
- Pregnancy Classes


Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
- Management of breech presentation
Evidence review M
NICE Guideline, No. 201
National Guideline Alliance (UK) .
- Copyright and Permissions
Review question
What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy?
Introduction
Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman’s and the baby’s health. The aim of this review is to determine the most effective way of managing a breech presentation in late pregnancy.
Summary of the protocol
Please see Table 1 for a summary of the Population, Intervention, Comparison and Outcome (PICO) characteristics of this review.
Summary of the protocol (PICO table).
For further details see the review protocol in appendix A .
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual 2014 . Methods specific to this review question are described in the review protocol in appendix A .
Declarations of interest were recorded according to NICE’s conflicts of interest policy .
Clinical evidence
Included studies.
Thirty-six randomised controlled trials (RCTs) were identified for this review.
The included studies are summarised in Table 2 .
Three studies reported on external cephalic version (ECV) versus no intervention ( Dafallah 2004 , Hofmeyr 1983 , Rita 2011 ). One study reported on a 4-arm trial comparing acupuncture, sweeping of fetal membranes, acupuncture plus sweeping, and no intervention ( Andersen 2013 ). Two studies reported on postural management versus no intervention ( Chenia 1987 , Smith 1999 ).
Seven studies reported on ECV plus anaesthesia ( Chalifoux 2017 , Dugoff 1999 , Khaw 2015 , Mancuso 2000 , Schorr 1997 , Sullivan 2009 , Weiniger 2010 ). Of these studies, 1 study compared ECV plus anaesthesia to ECV plus other dosages of the same anaesthetic ( Chalifoux 2017 ); 4 studies compared ECV plus anaesthesia to ECV only ( Dugoff 1999 , Mancuso 2000 , Schorr 1997 , Weiniger 2010 ); and 2 studies compared ECV plus anaesthesia to ECV plus a different anaesthetic ( Khaw 2015 , Sullivan 2009 ).
Ten studies reported ECV plus a β2 receptor agonist ( Brocks 1984 , Fernandez 1997 , Hindawi 2005 , Impey 2005 , Mahomed 1991 , Marquette 1996 , Nor Azlin 2005 , Robertson 1987 , Van Dorsten 1981 , Vani 2009 ). Of these studies, 5 studies compared ECV plus a β2 receptor agonist to ECV plus placebo ( Fernandez 1997 , Impey 2005 , Marquette 1996 , Nor Azlin 2005 , Vani 2009 ); 1 study compared ECV plus a β2 receptor agonist to ECV alone ( Robertson 1987 ); and 4 studies compared ECV plus a β2 receptor agonist to no intervention ( Brocks 1984 , Hindawi 2005 , Mahomed 1991 , Van Dorsten 1981 ).
One study reported on ECV plus Ca 2+ channel blocker versus ECV plus placebo ( Kok 2008 ). Two studies reported on ECV plus β2 receptor agonist versus ECV plus Ca 2+ channel blocker ( Collaris 2009 , Mohamed Ismail 2008 ). Four studies reported on ECV plus a µ-receptor agonist ( Burgos 2016 , Liu 2016 , Munoz 2014 , Wang 2017 ), of which 3 compared against ECV plus placebo ( Liu 2016 , Munoz 2014 , Wang 2017 ) and 1 compared to ECV plus nitrous oxide ( Burgos 2016 ).
Four studies reported on ECV plus nitroglycerin ( Bujold 2003a , Bujold 2003b , El-Sayed 2004 , Hilton 2009 ), of which 2 compared it to ECV plus β2 receptor agonist ( Bujold 2003b , El-Sayed 2004 ) and compared it to ECV plus placebo ( Bujold 2003a , Hilton 2009 ). One study compared ECV plus amnioinfusion versus ECV alone ( Diguisto 2018 ) and 1 study compared ECV plus talcum powder to ECV plus gel ( Vallikkannu 2014 ).
One study was conducted in Australia ( Smith 1999 ); 4 studies in Canada ( Bujold 2003a , Bujold 2003b , Hilton 2009 , Marquette 1996 ); 2 studies in China ( Liu 2016 , Wang 2017 ); 2 studies in Denmark ( Andersen 2013 , Brocks 1984 ); 1 study in France ( Diguisto 2018 ); 1 study in Hong Kong ( Khaw 2015 ); 1 study in India ( Rita 2011 ); 1 study in Israel ( Weiniger 2010 ); 1 study in Jordan ( Hindawi 2005 ); 5 studies in Malaysia ( Collaris 2009 , Mohamed Ismail 2008 , Nor Azlin 2005 , Vallikkannu 2014 , Vani 2009 ); 1 study in South Africa ( Hofmeyr 1983 ); 2 studies in Spain ( Burgos 2016 , Munoz 2014 ); 1 study in Sudan ( Dafallah 2004 ); 1 study in The Netherlands ( Kok 2008 ); 2 studies in the UK ( Impey 2005 , Chenia 1987 ); 9 studies in US ( Chalifoux 2017 , Dugoff 1999 , El-Sayed 2004 , Fernandez 1997 , Mancuso 2000 , Robertson 1987 , Schorr 1997 , Sullivan 2009 , Van Dorsten 1981 ); and 1 study in Zimbabwe ( Mahomed 1991 ).
The majority of studies were 2-arm trials, but there was one 3-arm trial ( Khaw 2015 ) and two 4-arm trials ( Andersen 2013 , Chalifoux 2017 ). All studies were conducted in a hospital or an outpatient ward connected to a hospital.
See the literature search strategy in appendix B and study selection flow chart in appendix C .
Excluded studies
Studies not included in this review with reasons for their exclusions are provided in appendix K .
Summary of clinical studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 2 .
Summary of included studies.
See the full evidence tables in appendix D and the forest plots in appendix E .
Quality assessment of clinical outcomes included in the evidence review
See the evidence profiles in appendix F .
Economic evidence
A systematic review of the economic literature was conducted but no economic studies were identified which were applicable to this review question.
A single economic search was undertaken for all topics included in the scope of this guideline. See supplementary material 2 for details.
Economic studies not included in this review are listed, and reasons for their exclusion are provided in appendix K .
Summary of studies included in the economic evidence review
No economic studies were identified which were applicable to this review question.
Economic model
No economic modelling was undertaken for this review because the committee agreed that other topics were higher priorities for economic evaluation.
Evidence statements
Clinical evidence statements, comparison 1. complementary therapy versus control (no intervention), critical outcomes, cephalic presentation in labour.
No evidence was identified to inform this outcome.
Method of birth
Caesarean section.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.74 (95% CI 0.38 to 1.43).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 1.29 (95% CI 0.73 to 2.29).
Admission to SCBU/NICU
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.19 (95% CI 0.02 to 1.62).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.40 (0.08 to 2.01).
Fetal death after 36 +0 weeks gestation
Infant death up to 4 weeks chronological age, important outcomes, apgar score <7 at 5 minutes.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.32 (95% CI 0.01 to 7.78).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.33 (0.01 to 8.09).
Birth before 39 +0 weeks of gestation
Comparison 2. complementary therapy versus other treatment.
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.64 (95% CI 0.34 to 1.22).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.57 (95% CI 0.30 to 1.07).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 1.13 (95% CI 0.66 to 1.94).
- Very low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.33 (95% CI 0.03 to 3.12).
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.48 (95% CI 0.04 to 5.22).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.69 (95% CI 0.12 to 4.02).
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 3. ECV versus no ECV
- Moderate quality evidence from 2 RCTs (N=680) showed that there is clinically important difference favouring ECV over no ECV on cephalic presentation in labour in pregnant women with breech presentation: RR 1.83 (95% CI 1.53 to 2.18).

Cephalic vaginal birth
- Very low quality evidence from 3 RCTs (N=740) showed that there is a clinically important difference favouring ECV over no ECV on cephalic vaginal birth in pregnant women with breech presentation: RR 1.67 (95% CI 1.20 to 2.31).
Breech vaginal birth
- Very low quality evidence from 2 RCTs (N=680) showed that there is no clinically important difference between ECV and no ECV on breech vaginal birth in pregnant women with breech presentation: RR 0.29 (95% CI 0.03 to 2.84).
- Very low quality evidence from 3 RCTs (N=740) showed that there is no clinically important difference between ECV and no ECV on the number of caesarean sections in pregnant women with breech presentation: RR 0.52 (95% CI 0.23 to 1.20).
- Very low quality evidence from 1 RCT (N=60) showed that there is no clinically important difference between ECV and no ECV on admission to SCBU//NICU in pregnant women with breech presentation: RR 0.50 (95% CI 0.14 to 1.82).
- Very low evidence from 3 RCTs (N=740) showed that there is no statistically significant difference between ECV and no ECV on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: Peto OR 0.29 (95% CI 0.05 to 1.73) p=0.18.
- Very low quality evidence from 2 RCTs (N=120) showed that there is no clinically important difference between ECV and no ECV on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.28 (95% CI 0.04 to 1.70).
Comparison 4. ECV + Amnioinfusion versus ECV only
- Very low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.74 (95% CI 0.74 to 4.12).
- Low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.95 (95% CI 0.75 to 1.19).
Comparison 5. ECV + Anaesthesia versus ECV only
- Very low quality evidence from 2 RCTs (N=210) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.16 (95% CI 0.56 to 2.41).
- Very low quality evidence from 5 RCTs (N=435) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.16 (95% CI 0.77 to 1.74).
- Very low quality evidence from 1 RCT (N=108) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on breech vaginal birth in pregnant women with breech presentation: RR 0.33 (95% CI 0.04 to 3.10).
- Very low quality evidence from 3 RCTs (N=263) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.76 (95% CI 0.42 to 1.38).
- Moderate quality evidence from 1 RCT (N=69) showed that there is a clinically important difference favouring ECV plus anaesthesia over ECV alone on admission to SCBU/NICU in pregnant women with breech presentation: MD −1.80 (95% CI −2.53 to −1.07).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 6. ECV + Anaesthesia versus ECV + Anaesthesia
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.13 (95% CI 0.73 to 1.74).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 0.05mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.69 (95% CI 0.37 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.19 (95% CI 0.79 to 1.79).
- Low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.92 (95% CI 0.68 to 1.24).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.08 (95% CI 0.78 to 1.50).
- Very low evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.70 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.17 (95% CI 0.86 to 1.61).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.03 (95% CI 0.77 to 1.37).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.88 (95% CI 0.64 to 1.20).
Comparison 7. ECV + β2 agonist versus Control (no intervention)
- Moderate quality evidence from 2 RCTs (N=256) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on cephalic presentation in labour in pregnant women with breech presentation: RR 4.83 (95% CI 3.27 to 7.11).
- Very low quality evidence from 3 RCTs (N=265) showed that there no clinically important difference between ECV plus β2 agonist and control (no intervention) on cephalic vaginal birth in pregnant women with breech presentation: RR 2.03 (95% CI 0.22 to 19.01).
- Very low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on breech vaginal birth in pregnant women with breech presentation: RR 0.38 (95% CI 0.20 to 0.69).
- Low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.53 (95% CI 0.41 to 0.67).
- Very low quality evidence from 1 RCT (N=48) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RD 0.00 (95% CI −0.08 to 0.08).
- Very low quality evidence from 3 RCTs (N=208) showed that there is no statistically significant difference between ECV plus β2 agonist and control (no intervention) on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD −0.01 (95% CI −0.03 to 0.01) p=0.66.
- Very low quality evidence from 2 RCTs (N=208) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.80 (95% CI 0.31 to 2.10).
Comparison 8. ECV + β2 agonist versus ECV only
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on cephalic vaginal birth in pregnant women with breech presentation: RR 1.32 (95% CI 0.67 to 2.62).
- Very low quality evidence from 1 RCT (N=58) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on breech vaginal birth in pregnant women with breech presentation: RR 0.75 (95% CI 0.22 to 2.50).
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 0.79 (95% CI 0.27 to 2.28).
- Very low quality evidence from 1 RCT (N=114) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.00 (95% CI 0.21 to 4.75).
Comparison 9. ECV + β2 agonist versus ECV + Placebo
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.54 (95% CI 0.24 to 9.76).
- Very low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 1.27 (95% CI 0.41 to 3.89).
- Very low quality evidence from 2 RCTs (N=227) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on breech vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.33 to 2.97).
- Low quality evidence from 4 RCTs (N=532) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.81 (95% CI 0.72 to 0.92)
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.78 (95% CI 0.17 to 3.63).
- Very low quality evidence from 1 RCT (N=124) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 10. ECV + Ca 2+ channel blocker versus ECV + Placebo
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.87 to 1.48).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.90 (95% CI 0.73 to 1.12).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 1.11 (95% CI 0.88 to 1.40).
- High quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: MD −0.20 (95% CI −0.70 to 0.30).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no statistically significant difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.01 to 0.01) p=1.00.
- Low quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.52 (95% 0.05 to 5.02).
Comparison 11. ECV + Ca2+ channel blocker versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=90) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on cephalic presentation in labour in pregnant women with breech presentation: RR 0.62 (95% CI 0.39 to 0.98).
- Very low quality evidence from 2 RCTs (N=126) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 1.26 (95% CI 0.55 to 2.89).
- Very low quality evidence from 2 RCTs (N=132) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on the number of caesarean sections in pregnant women with breech presentation: RR 1.42 (95% CI 1.06 to 1.91).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on admission to SCBU/NICU in pregnant women with breech presentation: Peto OR 0.53 (95% CI 0.05 to 5.22).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 12. ECV + µ-receptor agonist versus ECV only
- High quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.80 to 1.24).
- Low quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 1.00 (95% CI 0.42 to 2.40).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 13. ECV + µ-receptor agonist versus ECV + Placebo
Cephalic vaginal birth after successful ecv.
- High quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on cephalic vaginal birth after successful ECV in pregnant women with breech presentation: RR 1.00 (95% CI 0.86 to 1.17).
Caesarean section after successful ECV
- Low quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after successful ECV in pregnant women with breech presentation: RR 0.97 (95% CI 0.33 to 2.84).
Breech vaginal birth after unsuccessful ECV
- High quality evidence from 3 RCTs (N=186) showed that there is a clinically important difference favouring ECV plus µ-receptor agonist over ECV plus placebo on breech vaginal birth after unsuccessful ECV in pregnant women with breech presentation: RR 0.10 (95% CI 0.02 to 0.53).
Caesarean section after unsuccessful ECV
- Moderate quality evidence from 3 RCTs (N=186) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after unsuccessful ECV in pregnant women with breech presentation: RR 1.19 (95% CI 1.09 to 1.31).
- Low quality evidence from 1 RCT (N=137) showed that there is no statistically significant difference between ECV plus µ-receptor agonist and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03) p=1.00.
Comparison 14. ECV + µ-receptor agonist versus ECV + Anaesthesia
- Moderate quality evidence from 1 RCT (N=92) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on cephalic vaginal birth in pregnant women with breech presentation: RR 1.04 (95% CI 0.84 to 1.29).
- Very low quality evidence from 2 RCTs (N=212) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on the number of caesarean sections in pregnant women with breech presentation: RR 0.90 (95% CI 0.61 to 1.34).
- Very low quality evidence from 1 RCT (N=129) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on admission to SCBU/NICU in pregnant women with breech presentation: RR 2.30 (95% CI 0.21 to 24.74).
- Low quality evidence from 2 RCTs (N=255) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 15. ECV + Nitric oxide donor versus ECV + Placebo
- Very low quality evidence from 3 RCTs (N=224) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.59 to 2.16).
- Low quality evidence from 1 RCT (N=99) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.78 (95% CI 0.49 to 1.22).
- Low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.83 (95% CI 0.68 to 1.01).
Comparison 16. ECV + Nitric oxide donor versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=74) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus nitric oxide donor on cephalic presentation in labour in pregnant women with breech presentation: RR 0.56 (95% CI 0.29 to 1.09).
- Very low quality evidence from 2 RCTs (N=97) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 0.98 (95% CI 0.47 to 2.05).
- Very low quality evidence from 1 RCT (N=59) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on the number of caesarean sections in pregnant women with breech presentation: RR 1.07 (95% CI 0.73 to 1.57).
Comparison 17. ECV + Talcum powder versus ECV + Gel
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic presentation in labour in pregnant women with breech presentation: RR 1.02 (95% CI 0.68 to 1.53).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic vaginal birth in pregnant women with breech presentation: RR 1.08 (95% CI 0.67 to 1.74).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.67 to 1.33).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.96 (95% CI 0.38 to 10.19).
Comparison 18. Postural management versus No postural management
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic presentation in labour in pregnant women with breech presentation: RR 1.26 (95% CI 0.70 to 2.30).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic vaginal birth in pregnant women with breech presentation: RR 1.11 (95% CI 0.59 to 2.07).
Breech vaginal delivery
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on breech vaginal delivery in pregnant women with breech presentation: RR 1.15 (95% CI 0.67 to 1.99).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on the number of caesarean sections in pregnant women with breech presentation: RR 0.69 (95% CI 0.31 to 1.52).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.24 (95% CI 0.03 to 2.03).
Comparison 19. Postural management + ECV versus ECV only
- Moderate quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 1.05 (95% CI 0.80 to 1.38).
- Low quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.13 (95% CI 0.00 to 6.55).
Economic evidence statements
No economic evidence was identified which was applicable to this review question.
The committee’s discussion of the evidence
Interpreting the evidence, the outcomes that matter most.
Provision of antenatal care is important for the health and wellbeing of both mother and baby with the aim of avoiding adverse pregnancy outcomes and enhancing maternal satisfaction and wellbeing. Breech presentation in labour may be associated with adverse outcomes for the fetus, which has contributed to an increased likelihood of caesarean birth. The committee therefore agreed that cephalic presentation in labour and method of birth were critical outcomes for the woman, and admission to SCBU/NICU, fetal death after 36 +0 weeks gestation, and infant death up to 4 weeks chronological age were critical outcomes for the baby. Apgar score <7 at 5 minutes and birth before 39 +0 weeks of gestation were important outcomes for the baby.
The quality of the evidence
The quality of the evidence for interventions for managing a longitudinal lie fetal malpresentation (that is breech presentation) in late pregnancy ranged from very low to high, with most of the evidence being of a very low or low quality.
This was predominately due to serious overall risk of bias in some outcomes; imprecision around the effect estimate in some outcomes; indirect population in some outcomes; and the presence of serious heterogeneity in some outcomes, which was unresolved by subgroup analysis. The majority of included studies had a small sample size, which contributed to imprecision around the effect estimate.
No evidence was identified to inform the outcomes of infant death up to 4 weeks chronological age and birth before 39 +0 weeks of gestation.
There was no publication bias identified in the evidence. However, the committee noted the influence pharmacological developers may have in these trials as funders, and took this into account in their decision making.
Benefits and harms
The committee discussed that in the case of breech presentation, a discussion with the woman about the different options and their potential benefits, harms and implications is needed to ensure an informed decision. The committee discussed that some women may prefer a breech vaginal birth or choose an elective caesarean birth, and that her preferences should be supported, in line with shared decision making.
The committee discussed that external cephalic version is standard practice for managing breech presentation in uncomplicated singleton pregnancies at or after 36+0 weeks. The committee discussed that there could be variation in the success rates of ECV based on the experience of the healthcare professional providing the ECV. There was some evidence supporting the use of ECV for managing a breech presentation in late pregnancy. The evidence showed ECV had a clinically important benefit in terms of cephalic presentations in labour and cephalic vaginal deliveries, when compared to no intervention. The committee noted that the evidence suggested that ECV was not harmful to the baby, although the effect estimate was imprecise relating to the relative rarity of the fetal death as an outcome.
Cephalic (head-down) vaginal birth is preferred by many women and the evidence suggests that external cephalic version is an effective way to achieve this. The evidence suggested ECV increased the chance for a cephalic vaginal birth and the committee agreed that it was important to explain this to the woman during her consultation.
The committee discussed the optimum timing for ECV. Timing of ECV must take into account the likelihood of the baby turning naturally before a woman commences labour and the possibility of the baby turning back to a breech presentation after ECV if it is done too early. The committee noted that in their experience, current practice was to perform ECV at 37 gestational weeks. The majority of the evidence demonstrating a benefit of ECV in this review involved ECV performed around 37 gestational weeks, although the review did not look for studies directly comparing different timings of ECV and their relative success rates.
The evidence in this review excluded women with previous complicated pregnancies, such as those with previous caesarean section or uterine surgery. The committee discussed that a previous caesarean section indicates a complicated pregnancy and that this population of women are not the focus of this guideline, which concentrates on women with uncomplicated pregnancies.
The committee’s recommendations align with other NICE guidance and cross references to the NICE guideline on caesarean birth and the section on breech presenting in labour in the NICE guideline on intrapartum care for women with existing medical conditions or obstetric complications and their babies were made.
ECV combined with pharmacological agents
There were some small studies comparing a variety of pharmacological agents (including β2 agonists, Ca 2+ channel blockers, µ-receptor agonists and nitric oxide donors) given alongside ECV. Overall the evidence typically showed no clinically important benefit of adding any pharmacological agent to ECV except in comparisons with a control arm with no ECV where it was not possible to isolate the effect of the ECV versus the pharmacological agent. The evidence tended toward benefit most for β2 agonists and µ-receptor agonists however there was no consistent or high quality evidence of benefit even for these agents. The committee agreed that although these pharmacological agents are used in practice, there was insufficient evidence to make a recommendation supporting or refuting their use or on which pharmacological agent should be used.
The committee discussed that the evidence suggesting µ-receptor agonist, remifentanil, had a clinically important benefit in terms reducing breech vaginal births after unsuccessful ECV was biologically implausible. The committee noted that this pharmacological agent has strong sedative effects, depending on the dosage, and therefore studies comparing it to a placebo had possible design flaws as it would be obvious to all parties whether placebo or active drug had been received. The committee discussed that the risks associated with using remifentanil such as respiratory depression, likely outweigh any potential added benefit it may have on managing breech presentation.
There was some evidence comparing different anaesthetics together with ECV. Although there was little consistent evidence of benefit overall, one small study of low quality showed a combination of 2% lidocaine and epinephrine via epidural catheter (anaesthesia) with ECV showed a clinically important benefit in terms of cephalic presentations in labour and the method of birth. The committee discussed the evidence and agreed the use of anaesthesia via epidural catheter during ECV was uncommon practice in the UK and could be expensive, overall they agreed the strength of the evidence available was insufficient to support a change in practice.
Postural management
There was limited evidence on postural management as an intervention for managing breech presentation in late pregnancy, which showed no difference in effectiveness. Postural management was defined as ‘knee-chest position for 15 minutes, 3 times a day’. The committee agreed that in their experience women valued trying interventions at home first which might make postural management an attractive option for some women, however, there was no evidence that postural management was beneficial. The committee also noted that in their experience postural management can cause notable discomfort so it is not an intervention without disadvantages.
Cost effectiveness and resource use
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question.
The committee’s recommendations to offer external cephalic version reinforces current practice. The committee noted that, compared to no intervention, external cephalic version results in clinically important benefits and that there would also be overall downstream cost savings from lower adverse events. It was therefore the committee’s view that offering external cephalic version is cost effective and would not entail any resource impact.
Andersen 2013
Brocks 1984
Bujold 2003
Burgos 2016
Chalifoux 2017
Chenia 1987
Collaris 2009
Dafallah 2004
Diguisto 2018
Dugoff 1999
El-Sayed 2004
Fernandez 1997
Hindawi 2005
Hilton 2009
Hofmeyr 1983
Mahomed 1991
Mancuso 2000
Marquette 1996
Mohamed Ismail 2008
NorAzlin 2005
Robertson 1987
Schorr 1997
Sullivan 2009
VanDorsten 1981
Vallikkannu 2014
Weiniger 2010
Appendix A. Review protocols
Review protocol for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 260K)
Appendix B. Literature search strategies
Literature search strategies for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 281K)
Appendix C. Clinical evidence study selection
Clinical study selection for: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 113K)
Appendix D. Clinical evidence tables
Clinical evidence tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.2M)
Appendix E. Forest plots
Forest plots for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 678K)
Appendix F. GRADE tables
GRADE tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.0M)
Appendix G. Economic evidence study selection
Economic evidence study selection for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix h. economic evidence tables, economic evidence tables for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix i. economic evidence profiles, economic evidence profiles for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix j. economic analysis, economic evidence analysis for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No economic analysis was conducted for this review question.
Appendix K. Excluded studies
Excluded clinical and economic studies for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, clinical studies, table 24 excluded studies.
View in own window
Economic studies
No economic evidence was identified for this review.
Appendix L. Research recommendations
Research recommendations for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No research recommendations were made for this review question.
Evidence reviews underpinning recommendation 1.2.38
These evidence reviews were developed by the National Guideline Alliance, which is a part of the Royal College of Obstetricians and Gynaecologists
Disclaimer : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government , Scottish Government , and Northern Ireland Executive . All NICE guidance is subject to regular review and may be updated or withdrawn.
- Cite this Page National Guideline Alliance (UK). Management of breech presentation: Antenatal care: Evidence review M. London: National Institute for Health and Care Excellence (NICE); 2021 Aug. (NICE Guideline, No. 201.)
- PDF version of this title (2.2M)
In this Page
Other titles in this collection.
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 201: Antenatal care
Supplemental NICE documents
- Supplement 1: Methods (PDF)
- Supplement 2: Health economics (PDF)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Identification of breech presentation: Antenatal care: Evidence review L [ 2021] Review Identification of breech presentation: Antenatal care: Evidence review L National Guideline Alliance (UK). 2021 Aug
- Vaginal delivery of breech presentation. [J Obstet Gynaecol Can. 2009] Vaginal delivery of breech presentation. Kotaska A, Menticoglou S, Gagnon R, MATERNAL FETAL MEDICINE COMMITTEE. J Obstet Gynaecol Can. 2009 Jun; 31(6):557-566.
- Review Cephalic version by moxibustion for breech presentation. [Cochrane Database Syst Rev. 2005] Review Cephalic version by moxibustion for breech presentation. Coyle ME, Smith CA, Peat B. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD003928. Epub 2005 Apr 18.
- [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. [Gynecol Obstet Fertil Senol. 2...] [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. Riethmuller D, Ramanah R, Mottet N. Gynecol Obstet Fertil Senol. 2018 Dec; 46(12):937-947. Epub 2018 Oct 28.
- Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. [J Obstet Gynaecol Br Emp. 1961] Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. BAINBRIDGE MN, NIXON WC, SMYTH CN. J Obstet Gynaecol Br Emp. 1961 Oct; 68:748-54.
Recent Activity
- Management of breech presentation Management of breech presentation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Breech Presentation and Delivery
- First Online: 06 August 2021
Cite this chapter

- Uche A. Menakaya 5 , 6
1261 Accesses
Breech presentation refers to the presence of the fetal buttocks, knees or feet at the lower pole of the gravid uterus during pregnancy. At term, up to 4% of pregnancies are breech. The term breech foetus faces peculiar challenges in resource restricted countries with its lack of consensus on management and limited investments in health care systems and training of health care providers. This chapter describes the different types of breech presentation, the risk factors for term breech presentation and the antenatal management options including external cephalic version available to women presenting with a term breech foetus. The chapter also describes the techniques for performing external cephalic version and the maneuvers critical for a successful vaginal breech delivery and highlights the limitations of the evidence for and against vaginal breech delivery in the sub-Saharan continent.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Hofmeyr GJ, Lockwood CJ, Barss VA. Overview of issues related to breech presentation: Uptodate Topic 6776 Version 24.0.
Google Scholar
Scheer K, Nubar J. Variation of fetal presentation with gestational age. Am J Obstet Gynecol. 1976;125(2):269–70.
Article CAS PubMed Google Scholar
Hickok DE, Gordon DC, Milberg JA, Williams MA, Daling JR. The frequency of breech presentation by gestational age at birth: a large population-based study. Am J Obstet Gynecol. 1992;166(3):851–2.
Albrechtsen S, Rasmussen S, Dalaker K, Irgens LM. Reproductive career after breech presentation: subsequent pregnancy rates, inter pregnancy interval, and recurrence. Obstet Gynecol. 1998;92(3):345.
CAS PubMed Google Scholar
Ford JB, Roberts CL, Nassar N, Giles W, Morris JM. Recurrence of breech presentation in consecutive pregnancies. BJOG. 2010;117(7):830.
Article CAS PubMed PubMed Central Google Scholar
Nordtveit TI, Melve KK, Albrechtsen S, Skjaerven R. Maternal and paternal contribution to intergenerational recurrence of breech delivery: population based cohort study. BMJ. 2008;336(7649):872.
Article PubMed PubMed Central Google Scholar
Hofmeyr GJ. Abnormal fetal presentation and position. In: Chapter 34, Turnbull's obstetrics; 2000.
Thorp JM Jr, Jenkins T, Watson W. Utility of Leopold maneuvers in screening for malpresentation. Obstet Gynecol. 1991;78(3 Pt 1):394.
PubMed Google Scholar
Grootscholten K, Kok M, Oei SG, Mol BW, van der Post JA. External cephalic version-related risks: a meta-analysis. Obstet Gynecol. 2008;112(5):1143.
Article PubMed Google Scholar
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2015 Apr;4:CD000083.
De Hundt M, Velzel J, de Groot CJ, Mol BW, Kok M. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014;123(6):1327.
Article PubMed CAS Google Scholar
Tan JM, Macario A, Carvalho B, Druzin ML, El-Sayed YY. Cost-effectiveness of external cephalic version for term breech presentation. BMC Pregnancy Childbirth. 2010;10:3.
Gifford DS, Keeler E, Kahn KL. Reductions in cost and caesarean rate by routine use of external cephalic version: a decision analysis. Obstet Gynecol. 1995;85(6):930–6.
Ben-Meir A, Erez Y, Sela HY, Shveiky D, Tsafrir A, Ezra Y. Prognostic parameters for successful external cephalic version. J Matern Fetal Neonatal Med. 2008;21(9):660.
Kok M, Cnossen J, Gravendeel L, van der Post J, Opmeer B, Mol BW. Clinical factors to predict the outcome of external cephalic version: a meta-analysis. Am J Obstet Gynecol. 2008;199(6):630.e1.
Article Google Scholar
Ebner F, Friedl TW, Leinert E, Schramm A, Reister F, Lato K, Janni W, De Gregorio N. Predictors for a successful external cephalic version: a single centre experience. Arch Gynecol Obstet. 2016;293(4):749.
Buhimschi CS, Buhimschi IA, Wehrum MJ, Molaskey-Jones S, Sfakianaki AK, Pettker CM, Thung S, Campbell KH, Dulay AT, Funai EF, Bahtiyar MO. Ultrasonographic evaluation of myometrial thickness and prediction of a successful external cephalic version. Obstet Gynecol. 2011;118(4):913–20.
Fortunato SJ, Mercer LJ, Guzick DS. External cephalic version with tocolysis: factors associated with success. Obstet Gynecol. 1988;72(1):59.
Boucher M, Bujold E, Marquette GP, Vezina Y. The relationship between amniotic fluid index and successful external cephalic version: a 14-year experience. Am J Obstet Gynecol. 2003;189(3):751.
Hofmeyr GJ, Sadan O, Myer IG, Galal KC, Simko G. External cephalic version and spontaneous version rates: ethnic and other determinants. Br J Obstet Gynaecol. 1986;93(1):13.
Hofmeyr GJ. Effect of external cephalic version in late pregnancy on breech presentation and caesarean section rate: a controlled trial. Br J Obstet Gynaecol. 1983;90(5):392.
Collins S, Ellaway P, Harrington D, Pandit M, Impey LW. The complications of external cephalic version: results from 805 consecutive attempts. BJOG. 2007;114(5):636.
Holmes WR, Hofmeyr GJ. Management of breech presentation in areas with high prevalence of HIV infection. Int J Gynaecol Obstet. 2004;87(3):272.
American College of Obstetricians and Gynaecologists. External cephalic version. Practice Bulletin No. 161. Obstet Gynecol. 2016;127:e54.
Royal College of Obstetrics and Gynaecology. External Cephalic Version (ECV) and Reducing the Incidence of Breech Presentation (Green-top Guideline No. 20a). https://www.rcog.org.uk/en/guidelines-researchservices/guidelines/gtg20a/ . Accessed on 12 May 2016.
Ben-Meir A, Elram T, Tsafrir A, Elchalal U, Ezra Y. The incidence of spontaneous version after failed external cephalic version. Am J Obstet Gynecol. 2007;196(2):157.e1.
Hutton EK, Hannah ME, Ross SJ, Delisle MF, Carson GD, Windrim R, Ohlsson A, Willan AR, Gafni A, Sylvestre G, Natale R, Barrett Y, Pollard JK, Dunn MS, Turtle P. Early ECV2 Trial Collaborative Group. The Early External Cephalic Version (ECV) 2 Trial: an international multicentre randomised controlled trial of timing of ECV for breech pregnancies. BJOG. 2011;118(5):564.
Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev. 2015;7:CD000084.
Hutton EK, Kaufman K, Hodnett E, Amankwah K, Hewson SA, McKay D, Szalai JP, Hannah ME. External cephalic version beginning at 34 weeks' gestation versus 37 weeks' gestation: a randomized multicenter trial. Am J Obstet Gynecol. 2003;189(1):245.
Nassar N, Roberts CL, Raynes-Greenow CH, Barratt A, Peat B. Decision aid for breech presentation trial collaborators evaluation of a decision aid for women with breech presentation at term: a randomised controlled trial [ISRCTN14570598]. BJOG. 2007;114(3):325.
Cluver C, Gyte GM, Sinclair M, Dowswell T, Hofmeyr GJ. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb;2:CD000184.
Rosman AN, Vlemmix F, Fleuren MA, Rijnders ME, Beuckens A, Opmeer BC, Mol BW, van Zwieten MC, Kok M. Patients' and professionals' barriers and facilitators to external cephalic version for breech presentation at term, a qualitative analysis in the Netherlands. Midwifery. 2014;30(3):324.
Hofmeyr GJ. Sonnendecker EW Cardiotocographic changes after external cephalic version. Br J Obstet Gynaecol. 1983;90(10):914.
Menakaya UA, Trivedi A. Qualitative assessment of women experiences with ECV. Women Birth. 2013;26(1):41–4.
ACOG Committee on Obstetric Practice ACOG Committee Opinion No. 340. Mode of term singleton breech delivery. Obstet Gynecol. 2006;108 (1):235.
Royal College of Obstetricians and Gynaecologist (RCOG). The management of breech presentation. London: RCOG; 2006.
Westgren M, Edvall H, Nordström L, Svalenius E, Ranstam J. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol. 1985;92(1):19.
Coyle ME, Smith CA, Peat B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst Rev. 2012;5:CD003928.
Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012;10:CD000051.
Glezerman M. Five years to the term breech trial: the rise and fall of a randomized controlled trial. Am J Obstet Gynecol. 2006;194(1):20.
Menticoglou SM. Why vaginal breech delivery should still be offered. J Obstet Gynaecol Can. 2006;28(5):380.
Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group. Lancet. 2000;356(9239):1375.
Vlemmix F, Bergenhenegouwen L, Schaaf JM, Ensing S, Rosman AN, Ravelli AC, Van Der Post JA, Verhoeven A, Visser GH, Mol BW, Kok M. Term breech deliveries in the Netherlands: did the increased caesarean rate affect neonatal outcome? A population-based cohort study. Acta Obstet Gynecol Scand. 2014;93(9):888.
Whyte H, Hannah ME, Saigal S, Hannah WJ, Hewson S, Amankwah K, Cheng M, Gafni A, Guselle P, Helewa M, Hodnett ED, Hutton E, Kung R, McKay D, Ross S, Willan A, Term Breech Trial Collaborative Group. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: The International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004;191(3):864–71.
Adegbola O, Akindele OM. Outcome of term singleton breech deliveries at a University Teaching Hospital in Lagos. Nigeria Niger Postgrad Med J. 2009;16(2):154–7.
Hartnack Tharin JE, Rasmussen S, Krebs L. Consequences of the term breech trial in Denmark. Acta Obstet Gynecol Scand. 2011;90(7):767.
Vistad I, Klungsøyr K, Albrechtsen S, Skjeldestad FE. Neonatal outcome of singleton term breech deliveries in Norway from 1991 to 2011. Acta Obstet Gynecol Scand. 2015;94(9):997.
Lyons J, Pressey T, Bartholomew S, Liu S, Liston RM, Joseph KS. Canadian Perinatal Surveillance System (Public Health Agency of Canada) Delivery of breech presentation at term gestation in Canada, 2003-2011. Obstet Gynecol. 2015;125(5):1153.
Goffinet F, Carayol M, Foidart JM, Alexander S, Uzan S, Subtil D, Bréart G, PREMODA Study Group. Is planned vaginal delivery for breech presentation at term still an option? Results of an observational prospective survey in France and Belgium. Am J Obstet Gynecol. 2006;194(4):1002.
Kotaska A, Menticoglou S, Gagnon R, Farine D, Basso M, Bos H, Delisle MF, Grabowska K, Hudon L, Mundle W, Murphy-Kaulbeck L, Ouellet A, Pressey T, Roggensack A. Maternal Fetal Medicine Committee, Society of Obstetricians and Gynaecologists of Canada. Vaginal delivery of breech presentation. J Obstet Gynaecol Can. 2009;31 (6):557.
Goffinet F, Blondel B, Breart G. Breech presentation: questions raised by the controlled trial by Hannah et al. on systematic use of caesarean section for breech presentations. J Gynecol Obstet Biol Reprod. 2001;30:187–90.
CAS Google Scholar
Glezerman M. Five years to the term breech trial: the risk and fall of a randomised controlled trial. Am J Obstet Gynecol. 2006;194:20–5.
Hauth JC, Cunningham FG. Vaginal breech delivery is still justified. Obstet Gynecol. 2002;99:1115–6.
Hull AD, Moore TR. Multiple repeat caesareans and the threat of placenta accreta: incidence, diagnosis, management. Clin Perinatol. 2011;38(2):285.
Moore WT, Steptoe PP. The experience of the John Hopkins hospital with breech presentation: an analysis of 1444 cases. South Med J. 1943;36:295.
Piper EB, Bachman C. The prevention of fetal injuries in breech delivery. J Am Med Assoc. 1929;92:217–21.
DeLee JB. Year book of obstetrics and gynaecology. Chicago: Year Book Medical Publishers; 1939.
Azria E, Le Meaux JP, Khoshnood B, Alexander S, Subtil D, Goffinet F. PREMODA Study Group Factors associated with adverse perinatal outcomes for term breech fetuses with planned vaginal delivery. Am J Obstet Gynecol. 2012;207(4):285.e1–9. Epub 2012 Aug 17
Alarab M, Regan C, O'Connell MP, Keane DP, O'Herlihy C, Foley ME. Singleton vaginal breech delivery at term: still a safe option. Obstet Gynecol. 2004;103(3):407.
Hofmeyr GJ, Lockwood CJ, Barss VA. Delivery of the fetus in breech presentation. Uptodate.com 2016 Topic 5384 version 18.
De Hundt M, Vlemmix F, Bais JM, Hutton EK, de Groot CJ, Mol BW, Kok M. Risk factors for developmental dysplasia of the hip: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2012;165(1):8.
Kenfack B, Ateudjieu J, Ymele FF, et al. Does the advice to Assumethe knee-chest position at the 36th to 37th weeks of gestation reduce the incidence of breech presentation at delivery? Clin Mother Child Health. 2012;9:1–5.
Dobbit JS, Foumane P, Tochie JN, Mamoudou F, Mazou N, Temgoua MN, Tankeu R, Aletum V, Mboudou E. Maternal and neonatal outcomes of vaginal breech delivery for singleton term pregnancies in a carefully selected Cameroonian population: a cohort study. BMJ Open. 2017;7(11):e017198.
Download references
Author information
Authors and affiliations.
JUNIC Specialist Imaging and Women’s Centre, Coombs, ACT, Australia
Uche A. Menakaya
Calvary Public Hospital, Bruce, ACT, Australia
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Uche A. Menakaya .
Editor information
Editors and affiliations.
Centre of Excellence in Reproductive Health Innovation, Department of Obstetrics and Gynaecology, University of Benin, Benin City, Nigeria
Friday Okonofua
College of Health Sciences, Chicago State University, Chicago, IL, USA
Joseph A. Balogun
Roswell Park Cancer Institute, Buffalo, NY, USA
Kunle Odunsi
Clinical Obstetrics and Gynaecology, Weil Cornell Medicine, Doha, Qatar
Victor N. Chilaka
Rights and permissions
Reprints and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Menakaya, U.A. (2021). Breech Presentation and Delivery. In: Okonofua, F., Balogun, J.A., Odunsi, K., Chilaka, V.N. (eds) Contemporary Obstetrics and Gynecology for Developing Countries . Springer, Cham. https://doi.org/10.1007/978-3-030-75385-6_17
Download citation
DOI : https://doi.org/10.1007/978-3-030-75385-6_17
Published : 06 August 2021
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-75384-9
Online ISBN : 978-3-030-75385-6
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Breech - series—Types of breech presentation
- Go to slide 1 out of 7
- Go to slide 2 out of 7
- Go to slide 3 out of 7
- Go to slide 4 out of 7
- Go to slide 5 out of 7
- Go to slide 6 out of 7
- Go to slide 7 out of 7
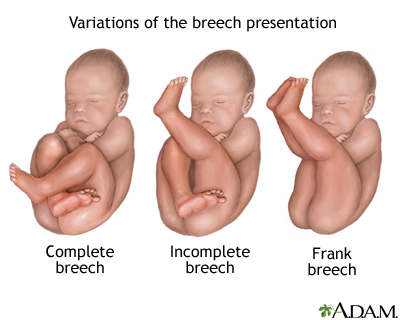
There are three types of breech presentation: complete, incomplete, and frank.
Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal.
Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
Frank breech is when the baby's legs are folded flat up against his head and his bottom is closest to the birth canal.
There is also footling breech where one or both feet are presenting.
Review Date 11/21/2022
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems

Uptodate Reference Title
Overview of breech presentation.
INTRODUCTION — Breech presentation, which occurs in approximately 3 percent of fetuses at term, describes the fetus whose presenting part is the buttocks and/or feet. Although most breech fetuses have normal anatomy, this presentation is associated with an increased risk for congenital malformations and mild deformations, torticollis, and developmental dysplasia of the hip. Pregnant people with fetuses in breech presentation at or near term are usually offered external cephalic version (ECV) because a persistent breech presentation is often delivered by planned cesarean, which is associated with a clinically significant decrease in perinatal/neonatal mortality and neonatal morbidity compared with vaginal birth.
This topic will provide an overview of major issues related to breech presentation, including choosing the best route for delivery. Techniques for breech delivery, with a focus on the technique for vaginal breech delivery, are discussed separately. (See "Delivery of the singleton fetus in breech presentation" .)
TYPES OF BREECH PRESENTATION — The main types of breech presentation are:
● Frank breech – Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term.
● Complete breech – Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
● Incomplete breech – One or both hips are not completely flexed ( figure 3 ); accounts for 10 to 40 percent of breech fetuses at term.
In the two nonfrank breech presentations, one or both feet (or rarely one or both knees) may present before the buttocks in the birth canal.
Significance — Because the hips are flexed and the knees are extended or flexed in the frank and complete breech presentations, the thighs and trunk pass through the birth canal simultaneously. If this large fetal diameter passes through the birth canal easily, then the aftercoming shoulders and head are likely to pass through easily as well, though a difficult delivery is still possible.
By contrast, in an incomplete breech presentation, one or both hips are not flexed; therefore, the thighs and trunk do not pass through the birth canal simultaneously. This smaller fetal diameter may easily pass through an incompletely dilated cervix (or an inadequate pelvis) followed by entrapment of the shoulders or head, which have larger diameters and require a fully dilated cervix and normal pelvic dimensions unless the fetus is small. Entrapment increases the risks for hypoxic injury and delivery-related trauma. Even before entrapment, the smaller fetal diameter provides space for umbilical cord prolapse, which can also result in hypoxic injury. In a series of planned vaginal breech deliveries (284 complete or incomplete breech, 884 frank breech), umbilical cord prolapse was more common in nonfrank breech presentations and was the reason for cesarean birth in 5/63 (7.9 percent) complete or incomplete breech presentations versus 3/222 (1.4 percent) frank breech presentations [ 1 ]. The overall cesarean birth rate was similar for both groups (nonfrank breech 22.2 percent, frank breech 25.1 percent). (See "Umbilical cord prolapse" .)
PREVALENCE — The prevalence of breech presentation at <28 weeks, 32 weeks, and term is approximately 20 to 25, 7 to 16, and 3 to 4 percent, respectively [ 2,3 ]. Breech presentation is more common earlier in pregnancy because the fetus can be highly mobile within the relatively large volume of amniotic fluid.
PATHOGENESIS — Breech presentation appears to be a chance occurrence in most pregnancies. In up to 15 percent of cases, however, it may be due to fetal, maternal, or placental abnormalities. It is hypothesized that a fetus with normal anatomy, activity, amniotic fluid volume, and placental location adopts the cephalic presentation near term because this position is the best fit for the intrauterine space, but if any of these variables is abnormal, then breech presentation is more likely.
RISK FACTORS — Multiple factors have been associated with an increased risk for breech presentation, including:
● Preterm gestation
● A previous sibling or either parent who was in breech presentation (see 'Risk of recurrence' below)
● Uterine abnormality (eg, bicornuate or septate uterus, fibroid) [ 4,5 ]
● Placental location (eg, placenta previa, cornual placenta) [ 6,7 ]
● Extremes of amniotic fluid volume (polyhydramnios, oligohydramnios)
● Nulliparity [ 8-10 ]
● Contracted maternal pelvis [ 11 ]
● Fetal anomaly (eg, anencephaly, hydrocephaly, sacrococcygeal teratoma, neck mass) [ 12 ]
● Extended fetal legs [ 13 ]
● Crowding from multiple gestation
● Fetal neurologic impairment
● Maternal hypothyroidism [ 8 ]
● Short umbilical cord [ 14 ]
● Fetal growth restriction [ 9 ]
● Fetal asphyxia [ 15 ]
● Female sex [ 9,16 ]
● Maternal anticonvulsant therapy [ 17 ]
● Older maternal age [ 9 ]
Risk of recurrence — Population-based registries indicate an increased risk of recurrent breech presentation [ 18,19 ]:
● After one pregnancy with breech presentation, the frequency of recurrence in the next pregnancy is approximately 9 percent
● After two consecutive pregnancies with breech presentation, the frequency of recurrence in the next pregnancy is approximately 25 percent
● After three consecutive pregnancies with breech presentation, the frequency of recurrence in the next pregnancy is almost 40 percent
By comparison, if the first pregnancy is not a breech presentation, the frequency of breech presentation in the next pregnancy is approximately 2 percent.
Recurrence is usually attributed to recurrent fetal, maternal, or placental abnormalities. However, the possibility of a heritable component to fetal presentation that can be transmitted from either parent was suggested by the observation that parents who themselves were delivered at term from breech presentation were twice as likely to have firstborn offspring in breech presentation compared with parents who were born as a cephalic presentation [ 20 ].
CLINICAL FINDINGS AND COURSE — Clinical assessment of fetal presentation should be a routine part of prenatal examination in late pregnancy since breech presentation affects antepartum and intrapartum management. (See 'Approach to management at or near term' below.)
Symptoms — Symptoms of breech presentation are most common in the third trimester. Patients often report subcostal discomfort because the fetal head is in the fundus [ 21 ]. They may also perceive kicking in the lower abdomen when the breech is complete or incomplete.
Physical examination — Breech presentation is most readily appreciated in the third trimester. However, abdominal palpation, even by an experienced clinician, may misdiagnose the presentation.
● On transabdominal examination of the lower uterine segment, breech presentation is characterized by the presence of a soft mass (ie, buttocks) and the absence of a hard fetal skull. In addition, a hollow (fetal neck) next to the presenting part is absent in a breech presentation and palpable in a cephalic presentation.
● On examination of the fundus, the fetal head can be readily balloted since it pivots on the neck and moves independently from the trunk. In comparison, in cephalic presentation, ballottement of the breech in the upper part of the uterus is typically sluggish because it is accompanied by movement of the entire trunk.
● On transvaginal examination, the soft buttocks, anal orifice, or feet may be identified when the cervix is dilated but can be difficult to palpate when the cervix is closed. A foot is differentiated from a hand by the presence of the heel, while palpating a fist or a grasp may identify a hand.
Imaging — Ultrasound clearly identifies the fetal head in the fundus, buttocks in the lower uterine segment, extension or flexion of each hip and knee, and location of each foot.
Hyperextension of the fetal head (defined by an extension angle greater than 90 degrees) is an important finding as it is a contraindication to vaginal birth. (See "Delivery of the singleton fetus in breech presentation", section on 'Criteria for minimizing risk in patients who opt for vaginal breech birth' .)
Natural history — Spontaneous version may occur at any time before labor, even after 40 weeks of gestation. In a prospective longitudinal study using serial ultrasound examinations, spontaneous version from breech to cephalic presentation after 36 weeks occurred in 25 percent of cases [ 13 ]. In the Term Breech Trial in which patients with breech presentation at ≥37 weeks of gestation were randomized to planned cesarean or vaginal birth, cephalic birth occurred in approximately 2 percent of those allocated to planned cesarean and 4 percent of the planned vaginal birth group, suggesting that additional spontaneous cephalic versions occurred during expectant management until the onset of spontaneous labor [ 22 ].
Characteristics that reduce the likelihood of spontaneous version include extended fetal legs, oligohydramnios, short umbilical cord, fetal/uterine abnormalities, and nulliparity.
DIAGNOSIS — The diagnosis of breech presentation should be suspected in patients who describe subcostal discomfort or kicking in the lower abdomen in late pregnancy. The diagnosis is confirmed by identifying the buttocks and/or feet as the presenting part on physical examination (transabdominal and/or transvaginal) or ultrasound examination (ultrasound is more reliable).
Our approach — Antepartum, our practice is to routinely perform a careful abdominal examination in late pregnancy to determine fetal presentation, with the addition of ultrasound examination if the presentation is not identifiable with certainty, as the diagnosis informs decision making around external cephalic version (ECV) and route of delivery. However, physical examination is not infallible [ 23,24 ]. In a study in which an experienced clinician examined 138 patients at 30 to 41 weeks of gestation immediately before an ultrasound examination, the examiner identified only three of eight breech presentations and falsely diagnosed six breeches [ 23 ]. Physical examination is fallible because characteristic findings of breech presentation on transabdominal examination may be obscured or distorted in patients with obesity, full bladder, leiomyoma, polyhydramnios, anterior placenta, or multiple gestation. Because ultrasound detects 100 percent of breech presentations at the time of the examination, performing ultrasound for fetal presentation in late pregnancy in conjunction with offering external cephalic version may be cost-effective [ 25,26 ].
We also routinely perform an ultrasound examination in laboring patients to confirm suspected breech presentation and the type of breech when physical findings are uncertain since sonographic confirmation of a previously unsuspected breech presentation should prompt a discussion about cesarean versus vaginal birth.
Intrapartum differential diagnosis
● Face presentation – On intrapartum transvaginal examination through a dilated cervix a frank breech presentation can feel like an edematous face presentation. A useful distinguishing characteristic is that the fetal greater trochanters and anal orifice form a straight line across the buttocks, whereas the malar bones and mouth form a triangle in the face. (See "Face and brow presentations in labor", section on 'Face presentation' .)
● Compound cephalic presentation – On intrapartum transvaginal examination through a dilated cervix, a foot suggests breech presentation but can also occur with a compound cephalic presentation, which often has one or both hands but may have one or both feet or a hand and a foot presenting alongside or in front of the head. A foot can be distinguished from a hand by its three bony protuberances (calcaneous, lateral and medial malleolus), the angle at the level of the calcaneous, and the toes, which are short and lie in the same line with no opposing thumb. On abdominal examination, the diagnosis of breech presentation is supported by palpation of the head in the fundus. Ultrasound confirms the diagnosis. (See "Compound fetal presentation", section on 'Differential diagnosis' .)
APPROACH TO MANAGEMENT AT OR NEAR TERM
Overview — There is general agreement that the breech fetus is at higher risk for asphyxia and traumatic injury during vaginal birth than the cephalic fetus (see 'Significance' above). To minimize the risk of these complications, the choice of delivery route for the term breech fetus is guided by patient values and preferences and provider experience, values, and preferences, taking into account the risks and benefits of the various approaches [ 27 ]. The pregnant person's choice of birth route should be informed by unbiased, noncoercive counseling [ 28 ]. The choice should be made with due consideration of specific health care environments, individual values and preferences [ 29 ], and the limitations inherent in the data described in the following sections of this topic [ 30-35 ]. Clinicians should be aware that people with breech presentation may experience a sense of loss of power and autonomy during this process [ 36 ].
Four strategies have evolved:
● External cephalic version (ECV) before labor, with a trial of labor if the version is successful and cesarean birth if unsuccessful. This is the most common approach in the United States and many other countries.
● ECV before labor, with a trial of labor if the version is successful. However, if the version is unsuccessful, a trial of labor and vaginal breech birth are offered to patients who have characteristics that are believed to place them at a low risk of labor and delivery-related complications. Cesarean birth is offered to higher risk patients and any patient who declines to attempt a vaginal breech birth. This is the author's approach. (See "Delivery of the singleton fetus in breech presentation", section on 'Criteria for minimizing risk in patients who opt for vaginal breech birth' .)
● Planned cesarean birth for breech presentation, without an attempt at ECV.
● A trial of labor and vaginal breech birth for patients who have characteristics that are believed to place them at a low risk of labor and delivery-related complications, without an attempt at ECV. (See "Delivery of the singleton fetus in breech presentation", section on 'Criteria for minimizing risk in patients who opt for vaginal breech birth' .)
Antepartum maternal postural changes, moxibustion, and acupuncture do not improve the chances of spontaneous version compared with expectant care alone. This evidence is reviewed separately. (See "External cephalic version", section on 'Postural maneuvers to facilitate spontaneous version' and "External cephalic version", section on 'Moxibustion and acupuncture' .)
Strategy #1: ECV, cesarean birth if unsuccessful — ECV at or near term, followed by a trial of vaginal birth if the version is successful and planned cesarean birth if breech presentation persists is the preferred approach to delivery of the term breech fetus in the United States, and many other countries [ 27 ]. Patients are encouraged to undergo ECV to convert a breech presentation to cephalic presentation and thus increase the likelihood of vaginal cephalic birth. If ECV is unsuccessful or the fetus reverts to breech, one or two retrials of version can be attempted in one or more days. In a meta-analysis of randomized trials, ECV at term resulted in a 60 percent reduction in noncephalic presentation at birth (relative risk [RR] 0.42, 95% CI 0.29-0.61) and a 40 percent reduction in cesarean birth (RR 0.57, 95% CI 0.40-0.82) [ 37 ]. Performing the version at 34 to 35 weeks of gestation, using a tocolytic drug, and/or administering neuraxial anesthesia increase the likelihood of success, but overall benefits are uncertain. These data and the timing and procedure for ECV are discussed separately. (See "External cephalic version" .)
Planned cesarean birth for persistent term breech presentation is associated with a clinically significant decrease in perinatal/neonatal mortality and neonatal morbidity, with only a modest increase in short-term maternal morbidity, compared with a policy of planned vaginal birth. It should be performed at ≥39+0 weeks of gestation to allow optimal physiologic maturation (unless there are specific indications for earlier delivery). Delaying cesarean birth until at least 39+0 weeks is particularly important when the indication is breech presentation, as spontaneous version may occur at any gestational age.
However, a policy of planned cesarean birth may not be affordable or feasible in resource-limited settings. On an individual-case basis, there may be clinical situations in which the maternal risks of cesarean or the patient's desire to avoid cesarean birth outweigh the newborn's risks from vaginal birth. Both birth routes have similar long-term maternal outcomes and childhood outcomes in survivors, and some data suggest some long-term health benefits from being born vaginally, including reduced risk of childhood conditions such as asthma and arthritis [ 38-40 ]. In addition, cesarean birth has implications for patients planning future pregnancies, including repeat cesarean birth and increased risks for serious morbidity and mortality associated with placenta accreta spectrum [ 41 ] and uterine rupture [ 42 ]. Pregnancies following preterm breech cesarean birth versus preterm breech vaginal birth have been associated with increased neonatal acidosis and intensive care admission [ 43 ] and other adverse neonatal and maternal outcomes [ 44 ]. Lastly, the current policy is largely based on a single randomized multicenter international trial (see 'Evidence' below). Increasing the magnitude of planned cesarean births worldwide will increase the absolute number of patients who develop rare but life-threatening complications of this major operative procedure [ 45,46 ]. For example, in Africa, overall maternal mortality from cesarean birth is 0.5 percent [ 47 ].
Evidence — The evidence supporting planned cesarean birth was provided by a systematic review of randomized trials of planned cesarean versus planned vaginal birth for term breech presentation (three trials, 2396 participants) [ 48 ]. In two of the trials, which were from the same unit, patients with frank [ 49 ] or nonfrank [ 50 ] breech presentation were randomly assigned to undergo planned cesarean birth or a protocol allowing vaginal birth within prescribed limitations, including the absence of diminished pelvic dimensions on radiographic pelvimetry. The third trial, the Term Breech Trial, was a large (2088 participants) multicenter, international trial comparing planned cesarean with planned vaginal birth by an experienced clinician following agreed upon clinical guidelines [ 22 ]. The participating countries were classified as having low or high perinatal mortality rates (low ≤20 deaths per 1000 live births plus late fetal deaths, high >20 deaths per 1000 live births plus late fetal deaths). Cesarean birth was performed in 550 of 1227 patients (45 percent) allocated to the vaginal birth protocol.
The key findings were as follows:
Compared with planned vaginal birth of breech presentation, planned cesarean [ 48 ]:
● Reduced perinatal/neonatal death (RR 0.29, 95% CI 0.10-0.86). Risk ratios were similar for countries with low versus high national perinatal mortality rates, but absolute mortality rates were higher in the latter. Subsequently, others estimated that 338 cesareans for breech presentation need to be performed to prevent one perinatal death [ 51 ].
● Reduced composite short-term outcome of perinatal/neonatal death or serious neonatal morbidity (RR 0.33, 95% CI 0.19-0.56). This result was largely driven by data from countries with low national perinatal mortality rates, where the comparative risk of the composite outcome was RR 0.07 (95% CI 0.02-0.29; 4/1000 for planned cesarean versus 57/1000 for planned vaginal birth). In countries with high national perinatal mortality rates, the comparative risk of the composite outcome was RR 0.66 (95% CI 0.35-1.24; 29/1000 for planned cesarean versus 44/1000 for planned vaginal birth). The unexpectedly low absolute composite mortality/morbidity rate with planned vaginal birth in high perinatal mortality rate countries may have been due to less macrosomia, more experience with vaginal breech birth, and documentation issues.
The number of adverse events in the meta-analysis was small, thus reducing the chances of detecting statistically significant reductions in birth trauma and brachial plexus injury with planned cesarean birth.
In addition:
● Route of planned birth had no significant effect on long-term outcome in offspring, except that infant medical problems were significantly increased following planned cesarean birth. The combined risk of death/neurodevelopmental delay was similar for the planned vaginal and planned cesarean groups at two years of age. Since there were few serious adverse events despite the large number of study participants and 17 of 18 neonates with serious early morbidity were neurologically normal at two years of age, a small difference between groups in long-term composite mortality/morbidity cannot be excluded.
● Route of planned birth had no significant effect on long-term maternal outcome. In the short-term, planned cesarean resulted in a small increase in some maternal morbidities (eg, hemorrhage, transfusion, infection), but less urinary incontinence and incontinence of flatus. Complications in future pregnancies related to scarring of the uterus were not assessed.
A meta-analysis of 21 cohort studies including nearly 400,000 pregnancies support these findings [ 52 ].
The Term Breech Trial impacted clinical practice worldwide: The rate of planned vaginal breech birth fell substantially since publication of this trial [ 53-57 ]. In 2016, the cesarean birth rate for breech presentation in European countries was ≥70 percent and approximately 95 percent in the United States [ 58 ]. Limited observational data suggest that this fall in planned vaginal breech birth has been accompanied by a fall in the morbidity and mortality of breech birth [ 51,53 ], especially if performed before labor begins [ 59 ].
Strategy #2: ECV, trial of vaginal birth for selected patients if unsuccessful — The author's preference is to offer ECV followed by a trial of vaginal birth if successful. If unsuccessful, he offers planned cesarean birth, and, for patients who meet criteria, he also offers a trial of labor and vaginal breech birth [ 30-35,38-40,42,45,46 ]. There is a general consensus that patients who choose to undergo a trial of labor and vaginal breech birth should be at low risk of complications from vaginal breech birth and their labor and birth should be supervised by a clinician with experience in vaginal breech birth. Whether such pregnancies can be identified and how the fetal risks from vaginal birth compare with maternal risks from cesarean birth have been debated for decades. (See "Delivery of the singleton fetus in breech presentation", section on 'Criteria for minimizing risk in patients who opt for vaginal breech birth' .)
Closely monitoring the progress of labor is particularly important in patients who attempt a vaginal breech birth. The author has a low threshold for performing a cesarean birth if he believes that labor progress is inadequate. His criteria for abnormal labor progress are described in detail separately. (See "Delivery of the singleton fetus in breech presentation", section on 'Labor management' .)
Evidence — The PREsentation et MODe d'Accouchement (PREMODA) study is often cited as the best evidence to support vaginal breech birth in selected patients [ 60 ]. The results of this observational study are less robust than those of the Term Breech Trial discussed above but provide information illustrating the magnitude of morbidity/mortality of planned vaginal birth in patients managed using the authors' protocol. Subsequent smaller prospective observational studies have also reported low rates of adverse outcome from planned vaginal breech birth that followed strict protocols [ 61-65 ], including first pregnancies [ 66 ] and pregnancies beyond the estimated due date [ 67 ].
PREMODA was a prospective observational multicenter study conducted in 174 centers in France and Belgium and including 8105 singleton breech fetuses at term [ 60 ]. The study evaluated the safety of vaginal breech birth using strict criteria ( table 1 ) for selecting patients for a trial of labor. Major findings were [ 60,68 ]:
● The composite outcome of fetal/neonatal mortality or serious neonatal morbidity was not significantly different for planned vaginal versus planned cesarean birth (1.60 versus 1.45 percent, odds ratio 1.10, 95% CI 0.75-1.61) after adjustment for geographic origin, gestational age less than 39 weeks at birth, birth weight less than the 10 th percentile, and an annual number of maternity unit births of less than 1500.
● Approximately 70 percent of the 2502 patients in the planned vaginal birth group delivered vaginally, and 165 (6.6 percent) of these pregnancies had an adverse perinatal outcome, including but not limited to brachial plexus injury (five infants), skull fracture (one infant), genital injury (two infants), intraventricular hemorrhage (one infant), seizure (four infants), and death (two infants). Factors associated with adverse perinatal outcome were geographic origin, delivery at <39 weeks of gestation, birth weight <10 th percentile, and annual number of maternity unit births <1500.
Strategy #3: Cesarean birth without ECV — Some patients may choose to undergo a planned cesarean birth without an attempt at ECV. Patients with a low likelihood of successful version or at increased risk of fetal harm from the procedure may reasonably avoid an attempt at version and choose cesarean birth. (See "External cephalic version", section on 'Candidates' .)
Strategy #4: Vaginal birth without ECV — Some patients may choose to undergo a trial of labor and vaginal breech birth without an attempt at ECV. Those with a low likelihood of successful version or at increased risk of fetal harm from the procedure may reasonably avoid the procedure and choose to attempt vaginal birth (see "External cephalic version", section on 'Candidates' ). As discussed above, there is a general consensus that patients who choose to undergo a trial of labor and vaginal breech birth should be at low risk of complications from vaginal breech birth and their labor and birth should be supervised by a clinician with experience in vaginal breech birth. (See "Delivery of the singleton fetus in breech presentation", section on 'Criteria for minimizing risk in patients who opt for vaginal breech birth' .)
APPROACH TO MANAGEMENT OF PRETERM BREECH BIRTH — In most cases, cesarean is preferred for birth of the preterm breech fetus because the body of evidence from observational studies suggests that vaginal birth of the very preterm breech fetus is likely associated with a small but significant increase in adverse outcome that can be avoided by cesarean birth. The preterm fetal head circumference-to-abdominal circumference ratio is larger than that of a term fetus; thus, the preterm breech head is more likely to be entrapped in a partially dilated cervix, resulting in birth trauma and/or acute asphyxia from compression of the umbilical cord [ 69,70 ].
● In a 2014 systematic review of seven observational studies (3557 participants) that evaluated cesarean versus vaginal birth of the preterm breech, the weighted risk of neonatal mortality was lower in the cesarean group than in the vaginal birth group (3.8 versus 11.5 percent, pooled relative risk 0.63, 95% CI 0.48-0.81) [ 71 ]. In one of the included studies, a retrospective study of patients delivering breech infants at 26 to 29 weeks of gestation, the rate of head entrapment was twofold higher in the planned vaginal birth group than in the planned cesarean birth group (11/84 [13 percent] versus 5/85 [6 percent]) [ 70 ]. Four neonatal deaths were attributed to head entrapment; three of these infants were delivered vaginally and died within an hour of birth (neonatal death related to head entrapment 3/45 vaginal births versus 1/124 cesarean births). The single infant that died after cesarean birth complicated by head entrapment died five days later because of sepsis and grade 3 intraventricular hemorrhage. Of note, approximately 50 percent of planned vaginal births ended in cesarean birth, while 6 percent of planned cesareans ended in vaginal birth.
The authors of the systematic review subsequently published a cohort study including over 8300 patients with a singleton preterm fetus in breech presentation who delivered at 26+0 to 36+6 weeks of gestation in the Netherlands from 2000 to 2011 [ 72 ]. A strength of this study is the large number of participants who intended to deliver vaginally (6421), although 2995 of these individuals delivered by emergency cesarean during labor. Compared with intended vaginal birth, intended cesarean birth was not associated with a significant reduction in perinatal mortality (1.3 versus 1.5 percent, adjusted odds ratio [OR] 0.97, 95% CI 0.60-1.57) or the composite outcome of perinatal mortality/severe morbidity (3.2 versus 4.1 percent, adjusted OR 0.76, 95% CI 0.56-1.03); however, when minor morbidities such as five-minute Apgar score <7 were also considered, intended cesarean birth reduced the rate of the composite outcome of perinatal mortality/morbidity (8.7 versus 10.4 percent, OR 0.77, 95% CI 0.63-0.93). A subgroup analysis based on gestational age found that perinatal mortality, morbidity, and severe morbidity were significantly reduced by cesarean at 28 to 32 weeks of gestation.
● In a 2018 meta-analysis to determine the safest route of delivery of actively resuscitated extremely preterm (23+0 to 27+6 weeks) breech singletons, cesarean was associated with reductions in the odds of death by 41 percent (OR 0.59, 95% CI 0.36-0.95, number needed to treat [NNT] 8) and of severe intraventricular hemorrhage by 49 percent (OR 0.51, 95% CI 0.29-0.91, NNT 12) [ 73 ]. Infants at lower gestational ages experienced the greatest benefit. Data from one randomized trial, one prospective cohort study, and 13 retrospective cohort studies were combined for the analysis.
TECHNIQUE FOR BREECH DELIVERY — (See "Delivery of the singleton fetus in breech presentation" .)
NEONATAL OUTCOME — Newborns that were in breech presentation have increased morbidity and mortality; however, breech presentation itself probably is not an independent risk factor for adverse neonatal outcome [ 74,75 ]. Rather, adverse outcomes are related, in part, to underlying conditions associated with breech presentation (eg, congenital anomalies, fetal growth restriction, preterm birth) and, in part, to birth trauma, which is often related to vaginal breech birth.
Regardless of route of birth, neonates who are breech in utero are more likely to have congenital anomalies [ 76 ] (4.4 versus 2.4 percent in vertex presentation [ 77 ]) and mild deformations (eg, frontal bossing, prominent occiput, upward slant, and low-set ears), torticollis, and developmental dysplasia of the hip [ 78-80 ], which may present late despite normal initial ultrasound evaluation [ 81 ]. Ultrasonography at four to six weeks of age (adjusted for preterm birth) has been recommended for infants with an abnormal hip examination or a normal examination and breech position at ≥34 weeks of gestation. (See "Congenital muscular torticollis: Clinical features and diagnosis" and "Developmental dysplasia of the hip: Epidemiology and pathogenesis", section on 'Breech position' .)
SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. (See "Society guideline links: Breech presentation and external cephalic version" .)
INFORMATION FOR PATIENTS — UpToDate offers two types of patient education materials, "The Basics" and "Beyond the Basics." The Basics patient education pieces are written in plain language, at the 5 th to 6 th grade reading level, and they answer the four or five key questions a patient might have about a given condition. These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. (You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword(s) of interest.)
● Basics topics (see "Patient education: Breech pregnancy (The Basics)" and "Patient education: External cephalic version (The Basics)" )
SUMMARY AND RECOMMENDATIONS
● Types – Breech presentation may be frank, complete, or incomplete ( figure 1 and figure 2 and figure 3 ). (See 'Types of breech presentation' above.)
● Prevalence – Breech presentation complicates 3 to 4 percent of pregnancies at term; the prevalence is inversely associated with gestational age. (See 'Prevalence' above.)
● Pathogenesis – In most pregnancies, breech presentation is a chance occurrence. In up to 15 percent of cases, it may be due to fetal, maternal, or placental abnormalities. (See 'Pathogenesis' above.)
● Symptoms – Symptoms of breech presentation include subcostal discomfort from the fetal head in the fundus and kicking in the lower abdomen when the breech is complete or incomplete. (See 'Symptoms' above.)
● Diagnosis – The diagnosis of breech presentation is based on identifying the buttocks and/or feet as the presenting part on physical examination (transabdominal or transvaginal) or ultrasound examination. (See 'Diagnosis' above and 'Physical examination' above and 'Imaging' above.)
● Management
• Overview – The management of breech presentation at term is guided by patient values and preferences and provider experience, values, and preferences after review of the evidence of the risks and benefits of available interventions. (See 'Approach to management at or near term' above.)
The choice of birth route should be made with due consideration of specific health care environments, individual patient values and preferences, and the limitations inherent in available evidence. A policy of planned cesarean birth may not be affordable or feasible in resource-limited settings. On an individual case basis, there may be clinical situations in which the risks of cesarean to the patient, or the patient's desire to avoid cesarean birth, may outweigh the newborn's short-term risks from vaginal birth. Both birth routes have similar long-term maternal and childhood outcomes, and some data suggest some long-term health benefits to being born vaginally. In addition, cesarean birth has implications for patients planning future pregnancies, including repeat cesarean birth and increased risks of placenta accreta spectrum and uterine rupture. (See 'Approach to management at or near term' above.)
• Role of external cephalic version – In the United States, clinician preference for pregnancies with breech presentation is to offer the patient external cephalic version (ECV) at or near term, followed by a trial of vaginal birth if the version is successful and planned cesarean if breech presentation persists because planned cesarean birth of the breech fetus reduces perinatal death or severe morbidity. (See 'Strategy #1: ECV, cesarean birth if unsuccessful' above.)
• Role of planned cesarean birth – Some patients may choose to undergo planned cesarean birth if the breech persists without an attempt at ECV. Patients with a low likelihood of successful version or at increased risk of fetal harm from the procedure may reasonably avoid the procedure. (See 'Strategy #3: Cesarean birth without ECV' above.)
• Role of vaginal breech birth – Some patients may choose to have a vaginal breech birth. There is a general consensus that these patients should be at low risk of complications from vaginal breech birth and their labor and delivery should be supervised by a clinician with experience in vaginal breech birth. (See 'Strategy #2: ECV, trial of vaginal birth for selected patients if unsuccessful' above.)
- Jennewein L, Allert R, Möllmann CJ, et al. The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term - A FRABAT prospective cohort study. PLoS One 2019; 14:e0225546.
- Scheer K, Nubar J. Variation of fetal presentation with gestational age. Am J Obstet Gynecol 1976; 125:269.
- Hickok DE, Gordon DC, Milberg JA, et al. The frequency of breech presentation by gestational age at birth: a large population-based study. Am J Obstet Gynecol 1992; 166:851.
- Ben-Rafael Z, Seidman DS, Recabi K, et al. Uterine anomalies. A retrospective, matched-control study. J Reprod Med 1991; 36:723.
- Michalas SP. Outcome of pregnancy in women with uterine malformation: evaluation of 62 cases. Int J Gynaecol Obstet 1991; 35:215.
- Fianu S, Václavínková V. The site of placental attachment as a factor in the aetiology of breech presentation. Acta Obstet Gynecol Scand 1978; 57:371.
- Sekulić S, Ilinčić M, Radeka G, et al. Breech presentation and the cornual-fundal location of the placenta. Croat Med J 2013; 54:198.
- Toijonen AE, Heinonen ST, Gissler MVM, Macharey G. A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case-control study. Arch Gynecol Obstet 2020; 301:393.
- Fruscalzo A, Londero AP, Salvador S, et al. New and old predictive factors for breech presentation: our experience in 14 433 singleton pregnancies and a literature review. J Matern Fetal Neonatal Med 2014; 27:167.
- Zhou Z, Wu J, Zhang G, Yang J. Spontaneous cephalic version and risk factors for persistent breech presentation: a longitudinal retrospective cohort study. J Matern Fetal Neonatal Med 2022; 35:9452.
- Ranney B. The gentle art of external cephalic version. Am J Obstet Gynecol 1973; 116:239.
- Mostello D, Chang JJ, Bai F, et al. Breech presentation at delivery: a marker for congenital anomaly? J Perinatol 2014; 34:11.
- Westgren M, Edvall H, Nordström L, et al. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol 1985; 92:19.
- Soernes T, Bakke T. The length of the human umbilical cord in vertex and breech presentations. Am J Obstet Gynecol 1986; 154:1086.
- Moessinger AC, Blanc WA, Marone PA, Polsen DC. Umbilical cord length as an index of fetal activity: experimental study and clinical implications. Pediatr Res 1982; 16:109.
- Hall MH, Carr-Hill R. Impact of sex ratio on onset and management of labour. Br Med J (Clin Res Ed) 1982; 285:401.
- Robertson IS. Breech presentation associated with anticonvulsant drugs. Am J Obstet Gynecol 1984; 4:174.
- Albrechtsen S, Rasmussen S, Dalaker K, Irgens LM. Reproductive career after breech presentation: subsequent pregnancy rates, interpregnancy interval, and recurrence. Obstet Gynecol 1998; 92:345.
- Ford JB, Roberts CL, Nassar N, et al. Recurrence of breech presentation in consecutive pregnancies. BJOG 2010; 117:830.
- Nordtveit TI, Melve KK, Albrechtsen S, Skjaerven R. Maternal and paternal contribution to intergenerational recurrence of breech delivery: population based cohort study. BMJ 2008; 336:872.
- Hofmeyr GJ. Abnormal fetal presentation and position. In: Chapter 34, Turnbull's Obstetrics, 2000.
- Hannah ME, Hannah WJ, Hewson SA, et al. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group. Lancet 2000; 356:1375.
- Thorp JM Jr, Jenkins T, Watson W. Utility of Leopold maneuvers in screening for malpresentation. Obstet Gynecol 1991; 78:394.
- Knights S, Prasad S, Kalafat E, et al. Impact of point-of-care ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes: An observational multicentre cohort study. PLoS Med 2023; 20:e1004192.
- Smith GC, Moraitis AA, Wastlund D, et al. Universal late pregnancy ultrasound screening to predict adverse outcomes in nulliparous women: a systematic review and cost-effectiveness analysis. Health Technol Assess 2021; 25:1.
- Salim I, Staines-Urias E, Mathewlynn S, et al. The impact of a routine late third trimester growth scan on the incidence, diagnosis, and management of breech presentation in Oxfordshire, UK: A cohort study. PLoS Med 2021; 18:e1003503.
- ACOG Committee Opinion No. 745: Mode of Term Singleton Breech Delivery. Obstet Gynecol 2018; 132:e60. Reaffirmed 2023.
- Powell R, Walker S, Barrett A. Informed consent to breech birth in New Zealand. N Z Med J 2015; 128:85.
- Wang XR, Cotter H, Fahey M. Women's Selection of Mode of Birth for their Breech Presentation. J Obstet Gynaecol Can 2021; 43:716.
- Glezerman M. Five years to the term breech trial: the rise and fall of a randomized controlled trial. Am J Obstet Gynecol 2006; 194:20.
- Lockwood CJ. The term, singleton, vaginal breech delivery controversy. J Matern Fetal Neonatal Med 2002; 12:75.
- Kotaska A. Inappropriate use of randomised trials to evaluate complex phenomena: case study of vaginal breech delivery. BMJ 2004; 329:1039.
- Hauth JC, Cunningham FG. Vaginal breech delivery is still justified. Obstet Gynecol 2002; 99:1115.
- van Roosmalen J, Rosendaal F. There is still room for disagreement about vaginal delivery of breech infants at term. BJOG 2002; 109:967.
- Menticoglou SM. Why vaginal breech delivery should still be offered. J Obstet Gynaecol Can 2006; 28:380.
- Morris S, Geraghty S, Sundin D. Women's experiences of breech birth and disciplinary power. J Adv Nurs 2021; 77:3116.
- Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev 2015; :CD000083.
- Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol 2004; 191:864.
- Negele K, Heinrich J, Borte M, et al. Mode of delivery and development of atopic disease during the first 2 years of life. Pediatr Allergy Immunol 2004; 15:48.
- Laubereau B, Filipiak-Pittroff B, von Berg A, et al. Caesarean section and gastrointestinal symptoms, atopic dermatitis, and sensitisation during the first year of life. Arch Dis Child 2004; 89:993.
- Matsuzaki S, Mandelbaum RS, Sangara RN, et al. Trends, characteristics, and outcomes of placenta accreta spectrum: a national study in the United States. Am J Obstet Gynecol 2021; 225:534.e1.
- Hull AD, Moore TR. Multiple repeat cesareans and the threat of placenta accreta: incidence, diagnosis, management. Clin Perinatol 2011; 38:285.
- Toijonen A, Hinnenberg P, Gissler M, et al. Maternal and neonatal outcomes in the following delivery after previous preterm caesarean breech birth: a national cohort study. J Obstet Gynaecol 2022; 42:49.
- Macharey G, Toijonen A, Hinnenberg P, et al. Term cesarean breech delivery in the first pregnancy is associated with an increased risk for maternal and neonatal morbidity in the subsequent delivery: a national cohort study. Arch Gynecol Obstet 2020; 302:85.
- Schutte JM, Steegers EA, Santema JG, et al. Maternal deaths after elective cesarean section for breech presentation in the Netherlands. Acta Obstet Gynecol Scand 2007; 86:240.
- Lawson GW. Report of a breech cesarean section maternal death. Birth 2011; 38:159.
- Bishop D, Dyer RA, Maswime S, et al. Maternal and neonatal outcomes after caesarean delivery in the African Surgical Outcomes Study: a 7-day prospective observational cohort study. Lancet Glob Health 2019; 7:e513.
- Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev 2015; :CD000166.
- Collea JV, Chein C, Quilligan EJ. The randomized management of term frank breech presentation: a study of 208 cases. Am J Obstet Gynecol 1980; 137:235.
- Gimovsky ML, Wallace RL, Schifrin BS, Paul RH. Randomized management of the nonfrank breech presentation at term: a preliminary report. Am J Obstet Gynecol 1983; 146:34.
- Vlemmix F, Bergenhenegouwen L, Schaaf JM, et al. Term breech deliveries in the Netherlands: did the increased cesarean rate affect neonatal outcome? A population-based cohort study. Acta Obstet Gynecol Scand 2014; 93:888.
- Wängberg Nordborg J, Svanberg T, Strandell A, Carlsson Y. Term breech presentation-Intended cesarean section versus intended vaginal delivery-A systematic review and meta-analysis. Acta Obstet Gynecol Scand 2022; 101:564.
- Hartnack Tharin JE, Rasmussen S, Krebs L. Consequences of the Term Breech Trial in Denmark. Acta Obstet Gynecol Scand 2011; 90:767.
- Vistad I, Klungsøyr K, Albrechtsen S, Skjeldestad FE. Neonatal outcome of singleton term breech deliveries in Norway from 1991 to 2011. Acta Obstet Gynecol Scand 2015; 94:997.
- Pasupathy D, Wood AM, Pell JP, et al. Time trend in the risk of delivery-related perinatal and neonatal death associated with breech presentation at term. Int J Epidemiol 2009; 38:490.
- Lansac J, Crenn-Hebert C, Rivière O, Vendittelli F. How singleton breech babies at term are born in France: a survey of data from the AUDIPOG network. Eur J Obstet Gynecol Reprod Biol 2015; 188:79.
- Hehir MP. Trends in vaginal breech delivery. J Epidemiol Community Health 2015; 69:1237.
- Weiniger CF, Lyell DJ, Tsen LC, et al. Maternal outcomes of term breech presentation delivery: impact of successful external cephalic version in a nationwide sample of delivery admissions in the United States. BMC Pregnancy Childbirth 2016; 16:150.
- Lyons J, Pressey T, Bartholomew S, et al. Delivery of breech presentation at term gestation in Canada, 2003-2011. Obstet Gynecol 2015; 125:1153.
- Goffinet F, Carayol M, Foidart JM, et al. Is planned vaginal delivery for breech presentation at term still an option? Results of an observational prospective survey in France and Belgium. Am J Obstet Gynecol 2006; 194:1002.
- Maier B, Georgoulopoulos A, Zajc M, et al. Fetal outcome for infants in breech by method of delivery: experiences with a stand-by service system of senior obstetricians and women's choices of mode of delivery. J Perinat Med 2011; 39:385.
- Michel S, Drain A, Closset E, et al. Evaluation of a decision protocol for type of delivery of infants in breech presentation at term. Eur J Obstet Gynecol Reprod Biol 2011; 158:194.
- Vistad I, Cvancarova M, Hustad BL, Henriksen T. Vaginal breech delivery: results of a prospective registration study. BMC Pregnancy Childbirth 2013; 13:153.
- Fonseca A, Silva R, Rato I, et al. Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes? Acta Med Port 2017; 30:479.
- Martel-Santiago CR, Arencibia-Díaz RD, Romero-Requejo A, et al. Delivery in breech presentation: Perinatal outcome and neurodevelopmental evaluation at 18 months of life. Eur J Obstet Gynecol Reprod Biol 2020; 255:147.
- Kielland-Kaisen U, Paul B, Jennewein L, et al. Maternal and neonatal outcome after vaginal breech delivery of nulliparous versus multiparous women of singletons at term-A prospective evaluation of the Frankfurt breech at term cohort (FRABAT). Eur J Obstet Gynecol Reprod Biol 2020; 252:583.
- Möllmann CJ, Kielland-Kaisen U, Paul B, et al. Vaginal breech delivery of pregnancy before and after the estimated due date-A prospective cohort study. Eur J Obstet Gynecol Reprod Biol 2020; 252:588.
- Azria E, Le Meaux JP, Khoshnood B, et al. Factors associated with adverse perinatal outcomes for term breech fetuses with planned vaginal delivery. Am J Obstet Gynecol 2012; 207:285.e1.
- Robilio PA, Boe NM, Danielsen B, Gilbert WM. Vaginal vs. cesarean delivery for preterm breech presentation of singleton infants in California: a population-based study. J Reprod Med 2007; 52:473.
- Kayem G, Baumann R, Goffinet F, et al. Early preterm breech delivery: is a policy of planned vaginal delivery associated with increased risk of neonatal death? Am J Obstet Gynecol 2008; 198:289.e1.
- Bergenhenegouwen LA, Meertens LJ, Schaaf J, et al. Vaginal delivery versus caesarean section in preterm breech delivery: a systematic review. Eur J Obstet Gynecol Reprod Biol 2014; 172:1.
- Bergenhenegouwen L, Vlemmix F, Ensing S, et al. Preterm Breech Presentation: A Comparison of Intended Vaginal and Intended Cesarean Delivery. Obstet Gynecol 2015; 126:1223.
- Grabovac M, Karim JN, Isayama T, et al. What is the safest mode of birth for extremely preterm breech singleton infants who are actively resuscitated? A systematic review and meta-analyses. BJOG 2018; 125:652.
- Azria E, Kayem G, Langer B, et al. Neonatal Mortality and Long-Term Outcome of Infants Born between 27 and 32 Weeks of Gestational Age in Breech Presentation: The EPIPAGE Cohort Study. PLoS One 2016; 11:e0145768.
- Macharey G, Gissler M, Rahkonen L, et al. Breech presentation at term and associated obstetric risks factors-a nationwide population based cohort study. Arch Gynecol Obstet 2017; 295:833.
- Macharey G, Gissler M, Toijonen A, et al. Congenital anomalies in breech presentation: A nationwide record linkage study. Congenit Anom (Kyoto) 2021; 61:112.
- Thesis: Term breech delivery in The Netherlands. Congenital malformations among infants in breech position: a study of 1.4 million newborns . Rietberg CC, Anthony S, Schonbeck Y, Visser GH.
- Hsieh YY, Tsai FJ, Lin CC, et al. Breech deformation complex in neonates. J Reprod Med 2000; 45:933.
- Fox AE, Paton RW. The relationship between mode of delivery and developmental dysplasia of the hip in breech infants: a four-year prospective cohort study. J Bone Joint Surg Br 2010; 92:1695.
- Humphry S, Hall T, Hall-Craggs MA, Roposch A. Predictors of Hip Dysplasia at 4 Years in Children with Perinatal Risk Factors. JB JS Open Access 2021; 6.
- Morris WZ, Mayfield L, Beckwith T, et al. Late Hip Dysplasia After Normal Ultrasound in Breech Babies: Implications on Surveillance Recommendations. J Pediatr Orthop 2021; 41:e304.
1 : The influence of the fetal leg position on the outcome in vaginally intended deliveries out of breech presentation at term - A FRABAT prospective cohort study.
2 : Variation of fetal presentation with gestational age.
3 : The frequency of breech presentation by gestational age at birth: a large population-based study.
4 : Uterine anomalies. A retrospective, matched-control study.
5 : Outcome of pregnancy in women with uterine malformation: evaluation of 62 cases.
6 : The site of placental attachment as a factor in the aetiology of breech presentation.
7 : Breech presentation and the cornual-fundal location of the placenta.
8 : A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case-control study.
9 : New and old predictive factors for breech presentation: our experience in 14 433 singleton pregnancies and a literature review.
10 : Spontaneous cephalic version and risk factors for persistent breech presentation: a longitudinal retrospective cohort study.
11 : The gentle art of external cephalic version.
12 : Breech presentation at delivery: a marker for congenital anomaly?
13 : Spontaneous cephalic version of breech presentation in the last trimester.
14 : The length of the human umbilical cord in vertex and breech presentations.
15 : Umbilical cord length as an index of fetal activity: experimental study and clinical implications.
16 : Impact of sex ratio on onset and management of labour.
17 : Breech presentation associated with anticonvulsant drugs
18 : Reproductive career after breech presentation: subsequent pregnancy rates, interpregnancy interval, and recurrence.
19 : Recurrence of breech presentation in consecutive pregnancies.
20 : Maternal and paternal contribution to intergenerational recurrence of breech delivery: population based cohort study.
21 : Maternal and paternal contribution to intergenerational recurrence of breech delivery: population based cohort study.
22 : Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group.
23 : Utility of Leopold maneuvers in screening for malpresentation.
24 : Impact of point-of-care ultrasound and routine third trimester ultrasound on undiagnosed breech presentation and perinatal outcomes: An observational multicentre cohort study.
25 : Universal late pregnancy ultrasound screening to predict adverse outcomes in nulliparous women: a systematic review and cost-effectiveness analysis.
26 : The impact of a routine late third trimester growth scan on the incidence, diagnosis, and management of breech presentation in Oxfordshire, UK: A cohort study.
27 : ACOG Committee Opinion No. 745: Mode of Term Singleton Breech Delivery.
28 : Informed consent to breech birth in New Zealand.
29 : Women's Selection of Mode of Birth for their Breech Presentation.
30 : Five years to the term breech trial: the rise and fall of a randomized controlled trial.
31 : The term, singleton, vaginal breech delivery controversy.
32 : Inappropriate use of randomised trials to evaluate complex phenomena: case study of vaginal breech delivery.
33 : Vaginal breech delivery is still justified.
34 : There is still room for disagreement about vaginal delivery of breech infants at term.
35 : Why vaginal breech delivery should still be offered.
36 : Women's experiences of breech birth and disciplinary power.
37 : External cephalic version for breech presentation at term.
38 : Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial.
39 : Mode of delivery and development of atopic disease during the first 2 years of life.
40 : Caesarean section and gastrointestinal symptoms, atopic dermatitis, and sensitisation during the first year of life.
41 : Trends, characteristics, and outcomes of placenta accreta spectrum: a national study in the United States.
42 : Multiple repeat cesareans and the threat of placenta accreta: incidence, diagnosis, management.
43 : Maternal and neonatal outcomes in the following delivery after previous preterm caesarean breech birth: a national cohort study.
44 : Term cesarean breech delivery in the first pregnancy is associated with an increased risk for maternal and neonatal morbidity in the subsequent delivery: a national cohort study.
45 : Maternal deaths after elective cesarean section for breech presentation in the Netherlands.
46 : Report of a breech cesarean section maternal death.
47 : Maternal and neonatal outcomes after caesarean delivery in the African Surgical Outcomes Study: a 7-day prospective observational cohort study.
48 : Planned caesarean section for term breech delivery.
49 : The randomized management of term frank breech presentation: a study of 208 cases.
50 : Randomized management of the nonfrank breech presentation at term: a preliminary report.
51 : Term breech deliveries in the Netherlands: did the increased cesarean rate affect neonatal outcome? A population-based cohort study.
52 : Term breech presentation-Intended cesarean section versus intended vaginal delivery-A systematic review and meta-analysis.
53 : Consequences of the Term Breech Trial in Denmark.
54 : Neonatal outcome of singleton term breech deliveries in Norway from 1991 to 2011.
55 : Time trend in the risk of delivery-related perinatal and neonatal death associated with breech presentation at term.
56 : How singleton breech babies at term are born in France: a survey of data from the AUDIPOG network.
57 : Trends in vaginal breech delivery.
58 : Maternal outcomes of term breech presentation delivery: impact of successful external cephalic version in a nationwide sample of delivery admissions in the United States.
59 : Delivery of breech presentation at term gestation in Canada, 2003-2011.
60 : Is planned vaginal delivery for breech presentation at term still an option? Results of an observational prospective survey in France and Belgium.
61 : Fetal outcome for infants in breech by method of delivery: experiences with a stand-by service system of senior obstetricians and women's choices of mode of delivery.
62 : Evaluation of a decision protocol for type of delivery of infants in breech presentation at term.
63 : Vaginal breech delivery: results of a prospective registration study.
64 : Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes?
65 : Delivery in breech presentation: Perinatal outcome and neurodevelopmental evaluation at 18 months of life.
66 : Maternal and neonatal outcome after vaginal breech delivery of nulliparous versus multiparous women of singletons at term-A prospective evaluation of the Frankfurt breech at term cohort (FRABAT).
67 : Vaginal breech delivery of pregnancy before and after the estimated due date-A prospective cohort study.
68 : Factors associated with adverse perinatal outcomes for term breech fetuses with planned vaginal delivery.
69 : Vaginal vs. cesarean delivery for preterm breech presentation of singleton infants in California: a population-based study.
70 : Early preterm breech delivery: is a policy of planned vaginal delivery associated with increased risk of neonatal death?
71 : Vaginal delivery versus caesarean section in preterm breech delivery: a systematic review.
72 : Preterm Breech Presentation: A Comparison of Intended Vaginal and Intended Cesarean Delivery.
73 : What is the safest mode of birth for extremely preterm breech singleton infants who are actively resuscitated? A systematic review and meta-analyses.
74 : Neonatal Mortality and Long-Term Outcome of Infants Born between 27 and 32 Weeks of Gestational Age in Breech Presentation: The EPIPAGE Cohort Study.
75 : Breech presentation at term and associated obstetric risks factors-a nationwide population based cohort study.
76 : Congenital anomalies in breech presentation: A nationwide record linkage study.
77 : Congenital anomalies in breech presentation: A nationwide record linkage study.
78 : Breech deformation complex in neonates.
79 : The relationship between mode of delivery and developmental dysplasia of the hip in breech infants: a four-year prospective cohort study.
80 : Predictors of Hip Dysplasia at 4 Years in Children with Perinatal Risk Factors.
81 : Late Hip Dysplasia After Normal Ultrasound in Breech Babies: Implications on Surveillance Recommendations.
آیا می خواهید مدیلیب را به صفحه اصلی خود اضافه کنید؟
اضافه کردن مدیلیب به صفحه اصلی


IMAGES
VIDEO
COMMENTS
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
Overview. Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of ...
No. 384 — management of breech presentation at term [2019] The Society of Obstetricians and Gynaecologists of Canada (SOGC) Canada: GRADE methodology framework: 1: 12/14 (85.7) 82: Y: National Clinical Guideline: the management of breech presentation [2017] Institute of Obstetrician and Gynaecologists, Royal College of Physicians of Ireland ...
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
Summary. Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head. Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal ...
Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. ... The effectiveness of moxibustion: an overview during 10 years, Evidence-Based Complementary & Alternative Medicine: eCAMEvid Based Complement Alternat Med, 2011, 306515, 2011 [PMC free article ...
Breech presentation is a type of malpresentation and occurs when the fetal head lies over the uterine fundus and fetal buttocks or feet present over the maternal pelvis (instead of cephalic/head presentation). The incidence in the United Kingdom of breech presentation is 3-4% of all fetuses. 1.
Breech Presentation Deformation. John M. Graham Jr MD, ScD, in Smith's Recognizable Patterns of Human Deformation (Third Edition), 2007 Genesis. The frequency of singleton breech presentation at term is 3.1% and rises to 6.2% when multiple births are included. 1-4 Breech presentation is an important cause of deformation, and fully one third of all deformations occur in babies who have been ...
1. Background. The management of breech presentation continues to cause academic and clinical contention globally [[1], [2], [3]].In recent years, research has shown that if certain criteria are met, and appropriately experienced and skilled clinicians are available, Vaginal Breech Birth (VBB) is a safe option [[4], [5], [6]].However, with Caesarean Section (C/S) rates for breech presentation ...
A breech baby (breech birth or breech presentation) is when a baby's feet or buttocks are positioned to come out of your vagina first. This means its head is up toward your chest and its lower body is closest to your vagina. Ideally, your baby is in a head down, or vertex presentation, at delivery. While most babies do eventually turn into this ...
The most widely quoted study regarding the management of breech presentation at term is the 'Term Breech Trial'. Published in 2000, this large, international multicenter randomised clinical trial compared a policy of planned vaginal delivery with planned caesarean section for selected breech presentations.
Overview Overview. Fetal malpresentation occurs in about 4% of all term pregnancies. The most common malpresentation by far is breech presentation, where the fetal longitudinal lie is oriented parallel to the long axis of the uterus and the buttocks are near the cervix. ... There are 3 types of breech presentation: frank (hips are flexed and ...
Breech presentation refers to the presence of the fetal buttocks, knees or feet at the lower pole of the gravid uterus during pregnancy. At term, up to 4% of pregnancies are breech. ... Overview of issues related to breech presentation: Uptodate Topic 6776 Version 24.0. Google Scholar Scheer K, Nubar J. Variation of fetal presentation with ...
Overview. There are three types of breech presentation: complete, incomplete, and frank. Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal. Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
This trend was accelerated by a 2000 study by Hannah et al. [] This randomized study of 2083 patients compared planned cesarean delivery (1041 patients) with planned vaginal birth (1042 patients) for breech presentation. The authors concluded, "Planned caesarean section is better than planned vaginal birth for the term fetus in the breech presentation; serious maternal complications are ...
BREECH PRESENTATION-An overview Umoh A. V, Abah M. G, Umoiyoho A.J ... Breech presentation is a form of mal-presentation in which the fetal buttocks or lower extremities occupy
INTRODUCTION — Breech presentation, which occurs in approximately 3 percent of fetuses at term, describes the fetus whose presenting part is the buttocks and/or feet. Although most breech fetuses have normal anatomy, this presentation is associated with an increased risk for congenital malformations and mild deformations, torticollis, and developmental dysplasia of the hip.
Breech presentation, which occurs in approximately 3 percent of fetuses at term, describes the fetus whose presenting part is the buttocks and/or feet. Although It seems to us that you have your JavaScript disabled on your browser.
A multivariable logistic regression analysis was used to calculate the risks of breech presentation. RESULTS The incidence of breech presentation at delivery decreased from 23.5% in pregnancy weeks 24-27 to 2.5% in term pregnancies. In gestational weeks 24-27, preterm premature rupture of membranes was associated with breech presentation.