Better Birth Blog
Information & Inspiration for Pregnancy, Birth & Parenting

Homeopathy for Breech

Natrum Muriaticum- a water balancing tissue salt for fluid imbalance (too much or too little amniotic fluid)
Ignatia Amara- 30c x 1 every two hours for fear, anxiety, or depression (related to suppressed grief, anger, or shock) which may be causing tightness of the lower uterine segment and keeping the baby high
Pulsatilla 6X 3-4x per day for 7-10 days combined with breech tilt 2x per day for 10 minutes (take Pulsatilla before beginning breech tilt) or 30c 2x per day for 3 days (up to 2 weeks) or 200c x1 every 3 days while doing breech tilt exercises or 200c x 1 for 2-3 days at 35-36 weeks or 1M x 1 Note: 30c or 200c can be given every 2 hours up to 6x in 1 day to turn a breech baby (do not take at this dosage level for more than 1 day)
Why it might work: In the homeopathic tradition, pulsatilla stimulates the uterine muscle to grow more evenly so the baby can naturally assume the best position if it hasn’t already.


Hi - My Account Log In / Register | Log out | Checkout
Using Homeopathy to Turn Babies
Editor’s note: This article first appeared in Midwifery Today , Issue 24, Spring 1993. Subscribe to Midwifery Today Magazine
The science of homeopathy is a perfect complement to the midwife’s art. Symptoms, in any part of the mind or body, are seen as part of a symptom-picture involving the whole person. The gentle action of homeopathic remedies can be used preventively or in acute situations to address any symptom-picture, weakness, or recurring tendency that is less than optimal.
While breech presentations are considered one variation of normal, many midwives are prevented by law from attending vaginal breech deliveries. Midwives who do attend breech births often say their hearts beat a little faster from worrying about possible complications.
In addition to breech, babies in posterior position are among the most challenging. It seems prudent to employ every gentle means available to get these babies to turn prenatally.
The windflower is one of the great homeopathic polychrests (drug of many uses). This herb has long been used to change unfavorable presentations prior to the onset of labor. The remedy is most effective when administered before the presenting occiput is deeply engaged in the pelvis and before the bag of waters ruptures.
How does it work? Pulsatilla is essentially soft and changeable. On the physical plane, the uterus grows asymmetrically, and the baby fits in there any way it can. Given in potency (a pharmaceutical process which progressively dilutes natural substances and then vigorously shakes them, thereby releasing dormant energy), pulsatilla stimulates the uterine muscle to grow more evenly. In response to a change in shape, the baby willingly and naturally assumes the most advantageous position—a gentle intervention.
Pulsatilla is always worth a try. Because you are giving the woman a non-material (dynamic) dose, you can cause no harm. The worst that can happen is that she simply will not respond to, or resonate with, the remedy. If the baby needs to remain in his present position for mechanical reasons, such as the location of the placenta or a tight cord wrap, the remedy will have no effect. The timing of the homeopathic intervention can coincide with other efforts you employ to turn babies. Usually you’ll try this at or near 35 weeks, or perhaps earlier if mom is small and the baby is persistent. Try one dose of the 200c potency. If there is no response in a few days, you can repeat it, or go to a 1M. If all you have on hand is 30c or lower, then try one or two doses a day for three days. There are no firm rules regarding dosage, but as a general guideline, do not repeat the high potencies (200c and above) more than twice or continue the lower potencies for more than two weeks. And stop all interventions once you have obtained results.
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
About Author: Patty Brennan
Patty Brennan is a practicing midwife and homeopathic educator from Michigan. She is co-author of “ Guide to Homeopathic Remedies for the Birth Bag ” and owner of Trusting Nature: Media and More, a store which carries homeopathic resources. View all posts by Patty Brennan
Get a membership! Read articles like this:

Subscribe to E-News :

Midwifery Today, Issue 149, Spring 2024
Donate to the Midwifery Today Scholarship Fund
Subscribe to our conference mailing list.
Sign up for our other lists .
Sign up to receive notification of new articles
Contact info, subscribe to e-news, privacy overview.
An informative newsletter delivered to your e-mail box every Wednesday. Learn about birth and midwifery with our articles, editorials, and Q&As with midwives. Keep up to date on our online magazine, books and other birth-related products.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
This topic will provide an overview of major issues related to breech presentation, including choosing the best route for delivery. Techniques for breech delivery, with a focus on the technique for vaginal breech delivery, are discussed separately. (See "Delivery of the singleton fetus in breech presentation" .)
TYPES OF BREECH PRESENTATION
● Frank breech – Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term.
● Complete breech – Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
When viewing this topic in a different language, you may notice some differences in the way the content is structured, but it still reflects the latest evidence-based guidance.
Breech presentation
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned cesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned cesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Breech presentation in pregnancy occurs when a baby presents with the buttocks or feet rather than the head first (cephalic presentation) and is associated with increased morbidity and mortality for both the mother and the baby. [1] Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997. [2] Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002. There is good current evidence regarding effective management of breech presentation in late pregnancy using external cephalic version and/or planned cesarean section.
History and exam
Key diagnostic factors.
- buttocks or feet as the presenting part
- fetal head under costal margin
- fetal heartbeat above the maternal umbilicus
Other diagnostic factors
- subcostal tenderness
- pelvic or bladder pain
Risk factors
- premature fetus
- small for gestational age fetus
- nulliparity
- fetal congenital anomalies
- previous breech delivery
- uterine abnormalities
- abnormal amniotic fluid volume
- placental abnormalities
- female fetus
Diagnostic investigations
1st investigations to order.
- transabdominal/transvaginal ultrasound
Treatment algorithm
<37 weeks' gestation, ≥37 weeks' gestation not in labor, ≥37 weeks' gestation in labor: no imminent delivery, ≥37 weeks' gestation in labor: imminent delivery, contributors, natasha nassar, phd.
Associate Professor
Menzies Centre for Health Policy
Sydney School of Public Health
University of Sydney
Disclosures
NN has received salary support from Australian National Health and a Medical Research Council Career Development Fellowship; she is an author of a number of references cited in this topic.
Christine L. Roberts, MBBS, FAFPHM, DrPH
Research Director
Clinical and Population Health Division
Perinatal Medicine Group
Kolling Institute of Medical Research
CLR declares that she has no competing interests.
Jonathan Morris, MBChB, FRANZCOG, PhD
Professor of Obstetrics and Gynaecology and Head of Department
JM declares that he has no competing interests.
Peer reviewers
John w. bachman, md.
Consultant in Family Medicine
Department of Family Medicine
Mayo Clinic
JWB declares that he has no competing interests.
Rhona Hughes, MBChB
Lead Obstetrician
Lothian Simpson Centre for Reproductive Health
The Royal Infirmary
RH declares that she has no competing interests.
Brian Peat, MD
Director of Obstetrics
Women's and Children's Hospital
North Adelaide
South Australia
BP declares that he has no competing interests.
Lelia Duley, MBChB
Professor of Obstetric Epidemiology
University of Leeds
Bradford Institute of Health Research
Temple Bank House
Bradford Royal Infirmary
LD declares that she has no competing interests.
Justus Hofmeyr, MD
Head of the Department of Obstetrics and Gynaecology
East London Private Hospital
East London
South Africa
JH is an author of a number of references cited in this topic.
Differentials
- Transverse lie
- Antenatal corticosteroids to reduce neonatal morbidity and mortality
- Caesarean birth
Use of this content is subject to our disclaimer
Help us improve BMJ Best Practice
Please complete all fields.
I have some feedback on:
We will respond to all feedback.
For any urgent enquiries please contact our customer services team who are ready to help with any problems.
Phone: +44 (0) 207 111 1105
Email: [email protected]
Your feedback has been submitted successfully.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Breech?
When a fetus is delivered buttocks or feet first
- Types of Presentation
Risk Factors
Complications.
Breech concerns the position of the fetus before labor . Typically, the fetus comes out headfirst, but in a breech delivery, the buttocks or feet come out first. This type of delivery is risky for both the pregnant person and the fetus.
This article discusses the different types of breech presentations, risk factors that might make a breech presentation more likely, treatment options, and complications associated with a breech delivery.
Verywell / Jessica Olah
Types of Breech Presentation
During the last few weeks of pregnancy, a fetus usually rotates so that the head is positioned downward to come out of the vagina first. This is called the vertex position.
In a breech presentation, the fetus does not turn to lie in the correct position. Instead, the fetus’s buttocks or feet are positioned to come out of the vagina first.
At 28 weeks of gestation, approximately 20% of fetuses are in a breech position. However, the majority of these rotate to the proper vertex position. At full term, around 3%–4% of births are breech.
The different types of breech presentations include:
- Complete : The fetus’s knees are bent, and the buttocks are presenting first.
- Frank : The fetus’s legs are stretched upward toward the head, and the buttocks are presenting first.
- Footling : The fetus’s foot is showing first.
Signs of Breech
There are no specific symptoms associated with a breech presentation.
Diagnosing breech before the last few weeks of pregnancy is not helpful, since the fetus is likely to turn to the proper vertex position before 35 weeks gestation.
A healthcare provider may be able to tell which direction the fetus is facing by touching a pregnant person’s abdomen. However, an ultrasound examination is the best way to determine how the fetus is lying in the uterus.
Most breech presentations are not related to any specific risk factor. However, certain circumstances can increase the risk for breech presentation.
These can include:
- Previous pregnancies
- Multiple fetuses in the uterus
- An abnormally shaped uterus
- Uterine fibroids , which are noncancerous growths of the uterus that usually appear during the childbearing years
- Placenta previa, a condition in which the placenta covers the opening to the uterus
- Preterm labor or prematurity of the fetus
- Too much or too little amniotic fluid (the liquid that surrounds the fetus during pregnancy)
- Fetal congenital abnormalities
Most fetuses that are breech are born by cesarean delivery (cesarean section or C-section), a surgical procedure in which the baby is born through an incision in the pregnant person’s abdomen.
In rare instances, a healthcare provider may plan a vaginal birth of a breech fetus. However, there are more risks associated with this type of delivery than there are with cesarean delivery.
Before cesarean delivery, a healthcare provider might utilize the external cephalic version (ECV) procedure to turn the fetus so that the head is down and in the vertex position. This procedure involves pushing on the pregnant person’s belly to turn the fetus while viewing the maneuvers on an ultrasound. This can be an uncomfortable procedure, and it is usually done around 37 weeks gestation.
ECV reduces the risks associated with having a cesarean delivery. It is successful approximately 40%–60% of the time. The procedure cannot be done once a pregnant person is in active labor.
Complications related to ECV are low and include the placenta tearing away from the uterine lining, changes in the fetus’s heart rate, and preterm labor.
ECV is usually not recommended if the:
- Pregnant person is carrying more than one fetus
- Placenta is in the wrong place
- Healthcare provider has concerns about the health of the fetus
- Pregnant person has specific abnormalities of the reproductive system
Recommendations for Previous C-Sections
The American College of Obstetricians and Gynecologists (ACOG) says that ECV can be considered if a person has had a previous cesarean delivery.
During a breech delivery, the umbilical cord might come out first and be pinched by the exiting fetus. This is called cord prolapse and puts the fetus at risk for decreased oxygen and blood flow. There’s also a risk that the fetus’s head or shoulders will get stuck inside the mother’s pelvis, leading to suffocation.
Complications associated with cesarean delivery include infection, bleeding, injury to other internal organs, and problems with future pregnancies.
A healthcare provider needs to weigh the risks and benefits of ECV, delivering a breech fetus vaginally, and cesarean delivery.
In a breech delivery, the fetus comes out buttocks or feet first rather than headfirst (vertex), the preferred and usual method. This type of delivery can be more dangerous than a vertex delivery and lead to complications. If your baby is in breech, your healthcare provider will likely recommend a C-section.
A Word From Verywell
Knowing that your baby is in the wrong position and that you may be facing a breech delivery can be extremely stressful. However, most fetuses turn to have their head down before a person goes into labor. It is not a cause for concern if your fetus is breech before 36 weeks. It is common for the fetus to move around in many different positions before that time.
At the end of your pregnancy, if your fetus is in a breech position, your healthcare provider can perform maneuvers to turn the fetus around. If these maneuvers are unsuccessful or not appropriate for your situation, cesarean delivery is most often recommended. Discussing all of these options in advance can help you feel prepared should you be faced with a breech delivery.
American College of Obstetricians and Gynecologists. If your baby is breech .
TeachMeObGyn. Breech presentation .
MedlinePlus. Breech birth .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term . Cochrane Database Syst Rev . 2015 Apr 1;2015(4):CD000083. doi:10.1002/14651858.CD000083.pub3
By Christine Zink, MD Dr. Zink is a board-certified emergency medicine physician with expertise in the wilderness and global medicine.
- Quickstart Guide
- Quickstart Guide Spanish
- What is Homeopathy?
- Testimonials
- Submit a Testimonial
- Gateway Study Group I
- Gateway Study Group II
Books & CDs
- Published Articles
- Newsletter Archive
- Resource Library
- Joette’s Blog
- Buster’s Blog
- Survival Medicine
- Professional
Birthing Series Part One: Turning a Breech Baby
May 21st, 2017 | 59 comments.

It was the best of times; it was the worst of times.
Hmmmm … I think that line’s already taken, so, let me be more specific.
Giving birth can be both the most magical time and the most stressful time of a woman’s life. Our bodies are changing by the moment, and any little out-of-the-ordinary pain or seeming delay can send even the most stoic amongst us into a tailspin of worry.
But there are women who came before us. Some women serve as emotional or educational support to enlighten us as to what to expect as we approach delivery.
But some women have taken it one step further by being pioneers in the medical field who have made delivery easier.
One such woman was Dr. Mercy B. Jackson (1802-1877). We touched on her contributions in our Mother’s Day tribute to a few stand-out women of homeopathy. Having given birth to 11 children, Dr. Jackson was understandably drawn toward a specialty in Obstetrics and Gynecology.
One of her greatest contributions was discovering that Pulsatilla can be used to turn breech babies in the womb and to speed labor.
Without this discovery, many women would have been subjected to unnecessary surgery in the delivery room. I’ve personally witnessed this phenomenon and can attest to its efficacy.
Pulsatilla is a uniquely feminine medicine. As such, it can help with so many physical issues that arise during pregnancy, such as bladder infections and indigestion.
It can also be extremely useful during periods of extreme emotion, especially weepiness (or what I like to call, feeling like “emotional mush.”) It can also help prevent a delayed labor.
If taken daily for the last month in an otherwise uneventful pregnancy, it sets the mother up so that when the time comes, her labor won’t lag.
But one of its most amazing uses (as Dr. Jackson discovered) comes into play when the baby is breech. I have no better example to share than that of one of my staff members, so here is Carrie’s story in her own words:
Two years ago, I was preparing to give birth to my third baby.
Having no need for interventions with my two previous homebirths, I proceeded to plan my third homebirth with the same midwife.
In the last month, I started to prepare for the birth: I purchased my birthing tub, attended hypnobirthing classes, and ordered any remedies I may need for the birth process — all in advance.
But at week 35, my midwife discovered that my baby was breech.
This threw my plans for a loop, as I was informed that unless the baby turned, I would not be able to birth at home.
I have always been a “good student” and immediately dedicated myself to the baby-turning methods described on Spinningbabies.com. I inverted myself daily, on an ironing board.
But the only thing that was spinning was my head!
After a week of practice, the baby still did not turn. I was getting anxious. That’s when I got the recommendation from Joette.
Alright midwives and expectant parents, get your pencils ready for this one: Pulsatilla 200 , twice daily.
You mean I don’t have to put myself through any uncomfortable positions or exercises?
This is what I realize time and again about homeopathy: It is just so easy.
And as for my third baby? I got to deliver him at home in my birth pool, just as planned. In fact, I’m pretty sure I felt him start to move into the correct position after taking my second dose of Pulsatilla.
Certainly, a good reason to keep Pulsatilla on hand during pregnancy.
If you are a midwife or expectant parent, be sure you stay tuned for our next two birth-related blogs.
The next blog will cover what I call the “premier” birth remedy. It’s the remedy you’ll want to be sure you have in several potencies for labor.
Should you be interested in learning more about the unique role homeopathy plays in the life of girls and women, and how to make health corrections with my simple practical homeopathy, consider my online course “Feminopathy.”
We owe it to ourselves (and to the family and friends who depend on us) to take care of and protect our bodies.
This is Practical Homeopathy® — proven, reproducible, effective protocols specific to women’s special health issues. Click here to learn more.
Call today and learn how homeopathy might just be the missing piece in your health strategy.
Joette is not a physician and the relationship between Joette and her clients is not of prescriber and patient, but as educator and client. It is fully the client's choice whether or not to take advantage of the information Joette presents. Homeopathy doesn't "treat" an illness; it addresses the entire person as a matter of wholeness that is an educational process, not a medical one. Joette believes that the advice and diagnosis of a physician is often in order.
We've provided links for your convenience but we do not receive any remuneration nor affiliation in payment from your purchase.
The Author disclaims all liability for any loss or risk, personal or otherwise incurred as a consequence of use of any material in this article. This information is not a substitute for professional medical advice, diagnosis or treatment.
Related Posts

59 thoughts on “Birthing Series Part One: Turning a Breech Baby”
I, too, used pulsatilla at 36 weeks for my fourth child who was breech. It worked! This was 29 years ago.
Happy birthday to your 29 year old!
Thank you Joette for your generosity and dedication your work is changing so many lives.
Great series! I’m due in 4 weeks. Will the other posts be out in that time?
Hold on! The next one will be next Sunday night.
Also worked for me exactly 32 years ago in Australia. My third baby was a shoulder presentation after two normal deliveries. Baby declined to turn when attempted manually by midwife and doctor. I was a bit sceptical (science + nursing background) when my lovely homebirth midwife gave me a dose of Pulsatilla 30c but we watched/felt as baby turned almost immediately. Within a few days she was back in shoulder presentation but turned with a second dose. Remained head down. She was a posterior presentation which made for a painful labour but at least I was able to have a normal delivery at home instead of a caesarian section thanks to my midwife’s homeopathic training and knowledge! I have been using homeopathy ever since. And have never stopped learning.
What a great story. Thanks for sharing.
Are you saying that a pregnant woman can use Pulsatilla daily for the last month and would that be 200C potency? Thank you for this info! My daughter is due in 10 days and I have set her up homeopathically so she may have a great recovery! She is having a homebirth
I like Pulsatilla 200 in the last month of pregnancy even if the baby is good position, but the Banerji Protocol is to use it every other day. There are others that are good to have on hand before during and after that you may or may not know about.
Joetta, the Feminopathy course looks amazing: I am a homebirth midwife in Georgia, USA. It doesn’t say, but does it provide CEUs?
There is no outside certification available at this time.
I’m 33 weeks and baby has turned transverse, would pulsatilla work for a transverse baby? Is it too early to take it? I tend to have large babies and worry she’ll get stuck like this and don’t want another cesarean. Thanks
I’m not able to give you personal advice on this forum. Read the post carefully and I’m sure you’ll find what you’re looking for.
The Pulsatilla card says 1 dose of 200C every other day (which you noted above is the Banerji protocol). Your article states 200C twice daily. Would you use the Banerji when everything looks good, and the twice daily if you know you have a breech presentation?
Would you use this in conjunction with the Caulophyllum 6x mentioned in your Baby Grande CD, or just pick one?
I should have clarified: This is my 3rd pregnancy. My due date was May 15th. Everything is normal; baby is in good position. I have been taking the Caulophyllum as you suggest in Baby Grande. I’m wondering if adding Pulsatilla is a good idea, or just stick with one remedy to aid in a faster, easier labor? Thanks!
If its clear that one is a better choice than the other, then go with that one. Having said this, I’ve used both in the last month and found the combo to be fruitful.
Just to let you know that the form to fill out for downloading the card does not appear when using Google Chrome. I switched to Microsoft Edge and was able to see it.
So grateful for this and future info! A rough and long labor was the reason I first started to study homeopathy, so this application of it never ceases to intrigue me.
Thank you, this is wonderful! I am expecting and 2 weeks away from my due date now. I know it is not preferred to deviate from Banerji protocol, but for overall body preparation these last few days would it be ok to take Pulsatilla 30 instead of 200 since that I all I have?
You may use whatever potency you choose, but if you hope to enjoy the results that the Banerjis and I have, it would behoove you to get the best potency.
Thank you Joette!
I hope the expectant mothers who have commented in these threads return and report!:) I am 40, and have been trying for a year to get pregnant with no luck so far. But I definitely want to use homeopathy!! My girls are 16, 17 1/2, and 19 and although each labor got shorter it was not ideal. Thank you!!
Homeopathy is over 230 years old, backed by data that has been gathered from the most influential and scientific organizations, and I offer information that represents that. I wouldn’t wait for someone on this blog to report back before giving it a go.
Oh I definitely plan to, but I have to get pregnant first:). I am using it for other acute situations that come up. I’ve only been aware of homeopathy for the last 4 or 5 weeks and am taking your beginner class, listening to the podcasts (I’ve listed to all at least once now) and ordering/reading books that are recommended. Now I am going through the blog posts and reading the comments. My comment was specifically in regards to labor. Thanks:)
What are the dosage instructions for the Pulsatilla 200ch? I am currently 37weeks 3 days and baby is breech. Doc says there is lots of room and baby is still very high. The bottle says to take 5 pellets 3 times a day but I am not sure. Is it 1 pellet just once or 5 pellets just once?
The information regarding frequency is in the article and the number of pills is printed on the label of the bottle.
According to the article Pulsatilla 200ch twice daily. And this should be continued until baby has turned?
Until the baby has turned or its ascertained that the baby cannot turn. Usually within a week or so.
Hi Joette, do you think or have you seen where Pulsatilla in the last month also helps with the hormone aspect of pregnancy that can result in mood swings or anxiety? I know from your classes that Ignatia is the go-to for anxiety and stress, but it hasn’t proven to be effective for me.
Pulsatilla is great for hormonal mood swings, etc. Read your materia medica; it will flesh out your understanding of Pulsatilla. Ignatia is only one of many.
Thanks for the reply! I did read again about Pulsatilla and I certainly identify with many aspects of it. I’m hopeful that it will help me.
I am 33 weeks 3 days with my 4th baby (6th pregnancy) and she has been in a breech position for 8 weeks – so I have been doing all the Spinning Babies things I can and seeing a Webster chiropractor. a mom today mentioned pulsatilla – I want to try! Is Boiron 200 the best brand to use? And should i do this twice daily or every other day? We will most likely be induced this birth at 39 weeks due to my history of loss, so I have about 5.5 weeks to get this baby turned for another vaginal birth (I’ve never had a surgical birth and usually birth with midwives out of the hospital, so am wanting to duplicate that with this hospital birth and our CNM as much as I can). <3
Your questions are answered in the article, including the link.
Thank you for replying! I did see the link to Boiron – I only asked if it is best because a holistic family group I’m in recommends other brands, so I wanted to double check before ordering 🙂 I also saw that in the article it recommends doing the dosing twice daily but in some of the comments it suggests every other day so before I begin I wanted to clarify. I re-read to check my understanding and realize the every other day refers to the Banerji protocol, so I’ll go with the twice daily per the article. Thank you for all the resources you provide!
‘Sounds like a plan. I like/trust Boiron.
Thank you!!
Any remedies on turning babies from a posterior “sunny side up” position? I had horrible back labor because of this with my first and my second, due in 4 weeks, seems to be in the same position. I tried getting the Baby Grande book (or cd?) and the feminopathy course but they are unavailable 🙁
https://feminopathy.joettecalabrese.com/
Dear Mrs. Calabrese,
If a breech was discovered during labor at a homebirth, would Pulsatilla 200 be used more frequently because of the urgent need for it to act?
Blessings & thank you.
I have no experience with an in labor breach but I would probably use it every few hours if there was that much time.
Thank you Mrs. Calabrese!
Does Pulsatilla 200 work for turning a posterior presentation or only on breech?
God bless you!
I believe it is specific for malpresentation, breech being one of the most common.
Thank you so much Mrs. Calabrese!! I was having THE HARDEST time deciding if Pulsatilla or Kali carb should be used. I’m still in a bit of a muddle, but your reply brings lots of clarity. Thank you again.
Mrs. Calabrese,
I just had to give you an update! PULSATILLA WORKED WONDERS!! The baby was Posterior at the beginning of labor & Pulsatilla corrected it. THREE more times, DURING ACTIVE LABOR, the baby reverted back and Pulsatilla corrected it every single time! The midwife was extremely impressed that it worked even though the head was very engaged, amazing!
Thank you for this article and answering my question about Posterior presentation in the nick of time. That mother & baby are also very grateful I am sure!
It doesn’t surprise me that it worked so well but it always brings a smile to my face hearing of one more. So far, its never failed me. A baby coming into the world with homeopathy at the helm is a wonderful start to life. I must also add that it was your perspicacity and the repetition that made it a success. I assume you’re in my online classes or one of my study groups, yes?
Can remedies be helpful to the fetus in utero for the condition diagnosed as “severe fetal hydronephrosis “ in my 33 yr. old daughter; 3rd trimester. Or is it suggested to wait for the baby to be born and decide if remedies are needed at that point? Thank you.
I can’t say I’ve witnessed this addressed in utero but it’s most definitely worth addressing during pregnancy.
Hi! I’m hoping you are still replying to comments as I’m desperate at the moment 🙂 I am expecting twins, 36 weeks and 5 days right now. Baby A iS breech and the OBs will do a c section if he remains in that position. They will not attempt to deliver vaginally. DO you know if 200 ck (which is what I’ve found, not 200 c or 200 cf) will be ok for this situation? Have you heard of success with pulsatilla helping flip a twin? Thank you!! Thank you so much!
I can’t offer you personal medical advice. This is a teaching forum where I share what I know.
Hello, My baby has been transverse for about 2.5 months from what I can tell. I am currently 34 weeks. Her head is in my right ribs for the last 2 weeks, and the week before that it was on my left side, and the week before that one it was on my right side (according to quick peek ultrasound confirmations) so she has moved somewhat like side to side but I never felt her head down. She was head down at her 23 week ultrasound. She flipped since that scan and has been transverse since. Since I tried all exercises and chiropractor many times and nothing happened, I decided to try the pulsatilla. I tried 30c for 1.5 weeks (twice a day), and nothing happened, so I bought the 200ck and did that twice a day for about 4-5 days. Still nothing. Would you suggest I keep going with the pulsatilla, or is it safe to assume if she hasn’t moved yet at this point after 1 month of trying including the pulsatilla for over 2 weeks, there is a reason she can’t turn? I’m just trying to figure out if it is safe to keep taking this for extended periods of time if nothing happened yet. Thanks!
If a woman is taking Cantharis as part of the protocol for interstitial cystitis, will it antidote Pulsatilla taken to turn a posterior baby? I know many “antidoting” comments are classical-based, but I need both protocols to work. 🙂 Thanks!!
We find that when remedies that would seemingly antidote each other are used in the same schedule they usually don’t do so when repeated as per protocols.
Hi, another woman asked this-she was expecting twins…i didnt notice a reply for this: do i purchase 200c or 200ck? thank you!!!
Either one.
Pulsatilla 2D to turn a transverse baby…Can I start at 33 weeks? Or wait until 36 weeks?
I’m 28 weeks and baby boy has been breech for both growth scans. Is it safe to try pulsatilla now, or should I wait until the last month of my pregnancy.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Follow Joette
- Online Courses
- Guided Study Groups
- Homeopathic Consultations

Joette’s Materia Medica

I designed it especially to provide a framework to guide you through your remedy choices. It is perfect for busy mothers and others who love curing their families themselves.
Protect Yourself from the Flu

Deal with the flu without drugs and expensive commercial products.
Combo Pack: Top 7 Products

Go from clueless to clued-in…in the fastest way possible.
Cell Salts: Learn Homeopathy at Home

The easiest, safest and most inexpensive way to treat your whole family.
Homeopathy in First Aid

Learn to choose the correct homeopathic remedy to give on the way to the emergency room or better yet, avoid the trip altogether.
Cure Yourself and Your Family with Homeopathy

Homeopathy is inexpensive, non-invasive and profoundly curative.
Secret Spoonfuls: Confessions of a Sneaky Mom with Kid Pleasing Recipes – CD & Booklet

Boost and maintain optimum health with simple foods, instead of vitamin pills.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
- Management of breech presentation
Evidence review M
NICE Guideline, No. 201
National Guideline Alliance (UK) .
- Copyright and Permissions
Review question
What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy?
Introduction
Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman’s and the baby’s health. The aim of this review is to determine the most effective way of managing a breech presentation in late pregnancy.
Summary of the protocol
Please see Table 1 for a summary of the Population, Intervention, Comparison and Outcome (PICO) characteristics of this review.
Summary of the protocol (PICO table).
For further details see the review protocol in appendix A .
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual 2014 . Methods specific to this review question are described in the review protocol in appendix A .
Declarations of interest were recorded according to NICE’s conflicts of interest policy .
Clinical evidence
Included studies.
Thirty-six randomised controlled trials (RCTs) were identified for this review.
The included studies are summarised in Table 2 .
Three studies reported on external cephalic version (ECV) versus no intervention ( Dafallah 2004 , Hofmeyr 1983 , Rita 2011 ). One study reported on a 4-arm trial comparing acupuncture, sweeping of fetal membranes, acupuncture plus sweeping, and no intervention ( Andersen 2013 ). Two studies reported on postural management versus no intervention ( Chenia 1987 , Smith 1999 ).
Seven studies reported on ECV plus anaesthesia ( Chalifoux 2017 , Dugoff 1999 , Khaw 2015 , Mancuso 2000 , Schorr 1997 , Sullivan 2009 , Weiniger 2010 ). Of these studies, 1 study compared ECV plus anaesthesia to ECV plus other dosages of the same anaesthetic ( Chalifoux 2017 ); 4 studies compared ECV plus anaesthesia to ECV only ( Dugoff 1999 , Mancuso 2000 , Schorr 1997 , Weiniger 2010 ); and 2 studies compared ECV plus anaesthesia to ECV plus a different anaesthetic ( Khaw 2015 , Sullivan 2009 ).
Ten studies reported ECV plus a β2 receptor agonist ( Brocks 1984 , Fernandez 1997 , Hindawi 2005 , Impey 2005 , Mahomed 1991 , Marquette 1996 , Nor Azlin 2005 , Robertson 1987 , Van Dorsten 1981 , Vani 2009 ). Of these studies, 5 studies compared ECV plus a β2 receptor agonist to ECV plus placebo ( Fernandez 1997 , Impey 2005 , Marquette 1996 , Nor Azlin 2005 , Vani 2009 ); 1 study compared ECV plus a β2 receptor agonist to ECV alone ( Robertson 1987 ); and 4 studies compared ECV plus a β2 receptor agonist to no intervention ( Brocks 1984 , Hindawi 2005 , Mahomed 1991 , Van Dorsten 1981 ).
One study reported on ECV plus Ca 2+ channel blocker versus ECV plus placebo ( Kok 2008 ). Two studies reported on ECV plus β2 receptor agonist versus ECV plus Ca 2+ channel blocker ( Collaris 2009 , Mohamed Ismail 2008 ). Four studies reported on ECV plus a µ-receptor agonist ( Burgos 2016 , Liu 2016 , Munoz 2014 , Wang 2017 ), of which 3 compared against ECV plus placebo ( Liu 2016 , Munoz 2014 , Wang 2017 ) and 1 compared to ECV plus nitrous oxide ( Burgos 2016 ).
Four studies reported on ECV plus nitroglycerin ( Bujold 2003a , Bujold 2003b , El-Sayed 2004 , Hilton 2009 ), of which 2 compared it to ECV plus β2 receptor agonist ( Bujold 2003b , El-Sayed 2004 ) and compared it to ECV plus placebo ( Bujold 2003a , Hilton 2009 ). One study compared ECV plus amnioinfusion versus ECV alone ( Diguisto 2018 ) and 1 study compared ECV plus talcum powder to ECV plus gel ( Vallikkannu 2014 ).
One study was conducted in Australia ( Smith 1999 ); 4 studies in Canada ( Bujold 2003a , Bujold 2003b , Hilton 2009 , Marquette 1996 ); 2 studies in China ( Liu 2016 , Wang 2017 ); 2 studies in Denmark ( Andersen 2013 , Brocks 1984 ); 1 study in France ( Diguisto 2018 ); 1 study in Hong Kong ( Khaw 2015 ); 1 study in India ( Rita 2011 ); 1 study in Israel ( Weiniger 2010 ); 1 study in Jordan ( Hindawi 2005 ); 5 studies in Malaysia ( Collaris 2009 , Mohamed Ismail 2008 , Nor Azlin 2005 , Vallikkannu 2014 , Vani 2009 ); 1 study in South Africa ( Hofmeyr 1983 ); 2 studies in Spain ( Burgos 2016 , Munoz 2014 ); 1 study in Sudan ( Dafallah 2004 ); 1 study in The Netherlands ( Kok 2008 ); 2 studies in the UK ( Impey 2005 , Chenia 1987 ); 9 studies in US ( Chalifoux 2017 , Dugoff 1999 , El-Sayed 2004 , Fernandez 1997 , Mancuso 2000 , Robertson 1987 , Schorr 1997 , Sullivan 2009 , Van Dorsten 1981 ); and 1 study in Zimbabwe ( Mahomed 1991 ).
The majority of studies were 2-arm trials, but there was one 3-arm trial ( Khaw 2015 ) and two 4-arm trials ( Andersen 2013 , Chalifoux 2017 ). All studies were conducted in a hospital or an outpatient ward connected to a hospital.
See the literature search strategy in appendix B and study selection flow chart in appendix C .
Excluded studies
Studies not included in this review with reasons for their exclusions are provided in appendix K .
Summary of clinical studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 2 .
Summary of included studies.
See the full evidence tables in appendix D and the forest plots in appendix E .
Quality assessment of clinical outcomes included in the evidence review
See the evidence profiles in appendix F .
Economic evidence
A systematic review of the economic literature was conducted but no economic studies were identified which were applicable to this review question.
A single economic search was undertaken for all topics included in the scope of this guideline. See supplementary material 2 for details.
Economic studies not included in this review are listed, and reasons for their exclusion are provided in appendix K .
Summary of studies included in the economic evidence review
No economic studies were identified which were applicable to this review question.
Economic model
No economic modelling was undertaken for this review because the committee agreed that other topics were higher priorities for economic evaluation.
Evidence statements
Clinical evidence statements, comparison 1. complementary therapy versus control (no intervention), critical outcomes, cephalic presentation in labour.
No evidence was identified to inform this outcome.
Method of birth
Caesarean section.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.74 (95% CI 0.38 to 1.43).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 1.29 (95% CI 0.73 to 2.29).
Admission to SCBU/NICU
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.19 (95% CI 0.02 to 1.62).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.40 (0.08 to 2.01).
Fetal death after 36 +0 weeks gestation
Infant death up to 4 weeks chronological age, important outcomes, apgar score <7 at 5 minutes.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.32 (95% CI 0.01 to 7.78).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.33 (0.01 to 8.09).
Birth before 39 +0 weeks of gestation
Comparison 2. complementary therapy versus other treatment.
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.64 (95% CI 0.34 to 1.22).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.57 (95% CI 0.30 to 1.07).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 1.13 (95% CI 0.66 to 1.94).
- Very low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.33 (95% CI 0.03 to 3.12).
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.48 (95% CI 0.04 to 5.22).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.69 (95% CI 0.12 to 4.02).
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 3. ECV versus no ECV
- Moderate quality evidence from 2 RCTs (N=680) showed that there is clinically important difference favouring ECV over no ECV on cephalic presentation in labour in pregnant women with breech presentation: RR 1.83 (95% CI 1.53 to 2.18).
Cephalic vaginal birth
- Very low quality evidence from 3 RCTs (N=740) showed that there is a clinically important difference favouring ECV over no ECV on cephalic vaginal birth in pregnant women with breech presentation: RR 1.67 (95% CI 1.20 to 2.31).
Breech vaginal birth
- Very low quality evidence from 2 RCTs (N=680) showed that there is no clinically important difference between ECV and no ECV on breech vaginal birth in pregnant women with breech presentation: RR 0.29 (95% CI 0.03 to 2.84).
- Very low quality evidence from 3 RCTs (N=740) showed that there is no clinically important difference between ECV and no ECV on the number of caesarean sections in pregnant women with breech presentation: RR 0.52 (95% CI 0.23 to 1.20).
- Very low quality evidence from 1 RCT (N=60) showed that there is no clinically important difference between ECV and no ECV on admission to SCBU//NICU in pregnant women with breech presentation: RR 0.50 (95% CI 0.14 to 1.82).
- Very low evidence from 3 RCTs (N=740) showed that there is no statistically significant difference between ECV and no ECV on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: Peto OR 0.29 (95% CI 0.05 to 1.73) p=0.18.
- Very low quality evidence from 2 RCTs (N=120) showed that there is no clinically important difference between ECV and no ECV on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.28 (95% CI 0.04 to 1.70).
Comparison 4. ECV + Amnioinfusion versus ECV only
- Very low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.74 (95% CI 0.74 to 4.12).
- Low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.95 (95% CI 0.75 to 1.19).

Comparison 5. ECV + Anaesthesia versus ECV only
- Very low quality evidence from 2 RCTs (N=210) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.16 (95% CI 0.56 to 2.41).
- Very low quality evidence from 5 RCTs (N=435) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.16 (95% CI 0.77 to 1.74).
- Very low quality evidence from 1 RCT (N=108) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on breech vaginal birth in pregnant women with breech presentation: RR 0.33 (95% CI 0.04 to 3.10).
- Very low quality evidence from 3 RCTs (N=263) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.76 (95% CI 0.42 to 1.38).
- Moderate quality evidence from 1 RCT (N=69) showed that there is a clinically important difference favouring ECV plus anaesthesia over ECV alone on admission to SCBU/NICU in pregnant women with breech presentation: MD −1.80 (95% CI −2.53 to −1.07).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 6. ECV + Anaesthesia versus ECV + Anaesthesia
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.13 (95% CI 0.73 to 1.74).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 0.05mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.69 (95% CI 0.37 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.19 (95% CI 0.79 to 1.79).
- Low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.92 (95% CI 0.68 to 1.24).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.08 (95% CI 0.78 to 1.50).
- Very low evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.70 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.17 (95% CI 0.86 to 1.61).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.03 (95% CI 0.77 to 1.37).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.88 (95% CI 0.64 to 1.20).
Comparison 7. ECV + β2 agonist versus Control (no intervention)
- Moderate quality evidence from 2 RCTs (N=256) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on cephalic presentation in labour in pregnant women with breech presentation: RR 4.83 (95% CI 3.27 to 7.11).
- Very low quality evidence from 3 RCTs (N=265) showed that there no clinically important difference between ECV plus β2 agonist and control (no intervention) on cephalic vaginal birth in pregnant women with breech presentation: RR 2.03 (95% CI 0.22 to 19.01).
- Very low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on breech vaginal birth in pregnant women with breech presentation: RR 0.38 (95% CI 0.20 to 0.69).
- Low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.53 (95% CI 0.41 to 0.67).
- Very low quality evidence from 1 RCT (N=48) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RD 0.00 (95% CI −0.08 to 0.08).
- Very low quality evidence from 3 RCTs (N=208) showed that there is no statistically significant difference between ECV plus β2 agonist and control (no intervention) on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD −0.01 (95% CI −0.03 to 0.01) p=0.66.
- Very low quality evidence from 2 RCTs (N=208) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.80 (95% CI 0.31 to 2.10).
Comparison 8. ECV + β2 agonist versus ECV only
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on cephalic vaginal birth in pregnant women with breech presentation: RR 1.32 (95% CI 0.67 to 2.62).
- Very low quality evidence from 1 RCT (N=58) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on breech vaginal birth in pregnant women with breech presentation: RR 0.75 (95% CI 0.22 to 2.50).
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 0.79 (95% CI 0.27 to 2.28).
- Very low quality evidence from 1 RCT (N=114) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.00 (95% CI 0.21 to 4.75).
Comparison 9. ECV + β2 agonist versus ECV + Placebo
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.54 (95% CI 0.24 to 9.76).
- Very low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 1.27 (95% CI 0.41 to 3.89).
- Very low quality evidence from 2 RCTs (N=227) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on breech vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.33 to 2.97).
- Low quality evidence from 4 RCTs (N=532) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.81 (95% CI 0.72 to 0.92)
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.78 (95% CI 0.17 to 3.63).
- Very low quality evidence from 1 RCT (N=124) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 10. ECV + Ca 2+ channel blocker versus ECV + Placebo
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.87 to 1.48).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.90 (95% CI 0.73 to 1.12).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 1.11 (95% CI 0.88 to 1.40).
- High quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: MD −0.20 (95% CI −0.70 to 0.30).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no statistically significant difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.01 to 0.01) p=1.00.
- Low quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.52 (95% 0.05 to 5.02).
Comparison 11. ECV + Ca2+ channel blocker versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=90) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on cephalic presentation in labour in pregnant women with breech presentation: RR 0.62 (95% CI 0.39 to 0.98).
- Very low quality evidence from 2 RCTs (N=126) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 1.26 (95% CI 0.55 to 2.89).
- Very low quality evidence from 2 RCTs (N=132) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on the number of caesarean sections in pregnant women with breech presentation: RR 1.42 (95% CI 1.06 to 1.91).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on admission to SCBU/NICU in pregnant women with breech presentation: Peto OR 0.53 (95% CI 0.05 to 5.22).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 12. ECV + µ-receptor agonist versus ECV only
- High quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.80 to 1.24).
- Low quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 1.00 (95% CI 0.42 to 2.40).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 13. ECV + µ-receptor agonist versus ECV + Placebo
Cephalic vaginal birth after successful ecv.
- High quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on cephalic vaginal birth after successful ECV in pregnant women with breech presentation: RR 1.00 (95% CI 0.86 to 1.17).
Caesarean section after successful ECV
- Low quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after successful ECV in pregnant women with breech presentation: RR 0.97 (95% CI 0.33 to 2.84).
Breech vaginal birth after unsuccessful ECV
- High quality evidence from 3 RCTs (N=186) showed that there is a clinically important difference favouring ECV plus µ-receptor agonist over ECV plus placebo on breech vaginal birth after unsuccessful ECV in pregnant women with breech presentation: RR 0.10 (95% CI 0.02 to 0.53).
Caesarean section after unsuccessful ECV
- Moderate quality evidence from 3 RCTs (N=186) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after unsuccessful ECV in pregnant women with breech presentation: RR 1.19 (95% CI 1.09 to 1.31).
- Low quality evidence from 1 RCT (N=137) showed that there is no statistically significant difference between ECV plus µ-receptor agonist and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03) p=1.00.
Comparison 14. ECV + µ-receptor agonist versus ECV + Anaesthesia
- Moderate quality evidence from 1 RCT (N=92) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on cephalic vaginal birth in pregnant women with breech presentation: RR 1.04 (95% CI 0.84 to 1.29).
- Very low quality evidence from 2 RCTs (N=212) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on the number of caesarean sections in pregnant women with breech presentation: RR 0.90 (95% CI 0.61 to 1.34).
- Very low quality evidence from 1 RCT (N=129) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on admission to SCBU/NICU in pregnant women with breech presentation: RR 2.30 (95% CI 0.21 to 24.74).
- Low quality evidence from 2 RCTs (N=255) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 15. ECV + Nitric oxide donor versus ECV + Placebo
- Very low quality evidence from 3 RCTs (N=224) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.59 to 2.16).
- Low quality evidence from 1 RCT (N=99) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.78 (95% CI 0.49 to 1.22).
- Low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.83 (95% CI 0.68 to 1.01).
Comparison 16. ECV + Nitric oxide donor versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=74) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus nitric oxide donor on cephalic presentation in labour in pregnant women with breech presentation: RR 0.56 (95% CI 0.29 to 1.09).
- Very low quality evidence from 2 RCTs (N=97) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 0.98 (95% CI 0.47 to 2.05).
- Very low quality evidence from 1 RCT (N=59) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on the number of caesarean sections in pregnant women with breech presentation: RR 1.07 (95% CI 0.73 to 1.57).
Comparison 17. ECV + Talcum powder versus ECV + Gel
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic presentation in labour in pregnant women with breech presentation: RR 1.02 (95% CI 0.68 to 1.53).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic vaginal birth in pregnant women with breech presentation: RR 1.08 (95% CI 0.67 to 1.74).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.67 to 1.33).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.96 (95% CI 0.38 to 10.19).
Comparison 18. Postural management versus No postural management
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic presentation in labour in pregnant women with breech presentation: RR 1.26 (95% CI 0.70 to 2.30).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic vaginal birth in pregnant women with breech presentation: RR 1.11 (95% CI 0.59 to 2.07).
Breech vaginal delivery
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on breech vaginal delivery in pregnant women with breech presentation: RR 1.15 (95% CI 0.67 to 1.99).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on the number of caesarean sections in pregnant women with breech presentation: RR 0.69 (95% CI 0.31 to 1.52).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.24 (95% CI 0.03 to 2.03).
Comparison 19. Postural management + ECV versus ECV only
- Moderate quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 1.05 (95% CI 0.80 to 1.38).
- Low quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.13 (95% CI 0.00 to 6.55).
Economic evidence statements
No economic evidence was identified which was applicable to this review question.
The committee’s discussion of the evidence
Interpreting the evidence, the outcomes that matter most.
Provision of antenatal care is important for the health and wellbeing of both mother and baby with the aim of avoiding adverse pregnancy outcomes and enhancing maternal satisfaction and wellbeing. Breech presentation in labour may be associated with adverse outcomes for the fetus, which has contributed to an increased likelihood of caesarean birth. The committee therefore agreed that cephalic presentation in labour and method of birth were critical outcomes for the woman, and admission to SCBU/NICU, fetal death after 36 +0 weeks gestation, and infant death up to 4 weeks chronological age were critical outcomes for the baby. Apgar score <7 at 5 minutes and birth before 39 +0 weeks of gestation were important outcomes for the baby.
The quality of the evidence
The quality of the evidence for interventions for managing a longitudinal lie fetal malpresentation (that is breech presentation) in late pregnancy ranged from very low to high, with most of the evidence being of a very low or low quality.
This was predominately due to serious overall risk of bias in some outcomes; imprecision around the effect estimate in some outcomes; indirect population in some outcomes; and the presence of serious heterogeneity in some outcomes, which was unresolved by subgroup analysis. The majority of included studies had a small sample size, which contributed to imprecision around the effect estimate.
No evidence was identified to inform the outcomes of infant death up to 4 weeks chronological age and birth before 39 +0 weeks of gestation.
There was no publication bias identified in the evidence. However, the committee noted the influence pharmacological developers may have in these trials as funders, and took this into account in their decision making.
Benefits and harms
The committee discussed that in the case of breech presentation, a discussion with the woman about the different options and their potential benefits, harms and implications is needed to ensure an informed decision. The committee discussed that some women may prefer a breech vaginal birth or choose an elective caesarean birth, and that her preferences should be supported, in line with shared decision making.
The committee discussed that external cephalic version is standard practice for managing breech presentation in uncomplicated singleton pregnancies at or after 36+0 weeks. The committee discussed that there could be variation in the success rates of ECV based on the experience of the healthcare professional providing the ECV. There was some evidence supporting the use of ECV for managing a breech presentation in late pregnancy. The evidence showed ECV had a clinically important benefit in terms of cephalic presentations in labour and cephalic vaginal deliveries, when compared to no intervention. The committee noted that the evidence suggested that ECV was not harmful to the baby, although the effect estimate was imprecise relating to the relative rarity of the fetal death as an outcome.
Cephalic (head-down) vaginal birth is preferred by many women and the evidence suggests that external cephalic version is an effective way to achieve this. The evidence suggested ECV increased the chance for a cephalic vaginal birth and the committee agreed that it was important to explain this to the woman during her consultation.
The committee discussed the optimum timing for ECV. Timing of ECV must take into account the likelihood of the baby turning naturally before a woman commences labour and the possibility of the baby turning back to a breech presentation after ECV if it is done too early. The committee noted that in their experience, current practice was to perform ECV at 37 gestational weeks. The majority of the evidence demonstrating a benefit of ECV in this review involved ECV performed around 37 gestational weeks, although the review did not look for studies directly comparing different timings of ECV and their relative success rates.
The evidence in this review excluded women with previous complicated pregnancies, such as those with previous caesarean section or uterine surgery. The committee discussed that a previous caesarean section indicates a complicated pregnancy and that this population of women are not the focus of this guideline, which concentrates on women with uncomplicated pregnancies.
The committee’s recommendations align with other NICE guidance and cross references to the NICE guideline on caesarean birth and the section on breech presenting in labour in the NICE guideline on intrapartum care for women with existing medical conditions or obstetric complications and their babies were made.
ECV combined with pharmacological agents
There were some small studies comparing a variety of pharmacological agents (including β2 agonists, Ca 2+ channel blockers, µ-receptor agonists and nitric oxide donors) given alongside ECV. Overall the evidence typically showed no clinically important benefit of adding any pharmacological agent to ECV except in comparisons with a control arm with no ECV where it was not possible to isolate the effect of the ECV versus the pharmacological agent. The evidence tended toward benefit most for β2 agonists and µ-receptor agonists however there was no consistent or high quality evidence of benefit even for these agents. The committee agreed that although these pharmacological agents are used in practice, there was insufficient evidence to make a recommendation supporting or refuting their use or on which pharmacological agent should be used.
The committee discussed that the evidence suggesting µ-receptor agonist, remifentanil, had a clinically important benefit in terms reducing breech vaginal births after unsuccessful ECV was biologically implausible. The committee noted that this pharmacological agent has strong sedative effects, depending on the dosage, and therefore studies comparing it to a placebo had possible design flaws as it would be obvious to all parties whether placebo or active drug had been received. The committee discussed that the risks associated with using remifentanil such as respiratory depression, likely outweigh any potential added benefit it may have on managing breech presentation.
There was some evidence comparing different anaesthetics together with ECV. Although there was little consistent evidence of benefit overall, one small study of low quality showed a combination of 2% lidocaine and epinephrine via epidural catheter (anaesthesia) with ECV showed a clinically important benefit in terms of cephalic presentations in labour and the method of birth. The committee discussed the evidence and agreed the use of anaesthesia via epidural catheter during ECV was uncommon practice in the UK and could be expensive, overall they agreed the strength of the evidence available was insufficient to support a change in practice.
Postural management
There was limited evidence on postural management as an intervention for managing breech presentation in late pregnancy, which showed no difference in effectiveness. Postural management was defined as ‘knee-chest position for 15 minutes, 3 times a day’. The committee agreed that in their experience women valued trying interventions at home first which might make postural management an attractive option for some women, however, there was no evidence that postural management was beneficial. The committee also noted that in their experience postural management can cause notable discomfort so it is not an intervention without disadvantages.
Cost effectiveness and resource use
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question.
The committee’s recommendations to offer external cephalic version reinforces current practice. The committee noted that, compared to no intervention, external cephalic version results in clinically important benefits and that there would also be overall downstream cost savings from lower adverse events. It was therefore the committee’s view that offering external cephalic version is cost effective and would not entail any resource impact.
Andersen 2013
Brocks 1984
Bujold 2003
Burgos 2016
Chalifoux 2017
Chenia 1987
Collaris 2009
Dafallah 2004
Diguisto 2018
Dugoff 1999
El-Sayed 2004
Fernandez 1997
Hindawi 2005
Hilton 2009
Hofmeyr 1983
Mahomed 1991
Mancuso 2000
Marquette 1996
Mohamed Ismail 2008
NorAzlin 2005
Robertson 1987
Schorr 1997
Sullivan 2009
VanDorsten 1981
Vallikkannu 2014
Weiniger 2010
Appendix A. Review protocols
Review protocol for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 260K)
Appendix B. Literature search strategies
Literature search strategies for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 281K)
Appendix C. Clinical evidence study selection
Clinical study selection for: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 113K)
Appendix D. Clinical evidence tables
Clinical evidence tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.2M)
Appendix E. Forest plots
Forest plots for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 678K)
Appendix F. GRADE tables
GRADE tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.0M)
Appendix G. Economic evidence study selection
Economic evidence study selection for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix h. economic evidence tables, economic evidence tables for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix i. economic evidence profiles, economic evidence profiles for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix j. economic analysis, economic evidence analysis for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No economic analysis was conducted for this review question.
Appendix K. Excluded studies
Excluded clinical and economic studies for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, clinical studies, table 24 excluded studies.
View in own window
Economic studies
No economic evidence was identified for this review.
Appendix L. Research recommendations
Research recommendations for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No research recommendations were made for this review question.
Evidence reviews underpinning recommendation 1.2.38
These evidence reviews were developed by the National Guideline Alliance, which is a part of the Royal College of Obstetricians and Gynaecologists
Disclaimer : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government , Scottish Government , and Northern Ireland Executive . All NICE guidance is subject to regular review and may be updated or withdrawn.
- Cite this Page National Guideline Alliance (UK). Management of breech presentation: Antenatal care: Evidence review M. London: National Institute for Health and Care Excellence (NICE); 2021 Aug. (NICE Guideline, No. 201.)
- PDF version of this title (2.2M)
In this Page
Other titles in this collection.
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 201: Antenatal care
Supplemental NICE documents
- Supplement 1: Methods (PDF)
- Supplement 2: Health economics (PDF)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Identification of breech presentation: Antenatal care: Evidence review L [ 2021] Review Identification of breech presentation: Antenatal care: Evidence review L National Guideline Alliance (UK). 2021 Aug
- Vaginal delivery of breech presentation. [J Obstet Gynaecol Can. 2009] Vaginal delivery of breech presentation. Kotaska A, Menticoglou S, Gagnon R, MATERNAL FETAL MEDICINE COMMITTEE. J Obstet Gynaecol Can. 2009 Jun; 31(6):557-566.
- Review Cephalic version by moxibustion for breech presentation. [Cochrane Database Syst Rev. 2005] Review Cephalic version by moxibustion for breech presentation. Coyle ME, Smith CA, Peat B. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD003928. Epub 2005 Apr 18.
- [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. [Gynecol Obstet Fertil Senol. 2...] [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. Riethmuller D, Ramanah R, Mottet N. Gynecol Obstet Fertil Senol. 2018 Dec; 46(12):937-947. Epub 2018 Oct 28.
- Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. [J Obstet Gynaecol Br Emp. 1961] Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. BAINBRIDGE MN, NIXON WC, SMYTH CN. J Obstet Gynaecol Br Emp. 1961 Oct; 68:748-54.
Recent Activity
- Management of breech presentation Management of breech presentation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Physician Physician Board Reviews Physician Associate Board Reviews CME Lifetime CME Free CME
- Student USMLE Step 1 USMLE Step 2 USMLE Step 3 COMLEX Level 1 COMLEX Level 2 COMLEX Level 3 96 Medical School Exams Student Resource Center NCLEX - RN NCLEX - LPN/LVN/PN 24 Nursing Exams
- Nurse Practitioner APRN/NP Board Reviews CNS Certification Reviews CE - Nurse Practitioner FREE CE
- Nurse RN Certification Reviews CE - Nurse FREE CE
- Pharmacist Pharmacy Board Exam Prep CE - Pharmacist
- Allied Allied Health Exam Prep Dentist Exams CE - Social Worker CE - Dentist
- Point of Care
- Free CME/CE
Breech Presentation
Introduction.
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the fetus sitting with flexion of both hips and both legs in a tuck position. Finally, the incomplete breech can have any combination of one or both hips extended, also known as footling (one leg extended) breech, or double footling breech (both legs extended). [1] [2] [3]
Register For Free And Read The Full Article
Learn more about a subscription to statpearls point-of-care.
Clinical conditions associated with breech presentation include those that may increase or decrease fetal motility, or affect the vertical polarity of the uterine cavity. Prematurity, multiple gestations, aneuploidies, congenital anomalies, Mullerian anomalies, uterine leiomyoma, and placental polarity as in placenta previa are most commonly associated with a breech presentation. Also, a previous history of breech presentation at term increases the risk of repeat breech presentation at term in subsequent pregnancies. [4] [5] These are discussed in more detail in the pathophysiology section.
Epidemiology
Breech presentation occurs in 3% to 4% of all term pregnancies. A higher percentage of breech presentations occurs with less advanced gestational age. At 32 weeks, 7% of fetuses are breech, and 28 weeks or less, 25% are breech.
Specifically, following one breech delivery, the recurrence rate for the second pregnancy was nearly 10%, and for a subsequent third pregnancy, it was 27%. Prior cesarean delivery has also been described by some to increase the incidence of breech presentation two-fold.
Pathophysiology
As mentioned previously, the most common clinical conditions or disease processes that result in the breech presentation are those that affect fetal motility or the vertical polarity of the uterine cavity. [6] [7]
Conditions that change the vertical polarity or the uterine cavity, or affect the ease or ability of the fetus to turn into the vertex presentation in the third trimester include:
- Mullerian anomalies: Septate uterus, bicornuate uterus, and didelphys uterus
- Placentation: Placenta previa as the placenta is occupying the inferior portion of the uterine cavity. Therefore, the presenting part cannot engage
- Uterine leiomyoma: Mainly larger myomas located in the lower uterine segment, often intramural or submucosal, that prevent engagement of the presenting part.
- Prematurity
- Aneuploidies and fetal neuromuscular disorders commonly cause hypotonia of the fetus, inability to move effectively
- Congenital anomalies: Fetal sacrococcygeal teratoma, fetal thyroid goiter
- Polyhydramnios: Fetus is often in unstable lie, unable to engage
- Oligohydramnios: Fetus is unable to turn to vertex due to lack of fluid
- Laxity of the maternal abdominal wall: Uterus falls forward, the fetus is unable to engage in the pelvis.
The risk of cord prolapse varies depending on the type of breech. Incomplete or footling breech carries the highest risk of cord prolapse at 15% to 18%, while complete breech is lower at 4% to 6%, and frank breech is uncommon at 0.5%.
History and Physical
During the physical exam, using the Leopold maneuvers, palpation of a hard, round, mobile structure at the fundus and the inability to palpate a presenting part in the lower abdomen superior to the pubic bone or the engaged breech in the same area, should raise suspicion of a breech presentation.
During a cervical exam, findings may include the lack of a palpable presenting part, palpation of a lower extremity, usually a foot, or for the engaged breech, palpation of the soft tissue of the fetal buttocks may be noted. If the patient has been laboring, caution is warranted as the soft tissue of the fetal buttocks may be interpreted as caput of the fetal vertex.
Any of these findings should raise suspicion and ultrasound should be performed.
Diagnosis of a breech presentation can be accomplished through abdominal exam using the Leopold maneuvers in combination with the cervical exam. Ultrasound should confirm the diagnosis.
On ultrasound, the fetal lie and presenting part should be visualized and documented. If breech presentation is diagnosed, specific information including the specific type of breech, the degree of flexion of the fetal head, estimated fetal weight, amniotic fluid volume, placental location, and fetal anatomy review (if not already done previously) should be documented.
Treatment / Management
Expertise in the delivery of the vaginal breech baby is becoming less common due to fewer vaginal breech deliveries being offered throughout the United States and in most industrialized countries. The Term Breech Trial (TBT), a well-designed, multicenter, international, randomized controlled trial published in 2000 compared planned vaginal delivery to planned cesarean delivery for the term breech infant. The investigators reported that delivery by planned cesarean resulted in significantly lower perinatal mortality, neonatal mortality, and serious neonatal morbidity. Also, there was no significant difference in maternal morbidity or mortality between the two groups. Since that time, the rate of term breech infants delivered by planned cesarean has increased dramatically. Follow-up studies to the TBT have been published looking at maternal morbidity and outcomes of the children at two years. Although these reports did not show any significant difference in the risk of death and neurodevelopmental, these studies were felt to be underpowered. [8] [9] [10] [11] (B2)
Since the TBT, many authors since have argued that there are still some specific situations that vaginal breech delivery is a potential, safe alternative to planned cesarean. Many smaller retrospective studies have reported no difference in neonatal morbidity or mortality using these specific criteria.
The initial criteria used in these reports were similar: gestational age greater than 37 weeks, frank or complete breech presentation, no fetal anomalies on ultrasound examination, adequate maternal pelvis, and estimated fetal weight between 2500 g and 4000 g. In addition, the protocol presented by one report required documentation of fetal head flexion and adequate amniotic fluid volume, defined as a 3-cm vertical pocket. Oxytocin induction or augmentation was not offered, and strict criteria were established for normal labor progress. CT pelvimetry did determine an adequate maternal pelvis.
Despite debate on both sides, the current recommendation for the breech presentation at term includes offering external cephalic version (ECV) to those patients that meet criteria, and for those whom are not candidates or decline external cephalic version, a planned cesarean section for delivery sometime after 39 weeks.
Regarding the premature breech, gestational age will determine the mode of delivery. Before 26 weeks, there is a lack of quality clinical evidence to guide mode of delivery. One large retrospective cohort study recently concluded that from 28 to 31 6/7 weeks, there is a significant decrease in perinatal morbidity and mortality in a planned cesarean delivery versus intended vaginal delivery, while there is no difference in perinatal morbidity and mortality in gestational age 32 to 36 weeks. Of note, due to lack of recruitment, no prospective clinical trials are examining this issue.
Differential Diagnosis
- Face and brow presentation
- Fetal anomalies
- Fetal death
- Grand multiparity
- Multiple pregnancies
- Oligohydramnios
- Pelvis Anatomy
- Preterm labor
- Primigravida
- Uterine anomalies
Pearls and Other Issues
In light of the decrease in planned vaginal breech deliveries, thus the decrease in expertise in managing this clinical scenario, it is prudent that policies requiring simulation and instruction in the delivery technique for vaginal breech birth are established to care for the emergency breech vaginal delivery.
Enhancing Healthcare Team Outcomes
A breech delivery is usually managed by an obstetrician, labor and delivery nurse, anesthesiologist and a neonatologist. The ultimate decison rests on the obstetrician. To prevent complications, today cesarean sections are performed and experienced with vaginal deliveries of breech presentation is limited. For healthcare workers including the midwife who has no experience with a breech delivery, it is vital to communicate with an obstetrician, otherwise one risks litigation if complications arise during delivery. [12] [13] [14]
Hinnenberg P, Toijonen A, Gissler M, Heinonen S, Macharey G. Outcome of small for gestational age-fetuses in breech presentation at term according to mode of delivery: a nationwide, population-based record linkage study. Archives of gynecology and obstetrics. 2019 Apr:299(4):969-974. doi: 10.1007/s00404-019-05091-2. Epub 2019 Feb 8 [PubMed PMID: 30734863]
Schlaeger JM, Stoffel CL, Bussell JL, Cai HY, Takayama M, Yajima H, Takakura N. Moxibustion for Cephalic Version of Breech Presentation. Journal of midwifery & women's health. 2018 May:63(3):309-322. doi: 10.1111/jmwh.12752. Epub 2018 May 18 [PubMed PMID: 29775226]
Niles KM, Barrett JFR, Ladhani NNN. Comparison of cesarean versus vaginal delivery of extremely preterm gestations in breech presentation: retrospective cohort study. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. 2019 Apr:32(7):1142-1147. doi: 10.1080/14767058.2017.1401997. Epub 2017 Nov 20 [PubMed PMID: 29157039]
Grabovac M, Karim JN, Isayama T, Liyanage SK, McDonald SD. What is the safest mode of birth for extremely preterm breech singleton infants who are actively resuscitated? A systematic review and meta-analyses. BJOG : an international journal of obstetrics and gynaecology. 2018 May:125(6):652-663. doi: 10.1111/1471-0528.14938. Epub 2017 Nov 2 [PubMed PMID: 28921813]
Andrews S, Leeman L, Yonke N. Finding the breech: Influence of breech presentation on mode of delivery based on timing of diagnosis, attempt at external cephalic version, and provider success with version. Birth (Berkeley, Calif.). 2017 Sep:44(3):222-229. doi: 10.1111/birt.12290. Epub 2017 May 8 [PubMed PMID: 28481464]
Walker S, Breslin E, Scamell M, Parker P. Effectiveness of vaginal breech birth training strategies: An integrative review of the literature. Birth (Berkeley, Calif.). 2017 Jun:44(2):101-109. doi: 10.1111/birt.12280. Epub 2017 Feb 17 [PubMed PMID: 28211102]
Hofmeyr GJ, Barrett JF, Crowther CA. Planned caesarean section for women with a twin pregnancy. The Cochrane database of systematic reviews. 2015 Dec 19:2015(12):CD006553. doi: 10.1002/14651858.CD006553.pub3. Epub 2015 Dec 19 [PubMed PMID: 26684389]
Ainsworth A, Sviggum HP, Tolcher MC, Weaver AL, Holman MA, Arendt KW. Lessons learned from a single institution's retrospective analysis of emergent cesarean delivery following external cephalic version with and without neuraxial anesthesia. International journal of obstetric anesthesia. 2017 May:31():57-62. doi: 10.1016/j.ijoa.2017.03.012. Epub 2017 Apr 2 [PubMed PMID: 28499551]
Hutton EK, Simioni JC, Thabane L. Predictors of success of external cephalic version and cephalic presentation at birth among 1253 women with non-cephalic presentation using logistic regression and classification tree analyses. Acta obstetricia et gynecologica Scandinavica. 2017 Aug:96(8):1012-1020. doi: 10.1111/aogs.13161. Epub 2017 May 27 [PubMed PMID: 28449212]
Adjaoud S, Demailly R, Michel-Semail S, Rakza T, Storme L, Deruelle P, Garabedian C, Subtil D. Is trial of labor harmful in breech delivery? A cohort comparison for breech and vertex presentations. Journal of gynecology obstetrics and human reproduction. 2017 May:46(5):445-448. doi: 10.1016/j.jogoh.2017.04.003. Epub 2017 Apr 13 [PubMed PMID: 28412313]
Poole KL, McDonald SD, Griffith LE, Hutton EK, Early ECV Pilot and ECV2 Trial Collaborative Group. Association of external cephalic version before term with late preterm birth. Acta obstetricia et gynecologica Scandinavica. 2017 Aug:96(8):998-1005. doi: 10.1111/aogs.13153. Epub 2017 May 16 [PubMed PMID: 28414857]
Domingues AP, Belo A, Moura P, Vieira DN. Medico-legal litigation in Obstetrics: a characterization analysis of a decade in Portugal. Revista brasileira de ginecologia e obstetricia : revista da Federacao Brasileira das Sociedades de Ginecologia e Obstetricia. 2015 May:37(5):241-6. doi: 10.1590/SO100-720320150005304. Epub [PubMed PMID: 26107576]
Delotte J, Oliver A, Boukaidi S, Mialon O, Breaud J, Benchimol D, Bongain A. [Who limit vaginal birth for breech presentation: medical practice or Law? Discussion between a medical doctor, a lawyer and the head chief of an university hospital]. Journal de gynecologie, obstetrique et biologie de la reproduction. 2011 Oct:40(6):587-9. doi: 10.1016/j.jgyn.2011.05.011. Epub 2011 Jul 16 [PubMed PMID: 21763083]
Burke G. The end of vaginal breech delivery. BJOG : an international journal of obstetrics and gynaecology. 2006 Aug:113(8):969-72 [PubMed PMID: 16827824]
Use the mouse wheel to zoom in and out, click and drag to pan the image
- Tel: +91 8446012817
- Tel: +91 9226482577
- Patient Login | Registration
PLEASE LOGIN FOR ONLINE TREATMENT
Get treated by the pioneer of Online treatment, who was first to start Online Medical practice in 1995. In a few clicks from now, you can get started with the journey to recovery.
Forgot Password
- INSIDE ASHER CLINIC
- TESTIMONIALS
- MISSION STATEMENT
- JOBS AT ASHER CLINIC
- Company Profile
- Our Mission
- Ethics and Values
- About Life Force Homeopathy
- About Dr. Asher
- Homeopathy Research
- Founder of Life Force
- Inside Life Force
- Articles and News
- Press and Media
- Jobs at Life Force
- Photo Gallery
- Testimonials
- Contact Information
Breech presentation
Breech presentation occurs when the fetus presents to the birth canal with buttocks or feet first. This presentation creates a mechanical problem in delivery of the fetus.
Factors that increase likelihood of breech delivery include the following:
Preterm delivery
Increased parity
Multiple gestations
Previous breech delivery
Pelvic tumors
Older maternal age
Pathophysiology
The buttocks and feet of the fetus do not provide an effective wedge to dilate the cervix. The umbilical cord may prolapse, and/or the aftercoming head may get trapped during delivery.
The 3 types of breech presentation are as follows:
Frank (65%): Hips of the fetus are flexed, and knees are extended.
Complete (10%): The hips and knees of the fetus are flexed.
Incomplete (25%): The feet or knees of the fetus are the lowermost presenting part.
Single footling: One of the lower extremities is lowermost.
Double footling: Both of the lower extremities are lowermost.
If a vaginal delivery is planned, or the fetus has an underlying concern leading to a breech presentation transport the mother to the nearest facility with neonatal intensive care.
If the mother is in the second-stage of labor or if amniotic membranes have ruptured, take the mother to the nearest hospital or urgent care center for emergency delivery.
Administer supportive oxygen and IV fluids.
Transport the mother in a comfortable position or in the left lateral decubitus position.
Inform the hospital of an impending arrival and of the clinical situation.
https://reference.medscape.com/article/797690-treatment
Find Dr. Asher opinion on your ailment.
Welcome to ighalo ™, order treatment online.

- Mission Statemnt
- What is homeopathy
- What is it not
- Photo gallery
- Case Studies
- Publications
- Diseases (A to Z)
- Tests and tools
- Case studies
- Get In Touch
- Book An Appointment
- Privacy Policy
- Patient's Login
- Book an Appointment
- Terms & Conditions
- Diseases A To Z
- Health Calculator
- FCurability Test
- Photos (Before-After)
Copyrights @ 2017. Asherclinic.com. All Rights Reserved.

- Service & Support

Book Online

Unlocking the Potential of Acupuncture: Managing Breech Presentations

Pregnancy is a remarkable journey filled with anticipation and joy, but it can also present certain challenges. One such challenge is the occurrence of a breech presentation, where the baby's position in the womb isn't head-down as expected for a smoother birth. However, recent research has shed light on a holistic and non-invasive approach to potentially manage this for women who do not have access to services that do not support vaginal breech birth —acupuncture.
A systematic of six randomised trials review delved into findings from six randomised trials, exploring the impact of acupuncture and moxibustion on breech presentations. The results were compelling. Among those receiving acupuncture and moxibustion treatments, only 34% showed breech positions, a significantly lower rate compared to the untreated group, where a striking 66% displayed breech presentations (van den Berg et al., 2008).
This evidence underscores the potential effectiveness of acupuncture as an intervention to influence foetal positioning during pregnancy. Acupuncture, an ancient Chinese practice entailing the precise insertion of fine needles into specific points on the body, when combined with moxibustion—a technique harnessing the therapeutic warmth from burning dried mugwort—offers a non-invasive and natural approach. This holistic method not only aims to encourage optimal foetal positioning but also aligns with traditional practices utilised to address babies in non-ideal positions, such as the posterior position (OP). We understand that pregnancies with babies in these positions potentially elevate the risk of medical interventions like caesarean sections or assisted vaginal births
The idea that such non-pharmacological and gentle methods might assist in reducing the incidence of breech presentations offers hope and a new avenue for expectant mothers. Moreover, the non-invasive nature of acupuncture and moxibustion aligns with the desire of many women for a holistic approach to prenatal care.
In conclusion, the findings from these trials highlight the potential of acupuncture and moxibustion as a gentle and non-invasive method for managing breech presentations during pregnancy. This ancient practice, when administered by a skilled professional, may offer expectant mothers an additional option in promoting optimal foetal positioning, potentially contributing to smoother and safer births.
The journey of pregnancy is one filled with choices, and acupuncture might just be the gentle nudge that some babies need for the right positioning before their grand entrance into the world.
References
van den Berg, I., Bosch, J.L., Jacobs, B., Bouman, I., Duvekot, J.J. and Hunink, M.M. (2008) 'Effectiveness of acupuncture-type interventions versus expectant management to correct breech presentation: a systematic review', Complementary Therapies in Medicine, 16(2), pp. 92-100.
About Us Acupuncture Chinese Medicine Conditions Contact Us
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Pregnancy Complications
Can Moxibustion Help Turn a Breech Baby?
The traditional Chinese medicine practice of moxibustion is one of the world's oldest techniques for turning a breech baby. Here's why OB-GYNs still prescribe it today.
Moxibustion for a Breech Baby
Trying moxibustion before ecv, is moxibustion safe, how moxibustion is performed, can moxibustion be done at home.
- Moxibustion Success Rate
Finding out that your baby is in a breech position with their feet or bottom facing down can be stressful. A baby that is still breech at term often requires a C-section delivery . However, there is some evidence moxibustion, a noninvasive traditional Chinese medicine practice, may help encourage breech babies to turn into a head-down position in time for delivery.
Read on to learn more about moxibustion, including what it is, how it works, and why some prenatal care providers recommend it in the third trimester for breech babies.
Many medical providers routinely refer their pregnant patients for moxibustion to treat breech presentation. "If I were to diagnose a breech presentation early in the third trimester, I would recommend acupuncture and the use of mugwort," says Marsha Granese, MD , an OB-GYN with Mission Hospital in Mission Viejo, California. "I would refer the patient to a Chinese medicine provider who knows the acupuncture points and herbs used to relax the uterus," Dr. Granese adds, noting that mugwort is a natural muscle relaxant.
What Is Moxibustion?
Moxibustion is a therapy from traditional Chinese medicine that involves burning the herb mugwort (or moxa) to warm specific points along a set of invisible vertical lines known as meridians that practitioners believe cross the body. These meridians are thought to correspond to specific organs and, when stimulated, can strengthen blood flow and prompt the release of certain hormones.
In the US, moxibustion is taught as part of the typical curriculum for a degree in acupuncture and only licensed acupuncturists can perform it. Moxibustion can be combined with acupuncture treatment or done on its own with moxa sticks.
There are several theories as to how moxibustion works for breech presentation. "It is thought that stimulating the last point on the bladder meridian brings movement to the kidney channel and helps the baby to turn," says Tom Ingegno , a licensed acupuncturist and doctor of acupuncture and Chinese medicine (DACM) with a master's in Oriental medicine (MSOM) who practices with Charm City Integrative Health in Baltimore.
"One theory, from a Western medical perspective, is that the heat encourages the release of two specific hormones in pregnancy: placental estrogen and prostaglandins," says Kristen Burris , a licensed acupuncturist with a master's in traditional oriental medicine (MSTOM) who practices with Eagle Acupuncture in Idaho. These hormones can lead to mild uterine contractions, helping the baby to move into an optimal, head-down position for a vaginal birth.
Many babies are in the breech (feet-down) position through early pregnancy and even up until 33 weeks . However, most babies turn into a head-down position (cephalic presentation) somewhere around 36 weeks gestation . But in about 3% to 4% of pregnancies, the baby remains breech even at full-term.
When a baby is still in the breech position at 36 weeks, a trained prenatal health care provider may use a technique called external cephalic version (ECV) , which is also referred to as a "version," to "turn" the baby by manipulating the pregnant person's abdomen externally with their hands. According to the American College of Obstetricians and Gynecologists (ACOG), ECV is successful just over 50% of the time.
Before then (usually between 33 to 35 weeks), health care providers may recommend trying moxibustion to encourage a breech baby to flip around on their own. Research has been mixed, but a 2023 Cochrane review concluded that moxibustion can reduce the risk of the baby staying breech.
Trying moxibustion for breech presentation has some advantages over waiting for an ECV as it is less painful and may increase your chances of getting your baby into an optimal position for birth.
According to a review published in Evidence-Based Complementary and Alternative Medicine in 2019, most of the evidence suggests that there are "no adverse effects directly related to acupuncture and moxibustion" in the treatment of breech presentation. That is to say that moxibustion is generally regarded as safe for use in pregnant people with breech babies.
When moxibustion is performed in a clinical setting, the risks are minimal. "They're hardly worth mentioning," says Burris. Those risks include coughing and nausea from the scent of burning mugwort and burns and blisters if the ignited herb comes in contact with the skin. "However, in 20 years of practice, none of my patients has ever experienced an inappropriate burn from moxibustion," Burris notes.
When moxibustion is combined with acupuncture, the practitioner wraps a small amount of dried mugwort atop a needle that is already in the acupuncture point and lights it. This creates a warming sensation in the skin.
A cone of moxa may also be placed directly on the acupuncture point and lit, with the practitioner taking care to extinguish it before it touches the skin. Another form of moxibustion, known as indirect moxibustion, involves lighting cigar-sized moxibustion sticks near the points and holding them close until their heat warms the skin.
At Integrative Acupuncture in Vermont, Kerry Boyle , a licensed acupuncturist and doctor of acupuncture (DAc), holds a moxibustion stick above the pregnant person's pinky toe when performing moxibustion for a breech baby. "Connective tissue and nerve channels link this area to the uterus and cause it to relax," says Boyle. "We add acupuncture needles to the ears and feet to further the relaxation."
Moxibustion for a breech baby is usually performed between weeks 33 and 36 of pregnancy and may be prescribed as an alternative or precursor to an ECV.
Whether or not it's safe to practice moxibustion at home depends on who you ask. The guidelines from reputable sources like the British Journal of Obstetrics and Gynaecology recommend moxibustion only be performed by a trained professional.
Burris says that although she's aware other practitioners give their patients moxibustion sticks to use at home, her practice advises against it. "Moxibustion only takes a few treatments in the office, and success rates are much higher and safer when performed by a professional," she claims.
But Ingegno says moxibustion that doesn't involve direct contact with the skin can be performed at home using sticks under the training and supervision of a licensed acupuncturist. "The moxa sticks need to be held at a comfortable distance to warm the area and not burn," says Ingegno. However, burning moxa directly on the point is not an at-home technique and should only be performed in a clinical setting, Ingegno warns.
Success Rate of Moxibustion for Breech Babies
Moxibustion doesn't always result in a breech baby turning head down but it's thought to increase the odds. When combined with in-office treatments and daily moxibustion at home, Ingegno says his practice has seen a 70% success rate with moxibustion for breech babies. "Modern studies confirm that moxibustion does increase the success of the fetus repositioning, but most of these studies are small," he says.
"Factors like how far along the pregnancy is can affect the outcome. The best success seems to occur when we intervene at 34 weeks. However, this leaves about a month and a half before the expected delivery date in which a decent percentage of babies would turn on their own [anyway]," explains Ingegno.
In other words, the farther out from their due date a baby is, the greater the chance that they will turn on their own without intervention. This is why treatment at 33 to 34 weeks will show a greater success rate than treatment after 35 weeks. The closer you get to 36 weeks and beyond, the less likely it is that a baby will be able to move to a head-down position as there is less space in the uterus to allow them to turn.
While research on the efficacy of moxibustion for breech babies is slim, there is some promising data. One 2013 study of 406 pregnant people with confirmed breech presentation showed that the moxibustion group had a significantly higher rate of success than those that had "sham moxibustion" or usual care. In fact, nearly 60% of the pregnant people in the moxibustion group had their babies turn while only about 45% of the people in the other groups experienced their breech babies turning head down.
At the end of the day, with both moxibustion or a version, the goal is to encourage the baby's movement to a head-first or "vertex" position so that a safe vaginal birth is possible. If both moxibustion and version are unsuccessful, a scheduled C-section delivery will likely be recommended.
Key Takeaway
If your baby is in a breech position, moxibustion can be used to encourage them to get into a better position for vaginal delivery. While success is not guaranteed, moxibustion can increase the odds that your baby will turn head down—and reduce the likelihood that you'll need a C-section for breech presentation. Talk to a prenatal health care provider about whether or not moxibustion is a good choice for you.
(Common Mugwort) in the History of Medicine and Its Possible Contemporary Applications Substantiated by Phytochemical and Pharmacological Studies . Molecules . 2020.
Moxibustion in Acupuncture: What You Should Know . American Institute of Alternative Medicine . 2019.
Physiology, Pregnancy Contractions . StatPearls Publishing . 2023.
Breech Presentation . StatPearls Publishing . 2023.
If Your Baby is Breech . American College of Obstetricians and Gynecologists. 2019.
Cephalic version by moxibustion for breech presentation . Cochrane Library . 2023.
Effectiveness and Safety of Acupuncture and Moxibustion in Pregnant Women with Noncephalic Presentation: An Overview of Systematic Reviews. Evid Based Complement Alternat Med . 2019.
Safety of moxibustion: a systematic review of case reports . Evid Based Complement Alternat Med . 2014.
External Cephalic Version and Reducing the Incidence of Term Breech Presentation . British Journal of Obstetrics and Gynaecology . 2017.
Does moxibustion work? An overview of systematic reviews . BMC Res Notes . 2010.
Using Moxibustion in Primary Healthcare to Correct Non-Vertex Presentation: A Multicentre Randomised Controlled Trial . Sage Journals . 2013.
Related Articles

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Breech - series—Types of breech presentation
- Go to slide 1 out of 7
- Go to slide 2 out of 7
- Go to slide 3 out of 7
- Go to slide 4 out of 7
- Go to slide 5 out of 7
- Go to slide 6 out of 7
- Go to slide 7 out of 7
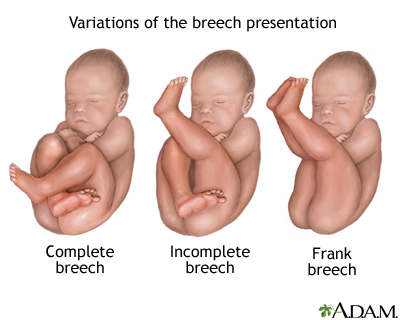
There are three types of breech presentation: complete, incomplete, and frank.
Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal.
Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
Frank breech is when the baby's legs are folded flat up against his head and his bottom is closest to the birth canal.
There is also footling breech where one or both feet are presenting.
Review Date 11/21/2022
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems

IMAGES
VIDEO
COMMENTS
Pulsatilla 6X 3-4x per day for 7-10 days combined with breech tilt 2x per day for 10 minutes (take Pulsatilla before beginning breech tilt) or 30c 2x per day for 3 days (up to 2 weeks) or 200c x1 every 3 days while doing breech tilt exercises or 200c x 1 for 2-3 days at 35-36 weeks or 1M x 1 Note: 30c or 200c can be given every 2 hours up to 6x ...
The gentle action of homeopathic remedies can be used preventively or in acute situations to address any symptom-picture, weakness, or recurring tendency that is less than optimal. While breech presentations are considered one variation of normal, many midwives are prevented by law from attending vaginal breech deliveries.
Other Research on Breech Presentation Outcomes by Delivery Method - Meta analysis 1: 24 studies published between 1966-199220 ... Homeopathic formulas pulsatilla and natrum muriaticum,33-36 Gentle ... Presenation: Preliminary Results. American Journal of Chinese Medicine, XIX(2), 105. 27. Cardini, F., & Hauang, W. (1998). Moxibustion for ...
Some breech births can happen vaginally, but there are risks. The risks of a vaginal breech birth include: Injuries to your baby's legs or arms such as dislocated or broken bones. Your baby's head can get stuck or trapped. Umbilical cord problems. The umbilical cord can flatten or twist during delivery.
If you do have after pains after the delivery, below are a few common homeopathic remedies you may need: Belladonna 30c or 200c - Is selected for pains that comes on quickly and then goes away quickly; similar to pains coming in like waves. Chamomilla 30c or 200c- Taken when you are unable to tolerate pains.
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
The ideal vaginal breech presentation is a frank breech position in which baby's buttocks are down and the legs in pike position, hips flexed and knees straight. Frank is the most common type of breech and with the buttocks about the same size as the head, this minimizes the concern that the cervix will not dilate enough and possibly trap the head.
Summary. Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head. Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal ...
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position. The complete breech has the ...
Homeopathic remedies. Homeopathy is a system of medicine based on using substances to treat "like with like", in that large doses of the substances used would actually cause a particular set of symptoms, but in a highly diluted and vigorously shaken (succussed) form, will treat that same set of symptoms. ... If the breech presentation ...
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
1. Background. The management of breech presentation continues to cause academic and clinical contention globally [[1], [2], [3]].In recent years, research has shown that if certain criteria are met, and appropriately experienced and skilled clinicians are available, Vaginal Breech Birth (VBB) is a safe option [[4], [5], [6]].However, with Caesarean Section (C/S) rates for breech presentation ...
We touched on her contributions in our Mother's Day tribute to a few stand-out women of homeopathy. Having given birth to 11 children, Dr. Jackson was understandably drawn toward a specialty in Obstetrics and Gynecology. One of her greatest contributions was discovering that Pulsatilla can be used to turn breech babies in the womb and to ...
Introduction. Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman's and the baby's health. The aim of this review is to determine the most ...
Point of Care - Clinical decision support for Breech Presentation. Treatment and management. Introduction, Etiology, Epidemiology, Pathophysiology, History and Physical, Evaluation, Treatment / Management, Differential Diagnosis, Pearls and Other Issues, Enhancing Healthcare Team Outcomes
If a vaginal delivery is planned, or the fetus has an underlying concern leading to a breech presentation transport the mother to the nearest facility with neonatal intensive care. If the mother is in the second-stage of labor or if amniotic membranes have ruptured, take the mother to the nearest hospital or urgent care center for emergency ...
Below is a list of common natural remedies used to treat or reduce the symptoms of Breech-Presentation. Follow the links to read common uses, side effects, dosage details and read user reviews for ...
Natural Techniques to try at home include: The Breech Tilt - Raise hips 12" or 30cm off the floor using large, solid pillows 3 times daily for 10-15 minutes each time. This is best done on an empty stomach, and at a time when your baby is active. Concentrate on your baby and not tensing your body, especially in the abdominal area.
The most widely quoted study regarding the management of breech presentation at term is the 'Term Breech Trial'. Published in 2000, this large, international multicenter randomised clinical trial compared a policy of planned vaginal delivery with planned caesarean section for selected breech presentations.
Pregnancy is a remarkable journey filled with anticipation and joy, but it can also present certain challenges. One such challenge is the occurrence of a breech presentation, where the baby's position in the womb isn't head-down as expected for a smoother birth. However, recent research has shed light on a holistic and non-invasive approach to potentially manage this for women who do not have ...
Learn about how the traditional Chinese practice of moxibustion can be used to turn a breech baby between weeks 34 and 36 of pregnancy, including the treatment's success rate, safety guidelines ...
Overview. There are three types of breech presentation: complete, incomplete, and frank. Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal. Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
A breech birth is when a baby is born bottom first instead of head first, as is normal. Around 3-5% of pregnant women at term (37-40 weeks pregnant) have a breech baby. Due to their higher than average rate of possible complications for the baby, breech births are generally considered higher risk. Breech births also occur in many other mammals such as dogs and horses, see veterinary ...