The Food and Nutrition Status in India: A Systematic Review
- First Online: 07 March 2023

Cite this chapter

- Shahnaz Basheer 6 ,
- V. V. Ashique 6 &
- Aakriti Grover 6 , 7
Part of the book series: Advances in Geographical and Environmental Sciences ((AGES))
338 Accesses
With undernutrition, overnutrition, and micronutrient deficiencies afflicting the country, India experiences a triple burden of malnutrition. Recent decades have seen modest progress when it comes to health in India, but progress has been uneven and inequitable. This study reviews food and nutrition status in India. The diversity in food is enabled by variety in nutrition, which is only possible with serious crop diversification. The nutrient uptake is majorly cereal-centric as food production, availability, and access are impacted by the agricultural policy that has placed a significant thrust on food grain production spurred by the green revolution and supported by the institutions. India is not only affected by malnutrition amongst the poor but also amongst all socio-economic groups. India ranks 101 out of 116 countries based on the Global Hunger Index 2020. The Global Nutrition Report 2018 clearly mentions that India is home to 46.6 million stunted children and 25.5 million wasted children. India ranks 103 out of 119 qualifying countries per the Global Hunger Index 2018. Malnutrition was the predominant risk factor for death in children younger than five years of age in every state of India in 2017 (GBD), accounting for 68.2% (95% UI 65.8–70.7) of the total under-5 deaths and the leading risk factor for health loss for all ages, responsible for 17.3% (16.3–18.2) of the entire disability-adjusted life years (DALYs). In India, nutrition status has deteriorated over decades because of ineffective policy interventions and inadequate food systems, which are neither affordable nor sustainable. There are severe gaps in India’s nutrition statistics, and even the most important nutrition trends are far from explicit; practical action in this field requires regular and reliable large-scale surveys that would make it possible to monitor the nutrition situation at the district levels at intervals.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
AbouZahr C, Boerma T (2005) Health information systems: the foundations of public health. Bull World Health Organ 83(8):578–583
Google Scholar
Arnold F, Parasuraman S, Arokiasamy P, Kothari M (2009) Nutrition in India. In: National Family Health Survey (NFHS-3), India, 2005–06. International Institute for Population Sciences, Mumbai; ICF Macro, Calverton, Maryland, USA
Battersby J (2019) Urban food systems governance and poverty in African Cities. pp 1–26. https://doi.org/10.4324/9781315191195
Black RE, Morris SS, Bryce J (2003) Where and why are 10 million children dying every year? Lancet 361(9376):2226–2234. https://doi.org/10.1016/S0140-6736(03)13779-8
Article Google Scholar
Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M et al (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371(9608):243–260. https://doi.org/10.1016/S0140-6736(07)61690-0
Brand C, Bricas N, Conaré D, Daviron B, Debru J, Michel J, Soulard C-T (ed) (2019) Designing urban food policies concepts and approaches, urban agriculture. Springer, Switzerland
Boerma JT, Stansfield SK (2007) Health statistics now: are we making the right investments? Lancet 369(9563):779–786. https://doi.org/10.1016/S0140-6736(07)60364-X
Capone R, Bilai HE, Debs P, Cardone G, Driouech N (2014) Food system sustainability and food security: connecting the dots. J Food Secur 2(1):13–22
Caulfield LE, de Onis M, Blossner M, Black RE (2004) Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am J Clin Nutr 80(1):193–198
Article CAS Google Scholar
Census of India (2011) Primary Census Abstract (PCA) directorate of census operations Kerala. https://censusindia.gov.in
Cesare Di M, Ghosh S, Osendarp S, Mozaffarian D (2021) A world free from malnutrition: an assessment of progress towards the global nutrition targets. https://globalnutritionreport.org/reports/2021-global-nutrition-report/assessing-progress-towards-the-global-nutrition-targets/
Christensson L, Unosson M, Ek AC (2002) Evaluation of nutritional assessment techniques in elderly people newly admitted to municipal care. Eur J Clin Nutr 56:810–881. https://doi.org/10.1038/sj.ejcn.1601394
Dambal S (2017) Malnutrition in India: an overview. Int J Med Pharm Sci (IJMPS) 7(6):41–52. www.tjprc.org
Deaton A, Drèze J (2008) Income, health, and well-being around the world: evidence from the gallup world poll. J Econ Perspect 22(2):53-72
Deaton A, Drèze J (2009) Nutrition in India: facts and interpretations, working paper no. 170. Econ Political Wkly 44(7):42–65
Ettinger AS (2004) Children’s health, the Nation’s wealth: assessing and improving child health. Environ Health Perspect 112(14)
Fogel RW (2004) Health, nutrition, and economic growth. Econ Dev Cult Change. 52(3). University of Chicago and National Bureau of Economic Research. https://doi.org/10.1086/383450
Food and Nutrition Security Analysis, India (2019) Ministry of statistics and programme implementation and the world food programme by the Government of India and World Food Programme. http://www.indiaenvironmentportal.org.in/files/file/Food%20and%20Nutrition%20Security%20Analysis.pdf
Ghosh S (2020) Factors responsible for childhood malnutrition: a review of the Literature. Curre Res Nutr Food Sci 8(2):360–370. https://doi.org/10.12944/CRNFSJ.8.2.01
Goli S, Doshi R, Perianayagam A (2013) Pathways of economic inequalities in maternal and child health in urban India: a decomposition analysis. PLoS ONE 8(3):e58573. https://doi.org/10.1371/journal.pone.0058573
Gómez MI, Barrett CB, Raney T, Pinstrup-Andersen P, Meerman J, Croppenstedt A, Lowder S, Carisma B, Thompson B (2013) Post-green revolution food systems and the triple burden of malnutrition. In: ESA Working Paper No. 13–02, Agricultural Development Economics Division Food and Agriculture Organization of the United Nations. www.fao.org/economic/esa
Gopalan C (2013) The changing nutrition scenario. Indian J Med Res 138(3):392–397
CAS Google Scholar
Huysentruyt K, Brunet-Wood K, Bandsma R, Gramlich L, Fleming-Carroll B, Hotson B, Byers R, Lovelace H, Persad R, Kalnins D, Martinez A, Marchand V, Vachon M, Hulst JM (2021) On behalf of the Canadian malnutrition task force-pediatric working group. Canadian nationwide survey on pediatric malnutrition management in tertiary hospitals. Nutrients 13:2635. https://doi.org/10.3390/nu13082635
Ighogboja SI (1992) Some factors contributing to protein-energy malnutrition in the middle belt of Nigeria. East Afr Med J 69(10):566–571
India State-Level Disease Burden Initiative Malnutrition Collaborators (2019) The burden of child and maternal malnutrition and trends in its indicators in the states of India: the global burden of disease study 1990–2017. Lancet Child Adolesc Health 3:855–870. https://doi.org/10.1016/S2352-4642(19)30273-1 . https://gdc.unicef.org/resource/burden-child-and-maternal-malnutrition-and-trends-its-indicators-states-india-global
International Institute for Population Sciences (IIPS) (1995) National family health survey (MCH and family planning), India 1992–93. IIPS, Mumbai
International Institute for Population Sciences (IIPS) and ICF (2017) National family health survey (NFHS-4), 2015–16: India. IIPS, Mumbai
International Institute for Population Sciences (IIPS) and ICF (2020) National family health survey (NFHS)-5, India and state factsheet compendium. IIPS, Mumbai
International Institute for Population Sciences (IIPS) and ORC Macro (2000) National family health survey (NFHS-2), 1998–99: India. IIPS, Mumbai
Jeejeebhoy KN, Detsky AS, Barker JP (1990) Assessment of nutritional status. J Parent Enternal Nutr 14:193–196
John A, E Knebel, L Haddad, Menon P (2015) An assessment of data sources to track progress towards global nutrition targets in India. POSHAN Research Note 6. International Food Policy Research Institute (IFPRI), New Delhi. http://ebrary.ifpri.org/cdm/ref/collection/p15738coll2/id/129722
Kapil U, Sachdev HP (2013) Massive dose vitamin A programme in India need for a targeted approach. Indian J Med Res 138(3):411–417
Kapil U, Chaturvedi S, Nayar D (1992) National nutrition supplementation programmes. Indian Pediatr 29:1601–1613. https://www.indianpediatrics.net/dec1992/1601.pdf
Kumar P (2017) Food and nutrition security in India: the way forward. Agric Econ Res Rev 30(1):1–21. https://doi.org/10.5958/0974-0279.2017.00001.5
McGuire S, FAO, IFAD, WFP (2015) The state of food insecurity in the world 2015: meeting the 2015 international hunger targets: taking stock of uneven progress. Adv Nutr 6(5):623–624. https://doi.org/10.3945/an.115.009936
Moestue H, Huttly S, Sarella L, Galab S (2007) ‘The bigger the better’-mothers’ social networks and child nutrition in Andhra Pradesh. Public Health Nutr 10(11):1274–1282
Muller O, Krawinkel M (2005) Malnutrition and health in developing countries. CMAJ 173(3):279–286. https://doi.org/10.1503/cmaj.050342
National Nutrition Policy (1993) Government of India Department of Women & Child Development Ministry of Human Resource Development New Delhi. https://wcd.nic.in/sites/default/files/nnp_0.pdf
National Policies and strategies, FAO (2001) https://www.fao.org/ag/AGN/nutrition/nationalpolicies_en.stm
Nguyen PH, Scott S, Headey D, Singh N, Tran LM, Menon P et al (2021) The double burden of malnutrition in India: trends and inequalities (2006–2016). PLoS ONE 16(2):e0247856. https://doi.org/10.1371/journal.pone.0247856
Popkin BM, Corvalan C, Grummer-Strawn LM (2020) Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 395(10217):65–74. https://doi.org/10.1016/S0140-6736(19)32497-3
Ramachandran P, Kalaivani K (2018) Nutrition transition in India: challenges in achieving global targets. Proc Indian Natn Sci Acad 84(4):821–833
Rikimaru T, Yartey JE, Taniguchi K, Kennedy DO, Nkrumah FK (1998) Risk factors for the prevalence of malnutrition among urban children in Ghana. J Nutr Sci Vitaminol (Tokyo) 44(3):391–407. https://doi.org/10.3177/jnsv.44.391
Ruel MT, Garrett JL, Yosef S, Olivier M (2017) Urbanization, food security, and nutrition. In: de Pee S, Taren D, Bloem MW (eds) Nutrition and health in a developing world, part VII, vol 705–735. New York. https://doi.org/10.1007/978-3-319-43739-2_32
Sobal J, Khan LK, Bisogni C (1998) A conceptual model of the food and nutrition system. Soc Sci Med 47(7):853–863. https://doi.org/10.1016/s0277-9536(98)00104-x
Söderström L, Rosenblad A, Adolfsson ET, Saletti A, Bergkvist L (2014) Nutritional status predicts preterm death in older people: a prospective cohort study. Clin Nutr 33(2):354–359. https://doi.org/10.1016/j.clnu.2013.06.004
Somalia, Mogadishu, Mohamud A, Ibrahim WM (2017) Study on risk factors for poor nutritional status among <5 children in Yaqshid district Mogadishu-Somalia. Dissertation. https://www.researchgate.net/publication/323831532_Study_on_risk_factors_for_Poor_Nutritional_Status_among_5_children_in_Yaqshid_district_Mogadishu-Somalia
Srilakshmi B (2006) Nutrition science, Revised 2nd edn. New Age International (P) Limited Publishers, New Delhi, India
Stansfield SK, Walsh J, Prata N, Evans T (2006) Information to improve decision making for health. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB et al (eds). Disease control priorities in developing countries, 2nd edn. The International Bank for Reconstruction and Development and The World Bank, Washington
Tette EM, Sifah EK, Nartey ET (2015) Factors affecting malnutrition in children and the uptake of interventions to prevent the condition. BMC Pediatr 15:189. https://doi.org/10.1186/s12887-015-0496-3
Tomkins A, Watson F (1989) Malnutrition and infection; a review. In: UN ACC/SCN. vol. Nutrition policy discussion paper. Administrative committee on coordination-subcommittee on nutrition, Geneva
The state of food security and nutrition in the world, UNICEF. https://www.unicef.org/reports/state-of-food-security-and-nutrition-2020
United Nations, Department of Economic and Social Affairs, Population Division (2018) World population prospects 2018: highlights (ST/ESA/SER.A/423)
Upadhyay R, Tripathi KD (2017) How can we assess the nutritional status of an individual? J Nutr Food Sci 7(6):1–2. https://doi.org/10.4172/2155-9600.1000640
Usmani G, Ahmad N (2018) Health status in India: a study of urban slum and non-slum population. J Nurs Res Pract 2(1):09–14
Webb P, Block S (2004) Nutrition information and formal schooling as inputs to child nutrition. Econ Dev Cult Change 52(4):801–820
WHO (2000) Nutrition for health and development: a global agenda for combating malnutrition. In: Sustainable development and healthy environments (SDE) for health and development. https://apps.who.int/iris/handle/10665/66509
WHO (2005) Vitamin and mineral requirements in human nutrition, 2nd edn. World Health Organization. https://apps.who.int/iris/handle/10665/42716
WHO (2007) Everybody’s business strengthening health systems to improve health outcomes: WHO’s framework for action. World Health Organization. https://apps.who.int/iris/handle/10665/43918
World population prospects (2019) Highlights, United Nations department of economic and social affairs, ministry of statistics and programme implementation UN. https://doi.org/10.18356/13bf5476-en . https://www.un.org
World urbanization prospects (2019) United Nations, department of economic and social affairs, population division. World urbanization prospects: the 2018 revision (ST/ESA/SER.A/420). New York, United Nations
Young MF, Nguyen P, Tran LM, Avula R, Menon PA (2020) Double-edged sword? Improvements in economic conditions over a decade in India led to declines in undernutrition as well as increases in overweight among adolescents and women. J Nutr 150(2):364–372. https://doi.org/10.1093/jn/nxz251
Zulkarnaen Z (2019) The influence of nutritional status on gross and fine motor skills development in early childhood. Asian Soc Sci 15(5):1–75
Download references
Author information
Authors and affiliations.
Department of Geography, School of Earth Sciences, Central University of Tamil Nadu, Thiruvarur, India
Shahnaz Basheer, V. V. Ashique & Aakriti Grover
School of Global Affairs, Dr. B.R. Ambedkar University, Delhi, India
Aakriti Grover
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Shahnaz Basheer .
Editor information
Editors and affiliations.
Dr. B.R. Ambedkar University,School of Global Affairs, New Delhi, India
Department of Geography, University of Delhi, Aditi Mahavidyalaya, Delhi, India
Department of Geography, University of Delhi, Delhi School of Economics, Delhi, India
R. B. Singh
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Basheer, S., Ashique, V.V., Grover, A. (2023). The Food and Nutrition Status in India: A Systematic Review. In: Grover, A., Singh, A., Singh, R.B. (eds) Sustainable Health Through Food, Nutrition, and Lifestyle. Advances in Geographical and Environmental Sciences. Springer, Singapore. https://doi.org/10.1007/978-981-19-7230-0_9
Download citation
DOI : https://doi.org/10.1007/978-981-19-7230-0_9
Published : 07 March 2023
Publisher Name : Springer, Singapore
Print ISBN : 978-981-19-7229-4
Online ISBN : 978-981-19-7230-0
eBook Packages : Earth and Environmental Science Earth and Environmental Science (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Research article
- Open access
- Published: 29 May 2020
A comparison of the Indian diet with the EAT-Lancet reference diet
- Manika Sharma ORCID: orcid.org/0000-0002-2841-8113 1 ,
- Avinash Kishore 1 ,
- Devesh Roy 1 &
- Kuhu Joshi 1
BMC Public Health volume 20 , Article number: 812 ( 2020 ) Cite this article
55k Accesses
103 Citations
276 Altmetric
Metrics details
The 2019 EAT-Lancet Commission report recommends healthy diets that can feed 10 billion people by 2050 from environmentally sustainable food systems. This study compares food consumption patterns in India, from different income groups, regions and sectors (rural/urban), with the EAT-Lancet reference diet and highlights the deviations.
The analysis was done using data from the Consumption Expenditure Survey (CES) of a nationally representative sample of 0.102 million households from 7469 villages and 5268 urban blocks of India conducted by the National Sample Survey Organization (NSSO) in 2011–12. This is the most recent nationally representative data on household consumption in India. Calorie consumption (kcal/capita/day) of each food group was calculated using the quantity of consumption from the data and nutritional values of food items provided by NSSO. Diets for rural and urban, poor and rich households across different regions were compared with EAT-Lancet reference diet.
The average daily calorie consumption in India is below the recommended 2503 kcal/capita/day across all groups compared, except for the richest 5% of the population. Calorie share of whole grains is significantly higher than the EAT-Lancet recommendations while those of fruits, vegetables, legumes, meat, fish and eggs are significantly lower. The share of calories from protein sources is only 6–8% in India compared to 29% in the reference diet. The imbalance is highest for the households in the lowest decile of consumption expenditure, but even the richest households in India do not consume adequate amounts of fruits, vegetables and non-cereal proteins in their diets. An average Indian household consumes more calories from processed foods than fruits.
Conclusions
Indian diets, across states and income groups, are unhealthy. Indians also consume excess amounts of cereals and not enough proteins, fruits, and vegetables. Importantly, unlike many countries, excess consumption of animal protein is not a problem in India. Indian policymakers need to accelerate food-system-wide efforts to make healthier and sustainable diets more affordable, accessible and acceptable.
Peer Review reports
A healthy diet is key for optimal nutrition and health outcomes through all stages of the lifecycle. Unhealthy diets are linked to all forms of malnutrition and various diseases [ 1 ]. World Health Organization (WHO) recognizes unhealthy diets along with inadequate physical activity as one of the risk factors for non-communicable diseases. High fat intake, low fruit and vegetable intake, overweight and obesity, physical inactivity, raised blood glucose, raised blood pressure, raised total cholesterol, high salt/sodium intake are amongst the exposures that lead to non-communicable diseases (NCDs) [ 2 ]. The prevalence of obesity and NCDs has been rising across the world [ 3 , 4 , 5 ] even as undernutrition and communicable disease burden remains high.
An analysis of India’s disease burden from 1990 to 2016 showed that heart diseases cause the most deaths in India while dietary iron deficiency is the biggest contributor to disability [ 6 ]. High prevalence of both anaemia and heart diseases shows the rising problem of the double burden of undernutrition and overnutrition in India. Unhealthy diets are a major contributor to this syndemic.
The global food system is unhealthy not only for humans, but also for the environment. On one hand, our existing diets contribute to multiple forms of malnutrition and the rising incidence of NCDs. On the other hand, food production has a large deleterious impact on multiple environmental variables like freshwater availability, soil quality, forest cover, biodiversity, coastal eutrophication, and climate change. Food, therefore, is as much an environmental issue as it is a health issue. This is the point of departure for the EAT-Lancet Commission. It sets two hard boundaries: first, the quantity and quality of foods and second, the environmental limits or the planetary boundaries. The Lancet Commission report (2019) sets out to answer the following question: What could we eat that would feed 10 billion people in 2050 a healthy diet within the environmental limits.
On the environment front, the commission has set scientific targets for the earth system processes - climate change, nitrogen and phosphorus cycling, freshwater use, biodiversity loss, and land-system change to lay the parameters necessary for sustainable food production [ 7 ].
On the consumption side, the report lays out a reference diet for individuals aged 2 years and above with reference range for food groups allowing for flexibility in its application while taking nutritional adequacy into account. It consists largely of plant-based foods: vegetables, fruits, whole grains, legumes, nuts, and unsaturated oils. It includes moderate amounts of seafood and poultry and no or small quantities of red meat, processed meat, added sugar, refined grains and starchy vegetables [ 7 ]. The EAT-Lancet Commission report acknowledges the challenges in defining a global reference diet owing to differences in body size, physical activity, disease status and needs of vulnerable populations like pregnant women and young children [ 7 ].
The reference diet as proposed is not aimed at providing national targets and allows for flexibility in its application. It does outline, in principle, the healthy diet with its relative food group composition. A big difference between the EAT-Lancet reference diet and the existing recommended dietary allowances (RDAs), like the one by the Indian Council of Medical Research (ICMR), is that the former also takes the environmental footprints of different foods into account while the latter focuses only on the human nutritional requirements. Accounting for environmental footprints makes EAT-Lancet recommend a more vegetarian diet than a typical RDA.
This paper does not discuss the environmental aspect of the reference diet and focusses exclusively on the divergence of the current Indian diets from the composition of the proposed reference diet by EAT-Lancet. From a public health perspective, this can clarify the policy and programmatic changes that might be needed in India for transformation to a healthier diet for better nutrition, health, and environmental outcomes.
The EAT-Lancet reference diet is made up of 8 food groups - whole grains, tubers and starchy vegetables, fruits, other vegetables, dairy foods, protein sources, added fats, and added sugars. Caloric intake (kcal/day) limits for each food group are given and add up to a 2500 kcal daily diet [ 7 ]. We compare the proportional calorie (daily per capita) shares of the food groups in the reference diet with similar food groups in Indian Diets.
We use data from the most recent round of the household Consumption Expenditure Survey (CES) conducted by the National Sample Survey Organization (NSSO) of India in 2011–12. NSS-CES has been conducted every 5 years from 1972 to 73 onwards. Each quinquennial round covers a nationally representative sample of more than 100 thousand households from both rural and urban areas of all states and union territories of India. The NSS-CES sample is also representative at the state level. Footnote 1
Data is collected from a random sample of households across India. Floating populations, foreign nationals and their domestic servants, soldiers in barracks, and kids in orphanages are excluded from the survey. This sample covers all kinds of households. A random 25% subsample of the total sampled households from each district of India are surveyed in all 4 quarters of the year to account for any seasonal variations in consumption patterns and obtain a more representative data of the usual intakes of households.
It is the primary source of public data on various indicators of the level of living of different segments of the population at national and state levels in India. This data has been extensively used for planning and policy formulation by government organizations, academicians, researchers, and scholars.
NSS-CES collects both 30-day and 7-day recall data on the quantity of consumption and the market value of 147 different food items by each household in the sample [ 8 ]. Detailed list of items in the expenditure survey helps get more accurate data. 30-day recall data is collected for cereals, legumes, milk & milk products, sugar, and salt while 7-day recall for edible oil, egg, fish, meat, vegetables, fruits, spices, beverages, and processed foods. The survey also records the value of purchased snacks and the number of meals eaten out of the home by household members.
We aggregated each of the 147 food items into 10 food groups. Eight food groups like the EAT-Lancet reference diet and two additional food groups: processed foods and spices. We included these two additional food groups because the consumption of processed foods is rising rapidly, and spices are an essential part of the Indian diet.
For Indian diets, the food group ‘whole grains’ comprises of cereals like rice, wheat, wheat flour and other cereals like jowar (sorghum), bajra (pearl millet), maize, barley, ragi (finger millets), other millets and other cereals. ‘Vegetables’ include all vegetables except for potatoes. ‘Fruits’ include all fresh fruits and dried fruits like dates, raisins, and other dry fruits. All beans, pulses, and groundnuts have been classified into ‘Legumes’. Food group ‘Tree nuts’ includes coconut, coconut-green, coconut- copra , walnuts, cashew nuts, and other nuts.
The food group ‘Added Fats’ in the EAT-Lancet reference diet includes palm oil, unsaturated oils, dairy fats and lard [ 7 ]. NSS-CES uses a different classification for edible oils and fats. For comparison with the reference diet, NSS-CES food items vanaspati (partially hydrogenated vegetable oil), refined and edible oil have been aggregated as ‘palm oil’ due to their high content of palm and palm olein oil [ 9 ] and mustard, groundnut and coconut oil as ‘unsaturated oil’ due to higher content of unsaturated fatty acids. It should be noted that many cooking oils used in India are a mixture of saturated and unsaturated oils which presents a limitation in this type of analysis [ 9 ].
The EAT-Lancet commission recommends “low” amounts of processed foods like refined grains, added sugar and highly processed foods. It has not been included as a part of the 2500 kcal reference diet [ 7 ]. It is, however, taken as a separate food group for Indian diets in this study as it forms a significant and growing portion of the total caloric intake by Indian households. It consists of processed cereals like maida, (refined wheat flour) and semolina along with packaged food like savouries ( namkeens ), chips, chocolates, sugary beverages, and other food consumed outside of the home. Another category of food that is not mentioned in the EAT-Lancet reference diet, but accounts for 1–2% of total calories in Indian diet is ‘spices’. Spices have been mentioned separately for the Indian diets.
The NSS dataset records the quantity of food items consumed by the household. This is given in grams or kilograms for the 30- or 7-day recall period, depending on the food item. We convert household consumption into per capita per day consumption and use sampling weights provided in the NSS dataset to estimate population averages. We then calculate the caloric intake of food items by multiplying per capita per day quantity consumed with the calorie content of each food item. We thus obtain total calorie intake per capita per day (kcal/capita/day) of food items. These are aggregated across the 10 food groups as mentioned above.
Calorie content of food items is taken from the NSS 68th round report based on “Nutritive Values of Indian Foods” by C. Gopalan, B.V. Ramasastry and S. C Balasubramanian, revised and updated by B.S. Narasinga, Y.G. Deosthale and K.C. Pant, 1991 [ 10 ].
NSS-CES reports consumption of some food items, like fruits and packaged foods, either in numbers or the money spent on them. This is the reason why we use calorie intake and not quantities consumed to compare the Indian diet with the reference diet. Differences are calculated as the simple difference and the percentage difference between the total calorie intake of the Indian diet and the EAT-Lancet reference diet.
There are large differences in dietary patterns of rural and urban households, rich and poor households, and people living in different parts of India [ 11 ]. Therefore, we also compare the EAT-Lancet reference diet with diets across regions, places of residence (urban and rural), and expenditure classes.
The average calorie intake/person/day in both rural (2214 kcal) and urban (2169 kcal) India is less than the reference diet (Table 1 ). In both rural and urban areas, people in rich households (top deciles of monthly per capita consumption expenditure (MPCE)) consume more than 3000 kcal/day i.e. 20% more than the reference diet. Their calorie intake/person/day is almost twice as high as their poorest counterparts (households in the bottom MPCE deciles) who consume only 1645 kcals/person/day (Table 1 ).
Why obesity is rising in India despite a lower average total calorie intake, as compared to the EAT-Lancet reference diet or even the ICMR recommendations, Footnote 2 is a question beyond the scope of this paper. However, it may be related to the fact that the reference diet is developed for individuals with moderate-to-high levels of activity, whereas available studies estimate high levels of inactivity amongst Indians. A Lancet study looking at trends of insufficient physical activity between 2001 and 2016 suggested that 34% of Indians are not sufficiently engaged in physical activity [ 12 ]. Similarly, a 2014 ICMR-INDIAB study indicates that more than half of all Indians are inactive. Lack of adequate physical activity is found to be more prevalent in urban areas and amongst females [ 13 ].
Calorie shares of different food groups
A healthy diet is diverse and has a balance in calorie shares of different food groups. Tables 2 and 3 show that except for the richest households in urban areas, whole grains (cereals) account for a very high share of total calories consumed by most Indian households. Indians also consume more starchy vegetables, dairy foods, and palm oil as compared to the reference diet. Consumption of processed foods is also high in India, especially among the richest urban households.
The average calorie intake from both plant and animal-based foods rich in protein is low in both rural and urban areas, across different income classes, and different parts of India. The same is true for the consumption of fruits and vegetables.
Interestingly, calorie shares of different food groups are similar between rural and urban households of similar per capita monthly expenditure levels. This is consistent with the results from a household survey in the state of Punjab that showed no significant rural-urban differences in diets [ 14 ].
The poorest 5% of the population in India consumes less than the suggested calories for all food groups except whole grains, tubers and starchy vegetables, and processed food. There is little rural-urban variation within this group.
Cereals and starchy vegetables
EAT-Lancet Commission recommends that about one-third (811 kcals) of the total daily calorie intake should come from whole grains. The average Indian households get almost half (47%) of their total calories from whole grains and the calorie share of cereals is as high as 70% for the poorest rural households (Tables 2 , 3 and 4 ).
Protein sources
When compared to the reference diet, low caloric intake from protein sources (both plant and animal-based) is common across all sectors, regions, and income groups of India (Tables 2 , 3 , and 4 and Figs. 1 and 2 ). The deficit is more in rural areas where only 6% of the total caloric intake comes from protein sources compared to 29% in the EAT-Lancet diet (Table 2 ).
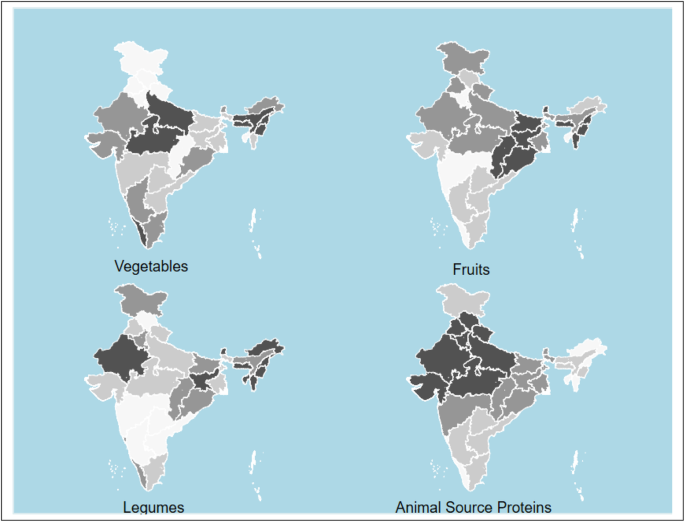
Caloric intake deficit* of vegetables, fruits, legumes and animal source proteins compared to reference diet. Animal source proteins include chicken, other poultry, eggs, lamb, beef, pork and fish. Darker colour depicts higher calorie difference between actual consumption and reference diet. Maps were generated using STATA statistical software version 15.0. *Difference between actual consumption and the daily per capita calorie intake suggested by the EAT-Lancet reference. State level caloric intake calculated using population weights for rural and urban populations. Values for Telangana same as that for Andhra Pradesh. NSS-CES sampling weights were applied in calculations
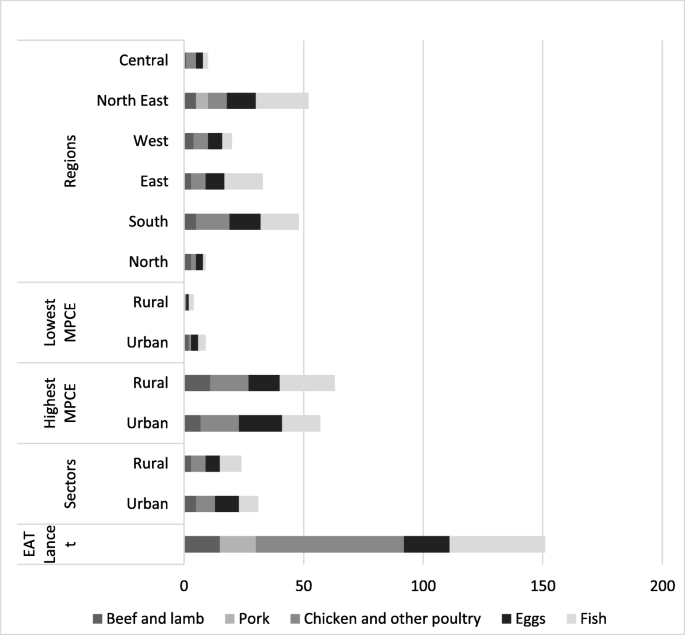
Caloric intake from various animal-based protein sources. Values in kcal. NSS-CES sampling weights were applied in calculations
Even for the richest 5% of India’s population, calories from protein sources is less than half of the 726 kcal in the reference diet. The poorest Indians get below 130 kcal per day (less than 20% of the recommendation) from protein sources. Among different regions of India, people in the North-east consume the lowest quantities of legumes (Fig. 1 and Table 5 ).
The rich in India get fewer calories from cereals and more calories from fruits, vegetables, animal source proteins, and fats compared to the poor. (Tables 2 and 3 ).
The EAT-Lancet reference diet advocates consumption of only “low to moderate” quantities of seafood and poultry and “no to low” amounts of red meat or processed meat. Animal-source proteins constitute 6% of the total caloric intake in the reference diet. Indian diets, across different types of households, have a lower share of calories from animal-based foods. Consumption of animal-based foods is relatively higher in South India and the North-Eastern region. The richest households in all parts of India consume more than average quantities (or calories) of meat. (Figs. 1 and 2 ). Consumption of red meat (beef, lamb and pork) is low in India (Table 2 , 3 and Fig. 2 ).
Fruits and vegetables
A diverse diet is a healthy diet [ 15 , 16 ]. The reference diet is largely plant-based with fruits and vegetables accounting for 204 kcal (8%) of the daily calorie intake. Most Indians, except the richest ones in urban areas, do not consume enough fruits. The average consumption of calories from fruits is less than 40% of what EAT-Lancet recommends (Table 2 , 3 and Fig. 3 ). The difference in caloric intake from vegetables is smaller than what it is for fruits, but under-consumption of vegetables is also common across all but the richest households in rural and urban areas (Fig. 3 ).
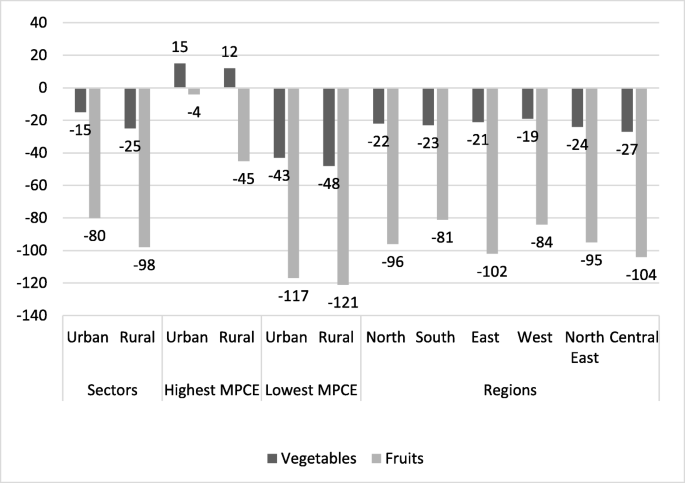
Difference in caloric intake from Vegetables and Fruits between EAT-Lancet reference diet and Indian diets. Caloric intake calculated as total kcal/person/day. NSS-CES sampling weights were applied in calculations
Oils and fats
Indians get fewer calories from added fats than what is recommended in the reference diet (Tables 2 and 3 ). This is despite an increase of 3.5% in the consumption of oils and fats between 1993 and 94 and 2011–12 in both rural and urban areas as per NSS reports. Figure 4 shows that Indians, in general, consume less of the healthier oils & fats and more of the unhealthier saturated fats like palm oil.
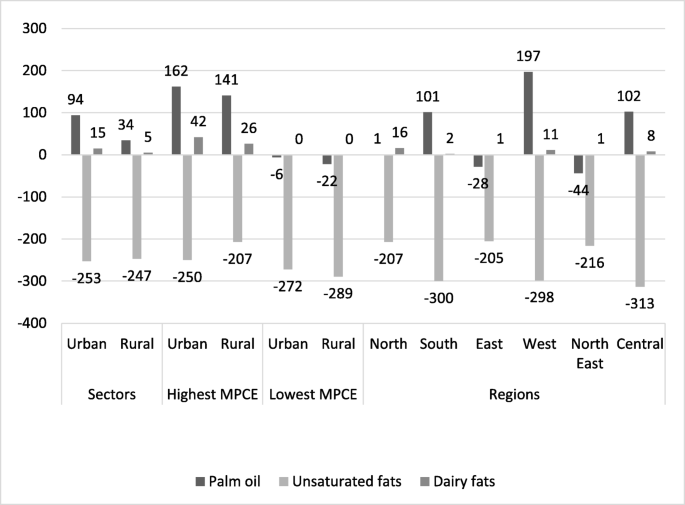
Caloric intake difference for added fats between Indian diets and proposed EAT-Lancet reference diet. Indian diets across sector, MPCE fractile classes and regions. Values in kcal. NSS-CES sampling weights were applied in calculations
Palm oil is high in unhealthy saturated fat and is the chief ingredient of the widely consumed vanaspati (partially hydrogenated vegetable oil) in India.
The consumption of vanaspati is known to have risen by 51% between 1993 and 94 and 2011–12 and it is widely used for cooking at home, in restaurants, by street vendors, and in the preparation of processed foods [ 17 ]. Figure 4 also shows that the highest caloric consumption of palm oil is among the highest income groups. Among different parts of India, consumption is highest in western India.
It should be noted that the consumption of fat in India might be higher than reflected in this data as the fat content of packaged food and meals consumed outside of the home is not accounted for.
- Processed food
EAT-Lancet commission recommends the consumption of only small amounts of processed food. Processed food is not even a separate food group in the reference diet. We report the consumption of processed food as a separate group in this paper because of its high and rising consumption in India. In the 68th round of NSS-CES, bread, bakery products, suji (semolina), maida (refined wheat flour), cold and hot beverages, outside cooked meals including snacks, prepared sweets, savouries ( namkeens ), chips, pickles, sauce, jams, jelly, ice cream, biscuits, chocolates have been included in the category of processed food along with meals consumed outside of the home. These types of foods, normally high in sugar, salt, saturated fats, and processed flour, are considered unhealthy and often linked to obesity/overweight and NCDs [ 2 , 18 , 19 , 20 , 21 , 22 , 23 ].
Processed food accounts for nearly 10% of the average total caloric intake in both rural and urban India (Table 2 , 3 and Fig. 5 ). Urban households in the highest income group consume almost 30% of their total daily calories from processed food (Fig. 5 ). Among different regions of India, the calorie share of processed food is highest in Southern Indian and the lowest in North-Eastern and Northern India (Tables 2 and 3 ).
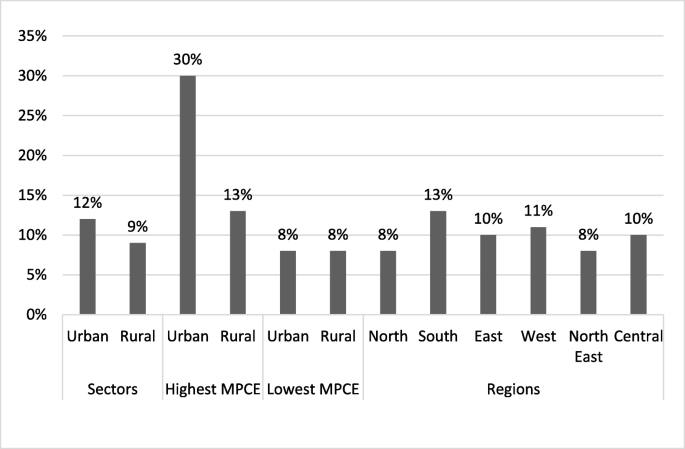
Proportion of daily per capita caloric intake from processed food in India. NSS-CES sampling weights were applied in calculations
Spices like ginger, garlic, coriander powder ( dhania) and turmeric constitute 2% of total caloric consumption in rural and urban India.
Diets in India are unhealthy and very different in their composition from the EAT-Lancet reference diet or even diets recommended by the ICMR. In a recent paper, Hirvonen et al. argue that the EAT-Lancet reference diets are not affordable for much of the world’s (and South Asia’s) low-income population. In South Asia, the reference diet will cost more than 60% of the mean daily per capita household income and cost more than 1.5 times the least-cost nutritionally adequate diet [ 24 ]. Hirvonen et al. also show that fruits, vegetables, and animal products are the most expensive among the major food groups across the world. Low affordability of healthy foods may be one of the reasons for their low consumption in India.
High subsidies on rice and wheat through the public distribution system and active management of the markets to keep market prices of cereals at low levels incentivize people to eat more rice and wheat.
Our analysis, however, shows that low affordability is not the only reason why Indian diets are so unhealthy. Even the richest 5% of households consume too little protein-rich food and too much processed foods. In rural areas, even the richest families eat more than recommended quantities of cereals and not enough fruits and vegetables. This points towards a lack of availability, accessibility, awareness, and acceptability as other major causes for the poor quality of diets.
Legumes are the main source of non-cereal plant protein in Indian diets. However, their consumption is low. The production of pulses has grown slower than the population, resulting in a steady decline in their per capita availability and consumption over the last five decades. Milk and other dairy products are the most common sources of animal protein in India. The majority of Indians now identify themselves as non-vegetarian [ 25 ]. Data from the National Family Health Survey conducted in 2015–16 in India supports this claim and indicates that only 20–30% population is vegetarian, having never had fish, chicken, meat, and eggs [ 25 ]. Yet, majority of the non-vegetarians report that they consume meat only occasionally. Meat production is projected to continue its fast growth at 3.1% p.a. up to 2023, with poultry dominating meat production. Per capita fish consumption is also expected to grow at 0.9% p.a. to reach 6.8 kg in 2023 [ 26 ]. This indicates that while the consumption of animal products is rising in India with rising incomes and urbanization, it is still significantly below the world average.
Rising imports of cheap palm oil have led to an increase in their consumption over the years—both in-home cooking and in the form of processed foods in India. Before 1992, edible oil was on the negative list and imports were disallowed. With liberalization, Palm oil is the largest food import in India [ 17 , 27 ] and more than half of domestic consumption of oil comprises imports.
Indian diets are unhealthy also because healthier calories are more expensive and their inflation is rising faster than cereals and edible oils [ 27 , 28 ].
Overall, dietary risks were responsible for 22% of all deaths and of all DALYs amongst adults [ 29 ]. Diets low in fruits, vegetables, and whole grains but high in salt, sugar, and fat (which constitute dietary risk) are also responsible for India’s increasing disease burden [ 23 ].
Our comparison of Indian diets with EAT-Lancet recommendations has several limitations. First, NSS-CES (and other consumption expenditure surveys) tend to underestimate total calorie consumption, especially calories consumed from meals taken outside home and from processed foods [ 30 ]. These differences are bigger for richer households. Second, NSS-CES uses 30-days and 7-days recall data when 24-h recall data is considered more accurate. There may be systematic errors due to a longer recall period in this data set. Third, there are significant gender and age-related differences in the diets within Indian households. Women eat a poorer diet than men in their families [ 31 , 32 ]. However, the NSS-CES data does not capture these intra-household differences as it only collects aggregate household consumption information. Finally, the latest available NSS-CES is already 8 years old and pre-dates the implementation of the National Food Security Act (NFSA)-2013 that led to a significant increase in the public distribution of highly subsidized rice and wheat, potentially affecting dietary patterns of the poorest two-thirds of Indian households. Therefore, recent changes in the dietary pattern and behaviour cannot be analysed.
Another limitation of this study is due to the nature of the EAT-Lancet reference diet itself. It pertains to a typical adult person, considers only a limited set of nutrients, and ignores differences in bioavailability across different food groups [ 24 ]. These limitations suggest the need for better, more disaggregated dietary data with a shorter recall period and more research to develop a better understanding of different nutritional requirements of different groups of people.
Two factors help with the reliability of estimates of dietary intake in this paper. First, NSS-CES visits each district 4 times in a year. The repeat visits increase the chance of capturing the usual consumption pattern of households and minimize any seasonal variations. Second, NSS-CES has a large sample size. Any underlying uncertainty is thus likely to be a function of measurement error rather than sample size. Our comparison of Indian diets with the EAT Lancet reference diets still provides important insights.
Promoting healthy diets requires a major policy reset in India. India’s food policies and budget allocations are focused almost entirely on ensuring the affordability of rice and wheat. Almost all food subsidy—both for farmers and consumers—is spent on promoting rice and wheat production and consumption. Trade policies work to ensure low prices for sugar and palm oil. Since the policy incentivizes farmers to grow more rice, wheat, and sugarcane, the production of healthier foods, like pulses, fruits, and vegetables is lower than what it would be without these policy distortions. Food policies need readjustments to ensure the availability of healthier foods at affordable prices.
Moreover, raising consumer awareness about the need for dietary diversification can encourage families to switch to healthier foods. The consumer subsidy on food should shift away from rice and wheat to healthier options. Cash transfers in combination with an intensive communication campaign can accelerate the shift to healthier diets.
The EAT-Lancet reference diet is described as a healthy and sustainable diet. Based on the analysis of consumption data, it is evident that Indian diets across urban-rural divide, regions, and income levels, deviate significantly from this reference diet and are far from being healthy for humans or the environment. Unhealthy diets are major contributors to persistently high levels of undernutrition (including micronutrient deficiencies) and rising levels of overweight and obesity in India.
As discussed in the paper, a shift to healthier diets will also require a change in production patterns. Currently, India produces too much rice and sugarcane and too little coarse cereals, pulses, fruits, and vegetables. Rice and sugarcane have big environmental footprints. Both are highly water intensive. Wet rice fields also emit methane, a powerful greenhouse gas. Moreover, rice farmers in many states of India burn rice residues emitting carbon dioxide and particulate matter creating severe air pollution. The shift in cropping patterns towards coarse cereals and pulses will make India’s food systems not only healthier but also environmentally more sustainable. Making food systems healthier and environmentally more sustainable requires public health and nutrition policies addressing malnutrition. It also requires agriculture, trade, and consumer awareness policies that can address the accessibility, acceptability, and affordability of healthier dietary options. A transformation of the Indian food system is much needed for both human health and environmental sustainability.
Availability of data and materials
The data used in this article is from the Household Consumer Expenditure, National Sample Survey, 68th Round, which contains anonymised data in the public domain. The survey is undertaken by the National Sample Survey Office (NSSO) of the Ministry of Statistics and Programme Implementation of the Government of India and is available from the Indian Council of Social Science Research (ICSSR): http://www.icssrdataservice.in/datarepository/index.php/catalog/135 . Unit-level data is also available at a nominal price from the Ministry of Statistics and Programme Implementation of India.
As the analysis is based on publicly available secondary data, ethics approval or consent to participate are not applicable.
Details about sampling, data collection, questionnaires, as well as reports of the NSS can be found on the website of the Indian Council of Social Science Research (ICSSR): http://www.icssrdataservice.in/datarepository/index.php/catalog/91 .
The Indian Council of Medical Research (ICMR) recommends per-person per-day calorie norms of 2400 kcal for rural areas and 2100 kcal for urban areas.
Abbreviations
National Sample Survey-Consumer Expenditure Survey
National Family Health Survey
Disability-adjusted life year
Non-communicable diseases
World Health Organization
Monthly per capita expenditure
Recommended Dietary Allowances RDAs
Indian Council of Medical Research
Development Initiatives. Global Nutrition Report: Shining a light to spur action on nutrition 2018. Bristol, UK; 2018. Available from: https://www.who.int/nutrition/globalnutritionreport/2018_Global_Nutrition_Report.pdf?ua=1 . [cited 2019 Apr 15].
WHO. A Comprehensive Global Monitoring Framework, including indicators, and a set of voluntary global targets for the prevention and control of noncommunicable diseases. 2012. Available from: http://www.who.int/nmh/events/2012/discussion_paper2_20120322.pdf .
Google Scholar
Doak CM, Adair LS, Bentley M, Monteiro C, Popkin BM. The dual burden household and the nutrition transition paradox. Int J Obes. 2005;29:129–36 Available from: https://www.nature.com/articles/0802824.pdf . [cited 2018 Apr 26].
CAS Google Scholar
Popkin BM. Contemporary nutritional transition: determinants of diet and its impact on body composition. In: Proceedings of the Nutrition Society; 2011. p. 82–91.
Popkin BM. Nutrition Transition and the Global Diabetes Epidemic. Curr Diab Rep. 2015;15(9):64 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26209940 . [cited 2019 Feb 11].
PubMed PubMed Central Google Scholar
Indian Council of Medical Research. Public Health Foundation of India; Institute for Health Metrics and Evaluation. New Delhi: Health of the Nation’s States - The India State-level Disease Burden Initiative; 2017.
Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, et al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019;6736:3–49. Available from: http://dx.doi.org/10.1016/ [cited 2019 Feb 5].
NSSO. Household Consumption of Various Goods and Services in India 2011-12 [Internet]. Vol. 558. New Delhi; 2014. Available from: http://mospi.nic.in/sites/default/files/publication_reports/Report_no558_rou68_30june14.pdf .
Saikia N. Fatty acids profile of Edible Oils and Fats in India. 2009;1–33.
National Sample Survey Office. Nutritional Intake in India, 2011-12. New Delhi; 2014. Available from: http://mospi.nic.in/sites/default/files/publication_reports/nss_report_560_19dec14.pdf . [cited 2019 May 13].
Green R, Milner J, Joy EJM, Agrawal S, Dangour AD. Dietary patterns in India: a systematic review. Br J Nutr. 2016;116(1):142–8.
CAS PubMed PubMed Central Google Scholar
Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. 2018; Available from: www.thelancet.com/lancetgh . [cited 2019 Jul 23].
Anjana RM, Pradeepa R, Das AK, Deepa M, Bhansali A, Joshi SR, et al. Physical activity and inactivity patterns in India - results from the ICMR-INDIAB study (Phase-1) [ICMR-INDIAB-5]. Int J Behav Nutr Phys Act. 2014;11(26). Available from: http://www.ijbnpa.org/content/11/1/26 . [cited 2019 Jul 23].
PubMed Google Scholar
Tripathy JP, Thakur JS, Jeet G, Chawla S, Jain S, Prasad R. Urban rural differences in diet, physical activity and obesity in India: are we witnessing the great Indian equalisation? Results from a cross-sectional STEPS survey. 2016; Available from: https://bmcpublichealth.biomedcentral.com/track/pdf/10.1186/s12889-016-3489-8 . [cited 2019 Apr 15].
WHO Technical Report S 880. R of a JFC. Preparation and Use of Food-Based Dietary Guidelines. Geneva; 1996. Available from: https://apps.who.int/iris/bitstream/handle/10665/42051/WHO_TRS_880.pdf;jsessionid=C101DC89C7F8261B46215E3B260F6A35?sequence=1 . [cited 2019 May 8].
Ruel MT. Operationalizing Dietary Diversity: A Review of Measurement Issues and Research Priorities 1,2. J Nutr. 2003;133:3911–26. Available from: https://academic.oup.com/jn/article-abstract/133/11/3911S/4818042 . [cited 2019 May 8].
CAS PubMed Google Scholar
Gaiha R, Kaicker N, Imai K, Kulkarni VS, Thapa G. Dietary Shift and Diet Quality in India: An Analysis Based on 50 th , 61 st and 66 th Rounds of NSS. 2012; Available from: https://taxpolicy.crawford.anu.edu.au/acde/asarc/pdf/papers/2012/WP2012_17.pdf . [cited 2018 May 23].
Kennedy G, Nantel G, Shetty P. Assessment of the double burden of malnutrition in six case study countries. FAO Food Nutr Pap 84. 2006.
Hawkes C. Uneven dietary development: linking the policies and processes of globalization with the nutrition transition, obesity and diet-related chronic diseases. Glob Health. 2006;2:1–18.
Moodie R, Stuckler D, Monteiro C, Sheron N, Neal B, Thamarangsi T, et al. Non-Communicable Diseases 4 Profi ts and pandemics: prevention of harmful eff ects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013;381:670–9. Available from: https://ac-els-cdn-com.ifpri.idm.oclc.org/S0140673612620893/1-s2.0-S0140673612620893-main.pdf?_tid=8f011665-4651-40d3-98c7-1773eab9d1d8&acdnat=1531892792_d4c508e5c873299a2df3dfaf453780c5 . [cited 2018 Jul 18].
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–14. Available from: https://doi.org/10.1016/S0140-6736(11)60813-1 .
Singh M, Chandorkar S. Is sodium and potassium content of commonly consumed processed packaged foods a cause of concern? Food Chem. 2018;238:117–24. https://doi.org/10.1016/j.foodchem.2016.11.108 .
Indian Council of Medical Research (ICMR), Public Health Foundation of India, Institute for Health metrics and Evaluation. India : Health of the Nation ’ s States, The Indian State-Level Disease Burden Initiative. 2017.
Registrar-General of India. Sample registration rystem, baseline report 2014. 2014. Available from: http://www.censusindia.gov.in/vital_statistics/BASELINE_TABLES07062016.pdf . [cited 2019 Apr 10].
International Institute for Population Sciences. National Family Health Survey (NFHS-4) [Internet]. 2017. Available from: http://rchiips.org/NFHS/NFHS-4Reports/India.pdf . [cited 2018 Jun 6].
OECD/Food and Agriculture Organization of the United Nations. OECD-FAO Agricultural Outlook 2014-2023; 2014. https://doi.org/10.1787/agr_outlook-2014-en . [cited 2019 Apr 10].
Prachi Mishra, Devesh Roy. Explaining Inflation in India: The Role of Food Prices. Vol. 8. New Delhi; 2011. Available from: http://testnew.ncaer.org/image/userfiles/file/IPF-Volumes/Volume 8/4_Prachi Mishra and Devesh Roy.pdf. [cited 2019 Aug 22].
Headey DD, Alderman HH. The Relative Caloric Prices of Healthy and Unhealthy Foods Differ Systematically across Income Levels and Continents. J Nutr. 2019. https://doi.org/10.1093/jn/nxz158 [cited 2019 Aug 22].
Afshin A, John Sur P, Fay KA, Cornaby L, Ferrara G, Salama JS, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019 [cited 2019 Apr 16]. https://doi.org/10.1016/S0140-6736 .
Deaton A, Drèze J. Food and Nutrition in india: Facts and interpretations. EPW Econ Polit Wkly. 2009;14(7). Available from: https://www.princeton.edu/~deaton/downloads/Food_and_Nutrition_in_India_Facts_and_Interpretations.pdf . [cited 2018 Jun 6].
Raskind IG, Patil SS, Haardörfer R, Cunningham SA. Unhealthy weight in Indian families: The role of the family environment in the context of the nutrition transition. Popul Res Policy Rev. 2018;37(2):157–80. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6023548/pdf/nihms937610.pdf . [cited 2019 Sep 3].
Aurino E. Do boys eat better than girls in India? Longitudinal evidence on dietary diversity and food consumption disparities among children and adolescents. 2016. https://doi.org/10.1016/j.ehb.2016.10.007 . [cited 2019 Sep 3].
Download references
Acknowledgements
The authors of this paper would like to acknowledge the support of Samuel Scott for his review and comments on the manuscript. Additionally, we are thankful for the guidance received from the participants in Food System for Healthier Diets meetings at Delhi, Dhaka and Wageningen University.
Funding for this paper was provided by the CGIAR Research Program on Agriculture for Nutrition and Health (A4NH), Led by International Food Policy Research Institute (IFPRI). A4NH works across five flagship research programs. This paper is under one of the five flagships – Food Systems for Healthier Diets. This flagship responds to concerns about global diet trends and demands from countries for systemic solutions that address problems, such as food insecurity, undernutrition, and overnutrition. Two of the authors involved in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript work for A4NH, IFPRI South Asia Region.
Author information
Authors and affiliations.
International Food Policy Research Institute, NASC Complex, CG Block, Dev Prakash Shastri Marg, Pusa, New Delhi, 110012, India
Manika Sharma, Avinash Kishore, Devesh Roy & Kuhu Joshi
You can also search for this author in PubMed Google Scholar
Contributions
MS conceived the study. AK DR MS KJ, analysed data, interpreted results and wrote the manuscript. All authors read and approved the final manuscript.
Authors’ information
Manika Sharma, CGIAR research program on Agriculture for Nutrition and Health, led by International Food Policy Research Institute.
Devesh Roy, CGIAR research program on Agriculture for Nutrition and Health, led by International Food Policy Research Institute.
Avinash Kishore, International Food Policy Research Institute.
Kuhu Joshi , International Food Policy Research Institute.
Corresponding author
Correspondence to Manika Sharma .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sharma, M., Kishore, A., Roy, D. et al. A comparison of the Indian diet with the EAT-Lancet reference diet. BMC Public Health 20 , 812 (2020). https://doi.org/10.1186/s12889-020-08951-8
Download citation
Received : 03 September 2019
Accepted : 18 May 2020
Published : 29 May 2020
DOI : https://doi.org/10.1186/s12889-020-08951-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Consumption
- Reference diet
- Food system
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Nutritional status of Indian adolescents (15-19 years) from National Family Health Surveys 3 and 4: Revised estimates using WHO 2007 Growth reference
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Software, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Department of Community Medicine, Yenepoya Medical College, Mangalore, Karnataka, India, Center for Nutrition Studies, Yenepoya (Deemed to be University), Mangalore, Karnataka, India
Roles Conceptualization, Data curation, Formal analysis, Methodology, Writing – review & editing
Affiliations Center for Nutrition Studies, Yenepoya (Deemed to be University), Mangalore, Karnataka, India, Department of General Medicine, Yenepoya Medical College, Mangalore, Karnataka, India
Roles Data curation, Methodology, Validation, Visualization, Writing – review & editing
Affiliation Yenepoya Research Centre, Yenepoya (Deemed to be University), Mangalore, Karnataka, India
Roles Data curation, Formal analysis, Methodology, Software, Visualization, Writing – review & editing
- Madhavi Bhargava,
- Anurag Bhargava,
- Sudeep D. Ghate,
- R. Shyama Prasad Rao

- Published: June 22, 2020
- https://doi.org/10.1371/journal.pone.0234570
- Peer Review
- Reader Comments
24 Sep 2020: Bhargava M, Bhargava A, Ghate SD, Rao RSP (2020) Correction: Nutritional status of Indian adolescents (15-19 years) from National Family Health Surveys 3 and 4: Revised estimates using WHO 2007 Growth reference. PLOS ONE 15(9): e0239923. https://doi.org/10.1371/journal.pone.0239923 View correction
The National Family Health Surveys (NFHS) in India apply adult cutoffs of nutritional status for the estimation of undernutrition/overweight in the 15–19 age group. The prevalence of thinness in boys and girls thus estimated is 58.1% and 46.8% in NFHS-3, and 45% and 42% in NFHS-4 respectively. But the WHO recommends using age and sex-specific reference for adolescents. We reanalyzed the nutritional status of the adolescents using the WHO 2007 Growth Reference to obtain revised estimates of thinness, overweight and stunting across states, rural-urban residence, and wealth quintiles.
Methods and findings
Demographic information, anthropometric data, and wealth index were accessed from the Demographic and Health Survey (DHS) database. We re-analyzed the anthropometric data using WHO AnthroPlus software which uses the WHO 2007 Growth reference. The revised estimates of thinness assessed by BMI-for-age z-scores in boys and girls was 22.3% (95%CI: 21.6, 23.0) and 9.9% (95%CI: 9.5, 10.3) in NFHS-3 and 16.5% (95%CI: 16.0,17.0) and 9% (95%CI: 8.9, 9.2) in NFHS-4 respectively. Stunting was found to be 32.2% (95% CI: 31.6, 32.9) in boys and 34.4% (95% CI: 34.2, 34.7) in girls in NFHS-4. This was higher than that in NFHS-3; 25.2% (95% CI: 24.4, 26) in boys and 31.2 (95% CI: 30.6, 31.8) in girls. There was a clear socioeconomic gradient as there were higher thinness and stunting in rural areas. There was wide variation among the states with pockets of a double burden of malnutrition.
Using the adult cutoffs significantly overestimates thinness in adolescents in the age group of 15–19 years old in India. Stunting, which is an indicator of long term nutrition is also widely prevalent in them. Future editions of DHS and NFHS should consider adolescents as a separate age group for nutritional assessment for a better understanding of nutritional transition in the population.
Citation: Bhargava M, Bhargava A, Ghate SD, Rao RSP (2020) Nutritional status of Indian adolescents (15-19 years) from National Family Health Surveys 3 and 4: Revised estimates using WHO 2007 Growth reference. PLoS ONE 15(6): e0234570. https://doi.org/10.1371/journal.pone.0234570
Editor: Vijayaprasad Gopichandran, ESIC Medical College & PGIMSR, INDIA
Received: March 31, 2020; Accepted: May 27, 2020; Published: June 22, 2020
Copyright: © 2020 Bhargava et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: MB received grant from The United Nations Children's Fund (UNICEF) SSFA/2019/07. URL of the website available at: https://unicef.in/Karnataka . The funders did not play any role in the design, analysis and preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The World Health Organization (WHO) defines adolescence as 10–19 years [ 1 ]. It is a key decade in the life course with implications on adult health, socio-economic well-being of a country and even the health of the future children. Adolescents comprise 16% of the total world population [ 2 ]. Asia has more than half of the world’s adolescents while according to the Census 2011, 20% of India’s population are adolescents [ 3 , 4 ].
Adolescence is a period of rapid growth and development, second only to infancy, with dramatic biological, psychological changes often shaped by socio-cultural factors. It is usually divided into two phases: early adolescence (10–14 years) and late adolescence (15–19 years) [ 5 ]. Physiologically, the early years are dominated by pubertal changes and the later stages by sexual maturation and development of adult roles and responsibilities. The nutritional issues in this age group have commonalities with children and adults with some added dimensions of puberty, psychological changes, and growth spurt which are crucial for current, future and intergeneration health [ 6 ]. Poor nutrition, on the one hand, can lead to delay or failure in achieving maturation with a stunted linear growth perpetuating the cycle of poverty and intergenerational undernutrition. On the other hand, there is an increased risk of non-communicable diseases (NCDs) [ 7 ]. The nutritional transition that is occurring in some low-middle income countries is resulting in a double burden of overweight and obesity in some population groups, along with the existing high proportion of undernutrition in others [ 8 – 10 ].
The National Family Health Surveys (NFHS)are periodic health and demographic surveys that include adult men and women in the age group of 15–54 years and 15–49 respectively and the adolescents (15–19 years) are included in them [ 11 , 12 ].The NFHS reports have so far used the adult cutoffs for nutritional assessment for this age group; i.e., those with a BMI <18.5 kg/m 2 are considered thin, those between 25–29.9 kg/m 2 are overweight, and BMI >30kg/m 2 are considered obese [ 11 – 13 ]. The proportions thus classified as thin were 58.1% and 46.8% in NFHS-3,and 45% and 42% in NFHS-4 in boys and girls respectively [ 11 , 12 ]. However, their nutritional assessment should be done using the WHO 2007 Growth reference curves [ 14 ].
We re-analyze the nutritional status of adolescents in the age group of 15–19 years(referred to as adolescents hereafter) included in NFHS-3 and 4 using the age and sex-specific WHO 2007 Growth reference to obtain revised estimates of thinness, overweight and stunting in boys and girls and compare them with currently reported estimates. We also compare these estimates across urban and rural populations, wealth quintiles and explore sub-national heterogeneity and inequalities based on socio-economic class.
Data source—National Family Health Survey
The NFHS is conducted at regular intervals in India since 1992–93 under the stewardship of the Ministry of Health and Family Welfare and coordinated by the International Institute of Population Sciences (IIPS), Mumbai. The NFHS-3 was conducted in 2005–6 and NFHS-4 in 2015–16. Data of both these surveys were extracted in Microsoft Excel from the Demographic and Health Surveys (DHS) database [ 15 ].
Study population and sample size
The NFHS-3 covered a representative sample of 109,041 households from the Census of 2001and included adult men and women in the age group of 15–54 years and15-49 years respectively. The number of boys and girls in the age group of 15–19 years was 26,086 and 26,238 respectively, making upa total of 52,324 participants.
TheNFHS-4 covered a representative sample of 601,509 households from the Census of 2011 with adult men and women in the same age categories as NFHS-3. A total of 277,059 adolescents in the age group of 15–19 years: 142,162 boys and 134,897 girls were included from these households.
Anthropometry
Trained field staff visited the households and any adult member capable of providing information served as the respondent for the ‘Household Questionnaire’. Other members were consulted only if necessary and this was followed by a ‘Biomarker or Measurement Questionnaire’. This included among other things, the measurement of weight and height using standard techniques for the available members in the under-five and 15-49-year-old adults. In the NFHS-3, weight was measured using a solar-powered electronic SECA scale with a digital screen (manufactured under the guidance of UNICEF) and measuring board designed by Shorr Productions for use in survey settings [ 11 ]. In the NFHS-4, digital weighing machine (SECA 874) to the nearest of one gram and stadiometer (SECA 213) to the nearest of 0.1cm were used. This was done by trained field staff and monitored by field supervisors. The percentage of missing anthropometric information was 6% in the under-five participants, 12.2% in men (15–54) and 5.7% in women (15–49) in NFHS-4 [ 12 ], but corresponding information for participants in the NFHS-3 is not available.
We used the WHO 2007 Growth Reference to assess the nutritional status of adolescents (14). Age, sex, weight, and height recorded in the NFHS-3 and NFHS-4 surveys, were accessed from DHS database, extracted in Microsoft Excel, and imported as a TXT file into the ‘nutritional survey tool’ of the WHO AnthroPlus software (v1.04) [ 16 ]. This is specifically used for children and adolescents in the age group of 6–19 years. Height-for-age z-scores (HAZ) and BMI-for-age z-scores (BAZ) were used to identify stunting and thinness (and overweight/obesity) respectively. The nutritional survey tool of the software generates ‘standard reports’ and gives the prevalence of nutritional abnormalities as percentages and confidence intervals (CI), stratified by sex along with mean z-scores and standard deviations (SD). The software uses default lower and upper SD boundary as flag limits to identify any extreme or potentially incorrect z-scores. These are -6SD and +6SD for HAZ scores and -5SD and +5SD for BAZ scores and any values beyond these limits get automatically removed.
Interpretation of anthropometric data
All the height-for-age z-scores <-2 SD compared to the WHO median were considered as stunting; while BAZ scores < -2SD and <-3SD defined thinness and severe thinness respectively [ 14 ]. The BAZ score at +1SD for 19 years coincides with the adult BMI of 25 kg/m 2 ; which is the cut-off for overweight in adults [ 13 ]. As a result, BAZ >+1SD was used to classify overweight and >+2SD for obesity [ 14 ].
Statistical analyses
We used descriptive statistics to describe stunting, thinness, and overweight and stratified these by sex, urban-rural residence, and wealth quintiles. An independent t-test was used to compare z-scores available as a continuous variable. ANOVA was used to test the means across the five wealth quintiles. A two-sided p-value of <0.05 was considered as statistically significant. The statistical analysis was done using StataCorp 2009 (Stata Statistical Software: Release 11. College Station, TX: StataCorp LP).
Data visualization
Z-score plots for boys and girls in comparison with the WHO reference curves were generated using the AnthroPlus Software (v 1.0.4). Representation of sub-national heterogeneity in nutritional status was done using R-Software in the form of maps and comparative bar-charts.
Ethics statement
The respondents in the NFHS undergo an informed consent process for participation in the survey after approval of the protocol by the institutional review board of the IIPS. These NFHS datasets are available for download from the DHS program after registration [ 15 ]. This study was a secondary data analysis of de-identified data; therefore ethics committee approval was not obtained.
Table 1 describes select demographic characteristics of the adolescent participants in NFHS-3 and 4. The NFHS-3 included 52,324 and NFHS-4 included 277,059 adolescents. There was more urban representation (23,802, 45.5%) in NFHS-3 as compared to NFHS-4 (76,095, 27.5%). The poorer and poorest quintiles together contributed 26% in NFHS-3 and 45% in NFHS-4.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0234570.t001
Nutritional status of adolescents (15–19 years) in NFHS-3 and NFHS-4 using WHO 2007 Growth reference
Data available for final analysis in the adolescents who underwent anthropometry and after removal of improbable values by AnthroPlus Software was 68% in NFHS-3 (48.4% boys; 87.4% girls) and 52% in NFHS-4 (13.4% boys; 92.9% girls).
Table 2 describes the mean BAZ and HAZ scores for the adolescents in NFHS-3 stratified by the urban-rural residence and the wealth quintiles. In the NFHS-3, the mean BAZ and HAZ scores were significantly lower in the rural adolescents and those in the poorer quintiles, and the mean HAZ score was significantly lower in the girls. The mean BAZ for boys was -1.17 (SD: 1.14) and that for girls was -0.71 (SD: 1.01) (p<0.001); mean HAZ score for girls was -1.58 (SD: 0.89) which was -1.63 (SD: 0.88) in rural girls. In NFHS-4 ( Table 3 ), the mean BAZ for the boys was -0.85 (SD: 1.2) and that in girls was -0.64 (SD: 1.03) (p<0.001). Stunting was consistently higher in the girls as compared to the boys (p<0.001) in all sub-groups; being highest in rural girls (mean HAZ -1.69; SD: 0.9) and lowest in urban boys (mean HAZ -1.45, SD: 1.06). The adolescents in the poorest quintile performed worse than their counterparts in the NFHS-3, the overall mean HAZ was -1.94 (SD: 0.88) and that in girls was -1.94 (SD: 0.87).
https://doi.org/10.1371/journal.pone.0234570.t002
https://doi.org/10.1371/journal.pone.0234570.t003
Figs 1A – 4B show the BAZ and HAZ curves of the urban and rural participants of both sexes compared to the WHO reference. There is a visible shift of curves to the left in both the NFHS.
A. BMI-for-age z-scores of rural adolescents (15–19 years), NFHS-3 (2005–6). B. BMI-for-age z-scores of urban adolescents (15–19 years), NFHS-3 (2005–6).
https://doi.org/10.1371/journal.pone.0234570.g001
A. Height-for-age z-scores of rural adolescents (15–19 years), NFHS-3 (2005–6). B. Height-for-age z-scores of urban adolescents (15–19 years), NFHS-3 (2005–6).
https://doi.org/10.1371/journal.pone.0234570.g002
A. BMI-for-age z-scores of rural adolescents (15–19 years), NFHS-4 (2015–16). B. BMI-for-age z-scores of urban adolescents (15–19 years), NFHS-4 (2015–16).
https://doi.org/10.1371/journal.pone.0234570.g003
A. Height-for-age z-score of rural adolescents (15–19 years) in NFHS-4 (2015–16). B. Height-for-age z-score of urban adolescents (15–19 years) in NFHS-4 (2015–16).
https://doi.org/10.1371/journal.pone.0234570.g004
Comparison of currently reported nutritional status of the adolescents in NFHS-3&4 with the revised estimates
Table 4 compares the burden of thinness in adolescents as reported by the NFHS-3 & 4 with the revised estimates using the WHO 2007 Growth reference. Using adult cut-offs for thinness this was 58.1% in boys and 46.8% in girls in NFHS-3. Using the WHO 2007 Growth reference, it was 22.3% (95%CI: 21.6, 23.0) in boys and 9.9% (95%CI: 9.5, 10.3) in girls. Similarly, NFHS-4 reported 44.8% in boys and 41.9% thinness in girls, which reduce to 16.5% (95%CI: 16.0,17.0) and 9% (95%CI: 8.9, 9.2) in boys and girls respectively.
https://doi.org/10.1371/journal.pone.0234570.t004
According to the NFHS reports the prevalence of short-statured women of reproductive age-group (< 145 cm) was 11.7% in NFHS-3 and 12.7% in NFHS-4. In the NFHS, data is available for stunting in the under-fives, but not for stunting in adolescents or adults. We found stunting to be 32.2% (95% CI: 31.6, 32.9) in boys and 34.4% (95% CI: 34.2, 34.7) in girls in the NFHS-4. This was higher than the corresponding prevalence in the NFHS-3; 25.2% (95% CI: 24.4, 26) in boys and 31.2% (95% CI: 30.6, 31.8). A significant increase in stunting from NFHS-3 to 4 for both sexes, urban/rural and within the wealth quintiles (p<0.001) was observed.
Table 5 compares the over-nutrition (overweight/obesity) in adolescents as reported currently in NFHS-3 and 4 with the revised estimates using WHO 2007 Growth reference. Overweight has been reported as 1.7%in boys and 2.4% in girls in the NFHS-3 which increased to3% (95% CI: 2.7, 3.3) and 4.3% (95% CI: 4, 4.6) respectively using WHO 2007 Growth reference. In NFHS-4, the same was 4.8%in boys and 4.2% in girls which increased to 6.2% (95% CI: 5.9, 6.4) and 5% (95% CI: 4.8, 5.1) respectively in the revised estimates.
https://doi.org/10.1371/journal.pone.0234570.t005
Sub-national revised estimates of thinness, overweight in thinness and stunting
Tables 6 and 7 describe thinness in adolescents across Indian states in NFHS-3 and 4. The overall thinness in NFHS-3 was 14.3% (95%CI: 13.9, 14.7). The state of Maharashtra had the highest levels of thinness: 24.9% (95% CI: 23.3, 26.5). It was the least in all the north-eastern states, Delhi, Jammu and Kashmir, and Punjab. In NFHS-4, the overall thinness was 10% (95%CI: 9.8. 10.1) and it was most pronounced in Gujarat: 19.3% (95%CI: 18.2, 20.5), Telangana (17.2; 95%CI: 15, 19.4), and Maharashtra (15.4; 95% CI: 14.4, 16.3) and again more in the boys. The Northeastern states had the least thinness. Thinness in less than 10% of adolescents was prevalent in 8 states in NFHS-3 and 20 states in the NFHS-4
https://doi.org/10.1371/journal.pone.0234570.t006
https://doi.org/10.1371/journal.pone.0234570.t007
The overall prevalence of overweight was 3.8% (95%CI: 3.6, 4) in NFHS-3 and 5.1 (95%CI: 4.9, 5.2) in NFHS-4. There were 15 states with overweight greater than the national average (highest in Punjab and Kerala) in the NFHS-3 while there were 29 states and union territories (UTs) with overweight more than the national average (highest in Chandigarh and Kerala) in the NFHS-4. None of the states had a prevalence of overweight/obesity of more than 10%in the former whereas there were 7 such states and UTs in the latter.
Fig 5 describes the sub-national distribution of thinness and overweight in NFHS-3 and 4.
Prevalence of thinness (A and C) and overweight (B and D) in adolescents (15–19 years) in NFHS-3 (A and B) NFHS-4 (C and D) using WHO 2007 Growth Reference.
https://doi.org/10.1371/journal.pone.0234570.g005
State-level stunting in the NFHS-3 is described in Table 8 and Fig 6 . The national prevalence of stunting in adolescents was 29.1% (95% CI: 28.6. 29.6) in NFHS-3 with range of 63.9% (95%CI: 60, 67.9)in Meghalaya to 14.6% (95%CI: 12.3%, 17%) in Punjab. Fifteen states had stunting greater than the national prevalence. Apart from the Northeastern states, these included Jharkhand (43.9%), Bihar (37.6%), West Bengal (36.8%), Orissa (34.8%), Chhattisgarh (32.2%), Uttar Pradesh (29.9%) and Delhi (29.8%). Six states had a prevalence of stunting of less than 20%.
https://doi.org/10.1371/journal.pone.0234570.g006
https://doi.org/10.1371/journal.pone.0234570.t008
State-level stunting in the NFHS-4 is described in Table 9 and Fig 6 . The national prevalence was 34.1% (95%CI: 33.9, 34.4). Meghalaya continued to top the list but with a marginal improvement compared to NFHS-3 (61.5%; 95%CI: 59.4, 63.7%). However, in NFHS-4, 11 states and UTs had stunting more than the national average. These included all the Northeastern states, Jharkhand (47.5%), Bihar (44.1%), Orissa (41.5%), West Bengal (38.8%), Chhattisgarh (38.6%), and Uttar Pradesh (38.2%). These states became worse-off as compared to NFHS-3 in terms of the burden of stunting. In the NFHS-4 were only three states that had a stunting prevalence of less than 20%.
https://doi.org/10.1371/journal.pone.0234570.t009
We conducted secondary data analyses of nutritional assessment of adolescents (15–19 years) available from the NFHS-3 and 4. We used the WHO 2007 Growth reference as against the adult cut-offs that are presently being used for adolescents in these surveys. Due to possible non-availability of this highly mobile age-group and removal of improbable values outside the default upper and lower boundaries, the anthropometric data available for final analysis was 68% in NFHS-3 (48.4% boys; 87.4% girls) and 52% in NFHS-4 (13.4% boys; 92.9% girls).
We found that the thinness in boys and girls was 22.3% and 9.9% in NFHS-3 and 16.5% and 9% in NFHS-4. The prevalence of stunting was 25.2% and 34.1% in NFHS-3; 32.2% and 34.4% in NFHS-4 in boys and girls respectively. These revised estimates indicate a dramatically different adolescent nutrition status in India as against what is currently reported. The problem of stunting in this age group is much bigger than thinness and there is a trend indicating an increase in overweight.
Overestimation of thinness when adult cut-offs are used for adolescents
The use of adult cut-offs rather than the recommended WHO 2007 Growth Reference seems to overestimate the thinness by almost 2.5 fold in the boys and 4 fold in the girls [ 11 , 12 ]. These are also more consistent and plausible with the trends in the older age groups (20–29, 30–39, 40–49 years) as seen in Fig 7 .Moreover, the over-estimation in one particular age-group (15–19 years) is likely to inflate the overall prevalence of thinness in adults and may not give an actual picture of the nutrition transition and evolving double burden of malnutrition in the country.
https://doi.org/10.1371/journal.pone.0234570.g007
The results of our re-analysis are comparable to those in other studies using the WHO 2007 Growth Reference. According to the Non-communicable Disease Risk Factor Collaboration (NCD-RisC), a database of 2416 population-based studies on cardio-metabolic risk factors, thinness in the age-group 5–19 years was 30.7% (95% CI: 23.5, 38.0) in boys and 22.7% (95%CI 16.7, 29.6) in girls for India [ 17 ]. These are higher but closer to our re-estimation than the currently reported thinness by the NFHS. In the Global School-Based survey, thinness in the age group 12–15 years was 17.2% (95%CI: 14.2, 20.8) in boys and 14.1% (95%CI: 11.4, 17.3) in girls in India using the WHO 2007 growth reference [ 18 ]. A recent study from Orissa and Chhattisgarh found thinness to be 9.6% in girls in 10–19 years age-group using BAZ and mid-upper arm circumference [ 19 ].Overall in South Asia, the prevalence of thinness has been higher in boys (28.6%) as compared to girls (20.3%) [ 17 ]. Among countries with comparable nutritional indicators, thinness was 32.4% in boys and 21.4% in girls (10–19 years) in Ethiopia,11.9% in girls (12–19 years) in Bangladesh, and 15.2% in Somalian refugee girls (10–19 years) [ 20 – 23 ].
Stunting estimates in adolescents and the trend over NFHS-3 and NFHS-4
Stunting is a robust indicator of long-term nutrition at the population level. In the NFHS the estimates of stunting are limited to the under-five children and no stunting is ever reported in any age-group other than the under-five at the national level.
Our analysis for the first time offers the estimates of stunting in adolescents in nationally representative samples. The overall prevalence of stunting in adolescents was 29.1% (25.2% in boys, 31.2% in girls) in NFHS-3 which increased to 34.1% in NFHS-4 (32.2% in boys and 34.4% in girls). The increase in stunting is supported by the fact that there were six states in NFHS-3that had stunting less than 20%, whereas there were only three such states in NFHS-4. This may be either a true increase but is confounded by the differing nature of populations sampled in both the surveys. The NFHS-4 sample was larger and had a greater representation of households from rural areas from poorer wealth quintiles. There was also a great subnational heterogeneity varying from 63.9% (NFHS-3) and 61.5% (NFHS-4) in Meghalaya to 14.6% in Punjab in the NFHS-3 and 15.9% in Chandigarh in the NFHS-4.
There is a paucity of data on adolescent/adult stunting in India. The National Nutritional Monitoring Bureau (NNMB) conducted a study comprising of diet and nutritional assessment in nine states in 2006 [ 24 ]. It reported increasing levels of stunting across childhood and adolescence. The prevalence of stunting was 30.1% in the 6–9 year age group, 34.2% in 10–13 and 36.8% in 14-17-year-olds, with no significant difference between sexes at any age. According to the Global School-Based survey, it was 14.2% (95%CI: 10.6, 18.8) in boys and 15.1% (95%CI: 9.9, 22.4) in girls in India, but this was in the age-group 12–15 years [ 18 ]. Levels of stunting reported in other studies have been higher in Asia; 48% in adolescents from rural Bangladesh[ 25 ] and 23.7% in Malaysia [ 26 ], compared to 12.2% in Ethiopian adolescent girls [ 20 ] and 9.7% in Somalian refugee camps [ 23 ].
Determinants of stunting in adolescents
The height attained in adulthood is a combination of pre-pubertal height and height attained during the pubertal growth spurt. India has a huge (46.6 million) population of under-five children with stunting [ 27 ]. The high levels of stunting in Indian adolescents could represent the persistence of pre-pubertal deficit. The pubertal growth spurt which can add 8.3 cm/year in girls and 9.5 cm/year in boys requires additional nutrition [ 28 ]. In countries with high levels of malnutrition, the adolescent growth period may be prolonged in duration and may continue till the late adolescence [ 29 ]. The NNMB study documented food intakes in 10-17-year-old adolescents. The median caloric intake in boys ranged from 1387 KCalories in the 10–12 years, 1611 in the 13–15 years, and 1832 in 16–17 year age groups. Similarly, protein intakes were 36 gm, 42 gm, and 50 gm in these age groups respectively [ 24 ]. These are substantially below the recommended allowance and the intakes in the girls were even lower.
Stunting in our analysis was worst in girls and adolescents from the rural areas and the poorer quintiles, reflecting the impact of gender, place of residence, and socioeconomic status on long-term nutrition. Stunting is an indicator that is affected by food security, education, water sanitation and hygiene, disparity, economic development, and women’s health and empowerment [ 30 ]. Stunting was similar in both the sexes in the under-five age group in both the NFHS, but the girls ended up being more stunted during adolescence as per our analysis [ 11 , 12 ]. This was also demonstrated in a review of the NNMB data (children 0–18 years over two surveys conducted in 1975–9 and 2012–13 [ 31 ]. The boys and girls had similar growth faltering compared to the WHO median till the age of 14 years but the boys grew better after that [ 31 ].
Implications of stunting in adolescents
Stunting in adolescents has received less attention as a public health problem in India, since there has been no nationally representative survey of adolescents. It also goes unrecognized in communities where it is common and gets normalized [ 30 ]. The first 1000 days are critical for growth and development in infants due to maximum growth velocity in early life [ 30 , 32 ]. It is however also recognized that the next 7000 days of childhood to adulthood are equally important for growth [ 33 ]. The growth velocity at puberty is similar to that in the first two years of life. While the brain attains 95% of its adult size by 6 years of age, memory, emotional processing, decision making, and higher executive functions develop during mid-childhood and adolescence [ 33 ]. An increase in height by one SD was associated with 5% points more likelihood of being able to write, indicating its role in cognitive development [ 34 ].There is a potential for catch up growth in adolescence in countries like India, where growth may continue to falter beyond the first 1000 days and it is an additional ‘window of opportunity’ for positive intervention and catch-up [ 29 ]. Its importance in adolescent girls is even more important given the inter-generational consequences [ 35 ]. The persistently high levels of stunting in Indian adolescents indicate a lost opportunity for normal growth and development, including cognitive development.
Stunting and its impact on estimates of thinness
Stunting and thinness are both indices of undernutrition in adolescents and both use the measurement of height. While lower HAZ score indicates chronic undernutrition, a low BAZ score is indicative of acute undernutrition. However stunting impacts the estimates of BAZ leading to underestimation of thinness, the mean BAZ may appear better in stunted populations than that might be in a population with better heights. This might be one of the reasons for low levels of thinness seen in our analysis, especially in the girls. The phenomenon where boys continue to gain height resulting in higher levels of thinness has also been seen in neighboring countries like Indonesia, Bangladesh and Nepal (11%, 19.6%, 37.8% in boys and 5%, 15.4% and 26.2% in girls) [ 36 – 38 ].
Over-nutrition using WHO 2007 Growth Reference in adolescents
The impact of the use of WHO 2007 Growth Reference on the prevalence of overweight in adolescents was modest, and more so for obesity. There is a trend of an increase in overweight in this age-group between the two surveys. While no state had overweight prevalence greater than 10% in the NFHS-3, there were seven such states and UTs in the NFHS-4. It continued to be less than 4% in states with a higher prevalence of thinness like Madhya Pradesh, Chhattisgarh, Rajasthan, Jharkhand, and Bihar.
A comparison with other studies needs to be done cautiously due to the use of different classifications and cut-offs for overweight/obesity. Studies have variously used the cut-offs recommended by the International Obesity Task Force (IOTF), CDC and occasionally national standards [ 39 – 42 ]. In subnational studies in India, the prevalence of overweight/obesity in adolescents was 7.8% in urban Gujarat and 15.6% in Uttarakhand using WHO growth reference [ 43 , 44 ]; 21% in urban Bihar using the CDC cut-offs [ 45 ]; 11% in urban Haryana [ 46 ] and 7.2% in Telangana using IOTF cut-offs [ 47 ].A large multi-centric study in affluent school going children (2–17 years) in India estimated the overall prevalence of overweight/obesity as 18.2% by IOTF classification and 23.9% by the WHO standards [ 48 ]. A systematic analysis of 1,769 global studies found the prevalence of overweight in children and adolescents in developing countries to have increased in boys from 8.1% (95%CI: 7.7, 8.6) to 12.9% (95%CI: 12.3, 13.5)in boys and from 8.4% (95%CI: 8.1, 8.8) to 13.4% (95%CI: 13.0, 13.9) in girls over 1980 to 2013 [ 49 ].
Double-burden of malnutrition
The WHO defines the double burden of malnutrition as the coexistence of undernutrition along with overweight, obesity or diet-related NCDs, within individuals, households, and populations and across the life-course [ 50 ]. In operational and statistical terms many surveys have defined double burden as the high prevalence of wasting, stunting or thinness as well as overweight in any population group. The cut-offs used to define the high prevalence of undernutrition are, for example, wasting >15%, thinness > 20%, stunting > 30%, and overweight in children or adults variously as more than 20%, 30%, or 40% [ 51 ]. India too is reported as having a double burden with a high prevalence of undernutrition in adults and children; emerging problems of overnutrition and NCDs, especially in the urban areas and high prevalence of micronutrient deficiency [ 52 ]. Our reanalysis of NFHS-3 and 4 show that there are increasing levels of overweight in some states along with the persistence of thinness and stunting in others. In states like Kerala, the persistence of thinness and stunting alongside overweight do suggest loci of a double burden of malnutrition. These are influenced by age, gender, residence, region, and income. In a study from urban Hyderabad (12–17 year), overweight was four times higher in the upper socio-economic class (OR: 4.1; 95%CI: 2.25,7.52) [ 47 ].A cross-sectional analysis of 57 DHS across low and middle-income countries conducted in 1994–2008 did not find a substantial co-existence of under and over-nutrition [ 53 ]. Moreover, with the high prevalence of stunting in the age-group which is at the threshold of adulthood, the prevalence of thinness needs interpretation with caution.
Poor growth and height are closely associated with poverty and deprivation, reflected in the phrase by Tanner, ‘growth is a mirror of the conditions of society’ [ 54 ]. In the present analysis, we found that stunting prevalence was either equal or higher in boys in the better performing states and it was more in girls in the worst-performing states. The Empowered Action Group states that are performing poorly in other social, economic and health indicators have higher stunting which has worsened from NFHS-3 to NFHS-4and this is corroborated by others [ 55 – 57 ].

Strengths and limitations
Our re-analysis used the recommended WHO 2007 Growth Reference for the characterization of the nutritional status of adolescents in successive editions of the NFHS across a span of 10 years. This is the first snapshot of the nutritional status of adolescents in nationally representative samples. This is an addition to the sparse literature in adolescent nutrition in India and abroad. According to a bibliometric analysis, only 1.2% of the publications were pertaining to adolescents as against more than 95% for the under-five [ 33 ].
However, there are several limitations to be considered in the interpretation of the findings. First, the NFHS covered only boys and girls in the late adolescence with no representation of 10–14 years age group. Also, anthropometry was available in a limited proportion of adolescents, especially boys. Second, the possibility of inaccurate age reporting cannot be ruled out. Third, the WHO 2007 Growth Reference has limitations as these do not account for the complex racial/ethnic variation across populations in the timing of the adolescent growth spurt and are not based on current or future health risks in them [ 58 ].
Conclusions
The revised national and sub-national estimates of thinness, stunting and overweight in the age-group of 15–19 years using the WHO 2007 Growth reference reveal several novel findings relevant for adolescent and adult health in India. The prevalence of thinness is 2.5–4 fold lower in boys and girls than what has been reported using the adult cutoffs in both NFHS-3 and NFHS-4. The prevalence of thinness is higher in the boys and that of stunting is higher in the girls. Stunting appears to have increased over the two surveys and affects one in three adolescents. It indicates a lost opportunity for undoing the damage of stunting in childhood and the potential for nutritional recovery in the second decade. Adolescents in rural India, living in poverty and the less developed states continue to suffer nutritional deprivation which has implications for their growth, development, predisposition to communicable and non-communicable diseases, and their escape from poverty. There is a need for nutritional interventions for improving adolescent nutrition in India which receives scant attention at the moment. These findings have future implications (NFHS-5) so that vital information on the nutritional status of adolescents and nutrition transition in the population is neither buried in the adult data nor does it influence adult means inappropriately.
Supporting information
S1 data. mean height-for-age and weight-for-age z-scores of all states in nfhs-3 and 4..
https://doi.org/10.1371/journal.pone.0234570.s001
Acknowledgments
Authors gratefully acknowledge comments and inputs of Dr. Anura Kurpad, Division of Nutrition, St John’s Research Institute, Bangalore.
- 1. WHO. The Second Decade: Improving Adolescent Health and Development. Geneva: World Health Organization, 2001. Available from https://apps.who.int/iris/bitstream/handle/10665/64320/WHO_FRH_ADH_98.18_Rev.1.pdf [Accessed on 30 Jun 2019].
- 2. United Nations, Department of Economic and Social Affairs, Population Division (2019). World Population Prospects 2019, Online Edition. Rev. 1.
- 3. UNICEF. Adolescent Demographics–UNICEF Data. 2016. Available at https://data.unicef.org/topic/adolescents/demographics/ [Accessed on 25 Jun 2019].
- 4. Office of Registrar General and Census Commissioner India. Population enumeration data (final population). 2015. Available from http://www.censusindia.gov.in/2011census/population_enumeration.html . [Accessed on 15 Jun 2019].
- View Article
- PubMed/NCBI
- Google Scholar
- 7. Story, M. 1992. Nutritional requirements during adolescence. In Textbook of Adolescent Medicine. E.R. McAnarney, R.E. Kreipe, D.E. Orr & G.D. Comerci, Eds.: 75–84. Saunders.
- 11. International Institute of Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-3), India (2005–6). Mumbai: IIPS; 2007.
- 12. International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4), India, 2015–16. Mumbai: IIPS; 2017.
- 13. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organization technical report series. 1995;854:1–452
- 15. The DHS Program, India: Standard DHS, 2015–16 Available at: https://dhsprogram.com/what-we-do/survey/survey-display-355.cfm [Accessed 2 Mar 2019]
- 16. WHO AnthroPlus for personal computers: Software for assessing growth of the world's children and adolescents. Geneva: WHO, 2009 ( http://www.who.int/growthref/tools/en/ ) [database on the Internet].
- 27. Fanzo J, Hawkes C, Udomkesmalee E, Afshin A, Allemandi L, Assery O, et al. Global Nutrition Report: Shining a light to spur action on nutrition. Bristol: Development Initiatives; 2018.
- 32. WHO (2009) WHO Child Growth Standards: Growth Velocity Based on Weight, Length and Head Circumference: Methods and Development. World Health Organization: Geneva.
- 40. International Obesity Task Force. Obesity: preventing and managing the global epidemic. Report of WHO consultation on obesity, Geneva, 3–5 June 1998. Geneva: WHO; 1998.
- 41. Department of Health and Human Services. Centers for Disease Control and Prevention, USA. CDC growth charts for the United States. Available from: http://www.cdc.gov/nchs/data/nhanes/growthcharts/zscore/bmiagerev.xls
- 50. World Health Organization. Double-duty actions for nutrition: policy brief. 2017. https://www.who.int/nutrition/publications/double-duty-actions-nutrition-policybrief/en/ [Accessed 7 Nov, 2019).
Need and Importance of Nutrition Informatics in India: A Perspective
Affiliations.
- 1 Population Health Informatics, City University of New York Graduate School of Public Health and Health Policy, New York, NY 10027, USA.
- 2 Department of Environmental, Occupational and Geospatial Health Sciences, City University of New York Graduate School of Public Health and Health Policy, New York, NY 10027, USA.
- 3 Foundations of Healthcare Technologies Society, New Delhi 110066, India.
- 4 Indian Council of Medical Research, New Delhi 110029, India.
- PMID: 34072133
- PMCID: PMC8230128
- DOI: 10.3390/nu13061836
Nutrition informatics (NI) is the effective retrieval, organization, storage, and optimum use of information, data and knowledge for food-and-nutrition-related problem-solving and decision-making. There is a growing opportunity to facilitate technology-enabled behavioral change interventions to support NI research and practice. This paper highlights the changing landscape of food and nutrition practices in India to prepare a NI workforce that could provide some valuable tools to address the double burden of nutrition. Management and interpretation of data could help clarify the relationships and interrelationships of diet and disease in India on both national and regional levels. Individuals with expertise in food and nutrition may receive training in informatics to develop national informatics systems. NI professionals develop tools and techniques, manage various projects and conduct informatics research. These professionals should be well prepared to work in technological settings and communicate data and information effectively. Opportunities for training in NI are very limited in developing countries. Given the current progress in developing platforms and informatics infrastructure, India could serve as an example to other countries to promote NI to support achieving SDGs and other public health initiatives.
Keywords: digital health; food and nutrition; nutrition informatics; workforce.
- Health Workforce
- Informatics*
- Nutritional Sciences*
C13, Qutab Institutional Area, New Delhi, 110016 [email protected] +91 9891485605

The Nutrition Foundation of India (NFI) is a non-governmental voluntary organization dedicated to improving the nutritional status of Indians by
- Carrying out research on major nutritional problems.
- Research to operationalize proven interventions to improve nutritional status in national programs.
- Evaluation of national nutrition programs.
- Capacity building to improve implementation of national programs to improve nutritional status.
Twenty-Five Year Report Festschrift for Dr Gopalan WHO SEARO Reports by Dr Gopalan Scientific Reports Special Publications Reports Report on Dual Nutrition Burden in India Nutrition Transition in India Policy Research Papers Evaluation Reports Training Manuals NFI Symposia Proceedings / Presentations / Videos

“NFI Bulletin” is a quarterly publication addressing important issues pertaining to the national policies and programs related to food security, dietary intake, physical activity, nutritional and health status of Indians.
Archives List of NFI Bulletins
Search By: Year Author
Total Visitors
- India Today
- Business Today
- Reader’s Digest
- Harper's Bazaar
- Brides Today
- Cosmopolitan
- Aaj Tak Campus
- India Today Hindi
ICMR released 17 dietary guidelines, urge Indians to reconsider dietary habits
Icmr has released 17 dietary guidelines and urges indians to reconsider their dietary habits, read to learn more..
Listen to Story

- Healthy diet and physical activity can reduce heart disease and hypertension
- Unhealthy diet causes 56.7% of disease burden in India
- Processed foods and limited physical activity worsening micronutrient deficiency
The latest study finds out, that 56.7 per cent of the disease burden in India is due to an unhealthy diet, as it releases the 17 necessary dietary guidelines to meet the essential requirement of a balanced diet and to prevent non-communicable diseases (NCDS) such as obesity and diabetes.
Nutrition plays an important role right from the time of a baby’s presence in the womb of the mother. A balanced diet helps in curing nutritional deficiencies and optimal growth for a child. Emphasis has been laid on the recommendations which can maximise protective effects in accordance with traditional habits.
The National Institute of Nutrition (NIN) under the apex body, said that healthy diets and physical activity can reduce the amount of coronary heart disease (CHD) and hypertension (HTN) and prevent 80% of 2 types of diabetes.
“The risk of premature deaths can be eliminated by using the right techniques of living”, it said, adding that the increase in consumption of processed foods encumbered with fats, sugar, and salt integrated with diminished physical activity and limited access to nutrients enrich food of diverse categories, worsening micronutrient deficiency and overweight problems.
ICMR’S 17 DIETARY GUIDELINES:
- Eat a variety of foods to ensure a balanced diet
- Pregnant women and new mothers should have access to extra food and healthcare
- Ensure exclusive breastfeeding for the first six months; continue breastfeeding till two years and beyond
- After six months of age, the infant should be fed homemade semi-solid complementary foods.
- Ensure adequate and appropriate diets for children and adolescents in health and sickness
- Eat plenty of vegetables and legumes
- Use oil/fats in moderation; choose a variety of oil seeds, nuts etc. to meet daily needs of fats and essential fatty acids
- Obtain good equality proteins and essential amino acids; avoid protein supplements to build muscle mass
- Adopt a healthy lifestyle to prevent abdominal obesity, overweight and overall obesity
- Be physically active, exercise regularly
- Restrict salt intake
- Consume safe and clean foods
- Ensure appropriate pre-cooking and cooking methods are used
- Drink plenty of water
- Minimise the consumption of ultra-processed foods and high-fat, sugar, salt
- Prioritise nutrient-rich foods in the diets of elderly people
- Read information on food labels
It also recommends adopting a healthy lifestyle to eradicate the risk of obesity, diabetes and other cardio problems. Consumers should read all the information labelled on the item to make informed and healthy food choices.
SEVENTEEN GUIDELINES HAVE BEEN LISTED IN THE DGI:
"Through the DGIs, we emphasise that the most logical, sustainable, and long-term solution to all forms of malnutrition is ensuring the availability, accessibility and affordability of nutrient-rich foods while promoting consumption of diverse foods. The guidelines contain in them scientific evidence-based information that would facilitate the attainment of goals stated in the National Nutrition Policy," Hemlatha said.
The dietary habits of Indians have undergone significant changes over the past few decades, leading to an increase in the prevalence of non-communicable diseases while some of the problems of undernutrition continue to persist, said Dr Rajiv Bahl, Director General, ICMR.
TO BE HIT, EAT FIT
A balanced diet should not provide more than 45% of calories from cereals and millet and up to 15% of calories from pulse, beans and meat. The rest must be confirmed by vegetables, nuts and fruit and milk products.
It has also been mentioned by NIN that Indians rely on cereals due to the high cost of meat, pulses and other enriched foods, resulti9ng in a poor intake of essential macronutrients and micronutrients.
- Weird But True
- Sex & Relationships
- Viral Trends
- Human Interest
- Fashion & Beauty
- Food & Drink
- Health Care
- Men’s Health
- Women’s Health
- Mental Health
- Health & Wellness Products
- Personal Care Products
trending now in Lifestyle

Doctor cancer-free one year after using own revolutionary...

'Anti-sex' beds have arrived at Paris Olympics — after horny...

Mother-in-law's 'unforgivable' wedding act stuns internet: 'Makes...

McDonald's is getting rid of free drink refills — and more...

University apologizes after wildly mispronouncing graduates'...

How to properly reheat leftover rice and prevent 'fried rice...

If you do this while driving, you might be a psychopath,...

World's tallest and fastest triple launch rollercoaster forced to...
These diets are best for lowering risk of diseases and cancer: study.
- View Author Archive
- Follow on Twitter
- Get author RSS feed
Thanks for contacting us. We've received your submission.

Turns out, vegan and vegetarian diets are un-beet-able when it comes to lowering the risk of cardiovascular diseases and cancer, new research has found .
Dr. Angelo Capodici, of the University of Bologna in Italy, and his colleagues reviewed 48 papers published between January 2000 and June 2023 that investigated the link between plant-based diets, cardiovascular health and cancer risk. They found “significant” health benefits in plant-based diets.

“Our umbrella review seems consistent with other primary evidence that links the consumption of red processed meats to an increased risk of cancers of the gastrointestinal tract,” Capodici and his team wrote in their findings, published Wednesday in PLOS One .
The World Health Organization’s International Agency for Research on Cancer classified processed meat as “carcinogenic to humans” in 2015 , noting that there is “sufficient evidence from epidemiological studies that eating processed meat causes colorectal cancer.” IARC also declared red meat as “probably carcinogenic to humans.”
Nevertheless, Capodici warned that “caution should be paid” before making a large-scale recommendation for plant-based diets because of limitations to the studies and potential vitamin and mineral deficiencies associated with these eating plans.
The pros of eating a diet rich in fruits, vegetables, nuts, seeds, oils, whole grains, legumes and beans have long been espoused.
Capodici and crew said lower blood pressure, better blood sugar management and a healthier body mass index are some outcomes of vegetarian and vegan diets.
They did point out that people who tend to follow these diets are “more prone to engage in healthy lifestyles,” such as regular exercise, avoidance of sugar-sweetened beverages and abstinence from alcohol and tobacco, which also reduces the risk of heart disease.
They also noted that pregnant women who adopted vegetarian diets did not lower their risk of developing gestational diabetes and hypertension compared to women who ate meat.

Get the latest breakthroughs in medicine, diet & nutrition tips and more.
Subscribe to our weekly Post Care newsletter!
Thanks for signing up!
Please provide a valid email address.
By clicking above you agree to the Terms of Use and Privacy Policy .
Never miss a story.
And vegans risk developing anemia due to a lack of vitamin B12, an essential nutrient naturally found in animal products. Vegans are encouraged to eat grains fortified with vitamin B12 or take a daily supplement .
Capodici’s team advised that more research is needed into the effects of vegetarian and vegan diets — they say the studies they analyzed differed in dietary patterns, sample size and participant demographics, among other factors.
Share this article:
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Sign up for alerts
- 13 May 2024
'Einstein’s death shattered Bose — he tore off an unpublished research paper in grief'
You can also search for this author in PubMed Google Scholar
Partha Ghose. Credit: Partha Ghose
Nature India : What inspired you to embark on a career in particle physics?
Partha Ghose : In 1961, I went to Imperial College London wanting to decipher what lies at the deepest core of matter. This was when physicists had already begun smashing atoms in colliders, churning out new transient particles to unveil the secrets of matter.
I was lucky to learn advanced physics from stalwarts in particle physics like Abdus Salam, P. T. Matthews and T. W. B. Kibble. In 1963, an opportunity to work briefly at CERN further spurred my interest in particle physics.
NI : How did you meet S. N. Bose?
PG : It was in mid-1963 that I met Bose, quite by chance. The famous Bengali pote Bishnu Dey, a relative of ours and Bose’s close friend, took me to meet Bose. They were immersed in discussion, and Bose suddenly turned to me and asked, ''Would you like to work with me?''. It was an offer I couldn’t refuse. He arranged everything very quickly and within days I joined his research group at the Saha Institute of Nuclear Physics in Calcutta as a junior scientist. I worked on particle physics, mainly on broken SU(3) symmetry which was in vogue at the time.
NI : How did Bose start interacting with Einstein and how was their relationship?
PG : Occasionally, Bose would reminisce about his interactions with Einstein. One day when I went to meet him at his residence, he started talking about the historic paper he sent to Einstein on 4 June 1924 along with a letter .
Bose told me that his deduction of the phase space factor in Planck’s law resulted in a factor of 4π instead of 8π. He went on to propose that the missing factor of 2 was due to the photon spin which could take only two values. In his letter back to Bose, “the old man” [Einstein] had crossed this portion out and said it was not necessary to talk about spin since the factor of 2 comes from the two states of polarisation of light.”
Bose said to me, ”I can understand a spinning particle, but what is the meaning of the polarization of a particle?” I asked him, "Sir, when the photon spin was eventually discovered, why didn’t you tell Einstein that you had already worked it out in 1924?” “How does it matter who discovered it,” he quipped. “It was eventually discovered, wasn’t it?”
In a second paper, which also Einstein translated into German and got published in Zeitschrift fur Physik , Bose proposed a probability law for interactions between matter and radiation. According to Einstein, it was inappropriate. He added a comment to the paper giving some reasons for his disagreement with Bose.
The first paper with Einstein’s strong endorsement made Bose famous. He moved to Paris on a two-year sabbatical from Dhaka University, worked in Maurice de Broglie’s and Marie Curie’s labs and arrived in Berlin in 1925 to finally meet Einstein. They discussed several issues including Bose’s new hypothesis of probabilistic interactions, but Einstein stuck to his point.
Despite their differences, Bose regarded Einstein as his master in physics. On 18 April 1955, Einstein died. The news shocked him into silence. He was writing a paper and was looking forward to discussing it with Einstein at a forthcoming conference in Switzerland to celebrate fifty years of Special Relativity. Bose tore that paper into shreds.
NI : Many say that S. N. Bose missed out on a Nobel Prize for physics.
PG : He deserved the prize for his seminal contribution to quantum theory. It led to the classification of particles into bosons and fermions and the prediction and discovery of Bose-Einstein condensates. Besides, his theories helped us understand superconductivity and superfluidity. Bose’s theories and insights shaped the works of many physicists. Some went on to win Nobel Prizes. But Bose, despite being recommended several times, was never considered for the prize.
NI : Apart from physics, you learned music, and played first-class cricket. Do you think science helps enrich music?
PG : Science can help explain music. The best example of this in India is Sir C. V. Raman who had a keen ear for Indian classical music. He could detect five harmonics in the 'mridangam' and the 'tabla' sounds. He did some experiments with Indian drums and circular membranes with central loads. He sprinkled white powder on them to see the patterns of vibrations formed as he kept changing the loads and the manner of striking. This led to a new understanding of the generation of harmonics in stretched membranes. His research in musical instruments earned him the Fellowship of the Royal Society of London even before he got the Nobel Prize for his work on light scattering.
NI : S. N. Bose advocated popularizing science in Bengali. Is it easier to communicate science through one’s mother tongue?
PG : Science is based on logic and requires precise language for its expression and understanding. Non-native speakers find it difficult to grasp the nuances of scientific terms in English. They often acquire wrong notions when they read science in English.
The language in which one dreams is one's mother tongue. Science can therefore take root and flourish in a country only when its citizens start dreaming about science in their mother tongue.
NI : What is your advice for young Indian students who want to pursue a career in physics?
PG : I will quote Bose’s last advice to me. ''Don't jump onto foreign bandwagons. Try to understand things in your way and say something new.''
Bose read the works of all leading quantum theorists of his time, including Einstein, with a critical mind, identified their shortcomings and went on to propose revolutionary new statistics. These days I see an undue rush to publish papers in reputed foreign journals, increase citations, and get quick recognition and promotion. This leads to derivative science.
doi: https://doi.org/10.1038/d44151-024-00054-2
Senior Research Assistant in Human Immunology (wet lab)
Senior Research Scientist in Human Immunology, high-dimensional (40+) cytometry, ICS and automated robotic platforms.
Boston, Massachusetts (US)
Boston University Atomic Lab
Postdoctoral Fellow in Systems Immunology (dry lab)
Postdoc in systems immunology with expertise in AI and data-driven approaches for deciphering human immune responses to vaccines and diseases.
Global Talent Recruitment of Xinjiang University in 2024
Recruitment involves disciplines that can contact the person in charge by phone.
Wulumuqi city, Ürümqi, Xinjiang Province, China
Xinjiang University
Tenure-Track Assistant Professor, Associate Professor, and Professor
Westlake Center for Genome Editing seeks exceptional scholars in the many areas.
Westlake Center for Genome Editing, Westlake University
Faculty Positions at SUSTech School of Medicine
SUSTech School of Medicine offers equal opportunities and welcome applicants from the world with all ethnic backgrounds.
Shenzhen, Guangdong, China
Southern University of Science and Technology, School of Medicine
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Evaluation of the Full-Frontal Crash Regulation for the M1 Category of Vehicles from an Indian Perspective
2024-01-2750.
- 1 What should be the appropriate test speed for the full-frontal test based on Indian accident data?
- 2 What is the suitable dummy configuration in terms of gender, seating position, and age to maximize occupant safety in full frontal accidents?
- 3 Is the proposed ATD’s anthropometry (weight and height) suitable, based on the people involved in full frontal cases in India?
- 4 What are occupant injury attributes in full-frontal accidents?
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10264273

Measuring Food Insecurity in India: A Systematic Review of the Current Evidence
Fiona h. mckay.
1 School of Health and Social Development, Faculty of Health, Deakin University, Victoria, Australia
2 Institute for Health Transformation, Faculty of Health, Deakin University, Victoria, Australia
Paige van der Pligt
3 Institute for Physical Activity and Nutrition (IPAN), School of Exercise and Nutrition Sciences, Deakin University, Geelong, Australia
Associated Data
Purpose of review.
India is home to an estimated 200 million malnourished people, suggesting widespread food insecurity. However, variations in the methods used for determining food insecurity status mean there is uncertainty in the data and severity of food insecurity across the country. This systematic review investigated the peer-reviewed literature examining food insecurity in India to identify both the breadth of research being conducted as well as the instruments used and the populations under study.
Recent Findings
Nine databases were searched in March 2020. After excluding articles that did not meet the inclusion criteria, 53 articles were reviewed. The most common tool for measuring food insecurity was the Household Food Insecurity Access Scale (HFIAS), followed by the Household Food Security Survey Module (HFSSM), and the Food Insecurity Experience Scale (FIES). Reported food insecurity ranged from 8.7 to 99% depending on the measurement tool and population under investigation. This study found variations in methods for the assessment of food insecurity in India and the reliance on cross-sectional studies.
Based on the findings of this review and the size and diversity of the Indian population, there is an opportunity for the development and implementation of an Indian-specific food security measure to allow researchers to collect better data on food insecurity. Considering India’s widespread malnutrition and high prevalence of food insecurity, the development of such a tool will go part of way in addressing nutrition-related public health in India.
Supplementary Information
The online version contains supplementary material available at 10.1007/s13668-023-00470-3.
Introduction
Food insecurity has been identified as a “pressing public health concern” in India [ 1 •]. At the household level, food security exists when all members, at all times, have access to enough food for an active, healthy life [ 2 ••]. Individuals who are food secure do not live with hunger or fear starvation. Across urban settings, the prevalence of food insecurity has been found to range from 51 to 77%, yet over 70% of India’s population resides rurally, where data concerning food insecurity is limited [ 3 ].
The concept of food security consists of six main dimensions: availability, access, utilization, stability, agency, and sustainability. The first three dimensions are interlinked and hierarchical. Food availability is concerned with ensuring that sufficient quantities of food of appropriate quality are supplied through domestic production or imports (including food aid). Access to food is necessary but not sufficient for access. Access is concerned with ensuring adequate resources, or entitlements, are available for the acquisition of appropriate foods for a nutritious diet. Access is necessary but not sufficient for utilization. Utilization is concerned with the ability of an individual to access an adequate diet, clean water, sanitation, and health care to reach a state of nutritional well-being. The three other concepts have become increasingly accepted as important, as risks such as climatic fluctuations, conflict, job loss, and epidemic disease can disrupt any one of the first three factors. Stability refers to the constancy of the first three dimensions. Agency is recognized as the capacity of individuals or groups to make their own food decisions, including about what they eat, what and how they produce food, and how that food is distributed within food systems and governance. Finally, sustainability refers to the long-term ability of food systems to provide food security and nutrition in a way that does not compromise the economic, social, and environmental bases that generate food security and nutrition for future generations [ 4 ••].
Two hundred million people living in India are estimated to be malnourished [ 5 •]. Poverty, a lack of clean drinking water, and poor sanitation have been identified as common factors contributing to malnutrition in India [ 1 •]. Yet to date, despite high rates of malnutrition pointing toward widespread food insecurity [ 6 ], the link between food insecurity and malnutrition in India has seldom been explored. Of the limited data available, associations have been found between household food insecurity and child stunting, wasting, and being underweight [ 7 ], highlighting the urgency of food insecurity as a public health priority.
Considering the high rates of child stunting, wasting, and overall malnutrition in India, exploring past and emerging research which has both assessed and addressed food insecurity is a crucial step in better understanding nutrition-related health at the population level. Currently, to the best of our knowledge, there is no published systematic review which has explored household food insecurity in India. To understand the factors that contribute to food insecurity at the household level, the related health and nutrition outcomes, and to conceptualize potential strategies which target food insecurity in India, a systematic review of published research undertaken to date which has focused on food insecurity in India is urgently needed. This review seeks to (1) systematically investigate the peer-reviewed literature that purports to investigate food insecurity in India, (2) identify the breadth of research being conducted in India, including the instruments used and the populations under study, and (3) provide an overview of the severity of food insecurity in India as presented by these studies.
A systematic search was undertaken to identify all food security research conducted at the household level in India. The search was conducted in March 2020. Key search terms were based on the FAO [ 8 ] definition of food security: “food access*,” OR “food afford*,” OR “food insecur*,” OR “food poverty*,” OR “food secur*,” OR “food suppl*,” OR “food sufficien*,” OR “food insufficien*,” OR “hung*” AND “household*” OR “house*” AND “India.” Searched databases included Academic Search Complete, CINAHL Complete, Global Health, MEDLINE, Embase, SCOPUS, ProQuest, PsychInfo, and Web of Science. To gain a full collection of articles that reported on research investigating household food security in India, no limits were placed on publication dates. Only peer-reviewed articles published in English were considered; unpublished articles, books, theses, dissertations, and non-peer-reviewed articles were excluded. This review adheres to the PRISMA statement [ 9 , 10 ], see Fig. Fig.1 for 1 for a flowchart describing the process of screened included and excluded articles.

Flow chart of articles meeting search criteria, number of articles excluded, and final number of articles meeting inclusion criteria for review
Two authors (FHM and AS) and a research assistant reviewed all articles to identify relevant studies. Articles underwent a three-step review process (see Fig. Fig.1). 1 ). All articles were downloaded into EndNote X7, duplicates were identified and removed, and the article titles, journal titles, year, and author names were then exported to Microsoft Excel 365 to facilitate reviewing. Articles were first screened by title and abstract based on the inclusion and exclusion criteria described above by two authors independently. Any article that clearly did not meet the inclusion criteria was removed at this stage, any that did, or possibly could meet the inclusion criteria on further inspection, were retained. The full text of the remaining articles was obtained, and at least two authors (FHM and AS) or a research assistant independently read all 161 articles that remained at this stage to determine if the article met the inclusion criteria. Any articles at this stage that clearly did not meet the inclusion criteria were removed. Any disagreements on those that were retained were discussed and settled by consensus between the authors.
Articles that discussed food insecurity in general but collected no new data (for example, Gopalan [ 11 ] and Gustafson [ 12 ]) were excluded, as were previously conducted reviews in the region (for example, del Ninno, Dorosh [ 13 ], Harris-Fry, Shrestha [ 14 ]). As this review was primarily interested in studies that purported to measure food insecurity in India, studies that discussed food insecurity, either as the standard measured construct or as a construct created by the authors but termed food insecurity, were included. While there are many non-government organizations and inter-government organizations that work to measure food or nutritional insecurity, the construct of “hunger,” the associated conditions of malnutrition (either with overweight or obesity) or conditions that might indicate malnutrition (including anemia or under-5 mortality), these reports generally do not include a complete description of the method used to collect data if data were collected at the household level and often use the sale or production of crops as a proxy; as such, these reports have been excluded from this review.
Data were extracted from each article by the three authors. Data were extracted into a Microsoft Excel 365 spreadsheet that allowed for the capture of specific information across all included articles. Data extracted at this stage included the following: location; population group; findings; measured food security (Y/N); method for determining food insecurity; and prevalence of food insecurity.
The search identified 1018 articles, of which 395 were duplicates. The titles and abstracts of the remaining 616 articles were read, with 518 articles excluded as they did not refer, either directly or indirectly, to food insecurity research in India, leaving 161 articles for further investigation. The full text of the 161 articles was reviewed; 108 articles were excluded as they did not meet the inclusion criteria. The remaining 53 articles were included in this review.
Most articles ( n = 48, 90%) were cross-sectional studies; three were longitudinal, with data covering 27 years [ 15 ], 11 years [ 16 ], and 4 years [ 17 ], and one was a randomized controlled trial [ 18 ]. Eight studies employed a mixed methods approach, seven were qualitative, and the remaining 38 were quantitative studies. Participant numbers ranged in size from the smallest study with 10 participants [ 19 ] to population-level studies with over 100,000 participants [ 15 , 20 ]. See the supplementary material for an overview of the studies included.
Most food insecurity research was conducted in the state of West Bengal, where 9 studies were conducted, followed by 6 studies each in Maharashtra and the union territory of Delhi (see Fig. Fig.2). 2 ). India consists of 28 states and 8 union territories; this review found research from 17 states and five union territories, as well as four nationwide studies showing good coverage across the country.

Distribution of studies exploring food insecurity in India
Measuring Food Insecurity
All studies included in this review purported to measure food insecurity directly, with the main aim of the majority ( n = 45, 85%) of articles to determine the prevalence of food insecurity. These articles employed a range of measurement tools to achieve this aim. The most common way to measure food insecurity was via the Household Food Insecurity Access Scale (HFIAS) which was employed in 17 studies. The second most common method employed to measure food insecurity was via the Household Food Security Survey Module (HFSSM), employed in 13 studies. Other measures of food insecurity include the Food Insecurity Experience Scale (FIES), used in three studies, the Comprehensive Nutrition Survey in Maharashtra used in two studies, and the Radimer/Cornell used in one study. The remaining 17 studies used a proxy measure, either one devised by the authors or by using data from the India National Sample Survey (NSS). See Table Table1 1 for an overview of these measurement tools.
Food insecurity measurement tools
The prevalence of food insecurity in these studies ranged from 8.7 to 99%; 13 studies stated that they measured food insecurity but did not report food insecurity results. The most common way for food insecurity to be measured in India was through employing Household Food Insecurity Access Scale (HFIAS). This experiential scale was designed to be used cross-culturally and consists of nine questions, with frequency questions asked if participants experience the condition. Responses to these questions are scored so that “never” receives a score of 0, “rarely” is scored 1, “sometimes” is scored 2, and “often” is scored 3, so that when summed, the lowest possible score is 0 and the highest is 27. A higher score represents greater food insecurity, with continuous scores typically divided into four categories, representing food-secure and mildly, moderately, and severely food-insecure households according to the scheme recommended by the HFIAS Indicator Guide [ 21 ]. The scale is based on a household’s experience of problems regarding access to food and represents three aspects of food insecurity found to be universal across cultures [ 22 – 24 ]. This scale measures feelings of uncertainty or anxiety about household food supplies, perceptions that household food is of insufficient quality, and insufficient food intake [ 21 ]. The questions asked in the HFIAS allow households to assign a score along a continuum of severity, from food secure to food insecure. Food insecurity measured via the HFIAS ranged from 77.2% in a population of 250 women who resided in an urban area in South Delhi [ 25 ] to 8.7% in Indian children [ 26 ].
The second most common measurement tool identified in this search is the US Household Food Security Survey Module (HFSSM). This tool was developed to measure whether households have enough food or money to meet basic food needs and what their behavioral and subjective responses to that condition were [ 27 ]. The HFSSM module consists of a set of 18 items, 8 of which are specific to households with children. It captures four types of household food insecurity experiences: (1) uncertainty and worry, (2) inadequate food quality, and insufficient food quantity for (3) adults and (4) children [ 28 ]. It is available in an 18-item and 6-item forms and allows households to be assigned a category of food insecurity: high food security, marginal food insecurity, low food insecurity, and very low food insecurity. In accordance with the method proposed by Coleman-Jensen et al. [ 29 ], food security scores are combined to create one measure for the level of food security for a household. Food security status is determined by the number of food-insecure conditions and behaviors that the household reports. Households are classified as food secure if they report fewer than two food-insecure conditions. They are classified as food insecure if they report three or more food-insecure conditions, or two or more food-insecure conditions if they have children. Food-insecure households are further classified as having either low food security if they report between three and five food-insecure conditions (or three and seven if they have children), or very low food security if they have six or more food-insecurity conditions (eight if they have children). Studies that employed the HFSSM reported food insecurity ranging from 15.4 [ 30 – 32 ] to over 80% of study participants [ 33 ]. The HFSSM is a commonly used measure of food insecurity and can be used in several valid forms. Studies included in this review used the 4-, 6-, and 18-item versions of the HFSSM.
The Food Insecurity Experience Scale (FIES) module was used by three studies included in this review. The FIES questions refer to the experiences of the individual or household. This scale was created by the Food and Agriculture Organization of the United Nations (FAO) and has been tested for use globally [ 28 ]. The questions focus on self-reported food-related behaviors and experiences associated with increasing difficulties in accessing food due to resource constraints. The FIES allows for the calibration of other measures, including the HFIAS and the HSSM with the FIES against a standard reference scale allowing for comparability of the estimated prevalence rates of food insecurity [ 34 ], as well as a raw score that can be used by authors as a way to create discrete categories of food insecurity severity [ 35 ]. The three studies that employed the FIES all reported food insecurity within a range of 66–77%, despite different population groups, locations, and sample sizes.
One study employed the Radimer/Cornell scale, a widely used and validated scale [ 36 ]. The scale includes ten items that relate to food anxiety and the quantity and quality of food available. The instrument allows for the categorization of households into four categories of food insecurity: food security, household food insecurity, individual food insecurity, and child hunger.
The Comprehensive National Nutrition Survey (CNNS) was used in two studies. It is a state-specific (Maharashtra) nutrition survey with a focus on infants and children under two and their mothers. The CNSM measured household food security using nine questions [ 37 ]. The questions capture experiences of uncertainty or anxiety over food, insufficient quality, insufficient quantity, and reductions in food intake [ 38 ]. Households are categorized as food secure, mildly food insecure, moderately food insecure, or severely food insecure.
The National Sample Survey (NSS) organization conducts nationwide household consumer expenditure surveys at regular intervals in “rounds,” typically 1 year. These surveys are conducted through interviews with a representative sample of households [ 20 ]. This survey includes only one question about household daily access to food [ 39 ], and while it does provide a method for estimating food insecurity in India, it assumes that financial access equates to physical access to available food; as such, this survey is unlikely to be able to comprehensively capture the intensity of household food insecurity in India [ 40 ]. Four studies employed the NSS. Given that these studies did not specifically collect food insecurity data, the use of the NSS has been considered a proxy indicator here as it generally reflects the measurement of food availability or acquisition rather than food insecurity per se.
Other proxy measures were commonly used. The variety of proxy measures included information on calorie intake, purchasing power, the quantity of food consumed, and agricultural productivity. These proxy measures provide only a partial, usually indirect, measure of food insecurity [ 41 ]. There are also challenges with these measures, as the relationship between food and caloric quantity and household food security is unpredictable [ 42 ]. For example, in a study of households in Gujarat, Sujoy [ 43 ] found that around 85% of households are food insecure at some point in a typical year. This study employed a range of measures to explore the experiences of hunger and food insecurity and the strategies employed by these population groups to mitigate hunger. Exploring the food insecurity experiences of farmers in Bihar, Sajjad and Nasreen [ 44 ] found that 75% of households had very low food security. While not using a standard measure, Sajjad and Nasreen [ 44 ] interviewed households alongside interviews with government officials, food production, food costs, and food acquisition to form an index of food security that could be applied at the household level. A study by George and Daga [ 45 ] using calorie consumption as a proxy for food security identified 57% of participants were food insecure, with the suggestion that income and family size play a role in food security among children. Of the 17 studies that employed a proxy measure of food insecurity, 10 provided no indication of the level of food security in their results.
Population Groups Under Investigation
Studies identified in this review included a variety of population groups. Most studies ( n = 30) focused on food insecurity at the household level; half of these studies employed one of the standard food insecurity measurement tools, while the other half relied on proxy measures.
Fourteen studies focused specifically on young children, and one on teenagers. These studies used a variety of methods to determine food insecurity among this population, with rates of food insecurity shown to range from 8.7 [ 26 ] to 80.3% [ 33 ]; within this range, most studies reported that food insecurity among children was in the range of 40 to 60%. Interestingly, while the study conducted by Humphries [ 26 ] reported lower levels of child food insecurity (8.7%) than the other studies included in this review, other findings of this study were consistent with other research reviewed. Across all studies that explored food insecurity among children and teenagers, findings suggest problematic infant and young child feeding practices, caregiving, and hygiene practices, with many studies reporting impaired growth in children and teenagers due to these practices.
Seven studies focused specifically on the experiences of women or used the experiences of women as an indicator of food insecurity in their households. All of these studies employed one of the standard measures of food insecurity, with food insecurity in these studies ranging from 32 [ 3 ] to 77.9% [ 46 ]. These studies identified a range of health outcomes related to food insecurity and hunger. For example, in a study of mothers of children under the age of 5, Das and Krishna [ 47 ] found that two-thirds of households were food insecure and that younger mothers were more likely to be food insecure, with the children of these mothers more likely to be underweight and stunted. Among mothers in a study by Chyne et al. [ 48 ], those who had low literacy levels, low income, and large family size were more likely to be food insecure, with many of the children of these mothers being vitamin A deficient, anemic, stunted, and/or wasted. This is consistent with the work of Chatterjee et al. [ 49 ] who found that food insecurity among women was associated with low income and a range of socioeconomic measures including education, employment, and relationship status.
Thirteen studies were conducted in slums. Four of these studies were conducted in slums in Delhi, finding that food insecurity among slum populations ranges between 12% among children aged 1–2 years [ 50 ] and 77% in households more broadly [ 25 ]. Three studies were located in slums in Kolkata, all conducted by Maitra and colleagues [ 30 – 32 ]. These studies found food insecurity to be 15.4%, finding that low income, household composition, and education are all predictors of household food insecurity. The remaining studies were conducted in slums in Jaipur [ 51 ], Mumbai [ 49 ], Varanasi [ 52 ], Vellore [ 53 ], and West Bengal [ 33 , 54 ]. Slums are an important setting for an exploration of food insecurity, especially in India, where 25% of the urban population resides in slums or slum-like settings. People living in slums have been found to have poorer quality of life, are generally lower income, and have lower educational attainment than non-slum-dwelling populations—all factors that are known to contribute to food insecurity [ 49 ].
Five studies explored food insecurity among people with an underlying health condition. Four of these explored food insecurity among people living with HIV/AIDS [ 55 – 58 ]. These studies found that food insecurity ranged from 16 to 99% with people who are food insecure and also living with HIV/AIDS more likely to experience depression and a lower quality of life [ 57 ] and that low income [ 58 ] and low education [ 55 ] are contributing factors to food insecurity, while ownership of a pressure cooker was found to be protective against food insecurity [ 56 ]. Finally, one study explored the experiences of food insecurity among people with tuberculosis [ 59 ]. This study found that around 34% of study participants were food insecure, with low income and employment being associated with food insecurity status.
India has seen massive growth and economic change over the past 2 decades; however, this increase in financial wealth has had little impact on food insecurity and population nutrition [ 60 ]. While India has increased production and, overall, the availability of food has increased [ 61 ], these increases have not yet translated into gains for the general population. Overall, India is seeing increasing income inequality which is having a negative impact on health [ 62 ]. As a result of the disconnect between economic growth and positive health outcomes, there has been an increased interest in food insecurity and nutrition in India over the past two decades, resulting in research that seeks to measure food insecurity.
The main finding of this study is the variation in the methods for the assessment of food insecurity prevalence in India and the reliance on cross-sectional studies to elicit food insecurity data. This may be explained by the fact that food security is notoriously difficult to measure. Initial descriptions of food insecurity were conceptualized through the lens of famine [ 63 ], meaning that solutions were often confined to domestic agriculture [ 41 ]. However, in an increasingly globalized world where countries easily sell and buy goods from each other, it is now important to consider food security in a holistic manner, incorporating the whole definition of food insecurity. By considering the six main dimensions of food security: availability, access, utilization, stability, agency, and sustainability, we can better understand the experiences and drivers of food security. However, as this review has found, few studies measure more than one dimension.
Studies included in this review utilized scales that focused on household food access or availability and were assessed through experience-based scales. Experiential food insecurity scales have been used since the 1990s [ 64 ], first used in the USA and later adopted for use in low- and middle-income countries [ 21 , 65 ]. Experiential measures are based on the notion that food insecurity is associated with a set of knowable and predictable characteristics that can be assessed and quantified [ 17 , 21 ]. This assumes that households will attempt to mitigate food insecurity through a generalizable or standard pattern of responses [ 17 , 22 ]. Strategies include reducing expenditure on education expenses [ 66 ], selling assets or seeking increased employment [ 67 ], and skipping meals or limiting the sizes of meals [ 68 ]. Measures of food insecurity that are based on experience seek to capture some of these strategies and actions, and compared to other metrics, such as agriculture production, caloric intake, or anthropometric measures, they enable direct measurement of the prevalence and severity of the extent of household food insecurity, as well as the perception of the quality of their diets [ 31 ].
Given the wide variety of measurement tools used, it is difficult to present a comprehensive understanding of food insecurity in India. What is clear is that some households are experiencing food insecurity but are not hungry, while others are both hungry and food insecure. Finding a way to identify and measure at-risk households and intervene to reduce hunger is essential to closing the economic-income gap in India. However, without a measure that can be used consistently across the country that takes into consideration each of the dimensions of food security and the diversity within the Indian population, this will not be possible.
Limitations
There are some limitations to this review that should also be acknowledged. While every attempt was made to ensure this review was comprehensive, additional articles may have been missed, particularly if articles were written in a language other than English. However, given that this is the first review of its kind, with the inclusion of several databases and broad key terms, the authors are confident that there is little information that is not presented here. The articles presented in this review are largely cross-sectional, and as such, the quality of the studies means that the conclusions drawn by their authors are limited to the study population and are not widely generalizable. The cross-sectional nature of many of the studies limited the potential impact of quality assessment; as such, no quality assessment was conducted. This is a limitation of both this review and the studies included, and in general, a reflection on the rigor with which food security research has been conducted in these settings. Given the variety of approaches taken to measure food insecurity as found in this review, there are challenges in comparing the outcomes of different studies; as such, this review has not sought to present a meta-analysis. If, in the future, there can be some consistency in the use of measurement tools by researchers and agencies, a meta-analysis may be appropriate. The authors do not feel this should invalidate these findings at this time.
An Indian-specific food security measure needs to be urgently developed and implemented so that food insecurity data can more accurately and consistently be collected and contrasted for the purpose of developing suitable responses to food insecurity. Considering India’s widespread malnutrition and high prevalence of food insecurity, future work should prioritize the development of such a tool in addressing nutrition-related public health in India.
Below is the link to the electronic supplementary material.
Open Access funding enabled and organized by CAUL and its Member Institutions.
Compliance with Ethical Standards
All authors have worked in paid and unpaid roles with not-for-profit food security organizations or with organizations that focus on pregnancy and/or nutrition outcomes. No other COI to declare.
This article does not contain any studies with human or animal subjects performed by any of the authors.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance

Department of Agricultural, Food, and Resource Economics Innovation Lab for Food Security Policy, Research, Capacity and Influence

Maize Price Shocks, Food Expenditure and the Mediating Role of Access to Market in Ghana
May 14, 2024 - Edward Martey, Justina Adwoa Onumah, Frank Adusah-Poku
The existing empirical literature on the impact of food price shocks on food consumption has primarily concentrated on market-purchased foods, offering limited insights into home-produced foods and food quality. Addressing this gap, our study employs panel data from Ghana to investigate the relationship between exposure to positive maize price shocks and price variability and household consumption patterns of nutrient-dense and less nutrient-dense diets, considering both market purchases and home production. Our findings indicate that maize price shocks lead to a reduction in households' consumption of purchased nutrient-dense and less nutrient-dense food groups, while increasing the consumption of home-produced nutrient-dense food groups. The effects of maize price shocks on diet consumption vary across household types, primary crop cultivation, and wealth status. Additionally, access to markets emerges as a crucial mechanism through which maize price shocks influence households' consumption of nutrient-dense and less nutrient-dense diets. The implications of our study underscore the significance of enhanced market access and policy interventions aimed at mitigating food price increases to improve food nutrition security.
maize price shocks; food consumption; nutrient-dense diets; market access; Ghana
DOWNLOAD FILE
Tags: prci research paper
new - method size: 1 - Random key: 0, method: personalized - key: 0
You Might Also Be Interested In
STAAARS+ RFP webinar Sept 14 2022
Published on September 15, 2022
PRCI STAAARS+ Teams Presentation Video 2022
Published on July 26, 2022

Scoping Study of Agriculture Development Strategy of Nepal (ADS) (Five-year achievements)
Published on February 1, 2023
Sugarcane Production and Food Security in Uganda
Published on September 1, 2023
Institutional Arrangements Between Sugarcane Growers and Millers in Uganda and Implications for Grower Productivity and Profitability
Rwanda Natural Forest Cover Dynamics between 2015 and 2020
Published on June 19, 2023
Accessibility Questions:
For questions about accessibility and/or if you need additional accommodations for a specific document, please send an email to ANR Communications & Marketing at [email protected] .
- prci research paper,
- innovation lab for food security policy research capacity & influence

COMMENTS
According to its annual report, the FAO estimates there are 189.2 million undernourished people in India (The State of Food Security and Nutrition in the World 2020 ). Approximately 14% of India's population (189.2 million) is undernourished, and Between 15 and 49 years old, 51.4% of women are anemic.
The 2017 National Nutrition Strategy and POSHAN Abhiyaan, India's national nutrition mission launched in early 2018, provide an updated strategic framework for action to improve nutritional outcomes by holistically addressing the multiple determinants of malnutrition through cross-sectoral convergence and contextualized planning at each level ...
Almost. one million children die every year in India before. completing one year o f their age. Half the children. population in India is affected by malnutrition. Of them, 43% are under weight ...
Why obesity is rising in India despite a lower average total calorie intake, as compared to the EAT-Lancet reference diet or even the ICMR recommendations, Footnote 2 is a question beyond the scope of this paper. However, it may be related to the fact that the reference diet is developed for individuals with moderate-to-high levels of activity, whereas available studies estimate high levels of ...
India is in a stage of nutrition transition. ... Studies were limited to primary research papers using any methods, articles published in English and only original studies conducted in India between 2015 and 2020 that were relevant to the present study objective. The recent nationally representative data available was NFHS-4 2015-2016.
India ranks 101 out of 116 countries based on the Global Hunger Index 2020. The Global Nutrition Report 2018 clearly mentions that India is home to 46.6 million stunted children and 25.5 million ...
There was wide variation among the states with pockets of a double burden of malnutrition. Conclusion Using the adult cutoffs significantly overestimates thinness in adolescents in the age group of 15-19 years old in India. Stunting, which is an indicator of long term nutrition is also widely prevalent in them.
Papers were considered for inclusion if they were published in English, Hindi, Urdu or Punjabi and were original scientific research papers (review papers were not included). Included studies were required to use dietary survey data from India to estimate at least two distinct dietary patterns in humans.
Children need age-specific adequate nutrition of acceptable quality and quantity to prevent malnutrition. 12 So far, nutrition programs in India have extensively focused on improving feeding practices and access to supplementary nutrition of pregnant and lactating mothers and children younger than 6 years, but the adequacy of nutritional intake ...
RESEARCH HIGHLIGHTS ICMR-National Institute of Nutrition 2020-21 (i) Nutrient Requirements for Indians ... rural India showed that an average adult from urban India consumed 1943 Kcal/day, 289 g carbohydrates, 51.6 g fat and 55.4 g protein. In rural region, an average adult consumed 2081 kcal/day, 368 g of carbohydrates, 36 g of fat and 69 ...
This research employed a mixed method approach to explore obesity, dietary intake, and food security status among women in India. The comprehensive study protocol for this study can be found elsewhere [ 17 ]. The main aims of this research are to determine the anthropomorphic status; and investigate the dietary patterns, food habits, and food ...
these papers, around 79 per cent of the outcomes were about coverage and participant uptake. India is a signatory to the global nutrition goals and has set ambitious national targets to improve maternal and child nutrition under the National Nutrition Mission, or POSHAN Abhiyaan,1 thus demonstrating a strong national policy commitment.
4 Indian Council of Medical Research, New Delhi 110029, India. PMID ... There is a growing opportunity to facilitate technology-enabled behavioral change interventions to support NI research and practice. This paper highlights the changing landscape of food and nutrition practices in India to prepare a NI workforce that could provide some ...
This is the first paper to examine large-scale relationships between soil mineral availability and human nutritional status in India, though scientists have speculated about the relationship ...
Concise Copy. Full Copy. (Nutritive Value Of Indian Foods) Book currently available at NIN's publications counter & Also available ONLINE! Nutrient Requirements for Indians. RDA and EAR 2020. Read. What India Eats Report. Macronutrient intake of different food groups for infant and children. Read.
Nutrition deficiency is commonly observed in lactating mothers and is a rising trend in India due to improper dietary patterns, physiological factors, socio-economic and demographic factors. The aim was to study the nutritional status and its related factors among lactating mothers in the urban areas of Delhi region, India.
Food Policy Research Institute in data validation for the preparedness score and other related inputs. AUTHORS. Abbreviations List of Figures & Tables EXECUTIVE SUMMARY 1. Introduction ... the nutrition outcome concerns in India. With a budget of Rs. 9046 crore, POSHAN Abhiyaan is
The most populous country in the world, India, is experiencing a nutrition transition that involves rapidly increasing prevalence of unhealthy packaged foods. To assist consumers in making healthier packaged food choices, the Government of India is in the process of designing and implementing a new front-of-pack nutrition labelling system.
elated ailments, among the growing geriatric population is a challenge. Ageing is associated with several changes in body composition including a decline in the lean body mass usually accompanied by an increase in body fat content which have a bearing on the nutrient requirements for the elderly. The nutrient requirements currently recommended for Indian adults are primarily computed using a ...
The Nutrition Foundation of India (NFI) is a non-governmental voluntary organization dedicated to improving the nutritional status of Indians by. Carrying out research on major nutritional problems. Research to operationalize proven interventions to improve nutritional status in national programs. Evaluation of national nutrition programs.
This paper presents the basic facts about growth, poverty and nutrition in India, it points to a number of puzzles, and it sketches a preliminary story that is consistent with the evidence. The reduction in calorie consumption cannot be attributed to declining real incomes, nor to any increase in the relative price of food.
To review the current evidence on the association between diet quality and economic costs in low- and middle-income countries, this paper first conducted a literature search to identify studies that include a dietary exposure, nutrition, or health outcome, and a cost estimate.
The latest study finds out, that 56.7 per cent of the disease burden in India is due to an unhealthy diet, as it releases the 17 necessary dietary guidelines to meet the essential requirement of a balanced diet and to prevent non-communicable diseases (NCDS) such as obesity and diabetes. ... Nutrition plays an important role right from the time ...
Researchers found "significant" health benefits of plant-based diets after reviewing 48 papers published between January 2000 and June 2023. Stock.adobe.com Turns out, vegan and vegetarian diets ...
A new book by Satyendra Nath Bose's student and particle physicist Partha Ghose talks of Bose's relations with Albert Einstein. Nature India caught up with Ghose to discuss some untold stories ...
India has a rich and highly varied cuisine, and its various diets are strongly related to social identity, religion and other cultural factors (1), as well as local agricultural practices and availability of diverse foods (2).The 'average diet' in a country as large and geographically diverse as India is therefore likely to be of little relevance from a public health nutrition perspective.
2.1. Review of Dietary Data from National Surveys. At the national level, the NNMB was established in 1972 by the National Institute of Nutrition and Indian Council of Medical Research to collect data on food and nutrient intakes in rural and tribal populations across 10 states (Kerala, Tamil Nadu, Karnataka, Andhra Pradesh, Maharashtra, Gujarat, Madhya Pradesh, Orissa, West Bengal, and Uttar ...
Background: The Indian automobile industry, including the auto component industry, is a significant part of the country's economy and has experienced growth over the years.India is now the world's 3 rd largest passenger car market and the world's second-largest two-wheeler market. Along with the boon, the bane of road accident fatalities is also a reality that needs urgent attention, as ...
India has seen massive growth and economic change over the past 2 decades; however, this increase in financial wealth has had little impact on food insecurity and population nutrition . While India has increased production and, overall, the availability of food has increased , these increases have not yet translated into gains for the general ...
The implications of our study underscore the significance of enhanced market access and policy interventions aimed at mitigating food price increases to improve food nutrition security. Keywords. maize price shocks; food consumption; nutrient-dense diets; market access; Ghana