
Get science-backed answers as you write with Paperpal's Research feature

How to Write a Conclusion for Research Papers (with Examples)
The conclusion of a research paper is a crucial section that plays a significant role in the overall impact and effectiveness of your research paper. However, this is also the section that typically receives less attention compared to the introduction and the body of the paper. The conclusion serves to provide a concise summary of the key findings, their significance, their implications, and a sense of closure to the study. Discussing how can the findings be applied in real-world scenarios or inform policy, practice, or decision-making is especially valuable to practitioners and policymakers. The research paper conclusion also provides researchers with clear insights and valuable information for their own work, which they can then build on and contribute to the advancement of knowledge in the field.
The research paper conclusion should explain the significance of your findings within the broader context of your field. It restates how your results contribute to the existing body of knowledge and whether they confirm or challenge existing theories or hypotheses. Also, by identifying unanswered questions or areas requiring further investigation, your awareness of the broader research landscape can be demonstrated.
Remember to tailor the research paper conclusion to the specific needs and interests of your intended audience, which may include researchers, practitioners, policymakers, or a combination of these.
Table of Contents
What is a conclusion in a research paper, summarizing conclusion, editorial conclusion, externalizing conclusion, importance of a good research paper conclusion, how to write a conclusion for your research paper, research paper conclusion examples.
- How to write a research paper conclusion with Paperpal?
Frequently Asked Questions
A conclusion in a research paper is the final section where you summarize and wrap up your research, presenting the key findings and insights derived from your study. The research paper conclusion is not the place to introduce new information or data that was not discussed in the main body of the paper. When working on how to conclude a research paper, remember to stick to summarizing and interpreting existing content. The research paper conclusion serves the following purposes: 1
- Warn readers of the possible consequences of not attending to the problem.
- Recommend specific course(s) of action.
- Restate key ideas to drive home the ultimate point of your research paper.
- Provide a “take-home” message that you want the readers to remember about your study.

Types of conclusions for research papers
In research papers, the conclusion provides closure to the reader. The type of research paper conclusion you choose depends on the nature of your study, your goals, and your target audience. I provide you with three common types of conclusions:
A summarizing conclusion is the most common type of conclusion in research papers. It involves summarizing the main points, reiterating the research question, and restating the significance of the findings. This common type of research paper conclusion is used across different disciplines.
An editorial conclusion is less common but can be used in research papers that are focused on proposing or advocating for a particular viewpoint or policy. It involves presenting a strong editorial or opinion based on the research findings and offering recommendations or calls to action.
An externalizing conclusion is a type of conclusion that extends the research beyond the scope of the paper by suggesting potential future research directions or discussing the broader implications of the findings. This type of conclusion is often used in more theoretical or exploratory research papers.
Align your conclusion’s tone with the rest of your research paper. Start Writing with Paperpal Now!
The conclusion in a research paper serves several important purposes:
- Offers Implications and Recommendations : Your research paper conclusion is an excellent place to discuss the broader implications of your research and suggest potential areas for further study. It’s also an opportunity to offer practical recommendations based on your findings.
- Provides Closure : A good research paper conclusion provides a sense of closure to your paper. It should leave the reader with a feeling that they have reached the end of a well-structured and thought-provoking research project.
- Leaves a Lasting Impression : Writing a well-crafted research paper conclusion leaves a lasting impression on your readers. It’s your final opportunity to leave them with a new idea, a call to action, or a memorable quote.

Writing a strong conclusion for your research paper is essential to leave a lasting impression on your readers. Here’s a step-by-step process to help you create and know what to put in the conclusion of a research paper: 2
- Research Statement : Begin your research paper conclusion by restating your research statement. This reminds the reader of the main point you’ve been trying to prove throughout your paper. Keep it concise and clear.
- Key Points : Summarize the main arguments and key points you’ve made in your paper. Avoid introducing new information in the research paper conclusion. Instead, provide a concise overview of what you’ve discussed in the body of your paper.
- Address the Research Questions : If your research paper is based on specific research questions or hypotheses, briefly address whether you’ve answered them or achieved your research goals. Discuss the significance of your findings in this context.
- Significance : Highlight the importance of your research and its relevance in the broader context. Explain why your findings matter and how they contribute to the existing knowledge in your field.
- Implications : Explore the practical or theoretical implications of your research. How might your findings impact future research, policy, or real-world applications? Consider the “so what?” question.
- Future Research : Offer suggestions for future research in your area. What questions or aspects remain unanswered or warrant further investigation? This shows that your work opens the door for future exploration.
- Closing Thought : Conclude your research paper conclusion with a thought-provoking or memorable statement. This can leave a lasting impression on your readers and wrap up your paper effectively. Avoid introducing new information or arguments here.
- Proofread and Revise : Carefully proofread your conclusion for grammar, spelling, and clarity. Ensure that your ideas flow smoothly and that your conclusion is coherent and well-structured.
Write your research paper conclusion 2x faster with Paperpal. Try it now!
Remember that a well-crafted research paper conclusion is a reflection of the strength of your research and your ability to communicate its significance effectively. It should leave a lasting impression on your readers and tie together all the threads of your paper. Now you know how to start the conclusion of a research paper and what elements to include to make it impactful, let’s look at a research paper conclusion sample.

How to write a research paper conclusion with Paperpal?
A research paper conclusion is not just a summary of your study, but a synthesis of the key findings that ties the research together and places it in a broader context. A research paper conclusion should be concise, typically around one paragraph in length. However, some complex topics may require a longer conclusion to ensure the reader is left with a clear understanding of the study’s significance. Paperpal, an AI writing assistant trusted by over 800,000 academics globally, can help you write a well-structured conclusion for your research paper.
- Sign Up or Log In: Create a new Paperpal account or login with your details.
- Navigate to Features : Once logged in, head over to the features’ side navigation pane. Click on Templates and you’ll find a suite of generative AI features to help you write better, faster.
- Generate an outline: Under Templates, select ‘Outlines’. Choose ‘Research article’ as your document type.
- Select your section: Since you’re focusing on the conclusion, select this section when prompted.
- Choose your field of study: Identifying your field of study allows Paperpal to provide more targeted suggestions, ensuring the relevance of your conclusion to your specific area of research.
- Provide a brief description of your study: Enter details about your research topic and findings. This information helps Paperpal generate a tailored outline that aligns with your paper’s content.
- Generate the conclusion outline: After entering all necessary details, click on ‘generate’. Paperpal will then create a structured outline for your conclusion, to help you start writing and build upon the outline.
- Write your conclusion: Use the generated outline to build your conclusion. The outline serves as a guide, ensuring you cover all critical aspects of a strong conclusion, from summarizing key findings to highlighting the research’s implications.
- Refine and enhance: Paperpal’s ‘Make Academic’ feature can be particularly useful in the final stages. Select any paragraph of your conclusion and use this feature to elevate the academic tone, ensuring your writing is aligned to the academic journal standards.
By following these steps, Paperpal not only simplifies the process of writing a research paper conclusion but also ensures it is impactful, concise, and aligned with academic standards. Sign up with Paperpal today and write your research paper conclusion 2x faster .
The research paper conclusion is a crucial part of your paper as it provides the final opportunity to leave a strong impression on your readers. In the research paper conclusion, summarize the main points of your research paper by restating your research statement, highlighting the most important findings, addressing the research questions or objectives, explaining the broader context of the study, discussing the significance of your findings, providing recommendations if applicable, and emphasizing the takeaway message. The main purpose of the conclusion is to remind the reader of the main point or argument of your paper and to provide a clear and concise summary of the key findings and their implications. All these elements should feature on your list of what to put in the conclusion of a research paper to create a strong final statement for your work.
A strong conclusion is a critical component of a research paper, as it provides an opportunity to wrap up your arguments, reiterate your main points, and leave a lasting impression on your readers. Here are the key elements of a strong research paper conclusion: 1. Conciseness : A research paper conclusion should be concise and to the point. It should not introduce new information or ideas that were not discussed in the body of the paper. 2. Summarization : The research paper conclusion should be comprehensive enough to give the reader a clear understanding of the research’s main contributions. 3 . Relevance : Ensure that the information included in the research paper conclusion is directly relevant to the research paper’s main topic and objectives; avoid unnecessary details. 4 . Connection to the Introduction : A well-structured research paper conclusion often revisits the key points made in the introduction and shows how the research has addressed the initial questions or objectives. 5. Emphasis : Highlight the significance and implications of your research. Why is your study important? What are the broader implications or applications of your findings? 6 . Call to Action : Include a call to action or a recommendation for future research or action based on your findings.
The length of a research paper conclusion can vary depending on several factors, including the overall length of the paper, the complexity of the research, and the specific journal requirements. While there is no strict rule for the length of a conclusion, but it’s generally advisable to keep it relatively short. A typical research paper conclusion might be around 5-10% of the paper’s total length. For example, if your paper is 10 pages long, the conclusion might be roughly half a page to one page in length.
In general, you do not need to include citations in the research paper conclusion. Citations are typically reserved for the body of the paper to support your arguments and provide evidence for your claims. However, there may be some exceptions to this rule: 1. If you are drawing a direct quote or paraphrasing a specific source in your research paper conclusion, you should include a citation to give proper credit to the original author. 2. If your conclusion refers to or discusses specific research, data, or sources that are crucial to the overall argument, citations can be included to reinforce your conclusion’s validity.
The conclusion of a research paper serves several important purposes: 1. Summarize the Key Points 2. Reinforce the Main Argument 3. Provide Closure 4. Offer Insights or Implications 5. Engage the Reader. 6. Reflect on Limitations
Remember that the primary purpose of the research paper conclusion is to leave a lasting impression on the reader, reinforcing the key points and providing closure to your research. It’s often the last part of the paper that the reader will see, so it should be strong and well-crafted.
- Makar, G., Foltz, C., Lendner, M., & Vaccaro, A. R. (2018). How to write effective discussion and conclusion sections. Clinical spine surgery, 31(8), 345-346.
- Bunton, D. (2005). The structure of PhD conclusion chapters. Journal of English for academic purposes , 4 (3), 207-224.
Paperpal is a comprehensive AI writing toolkit that helps students and researchers achieve 2x the writing in half the time. It leverages 21+ years of STM experience and insights from millions of research articles to provide in-depth academic writing, language editing, and submission readiness support to help you write better, faster.
Get accurate academic translations, rewriting support, grammar checks, vocabulary suggestions, and generative AI assistance that delivers human precision at machine speed. Try for free or upgrade to Paperpal Prime starting at US$19 a month to access premium features, including consistency, plagiarism, and 30+ submission readiness checks to help you succeed.
Experience the future of academic writing – Sign up to Paperpal and start writing for free!
Related Reads:
- 5 Reasons for Rejection After Peer Review
- Ethical Research Practices For Research with Human Subjects
7 Ways to Improve Your Academic Writing Process
- Paraphrasing in Academic Writing: Answering Top Author Queries
Preflight For Editorial Desk: The Perfect Hybrid (AI + Human) Assistance Against Compromised Manuscripts
You may also like, how to write a high-quality conference paper, academic editing: how to self-edit academic text with..., measuring academic success: definition & strategies for excellence, phd qualifying exam: tips for success , ai in education: it’s time to change the..., is it ethical to use ai-generated abstracts without..., what are journal guidelines on using generative ai..., quillbot review: features, pricing, and free alternatives, what is an academic paper types and elements , should you use ai tools like chatgpt for....
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- 9. The Conclusion
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
The conclusion is intended to help the reader understand why your research should matter to them after they have finished reading the paper. A conclusion is not merely a summary of the main topics covered or a re-statement of your research problem, but a synthesis of key points derived from the findings of your study and, if applicable, where you recommend new areas for future research. For most college-level research papers, two or three well-developed paragraphs is sufficient for a conclusion, although in some cases, more paragraphs may be required in describing the key findings and their significance.
Conclusions. The Writing Center. University of North Carolina; Conclusions. The Writing Lab and The OWL. Purdue University.
Importance of a Good Conclusion
A well-written conclusion provides you with important opportunities to demonstrate to the reader your understanding of the research problem. These include:
- Presenting the last word on the issues you raised in your paper . Just as the introduction gives a first impression to your reader, the conclusion offers a chance to leave a lasting impression. Do this, for example, by highlighting key findings in your analysis that advance new understanding about the research problem, that are unusual or unexpected, or that have important implications applied to practice.
- Summarizing your thoughts and conveying the larger significance of your study . The conclusion is an opportunity to succinctly re-emphasize your answer to the "So What?" question by placing the study within the context of how your research advances past research about the topic.
- Identifying how a gap in the literature has been addressed . The conclusion can be where you describe how a previously identified gap in the literature [first identified in your literature review section] has been addressed by your research and why this contribution is significant.
- Demonstrating the importance of your ideas . Don't be shy. The conclusion offers an opportunity to elaborate on the impact and significance of your findings. This is particularly important if your study approached examining the research problem from an unusual or innovative perspective.
- Introducing possible new or expanded ways of thinking about the research problem . This does not refer to introducing new information [which should be avoided], but to offer new insight and creative approaches for framing or contextualizing the research problem based on the results of your study.
Bunton, David. “The Structure of PhD Conclusion Chapters.” Journal of English for Academic Purposes 4 (July 2005): 207–224; Conclusions. The Writing Center. University of North Carolina; Kretchmer, Paul. Twelve Steps to Writing an Effective Conclusion. San Francisco Edit, 2003-2008; Conclusions. The Writing Lab and The OWL. Purdue University; Assan, Joseph. "Writing the Conclusion Chapter: The Good, the Bad and the Missing." Liverpool: Development Studies Association (2009): 1-8.
Structure and Writing Style
I. General Rules
The general function of your paper's conclusion is to restate the main argument . It reminds the reader of the strengths of your main argument(s) and reiterates the most important evidence supporting those argument(s). Do this by clearly summarizing the context, background, and necessity of pursuing the research problem you investigated in relation to an issue, controversy, or a gap found in the literature. However, make sure that your conclusion is not simply a repetitive summary of the findings. This reduces the impact of the argument(s) you have developed in your paper.
When writing the conclusion to your paper, follow these general rules:
- Present your conclusions in clear, concise language. Re-state the purpose of your study, then describe how your findings differ or support those of other studies and why [i.e., what were the unique, new, or crucial contributions your study made to the overall research about your topic?].
- Do not simply reiterate your findings or the discussion of your results. Provide a synthesis of arguments presented in the paper to show how these converge to address the research problem and the overall objectives of your study.
- Indicate opportunities for future research if you haven't already done so in the discussion section of your paper. Highlighting the need for further research provides the reader with evidence that you have an in-depth awareness of the research problem but that further investigations should take place beyond the scope of your investigation.
Consider the following points to help ensure your conclusion is presented well:
- If the argument or purpose of your paper is complex, you may need to summarize the argument for your reader.
- If, prior to your conclusion, you have not yet explained the significance of your findings or if you are proceeding inductively, use the end of your paper to describe your main points and explain their significance.
- Move from a detailed to a general level of consideration that returns the topic to the context provided by the introduction or within a new context that emerges from the data [this is opposite of the introduction, which begins with general discussion of the context and ends with a detailed description of the research problem].
The conclusion also provides a place for you to persuasively and succinctly restate the research problem, given that the reader has now been presented with all the information about the topic . Depending on the discipline you are writing in, the concluding paragraph may contain your reflections on the evidence presented. However, the nature of being introspective about the research you have conducted will depend on the topic and whether your professor wants you to express your observations in this way. If asked to think introspectively about the topics, do not delve into idle speculation. Being introspective means looking within yourself as an author to try and understand an issue more deeply, not to guess at possible outcomes or make up scenarios not supported by the evidence.
II. Developing a Compelling Conclusion
Although an effective conclusion needs to be clear and succinct, it does not need to be written passively or lack a compelling narrative. Strategies to help you move beyond merely summarizing the key points of your research paper may include any of the following:
- If your essay deals with a critical, contemporary problem, warn readers of the possible consequences of not attending to the problem proactively.
- Recommend a specific course or courses of action that, if adopted, could address a specific problem in practice or in the development of new knowledge leading to positive change.
- Cite a relevant quotation or expert opinion already noted in your paper in order to lend authority and support to the conclusion(s) you have reached [a good source would be from your literature review].
- Explain the consequences of your research in a way that elicits action or demonstrates urgency in seeking change.
- Restate a key statistic, fact, or visual image to emphasize the most important finding of your paper.
- If your discipline encourages personal reflection, illustrate your concluding point by drawing from your own life experiences.
- Return to an anecdote, an example, or a quotation that you presented in your introduction, but add further insight derived from the findings of your study; use your interpretation of results from your study to recast it in new or important ways.
- Provide a "take-home" message in the form of a succinct, declarative statement that you want the reader to remember about your study.
III. Problems to Avoid
Failure to be concise Your conclusion section should be concise and to the point. Conclusions that are too lengthy often have unnecessary information in them. The conclusion is not the place for details about your methodology or results. Although you should give a summary of what was learned from your research, this summary should be relatively brief, since the emphasis in the conclusion is on the implications, evaluations, insights, and other forms of analysis that you make. Strategies for writing concisely can be found here .
Failure to comment on larger, more significant issues In the introduction, your task was to move from the general [the field of study] to the specific [the research problem]. However, in the conclusion, your task is to move from a specific discussion [your research problem] back to a general discussion framed around the implications and significance of your findings [i.e., how your research contributes new understanding or fills an important gap in the literature]. In short, the conclusion is where you should place your research within a larger context [visualize your paper as an hourglass--start with a broad introduction and review of the literature, move to the specific analysis and discussion, conclude with a broad summary of the study's implications and significance].
Failure to reveal problems and negative results Negative aspects of the research process should never be ignored. These are problems, deficiencies, or challenges encountered during your study. They should be summarized as a way of qualifying your overall conclusions. If you encountered negative or unintended results [i.e., findings that are validated outside the research context in which they were generated], you must report them in the results section and discuss their implications in the discussion section of your paper. In the conclusion, use negative results as an opportunity to explain their possible significance and/or how they may form the basis for future research.
Failure to provide a clear summary of what was learned In order to be able to discuss how your research fits within your field of study [and possibly the world at large], you need to summarize briefly and succinctly how it contributes to new knowledge or a new understanding about the research problem. This element of your conclusion may be only a few sentences long.
Failure to match the objectives of your research Often research objectives in the social and behavioral sciences change while the research is being carried out. This is not a problem unless you forget to go back and refine the original objectives in your introduction. As these changes emerge they must be documented so that they accurately reflect what you were trying to accomplish in your research [not what you thought you might accomplish when you began].
Resist the urge to apologize If you've immersed yourself in studying the research problem, you presumably should know a good deal about it [perhaps even more than your professor!]. Nevertheless, by the time you have finished writing, you may be having some doubts about what you have produced. Repress those doubts! Don't undermine your authority as a researcher by saying something like, "This is just one approach to examining this problem; there may be other, much better approaches that...." The overall tone of your conclusion should convey confidence to the reader about the study's validity and realiability.
Assan, Joseph. "Writing the Conclusion Chapter: The Good, the Bad and the Missing." Liverpool: Development Studies Association (2009): 1-8; Concluding Paragraphs. College Writing Center at Meramec. St. Louis Community College; Conclusions. The Writing Center. University of North Carolina; Conclusions. The Writing Lab and The OWL. Purdue University; Freedman, Leora and Jerry Plotnick. Introductions and Conclusions. The Lab Report. University College Writing Centre. University of Toronto; Leibensperger, Summer. Draft Your Conclusion. Academic Center, the University of Houston-Victoria, 2003; Make Your Last Words Count. The Writer’s Handbook. Writing Center. University of Wisconsin Madison; Miquel, Fuster-Marquez and Carmen Gregori-Signes. “Chapter Six: ‘Last but Not Least:’ Writing the Conclusion of Your Paper.” In Writing an Applied Linguistics Thesis or Dissertation: A Guide to Presenting Empirical Research . John Bitchener, editor. (Basingstoke,UK: Palgrave Macmillan, 2010), pp. 93-105; Tips for Writing a Good Conclusion. Writing@CSU. Colorado State University; Kretchmer, Paul. Twelve Steps to Writing an Effective Conclusion. San Francisco Edit, 2003-2008; Writing Conclusions. Writing Tutorial Services, Center for Innovative Teaching and Learning. Indiana University; Writing: Considering Structure and Organization. Institute for Writing Rhetoric. Dartmouth College.
Writing Tip
Don't Belabor the Obvious!
Avoid phrases like "in conclusion...," "in summary...," or "in closing...." These phrases can be useful, even welcome, in oral presentations. But readers can see by the tell-tale section heading and number of pages remaining that they are reaching the end of your paper. You'll irritate your readers if you belabor the obvious.
Assan, Joseph. "Writing the Conclusion Chapter: The Good, the Bad and the Missing." Liverpool: Development Studies Association (2009): 1-8.
Another Writing Tip
New Insight, Not New Information!
Don't surprise the reader with new information in your conclusion that was never referenced anywhere else in the paper. This why the conclusion rarely has citations to sources. If you have new information to present, add it to the discussion or other appropriate section of the paper. Note that, although no new information is introduced, the conclusion, along with the discussion section, is where you offer your most "original" contributions in the paper; the conclusion is where you describe the value of your research, demonstrate that you understand the material that you’ve presented, and position your findings within the larger context of scholarship on the topic, including describing how your research contributes new insights to that scholarship.
Assan, Joseph. "Writing the Conclusion Chapter: The Good, the Bad and the Missing." Liverpool: Development Studies Association (2009): 1-8; Conclusions. The Writing Center. University of North Carolina.
- << Previous: Limitations of the Study
- Next: Appendices >>
- Last Updated: May 25, 2024 4:09 PM
- URL: https://libguides.usc.edu/writingguide
- Privacy Policy

Home » Research Paper Conclusion – Writing Guide and Examples
Research Paper Conclusion – Writing Guide and Examples
Table of Contents

Research Paper Conclusion
Definition:
A research paper conclusion is the final section of a research paper that summarizes the key findings, significance, and implications of the research. It is the writer’s opportunity to synthesize the information presented in the paper, draw conclusions, and make recommendations for future research or actions.
The conclusion should provide a clear and concise summary of the research paper, reiterating the research question or problem, the main results, and the significance of the findings. It should also discuss the limitations of the study and suggest areas for further research.
Parts of Research Paper Conclusion
The parts of a research paper conclusion typically include:
Restatement of the Thesis
The conclusion should begin by restating the thesis statement from the introduction in a different way. This helps to remind the reader of the main argument or purpose of the research.
Summary of Key Findings
The conclusion should summarize the main findings of the research, highlighting the most important results and conclusions. This section should be brief and to the point.
Implications and Significance
In this section, the researcher should explain the implications and significance of the research findings. This may include discussing the potential impact on the field or industry, highlighting new insights or knowledge gained, or pointing out areas for future research.
Limitations and Recommendations
It is important to acknowledge any limitations or weaknesses of the research and to make recommendations for how these could be addressed in future studies. This shows that the researcher is aware of the potential limitations of their work and is committed to improving the quality of research in their field.
Concluding Statement
The conclusion should end with a strong concluding statement that leaves a lasting impression on the reader. This could be a call to action, a recommendation for further research, or a final thought on the topic.
How to Write Research Paper Conclusion
Here are some steps you can follow to write an effective research paper conclusion:
- Restate the research problem or question: Begin by restating the research problem or question that you aimed to answer in your research. This will remind the reader of the purpose of your study.
- Summarize the main points: Summarize the key findings and results of your research. This can be done by highlighting the most important aspects of your research and the evidence that supports them.
- Discuss the implications: Discuss the implications of your findings for the research area and any potential applications of your research. You should also mention any limitations of your research that may affect the interpretation of your findings.
- Provide a conclusion : Provide a concise conclusion that summarizes the main points of your paper and emphasizes the significance of your research. This should be a strong and clear statement that leaves a lasting impression on the reader.
- Offer suggestions for future research: Lastly, offer suggestions for future research that could build on your findings and contribute to further advancements in the field.
Remember that the conclusion should be brief and to the point, while still effectively summarizing the key findings and implications of your research.
Example of Research Paper Conclusion
Here’s an example of a research paper conclusion:
Conclusion :
In conclusion, our study aimed to investigate the relationship between social media use and mental health among college students. Our findings suggest that there is a significant association between social media use and increased levels of anxiety and depression among college students. This highlights the need for increased awareness and education about the potential negative effects of social media use on mental health, particularly among college students.
Despite the limitations of our study, such as the small sample size and self-reported data, our findings have important implications for future research and practice. Future studies should aim to replicate our findings in larger, more diverse samples, and investigate the potential mechanisms underlying the association between social media use and mental health. In addition, interventions should be developed to promote healthy social media use among college students, such as mindfulness-based approaches and social media detox programs.
Overall, our study contributes to the growing body of research on the impact of social media on mental health, and highlights the importance of addressing this issue in the context of higher education. By raising awareness and promoting healthy social media use among college students, we can help to reduce the negative impact of social media on mental health and improve the well-being of young adults.
Purpose of Research Paper Conclusion
The purpose of a research paper conclusion is to provide a summary and synthesis of the key findings, significance, and implications of the research presented in the paper. The conclusion serves as the final opportunity for the writer to convey their message and leave a lasting impression on the reader.
The conclusion should restate the research problem or question, summarize the main results of the research, and explain their significance. It should also acknowledge the limitations of the study and suggest areas for future research or action.
Overall, the purpose of the conclusion is to provide a sense of closure to the research paper and to emphasize the importance of the research and its potential impact. It should leave the reader with a clear understanding of the main findings and why they matter. The conclusion serves as the writer’s opportunity to showcase their contribution to the field and to inspire further research and action.
When to Write Research Paper Conclusion
The conclusion of a research paper should be written after the body of the paper has been completed. It should not be written until the writer has thoroughly analyzed and interpreted their findings and has written a complete and cohesive discussion of the research.
Before writing the conclusion, the writer should review their research paper and consider the key points that they want to convey to the reader. They should also review the research question, hypotheses, and methodology to ensure that they have addressed all of the necessary components of the research.
Once the writer has a clear understanding of the main findings and their significance, they can begin writing the conclusion. The conclusion should be written in a clear and concise manner, and should reiterate the main points of the research while also providing insights and recommendations for future research or action.
Characteristics of Research Paper Conclusion
The characteristics of a research paper conclusion include:
- Clear and concise: The conclusion should be written in a clear and concise manner, summarizing the key findings and their significance.
- Comprehensive: The conclusion should address all of the main points of the research paper, including the research question or problem, the methodology, the main results, and their implications.
- Future-oriented : The conclusion should provide insights and recommendations for future research or action, based on the findings of the research.
- Impressive : The conclusion should leave a lasting impression on the reader, emphasizing the importance of the research and its potential impact.
- Objective : The conclusion should be based on the evidence presented in the research paper, and should avoid personal biases or opinions.
- Unique : The conclusion should be unique to the research paper and should not simply repeat information from the introduction or body of the paper.
Advantages of Research Paper Conclusion
The advantages of a research paper conclusion include:
- Summarizing the key findings : The conclusion provides a summary of the main findings of the research, making it easier for the reader to understand the key points of the study.
- Emphasizing the significance of the research: The conclusion emphasizes the importance of the research and its potential impact, making it more likely that readers will take the research seriously and consider its implications.
- Providing recommendations for future research or action : The conclusion suggests practical recommendations for future research or action, based on the findings of the study.
- Providing closure to the research paper : The conclusion provides a sense of closure to the research paper, tying together the different sections of the paper and leaving a lasting impression on the reader.
- Demonstrating the writer’s contribution to the field : The conclusion provides the writer with an opportunity to showcase their contribution to the field and to inspire further research and action.
Limitations of Research Paper Conclusion
While the conclusion of a research paper has many advantages, it also has some limitations that should be considered, including:
- I nability to address all aspects of the research: Due to the limited space available in the conclusion, it may not be possible to address all aspects of the research in detail.
- Subjectivity : While the conclusion should be objective, it may be influenced by the writer’s personal biases or opinions.
- Lack of new information: The conclusion should not introduce new information that has not been discussed in the body of the research paper.
- Lack of generalizability: The conclusions drawn from the research may not be applicable to other contexts or populations, limiting the generalizability of the study.
- Misinterpretation by the reader: The reader may misinterpret the conclusions drawn from the research, leading to a misunderstanding of the findings.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

How to Cite Research Paper – All Formats and...

Data Collection – Methods Types and Examples

Delimitations in Research – Types, Examples and...

Research Paper Format – Types, Examples and...

Research Process – Steps, Examples and Tips

Research Design – Types, Methods and Examples
When you choose to publish with PLOS, your research makes an impact. Make your work accessible to all, without restrictions, and accelerate scientific discovery with options like preprints and published peer review that make your work more Open.
- PLOS Biology
- PLOS Climate
- PLOS Complex Systems
- PLOS Computational Biology
- PLOS Digital Health
- PLOS Genetics
- PLOS Global Public Health
- PLOS Medicine
- PLOS Mental Health
- PLOS Neglected Tropical Diseases
- PLOS Pathogens
- PLOS Sustainability and Transformation
- PLOS Collections
- How to Write Discussions and Conclusions

The discussion section contains the results and outcomes of a study. An effective discussion informs readers what can be learned from your experiment and provides context for the results.
What makes an effective discussion?
When you’re ready to write your discussion, you’ve already introduced the purpose of your study and provided an in-depth description of the methodology. The discussion informs readers about the larger implications of your study based on the results. Highlighting these implications while not overstating the findings can be challenging, especially when you’re submitting to a journal that selects articles based on novelty or potential impact. Regardless of what journal you are submitting to, the discussion section always serves the same purpose: concluding what your study results actually mean.
A successful discussion section puts your findings in context. It should include:
- the results of your research,
- a discussion of related research, and
- a comparison between your results and initial hypothesis.
Tip: Not all journals share the same naming conventions.
You can apply the advice in this article to the conclusion, results or discussion sections of your manuscript.
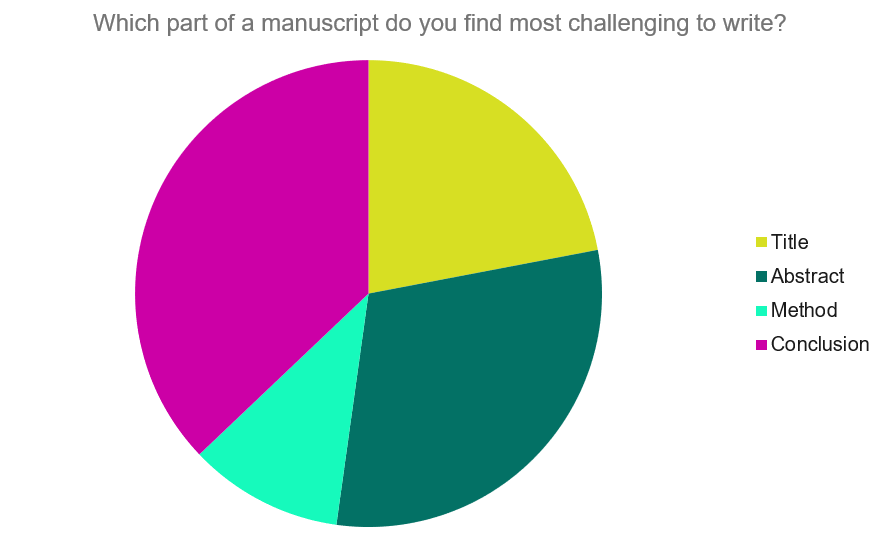
Our Early Career Researcher community tells us that the conclusion is often considered the most difficult aspect of a manuscript to write. To help, this guide provides questions to ask yourself, a basic structure to model your discussion off of and examples from published manuscripts.
Questions to ask yourself:
- Was my hypothesis correct?
- If my hypothesis is partially correct or entirely different, what can be learned from the results?
- How do the conclusions reshape or add onto the existing knowledge in the field? What does previous research say about the topic?
- Why are the results important or relevant to your audience? Do they add further evidence to a scientific consensus or disprove prior studies?
- How can future research build on these observations? What are the key experiments that must be done?
- What is the “take-home” message you want your reader to leave with?
How to structure a discussion
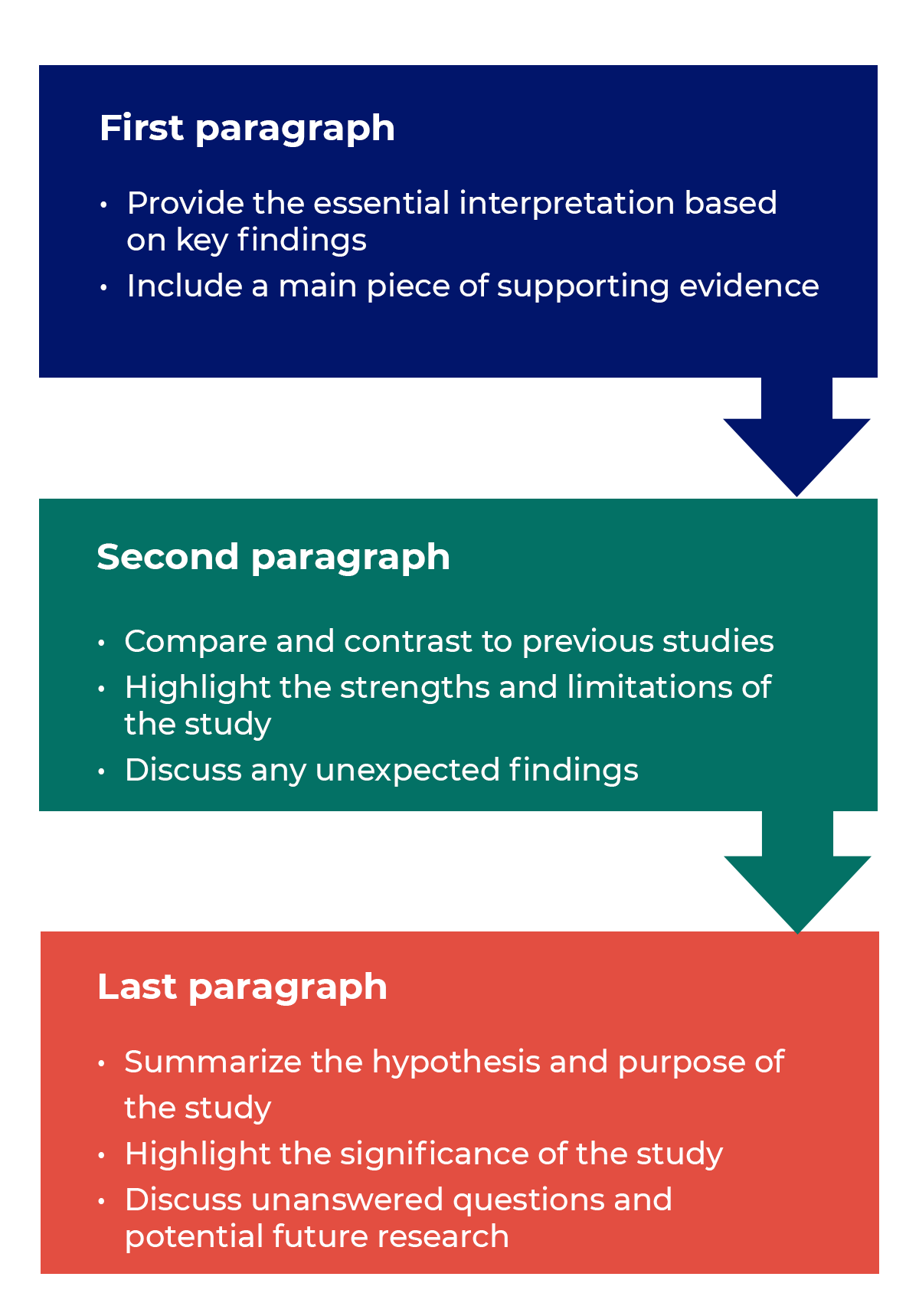
Trying to fit a complete discussion into a single paragraph can add unnecessary stress to the writing process. If possible, you’ll want to give yourself two or three paragraphs to give the reader a comprehensive understanding of your study as a whole. Here’s one way to structure an effective discussion:
Writing Tips
While the above sections can help you brainstorm and structure your discussion, there are many common mistakes that writers revert to when having difficulties with their paper. Writing a discussion can be a delicate balance between summarizing your results, providing proper context for your research and avoiding introducing new information. Remember that your paper should be both confident and honest about the results!

- Read the journal’s guidelines on the discussion and conclusion sections. If possible, learn about the guidelines before writing the discussion to ensure you’re writing to meet their expectations.
- Begin with a clear statement of the principal findings. This will reinforce the main take-away for the reader and set up the rest of the discussion.
- Explain why the outcomes of your study are important to the reader. Discuss the implications of your findings realistically based on previous literature, highlighting both the strengths and limitations of the research.
- State whether the results prove or disprove your hypothesis. If your hypothesis was disproved, what might be the reasons?
- Introduce new or expanded ways to think about the research question. Indicate what next steps can be taken to further pursue any unresolved questions.
- If dealing with a contemporary or ongoing problem, such as climate change, discuss possible consequences if the problem is avoided.
- Be concise. Adding unnecessary detail can distract from the main findings.

Don’t
- Rewrite your abstract. Statements with “we investigated” or “we studied” generally do not belong in the discussion.
- Include new arguments or evidence not previously discussed. Necessary information and evidence should be introduced in the main body of the paper.
- Apologize. Even if your research contains significant limitations, don’t undermine your authority by including statements that doubt your methodology or execution.
- Shy away from speaking on limitations or negative results. Including limitations and negative results will give readers a complete understanding of the presented research. Potential limitations include sources of potential bias, threats to internal or external validity, barriers to implementing an intervention and other issues inherent to the study design.
- Overstate the importance of your findings. Making grand statements about how a study will fully resolve large questions can lead readers to doubt the success of the research.
Snippets of Effective Discussions:
Consumer-based actions to reduce plastic pollution in rivers: A multi-criteria decision analysis approach
Identifying reliable indicators of fitness in polar bears
- How to Write a Great Title
- How to Write an Abstract
- How to Write Your Methods
- How to Report Statistics
- How to Edit Your Work
The contents of the Peer Review Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
The contents of the Writing Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
There’s a lot to consider when deciding where to submit your work. Learn how to choose a journal that will help your study reach its audience, while reflecting your values as a researcher…

Research Recommendations – Guiding policy-makers for evidence-based decision making
Research recommendations play a crucial role in guiding scholars and researchers toward fruitful avenues of exploration. In an era marked by rapid technological advancements and an ever-expanding knowledge base, refining the process of generating research recommendations becomes imperative.
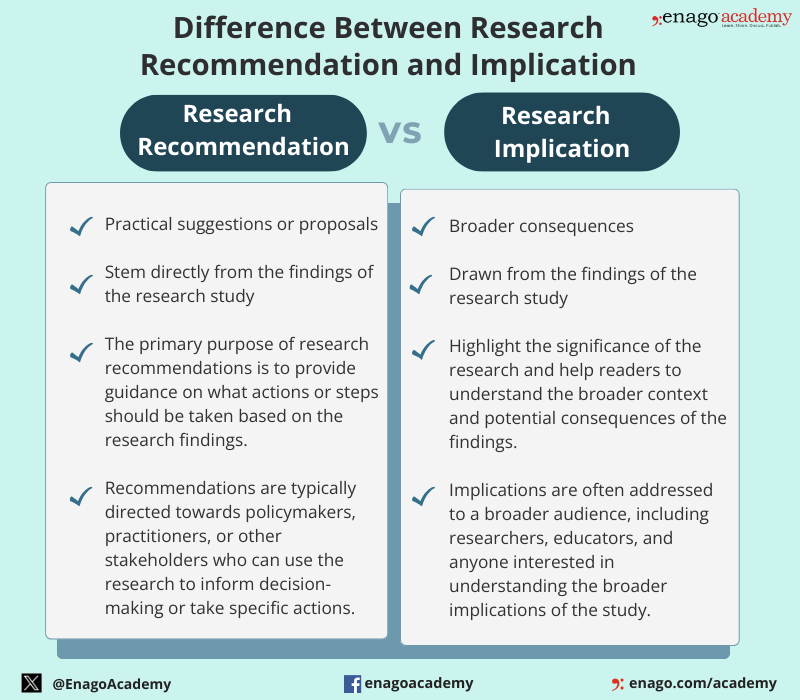
But, what is a research recommendation?
Research recommendations are suggestions or advice provided to researchers to guide their study on a specific topic . They are typically given by experts in the field. Research recommendations are more action-oriented and provide specific guidance for decision-makers, unlike implications that are broader and focus on the broader significance and consequences of the research findings. However, both are crucial components of a research study.
Difference Between Research Recommendations and Implication
Although research recommendations and implications are distinct components of a research study, they are closely related. The differences between them are as follows:
Types of Research Recommendations
Recommendations in research can take various forms, which are as follows:
These recommendations aim to assist researchers in navigating the vast landscape of academic knowledge.
Let us dive deeper to know about its key components and the steps to write an impactful research recommendation.
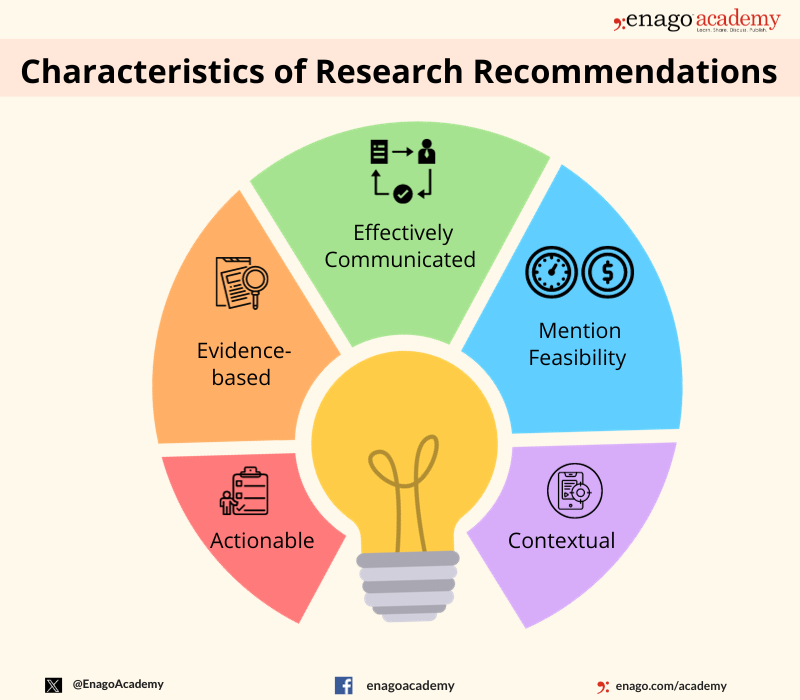
Key Components of Research Recommendations
The key components of research recommendations include defining the research question or objective, specifying research methods, outlining data collection and analysis processes, presenting results and conclusions, addressing limitations, and suggesting areas for future research. Here are some characteristics of research recommendations:
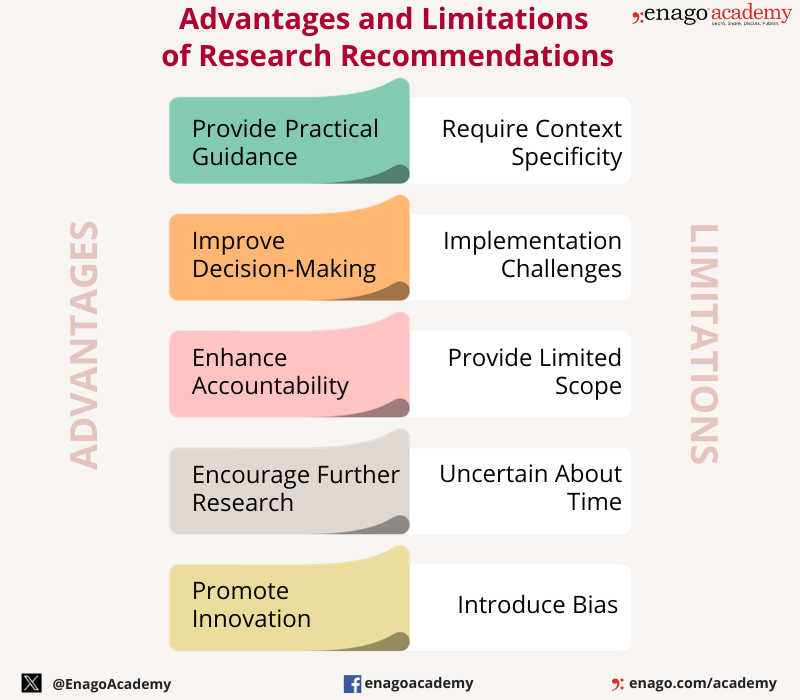
Research recommendations offer various advantages and play a crucial role in ensuring that research findings contribute to positive outcomes in various fields. However, they also have few limitations which highlights the significance of a well-crafted research recommendation in offering the promised advantages.
The importance of research recommendations ranges in various fields, influencing policy-making, program development, product development, marketing strategies, medical practice, and scientific research. Their purpose is to transfer knowledge from researchers to practitioners, policymakers, or stakeholders, facilitating informed decision-making and improving outcomes in different domains.
How to Write Research Recommendations?
Research recommendations can be generated through various means, including algorithmic approaches, expert opinions, or collaborative filtering techniques. Here is a step-wise guide to build your understanding on the development of research recommendations.
1. Understand the Research Question:
Understand the research question and objectives before writing recommendations. Also, ensure that your recommendations are relevant and directly address the goals of the study.
2. Review Existing Literature:
Familiarize yourself with relevant existing literature to help you identify gaps , and offer informed recommendations that contribute to the existing body of research.
3. Consider Research Methods:
Evaluate the appropriateness of different research methods in addressing the research question. Also, consider the nature of the data, the study design, and the specific objectives.
4. Identify Data Collection Techniques:
Gather dataset from diverse authentic sources. Include information such as keywords, abstracts, authors, publication dates, and citation metrics to provide a rich foundation for analysis.
5. Propose Data Analysis Methods:
Suggest appropriate data analysis methods based on the type of data collected. Consider whether statistical analysis, qualitative analysis, or a mixed-methods approach is most suitable.
6. Consider Limitations and Ethical Considerations:
Acknowledge any limitations and potential ethical considerations of the study. Furthermore, address these limitations or mitigate ethical concerns to ensure responsible research.
7. Justify Recommendations:
Explain how your recommendation contributes to addressing the research question or objective. Provide a strong rationale to help researchers understand the importance of following your suggestions.
8. Summarize Recommendations:
Provide a concise summary at the end of the report to emphasize how following these recommendations will contribute to the overall success of the research project.
By following these steps, you can create research recommendations that are actionable and contribute meaningfully to the success of the research project.
Download now to unlock some tips to improve your journey of writing research recommendations.
Example of a Research Recommendation
Here is an example of a research recommendation based on a hypothetical research to improve your understanding.
Research Recommendation: Enhancing Student Learning through Integrated Learning Platforms
Background:
The research study investigated the impact of an integrated learning platform on student learning outcomes in high school mathematics classes. The findings revealed a statistically significant improvement in student performance and engagement when compared to traditional teaching methods.
Recommendation:
In light of the research findings, it is recommended that educational institutions consider adopting and integrating the identified learning platform into their mathematics curriculum. The following specific recommendations are provided:
- Implementation of the Integrated Learning Platform:
Schools are encouraged to adopt the integrated learning platform in mathematics classrooms, ensuring proper training for teachers on its effective utilization.
- Professional Development for Educators:
Develop and implement professional programs to train educators in the effective use of the integrated learning platform to address any challenges teachers may face during the transition.
- Monitoring and Evaluation:
Establish a monitoring and evaluation system to track the impact of the integrated learning platform on student performance over time.
- Resource Allocation:
Allocate sufficient resources, both financial and technical, to support the widespread implementation of the integrated learning platform.
By implementing these recommendations, educational institutions can harness the potential of the integrated learning platform and enhance student learning experiences and academic achievements in mathematics.
This example covers the components of a research recommendation, providing specific actions based on the research findings, identifying the target audience, and outlining practical steps for implementation.
Using AI in Research Recommendation Writing
Enhancing research recommendations is an ongoing endeavor that requires the integration of cutting-edge technologies, collaborative efforts, and ethical considerations. By embracing data-driven approaches and leveraging advanced technologies, the research community can create more effective and personalized recommendation systems. However, it is accompanied by several limitations. Therefore, it is essential to approach the use of AI in research with a critical mindset, and complement its capabilities with human expertise and judgment.
Here are some limitations of integrating AI in writing research recommendation and some ways on how to counter them.
1. Data Bias
AI systems rely heavily on data for training. If the training data is biased or incomplete, the AI model may produce biased results or recommendations.
How to tackle: Audit regularly the model’s performance to identify any discrepancies and adjust the training data and algorithms accordingly.
2. Lack of Understanding of Context:
AI models may struggle to understand the nuanced context of a particular research problem. They may misinterpret information, leading to inaccurate recommendations.
How to tackle: Use AI to characterize research articles and topics. Employ them to extract features like keywords, authorship patterns and content-based details.
3. Ethical Considerations:
AI models might stereotype certain concepts or generate recommendations that could have negative consequences for certain individuals or groups.
How to tackle: Incorporate user feedback mechanisms to reduce redundancies. Establish an ethics review process for AI models in research recommendation writing.
4. Lack of Creativity and Intuition:
AI may struggle with tasks that require a deep understanding of the underlying principles or the ability to think outside the box.
How to tackle: Hybrid approaches can be employed by integrating AI in data analysis and identifying patterns for accelerating the data interpretation process.
5. Interpretability:
Many AI models, especially complex deep learning models, lack transparency on how the model arrived at a particular recommendation.
How to tackle: Implement models like decision trees or linear models. Provide clear explanation of the model architecture, training process, and decision-making criteria.
6. Dynamic Nature of Research:
Research fields are dynamic, and new information is constantly emerging. AI models may struggle to keep up with the rapidly changing landscape and may not be able to adapt to new developments.
How to tackle: Establish a feedback loop for continuous improvement. Regularly update the recommendation system based on user feedback and emerging research trends.
The integration of AI in research recommendation writing holds great promise for advancing knowledge and streamlining the research process. However, navigating these concerns is pivotal in ensuring the responsible deployment of these technologies. Researchers need to understand the use of responsible use of AI in research and must be aware of the ethical considerations.
Exploring research recommendations plays a critical role in shaping the trajectory of scientific inquiry. It serves as a compass, guiding researchers toward more robust methodologies, collaborative endeavors, and innovative approaches. Embracing these suggestions not only enhances the quality of individual studies but also contributes to the collective advancement of human understanding.
Frequently Asked Questions
The purpose of recommendations in research is to provide practical and actionable suggestions based on the study's findings, guiding future actions, policies, or interventions in a specific field or context. Recommendations bridges the gap between research outcomes and their real-world application.
To make a research recommendation, analyze your findings, identify key insights, and propose specific, evidence-based actions. Include the relevance of the recommendations to the study's objectives and provide practical steps for implementation.
Begin a recommendation by succinctly summarizing the key findings of the research. Clearly state the purpose of the recommendation and its intended impact. Use a direct and actionable language to convey the suggested course of action.
Rate this article Cancel Reply
Your email address will not be published.

Enago Academy's Most Popular Articles

- Reporting Research
Academic Essay Writing Made Simple: 4 types and tips
The pen is mightier than the sword, they say, and nowhere is this more evident…
![writing research conclusion and recommendation What is Academic Integrity and How to Uphold it [FREE CHECKLIST]](https://www.enago.com/academy/wp-content/uploads/2024/05/FeatureImages-59-210x136.png)
Ensuring Academic Integrity and Transparency in Academic Research: A comprehensive checklist for researchers
Academic integrity is the foundation upon which the credibility and value of scientific findings are…

- Industry News
- Publishing News
Unified AI Guidelines Crucial as Academic Writing Embraces Generative Tools
As generative artificial intelligence (AI) tools like ChatGPT are advancing at an accelerating pace, their…

How to Effectively Cite a PDF (APA, MLA, AMA, and Chicago Style)
The pressure to “publish or perish” is a well-known reality for academics, striking fear into…

- AI in Academia
- Trending Now
Using AI for Journal Selection — Simplifying your academic publishing journey in the smart way
Strategic journal selection plays a pivotal role in maximizing the impact of one’s scholarly work.…
How to Optimize Your Research Process: A step-by-step guide
Digital Citations: A comprehensive guide to citing of websites in APA, MLA, and CMOS…

Sign-up to read more
Subscribe for free to get unrestricted access to all our resources on research writing and academic publishing including:
- 2000+ blog articles
- 50+ Webinars
- 10+ Expert podcasts
- 50+ Infographics
- 10+ Checklists
- Research Guides
We hate spam too. We promise to protect your privacy and never spam you.
I am looking for Editing/ Proofreading services for my manuscript Tentative date of next journal submission:

As a researcher, what do you consider most when choosing an image manipulation detector?

Writing Effective Conclusions and Recommendations in a Thesis

Table of Contents
Have you ever experienced the triumphant moment of finishing a jigsaw puzzle , only to find that the final piece doesn’t quite fit? Such is the challenge when writing the conclusion and findings .">recommendations in your thesis . This final section isn’t just an endnote; it’s your opportunity to make your research resonate. Let’s explore how to craft a compelling conclusion that not only summarizes your findings but also sets the stage for future inquiry.
Understanding the weight of conclusions and recommendations
In the grand scheme of your thesis, the conclusion is your final act, your closing argument. It is here that you revisit your research objectives to demonstrate how your findings address them. But it’s not just a rehash of your research; it’s your chance to interpret the implications of your work and persuade your audience of its significance.
The art of summarizing findings
Begin by revisiting the questions you posed at the start of your journey. Summarize the answers you’ve uncovered, concisely distilling the essence of your research. This isn’t a place for exhaustive detail—that’s what the body of your thesis is for. Instead, think of it as the highlight reel, showcasing the most significant insights.
Drawing insightful conclusions
Conclusions are the thoughtful deductions you’ve drawn from your research. Linking back to your objectives, ask yourself: What have I learned? How have my findings contributed to the field? This is where you can shine a light on the larger implications of your work, the ‘so what?’ of your thesis.
Outlining clear and actionable recommendations
Your recommendations are your legacy, the path you lay for future research ers or practitioners. They should be clear, specific, and grounded in your findings. Think of them as a call to action—what should be done in light of your research? Whether it’s suggesting areas for further study or recommending changes to practice, your recommendations should inspire action.
Linking conclusions to research objectives
To ensure your conclusions are meaningful, they must be tethered to your research objectives. This alignment reinforces the relevance of your work and ensures you’re answering the questions you set out to explore.
Reflecting on research questions
Revisit your research questions or hypotheses . How have your findings addressed them? This reflection ensures your conclusions are directly tied to your initial inquiry, creating a cohesive narrative from start to finish.
Emphasizing the impact of your findings
Highlight the impact of your research. Have you filled a gap in knowledge? Challenged existing theories? Applied your findings to practice? Your conclusions should underscore the value of your work and its ripple effect in your field.
Formulating recommendations with purpose
Recommendations should never be an afterthought. They are your opportunity to influence the future, to suggest how the knowledge you’ve generated can be used to better understand or improve upon a particular issue.
Grounding recommendations in evidence
Ensure your recommendations are evidence\-based . They should flow naturally from the conclusions you’ve drawn, each one supported by the data you’ve collected.
Keeping recommendations achievable
Make your recommendations achievable. Pie-in-the-sky ideas might be inspirational, but they’re less helpful than practical, attainable suggestions that can be realistically implemented.
Setting the stage for future research
Use your recommendations to set the stage for future research. What questions have emerged from your study? Where are the knowledge gaps ? Propel the academic conversation forward by identifying the next steps.
Writing with clarity and conviction
The best conclusions and recommendations are those written with clarity and conviction. You’ve spent countless hours on your research—now’s the time to confidently present your findings and their implications.
Using precise language
Be precise in your language. Avoid ambiguity and make every word count. This precision not only makes your writing clearer but also reinforces the authority of your conclusions and recommendations.
Ensuring cohesiveness
Your conclusion should feel like a natural culmination of your thesis, not a separate entity. Ensure that it flows logically from the body of your work, with each part reinforcing the other.
Engaging the reader’s imagination
Engage your reader’s imagination by painting a picture of what could be. Use your recommendations to inspire visions of future possibilities, grounded in the solid foundation of your research.
In conclusion, remember that the final sections of your thesis are not mere formalities but the bridge between your research and its potential impact on the world. The conclusions and recommendations you write are your scholarly legacy , a testament to the hard work you’ve poured into your research. Approach them with the same rigor , creativity, and dedication as the rest of your thesis, and you’ll leave a lasting mark on your field.
What do you think? How do you approach writing conclusions and recommendations, and what strategies do you find most effective? Are there particular challenges you’ve faced in this part of the thesis-writing process?
How useful was this post?
Click on a star to rate it!
Average rating / 5. Vote count:
No votes so far! Be the first to rate this post.
We are sorry that this post was not useful for you!
Let us improve this post!
Tell us how we can improve this post?
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Submit Comment
Research Methodology
1 Introduction to Research in General
- Research in General
- Research Circle
- Tools of Research
- Methods: Quantitative or Qualitative
- The Product: Research Report or Papers
2 Original Unity of Philosophy and Science
- Myth Philosophy and Science: Original Unity
- The Myth: A Spiritual Metaphor
- Myth Philosophy and Science
- The Greek Quest for Unity
- The Ionian School
- Towards a Grand Unification Theory or Theory of Everything
- Einstein’s Perennial Quest for Unity
3 Evolution of the Distinct Methods of Science
- Definition of Scientific Method
- The Evolution of Scientific Methods
- Theory-Dependence of Observation
- Scope of Science and Scientific Methods
- Prevalent Mistakes in Applying the Scientific Method
4 Relation of Scientific and Philosophical Methods
- Definitions of Scientific and Philosophical method
- Philosophical method
- Scientific method
- The relation
- The Importance of Philosophical and scientific methods
5 Dialectical Method
- Introduction and a Brief Survey of the Method
- Types of Dialectics
- Dialectics in Classical Philosophy
- Dialectics in Modern Philosophy
- Critique of Dialectical Method
6 Rational Method
- Understanding Rationalism
- Rational Method of Investigation
- Descartes’ Rational Method
- Leibniz’ Aim of Philosophy
- Spinoza’ Aim of Philosophy
7 Empirical Method
- Common Features of Philosophical Method
- Empirical Method
- Exposition of Empiricism
- Locke’s Empirical Method
- Berkeley’s Empirical Method
- David Hume’s Empirical Method
8 Critical Method
- Basic Features of Critical Theory
- On Instrumental Reason
- Conception of Society
- Human History as Dialectic of Enlightenment
- Substantive Reason
- Habermasian Critical Theory
- Habermas’ Theory of Society
- Habermas’ Critique of Scientism
- Theory of Communicative Action
- Discourse Ethics of Habermas
9 Phenomenological Method (Western and Indian)
- Phenomenology in Philosophy
- Phenomenology as a Method
- Phenomenological Analysis of Knowledge
- Phenomenological Reduction
- Husserl’s Triad: Ego Cogito Cogitata
- Intentionality
- Understanding ‘Consciousness’
- Phenomenological Method in Indian Tradition
- Phenomenological Method in Religion
10 Analytical Method (Western and Indian)
- Analysis in History of Philosophy
- Conceptual Analysis
- Analysis as a Method
- Analysis in Logical Atomism and Logical Positivism
- Analytic Method in Ethics
- Language Analysis
- Quine’s Analytical Method
- Analysis in Indian Traditions
11 Hermeneutical Method (Western and Indian)
- The Power (Sakti) to Convey Meaning
- Three Meanings
- Pre-understanding
- The Semantic Autonomy of the Text
- Towards a Fusion of Horizons
- The Hermeneutical Circle
- The True Scandal of the Text
- Literary Forms
12 Deconstructive Method
- The Seminal Idea of Deconstruction in Heidegger
- Deconstruction in Derrida
- Structuralism and Post-structuralism
- Sign Signifier and Signified
- Writing and Trace
- Deconstruction as a Strategic Reading
- The Logic of Supplement
- No Outside-text
13 Method of Bibliography
- Preparing to Write
- Writing a Paper
- The Main Divisions of a Paper
- Writing Bibliography in Turabian and APA
- Sample Bibliography
14 Method of Footnotes
- Citations and Notes
- General Hints for Footnotes
- Writing Footnotes
- Examples of Footnote or Endnote
- Example of a Research Article
15 Method of Notes Taking
- Methods of Note-taking
- Note Book Style
- Note taking in a Computer
- Types of Note-taking
- Notes from Field Research
- Errors to be Avoided
16 Method of Thesis Proposal and Presentation
- Preliminary Section
- Presenting the Problem of the Thesis
- Design of the Study
- Main Body of the Thesis
- Conclusion Summary and Recommendations
- Reference Material
Share on Mastodon
How To Write The Conclusion Chapter
A Simple Explainer With Examples + Free Template
By: Jenna Crossley (PhD) | Reviewed By: Dr. Eunice Rautenbach | September 2021
So, you’ve wrapped up your results and discussion chapters, and you’re finally on the home stretch – the conclusion chapter . In this post, we’ll discuss everything you need to know to craft a high-quality conclusion chapter for your dissertation or thesis project.
Overview: The Conclusion Chapter
- What the thesis/dissertation conclusion chapter is
- What to include in your conclusion
- How to structure and write up your conclusion
- A few tips to help you ace the chapter
- FREE conclusion template
What is the conclusion chapter?
The conclusion chapter is typically the final major chapter of a dissertation or thesis. As such, it serves as a concluding summary of your research findings and wraps up the document. While some publications such as journal articles and research reports combine the discussion and conclusion sections, these are typically separate chapters in a dissertation or thesis. As always, be sure to check what your university’s structural preference is before you start writing up these chapters.
So, what’s the difference between the discussion and the conclusion chapter?
Well, the two chapters are quite similar , as they both discuss the key findings of the study. However, the conclusion chapter is typically more general and high-level in nature. In your discussion chapter, you’ll typically discuss the intricate details of your study, but in your conclusion chapter, you’ll take a broader perspective, reporting on the main research outcomes and how these addressed your research aim (or aims) .
A core function of the conclusion chapter is to synthesise all major points covered in your study and to tell the reader what they should take away from your work. Basically, you need to tell them what you found , why it’s valuable , how it can be applied , and what further research can be done.
Whatever you do, don’t just copy and paste what you’ve written in your discussion chapter! The conclusion chapter should not be a simple rehash of the discussion chapter. While the two chapters are similar, they have distinctly different functions.

What should I include in the conclusion chapter?
To understand what needs to go into your conclusion chapter, it’s useful to understand what the chapter needs to achieve. In general, a good dissertation conclusion chapter should achieve the following:
- Summarise the key findings of the study
- Explicitly answer the research question(s) and address the research aims
- Inform the reader of the study’s main contributions
- Discuss any limitations or weaknesses of the study
- Present recommendations for future research
Therefore, your conclusion chapter needs to cover these core components. Importantly, you need to be careful not to include any new findings or data points. Your conclusion chapter should be based purely on data and analysis findings that you’ve already presented in the earlier chapters. If there’s a new point you want to introduce, you’ll need to go back to your results and discussion chapters to weave the foundation in there.
In many cases, readers will jump from the introduction chapter directly to the conclusions chapter to get a quick overview of the study’s purpose and key findings. Therefore, when you write up your conclusion chapter, it’s useful to assume that the reader hasn’t consumed the inner chapters of your dissertation or thesis. In other words, craft your conclusion chapter such that there’s a strong connection and smooth flow between the introduction and conclusion chapters, even though they’re on opposite ends of your document.
Need a helping hand?
How to write the conclusion chapter
Now that you have a clearer view of what the conclusion chapter is about, let’s break down the structure of this chapter so that you can get writing. Keep in mind that this is merely a typical structure – it’s not set in stone or universal. Some universities will prefer that you cover some of these points in the discussion chapter , or that you cover the points at different levels in different chapters.
Step 1: Craft a brief introduction section
As with all chapters in your dissertation or thesis, the conclusions chapter needs to start with a brief introduction. In this introductory section, you’ll want to tell the reader what they can expect to find in the chapter, and in what order . Here’s an example of what this might look like:
This chapter will conclude the study by summarising the key research findings in relation to the research aims and questions and discussing the value and contribution thereof. It will also review the limitations of the study and propose opportunities for future research.
Importantly, the objective here is just to give the reader a taste of what’s to come (a roadmap of sorts), not a summary of the chapter. So, keep it short and sweet – a paragraph or two should be ample.
Step 2: Discuss the overall findings in relation to the research aims
The next step in writing your conclusions chapter is to discuss the overall findings of your study , as they relate to the research aims and research questions . You would have likely covered similar ground in the discussion chapter, so it’s important to zoom out a little bit here and focus on the broader findings – specifically, how these help address the research aims .
In practical terms, it’s useful to start this section by reminding your reader of your research aims and research questions, so that the findings are well contextualised. In this section, phrases such as, “This study aimed to…” and “the results indicate that…” will likely come in handy. For example, you could say something like the following:
This study aimed to investigate the feeding habits of the naked mole-rat. The results indicate that naked mole rats feed on underground roots and tubers. Further findings show that these creatures eat only a part of the plant, leaving essential parts to ensure long-term food stability.
Be careful not to make overly bold claims here. Avoid claims such as “this study proves that” or “the findings disprove existing the existing theory”. It’s seldom the case that a single study can prove or disprove something. Typically, this is achieved by a broader body of research, not a single study – especially not a dissertation or thesis which will inherently have significant limitations . We’ll discuss those limitations a little later.

Step 3: Discuss how your study contributes to the field
Next, you’ll need to discuss how your research has contributed to the field – both in terms of theory and practice . This involves talking about what you achieved in your study, highlighting why this is important and valuable, and how it can be used or applied.
In this section you’ll want to:
- Mention any research outputs created as a result of your study (e.g., articles, publications, etc.)
- Inform the reader on just how your research solves your research problem , and why that matters
- Reflect on gaps in the existing research and discuss how your study contributes towards addressing these gaps
- Discuss your study in relation to relevant theories . For example, does it confirm these theories or constructively challenge them?
- Discuss how your research findings can be applied in the real world . For example, what specific actions can practitioners take, based on your findings?
Be careful to strike a careful balance between being firm but humble in your arguments here. It’s unlikely that your one study will fundamentally change paradigms or shake up the discipline, so making claims to this effect will be frowned upon . At the same time though, you need to present your arguments with confidence, firmly asserting the contribution your research has made, however small that contribution may be. Simply put, you need to keep it balanced .
Step 4: Reflect on the limitations of your study
Now that you’ve pumped your research up, the next step is to critically reflect on the limitations and potential shortcomings of your study. You may have already covered this in the discussion chapter, depending on your university’s structural preferences, so be careful not to repeat yourself unnecessarily.
There are many potential limitations that can apply to any given study. Some common ones include:
- Sampling issues that reduce the generalisability of the findings (e.g., non-probability sampling )
- Insufficient sample size (e.g., not getting enough survey responses ) or limited data access
- Low-resolution data collection or analysis techniques
- Researcher bias or lack of experience
- Lack of access to research equipment
- Time constraints that limit the methodology (e.g. cross-sectional vs longitudinal time horizon)
- Budget constraints that limit various aspects of the study
Discussing the limitations of your research may feel self-defeating (no one wants to highlight their weaknesses, right), but it’s a critical component of high-quality research. It’s important to appreciate that all studies have limitations (even well-funded studies by expert researchers) – therefore acknowledging these limitations adds credibility to your research by showing that you understand the limitations of your research design .
That being said, keep an eye on your wording and make sure that you don’t undermine your research . It’s important to strike a balance between recognising the limitations, but also highlighting the value of your research despite those limitations. Show the reader that you understand the limitations, that these were justified given your constraints, and that you know how they can be improved upon – this will get you marks.

Next, you’ll need to make recommendations for future studies. This will largely be built on the limitations you just discussed. For example, if one of your study’s weaknesses was related to a specific data collection or analysis method, you can make a recommendation that future researchers undertake similar research using a more sophisticated method.
Another potential source of future research recommendations is any data points or analysis findings that were interesting or surprising , but not directly related to your study’s research aims and research questions. So, if you observed anything that “stood out” in your analysis, but you didn’t explore it in your discussion (due to a lack of relevance to your research aims), you can earmark that for further exploration in this section.
Essentially, this section is an opportunity to outline how other researchers can build on your study to take the research further and help develop the body of knowledge. So, think carefully about the new questions that your study has raised, and clearly outline these for future researchers to pick up on.
Step 6: Wrap up with a closing summary
Tips for a top-notch conclusion chapter
Now that we’ve covered the what , why and how of the conclusion chapter, here are some quick tips and suggestions to help you craft a rock-solid conclusion.
- Don’t ramble . The conclusion chapter usually consumes 5-7% of the total word count (although this will vary between universities), so you need to be concise. Edit this chapter thoroughly with a focus on brevity and clarity.
- Be very careful about the claims you make in terms of your study’s contribution. Nothing will make the marker’s eyes roll back faster than exaggerated or unfounded claims. Be humble but firm in your claim-making.
- Use clear and simple language that can be easily understood by an intelligent layman. Remember that not every reader will be an expert in your field, so it’s important to make your writing accessible. Bear in mind that no one knows your research better than you do, so it’s important to spell things out clearly for readers.
Hopefully, this post has given you some direction and confidence to take on the conclusion chapter of your dissertation or thesis with confidence. If you’re still feeling a little shaky and need a helping hand, consider booking a free initial consultation with a friendly Grad Coach to discuss how we can help you with hands-on, private coaching.

Psst... there’s more!
This post was based on one of our popular Research Bootcamps . If you're working on a research project, you'll definitely want to check this out ...
You Might Also Like:

17 Comments
Really you team are doing great!
Your guide on writing the concluding chapter of a research is really informative especially to the beginners who really do not know where to start. Im now ready to start. Keep it up guys
Really your team are doing great!
Very helpful guidelines, timely saved. Thanks so much for the tips.
This post was very helpful and informative. Thank you team.
A very enjoyable, understandable and crisp presentation on how to write a conclusion chapter. I thoroughly enjoyed it. Thanks Jenna.
This was a very helpful article which really gave me practical pointers for my concluding chapter. Keep doing what you are doing! It meant a lot to me to be able to have this guide. Thank you so much.
Nice content dealing with the conclusion chapter, it’s a relief after the streneous task of completing discussion part.Thanks for valuable guidance
Thanks for your guidance
I get all my doubts clarified regarding the conclusion chapter. It’s really amazing. Many thanks.
Very helpful tips. Thanks so much for the guidance
Thank you very much for this piece. It offers a very helpful starting point in writing the conclusion chapter of my thesis.
It’s awesome! Most useful and timely too. Thanks a million times
Bundle of thanks for your guidance. It was greatly helpful.
Wonderful, clear, practical guidance. So grateful to read this as I conclude my research. Thank you.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly

- Walden University
- Faculty Portal
Writing a Paper: Conclusions
Writing a conclusion.
A conclusion is an important part of the paper; it provides closure for the reader while reminding the reader of the contents and importance of the paper. It accomplishes this by stepping back from the specifics in order to view the bigger picture of the document. In other words, it is reminding the reader of the main argument. For most course papers, it is usually one paragraph that simply and succinctly restates the main ideas and arguments, pulling everything together to help clarify the thesis of the paper. A conclusion does not introduce new ideas; instead, it should clarify the intent and importance of the paper. It can also suggest possible future research on the topic.

An Easy Checklist for Writing a Conclusion
It is important to remind the reader of the thesis of the paper so he is reminded of the argument and solutions you proposed.
Think of the main points as puzzle pieces, and the conclusion is where they all fit together to create a bigger picture. The reader should walk away with the bigger picture in mind.
Make sure that the paper places its findings in the context of real social change.
Make sure the reader has a distinct sense that the paper has come to an end. It is important to not leave the reader hanging. (You don’t want her to have flip-the-page syndrome, where the reader turns the page, expecting the paper to continue. The paper should naturally come to an end.)
No new ideas should be introduced in the conclusion. It is simply a review of the material that is already present in the paper. The only new idea would be the suggesting of a direction for future research.
Conclusion Example
As addressed in my analysis of recent research, the advantages of a later starting time for high school students significantly outweigh the disadvantages. A later starting time would allow teens more time to sleep--something that is important for their physical and mental health--and ultimately improve their academic performance and behavior. The added transportation costs that result from this change can be absorbed through energy savings. The beneficial effects on the students’ academic performance and behavior validate this decision, but its effect on student motivation is still unknown. I would encourage an in-depth look at the reactions of students to such a change. This sort of study would help determine the actual effects of a later start time on the time management and sleep habits of students.
Related Webinar
Didn't find what you need? Email us at [email protected] .
- Previous Page: Thesis Statements
- Next Page: Writer's Block
- Office of Student Disability Services
Walden Resources
Departments.
- Academic Residencies
- Academic Skills
- Career Planning and Development
- Customer Care Team
- Field Experience
- Military Services
- Student Success Advising
- Writing Skills
Centers and Offices
- Center for Social Change
- Office of Academic Support and Instructional Services
- Office of Degree Acceleration
- Office of Research and Doctoral Services
- Office of Student Affairs
Student Resources
- Doctoral Writing Assessment
- Form & Style Review
- Quick Answers
- ScholarWorks
- SKIL Courses and Workshops
- Walden Bookstore
- Walden Catalog & Student Handbook
- Student Safety/Title IX
- Legal & Consumer Information
- Website Terms and Conditions
- Cookie Policy
- Accessibility
- Accreditation
- State Authorization
- Net Price Calculator
- Contact Walden
Walden University is a member of Adtalem Global Education, Inc. www.adtalem.com Walden University is certified to operate by SCHEV © 2024 Walden University LLC. All rights reserved.
Writing the parts of scientific reports
22 Writing the conclusion & recommendations
There are probably some overlaps between the Conclusion and the Discussion section. Nevertheless, this section gives you the opportunity to highlight the most important points in your report, and is sometimes the only section read. Think about what your research/ study has achieved, and the most important findings and ideas you want the reader to know. As all studies have limitations also think about what you were not able to cover (this shows that you are able to evaluate your own work objectively).
Possible structure of this section:
Use present perfect to sum up/ evaluate:
This study has explored/ has attempted …
Use past tense to state what your aim was and to refer to actions you carried out:
- This study was intended to analyse …
- The aim of this study was to …
Use present tense to evaluate your study and to state the generalizations and implications that you draw from your findings.
- The results add to the knowledge of …
- These findings s uggest that …
You can either use present tense or past tense to summarize your results.
- The findings reveal …
- It was found that …
Achievements of this study (positive)
- This study provides evidence that …
- This work has contributed to a number of key issues in the field such as …
Limitations of the study (negative)
- Several limitations should be noted. First …
Combine positive and negative remarks to give a balanced assessment:
- Although this research is somewhat limited in scope, its findings can provide a basis for future studies.
- Despite the limitations, findings from the present study can help us understand …
Use more cautious language (modal verbs may, can, could)
- There are a number of possible extensions of this research …
- The findings suggest the possibility for future research on …
- These results may be important for future studies on …
- Examining a wider context could/ would lead …
Or indicate that future research is needed
- There is still a need for future research to determine …
- Further studies should be undertaken to discover…
- It would be worthwhile to investigate …
Academic Writing in a Swiss University Context Copyright © 2018 by Irene Dietrichs. All Rights Reserved.
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Dissertation
- How to Write a Thesis or Dissertation Conclusion
How to Write a Dissertation Conclusion | Checklist and Examples
Published on 9 September 2022 by Tegan George and Shona McCombes. Revised on 10 October 2022.
The conclusion is the very last part of your thesis or dissertation . It should be concise and engaging, leaving your reader with a clear understanding of your main findings, as well as the answer to your research question .
In it, you should:
- Clearly state the answer to your main research question
- Summarise and reflect on your research process
- Make recommendations for future work on your topic
- Show what new knowledge you have contributed to your field
- Wrap up your thesis or dissertation
Instantly correct all language mistakes in your text
Be assured that you'll submit flawless writing. Upload your document to correct all your mistakes.

Table of contents
Discussion vs. conclusion, how long should your conclusion be, step 1: answer your research question, step 2: summarise and reflect on your research, step 3: make future recommendations, step 4: emphasise your contributions to your field, step 5: wrap up your thesis or dissertation, full conclusion example, conclusion checklist, frequently asked questions about conclusion sections.
While your conclusion contains similar elements to your discussion section , they are not the same thing.
Your conclusion should be shorter and more general than your discussion. Instead of repeating literature from your literature review , discussing specific research results , or interpreting your data in detail, concentrate on making broad statements that sum up the most important insights of your research.
As a rule of thumb, your conclusion should not introduce new data, interpretations, or arguments.
Prevent plagiarism, run a free check.
Depending on whether you are writing a thesis or dissertation, your length will vary. Generally, a conclusion should make up around 5–7% of your overall word count.
An empirical scientific study will often have a short conclusion, concisely stating the main findings and recommendations for future research. A humanities topic or systematic review , on the other hand, might require more space to conclude its analysis, tying all the previous sections together in an overall argument.
Your conclusion should begin with the main question that your thesis or dissertation aimed to address. This is your final chance to show that you’ve done what you set out to do, so make sure to formulate a clear, concise answer.
- Don’t repeat a list of all the results that you already discussed
- Do synthesise them into a final takeaway that the reader will remember.
An empirical thesis or dissertation conclusion may begin like this:
A case study –based thesis or dissertation conclusion may begin like this:
In the second example, the research aim is not directly restated, but rather added implicitly to the statement. To avoid repeating yourself, it is helpful to reformulate your aims and questions into an overall statement of what you did and how you did it.
Your conclusion is an opportunity to remind your reader why you took the approach you did, what you expected to find, and how well the results matched your expectations.
To avoid repetition , consider writing more reflectively here, rather than just writing a summary of each preceding section. Consider mentioning the effectiveness of your methodology , or perhaps any new questions or unexpected insights that arose in the process.
You can also mention any limitations of your research, but only if you haven’t already included these in the discussion. Don’t dwell on them at length, though – focus on the positives of your work.
- While x limits the generalisability of the results, this approach provides new insight into y .
- This research clearly illustrates x , but it also raises the question of y .
The only proofreading tool specialized in correcting academic writing
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Correct my document today
You may already have made a few recommendations for future research in your discussion section, but the conclusion is a good place to elaborate and look ahead, considering the implications of your findings in both theoretical and practical terms.
- Based on these conclusions, practitioners should consider …
- To better understand the implications of these results, future studies could address …
- Further research is needed to determine the causes of/effects of/relationship between …
When making recommendations for further research, be sure not to undermine your own work. Relatedly, while future studies might confirm, build on, or enrich your conclusions, they shouldn’t be required for your argument to feel complete. Your work should stand alone on its own merits.
Just as you should avoid too much self-criticism, you should also avoid exaggerating the applicability of your research. If you’re making recommendations for policy, business, or other practical implementations, it’s generally best to frame them as ‘shoulds’ rather than ‘musts’. All in all, the purpose of academic research is to inform, explain, and explore – not to demand.
Make sure your reader is left with a strong impression of what your research has contributed to the state of your field.
Some strategies to achieve this include:
- Returning to your problem statement to explain how your research helps solve the problem
- Referring back to the literature review and showing how you have addressed a gap in knowledge
- Discussing how your findings confirm or challenge an existing theory or assumption
Again, avoid simply repeating what you’ve already covered in the discussion in your conclusion. Instead, pick out the most important points and sum them up succinctly, situating your project in a broader context.
The end is near! Once you’ve finished writing your conclusion, it’s time to wrap up your thesis or dissertation with a few final steps:
- It’s a good idea to write your abstract next, while the research is still fresh in your mind.
- Next, make sure your reference list is complete and correctly formatted. To speed up the process, you can use our free APA citation generator .
- Once you’ve added any appendices , you can create a table of contents and title page .
- Finally, read through the whole document again to make sure your thesis is clearly written and free from language errors. You can proofread it yourself , ask a friend, or consider Scribbr’s proofreading and editing service .
Here is an example of how you can write your conclusion section. Notice how it includes everything mentioned above:
V. Conclusion
The current research aimed to identify acoustic speech characteristics which mark the beginning of an exacerbation in COPD patients.
The central questions for this research were as follows: 1. Which acoustic measures extracted from read speech differ between COPD speakers in stable condition and healthy speakers? 2. In what ways does the speech of COPD patients during an exacerbation differ from speech of COPD patients during stable periods?
All recordings were aligned using a script. Subsequently, they were manually annotated to indicate respiratory actions such as inhaling and exhaling. The recordings of 9 stable COPD patients reading aloud were then compared with the recordings of 5 healthy control subjects reading aloud. The results showed a significant effect of condition on the number of in- and exhalations per syllable, the number of non-linguistic in- and exhalations per syllable, and the ratio of voiced and silence intervals. The number of in- and exhalations per syllable and the number of non-linguistic in- and exhalations per syllable were higher for COPD patients than for healthy controls, which confirmed both hypotheses.
However, the higher ratio of voiced and silence intervals for COPD patients compared to healthy controls was not in line with the hypotheses. This unpredicted result might have been caused by the different reading materials or recording procedures for both groups, or by a difference in reading skills. Moreover, there was a trend regarding the effect of condition on the number of syllables per breath group. The number of syllables per breath group was higher for healthy controls than for COPD patients, which was in line with the hypothesis. There was no effect of condition on pitch, intensity, center of gravity, pitch variability, speaking rate, or articulation rate.
This research has shown that the speech of COPD patients in exacerbation differs from the speech of COPD patients in stable condition. This might have potential for the detection of exacerbations. However, sustained vowels rarely occur in spontaneous speech. Therefore, the last two outcome measures might have greater potential for the detection of beginning exacerbations, but further research on the different outcome measures and their potential for the detection of exacerbations is needed due to the limitations of the current study.
Checklist: Conclusion
I have clearly and concisely answered the main research question .
I have summarized my overall argument or key takeaways.
I have mentioned any important limitations of the research.
I have given relevant recommendations .
I have clearly explained what my research has contributed to my field.
I have not introduced any new data or arguments.
You've written a great conclusion! Use the other checklists to further improve your dissertation.
In a thesis or dissertation, the discussion is an in-depth exploration of the results, going into detail about the meaning of your findings and citing relevant sources to put them in context.
The conclusion is more shorter and more general: it concisely answers your main research question and makes recommendations based on your overall findings.
While it may be tempting to present new arguments or evidence in your thesis or disseration conclusion , especially if you have a particularly striking argument you’d like to finish your analysis with, you shouldn’t. Theses and dissertations follow a more formal structure than this.
All your findings and arguments should be presented in the body of the text (more specifically in the discussion section and results section .) The conclusion is meant to summarize and reflect on the evidence and arguments you have already presented, not introduce new ones.
For a stronger dissertation conclusion , avoid including:
- Generic concluding phrases (e.g. “In conclusion…”)
- Weak statements that undermine your argument (e.g. “There are good points on both sides of this issue.”)
Your conclusion should leave the reader with a strong, decisive impression of your work.
The conclusion of your thesis or dissertation shouldn’t take up more than 5-7% of your overall word count.
The conclusion of your thesis or dissertation should include the following:
- A restatement of your research question
- A summary of your key arguments and/or results
- A short discussion of the implications of your research
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
George, T. & McCombes, S. (2022, October 10). How to Write a Dissertation Conclusion | Checklist and Examples. Scribbr. Retrieved 26 May 2024, from https://www.scribbr.co.uk/thesis-dissertation/conclusion/
Is this article helpful?
Tegan George
Other students also liked, how to write a thesis or dissertation introduction, how to write a discussion section | tips & examples, how to write an abstract | steps & examples.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
6.6: Formal Report—Conclusion, Recommendations, References, and Appendices
Learning objectives.
- Examine the remaining report sections: conclusion, recommendation, reference list, appendices
What Are the Remaining Report Sections?
Conclusions and recommendations.
The conclusions and recommendations section conveys the key results from the analysis in the discussion section. Up to this point, readers have carefully reviewed the data in the report; they are now logically prepared to read the report’s conclusions and recommendations.
According to OACETT (2021), “Conclusions are reasoned judgment and fact, not opinion. Conclusions consider all of the variables and relate cause and effect. Conclusions analyze, evaluate, and make comparisons and contrasts” (p. 7) and “Recommendation(s) (if applicable) suggest a course of action and are provided when there are additional areas for study, or if the reason for the Technology Report was to determine the best action going forward” (p. 7).
You may present the conclusions and recommendations in a numbered or bulleted list to enhance readability.
Reference Page
All formal reports should include a reference page; this page documents the sources cited within the report. The recipient(s) of the report can also refer to this page to locate sources for further research.
Documenting your information sources is all about establishing, maintaining, and protecting your credibility in the profession. You must cite (“document”) borrowed information regardless of the shape or form in which you present it. Whether you directly quote it, paraphrase it, or summarize it—it’s still borrowed information. Whether it comes from a book, article, a diagram, a table, a web page, a product brochure, an expert whom you interview in person—it’s still borrowed information.
Documentation systems vary according to professionals and fields. In ENGL 250, we follow APA. Refer to a credible APA guide for support.
Appendices are those extra sections in a report that follow the conclusion. According to OACETT (2021), “Appendices can include detailed calculations, tables, drawings, specifications, and technical literature” (p. 7).
Anything that does not comfortably fit in the main part of the report but cannot be left out of the report altogether should go into the appendices. They are commonly used for large tables of data, big chunks of sample code, background that is too basic or too advanced for the body of the report, or large illustrations that just do not fit in the body of the report. Anything that you feel is too large for the main part of the report or that you think would be distracting and interrupt the flow of the report is a good candidate for an appendix.
References & Attributions
Blicq, R., & Moretto, L. (2012). Technically write. (8th Canadian Ed.). Pearson Canada.
OACETT. (2021). Technology report guidelines . https://www.oacett.org/getmedia/9f9623ac-73ab-4f99-acca-0d78dee161ab/TR_GUIDELINES_Final.pdf.aspx
Attributions
Content is adapted from Technical Writing by Allison Gross, Annemarie Hamlin, Billy Merck, Chris Rubio, Jodi Naas, Megan Savage, and Michele DeSilva, which is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
Writing in a Technical Environment (First Edition) Copyright © 2022 by Centennial College is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book
- How it works
- Pay for essays
- Do my homework
- Term Paper Writing Service
- Do my assignment
- Coursework help
- Our Writers

Research Paper Structure: The Complete Guide

A professional writer with ten years of experience and a Ph.D. in Modern History, Catharine Tawil writes engaging and insightful papers for academic exchange. With deep insight into the impact of historical events on the present, she provides a unique perspective in giving students a feel for the past. Her writing educates and stimulates critical thinking, making her a treasure to those wading through the complexities of history.
A research paper is an academic work depicting the design and results of a study. It can be an academic assignment in undergraduate and postgraduate programs. Moreover, it is an integral requirement in doctoral programs, where postgrads’ research papers are published in reputable journals to add credibility to their research findings.
Ordering different parts of a research paper is critical for fulfilling academic standards, streamlining your writing, and avoiding distractions and sidetracks. Although outlining may seem like a waste of time, it is the most efficient use of your time at the pre-writing stage, as it will help you order your thoughts and ideas and develop a plan of action to follow throughout the study.
In this post, we’ll cover the basics of the research paper formatting, provide a basic template of a research paper structure, and provide a detailed description of each section, including the title page and abstract, introduction and literature review, methodology, results, discussion, and conclusion. You can skip to a specific section if you have questions or concerns about it or check out the full article for an in-depth understanding of the full structure.
Essential Components of a Research Paper
Unlike other types of academic assignments, research papers have a structure more complex than a simple trio of introduction, body, and conclusion. You are expected to follow the established academic norms and include specific information for your paper to have any scientific value. The basic research paper structure example comprises the following parts:
Introduction
- Literature review
Methodology
- Acknowledgments
Please note that some sections of a research paper outlined above are optional. For example, you only need to include appendices if you wish to share a large volume of data that would make the paper unwieldy. You can also adjust this research paper setup to fit your study and word count requirements better. For instance, you can combine the results and discussion sections or the introduction and literature review.
Formatting Requirements
Although the research paper structure is basically the same for all fields of study and topics, the papers can look drastically different when following research paper formatting guidelines of various formatting styles, be it Chicago, MLA, or APA. You must learn the appropriate style at the onset of the writing process, so remember to ask your academic advisor about it if there’s no mention of the formatting style within general requirements.
Once you know which research paper formatting style to use, get your hands on the relevant formatting guidebook. You can find most of the requirements online or sign out a book from a college library. Considering most formatting guidebooks are huge, focus on the main aspects that can make or break your paper, such as:
- Margins, font, and spacing. Most research paper format guidelines require 1-inch margins on all sides, a legible font of at least 12 pt, and double-spaced lines.
- Page numbering. Requirements vary, but typically, you’ll need to include page numbers in the upper right-hand corner, half an inch from the corner.
- Headings and subheadings. Refer to MLA or APA handbooks to learn specific research paper headings requirements or ask your professor, as the guidelines differ greatly.
- In-text citations and reference list. In most cases, research paper in-text citations require the name of the main author along with the page number or the publication year. Reference list formatting varies across different styles, but you can use automatic citation generators to speed up the formatting process.
With formatting requirements out of the way, let’s now focus on individual components of a research paper to help you understand what each section should contain to be well received.
Title Page and Abstract
The research paper title page format depends on the required formatting style:
- MLA does not require a separate title page (unless specifically requested). Instead, in the upper left-hand corner of the first page, type your name, your instructor’s name, course name, and date (each on a new line, double-spaced). After that, center the title of the page and include its text.
- APA requires a separate title page, which should include the title of the paper, your name and affiliation, as well as the course name and number, your instructor’s name, and the assignment’s due date.
A research paper abstract is brief summary of the main points of the research paper. Depending on the formatting style, it can be from 100 to 250 words long, highlighting the research objective, key methodology, and results highlights. An abstract should help readers decide if your work is worth reading at a glance.
An APA research paper organization requires an abstract on a separate page, with the “Abstract” heading and the paper’s summary (without indent). Below the abstract, type “Keywords:” (in italics) and list the keywords researchers would use to find your paper in the library or online.
The opening section of the research paper outline gives students pause because they never know what the introduction should entail. If you’re stuck with writer’s block and don’t know how to start the paper, answer these four questions, and you’ll have all the major pieces necessary for the introduction:
- What’s the context of the problem? Open with a general view of the issue and its current state without going into too much detail (that’s what the literature review is for). The background information should fit within one or two paragraphs and lead directly to the next point.
- What is the issue? The problem statement or question is the core of this part of the research paper structure. Think of it as a thesis statement for an essay. Everything you write in other sections of a research paper should always tie to your problem statement.
- How do you plan to solve the problem? You can formulate research objectives or hypotheses that your study will try to achieve or prove. Short papers typically have one hypothesis, while longer works usually have two or more related objectives.
- How will your study improve the issue? The answer can circle back to the background you laid out at the beginning of the research paper introduction and highlight the benefits (and potential drawbacks and limitations) of your research. It’s the major “selling point” of the study, which should explain why anyone should care about it.
You can always leave the introduction for last and tackle it once the rest of the paper is done. That’s especially helpful if you use writer’s block as an excuse to procrastinate and put off writing other parts of a research paper.
Literature Review
The primary objective of a research paper literature review is to provide context and prove the relevance of your topic, as specified in the introduction. To that end, you need to find credible, objective, and relevant sources and synthesize any data pertaining to your research. It’s important to avoid simple paraphrasing or summarization of reference data and instead provide its analysis and synthesize your own hypothesis.
Aside from the similarities found in references, this part of the research paper structure should also focus on discrepancies, contradictions, and knowledge gaps. These will prove your study has merit and can resolve the existing issues. Moreover, the knowledge gaps will help lead up to your main research question, which you may repeat near the end of the literature review.
Depending on the topic of your study, you can organize the literature review:
- Chronologically. You can go from the oldest sources published to the latest or from the latest events to situations long past. This approach is often the easiest, but it doesn’t fit all topics and fields of study.
- Thematically. If you wish to cover two or more aspects of the issue, you can dedicate a subsection to each and analyze them together in the final subsection of the literature review. This is the most popular approach, as it can work for most topics.
- Methodologically. If you want to focus on the differences and similarities in research methodology, you can split the literature review into several subsections, devoting each one to a single methodology. This approach works for select subjects and can make the most of systemic studies.
If you’re working on an empirical study, you can stop there, but if your work is mostly theoretical, this stage of the research paper writing process could also involve developing a theoretical framework. It will help put your findings and results into perspective.
Although it may seem simple at first glance, a literature review takes a long time, most of which you’ll spend looking for reliable sources. Luckily, you can easily outsource this task. All you need to do is say, “Write my paper for me”, and our experts will take over ASAP.
The research paper methodology section is an integral part of the piece, as it helps ensure the reproducibility of your results and increases your credibility. This part should answer two main questions:
- What? What did your study involve? What resources, software, materials, or samples did you use? What were the ethical considerations of your research?
- How? How much time did your study take? How did you choose participants? How did you collect data and analyze it?
Keep these questions in mind when working out a research design, picking data collection procedures and analysis techniques. If you rely on standard methods, a quick description with a citation would be enough for the methodology part of the research paper structure. But if you employ a unique approach, make sure to describe it in minute detail to ensure anyone can repeat the process and achieve the same results.
For obvious reasons, the methodology section will differ greatly depending on your field of study and topic. For example, qualitative and quantitative research methods are vastly different. At the same time, quantitative analysis of sociology or linguistics research will be nothing like analyzing blood tests for nursing students or analyzing the success of a marketing campaign for a business and management class. While the tools (i.e., programming language or table processing software) may be similar, the application will be different, and you should highlight these distinctions in your methodology section.
Although you can put off working on this section of the structure of a research paper, it can be helpful to put your methodology on paper before embarking on the study. A clear idea of the protocols you plan to employ should keep your study on track and minimize methodological errors.
The research paper results present the study findings as the ultimate product of your research. Instead of the raw data, you can present analysis results and visual aids in the form of tables, figures, and graphs, provide statistical analysis results, and refer interested readers to appendices containing raw data.
Remember to follow the formatting style requirements for tables and figures, which differ for APA and MLA. The same applies to lists and other visual aids. You should also ensure these materials do not destroy your paper’s readability. For example, a three-page table is much more difficult to grasp than a couple of charts highlighting the same data. Moreover, if you plan to present your findings on a poster or a PowerPoint presentation, it pays to work out the best way to present your insights that will fit all formats, including print and projection.
It’s important to draw the line between the results and discussion parts of the research paper structure. The first presents analysis, while the latter relies on interpretations (or implications) of that analysis. Understanding the distinction can be quite challenging, especially if you’re working out the structure of a research paper for the first time.
Discussion and Conclusion
The research paper discussion connects the introduction and research question with the study results. Instead of merely analyzing data, this section should explain whether your initial hypothesis was correct or not. Moreover, the final section, along with the research paper conclusion, should cover the implications of the findings and their potential practical and theoretical applications. This part can also include the limitations of the study and the need for further research if you feel that it could be useful.
It may seem counterproductive, but you shouldn’t shy away from shortcomings, mistakes, and negative results achieved in your study. Instead of waiting for uncomfortable questions from your instructor, present the bad along with the good and hypothesize potential ways of correcting errors or minimizing the negative influences. In some cases, negative results can be just as valuable (if not more so) than positive findings.
Remember to include the research paper references and appendices after the conclusion to wrap up your work and make it better with careful editing, proofreading, and formatting.
What is the purpose of a research paper?
The main objective is to present and share research insights and discoveries, which you should account for when structuring a research paper. Adding literature review and methodology sections is critical for highlighting the study’s relevance and ensuring its reproducibility.
How do I structure the different sections of a research paper?
Structuring a research paper means adding an introduction, literature review, methodology, results, discussion, and conclusion. You can organize each of these sections thematically or chronologically or use a funnel structure, going from the broad context strokes to a narrow view of the problem.
What are the key formatting guidelines for a research paper?
Specific requirements for the structure of a research paper outline and its contents depend on the preferred formatting style. However, at its core, each formatting style focuses on readability. That’s where 12 pt to 14 pt font size and double line spacing come from. Refer to the relevant formatting style handbook for specific recommendations.
How do I effectively write the introduction and literature review?
The introduction is a critical part of the research paper structure that should include your primary research objective (or question), hypotheses, and the study’s relevance. A literature review is designed to support the claims you make within the introduction by generously using reference data.
What is the difference between the results and discussion sections?
Related posts

Research paper ideas: exploring innovative topics in modern academia

APA Proposal Format: All Writing Tips & Examples

Research paper format for students: key rules and guidelines to follow
What are you waiting for?
You are a couple of clicks away from tranquility at an affordable price!
- Open access
- Published: 21 May 2024
Efficacy of interventions and techniques on adherence to physiotherapy in adults: an overview of systematic reviews and panoramic meta-analysis
- Clemens Ley ORCID: orcid.org/0000-0003-1700-3905 1 &
- Peter Putz ORCID: orcid.org/0000-0003-2314-3293 2
Systematic Reviews volume 13 , Article number: 137 ( 2024 ) Cite this article
286 Accesses
3 Altmetric
Metrics details
Adherence to physiotherapeutic treatment and recommendations is crucial to achieving planned goals and desired health outcomes. This overview of systematic reviews synthesises the wide range of additional interventions and behaviour change techniques used in physiotherapy, exercise therapy and physical therapy to promote adherence and summarises the evidence of their efficacy.
Seven databases (PEDro, PubMed, Cochrane Library, Web of Science, Scopus, PsycINFO and CINAHL) were systematically searched with terms related to physiotherapy, motivation, behaviour change, adherence and efficacy (last searched on January 31, 2023). Only systematic reviews of randomised control trials with adults were included. The screening process and quality assessment with AMSTAR-2 were conducted independently by the two authors. The extracted data was synthesised narratively. In addition, four meta-analyses were pooled in a panoramic meta-analysis.
Of 187 reviews identified in the search, 19 were included, comprising 205 unique trials. Four meta-analyses on the effects of booster sessions, behaviour change techniques, goal setting and motivational interventions showed a significantly small overall effect (SMD 0.24, 95% CI 0.13, 0.34) and no statistical heterogeneity ( I 2 = 0%) in the panoramic meta-analysis. Narrative synthesis revealed substantial clinical and methodological diversity. In total, the certainty of evidence is low regarding the efficacy of the investigated interventions and techniques on adherence, due to various methodological flaws. Most of the RCTs that were included in the reviews analysed cognitive and behavioural interventions in patients with musculoskeletal diseases, indicating moderate evidence for the efficacy of some techniques, particularly, booster sessions, supervision and graded exercise. The reviews provided less evidence for the efficacy of educational and psychosocial interventions and partly inconsistent findings. Most of the available evidence refers to short to medium-term efficacy. The combination of a higher number of behaviour change techniques was more efficacious.
Conclusions
The overview of reviews synthesised various potentially efficacious techniques that may be combined for a holistic and patient-centred approach and may support tailoring complex interventions to the patient’s needs and dispositions. It also identifies various research gaps and calls for a more holistic approach to define and measure adherence in physiotherapy.
Systematic review registration
PROSPERO CRD42021267355.
Peer Review reports
Adherence to physiotherapeutic1 treatment and recommendations is crucial to achieving the planned goals and desired effects [ 1 , 2 ]. This is because the desired effects are usually only achieved in the long term if the recommended treatment and home-based exercises are carried out regularly. However, non-adherence in physiotherapy can be as high as 70%, particularly in unsupervised home exercise programmes [ 1 , 3 ] and may differ among medical conditions [ 4 ]. The World Health Organization defines adherence to therapy as ‘the extent to which a person’s behaviour—taking medication, following a diet and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider’ [ 5 ]. Long-term adherence often requires lifestyle changes, which can be supported by behaviour change techniques (BCTs). BCTs are considered the ‘active, replicable and measurable component of any intervention designed to modify behaviour’ ([ 6 ],cf. [ 7 ]). BCTs are defined and operationalised in the behaviour change taxonomy [ 8 ], based on theoretical underpinnings and a Delphi study. Theoretical models to explain (non-)adherence and (a) motivation as well as techniques to promote behaviour change have been extensively studied in health and exercise psychology [ 9 , 10 , 11 ]. Rhodes and Fiala [ 12 ] argue that despite several strong psychological theories that have been developed to explain behaviour, few provide guidance for the design and development of interventions. Furthermore, theories may not be equally applicable to all behavioural domains, therapeutic regimes and settings. For example, the factors determining adherence to (passive) medication use differ from those influencing adherence to (active) physical therapies and exercise behaviour (cf. [ 5 ]). This review specifically addresses the domain of physiotherapy and therapeutic exercise.
Existing reviews of predictive studies identified factors influencing adherence positively or negatively, showing the predominately conflicting and low evidence of a wide range of predictive factors for adherence [ 1 , 2 , 13 ]. Moderate to strong evidence was shown for some factors, referring to previous (adherence) behaviour and treatment experiences, physical activity level, social support and psychosocial conditions, number of exercises and motivational dispositions. Such predictive studies have identified the possible targets for intervention but do not provide evidence on the efficacy of interventions. In contrast, randomised control trials (RCTs) are recognized as the preferred study design for investigating the efficacy of interventions. Thus, this overview of reviews Footnote 1 aimed at providing a synthesis of reviews that examined RCTs, allowing for the discussion of the efficacy of different interventions and BCTs on adherence-related outcomes.
There are numerous reviews on adherence to physiotherapy and (home-based) exercise, and on BCTs to increase physical activity levels, therapeutic exercise or self-organised exercise [ 1 , 2 , 3 , 14 , 15 , 16 , 17 , 18 ]. Yet, no systematic overview of reviews has been identified that specifically synthesised the efficacy of interventions and techniques to enhance adherence to physiotherapy.
Objectives and research questions
Therefore, the aim of this overview of reviews was to synthesise the evidence on the efficacy of interventions and techniques on adherence in physiotherapy, to explore heterogeneity regarding the theoretical underpinnings, types of interventions used, and the adherence-related measures and outcomes reported, and finally to identify research gaps. Thus, the primary research question is the following: How efficacious are interventions and techniques in increasing adherence to physiotherapy? Secondary research questions are as follows: What types of intervention and behaviour change techniques were investigated? Which theoretical underpinning was reported? How was adherence defined and related outcomes measured?
This overview of reviews is guided by the research questions and aligns with the common purposes of overviews [ 19 , 20 ] and the three functions for overviews proposed by Ballard and Montgomery [ 21 ], i.e. to explore heterogeneity, to summarize the evidence and to identify gaps. This overview approach is appropriate for addressing the research questions specified above by exploring different types of interventions and behaviour change techniques and by synthesising the evidence from systematic reviews of RCTs on their efficacy. The review protocol was registered ahead of the screening process in PROSPERO (reg.nr. CRD42021267355). The only deviations from the registration were that we excluded reviews of only cohort studies, due to the already broad heterogeneity of intervention and outcome measures, and that we additionally performed a panoramic meta-analysis.
Information sources, search strategy and eligibility criteria
The search in seven databases, PEDro, PubMed, Cochrane Library, Web of Science, Scopus, PsycInfo and CINAHL (Cumulative Index to Nursing and Allied Health Literature), was last updated on January 31, 2023. The search strategy was structured according to the PICOS (Population, Intervention, Comparison, Outcome and Study Type) scheme. The search terms related to physiotherapy and motivation or behaviour change and adherence and effectiveness/efficacy (details on the searches are listed in Additional file 1 ). A filter was applied limiting the search to (systematic) reviews. No publication date restrictions were applied.
Table 1 outlines the study inclusion and exclusion criteria. Only studies published in peer-reviewed journals were included. The review addressed adult patients, with any illness, disease or injury, and thus excluded studies on healthy populations. Reviews in the field of physiotherapy, physical therapy or the therapeutic use of exercise or physical activity were included if they investigated adherence as a primary outcome. Studies measuring adherence as a secondary outcome were excluded as they do analyse interventions that were not primarily designed to promote adherence and thus are outside the scope of this overview. Reviews that analysed only studies on digital apps or tools (e.g. virtual reality, gamification, exergames or tele-rehabilitation) were excluded from this overview, as they were outside of the scope of this overview. Only systematic reviews that appraised RCTs were included. Reviews appraising RCTs and other study designs were included if RCT results could be extracted separately. Systematic reviews are in our understanding literature reviews of primary studies with a comprehensive description of objectives, materials and methods; considering the risk of bias and confidence in the findings; and reporting according to the PRISMA statement [ 22 , 23 , 24 ]. Adherence is defined as the extent to which a person’s behaviour corresponds with treatment goals, plans or recommendations [ 5 ]. Related terms used in the literature are compliance, maintenance, attendance, participation and behaviour change or lifestyle modification and were thus included in the search strategy.
Screening and selection process
Author CL conducted the search in the seven different databases and removed duplicates, using the Zotero bibliography management tool. Following this, authors CL and PP both independently screened the titles and abstracts of the resulting sources (see Fig. 1 Flow diagram). After removing the excluded studies, PP and CL independently screened the remaining full texts in an unblinded standardised manner. Reasons for exclusion were noted in a screening spreadsheet. Any discrepancy was discussed, verified and resolved by consensus.
Data collection process and data items
Data extraction was done by CL after agreeing with PP on the criteria. A spreadsheet was created with the following data extraction components: (i) objectives and main topic of the review; (ii) study design(s) and number of studies included and excluded; (iii) search strategies (incl. PICO); (iv) population including diagnosis, sample sizes and age; (v) intervention and comparison, theoretical foundations and models used for designing the intervention; (vi) time frames, including follow-up; (vii) adherence-related outcome and outcome measures; (viii) key findings; (ix) analysis of primary studies (meta-analytical, other statistical or narrative analysis); and (x) tools used for the quality assessment, risk of bias and evidence grading. Primary outcomes on adherence included, adherence rates or categories, engagement, attendance and participation, and accomplished physical activity levels. PP verified the data extraction results. The data was extracted as reported in the systematic reviews, then reformatted and displayed in the tables and used for the narrative synthesis.
Assessment of risk of bias across reviews
Systematic reviews of RCTs are ranked highest in the evidence level [ 25 ], but are subjected to risk of bias (RoB). In an overview of reviews of systematic reviews, there are further risks of bias, in addition to those deriving from the primary studies and those deriving from the review of those studies. Particularly, the overlap of reviews regarding the included individual studies may bias the findings. According to the purpose of this overview, i.e. to synthesise the wide range of interventions and behaviour change techniques used to promote adherence and to summarise the evidence of their efficacy, the overlap of reviews regarding intervention or population was not an exclusion criterion. For considering the overlap of primary studies among the reviews, CL extracted the primary RCTs from the included reviews, identified the unique trials and compared the frequency of their use across the reviews (see results overlap of review and Additional file 2 ). Furthermore, where two or more reviews provided findings on the same technique (e.g. on the efficacy of behavioural graded activities), the overlap of primary studies was assessed specifically for that finding. If the evidence came from the same study, this was taken into account and marked accordingly in Table 5 to avoid double counting and overestimation of evidence.
Assessment of risk of bias within the reviews
CL and PP independently assessed the quality and risk of bias of the systematic reviews included, using the AMSTAR-2 tool [ 26 ]. Any discrepancy was discussed and resolved by consensus. AMSTAR (A MeaSurement Tool to Assess systematic Reviews) was developed to evaluate systematic reviews of randomised trials. The AMSTAR-2 revision enables a more detailed assessment of systematic reviews which may also include non-randomised studies of healthcare interventions. The applied AMSTAR-2 checklist consists of 16 items, whereof seven are classified as critical, and the appraisal results in an overall confidence rating distinguishing between critically low, low, moderate or high [ 26 ]. In addition, the overall confidence in the review was stipulated by the number of positive assessments in relation to the applicable domains (depending if meta-analysis was performed or not) and considering whether an item represents a critical domain or not [ 26 ].
Synthesis methods
Panoramic meta-analysis.
Among the included reviews, there were four meta-analyses [ 7 , 16 , 27 , 28 ], which were pooled as a panoramic meta-analysis based on the reported effect sizes and standard errors using IBM SPSS Version 29 (IBM Corp., Armonk, NY, USA). All four meta-analyses used the standardized mean difference as effect size. Standard errors were calculated from the reported 95% CI as \(\frac{\mathrm{upper bound }-\mathrm{ lower bound}}{3.92}\) . Inverse variance was used to weight the meta-analyses, statistical heterogeneity was assessed by I -squared and a fixed-effects model was selected based on the absence of statistical heterogeneity of true effects. Eisele et al. [ 7 ] included 15 primary trials that examined the effect of BCTs on physical activity adherence. They pooled results for medium-term (3–6 months) and long-term (7–12 months) interventions, from which we selected the medium-term model that best matched the eligibility criteria of the other included meta-analyses. Levack et al. [ 27 ] included nine primary trials that examined the effect of goal-setting strategies on engagement in rehabilitation. Among models with other outcomes, we selected this model because it best matched the aim of this overview, and it was most consistent with the outcomes of the other included meta-analyses. McGrane et al. [ 28 ] included six primary trials, representing 378 subjects that examined the effects of motivational interventions on physiotherapy session attendance. They reported another model with perceived self-efficacy as an outcome, but we selected the attendance model because it best matched the aim of this overview, and it was most consistent with the outcomes of the other included meta-analyses. Nicolson et al. [ 16 ] included two primary trials that examined the effect of booster sessions on self-rated adherence. Results were summarized by a forest plot and publication bias was assessed graphically by a funnel plot, although the small number of individual meta-analyses included limits its interpretability. Alpha was set at 0.05.
Narrative synthesis
The narrative synthesis was performed by CL in constant dialogue with and verification of PP. Guided by the research questions, the narrative synthesis of the extracted data was manifold. First, we explored the heterogeneity of interventions, measures and adherence-related outcomes across and within the reviews using the data extraction table. Definitions and measures of adherence were compared among the reviews and discussed. Second, analysis of the descriptions of the interventions and their respective components/techniques, their theoretical underpinning and their objectives was used to classify the interventions according to different types of intervention, namely the informational/educational, the cognitive/behavioural/motivational and the relational/psychosocial intervention. Consequently, for each type of intervention, the results on the efficacy were narratively synthesised. In addition, reported differences in efficacy among medical conditions, theoretical underpinnings and physiotherapeutic settings were summarised based on the data extraction table. Third, the results on the efficacy of the interventions and BCTs were further summarised in a table and then restructured according to the evidence level as reported in the systematic reviews and the confidence in the reviews as analysed by the AMSTAR-2. Therefore, the levels of evidence were extracted as reported in the reviews, which are based on different evidence appraisal schemes: GRADE (high, moderate, low, very low certainty of evidence), Cochrane Collaboration Back Review Group Evidence Levels (strong, moderate, conflicting, limited, no evidence) and self-developed tools. Afterwards, they were compared for the respective intervention/technique across the relevant reviews, considering the confidence in the review and the comprehensiveness of the review as well. The levels of evidence are presented in the table with the categories high, moderate, low and very low. The efficacy supported by the evidence is also based on the results reported in the reviews. In case of overlapping reviews or discrepancies between the reviews, the primary studies were consulted. The category yes refers to results of merely positive effects, and inconsistent refers to findings of positive and no effects of the intervention (techniques) analysed. The category no indicates that the intervention was not efficacious. No negative effects (i.e. favouring the control condition) were reported for the intervention (techniques) shown.
The reporting of findings followed the PRIOR reporting guideline for overviews of reviews of healthcare interventions [ 29 ].
Study selection results
Of the 187 records screened, 19 were included (see Fig. 1 ). Main reasons for exclusion were not a systematic review of RCTs ( n = 79), adherence not the primary outcome ( n = 60), and lack of physiotherapy relevance ( n = 39) (see Fig. 1 ).
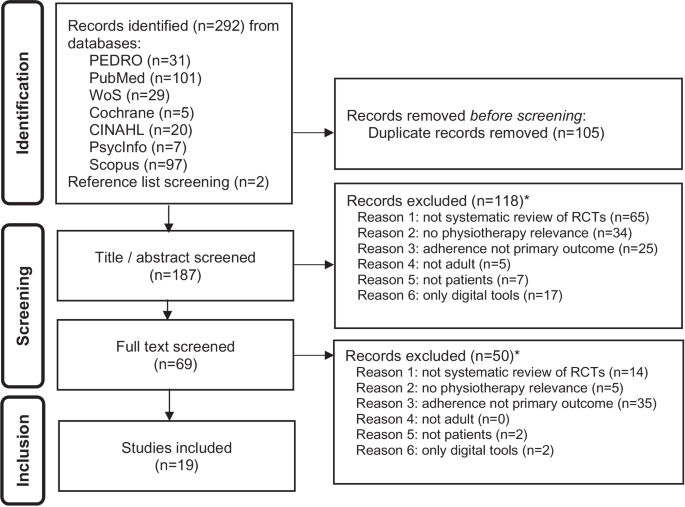
Flow diagram, based on PRISMA [ 24 ] and PRIOR [ 29 ] guidelines. Legend: *Multiple reasons for exclusion were possible
Characteristics and diversity of included reviews
The selection strategy resulted in a broad heterogeneity of included reviews. The 19 included reviews differed in their eligibility criteria of the primary studies as well, resulting in substantial clinical diversity, i.e. the inclusion of heterogenous conditions, intervention types and settings (see Table 2 ) and methodological diversity, i.e. the variability in study design, outcome measurements and risk of bias (see Tables 3 , 4 and 5 ). Musculoskeletal diseases [ 6 , 7 , 17 , 30 , 31 , 32 ] and pain [ 13 , 16 , 33 , 34 , 35 ] were the most investigated medical conditions. Those reviews that did not limit their search to a specific disease [ 12 , 27 , 28 , 36 , 37 , 38 , 39 , 40 ] yielded predominantly studies on musculoskeletal diseases. All reviews included adults only (18 and older). One focused on elderly (65 and older) people [ 40 ] and one on older (45 and older) adults [ 16 ]. Fourteen of the 19 reviews analysed RCTs only [ 6 , 7 , 16 , 17 , 27 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 40 ]; one also included besides RCT cohort studies [ 13 ] and three [ 12 , 37 , 38 ] also included any other quantitative study design (see Table 3 ). Four reviews performed a meta-analysis [ 7 , 16 , 27 , 28 ], and two studies were Cochrane Reviews [ 27 , 35 ]. Four reviews [ 6 , 7 , 17 , 40 ] analysed the use of BCTs and rated the interventions according to a BCT taxonomy [ 8 ].
Results of the individual reviews
The 19 reviews contained a total of 205 unique RCTs. Table 3 shows the main results of each review.
Results of quality assessment and confidence in the reviews
The critical appraisal with the AMSTAR-2 tool (see Table 4 ) showed that four reviews were rated with moderate to high quality [ 7 , 16 , 27 , 35 ], whereas all others resulted in a critically low to low overall confidence in the review. Frequent shortcomings were not explaining the reasons for the inclusion of primary study designs, and an insufficient discussion of the heterogeneity observed. Furthermore, as many reviews did not explicitly mention a pre-established, published or registered protocol or study plan, it is uncertain whether the research followed a pre-specified protocol and whether there were changes and/or deviations from it, and, if so, whether decisions during the review process may have biased the results [ 26 ].
Risk of bias and evidence assessment within reviews
The reviews used various approaches to appraise the evidence, particularly the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) system [ 13 , 16 , 26 , 27 ], the evidence levels by the Oxford Centre for Evidence-Based Medicine [ 28 ] or the system by Cochrane Collaboration Back Review Group [published by 25,30] [ 31 , 32 , 33 , 34 ]. Three reviews modified existing or developed their own tool or checklist [ 12 , 35 , 36 ]. For the assessment of the risk of bias and/or quality of the individual studies, the reviews used the following tools: PEDro Scale [ 7 , 13 , 26 , 32 , 37 ], Cochrane Collaboration Back Review Group Quality Assessment Tool [ 31 , 34 ], Cochrane Risk of Bias criteria [ 6 , 16 , 17 , 27 , 33 , 37 , 38 , 39 ], the Delphi List [ 40 ] or modified or developed own tools [ 12 , 35 , 36 ].
A recurring concern regarding potential performance bias was the lack of therapist blinding, which is almost impossible to implement in this research field [ 7 ]. Attrition bias, due to low sample size or drop-outs, and measurement bias, due to the mere use of subjective measures, were also highlighted in the reviews. Another concern was the availability and selection of adequate control groups. Control groups, such as usual practice, unspecific exercise group or alternative intervention commonly include varying numbers of BCTs which must be considered when assessing and comparing contents of interventions [ 7 ]. The comparability of the intervention and control group regarding adherence-related outcomes is further hindered by poor descriptions of the intervention, uncertainty about treatment fidelity and implementation processes, varying competences and proficiency of the therapist, and the diverse translation of theoretical models and use of intervention techniques [ 7 , 34 , 39 ]. Rhodes and Fiala [ 12 ] pointed out that procedures of RCTs, such as several pre-screenings and measurement batteries, may lead to a potential self-selecting of only the most motivated individuals. This may limit the ability to compare intervention to the control group, as both groups are (already) highly motivated, and to detect changes, due to the already high motivation and disposition to adhere. This may explain in part, that the reviews reported many studies that failed to provide evidence for intervention efficacy on adherence. In addition, the restricted timeline (limited duration for observation and follow-up) of the studies may confound/skew the results, as drop-out may occur shortly after the end of the study and long-term adherence is not measured [ 12 ].
Overlap of reviews
The 19 reviews included from 3 to 42 individual RCTs. In sum, the reviews included 261 RCTs (multiple publications on the same trial were counted as one; thus, the number of trials was counted), whereby 34 trials were included in various reviews (see Additional file 2 , Overlap of reviews), resulting in 205 unique RCTs. Of these 34 trials included in multiple reviews, 25 were included in two different reviews. The following trials were included more than twice: Basler et al. 2007 (8x), Friedrich et al. 1998 (7x), Schoo et al. 2005 (4x), Vong et al. 2011 (4x), Asenlof et al. 2005 (3x), Bassett and Petrie 1999 (3x), Brosseau et al. 2012 (3x), Bennell et al. 2017 (3x), Gohner and Schlicht 2006 (3x) and Duncan and Pozehl 2002, 2003 (3x).
In total, the overlap of primary trials in the reviews is considered low; except among reviews [ 27 , 39 ] and among reviews [ 12 , 16 , 28 , 30 ]. Two reviews [ 27 ] and [ 39 ] were conducted by the same authors, within the same field, i.e. goal planning and setting, however with a different approach and research question. Reviews [ 12 , 16 , 28 , 30 ] have a considerable amount of overlap. Still, each of these reviews included unique RCTs, not analysed in any of the other reviews, and they do focus on different research questions, foci and analyses. Therefore, we did not exclude an entire review due to an overlap of studies.
Synthesis of results
The synthesis focused on answering the research questions. We began by presenting the narrative synthesis findings on how adherence was measured, what types of intervention and BCTs were investigated, and which theoretical underpinnings were reported. Afterwards, we synthesised the evidence on the efficacy of the interventions and BCTs, both meta-analytically and narratively.
Measures of adherence and related outcomes
The reviews included studies with a heterogeneous use, breadth and measures of adherence. Mostly, they refer to adherence as the extent to which a person’s behaviour corresponds with treatment goals, plans or recommendations ([ 30 ],cf. [ 5 ]). McLean and colleagues [ 30 ] expressed that within physiotherapy, the concept of adherence is multi-dimensional and could refer to attending appointments, following advice or undertaking prescribed exercises. The terms adherence and compliance were sometimes used interchangeably, referring to the degree of treatment attendance or accomplishment of physical activity levels, participation and recommendations, irrespective of how the treatment goals and plans were established. Yet, for definition purposes, the distinction between agreed and prescribed goals and plans was occasionally used in the reviews to distinguish adherence from compliance .
For analytical purposes, adherence was frequently dichotomised, establishing a cutoff point or percentage used to distinguish adherence from non-adherence. One was considered adherent, for example, if he/she achieved more than 70% or 80% of the targeted, recommended or prescribed sessions. Few studies graded the degree of adherence according to multi-categorical cut-off points (e.g. very low, low, moderate and high adherence). Only in one review [ 13 ], one study was named that distinguished a certain fluctuation in the adherence pattern, i.e. Dalager et al. [ 41 ] included besides the minutes exercised in a week the regularity of participation, distinguishing regular from irregular participation. Self-reported diaries, exercise logs and attendance lists were the most commonly used data recording instruments [ 33 , 35 , 37 ]. Adherence to home-based programmes was mainly measured with self-reported diaries, which are problematic as the only source, due to poor completion rates, and the possibility of inaccurate recall and self-presentation bias [ 18 , 33 ]. Digital devices (e.g. accelerometers or pedometers) may be used additionally to measure adherence; however, their use may also be problematic, as they require certain adherence to a systematic use of the device and the mere use of the device also may increase adherence [ 18 , 33 ]. One study reported the use of the Sport Injury Rehabilitation Adherence Scale (SIRAS) [ 42 ], which measures the patients’ degree and manner of participation in a session and compliance with the therapist’s instructions and plan. Thus, it does not measure adherence over a certain period of time nor adherence to recommendations or home-based exercise, but it can be used to assess the intensity of rehabilitation exercises, the frequency with which they follow the practitioner’s instructions and advice, and their receptivity to changes in the rehabilitation programme during that day’s appointment [ 42 ].
Interventions used to promote adherence
The reviews included a wide range of different interventions, which we grouped into three different intervention types:
Information provision and patient education were investigated in seven reviews [ 12 , 13 , 30 , 31 , 33 , 34 , 36 ], including (i) video- and audio-assisted patient education, (ii) phone calls, (iii) use of supporting materials and spoken or graphically presented information or (iv) other didactical interventions. Patient education has been defined as ‘any combination of learning experiences designed to facilitate voluntary adoption of behaviour conducive to health’ [ 43 ]. Niedermann et al. [ 31 ] distinguished between ‘purely’ educational programs based on knowledge transfer and psychoeducational programs. In the latter, motivational techniques and shared knowledge-building processes are added to the educational programme, which is done similarly in health coaching [ 34 ], and thus also relate to the cognitive, behavioural and relational/psychosocial interventions.
Cognitive and behavioural motivational interventions were relating frequently to cognitive-behavioural and social-cognitive theories, and applied (i) behavioural graded exercise; (ii) booster sessions, refresher or follow-up in situ by the therapist or via phone call; (iii) behavioural counselling (focusing on readiness to change); (iv) psychoeducational counselling; (v) supervision; (vi) (unspecified) motivational intervention; (vii) positive reinforcement; (viii) action and coping planning; and (ix) goal setting [ 7 , 12 , 13 , 16 , 27 , 28 , 30 , 32 , 33 , 34 , 39 ].
Relational and psychosocial interventions were less investigated overall. Related aspects included (i) social support; (ii) patient-centeredness, in particular patient-led goal setting, motivational interviewing and the therapeutic or working alliance; and (iii) emotional components [ 6 , 13 , 17 , 33 ].
The included reviews focused either on one particular or several types of intervention. Particularly, four reviews [ 6 , 7 , 17 , 40 ], which used a BCT taxonomy to analyse the interventions of the primary studies, described BCTs relating to all three intervention types. While this distinction of different types of interventions is useful to showcase the range of diverse interventions and techniques, they do have a great overlap and include a mix of different BCTs. For example, the way of facilitation of information, supervision or goal setting was approached differently according to the relational approach, i.e. being more instructive, directive or more collaborative, participatory, patient-led ([ 31 ],cf. [ 34 ]).
Theoretical underpinning of interventions
No review focused on only one theoretical foundation or excluded studies based on any theoretical model or not underpinning the intervention. In total, the reviews included studies with diverse theoretical models and varying degrees of theoretical underpinning. References to the cognitive behavioural theory (CBT) and to the social-cognitive theory were frequent in the individual studies. Furthermore, the self-determination theory, the transtheoretical model, the health belief model, the social learning theory and the socioemotional selectivity theory were used in some individual studies (cf. [ 11 ]). The heterogeneity in the theoretical underpinning of the interventions is reinforced by the given overlap of the theories and models (cf. [ 11 ],[ 28 ]) and various BCTs are key components of several theories [ 17 ]. Furthermore, theories were not used enough to explicitly inform and underpin interventions and they were translated into practise in different ways; thus, interventions based on the same theory may differ substantially [ 17 ].
The BCT Taxonomy v1 [ 8 ], which relates to various theoretical models, was used in four reviews [ 6 , 7 , 17 , 40 ] to identify BCTs in interventions in a standardized manner. The Behaviour Change Wheel [ 44 ], which is linked to the BCT Taxonomy v1, was referred to in one review [ 40 ] pointing to its usefulness for designing a behaviour change intervention. The number of BCTs used appears to be relevant, as interventions using a higher number (≥ 8) of BCTs achieved a significant effect (pooled SMD = 0.29, 95% CI 0.19–0.40, p < 0.001), whereas interventions using a lower number (< 8) of BCTs did not (pooled SMD = 0.08, 95% CI -0.11 to 0.27, p = 0.41).
Overall efficacy and heterogeneity according to the panoramic meta-analysis
Although there was statistical heterogeneity ( I 2 from 41 to 63%) between the primary studies included in each meta-analysis [ 7 , 16 , 27 , 28 ], there was no heterogeneity between the pooled effects of these four meta-analyses ( I 2 0%). This means that all variability in the effect size estimates (SMD from 0.20 to 0.39) was attributable to sampling error, but there was no variability in the true effects. Although the interventions were selected based on different eligibility criteria (BCTs, goal-setting strategies, motivational interventions and booster sessions), they appear to be very similar in terms of the effects they trigger. There was no overlap between the primary trials included in the meta-analyses. The pooled SMD was 0.24 (95% CI 0.13, 0.34) (Fig. 2 ). Effect size estimates were somewhat larger in those meta-analyses with less weight in the model (i.e. due to a larger standard error). However, no obvious publication bias could be detected in the funnel plot (Fig. 3 ). Sensitivity analyses in the meta-analysis in Eisele et al. [ 7 ], considering only studies with PEDro scores of 6 or more, revealed slightly lower effect sizes but still statistically significant effect sizes regarding medium-term effects (SMD PEDro>=6 0.16, 95% CI 0.04–0.28, p < 0.01 versus SMD all 0.20, 95% CI 0.08–0.33, p < 0.01) and higher numbers of BCTs (SMD PEDro>=6 = 0.26, 95% CI 0.16–0.37, p < 0.001 versus SMD all = 0.29, 95% CI 0.19–0.40, p < 0.001), indicating that low-quality studies may tend to overestimate the efficacy ([ 7 ],cf. [ 31 ]).
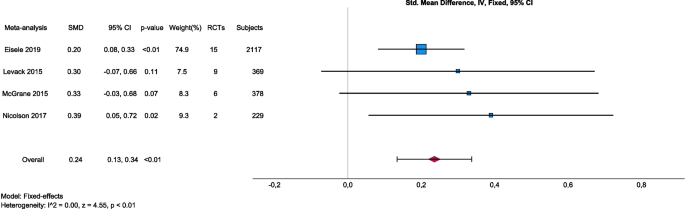
Forest plot of panoramic meta-analysis: interventions aiming at improving adherence, adherence-related outcomes
Legend: Eisele 2019. Intervention: Interventions aiming at improving physical activity levels or adherence, containing at least one BCT. Comparison: Usual care, minimal intervention, placebo or no intervention. Outcome: Any measure of physical activity level or adherence to any kind of physical activity. Levack 2015. Intervention: Goal setting (with or without strategies to enhance goal pursuit). Comparison: No goal setting. Outcome: Engagement in rehabilitation. McGrane 2015. Intervention: Motivational interventions as part of a package, psychological strategies, theory-based instructional manuals, Internet-based behavioural programmes and relapse prevention, and re-inforcement strategies. Comparison: Any comparison (not specified). Outcome: Attendance at physiotherapy sessions/exercise classes. Nicolson 2017. Intervention: Booster sessions to increase adherence to therapeutic exercise. Comparison: Contextually equivalent control treatments. Outcome: Self-rated adherence
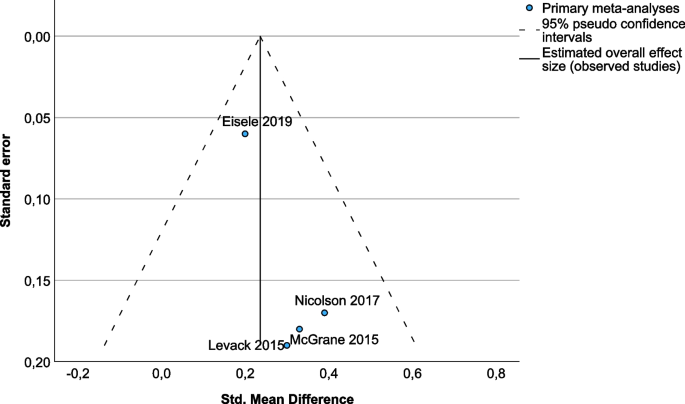
Funnel plot of publication bias
Efficacy of informational and educational interventions
The results of five—partly overlapping—reviews [ 12 , 30 , 31 , 34 , 36 ] showed, with a very low evidence base, that interventions that primarily aimed at information provision and knowledge transfer to the patient had limited efficacy on adherence-related outcomes. There was conflicting evidence and inconsistent efficacy of video-assisted patient education [ 36 ] and individualised exercise videos [ 12 , 30 ] in modifying behaviour or adherence. However, the authors identified the format in which the educational information is presented and the complexity of the addressed behaviour as crucial factors [ 36 ]. Videos that provide only spoken or graphically presented health information are inappropriate tools for changing patient behaviour. However, videos with a narrative format appear to be a powerful education tool [ 36 ]. Low evidence based on one study [ 12 , 30 ] indicates that additional written information seems superior to verbal instructions alone (mean difference between groups 39.3%, p < 0.001). With a high overlap of studies, two reviews [ 30 , 31 ] showed that there is limited evidence for long-term effects of patient education targeting knowledge acquisition. While the informative and instructive educational approach is an essential part of patient education, patient education often involves more than the transfer of knowledge [ 30 , 31 , 34 ]. Niedermann et al. [ 31 ] compared educational and psychoeducational interventions and provided arguments in favour of psychoeducational approaches that enrich patient education with motivational strategies and techniques (cf. [ 34 ]).
Efficacy of cognitive and behavioural motivational interventions
Several (though partly overlapping) reviews [ 12 , 16 , 28 , 30 , 33 , 37 ] examined studies on additional motivational interventions that were based on social-cognitive or cognitive-behavioural theories. McGrane et al. [ 28 ] concluded heterogeneity of motivational interventions, outcomes and measurements as potential causes for conflicting evidence regarding effects on exercise attendance and PT adherence, as they found no significant difference ( p = 0.07) in exercise attendance between additional motivational intervention groups and their controls (pooled SMD 0.33, 95% CI -0.03 to 0.68, I 2 62%), but a significant ( p < 0.01) medium-sized effect of additional motivational interventions on self-efficacy beliefs (pooled SMD 0.71, 95% CI 0.55 to 0.87, I 2 41%). The heterogeneity hindered in this meta-analysis the statistical analysis of subgroups to determine and compare the efficacy of different components and approaches to motivational interventions [ 28 ]. Another meta-analysis [ 16 ] found moderate-quality evidence that booster sessions with a physiotherapist helped people with hip/knee osteoarthritis to better adhere to therapeutic exercise (pooled SMD 0.39, 95% CI 0.05 to 0.72, p = 0.02, I 2 35%). Moderate evidence for the efficacy of supervision (2 studies, n = 193) favouring adherence was shown [ 13 , 33 , 35 ].
In four reviews [ 16 , 32 , 33 , 35 ], four unique high-quality trials supported the use of motivational strategies and behavioural graded exercise to improve adherence to exercise (effect sizes 0.26–1.23)[ 16 ]. Behavioural graded exercise includes a preset gradual increase of the physical activity through facility-based interventions followed by booster sessions [ 45 ] and uses principles of operant conditioning and self-regulation [ 16 ].
While cognitive behavioural programmes seem superior to exercise alone for short-term adherence and clinical attendance [ 30 ], behavioural counselling focusing on readiness to change, action and coping plans and/or audio/video exercise cues seem not to improve adherence significantly [ 16 ]. Holden [ 34 ] concludes inconsistent evidence for health coaching based on the transtheoretical model of change, with one RCT showing some efficacy on exercise compliance (SMD = 1.3). However, the frequently referred to study of Göhner and Schlicht [ 46 ], who analysed a cognitive-behavioural intervention with a strong emphasis on action and coping planning [ 12 ], showed no difference between experimental and control groups in the first 11 weeks, but a significant difference 5 months later on behaviour (SMD = 0.83) as well as differences over all time-points on self-efficacy (interaction effect of time by group, F (3, 43) 10.36, p < 0.001, n = 47) favouring the intervention [ 46 ]. Motivational interventions, including positive reinforcement, increased (i) adherence to home exercise in one RCT [ 33 ], (ii) reported frequency of exercise in two RCTs [ 35 ] and (iii) self-efficacy beliefs in two RCTs, in the short-term (SMD = 1.23) and in the long-term (SMD = 0.44) ([ 16 ],cf. [ 30 ]). Self-efficacy beliefs relate to the trust in one’s capacities/competencies to cope with daily demands [ 47 ] and are associated (moderate evidence) with adherence [ 13 , 48 ].
Levack et al. [ 27 ] conclude some evidence that goal planning/setting improves engagement in rehabilitation (motivation, involvement and adherence) over the duration of the programme (9 studies, 369 participants, SMD 0.30, 95% CI -0.07 to 0.66). Furthermore, they show a low-quality evidence for effects on patient self-efficacy from more structured goal setting compared to usual care with or without goal setting (2 studies, 134 participants; SMD 0.37, 95% CI 0.02 to 0.71) and from goal setting compared to no goal setting (3 studies; 108 participants; SMD 1.07, 95% CI 0.64 to 1.49). The review did not detect differences in efficacy between the approach taken to goal planning. However and similar to patient education [ 34 ], the review authors argue that the lack of clarity about the effects and the low evidence is due to the heterogeneity of the implementation of goal planning, lack of detailed descriptions of the goal-setting process in the intervention groups but also in the control groups, and methodological flaws ([ 27 , 39 ],cf. [ 13 ]).
The BCTs from the cluster goals and planning showed various positive effects, although not fully consistently [ 6 , 7 , 40 ]. Eisele et al. [ 7 ] identified goal setting (behaviour) , problem-solving , goal setting (outcome) , action planning and reviewing behaviour goal(s) as often used in non-effective interventions but also in effective ones. A trial that showed negative effects included problem-solving and goal setting (outcome) as well. Room et al. [ 40 ] found one study on older people and Thacker et al. [ 6 ] two home-exercise-related studies that used BCTs from the goals and planning cluster (i.e. problem-solving and action planning), but none of the studies found differences in favour of the intervention. Willett et al. [ 17 ] adjusted the BCTv1 taxonomy to differentiate patient-led and therapist-led goal setting and showed that patient-led goal setting (behaviour) achieved among the highest efficacy ratios across time points.
Efficacy of relational and psychosocial interventions
The BCT Social Support (unspecified) refers to ‘advise on, arrange or provide social support (e.g. from friends, relatives, colleagues, ’buddies’ or staff) or non-contingent praise or reward for the performance of the behaviour . It includes encouragement and counselling, but only when it is directed at the behaviour’ [8, Supplementary Material]. Eisele et al. [ 7 ] identified this BCT in 19 interventions and 10 control conditions. They found this BCT in three trials supporting efficacy and in seven trials supporting inefficacy. In contrast, Thacker et al. [ 6 ] found this BCT in all effective interventions but not in the non-effective ones. Willet et al. [ 17 ] concluded from their review that this BCT has among the highest efficacy ratios across time points to promote adherence to physical activity.
Social support may come along with monitoring and feedback, which can be graphically or narratively presented by the therapist. Willett et al. [ 17 ] recommend that self-monitoring (e.g. activity diaries), feedback on behaviour as well as social support should be used—beyond monitoring purposes—for explicit intervention purposes (e.g. to foster self-efficacy beliefs). Feedback on behaviour alone does not seem to be efficacious [ 6 ], but feedback can be efficacious for instance in combination with social support or goal setting and planning [ 17 , 40 ].
Patient-centred approaches were also included in the relational/psychosocial intervention type. Motivational interviewing, which is a collaborative, patient-centred communication style to promote behaviour change [ 49 ], was used in three studies, indicating positive effects on exercise compliance, physical activity and exercise at home in two trials, whereas no effect in a pilot study [ 28 ]. There is low evidence from three RCTs for positive effects of the therapist-patient alliance on global assessments; however, the efficacy on adherence-related outcomes is unclear [ 36 ]. The terms working or therapeutic alliance refer to the social connection or bond between therapist and patient/client, including reciprocal positive feelings, (assertive) communication, empathy, and mutual respect as well as collaboration, shared decision-making, agreement on the treatment goals and tasks [ 36 , 50 ]. The therapeutic alliance is a patient-centred approach as well. Patient-led goal setting was more often a component within efficacious interventions than therapist-led goal setting [ 17 ].
None of the included reviews focused specifically on affective interventions. However, some interventions relate to affective components, for example patient-led goal setting or motivational interviewing may cover emotional needs [ 27 ]; health coaching, therapeutic alliance or social support may include emotional support [ 13 , 34 , 35 , 38 ]; monitoring may consider emotional consequences [ 6 ]; or messaging and information provision may include emotional components [ 36 ]. Room et al. [ 40 ] included one RCT [ 51 ], comparing emotionally meaningful messages against factual informational messages, but with no significant differences between the groups.
Efficacy according to the theoretical underpinning
McGrane et al. [ 28 ] provide a narrative analysis of the efficacy of interventions according to the different theoretical underpinnings. In their review, the cognitive-behavioural theory (CBT) was the most popular theory (4 primary studies) and showed to be efficacious in improving self-efficacy and activity limitations, but not consistently regarding attendance and attrition [ 28 ]. The social-cognitive theory was used in three studies, showing improvements in self-efficacy, action and coping planning, and attendance, but conflicting results for exercising in the short and long term. One intervention [ 52 ] based on self-determination theory showed to be efficacious to improve adherence to physical activity. In contrast to McGrane et al. [ 28 ], the reviews [ 12 , 30 , 35 ] point to moderate to conflicting evidence for no or inconsistent efficacy of CBT-based approaches to physiotherapy programmes (see Efficacy of cognitive and behavioural motivational interventions ). Jordan [ 35 ] concluded that the addition of transtheoretical model-based counselling to physiotherapy is no more effective than physiotherapy and a sham intervention (GRADE: High (high quality); Silver). Notably, the interventions may not be representative of the theory described due to diverse translations of the theory into practice and the overlap of the same BCTs among the theories.
Various theories (e.g. the transtheoretical model or the Health Action Process Approach [ 53 ]) and studies [ 54 ] distinguish the action or adoption phase from the maintenance phase at 6 months. Interestingly, Willet et al. [ 17 ] found in total higher short (< 3 months) and long-term (12 months and more) than medium-term (around 6 months) efficacy ratios, pointing to the risk of drop-out when changing from the (short-term) adoption phase to the (long-term) maintenance phase [ 17 ]. Eisele et al. [ 7 ] divided in their meta-analysis the short-term (< 3 months), medium-term (3–6 months) and long-term (7–12 months post-intervention) differently, showing a small medium-term overall effect (pooled SMD 0.20, 95% CI 0.08–0.33, p < 0.01), but no significant long-term effect of interventions comprising BCTs in enhancing physical activity adherence (pooled SMD 0.13, 95% CI 0.02–0.28, p = 0.09).
Efficacy according to the different types of exercise, physiotherapeutic settings and medical condition
In their Cochrane review, Jordan et al. [ 35 ] compared the evidence for the efficacy of different types of exercises and physiotherapy settings. Graded exercise is beneficial for adherence (moderate evidence). The exercise type does not appear to play an important role (moderate evidence). Whether water-based exercise favours adherence is unclear (low evidence and inconsistent results). Furthermore, the supervision of exercising (moderate evidence) is beneficial for adherence, but also self-management programmes improve exercise frequency compared to waiting list or no-intervention control groups (moderate evidence). Exercising individually seems to improve attendance at exercise classes more than exercising in a group (moderate evidence), as individual sessions could be scheduled at more convenient times and missed sessions could be rescheduled, whereas group sessions were scheduled at relatively inflexible times, and missed sessions could not be rescheduled [ 35 ]. However, adding group exercise to a home exercise programme can increase overall physical activity levels (moderate evidence) [ 35 ]. While the results of home- versus clinic-based interventions were conflicting and confounded by the intervention approaches, a combination of home- and clinic-based approaches may be promising [ 12 ] and aligns with the moderate-quality evidence that self-management programmes, refresher or booster sessions with a physiotherapist assist people to better adhere to therapeutic exercise [ 16 ].
No study was identified in the reviews that compared other settings, such as private- and public-funded physiotherapy or primary care and rehabilitation settings regarding adherence outcomes. No review and no study comparing the same educational, motivational, or BCT-based intervention across different conditions were identified.
This overview of systematic reviews addresses adherence in the physiotherapy and therapeutic exercise domain, aiming to summarise the evidence on the efficacy of interventions, to explore heterogeneity and to identify research gaps. The overview of reviews provided an adequate approach to generate answers to the research questions. Nineteen reviews, covering 205 unique trials, were included and narratively synthesised. In addition, four meta-analyses were pooled in a panoramic meta-analysis. The findings provide an overview of the diverse interventions and techniques aiming to enhance adherence, ranging from informational/educational to cognitive/behavioural/motivational and to relational/psychosocial intervention types. Furthermore, it synthesised their efficacy in physiotherapy for adults.
Confidence in the reviews was rated moderate or high in four reviews [ 7 , 16 , 27 , 35 ], but low or very low in the others (Table 3 ). The individual reviews considered the evidence levels as mostly low or very low (Table 4 ; see Risk of bias and evidence assessment ). Table 5 summarizes the evidence on the efficacy of each intervention and technique according to (a) whether the evidence supports efficacy, (b) the evidence level based on the report in the systematic reviews and (c) the confidence in the reviews as assessed with AMSTAR-2. It must be noted that the components of the intervention which caused the efficacy were not always clear. Some interventions lacked detailed definitions and descriptions of the specific BCTs included [ 33 ]. A single technique or mechanism of action was not always identifiable; moreover, various techniques seem to influence each other in such a way that they achieved efficacy only jointly [ 17 , 40 ].
No clear conclusion can be drawn on the efficacy of informational/educational interventions. Five reviews [ 12 , 30 , 31 , 34 , 36 ] showed low evidence for the efficacy of interventions on knowledge acquisition and low evidence for limited short-term efficacy on adherence. Providing knowledge alone seems not enough and should be complemented with supportive material (very low evidence) and combined with other interventions (low evidence). Patient education should also include social-cognitive or cognitive-behavioural approaches, psychoeducational interventions and collaborative processes as it is included in the therapeutic alliance approach [ 31 , 34 , 36 ]. Patient education with a more constructive educational approach builds upon the knowledge of the patient, supporting him/her in exploring and co-constructing knowledge which is very relevant in physiotherapy as research has shown [ 55 , 56 ].
The reviews on additional motivational, cognitive and behavioural interventions showed findings ranging from non-efficacy of behavioural counselling based on readiness to change (with low to moderate evidence) to moderate efficacy for booster sessions and behavioural graded physical activity (with moderate evidence) (see Table 5 ). Overall, a small overall effect size (SMD 0.24) for motivational interventions is indicative of the findings of the panoramic meta-analysis. The four pooled meta-analyses [ 7 , 16 , 27 , 28 ] included studies analysing interventions with a considerable amount of content overlap (e.g. goal-setting and booster sessions are BCTs and often part of motivational interventions), and no statistical heterogeneity of the true effect was found. Nevertheless, the diversity of interventions and techniques included constrain the explanatory power for potential components responsible for the efficacy of adherence. The sensitivity analyses in the meta-analysis of Eisele et al. [ 7 ] indicate that low-quality studies tend to overestimate the efficacy (cf. [ 31 ]). While some evidence exists on short- and medium-term effects of motivational programmes on adherence, no clear evidence for long-term effects can be concluded [ 7 , 30 ]. Furthermore, there is moderate and low evidence that additional motivational interventions and goal planning/setting improve adherence to self-efficacy beliefs [ 27 , 28 , 39 ]. Since self-efficacy beliefs play an important role in motivation and adherence [ 13 , 48 ], the results are relevant for physiotherapists to promote motivation and adherence. Experiencing that one can reach the set goals and manage daily challenges, complemented with feedback and reinforcement from the therapist (or important others), may increase self-efficacy beliefs and human agency [ 48 , 57 , 58 , 59 ].
A closer look at how and in which manner goals and actions are planned and reviewed seems crucial. The patient-led approach was only reported in 5 of the 26 interventions that incorporated the BCT goal setting (behaviour) , although it is associated with greater engagement and achievement than goals which are set by the therapist [ 17 ]. Goal setting and action planning should be informed by the patient’s motives, interests and values in order to promote intrinsic motivation, self-determination and subsequently better adherence ([ 17 ],cf. [ 27 , 28 , 60 , 61 ]). The reviews on the BCTs displayed various positive effects relating to the BCT cluster goals and planning ; however, they point out that the BCT goal setting is not used alone but in connection with several other BCTs. Feedback on outcomes of behaviour , behavioural contract and non-specific reward as well as patient led-goal setting , self-monitoring of behaviour and social support (unspecified) was included in efficacious interventions [ 17 ]. Social support seems to have an important influence on adherence [ 6 , 7 , 17 , 40 ], for example through regular phone-calls or home visits, encouraging messaging, supervision or community-based group programs (cf. [ 1 , 2 , 3 ],[ 37 , 62 ]). Social support also relates to the promotion of self-efficacy beliefs, if it endorses confidence in own abilities and competences [ 6 ].
Some BCTs seem inherent to standard practices of physiotherapy [ 6 ] even though physiotherapists seem to use rather a small number of BCTs [ 15 ]. Control groups also contained BCTs [ 6 , 7 ]; in particular instruction on how to perform a behaviour , generalisation of the target behaviour and social support (unspecified) were frequently coded [ 6 ]. Thus, it seems difficult to identify those BCTs that are (most) efficacious in promoting adherence ([ 7 ],cf. [ 50 ]). Unsurprisingly, the reviews revealed conflicting results and a high risk of bias in the individual studies. However, combining a greater number of BCTs (≥ 8) can be highly recommended, as this achieved a larger effect than interventions using fewer BCTs [ 7 ]. It is fairly unlikely that any single BCT changes adherence [ 6 , 7 , 17 , 40 ]. In that regard, Ariie et al. [ 63 ] argue that not only the amount of BCTs but also the quality, appropriateness and feasibility of the use of the BCTs is crucial.
Meaningful combinations of several BCTs are required. However, the combinations of BCTs may also differ among conditions, personal factors and therapeutic interventions ([ 7 ],cf. [ 63 , 64 ], [ 64 , 65 , 66 ]), and over the time. Two reviews consistently point to the same crucial time point (i.e. after 6 months) when BCT efficacy seems to drop, and more attention is required to maintain adherence [ 7 , 17 ]. Action planning , feedback on behaviour and behavioural practice/rehearsal seem efficacious particularly on short-term. Patient led-goal setting , self-monitoring of behaviour and social support (unspecified) are among those BCTs that seem more efficacious at long-term [ 17 ]. These findings are also in line with findings in non-clinical adults [ 54 ] and with motivational theories (e.g. the Health Action Process Approach [ 53 ]).
Limitations
Conducting an overview of reviews is per se associated with methodological limitations. A limitation is that reviews were analysed and not the original RCTs, which adds further risks of bias domains such as selection, analysis and reporting bias. A specific potential source of bias in overviews of reviews is the overlap of primary studies among the included reviews. The small overlap, caused by a few reviews with similar thematic scope, was controlled for in the data analysis. The substantial non-overlap of primary studies across the reviews reflects the clinical and methodological diversity of the included reviews and showcases the efforts to address (a) motivation and (non-)adherence as complex phenomena and from various perspectives.
Another methodological limitation originates from the search strategies. Considering different health-care systems and delimitations of the physiotherapy profession among countries, divergences among the definitions of terms and the use of diverse approaches to physical therapy, physiotherapy or the therapeutic use of exercise and physical activity, made a clear delimitation in the search strategy and inclusion/exclusion criteria difficult. Therefore, we may have missed out some relevant reviews by reducing our search to the two terms physiotherapy and physical therapy. Equally, we may also have included some aspects that were not primarily investigated for physiotherapists or physical therapists. Including only studies with adults, the findings may not be applicable to promote adherence among children.
While we did not exclude reviews from another language, the search was conducted only in English, which may omit important reviews in other languages. All included reviews (and as far as reported, also the original RCTs) were conducted in economically developed countries; however, social-cultural and context-specific factors influence participation and adherence [ 67 , 68 , 69 , 70 , 71 ]. Furthermore, we are aware that our own cultural background and experiences may have influenced the analysis and synthesis of the results and that conclusions drawn in this overview of reviews may not be suitable for every setting around the world. Therefore, we encourage the readers to critically assess the applicability of the findings to their specific context.
Another gap in coverage of this overview is that interventions that were analysed in RCTs but not included in any systematic review are not considered in this overview. Thus, there may be new or alternative intervention approaches that resulted efficacious but were not covered by this overview. Furthermore, reviews that focused only on the use of digital apps or tools, e.g. virtual reality, gamification, exergames or tele-rehabilitation, were excluded from this overview. Several reviews in this field include adherence-related outcomes, showing potential efficacy as well as limitations of the use of digital tools [ 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 ].
Research gaps, recommendations and measuring adherence
This overview of reviews highlighted some gaps in the existing knowledge. First, there is a lack of clear evidence on the efficacy of the interventions. The use of BCTs in the intervention as well as in the control groups may be a reason for inconsistent findings and conflicting evidence. Furthermore, the clinical and methodological heterogeneity constrains drawing clear conclusions on the efficacy. Second (and related to the previous), interventions are insufficiently described regarding their theoretical underpinning and active ingredients/techniques and thus limit the comparison of interventions. Theoretical underpinnings were used partly and translated into practise differently. Difficulties concerning the derivation or deduction of concrete, practical techniques or strategies from the theories were reported. A broader use of the BCT taxonomies would make interventions more comparable. Recently, the BCT Ontology was published, which claims to provide a standard terminology and a comprehensive classification system for the content of behaviour change interventions, suitable for describing interventions [ 84 ]. Third, there is a need for studies on holistic approaches, complex interventions based on integrative theories and the combination of multiple BCTs. While many theories are based on cognitive and behavioural approaches, affective and psychosocial factors are hardly investigated, overlooked and probably underestimated. Rhodes and Fiala [ 12 ] call for studying the influences of affective attitudes on adherence (e.g. enjoyment and pleasing behaviour) which may oppose the more cognitive, instrumental attitudes (e.g. the utility of behaviour). Jordan et al. [ 35 ] refer to a meta-analysis in another therapeutic regime [ 85 ] to explicit the potential efficacy of affective interventions (e.g. appealing to feelings, emotions or social relationships and social supports) in combination with educational and behavioural interventions on patient adherence [ 35 ]. Fourth, more research in patient-led approaches to goal setting and action planning and the relationship of patient-centeredness to adherence is promising [ 60 , 61 , 86 , 87 ].
Fifth, the reviews reported many studies that failed to provide evidence for intervention efficacy on adherence, particularly on long-term adherence. There is a need for prolonged observation to investigate long-term effects on adherence. Probably, intervention or follow-up interventions (e.g. booster sessions) must also be prolonged or repeated to avoid drop out to medium-term follow-ups (around 6 months) and to maintain participation. Sixth, studies should pay more attention to the actual efficacy of adherent behaviour on the desired therapeutic outcomes.
Seventh, another research gap lies in the analysis of the potential variation of the intervention efficacy across medical conditions, physiotherapeutic settings, personal characteristics (e.g. age, gender, sociocultural background) and dispositions (e.g. motives, affective attitudes, previous behaviour) and diverse context-related factors. Huynh et al. [ 79 ] showed for the case of multiple sclerosis that the efficacy of BCTs is not investigated in all disease stages or throughout the disease course; participants with mild-to-moderate level disability were more frequently included in the studies (cf. [ 18 ]). Ariie et al. [ 73 ] stated that the response to BCTs may be different according to the condition (cf. [ 76 ]). On the one hand, studies analysing the use of the same intervention or same combination of BCTs in different intervention groups (according to the categories mentioned above) could be beneficial for comparison purposes. On the other hand, studies should analyse how to find the ‘right’ (ideally, the ‘most efficacious’) adherence promotion intervention for the patient or target group. Qualitative studies may explore adequate combinations of BCTs and contribute to the understanding of complex intervention processes. The findings showcased that different interventions and BCTs may contribute to adherence and that the BCT Taxonomy defines a wide range of techniques, providing the physiotherapists with an overview of which techniques are useable and thus may inspire and support them to develop additional interventions and to enrich their current physiotherapeutic practise. The physiotherapist may use this knowledge to tailor interventions in a patient-centred manner to promote adherence, and to adapt to the condition, characteristics, dispositions and context-related factors of the patient. Hence, experimental studies could compare the efficacy of tailored to not-tailored interventions.
Finally, the outcome adherence should be better defined and holistically assessed. The definition of adherence (as the extent to which a person’s behaviour corresponds with treatment goals or plans) and calculation of adherence rates (by reported exercise or attended sessions divided by the recommended or prescribed exercise or sessions) are simplifying a complex phenomenon. The average or the percentages of attended or completed sessions do not picture interruptions, regularity or periods of more and less adherence. Attendance regularity can change over the time and different participation and fluctuation patterns can be identified [ 88 , 89 ]. For example, an adherence rate of 50% can imply (a) that a person attended regularly every second session throughout the period of observation or (b) that a person attended all sessions of the first half of the observation period and then stopped attending. The underlying reasons and motivational factors may be quite different in these two cases. Besides assessing participation and fluctuation patterns, the three dimensions of the SIRAS scale [ 42 ], i.e. frequency, intensity and reciprocity, could be considered for a holistic account of adherence. The findings of this overview emphasized the importance of a patient-led goal setting and planning, which includes a shared decision-making process and the mutual agreement to adhere to the jointly established plan (cf. WHO definition of adherence, [ 5 ]). The measurement of adherence should be able to distinguish a patient-led approach from a therapist-led approach (cf. [ 17 ]) and to appraise the extent of a shared decision-making process. In conclusion, a holistic approach to measure adherence in physiotherapy may include measures of the frequency of attendance/exercising (e.g. attended sessions out of the prescribed/recommended sessions), the regularity of participation and fluctuation (e.g. timeline with pauses and interruptions, visualizing more and less adherent periods), the intensity of attendance/exercising (e.g. the number or the increment of exercises and repetitions performed in comparison to the plan), reciprocity and fidelity to the agreed goals and plan (e.g. therapist’s and patient’s subjective appraisal of the degree of accomplishment of the agreed plan) and persistence/perseverance over the time (e.g. measuring volition via questionnaires or rating persistence in participation in spite of the experienced challenges and barriers).
We conclude that moderate certainty of evidence supports that (i) additional motivational interventions and behaviour change programmes can increase adherence and patients’ self-efficacy beliefs and (ii) interventions applying BCTs increase adherence, particularly when using a greater number of BCTs and combining various BCTs, and particularly on short to medium term. The BCTs’ patient-led goal setting , self-monitoring of behaviour and social support seem promising to promote maintenance; (iii) graded activities, booster sessions with a physiotherapist and supervision foster adherence.
There is low certainty of evidence that (i) goal setting and planning improves adherence to treatment regimens, particularly if a patient-centred approach is taken; (ii) motivational interventions including various techniques, such as positive reinforcement, social support, monitoring or feedback, can foster adherence; (iii) social support seems to play an important role in promoting adherence; however, evidence is low as this BCT is frequently found in the control group; and (iv) information provision and transfer of knowledge to the patient may improve adherence-related outcomes when combined with motivational techniques, as in psychoeducational programmes. Additional written information is superior to verbal instructions alone; (v) a combination of home-based exercise programmes with clinical supervision, refresher or booster sessions, or/and self-management programmes seems promising to increase adherence.
Regarding the implications for future research, a holistic approach to measure adherence in physiotherapy and the investigation of clearly defined interventions combining multiple BCTs is recommended.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Overview of reviews, umbrella review and reviews of reviews are considered as synonyms in this article (cf. [ 19 ]).
Abbreviations
Behaviour change technique
Cognitive behavioural/cognitive behavioural theory
Control/comparator group
Grades of Recommendation, Assessment, Development and Evaluation
Intervention/experimental group
Physical activity
Preferred Reporting Items for Overviews of Reviews
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
Physiotherapy
Randomised controlled trial
Standardised mean difference
Systematic review
Essery R, Geraghty AW, Kirby S, Yardley L. Predictors of adherence to home-based physical therapies: a systematic review. Disabil Rehabil. 2017;39:519–34.
Article PubMed Google Scholar
Jack K, McLean SM, Moffett JK, Gardiner E. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther. 2010;15:220–8.
Article PubMed PubMed Central Google Scholar
Peek K, Sanson-Fisher R, Mackenzie L, Carey M. Interventions to aid patient adherence to physiotherapist prescribed self-management strategies: a systematic review. Physiotherapy. 2016;102:127–35.
Bullard T, Ji M, An R, Trinh L, Mackenzie M, Mullen SP. A systematic review and meta-analysis of adherence to physical activity interventions among three chronic conditions: cancer, cardiovascular disease, and diabetes. BMC Public Health. 2019;19:636.
World Health Organization. Adherence to long-term therapies: evidence for action. World Health Organization; 2003. Available from: https://apps.who.int/iris/handle/10665/42682
Thacker J, Bosello F, Ridehalgh C. Do behaviour change techniques increase adherence to home exercises in those with upper extremity musculoskeletal disorders? A systematic review. Musculoskeletal care. 2020;19(3):340-62.
Eisele A, Schagg D, Kramer L, Bengel J, Gohner W. Behaviour change techniques applied in interventions to enhance physical activity adherence in patients with chronic musculoskeletal conditions: a systematic review and meta-analysis. Patient Educ Couns. 2019;102:25–36.
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81–95.
Davis R, Campbell R, Hildon Z, Hobbs L, Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev. 2015;9:323–44.
Michie S, Johnston M. Theories and techniques of behaviour change: developing a cumulative science of behaviour change. Health Psychol Rev. 2012;6:1–6.
Article Google Scholar
Rhodes RE, McEwan D, Rebar AL. Theories of physical activity behaviour change: a history and synthesis of approaches. Psychol Sport Exerc. 2019;42:100–9.
Rhodes RE, Fiala B. Building motivation and sustainability into the prescription and recommendations for physical activity and exercise therapy: the evidence. Physiother Theory Pract. 2009;25:424–41.
Areerak K, Waongenngarm P, Janwantanakul P. Factors associated with exercise adherence to prevent or treat neck and low back pain: a systematic review. Musculoskeletal Science and Practice. 2021;52.
Husebø AML, Dyrstad SM, Søreide JA, Bru E. Predicting exercise adherence in cancer patients and survivors: a systematic review and meta-analysis of motivational and behavioural factors. J Clin Nurs. 2013;22:4–21.
Kunstler BE, Cook JL, Freene N, Finch CF, Kemp JL, O’Halloran PD, et al. Physiotherapists use a small number of behaviour change techniques when promoting physical activity: a systematic review comparing experimental and observational studies. J Sci Med Sport. 2018;21:609–15.
Nicolson PJA, Bennell KL, Dobson FL, Van Ginckel A, Holden MA, Hinman RS. Interventions to increase adherence to therapeutic exercise in older adults with low back pain and/or hip/knee osteoarthritis: a systematic review and meta-analysis. Br J Sports Med. 2017;51:791–9.
Willett M, Duda J, Fenton S, Gautrey C, Greig C, Rushton A. Effectiveness of behaviour change techniques in physiotherapy interventions to promote physical activity adherence in lower limb osteoarthritis patients: a systematic review. Regnaux J-P, editor. PLoS ONE. 2019;14:e0219482.
Kim Y, Mehta T, Lai B, Motl RW. Immediate and sustained effects of interventions for changing physical activity in people with multiple sclerosis: meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. 2020;101:1414–36.
Pollock M, Fernandes R, Becker L, Pieper D, Hartling L. Chapter V: overviews of reviews. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions version 63 (updated February 2022). Cochrane; 2022 [cited 2022 May 19]. Available from: https://training.cochrane.org/handbook/current/chapter-v
Aromataris E, Fernandez R, Godfrey C, Holly C, Khalil H, Tungpunkom P. Chapter 10: umbrella reviews. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI; 2020 [cited 2021 Apr 19]. Available from: https://jbi-global-wiki.refined.site/space/MANUAL/4687363/Chapter+10%3A+Umbrella+reviews
Ballard M, Montgomery P. Risk of bias in overviews of reviews: a scoping review of methodological guidance and four-item checklist. Res Synth Methods. 2017;8:92–108.
Centre for Reviews and Dissemination. Undertaking systematic reviews of research on effectiveness: CRD’s guidance for carrying out or commissioning reviews. York, UK: NHSCentre for Reviews and Dissemination, University of York; 2001 [cited 2023 Feb 20]. Available from: http://www.york.ac.uk/inst/crd/crdreports.htm
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane; 2022 [cited 2022 May 19]. Available from: www.training.cochrane.org/handbook
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, et al. 2015 Updated Method Guideline for Systematic Reviews in the Cochrane Back and Neck Group. Spine (Phila Pa 1976). 2015;40:1660–73.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Levack WMM, Weatherall M, Hay-Smith EJC, Dean SG, Mcpherson K, Siegert RJ. Goal setting and strategies to enhance goal pursuit for adults with acquired disability participating in rehabilitation. Cochrane Database of Systematic Reviews. 2015;2015.
McGrane N, Galvin R, Cusack T, Stokes E. Addition of motivational interventions to exercise and traditional Physiotherapy: a review and meta-analysis. Physiotherapy. 2015;101:1–12.
Article CAS PubMed Google Scholar
Gates M, Gates A, Pieper D, Fernandes RM, Tricco AC, Moher D, et al. Reporting guideline for overviews of reviews of healthcare interventions: development of the PRIOR statement. BMJ. 2022;378: e070849.
McLean SM, Burton M, Bradley L, Littlewood C. Interventions for enhancing adherence with physiotherapy: a systematic review. Man Ther. 2010;15:514–21.
Niedermann K, Fransen J, Knols R, Uebelhart D. Gap between short- and long-term effects of patient education in rheumatoid arthritis patients: a systematic review. Arthritis Care Res. 2004;51:388–98.
Cinthuja P, Krishnamoorthy N, Shivapatham G. Effective interventions to improve long-term physiotherapy exercise adherence among patients with lower limb osteoarthritis. A systematic review BMC Musculoskelet Disord. 2022;23:147.
Beinart NA, Goodchild CE, Weinman JA, Ayis S, Godfrey EL. Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: a systematic review. The Spine Journal. 2013;13:1940–50.
Holden J, Davidson M, O’Halloran PD. Health coaching for low back pain: a systematic review of the literature. Int J Clin Pract. 2014;68:950–62.
Jordan JL, Holden MA, Mason EE, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2010;CD005956.
Abu Abed M, Himmel W, Vormfelde S, Koschack J. Video-assisted patient education to modify behavior: a systematic review. Patient Educ Couns. 2014;97:16–22.
Bachmann C, Oesch P, Bachmann S. Recommendations for improving adherence to home-based exercise: a systematic review. Phys Med Rehab Kuror. 2018;28:20–31.
Hall AM, Ferreira PH, Maher CG, Latimer J, Ferreira ML. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys Ther. 2010;90:1099–110.
Levack WMM, Taylor K, Siegert RJ, Dean SG, McPherson KM, Weatherall M. Is goal planning in rehabilitation effective? A systematic review Clin Rehabil. 2006;20:739–55.
Room J, Hannink E, Dawes H, Barker K. What interventions are used to improve exercise adherence in older people and what behavioural techniques are they based on? A systematic review BMJ Open. 2017;7: e019221.
Dalager T, Bredahl TGV, Pedersen MT, Boyle E, Andersen LL, Sjøgaard G. Does training frequency and supervision affect compliance, performance and muscular health? A cluster randomized controlled trial. Man Ther. 2015;20:657–65.
Kolt GS, Brewer BW, Pizzari T, Schoo AMM, Garrett N. The Sport Injury Rehabilitation Adherence Scale: a reliable scale for use in clinical physiotherapy. Physiotherapy. 2007;93:17–22.
Green LW. Determining the impact and effectiveness of health education as it relates to federal policy. Health Educ Monogr. 1978;6:28–66.
Google Scholar
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
Pisters MF, Veenhof C, de Bakker DH, Schellevis FG, Dekker J. Behavioural graded activity results in better exercise adherence and more physical activity than usual care in people with osteoarthritis: a cluster-randomised trial. J Physiother. 2010;56:41–7.
Göhner W, Schlicht W. Preventing chronic back pain: evaluation of a theory-based cognitive-behavioural training programme for patients with subacute back pain. Patient Educ Couns. 2006;64:87–95.
Bandura A. Toward a psychology of human agency: pathways and reflections. Perspect Psychol Sci. 2018;13:130–6.
Ashford S, Edmunds J, French DP. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. Br J Health Psychol. 2010;15:265–88.
Frost H, Campbell P, Maxwell M, O’Carroll RE, Dombrowski SU, Williams B, et al. Effectiveness of motivational interviewing on adult behaviour change in health and social care settings: a systematic review of reviews. PLoS ONE. 2018;13: e0204890.
Michie S, West R, Sheals K, Godinho CA. Evaluating the effectiveness of behavior change techniques in health-related behavior: a scoping review of methods used. Translational Behavioral Medicine. 2018;8:212–24.
Gallagher KM. Helping older adults sustain their physical therapy gains: a theory-based intervention to promote adherence to home exercise following rehabilitation. Journal of Geriatric Physical Therapy. 2016;39:20–9.
Silva MN, Vieira PN, Coutinho SR, Minderico CS, Matos MG, Sardinha LB, et al. Using self-determination theory to promote physical activity and weight control: a randomized controlled trial in women. J Behav Med. 2010;33:110–22.
Schwarzer R, Lippke S, Luszczynska A. Mechanisms of health behavior change in persons with chronic illness or disability: the Health Action Process Approach (HAPA). Rehabil Psychol. 2011;56:161–70.
Murray JM, Brennan SF, French DP, Patterson CC, Kee F, Hunter RF. Effectiveness of physical activity interventions in achieving behaviour change maintenance in young and middle aged adults: a systematic review and meta-analysis. Soc Sci Med. 2017;192:125–33.
Areskoug Josefsson K, Andersson A-C. The co-constructive processes in physiotherapy. Lee A, editor. Cogent Medicine. 2017;4:1290308.
Qasem M. Constructivist learning theory in physiotherapy education: a critical evaluation of research. Journal of Novel Physiotherapies. 2015;5.
Brinkman C, Baez SE, Genoese F, Hoch JM. Use of goal setting to enhance self-efficacy after sports-related injury: a critically appraised topic. J Sport Rehabil. 2019;29:498–502.
Fillipas S, Oldmeadow LB, Bailey MJ, Cherry CL. A six-month, supervised, aerobic and resistance exercise program improves self-efficacy in people with human immunodeficiency virus: a randomised controlled trial. Australian Journal of Physiotherapy. 2006;52:185–90.
Ley C, Karus F, Wiesbauer L, Rato Barrio M, Spaaij R. Health, integration and agency: sport participation experiences of asylum seekers. J Refug Stud. 2021;34:4140–60.
Melin J, Nordin Å, Feldthusen C, Danielsson L. Goal-setting in physiotherapy: exploring a person-centered perspective. Physiother Theory Pract. 2021;37:863–80.
Wijma AJ, Bletterman AN, Clark JR, Vervoort SC, Beetsma A, Keizer D, et al. Patient-centeredness in physiotherapy: what does it entail? A systematic review of qualitative studies. Physiother Theory Pract. 2017;33:825–40.
Meade LB, Bearne LM, Sweeney LH, Alageel SH, Godfrey EL. Behaviour change techniques associated with adherence to prescribed exercise in patients with persistent musculoskeletal pain: systematic review. Br J Health Psychol. 2019;24:10–30.
Ariie T, Takasaki H, Okoba R, Chiba H, Handa Y, Miki T, et al. The effectiveness of exercise with behavior change techniques in people with knee osteoarthritis: a systematic review with meta-analysis. PM R. 2022;
Demmelmaier I, Iversen MD. How are behavioral theories used in interventions to promote physical activity in rheumatoid arthritis? A systematic review. Arthritis Care Res. 2018;70:185–96.
Larkin L, Gallagher S, Cramp F, Brand C, Fraser A, Kennedy N. Behaviour change interventions to promote physical activity in rheumatoid arthritis: a systematic review. Rheumatol Int. 2015;35:1631–40.
Rausch Osthoff A-K, Juhl CB, Knittle K, Dagfinrud H, Hurkmans E, Braun J, et al. Effects of exercise and physical activity promotion: meta-analysis informing the 2018 EULAR recommendations for physical activity in people with rheumatoid arthritis, spondyloarthritis and hip/knee osteoarthritis. RMD Open. 2018;4: e000713.
Armstrong TL, Swartzman LC. 3 - cross-cultural differences in illness models and expectations for the health care provider-client/patient interaction. In: Shané S. Kazarian, David R. Evans, editors. Handbook of Cultural Health Psychology. San Diego: Academic Press; 2001 [cited 2013 Aug 20]. p. 63–84. Available from: http://www.sciencedirect.com/science/article/pii/B9780124027718500052
Brady B, Veljanova I, Chipchase L. Culturally informed practice and physiotherapy. J Physiother. 2016;62:121–3.
Jimenez DE, Burrows K, Aschbrenner K, Barre LK, Pratt SI, Alegria M, et al. Health behavior change benefits: perspectives of Latinos with serious mental illness. Transcult Psychiatry. 2016;53:313–29.
Jorgensen P. Concepts of body and health in physiotherapy: the meaning of the social/cultural aspects of life. Physiother Theory Pract. 2000;16:105–15.
Teng B, Rosbergen ICM, Gomersall S, Hatton A, Brauer SG. Physiotherapists’ experiences and views of older peoples’ exercise adherence with respect to falls prevention in Singapore: a qualitative study. Disabil Rehabil. 2022;44:5530–8.
Alfieri FM, da Silva DC, de Oliveira NC, Battistella LR. Gamification in musculoskeletal rehabilitation. Curr Rev Musculoskelet Med. 2022;15:629–36.
Cox NS, Dal Corso S, Hansen H, McDonald CF, Hill CJ, Zanaboni P, et al. Telerehabilitation for chronic respiratory disease. Cochrane Database Syst Rev. 2021;1:CD013040.
Cruz-Cobo C, Bernal-Jiménez MÁ, Vázquez-García R, Santi-Cano MJ. Effectiveness of mHealth interventions in the control of lifestyle and cardiovascular risk factors in patients after a coronary event: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2022;10: e39593.
Darabseh MZ, Aburub A, Davies S. The effects of virtual reality physiotherapy interventions on cardiopulmonary function and breathing control in cystic fibrosis: a systematic review. Games Health J. 2023;12:13–24.
Fernandes CS, Magalhães B, Gomes JA, Santos C. Exergames to improve rehabilitation for shoulder injury: Systematic Review and GRADE Evidence Synthesis. REHABIL NURS. 2022;47:147–59.
García-Bravo S, Cuesta-Gómez A, Campuzano-Ruiz R, López-Navas MJ, Domínguez-Paniagua J, Araújo-Narváez A, et al. Virtual reality and video games in cardiac rehabilitation programs. A systematic review Disabil Rehabil. 2021;43:448–57.
Hawley-Hague H, Lasrado R, Martinez E, Stanmore E, Tyson S. A scoping review of the feasibility, acceptability, and effects of physiotherapy delivered remotely. Disability and Rehabilitation. 2022;
Melillo A, Chirico A, De Pietro G, Gallo L, Caggianese G, Barone D, et al. Virtual reality rehabilitation systems for cancer survivors: a narrative review of the literature. Cancers. 2022;14.
Moulaei K, Sheikhtaheri A, Nezhad MS, Haghdoost A, Gheysari M, Bahaadinbeigy K. Telerehabilitation for upper limb disabilities: a scoping review on functions, outcomes, and evaluation methods. Arch Public Health. 2022;80:196.
Patsaki I, Dimitriadi N, Despoti A, Tzoumi D, Leventakis N, Roussou G, et al. The effectiveness of immersive virtual reality in physical recovery of stroke patients: a systematic review. Frontiers in Systems Neuroscience. 2022;16.
Skov Schacksen C, Henneberg NC, Muthulingam JA, Morimoto Y, Sawa R, Saitoh M, et al. Effects of telerehabilitation interventions on heart failure management (2015–2020): scoping review. JMIR Rehabil Assist Technol. 2021;8: e29714.
Thompson D, Rattu S, Tower J, Egerton T, Francis J, Merolli M. Mobile app use to support therapeutic exercise for musculoskeletal pain conditions may help improve pain intensity and self-reported physical function: a systematic review. J Physiother. 2023;69:23–34.
Marques MM, Wright AJ, Corker E, Johnston M, West R, Hastings J, et al. The behaviour change technique ontology: transforming the behaviour change technique taxonomy v1. Wellcome Open Res. 2023;8:308.
Roter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, Svarstad B. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36:1138–61.
Hansen LS, Præstegaard J, Lehn-Christiansen S. Patient-centeredness in physiotherapy–a literature mapping review. Physiotherapy theory and practice. 2022;38(12):1843-56.
Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20:600–7.
Seelig H, Fuchs R. Physical exercise participation: a continuous or categorical phenomenon? Psychol Sport Exerc. 2011;12:115–23.
Shang B, Duan Y, Huang WY, Brehm W. Fluctuation – a common but neglected pattern of physical activity behaviour: an exploratory review of studies in recent 20 years. European Journal of Sport Science. 2018;18(2):266-78.
Download references
Acknowledgements
Not applicable
No funding was received.
Author information
Authors and affiliations.
Department Health Sciences, Physiotherapy, FH Campus Wien University of Applied Sciences, Favoritenstrasse 226, 1100, Vienna, Austria
Clemens Ley
Department Health Sciences, Competence Center INDICATION, FH Campus Wien, University of Applied Sciences, Favoritenstrasse 226, 1100, Vienna, Austria
You can also search for this author in PubMed Google Scholar
Contributions
CL and PP conceived and designed the review. CL did the database search and data extraction. CL and PP did screening and quality assessment. CL did the narrative synthesis and drafted the manuscript. PP conducted the panoramic meta-analysis and critically revised and substantially contributed throughout the writing of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Clemens Ley .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Search details
Additional file 2:
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ley, C., Putz, P. Efficacy of interventions and techniques on adherence to physiotherapy in adults: an overview of systematic reviews and panoramic meta-analysis. Syst Rev 13 , 137 (2024). https://doi.org/10.1186/s13643-024-02538-9
Download citation
Received : 29 November 2023
Accepted : 17 April 2024
Published : 21 May 2024
DOI : https://doi.org/10.1186/s13643-024-02538-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Umbrella review
- Physical therapy
- Rehabilitation
- Behaviour change techniques
- Effectiveness
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 83, Issue 6
- EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2023 update
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-4528-310X Laure Gossec 1 , 2 ,
- http://orcid.org/0000-0002-6685-8873 Andreas Kerschbaumer 3 ,
- http://orcid.org/0000-0002-2517-0247 Ricardo J O Ferreira 4 , 5 ,
- http://orcid.org/0000-0003-2108-0030 Daniel Aletaha 3 ,
- http://orcid.org/0000-0002-9475-9362 Xenofon Baraliakos 6 ,
- Heidi Bertheussen 7 ,
- Wolf-Henning Boehncke 8 ,
- http://orcid.org/0000-0001-5331-8221 Bente Appel Esbensen 9 , 10 ,
- Iain B McInnes 11 ,
- Dennis McGonagle 12 , 13 ,
- http://orcid.org/0000-0002-3892-6947 Kevin L Winthrop 14 ,
- Andra Balanescu 15 ,
- Peter V Balint 16 ,
- http://orcid.org/0000-0001-7518-1131 Gerd R Burmester 17 ,
- http://orcid.org/0000-0003-2606-0573 Juan D Cañete 18 , 19 ,
- Pascal Claudepierre 20 , 21 ,
- http://orcid.org/0000-0002-1473-1715 Lihi Eder 22 ,
- http://orcid.org/0000-0003-4229-6818 Merete Lund Hetland 23 , 24 ,
- http://orcid.org/0000-0001-5592-724X Annamaria Iagnocco 25 ,
- Lars Erik Kristensen 26 , 27 ,
- Rik Lories 28 , 29 ,
- http://orcid.org/0000-0002-8418-7145 Rubén Queiro 30 , 31 ,
- http://orcid.org/0000-0002-9022-8863 Daniele Mauro 32 ,
- http://orcid.org/0000-0002-9683-3407 Helena Marzo-Ortega 12 , 13 ,
- http://orcid.org/0000-0002-6620-0457 Philip J Mease 33 , 34 ,
- http://orcid.org/0000-0002-2571-788X Peter Nash 35 ,
- Wendy Wagenaar 36 , 37 ,
- Laura Savage 38 ,
- http://orcid.org/0000-0001-8740-9615 Georg Schett 39 ,
- http://orcid.org/0000-0002-9441-5535 Stephanie J W Shoop-Worrall 40 ,
- http://orcid.org/0000-0002-0807-7139 Yoshiya Tanaka 41 ,
- http://orcid.org/0000-0002-3561-5932 Filip E Van den Bosch 42 ,
- Annette van der Helm-van Mil 43 ,
- http://orcid.org/0000-0002-0573-464X Alen Zabotti 44 ,
- http://orcid.org/0000-0002-5781-158X Désirée van der Heijde 43 ,
- Josef S Smolen 3
- 1 INSERM, Institut Pierre Louis d'Epidémiologie et de Santé Publique , Sorbonne Universite , Paris , France
- 2 APHP, Rheumatology Department , Hopital Universitaire Pitie Salpetriere , Paris , France
- 3 Division of Rheumatology, Department of Medicine 3 , Medical University of Vienna , Vienna , Austria
- 4 Nursing Research, Innovation and Development Centre of Lisbon (CIDNUR) , Higher School of Nursing of Lisbon , Lisbon , Portugal
- 5 Rheumatology Department , Centro Hospitalar e Universitário de Coimbra EPE , Coimbra , Portugal
- 6 Rheumazentrum Ruhrgebiet , Ruhr University Bochum , Herne , Germany
- 7 EULAR Patient Research Partner , EULAR , Oslo , Norway
- 8 Dermatology and Venereology , Geneva University Hospitals , Geneva , Switzerland
- 9 Copenhagen Center for Arthritis Research, Center for Rheumatology and Spine Diseases, Centre for Head and Orthopaedics , Rigshospitalet , Glostrup , Denmark
- 10 Department of Clinical Medicine , University of Copenhagen , Copenhagen , Denmark
- 11 College of Medical Veterinary and Life Sciences , University of Glasgow , Glasgow , UK
- 12 LTHT , NIHR Leeds Biomedical Research Centre , Leeds , UK
- 13 Leeds Institute of Rheumatic and Musculoskeletal Medicine , University of Leeds , Leeds , UK
- 14 Division of Infectious Diseases, School of Medicine, School of Public Health , Oregon Health & Science University , Portland , Oregon , USA
- 15 Sf Maria Hospital , University of Medicine and Pharmacy Carol Davila Bucharest , Bucharest , Romania
- 16 Medical Imaging Centre, Semmelweis University, 3rd Rheumatology Department, National Institute of Musculoskeletal Diseases , Budapest , Hungary
- 17 Department of Rheumatology and Clinical Immunology, Freie Universität Berlin and Humboldt-Universität zu Berlin , Charité Universitätsmedizin Berlin , Berlin , Germany
- 18 Arthritis Unit, Department of Rheumatology , Hospital Clínic Barcelona , Barcelona , Spain
- 19 FCRB , IDIBAPS , Barcelona , Spain
- 20 Rheumatology , AP-HP, Henri Mondor University Hospital , Creteil , France
- 21 EA Epiderme , UPEC , Creteil , France
- 22 Department of Medicine, University of Toronto , Women's College Hospital , Toronto , Toronto , Canada
- 23 The Copenhagen Center for Arthritis Research, Center for Rheumatology and Spine Diseases, Centre of Head and Orthopedics , Rigshospitalet Glostrup , Glostrup , Denmark
- 24 Department of Clinical Medicine, Faculty of Health and Medical Sciences , University of Copenhagen , Copenhagen , Denmark
- 25 Academic Rheumatology Centre, Dipartimento Scienze Cliniche Biologiche , Università di Torino - AO Mauriziano Torino , Turin , Italy
- 26 The Parker Institute , Bispebjerg , Denmark
- 27 Frederiksberg Hospital , Copenhagen University , Copenhagen , Denmark
- 28 Laboratory of Tissue Homeostasis and Disease, Skeletal Biology and Engineering Research Center , KU Leuven , Leuven , Belgium
- 29 Division of Rheumatology , University Hospitals Leuven , Leuven , Belgium
- 30 Rheumatology , Hospital Universitario Central de Asturias , Oviedo , Spain
- 31 Translational Immunology Division, Biohealth Research Institute of the Principality of Asturias , Oviedo University School of Medicine , Oviedo , Spain
- 32 Department of Precision Medicine , University of Campania Luigi Vanvitelli , Naples , Italy
- 33 Rheumatology Research , Providence Swedish , Seattle , Washington , USA
- 34 University of Washington School of Medicine , Seattle , Washington , USA
- 35 School of Medicine , Griffith University , Brisbane , Queensland , Australia
- 36 Tranzo, Tilburg School of Social and Behavioral Sciences , Tilburg University , Tilburg , The Netherlands
- 37 Young PARE Patient Research Partner , EULAR , Zurich , Switzerland
- 38 School of Medicine and Dermatology, Leeds Teaching Hospitals NHS Trust , University of Leeds , Leeds , UK
- 39 Department of Internal Medicine 3, Rheumatology and Immunology and Universitätsklinikum Erlangen , Friedrich-Alexander-Universität Erlangen-Nürnberg , Erlangen , Germany
- 40 Children and Young Person’s Rheumatology Research Programme, Centre for Musculoskeletal Research , The University of Manchester , Manchester , UK
- 41 First Department of Internal Medicine , University of Occupational and Environmental Health, Japan , Kitakyushu , Japan
- 42 Department of Internal Medicine and Pediatrics, VIB Center for Inflammation Research , Ghent University , Gent , Belgium
- 43 Rheumatology , Leiden University Medical Center , Leiden , The Netherlands
- 44 Department of Medical and Biological Sciences , Azienda sanitaria universitaria Friuli Centrale , Udine , Italy
- Correspondence to Laure Gossec, INSERM, Institut Pierre Louis d'Epidémiologie et de Santé Publique, Sorbonne Universite, Paris, France; laure.gossec{at}aphp.fr
Objective New modes of action and more data on the efficacy and safety of existing drugs in psoriatic arthritis (PsA) required an update of the EULAR 2019 recommendations for the pharmacological treatment of PsA.
Methods Following EULAR standardised operating procedures, the process included a systematic literature review and a consensus meeting of 36 international experts in April 2023. Levels of evidence and grades of recommendations were determined.
Results The updated recommendations comprise 7 overarching principles and 11 recommendations, and provide a treatment strategy for pharmacological therapies. Non-steroidal anti-inflammatory drugs should be used in monotherapy only for mild PsA and in the short term; oral glucocorticoids are not recommended. In patients with peripheral arthritis, rapid initiation of conventional synthetic disease-modifying antirheumatic drugs is recommended and methotrexate preferred. If the treatment target is not achieved with this strategy, a biological disease-modifying antirheumatic drug (bDMARD) should be initiated, without preference among modes of action. Relevant skin psoriasis should orient towards bDMARDs targeting interleukin (IL)-23p40, IL-23p19, IL-17A and IL-17A/F inhibitors. In case of predominant axial or entheseal disease, an algorithm is also proposed. Use of Janus kinase inhibitors is proposed primarily after bDMARD failure, taking relevant risk factors into account, or in case bDMARDs are not an appropriate choice. Inflammatory bowel disease and uveitis, if present, should influence drug choices, with monoclonal tumour necrosis factor inhibitors proposed. Drug switches and tapering in sustained remission are also addressed.
Conclusion These updated recommendations integrate all currently available drugs in a practical and progressive approach, which will be helpful in the pharmacological management of PsA.
- Psoriatic Arthritis
- Biological Therapy
- Biosimilar Pharmaceuticals
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/ard-2024-225531
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Psoriatic arthritis (PsA) is a disease which has benefited from notable progress over recent years. Concepts have evolved, such as very early diagnosis and pre-PsA, as well as defining treatment targets and applying a holistic approach to comorbidity management. 1–4 Pharmacological options have extended, with the approval of new agents targeting various modes of action for PsA (as well as skin psoriasis). Drugs licensed for PsA now include (1) conventional synthetic (cs) disease-modifying antirheumatic drugs (DMARDs), such as methotrexate (MTX), sulfasalazine and leflunomide; (2) biological (b) DMARDs targeting tumour necrosis factor (TNF), the interleukin (IL)-12/23 or IL-23 pathway, and the IL-17A and IL-17A/F pathway; and (3) targeted synthetic (ts) DMARDs that inhibit Janus kinases (JAKs) or phosphodiesterase 4 (PDE4) ( table 1 ). 5 New safety data have emerged in inflammatory arthritis, particularly a worldwide cautionary comment regarding JAK inhibitors (JAKis), following a large randomised controlled trial (RCT) of tofacitinib in rheumatoid arthritis (RA). 6–8 Since the last EULAR recommendations for the pharmacological management of PsA in 2019, the field has changed significantly. 9–12 An update of the EULAR PsA management recommendations was therefore timely. 9
- View inline
Disease-modifying treatment options for psoriatic arthritis in 2023
This update addresses the non-topical, pharmacological management of PsA, with a specific focus on musculoskeletal (MSK) manifestations, while also addressing the spectrum of PsA, including how skin psoriasis, extra-MSK manifestations and comorbidities should influence treatment choices.
In accordance with the EULAR updated standardised operating procedures, 13 the process leading to this update included a data-driven approach and expert opinion.
After approval for an update by the EULAR Council in September 2022, taskforce members were selected by the convenor (JSS) and the methodologist (LG), to include more than one-third of new members, as well as country and gender representation. For the first time, experts from Australia, Japan and North America participated. Representatives from the health professionals in rheumatology (HPR) committee, patient research partners from PARE (People with Arthritis/Rheumatism) and young colleagues from the EMEUNET (EMerging EUlar NETwork) were included. Five members were recruited through an open call to EULAR countries via a competitive application process.
In October 2022, the steering group had its first meeting. The steering group consisted of seven rheumatologists (including the convenor, the methodologist and the fellow: JSS, LG, AK, DA, XB, IBM and DGM), a dermatologist (W-HB), an infectious disease specialist (KLW), an experienced fellow rheumatologist (AK), a patient research partner (HB) and two health professionals (BAE and RJOF, the latter acting in the capacity of a junior methodologist). Questions were then defined and addressed through a systematic literature review (SLR), performed by the fellow (AK) between November 2022 and April 2023, for the literature pertaining to pharmacological treatments of PsA and published since the previous SLR (ie, since the end of 2018). 5
The taskforce comprised the steering group and 23 other experts; members came from 19 different countries (of which 15 were EULAR countries), and included 27 rheumatology specialists, 2 dermatologists, 1 infectious disease specialist, 2 people affected with PsA acting as patient research partners, 2 HPRs and 3 rheumatology/epidemiology fellows/trainees. Overall, 47% of the taskforce members had not participated in the previous update in 2019. In April 2023, the taskforce met for a physical meeting to develop the updated bullet points. Each point was discussed in detail both in smaller (breakout) groups and in plenary sessions until consensus was reached. Group approval was sought through votes (by raised hands) for each bullet point; the limit for acceptance of individual recommendations was set at ≥75% majority among the taskforce for the first voting round; then (after discussions and potential reformulations) at ≥67% majority; and finally, if required, the last round of votes was accepted with >50% acceptance or else a proposal was rejected. 13
Although the SLR was a strong component of the discussions, the process was not only evidence-based but also experience-based and consensus-based, and included consideration of safety, efficacy, cost and long-term data. The levels of evidence (LoE) and grades of recommendation (GoR) were determined for each recommendation based on the Oxford Evidence Based System. 13 14 In May 2023, an anonymised email-based voting on the level of agreement (LoA) among the taskforce members was performed on a 0–10 scale (with 10 meaning full agreement) allowing calculation of mean LoA.
These recommendations address non-topical pharmacological treatments with a main focus on MSK manifestations. These recommendations concern stakeholders, such as experts involved in the care of patients with PsA, particularly rheumatologists and other health professionals (such as rheumatology nurses), general practitioners, dermatologists and other specialists; and also people with PsA as well as other stakeholders, for example, government and hospital officials, patient organisations, regulatory agencies and reimbursement institutions.
The overarching principles (OAPs) and recommendations are shown in table 2 , with LoE, GoR and LoA. The updated recommendations include 7 OAPs (vs 6 in 2019) and 11 recommendations (vs 12 in 2019, due to merges). Of the 11 recommendations, only 4 are unchanged compared with 2019 (the modifications compared with the 2019 recommendations are represented in table 3 ).
2023 updated EULAR recommendations for the pharmacological management of psoriatic arthritis
Comparison of the 2019 and 2023 EULAR recommendations for the management of psoriatic arthritis
Overarching principles
Of the seven OAPs, three remain unchanged, three were reworded and one has been added (overarching principle G). For more information on the thought process leading to the OAPs (unchanged or slightly changed), please refer to the 2015 and 2019 recommendations manuscripts. 9 15 Key points from the discussion of the OAPs are addressed in the following:
A. Psoriatic arthritis is a heterogeneous and potentially severe disease, which may require multidisciplinary treatment (unchanged) .
Although PsA is potentially severe, not all patients will develop severe forms. 16 17 Multidisciplinary management is helpful for many patients, through collaboration between physicians of different specialties and HPRs with the appropriate expertise. 18 19
B. Treatment of psoriatic arthritis patients should aim at the best care and must be based on a shared decision between the patient and the rheumatologist, considering efficacy, safety, patient preferences and costs.
This OAP was modified from 2019 to add patient preferences as an element to be considered and emphasise the importance of shared decision-making to maximise treatment adherence and efficacy while at the same time minimise complications driven by uncontrolled (active) disease as well as potential side effects of pharmacological drugs. 20 21
C. Rheumatologists are the specialists who should primarily care for the musculoskeletal manifestations of patients with psoriatic arthritis; in the presence of clinically relevant skin involvement, a rheumatologist and a dermatologist should collaborate in diagnosis and management.
We consider that rheumatology experts provide the best care for patients with PsA, given their experience with the many drugs used to treat these and other rheumatic and musculoskeletal diseases (RMDs), including the important aspects of safety and comorbidities. Consultation with dermatologists and sometimes other specialists may be helpful in individual clinical scenarios (see also overarching principles F and G). A very slight rewording was performed to discuss skin involvement as ‘clinically relevant’ rather than ‘clinically significant’ for more homogeneity with other bullet points. This bullet point does not address the role of HPRs, who are usually not prescribers in EULAR countries.
D. The primary goal of treating patients with psoriatic arthritis is to maximise health-related quality of life, through control of symptoms, prevention of structural damage, normalisation of function and social participation; abrogation of inflammation is an important component to achieve these goals (unchanged).
For more details, please see the 2019 update of these recommendations. 9
E. In managing patients with psoriatic arthritis, consideration should be given to each musculoskeletal manifestation and treatment decisions made accordingly (unchanged).
For more details, please refer to the 2019 update. 9
F. When managing patients with psoriatic arthritis, non-musculoskeletal manifestations (skin, eye and gastrointestinal tract) should be taken into account; comorbidities such as obesity, metabolic syndrome, cardiovascular disease or depression should also be considered.
The wording ‘such as obesity’ was added, since obesity is frequent in PsA and can influence outcomes. 22 23 Obesity concerns excess body fat, while metabolic syndrome is a collection of risk factors that increase the likelihood of developing cardiovascular disease and type 2 diabetes. Obesity is a significant contributor to the development of metabolic syndrome. The taskforce members discussed if other comorbidities should be added, but it was felt that the term ‘such as’ entails that comorbidities overall should be considered, without a need to list them. Depression and potentially other mental health issues may influence treatment choice. Central sensitisation to pain perception is frequent in PsA and also influences outcomes; this may lead to difficulties in disease management. 24 25 Bone health and malignancies were also specifically highlighted. The management of comorbidities poses specific issues, in particular as to who is responsible for managing distinct disease domains. Solutions need to be applied according to the individual patient, each country’s specific setting and healthcare system organisation.
G. The choice of treatment should take account of safety considerations regarding individual modes of action to optimise the benefit–risk profile (new).
Given new data on the safety of different modes of action, the taskforce proposed this new OAP to emphasise the importance of taking into account safety considerations for each patient. 6 The taskforce was aware that this item is somewhat redundant with overarching principle B but wished to emphasise the importance of benefit–risk assessment when considering the use of specific agents.
Recommendations
Of note, these recommendations are centred on non-topical pharmacological treatments; topical and non-pharmacological treatments are also important in PsA but are outside our scope. Figure 1 shows a summarised algorithm of the treatment proposals.
- Download figure
- Open in new tab
- Download powerpoint
2023 EULAR recommendations algorithm for the management of PsA. bDMARD, biological disease-modifying antirheumatic drug; csDMARD, conventional synthetic disease-modifying antirheumatic drug; IBD, inflammatory bowel disease; L, interleukin; JAK, Janus kinase inhibitor; JAKi, Janus kinase inhibitor; NSAID, non-steroidal anti-inflammatory drugs; TNF, tumour necrosis factor; TNFI, tumour necrosis factor inhibitor.
Some safety issues will be briefly addressed, but for a full picture of the adverse event profile of different drugs the package inserts should be consulted.
Recommendation 1
Treatment should be aimed at reaching the target of remission or, alternatively, low disease activity, by regular disease activity assessment and appropriate adjustment of therapy.
This (unchanged) recommendation is in keeping with the principles of treating-to-target. 26 27 Given the lack of new data to support treat-to-target in PsA, the LoE and GoR are also unchanged. The use of instruments to assess disease activity has been addressed in the treat-to-target recommendations. 26 The definition of remission in PsA remains a subject of debate. 28–30 For the context of these recommendations, remission should be seen as an abrogation of inflammation.
The taskforce members emphasised that disease activity should be regularly assessed across individual involved manifestations (eg, joints, skin, enthesitis, dactylitis, axial disease), and that treatment adjustments will depend on the predominant manifestation of the disease at a given moment. 31
Recommendation 2
Non-steroidal anti-inflammatory drugs may be used to relieve musculoskeletal signs and symptoms; local injections of glucocorticoids may be considered as adjunctive therapy.
This recommendation deals with the short-term use of symptomatic treatment. It was developed by merging the two previous recommendations 2 and 3, which dealt separately with non-steroidal anti-inflammatory drugs (NSAIDs) and glucocorticoids, as both only serve to relieve symptoms in the short term. It was decided to no longer allude to systemic glucocorticoids in a bullet point, since the data underlying the prescription of systemic glucocorticoids in PsA are scarce. Moreover, glucocorticoids harbour many potential safety issues, in particular when taking into account the high prevalence of comorbidities and cardiovascular risk factors in PsA. 3 32 However, the taskforce members agreed that, in some selected cases, systemic glucocorticoid therapy may be helpful for some patients, especially for polyarticular forms and/or as bridging therapy.
NSAIDs offer symptomatic relief to patients with MSK involvement, but have not shown any efficacy in psoriasis. NSAIDs and local glucocorticoid injections are useful to relieve symptoms and local inflammation temporarily, and may be used combined with DMARDs as needed (please see recommendation 3). However, the safety aspects of (potentially long-term) NSAID use have to be taken into account.
The taskforce emphasised that the vast majority of patients should not be treated with NSAIDs alone (without DMARDs), in keeping with a proactive treat-to-target approach to PsA. Only patients with very mild peripheral disease, or with predominant entheseal or axial disease, may sufficiently benefit from NSAIDs as monotherapy. Even in these cases, it is proposed that the use of symptomatic treatments alone should usually be short term, for example, limited to 4 weeks or so. In peripheral arthritis, this duration is based on the opinion of the group; in predominant axial disease, it is in keeping with the Assesment of Spondyloarthritis International Society (ASAS)/EULAR recommendations for axial spondyloarthritis (axSpA) whereby persistent disease after 4 weeks of treatment is considered a failure of NSAIDs. 33 On the other hand, for patients with predominant axial disease who experience significant improvement in clinical symptoms, continuous NSAID use may be proposed if needed to control symptoms, always taking the risks and benefits into account. Of note, data regarding the efficacy of NSAIDs in enthesitis are limited.
Recommendation 3
In patients with polyarthritis or those with monoarthritis/oligoarthritis and poor prognostic factors (eg, structural damage, elevated acute phase reactants, dactylitis or nail involvement), a csDMARD should be initiated rapidly, with methotrexate preferred in those with clinically relevant skin involvement.
Among patients with peripheral arthritis, 34 35 a distinction is made according to the number of swollen joints and according to prognostic factors. 36 In 2019, polyarthritis and monoarthritis/oligoarthritis with poor prognostic markers were addressed in separate bullet points, which were merged for clarity in this update ( table 3 ). Oligoarticular disease is defined as arthritis (swollen joints) of up to four (included) joints. 9 This definition applies to clinical detection (rather than imaging). The prognostic factors have also been previously defined 9 17 and are unchanged.
We recommend rapid csDMARD start, concomitant (or close) with the initiation of symptomatic therapy, for both patients with polyarticular disease and patients with oligoarticular disease and poor prognostic factors. Patients with oligoarticular disease and lack of poor prognostic factors should also receive a csDMARD, but there is less urgency for these patients given the more favourable long-term prognosis. The latter may receive csDMARDs after a longer delay, and potentially a period of symptomatic treatment alone (see recommendation 2). Since there is a lack of strong evidence to support this approach of rapid treatment introduction, this recommendation was mainly based on expert opinion.
Of note, there is no specific recommendation for dactylitis. We consider dactylitis as an association of (oligo)synovitis, tenosynovitis and enthesitis. Patients with isolated dactylitis should be treated similarly to patients with oligoarthritis; this includes the use of joint glucocorticoid injections and csDMARDs, which have shown efficacy in relieving dactylitis. 37
The first DMARD should be a csDMARD (meaning MTX, leflunomide or sulfasalazine). The decision concerning the first-line DMARD is important and led to much taskforce discussion, and has been put as an element for further research in the research agenda ( table 4 ). The continued prioritisation of csDMARDs reflects consensual expert opinion within the taskforce that favoured the benefit–risk–cost balance of csDMARDs and in particular MTX over targeted drugs. The absence of new data indicating the superiority of a b/tsDMARD as first-line, and in the presence of new data on MTX, was seen as confirming the efficacy of this drug in PsA. 5 37–39
Research agenda indicating priorities for future research in PsA
Since the EULAR recommendations adhere to a treat-to-target (T2T) approach which implies a reduction of disease activity by at least 50% within 3 months and reaching the treatment target within 6 months, a csDMARD should not be continued if these therapeutic goals are not attained. On csDMARD inefficacy, another DMARD, such as a bDMARD (see recommendation 4), can be rapidly instituted. Generally speaking, we recommend assessing the efficacy of the csDMARD and deciding if it should be pursued as monotherapy or not, after 12 weeks, in line with the T2T recommendations. 26 Although MTX use in PsA has typically been founded on evidence from other immune-mediated diseases such as RA and psoriasis, 40 there is also evidence for its efficacy in PsA, with recent confirmatory data both from observational data sources and from a randomised trial indicating that a proportion of patients will respond to escalation of doses of MTX. 39 41–43 The efficacy–safety balance of MTX should be assessed regularly, given the general metabolic profile of patients with PsA which can put them at a higher risk for adverse events such as hepatotoxicity. 42–44 The MTX dose should be sufficient, that is, usually between 20 mg and 25 mg weekly (about 0.3 mg/kg), and use of folate supplementation is recommended to reduce the adverse effects of MTX. 45
Other csDMARDs (ie, leflunomide and sulfasalazine) are potential treatment options and have demonstrated efficacy in PsA peripheral arthritis. 15 A recent trial of the combination of MTX with leflunomide indicated a low efficacy to safety ratio; thus, this association is not recommended. 38
Recommendation 4
In patients with peripheral arthritis and an inadequate response to at least one csDMARD, therapy with a bDMARD should be commenced.
This recommendation is relevant to patients with peripheral arthritis and therefore is meant to include both those with monoarticular/oligoarticular and those with polyarticular disease. However, where peripheral involvement is limited and without poor prognostic factors, it is not unreasonable to apply a second csDMARD course before initiating a bDMARD/tsDMARD, when this decision is agreed by the prescriber and the patient.
After failure of at least one csDMARD, the taskforce proposed as next step one of the many available bDMARDs ( table 1 ). 5
JAKi is efficacious in PsA, but the taskforce decided that at present the efficacy–safety balance, costs and long-term experience with many bDMARDs clearly favour their recommendation over JAKi. Relevant comorbidities in many patients with PsA also favour bDMARD selection.
Regarding bDMARDs, no order of preference is given since no bDMARD has demonstrated superiority for joint involvement over other bDMARDs ( table 1 ). 46–48 Herein they are listed in numeric order of the targeted cytokine, and not in order of preference. However, in the context of the present recommendation, CTLA4 (cytotoxic T-lymphocyte–associated antigen 4) inhibition is not considered a good option due to its limited efficacy in clinical trials. 49 The GoR is high for this bullet point, reflecting robust accrued data. 50
Unlike MSK manifestations, non-MSK domains of PsA allow differential order of bDMARD recommendation (se recommendation 9). 5 Two head-to-head trials of bDMARDs in PsA, both comparing an IL-17A inhibitor with adalimumab, showed similar efficacy for IL-17A inhibition and TNF inhibition, as regards efficacy on the joints, while skin responses are better with the former. 46 47 We also note that there is evidence on the better efficacy of a bDMARD compared with MTX in skin psoriasis (and evidence for differences between bDMARDs, please see recommendation 9). 51 52
All bDMARDs and JAKi showed efficacy regarding inhibition of radiographic progression; such data are lacking for apremilast.
The safety of the different available categories of bDMARDs appears acceptable in our SLR. 5 All bDMARDs increase the risk of infections. 5 The risks of TNF inhibitors (TNFis) are well known. Candidiasis (usually mucocutaneous) is more frequent with IL-17A and IL-17A/F inhibition, particularly the latter. 53 54 While IL-23-p19i is a more recent addition to the armament, its safety appears satisfactory, in line with ustekinumab which also interferes with IL-23 (p40 chain) whose adverse event profile is well known and appears satisfactory. 5
As a general rule, safety and comorbidities need to be taken into account when a decision to start a new drug is taken. More complete information regarding the safety aspects of bDMARDs is provided in the individual drug’s product information. Costs should also be taken into account, but these may vary at the country level; cost savings will occur in many countries due to the availability of biosimilar TNF blockers and potentially other biosimilars in due course. Personalised medicine, to facilitate an optimal choice of the first bDMARD, is currently difficult due to the lack of individualised predictors of response to treatment. 55 As previously discussed, it is of key importance to take into account the patient phenotype and potential extra-MSK features ( figure 1 ). Comorbidities are also to be considered. 23 56 More research is needed on the predictors of drug response, including the effect of sex. 57 58
Combination of a bDMARD with a csDMARD
First-line bDMARDs are often given in combination with csDMARDs, such as MTX. 41 59 However, there are conflicting data regarding the added benefit of concomitant MTX with targeted DMARDs in patients with peripheral disease and no evidence of a benefit of MTX in patients with axial symptoms. 33 60 61
MTX combination with bDMARDs has been explored mainly for TNFi; studies have generally found similar efficacy with or without concomitant MTX, although with increased drug survival when using MTX, in some studies. 41 59 62 A recent large study reported increased remission rates with TNFi plus MTX combination therapy. 59 With other modes of action, there is a lack of data to support comedication. Overall, the taskforce proposed to combine a first bDMARD with the previously prescribed csDMARD, in all cases where such a treatment has already been tolerated by the patient and in particular when the first bDMARD is a TNFi. For other modes of action, given the lack of data, we cannot recommend comedication, although the usual practice would be to continue a csDMARD when initiating a bDMARD (doses of the csDMARD can be diminished if needed).
Recommendation 5
In patients with peripheral arthritis and an inadequate response to at least one bDMARD, or when a bDMARD is not appropriate, a JAKi may be considered, taking safety considerations into account.
This recommendation elicited much debate. On the one hand, since 2019, new data have accrued on JAKis in terms of efficacy, such as the publication of positive trials on upadacitinib in PsA. 63 On the other hand, there is currently a worldwide cautionary statement issued by both the Food and Drug Administration and the European Medicine Agency restricting the use of JAKis in all diseases including PsA, based on an increased risk of cardiovascular and malignancy events observed with tofacitinib in older patients with RA with cardiovascular risk factors. 6–8 JAKis lead to increased general infection rates of similar magnitude to bDMARDs, but higher for herpes zoster infections. 5 Drug safety for the JAKis tofacitinib and upadacitinib in the specific context of PsA was recently reported and appeared reassuring; however, follow-up was short and further data are warranted. 64 65 While currently long-term extension data do not show increased cardiovascular/cancer risk related to JAKi use in PsA, there are no RCTs similar to the ORAL-Surveillance trial available at present in PsA. Therefore, the taskforce felt that the precautions related to RA also have to be taken for PsA, especially since various comorbidities important for the JAKi risk profile may be more prevalent in PsA than in RA (eg, obesity and cardiovascular risk factors). On the other hand, controlling inflammation is important to decrease cardiovascular risk.
Safety of JAKis should be carefully considered 66 ; we propose in table 2 and figure 1 a shortened version of the EMA warning/limitation to use, which includes age, smoking status and other cardiovascular/venous/cancer risk factors. 7 8
After much discussion, we considered that the efficacy–safety balance of JAKis did not justify putting JAKis on the same level as bDMARDs for order of choice (ie, proposing JAKis as usual treatment after insufficient response and/or intolerance to csDMARD treatment).
Therefore, JAKis are proposed usually as second-line targeted therapies (or third-line DMARDs). Of note, we recognise that, for some patients, JAKis may be a relevant option after a csDMARD; this is reflected in the wording of the bullet point (‘when a bDMARD is not appropriate’). This ‘non-appropriateness’ may include contraindications to bDMARDs, practical issues leading to a strong preference for oral administrations (eg, lack of proper conservation at regulated temperatures) and patient preferences, including risk of non-adherence to injections (in accordance with the first OAP concerning shared decision-making). Nevertheless, patients will have to weigh their preferences against potential risks.
The GoR was low for this recommendation, in particular regarding safety considerations, since the data are sparse in PsA and we had to rely on data taken from RA. The taskforce suggests using JAKi after bDMARDs have failed because several new bDMARDs with excellent effects on skin involvement and relatively good safety data are now available (IL-23, IL-17 inhibitors) and more long-term data on JAKi efficacy and safety are needed in PsA. The efficacy to safety ratio of JAKis was also put into the research agenda ( table 4 ).
Currently, drugs from the tyrosine kinase 2 (TYK2) pathway inhibition are being assessed in PsA 5 ; they are not currently licensed for use, and indeed the data are at this point limited in particular for safety (including in psoriasis where such therapy is licensed). Thus, we did not include TYK2 inhibition in the current recommendations.
Recommendation 6
In patients with mild disease and an inadequate response to at least one csDMARD, in whom neither a bDMARD nor a JAKi is appropriate, a PDE4 inhibitor may be considered.
This recommendation is unchanged from 2019, with unchanged LoE. ‘Mild disease’ is defined as oligoarticular or entheseal disease without poor prognostic factors and limited skin involvement. 9 67 The FOREMOST trial recently confirmed the efficacy of apremilast compared with placebo in oligoarticular PsA. 67 Nevertheless, the reason to place apremilast differently from bDMARDs or other tsDMARDs is not only based on its consistently relatively low efficacy, but also on the lack of structural efficacy data (thus putting the term ‘DMARD’ at risk since there are no data on inhibition of damage progression).
This recommendation received the lowest LoA within the taskforce, reflecting that more than a quarter of the taskforce participants were in favour of only discussing apremilast in the text without a specific bullet point.
The use of apremilast in combination with TNFi is off-label, and is a more costly drug combination with no supporting data and cannot be recommended.
Recommendation 7
In patients with unequivocal enthesitis and an insufficient response to NSAIDs or local glucocorticoid injections, therapy with a bDMARD should be considered.
This bullet point remains unchanged. Unequivocal enthesitis refers (as in 2019) to definite entheseal inflammation (which might need additional diagnostic imaging) to avoid overtreatment of entheseal pain not related to PsA (eg, in the context of widespread pain syndrome or repetitive mechanical stress). 68 69 In terms of treatment options, the taskforce discussed the recent data indicating indirectly some efficacy for MTX in enthesitis. 5 38 39 However, it was felt that the data for MTX were not sufficiently strong to propose MTX in the bullet point. We do acknowledge that, for some patients with enthesitis, MTX may be an option ( figure 1 ).
For unequivocal predominant enthesitis, the proposal is to introduce a bDMARD (without a preference for a specific mode of action) since all currently approved bDMARDs have demonstrated efficacy on enthesitis, with similar magnitudes of response, although head-to-head trials are missing ( figure 1 ). 5 Here, costs may be important, but other manifestations will also have to be taken into account (see recommendations 8 and 9). Of note, although tsDMARDs are not mentioned specifically in the bullet point, they are an option in some cases of enthesitis (always considering benefit to risk ratios, in particular for JAKis). 7 8
Recommendation 8
In patients with clinically relevant axial disease with an insufficient response to NSAIDs, therapy with an IL-17Ai, a TNFi, an IL-17 A/Fi or a JAKi should be considered.
The formulation for axial disease was modified from predominant to clinically relevant. For axial disease, in agreement also with the recently updated ASAS/EULAR axSpA recommendations, 33 we continue to judge csDMARDs as not relevant. bDMARDs targeting TNF and IL-17A and IL-17A/F as well as tsDMARDs targeting JAK are recommended. For JAKis, safety issues should be considered. Of note, we propose a choice between the drugs, not a combination of the drugs.
For this recommendation, the order of the drugs listed is of relevance, meaning that IL-17A inhibition has been put first due to the availability of currently only one trial specifically investigating axial PsA and using secukinumab (the MAXIMISE trial), 70 with the other drugs listed thereafter. Thus, the LoE is stronger for IL-17A inhibition than for the other drugs, where the data are derived from axial SpA. 33
The other drugs are listed with TNF inhibition first due to long-term safety data, then IL-17 A/F inhibition which has been recently licensed for axial SpA and JAK inhibition as an option taking into account safety. JAKis are here proposed in the same recommendation as bDMARDs, also reflecting that comorbidity profiles of patients with predominant or isolated axial PsA may be more comparable to patients with axial SpA and therefore may have a more favourable safety profile with respect to cardiovascular and cancer risks than many patients with predominant peripheral arthritis. The taskforce discussed the circumstantial evidence that IL-23 inhibition may be efficacious for axial PsA; however, given negative trials for IL-12/23 inhibition in axSpA, the IL-23 pathway is not recommended here. 33 71–73 Axial PsA remains a challenging form of PsA in terms of definition and differences with axial SpA; thus, this phenotype is part of the research agenda ( table 4 ).
Recommendation 9
The choice of the mode of action should reflect non-musculoskeletal manifestations related to PsA; with clinically relevant skin involvement, preference should be given to an IL-17A or IL-17A/F or IL-23 or IL-12/23 inhibitor; with uveitis to an anti-TNF monoclonal antibody; and with IBD to an anti-TNF monoclonal antibody or an IL-23 inhibitor or IL-12/23 inhibitor or a JAKi.
This is a new recommendation to clarify more visibly than in 2019 ( table 3 ) that the choice of drug should take into account not only the MSK PsA phenotype but also extra-MSK manifestations.
The first extra-MSK manifestation of interest in PsA is skin psoriasis. Although most patients with PsA present with skin psoriasis or have a personal history of skin psoriasis, registry data indicate that many patients with PsA have mild skin involvement. 74 However, even limited skin psoriasis can be troublesome, since relevant skin involvement is defined as either extensive (body surface area involvement >10%), or as important to the patient, that is, impacting negatively their quality of life (such as is the case with face or genital involvement). 9 For these patients, we recommend preferentially considering drugs targeting the IL-17A, IL-17A/F or IL-23 pathway (here, the order between drugs is cited in order of numbered cytokine, not preference). There are strong data, including head-to-head trials, in the field of skin psoriasis showing that drugs targeting the IL-23 and IL-17 pathways are superior to TNFis and to JAKis for skin psoriasis. 51 52 75–78 This justified proposing these modes of action preferentially in case of relevant skin involvement. This is in keeping with psoriasis recommendations. 79
Uveitis is not as frequent in PsA as it is in axial SpA; the prevalence is reported around 5%. 80 However, uveitis can be severe and should influence treatment decisions. Currently, the only mode of action with direct proof of efficacy on uveitis is TNF inhibition through monoclonal antibodies (ie, adalimumab and infliximab). Thus, for patients with uveitis, an anti-TNF monoclonal antibody is preferred.
Inflammatory bowel disease (IBD) concerns 2%–4% of patients with PsA. 80 The armamentarium for IBD has widened recently, and this recommendation reflects this fact, proposing that one of the modes of action currently licensed for IBD should be prescribed when it coexists with PsA. No order of preference is given here and prescribers are urged to adhere to EMA authorisations for IBD and take into account safety. For informative purposes, as of mid-2023, drugs authorised for IBD include anti-TNF monoclonal antibodies (ie, adalimumab and infliximab), the IL-12/23i ustekinumab, the IL-23i risankizumab (for Crohn’s disease) and two JAKis (one of which, tofacitinib, only for Crohn’s disease). 81–85 IL-17is (both A and A/F) are not recommended in case of active IBD, given indications of a heightened risk of flares. 86–88
Decisions for patients presenting with major skin involvement, with uveitis or with IBD should be discussed with the relevant specialist colleagues, as needed.
In all cases, the prescriber must refer to current drug authorisations and take into account safety and comorbidities.
To present an order for choosing drugs, we propose that the first element to take into account is the PsA subtype, then as a second element extra-MSK manifestations (always considering safety and comorbidities).
Recommendation 10
In patients with an inadequate response or intolerance to a bDMARD or a JAKi, switching to another bDMARD or JAKi should be considered, including one switch within a class.
This recommendation is unchanged from 2019, with unchanged LoE. 9 After failing one targeted drug, it is logical to switch to another targeted drug; there are currently no strong data to prefer a switch with a change in mode of action to a switch within the same mode of action. Of note, this recommendation does not limit the total number of switches for a given patient. It also does not necessarily mean that more switches within a class could not be done, but the taskforce felt that a switch should not necessarily be done after one drug of a class has failed. Switches can be made, as appropriate, between bDMARDs, or between bDMARDs and JAKis. We include abatacept as a treatment option ( table 1 ), 49 but note that it demonstrated modest efficacy and hence this is an option to be used only after failing one or more other targeted drugs. The efficacy of bimekizumab, the dual IL-17 A/F inhibitor, appeared similar in TNF-naïve and TNF-experienced populations; this will warrant confirmation. 53 54 Finally, a combination of bDMARDs is being explored, but cannot be recommended at this time.
Recommendation 11
In patients in sustained remission, tapering of DMARDs may be considered.
This bullet point is unchanged. However, more data have accrued on tapering, leading to a higher grade of recommendation. 89–91 By tapering we mean ‘dose reduction’ not drug discontinuation since the latter usually leads to flares. Drug tapering is a logical step when patients are doing well over time, from a safety and a cost perspective (tapering is often performed by the patient himself/herself alone). On the other hand, long-term data are missing and currently drug tapering is off-label. For all of these reasons, the taskforce kept the tentative wording of ‘may be considered’ (to ensure it is not made mandatory) and of course in the context of a shared decision with the patient (as is the case also for the other treatment decisions).
Research agenda
The taskforce felt that many issues needed more data, and an extensive research agenda was developed ( table 4 ).
This paper presents updated recommendations for the management of PsA, a treatment algorithm and a research agenda. This update addresses all currently available drugs and modes of action, and recommends an order to their use, taking into account the phenotype of the MSK and the non-MSK manifestations.
These elements should be helpful in the management of individual patients, but also in the advocacy for better access to care and for research.
This 2023 update is a major update since most of the recommendations were modified substantially. The EULAR standardised operating procedures propose a voting system for updates which discourages minor modifications for rewordings. 13 Since 2019, many new drugs have become available in PsA; the choice of which drug to prescribe to which patients rests on data related to efficacy, clinical phenotype, adverse event risk profile, tolerance, long-term data, cost and access. While laboratory biomarkers for stratified treatment approaches are lacking, the taskforce used clinical markers to develop clinical phenotypic preferences for specific drugs. In these updated recommendations, the taskforce applied expert opinion to the available data, to propose a pragmatic, logical order of a step-up approach to targeted treatments of PsA. The taskforce felt that proposing an order is helpful both for clinicians and to advocate for access to drugs for patients with PsA.
The drug options considered in these recommendations are currently licensed for PsA. We are aware that other drugs are being tested, or are available in other related conditions, especially skin psoriasis; however, these drugs are considered out of the scope of the present recommendations. Brodalumab was at the time of these recommendations only approved for psoriasis; TYK2 inhibitors such as deucravacitinib and brepocitinib have also been developed or in development for skin psoriasis and PsA; izokibep is a novel antibody mimetic, a small IL-17i currently undergoing testing; and an oral IL-23i is also in development. 5
The taskforce had extensive discussions on the positioning of JAKi in the recommendations. 63 92 We as a group feel that it is important to make haste slowly , and to uphold high safety standards when promoting drugs with only short-to-medium-term experience and for which long-term data are lacking—not least in PsA. In fact, this cautious attitude was also adhered to in the 2019 recommendations, and further safety developments have later confirmed that this attitude was appropriate. 7 8 It is of key importance to continue monitoring the drugs and, ideally, perform controlled trials, as only hard and high-level data can be reassuring.
Costs are also an important aspect in patient management, and it is generally recommended to prescribe the cheaper drug if two agents have similar efficacy and safety. Of note, even if one mode of action may have somewhat better efficacy on certain manifestations, a less expensive agent could still be preferred as long as it does not bear much lesser efficacy in that disease domain. Biosimilars are available for several TNFis and have led to significant reduction in expenditure and more use in many countries, while their price is not much lower than that of originators in many other ones. Tofacitinib will soon become generic, and the same is true for apremilast, which should also lower the costs for these agents and allow wider application especially in less affluent countries. Thus, overall, the taskforce felt that the prescription of drugs would account for the relationships between efficacy, safety and cost, in line with the OAPs and the 11 recommendations which are summarised in the algorithm ( figure 1 ). Many points are still to be confirmed in the management of PsA, leading to an extensive research agenda. 93
In conclusion, the updated 2023 recommendations should be helpful to clinicians but also to health professionals and patients when discussing treatment options. They can also be helpful to promote access to optimal care. As new data become available and new drugs are authorised in PsA, these recommendations should be again updated.
Ethics statements
Patient consent for publication.
Not required.
- Zabotti A ,
- De Marco G ,
- Gossec L , et al
- Alharbi S ,
- Lee K-A , et al
- Ferguson LD ,
- Siebert S ,
- McInnes IB , et al
- Lubrano E ,
- Scriffignano S ,
- de Vlam K , et al
- Kerschbaumer A ,
- Smolen JSS ,
- Ferreira JO , et al
- Ytterberg SR ,
- Mikuls TR , et al
- ↵ European Medicine Agency statement . Available : https://www.ema.europa.eu/en/medicines/human/referrals/janus-kinase-inhibitors-jaki [Accessed 7 Nov 2023 ].
- ↵ US food and Drug Administration . Available : https://www.fda.gov/safety/medical-product-safety-information/janus-kinase-jak-inhibitors-drug-safety-communication-fda-requires-warnings-about-increased-risk [Accessed 7 Nov 2023 ].
- Baraliakos X ,
- Kerschbaumer A , et al
- Coates LC ,
- Soriano ER ,
- Corp N , et al
- Ogdie A , et al
- ↵ Available : https://www.eular.org/web/static/lib/pdfjs/web/viewer.html?file=https://www.eular.org/document/download/680/b9eb08d0-faca-4606-8ed9-d0539b3f312a/660 [Accessed 1 Mar 2023 ].
- Chalmers I ,
- Glasziou P ,
- Greenhalgh T , et al
- Smolen JS ,
- Ramiro S , et al
- FitzGerald O ,
- Chandran V , et al
- Kerola AM ,
- Rollefstad S , et al
- Wendling D ,
- Hecquet S ,
- Fogel O , et al
- Gladman D ,
- McNeil HP , et al
- Chimenti MS ,
- Navarini L , et al
- Otero-Losada M ,
- Kölliker Frers RA , et al
- Orbai A-M , et al
- Trouvin AP ,
- Ballegaard C ,
- Skougaard M ,
- Guldberg-Møller J , et al
- Braun J , et al
- Moverley AR ,
- McParland L , et al
- Gayraud M , et al
- Landewé RBM ,
- van der Heijde D
- Orbai A-M ,
- Mease P , et al
- Vincken NLA ,
- Balak DMW ,
- Knulst AC , et al
- Nikiphorou E ,
- Sepriano A , et al
- de Vlam K ,
- Steinfeld S ,
- Toukap AN , et al
- Kishimoto M ,
- Deshpande GA ,
- Fukuoka K , et al
- Vieira-Sousa E ,
- Rodrigues AM , et al
- Mulder MLM ,
- Vriezekolk JE ,
- van Hal TW , et al
- Tillett W ,
- D’Agostino M-A , et al
- Bergstra SA , et al
- Lindström U ,
- di Giuseppe D ,
- Exarchou S , et al
- Wilsdon TD ,
- Whittle SL ,
- Thynne TR , et al
- Lambert De Cursay G ,
- Lespessailles E
- Curtis JR ,
- Beukelman T ,
- Onofrei A , et al
- Wang C , et al
- Behrens F , et al
- McInnes IB ,
- Behrens F ,
- Mease PJ , et al
- Bergmans P , et al
- Gottlieb AB ,
- van der Heijde D , et al
- Sawyer LM ,
- Markus K , et al
- Sbidian E ,
- Chaimani A ,
- Garcia-Doval I , et al
- Guelimi R , et al
- Asahina A ,
- Coates LC , et al
- Merola JF ,
- Landewé R ,
- Miyagawa I ,
- Nakayamada S ,
- Nakano K , et al
- Drosos GC ,
- Houben E , et al
- Tarannum S ,
- Leung Y-Y ,
- Johnson SR , et al
- Gorlier C , et al
- Di Giuseppe D ,
- Delcoigne B , et al
- Cañete JD ,
- Olivieri I , et al
- Rossmanith T ,
- Foldenauer AC , et al
- Fagerli KM ,
- Anderson JK ,
- Magrey M , et al
- Burmester GR ,
- Winthrop KL , et al
- Charles-Schoeman C ,
- Cohen S , et al
- Kristensen LE ,
- Yndestad A , et al
- Coates L , et al
- Lories RJ ,
- Marchesoni A ,
- Merashli M , et al
- Pournara E , et al
- Helliwell PS ,
- Gladman DD ,
- Chakravarty SD , et al
- Deodhar A ,
- Gensler LS ,
- Sieper J , et al
- Gladman DD , et al
- Love TJ , et al
- Bachelez H ,
- van de Kerkhof PCM ,
- Strohal R , et al
- Blauvelt A ,
- Bukhalo M , et al
- Reich K , et al
- Leonardi C ,
- Elewski B , et al
- Strober BE ,
- Kaplan DH , et al
- Harrison NL , et al
- Feagan BG ,
- Sandborn WJ ,
- Gasink C , et al
- Sands BE , et al
- Panaccione R , et al
- Vermeire S ,
- Zhou W , et al
- Loftus EV ,
- Lacerda AP , et al
- Letarouilly J-G ,
- Pierache A , et al
- Komaki Y , et al
- Tucker LJ ,
- Pillai SG ,
- Tahir H , et al
- Ruwaard J ,
- L’ Ami MJ ,
- Kneepkens EL , et al
- Fleishaker D , et al
- Widdifield J ,
- Wu CF , et al
Handling editor Dimitrios T Boumpas
X @LGossec, @FerreiraRJO, @lihi_eder, @dranielmar, @drpnash, @sshoopworrall
Contributors All authors have contributed to this work and approved the final version.
Funding Supported by EULAR (QoC016).
Competing interests No support to any author for the present work. Outside the submitted work: LG: research grants: AbbVie, Biogen, Lilly, Novartis, UCB; consulting fees: AbbVie, Amgen, BMS, Celltrion, Janssen, Lilly, MSD, Novartis, Pfizer, UCB; non-financial support: AbbVie, Amgen, Galapagos, Janssen, MSD, Novartis, Pfizer, UCB; membership on an entity’s Board of Directors or advisory committees: EULAR Treasurer. AK: speakers bureau, consultancy: AbbVie, Amgen, Galapagos, Janssen, Eli Lilly, MSD, Novartis, Pfizer, UCB. RJOF: research grants: Medac, Lilly; consulting fees: Sanofi. DA: research grants: Galapagos, Lilly; consulting fees: AbbVie, Gilead, Janssen, Lilly, Merck, Novartis, Sanofi. XB: research grants: AbbVie, MSD, Novartis; consultancies: AbbVie, Amgen, Celltrion, Chugai, Eli Lilly, Galapagos, Janssen, MSD, Novartis, Pfizer, Roche, Sandoz, UCB; membership on an entity’s Board of Directors or advisory committees: ASAS President, EULAR President Elect. W-HB: honoraria: AbbVie, Almirall, BMS, Janssen, Leo, Eli Lilly, Novartis, UCB; expert testimony: Novartis; participation on a Data Safety Monitoring Board or Advisory Board: AbbVie, Almirall, BMS, Janssen, Leo, Eli Lilly, Novartis, UCB. IBM: honoraria/consultation fees non-exec roles: NHS GGC Board Member, Evelo Board of Directors, Versus Arthritis Trustee Status; stock or stock options: Evelo, Cabaletta, Compugen, Causeway Therapeutics, Dextera. DGM: research grants: Janssen, AbbVie, Lilly, Novartis, UCB, BMS, Moonlake; consulting fees: Janssen, AbbVie, Lilly, Novartis, UCB, BMS, Moonlake, Celgene; honoraria: Janssen, AbbVie, Lilly, Novartis, UCB, BMS, Moonlake. KLW: research grants: BMS, Pfizer; consulting: Pfizer, AbbVie, AstraZeneca, BMS, Eli Lilly, Galapagos, GlaxoSmithKline (GSK), Gilead, Novartis, Moderna, Regeneron, Roche, Sanofi, UCB Pharma. AB: speakers fees: AbbVie, Amgen, AlphaSigma, AstraZeneca, Angelini, Biogen, BMS, Berlin-Chemie, Boehringer Ingelheim, Janssen, Lilly, MSD, Novartis, Pfizer, Roche, Sandoz, Teva, UCB, Zentiva; consultancies: Akros, AbbVie, Amgen, AlphaSigma, Biogen, Boehringer Ingelheim, Lilly, Mylan, MSD, Novartis, Pfizer, Roche, Sandoz, Sobi, UCB. PVB: consulting fees: AbbVie, Janssen-Cilag, Pfizer; honoraria: AbbVie, Bausch Health, Celltrion Healthcare, Eli Lilly, Gedeon Richter, IBSA Pharma, Infomed, Janssen-Cilag, Novartis, Pfizer, Sandoz; payment for expert testimony: Gedeon Richter; other: President, Hungarian Association of Rheumatologists. GRB: honoraria and/or speaker fees: AbbVie, BMS, Janssen, Lilly, Novartis, Pfizer. JDC: honoraria: UCB. PC: research grants: AbbVie, Amgen, Biogen, Jansen, Lilly, Novartis, UCB; consulting fees: AbbVie, Amgen, Celltrion, Janssen, Lilly, MSD, Novartis, Pfizer, UCB. LE: consultation fee/advisory board: AbbVie, Novartis, Janssen, UCB, BMS, Eli Lilly; research/educational grants: AbbVie, Fresenius Kabi, Janssen, Amgen, UCB, Novartis, Eli Lilly, Sandoz, Pfizer. MLH: grant support: AbbVie, Biogen, BMS, Celltrion, Eli Lilly, Janssen Biologics BV, Lundbeck Foundation, MSD, Pfizer, Roche, Samsung Bioepis, Sandoz, Novartis, Nordforsk; honoraria: Pfizer, Medac, Sandoz; advisory board: AbbVie; past-chair of the steering committee of the Danish Rheumatology Quality Registry (DANBIO, DRQ), which receives public funding from the hospital owners and funding from pharmaceutical companies; cochair of EuroSpA, partly funded by Novartis. AI: research grants from AbbVie, Pfizer, Novartis; honoraria for lectures, presentations, speakers bureaus from AbbVie, Alfasigma, BMS, Celgene, Celltrion, Eli Lilly, Galapagos, Gilead, Janssen, MSD, Novartis, Pfizer, Sanofi Genzyme, Sobi; EULAR Board Member; EULAR Congress Committee, Education Committee and Advocacy Committee Advisor; EULAR Past President. LEK: consultancies: AbbVie, Amgen, Biogen, BMS, Celgene, Eli Lilly, Pfizer, UCB, Sanofi, GSK, Galapagos, Forward Pharma, MSD, Novartis, Janssen; has been representing rheumatology FOREUM scientific chair. RQ: consultancy and/or speaker’s honoraria from and/or participated in clinical trials and/or research projects sponsored by AbbVie, Amgen-Celgene, Eli Lilly, Novartis, Janssen, Pfizer, MSD, UCB. DM: honoraria: UCB, Janssen, GSK, AstraZeneca, AbbVie; support to meetings: Janssen. HM-O: grant support: Janssen, Novartis, UCB; honoraria and/or speaker fees: AbbVie, Biogen, Eli Lilly, Janssen, Moonlake, Novartis, Pfizer, Takeda, UCB. PJM: grant support: AbbVie, Acelyrin, Amgen, Bristol Myers Squibb, Eli Lilly, Genascence, Janssen, Novartis, Pfizer, UCB; consulting fees: AbbVie, Acelyrin, Aclaris, Alumis, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly, Genascence, Inmagene, Janssen, Moonlake, Novartis, Pfizer, Takeda, UCB, Ventyx, Xinthera; honoraria: AbbVie, Amgen, Eli Lilly, Janssen, Novartis, Pfizer, UCB. PN: consulting fees and honoraria: AbbVie, Amgen, BMS, Lilly, Janssen, GSK, Novartis, UCB, Servatus; boards: Amgen, BMS, Janssen, GSK, Novartis, UCB; GRAPPA Steering Committee, Chair ASMPOC, ARA. LS: consulting fees: AbbVie, Almirall, Novartis, Janssen, Lilly, UCB, Pfizer, Bristol Myers Squibb, Boehringer Ingelheim; honoraria: AbbVie, Almirall, Novartis, Janssen, UCB, Pfizer, Takeda, Galderma, Biogen, Celgene, Celltrion, Lilly, Sanofi, Bristol Myers Squibb, Boehringer Ingelheim; support to attending meetings: AbbVie, Janssen, Lilly, Novartis, UCB, Galderma, Bristol Myers Squibb, Boehringer Ingelheim; participation in boards: AbbVie, Almirall, Novartis, Janssen, UCB, Pfizer, Galderma, Biogen, Lilly, Sanofi, Bristol Myers Squibb, Boehringer Ingelheim; GRAPPA Executive Board (elected), British Society for Medical Dermatology (BSMD) Committee. GS: honoraria: Novartis, Janssen. SJWS-W: grant support: Medical Research Council (MR/W027151/1). YT: research grants from Mitsubishi Tanabe, Eisai, Chugai, Taisho; speaking fees and/or honoraria from Eli Lilly, AstraZeneca, AbbVie, Gilead, Chugai, Boehringer Ingelheim, GlaxoSmithKline, Eisai, Taisho, Bristol Myers, Pfizer, Taiho. FEVdB: consultancy honoraria from AbbVie, Amgen, Eli Lilly, Galapagos, Janssen, Novartis, Pfizer, UCB. AZ: speakers bureau: AbbVie, Novartis, Janssen, Lilly, UCB, Amgen; paid instructor for AbbVie, Novartis, UCB. DvdH: consulting fees AbbVie, Argenx, Bayer, BMS, Galapagos, Gilead, GlaxoSmithKline, Janssen, Lilly, Novartis, Pfizer, Takeda, UCB Pharma; Director of Imaging Rheumatology bv; Associate Editor for Annals of the Rheumatic Diseases ; Editorial Board Member for Journal of Rheumatology and RMD Open ; Advisor Assessment Axial Spondyloarthritis International Society. JSS: research grants from AbbVie, AstraZeneca, Lilly, Galapagos; royalties from Elsevier (textbook); consulting fees from AbbVie, Galapagos/Gilead, Novartis-Sandoz, BMS, Samsung, Sanofi, Chugai, R-Pharma, Lilly; honoraria from Samsung, Lilly, R-Pharma, Chugai, MSD, Janssen, Novartis-Sandoz; participation in advisory board from AstraZeneca.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:

COMMENTS
Recommendations for future research should be: Concrete and specific. Supported with a clear rationale. Directly connected to your research. Overall, strive to highlight ways other researchers can reproduce or replicate your results to draw further conclusions, and suggest different directions that future research can take, if applicable.
Generate the conclusion outline: After entering all necessary details, click on 'generate'. Paperpal will then create a structured outline for your conclusion, to help you start writing and build upon the outline. Write your conclusion: Use the generated outline to build your conclusion.
Research recommendations are typically made at the end of a research study and are based on the conclusions drawn from the research data. The purpose of research recommendations is to provide actionable advice to individuals or organizations that can help them make informed decisions, develop effective strategies, or implement changes that ...
Having drawn your conclusions you can then make recommendations. These should flow from your conclusions. They are suggestions about action that might be taken by people or organizations in the light of the conclusions that you have drawn from the results of the research. Like the conclusions, the recommendations may be open to debate.
The conclusion is intended to help the reader understand why your research should matter to them after they have finished reading the paper. A conclusion is not merely a summary of the main topics covered or a re-statement of your research problem, but a synthesis of key points derived from the findings of your study and, if applicable, where you recommend new areas for future research.
The conclusion should end with a strong concluding statement that leaves a lasting impression on the reader. This could be a call to action, a recommendation for further research, or a final thought on the topic. How to Write Research Paper Conclusion. Here are some steps you can follow to write an effective research paper conclusion:
If possible, learn about the guidelines before writing the discussion to ensure you're writing to meet their expectations. Begin with a clear statement of the principal findings. This will reinforce the main take-away for the reader and set up the rest of the discussion. Explain why the outcomes of your study are important to the reader.
Here is a step-wise guide to build your understanding on the development of research recommendations. 1. Understand the Research Question: Understand the research question and objectives before writing recommendations. Also, ensure that your recommendations are relevant and directly address the goals of the study. 2.
The conclusions and recommendations you write are your scholarly legacy, a testament to the hard work you've poured into your research. Approach them with the same rigor , creativity, and dedication as the rest of your thesis, and you'll leave a lasting mark on your field.
Present recommendations for future research; Therefore, your conclusion chapter needs to cover these core components. Importantly, you need to be careful not to include any new findings or data points. Your conclusion chapter should be based purely on data and analysis findings that you've already presented in the earlier chapters. If there ...
The conclusion is where you describe the consequences of your arguments by justifying to your readers why your arguments matter (Hamilton College, 2014). Derntl (2014) also describes conclusion as the counterpart of the introduction. Using the Hourglass Model (Swales, 1993) as a visual reference, Derntl describes conclusion as the part of the ...
The best structure for a conclusion in a research paper is to draft your conclusion in such a way that it links back to your introduction and your introduction links back to it, just like a perfect cycle. This can be done by restating the question asked in the introduction. But in this section, you would be providing an answer that your readers ...
Writing a Conclusion. A conclusion is an important part of the paper; it provides closure for the reader while reminding the reader of the contents and importance of the paper. It accomplishes this by stepping back from the specifics in order to view the bigger picture of the document. In other words, it is reminding the reader of the main ...
22 Writing the conclusion & recommendations General. There are probably some overlaps between the Conclusion and the Discussion section. Nevertheless, this section gives you the opportunity to highlight the most important points in your report, and is sometimes the only section read. ... Suggestions for future research: Suggest how your work ...
PDF | Lesson 28 (Conclusion and recommendation) covers the following: definition of conclusion; general rules of structure and writing style of... | Find, read and cite all the research you need ...
The conclusion and recommendations sections are crucial components of a research paper. They mark the end of your research, leave a lasting impression on your readers, and should be approached with great care. No wonder many students search for information about how to write recommendations in research papers.
ISBN: 978-978-59429-9-6. CHAPTER FIVE. Summary, Conclusion and Recommendation. Aisha Ibrahim Zaid. Department of Adult Educ. & Ext. Services. Faculty of Education and Extension Services. Usmanu ...
Step 3: Make future recommendations. You may already have made a few recommendations for future research in your discussion section, but the conclusion is a good place to elaborate and look ahead, considering the implications of your findings in both theoretical and practical terms. Example: Recommendation sentence.
You may present the conclusions and recommendations in a numbered or bulleted list to enhance readability. Reference Page. All formal reports should include a reference page; this page documents the sources cited within the report. The recipient(s) of the report can also refer to this page to locate sources for further research.
The conclusions are as stated below: i. Students' use of language in the oral sessions depicted their beliefs and values. based on their intentions. The oral sessions prompted the students to be ...
The research paper title page format depends on the required formatting style: MLA does not require a separate title page (unless specifically requested). Instead, in the upper left-hand corner of the first page, type your name, your instructor's name, course name, and date (each on a new line, double-spaced).
Background Adherence to physiotherapeutic treatment and recommendations is crucial to achieving planned goals and desired health outcomes. This overview of systematic reviews synthesises the wide range of additional interventions and behaviour change techniques used in physiotherapy, exercise therapy and physical therapy to promote adherence and summarises the evidence of their efficacy ...
Objective New modes of action and more data on the efficacy and safety of existing drugs in psoriatic arthritis (PsA) required an update of the EULAR 2019 recommendations for the pharmacological treatment of PsA. Methods Following EULAR standardised operating procedures, the process included a systematic literature review and a consensus meeting of 36 international experts in April 2023 ...
Six steps to writing a project proposal: write the executive summary, explain the project background, present a solution, and define the project deliverables and resources needed. Top tips for writing a persuasive project proposal: know your audience, keep it simple and make it persuasive, do you research, use a template and cover letter.
purpose; a recommendation for graduate school admission may be more than a page long, whereas a work-related recommendation generally will be one page or less. You might structure your letter so that you have a short paragraph on in-class performance, then one on written work, then one on out-of-classroom activities.