Musculoskeletal Key
Fastest musculoskeletal insight engine.
- MANUAL THERAPIST
- MUSCULOSKELETAL MEDICINE
- PHYSICAL MEDICINE & REHABILITATION
- RHEUMATOLOGY
- SPORT MEDICINE
- Gold Membership

Case studies in a musculoskeletal out-patients setting
CHAPTER EIGHT Case studies in a musculoskeletal out-patients setting Adrian Schoo, Nick Taylor, Ken Niere, with a contribution from James Selfe Case study 1: Jaw Pain 217 Case study 2: Headache 218 Case study 3: Neck Pain – Case One 221 Case study 4: Neck Pain – Case Two 224 Case study 5: Thoracic Pain 226 Case study 6: Low Back Pain – Case One 228 Case study 7: Low Back Pain – Case Two 231 Case study 8: Shoulder Pain 234 Case study 9: Elbow Pain 237 Case study 10: Hand Weakness and Pain 239 Case study 11: Groin Pain 241 Case study 12: Hip and Thigh Pain 244 Case study 13: Medial Knee Pain 247 Case study 14: Anterior Knee Pain 249 Case study 15: Calf Pain 252 Case study 16: Achilles Pain 254 Case study 17: Ankle Sprain 256 Case study 18: Fibromyalgia 258 Introduction Musculoskeletal problems are very common, and can be encountered in hospital emergency departments, orthopaedics, and out-patient physiotherapy ( Carter & Rizzo 2007 ). It is not uncommon for in-patients who are admitted for another problem to be referred and treated in the ward or in the out-patient department for a musculoskeletal problem. The prevalence of specific conditions can vary between the different groups in the community. For example, sporting injuries are more likely to occur in the younger groups, whereas degenerative conditions such as osteoarthritis are more likely to occur as people progress in years. Musculoskeletal problems can result in pain and functional limitations (disability), and represent a major burden to the society due to associated health care costs and loss of productivity ( National Health Priority Action Council 2004 ). Musculoskeletal conditions, including arthritis, cause more disability than any other medical condition and affect one-third of all people with disability. Since part of the chronic disease burden is attributed to risk factors such as physical inactivity ( Bauman 2004 ) people with musculoskeletal conditions are often referred to physiotherapy out-patients for management of their conditions. As in other areas of physiotherapy practice, musculoskeletal assessment and treatment requires a systematic clinical reasoning approach ( Edwards et al 2004 ). The clinical reasoning approach used in this chapter considers: (i) differential diagnoses based on assessment and clinical presentation; (ii) intervention based on the best evidence available; (iii) constant evaluation of therapy outcomes; (iv) adjustment of intervention programme in line with diagnosis and stage of progress; and (v) referring to or working together with other disciplines to exclude and or address confounding problems. In assessing and treating common musculoskeletal conditions and measuring progress it is important to use outcome measures that are valid and reliable, and that consideration must be given to impairments of body structure and function as well as activity limitation and participation restriction, such as ability to return to work. The World Health Organization’s International Classification of Functioning, Disability and Health (ICF) provides a useful framework for physiotherapists in out-patients to assess patient functioning ( Jette 2006 ). Referral to or working with other disciplines may involve tests such as X-rays or dynamic ultrasound scans, or the provision of orthotics to improve biomechanics. In addition to specific techniques, treatment may require education, ergonomic advice and the instruction of a home exercise programme to improve outcomes on function and pain. There is an emerging and increasing body of research on the effectiveness of physiotherapy that provides the clinician in out-patients with an evidence base for their practice ( Herbert et al 2001 ). For example, there is high level evidence that therapeutic exercise can benefit clients across broad areas of physiotherapy practice ( Morris & Schoo 2004 , Taylor et al 2007 ). In prescribing exercises it can be important to know whether the exercise programme is performed correctly and adhered to by the client. Conditions such as back problems or tendinopathies may be negatively affected by incorrect activity performance. Additional problems that can affect health outcomes are incorrect belief systems and mental health problems. For instance, people with osteoarthritis may think that movement harms the joint, but by not moving they put themselves at risk of developing problems associated with physical inactivity (e.g. increased morbidity and mortality due to cardiovascular problems or falls) ( Philbin et al 1996 ). Also, people with chronic pain may be depressed and are, therefore, less likely to be interested in performing exercises, and may benefit from counselling (e.g. motivational interviewing). Screening patients for problems such as fear-avoidance behaviour and anxiety ( Andrews & Slade 2001 ), asking about past and current exercise performance, motivating them if needed (Friedrich et al 1998) and demonstrating the prescribed exercises can assist in determining the likelihood of correct and consistent programme performance (Friedrich et al 1996b, Schneiders et al 1998 ). We have selected common musculoskeletal conditions that are likely to be encountered in hospital out-patient departments. The different cases relate to younger and older people, females as well as males. A multitude of physical tests and outcome measures have been included together with clinical reasoning and evidence-based treatment options. CASE STUDY 1 Jaw pain Subjective examination Subject 34-year-old female office worker HPC Left sided headaches off and on for 3/12 Increasing pain of the left temporomandibular joint (TMJ) last 2/12 Pain at night, at rest, and when opening the mouth or chewing PMH Appendectomy Stress at work Aggravating factors Biting a big apple Chewing hard or tough food Easing factors Rest is better than chewing, although remains painful Drinking fluid Ice Night Wakes up because of pain Grinds teeth when asleep (according to partner) Daily pattern Constant pain that worsens during and directly after opening the mouth or chewing General health Using prescribed sedatives due stress at work. No other problems reported Attitude/expectations Given the symptoms she expects that it may take some time for them to settle Pain and dysfunction scores VAS current pain at rest = 3 VAS usual level of pain during chewing in the last week = 7 VAS worst level of pain during opening the mouth in the last week = 9 Objective examination Palpation Skin temperature (T sk ) normal Left TMJ painful on palpation TMJ movement and clicking can be felt when placing the index finger in the auditory canal and opening the mouth No signs of TMJ dislocation when comparing left with right Muscle length External pterygoid muscle feels tight and painful on opening of the mouth (palpation through the mouth) Functional testing, including ROM and strength Opening of the mouth is limited. It can accommodate two fingers only. Normally, the span is large enough to accommodate three fingers ( Hoppenfield 1986 ) Asymmetrical mandibular motion with severe swinging to the left when opening the mouth Questions 1. What is your provisional diagnosis? 2. What signs and symptoms lead you to this diagnosis? 3. How will you address these in your treatment plan? 4. What kind of common and less common problems need to be excluded? 5. How likely is it that the patient’s stress and teeth grinding contribute to the current complaint? 6. How will the expectations of the patient influence your treatment? 7. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 2 Headache Subjective examination Subject 29-year-old male working on Help Desk in Information and Computer Technology HPC Gradual onset of headaches and cervical pain about 3/52 ago Cannot recall precipitating incident Headaches becoming more frequent (now daily) and lasting longer (up to 3 hours) Has deep ache (non-throbbing) radiating from the back of the occiput to the right frontal region. Also complaining of stiffness like pain in the right side of the cervical spine. Neck pain and headache seem related (see Figure 8.1 ) FIGURE 8.1 Body chart – Case Study 2 . PMH Car accident 10 years ago which led to cervical pain for about 3/52. No problems since apart from an occasional stiff neck Aggravating factors Prolonged work at the computer (if more than 2 hours brings on headache) Reversing the car reproduces slight cervical stiffness Easing factors Analgesia dulls the headache Night Sleep undisturbed Daily pattern Seems to depend on how long he has spent at the computer General health In good health, no weight loss No complaints of dizziness, no nausea or vomiting Assessed as being depressed, has been taking antidepressants over the last 3/12 Investigations No X-rays or other investigations at this stage Attitude/expectations At the moment headache is not affecting him a lot but wanted to get it checked out in case it is something serious Keen not to miss any work Intends to continue normal recreation of sail boarding this weekend Pain and dysfunction scores Neck Disability Index: 14% Disability VAS level of pain when headache is most severe (after working at the computer for 2 hours) = 6 Physical examination Observation Forward head posture with a slouched sitting posture Palpation Hypo-mobility of upper cervical joints on the right, with reproduction of local cervical pain Increased muscle tone in right upper trapezius and right levator scapulae Movements Active movements Right cervical rotation equals 60° with slight stiffness in neck Left cervical rotation equals 75–80° Limited cervical retraction, feels stiff Muscle function Decreased strength and endurance of the deep cervical neck flexors as determined by the cranio-cervical flexion test ( Jull et al 1999 ) Neurodynamic testing Upper limb neurodynamic/tension test (base test): In 90° shoulder abduction and full external rotation, right elbow extension lacks 40° while left lacks 30°. Reproducing local neck pain, which is eased with cervical lateral flexion towards the right Neurological tests (tests of nerve conduction) Not assessed Questions 1. What is your provisional diagnosis? 2. What signs and symptoms led to your provisional diagnosis? 3. How will you address these in your treatment plan? 4. What kind of common and less common problems need to be excluded? 5. How relevant are work details for this patient? 6. How will the expectations of the patient influence your treatment? 7. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 3 Neck pain – case one Subjective examination Subject 32-year-old male accountant HPC Prolonged sitting (all day) at a conference 3/52 previously Noticed onset of left lower cervical and interscapular pain at the end of the day On waking the next morning pain had spread to the posterior aspect of the arm and forearm as far as the middle three fingers (see Figure 8.2 ) FIGURE 8.2 Body chart – Case Study 3 . Seen by doctor 1/52 ago. Doctor ordered plain X-rays including oblique views that did not show any abnormality Has not improved at all since onset of symptoms Medical history High cholesterol, overweight, sedentary lifestyle Minor neck complaints that usually settled within 2 or 3 days Aggravating factors Sitting for more than 10 minutes increases neck pain. More than 30 minutes increases arm pain Looking up or to the left increases neck and arm pain Lifting briefcase with left hand aggravates neck and interscapular pain Easing factors Neck pain relieved by lying supine Arm pain relieved by lying supine with left arm above head Night Can sleep 2–3 hours at a time before being woken by increased neck and interscapular pain Changing position helps to decrease the pain Daily pattern Increased symptoms with increased amounts of sitting, particularly if using computer Medication Was prescribed non-steroidal anti-inflammatory medication (Meloxicam) which helps take the edge off the neck pain Attitude/expectations Wants to know what the problem is, particularly as the X-rays did not show any abnormality Feels that something might be ‘out’ in his neck. If it could be ‘put back in’ the symptoms should resolve Physical examination Observation Sits with forward head posture Cervical active movements in sitting Extension reproduces pain in the neck and left arm at 30°. Movement occurs mainly in the upper and mid-cervical regions. Very little movement in the lower cervical or upper thoracic areas Right rotation produces a stretching in the left cervical region at 75° Left rotation reproduces left neck and interscapular pain at 40° Palpation Increased tone and tenderness noted in the left paraspinal muscles (cervical and upper thoracic) and left scalene muscles Local pain and left arm pain reproduced by postero-anterior (PA) pressures over the spinous processes of C6 and C7 and over the C6 and C7 articular pillars on the left Generalized stiffness noted with PA pressures in the mid and upper thoracic regions Segmental neurological examination Absent left triceps jerk Weakness in left triceps (25% of right side) Decreased sensation to light touch over the tip of the left middle finger Questions 1. What is the most likely source of the patient’s arm pain? 2. What is the most likely source of the patient’s neck and interscapular pain? 3. What are other possible symptoms sources? 4. Are there reasons to be cautious in administering physiotherapy treatment? 5. What would an appropriate initial physiotherapy treatment involve? 6. What would a longer-term management programme include? 7. What is the likely prognosis? 8. Is referral to other health professionals warranted? CASE STUDY 4 Neck pain – case two Subjective examination Subject 23-year-old female personal assistant HPC Rear end motor car accident 2/7 ago Immediate onset of cervical pain and stiffness (left and right). Both pain and stiffness have been increasing. Pain is now constant Vague headache started today (see Figure 8.3 ) FIGURE 8.3 Body chart – Case Study 4 . Seen by doctor yesterday who organised an X-ray (no abnormality detected) and referred patient to physiotherapy PMH Left knee reconstruction 3 years ago with good return of function since No past history of neck complaints Aggravating factors Turning head to either side, especially if movement is quick Travelling in car – took 20 minutes to settle after 30-minute car trip Easing factors Supine with head supported on one pillow Felt a bit easier under hot shower Night Wakes often due to discomfort Sleeps on 3 pillows Difficulty turning in bed due to pain Daily pattern Constant pain that gradually worsens during the day General health Taking non-prescription analgesics every 4 hours on advice of doctor. No other medications Not seeing the doctor for any other health problems Attitude/expectations Anxious about prognosis Worried about how much work she will have to miss as she only started in her current position 3/12 ago Pain and dysfunction scores VAS current pain at rest = 5 VAS level of pain after 30 minute car trip = 8.5 Physical examination Observation Walking slowly and all movements are guarded Removes jacket slowly and with great care Neck in slight protracted posture Palpation Generalized tenderness to light palpation of cervical spine (central, left and right) Increased muscle spasm left and right paraspinal muscles Further detailed palpation not possible because therapist wary of exacerbating symptoms Active movements Left rotation equals 30° before pain started increasing Right rotation equals 35° before pain started increasing Attempt to retract cervical spine caused increased pain No other movements tested today Questions 1. What is your provisional diagnosis? 2. Which of the signs and symptoms will you place on your priority list? 3. How will you address these in your treatment plan? 4. What kind of common and less common problems need to be excluded? 5. How relevant are work details for this patient? 6. How will the expectations of the patient influence your treatment? 7. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 5 Thoracic pain Subjective examination Subject 60-year-old male lawyer Presents with bilateral lower thoracic pain with radiation of symptoms anteriorly to the lower sternal area (see Figure 8.4 ) FIGURE 8.4 Body chart – Case Study 5 . Had a similar problem 5 years previously that settled with physiotherapy which resolved after three sessions of passive mobilisation directed to the thoracic spine HPC Noticed onset of symptoms 4/52 previously after lifting pots while gardening. Pain initially felt in sternal area, then onset of thoracic pain over the course of the day Pain initially intermittent, now constant at a level of VAS 2/10 at best and VAS 7/10 at worst Medical history Noticed 5 kg of weight loss in previous 4/52 that could not be explained by other factors Had noticed intermittent, generalised, mild (VAS 1–2/10), aches and pains in trunk, arms and legs over the previous 3/12 that had worsened slightly over the previous 4/52 Aggravating factors Prolonged sitting for greater than 20 minutes at work would increase posterior and anterior chest pains to VAS 6/10 Easing factors Standing and walking for 10 minutes decreases all symptoms to VAS 2/10 Night Wakes 3–4 times each night with increased symptoms in thoracic and sternal areas. Has to get out of bed and walk around to ease pain. Tends to notice generalised aches and pains associated with increased sweating at night Daily pattern Dependent on amount of sitting during the day. More thoracic and sternal pain at end of day when sitting a lot Medication Nil Attitude/expectations Expects that physiotherapy will ease symptoms as they did for a past episode of similar pain Physical examination Observation Increased thoracic kyphosis noted while sitting. Able to actively correct sitting posture, although this increases thoracic pain slightly Thoracic active movements in sitting Extension is restricted by about 50% and reproduces posterior thoracic pain with overpressures localised to the mid/lower thoracic spine Thoracic rotation feels stiff but no pain reproduced Flexion is normal in range and reproduces a stretching feeling in the mid thoracic area Palpation Generalised stiffness noted on midline and unilateral postero-anterior (PA) pressures from T2–T10 Posterior thoracic and anterior pain reproduced with midline PA pressures over T7–T8. These pains settled quickly once the pressure was released Palpation of the ribs, inferior part of the sternum and upper part of rectus abdominis did not reveal any increased tenderness Questions 1. What are your hypotheses regarding the likely source of the thoracic and sternal pains? 2. What would an appropriate initial physiotherapy treatment involve? 3. Are there examination findings that would make you suspect a non-musculoskeletal source of the symptoms? 4. What are red flags? 5. Is referral to other health professionals warranted? CASE STUDY 6 Low back pain – case one Subjective examination Subject 44-year-old male bank manager HPC 4/7 ago bent to reach into boot of car and felt slight backache. Thought it would settle so played golf anyway. Next morning severe low back pain with aching pain radiating down the back of the right leg to just below the knee. Has no pins and needles or numbness (see Figure 8.5 ) FIGURE 8.5 Body chart – Case Study 6 . PMH Has had four or five episodes of low back pain over the last 8 years, usually settles quickly in 2 or 3 days Has not required treatment with previous episodes Aggravating factors Finds it difficult to put shoes and socks on in the morning After driving to work (about 40 minutes) found leg pain had worsened Can only sit for about 15 to 20 minutes at a time at work Has noticed that sneezing increased back and leg pain Easing factors Lying on back eventually relieves the leg pain Standing and walking seem to help a little Night Pain gradually eases after initial discomfort Is waking at night but finds can get back to sleep quite quickly when changes position Daily pattern Back stiff and aches getting out of bed first thing in the morning but eases after shower Back pain is worse by the end of the day, and leg pain is more constant by the end of the day General health Taking non-steroidal anti-inflammatories (NSAIDs) with slight improvement At recent annual review doctor advised to increase physical activity to reduce weight (BMI 26.4) and adjust diet (cholesterol 6.4). Otherwise fit and well Attitude/expectations Very keen not to miss club Stableford golf competition this weekend (in 3/7) Intending to cope with work as best he can. Very busy at work so reluctant to take time off Pain and dysfunction scores Oswestry Disability Score: 36% Disability VAS level of pain after 40 minute car trip: back = 8, leg = 6 Physical examination Observation Slight left-sided contralateral list (when observed from behind in standing shoulders are to the left relative to the hips) Changes position regularly when in sitting position Palpation Increased tone, right erector spinae in the lumbar region Central postero-anterior pressures over the lumbar spine reproduced back pain (but not leg pain) at L4 and L5 Unilateral pressures were painful on the right at L4 and L5 Movements Active movements Lumbar flexion in standing limited (2 cm below the knee) Lumbar extension in standing markedly limited Left and right rotation (assessed in sitting) both more than 60° Attempt to correct contralateral list led to increased back pain Repeated active movements Flexion in standing repeated 10 times led to increased back pain and increase of leg pain Extension in standing repeated 15 times abolished leg pain, and increased range – back pain remained Repeated correction of contralateral list (side gliding to the right) led to reduced central back pain and slightly increased range Neurodynamic tests Straight leg raise: right = 70° left = 70° Slump test not evaluated Neurological tests (tests of nerve conduction) Muscle strength in myotomes L3 to S1, left = right Sensation in dermatomes L2 to S1, left = right Reflexes (patella tendon and Achilles), brisk left = right Questions 1. What is your provisional diagnosis? 2. What is the likely source of the right leg pain? 3. Which of the signs and symptoms will you place on your priority list? 4. How will you address these in your treatment plan? 5. What kind of common and less common problems need to be excluded? 6. How relevant are work details for this patient? 7. How will the expectations of the patient influence your treatment? 8. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 7 Low back pain – case two Subjective examination Subject 49-year-female assembly worker at automotive manufacturer HPC Complaining of increasing back pain over the last 14/12. Back pain is in the central low back region and radiates into both gluteal regions – no leg pain (see Figure 8.6 ). Has been off work for the last 6/12 with no improvement in pain FIGURE 8.6 Body chart – Case Study 7 . Injured back when installing car upholstery 14/12 ago. Initially had 3/7 off work and experienced some slow improvement over the first 3/12 Has had manipulative physiotherapy involving manipulation, mobilisation and traction with no benefit. Also tried chiropractic without benefit PMH 15-year history of intermittent low back pain usually no more than a few days off work Cholecystectomy 6 years ago Aggravating factors Prolonged walking or standing (more than 15 minutes) increases ache Prolonged sitting (more than 15 minutes) increases ache Unable to do weekly shopping or housework as these activities aggravate the ache Easing factors Lying down but only for about 30 minutes, as gets stiff when lying in one position for too long Night Finds it difficult to get comfortable, wakes when turning Not getting good-quality sleep any more Daily pattern Gradually worse by the end of the day General health Has gained weight over the last 14/12 (about 6 kg) Assessed as being depressed, has been taking antidepressants over the last 3/12 Investigations X-ray shows mild bilateral degeneration of the L4–5 facets CT scan shows a minor disc bulge at L4–5 and L5–S1 with no nerve root involvement Attitude/expectations Has reduced activity level to avoid aggravating back Believes that if she can find the right practitioner then they will fix her Very concerned with the CT scan report and the diagnosis of disc pathology Has been more short-tempered with family and friends since her back problem began Her spouse has been very supportive and has willingly taken over tasks such as housework and shopping Pain and dysfunction scores Oswestry Disability Score: 72% Disability VAS level of pain after 15 minutes of standing or sitting = 7.5 Physical examination Observation Exhibits pain behaviours including grimacing, and placing hand on back Changes position regularly when sitting and standing Walking pattern is slow and guarded Palpation Central palpation of the lumbar spine at L1, L2, L3, L4 and L5 painful Unilateral pressures are painful left and right at L1, L2, L3, L4 and L5 Movements Active movements Lumbar flexion in standing limited (2 cm above the knee) Lumbar extension in standing moderately limited (estimated half of expected range) Left and right rotation (assessed in sitting) both about 40° Neural mobility tests Straight leg raise on right = 50° left = 50° Able to fully extend knee in upright sitting Slump test not evaluated Neurological tests (tests of nerve conduction) • Normal no abnormality detected Questions 1. What is your provisional diagnosis? 2. How do you interpret the X-ray and CT scan reports? 3. Which of the signs and symptoms will you place on your priority list? 4. How will you address these in your treatment plan? 5. What kind of common and less common problems need to be excluded? 6. How relevant are work details for this patient? 7. What are yellow flags and how are they relevant for this patient? 8. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 8 Shoulder pain Subjective examination Subject 47-year-old female factory worker Right arm dominant HPC Right shoulder pain which started 1/52 ago when dragging a heavy item onto the conveyor belt. Routinely she has to pull, lift, and reach overhead PMH Low back pain episodes since work-related lifting injury Asthma and frequent coughing Aggravating factors At work: Overhead work, lifting and carrying boxes In transit: Driving car, riding a bike with wide handlebars. At home: Preparing meals, working at the computer, knitting Easing factors Rest Avoiding overhead work or holding elbows out when lifting or carrying items Night Wakes frequently because of pain, particularly when sleeping on the painful shoulder Daily pattern Constant nagging pain that worsens during activities as mentioned above (see aggravating factors ) General health Asthma attacks. Smokes. Using bronchodilatators as needed Attitude/expectations Is afraid that she may need to look for another job due to experiencing increasing shoulder problems at work Wants better duties within the factory as some of her colleagues have managed to do Pain and dysfunction scores VAS current pain at rest = 3 VAS usual level of pain during aggravating activity in the last week = 7 VAS worst level of pain in the last week = 9 Shoulder Pain and Disability Index (SPADI): Pain score = 60%, Disability score = 45%, Total score = 50.8% ( Roach et al 1991 ) Objective examination Standing with arms relaxed Shoulders protracted and depressed (right > left) Right shoulder abducted and elbow flexed Hyper kyphosis Shortness of breath with upper chest breathing Palpation Skin temperature (T sk ) normal Tenderness of subscapularis, supraspinatus and serratus posterior superior with palpable trigger points Painful insertion of subscapularis and supraspinatus on the humerus Palpable click on shoulder abduction Muscle length and strength Tightness of the subscapularis, pectoralis minor Weakness of rhomboids, supraspinatus Functional and other testing, including ROM Painful arc when abducting arm (90–115° abduction) with audible click (VAS rises to 6 during this impingement) Hawkins and Kennedy impingement test (compressing the subacromial tissues by internal rotation in 90° shoulder flexion) was positive ( Ginn 2003 ) and VAS rises to 8 Apprehension test for shoulder stability and SLAP lesion tests were negative, indicating integrity of joint capsule, labrum and ligaments ( Brukner et al 2001e , Ginn 2003 , Hoppenfield 1986 ) Shoulder elevation reduced by 10° with early scapular movement when comparing with left shoulder (VAS rises to 5) Pain on resistance against external rotation and abduction (VAS rises to 8) Reduced internal rotation and adduction strength when pushing palm of the hand on the table when sitting at the table (VAS rises to 7) Difficulty placing right hand behind back. Positive Gerbers’ test (resisting against hand when patient is pushing hand away from the spine (VAS rises to 8) Questions 1. What is your provisional diagnosis? 2. What signs and symptoms lead you to this diagnosis? 3. Describe the mechanism that can leads to this condition. 4. How will you address these signs and symptoms in your treatment plan? 5. What kind of common and less common problems need to be excluded? 6. Can patient’s asthma and hyper kyphosis contribute to the shoulder complaint? 7. How will the expectation of the patient influence your treatment? 8. Is it possible that outcome measures do not reflect the severity of pain and disability experienced by the patient? 9. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 9 Elbow pain Subjective examination Subject 39-year-old male carpenter Right hand dominant HPC Right lateral elbow pain off and on for at least 5/12. Insidious onset Worsened 4/52 ago when his nail gun broke down and he was forced to use a hammer all day Severe pain and reduced strength, particularly when using his arm during activities such as gripping, holding and lifting. Pain radiates into forearm No history of locking PMH Fractured ribs 3 years ago due to fall at work. Landed on his right side, and elbow was pushed into the ribs. No elbow symptoms until 5/12 ago Never experienced any symptoms of the cervical or thoracic spine Minor injuries such as an ankle sprain, mainly due to sport Aggravating factors Firm gripping (e.g. pliers) Hammering Screw driving Using a jackhammer Driving (car has no power steering) Closing a tap Knocking the elbow Easing factors Rest Ice Night Constant ache. Lying on elbow or pulling up the blanket makes it worse Daily pattern Constant pain that worsens during and directly after activity General health No other health problems reported. Not using any medication or receiving any other medical care Attitude/expectations Is disappointed that his elbow problem hasn’t improved over time as his other injuries did Experiencing increasing problems at work. Is afraid that he will lose his job One of his colleagues experienced major improvement after physiotherapy treatment and he hopes that it will help him too Expects that it may take some time since he wants to stay at work Pain and dysfunction scores VAS current pain at rest = 4 VAS usual level of pain during activity in the last week = 8 VAS worst level of pain in the last week = 9–10 Upper Extremity Functional Index (UEFI) 35/80 ( Stanford et al 2001 ) Objective examination Arm at rest while standing Elbow flexed (right > left) Wrist flexed (right > left) Forearm supinated (right > left) Palpation Skin temperature (T sk ) normal Lateral epicondyle extremely painful with some palpable swelling Tenderness extensor carpi radialis brevis and longus Thickening in extensor carpi radialis brevis (ECRB) Difficult to palpate for tenderness of capitellum radii due to surrounding tissue swelling and pain Muscle length ECRB – tight (flexion and ulnar deviation of the wrist, pronation of the forearm, and slight extension of elbow) Extensor carpi radialis longus – tight (flexion and ulnar deviation of the wrist, pronation of the forearm, and complete extension of elbow) Functional testing, including ROM and strength Elbow extension showed pain in at end of ROM (VAS rises to 6) Forearm pronation/supination showed full ROM (VAS rises to 5) Reduced grip strength (VAS rises from 4 to 9 during firm gripping) Difficulty opening pushing door handle and opening door (VAS rises to 7) Difficulty lifting an object with palm of hand facing down (VAS rises to 8) Resistance against dorsiflexion in a dorsiflexed position of the wrist, with fist closed, caused severe pain on the lateral side of the elbow Questions 1. What is your provisional diagnosis? 2. What signs and symptoms lead you to this diagnosis? 3. Describe the mechanism that can lead to the condition 4. What will you include in your treatment plan? 5. What kind of common and less common problems need to be excluded? 6. How likely does the patient’s previous fall contribute to the current complaint? 7. How will the expectations of the patient influence your treatment? 8. Is the patient likely to benefit from referral to other health professionals? CASE STUDY 10 Hand weakness and pain Subjective examination Subject 56-year-old woman who works part-time as a kindergarten assistant Right hand dominant HPC Pain, numbness and tingling noticed in right hand (particularly in the thumb, index and middle fingers) over the last 6/52, especially at night. Insidious onset Has started to have difficulty using right hand for gripping and it is starting to affect work as a kindergarten assistant and tennis Feels it is getting worse, because pain is now extending up the forearm. Is now waking her during the night PMH Diagnosed with non-insulin-dependent diabetes 5 years ago, currently well controlled with diet and exercise (walks for 45 minutes three times a week and plays social tennis twice a week) Knee arthroscopy with partial left medial menisectomy 12 years ago after tennis injury, recovered well Aggravating factors Gripping (tennis racquet after 1 set, a feeling of weakness) Opening jars Packing up play equipment at kindergarten Sleeping Easing factors Gets a little relief from changing position and shaking out wrist Aspirin (started aspirin 2/52 ago on advice of GP), may have helped a little Night Now waking every night (once only) with right wrist pain and numbness Daily pattern Symptoms are dependent on activity. Finds it is painful at end of shift at the kindergarten and after tennis. Otherwise not troubling too much during the day Attitude/expectations Enjoys her regular exercise (especially tennis) so is keen to get the problem fixed She has friends who had surgery for something that sounded similar so is not sure why she was referred to physiotherapy or how it might help Pain and dysfunction scores VAS current pain at rest = 1.5 VAS worst level of pain in the last week = 7 Levine symptom severity scale = 1.9/5.0 Levine functional status scale = 1.4/5.0 Physical examination Observation No abnormality detected No wasting of right thenar eminence Palpation Slight reduction to light touch on the palmar surface of the right thumb and 1st and 2nd finger Movement (right side) Wrist flexion = 60°, no pain Wrist extension = 55°, no pain Wrist supination = 90° from mid-prone, no pain Wrist pronation = 90° from mid-prone, no pain Finger IP flexion OK, no pain Finger MCP flexion OK, no pain Thumb flexion, abduction and opposition OK, no pain Functional testing, including ROM and strength Grip strength assessed on Jamar dynamometer (right = 27 kg with VAS = 3, left = 35 kg) Phalen’s test (sustained bilateral wrist flexion) reproduced numbness on palmar surface of index and middle after 45 seconds Upper limb tension test with a median nerve bias: reproduced right hand symptoms which eased on release of shoulder depression ( Butler 2000 ) Questions 1. What is your provisional diagnosis? 2. What are the anatomical relationships that explain your provisional diagnosis and the patient’s symptoms and signs? 3. Explain the significance of the night symptoms and the positive Phalen’s sign. 4. Are there other assessment techniques that could be used to confirm the provisional diagnosis? 5. Find out what items the Levine symptom severity and functional status scales assesses ( Levine et al 1993 ) and then discuss how this patient rates. 6. Which of the symptoms and signs will you place on your priority list? 7. How will you address these in your physiotherapy treatment plan? 8. Are there other problems that could be contributing to the symptoms? 9. The patient has some friends who had surgery for something similar. What is the role of surgery for this condition? CASE STUDY 11 Groin pain Subjective examination Subject 17-year-old male student Playing in high-level senior soccer team with training three times a week in addition to a match on the weekend Plays as midfielder Right foot dominant HPC About 4/12 ago noticed slight stiffness in groin the morning after a strenuous match. Insidious onset Gradually got worse until about 2/12 ago could not train or play without right-sided groin pain. Performance was also waning with a loss of power and acceleration On advice of team trainer rested from all training and playing for 6/52, but on resumption of training 2/52 ago groin pain returned immediately. Seen by GP who ordered X-rays and a bone scan, and referred him to physiotherapy PMH Well-controlled asthma. Uses one puff of a preventer daily (Flixitide). Rarely needs to use reliever (Ventolin) Episode of Osgood–Schlatters syndrome when 14 years old after joining soccer development squad. Resolved after 1 year through modification of activity Otherwise well and not seeing the doctor for any other condition Aggravating factors Running, especially when sprinting and when cutting (changing direction) Kicking, especially when taking a corner No pain on sneezing or coughing Easing factors Avoidance of aggravating activities Night Sleep unaffected Daily pattern Symptoms are dependent on activity. Now affecting whenever tries to run or kick a ball Notices in morning, takes 10 to 15 minutes to ease Attitude/expectations Concerned that the problem appears to be getting worse. Had thought it would just go away Receives payment for playing in soccer team which he had planned to continue to help support his studies at university Pain and dysfunction scores VAS current pain at rest = 0 VAS worst level of pain in the last week = 9 (kicking across from a corner) VAS worst level of pain in the last week = 8 (when attempting to sprint) Physical examination Observation In standing, no obvious wasting or pelvic asymmetry With walking, observed excessive pelvic tilting (obliquity) in the frontal plane Palpation Tender to palpation at tendon attaching to right medial inferior pubic ramus Trigger point tenderness to muscle belly distal to medial inferior pubic ramus Tender at right side of pubic symphysis Movement Right hip flexion = 130°, no pain = left Right hip extension = 25°, no pain = left Right hip abduction = 45°, pain (VAS = 3), left = 55° Right hip internal/external rotation = left Functional testing Squeeze test (patient supine with hip flexed 45°, examiner places fist between patient knees, and asks patient to bilaterally adduct) reproduced right groin pain (VAS = 4) Resisted straight-leg right hip adduction reproduced right groin pain (VAS = 4) Right hip quadrant (passive hip flexion, adduction and internal rotation) only very slight pain, similar to discomfort when tested on the left side Thomas test (slight restriction on right compared to left with only slight reproduction of pain (VAS = 0.5) when hip flexion resisted) Abdominal muscle testing: 1. global muscles, only slight pain (VAS = 1) on resisted abdominal flexion 2. stabilising muscles, assessed in supine with a pressure cuff biofeedback unit placed in the small of the back. He could increase the pressure in the cuff from 40 to 43 mmHg for 3 seconds 4 times before unwanted activity from global muscles was observed Standing on one leg (Trendelenburg test), only slight drop of pelvis observed, within normal limits (<10°) Investigations (completed 1/52 ago) X-ray: no abnormality detected Bone scan: indicated some increased uptake in the right inferior pubic region Questions 1. What is your provisional diagnosis? 2. What are the key findings from your examination that led to your provisional diagnosis? 3. What other common causes of groin pain did you consider in making your diagnosis? 4. What are some less common causes of groin pain that you need to consider when examining this patient? Briefly explain why these are considered unlikely at this stage. 5. What is Osgood–Schlatter’s disease and what is its relevance to the current condition? 6. What are the significance of the bone scan findings and the assessment of the abdominal stabilising muscles, and do these findings tie in with the other assessment findings? 7. Which of the symptoms and signs will you place on your priority list? 8. How will you address these in your physiotherapy treatment plan? CASE STUDY 12 Hip and thigh pain Subjective examination Subject 38-year-old female Right leg dominant HPC Right lateral hip and thigh pain that can radiate to knee Started approximately 1/12 ago Woke up with pain after a long shopping day PMH Overweight (BMI ≥27) Neck pain and headaches Aggravating factors Walking Sleeping on right side Sleeping on a hard mattress Easing factors Rest and ice Night Wakes up frequently, particularly when lying on right side, or on left side with right hip in adduction and knee resting on the mattress Daily pattern Pain during and after prolonged standing and walking General health Overweight. No other problems reported. Not using any medication Attitude/expectations Is not sure whether treatment will provide immediate relief, but hopes that at least she will be able to sleep better. Between pain experienced at night and her youngest child waking up and demanding attention she does not get much sleep and feels fatigued Pain and dysfunction scores VAS current pain at rest before activity = 2 VAS usual level of pain when waking up at night = 8 VAS usual level of pain during and after activity in the last week = 7 VAS worst level of pain in the last week = 9 Lower Extremity Functional Scale 48/80 ( Binkley et al 1999 ) Objective examination Standing Visibly overweight Wide hips, but knees are touching each other Valgus position of knees and ankles Pronated feet with reasonable longitudinal arches Palpation Although skin temperature (T sk ) around hip and along the thigh appeared normal, that of the posterior aspect of the trochanter may have been a little elevated Tenderness of the iliotibial tract and the bony posterior aspect of the greater trochanter, with a boggy feeling around the location of the bursa ( Hoppenfield 1986 )
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:

Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree


Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
12.1 Case Study: Muscles and Movement
Created by CK-12 Foundation/Adapted by Christine Miller
Case Study: Needing to Relax
This dog (Figure 12.1.1) is expressing his interest in something — perhaps a piece of food — by using the neck muscles to tilt its head in an adorable fashion. Humans also sometimes tilt their heads to express interest. But imagine how disturbing and painful it would be if your neck tilted involuntarily, without you being able to control it! Forty-three year old Edward unfortunately knows just how debilitating this can be.
Edward has a rare condition called cervical dystonia , which is also called spasmodic torticollis. In this condition, the muscles in the neck contract involuntarily, often causing the person’s head to twist to one side. Figure 12.1.2 shows one type of abnormal head positioning that can be caused by cervical dystonia. The muscles may contract in a sustained fashion, holding the head and neck in one position, or they may spasm repeatedly, causing jerky movements of the head and neck.
Cervical dystonia is painful and can significantly interfere with a person’s ability to carry out their usual daily activities. In Edward’s case, he can no longer drive a car, because his uncontrollable head and neck movements and abnormal head positioning prevent him from navigating the road safely. He also has severe neck and shoulder pain much of the time.
Although it can be caused by an injury, there is no known cause of cervical dystonia — and there is also no cure. Fortunately for Edward, and others who suffer from cervical dystonia, there is a treatment that can significantly reduce symptoms in many people. You may be surprised to learn that this treatment is the same substance which, when injected into the face, is used for cosmetic purposes to reduce wrinkles!
The substance is botulinum toxin, one preparation of which may be familiar to you by its brand name — Botox . It is a neurotoxin produced by the bacterium Clostridium botulinum , and can cause a life-threatening illness called botulism . However, when injected in very small amounts by a skilled medical professional, botulinum toxins have some safe and effective uses. In addition to cervical dystonia, botulinum toxins can be used to treat other disorders involving the muscular system, such as strabismus (misalignment of the eyes); eye twitches; excessive muscle contraction due to neurological conditions like cerebral palsy; and even overactive bladder.
Botulinum toxin has its effect on the muscular system by inhibiting muscle contractions. When used to treat wrinkles, it relaxes the muscles of the face, lessening the appearance of wrinkles. When used to treat cervical dystonia and other disorders involving excessive muscle contraction, it reduces the abnormal contractions.
In this chapter, you will learn about the muscles of the body, how they contract to produce movements and carry out their functions, and some disorders that affect the muscular system. At the end of the chapter, you will find out if botulinum toxin helped relieve Edward’s cervical dystonia, and how this toxin works to inhibit muscle contraction.
Chapter Overview: Muscular System
In this chapter, you will learn about the muscular system, which carries out both voluntary body movements and involuntary contractions of internal organs and structures. Specifically, you will learn about:
- The different types of muscle tissue — skeletal, cardiac, and smooth muscle — and their different characteristics and functions.
- How muscle cells are specialized to contract and cause voluntary and involuntary movements.
- The ways in which muscle contraction is controlled.
- How skeletal muscles can grow or shrink, causing changes in strength.
- The structure and organization of skeletal muscles, including the different types of muscle fibres, and how actin and myosin filaments move across each other — according to the sliding filament theory — to cause muscle contraction.
- Cardiac muscle tissue in the heart that contracts to pump blood through the body.
- Smooth muscle tissue that makes up internal organs and structures, such as the digestive system, blood vessels, and uterus.
- The physical and mental health benefits of aerobic and anaerobic exercise, such as running and weight lifting.
- How individuals vary in their response to exercise.
- Disorders of the muscular system, including musculoskeletal disorders (such as strains and carpal tunnel syndrome) and neuromuscular disorders (such as muscular dystrophy, myasthenia gravis, and Parkinson’s disease).
As you read the chapter, think about the following questions:
- How is the contraction of skeletal muscles controlled?
- Botulinum toxin works on the cellular and molecular level to inhibit muscle contraction. Based on what you learn about how muscle contraction works, can you think of some ways it could potentially be inhibited?
- What is one disorder involving a lack of sufficient muscle contraction? Why does it occur?
Attributions
Figure 12.1.1
Whiskey’s 2nd Birthday by Kelly Hunter on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 12.1.2
1024px-Dystonia2010 by James Heilman, MD on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
Botulism [online article]. (2018, January 10). World Health Organization (WHO). https://www.who.int/news-room/fact-sheets/detail/botulism
Mayo Clinic Staff. (n.d.) Cervical dystonia [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/cervical-dystonia/symptoms-causes/syc-20354123
A drug prepared from the bacterial toxin botulin, used medically to treat certain muscular conditions and cosmetically to remove wrinkles by temporarily paralyzing facial muscles.
A soft tissue that composes muscles in animal bodies, and gives rise to muscles' ability to contract. This is opposed to other components or tissues in muscle such as tendons or perimysium.
Actions which take place according to the one's desire or are under control.
Actions which are not under one's conscious control.
Voluntary, striated muscle that is attached to bones of the skeleton and helps the body move.
Involuntary, striated muscle found only in the walls of the heart; also called myocardium.
An involuntary, nonstriated muscle that is found in the walls of internal organs such as the stomach.
Human Biology Copyright © 2020 by Christine Miller is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
109 12.1 Case Study: Muscles and Movement
Created by CK-12 Foundation/Adapted by Christine Miller


Case Study: Needing to Relax
This dog (Figure 12.1.1) is expressing his interest in something — perhaps a piece of food — by using the neck muscles to tilt its head in an adorable fashion. Humans also sometimes tilt their heads to express interest. But imagine how disturbing and painful it would be if your neck tilted involuntarily, without you being able to control it! Forty-three year old Edward unfortunately knows just how debilitating this can be.
Edward has a rare condition called cervical dystonia , which is also called spasmodic torticollis. In this condition, the muscles in the neck contract involuntarily, often causing the person’s head to twist to one side. Figure 12.1.2 shows one type of abnormal head positioning that can be caused by cervical dystonia. The muscles may contract in a sustained fashion, holding the head and neck in one position, or they may spasm repeatedly, causing jerky movements of the head and neck.

Cervical dystonia is painful and can significantly interfere with a person’s ability to carry out their usual daily activities. In Edward’s case, he can no longer drive a car, because his uncontrollable head and neck movements and abnormal head positioning prevent him from navigating the road safely. He also has severe neck and shoulder pain much of the time.
Although it can be caused by an injury, there is no known cause of cervical dystonia — and there is also no cure. Fortunately for Edward, and others who suffer from cervical dystonia, there is a treatment that can significantly reduce symptoms in many people. You may be surprised to learn that this treatment is the same substance which, when injected into the face, is used for cosmetic purposes to reduce wrinkles!
The substance is botulinum toxin, one preparation of which may be familiar to you by its brand name — Botox . It is a neurotoxin produced by the bacterium Clostridium botulinum , and can cause a life-threatening illness called botulism . However, when injected in very small amounts by a skilled medical professional, botulinum toxins have some safe and effective uses. In addition to cervical dystonia, botulinum toxins can be used to treat other disorders involving the muscular system, such as strabismus (misalignment of the eyes); eye twitches; excessive muscle contraction due to neurological conditions like cerebral palsy; and even overactive bladder.
Botulinum toxin has its effect on the muscular system by inhibiting muscle contractions. When used to treat wrinkles, it relaxes the muscles of the face, lessening the appearance of wrinkles. When used to treat cervical dystonia and other disorders involving excessive muscle contraction, it reduces the abnormal contractions.
In this chapter, you will learn about the muscles of the body, how they contract to produce movements and carry out their functions, and some disorders that affect the muscular system. At the end of the chapter, you will find out if botulinum toxin helped relieve Edward’s cervical dystonia, and how this toxin works to inhibit muscle contraction.
Chapter Overview: Muscular System
In this chapter, you will learn about the muscular system, which carries out both voluntary body movements and involuntary contractions of internal organs and structures. Specifically, you will learn about:
- The different types of muscle tissue — skeletal, cardiac, and smooth muscle — and their different characteristics and functions.
- How muscle cells are specialized to contract and cause voluntary and involuntary movements.
- The ways in which muscle contraction is controlled.
- How skeletal muscles can grow or shrink, causing changes in strength.
- The structure and organization of skeletal muscles, including the different types of muscle fibres, and how actin and myosin filaments move across each other — according to the sliding filament theory — to cause muscle contraction.
- Cardiac muscle tissue in the heart that contracts to pump blood through the body.
- Smooth muscle tissue that makes up internal organs and structures, such as the digestive system, blood vessels, and uterus.
- The physical and mental health benefits of aerobic and anaerobic exercise, such as running and weight lifting.
- How individuals vary in their response to exercise.
- Disorders of the muscular system, including musculoskeletal disorders (such as strains and carpal tunnel syndrome) and neuromuscular disorders (such as muscular dystrophy, myasthenia gravis, and Parkinson’s disease).
As you read the chapter, think about the following questions:
- How is the contraction of skeletal muscles controlled?
- Botulinum toxin works on the cellular and molecular level to inhibit muscle contraction. Based on what you learn about how muscle contraction works, can you think of some ways it could potentially be inhibited?
- What is one disorder involving a lack of sufficient muscle contraction? Why does it occur?
Attributions
Figure 12.1.1
Whiskey’s 2nd Birthday by Kelly Hunter on Flickr is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0/) license.
Figure 12.1.2
1024px-Dystonia2010 by James Heilman, MD on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
Botulism [online article]. (2018, January 10). World Health Organization (WHO). https://www.who.int/news-room/fact-sheets/detail/botulism
Mayo Clinic Staff. (n.d.) Cervical dystonia [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/cervical-dystonia/symptoms-causes/syc-20354123
A drug prepared from the bacterial toxin botulin, used medically to treat certain muscular conditions and cosmetically to remove wrinkles by temporarily paralyzing facial muscles.
A soft tissue that composes muscles in animal bodies, and gives rise to muscles' ability to contract. This is opposed to other components or tissues in muscle such as tendons or perimysium.
Actions which take place according to the one's desire or are under control.
Actions which are not under one's conscious control.
Voluntary, striated muscle that is attached to bones of the skeleton and helps the body move.
Involuntary, striated muscle found only in the walls of the heart; also called myocardium.
An involuntary, nonstriated muscle that is found in the walls of internal organs such as the stomach.
Human Biology Copyright © 2020 by Christine Miller is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Case Studies in Management of Muscle Cramps
Affiliation.
- 1 Toronto General Hospital / University Health Network, Krembil Brain Institute, University of Toronto, 200 Elizabeth Street, 5ES-306, Toronto, Ontario M6S 4E6, Canada. Electronic address: [email protected].
- PMID: 32703476
- DOI: 10.1016/j.ncl.2020.03.011
Muscle cramps, defined as a painful contraction of a muscle or muscle group, are a common symptom most people have experienced throughout their lifespan. In some cases cramps can be frequent, severe, and disabling, thus requiring medical assessment and intervention. Physiologic states such as pregnancy and exercise are associated with excessive muscle cramps, as are numerous medical and neurologic conditions, medications such as diuretics and statins, and peripheral nerve hyperexcitability syndromes. Treatment options for muscle cramps are limited, although recent studies have shown that mexiletine could be a safe and efficient alternative for patients with amyotrophic lateral sclerosis.
Keywords: Charley horse; Contraction; Hyperexcitability; Muscle cramps; Spasms.
Copyright © 2020 Elsevier Inc. All rights reserved.
Publication types
- Case Reports
- Research Support, Non-U.S. Gov't
- Disease Management*
- Mexiletine / therapeutic use
- Middle Aged
- Muscle Cramp / diagnosis*
- Muscle Cramp / physiopathology
- Muscle Cramp / therapy*
- Voltage-Gated Sodium Channel Blockers / therapeutic use
- Young Adult
- Voltage-Gated Sodium Channel Blockers

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

Case Study: The Tired Swimmer
- Last updated
- Save as PDF
- Page ID 20316

- Shannan Muskopf
- Granite City School District via Biology Corner
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Part I: Meet Annie
Annie felt despondent. Her teammates were being kind to her, but she knew that she was the reason that her team lost the swim meet against the neighboring college. How many people could lose with a four-second lead against someone they had beaten so easily last year? As she walked out of the locker room she noticed that the blurred vision and eye strain had returned, even though she was wearing glasses instead of her usual contacts. Her eye strain had become worse over the past month. Over the last week she had had mid-term exams and papers to write and recently typing made her hands and fingers ache and they felt weak. Even swim practice, which helped relieve her stress in the past, had become taxing. Her coach noticed that her times were getting worse, even though he could see that she was working hard in practice.
As Annie walked out of the locker room she looked up and she saw her boyfriend, Matt, waiting for her. As they walked back to her dorm, Annie thought how nice it was to have Matt to support her during such a tough time. Annie was gasping for air and felt weaker than ever after they had walked up the two flights of stairs to her floor. She told herself that she must set some time aside next week to do something about this constant fatigue.
Annie had already packed her bags for the trip home and Matt was able to carry all of her stuff to his car in one trip. When he returned to the room he found Annie reclining on the bed with her eyes closed. He asked her if she was ready to go. “Sure, just can’t keep my eyes open these days. I am sure I’ll be better when we’re home.”
Matt knew that Annie liked to drive, so when they got to the car he handed her the keys. She tried to take them, but her fingers didn’t seem to work and she dropped his keys on the ground. Matt grabbed the keys and opened the passenger door for Annie. As they set off for home, Matt asked, “Are you feeling okay? You’re not usually so exhausted after a swim meet, and you seem to be having trouble catching your breath. I am worried about you.” Matt thought that this was probably the best time to suggest that she see a doctor.
- Summarize the setting (background) for this case.
- What symptoms does Annie exhibit? Prioritize these symptoms in order of what you think is the most concerning and the least concerning.
- What is the one common feature of all of her symptoms?
- When did Matt notice that Annie was having trouble breathing?
- List any diseases, disorders, or health problems that you can think of that might cause these symptoms.
Part II:The Doctor’s Office
On Monday afternoon, Matt drove Annie to her family doctor. She seemed to have slept for most of the weekend, and Matt thought that she looked much better than last Friday after the meet. In fact, she told him that she felt so much better that she really didn’t need to go to the doctor.
“Seriously, this is stupid. I’ve been feeling much better in the past few days. It’s amazing what some rest can do. That’s all I need; I really don’t need a doctor as long as I take a nap periodically. Let’s not waste his time; let’s just go home.” Matt looked at her with his eyebrows raised, “Let’s just hear what he has to say; better safe than sorry.”
Matt sat in the waiting room and Annie went with the nurse. After a few minutes Dr. Jones entered the cubicle, “Well, Annie, what seems to be the problem?”
“It’s nothing, really. I have just been tired lately. You know I’m going to college on a swimming scholarship, but my times have been getting worse this season, and I’ve been short of breath more than usual after my workouts. I think it’s just because I was stressed out over school; I have been feeling much better since I came home last Friday. “I see,” said the doctor. “Have you had any other problems?”
“Well, yes. My hands and fingers seem to get tired when I type, and a few days ago, after a swim meet, my fingers felt too weak to grab my boyfriend’s car keys when he offered them to me; but I was tired after a really hectic week.”
Dr. Jones looked pensive and asked, “Have you had any trouble with your eyes? Like have they been drooping?”
Annie looked confused. “I have had a lot of eye strain and double vision recently. It gets blurry when I stare at the computer screen too long; I seem to get a zillion papers every week. I also think the chlorine level in the pool is too high. Everyone on the team complains about it because, if your goggles come off , your eyes sting like mad.
The doctor smiled, “I swam before those goggles were even invented, so I know what you mean about stinging eyes. But, I think what you’re telling me goes beyond simple fatigue. I’m going to refer you to a neurologist at the hospital.”
5. What specific question does the doctor ask Annie?
6. What excuse does Annie give about her eye strain?
7. What is a neurologist?
8. Based on how the doctor responded, do you think he believes that Annie’s problems are caused by not getting enough sleep?
Part III—The Neurologist
Annie returned to the neurologist’s office with her mother. That morning Annie had been subjected to several different tests and she had been asked to return after lunch when the results would be in. The nurse told her that they were rushing this through because they knew that Annie was only home for a week. Annie and her mother sat in the waiting room for what seemed to be hours. At last the nurse came for them.
“Some of the results are here, and the rest are on their way,” she explained. “So the doctor will see you now.” Annie and her mother went into the doctor’s office and sat down.
“Well, Annie, I have read your family doctor’s notes, and we put you through a battery of tests this morning.” the neurologist skimmed through the chart, “Hmm, blurred vision, weak fingers, and decline in swimming performance. OK, let’s see what we found out today. First, the nerve conduction and the electromyography (emg) tests; these are the only results we have right now. This was the test when they put sticky electrodes on your skin, remember?” Annie nodded.
“Well, for the nerve conduction tests one set of electrodes stimulated the nerve and another recorded its response a little way down the nerve. The nerve conduction results are normal. There is no nerve fatigue and the conduction velocity is fine; nothing wrong with your nerves.”
Annie and her mother looked at each other and smiled with relief.
“Now, the electromyography test involves recording from a muscle; it was done in two stages. The first stage stimulated the muscle directly, and there isn’t too much out of the ordinary there. The second stage is when the nerves were stimulated and the muscle response was recorded. These results concern me because the muscle response decreased quickly during repeated nerve stimulation, indicating that your muscle response fatigued over time.”
8. Summarize the results of the nerve conduction test?
9. What is the EMG test? What did this test reveal about Annie’s muscles?
10. Based on these two tests, does Annie have a nerve problem or a muscle problem?
Part IV—The Neurologist Makes a Diagnosis
They heard a knock at the door and turned to see the nurse enter; she was holding a folder with the hospital’s stamp. The doctor looked over the lab results and then continued.
“I’m afraid I don’t have very good news. Do you remember when the nurse injected that solution into your arm and you said that suddenly you felt much stronger?” Annie nodded.
“That was the edrophonium test. It temporarily relieves symptoms of people who suffer from myasthenia gravis. I am afraid that the diagnosis is confirmed by these lab results, which show the disease.
The nurse handed Annie and her mother a pamphlet about myasthenia gravis while the doctor explained. “Myasthenia gravis causes your immune system to attack the acetylcholine receptors on your muscles. As these receptors stop working, the muscles fatigues easily. Often the first symptom is weakness of the eye muscle.” The doctor held a chart up showing the neuromuscular junction.
11. Label the image below that shows the neuromuscular junction: Sarcomere | Sarcolemma | Synapse | Motor End Plate | Nerve | Vesicles | T- Tubules
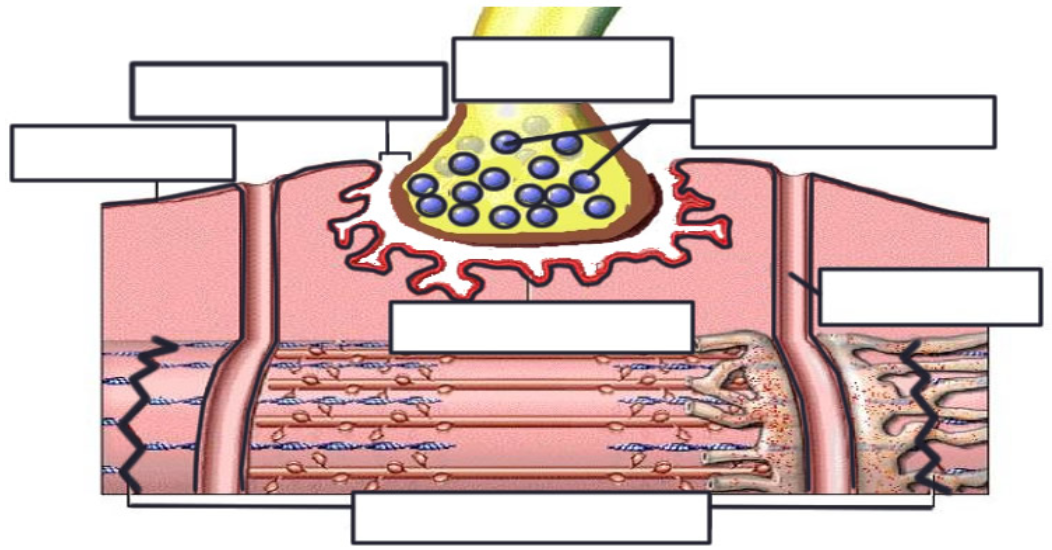
12. Add to the drawing by placing stars where the acetylcholine receptors would be located.
13. Edrophonium is a drug the blocks cholinesterase from breaking down acetylcholine in the muscles. Why does this improve Annie’s muscle function?
14. Why is myasthenia gravis called an autoimmune disease?
Modified from: A Case Study on the Nervous System

COMMENTS
Joint disease (53) arthropathy___ Muscle weakness (54)myasthenia____ Her osteoarthritis (55)OA has progressed, and she may be a candidate for a bilateral ... MUSCULOSKELETAL SYSTEM CASE STUDY—ANSWER KEY O: Doctor Rusk asks Mrs. Jenkins about her CC (17)chief complaint. She states, "My knees are killing me! I am having trouble getting around ...
Case Studies: Answers. Case 1: Acute joint disease. 1 The most crucial piece of information is that the patient is well. The diagnosis to rule out in every case is septic arthritis, and this seems unlikely in this scenario. However, his diabetes is a risk factor for infection, and a careful history of the previous injury might reveal a route of ...
Heart sounds were normal (no murmur). Shoulder, arm, and thigh. muscles appear slightly atrophied. Calf muscles appeared slightly enlarged. Muscle strength reduced in the biceps & triceps muscles (+4 on a scale from 0 to. +5, +5 being normal). MODULE 14: ANATOMY & PHYSIOLOGY. CASE STUDY #3: MUSCULAR SYSTEM.
View Guided Case Study Muscle Malady.pdf from GOV 106 at La Reina High School. Jaithan Phillips Grayson Guevara Guided Case Study: Muscle Malady 1.) ... Muscle case study Answer key (1).docx. Solutions Available. No School. AA 1. Research Paper 1.docx. Liberty University. MSCI 520. Bio 101 quiz 7.docx.
Presentation of Case. Dr. Chidiebere D. Akusobi (Medicine): A 44-year-old woman was evaluated in the rheumatology clinic of this hospital because of proximal muscle weakness and myalgia. The ...
The muscles may contract in a sustained fashion, holding the head and neck in one position, or they may spasm repeatedly, causing jerky movements of the head and neck. Figure 15.1.2 15.1. 2: Illustration from a medical book written around 1910, showing a person identified as having spasmodic torticollis. The person's neck is permanently tilted ...
Becker muscular dystrophy. similar to Duchenne but milder and progresses slower, occurs in teenage years or until the mid-20s or later. congenital. affects boys & girls. apparent at birth or before age of 2, can slowly cause mild disability to rapid severe impairment. Study with Quizlet and memorize flashcards containing terms like Skeletal ...
Becker's Muscular Dystrophy. A genetic disorder that is characterized by slowly progressive muscle paresis of legs and pelvis. This gene mutation causes a mutation of dystrophin, a protein that keeps muscle cells intact. Typically symptoms include weakness of hips and thighs, but they are typically milder than Duchene's.
Chapter 10 Case Studies Introduction Case 1. Shoulder Pain Case 2. Compromised Gait and Function Secondary to Muscle Weakness Case 3. Fatigue Secondary to Muscle Weakness Case 4. Muscle Weakness Following Nerve Injury Case 5. Muscle Weakness Following Hip Surgery Case 6. Muscle Weakness Following Childbirth Introduction This chapter serves as a brief summary of the muscle testing performance ...
Essentials of Medical Terminology Ch. 4 Muscular System Case Study Prof. Tolman Period: _____ Date: _____ CHAPTER 4: MUSCULOSKELETAL SYSTEM CASE STUDY—ANSWER KEY Directions: Read the case study. In each blank space, provide either the medical term, the definition of the medical term or the abbreviation for the bolded word(s).
Rahul is experiencing difficulty walking and an abnormal gait, which are symptoms of Duchenne Muscular Dystrophy (DMD).. 2. The blood test that was ordered specifically tests for the creatine-kinase (CK) enzyme linked to degeneration of muscles and provides a genetic analysis through DNA testing of the blood cells.
Duchenne muscular dystrophy (DMD) is an atypical inherited musculoskeletal disorder which shows clinical characteristics of progressive muscular weakness at an early stage and pathologic features of fibrosis and fatty replacement, particularly late in the disease course. It is a recessive X-linked disorder occurring 1 in every 3500 live male ...
CHAPTER EIGHT Case studies in a musculoskeletal out-patients setting. CHAPTER EIGHT. Case studies in a musculoskeletal out-patients setting. Case study 1: Jaw Pain 217. Case study 2: Headache 218. Case study 3: Neck Pain - Case One 221. Case study 4: Neck Pain - Case Two 224. Case study 5: Thoracic Pain 226. Case study 6: Low Back Pain ...
Muscle cramps, defined as a painful contraction of a muscle or muscle group, are a common symptom most people have experienced throughout their lifespan. In some cases cramps can be frequent, severe, and disabling, thus requiring medical assessment and intervention. Physiologic states such as pregnancy and exercise are associated with excessive muscle cramps, as are numerous medical and ...
Figure 12.1.2 shows one type of abnormal head positioning that can be caused by cervical dystonia. The muscles may contract in a sustained fashion, holding the head and neck in one position, or they may spasm repeatedly, causing jerky movements of the head and neck. Figure 12.1.2 Dystonia is a movement disorder in which a person's muscles ...
The current study's findings are consistent with the findings of the 2013 Global Burden of Disease Study which identified that in the Dominican Republic major depressive disorder (#1), low back pain (#2), anxiety (#4), neck pain (#8) and other musculoskeletal conditions (#10) were within the top 10 causes of years lived with disability .
muscle spasm. often result from injury to the musculoskeletal system—for example, overstretching a muscle, wrenching a joint, or tearing a tendon or ligament. These injuries can cause violent and painful involuntary muscle contractions. thought to be caused by the flood of sensory impulses coming to the spinal cord from the injured area ...
Figure 12.1.2 shows one type of abnormal head positioning that can be caused by cervical dystonia. The muscles may contract in a sustained fashion, holding the head and neck in one position, or they may spasm repeatedly, causing jerky movements of the head and neck. Figure 12.1.2 Dystonia is a movement disorder in which a person's muscles ...
Abstract. Muscle cramps, defined as a painful contraction of a muscle or muscle group, are a common symptom most people have experienced throughout their lifespan. In some cases cramps can be frequent, severe, and disabling, thus requiring medical assessment and intervention. Physiologic states such as pregnancy and exercise are associated with ...
Annie and her mother sat in the waiting room for what seemed to be hours. At last the nurse came for them. "Some of the results are here, and the rest are on their way," she explained. "So the doctor will see you now.". Annie and her mother went into the doctor's office and sat down.
Celiac disease is an autoimmune disease in genetically susceptible individuals caused by an immunological reaction to gluten. pathophysiology of celiac disease. Damage to villi when small intestine is exposed to components of gluten; reduced height, flattened. Decreased enzyme function and surface area. Maldigestion and malabsorption.