
Medical Devices News
Top headlines, latest headlines.
- Caffeine Affects Brain Dopamine Function
- Diet May Treat Pulmonary Hypertension
- New Sensor Detects Errors in MRI Scans
- Diamond Dust Imaging
- Miniature Brain Stimulator in Humans
- AI Makes Retinal Imaging 100 Times Faster
- Improving Endometriosis Evaluation
- Less Invasive Heart Bypass Surgery
- Removing Benign Pancreatic Tumors
- Revolutionizing Respiratory Disease Diagnoses
Earlier Headlines
Thursday, april 11, 2024.
- Novel CT Exam Reduces Need for Invasive Artery Treatment
Monday, March 11, 2024
- Wearable Tech Captures Real-Time Hemodynamics on the Go
- Would the Highly Sensitive Transparent Ultrasound Transducer Revolutionize Biomedical Imaging Technology?
Thursday, March 7, 2024
- Shape-Shifting Ultrasound Stickers Detect Post-Surgical Complications
- Doctors Can Now Watch Spinal Cord Activity During Surgery
Wednesday, March 6, 2024
- Amyloid Blood Levels Associated With Brain Changes in Alzheimer's Study
Tuesday, February 27, 2024
- New Study Links Placental Oxygen Levels to Fetal Brain Development
- Researchers Look at Environmental Impacts of AI Tools
Sunday, February 25, 2024
- Revolutionary Brain Stimulation Technique Shows Promise for Treating Brain Disorders
Wednesday, February 21, 2024
- Scientists Invent Ultra-Thin, Minimally-Invasive Pacemaker Controlled by Light
Tuesday, February 20, 2024
- Terahertz Biosensor Detects Skin Cancer With Remarkable Accuracy, Ushering in New Era of Early Detection
- Scientists Develop Novel Radiotracer for Earlier Detection of Disease
Friday, February 9, 2024
- Novel Technique Has Potential to Transform Breast Cancer Detection
Thursday, February 8, 2024
- New PET Tracer Detects Inflammatory Arthritis Before Symptoms Appear
- Visualising Multiple Sclerosis With a New MRI Procedure
Wednesday, February 7, 2024
- Knee Pain Explained: The Size of Your Meniscus Matters
Monday, February 5, 2024
- Scientist Shows Focused Ultrasound Can Reach Deep Into the Brain to Relieve Pain
Wednesday, January 17, 2024
- Pushing the Boundaries of Ultrasound Imaging: Breaking New Ground With Ultrafast Technology
Saturday, January 13, 2024
- Novel PET Tracer Enhances Lesion Detection in Medullary Thyroid Cancer, Offers Potential for Targeted Therapy
Friday, January 5, 2024
- Using Static Electricity to Enhance Biomedical Implant Durability
Wednesday, January 3, 2024
- Shining a Light on the Hidden Damage of Mild Brain Injuries
- Foundation Laid for Improved Diagnostic Imaging of Brain Tumors
Tuesday, December 12, 2023
- New Technique for Photon Detection
Monday, December 11, 2023
- Advanced MRI Technology Detects Changes in the Brain After COVID-19
Thursday, December 7, 2023
- Riding Sound Waves in the Brain
Monday, December 4, 2023
- Breakthroughs in Nanosized Contrast Agents and Drug Carriers Through Self-Folding Molecules
Wednesday, November 29, 2023
- Eye-Safe Laser Technology to Diagnose Traumatic Brain Injury
Friday, October 20, 2023
- Keeping a Human in the Loop: Managing the Ethics of AI in Medicine
Thursday, October 19, 2023
- A Miniature Magnetic Resonance Imager Made of Diamond
Tuesday, October 17, 2023
- Smarter CT Scans May Approach the Level of MRI
Monday, October 16, 2023
- A Powerful New Tool in the Fight Against One of the Deadliest Cancers
Thursday, October 12, 2023
- A Better 'map' Of the Lights You See When You Close Your Eyes Can Improve 'bionic Eye' Outcomes
Tuesday, October 10, 2023
- Medical Imaging Fails Dark Skin: Researchers Fixed It
Friday, September 29, 2023
- Novel Tau PET Tracer Exhibits High Sensitivity and Specificity, Allowing for Earlier Identification of Alzheimer's Disease
Monday, September 25, 2023
- Marker for Brain Inflammation Finally Decoded
Wednesday, September 13, 2023
- Researchers Use AI to Predict Recovery After Serious Brain Injury
Wednesday, August 30, 2023
- Researchers Identify the Link Between Memory and Appetite in the Human Brain to Explain Obesity
Monday, August 14, 2023
- Riding a Wave to Better Medical Diagnosis
Wednesday, August 9, 2023
- Tau-PET : Future of Alzheimer's Patients
Friday, July 28, 2023
- A Wearable Ultrasound Scanner Could Detect Breast Cancer Earlier
Wednesday, July 26, 2023
- A Quick Look Inside a Human Being
Monday, July 24, 2023
- Researchers Discover Specialized Immune Cells Patrolling the Human Eye
Tuesday, July 11, 2023
- Copper Could Help Create Clearer MRI Images and Improved Diagnosis
Tuesday, June 27, 2023
- Dogs and Humans Process Body Postures Similarly in Their Brains
- Molecular Imaging Identifies Brain Changes in Response to Food Cues; Offers Insight Into Obesity Interventions
Thursday, June 15, 2023
- New Discovery Can Help Detect Brain Tumors
Thursday, May 11, 2023
- The Technology That Can Detect Rapid Pressure Changes Inside Your Heart
Tuesday, May 2, 2023
- Wearable Ultrasound Patch Provide Non-Invasive Deep Tissue Monitoring
Tuesday, April 4, 2023
- Detecting, Predicting, and Preventing Aortic Ruptures With Computational Modeling
Tuesday, March 28, 2023
- Molecular Imaging Offers Insight Into Chemo-Brain
Monday, March 20, 2023
- Lighting Up Tumors Could Help Surgeons Remove Them More Precisely
Thursday, March 16, 2023
- Children at Risk of Multiple Sclerosis Often Go Undetected in Early Stages
Thursday, March 9, 2023
- Study Examines Heart Inflammation After COVID Vaccine
Tuesday, February 7, 2023
- AI Can Predict the Effectiveness of Breast Cancer Chemotherapy
Friday, January 27, 2023
- Study Shows FDA-Approved TB Regimen May Not Work Against the Deadliest Form of TB Due to Multidrug-Resistant Strains
Wednesday, January 25, 2023
- Wearable Sensor Uses Ultrasound to Provide Cardiac Imaging on the Go
Tuesday, January 24, 2023
- Potential Hidden Cause of Dementia Detected
Tuesday, January 17, 2023
- New Fluorescent Dye Can Light Up the Brain
Thursday, January 12, 2023
- MRI-Guided Radiotherapy Produces Fewer Side Effects and Better Quality of Life for Patients With Localized Prostate Cancer
Wednesday, January 11, 2023
- A New Ultrafast Camera With Multiple Applications
Tuesday, January 3, 2023
- Researchers Develop, Validate Tool to Visualize 3D Architectural Properties of Atherosclerosis Plaques
- Tracking Radiation Treatment in Real Time Promises Safer, More Effective Cancer Therapy
Thursday, December 22, 2022
- New Sensor Uses MRI to Detect Light Deep in the Brain
Friday, December 16, 2022
- Wearable Skin Patch Monitors Hemoglobin in Deep Tissues
Tuesday, December 6, 2022
- New X-Ray Technology Can Improve COVID-19 Diagnosis, Study Shows
Tuesday, November 29, 2022
- Machine Learning Model Builds on Imaging Methods to Better Detect Ovarian Lesions
Monday, November 28, 2022
- Machine Learning Gives Nuanced View of Alzheimer's Stages
Thursday, November 17, 2022
- Analysis of MRI Contrast Agents
Thursday, November 10, 2022
- Focused Ultrasound Treatment for Essential Tremor Highly Effective After 5 Years
Thursday, October 27, 2022
- Battery-Free, Light-Powered Pacemaker May Improve Quality of Life for Heart Disease Patients
Wednesday, October 19, 2022
- Novel PET Imaging Agent Detects Earliest Signs of Alzheimer's Disease
Friday, October 7, 2022
- Daylight Hours Impact Opioid Receptor Levels in Brown Fat
- Detecting Alzheimer's Disease from Blood Samples
Thursday, October 6, 2022
- Generative Design Offers Solution to Patient-Specific Knee Implants
- Radiotracer That Detects an Important Contributor to Neurological Diseases Tested for the First Time in Humans
Wednesday, September 21, 2022
- The Super-Fast MRI Scan That Could Revolutionize Heart Failure Diagnosis
Tuesday, September 13, 2022
- AI Helps Detect Pancreatic Cancer
Thursday, September 1, 2022
- Review Suggests 'parent-Centred' Approach to Medical Imaging Can Enhance Emotional Connection to the Unborn Baby During Pregnancy
Tuesday, August 30, 2022
- Researchers Visualize Alpha-Synuclein Pathology in Living Patients With a Neurodegenerative Disorder
- Breast MRI Illuminates Risk of Second Breast Cancer
Wednesday, August 17, 2022
- Smartphone Video Motion Analysis Detected Narrowed Neck Arteries That May Lead to Stroke
Wednesday, August 10, 2022
- PET Scan Visualization Can Measure Effects of STING-Activating Drugs
Thursday, July 28, 2022
- Engineers Develop Stickers That Can See Inside the Body
Friday, July 22, 2022
- Combing Through Brain Imaging Data to Discover Novel Patterns Linked to Mental Health Conditions
Wednesday, July 13, 2022
- Researchers Develop New Agent to Help Root out Hypertension-Causing Tumor
Tuesday, July 5, 2022
- Discovery Could Inspire New Way to Detect Brain Abnormalities
Thursday, June 30, 2022
- Optical Fiber Imaging Method Advances Studies of Alzheimer's Disease
Wednesday, June 15, 2022
- High-Intensity Focused Ultrasound (HIFU) Can Control Prostate Cancer With Fewer Side Effects
Tuesday, June 14, 2022
- Automating Renal Access in Kidney Stone Surgery Using AI-Enabled Surgical Robot
Monday, June 13, 2022
- Researchers Demonstrate Near-Non-Invasive In-Vivo Imaging in Mouse Cortex at an Unprecedented Depth
- Virtual CT Scans Cut Patient Radiation Exposure in Half During PET/CT Studies
Monday, June 6, 2022
- Chemists Design Chemical Probe for Detecting Minute Temperature Shifts in the Body
Thursday, June 2, 2022
- Researchers Take Optical Coherence Tomography to the Next Level
- Biomarker in Liquid Biopsy for Lung Cancer Appears More Accurate in Predicting Immunotherapy Response Than Tumor Biopsy
Wednesday, May 25, 2022
- Scientists Build Subcellular Map of Entire Brain Networks
- AI Can Predict Cancer Risk of Lung Nodules
Thursday, May 19, 2022
- Using Light and Sound to Reveal Rapid Brain Activity in Unprecedented Detail
Wednesday, May 18, 2022
- Study Reveals Imaging Approach With Potential to Detect Lung Cancer Earlier, at the Cellular Level
Thursday, May 5, 2022
- Active Brown Adipose Tissue Protects Against 'pre-Prediabetes'
- How MRI Could Revolutionize Heart Failure Diagnosis
- LATEST NEWS
- Health & Medicine
- Diseases & Conditions
- Alzheimer's Research
- Amyotrophic Lateral Sclerosis
- Attention Deficit Disorder
- Back and Neck Pain
- Birth Defects
- Bladder Disorders
- Blood Clots
- COVID and SARS
- Cervical Cancer
- Bladder Cancer
- Multiple Myeloma
- Pancreatic Cancer
- Brain Tumor
- Colon Cancer
- Breast Cancer
- Ovarian Cancer
- Lung Cancer
- Mesothelioma
- Skin Cancer
- Prostate Cancer
- Cerebral Palsy
- Chikungunya
- Chronic Fatigue Syndrome
- Cold and Flu
- Crohn's Disease
- Cystic Fibrosis
- Dengue Fever
- Down Syndrome
- Eating Disorder Research
- Encephalitis
- Epilepsy Research
- Erectile Dysfunction
- Fibromyalgia
- Gastrointestinal Problems
- HIV and AIDS
- Headache Research
- Hearing Loss
- Heart Health
- Cholesterol
- Stroke Prevention
- Heart Disease
- Hormone Disorders
- Hypertension
- Infectious Diseases
- Insomnia Research
- Irritable Bowel Syndrome
- Kidney Disease
- Liver Disease
- Lung Disease
- Lyme Disease
- Mental Health Research
- Multiple Sclerosis Research
- Mumps, Measles, Rubella
- Muscular Dystrophy
- Osteoporosis
- Parkinson's Research
- Prostate Health
- Restless Leg Syndrome
- Sickle Cell Anemia
- Sleep Disorder Research
- Thyroid Disease
- Triglycerides
- Tuberculosis
- Medical Topics
- Accident and Trauma
- Alternative Medicine
- Birth Control
- Bone and Spine
- Chronic Illness
- Controlled Substances
- Dietary Supplements and Minerals
- Epigenetics
- Food Additives
- Foodborne Illness
- Foot Health
- Gene Therapy
- Health Policy
- Human Biology
- Immune System
- Joint Health
- Medical Imaging
- Nervous System
- Pain Control
- Personalized Medicine
- Pharmacology
- Psychology Research
- Wounds and Healing
- PHYSICAL/TECH
- ENVIRONMENT
- SOCIETY & EDUCATION
- The Case of the Missing Black Holes
- Adjusting Sunglasses for Your Windows
- Novel Gene-Editing Tool Created
- How Hummingbirds Hover With Such Accuracy
- Complete X and Y Chromosomes of Great Apes
- Moonlets Stuck Together Orbit 'Dinky' Asteroid
- Orchids Aid Seedlings Through Fungal Networks
- Precise Maps of the Moon's Surface
- Amazing Expertise of Scent Detection Dogs
- Getting to Grips With a Handy Extra Thumb
Trending Topics
Strange & offbeat.
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Braunwald's Corner
- ESC Guidelines
- EHJ Dialogues
- Issue @ a Glance Podcasts
- CardioPulse
- Weekly Journal Scan
- European Heart Journal Supplements
- Year in Cardiovascular Medicine
- Asia in EHJ
- Most Cited Articles
- ESC Content Collections
- Author Guidelines
- Submission Site
- Why publish with EHJ?
- Open Access Options
- Submit from medRxiv or bioRxiv
- Author Resources
- Self-Archiving Policy
- Read & Publish
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Journals Career Network
- About European Heart Journal
- Editorial Board
- About the European Society of Cardiology
- ESC Publications
- War in Ukraine
- ESC Membership
- ESC Journals App
- Developing Countries Initiative
- Dispatch Dates
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, the expanding role of transcatheter heart valve interventions, innovation in imaging to assist device implantation, evaluation, and guidance, smart biomonitoring devices, patients’ perspectives and patient-reported outcomes, the changing regulatory environment and impact on innovation in europe, acknowledgements, supplementary data, declarations, data availability.
- < Previous
Device innovation in cardiovascular medicine: a report from the European Society of Cardiology Cardiovascular Round Table
- Article contents
- Figures & tables
- Supplementary Data
Stephan Windecker, Martine Gilard, Stephan Achenbach, Alain Cribier, Victoria Delgado, Nataliya Deych, Inga Drossart, Hélène Eltchaninoff, Alan G Fraser, Alexandra Goncalves, Gerhard Hindricks, Richard Holborow, Arie Pieter Kappetein, John Kilmartin, Jana Kurucova, Thomas F Lüscher, Roxana Mehran, Donal B O’Connor, Mark Perkins, Eigil Samset, Ralph Stephan von Bardeleben, Franz Weidinger, Device innovation in cardiovascular medicine: a report from the European Society of Cardiology Cardiovascular Round Table, European Heart Journal , Volume 45, Issue 13, 1 April 2024, Pages 1104–1115, https://doi.org/10.1093/eurheartj/ehae069
- Permissions Icon Permissions
Research performed in Europe has driven cardiovascular device innovation. This includes, but is not limited to, percutaneous coronary intervention, cardiac imaging, transcatheter heart valve implantation, and device therapy of cardiac arrhythmias and heart failure. An important part of future medical progress involves the evolution of medical technology and the ongoing development of artificial intelligence and machine learning. There is a need to foster an environment conducive to medical technology development and validation so that Europe can continue to play a major role in device innovation while providing high standards of safety. This paper summarizes viewpoints on the topic of device innovation in cardiovascular medicine at the European Society of Cardiology Cardiovascular Round Table, a strategic forum for high-level dialogue to discuss issues related to the future of cardiovascular health in Europe. Devices are developed and improved through an iterative process throughout their lifecycle. Early feasibility studies demonstrate proof of concept and help to optimize the design of a device. If successful, this should ideally be followed by randomized clinical trials comparing novel devices vs. accepted standards of care when available and the collection of post-market real-world evidence through registries. Unfortunately, standardized procedures for feasibility studies across various device categories have not yet been implemented in Europe. Cardiovascular imaging can be used to diagnose and characterize patients for interventions to improve procedural results and to monitor devices long term after implantation. Randomized clinical trials often use cardiac imaging-based inclusion criteria, while less frequently trials randomize patients to compare the diagnostic or prognostic value of different modalities. Applications using machine learning are increasingly important, but specific regulatory standards and pathways remain in development in both Europe and the USA. Standards are also needed for smart devices and digital technologies that support device-driven biomonitoring. Changes in device regulation introduced by the European Union aim to improve clinical evidence, transparency, and safety, but they may impact the speed of innovation, access, and availability. Device development programmes including dialogue on unmet needs and advice on study designs must be driven by a community of physicians, trialists, patients, regulators, payers, and industry to ensure that patients have access to innovative care.

European investigators have had a pioneering role in the history of cardiovascular device innovation and will continue to do so. AF, atrial fibrillation; AS, aortic stenosis; BAV, balloon aortic valvuloplasty.
European investigators have played a pioneering role in the history of cardiovascular (CV) device innovation and in advancing minimally invasive procedures in CV medicine, as summarized in Table 1 and Graphical Abstract . 1–7
European innovation in interventional cardiology
AF, atrial fibrillation; AS, aortic stenosis; BAV, balloon aortic valvuloplasty.
There are numerous other notable examples of advances in CV therapies that have improved clinical outcomes and quality of life, including demonstration of the superiority of primary percutaneous coronary intervention (PCI) over thrombolysis for acute ST-segment elevation myocardial infarction (MI); advances in cardiac resynchronization therapy (CRT) and implantable cardioverter defibrillator (ICD); the introduction of catheter ablation techniques for arrhythmias; percutaneous closure of the foramen ovale for prevention of paradoxical embolism; and device closure of the left atrial appendage for stroke prevention. 4 , 6 , 7 These types of interventions have provided evidence-based less invasive alternatives to cardiac surgery, allowing for more rapid recovery 8 and offering complementary strategies to optimized medical therapy that have influenced guidelines. 9 , 10
This paper summarizes viewpoints on the topic of device innovation in CV medicine discussed at a European Society of Cardiology (ESC) Cardiovascular Round Table (CRT), a strategic forum for high-level dialogue related to the future of CV health in Europe. It includes a summary of the discussions of innovative devices that are under investigation or in use in Europe and the influences of the changing regulatory environment. European Society of Cardiology CRT meetings do not develop official ESC policy; rather, they provide a forum for dialogue to better identify and discuss issues related to CV health in Europe. All CRT members that were included as authors actively contributed to the CRT meeting, which was chaired by S.W., M.G., A.P.K., J.K., M.P., and Marta Santiuste. The full agenda, as well as videos of the session, can be viewed online ( https://www.escardio.org/The-ESC/What-we-do/Cardiovascular-Round-Table-(CRT)/Events/device-innovation-in-cardiovascular-medicine ). The speakers were responsible for the views expressed at the meeting and in this manuscript, which do not necessarily represent the views or policies of the ESC or the institution to which the authors are affiliated.
Transcatheter aortic valve implantation (TAVI) provides a blueprint for future technological device development as it exemplifies innovation of a new device, followed by evidence generation and implementation as a new therapy ( Figure 1 ). 8–11 Transcatheter aortic valve implantation and surgical aortic valve interventions have been evaluated for patients across the surgical risk spectrum, with allocation to either therapy typically based on age, clinical status, and anatomical factors rather than estimated surgical risk. More recently, TAVI is being studied in patients with moderate and asymptomatic severe aortic stenosis (AS).

Evolution of transcatheter aortic valve implantation and surgical aortic valve replacement through evidence generation and guidelines. Based on Windecker et al. , 8 Vahanian et al. , 9 Otto et al. , 10 and Pilgrim et al. 11 EACTS, European Society of Cardio-Thoracic Surgery; ESC, European Society of Cardiology; RCT, randomised controlled trial; TAVI, transcatheter aortic valve implantation
Since the initial approval in Europe in 2007, the number of TAVI procedures has increased rapidly in both Europe and the USA. 12 More than 20 years after the first procedure, the use of TAVI continues to increase, with over 1.5 million patients treated in almost 80 countries worldwide as of August 2022. 13 Numbers are predicted to expand by ∼4%–10% per year, driven by the aging population, diagnostic and technical improvements, and interventions in younger patients. Nonetheless, according to a recent ESC heart valve disease survey, under treatment remains an issue for >20% of symptomatic patients with severe AS, who fulfil criteria for Class IA. 14
The advent of TAVI illustrates how innovation accompanied by clinical evidence generation is able to transform clinical practice by providing a safe and effective alternative to a previous gold standard therapy. The time delay between approval in Europe (2007) and the USA (2011) of 4 years is an expression of different regulatory processes applicable at that time and raises the question of the delicate balance between early access to promote innovation and a more cautious approach to market approval. Although the USA was the 42nd country worldwide to approve a TAVI device, it was the first country to approve TAVI for use in low-risk patients illustrating the impact of changes in regulatory pathways. 15
Transcatheter treatment options have also expanded to include the mitral valve. The first device to mimic surgical edge-to-edge repair by transcatheter technique was approved initially for treatment of patients with primary mitral regurgitation 16 and subsequently for secondary mitral regurgitation. Trials are ongoing to assess new generation mitral transcatheter edge-to-edge repair (TEER) devices compared with mitral valve surgery in patient with severe primary mitral regurgitation at low and intermediate surgical risk.
Transcatheter tricuspid valve interventions (TTVIs) are also being performed with increasing frequency. 8 , 9 Several randomized clinical trials (RCTs) are assessing the benefit of TTVI (leaflet coaptation, annuloplasty, and valve replacement) compared with medical therapy. Tricuspid TEER was shown to be safe and effective in reducing tricuspid regurgitation and in improving quality of life but without influencing heart failure (HF) hospitalization and mortality compared with medical treatment in the first RCT reported in 2023. 17
Transcatheter mitral and tricuspid technologies illustrate that the underlying disease and outcomes of interventions are more heterogeneous as compared with AS and continue to evolve in terms of technology as well as outcome assessment.
Imaging overview
In Western countries over the first decade of the 21st century, the use of computed tomography (CT) and magnetic resonance imaging (MRI) covering all body areas increased annually by around 10%. During the second decade, rates stabilized with annual growth of around 1%–5%. 18 , 19 The use of cardiac ultrasound also increased significantly, while the use of nuclear medicine imaging has declined. Current guidelines provide a Class I recommendation for non-invasive imaging techniques as the initial test to diagnose coronary artery disease (CAD), with invasive coronary angiography recommended as an alternative.
Recent technological advances have allowed characterization of coronary plaques, perivascular adipose tissue, and the haemodynamic consequences of coronary stenoses and have been useful to predict the risk of acute coronary events, to evaluate residual risk after implementation of lipid-lowering therapy, and to decide whether a coronary lesion needs revascularization or not. 20 , 21 Photon-counting CT is one of the latest advances to be introduced into clinical practice, providing superior image resolution, reduced radiation exposure, enhanced performance of myocardial perfusion CT, and reduced use of iodinated contrast. 22
Echocardiography remains the imaging technique of first choice in many CV conditions. Advanced methods such as strain imaging are used to detect subclinical disease or to refine the phenotype of CV conditions and suggest specific aetiologies, some of which can be confirmed by cardiac MRI or nuclear imaging (e.g. cardiac amyloidosis). 23 Multimodality imaging is also key in the diagnosis of the severity of heart valve disease, when echocardiography is inconclusive (e.g. assessment of aortic valve calcification with cardiac CT in severe AS). 24 Cardiac MRI has shown incremental diagnostic value in patients with mitral or aortic regurgitation. 25
Imaging contributes to improved procedural results when used in pre-procedural planning and to provide guidance during procedures. Cardiac CT, for example, is key in the selection of the prosthesis size and procedural access in transcatheter aortic, mitral, and tricuspid valve implantation. 26–28
Advanced echocardiographic techniques like strain echocardiography and cardiac MRI can help identify patients at risk of fatal cardiac events, such as CV death or ventricular arrhythmias, and refine the timing for intervention or indicate the need for an implantable cardioverter defibrillator (ICD). 29 Assessing myocardial fibrosis and/or scar by cardiac MRI in patients with ischaemic and non-ischaemic cardiomyopathies can help predict the risk of ventricular arrhythmias and need for ICD. 30 , 31
Imaging also plays an important role in device monitoring. 32 For instance, the durability of aortic bioprostheses is especially important in light of the increasing use of TAVI in younger patients. Cardiac CT to evaluate thrombosis or structural changes after TAVI implantation can help to confirm valve dysfunction. 33 The use of 18 F-sodium fluoride positron emission tomography has been shown to detect structural changes of aortic bioprostheses before overt bioprosthetic dysfunction occurs. 34
In the development of cardiac devices, the use of an appropriate imaging modality to demonstrate the effects of that device or treatment on the specific pathophysiological pathway or the natural course of the disease is crucial. Use of appropriate imaging techniques can reduce the costs of RCTs by reducing the numbers of patients needed or by providing validated surrogate outcomes such as angiographic restenosis for the clinical endpoint target lesion revascularization or left ventricular end-systolic volume index as outcome predictor in patients with ischaemic left ventricular dysfunction. Progress with new devices needs to be accompanied by innovations in imaging.
Fusion imaging combines echocardiography or CT and live fluoroscopy and does not require contrast injections. Fusion imaging can add soft tissue information from CT and echocardiography to aid orientation and determine landing zones during TEER, annuloplasty, and valve replacement.
In patients undergoing left atrial appendage closure, fusion imaging reduced procedural time and the amount of contrast medium used. 35 It has also been used in valve procedures, and work is underway on software to facilitate its use during mitral and tricuspid transcatheter interventions. 27 Figure 2 shows two examples of paravalvular leak closure. Other fusion technology merges fluoroscopy with ultrasound and is being successfully used during transcatheter procedures including mitral TEER, and CT is being combined with echocardiography and fluoroscopy to guide transcatheter tricuspid valve procedures. 27

Two examples of paravalvular leak closure using fusion technology. ( A ) Courtesy of New York University. ( B ) Courtesy of Katholisches Krankenhaus, Erfurt
Catheters are available that enable live 2D and 3D intravascular or intracardiac imaging that, when combined with virtual model rendering, provide 4D information. These systems offer image guidance for a wide range of procedures, including transcatheter mitral and tricuspid valve interventions and left atrial appendage occlusion, and they facilitate procedures in conscious patients.
Artificial intelligence and imaging
The number of artificial intelligence/machine learning (AI/ML)–based medical devices being approved in Europe and the USA has been steadily increasing ( Figure 3 ). 36 As of October 2023, there were 692 U.S. Food and Drug Administration (FDA)-approved AI/ML–enabled devices. 37

Number of approved (USA) and CE-marked (Europe) artificial intelligence/machine learning–based medical devices between 2015 and 2019. Data from Muehlematter et al. 36 The CE-mark year is considered the approval year for devices in Europe. AI/ML, artificial intelligence and machine learning
Machine learning algorithms are already an integral component in many acquisition, reconstruction, analysis, and reporting tools in imaging systems. Artificial intelligence systems can guide accurate acquisition of images using adaptive protocols, automated image acquisition, segmentation, and measurement, and image optimization can streamline the workflow. 38 In reconstruction, they can improve image quality, reduce noise, and improve resolution. 38 , 39 In a study using cardiac MRI scan:rescan data from 110 patients, automated ML analysis was 186 times faster than humans with similar accuracy. 39 There is also the potential for AI to predict outcomes based on imaging results. A deep learning approach using neural networks predicted survival curves from cardiac MRI images and clinical measures in patients with ischaemic heart disease. 40 Moreover, using AI/ML fat attenuation index (FAI) provides incremental prognostic information. 41
Artificial intelligence/machine learning–based medical innovation is growing rapidly, but challenges remain, including standardization of terminology and protocols, responsible data access, and technology and business model innovation. As of 2022, regulatory standards in both Europe and the USA remain in development, with neither jurisdiction having specific pathways for AI/ML–based medical devices (AI/MLMDs). 36 , 42 The FDA has proposed a ‘Predetermined Change Control Plan’ (PCCP) as part of its framework for regulating medical AI/ML, which would outline anticipated modifications and methods to implement changes over the algorithm’s lifecycle. 43 In April 2023, subsequent to the CRT meeting, the FDA posted draft PCCP guidance for public comment.
Smart devices encompass digital technologies that are used for biomonitoring. These devices may support diagnosis and treatment of CV disease, improve access to healthcare, and support self-care. Technologies include implantable devices with remote monitoring, as well as external devices worn for healthcare purposes (i.e. ‘wearables’). 44 The widespread use of smart phones and the development of AI/ML systems have expanded interest in self-assessment in the CV arena. Similar to diabetes, where patients measure glucose levels and self-adjust insulin, such strategies may help reduce the workload of cardiologists, particularly for monitoring chronic conditions such as HF.
A number of highly innovative devices are under investigation. Digital visual technology has the potential to ensure precise patient identification and could help in monitoring patients during follow-up and in self-assessment. For example, technology using the video camera from a smartphone was able to detect the presence of atrial fibrillation with sensitivity and specificity ≥90%. 45
Volatile organic compounds (VOCs) emitted from the human body reflect the metabolic condition of the individual and can be used as diagnostic olfactory biomarkers of diseases. 46 An electronic nose system differentiated patients with MI from those with stable CAD and from healthy individuals with 97% accuracy. 47
Heart failure affects the larynx and breathing and characteristics of speech. 48 In a small study, the status of HF patients was characterized from remote audio recordings using automated speech analysis technology. 49
This section only provides a few examples of the emerging field of biomonitoring technology and smart devices. An exhaustive overview is beyond the scope of this article.
At the centre of invasive CV procedures and device implantation are patients. Percutaneous coronary intervention, TAVI, mitral TEER, CV implantable electronic devices (CIEDs), and other procedures have made it possible for many patients to enjoy an improved quality of life. Innovations in devices allow critically ill patients, unfit to undergo major surgeries, to receive often life-saving treatment, and they generally result in less invasive and/or faster procedures enabling many patients to recover quickly.
Because of these benefits, patients may be willing to adopt a new technology early, despite a lack of long-term data, if it will improve their experience and outcomes. These outcomes may not only include death and hospitalization but also quality of life, relief of symptoms, and sometimes even aspects such as access to transmitted remote monitoring data, which current systems do not provide to patients. Thus, when developing new technologies, it is important to ensure they meet patients’ needs and expectations. Patients’ acceptance of a degree of risk and uncertainty is a key component of the early adoption of new technologies; further, this willingness has the potential to affect the stance of regulatory agencies as it pertains to innovation and expand the role of patient advocacy groups in the evaluation process.
Furthermore, the system and workforce must be ready and trained for the implementation of new technologies. For example, some patients with MRI-compatible CIEDs still face difficulties finding a hospital to do the procedure, despite this technology having been on the market for many years.
Finally, new technologies lead to an increasing number of treatment choices; hence, the decision-making processes are becoming more complex. Therefore, patients need better information around their specific case, and they must be aware of yet unknown risks associated with new devices. Patient involvement and shared decision-making are essential, including presentation of all available options and taking into consideration patients’ individual preferences and goals.
Interventional and device trials have traditionally reported on clinical outcomes, but as device technology improves and events become less common, larger and longer trials are needed to evaluate safety and efficacy. Focusing solely on clinical endpoints also neglects the impact of CV procedures on other patient outcomes like quality of life. 50 While patients consider clinical CV outcomes important, their expected initial benefits of having procedures are usually improvements in symptoms, function, and quality of life. Validated instruments exist to capture patients’ lived experiences, and such patient-reported outcomes need to be afforded greater weight in clinical trials and regulatory decisions. 51 For example, the FDA recognizes substantial and functional improvement as an acceptable endpoint for HF drug or device approval even in the absence of demonstrated effects on mortality or HF hospitalizations.
Regulatory challenges
The goals of the Medical Device Regulation (MDR) in Europe are to ensure a high level of health and safety while supporting innovation and cost-effectiveness. 52 Medical devices are vastly different from medicinal products and range from simple consumer products, such as bandages and dentures, to MRI and CT scanners, and CIED. Globally, there are estimated to be about 500 000 different types of medical devices compared with 20 000 medicinal products. 53 Device development is driven by an iterative process where technological advances of an approved device typically become available within 18–24 months of the previous version. Medicinal products tend to have longer product lifecycles with product development often taking decades prior to clinical use and with the final product remaining largely unchanged once placed on the market. This makes the regulatory process for devices (specifically high-risk devices) very different from that of drugs ( Table 2 ). 54
Comparison of the regulatory evaluation of pharmaceutical products and high-risk medical devices in the EU
Reprinted with permission from Fraser et al. 54
In 2017, the EU Medical Device Directives (MDDs) were replaced by the MDR. The EU Regulation on Medical Devices 2017/745 defines the requirements for approval of general medical devices 52 and 2017/746 defines the requirements for In Vitro Diagnostic Medical Devices (IVDRs). 55 Some of the key elements of the MDR changes are shown in Table 3 . 52 , 55–57
Key elements of Medical Device Regulation changes
From the European Union, 52 European Union, 55 Byrne, 56 and Fraser et al. 57
The MDR came into effect in May 2021, and the transition period was first scheduled to end in May 2023, 58 but there have been challenges including the limited capacity of notified bodies, which need to be redesignated to conduct conformity assessments of devices under the new regulation, increased costs, and delays by some manufacturers in applying. The backlog is extensive; in June 2023, notified bodies reported they had received over 13 000 applications for recertification but had issued fewer than 4000 certificates ( Figure 4 ). 59 However, many of the over 24 000 certificates expiring by May 2024 had not been submitted for recertification. In March 2023, the EU Commission approved an extension of the transition period to December 2027 for high-risk devices and to December 2028 for medium- and lower-risk devices. 60 These extensions were deemed necessary to prevent shortages of many legacy medical devices.

Number of applications received and certificates issued under the Medical Device Regulation according to a survey of Notified Bodies (June 2023). From the European Commission. 59 IVDR, In Vitro Diagnostic Medical Device
Regulatory system for high-risk devices
Figure 5 shows the EU system for the evaluation and approval of new high-risk medical devices. 57 The MDR mandates extensive clinical evaluation, conformity assessments, and stricter criteria for high-risk devices’ equivalence claims. More transparency is required through safety and performance documentation. Selected Class III implantable and active Class IIb devices require scrutiny by expert panels. Post-market clinical follow-up data must be continuously collected to assess the device’s safety throughout its lifecycle. Manufacturers must produce periodic safety update reports available to notified bodies, competent authorities, and to the public. 56 Transparency remains an issue that may be further improved. Although summaries of evidence must be made publicly available [Summaries of Safety and Clinical Performance (SSCP)], they are often extensively redacted to protect company intellectual property. 61

EU system for high-risk medical device evaluation and approval. Reprinted with permission from Fraser et al. 57 DG SANTE, Directorate-General for Health and Food Safety; NB, notified body
While the implementation of the MDR has been difficult, the principles espoused by the ESC are not. Indeed, there are genuine concerns about the lack of an early advice scheme (now being piloted by the European Medicines Agency (EMA) with the expert panels), lack of predictability of interpretation of evidence requirements by each notified body, lack of guidance on a specific device evaluation pathway from early experimental to first-in-human to pivotal studies, lack of distinction between innovative and established device categories, confusion between orphan devices and innovation, insufficient resources, and excessive costs.
The US FDA has a Breakthrough Devices Program designed to speed development, assessment, and approvals of more effective treatments of life-threatening or debilitating conditions. However, in Europe, there is currently no separate regulatory pathway specifically for innovative or disruptive device technology. However, the MDR does allow for scientific advice to be provided by the expert panels. Under the auspices of the EMA, a pilot facility is being launched in 2023 to assist developers of high-risk devices to seek guidance on their clinical development plans with the aim of increasing the reliability and predictability of bringing new devices to market. Innovative devices will be prioritized during this pilot phase. Further regulatory agility may be needed to facilitate a more accelerated pathway for innovative devices serving orphan indications or unmet needs together with enhanced interactive support tailored to the relevant stages of development and assessment, and regulators should work with clinical experts on initiatives in this area.
As early as 2011, the ESC Policy Conference published recommendations including two that suggested special provisions should be made in the new regulation for approval of devices that were genuine innovations or orphan products. 62 Neither was included in the 2017 MDR, but both recommendations are still relevant and now working groups of regulators are considering both options.
One recommendation has been to develop a central regulatory agency, or expansion of the EMA to cover devices. The 2011, the ESC Policy Conference group recommended ‘… a single, coordinated European system to oversee the evaluation and approval of medical devices.’ However, this was not done, and the opportunity for this may have passed. 62 Efforts are ongoing to encourage global regulatory convergence for device regulations, which is encouraged by the International Medical Device Regulators’ Forum and endorsed by the European Commission. 54
Initiatives such as the Coordinating Research and Evidence for Medical Devices (CORE-MD) project have been established to review and develop methods for the clinical evaluation of high-risk medical devices. 54 Although discussed at the CRT meeting, results were published afterwards. For example, a systematic evaluation of published evidence between 2000 and 2021 of seven selected classes of CV devices revealed that only a minority of 308 reports comprised randomized studies (19%) with no single RCT reported prior to CE mark approval. 63 Engagement by ESC and the Biomedical Alliance is supporting current EU regulators’ task forces that are evaluating shortcomings and promoting and supporting development of new policies to address the issues of non-availability of devices, orphan devices, and innovation. The gaps in the MDR may have resulted in part from insufficient engagement and influence from healthcare professionals when the legislation was being drafted. With a view to promoting global regulatory convergence, the consortium includes advisers from other jurisdictions. Their goal is to advise on study designs and data analysis methods to assess the safety and clinical effectiveness of medical devices. The project aims to provide improved regulatory guidance for developers by combining data from registries and other sources. For example, the group met in 2023 and produced expert consensus recommendations on the clinical evaluation of high-risk medical devices for children. 64
Registries are crucial for the post-market monitoring of the long-term safety of devices. However, there is a need for standardized reporting to provide quality evidence that could be used for regulatory purposes or clinical trials. 65 A CORE-MD systematic review of 20 CV registries found that a median of only 33% reported all 33 quality items. 65 The European Unified Registries for Heart Care Evaluation and Randomized Trials (EuroHeart, www.escardio.org/Research/euroheart ) is a Europe-wide programme that supports the development of local registries. EuroHeart has developed common data sets for CV diseases, including interventions such as TAVI and PCI. 66 , 67 Moreover, EuroHeart provides an opportunity to perform registry-based RCTs, which allow for more rapid inclusion of high patient numbers more closely resembling those encountered in clinical practice, and provides an opportunity for ongoing safety surveillance of devices.
Industry perspectives
The medical technology industry supports the goals of the new EU device regulations, including strengthening patient safety, as well as modernizing and building trust in the European regulatory system. However, there are concerns, particularly around the serious backlog of recertifications for existing devices. According to a 2022 survey of medical device manufacturers, fewer than 70 000 of the almost 500 000 devices requiring recertification under MDR had been completed. 68 The estimated time to certification was 13–18 months, which is twice as long as historically required. New devices and Class III devices were more likely to require longer certification times. The most important challenges with recertification have been the lack of predictability, lack of responsiveness, and the non-standardized interpretation of MDR and Medical Device Coordination Group (MDCG) guidance by notified bodies. Of the roughly 500 European medical technology companies, nearly half stated they are deprioritizing the EU market as their first choice for regulatory approval of new devices. Similarly, a survey of 104 company leaders found that 89% planned to prioritize US regulatory approval in the future, with 62% finding the US system predictable compared with only 22% for the EU. 69
In August 2022, the MDCG proposed 19 non-legislative solutions aimed at improving Notified Body capacity and access challenges. 70 In addition, in March 2023, the EU Commission approved extensions of the transition periods for devices as described above. 60
The ESC CRT Meetings bring together physicians, trialists, regulators, and industry to discuss landmark CV innovations, many of which originated in Europe. These treatments have improved the prognosis and quality of life for patients worldwide. Ongoing advances in implantable devices, imaging, smart devices, and AI/ML programmes continue to drive innovation in the field of CV medicine. As interventions become more complex and patients’ conditions become more advanced, device innovation must be driven by a collective effort among physicians, trialists, patients, regulators, and industry. This ensures a comprehensive understanding of patients’ needs, clinical expertise, science, engineering, and oversight, all of which are critical throughout the device development process.
Innovation must continue to flourish, and Europe must play a major role. However, innovation must be balanced against safety, and all stakeholders are committed to the highest standard of safety, yet equally committed to creating an environment conducive to innovation.
Devices evolve continuously throughout their lifecycle, in contrast to pharmaceuticals. Early feasibility studies are critical in promoting device innovation by providing proof of concept and aiding in device design optimization. 71 Such studies play a crucial role in the initial development of devices and are allowed by the FDA. However, Europe lacks a uniform protocol for an all-encompassing, device-specific strategy that encompasses early feasibility studies, RCTs, and real-world post-market registries.
What is imperative in Europe is for lawmakers to provide legislation that enables a structured device trial strategy including early feasibility studies with facilitation of their design while ensuring the necessary safety standards. To achieve this, it is necessary to work together as a community. Dialogue and open advice on unmet needs, the design of the device including the need for ongoing iterations, and the reliable establishment of the clinical development programme from early feasibility studies, to clinical trials, to post-marketing follow-up are all crucial elements including an agile and adaptive regulatory process with inclusion of all stakeholders. Joint efforts and advocacy from scientific societies, patient organizations, and industry are needed to call for more timely and effective legislation that ensures safety standards to be safeguarded while allowing more expeditious regulatory processes preventing critical shortage of devices and timely access to innovation.
This article was generated from discussions during an online Cardiovascular Round Table (CRT) event organized in November 2022 by the European Society of Cardiology (ESC). The ESC CRT is a strategic forum for high-level dialogue between 20 industry companies (pharmaceutical, devices, and diagnostics) and the ESC leadership to identify and discuss key strategic issues for the future of cardiovascular health in Europe. The authors alone are responsible for the views expressed in this manuscript, which do not necessarily represent the views or policies of the institution to which the authors are affiliated. The authors would like to thank Pauline Lavigne and Steven Portelance (unaffiliated, supported by the ESC) for their contributions to writing and editing the manuscript.
Supplementary data are not available at European Heart Journal online.
Disclosure of Interest
S.W.: institutional grants from Abbott, Abiomed, Amgen, AstraZeneca, Bayer, B. Braun, Biotronik, Boehringer Ingelheim, Boston Scientific, Bristol Myers Squibb, Cardinal Health, CardioValve, Cordis Medical, Corflow Therapeutics, CSL Behring, Daiichi Sankyo, Edwards Lifesciences, Farapulse Inc. Fumedica, Guerbet, Idorsia, Inari Medical, InfraRedx, Janssen-Cilag, Johnson & Johnson, MedAlliance, Medicure, Medtronic, Merck Sharp & Dohme, Miracor Medical, Novartis, Novo Nordisk, Organon, OrPha Suisse, Pharming Tech, Pfizer, Polares, Regeneron, sanofi-aventis, Servier, Sinomed, Terumo, Vifor, and V-Wave; advisory board participation for Abbott, Abiomed, Amgen, AstraZeneca, Bayer, Boston Scientific, Biotronik, Bristol Myers Squibb, Edwards Lifesciences, MedAlliance, Medtronic, Novartis, Polares, Recardio, Sinomed, Terumo, and V-Wave (all payments made to institution); and leadership roles with the European Society of Cardiology (vice president) and JACC CV Interventions (associate editor). M.G.: none. S.A.: none. A.C.: payment or honoraria for lectures, presentations, speakers bureaus, or other educational events from Meril Life Sciences; support for meeting attendance and/or travel from Meril Life Sciences; and participation on a data safety monitoring board or advisory board for Cardiawave and Meril Life Sciences. V.D.: consulting fees from Edwards Lifesciences and Novo Nordisk and payment or honoraria for lectures, presentations, speakers’ bureaus, or other educational events from Edwards Lifesciences, Medtronic, Philips, and Novartis. N.D.: stock or stock options from Edwards Lifesciences AG and Medtronic and employment with Edwards Lifesciences AG. I.D.: none. H.E.: institutional research grants (STOP-AS research programme) from Edwards Lifesciences and Medtronic and payment/honoraria and support for meeting attendance and/or travel from Edwards Lifesciences. A.G.F.: grants from the European Union Horizon 2020 programme (project grant 965246) for CORE-MD (Coordinating Research and Evidence for Medical Devices) and a leadership role (chairmanship) on the Regulatory Affairs Committee for the Biomedical Alliance in Europe. A.G.: stock or stock options from Philips Healthcare and employment with Philips Healthcare. GH: none. R.H.: none. A.P.K.: stock or stock options from Medtronic and employment with Medtronic. Jo.K.: stock or stock options from Medtronic and employment with Medtronic. Ja.K.: stock or stock options from Edwards Lifesciences AG and employment with Edwards Lifesciences AG. T.F.L.: educational or research grants from Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Sanofi, and Vifor; consulting fees from Acthera, Novo Nordisk, and Philips; and leadership positions with the European Society of Cardiology (president-elect), the Swiss Heart Foundation (research committee chairman), and the Foundation for CV Research—Zurich Heart House (president). R.M.: institutional research grants from Abbott, Abiomed, Alleviant Medical, Amgen, AM-Pharma, Applied Therapeutics, Arena Pharmaceuticals, AstraZeneca, Biosensors, Biotronik, Boston Scientific, Bristol Myers Squibb, Cardiawave, CeloNova, Chiesi, Concept Medical, CSL Behring, CytoSorbents, Daiichi Sankyo, Element Science, Faraday Pharmaceuticals, Humacyte, Idorsia Pharmaceuticals, I-Laser, Janssen, Magenta Medical, Mediasphere Medical, Medtelligence, Medtronic, Novartis, OrbusNeich, Penumbra, PhaseBio, Philips, Pi-Cardia, PLx Pharma, Protembis, RenalPro, RM Global, Shockwave, Transverse Medical, Vivasure, and ZOLL Medical; consulting fees from AstraZeneca, Novartis, Cine-Med Research, Ionis Pharmaceuticals, Novo Nordisk, Vectura Inc., and WebMD; honoraria from Novartis Pharmaceuticals, Philips Electronics, Biotronik Inc., and Bayer Healthcare Pharmaceuticals; advisory board participation for Humacyte Inc., PhaseBio, Faraday Pharmaceuticals, Medtronic, Philips, and PLx Pharma; participation on a data safety monitoring board for Pi-Cardia; a leadership role with the American Medical Association (JAMA Cardiology, associate editor), American College of Cardiology (BOT Member, SC Member CTR Program), and Society for Cardiovascular Angiography & Interventions (Women in Innovations Committee Member); stock or stock options from Applied Therapeutics, Elixir Medical, Stel, and ControlRad; and faculty membership with the Cardiovascular Research Foundation. D.B.O.: none. M.P.: stock or stock options from GE Healthcare, GE, and Boston Scientific and employment with GE Healthcare. E.S.: US patents (US20220319006A1, US20220319006A1); stock or stock options from GE Healthcare; and employment with GE Healthcare. R.S.v.B.: consulting for Abbott, Medtronic, Jenscare, Edwards Lifesciences, and Neochord; participation on a data safety monitoring board or advisory board for Abbott, Medtronic, Edwards Lifesciences, and Philips; and a leadership or fiduciary role with the Heart Valve Society (unpaid) and SHD Coalition (unpaid). F.W.: participation on a data safety monitoring board or advisory board for Biosensors Europe.
No data were generated or analysed for this manuscript.
All authors declare no funding for their contribution. This report was funded as part of the work of the CRT. The CRT is funded thanks to multisponsorship. Learn more at https://www.escardio.org/The-ESC/What-we-do/Cardiovascular-Round-Table-(CRT) .
Grüntzig A . Transluminal dilatation of coronary-artery stenosis . Lancet 1978 ; 311 : 263 . https://doi.org/10.1016/S0140-6736(78)90500-7
Google Scholar
Sigwart U , Puel J , Mirkovitch V , Joffre F , Kappenberger L . Intravascular stents to prevent occlusion and restenosis after transluminal angioplasty . N Engl J Med 1987 ; 316 : 701 – 6 . https://doi.org/10.1056/NEJM198703193161201
Sigwart U . Non-surgical myocardial reduction for hypertrophic obstructive cardiomyopathy . Lancet 1995 ; 346 : 211 – 4 . https://doi.org/10.1016/S0140-6736(95)91267-3
Haissaguerre M , Jais P , Shah DC , Takahashi A , Hocini M , Quiniou G , et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins . N Engl J Med 1998 ; 339 : 659 – 66 . https://doi.org/10.1056/NEJM199809033391003
Cribier A , Savin T , Saoudi N , Rocha P , Berland J , Letac B . Percutaneous transluminal valvuloplasty of acquired aortic stenosis in elderly patients: an alternative to valve replacement? Lancet 1986 ; 327 : 63 – 7 . https://doi.org/10.1016/S0140-6736(86)90716-6
Cribier A , Eltchaninoff H , Bash A , Borenstein N , Tron C , Bauer F , et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description . Circulation 2002 ; 106 : 3006 – 8 . https://doi.org/10.1161/01.CIR.0000047200.36165.B8
Sondergaard L , De Backer O , Franzen OW , Holme SJ , Ihlemann N , Vejlstrup NG , et al. First-in-human case of transfemoral CardiAQ mitral valve implantation . Circ Cardiovasc Interv 2015 ; 8 : e002135 . https://doi.org/10.1161/CIRCINTERVENTIONS.115.002135
Windecker S , Okuno T , Unbehaun A , Mack M , Kapadia S , Falk V . Which patients with aortic stenosis should be referred to surgery rather than transcatheter aortic valve implantation? Eur Heart J 2022 ; 43 : 2729 – 50 . https://doi.org/10.1093/eurheartj/ehac105
Vahanian A , Beyersdorf F , Praz F , Milojevic M , Baldus S , Bauersachs J , et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease . Eur Heart J 2022 ; 43 : 561 – 632 . https://doi.org/10.1093/eurheartj/ehab395
Otto CM , Nishimura RA , Bonow RO , Carabello BA , Erwin JP 3rd , Gentile F , et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines . Circulation 2021 ; 143 : e72 – 227 . https://doi.org/10.1161/CIR.0000000000000923
Pilgrim T , Siontis GCM , Windecker S . Transcatheter aortic valve implantation: a blueprint for evidence-based evaluation of technological innovation . Eur Heart J 2023 ; 44 : 853 – 5 . https://doi.org/10.1093/eurheartj/ehac635
Carroll JD , Mack MJ , Vemulapalli S , Herrmann HC , Gleason TG , Hanzel G , et al. STS-ACC TVT registry of transcatheter aortic valve replacement . Ann Thorac Surg 2021 ; 111 : 701 – 22 . https://doi.org/10.1016/j.athoracsur.2020.09.002
20 years of TAVR: an interview with Alain Cribier, MD, FACC, FESC . Cardiac Intervent Today 2022 ; 16 : 60 – 6 .
Iung B , Delgado V , Rosenhek R , Price S , Prendergast B , Wendler O , et al. Contemporary presentation and management of valvular heart disease: the EURObservational Research Programme Valvular Heart Disease II Survey . Circulation 2019 ; 140 : 1156 – 69 . https://doi.org/10.1161/CIRCULATIONAHA.119.041080
Wu C , Vasseur B , Maisel W . The march of transcatheter aortic valve replacement therapy—US Food and Drug Administration perspectives on device approval for patients at low surgical risk . JAMA Cardiol 2020 ; 5 : 5 – 6 . https://doi.org/10.1001/jamacardio.2019.4383
Ailawadi G , Lim DS , Mack MJ , Trento A , Kar S , Grayburn PA , et al. One-year outcomes after MitraClip for functional mitral regurgitation . Circulation 2019 ; 139 : 37 – 47 . https://doi.org/10.1161/CIRCULATIONAHA.117.031733
Sorajja P , Whisenant B , Hamid N , Naik H , Makkar R , Tadros P , et al. Transcatheter repair for patients with tricuspid regurgitation . N Engl J Med 2023 ; 388 : 1833 – 42 . https://doi.org/10.1056/NEJMoa2300525
Weir-McCall JR , Williams MC , Shah ASV , Roditi G , Rudd JHF , Newby DE , et al. National trends in coronary artery disease imaging: associations with health care outcomes and costs . JACC Cardiovasc Imaging 2023 ; 16 : 659 – 71 . https://doi.org/10.1016/j.jcmg.2022.10.022
Smith-Bindman R , Kwan ML , Marlow EC , Theis MK , Bolch W , Cheng SY , et al. Trends in use of medical imaging in US health care systems and in Ontario, Canada, 2000–2016 . JAMA 2019 ; 322 : 843 – 56 . https://doi.org/10.1001/jama.2019.11456
Serruys PW , Hara H , Garg S , Kawashima H , Norgaard BL , Dweck MR , et al. Coronary computed tomographic angiography for complete assessment of coronary artery disease: JACC state-of-the-art review . J Am Coll Cardiol 2021 ; 78 : 713 – 36 . https://doi.org/10.1016/j.jacc.2021.06.019
Antoniades C , Antonopoulos AS , Deanfield J . Imaging residual inflammatory cardiovascular risk . Eur Heart J 2020 ; 41 : 748 – 58 . https://doi.org/10.1093/eurheartj/ehz474
Si-Mohamed SA , Boccalini S , Lacombe H , Diaw A , Varasteh M , Rodesch PA , et al. Coronary CT angiography with photon-counting CT: first-in-human results . Radiology 2022 ; 303 : 303 – 13 . https://doi.org/10.1148/radiol.211780
Ioannou A , Patel RK , Razvi Y , Porcari A , Sinagra G , Venneri L , et al. Impact of earlier diagnosis in cardiac ATTR amyloidosis over the course of 20 years . Circulation 2022 ; 146 : 1657 – 70 . https://doi.org/10.1161/CIRCULATIONAHA.122.060852
Baumgartner HC , Hung JC-C , Bermejo J , Chambers JB , Edvardsen T , Goldstein S , et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography . Eur Heart J Cardiovasc Imaging 2017 ; 18 : 254 – 75 . https://doi.org/10.1093/ehjci/jew335
Lancellotti P , Pibarot P , Chambers J , La Canna G , Pepi M , Dulgheru R , et al. Multi-modality imaging assessment of native valvular regurgitation: an EACVI and ESC council of valvular heart disease position paper . Eur Heart J Cardiovasc Imaging 2022 ; 23 : e171 – 232 . https://doi.org/10.1093/ehjci/jeab253
Reid A , Ben Zekry S , Turaga M , Tarazi S , Bax JJ , Wang DD , et al. Neo-LVOT and transcatheter mitral valve replacement: expert recommendations . JACC Cardiovasc Imaging 2021 ; 14 : 854 – 66 . https://doi.org/10.1016/j.jcmg.2020.09.027
Hell MM , Emrich T , Kreidel F , Kreitner KF , Schoepf UJ , Munzel T , et al. Computed tomography imaging needs for novel transcatheter tricuspid valve repair and replacement therapies . Eur Heart J Cardiovasc Imaging 2021 ; 22 : 601 – 10 . https://doi.org/10.1093/ehjci/jeaa308
Blanke P , Weir-McCall JR , Achenbach S , Delgado V , Hausleiter J , Jilaihawi H , et al. Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR): an expert consensus document of the society of cardiovascular computed tomography . JACC Cardiovasc Imaging 2019 ; 12 : 1 – 24 . https://doi.org/10.1016/j.jcmg.2018.12.003
Bing R , Everett RJ , Tuck C , Semple S , Lewis S , Harkess R , et al. Rationale and design of the randomized, controlled early valve replacement guided by biomarkers of left ventricular decompensation in asymptomatic patients with severe aortic stenosis (EVOLVED) trial . Am Heart J 2019 ; 212 : 91 – 100 . https://doi.org/10.1016/j.ahj.2019.02.018
Klem I , Klein M , Khan M , Yang EY , Nabi F , Ivanov A , et al. Relationship of LVEF and myocardial scar to long-term mortality risk and mode of death in patients with nonischemic cardiomyopathy . Circulation 2021 ; 143 : 1343 – 58 . https://doi.org/10.1161/CIRCULATIONAHA.120.048477
Sanchez-Somonte P , Quinto L , Garre P , Zaraket F , Alarcon F , Borras R , et al. Scar channels in cardiac magnetic resonance to predict appropriate therapies in primary prevention . Heart Rhythm 2021 ; 18 : 1336 – 43 . https://doi.org/10.1016/j.hrthm.2021.04.017
Casenghi M , Popolo Rubbio A , Menicanti L , Bedogni F , Testa L . Durability of surgical and transcatheter aortic bioprostheses: a review of the literature . Cardiovasc Revasc Med 2022 ; 42 : 161 – 70 . https://doi.org/10.1016/j.carrev.2022.03.006
Pibarot P , Herrmann HC , Wu C , Hahn RT , Otto CM , Abbas AE , et al. Standardized definitions for bioprosthetic valve dysfunction following aortic or mitral valve replacement: JACC state-of-the-art review . J Am Coll Cardiol 2022 ; 80 : 545 – 61 . https://doi.org/10.1016/j.jacc.2022.06.002
Kwiecinski J , Tzolos E , Cartlidge TRG , Fletcher A , Doris MK , Bing R , et al. Native aortic valve disease progression and bioprosthetic valve degeneration in patients with transcatheter aortic valve implantation . Circulation 2021 ; 144 : 1396 – 408 . https://doi.org/10.1161/CIRCULATIONAHA.121.056891
Ebelt H , Domagala T , Offhaus A , Wiora M , Schwenzky A , Hoyme M , et al. Fusion imaging of x-ray and transesophageal echocardiography improves the procedure of left atrial appendage closure . Cardiovasc Drugs Ther 2020 ; 34 : 781 – 7 . https://doi.org/10.1007/s10557-020-07048-z
Muehlematter UJ , Daniore P , Vokinger KN . Approval of artificial intelligence and machine learning-based medical devices in the USA and Europe (2015–20): a comparative analysis . Lancet Digit Health 2021 ; 3 : e195 – 203 . https://doi.org/10.1016/S2589-7500(20)30292-2
US Food and Drug Administration . Artificial Intelligence and Machine Learning (AI/ML)-Enabled Medical Devices . 2023. https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-aiml-enabled-medical-devices (3 January 2024, date last accessed).
Zhou J , Du M , Chang S , Chen Z . Artificial intelligence in echocardiography: detection, functional evaluation, and disease diagnosis . Cardiovasc Ultrasound 2021 ; 19 : 29 . https://doi.org/10.1186/s12947-021-00261-2
Bhuva AN , Bai W , Lau C , Davies RH , Ye Y , Bulluck H , et al. A multicenter, scan-rescan, human and machine learning CMR study to test generalizability and precision in imaging biomarker analysis . Circ Cardiovasc Imaging 2019 ; 12 : e009214 . https://doi.org/10.1161/CIRCIMAGING.119.009214
Popescu DM , Shade JK , Lai C , Aronis KN , Ouyang D , Moorthy MV , et al. Arrhythmic sudden death survival prediction using deep learning analysis of scarring in the heart . Nat Cardiovasc Res 2022 ; 1 : 334 – 43 . https://doi.org/10.1038/s44161-022-00041-9
Oikonomou EK , Williams MC , Kotanidis CP , Desai MY , Marwan M , Antonopoulos AS , et al. A novel machine learning-derived radiotranscriptomic signature of perivascular fat improves cardiac risk prediction using coronary CT angiography . Eur Heart J 2019 ; 40 : 3529 – 43 . https://doi.org/10.1093/eurheartj/ehz592
Wellnhofer E . Real-world and regulatory perspectives of artificial intelligence in cardiovascular imaging . Front Cardiovasc Med 2022 ; 9 : 890809 . https://doi.org/10.3389/fcvm.2022.890809
US Food and Drug Administration . Artificial Intelligence/Machine Learning (AI/ML)-Based Software as a Medical Device (SaMD) Action Plan . 2021. https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-software-medical-device (3 January 2024, date last accessed).
Leclercq C , Witt H , Hindricks G , Katra RP , Albert D , Belliger A , et al. Wearables, telemedicine, and artificial intelligence in arrhythmias and heart failure: proceedings of the European Society of Cardiology Cardiovascular Round Table . Europace 2022 ; 24 : 1372 – 83 . https://doi.org/10.1093/europace/euac052
Couderc JP , Page A , Lutz M , Tsouri GR , Hall B . Assessment of facial video-based detection of atrial fibrillation across human complexion . Cardiovasc Digit Health J 2022 ; 3 : 305 – 12 . https://doi.org/10.1016/j.cvdhj.2022.08.003
Shirasu M , Touhara K . The scent of disease: volatile organic compounds of the human body related to disease and disorder . J Biochem 2011 ; 150 : 257 – 66 . https://doi.org/10.1093/jb/mvr090
Tozlu B , Simsek C , Aydemir O , Karavelioglu Y . A high performance electronic nose system for the recognition of myocardial infarction and coronary artery diseases . Biomed Signal Process Contol 2021 ; 64 : 102247 . https://doi.org/10.1016/j.bspc.2020.102247
Reddy M , Helkkula P , Keerthana Y , Kaitue K , Minkkinen M , Tolppanen H , et al. The automatic detection of heart failure using speech signals . Comput Speech Lang 2021 ; 69 : 101205 . https://doi.org/10.1016/j.csl.2021.101205
Amir O , Abraham WT , Azzam ZS , Berger G , Anker SD , Pinney SP , et al. Remote speech analysis in the evaluation of hospitalized patients with acute decompensated heart failure . JACC Heart Fail 2022 ; 10 : 41 – 9 . https://doi.org/10.1016/j.jchf.2021.08.008
Garcia-Garcia HM , McFadden EP , Farb A , Mehran R , Stone GW , Spertus J , et al. Standardized end point definitions for coronary intervention trials: the Academic Research Consortium-2 Consensus Document . Circulation 2018 ; 137 : 2635 – 50 . https://doi.org/10.1161/CIRCULATIONAHA.117.029289
Moons P , Norekval TM , Arbelo E , Borregaard B , Casadei B , Cosyns B , et al. Placing patient-reported outcomes at the centre of cardiovascular clinical practice: implications for quality of care and management . Eur Heart J 2023 ; 44 : 3405 – 22 . doi 10.1093/eurheartj/ehad514
European Union . Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on Medical Devices, Amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and Repealing Council Directives 90/385/EEC and 93/42/EEC . 2020. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A52023PC0010 (3 January 2024, date last accessed).
MedTech Europe . Medical Devices and Pharmaceuticals: Two Different Worlds in One Health Setting . 2015. https://www.medtecheurope.org/news-and-events/news/medical-devices-and-pharmaceuticals-two-different-worlds-in-one-health-setting/ (3 January 2024, date last accessed).
Fraser AG , Nelissen R , Kjaersgaard-Andersen P , Szymanski P , Melvin T , Piscoi P , et al. Improved clinical investigation and evaluation of high-risk medical devices: the rationale and objectives of CORE-MD (Coordinating Research and Evidence for Medical Devices) . Eur Heart J Qual Care Clin Outcomes 2022 ; 8 : 249 – 58 . https://doi.org/10.1093/ehjqcco/qcab059
European Union . Regulation (EU) 2017/746 of the European Parliament and of the Council of 5 April 2017 on In Vitro Diagnostic Medical Devices and Repealing Directive 98/79/EC and Commission Decision 2010/227/EU . 2022. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A02017R0746-20220128 (3 January 2024, date last accessed).
Byrne RA . Medical device regulation in Europe—what is changing and how can I become more involved? EuroIntervention 2019 ; 15 : 647 – 9 . https://doi.org/10.4244/EIJV15I8A118
Fraser AG , Byrne RA , Kautzner J , Butchart EG , Szymanski P , Leggeri I , et al. Implementing the new European Regulations on medical devices-clinical responsibilities for evidence-based practice: a report from the Regulatory Affairs Committee of the European Society of Cardiology . Eur Heart J 2020 ; 41 : 2589 – 96 . https://doi.org/10.1093/eurheartj/ehaa382
European Union . Proposal for a Regulation of the European Parliament and of the Council Amending Regulations (EU) 2017/745 and (EU) 2017/746 as Regards the Transitional Provisions for Certain Medical Devices and In Vitro Diagnostic Medical Devices . 2023. https://eur-lex.europa.eu/legal-content/EN/TXT/? uri=celex%3A52023PC0010 (3 January 2024, date last accessed).
European Commission . Notified Bodies Survey on Certifications and Applications. MDCG & Stakeholders . 2023. https://health.ec.europa.eu/system/files/2023-11/md_nb_survey_certifications_applications_en.pdf (3 January 2024, date last accessed).
European Union . Regulation (EU) 2023/607 of the European Parliament And Of The Council of 15 March 2023 Amending Regulations (EU) 2017/745 and (EU) 2017/746 as Regards the Transitional Provisions for Certain Medical Devices and In Vitro Diagnostic Medical Devices . 2023. https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32023R0607 (3 January 2024, date last accessed).
Fraser AG , Butchart EG , Szymanski P , Caiani EG , Crosby S , Kearney P , et al. The need for transparency of clinical evidence for medical devices in Europe . Lancet 2018 ; 392 : 521 – 30 . https://doi.org/10.1016/S0140-6736(18)31270-4
Fraser AG , Daubert JC , Van de Werf F , Estes NA 3rd , Smith SC Jr , Krucoff MW , et al. Clinical evaluation of cardiovascular devices: principles, problems, and proposals for European regulatory reform. Report of a policy conference of the European Society of Cardiology . Eur Heart J 2011 ; 32 : 1673 – 86 . https://doi.org/10.1093/eurheartj/ehr171
Siontis GC , Coles B , Haner JD , McGovern L , Bartkowiak J , Coughlan JJ , et al. Quality and transparency of evidence for implantable cardiovascular medical devices assessed by the CORE-MD consortium . Eur Heart J 2023 ; 45 : 161 – 77 . doi 10.1093/eurheartj/ehad567
Guerlich K , Patro-Golab B , Barnacle A , Baumann U , Eicken A , Fraser AG , et al. European expert recommendations on clinical investigation and evaluation of high-risk medical devices for children . Acta Paediatr 2023 ; 112 : 2440 – 8 . https://doi.org/10.1111/apa.16919
Hoogervorst LA , Geurkink TH , Lübbeke A , Buccheri S , Schoones JW , Torre M , et al. Quality and utility of European cardiovascular and orthopaedic registries for the regulatory evaluation of medical device safety and performance across the implant lifecycle: a systematic review . Int J Health Policy Manage 2023 ; 12 : 7648 – 11 . https://doi.org/10.34172/ijhpm.2023.7648
Batra G , Aktaa S , Wallentin L , Maggioni AP , Wilkinson C , Casadei B , et al. Methodology for the development of international clinical data standards for common cardiovascular conditions: European unified registries for heart care evaluation and randomised trials (EuroHeart) . Eur Heart J Qual Care Clin Outcomes 2023 ; 9 : 161 – 8 . https://doi.org/10.1093/ehjqcco/qcab052
Wallentin L , Gale CP , Maggioni A , Bardinet I , Casadei B . EuroHeart: European unified registries on heart care evaluation and randomized trials . Eur Heart J 2019 ; 40 : 2745 – 9 . https://doi.org/10.1093/eurheartj/ehz599
MedTech Europe . Survey Report Analysing the Availability of Medical Devices in 2022 in Connection to the Medical Device Regulation (MDR) Implementation . 2022. https://www.medtecheurope.org/wp-content/uploads/2022/07/medtech-europe-survey-report-analysing-the-availability-of-medical-devices-in-2022-in-connection-to-the-medical-device-regulation-mdr-implementation.pdf (3 January 2024, date last accessed).
Johnson C , McCaney J , Ulmer K , Eichelberger M , Lawyer P , Trommer G , et al. Interstates and Autobahns: Global Medtech Innovation and Regulation in the Digital Age . 2022. https://web-assets.bcg.com/8c/f0/06744e8848ea9654bbd0765bf285/bcg-interstates-and-autobahns-mar-2022.pdf (3 January 2024, date last accessed).
Medical Device Coordination Group . MDCG 2022–14: Transition to the MDR and IVDR-Notified Body Capacity and Availability of Medical Devices and IVDs . 2022. https://health.ec.europa.eu/latest-updates/mdcg-2022-14-transition-mdr-and-ivdr-notified-body-capacity-and-availability-medical-devices-and-2022-08-26_en (January 2024, date last accessed).
Callea G , Federici C , Freddi R , Tarricone R . Recommendations for the design and implementation of an Early Feasibility Studies program for medical devices in the European Union . Expert Rev Med Devices 2022 ; 19 : 315 – 25 . https://doi.org/10.1080/17434440.2022.2075729
- artificial intelligence
- cardiovascular system
- diagnostic imaging
- medical devices
- european society of cardiology

Email alerts
More on this topic, related articles in pubmed, citing articles via, looking for your next opportunity, affiliations.
- Online ISSN 1522-9645
- Print ISSN 0195-668X
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Public Health
Medical Device Development Process, and Associated Risks and Legislative Aspects-Systematic Review
Petra marešová.
1 Faculty of Informatics and Management, University of Hradec Kralove, Hradec Kralove, Czechia
Blanka Klímová
2 Biomedical Research Centrum, University Hospital Hradec Kralove, Hradec Kralove, Czechia
Kamil Kuča
Wan nur hidayah ibrahim.
3 Faculty of Computing, Universiti Teknologi Malaysia & Media and Game Innovation Centre of Excellence (MaGICX), Universiti Teknologi Malaysia, Kuala Lumpur, Malaysia
Ali Selamat
Objective: Medical device development, from the product's conception to release to market, is very complex and relies significantly on the application of exact processes. This paper aims to provide an analysis and summary of current research in the field of medical device development methodologies, discuss its phases, and evaluate the associated legislative and risk aspects.
Methods: The literature search was conducted to detect peer-reviewed studies in Scopus, Web of Science, and Science Direct, on content published between 2007 and November 2019. Based on exclusion and inclusion criteria, 13 papers were included in the first session and 11 were included in the second session. Thus, a total of 24 papers were analyzed. Most of the publications originated in the United States (7 out of 24).
Results: The medical device development process comprises one to seven stages. Six studies also contain a model of the medical device development process for all stages or for just some of the stages. These studies specifically describe the concept stage during which all uncertainties, such as the clinical need definition, customer requirements/needs, finances, reimbursement strategy, team selection, and legal aspects, must be considered.
Conclusion: The crucial factor in healthcare safety is the stability of factors over a long production time. Good manufacturing practices cannot be tested on individual batches of products; they must be inherently built into the manufacturing process. The key issues that must be addressed in the future are the consistency in the classification of devices throughout the EU and globally, and the transparency of approval processes.
Introduction
Each year, a considerable amount of medical technologies are developed ( 1 ), and billions of crowns are invested in their development to meet the increasing demand for medical technology innovation (MDI). Research shows that extensive implementation of healthcare services worldwide is heavily dependent on medical technologies. According to the healthcare use statistics provided by Organization for Economic Co-operation and Development (OECD) ( 2 ), numbers of medical technologies are constantly rising. As a result, more healthcare technology needs to be developed ( 3 ). Innovative processes in the pharmaceutical industry appear every 10–20 years, while medical technology becomes outdated within months. Thus, new medical device development processes, which meet the needs of contemporary drug treatments, are currently being investigated and developed.
Nevertheless, there are only a few technologies and resources that penetrate the market. Medical device development (MDD) is expensive and risky. High risk of technology failure in the market leads to the question: Would it be appropriate to create a process or guide to assess healthcare technology at the beginning of the development process so that the development process and future impacts can be addressed on time? ( 4 ).
Currently, around 88% of corporations that develop medical device technologies are not able to provide considerable returns for their investors ( 5 ). Companies mainly concentrate on regulatory approval targets, without careful scheduling that considers establishing a less costly and more sustainable process ( 6 ). Therefore, well-prepared and well-thought launch strategies that capture inefficiencies in a timely manner and lower total costs are crucial in ensuring a successful product development process and satisfying stakeholder requirements.
Product development, from conception to release to market, is a very complex process ( 7 , 8 ). It significantly relies on the application of exact processes that enable developers to optimally stage development, testing, validation, verification, and market release ( 9 ).
Current MDD processes have to respond to several process challenges ( 10 , 11 ); projects seldom advance as scheduled, and often modifications are introduced during the course of project development and implementation ( 12 ). These processes do not respect the current legislative changes that are taking place at the European Union (EU) level. Risk analysis is mostly separately addressed, with respect to specific phases of MDD.
The MDD process has been satisfactorily described in literature; however, there is a lack of comprehensive models that would support design teams with different experiences and backgrounds. In general, published studies in this area either address the MDD with a specific focus on regulations ( 9 , 13 , 14 ) or provide proposals for various approaches to MDD ( 9 , 15 , 16 ).
This paper provides an analysis and summary of current research in the field of MDD methodologies, discusses the phases of MDD, and evaluates associated legislative and risk aspects.
Research Strategy
The systematic review is based on PRISMA guidelines ( 17 , 18 ). The databases searched (by authors P.M. and W.N.) included Scopus (2007–2019) and Web of Science (2007–2019). In addition, legislative documents on the Research Topic, as well as the websites of medical companies dealing with the phases of MDD were explored. Keywords included the following collocations: “ medical device AND process AND development ” in Web of Knowledge and Scopus. Few more studies were found searching with the more specific keyword groups “ medical device AND process AND development AND investment evaluation ” and “ medical device AND stage development .” A Boolean operator procedure was used in the search. The database was searched from 1 October 2019 until 20 November 2019.
Research Questions
To achieve the objective of this review, the main research questions (RQ) were derived as follows:
- RQ1 What are the phases of the MDD process?
- RQ2 What are the regulation needs related to MDD?
- RQ3 What are the risk factors in MDD?
- RQ4 With which phases of the MDD process are regulation needs and risk factors associated?
Article Selection and Data Collection
The article selection process was divided into two sessions, and combined with an analysis, as shown in Figure 1 . In the first session, we searched for publications between 2007 and 2017, and in the second session, we searched for articles published between 2017 and 2019.

Illustration of search strategy.
The First Session
From the database/journal searches, 1,112 titles/abstracts were retrieved. The titles and abstracts of identified studies were checked by the lead author (J.K.) for relevance. Subsequently, the search was performed again, and it focused on the occurrence of at least one keyword in the title or abstract to significantly narrow down the selection. It provided the authors with a relevant entry-level file base. A total of 82 studies were found. The search procedure is illustrated below. As the search findings in:
Table 1 shows, most of the studies ( 19 ) were generated by the keyword string “medical device AND process AND development” in Web of Knowledge and Scopus. A few more studies were found by searching for a more specific keyword group: “medical device AND process AND development AND investment evaluation,” as well as by the search string “medical device AND stage development.”
An overview of distribution of publications found in the first session.
In cases of uncertainty, the full text of studies were checked for relevance. After removing duplicates and the titles/abstracts that were unrelated to the stages of the development process, we detected 38 peer-reviewed studies written in English. We included original articles and reviews. Of these, only 31 articles were relevant to the MDD process. These studies were investigated in full by BK and PM, with guidance from PM. Four more studies were detected from the references of the retrieved studies; thus, 35 articles were considered against our study's inclusion and exclusion criteria. On the basis of the criteria, 13 studies were included in the final analysis.
The Second Session
For articles published between 2017 and 2019, the search started with potential keywords based on the trends of the publication ( Table 2 ). Two keywords were used as the main keywords that best corresponded to the objective of this research. Then, the details and abstract of the publication were extracted, and we agreed to narrow down the selection to articles from the database. Only articles that had the string “medical device development” in their title or abstracts were selected. A total of 28 papers were detected to fulfill the criteria. Thereafter, we performed manual full-text analyses, leaving 12 papers after the inclusion and exclusion criteria check. These 12 papers were combined with the 13 papers that we extracted from the first session. The whole process for the first and second sessions is illustrated in Figure 1 .
An overview of publication distributions for the second session.
A combination of reviews and original studies were analyzed. Studies were selected on the basis of the following inclusion criteria:
- I1 The publication date of the article is between 2007 and 2017.
- I2 Reviewed full-text studies in scientific journals in English.
- I3 The aim of the research is to suggest MDD processes.
- I4 The study results proposed MDD processes or specifications associated with existing referenced phases of MDD.
- I5 The study aimed to provide an overview of existing approaches in relation to risks and valid legislation.
The studies with the following attributes were gradually excluded from the analysis:
- E1 The article was not written in English.
- E2 The article did not mention the main string (“medical device development”) in its title or abstract.
- E3 The article did not concern the research topic. For example,
- Cosgrove et al. ( 20 ) focused on a framework of key performance indicators to identify reductions in energy consumption in a medical device production facility;
- Songkajorn and Thawesaengskulthai ( 3 ) concentrated on one specific country and the development of medical devices according to the country's legislation;
- Cho and Kim ( 21 ) and Shaw ( 22 ) aimed at risk analysis;
- Songkajorn and Thawesaengskulthai ( 3 ) included incomplete data about the stages of MDD;
- Vaezi et al. ( 23 ) focused on the exploration of medical manufacturers' beliefs
- attitudes toward user involvement in the medical device design and development ( 24 );
- Bruse et al. ( 25 ) focused on data analysis of image processing that will assist clinicians in decision making during MDD;
- Ciubuc et al. ( 26 ) focused on theoretical and experimental approaches to the detection of dopamine.
- The article described the development of healthcare software [e.g., ( 27 , 28 )].
E4 The distribution of publications based on their origin is shown in Table 3 .
The distribution of the publication based on origin.
Text Analysis
During the review process, text analyses were performed to assist the reviewer's decision. We used VOSviewer software to extract the relation between the co-occurrence of keywords before we decided on the keywords to be used in our search. Figures 2 , ,3 3 show the mapping of keyword co-occurrence for keywords A and B for the analysis of the second session (publications, 2017–2019).

Keyword cluster for the second session; keyword A.

Keyword cluster for the second session; keyword B.
Keyword Clusters
Figure 4 shows the mapping of terms that co-occurred in the title and abstract during Step 5 of both sessions. A total of 61 non-duplicate publications were retrieved (35 from the first session and 28 from the second).

Title/abstract text-mapping in Step 5 (search strategy procedure).
In the abovementioned figures, one can observe the areas that are solved in the publications. After excluding the topics and areas that are directly related to the technical solutions of MDD (e.g., represented by biomaterial, diagnosis, therapy, computational fluid dynamics), two main areas of study remained: regulatory/legislative aspects and risk/risk management. These two areas are further specified as they are related to the stages of MDD.
We detected a total of 13 research studies on the topic. Five of them originated in the United States, four in the United Kingdom, one in Canada, one in Thailand, and one in Portugal. One study was of multiple origin, i.e., USA, Canada, and Denmark. According to these studies, the MDD process comprises one to seven stages. Six studies ( 3 , 9 , 29 – 32 ) also contained a model of the MDD process for all stages or just some of the stages. The findings of the selected studies, especially the stages of the development of new medical devices, and presence or absence of relevant legislative aspects and risks, are summarized in Table 4 below. The columns are ordered according to the alphabetical name of the first author of the selected study. To minimize bias or systematic error, every time we combined the published paper, the duplication check is performed automatically using JaBref's software and manually based on author, title, and DOI. Other than that, each author also plays a role in checking either the classification of term or the content of each table, interpreting the real content published. Other than that, we are analyzing all the published articles and explain the process step-by-step in this article.
Stages of MDD, an overview of the findings from the selected research studies.
The findings in Table 4 show that there is no agreement on the number of stages required for the development of medical devices. The number of product life cycle stages usually ranges from four to six. The study by Ocampo and Kaminski ( 42 ) suggests three stages—pre-development, development, and post-development (the PDP model). The specific medical device development is written in Table 4 . Some studies, such as that of Girling et al. ( 30 ), Hede et al. ( 34 ), and Johnson and Moultrie ( 35 ), focus only on one stage of the MDD process, especially the concept stage during which all uncertainties such as the clinical need definition, customer requirements and needs, finances, reimbursement strategy, team selection, or legal aspects must be considered. The most representative studies are that of Medina et al. ( 31 ) and Pietzsch et al. ( 9 ), which include all key phases of the MDD life cycle, as well as legal aspects and risk factors; other studies are less detailed, and their model often lacks case studies [e.g., ( 32 )]. Although Privitera et al. ( 38 ) reviews 18 medical devices as case studies and the reviews include legislative and risk analysis aspects, the research focuses only on the design stage of the MDD process. This is also true for the study by Panescu ( 37 ), whose descriptions of individual stages are very generic. He does not formulate a way to implement individual activities but only lists the activities and the order in which they should be performed. Moreover, the stages are not connected to specific legislative conditions or the type of medical device according to its level of risk.
According to Pietzsch et al. ( 9 ), the comprehensive MDD life cycle comprises five phases. Before the commencement of Phase 1, a clinical needs analysis must be conducted. Sometimes, this phase is referred to as Phase 0. Furthermore, preliminary market analysis must be conducted to check whether there is a satisfactory market opportunity for this clinical need and whether the new product is compatible with the company's strategy and ability to successfully commercialize this product. This phase is followed by Phase 1, with several important steps. These include a financial review and market analysis or competitive assessment that focuses on needs assessment and validation, demographics analysis, and SWOT analysis. These are followed by the legal intellectual property (IP) analysis and the regulatory review. The final step is to develop a business plan. In Phase 2, a cross-functional team is formed to formulate the concept, evaluate feasibility, and develop a design plan. Models and prototypes are made, and an initial design for manufacturing is developed. In addition, regulatory and reimbursement strategies from Phase 1 are further specified in this phase to comply with new requirements. In Phase 3, verification and validation tests are conducted to ensure that the quality of the device meets set standards and customer needs. In addition, regulatory and reimbursement activities continue in this phase. In Phase 4, formal design prints are made, and preparations are commenced for a medical device launch. The key step in this phase in the United States is the receipt of regulatory approval/clearance from the FDA. Phase 5 includes the product launch and post-market monitoring. If the device appears to succeed, it is distributed for widespread clinical use. Post-market activities involve post-market monitoring, quality audits, clinical validation, and the constant improvement of products and processes. Medina et al.'s ( 31 ) MDD stages resemble those of Pietzsch et al. ( 9 ). However, in comparison with Pietzsch et al.'s, they form the cross-functional team earlier on in Phase 1, while product launch preparation is a part of Phase 5.
Generally, the abovementioned linear stage-gate processes of the chosen authors have been used for almost three decades and been pivotal contributions for the medical device industry ( 49 ), because they are both conceptual and functional. Furthermore, they acknowledge that MDI is a manageable process ( 49 ).
Nevertheless, for the general model to be at least partially usable as a best practice, it must be updated to link to valid legislation, related risks, and valid changes in the management system of individual activities related to the audit trends and development of modern technologies, which affect most business activities.
The findings of the selected studies on the Research Topic show that the comprehensive MDD life cycle comprises five phases: opportunity and risk analysis phase, concept and feasibility phase, verification and validation phase, product launch preparation phase, and product launch and post-launch assessment phase. These individual MDD phases are linear and separated by gates that are characterized by certain set criteria that must be met before MDD can proceed further. That is why the whole MDD process is also called a linear stage-gate process, which is the most commonly used process in the development and innovation of medical devices.
However, Goldenberg and Gravagna ( 6 ) identified several gaps in the traditional stage-gate product development process. They point out that the stage-gate approach is linear, without a full life cycle plan and that companies, especially smaller ones, mainly focus on regulatory approval milestones than on providing significant returns to potential stakeholders. They suggest implementing an integrated customer engagement roadmap approach that identifies all stakeholder requirements/needs and device-specific marketing messages for product differentiation. Furthermore, detailed information on budget, timeline for data studies, and communications and marketing is included. Overall, a global launch strategy is implemented.
In addition, Cooper and Sommer ( 33 ) proposed the hybrid “agile-stage-gate” approach, which can be integrated into the traditional stage-gate model for the following benefits:
- It is built on customer needs in a cost-effective way.
- It reacts quickly to needs.
- It copes with uncertainty and ambiguity that are typical of innovative developments.
- It deals with resourcing issues more directly.
Furthermore, the sources of risks that can threaten the whole MDD process, in terms of price, timing, and quality, should be carefully considered to avoid failure. The key issue is meeting user needs. As far as the legislation aspects are concerned, the key issues are consistency in the classification of devices in the EU countries, as well as the transparency of the approval process worldwide.
Risk Aspects
Individual MDD phases are closely connected with risks ( 50 – 54 ) that the individual steps bring about. For example, developing a new medical device is quite costly and risky ( 36 ); its success significantly relies on the application of accurate processes ( 9 ). Product designers and developers attempt to reduce these risks; however, tough competition encourages them to investigate the sources of risks during the MDD process, which can threaten the MDD process in terms of price, timing, and quality ( 38 , 41 ). Aguwa et al. ( 55 ) reported that medical technology is quite unsuccessful (90%) during the first prototype test, which should be carefully considered by any MDD company. Some researchers have evaluated risks in medical device design. Privitera et al. ( 38 ) indicated the integration of human factors as one of the methods to reduce risks during the design stage of the MDD process; however, challenges exist because of the implementation of standards. These challenges can be solved if both parties, medical device developers and users, cooperate. Schmuland et al. ( 56 ) provided practical ideas to allow medical device manufacturers to evaluate residual risk of their devices. Risk analysis (ISO 14971) and failure analysis (FMEA) were combined by Chan et al. ( 57 ) to ensure device quality in the design phase of the MDD process, with a case study of a ventilation breathing circuit. Rane and Kirkire ( 41 ) summarized the key risks into three main groups: user-related sources of risks, internal sources of risks, and third party-related sources of risks. User-related risks include poor translation of user requirements or unmet user needs/requirements. Internal risks are due to the lack of application of adequate standards to check device performance; poor consideration of the effect of labeling and packaging; or poor communication among device developers, end users, and marketing. Third party-related sources of risks may include lack of training for end users; improper or poor assessment of progress by reviewers; and poor planning for regulatory and clinical approvals and tests. Their findings indicate that the most important source of risks is unmet user needs, which means that user needs should be met to successfully market any device.
The detection of risks and their sources in the MDD process plays a significant role, because it can prevent a lot of adverse effects of the use of medical devices by end users, save a lot of time on design and development of the medical device, and reduce costs during the MDD process. Therefore, the MDD process should be critically planned and modeled to decrease the number of risks and their severity.
Legislative Aspects
Global harmonization in the field of medical device regulation is following the pathway set by the pharmaceutical industry at the turn of the 1980s ( 58 ). In 1989, regulatory bodies of the United States, EU, and Japan came to the conclusion that it would be more effective for the industry to develop universal standards for all aspects of drug development, manufacturing, and pharmacovigilance, with the aim to bring more safety to the process of drug manufacturing ( Table 5 ).
The regulation in the European Union and in the United States of America.
Therefore, the International Council 1 for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH) was founded. Since then, almost all important pharmaceutical markets have closely similar legislation that stems from ICH guidelines. ICH plays a crucial role in adopting novel policies for the safety of pharmaceuticals.
The Global Harmonization Task Force (GHTF), founded in 1992, was replaced in 2011 by the International Medical Device Regulators Forum (IMDRF). In an ever-changing global market, focus on harmonization is needed to achieve the desired level of safety of medical devices. During the 1980s, almost no regulation of medical devices existed. Since the 1990s, some regulations have emerged mainly in the United States and the EU, as well as in the East Asia region, mainly in Japan and Taiwan. Since the beginning of the new millennium, one can observe convergence in the regulation of the medical devices industry owing to the work of the GHTF. However, a global world needs global approaches. That is why the IMDRF came to life. The two largest markets for medical devices are Europe and North America. Regulatory requirements converge on both sides of the Atlantic; yet, American rules had been stricter compared to European rules—until the recent approval of the new medical devices regulation (MDR) by the European Parliament. The rules concerning medical devices had been much more relaxed in the EU; however, after the large-scale scandal involving Poly Implant Prothèse (PIP)-manufactured breast implants, the European Union embarked on the path leading to the approval of the MDR. As thorough as it is, it is still inferior to Title 21, Part 812 and 820 of the Code of Federal Regulations set by the United States, also referred to as current good manufacturing practices (cGMP).
In the EU, the key role is versed on the so-called “accredited notified bodies” that are privately held for-profit companies. Their nature poses a great risk for the whole system. Since there is only a limited number of such bodies (gradually decreasing), and because of the mandatory re-evaluation of all medical devices approved in the EU common market, there will be shortages of available capacity for re-evaluation. Simultaneously, notified bodies would probably be less willing to inspect small companies, which make only a few types of medical devices and tend to be generally less prepared for the transition to novel regulations, because it will be much profitable to inspect large companies with diverse portfolios and better prepared paperwork.
Another limiting factor is the relatively large number of such bodies compared to the situation in the United States where all inspectors are employees of the Food and Drug Administration (FDA), and partially the Center for Devices and Radiological Health (CDRH). It seems plausible that there could be significant differences between the level of scrutiny among bodies based in distant parts of the EU. As such, the key factor of proposed regulation could be endangered by this flaw. Another issue that is addressed by the MDR is post-marketing vigilance of medical devices. The novel regulations impose the duty of post-marketing follow-up for all devices marketed in the EU.
Since the beginning of the PIP breast implant scandals, there has been a steady shift in the perception of how to achieve this goal within the industry. Before the MDR came into effect, the focus had been more on the safety of individual products. Thus, almost all effort was put to releasing the product by obtaining the CE mark. However, as a lesson learned from the pharmaceutical industry, safety should be achieved primarily by setting up a rigorous framework of rules for the whole product life cycle. A quick overview of the regulations in the EU and the United States could be seen in Table 5 . The EU and the United States were chosen because other states are modeling regulations after theirs. For further information on the topic, readers are kindly referred to the reviews by Gupta and Thomke ( 10 ) and Ocampo and Kaminski ( 42 ), which discuss the global regulation aspects of medical devices.
In Japan, as stated in Niimi ( 40 ), the risks are divided into four classes: Class I, Class II, Class III, and Class IV, where the highest risk is in Class III and Class IV, which are for highly controlled medical devices and need the approval from the minister and a review by the Pharmaceutical and Medical Devices Agency (PMDA).
Regarding the phases involved in MDD, and the related regulations and risk factors, the results indicate that the general model applied in the MDD process should follow the well-established linear stage-gate process, which is conceptual and manageable from the perspective of innovation. Nevertheless, the model should include recently suggested approaches such as implementing an integrated customer engagement roadmap. In addition, the model must respond to current valid legislation processes, their changes, and related risks, as well as to the valid changes in the management system of individual activities related to the audit trends and development of modern technologies, which affect most business activities. The crucial factor in healthcare safety ( 59 , 60 ) is the stability of factors over a long production time. Good manufacturing practices cannot be tested on individual batches of products; they must be inherently built into the manufacturing process. This is the goal that medical device regulations and cGMP are trying to achieve. The key issues that must be addressed in the future are consistency in the classification of devices throughout the EU and globally, and the transparency of the approval processes.
Strengths and Limitations of this Study
- This review presents in-depth specifications of the stages of the medical device development process and the associated risks, which are not described in organizational or managerial research. It provides a general point of view as opposed to large numbers of case studies.
- Research findings are strategically important for healthcare development, because they clearly state the requirements for medical device development and offer a way for researchers to apply this specific process in general managerial research.
- This study is limited in the sense that it cannot cover all consequences of changes in legislative aspects.
Author Contributions
PM and KK suggested the design of the study. WI wrote the methodology. WI and PM searched the databases. PM, AS, BK, JH, and KK prepared the tables, wrote the manuscript, and reviewed the paper. All authors approved this version of the paper.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The handling editor declared a past co-authorship with the author KK.
Abbreviations
1 Between 1990 and 2015, it was known as the International Conference on Harmonization.
Funding. This study was supported by the research project The Czech Science Foundation (GACR) 2017 No. 17-03037S Investment evaluation of medical device development run at the Faculty of Informatics and Management, University of Hradec Kralove, Czech Republic.
Tell Your Story.
- See us on facebook
- See us on twitter
- See us on linkedin
- See us on instagram
- See us on youtube
Biotechnology/Medical Devices: Research
Biotechnology Research | Medical Device Research | Desired Skills
Many non-academic (“industry”) research career options exist within the fields of drug development and medical-device development. Careers within the biotechnology and medical device fields are expected to grow faster than average. The challenge to these industries lies in strict regulatory requirements and the funding to bring new products to market.
Biotechnology Research
Discovery research, perhaps the most direct route from academic training into industrial research/biotechnology, offers career tracks throughout research and management. Unlike government research, which serves to drive policy, industry research is motivated by enterprise to develop useful products for the marketplace or to create entirely new markets based on an innovative technology.
Building on basic science, biotechnology companies use applied research to develop and commercialize cutting-edge products and technologies. Within therapeutic biotechnology, product development moves from discovery research to preclinical studies, into clinical development and regulatory affairs, and finally on to commercial operations (marketing, sales, and technical support). The process from conception to production can be a lengthy one, and legal and regulatory pressures, along with the public’s perception of emerging technologies, can influence the development and marketability of products and services.
Product development of instruments, reagents, diagnostics and platform technologies in nontherapeutic biotechnology is often a faster and less expensive process, as clinical trials are not required. The motivation behind product innovation is driven by market research, the expansion of an existing product line, or extant technical gaps. Components of the nontherapeutic development process include research/product development; manufacturing; and marketing, sales, and technical support. Industry research is largely collaborative, and project leaders often manage the process to completion.
Medical Device Research
The closely related and broad field of medical devices includes the development of healthcare products and procedures that diagnose, treat, cure, or prevent disease by means other than or in addition to pharmaceuticals or biologics. This field is an exciting place for researchers and biomedical engineers interested in bridging knowledge from many technical sources, as they conduct research or develop new medical products and procedures.
Product development within the medical device field begins with engineering and product design, undergoes clinical development/trials and regulatory affairs, and moves to sales and marketing.
In addition to scientific skills and training, it may be helpful to have an understanding of regulatory issues, safety standards, and project management. Medical device researchers may work in a single setting or in multiple diverse settings, including hospitals, laboratories, manufacturing, and business.
Desired Skills for Biotechnology and Medical Device Research
- Content: Familiarity with the diseases targeted and techniques used within the biotech/medical device organization. While general scientific skill sets are important, you may need to “market” these toward each organization’s needs.
- Analytical: The ability to analyze the needs of patients and customers, and to design appropriate experiments and solutions.
- Communication: Listening to and seeking out others’ ideas, and incorporating them into the problem-solving process. Expressing oneself clearly.
- Team Player: Contributing individual skill sets to come up with a proposed solution or plan of action.
Register for Upcoming Events
Click event titles for details & registration links. Click here for the full calendar .
Alumni in Biotechnology/ Medical Devices: Research
Suraj pradhan, neuroscience phd, mace cheng, genetics phd, julie granka, biology phd.
Biomedical Research
Research with device products.
Research involving the use of devices is complex and varied. Some protocols use marketed devices that are not generally considered to be medical devices, such as a Fitbit or virtual reality. Some devices are simply used to collect research data. On the other end of the spectrum, a device may be implanted into a participant. Some device use involves the return of results to participants (e.g., lab tests, MRIs, ECGs, etc.) while other device uses do not. Additionally, an algorithm, software or even artificial intelligence may be considered a device on a protocol, contingent upon its impact on prospective participants.

What is a Device?
A device might be an instrument, apparatus, implement, machine, contrivance, implant, in-vitro diagnostic, lab developed test, in vitro reagent, assay, software application, algorithm, or other similar or related article or component, part, or accessory.
Considerations for Research with Devices
Research with devices.
When evaluating a protocol, the IRB considers the following seven questions. Click here for a visual representation .
- What type of device is being used? (i.e., assay, MRI, software, etc.)
- How is the device used on the submitted protocol?
- Is it being used according to the definition of a medical device?
- If used as a medical device, is it the subject of the investigation?
- Is the device marketed? If yes, is it being used on label or being used in an investigational manner?
- Is the protocol subject to IDE regulations (requires an IDE) or is it exempt from IDE regulations (does not require an IDE)?
- If the protocol is subject to IDE regulations, what is the risk of the device, as used on the protocol? Device risk determinations are made on a protocol basis, not a device basis.
FDA Definition of a Medical Device
A medical device is:
- Recognized in the official National Formulary of the United States Pharmacopoeia ; OR
- Intended for use in the diagnosis, cure, mitigation, treatment or prevention of disease or other conditions; OR
- Intended to affect the structure or function of the body AND
- Does not achieve its primary intended purposes through chemical action within or on the body AND is not dependent upon being metabolized for the achievement of any of its primary intended purposes.
Exemption from IDE Regulations Guidance
An application to use a device in a study in order to collect safety or effectiveness data is called an investigational device exemption (IDE). The FDA regulations detailing these requirements also detail certain categories of research that do not require an IDE (i.e., exempt from IDE regulations). Click below for detailed guidance on the applicability of IDE regulations entitled, Exemption from IDE Regulations Guidance.
Requesting an Exemption from IDE Regulations Determination
Penn medicine office of clinical research regulatory services.
Penn Medicine Principal Investigators are recommended to request an exemption determination from the Office of Clinical Research Regulatory Services. OCR Regulatory will conduct exemption determinations for any product type.
Non-Penn Medicine Principal Investigators may request an exemption determination from the IRB. In order to request an exemption determination, submit the Research with Devices Form with your initial application.
Any Principal Investigators may seek an exemption determination directly from the FDA. See Additional Information section below.
Protocols that Require an IDE
If the protocol is not exempt from the IDE regulations, the IRB must determine the risk of the device as used on the protocol. NOTE: Risk determinations are not definitive and may change, should unanticipated adverse device effects occur, or evidence suggests that the risk of the device is greater or lower than originally anticipated.
Non-Significant Risk Protocol: Use of the device on the protocol does not meet the definition of significant risk.
Significant Risk Protocol: Use of an investigational device that presents a potential for serious risk* to the health, safety or welfare of a subject due to its intended use AND is used:
- As an implant OR
- For supporting or sustaining human life OR
- Of substantial importance in diagnosing, curing, mitigating, or treating disease or otherwise preventing impairment of human health OR
- Presents some other serious risk to patient’s health, safety, or welfare
Serious Risk
“Serious risk” is considered to be any risk that would be considered a serious adverse event.
- Is life-threatening, or cause death, or
- Causes hospitalization, disability or permanent damage, congenital anomaly/birth defect, or
- Requires a medical / surgical intervention to prevent permanent impairment or damage, or
- Is any other serious medical event that may adversely affect the safety or welfare of subjects.
- The device is a novel device with no predicate (a predicate is a medical device that may be legally marketed in the U.S. and is used as a point of comparison for new medical devices)
- A device used for an indication not previously evaluated by the research team, the FDA, or peer review, without medical and or scientific rational justifying the safety of the device(s)
Additional Information
Submitting a request for an exemption or risk determination to fda.
Unsure about risk of the device? Sponsors or sponsor-investigators can submit a Study Risk Determination Q Submission to the FDA. The only required documents consist of: Cover letter, device description, and protocol. A full IDE application is NOT required. FDA will determine whether the protocol qualifies for exemption and issue a determination letter. If the protocol is not exempt, FDA will provide a risk determination. Please review the FDA Guidance linked below.
Investigational Plans
IDE protocols require an investigational plan. See below for guidance on investigational plans. For guidance on submitting an IDE to the FDA, please contact the PSOM Office of Clinical Research, Regulatory Support Team. Regulatory Support
Treatment of a Patient with an Unapproved Device Product
An unapproved product can be administered for treatment purposes under the FDA’s expanded access program, if certain criteria are met. For more information, please click below.
Requirements for Conducting Clinical Investigations
Requirements for abbreviated ide holders.
For guidance on the Requirements for Abbreviated IDE Holders please contact the PSOM Office of Clinical Research, Regulatory Support Team.
PSOM Policies and Procedures
Perelman School of Medicine policies and procedures apply to device research when research involves Penn Medicine patients and / or PSOM faculty. This includes research that is led by Faculty from non-Penn Medicine schools such as School of Nursing, Engineering, or SAS. Questions about these policies and procedures can be directed to the Office of Clinical Research.
PI Acknowledgement of Responsibilities in Biomedical Research
The Principal Investigator is responsible for:
- Ensuring that an investigation is conducted according to the signed investigator statement, the investigational plan, and applicable regulations;
- Protecting the rights, safety, and welfare of subjects under the investigator’s care; and
- The control of drug(s) or device(s) used in the investigation.
The Principal Investigator’s Acknowledgement of Responsibilities document has been developed as a reminder of the responsibilities of the principal investigator in a clinical investigation.
Want to speak to an IRB staff member?
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Institutional Review Board
Investigational medical devices.
- What is a medical device?
- What is an investigational medical device?
- How are investigational medical devices classified?
- What is the Difference between Significant and Non-Significant Risk Devices?
- Does the FDA Have Ultimate Authority to Determine SR/NSR Classification?
- What is an Investigational Device Exemption (IDE)?
- What is “Compassionate Treatment Use” of a Device under an IDE?
- Are there investigational medical devices that are exempt from FDA IDE regulations?
- When must a Sponsor/Investigator apply for an IDE?
- What other Medical Device Studies may be conducted without an IDE?
- Do IDE regulations apply if the device has already been approved for a different use?
- IRB review of device studies
- Does Medicare cover investigational medical devices and related services?
1. What is a medical device?
The FDA regulations define items that are considered medical devices. A medical device is defined, in part, as any health care product that does not achieve its primary intended purposes by chemical action or by being metabolized. Medical devices include, among other things, surgical laser, wheelchairs, sutures, pacemakers, vascular grafts, intraocular lenses, and orthopedic pins. Medical devices also include diagnostic aids such as reagents and test kits for in vitro diagnosis (IVD) of disease and other medical conditions such as pregnancy. Clinical investigations of medical devices must comply with FDA informed consent and IRB regulations. Please note: The FDA regulations apply to ALL medical device studies, whether the device is marketed or not.
2. What is an investigational medical device?
An investigational medical device is one that is the subject of a clinical study designed to evaluate the effectiveness and/or safety of the device.
3. How are investigational medical devices classified?
There are two possible classifications for investigational medical devices:
- a) Significant Risk (SR) or
- b) Non-Significant Risk (NSR).
Please see the FDA Information Sheets for examples of SR and NSR devices.
[return to top]
4. What is the Difference between Significant and Non-Significant Risk Devices?
The distinctions between the two device risk categories are:
a) A SR device poses a “potential for serious risk to the health, safety, or welfare of a subject.” Such devices may only be studied under an Investigational Device Exemption (IDE) granted by the FDA. A device is SR ( and requires an IDE ) if it:
- is intended as an implant, or
- is purported or represented to be for a use in supporting or sustaining human life, or
- is for a use of substantial importance in diagnosing, curing, mitigating, or treating disease, or otherwise preventing impairment of human health; or
- otherwise presents a potential for serious risk to the health, safety, or welfare of a subject.
b) Non-significant risk devices do not meet the above definition. The assessment of whether or not a device study represents a NSR is initially made by the sponsor/investigator. The IRB will then determine if the NSR designation is appropriate. If the IRB disagrees with the NSR claim, it will require the sponsor/investigator to submit an IDE application to the FDA.
5. Does the FDA Have Ultimate Authority to Determine SR/NSR Classification?
The FDA has the ultimate authority to determine if a device study presents a “significant risk” or “nonsignificant risk.” If the FDA disagrees with the IRB’s decision that a device study presents a “nonsignificant risk”, an Investigational Device Exemption (IDE) application must be submitted to the FDA before the device is used in a clinical study. Additionally, if a sponsor/investigator presumes a device to be SR and submits an (IDE) to the FDA, the FDA may disagree and classify the device as “nonsignificant risk.” In this case, the FDA will return the IDE application with the recommendation that the device should be presented to the IRB as a “nonsignificant risk” device.
6. What is an Investigational Device Exemption (IDE)?
An IDE is issued by the FDA to allow the use investigational devices in human subjects. The IDE permits use of the device in a clinical investigation to evaluate the safety and/or efficacy of the investigational medical device. An IDE may be held either by a commercial sponsor or by a physician-investigator. Clinical studies of SR investigational devices must comply with FDA’s investigational device exemption (IDE) regulations and be conducted only with IRB approval. More information is available at this site: http://www.fda.gov/ . If an investigational device is a “non-significant risk device”, an investigator does not need to submit an IDE; the IDE will be “considered approved” under FDA regulations. Such devices do not have to comply with FDA premarket approval and performance standards prior to use in research studies. Such studies of devices “considered approved” by the FDA must still be submitted to the IRB for approval prior to use in human subject research. [return to top]
7. What is “Compassionate Treatment Use” of a Device under an IDE?
The FDA provides procedures for the use of an investigational device outside the parameters of an approved protocol. In the case of a serious disease, a device may be made available after the completion of all the clinical trials. If an “immediately life-threatening disease” presents, an investigational device may be made available for treatment use prior to the completion of the research.
Investigators must contact the FDA to discuss “ compassionate treatment ” using an investigational device outside of an IRB approved protocol and must obtain IRB approval for this use. The FDA will consider the use of an investigational device under a treatment IDE if:
a) the device is intended to treat or diagnose a serious or immediately life-threatening disease or condition; b) there is no comparable or satisfactory alternative device or other therapy available to treat or diagnose that stage of the disease or condition; c) the device is under investigation in a controlled clinical trial for the same use under an approved IDE, or such clinical trials have been completed; d) the sponsor of the investigation is actively pursuing marketing approval/clearance of the investigational device with due diligence.
FDA approval of compassionate use of an investigational device must precede use of that device. [return to top]
8. Are there investigational medical devices that are exempt from FDA IDE regulations?
There are five possible device studies that are exempt from the FDA regulations on IDEs. These exemptions apply only so long as the investigator remains qualified to conduct the research (see FDA regulations, 21 CFR 812.119 for Disqualification).
i. Devices, other than transitional devices * , in commercial distribution prior to May 28, 1976, when used or investigated in accordance with labeling in effect at that time;
ii. Devices, other than transitional devices * , introduced into commercial distribution on or after May 28, 1976, that the FDA determines to be substantially equivalent to a device in commercial distribution prior to May 28, 1976, and which is used or investigated in accordance with approved labeling;
iii. A diagnostic device (including in vitro diagnostic products in compliance with 21 CFR 809.10(c) if the testing:
a. Is non-invasive b. Does not require an invasive sampling procedure that presents significant risk c. Does not by design or intention introduce energy into a subject, and d. Is not used as a diagnostic procedure without confirmation of the diagnosis by another, medically established diagnostic product or procedure.
iv. Devices undergoing consumer preference testing, testing of a modification, or testing of a combination of two or more devices in commercial distribution , if the testing is not for the purpose of determining safety or effectiveness and does not put the subject at risk.
v. Custom devices, as defined by FDA in 21 CFR 812.3(b) , unless the device is being used to determine safety or effectiveness for commercial distribution.
9. When must a Sponsor/Investigator apply for an IDE?
A sponsor/investigator, must submit an application to the FDA for approval of an IDE if:
- an SR device is to be used in an investigational study,
- an investigation of a device is proposed to be conducted under the FDA regulations for emergency research,or
- the FDA notifies the sponsor/investigator that an IDE must be submitted for a proposed investigation
A sponsor/investigator may not begin a study for which FDA approval of an IDE application is required until the FDA has issued its approval and the IRB has approved the study. [return to top]
10. What other Medical Device Studies may be conducted without an IDE?
A device with an FDA 510(k) Designation.
FDA regulations allow a manufacturer/sponsor to claim that a new device is substantially equivalent to models that the FDA has already approved for marketing. Such devices are granted a 510(k) designation. The manufacturer/sponsor must apply to the FDA for this designation, and the FDA will provide a letter in response indicating whether or not it is granted. IRB approval is still required before an investigator may conduct research using a device with a 510(k) designation. [return to top]
11. Do IDE regulations apply if the device has already been approved for a different use?
Yes, the clinical study of a new indication for an already marketed device falls under the IDE regulation. The JHM IRB must review the device for its new investigational application. If there are questions, the investigator and/or the IRB may contact the FDA IDE Staff at :
9200 Corporate Blvd. Rockville, MD 20850 301-594-1190
12. IRB review of device studies:
Both SR and NSR device studies must be reviewed by a JHM IRB. In the case of an NSR claim, the initial assessment of whether or not the device study is NSR is made by the sponsor/investigator. The IRB then determines whether that assessment is appropriate. If an NSR study qualifies as “minimal risk” under Federal regulations; then the IRB may choose to use an expedited review procedure. The risk determination made by the IRB will be based upon both the nature of the device AND the proposed use of the device in the study. The Board’s finding will be documented in the meeting minutes.
All IRB requirements for human subject research apply to any medical device research study conducted at Hopkins regardless of whether investigators seek exemption from IDE requirements.
13. Does Medicare cover investigational medical devices and related services?
In 1995, the FDA and the Health Care Financing Agency (HCFA), now the Centers for Medicare & Medicaid Services (CMS), entered into an interagency agreement to categorize devices in clinical trials for purposes of eligibility for coverage by Medicare. There are two categories of devices: Category A (experimental/investigational devices for which there is no Medicare coverage); and Category B (non-experimental investigational devices). FDA will notify the sponsor (whether a commercial sponsor or a physician-investigator) of an investigational device clinical trial (i.e., a device with an IDE) of its decision regarding the category assigned to a device.
Category B devices will be eligible for Medicare coverage. The rule states that: " Payment for covered devices and related services will be based on, and may not exceed, the amount that would have been paid for a currently used FDA-approved device and related services serving the same medical purpose. " NSR device investigations for which the FDA does not require submission of an IDE are deemed to be in Category B. The JHM IRB must make the decision as to whether a device is SR or NSR.
Medicare will not provide payment for Category A devices , and will not pay for " services related to a non-covered device. " Investigators who wish to conduct clinical trials of devices that are determined to be Category A devices must address cost issues with the sponsor to assure that Medicare patients are not adversely affected by the decision to participate.
* Per FDA regulations, a transitional device is one that the FDA considered to be a new drug or an antibiotic drug before May 28, 1976 [return to top]
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
Adhesive coatings can prevent scarring around medical implants
Press contact :, media download.
*Terms of Use:
Images for download on the MIT News office website are made available to non-commercial entities, press and the general public under a Creative Commons Attribution Non-Commercial No Derivatives license . You may not alter the images provided, other than to crop them to size. A credit line must be used when reproducing images; if one is not provided below, credit the images to "MIT."
Previous image Next image
When medical devices such as pacemakers are implanted in the body, they usually provoke an immune response that leads to buildup of scar tissue around the implant. This scarring, known as fibrosis, can interfere with the devices’ function and may require them to be removed.
In an advance that could prevent that kind of device failure, MIT engineers have found a simple and general way to eliminate fibrosis by coating devices with a hydrogel adhesive. This adhesive binds the devices to tissue and prevents the immune system from attacking it.
“The dream of many research groups and companies is to implant something into the body that over the long term the body will not see, and the device can provide therapeutic or diagnostic functionality. Now we have such an ‘invisibility cloak,’ and this is very general: There’s no need for a drug, no need for a special polymer,” says Xuanhe Zhao, an MIT professor of mechanical engineering and of civil and environmental engineering.
The adhesive that the researchers used in this study is made from cross-linked polymers called hydrogels, and is similar to a surgical tape they previously developed to help seal internal wounds. Other types of hydrogel adhesives can also protect against fibrosis, the researchers found, and they believe this approach could be used for not only pacemakers but also sensors or devices that deliver drugs or therapeutic cells.
Zhao and Hyunwoo Yuk SM ’16, PhD ’21, a former MIT research scientist who is now the chief technology officer at SanaHeal, are the senior authors of the study, which appears today in Nature . MIT postdoc Jingjing Wu is the lead author of the paper.
Preventing fibrosis
In recent years, Zhao’s lab has developed adhesives for a variety of medical applications, including double-sided and single-sided tapes that could be used to heal surgical incisions or internal injuries. These adhesives work by rapidly absorbing water from wet tissues, using polyacrylic acid, an absorbent material used in diapers. Once the water is cleared, chemical groups called NHS esters embedded in the polyacrylic acid form strong bonds with proteins at the tissue surface. This process takes about five seconds.
Several years ago, Zhao and Yuk began exploring whether this kind of adhesive could also help keep medical implants in place and prevent fibrosis from occurring.
To test this idea, Wu coated polyurethane devices with their adhesive and implanted them on the abdominal wall, colon, stomach, lung, or heart of rats. Weeks later, they removed the device and found that there was no visible scar tissue. Additional tests with other animal models showed the same thing: Wherever the adhesive-coated devices were implanted, fibrosis did not occur, for up to three months.
“This work really has identified a very general strategy, not only for one animal model, one organ, or one application,” Wu says. “Across all of these animal models, we have consistent, reproducible results without any observable fibrotic capsule.”
Using bulk RNA sequencing and fluorescent imaging, the researchers analyzed the animals’ immune response and found that when devices with adhesive coatings were first implanted, immune cells such as neutrophils began to infiltrate the area. However, the attacks quickly quenched out before any scar tissue could form.
“For the adhered devices, there is an acute inflammatory response because it is a foreign material,” Yuk says. “However, very quickly that inflammatory response decayed, and then from that point you do not have this fibrosis formation.”
One application for this adhesive could be coatings for epicardial pacemakers — devices that are placed on the heart to help control the heart rate. The wires that contact the heart often become fibrotic, but the MIT team found that when they implanted adhesive-coated wires in rats, they remained functional for at least three months, with no scar tissue formation.
“The formation of fibrotic tissue at the interface between implanted medical devices and the target tissue is a longstanding problem that routinely causes failure of the device. The demonstration that robust adhesion between the device and the tissue obviates fibrotic tissue formation is an important observation that has many potential applications in the medical device space,” says David Mooney, a professor of bioengineering at Harvard University, who was not involved in the study.
Mechanical cues
The researchers also tested a hydrogel adhesive that includes chitosan, a naturally occurring polysaccharide, and found that this adhesive also eliminated fibrosis in animal studies. However, two commercially available tissue adhesives that they tested did not show this antifibrotic effect because the commercially available adhesives eventually detached from the tissue and allowed the immune system to attack.
In another experiment, the researchers coated implants in hydrogel adhesives but then soaked them in a solution that removed the polymers’ adhesive properties, while keeping their overall chemical structure the same. After being implanted in the body, where they were held in place by sutures, fibrotic scarring occurred. This suggests that there is something about the mechanical interaction between the adhesive and the tissue that prevents the immune system from attacking, the researchers say.
“Previous research in immunology has been focused on chemistry and biochemistry, but mechanics and physics may play equivalent roles, and we should pay attention to those mechanical and physical cues in immunological responses,” says Zhao, who now plans to further investigate how those mechanical cues affect the immune system.
Yuk, Zhao, and others have started a company called SanaHeal, which is now working on further developing tissue adhesives for medical applications.
“As a team, we are interested in reporting this to the community and sparking speculation and imagination as to where this can go,” Yuk says. “There are so many scenarios in which people want to interface with foreign or manmade material in the body, like implantable devices, drug depots, or cell depots.”
The research was funded by the National Institutes of Health and the National Science Foundation.
Share this news article on:
Press mentions, interesting engineering.
MIT engineers have developed a new adhesive, low-cost hydrogel that can stop fibrosis often experienced by people with pacemakers and other medical devices, reports for Maria Bolevich Interesting Engineering . “These findings may offer a promising strategy for long-term anti-fibrotic implant–tissue interfaces,” explains Prof. Xuanhe Zhao.
Previous item Next item
Related Links
- Xuanhe Zhao
- Hyunwoo Yuk
- Jingjing Wu
- Department of Mechanical Engineering
- Department of Civil and Environmental Engineering
Related Topics
- Mechanical engineering
- Civil and environmental engineering
- Biomedical engineering
- Medical devices
- National Institutes of Health (NIH)
- National Science Foundation (NSF)
Related Articles
Engineers develop surgical “duct tape” as an alternative to sutures

Double-sided tape for tissues could replace surgical sutures
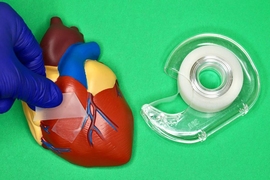
Super-strong surgical tape detaches on demand
Paper-folding art inspires better bandages
More mit news.

Scientists identify mechanism behind drug resistance in malaria parasite
Read full story →

Getting to systemic sustainability

New MIT-LUMA Lab created to address climate challenges in the Mediterranean region

MIT Press releases Direct to Open impact report

Modeling the threat of nuclear war
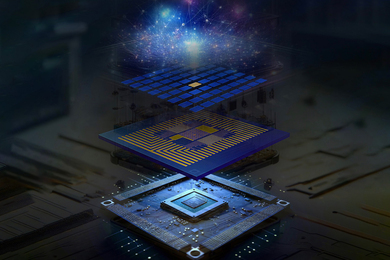
Modular, scalable hardware architecture for a quantum computer
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram

- HRP Staff Directory
- Office Hours
- Quality Improvement Project vs. Research
- Self Exempt & UROP
- Case Reports
- Commercial IRB Reliance Agreements
- National Cancer Institute Central IRB (CIRB) Independent Review Process
- UCI as the Reviewing IRB
- Submitting the Application
- Lead Researcher Eligibility
- Training & Education
- Ethical Guidelines, Regulations and Statutes
- Other Institutional Requirements
- Department of Defense Research Requirements
- Levels of Review
- Data Security
- Protected Health Information (HIPAA)
- European Union General Data Protection Regulation (EU GDPR)
- China’s Personal Information Protection Law
- Required Elements of Informed Consent
- Drafting the Informed Consent Form
- Consent and Non-English or Disabled Subjects
- Use Of Surrogate Consent In Research
- Vulnerable Populations
- Data and Safety Monitoring for Clinical Research
- Placebo-Controlled Studies
- Expanded Access to Unapproved Drugs or Biologics
- Right to Try: Unapproved Drugs or Biologics
- Use of Controlled Substances
- Expanded Access to Unapproved Medical Devices
- Humanitarian Use Devices
- Human Gene Transfer Research
- How To Register and Update Your Study
- Post-Review Responsibilities
Medical Devices Used in Clinical Investigations
Fda requirements for new medical devices.
A medical device is defined, in part, as any health care product that does not achieve its primary intended purposes by chemical action or by being metabolized. Medical devices include, among other things, surgical lasers, wheelchairs, sutures, pacemakers, vascular grafts, intraocular lenses, and orthopedic pins. Medical devices also include diagnostic aids such as reagents and test kits for in vitro diagnosis (IVD) of disease and other medical conditions such as pregnancy. Investigators interested in studying a new medical device are required to address additional information in KRP when completing the IRB application or when requesting an amendment to an IRB-approved study.
- Except for certain low risk devices, each manufacturer who wishes to introduce a new medical device to the market must submit a pre-market notification to FDA.
- FDA reviews these notifications to determine if the new device is " substantially equivalent " to a device that was marketed prior to passage of the Medical Device Amendments of 1976 and the Safe Medical Devices Act of 1990 (i.e., a "pre-amendments device").
- If the new device is deemed substantially equivalent to a pre-amendments device, it may be marketed immediately and is regulated in the same regulatory class as the pre-amendments device to which it is equivalent.
- The pre-market notification requirement for new devices and devices that are significant modifications of already marketed devices is set forth in section 510(k) of the Act.
- Devices determined by FDA to be substantially equivalent are often referred to as "510(k) devices."
- If the new device is deemed not to be substantially equivalent to a pre-amendments device, it must undergo clinical testing and pre-market approval before it can be marketed unless it is reclassified into a lower regulatory class.
An investigational device is a medical device which is the subject of a clinical study designed to evaluate the effectiveness and/or safety of the device.
- Clinical investigations undertaken to develop safety and effectiveness data for medical devices must be conducted according to the requirements of the FDA IDE regulations.
- An approved IDE permits a device that otherwise would be required to comply with a performance standard or to have pre-market approval to be shipped lawfully for the purpose of conducting investigations of that device.
- An IDE study may not necessarily commence 30 days after an IDE submission to FDA.
- Certain clinical investigations of devices (e.g., certain studies of lawfully marketed devices) may be exempt from FDA IDE regulations.
- The exemption applies only to investigations in which "510(k)'d" products are being used in accordance with the labeling cleared by FDA.
- Investigation of an off-label use of a 510(k) product takes it outside this exemption.
Non-significant Risk and Significant Device Classification
Unless exempt from IDE regulations, an investigational device must be categorized as either "significant risk" (SR) or "non-significant risk" (NSR).
Risk Device Studies
If the sponsor considers that a study is NSR, the UCI investigator must ask the sponsor to provide the IRB with an explanation of its determination and any other information that may assist the IRB in evaluating the risk of the study. The sponsor should provide the IRB with:
- a description of the device,
- reports of prior investigations with the device,
- the proposed investigational plan,
- a description of patient selection criteria and monitoring procedures, as well as
- any other information that the IRB deems necessary to make its decision.
The sponsor also should inform the UCI IRB whether other IRBs have reviewed the proposed study and what determination was made. The sponsor must inform the IRB of the FDA's assessment of the device's risk if such an assessment has been made. The IRB may also consult with the FDA for its opinion.
NSR studies do not require submission of an IDE application to the FDA. Instead, the sponsor is required to conduct the study in accordance with the "abbreviated requirements" of the FDA IDE regulations. Unless otherwise notified by the FDA, an NSR study is considered to have an approved IDE if the sponsor fulfills the abbreviated requirements.
SR device studies must be conducted in accordance with the full IDE requirements of the FDA and may not commence until 30 days following the sponsor's submission of an IDE application to the FDA.
- All SR risk studies require IRB full committee review.
- The IRB's risk determination is based on the proposed use of a device in an investigation, and not on the device alone. In deciding if a study poses an SR, the IRB must consider the nature of the harm that may result from use of the device.
- If the UCI IRB believes that a device study is SR, the investigation may not begin until both the IRB and FDA approve the investigation.
- Documentation of the FDA IDE number must be submitted to the IRB before UCI IRB approval will be granted.
- Reports: “Significant risk device determinations. If an IRB determines that a device is a significant risk device , and the sponsor had proposed that the IRB consider the device not to be a significant risk device, the sponsor shall submit to FDA a report of the IRB's determination within 5 working days after the sponsor first learns of the IRB's determination. ”
Abbreviated FDA requirements for NSR Devices
Below is a summary of the FDA abbreviated requirements [ 21 CFR 812.2(b) ] for NSR device studies:
- Sponsor and local investigator agree to provide the UCI IRB with a brief explanation of why the device is not a significant risk device, and to obtain and maintain UCI IRB approval;
- Sponsor labels the device in accordance with FDA requirements;
- Sponsor and local investigator ensure informed consent is obtained from each subject, unless documentation is waived by the IRB;
- Sponsor and local investigator comply with the FDA requirements for monitoring investigations, maintaining records and filing reports; and
- Sponsor complies with FDA regulations pertaining to the prohibition of promotion and other practices of the device.
- The investigation does not involve a device that was approved under an IND (on or before July 16, 1980).
FDA Definitions for Device Studies
The following definitions will assist investigators with the significant risk and non-significant risk classification:
Noninvasive when applied to a diagnostic device or procedure, means one that does not by design or intention:
- Penetrate or pierce the skin or mucous membranes of the body, the ocular cavity, or the urethra, or
- enter the ear beyond the external auditory canal, the nose beyond the nares, the mouth beyond the pharynx, the anal canal beyond the rectum, or the vagina beyond the cervical os.
- Blood sampling that involves simple venipuncture is considered noninvasive, and the use of surplus samples of body fluids or tissues that are left over from samples taken for non-investigational purposes is also considered noninvasive.
Significant risk device means an investigational device that:
- Is intended as an implant and presents a potential for serious risk to the health, safety, or welfare of a subject;
- Is purported or represented to be for a use in supporting or sustaining human life and presents a potential for serious risk to the health, safety, or welfare of a subject;
- Is for a use of substantial importance in diagnosing, curing, mitigating, or treating disease, or otherwise preventing impairment of human health and presents a potential for serious risk to the health, safety, or welfare of a subject; or
- Otherwise presents a potential for serious risk to the health, safety, or welfare of a subject.
Implant means a device that is placed into a surgically or naturally formed cavity of the human body if it is intended to remain there for a period of 30 days or more. FDA may, in order to protect public health, determine that devices placed in subjects for shorter periods are also "implants."
SR and NSR Examples
Below are several examples of SR and NSR devices.
Note: Inclusion of a device in the NSR category should not be viewed as a conclusive determination, because the proposed use of a device in a study is the ultimate determinant of the potential risk to subjects. It is unlikely that a device included in the SR category could be deemed NSR due to the inherent risks associated with most such devices.
Investigational Use of Marketed Medical Devices
The investigational use of approved, marketed devices requires consideration of whether an IND is required. When the principal intent of the investigational use of a medical device is to develop information about the product's safety or efficacy, submission of an IND or IDE may be required. Investigators interested in studying the above are also required to address additional information in Kuali Research (KR) Protocols when completing the IRB application or when requesting an amendment to an IRB-approved study.
Control of Investigational Devices
Research involving the use of investigational test articles (i.e., investigational drugs, biologics or devices) requires that the Investigator or other appropriate individual or entity (e.g., hospital pharmacy), provide appropriate control of test articles.
Note: An Investigational Device Accountability Log must be maintained, if the study includes a device.
UCIMC Policy for Control of Investigational Devices
Investigational devices are carefully regulated and must be appropriately managed by a qualified Investigator or other appropriate individual to ensure they are not co-mingled with similar approved devices. UCI Health Systems Control of Investigational Devices Policy can be found on the UCIMC website .
Lead Researcher (Investigator) Responsibilities
Lead Researchers (Investigators) conducting studies in which an investigational device will be used must ensure adequate control of the device. Adequate control and handling of investigational devices include all of the following:
- The investigator must ensure that the investigational device is used only in accordance with the UCI IRB approved protocol, the signed agreement, the investigational plan and applicable FDA regulations.
- The investigator must administer the investigational device only to participants under the investigator’s direct personal supervision or under the supervision of a sub-investigator directly responsible to the investigator.
- The investigator must not supply the investigational device to any person not authorized to receive it.
- The type and quantity of the device, the dates of its receipt, and the batch number or code mark.
- The names of all persons who received, used, or disposed of each device.
- Why and how many units of the device have been returned to the sponsor, repaired, or otherwise disposed of.
- If the investigation is terminated, suspended, discontinued, or completed, the investigator must return any unused stock of the investigational device to the study sponsor, or otherwise provide for disposition of the unused stock as directed by the sponsor.
Regulations
- Devices: FDA: 21 CFR 812
- HRP Guidance Document on Devices - IRB Member Desk Reference
- HRP Page: Humanitarian Use Devices
- FDA 510K Database Search
- FDA Guidance on Investigational Device Exemptions for Early Feasibility Studies
- FDA Information Sheet Guidance: FAQs About Medical Devices
- FDA Information Sheet Guidance: Significant Risk and Nonsignificant Risk
- FDA Information Sheet Guidance: Policy for Device Software Functions and Mobile Medical Applications
- FDA Information Sheet Guidance: Changes to Existing Medical Software Policies Resulting from Section 3060 of the 21st Century Cures Act
- NIH NHGRI IDE and Genomics Research ( pdf )
- Skip to main content
- Skip to secondary menu
- Skip to primary sidebar
- Skip to secondary sidebar
- Skip to footer

Medable Partners with Masimo to Bring Wearable Devices to Clinical Research, Capturing Better Data
by Fred Pennic 05/29/2024 Leave a Comment

What You Should Know:
– Medable Inc., a leader in modern clinical trial technology, has announced a groundbreaking partnership with Masimo (NASDAQ: MASI) to integrate medical-grade wearable devices into clinical research. This collaboration aims to streamline patient participation and enhance data collection for clinical trials.
– By offering a patient-centric approach and fostering richer data collection, this collaboration holds promise for faster drug development, improved patient experiences, and ultimately, advancements in healthcare.
Easing the Burden for Patients
Masimo’s MightySat® Rx pulse oximeter , a trusted medical device used by clinicians globally, is now being incorporated into Medable’s platform. This eliminates the need for frequent, often burdensome, trips to trial sites for routine testing, particularly beneficial for patients with serious illnesses like lung and breast cancer. Over 3,000 patients across eight major oncology trials in 25 countries are already benefiting from this technology.
A Multifaceted Approach to Data Collection
The partnership goes beyond wearables. Medable’s eCOA+ solution allows for subjective data capture through human interaction. When combined with Masimo’s objective sensor data, this creates a richer and more comprehensive dataset for researchers. Medable specifically chose Masimo for its Signal Extraction Technology®, known for delivering accurate readings even in challenging conditions.
Wearables Gaining Traction in Clinical Trials
The use of wearables in clinical trials is on the rise. Currently, 20% of trials utilizing Medable’s platform incorporate wearables, with 35% of those focused on oncology research. This trend highlights the growing recognition of wearables’ potential to improve patient experience and data collection.
Financial Advantages of Decentralized Trials
Research from the Tufts Center for the Study of Drug Development further strengthens the case for decentralized trials. Their findings suggest that decentralized trials can yield a net financial benefit of 5 to 13 times for Phase II and III trials, translating to a potential ROI of $10 million and $39 million respectively, with an average investment of $500,000 and $1.5 million for Phase II and III trials, respectively.
“Medable has always been a leader in digital and decentralized clinical trials, so we are excited to work with a forward-thinking organization with the ambition and ability to transform research,” said Dr. Daniel Cantillon, Chief Medical Officer at Masimo. “Clinical trials require top-in-class accuracy and data quality both on-site and off-site from clinical offices. Medable is solving this problem through its advocacy and by empowering more patients to participate in research. And, Medable’s flexible platform enables scalability and data aggregation for a holistic approach.”
Reader Interactions
- Advertise with Us
- Reprints and Permissions
- 2023 Editorial Calendar
- Submit An Op-Ed
Editorial Coverage
- Care Coordination
- Interoperability
- Population Health Management
- Revenue Cycle Management
- Artificial Intelligence
- Blockchain Tech
- Precision Medicine
- Accountable Care
- Medicare Advantage
Subscribe to HIT Consultant Media
Latest insightful articles delivered straight to your inbox weekly
Skip to Content
Charge your laptop in a minute or your EV in 10? Supercapacitors can help; new research offers clues

Imagine if your dead laptop or phone could charge in a minute or if an electric car could be fully powered in 10 minutes.
While not possible yet, new research by a team of CU Boulder scientists could potentially lead to such advances.
Published today in the Proceedings of the National Academy of Science , researchers in Ankur Gupta ’s lab discovered how tiny charged particles, called ions, move within a complex network of minuscule pores. The breakthrough could lead to the development of more efficient energy storage devices, such as supercapacitors, said Gupta, an assistant professor of chemical and biological engineering .

Gupta explained that several chemical engineering techniques are used to study flow in porous materials such as oil reservoirs and water filtration, but they have not been fully utilized in some energy storage systems.
The discovery is significant not only for storing energy in vehicles and electronic devices but also for power grids, where fluctuating energy demand requires efficient storage to avoid waste during periods of low demand and to ensure rapid supply during high demand.
Supercapacitors, energy storage devices that rely on ion accumulation in their pores, have rapid charging times and longer life spans compared to batteries.
“The primary appeal of supercapacitors lies in their speed,” Gupta said. “So how can we make their charging and release of energy faster? By the more efficient movement of ions.”
Their findings modify Kirchhoff’s law, which has governed current flow in electrical circuits since 1845 and is a staple in high school students’ science classes. Unlike electrons, ions move due to both electric fields and diffusion, and the researchers determined that their movements at pore intersections are different from what was described in Kirchhoff’s law.
Prior to the study, ion movements were only described in the literature in one straight pore. Through this research, ion movement in a complex network of thousands of interconnected pores can be simulated and predicted in a few minutes.
“That’s the leap of the work,” Gupta said. “We found the missing link.”
This work was funded by National Science Foundation CAREER Award # 2238412.
Apply Visit
Departments
- Ann and H.J. Smead Aerospace Engineering Sciences
- Chemical & Biological Engineering
- Civil, Environmental & Architectural Engineering
- Computer Science
- Electrical, Computer & Energy Engineering
- Paul M. Rady Mechanical Engineering
- Applied Mathematics
- Biomedical Engineering
- Creative Technology & Design
- Engineering Education
- Engineering Management
- Engineering Physics
- Integrated Design Engineering
- Environmental Engineering
- Materials Science & Engineering
Affiliates & Partners
- ATLAS Institute
- BOLD Center
- Colorado Mesa University
- Colorado Space Grant Consortium
- Discovery Learning
- Engineering Honors
- Engineering Leadership
- Entrepreneurship
- Herbst Program for Engineering, Ethics & Society
- Integrated Teaching and Learning
- Global Engineering
- Mortenson Center for Global Engineering
- National Center for Women & Information Technology
- Western Colorado University
- My View My View
- Following Following
- Saved Saved
Microsoft debuts 'Copilot+' PCs with AI features
- Medium Text

Sign up here.
Reporting by Max A. Cherney in Seattle; Additional reporting by Yuvraj Malik in Bengaluru and Stephen Nellis in San Francisco; Editing by Noel Randewich and Matthew Lewis
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab

Technology Chevron

Sony stresses PlayStation user engagement as hardware sales taper off
Japan's Sony on Thursday emphasised the strength of user engagement with its gaming platform as sales of the PlayStation 5 console taper off and companies in the sector look for recurring revenue.
Online betting company Sportsbet pledged to manage the risks associated with money laundering and terrorism financing in an undertaking given to Australian Transaction Reports and Analysis Centre, the financial crimes regulator said on Thursday.

Lithuanian webhosting firm Hostinger, which bills itself as a European rival to U.S. market leader GoDaddy , said on Thursday it had reached profitability for the first time, as European tech startups try and catch up with bigger U.S peers.


COMMENTS
Medical Device Regulatory Science Research Programs Conducted by OSEL. Goals, program areas, and initiatives aimed at improving methods and approaches for evaluating, manufacturing, and monitoring ...
Krucoff MW, Normand S-L, Edwards F, et al. Recommendations for a national medical device evaluation system: strategically coordinated registry networks to bridge clinical care and research: a ...
•Legally marketed devices used according to label •Certain diagnostic devices •Consumer preference testing, when not determining safety or effectiveness and does not put subjects at risk •Veterinary devices or research on/with laboratory animals intended solely for veterinary use •Custom devices (21 CFR 812.3(b)) 21 CFR 812.2(c) 14
2024 Regulatory Education for Industry (REdI) Conference. On May 29-30, 2024, hear from FDA's regulatory experts in medical product centers: devices, drugs, and biologics. The conference is free ...
Scientists Invent Ultra-Thin, Minimally-Invasive Pacemaker Controlled by Light. Feb. 21, 2024 — A team of researchers has developed a wireless device, powered by light, that can be implanted to ...
Main body. The evidence of HTA reports and journal publications on medical devices around the world has been growing. The challenges in assessing medical devices include scarcity of well-designed randomized controlled trials, inconsistent real-world evidence data sources and methods, device-user interaction, short product lifecycles, inexplicit target population, and a lack of direct medical ...
The Artificial Intelligence Program in the Center for Devices and Radiological Health (CDRH) conducts regulatory science research to help ensure patient access to innovative devices made using AI/ML.
A medical device can be any instrument, apparatus, implement, machine, appliance, implant, reagent for in vitro use, software, material or other similar or related article, intended by the manufacturer to be used, alone or in combination for a medical purpose. Fact sheets. Databases and tools. Initiatives and groups. Resolutions and decisions.
Medical Devices: Evidence and Research is an international, peer-reviewed, open access journal that focuses on evidence, technology, research, and expert opinion supporting use and application of medical devices. This informs advances in diagnosis, monitoring, treatment and management of clinical conditions and physiological processes.
A.G.F.: grants from the European Union Horizon 2020 programme (project grant 965246) for CORE-MD (Coordinating Research and Evidence for Medical Devices) and a leadership role (chairmanship) on the Regulatory Affairs Committee for the Biomedical Alliance in Europe. A.G.: stock or stock options from Philips Healthcare and employment with Philips ...
Objective: Medical device development, from the product's conception to release to market, is very complex and relies significantly on the application of exact processes. This paper aims to provide an analysis and summary of current research in the field of medical device development methodologies, discuss its phases, and evaluate the associated legislative and risk aspects.
An international, peer-reviewed, open access journal that focuses on the evidence, technology, research, and expert opinion supporting the use and application of medical devices in the diagnosis, monitoring, treatment and management of clinical conditions and physiological processes. This journal is a member of and subscribes to the principles ...
Medical Device Research. The closely related and broad field of medical devices includes the development of healthcare products and procedures that diagnose, treat, cure, or prevent disease by means other than or in addition to pharmaceuticals or biologics. This field is an exciting place for researchers and biomedical engineers interested in ...
Health equity considerations for medical device regulation. Disparities in access to medical devices and clinical outcomes of device use can manifest across multiple domains1 (Table 1). First, pre ...
Brief Overview. This guidance is intended to assist UCLA investigators in meeting the various Food and Drug Administration (FDA) requirements as well as UCLA requirements when using devices in clinical research (clinical investigations) and in treatment. FDA IDE regulations 21 CFR 812 contain procedures and requirements for the conduct of the ...
Medical device means any instrumen t, apparatus, machine, appliance, implant, reagent for in vitro use, software, material or other similar or related article, intended by the man ufacturer to be ...
Research involving the use of devices is complex and varied. Some protocols use marketed devices that are not generally considered to be medical devices, such as a Fitbit or virtual reality. Some devices are simply used to collect research data. On the other end of the spectrum, a device may be implanted into a participant.
Medical devices include, among other things, surgical laser, wheelchairs, sutures, pacemakers, vascular grafts, intraocular lenses, and orthopedic pins. Medical devices also include diagnostic aids such as reagents and test kits for in vitro diagnosis (IVD) of disease and other medical conditions such as pregnancy.
Linkedin. These Research Programs aim to ensure that patients have access to high quality, safe and effective medical devices. These programs advance regulatory science—the science of developing ...
"The dream of many research groups and companies is to implant something into the body that over the long term the body will not see, and the device can provide therapeutic or diagnostic functionality. ... the tissue obviates fibrotic tissue formation is an important observation that has many potential applications in the medical device space ...
Medical Devices Used in Clinical Investigations FDA Requirements for New Medical Devices A medical device is defined, in part, as any health care product that does not achieve its primary intended purposes by chemical action or by being metabolized. Medical devices include, among other things, surgical lasers, wheelchairs, sutures, pacemakers, vascular grafts, intraocular lenses, and…
AAOS Now / Issue: May 2024 / research01. At the AAOS-FDA Town Hall, held during the AAOS 2024 Annual Meeting, attendees gathered to hear from industry and regulatory leaders on the importance of collecting diverse real-world evidence to support the use of medical devices. AAOS Now. Published 5/29/2024.
The public's appetite for inexpensive and powerful electronic devices continues to grow. While silicon-based semiconductors have been key to satiating this demand, a superior alternative could be wide-bandgap semiconductors. ... Center for Computational Research (CCR) Center for Integrated Global Biomedical Sciences; Clinical Research ...
What is a medical device and an In-Vitro Diagnostic (IVD)? ... ResearchAndMarkets.com is the world's leading source for international market research reports and market data. We provide you with ...
Qualified Medical Device Development Tools (MDDTs) Regulatory science tools in the catalog may progress through the qualification process to become fully fledged medical device development tools ...
Print. What You Should Know: - Medable Inc., a leader in modern clinical trial technology, has announced a groundbreaking partnership with Masimo (NASDAQ: MASI) to integrate medical-grade ...
Study suggests innovation could improve photovoltaics, display screens, wireless communication devices, medical devices. The public's appetite for inexpensive and powerful electronic devices continues to grow. While silicon-based semiconductors have been key to satiating this demand, a superior alternative could be wide-bandgap semiconductors.
Published today in the Proceedings of the National Academy of Science, researchers in Ankur Gupta's lab discovered how ions move within a complex network of minuscule pores. The breakthrough could lead to the development of more efficient energy storage devices, such as supercapacitors, enabling fast charging of EVs and electronic devices.
CDRH's Innovation Initiative is designed to strengthen the U.S. medical device research infrastructure, promote regulatory science, streamline the conduct of clinical trials, improve the quality ...
Microsoft on Monday debuted a new category of personal computers with AI features as it rushes to build the emerging technology into products across its business and compete with Alphabet and Apple .