- Aims and scope
- About the journal
- Editorial board
- Best practice
- Editorial policy
- EnM Introduction Video & Testimonials
- Current issue
- Ahead-of print
- Article type
- Article category
- Guidelines in EnM
- COVID-19 in EnM
- Audioslides gallery
- Audio summary
- Funded articles
- Endocrinol Metab Search
- Author index
- Submission guidelines
- Research and publication ethics
- Permission guidelines
- Article-processing charge
- Author’s checklist
- Copyright transfer agreement
- E-submission

- E-SUBMISSION

- Author information
- Article notes
- Copyright and License information
1 Department of General Medicine, Government Medical College, Kozhikode, India.
2 Department of Internal Medicine, Badr Al Samaa Hospital, Barka, Oman.
3 Padma Yog Sadhana, A Unit of Terna Public Charitable Trust, Navi Mumbai, India.
4 Joshi Clinic, Lilavati Hospital and Bhatia Hospital, Mumbai, India.
Copyright © 2018 Korean Endocrine Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License ( http://creativecommons.org/licenses/by-nc/4.0/ ) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 11,680 Views
- 285 Download
- 45 Web of Science
- 60 Crossref
- Full Article
- Figure & data

INTRODUCTION
Yoga in type 2 diabetes, duration and frequency of yoga practice, mechanism of benefits and evidence from clinical trials, limitations of studies on yoga, conclusions, article information.
- Yoga originated in India more than 5,000 years ago and is a means of balancing and harmonizing the body, mind, and emotions. Yoga practice is useful in the management of various lifestyle diseases, including type 2 diabetes. Psycho-neuro-endocrine and immune mechanisms are involved in the beneficial effects of yoga on diabetes. Incorporation of yoga practice in daily life helps to attain glycaemic control and reduces the risk of complications in people with diabetes. In this review, we briefly describe the role of various yoga practices in the management of diabetes based on evidence from various clinical studies.
- Keywords : Yoga ; Diabetes mellitus ; Yoga asana ; Pranayama ; Meditation
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
- 1. International Diabetes Federation. Chapter 3, The global picture. IDF Diabetes Atlas; 8th ed. Brussels: International Diabetes Federation; 2017. p. 40–59.
- 2. Thangasami SR, Chandani AL, Thangasami S. Emphasis of yoga in the management of diabetes. J Diabetes Metab 2015;6:613. Article
- 3. Liu XC, Pan L, Hu Q, Dong WP, Yan JH, Dong L. Effects of yoga training in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Thorac Dis 2014;6:795–802. PubMed PMC
- 4. Jyotsna VP. Prediabetes and type 2 diabetes mellitus: evidence for effect of yoga. Indian J Endocrinol Metab 2014;18:745–749. Article PubMed PMC
- 5. Youngwanichsetha S, Phumdoung S, Ingkathawornwong T. The effects of mindfulness eating and yoga exercise on blood sugar levels of pregnant women with gestational diabetes mellitus. Appl Nurs Res 2014;27:227–230. Article PubMed
- 6. Miller CK, Kristeller JL, Headings A, Nagaraja H, Miser WF. Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a pilot study. J Acad Nutr Diet 2012;112:1835–1842. Article PubMed PMC
- 7. Jindal N, Joshi NP. Comparative study of Vamana and Virechanakarma in controlling blood sugar levels in diabetes mellitus. Ayu 2013;34:263–269. Article PubMed PMC
- 8. Shalinee , Mishra D, Kamal K, Gupta AK, Sharma KK. Shankhaprakshalana: a yogic karma for purification. Int J Ayurvedic Herb Med 2012;2:578–581.
- 9. Skoro-Kondza L, Tai SS, Gadelrab R, Drincevic D, Greenhalgh T. Community based yoga classes for type 2 diabetes: an exploratory randomised controlled trial. BMC Health Serv Res 2009;9:33 Article PubMed PMC PDF
- 10. Sreedevi A, Gopalakrishnan UA, Karimassery Ramaiyer S, Kamalamma L. A randomized controlled trial of the effect of yoga and peer support on glycaemic outcomes in women with type 2 diabetes mellitus: a feasibility study. BMC Complement Altern Med 2017;17:100 Article PubMed PMC PDF
- 11. Malhotra V, Singh S, Tandon OP, Sharma SB. The beneficial effect of yoga in diabetes. Nepal Med Coll J 2005;7:145–147. PubMed
- 12. Madhavi S, Raju PS, Reddy MV, Annapurna N, Sahay BK, Kumari DG, et al. Effect of yogic exercises on lean body mass. J Assoc Physicians India 1985;33:465–466. PubMed
- 13. Manjunatha S, Vempati RP, Ghosh D, Bijlani RL. An investigation into the acute and long-term effects of selected yogic postures on fasting and postprandial glycemia and insulinemia in healthy young subjects. Indian J Physiol Pharmacol 2005;49:319–324. PubMed
- 14. Mullur RS, Ames D. Impact of a 10 minute seated yoga practice in the management of diabetes. J Yoga Phys Ther 2016;6:1000224. Article PubMed PMC
- 15. Pal GK. Effects of pranayama on cardiovascular health. Int J Clin Exp Physiol 2016;3:57–58. Article
- 16. Bal BS. Effects of short term practice of Anuloma Viloma Pranayama on components of health-related fitness. Educ Prac Innov 2015;2:10–18. Article
- 17. Srivastava S, Goyal P, Tiwari SK, Patel AK. Interventional effect of Bhramari Pranayama on mental health among college students. Int J Ind Psychol 2017;4:29–33.
- 18. Nivethitha L, Mooventhan A, Manjunath NK. Effects of various PraXMLLink_XYZayama on cardiovascular and autonomic variables. Anc Sci Life 2016;36:72–77. Article PubMed PMC
- 19. Singh RB, Wilczynska-Kwiatek A, Fedacko J, Pella D, De Meester F. Pranayama: the power of breath. Int J Disabil Hum Dev 2009;8:141–153. Article PDF
- 20. Gurjar AA, Ladhake SA, Thakare AP. Analysis of acoustic of “OM” chant to study it's effect on nervous system. Int J Comput Sci Netw Secur 2009;9:363–367.
- 21. Bhavanani AB, Madanmohan , Sanjay Z, Vithiyalakshmi SL. Immediate cardiovascular effects of pranava relaxation in patients with hypertension and diabetes. Biomed Hum Kinet 2012;4:66–69. Article PDF
- 22. Mohanty S, Metri K, Nagaratna R, Nagendra HR. Immediate effect of mind sound resonance technique (MSRT-A yogic relaxation technique) on cognitive functions in type 2 diabetes. Voice Res 2015;4:44–45.
- 23. Jyotsna VP, Joshi A, Ambekar S, Kumar N, Dhawan A, Sreenivas V. Comprehensive yogic breathing program improves quality of life in patients with diabetes. Indian J Endocrinol Metab 2012;16:423–428. Article PubMed PMC
- 24. Ricard M, Lutz A, Davidson RJ. Mind of the meditator. Sci Am 2014;311:38–45. Article
- 25. Chung SC, Brooks MM, Rai M, Balk JL, Rai S. Effect of Sahaja yoga meditation on quality of life, anxiety, and blood pressure control. J Altern Complement Med 2012;18:589–596. Article PubMed
- 26. Keyworth C, Knopp J, Roughley K, Dickens C, Bold S, Coventry P. A mixed-methods pilot study of the acceptability and effectiveness of a brief meditation and mindfulness intervention for people with diabetes and coronary heart disease. Behav Med 2014;40:53–64. Article PubMed PMC
- 27. Amita S, Prabhakar S, Manoj I, Harminder S, Pavan T. Effect of yoga-nidra on blood glucose level in diabetic patients. Indian J Physiol Pharmacol 2009;53:97–101. PubMed
- 28. Singh K. Hasta Mudra's and respiratory system. Int J Phys Educ Sports Health 2015;1:83–86.
- 29. Vaishali K, Kumar KV, Adhikari P, UnniKrishnan B. Effects of yoga-based program on glycosylated hemoglobin level serum lipid profile in community dwelling elderly subjects with chronic type 2 diabetes mellitus: a randomized controlled trial. Phys Occup Ther Geriatr 2012;30:22–30. Article
- 30. Habibi N, Farsani ZH, Yazdani B, Arianshakib R, Noruozi P. The influence of yoga-on risk profiles programs in women with diabetes type II. Adv Environ Biol 2013;2013:550–556.
- 31. Subramaniyan TG, Subramaniyan N, Chidambaram M. Brisk walking and yoga as adjuvant therapy in management of type 2 diabetes mellitus. Int J Student Res 2012;2:43–46. Article
- 32. Angadi P, Jagannathan A, Thulasi A, Kumar V, Umamaheshwar K, Raghuram N. Adherence to yoga and its resultant effects on blood glucose in type 2 diabetes: a community-based follow-up study. Int J Yoga 2017;10:29–36. Article PubMed PMC
- 33. Shah NJ, Shah UN. Central retinal vein occlusion following Sirsasana (headstand posture). Indian J Ophthalmol 2009;57:69–70. Article PubMed PMC
- 34. Innes KE, Vincent HK. The influence of yoga-based programs on risk profiles in adults with type 2 diabetes mellitus: a systematic review. Evid Based Complement Alternat Med 2007;4:469–486. Article PubMed PDF
- 35. Aswathy S, Unnikrishnan AG, Kalra S. Effective management of type 2 DM in India: looking at low-cost adjunctive therapy. Indian J Endocrinol Metab 2013;17:149–152. Article PubMed PMC
- 36. Bystritsky A, Danial J, Kronemyer D. Interactions between diabetes and anxiety and depression: implications for treatment. Endocrinol Metab Clin North Am 2014;43:269–283. Article PubMed
- 37. Mahajan AS. Role of yoga in hormonal homeostasis. Int J Clin Exp Physiol 2014;1:173–178. Article
- 38. Innes KE, Bourguignon C, Taylor AG. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. J Am Board Fam Pract 2005;18:491–519. Article PubMed
- 39. Kosuri M, Sridhar GR. Yoga practice in diabetes improves physical and psychological outcomes. Metab Syndr Relat Disord 2009;7:515–517. Article PubMed
- 40. Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression. Part II: clinical applications and guidelines. J Altern Complement Med 2005;11:711–717. Article PubMed
- 41. Gangadhar BN, Naveen GH, Rao MG, Thirthalli J, Varambally S. Positive antidepressant effects of generic yoga in depressive out-patients: a comparative study. Indian J Psychiatry 2013;55(Suppl 3):S369–S373. Article PubMed PMC
- 42. Agrawal RP, Aradhana SH, Beniwal R, Sabir M, Kochar DK. Influence of yogic treatment on quality of life outcomes, glycaemic control and risk factors in diabetes mellitus. Int J Diab Dev Countries 2003;23:130–134.
- 43. Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. J Altern Complement Med 2010;16:3–12. Article PubMed
- 44. Kiecolt-Glaser JK, Christian LM, Andridge R, Hwang BS, Malarkey WB, Belury MA, et al. Adiponectin, leptin, and yoga practice. Physiol Behav 2012;107:809–813. Article PubMed PMC
- 45. Newberg AB, Iversen J. The neural basis of the complex mental task of meditation: neurotransmitter and neurochemical considerations. Med Hypotheses 2003;61:282–291. Article PubMed
- 46. Shree N, Bhonde RR. Can yoga therapy stimulate stem cell trafficking from bone marrow? J Ayurveda Integr Med 2016;7:181–184. Article PubMed PMC
- 47. Dusek JA, Otu HH, Wohlhueter AL, Bhasin M, Zerbini LF, Joseph MG, et al. Genomic counter-stress changes induced by the relaxation response. PLoS One 2008;3:e2576. Article PubMed PMC
- 48. Hegde SV, Adhikari P, Kotian S, Pinto VJ, D'Souza S, D'Souza V. Effect of 3-month yoga on oxidative stress in type 2 diabetes with or without complications: a controlled clinical trial. Diabetes Care 2011;34:2208–2210. Article PubMed PMC
- 49. Gordon L, Morrison EY, McGrowder D, Penas YF, Zamoraz EM, Garwood D, et al. Effect of yoga and traditional physical exercise on hormones and percentage insulin binding receptor in patients with type 2 diabetes. Am J Biochem Biotechnol 2008;4:35–42. Article PDF
- 50. Sahay BK. Yoga and diabetes. J Assoc Physicians India 1986;34:645–648. PubMed
- 51. Bhaskaracharyulu C, Raju PS, Madhavi S. The effect of yoga on lipoprotein profile in diabetics. J Diabet Assoc India 1986;XXVI:120–122.
- 52. Sahay BK. Role of yoga in diabetes. J Assoc Physicians India 2007;55:121–126. PubMed
- 53. Kapur A. Proceedings of novo nordisk diabetes update. Yoga and diabetes; Bombay: Health Care Communications; 1994. p. 159–167.
- 54. McDermott KA, Rao MR, Nagarathna R, Murphy EJ, Burke A, Nagendra RH, et al. A yoga intervention for type 2 diabetes risk reduction: a pilot randomized controlled trial. BMC Complement Altern Med 2014;14:212 Article PubMed PMC PDF
- 55. Vaibhavi B, Satyam T, Sanjibkumar P, Raghuram N, Ramarao NH. Effect of holistic module of yoga and Ayurvedic Panchakarma in type 2 diabetes mellitus: a pilot study. Open J Endocr Metab Dis 2013;3:90–98. Article
- 56. Cui J, Yan JH, Yan LM, Pan L, Le JJ, Guo YZ. Effects of yoga in adults with type 2 diabetes mellitus: a meta-analysis. J Diabetes Investig 2017;8:201–209. Article PubMed
- 57. Sahay BK, Murthy KJR, Raju PS, Madhavi S. Effect of yogic practices on exercises tolerance in diabetes. Diabetes 1991;40(Suppl 1):398.
- 58. Hagins M, States R, Selfe T, Innes K. Effectiveness of yoga for hypertension: systematic review and meta-analysis. Evid Based Complement Alternat Med 2013;2013:649836. Article PubMed PMC PDF
- 59. Cramer H, Lauche R, Haller H, Steckhan N, Michalsen A, Dobos G. Effects of yoga on cardiovascular disease risk factors: a systematic review and meta-analysis. Int J Cardiol 2014;173:170–183. Article PubMed
- 60. Chohan IS, Nayar HS, Thomas P, Geetha NS. Influence of yoga on blood coagulation. Thromb Haemost 1984;51:196–197. Article PubMed PDF
- 61. Patwardhan AR. Yoga research and public health: is research aligned with the stakeholders' needs? J Prim Care Community Health 2016 8 11 [Epub]. Article
Showing the mechanisms of benefits of yoga practice in type 2 diabetes. BP, blood pressure; HPA, hypothalamic-pituitary-adrenal; GH, growth hormone.

Some Yoga Practices Beneficial for the Management of Type 2 Diabetes Mellitus
Some of the beneficial effects of yoga practices on type 2 diabetes mellitus, figure & data.
- Yoga practice can reduce metabolic syndrome and cardiovascular risk in climacteric women Laura Alves Cota e Souza, Thiago Magalhães Gouvea, Francielle Caroline Fernandes, Maria Ruth Gonçalves Gaede Carrillo, Vanja Maria Veloso, Ariosvaldo Figueiredo Santos Filho, Angélica Alves Lima Journal of Behavioral Medicine .2024; 47(1): 94. CrossRef
- Clinical Practice Guidelines for mental health and well-being in patients with chronic medical illnesses Sandeep Grover, Ajit Avasthi, Abdul Majid Indian Journal of Psychiatry .2024; 66(Suppl 2): S338. CrossRef
- Complementary and alternative system of medicine for type 2 diabetes mellitus and its complications: A scoping review Shradha S Parsekar, Nachiket Gudi, Sujata Chodankar Walke, Prabhu Dutta Shaw, Aditi Hombali, Anupama V Nayak, Basavaraj S Hadapad F1000Research .2024; 11: 526. CrossRef
- CLINICAL STUDY OF YOGASANA AND PATHYAAHARA IN MANAGEMENT OF MADHUMEHA (DIABETES MELLITUS-2) Jyoti Prajapati, Pramod Kumar Mishra, Brahmanand Sharma International Ayurvedic Medical Journal .2024; 12(02): 346. CrossRef
- Therapeutic role of yoga in hypertension Anjali Mangesh Joshi, Arkiath Veettil Raveendran, Muruganathan Arumugam World Journal of Methodology .2024;[Epub] CrossRef
- The effect of yoga practices on health parameters: A review Gökhan Çetinoğlu, Emirhan Pehlivan Turkish Journal of Kinesiology .2024; 10(1): 41. CrossRef
- Managing Diabetic Complications with Alternative Therapeutic Strategies Shobhit Prakash Srivastava, Pawan Upadhyay, Shibu Das, Neha Tiwari, Sudhanshu Mishra, Shivendra Mani Tripathi Current Diabetes Reviews .2024;[Epub] CrossRef
- Novel Approaches to Control Diabetes Malissa Mathew Dmello, Geeta Bhagwat Current Diabetes Reviews .2024;[Epub] CrossRef
- A Study on Yoga-Based Lifestyle Intervention versus Dietary Intervention Alone on Cardiometabolic Risk Factors among People with Prediabetes Neha Saboo, Sudhanshu Kacker Annals of African Medicine .2024; 23(2): 202. CrossRef
- A self-management plus mind body intervention for adolescents and young adults with type 2 diabetes: Trial design and methodological report Molly McVoy, David Miller, Irina Bransteter, Rose Gubitosi-Klug, Tracy Segal, Jessica Surdam, Martha Sajatovic, Jeffery A. Dusek Contemporary Clinical Trials .2023; 133: 107317. CrossRef
- Epidemiology of type 2 diabetes mellitus and treatment utilization patterns among the elderly from the first wave of Longitudinal Aging study in India (2017-18)using a Heckman selection model Papai Barman, Milan Das, Madhur Verma BMC Public Health .2023;[Epub] CrossRef
- Is Type 2 Diabetes Mellitus a Behavioural Disorder? An Evidence Review for Type 2 Diabetes Mellitus Prevention and Remission through Lifestyle Modification Matthias Li, Mohammad Sadiq Jeeyavudeen, Ganesan Arunagirinathan, Joseph Pappachan European Endocrinology .2023; 19(1): 7. CrossRef
- Yogic practices for dyslipidemia in type 2 diabetes mellitus: A systematic review of randomized-controlled trials Bandana Sairem, Khushbu Jain BLDE University Journal of Health Sciences .2023; 8(1): 20. CrossRef
- Effect of yoga protocol in primary snoring: A pilot study JojanJ Jerone, Ashok Patil, SavitaS Angadi, AmalS Chandran Journal of Ayurveda .2023; 17(2): 114. CrossRef
- Effects of different mind-body exercises on glucose and lipid metabolism in patients with type 2 diabetes: A network meta-analysis Sijun Wu, Lin Wang, Yuxuan He, Fengrui Shi, Huiqi Zhuang, Linqi Mei, Youling Qian Complementary Therapies in Clinical Practice .2023; 53: 101802. CrossRef
- Mechanisms of improved body composition among perimenopausal women practicing Meditative Movement: a proposed biobehavioral model Dara L. James, Linda K. Larkey, Bronwynne Evans, Ann Sebren, Kimberley Goldsmith, Erica Ahlich, Nanako A. Hawley, Afton Kechter, Dorothy D. Sears Menopause .2023; 30(11): 1114. CrossRef
- A comparative analysis of Vamana and Shamana Chikitsa in prediabetes management: A randomized clinical trial Uttamram Yadav, Santosh Kumar Bhatted Journal of Ayurveda and Integrative Medicine .2023; 14(5): 100764. CrossRef
- Siddha Therapeutic Approach to Diabetic Nephropathy – A Review P. Parvathy, G. S. Lekha, S. Aparna, A. Kanagarajan Journal of Natural Remedies .2023; : 1359. CrossRef
- Enhancing Type 2 Diabetes Management: Exploring the Synergistic Impact of Vestibular Exercise and Yoga Athira MS, Sheela Joice P P, Mohan Varughese, Suresh Babu Sayana Cureus .2023;[Epub] CrossRef
- Dynamic In Silico Model of Type 2 Diabetes Treated With Metformin Combined With Exercise: A Sobol Sensitivity Analysis Darshna M. Joshi Avicenna Journal of Pharmaceutical Research .2023; 3(2): 91. CrossRef
- Complementary and alternative system of medicine for type 2 diabetes mellitus and its complications: A scoping review Shradha S Parsekar, Nachiket Gudi, Sujata Chodankar Walke, Prabhu Dutta Shaw, Aditi Hombali, Anupama V Nayak, Basavaraj S Hadapad F1000Research .2023; 11: 526. CrossRef
- Exploring the Impact of Combined Thai Yoga and Elastic Band Exercise on Physical Fitness and Exercise Capacity in Older Patients with Type 2 Diabetes Nattha Muangritdech, Tichanon Promsrisuk, Ratchaniporn Kongsui, Napatr Sriraksa, Sitthisak Thongrong, Arunrat Srithawong Physical Education Theory and Methodology .2023; 23(6): 894. CrossRef
- Role of Yoga and Its Plausible Mechanism in the Mitigation of DNA Damage in Type-2 Diabetes: A Randomized Clinical Trial Rajesh G Nair, Mithila M Vasudev, Ramesh Mavathur Annals of Behavioral Medicine .2022; 56(3): 235. CrossRef
- Efficacy of Integrated Ayurveda treatment protocol in type 2 Diabetes Mellitus – A case report Suketha Kumari, Laxmikant S.D, Sonika B, Suman Khanal Journal of Ayurveda and Integrative Medicine .2022; 13(1): 100512. CrossRef
- Role of structured exercise therapy on cognitive markers and stress parameters in young patients with Type 2 diabetes mellitus Harpreet Kour, VA Kothiwale, ShivaprasadS Goudar Indian Journal of Health Sciences and Biomedical Research (KLEU) .2022; 15(1): 70. CrossRef
- The Influence of Amateur Sports on Health Quality M. M. Vovchenko Ukraïnsʹkij žurnal medicini, bìologìï ta sportu .2022; 7(1): 8. CrossRef
- Complementary and alternative system of medicine for type 2 diabetes mellitus and its complications: A scoping review Shradha S Parsekar, Nachiket Gudi, Sujata Chodankar Walke, Prabhu Dutta Shaw, Aditi Hombali, Anupama V Nayak, Basavaraj S Hadapad F1000Research .2022; 11: 526. CrossRef
- Neuroimaging perspective in targeted treatment for type 2 diabetes melitus and sleep disorders Karen M. von Deneen, Malgorzata A. Garstka Intelligent Medicine .2022; 2(4): 209. CrossRef
- Efficacy of yoga practices on emotion regulation and mindfulness in type 2 diabetes mellitus patients Amit Kanthi, Singh Deepeshwar, Chidananda Kaligal, Mahadevappa Vidyashree, Dwivedi Krishna Yoga Mimamsa .2022; 54(1): 12. CrossRef
- Inside the diabetic brain: Insulin resistance and molecular mechanism associated with cognitive impairment and its possible therapeutic strategies Bhaskar Jyoti Dutta, Shamsher Singh, Sanket Seksaria, Ghanshyam Das Gupta, Amrita Singh Pharmacological Research .2022; 182: 106358. CrossRef
- LINKAGE OF YOGA TO OXIDATIVE STRESS IN PATIENTS WITH DIABETES MELLITUS, TYPE 2 Deepika Khatri, Yuliya Tyravska InterConf .2022; (15(117)): 215. CrossRef
- An Observational Study on the Effect of Yoga and Sudarshan Kriya in Type 2 Diabetes Mellitus Patients Meenakshi R Verma, Deepakkumar G Langade, Rahul D Rao, Shreya Shivangi, Sonali Khedkar, Divya Kanchibhotla Cureus .2022;[Epub] CrossRef
- The most effective exercise to prevent obesity: A longitudinal study of 33,731 Taiwan biobank participants Wan-Yu Lin Frontiers in Nutrition .2022;[Epub] CrossRef
- Type 2 diabetes mellitus, its impact on quality of life and how the disease can be managed-a review Priyanka Garg, Navneet Duggal Obesity Medicine .2022; 35: 100459. CrossRef
- Effect of om chanting and yoga nidra on blood pressure and lipid profile in hypertension – A randomized controlled trial K. Anjana, R. Archana, J.K. Mukkadan Journal of Ayurveda and Integrative Medicine .2022; 13(4): 100657. CrossRef
- Effect of yoga intervention on skeletal muscle linked glucose homeostasis in pre-diabetic individuals: Study protocol for a randomized controlled trial Supriya Bhalerao, Jayshree Kharche, Shubhangi Harke Advances in Integrative Medicine .2022; 9(4): 230. CrossRef
- Popular Complementary and Alternative Therapy Methods in Different Conditions Akın SÜZER, Nevriye ÜNAL SÜZER, Raziye ŞAVKIN, Nihal BÜKER International Journal of Traditional and Complementary Medicine Research .2022; 3(3): 201. CrossRef
- Add on Hypoglycemic effect of customized Yoga module in diabetes mellitus: A case report KK Resmi, MB Kavita, Gurubasavaraj Yalagachin Journal of Ayurveda Case Reports .2022; 5(4): 163. CrossRef
- Modern Postural Yoga and the Health-Spirituality-Neoliberalism Nexus Matteo Di Placido, Anna Strhan, Stefania Palmisano Fieldwork in Religion .2022;[Epub] CrossRef
- Metabolic syndrome and possible treatments (consecutive therapies): a literature review Jitender Sorout, Sudhanshu Kacker, Neha Saboo INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine) .2022; 18(6): 351. CrossRef
- Umbilical Cord-Mesenchymal Stem Cell-Conditioned Medium Improves Insulin Resistance in C2C12 Cell Kyung-Soo Kim, Yeon Kyung Choi, Mi Jin Kim, Jung Wook Hwang, Kyunghoon Min, Sang Youn Jung, Soo-Kyung Kim, Yong-Soo Choi, Yong-Wook Cho Diabetes & Metabolism Journal .2021; 45(2): 260. CrossRef
- Yoga as a complementary therapy for metabolic syndrome: A narrative review Dastan M. Khoshnaw, Abhijit A. Ghadge Journal of Integrative Medicine .2021; 19(1): 6. CrossRef
- Effect of yoga on glycemia and lipid parameters in type-2 diabetes: a meta-analysis Deep Dutta, Saptarshi Bhattacharya, Meha Sharma, Deepak Khandelwal, Vineet Surana, Sanjay Kalra Journal of Diabetes & Metabolic Disorders .2021; 20(1): 349. CrossRef
- Effect of Yoga on Glucose Control and Quality of Life in Patients of Prediabetes Rajesh Rajput, Karamvir Yadav, Meena Rajput, Jyoti Yadav, Neharika Saini Metabolic Syndrome and Related Disorders .2021; 19(8): 417. CrossRef
- Effect of long-term Yogic practices in type 2 diabetes mellitus: a single case study KetakiH Patil, Vidya Wasnik (Thatere), VijayG Patrikar Journal of Indian System of Medicine .2021; 9(2): 135. CrossRef
- Effectiveness of Yoga Lifestyle on Lipid Metabolism in a Vulnerable Population—A Community Based Multicenter Randomized Controlled Trial Raghuram Nagarathna, Saurabh Kumar, Akshay Anand, Ishwara N. Acharya, Amit Kumar Singh, Suchitra S. Patil, Ramesh H Latha, Purnima Datey, Hongasandra Ramarao Nagendra Medicines .2021; 8(7): 37. CrossRef
- Yoga for Healthy Aging: Science or Hype? Advances in Geriatric Medicine and Research .2021;[Epub] CrossRef
- A Prospective Study on Type-2 Diabetic Complications and Efficacy of Integrated Yoga: A Pan India 2017 Suchitra S. Patil, Nagarathna Raghuram, Amit Singh, S. K. Rajesh, Sabzar Ahmed, Nagendra Hongasandra Annals of Neurosciences .2021; 28(1-2): 21. CrossRef
- Effects of Yoga Therapy and Walking Therapy in Reducing Blood Sugar Levels on Diabetes Mellitus Patients in the Community Wachidah Yuniartika, Agus Sudaryanto, Abi Muhlisin, Dian Hudiyawati, Dimas Ria Angga Pribadi Open Access Macedonian Journal of Medical Sciences .2021; 9(E): 906. CrossRef
- Yoga nidra practice shows improvement in sleep in patients with chronic insomnia: A randomized controlled trial KARUNA DATTA, MANJARI TRIPATHI, MANSI VERMA, DEEPIKA MASIWAL, HRUDA NANDA MALLICK The National Medical Journal of India .2021; 34: 143. CrossRef
- MANAGEMENT THROUGH AYURVEDIC MEDICATIONS AND LIFESTYLE MODIFICATION (PATHYASEVANA AND YOGASANA) IN A CASE OF POST-COVID COMPLICATION DIABETES MELLITUS (TYPE 2 DM): A SINGLE CASE STUDY Prajakta D. Nimje, Vidya Wasnik (Thatere), Sumeeta Jain International Ayurvedic Medical Journal .2021; 9(10): 2619. CrossRef
- Efficacy of palliative herbal decoction (Darvyadi Kwatha) with lifestyle modification in the management of prediabetes (Prameha): a single-arm clinical trial Uttamram Yadav, SantoshK Bhatted Journal of Indian System of Medicine .2021; 9(4): 265. CrossRef
- Role of yoga as an adjuvant therapy in the management of metabolic syndrome – A randomized control pilot study Rajasekaran Balaji, Meena Ramanathan, AnandaBalayogi Bhavanani Yoga Mimamsa .2021; 53(2): 116. CrossRef
- Effect of an 8-Week Yoga-Based Lifestyle Intervention on Psycho-Neuro-Immune Axis, Disease Activity, and Perceived Quality of Life in Rheumatoid Arthritis Patients: A Randomized Controlled Trial Surabhi Gautam, Manoj Kumar, Uma Kumar, Rima Dada Frontiers in Psychology .2020;[Epub] CrossRef
- Type 2 diabetes mellitus: pathogenesis and genetic diagnosis D. Himanshu, Wahid Ali, Mohd Wamique Journal of Diabetes & Metabolic Disorders .2020; 19(2): 1959. CrossRef
- Prevalence and Awareness of Stroke and Other Comorbidities Associated with Diabetes in Northwest India Vivek Podder, Vinod Srivastava, Saurabh Kumar, Raghuram Nagarathna, Madhava Sai Sivapuram, Navneet Kaur, Kanupriya Sharma, Amit Kumar Singh, Neeru Malik, Akshay Anand, Hongasandra R. Nagendra Journal of Neurosciences in Rural Practice .2020; 11: 467. CrossRef
- Patterns of concomitant use of Ayurveda and conventional anti-diabetic formulations - Experiences at a tertiary care Ayurveda hospital, India R Galib, Poonam Dang, Vijay Kumar, Rakesh Rana, Pramod Yadav, PK Prajapati AYU (An international quarterly journal of research in Ayurveda) .2020; 41(2): 72. CrossRef
- A perspective on yoga as a preventive strategy for coronavirus disease 2019 R Nagarathna, HR Nagendra, Vijaya Majumdar International Journal of Yoga .2020; 13(2): 89. CrossRef
- Effect of Ayurveda intervention, lifestyle modification and Yoga in prediabetic and type 2 diabetes under the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS)–AYUSH integration project Ramavtar Sharma, VinodKumar Shahi, Shruti Khanduri, Arun Goyal, Suhas Chaudhary, RakeshKumar Rana, Richa Singhal, Narayanam Srikanth, KartarSingh Dhiman AYU (An international quarterly journal of research in Ayurveda) .2019; 40(1): 8. CrossRef
- Type 2 diabetes mellitus, physical activity, yoga and telomere length: A literature review Reepa A. Ughreja, Reena A. Ughreja Journal of Metabolic Health .2019;[Epub] CrossRef

- Initial Combination Therapy in Type 2 Diabetes
- Skeletal Senescence with Aging and Type 2 Diabetes

- Short report
- Open access
- Published: 23 December 2021
Diabetic yoga protocol improves glycemic, anthropometric and lipid levels in high risk individuals for diabetes: a randomized controlled trial from Northern India
- Navneet Kaur 1 , 4 ,
- Vijaya Majumdar 2 ,
- Raghuram Nagarathna 2 ,
- Neeru Malik 3 ,
- Akshay Anand 4 &
- Hongasandra Ramarao Nagendra 2
Diabetology & Metabolic Syndrome volume 13 , Article number: 149 ( 2021 ) Cite this article
2986 Accesses
6 Citations
Metrics details
To study the effectiveness of diabetic yoga protocol (DYP) against management of cardiovascular risk profile in a high-risk community for diabetes, from Chandigarh, India.
The study was a randomized controlled trial, conducted as a sub study of the Pan India trial Niyantrita Madhumeha Bharath (NMB) . The cohort was identified through the Indian Diabetes Risk Scoring (IDRS) (≥ 60) and a total of 184 individuals were randomized into intervention (n = 91) and control groups (n = 93). The DYP group underwent the specific DYP training whereas the control group followed their daily regimen. The study outcomes included changes in glycemic and lipid profile. Analysis was done under intent-to-treat principle.
The 3 months DYP practice showed diverse results showing glycemic and lipid profile of the high risk individuals. Three months of DYP intervention was found to significantly reduce the levels of post-prandial glucose levels (p = 0.035) and LDL-c levels (p = 0.014) and waist circumference (P = 0.001).
The findings indicate that the DYP intervention could improve the metabolic status of the high-diabetes-risk individuals with respect to their glucose tolerance and lipid levels, partially explained by the reduction in abdominal obesity. The study highlights the potential role of yoga intervention in real time improvement of cardiovascular profile in a high diabetes risk cohort.
Trial registration: CTRI, CTRI/2018/03/012804. Registered 01 March 2018—Retrospectively registered, http://www.ctri.nic.in/ CTRI/2018/03/012804.
Introduction
The rise of diabetes in the developing world poses a threat to meager health budgets. Owing to the strong association between various morbidity and mortality outcomes as complications of this dreaded disease, early detection of diabetes risk through non-invasive parameters is a primary requisite. Observational studies show that the risk reduction for diabetes can be decreased by 58% or 63–65% if risk factors could be controlled [ 1 , 2 ]. Many argue that such experimental strategies for the possible halting of conversion of prediabetes into diabetes must continue to include pharmacological interventions even though the rates have not been compared [ 3 ]. Identification of individuals at increased risk for the disease with invasive measurements of fasting and post challenge (postprandial) blood glucose are costly and time consuming. Hence, it has been advocated that the realistic prevention of diabetes should identify high-risk subjects with the use of the non-invasive risk scores [ 4 ]. Such studies should also target subjects with normoglycemia and prevent their progression to poor glycemic status [ 4 ].
Yoga plays a promising role in minimizing the risk of Diabetes for high-risk individuals with prediabetes [ 5 , 6 ]. It reduces body weight, glucose, and lipid levels, though, most of these studies comply with the guidelines of randomized controlled trials adhered to the CONSORT statements [ 7 , 8 , 9 , 10 , 11 ] whereas majority of studies have not reported as per CONSORT statements [ 12 , 13 , 14 , 15 ]. Several review of published studies, in people with diabetes and prediabetes, have concluded that the practice of yoga may reduce insulin resistance and related cardiovascular disease (CVD) risk factors and improve clinical outcomes [ 16 ]. Specifically, reports suggest that a yoga-based lifestyle intervention reduces body weight, glucose and lipid levels that should reduce diabetes risk. Keeping in view the high transition rates of diabetes in India, we selected a high-risk cohort from Chandigarh, one of the most affluent Union Territories of India with highest reported prevalence of diabetes in order to establish the efficacy of yoga to alleviate the cardiovascular disease. Indian Diabetes Risk Score (IDRS), specific for Indian ethnicity a validated tool was used for identification of the high-risk population [ 17 ]. We developed a national consensus ‘Diabetes Yoga protocol’ based on published reports and classical literature with an aim to stimulate weight reduction by combination of postures and meditation techniques [ 18 , 19 ]. Additionally, cardiometabolic risk reduction has also been recognized as one of the potential outcomes of yoga-based interventions [ 20 ]. Yoga has been shown to be regulating the risk parameters of diabetes, waist circumference (WC), body mass index (BMI), oxidative stress, fasting blood sugar (FBS) and systolic blood pressure (SBP) respectively [ 21 ]. Hence, in this study we tested the efficacy of diabetic yoga protocol (DYP) on alleviation of glycemic and lipid imbalances in individuals at high risk of diabetes.
Materials and methods
Study population.
Under the multi-region survey of Niyantarita Maduhmeha Bharat (NMB-2017) a door-to-door screening was carried out for the identification of high risk individuals among the population of Chandigarh (U.T) and Panchkula (District in Haryana state) on the basis of Indian Diabetes Risk Score (IDRS). The data collection was carried out by well trained yoga volunteers for diabetes management (YVDMs). Written informed consents were taken from every subject during door to door screening as well as at the time of registration. All the experimental protocol, methods and procedures were approved by Ethics committee of Indian Yoga Association (IYA) (ID: RES/IEC-IYA/001). All experiments methods and procedures were carried out in accordance with relevant guidelines and regulations of ethics committee. The study was registered at clinical trial registry of India, CTRI/2018/03/012804 (dated: 01/03/2018).
Study design
The present study is the two-armed randomized controlled trial conducted in the population of Chandigarh and Panchkula regions of northern India. Indian Diabetes Risk Score (IDRS) was used for detection of high risk (≥ 60 score) individuals from the study. Self-declared diabetics and low (< 30 score) and moderate [between 30–50 score] risk individuals were excluded from the study. As evident from the flow of patients presented in the flowchart, out of 1214 eligible subjects, there was approximately 50% loss of sample data due to error in the sampling. Further out of 564, we had to exclude as they were self-declared patients with diabetes and did not further participate in the study. However, this led to final participation of only 184 subjects in the study and allocation of these subjects diminishing the random selection of the study cohort. A cohort of high diabetes-risk cohort consisting of n = 184 participants was randomized into the interventional and control groups (n = 91:93). After excluding the dropouts from the study, based on CONSORT guidelines, the remaining subjects in the DYP and control group were further assessed for selected anthropometric, glycemic and lipid parameters. The intervention group was given the Diabetic Yoga Protocol for three months and control group continued with their daily routine activities. The detailed categorization of the samples is shown in Fig. 1 . The control group was waitlisted for yoga.
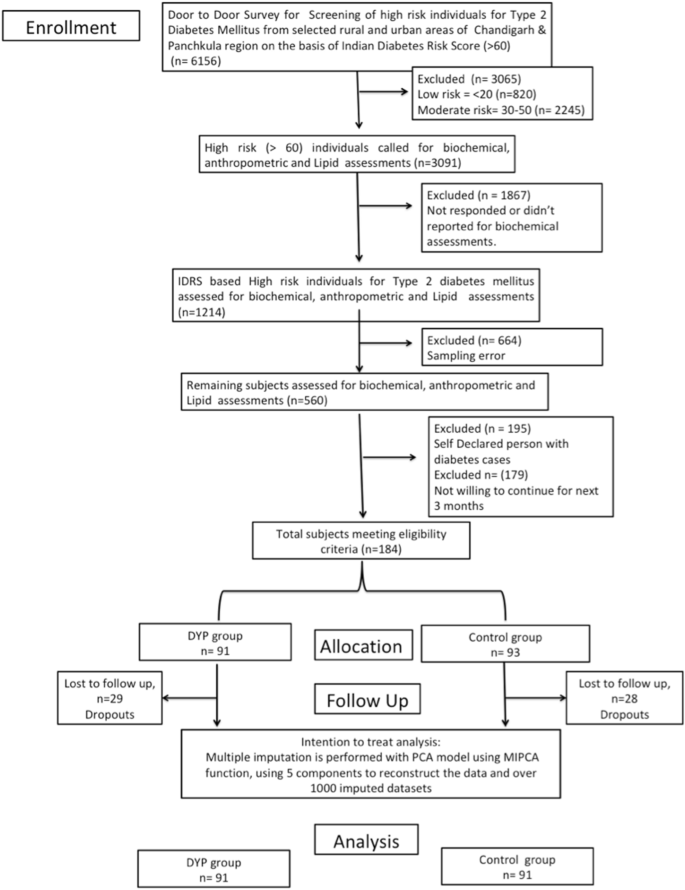
Flowchart of study design. PCA principal component analysis, MIPCA multiple imputations with PCA
Randomization
Simple randomization technique was used to allocate participants into the intervention and the control groups. An independent statistician generated a computer-generated random number sequence and the sequence was given to an external staff who had no involvement in the study procedures. The participants were allocated their consecutive numbers, after baseline measurements. Blinding of the participants was not possible due to the nature of the intervention. However, the outcome assessors were blinded.
Risk assessment
To identify the individuals at high-risk of diabetes, Indian Diabetes Risk Score (IDRS) was administered as proposed by Mohan et al. [ 22 ]. It consisted of two unmodifiable (i.e. age, and family history) and two modifiable (physical activity and waist circumference) risk factors for diabetes, which can predict the level of risk for the development of diabetes in the community. The IDRS is one of the easily accessible and budget friendly questionnaire to be administered. The aggregate score of the unmodifiable and modifiable risk used to probe the level of risk among the population (i.e. High risk > 60, Moderate risk-30–50, Low risk < 30).
Sample size
Sample size estimation for the main Pan India study was focused for prediabetes subjects [ 23 ]. However, for the present pilot scale study we calculated sample size assuming a small effect size 0.3 [ 5 ] of DYP vs waitlist control 0.25, α = 0.80 as 180 (n = 90:90). Further, assuming an attrition rate of 20%, the final sample size was n = 220.
Study outcomes
Changes in the glycemic and other metabolic variables (anthropometric and lipid) over 3 months were documented. The fasting blood sample was withdrawn. For glucose analysis, fasting samples for 10–12 h were taken early in the morning for the estimation of FBS and afterwards 75 g glucose was given to the participants. The blood sampling was repeated after 2 h. for estimation of OGTT.
Biochemical analysis
For the estimation of biochemical parameters viz. FBS (Fasting Blood Sugar, Rxl-Max 500), OGTT (Oral Glucose Tolerance Test), HbA1c (Bio-Rad D-10), Triglycerides, Cholesterol, HDL, LDL, Chol/HDL ratio, HDL/LDL ratio (Rxl-Max 500) and VLDL about 9 ml of blood was drawn and analyzed by phlebotomist of Sisco Research Laboratories (SRL) of Chandigarh. Anthropometric measurements were also obtained (i.e. height, weight, waist circumference) by trained researcher. The waist circumference (WC) was reported in centimeters. The BMI was obtained by using the formula (weight in kg/height (meter) 2 ).
Interventions
The study protocol consisted of Diabetic Yoga Protocol (DYP) approved by the Ministry of AYUSH and Quality Council of India as shown in Table 1 . This is the first protocol to be made specifically for the prediabetics and diabetics. The complete sequence of prayer, yogic postures, breathing and meditative techniques, along with specified time, was shown in previously published paper [ 24 ]. The Yogic practices were performed for 3 months for 60 min. Certified yoga instructors took the yoga classes and they recorded regular attendance. Randomization was done through a computer-generated list of random numbers and allocation was concealed to the participants until the completion of the baseline assessment.
Statistical analysis
For the analysis of data SPSS for Windows (version 22; IBM SPSS Inc., Chicago IL) 0 and R statistical package were used. The normality of data was analyzed using Kolmogorov–Smirnov test. The paired t-test was used to estimate the Baseline and posttest differences of DYP, and control group and the significant level was set at ≤ 0.05. The trial outcomes were analyzed according to the intention-to-treat principle; hence multiple imputation was carried for the missing variables accounting for the loss to follow up. We used absolute change (time and treatment interaction), to estimate intervention effects refers to the difference in the outcome of the intervention and control over different time-points of assessment. Absolute change was determined as follows: absolute change = [(intervention group follow-up) – (intervention group baseline)] – [(control group follow-up) – (control group baseline)]. The percentage change, also called the relative change was determined as relative change = (absolute change / intervention group baseline) × 100%. To evaluate the influence of missing data, we applied multiple imputations to the data using missMDA R package (v1.13) based on the principal component analysis method [ 25 ] from the package, using 5 components to reconstruct the data and over 1000 imputed datasets. One-way multivariate analysis of covariance (MANCOVA) was conducted to compare the effects of the DYP with control group glycemic and metabolic measures, while controlling for the age, gender and baseline values of the covariates.
Baseline characteristics
The data used in this study was collected in (NMB-2017) the northern region of India i.e. Chandigarh and Panchkula. The age range of participants was 3–70 years; [mean age 48.51 (SD 10.08) years]with baseline characteristics of the yoga and control groups as shown in Table 2 . Mean HbA1c of the high-risk cohort was 5.64% (0.38), mean FBS was 97.13 mg/dl (SD 11.10), and mean PPBS were 108.40 mg/dl (SD 28.79). Distributions of age and gender was similar between the intervention and the control groups. The IDRS and anthropometric values were also similarly distributed between the groups. Overall, there was no significant difference in the distribution of demographic, anthropometric, or biochemical parameters between the DYP and the control groups at the baseline.
When analyzed by multivariate analysis of covariance (MANCOVA), adjusting for age, gender and status of diabetes/prediabetes/normoglycemia, and baseline values of the covariates, yoga intervention was found to have significant influence on few cardinal parameters related to glycemic control (PPBS), and lipid control (LDL-C) as shown in Table 3 . We also observed a significant influence of DPP on waist circumference reduction [relative changes, − 1.94%. Compared to the control, DYP also resulted in significant reductions in LDL-C and, − 0.16% and − 2.81%, for LDL-Cholesterol and post-prandial blood glucose levels from baseline to 3 months [absolute changes, − 0.18% and − 3.08%, respectively and relative changes, − 0.16% and − 2.81%, respectively].
We examined the effect of Diabetic Yoga Protocol on baseline and post (3 months) levels of HbA1c and other glycemic (OGTT and FBS), Lipid (Total cholesterol, triglycerides, HDL-c, LDL-c, and VLDL-c, CDL/HDL, LDL/HDL) and anthropometric parameters (BMI). In the present study, we show the efficacy of DYP in substantial improvement in the waist circumference in a high-risk diabetes population from Chandigarh (relative change of 1.94 cm). We could also demonstrate a significant decline in the worsening of post prandial glucose levels with yoga intervention as compared to the wait-list control group (relative change of 2.82 mg/ml). However, for LDL-c levels, there were clinically significant improvements by 0.16 units. Notably, over 3 months study duration there was an overall increase in the levels of total cholesterol, triglyceride and VLDL means in the study cohort, while HDL levels had decreased. In particular TG levels have gone from normal range to mildly high (> 150 mg/dl) [ 26 ] which draws our attention towards accelerated pace of metabolic dysfunction in the high risk population. These findings comply with Chandigarh being an affluent union territory of India with high per-capita GDP and has been documented to have highest prevalence of diabetes 13.6%, 12.8–15·2 as compared to other Indian states [ 27 ]. As mentioned above, there was a significant influence of DYP on the waist circumference, one of the two important modifiable parameters of Indian Diabetes Risk Score [ 17 ]. The relevance of WC reduction in context of reduced risk of CVD is well established; a 1 cm increase in WC has been associated with a 2% increase in the relative risk of future CVD [ 28 ]. The visceral adipose tissue is a primary source of cytokine production and insulin resistance (IR) [ 29 ]. Given the higher susceptibility towards visceral fat accumulation and insulin resistance in Asian populations as compared to their Caucasian counterparts, the observed influence of DYP on WC is of particular relevance to the metabolically obese phenotype of Asian Indians [ 30 ].
In relation to the glucose metabolism, we could also demonstrate a significant decline in the worsening of post prandial glucose levels with DYP as compared to the wait-list control group (relative change = − 2.81%, P < 0.05); however, no significant influence could be established for fasting blood glucose concentration. These findings could be justified by the phenotypic differences underlying fasting and post-challenge hyperglycemia that represent distinct natural histories in the evolution of type 2 diabetes [ 31 ]. Postprandial glucose disposal is the primary pathogenic manifestation in impaired glucose tolerance (IGT), and impaired fasting glucose (IFG) merely signifies an abnormal glucose set point [ 31 , 32 ]. Our relevance of the study findings is further underlined by the previous results wherein PPG has been reported to contribute more than FBS to overall hyperglycemia and its control was found essential either to decrease or to obtain HbA1c goals of < 7 [ 33 ]. Several epidemiological studies have suggested that increased glycemic exposure, especially post challenge or postprandial hyperglycemia, is an independent risk factor for macrovascular disease with no apparent upper or lower threshold. Our results indicate a significant influence of yoga on glycemic control integrating postprandial glycemic alterations in the high diabetes risk group. Since in the present study the high-risk cohort was selected through A1c based diagnosis, and IGT was not a primary manifestation in the cohort, hence, the overall improvement in postprandial glucose should be specifically tested in an IGT cohort. The findings of the current study with a 3-month intervention of yoga on postprandial measures of glucose at-risk population deserves clinical attention. Increase in the glucose concentration even in the prediabetes stage, manifests as a chronic inflammatory condition and predisposes an individual to the risk of pathogenic infections [ 32 , 34 , 35 ].
The simultaneous reduction in waist circumference observed in the cohort, is also consistent with the observation of an association between abdominal obesity and the risk of IGT. Based on a significant association between IGT and CVD risk [ 32 , 33 , 36 ], we note a significant improvement in lipid concentrations [LDL-c] by the DYP protocol as compared to the control group. These results are consistent with the previously reported overall beneficial effect of yoga in the management of hyperlipidemia [ 36 ]. These results need validation at larger scale and to ascertain the mechanistic insights into the action of yoga, the indices of monocyte chemotaxis, endothelial inflammation, oxidation, nitric oxide production, and thrombosis should also be explored [ 37 ], including animal models, invitro systems and other approaches [ 38 , 39 , 40 , 41 , 42 , 43 , 44 ].
The findings of the present study indicate that identification of high-risk group through IDRS and consequent intervention of Yoga based lifestyle protocol could be an effective strategy to combat the metabolic perturbations associated with diabetes, whose co-morbidity is also being reported to be associated with increasing vulnerability to the emerging viral pandemic of COVID-19. Lifestyle interventions are reported to reduce the risk of Type 2 diabetes in high-risk individuals after mid and long-term follow-up. Information on determinants of intervention outcome, adherence and the mechanisms underlying diabetes progression are valuable for a more targeted implementation. Weight loss is a major contributor in the prevention and management of type 2 diabetes. In many of the earlier lifestyle intervention group of the DPP, weight loss was the dominant predictor of reduced diabetes risk, with a 16% reduction observed for every kilogram of weight loss during the 3.2-year follow-up [ 45 ]. Though we failed to observe a significant weight loss over 3 months of DYP intervention, the significant reductions in WC indicate the plausibility of significant weight loss on longer interventions and follow ups.
Whether Yoga alters the conversion of prediabetics into healthy status and if it helps in maintenance of glycemic index can be assessed by longitudinal studies. There was a significant improvement in the glycemic status of the high risk population at administration of DYP. The analysis shows the aptness of Diabetic protocol which is apparently superior to previous studies where no standardized protocols were used for intervention [ 46 , 47 ]. The findings suggest that there is potential of DYP to manage glucose levels in diabetes patients if public intervention is planned through forthcoming wellness centers in India. There are additional studies showing beneficial effects of Yoga on FBS [ 48 ], PPBS [ 49 , 50 , 51 ], HbA1c [ 50 , 51 ], total cholesterol, LDL [ 50 , 51 ]. The analysis of the yoga protocols used in above said studies reveal the incorporation of some common and important postures in DYP, which seem to be important in managing the disease. It is also the possible that the beneficial effects of mind body techniques are sensitive to mental disposition of subjects and has been characterized by various measures like psychometric analysis [ 52 , 53 ], namely, Tridosha and Triguna scoring [ 54 , 55 ]. These were not analyzed in this study.
Briefly, DYP’s promising efficacy on glycemic and metabolic parameters requires mechanistic insights. This can be examined by further studies, and long term follow up which was not possible in this study. As DYP is a non-pharmacological, cost-effective method to halt the conversion of early diabetes into prediabetes and/or healthy individuals, the success of its integration into public health policy will depend on its wider acceptability and perception of benefits by both public as well as healthcare workers [ 56 , 57 , 58 , 59 ]. Yoga’s benefits in maintaining and regulation of the glycemic status are supported by several other studies [ 49 , 50 ], which might enable its inclusion in the National Ayushman Bharat scheme or as part COVID pandemic management protocol in which a large number of individuals with diabetes and heart disease are falling prey [ 60 , 61 ]. This will further encourage molecular and Ayurgenomic studies which presumably underlie the stated clinical outcome.
Limitations
Moreover, there are some limitations of our study that we only studied in two regions of North India and thus the result of this study cannot be generalized on the remaining population. Further, in this study, the socio economic status and psychological assessments were not carried out. We were not able to control for the dietary habits and psychological status of the study participants. However, the small sample size and absence of long term evaluations limit the strength of the study.
Availability of data and materials
The datasets used during the present study are available from the corresponding author on reasonable request.
Abbreviations
American Diabetes Association
Body mass Index
Cardiovascular disease
- Diabetic yoga protocol
Fasting blood sugar
- Glycated hemoglobin
High density lipid-cholesterol
Indian Diabetes Risk Score
Impaired fasting glucose
Impaired glucose tolerance
Indian Yoga Association
Low density lipid-cholesterol
Niyantarita Maduhmeha Bharat
Oral glucose tolerance test
Postprandial blood glucose
Systolic blood pressure
Very low density lipid-cholesterol
Waist circumference
Yoga volunteers for diabetes management
Laaksonen DE, Lindström J, Lakka TA, Eriksson JG, Niskanen L, Wikström K, Aunola S, Keinänen-Kiukaanniemi S, Laakso M, Valle TT, Ilanne-Parikka P. Physical activity in the prevention of type 2 diabetes: the Finnish diabetes prevention study. Diabetes. 2005;54(1):158–65.
CAS PubMed Google Scholar
Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, Hämäläinen H, Härkönen P, Keinänen-Kiukaanniemi S, Laakso M, Louheranta A. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006;368(9548):1673–9.
PubMed Google Scholar
DREAM (Diabetes REduction Assessment with ramipril and rosiglitazone Medication) Trial Investigators. Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet. 2006;368(9541):1096–105.
Google Scholar
Lindström J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care. 2003;26(3):725–31.
McDermott KA, Rao MR, Nagarathna R, Murphy EJ, Burke A, Nagendra RH, Hecht FM. A yoga intervention for type 2 diabetes risk reduction: a pilot randomized controlled trial. BMC Complement Altern Med. 2014;14(1):1–4.
Jyotsna VP. Prediabetes and type 2 diabetes mellitus: evidence for effect of yoga. Indian J Endocrinol Metab. 2014;18(6):745.
PubMed PubMed Central Google Scholar
Thind H, Lantini R, Balletto BL, Donahue ML, Salmoirago-Blotcher E, Bock BC, Scott-Sheldon LA. The effects of yoga among adults with type 2 diabetes: a systematic review and meta-analysis. Prev Med. 2017;1(105):116–26.
Singh VP, Khandelwal B. Effect of yoga and exercise on glycemic control and psychosocial parameters in type 2 diabetes mellitus: a randomized controlled study. Int J Yoga. 2020;13(2):144.
Chen N, Xia X, Qin L, Luo L, Han S, Wang G, Zhang R, Wan Z. Effects of 8-week Hatha yoga training on metabolic and inflammatory markers in healthy, female Chinese subjects: a randomized clinical trial. BioMed Res Int. 2016. https://doi.org/10.1155/2016/5387258 .
Article PubMed PubMed Central Google Scholar
Ramamoorthi R, Gahreman D, Skinner T, Moss S. Development of Sham yoga poses to assess the benefits of yoga in future randomized controlled trial studies. Life. 2021;11(2):130.
Sreedevi A, Gopalakrishnan UA, Ramaiyer SK, Kamalamma L. A randomized controlled trial of the effect of yoga and peer support on glycaemic outcomes in women with type 2 diabetes mellitus: a feasibility study. BMC Complement Altern Med. 2017;17(1):1–8.
Ramamoorthi R, Gahreman D, Skinner T, Moss S. The effect of yoga practice on glycemic control and other health parameters in the prediabetic state: a systematic review and meta-analysis. PLoS ONE. 2019;14(10): e0221067.
CAS PubMed PubMed Central Google Scholar
Chimkode SM, Kumaran SD, Kanhere VV, Shivanna R. Effect of yoga on blood glucose levels in patients with type 2 diabetes mellitus. J Clin Diagn Res JCDR. 2015;9(4):CC01.
Kacker S, Saboo N, Sharma S, Sorout J. Quasi prospective comparative study on effect of yoga among prediabetics on progression of cardiovascular risk factors. Int J Yoga. 2019;12(2):114.
Ebrahimi M, Guilan-Nejad TN, Pordanjani AF. Effect of yoga and aerobics exercise on sleep quality in women with Type 2 diabetes: a randomized controlled trial. Sleep Sci. 2017;10(2):68.
Innes KE, Vincent HK. The influence of yoga-based programs on risk profiles in adults with type 2 diabetes mellitus: a systematic review. Evid-Based Complementary Altern Med. 2007;4(4):469–86.
Mohan V, Anbalagan VP. Expanding role of the Madras diabetes research foundation-Indian diabetes risk score in clinical practice. Indian J Endocrinol Metab. 2013;17(1):31.
Wilson PW, Meigs JB, Sullivan L, Fox CS, Nathan DM, D’Agostino RB. Prediction of incident diabetes mellitus in middle-aged adults: the Framingham Offspring Study. Arch Intern Med. 2007;167(10):1068–74.
Chen L, Magliano DJ, Balkau B, Colagiuri S, Zimmet PZ, Tonkin AM, Mitchell P, Phillips PJ, Shaw JE. AUSDRISK: an Australian Type 2 Diabetes Risk Assessment Tool based on demographic, lifestyle and simple anthropometric measures. Med J Aust. 2010;192(4):197–202.
Yang K, Bernardo LM, Sereika SM, Conroy MB, Balk J, Burke LE. Utilization of 3-month yoga program for adults at high risk for type 2 diabetes: a pilot study. Evid-Based Complementary Altern Med. 2011;1:2011.
Hegde SV, Adhikari P, Shetty S, Manjrekar P, D’Souza V. Effect of community-based yoga intervention on oxidative stress and glycemic parameters in prediabetes: a randomized controlled trial. Complement Ther Med. 2013;21(6):571–6.
Mohan V, Deepa R, Deepa M, Somannavar S, Datta M. A simplified Indian Diabetes Risk Score for screening for undiagnosed diabetic subjects. J Assoc Phys India. 2005;53:759–63.
CAS Google Scholar
Nagarathna R, Rajesh SK, Amit S, Patil S, Anand A, Nagendra HR. Methodology of Niyantrita Madhumeha Bharata Abhiyaan-2017, a nationwide multicentric trial on the effect of a validated culturally acceptable lifestyle intervention for primary prevention of diabetes: Part 2. Int J Yoga. 2019;12(3):193.
Nagarathna Raghuram VR, Vijaya Majumdar RS, Amit Singh SP, Akshay Anand IJ, Srikanta Bhaskara JR. Effectiveness of a yoga-based lifestyle protocol (YLP) in preventing diabetes in a high-risk Indian cohort: a multicenter cluster-randomized controlled trial (NMB-trial). Front Endocrinol. 2021. https://doi.org/10.3389/fendo.2021.664657 .
Article Google Scholar
Josse J, Husson F. missMDA: a package for handling missing values in multivariate data analysis. J Stat Softw. 2016;70(1):31.
Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al., ICMR–INDIAB Collaborative Study Group. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54(12):3022–7. https://doi.org/10.1007/s00125-011-2291-5 . Epub 2011 Sep 30. PMID: 21959957.
Rygiel K. Hypertriglyceridemia—common causes, prevention and treatment strategies. Curr Cardiol Rev. 2018;14(1):67–76.
De Koning L, Merchant AT, Pogue J, Anand SS. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur Heart J. 2007;28(7):850–6.
McLaughlin T, Lamendola C, Liu A, Abbasi F. Preferential fat deposition in subcutaneous versus visceral depots is associated with insulin sensitivity. J Clin Endocrinol Metab. 2011;96(11):E1756–60.
Jeon J, Jung KJ, Jee SH. Waist circumference trajectories and risk of type 2 diabetes mellitus in Korean population: the Korean genome and epidemiology study (KoGES). BMC Public Health. 2019;19(1):1–1.
Roumen C, Corpeleijn E, Feskens EJ, Mensink M, Saris WH, Blaak EE. Impact of 3-year lifestyle intervention on postprandial glucose metabolism: the SLIM study. Diabet Med. 2008;25(5):597–605.
Bock G, Dalla Man C, Campioni M, Chittilapilly E, Basu R, Toffolo G, et al. Pathogenesis of pre-diabetes: mechanisms of fasting and postprandial hyperglycemia in people with impaired fasting glucose and/or impaired glucose tolerance. Diabetes. 2006;55:3536–49.
Gerich JE. The importance of tight glycemic control. Am J Med. 2005;118(9):7–11.
Buysschaert M, Medina JL, Bergman M, Shah A, Lonier J. Prediabetes and associated disorders. Endocrine. 2015;48(2):371–93.
Diabetes D. Learning about prediabetes. American Diabetes Association website http://www.diabetes.org/diabetes-basics/diagnosis . 2014.
Shantakumari N, Sequeira S. Effects of a yoga intervention on lipid profiles of diabetes patients with dyslipidemia. Indian Heart J. 2013;65(2):127–31.
DeGoma EM, Degoma RL, Rader DJ. Beyond high-density lipoprotein cholesterol levels: evaluating high-density lipoprotein function as influenced by novel therapeutic approaches. J Am Coll Cardiol. 2008;51(23):2199–211.
Anand A, Saraf MK, Prabhakar S. Sustained inhibition of brotizolam induced anterograde amnesia by norharmane and retrograde amnesia by l-glutamic acid in mice. Behav Brain Res. 2007;182(1):12–20.
Anand A, Saraf MK, Prabhakar S. Antiamnesic effect of B. monniera on L-NNA induced amnesia involves calmodulin. Neurochem Res. 2010;35(8):1172–81.
Goyal K, Koul V, Singh Y, Anand A. Targeted drug delivery to central nervous system (CNS) for the treatment of neurodegenerative disorders: trends and advances. Cent Nerv Syst Agents Med Chem (Formerly Current Medicinal Chemistry-Central Nervous System Agents). 2014;14(1):43–59.
Gupta PK, Prabhakar S, Abburi C, Sharma NK, Anand A. Vascular endothelial growth factor-A and chemokine ligand (CCL2) genes are upregulated in peripheral blood mononuclear cells in Indian amyotrophic lateral sclerosis patients. J Neuroinflammation. 2011;8(1):1–6.
Kumar S, Modgil S, Bammidi S, Minhas G, Shri R, Kaushik S, Singh V, Anand A. Allium cepa exerts neuroprotective effect on retinal ganglion cells of pterygopalatine artery (PPA) ligated mice. J Ayurveda Integr Med. 2020;11(4):489–94.
Saraf MK, Prabhakar S, Anand A. Neuroprotective effect of Bacopa monniera on ischemia induced brain injury. Pharmacol Biochem Behav. 2010;97(2):192–7.
Singh T, Prabhakar S, Gupta A, Anand A. Recruitment of stem cells into the injured retina after laser injury. Stem Cells Dev. 2012;21(3):448–54.
Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–86.
Hegde SV, Adhikari P, Kotian S, Pinto VJ, D’Souza S, D’Souza V. Effect of 3-month yoga on oxidative stress in type 2 diabetes with or without complications: a controlled clinical trial. Diabetes Care. 2011;34(10):2208–10.
Sharma M, Knowlden AP. Role of yoga in preventing and controlling type 2 diabetes mellitus. J Evid-Based Complementary Altern Med. 2012;17(2):88–95.
Keerthi GS, Pal P, Pal GK, Sahoo JP, Sridhar MG, Balachander J. Effect of 12 Weeks of yoga therapy on quality of life and Indian diabetes risk score in normotensive Indian young adult prediabetics and diabetics: randomized control trial. J Clin Diagn Res. 2017;11(9):CC10.
Sahay BK. Role of yoga in diabetes. JAPI. 2007;55:121–6.
Balaji PA. Effects of yoga-pranayama practices on metabolic parameters and anthropometry in type 2 diabetes. Int Multidiscipl Res J. 2011;1(10).
Cui J, Yan JH, Yan LM, Pan L, Le JJ, Guo YZ. Effects of yoga in adults with type 2 diabetes mellitus: a meta-analysis. J Diabet Investig. 2017;8(2):201–9.
Sedlmeier P, Eberth J, Schwarz M, Zimmermann D, Haarig F, Jaeger S, Kunze S. The psychological effects of meditation: a meta-analysis. Psychol Bull. 2012;138(6):1139.
Bonura KB, Tenenbaum G. Effects of yoga on psychological health in older adults. J Phys Act Health. 2014;11(7):1334–41.
Rastogi S. Development and validation of a Prototype Prakriti Analysis Tool (PPAT): Inferences from a pilot study. AYU. 2012;33(2):209.
Govindaraj P, Nizamuddin S, Sharath A, Jyothi V, Rotti H, Raval R, Nayak J, Bhat BK, Prasanna BV, Shintre P, Sule M. Genome-wide analysis correlates Ayurveda Prakriti. Sci Rep. 2015;5(1):1–2.
Singh AK, Kaur N, Kaushal S, Tyagi R, Mathur D, Sivapuram MS, Metri K, Bammidi S, Podder V, Modgil S, Khosla R. Partitioning of radiological, stress and biochemical changes in pre-diabetic women subjected to Diabetic Yoga Protocol. Diabetes Metab Syndr. 2019;13(4):2705–13.
Pal DK, Bhalla A, Bammidi S, Telles S, Kohli A, Kumar S, Devi P, Kaur N, Sharma K, Kumar R, Malik N. Can yoga-based diabetes management studies facilitate integrative medicine in India current status and future directions. Integr Med Int. 2017;4(3–4):125–41.
Bali P, Kaur N, Tiwari A, Bammidi S, Podder V, Devi C, Kumar S, Sivapuram MS, Ghani A, Modgil S, Malik N. Effectiveness of yoga as the public health intervention module in the management of diabetes and diabetes associated dementia in South East Asia: a narrative review. Neuroepidemiology. 2020;54(4):287–303.
Anand A. Narendra Modi’s citizen centered Yoga-Diabetes Management Program: will Indian state install integrative medicine in premier institutes? Ann Neurosci. 2019;26(2):47–8.
Bansal M. Cardiovascular disease and COVID-19. Diabetes Metab Syndr. 2020;14(3):247–50.
Peric S, Stulnig TM. Diabetes and COVID-19. Wien Klin Wochenschr. 2020;132(13):356–61.
Download references
Acknowledgements
The authors would like to thank Central Council for Research in Yoga & Naturopathy (CCRYN) for their support for man power, Ministry of Health and Family Welfare (MOHFW) for support the cost of investigations and Indian Yoga Association (IYA) for the overall project implementation. The authors also like to thank to thank Yoga Volunteer for Diabetes Management (YVDMs) for helping in collection of data and also for training participants for yoga.
The Project was funded by Ministry of AYUSH, Government of India (grant number 16-63/2016-17/CCRYN/RES/Y&D/ MCT/).
Author information
Authors and affiliations.
Department of Physical Education, Panjab University, Chandigarh, 160014, India
Navneet Kaur
Division of Life Sciences, Swami Vivekananda Yoga Anusandhana Samsathana, Bengaluru, Karnataka, 560106, India
Vijaya Majumdar, Raghuram Nagarathna & Hongasandra Ramarao Nagendra
Dev Samaj College of Education, Sector 36B, Chandigarh, 160036, India
Neeru Malik
Department of Neurology, Neuroscience Research Lab, Postgraduate Institute of Medical Education and Research, Chandigarh, 160012, India
Navneet Kaur & Akshay Anand
You can also search for this author in PubMed Google Scholar
Contributions
NK: writing of manuscript, collection of data. VM: writing of manuscript, analysis. RN: conceptualization of manuscript, supervision and study design. NM: co-conceptualization of manuscript. AA: conceptualization of manuscript. HRN: supervision. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Raghuram Nagarathna or Akshay Anand .
Ethics declarations
Ethics approval and consent to participate.
Written informed consents were taken from every subject during door to door screening as well as at the time of registration. All the experimental protocol, methods and procedures were approved by Ethics committee of Indian Yoga Association (IYA) (ID: RES/IEC-IYA/001). All experiments methods and procedures were carried out in accordance with relevant guidelines and regulations of ethics committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kaur, N., Majumdar, V., Nagarathna, R. et al. Diabetic yoga protocol improves glycemic, anthropometric and lipid levels in high risk individuals for diabetes: a randomized controlled trial from Northern India. Diabetol Metab Syndr 13 , 149 (2021). https://doi.org/10.1186/s13098-021-00761-1
Download citation
Received : 26 August 2021
Accepted : 17 November 2021
Published : 23 December 2021
DOI : https://doi.org/10.1186/s13098-021-00761-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Indian diabetes risk score
- Prediabetes
Diabetology & Metabolic Syndrome
ISSN: 1758-5996
- Submission enquiries: [email protected]

- Previous Article
- Next Article
RESEARCH DESIGN AND METHODS
Conclusions, acknowledgments, effect of 3-month yoga on oxidative stress in type 2 diabetes with or without complications : a controlled clinical trial.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Shreelaxmi V. Hegde , Prabha Adhikari , Shashidhar Kotian , Veena J. Pinto , Sydney D’Souza , Vivian D’Souza; Effect of 3-Month Yoga on Oxidative Stress in Type 2 Diabetes With or Without Complications : A controlled clinical trial . Diabetes Care 1 October 2011; 34 (10): 2208–2210. https://doi.org/10.2337/dc10-2430
Download citation file:
- Ris (Zotero)
- Reference Manager
To assess the effect of yoga on anthropometry, blood pressure, glycemic control, and oxidative stress in type 2 diabetic patients on standard care in comparison with standard care alone.
The study involved 123 patients stratified according to groups with microvascular complications, macrovascular complications, and peripheral neuropathy and without complications and assigned to receive either standard care or standard care along with additional yoga for 3 months.
In comparison with standard care alone, yoga resulted in significant reduction in BMI, glycemic control, and malondialdehyde and increase in glutathione and vitamin C. There were no differences in waist circumference, waist-to-hip ratio, blood pressure, vitamin E, or superoxide dismutase in the yoga group at follow-up.
Yoga can be used as an effective therapy in reducing oxidative stress in type 2 diabetes. Yoga in addition to standard care helps reduce BMI and improve glycemic control in type 2 diabetic patients.
Oxidative stress has been implicated as the root cause underlying the development of insulin resistance, β-cell dysfunction, diabetes, and its associated clinical conditions such as atherosclerosis, microvascular complications, and neuropathy ( 1 , 2 ). Yoga has been found to be beneficial in reducing oxidative stress in type 2 diabetes ( 3 , 4 ), but there is a lack of controlled trials to demonstrate the same. This report describes the effect of yoga on oxidative stress, glycemic control, blood pressure control, and anthropometry in type 2 diabetic patients with or without complications compared with control subjects on standard care.
This study was conducted at the diabetes clinic of Kasturba Medical College hospital and at four community diabetes clinics offering primary care to diabetic patients in Mangalore, India. A total of 123 type 2 diabetic patients aged between 40 and 75 years, none of whom were alcoholics or smokers, gave written informed consent and were included. Patients with acute macrovascular complications, cancer, pulmonary tuberculosis, and rheumatoid arthritis and those who were unable to perform yoga were excluded. Patients were grouped as 60 for yoga and 63 for control. Stratified sampling was used at the time of allocation to maintain an equal number of patients with uncomplicated diabetes and with microvascular, macrovascular, and peripheral neuropathy in these groups.
Three months’ yoga included tadasana, padahastasana, vrikshasana, trikonasana, parshvothanasana, vajrasana, vakrasana, gomukasana, paschimotasana, uttanapadasana, pawanamuktasana, bhujangasana, shalabasana, dhanurasana, viparitakarani, sitkari and bhramari pranayama, anuloma viloma, and shavasana poses. The control group at their baseline visit was given general oral and written information about diet and exercise. Compliance with the intervention was defined as attendance for at least 3 days/week at the yoga center for 3 months. Drug dosages with regard to diabetes and blood pressure were kept constant throughout the study period.
Malondialdehyde ( 5 ), glutathione ( 6 ), superoxide dismutase ( 7 ), vitamin C ( 8 ), and vitamin E ( 9 ) were measured to assess the oxidative stress and antioxidant status. BMI, waist circumference, waist-to-hip ratio, blood pressure, fasting plasma glucose (FPG), postprandial plasma glucose (PPPG), and HbA 1c were analyzed.
Data were analyzed using SPSS version 11.0. Paired t test was used to compare the continuous variables from baseline to follow-up. Mann-Whitney U test, a nonparametric test, was used to compare the differences in various parameters before and after intervention between the two groups.
Three participants withdrew from yoga intervention during the first month of the study and were not included in the final analysis. Among these, two moved their residence and one reported illness unrelated to the study. Mean ± SD age was 59.8 ± 9.9 years for the yoga group and 57.5 ± 8.9 years in the control group. There were no significant differences in sex, duration of diabetes, or hypertension between the groups at baseline. Average attendance at the yoga classes was 82–88%.
Yoga practitioners achieved significant improvements in BMI, FPG, PPPG, HbA 1c , malondialdehyde, glutathione, and vitamin C at 3 months compared with the standard care group ( Table 1 ). In the yoga group, the mean percentage reduction in malondialdehyde was 20% (−10.8 ± 1.4 μmol/L) and in HbA 1c 1.4% (−0.1 ± 0.2%). In the control group, the mean percentage increase in malondialdehyde was 3.2% (1.6 ± 1.6 μmol/L) and in HbA 1c 6.25% (0.5 ± 0.3%). Significant reductions in glutathione and vitamin C were seen in control subjects. No significant changes in waist circumference, waist-to-hip ratio, blood pressure, vitamin E, or superoxide dismutase were observed in the yoga group compared with control subjects. No adverse events were observed during the intervention period.
Parameters at baseline and after 3 months
Data are means ± SD. P values are significance values in yoga group compared with the control group.
Yoga practitioners achieved a 20% reduction in oxidative stress, which is similar to the findings of Gordon et al. ( 10 ): 6 months of yoga in type 2 diabetic subjects showed a 19.9% reduction in oxidative stress. Other lifestyle interventions such as aerobic exercise and resistance training are known to increase stress parameters ( 11 , 12 ). Antioxidants like glutathione and vitamin C improved by 15 and nearly 60% compared with standard care. To the best of our knowledge, to date there are no reports of the effect of yoga on glutathione and vitamin status in type 2 diabetes. In this study, yoga improved the antioxidant levels, thereby reducing the oxidative stress in type 2 diabetic patients.
The effect on glycemic control and BMI was marginal compared with results obtained by other lifestyle interventions such as aerobic exercise and resistance training. In the current study, mean percentage reduction in HbA 1c was 1.4% in the yoga group, whereas it increased by 6.25% in the control group. From a clinical perspective, this represents a small change. However, long-term, regular practice of yoga can sustain the improved glycemic control brought about by standard care. Greatest improvements in HbA 1c values after yoga in type 2 diabetes have come from studies in which the sample sizes are small, about 10–30 in each group ( 4 , 13 ) and from studies where yoga was delivered along with exercises ( 14 ).
Skora-Kondza et al. ( 15 ) observed difficulty with adherence of patients to yoga intervention. This was overcome in our study because yoga classes were held at several community centers in the city, which made it easy for the patients to attend the classes; in addition, culturally, Indian patients would accept yoga better than the Western population.
Our study is limited by the fact that the allocation to the groups was not randomized. Random allocation in community settings is difficult. In this study, social and environmental factors during these training sessions may have a beneficial influence on oxidative stress. The strength of our study was the stratification of sample according to complications. Participants with various complications may have increased oxidative stress; stratification made the two groups identical.
In conclusion, yoga can be used as an effective therapy in reducing oxidative stress in type 2 diabetes. Yoga is also beneficial in improving glycemic parameters and BMI and can be administered as an add-on therapy to standard lifestyle interventions. Yoga was not beneficial in reducing the blood pressure or waist circumference in this short-term study. Further studies are needed to confirm that yoga is beneficial in preventing the progression of diabetes and its complications.
Clinical trial reg. no. CTRI/2011/05/001739, ctri.nic.in .
This study was funded by a grant from Manipal University (431/013/2007).
No potential conflicts of interest relevant to this article were reported.
S.V.H. designed the study, acquired and interpreted data, and wrote the manuscript. P.A. developed the protocol, designed the study, interpreted data, and reviewed and edited the manuscript. S.K. analyzed data. V.J.P. acquired data and contributed to discussion. S.D. and V.D. reviewed and edited the manuscript.
The authors thank Laura Prakash, School of Public Health, University of Minnesota, Minneapolis, MN, for her contribution to the study. The authors express appreciation to the participants whose cooperation and dedication made this study possible. The authors also acknowledge International Training and Research In Environmental and Occupational Health (ITREOH) training grant from Fogarty Foundation, which was responsible for their training in medical writing.

Email alerts
- Online ISSN 1935-5548
- Print ISSN 0149-5992
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center
The Effect of Yoga on Health-Related Fitness among Patients with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis

2022, International Journal of Environmental Research and Public Health
Related Papers
Diabetes & metabolic syndrome
Priyanga Ranasinghe
Yoga is increasingly used as an adjunctive therapy in the management of Type-2 Diabetes Mellitus (T2DM). The present study aims to systematically evaluate the literature and perform a meta-analysis on the effects of yoga practice compared to physical exercise in the management of T2DM. Data were obtained using a stepwise search process using keywords in the following online medical databases; PubMed, Web of Science and Scopus. All controlled clinical trials involving patients with T2DM, comparing yoga as an intervention with physical exercise and evaluating glycaemic control and other outcomes between the intervention and control groups were included in the analysis. Eight studies were eligible to be included in the systematic review. In total, 842 participants were assigned to a Yoga intervention or a control group with an Exercise intervention and the age range of participants was 30-78 years. A significant reduction in FBG (15.16 mg/dl), PPBG (28.66 mg/dl), HbA1c (0.39%) and BMI ...
Clinical Diabetology
Sridip Chatterjee
TMR Non-Drug Therapy
Ayush Anand
BMC complementary and alternative medicine
raghavendra Rao
Type 2 diabetes is a major health problem in many countries including India. Yoga may be an effective type 2 diabetes prevention strategy in India, particularly given its cultural familiarity. This was a parallel, randomized controlled pilot study to collect feasibility and preliminary efficacy data on yoga for diabetes risk factors among people at high risk of diabetes. Primary outcomes included: changes in BMI, waist circumference, fasting blood glucose, postprandial blood glucose, insulin, insulin resistance, blood pressure, and cholesterol. We also looked at measures of psychological well-being including changes in depression, anxiety, positive and negative affect and perceived stress. Forty-one participants with elevated fasting blood glucose in Bangalore, India were randomized to either yoga (n = 21) or a walking control (n = 20). Participants were asked to either attend yoga classes or complete monitored walking 3-6 days per week for eight weeks. Randomization and allocation ...
Evidence-Based Complementary and Alternative Medicine
Badr Aljasir
The effect of practicing yoga for the management of type II Diabetes was assessed in this systematic review through searching related electronic databases and the grey literature to the end of May 2007 using Ovid. All randomized controlled clinical trials (RCTs) comparing yoga practice with other type of intervention or with regular practice or both, were included regardless of language or type of publication. Each study was assessed for quality by two independent reviewers. Mean difference was used for summarizing the effect of each study outcomes with 95% confidence intervals. Pooling of the studies did not take place due to the wide clinical variation between the studies. Publication bias was assessed by statistical methods. Five trials with 363 participants met the inclusion criteria with medium to high risk of bias and different intervention characteristics. The studies’ results show improvement in outcomes among patients with diabetes type II. These improvements were mainly am...
Lisa Bernardo
Journal of Evidence Based Medicine and Healthcare
sonal bhardwaj
BACKGROUND Psychosocial variables characterized by different emotional, cognitive and behavioural changes are highly persistent / or recurrent in diabetics. An important aspect of diabetes care is assessing symptoms related to these with the use of reliable and valid instruments. Treatment and control of Type 2 diabetes mellitus (T2DM) focuses on lifestyle changes. Yoga practice, a cost-effective method has a role in the prevention of diabetes, lowering glucose levels, and in improving health. We studied the effects of yoga practice on psychosocial factors and Quality of Life (QoL) in participants of T2DM. METHODS This is a prospective randomized hospital based trial. It was conducted on 104 participants of T2DM (age of study participants 30 - 65 years of both gender) which were randomized into two study groups viz. Control and Yoga active group. Approximately 40 minutes of yogasana, five days (minimum) a week for six months was performed in yoga active group. Fasting & postprandial...
BMC health services research
Trish Greenhalgh
Journal of physical activity & health
Pamela Kulbok , Gina Alexander
The current study described patterns of yoga practice and examined differences in physical activity over time between individuals with or at risk for type 2 diabetes who completed an 8-week yoga intervention compared with controls. A longitudinal comparative design measured the effect of a yoga intervention on yoga practice and physical activity, using data at baseline and postintervention months 3, 6, and 15. Disparate patterns of yoga practice occurred between intervention and control participants over time, but the subjective definition of yoga practice limits interpretation. Multilevel model estimates indicated that treatment group did not have a significant influence in the rate of change in physical activity over the study period. While age and education were not significant individual predictors, the inclusion of these variables in the model did improve fit. Findings indicate that an 8-week yoga intervention had little effect on physical activity over time. Further research i...
National Journal of Community Medicine
Padmaja Walveka
Context/Background: Lifestyle interventions have proven to reduce the incidence of type 2 diabetes mellitus and prevent the complications. Yoga is considered safe, simple to learn, and can be practiced even by ill, obese, elderly, or disabled persons at home. The present study was conducted to assess the effect of one year of yoga therapy on lipid profile, BMI, and blood pressure in subjects with type 2 diabetes mellitus. Methodology: This randomized controlled trial was conducted in an Urban Health center, Belagavi from July 2018 to December 2019. Around 120 participants diagnosed with type 2 diabetes mellitus were randomized into “Yoga” and “Exercise” groups. Fasting lipid profile, BMI, and blood pressure were examined at baseline, six months, and after one year of intervention. Results: GEE model analysis showed that there were significant effects of Intervention × Time on Cholesterol (p=0.001), LDL (p=0.006) and VLDL (p=0.000). It was identified that the exercise intervention wa...
RELATED PAPERS
Paola Calderón
Shemaraiah Johnson
Seminar Nasional Pengabdian Kepada Masyarakat
Andi Cudai Nur
SSRN Electronic Journal
Benjamin Grosof
Journal of the City Planning Institute of Japan
minami narita
International journal of health & medical sciences
Lilis Candrayanti
Faculdades EST
Edson Ponick
The International Journal of Academic Research in Business and Social Sciences
ABUZAR ABDUL HALIM
Experimental Biology and Medicine
Astrophysics and Space Science
Himadri Sekhar Das
2008 Sixth IEEE International Conference on Software Engineering and Formal Methods
Hung Dang Van
International Journal of Information Technology and Web Engineering
Dr. Ravirajsinh Vaghela
Selly Indah
Journal of Virology
David Milich
실시간카지노 토토사이트
Todd Brusko
zairol yusoff
Entomologia Experimentalis et Applicata
Value in Health
Antonio Bertolotto
hgtyfrf fggfhhfg
Pharmacology & Pharmacy
Ahmed Fathelrahman
Open Journal of Forestry
Vanessa Rodrigues Pereira
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Yoga Programme for Type 2 Diabetes Prevention (YOGA-DP) Among High-Risk People in India: A Multicenter Feasibility Randomized Controlled Trial
- Original Research
- Open access
- Published: 31 March 2023
- Volume 14 , pages 1137–1154, ( 2023 )
Cite this article
You have full access to this open access article

- Kaushik Chattopadhyay ORCID: orcid.org/0000-0002-3235-8168 1 ,
- Pallavi Mishra 2 ,
- Kavita Singh 2 ,
- Kalpana Singh 2 ,
- Tess Harris 3 ,
- Mark Hamer 4 ,
- Sheila Margaret Greenfield 5 ,
- Nandi Krishnamurthy Manjunath 6 ,
- Rukamani Nair 7 ,
- Somnath Mukherjee 7 ,
- Nikhil Tandon 8 ,
- Sarah Anne Lewis 1 ,
- Sanjay Kinra 9 ,
- Dorairaj Prabhakaran 2 &
YOGA-DP Study Team
2488 Accesses
2 Citations
3 Altmetric
Explore all metrics
A Publisher Correction to this article was published on 24 May 2023
This article has been updated
Introduction
Many Indians are at high risk of type 2 diabetes mellitus (T2DM). The blood glucose level can be improved through a healthy lifestyle (such as physical activity and a healthy diet). Yoga can help in T2DM prevention, being a culturally appropriate approach to improving lifestyle. We developed the Yoga Programme for T2DM Prevention (YOGA-DP), a 24-week structured lifestyle education and exercise (Yoga) program that included 27 group Yoga sessions and self-practice of Yoga at home. In this study, the feasibility of undertaking a definitive randomized controlled trial (RCT) was explored that will evaluate the intervention’s effectiveness among high-risk individuals in India.
A multicenter, two-arm, parallel-group, feasibility RCT was conducted in India. The outcome assessors and data analysts were blinded. Adults with a fasting blood glucose level of 100–125 mg/dL (i.e., at high risk of T2DM) were eligible. Participants were randomized centrally using a computer-generated randomization schedule. In the intervention group, participants received YOGA-DP. In the control group, participants received enhanced standard care.
In this feasibility trial, the recruitment of participants took 4 months (from May to September 2019). We screened 711 people and assessed 160 for eligibility. Sixty-five participants (33 in the intervention group and 32 in the control group) were randomized, and 57 (88%) participants were followed up for 6 months (32 in the intervention group and 25 in the control group). In the intervention group, the group Yoga sessions were continuously attended by 32 (97%) participants (median (interquartile range, IQR) number of sessions attended = 27 (3)). In the intervention group, Yoga was self-practiced at home by 30 (91%) participants (median (IQR) number of days per week and minutes per day self-practiced = 2 (2) and 35 (15), respectively). In the control group, one (3%) participant attended external Yoga sessions (on Pranayama) for 1 week during the feasibility trial period. There was no serious adverse event.
Conclusions
The participant recruitment and follow-up and adherence to the intervention were promising in this feasibility study. In the control group, the potential contamination was low. Therefore, it should be feasible to undertake a definitive RCT in the future that will evaluate YOGA-DP’s effectiveness among high-risk people in India.
Feasibility Trial Registration
Clinical Trials Registry—India (CTRI) CTRI/2019/05/018893; registered on May 1, 2019.
Similar content being viewed by others
A yoga intervention for type 2 diabetes risk reduction: a pilot randomized controlled trial
Yoga-based lifestyle treatment and composite treatment goals in Type 2 Diabetes in a rural South Indian setup- a retrospective study

A multicentric, randomized, controlled trial of yoga and fenugreek in prevention of type 2 diabetes mellitus: methodological details—the Indian Prevention of Diabetes Study (IPDS)
Avoid common mistakes on your manuscript.
Type 2 diabetes mellitus (T2DM) is a complex metabolic disorder with significant health and socioeconomic consequences, and India has the second-largest T2DM population in the world [ 1 ]. An individual at high risk of T2DM has a higher blood glucose level than normal but lower than the level for T2DM, and more than 77 million people in India are at high risk of T2DM [ 2 ]. The chances of developing T2DM and its complications are higher among these people compared to individuals with a normal blood glucose level [ 3 ]. Indians rapidly develop T2DM from the high-risk state and have one of the highest rates across many ethnicities [ 4 ]. The major risk factors for T2DM are physical inactivity and an unhealthy diet, i.e., an unhealthy lifestyle [ 3 ]. A cost-effective and sustainable strategy is to screen individuals at high risk of T2DM and provide a lifestyle intervention that is effective [ 3 , 5 , 6 ]. Effective lifestyle interventions can improve their blood glucose level and can have other health benefits [ 7 , 8 , 9 ]. However, Indians usually have a low physical activity level, and they usually consume an unhealthy diet [ 10 , 11 , 12 ].
Yoga, an ancient mind–body discipline, originated in the Indian subcontinent and incorporates physical activity and a healthy diet [ 13 ]. Various styles of Yoga are practiced, but one style is not necessarily superior or more authentic than another, and all focus on the same important topic, i.e., a healthy lifestyle [ 14 ]. In general, Yoga’s acceptability is high in India as it fits people’s health beliefs and culture [ 15 , 16 ]. A gentle approach is used in Yoga, and it is safe and easy to learn, requires minimal guidance and maintenance costs, and can be practiced indoors as well as outdoors [ 15 ]. People who are old or with comorbidities can practice it [ 14 , 15 ]. Yoga includes low-intensity and moderate-intensity practices (< 3.5 kcal/min and 3.5–7.0 kcal/min, respectively) [ 14 , 17 , 18 , 19 ]. In addition, it is an activity that strengthens the muscles [ 14 ]. Therefore, Yoga can contribute to the goal of routine lifestyle advice which is given to individuals at high risk of T2DM to prevent it.
Yoga’s mechanism of action in T2DM and related conditions has been reported before [ 20 ]. Briefly, its benefits on T2DM-related risk profiles seem to occur predominantly through the following pathways: (1) by decreasing the activation and reactivity of the sympathoadrenal system and the hypothalamic–pituitary–adrenal axis, and by fostering feelings of well-being, it may lessen the effects of stress and promote multiple beneficial downstream effects on the neuroendocrine status, metabolic function, and related systemic inflammatory responses; (2) by directly stimulating the vagus nerve, it may improve the parasympathetic activity and lead to beneficial changes in the cardiovagal function, energy state, mood, and related neuroendocrine, metabolic, and inflammatory responses. Furthermore, Yoga may reduce body mass index (BMI), and the reduction in BMI lowers the risk of T2DM [ 3 ].
Effectiveness systematic reviews suggest the benefits and safety of Yoga in T2DM and related conditions [ 21 , 22 , 24 ]. However, the duration of most of the primary studies was short (≤ 3 months), and these studies often had significant methodological limitations. In addition, the intervention development process was not always reported, and some did not describe the intervention in detail. Even if they did, the interventions were heterogeneous. Therefore, robustly designed studies are needed to evaluate the utility of Yoga for preventing T2DM among high-risk individuals. We systematically developed the Yoga Programme for T2DM Prevention (YOGA-DP) [ 25 ]. Our aim is to conduct a definitive randomized controlled trial (RCT) in the future that will evaluate YOGA-DP’s effectiveness among high-risk individuals in India compared to enhanced standard care. The chances of successful completion of the definitive RCT will improve if the feasibility of its key elements is tested before commencement [ 26 , 27 ]. Therefore, the feasibility of undertaking the definitive RCT was explored in this study.
The feasibility study protocol is published elsewhere [ 28 ].
Study Design
A multicenter, two-arm, parallel-group, feasibility RCT was conducted. The outcome assessors and data analysts were blinded.
Study Setting
We conducted this feasibility study at two Yoga centers in India, namely Bapu Nature Cure Hospital and Yogashram (BNCHY, New Delhi) in north India and Swami Vivekananda Yoga Anusandhana Samsthana (S-VYASA, Bengaluru) in south India. These centers are accessed by individuals from a range of socioeconomic backgrounds. We used three languages (English, Hindi, and Kannada) in conducting this feasibility study.
Sample Size
In a feasibility trial, a formal sample size estimation is not usually needed [ 29 ]. It is recommended to recruit at least 50 participants in a feasibility trial [ 30 ]. Thus, we recruited a total of 65 participants in this feasibility trial, after taking into consideration the loss to follow-up.
Screening and Recruitment Strategies
The following strategies were used to inform people about this feasibility study: posters were placed and pamphlets were distributed at several locations (such as in these Yoga centers, health clinics, communities, parks, and religious places) and door-to-door visits were conducted in several communities at different times of the day. Screening camps were organized at several places (such as in these Yoga centers, communities, and religious places) for identifying potential participants. After giving the participant information sheet to potential participants, describing this feasibility study to them, and answering their questions, we requested that those interested in this feasibility trial provide written informed consent. The screening was conducted after receiving written informed consent, i.e., the fasting blood glucose level was assessed using a glucometer (by finger-prick; using either HemoCue Glucose 201 + System or Accu-Chek Active) [ 31 , 32 ]. People with a fasting blood glucose level of 100–125 mg/dL (i.e., potentially at high risk of T2DM) [ 33 ] were requested to visit the Yoga center for eligibility assessment, including a confirmatory venous blood test using the standardized glucose oxidase–peroxidase method. This eligibility assessment was conducted after receiving further written informed consent. Blood samples collected were sent immediately to the accredited laboratories for analysis within an hour. If this was not possible for any reason, the serum was immediately separated by centrifugation and stored in a − 80 °C freezer for analysis on the next day.
Eligibility Criteria
People aged 18–74 years, with a fasting blood glucose level of 100–125 mg/dL (i.e., at high risk of T2DM) [ 33 ], and who were safe to do physical activities (checked using the Physical Activity Readiness Questionnaire (PAR-Q)/clinician) [ 34 ], willing and able to attend the intervention/control sessions on their own, and able to provide written informed consent were included in this feasibility study. The following people were excluded: pregnant women, those with glycated hemoglobin (HbA1c) ≥ 6.5% (i.e., with T2DM [ 33 ]; venous blood test using the high-performance liquid chromatography method) or a serious or uncontrolled medical condition (e.g., cancer), or those who regularly practiced Yoga (i.e., ≥ 150 min/week) or were receiving (or had plans to receive during the feasibility trial period) any related non-pharmaceutical/pharmaceutical intervention (e.g., glucose-lowering medication).
Randomization
A computer-generated randomization schedule was used to randomize eligible participants to the intervention or control group (1:1, block randomization, stratified by sex and site). Sequential random sampling (140/group) was used, with 35 equal blocks generated using STATA V.15. The block size was four and fixed. This central randomization was performed by an independent statistician, based at the Centre for Chronic Disease Control (CCDC), New Delhi, India, and the allocation was accessed by the recruiting site staff by telephone call. There was an exception to this rule to avoid contamination, i.e., people recruited from the same household or who were close relatives or friends were randomized to the same group. Baseline data were collected after randomization. Participants and intervention/control providers were not blinded to group allocation, but the outcome assessors and data analysts were blinded to the feasibility trial assignment.
Interventions
Intervention (yoga-dp).
Intervention details are published elsewhere [ 25 ]. Briefly, YOGA-DP was a 24-week structured lifestyle education and exercise (Yoga) program and included 27 group Yoga sessions and self-practice of Yoga at home using the program booklet and a video. The intervention was delivered by YOGA-DP instructors, qualified and experienced Yoga teachers with formal training received on the program. The program included Shithilikarana Vyayama (loosening exercises), Surya Namaskar (sun salutation exercises), Asana (Yogic poses), Pranayama (breathing practices), and Dhyana (meditation) and relaxation practices. Female instructors were available for women. Group sessions were delivered locally (e.g., at these Yoga centers and community centers). Participants were able to join at their convenience as these sessions were run at different time points of the day (including evening and weekend sessions). We reimbursed participants’ local travel costs to attend these sessions. We also invited a family member or someone close to the participant to join him/her in these sessions. After completing the program, participants were strongly encouraged to use the intervention materials and maintain a healthy lifestyle in the long term.
We ensured intervention fidelity, and YOGA-DP instructors were regularly trained on the basis of an instructor manual. In addition, we regularly observed and evaluated these sessions using a checklist to ensure delivery according to the manual. Structured and instructive feedback was provided to them to improve their performance.

Control (Enhanced Standard Care)
No formal T2DM prevention program is available in India, although some healthcare professionals offer rudimentary advice. Therefore, in the control group, participants received the routine lifestyle advice to prevent T2DM among them in the form of a leaflet, provided by another team member (i.e., different from the YOGA-DP instructor) to avoid contamination.
Study Parameters and Data Collection
We estimated the essential parameters needed for designing the definitive RCT, e.g., participant recruitment and follow-up (for 6 months), adherence to the intervention, potential contamination in the control group, and standard deviations (SDs) of the outcomes. Details are provided in the feasibility study protocol [ 28 ]. Briefly, the following outcomes were assessed: biochemical parameters (fasting blood glucose, HbA1c, total cholesterol, high-density lipoprotein, low-density lipoprotein, very low-density lipoprotein, and triglyceride), physiological parameters (systolic blood pressure, diastolic blood pressure, and heart rate), anthropometric parameters (weight, BMI, and waist circumference), lifestyle (diet, physical activity (the International Physical Activity Questionnaire (IPAQ)-Short was used and categorized into low and moderate/high and vigorous, moderate, walking, and sitting) [ 35 ], tobacco usage, and alcohol consumption), health-related quality-of-life (the EuroQol-5D (EQ-5D) dimensions were categorized into no (level 1; no problems) and yes (level 2 to 5; problems)) [ 36 ], depression, anxiety, and stress (the Depression, Anxiety and Stress Scale (DASS) dimensions were categorized into normal and mild/moderate/severe/extremely severe) [ 37 ], and self-efficacy (for assessing confidence in participant’s ability to practice Yoga) [ 38 ].
Data Analyses and Reporting
For categorical data, numbers and percentages were calculated. For continuous data, summary measures of mean or median and spread were calculated. In terms of the percentage of loss to follow-up and withdrawal, the two groups were compared using the chi-squared test. Being a feasibility trial, it was not powered to find a difference in trial outcomes at 6 months between the two trial arms. However, unadjusted mean difference (MD) or odds ratio (OR) with a 95% confidence interval (CI) were reported to indicate initial estimates of effects. Subsequently, we conducted the analysis of covariance (ANCOVA) for four critical outcomes (fasting blood glucose, HbA1c, BMI, and waist circumference), and regression coefficient and 95% CI were reported. In model 1, the respective baseline value was adjusted for; in model 2, the respective baseline value and age were adjusted for. The analysis was based on the intention-to-treat principle. There was no plan to conduct an interim analysis. STATA V.15 was used to analyze the data. The extension of the Consolidated Standards of Reporting Trials (CONSORT) statement for randomized pilot and feasibility trials was used to report the results [ 39 ].
Ethics and Related Issues
The study was conducted in accordance with the Declaration of Helsinki. The research ethics committees of the following institutes gave ethics approval: Faculty of Medicine and Health Sciences, University of Nottingham (UK), CCDC (India), BNCHY (India), and S-VYASA (India). This feasibility study was performed in accordance with relevant guidelines and regulations. We obtained written informed consent from participants. This feasibility trial was registered with the Clinical Trials Registry—India (CTRI) (CTRI/2019/05/018893; registered on May 1, 2019). India’s Health Ministry’s Screening Committee (HMSC) also approved this feasibility study. The independent Trial Steering Committee (TSC) monitored and supervised this feasibility study.
Serious Adverse Events
We planned to collect information on serious adverse events (including hospitalization for at least 24 h and mortality) occurring in the feasibility trial participants that might be attributed to the interventions. An independent clinician was to adjudicate the association of any such event to the interventions on the basis of medical and scientific judgment.
Participant Withdrawal
We planned to withdraw participants from the feasibility trial on the basis of their request or at the discretion of the site investigator, e.g., in case the participant was no longer safe to do physical activities (determined by PAR-Q/clinician) [ 34 ] or was diagnosed with diabetes (and would receive the standard treatment).
Recruitment and Follow-up
In this feasibility trial, participants were recruited from 18 May 2019 to 19 September 2019 (i.e., when the first person was approached to participate and the last participant was randomized, respectively). It took 4 months and 2 days to recruit participants. We approached 727 people to participate. Of these, 711 were screened before eligibility assessment and 160 were assessed for eligibility. Sixty-five participants (33 in the intervention group and 32 in the control group) were randomized, and this excludes deregistered participants who did not meet the inclusion criteria but were recruited or who were recruited late. Five participants were randomized to the same group as the first participant (as either they were from the same household or were close relatives or friends). Fifty-seven (88%) participants were followed up for 6 months (32 in the intervention group and 25 in the control group). There was one (3%) loss to follow-up in the intervention group and six (19%) loss to follow-up in the control group, and the difference was statistically significant ( p = 0.04). There was no withdrawal in the intervention group and one (3%) withdrawal in the control group, but the difference was statistically insignificant ( p = 0.31) (see Fig. 1 CONSORT flowchart for details). As a result of the COVID-19 lockdown in India, the follow-up of one intervention group participant was delayed and limited information was collected over the telephone from two intervention group participants and one control group participant.
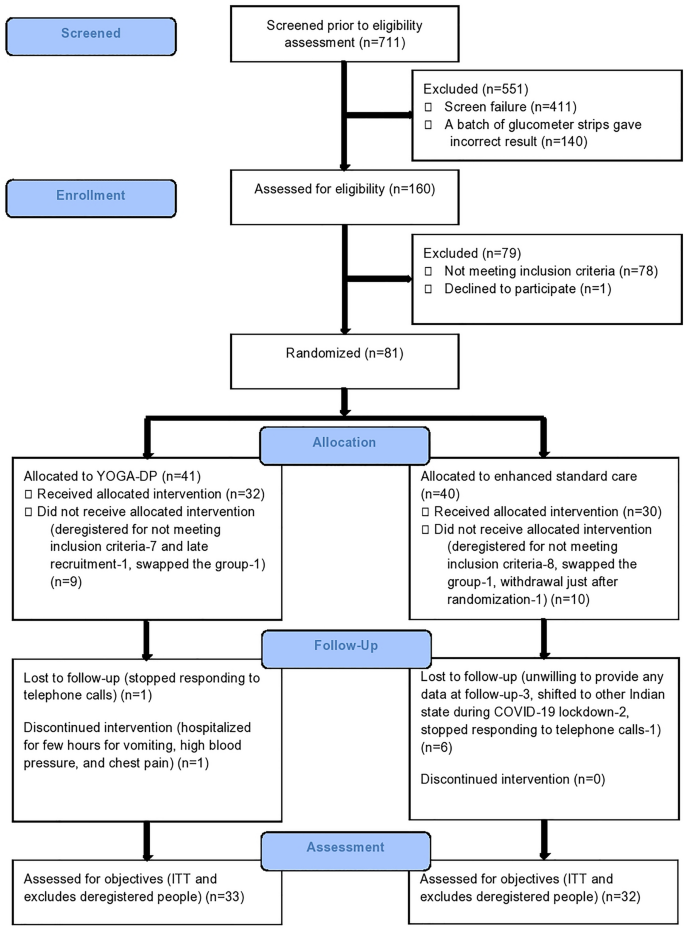
CONSORT flowchart
Intervention Adherence
In this feasibility study, the group Yoga sessions were continuously attended by 32 (97%) participants, and one participant discontinued because of hospitalization for a few hours for vomiting, high blood pressure, and chest pain (this was not counted as a serious adverse event). The median (interquartile range, IQR) number of group Yoga sessions attended was 27 (3). Yoga was self-practiced at home by 30 (91%) participants, and the median (IQR) number of days per week and minutes per day self-practiced was 2 (2) and 35 (15), respectively.
Potential Contamination in the Control Group
One (3%) participant attended external Yoga sessions (on Pranayama) for 1 week during the feasibility trial period (self-reported). Yoga classes were available outside, but YOGA-DP was not available externally.
Table 1 reports the baseline characteristics of the feasibility trial participants. The mean (± SD) age of participants was 42.1 (7.7) years, and 25 (38%) were female. The mean (± SD) fasting blood glucose was 110.3 (8.3) mg/dL, HbA1c was 5.9 (0.3) %, BMI was 27.6 (5) kg/m 2 , and waist circumference was 93 (13.2) cm. At baseline, the two groups were mostly similar except for a few variables, which could be due to the small sample size.
Table 2 reports the unadjusted outcomes at 6 months.
Biochemical, physiological, and anthropometric parameters—The fasting blood glucose, HbA1c, weight, BMI, and waist circumference were lower in the intervention group compared to the control, but the differences were statistically insignificant. The high-density lipoprotein was higher in the intervention group compared to the control, but the difference was statistically insignificant.
Lifestyle—The percentage of participants reporting no/occasional intake of high-fat/deep-fried food was higher in the intervention group compared to the control. The moderate physical activity time was higher in the intervention group compared to the control, but the difference was statistically insignificant. Sitting time was lower in the intervention group compared to the control, but the difference was statistically insignificant. The percentage of participants reporting no tobacco usage was higher in the intervention group compared to the control. In addition, the odds of tobacco usage were lower in the intervention group compared to the control, but the difference was statistically insignificant.
Health-related quality-of-life—The percentage of participants reporting no problems in all five dimensions of EQ-5D was higher in the intervention group compared to the control. In addition, the odds of problems in the three dimensions (mobility problems, problems in taking self-care, and problems in doing usual activities) were lower in the intervention group compared to the control, but the differences were statistically insignificant. The visual analog scale score was higher in the intervention group compared to the control, but the difference was statistically insignificant.
Depression, anxiety, and stress—The percentage of participants reporting no problems in all three dimensions of DASS was higher in the intervention group compared to the control.
Self-efficacy in Yoga practice—The self-efficacy was higher in the intervention group compared to the control, but the difference was statistically insignificant.
Table 3 reports the adjusted four critical outcomes at 6 months.
Fasting blood glucose, HbA1c, BMI, and waist circumference—After adjustment for the respective baseline value (model 1) and baseline value and age (model 2), BMI was found to be lower in the intervention group compared to the control, and the difference was statistically significant (regression coefficient − 0.56; 95% CI − 1.00 to − 0.11 and regression coefficient − 0.56; 95% CI − 1.02 to − 0.11, respectively). In addition, fasting blood glucose, HbA1c, and waist circumference were lower, but the differences were statistically insignificant.
There was no serious adverse event.
We conducted a multicenter feasibility RCT in India to assess the feasibility of undertaking the definitive RCT in the future that will evaluate YOGA-DP’s effectiveness among high-risk individuals in India. The participant recruitment and follow-up and adherence to the intervention were promising in this feasibility study. There was low potential contamination in the control group. Compared to other T2DM prevention RCTs in India and globally [ 27 , 40 ], the recruitment in this feasibility trial was without any major hurdles. In this feasibility study, the dropout rate was 12% which is consistent with the findings of a systematic review (less than 15–20% in most RCTs on Yoga interventions) [ 41 ]. The only follow-up-related challenge we faced was towards the end of this feasibility trial, and this was due to the COVID-19 lockdown in India. Therefore, it should be feasible to undertake a definitive RCT. This feasibility study provided estimates of important parameters needed for designing the definitive RCT.
In the definitive RCT, the first co-primary outcome will be the incidence of T2DM, indicated by either a fasting blood glucose level of at least 126 mg/dL or an HbA1c level of at least 6.5% at 1-year follow-up [ 3 ]. Repeat testing will be conducted in asymptomatic participants to confirm the diagnosis [ 3 ], and they will only be included as achieving the co-primary outcome if repeat testing of either fasting blood glucose or HbA1c is above the cutoff. The second co-primary outcome will be BMI at 1-year follow-up [ 42 ]. The reduction in BMI lowers the risk of T2DM [ 3 ]. It should be noted that compared to other ethnicities, South Asians are at higher risk of T2DM at equivalent BMI levels [ 43 ]. We expect that the cumulative incidence of T2DM over 1 year will be 18% in the control group [ 44 , 45 ]. In the intervention group, we will be interested in a 50% reduction in the cumulative incidence of T2DM [ 46 , 47 ]. Therefore, in the definitive RCT, we will need to recruit at least 356 participants per group (a total of 712), with 90% power and assuming significance (alpha; two-tailed) of 2.5% to conservatively allow for co-primary outcomes. This sample size will be sufficient for the other primary outcome, considering the mean (± SD) BMI at the baseline was 27.6 (5) kg/m 2 in this feasibility trial and our interest in at least a 5% reduction in BMI at 1 year in the intervention group [ 42 , 48 ].
Initial estimates (as this feasibility trial was not powered for effectiveness) show some beneficial effects of the intervention on many critical outcomes, including fasting blood glucose, HbA1c, BMI, and waist circumference. In the adjusted models, BMI was lower in the intervention group compared to the control and the difference was statistically significant. No serious adverse events occurred. Similar beneficial effects and safety of Yoga on T2DM-related outcomes have been synthesized in several effectiveness systematic reviews [ 21 , 22 , 24 ]. In the future, the adequately powered definitive RCT will be able to provide a clear answer.
In the definitive RCT, if YOGA-DP is found to be effective, it will be a need-sensitive and evidence-based intervention for preventing T2DM among high-risk individuals, not only in India but also globally. Yoga’s popularity is not restricted to India and other South Asian countries, and it is increasingly becoming popular in other nations [ 49 , 50 ]. T2DM and its associated costs are global concerns, and a low-cost intervention to prevent T2DM will be of worldwide interest. More evidence-based choices will be available to people for preventing T2DM. The future burden of T2DM (such as clinical, personal, and economic) on patients, families, health systems, and economies will be prevented. The prevention of T2DM may extend to the prevention of its complications. Individuals will become healthier overall, and the intervention may empower people at the same time for managing their health. The intervention has become even more relevant during the COVID-19 pandemic, as it can be delivered online or in-person (outdoors or indoors by following the social distancing rules), and Yoga can be self-practiced at home.
Semi-structured qualitative interviews (as part of the qualitative process evaluation) were conducted with feasibility trial non-participants, participants, YOGA-DP instructors, and staff to explore trial- and intervention-related barriers and facilitators [ 28 , 51 , 52 ]. The findings will inform decisions on modifying the definitive RCT and intervention to further improve participation and adherence. For example, the intervention duration was 6 months in this feasibility trial, and we intend to deliver a year-long intervention in the definitive RCT. The relatively short-term follow-up was another limitation in this feasibility trial, and we intend to do long-term follow-ups (at least for a year) in the definitive RCT. In terms of glycemic control, this feasibility trial gave some hints about the effectiveness of the intervention, and we intend to assess the cumulative incidence of T2DM in the definitive RCT as a co-primary outcome. We reimbursed participants’ local travel costs for attending the Yoga sessions at BNCHY, and at SVYASA, Yoga sessions were run locally and close to their residence. The reimbursement could have boosted participant recruitment and follow-up in this feasibility trial and adherence to the intervention; however, this would not be available in real-world settings.
The participant recruitment and follow-up and adherence to the intervention were promising in this feasibility study. In the control group, the potential contamination was low. Therefore, it should be feasible to undertake a definitive RCT in the future that will evaluate YOGA-DP’s effectiveness among high-risk individuals in India.
Change history
24 may 2023.
A Correction to this paper has been published: https://doi.org/10.1007/s13300-023-01420-6
International Diabetes Federation (IDF). IDF diabetes atlas. 9th ed. Brussels: IDF; 2019.
Google Scholar
Anjana RM, Pradeepa R, Deepa M, et al. Prevalence of diabetes and prediabetes in urban and rural India: phase I results of the ICMR-INDIAB study. Diabetologia. 2011;54:3022–7.
Article CAS PubMed Google Scholar
National Institute for Health and Care Excellence (NICE). Preventing type 2 diabetes: risk identification and interventions for individuals at high-risk. Manchester: NICE; 2012.
Anjana RM, Shanthi Rani CS, Deepa M, et al. Incidence of diabetes and prediabetes and predictors of progression among Asian Indians: 10-year follow-up of the Chennai Urban Rural Epidemiology Study (CURES). Diabetes Care. 2015;38(8):1441–8.
Article PubMed Google Scholar
Haw JS, Galaviz KI, Straus AN, et al. Long-term sustainability of diabetes prevention approaches: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2017;177(12):1808–17.
Article PubMed PubMed Central Google Scholar
Galaviz KI, Weber MB, Straus A, et al. Global diabetes prevention interventions: a systematic review and network meta-analysis of the real-world impact on incidence, weight, and glucose. Diabetes Care. 2018;41(7):1526–34.
Gong QH, Kang JF, Ying YY, et al. Lifestyle interventions for adults with impaired glucose tolerance: a systematic review and meta-analysis of the effects on glycemic control. Intern Med. 2015;54:303–10.
World Health Organization (WHO). Global strategy on diet, physical activity and health. Geneva: WHO; 2015.
Mudaliar U, Zabetian A, Goodman M, et al. Cardiometabolic risk factor changes observed in diabetes prevention programs in US settings: a systematic review and meta-analysis. PLoS Med. 2016;13(7):e1002095.
Anjana RM, Pradeepa R, Das AK, et al. Physical activity and inactivity patterns in India: results from the ICMR-INDIAB study (Phase-1) [ICMR-INDIAB-5]. Int J Behav Nutr Phys Act. 2014;11:26.
Gulati S, Misra A, Sharma M. Dietary fats and oils in India. Curr Diabetes Rev. 2017;13(5):438–43.
Minocha S, Thomas T, Kurpad AV. Are “fruits and vegetables” intake really what they seem in India? Eur J Clin Nutr. 2018;72:603–8.
Feuerstein G. The deeper dimensions of Yoga: theory and practice. Boston: Shambhala Publications; 2003.
National Health Service (NHS). A guide to Yoga: exercise. UK: NHS. 2018. https://www.nhs.uk/live-well/exercise/guide-to-yoga/ . Accessed 12 Jul 2021.
Anderson JG, Taylor AG. The metabolic syndrome and mind-body therapies: a systematic review. J Nutr Metab. 2011;2011:276419.
Anjana RM, Ranjani H, Unnikrishnan R, et al. Exercise patterns and behaviour in Asian Indians: data from the baseline survey of the Diabetes Community Lifestyle Improvement Program. Diabetes Res Clin Pract. 2015;107:77–84.
Centers for Disease Control and Prevention (CDC) and American College of Sports Medicine (ACSM). General physical activities defined by level of intensity. Atlanta: CDC; 2015.
Sinha B, Ray US, Pathak A, et al. Energy cost and cardiorespiratory changes during the practice of Surya Namaskar. Indian J Physiol Pharmacol. 2004;48:184–90.
CAS PubMed Google Scholar
Mody BS. Acute effects of Surya Namaskar on the cardiovascular and metabolic system. J Bodyw Mov Ther. 2011;15:343–7.
Cramer H, Innes KE, Michalsen A, et al. Yoga for adults with type 2 diabetes mellitus (protocol). Cochrane Database Syst Rev. 2015;4:CD011658.
Cramer H, Lauche R, Haller H, et al. Effects of Yoga on cardiovascular disease risk factors: a systematic review and meta-analysis. Int J Cardiol. 2014;173:170–83.
Cramer H, Langhorst J, Dobos G, et al. Yoga for metabolic syndrome: a systematic review and meta-analysis. Eur J Prev Cardiol. 2016;23:1982–93.
Kumar V, Jagannathan A, Philip M, et al. Role of Yoga for patients with type II diabetes mellitus: a systematic review and meta-analysis. Complement Ther Med. 2016;25:104–12.
Cui J, Yan JH, Yan LM, et al. Effects of Yoga in adults with type 2 diabetes mellitus: a meta-analysis. J Diabetes Investig. 2017;8:201–9.
Chattopadhyay K, Mishra P, Manjunath NK, et al. Development of a Yoga Program for Type-2 Diabetes Prevention (YOGA-DP) among high-risk people in India. Front Public Health. 2020;8:548674.
National Institute for Health Research (NIHR). Feasibility and pilot studies. London: NIHR; 2014.
Ranjani H, Weber MB, Anjana RM, et al. Recruitment challenges in a diabetes prevention trial in a low- and middle-income setting. Diabetes Res Clin Pract. 2015;110:51–9.
Chattopadhyay K, Mishra P, Singh K, et al. Yoga Programme for Type-2 Diabetes Prevention (YOGA-DP) among high risk people in India: a multicentre feasibility randomised controlled trial protocol. BMJ Open. 2020;10(9):e036277.
Thabane L, Ma J, Chu R, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10(1):1.
Hooper R. Justifying sample size for a feasibility study. London: NIHR; 2014.
Horovskaia LA, Lobachevskaia TV, Chernichuk OV. The analytical quality and comparability value of four glucometers from different manufacturers. Klin Lab Diagn. 2015;60(1):60–3.
Baumstark A, Jendrike N, Kamecke U, et al. Measurement accuracy of two professional-use systems for point-of-care testing of blood glucose. Clin Chem Lab Med. 2020;58(3):445–55.
Buysschaert M, Medina JL, Buysschaert B, et al. Definitions (and current controversies) of diabetes and prediabetes. Curr Diabetes Rev. 2016;12:8–13.
Adams R. Revised Physical Activity Readiness Questionnaire. Can Fam Physician. 1999;45:992, 995, 1004–5.
CAS PubMed PubMed Central Google Scholar
Craig CL, Marshall AL, Sjöström M, et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20:1727–36.
Article CAS PubMed PubMed Central Google Scholar
Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–39.
Bandura A. Guide for constructing self-efficacy scales. In: Pajares F, Urdan T, editors. Self-efficacy beliefs of adolescents. Greenwich: Information Age Publishing; 2006. p. 307–37.
Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ. 2016;355:i5239.
Douglas A, Bhopal RS, Bhopal R, et al. Recruiting South Asians to a lifestyle intervention trial: experiences and lessons from PODOSA (Prevention of Diabetes & Obesity in South Asians). Trials. 2011;12:220.
Cramer H, Haller H, Dobos G, et al. A systematic review and meta-analysis estimating the expected dropout rates in randomized controlled trials on Yoga interventions. Evid Based Complement Alternat Med. 2016;2016:5859729.
Ryan DH, Yockey SR. Weight loss and improvement in comorbidity: differences at 5%, 10%, 15%, and over. Curr Obes Rep. 2017;6(2):187–94.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Article Google Scholar
Ramachandran A, Snehalatha C, Mary S, et al. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006;49(2):289–97.
Ramachandran A, Snehalatha C, Ram J, et al. Effectiveness of mobile phone messaging in prevention of type 2 diabetes by lifestyle modification in men in India: a prospective, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol. 2013;1(3):191–8.
Glechner A, Keuchel L, Affengruber L, et al. Effects of lifestyle changes on adults with prediabetes: a systematic review and meta-analysis. Prim Care Diabetes. 2018;12(5):393–408.
Uusitupa M, Khan TA, Viguiliouk E, et al. Prevention of type 2 diabetes by lifestyle changes: a systematic review and meta-analysis. Nutrients. 2019;11(11):2611.
European Medicines Agency (EMA). Guideline on clinical evaluation of medicinal products used in weight management. London: EMA; 2016.
Birdee GS, Legedza AT, Saper RB, et al. Characteristics of Yoga users: results of a national survey. J Gen Intern Med. 2008;23:1653–8.
Ding D, Stamatakis E. Yoga practice in England 1997–2008: prevalence, temporal trends, and correlates of participation. BMC Res Notes. 2014;7:172.
Mishra P, Greenfield SM, Harris T, et al. Yoga program for type 2 diabetes prevention (YOGA-DP) among high-risk people: qualitative study to explore reasons for non-participation in a feasibility randomized controlled trial in India. Front Public Health. 2021;9:682203.
Mishra P, Harris T, Greenfield SM, et al. Feasibility trial of Yoga programme for type 2 diabetes prevention (YOGA-DP) among high-risk people in India: a qualitative study to explore participants’ trial- and intervention-related barriers and facilitators. Int J Environ Res Public Health. 2022;19(9):5514.
Download references
Acknowledgment
The authors would like to thank the funding agencies, participants, and TSC members, namely Prof. Nitin Kapoor (chair), Prof. Mohammed K Ali, Dr. Ajay Vamadevan, and Dr. Dimple Kondal.
The study was funded by the UK’s FCDO/MRC/NIHR/Wellcome Trust Joint Global Health Trials (MR/R018278/1). The funding agencies had no role in designing the study or in writing the manuscript. The publication fee was covered through the UKRI block grant.
Author Contributions
KC wrote the first draft of the manuscript. PM, KavS, KalS, TH, MH, SMG, NKM, RN, SM, NT, SAL, SK, and DP contributed significantly to the revision of the manuscript. All the authors read and approved the final manuscript.
List of Investigators
KC (Principal Investigator) conceptualized and designed the study with the help of Co-Investigators (TH, MH, SMG, NKM, NT, SAL, SK, and DP).
Prior Presentation
The study abstract was selected for presentation at the International Diabetes Federation (IDF) Congress 2021 (held virtually from 6 to 11 December 2021 due to the COVID-19 pandemic) and published in the event material. https://doi.org/10.26226/morressier.617c37317c09fc044a9751b2 .
Disclosures
KC, PM, KavS, KalS, TH, MH, SMG, NKM, RN, SM, NT, SAL, SK, and DP have nothing to disclose.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Declaration of Helsinki. The research ethics committees of the following institutes gave ethics approval: Faculty of Medicine and Health Sciences, University of Nottingham, UK (14-1805); CCDC, India (CCDC_IEC_09_2018); BNCHY, India (BNCHY/IEC/2/2019); and S-VYASA, India (RES/IEC-SVYASA/138/2018). We obtained written informed consent from participants.
Data Availability
The data set generated during the current study is available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
Lifespan and Population Health Academic Unit, University of Nottingham, Nottingham, UK
Kaushik Chattopadhyay & Sarah Anne Lewis
Centre for Chronic Disease Control, New Delhi, India
Pallavi Mishra, Kavita Singh, Kalpana Singh & Dorairaj Prabhakaran
Population Health Research Institute, St. George’s University of London, London, UK
Tess Harris
Division of Surgery and Interventional Science, Institute of Sport, Exercise and Health, University College London, London, UK
Institute of Applied Health Research, University of Birmingham, Birmingham, UK
Sheila Margaret Greenfield
Swami Vivekananda Yoga Anusandhana Samsthana, Bengaluru, India
Nandi Krishnamurthy Manjunath
Bapu Nature Cure Hospital and Yogashram, New Delhi, India
Rukamani Nair & Somnath Mukherjee
Department of Endocrinology, Metabolism and Diabetes, All India Institute of Medical Sciences, New Delhi, India
Nikhil Tandon
Department of Non-communicable Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, UK
Sanjay Kinra
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Kaushik Chattopadhyay .
Additional information
The original online version of this article was revised due to update in author group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Chattopadhyay, K., Mishra, P., Singh, K. et al. Yoga Programme for Type 2 Diabetes Prevention (YOGA-DP) Among High-Risk People in India: A Multicenter Feasibility Randomized Controlled Trial. Diabetes Ther 14 , 1137–1154 (2023). https://doi.org/10.1007/s13300-023-01395-4
Download citation
Received : 19 February 2023
Accepted : 08 March 2023
Published : 31 March 2023
Issue Date : July 2023
DOI : https://doi.org/10.1007/s13300-023-01395-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Blood glucose
- Prediabetes
- Physical activity
- Feasibility study
- Randomized controlled trial
- Find a journal
- Publish with us
- Track your research
Welcome, Please Sign In

Scientific Research on Yoga > Disease and Disorders > Diabetes and Endocrine
Other Research Categories
Diabetes and endocrine type 1 and 2 diabetes, metabolic syndrome/prediabetes, endocrine conditions.
Our hope is for yoga schools and yoga teachers to utilize this impactful content in their teachings to promote and highlight yoga's evident multi-faceted ability to improve lives. Let us know how research on yoga is important or valuable to you on social media (@YogaAlliance) or by emailing us at [email protected] . We honor and value your personal experiences and look forward to featuring your stories.
These citations were curated by Yoga Alliance's Director of Yoga Research, Dr. Sat Bir Singh Khalsa .
Main Research Categories

Review Papers (What's this?)
Effectiveness of Yoga as the Public Health Intervention Module in the Management of Diabetes and Diabetes Associated Dementia in South East Asia: A Narrative Review. Bali P, Kaur N, Tiwari A, Bammidi S, Podder V, Devi C, Kumar S, Sivapuram MS, Ghani A, Modgil S, Malik N, Anand A. Neuroepidemiology. 2020 Feb 19:1-17. [ full text ]
The effect of yoga practice on glycemic control and other health parameters in the prediabetic state: A systematic review and meta-analysis. Ramamoorthi R, Gahreman D, Skinner T, Moss S. PLoS One. 2019 Oct 16;14(10):e0221067. [ full text ]
Therapeutic Role of Yoga in Type 2 Diabetes. Raveendran AV, Deshpandae A, Joshi SR. Endocrinol Metab (Seoul). 2018 Sep;33(3):307-317. [ full text ]
The benefits of yoga practice compared to physical exercise in the management of type 2 Diabetes Mellitus: A systematic review and meta-analysis. Jayawardena R, Ranasinghe P, Chathuranga T, Atapattu PM, Misra A. Diabetes Metab Syndr. 2018 Sep;12(5):795-805. [ abstract ]
The effects of yoga among adults with type 2 diabetes: A systematic review and meta-analysis. Thind H, Lantini R, Balletto BL, Donahue ML, Salmoirago-Blotcher E, Bock BC, Scott-Sheldon LAJ. Prev Med. 2017 Dec;105:116-126. [ abstract ]
A narrative review on role of Yoga as an adjuvant in the management of risk factor, disease progression and the complications of type 2 diabetes mellitus. Mooventhan A. Diabetes Metab Syndr. 2017 Nov;11 Suppl 1:S343-S346. [ abstract ]
The effect of yoga practice on glycemic control and other health parameters in Type 2 diabetes mellitus patients: A systematic review and meta-analysis. Vizcaino M, Stover E. Complement Ther Med. 2016 Oct;28:57-66. doi: 10.1016/j.ctim.2016.06.007. [ abstract ]
Yoga for metabolic syndrome: A systematic review and meta-analysis. Cramer H, Langhorst J, Dobos G, Lauche R. Eur J Prev Cardiol. 2016 Dec;23(18):1982-1993. [ abstract ]
Role of yoga for patients with type II diabetes mellitus: A systematic review and meta-analysis. Kumar V, Jagannathan A, Philip M, Thulasi A, Angadi P, Raghuram N. Complement Ther Med. 2016 Apr;25:104-12. [ abstract ]
Yoga for Adults with Type 2 Diabetes: A Systematic Review of Controlled Trials. Innes KE, Selfe TK. J Diabetes Res. 2016;2016:6979370. [ full text ]
Psycho-neuro-endocrine-immune mechanisms of action of yoga in type II diabetes. Singh VP, Khandelwal B, Sherpa NT. Anc Sci Life. 2015 Jul-Sep;35(1):12-7. [ full text ]
The benefits of yoga for adults with type 2 diabetes: a review of the evidence and call for a collaborative, integrated research initiative. de G R Hansen E, Innes KE. Int J Yoga Therap. 2013;(23):71-83. [ full text ]
Male reproductive health and yoga. Sengupta P, Chaudhuri P, Bhattacharya K. Int J Yoga. 2013 Jul;6(2):87-95. [ full text ]
Notable Publications (What's this?)
Effect of an Integrated Naturopathy and Yoga Program on Long-Term Glycemic Control in Type 2 Diabetes Mellitus Patients: A Prospective Cohort Study. Bairy S, Rao MR, Edla SR, Manthena SR, Tatavarti NVGD. Int J Yoga. 2020 Jan-Apr;13(1):42-49. doi: 10.4103/ijoy.IJOY_32_19. [ full text ]
Randomized Controlled Trial of A 12-Week Yoga-Based (Including Diet) Lifestyle vs. Dietary Intervention on Cardio-Metabolic Risk Factors and Continuous Risk Score in Indian Adults with Metabolic Syndrome. Yadav R, Yadav RK, Khadgawat R, Pandey RM, Upadhyay AD, Mehta N. Behav Med. 2020 Jan-Mar;46(1):9-20. [ abstract ]
Efficacy of a Validated Yoga Protocol on Dyslipidemia in Diabetes Patients: NMB-2017 India Trial. Nagarathna R, Tyagi R, Kaur G, Vendan V, Acharya IN, Anand A, Singh A, Nagendra HR. Medicines (Basel). 2019 Oct 11;6(4). [ full text ]
Partitioning of radiological, stress and biochemical changes in pre-diabetic women subjected to Diabetic Yoga Protocol. Singh AK, Kaur N, Kaushal S, Tyagi R, Mathur D, Sivapuram MS, Metri K, Bammidi S, Podder V, Modgil S, Khosla R, Sharma K, Anand A, Malik N, Boroiah V, Nagarathna R, Nagendra HR, Anand A. Diabetes Metab Syndr. 2019 Jul - Aug;13(4):2705-2713. [ abstract ]
Comparative efficacy of a 12 week yoga-based lifestyle intervention and dietary intervention on adipokines, inflammation, and oxidative stress in adults with metabolic syndrome: a randomized controlled trial. Yadav R, Yadav RK, Khadgawat R, Pandey RM. Transl Behav Med. 2019 Jul 16;9(4):594-604. [ full text ]
Effectiveness of Adjuvant Yoga Therapy in Diabetic Lung: A Randomized Control Trial. Balaji R, Ramanathan M, Bhavanani AB, Ranganadin P, Balachandran K. Int J Yoga. 2019 May-Aug;12(2):96-102. [ full text ]
"I can do almost anything": The experience of adults with type 2 diabetes with a yoga intervention. Thind H, Guthrie KM, Horowitz S, Conrad M, Bock BC. Complement Ther Clin Pract. 2019 Feb;34:116-122. [ full text ]
Feasibility of yoga as a complementary therapy for patients with type 2 diabetes: The Healthy Active and in Control (HA1C) study. Bock BC, Thind H, Fava JL, Dunsiger S, Guthrie KM, Stroud L, Gopalakrishnan G, Sillice M, Wu W. Complement Ther Med. 2019 Feb;42:125-131. [ full text ]
Effect of Ayurveda intervention, lifestyle modification and Yoga in prediabetic and type 2 diabetes under the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS)-AYUSH integration project. Sharma R, Shahi VK, Khanduri S, Goyal A, Chaudhary S, Rana RK, Singhal R, Srikanth N, Dhiman KS. Ayu. 2019 Jan-Mar;40(1):8-15. [ full text ]
One Year of Yoga Training Alters Ghrelin Axis in Centrally Obese Adults With Metabolic Syndrome. Yu AP, Ugwu FN, Tam BT, Lee PH, Lai CW, Wong CSC, Lam WW, Sheridan S, Siu PM. Front Physiol. 2018 Sep 20;9:1321. [ full text ]
Influence of Time of Yoga Practice and Gender Differences on Blood Glucose Levels in Type 2 Diabetes Mellitus and Normal Healthy Adults. Vijayakumar V, Mooventhan A, Raghuram N. Explore (NY). 2018 Jul - Aug;14(4):283-288. [ abstract ]
Multidimensional Improvements in Health Following Hatha Yoga for Individuals with Diabetic Peripheral Neuropathy. Van Puymbroeck M, Atler K, Portz JD, Schmid AA. Int J Yoga Therap. 2018 Nov;28(1):71-78. [ abstract ]
Effect of 12 Weeks of Yoga Therapy on Quality of Life and Indian Diabetes Risk Score in Normotensive Indian Young Adult Prediabetics and Diabetics: Randomized Control Trial. Keerthi GS, Pal P, Pal GK, Sahoo JP, Sridhar MG, Balachander J. J Clin Diagn Res. 2017 Sep;11(9):CC10-CC14. [ full text ]
Effect of yoga and aerobics exercise on sleep quality in women with Type 2 diabetes: a randomized controlled trial. Ebrahimi M, Guilan-Nejad TN, Pordanjani AF. Sleep Sci. 2017 Apr-Jun;10(2):68-72. doi: 10.5935/1984-0063.20170012. [ full text ]
A Randomized controlled trial of the effect of yoga and peer support on glycaemic outcomes in women with type 2 diabetes mellitus: a feasibility study. Sreedevi A, Gopalakrishnan UA, Karimassery Ramaiyer S, Kamalamma L. BMC Complement Altern Med. 2017 Feb 7;17(1):100. [ full text ]
Yoga for Risk Reduction of Metabolic Syndrome: Patient-Reported Outcomes from a Randomized Controlled Pilot Study. Sohl SJ, Wallston KA, Watkins K, Birdee GS. Evid Based Complement Alternat Med. 2016;2016:3094589. [ full text ]
Impact of individualized yoga therapy on perceived quality of life performance on cognitive tasks and depression among Type II diabetic patients. Satish L, Lakshmi VS. Int J Yoga. 2016 Jul-Dec;9(2):130-6. [ full text ]
Effect of 6 months intense Yoga practice on lipid profile, thyroxine medication and serum TSH level in women suffering from hypothyroidism: A pilot study. Nilakanthan S, Metri K, Raghuram N, Hongasandra N. J Complement Integr Med. 2016 Jun 1;13(2):189-93. [ abstract ]
Effects of a 12-Week Hatha Yoga Intervention on Metabolic Risk and Quality of Life in Hong Kong Chinese Adults with and without Metabolic Syndrome. Lau C, Yu R, Woo. PLoS One. 2015 Jun 25;10(6):e0130731. [ full text ]
Effects of 1-year yoga on cardiovascular risk factors in middle-aged and older adults with metabolic syndrome: a randomized trial. Siu PM, Yu AP, Benzie IF, Woo J. Diabetol Metab Syndr. 2015 Apr 30;7:40. [ full text ]
Completion report: Effect of Comprehensive Yogic Breathing program on type 2 diabetes: A randomized control trial. Jyotsna VP, Dhawan A, Sreenivas V, Deepak KK, Singla R. Indian J Endocrinol Metab. 2014 Jul;18(4):582-4. [ full text ]
Effect of restorative yoga vs. stretching on diurnal cortisol dynamics and psychosocial outcomes in individuals with the metabolic syndrome: the PRYSMS randomized controlled trial. Corey SM, Epel E, Schembri M, Pawlowsky SB, Cole RJ, Araneta MR, Barrett-Connor E, Kanaya AM. Psychoneuroendocrinology. 2014 Nov;49:260-71. [ full text ]
A yoga intervention for type 2 diabetes risk reduction: a pilot randomized controlled trial. McDermott KA, Rao MR, Nagarathna R, Murphy EJ, Burke A, Nagendra RH, Hecht FM. BMC Complement Altern Med. 2014 Jul 1;14:212. [ full text ]
Restorative yoga and metabolic risk factors: the Practicing Restorative Yoga vs. Stretching for the Metabolic Syndrome (PRYSMS) randomized trial. Kanaya AM, Araneta MR, Pawlowsky SB, Barrett-Connor E, Grady D, Vittinghoff E, Schembri M, Chang A, Carrion-Petersen ML, Coggins T, Tanori D, Armas JM, Cole RJ. J Diabetes Complications. 2014 May-Jun;28(3):406-12. [ full text ]
Effect of regular yogic training on growth hormone and dehydroepiandrosterone sulfate as an endocrine marker of aging. Chatterjee S, Mondal S. Evid Based Complement Alternat Med. 2014;2014:240581. [ full text ]
Stay Connected
Have questions.
Visit our Help Center .
Media Inquiries
Stay up-to-date on the latest from Yoga Alliance, subscribe to our newsletters.
A Comprehensive Review of Yoga Research in 2020
Affiliations.
- 1 Advanced Yoga Research Council, AAYM, Germantown, TN, USA.
- 2 Department of Research, Government Yoga and Naturopathy Medical College, Chennai, India.
- 3 Department of Cardiology, NRS Medical College, Kolkata, India.
- 4 Department of Yoga, Central University of Rajasthan, Ajmer, India.
- 5 Department of Yoga, Manipur University, Imphal, India.
- 6 Department of Cardiology, Memphis VA Medical Center, Memphis, TN, USA.
- 7 School of Public Health, The University of Memphis, Memphis, TN, USA.
- 8 Integrative Cardiology, All India Institute of Medical Sciences, Rishikesh, India.
- PMID: 35099279
- DOI: 10.1089/jicm.2021.0420
Objectives: Accumulated evidence garnered in the last few decades has highlighted the role of yoga in health and disease. The overwhelming mortality and morbidity mediated by noncommunicable epidemics such as heart disease and cancer have fostered a search for mechanisms to attenuate them. Despite overwhelming success in acute care, the efficacy of modern medicines has been limited on this front. Yoga is one of the integrative therapies that has come to light as having a substantial role in preventing and mitigating such disorders. It thus seems trite to analyze and discuss the research advancements in yoga for 2020. The present review attempts to distill recent research highlights from voluminous literature generated in 2020. Methods: This review was conducted on the articles published or assigned to an issue in 2020. The authors searched the PubMed database for clinical studies published in the English language, using yoga (including meditation) as the intervention, and having an adequate description of the intervention. Then, they extracted data from each study into a standardized Google sheet. Results: A total of 1149 citations were retrieved in the initial search. Of these, 46 studies met eligibility criteria and were finally included. The studies were predominantly on mental health and neuropsychology, addressing various issues such as anxiety, postural balance, migraine, academic performance, and childhood neglect. Anxiety, stress, and depression were other common denominators. Eight studies were on cardiorespiratory systems, including exercise capacity, cardiac rehabilitation, myocardial infarction, and hypertension. Three studies were on diabetes, evaluating the effect of yoga. Five studies focused on cognition, health status, and autonomic regulation and few others included cancers, infertility, ulcerative colitis, urinary incontinence, restless leg syndrome, rheumatoid arthritis, chronic pain, and metabolic syndrome. Finally, most studies were on noncommunicable diseases with one exception, human immunodeficiency virus; two randomized controlled trials were dedicated to it. Conclusions: Yoga has been studied under a wide variety of clinicopathological conditions in the year 2020. This landscape review intends to provide an idea of the role of yoga in various clinical conditions and its future therapeutic implications.
Keywords: clinical research; meditation; trials; yoga.
Publication types
- Chronic Pain*
- Meditation*
- Mental Health
50% Off Selected ELC courses in March
- Globally Accessible Kundalini Yoga | Health. Self Awareness. Education.

- All ATA Academy Best Sellers Books & Manuals Bundles Chakras Courses Deep Dive Immersion Digital Products English KRI Products Kundalini Yoga for Healing Kundalini Yoga Teacher Resources Libros en Español Other Self Care Products Specialty Items Teacher Training Course Teacher Training Material Yoga for Women Yogi Bhajan Search for:
No products in the cart.
- Make A Donation

- How To Become a Teacher Trainer
- The Aquarian Teacher | Overview
- What is Level One?
- KRI Level One
- Level One Bali Immersion 2024
- Level One Mexico Hybrid 2024
- What is Level Two?
- Level Two Conscious Communication 2024
- Level Two Mind & Meditation India 2024
- What is Level Three?
- 2024 Upcoming Melas
- 21 Stages of Meditation
- 21 Etapas de la Meditación Mexico 2024
- KRI Approved Specialty Courses
- International Trainer & Program Directory
- EPS Ethics and Anti Harassment Training
- Research Symposium
- Research Papers
- E-learning Center
- KRI Board of Directors
- KRI History
- News and Updates
- Seva Projects
- Diversity, Equity & Inclusion
- Free Resources
- Kundalini Beyond Borders
- About Kundalini Yoga
- Library of Teachings
- EBook Store
- KRI Wholesaler Program
Yoga for Type 2 Diabetes: Scientific Rationale and Clinical Research Evidence
By Nikhil Rayburn and Sat Bir Singh Khalsa, Ph.D.
Type 2 Diabetes Mellitus (DM2), also called adult-onset diabetes, is a metabolic disease that was formerly only diagnosed in midlife but is now impacting younger adults and even children. This disorder is characterized by defects in insulin production and action, resulting in elevated blood glucose levels, which can lead to serious medical consequences. Long-term complications from diabetes account for more adult cases of vision loss, end-stage kidney disease, and amputations than any other disease. In addition, diabetes significantly increases the risk of cardiovascular disease and may be linked to cancer.
DM2 is largely a lifestyle disease caused by inadequate physical activity, diets rich in highly-processed foods and refined sugars, and elevated levels of life-stress. Twenty-eight million people in the United States have DM2, and more than 80 million are considered to be at high risk of developing it, a state called prediabetes or metabolic syndrome. Worldwide, more than 350 million people are estimated to have DM2, a disease affecting many developing countries with limited resources. The high cost and relatively low effectiveness of conventional treatment have resulted in an economic burden estimated to total $322 billion annually in the United States. Conventional treatment aims at controlling glucose levels through medications, education, and behavior change schemes. However, behavior change is notoriously hard to enact because the same environmental and social conditions that gave rise to the disease-causing behavior are still in place. Pharmaceutical treatment drawbacks include dependency, resistance, and adverse long-term effects. Consequently, there has been a concentrated search for non-pharmaceutical treatment and preventative measures. Behavioral treatments such as lifestyle interventions addressing the risk factors of obesity and sedentary activity reduce the development of diabetes by as much as 58% and decrease the need for medications. However, current conventional behavioral lifestyle interventions have limited effectiveness; this is a factor that may likely be improved with yoga.
Yoga interventions address several DM2 risk factors and bring a much-needed holistic approach to DM2 treatment. In yoga, physical exercises are linked to lifestyle and behavioral changes that include diet, relaxation, and stress management. A lesser-known aspect of yoga is the social support that a yoga class or community provides and social support is strongly linked to improved diabetes self-care and clinical outcomes. Yoga is better known for increasing fitness and physical function, thereby improving both glucose metabolism and psychological health. At the same time, yoga promotes and supports weight loss and thereby addresses obesity which is a major cause of DM2 onset and complications. Finally, the two most beneficial and consistent outcomes of yoga are an increase in mind-body awareness and stress-coping ability. This leads to a host of positive downstream effects including improvements in healthy behaviors, avoidance of unhealthy behaviors, better sleep cycles, balanced neuroendocrine status, improved metabolic function, and reduced inflammatory responses.
There is convincing research that shows that yoga improves mindfulness and mind-body awareness, and this may well encourage individuals to gravitate to healthy behaviors such as exercise and healthy food choices, and away from unhealthy habits such as consuming junk food. This is all due to their enhanced experience of the positive effects of these behaviors. Evidence suggests that stress may play a major role in the development of diabetes, which is why relaxation techniques, such as are found in yoga, could serve as a very effective complement to other lifestyle modifications. Therefore, there is every reason to believe that yoga should be efficacious in preventing and treating DM2.
Metabolic Regulation
Studies evaluating yoga interventions in patients with DM2 found that yoga normalized metabolic functions which resulted in increased insulin sensitivity, glucose tolerance, and improved lipid profiles. These beneficial effects of yoga on glycemic control are well documented. A recent review in the International Journal of Yoga Therapy looked at the evidence for the benefits of yoga in adults with DM2. Peer-reviewed studies published between 1970 and 2006 looked at the effects of yoga on diabetes and diabetes risk factors in a broad range of outcomes, such as insulin resistance, glucose intolerance, elevated blood pressure, and excess body weight. Each of these factors is strongly implicated in the development and progression of DM2.
Despite considerable variability in design, clinical measures, and target populations, most trials reported positive changes in at least one of the outcomes related to DM2 and in clinical outcomes as well. The most recent review of research on yoga therapy for DM2 was published this year by Kim Innes of West Virginia University in the Journal of Diabetes Research. Researchers found 33 papers reporting findings from 25 controlled trials (12 of them RCTs) representing 2170 participating research subjects and concluded that “collectively, the findings suggest that yogic practices may promote significant improvements in several indices of importance in DM2 management, including glycemic control, lipid levels, and body composition.
More limited data suggest that yoga may also lower oxidative stress and blood pressure; enhance pulmonary and autonomic function, mood, sleep, and quality of life; and reduce medication use in adults with DM2.”
Improved Sense of Well-Being
In a pilot study conducted by Shanti Shanti Kaur Khalsa and Guru Parkash Kaur of the Guru Ram Das Center for Medicine and Humanology (founded by Yogi Bhajan in Espanola, New Mexico to apply the practices of Kundalini Yoga for therapeutic populations), they applied 3 questionnaires to evaluate the effectiveness of an 8-week Kundalini Yoga and lifestyle intervention program in diabetic patients. One of these was the Audit of Diabetes Dependent Quality of Life, which measures individuals’ perception of the impact of diabetes on their quality of life. Improvement in quality of life was measured in 9 of 11 participants.
The second scale was the Profile of Mood States which consists of subscales measuring the following moods: anger, confusion, depression, fatigue, anxiety, and vigor. There was a statistically significant improvement in all of the above mood states following participation in the diabetes program. The third measure was the Functional Assessment of Chronic Illness Therapy – Spiritual Well-Being, which measures a faith factor as well as a meaning-and-peace factor. There was a statistically significant improvement in spiritual well-being following participation in the diabetes program as measured by this scale.
The evaluation showed that most participants found the components of the program extremely helpful especially in the areas of mood, stress management, quality of life, and ability to relax. Although such findings support the efficacy of yoga as a therapeutic intervention to improve quality of life and stress management, larger randomized control trials are required to substantiate the results.
Assist Controlling Glucose Levels
There is now a growing number of studies with larger sample sizes showing that yoga can have a positive impact on diabetes. For example, an Indian study from 2015 highlights the efficacy of yoga in controlling blood glucose levels in patients with DM2. The study was conducted at the Department of Physiology and Diabetic clinic of a teaching hospital over a period of two years. The subjects were 30 middle-aged male diabetic patients and an equal number of non-diabetic volunteers made up the control group. The significant decrease in blood glucose levels after yoga in both the experimental and control groups indicates the potential role of yoga as preventive and treatment strategies for DM2. In addition, there is some reason to believe that yoga may rejuvenate or regenerate beta cells of the pancreas which can normalize insulin production.
Given its positive effects on metabolic regulation, physical well-being, and mental health, yoga can be considered as a cost-effective and non-invasive adjunct therapy for treating DM2. With few exceptions, the studies document beneficial changes in yoga program participants and suggest improvements in several risk indices mentioned previously such as glucose tolerance, insulin sensitivity, lipid profiles, blood pressure, oxidative stress, and pulmonary function. However, several of the current studies have small sample sizes which prevent the generalization of findings. The therapeutic potential of yoga in the face of a worldwide epidemic of diabetes warrants additional research, which will require more funding from our public health institutions. This would likely prove to be a valuable investment given that conventional pharmaceutical treatment comes with a number of side effects and limited efficacy. Yoga is potentially a highly cost-effective protocol to treat and prevent DM2 since it addresses the underlying causes along with symptoms.
Nikhil Rayburn grew up practicing yoga under mango trees in the tropics. He is a certified Kundalini Yoga teacher and has taught yoga to children and adults in Vermont, New Mexico, Connecticut, India, France, and Mauritius. He is a regular contributor to the Kundalini Research Institute newsletter and explores current yoga research.
Sat Bir Singh Khalsa, Ph.D. is the KRI Director of Research, Research Director for the Kripalu Center for Yoga & Health, and Assistant Professor of Medicine at Harvard Medical School. He has practiced a Kundalini Yoga lifestyle since 1973 and is a KRI certified Kundalini Yoga instructor. He has conducted research on yoga for insomnia, stress, anxiety disorders, and yoga in public schools. He is editor in chief of the International Journal of Yoga Therapy and The Principles and Practice of Yoga in Health Care and author of the Harvard Medical School ebook Your Brain on Yoga.
Kundalini Research Institute
KRI is a non-profit organization that holds the teachings of Yogi Bhajan and provides accessible and relevant resources to teachers and students of Kundalini Yoga.
See author's posts
More Related Blogs

Sign up form for Mexico Hybrid
Want to know more.
Subscribe to get free
Kundalini Yoga sets and meditations + special offers for Level One!
We respect your privacy. Unsubscribe at any time.
This will close in 0 seconds
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Diabetol Metab Syndr

Diabetic yoga protocol improves glycemic, anthropometric and lipid levels in high risk individuals for diabetes: a randomized controlled trial from Northern India
Navneet kaur.
1 Department of Physical Education, Panjab University, Chandigarh, 160014 India
4 Department of Neurology, Neuroscience Research Lab, Postgraduate Institute of Medical Education and Research, Chandigarh, 160012 India
Vijaya Majumdar
2 Division of Life Sciences, Swami Vivekananda Yoga Anusandhana Samsathana, Bengaluru, Karnataka 560106 India
Raghuram Nagarathna
Neeru malik.
3 Dev Samaj College of Education, Sector 36B, Chandigarh, 160036 India
Akshay Anand
Hongasandra ramarao nagendra, associated data.
The datasets used during the present study are available from the corresponding author on reasonable request.
To study the effectiveness of diabetic yoga protocol (DYP) against management of cardiovascular risk profile in a high-risk community for diabetes, from Chandigarh, India.
The study was a randomized controlled trial, conducted as a sub study of the Pan India trial Niyantrita Madhumeha Bharath (NMB) . The cohort was identified through the Indian Diabetes Risk Scoring (IDRS) (≥ 60) and a total of 184 individuals were randomized into intervention (n = 91) and control groups (n = 93). The DYP group underwent the specific DYP training whereas the control group followed their daily regimen. The study outcomes included changes in glycemic and lipid profile. Analysis was done under intent-to-treat principle.
The 3 months DYP practice showed diverse results showing glycemic and lipid profile of the high risk individuals. Three months of DYP intervention was found to significantly reduce the levels of post-prandial glucose levels (p = 0.035) and LDL-c levels (p = 0.014) and waist circumference (P = 0.001).
The findings indicate that the DYP intervention could improve the metabolic status of the high-diabetes-risk individuals with respect to their glucose tolerance and lipid levels, partially explained by the reduction in abdominal obesity. The study highlights the potential role of yoga intervention in real time improvement of cardiovascular profile in a high diabetes risk cohort.
Trial registration: CTRI, CTRI/2018/03/012804. Registered 01 March 2018—Retrospectively registered, http://www.ctri.nic.in/ CTRI/2018/03/012804.
Introduction
The rise of diabetes in the developing world poses a threat to meager health budgets. Owing to the strong association between various morbidity and mortality outcomes as complications of this dreaded disease, early detection of diabetes risk through non-invasive parameters is a primary requisite. Observational studies show that the risk reduction for diabetes can be decreased by 58% or 63–65% if risk factors could be controlled [ 1 , 2 ]. Many argue that such experimental strategies for the possible halting of conversion of prediabetes into diabetes must continue to include pharmacological interventions even though the rates have not been compared [ 3 ]. Identification of individuals at increased risk for the disease with invasive measurements of fasting and post challenge (postprandial) blood glucose are costly and time consuming. Hence, it has been advocated that the realistic prevention of diabetes should identify high-risk subjects with the use of the non-invasive risk scores [ 4 ]. Such studies should also target subjects with normoglycemia and prevent their progression to poor glycemic status [ 4 ].
Yoga plays a promising role in minimizing the risk of Diabetes for high-risk individuals with prediabetes [ 5 , 6 ]. It reduces body weight, glucose, and lipid levels, though, most of these studies comply with the guidelines of randomized controlled trials adhered to the CONSORT statements [ 7 – 11 ] whereas majority of studies have not reported as per CONSORT statements [ 12 – 15 ]. Several review of published studies, in people with diabetes and prediabetes, have concluded that the practice of yoga may reduce insulin resistance and related cardiovascular disease (CVD) risk factors and improve clinical outcomes [ 16 ]. Specifically, reports suggest that a yoga-based lifestyle intervention reduces body weight, glucose and lipid levels that should reduce diabetes risk. Keeping in view the high transition rates of diabetes in India, we selected a high-risk cohort from Chandigarh, one of the most affluent Union Territories of India with highest reported prevalence of diabetes in order to establish the efficacy of yoga to alleviate the cardiovascular disease. Indian Diabetes Risk Score (IDRS), specific for Indian ethnicity a validated tool was used for identification of the high-risk population [ 17 ]. We developed a national consensus ‘Diabetes Yoga protocol’ based on published reports and classical literature with an aim to stimulate weight reduction by combination of postures and meditation techniques [ 18 , 19 ]. Additionally, cardiometabolic risk reduction has also been recognized as one of the potential outcomes of yoga-based interventions [ 20 ]. Yoga has been shown to be regulating the risk parameters of diabetes, waist circumference (WC), body mass index (BMI), oxidative stress, fasting blood sugar (FBS) and systolic blood pressure (SBP) respectively [ 21 ]. Hence, in this study we tested the efficacy of diabetic yoga protocol (DYP) on alleviation of glycemic and lipid imbalances in individuals at high risk of diabetes.
Materials and methods
Study population.
Under the multi-region survey of Niyantarita Maduhmeha Bharat (NMB-2017) a door-to-door screening was carried out for the identification of high risk individuals among the population of Chandigarh (U.T) and Panchkula (District in Haryana state) on the basis of Indian Diabetes Risk Score (IDRS). The data collection was carried out by well trained yoga volunteers for diabetes management (YVDMs). Written informed consents were taken from every subject during door to door screening as well as at the time of registration. All the experimental protocol, methods and procedures were approved by Ethics committee of Indian Yoga Association (IYA) (ID: RES/IEC-IYA/001). All experiments methods and procedures were carried out in accordance with relevant guidelines and regulations of ethics committee. The study was registered at clinical trial registry of India, CTRI/2018/03/012804 (dated: 01/03/2018).
Study design
The present study is the two-armed randomized controlled trial conducted in the population of Chandigarh and Panchkula regions of northern India. Indian Diabetes Risk Score (IDRS) was used for detection of high risk (≥ 60 score) individuals from the study. Self-declared diabetics and low (< 30 score) and moderate [between 30–50 score] risk individuals were excluded from the study. As evident from the flow of patients presented in the flowchart, out of 1214 eligible subjects, there was approximately 50% loss of sample data due to error in the sampling. Further out of 564, we had to exclude as they were self-declared patients with diabetes and did not further participate in the study. However, this led to final participation of only 184 subjects in the study and allocation of these subjects diminishing the random selection of the study cohort. A cohort of high diabetes-risk cohort consisting of n = 184 participants was randomized into the interventional and control groups (n = 91:93). After excluding the dropouts from the study, based on CONSORT guidelines, the remaining subjects in the DYP and control group were further assessed for selected anthropometric, glycemic and lipid parameters. The intervention group was given the Diabetic Yoga Protocol for three months and control group continued with their daily routine activities. The detailed categorization of the samples is shown in Fig. 1 . The control group was waitlisted for yoga.

Flowchart of study design. PCA principal component analysis, MIPCA multiple imputations with PCA
Randomization
Simple randomization technique was used to allocate participants into the intervention and the control groups. An independent statistician generated a computer-generated random number sequence and the sequence was given to an external staff who had no involvement in the study procedures. The participants were allocated their consecutive numbers, after baseline measurements. Blinding of the participants was not possible due to the nature of the intervention. However, the outcome assessors were blinded.
Risk assessment
To identify the individuals at high-risk of diabetes, Indian Diabetes Risk Score (IDRS) was administered as proposed by Mohan et al. [ 22 ]. It consisted of two unmodifiable (i.e. age, and family history) and two modifiable (physical activity and waist circumference) risk factors for diabetes, which can predict the level of risk for the development of diabetes in the community. The IDRS is one of the easily accessible and budget friendly questionnaire to be administered. The aggregate score of the unmodifiable and modifiable risk used to probe the level of risk among the population (i.e. High risk > 60, Moderate risk-30–50, Low risk < 30).
Sample size
Sample size estimation for the main Pan India study was focused for prediabetes subjects [ 23 ]. However, for the present pilot scale study we calculated sample size assuming a small effect size 0.3 [ 5 ] of DYP vs waitlist control 0.25, α = 0.80 as 180 (n = 90:90). Further, assuming an attrition rate of 20%, the final sample size was n = 220.
Study outcomes
Changes in the glycemic and other metabolic variables (anthropometric and lipid) over 3 months were documented. The fasting blood sample was withdrawn. For glucose analysis, fasting samples for 10–12 h were taken early in the morning for the estimation of FBS and afterwards 75 g glucose was given to the participants. The blood sampling was repeated after 2 h. for estimation of OGTT.
Biochemical analysis
For the estimation of biochemical parameters viz. FBS (Fasting Blood Sugar, Rxl-Max 500), OGTT (Oral Glucose Tolerance Test), HbA1c (Bio-Rad D-10), Triglycerides, Cholesterol, HDL, LDL, Chol/HDL ratio, HDL/LDL ratio (Rxl-Max 500) and VLDL about 9 ml of blood was drawn and analyzed by phlebotomist of Sisco Research Laboratories (SRL) of Chandigarh. Anthropometric measurements were also obtained (i.e. height, weight, waist circumference) by trained researcher. The waist circumference (WC) was reported in centimeters. The BMI was obtained by using the formula (weight in kg/height (meter) 2 ).
Interventions
The study protocol consisted of Diabetic Yoga Protocol (DYP) approved by the Ministry of AYUSH and Quality Council of India as shown in Table Table1. 1 . This is the first protocol to be made specifically for the prediabetics and diabetics. The complete sequence of prayer, yogic postures, breathing and meditative techniques, along with specified time, was shown in previously published paper [ 24 ]. The Yogic practices were performed for 3 months for 60 min. Certified yoga instructors took the yoga classes and they recorded regular attendance. Randomization was done through a computer-generated list of random numbers and allocation was concealed to the participants until the completion of the baseline assessment.
Diabetic yoga protocol (DYP)
Statistical analysis
For the analysis of data SPSS for Windows (version 22; IBM SPSS Inc., Chicago IL) 0 and R statistical package were used. The normality of data was analyzed using Kolmogorov–Smirnov test. The paired t-test was used to estimate the Baseline and posttest differences of DYP, and control group and the significant level was set at ≤ 0.05. The trial outcomes were analyzed according to the intention-to-treat principle; hence multiple imputation was carried for the missing variables accounting for the loss to follow up. We used absolute change (time and treatment interaction), to estimate intervention effects refers to the difference in the outcome of the intervention and control over different time-points of assessment. Absolute change was determined as follows: absolute change = [(intervention group follow-up) – (intervention group baseline)] – [(control group follow-up) – (control group baseline)]. The percentage change, also called the relative change was determined as relative change = (absolute change / intervention group baseline) × 100%. To evaluate the influence of missing data, we applied multiple imputations to the data using missMDA R package (v1.13) based on the principal component analysis method [ 25 ] from the package, using 5 components to reconstruct the data and over 1000 imputed datasets. One-way multivariate analysis of covariance (MANCOVA) was conducted to compare the effects of the DYP with control group glycemic and metabolic measures, while controlling for the age, gender and baseline values of the covariates.
Baseline characteristics
The data used in this study was collected in (NMB-2017) the northern region of India i.e. Chandigarh and Panchkula. The age range of participants was 3–70 years; [mean age 48.51 (SD 10.08) years]with baseline characteristics of the yoga and control groups as shown in Table Table2. 2 . Mean HbA1c of the high-risk cohort was 5.64% (0.38), mean FBS was 97.13 mg/dl (SD 11.10), and mean PPBS were 108.40 mg/dl (SD 28.79). Distributions of age and gender was similar between the intervention and the control groups. The IDRS and anthropometric values were also similarly distributed between the groups. Overall, there was no significant difference in the distribution of demographic, anthropometric, or biochemical parameters between the DYP and the control groups at the baseline.
Baseline characteristics of the participants in the intervention and control group
Continuous variables are represented as mean (SD) and compared using independent t-test. Categorical variables are represented as number (percentages) and compared using chi-square test. P value < 0.05 were considered significant. FBS fasting blood sugar, PPBG postprandial blood glucose, HbA1c glycated hemoglobin, HDL-c high density lipid-cholesterol, LDL-c low density lipid-cholesterol, VLDL very low density lipid-cholesterol, IDRS Indian diabetes risk score
When analyzed by multivariate analysis of covariance (MANCOVA), adjusting for age, gender and status of diabetes/prediabetes/normoglycemia, and baseline values of the covariates, yoga intervention was found to have significant influence on few cardinal parameters related to glycemic control (PPBS), and lipid control (LDL-C) as shown in Table Table3. 3 . We also observed a significant influence of DPP on waist circumference reduction [relative changes, − 1.94%. Compared to the control, DYP also resulted in significant reductions in LDL-C and, − 0.16% and − 2.81%, for LDL-Cholesterol and post-prandial blood glucose levels from baseline to 3 months [absolute changes, − 0.18% and − 3.08%, respectively and relative changes, − 0.16% and − 2.81%, respectively].
Comparative assessment of influence of DYP on biochemical and weight related variables with the control group
Absolute change = [(intervention group follow-up) – (intervention group baseline)] – [(control group follow-up) – (control group baseline)]. Relative change = (absolute change / intervention group baseline) × 100%; p value for difference between the intervention and the control groups by MANCOVA adjusting for age, gender, status of diabetes/prediabetes/normoglycemia baseline values of glycemic and lipid variables, length of time having had prior exposure of yoga
We examined the effect of Diabetic Yoga Protocol on baseline and post (3 months) levels of HbA1c and other glycemic (OGTT and FBS), Lipid (Total cholesterol, triglycerides, HDL-c, LDL-c, and VLDL-c, CDL/HDL, LDL/HDL) and anthropometric parameters (BMI). In the present study, we show the efficacy of DYP in substantial improvement in the waist circumference in a high-risk diabetes population from Chandigarh (relative change of 1.94 cm). We could also demonstrate a significant decline in the worsening of post prandial glucose levels with yoga intervention as compared to the wait-list control group (relative change of 2.82 mg/ml). However, for LDL-c levels, there were clinically significant improvements by 0.16 units. Notably, over 3 months study duration there was an overall increase in the levels of total cholesterol, triglyceride and VLDL means in the study cohort, while HDL levels had decreased. In particular TG levels have gone from normal range to mildly high (> 150 mg/dl) [ 26 ] which draws our attention towards accelerated pace of metabolic dysfunction in the high risk population. These findings comply with Chandigarh being an affluent union territory of India with high per-capita GDP and has been documented to have highest prevalence of diabetes 13.6%, 12.8–15·2 as compared to other Indian states [ 27 ]. As mentioned above, there was a significant influence of DYP on the waist circumference, one of the two important modifiable parameters of Indian Diabetes Risk Score [ 17 ]. The relevance of WC reduction in context of reduced risk of CVD is well established; a 1 cm increase in WC has been associated with a 2% increase in the relative risk of future CVD [ 28 ]. The visceral adipose tissue is a primary source of cytokine production and insulin resistance (IR) [ 29 ]. Given the higher susceptibility towards visceral fat accumulation and insulin resistance in Asian populations as compared to their Caucasian counterparts, the observed influence of DYP on WC is of particular relevance to the metabolically obese phenotype of Asian Indians [ 30 ].
In relation to the glucose metabolism, we could also demonstrate a significant decline in the worsening of post prandial glucose levels with DYP as compared to the wait-list control group (relative change = − 2.81%, P < 0.05); however, no significant influence could be established for fasting blood glucose concentration. These findings could be justified by the phenotypic differences underlying fasting and post-challenge hyperglycemia that represent distinct natural histories in the evolution of type 2 diabetes [ 31 ]. Postprandial glucose disposal is the primary pathogenic manifestation in impaired glucose tolerance (IGT), and impaired fasting glucose (IFG) merely signifies an abnormal glucose set point [ 31 , 32 ]. Our relevance of the study findings is further underlined by the previous results wherein PPG has been reported to contribute more than FBS to overall hyperglycemia and its control was found essential either to decrease or to obtain HbA1c goals of < 7 [ 33 ]. Several epidemiological studies have suggested that increased glycemic exposure, especially post challenge or postprandial hyperglycemia, is an independent risk factor for macrovascular disease with no apparent upper or lower threshold. Our results indicate a significant influence of yoga on glycemic control integrating postprandial glycemic alterations in the high diabetes risk group. Since in the present study the high-risk cohort was selected through A1c based diagnosis, and IGT was not a primary manifestation in the cohort, hence, the overall improvement in postprandial glucose should be specifically tested in an IGT cohort. The findings of the current study with a 3-month intervention of yoga on postprandial measures of glucose at-risk population deserves clinical attention. Increase in the glucose concentration even in the prediabetes stage, manifests as a chronic inflammatory condition and predisposes an individual to the risk of pathogenic infections [ 32 , 34 , 35 ].
The simultaneous reduction in waist circumference observed in the cohort, is also consistent with the observation of an association between abdominal obesity and the risk of IGT. Based on a significant association between IGT and CVD risk [ 32 , 33 , 36 ], we note a significant improvement in lipid concentrations [LDL-c] by the DYP protocol as compared to the control group. These results are consistent with the previously reported overall beneficial effect of yoga in the management of hyperlipidemia [ 36 ]. These results need validation at larger scale and to ascertain the mechanistic insights into the action of yoga, the indices of monocyte chemotaxis, endothelial inflammation, oxidation, nitric oxide production, and thrombosis should also be explored [ 37 ], including animal models, invitro systems and other approaches [ 38 – 44 ].
The findings of the present study indicate that identification of high-risk group through IDRS and consequent intervention of Yoga based lifestyle protocol could be an effective strategy to combat the metabolic perturbations associated with diabetes, whose co-morbidity is also being reported to be associated with increasing vulnerability to the emerging viral pandemic of COVID-19. Lifestyle interventions are reported to reduce the risk of Type 2 diabetes in high-risk individuals after mid and long-term follow-up. Information on determinants of intervention outcome, adherence and the mechanisms underlying diabetes progression are valuable for a more targeted implementation. Weight loss is a major contributor in the prevention and management of type 2 diabetes. In many of the earlier lifestyle intervention group of the DPP, weight loss was the dominant predictor of reduced diabetes risk, with a 16% reduction observed for every kilogram of weight loss during the 3.2-year follow-up [ 45 ]. Though we failed to observe a significant weight loss over 3 months of DYP intervention, the significant reductions in WC indicate the plausibility of significant weight loss on longer interventions and follow ups.
Whether Yoga alters the conversion of prediabetics into healthy status and if it helps in maintenance of glycemic index can be assessed by longitudinal studies. There was a significant improvement in the glycemic status of the high risk population at administration of DYP. The analysis shows the aptness of Diabetic protocol which is apparently superior to previous studies where no standardized protocols were used for intervention [ 46 , 47 ]. The findings suggest that there is potential of DYP to manage glucose levels in diabetes patients if public intervention is planned through forthcoming wellness centers in India. There are additional studies showing beneficial effects of Yoga on FBS [ 48 ], PPBS [ 49 – 51 ], HbA1c [ 50 , 51 ], total cholesterol, LDL [ 50 , 51 ]. The analysis of the yoga protocols used in above said studies reveal the incorporation of some common and important postures in DYP, which seem to be important in managing the disease. It is also the possible that the beneficial effects of mind body techniques are sensitive to mental disposition of subjects and has been characterized by various measures like psychometric analysis [ 52 , 53 ], namely, Tridosha and Triguna scoring [ 54 , 55 ]. These were not analyzed in this study.
Briefly, DYP’s promising efficacy on glycemic and metabolic parameters requires mechanistic insights. This can be examined by further studies, and long term follow up which was not possible in this study. As DYP is a non-pharmacological, cost-effective method to halt the conversion of early diabetes into prediabetes and/or healthy individuals, the success of its integration into public health policy will depend on its wider acceptability and perception of benefits by both public as well as healthcare workers [ 56 – 59 ]. Yoga’s benefits in maintaining and regulation of the glycemic status are supported by several other studies [ 49 , 50 ], which might enable its inclusion in the National Ayushman Bharat scheme or as part COVID pandemic management protocol in which a large number of individuals with diabetes and heart disease are falling prey [ 60 , 61 ]. This will further encourage molecular and Ayurgenomic studies which presumably underlie the stated clinical outcome.
Limitations
Moreover, there are some limitations of our study that we only studied in two regions of North India and thus the result of this study cannot be generalized on the remaining population. Further, in this study, the socio economic status and psychological assessments were not carried out. We were not able to control for the dietary habits and psychological status of the study participants. However, the small sample size and absence of long term evaluations limit the strength of the study.
Acknowledgements
The authors would like to thank Central Council for Research in Yoga & Naturopathy (CCRYN) for their support for man power, Ministry of Health and Family Welfare (MOHFW) for support the cost of investigations and Indian Yoga Association (IYA) for the overall project implementation. The authors also like to thank to thank Yoga Volunteer for Diabetes Management (YVDMs) for helping in collection of data and also for training participants for yoga.
Abbreviations
Authors' contributions.
NK: writing of manuscript, collection of data. VM: writing of manuscript, analysis. RN: conceptualization of manuscript, supervision and study design. NM: co-conceptualization of manuscript. AA: conceptualization of manuscript. HRN: supervision. All authors read and approved the final manuscript.
The Project was funded by Ministry of AYUSH, Government of India (grant number 16-63/2016-17/CCRYN/RES/Y&D/ MCT/).
Availability of data and materials
Declarations.
Written informed consents were taken from every subject during door to door screening as well as at the time of registration. All the experimental protocol, methods and procedures were approved by Ethics committee of Indian Yoga Association (IYA) (ID: RES/IEC-IYA/001). All experiments methods and procedures were carried out in accordance with relevant guidelines and regulations of ethics committee.
Not applicable.
The authors declare that they have no competing interests.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Raghuram Nagarathna, Email: moc.liamg@antaraganr .
Akshay Anand, Email: moc.liamffider@dnana1yahska .

COMMENTS
Yoga improves cell-mediated immunity, as demonstrated by improvements in the lymphocyte migration test in people with type 2 diabetes [ 53 ]. Yoga also prevents the development of diabetes in high-risk individuals [ 54 ]. It was found to improve symptom scores in people with diabetes [ 55 ].
Abstract. A growing body of evidence suggests yogic practices may benefit adults with type 2 diabetes (DM2). In this systematic review, we evaluate available evidence from prospective controlled trials regarding the effects of yoga-based programs on specific health outcomes pertinent to DM2 management. To identify qualifying studies, we ...
The benefit of yoga for diabetes management has also been found in recent reviews. Innes and Selfe (2016) showed that yoga may improve ... The research reported in this paper was supported by the National Center for Complementary and Integrative Health of the National Institutes of Health under award number R01-AT008815 to Lori A. J. Scott ...
Abstract and Figures. Yoga originated in India more than 5,000 years ago and is a means of balancing and harmonizing the body, mind, and emotions. Yoga practice is useful in the management of ...
Abstract. A growing body of evidence suggests yogic practices may benefit adults with type 2 diabetes (DM2). In this systematic review, we evaluate available evidence from prospective controlled trials regarding the effects of yoga-based programs on specific health outcomes pertinent to DM2 management. To identify qualifying studies, we ...
Abstract. The purpose of this meta-analysis was to examine the effects of yoga for glycemic control among adults with type 2 diabetes (T2DM). Comprehensive electronic databases searches located 2559 unique studies with relevant key terms. Studies were included if they (1) evaluated a yoga intervention to promote T2DM management, (2) used a ...
Yoga practice is useful in the management of various lifestyle diseases, including type 2 diabetes. Psycho-neuro-endocrine and immune mechanisms are involved in the beneficial effects of yoga on diabetes. Incorporation of yoga practice in daily life helps to attain glycaemic control and reduces the risk of complications in people with diabetes.
A growing body of evidence suggests yogic practices may benefit adults with type 2 diabetes (DM2). In this systematic review, we evaluate available evidence from prospective controlled trials regarding the effects of yoga-based programs on specific health outcomes pertinent to DM2 management. To identify qualifying studies, we searched nine databases and scanned bibliographies of relevant ...
To study the effectiveness of diabetic yoga protocol (DYP) against management of cardiovascular risk profile in a high-risk community for diabetes, from Chandigarh, India. The study was a randomized controlled trial, conducted as a sub study of the Pan India trial Niyantrita Madhumeha Bharath (NMB). The cohort was identified through the Indian Diabetes Risk Scoring (IDRS) (≥ 60) and a total ...
Benefits of Yoga for Diabetes § Deep focused breath, stretching, strengthening muscles, and non- judgmental awareness § Switching between asanas (poses) contracts and relaxes specific areas, increases oxygenated supply to cells and organ, uses glucose § Stretching triggers endorphins and makes you feel good § Stress = ↑BG. Consistent practice, especially Pranayama (Yogic
Diabetes mellitus (DM) is a group of metabolic disorders characterized by chronic hyperglycemia due to relative insulin deficiency or resistance or both. India with an estimated 31million diabetics in 2000 and 79 mllions by the year 2030 has the highest number of type 2 diabetics in the world. Although patients with DM can have a reasonably ...
Academia.edu is a platform for academics to share research papers. Effect of Yoga on Insulin Resistance in Type 2 Diabetes: A Systematic Review and Meta-Analysis (PDF) Effect of Yoga on Insulin Resistance in Type 2 Diabetes: A Systematic Review and Meta-Analysis | Sridip Chatterjee - Academia.edu
Oxidative stress has been implicated as the root cause underlying the development of insulin resistance, β-cell dysfunction, diabetes, and its associated clinical conditions such as atherosclerosis, microvascular complications, and neuropathy (1,2).Yoga has been found to be beneficial in reducing oxidative stress in type 2 diabetes (3,4), but there is a lack of controlled trials to ...
Academia.edu is a platform for academics to share research papers. The Effect of Yoga on Health-Related Fitness among Patients with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis ... randomized controlled pilot study to collect feasibility and preliminary efficacy data on yoga for diabetes risk factors among people at high risk ...
Introduction Many Indians are at high risk of type 2 diabetes mellitus (T2DM). The blood glucose level can be improved through a healthy lifestyle (such as physical activity and a healthy diet). Yoga can help in T2DM prevention, being a culturally appropriate approach to improving lifestyle. We developed the Yoga Programme for T2DM Prevention (YOGA-DP), a 24-week structured lifestyle education ...
Serum insulin, plasma fasting and one hour postprandial blood glucose levels and anthropometric parameters were measured before and after yoga asanas. The results indicate that there was significant decrease in fasting glucose levels from basal 208.3 +/- 20.0 to 171.7 +/- 19.5 mg/dl and one hour postprandial blood glucose levels decreased from ...
Abstract. This article provides a review of literature both to identify the effects of yoga-based therapy on the management of type 2 diabetes mellitus and to examine the social context of physical activity. Findings from the review indicate that yoga has a positive short-term effect on multiple diabetes-related outcomes; however, long-term ...
THE EFFECT OF YOGA IN DIABETES. B.K.SAHAY, RAMANANDA YOGI, P.S. RA JU, MADHAVI SUNITHA, C.BHASKARACHARYULU, B.SADASIVUDU AN D K.J.R. MURTHY. Vemana Yoga Research Institute, Market Street ...
Type 1 and 2 Diabetes, Metabolic Syndrome/Prediabetes, Endocrine Conditions. Our hope is for yoga schools and yoga teachers to utilize this impactful content in their teachings to promote and highlight yoga's evident multi-faceted ability to improve lives. Let us know how research on yoga is important or valuable to you on social media ...
Conclusions: Yoga has been studied under a wide variety of clinicopathological conditions in the year 2020. This landscape review intends to provide an idea of the role of yoga in various clinical conditions and its future therapeutic implications. Keywords: clinical research; meditation; trials; yoga.
The American Diabetes Association Position Statement ( 38) recommends that the use of adjuvant therapies be based on evidence from clinical research and presently there is no comprehensive, systematic review in the existing literature that addresses the effectiveness of yoga practice in diabetes mellitus management.
Peer-reviewed studies published between 1970 and 2006 looked at the effects of yoga on diabetes and diabetes risk factors in a broad range of outcomes, such as insulin resistance, glucose intolerance, elevated blood pressure, and excess body weight. ... The most recent review of research on yoga therapy for DM2 was published this year by Kim ...
We developed a national consensus 'Diabetes Yoga protocol' based on published reports and classical literature with an aim to ... along with specified time, was shown in previously published paper ... in urban and rural India: phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54 ...