Case Study: A Systematic Approach to Early Recognition and Treatment of Sepsis
Submitted by Madeleine Augier RN BSN
Tags: assessment Case Study emergency department guidelines mortality prevention risk factors sepsis standard of care treatment

Share Article:
Sepsis is a serious medical condition that affects 30 million people annually, with a mortality rate of approximately 16 percent worldwide (Reinhart, 2017). The severity of this disease process is not well known to the public or health care workers. Often, health care providers find sepsis difficult to diagnose with certainty. Deaths related to sepsis can be prevented with accurate assessments and timely treatment. Sepsis must be considered an immediate life-threatening condition and needs to be treated as a true emergency.

Relevance and Significance
Sepsis is defined as “the life-threatening organ dysfunction resulting from a dysregulated host response to infection” (Kleinpell, Schorr, & Balk, 2016, p. 459). Jones (2017) study of managing sepsis affirms that the presence of sepsis requires a suspected source of infection plus two or more of the following: hyperthermia (>38.1 degrees Celsius) or hypothermia (<36 degrees Celsius), tachycardia (>91 beats per minute), leukocytosis or leukopenia, altered mental status, tachypnea (>21 breaths per minute), or no urine output for 12 hours. If the infection persists, acute organ dysfunction or failure occurs from widespread inflammation, eventually leading to septic shock (Palleschi, Sirianni, O’Connor, Dunn, & Hasenau, 2013). Palleschi et al. (2013) states that during septic shock, “the cardiovascular system fails, resulting in hypotension, depriving vitals organs of an adequate supply of oxygenated blood” (p. 23). Ultimately the body can go into multiple organ dysfunction syndrome (MODS), leading to death if there is inaccurate assessment and inadequate treatment.
The purpose of this case study is to make the nurse practitioner aware of the severity sepsis, and how to accurately diagnose and treat using evidence-based data. Sepsis can affect everyone, despite his or her age or comorbidity. Center for Medicare and Medicaid Services (CMS) has diagnosed this problem as a priority and uses sepsis management in determining payment to providers (Tedesco, Whiteman, Heuston, Swanson-Biearman, & Stephens, 2017). This medical diagnosis is unpredictable and presents a challenge to nurse practitioners worldwide. Early recognition and treatment of sepsis by the nurse practitioner is critical to decrease morbidity and mortality.
After completing this case study, the reader should be able to:
- Identify the risk factors of sepsis
- Identify the signs and symptoms of sepsis
- Identify the treatment course of sepsis
Case Presentation
A 65-year-old Asian female presented to the emergency department accompanied by her husband with a chief complaint of altered mental status. Upon assessment, the patient was lethargic, and alert and oriented to person only. The patient’s heart rate was 136, blood pressure 104/50, oral temperature 99 degrees Fahrenheit, oxygen saturation 97% on 4 liters nasal cannula, and respirations 26 per minute. The patient’s blood glucose was obtained with a result 454.
Further orders, such as labs and imaging were made by the provider to rule out potential diagnoses. A rectal temperature was obtained revealing a fever of 103.7 degrees Fahrenheit. The patient remained restless on the stretcher. After one hour in the emergency department, her heart rate spiked to 203 beats per minute, respirations became more rapid and shallow, and she became more lethargic. The patient’s altered mental status, increasing heart rate and respirations caused the providers to act rapidly.
Medical History
The patient’s husband reports that she is a type one diabetic, he denies any other medical conditions. In addition, the patient’s husband states that she has not been exposed to any sick individuals in the past few weeks. The husband reports a family history of diabetes, other wise no significant familial history. No history of smoking, drinking, or illicit drug use was to be noted.
Physical Assessment Findings
The patient appeared lethargic and confused with a Glasgow Coma Scale of 12. She appeared tachypnic, with shallow respirations, and a rate of 28 breaths per minute. Upon auscultation, breath sounds were coarse. Her abdomen was soft and non-tender, no nausea or vomiting noted. The patient appeared diaphoretic, and her legs were mottled.
Laboratory and Diagnostic Testing and Results
During the initial assessment, a complete blood count (CBC), basic metabolic panel (BMP), and lactic acid level were ordered for blood work. A STAT electrocardiogram (EKG), urinalysis, and a chest X-ray were ordered to differentiate possible diagnoses. The CBC revealed leukocytosis with a white blood cell count of 23,000 and an increased lactic acid level of 4.3. The anion gap and potassium level remained within a normal limit, ruling out the possibility of diabetic ketoacidosis (DKA). The patient’s EKG showed supraventricular tachycardia (SVT). The chest X-ray revealed infiltrates to the right lung. The urinalysis was free from leukocytes or nitrites. Blood cultures were ordered to confirm their hypothesized diagnosis, septicemia.
Pharmacology
The provider initiated intravenous (IV) fluid treatment with Lactated Ringers at a bolus of 30 mL/kg. Because the patient’s heart rate was elevated, 6 mg of adenosine was ordered to combat the SVT. Additionally, broad-spectrum IV antibiotics were initiated. One gram of vancomycin and 3.375 grams of piperacillin-tazobactam were the preferred antibiotics of choice.
Final Diagnosis
Upon arrival, the providers were ruling out DKA and sepsis, given the patient’s history.
The patient’s elevated white blood cell counts, temperature, lactic acid level, heart/respiratory rate, and altered mental status were all clinical indicators of sepsis. The chest X-ray revealed a right lung infiltrate, persuading the providers to diagnose the patient with sepsis secondary to pneumonia.
Patient Management
After sepsis was ruled as the patient’s diagnosis, rapid antibiotic administration and IV fluid treatment became priority after the patient’s heart rate was controlled. A cooling blanket and a temperature sensing urinary catheter was placed to continuously monitor and control the patient’s fever. Later, the patient was transferred to a critical care unit for further treatment. Shortly after being transferred, the patient went into respiratory failure and was placed on a ventilator. After two days in the ICU, the patient remained in septic shock, and died from multisystem organ failure.
When the patient initially presented to the emergency department, accurate and rapid diagnosis of sepsis was critical in order to stabilize the patient and prevent mortality. A challenge was presented to the provider regarding a rapid diagnosis due to the patient’s history and her presenting signs and symptoms. Increased awareness and interprofessional education regarding sepsis and its’ treatment is vital to decrease mortality. Health care providers need to be competent in recognizing and accurately treating sepsis in a rapid manner.
Research shows that outcomes in sepsis are improved with timely recognition and early resuscitation (Javed et al., 2017). It is important for the provider to identify certain risk factors and symptoms to easily diagnose sepsis. A research study by Henriksen et al. (2015) proved that age, and comorbidities including psychotic disorders, immunosuppression, diabetes, and alcohol abuse served as top risk factors for sepsis.
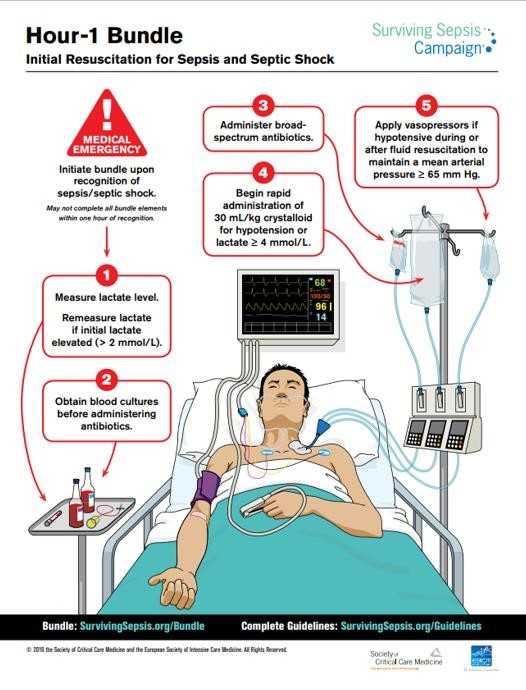
Once the diagnosis of sepsis is determined, rapid treatment must be initiated. The golden standard of treatment consists of a bundle of care that includes blood cultures, broad-spectrum antibiotic agents, and lactate measurement completed within 3 hours as described by Henriksen et al. (2015). A study by Seymour et al. (2017) showed that the more rapid administration of the bundle of care is correlated with a decreased mortality rate. In addition, The Survival of Sepsis Campaign formed a guideline to sepsis treatment; Rhodes et al. (2016) suggests giving a 30 mL/kg of IV crystalloid fluid for hypoperfusion. If hypotension persists (mean arterial pressure <65), vasopressors, preferably norepinephrine, should be initiated (Rhodes et al., 2016). Prompt recognition of sepsis and implementation of the bundle of care can help reduce avoidable deaths.
To increase awareness, interprofessional education regarding sepsis and its’ common signs and symptoms needs to be established. Evidence-based protocols should be utilized in hospital care settings that provide nurse practitioners with a guideline to follow to ensure rapid and accurate treatment is given. Increased awareness and education helps providers and other healthcare workers to properly identify and accurately treat sepsis.
The public and health care providers must become more aware and educated on the severity of sepsis. It is crucial to be able to recognize signs and symptoms of sepsis to prevent further complications such as septic shock and multi-organ failure. Increased awareness, interprofessional education, accurate assessment, and rapid treatment can help reduce incidence and mortality. Sepsis management must focus upon early goal-directed therapy (antibiotic administration, fluid resuscitation, blood cultures, lactate level) and individualized management pertaining to the patient’s history and assessment (Head & Coopersmith, 2016). Misdiagnosis and delay in emergency treatment can result in missed opportunities to save lives.
- Head, L. W., & Coopersmith, C. M. (2016). Evolution of sepsis management:from early goal-directed therapy personalized care. Advances in Surgery, 50 (1), 221-234. doi:10.1016/j.yasu.2016.04.002
- Henriksen, D. P., Pottegard, A., Laursen, C. B., Jensen, T. G., Hallas, J., Pedersen, C., & Lassen, A. T. (2015). Risk factors for hospitalization due to community-acquired sepsis-a population-based case-control study. PLOS ONE, 10 (4), 1-12. doi:10.1371/journal.pone.0124838
- Javed, A., Guirgis, F. W., Sterling, S. A., Puskarich, M. A., Bowman, J., Robinson, T., & Jones, A. E. (2017). Clinical predictors of early death from sepsis. Journal of Critical Care, 42 , 30-34. doi:10.1016/j.jcrc.2017.06.024
- Jones, J. (2017). Managing sepsis effectively with national early warning scores and screening tools. British Journal of Community Nursing, 22 (6), 278-281. doi:10.12968/bjcn.2017.22.6.278
- Kleinpell, R. M., Schorr, C. A., & Balk, R. A. (2016). The new sepsis definitions: Implications for critical care. American Journal of Critical Care, 25 (5), 457-464. doi:10.4037/ajcc2016574
- Palleschi, M. T., Sirianni, S., O'Connor, N., Dunn, D., & Hasenau, S. M. (2013). An interprofessioal process to improve early identification and treatment for sepsis. Journal for Healthcare quality, 36 (4), 23-31. doi:10.1111/jhq.12006
- Reinhart, K., Daniels, R., Kissoon, N., Machado, F. R., Schachter, R. D., & Finfer, S. (2017). Recognizing sepsis as a global health priority-A WHO resolution. The New England Journal of Medicine, 377 (5), 414-417. doi:10.1056/NEJMp1707170
- Rhodes, A., Evans, L. E., Alhazzani, W., Levy, M. M., Anotnelli, M., Ferrer, R.,...Beale, R. (2017). Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Medicine, 43 (3), 304-377. doi:10.1007/s00134-017-4683-6
- Seymour, C. W., Gesten, F., Prescott, H. C., Friedrich, M. E., Iwashyna, T. J., Phillips, G. S.,...Levy, M. M. (2017). Time to treatment and mortality during mandated emergency care for sepsis. The New England Journal of Medicine, 376 (23), 2235-2244. doi:10.1056/NEJMoal1703058
- Tedesco, E. R., Whiteman, K., Heuston, M., Swanson-Biearman, B., & Stephens, K. (2017). Interprofessional collaboration to improve sepsis care and survival within a tertiary care emergency department. Journal of Emergency Nursing, 43 (6), 532-538. doi:10.1016/j.jen.2017.04.014
Career Opportunities

More Like This

Sepsis and Septic Shock
Sepsis and septic shock stand as life-threatening conditions that demand swift and vigilant action from healthcare providers, with nurses playing a pivotal role in their management. As frontline caregivers , nurses are essential in recognizing early signs of sepsis, initiating prompt interventions, and providing comprehensive care to improve patient outcomes.
This article aims to highlight the critical importance of nursing in battling sepsis and septic shock, shedding light on the pathophysiology, risk factors, clinical presentations, and evidence-based interventions. By fostering a comprehensive understanding of these conditions, nurses can proactively contribute to saving lives and minimizing the burden of sepsis on patients and healthcare systems.
Table of Contents
- What is Sepsis and Septic Shock?
Pathophysiology
Epidemiology, clinical manifestations, complications, assessment and diagnostic findings, medical management, nursing assessment, planning & goals, nursing interventions, discharge and home care guidelines, documentation guidelines, what is sepsis and septic shock .
One of the most common types of circulatory shock and the incidences of this disease continue to rise despite the technology.
- Sepsis is a systemic response to infection. It is manifested by two or more of the SIRS (Systemic Inflammatory Response Syndrome) criteria as a consequence of documented or presumed infection.
- Septic shock is associated with sepsis. It is characterized by symptoms of sepsis plus hypotension and hypoperfusion despite adequate fluid volume replacement.
The pathophysiology of sepsis involves an evolving process. The following shows the process of how sepsis works its way inside of our body.
- Microorganisms invade the body tissues and in turn, patients exhibit an immune response.
- The immune response provokes the activation of biochemical cytokines and mediators associated with an inflammatory response.
- Increased capillary permeability and vasodilation interrupt the body’s ability to provide adequate perfusion, oxygen, and nutrients to the tissues and cells.
- Proinflammatory and anti-inflammatory cytokines released during the inflammatory response and activates the coagulation system that forms clots whether or not there is bleeding .
- The imbalance of the inflammatory response and the clotting and fibrinolysis cascades are critical elements of the physiologic progression of sepsis in affected patients.
Sepsis has affected a lot of people in the United States and around the world as well. The rise in the numbers of those affected with sepsis is alarming and should be given utmost attention.
- Annually, an estimated 750, 000 people in the United States are affected by sepsis.
- By 2010, the rate may increase up to 1 million cases every year.
- Elderly patients are at most risk for developing sepsis because of decreased physiologic reserves and an aging immune system.
- Gram-positive bacteria accounts for 50% of cases of septic shock.
- It is also estimated that 20% to 30% with severe sepsis may never identify the site of infection.
There are several factors that can put the patient at risk for septic shock, and these include:
- Patients with immunosuppression have greater chances of acquiring septic shock because they have decreased immune system, making it easier for microorganisms to invade the body tissues.
- Extremes of age. Elderly people and infants are more prone to septic shock because of their weak immune system .
- Malnourishment . Malnourishment can lower the body’s defenses, making it susceptible to the invasion of pathogens.
- Chronic illness. Patients with a longstanding illness are put at risk for sepsis because the body’s immune system is already weakened by the existing pathogens.
- Invasive procedures. Invasive procedures can introduce microorganisms inside the body that could lead to sepsis.
The signs and symptoms that are associated with septic shock and sepsis include the following:
- Since the ability of the body to provide oxygen and nutrients is interrupted, the heart compensates by pumping faster.
- Hypotension occurs because of vasodilation .
- To compensate for the decreased oxygen concentration, the patient tends to breathe faster, and also to eliminate more carbon dioxide from the body.
- The inflammatory response is activated because of the invasion of pathogens.
- Decreased urine output. The body conserves water to avoid undergoing dehydration because of the inflammatory process.
- Changes in mentation . As the body slowly becomes acidotic, the patient’s mental status also deteriorates.
- Elevated lactate level. The lactate level is elevated because there is maldistribution of blood .
Before sepsis could invade a patient’s body, it is better to prevent its occurrence here are some ways to prevent sepsis and septic shock.
- Strict infection control practices. To prevent the invasion of microorganisms inside the body, infection must be put at bay through effective aseptic techniques and interventions.
- Prevent central line infections . Hospitals must implement efficient programs to prevent central line infections, which is the most dangerous route that can be involved in sepsis.
- Early debriding of wounds. Wounds should be debrided early so that necrotic tissue would be removed.
- Equipment cleanliness. Equipment used for the patient, especially the ones involved in invasive procedures, must be properly cleaned and maintained to avoid harboring harmful microorganisms that can enter the body.
Complications could happen in a patient with sepsis if it is not properly treated or not treated at all.
- Severe sepsis. Sepsis could progress to severe sepsis with symptoms of organ dysfunction, hypotension or hypoperfusion, lactic acidosis, oliguria, altered level of consciousness, coagulation disorders, and altered hepatic functions.
- Multiple organ dysfunction syndrome . This refers to the presence of altered function of one or more organs in an acutely ill patient requiring intervention and support of organs to achieve physiologic functioning required for homeostasis .
Early assessment and diagnosis of the infection must be established to avoid its progression.
- Blood culture. To identify the microorganism responsible for the disease, a blood culture must be performed.
- Liver function test. This should be performed to detect any alteration in the function of the liver.
- Blood studies. Hematologic test must also be performed to check on the perfusion of the blood.
The current treatment of septic shock and sepsis include identification and elimination of the cause of infection.
- Fluid replacement therapy . The therapy is done to correct the tissue hypoperfusion, so aggressive fluid resuscitation must be implemented.
- Nutritional therapy . Aggressive nutritional supplementation is critical in the management of septic shock because malnutrition further impairs the patient’s resistance to infection.
Nursing Management
Nurses must keep in mind that the risks of sepsis and the high mortality rate associated with sepsis, severe sepsis, and septic shock.
Assessment is one of the nurse ’s primary responsibilities, and this must be done precisely and diligently.
- Signs and symptoms . Assess if the patient has positive blood culture, currently receiving antibiotics , had an examination or chest x-ray , or has a suspected infected wound.
- Signs of acute organ dysfunction . Assess for presence of hypotension, tachypnea , tachycardia, decreased urine output, clotting disorder, and hepatic abnormalities.
Sepsis can affect a lot of body systems and even cause their failure, so diagnosis is an important part of the process to establish the presence of sepsis.
- Risk for deficient fluid volume related to massive vasodilation.
- Risk for decreased cardiac output related to decreased preload.
- Impaired gas exchange related to interference with oxygen delivery.
- Risk for shock related to infection.
Healthcare team members should be prepared with a care plan for the patient for a more systematic and detailed achievement of the goals.
- Patient will display hemodynamic stability.
- Patient will verbalize understanding of the disease process.
- Patient will achieve timely wound healing .
Nursing interventions pertaining to sepsis should be done timely and appropriately to maximize its effectivity.
- Infection control . All invasive procedures must be carried out with aseptic technique after careful hand hygiene .
- Collaboration . The nurse must collaborate with the other members of the healthcare team to identify the site and source of sepsis and specific organisms involved.
- Management of fever . The nurse must monitor the patient closely for shivering.
- Pharmacologic therapy . The nurse should administer prescribed IV fluids and medications including antibiotic agents and vasoactive medications.
- Monitor blood levels . The nurse must monitor antibiotic toxicity, BUN, creatinine , WBC, hemoglobin, hematocrit, platelet levels, and coagulation studies.
- Assess physiologic status . The nurse should assess the patient’s hemodynamic status, fluid intake and output , and nutritional status.
After implementation of the interventions, the nurse must evaluate their effectiveness.
- Patient displayed hemodynamic stability.
- Patient verbalized understanding of the disease process.
- Patient achieved timely wound healing.
Even after discharge, the patient must still be taught how to establish home and community care regimen.
- Prevent shock episodes . The nurse should instruct the patient and the family strategies to prevent shock episodes through identifying the factors implicated in the initial episodes.
- Instructions on assessment . The patient and the family should be taught about assessments needed to identify the complications that may occur after discharge.
- Treatment modalities . The nurse must teach the patient and the family about treatment modalities such as emergency administration of medications, IV therapy, parenteral or enteral nutrition , skin care, exercise, and ambulation .
Proper documentation must be established both for legal protection and data organization.
- Document individual risk factors.
- Document assessment findings.
- Document results of the laboratory tests and diagnostic studies.
- Document plan of care and teaching plan.
- Document client’s responses to treatment, teaching, and actions performed.
- Document modifications in the plan of care.
Posts related to Sepsis and Septic Shock:
- Risk for Infection
1 thought on “Sepsis and Septic Shock”
I’m not sure if you are aware, but under “Medical Management: Pharmacologic Therapy” Drotrecogin alfa by Eli Lily & Company (pharm company) was taken off the market on Oct of 2011. Good luck with all your endeavors and keep up the good work!
Leave a Comment Cancel reply
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Sepsis assessment and management in critically Ill adults: A systematic review
Contributed equally to this work with: Mohammad Rababa, Dania Bani Hamad, Audai A. Hayajneh
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Adult Health Nursing Department, Faculty of Nursing, Jordan University of Science and Technology, Irbid, Jordan
Roles Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing
- Mohammad Rababa,
- Dania Bani Hamad,
- Audai A. Hayajneh

- Published: July 1, 2022
- https://doi.org/10.1371/journal.pone.0270711
- Reader Comments
Early assessment and management of patients with sepsis can significantly reduce its high mortality rates and improve patient outcomes and quality of life.
The purposes of this review are to: (1) explore nurses’ knowledge, attitude, practice, and perceived barriers and facilitators related to early recognition and management of sepsis, (2) explore different interventions directed at nurses to improve sepsis management.
A systematic review method according to the PRISMA guidelines was used. An electronic search was conducted in March 2021 on several databases using combinations of keywords. Two researchers independently selected and screened the articles according to the eligibility criteria.
Nurses reported an adequate of knowledge in certain areas of sepsis assessment and management in critically ill adult patients. Also, nurses’ attitudes toward sepsis assessment and management were positive in general, but they reported some misconceptions regarding antibiotic use for patients with sepsis, and that sepsis was inevitable for critically ill adult patients. Furthermore, nurses reported they either were not well-prepared or confident enough to effectively recognize and promptly manage sepsis. Also, there are different kinds of nurses’ perceived barriers and facilitators related to sepsis assessment and management: nurse, patient, physician, and system-related. There are different interventions directed at nurses to help in improving nurses’ knowledge, attitudes, and practice of sepsis assessment and management. These interventions include education sessions, simulation, decision support or screening tools for sepsis, and evidence-based treatment protocols/guidelines.
Our findings could help hospital managers in developing continuous education and staff development training programs on assessing and managing sepsis in critical care patients.
Nurses have poor to good knowledge, practices, and attitudes toward sepsis as well as report many barriers related to sepsis management in adult critically ill patients. Despite all education interventions, no study has collectively targeted critical care nurses’ knowledge, attitudes, and practice of sepsis management.
Citation: Rababa M, Bani Hamad D, Hayajneh AA (2022) Sepsis assessment and management in critically Ill adults: A systematic review. PLoS ONE 17(7): e0270711. https://doi.org/10.1371/journal.pone.0270711
Editor: Paavani Atluri, Bay Area Hospital, North Bend Medical Center, UNITED STATES
Received: December 1, 2021; Accepted: June 14, 2022; Published: July 1, 2022
Copyright: © 2022 Rababa et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the article and its files.
Funding: This study was funded by The deanship of research at Jordan University of Science and Technology (grant number 20200668).
Competing interests: The authors have declared that no competing interests exist.
Introduction
Sepsis is a global health problem that increases morbidity and mortality rates worldwide and which is one of the most common complications documented in intensive care units (ICUs) [ 1 ]. About 48.9 million cases of sepsis and 11 million sepsis-related deaths were documented in 2017 worldwide [ 2 ]. Sepsis is an emergency condition leading to several life-threatening complications, such as septic shock and multiple organ dysfunction and failure [ 3 ]. Sepsis has negative physiological, psychological, and economic consequences. Untreated sepsis can lead to septic shock; multiple organ failure, such as acute renal failure [ 4 ]; respiratory distress syndrome [ 5 ]; cardiac arrhythmia (e.g. Atrial Fibrillation) [ 6 ]; and disseminated intravascular coagulation (DIC) [ 7 ]. Also, sepsis is associated with anxiety, depression, and post-traumatic stress disorder [ 8 ]. As for the financial burden of sepsis on the healthcare system, the cost of healthcare services and supplies for ICU critical care patients with sepsis is high [ 1 ]. In 2017, the estimated annual cost of sepsis in the United States (US) was over $24 billion [ 2 ].
Previous studies have shown that among nurses, misunderstanding and misinterpretation of the early clinical manifestations of sepsis, poor knowledge, attitudes, and practices related to sepsis, and inadequate training might lead to delayed assessment and management of sepsis [ 9 – 11 ]. Moreover, the limited numbers of specific and sensitive assessment tools and standard protocols for the early identification and assessment of sepsis in critical care patients leads to delayed management, therefore increasing sepsis-related mortality rates [ 10 ].
Critical care nurses, as frontline providers of patient care, play a vital role in the decision-making process for the early identification and prompt management of sepsis [ 11 ]. Therefore, improving nurses’ knowledge, attitudes, and practices related to the early identification and management of sepsis is associated with improved patient outcomes [ 12 , 13 ]. To date, there remains a wide gap between the findings of previous research and sepsis-related clinical practice in critical care units (CCUs). Furthermore, there is no evidence in the nursing literature regarding nurses’ knowledge, attitudes, and practices related to the early identification and management of sepsis in adult critical care patients and the association of these factors with patient health outcomes. Therefore, summarizing and synthesizing the existing research on sepsis assessment and management among adult critical care patients is needed to guide future directions of sepsis-related clinical practice and research. Accordingly, this review aims to identify nurses’ knowledge, and attitudes, practices related to the early identification and management of sepsis in adult critical care patients.
Materials and methods
The present review used a systematic review design guided by structured questions constructed after reviewing the nursing literature relevant to sepsis assessment and management in adult critical care patients. The authors (MR, DB, AH) carefully reviewed and evaluated the selected articles and synthesized and analyzed their findings to reach a consensus. This review was guided by the following questions: (a) what are nurses’ knowledge, attitudes, and practices related to sepsis assessment and management in adult critical care patients?, (b) what are the perceived facilitators of and barriers to the early identification and effective management of sepsis in adult critical care units?, and (c) what are the interventions directed at improving nurses’ sepsis assessment and management?
Eligibility criteria
The review questions were developed according to the PICOS (Participants, Interventions, Comparisons, Outcome, and Study Design) framework, as displayed in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0270711.t001
Inclusion criteria.
The articles were retrieved and assessed independently by two researchers (MR, DB) according to the following inclusion criteria: (1) being written in English, (2) having an abstract and reference list, (3) having been published during the past 10 years, (4) focusing on critical care nurses as a target population, (5) examining knowledge, attitudes, and practices related to the assessment and management of sepsis, and (6) having been conducted in adult critical care units.
Exclusion criteria.
Studies were excluded if they were (1) written in languages other than English, and (2) conducted in pediatric critical care units or non-ICU. Dissertations, reports, reviews, editorials, and brief communications were also excluded.
Search strategy.
An electronic search of the databases CINAHL, MEDLINE/PubMed, EBSCO, Embase, Cochrane, Scopus, Web of Science, and Google Scholar was conducted using combinations of the following keywords: critical care, intensive care, critically ill, critical illness, knowledge, awareness, perception, understanding, attitudes, opinion, beliefs, thoughts, views, practice, skills, strategies, approaches, barriers, obstacles, challenges, difficulties, issues, problems, limitations, facilitators, motivators, enablers, sepsis, septic, septic shock, and septicemia. The search terms used in this review were described in S1 File . The search was initially conducted in March 2021, and a search re-run was conducted in April 2022. The search was conducted in the selected databases from inception to 4/2022. The initial search, using the keywords independently, resulted in 1579 articles, and after using the keyword combinations, this number was reduced to 241 articles. Then, after applying the inclusion and exclusion criteria, the number of articles was reduced to 92. A manual search of the reference lists of the 92 articles was carried out to identify any relevant publications not identified through the search. The researcher (MR) used the function “cited by” on Google Scholar to explore these publications in more depth. The researchers (MR, DB) then screened the identified citations of these publications, applying the eligibility criteria. In case of discrepancies, the researchers (MR, DB) discussed their conflicting points of view until a consensus was reached. Then, after careful reading of the article abstracts, 61 irrelevant articles were excluded, and a total of 31 articles were included in this review. Fig 1 below shows the Preferred Reporting Items for Meta-Analysis (PRISMA) checklist and flow chart used as a method of screening and selecting the eligible studies.
https://doi.org/10.1371/journal.pone.0270711.g001
Data extraction
The following data were extracted from each of the selected studies: (1) the general features of the article, including the authors and publication year; (2) the characteristics of the study setting (e.g., single vs. multisite); (3) the sociodemographic and clinical characteristics of the target population, including mean age, and medical diagnosis (e.g., sepsis, septic shock, and SIRS); (4) the name of the sepsis protocol used, if any; (5) the characteristics of the study methodology (e.g., sample size and measurements); (7) the main significant findings of the study; and (8) the study strengths and limitations. All extracted data were summarized in an evidence-based table ( Table 2 ). Data extraction was performed by two researchers (MR, DB). An expert third researcher (AH) was consulted to reach a consensus between the two researchers throughout the process of data extraction.
https://doi.org/10.1371/journal.pone.0270711.t002
Ethical considerations
There was no need to obtain ethical approval to conduct this systematic review since no human subjects were involved.
Quality assessment and data synthesis
A quality assessment of the selected studies was performed independently by two researchers based on the guidelines of Melnyk and Fineout-Overholt [ 14 ]. Disagreements between the two researchers (MR, DB) were identified and resolved through a detailed discussion held during a face-to-face meeting. For complicated cases, the researchers (MR, DB) requested a second opinion from a third researcher (AH). According to the guidelines of Melnyk and Fineout-Overholt [ 14 ], twelve of the studies were at level 3 in terms of quality, four studies at level 5, and nine studies at level 6.
A qualitative synthesis was performed to synthesize the findings of the reviewed studies. The following steps were applied throughout the process of data synthesis:
- The data in the selected studies were assessed, evaluated, contrasted, compared, and summarized in a table ( Table 2 ). This data included the design, purpose, sample, main findings, strengths/limitations, and level of evidence for each of the studies.
- The similarities and differences between the main findings of the selected studies were highlighted.
- The strengths and limitations of the reviewed studies were discussed.
Description of the selected studies
Most of the reviewed studies were conducted in Western countries [ 9 , 11 , 12 ], with only one study conducted in Eastern countries [ 1 ], and two in Middle-Eastern countries [ 15 , 16 ]. The detailed geographical distribution of the studies and other characteristics are described in Table 2 .
Nurses’ knowledge, attitudes, and practices
Nine of the selected studies assessed nurses’ knowledge and attitudes related to sepsis assessment and management in critically ill adult patients [ 1 , 9 , 12 , 15 , 17 – 21 ] ( Table 3 ) . Nucera et al. [ 18 ] found that ICU nurses had poor attitudes towards blood culture collection techniques and timing and poor levels of knowledge related to the early identification, diagnosis, and management of sepsis. For example, the majority of nurses reported that there is no need to sterilize the tops of culture bottles, and there is no specific time for specimen collection [ 18 ]. However, the participating nurses reported good levels of knowledge related to blood culture procedures and the risk factors for sepsis. Similarly, R. J. Roberts et al. [ 19 ] found the participating nurses to have good knowledge of septic shock and good attitudes toward the initiation of antibiotics for critically ill adult patients with sepsis. Only two studies assessed nurses’ practices related to sepsis assessment and management [ 15 , 19 ]. For example, in the study of R. J. Roberts et al. [ 19 ], 40% of the nurse participants reported that they were aware of the importance of initiating antibiotics and IV fluid within one hour of septic shock recognition [ 20 ]. Also, Yousefi et al. [ 15 ] found the participating nurses to have good practices related to sepsis assessment and management.
https://doi.org/10.1371/journal.pone.0270711.t003
Barriers to and facilitators of sepsis assessment and management
The reviewed studies identified three types of barriers to the early identification and management of sepsis, namely patient-, nurse-, and system-related barriers ( Table 4 ). Meanwhile, only nurse- and system-related facilitators were reported in the reviewed studies. The most-reported barriers and facilitators were system-related. The reported barriers included (a) the lack of written sepsis treatment protocols or guidelines adopted as hospital policy [ 22 , 23 ]; (b) the complexity and atypical presentation of the early symptoms of sepsis [ 19 ]; (c) nurses’ poor level of education and clinical experience [ 1 , 12 ]; (d) the lack of sepsis educational programs or training workshops for nurses [ 22 , 23 ]; (e) the high comorbid burden among patients with sepsis, which complicates the critical thinking process of sepsis management [ 19 ]; (f) nurses’ deficits in knowledge related to sepsis treatment protocols and guidelines [ 22 – 24 ]; (g) the lack of mentorship programs in which junior nurses’ actions/activities are strictly supervised by experienced nurses [ 17 , 23 ]; (h) heavy workloads or high patient-nurse ratios [ 22 ]; (i) the shortage of well-trained and experienced physicians, particularly in EDs [ 19 , 22 , 23 ]; (j) the lack of awareness related to antibiotic use for patients with sepsis [ 19 , 22 ]; (k) the lack of IV access and unavailability of ICU beds [ 25 ]; (l) the non-use of drug combinations for the treatment of sepsis [ 22 , 26 , 27 ], and (m) poor teamwork and communication skills among healthcare professionals [ 22 , 26 ]. Only three facilitators of sepsis assessment and management were identified in the reviewed studies. These facilitators were (1) nurses’ improved confidence in caring for patients with sepsis, (2) increased consistency in sepsis treatment, and (3) positive enforcement of successful stories of sepsis management [ 22 , 27 ].
https://doi.org/10.1371/journal.pone.0270711.t004
Measurement tools of sepsis-related knowledge, attitudes, and practices
One of the reviewed studies used a Knowledge, Attitudes, and Practice (KAP) questionnaire developed according to the Surviving Sepsis Campaign (SSC) guidelines [ 15 ] to measure nurses’ knowledge, attitudes, and practices related to sepsis assessment and management. Meanwhile, eight studies [ 1 , 9 , 12 , 17 – 21 ] used self-developed questionnaires based on the literature and SSC guidelines and validated by expert panels. Details of these measurement tools and their psychometric properties are summarized in Table 5 .
https://doi.org/10.1371/journal.pone.0270711.t005
Interventions directed at improving nurses’ sepsis assessment and management
Educational programs..
Only four of the selected studies examined the impact of educational programs on nurses’ knowledge, attitudes, and practices related to sepsis management and found significant improvements in nurses’ posttest scores ( Table 6 ) [ 11 , 15 , 28 , 29 ]. For example, Drahnak’s study [ 28 ] implemented an educational program developed by the authors and integrated with patients’ health electronic records (HER) and found significant improvements in nurses’ post-test nursing knowledge scores. Another educational program developed by the authors was implemented to improve ICU nurses’ knowledge, attitudes, and practices related to sepsis and found a significant improvement in posttest scores among the intervention group [ 15 ]. Another study was designed to examine the effectiveness of the Taming Sepsis Educational Program® (TSEP™) in improving nurses’ knowledge of sepsis [ 11 ]. A 15-minute structured educational session was developed to decrease the mean time needed to order a sepsis order set for critically ill patients through improving ER nurses’ knowledge about SSC guidelines and found that the mean time was reduced by 33 minutes among the intervention group [ 29 ].
https://doi.org/10.1371/journal.pone.0270711.t006
Simulation.
Only two studies examined the effect of using simulation in improving the early recognition and prompt treatment of sepsis by critical care nurses ( Table 6 ) [ 30 , 31 ]. Vanderzwan et al. [ 30 ] assessed the effect of a medium-fidelity simulation incorporated into a multimodel nursing pedagogy on nurses’ knowledge of sepsis and showed significant improvements in six of the nine questionnaire items. While Giuliano et al. examined the difference in mean times required for sepsis recognition and treatment initiation between nurses exposed to two different monitor displays in response to simulated case scenarios of sepsis and showed a significant reduction in the mean times required for sepsis recognition and treatment initiation by those nurses who were exposed to enhanced bedside monitor (EBM) display [ 31 ].
Decision support tools.
Four of the selected studies examined the effectiveness of decision support tools, adapted based on the SSC guidelines and the “sepsis alert protocol”, on the early identification and management of sepsis and confirmed the effectiveness of these tools ( Table 7 ) [ 32 – 35 ]. The decision support tools used in three of the studies guided the nurses throughout their decision-making processes to reach effective assessment, high quality and timely management of sepsis, and, in turn, optimal patient outcomes [ 32 , 33 , 35 ]. However, no significant differences in the time of blood culture collection and antibiotic administration were reported between the intervention and control groups in the study of Delawder et al. [ 34 ].
https://doi.org/10.1371/journal.pone.0270711.t007
Sepsis protocols.
Eight of the selected studies examined the effectiveness of sepsis protocols [ 24 , 36 – 38 ] and sepsis screening tools [ 16 , 39 – 41 ] for the early assessment and management of sepsis ( Table 7 ). All of these articles revealed that the implementation of sepsis screening tools or protocols based on the SSC guidelines leads to the early identification and timely management of sepsis, as well as the improvement in nurses’ compliance to the SSC guidelines for the detection and management of sepsis. For example, in one study, patients who received Early Goal-Directed Therapy (EGDT) had a lower mortality rate as compared to patients who received usual care [ 16 ]. The sepsis screening tools and guidelines were also tested to examine their impact on some patient outcomes, and variabilities were identified. For example, the use of the Modified Early Warning Score (MEW-S) tool revealed no significant improvement in patient mortality rate [ 41 ]. In contrast, mortality rates were decreased by using the Nurse Driven Sepsis Protocol (NDS) [ 40 ], Quality Improvement (QI) initiative [ 38 ], and a computerized protocol [ 37 ]. In addition, nurses in the computerized protocol group had better compliance with the SSC guidelines than did nurses in the paper-based group [ 37 ]. One of the selected studies compared between a paper-based sepsis protocol and a computer-based protocol and found that antibiotic administration, blood cultures, and lactate level checks were conducted more often and sooner by nurses in the computerized protocol group [ 37 ]. Two of the selected studies used the EGDT as a screening tool for sepsis and found no significant differences in times of diagnosis, blood culture collection, or lactate measurements between the control and intervention groups [ 16 , 24 ]. However, significant differences were found in the time of antibiotic administration in the study of Oliver et al. [ 24 ]. Although El-khuri et al. [ 16 ] revealed no significant differences in the time of antibiotic administration, the mortality rate among patients in the intervention group declined significantly.
Most of the reviewed studies focused on assessing critical care nurses’ knowledge, attitudes, and practices related to sepsis assessment and management, revealing poor levels of knowledge, moderate attitude levels, and good practices. Also, this review revealed that the three most common barriers to effective sepsis assessment and management were nursing staff shortages, delayed initiation of antibiotics, and poor teamwork skills. Meanwhile, the three most common facilitators of sepsis assessment and management were the presence of standard sepsis management protocols, professional training and staff development, and positive enforcement of successful stories of sepsis treatment. Moreover, this review reported on a wide variety of interventions directed at improving sepsis management among nurses, including educational sessions, simulations, screening or decision support tools, and intervention protocols. The impacts of these interventions on patient outcomes were also explored.
The findings of our review are consistent with the findings of previous studies which have explored critical care nurses’ knowledge related to sepsis assessment and management [ 42 ]. Also, recent studies conducted in different clinical settings support the findings of our review regarding nurses’ knowledge of sepsis. For example, a recent study conducted in a medical-surgical unit revealed that nurses had good knowledge of early sepsis identification in non-ICU adult patients [ 43 ]. The variations in nurses’ levels of knowledge related to sepsis assessment were attributed to variations in educational level and work environment (i.e., ICU vs. non-ICU).
The evidence indicates that the successful treatment of critically ill patients with suspected or actual sepsis requires early identification or assessment [ 44 , 45 ]. Early assessment is a critical step for the initiation of antibiotics for patients with sepsis, leading to improved patient outcomes and a decline in mortality rates [ 44 ]. The current review also revealed the significant role of educational programs in improving nurses’ knowledge, attitudes, and practices related to the early recognition and management of sepsis. These findings are in line with the findings of another study, which tested the impact of e-learning educational modules on pediatric nurses’ retention of knowledge about sepsis [ 45 ]. The study revealed that the educational modules improved the nurses’ knowledge acquisition and retention and clinical performance related to sepsis management [ 45 ]. The findings of our review related to sepsis screening and decision support tools are in congruence with the findings of a previous clinical trial which assessed the impact of a prompt telephone call from a microbiologist upon a positive blood culture test on sepsis management [ 46 ]. The study revealed that this screening tool contributed to the prompt diagnosis of sepsis and antibiotic administration, improved patient outcomes, and reduced healthcare costs [ 46 ]. The findings of our review related to the effectiveness of educational programs in improving the assessment and management of sepsis were consistent with the findings of a recent quasi-experimental study. The study found that incorporating sepsis-related case scenarios in ongoing educational and professional training programs improved nurses’ self-efficacy and led to a prompt and accurate assessment of sepsis [ 47 ]. One of the interventions explored in this review was a simulation that facilitated decision-making related to sepsis management. The simulation was found to be effective in mimicking the real stories of patients with sepsis and proved to be a safe learning environment for inexperienced nurses before encountering real patients, increasing nurses’ competency, self-confidence, and critical thinking skills [ 48 ]. Also, a recent study showed that the combination of different interventions aimed at targeting sepsis assessment and management, including educational programs and simulation, may lead to optimal nurse and patient outcomes [ 49 ].
Limitations
The present review has several limitations. There is limited variability in the findings of the reviewed studies in terms of the main variable, sepsis. Moreover, the review excluded studies written in languages other than English and conducted among populations other than critical care nurses. However, there may be studies written in other languages which may have significant findings not considered in this review. Further, only eight databases were used to search for articles related to the topic of interest, which may have limited the number of retrieved studies. Finally, due to the heterogeneity between the selected studies, a meta-analysis was not performed.
Relevance to clinical practice
Our findings could help hospital managers in developing continuous education and staff development training programs on assessing and managing sepsis for critical care patients. Establishing continuous education, workshops, professional developmental lectures focusing on sepsis assessment and management for critical care nurses, as well as training courses on how to use evidence-based sepsis protocol and decision support and screening tools for sepsis, especially for critical care patients are highly recommended. Also, our findings could be used to development of an evidence-based standard sepsis management protocol tailored to the unmet healthcare need of patients with sepsis.
To date, nurses remain to have poor to good knowledge of and attitudes towards sepsis and report many barriers related to the early recognition and management of sepsis in adult critically ill patients. The most-reported barriers were system-related, pertaining to the implementation of evidence-based sepsis treatment protocols or guidelines. Our review indicated that despite all educational interventions, no study has collectively targeted nurses’ knowledge, attitudes, and practices related to the assessment and treatment of sepsis using a multicomponent interactive teaching method. Such a method would aim to guide nurses’ decision-making and critical thinking step by step until a prompt and effective treatment of sepsis is delivered. Also, despite all available protocols and guidelines, no study has used a multicomponent intervention to improve health outcomes in adult critically ill patients. Future research should focus on sepsis-related nurse and patient outcomes using a multilevel approach, which may include the provision of ongoing education and professional training for nurses and the implementation of a multidisciplinary sepsis treatment protocol.
Supporting information
S1 checklist. prisma 2020 checklist..
https://doi.org/10.1371/journal.pone.0270711.s001
S1 File. Search strategies.
https://doi.org/10.1371/journal.pone.0270711.s002
Acknowledgments
The authors want to thank the Liberian of Jordan University of Science and Technology for his help in conducting this review.
- View Article
- PubMed/NCBI
- Google Scholar
- 14. Melnyk BM, Fineout-Overholt E, editors. Evidence-based practice in nursing & healthcare: A guide to best practice. Lippincott Williams & Wilkins; 2011.
Early Recognition and Management of Sepsis in the Elderly: A Case Study
Affiliation.
- 1 Alice M. Onawola, College of Nursing, The University of Alabama in Huntsville.
- PMID: 33595964
- DOI: 10.1097/CNQ.0000000000000351
Sepsis is a life-threatening and debilitating sickness in the elderly. This case study explores the importance of adequate assessment of patients on their initial presentation to the emergency department, during hospitalization, and before discharge. The clinical evaluation, recognition, and management of sepsis continue to be essential for patient survival to prevent and decrease the mortality rate. Some changes go on in the elderly organ systems and can lead to delay in identifying and treatment implementation. The use of the Third International Consensus Definition for Sepsis and Septic Shock (Sepsis-3) to anticipate outcomes in septic patients and the use of the Survival Sepsis Campaign for treatment guidelines promptly to improve outcomes are crucial. This article aims to inform clinicians and nurses of the importance of early recognition of subtle signs and symptoms and the management of sepsis in the elderly.
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.
- Emergency Service, Hospital
- Shock, Septic

- View All Courses
- Courses by Topic
- Live Webinars
- CE Enduring Activities
- Sponsor Courses
- Virtual Conferences
- Virtual Symposia
- Discussions
- Log In / Home
- Cart (0 items)
- Contact Sepsis Alliance

Sepsis Case Studies
Product not yet rated
Recorded On: 03/18/2020
- CE Information
- Course Contents
Description:
Delve into sepsis case studies that illustrate common assessments and tools used to care for sepsis. This presentation details case studies that cover three different healthcare areas, as well as the team members involved in the assessment, diagnosis, and treatment of patients with sepsis. These cases highlight the need for all members of the healthcare team to be aware of acute changes, and the need to communicate them to the appropriate provider. It is also a reminder that patients need to be assessed at every shift for early identification and early treatment.
Learning Objectives:
At the end of the activity, the learner should be able to:
- Identify SIRS and qSOFA criteria;
- Restate the importance of early identification and treatment of sepsis across the continuum of care;
- List clinical pearls from sepsis case studies across different healthcare settings.
Target Audience:
Nurses, advanced practice providers, physicians, emergency responders, pharmacists, medical technologists, respiratory therapists, physical/occupational therapists, infection prevention specialists, data/quality specialists, and more.
Webinar Supporter:
Sepsis Alliance gratefully acknowledges the support provided for this webinar by bioMérieux.
Lori Muhr, DNP, MHSM/MHA
Sepsis program coordinator, jps health network.
Lori brings over 30 years of clinical, managerial, and educational experience to this project. She has a Doctorate Degree in Nursing Practice, a dual Master’s Degree in Management and Administration, is certified Adult Clinical Nurse Specialist, and works as an Advance Practice Nurse. She has experience in ED, Critical Care, and Community Health. Lori has experience working in rural hospitals, Level 1 Trauma centers, For-Profit and Not-for-profit organizations, all of which bring a unique perspective in her ability to reach all levels of healthcare providers. She has recently led JPS Hospital to achieve Joint Commission - Disease Specific Certification in Sepsis and has led them to be the first community safety net hospital to receive this designation. Her ability to simplify complex issues and passion for teaching comes through in her energetic and motivational style.
Provider approved by the California Board of Registered Nursing, Provider Number CEP17068 for 1.6 contact hours.
Other healthcare professionals will receive a certificate of attendance for 1.25 contact hours.
- Medical Disclaimer
The information on or available through this site is intended for educational purposes only. Sepsis Alliance does not represent or guarantee that information on or available through this site is applicable to any specific patient’s care or treatment. The educational content on or available through this site does not constitute medical advice from a physician and is not to be used as a substitute for treatment or advice from a practicing physician or other healthcare professional. Sepsis Alliance recommends users consult their physician or healthcare professional regarding any questions about whether the information on or available through this site might apply to their individual treatment or care.
Please Log In
Find sepsis education.
- Sepsis Program Overviews and Performance Improvement
- Sepsis Core Measure and Surviving Sepsis Campaign Guidelines
- Sepsis and Technology
- Infection Prevention and Sepsis Prevention
- Sepsis Recognition, Diagnosis, Treatment, and Monitoring
- Sepsis Populations and Comorbidities
- Pre-Hospital and Post-Acute Sepsis
- Specialty Topics
- Sepsis Stories (Patients, Family, and Caregivers)
- CE Enduring Courses
- Courses by Speaker
- Privacy Policy
- Funding and Sponsorship Policy
Copyright ©2024 Sepsis Alliance. All rights reserved.
Sepsis Alliance is a tax-exempt organization under Sections 501(c)(3) of the Internal Revenue Code. Contributions are deductible for computing income estate taxes. Sepsis Alliance tax ID 38-3110993
Sepsis Patient Case Study


Executive Summary
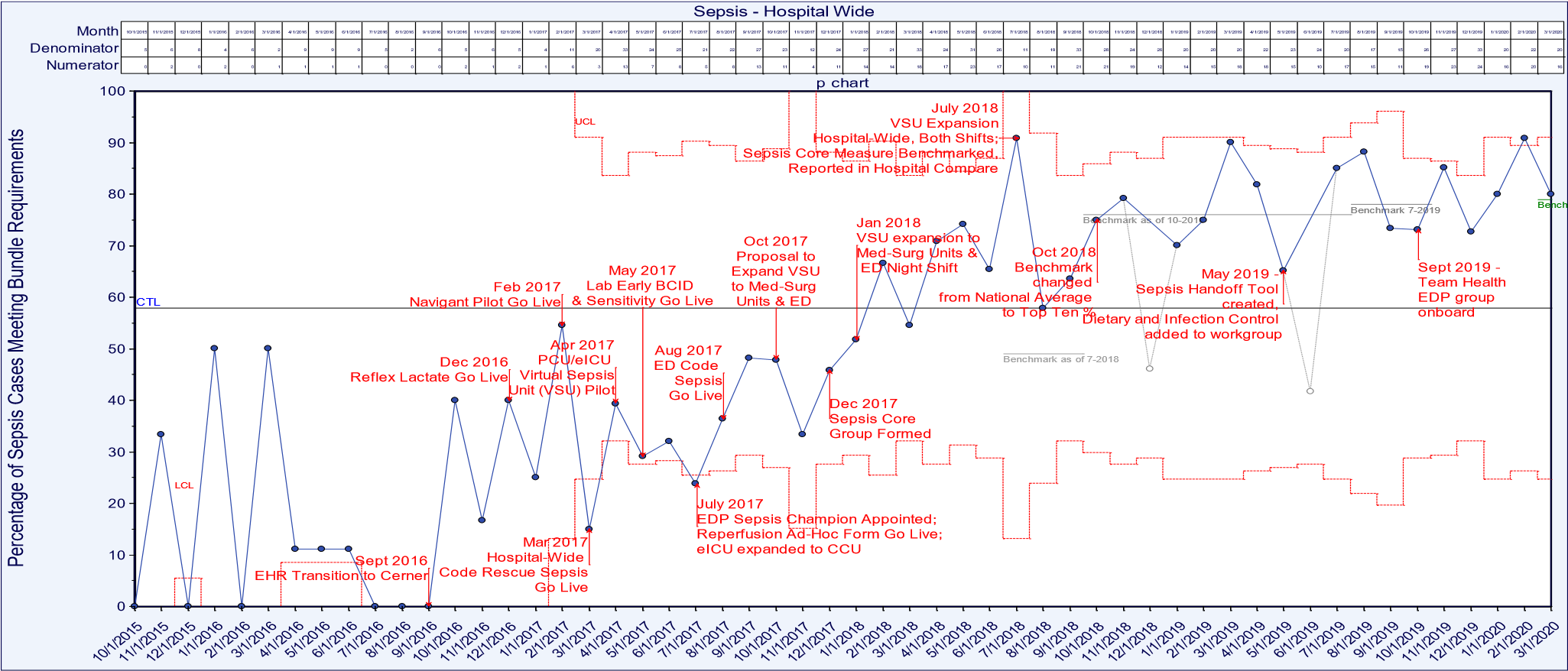
The percentage of sepsis patient cases meeting bundle requirements was below benchmark and there was opportunity to improve both mortality and length of stay (LOS).
Key Stakeholders
Medical Staff, nursing, performance improvement, virtual sepsis unit (VSU), healthcare informatics, laboratory personnel, pharmacy and patients.
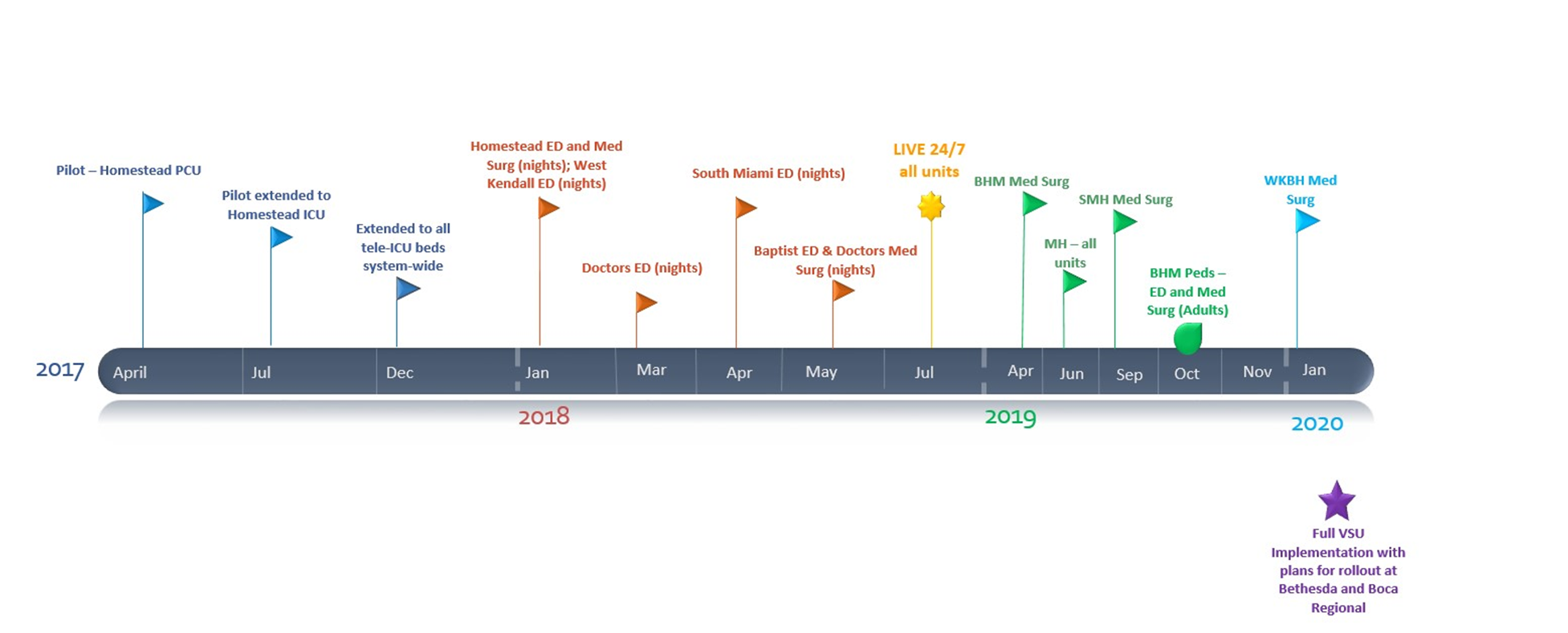
People, Process and Technology
- Interdisciplinary Committee, established December 2017
- Assign patient champions
- Ongoing Physician Education (Team Health EDP group onboard)
- VSU/eICU (PCU/ICU and Med-Surg Units) April 2017; January 2018
- Sepsis Handoff Tool – May 2019
- Sepsis Bundles
- Device integration
- Bedside specimen collection and scanning
- Clinical decision support (CDS)–Alerts
- Care team communication
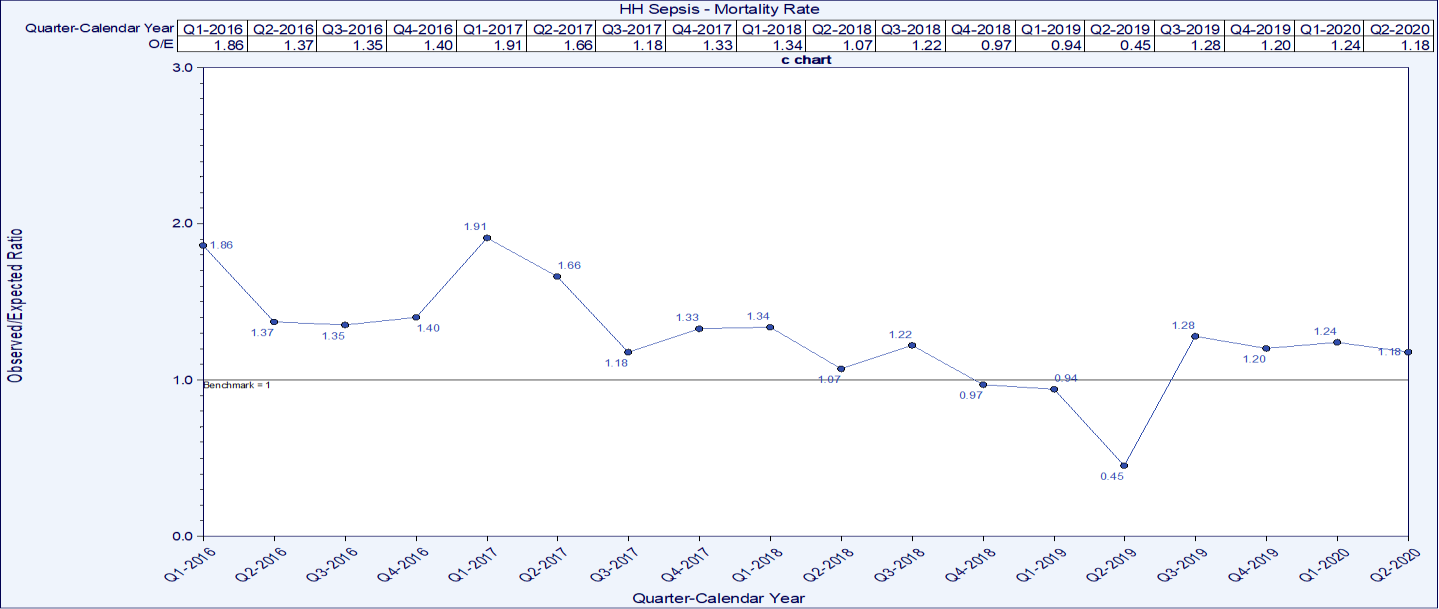
The sepsis patient mortality rate decreased from as high as 1.91 in Q1 2017 to as low as 0.45 in 2019. Cases meeting the bundle compliance increased from as low as 52% in Jan 2018 to as high as 88% in August 2019. LOS also decreased from a high of 6.83 days on average in January of 2017 to as low as 3.88 days on average in August of 2019.
Lesson Learned
- Teamwork and collaboration were instrumental in the success of bundle build and increasing bundle compliance. Accountability and the ability to measure outcomes and compliance are critical
- Assign a patient champion who is an expert in sepsis management
- Utilization of a VSU such as an eICU provides another layer of surveillance.
- CDS, alerts, dashboards and direct communication with the care teams are part of the direct communication in place to improve care.
Define the Clinical Problem and Pre-Implementation Performance
Local problem.
Our goal was to reduce clinical variation in the care of sepsis patients at Homestead Hospital and throughout the system at Baptist Health South Florida (BHSF). We engaged the care team in improving processes related to the treatment of patients presenting to respective Emergency Departments (ED), via direct admission, or who become septic during their stay.
Sepsis affects over 26 million people worldwide every year, and the organization treats over 3,000 patients annually with sepsis, severe sepsis or septic shock. Sepsis is the body’s response to an infection that has become overwhelming and can lead to tissue damage, organ failure, amputations and death. Mortality increases 8% for every hour that treatment is delayed and as many as 80% of sepsis deaths could have been prevented with rapid diagnosis and treatment. Sepsis patients have the largest cost of hospitalizations in the United States consuming more than $24 billion dollars each year. Sepsis patients also have almost double the average cost per stay at around $18,400 per admission.
Previous work to improve bundle compliance was achieved through the BHSF Accelerated Change Team (ACT), which developed system wide order sets. The reflex lactate was also implemented through the BHSF ACT enabling lab to automatically order a timed lactate to achieve follow-up lactate compliance.
Homestead Hospital has a robust sepsis patient committee that meets monthly, reviewing outcome measures and providing education, mock codes, as well as reviewing cases month to month. The organization partnered with Navigant on the T2020 initiative which includes redesigning care for select DRGs. Navigant and the organization decided upon a structure of a Sepsis Steering Committee as well as two design groups: An ED team and an inpatient and ICU team. These teams collaborated on creating clinical specification to ensure sepsis patients got the same care every patient, every time. BHSF facilities such as Homestead Hospital had varied levels of success in completing the Centers for Medicare and Medicaid Services (CMS) 3-hour and 6-hour bundles for patients identified as septic. The inconsistency of implementing the two bundles in a timely manner led to significant LOS and improved mortality opportunities. Earlier identification and implementation of the interventions described in the bundles led to better outcomes for sepsis patients and a decrease in the LOS.
The mortality rate decreased from as high as 1.91 in Q1 2017 to as low as 0.45 in 2019. Sepsis patient cases meeting bundle compliance increased from as low as 52% in Jan 2018 to as high as 88% in August 2019. LOS also decreased from a high of 6.83 days on average in January of 2017 to as low as 3.88 days on average in August of 2019.
All patients >18 years of age are screened for sepsis, the numerator is the total count of patients treated in compliance with the bundle and the denominator includes all patients with the MS-DRG of sepsis (positive screen). Mortality rates are based on severity adjusted benchmarks and LOS is based on the average LOS against the benchmark of CMS and Premier.
Targeted performance
To meet and/or exceed the benchmark.
Benchmark data
BHSF benchmarks sepsis patient data against CMS, the Acute Physiology And Chronic Health Evaluation (APACHE) IV severity of disease classification system (ICU/PCU), Premier, and internal goals.
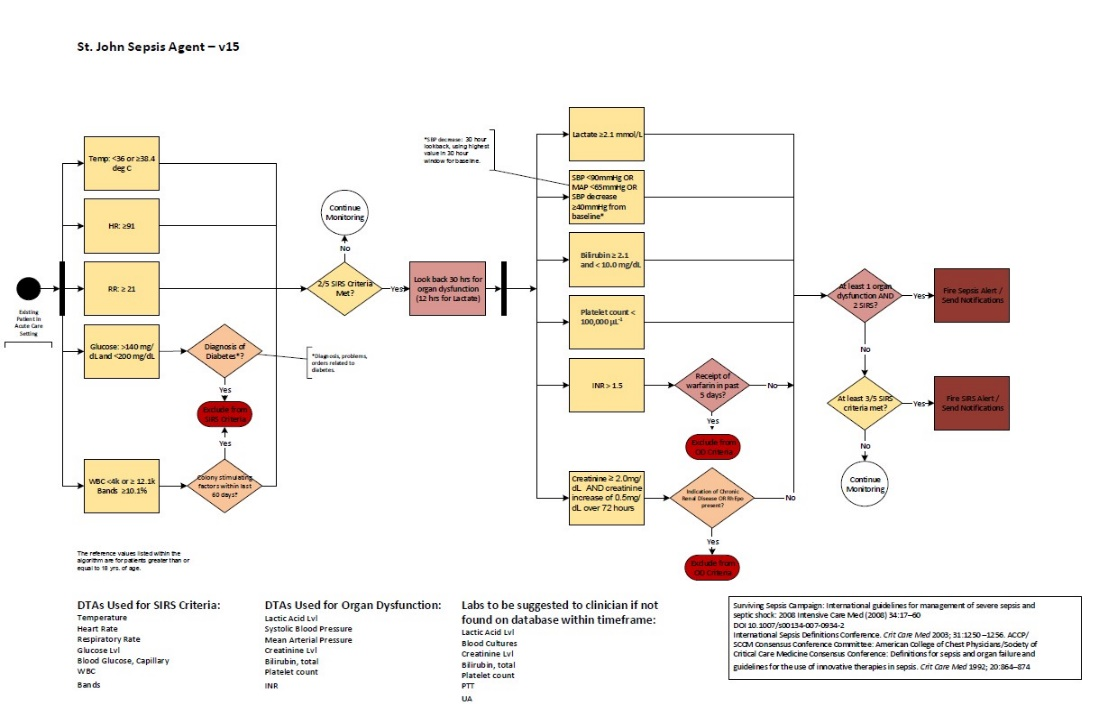
Technology initiatives
Electronic health record (EHR) data, CDS such as the St. Johns Sepsis Alert, clinical dashboards, Ascom phones for communication, the eICU for virtual care management, bedside specimen collection scanning, device integration for clinical data and bundle management via PowerPlans™.
People and Process
The evidence-based clinical care (EBCC) committee oversees the organizational structure for process waves which identify areas for improvement. The VSU is a component that enhances people, process and technology. The sepsis patient champions help to optimize infection management and emphasize the importance of early recognition and timely treatment, they also facilitate sepsis patient care and optimize patient outcomes. Ongoing physician and team education are available via lunch and learns with classroom time, elbow to elbow support, web-based learning, online formats on the EBCC website via the intranet and on the Baptist Health South website which is available in the public domain. The continuing education is a vital component to the hospital-wide code rescue response team.
Design and Implementation Model Practices and Governance
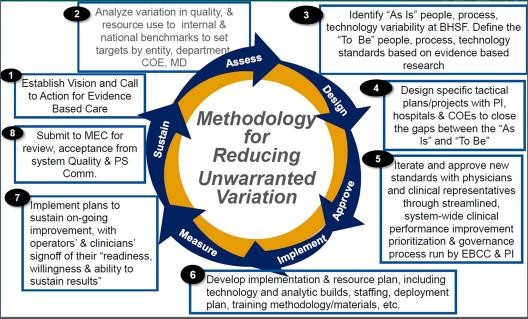
Baptist Health South Florida’s EBCC initiative is a strategic system-wide standardization effort to reduce variation and unnecessary costs while focusing on evidence-based, quality care. The process is driven by key stakeholders and is supported by real-time, statistically supported benchmarked data. The charter was signed in 2016 and provides the foundation for a methodical approach to improve patient outcomes (Figure 1).
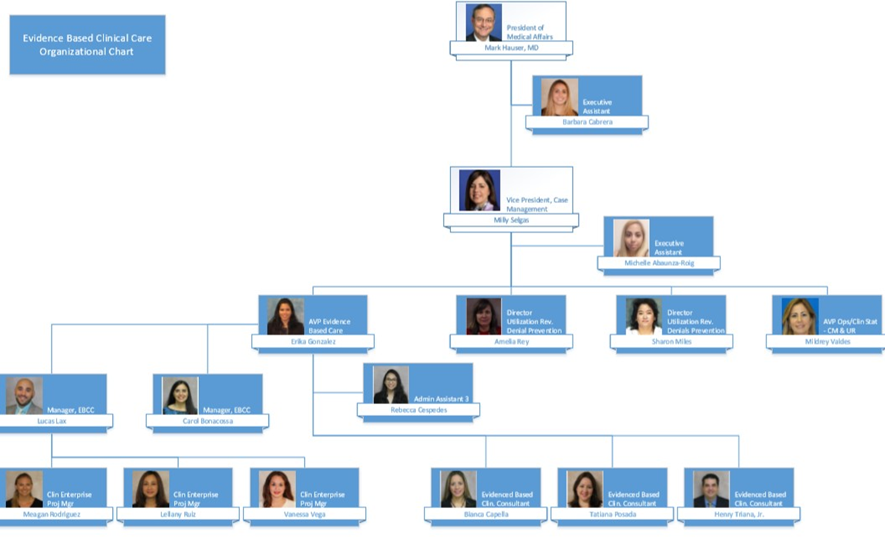
The methodology begins with a call to action to for an evidenced based care assessment of current and future state, design plan, team approval, development of an implementation plan, measurement and sustainment plans (Figure 2).
Each specific project is supported by a sub-group who are experts in on the focus topic. The Service Line Collaborative includes:
- Cardiac and Vascular
- Critical Care
- Emergency Department
- Gastrointestinal
- Infectious Disease
- Neonatology
- Neuroscience
- Orthopedics
- Surgery/PEI/ERAS/NSQIP
Navigant and BHSF decided upon a structure for a Sepsis Steering Committee to reduce variation in the management of sepsis to improve the sepsis patient mortality rate.
Education was completed via lunch and learns with classroom time, online formats on the EBCC website via the intranet and on the organization’s website which is available in the public domain.
PowerPlan™ education is a consistent part of physician education and CME education is available with every MS-DRG or pathway as it rolls out. The pilot for the sepsis patient go-live began in February 2017 and the hospital wide go-live was April 2017. The iterations over time have continued based on new benchmarks and evidence as it becomes available.
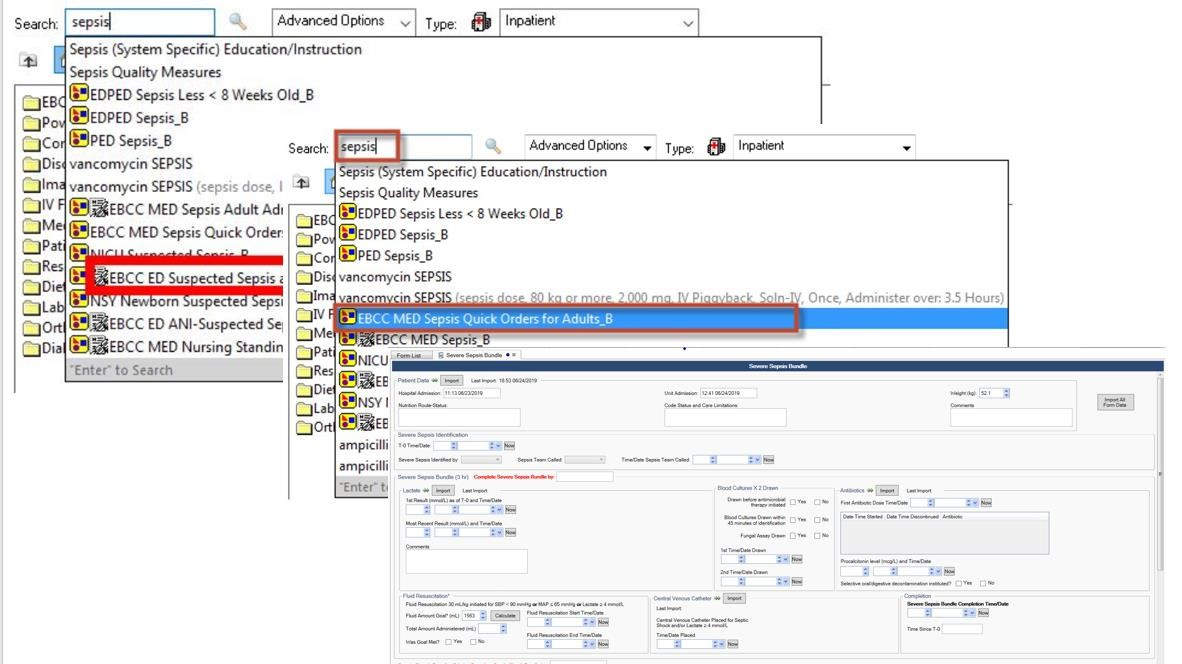
Technologies include: the physiologic data within the EHR, device integration, CDS, bedside specimen collection, sepsis algorithm, support from the eICU/VSU, dashboards and PowerPlans™ for the care bundle.
Clinical Transformation enabled through Information and Technology
To reduce clinical variation in the care of sepsis patients throughout the health system at BHSF, we engaged the care teams to improve processes related to the treatment of patients presenting to respective EDs, via direct admission, or who become septic during their stay. The workflows are geared to meet the care requirements as outlined by the industry in evidenced based research such as CMS and the Society of Critical Care Medicine’s Surviving Sepsis Campaign (Figure 3). While the overarching goal is the same throughout the venues of care, the workflows are created to meet clinical specification to ensure sepsis patients get the same care—every patient, every time. The utilization of the bundle is the foundation for minimizing the variation in care, and the people, process and technology as overseen by the EBCC committee provides the balance to drive action.
The workflows for the ED begin at triage and lead to the engagement of the VSU (Figure 4). The VSU is “air traffic control” for compliance and workflows are also designed for the ICU/PCU and med/surg areas (Figures 5 and 6). The VSU is operated out of the eICU and the virtual team streamlines the workflows to improve compliance to CMS guidelines, improving outcomes and reducing reimbursement penalties.
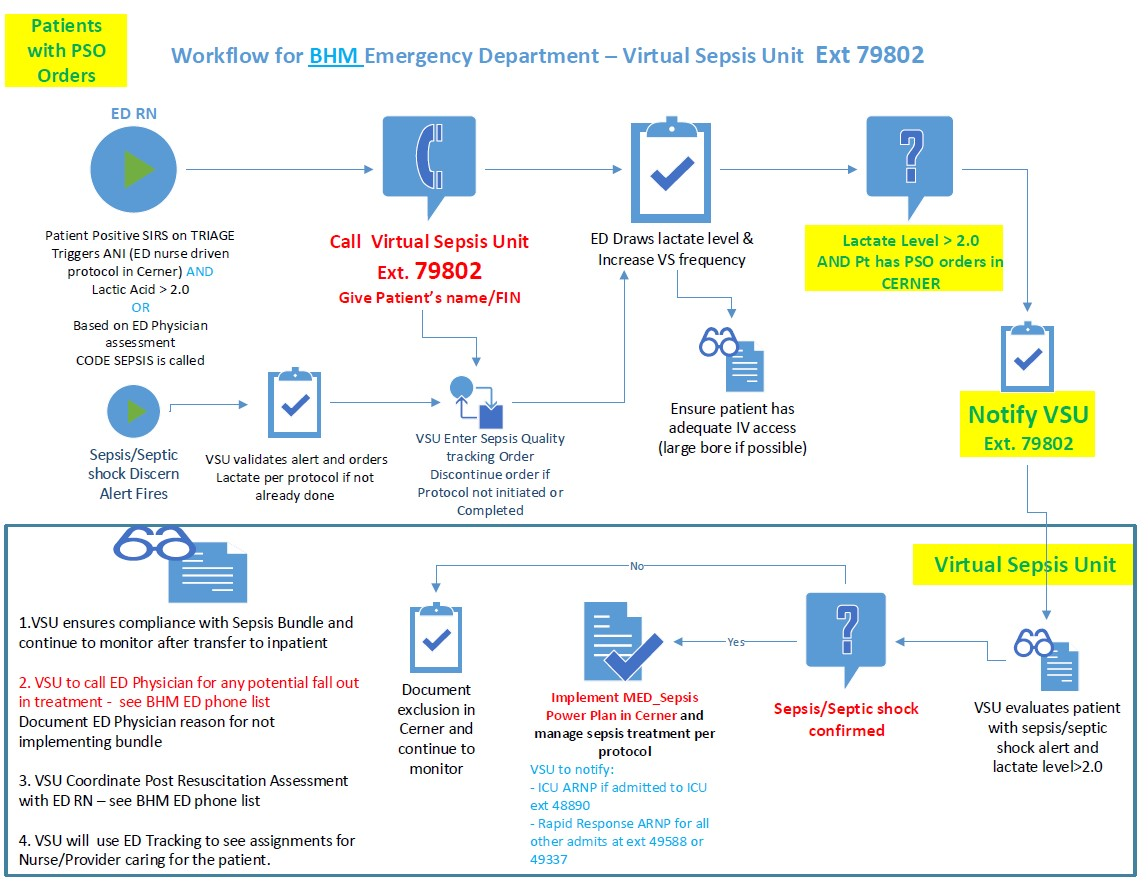
The algorithm that drives the alert is embedded into the EHR (Figure 7). The EHR supplies the clinical data required for the alert by integrating technologies such as vital sign devices, bedside specimen collection and scanning and lab values. Dashboards are available in the VSU, ED and nursing units to enhance access to the alerts, as well as alerting within the EHR.
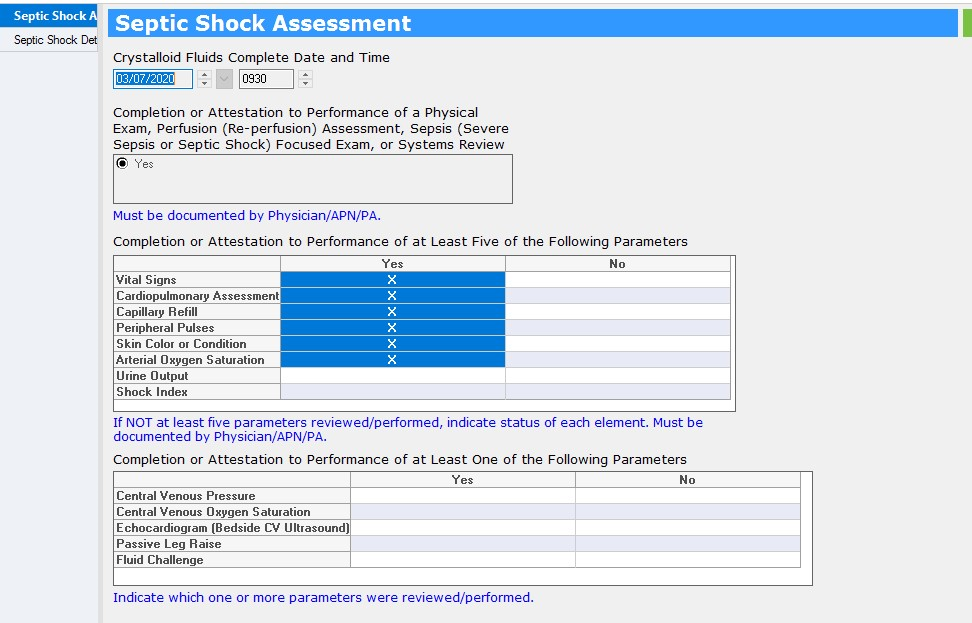
Documentation of care takes place in the EHR and the CDS for the algorithm generates the alert (Figure 8).
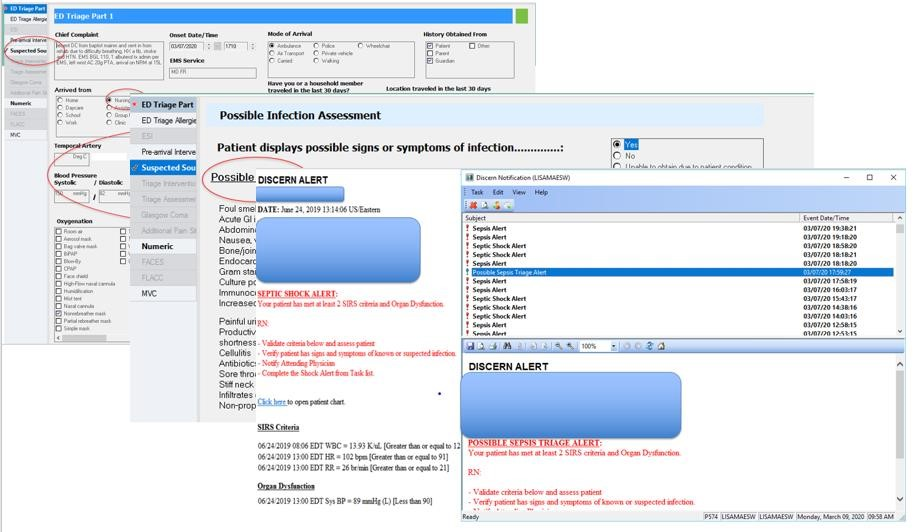
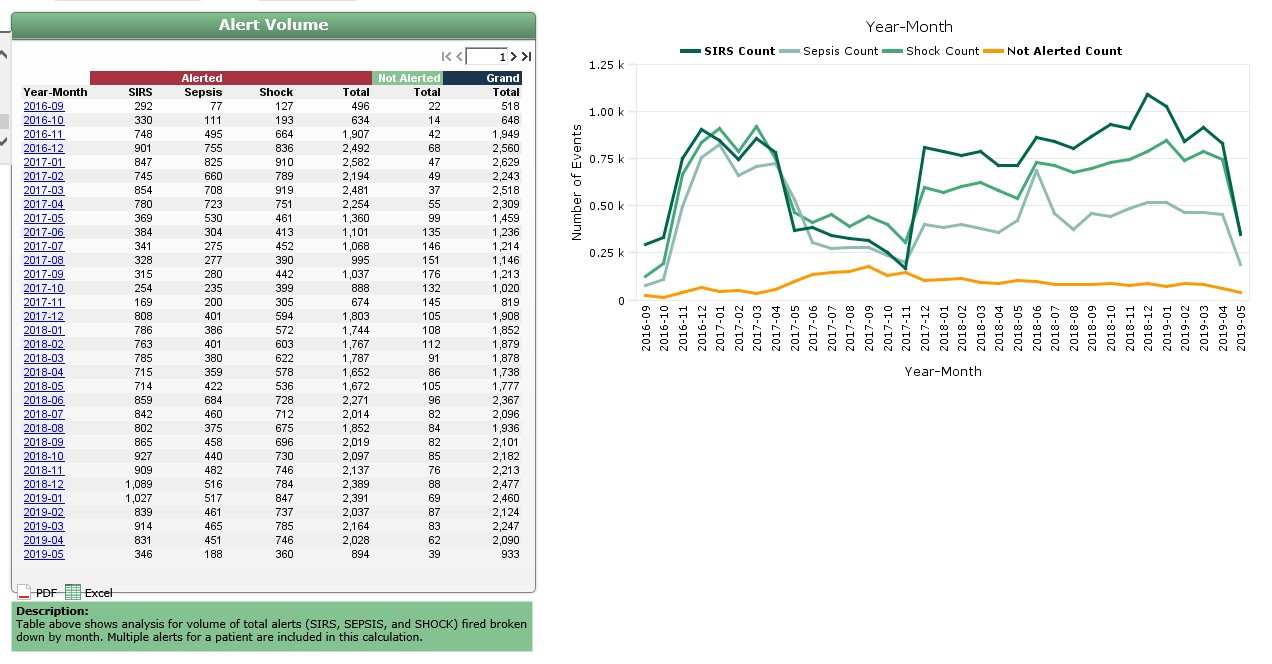
Managing the alert volume to prevent alert fatigue is a key responsibility of the VSU. The VSU reduces the number of non-actionable alerts going to physicians and nurses. Fewer alerts help to improve the specificity of the alert and provides clinical validation. (Figure 9).
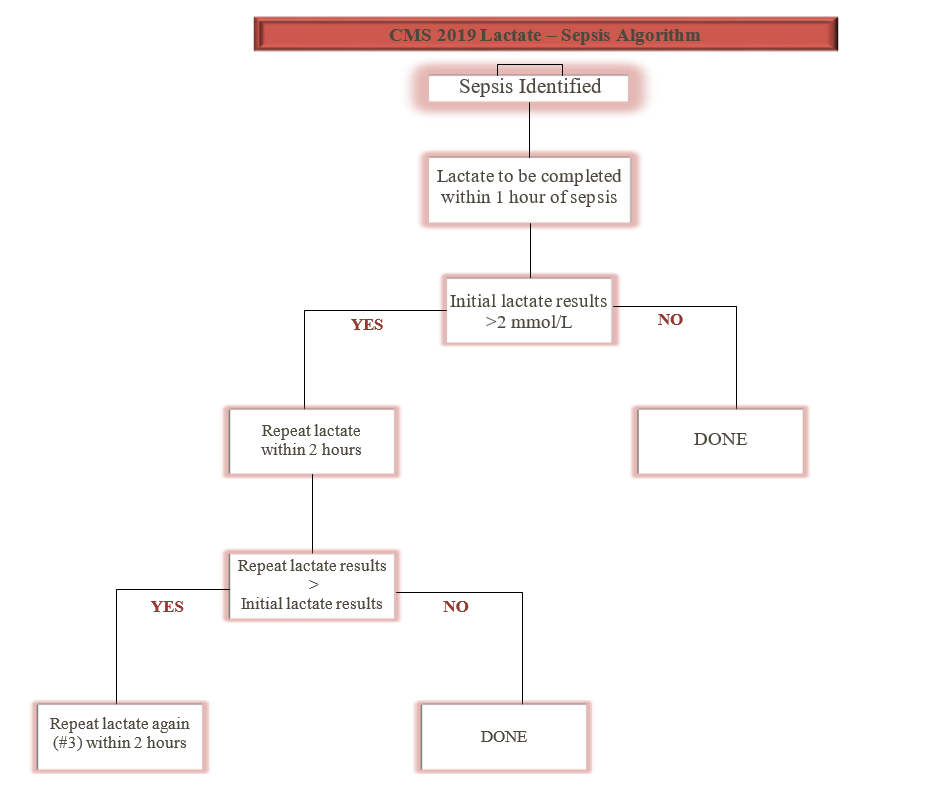
In 2019, new guidelines were released for the recommendation of lactate measures and these recommendations were built into the bundle and the workflows (Figure 10).
Examples of documentation for the bundle includes suspected sepsis patient and a quick bundle (Figure 9). Education for all care is available in the electronic version of ‘what I need to know’ (eWINK), a BHSF online education tool in the public domain which also offers CMEs/CEUs. Education for staff also includes lunch and learns with classroom time, elbow to elbow support and online formats on the EBCC website via the intranet. PowerPlan™ education is a consistent part of physician education and WINK collateral, CME education is available with every MS-DRG or pathway as it rolls out (Figure 11).
Using existing infrastructure of the eICU, virtual sepsis management was incorporated into exiting workflows. PowerPlans™ are used for bundle documentation, integration of clinical data within the EHR is supported by device integration and specimen collection and the EBCC drives pushing the current evidence to the point of care and keeps the educational material up to date.
Improving Adherence to the Standard of Care
All patients >18 years of age are screened for sepsis upon triage in the ED and all inpatients >18 years of age are monitored via CDS surveillance with the sepsis alert running within the EHR. The numerator is the total count of patients treated in compliance with the bundle and the denominator includes all patients with the MS-DRG of sepsis (positive screen). The organization transitioned to the current EHR in September of 2016 and implemented the bundle PowerPlans™ and sepsis initiative in 2017. Prior data indicated the facilities had varied levels of success in completing the bundles for patients identified as septic and the inconsistency led to opportunities to improve LOS and mortality rate.
Over time, at Homestead Hospital the compliance rate for the CMS 3-hour sepsis bundle increased from ~35% in 2015 to >90% in February 2020, with the data steward being CMS (Figure 12).
Homestead Hospital followed the standard process of change management and care redesign as outlined in the EBCC methodology. The EBCC is the governing body driving the utilization of evidence-based care focused on eliminating variation in care delivery.
Improving Patient Outcomes
The sepsis severity adjusted mortality rate decreased from as high as 1.91 in Q1 2017 to as low as 0.45 in 2019 (Figure 13). Average LOS also decreased from a high of 6.83 days on average in January of 2017 to as low as 3.88 days on average in August of 2019 (Figure 14). The risk adjusted mortality and O:E ratio are generated from Premier data.
Accountability and Driving Resilient Care Redesign
BHSF and Homestead Hospital rely on a data driven and evidence based clinical care approach to guide the design and implementation of sepsis patient care bundles. The goals of the organization’s EBCC are to decrease variation across the clinical areas and provide predictable, data-driven high quality, affordable care. Having the tools to collect as close to real-time as possible compliance data and report on that data in near-real-time reflects the ability of the organization to target and successfully improve care delivery, and ultimately improve the clinical outcomes.
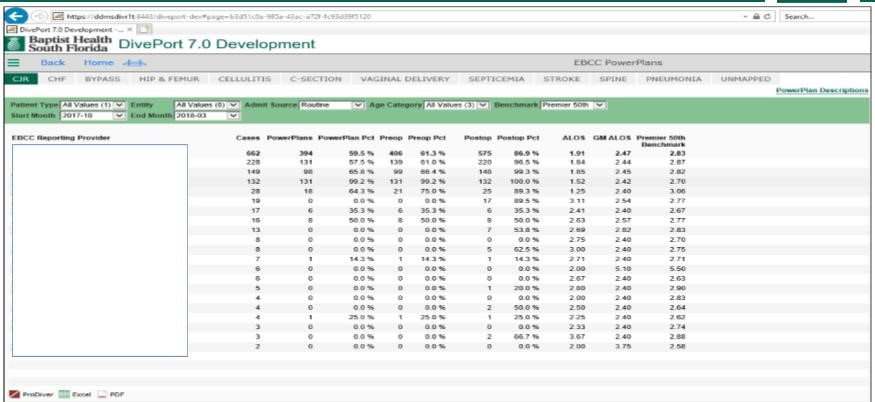
In near-real-time, the clinical team document the compliance of bundle utilization and the data is then accessible in their DivePort analytics dashboard (Figures 15 and 16). The dashboard is designed to provide statistical analysis, benchmark information and severity adjusted data with the capability to drill in multiple layers.
PowerPlans™ and bundle utilization is also available in DivePort, lending to the capability of measuring and reporting not only on the outcomes, but also to the compliance of the guidelines (Figure 17).
Using analytics to find variation
- APR-DRG Population Group is identified based on cost opportunity when compared to HCUP 40th percentile (Total Cost Per Case and ALOS).
- EBCC and Analytics Integrity Committee members review MS-DRG specific groupings that correspond with APR-DRG grouping.
- Premier benchmark levels of 50th and 75th percentile variable cost opportunities are used to further validate the data.
- MS-DRGs are recommended for EBCC team redesign based on variable cost opportunity, average LOS and volume.
- EBCC DivePort 7.0 Portal reporting is updated as DRGs waves are defined for tracking outcomes.
The rollout of the VSU is an example of using data to further refine the care redesign to complement the people, process and technology to enhance care delivery (Figure 18).
The views and opinions expressed in this content or by commenters are those of the author and do not necessarily reflect the official policy or position of HIMSS or its affiliates.
HIMSS Davies Awards
The HIMSS Davies Award showcases the thoughtful application of health information and technology to substantially improve clinical care delivery, patient outcomes and population health.
Begin Your Path to a Davies Award

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

7: Case Study #6- Sepsis
- Last updated
- Save as PDF
- Page ID 9901
- 7.1: Learning Objectives
- 7.2: Patient- George Thomas
- 7.3: Sleepy Hollow Care Facility
- 7.4: Emergency Room
- 7.5: Day 1- Medical Ward
- 7.6: Day 2- Medical Ward
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Berg D, Gerlach H. Recent advances in understanding and managing sepsis [version 1; peer review: 3 approved].: F1000 Research; 2018 https://doi.org/10.12688/f1000research.15758.1
Churpek MM, Snyder A, Han X Quick sepsis-related organ failure assessment, systemic inflammatory response syndrome, and early warning scores for detecting clinical deterioration in infected patients outside the intensive care unit. Am J Respir Crit Care Med.. 2017; 195:(7)906-911 https://doi.org/10.1164/rccm.201604-0854OC
Daniels R, Nutbeam T, McNamara G, Galvin C. The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emerg Med J.. 2011; 28:(6)507-512 https://doi.org/10.1136/emj.2010.095067
The sepsis manual. 2019. https://sepsistrust.org/wp-content/uploads/2020/01/5th-Edition-manual-080120.pdf (accessed 10 November 2020)
Gotts JE, Matthay MA. Sepsis: pathophysiology and clinical management. BMJ.. 2016; 353 https://doi.org/10.1136/bmj.i1585
Gyawali B, Ramakrishna K, Dhamoon AS. Sepsis: The evolution in definition, pathophysiology, and management. SAGE Open Med.. 2019; 21:(7) https://doi.org/10.1177/2050312119835043
Kumar P, Jordan M, Caesar J, Miller S. Improving the management of sepsis in a district general hospital by implementing the ‘Sepsis Six’ recommendations. BMJ Qual Improv Rep.. 2015; 4:(1) https://doi.org/10.1136/bmjquality.u207871.w4032
Lavallée JF, Gray TA, Dumville J, Russell W, Cullum N. The effects of care bundles on patient outcomes: a systematic review and meta-analysis. Implement Sci.. 2017; 12:(1) https://doi.org/10.1186/s13012-017-0670–0
Lee SM, An WS. New clinical criteria for septic shock: serum lactate level as new emerging vital sign. J Thorac Dis.. 2016; 8:(7)1388-90 https://doi.org/10.21037/jtd.2016.05.55
NHS England. Improving outcomes for patients with sepsis: a cross-system action plan. 2015. https://tinyurl.com/gm4zkps (accessed 10 November 2020)
National Institute for Health and Care Excellence. Neutropenic sepsis: prevention and management in people with cancer. Clinical guideline CG151. 2012. https://www.nice.org.uk/guidance/cg151 (accessed 10 November 2020)
National Institute for Health and Care Excellence. Sepsis: recognition, diagnosis and early management. NICE guideline NG51. 2016. https://www.nice.org.uk/guidance/ng51 (accessed 10 November 2020)
Porth CM. Essentials of pathophysiology, 4th edn. Philadelphia (PA): Wolters Kluwer; 2015
Royal College of Physicians. National Early Warning Score (NEWS) 2. Standardising the assessment of acute-illness severity in the NHS. Updated report of a working party. 2017. https://tinyurl.com/y5kbsnoa (accessed 10 November 2020)
Singer M, Deutschman CS, Seymour CW The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA.. 2016; 315:(8)801-810 https://doi.org/10.1001/jama.2016.0287
Stearns-Kurosawa DJ, Osuchowski MF, Valentine C, Kurosawa S, Remick DG. The pathogenesis of sepsis. Annu Rev Pathol.. 2011; 6:19-48 https://doi.org/10.1146/annurev-pathol-011110-130327
Thompson K, Venkatesh B, Finfer S. Sepsis and septic shock: current approaches to management. Intern Med J.. 2019; 49:(2)160-170
UK Sepsis Trust. Clinical resources. 2020. https://sepsistrust.org/professional-resources/clinical/ (accessed 10 November 2020)
Wentowski C, Mewada N, Nielsen N. Sepsis in 2018: a review. Anaesthesia and Intensive Care Medicine. 2018; 20:(1)6-13
Recognition and management of sepsis: the nurse's role
Greg Bleakley
Lecturer in Adult Nursing, University of Manchester
View articles · Email Greg
Senior Lecturer in Nursing, University of Manchester
View articles
Caring for a patient with suspected sepsis is a challenging nursing role. Early recognition and appropriate management of a patient with sepsis saves lives. Nurses play a fundamental role in detecting changes in physiological observations that could indicate the onset of sepsis. Additionally, an awareness of the pathophysiology of sepsis allows the nurse to better understand how rapid intervention prevents the onset of septic shock. Furthermore, knowledge and use of clinical guidelines and sepsis screening tools are established methods to help reduce patient mortality. Nurse familiarity with ‘red flag’ criteria for sepsis and thorough completion of early warning scores facilitate earlier recognition and time critical intervention. Delivery of the ‘sepsis six’ within 1 hour of suspected sepsis saves lives.
Sepsis can be defined as a life-threatening organ dysfunction that is caused by a dysregulated host response to infection ( Singer et al, 2016 ). Despite notable improvements in our understanding of the pathophysiology of sepsis, innovations in haemodynamic monitoring and methods of resuscitation, as well as pharmacological and surgical interventions, it remains one of the major causes of morbidity and mortality in critically ill patients. The global incidence of this clinical syndrome has been placed at 30 million patients each year with up to 6 million deaths. In the UK, this translates to 200 000 cases, 70% of which arise in the community and an estimated 52 000 deaths ( Daniels and Nutbeam, 2019:9 ). The annual economic burden may be as high as £2 billion and this may rise to £15.6 billion if the long-term effects on survivors is taken into account ( Daniels and Nutbeam, 2019:10 ). Despite the significant morbidity, mortality and economic costs associated with sepsis, 10 000 deaths are thought to be preventable and the care improved in 2 out of 3 patients ( NHS England, 2015 ). It is generally agreed that the crux of improving outcomes associated with sepsis is its early identification, coupled with prompt diagnostic testing, antimicrobial therapy and haemodynamic resuscitation ( Wentowski et al, 2018 ). In essence, it is vital to recognise and act before significant organ failure has occurred. Early appropriate management saves lives. Delay costs lives. Sepsis is life-threatening and time-critical ( Daniels and Nutbeam, 2019:53 ).
Early appropriate management, however, is not without challenges. Sepsis recognition and management often takes place in busy healthcare settings and it can be difficult at first presentation to distinguish between sepsis and severe infection. Moreover, sepsis has a highly complex set of pathophysiological pathways. It is not so much an illness as a syndrome that can manifest itself through a number of nonspecific symptoms ( Berg and Gerlach, 2018 ). A plethora of health professionals will come in contact with sepsis but it is nurses who take an inimitable position because of the constant interaction they have with patients.
The thrust of sepsis guidance is its proactive management. That is, ‘think sepsis’ if a patient presents with signs and symptoms that indicate possible infection. However, the Sepsis Manual ( Daniels and Nutbeam, 2019 ) highlights the challenge in differentiating between ‘infection’ and ‘sepsis’. Infection is defined as:
‘The invasion of a normally sterile cavity by organisms, or inflammation caused by organisms in parts of the body which are not normally sterile.’
and sepsis as:
‘A deterioration in the Sequential Organ Failure Assessment score of 2 points.’
The quick Sequential Organ Failure Assessment (qSOFA) score is a prompt bedside assessment for patients with suspected infection; qSOFA is considered positive if the patient has at least two of the following clinical criteria ( Daniels and Nutbeam, 2019:16 ):
- Low blood pressure (systolic blood pressure below 100 mmHg)
- High respiratory rate above 22 breaths per minute (bpm)
- Reduced conscious level (Glasgow Coma Scale below 15).
This article will provide a brief overview of the pathophysiology of sepsis and septic shock. It will then outline high risk groups, the importance of early warning scores and red flags to aid a structured assessment and a prompt diagnosis. Finally, it will introduce the Sepsis six care bundle and highlight how it has been shown to improve patient mortality.
Pathophysiology of sepsis
Sepsis occurs when infective pathogens trigger a localised inflammatory reaction that stimulates a wider systemic inflammatory response (SIR). Physiologically, a bacterial pathogen enters the body and resident macrophages initiate a localised inflammatory response ( Stearns-Kurosawa et al, 2011 ; Porth, 2015 ). Receptors in the lining of blood vessels detect infective agents on the cell wall of pathogens. The response from the host immune system is to infiltrate the local area with macrophages, leukocytes and neutrophils. Macrophages are specialised cells linked to the detection, phagocytosis and destruction of pathogens. Essentially, macrophage cells ingest (phagocytose) infective bacteria and create a series of pro-inflammatory cytokines which stimulate a SIR. In a similar way, leukocytes are white blood cells connected to pathogen recognition and destruction. Neutrophils are among the first specialist white blood cells to migrate to the site of infection and destroy invading micro-organisms ( Gotts and Matthay, 2016 ). Interestingly, some forms of cancer treatments can suppress the ability of bone marrow to respond to infection. People receiving chemotherapy and health professionals providing care need to be aware of the risk of neutropenic sepsis. Neutropenic sepsis is an overwhelming infection that affects people with a low neutrophil count and is a potentially fatal complication of anticancer treatment ( National Institute for Health and Care Excellence (NICE), 2012 ).
Infective agents can give rise to sepsis via a number of sources. These include: skin and joint infection, meningitis, respiratory tract (lungs), endocarditis, urinary tract infection (UTI) and healthcare device-related infection. Sometimes there may be a clinical suspicion of infection, but the source is unknown. Clinically, such patients may have a history of pyrexia (fever), diaphoresis or appear flushed. The Sepsis Manual reports that a ‘clinical suspicion of an infection is all that's needed’ to trigger further investigations to exclude sepsis ( Daniels and Nutbeam, 2019:20 ).
The systemic immune response is characterised by the mobilising of white blood cells (neutrophils and monocytes) to the site of injured tissue to destroy pathogens. The proliferation of white blood cells due to the SIR is referred to as leukocytosis ( Porth, 2015 ). Although increases in white cell count attempt to destroy the invasive pathogens, they can harm the cells that line blood vessels (endothelium). Critically, damage to the endothelium enhances vascular permeability causing capillaries to become ‘leaky’ ( Daniels and Nutbeam, 2019:20 ). Damaged endothelial cells produce excesses of nitric oxide and other cytokines, which in turn, act as an effective vasodilator and key determinant in developing sepsis ( Porth, 2015 ). Updated evidence from the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) suggests abandoning use of host inflammatory response syndrome criteria (systemic inflammatory response syndrome (SIRS)) in the identification of sepsis and, furthermore, eliminate the term ‘severe sepsis’ from existing terminology. This is particularly significant when discussing the progression of sepsis through to septic shock ( Singer et al, 2016 ). Table 1 highlights the molecules and cytokines that are released during the SIRS phase.
It is important to note that primary care settings have a different pre-hospital sepsis screening tool and action tool. If the NEWS score is above 3 and/or the patient looks sick then sepsis should be considered. Significantly, the prehospital sepsis screening tool advises practitioners to arrange immediate transfer of the patient to a ‘designated destination’ and ‘communicate likelihood of sepsis at handover’ ( Daniels and Nutbeam, 2019: 29 ).
Sepsis remains a significant healthcare challenge and economic burden. This article has explained how a sound understanding of the pathophysiology of sepsis can equip the nurse with the knowledge needed to ensure prompt action and save lives. Nurses are the health professional that has greatest contact with high-risk patients. As such, they are uniquely placed to use clinical guidelines and make a rapid detection of the syndrome and then activate appropriate interventions. In particular, the integration of early warning scores is a proven template that can ‘track and trigger’ clinical deterioration and ensure patient safety and timely intervention.
- Early appropriate management of sepsis saves lives. Delay costs lives
- Septic shock is a life-threatening clinical emergency that occurs when the blood pressure drops to dangerously low level following an infection
- ‘Think sepsis’ has entered healthcare language and the nurse should combine this approach with a knowledge of at risk groups by using validated screening tools and their own clinical acumen
- The National Early Warning Score (NEWS) is the most accurate tool for predicting in-hospital mortality
- The Sepsis six need to be delivered within 1 hour to control the source of infection, restore circulation and promote oxygen delivery
CPD reflective questions
- Are you aware of your hospital's policy on sepsis? Reflect on how you treat patients with suspected sepsis in your clinical area
- Can you and members of your team identify any sepsis ‘red flag’ criteria?
- Can you identify the difference between ‘infection’ and ‘sepsis’ when communicating with the wider healthcare team?
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
The following scenario is about a patient who experienced sepsis secondary to a UTI. The patient, Mrs. June Peters (84), was found by her daughter, Mary Jones, in her apartment in a a state of acute confusion. She was admitted to the ED with nausea, vomiting, acute confusion, shivering, severe right flank pain 8/10, pale and mottled skin, tachypnea, tachycardia, and elevated temperature. Her vital signs were: Temp 102, HR 112, RR 28, BP 85/52 (63), SaO2: 92% on room air. The Physician suspected a possible UTI.
Question 1: Given this information, what should be done?
Code Sepsis was called and orders were placed for the following tests and diagnostics: CBC, lactate level, ABGs, CMP, coagulation screen, C-reactive protein, Procalcitonin, Gram stains/cultures, blood culture, urinalysis & urine culture, ultrasound of the abdomen and pelvis, and 2 L O2 with nasal cannula. While results were pending, patient was started on Zosyn (Piperacillin-tazobactam 4.5g IV Q8H extended infusion).
When the labs and diagnostic results returned, significant findings were as follows: WBC 13.5, Lactic acid 9.8, CRP 120, urine culture cloudy with sediment and positive for E. coli., ProCT 8.7, blood culture positive for E. coli., creat 2.0, BUN 45, and the ultrasound demonstrated findings of right kidney infection. Mrs. Peters is transferred to the ICU.
Overnight, Mrs. Peters’ status has declined. Her SpO2 was consistently at 76% on 6 L NC, so she was switched to a non-rebreather mask at 10 L O2. The SpO2 remained at 77% with a respiratory rate of 10 and the doctor was called. He decided to put the patient on the ventilator and sedated the patient with propofol before intubation. A chest x-ray was done, which confirmed correct placement of the ET. The patient was placed on the A/C setting on the ventilator and continuous ABG monitoring was ordered. In addition, her blood pressure was unresponsive to the crystalloid ordered the day before as part of the 3-hour sepsis bundle.
Question 2: The nurse would expect what additional new orders since Mrs. Peters was still presenting with hypotension and elevated lactate level even after the 3 hour sepsis bundle was followed?
Doctor’s orders were to initiate endotracheal tube placement, ventilator (Settings: mode – A/C, Rate – 16, TV: 500ml, FiO2: 30%, PEEP: 10), Propofol 20 mcg/kg/min, chest x-ray, monitor V/S Q 15 min x4 at the start of ventilation, then Q 2 hours. Vasopressin 0.01 un/min and titrate by 0.005 un/min Q 10-15 min until target BP achieved.
Nursing actions were to monitor V/S, administer propofol 20 mcg/kg/min IV drip, oral care, reposition patient Q2 hrs, suction patient PRN, and titrate vasopressin to maintain MAP ≥ 65.
On the fifth day, the patient remained in the ICU and was lethargic & sedated. While she spontaneously opened her eyes in response to her name, she didn’t stay alert for very long before dozing off again. After performing a HTT the nurse found that the patient had a heart rate of 106, a BP of 89/38, and a temperature of 99.8. Doctor notified. Skin was warm and sweaty. Pulses were rapid and +2. Patient had a Foley draining cloudy urine at approximately 30 ml/hr. Respirations were clear. She had no significant GI findings. The ventilator settings were on AC control, PEEP of 6. Tidal volume of 410. FiO2 of 35%. Lactic acid was trending down (1.5) as well as WBC count (12.4). The nurse administered Zosyn, Vasopressin and Tyleonl. The Vasopressin helped regulate the patient’s BP and HR and the Tylenol lowered the patient’s temperature.
The nurse referred the caseworker to talk with the daughter as she expressed concern about her mother returning home to her own apartment. The caseworker came to speak with the daughter and asked about her mother’s living situation. The daughter explained that her mother lived by herself on the 2nd floor of the apartment complex, but the elevator works most of the time. She told the caseworker that she had to help her mother with groceries, cooking, and laundry, but that she is fine by herself. After hearing this, the caseworker told the daughter that it would be advisable for her mother to be moved to an assisted living facility. The daughter became very frustrated and told the caseworker that she was not going to abandon her mother like that. The caseworker was silent and listened until the daughter was done talking. She expressed to the daughter that she seemed frustrated and that this was not the intent of the conversation. She said that the goal was to decide what is best for her mother and she explained that they will include her mother in this conversation once she became more alert. Upon hearing this, the daughter acknowledged that the caseworker was right and that her mother does need more help than she is able to provide. She agreed to hear the options for an assisted living facility.
Question 3: How was therapeutic communication used by the caseworker in this conversation? What types of therapeutic communication did she use?
On day 10, after being extubated for 2 days, Mrs. Peters was discharged from the hospital. She and her daughter decided that she would move into an assisted living facility nearby. The nurse gathered all the discharge paperwork and provided Mrs. Peters with education on UTIs and how to prevent them.
Answer Key:
Question 1: Initiation of Code Sepsis
Question 2: The MD placed new orders to maintain the MAP ≥ 65 using Vasopressin. Mrs. Peters perfusion and volume status were reassessed and documented by the physician. Her lactate level was redrawn.
Question 3: The caseworker used therapeutic communication to diffuse a tense conversation. She was able to help the daughter come to terms with her mother’s changing situation and she helped the daughter focus on doing what was best for her mother. She used the techniques of focusing, restating, recognition, and silence.
By Genevieve Cragoe
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Sepsis Performance Improvement Programs: From Evidence Toward Clinical Implementation
Michiel schinkel.
1 Center for Experimental and Molecular Medicine, Amsterdam UMC, Location Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands
2 Section General Internal Medicine, Department of Internal Medicine, Amsterdam Public Health Research Institute, Amsterdam UMC, Location VU University Medical Center, Amsterdam, The Netherlands
Prabath W. B. Nanayakkara
W. joost wiersinga.
3 Department of Medicine, Division of Infectious Diseases, Amsterdam UMC, Location Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands
Associated Data
Not applicable.
This article is one of ten reviews selected from the Annual Update in Intensive Care and Emergency Medicine 2022. Other selected articles can be found online at https://www.biomedcentral.com/collections/annualupdate2022 . Further information about the Annual Update in Intensive Care and Emergency Medicine is available from https://link.springer.com/bookseries/8901 .
Introduction
Since its launch in the early 2000s, the international Surviving Sepsis Campaign (SSC) has provided guidelines for the management of sepsis, most recently updated in 2021 [ 1 ]. The SSC aims to provide a standard of care for sepsis while increasing awareness among healthcare professionals and the general public. The goal is to reduce morbidity and mortality from sepsis and septic shock worldwide [ 2 ].
To facilitate the clinical implementation of the guidelines, the SSC bundles their recommendations into small groups of care processes that physicians should perform within a specific timeframe and that provides them with a concrete plan of action [ 1 , 2 ]. Despite efforts to facilitate the successful implementation of the guidelines, adherence has been suboptimal, particularly regarding the microbiological work-up and administration of appropriate antibiotics [ 3 ]. Non-compliance to the SSC guidelines seems most prominent among emergency medicine and internal medicine physicians [ 4 ].
In response to the low adoption rates of (SSC) sepsis guidelines, individual hospitals and organizations have introduced sepsis performance improvement programs. Usually, dedicated physicians or research teams lead these initiatives and use screening tools, process changes in sepsis care pathways, and sepsis educational programs to optimize adherence to the standard of care [ 5 ]. The latest update of the SSC guidelines recommends that all hospitals and health systems have sepsis performance improvement programs [ 1 ].
In this chapter, we discuss the literature on the use and benefits of sepsis performance improvement programs to improve protocol adherence and provide practical insights for the clinical implementation of such programs in your hospital.
Do ‘One-Size-Fits-All’ Care Bundles Improve Sepsis Outcomes?
Sepsis performance improvement programs aim to improve adherence to a guideline or protocol for sepsis care, and they are almost exclusively studied in the context of the SSC care bundles [ 5 ]. When one aims to improve compliance rates to any guideline, one should first be convinced that this is a goal worth pursuing. In the case of the SSC guidelines, this debate has been ongoing for many years, and this paragraph presents only a brief overview of this reflective and meaningful discussion [ 6 , 7 ].
Expert panelists on sepsis have created the SSC bundles, spearheaded by the Society of Critical Care Medicine (SCCM) and European Society of Intensive Care Medicine (ESICM), and endorsed by numerous medical societies [ 1 , 6 ]. However, the evidence base for these bundles and the timeframes in which they should be performed have been a matter of debate [ 7 – 9 ]. One prominent example concerns adherence to early goal-directed therapy (EDGT), an early form of bundled care that was associated with significantly lower in-hospital mortality rates (30.5% vs. 46.5% in the usual care group) in a randomized study of 263 patients with sepsis or septic shock presenting to the emergency department of a tertiary hospital in the United States [ 10 ]. However, these results were not replicated in subsequent large randomized trials and meta-analyses [ 11 – 13 ]. Furthermore, the value of individual bundle items, such as the 30 ml/kg fluid bolus and administration of antibiotics within 1 h to all patients, has been heavily debated because of conflicting results regarding the benefits [ 7 , 14 – 16 ]. Moreover, fear exists that pressure to perform bundle items within a specific timeframe may promote harmful diagnostic tests and treatments, as was the case with the 2002 quality measure for the management of community-acquired pneumonia by the Centers for Medicare & Medicaid Services, which was later removed [ 9 , 17 ].
Despite the limited evidence base that underlies some of the recommendations in the SSC bundles, the overall consensus, underscored by the endorsements from 35 international medical societies, seems to be that most of the care processes in the bundles will positively contribute to the management of the majority of sepsis patients [ 6 ]. Numerous observational studies have shown associations between improved bundle compliance and a reduction in mortality. An extensive 7.5-year study in 280 hospitals across Europe, South America, and the United States showed that overall mortality was significantly lower in high-compliance hospitals (29.0%) compared with low-compliance hospitals (38.6%) [ 18 ]. This study included 29,470 patients with sepsis or septic shock from emergency departments, regular wards, and intensive care units (ICUs) between January 1st 2005 and June 30th 2021. Notably, compliance was defined as high when sites completed the resuscitation bundle within 6 h for as few as 15% of their patients, suggesting that complete bundle adherence is only practical in a small subset of patients [ 18 ]. A similar project in Portugal studied the effects of adherence to the 6-h bundle in 897 patients with community-acquired sepsis in 17 ICUs [ 19 ]. Among those 897 patients, the core bundle was only completed within 6 h in 12% of the patients. The highest compliance was seen for the administration of vasopressors (78%) and the collection of cultures before antibiotic treatment (77%). In comparison, the lowest adherence was seen for blood culture collection in general (48%) and administration of antibiotics (52%) [ 19 ]. Compliance with the complete bundle was associated with decreased 28-day mortality, with an adjusted odds ratio (OR) of 0.44 (95% confidence interval [CI] 0.24–0.80) in sepsis and 0.49 (95% CI 0.25–0.95) in septic shock. Other studies have found similar mortality benefits associated with improved SSC bundle adherence [ 20 – 22 ].
Sepsis Improvement Programs: What Is the Evidence?
Adherence to the SSC guidelines in hospitals and healthcare systems that have adopted them is still suboptimal [ 3 , 5 ]. For example, a nationwide study in Finland showed complete guideline adherence in only 6 out of 92 ICU patients during the four-month study period, similar to rates found in other studies [ 5 , 23 ]. Sepsis performance improvement programs may help improve compliance, and a 2015 systematic review and meta-analysis by Damiani and colleagues tried to quantify this effect [ 5 ]. The reviewers identified 50 observational studies with highly diverse improvement programs and study designs. Despite this heterogeneity, the meta-analysis showed that sepsis performance improvement programs were consistently associated with increased compliance with 6-h (OR 4.12, 95% CI 2.95–5.76) and 24-h (OR 2.57, 95%-CI 1.74–3.77) bundles and with reduced mortality (OR 0.66, 95%-CI 0.61–0.72). The mortality estimates are hard to interpret in this meta-analysis since they include in-hospital mortality as well as short- and long-term mortality.
Among the 50 studies included in the systematic review of Damiani et al., combinations of interventions using screening tools, process changes, and educational programs were independently associated with increased bundle compliance and reduced mortality [ 5 ]. It thus appears that having a sepsis performance improvement program in itself is more important than the specific content of the program. However, the best results were observed in programs with various simultaneous interventions for performance improvement and in hospitals where the initial compliance was lowest [ 5 ]. The following sections will discuss the most-studied interventions (implementation of sepsis screening tools, process changes in sepsis care pathways, and educational programs) and their effects in further detail.
Sepsis Screening Tools
A primary focus of many performance improvement programs is using screening tools to identify sepsis early. Correct treatment can be initiated earlier if sepsis is recognized sooner, which is expected to improve patient outcomes [ 2 ]. Three randomized controlled trials (RCTs) have studied whether the use of screening tools can improve patient outcomes in sepsis [ 24 – 26 ]. Downing et al. used an electronic health record (EHR) alert to detect sepsis early in medical and surgical wards, based on modified sepsis criteria including laboratory results and vital signs [ 24 ]. However, the alert did not result in improved performance measures or patient outcomes.
Hooper and colleagues studied the effects of pager alerts whenever a patient in the medical ICU satisfied a modified version of the systemic inflammatory response syndrome (SIRS) criteria [ 25 ]. Again, the alerts did not result in any improved performance measures or decreased mortality rates. Only Shimabukuro and colleagues were able to show improvements in patient outcomes using automatically generated alerts in the EHR with their machine learning-based sepsis screening tool [ 26 ].
Among 142 patients in the US-based medical-surgical ICUs, the hospital length-of-stay (− 2.30 days), ICU length-of-stay (− 2.09 days), and in-hospital mortality (− 12.3%, absolute) were all significantly lower in the intervention group that used the automated sepsis screening tool [ 26 ]. One explanation for why this study was able to find beneficial effects is that it was the only one of the three to combine the alert with a mandatory and immediate evaluation of the patient to specifically address the potential diagnosis of sepsis, which can be regarded as an additional process change.
A problem in sepsis screening is that there is a plethora of different risk scores and screening tools which are currently used, such as the SIRS criteria, Modified Early Warning Score (MEWS), National Early Warning Score (NEWS), and quick Sequential Organ Failure Score (qSOFA). The accuracy of these risk scores is highly variable in the emergency department, regular wards, and the ICU [ 27 ].
Several extensive studies and reviews have evaluated which screening tool is most effective for suspected infection or sepsis [ 27 – 31 ]. The NEWS and MEWS consistently show a balance between sensitivity and specificity, both usually ranging between 0.40 and 0.80 [ 27 , 29 ]. SIRS is more sensitive than specific, and qSOFA more specific than sensitive. None of these instruments seems superior to the others in identifying sepsis across studies [ 27 – 31 ]. The SSC guideline consequently does not recommend using a particular tool [ 1 ]. Physicians should be aware of the benefits and limitations of the tools they use, and choices should be based on local preferences. The only exception is the use of qSOFA, which the guideline recommends against as a screening tool [ 1 ]. Although the qSOFA is highly specific, the poor sensitivity makes it unsuitable for screening purposes.
A limitation to all currently used tools is that they are susceptible to false positives because of the relatively low prevalence of sepsis, particularly in the general emergency department and ward populations [ 30 ]. Advanced computational approaches such as machine learning could provide a solution for this and may eventually replace the current, less complex risk scores. A systematic review and meta-analysis evaluating seven studies showed that machine learning algorithms outperform MEWS, SIRS, and qSOFA for sepsis prediction [ 32 ]. Additionally, monitoring through EHR systems with continuous data streams can detect sepsis even earlier than static risk scores. Van Wyk et al. showed this when their algorithm predicted sepsis onset in 377 ICU patients in the USA on average 205 min earlier than SIRS criteria would have [ 33 ]. However, many challenges still need to be overcome before safely introducing machine learning tools for sepsis into everyday clinical practice [ 34 ]. Some of these challenges were recently illustrated by the external validation of the Epic Sepsis Model, the machine learning-based screening tool for sepsis provided by the EHR vendor, Epic (Verona, WI, USA) [ 35 ]. This algorithm is widely adopted for sepsis screening, particularly in the USA. In a population of 2552 sepsis patients among 38,455 hospitalizations, the Epic Sepsis Model reached an area under the curve (AUC) of only 0.63 for sepsis recognition in an external validation [ 35 ]. Physicians using this tool evaluated an average of 109 patients based on sepsis screening alerts to detect only one case earlier than they would have without, putting a disproportionate burden on the healthcare system.
Process Changes in Sepsis Care Pathways
Several studies have examined the effect of sepsis performance improvement programs using process changes to improve adherence to the SSC care bundles. After identifying a patient who may have sepsis, the diagnostic work-up and treatments should be promptly initiated. The most critical process change in sepsis care pathways studied in this regard is the implementation of sepsis (response) teams. Instead of putting the responsibility to act on a sepsis screening alert on one consulting physician, who may already care for multiple patients, dedicated teams are created to respond to sepsis alerts collectively. A pre-post study by Viale et al. in Italian emergency departments showed that implementing a dedicated sepsis response team was associated with increased bundle adherence from 4.6 to 32%, improved appropriateness of the initial antibiotic therapy from 30 to 79%, and a hazard ratio of 0.64 (95% CI 0.43–0.94) for 14-day all-cause mortality [ 3 ]. In another study from Italy, these results were replicated in a multidisciplinary ICU [ 36 ]. In this setting, implementing a dedicated sepsis team was reported to be associated with a significant decrease in in-hospital mortality from 68 to 23%. Furthermore, the use of the dedicated sepsis team was significantly associated with decreased mortality in univariate logistic analysis (OR 0.28, 95% CI 0.10–0.79) [ 36 ]. However, the results of these studies should be interpreted cautiously, given their observational design and potential for confounding by indication.
Process changes other than implementing a dedicated sepsis team may also contribute to better bundle adherence when they improve the efficiency of the care workflow. Examples that have been extensively studied are printed or easily accessible protocols, standardized EHR order sets, daily auditing with weekly feedback, and nurse-driven sepsis protocols [ 5 ]. Nurse-driven sepsis protocols are a practical approach that acknowledges the essential role of nurses in the sepsis care pathways [ 37 ]. Their role is not formally described in the SSC guidelines, but they are often the first to triage patients and respond to their deteriorating condition. As an example, a Dutch study by Tromp et al. showed that a nurse-driven sepsis care bundle increased compliance with the complete bundle from 3.5 to 12.4% and the mean number of performed bundle elements within the appropriate timeframe from 3.0 to 4.2 [ 37 ]. Completion of four of the six individual bundle items, such as the measurement of serum lactate (23% to 80%) and the start of antibiotics within 3 h (38% to 56%), increased significantly. No significant changes in the in-hospital mortality rates or hospital length of stay were observed [ 37 ].
Sepsis Educational Programs
Arguably, increased sepsis awareness is one of the primary reasons for better patient outcomes through SSC care bundle use. Therefore, education is an essential aspect of sepsis performance improvement programs, as it helps raise awareness among healthcare professionals. The 2015 systematic review about sepsis performance improvement programs by Damiani et al. included 17 studies in which only educational programs were used [ 5 ]. These included educational materials, lectures, bedside teaching, and simulation training, among others. Many of these education-only programs showed significantly increased bundle adherence and decreased mortality rates. An early observational cohort study in the USA by Nguyen et al. studied the effects of a comprehensive sepsis education program in a small cohort of 96 patients with sepsis in their ICU [ 38 ]. A mortality rate of 45% was observed when the compliance with SSC care bundles was high, but was 73% when SSC guidelines were largely disregarded ( p = 0.006). Another example of the effects of educational programs is the more extensive study by van Zanten and colleagues, which also reduced the limitations of the observational approach by using control groups and propensity score matching [ 22 ]. Implementation of educational programs in 52 participating hospitals was associated with an absolute increase of 23.6% in SSC bundle adherence and an absolute decrease in mortality rates of 5.8% in 8031 ICU patients with sepsis during the study period. No such associations were found in 8387 ICU patients in 30 non-participating hospitals over the same period.
The Road Ahead
The discussion about the precise value of the SSC care bundles and the care processes within them will inevitably continue [ 6 , 7 ]. Standardized expert care recommendations are indispensable for a syndrome with a mortality rate as high as it is in sepsis. However, such recommendations are often challenging to develop given the heterogeneity of sepsis and the weak and often contradicting evidence for its different treatment modalities [ 1 , 13 , 39 ]. Still, bundle adherence has consistently been associated with improved patient outcomes. An unanswered question is whether improved patient outcomes are caused by the items in the care bundles, by increased awareness irrespective of bundle adherence, or whether they are just artifacts of confounding by indication. Well-controlled trials could potentially find a definitive answer to this question, further determining what matters most while implementing sepsis performance improvement programs. Such a trial will, however, be hard to carry out and needs sophisticated methodological design.
Sepsis improvement programs are associated with improved protocol compliance and can be helpful to improve protocol adherence when a hospital or healthcare system implements either the SSC sepsis guidelines or their version of a protocol for sepsis detection and treatment. Therefore, these programs should be used in any hospital with low adherence rates to local protocols. The program should ideally consist of various simultaneous interventions to promote bundle compliance optimally [ 5 ]. Those interventions can be sepsis screening tools, process changes in sepsis care pathways, and sepsis educational programs. However, the goal should never be to mandate 100% guideline adherence but to leave room to deviate from standardized protocols when appropriate.
In our university medical center, we initiated a sepsis performance improvement program in 2021. As an illustration, we provide the details about this program, including early lessons learned from the implementation process in Box Box1. 1 . The flowchart for our sepsis response team set-up is visually presented in Fig. 1 . A major takeaway is that the engagement of only a few clinical leaders per department seems insufficient in an emergency department’s dynamic and continuous environment. Furthermore, the involvement of patient representatives is important when initiating a sepsis performance improvement program, as the values and perspectives of the main stakeholder should not be overlooked. In high-pressure situations, such as acute care for patients with suspected sepsis in the emergency department, treatment of the patient’s physical state is prioritized over the mental state. However, systematically addressing important questions the patient may have could alleviate much of the mental stress they will likely experience. In Box Box2, 2 , we summarize important questions to address from the viewpoint of a sepsis survivor who has been involved with our sepsis performance improvement program.
An example from the emergency department: creating a sepsis performance improvement program in a large university medical center. The different phases of implementing a sepsis performance improvement program in the Amsterdam University Medical Center
Essential aspects of emergency department sepsis care from the patient’s point of view. A summary of aspects to address during the evaluation of and conversation with a patient who may have sepsis

Flowchart of sepsis response team involvement in a large teaching university medical center. A practical example from Amsterdam University Medical Center including all aspects from early detection to the diagnostic work-up and treatment decisions. ED emergency department, MEWS Modified Early Warning Score
Finally, most studies investigating the benefits of bundled care and sepsis performance improvement programs used mortality reduction as an endpoint [ 5 ]. Already in 2005, an International Sepsis Forum (ISF) colloquium provided a broad set of outcome measures that sepsis studies can use beyond survival as the only and ultimate goal of sepsis care [ 40 ]. Nevertheless, the literature is still dominated by the pursuit of short-term survival benefits. During the coronavirus disease 2019 (COVID-19) pandemic, the ISF proposed an adjusted version of the original outcome set, which was adopted globally [ 40 , 41 ]. Improving outcome parameters such as resource use, duration of invasive treatments, and the development of organ dysfunction that requires higher levels of care, suddenly became extremely valuable in a resource-scarce setting [ 42 ]. Future studies on sepsis performance improvement programs and sepsis care bundles should similarly expand the core set of outcome measures to capture these additional benefits. In the era of shared decision-making and patient-centered care, we should acknowledge that there is more to life than death [ 43 ].
Sepsis performance improvement programs can optimize compliance to sepsis care protocols, which have been associated with improved patient outcomes in various studies. These programs should ideally combine screening tools, process changes in sepsis care pathways, and educational programs to create awareness about sepsis care. The consequent gains through swift and adequate recognition of sepsis can be used to diagnose and treat patients accurately and timely according to (SSC) care protocols and deliberately think about when it is necessary to deviate from the general recommendations. Trust and behavior change are essential aspects of implementing sepsis care bundles. These aspects can be reinforced by performance improvement programs but need time. Engaging a large group of multidisciplinary clinical leaders for sepsis improvement programs seems essential for their success.
Acknowledgements
This work is supported by an innovation grant from the Amsterdam UMC. We would also like to thank Idelette Nutma, patient representative and sepsis survivor, for contributing to this work.
Authors' contributions
MS and WJW conceived the study. MS, PWBN, and WJW analysed and interpreted the literature. MS drafted the work. PWBN and WJW substantially revised the work. MS, PWBN, and WJW all read and approved the final version of the manuscript and agree to be accountable for the integrity of the work. All authors read and approved the final manuscript.
Publication costs were funded by the 2019 Amsterdam UMC Innovation Grant: “Het Sepsis Team: Betere Overleving Door Snelle Behandeling” (Project No: 23297).
Availability of data and material
Declarations.
PWBN and WJW declare that they have received an innovation grant from the Amsterdam UMC to study the effects of a sepsis improvement program. MS’s Ph.D. studies are funded by this grant.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Case-based learning: recognising sepsis
Sepsis can lead to organ failure and death. However, early diagnosis and recognition may help prevent these potentially fatal consequences.

JL / Science Photo Library / Shutterstock.com
Several personal stories of sepsis survivors and deaths from sepsis have been published in the media, highlighting the importance of sepsis as a major cause of preventable deaths in the UK. This article will provide an overview of sepsis with particular focus on the role of pharmacy professionals in recognition and referral.
Pathophysiology
Sepsis is characterised by a systemic inflammatory response to an invasive infection that has become unregulated [1] . White blood cells and pro-inflammatory cytokines are released causing widespread vasodilation and an increase in capillary permeability, resulting in the loss of fluid from circulation. This results in hypovolaemia and a fall in systemic vascular resistance, which in turn leads to a fall in blood pressure and a decrease in organ perfusion, culminating in tissue hypoxia and organ failure [1] .
There are around 250,000 cases of sepsis annually in the UK, 20% of which are fatal [1], [2] . The UK Sepsis Trust estimates that early diagnosis of sepsis and the application of evidence-based treatment could save 14,000 lives per year [2] . Therefore, the timely identification of sepsis can lead to rapid treatment and potential mortality reduction.
Initial recognition of sepsis relies on identifying symptoms, which presents challenges for healthcare professionals as the common symptoms are not specific to sepsis and could be caused by non-infective pathology (e.g. trauma, pancreatitis, burns ) [3] .
The inflammatory-response-induced hypovolaemia affects the brain and can cause confusion, slurred speech and loss of consciousness. Similarly, as the kidneys are affected, there is a reduction in glomerular filtration resulting in a drop in urine output and development of acute kidney injury [1] , [3] .
Gas exchange across the alveoli is compromised as fluid and proteins leak into the lungs, causing a drop in systemic oxygen saturation and a rise in carbon dioxide levels. The body attempts to compensate by increasing its respiratory rate, but the problem is ultimately compounded as the drop in organ perfusion affects the lungs, meaning that even if oxygen-rich air is present, there is little blood flow with which gas exchange can take place [1] , [3] .
Initially, the heart rate increases in an attempt to compensate for the drop in blood pressure. However, the reduction in circulating volume and the fall in systemic vascular resistance ultimately undermine this action. This is because a reduction in venous return prevents the ventricles from properly filling before they contract, reducing the cardiac output [1] .
The typical signs and symptoms of sepsis may vary across different age groups, be general or may not all be present. Examples of moderate- and high-risk symptoms include:
- Reduced urine output (e.g. dry nappies in babies and toddlers);
- Feeling cold with shivering or chills;
- Rapid breathing (increased resting breaths per minute);
- Rapid heart rate (increased resting heart rate per minute);
- Mottled (see Photoguide A) or ashen appearance;
- Cyanosis (blue tint) of skin, lips or tongue (see Photoguide B);
- Non-blanching rash (see Photoguide C) [1] , [4] , [5] .
Additional signs in babies and young children (aged under five years)
- Not responding normally to social cues (e.g. does not smile);
- Visibly unwell (e.g. floppy or overly passive);
- Wakes only with prolonged stimulation or, if roused, does not stay awake;
- Weak high-pitched or continuous cry;
- Parent or carer is concerned that the child is behaving differently from normal;
- Has a seizure or convulsion;
- Pallor of the skin, lips or tongue;
- Cold extremities, but head and torso may be hot to the touch;
- Change in temperature (e.g. red flag temperatures are over 38 o C in those aged under 3 months, 39 o C in those aged 3–6 months and less than 36 o C for any age) [1] , [4] , [5] .
Additional signs that can affect patients aged over five years
- Evidence of new-onset confusion (history may be from a parent, carer, relative or friend);
- Slurred speech;
- Signs of potential infection (e.g. redness, swelling or discharge at surgical site, breakdown of the wound);
- Tympanic temperature less than 36 o C;
- New onset arrhythmia [1] , [4] , [5] .
If sepsis is suspected, the patient should be immediately referred for emergency medical assessment.
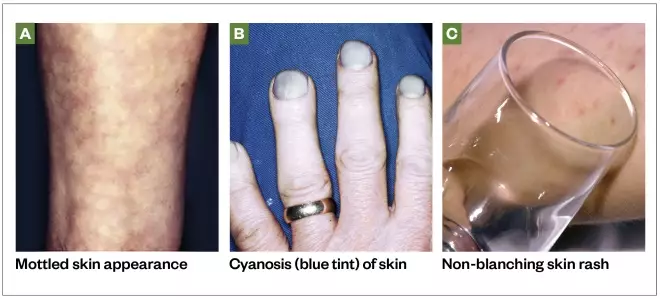
Photoguide: symptoms of sepsis
Source: Science Photo Library / Shutterstock.com
At-risk groups
Sepsis can affect anyone, but there are some patient groups that should be considered to be more susceptible to the development of sepsis, including:
- Very young children (aged under 1 year);
- Frail or older people (aged over 75 years);
- Immunocompromised people (e.g. those being treated for cancer with or without chemotherapy, post-splenectomy, taking long-term steroids or other immunosuppressant drugs);
- People who have had surgery or other invasive procedures in the past six weeks;
- People with any breach of skin integrity (e.g. cuts, burns, blisters or skin infections);
- People who misuse drugs intravenously;
- People with indwelling lines or catheters;
- Pregnant women;
- Women who have given birth or who have had a termination of pregnancy or miscarriage in the past six weeks [4] .
Understanding the patient risk factors may help improve timely diagnosis of suspected sepsis.
Sepsis can occur in response to a wide range of infections, but is most commonly associated with bacterial infection of the lungs, urinary tract, abdomen, central nervous system, or skin and soft tissues [1] . It is primarily diagnosed by a clinical assessment. Any number or combination of signs and symptoms may be present on diagnosis.
The National Institute of Health and Care Excellence (NICE) and the UK Sepsis Trust have published risk stratification tools to facilitate appropriate recognition of sepsis and the level of risk to the patient. Most NHS organisations use these tools or a locally approved variation of them [1] , [4] . These tools cater to a wide range of patients of different ages and the recommended action differs depending on whether patients’ symptoms are recognised in the primary or secondary care setting.
Patients who meet the high-risk criteria (see Box for the criteria for children aged under five years) should be sent urgently for emergency care (at a setting with resuscitation facilities). These patients should receive intravenous antibiotics with an appropriate level of cover within one hour of recognition of sepsis, along with other treatments and investigations [1] , [4] .
Box: high-risk criteria for children aged under five years outside of the hospital setting
- No response to social cues;
- Appears ill to a healthcare professional;
- Does not wake, or if roused, does not stay awake;
- Weak high-pitched or continuous cry.
- Aged under one year: 160 beats per minute or more;
- Aged one to two years: 150 beats per minute or more;
- Aged three to four years: 140 beats per minute or more;
- Heart rate less than 60 beats per minute at any age.
Respiratory rate
- Aged under one year: 60 breaths per minute or more;
- Aged one to two years: 50 breaths per minute or more;
- Aged three to four years: 40 breaths per minute or more;
- Oxygen saturation of less than 90% in air or increased oxygen requirement over baseline.
Temperature
- Aged under three months: 38°C or more;
- Any age: less than 36°C.
To see examples of mottled skin or ashen appearance, non-blanching rash of the skin, and cyanosis of the skin, lips or tongue, see the Photoguide.
Source: National Institute for Health and Care Excellence [8]
Initial blood tests should be requested to aid diagnosis and further inform on the likelihood of infection and prognosis. These should include:
- C-reactive protein — to detect inflammatory response;
- Full blood count — to detect immune response;
- Lactate — to detect tissue hypoxia.
Other investigations, such as a chest X-ray or lumbar puncture, may also be indicated depending on the likely focus of the suspected infection.
Point-of-care testing and future diagnostics
In the future, point-of-care testing facilities for key biomarkers may have a greater role in both primary care and hospital emergency departments, aiding healthcare professionals in diagnosing infection and sepsis. Recently published research into the use of sensor technologies designed to rapidly report on raised levels of biomarkers closely associated with sepsis (notably interleukin-6) may have the potential to aid sepsis diagnosis in the future [6] , [7] .
Case studies
Case study 1: a 12-month-old baby with suspected sepsis.
A mother brings her 12-month-old daughter Alice* into the pharmacy and asks to speak to the pharmacist. The mother clearly appears concerned and expresses that Alice seems very poorly and is not her usual self.
Consultation
The mother explains that her daughter attended nursery today and the nursery staff phoned in the afternoon to report that Alice was not feeling well. As she had a temperature of 39 o C, they administered a dose of paracetamol. The nursery staff also said that Alice had not been eating or drinking well and her nappies were dry all day.
Alice takes no regular medicine and has no ongoing health problems. She seems withdrawn and is not smiling or engaging with anyone, which the mother insists is unusual behaviour.
When assessing the patient, Alice’s hands feel cold despite her body and head feeling hot. During the interaction with Alice, she is noticeably very passive and inactive, and seems floppy in her mother’s arms. Alice does not appear to have a rash, though her skin appears pale.
Alice’s breathing appears very rapid.
Information given in the consultation suggests that Alice may have sepsis. Use the National Institute for Health and Care Excellence ‘Sepsis risk stratification tool’ for children aged under five years out of hospital and compare it to the information obtained during the consultation [8] . By doing so, it is apparent that the following moderate-to-high risk criteria were demonstrated by the patient:
- Behaviour: parent or carer concern that the child is behaving differently than usual; not responding normally to social cues; no smile; and decreased activity;
- Cold hands or feet;
- Reduced urine output;
- Between 40 and 49 breaths per minute (normal resting respiratory rate for a 12-month-old is typically 20–40 breaths per minute);
- Pallor of skin, lips or tongue.
Although her temperature was high (39 o C), this would only be a moderate-risk criterion if Alice was aged between 3–6 months of age outside the hospital setting.
Advice and recommendations
Alice’s symptoms clearly indicate moderate-to-high risk of sepsis. According to the risk stratification tool, Alice should be referred either for a definitive diagnosis for treatment outside the hospital (i.e. to the patient’s GP), or to hospital for further review.
Considering the risk of sepsis and the importance of timely management, referral to hospital is the best choice for this patient. Calmly and clearly explain to the mother that Alice may have a serious infection and that the best course is for her to go to the hospital immediately.
Case study 2: an 11-year-old child with a viral infection
An 11-year-old boy called Liam* is brought into the pharmacy by his parents. They explain that he has not been feeling well for the past few days. The parents want to know if Liam’s symptoms can be treated with an over-the-counter (OTC) product or whether they should take him to the GP.
Liam has been unwell for the past three or four days and his condition does not seem to be improving. He has not yet taken any medicine for this illness. His temperature was 37.8 o C when most recently checked using an ear thermometer at home.
Liam says that he has a sore throat, a cough and a blocked nose. Liam describes the severity of his throat pain as three out of ten. Liam has been eating and drinking normally, has no long-term medical conditions and takes no regular medicine.
Liam and his parents agree that his behaviour and function are normal and he appears alert and coherent through the consultation. Liam’s breathing rate does not appear to be raised and his skin and lips appear normal, with no signs of a rash.
Liam may have an infection, which is likely to be viral, but does not require medical attention at present. However, to rule out sepsis, use the National Institute for Health and Care Excellence ‘Sepsis risk stratification tool’ for children aged 5–11 years out of hospital and compare this to the information obtained during the consultation [8] . By doing so, it is apparent that no moderate-to-high risk criteria were demonstrated by the patient.
Liam can be treated with OTC analgesics to alleviate his throat pain and his raised temperature. Liam’s parents should ensure he is taking plenty of fluids and continue to monitor his temperature. If they become concerned about his condition, his behaviour or general functional ability, they should return to or call the pharmacy. Particular symptoms you advise them to look out for include development of a rash, if his skin becomes pale or mottled, his urine output drops, his breathing rate increases, or any general concern that mental state or activity is not normal.
Case study 3: an adult with red flag sepsis
Rahul*, a 28-year-old man, comes into the pharmacy and asks to see the pharmacist as he has begun to feel very unwell.
Rahul works as a driver, and he fell and scraped his leg while getting out of his van the previous day. Rahul explains that at the time he did not think much about the cut, so he did not clean or dress the wound and has not yet taken any medicine for it. Although the wound began to swell and weep overnight, Rahul went into work this morning, but left when he suddenly started to feel seriously unwell — around an hour ago.
Rahul says the wound now looks much worse than it previously did. On examination you find the wound is very red and swollen, the tissue around the wound is blistering and weeping, and there are red track marks extending further up Rahul’s leg. It is clear that this wound is infected.
Rahul uses inhalers for mild asthma, but otherwise takes no regular medicine.
Rahul says he is feeling hot and sluggish, and is clearly struggling to maintain his train of thought. His condition appears to be worsening by the minute. He needs to be referred for further help, but more information is required to decide whether he is referred to his GP or to a hospital emergency department.
Rahul’s temperature is 35.8 o C. His breathing appears to be rapid. His blood pressure is 92/58mmHg and his heart rate is 140 beats per minute. Rahul does not appear to have a skin rash, although his lips seem to have a blue tint.
Rahul is likely to have a serious infection, which requires urgent attention. Use the National Institute for Health and Care Excellence ‘Sepsis risk stratification tool’ for people aged 18 years and over outside of the hospital setting and compare this to the information obtained during the consultation [8] . The patient has moderate- to high-risk criteria, such as tympanic temperature less than 36 o C and signs of potential infection. He also has several high-risk criteria that require urgent referral to emergency care:
- Altered behaviour or mental state;
- Respiratory rate over 25 breaths per minute;
- Heart rate more than 130 beats per minute;
- Cyanosis of skin, lips or tongue.
Tell Rahul that it is likely that he has a serious infection, and ask him to sit and wait in the pharmacy while an ambulance is called. It is not safe for him to drive to hospital. Share his information with the 999 operator and make another note of the details gathered during the consultation to hand over to the ambulance team upon arrival.
*All cases are fictional
Useful additional resources
- The UK Sepsis Trust. The Sepsis Manual. 2017–2018: Available at: https://sepsistrust.org/wp-content/uploads/2018/06/Sepsis_Manual_2017_web_download.pdf
- National Institute for Health and Care Excellence. Sepsis: risk stratification tools. Available at: https://www.nice.org.uk/guidance/ng51/resources/algorithms-and-risk-stratification-tables-compiled-version-2551488301
- For patients who are interested in finding out more about sepsis you can direct them to the NHS website. Available at: https://www.nhs.uk/conditions/sepsis/
[1] The UK Sepsis Trust. The Sepsis Manual. 2017–2018. 2017. Available at: https://sepsistrust.org/wp-content/uploads/2018/06/Sepsis_Manual_2017_web_download.pdf (accessed October 2019)
[2] The UK Sepsis Trust. Professional Resources. Available at: https://sepsistrust.org/professional-resources/ (accessed October 2019)
[3] Gotts JE & Matthay MA. Sepsis: pathophysiology and clinical management. BMJ 2016;353:i1585. doi: 10.1136/bmj.i1585
[4] National Institute for Health and Care Excellence. Sepsis: recognition, diagnosis and early management. NICE guideline [NG51]. 2016. Available at: https://www.nice.org.uk/Guidance/NG51 (accessed October 2019)
[5] National Health Service: Overview — Sepsis. 2019. Available at: https://www.nhs.uk/conditions/sepsis/ (accessed October 2019)
[6] Russell C, Ward AC, Vezza V et al . Development of a needle shaped microelectrode for electrochemical detection of the sepsis biomarker interleukin-6 (IL-6) in real time. Biosens Bioelectron 2019;126:806–814. doi: 10.1016/j.bios.2018.11.053
[7] Dolin H, Papadimos T, Stepkowski S et al. A novel combination of biomarkers to herald the onset of sepsis prior to the manifestation of symptoms. Shock 2018;49(4):364–370. doi: 10.1097/SHK.0000000000001010
[8] National Institute for Health and Care Excellence. Sepsis: Risk stratification tools. 2017. Available at: https://www.nice.org.uk/guidance/ng51/resources/algorithms-and-risk-stratification-tables-compiled-version-2551488301 (accessed October 2019)
You might also be interested in…

How the London Ambulance Service is working to transform medicines management

All emergency departments must have dedicated pharmacist, royal college and UKCPA say

Hyponatraemia: clinical presentation, diagnosis and treatment

IMAGES
VIDEO
COMMENTS
The patient arrives to the emergency room within 15 minutes and is admitted for treatment at 1000. On the unit, Code Sepsis is called, and the agency's sepsis protocol based on the Surviving Sepsis campaign is implemented. The patient's vitals are now a temperature of 102F, heart rate of 140, respiratory rate of 34, and blood pressure of 96/42.
This septic shock case study is designed to help the nursing student better understand nursing care for a patient with sepsis. Mr. McMillan, a 92-year old male, presents to the Emergency Department (ED) with urinary hesitancy and burning and a fever at home of 101.6°F. His caregiver states "he just doesn't seem like himself".
A study by Seymour et al. (2017) showed that the more rapid administration of the bundle of care is correlated with a decreased mortality rate. In addition, The Survival of Sepsis Campaign formed a guideline to sepsis treatment; Rhodes et al. (2016) suggests giving a 30 mL/kg of IV crystalloid fluid for hypoperfusion.
Sepsis is a systemic response to infection. It is manifested by two or more of the SIRS (Systemic Inflammatory Response Syndrome) criteria as a consequence of documented or presumed infection. Septic shock is associated with sepsis. It is characterized by symptoms of sepsis plus hypotension and hypoperfusion despite adequate fluid volume ...
This case study explores the importance of adequate assessment of patients on their initial presentation to the emergency department, during hospitalization, and before discharge. The clinical evaluation, recognition, and management of sepsis continue to be essential for patient survival to prevent and decrease the mortality rate.
Sepsis syndromes span a clinical continuum with variable prognoses. Septic shock, the most severe complication of sepsis, carries a high mortality. In response to an inciting agent, pro-inflammatory and anti-inflammatory arms of the immune system are activated in concert with the activation of monocytes, macrophages, and neutrophils that interact with the endothelium through pathogen ...
The study found that incorporating sepsis-related case scenarios in ongoing educational and professional training programs improved nurses' self-efficacy and led to a prompt and accurate assessment of sepsis . One of the interventions explored in this review was a simulation that facilitated decision-making related to sepsis management.
Abstract. Caring for a patient with suspected sepsis is a challenging nursing role. Early recognition and appropriate management of a patient with sepsis saves lives. Nurses play a fundamental role in detecting changes in physiological observations that could indicate the onset of sepsis. Additionally, an awareness of the pathophysiology of ...
Sepsis is a life-threatening and debilitating sickness in the elderly. This case study explores the importance of adequate assessment of patients on their initial presentation to the emergency department, during hospitalization, and before discharge. The clinical evaluation, recognition, and management of sepsis continue to be essential for ...
Description: Delve into sepsis case studies that illustrate common assessments and tools used to care for sepsis. This presentation details case studies that cover three different healthcare areas, as well as the team members involved in the assessment, diagnosis, and treatment of patients with sepsis. These cases highlight the need for all ...
The sepsis patient mortality rate decreased from as high as 1.91 in Q1 2017 to as low as 0.45 in 2019. Cases meeting the bundle compliance increased from as low as 52% in Jan 2018 to as high as 88% in August 2019. LOS also decreased from a high of 6.83 days on average in January of 2017 to as low as 3.88 days on average in August of 2019.
Core case: Change in condition - recognition early sepsis . Brief Summary of Case: 78-year-old widower with a 2-year history of Alzheimer's disease, HTN, Type 2 DM. ... Nursing role in early sepsis screening ... 4. Laboratory, Diagnostic Study Results Na: 142 K: 4.2 Cl: 101 HCO3: 20 BUN: 22 Cr: 0.9
This case study explores the importance of adequate assessment of patients on their initial presentation to the emergency department, during hospitalization, and before discharge. The clinical evaluation, recognition, and management of sepsis continue to be essential for patient survival to prevent and decrease the mortality rate.
This page titled 7: Case Study #6- Sepsis is shared under a CC BY-SA 4.0 license and was authored, remixed, and/or curated by Glynda Rees, Rob Kruger, and Janet Morrison via source content that was edited to the style and standards of the LibreTexts platform; a detailed edit history is available upon request.
The selected respondents were 618 undergraduate nursing students. All three years of study, and full-time and part-time (students employed in the healthcare system) students, were included. ... Clinical exercises provide students with the opportunity to directly interact with patient situational factors, in this case, sepsis, ...
Nurses play a fundamental role in detecting changes in physiological observations that could indicate the onset of sepsis. Additionally, an awareness of the pathophysiology of sepsis allows the nurse to better understand how rapid intervention prevents the onset of septic shock. Furthermore, knowledge and use of clinical guidelines and sepsis ...
This case study learning activity reviews the definition, pathophysiology, and management of sepsis and sepsis-related syndromes using the case study of a 54-year-old man. It emphasizes the early recognition of sepsis using physical assessment, hemodynamic parameters, and laboratory findings. ... list priority nursing interventions for the ...
The patient, Mrs. June Peters (84), was found by her daughter, Mary Jones, in her apartment in a a state of acute confusion. She was admitted to the ED with nausea, vomiting, acute confusion, shivering, severe right flank pain 8/10, pale and mottled skin, tachypnea, tachycardia, and elevated temperature. Her vital signs were: Temp 102, HR 112 ...
The reviewers identified 50 observational studies with highly diverse improvement programs and study designs. Despite this heterogeneity, the meta-analysis showed that sepsis performance improvement programs were consistently associated with increased compliance with 6-h (OR 4.12, 95% CI 2.95-5.76) and 24-h (OR 2.57, 95%-CI 1.74-3.77 ...
Keith RN Case Study shock case study leesa green shock unfolding reasoning case study student jack holmes, 72 years old primary concept perfusion interrelated ... Sepsis Case Study #3. Keith RN Case Study. Course. Professional Nursing Concepts IV (4-11-8) (HSNS 2218) ... What nursing priority (ies) will guide your plan of care? (Management of Care)
Case study 1: a 12-month-old baby with suspected sepsis. A mother brings her 12-month-old daughter Alice* into the pharmacy and asks to speak to the pharmacist. The mother clearly appears concerned and expresses that Alice seems very poorly and is not her usual self. Consultation.
case study about sepsis Jack Holmes a 72-year-old Caucasian male brought to the ED by ambulance from a skilled nursing facility (SNF). According to report from
The article depicts a case study of a 21-month-old male child presenting with these signs and symptoms that ultimately resulted in a diagnosis of septic shock. The importance of physical assessment, rapid response to findings with time-constrained empirical interventions, the relevance of pediatric sepsis to the provider, the consideration of ...