An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection


The COVID-19 pandemic in Ireland: An overview of the health service and economic policy response
Brendan kennelly.
a J.E. Cairnes School of Business and Economics, National University of Ireland Galway, Galway, Ireland
Mike O'Callaghan
b Graduate Entry Medical School and Health Research Institute, University of Limerick, Limerick, Ireland
Diarmuid Coughlan
c Health Economics and Evidence Synthesis (HEES) Group, Population Health Sciences Institute, Newcastle University, Baddiley-Clark Building, Newcastle upon Tyne, NE2 4AX, UK
John Cullinan
Edel doherty, eoin moloney, michelle queally.
- • Very significant effects on health and well-being from the COVID-19 virus and the associated lockdown.
- • As of July 19th, 1,753 people have died and 25,766 have tested positive with the virus.
- • Raid growth in new cases and deaths in the first six weeks of the pandemic.
- • Subsequent fall in cases and deaths until late July.
- • Generally a very high level of compliance with public health measures.
To outline the situation in Ireland with regard to the COVID-19 pandemic.
Analyse the evolution of the COVID-19 pandemic in Ireland. Review the key public health and health system responses.
Over 1700 people have died with COVID-19 by July 19th while almost 3000 people had been admitted to hospital with COVID-19. A high proportion of the deaths occurred in nursing homes and other residential centres who did not receive sufficient attention during the early phase of the pandemic.
Conclusions
Ireland's response to the COVID-19 crisis has been comprehensive and timely. Transparency, a commitment to a relatively open data policy, the use of traditional and social media to inform the population, and the frequency of updates from the Department of Health and the Health Services Executive are all commendable and have led to a high level of compliance among the general public with the various non-medical measures introduced by the government.
Introduction
This paper outlines the situation in Ireland with regard to the COVID-19 pandemic. We begin by outlining some key indicators of population health in Ireland and a brief description of the health system. We then discuss the key health policy and health technology aspects of the pandemic in Ireland. We analyse the available data on cases, hospitalisations and deaths, and outline the key public health initiatives undertaken by the government in Ireland. Our data analysis covers the period from February 29 when the first case was reported up to July 19. The response of the health system is explored in detail. We also discuss the economic impact of the virus to date and outline the very substantial financial measures that have been implemented by the government to ameliorate some of the effects of the pandemic, and the related lockdown, on individuals and businesses. The final section contains suggestions for how the country may cope with the continuing presence of the virus.
Country description
Sociodemographic profile of ireland.
According to the most recent census there were 4,689,921 people classified as usually resident in Ireland in 2016. The Central Statistics Office (CSO) estimates that the population increased by 3.8% since then [1] . The breakdown of the 2019 estimates by region and age group is contained in Table 1 . There is a heavy concentration of the population in Dublin and the Mid-East region that surrounds Dublin, with over 43% of the population living in that area. Overall, the population density is 72 people per square kilometre. The proportion of the population aged 65 or older is a little over 14% while the proportion aged over 85 is just over 1.5%. Almost 400,000 people (8.5% of the total population) lived alone in 2016 and, of these, 39% were aged 65 or older. Just over 41% of the population aged 15+ were single while 47.7% of this age group were married. There were almost 219,000 one-parent families in 2016, 86% of which were headed by a female [1] .
Population estimates (‘000 s) for regions by age group, 2019.
There were 44,531 people with at least one disability living in a communal establishment in 2016. Almost 70% of these were aged 65 or older. There were approximately 10,000 homeless people in Ireland at the beginning of 2020, most of whom were living in temporary accommodation. Around 6000 people seeking asylum in Ireland were living in Direct Provision Centres at the end of 2019, with a further 1500 living in Emergency Accommodation Centres. There were almost 31,000 members of the Traveller community in Ireland in 2016. 11.4% of the population in 2016 were born outside of Ireland, mainly elsewhere in Europe [1] .
Health profile of the country
Life expectancy at birth was 82.2 years for the whole population in 2017, 84.0 years for females and 80.4 years for males [2] . People aged 65 can expect to live for another 21.4 years on average for women, and 19.0 years for men. Just under 28% of the population report having a chronic illness or health problem. The percentage of the adult population that are smokers has declined steadily in recent years and now stands at 17%. Approximately 23% of the population in Ireland are obese. In 2016, 18.5% of the Irish population experienced some type of mental health disorder such as anxiety, schizophrenia, depression, alcohol abuse or drug abuse [2] .
Overview of the health system
Health policy in Ireland is determined by the Department of Health, headed by a Minister of Health, and publicly funded healthcare is delivered by the Health Services Executive (HSE). There is also substantial private sector involvement in the delivery of healthcare, ranging from GPs to allied healthcare professionals to private hospitals.
The Irish health system incorporates public, voluntary and private elements in the production, delivery and financing of healthcare. People in Category I (which includes 36% of the population) are eligible for free healthcare in the public system (with significant co-payments for medicines). Most people who qualify for Category I entitlements do so on the basis of a means test while others do so depending on a diagnosis of a specified chronic illness. A further 10% of the population have a limited form of eligibility in Category 1 which entitles them to free GP visits [3] .
The remainder of the population are in Category II, which entitles them to care in the public hospital system subject to a co-payment. They pay a full fee for visits to a GP. Many people in Category II as well as a minority of people in Category I buy private health insurance which gives them access to privately supplied care, some of which is provided in private hospitals but much of it is provided in public hospitals. Approximately 74% of healthcare expenditure is funded by taxation, 14% by private health insurance and the remaining 12% of expenditure by out-of-pocket payments. Further details about the Irish health system and proposals to reform it can be found in Connolly and Wren [3] , Cullinan et al. [4] and Burke et al. [5] . The CSO recommends that modified Gross National Income be used as a measure of overall economic activity rather than Gross Domestic Product (GDP) because of the disproportionate effect of globalisation on Irish GDP. The proportion of modified Gross National Income that is spent on healthcare in Ireland was 12% in 2018 [6] . Per capita expenditure on health (adjusted for purchasing power parities) was estimated to be $4915 in 2018 [2] .
The number of practicing doctors in Ireland is 3.1 per 1000, a relatively low figure by international standards. The number of nurses, 12.2 per 1000, is higher than the average in the OECD. There were a total of just over 10,000 hospital doctors in Ireland in September 2019, 32% of whom were consultants. There were 2.9 hospital beds per 1000 inhabitants in Ireland in 2018 [2] . A particular concern at the beginning of the pandemic was the low number of ICU beds in Ireland. The total number of ICU beds in the public health system was estimated to be 255 in February 2020 or 5.5 ICU beds per 100,000 people. Long-term residential care in Ireland is provided by publicly-owned, privately-owned and voluntary (not-for-profit) care homes. There are approximately 25,000 people living in nursing homes run by private and voluntary organisations and a further 5000 people living in public nursing homes. Pearce et al. [7] estimated that a significant proportion (between one half and two thirds) of nursing home residents have dementia.
Organizational structure of the public health policy response to COVID-19
The National Public Health Emergency Team (NPHET), a body of approximately 30 medical, science and health service professionals, was activated in January 2020 to deal with the COVID-19 virus. Its chairman is the State's Chief Medical Officer, Dr. Tony Holohan. NPHET is supported by an Expert Advisory Group as well as 11 sub-groups, including an expert modelling group. NPHET works closely with the HSE National Crisis Management Team which manages the HSE's response. Questions have been raised in Dáil Éireann (the Irish parliament) about the membership of NPHET and the delay in minutes of meetings being released. The Department of the Taoiseach (Prime Minster) has given regular press briefings since March 12th. These typically include details of financial supports for individuals and businesses. In May, a special parliamentary committee was established to consider the State's response to the pandemic. The committee has been meeting weekly and its proceedings are streamed live.
COVID-19 data sources and trends
Overview of data availability.
There are four publicly available official online data sources relating to Ireland's experience of the COVID-19 pandemic:
- 1 Health Protection Surveillance Centre (HPSC) website: www.hpsc.ie/
- 2 Department of Health (DoH) website: https://www.gov.ie/en/organisation/department-of-health/
- 3 Irish government's open data portal: https://data.gov.ie/
- 4 Health Service Executive (HSE) Daily Operations COVID-19 Update: https://www.hse.ie/eng/services/news/newsfeatures/covid19-updates/
The HPSC, an agency within the HSE, is Ireland's specialist agency for the surveillance of all communicable diseases. The HPSC data forms the foundation for the other three sources as it collates data relating to all confirmed and probable cases of COVID-19 in Ireland. The DoH updates, the governmental open data platform, and the HSE daily operations updates all have additional unique features that make them useful in the context of data collection and transparency. Since March 23rd, the HPSC has published daily update reports for NPHET on their website [8] . These reports provide the following data specifically related to COVID-19:
- • number of new cases and cumulative number of cases.
- • number of new deaths and cumulative number of deaths.
- • number of hospitalisations and ICU admissions.
- • number of clusters of infection, broken down by geographic region and the number of clusters in settings such as nursing homes.
- • breakdown of number of cases by age, range, gender and county.
- • breakdown of mode of transmission – community transmission, close contact with confirmed case or travel-related.
The daily briefings from NPHET, which are also posted on the DoH website, are subsets of the HPSC reports, but sometimes contain additional data such as the numbers of tests completed, the number of recovered cases and more detailed information on special groups, such as those in residential care settings or healthcare workers. However, these are not consistently reported. Data on recovered and active cases was very slow to emerge in the beginning but have been reported on a more regular basis since April 21st. The DoH also uses its website to update the general public about the findings of bi-weekly population surveys about public sentiment relating to the COVID-19 response and related restrictions in place. Finally, minutes of NPHET meetings are published on the DOH website with, at times, a considerable lag.
The Irish government's open data portal ( https://data.gov.ie/ ) is designed to provide easy access to datasets held by public bodies in Ireland. These datasets are free to use, reuse, and redistribute. Since late March, the Health section of the open data portal has featured several datasets relating to the COVID-19 pandemic which can easily be used for analysis by researchers and the general public. Since mid-May, the Central Statistics Office have published a series of information bulletins containing an analysis of people who have died or contracted COVID-19 [9] . These bulletins contain data not previously available, such as a breakdown of deaths by county.
Since April 13th, the HSE has released daily updates [10] describing the acute hospital activity related to COVID-19. These updates offer a succinct summary of the situation in each of Ireland's public hospitals and critical care units in relation to COVID-19. Current COVID-19 admissions, occupancy due to COVID-19 and non-COVID disease, and available bed capacity in terms of regular beds and critical care beds are all included in these updates. Individual hospitals are listed by name and this offers some additional visibility on where in the country COVID-19 is most active.
How has the virus spread?
Our data analysis covers the period from February 29, when the first case was reported, up to July 19. From the outset, cases were defined as people who had tested positive for COVID-19. Despite initial ambitious plans by the HSE to test widely, it became clear quite quickly that laboratory capacity could not meet the demand created by the broad definition of criteria for testing. GPs quickly identified thousands of patients with respiratory symptoms as part of the first wave of the COVID-19 pandemic. These patients were referred for testing before the capacity existed to either conduct or to analyse this level of testing in a timely fashion, which meant there were considerable delays in the system. Testing criteria were changed on March 24th. The new criteria stated that individuals must be suffering from two symptoms, have a respiratory disease, and be a contact of a confirmed or suspected case, and also be in a priority group to be eligible for testing. Some testing was outsourced to German laboratories to clear the backlog. These outsourced test results were delayed coming back into the system which created a 10-day period in mid-April where these test results were returned in bulk and reported in the daily HPSC and DoH updates. This led to a spike in apparent virus activity which was, in fact, an artefact of the delays.
Initially, for a death to be classified as a COVID-19 death, it was contingent on the patient having a laboratory-confirmed diagnosis of COVID-19 before their death. Since April 24th, the HPSC have included ‘probable’ deaths (i.e. deaths where the cause was likely COVID-19 but where the patient was not tested before death) in the total deaths tally. Deaths include people who died in either private homes or long term residential institutions in the community as well as people who died in hospital. This complete tally of hospital patients, community patients and probable cases has remained the standard reporting format since April 24th.
The majority of cases in Ireland have been in the east of the country, with 48% of cases occurring in Dublin. More broadly, a block of ten counties in the east, north-east and midlands, account for almost 75% of the total number of cases (see Fig. 1 ). Initially, most cases had a history of foreign travel, most notably to Northern Italy, but by the end of April community transmission accounted for almost two-thirds of total cases. Fig. 2 shows the number of new cases each day. The peak of new cases occurred in mid-April. However, positive COVID-19 results returning in bulk from foreign laboratories around this time complicates this somewhat, as date of reporting lagged significantly behind date of sampling. While the large majority of cases recovered without needing to be hospitalised, 12.9% of cases did require hospitalisation while 1.6% of cases were admitted to ICU [8] . Reporting of cumulative COVID-19 deaths also rose sharply on April 22nd (see Fig. 3 ). This is due to the fact that at this point the HPSC and DOH began reporting “probable” deaths, where patients died of a COVID-19-like illness prior to testing positive for COVID-19.

Cases by county.

Cases per day.

Deaths per day.
As seen in Figs. 4 and and5 , 5 , COVID-19 hospitalisations and ICU admissions both began to decrease in the second week of April. While the complications of infection of COVID-19 lag behind the emergence of first symptoms by 7 to 10 days, hospitalisations and ICU admissions are less prone to the nuances of the variations in COVID-19 testing strategies and reporting dates.

Hospitalisations per day.

ICU Admissions per day.
The initial focus in Ireland was on how the virus was spreading in the general community, but by the end of March it was clear that the virus has spread widely in a substantial number of long-term residential settings. There have been 257 clusters (defined as 5 or more cases) in nursing homes and 184 clusters in other residential settings. Nursing homes and residential settings in the east and north-east have been especially vulnerable, with 67% of the clusters in long-term residential settings occurring in these areas. Healthcare workers in Ireland have also been disproportionately affected by COVID-19, with 32% of cases being detected in healthcare staff [8] .
The HSE daily operations update [10] offers the most granular breakdown of hospital activity related to COVID-19, particularly critical care activity. It includes the measure “Total Critical Care Beds Open & Staffed”, which is arguably a more important measure than ventilator availability. No figures are available as to the number of people isolating at home. This may become a more relevant measure as society-wide restrictions are relaxed and more focused efforts are employed to control COVID-19 activity.
Initially, the number of new cases grew rapidly and increases exceeded 40% on some days. The public health restrictions imposed by the government and the high level of compliance with these restrictions and general public health advice slowed the spread of the virus very significantly. On April 24th, the daily increase in cases fell below 5%, and dropped sharply thereafter, falling below 1% growth consistently since mid-May. Similar trends can be seen in the “flattening of the curve” of new hospitalisations and new admissions to ICU. The growth in new cases fell to around 0.1% in the first two weeks of June and has remained very low since. An increase in the number of new cases in the first two weeks of July followed an easing of lockdown restrictions and led to a postponement of the final phase of a plan to re-open the economy (see Section 4 below).
Table 2 provides a breakdown by age range of cases and deaths. It is clear that older Irish patients are at a far higher risk of requiring hospital care and of dying from COVID-19. The mean and median ages of people who have died is 82 and 84 years respectively [8] (this only refers to deaths where a laboratory test confirmed the presence of COVID-19). Over 45% of people who died were aged 85 or older even though this group only accounted for 9.2% of cases. Males make up 43% of cases while they account for 49% of deaths. Fig. 6 shows the distribution of deaths by county as of July 3rd. The distribution of deaths closely matches the distribution of cases with a large proportion of deaths occurring in the north-east and east of the country. Information on the presence of co-morbidities is available for about 75% of cases and 82% of deaths. As of June 10th, 42% of patients who have died from COVID-19 had chronic heart disease, 31% suffered from a chronic neurological condition and 17% had a chronic respiratory disease. The CSO has analysed the spatial distribution of standard mortality rates according to the deprivation level of the area that the person who died was normally resident in [9] . The analysis was carried out using deprivation indexes for small areas. Nationally, standard mortality rates have been highest in the least deprived quintile and second highest in the most deprived quintile. So far, no individual-level analysis of the socio-economic background of people who have died has been possible as the data has not been released.
Age breakdown of cases, hospitalisations and deaths (as of July 19th).

Deaths by county.
8144 of the 25,333 (32%) cases relate to healthcare workers. Of the 8018 healthcare workers infected up to May 30th, 88% got the virus in a healthcare setting, 4% got the virus from contact with a confirmed case, 3% got the virus from travel, 3% got the virus from community transmission and 1% got the virus from a healthcare setting as a patient. Seven healthcare workers have died from the virus. Over a third of the healthcare workers infected by the end of April were nurses while almost a quarter were healthcare assistants [8] .
Policy and technology road map
Ireland has followed a multi-faceted approach to the COVID-19 crisis involving measures to: 1) limit the spread of the virus in the community and specific institutional settings, 2) test and trace suspected contacts, 3) ensure that there were adequate healthcare services and equipment available for people who became seriously ill with the virus, and 4) limit the financial burden on individuals and businesses due to the response to the virus. Extensive use of a large number of health and non-health technologies have been employed including diagnostic testing and the use of medical devices. In the period immediately after the first cases were reported in Ireland, the Government and the Public Health authorities tried to delay as much as possible the disease (this period is known as the ‘delay phase’). Approximately one month after the first case, the Government and the Public Health authorities moved to the ‘mitigation phase’ where the main goal was to contain as much as possible the health and economic impact of the pandemic.
Health policy developments during the COVID-19 delay phase
From the outset, public health advice from the Government and the HSE to the community at large has emphasised frequent hand-washing, appropriate respiratory etiquette (recommending that people cover their mouth and nose with a tissue or sleeve when coughing or sneezing), the importance of maintaining a two metre distance between people, and the need to avoid touching one's eyes, nose and mouth [11] . More recently, the importance of wearing face coverings on public transport and in indoor settings has been emphasised. Traditional and social media have been extensively used to convey basic public health messages. Table 3 summarises the key health policy initiatives that have been implemented in Ireland since the beginning of March. The table follows the classification system developed by Moy et al. [12] . They classify measures based on their impact; minimal, medium, significant or very significant, and which category the measure falls into; containment, economic impact, prevention and care and health technology and finally whether the measure represents an escalation (increasing measures to respond to increases in active cases) or de-escalation (easement of measures). See Moy et al. [12] for a further explanation.
List of key measures introduced in Ireland and categorised based on the classification system developed by Moy et al., (2020).
On March 9th, the annual St Patrick's Day parades were cancelled and an initial increase of €435 million in funding to deal with the impact of COVID-19 was announced for the HSE. On March 12th, Ireland entered the delay phase of dealing with the pandemic. The government ordered schools, colleges, childcare facilities and state-run cultural institutions to close. Indoor gatherings of more than 100 people and outdoor gatherings of more than 500 people were banned. Mandatory closure of pubs was announced on March 15th.
On March 24th the government introduced a second raft of mandatory measures. These included the closure of non-essential businesses such as retail outlets, gyms, hairdressers, outdoor markets and libraries while hotels were limited to cater for essential non-social and non-tourist guests. Cafés and restaurants were only permitted to supply take-away food and delivery. All indoor and outdoor sporting activities were cancelled. All playgrounds were closed and places of worship were required to restrict numbers and adhere to physical distancing. Essential services (such as supermarkets) were required to implement physical distancing. Individuals were not permitted to take unnecessary travel either within Ireland or overseas. Physical distancing was required when outside and social gatherings of more than four individuals were prohibited (except for members of the same household). Individuals were required to work from home unless they worked in essential services.
Policy developments during the COVID-19 mitigation phase
On March 27th Ireland moved to the mitigation phase and introduced a third range of additional measures [13] . People were asked to stay at home unless to undertake essential work or access essential services. Exercise and travel were restricted to 2 kilometres of an individual's home and individuals were not permitted to arrange gatherings with anyone outside their households. The government issued cocooning guidelines for anyone over 70 or medically vulnerable, asking them not to leave their houses. To ease the burden of cocooning, a community call initiative was introduced on April 2nd to mobilise volunteers to help cocooning citizens.
To enhance compliance with the measures, An Garda Síochána (the Irish Police Service) was given additional powers including arrest without warrant. Non-compliance with a direction of a Garda without a lawful excuse is considered a criminal offence and is punishable by a fine of up to €2500, up to six months imprisonment, or a combination of both. The Government also had the power to detain a person who refuses to remain in a specific place (such as a home or a hospital) if they are deemed by a medical professional to be a potential source of infection and/or a risk to public health, and detention is necessary to slow the spread of COVID-19. As of July 1st, 320 people had been arrested for breaching the restrictions [14] .
On May 1st the Taoiseach announced a Roadmap to reopen the economy and society [15] . Initially, the roadmap contained a five phase reopening process with the first phase beginning on May 18th and the final phase on 10th August with three week periods between phases. On June 8th, the government announced an accelerated re-opening with a four phase process rather than five phases and with the final phase scheduled to begin on July 20th. An additional acceleration of the re-opening was announced on June 19th which meant that most commercial activity was able to resume in some form or other from June 29th. However, on July 15th, the government announced that the final (fourth) phase of re-opening would not in fact begin until August 10th. Details of what are included in the phases of the roadmap are included in Table 3 .
Use of technology in disease detection and prevention
Technology has played a major role in Ireland's response to the pandemic. In the health sector, diagnostic testing, clinical trials, use of medical devices and eHealth systems have all been employed to combat the effects of the pandemic. As the pandemic progressed, the use of technology has evolved. A number of Irish organisations have provided rapid evidence reviews of health technology assessment and health queries about the coronavirus and COVID-19 disease including the National Health Library and Knowledge Service [16] , the Health Information and Quality Authority (HIQA) [17] , iHealthFacts [18] and Cochrane Ireland [19] .
During the first month of the crisis, around 1400 public service workers received training in contact tracing. Many of these have been deployed along with existing HSE staff in a series of contact tracing centres that have been set up countrywide. A special mobile phone app to track and trace Covid-19 infections was developed by a collaboration between the private sector and health authorities and was launched on July 7th. Over 25% of the population downloaded the app in the week after it was launched [20] . A recurring concern in Ireland has been the availability of personal protective equipment (PPE), which is a particular issue in long-term residential care homes. The Health Research Board have funded local projects that avail of technology such as AI-enabled analysis and participation in international consortium clinical trials treating COVID-19 in ICU [21] .
Healthcare system response
As noted earlier, the low number of ICU beds in the public health system (255 in total or 5.5 per 100,000) was a particularly pressing issue in Ireland at the beginning of the pandemic. On March 24th, the government announced that private hospitals had in effect been incorporated into the public hospital system for the duration of the crisis. In addition, many of the public hospitals increased the number of ICU beds in their own hospitals or identified additional beds that could be used as ICU beds if there was a surge in admissions. The number of ICU beds occupied by confirmed and suspected COVID-19 patients peaked in the second week of April and has steadily declined since then. The increase in the number of ICU beds meant that there were always at least 90 ICU beds available on any particular day [10] . As far as we know, no hospital ever exceeded its ICU capacity.
Recruiting additional healthcare workers
The Irish government took a number of steps to try to maintain and enhance the workforce capacity to deal with the COVID-19 pandemic. On March 17th, the Health Service Executive launched an international recruitment campaign, “Be on call for Ireland” to encourage healthcare professionals at home and abroad to come and work in the public health service [22] . The number of applicants for the Be on Call for Ireland initiative was approximately 73,000. However, the vast majority of these were not healthcare professionals. According to the Irish Medical Council, 397 doctors registered with the Council under this initiative. About one third of these were retired doctors returning to work. In addition to the Be on Call initiative, a number of other recruitment initiatives took place to maximise the current work force and increase capacity across both the public and private healthcare providers. These included increasing the hours of part time staff, maximising agency usage, rehiring of retired clinicians, redeployment of staff and encouraging those on career break to return early.
Changing requisites to practice medicine
The Government reached an agreement in March with the Private Hospitals Association to use its facilities for the treatment of both Covid-19 and non Covid-19 patients. Under the deal, 19 private hospitals essentially operated as public hospitals for a three month period. The arrangements between the State and private hospitals however did not cover 600 consultants who work exclusively in the private sector. By April 23rd about one quarter of these consultants had signed up to a contract offered to them. There have been ongoing discussions around the problem of how to ensure that formerly private consultants are able to continue their care relationship with their patients with many consultants strongly criticizing the arrangement between the State and the private hospitals. The deal has been criticised over its costs (€115 million cost per month) and the relatively few patients treated in these facilities [23] . The agreement lapsed at the end of June 2020.
Other actions pertaining to changing requisites in Ireland include:
- - Bringing forward exams for final year medical students to enable them to join the workforce.
- - All student nurses were hired as healthcare assistants.
- - Reassignment of healthcare workers from private sector, and other external staffing supports on a needs basis.
- - Cross training of healthcare workers where needed, for example where retraining has occurred e.g. theatre nurses to be ICU nurses.
GP / Specialists operational changes
Individuals who suspect that they have the virus are strongly encouraged to contact their GP as the first point of contact. Since mid-March, GPs have been providing the majority of their consultations over the phone or via video link. A number of Community Hubs were established around the country. In these hubs, patients can be seen by a GP who can refer them to an acute hospital. There has been ongoing concern over people delaying seeking medical help because of fear of contracting COVID-19 if they attended a hospital or other medical clinic [24] .
Changes in utilisation of non COVID-19 healthcare
Systematic evidence for changes in the demand or need for other types of medical care or pharmaceuticals is limited. A large online survey with over 35,000 respondents conducted in the third week of April found that about 32% of respondents had postponed medical treatment or check-ups [20] . Most of the appointments that were postponed were routine medical examinations such as a consultation with a GP or a dentist or a post-operation follow-up. Parents reported that vaccinations had frequently been postponed as had some pre- and post-natal appointments. Almost 5% said that a medical examination in a hospital had been postponed and 2% had an operation postponed. The Irish Cancer Society has claimed that more than 450 cancers have remained undetected due to the suspension of cancer screening services [25] .
Many mental health organizations have reported an increase in the use of their online and telephone services. SpunOut, which provides information on a broad range of issues to young people, said that there had been a 100% increase in people contacting them due to anxiety and depression. ALONE, an organization which supports older people, reported on April 27th that there had been a large increase in the number of older people contacting them about social isolation and loneliness. The number of calls they were receiving from people with suicidal ideation had also shown a large increase. The Samaritans have also reported an increase in calls to their helpline [26] . In April, the Government announced additional funding for online mental health services to support people, especially health services staff, during the pandemic. There has been a large fall in the proportion of adults reporting their satisfaction with life as ‘high’ with particularly large falls among younger people [27] . Only 12% of adults reported a high level of overall life satisfaction compared to over 44% in 2018.
A survey of almost 200 psychiatrists published in the middle of June 2020 found that there had been a significant increase in the number of referrals and emergency presentations for psychiatric services in the third month of the pandemic. The main factors identified as influencing the increase in emergency referrals were increased social isolation and reduced access to community-based mental health services [28] .
Economic and financial fluctuation
Economic impact.
Ireland has experienced considerable economic disruption from the COVID-19 pandemic, with significant challenges for households, businesses, and policymakers. A report published on April 21st 2020 by the Department of Finance [29] set out a macroeconomic and fiscal scenario for the period 2020–2021, incorporating the potential impact of COVID-19. A significant contraction in modified domestic demand of 15.1% was projected for 2020 (see Table 4 ), resulting from domestic and international efforts to combat the virus. Notably, this ‘baseline’ projection assumed a transient shock to the Irish economy, whereby activity bottoms out in the second quarter of 2020 and is followed by recovery, both domestically and internationally, later in the year. Based on such a scenario, the Department forecasts economic growth of 6% in GDP in 2021 and a restoration of overall economic activity to pre-pandemic levels in 2022 [29] . However, it warns this is based on successful containment of the virus. In May, the Economic and Social Research Institute's forecast that real GDP would decline by over 12% in 2020 under a baseline scenario that reflects continued physical distancing and containment measures to the end of 2020 [30] .
Summary of key economic activity and public finance variables.
From a position of full-employment at the start of 2020, unemployment hit a record high of 28.2% in April and is set to average 17.4% for 2020, with young adults disproportionately affected [31] . At a sectoral level, non-food retail, entertainment and hospitality are among those sectors that have been hardest hit, both in terms of economic activity and employment.
Economic policy response
In terms of economic policy responses, there have been a number of measures introduced to reduce the impact on households, businesses, and the economy. Broadly speaking, the Government's response to the crisis at an economic level has involved attempting to reduce the impact of COVID-19-related restrictions on household incomes, and on helping businesses and firms survive until restrictions are relaxed [32] . This has included, for example, income supports in the form of a flat-rate Pandemic Unemployment Payment of €350 per week for individuals who lose their jobs due to the pandemic, as well as a Temporary Wage Subsidy Scheme , which enables employees, whose employers are affected by the pandemic, to receive significant supports directly from their employer through the payroll system. Other measures undertaken include payment breaks on mortgage, personal, and business loans, liquidity funding for businesses, guaranteed loan schemes and deferred tax payments, as well as moratoriums on evictions and rent increases.
Beirne et al. [33] found that the measures announced by the Government, and in particular the Pandemic Unemployment Payment , reduced the numbers exposed to extreme income losses by about a third. Nonetheless, more than 150,000 households lost between 20% and 40% of their incomes, with smaller numbers suffering even heavier losses. The Department of Finance [29] announced increased expenditure of €8 billion to account for measures taken in response to COVID-19, including income supports. It estimates that the general government deficit could increase to 7.4% of GDP this year (see Table 4 ), or possibly as much as 10% if the easing of restrictions is delayed and large parts of the economy remain closed. This large deficit is driven by both the expenditure measures implemented by the Government and decreases in taxation revenue arising from reduced economic activity, and will lead to an increase in the debt-to-GDP ratio to an estimated 69%.
Overall, the consensus amongst economic commentators, including the Irish Fiscal Advisory Council (IFAC) [ 34 , 35 ], appears to be that Ireland, given its recent strong economic performance and relatively healthy public finances, is reasonably well positioned to meet the economic challenges of COVID-19 and that it should be possible to avoid a return to severe fiscal adjustments. Nonetheless, this is predicated on the containment of the virus and a return to normal patterns of economic activity in the second half of 2020.
Conclusions and policy implications
Ireland has suffered substantial loss of life and health since the beginning of the COVID-19 pandemic. As of July 19th, 1753 people have died with either a confirmed or suspected infection of COVID-19 and 25,766 have tested positive with the virus. The effects on health and well-being from the effective lockdown of large parts of normal economic and social life are also very significant. Already, there is some evidence of an increase in mental health difficulties experienced by people during the crisis. There has been a large fall in the proportion of adults reporting their satisfaction with life as ‘high’ with particularly large falls among younger people. To date, there have not been any estimates of the total loss of a broad measure of health such as QALYs nor has anybody published a comparison of the loss of well-being due to the lockdown relative to a counterfactual where a different kind of a lockdown or no lockdown at all had been imposed.
In general, compliance with the various public health measures has been very high. At a policy level, there has been little disagreement about the various steps that have been implemented. Many of the limited disagreements have been more about the timing of particular measures than the merits of the measures themselves. There is a very high level of trust in NPHET and politicians from all parties were generally supportive of the caretaker Government's handling of the pandemic, with a strong sense of national solidarity during the crisis.
Ireland's response to the COVID-19 crisis has been comprehensive and timely in many respects. Transparency, a commitment to a relatively open data policy, the use of traditional and social media to inform the population, and the frequency of updates from the Department of Health and the HSE are all commendable. Other areas such as testing and contact tracing took some time to work effectively but have been operating efficiently in recent weeks.
A striking feature of how the health system has prepared for and responded to the COVID 19 situation is that essentially it has been identical to what a tax-financed public health system would involve. People have not been charged for any aspect of care associated with the virus. The HSE took over the operation of private hospitals early in the crisis to increase capacity. While the universal, free-to-the-user nature of care for COVID-19 patients may bolster the case for a one-tier health system financed primarily by taxation, the difficulties of moving to such a system can be seen in the anomalous position that many patients in the private health system found themselves in.
Ireland's land border with Northern Ireland is another area which deserves close attention during this health emergency. Counties along the border with Northern Ireland are among those with the highest rate of cases and deaths per capita (see Figs. 1 and and6). 6 ). Free movement across this border is an obvious cause for concern, particularly when two different public health and testing strategies are being pursued in the jurisdictions. Northern Ireland has thus far carried out less community testing. As of July 23rd, Northern Ireland had completed 170,000 tests (90 tests per 1000 inhabitants) [36] while the equivalent figure for the Republic was 580,000 tests (118 tests per 1000 inhabitants). There are also significant differences in death rates between Ireland and Northern Ireland and between Ireland and the UK mainland [37] .
Much of the response by healthcare decision-makers in Ireland, particularly in the first month of the pandemic, focused on hospital-related issues. This was certainly understandable given the unfolding situation in some other countries. Nursing homes and other residential centres did not receive sufficient attention during that phase of the pandemic. The focus of attention on the hospital system can at times obscure the fact that the real battle needs to take place upstream in our communities, including long-term residencies. Further study of the individual components of public health advice that has clearly worked is required so we can be more focused in our response to further outbreaks of COVID-19. Improved information on symptoms reporting by the general public or likely diagnoses observed by GPs and other healthcare workers in our communities, along with better and more regular updates on testing and contact tracing will all contribute to better understanding of what is happening in our communities, the breeding ground for COVID-19. A further area of promise is the introduction of a contact tracing app which was downloaded by over a quarter of the population within a week of being launched. All of this additional data and research will be of utmost importance if we wish to be able to employ more focused yet effective measures rather than relying on a national lockdown.
To conclude, we offer some brief thoughts on what lessons we have learned that might help Ireland respond to a potential second or third wave of the pandemic. These observations, speculative as they might be, may also be useful to readers and policy makers in other countries.
- 1 The rapid fall in the number of new cases, hospitalisations and deaths per day, evident in Fig. 2 , Fig. 3 , Fig. 4 , has been achieved in large part by the collective action of an overwhelming majority of people in Ireland. A powerful solidarity with family, neighbours and fellow citizens emerged quickly once the country's leaders and its public health officials explained clearly what the problem was and what was needed to mitigate the problem. We are hopeful that a similar sense of solidarity could be drawn on if a second or subsequent wave emerged.
- 2 Continuing to have regular clear updates on the public health situation is of vital importance in maintaining the high level of acceptance by the public of the various non-medical interventions that are required to keep the virus transmission at his currently low level. This will be particularly important as people get annoyed with the longevity of various restrictions and measures such as being required to wear masks. People will need to be reminded about why they are being asked to do what they are doing. Successes, such as instances where the COVID tracker App helps contact tracers, should be acknowledged and celebrated.
- 3 The hospital and long-term care system in Ireland has suffered from significant under-investment for many years. A second wave during the winter when the public hospital system has historically operated near or beyond capacity is likely to prove a much more serious challenge than that posed by the first wave. The pandemic may have strengthened the case for a universal health system but it has also underlined how difficult bringing that about will be given the current hybrid model of health care provision and financing. Short-term interventions, such as the raid development of Respiratory Hubs in the community, need to be prioritised and adequately resourced.
- 4 The public health system itself is another area that has suffered from many years of significant under-investment. One area of particular concern that the pandemic has highlighted is the lack of a comprehensive electronic health record system. The absence of such a system will make dealing with a second wave much more challenging.
- 5 As hope rise around the world that some vaccines may be available by early 2021 and as doctors learn more about possible treatments for people with the virus, we think that Ireland and other countries should remain on a very high state of alert and caution. It is not yet time to consider any kind of a return to normal business and social life. Money is cheap and states should continue to borrow large sums to protect individuals and businesses for what we tentatively hope may be a relatively short period.
Author Statements
Declaration of competing interest.
None declared.
Ethical approval
Not required.
Reform of the Irish Healthcare System: What Reform?
- First Online: 05 October 2016
Cite this chapter

- Sara Burke 3
379 Accesses
2 Citations
This chapter outlines what happened to the Irish health system over the last decade, detailing the constant reorganising and restructuring which had little positive impact on patient care. It chronicles Ireland’s unusual public–private mix, an outlier in a European and OECD context, in that there is no universal access to healthcare. The impact of the economic crisis on health is assessed, demonstrating how during austerity inequalities in access to healthcare persisted and resulted in people paying more and waiting for longer for some aspects of essential care. It concludes by proposing that Ireland is at a critical juncture where it can maintain the status quo or pursue a path towards universal access to healthcare.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Barrington, R. (1987). Health, medicine and politics in Ireland 1900–1970 . Dublin: IPA.
Google Scholar
Brick, A., Nolan, A., O’Reilly, J., & Smith, S. (2010). Resource allocation, financing and sustainability in health care. Evidence for the expert group, volume 1 . Dublin: DHC/ESRI.
Brick, A., Gorecki, P., & Nolan, A. (2014). Ireland: Pharmaceutical prices, prescribing practices and usage of generics in a comparative context . Dublin: ESRI.
Burke, S. (2009). Irish apartheid. Healthcare inequality in Ireland . Dublin: New Island.
Burke, S. (2013). How three policies aimed at increasing for-profit hospital care became an accepted method of reform in Ireland between 2000 and 2005. ‘How many ditches do you die on?’. Ph.D, TCD.
Burke, S. (2014) There was absolutely nothing natural about the death of Dhara Kivlehan. Irish Independent , 4 October.
Burke, S., Barry, S., Thomas, S. (2014a). Indicators of health system coverage and activity in Ireland during the economic crisis, 2008–2014—From “more with less” to “less with less”. Health Policy , 117 (3), 275–278
Burke, S., Thomas, S., Barry, S., & Keegan, C. (2014b). Overview of resilience project: Concepts, research stages and initial findings, Presentation to the HSE Masterclass 24 May, Dublin Convention Centre: HSE/Trinity.
Children’s Mental Health Coalition. (2015). Meeting the mental health support needs of children and adolescents: A children’s mental health coalition view . Dublin: Children’s Mental Health Coalition.
Connor, M. (2014). Is the Irish health system at an inflection point? Is further consolidation safe? Unpublished: Griffith University, Australia.
DH. (2012a). Future health: A strategic framework for reform of the health service 2012–2015 . Dublin: DH.
DH. (2012b). National carers strategy . Dublin: DH.
DH. (2013a). Healthy Ireland—A framework for improved health and well-being 2013–2025 . Dublin: DH.
DH. (2013b). The establishment of hospital groups as a transition to independent hospital trusts . Dublin: DH.
DH. (2013c). Securing the future of small hospitals . Dublin: DH.
DH. (2014). The pathway to universal healthcare: White paper on universal health insurance . Dublin: DH.
DH. (2015a). Emergency department task force report . Dublin: DH.
DH. (2015b). Healthcare quality indicators in the Irish health system . Dublin: DH.
DHC. (2001a). Quality and fairness a health system for you . Dublin: DHC.
DHC. (2001b). Primary care a new direction . Dublin: DHC.
DHC. (2003a). Audit and structures and functions in the health system (the prospectus report) . Dublin: DHC.
DHC. (2003b). Commission on financial management and control systems in the health service (Brennan Report) . Dublin: DHC.
DHC. (2003c). Report of national task force on medical staffing (Hanly Report) . Dublin: DHC.
DHC. (2006). A vision for change . Dublin: DHC.
EC. (2013). The impact of the financial crisis on unmet needs for healthcare . Athens/Brussels: EC Employment, Social Affairs and Inclusion.
GoI. (2011). Government for national recovery 2011–2016 . Dublin: FG/LP.
HIA. (2013). HIA annual report and accounts 2012 . Dublin: HIAI.
HIAI. (2015). Market statistics for number of people with private health insurance inpatient cover. http://www.hia.ie/sites/default/files/Website%20Statistics%20270315.pdf . Accessed 27 Apr 2015.
HIQA. (2013). Investigation into the care and treatment of Savita Halappanavar in University College Galway Hospital and 19 other maternity units in Ireland . Dublin: HIQA.
HIQA. (2015). Report of the investigation into the safety, quality and standards of services provided by the health service executive to patients in the Midlands Regional Hospital, Portlaoise . Dublin: HIQA.
HSE. (2006). The health service reform programme . Dublin: HSE.
HSE. (2009). HSE national service plan 2009 . Dublin: HSE.
HSE. (2014a). Community healthcare organisations—Report and recommendations of the integrated service area review group . Dublin: HSE.
HSE. (2014b). Health service executive plan for acute services 2014 . Dublin: HSE.
HSE. (2014c). HSE national service plan 2015 . Dublin: HSE.
HSE. (2015a). Health service performance report, April 2015 . Dublin: HSE.
HSE. (2015b). Health service performance report, January 2015 . Dublin: HSE.
HSE. (2015c). Primary care reimbursement service statistical analysis of claims and payments 2013 . Dublin: HSE.
Keane, F. (2014). Report of the expert panel on medical need for medical card eligibility . Dublin: HSE.
Layte, R., Nolan, A., & Nolan, B. (2007). Poor prescriptions. Poverty and access to community health services . Dublin: Combat Poverty Agency.
Maarse, M., & Normand, C. (2009). Market competition in European hospital care. In B. Rechel, S. Wright, N. Edwards, B. Dowdeswell, & M. McKee (Eds.), Investing in hospitals in the future (pp. 103–122). Copenhagen: European Observatory on Health Systems and Policies/WHO.
Mental Health Commission. (2015). Mental health commission annual report 2014, including report of the inspector of mental health services . Dublin: Mental Health Commission.
Murphy, C., Moore, P., McHugh, S., & Nolan, H. (2014). Health and social care utilisation. In A. Nolan, C. O’Regan, C. Dooley, D. Wallace, A. Hever, H. Cronin, E. Hudson, & R. A. Kenny (Eds.), The over 50s in a changing Ireland. Economic circumstances, health and well-being 2014 . Dublin: TILDA.
NHI. (2011). Annual private nursing homes survey 2009/2010 . Dublin: NHI.
Nolan, A., Barry, S., Burke, S., & Thomas, S. (2014). Observatory-WHO study on the impact of the financial crisis on health and health systems in Europe. Case study Ireland . London: WHO European Observatory on Health Systems.
Normand, C. (2015). Funding universal health and social care in Ireland: Ageing, dying and affordability (NERI research seminar). Dublin: NERI.
Normand, C., & Thomas, S. (2009). Health care financing and the health system. In G. Carrin, K. Buse, H. K. Heggenhougen, & S. R. Quah (Eds.), Health systems policy, finance, and organization . Oxford: Elsevier.
NTPF. (2015a). Outpatient national waiting list figures by group/hospitals as at 26/03/2015 . Dublin: NTPF.
NTPF. (2015b). Inpatient/day case national waiting times by group/hospital as at 26/05/2015 . Dublin: NTPF.
O’Brien, T. (2013). Tony O’Brien HSE Director General commenting on the publication of the HIQA report into the death of Savita Halappanavar, 9 November . Dublin: HSE.
O’Riordan, M., Collins, C., & Doran, G. (2013). Access to diagnostics—A key enabler for a primary care led health service . Dublin: ICGP.
Organisation for Economic Co-operation and Development (OECD). (2015). Health at a glance 2015 . Paris: OECD.
Revenue Commissioners. (2015). Costs of credits, allowances and reliefs . Dublin: Revenue Commissioners.
Smith, S., & Normand, C. (2010). Equity in health care: The Irish perspective. Health Economics, Policy and Law, 5 (2), 149–169.
Article Google Scholar
Thomas, S., Burke, S., & Barry, S. (2014). The Irish health-care system and austerity: Sharing the pain. The Lancet, 383 , 1545–1546.
Thomson, S., Jowett, M., & Mladovsky, P. (2014). Health system responses to financial pressures in Ireland. Policy options in an international context . Copenhagen: WHO.
Tussing, D. A., & Wren, M. A. (2005). How Ireland cares. The case for healthcare reform . Dublin: New Island.
WHO. (2015). National health accounts indicators . Geneva: WHO.
Wren, M. A. (2003). Unhealthy state. Anatomy of a sick society . Dublin: New Island.
Download references
Author information
Authors and affiliations.
Centre for Health Policy and Management, Trinity College Dublin, Dublin, Ireland
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sara Burke .
Editor information
Editors and affiliations.
Department of Sociology, Maynooth University, Maynooth, Ireland
Mary P. Murphy
School of Applied Social Studies, University College Cork, Cork, Ireland
Fiona Dukelow
Copyright information
© 2016 The Author(s)
About this chapter
Burke, S. (2016). Reform of the Irish Healthcare System: What Reform?. In: Murphy, M., Dukelow, F. (eds) The Irish Welfare State in the Twenty-First Century. Palgrave Macmillan, London. https://doi.org/10.1057/978-1-137-57138-0_8
Download citation
DOI : https://doi.org/10.1057/978-1-137-57138-0_8
Published : 05 October 2016
Publisher Name : Palgrave Macmillan, London
Print ISBN : 978-1-137-57137-3
Online ISBN : 978-1-137-57138-0
eBook Packages : Social Sciences Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
We need your help now
Support from readers like you keeps The Journal open.
You are visiting us because we have something you value. Independent, unbiased news that tells the truth. Advertising revenue goes some way to support our mission, but this year it has not been enough.
If you've seen value in our reporting, please contribute what you can, so we can continue to produce accurate and meaningful journalism. For everyone who needs it.
- Temperature Check
- The Stardust Inquests
- Inside The Newsroom
- Climate Crisis
- International

Ireland's healthcare system: What exactly are we doing wrong?
WHAT IS WRONG with Ireland’s healthcare system?
Long waiting lists, healthcare professionals under pressure, and emergency services at breaking point are some of the most common complaints that we hear about, but what can we do to change it?
And before you say ‘money’, the short response to that is it’s not the main problem – a recent report seriously questioned whether increasing the money going into the healthcare system would make things better by the same proportion.
Using some of the metrics that Ireland scored the lowest on as part of the EuroHealth Consumer Index 2016 , we’ve taken a look at what are the worst aspects of our healthcare system, and what we could do to change it (with a quick reminder that it’s not just the healthcare system at fault, either).
What did we score worst on?
In the EuroHealth report, a ‘matrix’ shows how each of the 35 countries surveyed scored under six main headings, marking them with a green, yellow or red mark to represent ‘good’, ‘intermediary’ or ‘not-so-good’ respectively.

To view this image in Full click here.
The matrix is broken down into six headings and the number of subheadings, and out of those six headings, Ireland scored ‘not-so-good’ on the following:
1. Patient Rights and Information (12)
- No-fault malpractice insurance
- Right to second opinion
- Online booking of appointments
- e-prescriptions
2. Accessibility (6)
- Direct access to specialist
- Major elective surgery <90 days
- CT scan <7 days
- A&E waiting times
3. Outcomes (9)
COPD mortality
4. Range and Reach of Services (8)
- Equity of healthcare systems
- Cataract operations per 100,000 age 65+
5. Prevention (7)
- Physical activity
We were given all ‘intermediate’ or ‘good’ marks under the sixth category; Pharmaceuticals.
Based on this score sheet, we grouped some of those subheadings together, had a look at what we’re doing wrong, and possible ways of fixing it.
Accessibility is the main issue for the Irish healthcare system (we scored badly on 4/6 criteria); patient rights were an issue too.
We also had a quick look at what we scored badly on that don’t have anything to do with the healthcare system: COPD mortality attitudes to alcohol and exercise.
Lastly, there’s a general look at what needs to be done to improve the Irish healthcare system, and Simon Harris’ attitude towards it.
Accessibility

Ireland ranked the worst in a survey of European countries for long waiting list times: both in terms of the number of people waiting and the length of time.
This isn’t a problem that can be solved by money or funding (there’s no obvious link between access to healthcare and healthcare funding), but rather it’s an issue of system or management reform.
One major difference between the four countries with the worst waiting times and those with the best is that the latter never had systems where hospitals/clinics were financed beforehand to provide healthcare for citizens.
Dr Arne Björnberg used to be European Manager for healthcare solutions for IBM back in the 1990s and is now Chairman of the Health Consumer Powerhouse. He explains:
On the contrary, their hospitals and primary care doctors were always remunerated for services provided, so that in Belgium, Switzerland, Germany and Austria waiting lists are short or non-existent.
So basically, if people are on waiting lists for prolonged periods of time, it means hospitals aren’t getting money. They have to see and treat patients to get paid by the state.
To show how much of a difference this approach to healthcare makes, Germany’s waiting times to see your primary care doctor were measured in minutes, not weeks.
Again; this isn’t a funding issue as Macedonia, which isn’t a particularly wealthy country has one of the best rates of accessible healthcare, while Sweden has one of the worst.

The Irish Nurses and Midwives Organisation and the Irish Medical Organisation say that most accessibility problems come down to staffing issues – that there are simply not enough staff in proportion to patients.
That’s difficult to compare to other countries, but a recent FactCheck from the end of last year showed that there has only been a slight decrease in the numbers of whole time equivalent staff working in the healthcare system.
Patient rights and information
Under this heading, Ireland doesn’t have access to no-fault malpractice insurance, a right to second opinion, online booking of appointments or e-prescriptions.
In countries such as Norway (which topped the list on patients the information and rights) they offer insurance that covers a patient who suffers because of treatment – even though there might be no one at fault.
The Nordic countries are good examples for patient malpractice insurance, where the issue of ’who might have made an error’ is separated from the issue ‘has the patient suffered because of preventive causes?’.
Nordic healthcare institutions are carrying insurance for the latter circumstance, meaning that it is very rare for patients having to enlist expensive lawyers to push malpractice cases.
In Norway, you’re also entitled to a second opinion if your request for a referral has been rejected. You can speak with any doctor for a second opinion including an emergency doctor, private doctor, or online doctor.
Macedonia and Serbia have implemented a system which displays where healthcare specialists around the country are, with their availability displayed to view. GPs can book a patient for a referral if needed, so that the patient leaves the office with a date and time.
Macedonia also have an e-prescriptions facility, meaning patients who have repeat prescriptions can apply for them from their home, meaning patients don’t have to book GP appointments just to get prescriptions.
“These are important,” says Björnberg. “If you agree that patients are grown-ups who should be supported at taking their own decisions on their health.”
It’s not all the healthcare system’s fault though and some things made it to the list that aren’t under the Department of Health’s remit.
Chronic Obstructive Pulmonary Disease deaths, although recorded included in the report, doesn’t make up the ‘final score’ for countries assessed as part of the Euro Health Index. This is because the data is so poor; very heavy smokers Bulgaria, for example, report very low rates of COPD death, which is simply not possible.
What makes it worth mentioning here, though, is that Ireland and Britain have had the highest COPD death rates in Europe for years – and we’re unsure as to why.
You do have a lot of rain, damp and draughty houses,” says Dr Björnberg. “But the connection of that to COPD is not proven.
COPD is a disease that makes it hard to empty air out of your lungs. This is because the airways get smaller leading to airflow obstruction, which can result in shortness of breath as you try to push the air through a smaller gap.
Most people with COPD are smokers or have smoked in the past. Sometimes COPD is caused by working or living for many years in an environment where there is exposure to smoke, dust or other fumes.
So cold and damp weather is worth being wary of.
Alcohol and exercise

Ireland also scored badly in terms of alcohol consumption and physical activity, which are preventative healthcare measures.
In Ireland, it’s not the alcohol intake in itself that’s the problem, but rather the massive drinking sessions in one go, compared to the Mediterranean’s moderate intake that’s spread out over time.
“A steady moderate alcohol intake seems to be beneficial against Cardiovascular Disease, and thus having a positive effect on public health,” says Björnberg.
Alcohol intake is the cause of around 900 incidences of cancer in Ireland each year, and 500 of these patients will die of their disease.
Ireland has also a rising rate of obesity: with the Royal College of Physicians warning that Ireland could become the fattest country in Europe by 2030 if urgent action isn’t taken.
Efforts have been made to curb this rate by promoting exercise among young people, and imposing more regulations on sugary and fatty foods.
Health Minister’s mission
Björnberg’s major assertion on how to fix healthcare systems revolves around two key concepts: demanding better management results, something he says all healthcare systems are looking at, and taking politics out of the healthcare system.
If that sounds familiar, it’s because it echoes previous promises made by health minister Simon Harris: who upon his appointment, promised to fix the healthcare system by taking the political element out of it, and more recently, asked for improvements from hospital managers.
Harris clarified that this didn’t mean firing managers, but asking them to improve their way of operating, and looking at other hospitals’ examples of how to improve conditions, like any other business would.
“It’s not difficult,” according to Björnberg. ”You just need to manage in a way that motivates staff, maximises production, keeps costs down, and monitors the output of healthcare.”
Apart from that, just stand in the main entrance of the hospital with a cane to keep amateurs out and let the professionals do their jobs.
“And by amateurs, I mean politicians.”
Read: How Ireland’s hospitals are massaging the numbers of people on trolleys
Factcheck: nursing union leader liam doran’s claims about the irish health service, making a difference, a mix of advertising and supporting contributions helps keep paywalls away from valuable information like this article. over 5,000 readers like you have already stepped up and support us with a monthly payment or a once-off donation..
For the price of one cup of coffee each week you can make sure we can keep reliable, meaningful news open to everyone regardless of their ability to pay.

To embed this post, copy the code below on your site
600px wide <iframe width="600" height="460" frameborder="0" style="border:0px;" src="https://www.thejournal.ie/https://www.thejournal.ie/irish-healthcare-system-3242479-Feb2017/?embedpost=3242479&width=600&height=460" ></iframe>
400px wide <iframe width="600" height="460" frameborder="0" style="border:0px;" src="https://www.thejournal.ie/https://www.thejournal.ie/irish-healthcare-system-3242479-Feb2017/?embedpost=3242479&width=400&height=460" ></iframe>
300px wide <iframe width="600" height="460" frameborder="0" style="border:0px;" src="https://www.thejournal.ie/https://www.thejournal.ie/irish-healthcare-system-3242479-Feb2017/?embedpost=3242479&width=300&height=460" ></iframe>
- Defamation Damaging the good reputation of someone, slander, or libel.
- Racism or Hate speech An attack on an individual or group based on religion, race, gender, or beliefs.
- Trolling or Off-topic An attempt to derail the discussion.
- Inappropriate language Profanity, obscenity, vulgarity, or slurs.
- Spam Advertising, phishing, scamming, bots, or repetitive posts.
Create an email alert based on the current article
- Find Flashcards
- Why It Works
- Tutors & resellers
- Content partnerships
- Teachers & professors
- Employee training
Brainscape's Knowledge Genome TM
- Entrance Exams
- Professional Certifications
- Foreign Languages
- Medical & Nursing
- Humanities & Social Studies
- Mathematics
- Health & Fitness
- Business & Finance
- Technology & Engineering
- Food & Beverage
- Random Knowledge
See full index
Learn irish essay.
Irish: Essay Vocabulary
By: allan haydenerd.
Irish: Essay Writing
Irish essay writing, by: aoife luc, irish essay vocab, by: alex caverly, irish: essay - seandaoine, irish: essay - an foréigean, irish essay, by: hagahs green.
Irish: Essay - Daoine gan Dídean & Óráid
Irish: essay - an timpeallacht, irish essays, by: aoife lambe.
Irish: Essay - An Córas Oideachais - 10 Week Assessment Subject Notes
Irish: essay - an ciníochas, irish: essay - fadhb na ndrugaí agus an alcóil.
CCEA GCSE (S1)
By: james brewster, by: sarah oliver.
Leaving Cert Irish
By: shane mc dermott, by: laura connolly.
Higher History
By: liza angelica solas, by: rory doran, by: adam greaney.
History A Level
By: finyl vinyl, all subjects, by: meril jacob, by: ella dillon, politics and society, by: sam keogh, by: laura baginska, by: anna lenkovska, by: nathan walsh, by: paddy kelly, knowledge genome.
- Corporate Training
- Teachers & Schools
- Android App
- Help Center
- Law Education
- All Subjects A-Z
- All Certified Classes
- Earn Money!
- français
- español
- português
Related Links
Russian federation: health system review.

View Statistics
Description, more languages, collections.
- Publications
Show Statistical Information
- 5. Regional Office for Europe
- Court & Crime
Ireland's mental health system is broken, says man whose wife took her own life

Darren Coleman( left) was speaking in the High Court as he settled an action over the care received by his 34-year-old wife Nicola Keane (right) who had post-natal depression and psychosis after the birth of their baby boy, Henry. File picture: Colin Keegan, Collins Dublin
A man whose wife took her own life and whose seven-month-old baby son died has told a High Court judge that the mental health system in Ireland is broken.
Darren Coleman was speaking in the High Court as he settled an action over the care received by his 34-year-old wife Nicola Keane who had post-natal depression and psychosis after the birth of their baby boy, Henry.
Nicola’s body was discovered at Lower Rd Strawberry Beds in west Dublin on October 22, 2020, at 3.45am. When gardaí called to her home in Lucan, Co Dublin, to inform her husband of her death, Darren Coleman, who had been asleep, found his son Henry lifeless in the back bedroom.
Counsel Bruce Antoniotti SC, instructed by Rachael Liston solicitor, said the facts were both harrowing and distressing. He said Mr Coleman has been living a nightmare since October 2020.
Counsel said on October 21, 2020, Ms Keane, a paediatric nurse had offered to go to the spare room with Baby Henry who had become unsettled late at night. Counsel said Ms Keane administered a lethal level of medication to the baby before she left the house.
Mr Darren Coleman from Lucan, Dublin, sued Children’s Health Ireland and the HSE over the circumstances leading to the death of his wife Nicole Coleman Keane and the aftermath.
It was claimed that the mother and baby were owed a duty of care in and about the investigation, diagnosis, management, treatment and care of the mother’s severe mental illness and the identification of the risk of the mother committing infanticide and the risk of suicide.
Children’s Health Ireland denied all claims but the HSE admitted a breach of duty by failing to appreciate that Ms Keane had suffered from psychotic depression, failing to communicate this to her husband and failing to ensure she received in patient treatment before October 13, 2020.
An apology on behalf of the Dublin South, Kildare and West Wicklow Mental Health Services was read to the court.
Mr Coleman who settled his action after mediation told the judge: “I am Henry Coleman's father and Nicola Keane’s husband. I'm a widower and a father of a deceased seven-month-old baby boy.
"Nicola had post partum psychosis after our son Henry's birth. She never hid her illness from her medical team. She repeatedly told them she wasn't getting better and spoke about the concerning thoughts she had,” he said.
He described his son as beautiful and inquisitive and said people complimented that he was gorgeous.
He told Mr Justice Coffey:
The mental health system in Ireland is broken. Mental health is not a priority in this country.
"Investment in mental health is a necessity. People with mental health issues don't receive the same level of care as those who have a physical condition.”
He also told those involved in his wife’s care not to blame themselves. “I'm not here to blame any individual involved in Nicola and Henry's care in the HSE. You are not to blame yourselves,” he said.
Counsel told the court that in August 2020 when Mr Coleman told the care team he was going back to work he was told everything was fine and his wife’s post-natal depression had improved.
Counsel said Mr Coleman completely trusted his care team but actually between September and October 2020 Ms Keane’s medication was increased twice as her mental state deteriorated. Counsel said if Mr Coleman had been told of his wife’s condition he would not gone back to work.
“She was deteriorating unbeknownst to her husband,” counsel said.
Noting the settlement, Mr Justice Paul Coffey said it was a tragic and distressing case and he extended his deepest sympathy to Mr Coleman and the extended families.
- If you are affected by any of the issues raised in this article, please click here for a list of support services.

Irish Examiner’s WhatsApp channel
Follow and share the latest news and stories
More in this section

€1m cannabis haul seized in Meath
Lunchtime news.
Sign up to the best reads of the week from irishexaminer.com selected just for you.
Please click here for our privacy statement.
FOLLOW IRISH EXAMINER

Select your favourite newsletters and get the best of Irish Examiner delivered to your inbox

Sunday, May 19, 2024 - 10:00 PM

Sunday, May 19, 2024 - 7:00 PM

Family Notices
© Examiner Echo Group Limited
- Open access
- Published: 08 May 2024
The digital transformation in pharmacy: embracing online platforms and the cosmeceutical paradigm shift
- Ahmad Almeman ORCID: orcid.org/0000-0002-6521-9463 1
Journal of Health, Population and Nutrition volume 43 , Article number: 60 ( 2024 ) Cite this article
682 Accesses
3 Altmetric
Metrics details
In the face of rapid technological advancement, the pharmacy sector is undergoing a significant digital transformation. This review explores the transformative impact of digitalization in the global pharmacy sector. We illustrated how advancements in technologies like artificial intelligence, blockchain, and online platforms are reshaping pharmacy services and education. The paper provides a comprehensive overview of the growth of online pharmacy platforms and the pivotal role of telepharmacy and telehealth during the COVID-19 pandemic. Additionally, it discusses the burgeoning cosmeceutical market within online pharmacies, the regulatory challenges faced globally, and the private sector’s influence on healthcare technology. Conclusively, the paper highlights future trends and technological innovations, underscoring the dynamic evolution of the pharmacy landscape in response to digital transformation.
Introduction
Digital technology is driving a massive shift in the worldwide pharmacy industry with the goal of improving productivity, efficiency, and flexibility in healthcare delivery. In the pharmacy industry, implementing digital technologies like automation, computerization, and robotics is essential to cutting expenses and enhancing service delivery [ 1 ]. With a predicted 14.42% annual growth rate, the digital pharmacy market is expanding significantly and is expected to reach a market volume of about $35.33 billion by 2026. This expansion reflects the pharmacy industry’s growing reliance on and promise for digital technologies [ 2 ].
Pharmacy services have always been focused on face-to-face communication and paper-based procedures. However, the drive for more effective, transparent, and patient-centered healthcare is clear evidence of the growing need for digital transformation. Breakthroughs like mobile communications, cloud computing, advanced analytics, and the Internet of Things (IoT) are reshaping the healthcare sector. These breakthroughs have the potential to greatly improve patient care and service delivery, as demonstrated in other industries including banking, retail, and media [ 3 ].
In the pharmacy industry, a number of significant factors are hastening this digital transition. Important concerns include the desire for cost-effectiveness, enhanced patient care, and more transparency and efficiency in medication development and manufacture. This change has been made even more rapid by the COVID-19 pandemic, which has highlighted the necessity for digital solutions to address the difficulties associated with providing healthcare in emergency situations [ 4 ].
In terms of specific technologies being adopted, artificial intelligence (AI) and machine learning are playing a pivotal role. The McKinsey Global Institute estimates that AI in the pharmaceutical industry could generate nearly $100 billion annually across the U.S. healthcare system. The use of AI and machine learning enhances decision-making, optimizes innovation, and improves the efficiency of research and clinical trials. This results in more effective patient care and a more streamlined drug development process [ 5 ].
The digital transformation in the pharmacy sector represents a pivotal shift in the delivery and experience of healthcare services. This evolution is more than a transient trend; it’s a fundamental alteration in the healthcare landscape [ 6 ]. The adoption of digital technologies is reshaping aspects of healthcare, including patient engagement and medication adherence, leading to enhanced healthcare outcomes. Research indicates that digital tools in pharmacy practices have resulted in more individualized and efficient patient care. Telehealth platforms, exemplified by companies like HealthTap, are being increasingly incorporated by pharmacies to augment patient care via technological solutions. The contribution of digital health technology to medication adherence is notable, employing a variety of tools such as SMS, mobile applications, and innovative devices like virtual pillboxes and intelligent pill bottles. These advancements are pivotal in addressing the critical issue of medication nonadherence in healthcare. Furthermore, digital health tools are empowering pharmacists with expanded clinical responsibilities, particularly in the management of chronic diseases like diabetes, where apps and smart devices provide essential features such as blood glucose tracking and medication reminders. This comprehensive integration of digital health into pharmacy practice signifies a transformative era in healthcare delivery and patient management [ 7 ].
Online platforms are being used increasingly by the pharmaceutical sector and educational institutions to improve efficiency, flexibility, and accessibility. The telepharmacy program at CVS Pharmacy is an example of how telepharmacy services, which provide remote counseling and prescription verification, bring pharmaceutical care to underprivileged communities [ 8 ]. Prescription accuracy and drug management are enhanced by e-prescribing software like Epic’s MyChart and digital health apps like Medisafe [ 9 ; 10 ]. Blockchain technology is also being investigated for transparent and safe supply chain management. Continuous learning and professional networking are made possible in education by Virtual Learning Environments (VLEs) like Moodle [ 11 ], simulation software like SimMan 3G Plus [ 12 ], Continuing Professional Development (CPD) platforms like the American Pharmacists Association [ 13 ], and online conference platforms, as shown in Fig. 1 . While these platforms offer significant benefits like enhanced access and cost-effectiveness, they also present challenges, including addressing the digital divide and ensuring the quality and credibility of online services to maintain professional standards and patient safety.
In this review, we summarized the digital transformation in the pharmacy sector, emphasizing the integration of online platforms and the emerging significance of cosmeceuticals. We discussed the global shift towards digital healthcare, including telehealth and online pharmacy services, and how these changes have been accelerated by the COVID-19 pandemic. The paper also examined the impact of digital technologies on pharmacy practice and education, with a focus on telepharmacy services, e-prescribing software, and digital health apps. Additionally, it addresses the challenges and opportunities presented by this transformation, including regulatory and safety concerns, and the need for continuous professional development in the digital era.
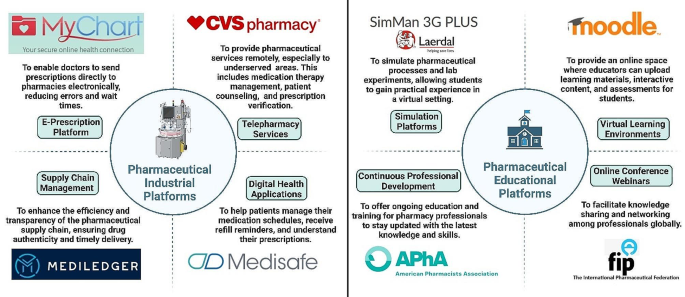
Comprehensive overview of different platforms in the pharmaceutical industry and education illustrating purposes and exemplary cases
The global impact of online pharmacy platforms
In recent years, the landscape of pharmacy practice and education has undergone a significant transformation, driven by technological advancements and catalyzed by the global COVID-19 pandemic. A study highlighting the increasing consumer trust in online medication purchases pre, during, and post-pandemic reveals a shift in consumer behavior towards online pharmacies [ 14 ]. This trend underscores a greater reliance on these platforms, where the perceived benefits significantly outweigh the perceived risks, indicating a positive reception and growing trust in digital healthcare solutions.
The adoption of telehealth, including telepharmacy, exemplifies this shift. In the United States, patient adoption of telehealth services surged from 11% in 2019 to 46%, with healthcare providers expanding their telehealth visits [ 15 ]. This shift is a reflection of how adaptable the healthcare sector is to digital platforms and how customer acceptance is increasing. The epidemic has also served as a catalyst, hastening the creation and uptake of online telepharmacy services throughout the world. The “new normal” has forced the addition of new platforms to support established sources of health information. The creation and evaluation of an online telepharmacy service in the Philippines during the pandemic serves as an example of this, demonstrating how quickly the global pharmacy industry adopted digital solutions. These services are essential for providing and elucidating pharmaceutical information within the context of primary healthcare delivery; they are not merely supplementary [ 16 ].
Simultaneously, pharmacist-led companies such as MedEssist and MedMehave, innovated digital platforms to facilitate services like flu shots or COVID-19 tests, reflecting a move towards customer-centric, digital-first services [ 17 ]. This transition enhances convenience and access to care but also introduces significant regulatory challenges. As the growth of online medicine sales disrupts traditional pharmacy markets, navigating these challenges becomes crucial for maintaining patient safety, quality standards, and fostering a trustworthy online healthcare environment [ 18 ].
Parallel to the practice changes, educational platforms for pharmacy have also evolved, especially under the impetus of the pandemic. These platforms have integrated a mix of traditional and student-centered teaching methodologies, including remote didactic lectures and on-site experiential training. The implementation of blended learning approaches, which combine remote lectures with on-site laboratory classes, reflects a broader educational trend towards hybrid models. This approach aims to leverage the advantages of both online and traditional methods, offering a more flexible and potentially more effective educational experience [ 19 ].
It takes more than just implementing new tools to integrate educational technology into pharmacy education, it also requires understanding how these technologies affect instruction and student learning. To effectively improve the educational experience, their utilization must have a purpose. There is an increasing amount of scholarly interest in this field, as evidenced by systematic reviews of the effects of new technologies on undergraduate pharmacy teaching and learning [ 20 ]. These digital platforms will probably become more significant in the future of pharmacy education, helping to mold the profession and guaranteeing that pharmacists are equipped to fulfill the ever-changing demands of the healthcare system. This development is indicative of a larger trend in the healthcare industry toward a more flexible, patient-focused, and technologically advanced environment [ 21 ].
Digital transformation in global healthcare
The recent advancements in digital transformation within global healthcare are significantly reshaping the landscape of healthcare and pharmacy services. These transformations are largely driven by the integration of digital technologies, which are redefining the tools and methods used in health, medicine, and biomedical science, ultimately aiming to create a healthier future for people worldwide [ 22 ]. In a 2018 report [ 23 ], Amazon’s potential entry into the $500 billion U.S. pharmacy market, the second-largest retail category, through mail-order and online pharmacies was highlighted as a significant industry disruptor. With licenses in at least 12 states in the US and a strategy focused on bypassing middlemen, Amazon’s historical success positions it to transform the pharmacy landscape, promising enhanced efficiency and cost savings for consumers.
One of the critical areas identified in recent research is the establishment of five priorities of e-health policy making: strategy, consensus-building, decision-making, implementation, and evaluation. These priorities emerged from stakeholders’ perceptions and are crucial for the effective integration and adoption of digital health technologies [ 24 ]. This holistic approach is increasingly relevant for scholars and practitioners, suggesting a focus on how multiple stakeholders implement digital technologies for management and business purposes in the healthcare sector [ 25 ]. The deployment of technological modalities, encompassed within five distinct clusters, can facilitate the development of a digital transformation model. This model ensures operational efficiency through several dimensions: enhanced operational efficacy by healthcare providers, the adoption of patient-centered methodologies, the integration of organizational factors and managerial implications, the refinement of workforce practices, and the consideration of socio-economic factors [ 25 ].
Studies focusing on value creation through digital means suggest healthcare as a consumer-centric realm ripe for center-edge transformations, characterized by self-service and feedback cycles. These transformations are vital in addressing inherent tensions between patients and physicians, steering the focus towards value co-creation and service-dominant logic [ 26 ]. Participatory design and decision-making approaches are emphasized for enhancing health information technology’s performance and institutional healthcare innovation. Such approaches are particularly crucial in developing national electronic medical record systems and improving chronic disease treatment through electronic health records. Additionally, telehealth research integrates patients’ perceptions, contributing to the understanding of technology, bureaucracy, and professionalism within healthcare [ 27 ].
The impact of health information technology (HIT) on operational efficiencies is profound. Empirical studies, such as those by Hong and Lee [ 28 ], Laurenza et al. [ 29 ], and Mazor et al. [ 30 ], demonstrate positive correlations between HIT and patient satisfaction, quality of care, and operational efficiency. However, challenges remain, as Rubbio et al. [ 31 ] highlight deficiencies in resilience-oriented practices for patient safety. Organizational and managerial factors in digital healthcare transformation also receive significant attention. Hikmet et al. [ 32 ] and Agarwal et al. [ 33 ] investigate the role of organizational variables and barriers in HIT adoption, whereas Cucciniello et al. [ 34 ] delve into the interdependence between implementing electronic medical records (EMR) systems and organizational conditions. Further, Eden et al. [ 35 ] and Huber and Gärtner [ 36 ] explore workforce adaptations and the implications of health information systems in hospitals that can increases transparency of work processes and accountability. Lastly, examining healthcare financialization and digital division provides an international perspective, contrasting the regulated environment in the EU with the US’s use of online medical crowdfunding as a potential solution to reduce bankruptcy [ 37 ; 38 ]. Collectively, these studies suggest a comprehensive model where stakeholders leverage digital transformation for management, enhancing operational efficiency in healthcare service providers.
Marques and Ferreira [ 39 ] performed a systematic literature review of digital transformation in healthcare, spanning the period from 1973 to 2018. Utilizing the SMARTER (Simple Multi-attribute Rating Technique Exploiting Ranks) method, 749 potential articles were analyzed, culminating in the prioritization and selection of 53 articles for detailed examination. The literature was organized into seven thematic areas: (1) Integrated management of IT in healthcare, (2) Medical images, (3) Electronic medical records, (4) IT and portable devices in healthcare, (5) Access to e-health, (6) Telemedicine, and (7) Privacy of medical data. It was observed that the predominant focus of research resides in the domains of integrated management, electronic medical records, and medical images. Concurrently, emerging trends were identified, notably the utilization of portable devices, the proliferation of virtual services, and the escalating concerns surrounding privacy. See Fig. 2 for visual representation of multifaceted digital transformation in healthcare.
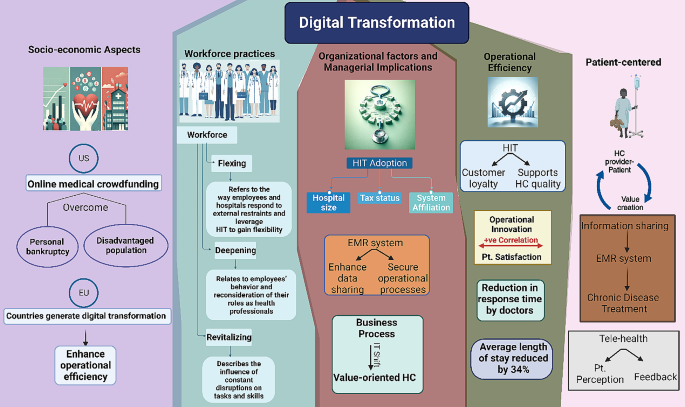
Visual representation of multifaceted digital transformation in healthcare: a synthesis of provider-patient dynamics, HIT impact, and strategic management. HIT; health information technology, HC; healthcare, EMR; electronic medical records. IT; information technology, Pt.; patient
Telehealth and online pharmacy advancements in pandemic management
In the realm of online pharmacies and telehealth, digital health technologies have been instrumental in managing the COVID-19 pandemic through surveillance, contact tracing, diagnosis, treatment, and prevention. These technologies ensure that healthcare, including pharmacy services, is delivered more effectively, addressing the challenges of accessibility and timely care. The role of telemedicine and e-pharmacies, in particular, has been emphasized in improving access to care worldwide. By enabling remote consultations and drug delivery, these platforms are making healthcare more accessible, especially in regions where traditional healthcare infrastructure is limited or overstretched [ 40 ].
The Canadian Virtual Care Policy Framework advocates for the swift adoption and integration of virtual care, propelled by the COVID-19 pandemic. It emphasizes enhancing access and quality, ensuring equity and privacy, and devising appropriate remuneration models, employing a collaborative, patient-centered approach while addressing digital disparities. During the COVID-19 pandemic, Canadian provinces and territories rapidly adopted virtual health care, leading to 60% of visits being virtual by April 2020, up from 10 to 20% in 2019. However, these implementations were often temporary and not fully integrated into healthcare systems. By August 2020, virtual visits decreased to 40%, with variations across regions, while provinces and territories used temporary billing codes for these services. The framework’s “Diagnostique” provides a thorough analysis of policy enablers and strategies for virtual care, underscoring the need for comprehensive policy and partnership engagement [ 41 ]. In the context of digital transformation in pharmacy, the Hospital News article outlines the application and infrastructure of telepharmacy services in Canada, highlighting the geographical challenges and the early adoption of telepharmacy in certain regions since 2003. It notes the use of various technologies like Medication Order Management, Videoconferencing, and Remote Camera Verification. Although lacking specific quantitative data, the article underscores the necessity for expanded telepharmacy services to ensure uniform care quality across diverse locations [ 42 ].
Similarly, Telehealth offers extensive resources for patients and providers in the United States, emphasizing programs like the Affordable Connectivity Program and Lifeline to facilitate access. The Health Resources and Services Administration enhances telehealth through support services, research, and technical assistance, reflecting a significant outreach impact [ 43 ]. The Office for the Advancement of Telehealth (OAT) under Health Resources and Services Administration (HRSA) works to improve access to quality health care through integrated telehealth services in the US. It supports direct services, research, and technical assistance, with over 6,000 telehealth technical assistance requests sent to Telehealth Resource Centers and approximately 22,000 patients served [ 44 ].
Internationally, In the UK, the National Health Service (NHS) spearheads digital health and care, providing significant innovation opportunities through vast data management. Support for digital health spans various stages, from discovery with organizations like Biotechnology and Biological Sciences Research Council (BBSRC) and Intelligent Data Analysis (IDA) research group, to development with networks such as Catapults and CPRD, and delivery with entities like the Academic Health Science Networks (AHSNs) and DigitalHealth.London. Regulatory bodies like the Medicines and Healthcare products Regulatory Agency (MHRA) and NICE ensure safety and efficacy. The collaborative ecosystem involves academic, healthcare, and industry stakeholders, aiming to enhance health and care services through technology and innovation [ 45 ].
In Australia, the government’s investment of over $4 billion into COVID-19 telehealth measures has facilitated universal access to quality healthcare. This initiative has provided over 85 million telehealth services to more than 16 million patients, with approximately 89,000 healthcare providers engaging in this service delivery. From 1 January 2022, telehealth services, initially introduced in response to COVID-19, will become an ongoing part of Medicare. This will allow eligible patients across Australia continued access to general practice (GP), nursing, midwifery, and allied health services via telehealth, deemed clinically appropriate by the health professional [ 46 ].
European nations such as the Netherlands, Austria, and Italy are at the forefront of implementing cross-organizational patient records, significantly enhancing telehealth communication and facilitating cross-border healthcare. The role of strong government support in advancing telehealth is pivotal. Ursula von der Leyen, the President of the European Commission, has been a prominent advocate for eHealth. She proposed the establishment of a European Health Data Space to streamline health data exchange across member states. France, a leader in telehealth legislation for nearly a decade, has pioneered a public funding scheme for tele-expertise at a national scale. Despite these advancements, challenges like legislative barriers and the lack of consistent political direction continue to impede progress in the telehealth domain [ 47 ].
The Asia-Pacific region anticipates a surge in telehealth adoption driven by digital demand and pandemic-induced behavioral changes, while South East Asia exhibits widespread telehealth growth across healthcare aspects [ 48 ]. The telehealth adoption across the Asia-Pacific region has shown remarkable growth between 2019 and 2021 and is projected to continue rising by 2024. China’s adoption nearly doubled to 47% and is expected to reach 76%. Indonesia’s usage more than doubled to 51%, with a forecast of 72%. Malaysia and the Philippines both anticipate reaching a 70% adoption rate, increasing from 30% to 29%, respectively. India’s adoption is projected to more than double to 68%, while Singapore, which had a significant increase from 5 to 45%, is expected to achieve a 60% adoption rate. This trend indicates a robust uptake of telehealth services in the region [ 48 ].
Global telemedicine and E-pharmacy policy dynamics
In the context of telemedicine and e-pharmacy regulations within South East Asia, a notable distinction emerges with Singapore, Malaysia, and Indonesia being the only countries to have formalized legal frameworks governing both telemedicine practices and the dissemination of electronic information. In these countries, tele-consultation is restricted to patients already under the care of healthcare practitioners or as part of ongoing treatment, specifically in Singapore and Malaysia. Additionally, for scenarios requiring more intensive medical intervention, such as new referrals, emergency cases, or invasive procedures, both Malaysia and Indonesia mandate physical presence and face-to-face consultations, emphasizing a cautious and regulated approach to remote healthcare. In Malaysia, the regulations further stipulate that online prescriptions, excluding narcotics and psychotropic substances, are permissible solely under the continuation of care model, reflecting a judicious use of digital prescription services [ 49 ].
In Central and Eastern Europe (CEE), telemedicine has experienced substantial growth, primarily catalyzed by the COVID-19 pandemic, which necessitated rapid advancements in technology and alterations in healthcare practices. The region’s robust digital infrastructure, coupled with the innovative drive of local companies and the challenges posed by an aging demographic, has significantly contributed to this expansion. According to the European Commission’s Market Study on Telemedicine, the global telemedicine market was projected to grow annually by 14% by 2021, a rate that was likely surpassed due to the pandemic’s impact. More specifically, the Europe Telehealth Market, valued at US $6,185.4 million in 2019, is anticipated to witness an annual growth rate of 18.9% from 2020 to 2030. This trend underscores the increasing reliance on and potential of telemedicine in addressing healthcare needs in the CEE region [ 50 ].
In the Middle East, telehealth and telepharmacy, have seen varied degrees of adoption and progress. Despite attempts to reform healthcare delivery in the region, the progress of telemedicine has been somewhat slow, with certain expectations yet to be fully realized. However, there has been notable development in the use and adoption of these technologies [ 51 ]. In a survey comparing the utilization of digital-health applications in Saudi Arabia and the United Arab Emirates (UAE), it was observed that a higher percentage of Saudi participants have utilized online pharmacy services (48%) compared to the UAE (36%). Conversely, awareness of teleconsultation services without prior use was higher in the UAE (43%) than in Saudi Arabia (35%). Retention data indicates that a significant proportion of users in both countries continue to engage with these services, with 80% of Saudi participants and 71% of UAE participants using teleconsultations at varying frequencies. Notably, a substantial majority of users in Saudi Arabia reported regular use of online pharmacies (90%), slightly higher than the UAE (78%), reflecting robust ongoing engagement with these digital health modalities. Notably, consumer adoption of telehealth products is primarily driven by time savings (48%) and convenience (47%), with 24-hour accessibility and efficacy both influencing 34% of users. Affordability and personal recommendations are also notable factors, while a wide range of options and quality are lesser but relevant considerations [ 52 ].
In response to the COVID-19 pandemic, a cross-sectional study was conducted among 391 licensed community pharmacists in the United Arab Emirates to assess the adoption and impact of telepharmacy services. The study revealed a predominant use of telepharmacy services, particularly via phone (95.6%) and messaging applications (80.0%). The findings highlighted that pharmacies with more pharmacists and those operating as part of a group or chain were more likely to implement a diverse range of telepharmacy services. The study identified significant barriers to telepharmacy adoption in individual pharmacies, including limited time, inadequate training, and financial constraints. There was a noticeable shift in service provision during the lockdown, with an increased reliance on telepharmacy, especially among pharmacies serving 50–100 patients per day. However, a reduction in services such as managing mild diseases and selling health products was observed during the lockdown period. The study concluded that telepharmacy played a pivotal role in supporting community pharmacies during the pandemic, with its expansion facilitated by the UAE’s advanced internet infrastructure, supportive health policies, and widespread digital connectivity [ 53 ]. Collectively, these insights reflect a global shift towards integrating and enhancing telehealth services as a response to emerging healthcare needs and technological advancements.
Unni et al. [ 54 ] provided an extensive review of telepharmacy initiatives adopted globally during the COVID-19 pandemic. Predominantly, virtual consultations were utilized to enable at-risk patients and others to remotely access pharmacists, thereby monitoring chronic illnesses, optimizing medication usage, and providing educational support [ 55 ]. Home delivery of medicines was widely implemented to decrease the necessity for in-person visits and mitigate exposure risks [ 56 ]. Additionally, patient education was prioritized to ensure effective management of health conditions from a distance [ 57 ]. Notably, a network of hospitals in China developed cloud-pharmacy care, allowing patients to consult pharmacists via text and the internet, while Spain utilized information and communication technologies for remote pharmaceutical care [ 58 ; 59 ]. Zero-contact pharmaceutical care, introduced in China, facilitated online medication consultations, eliminating direct contact [ 60 ]. The Kingdom of Saudi Arabia and other regions adapted new e-tools and teleprescriptions to enhance service accessibility [ 61 ]. The U.S. focused on credentialing pharmacists for telehealth to ensure competent service provision, and New Zealand implemented hotline numbers for phone consultations to further reduce physical visits [ 62 ; 63 ]. These initiatives reflect a significant shift towards innovative, technology-driven solutions in pharmaceutical care during a global health crisis. Refer to Fig. 3 for a graphical depiction of the worldwide distribution and applications of telepharmacy initiatives.
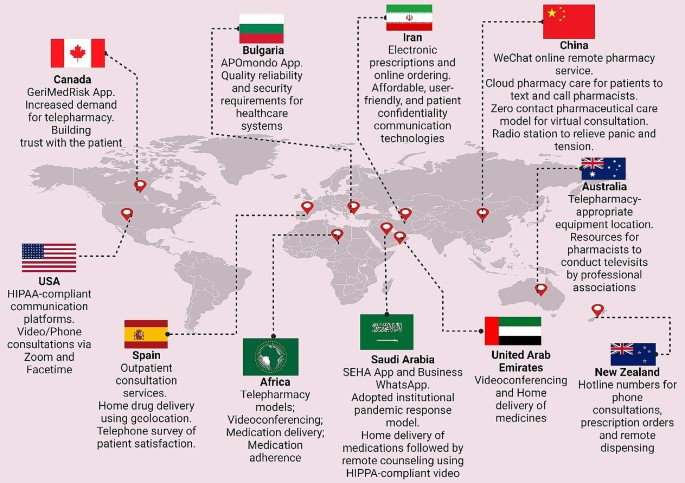
The global distribution of telepharmacy programs with an analysis of geographical distribution, technological applications, and associated benefits
Tracing the Private Sector’s Impact on Healthcare’s Technological Transformation
The role of the private sector in the fourth industrial revolution.
The World Economic Forum underscores the private sector’s leading role in digital inclusion and the acceleration of actions pertinent to the Fourth Industrial Revolution. This revolution affects economies, industries, and global issues profoundly, indicating the private sector’s critical role in driving technological advancements and digital platforms that deliver impactful healthcare solutions [ 64 ].
Mapping digital transformation in healthcare
A comprehensive analysis performed by Dal Mas et al. [ 65 ] meticulously maps the intricate terrain of digital transformation in healthcare, spotlighting the private sector’s instrumental role. Initially, the investigation encompassed an extensive array of diverse studies, leading to the identification of five main areas of digital technologies: smart health technologies, data-enabled and data collection technologies, Industry 4.0 tools and technologies, cognitive technologies, and drug & disease technologies. These domains frame the future research pathways, primarily steered by the private sector’s innovative drive. A significant proportion of the literature addresses healthcare broadly, suitable for both private and public sectors, yet a notable segment specifically focuses on the private sector’s endeavors, with a pronounced emphasis on the pharmaceutical domain [ 66 ; 67 ].

Public-private partnerships in healthcare delivery
The highlighted technologies, including digital platforms and telemedicine, exemplify the private sector’s trailblazing contributions to digital healthcare advancements. For instance, public-private partnerships (PPP) in India have emerged as a pivotal model for realizing universal healthcare (UHC), especially against the backdrop of acute healthcare shortages and urban-rural divides. Notably, mega PPP projects have successfully deployed technology-enabled remote healthcare (TeRHC), demonstrating its feasibility and impact in reaching isolated communities. These initiatives, overcoming various challenges, serve as a compelling example for global adoption, underscoring the transformative role of PPP in healthcare delivery [ 68 ].. Furthermore, a considerable majority of the literature in telemedicine underscores the necessity for profound research implications, yet a significant minority suggests policy implications [ 69 ; 70 ], reflecting a complex synergy between the private and public sectors in sculpting the digital healthcare framework [ 71 ]. This synthesis underscores the private sector’s critical influence in propelling the digital transformation in healthcare, charting a course that progressively fuses technological innovation with healthcare provision.
A study highlights Indonesia’s strategic initiatives to capitalize on telehealth business opportunities, driven by the Ministry of Research and Technology’s robust support for Technology-Based Start-up Company schemes [ 72 ]. With a demographic boon of 298 million from 2020 to 2024, escalating non-communicable diseases (71%), and a growing base of 222.4 million JKN participants, the stage is set for transformative growth. Despite a critical shortage of health workers (0.4 doctors per 1000 population), the enthusiasm for telemedicine is evident, with 71% satisfaction in hospital telemedicine and 32 million active telehealth users. The Ministry’s foresight in fostering technology start-ups, exemplified by the TEMENIN platform with its 11 health platforms, is steering Indonesia towards a future where high-quality healthcare is accessible and sustainable.
Lab@AOR: a model for PPPs in healthcare sector
The “Lab@AOR” initiative stands as a paradigmatic example of PPPs effectuating digital transformation within the healthcare sector. This strategic collaboration, between the University Hospital of Marche and Loccioni [ 73 ], a private entity, underscores the capacity of PPPs to navigate intricate challenges, stimulate international cooperation, and contribute to the development of sustainable, patient-centric healthcare solutions. Specifically, Lab@AOR was instituted to confront the nuanced challenges associated with the robotization of healthcare service delivery, highlighting the initiative’s role in fostering technological advancement through public and private sector synergy [ 74 ]. The project illustrates the evolution of Lab@AOR through three main phases: the pioneering stage, where groundwork for collaboration was laid; the nurturing stage, where collaborative exchanges were fostered; and the harvesting stage, wherein the potential of the PPP was fully unleashed. In the pioneering stage, Lab@AOR focused on a critical healthcare service component: the in-hospital preparation of medications for oncological patients. The University Hospital of Marche identified a need for innovation to improve service quality, efficiency, and safety, while Loccioni sought a real-life setting to test and refine its robotized system, APOTECAchemo [ 75 ]. This convergence of needs led to a symbiotic partnership aiming to enhance healthcare delivery through technological advancement.
During the nurturing stage, the partnership expanded the scope of APOTECAchemo to include non-oncological medications and developed additional tools like APOTECAps for manual preparation support. This phase was characterized by intensive collaboration, knowledge sharing, and continuous innovation, demonstrating the dynamic capability of the PPP to adapt and evolve in response to emerging healthcare challenges. The harvesting stage marked the international expansion of Lab@AOR, transforming it from a local initiative to an international community focused on leveraging digitalization and robotization to improve care quality and patient-centeredness. The PPP’s growth was catalyzed by its open perspective and inclusive approach, engaging entities from various cultural and institutional contexts, and fostering a network of 31 nodes across 19 countries and 3 continents.
Advancements in telehealth business models and frameworks
In their investigative study, Velayati et al. [ 76 ] delved into the articulation of emergent business models in telehealth and scrutinized the deployment of established frameworks across a variety of telehealth segments. The research spanned an extensive range of sectors, notably telemonitoring, telemedicine, mobile health, and telerehabilitation, alongside telehealth more broadly. The scope further extended to encompass niche areas such as assisted living technologies, sensor-based systems, and specific fields like mobile teledermoscopy, teleradiology, telecardiology, and teletreatment, presenting a thorough analysis of the telehealth landscape. Within the telemedicine and telehealth services sector, Barker et al. [ 77 ] introduced the Arizona Telemedicine Program (ATP) Model, a quintet-layer approach aimed at efficiently distributing telemedicine services throughout Arizona. Complementing this, Lee and Chang [ 78 ] proposed a four-component model specifically tailored for mobile health (mHealth) services pertaining to chronic kidney disease, focusing on offering a cost-effective platform for disease support and management. In the realm of telemonitoring, Dijkstra et al. [ 79 ] utilized the Freeband Business Blueprint Method (FBBM), which includes service, technological, organizational, and financial domains, to facilitate multiple telemonitoring services. Furthermore, the systemic and economic differences were explored in care coordination through Business to customer (B2C) and business (B2B) models for telemonitoring patients with chronic diseases, with the B2C model’s economic advantages were highlighted [ 80 ].
General telemedicine frameworks also received attention. Lin et al. [ 81 ] constructed a six-component framework analyzing major telemedicine projects in Taiwan, while Peters et al. [ 82 ] developed the CompBizMod Framework in Germany, encompassing value proposition, co-creation, communication and transfer, and value capture, designed to evaluate and enhance competitive advantages in telemedicine. In the specialized field of telecardiology, a comprehensive nine-component sustainable business model was crafted to facilitate mutual benefits for service providers and patients. This model emphasizes the importance of a holistic approach in ensuring the longevity and effectiveness of healthcare delivery within this domain [ 83 ]. Meanwhile, Mun et al. [ 84 ] presented a suite of five teleradiology business models aimed at providing effective, high-quality, and cost-efficient diagnoses.
The teletreatment sector saw innovative models from Kijl et al. [ 85 ], who designed a model for treating patients with chronic pain, focusing on the interrelation of components in the value network and the role of information technology. Complementarily, Fusco and Turchetti [ 86 ] introduced four models for telerehabilitation post-total knee replacement, emphasizing partnerships between care units and equipment suppliers to reduce costs and waiting lists. The mHealth and assisted living technology sector witnessed the introduction of a wearable biofeedback system model by Hidefjäll and Titkova [ 87 ], which employed Alexander Osterwalder’s Business Model Canvas and focused on a comprehensive commercialization process. Additionally, Oderanti and Li [ 88 ] presented a seven-component sustainable business model for assisted living technologies, aimed at encouraging older individuals to invest in eHealth services while reducing the pressure on health systems. These diverse clusters and models reflect the multifaceted nature of telehealth, each tailoring its approach to meet the unique demands of its domain. They collectively aim to optimize service delivery, stakeholder involvement, cost efficiency, and patient care quality, marking significant strides in the ongoing evolution of digital healthcare.
Challenges and biases in healthcare technology
One key aspect is the emergence of novel medical technologies and their potential biases. These biases are often a result of insufficient consideration of patient diversity in the development and testing phases. For example, disparities in the performance of medical devices like pulse oximeters among different racial groups have been observed, potentially due to a lack of diverse representation in clinical trials. This indicates a tendency for the development of healthcare technologies that may not adequately serve all patient populations [ 89 ]. A study on the profitability and risk-return comparison across health care industries highlights the use of return on equity (ROE) as a measure of profitability from a shareholder’s perspective. This measure combines profit margin, asset utilization, and financial leverage. The study analyzed financial data of publicly traded healthcare companies, providing insights into the financial dynamics of the healthcare sector. It revealed that while companies like Pfizer Inc. and UnitedHealth Group reported similar profitability, they had substantial differences in profit margin and asset utilization, indicating diverse financial strategies within the healthcare sector. This study underscores the complexity of financial performance in healthcare, where profitability measures need to be balanced with risk assessment and the broader impact on healthcare provision [ 90 ].
Additionally, an article discusses the benefits, pitfalls, and potential biases in healthcare AI. It emphasizes that as the healthcare industry adopts AI, machine learning, and other modeling techniques, it is seeing benefits for both patient outcomes and cost reduction. However, the industry must be mindful of managing the risks, including biases that may arise during the implementation of AI. Lessons from other industries can provide a framework for acknowledging and managing data, machine, and human biases in AI. This perspective is crucial in understanding how the integration of advanced technologies in healthcare can be influenced by the drive for profitability and efficiency, possibly at the expense of equitable and patient-centered care [ 91 ; 92 ].
Cosmeceuticals in the online pharmacy market
Cosmeceuticals, a term derived from the combination of cosmetics and pharmaceuticals, refer to a category of products that are formulated to provide both aesthetic improvements and therapeutic benefits. These products, typically applied topically, are designed to enhance the health and beauty of the skin, going beyond the mere cosmetic appearance. The exploration of cosmeceuticals in the online pharmacy market reveals a multifaceted and rapidly expanding industry. Bridging the gap between cosmetics and pharmaceuticals, they form a significant portion of the skincare industry. Cosmeceuticals are formulated from various ingredients, with their main categories being constantly discussed and analyzed in the scientific community [ 93 ]. They have taken a considerable share of the personal care industry globally, constituting a significant part of dermatologists’ prescriptions worldwide [ 94 ]. This surge is further fueled by increasing consumer demand for effective and safe products, including anti-aging skincare cosmeceuticals, a need which has been intensified by concerns over pollution, climate change, and the COVID-19 pandemic [ 95 ].
The global cosmeceuticals market is experiencing robust growth. Valued at USD 56.78 billion in 2022, it’s projected to expand to USD 95.75 billion by 2030, with a compound annual growth rate (CAGR) of 7.45%. This growth trajectory is propelled by the innovative integration of bioactive ingredients known for their medical benefits [ 96 ]. Another report confirms this upward trend, indicating the market was worth $45.56 billion in 2021 and is on a path of significant growth to USD 114 billion by 2030. The global disease burden is significantly impacted by various skin diseases, with dermatitis, psoriasis, and acne vulgaris among the most prevalent, contributing 0.38%, 0.19%, and 0.29% respectively. The pervasive nature of these conditions drives a substantial demand for effective treatments, propelling the integration of cosmeceuticals into the online pharmacy market. This integration not only offers convenient access to a range of therapeutic skincare products but also caters to the rising consumer inclination towards self-care and preventive healthcare. As a result, the online availability of cosmeceuticals is not just addressing the immediate needs of individuals suffering from skin conditions but is also reshaping the landscape of personal healthcare by making specialized treatments more accessible and customizable [ 97 ]. See Fig. 4 .
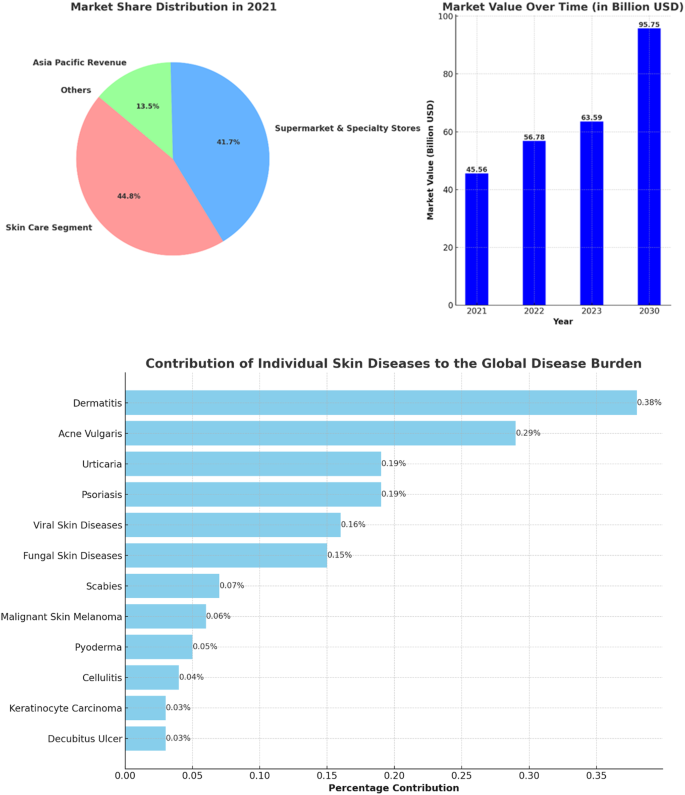
The left panel presents the market share distribution for key segments in the cosmeceuticals industry in 2021, including Skin Care Segment, and Supermarket & Specialty Stores, for Asia Pacific Revenue, with percentages for each category. The right panel displays the market value progression over time from 2021 to the projected value in 2030, with bold numbers indicating the value in billion USD for each year. The lower horizontal bar chart depicts the percentage contribution of various skin diseases to the global disease burden
Several factors are contributing to this expansion of the cosmeceuticals market. The market is driven by innovation in natural ingredients and a significant penetration of internet, smartphone, and social media applications, which attract potential consumer populations and reflect constantly changing consumer behavior [ 98 ]. The cosmeceuticals market’s robust CAGR and revenue share, especially in regions like Asia Pacific, further signify its burgeoning presence and potential within the global market [ 99 ]. Integration into online pharmacies is a key aspect of this market’s evolution, offering easier access to these products for a wider customer base. As the market continues to grow, it’s anticipated that the blend of cosmeceuticals with online pharmaceutical platforms will become increasingly seamless, offering consumers a diverse range of accessible, effective, and beneficial skincare and health products. This integration is likely to be driven by the growing trend of e-commerce and digitalization in healthcare and personal care sectors.
The landscape of online pharmacies, particularly concerning cosmeceuticals, is evolving. While the overall penetration for non-specialty drugs in mail-order and online pharmacies is low, they represent a significant portion of specialty prescription revenues at 37%. Despite this, only 13% of consumers consider these as their primary pharmacy choice, indicating a growing but still emerging market. Strategies are in place to enhance the market appeal of these pharmacies, focusing on speed, convenience, and personalized experiences, such as video telehealth visits, to attract a broader consumer base [ 100 ].
The dissertation “L’Oréal Portugal: A Digital Challenge for the Active Cosmetics Division” authored by Ascenso [ 101 ] provides an in-depth examination of the impact of digital evolution on the Portuguese cosmeceutical sector and its implications for L’Oréal, a significant cosmetics company. It posits that while L’Oréal has foundational digital competencies, the rapidly evolving digital landscape presents a broad spectrum of potential risks and opportunities. The study details the operations of L’Oréal’s Active Cosmetics Division, which manages brands predominantly sold in pharmacies and parapharmacies, and explores the potential repercussions of digitalization on L’Oréal Portugal’s strategic and operational frameworks. Furthermore, the thesis highlights the expanding role of e-pharmacies and the need for legal reforms to facilitate their operation. It discusses the prevalent trends in the cosmetic industry, such as the increasing demand for natural, male-focused, and environmentally friendly products. The dissertation scrutinizes L’Oréal’s strategic pillars, including innovation, acquisition, and regional growth, emphasizing the need for the company to integrate advanced technologies and recalibrate its business methodologies in light of digital progression [ 101 ]. Although L’Oréal has initiated some digital strategies targeting consumers and pharmacies, there’s a recognized need for an intensified focus on digital marketing aimed at clients. An exploratory attempt by L’Oréal to implement an online ordering platform for pharmacies did not meet success, indicating possible industry unreadiness for such advancements. This case study serves as a critical examination of how traditional companies in the pharmaceutical and cosmetics sectors must adapt to the digital age’s challenges and opportunities [ 101 ].
In a collaborative endeavor with L’Oréal, an associated digital agency provided a comprehensive suite of services that encompasses the full management of social media pages, the development of e-commerce websites, the establishment of Customer Relationship Management (CRM) platforms tailored for pharmacies, and the execution of digital campaigns leveraging QR codes, SMS marketing, and newsletters. These digital tools confer a competitive edge, facilitating a deeper comprehension of consumer behavior and the potential to augment value extraction from customer interactions. For the laboratories, particularly those associated with cosmetics, the advantages are twofold: an increase in sell-out figures, thereby enhancing direct sales to end consumers, and a boost in sell-in metrics, reflecting a rise in transactions to pharmacies or wholesalers. The online ordering feature, as noted by João Roma, a manager at La Roche-Posay, could result in a cacophony of processes if laboratories were to individually develop distinct methods. He advocates for the utilization of pre-existing platforms, such as the established e-learning infrastructure, to spearhead ventures into the online marketplace [ 101 ].
A survey conducted specifically for L’Oréal’s e-learning platform, cosmeticaactiva.pt [ 102 ], across the Portuguese landscape garnered responses from 324 participants, comprising 71% general pharmacists, 13% technical assistants, 8% directors, 7% individuals responsible for procurement from laboratories, and 2% beauty/cosmetic advisors. The findings from this survey underscore the pervasive adoption of digital tools within the pharmacy sector: 82% of respondents affirmed the presence of their pharmacies on social media platforms, 80% reported the use of basic management software, 64% indicated the deployment of advanced management systems, 61% were conversant with online ordering systems directed at laboratories, 38% utilized a store locator, 28% had an established website presence, and a smaller segment of 12% offered online shopping facilities.
Another survey conducted within this study to evaluate the significance of dermocosmetic products in pharmacies yielded a mean importance rating of 4.38 out of 5, indicating that a majority of pharmacists consider these products to be highly important to their business operations. Factors critical to the differentiation of a proficient laboratory/supplier were innovation and cost-effectiveness, with mean scores of 1.9 and 2.7 respectively, on a scale from 1 (most important) to 5 (least important). A substantial majority of pharmacists, amounting to 81.8%, perceive their pharmacies as beacons of innovation and modernity. Detailed interviews elucidated that digital tools are indispensable in augmenting sales for cosmeceutical products by catalyzing demand—a dynamic not feasible with medicinal products. These tools are paramount in managing customer loyalty, facilitating enhanced communication with existing clients via online and mobile channels. Despite the challenges posed by digitalization, particularly in the realms of logistics and human resources, the management at L’Oréal is well-equipped to swiftly adapt to the evolving business landscape, as evidenced by the proactive adoption and integration of these digital strategies [ 101 ] as illustrated in Fig. 5 .
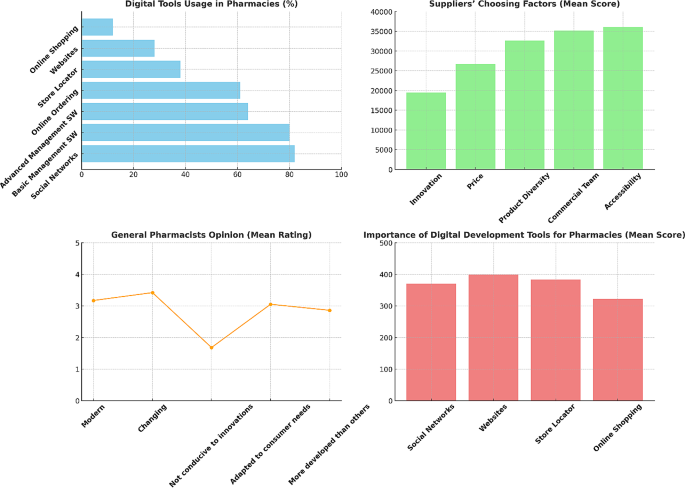
Results from Ascenso [ 101 ] survey assessing digital challenges for L’Oréal in the Portuguese cosmeceutical sector. Digital Tools Usage in Pharmacies (upper left) : the bar chart showing the percentage of respondents using various digital tools in pharmacies. Suppliers’ Choosing Factors (upper right) : the bar chart displaying the mean scores of factors that distinguish a good laboratory/supplier. General Pharmacists Opinion (lower left) : A line chart illustrating the mean ratings of pharmacists’ opinions on whether the pharmaceutical sector is modern, changing, conducive to innovations, adapted to consumer needs, and more developed than other sectors. Importance of Digital Development Tools for Pharmacies (lower right) : A vertical bar chart demonstrating the mean scores for the importance of different digital development tools for pharmacies
The digital transformation strategies, exemplified by companies like L’Oréal, extend beyond the mere targeting of end consumers, encompassing the perspectives of various stakeholders, including retailers. This broadened focus reflects a holistic and integrated approach to digital marketing and customer engagement, indicative of a larger trend within the market. The significance of digital channels in facilitating comprehensive customer interaction and brand development is increasingly recognized. The distinction of organizations such as L’Oréal in their digital initiatives highlights the competitive advantage that can be garnered through innovative digital strategies.
The receptiveness of industry professionals, such as pharmacists, to emerging digital trends, along with the readiness of companies to engage in non-face-to-face sales models, marks a paradigm shift in traditional sales and distribution methods. This shift is reflective of a broader market trend where digital platforms are becoming integral to the customer journey. Furthermore, the potential for online sales in specialized sectors, such as dermocosmetics, and the benefits that organizations derive from the technological advancement of their client base, underscore an escalating acknowledgment of e-commerce and digital tools as crucial elements of a business strategy. This trend, with L’Oréal as a prime example, emphasizes the broader market movement towards digital transformation, not merely as an option but as a necessity for maintaining relevance and competitiveness in an ever-evolving market landscape.
The global regulatory landscape for cosmeceuticals
Sophisticated regulatory legislation and enforcement mechanisms characterize many developed countries such as the USA, EU Member States, Canada, and Japan. These nations, along with influential organizations like the World Health Organization (WHO), significantly shape international market rules and regulations due to their market size and regulatory capacity [ 103 ]. The WHO is particularly noted for its crucial role in setting global standards, with a focus on developing and promoting international standards related to food, biological, pharmaceutical, and similar products [ 104 ]. In contrast to pharmaceuticals, the cosmetic industry necessitates a more advanced international regulatory framework due to consumers’ extensive exposure to these products. The distinction between cosmetics and pharmaceuticals varies significantly across different countries, with the USA employing a voluntary registration system for cosmetics and the EU and Japan requiring mandatory product filings prior to marketing [ 105 ]. Concerns over the safety of pharmaceutical and cosmetic products are highlighted, with an increasing consumer focus on “natural, ecological, and clean” products [ 106 ]. However, the lack of a regulatory framework for these categories underscores the need for more advanced regulations to mitigate health risks.
Intergovernmental cooperation is emphasized, with the US and EU portrayed as dominant players in the pharmaceutical and cosmetic industries, respectively. Regulatory capacity, which is essential for defining, implementing, and monitoring market rules, varies among countries and markets. This capacity depends on several factors, including staff expertise, statutory sanctioning authority, and the degree of centralization of regulatory authority [ 103 ]. The regulatory systems of the EU and US are explored, focusing on their unique approaches to medicine authorization and regulation. The European Medicines Agency (EMA) in the EU and the Food and Drug Administration (FDA) in the US serve as pivotal regulatory bodies [ 107 ; 108 ]. The EMA’s centralized procedure and the FDA’s premarket approval process are detailed, along with subsequent postmarket regulatory procedures. For instance, EU and US cosmetic regulations are compared, revealing differences in their approaches and the evolution of the EU’s regulatory landscape through various amendments and directives. In particular, directive 76/768/EC has been superseded by Regulation (EC) N° 1223/2009, serving as the principal regulatory framework for finished cosmetic products in the EU market. This regulation enhances product safety, optimizes the sector’s framework, and eases procedures to promote the internal cosmetic market. Incorporating recent technological advancements, including nanomaterials, it maintains an internationally acknowledged regime focused on product safety without altering existing animal testing prohibitions [ 109 ].
The Eurasian Economic Union’s (EAEU) regulatory framework for medicines and medical devices is detailed, including the legal framework established for regulating the circulation of these products. The conformity assessment methods, such as the EAC Declaration and the State Registration process, are required for manufacturers to demonstrate their products’ compliance with the standards [ 110 ]. Armenia is also part of the EAEU’s legal framework, which aims to unify regulations for the production and registration of pharmaceuticals and medical products by 2025. This unification is expected to reduce administrative costs for manufacturers and improve medicinal products for patients. Despite significant developments in the cosmetics industry, Armenia does not have an extensive regulatory framework for it. Prior to joining the EAEU, the only regulation concerning cosmetic products was the Order of the Minister of Health of the Republic of Armenia on “Hygiene Requirements of the Production and Safety of Perfume-Cosmetic Products.” Since joining the EAEU, Armenia has unified its national legislation with EAEU regulations, but there are challenges and gaps in the direct applicability of the EAEU’s technical regulations in the country [ 111 ].
In the context of the necessity for clear regulatory framework stems from two reasons. Firstly, cosmeceuticals - products straddling cosmetics and drugs - demand intensified regulatory attention. Examples include the 2007 FDA seizure of Jan Marini’s Age Intervention Eyelash, which contained the drug ingredient bimatoprost, and products boasting human stem cell cultured media, which claim rejuvenating effects but may pose safety risks due to minimal oversight [ 112 ]. A noted 1450% increase in FDA warnings (from 4 to 62 letters) between 2007 and 2011 and 2012–2017, with 8 targeting stem cell ingredient promotions, underscores the growing concern [ 113 ]. The FDA’s limited capacity to identify and assess potential drug-adulterated cosmetics raises concerns.
The second aspect focuses on the necessity for a more comprehensive and unbiased scientific and medical perspective in the FDA’s ingredient review process. The Personal Care Products Safety Act proposes a balanced committee formation including industry, consumer, and medical representatives, yet advocates for the inclusion of specialized professionals like chemists, dermatologists, toxicologists, and endocrinologists. Specific ingredients like diazolidinyl urea and quarternium-15, although effective antimicrobials, are flagged for potential skin allergy risks and formaldehyde release. The preservative 4-methylisothiazolinone, banned in Europe for rinse-off products, is noted for increasing allergic contact dermatitis cases in the US [ 114 ]. The lag in US cosmetic regulation compared to the EU is acknowledged, with the Personal Care Products Safety Act considered a significant advancement, albeit in need of further refinement [ 115 ].
The importance of consumer safety in the global regulatory landscape for cosmeceuticals, particularly for products that blur the line between cosmetics and pharmaceuticals, is a critical issue due to several key factors. Firstly, the cosmeceutical market is expanding rapidly, driven by new ingredients promising various skincare benefits like anti-aging and photoprotection. This growth necessitates clear regulatory guidelines to ensure that these products are safe and their claims are clinically proven. The FDA, for instance, differentiates between cosmetics and cosmeceuticals based on their intended use, particularly if a product is marketed as a cosmetic but functions in a way that affects the structure of the human body, classifying it as a cosmeceutical [ 116 ].
Secondly, the legal and regulatory distinctions between drugs and cosmetics are significant. Drugs are subject to FDA approval based on their intended use in treating diseases or affecting the body’s structure or function, whereas cosmetics are not. This difference becomes crucial when products are marketed with drug-like claims but are not regulated as drugs, potentially leading to consumer safety issues. For example, botanical cosmeceuticals, which contain natural ingredients like herbal extracts, need thorough evaluation to ensure consistency in therapeutic effects [ 117 ]. Additionally, cosmeceutical manufacturers must be careful with marketing and advertising claims to avoid legal implications. Misleading claims can lead to lawsuits and regulatory actions, as seen in past cases where companies faced consequences for unfounded product claims. Moreover, the FDA advises cosmeceutical manufacturers to follow Good Manufacturing Practices (GMP) to reduce the risk of misbranding or mislabeling. These guidelines include production practices and specific warning statement guidelines, emphasizing the importance of substantiating the safety of these products [ 118 ].
The global regulatory landscape for online pharmacy
Online pharmacies pose various risks to consumers, including the potential health hazards from counterfeit or substandard medications and the inappropriate use of prescription drugs. The regulatory landscape for these pharmacies varies significantly across nations, with some countries like the United States implementing specific laws, while others, such as France, have instituted outright bans [ 119 ]. The European Union, for instance, has implemented a mandate effective from 1 July 2015, which requires member states to adhere to legal provisions for a common logo specific to online pharmacies. This is coupled with an obligation for national regulatory authorities to maintain a registry of all registered online medicine retailers, as detailed by the European Medicines Agency [ 120 ]. Furthermore, the sale of certain medications online within the EU is permissible, contingent upon the registration of the pharmacy or retailer with respective national authorities [ 121 ]. Additionally, the Council of Europe’s MEDICRIME Convention introduces an international treaty that criminalizes the online sale of counterfeit medicinal products, enforcing prosecution irrespective of the country in which the crime is perpetrated [ 122 ].
Switzerland presents a unique stance, where Swissmedic strongly advises against the online purchase of medicines due to the high risk of illegal sourcing and poor quality. However, Swiss mail-order pharmacies with a valid cantonal license to operate a mail-order business are exempted from this advisory [ 123 ]. The Swiss Mail-Order Pharmacists Association and its affiliates, such as Zur Rose AG and MediService AG, actively advocate for a modern and equitable regulation of mail-order medicine sales [ 124 ]. The legislative framework is further bolstered by the Federal Act on Medicinal Products and Medical Devices, which regulates therapeutic products to guarantee their quality, safety, and efficacy [ 125 ]. In the Middle East, community pharmacy practice is predominantly governed by national Ministries of Public Health or equivalent governmental entities, with most community pharmacies being privately owned [ 126 ]. The region’s involvement in the Global Cooperation Group, which encompasses various international regulatory bodies like the EMA and USFDA, signifies a collaborative approach towards drug regulatory affairs in the MENA region [ 127 ]. Despite these advances in regulatory collaboration, it is notable that currently no specific regulations have been detected for online purchases from online pharmacies in the Middle East, highlighting a significant area for potential regulatory development. Furthermore, a notable transition is observed in pharmacy education across several Middle Eastern nations, with an inclination towards introducing Pharm.D degrees to replace traditional pharmacy degrees, reflective of evolving educational standards in the pharmaceutical field [ 128 ]. This shift in education parallels the need for updated regulatory frameworks, especially in the context of the burgeoning online pharmacy sector.
Furthermore, Australia permits the sale of both Prescription-Only Medicines (POMs) and Over-the-Counter (OTC) medications online, provided that brick-and-mortar pharmacies comply with all relevant laws and practice standards [ 129 ]. In contrast, South Korea maintains a stringent stance, prohibiting the online sale of both POMs and OTC medicines, with sales confined exclusively to physical stores registered with the Regulatory Authority (RA) [ 130 ]. China, Japan, Russia, Singapore, and Malaysia exhibit a more selective regulatory framework. China and Russia allow the online sale of OTC medicines only, with China imposing additional restrictions on third-party e-commerce platforms and Russia having introduced a draft law in December 2017 to formalize this practice [ 131 ; 132 ]. Japan permits the online sale of certain OTC medicines, explicitly excluding specific substances such as fexofenadine and loratadine [ 133 ]. Similarly, Singapore and Malaysia endorse the online sale of specific OTC medicines only, adopting a “buyers beware” approach to caution consumers about the associated risks [ 134 ; 135 ]. Lastly, the legal landscapes in India and Indonesia remain ambiguous. India’s RA has effectively banned the online sale of medicinal products, yet this prohibition lacks legislative backing. Indonesia, too, grapples with unclear regulations, leaving the legal status of online pharmacies indeterminate [ 136 ].
In response to these risks, several initiatives have been developed to guide and certify online pharmacies. In the United States, LegitScript offers certification to online pharmacies that comply with criteria such as appropriate licensing and registration [ 137 ]. Similarly, the Verified Internet Pharmacy Practice Sites (VIPPS) program, accredited by the National Association of Boards of Pharmacy, ensures pharmacies adhere to licensing requirements in the states where they dispense medications [ 138 ]. Internationally, the Health On the Net Foundation has introduced the HONcode, an ethical standard for health websites globally. This code certifies sites that provide transparent and qualified information. However, due to the absence of international harmonization, the HONcode’s certification is limited to US and Canadian pharmacies verified by VIPPS [ 139 ]. The lack of a harmonized international approach presents significant challenges. Consumers do not have access to a comprehensive, global repository of all certified pharmacies. The diverse certification schemes are not well articulated or interconnected, leading to consumer unawareness about their significance or existence. Moreover, enforcing standards across different legal jurisdictions is complex without a unified agreement. To enhance consumer protection, it is imperative to develop and promote a standardized, minimal international code of conduct for online pharmacies. Such a code would unify requirements and allow all initiatives to clarify their roles under a common framework. Adequate oversight in the borderless online pharmacy market can only be achieved through collaborative efforts. To visualize the infographic of the global regularity landscape for the online pharmacy see Fig. 6 .
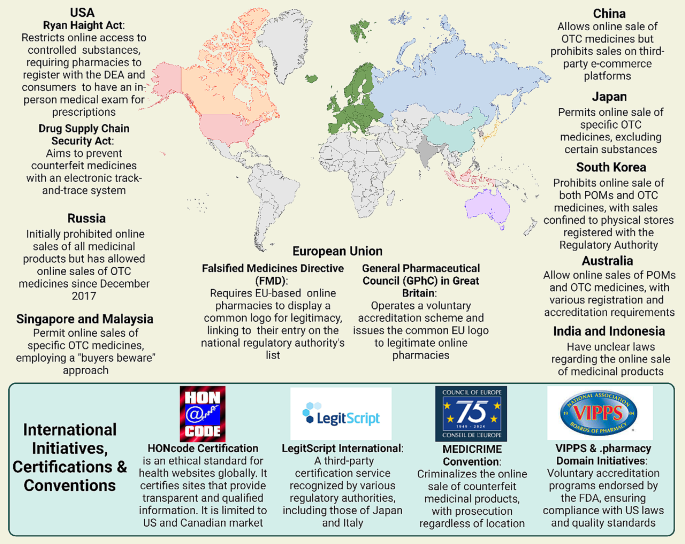
Comprehensive representation of the regulatory landscape for global online pharmacies, detailing international and national initiatives, certification programs, and conventions aimed at minimizing risks associated with the purchase of medications via online platforms
Technological innovations and Future trends in global pharmacy
The global pharmacy sector is undergoing a transformative shift, driven by the rapid advancement of technological innovations. As the world becomes increasingly digital, the integration of cutting-edge technologies like Artificial Intelligence (AI) and blockchain is setting the stage for a new era in pharmaceutical care and management. These advancements promise to revolutionize the industry by enhancing efficiency, accuracy, and security, ultimately leading to improved patient outcomes and a more streamlined healthcare experience [ 140 ].
Walgreens, in partnership with Medline, a telehealth firm, has developed a platform for patient interaction with healthcare professionals via video chat. AI’s role extends to inventory management in retail pharmacies, allowing pharmacists to predict patient needs, stock appropriately, and use personalized software for patient reminders. Although not all inventory management software in retail pharmacies utilizes AI, some, like Blue Yonder’s software developed for Otto group, demonstrate the potential of AI in predicting product sales with high accuracy, thus enhancing supply chain efficiency [ 141 ; 142 ]. At the University of California San Francisco (UCSF) Medical Center, robotic technology is employed to improve patient safety in medication preparation and tracking. This technology has prepared medication doses with a notable error-free record and surpasses human capabilities in accuracy and efficiency. It prepares both oral and injectable medicines, including chemotherapy drugs, freeing pharmacists and nurses to focus on direct patient care. The automated system at UCSF receives electronic medication orders, with robotics handling the picking, packaging, and dispensing of individual doses. This system also assembles medications on bar-coded rings for 12-hour patient intervals and prepares sterile preparations for chemotherapy and intravascular syringes [ 143 ].
In the realm of global pharmacy, blockchain technology emerges as a pivotal force, driving advancements across various facets of healthcare and pharmaceuticals. At the forefront of its application is the enhancement of supply chain transparency [ 144 ]. Blockchain’s immutable ledger ensures the provenance and legitimacy of medical commodities, offering an unprecedented level of visibility from manufacturing to distribution. This is particularly vital in areas plagued by counterfeit drugs, where systems like MediLedger are instrumental in verifying the legality and essential details of medicines [ 145 ].
The utility of blockchain extends to the implementation of smart contracts — scripts processed on the blockchain that bolster transparency in medical studies and secure patient data management [ 146 ]. These contracts find extensive use in advanced medical settings, as evidenced by a blockchain-based telemonitoring system for remote patients and Dermonet, an online platform for dermatological consultation [ 147 ].
Furthermore, blockchain is revolutionizing patient care through patient-centric Electronic Health Records (EHRs). By decentralizing EHR maintenance, blockchain empowers patients with secure access to their historical and current health records [ 148 ]. Prototypes like MedRec and systems such as MeD Share exemplify how blockchain can provide complete, permanent access to clinical documents and facilitate the sharing of medical data between untrusted parties, respectively, ensuring high information authenticity and minimal privacy risks [ 149 ; 150 ]. In verifying medical staff credentials, blockchain again proves invaluable. Systems like ProCredEx, based on the R3 Corda blockchain protocol, streamline the credentialing process, offering rapid verification while allowing healthcare entities to leverage their existing data for enhanced transparency and assurance about medical staff experience [ 151 ].
The integration of blockchain with Internet of Things devices for remote monitoring marks another leap forward, significantly bolstering data security. By safeguarding the integrity and privacy of patient data collected by these devices, blockchain mitigates the risk of tampering and ensures that only authorized parties can access sensitive information [ 152 ]. Besides, a blockchain-based drug supply chain initiative, PharmaChain, utilizes AI for approaches against drug counterfeit and ensures the drug supply chain is more traceable, visible, and secure. For online pharmacies, this means a more reliable supply chain and assurance of drug authenticity, crucial for maintaining trust and safety [ 153 ].
In response to the COVID-19 pandemic, the PharmaGo platform has emerged as an innovative solution in Sri Lanka, revolutionizing the delivery of pharmacy services. As traditional pharmacies grapple with the challenges of meeting all customer needs in one location, PharmaGo addresses this by providing a comprehensive online pharmaceutical service. It allows customers to access a wide range of medications through a single platform, reducing the need to visit multiple pharmacies. Utilizing image processing technology, pharmacy owners can accurately identify prescribed medicines, while the system’s predictive analytics forecasts future drug demands, enhancing stock management. Additionally, PharmaGo’s AI-powered medical chatbot offers real-time guidance, ensuring a seamless and efficient customer experience. This platform represents a significant advancement in healthcare accessibility and pharmacy service delivery in the pandemic era [ 154 ]. In the same context, ontology-based medicine information system, enhancing search relevance through a chatbot interface was presented by Amalia et al. [ 155 ]. Addressing conventional search engines’ limitations in interpreting data relationships, it employs semantic technology to represent metadata informatively. The ontology as a knowledge base effectively delineates disease-medicine relationships, with evaluations indicating a 90% response validity from the chatbot, offering a robust reference for medical information retrieval and its semantic associations.
Future trends for the digital transformation of in the pharmaceutical sector
Future trends for the digital transformation of pharmacies globally are heavily influenced by the transformative impact of digital technologies on healthcare delivery. The integration of telemedicine, electronic health records, and mobile health applications is pivotal in enhancing patient care. These technologies are instrumental in improving data sharing and collaboration among healthcare professionals, increasing the efficiency of healthcare services. Additionally, they offer significant potential for personalized medicine through data analytics and play a crucial role in patient engagement and self-management of health. The importance of these technologies in creating a more connected and efficient healthcare system is underscored, marking a significant shift in the global healthcare landscape [ 156 ].
In the pharmaceutical sector, the COVID-19 pandemic has catalyzed a significant shift towards Pharmaceutical Digital Marketing (PDM), particularly for over-the-counter drugs. This shift focuses on utilizing online pharmacies and digital platforms for targeted advertising, directly reaching consumers. The trend towards purchasing OTC drugs online has grown, driven by the convenience and efficiency of digital channels. While PDM faces challenges like regulatory constraints and the need for digital proficiency, it offers substantial opportunities in enhancing customer engagement and precise marketing. The future of PDM is poised to be more consumer-centric, integrating advanced technologies like AI, and emphasizing personalized marketing strategies to strengthen brand engagement and customer interaction [ 157 ].
Artificial intelligence holds immense potential to revolutionize the field of pharmacy, offering numerous benefits that can significantly enhance efficiency and patient care. One of the primary applications of AI in this sector is the automation of routine tasks. By utilizing AI, pharmacies can automate critical processes such as prescription processing, checking for drug interactions, and managing inventory. This automation not only streamlines operations but also minimizes the likelihood of human error, thereby increasing the overall efficiency of pharmacies [ 158 ].
Furthermore, AI can play a pivotal role in personalized medication management. This is particularly beneficial for patients with chronic conditions such as diabetes who require careful management of their insulin dosages, as fluctuations in blood sugar levels can lead to serious complications. AI systems can monitor patients continuously, provide timely reminders for medication intake, and dynamically adjust treatment plans based on individual health data. Such personalized management ensures that patients receive optimal care tailored to their specific needs, potentially improving treatment outcomes. Incorporation of AI into electronic health records presents another significant advancement. By integrating AI with EHRs, healthcare providers can access real-time patient data. This integration empowers healthcare professionals to make more informed care decisions, enhancing the quality of patient care. Moreover, it significantly reduces the likelihood of medication errors, a critical concern in healthcare.
Likewise, AI’s capability to analyze extensive patient data is invaluable. It can identify patterns and trends in medication adherence, detect potential drug interactions, and pinpoint adverse drug reactions. These insights are crucial for healthcare professionals and researchers. By understanding these patterns, they can develop more effective medication adherence strategies and support systems, contributing to better patient outcomes and advancing the overall field of pharmaceutical care.
In the expansive realm of chemical space, the pharmaceutical industry faces the continual challenge of identifying new active pharmaceutical ingredients (APIs) for diverse diseases [ 159 ]. High throughput screening (HTS), despite its advancements in recent decades, remains resource-intensive and often yields unsuitable hits for drug development. The failure rate of investigational compounds remains high, with a study citing only a 6.2% success rate for orphan drugs progressing from phase I to market approval [ 160 , 161 ].
Machine learning presents a transformative approach to this challenge. It offers an alternative to manual HTS through in silico methodologies. ML-driven drug discovery boasts several advantages: it operates continuously, surpasses the capacity of manual methods, reduces costs by decreasing the number of physical compounds tested, and early identifies negative characteristics of compounds, such as off-target effects and sex-dependent variability [ 162 ].
A substantial advancement in the realm of machine learning has emerged from major pharmaceutical entities, notably AstraZeneca, in conjunction with research institutions. This progress is evidenced by the development of an innovative algorithm that demonstrates both time efficiency and effectiveness in the sphere of drug discovery. The recent introduction of this algorithm significantly enhances the process of determining binding affinities between investigational compounds and therapeutic targets. It surpasses traditional in silico methods in terms of performance. The application of this algorithm underscores the remarkable potential of machine learning in accelerating the identification and development of novel therapeutic agents [ 163 ].
Moreover, the proficiency of machine learning in managing vast and intricate datasets has rendered it indispensable in research focused on cancer targets, utilizing diverse and extensive datasets. This approach is fundamental in numerous drug discovery initiatives, especially those targeting various forms of cancer. A wide array of ML techniques, ranging from supervised to unsupervised learning, are employed to discern chemical attributes that are indicative of potential therapeutic efficacy against a spectrum of cancer targets. This methodology is crucial in identifying novel compounds that could be effective in cancer treatment, leveraging the rich and complex data available in oncological research [ 164 ].
The digital transformation in the pharmacy sector is significantly reshaping healthcare delivery, driven by the integration of cutting-edge technologies like Artificial Intelligence and blockchain. This transformation is marked by a substantial growth in the digital pharmacy market, with a projected annual growth rate of 14.42%, leading to a market volume of approximately $35.33 billion by 2026.
One major aspect of this transformation is the growing reliance on online pharmacy platforms, largely influenced by the COVID-19 pandemic. Consumer trust in online medication purchases has significantly increased, indicating a shift towards digital healthcare solutions. The adoption of telehealth services, including telepharmacy, has surged, with patient adoption in the United States increasing from 11% in 2019 to 46%. This shift towards digital-first services enhances convenience and access to care but also introduces regulatory challenges, particularly in maintaining patient safety and quality standards in the rapidly evolving online healthcare environment.
The cosmeceuticals market, a segment within online pharmacies, is experiencing robust growth. Cosmeceuticals, which bridge the gap between cosmetics and pharmaceuticals, have become a significant part of the skincare industry. The market, valued at USD 56.78 billion in 2022, is projected to expand to USD 95.75 billion by 2030. This expansion is driven by factors like innovation in natural ingredients and significant penetration of internet, smartphone, and social media applications. Despite the growth, the overall penetration for non-specialty drugs in mail-order and online pharmacies remains low, representing a significant portion of specialty prescription revenues. The evolving landscape of online pharmacies in the cosmeceuticals sector reflects a trend towards more accessible and customizable personal healthcare solutions.
Technological innovations are setting the stage for a new era in pharmaceutical care and management. AI’s role extends to areas like inventory management in retail pharmacies, where it predicts patient needs and enhances supply chain efficiency. Blockchain technology enhances supply chain transparency and legitimizes medical commodities, especially crucial in areas affected by counterfeit drugs. Blockchain also plays a vital role in patient-centric Electronic Health Records and telemonitoring systems. For instance, PharmaGo, an innovative platform developed in response to the pandemic, provides a comprehensive online pharmaceutical service, demonstrating the significant advancements in healthcare accessibility and pharmacy service delivery.
These technological advancements are instrumental in improving data sharing and collaboration among healthcare professionals. They offer significant potential for personalized medicine through data analytics, playing a crucial role in patient engagement and self-management of health. The future trends in the pharmaceutical sector, particularly influenced by the COVID-19 pandemic, indicate a shift towards Pharmaceutical Digital Marketing (PDM) and a more consumer-centric approach. AI’s potential in revolutionizing pharmacy includes automation of routine tasks, personalized medication management, real-time patient data access, and the identification of patterns in medication adherence and potential drug interactions.
Data availability
No datasets were generated or analysed during the current study.
Hole G, Hole AS, McFalone-Shaw I. Digitalization in pharmaceutical industry: what to focus on under the digital implementation process? Int J Pharmaceutics: X. 2021;3:100095.
CAS Google Scholar
Shambhavi. Digital Pharmacy on the rise: transforming the Pharma Sector. Brillio.com; Oct. 2022.
Champagne HA, Leclerc D. O., The road to digital success in pharma [Internet]. https://www.mckinsey.com/industries/life-sciences/our-insights/the-road-to-digital-success-in-pharma# ~:text=Mobile%20communications%2 C%20the%20cloud%2 C%20advanced,media%2 C%20retail%2 C%20and%20banking%20industries, August 1, 2015.
COVID-19 accelerated. digital transformation of the pharma industry by five years: Poll, Available from: http://www.pharmaceutical-technology.com/news/covid-19-accelerated-digital-transformation-of-the-pharma-industry-by-five-years-poll/#:~:text=Digital%20transformation%20in%20the%20pharmaceutical,powerful%20analytics%20than%20ever%20before?cf-view&acf-closed , March 9, 2021.
Raza MA, Aziz S, Noreen M, Saeed A, Anjum I, Ahmed M, Raza SM. Artificial Intelligence (AI) in pharmacy: an overview of innovations. INNOVATIONS Pharm 13 (2022).
Zhang X. Investment analysis based on intrinsic value in the Information Technology and Pharmaceutical sectors for advancements in Digital Healthcare. Finance Econ 1 (2023).
Clark M, Clark T, Bhatti A, Aungst T. The rise of digital health and potential implications for pharmacy practice. J Contemp Pharm Pract. 2017;64:32–40.
Article Google Scholar
Health C, Pharmacy CVS. USA, 2023.
MyChart. Epic’s MyChart software system, USA, 2023.
Medisafe MD, Companion. USA, 2023.
Moodle. Moodle open source learning management system, USA, 2023.
PLUS SG. SimMan 3G PLUS advanced emergency care patient simulators, USA, 2023.
Association AP. American Pharmacists Association, USA, 2023.
Fittler A, Ambrus T, Serefko A, Smejkalová L, Kijewska A, Szopa A, Káplár M. Attitudes and behaviors regarding online pharmacies in the aftermath of COVID-19 pandemic: at the tipping point towards the new normal. Front Pharmacol. 2022;13:1070473.
Article PubMed PubMed Central Google Scholar
Hiskey O. The era of telehealth pharmacy practice. J Am Pharmacists Association. 2022;62:10–1.
Plantado ANR, de Guzman HJd, Mariano JEC, Salvan MRAR, Benosa CAC, Robles YR. Development of an online telepharmacy service in the Philippines and analysis of its usage during the COVID-19 pandemic. J Pharm Pract. 2023;36:227–37.
Article PubMed Google Scholar
Zhang PC. The future of pharmacy is intertwined with digital health innovation. Can Pharmacists Journal/Revue Des Pharmaciens Du Can. 2022;155:7–8.
Miller R, Wafula F, Onoka CA, Saligram P, Musiega A, Ogira D, Okpani I, Ejughemre U, Murthy S, Garimella S. When technology precedes regulation: the challenges and opportunities of e-pharmacy in low-income and middle-income countries. BMJ Global Health 6 (2021).
Shawaqfeh MS, Al Bekairy AM, Al-Azayzih A, Alkatheri AA, Qandil AM, Obaidat AA, Harbi SA, Muflih SM. Pharmacy students perceptions of their distance online learning experience during the COVID-19 pandemic: a cross-sectional survey study. J Med Educ Curric Dev. 2020;7:2382120520963039.
Lee CY, Lee SWH. Impact of the educational technology use in undergraduate pharmacy teaching and learning–A systematic review. Pharm Educ. 2021;21:159–68.
Strawbridge J, Hayden JC, Robson T, Flood M, Cullinan S, Lynch M, Morgan AT, O’Brien F, Reynolds R, Kerrigan SW. Educating pharmacy students through a pandemic: reflecting on our COVID-19 experience. Res Social Administrative Pharm. 2022;18:3204–9.
Lin B, Wu S. Digital transformation in personalized medicine with artificial intelligence and the internet of medical things. OMICS. 2022;26:77–81.
Article CAS PubMed Google Scholar
Company M. Trends disrupting pharmacy value pools and potential implications for the value chain, 2018.
Stoumpos AI, Kitsios F, Talias MA. Digital Transformation in Healthcare: Technology Acceptance and its applications. Int J Environ Res Public Health. 2023;20:3407.
Kraus S, Schiavone F, Pluzhnikova A, Invernizzi AC. Digital transformation in healthcare: analyzing the current state-of-research. J Bus Res. 2021;123:557–67.
Jefferies JG, Bishop S, Hibbert S. Customer boundary work to navigate institutional arrangements around service interactions: exploring the case of telehealth. J Bus Res. 2019;105:420–33.
Patrício L, Teixeira JG, Vink J. A service design approach to healthcare innovation: from decision-making to sense-making and institutional change. AMS Rev. 2019;9:115–20.
Hong KS, Lee D. Impact of operational innovations on customer loyalty in the healthcare sector. Service Bus. 2018;12:575–600.
Laurenza E, Quintano M, Schiavone F, Vrontis D. The effect of digital technologies adoption in healthcare industry: a case based analysis. Bus Process Manage J. 2018;24:1124–44.
Mazor I, Heart T, Even A. Simulating the impact of an online digital dashboard in emergency departments on patients length of stay. J Decis Syst. 2016;25:343–53.
Rubbio I, Bruccoleri M, Pietrosi A, Ragonese B. Digital health technology enhances resilient behaviour: evidence from the ward. Int J Oper Prod Manage. 2020;40:34–67.
Hikmet N, Bhattacherjee A, Menachemi N, Kayhan VO, Brooks RG. The role of organizational factors in the adoption of healthcare information technology in Florida hospitals. Health Care Manag Sci. 2008;11:1–9.
Agarwal R, Gao G, DesRoches C, Jha AK. Research commentary—the digital transformation of healthcare: current status and the road ahead. Inform Syst Res. 2010;21:796–809.
Cucciniello M, Lapsley I, Nasi G. Managing health care in the digital world: a comparative analysis. Health Serv Manage Res. 2016;29:132–42.
Eden R, Burton-Jones A, Casey V, Draheim M. Digital transformation requires workforce transformation. MIS Q Exec. 2019;18:1–17.
Google Scholar
Huber C, Gärtner C. Digital transformations in healthcare professionals’ work: Dynamics of autonomy, control and accountability. Manage Revue. 2018;29:139–61.
Burtch G, Chan J. Investigating the relationship between medical crowdfunding and personal bankruptcy in the United States: evidence of a digital divide. MIS Quarterly (Forthcoming; 2018.
Seddon JJJM, Currie WL. Healthcare financialisation and the digital divide in the European Union: narrative and numbers. Inf Manag. 2017;54:1084–96.
Marques IC, Ferreira JJ. Digital transformation in the area of health: systematic review of 45 years of evolution. Health Technol. 2020;10:575–86.
Naik N, Hameed B, Sooriyaperakasam N, Vinayahalingam S, Patil V, Smriti K, Saxena J, Shah M, Ibrahim S, Singh A. Transforming healthcare through a digital revolution: a review of digital healthcare technologies and solutions. Front Digit Health. 2022;4:919985.
Canada. Virtual care policy framework, Canada, 2023.
Dhaliwall S. Telepharmacy services in Canada. Canada: Hospital News; 2018.
Telehealth HHSgov. Telehealth services in the United States, USA, 2023.
HRSA. Health Resources & Services Administration, USA, 2023.
UK.digital. health, Digital health and care, UK, 2023.
Australia AT, Services. Australia, 2023.
Imenokhoeva M. Telehealth in the European Union: Improving Access to Healthcare, HIMSS, EU, 2020.
Lucy d’Arville, Boulton A, Kapur V. Asia Pacific, Telehealth Adoption is expected to soar through 2024. BIAN and Company; 2022.
Intan Sabrina M, Defi IR. Telemedicine guidelines in South East Asia—a scoping review. Front Neurol. 2021;11:581649.
Wolf.Theiss. Telemedicine– the future of healthcare in Central and Eastern Europe, 2022.
Al-Samarraie H, Ghazal S, Alzahrani AI, Moody L. Telemedicine in Middle Eastern countries: Progress, barriers, and policy recommendations. Int J Med Informatics. 2020;141:104232.
Mahdi AlBasri H, Elwan P, Georgiev, Ustun A. Growth opportunities for digital health in KSA and UAE. McKinsey: McKinsey; 2022.
Ibrahim OM, Ibrahim RM, Al Meslamani AZ, Al Mazrouei N. Role of telepharmacy in pharmacist counselling to coronavirus disease 2019 patients and medication dispensing errors. J Telemed Telecare. 2023;29:18–27.
Unni EJ, Patel K, Beazer IR. Hung, Telepharmacy during COVID-19: a scoping review. Pharmacy. 2021;9:183.
Leila Shafiee Hanjani JS, Bell, Freeman CR. Undertaking medication review by telehealth. Australian J Gen Pract. 2020;49:826–31.
Bejarano AP, Santos PV, Robustillo-Cortés MdlA, Gómez ES, Rubio MDS. Implementation of a novel home delivery service during pandemic. Eur J Hosp Pharm (2020) ejhpharm–2020.
Elson EC, Oermann C, Duehlmeyer S, Bledsoe S. Use of telemedicine to provide clinical pharmacy services during the SARS-CoV-2 pandemic. Am J Health-System Pharm. 2020;77:1005–6.
Li H, Zheng S, Liu F, Liu W, Zhao R. Fighting against COVID-19: innovative strategies for clinical pharmacists. Res Social Administrative Pharm. 2021;17:1813–8.
Margusino-Framiñán L, Illarro-Uranga A, Lorenzo-Lorenzo K, Monte-Boquet E, Márquez-Saavedra E, Fernández-Bargiela N, Gómez-Gómez D, Lago-Rivero N, Poveda-Andrés JL, Díaz-Acedo R, Hurtado-Bouza JL, Sánchez-Gundín J, Casanova-Martínez C. Morillo-Verdugo, Pharmaceutical care to hospital outpatients during the COVID-19 pandemic. Telepharmacy Farmacia Hospitalaria. 2020;44:61–5.
PubMed Google Scholar
Hua X, Gu M, Zeng F, Hu H, Zhou T, Zhang Y, Shi C. Pharmacy administration and pharmaceutical care practice in a module hospital during the COVID-19 epidemic. J Am Pharmacists Association. 2020;60:431–e4381.
Asseri AA, Manna MM, Yasin IM, Moustafa MM, Roubie FM, El-Anssasy SM, Baqawie SK. Implementation and evaluation of telepharmacy during COVID-19 pandemic in an academic medical city in the Kingdom of Saudi Arabia: paving the way for telepharmacy. World J Adv Res Reviews. 2020;7:218–26.
Segal EM, Alwan L, Pitney C, Taketa C, Indorf A, Held L, Lee KS, Son M, Chi M, Diamantides E, Gosser R. Establishing clinical pharmacist telehealth services during the COVID-19 pandemic. Am J Health-System Pharm. 2020;77:1403–8.
Bukhari N, Rasheed H, Nayyer B, Babar Z-U-D. Pharmacists at the frontline beating the COVID-19 pandemic. J Pharm Policy Pract. 2020;13:8.
Smith RF. The private sector is taking the lead on enabling digital inclusion. Here’s how. in: W.E. Forum, editor, World Economic Forum, 2021.
Dal Mas F, Massaro M, Rippa P, Secundo G. The challenges of digital transformation in healthcare: an interdisciplinary literature review, framework, and future research agenda. Technovation. 2023;123:102716.
Ianculescu M, Alexandru A. Microservices–A Catalyzer for Better Managing Healthcare Data Empowerment. Stud Inf Control. 2020;29:231–42.
López-Martínez F, Núñez-Valdez ER, García-Díaz V, Bursac Z. A case study for a big data and machine learning platform to improve medical decision support in population health management. Algorithms. 2020;13:102.
Ganapathy K, Reddy S. Technology enabled remote healthcare in public private partnership mode: A story from India. Telemedicine, Telehealth and Telepresence: Principles, Strategies, Applications, and New Directions (2021) 197–233.
Gleiss A, Kohlhagen M, Pousttchi K. An apple a day–how the platform economy impacts value creation in the healthcare market. Electron Markets. 2021;31:849–76.
Bonacina S, Koch S, Meneses I, Chronaki C. Can the European EHR exchange format support shared decision making and citizen-driven health science? Public Health and Informatics, IOS; 2021. pp. 1056–60.
Samuel L, TRANSFORMING THE HEALTHCARE SYSTEM: THE PUBLIC-PRIVATE HEALTHCARE DICHOTOMY IN INDIA IN THE ERA OF DIGITAL HEALTH., Proceedings of the International Conference on Public Health, 2020, pp. 18–31.
Antarsih NR, Setyawati SP, Ningsih S, Sulaiman E, Pujiastuti N. Telehealth Business Potential in Indonesia, International Conference on Social, Economics, Business, and Education (ICSEBE 2021), Atlantis Press, 2022, pp. 73–78.
Loccioni LG. Italy, 2023.
Casprini E, Palumbo R. Reaping the benefits of digital transformation through Public-Private Partnership: A service ecosystem view applied to healthcare. Global Public Policy Gov. 2022;2:453–76.
APOTECAchemo. APOTECAchemo Advanced Robotic Chemotherapy Drug Compounding Systems, Italy, 2023.
Velayati F, Ayatollahi H, Hemmat M, Dehghan R. Telehealth business models and their components: systematic review. J Med Internet Res. 2022;24:e33128.
Barker GP, Krupinski EA, McNeely RA, Holcomb MJ, Lopez AM, Weinstein RS. The Arizona telemedicine program business model. J Telemed Telecare. 2005;11:397–402.
Lee Y-L, Chang P. Modeling a mobile health management business model for chronic kidney disease, Nursing Informatics 2016, IOS Press, 2016, pp. 1047–1048.
Dijkstra SJ, Jurriëns JA, van der Mei RD. A business model for telemonitoring services, 14th Annual High Technology Small Firms Conference, HTSF 2006, University of Twente, 2006.
Grustam AS, Vrijhoef HJ, Poulikidis V, Koymans R, Severens JL. Extending the business-to-business (B2B) model towards a business-to-consumer (B2C) model for telemonitoring patients with chronic heart failure. J Bus Models. 2018;6:106–29.
Lin T-C, Chang H-J, Huang C-C. An analysis of telemedicine in Taiwan: a business model perspective. Int J Gerontol. 2011;5:189–92.
Peters C, Blohm I, Leimeister JM. Anatomy of successful business models for complex services: insights from the telemedicine field. J Manage Inform Syst. 2015;32:75–104.
Lin S-H, Liu J-H, Wei J, Yin W-H, Chen H-H, Chiu W-T. A business model analysis of telecardiology service. Telemedicine e-Health. 2010;16:1067–73.
Mun SK, Tohme WG, Platenberg RC, Choi I. Teleradiology and emerging business models. J Telemed Telecare. 2005;11:271.
Kijl B, Nieuwenhuis LJ, Veld RM, Hermens HJ. and M.M. Vollenbroek-Hutten, Deployment of e-health services–a business model engineering strategy. Journal of telemedicine and telecare 16 (2010) 344–353.
Fusco F, Turchetti G, Interactive Business Models for Telerehabilitation after Total Knee Replacement.: Preliminary Results from Tuscany, Bioinformatics and Biomedical Engineering: Third International Conference, IWBBIO 2015, Granada, Spain, April 15–17, 2015. Proceedings, Part II 3, Springer, 2015, pp. 502–511.
Hidefjäll P, Titkova D. Business model design for a wearable biofeedback system, pHealth, 2015, pp. 213–224.
Oderanti FO, Li F. A holistic review and framework for sustainable business models for assisted living technologies and services. Int J Healthc Technol Manage. 2016;15:273–307.
Valbuena VS, Seelye S, Sjoding MW, Valley TS, Dickson RP, Gay SE, Claar D, Prescott HC, Iwashyna TJ. Racial bias and reproducibility in pulse oximetry among medical and surgical inpatients in general care in the Veterans Health Administration 2013-19: multicenter, retrospective cohort study. BMJ 378 (2022).
Bai G, Rajgopal S, Srivastava A, Zhao R. Profitability and risk-return comparison across health care industries, evidence from publicly traded companies 2010–2019. PLoS ONE. 2022;17:e0275245.
Article CAS PubMed PubMed Central Google Scholar
McCall CJ, DeCaprio D, Gartner J. The Measurement and Mitigation of Algorithmic Bias and Unfairness in Healthcare AI Models Developed for the CMS AI Health Outcomes Challenge. medRxiv (2022) 2022.09. 29.22280537.
Hsueh P-YS. Ecosystem of patient-centered research and information System Design, Personal Health Informatics: patient participation in Precision Health. Springer; 2022. pp. 329–51.
Martin KI, Glaser DA. Cosmeceuticals: the new medicine of beauty. Mo Med. 2011;108:60.
PubMed PubMed Central Google Scholar
Pandey A, Jatana GK, Sonthalia S, Cosmeceuticals SP. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC., Treasure Island (FL) ineligible companies. Disclosure: Gurpoonam Jatana declares no relevant financial relationships with ineligible companies. Disclosure: Sidharth Sonthalia declares no relevant financial relationships with ineligible companies., 2023.
Morganti P, Morganti G, Gagliardini A, Lohani A. From cosmetics to innovative cosmeceuticals—Non-woven tissues as New Biodegradable Carriers. Cosmetics. 2021;8:65.
Article CAS Google Scholar
Market C. Fortune Business Insights., Cosmeceuticals Market, 2023.
LLP SMR. Global Cosmeceuticals Market, A $95.75 Billion Industry Opportunity by 2030., 2022.
R.a. Markets, Global Cosmeceuticals Market - Outlook & Forecast 2023–2028, 2023.
Research SM. Industry Report and Statistics (Facts & Figures) - Number of Users, Price, Demand & Sales Analysis by Product & Distribution Channel, 2021.
Company M. Meeting changing consumer needs: The US retail pharmacy of the future, 2023.
Ascenso FNS. L’Oréal Portugal: a digital challenge for the active cosmetics division, 2016.
cosmeticaactiva. L’Oreal E-Learning Platform in Portugal, 2023.
Bach D, Newman AL. Governing lipitor and lipstick: capacity, sequencing, and power in international pharmaceutical and cosmetics regulation. Rev Int Polit Econ. 2010;17:665–95.
Organization WH. Quality assurance of pharmaceuticals. a compendium of guidelines and related materials: Good manufacturing practices and inspection, 2007.
Rai S, Gupta A, Punetha V. Regulations of Cosmetics across the Globe. Applied Clinical Research. Clin Trials Regul Affairs. 2015;2:137–44.
Natural VLAMBERT. & Organic Living; Say ‘No’ To Chemicals For A Healthy Life. in: Raconteur, editor, 2016.
Agency EM. The European regulatory system for medicines, 2023.
FDA, Food and Drug Adimenstration in the United States of America, 2023.
Cosmetics I, Market. Industry, Entrepreneurship and SMEs, EU, European Commission 2023.
EEU EEU. TECHNICAL REGULATION ON THE SAFETY OF COSMETICS AND PERFUMERY, 2015.
Danghyan L. Armenian regulatory framework of the cosmetics and pharmaceutical industries, and its compliance with international regulations. Whether the existing regulatory framework of cosmetics and pharmaceutical industries complies with international best practice and ensures product safety and consumer protection. American University of Armenia; 2020.
TGA. Australian Public Assessment Report for Bimatoprost, 2017.
Kwa M, Welty LJ, Xu S. Adverse events reported to the US Food and Drug Administration for cosmetics and personal care products. JAMA Intern Med. 2017;177:1202–4.
DeKoven JG, Warshaw EM, Belsito DV, Sasseville D, Maibach HI, Taylor JS, Marks JG, Fowler JF, Mathias CT, DeLeo VA. North American contact dermatitis group patch test results 2013–2014. Dermatitis. 2017;28:33–46.
Janetos TM, Kwa M, Xu S. Regulation of cosmetics. JAMA Intern Med. 2018;178:1000–1.
Daum C. Self-Regulation in the Cosmetic Industry: A Necessary Reality or a Cosmetic Illusion? 2006.
Schaffer S, Reading Our Lips.: The History of Lipstick Regulation in Western Seats of Power, 2006.
Lincoln JE. Overview of the us fda gmps: good manufacturing practice (gmp)/quality system (qs) regulation (21 CFR part 820). J Validation Technol. 2012;18:17.
van der Heijden I, Pletneva N, Boyer C. How to protect consumers against the risks posed by the online pharmacy market. Swiss Med Inf 29 (2013).
Agency EM. Buying medicines online, 2015.
Union E. Buying medicine online, 2023.
ISPE. Regulating Online Pharmacies & Medicinal Product E-Commerce, 2019.
Swissmedic. Guideline on medicines and the Internet, 2020.
Kulali H. Online Pharmacy in Switzerland: A Full Guide. 2023, Pharmapidya, 2023.
Swissmedic. Current law, 2019.
El Hajj MS, Mekkawi R, Elkaffash R, Saleh R, Awaisi AE, Wilbur K. Public attitudes towards community pharmacy in Arabic speaking Middle Eastern countries: a systematic review. Res Social Administrative Pharm. 2021;17:1373–95.
DelveInsight. The Regulatory process for drug approval in the MENA region, DelveInsight, 2019.
Sallom H, Abdi A, Halboup AM, Başgut B. Evaluation of pharmaceutical care services in the Middle East Countries: a review of studies of 2013–2020. BMC Public Health. 2023;23:1364.
P.B.o. Australia, Guidelines for Dispensing of Medicines., 2019.
Center KLT. Statutes of the Republic of Korea. Pharmaceutical Affairs Act; 2016.
Goryachev I. Russia Federation: Telemedicine Law in Russia, Mondaq, 2018.
Jing M. China FDA stops online med sales, 2016.
L.a.W. o.J. Ministry of Health, List of Sales Sites for over-the-counter Drugs, 2020.
H.S.A.o, Singapore. Dangers of Buying Health Products Online, 2023.
M.o.H.o. Malaysia, Buying Medicines Online: Beware., 2023.
Ganapathy N. India’s pharmacies do battle with online rivals Straitimes, India, 2017.
LegitScript LS. Industry-Leading Certification, 2023.
NABP. The Verified Internet Pharmacy Practice Sites, 2012.
Boyer C, Baujard V, Geissbuhler A. Evolution of health web certification through the HONcode experience. Stud Health Technol Inf. 2011;169:53–7.
Tagde P, Tagde S, Bhattacharya T, Tagde P, Chopra H, Akter R, Kaushik D, Rahman MH. Blockchain and artificial intelligence technology in e-Health. Environ Sci Pollut Res. 2021;28:52810–31.
Walgreen. Convenient virtual care., 2023.
Group O. Otto Group, 2023.
U.o.C.S, Francisco, New UCSF. Robotic Pharmacy Aims to Improve Patient Safety, 2011.
Narayanaswami C, Nooyi R, Govindaswamy SR, Viswanathan R. Blockchain anchored supply chain automation. IBM J Res Dev. 2019;63:7: 1–7.
Khezr S, Moniruzzaman M, Yassine A, Benlamri R. Blockchain technology in healthcare: a comprehensive review and directions for future research. Appl Sci. 2019;9:1736.
Xia Q, Sifah EB, Asamoah KO, Gao J, Du X, Guizani M. MeDShare: Trust-less medical data sharing among cloud service providers via blockchain. IEEE access 5 (2017) 14757–14767.
Mannaro K, Pinna A, Marchesi M. Crypto-trading: Blockchain-oriented energy market, 2017 AEIT International Annual Conference, IEEE, 2017, pp. 1–5.
Rallapalli S, Minalkar A. Improving Healthcare-Big Data Analytics for. J Adv Inform Technol 7 (2016).
Wang H, Song Y. Secure cloud-based EHR system using attribute-based cryptosystem and blockchain. J Med Syst. 2018;42:152.
Cyran MA. Blockchain as a foundation for sharing healthcare data. Blockchain Healthc Today (2018).
Funk E, Riddell J, Ankel F, Cabrera D. Blockchain technology: a data framework to improve validity, trust, and accountability of information exchange in health professions education. Acad Med. 2018;93:1791–4.
Khan PW, Byun Y. A blockchain-based secure image encryption scheme for the industrial internet of things. Entropy. 2020;22:175.
Gomasta SS, Dhali A, Tahlil T, Anwar MM, Ali ABMS. PharmaChain: Blockchain-based drug supply chain provenance verification system. Heliyon. 2023;9:e17957.
Gamage RG, Bandara NS, Diyamullage DD, Senadeera KU, Abeywardena KY, Amarasena N. PharmaGo-An Online Pharmaceutical Ordering Platform, 2021 3rd International Conference on Advancements in Computing (ICAC), IEEE, 2021, pp. 365–370.
Amalia A, Sipahutar PYC, Elviwani E, Purnamasari F. Chatbot Implementation with Semantic Technology for Drugs Information Searching System. Journal of Physics: Conference Series 1566 (2020) 012077.
Trenfield SJ, Awad A, McCoubrey LE, Elbadawi M, Goyanes A, Gaisford S, Basit AW. Advancing pharmacy and healthcare with virtual digital technologies. Adv Drug Deliv Rev. 2022;182:114098.
Anis MS, Hassali MA. Pharmaceutical marketing of over-the-counter drugs in the current digital era: a review. Pharm Sci Asia 49 (2022).
Khan O, Parvez M, Kumari P, Parvez S, Ahmad S. The future of pharmacy: how AI is revolutionizing the industry. Intell Pharm. 2023;1:32–40.
Moshawih S, Hadikhani P, Fatima A, Goh HP, Kifli N, Kotra V, Goh KW, Ming LC. Comparative analysis of an anthraquinone and chalcone derivatives-based virtual combinatorial library. A cheminformatics proof-of-concept study. J Mol Graph Model. 2022;117:108307.
Moshawih S, Goh HP, Kifli N, Idris AC, Yassin H, Kotra V, Goh KW, Liew KB, Ming LC. Synergy between machine learning and Natural products Cheminformatics: application to the lead Discovery of anthraquinone derivatives. Chemical Biology & Drug Design; 2022.
Wong CH, Siah KW, Lo AW. Estimation of clinical trial success rates and related parameters. Biostatistics. 2019;20:273–86.
Moshawih S, Goh HP, Kifli N, Darwesh MAE, Ardianto C, Goh KW, Ming LC. Identification and optimization of TDP1 inhibitors from anthraquinone and chalcone derivatives: consensus scoring virtual screening and molecular simulations. J Biomol Struct Dynamics (2023) 1–25.
Moore JH, Margreitter C, Janet JP, Engkvist O, de Groot BL, Gapsys V. Automated relative binding free energy calculations from SMILES to ∆∆G. Commun Chem. 2023;6:82.
Moshawih S, Lim AF, Ardianto C, Goh KW, Kifli N, Goh HP, Jarrar Q, Ming LC. Target-based small Molecule Drug Discovery for Colorectal Cancer: a review of Molecular pathways and in Silico studies. Biomolecules. 2022;12:878.
Download references
Acknowledgements
The researcher would like to thank the Deanship of Scientific Research, Qassim University for funding the publication of this project.
Deanship of Scientific Research, Qassim University
Author information
Authors and affiliations.
Department of Pharmacology, College of Medicine, Qassim University, Buraydah, Saudi Arabia
Ahmad Almeman
You can also search for this author in PubMed Google Scholar
Contributions
Conceived the conceptual framework, Wrote the paper, Designed search strategies, Critically reviewed the manuscript for important intellectual content: A.A.
Corresponding author
Correspondence to Ahmad Almeman .
Ethics declarations
Ethical approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The author declares no competing interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Almeman, A. The digital transformation in pharmacy: embracing online platforms and the cosmeceutical paradigm shift. J Health Popul Nutr 43 , 60 (2024). https://doi.org/10.1186/s41043-024-00550-2
Download citation
Received : 14 February 2024
Accepted : 09 April 2024
Published : 08 May 2024
DOI : https://doi.org/10.1186/s41043-024-00550-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Digital transformation
- Healthcare technology
- Cosmeceuticals
- Global health
- Patient care
- 2019 novel coronavirus
- Drug safety
Journal of Health, Population and Nutrition
ISSN: 2072-1315
- Submission enquiries: [email protected]
- General enquiries: [email protected]
We will keep fighting for all libraries - stand with us!
Internet Archive Audio

- This Just In
- Grateful Dead
- Old Time Radio
- 78 RPMs and Cylinder Recordings
- Audio Books & Poetry
- Computers, Technology and Science
- Music, Arts & Culture
- News & Public Affairs
- Spirituality & Religion
- Radio News Archive

- Flickr Commons
- Occupy Wall Street Flickr
- NASA Images
- Solar System Collection
- Ames Research Center

- All Software
- Old School Emulation
- MS-DOS Games
- Historical Software
- Classic PC Games
- Software Library
- Kodi Archive and Support File
- Vintage Software
- CD-ROM Software
- CD-ROM Software Library
- Software Sites
- Tucows Software Library
- Shareware CD-ROMs
- Software Capsules Compilation
- CD-ROM Images
- ZX Spectrum
- DOOM Level CD

- Smithsonian Libraries
- FEDLINK (US)
- Lincoln Collection
- American Libraries
- Canadian Libraries
- Universal Library
- Project Gutenberg
- Children's Library
- Biodiversity Heritage Library
- Books by Language
- Additional Collections

- Prelinger Archives
- Democracy Now!
- Occupy Wall Street
- TV NSA Clip Library
- Animation & Cartoons
- Arts & Music
- Computers & Technology
- Cultural & Academic Films
- Ephemeral Films
- Sports Videos
- Videogame Videos
- Youth Media
Search the history of over 866 billion web pages on the Internet.
Mobile Apps
- Wayback Machine (iOS)
- Wayback Machine (Android)
Browser Extensions
Archive-it subscription.
- Explore the Collections
- Build Collections
Save Page Now
Capture a web page as it appears now for use as a trusted citation in the future.
Please enter a valid web address
- Donate Donate icon An illustration of a heart shape
Ireland and the Irish Question
Bookreader item preview, share or embed this item, flag this item for.
- Graphic Violence
- Explicit Sexual Content
- Hate Speech
- Misinformation/Disinformation
- Marketing/Phishing/Advertising
- Misleading/Inaccurate/Missing Metadata
plus-circle Add Review comment Reviews
4 Favorites
DOWNLOAD OPTIONS
In collections.
Uploaded by Some place else on January 12, 2022
SIMILAR ITEMS (based on metadata)

Listen Live
Climate one.
Climate One is a one-hour weekly public radio program about energy, economy and the environment from Climate One at the Commonwealth Club of California. Each week listeners will get a candid discussion among climate scientists, policy makers, activists and concerned citizens, hosted by Climate One founder Greg Dalton.
- Health Care
Citing ‘burnout,’ doctors with ChristianaCare file papers to form system’s first labor union
Two-thirds of the more than 400 doctors on staff at the health system’s major delaware operations, including christiana and wilmington hospitals, would be covered..

- Cris Barrish

Doctors on staff at Christiana Hospital and other Christiana Care facilities in Delaware are seeking to unionize. (Cris Barrish/WHYY)

Related Content

Delaware faces persistent health disparities, particularly for Black maternal health
Health disparities for Black maternity remain a challenge in Delaware. Advocates say the problem stems from systemic racism, implicit bias and injustice.
1 month ago
- The erosion of the physician-led model of care and the threat of corporate influence on medical decision-making.
- Limited input and decision-making power in matters affecting patient care, physician safety and professional autonomy.
- The moral injury caused by the pressure to prioritize productivity and profit over patient needs and values, and from a lack of support and resources to provide high-quality care.

Get daily updates from WHYY News!
The free WHYY News Daily newsletter delivers the most important local stories to your inbox.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.
You may also like

Delaware hospital cost review board one step closer to governor’s desk
The bill heads back to the House for approval of a Senate amendment. Hospitals are neutral on the bill after fierce opposition.

Study: Low pay a driving factor in N.J.’s primary care shortage
The report found that New Jersey has around 17 primary care physicians for every 100,000 people, which is far below previous estimates.
2 months ago

Delaware responds to nursing shortage with ‘Tuition Incentive Program’
Delaware's 'Tuition Incentive Program' aims to alleviate nurse shortages by offering financial support for CNA training and workforce development.
5 months ago
About Cris Barrish

Want a digest of WHYY’s programs, events & stories? Sign up for our weekly newsletter.
Together we can reach 100% of WHYY’s fiscal year goal
Advertisement
Supported by
There’s a New Covid Variant. What Will That Mean for Spring and Summer?
Experts are closely watching KP.2, now the leading variant.
- Share full article

By Dani Blum
For most of this year, the JN.1 variant of the coronavirus accounted for an overwhelming majority of Covid cases . But now, an offshoot variant called KP.2 is taking off. The variant, which made up just one percent of cases in the United States in mid-March, now makes up over a quarter.
KP.2 belongs to a subset of Covid variants that scientists have cheekily nicknamed “FLiRT,” drawn from the letters in the names of their mutations. They are descendants of JN.1, and KP.2 is “very, very close” to JN.1, said Dr. David Ho, a virologist at Columbia University. But Dr. Ho has conducted early lab tests in cells that suggest that slight differences in KP.2’s spike protein might make it better at evading our immune defenses and slightly more infectious than JN.1.
While cases currently don’t appear to be on the rise, researchers and physicians are closely watching whether the variant will drive a summer surge.
“I don’t think anybody’s expecting things to change abruptly, necessarily,” said Dr. Marc Sala, co-director of the Northwestern Medicine Comprehensive Covid-19 Center in Chicago. But KP.2 will most likely “be our new norm,’” he said. Here’s what to know.
The current spread of Covid
Experts said it would take several weeks to see whether KP.2 might lead to a rise in Covid cases, and noted that we have only a limited understanding of how the virus is spreading. Since the public health emergency ended , there is less robust data available on cases, and doctors said fewer people were using Covid tests.
But what we do know is reassuring: Despite the shift in variants, data from the C.D.C. suggests there are only “minimal ” levels of the virus circulating in wastewater nationally, and emergency department visits and hospitalizations fell between early March and late April.
“I don’t want to say that we already know everything about KP.2,” said Dr. Ziyad Al-Aly, the chief of research and development at the Veterans Affairs St. Louis Healthcare System. “But at this time, I’m not seeing any major indications of anything ominous.”
Protection from vaccines and past infections
Experts said that even if you had JN.1, you may still get reinfected with KP.2 — particularly if it’s been several months or longer since your last bout of Covid.
KP.2 could infect even people who got the most updated vaccine, Dr. Ho said, since that shot targets XBB.1.5, a variant that is notably different from JN.1 and its descendants. An early version of a paper released in April by researchers in Japan suggested that KP.2 might be more adept than JN.1 at infecting people who received the most recent Covid vaccine. (The research has not yet been peer-reviewed or published.) A spokesperson for the C.D.C. said the agency was continuing to monitor how vaccines perform against KP.2.
Still, the shot does provide some protection, especially against severe disease, doctors said, as do previous infections. At this point, there isn’t reason to believe that KP.2 would cause more severe illness than other strains, the C.D.C. spokesperson said. But people who are 65 and older, pregnant or immunocompromised remain at higher risk of serious complications from Covid.
Those groups, in particular, may want to get the updated vaccine if they haven’t yet, said Dr. Peter Chin-Hong, an infectious disease specialist at the University of California, San Francisco. The C.D.C. has recommended t hat people 65 and older who already received one dose of the updated vaccine get an additional shot at least four months later.
“Even though it’s the lowest level of deaths and hospitalizations we’ve seen, I’m still taking care of sick people with Covid,” he said. “And they all have one unifying theme, which is that they’re older and they didn’t get the latest shot.”
The latest on symptoms and long Covid
Doctors said that the symptoms of both KP.2 and JN.1 — which now makes up around 16 percent of cases — are most likely similar to those seen with other variants . These include sore throat, runny nose, coughing, head and body aches, fever, congestion, fatigue and in severe cases, shortness of breath. Fewer people lose their sense of taste and smell now than did at the start of the pandemic, but some people will still experience those symptoms.
Dr. Chin-Hong said that patients were often surprised that diarrhea, nausea and vomiting could be Covid symptoms as well, and that they sometimes confused those issues as signs that they had norovirus .
For many people who’ve already had Covid, a reinfection is often as mild or milder than their first case. While new cases of long Covid are less common now than they were at the start of the pandemic, repeat infections do raise the risk of developing long Covid, said Fikadu Tafesse, a virologist at Oregon Health & Science University. But researchers are still trying to determine by how much — one of many issues scientists are trying to untangle as the pandemic continues to evolve.
“That’s the nature of the virus,” Dr. Tafesse said. “It keeps mutating.”
Dani Blum is a health reporter for The Times. More about Dani Blum
Irish embassy in Moscow concerned about ‘food safety’ in wake of Chernobyl
State papers 1986: ambassador wrote that russian authorities treated disaster as ‘violation of party rules’.
The Chernobyl nuclear power plant in Ukraine, scene of the world’s worst nuclear accident in April 1986. Photograph: AP Photo/Efrem Lukatsky/File
In the wake of the Chernobyl nuclear explosion in April 1986, the Irish embassy in Moscow sourced its food from Finland, State papers show.
The documents show the then Irish ambassador in Moscow, Tadhg O'Sullivan, said Pravda treated the disaster as "a violation of party rules".
In the early hours of April 26th, the world's largest ever nuclear disaster occurred at Chernobyl in Ukraine, when an explosion destroyed reactor four at the nuclear plant.
Fallout spewed high into the atmosphere and spread widely across the then USSR and Europe. Territory in parts of Ukraine, Belarus and Russia are still contaminated.
State Papers: Garda killer’s 1985 death sentence commuted
:quality(70)/cloudfront-eu-central-1.images.arcpublishing.com/irishtimes/WGXNSAKOPWDLHYVC6JSPDJN2IQ.jpg)
Anglo-Irish relations seen as ‘a nuisance’ by British officials
:quality(70)/cloudfront-eu-central-1.images.arcpublishing.com/irishtimes/WES3RVYVBQLJLT4GGG7PDMCXH4.jpg)
Ian Paisley criticised for ‘intemperate tone’ in attack on Bishop Daly
:quality(70)/cloudfront-eu-central-1.images.arcpublishing.com/irishtimes/PYYLVO7NWLS7GIKF3D3DU4AELE.jpg)
Government considered citing Aids in David Norris case
:quality(70)/cloudfront-eu-central-1.images.arcpublishing.com/irishtimes/LYPHA2GGNE2GLF3FFHZKUU7EEQ.jpg)
A combination of design faults and human error triggered the meltdown and an estimated 30 people died in the immediate aftermath of the event. But there are no agreed figures on the long-term death toll. The World Health Organisation recognises a "dramatic increase in thyroid cancer . . . among those exposed at a young age" to the fallout, and "some indication of increased leukaemia and cataract incidence among workers" in the clean-up operation.
Other groups, including Greenpeace, predict that tens of thousands of people will die as a result of health issues linked to radiation released by the disaster.
A letter from Mr O’Sullivan, dated June 18th, 1986, raised concerns about food safety in the capital.
He said German embassy monitoring had brought to light a localised high radiation level, 10 times the normal level, in a patch of ground on the embassy premises and a soil sample had been sent to Bonn for analysis.
“EC ambassadors at their last meeting had a lengthy discussion on whether to bring findings of contaminated food to the attention of the Soviet authorities,” he said.
“It was concluded that the reaction of the latter would be unfavourable, for political reasons, and it was decided that any such findings should be reported to the presidency capital for appropriate action . . .”
Purchase of meat
Mr O’Sullivan said he’d read a newspaper report saying the British embassy circular had advised against the purchase of meat in local markets, and he would try to get a copy of the circular.
"So far as this embassy is concerned, food supplies are being ordered from Stockmann's of Helsinki. and the first consignment of beef has arrived from Ireland, " he said.
He also asked that to enable the embassy “cope with food shortages and to ensure food safety”, allowances in future should be “related to Helsinki” and the cost of transport of fresh food supplies should be reimbursed by the department.
In a letter of July 23rd, Mr O'Sullivan said a report from the Shcherbina Commission, tasked with investigating the Chernobyl disaster, had been discussed by the Politburo and state organisation Pravda had reported on that meeting.
" Pravda describes the cause of the accident as "a whole series of gross violations of the operating rules by the staff of the station", and its account basically consists of the punishments and disciplinary measures meted out to these," Mr O'Sullivan said.
"The disaster at Chernobyl is thus treated by Pravda in terms of a violation of party rules, for which those concerned are to be punished, and as a lesson in the need for strict observance of party discipline in the future."
He said the approach was typical of Soviet methods of explaining failures in public policy.
“There is no criticism of the system, nor any challenge to the party leadership,” he said. It was noteworthy, Mr O’Sullivan said, that the manager of the nuclear power station, who was expelled from the party, had repeatedly drawn attention to defects in the design of the reactor.
“To pick out scapegoats is a classic Soviet way of dealing with such situations, but it is unlikely to satisfy the international community in its concern over safety standards in the nuclear industry in this country,” he concluded.
Fiona Gartland
Fiona Gartland is a crime writer and former Irish Times journalist
State Papers: Row over registration of Irish emblems
State papers: hussey complained of conflict and lack of direction, tolerant berlin appears latest terrorist target, tánaiste describes berlin attack as ‘unspeakably evil’, bill to ban domestic abusers contacting victims by phone, web, garda strike restrictions to be discussed by cabinet, in this section, spending limits for local election candidates increase to as much as €15,350, withdrawing irish troops from lebanon due to israel-hamas war may cause added ‘carnage’, says martin, no wish to cut diplomatic ties with israel as ireland proceeds with plan to recognise palestine, says harris, ‘common sense’ needed on number of asylum seekers entering ireland, says harris, local elections: record numbers of women run for council seats, bruce springsteen in croke park review: blockbuster performance closes irish tour on an emotion-filled evening, moving back to ireland would mean working till 10pm, no home of my own and bad coffee, teen hospitalised after stabbing in dublin city centre, motorcyclist killed in m50 crash named locally, bishop describes as ‘shameful’ church of ireland rejection of motion on baptism for children of unmarried mothers, latest stories, gníomh cogaidh, an coimisinéir teanga: ‘cruthaíonn muinín éileamh’, xander schauffele holds off bryson dechambeau at us pga to win his first major, rent increases likely to accelerate as supply of new homes dries up, says daft.ie report.
:quality(70)/cloudfront-eu-central-1.images.arcpublishing.com/irishtimes/MOENYACS6VA77KV7ZXJ7HWR6UM.png)
- Terms & Conditions
- Privacy Policy
- Cookie Information
- Cookie Settings
- Community Standards

Cost of living help and a future made in Australia
Strengthening medicare and the care economy.
Building a better health system than improves outcomes
Print or save page
On this page
High‑quality health services through Medicare
Boosting access to essential health services
Building a better healthcare system
The Government is investing $2.8 billion to continue its commitment to strengthen Medicare. This includes the $1.2 billion package to address pressures facing the health system, which provides:
- $882.2 million to support older Australians avoid hospital admission, be discharged from hospital earlier and improve their transition out of hospital to other appropriate care.
- $227 million to deliver a further 29 Medicare Urgent Care Clinics and boost support for regional and remote clinics. This will increase the total number of clinics across Australia to 87. Since commencing last year, existing clinics have already provided almost 400,000 bulk‑billed visits.
- $90 million to address health workforce shortages by making it simpler and quicker for international health practitioners to work in Australia.

Rohan’s daughter Zoya has been off school with a runny nose and a cough. By 6pm, she is lethargic and has a fever.
Rohan is concerned because his regular GP is now closed. Instead of waiting for hours at the emergency department, he takes Zoya to a Medicare Urgent Care Clinic, without having to make an appointment.
During the bulk billed visit, Zoya is diagnosed with an infection by the doctor and prescribed appropriate medication. Rohan and Zoya leave within an hour of arrival. Zoya makes a full recovery.
Improving health outcomes
Almost half of Australians live with a chronic condition. This Budget will provide $141.1 million for research and services for people living with chronic conditions, including bowel and skin cancer, diabetes and dementia.
To improve health outcomes, the Government is providing:
- Support for Australians to enjoy healthier, more active lives by investing $132.7 million in sport participation and performance programs.
- $825.7 million to ensure Australians can continue to access testing for and vaccinations against COVID‑19. The Government is also ensuring continued access to oral antiviral medicines on the Pharmaceutical Benefits Scheme.
- $41.6 million over two years to continue funding for alcohol and other drug treatment and support services, including the Good Sports alcohol management program for community sporting clubs.
The Government is allocating an additional $411.6 million (for a total $1.6 billion over 13 years) through the Medical Research Future Fund to continue existing research and introduce two new research missions for low‑survival cancers and reducing health inequities.
Improving access to medicines
The Government is investing $3.4 billion for new and amended listings to the Pharmaceutical Benefits Scheme, which means eligible patients can save on treatment costs.
By expanding the Closing the Gap Pharmaceutical Benefits Scheme Co‑payment Program, eligible First Nations patients will have free or cheaper access to all Pharmaceutical Benefits Scheme medicines.
Australians will benefit from $141.1 million to support and expand the National Immunisation Program.
Mental health support
The Government’s $888.1 million mental health package over eight years will help people get the care they need, while relieving pressure on the Better Access initiative and making it easier to access services.
A free, low‑intensity digital service will be established to address the gap for people with mild mental health concerns. From 1 January 2026, Australians will be able to access the service without a referral and receive timely, high‑quality mental health support. Once fully established, 150,000 people are expected to make use of this service each year.
The Government is improving access to free mental health services through a network of walk‑in Medicare Mental Health Centres, built on the established Head to Health network. The upgraded national network of 61 Medicare Mental Health Centres will open by 30 June 2026. They will provide clinical services for adults with moderate‑to‑severe mental health needs.
For Australians with complex mental health needs, funding will be provided for Primary Health Networks to partner with GPs to deliver multidisciplinary, wraparound support services and care coordination.
Improving the aged care system
Providing quality care
The Budget provides $2.2 billion to deliver aged care reforms and continue implementing recommendations from the Royal Commission into Aged Care Quality and Safety.
The new Aged Care Act will put the rights and needs of older people at the centre of the aged care system. The new Act will provide the framework for fundamental change within the aged care sector.
More Home Care Packages
The Government is investing $531.4 million to release an additional 24,100 Home Care Packages in 2024–25. This will help reduce average wait times and enable people to age at home if they prefer to do so.
Improving aged care regulation
Funding of $110.9 million over four years will support an increase in the Aged Care Quality and Safety Commission’s regulatory capabilities.
The Government is investing $1.2 billion in critical digital systems to support the introduction of the new Aged Care Act and contemporary IT systems.
The My Aged Care Contact Centre will receive $37 million to reduce call‑waiting times for people seeking information and access to aged care.
Higher wages for aged care workers
The Government has committed to fund the Fair Work Commission decision to increase the award wage for direct and indirect aged care workers once the final determination is made. This will build on the $11.3 billion already allocated to support the interim 15 per cent wage increase for aged care workers.
The Government is providing $87.2 million for workforce initiatives to attract nurses and other workers into aged care.
Reforming the disability sector
Better and more sustainable services
Getting the National Disability Insurance Scheme (NDIS) back on track
A further $468.7 million is being provided to support people with disability and get the NDIS back on track. This includes:
- $214 million over two years to fight fraud and to co‑design NDIS reforms with people with disability, announced earlier this year
- $160.7 million to upgrade the NDIS Quality and Safeguards Commission’s information technology
- $45.5 million to establish a NDIS Evidence Advisory Committee
- $20 million to start consultation and design on reforms to help NDIS participants and people with disability navigate services.
This builds on $732.9 million provided in the 2023–24 Budget.
In December 2023, National Cabinet agreed to work together to improve the experience of participants and restore the original intent of the Scheme to support people with permanent and significant disability, within a broader ecosystem of supports. This builds on an earlier decision by National Cabinet to ensure Scheme sustainability and achieve an 8 per cent growth target by 1 July 2026, with further moderation as the NDIS matures.
Improving employment for people with disability
A $227.6 million investment will support a new specialised disability employment program to replace the existing Disability Employment Services program by 1 July 2025. This includes a modern digital platform for providers and participants. These reforms will support more people with disability into sustainable work, through a program with greater flexibility, increased individual supports, and better service quality. Eligibility will be expanded to include volunteers outside the income support system and those with less than eight hours per week work capacity.
Delivering essential services
Investing in reliability and security
Strengthening resourcing for Services Australia
The Government is delivering safer and more efficient government services for all Australians.
A $1.8 billion provision will support delivery of customer and payment services. This includes funding for frontline and service delivery staff to manage claims, respond to natural disasters and improve the cyber security environment. The Government is providing $314.1 million over two years to strengthen safety and security at Services Australia centres.
The Government is investing $580.3 million over four years and $139.6 million per year ongoing to sustain the myGov platform and identify potential enhancements. A further $50 million will improve usability, safety and security of the myGov platform and ensure Services Australia can support people to protect their information and privacy.
Strengthening the Australian Taxation Office (ATO) against fraud
There will be $187.4 million to better protect taxpayer data and Commonwealth revenue against fraudulent attacks on the tax and superannuation systems. Funding will upgrade the ATO’s information and communications technologies and increase fraud prevention capabilities to manage increasing risk, prevent revenue loss, and support victims of fraud and cyber crime.
Looking after our veterans
Veterans’ claims processing is prioritised with an additional $186 million for staffing resources and $8.4 million to improve case management and protect against cyber risk. The Government will provide $222 million to harmonise veterans’ compensation and rehabilitation legislation.
A further $48.4 million will be available for Veterans’ Home Care and Community Nursing programs and $10.2 million to provide access to funded medical treatment for ill and injured veterans while their claims for liability are processed.
Back to top

IMAGES
VIDEO
COMMENTS
1. It is clear that time must be spent on a discussion about the health system and the political system and of course the about politicians themselves, and its widely believed throughout the country that the government is working for the good of the people but only for the good of themselves. Click the card to flip 👆. 1 / 7.
Study with Quizlet and memorize flashcards containing terms like There is not a day that passes by were we do not hear about the healthcare system in Ireland., It is no exaggeration, I think, that there is a problem with the system here in Ireland., On the other hand, we cannot forget the good work done by the healthcare workers. and more.
Previous analyses of the Irish health system noted the barriers to the delivery of integrated care, such as incompatible financial incentives (on the part of both users and providers), human resource constraints and poorly developed community care services (Ruane, 2010; Brick et al., 2012). Such issues will have to be resolved to secure the ...
Irish essay on the health system. 7 terms. hannahconroy2021. Preview. Irish Essay - Healthcare System. 15 terms. lucyrocke. Preview. Straith pictiúr - Cuairt ar Aintín i Nua-Eabhrac . 18 terms. Megan_Greene401. Preview. Cluastuiscint 2022 Deferred Paper FOCLÓIR. 39 terms. cennis30.
The Irish health system incorporates public, voluntary and private elements in the production, delivery and financing of healthcare. People in Category I (which includes 36% of the population) are eligible for free healthcare in the public system (with significant co-payments for medicines). Most people who qualify for Category I entitlements ...
Anne Nolan and Brian Nolan1. 1. Introduction. A variety of recent reports and strategy documents have highlighted the intimidating range of challenges facing Ireland's health system as it seeks to improve its performance. In this short paper we cannot deal with these in any comprehensive fashion, but instead focus on three specific issues.
Soon after becoming the leader of the newly established Irish Free State in 1922, W.T. Cosgrave believed that such reforms would "win for themselves the confidence of the people". These boards ...
focuses on health insurance and the Irish health system more widely, has been published nationally and internationally and he is a frequent contributor to national media discussions on the Irish health system. Brian is also co-director of the Postgraduate Diploma/MSc in Health Economics ... In an essay published in 1733, Jonathan Swift
The Irish Government has also been overseeing the implementation of its 10-year programme to create a universally accessible health-care system, entitled Sláintecare—sláinte meaning health in Gaelic. Adopted in 2018, the overarching idea was to reorientate the two-tier system, with a reliance on an insurance-based system of private care dominated by hospital services, to a publicly funded ...
Data, policy advice and research on Ireland including economy, education, employment, environment, health, tax, trade, GDP, unemployment rate, inflation and PISA., This profile provides a concise and policy-relevant overview of health and the health system in Ireland as part of the broader series of the State of Health in the EU country profiles.
The health section in the PfG and Future Health, if delivered, could have resulted in radical change of the Irish health system. The 2011 PfG, which at the time of writing was four years old, remains largely unimplemented. Of its 85 health actions, just 17 of them had been acted upon.
The American advocacy group, Physicians for a National Health Program, notes that the world's healthcare systems can be categorized into 4 models. As well as the Bismarck and Beveridge systems, there is a national health insurance system, and an out of pocket system. In the former, private healthcare providers are paid by nonprofit insurance ...
The education system in Ireland - advantages, disadvantages, stress of young people; Sport - benefits, drawbacks, sport in Irish society, women in sport, scandals in sport *NOTE* - an essay on young people comes up almost every year so it is a good idea to be able to slant any essay to how it effects young people e.g. how young people use ...
Accessibility is the main issue for the Irish healthcare system (we scored badly on 4/6 criteria); patient rights were an issue too. We also had a quick look at what we scored badly on that don ...
Study Irish Essay using smart web & mobile flashcards created by top students, teachers, and professors. Prep for a quiz or learn for fun! ... Sample Decks: Poverty, Education System, The Health System Show Class Irish: Essay Writing. Irish: Essay Writing By: Allan Haydenerd. 112 Cards - 8 Decks - 38 Learners
While the health system has evolved significantly since the early 1990s, the legacy of a highly centralized system focused on universal access to basic care remains. High energy prices on world markets have ensured greater macroeconomic stability, a budget surplus and improvements in living standards for most of the Russian population. ...
Study with Quizlet and memorize flashcards containing terms like They have to wait again, waiting room, waiting and more.
Irish Examiner's WhatsApp channel. Follow and share the latest news and stories. Darren Coleman told the High Court: 'The mental health system in Ireland is broken. Mental health is not a ...
In the face of rapid technological advancement, the pharmacy sector is undergoing a significant digital transformation. This review explores the transformative impact of digitalization in the global pharmacy sector. We illustrated how advancements in technologies like artificial intelligence, blockchain, and online platforms are reshaping pharmacy services and education. The paper provides a ...
Country's asylum system at crisis point as it grapples with unprecedented numbers. Eir Nolsøe 19 May 2024 • 6:00am. 2203. Pub landlord Brian Moore, 54, is busy with customers enjoying a late ...
The health insurer said its price hike will result in an average increase of 5.3% on its gross adult premium. But it added that the price increase across its various plans will range from between ...
There are many reasons why the publication in one volume of the writings of Marx and Engels on Ireland is to be welcomed. It is timely since the myth that the Irish national struggle was over has been exploded by events in "Northern Ireland", the area, since the partition of 1921, still held within the Union.
The number of mental health professionals has reduced in recent years. According to the World Health Organization, there are currently 8.5 psychiatrists and 4.6 psychologists per 100,000 of the population. If you need mental health treatment in Russia, you can visit your GP who will refer you for necessary treatment.
Let us know! Doctors employed by Delaware's dominant medical system, ChristianaCare, have petitioned the National Labor Relations Board to vote on forming a union, WHYY News has learned. Two-thirds of the more than 400 physicians who are on staff at the health care system's main Delaware operations — Christiana and Wilmington hospitals ...
Nurses. Nua- cháilithe. Newly qualified. Deireadh leis na liostaí fada fanachta chun coinne a fháil le dochtúir. The long waiting lists for an appointment with a doctor would end. a léitheoir. reader. Study with Quizlet and memorize flashcards containing terms like Caithear go leor ama, ag plé, Cúrsaí polaitíochta and more.
The latest on symptoms and long Covid. Doctors said that the symptoms of both KP.2 and JN.1 — which now makes up around 16 percent of cases — are most likely similar to those seen with other ...
In the wake of the Chernobyl nuclear explosion in April 1986, the Irish embassy in Moscow sourced its food from Finland, State papers show. The documents show the then Irish ambassador in Moscow ...
Terms in this set (16) Study with Quizlet and memorize flashcards containing terms like Feidhmeannacht na Seirbhíse Sláinte, athstruchtúrú an chórais leighis, haonaid éigeandála and more.
The Government is investing $2.8 billion to continue its commitment to strengthen Medicare. This includes the $1.2 billion package to address pressures facing the health system, which provides: $882.2 million to support older Australians avoid hospital admission, be discharged from hospital earlier and improve their transition out of hospital ...
To get a better job abroad. Chun post níos fearr a fháil thar lear. Underpaid. Réamhíochta. unfair. éagórach. Is it not the responsibility. Nach bhfuil freagracht ar... Study with Quizlet and memorize flashcards containing terms like This is a great scandal, Definite date, They have to wait again and more.