- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram

Stanford Medicine teams find biomarkers that predict common, severe pregnancy complication
Biological molecules in urine and gene-activity signals in blood can predict early in pregnancy which women develop preeclampsia, Stanford Medicine researchers found.
December 9, 2022 - By Erin Digitale

Pregnant women in developing countries who live far from hospitals are at particularly high risk of dying from maternal complications. A study by Stanford researchers may lead to an early-pregnancy urine test that predicts who will develop preeclampsia, a potentially fatal complication of pregnancy. Health care workers can help those at risk get to a hospital. Belen B Massieu/Shutterstock.com
A discovery by Stanford School of Medicine researchers of biomarkers in the blood and urine of women with a dangerous complication of pregnancy could lead to a low-cost test to predict the condition.
The findings, which published online Dec. 9 in Patterns , lay the groundwork for predicting preeclampsia — one of the top three causes of maternal death worldwide — months before a pregnant woman shows symptoms. Predictive testing would enable better pregnancy monitoring and the development of more effective treatments.
Preeclampsia is characterized by high blood pressure late in pregnancy. It affects 3% to 5% of pregnancies in the United States and up to 8% of pregnancies worldwide, and it can lead to eclampsia, an obstetric emergency linked to seizures, strokes, permanent organ damage and death. At present, preeclampsia can be diagnosed only in the second half of pregnancy, and the sole treatment is to deliver the baby, putting infants at risk from premature birth.
“The advantage of predicting early in pregnancy who will get preeclampsia is that we could follow moms more closely for early symptoms,” said the study’s co-lead author, Ivana Marić , PhD, a senior research scientist in pediatrics at Stanford Medicine. In addition, taking low-dose aspirin starting early in pregnancy may lower preeclampsia rates in women at risk for the condition, but pinpointing who could benefit has been challenging, Marić said.
“There is really a need to identify those pregnancies to prevent tragic outcomes for mothers, and preterm births for babies, which can be very dangerous.”
Marić shares lead authorship of the study with Kévin Contrepois, PhD, former scientific director of the Stanford Medicine Metabolic Health Center . The study’s senior authors are Nima Aghaeepour , PhD, associate professor of pediatrics and of anesthesiology, perioperative and pain medicine; Brice Gaudilliere , MD, PhD, associate professor of anesthesiology, perioperative and pain medicine; and David Stevenson , MD, professor of pediatrics and director of the March of Dimes Prematurity Research Center at Stanford University School of Medicine, which supported the research.
“When you reduce preeclampsia, you also likely reduce preterm birth,” Stevenson said. “It’s a double whammy of good impacts.”
To figure out which biological signals could provide an early warning system for preeclampsia, the Stanford Medicine research team collected biological samples from pregnant women who did and did not develop preeclampsia. They conducted highly detailed analyses of all the samples, measuring changes in as many biological signals as possible, then zeroing in on a small set of the most useful predictive signals.
“We used a number of cutting-edge technologies on Stanford University’s campus to analyze preeclampsia at an unprecedented level of biological detail,” Aghaeepour said. “We learned that a urine test fairly early on during pregnancy has a strong statistical power for predicting preeclampsia.”
Measuring everything that changes in pregnancy
The research team collected biological samples at two or three points in pregnancy (early, mid and late) in 49 women, of whom 29 developed preeclampsia during their pregnancies and 20 did not. The participants were selected from a larger cohort of women who had donated biological samples for pregnancy research at Stanford Medicine.
For each time point, the participants gave blood, urine and vaginal swab samples. The samples were used to measure six types of biological signals: all cell-free RNA in blood plasma, a measure of which genes are active; all proteins in plasma; all metabolic products in plasma; all metabolic products in urine; all fat-like molecules in plasma; and all microbes/bacteria in vaginal swabs. The scientists also conducted measurements of all immune cells in plasma in a subset of 19 of the participants.
Using the resulting thousands of measurements, as well as information about which participants developed preeclampsia and when in pregnancy each sample was collected, the scientists used machine learning to determine which biological signals best predicted who progressed to preeclampsia.
They aimed to identify a small set of signals detectable in the first 16 weeks of pregnancy that could form the basis for a simple, low-cost diagnostic test feasible to use in low-, middle- and high-income countries. To estimate the accuracy of the machine learning models, the researchers initially constructed the models with data from the discovery cohort, then confirmed the results by testing their performance on data from women in the validation cohort.
When you reduce preeclampsia, you also likely reduce preterm birth. It’s a double whammy of good impacts.
A prediction model using a set of nine urine metabolites was highly accurate, the researchers found. These urine markers, in samples collected before week 16 of pregnancy, strongly predicted who later developed preeclampsia. The performance of the test was measured by a statistical standard used in machine learning known as area under the characteristic curve. An AUC of 1 for a test with two possible outcomes indicates perfect prediction, whereas an AUC of 0.5 indicates no predictive value, the same as the results obtained from a coin toss. For the urine markers, the AUC was 0.88 in the discovery cohort and 0.83 in the validation cohort, indicating high prediction capability.
Measuring the same set of urine metabolites in samples collected throughout pregnancy produced similar predictive power, with an AUC of 0.89 in the discovery cohort and 0.87 in the validation cohort.
The researchers confirmed that their model had stronger predictive power than using only clinical features linked to a pregnant woman’s preeclampsia risk, such as chronic hypertension, high body mass index and carrying twins.
A set of nine proteins measured in blood performed almost as strongly, with an AUC of 0.84.
The researchers also created a predictive model that combined participants’ clinical features with urine metabolites, which enabled them to predict preeclampsia starting early in pregnancy with an AUC of 0.96. The clinical features in the combined model are data that are already collected as part of standard medical records, such as patients’ age, height, body mass index and pre-pregnancy hypertension.
“This data collection is routine and could serve as the first level of triage,” Agheeapour said. “We envision that patients whom the data show as at risk could receive the more extensive urine assay.”
Uncovering the disease biology
Stanford Medicine researchers are also opening windows into the biology of preeclampsia. Another study , published in February in Nature , used cell-free RNA measurements to reveal biological clues as to how preeclampsia originates.
“The ability to eavesdrop on the conversation during pregnancy, synchronously measuring molecules from the pregnant woman, fetus and placenta, is very helpful for giving us hints about what biological changes contribute to the disease,” said Mira Moufarrej , PhD, lead author of the Nature paper, who was a graduate student in bioengineering when the research was conducted. The paper’s senior author is Stephen Quake , DPhil, professor of bioengineering and of applied physics.
“The most striking changes occurred before 20 weeks’ gestation, whereas a preeclampsia diagnosis is usually made at 30-plus weeks of pregnancy,” Moufarrej said. “That was surprising. We would expect changes in gene signals when you see clinical symptoms, and this was happening much earlier in pregnancy.”
Using 404 blood samples from 199 pregnant women, Moufarrej and her colleagues identified a set of 18 genes whose activity in early pregnancy predicted the development of preeclampsia.
The genes are consistent with what is known about the biology of how the disorder develops, she noted.
Scientists hypothesize that in preeclamptic pregnancies, the placenta doesn’t fully develop; its blood vessels may be too small. At first, this is OK because the fetus is small and doesn’t need much nutrition.
“But later in pregnancy, the fetus has grown, sending signals for more nutrition,” Moufarrej said. “At that point, the only solution to small blood vessels is more blood flow, so we see high blood pressure.” In severe cases, the pressure can lead to a premature separation of the placenta from the uterine lining, creating an emergency in which the baby must be delivered immediately.
The gene activity signals that Moufarrej and her colleagues identified came from genes involved in pathways consistent with the development of preeclampsia, such as tissues related to the endothelial system, placenta and brain. (The brain is relevant because full-blown eclampsia causes seizures.) The scientists plan to use the work as a foundation for future studies into the way the condition develops.
Worldwide benefits
The scientists involved in both studies will validate their predictive tests in much larger, more diverse populations of women, with the goal of creating tests for universal use.
Knowing more about how preeclampsia develops, and how to predict it, could have profound benefits for the world’s most vulnerable moms, the researchers said, noting that an estimated 86% of maternal deaths worldwide occur in Asia and sub-Saharan Africa.
“This is where this type of test is really needed, where resources are very scarce,” Marić said. Unlike women in high-income countries, many women in low-income regions give birth far from hospitals, limiting their access to emergency care when they show symptoms of preeclampsia or eclampsia. “If we can identify which pregnancies are at high risk early on, we can help get those women to health care facilities and prevent deaths.”
The Patterns study was supported by the March of Dimes Prematurity Research Center at Stanford University School of Medicine, the Stanford Maternal and Child Health Research Institute, the Christopher Hess Research Fund, the National Institutes of Health (grants 1R01HL139844, 5RM1HG00773507 and R35GM138353), Burroughs Wellcome Fund, the Alfred E. Mann Foundation, the Bill and Melinda Gates Foundation, the Thomas C. and Joan M. Merigan Endowment at Stanford University, and the Chan Zuckerburg Biohub Microbiome Initiative.
The Nature study was supported by the Chan Zuckerberg Biohub, the Global Alliance to Prevent Prematurity and Stillbirth, the March of Dimes Foundation, the National Science Foundation (grant DGE 1656518), the Benchmark Stanford Graduate Fellowship, the Stanford ChEM-H Chemistry Biology Interface Training Program, and the H&H Evergreen Fund.

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Hope amid crisis
Psychiatry’s new frontiers

- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 6, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Personalized screening early in pregnancy may improve preeclampsia detection
by American Heart Association

A new screening algorithm for preeclampsia combining maternal history, ultrasound data and several tests for blood markers may better predict the majority of preeclampsia cases in the first trimester of pregnancy, when it may still be preventable, according to new research published in Hypertension .
Preeclampsia is the most dangerous form of high blood pressure during pregnancy (blood pressure measures ≥140/90 mm Hg), and it is a leading cause of maternal death worldwide. Preeclampsia is potentially life-threatening when untreated. It affects one in 25 pregnancies in the U.S. and is more common in first-time pregnancies.
Symptoms include headaches, vision changes and swelling of the mother's hands, feet, face or eyes; or a change in the well-being of the baby. Recent research has found that preeclampsia can be linked to an increased risk of developing cardiovascular complications for women later in life.
"Preeclampsia is one of the most severe illnesses of pregnancy and may lead to preterm birth and/or maternal death," said senior study author Emmanuel Bujold, M.D., M.Sc., professor in the department of obstetrics and gynecology at the Université Laval in Québec City, Canada.
The biological mechanisms that lead preeclampsia usually start in the first trimester of pregnancy (weeks one through 12), however, the initial symptoms of preeclampsia most often do not appear before week 20, Bujold noted.
The current risk factor-based guidelines from the American College of Obstetricians and Gynecologists (ACOG) recommend pregnant women take aspirin if they have a major risk factor such as chronic high blood pressure, type 2 diabetes, chronic kidney disease , lupus or preeclampsia in a prior pregnancy. Aspirin is also recommended by ACOG for pregnant women with two moderate risk factors such as being a Black woman, having a sister or mother with history of preeclampsia, having a first pregnancy, obesity or an IVF pregnancy.
"Following those guidelines, almost all Black women should take aspirin during pregnancy, as should about one-third of all women of other races and ethnicities," Bujold said.
Previous studies from the Fetal Medicine Foundation have found that preterm preeclampsia, defined as developing preeclampsia before 37 weeks of gestation, can be predicted in the first trimester using a combination of ultrasound and blood biomarker tests.
In this study, researchers recruited over 7,000 women with first-time pregnancies across Canada who were between 11 and 14 weeks pregnant to evaluate the Fetal Medicine Foundation's screening model. The model consisted of maternal history, ultrasound data and several tests for blood markers.
The study found:
- Using the Fetal Medicine Foundation's screening model for participants between 11 and 13 weeks of pregnancy, the preeclampsia detection rate was 63.1% for preterm preeclampsia (before 37 weeks of gestation) and 77.3% for early preeclampsia (before 34 weeks of gestation). The false positive rate was 15.8%.
- Using the risk factor-based guidelines from the American College of Obstetricians and Gynecologists, the detection rate for preterm preeclampsia would be 61.5% and 59.1% for early preeclampsia, with a false-positive rate of 34.3%. This would be more than twice the false-positive rate of the Fetal Medicine Foundation's screening model.
The only way to resolve preeclampsia once it has developed is to deliver the baby. A previous meta-analysis by the study authors found that taking one low-dose aspirin daily may reduce the risk of developing preeclampsia by up to 53%.
"Using this new screening model, treatment decisions were based on each individual's personal risk," Bujold said. "With their personal risk calculated, it's much easier for a woman to make the right decision, for example, if she chooses to take daily low-dose aspirin, she is much more likely to follow through because it's based on personalized screening test."
Study background and details:
- The study was conducted between 2014 and 2020 at five health centers across Canada. Of note: Canada has a national health care service, and coverage is universal for all Canadian citizens and permanent residents.
- 7,554 women who were pregnant for the first time were recruited between 11 and 14 weeks of pregnancy. 7,325 delivered after 20 weeks and remained eligible for the final analysis; 229 had pregnancies with fetal anomalies and were excluded from the analyses for the study.
- At time of enrollment in the study, participants underwent screening for preeclampsia. The data collected included age, weight, ethnicity, smoking status and chronic health conditions (chronic hypertension, type 1 diabetes or type 2 diabetes and antiphospholipid syndrome, an autoimmune disease that may be associated with pregnancy complications).
- The study participants had an average age of 29 years. 92% of participants self-identified as white; 4% as Black; 2.6% as South Asian; 0.9% as East Asian; 0.3% as First Nations; and 0.2% as mixed race or undetermined.
- The study excluded women who were taking antihypertensive medication for chronic hypertension, low-dose aspirin or low-molecular-weight-heparin (a blood thinner) on a daily basis were excluded from the study.
- Participants were followed until delivery. The primary outcome was preterm preeclampsia. The secondary outcome was early preeclampsia.
- Of the 7,325 women included in the analysis, 65 (0.9%) developed preterm preeclampsia, and 22 (0.3%) developed early preeclampsia.
Among the study's limitations, several women with risk factors for preeclampsia, such as high blood pressure and type 2 diabetes before pregnancy, were not included in the study if they were already taking aspirin for preeclampsia prevention. This would make it difficult to determine whether this population would rely solely on the Fetal Medicine Foundation's screening model to decide whether or not to take daily, low-dose aspirin , Bujold noted.
Additionally, only one lab was used to analyze blood samples , and blood samples collected at other centers across Canada were frozen and shipped for analysis, meaning that biomarkers were measured several weeks after the blood was drawn, which may have affected the results.
"It's reasonable to believe that the inclusion of the entire population and immediate analysis of blood samples may both have improved the screening process. If we implemented a screening program in big cities across North America, the screening would be expected to be even better and more accurate," Bujold said.
"The good news is that we now have a more precise screening approach using existing tests that can predict preeclampsia early in pregnancy. The next step is to make this screening available to all pregnant women so that more women could receive a diagnosis early in pregnancy and begin preventative aspirin treatment, potentially preventing complications of severe preeclampsia."
According to Sadiya S. Khan, M.D., M.Sc., FAHA, chair of the writing group for the Association's 2023 scientific statement on Optimizing Prepregnancy Cardiovascular Health to Improve Outcomes in Pregnant and Postpartum Individuals and Offspring, predicting risk for term and preterm preeclampsia remains an important goal and priority to improve maternal health and mitigate disparities.
Khan is the Magerstadt Professor of Cardiovascular Epidemiology and an associate professor of medicine and preventive medicine at the Northwestern University Feinberg School of Medicine in Chicago and a preventive cardiologist at Northwestern Medicine.
"Since the risks for preeclampsia may be largely influenced by health before pregnancy, the ability of a screening model to be applied in early pregnancy is very helpful and can initiate conversations between the clinician and patient about strategies to optimize heart health," Khan said.
"However, challenges remain with implementation of models such as this one that integrate biomarkers that are not routinely assessed and may not be widely available, especially among people in vulnerable populations who are most likely to have the highest risk for preterm preeclampsia."
Explore further
Feedback to editors

New vaccine could protect against coronaviruses that haven't even emerged yet
9 hours ago

Study links organization of neurotypical brains to genes involved in autism and schizophrenia
12 hours ago

Study traces an infectious language epidemic
21 hours ago

Visual experiences unique to early infancy provide building blocks of human vision, study finds
May 10, 2024

Study points to personalized treatment opportunities for glioblastoma

Research team introduces new tool to boost battle against childhood undernutrition

How herpes hijacks a ride into cells

How the brain is flexible enough for a complex world, without being thrown into chaos

Researchers create AI model to understand how brain activity relates to illness

Study reveals need to review temperature control measures in hospitals to manage Legionella
Related stories.

Blood test reveals which women are at higher risk of preeclampsia in the later stages of pregnancy
Aug 29, 2023

Patients interested in learning about preeclampsia risk, shows study
Mar 27, 2024

Screening test predicts preterm preeclampsia during pregnancy
Oct 4, 2023

Lipid test can reveal risk of preeclampsia, a potentially deadly pregnancy complication
Jul 14, 2023

ACOG updates guidelines for gestational HTN, preeclampsia
Dec 29, 2018

FDA approves first blood test to predict preeclampsia in pregnant women
Jul 5, 2023
Recommended for you

Serotonergic neuron findings suggest possible treatment for depression-related infertility
May 8, 2024

Researchers find that a new mother's immune status varies with her feeding strategy

About 90% of US adults are on the way to heart disease, study suggests

Intervention in Navajo Nation boosts uptake for heart failure drugs by 53%

Cannabis, nicotine use during pregnancy found to increase rate of infant death fourfold
May 7, 2024

AI may help physicians detect abnormal heart rhythms earlier
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

Personalized screening early in pregnancy may improve preeclampsia detection
Study suggests more extensive screening method in the first trimester of pregnancy may improve detection of preeclampsia.
A new screening algorithm for preeclampsia combining maternal history, ultrasound data and several tests for blood markers may better predict the majority of preeclampsia cases in the first trimester of pregnancy, when it may still be preventable, according to new research published today in Hypertension , an American Heart Association journal.
Preeclampsia is the most dangerous form of high blood pressure during pregnancy (blood pressure measures ≥140/90 mm Hg), and it is a leading cause of maternal death worldwide. Preeclampsia is potentially life-threatening when untreated. It affects 1 in 25 pregnancies in the U.S. and is more common in first-time pregnancies. Symptoms include headaches, vision changes and swelling of the mother's hands, feet, face or eyes; or a change in the well-being of the baby. Recent research has found that preeclampsia can be linked to an increased risk of developing cardiovascular complications for women later in life.
"Preeclampsia is one of the most severe illnesses of pregnancy and may lead to preterm birth and/or maternal death," said senior study author Emmanuel Bujold, M.D., M.Sc . , professor in the department of obstetrics and gynecology at the Université Laval in Québec City, Canada.
The biological mechanisms that lead preeclampsia usually start in the first trimester of pregnancy (weeks 1 through 12), however, the initial symptoms of preeclampsia most often do not appear before week 20, Bujold noted.
The current risk factor-based guidelines from the American College of Obstetricians and Gynecologists (ACOG) recommend pregnant women take aspirin if they have a major risk factor such as chronic high blood pressure, Type 2 diabetes, chronic kidney disease, lupus or preeclampsia in a prior pregnancy. Aspirin is also recommended by ACOG for pregnant women with two moderate risk factors such as being a Black woman, having a sister or mother with history of preeclampsia, having a first pregnancy, obesity or an IVF pregnancy.
"Following those guidelines, almost all Black women should take aspirin during pregnancy, as should about one-third of all women of other races and ethnicities," Bujold said.
Previous studies from the Fetal Medicine Foundation have found that preterm preeclampsia, defined as developing preeclampsia before 37 weeks of gestation, can be predicted in the first trimester using a combination of ultrasound and blood biomarker tests. In this study, researchers recruited over 7,000 women with first-time pregnancies across Canada who were between 11 and 14 weeks pregnant to evaluate the Fetal Medicine Foundation's screening model. The model consisted of maternal history, ultrasound data and several tests for blood markers.
The study found:
- Using the Fetal Medicine Foundation's screening model for participants between 11 and 13 weeks of pregnancy, the preeclampsia detection rate was 63.1% for preterm preeclampsia (before 37 weeks of gestation) and 77.3% for early preeclampsia (before 34 weeks of gestation). The false positive rate was 15.8%.
- Using the risk factor-based guidelines from the American College of Obstetricians and Gynecologists, the detection rate for preterm preeclampsia would be 61.5% and 59.1% for early preeclampsia, with a false-positive rate of 34.3%. This would be more than twice the false-positive rate of the Fetal Medicine Foundation's screening model.
The only way to resolve preeclampsia once it has developed is to deliver the baby. A previous meta-analysis by the study authors found that taking one low-dose aspirin daily may reduce the risk of developing preeclampsia by up to 53%.
"Using this new screening model, treatment decisions were based on each individual's personal risk," Bujold said. "With their personal risk calculated, it's much easier for a woman to make the right decision, for example, if she chooses to take daily low-dose aspirin, she is much more likely to follow through because it's based on personalized screening test."
Study background and details:
- The study was conducted between 2014 and 2020 at five health centers across Canada. Of note: Canada has a national health care service, and coverage is universal for all Canadian citizens and permanent residents.
- 7,554 women who were pregnant for the first time were recruited between 11 and 14 weeks of pregnancy. 7,325 delivered after 20 weeks and remained eligible for the final analysis; 229 had pregnancies with fetal anomalies and were excluded from the analyses for the study.
- At time of enrollment in the study, participants underwent screening for preeclampsia. The data collected included age, weight, ethnicity, smoking status and chronic health conditions (chronic hypertension, Type 1 diabetes or Type 2 diabetes and antiphospholipid syndrome, an autoimmune disease that may be associated with pregnancy complications).
- The study participants had an average age of 29 years. 92% of participants self-identified as white; 4% as Black; 2.6% as South Asian; 0.9% as East Asian; 0.3% as First Nations; and 0.2% as mixed race or undetermined.
- The study excluded women who were taking antihypertensive medication for chronic hypertension, low-dose aspirin or low-molecular-weight-heparin (a blood thinner) on a daily basis were excluded from the study.
- Participants were followed until delivery. The primary outcome was preterm preeclampsia. The secondary outcome was early preeclampsia.
- Of the 7,325 women included in the analysis, 65 (0.9%) developed preterm preeclampsia, and 22 (0.3%) developed early preeclampsia.
Among the study's limitations, several women with risk factors for preeclampsia, such as high blood pressure and Type 2 diabetes before pregnancy, were not included in the study if they were already taking aspirin for preeclampsia prevention. This would make it difficult to determine whether this population would rely solely on the Fetal Medicine Foundation's screening model to decide whether or not to take daily, low-dose aspirin, Bujold noted. Additionally, only one lab was used to analyze blood samples, and blood samples collected at other centers across Canada were frozen and shipped for analysis, meaning that biomarkers were measured several weeks after the blood was drawn, which may have affected the results.
"It's reasonable to believe that the inclusion of the entire population and immediate analysis of blood samples may both have improved the screening process. If we implemented a screening program in big cities across North America, the screening would be expected to be even better and more accurate," Bujold said. "The good news is that we now have a more precise screening approach using existing tests that can predict preeclampsia early in pregnancy. The next step is to make this screening available to all pregnant women so that more women could receive a diagnosis early in pregnancy and begin preventative aspirin treatment, potentially preventing complications of severe preeclampsia."
According to Sadiya S. Khan, M.D., M.Sc., FAHA, chair of the writing group for the Association's 2023 scientific statement on Optimizing Prepregnancy Cardiovascular Health to Improve Outcomes in Pregnant and Postpartum Individuals and Offspring, predicting risk for term and preterm preeclampsia remains an important goal and priority to improve maternal health and mitigate disparities. Khan is the Magerstadt Professor of Cardiovascular Epidemiology and an associate professor of medicine and preventive medicine at the Northwestern University Feinberg School of Medicine in Chicago and a preventive cardiologist at Northwestern Medicine.
"Since the risks for preeclampsia may be largely influenced by health before pregnancy, the ability of a screening model to be applied in early pregnancy is very helpful and can initiate conversations between the clinician and patient about strategies to optimize heart health," Khan said. "However, challenges remain with implementation of models such as this one that integrate biomarkers that are not routinely assessed and may not be widely available, especially among people in vulnerable populations who are most likely to have the highest risk for preterm preeclampsia."
- Pregnancy and Childbirth
- Hypertension
- Heart Disease
- Diseases and Conditions
- Teen Health
- Personalized Medicine
- Birth Defects
- Mammography
- Nutrition and pregnancy
- Miscarriage
- Facial symmetry
- Health science
Story Source:
Materials provided by American Heart Association . Note: Content may be edited for style and length.
Journal Reference :
- Paul Guerby, Francois Audibert, Jo-Ann Johnson, Nanette Okun, Yves Giguère, Jean-Claude Forest, Nils Chaillet, Benoit Mâsse, David Wright, Louise Ghesquiere, Emmanuel Bujold. Prospective Validation of First-Trimester Screening for Preterm Preeclampsia in Nulliparous Women (PREDICTION Study) . Hypertension , 2024; DOI: 10.1161/HYPERTENSIONAHA.123.22584
Cite This Page :
Explore More
- Controlling Shape-Shifting Soft Robots
- Brain Flexibility for a Complex World
- ONe Nova to Rule Them All
- AI Systems Are Skilled at Manipulating Humans
- Planet Glows With Molten Lava
- A Fragment of Human Brain, Mapped
- Symbiosis Solves Long-Standing Marine Mystery
- Surprising Common Ideas in Environmental ...
- 2D All-Organic Perovskites: 2D Electronics
- Generative AI That Imitates Human Motion
Trending Topics
Strange & offbeat.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 27 October 2023
Mitigating preeclampsia risk through effective uncontrolled blood pressure management
- Mariane Bertagnolli 1
Hypertension Research volume 47 , pages 545–547 ( 2024 ) Cite this article
738 Accesses
4 Altmetric
Metrics details
The Original Article was published on 02 October 2023
Hypertensive disorders of pregnancy include chronic hypertension, gestational hypertension, preeclampsia/eclampsia, and preeclampsia superimposed on chronic hypertension [ 1 ]. Hypertension in pregnancy is defined by the most guidelines as blood pressure ≥140/90 mmHg. Nevertheless, the initiation of antihypertensive treatment during pregnancy exhibits a degree of variability. This variability stems from the prevailing uncertainty regarding the advantages of lowering maternal blood pressure and the potential fetal risks associated with the impact of antihypertensive medications on utero-placental circulation, as well as the reported alterations in fetal growth resulting from in utero exposure to such medications. This is important because hypertensive disorders affect up to 10% of pregnancies worldwide, being a major health problem for women and their infants and causing increased maternal and infant morbidity and mortality [ 2 ]. Hence, enhancements in the identification and management of risks have the potential to markedly alleviate the burden imposed by hypertensive disorders during pregnancy.
The present study by Salazar et al. [ 3 ] provides insights into the benefits of treating mild chronic hypertension during pregnancy. This debate has been fueled by recent discrepant findings that describe the beneficial effects of pharmacologically treating pregnant women with mild chronic hypertension on the reduction of preeclampsia/eclampsia risk and the risk of small-for-gestational-age infants [ 4 , 5 ]. Salazar and colleagues conducted an analysis to investigate the correlation between the blood pressure levels achieved through antihypertensive treatment and the risk of developing preeclampsia/eclampsia in pregnant women with chronic hypertension. They conducted a historical cohort study on pregnant women undergoing treatment for chronic hypertension, incorporating both office blood pressure readings and ambulatory blood pressure monitoring (ABPM) after 20 weeks of gestation. This allowed them to categorize the cohort into four groups: controlled hypertension, white-coat uncontrolled hypertension, masked uncontrolled hypertension, and sustained hypertension.
Their findings revealed that sustained uncontrolled hypertension (defined as office blood pressure ≥ 140/90 mmHg and 24-h ABPM ≥ 130/80 mmHg) and masked uncontrolled hypertension (defined as office blood pressure < 140/90 mmHg and 24-hour ABPM ≥ 130/80 mmHg) were associated with a similar increase in the risk of preeclampsia/eclampsia. Controlled hypertension (office blood pressure < 140/90 mmHg and 24-h ABPM < 130/80 mmHg) or white-coat uncontrolled hypertension (office blood pressure ≥ 140/90 mmHg and 24-h ABPM < 130/80 mmHg) did not exhibit a significant risk of preeclampsia/eclampsia. Furthermore, within this cohort, nocturnal hypertension and blood pressure levels achieved during the nighttime period emerged as the most robust predictors for the development of preeclampsia/eclampsia.
Based on the compelling findings presented by Salazar et al. [ 3 ], three pivotal considerations should be taken into account when diagnosing and managing chronic hypertension during pregnancy (as illustrated in Fig. 1 ). The first critical issue revolves around the methodology employed for diagnosing and monitoring uncontrolled blood pressure. This underscores the importance of employing accurate techniques for early-gestation blood pressure measurement to correctly diagnose chronic hypertension and identify individuals with uncontrolled and masked uncontrolled elevated blood pressure. Ambulatory blood pressure monitoring (ABPM) has been demonstrated to enhance both diagnosis and risk prediction in general hypertension, with additional evidence supporting its utility in managing hypertensive disorders during pregnancy. In the context of pregnancy, ABPM is recommended for identifying white-coat hypertension. However, Salazar and colleagues previously published data have underscored the indispensable role of ABPM in uncovering masked hypertension when out-of-office values are elevated but office blood pressure remains within the normal range [ 6 ]. More specifically, they have documented that nearly 60% of pregnancies initially classified as gestational hypertensive (according to current guidelines) were, in fact, cases of masked chronic hypertension. This finding holds significant importance, as masked uncontrolled hypertension, as highlighted by this study and others, has been associated with an increased risk of preeclampsia during pregnancy. Furthermore, the markedly elevated risk of preeclampsia in pregnancies with persistently elevated nighttime blood pressure values, as demonstrated by Salazar et al. [ 3 ], sheds additional light on the necessity for stringent blood pressure monitoring, including 24-h assessment, in women with uncontrolled blood pressure.
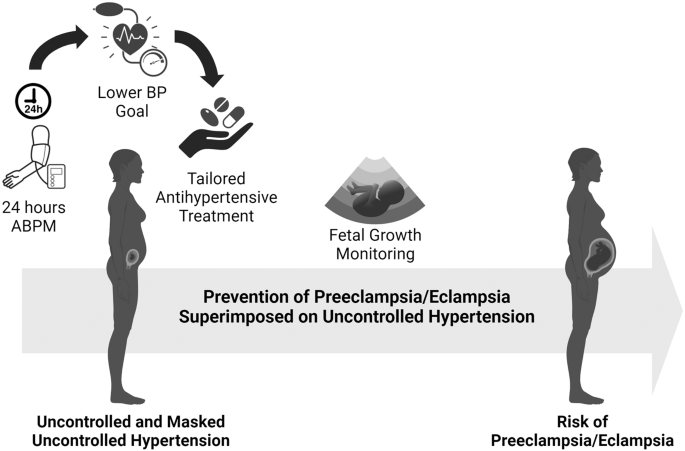
Considerations when diagnosing and managing uncontrolled hypertension during pregnancy and the associated risk of developing preeclampsia/eclampsia. ABPM ambulatory blood pressure monitoring, BP blood pressure
The second crucial issue under consideration pertains to the necessity of lowering the targeted blood pressure goals for managing treated chronic hypertension during pregnancy. This proposition gains substantial support from Tita et al. [ 4 ] findings, which demonstrated that aiming for a blood pressure goal lower than 140 mmHg reduced the risk of preeclampsia in pregnant women receiving treatment. Moreover, the study of Ueda et al. [ 7 ] further reinforces this argument by highlighting the positive effects of even more stringent blood pressure goals. According to their research, women with systolic blood pressure levels below 130 mmHg at 16–19 weeks of gestation exhibited a significantly reduced risk of early-onset superimposed preeclampsia compared to those with systolic blood pressure readings exceeding 140 mmHg. These findings align with the results of a meta-analysis, which indicated that blood pressure-lowering treatment during pregnancy, aiming for an achieved systolic blood pressure below 130 mmHg, reduced the risk of severe hypertension to nearly one-third when compared to maintaining systolic blood pressure levels above 140 mmHg [ 8 ]. It is worth noting, however, that this approach was associated with an increased risk of infants being born small for their gestational age. This collective body of evidence suggests that targeting a systolic blood pressure below 130 mmHg during pregnancy through blood pressure-lowering treatment may significantly decrease the risk of preeclampsia. Nonetheless, it is essential to accompany this approach with meticulous monitoring of fetal growth due to the identified increased risk of infants being small for their gestational age.
The third critical issue addressed pertains to the selection and adherence to antihypertensive treatment during pregnancy. Concerns regarding the potential association between aggressive blood pressure reduction and fetal growth restriction represent significant barriers to the consistent use of antihypertensive medications during pregnancy. The present study of Salazar et al. [ 3 ] made an important observation by noting a trend towards a higher prevalence of neonates classified as small for their gestational age among women with uncontrolled hypertension who were also taking multiple antihypertensive drugs. The mechanisms responsible for fetal growth restriction in women treated with antihypertensive drugs during pregnancy remain incompletely understood. Furthermore, whether such adverse effects are dependent on the specific type of antihypertensive agent remains an open question. The available options for antihypertensive treatment during hypertensive pregnancies are limited and include medications like methyldopa, calcium channel blockers, β-blockers, and diuretics. It’s worth noting that first-line antihypertensive drugs that block the renin-angiotensin system, such as angiotensin-converting-enzyme inhibitors and angiotensin receptor blockers, are contraindicated due to their known teratogenic effects [ 1 ]. A systematic review comparing the effects of available antihypertensive drugs for pregnancy revealed that both atenolol and labetalol, which are both β-blockers, significantly increased the risk of neonates being classified as small for their gestational age [ 9 ]. Additionally, these drugs were associated with elevated rates of caesarean delivery. It is hypothesized that β-blockers’ negative inotropic and chronotropic properties can reduce maternal cardiac output, subsequently affecting placental perfusion and fetal growth [ 10 ].
In conclusion, the choice and adherence to antihypertensive treatment during pregnancy present complex challenges, particularly in light of concerns about potential fetal growth restrictions associated with certain medications. Further research is needed to better understand the mechanisms at play and to refine treatment approaches for pregnant women with chronic hypertension.
Magee LA, Pels A, Helewa M, Rey E, von Dadelszen P, Committee SHG. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: executive summary. J Obstet Gynaecol Can : JOGC = J d’obstetrique et gynecologie du Can : JOGC. 2014;36:575–6.
Article Google Scholar
Abalos E, Cuesta C, Carroli G, Qureshi Z, Widmer M, Vogel JP, et al. Pre-eclampsia, eclampsia and adverse maternal and perinatal outcomes: a secondary analysis of the world health organization multicountry survey on maternal and newborn health. BJOG : Int J Obstet Gynaecol. 2014;121:14–24.
Salazar MR, Espeche WG, Minetto J, Carrera PR, Cerri G, Leiva Sisnieguez CB, et al. Uncontrolled and masked uncontrolled blood pressure in treated pregnant women with chronic hypertension and risk for preeclampsia/eclampsia. Hypertens Res. 2023. https://doi.org/10.1038/s41440-023-01443-3 .
Tita AT, Szychowski JM, Boggess K, Dugoff L, Sibai B, Lawrence K, et al. Treatment for mild chronic hypertension during pregnancy. N Engl J Med. 2022;386:1781–92.
Article CAS PubMed PubMed Central Google Scholar
Webster LM, Conti-Ramsden F, Seed PT, Webb AJ, Nelson-Piercy C, Chappell LC. Impact of antihypertensive treatment on maternal and perinatal outcomes in pregnancy complicated by chronic hypertension: a systematic review and meta-analysis. J. Am Heart Assoc. 2017;6:e005526.
Article PubMed PubMed Central Google Scholar
Espeche WG, Salazar MR, Minetto J, Leiva Sisnieguez CE, Cerri G, Balbin E, et al. Hypertension arising after 20 weeks of gestation: gestational hypertension or masked chronic hypertension? J Hum Hypertens. 2023;37:813–7.
Article PubMed Google Scholar
Ueda A, Hasegawa M, Matsumura N, Sato H, Kosaka K, Abiko K, et al. Lower systolic blood pressure levels in early pregnancy are associated with a decreased risk of early-onset superimposed preeclampsia in women with chronic hypertension: a multicenter retrospective study. Hypertens Res : Off J Jpn Soc Hypertens. 2022;45:135–45.
Abe M, Arima H, Yoshida Y, Fukami A, Sakima A, Metoki H, et al. Optimal blood pressure target to prevent severe hypertension in pregnancy: a systematic review and meta-analysis. Hypertens Res : Off J Jpn Soc Hypertens. 2022;45:887–99.
Bellos I, Pergialiotis V, Papapanagiotou A, Loutradis D, Daskalakis G. Comparative efficacy and safety of oral antihypertensive agents in pregnant women with chronic hypertension: a network metaanalysis. Am J Obstet Gynecol. 2020;223:525–37.
Article CAS PubMed Google Scholar
Carr DB, Tran LT, Brateng DA, Kawamura C, Shofer JB, Karumanchi SA, et al. Hemodynamically-directed atenolol therapy is associated with a blunted rise in maternal sFLT-1 levels during pregnancy. Hypertens Pregnancy. 2009;28:42–55.
Download references
Author information
Authors and affiliations.
School of Physical and Occupational Therapy, Faculty of Medicine and Health Sciences, McGill University, Montreal, QC, Canada
Mariane Bertagnolli
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Mariane Bertagnolli .
Ethics declarations
Conflict of interest.
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Bertagnolli, M. Mitigating preeclampsia risk through effective uncontrolled blood pressure management. Hypertens Res 47 , 545–547 (2024). https://doi.org/10.1038/s41440-023-01489-3
Download citation
Received : 29 September 2023
Accepted : 04 October 2023
Published : 27 October 2023
Issue Date : February 2024
DOI : https://doi.org/10.1038/s41440-023-01489-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
- Preeclampsia
- Small-for-gestational-age
- Antihypertensive drugs
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

- News Releases
Personalized screening early in pregnancy may improve preeclampsia detection
Study suggests more extensive screening method in the first trimester of pregnancy may improve detection of preeclampsia
American Heart Association
Research Highlights:
- A personalized screening algorithm for preeclampsia in the first trimester of pregnancy may help clinicians better predict who is at risk for developing the condition and who may benefit from treatment with a daily, low-dose aspirin.
- In this study of more than 7,000 women, the new screening method, which combined maternal history, biomarker tests and ultrasound tests, was better at identifying preeclampsia risk in than current risk factor-based guidelines.
Embargoed until 4 a.m. CT/5 a.m. ET Monday, May 6, 2024
DALLAS, May 6, 2024 — A new screening algorithm for preeclampsia combining maternal history, ultrasound data and several tests for blood markers may better predict the majority of preeclampsia cases in the first trimester of pregnancy, when it may still be preventable, according to new research published today in Hypertension , an American Heart Association journal.
Preeclampsia is the most dangerous form of high blood pressure during pregnancy (blood pressure measures ≥140/90 mm Hg), and it is a leading cause of maternal death worldwide. Preeclampsia is potentially life-threatening when untreated. It affects 1 in 25 pregnancies in the U.S. and is more common in first-time pregnancies. Symptoms include headaches, vision changes and swelling of the mother’s hands, feet, face or eyes; or a change in the well-being of the baby. Recent research has found that preeclampsia can be linked to an increased risk of developing cardiovascular complications for women later in life.
“Preeclampsia is one of the most severe illnesses of pregnancy and may lead to preterm birth and/or maternal death,” said senior study author Emmanuel Bujold, M.D., M.Sc . , professor in the department of obstetrics and gynecology at the Université Laval in Québec City, Canada.
The biological mechanisms that lead preeclampsia usually start in the first trimester of pregnancy (weeks 1 through 12), however, the initial symptoms of preeclampsia most often do not appear before week 20, Bujold noted.
The current risk factor-based guidelines from the American College of Obstetricians and Gynecologists (ACOG) recommend pregnant women take aspirin if they have a major risk factor such as chronic high blood pressure, Type 2 diabetes, chronic kidney disease, lupus or preeclampsia in a prior pregnancy. Aspirin is also recommended by ACOG for pregnant women with two moderate risk factors such as being a Black woman, having a sister or mother with history of preeclampsia, having a first pregnancy, obesity or an IVF pregnancy.
“Following those guidelines, almost all Black women should take aspirin during pregnancy, as should about one-third of all women of other races and ethnicities,” Bujold said.
Previous studies from the Fetal Medicine Foundation have found that preterm preeclampsia, defined as developing preeclampsia before 37 weeks of gestation, can be predicted in the first trimester using a combination of ultrasound and blood biomarker tests. In this study, researchers recruited over 7,000 women with first-time pregnancies across Canada who were between 11 and 14 weeks pregnant to evaluate the Fetal Medicine Foundation’s screening model. The model consisted of maternal history, ultrasound data and several tests for blood markers.
The study found:
- Using the Fetal Medicine Foundation’s screening model for participants between 11 and 13 weeks of pregnancy, the preeclampsia detection rate was 63.1% for preterm preeclampsia (before 37 weeks of gestation) and 77.3% for early preeclampsia (before 34 weeks of gestation). The false positive rate was 15.8%.
- Using the risk factor-based guidelines from the American College of Obstetricians and Gynecologists, the detection rate for preterm preeclampsia would be 61.5% and 59.1% for early preeclampsia, with a false-positive rate of 34.3%. This would be more than twice the false-positive rate of the Fetal Medicine Foundation’s screening model.
The only way to resolve preeclampsia once it has developed is to deliver the baby. A previous meta-analysis by the study authors found that taking one low-dose aspirin daily may reduce the risk of developing preeclampsia by up to 53%.
“Using this new screening model, treatment decisions were based on each individual’s personal risk,” Bujold said. “With their personal risk calculated, it’s much easier for a woman to make the right decision, for example, if she chooses to take daily low-dose aspirin, she is much more likely to follow through because it’s based on personalized screening test.”
Study background and details:
- The study was conducted between 2014 and 2020 at five health centers across Canada. Of note: Canada has a national health care service, and coverage is universal for all Canadian citizens and permanent residents.
- 7,554 women who were pregnant for the first time were recruited between 11 and 14 weeks of pregnancy. 7,325 delivered after 20 weeks and remained eligible for the final analysis; 229 had pregnancies with fetal anomalies and were excluded from the analyses for the study.
- At time of enrollment in the study, participants underwent screening for preeclampsia. The data collected included age, weight, ethnicity, smoking status and chronic health conditions (chronic hypertension, Type 1 diabetes or Type 2 diabetes and antiphospholipid syndrome, an autoimmune disease that may be associated with pregnancy complications).
- The study participants had an average age of 29 years. 92% of participants self-identified as white; 4% as Black; 2.6% as South Asian; 0.9% as East Asian; 0.3% as First Nations; and 0.2% as mixed race or undetermined.
- The study excluded women who were taking antihypertensive medication for chronic hypertension, low-dose aspirin or low-molecular-weight-heparin (a blood thinner) on a daily basis were excluded from the study.
- Participants were followed until delivery. The primary outcome was preterm preeclampsia. The secondary outcome was early preeclampsia.
- Of the 7,325 women included in the analysis, 65 (0.9%) developed preterm preeclampsia, and 22 (0.3%) developed early preeclampsia.
Among the study’s limitations, several women with risk factors for preeclampsia, such as high blood pressure and Type 2 diabetes before pregnancy, were not included in the study if they were already taking aspirin for preeclampsia prevention. This would make it difficult to determine whether this population would rely solely on the Fetal Medicine Foundation’s screening model to decide whether or not to take daily, low-dose aspirin, Bujold noted. Additionally, only one lab was used to analyze blood samples, and blood samples collected at other centers across Canada were frozen and shipped for analysis, meaning that biomarkers were measured several weeks after the blood was drawn, which may have affected the results.
“It's reasonable to believe that the inclusion of the entire population and immediate analysis of blood samples may both have improved the screening process. If we implemented a screening program in big cities across North America, the screening would be expected to be even better and more accurate,” Bujold said. “The good news is that we now have a more precise screening approach using existing tests that can predict preeclampsia early in pregnancy. The next step is to make this screening available to all pregnant women so that more women could receive a diagnosis early in pregnancy and begin preventative aspirin treatment, potentially preventing complications of severe preeclampsia.”
According to Sadiya S. Khan, M.D., M.Sc., FAHA, chair of the writing group for the Association’s 2023 scientific statement on Optimizing Prepregnancy Cardiovascular Health to Improve Outcomes in Pregnant and Postpartum Individuals and Offspring, predicting risk for term and preterm preeclampsia remains an important goal and priority to improve maternal health and mitigate disparities. Khan is the Magerstadt Professor of Cardiovascular Epidemiology and an associate professor of medicine and preventive medicine at the Northwestern University Feinberg School of Medicine in Chicago and a preventive cardiologist at Northwestern Medicine.
“Since the risks for preeclampsia may be largely influenced by health before pregnancy, the ability of a screening model to be applied in early pregnancy is very helpful and can initiate conversations between the clinician and patient about strategies to optimize heart health,” Khan said. “However, challenges remain with implementation of models such as this one that integrate biomarkers that are not routinely assessed and may not be widely available, especially among people in vulnerable populations who are most likely to have the highest risk for preterm preeclampsia.”
Co-authors, disclosures and funding sources are listed in the manuscript.
Studies published in the American Heart Association’s scientific journals are peer-reviewed. The statements and conclusions in each manuscript are solely those of the study authors and do not necessarily reflect the Association’s policy or position. The Association makes no representation or guarantee as to their accuracy or reliability. The Association receives funding primarily from individuals; foundations and corporations (including pharmaceutical, device manufacturers and other companies) also make donations and fund specific Association programs and events. The Association has strict policies to prevent these relationships from influencing the science content. Revenues from pharmaceutical and biotech companies, device manufacturers and health insurance providers and the Association’s overall financial information are available here .
Additional Resources:
- Multimedia is available on the right column of release link http://newsroom.heart.org/news/personalized-screening-early-in-pregnancy-may-improve-preeclampsia-detection?preview=3ce33b2428f817ce1d7a432efe2ced08
- After May 6, 2024, view the manuscript online .
- AHA news release: Scheduled childbirth may greatly reduce preeclampsia, a leading cause of maternal death (April 2023)
- AHA news release: Severe preeclampsia treated safely with nifedipine during labor and delivery (October 2022)
- AHA news release: Following a Mediterranean-style diet during pregnancy may reduce the risk of preeclampsia (April 2022)
- AHA health information: Preeclampsia and High Blood Pressure
- Follow AHA/ASA news on X (formerly known as Twitter) @HeartNews
- Follow news from AHA’s Hypertension journal @HyperAHA
About the American Heart Association
The American Heart Association is a relentless force for a world of longer, healthier lives. We are dedicated to ensuring equitable health in all communities. Through collaboration with numerous organizations, and powered by millions of volunteers, we fund innovative research, advocate for the public’s health and share lifesaving resources. The Dallas-based organization has been a leading source of health information for a century. During 2024 - our Centennial year - we celebrate our rich 100-year history and accomplishments. As we forge ahead into our second century of bold discovery and impact, our vision is to advance health and hope for everyone, everywhere. Connect with us on heart.org , Facebook , X or by calling 1-800-AHA-USA1.
Hypertension
10.1161/HYPERTENSIONAHA.123.22584
Article Title
Prospective Validation of First-Trimester Screening for Preterm Preeclampsia in Nulliparous Women (PREDICTION Study)
Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system.
Original Source
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Research Adds Insights Into Preeclampsia, a Deadly Pregnancy Complication
Hydroxychloroquine is a potential treatment.
Preeclampsia is a dangerous complication during pregnancy that endangers both the mother and fetus, but clinicians still don’t have an effective way of predicting who will develop it. New research has uncovered a possible mechanism for how this potentially life-threatening condition occurs and the potential of the immunosuppressive drug hydroxychloroquine to treat it.
Researchers knew that in pregnancies complicated by preeclampsia, the development of the placenta is impaired, but they know little about how this happens. Furthermore, they knew that levels of placental DNA in the mother’s blood, known as cell-free fetal DNA (cffDNA), are significantly higher in women who experience preeclampsia. So, a team led by Vikki Abrahams, PhD , professor of obstetrics, gynecology & reproductive sciences, studied the interactions of cultured placental cells called trophoblasts with levels of cffDNA observed in preeclampsia, and they found that this significantly inhibited the movement of the trophoblasts. The team also found that treatment with hydroxychloroquine reversed the effects of cffDNA on the trophoblasts. They published their findings in the Journal of Reproductive Immunology on April 5.
All of these pathological processes seemed to be coming from the placenta, but we didn’t know how or why. Vikki Abrahams, PhD
“Our research is giving us insight into how high levels of cffDNA that we see in women with preeclampsia might be acting in a pathological way,” says Abrahams, who was the paper’s senior author. “It’s informing us about how cell-free fetal DNA is negatively impacting trophoblast function and the process of placentation, as well as some insight into a potential therapeutic that could be used to at least stop that part of the disease.”
Preeclampsia Symptoms Are Linked to the Placenta
Preeclampsia, in which women experience highly elevated blood pressure, is a condition that normally manifests in the late second, or third, trimester of pregnancy. If not adequately controlled, it can cause the mother to have seizures and also harm the developing fetus. The only current remedy for the condition is to deliver the baby and placenta.
Scientists have made an intriguing observation that if a clinician delivers the baby but not the placenta, women will continue to experience symptoms of preeclampsia until the placenta is also delivered. “All of these pathological processes seemed to be coming from the placenta, but we didn’t know how or why,” says Abrahams.
While preeclampsia develops later during pregnancy, researchers believe that the origins of the disease may occur much earlier, during implantation and placental development. In women with preeclampsia, researchers have noticed abnormalities at the maternal-fetal interface—where the placenta and maternal endometrium [mucus membrane lining the uterus] meet. During a normal pregnancy, trophoblasts migrate into the endometrium, an essential process for anchoring the placenta and allowing the placental cells to interact with maternal immune cells that is necessary. However, in cases of preeclampsia, there is insufficient migration of the trophoblasts, which impairs normal placental development. Furthermore, research has shown a strong inflammatory response at the maternal-fetal interface in cases of preeclampsia.
During a normal pregnancy, the placenta continuously sheds material, including cffDNA, from its surface. It enters the mother’s blood stream and circulates throughout her body. Throughout the pregnancy, levels of cffDNA rise as the placenta grows and sheds more material, and after delivery, the levels completely drop off. In cases of preeclampsia, the levels of cffDNA rise significantly higher compared to a normal pregnancy. “We wondered if cffDNA was having a functional effect that was leading to the development of preeclampsia,” says Abrahams. “So, we decided to examine this locally in terms of placentation.”
Identifying Potential Mechanism for Impaired Placental Development
In their latest study, Abrahams’ team isolated cffDNA and added it to fresh cultures of trophoblast cells. Then, they measured the ability of the trophoblasts to spontaneously migrate in the presence and absence of the cffDNA. They found that cffDNA significantly inhibited the trophoblasts' ability to migrate.
This finding uncovered clues about preeclampsia’s mechanism. cffDNA, says Abrahams, is different from adult DNA. The differences in structure of cffDNA have similarities to bacterial DNA, and consequentially, it gets recognized as such by an innate immune receptor called Toll-like receptor 9 (TLR9).
Intrigued, the team added a synthetic TLR9 inhibitor to the culture and found that it reversed the inhibition of trophoblast migration. “We found that the inhibition of trophoblast migration by cffDNA is TLR9-mediated,” says Abrahams. “Its interaction with cffDNA causes a downregulation of the ability of trophoblast cells to spontaneously migrate.”
Hydroxychloroquine Reverses Pathological Mechanism of Preeclampsia
Next, the team examined whether various therapeutics may be useful in treating this pathological mechanism, including aspirin and hydroxychloroquine. Previous research suggested that aspirin, an anti-inflammatory drug, may be useful in preventing symptoms of preeclampsia in women at high risk. So, they added aspirin to the trophoblast cultures to see if it would reverse the effects of cffDNA on migration, but it had no effect.
The team then turned their attention to hydroxychloroquine, a drug that is often given to patients with autoimmune diseases such as lupus and is safe to use during pregnancy. It also is a TLR9 inhibitor. They found that this medication did indeed restore the trophoblasts’ ability to migrate. “This not only underscores the role of TLR9 as the mechanism by which cffDNA is inhibiting trophoblast migration, but also gives us a potential therapeutic that could be useful in a targeted way if given early in pregnancy,” says Abrahams.
Abrahams hopes her work will lead to finding better ways for treating women with preeclampsia. “Now that we have an idea of how this cffDNA might be functioning during pregnancy, I’m hoping we can turn it into more studies to help us gain a better understanding of cffDNA function at the maternal-fetal interface, so that we can figure out more ways to promote healthy pregnancies in women,” she says.
Featured in this article
- Vikki M Abrahams, PhD Professor, Obstetrics, Gynecology & Reproductive Sciences; Director, Division of Reproductive Sciences, Department of Obstetrics, Gynecology & Reproductive Sciences; Co-Vice Chair of Faculty Development, Department of Obstetrics, Gynecology & Reproductive Sciences

Risk of adverse pre-eclampsia outcomes accurately identified through new AI model
A potentially lifesaving model for identifying maternal risk in pregnant women with pre-eclampsia has been developed by researchers.
More than 8,800 women in 11 countries took part in the study, which accurately classified women's risk of adverse outcomes of the blood pressure condition in five categories, ranging from very low to very high, within two days of their first assessment.
Pre-eclampsia occurs in between 2% and 4% of pregnancies and is a leading global cause of maternal morbidity and mortality. It causes an estimated 46,000 maternal deaths, and half a million stillbirths and newborn deaths a year, nearly all occurring in low- and middle-income countries.
The majority of the pregnant women who develop pre-eclampsia have mild disease which ends soon after they give birth. However, about 1 in 10 of these women in the U.K. experience life-threatening or life-changing complications, such as stroke.
The new risk-prediction model has been designed to be used internationally and its operation is based on machine learning, a form of AI.
The researchers from the University of Strathclyde in Glasgow, and King's College London now aim to develop an app for determining an individual woman's risk of suffering adverse outcomes of pre-eclampsia after they are diagnosed.
The model, named PIERS-ML (Pre-eclampsia Integrated Estimate of Risk—Machine Learning), consolidates two previous versions of the model. The research paper has been published in The Lancet Digital Health .
Tunde Csobán, a Research Assistant in Strathclyde's Department of Mathematics and Statistics, the lead author of the paper, said, "Pre-eclampsia presents considerable, often fatal, risks to women and their children. There is an urgent need for an effective means of assessing these risks, so that they can be managed and support can be offered."
Dr. Kimberley Kavanagh, Senior Lecturer in Strathclyde's Department of Mathematics and Statistics and a co-author of the paper, said, "The model we have developed has been rigorously tested and shown to deliver fast, precise predictions of the risks, in a way which can be adapted to the individual circumstances of women around the world.
"We hope to make it available on an app which can be used in clinical settings—and potentially save many lives."
The project's Principal Investigator, Professor Peter von Dadelszen, Professor of Global Women's Health, King's College London, said, "The longer a woman remains pregnant, generally the better the outcome is for the baby but in pre-eclampsia, the placental problems that are underlying the process are getting worse.
"We started developing a model that would objectively measure the risks of pre-eclampsia in 2001. We have now taken the data we obtained from the previous versions, fullPIERS and miniPIERS, and came up with the machine learning approach that produced the best model."
"One of the innovative things we have done with the modeling is to include the countries' GDPs and their national maternal mortality ratios. Including these variables means that the model automatically adjusts according to where a woman is living and makes it a globally relevant model. This is a very important research paper and is probably the most generalizable model there is for pre-eclampsia. It's fantastic to see how well it works."
The study recruited 8,843 women from 53 maternity units in 11 low-income, middle-income countries, and high-income countries: Brazil; Fiji; Pakistan; South Africa; Uganda; Australia; Canada; Finland; New Zealand; the UK and the US. The maternal risk categories were defined as very low, low, moderate, high or very high.
The records of a further 2,901 women from South-East England were used for an externally validation exercise for the model, which confirmed the performance of the main study.
More information: Tünde Montgomery-Csobán et al, Machine learning-enabled maternal risk assessment for women with pre-eclampsia (the PIERS-ML model): a modelling study, The Lancet Digital Health (2024). DOI: 10.1016/S2589-7500(23)00267-4
Provided by University of Strathclyde, Glasgow


- JOIN A PROMISE WALK
- WOMEN & FAMILIES
- HEALTHCARE PROVIDERS
- Signs & Symptoms
- What is Preeclampsia
- What is Eclampsia
- HELLP Syndrome
- Postpartum Preeclampsia
- Preeclampsia Tests
- Long Term Impact
- Taking Your Blood Pressure
- COVID & preeclampsia
- Birth Trauma Resources
- Our Stories
- Ask a Support Question
- The Patient Journey
- Support Articles
- Participate in Research
- Share your Story
- Policy Priorities
- Materials for Advocates
- Other Resources
- Advocacy History
- Corporate Partners
- Ways to Give
- Do It Yourself Fundraising
- Shop for the Cause
- Become a Trained Advocate
- News & Events
- The Cuff Kit™
- Current Guidelines
- Prenatal Aspirin
- Blood Pressure
- Postpartum Care
- Educating Patients
- Mommas Voices
- Nurse Resources
- Doula Resources
- About the Registry
- Registry Privacy Policy
- Preeclampsia Registry FAQs
- Take 10 for Preeclampsia Research
- Peter J. Pappas recipients
- Vision Grant recipients
- Research Results
- Research Roundup
- Ask an Expert
- Press Releases
- Video Library
- Awareness Month
- Start a Promise Walk
- Host a fundraiser
- Ways to give
- Give Every Month
- Board of Directors
- Patient Advisory Council
- Medical Advisory Board
1591366604.png)
Research News
Keeping current on all preeclampsia research.

Preeclampsia is a life-threatening hypertensive disorder, affecting 2%–5% of pregnancies, that remains poorly understood. In a recent study published by Physiological Genomics that was partially funded by the Preeclampsia Foundation's...
Echocardiography, commonly referred to as cardiac ultrasound or an “echo”, generates visual images of the heart known as echocardiograms. This imaging technique is especially informative during the peripartum period, the time encompassing...

There is an increased cardiovascular risk after a pregnant woman has preeclampsia. Previous research found that there are signs of early cardiovascular aging when a woman is six months postpartum. This study looked at women when they were six mo...

The accuracy of medical history is critical for the care of any patient. Preeclampsia increases the risk of complications in future pregnancies and is also associated with an increased risk of cardiovascular disease (CVD). The ability of patients to...

The authors of this paper note that an increasing number of people are being readmitted to the hospital within six weeks of discharge home after delivery and that many of these persons had a hypertensive disorder of pregnancy (HDP). Utilizing data fr...

This study aimed to examine the performance of two algorithms for diagnosis of hypertensive disorders of pregnancy (HDP) with medical record data from a large cohort of pregnant women. In this article, the researchers emphasize the importan...

New Preeclampsia Research Funded to Investigate Genetic Targets to Develop Potential Therapeutics
1707833797.png)
Research Funding Available for Preeclampsia and Related Pregnancy Disorders
North Bethesda, MD – February 10, 2024—The Foundation for the National Institutes of Health (FNIH) today announced the launch of a new public-private partnership to develop tools to identify pregnant women at high risk of early-onset pree...

A study between the UNC Chapel-Hill and Orange County Health Department, called “Thriving Hearts: Healing-Centered, Integrated, Community Maternity Care,” has been approved for a $21-million funding award from the Patient-Centered Outcome...

Preeclampsia Foundation Canada has announced that Kylie Belchamber, PhD of University of Birmingham, and Serena Gundy, MD, FRCP of McMaster University, are their 2023 Vision Grant research award recipients. These highly competitive monetary awards re...
New preeclampsia research funded by Preeclampsia Foundation Peter J. Pappas grant finds distinct genetic traits of early-onset preeclampsia.
- Share full article
Advertisement
Supported by
Aspirin Can Prevent a Deadly Pregnancy Complication. Why Aren’t Women Told?

By Roni Caryn Rabin
Baby aspirin is routinely prescribed to people who survive heart attacks. But there’s another vulnerable group who benefit from daily low-dose aspirin: pregnant women at risk of developing pre-eclampsia, life-threatening high blood pressure.
It’s a factor in up to one in 20 pregnancies in the United States, and one of the leading causes of maternal mortality nationwide . Pre-eclampsia is the top cause of maternal death among Black women, who die of pregnancy-related complications at rates almost triple those of white women.
But not enough pregnant women are getting the word that low-dose aspirin can help. Now leading experts are hoping to change that.

Back Story: Aspirin reduces the odds of certain complications.
The U.S. Preventive Services Task Force, an influential panel of experts that issues national guidance, has for 10 years been recommending that women who are at risk for pre-eclampsia start taking baby aspirin when they are 12 weeks pregnant.
Both the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine support the recommendation, saying low-dose aspirin is safe and not likely to cause complications. The optimal time to start is before 16 weeks of pregnancy, though it can be initiated later, the groups advise.
Those at risk for developing pre-eclampsia include anyone who had pre-eclampsia during a previous pregnancy, as well as those carrying twins, triplets or other multiples; those who have kidney disease, autoimmune disease, Type 1 or Type 2 diabetes; and those with chronic hypertension.
A pregnant woman may also be at risk if she is pregnant for the first time, is 35 or older, has a body mass index greater than 30, or has a family history of pre-eclampsia.
Taking aspirin reduces the risk of pre-eclampsia by 15 percent , while reducing the risk of premature birth by 20 percent and reducing the risk of another complication, intrauterine growth restriction, by 18 percent, studies have found.
The Problem: Women and their doctors haven’t gotten the news.
Despite all the data, too few pregnant women at risk are taking baby aspirin, and too few doctors recommend it. A 2022 study found that Black women are less likely to be told to take baby aspirin, even when they meet the criteria.
Pre-eclampsia itself is far from a household term: One in five families, and one in four Black families, has never heard of it, according to a new survey conducted by the Harris Poll for the March of Dimes.
In addition, only about one in five families surveyed said they were familiar with interventions like baby aspirin.
“Baby aspirin has been out there for a while, but a lot of patients don’t know about it and a lot of providers aren’t screening patients appropriately,” said Dr. Elizabeth Cherot, president and chief executive of the March of Dimes.
“It’s low-dose aspirin,” she added. “It’s over-the-counter, it’s available, it’s accessible. But there seem to be barriers preventing high-risk patients from taking it as a preventive measure.”
The Fix: A national campaign to raise awareness.
The March of Dimes, which fights for the health of mothers and babies, on Wednesday announced it was starting a campaign called “Low Dose, Big Benefits,” to raise awareness among health providers and pregnant women regarding the benefits of low-dose aspirin.
The campaign features the U.S. Olympian Allyson Felix, who developed pre-eclampsia during her first pregnancy and had to have an emergency cesarean section at 32 weeks.
Having had the condition once, Ms. Felix knew she might develop it again during her second pregnancy, so she decided to take baby aspirin. She had a normal full-term pregnancy with her second child, who was born on April 10.
“This project is about getting the message out there for families and pregnant people as well as health care personnel,” Dr. Cherot said. “Patients should be asking their providers about low-dose aspirin.”
Roni Caryn Rabin is a Times health reporter focused on maternal and child health, racial and economic disparities in health care, and the influence of money on medicine. More about Roni Caryn Rabin
Pregnancy, Childbirth and Postpartum Experiences
Aspirin’s Benefits: Not enough pregnant women at risk of developing pre-eclampsia, life-threatening high blood pressure, know that low-dose aspirin can help lower that risk. Leading experts are hoping to change that.
‘A Chance to Live’: Cases of trisomy 18 may rise as many states restrict abortion. Some women have chosen to have these babies , love them tenderly and care for them devotedly.
Teen Pregnancies: A large study in Canada found that women who were pregnant as teenagers were more likely to die before turning 31 .
Weight-Loss Drugs: Doctors say they are seeing more women try weight-loss medications in the hopes of having a healthy pregnancy. But little is known about the impact of those drugs on a fetus.
Premature Births: After years of steady decline, premature births rose sharply in the United States between 2014 and 2022. Experts said the shift might be partly the result of a growing prevalence of health complications among mothers .
Depression and Suicide: Women who experience depression during pregnancy or in the year after giving birth have a greater risk of suicide and attempted suicide .
New Screening For A Dangerous Pregnancy Condition Could Save Lives
Parenting reporter

It’s difficult to imagine someone in better physical condition than an Olympic athlete, which is why it came as a shock last year when three-time medalist Tori Bowie died from complications in childbirth at the age of 32. Bowie’s death may have been caused by eclampsia, a life-threatening condition that can develop from preeclampsia, which is a disease of pregnancy marked by high blood pressure and impaired kidney function.
Dr. Christine Greves , an OB-GYN at Orlando Health Women’s Institute in Florida, explained to HuffPost: “Eclampsia means seizure. So [preeclampsia is] what you experience before you have a seizure. Obviously, we do not want anybody to have a seizure.” This kind of seizure can be fatal.
Preeclampsia affects approximately 5% of pregnant people, with a disproportionate number of Black people impacted. (Overall, Black women and birthing people in the U.S. are three times more likely than white people to die of pregnancy complications.) The reasons for this racial disparity are poorly understood.
“Research is needed to explore why biological and psychological [and] social determinants of health [are] contributing to pregnancy-related disparities in preeclampsia,” Greves said.
The disparities are clear, she continued, but “we need to understand the why in order to try to help more.”
She added, “Some centers like ours recognize the disparities and are incorporating strategies with more access to help.”
Preeclampsia is also a leading cause of maternal mortality worldwide.
If you’ve been pregnant, you know that prenatal visits always involve taking your blood pressure and testing a urine sample. These procedures detect those two major markers of preeclampsia: high blood pressure and protein in the urine. Because preeclampsia can become life-threatening, health care providers are eager to catch it early so that they can monitor patients closely.
Now, researchers have discovered a new screening method that is able to detect signs of preeclampsia more effectively and even earlier in pregnancy, giving doctors a chance to prevent the condition from developing — and potentially saving lives. Here’s what you need to know.
What preeclampsia screening and treatment currently look like.
Providers monitor patients’ blood pressure and check their urine throughout pregnancy, and with greater frequency towards the end of pregnancy, when preeclampsia is most likely to develop. Preeclampsia can even occur postpartum, after delivery.
In addition, patients with risk factors for developing preeclampsia are given a daily dose of aspirin, starting by the 16th week of their pregnancy, as previous research has shown that it effectively reduces the rate of preeclampsia in people who are at risk.
“A spirin prevents the majority of preeclampsias when started in the first trimester of pregnancy,” Dr. Emmanuel Bujold, one of the study’s authors, told HuffPost.
For this reason, currently, pregnant people who meet one or more of the following severe risk factors, or two or more of the following moderate risk factors are advised to start taking aspirin by 16 weeks, Bujold said.
Moderate risk factors:
- It is your first pregnancy
- You are Black
- You have obesity
- You became pregnant through IVF
- You are over 40 or under 18 years old
- There is a family history of preeclampsia
Severe risk factors:
- You have a personal history of preeclampsia (a previous pregnancy with preeclampsia)
- You have chronic hypertension
- You have diabetes
- You have Lupus
Other diseases and conditions can also increase risk. Greves noted that even a mental health condition, post-traumatic stress disorder, has been correlated with an increased risk of preeclampsia.
Bujold explained that by these criteria, about 35% of non-Black pregnant people, and over 50% of Black pregnant people, are advised to take aspirin.
The aspirin treatment is “ relatively safe and highly effective,” Bujold said.
You might wonder, if aspirin is so safe, why all pregnant people aren’t simply told to take it starting at 16 weeks. Bujold says this has been proposed in some places, such as Brazil, but has met with little success.
“I n the absence of screening, compliance with treatment is much poorer, follow-up is absent, and the risk of incorrect dosage and errors is high,” he said. In other words, p eople are less likely to follow through on a blanket recommendation than they are on one that is based on their own, personal risk. Greves also mentioned that while small, there is a risk of bleeding from taking aspirin.
If preeclampsia does develop, doctors will monitor a patient closely and treat their symptoms, but, unfortunately the only cure is delivery. This can leave doctors and patients in an impossible bind. You want to deliver the baby before the pregnant person becomes seriously ill, but you also want to delay delivery as long as possible for the health of the baby. Babies born at 28 weeks of gestation or later have 80-90% odds of survival , whereas babies born before 24 weeks have odds below 50%, in addition to a 40% chance of developing long-term health problems.
How the newly-proposed screening method would work.
Bujold and his co-authors conducted a study of over 7,000 Canadian women. Some were screened for preeclampsia using only a tally of the risk factors, as explained above. Others were also given a blood test which identified biomarkers associated with preeclampsia.
The results of this blood test, along with those from an ultrasound, a blood pressure reading, and the patient’s health history were then “ integrated into a computer algorithm that indicates whether or not the woman is at risk,” Bujold said.
Using the new screening method, Bujold said, researchers were able to detect about two-thirds of the cases of severe (before 37 weeks) cases of preeclampsia and about three-quarters of very severe (before 34 weeks) cases. This represents a significant improvement over the current screening method based on risk factors alone, which identifies about half of cases.
The rate of false positives — a person is labeled at risk but does not go on to develop preeclampsia — is also lower using the new screening method. Its rate of false positives is around 16%, meaning “one woman in six is worried when she won’t develop preeclampsia,” explained Bujold, while the rate of false positives for the current method is twice as high: 34%, or 1 in 3.
What patients need to know.
While the ability to test for these biomarkers and calculate a person’s individual risk of developing preeclampsia is promising, these tests are not widely available yet. For now, Greves said, if you are pregnant, the most important things are to listen to your health care provider and to your body. If you are having headaches that don’t go away with Tylenol, or other symptoms, let your provider know. And if your provider asks you to take aspirin or check your blood pressure, it’s important that you follow through.
Screening can prevent some, but not all, cases of preeclampsia.
“Recognize that it doesn’t mean you did anything wrong if you have it,” Greves said. “Some people are just more predisposed than others.”
Engaging in regular physical activity, going to all of your prenatal appointments, following your provider’s recommendations and reporting any worrisome symptoms to them are things you can do to increase your chances of a healthy pregnancy, whether or not you happen to have any risk factors.
Our 2024 Coverage Needs You
It's another trump-biden showdown — and we need your help, the future of democracy is at stake, your loyalty means the world to us.
As Americans head to the polls in 2024, the very future of our country is at stake. At HuffPost, we believe that a free press is critical to creating well-informed voters. That's why our journalism is free for everyone, even though other newsrooms retreat behind expensive paywalls.
Our journalists will continue to cover the twists and turns during this historic presidential election. With your help, we'll bring you hard-hitting investigations, well-researched analysis and timely takes you can't find elsewhere. Reporting in this current political climate is a responsibility we do not take lightly, and we thank you for your support.
Contribute as little as $2 to keep our news free for all.
Can't afford to donate? Support HuffPost by creating a free account and log in while you read.
The 2024 election is heating up, and women's rights, health care, voting rights, and the very future of democracy are all at stake. Donald Trump will face Joe Biden in the most consequential vote of our time. And HuffPost will be there, covering every twist and turn. America's future hangs in the balance. Would you consider contributing to support our journalism and keep it free for all during this critical season?
HuffPost believes news should be accessible to everyone, regardless of their ability to pay for it. We rely on readers like you to help fund our work. Any contribution you can make — even as little as $2 — goes directly toward supporting the impactful journalism that we will continue to produce this year. Thank you for being part of our story.
It's official: Donald Trump will face Joe Biden this fall in the presidential election. As we face the most consequential presidential election of our time, HuffPost is committed to bringing you up-to-date, accurate news about the 2024 race. While other outlets have retreated behind paywalls, you can trust our news will stay free.
But we can't do it without your help. Reader funding is one of the key ways we support our newsroom. Would you consider making a donation to help fund our news during this critical time? Your contributions are vital to supporting a free press.
Contribute as little as $2 to keep our journalism free and accessible to all.
Dear HuffPost Reader
Thank you for your past contribution to HuffPost. We are sincerely grateful for readers like you who help us ensure that we can keep our journalism free for everyone.
The stakes are high this year, and our 2024 coverage could use continued support. Would you consider becoming a regular HuffPost contributor?
The stakes are high this year, and our 2024 coverage could use continued support. If circumstances have changed since you last contributed, we hope you'll consider contributing to HuffPost once more.
Already contributed? Log in to hide these messages.
Popular in the Community
From our partner, huffpost shopping’s best finds, more in life.

IMAGES
VIDEO
COMMENTS
Preeclampsia should be viewed as a disease spectrum in which different subtypes may vary greatly in disease mechanisms and clinical presentations. The status of a previously normotensive pregnant woman developing new onset of hypertension after GA 20 weeks is termed "gestational hypertension" or "pregnancy induced hypertension".
The women, who were an average 29 years old and mostly white, were between 11 and 14 weeks pregnant when the study began. Preterm preeclampsia developed in 65 women and early-onset preeclampsia occurred in 22. The new screening model predicted preterm preeclampsia in 63% of cases and early-onset preeclampsia in 77%, with a false positive rate ...
Preeclampsia complicates 2 to 4% of all pregnancies and accounts for about 46,000 maternal deaths and 500,000 fetal or newborn deaths each year. Antihypertensive agents and magnesium sulfate can he...
Future research must investigate the pathogenesis of pre-eclampsia, in particular of term and postpartum pre-eclampsia, and evaluate new prognostic tests and treatments in adequately powered ...
DALLAS, May 6, 2024 — A new screening algorithm for preeclampsia combining maternal history, ultrasound data and several tests for blood markers may better predict the majority of preeclampsia cases in the first trimester of pregnancy, when it may still be preventable, according to new research published today in Hypertension, an American ...
Reviewed by Emily Henderson, B.Sc. Apr 28 2023. A new special report published in the American Journal of Obstetrics and Gynecology ( AJOG) provides a groundbreaking approach to preeclampsia, one ...
Pre-eclampsia is a heterogeneous, multisystemic disorder characterized by the onset of hypertension (high blood pressure) and proteinuria (protein in the urine) in a pregnant women in the second ...
Hypertension Research - HTN hypertension, HDP hypertensive disorders of pregnancy, PE preeclampsia, BP blood pressure, cfDNA cell-free DNA, ST2 human suppression of tumorigenesis 2, sFlt-1 soluble ...
Hydroxychloroquine in Lupus Pregnancy and Risk of Preeclampsia. Last Updated on January 25, 2024. Using a large insurance-based database, we did not observe a decreased risk of preeclampsia associated with HCQ treatment in pregnancy, although we cannot rule out residual and unmeasured confounding and misclassification.
Preeclampsia is pregnancy-specific, and significantly contributes to maternal, and perinatal morbidity and mortality worldwide. An effective predictive test for preeclampsia would facilitate early diagnosis, targeted surveillance and timely delivery; however limited options currently exist. A first-trimester screening algorithm has been developed and validated to predict preterm preeclampsia ...
In 2016, Sharma, a leading preeclampsia researcher, and his team had identified that preeclampsia and diseases like Alzheimer's had similar root causes related to protein issues. This research ...
Preeclampsia, in particular, is one of the most feared complications of pregnancy. Often presenting as new-onset hypertension and proteinuria during the third trimester, preeclampsia can progress rapidly to serious complications, including death of both mother and fetus.
The research team collected biological samples at two or three points in pregnancy (early, mid and late) in 49 women, of whom 29 developed preeclampsia during their pregnancies and 20 did not. The participants were selected from a larger cohort of women who had donated biological samples for pregnancy research at Stanford Medicine.
Using the Fetal Medicine Foundation's screening model for participants between 11 and 13 weeks of pregnancy, the preeclampsia detection rate was 63.1% for preterm preeclampsia (before 37 weeks of ...
Abstract. To the Editor: Omitted from the list of "factors conferring maternal predisposition" to preeclampsia in the review article by Magee et al. (May 12 issue) 1 was a well-established ...
July 3, 2023. The Food and Drug Administration has approved a blood test that can identify pregnant women who are at imminent risk of developing a severe form of high blood pressure called pre ...
A new screening algorithm for preeclampsia combining maternal history, ultrasound data and several tests for blood markers may better predict the majority of preeclampsia cases in the first ...
Orlando, FL - February 2, 2022 - The Preeclampsia Foundation announced today the recipients of its 2022 Peter Joseph Pappas Research Grants at the Society for Maternal Fetal Medicine 42nd Annual Pregnancy Meeting. Based on the recommendations of its Preeclampsia Registry Advisory Council, the Preeclampsia Foundation awarded these two-year grants totaling $195,025 USD to Brian Cox, PhD ...
The Research Roundup team consists of diverse researchers who scour the peer-reviewed research journals to highlight the most important, recently published studies in the field of preeclampsia. The results of these studies, which cover everything from basic science to clinical care practices, are summarized in plain language with an explanation ...
According to their research, women with systolic blood pressure levels below 130 mmHg at 16-19 weeks of gestation exhibited a significantly reduced risk of early-onset superimposed preeclampsia ...
Using the Fetal Medicine Foundation's screening model for participants between 11 and 13 weeks of pregnancy, the preeclampsia detection rate was 63.1% for preterm preeclampsia (before 37 weeks ...
New research has uncovered a possible mechanism for how this potentially life-threatening condition occurs and the potential of the immunosuppressive drug hydroxychloroquine to treat it. Researchers knew that in pregnancies complicated by preeclampsia, the development of the placenta is impaired, but they know little about how this happens.
A potentially dangerous spike in blood pressure known as preeclampsia can occur in 1 in every 25 pregnancies, but an accurate test to spot those women at highest risk has remained elusive.
Tunde Csobán, a Research Assistant in Strathclyde's Department of Mathematics and Statistics, the lead author of the paper, said, "Pre-eclampsia presents considerable, often fatal, risks to women ...
Keeping current on all preeclampsia research. April 30, 2024. New Study Reveals Key Genetic Markers for Preeclampsia, Paving Way for Biomarker Development for Preeclampsia. Preeclampsia is a life-threatening hypertensive disorder, affecting 2%-5% of pregnancies, that remains poorly understood. In a recent study published by Physiological ...
Pre-eclampsia itself is far from a household term: One in five families, and one in four Black families, has never heard of it, according to a new survey conducted by the Harris Poll for the March ...
"Research is needed to explore why biological and psychological [and] social determinants of health [are] contributing to pregnancy-related disparities in preeclampsia," Greves said. ... The rate of false positives — a person is labeled at risk but does not go on to develop preeclampsia — is also lower using the new screening method ...