Current SWHPN Members: We have switched platforms. Your old login will no longer work. Contact [email protected] to access your account.

We're on a mission to revolutionize hospice and palliative care by making it a more equitable experience for everyone involved, including the clinicians at its heart.
If you're a healthcare provider committed to dismantling structures of oppression and crave the support you need for a fulfilling career instead of a draining one, you’re in the right place.

About SWHPN
We offer membership, small group support and continuing education for hospice + palliative care social workers and clinicians making an impact.
Our mission is to enhance hospice and palliative care social work through mentorship, education, community building and advocacy as change agents committed to equity and anti-racism. We start with ourselves to dismantle harms perpetuated within the systems in which we exist.
Join us in defining the future of compassionate, whole-person healthcare — and get the support you need for a sustainable career while you're at it.
Membership Options
Becoming a SWHPN member offers you access to the sweetest + boldest community you've ever met, support for a sustainable career, resources valued at over $1000 per year and more.
Learn With Us
At least once a month we offer continuing education programming that covers the topics that really matter, such as cultivating cultural responsiveness in your practice and how to take care of yourself in ways that actually work.
Support Our Work
Your tax deductible donation fuels the development of anti-oppression curriculum, supports advocacy efforts for healthcare equity, provides genuine assistance to hospice + palliative care clinicians and offers valuable resources to those in need.
What we offer
MENTORSHIP PROGRAM
Applications for our 2024-2025 Mentor-Mentee Cohort are now closed
As a benefit of SWHPN membership, we pair mentors + mentees together for a year long relationship to enhance professional practice.
Thank you to all who applied!
We will be accepting 10 pairs for the 2024-2025 cohort which will run from June 2024 through the SWHPN Annual Conference in 2025.
If you submitted an application you can expect an email with an update by the end of May.
.jpg)
The only evidence based certification for hospice + palliative care workers
Social workers are essential to the practice of hospice and palliative care. The APHSW-C certification recognizes bachelor’s and master’s level social workers with experience, specialized skills and competency in hospice and palliative social work. The APHSW-C assures the public that certified practitioners have the knowledge and skills to provide safe, high-quality care at an advanced level and we have the resources you need to prepare for your exam.

TESTIMONIALS
What people are saying
Alisha McGuire
I joined SWHPN when I transitioned into the world of palliative (and hospice) social work. I have gotten so much out of my membership; ranging from education, professional/career development, mentorship, and lifelong friendships. SWHPN has helped be the platform in the "next steps" of my career from the micro to the macro!

Arika Patneaude
I joined SWHPN because I wanted to be in community with other HAPC social workers and interprofessional colleagues. I remain a SWHPN member because I want to make an impact on HAPC as a field in engaging in and committing to anti-oppression and anti-racist end-of-life care with colleagues and an organization that are committed to this as a mission. As HAPC professionals we cannot provide high quality serious illness care from diagnosis to death without being culturally responsive and anti-racist.

Jennifer Hill Buehrer
Social work in the medical field is lonely - palliative care social work even more so! I love the chance to connect with other professionals who understand that, and who do the same really difficult, emotionally challenging work I do.

STAY IN THE LOOP
Sign up for our newsletter
You Can Also Sign Up For Our Friday Weekly News Brief Here
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Institute of Medicine (US) and National Research Council (US) National Cancer Policy Board; Foley KM, Gelband H, editors. Improving Palliative Care for Cancer. Washington (DC): National Academies Press (US); 2001.

Improving Palliative Care for Cancer.
- Hardcopy Version at National Academies Press
9 Professional Education in Palliative and End-of-Life Care for Physicians, Nurses, and Social Workers
Hellen Gelband
Institute of Medicine
- INTRODUCTION
In 1997, the Institute of Medicine (IOM, 1997) described a system of professional end-of-life care whose major deficiencies included
- a curriculum in which death is conspicuous mainly by its relative absence;
- educational materials that are notable for their inattention to the end stages of most diseases and their neglect of palliative strategies; and
- clinical experiences for students and residents that largely ignore dying patients and those close to them.
However, it also reported “increasing acknowledgement by practitioners and educators of the compelling need to better prepare clinicians to assess and manage symptoms, to communicate with patients and families, and to participate in interdisciplinary caregiving that meets the varied needs of dying patients and those close to them.” The increasing interest had already translated into new programs by professional societies, medical schools, and private foundations, and these continue. However, impressive as the initiatives are, they are small in scale compared with national needs. The IOM report cautioned that “persistence in their implementation, evaluation, redesign, and extension will be necessary to keep the promise from fading once initial enthusiasm subsides,” and this caution remains appropriate in 2001. This chapter takes as a starting point one of the 1997 report's major recommendations:
Educators and other health professionals should initiate changes in undergraduate, graduate, and continuing education to ensure that practitioners have relevant attitudes, knowledge, and skills to care well for dying patients.
Within medicine, nursing, and social work, the recognition of deficiencies in education are well known, and each profession has at least initiated efforts to improve the status quo. However, the recognition that improvements are needed does not bring the knowledge and tools necessary to accomplish those ends. This is the task that lies ahead and that will require persistent effort and increased and sustained funding for a wide range of activities. Thus far, funding for the major initiatives have been led by private foundations. With successful programs started and ideas for new approaches proliferating however, the amount of funding that can be put to productive use is much greater. Sustained progress at this juncture requires a substantial commitment of support from the public sector as well as continued support for innovation from the private sector.
- PHYSICIAN EDUCATION IN END-OF-LIFE CARE
Most U.S. physicians—oncologists, other specialists, and generalists alike—are not prepared by education or experience to satisfy the palliative care needs of dying cancer patients or even to help them get needed services from other providers. With half a million people dying from cancer each year in this country, this is a stark, but robust finding. The strongest sources of supporting evidence are
- studies during the late 1990s documenting end-of-life and palliative care content in undergraduate and residency coursework, and
- studies during the late 1990s of medical textbook content on end-of-life and palliative care.
Consistent with these sources are responses given by oncologists to American Society of Clinical Oncology (ASCO) 1998 survey questions about their training in end-of-life and palliative care and their abilities to provide appropriate care of this type (Emanuel, 2000). The evidence is consistent with a lack of funding for end-of-life and palliative care educational initiatives, which has begun to change only recently. Even in 2001, however, the programs are small and funded largely by private grant-making organizations, with little contribution by the federal government. Perhaps even more persuasive is the complete lack of documented disagreement about the poor state of end-of-life medical education.
End-of-Life Care Education During Medical School and Residency Programs
The subject of “death and dying” first entered the medical school curriculum in the 1960s, as a topic of discussion in preclinical coursework. Movement toward integrating end-of-life and palliative care into the clinical curriculum has begun much more recently. In 1999, the Medical School Objectives Project identified “knowledge…of the major ethical dilemmas in medicine, particularly those that arise at the beginning and end of life…” and “knowledge about relieving pain and ameliorating the suffering of patients” as subjects that should be mastered by all undergraduate medical students (Medical School Objectives Writing Group, 1999).
Students in some programs may get the training and opportunities needed, but according to the most recent and most complete survey of medical school and residency end-of-life and palliative care curricula, most do not. Barzansky and colleagues (1999) used three annual surveys that collectively cover all medical school and residency programs to analyze end-of-life and palliative care content. Results for undergraduate medical education and residency programs are summarized separately.
Undergraduate Medical Education
Two surveys provide information on medical school curricula: the Liaison Committee on Medical Education (LCME) Annual Medical School Questionnaires for years 1997–1998 and 1998–1999, and the 1998 Association of American Medical Colleges (AAMC) Graduation Questionnaire. The LCME survey goes to the deans of all 125 LCME-accredited medical schools each year, and in the two years described here, all deans responded. The AAMC questionnaire went to all 14,040 students graduating from the 125 medical schools, of whom 88 percent responded.
The LCME survey asked different questions about end-of-life and palliative care in each of the two years. In 1997–1998, the question was whether selected topics related to end-of-life care were included in the curriculum as courses that were required, parts of required courses, electives, or a combination of these. In the second year, schools were asked (1) whether certain topics related to the care of terminally ill patients were covered in required lectures or conferences and (2) whether students spent time during required courses or clerkships in clinical units devoted to care of terminally ill patients. The 1998 AAMC survey asked students to rate the level of time devoted to end-of-life issues (among others) as either inadequate, appropriate, or excessive.
LCME S URVEYS At all schools, students have some exposure to end-of-life coursework, but it is overwhelmingly in broader courses, not in required courses on end-of-life topics ( Table 9-1 ). More than half the schools do not offer even one elective course devoted to end-of-life issues. The survey provides no information on how much time was spent on relevant topics or how they were covered but does suggest that there are substantial gaps. For instance, 30 percent of the schools appear to have no required instruction on at least one of the three topics asked about in 1997–1998. The 1998– 1999 survey also asked about direct experience with patients in hospice care (or other settings in which the focus was on end-of-life or palliative care) ( Table 9-2 ). At 20 percent of the schools, such experience was required, and at another 20 percent, it was not available at all. No information was gathered on the percentage of students who took advantage of the elective opportunity offered in the remaining three-fifths of the schools.
LCME Annual Medical School Questionnaire—Course Content (125 Schools=100%).
LCME Annual Medical School Questionnaire: Experience in Hospice or Other End-of-Life Care Setting, 1998–1999 Survey (125 Schools=100%).
AAMC M EDICAL S CHOOL G RADUATION Q UESTIONNAIRE The AAMC annual survey asks graduating medical students to rate the adequacy of instruction in various areas. In 1998, they were asked about death and dying, and pain management ( Table 9-3 ). The responses are subjective, but again, they suggest strongly that students are not prepared to care for dying patients as well as they could be during their undergraduate medical education.
AAMC Medical School Graduation Questionnaire: Level of Coverage of Death and Dying and Pain Management 1998 Survey (N= 13,861 responses out of 14,040 eligible).
Residency Programs
The 1997–1998 American Medical Association (AMA) Annual Survey of Graduate Medical Education was sent to 7,861 residency programs (all of those accredited by the Accreditation Council on Graduate Medical Education), of which 96.5 percent responded. The survey asked whether each program had a structured curriculum in end-of-life care. (No more specific definitions of what might be included in an end-of-life curriculum were provided, so the term may have been interpreted differently by different respondents.)
Overall, 60 percent of programs reported that they did have a structured curriculum, but there was tremendous variability among programs in different specialties. Of the types of physicians most likely to care for dying patients
- 92 percent of programs in family practice and internal medicine and 98 percent in critical care medicine reported positively, and
- between 60 percent and 70 percent of programs in obstetrics-gynecology, pediatrics, psychiatry, and surgery reported positively.
The results of these recent surveys suggest that undergraduate medical and residency training lacks adequate content in end-of-life care, but without much detail. One would like to know what topics are covered in end-of-life education, the format (i.e., lectures, discussions, clinical experience), how much time is devoted to each subject, and how well students are prepared by the extent and types of training they receive. This information has not been assembled in a comprehensive way, but pieces of it are explored in the recent literature in different ways. A wide-ranging review of published literature and grant proposals for end-of-life care by Billings and Block (1997) has brought together the relevant material.
Billings and Block (1997) searched the published literature for articles on palliative care and related topics for the years 1980 through 1995 and reviewed palliative care education grants funded by the National Cancer Institute or submitted for funding to the Project on Death in America. One hundred eighty articles—culled from more than 9,000 potentially relevant citations—form the basis of their analysis. Their findings, which complement and support the findings of the recent surveys discussed earlier, are summarized here.
C URRICULUM IN E ND - OF -L IFE C ARE Some of the literature reviewed by Billings and Block (1997) represented reports of the surveys of medical school deans in years earlier than those characterized by Barzansky and colleagues (1999). The following findings were reported from the 1989 survey of medical school deans, which at the time numbered 124, of whom 111 responded (Mermann et al., 1991).
Twelve of the schools had no curriculum at all in death and dying. In 30 schools, one or two lectures on death and dying were included in other courses. In 51 schools, it was taught as a distinct module in a required course, consisting of four to six lectures or a combined lecture and seminar series with small-group discussion. Eighteen schools offered a separate course on death and dying, which was required in the first two years by nearly half of the schools. The format varied from a one-weekend workshop to semester-long lecture and seminar classes, with the lecture format predominating (15 schools). There was very little contact with dying patients in any program.
The class presidents of all U.S. medical schools were polled in 1991 about terminal care education (Holleman et al., 1994). Among the findings highlighted by Billings and Block are
- more than one-quarter reported one hour or less of class time,
- 39 percent recalled some reading on the topic, and
- 37 percent rated the quality of teaching “ineffective” and 3 percent rated it “very effective.”
In contrast to the students' evaluations, a national sample of cancer center directors and directors of nursing oncology reported high levels of satisfaction with supportive care instruction (greater than 90 percent) (Belani et al., 1994). However, in the one institution where students were actually studied, the level of satisfaction was 27 percent.
R ELATED F INDINGS When Billings and Block reviewed the literature in the mid-1990s, they found a number of small, more detailed studies, all of which lend support to the need for more attention to end-of-life care. Their findings span research published from 1980 through 1995; thus, some findings may be less relevant in 2001 than when published, but the pace of change has not been so great that this is necessarily so. Following are some provocative observations from individual studies:
- 30 percent of a random sample of generalists in Oregon recalled medical school training in dealing with dying patients, and 87 percent thought that more such instruction should be given in medical school;
- 39 percent of a sample of young physicians felt they had good or excellent preparation for managing the care of patients who want to die;
- 41 percent of students completing third-year clerkships were never present when an attending physician talked with a dying person, 35 percent had never discussed with an attending physician how to deal with terminally ill patients, 73 percent had never been present when a surgeon told a family about bad news after an operation, and one-third could not identify problems that would arise for family members when a dying patient was discharged to go home.
Articles on end-of-life care during residency reviewed by Billings and Block (1997) are consistent with the more recent survey findings. A similar survey of 1,068 accredited residency programs in family medicine, internal medicine, pediatrics, and geriatrics, published in 1995 (Hill, 1995) found that
- 26 percent of all residency programs in the United States offer a standard course in end-of-life care,
- almost 15 percent of programs offer no formal training in care of terminally ill patients, and
- 8 percent require a hospice rotation and 9 percent offer an elective one.
More than 1,400 residents in 55 internal medicine residency programs were surveyed by the American Board of Internal Medicine about the adequacy of their training in end-of-life care (reported in Foley, 1997). The percentage of residents reporting “adequate training” in specific areas was
- 72 percent, managing pain and other symptoms;
- 62 percent, telling patients that they are dying;
- 38 percent, describing what the dying process will be like; and
- 32 percent, talking to patients who request assistance in dying.
Conclusions
Most new physicians leave medical school and residency programs with little training or experience in caring for dying patients. In most cases, a few lectures are folded into other courses (in many cases in psychiatry and behavioral sciences, ethics, or the humanities). A few schools offer full-length courses on end-of-life care, but they are nearly all electives. According to the limited information available, most end-of-life training is provided in lectures only. Contact with dying patients, particularly for undergraduate medical students, if any, is limited.
Formal curriculum in end-of-life care is presented predominantly in preclinical years. In clinical training, which tends to be more informal and less systematic, teachers may have no special interest or expertise in end-of-life care. The importance of role models and mentors who are enthusiastic about caring for dying patients has largely been overlooked. There is a tremendous opportunity to train the next generation of physicians in the care of dying patients. At the same time, opportunities must be created to improve the competence of physicians who are already practicing, but who have had inadequate preparation in end-of-life care.
End-of-Life Care in Medical Textbooks
Textbooks play an important role both in educating medical students and in informing practicing physicians of the standard of care for each disease covered. The topics included in textbooks and the way information is organized may be strong influences on the practice of medicine. In the past few years, researchers have looked systematically at the information relating to end-of-life issues that is contained in a variety of medical textbooks. Two landmark studies, one of general medical texts and the other of medical specialty texts, which are the most recent and comprehensive, are presented here (a similar analysis of nursing texts is discussed later in this chapter). Both studies included specific cancers in their analyses.
End-of-Life Content in Four General Medical Textbooks
The study of general medical textbooks (Carron et al., 1999) focused on four widely used books: Harrison's Principles of Internal Medicine (Isselbacher et al., 1994), the Merck Manual (Berkow, 1992), Scientific American Medicine on CD-ROM (SAM-CD, 1994), and Manual of Medical Therapeutics (Ewald and McKenzie, 1995; also known as the Washington Manual ). In addition, the authors reviewed (although not in the same quantitative format as the target texts) William Osler's (1899) Principles and Practice of Medicine, and the Mayo Clinic Family Health Book (Larson, 1996) a medical reference for nonprofessionals.
Information was sought from each book on 12 of the leading causes of death in the United States, and for each disease, nine “content domains” were assessed ( Table 9-4 ). In addition to displaying the content score for each domain by disease, a rough overall score was calculated for each book by assigning a value of 1 for each “+” rating and 2 for each “++” rating and dividing the total by the total possible score (i.e., a rating of ++ in each category).
End-of-Life Care in General Medical Textbooks.
The following are some general findings (Carron et al., 1999):
- Harrison's Principles of Internal Medicine, the Merck Manual, and Scientific American Medicine characterized medical interventions and prognostic factors but often did not mention decisionmaking or the effect of death and dying on the patient's family.
- The Washington Manual “offered almost no helpful information.”
- Dementia, AIDS, lung cancer, and breast cancer received the most comprehensive coverage of issues related to dying. However, “the best coverage…was scored as presenting useful information in only five of the nine domains.”
Overall scores ranged from 11 percent for The Washington Manual to 38 percent for Harrison's Principles of Internal Medicine.
In contrast to the lack of coverage in medical textbooks, the Mayo Clinic Family Health Book contains a chapter on death and dying with a comprehensive discussion of “pain control in a terminal patient, the emotions of a dying patient, hospice care, funeral arrangements, when and how to tell the patient about a terminal diagnosis, and what the family should expect” (Carron et al., 1999).
Osler's 1899 textbook was found to be more straightforward about the fact of death but generally not about how to help patients cope with dying. One exception is Osler's admonition to use opiates for patients dying of hemorrhage into the lungs, to suppress terror and dyspnea. This information did not appear in any other text.
End-of-Life Content in 50 Medical Specialty Textbooks
The end-of-life content of 50 top-selling textbooks in a variety of specialties ( Table 9-5 ) was the subject of the second major review (Rabow et al., 2000). The methodology followed closely the methods used by Carron and colleagues in their study of general medical textbooks, but the content domains were expanded and the medical conditions studied necessarily varied from book to book and were chosen to represent the common causes of death in each specialty. The authors also reviewed the tables of contents for chapters dealing specifically with end-of-life care and searched the indexes for 18 relevant key words. In scoring, rather than calculating an overall score for each book (as Carron and colleagues did), the results are presented as the percentage of instances of “absent,” “minimal,” and “helpful” information.
End-of-Life Care Content of 50 Textbooks: Specialties, Content Domains, Scoring.
When the overall scores for each specialty were calculated (the average of the individual textbook scores in each specialty), there were some differences among specialties but a generalized pattern of 50–70 percent absent content and lower scores (i.e., poorer ratings) for minimal or helpful content (see Rabow et al., 2000, figure 1). Although the differences were not large, the authors noted that textbooks with the least end-of-life content were in the specialties of infectious diseases and AIDS, oncology and hematology, and surgery.
Information on how each domain was covered was presented for the six internal medicine textbooks. The 14 conditions analyzed in these texts included three cancers (breast, colon, and lung). The best-covered domains were epidemiology and natural history (i.e., consistent ratings of 2), and the worst were social, spiritual, and family issues; ethics, and physician responsibilities. In the remaining domains, minimal information (a rating of 1) was most common.
Ten conditions were appropriate to more than one specialty, and these included two cancers: lung cancer and leukemia. Lung cancer was covered in family and primary care medicine, internal medicine, and oncology-hematology; leukemia in family and primary care medicine and pediatrics, in addition to oncology-hematology. For lung cancer, oncology-hematology had the lowest helpful score (11.6 percent), followed by internal medicine (20.5 percent), and family and primary care had the best helpful score (28.2 percent). For leukemia, pediatrics and oncology-hematology helpful scores were similar (21.2 percent and 20.5 percent, respectively), and the lowest score was in family and primary care medicine (10.3 percent).
The analysis of key end-of-life index words showed an overall paucity of references, consistent with the content domain analyses.
Comment on Textbook Studies
A physician consulting a textbook on the treatment of a potentially fatal condition is most likely to find no specific information that will help care for the patient who does, indeed, die. In a minority of cases, useful information may be found. In both studies (Carron et al., 1999; Rabow et al., 2000), the scoring was generous, erring on the side of giving higher rather than lower scores, so even these scores may overestimate the useful content. The investigators also did not rate how useful or complete the information was. However, Carron and colleagues found that more often than not, when information about prognostic factors and disease progression was present, it was vague and would not be helpful in caring for a patient (e.g., the admonition that “supportive care is all that can be offered at this point”).
Knowing that many physicians have little experience with dying and little training to help them, Carron and colleagues commented that “standard reference textbooks should provide at least the essentials of good practice.” Yet, in fact, physicians cannot rely on these texts for much-needed information: on advance care planning, decisionmaking, the effect of death and dying on a patient's family, or symptom management. Most texts do not describe the way that people with a disease generally die.
The findings from these textbook reviews are so stark that they cannot, and in fact have not, been ignored. Partly in response to these studies, some textbook publishers have commissioned updates for particular chapters. In addition, the Robert Wood Johnson Foundation has begun a Textbook Revisions Project with the goal of working with publishers and editors to ensure that end-of-life chapters are added to textbooks and that end-of-life information is added to other chapters as appropriate (Gibson, 2000).
The 1998 ASCO Survey
In 1998, American Society of Clinical Oncology conducted the first and only large-scale survey of U.S. oncologists about their experiences in providing care to dying patients. The questionnaire consisted of 118 questions about end-of-life care under eight headings, one of which was education and training (Hilden et al., 2001). All U.S. oncologists who reported that they managed patients at the end of life, and were ASCO members, were eligible for the survey, a total of 6,645 (the small number of ASCO members from England and Canada was also included). About 40 percent (2,645) responded (see table below) (Emanuel, 2000). No information is available to compare the characteristics of those who responded with those who did not.
This survey documented serious shortcomings in the training and current practices of a large proportion of oncologists who responded. Among the key findings are the following:
- Most oncologists have not had adequate formal training in the key skills needed for them to provide excellent palliative and end-of-life care. Less than one-third reported their formal training “very helpful” in communicating with dying patients, coordinating their care, shifting to palliative care, or beginning hospice care. About 40 percent found their training very helpful in managing dying patients' symptoms.
- Slightly more than half (56 percent) reported “trial and error in clinical practice” as one important source of learning about end-of-life care. About 45 percent also ranked role models during fellowships and in practice as important. Traumatic patient experiences ranked higher as a source of learning than did lectures during fellowship, medical school role models, and clinical clerkships.
Recommendations to Improve End-of-Life Medical Education
In 1997, the Robert Wood Johnson Foundation and the Project on Death in America brought together 94 academic leaders (selected through a structured nomination process) in a national consensus conference on medical education for end-of-life care (Barnard et al., 1999). Their task was to develop recommendations to guide teaching in end-of-life care, based on evidence from the literature and expert opinion. The work was carried out by eight working groups in the following areas:
Preclinical years
Primary care and ambulatory care
Acute care hospitals
Emergency medicine
Intensive care
Long-term institutional care
Home care and hospice care
Each working group addressed five questions:
How do death and dying manifest themselves in your setting?
What are the tasks of end-of-life care in your setting?
What are the major opportunities and barriers to learning about end-of-life care?
What can be done to improve teaching about end-of-life care in your setting?
What currently available and new resources are needed to facilitate change?
A set of guiding principles for undergraduate medical education provides a framework for the recommendations of all the working groups (Billings and Block, 1997). The recommendations at the end of this chapter address how these principles might be advanced. This report does not make recommendations about the precise content of educational materials or programs, but the general skills and knowledge required are summarized well in the IOM report, Approaching Death (IOM, 1997).
Basic Principles for Enhancing Undergraduate Medical Education in Palliative Care 1
The care of dying persons and their families is a core professional task of physicians. Medical schools have a responsibility to prepare students to provide skilled, compassionate end-of-life care.
The following key content areas related to end-of-life care must be appropriately addressed in undergraduate medical education (NOTE: this list will differ depending on the setting and to some extent, patient population, e.g., children vs. adults.)
Medical education should encourage students to develop positive feelings about dying patients and their families and about the role of the physician in terminal care.
Enhanced teaching about death, dying, and bereavement should occur throughout the span of medical education.
Educational content and process should be tailored to students' developmental stage.
The best learning grows out of direct experiences with patients and families, particularly when students have an opportunity to follow patients longitudinally and develop a sense of intimacy and manageable personal responsibility for suffering persons.
Teaching and learning about death, dying, and bereavement should emphasize humanistic attitudes.
Teaching should address communication skills.
Students need to see physicians offering excellent medical care to dying people and their families, and finding meaning in their work.
Medical education should foster respect for patients' personal values and an appreciation of cultural and spiritual diversity in approaching death and dying.
The teaching process itself should mirror the values to which physicians aspire in working with patients.
A comprehensive, integrated understanding of and approach to death, dying, and bereavement is enhanced when students are exposed to the perspectives of multiple disciplines working together.
Faculty should be taught how to teach about end-of-life care, including how to be mentors and to model ideal behaviors and skills.
Student competence in managing prototypical clinical settings related to death, dying, and bereavement should be evaluated.
Educational programs should be evaluated using state-of-the-art methods.
Additional resources will be required to implement these changes.
Programs and Activities Needed to Advance End-of-Life Medical Education 2
Faculty development.
Few medical faculty, at either the undergraduate or the graduate level, are knowledgeable and enthusiastic about end-of-life care and therefore are not likely to be effective teachers. To compound this, there is little end-of-life care included in the grand rounds, teaching conferences, or journal clubs of traditional continuing medical education (CME) programs.
The end-of-life skills of interns and residents, who often act as role models for medical students in hospitals, may be lacking and should also be enhanced through special programs for house staff (Weissman et al., 1999).
More intense faculty development programs should be offered to improve communication, mentoring, and other teaching skills. Educators need ready access to end-of-life educational resource materials (e.g., handouts, pocket guides).
Improved Educational Materials
New materials have to be created and existing materials improved for training new and practicing physicians. This includes adding end-of-life content to medical textbooks, producing pocket guides and other references for interns and residents, and developing continuing education materials for practicing physicians.
Coordination of Medical Schools and Teaching Hospitals
Medical education takes place in a number of settings throughout the schooling process. Each medical school should develop a plan for teaching end-of-life care. This could be overseen by a committee with responsibility to review content across the entire curriculum, including preclinical and all phases of clinical education in outpatient, acute care hospital, long-term care, and home and hospice settings.
Coordination should also emphasize the need for interdisciplinary teamwork in caring for dying patients. Students should experience working together with physicians of different specialties, nurses, social workers, psychologists, other mental health workers, and clergy. They should also be instructed in caring for, and have opportunities to interact with, dying patients and their families (Weissman et al., 1999).
Residency Program Guidelines
The residency review committees that establish guidelines for clinical training have generally not mandated the inclusion of end-of-life and palliative care instruction. Perhaps presaging change, however, the internal medicine residency review committee has revised its guidelines to require instruction in palliative care and recommend clinical experience in hospice and home care.
Evaluation of Clinical Competence in End-of-Life and Palliative Care
Competence in these areas should be tested in the same way as for other clinical topics. Structured clinical examinations should be designed to assess the relevant skills in clinical care, decisionmaking, reasoning, and ethical problem solving.
In the hospital setting, communication and clinical decisionmaking skills can be observed by attending physicians or residents and they can give immediate feedback to students. Students' attitudes can be assessed by consulting hospital staff, patients, and family members, and medical charts can be reviewed to evaluate clinical practice (Weissman et al., 1999).
Licensing and Certifying Examinations
Both undergraduate licensing and graduate certification examinations have begun to include more questions on end-of-life care, but the content is still minimal. More questions on these exams will likely promote appropriate additions to the curriculum.
Improving the Research Base for Palliative Care Education
In addition to the many unanswered clinical questions surrounding end-of-life care, there is research to be done that could directly benefit the education process. The “epidemiology of dying” would describe where, how, and under whose care patients die in different settings, including the interactions of physicians, nurses, social workers, clergy, family, and other caregivers. Information about the effect on physicians (and others) of caring for dying patients could also help guide medical education.
The transition period of “prognostic uncertainty,” when choices must be made in the face of an uncertain outcome, is relatively unstudied in terms of the choices for patients and physicians.
Activities of Professional Organizations
Medical societies of various kinds, as well as societies of medical educators, can take a leadership role in placing end-of-life care prominently on the educational agenda. They can assess the educational needs of their members, develop clinical practice guidelines, encourage research, highlight end-of-life care at annual and other meetings, and undertake other activities (Weissman et al., 1999).
Standard-setting organizations, such as the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) can promote more comprehensive end-of-life care requirements for hospitals, nursing homes, and other institutions. They also can help to educate medical administrators about quality end-of-life care (Weissman et al., 1999).
Recent and Ongoing End-of-Life Medical Education Project: Funding and Aims
Work on many of the identified needs has been started, mainly through foundation grants. These projects have succeeded in raising awareness of the need for improvement and stimulating innovative ideas. The major projects and funding sources are characterized in Table 9-6 . The National Cancer Institute also funded a group of grants through a one-time initiative but has no ongoing program for soliciting proposals in this area.
Recent and Ongoing End-of-Life Medical Education Projects.
- NURSING EDUCATION IN END-OF-LIFE CARE
Nurses are expected to provide physical, emotional, spiritual, and practical care for patients in every phase of life. They spend more time with patients near the end of life than do any other health professionals. Yet, like physicians, most nurses in the United States do not receive the training and practical experience they need to carry out these duties in the best fashion. The nursing curriculum has been less studied than the medical curriculum, but this has been changing, particularly in response to debates about assisted suicide and euthanasia (Ferrell et al., 2000).
The 1997 Institute of Medicine report (IOM, 1997) reviewed studies of the nursing curriculum and found that coursework varied greatly from school to school. Nurses were found to have had little supervised clinical experience with dying patients and had been given minimal guidance on handling their personal reactions and involvement with dying patients. Criticisms were also raised that the end-of-life curriculum is out of date and not based on current models of death education.
End-of-Life Nursing Curriculum and Nurses' Preparedness for End-of-Life Care
Analytical studies of the U.S. nursing curriculum for end-of-life content have not yet been done, but a recent survey of nursing faculty and members of state nursing boards about their perceptions of this content provides a useful starting point (Ferrell et al., 1999). The survey is part of a larger project (funded by the Robert Wood Johnson Foundation) in which the three main nursing education associations are taking part, and the members of these three organizations were surveyed: the National Council of State Boards of Nursing, Inc.; the American Association of Colleges of Nursing; and the National League for Nursing Accreditation Commission.
Of the 725 respondents (the number surveyed was not reported), one-third were deans or chairpersons of schools of nursing, just over half were faculty members, and four percent were consultants or staff of state nursing boards (the rest had various roles). The key finding was that the adequacy of end-of-life content in these schools was rated at 6–7 on a scale of 0 (not adequate) to 10 (very adequate). This held for each of 10 specific content areas (e.g., death and dying, pain management, ethical issues).
The survey respondents also called for resources to help faculty improve end-of-life content in the form of
- Case studies
- Access to clinical sites
- Internet resources
- Audiovisuals
- Access to speakers, experts
- Lecture guides or outlines on end-of-life topics
- Computer-assisted instruction
- Standardized curriculum
As part of the same overall project, a sample of nurses completed a survey on a number of end-of-life topics, including their assessment of the effectiveness of nursing education in this area. The nurses surveyed included volunteers (300 who mailed in the survey, which was published in two general nursing journals) and 2,033 oncology nurses solicited directly (out of 5,000 who were mailed the survey), so the results should be considered descriptive only. They were asked about nine aspects of nursing education:
pain management,
overall content,
role and needs of family caregivers,
other symptom management,
grief and bereavement,
understanding the goals of palliative care,
ethical issues,
care of patients at time of death, and
communication with patients and families.
Less than 13 percent of those responding rated their education in all nine aspects as adequate. Most frequently rated as not adequate were pain management (71 percent), overall content (62 percent), and roles and needs of family caregivers (61 percent), but more than half reported “not adequate” education in each of the nine areas.
Most other relevant studies have focused on nurses' knowledge in the area of cancer pain management and palliative care, and these have found major deficiencies, most likely resulting from deficiencies in training (see, e.g., Ferrell and McCaffery, 1997; McCaffery and Ferrell, 1995).
End-of-Life Care in Nursing Textbooks
A major review of nursing textbooks for end-of-life content was completed recently (Ferrell et al., 1999b). Fifty current nursing textbooks, both general and specialty, used heavily in nursing programs were selected for analysis ( Table 9-7 ). “Critical content areas” were identified as key items that should appear in complete discussions of each content area (the pharmacology texts were treated somewhat differently, appropriate to their different scope), and included:
End-of-Life Care Content in 50 Nursing Textbooks.
- Palliative care defined
- Quality of life
- Other symptom assessment and management
- Communication with dying patients and their family members
- Role/needs of caregivers in end-of-life care
- Issues of policy, ethics, and law
- Bereavement
For each critical content area, a list of specific types of information were prespecified as important for inclusion in a text. For examples, under “Pain,” the topics identified were:
- definition of pain;
- assessment of pain—physical;
- assessment of meaning of pain—scales;
- pharmacologic management of pain at end of life (classes of analgesics);
- use of invasive techniques;
- principles of addiction, tolerance, and dependence;
- nonpharmacologic management of pain at end of life;
- physical pain versus suffering;
- side effects of opioids;
- barriers to pain management;
- fear of opioids hastening death or opioids near death;
- equianalgesia; and
- recognition of nurses' own burden in pain management.
The authors tallied the presence of end-of-life information in various ways, including examining tables of contents and indexes for mentions, as well as analyzing each text for the critical content areas. Among the key findings are the following:
- 1.4 percent of all chapters (24 out of 1,750) and 2 percent of all content (902 out of 45,683 pages) were devoted to any end-of-life topic;
- 30 percent of the texts had at least one chapter devoted to end-of-life issues (the vast majority were devoted only to pain);
- the strongest coverage was in the two areas of pain and issues of policy or ethics; end-of-life topics with the poorest coverage were quality of life issues and role and needs of family caregivers; and
- overall, 74 percent of the prespecified content was absent, 15 percent was present and 11 percent was present and useful or commendable.
The authors also qualitatively analyzed the information that was found in the texts, drawing a number of conclusions, among them:
- most end-of-life content focused only on cancer and AIDS;
- although pain was frequently discussed, the text referred mainly to acute or chronic pain, and not pain at the end of life; minimal content was found on pain assessment, neuropathic pain, or pain assessment in the cognitively impaired or nonverbal patient;
- outdated drug approaches were frequently recommended, and there was virtually no information on pain management at the end of life;
- minimal information was found on symptoms other than pain at the end of life; and
- the four pharmacology texts all included erroneous information and lacked information on current approaches to pain and symptom management.
The overarching finding was a lack of content on essential topics for end-of-life care.
Ongoing Programs and Initiatives
As is the case for education programs for physicians, much of support for nursing education comes from private foundations ( Table 9-8 ).
Major Recent and Ongoing End-of-Life Nursing Education Projects.
- SOCIAL WORK EDUCATION IN END-OF-LIFE CARE
Social workers are central to counseling, case management, and advocacy services for the dying and for bereaved families. With their focus on the psychosocial aspects of the dying process, they work not only with patients but with those around them in making decisions about treatment options, marshaling resources, helping families cope with terminal illness and death of a relative, and generally encouraging the best quality of life for all concerned. The demands on social workers have changed over time. A major reason is the shift from largely hospital-based care for those who are dying to home, hospice, and other settings, which has required social workers to coordinate a broadening array of services and providers and to navigate a more complex set of rules and regulations.
Just as nursing and medicine have begun to do, the social work profession has been examining its education process for preparing practitioners to care for dying patients and their families. Efforts to improve undergraduate and master's level social work training in this area are just getting under way in the United States, in comparison to the more mature field in Canada and England, and in comparison to medical and nursing education. Quite recently, opportunities have been identified, and some programs initiated, to begin making the needed changes.
End-of-Life Care Training in Social Work Education 3
Studies in the 1990s began to look at the end-of-life content of social work education and the preparedness of social workers to care for dying patients and their bereaved families. Four small but prominent studies set the stage for the most definitive review of this issue, by Christ and Sormanti (1999).
Briefly, of the four earlier studies, one was a survey of 108 hospice social workers from around the country, which found a uniform lack of preparation at the master's level for end-of-life care (Kovacs and Bronstein, 1998). The second consisted of a focus group of 10 oncology social work supervisors who described serious gaps in the social work curriculum related to end-of-life care (Sormanti, 1995).
A survey of social work programs found that in most, the end-of-life content was folded into courses on “human behavior and the social environment” or into gerontology courses. Less than a quarter of all students enrolled in these courses when they were electives (Dickinson et al., 1992). The last study was based on a questionnaire given to 50 M.S.W. students at the beginning of the second year, who reported feeling “a little” or “somewhat” prepared to deal with dying patients and their families (Kramer, 1998).
Though small and of varied types, these studies suggest that, like medicine and nursing, social work students have insufficient training—both didactic and practical—to provide the best care at the end of life. (No studies of social work textbooks for end-of-life care content have yet been carried out.)
Christ and Sormanti (1999) extended the earlier efforts with surveys and focus groups designed to address the following issues (of which the last two are of most interest in this section):
barriers to effective social work practice in palliative care and care of the bereaved,
the adequacy of M.S.W. practitioners' preparedness for this work, and
the extent of social work educators' experiences in teaching and research in bereavement and end-of-life care.
The first survey involved 48 oncology social workers attending the 1998 annual meeting of the Association of Oncology Social Workers. Regarding education, they were asked about their preparation in M.S.W. programs and about postgraduate training and educational opportunities. The practitioners uniformly reported insufficient training in end-of-life issues to prepare them for the work they were doing. None except for the few who had trained in hospice settings had clinical experience with dying patients. The respondents were asked about their preparation in 10 skill categories, with the result that in only two—supportive counseling and advocacy—did less than half rate their preparation as “unsatisfactory.” At least 50 percent rated end-of-life training in symptom management, communication, bereavement, education, ethics, case management, decisionmaking, and discharge planning as unsatisfactory.
Only one continuing education program associated with a school of social work was identified among the 48 participants. Overall, most lacked access to continuing education programs that were at all satisfactory. Even where programs exist, finding funds to attend and being able to take time away from work are significant barriers. In addition, most programs highlight medicine and nursing, and few social workers speak in the relevant courses. Five focus groups were held with social workers who provide end-of-life services, and they largely corroborated the findings of the survey.
Finally, 35 faculty members from 30 schools of social work were surveyed about end-of-life care content in their own programs and about research on related topics. They reported that only a small proportion of students receive instruction in end-of-life issues and that it comes in small parts of courses on human behavior and the social environment, policy, and practice. It usually consists of one or two lectures. More comprehensive elective courses were taken by a minority of students. Only one-quarter of survey participants believed that their schools adequately prepared students for end-of-life work.
Research funding was a very scarce commodity: about one-quarter reported even modest monetary support for their ongoing research. They reported that they were aware of no money targeted specifically for end-of-life research in social work.
Opportunities for Improving Social Work End-of-Life Education
Some specific areas that could benefit from funding and development of programs are
- better undergraduate and master's level curricula in end-of-life care;
- innovative programs that integrate coursework with clinical work through alliances between schools and practice sites;
- accessible continuing education designed and provided by social work experts in end-of-life care; and
- collaborative educational programs with other professions working with dying patients and bereaved families.
Also key is funding earmarked for social work research to provide a better foundation for the development of innovative methods of care.
The Project on Death in America has begun a program of Social Work Leadership Development Awards to promote innovative research and training projects for collaborations between schools of social work and practice sites that will advance the ongoing development of social work practice, education, and training in the care of the dying. The Hartford Foundation also provides support for gerontology social workers. The National Cancer Institute does not currently fund any social work education projects.
- RECOMMENDATIONS FOR IMPROVING PROFESSIONAL EDUCATION FOR PHYSICIANS, NURSES, AND SOCIAL WORKERS IN END-OF-LIFE CARE
Leaders in medicine, nursing, and social work have recognized that training in end-of-life care has been inadequate. These leaders have systematically documented at least some of the shortcomings in the education process and continue to add to the information base. This has been effective both in broadening recognition among the professions of the need for improvements and in serving as a basis for determining what tasks must be accomplished to effect improvements. The work has been concentrated among a small group of experts nationwide, and funding has come almost exclusively from private foundations, which have catalyzed these movements. At this point, the groundwork has been laid for larger-scale activities, which could move quickly with significant funding from the federal government, in particular, the National Cancer Institute (NCI) and other National Institutes of Health.
Few medical, nursing, or social work faculty, either at the undergraduate or graduate level, are knowledgeable and enthusiastic about end-of-life care and therefore are unlikely to be effective teachers. To compound this, little end-of-life care is included in the grand rounds, teaching conferences, or journals clubs of traditional continuing education programs. More intense faculty development programs should be offered to improve communication, mentoring, and other teaching skills.
Recommendation: NCI should fund a national oncology faculty development programs along the lines of the Project on Death in America Faculty Scholars Program.
New materials have to be created and existing materials improved for training new and practicing physicians, nurses, and social workers. This includes adding end-of-life content to textbooks, producing pocket guides and other references, and developing continuing education materials for practicing professionals.
Recommendation: NCI should make funding available for the development of appropriate materials, which could be pilot-tested by students and fellows in NCI-designated cancer centers. This could be accomplished through the “R25” mechanism, which was used to fund a small number of recent grants after a one-time call for proposals.
Coordination of Medical, Nursing, and Social Work Schools and Teaching Hospitals
Education takes place in a number of settings throughout the schooling process. Each medical, nursing, and social work school should develop a plan for teaching end-of-life care. This could be overseen by a committee with responsibility to review content across the entire curriculum, including preclinical and all phases of clinical education in outpatient, acute care hospital, long-term care, and home and hospice settings.
Coordination should also emphasize the need for interdisciplinary teamwork in caring for dying patients. Students should experience working together with physicians of different specialties, nurses, social workers, psychologists, other mental health workers, and clergy. They should also be instructed in caring for and have opportunities to interact with, dying patients and their families (Weissman et al., 1999).
Recommendation: In addition to coordination by the schools themselves, NCI should provide clinical training fellowship slots at all NCI-designated cancer centers that have clinical programs, including training in both clinical care and palliative or end-of-life care research for all of the relevant professions. Specific cancer centers could also be developed as “centers of excellence” for palliative and end-of-life care training and research.
The residency review committees that establish guidelines for clinical training have generally not mandated the inclusion of end-of-life or palliative care instruction. Perhaps presaging change, however, the internal medicine residency review committee has revised its guidelines to require instruction in palliative care and recommend clinical experiences in hospice and home care.
Recommendation: All residency review committees should be canvassed to determine the status of end-of-life care in each set of guidelines. Each specialty should be encouraged to consider appropriate changes, and technical assistance should be offered, if necessary. This activity would not require large amounts of funding, but some money for coordination and consultation should be made available by either the government, academic institutions, or foundations.
Both undergraduate licensing and graduate certification examinations have begun to include more questions on end-of-life care, but the content is still minimal. More questions on these exams will likely promote appropriate additions to the curricula.
Recommendation: Licensing and certifying bodies should be encouraged and assisted in developing appropriate examination questions.
This should be coordinated with curriculum development and textbook revisions. A coordinating function might be helpful in ensuring communication among the key players, funded by public or private sector sources.
In addition to the many unanswered clinical questions surrounding end-of-life care, there is research to be done that could directly benefit the education process. The “epidemiology of dying” would describe where, how, and under whose care patients die in different settings, including the interactions of physicians, nurses, social workers, clergy, family, and other caregivers. Information about the effect on physicians and other caregivers of caring for dying patients could also help guide education.
The transition period of “prognostic uncertainty,” when choices must be made in the face of an uncertain outcome, is relatively unstudied in terms of what the choices are for patients and physicians.
Recommendation: NCI should initiate a grant program for these activities by issuing a request for proposals in this area and by continuing such a program over the long term.
Standard-setting organizations such as JCAHO can promote more comprehensive end-of-life care requirements for hospitals, nursing homes, and other institutions. They also can help to educate medical administrators about quality end-of-life care (Weissman et al., 1999).
Recommendation: Private sector organizations should be encouraged by government to undertake these activities and should be provided with technical assistance, if needed. Funding could come from either public or private sector sources.
- American Medical Association. The EPEC Project . 2000. Web page, http://222 .ama-asn.org/ethic/epec/epec .htm .
- Barnard D, Quill T, Hafferty FW, et al. Preparing the ground: contributions of the preclinical years to medical education for care near the end of life . Academic Medicine 1999 ; 74:499– 505. [ PubMed : 10353280 ]
- Barzansky B, Veloski JJ, Miller R, Jonas HS. Palliative care and end-of-life education . Aca demic Medicine 1999 ; 74(10):S102–104. [ PubMed : 10536608 ]
- Begg L. National Cancer Institute, Cancer Training Branch. Personal communication, June 21, 2000.
- Belani CP, Belcher AE, Sridhara R, Schimper SC. Instruction in the techniques and concept of supportive care in oncology . Supportive Care Cancer . 1994; 2:50–55. Cited in Billings and Block (1997). [ PubMed : 8156257 ]
- Berkow R, editor. , ed. 1992. The Merck Manual of Diagnosis and Therapy . 16 th ed. Rahway, NJ: Merck Research Laboratories.
- Billings, JS, Block S. Palliative care in undergraduate medical education . JAMA 1997 ; 28:733– 738. [ PubMed : 9286833 ]
- Block SD, Bernier GM, Crawley LM. Incorporating palliative care into primary care education . JGIM; 1998 ; 13:768–773. [ PMC free article : PMC1497022 ] [ PubMed : 9824524 ]
- Carron AT, Lynn J, Keaney P. End-of-life care in medical textbooks . Arch Intern Med 1999 ; 130:82–6. [ PubMed : 9890873 ]
- Christ GH, Sormanti M. Advancing social work practice in end-of-life care . Social Work in Health Care 1999 ; 30(2):81–99. [ PubMed : 10839248 ]
- Dickinson G, Sumner E, Frederick L. Death education in selected health professions . Death Studies 1992 ; 16:281–289. Cited in Christ and Sormanti (1999). [ PubMed : 10118944 ]
- Emanuel EJ. National Cancer Institute. Personal communication (unpublished data), 2000.
- Ewald GA, editor; , McKenzie CR, editor. , eds. 1995. Manual of Medical Therapeutics . 28 th edition. Boston: Little, Brown.
- Ferrell BR, Grant M, Virani R. Strengthening nursing education to improve end-of-life care . Nursing Outlook 1999a ; 47:252–256. [ PubMed : 10626282 ]
- Ferrell BR, McCaffery M. Nurses' knowledge about equianalgesia and opioid dosing . Cancer Nursing 1997 ; 20(3):201–212. [ PubMed : 9190095 ]
- Ferrell B, Virani R, Grant M. Analysis of end-of-life content in nursing textbooks . Oncol Nurs Forum 1999b ; 26(5):869–876. [ PubMed : 10382185 ]
- Ferrell B, Virani R, Grant M, et al. Beyond the Supreme Court decision: nursing perspectives on end-of-life care . Oncology Nursing Forum 2000 ; 27(3):445–455. [ PubMed : 10785899 ]
- Foley KM. Competent care for the dying instead of physician-assisted suicide . New England Journal of Medicine 1997 ; 336:54–58. [ PubMed : 8970941 ]
- Gibson R. Robert Wood Johnson Foundation projects to promote professional education and training. Personal communication, June 2000.
- Hilden JM, Emanuel EJ, Fairclough DL, Link MP, Foley KM, Clarridge BC, Schnipper LE, Mayer RJ. Attitudes and practices among pediatric oncologists regarding end-of-life care: results of the 1998 American Society of Clinical Oncology survey . JCO 2001 ; 19: 205–212. [ PubMed : 11134214 ]
- Hill TP. Treating the dying patient: the challenge for medical education . Arch Intern Med 1995 ; 155:1265–1269. Cited in Billings and Block (1997). [ PubMed : 7778956 ]
- Holleman WL, Holleman MC, Gershenshorn S. Death education curricula in U.S. medical schools . Teaching Learning Med 1994 ; 6:260–263. Cited in Billings and Block (1997).
- Institute of Medicine (IOM). 1997. Approaching Death: Improving Care at the End of Life , Field MJ, editor; , Cassel CK, editor. , eds. Washington, D.C.: National Academy Press. [ PubMed : 25121204 ]
- Isselbacher K, editor; , Martin W, editor; , Kasper F, editor. , eds. 1994. Harrison's principles of internal medicine , 13th ed . New York: McGraw-Hill.
- Kovacs P, Bronstein L. Preparation for oncology settings: what hospice social workers say they need . Social Work in Health Care 1999 ; 24(1):57–64. Cited in Christ and Sormanti (1999). [ PubMed : 14533420 ]
- Kramer B. Preparing social workers for the inevitable: A preliminary investigation of a course on grief, death, and loss . Journal of Social Work Education 1998 ; 34(2):1–17. Cited in Christ and Sormanti (1999).
- Larson DE, editor. , ed. 1996. Mayo Clinic Family Health Book . 2 nd edition. New York: W.Morrow.
- McCaffery M, Ferrell BR. Nurses' knowledge about cancer pain: a survey of five countries . Journal of Pain and Symptom Management 1995 ; 10(5):356–369. [ PubMed : 7673768 ]
- Medical School Objectives Writing Group. Learning objectives for medical student education: guidelines for medical schools. Report I of the Medical School Objectives Project . Aca demic Medicine 1999 ; 74:418–422. [ PubMed : 9934288 ]
- Mermann AC, Gunn DB, Dickinson GE. Learning to care for the dying: a survey of medical schools and a model course . Academic Medicine 1991 ; 66(1):25–28. [ PubMed : 1985674 ]
- Osler W. 1899. Principles and Practice of Medicine , 3 rd edition. New York: D.Appleton.
- Rabow MW, Hadie GE, Fair JM, McPhee SJ. End-of-life care content in 50 textbooks from multiple specialties . JAMA 2000 ; 283:771–778. [ PubMed : 10683056 ]
- SAM-CD. 1994. Scientific American Medicine on CD-ROM: A Comprehensive Knowledge- Base of Internal Medicine . New York: Scientific American Medicine.
- Sormanti M. Fieldwork instruction in oncology social work: supervisory issues . Journal of Psychosocial Oncology 1994 ; 12(3):73–87. Cited in Christ and Sormanti (1999).
- Weissman DE, Block SD, Blank L et al. Recommendations for incorporating palliative care education into the acute care hospital setting . Academic Medicine 1999 ; 74:871–877. [ PubMed : 10495725 ]
The section is taken verbatim from Billings and Block (1997).
Drawn and adapted largely from Block et al. (1998) except as noted.
This section is largely based on the work of Christ and Sormanti (1999).
- Cite this Page Institute of Medicine (US) and National Research Council (US) National Cancer Policy Board; Foley KM, Gelband H, editors. Improving Palliative Care for Cancer. Washington (DC): National Academies Press (US); 2001. 9, Professional Education in Palliative and End-of-Life Care for Physicians, Nurses, and Social Workers.
- PDF version of this title (6.2M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Professional Education in Palliative and End-of-Life Care for Physicians, Nurses... Professional Education in Palliative and End-of-Life Care for Physicians, Nurses, and Social Workers - Improving Palliative Care for Cancer
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

- What Is Social Work?
- How Long Does it Take to Become a Social Worker?
- LMSW vs. LCSW: What’s the difference?
- Macro, Mezzo, and Micro Social Work
- Associate Degree in Social Work (ASW)
- Online BSW Programs
- Online Clinical MSW Programs
- Advanced Standing Online MSW Programs
- Online MSW Programs with No GRE Required
- SocialWork@Simmons
- Howard University’s Online MSW
- OnlineMSW@Fordham
- Syracuse University’s Online MSW
- Online Social Work at CWRU
- Is an Online Master’s in Social Work (MSW) Degree Worth it?
- MSW Programs in California
- MSW Programs in Colorado
- MSW Programs in Massachusetts
- MSW Programs in New York
- MSW Programs in Ohio
- MSW Programs in Texas
- MSW vs LCSW
- What is a Master of Social Work (MSW) Degree?
- What Can I Do with an MSW Degree? MSW Career Paths
- HBCU MSW Programs – Online and On-Campus Guide
- DSW vs. Ph.D. in Social Work
- Ph.D. in Social Work
- Social Work Continuing Education
- Social Work Licensure
- How to Become a Licensed Clinical Social Worker (LCSW)
- Community Social Worker
- Child and Family Social Worker
- Forensic Social Worker
- Geriatric Social Worker
- Hospice Social Worker
- Medical Social Worker
- Mental Health Social Worker
- Resources for Military Social Workers
- Oncology Social Worker
- Psychiatric Social Worker
- Resources for School Social Workers
- Social Work Administrator
- Social Work vs. Therapy
- Social Work Salary
- Social Work Collaborations
- Social Work Career Pathways
- Social Work vs. Sociology
- Benefits of a Part-Time MSW Program
- MSW vs. MPH
- Social Work vs. Counseling
- Social Work vs. Psychology
- Bachelor’s in Psychology Programs Online
- Master’s Degree in Counseling
- Become a School Counselor
- School Counselor Salary
- Become a Mental Health Counselor
- Advantages of Veterinary Social Work
- Practicing Anti-Racism in Social Work: A Guide
- Social Work License Exam Prep
- Theoretical Approaches in Social Work: Systems Theory
- Social Learning Theory
- Sarah Frazell on Racism
- Lisa Primm on Macro Social Work
- Jessica Holton on Working With Clients Who Are Deaf and Hard of Hearing
- Cornell Davis III on Misperceptions About the Child Welfare Field
- Morgan Gregg on Working with Law Enforcement
- Social Work Grants
- Social Work Scholarships
- Social Work Internships
- Social Work Organizations
- Social Work Volunteer Opportunities
- Social Worker Blogs
- Social Work Podcasts
- Social Workers on Twitter
- Ethnic and Minority Social Work Resources
- Resources for LGBTQIA Social Work
- Mental Health Resources List
Home / Social Work Careers / Hospice Social Worker
Guide to Becoming a Hospice and Palliative Care Social Worker
Hospice and palliative care social workers work alongside medical workers to provide end-of-life care for patients. If you decide to pursue this challenging and rewarding branch of social work, you may need additional training and certification depending on your educational background. Below, we provide you with some resources to help you pursue your career as a hospice and palliative care social worker.
What is a Palliative and Hospice Social Worker?
Palliative social work and hospice social work have subtle, usually overlapping distinctions. Hospice social work is a category within palliative care that specifically deals with end-of-life care for people with terminal illnesses. Palliative care may or may not deal with people suffering from terminal illnesses; the focus is on managing symptoms rather than curing a condition that might be incurable.
Your day-to-day responsibilities in this field will vary. In general, social workers in palliative care settings help all parties—patients, medical professionals, families—communicate with each other.
Sponsored online social work programs
University of Denver
Master of social work (msw).
The University of Denver’s Online MSW Program is delivered by its top-ranked school of social work and offers two programs. Students can earn their degree in as few as 12 months for the Online Advanced-Standing MSW or 27 months for the Online MSW.
- Complete the Online Advanced-Standing MSW in as few as 12 months if you have a BSW; if you do not have a BSW, the Online MSW Program may be completed in as few as 27 months.
- No GRE Required
- Customizable pathway options include Mental Health and Trauma or Health, Equity and Wellness concentrations
Fordham University
Fordham’s skills-based, online MSW program integrates advanced relevant social work competencies, preparing students to serve individuals and communities while moving the profession forward. This program includes advanced standing and traditional MSW options.
- Traditional and advanced standing online MSW options are available.
- There are four areas of focus: Individuals and Families, Organizations and Community, Evaluation, and Policy Practice and Advocacy.
- Pursue the degree on a full-time or part-time track.
Hawaii Pacific University
Master of social work.
The online Master of Social Work prepares aspiring social work leaders to develop a multicultural social work practice, advocate for social and economic justice, and empower diverse communities affected by systemic inequities within civilian and military-focused areas.
- Learn how to develop a multicultural social work practice.
- Pending accreditation by the Council on Social Work Education (CSWE).
- Complete in 18 months full time, or in 36 months part time on the traditional track.
- Complete in 12 months full time or 24 months part time on the Advanced Standing Track.
Simmons University
Aspiring direct practitioners can earn their MSW online from Simmons University in as few as 9 months . GRE scores are not required, and the program offers full-time, part-time, accelerated, and advanced standing tracks.
- Prepares students to pursue licensure, including LCSW
- Full-time, part-time, and accelerated tracks
- Minimum completion time: 9 months
Howard University
The online Master of Social Work program from Howard University School of Social Work prepares students for advanced direct or macro practice in culturally diverse communities. Two concentrations available: Direct Practice and Community, Administration, and Policy Practice. No GRE. Complete in as few as 12 months.
- Concentrations: Direct Practice and Community, Administration, and Policy Practice
- Complete at least 777-1,000 hours of agency-based field education
- Earn your degree in as few as 12 months
Syracuse University
Syracuse University’s online Master of Social Work program does not require GRE scores to apply and is focused on preparing social workers who embrace technology as an important part of the future of the profession. Traditional and Advanced Standing tracks are available.
- Traditional and Advanced Standing tracks
- No GRE required
- Concentrate your degree in integrated practice or clinical practice
Case Western Reserve University
In as few as a year and a half, you can prepare for social work leadership by earning your Master of Social Work online from Case Western Reserve University’s school of social work.
- CSWE-accredited
- No GRE requirement
- Complete in as few as one and a half years
info SPONSORED
Steps to Become a Palliative Care and Hospice Social Worker
Below are some common steps to become a palliative care and hospice social worker:
1. Complete Your Social Work Education
A common first step to becoming a palliative care or hospice care social worker is obtaining an appropriate background in generalized social work education at an accredited school. For some entry-level jobs, a bachelor’s degree in social work or a related major, such as psychology, is sufficient; some jobs in the social work field (such as aides) may only require a high school diploma. More commonly, however, social workers obtain a Master of Social Work (MSW) to meet state licensing guidelines.
2. Gain Fieldwork Experience
Education may need to be supplemented with fieldwork, which both BSW and MSW programs will likely require. Specifications for required hours will vary by state, requirements such as these are not uncommon.
3. Apply for and Pass the ASWB Exam
To obtain a social work license, you likely will need to pass a licensing exam administered by the Association of Social Work Boards (ASWB).
4. Apply for Licensure
Once you pass your ASWB exam and scores are sent to your state of practice, you may then apply for state licensure as a licensed social worker.
5. Pursue Employment
Finally, you will need to look for work in palliative care or at a hospice. You may already have contacts through your fieldwork; otherwise, you can search for jobs using keywords such as “hospice social worker,” “end-of-life social worker,” or “palliative care social worker.”
Should I Become a Hospice Social Worker?
If you have already decided you would like to become a social worker , you should evaluate other branches of social work before you settle on your social work career . Social workers deal with all kinds of societal issues, and their specializations may include foster care, education, homelessness, mental illness and substance abuse. Social workers may also choose to focus on the same problem from different scales—for example, a substance abuse social worker could work one-on-one with people with addiction issues, or help develop programs to treat addiction.
You should also evaluate the type of social work degree you’d like to pursue. Careers for those with a BSW will vary from careers for those with a Doctorate of Social Work (DSW).
Degree Programs for Hospice and Palliative Social Workers
Most people interested in earning a social work degree after their bachelor’s education may then choose to earn a Master of Social Work (MSW). There are different types of master’s degrees that meet different needs. Some of these include:
- Master of Social Work (MSW) programs : These are what you typically think of when you think of graduate school – in-person classes, on a campus. These can provide networking and teaching opportunities that online MSW programs don’t have.
- Online MSW programs : These are particularly good for those who don’t live near a major university, or who already have a full-time job and want the flexibility of online classes.
- MSW programs with no GRE requirement : For many master’s degree programs, applicants need to take the Graduate Record Examinations (GRE), a lengthy standardized test. MSW programs without this requirement can save you time when you’re applying for schools.
- Advanced standing MSW programs : These are for people who studied social work or a related field in their undergraduate education. These degrees can be completed more quickly than a traditional MSW program.
You can also apply for Doctorate of Social Work (DSW) programs , which take longer to complete and are more challenging but necessary for many academic and research-oriented social work jobs.
Skills Needed for Hospice and Palliative Care
Though the skills you will use may vary from job to job, there are some skills that all hospice social workers and palliative social workers would do well to learn, retrieved from the National Association of Social Work (NASW) Social Workers in Hospice and Palliative Care Occupational Profile (PDF, 4.6 MB) :
- Counseling and psychotherapy
- Providing psychosocial education
- Facilitation of advance care planning and lifespan planning
- Crisis intervention
- Conflict mediation
- Patient advocacy
- Interdisciplinary communication
What is the Role of a Hospice Social Worker?
Hospice social workers act as advocates for patients and their families dealing with end-of-life decisions, emotions and medical care. Social workers can also ensure that patients and families get the care they need beyond physical care—making sure they have a connection to their communities, for instance, or have appropriate mental health treatment. This can mean that hospice social workers sometimes act as facilitators between a patient and other resources and organizations.
Work Settings of a Hospice Social Worker
Typically, these kinds of hospice and palliative social workers work in a hospice—a hospital alternative focused entirely on end-of-life care. The amount of palliative care programs in hospitals has been rising since 2000. Nursing homes and assisted living facilities also hire palliative care workers. Additionally, many palliative social workers work in more traditional homes, helping to ensure that patients have access to appropriate medical care and other necessities and comforts.
How Much do Hospice Social Workers make?
According to the Bureau of Labor Statistics (BLS), the median pay of all social workers is $51,760 per year —though the BLS doesn’t break down this median pay by specialization, and your salary may vary based on location. You will want to consider your potential salary as a social worker when applying for graduate programs, some of which may cost as much as your expected annual pay.
Hospice Social Work Certification
Licensing requirements vary by state . The two types of licenses you may find are licensed master social worker (LMSW) and licensed clinical social worker (LCSW) , the difference generally being that social workers with an LCSW can apply clinical services in therapy for clients. To obtain one of these licenses, social workers must pass their appropriate ASWB Social Work Exam.
There are additional certifications social workers can receive that are specifically for palliative care and hospice social work. For instance, the NASW offers a Certified Hospice and Palliative Social Worker (CHP-SW) credential, as does the Center to Advance Palliative Care (CAPC) . This certification is not a requirement to work in palliative care and hospice social work, but it can be useful for job seekers and those who wish to further hone their skills.
Hospice Social Work Resources
Hospice social workers have dedicated and established professional organizations that can assist them throughout their careers. Some of these include:
- Center to Advance Palliative Care (CAPC) : In addition to the certification program mentioned above, CAPC offers events, seminars, training and job opportunities to members. CAPC’s resources include more than 500 online courses and tools.
- National Coalition for Hospice and Palliative Care : This organization—an umbrella organization for 12 hospice and palliative care groups—is focused on advocacy for hospice and palliative care workers of all types.
- Social Work Hospice and Palliative Care Network (SWHPN) : SWHPN provides resources specific to hospice and palliative care social workers, including industry news, mentorship programs, career opportunities and certification.
Information on this page was last updated in June 2021.
Visit smith.edu
Master of Social Work Program
- Curriculum, Core Courses and Advising
- Practicum Sequence
- HBSE Sequence
- Practice Sequence
- Research Sequence
- Policy Sequence
- Summer at Smith SSW
- Admission Process, Dates and Deadlines
- Begin Your Application
- Meet a Current Student
- Contact an Alum
- Refer A Student
- Request Information
- Cost of Attendance
- Financial Aid and Scholarships
- Student Accounts
Doctoral Program
- Curriculum and Core Courses
- Dissertation
- Summer on Campus
- Internships
- Financial Aid
Professional Education
- Advanced Clinical Supervision Certificate
Palliative and End-of-Life Care Certificate
- Foundations of Clinical Supervision Certificate
- Upcoming Trainings
- Deepening Clinical Practice Conference
- Recorded Webinars
- Sign Up for Mailing List
- Submit a Professional Education Proposal
News & Events
- InDepth Magazine
- Tell Us Your News!
- Admission Events
- Alumni Events
- Public Community Events
- Continuing Education
- Commencement Speakers
- Parking for Commencement
- Office of the Deans
- Sotomayor Collective
- Staff and Administration
- Core Principles
- Statement of Purpose
- Community Agreement
- Strategic Plan
- Studies in Clinical Social Work
- Accreditation
- Academic Calendars
- M.S.W. Tuition and Financial Aid
- M.S.W. Admission
- M.S.W. Financial Aid
- M.S.W. Housing
- M.S.W. Dates and Deadlines

Social workers encounter situations of life threatening illness, death, dying and bereavement in every setting in which they work. The Certificate in Palliative and End-of-Life Care provides an opportunity for social workers to deepen clinical and leadership skills in palliative care and participate in relational ways of learning in a community of colleagues with an outstanding faculty of leaders.
There are a growing number of individuals and families in need of palliative care. Clinical social work interventions have never been more needed, yet there is a lack of highly-trained clinical social workers prepared to effectively address the complex needs of those facing end of life. The person who is ill, their family, social supports, health care providers and clergy members all benefit from the skills of social workers specially trained in this area.
Coursework takes place on Zoom in three intensive teaching sessions, addressing issues of diversity throughout instruction. During the months between classes, students participate in clinical advisement sessions at which they will work on clinical case studies (patients and families) and further integrate learning. Two to three students are paired with experienced clinical advisers and, each month, receive two hours of clinical advisement via telephone, for a total of 12 sessions, ten group and two individual. The program's primary focus is on interactive learning, which enhances professional use of self, deepens clinical skills and promotes leadership in the field.
The program offers 15 courses and 12 advisement sessions, which makes it one of the most comprehensive programs in the country. The academic content includes theoretical views on end of life care and bereavement, pediatric palliative care and bereavement, geriatric palliative care and bereavement, spirituality, legal and ethical issues, pain management, leadership in palliative care, and racism as a public health issue. Graduates of the program have gone on to assume leadership positions, write grants, develop programs, provide clinical supervision, teaching and engage in research and writing for publication.
Session I: November 8-10, 2024
Session II: January 31-February 2, 2025
Session III: April 25-27, 2025
Format: Live interactive webinars
CEs: Up to 45 CEs available.
Hospice & Palliative Care
Online continuing education, learn anytime. earn credits. improve practice..
The MJHS Institute for Innovation in Palliative Care is pleased to offer free interdisciplinary palliative care webinars, live and on demand , delivered by frontline experts, typically offering 1.0 AMA PRA Category 1 Credit™ for Continuing Medical Education (CME), Nursing continuing education (CE), Social Work CE credits, Case Manager CCMC CE credits, and Music Therapy CE credits.
Our free interactive multimedia modules on Community-Based Palliative Care Program Development and Caring for Holocaust Survivors With Sensitivity at End of Life offer up to 9.75 CE credits.
Free pdf downloads now available: 15 palliative care professional factsheets and patient education handouts on 18 topics in English, Spanish, Haitian Creole, Arabic, French, and Russian.
Serious Illness Discussions
Live webinar 5/30/24, palliative care in dementia, live webinar 6/13/24, psychosocial needs of cancer patients from an ethnically diverse underserved community, live webinar 6/27/24, ethical decision-making when advance directives may no longer apply, live webinar 8/15/24, cystic fibrosis palliative care series, webinar package, palliative care training for cnas, palliative care for case managers, palliative care in nursing homes, a 69-year-old male with lung cancer..., on-demand webinar, a 69-year-old man with a history of alcoholism..., a 71-year-old man with class iv chf, and no advance directives..., advance care planning: the advance directive, an 80-year-old woman with copd and dyspnea..., an 86-year-old woman with moderate dementia..., anticipatory mourning at end-of-life, anxiety in palliative care, artificial nutrition and hydration in palliative care and hospice, assessment and management of dyspnea in advanced illness, bereavement: contributing factors that affect how one grieves, bias: achieving success despite historical discrimination, cardiac devices and palliative care, care of families during end-of-life vigils, caregiver burnout, caring for family caregivers while caring for ourselves, caring for patients with hiv, communication in palliative care: serious illness discussions, communication with patients and families at end-of-life, cultural humility in end-of-life care, culturally relevant pain assessment and management, culture: end-of-life care through a cultural lens, cystic fibrosis: mental health and palliative care though the lifespan, dvt: a patient with deep venous thrombosis and kennedy terminal ulcer, delirium: assessment, diagnosis, and treatment in seriously ill patients, deprescribing: identifying inappropriate medications and strategies, depression and anxiety, depression in palliative care, end-stage liver disease and palliative care, ethics: applying a “dignity of risk” framework in home hospice care, evidence-based advocacy, faith in terms of death and dying, family caregiving: what is trending, family meeting in palliative care: best practices, frailty in palliative care, goodbyes and condolences in palliative and hospice care, holocaust: the liberator and the liberated – 75 years post wwii, home care: the family meeting, hospice 101: levels of care across settings, hospice and palliative care in the covid-19 pandemic, hospice: current perspective, hospice: understanding and improving underutilization, impending death, interprofessional team conflict, ketamine use for pain, lgbtq-inclusive hospice and palliative care, lgbtq: end-of-life care, lgbtq: optimizing access to palliative care, lgbtq: sexual orientation and gender identity in the health record, management of mucositis and candidiasis, music therapy: caring for nursing home residents with alzheimer’s and related dementias, music therapy: patient-preferred music to address therapeutic goals, music therapy: songwriting as emotional expression for hospice patients, nausea pathophysiology and management, new york state hospice utilization and updates, nursing assessment and case management, nursing care in the final hours of life, nursing: pain assessment and management in advanced illness, nursing: spirituality and culture in nursing assessment and interventions, opioid therapy in the medically ill: side effect management, opioid therapy in the seriously ill: balancing benefit and harms, outpatient palliative and supportive care clinics: current state, pain: its multifaceted nature, pain: nursing assessment and management, palliative care in amyotrophic lateral sclerosis (als), palliative care in coma and disorders of consciousness, palliative care in parkinson’s disease and other neurodegenerative diseases, palliative care in the elderly sickle cell patient, palliative radiation therapy, palliative sedation: medical, ethical, and legal issues, patient eligibility and referral for hospice and palliative care, pediatric pain management, pediatric palliative care, pediatric symptom management, prescription drug abuse: what the palliative care specialist needs to know, professional caregivers: looking at our coping through a disaster psychology lens, prognostication: the art and science, psychological and psychiatric risk factors in patients and families, racial and ethnic disparities in end-of-life care, ritual at end of life, role of medical cannabis for the seriously ill, role of specialist palliative care in heart failure, role of the music therapist, role of the nurse in advance directives, role of the social worker in advance care planning, role of the social worker in care transition: hospital, etc., seizures in far-advanced disease, self-care for clinicians, symptom assessment and management for nurses, symptom distress through the prism of culture, teamwork and the interdisciplinary team, the role of the nurse, trauma-informed care: understanding the impact of trauma on holocaust survivors facing the end of life, update on adjuvant analgesics in advanced illness, withholding and withdrawing life-sustaining therapies in the setting of home hospice, wound care in advanced illness.

Congratulations to Marycarol Reeder, Recipient of the 2023 Doris A. Howell Award

Shaping Palliative Care Education for Current and Future Professionals

Sponsoring Compassionate Palliative Care Curriculum Through Community

Building Awareness Through Campus Partnerships

Palliative Care Education, Anytime.

Palliative Care Education, Anywhere.

Make an Impact by Helping Fund our Mission
Our mission.
The CSU Shiley Haynes Institute for Palliative Care Provides High-Quality Education to Healthcare Professionals and Students, Builds Advocacy, and Promotes Research to Advance the Care of Those Living with Serious Illness and Their Communities.
Palliative Care Education for Current Professionals, Future Professionals & the Community. All Backed by the Standards of California State University.
Select A Discipline:
- All Courses
- Care Management
- Groups and Teams
- Interdisciplinary Teams
- Nursing Professionals
- Physicians/PAs/NPs
- Social Workers
- Spiritual Care
- All Professionals
- Instructor-Led
- Open To All
- Foundational
- Introductions to Palliative Care
- Advanced Clinical Skills
- Program Design & Implementation
- Teams and Interdisciplinary Training
Communication and Advance Care Planning
Physical aspects of care.
- Psychological Aspects of Care
Social Aspects of Care
- Spiritual Aspects of Care
Cultural Aspects of Care
- End-of-Life Patient Care
- Pediatric Palliative Care
- Integrative Therapies & Approaches
Beyond Cultural Humility: Diversity, Inclusivity, and Navigating Bias in Care
Excellence in interprofessional palliative care documentation, telemedicine skills for clinicians, self-care and resilience, advanced concepts in easing suffering and promoting healing for pediatric patients, advanced communication skills for pediatric patient and family support, advanced pediatric care delivery, advanced pediatric pain and symptom assessment and management, advanced practice palliative care certificate for social workers, advanced practice rn certificate in palliative care, applying motivational interviewing techniques and interventions in palliative care, aromatherapy in palliative care, basic communication skills for pediatric patient and family support, basic concepts of easing suffering and promoting healing for pediatric patients, basic pediatric care delivery, basic pediatric pain and symptom assessment and management, billing for advance care planning conversations, care of the patient at the end of life, certificate in clinical pediatric palliative care, communication strategies for shared and informed decision making, core concepts in palliative care – all health professionals, core concepts in palliative care – chaplains, core concepts in palliative care – nurses, core concepts in palliative care – social workers, effective advance care planning fundamentals, essentials of palliative care chaplaincy, facilitating an advance care planning conversation, food is medicine series – nutrition in palliative care, foundational communication skills for pediatric patient and family support, foundational concepts of easing suffering and promoting healing for pediatric patients, foundational pediatric care delivery, foundational pediatric pain and symptom assessment and management, healing through art, integrating advance care planning into your medical practice, integrating palliative care into practice, introduction to primary palliative care, introduction to pediatric palliative care, multidisciplinary certificate in pediatric palliative care, palliative care for care managers, pediatric ethical principles and challenges, pediatric team support, pa certificate in palliative and serious illness care, primary palliative care skills for every provider, rn certificate in palliative care, self-care and resilience skills for palliative care clinicians, sharing serious news, spiritual, religious, and existential aspects of care, the business case for palliative care, the evidence for nutrition in palliative care, understanding food choices and chronic or complex illness, what every aprn needs to know about palliative care, what every chaplain needs to know about palliative care, what every health professional needs to know about palliative care, what every nurse needs to know about palliative care, what every physician needs to know about palliative care, what every pa needs to know about palliative care, what every social worker needs to know about palliative care, working with polst, workforce solutions, empowering your staff.
As a California State University institute, we provide innovative palliative care education, delivered through a state-of-the-art online learning platform with customized programs and top-tier instructional support tailored to your organization’s unique needs.
Partnering with us couldn’t be easier. We collaborate closely with our corporate clients to understand their vision, assess their needs, deliver convenient and effective distance-learning solutions, and help measure results.
Adapting to Your Needs
Our instructor-led courses offer students rigorous content and personalized feedback that rivals clinical programs, all with the convenience and flexibility of online learning. Class sizes are limited, so students receive quality, personalized instruction. Students complete weekly lessons on their own schedule, participate in online discussions with their peers, and get guidance from their instructor on practical ways to apply their new skills.
Our self-paced courses allow students to work on their own time and schedule. Based on the latest research and skill-building practices, our courses are delivered through a state-of-the-art learning platform with interactive features designed to reinforce learning and retention.
Custom Training
- Special packaging and group pricing of all available courses
- Dedicated instructor-led courses reserved for your employees
- Custom-developed online or in-person training designed for your unique needs
- Courses customized to reflect your organization’s practices and policies
- Supplemental toolkits for team leaders and managers to reinforce staff learning
Building Strategic Skills
We offer convenient and effective workforce education programs designed to empower your team to deliver the best patient-centered care for individuals with serious illnesses.
Our self-paced and instructor-led courses deliver real-world clinical skills for nurses, social workers, physicians, chaplains, and other health professionals, helping employers build staff resilience, improve care delivery, boost quality metrics, and achieve operational goals.
Our customized training solutions deliver flexible, affordable, targeted learning that supports your employees and helps your organization meet strategic benchmarks.
Learning Experience
Defining excellence.
Our online courses are packed with interactive exercises, evidence-based tools and resources, case studies, and other strategies designed to expertly engage adult learners and reinforce retention. Courses are tailored to help nurses, social workers, physicians, chaplains, and other busy health professionals make a measurable impact on care delivery.
Yielding Results
Research shows companies with strong staff development programs reap multiple benefits, including better employee retention, increased job satisfaction, and enhanced team performance. All are vital for healthcare organizations that care for people with serious illnesses. We are devoted to helping you reach your goals.
Palliative Care saved this hospital $2M in one year
The CSU Shiley Haynes Institute for Palliative Care has a proven track record. Read this case study to learn how an Institute course helped a strategic team from a South Carolina hospital make the business case for palliative care by showing their palliative care pilot program saved the hospital $2 million in its first year.
Request Our Newsletter
333 S. Twin Oaks Valley Road San Marcos, CA, 92096 Call: (760) 750-4006
Giving the Gift of Palliative Care Education
The Institute offers scholarships to cover the full cost of tuition in any Institute course, funded by philanthropist Darlene Marcos Shiley to provide training that can enhance care for patients and families in the San Diego region. Join the interest list below.
Alumni: Guiding the Next Generation
If you’ve taken a palliative care course through the Institute, you are part of a movement to transform care for people with serious illnesses and their families. We are invested in your success! Stay connected with us for support, new practice strategies, special offers, and more.
Inspiring Exceptional Whole Person Care
Individuals and organizations committed to improving care and quality of life for people with serious illnesses have supported the CSU Shiley Haynes Institute for Palliative Care since its inception. Their generosity has helped the Institute further its mission and create new palliative care courses that address critical healthcare needs.
Training Your Team with Our Custom Solutions
Sharing resources: request a free demo, want to learn more connect with us to get started…, sharing resources, personally and professionally.
These free resources explore palliative care topics and strategies designed to inspire exceptional whole person care. Stay engaged with us to access new resources as they become available.
Join Our Mission
If you’re passionate about palliative care education and innovation, join our mission to advance and enhance palliative care by educating current and future healthcare professionals, we’d love to connect with you!
Sharing Experiences, Personally and Professionally
The Institute is a respected source of palliative care expertise. If you’re a media professional writing about palliative care, we’re glad to connect you with our staff, faculty, and/or subject matter experts to answer questions or provide a quote.
Contribute to the Discussion, Post or Share a Story Idea
If you’re a palliative care clinician interested in advancing serious illness care by contributing a blog post or suggesting a story idea, we want to hear from you!
Sharing Resources: Request a Faculty Toolkit
The Institute and its Campus Partners began work in 2018 on a pilot program for an online Faculty Toolkit to help college and university faculty integrate palliative care content into classes in multiple disciplines. The online modules include resources and interactive learning activities that focus on the basics of palliative care and health disparities in palliative care.
Disability Accommodations or Special Needs
It is requested that anyone who requires auxiliary aids such as sign language interpreters and alternative format materials notify the event sponsor at least seven business days in advance. Every reasonable effort will be made to provide reasonable accommodations.
Building Palliative Care Awareness at the Local Level
Campus partners build awareness of palliative care through programs for students, faculty, health professionals, and caregivers in their communities.
If you’re a CSU faculty member who is passionate about palliative care, we’d love to talk with you about creating a Campus Partner Institute on your campus. The Institute supports its Campus Partners in several ways, including identifying funders for research, helping with grantwriting, and sharing faculty resources.
Join Our Community of Contributors Passionate About Palliative Care
If you’re passionate about palliative care education and innovation and have specific skills that complement our mission to advance and enhance palliative care by educating current and future healthcare professionals, we’d love to connect with you!
The CSU Shiley Haynes Institute for Palliative Care is continuously seeking to expand our network of content contributors, and freelancers who are skilled in the following areas:
- Subject-matter experts in palliative care or case management
- Online instructors including physicians, clinical social workers, RNs, APRNs, and chaplains with experience in palliative care
- Content and curriculum developers
- Healthcare writers and editors
- Instructional designers

Thank you for your Support!
We are so grateful that you are helping support scholarships for healthcare professionals who need financial assistance to deepen their skills in caring for people with serious illnesses and their families.
Here are some helpful instructions:

- Latest News
- Employer Partnership Program

- About the APHSW-C
The APHSW Certification
Social workers are essential to the practice of hospice and palliative care. The APHSW-C certification recognizes bachelor’s and master’s level social workers with experience, specialized skills, and competency in hospice and palliative social work. The APHSW-C assures the public that certified practitioners have the knowledge and skills to provide safe, high-quality care at an advanced level. Individuals eligible for certification include experienced hospice and palliative care social workers that practice in clinical and academic settings in the United States and Canada.
Holding the APHSW-C certification demonstrates to patients, their families and caregivers, employers, colleagues, and the public at large that a practitioner has met the highest standards of professional practice and has obtained objective validation of their expertise in providing advanced palliative and hospice social work services by:
- Having earned a Bachelor’s or Master’s degree in Social Work;
- Completing a minimum of post-degree experience in hospice and/or palliative social work determined by the degree earned;
- Attesting to practice in accordance to the National Association of Social Workers (NASW) Code of Ethics;
- Holding state licensure in good standing to practice, if required for employment;
- Successfully passing a certification exam; and,
- Committing to ongoing professional development.
Recertification is required every 4 years, which includes an application and 40CE credits. You do not take the exam again for recertification.
Information sheets about the certification.
The APHSW Certification This one page document lists the key discussion points of the APHSW Certification. How it was developed, eligibility requirements, veracity of the exam, employer benefits and more.
Benifits of APHSW This one page quick resource outlines some of the benefits of the APHSW Certification. Great resource for quickly explaining the purpose of the certification!
APHSW overview : This is a good one page, quick, resource to share with your colleagues about the development and validity of the certification for the field of Hospice and Palliative Care.
Toggle Content
Are you a member of a social work organization?
Thank you to the following social work organizations who have partnered with APHSWC to offer a discount on the the application as a member benefit!!
These members receive a 25% discount on the application!
Look for instructions on the Application Page for more details.
Social Work Hospice & Palliative Care Network
Click here for more information about SWHPN membership!
Association of Oncology Social Work
Click here for more information about AOSW membership!
Society for Social Work Leadership in Health Care
Click here for more information about SSWLHC membership!
Where are the APHSW-C Certificate Holders?
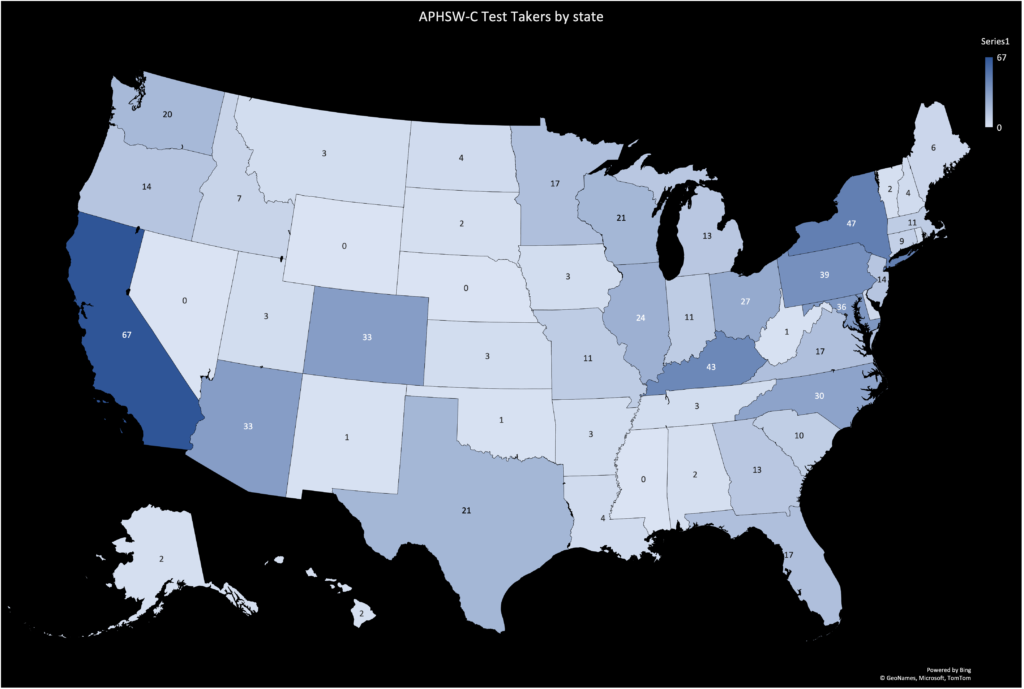
Upcoming Events
- Next Application Window: July 1, 2022
- APHSW-C Information Session on June 28th at 3pm. Hosted by SWHPN.
- The APHSW-C Candidate Handbook
- Recertification Guide
- Test Specifications for the APHSW-C
- Article: Job Analysis Research 2019
- References List for Exam
- Clinical Practice Guidelines for Quality Palliative Care, 4th Edition
Twitter Feed
Join our mailing list.
Sign up for our newsletter and stay up to date on the latest news.
The first evidence-based certification for social workers in hospice and palliative care.
Quick Links
- The APHSW Board
- Eligibility
- APHSW-C Exam
- Application
- Learn About Recertification
- Certification Verification
- Candidate Handbook
Useful Links
- Newsletters
- Email: [email protected]
Our Mission
Identify and recognize the special skills and knowledge that social workers bring to the practice of palliative and hospice care through a rigorous certification process.
All seriously ill and dying patients receive and have access to quality psychosocial care. We recognize that poverty, discrimination, oppression, and injustice can interfere with this vision and we strive to overcome these obstacles by incorporating a lens of equity in all of our activities.
Social Work Competencies on Palliative Education – SCOPE

The evidence supporting social work involvement in end of life care is primarily anecdotal and experience-based and derives from the experiences of clients and professionals themselves. However, a review of evidence-based research literature by Rizzo and Rowe found that social work interventions had a positive and significant impact on quality of life and health care costs and use for aging individuals and their caregivers. A further study by Reese and Raymer demonstrated that increased social work involvement in hospice care was significantly associated with lower hospice costs, improved team functioning, reduced medical services, fewer visits for other team members and lower severity of case. The ability of social workers to make psychosocial assessments generally improved planning and, ultimately, care. Other articles examine the general benefits of early social worker assessment and intervention, which can be assumed to apply to end-of-life care. Planning and intervention from those skilled and knowledgeable regarding the psychosocial needs of patients and families increase family cooperation and patient satisfaction, decrease the need for crisis management and reduce the need for contact from other disciplines.
While this project is aimed at general social work curriculum, the competencies upon which it is to be based are derived from the practice of palliative care social workers. One would assume that the outcome of this education will serve to advance the practice of all social workers in the area of end-of-life care. Opportunities for social workers to better understand psychosocial care at the end-of-life and their role and practice within that will further help them articulate their contribution and expertise to clients and their families, colleagues and policy makers.
Despite the prevalence of social work interactions with individuals and families facing end-of-life, the existing education for social workers in HPCis inconsistent and limited. This is true in Canadian university schools of social work, regional college programs and in social work continuing education programs.
From the work done to date on the competency development, there are reports from both practitioners and educators that gaps exist in current social work programs. Practitioners said they learned about end-of-life issues through experience and often felt ill-prepared to deal with them. Educators indicated a need for resources that can be used within existing courses. Field instructors reported students expressing frustration with the lack of preparation in undergraduate programs to work with issues of grief and loss, death and dying, and family issues.
To address this gap, in 2005 Health Canada’s Secretariat on Palliative and End-of-Life Care funded a task group, known as the SCOPE (Social Work Competencies on Palliative Education) team, to conduct national research aimed at developing a set of core social work competencies to guide education for practice with people facing end-of-life issues. The SCOPE team, lead by Wendy Wainwright of Victoria Hospice and Dr. Susan Cadell, who was then at the University of British Columbia, consisted of nine social work educators and practitioners. In this first phase, the (2002) Canadian Hospice Palliative Care Association (CHPCA) Standards – A Model to Guide Hospice Palliative care: Based on National Principles and Norms of Practice framework was used as the foundation for the development of 11 core competencies essential to social work practice in HPC. National consensus regarding these competencies was sought using a modified Delphi technique, focus groups and surveys. Each competency included the values, knowledge and skills most salient to it. The 11 core competencies developed as a result of this research were: Advocacy; Assessment; Care Delivery; Care Planning; Community Capacity Building; Decision-Making; Evaluation; Education and Research; Information Sharing; Interdisciplinary Teamwork; and Self-Reflective Practice (Appendix 4).
In 2008 the Canadian Partnership Against Cancer funded a second phase of this project. This phase was based at Lakehead University and was led by Dr. Mary Lou Kelley and members of the SCOPE team. It built upon phase one and extended the development of social work competencies by undertaking a national consultation process to validate them and to create a strategic plan for implementing them in education and practice settings.
That consultation process engaged four groups with the following purposes: 1) social workers across Canada – to validate the competencies across jurisdictions and settings of care, and to identify effective strategies for implementing them in the workplace; 2) oncology patients facing end of life and their families-to validate the competencies based on their lived experience; 3) social work educators – to disseminate the competencies and consult about effective strategies to incorporate them into curricula of schools of social work; and 4) professional social work associations and others responsible for the continuing education of social workers- to consult about effective strategies to make competency-based education accessible through their programs. The consultations involved national workshops, telephone and face-to-face interviews, and online surveys.
The project was completed in June 2009. The consultations provided a broad validation of the original competencies with their purpose more clearly articulated, and resulted in the preliminary development of a strategic plan with the schools of social work regarding their implementation into formal curricula. The consultation process served to engage social work educators and professional associations in planning an implementation process and began to create a foundation for developing system partnerships between practitioners, educators, and professional associations. In particular, developing a partnership with the Canadian Association of Social Work Education (CASWE) to influence the use of the competencies in curriculum development at all levels of social work education and training was seen as a positive next step. Both educators and practitioners across the country were clear in their conclusion that, while palliative care social work is a small speciality area within the profession, all social workers need and would benefit from education in end-of-life issues, approaches and interventions.
The third phase of the project, Implementation of Canadian Social Work End-of-Life Competencies into Professional Education Curricula, involved the development and evaluation of model curricula based on the competencies that can be used in schools of social work at the undergraduate and graduate levels, as well as in continuing professional education.
Now completed, this three-phase project will result in the advancement of education and training for social work practitioners caring for Canadians who are faced with progressive life-limiting illness, dying, death and bereavement. Ultimately, this work will build capacity and support system change by increasing the number of expertly trained/educated social workers who provide hospice palliative care and psychosocial end-of-life care.
The National Team is now ready to launch their newly created educational learning modules – available April 1, 2011. This unit contains a series of five teaching modules specific to hospice palliative care that can be used to enhance Social Work competencies with people at end of life. The unit was developed with the knowledge that all Social Workers, at some point in their careers, will work with people facing life-limiting illness, death, and bereavement.
The information and tools included aim to enhance knowledge, skills, and practice fundamental to hospice palliative care. The modules can be used together as a unit, or each module can stand alone and be used individually. The intent of this teaching unit is to make competency-based, end of life care content and materials available to social work education programs in Canada, without requiring the addition of new courses to existing curricula.
The five unit modules are as follows:
- Module 1: Fundamentals of Social Work in End of Life Care
- Module 2: Communication
- Module 3: Care Planning and Delivery
- Module 4: Advocacy
- Module 5: Evaluation and Self-Reflective Practice
Modules are available on the CHPCA Marketplace
Journal Article in Palliative Medicine: Creating Social Work Competencies for Practice in Hospice Palliative Care
May 14, 2024
Patients Fare Better When They Get Palliative Care Sooner, Not Later
Supportive care is often started late in an illness, but that may not be the best way
By Lydia Denworth

In the last months of my mother’s life, before she went into hospice, she was seen at home by a nurse practitioner who specialized in palliative care. The focus is on improving patients’ quality of life and reducing pain rather than on treating disease. Mom had end-stage Alzheimer’s disease and could no longer communicate. It was a relief to have someone on hand who knew how to read her behavior (she ground her teeth, for instance, a possible sign of pain) for clues as to what she might be experiencing.
I was happy to have the help but wished it had been available earlier. I’m not alone in that. Evidence of the benefits of palliative care continues to grow. For people with advanced illnesses, it helps to control physical symptoms such as pain and shortness of breath. It addresses mental health issues, including depression and anxiety. And it can reduce unnecessary trips to the hospital. But barriers to access persist—especially a lack of providers. As a result, palliative care is too often offered late, when “the opportunity to benefit is limited,” says physician Kate Courtright of the Perelman School of Medicine at the University of Pennsylvania.
In 2021 only an estimated one in 10 people worldwide who needed palliative care received it, according to the World Health Organization. In the U.S., the numbers are better—the great majority of large hospitals include palliative care units—but it’s still hard for people who depend on small local hospitals or live in rural areas. Outpatient palliative care is especially hard to find.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Experts are also working to correct misconceptions. “When people hear the words ‘palliative care,’ they think ‘end-of-life care—I’m going to die,’ ” says physician Helen Senderovich, a palliative care expert at the University of Toronto. Although palliative medicine grew out of the hospice movement, it has evolved into a multidisciplinary specialty encompassing physical, psychological and spiritual needs of patients and their families throughout the trajectory of disease, Senderovich says. That path includes the time when treatments are still being tried.
So palliative care specialists have begun referring broadly to “supportive care”— “anything that is not directly modifying the disease,” says medical oncologist and palliative care specialist David Hui of the MD Anderson Cancer Center. For example, wound care and infusions to improve red blood cell counts in cancer patients are supportive; chemotherapy is not.
Generally, the earlier that supportive care is offered, the more satisfied patients report feeling. And ideally, people who need it now get referred to palliative medicine around the time they are diagnosed with a serious illness. An influential study in 2010 found that patients with lung cancer who received palliative care within eight weeks of diagnosis showed significant improvements in both quality of life and mood compared with patients who got only standard cancer care. Even though those receiving early palliative care had less aggressive care at the end of life, they lived an average of almost three months longer.
More recent studies have confirmed the life-quality advantages of earlier palliative care, although not all studies have shown longer survival. “Patients don’t just start having pain and anxiety and weight loss and tiredness only in the last days of life,” Hui says. Starting palliative care earlier allows patients and the care team to “think ahead and plan a little bit,” he adds.
Nor is palliative care effective only for cancer, although that’s where much of the research has been done. It benefits those with heart failure, chronic kidney disease, dementia, chronic obstructive pulmonary disease (COPD), Parkinson’s, and other serious illnesses.
In January 2024 the Journal of the American Medical Association published a pair of studies that broke “new ground” in developing sustainable, scalable palliative care programs, according to an accompanying editorial. One, the largest-ever randomized trial of palliative care, included more than 24,000 people with COPD, kidney failure and dementia across 11 hospitals in eight states. The researchers made palliative care an automated order, where doctors had to opt out of such care for their patients instead of going through an extra step of opting in. The rate of referrals to palliative care increased from 16.6 to 43.9 percent, says Courtright, lead author of the study. Length of hospital stay did not decline overall, but it did drop by 9.6 percent among those who received palliative care only because of the automated order.
The second study looked at 306 patients with advanced COPD, heart failure or interstitial lung disease. Half these people participated in palliative care via telehealth visits with a nurse to handle symptom management and a social worker to address psychosocial needs; the other people in the study did not get such care. Those who received the calls quickly showed improved quality of life, and the positive effects persisted for months after the calls concluded.
Because there are not enough palliative care providers, Hui advocates for a system that directs them to patients who would benefit most. Usually, and not surprisingly, those are people with the most severe symptoms. This system uses early screening of symptoms to identify these people. Hui calls the approach “timely” palliative care. “In reality, not every patient needs palliative care up front,” Hui says, so timely care uses scarce resources as effectively as possible.
I don’t know exactly when my mother needed to start palliative care, but I hope that going forward more caregivers and more families know to ask about it sooner.
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.
- Asia - Pacific
- Middle East - Africa
- Apologetics
- Benedict XVI
- Catholic Links
- Church Fathers
- Life & Family
- Liturgical Calendar
- Pope Francis
- CNA Newsletter
- Editors Service About Us Advertise Privacy

Hospice and palliative care: A look at ‘absolutely vital’ end-of-life support

By Daniel Payne
CNA Staff, May 19, 2024 / 05:00 am
As assisted suicide and euthanasia continue to grow more common throughout much of the developed world, services like palliative and hospice care serve as a vital counterweight to those trends, offering what one provider calls care for “the whole person” that’s respectful of both a patient’s life — and death.
Assisted suicide and euthanasia have been legalized in countries such as Canada, Australia, Spain, Belgium, and in multiple U.S. states, permitting patients to take their own lives or allowing doctors to kill them outright.
In contrast, services such as palliative care and end-of-life hospice care seek to uphold the dignity of each human life, especially as it nears its end.
What is palliative care? What about hospice?
Dian Backoff told CNA that both palliative and hospice providers are trained to minister to the “psychosocial, spiritual, and financial needs” of patients facing debilitating or terminal illnesses.
Backoff, the executive director of Catholic Hospice for Catholic Health Services in Fort Lauderdale, Florida, told CNA that palliative care is meant to address “what the whole patient wants during the treatment of an illness,” whether or not the patient is terminally ill or dealing with a long-term affliction.
Oftentimes a patient suffering from a severe illness has multiple doctors from multiple disciplines, such as neuroscientists and cardiac experts, Backoff pointed out.
“Palliative care has someone bring all that specialty work together so that we don’t forget there’s a person behind the brain, behind the liver, behind the heart,” she said.
Backoff said hospice is a part of palliative care, one that arises at the end of a patient’s life. A significant part of hospice service, she said, involves ensuring that dying patients have medication to alleviate any pain or suffering they may have as death nears.
But, she noted, “all of the services that are applied to the patient, other than clinical, are also applied to the family.”
“How are you going to cope with the death? Is there anticipatory grief? Is there complicated grief pending because there are unresolved family issues?” she said.
Hospice workers “make sure coping mechanisms are appropriate” and that family members are “grieving appropriately instead of dealing with something years down the road.”
Hospice ‘absolutely vital,’ in line with Catholic teaching
Joe Zalot, an ethicist and the director of education at the National Catholic Bioethics Center, said that hospice, when done right, is “very, very important” for both dying patients and families.
“Hospice, when done correctly, is proper accompaniment at the end of life,” Zalot said. “It’s palliating symptoms, it’s providing spiritual care, it’s helping people live the most full possible life that they can given the limitations of their illness. It’s helping them and their family prepare well for death.”
“When done well, it’s absolutely vital and very much in line with Catholic teaching,” he said.
Zalot warned, however, that there are “not-so-good” hospice practices on the market as well.

Pope Francis appoints Cardinal Tagle as special envoy to National Eucharistic Congress
“We get calls on our consult line and we hear horror stories, from families and doctors, where people go in and they’re medicated for whatever reason, there’s questions about nutrition and hydration, any number of different things,” he said.
Zalot said the best hospice workers are those who support the family unobtrusively. “If you don’t know what they did, they probably did their job correctly,” he said.
Among the best practices of hospice, he said, are symptom management, relief from pain and nausea, and relief from complications that arise from one’s pain, conditions, or treatments.
“Another essential element is to help family members and support them as they journey with their loved ones,” he said.
“Specifically from a Catholic perspective, a very good-quality hospice is one that provides spiritual care and access to the sacraments, through chaplains,” Zalot noted.
Backoff said their patients are split between home and hospital settings, with the majority in the former. “We have 750 patients, and all but about 120 are at home,” she said. “The rest are in nursing homes or in our hospice facility.”
“The average length of stay for us is about 70 days,” she said. “That’s average for us, and probably it’s fairly consistent around the country.”
(Story continues below)
Subscribe to our daily newsletter
Zalot said the Church’s opposition to euthanasia and assisted suicide is because those procedures are quite literally homicide. “You’re killing people,” he said.
“It’s sort of like abortion,” Zalot said. “We have all of these euphemisms — ’reproductive rights,’ et cetera. It’s the same thing with assisted suicide and euthanasia: ‘Death with dignity,’ ‘medical aid in dying.’”
“Euthanasia and assisted suicide are killing people,” he said. “They are actions that kill people. And the Fifth Commandment says that thou shalt not kill. And that’s the bottom line.”
- Catholic News ,
- Palliative Care ,
- Euthanasia ,
- End of Life ,
- Death and Dying

Our mission is the truth. Join us!
Your monthly donation will help our team continue reporting the truth, with fairness, integrity, and fidelity to Jesus Christ and his Church.
You may also like

Hospice leader in Canada promotes anti-euthanasia film: ‘My life’s work’
The president of Delta Hospice Society is promoting a new film to raise awareness of the “predatory doctor-assisted suicide regime” of the Canadian government.

Archdiocese of Montreal sues Quebec government over MAID forced upon hospice
Montreal’s Archbishop Christian Lépine is taking on the attorney general of Quebec.

New palliative care hospital brings ‘sweetness of Mary’ to poorest in Peru
In the context of the recent news of the death of Ana Estrada, the first person to request and receive euthanasia in Peru, there is a contrasting story to tell.
Palliative care isn't just for the dying: Demystifying what it means to get help
When Despina Liberopoulos-Shousha first found out that she had stage four lung cancer and needed palliative care, her first thought was, "But I'm not dying."
"The stigma of palliative care is it's your final days and it's the last place you can have the best quality of life," she said. "You're dying and it's just a matter of time."
The mother of two says when doctors found her cancer in February 2022, it had already metastasized to her brain, bones, liver and abdomen.
"I was shocked because I'd never been ill, I'd never been hospitalized," she tells CTV News. "I was totally taken aback."
Since then, the cancer has spread to her pancreas, the lining of her gut and her adrenal glands.
The Beaconsfield resident admits that every now and then she throws herself a "pity party" and then picks herself up to face her new life head-on -- with the support of doctors and caregivers at the McGill University Health Centre (MUHC) palliative care department.
"I don't like to look at it like it's not good," she said. "As long as they can continue to find treatments for me, then I'm in the game, and as long as I'm in the game, I'm fighting the fight and I have a very positive attitude and I don't let any of this get me down."
She says palliative care has helped her mostly with the physical side effects of her treatment.
"If you're feeling good physically then you're feeling good mentally and you can face the challenge," she said.
Am I dying?
Dr. Justin Sanders, the director of Palliative Care McGill, says the number one worry people have when they are referred to him is: am I dying?
He notes palliative care, which is offered when someone is diagnosed with a serious illness, often gets confused with hospice care, which is comfort without curative intent.
Sanders classifies "serious illness" as a grave diagnosis -- but not one that necessarily means death is imminent.
"Palliative care should be provided alongside 'active treatment' or disease-directed treatment in order to get the best outcome from that treatment," he tells CTV News. "When studies compare people who get palliative care versus those who do not, the people who get palliative care are, on average, likely to live longer."

Sanders notes palliative care helps people take care of their physical ailments, have it be nausea or other maladies associated with their illness or treatment.
Additionally, some of the most important work his team does is taking care of people's emotional and mental states.
"Sometimes it's the existential concerns about what comes next after we die," he said. "When we don't create space to talk about those things, we leave people to suffer alone."
Improving quality of life
Sanders notes he strongly believes that with proper palliative care, people are less likely to fall into distress or ask for medical aid in dying (MAID).
"Quebec has the highest rates of medical aid in dying in the world," he tells CTV News. "I don't think it's unrelated that people bring to their illness experience a lot of fear about what it means to die, and there are a lot of perceptions that dying is a process characterized only by suffering."
The irony of facing death, Sanders adds, is that people can still thrive.
"It's not uncommon that we hear people say, at the end of a year of cancer treatment, or as they approach the end of their life, 'this last year was the best year of my life,'" he said. "I think something that we're all striving for in our lives is how to make meaning of what it is that we're going through."
Sanders says with the integration of Santé-Québec into the province's health system, he hopes to bring the importance of palliative care to the forefront of people's minds.
"There's an enormous opportunity for them to integrate palliative care," he said, adding that every Quebecer has a right to seek help.
"If you have a serious illness and you don't have access to palliative care, then you really don't have access to the best care," he notes. "It's really important for people to advocate for themselves and for their loved ones, and make sure that they have access to palliative care."
Palliative care as an umbrella
Sanders recalls a colleague of his who once perfectly articulated a simple way to explain palliative care:
"Palliative care is the umbrella, not the rain. What we know is that when the rain comes, if you're stuck out and you get soaked, and someone gives you an umbrella, then it's really too late," he recounts. "But if you have that umbrella early and you can carry it alongside you unfolded, then when it starts to rain, and you can raise that umbrella, you can stay dry."
As she continues persevering, Liberopoulos-Shousha has some parting words for anyone diagnosed with a serious illness: "Get in the system...If you need anything, they'll be there for you."
"Cancer has really made me stop and think about a lot of things," she said. "[It has] given me patience and humility and I know there's a lesson here."
Montreal Top Stories

Quebec has more health care workers per capita than 30 years ago: IRIS

Child dies after being found in residential pool

Cardinal Lacroix cleared after investigation ordered by the Pope

Desjardins apologizes for using Canada flag in Patriots' Day poster

SOPFEU urges fire caution in the face of hot, dry weather

McGill says pro-Palestinian protest outside senior administrator's home 'crosses the line'

Jury finds Andrei Donet guilty of second-degree murder in stabbing death of Montreal teen

Woman, 35, in critical condition after her truck collided with a Via Rail train near Montreal
Ctvnews.ca top stories.

Feels like mid-30s in parts of Canada, while other areas expecting snow
Anything is possible this week, as far as Canada's weather is concerned, with forecasts ranging from scorching heat in some parts of the country to rain and snow in others.
Independent stores and grocery alternatives see sales boost amid Loblaw boycott
As the month-long boycott of Loblaw-owned stores wears on, small independent food retailers and alternative grocery options say they're seeing a boost in traffic and sales.
1 dead, others injured after London-Singapore flight hit severe turbulence, Singapore Airlines says
One person has died aboard a London-Singapore flight that encountered severe turbulence, Singapore Airlines said Tuesday. The plane was diverted to Bangkok, where emergency crews rushed to help injured passengers amid stormy weather.
What is BORG drinking, and why is it a dangerous trend? An expert explains
If you've been to a party lately and haven't seen someone drinking a BORG, you're likely not partying with college students.
How to check the Air Quality Health Index and assess your health risks
As we enter another wildfire season, Environment and Climate Change Canada is advising people to pay attention to air pollution levels and check the Air Quality Health Index – especially on smoky days.
The Vatican has announced that the investigation it commissioned into allegations of sexual touching against Cardinal Gerald Cyprien Lacroix did not confirm any act constituting misconduct or abuse on the part of the Vatican.
Trudeau making 'Team Canada' charm offensive in visit to Philadelphia
Prime Minister Justin Trudeau is in Philadelphia today, on his first trip south of the border since his government launched a new 'Team Canada' charm offensive in the United States.
Oilers win Game 7 over Canucks, advance to Western Conference Final
The Edmonton Oilers weathered a late Vancouver Canucks charge on Monday night, beating the hosts 3-2 to win their seven-game second-round playoff series in the decisive showdown.
Katy Perry sings goodbye to 'American Idol'
Katy Perry said her goodbyes on 'American Idol' after seven seasons. On Sunday night’s live 'idol' season finale, a medley of Perry's hit songs were performed, including 'Teenage Dream,' 'Dark Horse' and 'California Gurls.'
Shopping Trends
The Shopping Trends team is independent of the journalists at CTV News. We may earn a commission when you use our links to shop. Read about us.
Editor's Picks
13 blackout curtains for anyone who needs complete darkness to fall asleep, 17 backyard decor and furniture pieces you need before summer arrives, 20 affordable amazon beauty and skincare products you'll probably repurchase over and over again, 12 organization products that'll keep your pantry in order, here are the best, most practical patio furniture sets we found online, 18 budget-friendly products that are bound to come in handy, 15 unique father's day gifts they're guaranteed to love, 18 brilliant birthday gifts for the person on your list who is impossible to shop for, 15 birthday gifts that prove good things come in small packages, i tried 7 of the most popular eye creams on amazon canada, and here are my thoughts, our guide to the best beard trimmers in canada in 2024 (and where to get them), 13 inexpensive beauty products that feel luxurious, health & fitness, 15 of the best bike helmets, according to actual cyclists, 12 of the best pickleball sets you can get online right now, our guide to the best bike trailers in canada in 2024 (and where to get them).

Toronto to see blast of heat on Tuesday
Hot and humid weather is in the forecast for Toronto early this week before a return to more seasonable temperatures this weekend.
Altercation over fireworks led to stabbing at Toronto waterfront: police
An altercation over fireworks led to a stabbing at Toronto's waterfront late Monday night, Toronto police say.

Here's what you need to know about Ottawa's new 3-item garbage limit
Ottawa residents have four months to adjust their garbage disposal habits before a new three-garbage item limit is imposed on curbside waste this fall.
Hot and humid start to the short work week in Ottawa
The hot and humid weather will continue to grip Ottawa over the next two days, but there is relief on the way ahead of Ottawa Race Weekend this weekend.
Fewer accidental 9-1-1 calls to Ottawa police in first 3 months of 2024
Ottawa police received fewer accidental 9-1-1 calls in the first three months of the year following an update to the automatic SOS function in Android devices, according to a new report.

Voters in Pictou West prepare to cast ballots in Nova Scotia byelection
Voters in the rural Nova Scotia electoral district of Pictou West will head to the polls for a byelection today to replace the recently retired legislative speaker.
Newfoundland grandmothers can wail on the accordion. A historian wants them on stage
79-year-old Madonna Wilkinson has been playing the accordion since she was 15, when she picked one up that had been left behind at one of her parents' rollicking parties in the oceanside town about 25 kilometres north of St. John's, N.L. She has played Sunday masses and St. Patrick's Day parties, and community events of all kinds.

The latest advice for expecting parents? Sign up for child care as soon as you're pregnant
Canada's new $10-a-day child care program is expanding, but there's growing evidence that demand for the program is rising even faster, leaving many parents on the outside looking in.
Study says aquaculture likely driving wild salmon extinction in Newfoundland
A new study shows an Atlantic salmon population in southern Newfoundland is disappearing, and it says nearby aquaculture operations are a likely contributor to the decline.
Northern Ontario

Sudbury MPP says tenants need more protection from landlords
A northern Ontario NDP MPP says the province needs to tackle the issue of predatory landlords.
Neighbour dispute leads to charges in northern Ont.
East Algoma Ontario Provincial Police have charged one person in Elliot Lake in connection with an ongoing neighbour dispute.
Medical emergency prompts SIU to invoke mandate in London arrest
For the second day in a row, the province’s Special Investigations Unit (SIU) has invoked its mandate following an arrest in London. According to London police, a 38-year-old man was taken to hospital on Monday as a result of a medical emergency that took place while he was in police custody.
Hot and humid conditions trigger special weather statement
London-Middlesex and Sarnia-Lambton are under a special weather statement from Environment Canada. Hot and humid conditions are expected Tuesday as an air mass moves into southwestern Ontario.
Highway in South Huron reopens following crash involving a motorcycle
A busy section of Dashwood Road/Highway 83 in South Huron has reopened following a crash on Monday. Crews were called to the scene near Goshen Line around 4 p.m. for what was described as a "serious collision" between a pickup truck and a motorcycle.

Developing | One person in hospital following overnight shooting in Kitchener: police
Waterloo Regional Police are investigating after a reported Victoria Day shooting in Kitchener.
Man suffers serious injuries following single vehicle collision in Woolwich Township
Waterloo Regional Police is continuing to investigate a single motor vehicle collision in Woolwich Township.
Rope Skipping Canada hosts national championship in Waterloo
Hundreds of Canada’s best jumpers were in Waterloo this weekend for Rope Skipping Canada’s national championships.

Special weather statement for Windsor-Essex, Chatham-Kent
Windsor-Essex and Chatham-Kent are under a special weather statement as hot and humid conditons are expected Tuesday.
Multiple shots fired at vehicle on Erie Street: WPS
Windsor police officers are investigating after multiple shots were fired at a vehicle on Erie Street.
Road scanning taking place this week. Here’s why:
The Town of Tecumseh is all having roadways inspected using automated road scanning technology.

Barrie residents asked to be good neighbours
Barrie reminds its residents about fines for not following bylaws.
Boaters issued tickets for alcohol consumption over long weekend
OPP monitored the waters of Georgian Bay during the Victoria Day long weekend and issued tickets to boaters who consumed alcohol.
19-year-old driver caught speeding double the posted limit
A 19-year-old driver was caught driving double the posted speed limit in Innisfil on Sunday.

Vancouver Canucks eliminated from Stanley Cup playoffs
A 3-2 defeat by the Edmonton Oilers Monday night ended the playoff run for the Vancouver Canucks.
Sea-to-Sky Highway crash sends 2 to hospital, major delays expected
Two people were transported to hospital Monday, including one in an air ambulance, after a serious crash closed the Sea-to-Sky Highway in both directions.
Mounties searching for vehicle after 'firearms incident' near Cranbrook, B.C.
Mounties in southeastern British Columbia are searching for the occupants of a vehicle that allegedly fled from police after a reported "firearms incident" on Monday.
Vancouver Island

B.C. mayor says drones endangering wildfire helicopter pilots, pleads for patience
The mayor of the Northern Rockies Regional Municipality in British Columbia says drones are endangering helicopters being used to fight wildfires near Fort Nelson, which was ordered evacuated earlier this month.
'Next man up': Canucks coach, teammates bracing for Game 7 without Brock Boeser
Questions about how the team is going to handle the absence of star winger Brock Boeser from a do-or-die game seven dominated pre-game interviews with the Vancouver Canucks coach and players Monday morning.

Premier Kinew announces byelection date for Heather Stefanson's former constituency
Premier Wab Kinew announced Monday a byelection will be held in Tuxedo on June 18.
Pedestrian dies after being hit by vehicle along Portage Avenue: Winnipeg police
Winnipeg police is investigating after a woman was hit by a vehicle and later died from her injuries Sunday.
'A special bird': The unbreakable bond between purple martins and humans
Flashes of purple darting across the sky mixed with the serenading sound of songs will be noticed more with spring in full force in Manitoba.

Calgary youth slings lemonade to raise money for Autism Asperger's Friendship Society
Inflation does not appear to exist at Dane's Lemonade Stand. "No, it does not," Dane Benesh said. Monday, in Copperfield, a tall glass of his lemonade cost the same $1 it did when he started in 2018.
Family Fun Day at Genesis Centre puts focus on safety and inclusion for special-needs children
The goal at Calgary's Genesis Centre on Monday was to make sure every single kid who walked through the doors felt included.

Status of wildfire that threatened Fort McMurray changed to 'being held'
A wildfire that forced thousands of people to evacuate several Fort McMurray neighbourhoods last week is no longer classified as out-of-control.
Alberta wild food guide teaches others to forage for everyday ingredients
Kevin Kossowan isn't going to the grocery store to find ingredients for dinner. Instead, he's searching for them in the wild in places such forested land he owns north of Rochester, Alta.

Touchwood First Nations address overdose deaths at public meeting
Close to 200 people showed up at the Muskowekwan Bingo Hall on Monday to address the weekly drug-related deaths casting a shadow on their communities.
Nearly half of Sask. Party members elected in 2020 will not be on the ballot in 2024
There's bound to be many new faces in the province's legislature later this year. Nearly half of Saskatchewan Party members elected in 2020 will not be representing the party on the ballot this fall.
'He was laying on the ground': Regina resident reports hearing gunshots during police operation on Garry Street
The Regina Police Service (RPS) has released very few details surrounding a shooting involving the service's Special Weapons and Tactics Team (SWAT).

Environment Canada warns of potential for funnel clouds over Saskatoon
Canada’s weather service has issued an advisory about the potential of funnel clouds forming over the City of Saskatoon.
Court eases internet restrictions for Sask. man who matched with a 15-year-old girl on Tinder
A Saskatchewan man who had a sexual encounter with a 15-year-old girl he met on Tinder successfully appealed to shorten release conditions barring him from online dating.
Thousands from Saskatoon Sikh community celebrate annual Nagar Kirtan parade
The Sikh culture in Saskatoon is growing, and the massive turnout at the Nagar Kirtan parade on Sunday put the strength of their community on full display, as thousands walked up a span of Attridge Drive.
Bishop Simard: Palliative care seeks to accompany people
By Christopher Wells
Palliative care is not about “terminating someone’s life,” says Bishop Noël Simard. Instead, it means accompanying each person as their earthly life draws to a close, and attending to their physical, emotional, psychological, social, and spiritual needs.
The Bishop of Valleyfield, Quebec, Canada, is chairing a Symposium on Palliative Care taking place this week in Canada, under the auspices of the Canadian Conference of Catholic Bishops and the Pontifical Academy for Life.
In an interview with Vatican News ahead of the event, Bishop Simard noted the confusion around palliative care, where euthanasia is permitted under the euphemism “medical assistance in dying,” or MAID. The practice involves doctors or nurse practitioners to either administer drugs to end a patient’s life, or provide drugs that are administered by the patients themselves.
Palliative care, by contrast, “is accompanying people’s lives,” said Bishop Simard, attempting to respond to all the person’s need. “So yes, we need to answer the problem of suffering and pain,” the Bishop says, “but at the same time, there are many other needs” that must be addressed.
This week’s conference, entitled “Towards a Narrative of Hope: An International Interfaith Symposium on Palliative Care,” is aimed at promoting good palliative care, while also working to develop “a culture of responsibility” with regard to end-of-life care.”
Accompaniment is one of the major themes of the Symposium, and Bishop Simard was careful to explain what the term means. A key part of accompaniment is assuring the dying that they are not a burden to others but instead have dignity, which is never lost.
“We are telling them: ‘You are still a person loved by God. You have your place in society. And we are here to tell you that we love you,’” the Bishop said.
It also means assuring them that they are not alone and expressing to them the compassion and tenderness of God that never leaves them.
Bishop Simard likewise highlighted the importance of listening to the person, “to her fears, to her anxiety, and also to what she is unable to say... accompanying helps them to express” their hopes and fears as they approach the end of their lives.
Palliative care, he continued, is also concerned for family members and other caregivers, for whom accompaniment can be a challenge. “We have to be there to listen to them and maybe offer them some respite,” he said, adding that listening to all those involved in palliative care is “essential.”
The Canadian Bishop also emphasized the necessity of accompaniment in the dying person’s spiritual life. Prayer and the reception of the Sacraments are important means to help the person prepare themselves “to go and join the Lord in glory,” reflecting the “very important role” of palliative care for the spiritual life.
Bishop Simard concluded the interview by recalling Pope Francis’ regular calls for “closeness,” and highlighting the importance of being present, of holding a loved one’s hand and assuring them that they are not alone.
Thank you for reading our article. You can keep up-to-date by subscribing to our daily newsletter. Just click here

More upcoming events:

Listen to our podcasts

Subscribe to our newsletters
To get the latest news

Papal audiences

Daily readings

Saint of the day

Australian Government Department of Health and Aged Care
National Palliative Care Week 2024
It’s National Palliative Care Week – a timely reminder that it’s never too soon to start the conversation about matters of life and death.

National Palliative Care Week is running from 19 to 25 May 2024.
Palliative care focuses on physical, emotional, spiritual and social aspects of care.
Palliative care is family-centred. Family, loved ones and carers can also receive practical and emotional support.
Early access to palliative care helps people to maintain quality of life by managing pain and symptoms.
It’s never too soon to start the conversation about matters of life and death.
For advice, tools and support visit the Palliative Care Australia website .
- Palliative care
Is there anything wrong with this page?
Help us improve health.gov.au
If you would like a response please use the enquiries form instead.
New palliative care nonprofit encourages open, candid conversations about death, dying
by Kimberly King

SWANNANOA, N.C. (WLOS) — There’s a national movement among a segment of palliative and hospice care workers to help people facing a terminal illness find the strength to have more candid conversations around death. The goal is to ease the final days not only for the individual dying but for their loved ones at a most painful time.
Dr. Aditi Sethi, a physician specializing in hospice and palliative care, founded the nonprofit Center for Conscious Living and Dying (CCLD) based in Swannanoa. Sethi’s work focuses on helping people come to terms with mortality and break the stigma of avoiding the hard conversations about it.
“I worked in an in-patient hospice facility with 26 beds here in Asheville,” Sethi said Wednesday, May 15, “and I noticed people were coming to us unprepared for death and terrified of dying. They had this crisis-driven response to this natural, inevitable experience we all have. And that didn’t sit well with me.”
After 10 years working as an MD in hospice care, Sethi, also trained as an end-of-life doula, decided it would be her life’s work to help people become more emotionally comfortable in their days before death. Sethi, along with a board of directors, opened The Sanctuary on a tranquil six-acre site in Swannanoa. It will hold a grand opening Thursday, May 17 .
ADVENTHEALTH TO HOLD LISTENING SESSIONS FOR MORE INPUT ON BUNCOMBE COUNTY HOSPITAL
“We are offering community-supported end-of-life care, free of charge, to the person who is dying and their family,” said Sethi. “Anyone who wants or needs this type of care is welcome here, unhoused, uninsured or single. This is a residential home that is run and supported by volunteers. We do have a small staff as part of the nonprofit.”
The facility is collaborating with area hospice agencies in which trained workers come to the site and provide care to those who’ve come to live out their final days. Sethi credits CCLD’s main benefactor David Case with helping her and her team make the center a reality.
Linda Solomon has lived in the Asheville area for years. But several years ago, while maintaining a very close bond with her ex-husband, David, who lived in Dallas, her personal journey around death was about to hit close to home.
“About a year ago, we sat down and he said, 'You know I’m dying, and I’ve decided what I want that to look like,'" Solomon said.
FOUR SEASONS UNVEILS NEW MOBILE MEDICAL UNIT, HELPING BRING CARE TO MORE RURAL AREAS (2023)
David was diagnosed with Parkinson's several years ago. The disease was steadily ravaging his body. Before Parkinson's, photos Linda has kept show a handsome, vital, athletic man who loved dogs, nature and life.
“He was executive vice president of worldwide human resources for a company that had five locations around the world. He was a gentle soul. He was pragmatic, he was a deep thinker. He was very private and he very much wanted to march to the beat of his own drum.”
Linda said he candidly discussed his declining health with her. While they were no longer a couple, Linda said they remained extremely close. She generously told David she’d be his primary support system as he faced the final stages of his life with Parkinson’s. He moved to the Asheville area. Last fall the two found The Sanctuary as the place David felt most at peace for his final days.
“It’s very emotional for me even now,” said Solomon. “But David was a planner, he’s pragmatic. He thought about this, I’m sure, for weeks and months and finally verbalized it to me.”
Linda said it was the right choice. She said the team led by Dr. Aditi was respectful, compassionate and honored all of David’s wishes at the end of his life. She said David’s decision to be open about his own mortality has enlightened her to the gift a terminally ill person can give to their loved ones by bravely being open about their wishes at the end of their life.
“There are a lot of things we don’t want to talk about in life,” said Solomon. “But we do better to talk about the truth. There’s less confusion, fewer decisions for families. It’s a gift to share with them some of your true needs and wants and wishes.”
CCLD has become a model for other communities. The Sanctuary is holding an official opening of services Thursday, May 17 , at the site in Swannanoa from 5:30 to 10 p.m. at 83 Sanctuary Road in Swannanoa.

IMAGES
VIDEO
COMMENTS
Course Overview. ESPEC is a state-of-the art curriculum providing Interactive coursework with engaging videos of patient and family encounters, highlighting best social work practices using the eight domains of palliative care as the framework. Learners must complete Part I before registering for Part II and complete Part II before registering ...
Social workers are integral members of the interdisciplinary palliative care team (IDT), addressing psychological and social needs to support patients living with serious illness, and their families. Because of their specialized training, social workers play a critical role on the team—communicating with patients and families.
From the inception of palliative care in the latter half of the 20th century, social workers have always been involved 5-7 and today they can even be described as core members in this field of practice. 7,8 Brandsen 9 discerned three major social work roles in palliative care: social workers address psychosocial concerns of clients and their relatives; they promote and contribute to advanced ...
We offer membership, small group support and continuing education for hospice + palliative care social workers and clinicians making an impact. Our mission is to enhance hospice and palliative care social work through mentorship, education, community building and advocacy as change agents committed to equity and anti-racism.
Palliative care social workers help ensure individuals with serious illnesses get compassionate, whole-person care that addresses their symptoms, reflects their care wishes, and supports their families and caregivers. ... If you're passionate about palliative care education and innovation and have specific skills that complement our mission ...
Studies in the 1990s began to look at the end-of-life content of social work education and the preparedness of social workers to care for dying patients and their bereaved families. Four small but prominent studies set the stage for the most definitive review of this issue, by Christ and Sormanti (1999).
Below are some common steps to become a palliative care and hospice social worker: 1. Complete Your Social Work Education. A common first step to becoming a palliative care or hospice care social worker is obtaining an appropriate background in generalized social work education at an accredited school.
Social workers encounter situations of life threatening illness, death, dying and bereavement in every setting in which they work. The Certificate in Palliative and End-of-Life Care provides an opportunity for social workers to deepen clinical and leadership skills in palliative care and participate in relational ways of learning in a community of colleagues with an outstanding faculty of leaders.
Here are the general steps for becoming a palliative care social worker: 1. Earn a degree. Palliative care social workers must have a bachelor's degree in social work (BSW) or a master's degree in social works (MSW). The Council for Social Work Education (SCWE) must accredit the bachelor's or master's degree program.
We are pleased to offer our highly rated 2023-2024 free and fee-based palliative care webinar series, presented live and on-demand (typically 1.0 AMA PRA Category 1 Credit™ for CME, Nursing CE, and Social Work CE credits). Access free interactive learning modules on palliative care program development and trauma-informed end-of-life care.
Gain expert skills in palliative care social work and learn how to navigate the diverse demands of your role, assess psychosocial distress, apply appropriate interventions to support patients and families, and emerge as a leader on a palliative care team. ... If you're passionate about palliative care education and innovation and have ...
The APHSW Certification Social workers are essential to the practice of hospice and palliative care. The APHSW-C certification recognizes bachelor's and master's level social workers with experience, specialized skills, and competency in hospice and palliative social work. The APHSW-C assures the public that certified practitioners have the knowledge and skills to provide safe, high ...
Social Workers have been recognized by the CHPCA as core members of the inter-professional palliative care team in all settings of care-residential hospice, acute and long-term care facilities, cancer centres and community care. The intent of this research is to make competency-based, end of life care content and materials available to social work education programs in Canada, without ...
Palliative Care Education and Practice (PCEP) is a comprehensive course delivered by expert palliative care clinicians and educators who create a warm, welcoming environment conducive to deep learning and growth. PCEP provides physicians, nurses, and social workers a structure to efficiently acquire the skills and perspectives necessary to ...
The rate of referrals to palliative care increased from 16.6 to 43.9 percent, says Courtright, lead author of the study. Length of hospital stay did not decline overall, but it did drop by 9.6 ...
The New York State Palliative Care Education and Training Council was created by Public Health Law, Section 2807-n. in 2007. Council members were appointed by the Commissioner of Health and in accordance with the law included representatives from the following types of organizations and/or with subject-matter expertise in the following areas ...
Population need for community palliative and end of life care is rising, with aging, frailty, rising health-related suffering and increasing numbers of people dying at home. 1,2 Access to good community palliative and end of life care is inconsistent and there are longstanding inequalities (unfair and avoidable differences) in access to specialist palliative care services for people with non ...
Backoff said hospice is a part of palliative care, one that arises at the end of a patient's life. A significant part of hospice service, she said, involves ensuring that dying patients have ...
Feudtner C, Rosenberg AR, Boss RD, et al. Challenges and priorities for pediatric palliative care research in the U.S. and similar practice settings: report from a pediatric palliative care research network workshop. J Pain Symptom Manage 2019; 58: 909.e3-917.e3.
Updated evidence-based recommendations were developed to reflect new evidence published since the 2016 guideline, address new research questions, and further clarify the role of palliative care in oncology. 1 The update provides oncology clinicians and researchers, patients, family caregivers, and policymakers with recommendations regarding how and when to integrate palliative care for ...
Patients with hematologic malignancies (HMs) struggle with immense physical and psychological symptom burden, which negatively affect their quality of life (QOL) throughout the continuum of illness. These patients are often faced with substantial prognostic uncertainty as they navigate their illness course, which further complicates their medical decision making, especially at the end of life ...
These social media tiles are part of the palliative care education and training communication toolkits. Use them to encourage people who work in palliative care to complete training to help them deliver high-quality care.
Palliative care isn't just for the dying: Demystifying what it means to get help. When Despina Liberopoulos-Shousha first found out that she had stage four lung cancer and needed palliative care ...
Palliative care seeks to accompany men and women in the final moments of their life, according to Canadian Bishop Noël Simard, ahead of a Symposium on Palliative Care taking place this week in Toronto. By Christopher Wells. Palliative care is not about "terminating someone's life," says Bishop Noël Simard. Instead, it means accompanying ...
General public. National Palliative Care Week is running from 19 to 25 May 2024. Palliative care focuses on physical, emotional, spiritual and social aspects of care. Palliative care is family-centred. Family, loved ones and carers can also receive practical and emotional support. Early access to palliative care helps people to maintain quality ...
Social work in hospice and palliative care can be defined as the discipline that provides a professional continuum ... Council on Social Work Education . 1701 Duke Street, Suite 200 Alexandria, VA 22314 Telephone: 703.683.8080 • Fax: 703.683.8099 www.cswe.org
After 10 years working as an MD in hospice care, Sethi, also trained as an end-of-life doula, decided it would be her life's work to help people become more emotionally comfortable in their days ...