- Effectiveness of situated e-learning on medical and nursing education
- Benefits of cultural competence training among nurses on the patient satisfaction
- Experiences and attitudes of student nurses on formal preceptor programs
- The effectiveness of using virtual and augmented reality in nursing education
- Strategies to attract, train, and retain student nurses until retirement
- The application of gamification in nursing training
- Should nurses be taught basic coding concepts?
- Inclusion of LGBTQ student nurses in clinical settings
- The use of social media to facilitate learning among nursing students
- Benefits of introducing students to reflective nursing practice
- Benefits of e-learning for nursing education
- Online nursing programs as a means to prepare nurses for leadership roles
- The nurse training pipeline is an essential aspect of addressing nurse shortages
- Discrimination among nurse student acceptance of some programs/nursing schools
- Factors affecting the progress of nursing students in the USA
- Should the nursing career be ubiquitous globally?
- Student nurses should join professional organizations that advocate for their rights
- Steps to improve collaboration and teamwork among nurse students
Pain Management Evidence-Based Topics
- Effectiveness of ERAS in postoperative pain management
- Non-pharmacological methods and perceived barriers in pain management by nurses
- Psychological and behavioral pain management strategies in pediatric oncology departments
- Mindfulness mediation as a strategy for chronic pain management
- Impacts of relaxation techniques for pain management during labor
- The efficacy of cannabis-based medicines for pain management
- Use of music therapy during labor
- Impacts of massage therapy on cancer pain management
- The effectiveness of craniosacral therapy for chronic pain management
- Effectiveness of manual therapy vs. exercise therapy in the management of adult neck-pain
- Non-pharmacological pain management approaches for cancer patients
- Music-induced analgesia in chronic pain management
- The effectiveness of transcutaneous electric nerve stimulation for cancer pain
- The efficacy of acupuncture in the management of postoperative pain
- The application of cannabinoids in pain management
- Acupressure for pain management during labor
Pediatrics Evidence-Based Topics
- Practical strategies for preventing failure to rescue obstetric patients
- Effectiveness of neonatal pain management via oral sucrose
- Benefits of nutritional assessment and intervention in a pediatric oncology unit
- Strategies to manage inguinal hernias in children
- Impacts of clinical settings appearance on the anxiety of kids in cancer care facilities
- Evidence-based strategies for the management of the acute phase of Kawasaki disease
- Strategies to address diabetes ketoacidosis among pediatric patients
- The use of virtual reality in managing anxiety among pediatric patients
- The use of probiotics in the prevention of diarrhea among children
- The efficiency of using gastronomy tubes among pediatric patients
- Best strategies to treat and manage infant colic
- Management of ventilator-associated pneumonia (VAP) among neonates and children
- Strategies parents can use to cope during acute pediatric hospitalizations
- Strategies to address childhood constipation
- Strategies to prevent SIDS during breastfeeding
- The safety of corticosteroids in young children with acute respiratory conditions
- Management of hospital-acquired venous thromboembolism in pediatric patients
- Efficacy of insertion and maintenance bundles in preventing central-line associated bloodstream infections in critically ill pediatric patients
- Prevalent and management strategies for burnout among pediatric nurses
- The efficacy of magnesium supplementation in addressing postoperative arrhythmias after cardiopulmonary bypass among pediatric patients
As we come to the End of this Article '
You can select a topic among the ones we have listed above or get inspired to select a topic whose research direction interests you. If you need unique topics, kindly place a one-page order and get 3-4 topics researched, suggested, and listed by an expert based on your preferences.
Nobody understands evidence-based nursing practice more than our online nursing writers. Through the years, we have helped students at the ADN, BSN, MSN, DNP, and Ph.D. nursing levels access unique and exciting evidence-based topics. What's more, if you need help writing an evidence-based practice paper (report, term paper, change project, thesis, research paper, or dissertation), our astute writers can help you. You will get a 100% original, well-formatted (in APA or Harvard format), and edited paper that meets your rubric requirements.
Struggling with
Related Articles
Integrating Spiritual Texts in a Nursing Paper (A Guide)
Making Concept Map for Nursing School : A Nursing Student's guide

Tips for Passing NCLX RN exam on first attempt
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
📕 Studying HQ
Evidence based practice nursing topics and ideas, rachel r.n..
- May 28, 2024
- Essay Topics and Ideas
Evidence-based practice (EBP) is a systematic approach to clinical decision-making that integrates the best available research evidence with a nurse’s clinical expertise and patient preferences and values. It involves the ongoing process of formulating clinical questions, searching and critically appraising relevant research, and applying the findings to improve patient care.
What You'll Learn
key components of EBP
- Best Research Evidence: This includes findings from high-quality research studies, such as randomized controlled trials, systematic reviews, and meta-analyses, as well as clinical practice guidelines developed by reputable organizations. These sources provide reliable information about the effectiveness, risks, and benefits of various interventions, treatments, or nursing practices.
Example: A systematic review and meta-analysis of multiple studies may provide strong evidence that early mobilization after surgery reduces the risk of postoperative complications and shortens hospital stays.
- Clinical Expertise: Nurses bring their cumulative knowledge, skills, and experience to the decision-making process. This expertise allows them to interpret and apply research evidence in the context of individual patient situations, taking into account factors such as comorbidities, psychosocial considerations, and available resources.
Example: A nurse with extensive experience in wound care may use their expertise to appropriately modify an evidence-based dressing protocol based on a patient’s specific wound characteristics or risk factors.
- Patient Preferences and Values: Effective EBP considers the unique needs, preferences, cultural beliefs, and values of each patient. By involving patients in the decision-making process and respecting their autonomy, nurses can provide care that aligns with the patient’s goals and values.
Example: A patient with a strong preference for complementary therapies may choose to incorporate evidence-based practices like aromatherapy or music therapy alongside conventional treatments, if appropriate and supported by research.
Importance of Evidence-Based Practice in Nursing
Implementing EBP in nursing has several crucial benefits:
- Improved Patient Outcomes: By relying on interventions and practices that have been proven effective through high-quality research, nurses can provide care that is more likely to achieve positive patient outcomes, such as faster recovery times, reduced complications, better symptom management, and improved quality of life.
- Consistency and Quality of Care: EBP promotes the delivery of consistent, high-quality care across different healthcare settings by standardizing practices based on the best available scientific evidence. This helps reduce variation in care and ensures that patients receive the most appropriate and effective interventions, regardless of where they are treated.
- Cost-Effectiveness: EBP can help reduce the use of ineffective or unnecessary interventions, leading to more efficient allocation of healthcare resources and potential cost savings for patients, healthcare organizations, and society as a whole.
- Professional Development: Engaging in EBP encourages nurses to continuously learn, update their knowledge, and develop critical thinking and research appraisal skills, contributing to their professional growth and advancement.
- Evidence-Based Policies and Guidelines: Findings from EBP can inform the development of evidence-based policies, protocols, and clinical practice guidelines at the organizational or national level, promoting standardization and quality improvement across the healthcare system.
Steps in Evidence-Based Practice
The EBP process typically involves the following steps:
- Formulating a Clinical Question: Nurses start by identifying a specific patient problem, clinical issue, or knowledge gap and formulating a clear, answerable question using frameworks like PICO (Patient, Intervention, Comparison, Outcome) or PICOT (adding Time).
Example: In postoperative patients (P), how does the use of multimodal analgesia (I) compared to single-agent pain medication (C) affect pain levels and opioid-related side effects (O) within the first 48 hours after surgery (T)?
- Searching for Evidence: Nurses conduct systematic searches of relevant databases, such as PubMed, CINAHL, Cochrane Library, or discipline-specific databases, to find the most current and reliable research evidence related to their clinical question. They may also consult evidence-based practice guidelines, systematic reviews, and other secondary sources.
- Critically Appraising the Evidence: Nurses evaluate the quality, validity, and relevance of the research studies or guidelines they have found. This involves assessing factors such as study design, sample size, methodology, potential biases, statistical analyses, and the strength of the findings. Critical appraisal tools, like those developed by the Joanna Briggs Institute or the Critical Appraisal Skills Programme (CASP), can aid in this process.
- Integrating the Evidence: After appraising the evidence, nurses synthesize the findings and integrate them with their clinical expertise and patient preferences to make informed clinical decisions. This may involve weighing the potential benefits and risks of different interventions, considering patient values and goals, and determining the most appropriate course of action.
Example: Based on the evidence, a nurse might recommend a multimodal approach combining pharmacological (e.g., non-opioid analgesics) and non-pharmacological (e.g., ice packs, repositioning) interventions for effective postoperative pain management, while considering the patient’s preferences and risk factors.
- Implementing the Evidence: Nurses put the evidence-based intervention or practice into action, ensuring proper documentation, patient education, and monitoring of patient outcomes. This may involve developing protocols, training staff, and establishing systems for consistent implementation.
- Evaluating Outcomes: Nurses assess the effectiveness of the implemented intervention or practice by measuring and evaluating relevant patient outcomes, such as pain levels, functional status, quality of life, or adverse events. This evaluation may involve collecting data through patient self-reports, clinical assessments, or objective measures.
- Disseminating Findings: Nurses share their experiences and findings with colleagues through presentations, publications, or informal discussions, contributing to the body of nursing knowledge and promoting the continued advancement of EBP. This can help facilitate the adoption of successful evidence-based practices in other settings.
Example: A nurse-led EBP project implementing a new evidence-based protocol for preventing pressure injuries in the intensive care unit could be presented at a nursing conference or published in a peer-reviewed journal, allowing other healthcare organizations to learn from the experience and potentially adopt the protocol.
Related Articles Understanding the Different Types of Assignments in Detail
A Comprehensive Guide to Writing a Nursing Research Paper
Types of Assignment
100 potential evidence-based practice nursing topics
- Early mobilization strategies for postoperative patients
- Effective pain management approaches in the elderly
- Interventions to prevent catheter-associated urinary tract infections
- Strategies for reducing medication errors in nursing practice
- Wound care management for diabetic foot ulcers
- Effects of nurse-led discharge planning on hospital readmissions
- Interventions for preventing and managing delirium in hospitalized patients
- Approaches to improve medication adherence in chronic disease management
- Strategies for preventing falls in long-term care facilities
- Effectiveness of nurse-led education on self-management in chronic obstructive pulmonary disease
- Interventions for managing chemotherapy-induced nausea and vomiting
- Approaches to improve communication and shared decision-making with patients
- Strategies for promoting breastfeeding among new mothers
- Interventions for managing behavioral and psychological symptoms in dementia
- Effectiveness of early mobility protocols in intensive care units
- Approaches to improve pain management in pediatric patients
- Interventions for preventing and managing pressure injuries
- Strategies for improving sleep quality in hospitalized patients
- Effectiveness of nurse-led interventions for smoking cessation
- Approaches to manage anxiety and depression in cancer patients
- Interventions for promoting healthy weight management in nursing practice
- Strategies for improving medication reconciliation during care transitions
- Effectiveness of nurse-led interventions for diabetes self-management education
- Approaches to manage symptoms and improve quality of life in palliative care
- Interventions for promoting physical activity and exercise in older adults
- Strategies for preventing and managing delirium in the intensive care unit
- Effectiveness of nurse-led interventions for asthma management
- Approaches to improve patient education and self-care for chronic heart failure
- Interventions for promoting early mobilization in stroke patients
- Strategies for improving communication and collaboration in interprofessional teams
- Effectiveness of nurse-led interventions for managing chronic pain
- Approaches to improve infection control practices in healthcare settings
- Interventions for promoting healthy lifestyle behaviors in adolescents
- Strategies for improving medication management in older adults
- Effectiveness of nurse-led interventions for managing urinary incontinence
- Approaches to improve patient education and self-care for chronic kidney disease
- Interventions for promoting mental health and well-being in nursing practice
- Strategies for improving care coordination and transition planning
- Effectiveness of nurse-led interventions for managing osteoarthritis
- Approaches to improve patient education and self-care for chronic respiratory diseases
- Interventions for promoting healthy eating habits and nutrition in nursing practice
- Strategies for improving patient satisfaction and experience
- Effectiveness of nurse-led interventions for managing hypertension
- Approaches to improve patient education and self-care for chronic liver diseases
- Interventions for promoting physical activity and exercise in cardiac rehabilitation
- Strategies for improving communication and support for caregivers
- Effectiveness of nurse-led interventions for managing obesity
- Approaches to improve patient education and self-care for multiple sclerosis
- Interventions for promoting mental health and well-being in the workplace
- Strategies for improving end-of-life care and advance care planning
- Effectiveness of nurse-led interventions for managing rheumatoid arthritis
- Approaches to improve patient education and self-care for Parkinson’s disease
- Interventions for promoting healthy aging and preventing frailty
- Strategies for improving medication management in patients with cognitive impairment
- Effectiveness of nurse-led interventions for managing chronic obstructive pulmonary disease
- Approaches to improve patient education and self-care for inflammatory bowel diseases
- Interventions for promoting mental health and well-being in the LGBTQ+ community
- Strategies for improving care coordination for patients with complex medical conditions
- Effectiveness of nurse-led interventions for managing diabetes in pregnancy
- Approaches to improve patient education and self-care for epilepsy
- Interventions for promoting physical activity and exercise in patients with mental health disorders
- Strategies for improving medication management in patients with substance use disorders
- Effectiveness of nurse-led interventions for managing chronic kidney disease
- Approaches to improve patient education and self-care for lupus
- Interventions for promoting mental health and well-being in underserved communities
- Strategies for improving care coordination for patients with intellectual and developmental disabilities
- Effectiveness of nurse-led interventions for managing sickle cell disease
- Approaches to improve patient education and self-care for HIV/AIDS
- Interventions for promoting physical activity and exercise in patients with cancer
- Effectiveness of nurse-led interventions for managing chronic fatigue syndrome
- Approaches to improve patient education and self-care for fibromyalgia
- Interventions for promoting mental health and well-being in veterans and military personnel
- Strategies for improving care coordination for patients with rare diseases
- Effectiveness of nurse-led interventions for managing chronic pain in children
- Effectiveness of nurse-led interventions for managing chronic kidney disease in children
- Effectiveness of nurse-led interventions for managing sickle cell disease in children
- Approaches to improve patient education and self-care for HIV/AIDS in adolescents
- Interventions for promoting physical activity and exercise in patients with cancer during treatment
- Strategies for improving medication management in patients with cognitive impairment due to traumatic brain injury
- Effectiveness of nurse-led interventions for managing chronic fatigue syndrome in adolescents
- Approaches to improve patient education and self-care for fibromyalgia in older adults
- Interventions for promoting mental health and well-being in LGBTQ+ youth
- Strategies for improving care coordination for patients with rare diseases in rural areas
- Effectiveness of nurse-led interventions for managing chronic pain in children with developmental disabilities
- Approaches to improve patient education and self-care for multiple sclerosis in pregnancy
- Interventions for promoting physical activity and exercise in patients with mental health disorders during inpatient treatment
- Strategies for improving medication management in patients with substance use disorders and comorbid mental health conditions
- Effectiveness of nurse-led interventions for managing chronic kidney disease in patients with diabetes
- Approaches to improve patient education and self-care for lupus in underserved communities
- Interventions for promoting mental health and well-being in immigrants and refugees
- Strategies for improving care coordination for patients with intellectual and developmental disabilities in long-term care facilities
- Effectiveness of nurse-led interventions for managing sickle cell disease in adults
- Approaches to improve patient education and self-care for HIV/AIDS in older adults
Start by filling this short order form order.studyinghq.com
And then follow the progressive flow.
Having an issue, chat with us here
Cathy, CS.
New Concept ? Let a subject expert write your paper for You
Have a subject expert write for you now, have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, popular topics.
Business Analysis Examples Essay Topics and Ideas How to Guides Nursing
- Nursing Solutions
- Study Guides
- Free College Essay Examples
- Privacy Policy
- Writing Service
- Discounts / Offers
Study Hub:
- Studying Blog
- Topic Ideas
- How to Guides
- Business Studying
- Nursing Studying
- Literature and English Studying
Writing Tools
- Citation Generator
- Topic Generator
- Paraphrasing Tool
- Conclusion Maker
- Research Title Generator
- Thesis Statement Generator
- Summarizing Tool
- Terms and Conditions
- Confidentiality Policy
- Cookies Policy
- Refund and Revision Policy
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Contact Us:
📞 +15512677917
2012-2024 © studyinghq.com. All rights reserved
- Call to +1 844 889-9952
191 Evidence-Based Practice Research Topics & Essay Examples
📝 evidence-based practice research papers examples, 💡 essay ideas on evidence-based practice, 👍 good evidence-based practice essay topics to write about, 🏆 best evidence-based practice essay titles, 🎓 simple research topics about evidence-based practice, ❓ evidence-based practice research questions.
- Chronic Diseases: Evidence-Based Project Chronic diseases become one of the most threatening health issues all over the globe. In particular, insufficient health literacy unreasonably impacts older adults in the USA.
- Evidence-Based Clinical Intervention in Umbilical Hernia The role of organizational work as it is conducted in various modern companies is primarily determined by the qualifications of the employees performing specific duties.
- Contraceptive Options and Evidence-Based Prescription The purpose of this paper is to provide an evidence-based decision on which contraceptive option should be prescribed.
- Evidence-Based Practice in Nursing This study describes the importance of evidence-based projects in nursing, as it presents new ideas that can guide and empower future researchers to address issues in healthcare.
- Ask Clinical Question in Evidence-Based Nursing The PICOT format is beneficial to identify a clinical problem and pinpoint all details. It allows formulating the problem in a way that ensures attention to the intervention.
- Evidence-Based Practice for Obese African Americans Evidence-based nursing empowers clinicians to apply interventions that can address patients’ needs. This paper discusses how such practices can empower diabetic African Americans to manage the condition.
- Evidence-Based Nursing and Personal Philosophy This paper discusses the domains of nursing, the assumptions, and challenges associated with the practice, and goals for professional development.
- Evidence-Based Practice in the Clinical Setting Evidence-based practice models were created to describe the process of evaluating the evidence and implementing it in the clinical setting.
- Human Factor and Systems Management in Evidence-Based Practice Within the advanced nursing practice environment, the human factor is often considered a restricting phenomenon since it is prone to result in mistakes.
- Evidence-Based Nursing in Intensive Care Unit Evidence-based practice does not imply that nurses abandon the principles and knowledge obtained during training.
- Evidence-Based Practice in Intensive Care Unit Physicians must take part in Evidence-Based Practice in an ICU in order for them to give high quality services to their clients.
- Information Systems for Evidence-Based Practice Information systems can be viewed as a part of the evidence-based practice since their introduction in nursing processes tends to enhance the latter.
- Evidence-Based Care in Intensive Treatment Unit The nurse manager should make the nurse understand that research does not prevent him/her from practicing his/her profession in any way.
- Evidence-Based Nursing in Intensive Therapy Unit EBP is not a separate practice from nursing; in fact, it is based on the core teachings of nursing in which nurses are supposed to provide personalized care.
- Case Management Programs and Evidence-Based Practice Strategies for expanding an evidence-based program include concentrating on the practitioner’s experience and search and application of the most recent evidence.
- Hospital Readmission Prevention: Study Design The problem of high readmission rates among patients with chronic heart failure (CHF) is a pressing issue in modern nursing practice.
- Hypertensive Patients' Education and Evidence-Based Care The PICOT question concerns educational protocol and counselling sessions for hypertensive patients who fail to follow treatment rules.
- Elderly Education and Evidence-Based Care The research explores whether in elderly patients with chronic diseases patient education compared to only medication treatments improves their health status.
- “Baby Blues” or Postpartum Depression and Evidence-Based Care Want to learn about postpartum depression and a picot question format? 😐 Read this article to get to know more about the topic! ➞ Here you’ll also find great paper samples for students! 📝
- Evidence-Based Practice Adoption and Barriers The recommendations made in this study are significant to nursing because they explain what nurses should do to apply EBP in their respective places of work.
- Evidence-Based Practice and Barriers to Its Implementation Evidence-based practice (EBP) comprises five major steps: identifying practice needs and formulating a relevant question, searching for the best available evidence,
- Patient Portals in Evidence-Based Practice With functioning patient portals, patients are more likely to follow treatment plans because they can log in at any time and view instructions given by primary care providers.
- Hypothermia Therapy in Evidence-Based Practice Hypothermia therapy is recognized to be effective when applying to trauma patients with serious injuries leading to decrease of mortality cases.
- Telehealth for Cardiac Patients: Change Model The program for helping patients with CHF via the telehealth protocol and aimed at reducing the level of readmission can be useful.
- Evidence-Based Practice in Nursing Care Evidence-based practice (EBP) is gaining more and more important both in scholarly research and professional environment.
- Pressure Ulcers Evidence-Based Management Proper patient care is the basis and key to the successful treatment of PUs; for that reason, it is necessary to employ effective nursing interventions to combat the problem.
- Diabetes Evidence-Based Treatment Outcomes Diabetes is associated with a decline in health-related quality of life, so after the intervention, it is reasonable to expect improvements in several areas.
- Hospital Readmissions Evidence-Based Care Project Possible interventions that could change patient outcomes include weekly home visits, post-discharge telephone counseling, drug counseling, and cognitive approaches.
- Breast Cancer Detection: Evidence-Based Project The research is expected to expand the knowledge on the role of healthcare specialists in the early detection of breast cancer in adult women belonging to minority groups.
- Evidence-Based Nursing Practice in the United States The concept of caring undergoes certain contributions and improvement safety is promoted through high education, evidence-based practice, and the exchange of experience.
- APN Clinical Roles, Evidence-Based Strategies for Achieving Continuity The paper describes the changing landscape of nursing requires improved services and an assessment of nurses’ skills and competencies is required.
- Breastfeeding: Evidence-Based Project Results The study compares breastfeeding and the use of the formula in regard to the effects on a child’s propensity toward contracting gastroenterological infections.
- Clinical Point of Care and Evidence-Based Practice The paper investigates whether point-of-care clinicians benefit from training on research aspects and the impact of the same on evidence-based practice.
- Evidence-Based Geriatric Nursing Protocols for Best Practice To support the patient and provide the necessary portion of help, the referral to geriatric medicine is required.
- Application of Analytic Methods: Using the Johns Hopkins Nursing Evidence-Based Practice Individual Evidence Summary Tool The issue of patient falls remains a problem for modern using, yet the integration of patient and nurse education techniques will help to counteract the current situation with fall management.
- Refinement of a Nursing Concern Into an Evidence-Based Practice: Formula vs. Human Milk During Infancy and Gastrointestinal Complications The investigation of the connection between feeding and gastrointestinal infections with the help of the evidence-based practice and the theory of planned behavior has its positive outcomes in nursing.
- Chronic Pulmonary Obstructive Disease: Evidence-Based Integration Chronic pulmonary obstructive disease (COPD) is a serious condition characterized by airflow blockage and various breathing-related problems.
- Geriatric Diabetes Management: Evidence-Based Project The presence of diabetes may provoke several complications such as an increase in the levels of blood sugar and blood glucose.
- Asthma in Evidence-Based Practice In patients with asthma, the disease causes the inflammation of air passages followed by the significant narrowing of airways.
- Evidence-Based Practice and Quality Organizations The paper discusses governmental agencies and non-governmental organizations for evidence-based practice, quality improvement, and patient safety.
- “Acupuncture and Moxibustion as an Evidence-Based Therapy for Cancer” by William Cho “Acupuncture and Moxibustion as an Evidence-Based Therapy for Cancer” by William Cho shows us both the negative and positive sides of acupuncture and moxibustion.
- Importance of Nursing Research and Evidence-Based Practice Nursing research involves looking for ways of improving the provision of health care services and maintaining professional conduct.
- Evidence-Based Practice Interventions for Diabetes: CLC Assignment in Nursing Looking for evidence-based practice interventions for diabetes? ➤ Read our project paper example to ✅ learn about mobile health interventions in diabetes care.
- Research, Evidence-Based Practice, and Quality Improvement Evidence-based practice (EBP), research, and quality improvement are useful methods to enhance patient outcomes.
- Evidence-Based Practice Change in Nursing At the present time, low nurse staffing rates are concerned with the increased reports of missed care, with chronic illnesses often being left unnoticed because they are not urgent.
- Evidence-Based Practice Beliefs and Implementation. Article Critique The article "Evidence-based practice beliefs and implementation" addresses the problem of evidence-based practice knowledge, beliefs, and implementation in oncology nurses.
- Evidence-Based Practice (EBP) and Global Health Even though Evidence Based Practice has led to considerable improvements in healthcare in general and nursing in particular, the concept of informed instruction.
- Evidence Based Practices in Care Delivery According to Burns and Grove (2010), various methods have been proposed to use to expand the use of evidence based practices in healthcare care delivery.
- Evidence-Based Nursing Practice in Future The significance of the evidence-based practice as the foundation for the further development of the healthcare field can hardly be underrated.
- Evidence-Based Medicine Skills for Healthcare Professionals The following paper is an analysis of key elements of a systematic peer-reviewed article. The analysis includes the validity and reliability of the study.
- The Evidence-Based Practice in Nursing The purpose of the study was to present the nurses’ attitudes and perceptions of their skills regarding the use of evidence-based practices in the administration of healthcare.
- Evidence-Based Practice in Nursing The purpose of the paper is to review peer-reviewed articles to get a better understanding of the relationship between nursing and evidence-based practice.
- Acute Stroke: An Evidence-Based Practice The study uses a pretest/post-test research design, with the aim to improve the quality of care provided by nurses to patients presenting in emergency department settings with acute stroke.
- Evidence-Based Practices for Deep Vein Thrombosis Prevention This paper develops an in-depth analysis of the use and application of evidence-based practice in the management and prevention of deep vein thrombosis.
- The Evidence-Based Practice in Nursing Nurses use evidence-based practice to treat and guide patients. They use EBP to evaluate different medical interventions and settle for the most effective.
- Critique of the Evidence-Based Practice in Pre-Hospital Delay The objective of the article is that of demonstrating several reasons for the extended pre-hospital delay in patients suffering from myocardial infarction.
- “Practice Nurse Use of Evidence in Clinical Practice”: The Integration of Evidence-based Practice This paper is a critique of a “Practice Nurse Use of Evidence in Clinical Practice” article aimed at evaluating influential factors to the integration of Evidence-based Practice.
- Evidence-Based Practice (EBP) & Global Health Health care provisions vary significantly across the world. This paper will analyse the global EBP and highlight the gaps that exist in its application.
- Evidence-Based Practice Among Faculty Members Awareness of faculty members with regards to evidence-based practice (EBP) in the teaching of baccalaureate nursing is yet to be conclusively determined.
- Evidence-Based Nursing: Barriers and Enablers This study aimed at establishing the enablers and barriers of guideline implementation in a primary healthcare setting.
- “The Role of the Clinical Nurse in Promoting Evidence-Based Practice” by LaSala “The Role of the Clinical Nurse in Promoting Evidence-Based Practice” idea is to describe how clinical nurses promote evidence-based practice in nursing in a hospital scenario.
- Fall Risk Prevention in Evidence-Based Practice This research investigates how the usage of alarm bells reduces the risk of future falls compared to frequent rounding in an acute care setting for age 65 years and older.
- Theories, Risks, and Measurement of Care Quality This paper discusses the role in the development and implementation, components and tools, risk and quality, and the role of evidence-based practice.
- The Use of Kotter 8-Step Change Model to Promote Scholarship Pertaining This research paper addresses the need for nurses not only to use EBP but also to participate in its creation.
- Evidence-Based Nursing Practice for Pressure Ulcer Prevention To develop evidence-based practice, a nurse should establish the question first, which is how to minimize the prevalence of pressure ulcers in immobile patients.
- Baltimore City: Evidence-Based Population Health Improvement Plan The Baltimore City Health Department conducted a comprehensive health needs assessment in the community and identified six major health concerns and their intervention.
- PTSD: Application of the Public Health Improvement Initiatives This report provides details on the Safe Headspace PHII for combat veterans and then gives a rationale for applying it to the Posttraumatic Stress Disorder patient care plan.
- Medication Errors as a Health Care Issue of Evidence-Based Practice It goes without saying that patient-centered nursing practice is based on the ethical principles of beneficence and nonmaleficence.
- Research in the Nursing Profession Qualitative research is the inquiry of social phenomena as it exists in the natural setting, for example, the beliefs and practices of doctors on a certain aspect of health
- Practicing Nurses: The Evidence-Based Practice in Primary Healthcare The study aims to evaluate the perceptions, attitudes and the knowledge level of practicing nurses towards the use of evidence-based practice in primary healthcare.
- Problem-Intervention-Comparison-Outcome-Time Format for Evidence-Based Nursing Practice PICOT(Problem-Intervention-Comparison-Outcome-Time) is a specific acronym used in nursing that is traditionally applied for the creation of a clinical question.
- Recommendation for an Evidence-Based Practice Change This presentation will explore the PICOT question related to the potential improvements in the quality of life of a target population.
- The Nursing Theory: The Diffusion of Innovation The paper discusses that the nursing theory applied within the current proposal is the diffusion of innovation. It explores the benefits of retaining employees.
- ICARE in the ICU Relations This paper explores how the iCARE concept could improve interprofessional care in the ICU, particularly in enhancing communication.
- Quality Management and Nurse Administrator’s Role This paper analyzes the nurse administrator’s role in risk and quality management and the relationship between theory and change management.
- Transcultural Nursing Theory by Madeleine Leininger Madeleine Leininger's theory appears to be a useful contribution to nursing education and has provided new insight into the clinical setting.
- Depression Screening Tool for Primary Care Center The present paper offers an overview of the literature on the topic and details an action plan with a timetable based on the IOWA model and Kurt Lewin’s model.
- Scope Course Reflection. Nursing Practice This reflection’s purpose is to gain an understanding of my preparedness to perform nursing activities through competencies.
- Translating Evidence Into Practice Falls are the primary cause of death from injuries in patients aged 64 and over and the leading cause of hospital admissions because of trauma.
- Reducing Hospital Acquired and Surgical Site Infections New guidelines have provided new insights into infections’ microbial mechanisms and specific mechanisms of some disease processes that may cause increased infection rates.
- The Efficacy of Iron Supplementation to Reduce Vulnerability to Anxiety in Women with Heavy Menses The women of reproductive age who experience excessive menstrual bleeding are most susceptible to this mineral deficiency.
- Bullying and Cyberbullying in Healthcare Nurse bullying is a systemic challenge that begins before the commencement of nursing school and lasts throughout the career of a care practitioner.
- Evidence-Based Project: How to Decrease Burnout in Nurses Nursing burnout is a widespread problem. Different methods of stress reduction are used to reduce the stress level and to overcome the problem.
- The ACE Star Model of Knowledge Transformation Analysis of The ACE Star Model of Knowledge Transformation. The ACE Star Model focuses to enhance the use of EBP in a distinctive way for the community nurses.
- Diabetes Intervention as Evidence-Based Practice Project The development of artificial pancreas technology provides an opportunity for more effective and safe treatment that is ongoing 24/7.
- Evidence-Based Practice in Nursing Culture Evidence-based practice is one of the commonly used decision-making methods to define and integrate the results of efficient studies with clinical and patient expertise.
- Fall Prevention Program for the Elderly Falls of older people often cause loss of their independence, disability, and even mortality. Nurses are critical to preventing drops in older people.
- Disseminating the Results of a Practice Improvement Project This paper discusses the approach to disseminating results and its effect on the promotion of EBP, keeping the spirit of inquiry alive, and mentoring for EBP.
- Pediatric Nurse Specialization & Evidence-Based Projects The presentation will focus on the pediatric nurse specialization; generally, their role is to treat, observe and diagnose young patients.
- Dealing With the Understaffing of Nurses The paper describes the applicable change, a proposed implementation plan with outcome measures, and a method for evaluating the proposed nursing intervention.
- External Urinary Collection Device as an Alternative to Indwelling Catheters Catheter-associated urinary tract infection (CAUTI) is a major health concern among mixed-gender patients in the long-term acute care setting (LTAC).
- Determining the Credibility of Evidence and Resources The paper discusses the criteria that should be considered when determining the credibility of information sources and provides an example of sources related to the safety issue.
- EBP: Training Program, Implementation, Nursing Student Stressors This paper summarizes articles about evidence-based practice, promoting EBP through a research training program, and graduate nursing student stressors during the COVID-19 pandemic.
- Remote Collaboration and Evidence-Based Care Developing methods to improve patient outcomes and safety is a priority. There is the implementation of software and personnel actions.
- Enhancing Remote Healthcare: Evidence-Based Strategies Considering the service delivery sector’s orientation towards remote service provision, it is essential to know strategies to improve remote health care service delivery.
- Nurse Staffing Level in Relation to COVID-19 Patients’ Condition The paper aims to answer the question: “In urgent patients during the COVID-19 pandemic, how adequate nurse staffing level can improve patient safety within six months”?
- Mentorship Increasing Job Confidence of New Nurses This project paper discusses the problem in the medical institution to get an in-depth understanding of a program that can tackle the issue of job confidence among new nurses.
- Nursing Interventions to Alleviate Pain The ability to alleviate pain through distraction and verbal reassurance is a powerful tool for nurses. This method can ease the pain and discomfort.
- Handwashing Regulations: The Nursing Intervention Handwashing regulations are an essential condition for preventing the spread of various diseases, which is especially critical at the time of the ongoing pandemic.
- Nursing Shortage and Change Project The shortage of nurses has become one of the most acute problems on a global scale. According to the World Health Organization, the global nurse shortage could widen to 13 million.
- Increasing Job Confidence of New Nurses with Mentorship The project aims to increase job confidence among new nurses by implementing a structured mentorship program introduced in the hospital for the first ten weeks after orientation.
- Leininger's Cultural Care Diversity Theory Leininger's Culture Care Theory provides nursing which follows all cultural traditions. The main aspect of Leininger's Culture Care Theory is cultural diversity.
- Evidence-Based Practice and Barriers in Nursing Evidence-based practice is a method used by nurse practitioners to utilize the most current and effective care for their patients.
- Mentoring Nurses for Quincke's Edema: Research Strategies Evidence-based practice approaches quality decision-making and nursing care based on personal clinical experience.
- Creating Awareness of Data Security Violations The intended outcome of the proposed project is to increase knowledge and create awareness of data security violations involving patient information.
- The Issue of the Nursing Shortage The paper aims to establish the dependence between nursing shortage and the health outcomes of patients since lack of staff is a significant problem in the U.S.
- Evidence-Based Practice in Colorectal Cancer Implementation of evidence-based methods in the treatment of colorectal cancer is an effective strategy for minimizing the risks of medical errors.
- Locating Credible Databases and Research Evidence-based practice (EBP) is the best way to provide high-quality, credible healthcare services for nurses and doctors.
- Contemporary Nursing Profession Nursing practice is a caring-based profession whereby methods of management and therapy are used in public health and sickness situations.
- Contemporary Nursing Practice and Evolution This paper discusses contemporary nursing practice in aspects of the evolution of nursing practice, features of BSN and ADN practices, collaboration with interdisciplinary teams.
- The Nursing Shortage Issue Analysis Expanding the size of the staff and offering favorable employment conditions can help resolve the problem of the shortage of nurses in clinics.
- Colorectal Cancer: Evidence-Based Practice Intervention The proposed intervention aims to raise public awareness regarding the importance of colorectal screening, especially among older adults.
- The COVID-19 Condition and Nursing The paper discusses how COVID-19 is likely to impact quality care, patient safety, and costs to individuals and the healthcare system.
- The Use of Evidence-Based Practice in Nursing The use of Evidence-Based Practice will ensure the proper use of resources, which will be of great benefit to all involved in the medical process.
- Medication Rehabilitation and Hospital Readmissions To what extent can utilizing medication rehabilitation reduce the risk of hospital readmissions in US adults discharged from a hospital undergoing usual care within 30 days?
- Late Referrals to Hospice: Clinical (PICOT) Question Late referrals to hospice have severe consequences as the lack of timely medical help results in conditions worsening and irreversible damage for patients with chronic diseases.
- Patient Falls in the Hospitals Patient falls in the hospitals prominently impact the individuals mainly because of the risk of incurring further injuries and medical complications.
- The Problem of Late Referrals to Hospice Late referrals to hospice are a significant issue that adversely affects people’s health. That is why the given project focuses on this problem.
- Watson's Theory to Support Evidence-Based Practice Watson's nursing theory is founded on the concept of empathy and defines the significance of the environment, connections, and disease avoidance as its guiding principles.
- Evidence-Based Practice and Mentorship in Nursing The main idea of this work is to analyze the importance of evidence-based practice beliefs and implementations using the Doctor of Nursing Practice as a mentoring strategy.
- Clinical Decision-Making Using Evidence-Based Practice
- Evidence-Based Practice and Empirically Supported Treatment in Future Practice
- Ethical Considerations of Evidence-Based Practice in Nursing
- Evidence-Based Practice and Psychological Treatments: The Imperatives of Informed Consent
- Evidence-Based Interventions on Anxiety Disorders According to the Australian Institute of Health and Welfare, anxiety disorder accounts for approximately 14.4% of Australians’ general disease prevalence.
- Similarities and Differences between Evidence-Based and Reflective Practice
- Staff Nurses’ Use of Research to Facilitate Evidence-Based Practice
- Evidence-Based Medicine for Occupational Health
- Toward a Transdisciplinary Model of Evidence-Based Practice
- Promoting Patient Safety and Enabling Evidence-Based Practice through Informatics
- Factors in the Utilization and Integration of Evidence-Based Practice in Nursing
- Research Methods in Evidence-Based Practice: Understanding the Evidence
- Using Evidence-Based Practice to Reduce Catheter-Associated Urinary Tract Infections
- Evidence-Based Screening for Depression in Acute Care EB analysis for the topic of depression to identify the need for an appropriate screening tool in addition to the PHQ-9 in the assessment evaluation process.
- Evidence-Based Practice in Health Education and Promotion
- Examining the Support for Evidence-Based Nursing Practice
- Improving the Self-Efficacy of Caregivers Using Evidence-Based Practice
- Evidence-Based Practice Competency and Related Factors among Nurses
- Organization-Level Factors in the Adoption of Evidence-Based Care for Depression in Primary Care
- Evidence-Based Practice in Improving Patient Outcomes
- Implementing Evidence-Based Practice in Home Care
- Challenges of the Nurse Manager in Implementation of Evidence-Based Nursing Practice
- The Iowa Model of Evidence-Based Practice to Promote Quality Care
- Evidence-Based Clinical Practice in Counselling Care
- Discharge Planning Process: Applying a Model for Evidence-Based Practice
- Qualitative Health Research in the Era of Evidence-Based Practice
- Evidence-Based Practice in Child and Adolescent Mental Health Services
- Effect of an Evidence-Based Practice Educational Program on the Competence of Nursing Students
- Evidence-Based Practice as a Viable Tool to Manage the COVID-19 Pandemic
- Bridging the Theory–Practice Gap with Evidence-Based Practice
- Enhancing Healthcare through Evidence-Based Practice: A Comprehensive Review
- Evidence-Based Practice for Rehabilitation Professionals: Concepts and Controversies
- Implementation of Evidence-Based Medicine in Everyday Clinical Practice
- Evidence-Based Practice Competencies among Nutrition Professionals
- Recent Developments in Family Psychoeducation as an Evidence‐Based Practice
- Evidence-Based Practice: The Role of Staff Development
- Autism Spectrum Disorder: Advances in Evidence-Based Practice
- Managing Anxiety in Evidence-Based Practice This EBP project proposal focuses on nonpharmacological treatment that does not involve the administration of drugs. It tries to effectively manage anxiety.
- Implementation of Evidence‐Based Practice in Nursing Using Action Research
- Cost-Effective Care: Between Evidence-Based Practice and TQM
- Facilitation as a Role and Process in Achieving Evidence‐Based Practice in Nursing
- Preventing Respiratory Complications of Tube Feedings: Evidence-Based Practice
- Evidence-Based Practice in Mental Health Care to Ethnic Minority Communities
- Strategies for Starting a Successful Evidence-Based Practice Program
- Care Bundles in Critical Care: A Practical Approach to Evidence-Based Practice
- Evidence-Based Approaches to Palliative Care Nursing
- Community- and Hospital-Based Nurses’ Implementation of Evidence-Based Practice
- Impact of Introducing Multiple Evidence-Based Clinical Practice Protocols in a Medical ICU
- What Contribution Can Quantitative Research Make to Evidence-Based Practice?
- Does Clinical Simulation Learning Enhance Evidence-Based Practice?
- How Do Patients Benefit from Evidence-Based Practice?
- What Are the Primary Ethical Considerations of Evidence-Based Practice and Practice-Based Evidence?
- Is the Evidence-Based Practice Movement Doing More Good than Harm?
- What Are the Pathways and Barriers to Implementing Evidence-Based Practice in Psychotherapy?
- What Is the Ultimate Goal of Evidence-Based Practice?
- How Can We Achieve Evidence‐Based Practice If We Have a Theory–Practice Gap in Nursing Today?
- What Is the Relation between Practice-Based Evidence and Evidence-Based Practice?
- How to Proceed When Evidence-Based Practice Is Required but Very Little Evidence Available?
- Why Many Clinical Psychologists Are Resistant to Evidence-Based Practice?
- How Is Qualitative Evidence Used in Evidence-Based Practice?
- What Are the Factors of Organizational Culture in Health Care That Act as Barriers to the Implementation of Evidence-Based Practice?
- How Does Evidence-Based Practice Promote Change?
- Can We Make Better Public Health Decisions Using the Principles of Evidence-Based Practice?
- What Is the Importance of Using Evidence-Based Practices in Nursing?
- Who Are the Stakeholders in Evidence-Based Practice?
- How Does Health Information Technology Support Evidence-Based Practice?
- What Are the Reasons for the Current Emphasis on Evidence-Based Practice in Therapy?
- How Do You Evaluate the Effectiveness of Evidence-Based Practice?
- What Is the Role of Evidence-Based Practice in Modern Psychiatry?
- What Challenges Do Nurses Face as They Transition to Evidence-Based Practice?
- How Has Evidence-Based Practice Evolved within the Nursing Profession?
Cite this page
Select style
- Chicago (A-D)
- Chicago (N-B)
NursingBird. (2024, May 23). 191 Evidence-Based Practice Research Topics & Essay Examples. https://nursingbird.com/topics/evidence-based-practice-research-topics/
"191 Evidence-Based Practice Research Topics & Essay Examples." NursingBird , 23 May 2024, nursingbird.com/topics/evidence-based-practice-research-topics/.
NursingBird . (2024) '191 Evidence-Based Practice Research Topics & Essay Examples'. 23 May.
NursingBird . 2024. "191 Evidence-Based Practice Research Topics & Essay Examples." May 23, 2024. https://nursingbird.com/topics/evidence-based-practice-research-topics/.
1. NursingBird . "191 Evidence-Based Practice Research Topics & Essay Examples." May 23, 2024. https://nursingbird.com/topics/evidence-based-practice-research-topics/.
Bibliography
NursingBird . "191 Evidence-Based Practice Research Topics & Essay Examples." May 23, 2024. https://nursingbird.com/topics/evidence-based-practice-research-topics/.
- Healthcare Policy
- Patient Safety
- Nursing Care Plan
- Nursing Theory
- Breast Cancer
- Health Insurance
- Reproductive Health
What is Evidence-Based Practice in Nursing? (With Examples, Benefits, & Challenges)

Are you a nurse looking for ways to increase patient satisfaction, improve patient outcomes, and impact the profession? Have you found yourself caught between traditional nursing approaches and new patient care practices? Although evidence-based practices have been used for years, this concept is the focus of patient care today more than ever. Perhaps you are wondering, “What is evidence-based practice in nursing?” In this article, I will share information to help you begin understanding evidence-based practice in nursing + 10 examples about how to implement EBP.
What Is Evidence-Based Practice In Nursing?
When was evidence-based practice first introduced in nursing, who introduced evidence-based practice in nursing, what is the difference between evidence-based practice in nursing and research in nursing, what are the benefits of evidence-based practice in nursing, top 5 benefits to the patient, top 5 benefits to the nurse, top 5 benefits to the healthcare organization, 10 strategies nursing schools employ to teach evidence-based practices, 1. assigning case studies:, 2. journal clubs:, 3. clinical presentations:, 4. quizzes:, 5. on-campus laboratory intensives:, 6. creating small work groups:, 7. interactive lectures:, 8. teaching research methods:, 9. requiring collaboration with a clinical preceptor:, 10. research papers:, what are the 5 main skills required for evidence-based practice in nursing, 1. critical thinking:, 2. scientific mindset:, 3. effective written and verbal communication:, 4. ability to identify knowledge gaps:, 5. ability to integrate findings into practice relevant to the patient’s problem:, what are 5 main components of evidence-based practice in nursing, 1. clinical expertise:, 2. management of patient values, circumstances, and wants when deciding to utilize evidence for patient care:, 3. practice management:, 4. decision-making:, 5. integration of best available evidence:, what are some examples of evidence-based practice in nursing, 1. elevating the head of a patient’s bed between 30 and 45 degrees, 2. implementing measures to reduce impaired skin integrity, 3. implementing techniques to improve infection control practices, 4. administering oxygen to a client with chronic obstructive pulmonary disease (copd), 5. avoiding frequently scheduled ventilator circuit changes, 6. updating methods for bathing inpatient bedbound clients, 7. performing appropriate patient assessments before and after administering medication, 8. restricting the use of urinary catheterizations, when possible, 9. encouraging well-balanced diets as soon as possible for children with gastrointestinal symptoms, 10. implementing and educating patients about safety measures at home and in healthcare facilities, how to use evidence-based knowledge in nursing practice, step #1: assessing the patient and developing clinical questions:, step #2: finding relevant evidence to answer the clinical question:, step #3: acquire evidence and validate its relevance to the patient’s specific situation:, step #4: appraise the quality of evidence and decide whether to apply the evidence:, step #5: apply the evidence to patient care:, step #6: evaluating effectiveness of the plan:, 10 major challenges nurses face in the implementation of evidence-based practice, 1. not understanding the importance of the impact of evidence-based practice in nursing:, 2. fear of not being accepted:, 3. negative attitudes about research and evidence-based practice in nursing and its impact on patient outcomes:, 4. lack of knowledge on how to carry out research:, 5. resource constraints within a healthcare organization:, 6. work overload:, 7. inaccurate or incomplete research findings:, 8. patient demands do not align with evidence-based practices in nursing:, 9. lack of internet access while in the clinical setting:, 10. some nursing supervisors/managers may not support the concept of evidence-based nursing practices:, 12 ways nurse leaders can promote evidence-based practice in nursing, 1. be open-minded when nurses on your teams make suggestions., 2. mentor other nurses., 3. support and promote opportunities for educational growth., 4. ask for increased resources., 5. be research-oriented., 6. think of ways to make your work environment research-friendly., 7. promote ebp competency by offering strategy sessions with staff., 8. stay up-to-date about healthcare issues and research., 9. actively use information to demonstrate ebp within your team., 10. create opportunities to reinforce skills., 11. develop templates or other written tools that support evidence-based decision-making., 12. review evidence for its relevance to your organization., bonus 8 top suggestions from a nurse to improve your evidence-based practices in nursing, 1. subscribe to nursing journals., 2. offer to be involved with research studies., 3. be intentional about learning., 4. find a mentor., 5. ask questions, 6. attend nursing workshops and conferences., 7. join professional nursing organizations., 8. be honest with yourself about your ability to independently implement evidence-based practice in nursing., useful resources to stay up to date with evidence-based practices in nursing, professional organizations & associations, blogs/websites, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. what did nurses do before evidence-based practice, 2. how did florence nightingale use evidence-based practice, 3. what is the main limitation of evidence-based practice in nursing, 4. what are the common misconceptions about evidence-based practice in nursing, 5. are all types of nurses required to use evidence-based knowledge in their nursing practice, 6. will lack of evidence-based knowledge impact my nursing career, 7. i do not have access to research databases, how do i improve my evidence-based practice in nursing, 7. are there different levels of evidence-based practices in nursing.
• Level One: Meta-analysis of random clinical trials and experimental studies • Level Two: Quasi-experimental studies- These are focused studies used to evaluate interventions. • Level Three: Non-experimental or qualitative studies. • Level Four: Opinions of nationally recognized experts based on research. • Level Five: Opinions of individual experts based on non-research evidence such as literature reviews, case studies, organizational experiences, and personal experiences.
8. How Can I Assess My Evidence-Based Knowledge In Nursing Practice?

We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essay Examples >
- Essays Topics >
- Essay on Medicine
Example Of Essay On Evidence Based Practice
Type of paper: Essay
Topic: Medicine , Nursing , Education , Patient , Belief , Customers , Training , Evidence
Published: 12/02/2019
ORDER PAPER LIKE THIS
Evidence Based Practice
Evidence Based Practice (EBP), involves the use of current research data or findings from day to day life in making decisions concerning patient care (Brown & Schmidt, 2011, p. 9). It is an integration of knowledge gained from the clinical field, patient values, and the most reliable scientific information to come up with a comprehensive decision making process concerning patient welfare. Barriers to practice or positive customer outcomes are common and can be identified through observing clinical practice in action, running a focus group, through brainstorming, talking to key individuals and by using questionnaires. One major barrier to practice or positive customer outcomes is acceptance and beliefs. Acceptance and beliefs are the beliefs and attitudes of individuals which have significance on the way people behave and carry out their duties. Many healthcare practitioners have a hard time accepting and applying new policies and research recommendations if there is a discrepancy between these policies and recommendations with other existing ones issued by professional bodies or the opinion of an influential colleague. Some professionals believe that recommendations don’t reflect the evidence and as such will not achieve better patient outcomes (Ladwig & Ackley, 2010, p. 518). An individual’s attitude towards change and belief in their own ability to adopt a new behavior also has an impact. The barriers to practice or positive customer outcomes can be addressed through various ways that support evidence based practice. These approaches include; educational meetings, clinical audit and feedback, educational materials, patient-mediated strategies, opinion leaders, educational outreach visits and reminder systems (Townsend, 2011, p. 75). There is no one way of overcoming barriers and so use of different methods can be used by different people in varied situations. The combination of different approaches to overcoming barriers has proven to have positive results and a huge impact within a shorter length of time. Patient involvement in coming up with strategies to improve patient care is very important in EBP as past patient experience and their expectations have a huge significance in formulating best practices when integrated with clinical expertise and best research evidence.
Brown, J. & Schmidt, N. (2011). Evidence-Based Practice for Nurses: Appraisal and Application Research. Burlington, MA. Townsend, M. (2011). Psychiatric Mental Health Nursing: Concepts of Care in Evidence-Based Practice. Philadelphia, PA: F. A. Davis Company Ladwig, G. & Ackley, B. (2010). Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care. Philadelphia, PA: Mosby Publishing

Cite this page
Share with friends using:
Removal Request

Finished papers: 1596
This paper is created by writer with
ID 253832377
If you want your paper to be:
Well-researched, fact-checked, and accurate
Original, fresh, based on current data
Eloquently written and immaculately formatted
275 words = 1 page double-spaced

Get your papers done by pros!
Other Pages
Killing us softly 4 essay, protecting personal information ppi applicability in electronic medical records research papers example, free paper essay sample 2, post operative for acute cholecystitis patients research paper sample, free essay on website analysis, free essay on the texas revolution, sample essay on statistics 3, good example of essay on origins of the first person shooter summary and response, good case study about detailed analysis of the social contract underpinning each stakeholder relationship, sample essay on physical security paper, the eu regional policy essays examples, example of report on production, horror and terror essays, wounded knee massacre essays, wounded knee essays, pine ridge essays, diffraction grating essays, alien essays, fugitive essays, potatoes essays, alien abduction essays, teri garr essays, dreyfuss essays, going home essays, neoclassical essays, minn essays, wilmington essays, mankato essays, clara essays, ethnomethodology essays, amdur essays, burr essays, milieu college essays, potash college essays, decisiveness college essays, gore college essays, glucagon college essays, inferiority complex college essays, timelessness college essays, air travel college essays, transcendence college essays, electron college essays, electron microscope college essays.
Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline
67 Critical Care Research Topics & Essay Ideas
🏆 best critical care research topics, ✍️ critical care essay topics for college, 🎓 hot icu evidence-based practice topics, 💡 simple icu nursing research topics.
- Intensive Care Unit Nursing ( ICU)
- Physical Versus Chemical Restraints in Intensive Care Unit
- The Intensive Care Unit: Nurses’ Responsibilities
- Intensive Care Unit Quality Improvement Checklist
- Implementation of Cycled Lighting in Intensive Care Units
- Intensive Care Units: Quantitative and Qualitative Research Applications
- Analysis of Leadership in the Intensive Care Unit
- Hospital-Acquired Infections Prevention in Intensive Care Unit Patients The purpose of this project is to reduce the prevalence and incidences of hospital-acquired infections among intensive care unit patients.
- The Intensive Care Unit: Intelligent Hospital Pavilion The Intensive Care Unit (ICU) is designed in such a way that it can provide adequate and timely care to high-risk patients.
- Using Information Technology and Artificial Intelligence in Critical Care Medicine Artificial Intelligence in critical care is helping to care for patients faster, supervise more patients, calculate the exact dosage for patients, and collect more detailed data.
- Children’s Weight Estimation in Intensive Care Units Due to the fact that a large standard deviation is always present in the children’s group, the mean weight itself is not a reliable value.
- Opinion Leadership in Intensive Care Unit The paper aims to explore the concept of an opinion leader with references to scholarly literature as well as personal working experience.
- Intensive Care Unit: Evidence-Based Practice’ Environment Among the EBP practices employed in the unit, it is possible to recognize the moderation of noise in the area and reevaluation of the demand for the medical supplies required for the unit operations.
- Cardiac Intensive Care Unit Case Study This essay discusses the steps a cardiac intensive care unit manager would take when planning the annual budget, including reviewing income statements, analyzing expenses.
- Troubles in the Intensive Care Unit The team is hesitant to perform intubation due to the man’s advance directive expressing his wish to refuse artificial life support.
- Ethical and Justice Considerations of Triage of Critical Care Resources The rising scale of the pandemic causes problems with resource allocation when providing health care to the continuously increasing number of patients impacted by the coronavirus.
- Physical Restraints in Acute and Intensive Care Units The issue of using physical restraints in health care institutions is a rather debatable topic, and some experts consider it a necessity for managing some patients.
- Decreasing Ventilator Pneumonia in the Intensive Care Units This article is a proposed protocol for implementation in US hospitals to reduce the risk of ventilatory pneumonia in intensive care units.
- Interview of Nurse of the Intensive Care Unit As the subject of the interview, the senior nurse of the intensive care unit (ICU) of a Miami hospital, Mrs. S., is engaged. Mrs. S. is a registered nurse with a BSN degree.
- Nosocomial Infections in Neonatal Intensive Care Units The Centre for Disease Control defines Nosocomial infections as diseases that occur three days or more after birth usually in a neonatal intensive care unit (NICU) setting.
- Plan of Interview the Intensive Care Unit Nurse Plan of the interview with the intensive care unit nurse. The question where the candidate must provide the most precise response would involve a real-life scenario.
- Effectiveness of Supporting Intensive Care Units Medicine appears to be the sphere of active developments and constant improvements, as high quality of service presents a matter of importance.
- Enteral Feeding in Paediatric Intensive Care The nasogastric tube is a safe and effective method for short-term feeding in children with a variety of chronic conditions that can be regularly used at home and in hospital.
- Intelligent Hospital Pavilion for Intensive Care Given the advantages of computerized systems for intensive care units, the latter significantly improve patient outcomes and reduce the impact of human factors on nurses’ work.
- National Patient Safety Goals: Critical Care Access Limited access to healthcare services has been on the agenda of the modern healthcare system for quite a long, warranting the status of critical concern.
- Compassion Fatigue in Pediatric and Intensive Care Units Compassion fatigue deserves attention in the healthcare sector and requires taking relevant measures, particularly in pediatric departments and intensive care units.
- Dry Eye in Critical Care: Evidence-Based Practice A common problem for ICU patients is dry eye due to their conditions or medications that block physical mechanisms of maintaining moisture in the eyes.
- Team Nursing Model in Intensive Care Unit The team nursing model involves the creation of teams whose members work together and are responsible for a limited number of patients.
- Interprofessional Teams and iCare in Intensive Care Units The intensive care unit (ICU) is a highly complex dynamic work environment that requires highly sophisticated and engaged interprofessional team functioning.
- Hand Hygiene Compliance in Neonatal Intensive Care Unit Simple handwashing education may be an effective intervention method to increase the literacy of staff and visitors regarding the problem in question.
- Evidence-Based Practice Employed in Intensive Care The nurse manager should encourage all nurses to practice evidence-based nursing through conducting research training.
- Safe Medication in Intensive Care Unit In this paper, safe medication use in intensive care units (ICUs) the CPG was selected due to its relevance to the current needs of inpatient care.
- Electronic Intensive Care Unit Benefits An Electronic Intensive Care Unit (eICU) represents a type of a healthcare setting that uses the latest technologies with the purpose of providing top quality care to patients.
- The Needs of Family Members of Patients in Intensive Care The intensive (critical) care unit (ICU) could be a challenging setting for the family members of patients, particularly when the loved ones are at an immense risk of death.
- Nurses Role Overload and Burnout in Intensive Care This paper critiques the article “Relationship among nurses role overload, burnout, and managerial coping strategies at intensive care units” by Mohamed.
- Moral Distress and Effects on Critical Care Nurses Wiegand and Funk explore the moral distress experiences of nurses, the causes of such experiences, and the effects they had on nurses’ practice, attitude, and future decisions.
- Psychological Flexibility and Its Relationship to Distress and Work Engagement Among Intensive Care Medical Staff
- Intensive Care Unit Related Post Traumatic Stress Disorder
- Pain, Parental Involvement, and Oxytocin in the Neonatal Intensive Care Unit
- Pediatric Intensive Care: Immunomodulation With Activated Protein C Ex Vivo
- Preventing Catheter-Related Bloodstream Infections in Intensive Care Unit
- Moral Distress Among European Intensive Care Nurses
- Intensive Care Nurses and Technology BSC
- Nurse Burnout and Stress in Neonatal Intensive Care
- Preventing Ventilator-Associated Pneumonia in the Intensive Care Unit
- Intensive Care Nurse’s Views and Practices for Eye Care: An International Comparison
- Prevention, Identification, and Treatment of Sepsis in Intensive Care Unit (ICU) Patients
- Premature Triplets: Neonatal Intensive Care Unit at Cook Children’s Hospital
- Abuse of Drugs and Alcohol in Intensive Care Unit
- Medical Imaging During Intensive Care Unit (ICU)
- The Assessment Process Of Patients In Intensive Care
- Neonatal Intensive Care Unit Evacuation and Care During a Natural Disaster: The Experience of Cyclone Idai in Beira, Mozambique
- Nursing and the Importance of Intensive Care and Critical Care Skills
- Hospital Neonatal Intensive Care Unit and the Inclusion of a Child Life Therapist
- Physician Scheduling for Continuity: An Application in Pediatric Intensive Care
- Intensive Care Unit: Stress Meeting Needs of Family and Coping
- Nosocomial Infections and the Infant Intensive Care Unit (NICU)
- Horizontal Violence Experienced During Orientation in Intensive Care Units
- Risk Factors for Intensive Care Unit Admission in Patients With Autoimmune Encephalitis
- Intensive Care Admission and Early Neuro-Rehabilitation
- Simulating Neonatal Intensive Care Capacity in British Columbia
- Safety Score Improvement Plan For By-Faith Intensive Care Unit (ICU)
- Continuous Renal Replacement Therapy in the Intensive Care Unit
- Care for Critical Ill Patients With COVID-19: Establishment of a Temporary Intensive Care Unit in an Isolated Hospital
- Modeling the Requirement for Supplementary Nurses in an Intensive Care Unit
- Preventing and Assessing Intensive Care Unit Delirium
Cite this post
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, May 10). 67 Critical Care Research Topics & Essay Ideas. https://studycorgi.com/ideas/intensive-care-essay-topics/
"67 Critical Care Research Topics & Essay Ideas." StudyCorgi , 10 May 2022, studycorgi.com/ideas/intensive-care-essay-topics/.
StudyCorgi . (2022) '67 Critical Care Research Topics & Essay Ideas'. 10 May.
1. StudyCorgi . "67 Critical Care Research Topics & Essay Ideas." May 10, 2022. https://studycorgi.com/ideas/intensive-care-essay-topics/.
Bibliography
StudyCorgi . "67 Critical Care Research Topics & Essay Ideas." May 10, 2022. https://studycorgi.com/ideas/intensive-care-essay-topics/.
StudyCorgi . 2022. "67 Critical Care Research Topics & Essay Ideas." May 10, 2022. https://studycorgi.com/ideas/intensive-care-essay-topics/.
These essay examples and topics on Critical Care were carefully selected by the StudyCorgi editorial team. They meet our highest standards in terms of grammar, punctuation, style, and fact accuracy. Please ensure you properly reference the materials if you’re using them to write your assignment.
This essay topic collection was updated on January 5, 2024 .
- How it works

Useful Links
How much will your dissertation cost?
Have an expert academic write your dissertation paper!
Dissertation Services
Get unlimited topic ideas and a dissertation plan for just £45.00
Order topics and plan
Get 1 free topic in your area of study with aim and justification
Yes I want the free topic
Evidence-based Practice Nursing Dissertation Topics
Published by Owen Ingram at January 3rd, 2023 , Revised On August 16, 2023
Nurses provide daily clinical care to patients based on evidence-based practices. This article encourages you to consider a career as an EBP nurse to contribute to the healthcare industry and look at the various evidence-based nursing dissertation topics for your thesis paper.
Evidence-based practice nursing involves integrating the use of the best available evidence into the care of patients. The subject is not new and has been around for several decades. It is now becoming a career option for many healthcare professionals. Evidence-based practice nursing improves patient outcomes, reduces costs, and enhances a hospital’s reputation.
Evidence-based practice nursing incorporates four fundamental principles:
The use of the best available evidence to make decisions about care for patients with specific health problems;
- The ability to recognise gaps in knowledge about how to provide safe and effective patient care;
- The ability to identify potential barriers that may interfere with implementing evidence-based practices; and
- The ability to translate research findings into clinical practice guidelines and other practical resources
Possible Evidence-Based Practice Nursing Issues
EBP includes many studies, including those of low methodological quality, to inform clinical decision-making in each care area. In other words, it incorporates the best research evidence into clinical decision-making to treat a patient on time. It is best to use a clearly defined decision tree or matrix based on a previous literature review when performing EBP.
Evidence-based practice (EBP) is becoming increasingly important in nursing as the role evolves. EBP expertise is expected of nurse practitioners (NPs), certified nurse midwives (CNMs), and certified registered nurse anaesthetists (CRNAs). Nurses must prepare for the changes the profession is undergoing.
Care providers in this field are encouraged to apply their knowledge and expertise. In addition, you gain experience and confidence in your judgment. Due to this, more emphasis is placed on what works in practice than on what doesn’t. By teaching best practices, nurses can become leaders in their field by challenging their beliefs and experiences.
- Child Health Nursing Dissertation Topics
- Adult Nursing Dissertation Topics
- Critical Care Nursing Dissertation Topics
- Dementia Nursing Dissertation Topics
- Midwifery Dissertation Topics
- Palliative Care Nursing Dissertation Topics
- Mental Health Nursing Dissertation Topics
- Nursing Dissertation Topics
- Coronavirus (COVID-19) Nursing Dissertation Topics
Evidence-Based Nursing Dissertation Topics
Topic:1 reducing falls in combative dementia patients.
Research Aim: Studying all the preventive measures to protect dementia patients from accidental falls and injuries with severe cognitive impairments.
Topic:2 Palliative oxygen usage: nasal cannula vs masks
Research Aim: Understanding the importance of the nasal canal for high flow rates of oxygen for those with breathing difficulties.
Topic:3 Early care of intoxicated patients
Research Aim: Studying the management of intoxicated patients admitted to intensive care units because of causative diseases, mortality issues and others.
Topic:4 Delirium Prevention
Research Aim: Learning the sensitivity of the topic of delirium and finding ways to prevent it with the help of sensory impairment, regular continence, hydration and others.
Topic:5 Choosing the correct catheter size of IVs
Research Aim: Measuring the accurate vessel size with respect to the length of the catheter for reducing dislodgement.
Topic:6 Reducing CAUTI's (Catheter acquired UTI)
Research Aim: Studying the intervention and the use of chlorhexidine mixture to treat the catheter associated with urinary tract infections with special tricks and techniques.
Topic:7 Alternative interventions to SOB for COPD patients
Research Aim: Differentiating between the pharma-logical and non-pharmacological interventions to treat breathlessness through different medical procedures.
Topic:8 Effect of visiting hours on patient outcomes
Research Aim: Studying the horrendous effect of visiting hours on patient outcomes because of the visiting policies made years ago.
Topic:9 Reducing pressure ulcerations
Research Aim: Finding out all the possible ways to reduce pressure ulcerations with the help of common practices like hydration, moisturisation, using skin Protestants and others.
Topic:10 Offering pain medication for hospitalised patients
Research Aim: Search for useful ways to improve pain management for hospitalized patients with acute needs to be fulfilled
Topic:11 Nonpharmacologic intervention for pain
Research Aim: Understanding the meaning of nonpharmacological pain management with different educational and psychological hypnosis conditions.
Topic:12 Discharge on heart failure and readmission rates
Research Aim: Learning different insights on the discharge education program for patients suffering from serious health problems like heart failure and terms and policies for readmission.
Topic:13 NPO status and hypoglycemic rates
Research Aim: Understanding the need of hypoglycemia in hospitalized patients and injecting into the patient’s blood glucose.
Topic:14 Ambulations after surgery
Research Aim:
Studying different body systems and the role of ambulation to get the blood system flow smoothly throughout the body after surgery or any medical procedure.

Topic:15 Reducing HAP And VAP for medical treatments
Research Aim: Understanding the difference between hospital-acquired pneumonia and ventilator-acquired pneumonia with their respective treatments through antibiotics and other medical procedures.
I/O Example
To become an Evidence-based practice nurse, you need to be able to:
- Understand the importance of evidence-based practice
- Develop a clear understanding of the clinical decision-making process and how it relates to nursing research and evidence-based practice.
- Use principles from evidence-based practice to make decisions about patient care.
- Recognize potential problems in applying evidence-based practice and be able to respond appropriately.
You will also need to gain hands-on experience in a clinical setting in order to become an evidence-based practice nurse.
A nurse who practices evidence-based practice can earn $53,000 annually. In the United States, this is the average wage for nurses, according to the Bureau of Labor Statistics.
A registered nurse’s average salary in 2014 was $58,790. According to the Bureau of Labor Statistics, registered nurses have earned an average of $51,230 over the past five years.
It is a rewarding and fulfilling career to work in evidence-based nursing. Nurses can make a significant impact on their patients’ lives through this field. There is a high demand for nurses with strong clinical skills and an understanding of evidence-based practice in today’s nursing market.
If you need help with the complete dissertation writing process, you may want to additionally read about our proposal writing service and the full dissertation writing service .
Free Dissertation Topic
Phone Number
Academic Level Select Academic Level Undergraduate Graduate PHD
Academic Subject
Area of Research
Frequently Asked Questions
How to find evidence based practice nursing dissertation topics.
For evidence-based practice nursing dissertation topics:
- Identify healthcare gaps.
- Review clinical problems.
- Explore recent research.
- Focus on patient outcomes.
- Consider innovations.
- Choose a topic with available data and relevance.
You May Also Like
Urban planning is an essential tool in creating vibrant and healthy communities. It is the practice of balancing the needs of a society with limited resources to ensure equitable development and long-term sustainability.
Need interesting and manageable HRM dissertation topics or thesis? Here are the trending HRM dissertation titles so you can choose the most suitable one.
In this article, we suggest some topics regarding USA’s Withdrawal From Afghanistan so you can kick start your dissertation without any delay.
USEFUL LINKS
LEARNING RESOURCES

COMPANY DETAILS

- How It Works
72 Intensive Care Essay Topic Ideas & Examples
🏆 best intensive care topic ideas & essay examples, 👍 good essay topics on intensive care, ⭐ simple & easy intensive care essay titles.
- Intensive Care & Critical Care Skills in Nursing Therefore, the current research examines the importance of intensive and critical care skills in nursing. Due to this, ICU and critical care training can be considered most beneficial in nursing.
- Palliative Care in Intensive Care Unit Palliative care is an important field of the healthcare industry that allows terminally ill patients and their families to feel cared for, which is why the services at this unit should be of the highest […]
- The Nurse Manager’s Role in a Pediatric Intensive Care Unit On the basis of the observation of Anderson’s skills, behaviors, and strategies that this leader exhibits, it is possible to say that he may be regarded as an efficient leader and nurse manager who obtains […]
- The Nursing Workflow in the Intensive Care Unit This article summarizes the nursing workflow in the intensive care unit among the enlisted nurses in research conducted in mainland China.
- Why Intensive Care Unit Nurses Have Low Work Morale The diagram above analyzes the root causes of the low work morale of nurses working in the intensive care unit at the hospital where I am employed.
- Actors Influencing How Intensive Care Unit Nurses Allocate Their Time Show Less Given the importance of all of the above factors, the purpose of my work is to determine whether the allocation of nurses and patients is adequate to provide quality services.
- Confusion Assessment Method in Intensive Care Unit According to Richardson et al, the reliability of a screening tool is confirmed by comparing the results to the gold standard of diagnosis.
- Use of BIS Brain Monitors in Intensive Care Unit The objectives of the innovation project are to measure the present use of BIS in sedation at a specific facility and evaluate patient outcomes for BIS-guided sedation compared to routine clinical assessment.
- Nosocomial Infections in Intensive Care Units The choice to insert the urinary catheter ought to be made with the awareness that it entails the risk of causing infections with a prolonged hospital stay.
- Hiring New Registered Nurses for Intensive Care Unit The purpose of this paper is to outline methods for analyzing the ICU job, drafting the job description, and future changes that may affect the future of the job description.
- Intensive Care Units Standards and Services Thus, in the cases of unplanned extubation, both self and accidental, the quality of care is observed through the nurse’s ability to react according to an incidence, with emphasis on the patient’s safety and the […]
- Comfort Care of the Patient in Intensive Care The relationship between nurses’ comforting interventions and the patients’ comfort is the foundation of the theory. The purpose of the comfort theory is to establish the link between nursing interventions and patients’ comfort.
- Resuscitation of Patients in Intensive Care Units The project utilizes a quasi-experimental design to choose the sample and manipulate the independent variable, the nursing training program of capnography use during CPR, to influence the dependent variable, the number of CPR cases with […]
- Public Health: The Intensive Care Units To achieve this, the program will transform the work culture within the ICU to be more rigorous and goal oriented. It is important that all of the hospital critical-care stakeholders to distinguish and enforce imperative […]
- Nurse Staffing, Medical Staffing and Mortality in Intensive Care In order to discuss the contribution of different types of personnel to the survival of patients in ICUs, the researchers provided different hypotheses for the relationship between the number of nurses and rates of patient […]
- Clinical Personal Experience in a Pediatric Intensive Care Unit I had the opportunity to provide adequate care and patient support in the ICU. Such leadership styles are applicable in health care organizations to promote the quality of care provided to patients.
- Ethics Review: ‘Living Wills’ and Intensive Care However, some opponents of the move to legalize advance decisions in England and Wales are of the idea that legalizing advance decisions will be tantamount to euthanizing the patients illegally.
- Having Visiting Hours in the Intensive Care Unit A family member selected to visit the patient will be in position to give feedback concerning the patient to the rest of the family members and friends.
- Nurse Practitioners and Physician Assistants in the Intensive Care Unit Kleinpell and Robert Grabenkort, the authors of the article under consideration, tell that nursing practitioners and physician assistants play a very important role in the intensive care unit, however, their participation is still not well […]
- Intensive Care Unit Nurses’ Education Needs The reason for choosing this target group is the affiliation of the researcher: since the researcher is a nurse who works in the ICU of KFH, the analysis of the educational needs of the nurses […]
- Medication Errors in Intensive Care Unit The majority of medication errors take place at the stage of administration; however, mistakes also occur during prescription, preparation of medication, and transcription.
- Cross-Training in Intensive Care Unit The students who took this course will exhibit the mastery of: Assessment of the need for care under time constraints and in adverse conditions; Provision of assistance to critically ill individuals with precision, speed, and […]
- Constructive Alignment in Intensive Care Nursing Education Given the potential benefits of CA for education, CA needs to be considered in terms of ICU nurse training to determine if it applies to the settings of ICU.
- Evidence-Based Practice in the Intensive Care Unit The purpose of this paper is to identify challenges that are associated with the implementation of an evidence-based approach in a clinical environment and describe strategies that can be used for implementing this approach.
- Intensive Care Unit Patients Therapy Differences The meta-analysis study explored the differences between burn ICU and general ICU patients. The differences are brought about by the fact that the injuries of burn patients are both external and internal.
- Bloodstream Infections in Intensive Care Department The scope of the essay is limited to the discussion of the risks of contract in infectious diseases, which nurses may face in the context of the ICU environment in a hospital.
- Management of Burns in Intensive and Acute Care The article can be viewed as the review of the currently used practices to cope with burns in intensive care units, and the author describes procedures that are necessary in order to provide the respiratory […]
- Early Mobilization Therapy for Severely Injured Patients The PDSA plan will be as follows: Plan: It will be needed to identify the setting, sample selection criteria, the intervention, and the type of data to be collected.
- Early Mobility Therapy in the Intensive Care Unit Particularly, the advantages and the disadvantages of the early mobility therapy compared to the non-early mobility therapy for patients who are in intensive care will be analyzed.
- Implementation of Physical Restraints in the Intensive Care Unit Once the tool determines the total number of FTEs needed for the ICU patients, they will be distributed throughout the day according to the trends of the patient volume.
- Pain Management at a Neonatal Intensive Care Unit
- Safety Score Improvement Plan For By-Faith Intensive Care Unit (ICU)
- Seizure Detection in a Pediatric Intensive Care Unit
- The Association Between Brain Volumes and Posttraumatic Stress Disorder in Intensive Care Unit
- Measuring Parent Satisfaction With Care in Neonatal Intensive Care Units
- Nurse Burnout and Stress in Neonatal Intensive Care Unit
- Care for Critical Ill Patients With COVID-19 in Intensive Care Unit
- Early Neonatal Intensive Care Unit Therapy
- Implementation of an Intensive Care Unit Pharmaceutical Care Model
- Premature Triplets: Neonatal Intensive Care Unit at Cook
- Continuous Renal Replacement Therapy in the Intensive Care Unit
- The Nature of Caring Work in an Intensive Care Unit
- Intensive Care Admission and Early Neuro-Rehabilitation
- Alarm Problems Going Off in the Intensive Care Unit
- Patients With Traumatic Brain Injury Admitted to the Ward or Intensive Care Unit
- Stress and Burnout of Nurses in the Intensive Care Unit
- Pain-Related Stress During the Neonatal Intensive Care Unit Stay
- Expert and Competent Non-expert Visual Cues During Simulated Diagnosis in Intensive Care
- Preventing Ventilator-Associated Pneumonia in the Intensive Care Unit
- Intensive Care Nurses’ Views and Practices on Eye Care
- Risk Factors for Intensive Care Unit Admission in Patients With Autoimmune Encephalitis
- Chronic Pain and Chronic Opioid Use After Intensive Care
- Premature Infants’ Physiologic Outcomes in the Neonatal Intensive Care Unit
- The Relationship Between Safety Climate and Performance in Intensive Care Units
- Intensive Care Unit Related Post Traumatic Stress Disorder
- Treatment of Severe Infections in the Intensive Care
- The Needs of Bereaved Parents in the Pediatric Intensive Care Unit
- Intensive Care Unit-Acquired Weakness
- Nosocomial Infections and the Infant Intensive Care Unit
- Complications and In-Hospital Mortality in Trauma Patients Treated in Intensive Care Units
- The Uniform Need for Critical and Intensive Care Skills in All Branches of Nursing
- Moral Distress Among European Intensive Care Nurses
- Capacity Planning for Intensive Care Units
- Real-Time Predictive Analytics for Therapeutic Plans in Intensive Care
- Nursing and the Importance of Intensive Care
- Abuse of Drugs and Alcohol in Intensive Care Unit
- Physician Scheduling for Continuity: An Application in Pediatric Intensive Care
- Monitoring Oxygenation and Gas Exchange in Neonatal Intensive Care Units
- Mortality in Intensive Care Unit Patients
- The Requirement for Supplementary Nurses in an Intensive Care Unit
- Respiratory Disorders Research Topics
- Affordable Care Act Essay Titles
- Biomedicine Essay Topics
- Asthma Paper Topics
- Health Promotion Research Topics
- Nursing Theory Questions
- Occupational Therapy Titles
- Wellness Essay Topics
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 28). 72 Intensive Care Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/intensive-care-essay-topics/
"72 Intensive Care Essay Topic Ideas & Examples." IvyPanda , 28 Feb. 2024, ivypanda.com/essays/topic/intensive-care-essay-topics/.
IvyPanda . (2024) '72 Intensive Care Essay Topic Ideas & Examples'. 28 February.
IvyPanda . 2024. "72 Intensive Care Essay Topic Ideas & Examples." February 28, 2024. https://ivypanda.com/essays/topic/intensive-care-essay-topics/.
1. IvyPanda . "72 Intensive Care Essay Topic Ideas & Examples." February 28, 2024. https://ivypanda.com/essays/topic/intensive-care-essay-topics/.
Bibliography
IvyPanda . "72 Intensive Care Essay Topic Ideas & Examples." February 28, 2024. https://ivypanda.com/essays/topic/intensive-care-essay-topics/.
Questions? Call us:
Email:
- How it works
- Testimonials
Essay Writing
- Essay service
- Essay writers
- College essay service
- Write my essay
- Pay for essay
- Essay topics
Term Paper Writing
- Term paper service
- Buy term papers
- Term paper help
- Term paper writers
- College term papers
- Write my term paper
- Pay for term paper
- Term paper topic
Research Paper Writing
- Research paper service
- Buy research paper
- Research paper help
- Research paper writers
- College research papers
- Write my research paper
- Pay for research paper
- Research paper topics
Dissertation Writing
- Dissertation service
- Buy dissertation
- Dissertation help
- Dissertation writers
- College thesis
- Write my dissertation
- Pay for dissertation
- Dissertation topics
Other Services
- Custom writing services
- Speech writing service
- Movie review writing
- Editing service
- Assignment writing
- Article writing service
- Book report writing
- Book review writing
Popular request:
The 100 nursing research topics you need this semester.
December 19, 2019

Most students are writing their essays on the same couple of topics, and this is driving professors crazy. It doesn’t matter if we’re talking about evidence based practice nursing topics or about ethical topics in nursing. The truth of the matter is that students who want a top grade on their essay should focus on finding an exceptional topic. But what makes nursing paper topics exceptional? Here are some things to keep in mind:
- The topic for the nursing research paper must be original and very interesting. Find something that can pique the interest of your professor.
- Don’t pick the easiest topics. You won’t have much to write about and your professor will figure out that you just wanted to get the paper done as soon as possible.
- Don’t pick the most difficult nursing paper topics either. You will have a lot of work to do and it can take you days to complete the essay.
- Find a topic that is of interest today. Avoid discussing issues that don’t interest anyone in the present. Remember that your research must bring value the academic community.
- It’s difficult to do, but try to find nursing topics that are focused and narrow. Broad topics are too general and your professor won’t appreciate them. Narrow down the topic by geographical area, time frame, culture, and so on.
Only the Best Nursing Research Topics for Students
Whether you’re looking for quantitative nursing research topics or qualitative topics, you need to be aware that the topic you pick has a great influence on the final grade you get on your essay. Why? It’s pretty simple actually; professors want something new. They want you to be original. They want to be surprised. Wouldn’t you get bored reading papers on the same nursing research topics over and over again?
By taking the time to search for an original, interesting topic, you are showing to your teacher that you really did put in the effort to write an excellent academic paper. In most cases, you will get some bonus points just for this. This is why our list of 100 nursing research topics is so important. And remember, the topics are 100% free, so you can use them right now as you see fit.
Mental Health Topics
Mental health can be difficult to write about. However, the grade you can get on such a paper can be great for your GPA. Here are some topics about mental health that are relatively easy to tackle:
- The link between violent video games and mental health.
- Stress in law enforcement officers.
- The causes of PTSD in army veterans.
- What causes depression?
- What is bipolar disorder and how can it be alleviated.
- Testing for schizophrenia.
- Ethics concerns for psychiatric patients.
Controversial Nursing Topics
Every one of these evidence based practice nursing research topics is a hot potato. You should be very careful when writing an academic paper on these because it’s very easy to offend some of your audience. Here are the controversial essay topics you can try your hand at:
- Does short staffing affect nurses at the work place?
- Working long shifts decreases patient care quality.
- Nurses should receive bonuses related to patient outcome.
- Nurses should be allowed to prescribe medicine.
- Sometimes nurses are more important than doctors.
- Is nursing a women’s job?
- Should nurses get the same wages as doctors?
Elderly Care
These nursing evidence based practice topics are related to elders. If you are interested in providing better care for elderly people, these are the topics for you. You can help make a change in the world by writing on any of the topics below:
- Reducing cardiovascular risks in elderly patients.
- What are the requirements for critical care?
- How to protect against Parkinson’s Disease?
- A study about joint disorders.
- What is the Restless Legs Syndrome?
- An in-depth analysis of atrial fibrillation.
- Three ways to defend against a stroke.
Nursing Careers
Do you have some advice about people looking at a nursing career? Why don’t you write an essay on a topic like:
- Does it pay off to become a nurse?
- Analyzing diversity in the nursing environment.
- The difficulties faced by nursing practitioners.
- The stress effects of night shifts.
- What is a remote intensive care unit?
- 10 things to do with your nursing degree.
- The three unique nursing career options.
Ethics Topics in Nursing
Ethics is a major talking point when it comes to nursing. There are many controversies surrounding certain practices and opinions are split. Why don’t you shed some light on topics such as:
- The personal values of nurses.
- Do nurses have contractual relationships with patients?
- When can nurses refuse care?
- Ethics is vital for the foundation of nursing.
- Ethics problems that are making nurses quit.
- Should nurses discuss ethics with their family?
- The three ethics issues nurses face every day.
Pediatric Nursing Research Topics
If you like children and you want to make a difference, there are some pediatric nursing research topics you can write about right now. Here are some of the topics we consider to be the best candidates for an A+ paper:
- What causes ADHD in children?
- Fighting against child obesity: top 3 methods.
- The ethics of pediatric care nurses.
- The link between vaccination and authism.
- What causes seizures in children?
- Social media and it’s effects on children’s psychology.
- The best treatment for speech disorders.
- What causes antibiotic resistance in children?
- Does healthy eating really prevent obesity?
Nursing Quality Improvement Topics
These research topics in nursing are an excellent choice for many students. If you are worried about the quality of the nursing service, write about any of these topics:
- Improving the quality of pain management in children.
- An analysis of the human pain limits.
- What does it take to improve nursing care?
- Nurses need to speak up about quality problems.
- Best exercises that improve mental health.
- Limiting long night shifts and focusing on individual patients.
- The role of nurses in improving medical services quality.
- The tools nurses can use to improve care quality.
Easily Researchable Topics in Nursing
You want some nursing research paper topics, but don’t want to spend more than a day or two working on your paper? Here are some easy nursing topics that you can use right now:
- What are Phantom Pains and why do they appear?
- Three symptoms in the ER that medicine can’t explain.
- The dangers of pre-term labor.
- Is telemedicine really effective?
- The problems with the telemedicine system.
- The best 3 disease control methods.
- Do opioids aid in bone healing?
- The future of nursing in the digital age.
Adult Nursing Research Topics
There are plenty of good nursing research topics out there, and plenty of them are about adult nursing. Here are some of the topics your writers consider to be the most interesting for high school and college students:
- Analyzing the lack of dental care in the United States.
- The roles of clinical nurses in the UK.
- How do you treat sleep disorders effectively?
- Here is how you control your blood pressure at home.
- Providing treatment to homeless people.
- The most effective headache treatments.
- The disastrous consequences of abortion.
- Analyzing the main symptoms of autism.
- Effective ways to treat patients in prison.
Hot Topics in Nursing
These evidence based nursing topics are hot. They are trending right now. Consequently, it makes a lot of sense to write an essay on any of these topics:
- Private nursing homes are the best choice.
- Online training is excellent for future nurses.
- What is art therapy and how does it work?
- The benefits of music theraphy.
- We are seeing a reduction in experienced nurses.
- Nurses are doing more than ever before.
- Analyzing the gender pay gap in nursing.
- Let’s take a closer look at Holistic Care.
Women’s Health
Are you interested in women’s health? Do you know about something that should be changed? Then why not write a nursing essay on a topic about women’s health? Here are some ideas for you:
- The prognosis for breast cancer.
- What causes sleep disorders in women?
- The newest neonatal practices.
- Three effective pregnancy prevention methods.
- The many challenges of menopause.
- The causes for vaginal atrophy.
- The three effective ways to prevent breast cancer.
Healthcare Management
Perhaps you consider healthcare management lacking. Don’t worry, you are definitely not the only one. But while other people just complain and don’t do anything about it, you have the chance to write an academic paper on this:
- The effects of gender bias on nurses.
- Medicare benefits of nurses.
- How effective is home service really?
- Uniform code regulations for nurses.
- How to start your own medical practice.
- Non-english patients can pose legal issues.
- Regulations about medical marijuana every nurse needs to know.
- Home nursing needs more oversight.
Other Nursing Topics
- These are the topics that don’t really fall into any of the categories above:
- The role of the nurse in palliative care.
- Should nurses be checked for drugs periodically?
- The effects of a smiling face.
- What does an emergency room nurse do in the US?
- Time management in the nursing profession.
- Is pediatric nursing different than regular nursing?
- How to deal with abusive patients as a nurse?
It doesn’t matter whether you are writing your essay on controversial topics in nursing or on pediatrics topics. What matters the most is the quality of the topic and the quality of the writing. As such, you should do your homework and learn how to write an essay the proper way. Citation and bibliography mistakes will not be tolerated. Tone, style and vocabulary are also very important. As you probably already know, academic writing has a very large set of rules and guidelines that you should strictly abide by.
In case you need some research topics for nursing students, or if you need help with writing the essays, you should get high quality help from a professional nursing writer. An academic writer can compose your nursing term paper or give you a lengthy list of nursing capstone project topics in just a day or two. You can easily save a lot of time and get a better grade simply by enlisting the help of such an experienced professional.
It’s time to nail your grades! Get your 20% discount on a nursing writing assignment with promo “ ewriting20 ” – and enjoy your college life!

Take a break from writing.
Top academic experts are here for you.
- How To Write An Autobiography Guideline And Useful Advice
- 182 Best Classification Essay Topics To Learn And Write About
- How To Manage Stress In College: Top Practical Tips
- How To Write A Narrative Essay: Definition, Tips, And A Step-by-Step Guide
- How To Write Article Review Like Professional
- Great Problem Solution Essay Topics
- Creating Best Stanford Roommate Essay
- Costco Essay – Best Writing Guide
- How To Quote A Dialogue
- Wonderful Expository Essay Topics
- Research Paper Topics For 2020
- Interesting Persuasive Essay Topics
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Brechin A. Introducing critical practice. In: Brechin A, Brown H, Eby MA (eds). London: Sage/Open University; 2000
Introduction to evidence informed decision making. 2012. https://cihr-irsc.gc.ca/e/45245.html (accessed 8 March 2022)
Cullen L, Adams SL. Planning for implementation of evidence-based practice. JONA: The Journal of Nursing Administration. 2012; 42:(4)222-230 https://doi.org/10.1097/NNA.0b013e31824ccd0a
DiCenso A, Guyatt G, Ciliska D. Evidence-based nursing. A guide to clinical practice.St. Louis (MO): Mosby; 2005
Implementing evidence-informed practice: International perspectives. In: Dill K, Shera W (eds). Toronto, Canada: Canadian Scholars Press; 2012
Dufault M. Testing a collaborative research utilization model to translate best practices in pain management. Worldviews Evid Based Nurs. 2004; 1:S26-S32 https://doi.org/10.1111/j.1524-475X.2004.04049.x
Epstein I. Promoting harmony where there is commonly conflict: evidence-informed practice as an integrative strategy. Soc Work Health Care. 2009; 48:(3)216-231 https://doi.org/10.1080/00981380802589845
Epstein I. Reconciling evidence-based practice, evidence-informed practice, and practice-based research: the role of clinical data-mining. Social Work. 2011; 56:(3)284-288 https://doi.org/10.1093/sw/56.3.284
Implementation research: a synthesis of the literature. 2005. https://tinyurl.com/mwpf4be4 (accessed 6 March 2022)
Graham ID, Logan J, Harrison MB Lost in knowledge translation: time for a map?. J Contin Educ Health Prof. 2006; 26:(1)13-24 https://doi.org/10.1002/chp.47
Greenhalgh T, Robert G, Bate P, MacFarlane F, Kyriakidou O. Diffusion of innovations in health service organisations. A systematic literature review.Malden (MA): Blackwell; 2005
Greenhalgh T, Howick J, Maskrey N. Evidence based medicine: a movement in crisis?. BMJ. 2014; 348 https://doi.org/10.1136/bmj.g3725
Haynes RB, Devereaux PJ, Guyatt GH. Clinical expertise in the era of evidence-based medicine and patient choice. BMJ Evidence-Based Medicine. 2002; 7:36-38 https://doi.org/10.1136/ebm.7.2.36
Hitch D, Nicola-Richmond K. Instructional practices for evidence-based practice with pre-registration allied health students: a review of recent research and developments. Adv Health Sci Educ Theory Pract. 2017; 22:(4)1031-1045 https://doi.org/10.1007/s10459-016-9702-9
Jerkert J. Negative mechanistic reasoning in medical intervention assessment. Theor Med Bioeth. 2015; 36:(6)425-437 https://doi.org/10.1007/s11017-015-9348-2
McSherry R, Artley A, Holloran J. Research awareness: an important factor for evidence-based practice?. Worldviews Evid Based Nurs. 2006; 3:(3)103-115 https://doi.org/10.1111/j.1741-6787.2006.00059.x
McSherry R, Simmons M, Pearce P. An introduction to evidence-informed nursing. In: McSherry R, Simmons M, Abbott P London: Routledge; 2002
Implementing excellence in your health care organization: managing, leading and collaborating. In: McSherry R, Warr J (eds). Maidenhead: Open University Press; 2010
Melnyk BM, Fineout-Overholt E, Stillwell SB, Williamson KM. Evidence-based practice: step by step: the seven steps of evidence-based practice. AJN, American Journal of Nursing. 2010; 110:(1)51-53 https://doi.org/10.1097/01.NAJ.0000366056.06605.d2
Implementing evidence-based practices: six ‘drivers’ of success. Part 3 in a Series on Fostering the Adoption of Evidence-Based Practices in Out-Of-School Time Programs. 2007. https://tinyurl.com/mu2y6ahk (accessed 8 March 2022)
Muir-Gray JA. Evidence-based healthcare. How to make health policy and management decisions.Edinburgh: Churchill Livingstone; 1997
Nevo I, Slonim-Nevo V. The myth of evidence-based practice: towards evidence-informed practice. British Journal of Social Work. 2011; 41:(6)1176-1197 https://doi.org/10.1093/bjsw/bcq149
Newhouse RP, Dearholt S, Poe S, Pugh LC, White K. The Johns Hopkins Nursing Evidence-based Practice Rating Scale.: The Johns Hopkins Hospital: Johns Hopkins University School of Nursing; 2005
Nursing and Midwifery Council. The Code. 2018. https://www.nmc.org.uk/standards/code (accessed 7 March 2022)
Nutley S, Walter I, Davies HTO. Promoting evidence-based practice: models and mechanisms from cross-sector review. Research on Social Work Practice. 2009; 19:(5)552-559 https://doi.org/10.1177/1049731509335496
Reed JE, Howe C, Doyle C, Bell D. Successful Healthcare Improvements From Translating Evidence in complex systems (SHIFT-Evidence): simple rules to guide practice and research. Int J Qual Health Care. 2019; 31:(3)238-244 https://doi.org/10.1093/intqhc/mzy160
Rosswurm MA, Larrabee JH. A model for change to evidence-based practice. Image J Nurs Sch. 1999; 31:(4)317-322 https://doi.org/10.1111/j.1547-5069.1999.tb00510.x
Rubin A. Improving the teaching of evidence-based practice: introduction to the special issue. Research on Social Work Practice. 2007; 17:(5)541-547 https://doi.org/10.1177/1049731507300145
Shlonsky A, Mildon R. Methodological pluralism in the age of evidence-informed practice and policy. Scand J Public Health. 2014; 42:18-27 https://doi.org/10.1177/1403494813516716
Straus SE, Tetroe J, Graham I. Defining knowledge translation. CMAJ. 2009; 181:(3-4)165-168 https://doi.org/10.1503/cmaj.081229
Titler MG, Everett LQ. Translating research into practice. Considerations for critical care investigators. Crit Care Nurs Clin North Am. 2001; 13:(4)587-604 https://doi.org/10.1016/S0899-5885(18)30026-1
Titler MG, Kleiber C, Steelman V Infusing research into practice to promote quality care. Nurs Res. 1994; 43:(5)307-313 https://doi.org/10.1097/00006199-199409000-00009
Titler MG, Kleiber C, Steelman VJ The Iowa model of evidence-based practice to promote quality care. Crit Care Nurs Clin North Am. 2001; 13:(4)497-509 https://doi.org/10.1016/S0899-5885(18)30017-0
Ubbink DT, Guyatt GH, Vermeulen H. Framework of policy recommendations for implementation of evidence-based practice: a systematic scoping review. BMJ Open. 2013; 3:(1) https://doi.org/10.1136/bmjopen-2012-001881
Wang LP, Jiang XL, Wang L, Wang GR, Bai YJ. Barriers to and facilitators of research utilization: a survey of registered nurses in China. PLoS One. 2013; 8:(11) https://doi.org/10.1371/journal.pone.0081908
Warren JI, McLaughlin M, Bardsley J, Eich J, Esche CA, Kropkowski L, Risch S. The strengths and challenges of implementing EBP in healthcare systems. Worldviews Evid Based Nurs. 2016; 13:(1)15-24 https://doi.org/10.1111/wvn.12149
Webber M, Carr S. Applying research evidence in social work practice: Seeing beyond paradigms. In: Webber M (ed). London: Palgrave; 2015
Evidence-based practice vs. evidence-based practice: what's the difference?. 2014. https://tinyurl.com/2p8msjaf (accessed 8 March 2022)
Evidence-informed practice: simplifying and applying the concept for nursing students and academics
Elizabeth Adjoa Kumah
Nurse Researcher, Faculty of Health and Social Care, University of Chester, Chester
View articles · Email Elizabeth Adjoa
Robert McSherry
Professor of Nursing and Practice Development, Faculty of Health and Social Care, University of Chester, Chester
View articles
Josette Bettany-Saltikov
Senior Lecturer, School of Health and Social Care, Teesside University, Middlesbrough
Paul van Schaik
Professor of Research, School of Social Sciences, Humanities and Law, Teesside University, Middlesbrough

Background:
Nurses' ability to apply evidence effectively in practice is a critical factor in delivering high-quality patient care. Evidence-based practice (EBP) is recognised as the gold standard for the delivery of safe and effective person-centred care. However, decades following its inception, nurses continue to encounter difficulties in implementing EBP and, although models for its implementation offer stepwise approaches, factors, such as the context of care and its mechanistic nature, act as barriers to effective and consistent implementation. It is, therefore, imperative to find a solution to the way evidence is applied in practice. Evidence-informed practice (EIP) has been mooted as an alternative to EBP, prompting debate as to which approach better enables the transfer of evidence into practice. Although there are several EBP models and educational interventions, research on the concept of EIP is limited. This article seeks to clarify the concept of EIP and provide an integrated systems-based model of EIP for the application of evidence in clinical nursing practice, by presenting the systems and processes of the EIP model. Two scenarios are used to demonstrate the factors and elements of the EIP model and define how it facilitates the application of evidence to practice. The EIP model provides a framework to deliver clinically effective care, and the ability to justify the processes used and the service provided by referring to reliable evidence.
Evidence-based practice (EBP) was first mentioned in the literature by Muir-Gray, who defined EBP as ‘an approach to decision-making in which the clinician uses the best available evidence in consultation with the patient to decide upon the option which suits the patient best’ (1997:97). Since this initial definition was set out in 1997, EBP has gained prominence as the gold standard for the delivery of safe and effective health care.
There are several models for implementing EBP. Examples include:
- Rosswurm and Larrabee's (1999) model
- The Iowa model ( Titler et al, 2001 )
- Collaborative research utilisation model ( Dufault, 2004 ); DiCenso et al's (2005) model
- Greenhalgh et al's (2005) model
- Johns Hopkins Nursing model ( Newhouse et al, 2005 )
- Melnyk et al's (2010) model.
Although a comprehensive review of these models is beyond the scope of this article, a brief assessment reveals some commonalities among them. These include a) asking or selecting a practice question, b) searching for the best evidence, c) critically appraising and applying the evidence, d) evaluating the outcome(s) of patient care delivery, and e) disseminating the outcome(s).
Regardless of the benefits of EBP, and the existence of multiple EBP models intended to facilitate the application of evidence into practice, health professionals, including nurses, continue to struggle to implement it effectively ( Ubbink et al, 2013 ). Critics of EBP have questioned its validity ( Rubin, 2007 ; Nevo and Slonim-Nevo, 2011 ); the best practice and setting to support its use ( Nutley et al, 2009 ); its failure to address the complexity of health and health care, as well as the patient's context ( Muir-Gray, 1997 ; Reed et al, 2019 ), and its mechanistic approach ( Epstein, 2009 ; Jerkert, 2015 ). Some of these criticisms are outlined below.
For example, previous studies have reported the barriers health professionals face to successfully implement EBP. Ubbink et al (2013) conducted a systematic review to determine nurses' and doctors' views on knowledge, attitudes, skills, barriers, and behaviour required to implement EBP. The review included 31 studies from 17 countries: eight from North America and 11 from Europe. The results revealed that organisational and individual barriers prevent uptake of EBP among nurses and doctors. These barriers included the lack of material and human resources, and lack of support from managers and leaders; individual barriers included knowledge deficit regarding EBP, time and workload ( Ubbink et al, 2013 ). Researchers such as Hitch and Nicola-Richmond (2017) and Warren et al (2016) found similar barriers to implementing EBP reported by health professionals.
Effective and consistent implementation of EBP in healthcare settings depends on complex interdependent factors, such as the characteristics of an organisation (eg the internal and external healthcare environment, and organisational structures and values); the EBP intervention (eg reduction of hospital-acquired infections); and the attitudes of the individual practitioner towards EBP ( Titler and Everett, 2001 ; Cullen and Adams, 2012 ). Yet, existing approaches of EBP have been ineffective in facilitating its implementation ( Greenhalgh et al, 2014 ).
Consequently, authors such as Cullen and Adams (2012) and Greenhalgh et al (2014) have called for a resurgence of the concept, especially concerning the components of EBP associated with involving patients in decision-making, and with expert judgement and experience. Greenhalgh et al (2014:3) consider it is time to return to implementing ‘real EBP’, where person-centred care is the priority, and health professionals and their patients ‘are free to make appropriate care decisions that may not match what best evidence seems to suggest’. Nonetheless, researchers including McSherry et al (2002) , Epstein (2009) and Nevo and Slonim-Nevo (2011) have proposed an alternative, holistic approach to the application of evidence into practice, termed evidence-informed practice (EIP).
Journey towards evidence-informed practice
The problems with the uptake and effective implementation of EBP led to the emergence of the EIP concept. This concept is based on the premise that healthcare practice should, as a matter of principle, be informed by, rather than based on, evidence ( Nevo and Slonim-Nevo, 2011 ). This implies that other forms of evidence (for example, patient experiences, the nurse's expertise and experiences), not just the ‘research evidence’, should be considered in applying evidence in practice.
McSherry et al (2002) defined EIP as the assimilation of professional judgment and research evidence regarding the efficiency of interventions. This definition was further elaborated as an approach to patient care where:
‘Practitioners are encouraged to be knowledgeable about findings coming from all types of studies and to use them in an integrative manner, taking into consideration clinical experience and judgment, clients' preferences and values, and context of the interventions.’
Nevo and Slonim-Nevo (2011:18)
It has been over two decades since EIP emerged in the literature, however, primary research on the concept has been limited. Hence, although the term EIP has gained momentum in recent times, the methods needed to implement it effectively are not widely known ( McSherry, 2007 ; Woodbury and Kuhnke, 2014 ). While some proponents of EIP (eg Epstein 2011 ; Webber and Carr 2015 ) have identified significant differences between EBP and EIP, most researchers (eg Ciliska, 2012 ; Shlonsky and Mildon, 2014 ) have used the terms interchangeably.
Ciliska (2012) , for instance, developed an evidence-informed decision making (EIDM) module, but referred to the steps of EBP (ie Ask, Acquire, Appraise, Integrate, Adapt, Apply, Analyse) as the processes to be followed in implementing EIDM. Ciliska (2012) explained that the term EIDM was adopted to signify that other types of evidence are useful in clinical decision-making and to attempt to get beyond the criticisms of EBP. This notwithstanding, the author maintained the existing process for implementing EBP. Similarly, Shlonsky and Mildon (2014) used the terms EBP and EIP interchangeably, as they consistently referred to an EBP approach as EIP. Examples include referring to the steps of EBP as ‘the steps of EIP’ ( Shlonsky and Mildon, 2014:3 ) and referring to Haynes et al's (2002) expanded EBP model as a ‘revised EIP model’ ( Shlonsky and Mildon, 2014:2 ).
Another term that is often used interchangeably with EIP is ‘knowledge translation’. This term has been explored extensively. For example, the Canadian Institute of Health Research (CIHR) has adopted knowledge translation to signify the use of high-quality research evidence to make informed decisions ( Straus et al, 2009 ). The CIHR ( Graham et al, 2006 ) developed a ‘knowledge to action’ model intended to integrate the creation and application of knowledge. The model acknowledges the non-linear process of applying evidence in practice, where each stage is influenced by the next, as well as the preceding, stage. In a typical clinical setting, the actual process of applying evidence in practice is not linear, as acknowledged by the proponents of EBP, but cyclical and interdependent. Ciliska (2012) linked Graham et al's (2006) model to the components of evidence-informed decision-making. According to Ciliska (2012:7) , the knowledge-to-action model ‘fits with the steps of evidence-informed decision-making’. However, like EBP, the term ‘knowledge translation’, differs significantly from the EIP concept because it focuses on the ‘research evidence’ in decision-making.
The apparent confusion surrounding EIP is due to inadequate information about its components and the methods involved in implementing the concept. To foster a culture of EIP among health professionals, they must first be made aware of the actual components of the concept and the strategies involved in its successful implementation. The following section uses case scenarios to provide a description of the factors and elements of the EIP model and defines how it facilitates the application of evidence into clinical nursing practice.
Systems thinking
The clinical setting within which nurses work is a complex system made up of several interdependent and inter-related parts. Problems with healthcare delivery and management must therefore be perceived as a consequence of the exchanges between elements of the systems, instead of an outcome or the malfunctioning of a particular element. This, McSherry and Warr (2010) , have referred to as ‘systems thinking’.
Effective implementation of EIP demands an understanding of the various parts of the system that come together to aid the application of evidence in practice.
The evidence-informed practice model
The original model.
The earliest version of the evidence-informed practice model is depicted in Figure 1 . This was developed specifically for nurses and was originally named ‘the evidence-informed nursing model’. The model presented in Figure 1 was developed through PhD research conducted by Robert McSherry (2007) , with the aim to explore, through a mixed-methods study design, why the use of research as evidence in support of clinical nursing practice remains problematic. Study participants were registered nurses practising in a hospital trust located in north-east England.
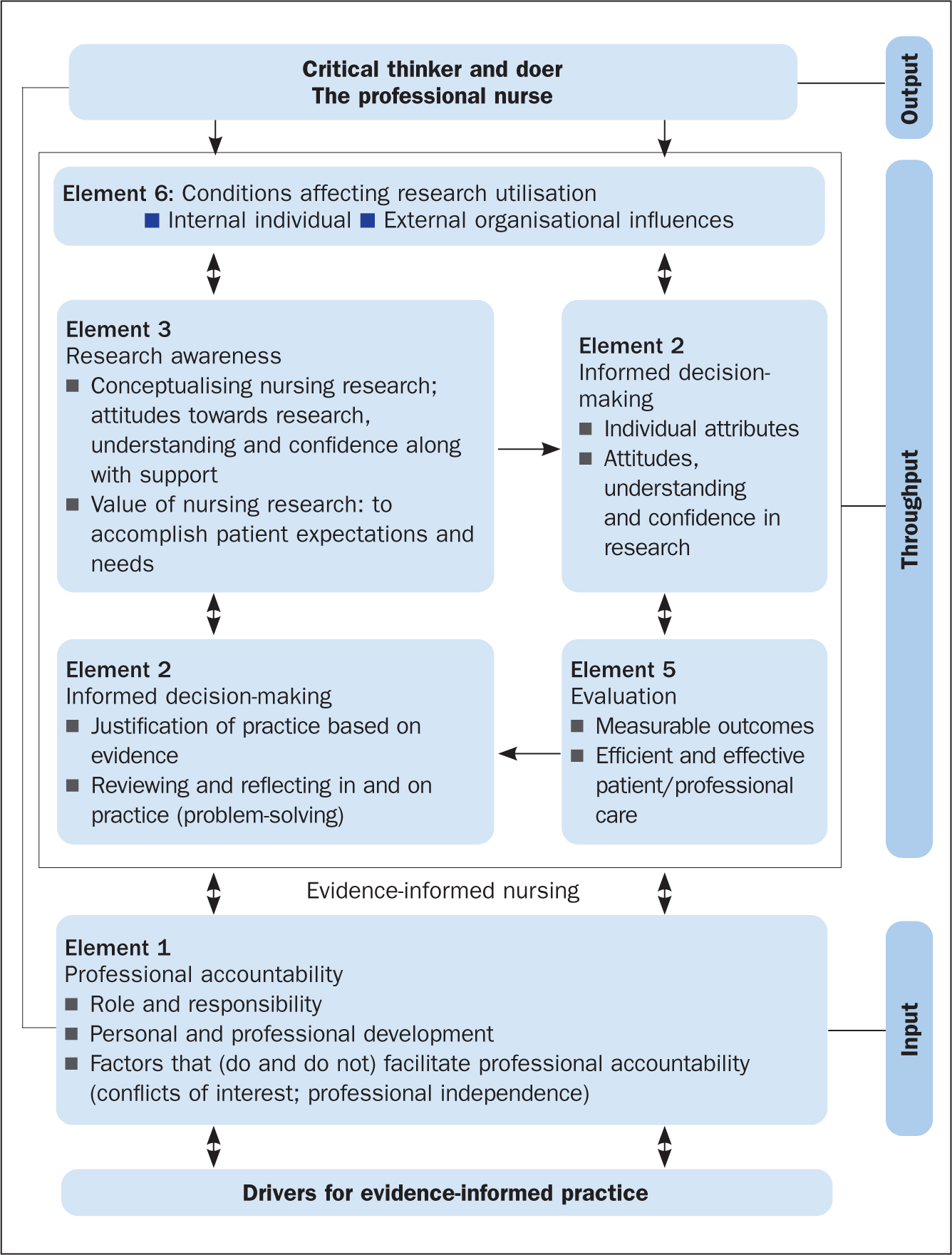
The results of McSherry's (2007) study showed that, to effectively apply evidence in clinical nursing practice, nurses needed to be informed of, and be able to interact with, several key elements. The evidence-informed nursing model was developed as an alternative framework for facilitating the application of evidence in clinical nursing practice and was grounded in the principles and practices of systems thinking. This is because, primarily, the model provided an integrated process to applying evidence into practice, consisting of:
- A clearly defined input; to encourage nurses to use evidence in practice
- Throughput; facilitation of the processes associated with the elements
- Output; improved standards of professional practice
The revised model
The evidence-informed nursing model has been adapted to the evidence-informed practice model. The new model ( Figure 2 ) is adapted in several ways. First, it has been modified to be all-inclusive, so it could be applied to any health profession. Second, the model has been simplified to show the interconnectedness of the various factors and elements that enable a professional to use evidence in support of their clinical decision-making. Third, the model demonstrates the ongoing complexity that health professionals find themselves working in, in the quest to apply evidence to clinical practice. Last, the EIP model incorporates the principles and components of EBP, which is particularly evident in the EIP cycle (the throughput phase of the model).
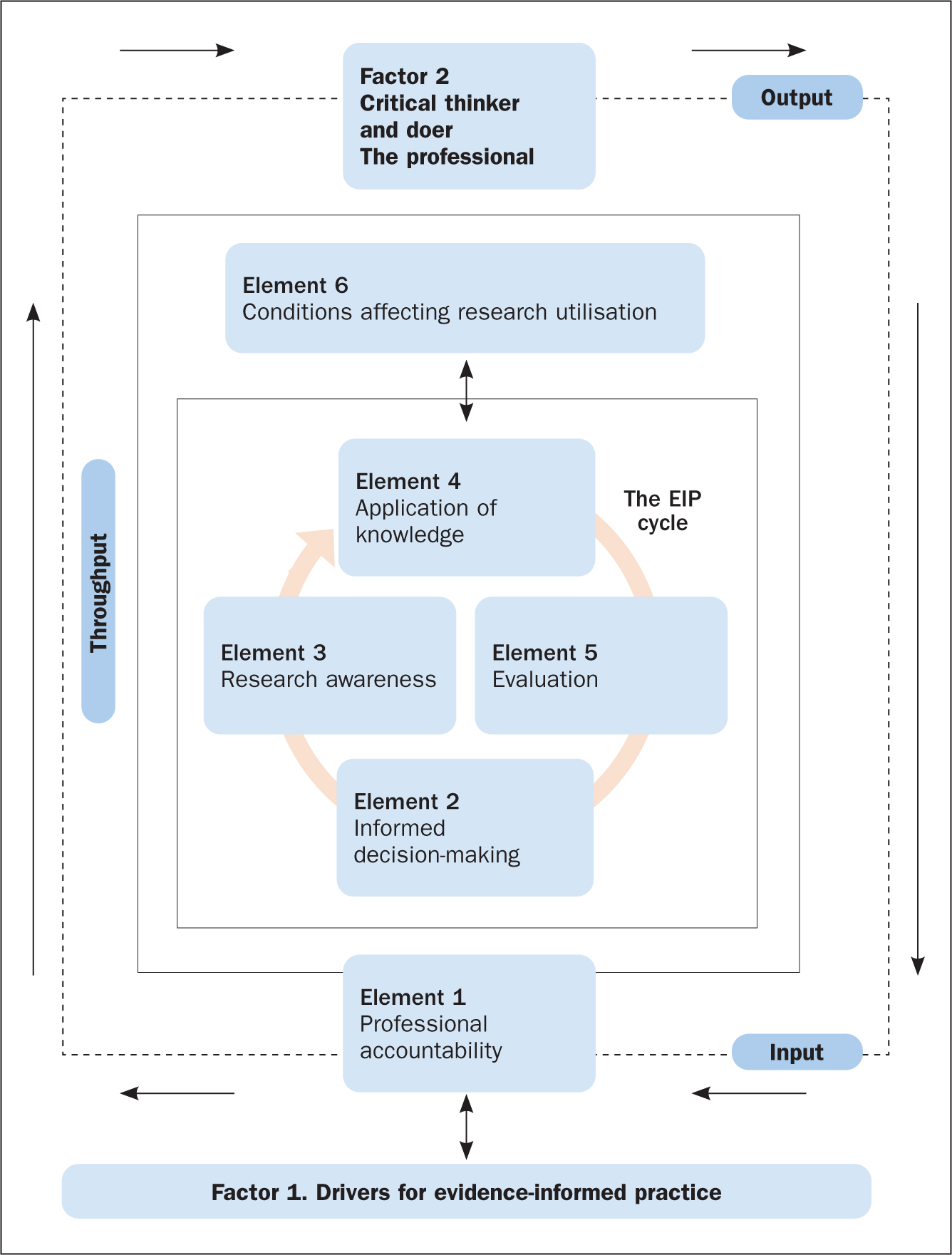
The factors and elements of the EIP model ( Figure 2 ) are explored in more detail below with reference to two scenarios, which are used to apply the EIP model to clinical nursing practice within both a scientific and the wider context within which nursing care takes place.
The first factor of the EIP model is ‘Factor 1. Drivers for evidence-informed practice’ ( Figure 2 ). In order for nurses to enhance patient care and experiences, along with improving their knowledge and skills of the patient's condition and associated signs and symptoms, they need to be aware of what EIP is, what it involves, and the principles required to make it happen. Applying the scenarios, it is essential that the nurse understands and can identify the key elements that drive successful implementation of the EIP concept. This is referred to as the drivers for EIP, which are illustrated in Figure 3 and discussed below.
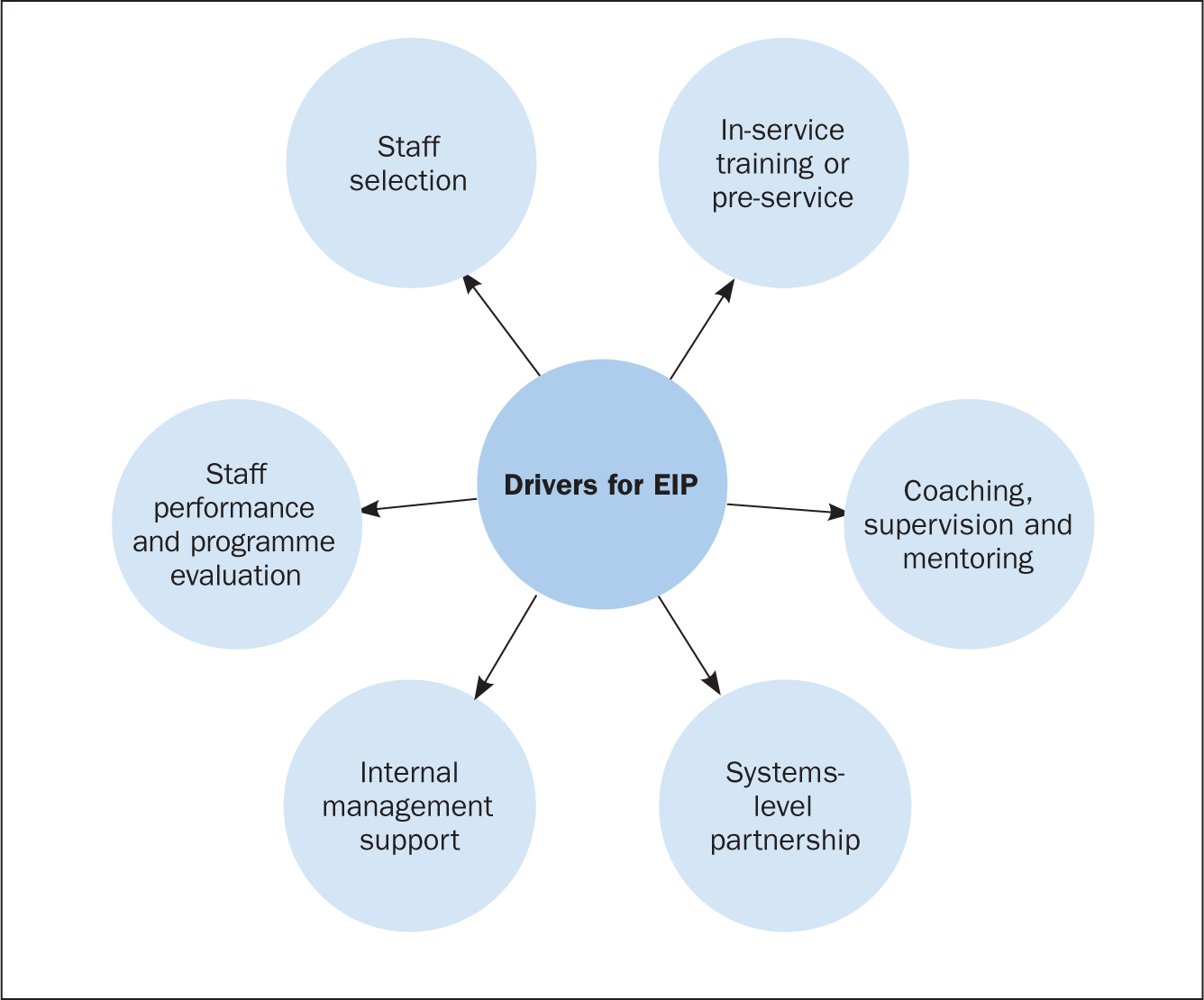
Drivers for EIP
Staff selection.
Recruiting, interviewing and redeploying existing staff or hiring new staff are part of the staff selection process ( Dill and Shera, 2012 ). The importance of this driver is to identify personnel who qualify to implement the EIP programme or model. Additionally, it aims at selecting individuals within the organisation (for example coaches, supervisors, and trainers), who will ensure that the required organisational changes to support nurses in the effective implementation of EIP are done.
In-service training or pre-service
Training on EIP programmes involves activities that are related to offering instruction, providing specialist information or skills development in a structured manner to nurses and other key healthcare staff involved in the EIP programme. Nurses, as well as other members of staff, must learn when, how, where, and with whom to use new approaches and skills in applying evidence to practice ( Metz et al, 2007 ).
Coaching, supervision and mentoring
The coaching and mentoring approach enables new skills to be introduced to nurses on the ward with the support of a coach. The duty of a coach is to offer expert information and support, together with encouragement, opportunities and advice to practise and apply skills that are specific to the EIP programme. Effective implementation of human service interventions (such as EIP) requires changes in behaviour at administrative, supervisory and practitioner levels ( Dill and Shera, 2012 ). Coaching and mentoring are the main ways to bring about a change in behaviour for staff who have been successfully involved in the beginning stage of the implementation process and throughout the life of the EIP programme.
Systems-level partnership
This refers to the improvement of partnerships with the broader and immediate systems to ensure access to required funds, and institutional and human resources necessary to support nurses' work. The immediate systems-level partnership refers to working with individuals or organisations that directly influence healthcare delivery (for example, nurses and doctors).
Partnerships within the broader system, on the other hand, refer to policymakers, funders or other organisations that may support the EIP programme, but are not directly involved in delivering health care. A variety of activities may be conducted as part of the development of systems-level partnerships to aid the implementation of EIP. These may include fundraising activities to support the implementation of EIP programmes, as well as the use of external coaches and consultants to assist with mentoring, technical assistance and training on an ongoing basis.
Internal management support
This involves activities that are associated with establishing processes and structures within an EIP programme to enhance effective implementation of the programme. This is necessary in order to inform healthcare decision-making as well as keep staff organised and focussed on desired care outcomes ( Fixsen et al, 2005 ). Instances of internal management support include the formation of institutional structures and processes, the allocation of resources to support selection of suitable staff, and administrative support for efficient training.
Staff performance and programme evaluation
This involves evaluation of staff performance and the overall EIP programme to determine whether the objectives of the programme have been achieved. To do this effectively, it is important to evaluate the outcomes of the above-defined drivers, in particular, staff selection, in-service training, as well as coaching and mentoring. This will offer managers and stakeholders insight about the effectiveness of staff selection, training, and mentoring in facilitating the application of evidence into clinical practice ( Dill and Shera, 2012 ).
Elements of the EIP model
The first element of the EIP model is professional accountability, depicted as an ‘input’ in Figure 2 . This is an essential part of a nurse's roles and responsibilities and is reaffirmed in the nursing Code ( Nursing and Midwifery Council, 2018 ) of professional practice, the contract of employment and job description. In both case scenarios involving Mitchell and Yvonne ( Box 1 ), professional accountability is evident on several fronts: the nurse must establish a caring, compassionate and therapeutic relationship with the patients by involving and engaging them in shared decision-making regarding all aspects of their care, treatments, and interventions; the nurse is accountable and answerable to the patient and his or her professional colleagues throughout the patient's journey.
Box 1.Patient scenariosScenario 1Yvonne, aged 31, is admitted to the emergency medical unit following a visit to her GP for a non-healing wound to her right big toe. The GP also reported that Yvonne has had a recurring sore throat, extreme tiredness and a low white blood cell count.The GP requested an urgent investigation of these symptoms. Yvonne was placed in a side room for precaution.Scenario 2Mitchell, aged 58, arrives in the emergency department complaining of severe chest pain. He is diaphoretic (sweating excessively) and says his pain is radiating down his left arm and up into his jaw, and he adds that he feels nauseated. A few minutes after admission, he suffers a cardiac arrest.He is resuscitated and transferred to the intensive care unit. He is intubated, is placed on a ventilator and has a central line catheter in place.
Throughput: the evidence-informed practice cycle
The EIP cycle (located in the ‘throughput’ of Figure 2 ) involves the processes or methods through which nurses apply evidence in support of their decision-making in clinical nursing practice. This often occurs in a clinical nursing environment that is complex, constantly changing, and involves numerous members of the multidisciplinary team, patients and their family. Effective communication (verbal and written) is essential for ensuring that the various elements are interchanging, interconnecting and communicating between, and with, each other. For example, the case of Yvonne in scenario 1 ( Box 1 ) can be used as an example to underline the importance of good communication. It is important to explain to the patient and her family the reason for nursing her in a side room rather than the main ward. In this situation, avoiding and preventing cross-infection is essential to safeguard Yvonne from harm.
To ensure the EIP cycle proceeds effectively requires that the nurse (the health professional) acts as the conduit for the interplay between the different elements of the model (ie Element 2: informed decision-making; Element 3: research awareness; Element 4: application of knowledge; and Element 5: evaluation). These elements will be further explored.
Element 2. Informed decision-making
This involves two-way communication between the nurse and the patient(s), and is critical in ensuring there is a robust relationship (honesty, openness, transparency) founded on the principles of person-centred care ( McSherry and Warr, 2010 ). It reaffirms the ethical principle of a patient's right to make an informed decision about what is suitable for them, and takes into account their beliefs, values, priorities and personal circumstances. In case scenario 2, applying the EIP model, the critical care nurse will be expected to involve Mitchell's (the patient's) relatives, medical staff and other members of the healthcare team in making decisions about, for example, ventilator management and care of the central line catheter. However, decision-making in an intensive care unit can be complex, and some of the decisions may involve the nurse only. Similarly, applying the EIP model in case scenario 1, the nurse will be expected to communicate with the patient (Yvonne), carers and colleagues about the importance of hand hygiene, wound care and the importance of using precautions to avoid hospital-acquired infections when caring for the patient.
In both case scenarios, the nurse must endeavour to involve the patient/family members in the process of decision-making by providing them with timely, appropriate and relevant information needed to make often complex and life-changing decisions.
Element 3. Research awareness
This element refers to motivating practitioners to acquire skills and knowledge, as well as to conceptualise what research and evidence involves and the significance they have in improving standards of healthcare practice ( McSherry et al, 2006 ). Research awareness is reliant on the nurse's attitudes towards research, the acquisition of knowledge and confidence about the value of research to practice, and on having supportive managers and colleagues.
This element of the EIP cycle, contained within the model, incorporates three of the steps (Research awareness) of EBP: ask a clinical question, search the literature for research evidence to answer the question, and critically appraise the evidence obtained). Although the nurse is not required to be a researcher to implement the EIP model effectively, they must be knowledgeable about relevant databases and search engines (such as Medline and Google), as well as critical appraisal tools, in order to be able to include high-quality research evidence when making patient care decisions.
However, the EIP model acknowledges the fact that research evidence may not always be readily available, and nurses may not have the necessary hardware and software in the care environment to enable them to search for research evidence. Hence, recommendations by Greenhalgh et al (2014) led to inclusion, within the EIP model, of nurses as critical thinkers and doers which, therefore, allows them to make appropriate care decisions based on patient preferences and actions, the clinical state, clinical setting and circumstances, and advocates that nurses apply their own knowledge, expertise and clinical experiences in clinical decision-making, which may not necessarily match what the research evidence seems to suggest.
With reference to scenario 2 (and similarly for scenario 1), to adhere to the EIP model the nurse would take the following steps:
- Update his/her knowledge about Mitchell's clinical presentation
- Search Medline for research evidence on ‘chest pain’, and ‘cardiac arrest’ and its associated symptoms. Based on the number of articles obtained, the nurse reads the titles and abstracts, and then, the full text of selected articles to exclude irrelevant articles. The remaining articles are then critically appraised to include the best research evidence in patient care decisions.
In situations where the above steps are not possible, the model advocates that the nurse endeavours to make the best care decisions possible based on patient preferences, clinical state, context and circumstances, and the nurse's own expertise and experience, as well as the experience of the patient and family members where possible.
Element 4. Application of knowledge
This is a complex element that requires the gathering and assimilation of various sources of information, evidence, quality and standards, and policy and guidance, to support the nurse's decision-making in clinical practice. In relation to both scenarios, the nurse would need to:
- Apply knowledge acquired from the patients (Mitchell and Yvonne), along with information from their relatives
- Apply evidence from reviewing the findings from research
- Take into account information gleaned from engaging with the multidisciplinary team
- Ensure they follow recommended local and national guidance and policy on the management of each patient's condition.
It is imperative that the nurse is experienced, knowledgeable, and competent in order to make the most appropriate care decisions together with the patient, the family and the wider multidisciplinary team. To do this effectively, the nurse requires certain personal attributes, it is also important for the organisation within which the nurse works to have specific institutional characteristics. Institutional features include culture, education and training, and workload/skill mix, whereas personal characteristics include improved confidence, attitude, understanding and behaviour towards the application of evidence into practice.
Element 5. Evaluation
This element of the EIP cycle within the model measures the effects of decision-making and actions of the nurse on care outcomes and in creating an optimal care environment. In both scenarios, the nurse would need to periodically evaluate specific processes and outcomes of care. For example, with regards to scenario 2, this would include:
- Monitoring how Mitchell is performing on the ventilator
- Taking the necessary infection prevention precautions to avoid the development of infections related to the insertion of a central line and transmission of hospital-acquired infection
- Monitoring improvement in Mitchell's general wellbeing.
Depending on the outcome of the evaluation, Mitchell's care plan would be either revised or continued.
Element 6. Conditions affecting research utilisation
Research utilisation involves critically appraising research findings, disseminating, and using the knowledge obtained from research to cause changes in an existing healthcare practice ( Titler et al, 1994 ). The conditions that affect research utilisation are grouped into five domains ( Wang et al, 2013 ):
- The process involved in utilising research findings
- Accessibility to research
- The quality of research
- The knowledge and attitudes of the nurse (health professional) regarding the use of research findings
- The organisation within which the findings of research are to be implemented.
In the two scenarios ( Box 1 ), the nurse needs to be aware of the potential barriers to research utilisation and identify ways to overcome these in order to effectively apply evidence to healthcare practice. In addition, the clinical environment within which nurses work must provide sufficient support in order to enhance the effective and consistent application of evidence to practice. Nurses must be supported to acquire the necessary knowledge, skills, and understanding needed to practise safely (ie competently and confidently). In addition, the resources necessary to obtain research evidence, such as IT (computers and internet), must be readily available in the clinical setting for easy access to information.
Factor 2 (Output). Critical thinker and doer, the professional nurse
To ensure that nurses inform their decisions with the best available evidence, it is imperative that they have a sound understanding and knowledge of what constitutes the EIP model ( Figure 2 ). Successfully engaging with the various factors and elements of this model will lead to the desired outcome—that of a professional who is a critical thinker and doer, a professional nurse who, as argued by Brechin (2000:44) , is ‘knowledgeable and skilled, yet welcomes alternative ideas and belief systems, appreciating and respecting alternative views’. In this context, it is about creating a caring and compassionate environment in which excellence in nursing practice occurs. This can only be exemplified by ensuring that decisions and actions are based on the best available evidence.
The benefits of the EIP model for the nurse, patient and family are that it simplifies a highly complex series of systems and processes pertaining to how evidence is used to support decisions made in clinical practice. The EIP model simply illustrates the why, the how and the sequencing of getting evidence into clinical practice. It also complements the evidence-based movement by offering a holistic systems-based approach to facilitating the application of evidence into clinical practice.
EIP is a holistic integrated approach to applying evidence into practice, which incorporates the steps of EBP within its system and processes. In other words, EBP is a subset of the EIP model, made explicit within the EIP cycle. Thus, EIP is neither an alternative to, nor a replacement for, EBP. The EIP model provides a framework for nurses (indeed all health practitioners) to deliver clinically effective care and enable them to justify the processes used and the service provided by referring to reliable evidence. Using two scenarios, this article demonstrated how the EIP model can be applied to clinical nursing practice. Future initiatives should focus on developing EIP educational interventions and determining the effects of such interventions on healthcare students' knowledge of, and attitudes towards, the application of evidence to practice.
- Two main concepts have been associated with the application of evidence into practice: evidence-based practice (EBP) and evidence-informed practice (EIP)
- The main feature that distinguishes EIP from EBP is the processes used in implementing the concepts
- EIP provides the mechanisms or processes to follow in implementing EBP
- EIP is not a substitute or replacement for EBP. EIP is an integrated approach to applying evidence to practice, which incorporates the steps of EBP in its processes
CPD reflective questions
- Make a list of the challenges you encounter in implementing EBP
- Use the same list and indicate how these challenges prevent you from using evidence to support your nursing clinical decisions and actions in practice
- How does viewing health and healthcare delivery as a complex system impact on your patient care?
- Make a list of the drivers that are encouraging you to support your clinical nursing decisions and actions with evidence
- Using your own experience to date and the information presented in the text, make a list of why and how you think evidence-informed practice forms part of your professional accountability and professional registration
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.

Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
Chapter 7 the evidence for evidence-based practice implementation.
Marita G. Titler .
Affiliations
Overview of evidence-based practice.
Evidence-based health care practices are available for a number of conditions such as asthma, heart failure, and diabetes. However, these practices are not always implemented in care delivery, and variation in practices abound. 1–4 Traditionally, patient safety research has focused on data analyses to identify patient safety issues and to demonstrate that a new practice will lead to improved quality and patient safety. 5 Much less research attention has been paid to how to implement practices. Yet, only by putting into practice what is learned from research will care be made safer. 5 Implementing evidence-based safety practices are difficult and need strategies that address the complexity of systems of care, individual practitioners, senior leadership, and—ultimately—changing health care cultures to be evidence-based safety practice environments. 5
Nursing has a rich history of using research in practice, pioneered by Florence Nightingale. 6–9 Although during the early and mid-1900s, few nurses contributed to this foundation initiated by Nightingale, 10 the nursing profession has more recently provided major leadership for improving care through application of research findings in practice. 11
Evidence-based practice (EBP) is the conscientious and judicious use of current best evidence in conjunction with clinical expertise and patient values to guide health care decisions. 12–15 Best evidence includes empirical evidence from randomized controlled trials; evidence from other scientific methods such as descriptive and qualitative research; as well as use of information from case reports, scientific principles, and expert opinion. When enough research evidence is available, the practice should be guided by research evidence in conjunction with clinical expertise and patient values. In some cases, however, a sufficient research base may not be available, and health care decision making is derived principally from nonresearch evidence sources such as expert opinion and scientific principles. 16 As more research is done in a specific area, the research evidence must be incorporated into the EBP. 15
Models of Evidence-Based Practice
Multiple models of EBP are available and have been used in a variety of clinical settings. 16–36 Although review of these models is beyond the scope of this chapter, common elements of these models are selecting a practice topic (e.g., discharge instructions for individuals with heart failure), critique and syntheses of evidence, implementation, evaluation of the impact on patient care and provider performance, and consideration of the context/setting in which the practice is implemented. 15 , 17 The learning that occurs during the process of translating research into practice is valuable information to capture and feed back into the process, so that others can adapt the evidence-based guideline and/or the implementation strategies.
A recent conceptual framework for maximizing and accelerating the transfer of research results from the Agency for Healthcare Research and Quality (AHRQ) patient safety research portfolio to health care delivery was developed by the dissemination subcommittee of the AHRQ Patient Safety Research Coordinating Committee. 37 This model is a synthesis of concepts from scientific information on knowledge transfer, social marketing, social and organizational innovation, and behavior change (see Figure 1 ). 37 Although the framework is portrayed as a series of stages, the authors of this framework do not believe that the knowledge transfer process is linear; rather, activities occur simultaneously or in different sequences, with implementation of EBPs being a multifaceted process with many actors and systems.
AHRQ Model of Knowledge Transfer Adapted from Nieva, V., Murphy, R., Ridley, N., et al. Used with permission. http://www.ahrq.gov/qual/advances/
Steps of Evidence-Based Practice
Steps of promoting adoption of EBPs can be viewed from the perspective of those who conduct research or generate knowledge, 23 , 37 those who use the evidence-based information in practice, 16 , 31 and those who serve as boundary spanners to link knowledge generators with knowledge users. 19
Steps of knowledge transfer in the AHRQ model 37 represent three major stages: (1) knowledge creation and distillation, (2) diffusion and dissemination, and (3) organizational adoption and implementation. These stages of knowledge transfer are viewed through the lens of researchers/creators of new knowledge and begin with determining what findings from the patient safety portfolio or individual research projects ought to be disseminated.
Knowledge creation and distillation is conducting research (with expected variation in readiness for use in health care delivery systems) and then packaging relevant research findings into products that can be put into action—such as specific practice recommendations—thereby increasing the likelihood that research evidence will find its way into practice. 37 It is essential that the knowledge distillation process be informed and guided by end users for research findings to be implemented in care delivery. The criteria used in knowledge distillation should include perspectives of the end users (e.g., transportability to the real-world health care setting, feasibility, volume of evidence needed by health care organizations and clinicians), as well as traditional knowledge generation considerations (e.g., strength of the evidence, generalizability).
Diffusion and dissemination involves partnering with professional opinion leaders and health care organizations to disseminate knowledge that can form the basis of action (e.g., essential elements for discharge teaching for hospitalized patient with heart failure) to potential users. Dissemination partnerships link researchers with intermediaries that can function as knowledge brokers and connectors to the practitioners and health care delivery organizations. Intermediaries can be professional organizations such as the National Patient Safety Foundation or multidisciplinary knowledge transfer teams such as those that are effective in disseminating research-based cancer prevention programs. In this model, dissemination partnerships provide an authoritative seal of approval for new knowledge and help identify influential groups and communities that can create a demand for application of the evidence in practice. Both mass communication and targeted dissemination are used to reach audiences with the anticipation that early users will influence the latter adopters of the new usable, evidence-based research findings. Targeted dissemination efforts must use multifaceted dissemination strategies, with an emphasis on channels and media that are most effective for particular user segments (e.g., nurses, physicians, pharmacists).
End user adoption, implementation, and institutionalization is the final stage of the knowledge transfer process. 37 This stage focuses on getting organizations, teams, and individuals to adopt and consistently use evidence-based research findings and innovations in everyday practice. Implementing and sustaining EBPs in health care settings involves complex interrelationships among the EBP topic (e.g., reduction of medication errors), the organizational social system characteristics (such as operational structures and values, the external health care environment), and the individual clinicians. 35 , 37–39 A variety of strategies for implementation include using a change champion in the organization who can address potential implementation challenges, piloting/trying the change in a particular patient care area of the organization, and using multidisciplinary implementation teams to assist in the practical aspects of embedding innovations into ongoing organizational processes. 35 , 37 Changing practice takes considerable effort at both the individual and organizational level to apply evidence-based information and products in a particular context. 22 When improvements in care are demonstrated in the pilot studies and communicated to other relevant units in the organization, key personnel may then agree to fully adopt and sustain the change in practice. Once the EBP change is incorporated into the structure of the organization, the change is no longer considered an innovation but a standard of care. 22 , 37
In comparison, other models of EBP (e.g., Iowa Model of Evidence-based Practice to Promote Quality of Care 16 ) view the steps of the EBP process from the perspective of clinicians and/or organizational/clinical contexts of care delivery. When viewing steps of the EBP process through the lens of an end user, the process begins with selecting an area for improving care based on evidence (rather than asking what findings ought to be disseminated); determining the priority of the potential topic for the organization; formulating an EBP team composed of key stakeholders; finding, critiquing, and synthesizing the evidence; setting forth EBP recommendations, with the type and strength of evidence used to support each clearly documented; determining if the evidence findings are appropriate for use in practice; writing an EBP standard specific to the organization; piloting the change in practice; implementing changes in practice in other relevant practice areas (depending on the outcome of the pilot); evaluating the EBP changes; and transitioning ongoing quality improvement (QI) monitoring, staff education, and competency review of the EBP topic to appropriate organizational groups as defined by the organizational structure. 15 , 40 The work of EBP implementation from the perspective of the end user is greatly facilitated by efforts of AHRQ, professional nursing organizations (e.g., Oncology Nursing Society), and others that distill and package research findings into useful products and tools for use at the point of care delivery.
When the clinical questions of end users can be addressed through use of existing evidence that is packaged with end users in mind, steps of the EBP process take less time and more effort can be directed toward the implementation, evaluation, and sustainability components of the process. For example, finding, critiquing, and synthesizing the evidence; setting forth EBP recommendations with documentation of the type and strength of evidence for each recommendation; and determining appropriateness of the evidence for use in practice are accelerated when the knowledge-based information is readily available. Some distilled research findings also include quick reference guides that can be used at the point of care and/or integrated into health care information systems, which also helps with implementation. 41 , 42
Translation Science: An Overview
Translation science is the investigation of methods, interventions, and variables that influence adoption by individuals and organizations of EBPs to improve clinical and operational decisionmaking in health care. 35 , 43–46 This includes testing the effect of interventions on promoting and sustaining adoption of EBPs. Examples of translation studies include describing facilitators and barriers to knowledge uptake and use, organizational predictors of adherence to EBP guidelines, attitudes toward EBPs, and defining the structure of the scientific field. 11 , 47–49
Translation science must be guided by a conceptual model that organizes the strategies being tested, elucidates the extraneous variables (e.g., behaviors and facilitators) that may influence adoption of EBPs (e.g., organizational size, characteristics of users), and builds a scientific knowledge base for this field of inquiry. 15 , 50 Conceptual models used in the translating-research-into-practice studies funded by AHRQ were adult learning, health education, social influence, marketing, and organizational and behavior theories. 51 Investigators have used Rogers’s Diffusion of Innovation model, 35 , 39 , 52–55 the Promoting Action on Research Implementation in Health Services (PARIHS) model, 29 the push/pull framework, 23 , 56 , 57 the decisionmaking framework, 58 and the Institute for Healthcare Improvement (IHI) model 59 in translation science.
Study findings regarding evidence-based practices in a diversity of health care settings are building an empirical foundation of translation science. 19 , 43 , 51 , 60–83 These investigations and others 18 , 84–86 provide initial scientific knowledge to guide us in how to best promote use of evidence in practice. To advance knowledge about promoting and sustaining adoption of EBPs in health care, translation science needs more studies that test translating research into practice (TRIP) interventions: studies that investigate what TRIP interventions work, for whom, in what circumstances, in what types of settings; and studies that explain the underlying mechanisms of effective TRIP interventions. 35 , 49 , 79 , 87 Partnership models, which encourage ongoing interaction between researchers and practitioners, may be the way forward to carry out such studies. 56 Challenges, issues, methods, and instruments used in translation research are described elsewhere. 11 , 19 , 49 , 78 , 88–97
- Research Evidence
What Is Known About Implementing Evidence-Based Practices?
Multifaceted implementation strategies are needed to promote use of research evidence in clinical and administrative health care decisionmaking. 15 , 22 , 37 , 45 , 64 , 72 , 77 , 79 , 98 , 99 Although Grimshaw and colleagues 65 suggest that multifaceted interventions are no more effective than single interventions, context (site of care delivery) was not incorporated in the synthesis methodology. As noted by others, the same TRIP intervention may meet with varying degrees of effectiveness when applied in different contexts. 35 , 49 , 79 , 80 , 87 , 100 , 101 Implementation strategies also need to address both the individual practitioner and organizational perspective. 15 , 22 , 37 , 64 , 72 , 77 , 79 , 98 When practitioners decide individually what evidence to use in practice, considerable variability in practice patterns result, 71 potentially resulting in adverse patient outcomes.
For example, an “individual” perspective of EBP would leave the decision about use of evidence-based endotracheal suctioning techniques to each nurse and respiratory therapist. Some individuals may be familiar with the research findings for endotracheal suctioning while others may not. This is likely to result in different and conflicting practices being used as people change shifts every 8 to 12 hours. From an organizational perspective, endotracheal suctioning policies and procedures based on research are written, the evidence-based information is integrated into the clinical information systems, and adoption of these practices by nurses and other practitioners is systematically promoted in the organization. This includes assuring that practitioners have the necessary knowledge, skills, and equipment to carry out the evidence-based endotracheal suctioning practice. The organizational governance supports use of these practices through various councils and committees such as the Practice Committee, Staff Education Committee, and interdisciplinary EBP work groups.
The Translation Research Model, 35 built on Rogers’s seminal work on diffusion of innovations, 39 provides a guiding framework for testing and selecting strategies to promote adoption of EBPs. According to the Translation Research Model, adoption of innovations such as EBPs are influenced by the nature of the innovation (e.g., the type and strength of evidence, the clinical topic) and the manner in which it is communicated (disseminated) to members (nurses) of a social system (organization, nursing profession). 35 Strategies for promoting adoption of EBPs must address these four areas (nature of the EBP topic; users of the evidence; communication; social system) within a context of participative change (see Figure 2 ). This model provided the framework for a multisite study that tested the effectiveness of a multifaceted TRIP intervention designed to promote adoption of evidence-based acute pain management practices for hospitalized older adults. The intervention improved the quality of acute pain management practices and reduced costs. 81 The model is currently being used to test the effectiveness of a multifaceted TRIP intervention to promote evidence-based cancer pain management of older adults in home hospice settings. * This guiding framework is used herein to overview what is known about implementation interventions to promote use of EBPs in health care systems (see Evidence Table ).
*Implementation Model Redrawn from Rogers EM. Diffusion of innovations. 5th ed. New York: The Free Press; 2003; Titler MG, Everett LQ. Translating research into practice: considerations for critical care investigators. Crit Care Nurs Clin North Am 2001a;13(4):587-604. (more...)
Evidence Table
Evidence-Based Practice in Nursing
Nature of the Innovation or Evidence-Based Practice
Characteristics of an innovation or EBP topic that affect adoption include the relative advantage of the EBP (e.g., effectiveness, relevance to the task, social prestige); the compatibility with values, norms, work, and perceived needs of users; and complexity of the EBP topic. 39 For example, EBP topics that are perceived by users as relatively simple (e.g., influenza vaccines for older adults) are more easily adopted in less time than those that are more complex (acute pain management for hospitalized older adults). Strategies to promote adoption of EBPs related to characteristics of the topic include practitioner review and “reinvention” of the EBP guideline to fit the local context, use of quick reference guides and decision aids, and use of clinical reminders. 53 , 59 , 60 , 65 , 74 , 82 , 102–107 An important principle to remember when planning implementation of an EBP is that the attributes of the EBP topic as perceived by users and stakeholders (e.g., ease of use, valued part of practice) are neither stable features nor sure determinants of their adoption. Rather it is the interaction among the characteristics of the EBP topic, the intended users, and a particular context of practice that determines the rate and extent of adoption. 22 , 35 , 39
Studies suggest that clinical systems, computerized decision support, and prompts that support practice (e.g., decisionmaking algorithms, paper reminders) have a positive effect on aligning practices with the evidence base. 15 , 51 , 65 , 74 , 80 , 82 , 102 , 104 , 107–110 Computerized knowledge management has consistently demonstrated significant improvements in provider performance and patient outcomes. 82 Feldman and colleagues, using a just-in-time e-mail reminder in home health care, have demonstrated (1) improvements in evidence-based care and outcomes for patients with heart failure, 64 , 77 and (2) reduced pain intensity for cancer patients. 75 Clinical information systems should deploy the evidence base to the point of care and incorporate computer decision-support software that integrates evidence for use in clinical decisionmaking about individual patients. 40 , 104 , 111–114 There is still much to learn about the “best” manner of deploying evidence-based information through electronic clinical information systems to support evidence-based care. 115
Methods of Communication
Interpersonal communication channels, methods of communication, and influence among social networks of users affect adoption of EBPs. 39 Use of mass media, opinion leaders, change champions, and consultation by experts along with education are among strategies tested to promote use of EBPs. Education is necessary but not sufficient to change practice, and didactic continuing education alone does little to change practice behavior. 61 , 116 There is little evidence that interprofessional education as compared to discipline-specific education improves EBP. 117 Interactive education, used in combination with other practice-reinforcing strategies, has more positive effects on improving EBP than didactic education alone. 66 , 68 , 71 , 74 , 118 , 119 There is evidence that mass media messages (e.g., television, radio, newspapers, leaflets, posters and pamphlets), targeted at the health care consumer population, have some effect on use of health services for the targeted behavior (e.g., colorectal cancer screening). However, little empirical evidence is available to guide framing of messages communicated through planned mass media campaigns to achieve the intended change. 120
Several studies have demonstrated that opinion leaders are effective in changing behaviors of health care practitioners, 22 , 68 , 79 , 100 , 116 , 121–123 especially in combination with educational outreach or performance feedback. Opinion leaders are from the local peer group, viewed as a respected source of influence, considered by associates as technically competent, and trusted to judge the fit between the innovation and the local situation. 39 , 116 , 121 , 124–127 With their wide sphere of influence across several microsystems/units, opinion leaders’ use of the innovation influences peers and alters group norms. 39 , 128 The key characteristic of an opinion leader is that he or she is trusted to evaluate new information in the context of group norms. Opinion leadership is multifaceted and complex, with role functions varying by the circumstances, but few successful projects to implement innovations in organizations have managed without the input of identifiable opinion leaders. 22 , 35 , 39 , 81 , 96 Social interactions such as “hallway chats,” one-on-one discussions, and addressing questions are important, yet often overlooked components of translation. 39 , 59 Thus, having local opinion leaders discuss the EBPs with members of their peer group is necessary to translate research into practice. If the EBP that is being implemented is interdisciplinary in nature, discipline-specific opinion leaders should be used to promote the change in practice. 39
Change champions are also helpful for implementing innovations. 39 , 49 , 81 , 129–131 They are practitioners within the local group setting (e.g., clinic, patient care unit) who are expert clinicians, passionate about the innovation, committed to improving quality of care, and have a positive working relationship with other health care professionals. 39 , 125 , 131 , 132 They circulate information, encourage peers to adopt the innovation, arrange demonstrations, and orient staff to the innovation. 49 , 130 The change champion believes in an idea; will not take “no” for an answer; is undaunted by insults and rebuffs; and, above all, persists. 133 Because nurses prefer interpersonal contact and communication with colleagues rather than Internet or traditional sources of practice knowledge, 134–137 it is imperative that one or two change champions be identified for each patient care unit or clinic where the change is being made for EBPs to be enacted by direct care providers. 81 , 138 Conferencing with opinion leaders and change champions periodically during implementation is helpful to address questions and provide guidance as needed. 35 , 66 , 81 , 106
Because nurses’ preferred information source is through peers and social interactions, 134–137 , 139 , 140 using a core group in conjunction with change champions is also helpful for implementing the practice change. 16 , 110 , 141 A core group is a select group of practitioners with the mutual goal of disseminating information regarding a practice change and facilitating the change by other staff in their unit/microsystem. 142 Core group members represent various shifts and days of the week and become knowledgeable about the scientific basis for the practice; the change champion educates and assists them in using practices that are aligned with the evidence. Each member of the core group, in turn, takes the responsibility for imparting evidence-based information and effecting practice change with two or three of their peers. Members assist the change champion and opinion leader with disseminating the EBP information to other staff, reinforce the practice change on a daily basis, and provide positive feedback to those who align their practice with the evidence base. 15 Using a core-group approach in conjunction with a change champion results in a critical mass of practitioners promoting adoption of the EBP. 39
Educational outreach, also known as academic detailing, promotes positive changes in practice behaviors of nurses and physicians. 22 , 64 , 66 , 71 , 74 , 75 , 77 , 81 , 119 , 143 Academic detailing is done by a topic expert, knowledgeable of the research base (e.g., cancer pain management), who may be external to the practice setting; he or she meets one-on-one with practitioners in their setting to provide information about the EBP topic. These individuals are able to explain the research base for the EBPs to others and are able to respond convincingly to challenges and debates. 22 This strategy may include providing feedback on provider or team performance with respect to selected EBP indicators (e.g., frequency of pain assessment). 66 , 81 , 119
Users of the Innovation or Evidence-Based Practice
Members of a social system (e.g., nurses, physicians, clerical staff) influence how quickly and widely EBPs are adopted. 39 Audit and feedback, performance gap assessment (PGA), and trying the EBP are strategies that have been tested. 15 , 22 , 65 , 66 , 70–72 , 81 , 98 , 124 , 144 PGA and audit and feedback have consistently shown a positive effect on changing practice behavior of providers. 65 , 66 , 70 , 72 , 81 , 98 , 124 , 144 , 145 PGA (baseline practice performance) informs members, at the beginning of change, about a practice performance and opportunities for improvement. Specific practice indicators selected for PGA are related to the practices that are the focus of evidence-based practice change, such as every-4-hour pain assessment for acute pain management. 15 , 66 , 81
Auditing and feedback are ongoing processes of using and assessing performance indicators (e.g., every-4-hour pain assessment), aggregating data into reports, and discussing the findings with practitioners during the practice change. 22 , 49 , 66 , 70 , 72 , 81 , 98 , 145 This strategy helps staff know and see how their efforts to improve care and patient outcomes are progressing throughout the implementation process. Although there is no clear empirical evidence for how to provide audit and feedback, 70 , 146 effects may be larger when clinicians are active participants in implementing change and discuss the data rather than being passive recipients of feedback reports. 67 , 70 Qualitative studies provide some insight into use of audit and feedback. 60 , 67 One study on use of data feedback for improving treatment of acute myocardial infarction found that (1) feedback data must be perceived by physicians as important and valid, (2) the data source and timeliness of data feedback are critical to perceived validity, (3) time is required to establish credibility of data within a hospital, (4) benchmarking improves the validity of the data feedback, and (5) physician leaders can enhance the effectiveness of data feedback. Data feedback that profiles an individual physician’s practices can be effective but may be perceived as punitive; data feedback must persist to sustain improved performance; and effectiveness of data feedback is intertwined with the organizational context, including physician leadership and organizational culture. 60 Hysong and colleagues 67 found that high-performing institutions provided timely, individualized, nonpunitive feedback to providers, whereas low performers were more variable in their timeliness and nonpunitiveness and relied more on standardized, facility-level reports. The concept of useful feedback emerged as the core concept around which timeliness, individualization, nonpunitiveness, and customizability are important.
Users of an innovation usually try it for a period of time before adopting it in their practice. 22 , 39 , 147 When “trying an EBP” (piloting the change) is incorporated as part of the implementation process, users have an opportunity to use it for a period of time, provide feedback to those in charge of implementation, and modify the practice if necessary. 148 Piloting the EBP as part of implementation has a positive influence on the extent of adoption of the new practice. 22 , 39 , 148
Characteristics of users such as educational preparation, practice specialty, and views on innovativeness may influence adoption of an EBP, although findings are equivocal. 27 , 39 , 130 , 149–153 Nurses’ disposition to critical thinking is, however, positively correlated with research use, 154 and those in clinical educator roles are more likely to use research than staff nurses or nurse managers. 155
Social System
Clearly, the social system or context of care delivery matters when implementing EBPs. 2 , 30 , 33 , 39 , 60 , 84 , 85 , 91 , 92 , 101 , 156–163 For example, investigators demonstrated the effectiveness of a prompted voiding intervention for urinary incontinence in nursing homes, but sustaining the intervention in day-to-day practice was limited when the responsibility of carrying out the intervention was shifted to nursing home staff (rather than the investigative team) and required staffing levels in excess of a majority of nursing home settings. 164 This illustrates the importance of embedding interventions into ongoing processes of care.
Several organizational factors affect adoption of EBPs. 22 , 39 , 79 , 134 , 165–167 Vaughn and colleagues 101 demonstrated that organizational resources, physician full-time employees (FTEs) per 1,000 patient visits, organizational size, and whether the facility was located in or near a city affected use of evidence in the health care system of the Department of Veterans Affairs (VA). Large, mature, functionally differentiated organizations (e.g., divided into semiautonomous departments and units) that are specialized, with a focus of professional knowledge, slack resources to channel into new projects, decentralized decisionmaking, and low levels of formalization will more readily adopt innovations such as new practices based on evidence. Larger organizations are generally more innovative because size increases the likelihood that other predictors of innovation adoption—such as slack financial and human resources and differentiation—will be present. However, these organizational determinants account for only about 15 percent of the variation in innovation adoption between comparable organizations. 22 Adler and colleagues 168 hypothesize that while more structurally complex organizations may be more innovative and hence adopt EBPs relatively early, less structurally complex organizations may be able to diffuse EBPs more effectively. Establishing semiautonomous teams is associated with successful implementation of EBPs, and thus should be considered in managing organizational units. 168–170
As part of the work of implementing EBPs, it is important that the social system—unit, service line, or clinic—ensures that policies, procedures, standards, clinical pathways, and documentation systems support the use of the EBPs. 49 , 68 , 72 , 73 , 103 , 140 , 171 Documentation forms or clinical information systems may need revision to support changes in practice; documentation systems that fail to readily support the new practice thwart change. 82
Absorptive capacity for new knowledge is another social system factor that affects adoption of EBPs. Absorptive capacity is the knowledge and skills to enact the EBPs; the strength of evidence alone will not promote adoption. An organization that is able to systematically identify, capture, interpret, share, reframe, and recodify new knowledge, and put it to appropriate use, will be better able to assimilate EBPs. 82 , 103 , 172 , 173 A learning organizational culture and proactive leadership that promotes knowledge sharing are important components of building absorptive capacity for new knowledge. 66 , 139 , 142 , 174 Components of a receptive context for EBP include strong leadership, clear strategic vision, good managerial relations, visionary staff in key positions, a climate conducive to experimentation and risk taking, and effective data capture systems. Leadership is critical in encouraging organizational members to break out of the convergent thinking and routines that are the norm in large, well-established organizations. 4 , 22 , 39 , 122 , 148 , 163 , 175
An organization may be generally amenable to innovations but not ready or willing to assimilate a particular EBP. Elements of system readiness include tension for change, EBP-system fit, assessment of implications, support and advocacy for the EBP, dedicated time and resources, and capacity to evaluate the impact of the EBP during and following implementation. If there is tension around specific work or clinical issues and staff perceive that the situation is intolerable, a potential EBP is likely to be assimilated if it can successfully address the issues, and thereby reduce the tension. 22 , 175
Assessing and structuring workflow to fit with a potential EBP is an important component of fostering adoption. If implications of the EBP are fully assessed, anticipated, and planned for, the practice is more likely to be adopted. 148 , 162 , 176 If supporters for a specific EBP outnumber and are more strategically placed within the organizational power base than opponents, the EBP is more likely to be adopted by the organization. 60 , 175 Organizations that have the capacity to evaluate the impact of the EBP change are more likely to assimilate it. Effective implementation needs both a receptive climate and a good fit between the EBP and intended adopters’ needs and values. 22 , 60 , 140 , 175 , 177
Leadership support is critical for promoting use of EBPs. 33 , 59 , 72 , 85 , 98 , 122 , 178–181 This support, which is expressed verbally, provides necessary resources, materials, and time to fulfill assigned responsibilities. 148 , 171 , 182 , 183 Senior leaders need to create an organizational mission, vision, and strategic plan that incorporate EBP; implement performance expectations for staff that include EBP work; integrate the work of EBP into the governance structure of the health care system; demonstrate the value of EBPs through administrative behaviors; and establish explicit expectations that nurse leaders will create microsystems that value and support clinical inquiry. 122 , 183 , 184
A recent review of organizational interventions to implement EBPs for improving patient care examined five major aspects of patient care. The review suggests that revision of professional roles (changing responsibilities and work of health professionals such as expanding roles of nurses and pharmacists) improved processes of care, but it was less clear about the effect on improvement of patient outcomes. Multidisciplinary teams (collaborative practice teams of physicians, nurses, and allied health professionals) treating mostly patients with prevalent chronic diseases resulted in improved patient outcomes. Integrated care services (e.g., disease management and case management) resulted in improved patient outcomes and cost savings. Interventions aimed at knowledge management (principally via use of technology to support patient care) resulted in improved adherence to EBPs and patient outcomes. The last aspect, quality management, had the fewest reviews available, with the results uncertain. A number of organizational interventions were not included in this review (e.g., leadership, process redesign, organizational learning), and the authors note that the lack of a widely accepted taxonomy of organizational interventions is a problem in examining effectiveness across studies. 82
An organizational intervention that is receiving increasing attention is tailored interventions to overcome barriers to change. 162 , 175 , 185 This type of intervention focuses on first assessing needs in terms of what is causing the gap between current practice and EBP for a specified topic, what behaviors and/or mechanism need to change, what organizational units and persons should be involved, and identification of ways to facilitate the changes. This information is then used in tailoring an intervention for the setting that will promote use of the specified EBP. Based on a recent systematic review, effectiveness of tailored implementation interventions remains uncertain. 185
In summary, making an evidence-based change in practice involves a series of action steps and a complex, nonlinear process. Implementing the change will take several weeks to months, depending on the nature of the practice change. Increasing staff knowledge about a specific EBP and passive dissemination strategies are not likely to work, particularly in complex health care settings. Strategies that seem to have a positive effect on promoting use of EBPs include audit and feedback, use of clinical reminders and practice prompts, opinion leaders, change champions, interactive education, mass media, educational outreach/academic detailing, and characteristics of the context of care delivery (e.g., leadership, learning, questioning). It is important that senior leadership and those leading EBP improvements are aware of change as a process and continue to encourage and teach peers about the change in practice. The new practice must be continually reinforced and sustained or the practice change will be intermittent and soon fade, allowing more traditional methods of care to return. 15
- Practice Implications From Translation Science
Principles of Evidence-Based Practice for Patient Safety
Several translation science principles are informative for implementing patient safety initiatives:
- First, consider the context and engage health care personnel who are at the point of care in selecting and prioritizing patient safety initiatives, clearly communicating the evidence base (strength and type) for the patient safety practice topic(s) and the conditions or setting to which it applies. These communication messages need to be carefully designed and targeted to each stakeholder user group.
- Second, illustrate, through qualitative or quantitative data (e.g., near misses, sentinel events, adverse events, injuries from adverse events), the reason the organization and individuals within the organization should commit to an evidence-based safety practice topic. Clinicians tend to be more engaged in adopting patient safety initiatives when they understand the evidence base of the practice, in contrast to administrators saying, “We must do this because it is an external regulatory requirement.” For example, it is critical to converse with busy clinicians about the evidence-based rationale for doing fall-risk assessment, and to help them understand that fall-risk assessment is an external regulatory agency expectation because the strength of the evidence supports this patient safety practice.
- Third, didactic education alone is never enough to change practice; one-time education on a specific safety initiative is not enough. Simply improving knowledge does not necessarily improve practice. Rather, organizations must invest in the tools and skills needed to create a culture of evidence-based patient safety practices where questions are encouraged and systems are created to make it easy to do the right thing.
- Fourth, the context of EBP improvements in patient safety need to be addressed at each step of the implementation process; piloting the change in practice is essential to determine the fit between the EBP patient safety information/innovation and the setting of care delivery. There is no one way to implement, and what works in one agency may need modification to fit the organizational culture of another context.
- Finally, it is important to evaluate the processes and outcomes of implementation. Users and stakeholders need to know that the efforts to improve patient safety have a positive impact on quality of care. For example, if a new barcoding system is being used to administer blood products, it is imperative to know that the steps in the process are being followed (process indicators) and that the change in practice is resulting in fewer blood product transfusion errors (outcome indicators).
Research Implications
Translation science is young, and although there is a growing body of knowledge in this area, we have, to date, many unanswered questions. These include the type of audit and feedback (e.g., frequency, content, format) strategies that are most effective, the characteristics of opinion leaders that are critical for success, the role of specific context variables, and the combination of strategies that are most effective. We also know very little about use of tailored implementation interventions, or the key context attributes to assess and use in developing and testing tailored interventions. The types of clinical reminders that are most effective for making EBP knowledge available at the point of care require further empirical explanation. We also know very little about the intensity and intervention dose of single and multifaceted strategies that are effective for promoting and sustaining use of EBPs or how the effectiveness differs by type of topic (e.g., simple versus complex). Only recently has the context of care delivery been acknowledged as affecting use of evidence, and further empirical work is needed in this area to understand how complex adaptive systems of practice incorporate knowledge acquisition and use. Lastly, we do not know what strategies or combination of strategies work for whom, in what context, why they work in some settings or cases and not others, and what is the mechanism by which these strategies or combination of strategies work.
This is an exciting area of investigation that has a direct impact on implementing patient safety practices. In planning investigations, researchers must use a conceptual model to guide the research and add to the empirical and theoretical understanding of this field of inquiry. Additionally, funding is needed for implementation studies that focus on evidence-based patient safety practices as the topic of concern. To generalize empirical findings from patient safety implementation studies, we must have a better understanding of what implementation strategies work, with whom, and in what types of settings, and we must investigate the underlying mechanisms of these strategies. This is likely to require mixed methods, a better understanding of complexity science, and greater appreciation for nontraditional methods and realistic inquiry. 87
Although the science of translating research into practice is fairly new, there is some guiding evidence of what implementation interventions to use in promoting patient safety practices. However, there is no magic bullet for translating what is known from research into practice. To move evidence-based interventions into practice, several strategies may be needed. Additionally, what works in one context of care may or may not work in another setting, thereby suggesting that context variables matter in implementation. 80
- Search Strategy
Several electronic databases were searched (MEDLINE ® , CINAHL ® , PubMed ® ) using terms of evidence-based practice research, implementation research, and patient safety. (The terms “quality improvement” or “quality improvement intervention research” were not used.) The Cochrane Collaboration–Cochrane Reviews was also searched to look for systematic reviews of specific implementation strategies, and the Journal of Implementation Science was also reviewed. I also requested the final reports of the TRIP I and TRIP II studies funded by AHRQ. Classic articles known to the author were also included in this chapter (e.g.,Locock et al. 123 ).
*Principal Investigator: Keela Herr (R01 grant no. CA115363-01; National Cancer Institute (NCI))Background
- Cite this Page Titler MG. The Evidence for Evidence-Based Practice Implementation. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 7.
- PDF version of this page (470K)
In this Page
Other titles in this collection.
- Advances in Patient Safety
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- It Is Not That Simple nor Compelling! Comment on "Translating Evidence Into Healthcare Policy and Practice: Single Versus Multi-faceted Implementation Strategies - Is There a Simple Answer to a Complex Question?". [Int J Health Policy Manag. 2015] It Is Not That Simple nor Compelling! Comment on "Translating Evidence Into Healthcare Policy and Practice: Single Versus Multi-faceted Implementation Strategies - Is There a Simple Answer to a Complex Question?". Bucknall T, Fossum M. Int J Health Policy Manag. 2015 Jul 28; 4(11):787-8. Epub 2015 Jul 28.
- Nursing implementation science: how evidence-based nursing requires evidence-based implementation. [J Nurs Scholarsh. 2008] Nursing implementation science: how evidence-based nursing requires evidence-based implementation. van Achterberg T, Schoonhoven L, Grol R. J Nurs Scholarsh. 2008; 40(4):302-10.
- Review The science of implementation: changing the practice of critical care. [Curr Opin Crit Care. 2008] Review The science of implementation: changing the practice of critical care. Weinert CR, Mann HJ. Curr Opin Crit Care. 2008 Aug; 14(4):460-5.
- Review Integrative review of implementation strategies for translation of research-based evidence by nurses. [Clin Nurse Spec. 2014] Review Integrative review of implementation strategies for translation of research-based evidence by nurses. Wuchner SS. Clin Nurse Spec. 2014 Jul-Aug; 28(4):214-23.
- Review A realist analysis of hospital patient safety in Wales: applied learning for alternative contexts from a multisite case study [ 2015] Review A realist analysis of hospital patient safety in Wales: applied learning for alternative contexts from a multisite case study Herepath A, Kitchener M, Waring J. 2015 Sep
Recent Activity
- The Evidence for Evidence-Based Practice Implementation - Patient Safety and Qua... The Evidence for Evidence-Based Practice Implementation - Patient Safety and Quality
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Evidence-based practice takes advantage of new knowledge developments and keeps the medical field up to date with the latest technological advances. Sustaining Evidence-Based Practice Change. While short-term results of EBP change implementation may be promising, the pace may change after the initial six months.
Nursing EBP Topics You Can Use in Your Essay. Here are some of the latest evidence-based practice nursing research topics that you can use in your essay or explore further in your own research: The impact of telehealth on patient outcomes in primary care; The use of music therapy to manage pain in post-operative patients
One effective way to do this is through writing essays on EBP topics. To help you get started, here are 103 evidence-based practice essay topic ideas and examples: The importance of evidence-based practice in healthcare. The history and evolution of evidence-based practice.
Cardiovascular and Respiratory Evidence-Based Topics. Improving the quality of cardiovascular care through evidence-based practice. Addressing social determinants of health as a means of addressing cardiovascular diseases. Effects of listening to music during cardiac rehabilitation on clinical outcomes.
Evidence-based practice (EBP) is a decision-making approach that uses the best evidence from research and clinical expertise to improve healthcare delivery. Our examples of evidence-based practice nursing topics let you explore the significance, challenges, and ethical aspects of EBP.
Rachel R.N. May 28, 2024. Essay Topics and Ideas. Evidence-based practice (EBP) is a systematic approach to clinical decision-making that integrates the best available research evidence with a nurse's clinical expertise and patient preferences and values. It involves the ongoing process of formulating clinical questions, searching and ...
Looking for Evidence-Based Practice essay topics? ⏰ We've gathered a collection of research topics & essay examples on Evidence-Based Practice. ️ Write your A+ nursing essay with us! Call to +1 844 889-9952 +1 844 889-9952 Writing Services. Services Pricing Reviews Experts About ...
Top 5 Benefits To The Nurse. 1. Evidence-based practice in nursing provides nurses with scientifically supported research to help them make well-educated decisions. 2. EBP in nursing helps nurses stay up-to-date about new nursing interventions and protocols used in patient care. 3.
Evidence-based clinical practice or evidence-based medicine is the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients" (Sackett et al., 1996). The beginning of Evidence-Based Practice (EBP), formerly known as evidence-based medicine, was initiated by Archie Cochrane in ...
The authors describe a new course (Evidence-Based Nursing 1) that was implemented as part of an undergraduate nursing program. The researchers observed that the targeted learners were willing to make evidence-based practices part of their nursing philosophies after completing the course. The practice can encourage practitioners to integrate EBP ...
EBP is a process used to review, analyze, and translate the latest scientific evidence. The goal is to quickly incorporate the best available research, along with clinical experience and patient preference, into clinical practice, so nurses can make informed patient-care decisions ( Dang et al., 2022 ). EBP is the cornerstone of clinical practice.
Evidence-based practice (EBP) in health care has become imperative for patient safety. ... writing Bachelor's degree, essays and establishing teaching modules related to the research process (concept analysis, identifying evidence-based quantitative and qualitative research, critical assessment, identifying discourses in documents and ...
Evidence Based Practice (EBP), involves the use of current research data or findings from day to day life in making decisions concerning patient care (Brown & Schmidt, 2011, p. 9). It is an integration of knowledge gained from the clinical field, patient values, and the most reliable scientific information to come up with a comprehensive ...
1. Introduction. Evidence-based practice (EBP) is defined as "clinical decision-making that considers the best available evidence; the context in which the care is delivered; client preference; and the professional judgment of the health professional" [] (p. 2).EBP implementation is recommended in clinical settings [2,3,4,5] as it has been attributed to promoting high-value health care ...
The nurse manager should encourage all nurses to practice evidence-based nursing through conducting research training. Safe Medication in Intensive Care Unit. In this paper, safe medication use in intensive care units (ICUs) the CPG was selected due to its relevance to the current needs of inpatient care. Electronic Intensive Care Unit Benefits.
The importance of evidence based practice is to enable nurses to provide high quality care, improve outcomes for patient and families and to run a more efficient health service. Therefore other agencies within the health service will benefit when interventions and care is based on research (Burns & Grove 2007).
A nurse who practices evidence-based practice can earn $53,000 annually. In the United States, this is the average wage for nurses, according to the Bureau of Labor Statistics. A registered nurse's average salary in 2014 was $58,790. According to the Bureau of Labor Statistics, registered nurses have earned an average of $51,230 over the past ...
5 min read • June, 01 2023. Evidence-based practice in nursing involves providing holistic, quality care based on the most up-to-date research and knowledge rather than traditional methods, advice from colleagues, or personal beliefs. Nurses can expand their knowledge and improve their clinical practice experience by collecting, processing ...
Evidence-Based Practice Is an Approach That Has. PAGES 4 WORDS 1341. Evidence-based practice is an approach that has been applied to clinical practice and nursing. Evidence-based practice started initially in medicine and went to fields like education, psychology, nursing and dentistry.
Looking for a good essay, research or speech topic on Intensive Care? Check our list of 72 interesting Intensive Care title ideas to write about! Clear. Writing Help Login ... Evidence-Based Practice Titles Sepsis Ideas 72 Intensive Care Essay Topic Ideas & Examples Updated: Feb 28th, 2024 6 min. Table of Contents ...
Most students are writing their essays on the same couple of topics, and this is driving professors crazy. It doesn't matter if we're talking about evidence based practice nursing topics or about ethical topics in nursing. The truth of the matter is that students who want a top grade on their essay should focus on finding an exceptional topic.
The problems with the uptake and effective implementation of EBP led to the emergence of the EIP concept. This concept is based on the premise that healthcare practice should, as a matter of principle, be informed by, rather than based on, evidence (Nevo and Slonim-Nevo, 2011). This implies that other forms of evidence (for example, patient experiences, the nurse's expertise and experiences ...
Models of Evidence-Based Practice. Multiple models of EBP are available and have been used in a variety of clinical settings. 16-36 Although review of these models is beyond the scope of this chapter, common elements of these models are selecting a practice topic (e.g., discharge instructions for individuals with heart failure), critique and syntheses of evidence, implementation, evaluation ...