An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings

Trending Articles
- Association between pretreatment emotional distress and immune checkpoint inhibitor response in non-small-cell lung cancer. Zeng Y, et al. Nat Med. 2024. PMID: 38740994
- Characteristics, treatment, and outcomes of early vs. late enrollees of the STRONG-HF trial. Arrigo M, et al. Am Heart J. 2024. PMID: 38740532
- An age-progressive platelet differentiation path from hematopoietic stem cells causes exacerbated thrombosis. Poscablo DM, et al. Cell. 2024. PMID: 38749423
- A Direct Link Implicating Loss of SLC26A6 to Gut Microbial Dysbiosis, Compromised Barrier Integrity and Inflammation. Anbazhagan AN, et al. Gastroenterology. 2024. PMID: 38735402
- Andexanet for Factor Xa Inhibitor-Associated Acute Intracerebral Hemorrhage. Connolly SJ, et al. N Engl J Med. 2024. PMID: 38749032 Clinical Trial.
Latest Literature
- Arch Phys Med Rehabil (1)
- Gastroenterology (2)
- J Am Coll Cardiol (2)
- J Biol Chem (1)
- J Neurosci (2)
- Nat Commun (54)
- Neuron (10)
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

MEDLINE is the National Library of Medicine's (NLM) premier bibliographic database that contains references to journal articles in life sciences, with a concentration on biomedicine. See the MEDLINE Overview page for more information about MEDLINE.
MEDLINE content is searchable via PubMed and constitutes the primary component of PubMed, a literature database developed and maintained by the NLM National Center for Biotechnology Information (NCBI).
Last Reviewed: February 5, 2024
When you choose to publish with PLOS, your research makes an impact. Make your work accessible to all, without restrictions, and accelerate scientific discovery with options like preprints and published peer review that make your work more Open.
- PLOS Biology
- PLOS Climate
- PLOS Complex Systems
- PLOS Computational Biology
- PLOS Digital Health
- PLOS Genetics
- PLOS Global Public Health
- PLOS Medicine
- PLOS Mental Health
- PLOS Neglected Tropical Diseases
- PLOS Pathogens
- PLOS Sustainability and Transformation
- PLOS Collections
Breaking boundaries. Empowering researchers. Opening Science.
PLOS is a nonprofit, Open Access publisher empowering researchers to accelerate progress in science and medicine by leading a transformation in research communication.
Every country. Every career stage. Every area of science. Hundreds of thousands of researchers choose PLOS to share and discuss their work. Together, we collaborate to make science, and the process of publishing science, fair, equitable, and accessible for the whole community.
FEATURED COMMUNITIES
- Molecular Biology
- Microbiology
- Neuroscience
- Cancer Treatment and Research
RECENT ANNOUNCEMENTS
Written by Lindsay Morton Over 4 years: 74k+ eligible articles. Nearly 85k signed reviews. More than 30k published peer review history…
The latest quarterly update to the Open Science Indicators (OSIs) dataset was released in December, marking the one year anniversary of OSIs…
PLOS JOURNALS
PLOS publishes a suite of influential Open Access journals across all areas of science and medicine. Rigorously reported, peer reviewed and immediately available without restrictions, promoting the widest readership and impact possible. We encourage you to consider the scope of each journal before submission, as journals are editorially independent and specialized in their publication criteria and breadth of content.
PLOS Biology PLOS Climate PLOS Computational Biology PLOS Digital Health PLOS Genetics PLOS Global Public Health PLOS Medicine PLOS Neglected Tropical Diseases PLOS ONE PLOS Pathogens PLOS Sustainability and Transformation PLOS Water
Now open for submissions:
PLOS Complex Systems PLOS Mental Health
ADVANCING OPEN SCIENCE
Open opportunities for your community to see, cite, share, and build on your research. PLOS gives you more control over how and when your work becomes available.
Ready, set, share your preprint. Authors of most PLOS journals can now opt-in at submission to have PLOS post their manuscript as a preprint to bioRxiv or medRxiv.
All PLOS journals offer authors the opportunity to increase the transparency of the evaluation process by publishing their peer review history.
We have everything you need to amplify your reviews, increase the visibility of your work through PLOS, and join the movement to advance Open Science.
FEATURED RESOURCES
Ready to submit your manuscript to PLOS? Find everything you need to choose the journal that’s right for you as well as information about publication fees, metrics, and other FAQs here.
We have everything you need to write your first review, increase the visibility of your work through PLOS, and join the movement to advance Open Science.
Transform your research with PLOS. Submit your manuscript
Navigation group
Home banner.

Where scientists empower society
Creating solutions for healthy lives on a healthy planet.
most-cited publisher
largest publisher
2.5 billion
article views and downloads
Main Content
- Editors and reviewers
- Collaborators

Find a journal
We have a home for your research. Our community led journals cover more than 1,500 academic disciplines and are some of the largest and most cited in their fields.

Submit your research
Start your submission and get more impact for your research by publishing with us.

Author guidelines
Ready to publish? Check our author guidelines for everything you need to know about submitting, from choosing a journal and section to preparing your manuscript.

Peer review
Our efficient collaborative peer review means you’ll get a decision on your manuscript in an average of 61 days.

Article publishing charges (APCs) apply to articles that are accepted for publication by our external and independent editorial boards

Press office
Visit our press office for key media contact information, as well as Frontiers’ media kit, including our embargo policy, logos, key facts, leadership bios, and imagery.

Institutional partnerships
Join more than 555 institutions around the world already benefiting from an institutional membership with Frontiers, including CERN, Max Planck Society, and the University of Oxford.

Publishing partnerships
Partner with Frontiers and make your society’s transition to open access a reality with our custom-built platform and publishing expertise.

Policy Labs
Connecting experts from business, science, and policy to strengthen the dialogue between scientific research and informed policymaking.

How we publish
All Frontiers journals are community-run and fully open access, so every research article we publish is immediately and permanently free to read.

Editor guidelines
Reviewing a manuscript? See our guidelines for everything you need to know about our peer review process.

Become an editor
Apply to join an editorial board and collaborate with an international team of carefully selected independent researchers.

My assignments
It’s easy to find and track your editorial assignments with our platform, 'My Frontiers' – saving you time to spend on your own research.

Experts call for global genetic warning system to combat the next pandemic and antimicrobial resistance
Scientists champion global genomic surveillance using latest technologies and a “One Health” approach to protect against novel pathogens like avian influenza and antimicrobial resistance, catching epidemics before they start.

Safeguarding peer review to ensure quality at scale
Making scientific research open has never been more important. But for research to be trusted, it must be of the highest quality. Facing an industry-wide rise in fraudulent science, Frontiers has increased its focus on safeguarding quality.

Scientists call for urgent action to prevent immune-mediated illnesses caused by climate change and biodiversity loss
Climate change, pollution, and collapsing biodiversity are damaging our immune systems, but improving the environment offers effective and fast-acting protection.

Baby sharks prefer being closer to shore, show scientists
marine scientists have shown for the first time that juvenile great white sharks select warm and shallow waters to aggregate within one kilometer from the shore.

Puzzling link between depression and cardiovascular disease explained at last
It’s long been known that depression and cardiovascular disease are somehow related, though exactly how remained a puzzle. Now, researchers have identified a ‘gene module’ which is part of the developmental program of both diseases.

Air pollution could increase the risk of neurological disorders: Here are five Frontiers articles you won’t want to miss this Earth Day
At Frontiers, we bring some of the world’s best research to a global audience. But with tens of thousands of articles published each year, it’s impossible to cover all of them. Here are just five amazing papers you may have missed.

Opening health for all: 7 Research Topics shaping a healthier world
We have picked 7 Research Topics that tackle some of the world's toughest healthcare challenges. These topics champion everyone's access to healthcare, life-limiting illness as a public health challenge, and the ethical challenges in digital public health.
Get the latest research updates, subscribe to our newsletter
Reference management. Clean and simple.
The top list of research databases for medicine and healthcare
3. Cochrane Library
4. pubmed central (pmc), 5. uptodate, frequently asked questions about research databases for medicine and healthcare, related articles.
Web of Science and Scopus are interdisciplinary research databases and have a broad scope. For biomedical research, medicine, and healthcare there are a couple of outstanding academic databases that provide true value in your daily research.
Scholarly databases can help you find scientific articles, research papers , conference proceedings, reviews and much more. We have compiled a list of the top 5 research databases with a special focus on healthcare and medicine.
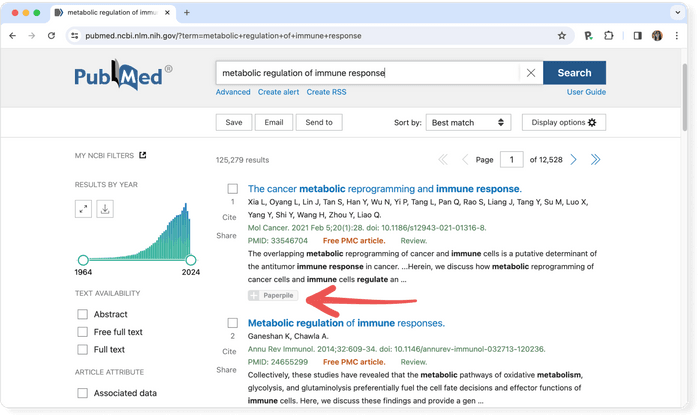
PubMed is the number one source for medical and healthcare research. It is hosted by the National Institutes of Health (NIH) and provides bibliographic information including abstracts and links to the full text publisher websites for more than 28 million articles.
- Coverage: around 35 million items
- Abstracts: ✔
- Related articles: ✔
- References: ✘
- Cited by: ✘
- Links to full text: ✔
- Export formats: XML, NBIB
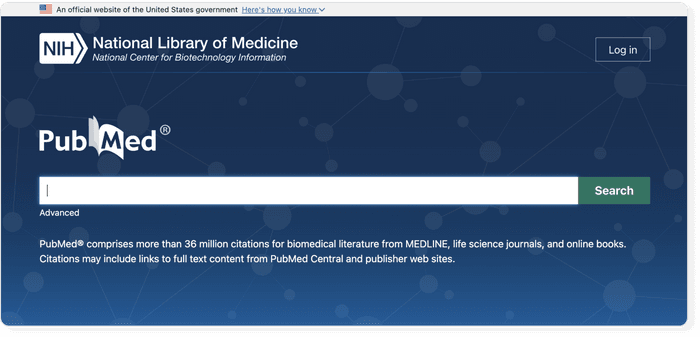
Pro tip: Use a reference manager like Paperpile to keep track of all your sources. Paperpile integrates with PubMed and many popular databases. You can save references and PDFs directly to your library using the Paperpile buttons and later cite them in thousands of citation styles:
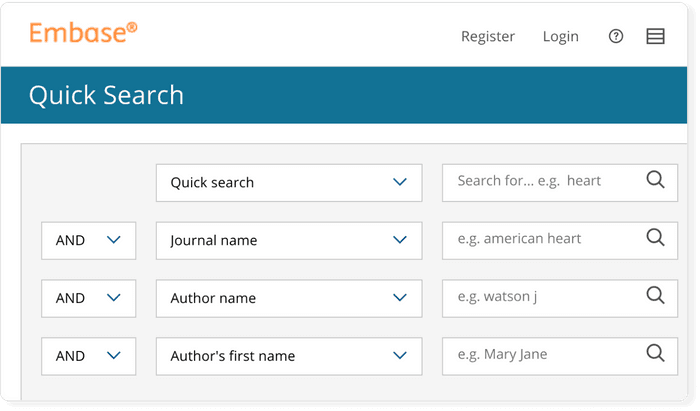
EMBASE (Excerpta Medica Database) is a proprietary research database that also includes PubMed. It can also be accessed by other database providers such as Ovid .
- Coverage: 38 million articles
- References: ✔
- Cited by: ✔
- Full text: ✔ (requires institutional subscription to EMBASE and individual publishers)
- Export formats: RIS
The Cochrane Library is best know for its systematic reviews. There are 53 review groups around the world that ensure that the published reviews are of high-quality and evidence based. Articles are updated over time to reflect new research.
- Coverage: several thousand high quality reviews
- Full text: ✔
- Export formats: RIS, BibTeX
PubMed Central is the free, open access branch of PubMed. It includes full-text versions for all indexed papers. You might also want to check out its sister site Europe PMC .
- Coverage: more than 8 million articles
- Export formats: APA, MLA, AMA, RIS, NBIB
Like the Cochrane Library, UpToDate provides detailed reviews for clinical topics. Reviews are constantly updated to provide an up-to-date view.
- Coverage: several thousand articles from over 420 peer-reviewed journals
- Related articles: ✘
- Full text: ✔ (requires institutional subscription)
- Export formats: ✘
PubMed is the number one source for medical and healthcare research. It is hosted at the National Institutes of Health (NIH) and provides bibliographic information including abstracts and links to the full text publisher websites for more than 35 million items.
EMBASE (Excerpta Medica Database) is a proprietary research database that also includes in its corpus PubMed. It can also be accessed by other database providers such as Ovid.
Journal of Medical Internet Research
The leading peer-reviewed journal for digital medicine and health and health care in the internet age. .
Gunther Eysenbach, MD, MPH, FACMI, Founding Editor and Publisher; Adjunct Professor, School of Health Information Science, University of Victoria, Canada
The Journal of Medical Internet Research (JMIR) is the pioneer open access eHealth journal and is the flagship journal of JMIR Publications. It is a leading health services and digital health journal globally in terms of quality/visibility ( Journal Impact Factor™ 7.4 (Clarivate, 2023) ) and is also the largest journal in the field. The journal is ranked #1 on Google Scholar in the 'Medical Informatics' discipline. The journal focuses on emerging technologies, medical devices, apps, engineering, telehealth and informatics applications for patient education, prevention, population health and clinical care.
JMIR is indexed in all major literature indices including National Library of Medicine(NLM)/MEDLINE , Sherpa/Romeo, PubMed, PMC , Scopus , Psycinfo, Clarivate (which includes Web of Science (WoS)/ESCI/SCIE) , EBSCO/EBSCO Essentials, DOAJ , GoOA and others. As a leading high-impact journal in its disciplines, ranking Q1 in both the 'Medical Informatics' and 'Health Care Sciences and Services' categories, it is a selective journal complemented by almost 30 specialty JMIR sister journals , which have a broader scope, and which together receive over 6.000 submissions a year.
As an open access journal, we are read by clinicians, allied health professionals, informal caregivers, and patients alike, and have (as with all JMIR journals) a focus on readable and applied science reporting the design and evaluation of health innovations and emerging technologies. We publish original research, viewpoints, and reviews (both literature reviews and medical device/technology/app reviews). Peer-review reports are portable across JMIR journals and papers can be transferred, so authors save time by not having to resubmit a paper to a different journal but can simply transfer it between journals.
We are also a leader in participatory and open science approaches, and offer the option to publish new submissions immediately as preprints , which receive DOIs for immediate citation (eg, in grant proposals), and for open peer-review purposes. We also invite patients to participate (eg, as peer-reviewers) and have patient representatives on editorial boards.
As all JMIR journals, the journal encourages Open Science principles and strongly encourages publication of a protocol before data collection. Authors who have published a protocol in JMIR Research Protocols get a discount of 20% on the Article Processing Fee when publishing a subsequent results paper in any JMIR journal.
Be a widely cited leader in the digital health revolution and submit your paper today !
Recent Articles
Limiting in-person contact was a key strategy for controlling the spread of the highly infectious novel coronavirus (COVID-19). To protect patients and staff from the risk of infection while providing continued access to necessary health care services, we implemented a new electronic consultation (e-consult) service that allowed referring providers to receive subspecialty consultations for patients who are hospitalized and do not require in-person evaluation by the specialist.
The increased pervasiveness of digital health technology is producing large amounts of person-generated health data (PGHD). These data can empower people to monitor their health to promote prevention and management of disease. Women make up one of the largest groups of consumers of digital self-tracking technology.
Telemedicine offers a multitude of potential advantages, such as enhanced health care accessibility, cost reduction, and improved patient outcomes. The significance of telemedicine has been underscored by the COVID-19 pandemic, as it plays a crucial role in maintaining uninterrupted care while minimizing the risk of viral exposure. However, the adoption and implementation of telemedicine have been relatively sluggish in certain areas. Assessing the level of interest in telemedicine can provide valuable insights into areas that require enhancement.
Digital health and telemedicine are potentially important strategies to decrease health care’s environmental impact and contribution to climate change by reducing transportation-related air pollution and greenhouse gas emissions. However, we currently lack robust national estimates of emissions savings attributable to telemedicine.
The information epidemic emerged along with the COVID-19 pandemic. While controlling the spread of COVID-19, the secondary harm of epidemic rumors to social order cannot be ignored.
Building therapeutic relationships and social presence are challenging in digital services and maybe even more difficult in written services. Despite these difficulties, in-person care may not be feasible or accessible in all situations.
Whether and how the uncertainty about a public health crisis should be communicated to the general public have been important and yet unanswered questions arising over the past few years. As the most threatening contemporary public health crisis, the COVID-19 pandemic has renewed interest in these unresolved issues by both academic scholars and public health practitioners.
No preview text available.
The use of triage systems such as the Manchester Triage System (MTS) is a standard procedure to determine the sequence of treatment in emergency departments (EDs). When using the MTS, time targets for treatment are determined. These are commonly displayed in the ED information system (EDIS) to ED staff. Using measurements as targets has been associated with a decline in meeting those targets.
Artificial intelligence (AI)–based medical devices have garnered attention due to their ability to revolutionize medicine. Their health technology assessment framework is lacking.
Digital twins have emerged as a groundbreaking concept in personalized medicine, offering immense potential to transform health care delivery and improve patient outcomes. It is important to highlight the impact of digital twins on personalized medicine across the understanding of patient health, risk assessment, clinical trials and drug development, and patient monitoring. By mirroring individual health profiles, digital twins offer unparalleled insights into patient-specific conditions, enabling more accurate risk assessments and tailored interventions. However, their application extends beyond clinical benefits, prompting significant ethical debates over data privacy, consent, and potential biases in health care. The rapid evolution of this technology necessitates a careful balancing act between innovation and ethical responsibility. As the field of personalized medicine continues to evolve, digital twins hold tremendous promise in transforming health care delivery and revolutionizing patient care. While challenges exist, the continued development and integration of digital twins hold the potential to revolutionize personalized medicine, ushering in an era of tailored treatments and improved patient well-being. Digital twins can assist in recognizing trends and indicators that might signal the presence of diseases or forecast the likelihood of developing specific medical conditions, along with the progression of such diseases. Nevertheless, the use of human digital twins gives rise to ethical dilemmas related to informed consent, data ownership, and the potential for discrimination based on health profiles. There is a critical need for robust guidelines and regulations to navigate these challenges, ensuring that the pursuit of advanced health care solutions does not compromise patient rights and well-being. This viewpoint aims to ignite a comprehensive dialogue on the responsible integration of digital twins in medicine, advocating for a future where technology serves as a cornerstone for personalized, ethical, and effective patient care.
Large language models showed interpretative reasoning in solving diagnostically challenging medical cases.
Preprints Open for Peer-Review
Open Peer Review Period:
May 16, 2024 - July 11, 2024
May 15, 2024 - July 10, 2024
May 14, 2024 - July 09, 2024
May 09, 2024 - July 04, 2024
May 07, 2024 - July 02, 2024
May 05, 2024 - June 30, 2024
May 03, 2024 - June 28, 2024
May 02, 2024 - June 27, 2024
May 01, 2024 - June 26, 2024
We are working in partnership with

This journal is indexed in

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Med Inform Decis Mak

Who can you trust? A review of free online sources of “trustworthy” information about treatment effects for patients and the public
Andrew d. oxman.
1 Centre for Informed Health Choices, Norwegian Institute of Public Health, PO Box 4404, Nydalen, N-0403 Oslo, Norway
2 University of Oslo, Oslo, Norway
Elizabeth J. Paulsen
Associated data.
All data generated or analysed during this study are included in this published article and the Additional file 1 .
Information about effects of treatments based on unsystematic reviews of research evidence may be misleading. However, finding trustworthy information about the effects of treatments based on systematic reviews, which is accessible to patients and the public can be difficult. The objectives of this study were to identify and evaluate free sources of health information for patients and the public that provide information about effects of treatments based on systematic reviews.
We reviewed websites that we and our colleagues knew of, searched for government sponsored health information websites, and searched for online sources of health information that provide evidence-based information. To be included in our review, a website had to be available in English, freely accessible, and intended for patients and the public. In addition, it had to have a broad scope, not limited to specific conditions or types of treatments. It had to include a description of how the information is prepared and the description had to include a statement about using systematic reviews. We compared the included websites by searching for information about the effects of eight treatments.
Three websites met our inclusion criteria: Cochrane Evidence , Informed Health , and PubMed Health . The first two websites produce content, whereas PubMed Health aggregated content. A fourth website that met our inclusion criteria, CureFacts , was under development. Cochrane Evidence provides plain language summaries of Cochrane Reviews (i.e. summaries that are intended for patients and the public). They are translated to several other languages. No information besides treatment effects is provided. Informed Health provides information about treatment effects together with other information for a wide range of topics. PubMed Health was discontinued in October 2018. It included a large number of systematic reviews of treatment effects with plain language summaries for Cochrane Reviews and some other reviews. None of the three websites included links to ongoing trials, and information about treatment effects was not reported consistently on any of the websites.
It is possible for patients and the public to access trustworthy information about the effects of treatments using the two of the websites included in this review.
Electronic supplementary material
The online version of this article (10.1186/s12911-019-0772-5) contains supplementary material, which is available to authorized users.
Patients and the public must make choices among different treatment options. We define “treatment” broadly, as any preventive, therapeutic, rehabilitative, or palliative action intended to improve the health or wellbeing of individuals or communities [ 1 ]. This includes, for example, drugs, surgery and other types of “modern medicine”; lifestyle changes, such as changes to what you eat or how you exercise; herbal remedies and other types of “traditional” or “alternative medicine”, and public health interventions. Few people would prefer that decisions about what they should and should not do for their health should be uninformed. Yet, if a decision is going to be well informed rather than misinformed, they need information that is relevant, trustworthy, and accessible. They also need to be able to distinguish between claims about the effects of treatments that are trustworthy and those that are not [ 2 ].
Often the problem is too much information rather than too little. For example, a Google search for “back pain” yields over 60 million hits [ 3 ]. PubMed, a free search engine for accessing MEDLINE and other databases maintained by the United States National Library of Medicine, includes over 27 million citations [ 4 ], and this represents only a fraction of the biomedical literature. The Cochrane Central Register of Controlled Trials, a bibliographic database that is restricted to controlled trials of treatments, contains over a million citations [ 5 ]. It is not practical for people making decisions about treatments to use search engines or databases such as these to find relevant information, critically appraise the studies they find, synthesize them, and interpret the results.
Systematic reviews reduce the risk of being misled by bias (systematic errors) and the play of chance (random errors), by using systematic and explicit methods to identify, select, and critically appraise relevant studies, and to collect and analyse data from them [ 6 ]. For information about treatment effects to be trustworthy, it should be based on systematic reviews. For it to be accessible to patients and the public, it should be easy to find and should be clearly communicated in plain language [ 7 ].
Unfortunately, a large amount of information about treatment effects is not based on systematic reviews and is not trustworthy [ 8 – 19 ]. This includes handouts for patients [ 8 , 9 ], internet-based information [ 10 , 11 ], information in social and mass media [ 12 – 18 ], information produced by patient organisations [ 8 , 9 , 12 ]. press releases [ 18 ], and advertisements [ 19 ]. Studies of the trustworthiness of health information have used a variety of criteria, but have consistently found important limitations [ 8 – 19 ]. Although trustworthy information about treatment effects can be found, evidence-based information is frequently written for health professionals or researchers, rather than for patients and the public [ 7 ].
There is an abundance of health information on the internet, which has become an important source of health information over the past two decades [ 10 , 11 , 20 – 24 ], but patients and the public find it difficult to search the internet for trustworthy information [ 21 – 23 ], and are unlikely to critically appraise the information that they do find [ 22 , 23 ].
There are a number of websites that aim to improve access to trustworthy health information for patients and the public. The objectives of this study were to identify free sources of health information for patients and the public which provide information about the effects of treatments based on systematic reviews, and to evaluate those websites.
Our motivation for undertaking this review grew out of a desire to respond to people who were looking for trustworthy information about the effects of specific treatments and landed on Testing Treatments international [ 25 ], a website for promoting critical thinking about treatment claims. Rather than simply noting that the Testing Treatments website does not provide the information they were seeking, we wanted to help them by directing them to sources that do provide this information. Given this motivation, we restricted our review of websites to ones with a broad scope. There were two reasons for this. First, websites with a broad scope can meet the needs of most people seeking trustworthy information about treatment effects. Furthermore, although disease-specific websites can be useful, it would be impractical to assess any more than a small sample of websites for specific conditions or types of treatments. Second, it is easier to become familiar with one or a small number of websites than it is to use multiple websites for questions about different conditions or types of treatments.
We considered any website that defined itself as providing “health information”, which included information about treatments. To be included in this review a website needed to be:
- Available in English
- Freely accessible (i.e. non-commercial with no cost to users or membership fees)
- That described itself as being intended for patients and the public
- Broad in scope (not limited to specific conditions or types of treatments)
- Explicitly based on systematic reviews (i.e. there had to be a description of how the information is prepared and the description had to include a statement about using systematic reviews)
We identified websites that potentially met those criteria by considering websites that we and our colleagues (see Acknowledgements) knew of. The first author (AO) searched for government sponsored websites in English speaking countries (including Australia, Canada, Ireland, New Zealand, the UK, and the USA); searched Google for “health information” and “patient information” to identify websites that are frequently accessed for health information; and checked links to other websites on the websites that were identified. On 29 January 2018, AO conducted a final set of searches using the following terms: “health information”, “patient information”, “evidence-based health information”, and “evidence-based patient information”; and these search engines: Google [ 3 ], Bing [ 26 ], DuckDuckGo [ 27 ], and HONsearch patients [ 28 ]. Google and Bing are the two most popular search engines, DuckDuckGo is not affected by your previous search history, and HONsearch searches “trustworthy” health websites. The first 20 hits for each search were screened, and any websites that looked like they might meet our inclusion criteria were checked.
AO assessed each identified website for inclusion and the second author (EP) checked those judgements using information provided on the websites. In addition, we emailed each excluded website to confirm that our reason for excluding it was correct.
AO collected the following information for each included website:
- The stated purpose
- A statement that information about treatment effects is based on systematic reviews
- Availability of links to the systematic reviews
- Reporting size of effects
- Reporting certainty of the evidence; i.e. a judgement using GRADE (Grading of Recommendations Assessment, Development and Evaluation) [ 29 – 31 ] or another formal approach or an informal judgement about how sure we can be about the reported effects
- Availability of links to ongoing trials
- Information about how up-to-date information about treatment effects is
- What other information is provided
- What tools there are for searching, sorting, and filtering information
- Use of plain language (i.e. summaries written for patients and the public) and the availability of a glossary
EP checked all of the information that was recorded and the judgements that were made. To inform these judgements, both authors independently searched each included website for eight questions about treatments to assess the ease of finding information (AO on 22 December 2017 and EP on 9 January 2018). We selected the eight questions by searching Google for “common health questions” and selecting the first relevant list that we found ( 25 Questions About Your Health Answered - Oprah.com ). Many of the questions in that list were not about treatment effects and we modified some of the questions with the intention of having a variety of questions for different types of conditions and treatments. Table 1 shows the original question from that list, our question, the conditions, the treatments, and the initial search terms that we used to find information about treatment effects on each website.
Questions about treatments used to assess the included websites
We then independently assessed what was reported about treatment effects, the consistency of reporting, and the advantages and disadvantages of each website. Disagreements were resolved by discussion. Based on these assessments and the information we had collected for each website we suggested how the websites could be improved and provided tips for website users.
For each question, we searched for information using plain language terms without Boolean logic (using the first terms shown for each question in the last column of Table Table1). 1 ). We recorded the number of hits for each search and each relevant summary that we found. We assessed the search as easy if we found relevant information using plain language terms without Boolean logic and the relevant information was one of the first few hits. We assessed searches as hard if we had to use technical terms or Boolean logic, or if we could not find relevant information; and as moderate if finding relevant information required some minor fiddling with the search terms or screening more than a few hits.
For each relevant summary that we found, we recorded whether any information was provided about benefits of the treatment and harms of the treatment, whether quantitative information was provided for at least one outcome, and whether a formal or informal assessment of the certainty of the evidence was provided. We then ranked the three websites for each question based on an overall assessment of how hard it was to find relevant information and the completeness of the information about the effects of the treatments.
We considered 35 websites for inclusion. Of these, 26 were excluded because information about treatment effects was not explicitly based on systematic reviews (Table 2 ), five were excluded because they were not intended for patients and the public (Table 3 ), and one was under development (Table 4 ). Three of the 34 websites met our inclusion criteria: Cochrane Evidence , Informed Health , and PubMed Health (Table 5 ). Cochrane Evidence and Informed Health produce content, whereas PubMed Health , which was discontinued in October 2018, aggregated content, including content from the first two websites.
Websites excluded because they are not explicitly based on systematic reviews a
a These websites were excluded because they do not include a description of how information is prepared that includes a statement about using or being based on systematic reviews of research evidence. It is unclear to what extent information about treatment effects on these websites is based on systematic reviews
Websites excluded because they are not intended for patients and the public a
a These websites were excluded because they are not primarily intended for patients and the general public. However, some patients and members of the general public use these databases
Websites under development a
a Last accessed 14 February 2018
Included websites
a The headings used were inconsistent for all three
b We got an error message (“A technical error has occurred. Please try again later.”) when we used AND to limit searches on Informed Health , and no search results when we used quotation marks (e.g. “back pain”). It was possible to use this logic on the other two websites
Cochrane Evidence provides plain language summaries of over 7500 Cochrane Reviews, most of which are systematic reviews of the effects of treatments. The systematic reviews and the plain language summaries are prepared and updated by Cochrane review groups. Cochrane is a global independent network of researchers, professionals, patients, carers, and people interested in health, with over 37,000 contributors from more than 130 countries.
The plain language summaries include links to the full reviews. The full reviews are available in The Cochrane Library, which can be accessed for free in countries that have a national subscription or if the review or an update was published more than one year previously. The headings and content of the plain language summaries are inconsistent. The summaries include some background information, the authors’ conclusions, and links to other summaries that may be of interest. There is variability in the quality of the summaries. Some summaries include pop-up definitions (but not links to longer explanations) for some research and medical terms, and there is a glossary of terms relevant for Cochrane Reviews available on the Cochrane website. The summaries are translated into Chinese, Croatian, Czech, French, German, Japanese, Korean, Malay, Polish, Portuguese, Romanian, Russian, Spanish, Tamil, and Thai. The glossary is only in English.
No other information regarding treatments is provided in Cochrane Evidence , besides the plain language summaries of Cochrane Reviews. Cochrane website, where Cochrane Evidence is found has other information about the Cochrane Colaboration. Navigation tools for Cochrane Evidence are limited to a simple search for the entire Cochrane website. It is possible to sort findings by relevance, alphabetically, or by date of publication; and to filter the summaries by broad health topics and whether the reviews are new or updated.
Informed Health is the English-language version of the German website Gesundheitsinformation.de. The website is prepared by the Institute for Quality and Efficiency in Health Care (IQWiG) in Germany. IQWiG is a professionally-independent, scientific institute established under the Health Care Reform 2004.
The Informed Health website provides information about treatment effects together with other information for a wide range of topics. The website includes “research summaries” for some but not all treatments. “These are objective, brief summaries of the latest findings on a research question described in the title. They usually summarize the results of studies, for instance the results of one or (rarely) several systematic reviews or IQWiG reports. They also describe the study/studies in more detail and explain how the researchers came to their conclusions.” The website states that they “mainly use systematic reviews of studies to answer questions about the benefits and harms of medical interventions.” Links to systematic reviews are provided when these are used, but the reviews may not be freely available.
All of the research summaries that we examined (Additional file 1 ) included quantitative information about the size of the benefits, and they included frequencies for at least one outcome, but most often only for one outcome. The certainty of the evidence is not reported. All of the information is in plain language, written for patients and the public. There are hyperlinks to background information (but not pop-up definitions). There is a glossary of “medical and scientific” terms that includes primarily medical terms and few research terms.
In addition to information about treatments, Informed Health includes information about symptoms, causes, outlook, diagnosis, everyday life, where to learn more, and explanations (“Extras”) of topics such as how the body works, how treatments work, and types of treatments. Navigation tools for Informed Health include browsing by broad topic areas, an index (A to Z list) and a simple search. Search results can be sorted by relevance, the date information on the website was created, or the date it was updated.
PubMed Health specialized in systematic reviews of clinical effectiveness research. It included plain language summaries and abstracts of Cochrane Reviews; abstracts (technical summaries) of systematic reviews in the Database of Abstracts of Reviews of Effects (DARE) up to 31 March 2015; full texts of reviews from public agencies; information developed by public agencies for consumers and clinicians based on systematic reviews; and methods resources about the best research and statistical techniques for systematic reviews and clinical effectiveness research. PubMed Health was a service provided by the National Center for Biotechnology Information at the U.S. National Library of Medicine. It was discontinued October 31, 2018 “in an effort to consolidate similar resources and make information easier to find”. It included information from over 40,000 systematic reviews from a variety of sources, but plain language summaries were not available for most of those reviews. Links to the systematic reviews were provided, but not all of the reviews were freely available.
The reporting was inconsistent. Headings, reporting of effects, and reporting of the certainty of the evidence were inconsistent. PubMed Health had an extensive glossary (Health A – Z) and background information on drugs. Navigation tools included a simple search. Search results could be sorted by date of publication and filtered by Article types (including “Consumer information”); when information was added to PubMed Health , Content providers (including Cochrane and IQWiG); and Reviews with a quality assessment.
None of the three included websites includes links to ongoing trials and adverse effects are not consistently reported on any of the websites. All three include information about how up-to-date the information about treatment effects is.
PubMed Health was the easiest website to search, despite the large number of records that it includes. However, we had difficulties searching all three websites. We found information easily in Cochrane Evidence and Informed Health for one of the eight questions in Table Table1, 1 , and for three of the questions in PubMed Health (Additional file 1 ). Conversely, it was hard to find information (or we did not find any information) for the five questions in Cochrane Evidence , six questions in Informed Health , and three questions in PubMed Health . It was not possible to use Boolean logic when searching Informed Health . This was possible on the other two websites, but none of the three provided any instructions or help for searching.
When we found information, it was consistently available about benefits, but only Informed Health consistently reported this information quantitatively in the plain language summaries. Quantitative information was provided in the linked scientific abstracts. None of the websites consistently reported information about harms or the certainty of the evidence, although Cochrane plain language summaries in Cochrane Evidence and PubMed Health frequently reported the certainty of the evidence. When the certainty of the evidence was reported using GRADE or another systematic approach, there was not a link to an explanation of what the grade means.
Overall we were most satisfied with Cochrane Evidence for 2 questions, with Informed Health for one question, and with PubMed Health for 3 of our questions. We did not find information about treatment effects on any of the three websites for two questions: “Should I stop using phone, tablet, computer, and TV screens before going to bed (for insomnia)?” and “Should I get my osteoarthritic knee replaced?” Informed Health provided advice for the first question (“For instance, it might help to only listen to relaxing music before going to bed and keep from talking on the phone or playing computer or mobile phone games”), but no reference to research evidence for that advice. We easily found relevant systematic reviews for both of these questions in Epistemonikos (Additional file 1 ).
We identified three websites for patients and the public that provide free information about treatment effects based on systematic reviews. A fourth, promising website, CureFacts, was under development (Table (Table4), 4 ), and is still under development as of February 2019. Twenty-two other websites that provide free information for patients and the public claim to provide trustworthy, evidence-based information. However, it is not possible to know the extent to which the information they provide about treatment effects is based on systematic reviews, so is therefore less likely to be trustworthy. We considered four websites that provide access to systematic reviews, but none of these is intended for patients and the public (Table (Table3). 3 ). Nonetheless, some people may find these useful, particularly Epistemonikos . It includes over 100,000 systematic reviews with the abstracts translated to Arabic, Chinese, Dutch, French, German, Italian, Portuguese, and Spanish. It is aimed for health professionals, researchers and policymakers but plain language summaries are not available for most of the reviews. Although it is not intended for patients and the public, it “has been used by well-informed lay people and journalists successfully” (Table (Table3 3 ).
We did not consider databases that are not free, such as Trip Pro, which includes access to over 100,000 systematic reviews; or patient information from web-based medical compendia for clinicians, such as Best Practice , Dynamed , and UptoDate. We also did not consider websites that provide information for patients and the public based on guidelines, such as the UK National Institute for Health and Care Excellence (NICE) guidance for patients; or websites that are limited to specific conditions or types of treatments.
The three websites for patients and the public that explicitly provided information about treatment effects based on systematic reviews were likely to appeal to different people and their appeal may vary depending on the question being asked. We found that we preferred each of the websites for at least one of the eight questions we used as test cases (Table (Table1). 1 ). We found PubMed Health somewhat easier to search, despite the large number of records it includes, and we found both Cochrane plain language summaries and Health Information research summaries when searching PubMed Health . Simple instructions regarding the use of Boolean logic and the use of quotations to limit searches would help improve the ease of use for all three websites. For example, the default for Cochrane Evidence appears to be to insert OR between words, resulting in large numbers of irrelevant hits.
All of the websites could be improved by more consistent use of headings and consistent reporting of both benefits and (especially) harms; inclusion of quantitative information about the size of the effects; and information about the certainty of the evidence based on the use of a consistent set of criteria, such as GRADE [ 29 – 31 ], and links to explanations of what the grades mean. Because many systematic reviews, including Cochrane Reviews, do not consistently provide this information, plain language summaries based on systematic reviews cannot always provide this information. However, they can alert users to the absence of trustworthy information about adverse effects, when this is the case, and it is possible to provide an assessment of the certainty of the evidence even when review authors have not done this [ 32 , 33 ].
All three websites provided plain language summaries of systematic reviews and all three had glossaries. However, none of the websites included both pop-up short definitions (which can be quickly accessed and read as scroll overs without having to go to another webpage) and links to longer explanations (that can be easily accessed when needed).
None of the websites included links to ongoing trials. This is something that, for example, NHS Choices does [ 34 ]. This is important because when there is important uncertainty about the effects of treatments, participating in a randomised trial may be the best option for patients [ 35 , 36 ].
We are not aware of any other studies that have attempted to systematically identify and evaluate websites that provide free access to information about the effects of treatments for patients and the public which is based on systematic reviews. There are thousands of websites that provide health information and we did not systematically screen all of these. Although we believe it is unlikely that there are other websites that meet our inclusion criteria, we did not consider websites for specific conditions or types of interventions, non-English language websites, or websites that were not freely accessible. Others might want to assess these and other sources of information about treatment effects in future studies.
"The evaluation criteria that we used were based on our judgement about what information is important and what is needed to make that information accessible. For example, providing a link to the systematic review enables people to go to the source of information about treatment effects for more information, if they desire. It also makes the basis of the information clear. Information about the size of effects and the certainty of the evidence is essential for making well-informed decisions. Basic search tools are necessary to make it easy to find information on the websites, and summaries that are written in plain language for patients and the public are more likely to be understandable than abstracts written for researchers or health professionals. Consistent headings, content, and use of language make it easier for users to become familiar with the websites and to find and understand information.
Our evaluation was based in part on searching for answers for eight treatment questions (Table (Table1). 1 ). The criteria that we used to assess what we found for each question did not require a great deal of judgement. Consequently, there were only minor disagreements in our assessments (Additional file 1 ), and those were easily resolved. It is uncertain how representative what we found for those questions is for what would be found for other treatment questions, but we believe they provided a fair basis for assessing the websites. Moreover, we sent full drafts of this report to people responsible for each website and their corrections did not substantially alter our assessments or conclusions.
We did not evaluate the readability of the plain language summaries and, although we described other information that each website provides, we did not evaluate whether the websites provided other information that patients and the public want or need to make informed decisions; for example, information about other treatment alternatives, costs, and people’s experiences with the treatment [ 37 , 38 ]. We also did not evaluate how users of the websites experience them [ 39 ]. All of these are potential areas for future research."
Conclusions
It is possible for patients and the public to access trustworthy information about the effects of treatments based on systematic reviews using two of the three websites included in this review. However, all three of these websites could be improved and made more useful and easier to use by consistently reporting information about the size of both the benefits and harms of treatments and the certainty of the evidence, and by making it easier to find relevant information.
Searching the three websites frequently yielded much irrelevant information. Users can limit searches by using Boolean logic - inserting AND between terms (e.g. for the condition and for the treatment) and quotation marks to indicate that words need to be next to each other; e.g. “back pain”. However, this is unlikely to be obvious to novice users. Some users may want to use sources that are not intended for patients and the public, such as Epistemonikos , if they are unable to find information on one of these websites. They also might want to consider searching for ongoing trials, if there is important uncertainty about the effects of relevant treatments.
There are many other websites that claim to provide evidence-based or reliable information about treatments, but it is difficult to assess the reliability of the information about treatment effects provided on those websites since they do not explicitly base that information on systematic reviews.
Additional file
Appendix review of online evidence-based patient info. Assessments of three included websites. Description of data: Search results and assessments of the information found in the three included websites for eight common health questions. (XLSX 29 kb)
Acknowledgements
With support from the James Lind Initiative, Anita Peerson prepared an earlier unpublished version of this review with advice from Iain Chalmers, Douglas Badenoch, Sarah Rosenbaum, and Astrid Austvoll-Dahlgren. We would like to thank the following colleagues for helpful comments on an earlier version of this paper: Astrid Austvoll-Dahlgren, Atle Fretheim, Claire Glenton, Hilda Bastian, Iain Chalmers, Jon Brasey, Karla Soares-Weiser, Marit Johansen, Marita Sporstøl Fønhus, Sarah Rosenbaum, Signe Flottorp.
Not applicable.
Availability of data and materials
Abbreviations, authors’ contributions.
AO made all of the initial assessments and wrote the first draft of this report. EP checked all of the assessments and contributed to revisions of this report. Both authors read and approved the final manuscript.
Ethics approval and consent to participate
Consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Andrew D. Oxman, Email: on.enilno@namxo .
Elizabeth J. Paulsen, Email: [email protected] .
is an online, open access journal, dedicated to publishing medical research from all disciplines and therapeutic areas.
Impact Factor: 2.9 Citescore: 4.4 All metrics >>
The journal publishes all research study types, from protocols through phase I trials to meta-analyses, including small, specialist studies, and negative studies. Publishing procedures are built around fully open peer review and continuous publication, publishing research online as soon as the article is ready.
BMJ Open aims to promote transparency in the publication process by publishing reviewer reports and previous versions of manuscripts as pre-publication histories. Authors are asked to pay article-publishing charges on acceptance; the ability to pay does not influence editorial decisions.
All papers are included in MEDLINE/PubMed and Science Citation Index Expanded (Web of Science).

BMJ Open accepts submissions on a range of article types, including original research, cohort profiles and protocols.
The Author Information section provides specific article requirements to help you turn your research into an article suitable for BMJ Open.
Information is also provided on editorial policies and open access .
Press Releases
Health policy :
16 April 2024
Epidemiology :
26 March 2024
Complementary medicine :
13 February 2024
9 February 2024
Most Read Articles
Public health :
16 May 2023
Cardiovascular medicine :
28 March 2024
Evidence based practice :
22 May 2023
30 March 2024
Mental Health
Mental health :
15 May 2024
Recent Articles
17 May 2024
Anaesthesia :
Renal medicine :
General practice / Family practice :
Health services research :
Content Editors picks Highly accessed Open access
29 April 2024
Highly accessed Press release
17 April 2024
In the news Press release
27 March 2024
Highly accessed

Related Journals

BMJ Open Respiratory Research

BMJ Open Sport & Exercise Medicine

Isle of Man (GB) (IM)
Recruiter: Peel Medical Group Practice
Recruiter: Cwm Taf Morgannwg University Health Board
Worcester, Worcestershire
Recruiter: University of Worcester
Recruiter: Elysium Healthcare
Recruiter: The Shrewsbury and Telford Hospital NHS Trust
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Welcome to MedlinePlus
MedlinePlus is an online health information resource for patients and their families and friends. It is a service of the National Library of Medicine (NLM), the world's largest medical library, which is part of the National Institutes of Health (NIH). Learn more about MedlinePlus


For Businesses
For students & teachers, how to find credible medical websites for research.
EVERFI Content Team
The Internet is a powerful tool, but it is not without pitfalls. It is no secret that the Internet is the primary form of research for our students — medical information included.
Teaching our students how to use the Internet for medical information comes with a unique set of challenges. Below, we’ll break down how to judge the credibility of online sources.
What Do We Risk?
In a world defined by instant access to communication, we run the risk of our students leaping to incorrect conclusions. For medical information (used to inform medical decisions), this is incredibly dangerous.
Wrong, unsafe, or incorrectly understood medical information can have a very real impact on the lives of our students.
Online Medical Information: How Do We Determine Credibility?
The Who: Always Look to the Source First
The first step in gauging credibility is to analyze the source. Consider publications from the following:
- Mayo Clinic, a nonprofit academic medical center
- National Institutes of Health (NIH), a part of U.S. Department of Health and Human Services
- Johns Hopkins Hospital, one of the world’s premier teaching and biomedical research hospitals
The above institutions are examples of nonprofit, publicly funded, or university-affiliated medical centers. As a general rule of thumb, students can consider information from these sources to be impartial and accurate.
On the other hand, imagine information from the following fictional organizations:
- The Academy of Tobacco Studies, a for-profit research center funded by tobacco companies
- “Aunt Betsy Knows Best”, a blog selling herbal remedies for serious medical conditions
Clearly, these are not credible medical websites for research!
Yes, the examples are extreme. The core approach, however, remains the same — look to the source. If the source has an agenda, the website may lack credibility.
Tip: Websites ending in “.gov” (government) or “.edu” (top level domain for education) tend to be the most credible.
The What: What Information is Offered?
Consider the information offered by the website. For example, this article on the common cold from the Mayo Clinic gives a comprehensive overview of the disease. It offers general treatment tips, of course, but it doesn’t push a product — at best, it briefly mentions a generic medicine brand once or twice.
Tip: If a medical information website is telling the visitor to buy a specific product, it’s likely best to run in the other direction.
The When: Is the Information Current?
Outdated medical information is as potentially hazardous as incorrect content. It’s best to teach students to always check for a publication date.
Tip: The most credible online medical resources probably have the budget for quality web design. If the website looks and feels questionable, it probably is.
The Where: Where Did the Information Come From?
A few minutes spent poking around online can yield “evidence” that the 1969 Moon Landing is a government conspiracy and that smoking is good for your health. It’s vital that students understand where information comes from.
When our students stumble across medical information online, have them consider the following:
- What evidence does it provide?
- Is the evidence from a respectable, peer-reviewed medical publication?
- If the website provides studies as sources, do the studies back up the website author’s claims?
Tip: Medical studies have published abstracts — taking a minute to verify a study supports a website’s information is quick and easy.
The Why: Why Does This Website Exist?
As a pair of general rules:
- Credible online medical resources inform; they do not diagnose.
- Credible sources may recommend treatments; they do not sell medication.
Ask your students to take a minute and consider why a medical website exists. Informative articles from the Mayo Clinic, NIH, or Johns Hopkins exist to provide an objective understanding of a medical issue.
The more we instill a healthy sense of skepticism in our students, the better equipped they will be.
Tip: If a website pushes a treatment or recommends self-diagnosis without a doctor present, run for the hills!
What Are Some Credible Medical Websites For Research?
Our students can develop an appreciation for quality online medical information below:
- Johns Hopkins Medicine : premier teaching and biomedical research center
- Mayo Clinic : Nonprofit medical center
- DailyMed : Government-run drug information website
- MedlinePlus : Government-run health information website
- National Institutes of Health : Government-run health information website
Better Students, Better Research
There’s a lot of medical information on the Internet. Instilling our students with the right mindset for how to find credible medical information online is vital.
If our students can differentiate between credible medical websites and illegitimate ones, we can breathe a sigh of relief.
Real World Learning Matters
EVERFI empowers teachers to bring critical skills education into their classrooms at no cost. Get activated and join 50,000+ educators across North America!
Credible Sources for Students FAQs
Why do students need credible sources in their research papers.
Incorporating credible sources into research papers is a crucial aspect of academic writing. It serves multiple purposes, such as ensuring the accuracy and validity of the information presented, avoiding plagiarism, developing critical thinking skills, and building a strong academic reputation.
Want to prepare students for career and life success, but short on time?
Busy teachers use EVERFI’s standards-aligned, ready-made digital lessons to teach students to thrive in an ever-changing world.
Explore More Resources
10 teacher tips to encourage self-awareness in teens.
Check out these 10 tips for teachers to help guide teenagers toward becoming independent, healthy, and happy adults.
10 Teacher Mental Health Tips You Can Put Into Practice Today
There has been little focus on teachers balancing COVID-19 & remote teaching. That’s why we put together ten mental health tips for t ...
Elementary Schooled Podcast: What is the NFL Character Playbook Program for Students? with ...
Character Playbook course for middle and high school students, where students learn about character building and specific skills for ...
Teaching Data Literacy Skills
Students aren’t equipped with the best analytical tool kit to take in and process all this information. How do we go about teaching d ...
Teaching Budgeting: 3 Ways Educators Bring Budgeting to Life
A budget is just a plan for our money. When we are teaching budgeting basics to our students, we can frame that plan the way we would ...
Class Activities for Teaching the Psychology of Spending Money
Here are some interesting findings we can share with our students to help them understand spending habits and lesson ideas to help th ...
- Open access
- Published: 05 May 2024
The quality of life of men experiencing infertility: a systematic review
- Zahra Kiani ORCID: orcid.org/0000-0002-4548-7305 1 ,
- Masoumeh Simbar ORCID: orcid.org/0000-0003-2843-3150 2 ,
- Farzaneh Rashidi ORCID: orcid.org/0000-0001-7497-4180 3 ,
- Farid Zayeri ORCID: orcid.org/0000-0002-7791-8122 4 &
- Homayoon Banaderakhsh ORCID: orcid.org/0000-0001-8982-9381 5
BMC Public Health volume 24 , Article number: 1236 ( 2024 ) Cite this article
414 Accesses
Metrics details
Men experiencing infertility encounter numerous problems at the individual, family, and social levels as well as quality of life (QOL). This study was designed to investigate the QOL of men experiencing infertility through a systematic review.
Materials and methods
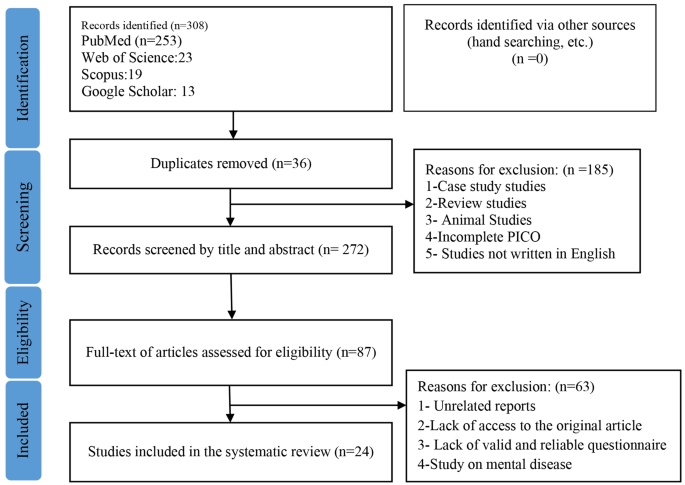
This systematic review was conducted without any time limitation (Retrieval date: July 1, 2023) in international databases such as Scopus, Web of Science, PubMed, and Google Scholar. The search was performed by two reviewers separately using keywords such as QOL, infertility, and men. Studies were selected based on inclusion and exclusion criteria. The quality of the articles were evaluated based on the Newcastle-Ottawa Scale. In the initial search, 308 studies were reviewed, and after removing duplicates and checking the title and abstract, the full text of 87 studies were evaluated.
Finally, 24 studies were included in the final review based on the research objectives. Based on the results, men’s QOL scores in different studies varied from 55.15 ± 13.52 to 91.45 ± 13.66%. Of the total reviewed articles, the lowest and highest scores were related to mental health problems and physical dimensions, respectively.
The reported findings vary across various studies conducted in different countries. Analysis of the factors affecting these differences is necessary, and it is recommended to design a standard tool for assessing the quality of life of infertile men. Given the importance of the QOL in men experiencing infertility, it is crucial to consider it in the health system. Moreover, a plan should be designed, implemented and evaluated according to each country’s contex to improve the quality of life of infertile men.
Peer Review reports
Introduction
Defined as the absence of pregnancy after one or two years of unprotected sexual intercourse (without the use of contraceptive methods) [ 1 ], infertility is recognized as both a medical and social issue [ 2 ]. Based on the latest Word Health Organization (WHO) report in 2023, the pooled lifetime and period prevalence of infrtility are reported as 17.5% and 12.6%, respectively [ 3 ]. In this regard, male factors play a role in 50% of infertilities [ 4 ].
Complicated treatment protocol, difficult treatment process, semen analysis, multiple ultrasounds, invasive treatments, long waiting lists, and high financial costs for the clients who seek assisted reproductive techniques have been described as psychological stresses for infertile couples [ 5 , 6 ]. Moreover, the diagnosis and treatment of infertility can have negative impact on the frequency of sexual intercourse, self-esteem, and body image [ 5 ]. However, these men usually tend to suppress or deny their problems which may diminish their quality of life (QOL) over time [ 7 ]. This decreased QOL, in turn, can have a detrimental effect on their response to treatment [ 8 ].
The function of infertile people is under the influence of society, family, and the society culture. In many societies, infertility is primarily viewed as a medical problem, often neglecting its individual and social dimensions [ 9 ]. In other words, despite having the right attitude toward infertility, infertile people sometimes cannot adapt to the problem. Thus, non-compliance during the behavioral process may lead to additional problems and impair one’s QOL [ 10 ].
The WHO describes the QOL as people’s perspective of their life circumstances in terms of the cultural systems and standards of their environment, and how these perspectives are associated with their objectives, prospects, ideals, and apprehensions [ 11 ]. Recently, the QOL of men experiencing infertility as a main subject has been carefully considered by health investigators. Furthermore, because of men’s essential role in future phases of life, their QOL can significantly affect their health at both individual and societal levels [ 12 ].
Given the significance of QOL, its precise measurement is substantially important. In this regard, various tools have been designed and used in studies to examine this concept. A systematic study used the World Health Organization Quality Of Life )WHOQOL), 36-Item Short Form Survey (SF-36 ), and general QOL questionnaires. Based on the results, the QOL of men experiencing infertility was reported to be low in two studies that had used the SF-36 questionnaire. By contrast, the QOL of these men was high in a study that used the WHOQOL questionnaire. It was noted in this systematic review that although infertility has a negative effect on the mental health and sexual relationships of couples, there is no consensus regarding its effect on the QOL of infertile couples [ 13 ].
In Almutawa et al.‘s systematic review and meta-analysis 2023, it has been shown that the psychological disturbances in infertile women are higher than in men, and this difference in couples needs further investigation [ 14 ]. Chachavomich et al. 2010 showed that women’s quality of life is more affected by infertility than men study, which was a systematic review [ 12 ], . This study was conducted 14 years ago and due to the increase in the number of articles in this field, it needs to be re-examined.Given that no systematic review had been conducted to address the QOL of men experiencing infertility and considering the significance of this issue in therapeutic responses, this study examined the QOL of men experiencing infertility in the form of a systematic review.
Search strategy
To search and review the studies, reputable international databases and sites such as Scopus, Web of Science, PubMed, and Google Scholar were used. The search was performed using keywords such as QOL, infertility, and men (Table 1 ), without time limitation (Retrieval date: July 1, 2023), and using AND and OR operators, and specific search strategies were used for each database.
The search strategy of PubMed, Web of Science, and Scopus databases is as follows:
Pubmed (retrieval date: July 1, 2023)
Male [tiab] OR Males [tiab] OR Men [tiab] OR Man [tiab] OR Boy [tiab] OR Boys [tiab] AND Quality of Life [tiab] OR Health-Related Quality of Life [tiab] AND Infertility [tiab] OR Sterility OR Reproductive [tiab] OR Reproductive Sterility [tiab] OR Subfertility [tiab] Sub-Fertility [tiab].
Web of science (retrieval date: July 1, 2023)
((TI=(male OR males OR man OR men OR boy OR boys)) AND TI=(Quality of Life OR Health-Related Quality of Life OR Health-Related Quality of Life)) AND TI=(Infertility OR Sterility OR Reproductive OR Reproductive Sterility).
Scopus (retrieval date: July 1, 2023)
TITLE ( male OR males OR men OR man OR boy OR boys ) AND TITLE (quality AND of AND life OR health-related AND quality AND of AND life ) AND TITLE ( infertility OR sterility OR reproductive).
The method of presenting the article, describing the problem, data collection, data analysis, discussion, and conclusion of the findings were based on preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2020 [ 15 ]. The reviews were conducted separately by two reviewers, and the third reviewer was also used in case of disagreement between them.
Inclusion and exclusion criteria
Those studies with the following criteria were included in the review: (1) Observational studies; (2) Cross-sectional data from longitudinal studies; (3) Using valid tools for measuring the QOL; (4) Studies conducted on men of infertile couples (by men experiencing infertility we mean those men whose unprotected sexual intercourse during the past year did not lead to any pregnancy); (5) Minimum sample size of 30 subjects; (6) Subjects with no chronic disease, and (7) those men of infertile couples who were within the diagnostic process for infertility and before starting infertility treatment. The search and review process for this study were conducted in English, and there were no restrictions imposed on the inclusion of open-access studies.
Exclusion criteria included: (1) Case report studies; (2) Review studies; (3) Animal studies; (4) Studies on mental syndromes; (5) Studies not written in English; (6) Lack of access to the full text of the article, and (7) Unrelated reports.
The patient, intervention, comparison, outcome, and study design (PICOS)
PICOS model was used to help break down the searchable elements of the research question into (P) participants: men experiencing infertility (primary or secondary infertility) (I) intervention/exposure: not applicable; (C) control group: not applicable; (O) outcomes: evaluate infertile men’s QOL, which was measured using standard tools such as general or specific QOL questionnaire and (S) study type: Observational studies and Cross-sectional data from longitudinal studies.
Data extraction
The two reviewers independently reviewed the titles and abstracts of the articles following the inclusion criteria, and the studies which did not have the required criteria were excluded. Then, the full text of the articles with inclusion criteria was reviewed and if appropriate, they were included in the study.
Required information, including authors’ names, year of publication, research location, sample size, QOL score, type of tool, type of infertility, mean age of men, and duration of infertility, were extracted from the studies.
Outcome measurement
The main outcome of this study was to evaluate QOL of men experiencing infertility, which was measured using standard tools such as a general or specific QOL questionnaire.
Quality evaluation
The Newcastle-Ottawa Scale checklist was used to assess the quality of nonrandomized studies in meta-analyses [ 16 ]. This checklist consists of 5 parts that are representativeness of the sample, sample size, non-respondents, ascertainment of anxiety, and quality of descriptive statistics reporting. Each part gets a score of zero and one. Given the fact that the checklist has 5 items, the minimum, and maximum scores are 0 and 5, respectively. Then, studies were divided into high- and low-risk groups if their scores were ≤ 3 and more than 3 [ 16 ]. The quality assessment in this study was performed by two reviewers independently, and in case of disagreement between them, the third reviewer was asked to help. The coefficient of agreement of 0.7 and more among the reviewers was acceptable.
Ethical consideration
Ethics approval was obtained from the Ethics Committee, Faculty of Pharmacy and Nursing.
Midwifery, Shahid Beheshti University (Ethical code: IR.SBMU.PHARMACY.REC.1400.214). All methods were carried out in accordance with relevant guidelines and regulations.
After reviewing the title, abstract, and text of the articles in different stages (Fig. 1 ), finally, 24 articles were reviewed based on the inclusion criteria and research objectives and the coefficient of agreement among the reviewers was K = 0.81 (Table 2 ).
Flowchart for selection of studies
The smallest and largest sample size were 30 [ 19 ] and 1,000 [ 40 ], respectively. Seven studies were conducted in low- and middle-income countries, two studies in upper-middle-income, and 15 studies in high-income countries. High-income countries had a higher quality of life score compared to low- and middle-income countries countries. In all studies, QOL scores were calculated based on 100, and the highest score (91.45 ± 13.66%) obtained from the Fertility quality of life (FertiQoL) questionnaire in South Korea as a high-income country [ 25 ]. Most of the studies showed that education, family income and proper marital relations improved the quality of life of infertile men. Out of 24 reviewed articles, 12 articles used the FertiQoL questionnaire, 7 articles SF-36, and 6 articles WHOQOL-BREF. One study [ 36 ] used SF-36 and WHOQOL-BREF questionnaires simultaneously.
Out of the total articles reviewed, the lowest scores were attributed to different domains. Accordingly, the lowest score in 11 articles was related to mental health problems, in 8 articles it was related to social problems, and 3 articles to communication problems.Some articles did not report the scores based on the dimensions. Based on the results, men’s QOL scores in different studies varied from 55.15 ± 13.52 to 91.45 ± 13.66%. In the total reviewed articles, the lowest and highest scores were related to mental health problems and physical dimensions, respectively.
In most of the studies using the FertiQoL questionnaire, it was observed that the lowest scores belonged to the social and communication dimensions. The FertiQoL questionnaire was developed and psychometrically evaluated in a survey study conducted in the United States. FertiQoL is a 36-item scale with Six dimension: (1) Emotional; (2) Mind-body; (3) Relational; (4) Social; (5) Environment; and (6) Treatment tolerability. A 5-point Likert scale (0–4) was used in the questionnaire, and the total score was between 0 and 100, where the higher the score, the better was the QOL [ 41 ]. This questionnaire has been translated into different languages in the world and has obtained the required validity (content, face, and construct) and reliability (with Cronbach’s alpha of 0.7–0.9) in different populations [ 42 , 43 , 44 , 45 ].
In the studies where the SF-36 and WHOQOL-BREF questionnaires had been used, the lowest scores belonged to the dimensions of limitations in usual role activities because of emotional problems and social relationships. On the other hand, the highest scores in the questionnaires were related to physical dimensions. The SF-36 questionnaire has been considered for clinical investigation, health policy assessments, and surveys. The 8 dimensions of this questionnaire are as follows: Restrictions in physical activities; Restrictions in social activities; Restrictions in standard role activities; Physical pain; General mental health; Restrictions in standard role activities; Vitality; and Common health perceptions. The final scores of the questionnaire are standardized based on 100 [ 46 ]. This questionnaire has been translated into different languages in the world and has obtained validity (content and face) and reliability (Cronbach’s alpha of 0.8–0.95) in different populations [ 47 , 48 , 49 , 50 , 51 , 52 ]. The 26-item version of WHOQOL-BREF was developed in the following four dimensions: physical health, mental health, social connections, and environmental health, and two items associated with common QOL and general health [ 53 ]. The questionnaire has been translated into different languages of the world and has obtained validity (content and face) and reliability (Cronbach’s alpha of 0.74–0.88) in different populations [ 54 , 55 , 56 , 57 ].
This systematic review study investigated the quality of life of infertile men. Based on the results, men’s quality of life scores in different studies varied from 55.15 ± 13.52 to 91.45 ± 13.66%. However, men’s quality of life scores was reported to be between 70 and 80% in the majority of the studies. As one of the health indicators with a combination of each person’s knowledge in different aspects of life and performance in human, work and social relations, quality of life is essentially important for the continuation of an optimal life and well-being of the individuals. Moreover, quality of life is strongly influenced by demographic, social, economic, and cultural variables, as well as the variables related to health and disease, and its measurement is, thus, substantially important [ 58 ]. Quality of life is a reflection of the desires, hopes, and expectations of individuals regarding their current and future life situation, and is influenced by factors such as age, personal and family characteristics, socio-economic status, and time [ 59 ].
In this systematic review, the lowest scores of men’s quality of life belonged to the psychological and emotional dimensions and then to the social and communication dimensions. Although the reviewed studies had used different tools, these tools were essentially similar in these dimensions, indicating the problems of men in these areas. Fertility is highly valued in most cultures and the desire for having a child is one of the human stimuli in the continuation of life. If efforts for fertility do not lead to success, they can have adverse effects on mental health as well as family and social relationships [ 60 ].
The reviewed studies indicated that education has a significantly positive effect on the quality of life of infertile men. Higher levels of education are associated with increased awareness and better decision-making abilities [ 25 ], and improved coping strategies for dealing with infertility-related challenges [ 38 ]. Infertile men with higher education are also more likely to seek treatment, and remain hopeful that treatment will improve their quality of life [ 28 ].
The results of most studies showed the positive and significant relationship between family income and quality of life.The costs of infertility treatment and the potential need for repeated treatment can lead to concerns and anxieties among men and reduce their quality of life [ 61 ]. If men have fewer concerns about the cost of treatment, they are more inclined to pursue infertility treatment. In the International Conference on Population and Development held in Cairo in 1994, addressing the issue of infertility was emphasized as an important health priority. However, it is unfortunate that infertility problems have been overlooked not only in developing countries but also at various levels of international health management [ 62 ].
The results of the study regarding the countries’ income showed that the quality of life score of men in infertile couples residing in low-income countries was lower compared to those in high-income countries. Current infertility policies in the treatment and distribution sector are uncoordinated, which has led to improper distribution of public and private centers in low- and middle-income countery [ 63 ]. This point of view is a kind of simplistic calculation of the problem of infertility that justifies the lack of public centers, inadwquate finantial sources, specialists and affordable treatment options [ 64 ], requireing serious attention and careful planning, especially in low- and middle-income countries.
The results of the studies showed that marital relationships have a positive and significant impact on the quality of life of infertile men. Sometimes, infertile men may experience a lack of sexual attraction, and due to irrational thoughts, they might abstain from having sexual relations with their partners or try to suppress their sexual desires. Sexual desire is a significant aspect of life that can affect the quality of life [ 65 ]. Some studies have indicated that the quality of marital relations is higher among infertile couples than the fertile ones, and infertility can bring couples closer together and encourage more open communication about their concerns and plans for the future [ 33 , 66 ]. Further research is recommended to gain a deeper understanding in this area.
Infertility presents people with a new and challenging world [ 28 ]. In this regard, infertility is characterized as a long-term process that involves time-consuming treatments, fluctuations between hope and disappointment, loss of control over reproductive outcomes, inability to plan for future, and significant shifts in personal identity and worldview [ 28 , 32 , 63 ]. Long working hours, work-caused exhaustion, along with infertility, can exacerbate men’s problems. These problems affect their quality of life, though they may deny the problems [ 67 ].
Given the significance of quality of life, its accurate measurement is essentially important. In this regard, various tools have been designed to investigate this concept and have been used in several studies. The noteworthy point in this systematic review was the use of different measurement tools in various studies. In the majority of the studies, Boivin’s FertiQoL [ 41 ] was used as a specific tool for measuring the quality of life of infertile couples. Covering emotional, physical, communicational, social, environmental, and acceptability dimensions, this questionnaire has been designed for infertile couples and does not specifically assess the quality of life of infertile men. Other studies have used a general quality-of-life questionnaire (SF-36 and WHOQOL-BREF). WHOQOL questionnaire has been designed in 4 dimensions of physical health, psychological health, social relationships, and environmental health [ 53 ]. SF-36 questionnaire also has 8 dimensions of Limitations in physical activities because of health problems; 2) Limitations in social activities because of physical or emotional problems; 3) Limitations in usual role activities because of physical health problems; 4) Bodily pain; 5) General mental health (psychological distress and well-being); 6) Limitations in usual role activities because of emotional problems; 7) Vitality (energy and fatigue); and 8) General health perceptions [ 46 ]. The main drawback of these tools is that they ignore significant dimensions such as sexual and socio-economic dimensions which are important for certain groups including infertile men. Additionally, the other dimensions of the questionnaire are not sensitive enough to measure changes in the quality of life of people with various diseases [ 68 ].
Health researchers have recently paid much attention to the examination of the quality of life and the design of a questionnaire to measure this concept. This measurement can improve clinical decision-making, estimate healthcare in a particular population, perceive different health causes and consequences, and, finally, promote health policy. All of these objectives will be achieved in light of a specific tool in this regard. However, according to the review, no questionnaire has hitherto been designed to measure the quality of life in infertile men. Specific questionnaires for infertile couples or general quality of life questionnaires have been used in different studies. Given the concept of quality of life and its changes over time as well as the expansion of tool-making knowledge, there is a need to design specific tools to measure the quality of life of infertile men by using mixed methods. We hope that more attention will be given to this significant issue in future. Polit and Beck argue that one of the main applications of exploratory mixed methods is in instrument making. They maintain that when a new tool is developed to explain a health-related concept, the complexity of this concept must be carefully explained [ 69 ].
Furthermore, it seems that the concept of men’s quality of life needs more investigation and also this concept may change over time and impact on their life. Besides, the studies demonstrated specific concerns among infertile men such as decreased self-esteem, Fertility- related stress, masculinity identity, hiding the infertility problem, resistance to the treatment, and cost of treatment [ 70 , 71 ]. These concerns could be the specific items for the infertile men-related quality of life questionnaire.
Research limitations
The impossibility of meta-analysis was because of several limitations in the study: (1) Variety of tools and small sample size in each subgroup; (2) Inaccurate report of information; and (3) -heterogeneity of the studies. Other limitation in this systematic review was that the reviewed papers were confined to English literature; thus, it is possible that some relevant non-English language studies were missed.
The systematic review strategies and solutions
The quality of life of men is one of the basic issues in their life. Assessing the quality of life of men should be done during the initial evaluation of infertility, and if necessary, interventions should be made to improve their quality of life. It is recommended that researchers, using qualitative-quantitative methods, first explain the concept of the QOL of men with infertility and then design and psychometrically evaluate the QOL tool for men experiencing infertility. Based on its context, each country should design a suitable program to improve the quality of life of men.
Data availability
All data related to this review is included in the result section of the manuscript. If any further data is needed it can be accessible via the corresponding author on request.
Abbreviations
World Health Organization
The Newcastle-Ottawa Scale
Preferred reporting items for systematic reviews and meta-analyses
Not reported
The Health Survey Short Form
World Health Organization Quality of Life Instruments
The Fertility Quality of Life tool
Berek JS. Berek & Novak’s gynecology. Lippincott Williams & Wilkins; 2019.
Kiani Z, Simbar M, Hajian S, Zayeri F. The prevalence of depression symptoms among infertile women: a systematic review and meta-analysis. Fertility Res Pract. 2021;7(1):1–10.
Google Scholar
World Health Organization. Infertility prevalence estimates: 1990–2021. 2023.
Santi D, Granata A, Simoni M. FSH treatment of male idiopathic infertility improves pregnancy rate: a meta-analysis. Endocr Connections. 2015;4(3):R46–58.
Article CAS Google Scholar
Hayden RP, Flannigan R, Schlegel PN. The role of lifestyle in male infertility: diet, physical activity, and body habitus. Curr Urol Rep. 2018;19(7):1–10.
Article Google Scholar
Kiani Z, Simbar M, Hajian S, Zayeri F, Shahidi M, Saei Ghare Naz M, et al. The prevalence of anxiety symptoms in infertile women: a systematic review and meta-analysis. Fertility Res Pract. 2020;6(1):1–10.
Ilacqua A, Izzo G, Emerenziani GP, Baldari C, Aversa A. Lifestyle and fertility: the influence of stress and quality of life on male fertility. Reproductive Biology Endocrinol. 2018;16(1):1–11.
https:// www.skillsyouneed.com/ips/relationship-skills.html,Accessed , 14 September 2023.
Hasanpoor-Azghady SB, Simbar M, Abou Ali Vedadhir SAA, Amiri-Farahani L. The social construction of infertility among Iranian infertile women: a qualitative study. J Reprod Infertility. 2019;20(3):178.
Lawshe CH. A quantitative approach to content validity 1. Pers Psychol. 1975;28(4):563–75.
World Health Organization. The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998;46(12):1569–85.
Chachamovich JR, Chachamovich E, Ezer H, Fleck MP, Knauth D, Passos EP. Investigating quality of life and health-related quality of life in infertility: a systematic review. J Psychosom Obstet Gynecol. 2010;31(2):101–10.
Luk BH-K, Loke AY. The impact of infertility on the psychological well-being, marital relationships, sexual relationships, and quality of life of couples: a systematic review. J Sex Marital Ther. 2015;41(6):610–25.
Article PubMed Google Scholar
Almutawa YM, AlGhareeb M, Daraj LR, Karaidi N, Jahrami H, Karaidi NA. A systematic review and Meta-analysis of the Psychiatric morbidities and Quality of Life Differences between Men and Women in infertile couples. Cureus. 2023;15(4).
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372.
Zhang L, Fu T, Yin R, Zhang Q, Shen B. Prevalence of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysis. BMC Psychiatry. 2017;17(1):1–14.
Andrei F, Salvatori P, Cipriani L, Damiano G, Dirodi M, Trombini E, et al. Self-efficacy, coping strategies and quality of life in women and men requiring assisted reproductive technology treatments for anatomical or non-anatomical infertility. Eur J Obstet Gynecol Reproductive Biology. 2021;264:241–6.
Warchol-Biedermann K. The etiology of infertility affects fertility quality of life of males undergoing fertility workup and treatment. Am J Men’s Health. 2021;15(2):1557988320982167.
Asazawa K, Jitsuzaki M, Mori A, Ichikawa T, Shinozaki K. Effectiveness of a spousal support program in improving the quality of life of male patients undergoing infertility treatment: a pilot study. Int J Community Based Nurs Midwifery. 2020;8(1):23.
PubMed Google Scholar
Cusatis R, Fergestrom N, Cooper A, Schoyer KD, Kruper A, Sandlow J, et al. Too much time? Time use and fertility-specific quality of life among men and women seeking specialty care for infertility. BMC Psychol. 2019;7(1):1–9.
Asazawa K, Jitsuzaki M, Mori A, Ichikawa T, Shinozaki K, Porter SE. Quality-of‐life predictors for men undergoing infertility treatment in Japan. Japan J Nurs Sci. 2019;16(3):329–41.
Shahraki Z, Afshari M, Ghajarzadeh M, Tanha FD. How different are men with infertility-related problems from fertile men in prevalence of Depression, anxiety and quality of life? Maedica. 2019;14(1):26.
PubMed PubMed Central Google Scholar
Jahromi BN, Mansouri M, Forouhari S, Poordast T, Salehi A. Quality of life and its influencing factors of couples referred to an infertility center in Shiraz. Iran Int J Fertility Steril. 2018;11(4):293.
Goker A, Yanikkerem E, Birge O, Kuscu NK. Quality of life in Turkish infertile couples and related factors. Hum Fertility. 2018;21(3):195–203.
Kim JH, Shin HS, Yun EK. A dyadic approach to infertility stress, marital adjustment, and depression on quality of life in infertile couples. J Holist Nurs. 2018;36(1):6–14.
Casu G, Ulivi G, Zaia V, Fernandes Martins MdC, Parente Barbosa C, Gremigni P. Spirituality, infertility-related stress, and quality of life in Brazilian infertile couples: analysis using the actor‐partner interdependence mediation model. Res Nurs Health. 2018;41(2):156–65.
Maroufizadeh S, Hosseini M, Foroushani AR, Omani-Samani R, Amini P. The effect of depression on quality of life in infertile couples: an actor-partner interdependence model approach. Health Qual Life Outcomes. 2018;16(1):1–7.
Zurlo MC, Della Volta MFC, Vallone F. Predictors of quality of life and psychological health in infertile couples: the moderating role of duration of infertility. Qual Life Res. 2018;27(4):945–54.
Madero S, Gameiro S, García D, Cirera D, Vassena R, Rodríguez A. Quality of life, anxiety and depression of German, Italian and French couples undergoing cross-border oocyte donation in Spain. Hum Reprod. 2017;32(9):1862–70.
Article CAS PubMed Google Scholar
Agostini F, Monti F, Andrei F, Paterlini M, Palomba S, La Sala GB. Assisted reproductive technology treatments and quality of life: a longitudinal study among subfertile women and men. J Assist Reprod Genet. 2017;34:1307–15.
Article PubMed PubMed Central Google Scholar
El Kissi Y, Amamou B, Hidar S, Idrissi KA, Khairi H, Ali BBH. Quality of life of infertile Tunisian couples and differences according to gender. Int J Gynecol Obstet. 2014;125(2):134–7.
Huppelschoten AG, Van Dongen A, Verhaak C, Smeenk J, Kremer J, Nelen W. Differences in quality of life and emotional status between infertile women and their partners. Hum Reprod. 2013;28(8):2168–76.
Onat G, Beji NK. Effects of infertility on gender differences in marital relationship and quality of life: a case-control study of Turkish couples. Eur J Obstet Gynecol Reproductive Biology. 2012;165(2):243–8.
Herrmann D, Scherg H, Verres R, Von Hagens C, Strowitzki T, Wischmann T. Resilience in infertile couples acts as a protective factor against infertility-specific distress and impaired quality of life. J Assist Reprod Genet. 2011;28(11):1111–7.
Bolsoy N, Taspinar A, Kavlak O, Sirin A. Differences in quality of life between infertile women and men in Turkey. J Obstetric Gynecologic Neonatal Nurs. 2010;39(2):191–8.
Chachamovich JL, Chachamovich E, Ezer H, Cordova FP, Fleck MM, Knauth DR, et al. Psychological distress as predictor of quality of life in men experiencing infertility: a cross-sectional survey. Reproductive Health. 2010;7(1):1–9.
Chachamovich J, Chachamovich E, Fleck M, Cordova FP, Knauth D, Passos E. Congruence of quality of life among infertile men and women: findings from a couple-based study. Hum Reprod. 2009;24(9):2151–7.
Drosdzol A, Skrzypulec V. Quality of life and sexual functioning of Polish infertile couples. Eur J Contracept Reproductive Health Care. 2008;13(3):271–81.
Rashidi B, Montazeri A, Ramezanzadeh F, Shariat M, Abedinia N, Ashrafi M. Health-related quality of life in infertile couples receiving IVF or ICSI treatment. BMC Health Serv Res. 2008;8(1):1–6.
Ragni G, Mosconi P, Baldini MP, Somigliana E, Vegetti W, Caliari I, et al. Health-related quality of life and need for IVF in 1000 Italian infertile couples. Hum Reprod. 2005;20(5):1286–91.
Boivin J, Takefman J, Braverman A. The fertility quality of life (FertiQoL) tool: development and general psychometric properties. Hum Reprod. 2011;26(8):2084–91.
Hsu P-Y, Lin M-W, Hwang J-L, Lee M-S, Wu M-H. The fertility quality of life (FertiQoL) questionnaire in Taiwanese infertile couples. Taiwan J Obstet Gynecol. 2013;52(2):204–9.
Maroufizadeh S, Ghaheri A, Amini P, Samani RO. Psychometric properties of the fertility quality of life instrument in infertile Iranian women. Int J Fertility Steril. 2017;10(4):371.
Asazawa K, Jitsuzaki M, Mori A, Ichikawa T, Shinozaki K, Yoshida A, et al. Validity and reliability of the Japanese version of the fertility quality of life (FertiQoL) tool for couples undergoing fertility treatment. Open J Nurs. 2018;8(9):616–28.
Gao M, Ji X, Zhou L, Zhang Z. AB084. The fertility quality of life (FertiQol) in Chinese infertile women. Translational Androl Urol. 2016;5(Suppl 1).
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical care. 1992:473 – 83.
Jenkinson C, Stewart-Brown S, Petersen S, Paice C. Assessment of the SF-36 version 2 in the United Kingdom. J Epidemiol Community Health. 1999;53(1):46–50.
Article CAS PubMed PubMed Central Google Scholar
Alonso J, Prieto L, Anto J. The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire): an instrument for measuring clinical results. Medicina Clínica. 1995;104(20):771–6.
CAS PubMed Google Scholar
Shayan NA, Arslan UE, Hooshmand AM, Arshad MZ, Ozcebe H. The short form health survey (SF-36): translation and validation study in Afghanistan. East Mediterr Health J. 2020;26(8):899–908.
HÅvard Loge J, Kaasa S. Short form 36 (SF-36) health survey: normative data from the general Norwegian population. Scand J Soc Med. 1998;26(4):250–8.
Bjorner JB, Thunedborg K, Kristensen TS, Modvig J, Bech P. The Danish SF-36 Health Survey: translation and preliminary validity studies. J Clin Epidemiol. 1998;51(11):991–9.
Apolone G, Mosconi P. The Italian SF-36 Health Survey: translation, validation and norming. J Clin Epidemiol. 1998;51(11):1025–36.
Organization WH. WHOQOL-BREF: introduction, administration, scoring and generic version of the assessment: field trial version, December 1996. World Health Organization; 1996.
Kim WH, Hahn SJ, Im HJ, Yang KS. Reliability and validity of the Korean World Health Organization Quality of Life (WHOQOL)-BREF in people with physical impairments. Annals Rehabilitation Med. 2013;37(4):488.
Yao G, Chung C-W, Yu C-F, Wang J-D. Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. J Formos Med Assoc. 2002;101(5):342–51.
Usefy A, Ghassemi GR, Sarrafzadegan N, Mallik S, Baghaei A, Rabiei K. Psychometric properties of the WHOQOL-BREF in an Iranian adult sample. Commun Ment Health J. 2010;46(2):139–47.
Jaracz K, Kalfoss M, Górna K, Bączyk G. Quality of life in Polish respondents: psychometric properties of the Polish WHOQOL–Bref. Scand J Caring Sci. 2006;20(3):251–60.
Khayata G, Rizk D, Hasan M, Ghazal-Aswad S, Asaad M. Factors influencing the quality of life of infertile women in United Arab Emirates. Int J Gynecol Obstet. 2003;80(2):183–8.
Li Y, Zhang X, Shi M, Guo S, Wang L. Resilience acts as a moderator in the relationship between infertility-related stress and fertility quality of life among women with infertility: a cross-sectional study. Health Qual Life Outcomes. 2019;17(1):1–9.
Dyer S, Chambers GM, Adamson GD, Banker M, De Mouzon J, Ishihara O, et al. ART utilization: an indicator of access to infertility care. Reprod Biomed Online. 2020;41(1):6–9.
Kiani Z, Fakari FR, Hakimzadeh A, Hajian S, Fakari FR, Nasiri M. Prevalence of depression in infertile men: a systematic review and meta-analysis. BMC Public Health. 2023;23(1):1972.
Widge A, Cleland J. The public sector’s role in infertility management in India. Health Policy Plann. 2009;24(2):108–15.
Kiani Z, Simbar M, Hajian S, Zayeri F. Quality of life among infertile women living in a paradox of concerns and dealing strategies: a qualitative study. Nurs Open. 2021;8(1):251–61.
De Berardis D, Mazza M, Marini S, Del Nibletto L, Serroni N, Pino M, et al. Psychopathology, emotional aspects and psychological counselling in infertility: a review. Clin Ter. 2014;165(3):163–9.
Starc A, Trampuš M, Pavan Jukić D, Grgas-Bile C, Jukić T. Polona Mivšek A. Infertility and sexual dysfunctions: a systematic literature review. Acta Clin Croatica. 2019;58(3):508–15.
Drosdzol A, Skrzypulec V. Evaluation of marital and sexual interactions of Polish infertile couples. J Sex Med. 2009;6(12):3335–46.
Wischmann T, Thorn P. (Male) infertility: what does it mean to men? New evidence from quantitative and qualitative studies. Reprod Biomed Online. 2013;27(3):236–43.
Streiner D, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. Aust NZJ Public Health. 2016.
Polit D, Beck C. Essentials of nursing research: appraising evidence for nursing practice. Lippincott Williams & Wilkins; 2020.
Wu W, La J, Schubach KM, Lantsberg D, Katz DJ. Psychological, social, and sexual challenges affecting men receiving male infertility treatment: a systematic review and implications for clinical care. Asian J Androl. 2023;25(4):448–53.
Biggs SN, Halliday J, Hammarberg K. Psychological consequences of a diagnosis of infertility in men: a systematic analysis. Asian J Androl. 2024;26(1):10–9.
Download references
Acknowledgements
The authors would like to express their gratitude and thank to the cooperation and assistance of the officials of faculty, library and computer ward at Shahid Beheshti University of Medical Sciences.
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and affiliations.
Midwifery and Reproductive Health Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Zahra Kiani
Midwifery and Reproductive Health Research Center, Department of Midwifery, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Masoumeh Simbar
Department of Midwifery, School of Medicine, North Khorasan University of Medical Sciences, Bojnurd, Iran
Farzaneh Rashidi
Proteomics Research Center, Department of Biostatistics, Faculty of Allied Medical Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Farid Zayeri
Department of Anesthesia and Operating Room, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Homayoon Banaderakhsh
You can also search for this author in PubMed Google Scholar
Contributions
ZK: Project development, Data Collection, Manuscript writing MS: Project administration, writing-review, and editing, supervision FR: Project administration, writing-review, and editing, supervision FZ: Project development, Data Collection, Manuscript writing HB: Project development, Data Collection, Manuscript writing All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Masoumeh Simbar .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Not applicable.

Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kiani, Z., Simbar, M., Rashidi, F. et al. The quality of life of men experiencing infertility: a systematic review. BMC Public Health 24 , 1236 (2024). https://doi.org/10.1186/s12889-024-18758-6
Download citation
Received : 21 September 2023
Accepted : 02 May 2024
Published : 05 May 2024
DOI : https://doi.org/10.1186/s12889-024-18758-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality of life
- Infertility
- Systematic review
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Effect of the HPV...
Effect of the HPV vaccination programme on incidence of cervical cancer and grade 3 cervical intraepithelial neoplasia by socioeconomic deprivation in England: population based observational study
Linked editorial.
HPV vaccine: the key to eliminating cervical cancer inequities
- Related content
- Peer review
- Milena Falcaro , senior statistician 1 ,
- Kate Soldan , scientist and epidemiologist 2 ,
- Busani Ndlela , cancer information analyst 3 ,
- Peter Sasieni , professor of cancer epidemiology 1
- 1 Centre for Cancer Screening, Prevention and Early Diagnosis, Wolfson Institute of Population Health, Queen Mary University of London, London EC1M 6BQ, UK
- 2 Blood Safety, Hepatitis, Sexually Transmitted Infections and HIV Division, UK Health Security Agency (UKHSA), London, UK
- 3 National Disease Registration Service (NDRS), NHS England, London, UK
- Correspondence to: P Sasieni p.sasieni{at}qmul.ac.uk (or @petersasieni on X)
- Accepted 27 March 2024
Objectives To replicate previous analyses on the effectiveness of the English human papillomavirus (HPV) vaccination programme on incidence of cervical cancer and grade 3 cervical intraepithelial neoplasia (CIN3) using 12 additional months of follow-up, and to investigate effectiveness across levels of socioeconomic deprivation.
Design Observational study.
Setting England, UK.
Participants Women aged 20-64 years resident in England between January 2006 and June 2020 including 29 968 with a diagnosis of cervical cancer and 335 228 with a diagnosis of CIN3. In England, HPV vaccination was introduced nationally in 2008 and was offered routinely to girls aged 12-13 years, with catch-up campaigns during 2008-10 targeting older teenagers aged <19 years.
Main outcome measures Incidence of invasive cervical cancer and CIN3.
Results In England, 29 968 women aged 20-64 years received a diagnosis of cervical cancer and 335 228 a diagnosis of CIN3 between 1 January 2006 and 30 June 2020. In the birth cohort of women offered vaccination routinely at age 12-13 years, adjusted age standardised incidence rates of cervical cancer and CIN3 in the additional 12 months of follow-up (1 July 2019 to 30 June 2020) were, respectively, 83.9% (95% confidence interval (CI) 63.8% to 92.8%) and 94.3% (92.6% to 95.7%) lower than in the reference cohort of women who were never offered HPV vaccination. By mid-2020, HPV vaccination had prevented an estimated 687 (95% CI 556 to 819) cervical cancers and 23 192 (22 163 to 24 220) CIN3s. The highest rates remained among women living in the most deprived areas, but the HPV vaccination programme had a large effect in all five levels of deprivation. In women offered catch-up vaccination, CIN3 rates decreased more in those from the least deprived areas than from the most deprived areas (reductions of 40.6% v 29.6% and 72.8% v 67.7% for women offered vaccination at age 16-18 and 14-16, respectively). The strong downward gradient in cervical cancer incidence from high to low deprivation in the reference unvaccinated group was no longer present among those offered the vaccine.
Conclusions The high effectiveness of the national HPV vaccination programme previously seen in England continued during the additional 12 months of follow-up. HPV vaccination was associated with a substantially reduced incidence of cervical cancer and CIN3 across all five deprivation groups, especially in women offered routine vaccination.
Introduction
Human papillomavirus (HPV) comprises a family of viruses, a subset of which are responsible for virtually all cervical and some anogenital and oropharyngeal cancers. 1 More than 100 countries worldwide have introduced prophylactic HPV vaccination as part of routine immunisation schedules. 2 One important outcome yet to be reported is whether vaccination has reduced or increased the inequalities seen for cervical disease in the UK and elsewhere.
In England, the national HPV vaccination programme started in 2008 using the bivalent Cervarix vaccine to prevent infections due to HPV types 16 and 18, which are estimated to cause around 80% of all cervical cancers in the UK. 3 Vaccination was offered routinely to 12-13 year old (school year 8) girls and as part of a catch-up campaign to those aged <19 years. 4 In September 2012 the programme switched to the quadrivalent vaccine (Gardasil), which additionally protects against HPV types 6 and 11 (responsible for genital warts), and in 2019 the programme was extended to 12-13 year old boys. Those who are eligible but not vaccinated can receive the vaccine free of charge from their general practitioner until their 25th birthday. 5
The introduction and implementation of HPV immunisation in this way means that noticeable discontinuities exist in the proportion of women vaccinated by date of birth, enabling a rigorous evaluation of the effectiveness of the programme. 6 For example, women born in August 1990 are unlikely to have received HPV vaccination, whereas among those born in the year from 1 September 1990 nearly 70% have received at least one dose of the vaccine.
Findings on the early effect of national HPV vaccination programmes have been encouraging. A wealth of real world evidence for the effect of vaccination on HPV prevalence exists 7 8 9 10 11 and evidence is growing for its effectiveness in reducing high grade cervical intraepithelial neoplasia (CIN) 12 13 14 15 and cervical cancer in vaccinated women. 14 16 17 18 19 For instance, we found that in England rates of grade 3 CIN (CIN3) and of cervical cancer were greatly reduced among those who were offered HPV vaccination, and that the magnitude of the reduction was greatest in the cohorts with the highest uptake and younger age at vaccination. 14 We estimated that by mid-2019 the immunisation programme had prevented cervical cancer in nearly 450 women and CIN3 in around 17 000 women.
Along with preventing ill health, a key aim of the NHS is to reduce health inequalities. 20 To this end, we investigated whether the effect of immunisation against HPV has resulted in a reduction in inequalities in cervical disease or a widening. Concern has been expressed that if the uptake of HPV vaccination is lower in those at greatest risk of cervical cancer, as has been seen in the US, 21 this could accentuate health inequalities. One study found that the introduction of HPV immunisation in England might initially have increased inequities in HPV related cancer incidence among ethnic minority groups because of the differential effect of herd protection in subpopulations with dissimilar vaccination coverage. 22 Previous studies have suggested that white people have a higher awareness of HPV and acceptance of the immunisation 23 and that vaccination uptake is lower in women from ethnic minority groups and more deprived areas. 24 Using data on HPV vaccination coverage by local area, however, a study found little variation by deprivation score in women offered routine vaccination (83% v 86% for most and least deprived areas, respectively) and only a small negative correlation between deprivation and vaccine uptake in those offered catch-up vaccination (47% v 53% for most and least deprived areas, respectively). 25 A full understanding of the effect of HPV vaccination across different socioeconomic groups is complicated by the poor uptake of cervical screening observed among younger women in the most deprived areas, leading to lower rates of screen detected cervical cancer and CIN3 at age 25 years compared with women in less deprived areas. 26 27
We replicated results from an analysis of population based cancer registry data to evaluate if the high vaccination effectiveness seen previously continued during an additional year of follow-up. The combined data were also used to investigate the effect of the vaccination programme by socioeconomic deprivation.
To represent socioeconomic deprivation, we used the index of multiple deprivation, a small area measure based on several domains of deprivation, such as income, employment, and health. The index is determined by using a standard statistical geographical unit, called lower super output area, which divides England into small areas of similar sized populations (on average about 1500 residents, or 650 households). 28 The lower super output areas are then ranked from the most to the least deprived and divided into five equal groups. The first and fifth groups correspond to the 20% most deprived and 20% least deprived lower super output areas in England, respectively.
We retrieved the records of all women aged 20-64 years resident in England with a diagnosis of invasive cervical cancer (ICD-10 (international classification of diseases, 10th revision) code C53) or CIN3 (ICD-10 code D06) between 1 January 2006 and 30 June 2020. These records are stored in the database managed by NHS England’s National Disease Registration Service, 29 and for each patient included information on index of multiple deprivation derived from the patient’s home postcode at the time of diagnosis. To convert these counts into rates, we used mid-year estimates of the female population for England by single year of age, calendar year (January 2006 to June 2020), and index of multiple deprivation (five groups). These estimates were retrieved from multiple tables publicly available on the website of the UK’s Office for National Statistics (ONS). 30 The supplementary material provides more details about the index of multiple deprivation versions used by the National Disease Registration Service and ONS, along with information on how we derived the population estimates required in our statistical analysis.
Statistical analysis
We separately analysed incidence rates of cervical cancer and CIN3 by using extensions of our previously described age-period-cohort Poisson model. 14 31 32 Data on women with cancer or CIN3 were aggregated by single month of age, calendar time (period), and date of birth (cohort). We derived the corresponding population risk time by subdividing the mid-year ONS population estimates into one month intervals for age, period, and cohort. For the analysis of the effectiveness by deprivation, we further split both the data on women with cancer or CIN3 and the population estimates by deprivation group (fifths). We then used the population risk time as the denominator for calculating rates (formally, the subdivided population estimates were log transformed and included in the Poisson regression model as an offset). Confidence intervals were computed using robust standard errors. 33 34
The code for the analysis was written and tested on synthetic data (extending the Simulacrum dataset) 35 by a statistician (MF) at King’s College London and then run on the real dataset by an analyst (BN) at the National Disease Registration Service.
We started by considering a core model where we included the main effects for age, period, and birth cohort, along with selected age by cohort and age by period interactions (see supplementary table S1). The interaction terms were included to account for variations in screening policy and historical events that affected cervical cancer rates. Specifically, we defined seven birth cohorts to capture differences in the age at first invitation to screening and the school years in which HPV vaccination was offered (see table 1 ). We added terms for seasonality and for events that may have affected registrations for cervical cancer and CIN3, such as the covid-19 lockdown, the “Jade Goody effect,” 36 37 and the 2019 cervical screening awareness campaign. In our previous paper, 14 we used several similar regression models to study the sensitivity of results to the precise way in which we adjusted for potential confounding factors. Because we found that the estimates of the cohort specific incidence rate ratios changed little across the various models, here we report on only a single model adjustment for confounders.
Characteristics of the birth cohorts
- View inline
Using the core model described, we investigated if the high effectiveness of the HPV immunisation programme reported previously 14 continued during an additional 12 months of follow-up. To do this we split the main effect of each cohort offered vaccination into two subgroup effects depending on whether the data related to the periods 1 January 2006 to 30 June 2019 or 1 July 2019 to 30 June 2020; this approach corresponded to adding three cohort by period interaction terms.
To evaluate the impact of socioeconomic deprivation on incidences of cervical cancer and CIN3, we extended the core model by adding main effects for deprivation and deprivation by cohort interactions. Specifically, we allowed the effect of each deprivation level to vary between unvaccinated women (cohorts 1-4) and those offered vaccination (cohorts 5-7), but we assumed it was otherwise constant within these two groups. We did not include further interactions between deprivation and other covariates as they were not of primary interest in this analysis. Using the fitted Poisson regression models, we made “what if” predictions by changing the value of one or more predictors and by leaving the others as observed. In this way it was possible to compare what happened (factual scenario) with what would have happened under an alternative (counterfactual) scenario.
We also carried out a sensitivity analysis where the effects of these deprivation by cohort interactions were allowed to vary across the three different groups offered vaccination (ie, we used 15 terms instead of five). For cervical cancer, owing to small numbers in cohort 7, we fitted a reduced model where the effects of these interactions were constrained to be the same for cohorts 6 and 7.
All analyses were performed in Stata, version 17. 38
Patient and public involvement
Patient and public involvement contributors were not formally involved in this research. We did, however, engage with Cancer Research UK (CRUK), Jo’s Cervical Cancer Trust, and the HPV Coalition on the importance of these analyses and the dissemination of the results. This included taking part in a video produced by ITN Business for World Cancer Day 2023, writing a piece for the 20th anniversary of the creation of CRUK, and engaging with international media about our research findings on the effect of the English HPV vaccination programme. We have also discussed the research and a draft of this paper with individual patients, journalists, and patient and public involvement representatives linked to broader research programmes.
Table 1 lists the characteristics of the birth cohorts included in the study. We defined the different cohorts so that each cohort is homogeneous in terms of the age women would have been offered HPV vaccination (if at all) and the age at which they would have first been invited for cervical screening.
Overall, there were 231.1 million women years of observation between 1 January 2006 and 30 June 2020 on women aged 20-64 years in England. During this time, 29 968 women received a diagnosis of invasive cervical cancer and 335 228 a diagnosis of CIN3 ( table 2 ). Observations between 1 July 2019 and 30 June 2020 have not been reported previously. With these additional 12 months of follow-up, there are, in the routine vaccination group (cohort 7), about twice the number of diagnoses compared with the same group in our previous study (we now have 13 v 7 previously for cervical cancer, 109 v 49 for CIN3; see supplementary table S2).
Summary statistics of study population
Our previously published findings on the effect of the national HPV vaccination were largely confirmed with the new data ( table 3 , also see supplementary table S3). The analysis showed that the previously observed low rates of disease and the estimated high effectiveness of the immunisation programme continued during the additional 12 months of follow-up (diagnoses in July 2019 to June 2020) among women born since 1 September 1990. In particular, the estimated effects of vaccination for that later period in cohort 7 (those born since 1 September 1995) imply a reduction in incidence of 83.9% (95% confidence interval (CI) 63.8% to 92.8%) for cervical cancer and 94.3% (92.6% to 95.7%) for CIN3 ( table 3 ). The relative risk reduction estimates for the earlier period are not identical to those reported previously because we also had new data for the unvaccinated cohorts that affected the baseline rates.
Estimated relative risk reductions (percentages) in incidence of invasive cervical cancer and CIN3 in the three cohorts offered HPV vaccination compared with the most recent unvaccinated cohort
Supplementary table S4 shows the full estimates from modelling the effects of vaccination in different levels of socioeconomic deprivation, with summary results reported in table 4 , table 5 , and table 6 . The highest incidence rates for invasive cervical cancer were observed among women living in the most deprived areas (first fifth) but, while in the reference unvaccinated group there was a strong downward gradient moving from women in the most deprived areas to those in the least deprived, little difference was found between the second and fifth fifths of deprivation in the groups offered vaccination. In both the reference and the vaccination cohorts the highest rates of CIN3 occurred in those from the most deprived areas, but no clear trend was observed among the other four fifths of deprivation (see supplementary tables S5 and S6).
Estimated number of invasive cervical cancers and CIN3s predicted and prevented by mid-2020 in the three cohorts of women offered HPV vaccination
Estimated cohort specific numbers of invasive cervical cancers predicted and prevented by mid-2020 among women in the least and most deprived areas
Estimated cohort specific numbers of CIN3 predicted and prevented by mid-2020 among women in the least and most deprived areas
Overall, our model estimated that 687 (95% CI 556 to 819) cervical cancers and 23 192 (22 163 to 24 220) CIN3s had been prevented by the vaccination programme up to mid-2020 among young women in England ( table 4 ). The greatest numbers for cervical cancer were prevented in women in the most deprived areas (192 and 199 for first and second fifths, respectively) and the fewest in women in the least deprived fifth (61 cancers prevented). The number of women with CIN3 prevented was high across all deprivation groups but greatest among women living in the more deprived areas: 5121 and 5773 for first and second fifths, respectively, compared with 4173 and 3309 in the fourth and fifth fifths, respectively. When we looked at the corresponding cohort specific figures ( table 5 and table 6 ), we noticed differences between the cohorts, particularly for CIN3. In all three cohorts offered vaccination the numbers and rates of prevented cervical cancers were much higher in women from the most deprived areas than least deprived areas ( table 5 ). The proportion of women with prevented cervical cancer in each cohort was, however, similar between the first and fifth fifths of deprivation. For CIN3 ( table 6 ), the results were more complicated. In women offered vaccination at age 16-18 years (cohort 5), the proportion of cervical cancers prevented was substantially less in those from the most deprived areas (29.6%) compared with those from the least deprived areas (40.6%). An inequality still existed in cohorts 6 and 7, but it was greatly reduced (67.7% v 72.8% in cohort 6 and 95.3% v 96.1% in cohort 7).
In England, the social-class gradient for cervical cancer is one of the steepest of any cancers: women in the most deprived fifth have had double the risk of those in the least deprived fifth. 39 40 Some of this results from differences in exposure to HPV and risk of an infection becoming persistent, 41 but differential uptake of cervical screening has also been an important factor. Previous research has highlighted the need for new engagement strategies to improve attendance for cervical screening among young women living in more socially deprived areas. 42 Encouragingly, the coverage of HPV vaccination has been (at least for the routine campaign and before the covid-19 pandemic) uniformly high. 43 It is, however, important to investigate whether immunisation—including the indirect effects achieved by high uptake—is helping to reduce health inequalities.
Using population based cancer registrations updated to mid-2020, which provided information on about twice the expected number of cancers in women offered HPV vaccination aged 12-13 years than in our previous analysis, we were able to show that the high vaccination effectiveness seen previously was confirmed with more recent data. The largest differences between the old and the new data were found for cohort 6 (the catch-up group offered the vaccine at age 14-16 years): for cervical cancer the estimated effectiveness increased, whereas for CIN3 it decreased. The reasons behind these differences are unclear. The results for cohorts 6 and 7 in the new data are more in keeping with what we would have expected given that the proportion of disease caused by HPV types 16 and 18 is greater for invasive cancer than for CIN3.
We also investigated the effect of the HPV immunisation programme by socioeconomic deprivation. Overall, we found that the programme was associated with a substantial reduction in the expected number of women with cervical cancers and CIN3 in all fifths of deprivation. For cervical cancer before vaccination, the downward gradient with decreasing deprivation was strong. In all cohorts offered vaccination, the highest rate was still seen among women living in the most deprived areas, but little difference was observed between women living in the second to fifth deprived areas. For CIN3, similar patterns were observed for the reference unvaccinated group and the three cohorts offered vaccination, but rates were greatly reduced in all fifths of deprivation in the latter. When we compared women in the most deprived areas with those in the least deprived areas in terms of percentage of disease averted, we observed differences across the cohorts for CIN3, with women in the least deprived areas in the older catch-up cohort (vaccine offered at age 16-18 years) having a greater proportion of averted CIN3s after HPV immunisation than women in the most deprived area (40.6% v 29.6%). The same, although to a much less extent, was observed for the younger catch-up cohort (72.8% v 67.7%). For invasive cervical cancer, we found no evidence of a less beneficial impact (in terms of percentage of cases averted) of the vaccination in women living in the most deprived areas; in fact, especially for the older catch-up cohort, the percentage was slightly higher in women in the most deprived areas compared with those in the least deprived areas.
The observed incidences of cervical cancer and CIN3 depend on three key factors: the intensity of exposure to HPV infections (including age at first exposure), the uptake of cervical screening, and HPV vaccination coverage. It is therefore difficult to disentangle the effects of these three drivers on the index of multiple deprivation specific rates with the data at hand. The health inequality in CIN3 in cohort 5 might result from the lower vaccination coverage among women in the most deprived areas since at age 16-18 years when they became eligible for vaccination more of those from the most deprived fifth may not have been in school or, for other reasons, may have missed the offer of HPV immunisation. These observations are consistent with previous understanding that higher uptake of catch-up vaccination was associated, although not as strongly as in some countries, with lower deprivation. 25 It is, however, reassuring that cohorts 6 and 7 showed little inequality in relative reductions in cancer (as in vaccination coverage).
However, since the UK has recently announced a change to a one dose schedule for routine HPV vaccination, ensuring this change achieves high coverage (including in the birth cohorts currently with lower coverage owing to covid-19 related interruption to schooling, and to immunisation services) is important to maintain the effects we have seen on cervical disease and on inequalities. Further investigations could be carried out in the future to check for any effect on cancer incidence caused by covid-19, gender neutral vaccination (since 2019), a change in the type of vaccine used, or reduced dose schedules.
Strengths and limitations of this study
Our analysis has several strengths. Our study provides direct evidence for the effect of a public health intervention (such as HPV vaccination) on cancer rates by deprivation. We used high quality data from population based cancer registries and were able to investigate the extent of socioeconomic inequalities in cohorts offered vaccination and whether the effectiveness of the HPV immunisation continued in an additional year of follow-up. The code for the analysis was written and tested using simulated data and an independent analyst later ran the code on the real dataset, guaranteeing reliable and robust results and preserving patient confidentiality.
The main limitations of our study are that it was observational and individual level data on vaccination status were not available. However, previous published research 14 provided detailed information on potential confounding factors and the best way to adjust for these in the analysis. Additionally, the discontinuities in vaccine uptake with date of birth makes this study powerful and less prone to biases from unobserved confounders than an analysis based on individual level data on HPV vaccination status.
Women born after 1 September 1999 were offered the Gardasil vaccine from 1 September 2012. As these women were at most aged 20 years and 10 months at the end of the study follow-up (30 June 2020), it is not yet possible with the data available to compare the effectiveness of the programme among those offered Cervarix and those offered Gardasil. This additional comparative analysis will become feasible with a longer follow-up on the recipients of Gardasil.
Policy implications
We found that the high effectiveness of the national HPV immunisation continued in the additional year of follow-up (July 2019 to June 2020). This is encouraging as it validates the previously published results and further supports consideration of more limited cervical screening for cohorts with high vaccination coverage aged 12-13 years. Moreover, although women living in the most deprived areas are still at higher risk of cervical cancer than those in less deprived areas, the HPV vaccination programme is associated with substantially lowered rates of disease across all fifths of socioeconomic deprivation. For cervical cancer, this has led to the levelling-up of the rates across the second to fifth fifths of deprivation so that the strong downward gradient observed in the reference unvaccinated cohort is no longer present in the cohorts offered vaccination. For CIN3, in the older catch-up cohorts women living in the least deprived areas seem to have benefited more from vaccination than those living in the most deprived areas, but the rates were still greatly reduced in all socioeconomic groups. Cervical screening strategies for women offered vaccination should carefully consider the differential effect both on rates of disease and on inequalities that are evident among women offered catch-up vaccination.
Conclusions
The HPV vaccination programme in England has not only been associated with a substantial reduction in incidence of cervical neoplasia in targeted cohorts, but also in all socioeconomic groups. This shows that well planned and executed public health interventions can both improve health and reduce health inequalities.
What is already known on this topic
In England, immunisation against human papillomavirus (HPV) has been associated with greatly reduced incidence rates of cervical cancer and grade 3 cervical intraepithelial neoplasia (CIN3) up to June 2019, especially among women offered routine vaccination at age 12-13 years
The social-class gradient for cervical cancer incidence has been one of the steepest of any cancers
Concern has been raised that HPV vaccination could least benefit those at highest risk of cervical cancer
What this study adds
The high effectiveness of vaccination against HPV seen previously continued during an additional year of follow-up, from July 2019 to June 2020
The English HPV vaccination programme was associated with substantially lower rates of cervical cancer and CIN3 in all fifths of socioeconomic deprivation, although the highest rates remained among women in the most deprived areas
For cervical cancer, the strong downward gradient from high to low deprivation observed in the reference unvaccinated cohort was no longer present among those offered vaccination
Ethics statements
Ethical approval.
Not required as the study used aggregated data from the National Disease Registration Service as well as publicly available information from the Office for National Statistics website.
Data availability statement
The cancer registry data analysed for this paper are securely held by the National Disease Registration Service (NDRS). Requests to access the data can be made through NHS England’s DARS service ( https://digital.nhs.uk/services/data-access-request-service-dars ). The Simulacrum ( https://simulacrum.healthdatainsight.org.uk/ ) is a synthetic dataset developed by Health Data Insight and derived from anonymous cancer data provided by NHS England’s NDRS. Mid-year population estimates are freely downloadable from the Office for National Statistics website ( https://www.ons.gov.uk/ ).
Acknowledgments
We thank Alejandra Castañon (LCP Health Analytics), Marta Checchi (UK Health Security Agency), and Lucy Elliss-Brookes (NHS England) for helpful comments on the study protocol, and Kwok Wong (NHS England) for contributing to the quality assurance of the data extraction code.
Contributors: PS had the original idea. He is the guarantor. MF and PS conceptualised the study and prepared the study protocol, which was subsequently reviewed by the other co-authors. MF wrote and tested the Stata code (checked by PS) for the data analysis and drafted the manuscript. BN extracted the dataset and ran the Stata code on it. All authors critically reviewed and approved the final submitted version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This work was supported by Cancer Research UK (grant No C8162/A27047). The funder had no role in the study design or in the collection, analysis, interpretation of data, writing of the report or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare support from Cancer Research UK for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Transparency: The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: The results of this research will be disseminated through the media, blogs and scientific meetings and will inform the design and implementation of interventions to reduce health inequalities. We will also work with others to produce information for the public to support human papillomavirus immunisation and cervical screening programmes and, if the opportunity arises, to contribute summary data for an international meta-analysis of similar studies.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/ .
- ↵ IARC. Human papillomaviruses. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, Volume 90. 2007.
- ↵ World Health Organization (WHO). Global Market Study: HPV 2022 https://cdn.who.int/media/docs/default-source/immunization/mi4a/who-mi4a-global-market-study-hpv.pdf?sfvrsn=649561b3_1&download=true .
- Cuschieri K ,
- Hibbitts S ,
- ↵ Public Health England (PHE). Human Papillomavirus (HPV) vaccine coverage in England, 2008/09 to 2013/14. A review of the full six years of the three-dose schedule: Public Health England (PHE); 2015. https://www.gov.uk/government/publications/human-papillomavirus-hpv-immunisation-programme-review-2008-to-2014 ; accessed 6 January 2021.
- ↵ UK Health Security Agency. HPV vaccination: guidance for healthcare practitioners (version 6) 2022 [updated April 2022]. https://www.gov.uk/government/publications/hpv-universal-vaccination-guidance-for-health-professionals ; accessed 24 August 2022.
- Lévesque LE ,
- Kaufman JS ,
- Brisson M ,
- HPV Vaccination Impact Study Group
- Thomas SL ,
- Tabrizi SN ,
- Brotherton JM ,
- Kaldor JM ,
- Markowitz LE ,
- Steinau M ,
- Hernandez-Aguado JJ ,
- Sánchez Torres DA ,
- Martínez Lamela E ,
- Lehtinen M ,
- Lagheden C ,
- Luostarinen T ,
- Falcaro M ,
- Castañon A ,
- Wallace L ,
- Pollock KG ,
- Elfström KM ,
- Skorstengaard M ,
- Thamsborg LH ,
- Dillner J ,
- Dehlendorff C ,
- Belmonte F ,
- ↵ NHS. The NHS long term plan 2019. https://www.longtermplan.nhs.uk/ ; accessed 24 August 2022.
- Johnson HC ,
- Lafferty EI ,
- Roberts SA ,
- Stretch R ,
- Sheridan A ,
- Pappas-Gogos G ,
- Douglas E ,
- McLennan D ,
- Henson KE ,
- Elliss-Brookes L ,
- Coupland VH ,
- ↵ Office for National Statistics. https://www.ons.gov.uk/ ; accessed 24 October 2022.
- Carstensen B
- Sasieni P ,
- ↵ Huber P. The behavior of maximum likelihood estimates under nonstandard conditions. Proceedings of the 5th Berkeley Symposium on Mathematical Statistics and Probability: University of California Press, 1967:221-33.
- Health Data Insight
- Lancucki L ,
- Patnick J ,
- Castanon A ,
- Thomson CS ,
- UK Association of Cancer Registries
- ↵ Cancer Research UK. Cervical Cancer Incidence Statistics 2015. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer/incidence ; accessed 14 March 2023.
- Currin LG ,
- Linklater KM ,
- Rahman MA ,
- Paranjothy S
- ↵ UK Health Security Agency (UKHSA). HPV vaccine uptake 2023. https://www.gov.uk/government/collections/vaccine-uptake#hpv-vaccine-uptake ; accessed 12 March 2023.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 6, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Online patient portal usage increasing, study shows
by UT Southwestern Medical Center
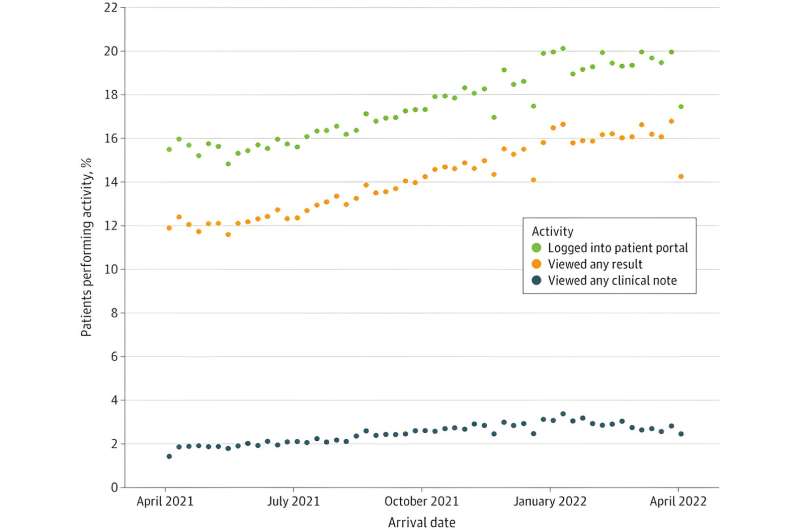
More people are using online patient portals to view their information while in the emergency room, but access is challenging for members of medically underserved communities and the elderly, UT Southwestern Medical Center researchers and national colleagues found in a new study.
"Patient portals such as Epic's MyChart have grown in popularity in recent years, but they are still often seen as a tool for ambulatory chronic disease management," said Robert Turer, M.D., Assistant Professor of Emergency Medicine at UT Southwestern and the study's corresponding author.
"Our research suggests portals can be an asset in emergency medicine too, both to help patients with exacerbations of chronic conditions and to support those experiencing acute illness during and after the emergency department (ED) visit."
The research, published in JAMA Network Open , studied patient data from 36 teaching and community EDs affiliated with eight academic medical centers in seven states over the year ending in April 2022. Researchers found that 17.4% of the 1,280,924 adults who visited participating EDs logged into their patient portals to view test results or read clinical notes while at the hospital, and participation increased as the study progressed.
The research also found that most portal users were white, insured, and English-speaking and had portal accounts before arriving at the emergency room. Patients who were male or Black or had no insurance logged in at lower rates, as did older patients.
"Emergency departments often serve as a safety net for patients without an ongoing relationship with a health care provider , so they have no patient portal account," Dr. Turer said. "Or, in many cases, there is a lack of familiarity with technology—which is especially true with older patients . There is a tremendous opportunity for EDs to help bridge this gap by supporting and aiding enrollment and educating patients on the portal's key functions, using patient navigators or registration staff."
The study—the largest and most representative evaluation of real-time portal use among ED patients in the U.S.—builds on earlier single-site research at UT Southwestern that had similar results.
"Our findings in both studies support the need for further research to help us better understand portal features that are most useful within the ED," Dr. Turer said. "For example, status updates, point-of-care education, and coordination of follow-up appointments are potential solutions to explore."
Explore further
Feedback to editors

New blood test for stroke detection combines blood-based biomarkers with a clinical score
42 minutes ago

The neural signature of subjective disgust could apply to both sensory and socio-moral experiences

Likelihood of kids and young people smoking and vaping linked to social media use
14 hours ago

Primary health coverage found to have prevented more than 300,000 child deaths in four Latin American countries

Global life expectancy projected to increase by nearly 5 years by 2050 despite various threats

Number of people experiencing poor health, early death from metabolism-related risk factors has increased since 2000

Men at greater risk of major health effects of diabetes than women, study suggests

Discovery of a master neuron that controls movement in worms has implications for human disease
15 hours ago

First US trial of varenicline for e-cigarette cessation shows positive results
16 hours ago

Examining the mechanisms and clinical potential of a promising non-opioid pain therapy candidate
Related stories.

Do you use a patient portal? Study finds differences between portal users versus nonusers
Jun 9, 2023

Higher use of health care portal seen during COVID-19 pandemic
Mar 6, 2024

Patient portal use explored for older adults with dementia diagnosis
Jul 7, 2023

Medicare pays for message-based e-visits. Are older adults using them?
Apr 8, 2024

Electronic portals may help patients with multiple complex conditions
Jun 19, 2019

Logging on for health: More older adults use patient portals, but access and attitudes vary widely
May 24, 2023
Recommended for you

AI may improve doctor–patient interactions for older adults with cancer
May 15, 2024

New tool can help surgeons quickly search videos and create interactive feedback

Artificial intelligence tool detects sex-related differences in brain structure
May 14, 2024

Machine learning sheds light on gene transcription
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Introduction
- Article Information
Data source was OnPoint overdose prevention center enrollment, November 30, 2021, to January 31, 2022. Additional categories not displayed in this figure are other (0.6%) and missing or decline to answer (2.5%). Private space indicates own residence or other’s residence; public space, street, sidewalk, underpass, park, or between cars; semipublic space, public bathroom, subway station, syringe service program bathroom, hotel, shelter, or building roof, hallway, or basement.
- Overdose Prevention Centers: An Essential Strategy to Address the Overdose Crisis JAMA Network Open Invited Commentary July 15, 2022 Elizabeth A. Samuels, MD, MPH, MHS; Dennis A. Bailer, PRS; Annajane Yolken, MPH
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Harocopos A , Gibson BE , Saha N, et al. First 2 Months of Operation at First Publicly Recognized Overdose Prevention Centers in US. JAMA Netw Open. 2022;5(7):e2222149. doi:10.1001/jamanetworkopen.2022.22149
Manage citations:
© 2024
- Permissions
First 2 Months of Operation at First Publicly Recognized Overdose Prevention Centers in US
- 1 New York City Department of Health and Mental Hygiene, Queens, New York
- 2 OnPoint NYC, New York, New York
- Invited Commentary Overdose Prevention Centers: An Essential Strategy to Address the Overdose Crisis Elizabeth A. Samuels, MD, MPH, MHS; Dennis A. Bailer, PRS; Annajane Yolken, MPH JAMA Network Open
In New York City (NYC), there were 2062 overdose fatalities in 2020, the deadliest year on record for NYC and the US. 1 Fentanyl and its analogs were the most common substances involved in overdose deaths in NYC, present in 77% of such deaths in 2020. 1 A characteristic of fentanyl-involved overdose is rapid onset of overdose symptoms 2 ; however, with timely administration of oxygen or naloxone, deaths can be averted.
In response to unprecedented numbers of overdose deaths, on November 30, 2021, NYC implemented overdose prevention center (OPC) services at 2 syringe service programs operated by OnPoint NYC. Also known as supervised consumption sites, OPCs are health care facilities that aim to improve individual and community health, increase public safety, and reduce consequences of drug use, including overdose deaths, public drug use, and syringe litter. 3 , 4 Operating in more than 10 countries, OPCs offer supervised, hygienic spaces in which people can use preobtained drugs and access services, onsite or by referral, to health and mental health care, drug treatment, and other social supports. 3 , 4 While previous research documented operations at an underground US OPC, 5 use of sanctioned sites has not yet been studied, to our knowledge. This study describes the first 2 months of operation and use at the first 2 publicly recognized US OPCs.
Because data were collected for program evaluation and presented in aggregate, the NYC Department of Health and Mental Hygiene Institutional Review Board (IRB) determined that this quality improvement study was not human participants research and so IRB approval and informed consent were not required. This study is reported following the SQUIRE reporting guideline.
Data were collected by program staff from individuals using services at 2 OPC sites at intake and before each subsequent use of OPC services. Outcome data related to OPC visits (eg, staff interventions to mitigate overdose risk) were also recorded. Using a unique identifier, OPC participant data were then matched with data indicating uptake of additional services provided at the syringe service program. Descriptive statistics (frequencies and percentages) were calculated using SAS statistical software version 9.4 (SAS Institute).
Between November 30, 2021, and January 31, 2022, 613 individuals used OPC services 5975 times across 2 sites. Most individuals identified as male (78.0%), and 55.3% identified as Hispanic, Latino, or Latina. The mean (range) age was 42.5 (18-71) years. A plurality of individuals (36.9%) reported being street homeless. Fewer than one-fifth of individuals (17.8%) were living in their own rooms or apartments ( Table ).
In self-reported data, the drug most commonly used across 2 sites was heroin or fentanyl (73.7%) and the most frequent route of drug administration at the OPC was injection (65.0%). Among all participants, 75.9% reported that they would have used their drugs in a public or semipublic location if OPC services had not been available ( Figure ).
During the first 2 months of OPC operation, trained staff responded 125 times to mitigate overdose risk. In response to opioid-involved symptoms of overdose, naloxone was administered 19 times and oxygen 35 times, while respiration or blood oxygen levels were monitored 26 times. In response to stimulant-involved symptoms of overdose (also known as overamping), staff intervened 45 times to provide hydration, cooling, and de-escalation as needed. Emergency medical services responded 5 times, and participants were transported to emergency departments 3 times. No fatal overdoses occurred in OPCs or among individuals transported to hospitals.
More than half of individuals using OPC services (52.5%) received additional support during their visit. This included, but was not limited to naloxone distribution, counseling, hepatitis C testing, medical care, and holistic services (eg, auricular acupuncture).
This quality improvement study found that during the first 2 months of operations, services at 2 OPCs in NYC were heavily used, with early data suggesting that supervised consumption in these settings was associated with decreased overdose risk. Data also suggested that OPCs were associated with decreased prevalence of public drug use. Findings are limited by the short study period and lack of a comparison group with individuals not participating in OPC services. Additional evaluation may explore whether OPC services are associated with improved overall health outcomes for participants, as well as neighborhood-level outcomes, including public drug use, improperly discarded syringes, and drug-related crime.
Accepted for Publication: May 26, 2022.
Published: July 15, 2022. doi:10.1001/jamanetworkopen.2022.22149
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2022 Harocopos A et al. JAMA Network Open .
Corresponding Author: Alex Harocopos, PhD, MSc, New York City Department of Health and Mental Hygiene, 42-09 28th St, Floor 19-81, Queens, NY 11101 ( [email protected] ).
Author Contributions : Drs Harocopos and Gibson had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: All authors.
Acquisition, analysis, or interpretation of data: Harocopos, Gibson, See, Rivera, Chokshi.
Drafting of the manuscript: Harocopos.
Critical revision of the manuscript for important intellectual content: Gibson, Saha, McRae, See, Rivera, Chokshi.
Statistical analysis: Gibson.
Administrative, technical, or material support: Harocopos, Gibson, Saha, See, Chokshi.
Supervision: McRae, See, Rivera, Chokshi.
Conflict of Interest Disclosures: Dr Gibson reported working for OnPoint NYC, which receives core funding from the New York City (NYC) Department of Health and Mental Hygiene. Dr Chokshi reported serving as NYC health commissioner when the first overdose prevention centers were launched in NYC and serving currently as visiting fellow at the New York Health Foundation, which has financially supported overdose prevention centers. No other disclosures were reported.
Additional Contributions: We thank Jonathan McAteer, MPH; Shivani Mantha, MPH; Ajani Benjamin, MSW; and Casey Fulmer, MPH (New York City Department of Health and Mental Hygiene), for their assistance with preparing this manuscript and OnPoint NYC staff for their dedication to serving people who use drugs. No contributors were compensated beyond their salaried positions.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
A review of medication errors and the second victim in pediatric pharmacy.
Bredenkamp K, Raschka MJ, Holmes A. A review of medication errors and the second victim in pediatric pharmacy. J Pediatr Pharmacol Ther. 2024;29(2):100-106. doi:10.5863/1551-6776-29.2.100.
Even with technology designed to prevent them, medication errors continue to occur, often causing staff involved to experience " second victim " syndrome. This article, with a focus on pediatric pharmacists, presents four programs designed to support second victims: MU Health’s forYOU , Johns Hopkins’ RISE , Nationwide Children’s YOU Matter, and Children’s Minnesota’s (Children’s MN’s) P2P (peer-to-peer) program. The authors also present options for support that individuals can access if their institution does not have a formal second victim program.
Evaluating the implementation of Project Re-Engineered Discharge (RED) in five Veterans Health Administration (VHA) hospitals. October 17, 2018
Medical misadventures as errors and mistakes and motor vehicular accidents in the disproportionate burden of childhood mortality among Blacks/African Americans in the United States: CDC Dataset, 1968-2015. March 13, 2024
Implementation of the I-PASS handoff program in diverse clinical environments: a multicenter prospective effectiveness implementation study. November 16, 2022
Families as partners in hospital error and adverse event surveillance. March 8, 2017
Misdiagnosis, mistreatment, and harm - when medical care ignores social forces. April 8, 2020
A survey of hospital quality improvement activities. July 30, 2008
Preferred language and diagnostic errors in the pediatric emergency department. November 8, 2023
Impact of online education on intern behaviour around Joint Commission national patient safety goals: a randomised trial. June 27, 2012
Multiple-institution comparison of resident and faculty perceptions of burnout and depression during surgical training. May 16, 2018
Is disruptive behavior inherent to the surgeon or the environment? Analysis of 314 events at a single academic medical center. September 4, 2019
Health economic evaluation of an infection prevention and control program: are quality and patient safety programs worth the investment? September 25, 2013
Racial and ethnic differences in emergency department pain management of children with fractures. April 22, 2020
Operating room traffic as a modifiable risk factor for surgical site infection. January 11, 2017
Recommendations to improve the usability of drug–drug interaction clinical decision support alerts. November 25, 2015
The impact of resident duty hour reform on hospital readmission rates among Medicare beneficiaries. April 27, 2011
Safety of overlapping surgery at a high-volume referral center. January 18, 2017
To do no harm - and the most good - with AI in health care. March 13, 2024
Improving handoffs in the perioperative environment: a conceptual framework of key theories, system factors, methods, and core interventions to ensure success. July 19, 2023
Association between long-term opioid use in family members and persistent opioid use after surgery among adolescents and young adults. March 13, 2019
Effects on resident work hours, sleep duration and work experience in a Randomized Order Safety Trial Evaluating Resident-physician Schedules (ROSTERS). June 26, 2019
Prolonged hospital stay and the resident duty hour rules of 2003. January 13, 2010
Did duty hour reform lead to better outcomes among the highest risk patients? November 4, 2009
Principles of conservative prescribing. June 29, 2011
Automated identification of postoperative complications within an electronic medical record using natural language processing. August 31, 2011
Effect of clinical decision-support systems: a systematic review. July 18, 2012
Teaching hospital five-year mortality trends in the wake of duty hour reforms. August 7, 2013
Teaching hospital financial status and patient outcomes following ACGME duty hour reform. September 26, 2012
A usability and safety analysis of electronic health records: a multi-center study. September 19, 2018
Leapfrog Hospital Safety Score, Magnet designation, and healthcare-associated infections in United States hospitals. May 17, 2017
New persistent opioid use after minor and major surgical procedures in US adults. April 26, 2017
Effects of resident duty hour reform on surgical and procedural patient safety indicators among hospitalized Veterans Health Administration and Medicare patients. July 1, 2009
Standardizing patient safety event reporting between care delivered or purchased by the Veterans Health Administration (VHA). April 10, 2024
Medical team training: applying crew resource management in the Veterans Health Administration. May 30, 2007
The effect of a rapid response team on major clinical outcome measures in a community hospital. September 5, 2007
Facing ambiguous threats. December 13, 2006
Misdiagnosis of thoracic aortic emergencies occurs frequently among transfers to aortic referral centers: an analysis of over 3700 patients. October 12, 2022
Value of improving patient safety: health economic considerations for rapid response systems-a rapid review of the literature and expert round table. May 3, 2023
Defining the incidence of cardiorespiratory instability in patients in step-down units using an electronic integrated monitoring system. December 17, 2008
Nurse sensemaking for responding to patient and family safety concerns. March 17, 2021
Interprofessional learning in multidisciplinary healthcare teams is associated with reduced patient mortality: a quantitative systematic review and meta-analysis. January 24, 2024
Prescribing decision making by medical residents on night shifts: a qualitative study. November 9, 2022
Clinical pathway adherence and missed diagnostic opportunities among children with musculoskeletal infections. September 6, 2023
Impact of a drug shortage on medication errors and clinical outcomes in the pediatric intensive care unit. February 3, 2016
Implementing a surgical checklist: more than checking a box. November 7, 2012
Using an objective structured clinical examination to test adherence to Joint Commission National Patient Safety Goal–associated behaviors. September 5, 2012
Incidence of clinically relevant medication errors in the era of electronically prepopulated medication reconciliation forms: a retrospective chart review. May 17, 2017
Quality measures of clinical pharmacy services during transitions of care. June 1, 2021
Extended work shifts and neurobehavioral performance in resident-physicians. March 10, 2021
Missing the near miss: recognizing valuable learning opportunities in radiation oncology. December 16, 2020
Resilience vs. vulnerability: psychological safety and reporting of near misses with varying proximity to harm in radiation oncology. November 18, 2020
Cumulative effect of flexible duty-hour policies on resident outcomes: long-term follow-up results from the FIRST trial. July 15, 2020
Family safety reporting in hospitalized children with medical complexity. July 20, 2022
A cluster randomized trial of two implementation strategies to deliver audit and feedback in the EQUIPPED medication safety program. April 26, 2023
Effect on patient safety of a resident physician schedule without 24-hour shifts. July 15, 2020
How hospitals select their patient safety priorities: an exploratory study of four Veterans Health Administration hospitals. September 25, 2019
Partnering with VA stakeholders to develop a comprehensive patient safety data display: lessons learned from the field. February 11, 2015
A systematic review of patient safety measures in adult primary care. May 18, 2016
Using estimated true safety event rates versus flagged safety event rates: does it change hospital profiling and payment? May 21, 2014
Medication-error alerts for warfarin orders detected by a bar-code-assisted medication administration system. March 9, 2011
Vital signs: improving antibiotic use among hospitalized patients. March 26, 2014
The impact of drug shortages on children with cancer—the example of mechlorethamine. January 16, 2013
Influence of state laws mandating reporting of healthcare-associated infections: the case of central line–associated bloodstream infections. July 31, 2013
Validating the Patient Safety Indicators in the Veterans Health Administration: do they accurately identify true safety events? November 2, 2011
Examining the impact of the AHRQ Patient Safety Indicators (PSIs) on the Veterans Health Administration: the case of readmissions. October 17, 2012
Redesigning rounds in the ICU: standardizing key elements improves interdisciplinary communication. October 3, 2018
Supporting clinicians after adverse events: development of a clinician peer support program. September 5, 2018
Impact of the Opioid Safety Initiative on opioid-related prescribing in veterans. March 22, 2017
Using harm-based weights for the AHRQ Patient Safety for Selected Indicators composite (PSI-90): does it affect assessment of hospital performance and financial penalties in Veterans Health Administration hospitals? February 1, 2017
Improving administration and documentation of enteral nutrition support therapy in a Veteran Affairs health care system: use of medication administration record and bar code scanning technology. February 1, 2023
Survival from in-hospital cardiac arrest during nights and weekends. February 27, 2008
Patient safety after implementation of a coproduced family centered communication programme: multicenter before and after intervention study. December 19, 2018
Patient safety in chiropractic teaching programs: a mixed methods study. December 23, 2020
Role of nursing home quality on COVID-19 cases and deaths: evidence from Florida nursing homes. September 22, 2021
A simulation systems testing program using HFMEA methodology can effectively identify and mitigate latent safety threats for a new on-site helipad. January 12, 2022
Psychological safety and hierarchy in operating room debriefing: reflexive thematic analysis. January 31, 2024
A longitudinal study of a multifaceted intervention to reduce newborn falls while preserving rooming-in on a mother-baby unit. October 5, 2022
Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. March 11, 2015
Impact of organizations on healthcare-associated infections. April 1, 2015
Good people who try their best can have problems: recognition of human factors and how to minimise error. January 27, 2016
Antimicrobial stewardship: another focus for patient safety? July 9, 2014
Changing cardiac arrest and hospital mortality rates through a medical emergency team takes time and constant review. February 3, 2010
Physician attitudes toward family-activated medical emergency teams for hospitalized children. April 2, 2014
Addressing healthcare-associated infections and antimicrobial resistance from an organizational perspective: progress and challenges. September 12, 2012
Video analysis of factors associated with response time to physiologic monitor alarms in a children's hospital. April 19, 2017
Association between mobile telephone interruptions and medication administration errors in a pediatric intensive care unit. January 15, 2020
Is health care getting safer? November 26, 2008
Reduced postdischarge incidents after implementation of a hospital-to-home transition intervention for children with medical complexity. October 4, 2023
Assessing the potential adoption and usefulness of concurrent, action-oriented, electronic adverse drug event triggers designed for the outpatient setting. June 24, 2015
Development of trigger tools for surveillance of adverse events in ambulatory surgery. November 10, 2010
Applying trigger tools to detect adverse events associated with outpatient surgery. March 16, 2011
A randomized controlled trial on the effect of a double check on the detection of medication errors. August 23, 2017
Physician and nurse well-being and preferred interventions to address burnout in hospital practice: factors associated with turnover, outcomes, and patient safety. July 19, 2023
Association of patient and family reports of hospital safety climate with language proficiency in the US. June 29, 2022
Complexity and challenges of the clinical diagnosis and management of Long COVID. November 30, 2022
Reporting and disclosing medical errors: pediatricians' attitudes and behaviors. February 7, 2007
Clarifying radiology's role in safety events: a 5-year retrospective common cause analysis of safety events at a pediatric hospital. September 2, 2020
I-PASS Mentored Implementation Handoff Curriculum: implementation guide and resources. March 10, 2019
Use of the revised second victim experience and support tool to examine second victim experiences of respiratory therapists. April 26, 2023
ASPEN Safe Practices for Enteral Nutrition Therapy. December 14, 2016
Changes in medical errors after implementation of a handoff program. November 12, 2014
Perceptions of U.S. and U.K. incident reporting systems: a scoping review. May 15, 2024
Paediatric medication incident reporting: a multicentre comparison study of medication errors identified at audit, detected by staff and reported to an incident system. May 1, 2024
Bad behavior in healthcare: an insidious threat to patients, staff, and organizations. April 17, 2024
Support and recovery strategies for second victims. April 3, 2024
Annual Perspective
Scoping review of the second victim syndrome among surgeons: understanding the impact, responses, and support systems. March 27, 2024
Nurse leader attitudes and beliefs regarding medical errors. March 6, 2024
Second-victim phenomenon. February 28, 2024
Interventions to support nurses as second victims of patient safety incidents: a qualitative study of nurse managers' perceptions. February 7, 2024
Prospective study of the multisite spread of a medication safety intervention: factors common to hospitals with improved outcomes. February 7, 2024
Factors influencing second victim experiences and support needs of OB/GYN and pediatric healthcare professionals after adverse patient events. January 17, 2024
Key factors for effective implementation of healthcare workers support interventions after patient safety incidents in health organisations: a scoping review. January 10, 2024
Validation and use of the Second Victim Experience and Support Tool questionnaire: a scoping review. December 20, 2023
System planning for modern-day Just Culture to mitigate worker distress and second victim response. November 29, 2023
Psychological safety as a new ACGME requirement: a comprehensive all-in-one guide to radiology residency programs. November 8, 2023
Use of the Second Victim Experience and Support Tool (SVEST) to assess the impact of a departmental peer support program on anesthesia professionals' second victim experiences (SVEs) and perceptions of support two years after implementation. November 8, 2023
Second victim syndrome in intensive care unit healthcare workers: a systematic review and meta-analysis on types, prevalence, risk factors, and recovery time. October 25, 2023
Achieving a successful patient safety program with implementation of a harm reduction strategy. October 25, 2023
In search of an international multidimensional action plan for second victim support: a narrative review. September 13, 2023
In their own words: safety and quality perspectives from families of hospitalized children with medical complexity. September 6, 2023
Patient, carer and family experiences of seeking redress and reconciliation following a life-changing event: systematic review of qualitative evidence. August 2, 2023
Emotional responses and support needs of healthcare professionals after adverse or traumatic experiences in healthcare-evidence from seminars on peer support. June 28, 2023
Individual characteristics that promote or prevent psychological safety and error reporting in healthcare: a systematic review. May 10, 2023
Improving medication safety in a paediatric hospital: a mixed-methods evaluation of a newly implemented computerised provider order entry system. April 12, 2023
Few hospitals are willing to bear the cost of providing psychiatric care for kids. March 22, 2023
Perspectives on Safety
Medication rounds: a tool to promote medication safety for children with medical complexity. March 8, 2023
Incidence and characteristics of adverse events in paediatric inpatient care: a systematic review and meta-analysis. January 25, 2023
A failure in the medication delivery system-how disclosure and systems investigation improve patient safety. January 11, 2023

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
- Open access
- Published: 15 May 2024
Effectiveness of a flipped classroom for undergraduate in implant dentistry hands-on course
- Tao Wu 1 , 2 ,
- Haibin Xia 1 , 3 ,
- Wei Sun 1 , 3 ,
- Chun Liu 1 ,
- Fengxiao He 1 ,
- Tiange Cheng 1 ,
- Yi Zhao 1 , 4 &
- Si Chen 1 , 3
BMC Medical Education volume 24 , Article number: 545 ( 2024 ) Cite this article
Metrics details
The purpose of this study was to compare the learning in the implant dentistry hands-on course to that of the flipped classroom (FC) and the traditional lecture cohorts (control).
Materials and methods
In this study,80 students were enrolled for the first time in an implant dentistry program. Subsequently, they were divided into two groups. The first, the FC group, which had free access to a video with a PowerPoint presentation on the Chaoxing-WHU-MOOC platform about the implant placement on first molar sites before class. The second, the control group, which attended a didactic lecture describing implant practice on the first molar site via a bidirectional multimedia interactive teaching demonstration and then operated on a simulation model. Cone beam computed tomography (CBCT) and the deviation gauge were utilized to analyze the accuracy of the implant placement in the students’ models. An online satisfaction questionnaire was distributed to both groups one week after the class.
The linear deviation of the CBCT examination did not show any statistical difference between the two groups concerning cervical, apex, and angular. A significant buccal deviation was observed in the control group compared with the FC group (mean: 0.7436 mm vs. 0.2875 mm, p = 0.0035), according to the restoration-level deviation gauge. A total of 74.36% of students in the FC group placed implant within 0.5 mm buccal-to-lingual deviations, but only 41.03% of students in the control group reached within 0.5 mm buccal-to-lingual deviation ranges. Additionally, 91.67% of the students in the FC group and 97.5% of the students in the control group were satisfied with the practical implant class.
FC was more effective than a didactic lecture for implant dentistry practical skill acquisition.
Peer Review reports
Introduction
Teaching methodology in dentistry faces significant challenges because of the advancement of media technologies. Students must develop abilities in critical thinking and problems-solving abilities independently. Instead of holding classroom lectures and having students apply the content in homework, students prereview the material (e.g., audiovisual presentations, videos, and websites, etc.) at home, and then have small-group discussions occur in the classroom resulting from flipped classroom (FC) learning [ 1 , 2 , 3 , 4 , 5 ]. The primary goal of FC is to shift learning from an instructor-centered model to a learner-centered model involving individual or team-based collaborative learning [ 4 ]. In the last two decades, FC has been introduced in different fields of dentistry, such as periodontics [ 3 ], dental anatomy [ 6 ], orthodontics [ 7 , 8 ], paediatric dentistry [ 9 ], maxillofacial surgery [ 10 ], prosthodontics [ 11 , 12 ], dental local anaesthetic [ 13 ]. However, it still has few applications in implant dentistry, especially in terms of hands-on learning.
As an emerging independent branch of dental, implant dentistry has advanced in education and practice over generations [ 14 ]. This course requires a combination of theory and practice, specifically students’ clinical and practical skills training. A study included 1015 respondents from 84 countries found that didactic lectures or theory-based training were the most common [ 14 ]. In recent years, the teaching mode of theoretical courses has evolved from the traditional way to a blended teaching model such as problem-based learning (PBL) and case-based learning (CBL), and various online applications have been added [ 15 ]. However, few studies have been reported about teaching method innovation in implant dentistry. It also determined that the most frequent challenge was the “identification of implant position” [ 14 ]. An overview of the U.S. predoctoral dental implant program established that 90.4% would conduct simulation exercises without direct patient care [ 16 ]. In China, students take oral implant placement hands-on classes on simulation models before attending a senior undergraduate implant teaching in their fourth or fifth years. This kind of hands-on course enables unskilled students to grasp anatomy characteristics and operation skills comprehensively for future safe clinical practice [ 17 ]. Traditionally, the teacher first demonstrates face-to-face how to perform the implant surgery on a simulation model, and then the students operate independently. Due to venue and time constraints, students may ignore the details of the operation in the short class time, and some students have poor learning initiative and lack experience. Besides, students lack initiative and a sense of self-inquiry. Therefore, a reform of the existing teaching methodology is necessary.
The combination of implantology theory and practical skill is a significant challenge; thus, exploring implant dentistry practice teaching methods is essential. However, no study in the literature has been conducted on the FC approach to implant dentistry practical skill teaching. We hypothesize that the implementation of the FC teaching method will improve students’ performances in implant dentistry practical skills. This study aimed to compare students’ learning in implant placement practice classes between an FC and a TL cohort, and assess the effectiveness of the FC methodology in implant dentistry hands-on course.
Student recruitment
The trial involved 80 undergraduates in their fourth year at Wuhan University from November 2022 to April 2023. Inclusion was achieved through volunteering, and exclusion involved refusal to participate. Two cohorts of participants ( N = 80 in total, N = 40 per group) were randomly allocated to the FC cohort and the TL cohort to complete the oral implant practice course (surgical implantation at the mandibular molar). Informed consent was obtained from all the participants. This study was approved by the Ethics Committee at the School and Hospital of Stomatology, Wuhan University (No. [2022] B73).
Interventions
The interventions were as follows:
The subjects included in this pedagogical study had previously completed theoretical teaching related to oral implantology. The FC group had access to pre-class videos and a related PowerPoint of an implant surgery operation on Chaoxing-WHU-MOOC platform online one week before class. After the self-study, students summarized the operation’s key points and collected the problems and difficulties. During the hands-on practice, the teacher answered common questions at the beginning of the course, and students discussed in small groups (eight persons per group). Then, students operated on a simulation model independently for 90 min (two people per implant machine). One week after the class, a satisfaction questionnaire was taken online.
The control group attended a didactic lecture about the ideal management of implant practice on the first molar site via a 30-minute bidirectional multimedia interactive teaching demonstration, and then operated on the simulation model independently for two hours (two persons per implant machine). One week after the class, a satisfaction questionnaire was taken online.
CBCT matching
A file containing an ideal implant 3D position design file was imported into the implant navigation design software, and the teacher performed the implant placement on the posterior mandibular simulation model under navigational guidance. This model was used as a standard reference model. For the two different teaching approaches, a CBCT examination of models of students placing implants was taken; and then matched with the CBCT file of the standard model to analyze the linear deviations.
Restoration deviation gauge
In addition to detecting deviations of the implants in the simulated bone with CBCT, a novel gauge was invented to analyze deviations in the penetration position of the dental implant restorations (Fig. 1 ). After implant placement, an implant carrier was inserted into the implant to check buccal-lingual, mesial-distal, and coronal-root depth deviations.
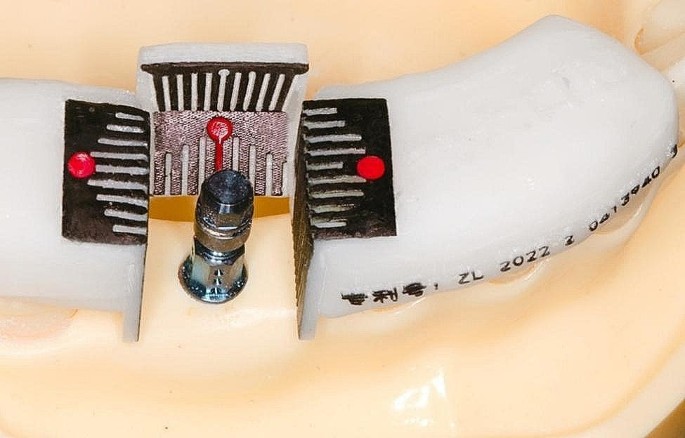
Restoration deviation measuring gauge (the red point refers to the ideal restoration position)
Satisfaction questionnaire
A satisfaction questionnaire was developed so that the students could evaluate the clinical practice skill process one week after class (Table 1 ). The first question was “What is your overall feeling about this practical implant class?”, which intended to evaluate students’ overall impression of the teaching approach. The second question, “What do you think about the teaching model self-study to self-summary to hands-on practice?” was used to assess students’ attitudes and gains from the FC approach during the learning process. The third question, “How do you feel about the teaching model in which the teacher shows and then performs the hands-on?” was designed to obtain students’ feedback on the traditional teaching method in the implant dentistry hands-on course.
Statistical analysis
SPSS 26 statistical software was used to analyze the data. The Shapiro-Wilk test determined whether the study subjects conformed to the normal distribution, and a t-test analyzed the results. A statistically significant difference was indicated by P < 0.05.
Participants attendance
A total of 80 students were included in the study. Of the 80 students who participated in the implantation hands-on class, one model in the control group was discarded because of operational mishandling. A total of 76 students provided feedback via the satisfactory questionnaire: 36 students in the FC group and 40 in the control group.
Implant linear deviations
To analyze the accuracy of implant placement, CBCT of students’ models was used to match the standard model which was placed by the teacher under dynamic navigation (Fig. 2 ). The mean linear deviation at the coronal implant region was 1.016 mm in the FC group and 1.018 mm in the control group respectively ( p = 0.9882). The mean linear deviation at the apex was 1.173 mm in the FC group and 1.058 mm in the control group, respectively ( p = 0.3413). The mean angular deviation was 4.321 degrees in the FC group and 4.183 degrees in the control group, respectively ( p = 0.7817).
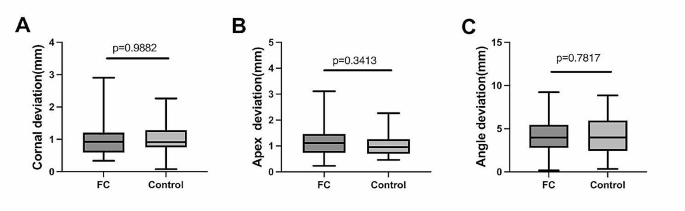
CBCT analysis of implant linear deviations between the two groups. Implant linear deviation between the FC and the control group at the coronal implant region ( A ), at the apex implant region ( B ), and at the angular level ( C )
Prosthetic deviations
Apart from using CBCT to examine each group’s implant linear deviation, a novel restoration-level deviation gauge was utilized to check the students’ implant prosthetic-level accuracy (Fig. 1 ). The results showed that a significant buccal deviation was observed in the control group compared to the FC group (buccal deviation mean: 0.7436 mm v.s.0.2875 mm, p = 0.0035) (Fig. 3 A). However, no statistical difference was observed between the FC group (mean = 0.0625 mm distal deviation) and the control group (mean = 0.2436 mm distal deviation) for mesial-distal deviation ( p = 0.1939) (Fig. 3 B). The difference in implantation depth in the coronal-apical direction between the two groups was the minimum ( p = 0.6502) (Fig. 3 C).
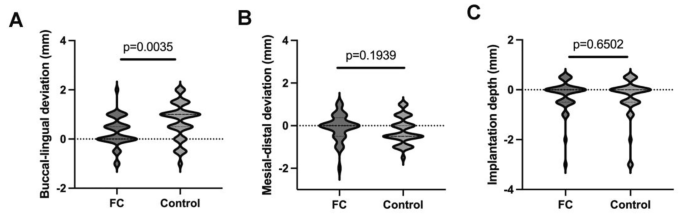
Semiquantitative restoration deviation measurement by the novel gauge between the FC and the control group. The deviation at buccal-lingual direction ( A ), Mesial-distal direction ( B ), and coronal-apex direction ( C ). (Direction illustration: + referring to buccal, - referring to lingual in figure A ; (+ referring to mesial, - referring to distal in figure B ; + referring to coronal, - referring to apex in figure C )
Considering the measurement discernible to the naked eye, the restoration deviation accuracy was graded at every 0.5 mm. The percentage distribution of the restoration linear deviation was also analyzed. In the FC group, 74.36% of the participants placed implants within 0.5 mm of buccal-to-lingual deviations, but only 41.03% of the control group (29 students) did the same (Fig. 4 ). A total of 41.03% of the FC group (16 students) achieved implant placement with no visually visible discrepancy, but only 10.26% of the control group (4 students) achieved this (Fig. 4 ). Students in the control group pretended to place implants more buccally than those in the FC group. Thus, the FC approach could significantly improve students’ control of buccal deviation at the restoration level.
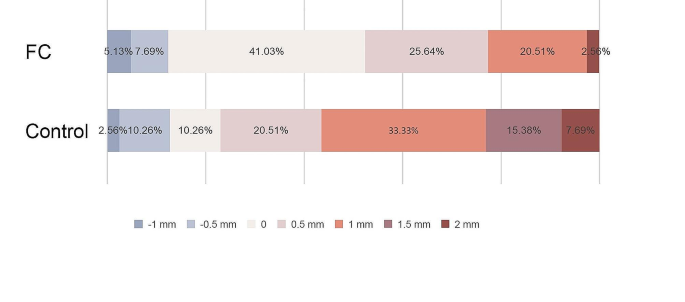
The percentage distribution of restoration linear deviation at the buccal-lingual direction (+ referring to buccal deviation, - referring to lingual deviation)
As for the mesial-distal of the restoration linear deviation, the distal deviation was greater than the mesial deviation in both groups (Fig. 5 ). In the FC group, 87.5% of students (34 students) placed implants within 0.5 mm of mesial-to-distal deviations, and in the control group, 74.39% of the students (29 students) did the same (Fig. 5 ). The implant placement deviation was greater than 1 mm for 20.51% of the control group and only 5% for the FC group (Fig. 5 ).
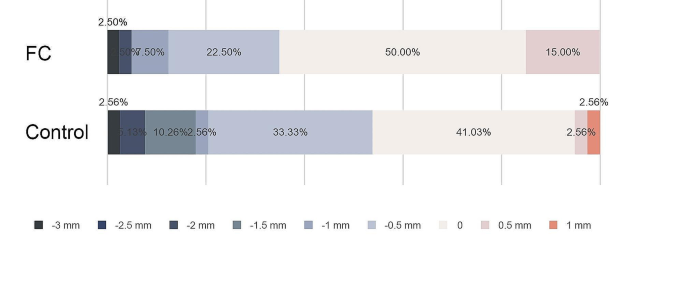
The percentage distribution of restoration linear deviation at the mesial-distal direction (+ referring to mesial deviation, - referring to distal deviation)
A total of 47.5% of students in the FC group were able to control the implant platform flush with the alveolar crest level, compared to 20.51% of students in the control group. Interestingly, the students preferred to place the implant 0.5 mm beneath the alveolar crest level in the control group (Fig. 6 ).
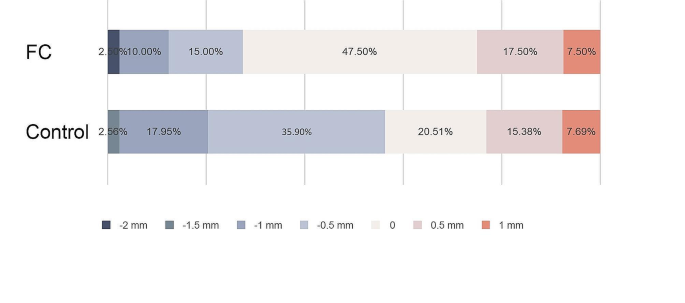
The percentage distribution of restoration linear deviation at the coronal-apex direction (+ referring to coronal deviation, - referring to apex deviation)
Satisfaction questionnaire results
According to the satisfaction survey (Table 1 ), 91.67% of the students in the FC group felt positive about the implant hands-on course, while 97.5% of the students in the control group agreed. A total of 77.78% of students in the FC group thought that this teaching method could promote their pre-reading and reflection, 91.67% of students indicated videos can be studied repeatedly, 83.33% found that videos were more convenient for learning, 22.22% thought that the flipped classroom approach could stimulate self-learning and enhance confidence, and only 5.56% of the students did not like pre-class self-study (Table 1 ). In the control group, over 80% of students noted that their teacher’s explanation can make the class clearer, and give more details of the operation, 85% considered the teacher’s explanations made more understandable, and 60% stated they could master the operation the first time because of the teacher’s clear instructions. However, 30% of students indicated that the teacher’s one-time demonstration could not be repeated for reviews if they missed it (Table 1 ).
The core features of the FC approach include students’ previewing teaching content (e.g., a pre-recorded lecture, PowerPoint presentations, websites, and bibliographic references, et al.) in advance, and the teacher was aware of students’ understanding and learning status during the flipped learning activities [ 9 ]. Videos have been frequently validated for dentistry teaching when a practical component is essential [ 3 ]. Accordingly, our study focused on the application of instructional videos in the FC approach to implant dentistry hands-on teaching.
The status of implant dentistry education among undergraduates from 34 institutions in 18 European countries was assessed. The average amount of time assigned to implant dentistry was 36 h, with a range of 3 to 120 h. All the institutions provided theoretical courses, but only 65% offered pre-clinical training. Half of the schools permitted students to assist in implant surgery and prosthetic treatment sessions, but less than one-third of the schools allowed students to treat clinical patients [ 3 ]. It has become a mandatory curriculum at Wuhan University for postgraduate students since the year 2016, and for undergraduate students since the year 2021. In senior undergraduate implant teaching (the fourth or fifth year), students are arranged for implant placement hands-on classes on simulation models before attending the clinic. The traditional teaching mode is widely used for dental implantology practice in China. The advantage of this teaching model is that the teacher’s on-site demonstration can bring a deep impression, while the disadvantage is that it leads to a lack of independent learning and self-exploration of the students. The Association for Dental Education in Europe (ADEE) proposed a consensus on guidelines for the teaching and assessment of implant dentistry at the undergraduate level. The consensus concerning implant surgical procedures demonstrated that the undergraduate should handle the surgical principles and major techniques for the surgical placement of dental implants [ 18 ]. Thus, pre-clinical training on the simulation model has a positive influence on the attitude toward implant dentistry surgical knowledge [ 19 ]. The FC teaching approach usually applied to theory teaching, may have a different effect when applied to dental implant practice courses.
Clinical practice skill requires tight integration of theoretical knowledge with hand-eye-brain coordination in clinical realities [ 20 ]. The FC model could serve as a student-centered method in clinical hands-on skills. In our study, the analysis of the results of implant deviation via CBCT did not indicate a statistical difference between the FC and the control group. However, the FC group took less time than the control group (1.5 h vs. 2.5 h) to reach a similar learning goal. Research exploring the FC approach in clinical practical skill teaching is scant. A recent study emphasized the FC approach resulted in better student performance in five areas of clinical skills: intravenous catheterization (IV), IV blood collection, blood pressure measurement from the brachial artery, intramuscular injection into the ventrogluteal region, and urinary catheterization in women [ 20 ]. Another study exploring third-year undergraduate dental students fabricating orthodontic wire-bending skills also compared FC with the live demonstration (LD) approach, and concluded that the FC outperformed the LD approach in fostering personalized learning and improving the efficacy of physical class time, but LD was more advantageous than FC in allowing immediate question and answer [ 21 ].
To more accurately and quickly assess students’ practical deviations, a novel deviation-measuring gauge was invented that could offer more timely feedback to the students and timely correction of errors compared with a periodontal probe (Fig. 1 ). This unique gauge is made of resin, and fixed on the neighboring teeth on either side. To facilitate observation and accurate reading, an evaluation scale was provided on each side wall, and a conspicuous red sign was stamped on the center. Once the implant is connected to the transfer bar, the implantation deviation can be measured on the restoration. With this gauge, students can achieve timely self-evaluation in the classroom, analyze the reasons for mistakes, self-summarize, and make practical skill improvements. Thus, teachers can accurately analyze the implant position, depth, and angular deviation, and correspondingly help students improve their knowledge of implantation technology. Rather than taking a CBCT after class, teachers can use this gauge to assist in judging implant placement accuracy based on restoration-level deviation. In our study, a significant difference was found when we penetrated the implant out to the position of the crown to judge the restoration-level deviation. Regarding this phenomenon, we speculate that these differences occurred because students could view the video several times, focus on more surgical details, and learn at their own pace (by pausing, rewinding, and replaying the video), unlike with the one-time on-the-spot surgery demonstration.
Most of the students found the two teaching methods interesting because oral implantology hands-on practice was completely new to them. The majority of the students (91.67%) in the FC group responded “It’s great. I love it”, and a higher percentage in the control group (97.5%) chose this option. These responses may be due to the FC approach requiring students to think independently and interact actively. A total of 91.67% of students agreed that the FC teaching method could allow the instructional video to be repeated, and 83.33% of students thought these repeats could bring more convenience. These results coincide with those obtained in the pediatric dentistry course, in which students stated the video was a very useful tool [ 9 ]. Faraone et al. implemented a blended curriculum model on complete denture prosthodontics, in which audio-visual and written materials were provided at the beginning of the semester. Students on this course were satisfied with comments like “This course allowed me to move at my own pace. I was having difficulty with a few procedures so I watched and re-watched the videos and reviewed the lectures at home and then went back to the school to master those steps. The asynchronous structure of this course was very conducive to my productivity and progress” [ 11 ]. Pre-class video lectures can be accessed at any time and as often as students desire. Students also highly appreciated the use of small-group discussion-based activities in the FC face-to-face sessions because these sessions helped increase their interest in subject and their motivation to learn.
The FC teaching approach can improve students’ engagement inside and outside the classroom, and cultivate critical thinking and problem-solving abilities through small-group discussion and the instructor’s assistance [ 9 ]. With the traditional lecture method, students can only focus on teaching for approximately 15 min and only 20% retained the content. However, the FC teaching approach engages students in the classroom with various activities related to the previous homework assignment so that students can concentrate for a longer time and knowledge can be better retained because of active engagement [ 22 ]. Introducing the FC teaching approach to the implant dentistry practical course not only allows students to get more opportunities for practical exercise and skills within the limited class time, but also stimulates the students’ subjective initiative, which creates positive feedback. Precise surgical operation and subjective initiative are both significant abilities for a qualified surgeon, and the FC teaching method applied to the implant dentistry practical course exactly focuses on the development of these two aspects of the student’s ability. In addition, this study will provide an important reference for the reform of teaching methodology in oral implant practice and expand the application of the FC teaching approach.
Even though the FC teaching approach was an effective model for learning implant dentistry through hands-on courses, it has limitations. Firstly, a well-organized video presentation and logistical planning required more input from teachers than traditional lectures. Secondly, it requires more classrooms to facilitate small-group discussions [ 3 ]. Thirdly, students were unwilling to work at home as is typically done in a traditional face-to-face class, and considered watching the pre-class videos to be a time [ 22 ]. Fourthly, the FC approach did not allow students to ask questions and receive immediate answers [ 21 ]. Finally, the online video demonstration is 2D, thus limiting the accurate representation of an actual 3D demonstration. As for the limitations of this study, on one hand, the summary debriefing of the practical course presented by each group tends to be homogeneous, lacking personalized viewpoints and extended discussion on the implementation of skills. On the other hand, we only compared the two teaching methods for the simulated placement of implants on the mandibular first molar. The problems in clinical are complex, and the results of this study cannot represent other complex situations Thus, more studies need to be applied to different degrees of difficulty in the classroom such as anterior aesthetic zone implantation and multi-tooth implantation to observe the effect FC approach in the dental implantology practice course.
Conclusions
In conclusion, implementing the FC teaching approach in implant dentistry hands-on course improved learning efficiency more than the traditional approach in limited class time. Although students were less satisfied with the application of the FC teaching method to implant dentistry practical courses than the traditional teaching method due to an additional study burden and the requirement to think independently, the majority of students appreciated pre-class video lectures. Therefore, the FC approach can be applied as in clinical practical skills training as an available teaching method.
Data availability
The authors declare that all the data and materials supporting the findings of this study are available within the article and are available from the corresponding author upon request.
Othman SA, Kamarudin Y, Sivarajan S, Soh EX, Lau MN, Zakaria NN, Wey MC, Wan Hassan WN, Bahar AD, Mohd Tahir NNZ, et al. Students’ perception on flipped classroom with formative assessment: a focus group study. Eur J Dent Educ. 2023;27(3):419–27.
Article Google Scholar
Lundegren N, Jönsson A, Lindberg P. An upgrade of the Malmö model by implementing case-based teaching and learning, in an undergraduate dental education. Eur J Dent Educ. 2021;25(4):649–56.
Lee C, Kim S-W. Effectiveness of a flipped classroom in learning periodontal diagnosis and treatment planning. J Dent Educ. 2018;82(6):614–20.
Vanka A, Vanka S, Wali O. Flipped classroom in dental education: a scoping review. Eur J Dent Educ. 2020;24(2):213–26.
O’Flaherty J, Phillips C. The use of flipped classrooms in higher education: a scoping review. Internet High Educ. 2015;25:85–95.
Chutinan S, Riedy C, Park S. Student performance in a flipped classroom dental anatomy course. Eur J Dent Educ. 2018;22(3):e343–9.
Arqub SA, Waleed M, Al-Abedalla K, Iverson MG, Uribe F. Insight on the influence of technology‐enhanced learning in orthodontics’ education: A systematic review. Eur J Dent Educ 2022.
Isherwood G, Taylor K, Burnside G, Fitzgerald R, Flannigan N. Teaching orthodontic emergencies using the flipped classroom method of teaching—A mixed methods RCT. Eur J Dent Educ. 2020;24(1):53–62.
Gallardo López NE, Caleya Zambrano AM, Sánchez Sánchez E. Feijóo García G: learning of paediatric dentistry with the flipped classroom model. Ene. 2022;8:53.
Google Scholar
Elledge R, Houlton S, Hackett S, Evans MJ. Flipped classrooms in training in maxillofacial surgery: preparation before the traditional didactic lecture? Br J Oral Maxillofac Surg. 2018;56(5):384–7.
Faraone K, Garrett P, Romberg E. A blended learning approach to teaching pre-clinical complete denture prosthodontics. Eur J Dent Educ. 2013;17(1):e22–7.
Nishigawa K, Omoto K, Hayama R, Okura K, Tajima T, Suzuki Y, Hosoki M, Shigemoto S, Ueda M, Rodis OMM, et al. Comparison between flipped classroom and team-based learning in fixed prosthodontic education. J Prosthodont Res. 2017;61(2):217–22.
Wong G, Apthorpe HC, Ruiz K, Nanayakkara S. An innovative educational approach in using instructional videos to teach dental local anaesthetic skills. Eur J Dent Educ. 2019;23(1):28–34.
Dragan IF, Pirc M, Rizea C, Yao J, Acharya A, Mattheos N. A global perspective on implant education: cluster analysis of the first dental implant experience of dentists from 84 nationalities. Eur J Dent Educ. 2019;23(3):251–65.
Ferro AS, Nicholson K, Koka S. Innovative trends in Implant Dentistry Training and Education: a narrative review. J Clin Med 2019, 8(10).
Barwacz CA, Avila-Ortiz G, Allareddy V, Tamegnon M, Hoogeveen K. An overview of U.S. predoctoral dental implant programs and their directors. J Dent Educ. 2015;79(3):265–77.
Hu L, Rong R, Song W, Wu H, Jia S, He Z, Sa Y. Patient-specific 3D printed models for enhanced learning of immediate implant procedures and provisionalization. Eur J Dent Educ 2023.
Mattheos N, Albrektsson T, Buser D, De Bruyn H, Donos N, Hjørting Hansen E, Lang NP, Sanz M, Nattestad A. Teaching and assessment of implant dentistry in undergraduate and postgraduate education: a European consensus. Eur J Dent Educ. 2009;13(Suppl 1):11–7.
Yuan JC, Kaste LM, Lee DJ, Harlow RF, Knoernschild KL, Campbell SD, Sukotjo C. Dental student perceptions of predoctoral implant education and plans for providing implant treatment. J Dent Educ. 2011;75(6):750–60.
Kaplan A, Özdemir C, Kaplan Ö. The Effect of the flipped Classroom Model on Teaching Clinical Practice skills. J Emerg Nurs. 2023;49(1):124–33.
Lau MN, Sivarajan S, Kamarudin Y, Othman SA, Wan Hassan WN, Soh EX, Zakaria NN, Wey MC, Bahar AD. Students’ perception on flipped classroom in contrast to live demonstration for teaching orthodontic wire-bending skills: a focus group study. J Dent Educ. 2022;86(11):1477–87.
Aljabr A. Flipped Classroom experiences in Clinical Dentistry – A Strategic Mini-review. Open Dentistry J. 2021;15(1):717–27.
Download references
Acknowledgements
We thank all participating students and teachers for supporting our study. This project was supported by the Medical Education Research Project of the Chinese Medical Association Medical Education Branch and the National Center for Development of Medical Education in 2023 (Number: 2023B278) and by the National Natural Science Foundation of China (No. 82201103).
Author information
Authors and affiliations.
State Key Laboratory of Oral & Maxillofacial Reconstruction and Regeneration, Key Laboratory of Oral Biomedicine Ministry of Education, Hubei Key Laboratory of Stomatology, School & Hospital of Stomatology, Wuhan University, 237 Luoyu Road, Wuhan, 430079, P. R. China
Tao Wu, Haibin Xia, Wei Sun, Chun Liu, Fengxiao He, Tiange Cheng, Yi Zhao & Si Chen
Center for Prosthodontics and Implant Dentistry, Optics Valley Branch, School and Hospital of Stomatology, Wuhan University, Wuhan, 430079, P. R. China
Department of Oral Implantology, School &Hospital of Stomatology, Wuhan University, Wuhan, 430079, P.R. China
Haibin Xia, Wei Sun, Yan Ge & Si Chen
Department of Prosthodontics, School &Hospital of Stomatology, Wuhan University, Wuhan, 430079, P. R. China
You can also search for this author in PubMed Google Scholar
Contributions
Study design: Si Chen. Study conduct: Si Chen, Tao Wu, Wei Sun, Yan Ge, Chun Liu. Data collection: Tao Wu, Chun Liu, Fengxiao He. Data analysis: Tao Wu, Tiange Cheng. Revising manuscript content: Si Chen, Haibin Xia Approving the final version of the manuscript: Si Chen, Yi Zhao.
Corresponding authors
Correspondence to Yi Zhao or Si Chen .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all participants at the beginning of the study. All experimental protocols were approved by the Ethics Committee at the School and Hospital of Stomatology, Wuhan University (No. [2022] B73).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wu, T., Xia, H., Sun, W. et al. Effectiveness of a flipped classroom for undergraduate in implant dentistry hands-on course. BMC Med Educ 24 , 545 (2024). https://doi.org/10.1186/s12909-024-05536-6
Download citation
Received : 09 October 2023
Accepted : 08 May 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12909-024-05536-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Implant dentistry
- Hands-on course
- Flipped classroom
- Teaching methods
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Signs and Symptoms
- Living with Autism Spectrum Disorder
- Frequently Asked Questions (FAQs)
- Data and Statistics on Autism Spectrum Disorder
- Autism Materials and Resources
- Diagnosis ASD
- Information on ASD for Healthcare Providers
- Acceptance Month Partner Toolkit
- 2023 Community Report on Autism
- Autism Data Visualization Tool
Autism Prevalence Studies Data Table
What to know.
- This data table summarizes information from peer-reviewed autism prevalence studies. Information reported from each study includes the autism prevalence estimate and additional study characteristics (such as case ascertainment and criteria).
- The information on this page is intended for healthcare providers, public health professionals, and those interested in reviewing additional scientific articles about ASD.

A PubMed search was conducted to identify studies using the search terms: autism (title/abstract) OR autistic (title/abstract) AND prevalence (title/abstract). Data were abstracted and included if the study fulfilled the following criteria:
- The study was published in English;
- The study produced at least one autism prevalence estimate; and
- The study was population-based (any age range) within a defined geographic area.
Autism prevalence studies data table
Originating source: https://data.cdc.gov/Public-Health-Surveillance/autism-prevalence-studies/9mw4-6adp
To suggest additional autism prevalence studies for inclusion in the data table, please email [email protected] .
Description of data table
Data column descriptions.
Note: blank cells indicate data not available.
Title —publication title
Year published —publication year
Country —country where the study was conducted
Area(s) —the city or specific geographical area(s) where the study was conducted
Age range (years) —age range (in years) of the population studied
Study years —the study period (in years)
Case identification method —study source record(s)* used to identify individuals with autism (registry; health records; education records; survey [specify type: in-person, phone, mail, online]; service provider records; other [define]) *more than one method may be used
Case criterion —criteria* used to identify individuals with autism (DSM [specify edition]; ICD [specify version]; Rutter(1); Kanner(2); clinical impression; autism test [specify test]; special education classification; self-report; parental report; receipt of autism-specific services; other [define]) * more than one case criterion may be used
- Rutter M. Diagnosis and definition of childhood autism. Journal of Autism and Childhood Schizophrenia. 1978;8(2):139-161.
- Kanner L. Autistic disturbances of affective contact. Nervous Child. 1943;2:217-250.
Sample size —study population size (prevalence denominator)
Number of cases —individuals with autism (prevalence numerator)
Autism prevalence estimate —autism prevalence estimate per 1,000 population; autism prevalence estimates were reported or calculated by CDC under the following conditions. Autism prevalence was reported separately for multiple study years with no overall estimate (data from the most recent study year was reported to highlight the most up-to-date data); autism prevalence for multiple age ranges was reported separately with no overall estimate (the age range with the largest sample size or best quality data, as reported by study authors, was used); autism prevalence for multiple birth cohorts of data was reported separately with no overall estimate (the most recent birth cohort to date was used to highlight the most-up-to-date data); autism prevalence was reported separately by subtype of autism or separately by geographic area with no overall estimate (number of individuals with autism in each subgroup combined or combined geographic areas were used to estimate autism prevalence if possible. If not possible [for example, denominator for subgroup was not available], the estimate with the best quality data, as indicated by the author, was reported)
Confidence interval (CI) —95% confidence interval (CI) for the autism prevalence estimate; if a CI was not reported in the study, a CI was calculated using the Wilson method with this online tool: http://www.hutchon.net/Wilsons.htm
Male:female ratio —male to female ratio of individuals with autism
Non-Hispanic White:Hispanic prevalence ratio —non-Hispanic White to Hispanic ethnicity autism prevalence ratio
White:Black prevalence ratio —White to Black race autism prevalence ratio
Diagnosis age range (months) —age range (in months) of cases at time of autism diagnosis
Diagnosis mean age (months) —mean age (in months) of cases at time of autism diagnosis
Diagnosis median age (months) —median age (in months) of cases at time of autism diagnosis
IQ <70 (%) —percentage of individuals with autism with an IQ (intelligence quotient) less than 70
Adaptive score <70 (%) —percentage of individuals with autism with an adaptive score less than 70
Non-verbal or minimally verbal (%) —percentage of individuals with autism that are non-verbal or minimally verbal
Percentage of individual co-occurring conditions (%) —percentage of co-occurring conditions reported in individuals with autism (attention deficit disorder [ADD] or attention deficit hyperactivity disorder [ADHD]; anxiety; cerebral palsy [CP]; congenital rubella; depression; Down syndrome; encephalopathy; epilepsy/seizure disorder; fetal alcohol syndrome; fragile X; language delay; learning disability; mood disorder; neonatal abstinence syndrome; obsessive compulsive disorder [OCD]; oppositional defiant disorder [ODD]; prematurity; Rett syndrome*; sudden infant death syndrome [SIDS]; sickle cell disease [SCD]; Tourette syndrome; tuberous sclerosis) * For cases of Rett syndrome: if Rett syndrome cases were included in the autism prevalence estimate, Rett syndrome was not included as a co-occurring condition. If authors separated Rett syndrome from the autism prevalence estimate, it was included as a co-occurring condition and excluded from the prevalence estimate.
Autism types included —subtypes of autism included in the study as reported by the authors (early or classic infantile autism, autistic syndrome, autistic mental retardation, childhood autism, autistic-like conditions, pervasive developmental disorder [PDD], pervasive developmental disorder–not otherwise specified [PDD-NOS], autistic disorder, atypical autism, Asperger's syndrome, childhood disintegrative disorder [CDD], autism spectrum disorder [ASD])
Publication link —link to publication
CDC calculated values —indicates values calculated by CDC's abstractor (e.g., converting age range from months to years, calculating confidence interval [CI], calculating overall autism prevalence estimate when prevalence was reported separately for autism subtype or for geographic study area; calculating percentages of individuals with autism by IQ categories or with co-occurring conditions when only individual case numbers are reported)
Autism Spectrum Disorder (ASD)
Autism spectrum disorder (ASD) is a developmental disability that can cause significant social, communication and behavioral challenges. CDC is committed to continuing to provide essential data on ASD and develop resources that help identify children with ASD as early as possible.
For Everyone
Health care providers, public health.

IMAGES
VIDEO
COMMENTS
PubMed is a comprehensive database of biomedical literature from various sources, including MEDLINE, life science journals, and online books. You can search for citations, access full text content, and explore topics related to health, medicine, and biology. PubMed also provides advanced search options and tools for researchers and clinicians.
The New England Journal of Medicine (NEJM) is a weekly general medical journal that publishes new medical research and review articles, and editorial opinion on a wide variety of topics of ...
Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site. ... (PMC) is a free full-text archive of biomedical and life sciences journal literature at the U.S. National Institutes of Health's National Library of Medicine (NIH/NLM)
AJM is the official journal of the Alliance for Academic Internal Medicine, a prestigious group comprising internal medicine department chairs at more than 125 medical schools across the U.S. Each issue carries useful reviews as well as seminal articles of immediate interest to the practicing physician, including peer-reviewed, original ...
21,857. 21,285. Explore the latest in medicine including the JNC8 blood pressure guideline, sepsis and ARDS definitions, autism science, cancer screening guidelines, and.
MEDLINE is the National Library of Medicine's (NLM) premier bibliographic database that contains references to journal articles in life sciences, with a concentration on biomedicine. See the MEDLINE Overview page for more information about MEDLINE.. MEDLINE content is searchable via PubMed and constitutes the primary component of PubMed, a literature database developed and maintained by the ...
Find comprehensive medical reference information including disease symptoms, diagnoses, treatments, and follow-up; plus drug and medication dosing, interactions, adverse effects, and more on Medscape, a free, comprehensive, and current resource for physicians and other healthcare professionals.
Rigorously reported, peer reviewed and immediately available without restrictions, promoting the widest readership and impact possible. We encourage you to consider the scope of each journal before submission, as journals are editorially independent and specialized in their publication criteria and breadth of content. ... PLOS Mental Health ...
The New England Journal of Medicine (NEJM) is recognized as the world's leading medical journal and website. Published continuously for over 200 years, NEJM delivers high-quality, peer-reviewed ...
Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and SARS-CoV-2 positive testing: self-controlled case series study. Aug 26, 2021. High impact medical journal. Champion of better research, clinical practice & healthcare policy since 1840. For GPs, hospital doctors, educators, policymakers.
Open access publisher of peer-reviewed scientific articles across the entire spectrum of academia. Research network for academics to stay up-to-date with the latest scientific publications, events, blogs and news. ... Opening health for all: 7 Research Topics shaping a healthier world.
3.3 million articles on ScienceDirect are open access. Articles published open access are peer-reviewed and made freely available for everyone to read, download and reuse in line with the user license displayed on the article. ScienceDirect is the world's leading source for scientific, technical, and medical research.
One of the premier peer-reviewed clinical journals in general and internal medicine, Mayo Clinic Proceedings is among the most widely read and highly cited scientific publications for physicians. While the Proceedings is sponsored by Mayo Clinic, it welcomes submissions from authors worldwide, publishing articles that focus on clinical medicine and support the professional and educational ...
PubMed is the number one source for medical and healthcare research. It is hosted by the National Institutes of Health (NIH) and provides bibliographic information including abstracts and links to the full text publisher websites for more than 28 million articles. ... Coverage: several thousand articles from over 420 peer-reviewed journals;
The leading peer-reviewed journal for digital medicine and health and health care in the internet age. Editor-in-Chief: ... Adjunct Professor, School of Health Information Science, University of Victoria, Canada. Impact Factor 7.4. The Journal of Medical Internet Research (JMIR) is the pioneer open access eHealth journal and is the ...
Prevalence of Short Peer Reviews in 3 Leading General Medical Journals. JAMA Network Open. Research. December 14, 2023. This cross-sectional study examines the prevalence of very short peer reviews (<200 words) from 3 general medical journals as a measure of peer review quality. Research, Methods, Statistics.
Investigation of the effect of circadian rhythm on the performances of NBA teams. Fırat Özdalyan, Erhan Çene, Hikmet Gümüş & Osman Açıkgöz. Published online: 30 Apr 2024. Search and explore the millions of quality, peer-reviewed journal articles published under the Taylor & Francis, Routledge and Dove Medical Press imprints.
We reviewed websites that we and our colleagues knew of, searched for government sponsored health information websites, and searched for online sources of health information that provide evidence-based information. To be included in our review, a website had to be available in English, freely accessible, and intended for patients and the public.
BMJ Open is a leading multidisciplinary open access medical journal publishing high-quality peer-reviewed content. Validation period: 5/16/2024, 3:28:02 PM - 5/16/2024, 9:28:02 PM. Search. ... Publishing procedures are built around fully open peer review and continuous publication, publishing research online as soon as the article is ready. ...
Office of Disease Prevention and Health Promotion (ODPHP) 240-453-8280 [email protected] https://health.gov/. USA.gov 844-872-4681 www.usa.gov. This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
MedlinePlus is an online health information resource for patients and their families and friends. It is a service of the National Library of Medicine (NLM), the world's largest medical library, which is part of the National Institutes of Health (NIH). Learn more about MedlinePlus. FEATURED TOPIC.
The first step in gauging credibility is to analyze the source. Consider publications from the following: Mayo Clinic, a nonprofit academic medical center. National Institutes of Health (NIH), a part of U.S. Department of Health and Human Services. Johns Hopkins Hospital, one of the world's premier teaching and biomedical research hospitals.
Finally, 24 studies were included in the final review based on the research objectives. Based on the results, men's QOL scores in different studies varied from 55.15 ± 13.52 to 91.45 ± 13.66%. Of the total reviewed articles, the lowest and highest scores were related to mental health problems and physical dimensions, respectively.
Objectives To replicate previous analyses on the effectiveness of the English human papillomavirus (HPV) vaccination programme on incidence of cervical cancer and grade 3 cervical intraepithelial neoplasia (CIN3) using 12 additional months of follow-up, and to investigate effectiveness across levels of socioeconomic deprivation. Design Observational study. Setting England, UK. Participants ...
Temporal Trends of Real-Time Emergency Department Patient Portal Use. Credit: JAMA Network Open (2024). DOI: 10.1001/jamanetworkopen.2024.9831
Also known as supervised consumption sites, OPCs are health care facilities that aim to improve individual and community health, increase public safety, and reduce consequences of drug use, including overdose deaths, public drug use, and syringe litter. 3,4 Operating in more than 10 countries, OPCs offer supervised, hygienic spaces in which ...
This article, with a focus on pediatric pharmacists, presents four programs designed to support second victims: MU Health's forYOU, Johns Hopkins' RISE, Nationwide Children's YOU Matter, and Children's Minnesota's (Children's MN's) P2P (peer-to-peer) program. The authors also present options for support that individuals can access ...
The purpose of this study was to compare the learning in the implant dentistry hands-on course to that of the flipped classroom (FC) and the traditional lecture cohorts (control). In this study,80 students were enrolled for the first time in an implant dentistry program. Subsequently, they were divided into two groups. The first, the FC group, which had free access to a video with a PowerPoint ...
The information on this page is intended for healthcare providers, public health professionals, and those interested in reviewing additional scientific articles about ASD. Data table A PubMed search was conducted to identify studies using the search terms: autism (title/abstract) OR autistic (title/abstract) AND prevalence (title/abstract).