Personal Health Change Autobiography Essay
Introduction, chosen healthy behavior, reasons for making this health change, challenges likely to be faced, ways of overcoming the challenges, benefits of healthy behavior.
Improving the quality of one’s life is imperative in the present century. Education, establishment of more employment opportunities and private health in life are among the objectives which self-gratify an individual. The lifestyles individuals are accustomed to and their environment impact healthy behavior.
However, there are several ways of improving personal health, which may at times present challenges in their implementation. The benefits of most of these healthy behaviors nevertheless obscure the impediments which are faced.
I would like to exercise more routinely (5-7 times a week), while trying to develop a nutritional plan. This calls for having a meaningful vision and acquiring skills necessary to achieve the desired wellness. Physical activity, aerobics and muscle training are some of the divisions of exercise which include a painless 20 minute walk to an intensified work out in the gym.
Dancing and engaging in a physical sport like basketball or tennis is also forms of indirect exercise. The beauty of some exercises is that they do not necessarily involve a routine. Walking, for example, may be administered whenever an opportunity carves itself out.
These forms of physical activity stimulate hormones which are necessary for proper growth. Its other benefits like feeling and looking better lift composure and improves character, traits which are critical in the normal human socialization process. Using the stairs instead of the elevator and cycling to work are other valuable processes which are not that hard to achieve.
My main focus will be engaging in exercise, but I will also try maintaining a good diet. My nutritional project involves taking more fruits and vegetables and avoiding junk food which usually has a lot of fat. I have thought out turning into vegetarianism, but it has proven to yield more challenges than benefits, so I will prefer adding more vitamins in my diet.
Health is not just about whether a person is challenged by a disease. I chose to make this condition change in order to further my physical, social and emotional well being. Physical activities help reduce weight and promote better sleep regardless of age or masculinity. I would like to reduce 30 pounds that I am overweight, and while keeping a diet may be forceful and not so feasible, employing straightforward exercise strategies will be my first choice of a health change.
Being proud of my physique would significantly assist in developing the social interactions I want. The observations I have made on the behavior of overweight students in school is not so attractive. They tend to cluster together and receive taunting comments, which lower their faith in life. I want to make a health change in order to maintain satisfactory relationships with my present friends and be able to communicate confidently with others.
Emotional support and the behavior other people rally will unquestionably present a challenge. Close friends and associations will play a central role in influencing my training schedule and the diet I intend to maintain. Group activities would thus cease, because my schedule will need individual effort without distractions. However, the greatest challenge will be choosing the most appropriate exercise to practice regularly. It would be essential to have a regular plan if I am to achieve my objectives.
Scheduling, discipline and determination will be the factors considered in choosing an applicable practice. It would be useless reasonably to engage in a strenuous muscle application and put in lots of hours in the gym only to give up after a week. Making the decision would be exceedingly difficult, considering I have not engaged in any practical exercise for a while.
Time will also be an obstacle as I am significantly engaged with either homework or domestic duties. Whenever one gets busy, the time delegated for work-outs is usually sacrificed.
I have reviewed specific medical articles, and the negative impacts of exercise others have experienced significantly scare me off. There are those who experience colds or running noses in the middle of training sessions. Other trainers complain about breathing problems and splitting headaches after sessions. Experiencing no changes as soon as they expect them will prove frustrating. In case the practice I employ does not yield visible results within the first month, then I may change the form of exercise or plainly relinquish.
My present physical condition demands for regular exercise notwithstanding the challenges I would face. I have high cholesterol for a young 25 year old, so in order to live longer and healthier, I have to take part in some form of physical activity. The bigger one gets, the harder it would be to practice some routines. I would be thus required to complete a substantial health change before I start suffering unnecessary mortifications.
Exercise is usually strenuous and may involve a lot of wearisome activity. This will prove boring and I predict avoiding some responsibilities. However, devising methods to make it enjoyable would be meaningful. Exercising while having fun would unquestionably inspire me in the initiative to improve health.
I consider doing my exercises at home through the use of exercise videos. This will reduce the uncomfortable situations experienced in gyms which may make one uncomfortable. The use of some complex machines may also reduce the esteem of an individual.
Setting realistic fitness goals would be required depending on the pattern of physical activity. Studies indicate that most forms of practice would require consistency for around four months before producing physical benefits. It would be required to understand how different techniques work, how long they take to present visible or mental results, and how best to preserve the process.
The cholesterol issue will go away; I will look healthier and sexier and will have a strong body just like in high school, and will live longer. Having a fit body, proper posture, agility and muscles will transparently create the impact I desire with the opposite sex. Engaging in physical activity will help me burn the extra calories hence assist in the supervision of my weight, which is a considerable problem at present.
Physical activity improves concentration; any activity, which involves attentiveness, boosts the psychiatric process hence increasing sharpness and academic focus both in class and later years. Strength is also increased substantially when one specializes in meticulous work-outs of the muscles and stiff joints.
Proper combination of healthful food and appropriate muscles training has traditionally proven to increase the endurance of people. A chance of catching a cold is substantially reduced as the immune system is generally jump-started by regular exercises.
Exercising and eating healthy have been proven to progress physical health. Nevertheless, there are several other minor details which affect people’s healthiness. Personal hygiene and social participation have traditionally fostered health in diverse ways. Keeping one’s body clean to thwart illnesses and avoid infections is imperative. Cleaning hands, brushing teeth, cleaning cutlery helps in preventing infections.
One should strive to avoid the appearance of microbes in the body. Establishing social relationships prolongs life and increases productivity and positivism in life. Socialization may also increase knowledge, develop character and make an individual significantly healthy.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, July 5). Personal Health Change. https://ivypanda.com/essays/personal-health-change/
"Personal Health Change." IvyPanda , 5 July 2018, ivypanda.com/essays/personal-health-change/.
IvyPanda . (2018) 'Personal Health Change'. 5 July.
IvyPanda . 2018. "Personal Health Change." July 5, 2018. https://ivypanda.com/essays/personal-health-change/.
1. IvyPanda . "Personal Health Change." July 5, 2018. https://ivypanda.com/essays/personal-health-change/.
Bibliography
IvyPanda . "Personal Health Change." July 5, 2018. https://ivypanda.com/essays/personal-health-change/.
- Safety of Silver’s Gym
- Going to the Gym: What Health Effects to Expect
- David Barton Gym’s Marketing and Communication
- HIV/AIDS Issues in African Women
- Smoking and Its Negative Effects on Human Beings
- Ethnic Disparities in Women's Health Care
- Langley Park: Public Health Services
- Importance of Nutrition and Exercise in the Society

Using these brief interventions, you can help your patients make healthy behavior changes.
STEPHANIE A. HOOKER, PHD, MPH, ANJOLI PUNJABI, PHARMD, MPH, KACEY JUSTESEN, MD, LUCAS BOYLE, MD, AND MICHELLE D. SHERMAN, PHD, ABPP
Fam Pract Manag. 2018;25(2):31-36
Author disclosures: no relevant financial affiliations disclosed.

Effectively encouraging patients to change their health behavior is a critical skill for primary care physicians. Modifiable health behaviors contribute to an estimated 40 percent of deaths in the United States. 1 Tobacco use, poor diet, physical inactivity, poor sleep, poor adherence to medication, and similar behaviors are prevalent and can diminish the quality and length of patients' lives. Research has found an inverse relationship between the risk of all-cause mortality and the number of healthy lifestyle behaviors a patient follows. 2
Family physicians regularly encounter patients who engage in unhealthy behaviors; evidence-based interventions may help patients succeed in making lasting changes. This article will describe brief, evidence-based techniques that family physicians can use to help patients make selected health behavior changes. (See “ Brief evidence-based interventions for health behavior change .”)
Modifiable health behaviors, such as poor diet or smoking, are significant contributors to poor outcomes.
Family physicians can use brief, evidence-based techniques to encourage patients to change their unhealthy behaviors.
Working with patients to develop health goals, eliminate barriers, and track their own behavior can be beneficial.
Interventions that target specific behaviors, such as prescribing physical activity for patients who don't get enough exercise or providing patient education for better medication adherence, can help patients to improve their health.

CROSS-BEHAVIOR TECHNIQUES
Although many interventions target specific behaviors, three techniques can be useful across a variety of behavioral change endeavors.
“SMART” goal setting . Goal setting is a key intervention for patients looking to make behavioral changes. 3 Helping patients visualize what they need to do to reach their goals may make it more likely that they will succeed. The acronym SMART can be used to guide patients through the goal-setting process:
Specific. Encourage patients to get as specific as possible about their goals. If patients want to be more active or lose weight, how active do they want to be and how much weight do they want to lose?
Measurable. Ensure that the goal is measurable. For how many minutes will they exercise and how many times a week?
Attainable. Make sure patients can reasonably reach their goals. If patients commit to going to the gym daily, how realistic is this goal given their schedule? What would be a more attainable goal?
Relevant. Ensure that the goal is relevant to the patient. Why does the person want to make this change? How will this change improve his or her life?
Timely. Help patients define a specific timeline for the goal. When do they want to reach their goal? When will you follow-up with them? Proximal, rather than distal, goals are preferred. Helping patients set a goal to lose five pounds in the next month may feel less overwhelming than a goal of losing 50 pounds in the next year.
Problem-solving barriers . Physicians may eagerly talk with patients about making changes — only to become disillusioned when patients do not follow through. Both physicians and patients may grow frustrated and less motivated to work on the problem. One way to prevent this common phenomenon and set patients up for success is to brainstorm possible obstacles to behavior change during visits.
After offering a suggestion or co-creating a plan, physicians can ask simple, respectful questions such as, “What might get in the way of your [insert behavior change]?” or “What might make it hard to [insert specific step]?” Physicians may anticipate some common barriers raised by patients but be surprised by others. Once the barriers are defined, the physician and patient can develop potential solutions, or if a particular barrier cannot be overcome, reevaluate or change the goal. This approach can improve clinical outcomes for numerous medical conditions and for patients of various income levels. 4
For example, a patient wanting to lose weight may commit to regular short walks around the block. Upon further discussion, the patient shares that the cold Minnesota winters and the violence in her neighborhood make walking in her area difficult. The physician and patient may consider other options such as walking around a local mall or walking with a family member instead. Anticipating every barrier may be impossible, and the problem-solving process may unfold over several sessions; however, exploring potential challenges during the initial goal setting can be helpful.
Self-monitoring . Another effective strategy for facilitating a variety of behavioral changes involves self-monitoring, defined as regularly tracking some specific element of behavior (e.g., minutes of exercise, number of cigarettes smoked) or a more distal outcome (e.g., weight). Having patients keep diaries of their behavior over a short period rather than asking them to remember it at a visit can provide more accurate and valuable data, as well as provide a baseline from which to track change.
When patients agree to self-monitor their behavior, physicians can increase the chance of success by discussing the specifics of the plan. For example, at what time of day will the patient log his or her behavior? How will the patient remember to observe and record the behavior? What will the patient write on the log? Logging the behavior soon after it occurs will provide the most accurate data. Although patients may be tempted to omit unhealthy behaviors or exaggerate healthy ones, physicians should encourage patients to be completely honest to maximize their records' usefulness. For self-monitoring to be most effective, physicians should ask patients to bring their tracking forms to follow-up visits, review them together, celebrate successes, discuss challenges, and co-create plans for next steps. (Several diary forms are available in the Patient Handouts section of the FPM Toolbox .)
A variety of digital tracking tools exist, including online programs, smart-phone apps, and smart-watch functions. Physicians can help patients select which method is most convenient for daily use. Most online programs can present data in charts or graphs, allowing patients and physicians to easily track change over time. SuperTracker , a free online program created by the U.S. Department of Agriculture, helps patients track nutrition and physical activity plans, set goals, and work with a group leader or coach. Apps like Lose It! or MyFitnessPal can also help.
The process of consistently tracking one's behavior is sometimes an intervention itself, with patients often sharing that it created self-reflection and resulted in some changes. Research shows self-monitoring is effective across several health behaviors, especially using food intake monitoring to produce weight loss. 5
BEHAVIOR-SPECIFIC TECHNIQUES
The following evidence-based approaches can be useful in encouraging patients to adopt specific health behaviors.
Physical activity prescriptions . Many Americans do not engage in the recommended amounts of physical activity, which can affect their physical and psychological health. Physicians, however, rarely discuss physical activity with their patients. 6 Clinicians ought to act as guides and work with patients to develop personalized physical activity prescriptions, which have the potential to increase patients' activity levels. 7 These prescriptions should list creative options for exercise based on the patient's experiences, strengths, values, and goals and be adapted to a patient's condition and treatment goals over time. For example, a physician working with a patient who has asthma could prescribe tai chi to help the patient with breathing control as well as balance and anxiety.
In creating these prescriptions, physicians should help the patient recognize the personal benefits of physical activity; identify barriers to physical activity and how to overcome them; set small, achievable goals; and give patients the confidence to attempt their chosen activity. Physicians should also put the prescriptions in writing, give patients logs to track their activity, and ask them to bring those logs to follow-up appointments for further discussion and coaching. 8 More information about exercise prescriptions and sample forms are available online.
Healthy eating goals . Persuading patients to change their diets is daunting enough without unrealistic expectations and the constant bombardment of fad diets, cleanses, fasts, and other food trends that often leave both patients and physicians uncertain about which food options are actually healthy. Moreover, physicians in training receive little instruction on what constitutes sound eating advice and ideal nutrition. 9 This confusion can prevent physicians from broaching the topic with patients. Even if they identify healthy options, common setbacks can leave both patients and physicians less motivated to readdress the issue. However, physicians can help patients set realistic healthy eating goals using two simple methods:
Small steps. Studies have shown that one way to combat the inertia of unhealthy eating is to help patients commit to small, actionable, and measurable steps. 10 First, ask the patient what small change he or she would like to make — for example, decrease the number of desserts per week by one, eat one more fruit or vegetable serving per day, or swap one fast food meal per week with a homemade sandwich or salad. 11 Agree on these small changes to empower patients to take control of their diets.
The Plate Method. This model of meal design encourages patients to visualize their plates split into the following components: 50 percent fruits and non-starchy vegetables, 25 percent protein, and 25 percent grains or starchy foods. 12 Discuss healthy options that would fit in each of the categories, or combine this method with the small steps described above. By providing a standard approach that patients can adapt to many forms of cuisine, the model helps physicians empower their patients to assess their food options and adopt healthy eating behaviors.
Brief behavioral therapy for insomnia . Many adults struggle with insufficient or unrestful sleep, and approximately 18.8 percent of adults in the United States meet the criteria for an insomnia disorder. 13 The first-line treatment for insomnia is Cognitive Behavioral Therapy for Insomnia (CBT-I), which involves changing patients' behaviors and thoughts related to their sleep and is delivered by a trained mental health professional. A physician in a clinic visit can easily administer shorter versions of CBT-I, such as Brief Behavioral Therapy for Insomnia (BBT-I). 14 BBT-I is a structured therapy that includes restricting the amount of time spent in bed but not asleep and maintaining a regular sleep schedule from night to night. Here's how it works:
Sleep diary. Have patients maintain a sleep diary for two weeks before starting the treatment. Patients should track when they got in bed, how long it took to fall asleep, how frequently they woke up and for how long, what time they woke up for the day, and what time they got out of bed. Many different sleep diaries exist, but the American Academy of Sleep Medicine's version is especially user-friendly.
Education. In the next clinic appointment, briefly explain how the body regulates sleep. This includes the sleep drive (how the pressure to sleep is based on how long the person has been awake) and circadian rhythms (the 24-hour biological clock that regulates the sleep-wake cycle).
Set a wake-up time. Have patients pick a wake-up time that will work for them every day. Encourage them to set an alarm for that time and get up at that time every day, no matter how the previous night went.
Limit “total time in bed.” Review the patient's sleep diary and calculate the average number of hours per night the patient slept in the past two weeks. Add 30 minutes to that average and explain that the patient should be in bed only for that amount of time per night until your next appointment.
Set a target bedtime. Subtract the total time in bed from the chosen wake-up time, and encourage patients to go to bed at that “target” time only if they are sleepy and definitely not any earlier.
For example, if a patient brings in a sleep diary with an average of six hours of sleep per night for the past two weeks, her recommended total time in bed will be 6.5 hours. If she picks a wake-up time of 7 a.m., her target bedtime would be 12:30 a.m. It usually takes up to three weeks of regular sleep scheduling and sleep restriction for patients to start seeing improvements in their sleep. As patients' sleep routines become more solid (i.e., they are falling asleep quickly and sleeping more than 90 percent of the time they are in bed), slowly increase the total time in bed to possibly increase time asleep. Physicians should encourage patients to increase time in bed in increments of 15 to 30 minutes per week until the ideal amount of sleep is reached. This amount is different for each patient, but patients generally have reached their ideal amount of sleep when they are sleeping more than 85 percent of the time in bed and feel rested during the day.
Patient education to prevent medication nonadherence . Medication adherence can be challenging for many patients. In fact, approximately 20 percent to 30 percent of prescriptions are never picked up from the pharmacy, and 50 percent of medications for chronic diseases are not taken as prescribed. 15 Nonadherence is associated with poor therapeutic outcomes, further progression of disease, and decreased quality of life. To help patients improve medication adherence, physicians must determine the reason for nonadherence. The most common reasons are forgetfulness, fear of side effects, high drug costs, and a perceived lack of efficacy. To help patients change these beliefs, physicians can take several steps:
Educate patients on four key aspects of drug therapy — the reason for taking it (indication), what they should expect (efficacy), side effects and interactions (safety), and how it structurally and financially fits into their lifestyle (convenience). 16
Help patients make taking their medication a routine of their daily life. For example, if a patient needs to use a controller inhaler twice daily, recommend using the inhaler before brushing his or her teeth each morning and night. Ask patients to describe their day, including morning routines, work hours, and other responsibilities to find optimal opportunities to integrate this new behavior.
Ask patients, “Who can help you manage your medications?” Social networks, including family members or close friends, can help patients set up pillboxes or provide medication reminders.
The five Rs to quitting smoking . Despite the well-known consequences of smoking and nationwide efforts to reduce smoking rates, approximately 15 percent of U.S. adults still smoke cigarettes. 17 As with all kinds of behavioral change, patients present in different stages of readiness to quit smoking. Motivational interviewing techniques can be useful to explore a patient's ambivalence in a way that respects his or her autonomy and bolsters self-efficacy. Discussing the five Rs is a helpful approach for exploring ambivalence with patients: 18
Relevance. Explore why quitting smoking is personally relevant to the patient.
Risks. Advise the patient on negative consequences of continuing to smoke.
Rewards. Ask the patient to identify the benefits of quitting smoking.
Roadblocks. Help the patient determine obstacles he or she may face when quitting. Common barriers include weight gain, stress, fear of withdrawal, fear of failure, and having other smokers such as coworkers or family in close proximity.
Repeat. Incorporate these aspects into each clinical contact with the patient.
Many patients opt to cut back on the amount of tobacco they use before their quit date. However, research shows that cutting back on the number of cigarettes is no more effective than quitting abruptly, and setting a quit date is associated with greater long-term success. 19
Once the patient sets a quit date, repeated physician contact to reinforce smoking cessation messages is key. Physicians, care coordinators, or clinical staff should consider calling or seeing the patient within one to three days of the quit date to encourage continued efforts to quit, as this time period has the highest risk for relapse. Evidence shows that contacting the patient four or more times increases the success rate in staying abstinent. 18 Quitting for good may take multiple a empts, but continued encouragement and efforts such as setting new quit dates or offering other pharmacologic and behavioral therapies can be helpful.
GETTING STARTED
Family physicians are uniquely positioned to provide encouragement and evidence-based advice to patients to change unhealthy behaviors. The proven techniques described in this article are brief enough to attempt during clinic visits. They can be used to encourage physical activity, healthy eating, better sleep, medication adherence, and smoking cessation, and they can help patients adjust their lifestyle, improve their quality of life, and, ultimately, lower their risk of early mortality.
Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all-cause mortality: a systematic review and meta-analysis. Prev Med . 2012;55(3):163-170.
Bodenheimer T, Handley MA. Goal-setting for behavior change in primary care: an exploration and status report. Patient Educ Couns . 2009;76(2):174-180.
Lilly CL, Bryant LL, Leary JM, et al.; Evaluation of the effectiveness of a problem-solving intervention addressing barriers to cardiovascular disease prevention behaviors in three underserved populations: Colorado, North Carolina, West Virginia, 2009. Prev Chronic Dis . 2014;11:E32.
U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans (7th Ed). Washington, D.C: U.S. Government Printing Office; 2010.
Sreedhara M, Silfee VJ, Rosal MC, Waring ME, Lemon SC. Does provider advice to increase physical activity differ by activity level among U.S. adults with cardiovascular disease risk factors? Fam Pract . 2018;35(4):420-425.
Pinto BM, Lynn H, Marcus BH, DePue J, Goldstein MG. Physician-based activity counseling: intervention effects on mediators of motivational readiness for physical activity. Ann Behav Med . 2001;23(1):2-10.
Hechanova RL, Wegler JL, Forest CP. Exercise: a vitally important prescription. JAAPA . 2017;30(4):17-22.
Guo H, Pavek M, Loth K. Management of childhood obesity and overweight in primary care visits: gaps between recommended care and typical practice. Curr Nutr Rep . 2017;6(4):307-314.
Perkins-Porras L, Cappuccio FP, Rink E, Hilton S, McKay C, Steptoe A. Does the effect of behavioral counseling on fruit and vegetable intake vary with stage of readiness to change?. Prev Med . 2005;40(3):314-320.
Kahan S, Manson JE. Nutrition counseling in clinical practice: how clinicians can do better. JAMA . 2017;318(12):1101-1102.
Choose My Plate. U.S. Department of Agriculture website. https://www.choosemyplate.gov/ . Updated January 31, 2018. Accessed February 1, 2018.
Ford ES, Cunningham TJ, Giles WH, Croff JB. Trends in insomnia and excessive daytime sleepiness among U.S. adults from 2002 to 2012. Sleep Med . 2015;16(3):372-378.
Edinger JD, Sampson WS. A primary care “friendly” cognitive behavioral insomnia therapy. Sleep . 2003;26(2):177-182.
Viswanathan M, Golin CE, Jones CD, et al.; Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med . 2012;157(11):785-795.
Cipolle RJ, Strand LM, Morley PC. Pharmaceutical care practice: the patient-centered approach to medication management services . 3rd ed. New York: McGraw-Hill; 2012.
Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current cigarette smoking among adults — United States, 2005–2015. MMWR Morb Mortal Wkly Rep . 2016;65(44):1205-1211.
Patients not ready to make a quit attempt now (the “5 Rs”). Agency for Healthcare Research and Quality website. http://bit.ly/2jVvpoY . Updated December 2012. Accessed February 2, 2018.
Larzelere MM, Williams DE. Promoting smoking cessation. Am Fam Physician . 2012;85(6):591-598.
Continue Reading
More in FPM
More in pubmed.
Copyright © 2018 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Public Policy
- Public Administration
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >
24 Health Behavior Change
Ralf Schwarzer is a professor in the Department of Psychology at Freie Universitat Berlin in Berlin, Germany.
- Published: 18 September 2012
- Cite Icon Cite
- Permissions Icon Permissions
An overview of theoretical constructs and mechanisms of health behavior change is provided, based on a self-regulation framework that makes a distinction between goal setting and goal pursuit. Risk perception, outcome expectancies, and task self-efficacy are seen as predisposing factors in the goal setting phase (motivational phase), whereas planning, action control, and maintenance/recovery self-efficacy are regarded as influential in the goal pursuit phase (volitional phase). The first phase leads to forming an intention, and the second phase leads to actual behavior change. Such a mediator model serves to explain social-cognitive processes in health behavior change. Adding a second layer on top of it, a moderator model is provided in which three stages are distinguished to segment the audience for tailored interventions. Identifying persons as preintenders, intenders, or actors offers an opportunity to match theory-based treatments to specific target groups. Research examples serve to illustrate the application of the model to health promotion.
Many health conditions are caused by risk behaviors, such as problem drinking, substance use, smoking, reckless driving, overeating, or unprotected sexual intercourse. The key question in health behavior research is how to predict and modify the adoption and maintenance of health behaviors. Fortunately, human beings have, in principle, control over their conduct. Health-compromising behaviors can be eliminated by self-regulatory efforts, and health-enhancing behaviors can be adopted instead, such as physical exercise, weight control, preventive nutrition, dental hygiene, condom use, or accident prevention. Health self-regulation refers to the motivational, volitional, and actional processes of abandoning such health-compromising behaviors in favor of adopting and maintaining health-enhancing behaviors (Leventhal, Weinman, Leventhal, & Phillips, 2008 ).
This chapter highlights some current issues in health behavior research. In the first section, various psychological constructs are described that have been found useful. These are intention, risk perception, outcome expectancies, perceived self-efficacy, and planning. In the second section, theoretical perspectives on the health behavior change process are discussed. From a metatheoretical viewpoint, stage models are contrasted to continuum models. Following is one example of a continuum model (theory of planned behavior) and one example of a stage model (transtheoretical model). Then a two-layer hybrid framework is introduced (health action process approach). In the third section, some unresolved issues in health behavior research are discussed. All sections are illustrated by research findings and suggestions for further research.
Constructs and Principles
Intention, motivation, volition.
Changes in health behaviors can be influenced by opportunities and barriers, by explicit decisions, or by random events. In this chapter, we are dealing solely with intentional changes that happen when people become motivated to alter their previous way of life and set goals for a different course of action. For example, they may consider to quit smoking, or they make an effort to do so. Thus, intention represents a key factor in health behavior change. This construct had been suggested by Fishbein and Ajzen ( 1975 ) to operate as a mediator to overcome the attitude–behavior gap. Since behaviors could not be well predicted by attitudes, intention appeared to be a useful mediator and a better proximal predictor of many behaviors. Since then, there is consensus that intention is an indispensable variable when it comes to explaining and predicting behaviors. In the process of motivation, intention has been regarded as a kind of “watershed” between an initial goal setting phase and a subsequent goal pursuit phase. Lewin, Dembo, Festinger, and Sears ( 1944 ) described a motivation phase of goal setting that is followed by a volition phase of goal pursuit. This distinction has been elaborated and called the Rubicon model by Heckhausen ( 1980 , 1991 ), Heckhausen and Gollwitzer ( 1987 ), and Kuhl ( 1983 ). Motivation is a preintentional process, whereas volition refers to a postintentional process. When describing health behavior change, it is most helpful to follow this distinction. For example, to gauge the progress of an individual who is supposed to quit smoking and to design therapeutic interventions, the first question to ask should be whether this person is either preintentional or postintentional. To which degree is the person motivated (goal setting), or to which degree is the person making explicit efforts to quit (goal pursuing)? The terms motivation and goal setting pertain to the preintentional phase, whereas the terms volition and goal pursuit pertain to the postintentional phase. These distinctions will be discussed in more detail in the section on stage models.
Although the construct of intention is indispensable in explaining health behavior change, its predictive value is limited (Schwarzer, 1992 ; Sheeran, 2002 ). When trying to translate intentions into behavior, individuals are faced with various obstacles, such as distractions, forgetting, or conflicting bad habits. Godin and Kok ( 1996 ), who reviewed 19 studies, found a mean correlation of .46 between intention and health behavior, such as exercise, screening attendance, and addictions. Abraham and Sheeran ( 2000 ) reported behavioral intention measures to account for 20%–25% of the variance in health behavior measures. If not equipped with means to meet these obstacles, motivation alone does not suffice to change behavior (Baumeister, Heatherton & Tice, 1994 ). To overcome this limitation, further constructs are required that operate in concert with the intention. Volitional factors can help to bridge the intention–behavior gap (Sheeran, 2002 ) since people do not fully act upon their intentions (e.g., Abraham, Sheeran, & Johnston, 1998 ). Implementation intentions are one such volitional factor (Gollwitzer, 1999 ) that can be interpreted as postintentional mental simulation or planning strategies. A detailed discussion follows below in the section on planning.
A concept related to intention is behavioral willingness (Gibbons & Gerrard, 1997 ; Gibbons, Gerrard, & Lane, 2003 ). The authors believe that health-compromising behavior is often not intentional, but is rather a spontaneous reaction to social circumstances. Gibbons and Gerrard define behavioral willingness as an openness to risk opportunity (i.e., what an individual would be willing to do under certain circumstances).
Risk Perception
At first glance, perceiving a health threat seems to be the most obvious prerequisite for the motivation to overcome a risk behavior (e.g., smoking). Consequently, a central task for health communication is not only to provide information about the existence and magnitude of a certain risk, but also to increase the subjective relevance of a health issue to focus the individuals’ attention on information pertaining directly to their own risk. However, general perceptions of risk (e.g., “Smoking is dangerous”) and personal perceptions of risk (e.g., “I am at risk because I am a smoker”) often differ to a great extent. Individuals could be well informed about general aspects of certain risks and precautions (e.g., most smokers acknowledge that smoking can cause diseases), but, nevertheless, many might not feel personally at risk (Klein & Cerully, 2007 ).
Especially when it comes to a comparison with similar others, one’s view of the risk is somewhat distorted (see Suls, 2011 , Chapter 12 , this volume). On average, individuals tend to see themselves as being less likely than others to experience health problems in the future. For example, when asked how they judge their risk of becoming infected with human immunodeficiency virus (HIV) compared to an average peer of the same sex and age (the average risk ), participants typically give a below-average estimate (e.g., Hahn & Renner, 1998 ). This has been coined “unrealistic optimism” or “optimistic bias” (Weinstein, 1980 , 1988 ). It reflects the difference between the perceived risk for oneself and that for others, belonging to the broader construct of defensive optimism (Taylor & Brown, 1994 ).
Defensive optimism represents an underestimation of risk that hinders the adoption of precautionary behaviors, whereas functional optimism promotes their adoption (Radcliffe & Klein, 2002 ; Schwarzer, 1994 ). People who are optimistic may be so in two ways: They underestimate risks, but are optimistic about their capability to overcome their bad habits. Since both kinds of optimism are confounded, risk perceptions are often poor predictors of behavior.
People with a high-risk status (e.g., high blood pressure, obesity, and high cholesterol) should perceive a higher pressure to act, and they are more inclined to form an intention to change their habits than are people who are not at risk (cf. Croyle, Sun, & Louie, 1993 ; Renner, 2004 ). The actual risk status should be related to perceived risk for future health problems and diseases. However, the relationship between current objective risk status and risk perception varies considerably, suggesting that they might contribute differently to intention forming.
Renner and Schwarzer ( 2005 ) found that objective risk predicted risk perception, but the latter did not translate into an intention to eat a healthy diet. Thus, risk communication might be a dead end, resulting in higher risk perception, but not leading to intention formation. The relation between objective risk status, risk perception, and risk behavior is still not well understood and represents a challenge for further research (Brewer, Weinstein, Cuite, & Herrington, 2004 ; Panzer & Renner, 2008 ). Both the objective and subjective risk may not be functional for health behavior change if not accompanied by other motivational and volitional factors.
An example for the ambiguous role of fear appeals in health promotion is the current debate on the introduction of graphic warning labels on cigarette packs. Although good research on fear appeals has been published for half a century (e.g., Leventhal, Singer, & Jones, 1965 ), public health agents seem to be unaware of the psychological mechanisms that are involved in risk communication. Some epidemiological studies provide evidence for the effectiveness of graphic warning labels. However, this kind of evidence is methodologically weak because studies are nonexperimental and do not allow for causal inferences. Typically, in such studies telephone interviews are conducted based on random-digit dialing, and a subsample of volunteers report about reading warning labels and what they believe is the impact on their intentions not to smoke, and eventually, on their attempts at quitting. It can be assumed that respondents constitute a positive selection of intenders or contemplators who are interested in the topic, and who consider quitting anyway. Such studies are typically not guided by health behavior theories but are rather data driven. It is indeed very hard to collect valid data on this issue because there might be no good way to design a randomized controlled trial. Experimental work on risk communication mainly takes place in the laboratory, where internal validity is high, but external (ecological) validity is low. One such experiment was recently conducted to investigate the impact of cigarette warning labels on cognitive dissonance in smokers. Smokers’ and nonsmokers’ risk perceptions with regard to smoking-related diseases were measured with response latencies before and after presentation of warning labels. Responses showed an impact of confrontation with smoking-related health risks rather than an impact of warning labels themselves.
The adoption of health behaviors should not be viewed simplistically as a response to a health threat. Risk information alone does not help people to change risky behaviors because it does not provide meaningful information about how to manage behavioral changes. Initial risk perception seems to be advantageous in helping people become motivated to change, but later, other factors are more influential in the self-regulation process. This state of affairs has encouraged health psychologists to design more complex models that combine risk perception with other determinants and processes of change.
Outcome Expectancies
In addition to being aware of a health threat, people also need to know how to regulate their behavior. They need to understand the links between actions and subsequent outcomes. These outcome expectancies can be the most influential beliefs in the motivation to change. The term outcome expectancies is most common in social-cognitive theory (Bandura, 1997 ). The equivalent terms pros and cons are used in the transtheoretical model (Prochaska & Velicer, 1997 ), in which they represent the decisional balance in people who are contemplating whether to adopt a novel behavior or not. In the theory of reasoned action (Fishbein & Ajzen, 1975 ), the corresponding term is behavioral beliefs that act as precursors of attitudes.
The pros and cons represent positive and negative outcome expectancies. A smoker may find more good reasons to quit (“If I quit smoking, then my friend will like me much more”) than reasons to continue smoking (“If I quit, I will become more tense and irritated”). This imbalance in favor of positive outcome expectancies will not lead directly to action, but it can help to generate the intention to quit. Outcome expectancies can also be understood as means–ends relationships, indicating that people know proper strategies to produce the desired effects. Many of those cognitions represent social outcome expectancies (normative beliefs) by pertaining to the social consequences of a particular behavior (Trafimow & Fishbein, 1995 ).
The perceived contingencies between actions and outcomes need not be explicitly worded; they can also be rather diffuse mental representations, loaded with emotions (Trafimow & Sheeran, 1998 ). Social cognition models are often misunderstood as being rational models that deal with “cold cognitions.” In line with the “bounded rationality” view, emotions would only be an error term. In contrast, health behavior change, to a large degree, is an emotional process that turns into a cognitive one after people have been asked about their thoughts and feelings, thus making them aware of what is going on emotionally. Recent studies have, therefore, focused on emotional outcome expectancies (Dunton & Vaughan, 2008 ; Lawton, Conner, & McEachan, 2009 ; Trafimow et al., 2004 ). An example of an emotional outcome expectancy is anticipated regret (“If I do not use a condom tonight, then I will regret it tomorrow”). Behavior is followed by an expected emotion (Abraham & Sheeran, 2003 ; Conner, Sandberg, McMillan, & Higgins, 2006 ). Emotional content of outcome expectancies seems to be most influential in intention formation.
Another important aspect of outcome expectancies is the focus on either gains or losses. A gain-framed message refers to a positive outcome expectancy, such as “Protect yourself from the sun and you will help yourself stay healthy,” whereas a loss-framed message can be a negative outcome expectancy, such as “Expose yourself to the sun and you will risk becoming sick” (item examples from Detweiler, Bedell, Salovey, Pronin, & Rothman, 1999 ). A similar distinction is the promotion versus prevention focus of outcome expectancies or health messages.
Outcome expectancies change over time. The distance between cognitions and actions plays a role for the decisional balance. When thinking of the consequences of lifestyle changes such as more physical activity and dietary improvements, the positive side is more valued. However, when it comes to micro-level intentions, when imminent health behaviors are at stake, the negative side comes into play. When people contemplate long-term outcomes (e.g., “I will stay slim and become healthier”), the pros might dominate the cons. When they anticipate immediate outcomes (e.g., “I will be exhausted; desserts are tempting”), the cons move into the foreground. This instability of the decisional balance changes the intention levels and reduces the subsequent likelihood of taking action. Thus, failure to act upon one’s intentions can be due to intention instability, which, in turn, emerges as a result of the reevaluation of the pros and cons, as the situation for the intended action approaches. This is in line with construal level theory (Eyal, Liberman, Trope, & Walther, 2004 ). According to this theory, mental representations of an event depend on psychological distance, which may be more or less the temporal distance to the event. More distal events are construed at a high level, whereas more proximal events are construed at a low level. Low-level construals are contextualized, concrete, and often short-term outcomes, whereas high-level construals are more decontextualized, abstract, and often long-term outcomes. Pros about an event tend to represent higher-level construals, whereas cons represent lower-level construals (Eyal et al., 2004 ). As a consequence for the design of interventions, one would make short-term and emotional outcome expectancies more salient (e.g., “You will feel more energetic after exercise; you will enjoy the taste of fresh fruits; you will regret not having used a condom”). A favorable decisional balance can be achieved even by parsimonious interventions (Göhner, Seelig, & Fuchs, 2009 ).
Perceived Self-efficacy
Perceived self-efficacy portrays individuals’ beliefs in their capabilities to exercise control over challenging demands and over their own functioning (Bandura, 1997 , 2000 ). It involves the regulation of thought processes, affective states, motivation, behavior, or changing environmental conditions. These beliefs are critical in approaching novel or difficult situations, or in adopting a strenuous self-regimen. People make an internal attribution in terms of personal competence when forecasting their behavior (e.g., “I am certain that I can quit smoking even if my friend continues to smoke”). Such optimistic self-beliefs influence the goals people set for themselves, what courses of action they choose to pursue, how much effort they invest in given endeavors, and how long they persevere in the face of barriers and setbacks. Self-efficacy influences the challenges that people take on, as well as how high they set their goals (e.g., “I intend to reduce my smoking,” or “I intend to quit smoking altogether”). Some people harbor self-doubts and cannot motivate themselves. They see little point in even setting a goal if they believe they do not have what it takes to succeed. Thus, the intention to change a habit that affects health depends to some degree on a firm belief in one’s capability to exercise control over that habit.
Perceived self-efficacy has been found to be important at all stages in the health behavior change process (Bandura, 1997 ), but it does not always constitute exactly the same construct. Its meaning depends on the particular situation of individuals who may be more or less advanced in the change process. The distinction between action self-efficacy, coping self-efficacy, and recovery self-efficacy has been brought up by Marlatt, Baer, and Quigley ( 1995 ) in the domain of addictive behaviors. The rationale for the distinction between several phase-specific self-efficacy beliefs is that, during the course of health behavior change, different tasks have to be mastered and different self-efficacy beliefs are required to master these tasks successfully. For example, a person might be confident in his or her capability to be physically active in general (i.e., high action self-efficacy), but might not be very confident to resume physical activity after a setback (low recovery self-efficacy).
Action self-efficacy (also called “preaction self-efficacy”) refers to the first phase of the process, in which an individual does not yet act, but develops a motivation to do so. It is an optimistic belief during the preactional phase. Individuals high in action self-efficacy imagine success, anticipate potential outcomes of diverse strategies, and are more likely to initiate a new behavior. Those with less self-efficacy imagine failure, harbor self-doubts, and tend to procrastinate. Although preaction self-efficacy is instrumental in the motivation phase, the two following constructs are instrumental in the subsequent volition phase and can, therefore, also by summarized under the heading of volitional self-efficacy.
Maintenance self-efficacy represents optimistic beliefs about one’s capability to cope with barriers that arise during the maintenance period. (The equivalent term “coping self-efficacy” has also been used in a different sense; therefore, we now prefer the term “maintenance self-efficacy.”) A new health behavior might turn out to be much more difficult to adhere to than expected, but a self-efficacious person responds confidently with better strategies, more effort, and prolonged persistence to overcome such hurdles. Once an action has been taken, individuals with high maintenance self-efficacy invest more effort and persist longer than those who are less self-efficacious.
Recovery self-efficacy addresses the experience of failure and recovery from setbacks. If a lapse occurs, individuals can fall prey to the “abstinence violation effect,” that is, they attribute their lapse to internal, stable, and global causes, dramatize the event, and interpret it as a full-blown relapse (Marlatt et al., 1995 ). Highly self-efficacious individuals, however, avoid this effect by attributing the lapse to an external high-risk situation and by finding ways to control the damage and to restore hope. Recovery self-efficacy pertains to one’s conviction to get back on track after being derailed. The person trusts his or her competence to regain control after a setback or failure and to reduce harm (Marlatt, 2002 ).
A functional difference exists between these self-efficacy constructs, whereas their temporal sequence is less important. Different phase-specific self-efficacy beliefs may be harbored at the same point in time. The assumption is that they operate in a different manner. For example, recovery self-efficacy is most functional when it comes to resuming an interrupted chain of action, whereas action self-efficacy is most functional when facing a novel challenging demand (Luszczynska, Mazurkiewicz, Ziegelmann, & Schwarzer, 2007 ).
This distinction between phase-specific self-efficacy beliefs has proven useful in various domains of behavior change. Action self-efficacy tends to predict intentions, whereas maintenance self-efficacy tends to predict behaviors. Individuals who had recovered from a setback needed different self-beliefs than did those who had maintained theirs levels of activity (Scholz, Sniehotta, & Schwarzer, 2005 ). Several authors (Rodgers, Hall, Blanchard, McAuley, & Munroe, 2002 ; Rodgers & Sullivan, 2001 ; Rodgers, Murray, Courneya, Bell, & Harber, 2009 ) have found evidence for phase-specific self-efficacy beliefs in the domain of exercise behavior (i.e., task self-efficacy, coping self-efficacy, and scheduling self-efficacy). Phase-specific self-efficacy differed in the effects on various preventive health behaviors, such as breast self-examination (Luszczynska & Schwarzer, 2003 ), dietary behaviors (Schwarzer & Renner, 2000 ), and physical exercise (Scholz et al., 2005 ).
Good intentions are more likely to be translated into action when people develop success scenarios and preparatory strategies of approaching a difficult task. Mental simulation helps to identify cues for action. The terms planning and implementation intentions have been used to address this phenomenon. Research on action plans for health behaviors has been suggested by Lewin ( 1947 ), for example, in the context of food choice. Lewin distinguished between an overall plan and a specific plan to take the first step toward a dietary goal. Leventhal, Singer, and Jones ( 1965 ) have argued that fear appeals can facilitate health behavior change only when combined with action plans; that is, specific instructions on when, where, and how to perform them.
Renewed attention to planning emerged when the concept of implementation intentions was introduced from the perspective of motivation psychology (Gollwitzer, 1999 ). An implementation intention represents a mental “if-then” association that links the when and where of a situation (if-condition) to a specific action (then-condition). Holding an if-then cognition in a critical situation is assumed to lead to a behavioral response without much conscious awareness. An if-then cognition facilitates increased information processing in terms of enhanced accessibility, detection, and discrimination of critical cues (Webb, Hendricks, & Brandon, 2007 ). To date, research has accumulated abundant evidence for the effectiveness of implementation intentions in the laboratory, as well as in the field where participants generate plans themselves (Wiedemann, Schüz, Sniehotta, Scholz, & Schwarzer, 2009 ). In many studies, action planning was found to mediate the relations between intentions and behaviors, such as physical activity (Conner & Norman, 2005 ; Norman & Conner, 2005 ). Meta-analyses have summarized their effects on health behaviors (for an overview, see Gollwitzer & Sheeran, 2006 ).
Another way of planning is the anticipation of barriers and the generation of alternative behaviors to overcome them. This has been called coping planning (Scholz, Sniehotta, Burkert, & Schwarzer, 2007 ; Sniehotta, Scholz, & Schwarzer, 2006 ; Sniehotta , Schwarzer, Scholz, & Schüz, 2005 ). People imagine scenarios that hinder them in performing their intended behavior, and they develop one or more plans to cope with such a challenging situation. For example: “If I plan to run on Sunday, but the weather does not permit it, I will go swimming instead,” or “If there is something exciting on TV tonight that I do not want to miss, I will reschedule my workout to the afternoon.” Coping planning might be a more effective self-regulatory strategy than action planning, partly because it implies action planning. After people contemplate the when, where, and how of action, they imagine possible barriers and generate coping strategies. Thus, coping planning comes on top of action planning (Scholz, Schüz, Ziegelmann, Lippke, & Schwarzer, 2008 ). Planning is an alterable variable. It can be easily communicated to individuals with self-regulatory deficits. Quite a few randomized controlled trials have documented the evidence in favor of such planning interventions (e.g., Chapman, Armitage, & Norman, 2009 ; Luszczynska, 2006 ; Luszczynska, Tryburcy, & Schwarzer, 2007 ; Van Osch, Lechner, Reubsaet, Wigger, & de Vries, 2008 ). It has also been found that action planning and coping planning have a synergistic effect on physical activity (Araújo-Soares, McIntyre, & Sniehotta, 2009 ).
Mechanisms and Models of Health Behavior Change
Meta theory: stage models and continuum models.
Health behavior change encompasses a variety of social, emotional, and cognitive factors. Some of these determinants are assumed to operate in concert. Therefore, researchers have aimed at identifying the optimal set of factors that allow for the best prediction or explanation of health behavior change. Such models or theories are subject to debate in health psychology. For example, which model is the most parsimonious and makes the best prediction of regular condom use? From which model can we derive clinical strategies to modify refractory dietary risk behaviors? Which model suggests a good policy to promote smoking cessation at the workplace? The models of health behavior change preferred currently overlap in terms of some of the crucial factors, but major differences are found in terms of the underlying philosophy. This section provides a brief overview of some models.
Models of health behavior change postulate a pattern of factors that may improve motivation and that would eventually lead to sustained behavior change. A distinction is made between stage models and continuum models. In continuum models, individuals are placed along a range that reflects the likelihood of action. Influential predictor variables are identified and combined in one prediction equation. The goal of an intervention is to move the individual along this route toward action. Such models assume that a person’s behavior is the outcome of an intention (e.g., “I intend to run four times a week for at least 30 minutes each time”). Intention forming is seen as being determined by beliefs and attitudes (Fishbein & Ajzen, 1975 ). Therefore, the focus is on identifying a parsimonious set of predictors that includes constructs such as perceived barriers, social norms, disease severity, personal vulnerability, attitudes, or perceived self-efficacy. These are then combined into a prediction equation for explaining behavioral intention and behavior change. The most prominent approach of this kind is the theory of planned behavior (see below). A general characteristic of continuum models is that they better account for intention variance than for behavior variance.
There are two debatable aspects of continuum models. First, a single prediction rule for describing behavior change implies that cognitive and behavioral changes occur in a linear fashion, and that a “one-size-fits-all” intervention approach is suitable for all individuals engaging in unhealthy behaviors. Consequently, it excludes qualitative changes during the course of time, such as changing mindsets, phase transitions, or recycling back and forth. According to continuum models, it is not important whether an intervention approach is targeted first toward changing perceived vulnerability, perceived consequences, or perceived self-efficacy. Hence, interventions are not required to move forward in any certain sequence, but they could be applied in any order, or even simultaneously.
Second, traditional continuum models typically did not account for the postintentional phase, in which goals are translated into action. The segment between intentions and behaviors is a black box, also called the intention–behavior gap (Sheeran, 2002 ). It is quite common that people do not behave in accordance with their intentions. For example, unforeseen barriers emerge, and people give in to temptations. In a postintentional phase, various factors can compromise or facilitate the translation of intentions into action. Some of these postintentional factors have been identified, such as maintenance self-efficacy and recovery self-efficacy (Luszczynska & Schwarzer, 2003 ; Scholz, Sniehotta, & Schwarzer, 2005 ), as well as action planning and coping planning (Lippke, Ziegelmann, & Schwarzer, 2004 , 2005 ; Luszczynska, Sobczyk, & Abraham, 2007 ; Sniehotta, Scholz, & Schwarzer, 2005 , 2006 ; Ziegelmann, Lippke, & Schwarzer, 2006 ). Theorizing about health behavior change should not be reduced to the motivation phase only, while omitting the subsequent action phase that is more decisive for behavior change. Advanced continuum models, therefore, need to include factors that help to bridge the intention–behavior gap (Sniehotta, 2009a ). In doing so, it is implicitly assumed that there are at least two phases of behavior change: a motivational one that ends with an intention, and a volitional one that ends with successful performance. Thus, any extension of traditional continuum models into this direction implicitly adopts the idea of distinct processes, stages, or phases in health behavior change.
To overcome the limitations of continuum models, stage theorists have made an attempt to consider process characteristics by proposing a number of qualitative stages. The transtheoretical model of behavior change (TTM; e.g., DiClemente & Prochaska, 1982 ; Prochaska & DiClemente, 1983 ; Prochaska, DiClemente, & Norcross, 1992 ; Velicer, Prochaska, & Redding, 2006 ) has become the most popular stage model. Stage models can only be seen as superior to continuum models if empirical evidence emerges that attests to the discontinuity between stages and to the successful tailoring of interventions to subgroups of individuals who have been identified at such stages. Moreover, the critical factors that move people from one stage to another need to be identified (Armitage & Arden, 2002 ).
Whereas the focus of continuum models lies in the prediction of intention and behaviors, the focus of stage models lies in stage-matched interventions. However, administering matched treatments may not necessarily be the most productive approach to encourage health behavior change—combination treatments might be even more successful. In terms of utility, Abraham ( 2008 ) argued that as long as targeting stage-defined audiences is problematic and causes additional costs, investment in stage-specific interventions is not justified. Combining interventions that are designed to promote a variety of cognitive changes might be less expensive, since this does not require prior screening for action preparedness within the audience. Above all, they might be even more successful. Nonetheless, it would be premature to conclude that stage-tailored interventions are not useful since they can only be as good as the underlying stage definitions. Refining stage definitions or different stage conceptions might generate stronger support for the stage framework.
A variety of stage models have been proposed, for example the precaution adoption process approach (PAPM; Weinstein, 1988 ). Another older stage model has only recently been applied to health behaviors is the model of action phases (MAP), also called the Rubicon model. Heckhausen ( 1980 , 1991 ), Heckhausen and Gollwitzer ( 1987 ), and Kuhl ( 1983 ) have distinguished between a motivation phase of goal setting that is followed by a volition phase of goal pursuit. This approach has evolved from German motivation psychology since the early 20th century (e.g., Lewin et al., 1944 ), and it has inspired the health action process approach (HAPA; Schwarzer, 1992 ).
Overviews of leading health behavior theories are provided in some book chapters (health belief model, reviewed by Abraham & Sheeran, 2005 ; protection motivation theory, reviewed by Norman, Boer, & Seydel, 2005 ; social cognitive theory, reviewed by Luszczynska & Schwarzer, 2005 ; transtheoretical model, reviewed by Sutton, 2005 ; theory of planned behavior, reviewed by Conner & Sparks, 2005 ; Biddle, & Fuchs, 2009 ; Sniehotta, 2009b ). In the following sections, three models will be described briefly.
Theory of Planned Behavior
The theory of planned behavior (TPB; Ajzen, 1991 ) represents a revised version of the theory of reasoned action (TRA; Fishbein & Ajzen, 1975 ). It is a continuum model that includes distal and proximal antecedents of a given behavior. The core of the model consists of eight variables (see Figure 24.1 ).ntention reflects a person’s readiness to perform a health behavior. The intention is based on attitude toward the behavior, subjective norm, and perceived behavioral control. Intention mediates between these three factors and the behavior. Attitude toward a behavior is an indicator of the positive or negative value that is associated with the performance of the behavior. It is determined by a set of behavioral beliefs. Subjective norm is the perceived social pressure to engage or not to engage in a behavior. It is determined by a set of normative beliefs. Perceived behavioral control pertains to one’s perceptions of the ability to perform a health behavior. It is determined by a set of control beliefs. It is about the same as perceived self-efficacy (Bandura, 1997 ). Behavioral beliefs reflect the contingency between a behavior and expected outcomes. Thus, this is the same as outcome expectancies (Bandura, 1997 ). These beliefs are multiplied with the subjective values of the expected outcomes. This product is seen to determine the attitude toward the behavior. Normative beliefs pertain to the perceived behavioral expectations of significant others such as a partner, coworker, teacher, or friend. These beliefs are multiplied with one’s motivation to comply with these specific expectations. This product, then, is seen to determine the subjective norm. Control beliefs refer to factors that may facilitate or impede performance of a behavior. These beliefs are multiplied with the perceived power of each control factor. This product is seen to determine the perceived behavioral control.
The TPB has been applied to many health behaviors, and it has become the most frequently used continuum model. There are more than one thousand publications referring to this model. The model has been evaluated as being successful in predicting intentions, but less successful in predicting behaviors, which is obvious because there are no postintentional variables in the model. In a meta-analysis, Armitage and Conner ( 2001 ) reported an average of 39 percent of explained intention variance, as opposed to an average of 27 percent explained behavior variance. These percentages are high because many studies in this area are only cross-sectional correlation studies based upon self-reports. Due to such research designs, the coefficients are inflated, whereas in longitudinal studies, using objective behavioral outcomes, and in experimental studies, the predictive value of the theory is very limited (Sniehotta, 2009b ). Thus, the TPB is mainly an intention theory. To transform it into a more powerful behavior change theory, it needs to be extended by postintentional predictors that are more proximal to the behavior in question. Several recent studies have added action planning as a mediator between intentions and behavior, which has made a substantial improvement (Sheeran, Milne, Webb, & Gollwitzer, 2005 ).
Theory of planned behavior (TPB).
The Transtheoretical Model of Behavior Change
To overcome the limitations of continuum models, stage theories offer an alternative that address the existence or usefulness of action phases or stages. One such approach is based on clinical research on addictions, and now has become the dominant model of health behavior change: the transtheoretical model of behavior change (TTM), also called stages of change (SOC) model (DiClemente & Prochaska, 1982 ; Prochaska, & Velicer, 1997 ). Its main feature is the implication that different types of cognitions and behaviors may be important at different stages of the health behavior change process. The most common version of the TTM includes five discrete stages of health behavior change that are defined in terms of one’s past behavior and future plans (precontemplation, contemplation, preparation, action, maintenance; see Figure 24.2 ). For example, at the precontemplation stage, a problem drinker does not think about quitting in the future. At the contemplation stage, he or she reflects about quitting sometime within the next 6 months, but does not make any specific plans for behavior change. At the preparation stage, the problem drinker resolves to quit within the next month and prepares for this step. The action stage includes individuals who have taken successful action for any period of time. If abstinence has lasted for more than 6 months, the person is categorized as being in the maintenance stage. The five stages are expected to be mutually exclusive and qualitatively different. Sometimes a termination stage is added, for example in the case of smokers who have been abstinent for at least 5 years.
People could make multiple attempts to progress from preaction to action stages. However, relapses could occur anytime, resulting in a spiral-like progression through the behavior-change process. In contrast to continuum models, stage models such as the transtheoretical model assume that factors producing movement toward action differ in respect to a person’s stage. The identification of stages bears implications for interventions because matching a treatment to the current stage of a target group would lead to better outcomes.
In addition to the described basic stages of change, the TTM also includes ten processes of change, decisional balance (the perceived pros and cons of changing), perceived self-efficacy, and temptation. Processes of change are conceptualized as causes for the transitions between the stages, whereby it is assumed that different factors influence different stage transitions.
Decisional balance, as well as self-efficacy/temptation, are usually described as dependent variables. Thus, as people move through stages, they arrive at a more favorable decisional balance and at higher levels of self-efficacy. On the other hand, is seems more plausible to understand these factors as causes of stage movement. Decisional balance is one of the oldest constructs in psychology. Benjamin Franklin (1706–1790) had already suggested to list all the pros and cons on a sheet of paper when it comes to making a difficult decision (that’s why it is also called the Franklin method ). In decision making theories, balancing plays a key role (Janis & Mann, 1977 ). Thus, it can be assumed that balancing is mainly a preintentional process, in particular in the contemplation stage, and that it facilitates intention formation.
The transtheoretical model (TTM).
In TTM, the ten processes of change constitute clusters of treatment strategies that were derived from an examination of 24 psychotherapy models (Prochaska & DiClemente, 1983 ). These are consciousness raising (the extent to which people seek and assimilate new information), dramatic relief (identification and expression of emotions pertaining to the problem behavior), environmental reevaluation (gauging the effects of the risk behavior on the physical and social environment), self-reevaluation (appraising one’s values in terms of a problem behavior), social liberation (perceptions of whether the social world is supportive of a person’s choices), counter-conditioning (substituting the problem behavior with alternatives), helping relationships (provision and use of social support), reinforcement management (use of rewards in making changes), self-liberation (commitment to changing the problem behavior), and stimulus control (controlling the situation that evokes the problem behavior).
An abundance of studies have used the TTM, providing support for the usefulness of stages. Evidence has emerged suggesting that the notion of stages of behavior change is meaningful and has pragmatic value (Velicer, Redding, Sun, & Prochaska, 2007 ). A meta-analysis on tailoring interventions pointed to empirical evidence in favor of stage-matched treatments (Noar, Benac, & Harris, 2007 ). The TTM’s practicability for interventions is very appealing.
The TTM has been criticized by some researchers (e.g., Adams & White, 2003 ; Bandura, 1997 ). Weinstein, Rothman, and Sutton ( 1998 ) and Sutton ( 2005 ) argued that the stages might not be genuinely qualitative, but are rather arbitrary distinctions within a continuous process. In particular, passage of time might not be the ideal criterion for defining stages (Lippke, Ziegelmann, Schwarzer, & Velicer, 2009 ). Kraft, Sutton, and McCreath Reynolds ( 1999 ) demonstrated within a sample of daily smokers that precontemplators, contemplators, and preparers were not at different qualitative stages, but rather at different places along an underlying continuum. Similarly, Courneya, Nigg, and Estabrooks ( 1998 ) reported that continuous measures of intention explained more variance in exercise behavior than did the stage algorithm proposed by the TTM. Armitage and Arden ( 2008 ) found a correlation of .78 between intention and stages of change, indicating that the stages seem to reflect a linear process of readiness for change. However, such a high correlation sheds doubt on the usefulness of the stage construct because arbitrary cutoffs of a behavioral intention measure would then become an equivalent means to segment the audience into more homogeneous target groups for interventions (Armitage, 2009 ). The stages of change construct is supposed to be a “fast and frugal decision tree” blending intentions (precontemplation, contemplation, preparation) and behavior (action, maintenance). Therefore, it should be sufficiently distinct from any behavioral intention measure. In other words, a moderate intercorrelation between intentions and stages would reflect discriminant validity. Other researchers have found that processes of change did not predict smoking stage movements (Herzog & Blagg, 2007 ), and that stage-matched and stage-mismatched interventions with young adult smokers did not yield the hypothesized results (Quinlan & McCaul, 2000 ). Stages of change did not predict success in weight control in adult women (Jeffery, French, & Rothman, 1999 ). De Vet, de Nooijer, de Vries, and Brug ( 2008 ) provided matched versus mismatched treatments for precontemplators, contemplators, and actors, but they did not find that matching was superior.
Thus, evidence in favor of the TTM is mixed. The critique mainly addresses the conceptual notion of stages, their operationalization, the failure to move people from one stage to the next, or the failure to achieve stage-matched effects. A major problem that TTM shares with all other models is the validity of the key constructs. Stage allocation is based on a simple algorithm (a fast and frugal decision tree) asking people whether they act or not, and if not, whether they intend to do so or not, etc. Sensitivity and specificity need to be addressed to determine the number of false positives, for example. Passage of time might not be the ideal criterion to identify cutoff points in the process of change (Lippke, Ziegelmann, Schwarzer, & Velicer, 2009 ). Self-reports for stages or intentions are subject to intraindividual fluctuation and, therefore, may result in different decisions depending on the time of day, mood, or social influence. Thus, if a particular stage algorithm is not sufficiently valid in a particular health promotion setting, any stage-matched intervention will fail. Moreover, if validity is perfect, but the treatment contents or implementation methods are not well designed, the interventions will also fail. Also, tailoring per se may have a placebo effect that undermines the genuine effects of the matched treatments (Webb, Hendricks, & Brandon, 2007 ). Thus, an unsuccessful research project based on a stage of change model should not be counted as a disconfirmation of the theory.
Some authors have been critical about the assumption of stages and have discarded the TTM as a whole. This is unjustified because it not only consists of the five stages, but also of ten processes of change and decisional balance, and self-efficacy/temptation. The TTM had been proposed as an integration of theories (Prochaska & Velicer, 1997 ). It includes a number of promising components that are not yet well tested and deserve more experimental scrutiny.
Processes such as stimulus control, counter-conditioning, consciousness raising, and receipt of social support are included as components in many interventions without explicitly referring to TTM. Planning, for example, can involve content that reflects some of the ten processes. Armitage ( 2008 ) has studied implementation intentions that were inspired by TTM processes. Thus, many components of the TTM appear in studies without an explicit link to this model. It does not come as a surprise that specific components have been found successful, given the fact that they were originally taken from leading psychotherapy models. All 14 variables of the TTM as a whole are hard to test. Therefore, the TTM might be seen rather as a useful heuristic framework than as a closed, testable theory (Armitage, 2009 ; Lippke & Ziegelmann, 2008 ).
The Health Action Process Approach: A Two-layer Framework
The traditional continuum models have been mainly criticized because of the intention–behavior gap. A model that explicitly includes postintentional factors to overcome this gap is the HAPA (Schwarzer, 2008 ). The model suggests a distinction between (a) preintentional motivation processes that lead to a behavioral intention and (b) postintentional volition processes that lead to the actual health behavior. Within the two phases, different patterns of social-cognitive predictors may emerge (see Figure 24.3 ). In the initial motivation phase, a person develops an intention to act. In this phase, risk perception is seen as a distal antecedent (e.g., “I am at risk for cardiovascular disease”). Risk perception in itself is insufficient to enable a person to form an intention. Rather, it sets the stage for a contemplation process and further elaboration of thoughts about consequences and competencies. Similarly, positive outcome expectancies (e.g., “If I exercise five times per week, I will reduce my cardiovascular risk”) are chiefly seen as being important in the motivation phase, when a person balances the pros and cons of certain behavioral outcomes. Further, one needs to believe in one’s capability to perform a desired action (perceived self-efficacy, e.g., “I am capable of adhering to my exercise schedule in spite of the temptation to watch TV”). Perceived self-efficacy operates in concert with positive outcome expectancies, both of which contribute substantially to forming an intention. Both beliefs are needed for forming intentions to adopt difficult behaviors, such as regular physical exercise.
After a person develops an inclination toward a particular health behavior, the “good intention” has to be transformed into detailed instructions on how to perform the desired action. Once an action has been initiated, it has to be maintained. This is not achieved through a single act of will, but involves self-regulatory skills and strategies. Thus, the postintentional phase should be further broken down into more proximal factors, such as planning and recovery self-efficacy. Other social cognition models do not address explicitly postintentional factors (Luszczynska & Schwarzer, 2005 ).
The continuum layer of the health action process approach (HAPA).
Including planning and self-efficacy as volitional mediators renders the model into an implicit stage model because it implies the existence of (at least) two phases: a motivational one and a volitional one. The purpose of such a model is twofold: It allows a better prediction of behavior, and it reflects the assumed causal mechanism of behavior change. Research based on this model, therefore, employs path-analytic methods (e.g., Lippke, Ziegelmann, & Schwarzer, 2005 ; Luszczynska & Schwarzer, 2003 ; Renner et al., 2008 ; Richert, Reuter, Wiedemann, Lippke, Ziegelmann, & Schwarzer, 2010 ; Schwarzer et al., 2007 ; Schwarzer et al., 2010 ).
However, when it comes to the design of interventions, one can consider turning the implicit stage model into an explicit one. This is done by identifying individuals who reside either at the motivational stage or the volitional stage. Then, each group becomes the target of a specific treatment that is tailored to this group. Moreover, it is theoretically meaningful, and has been found to be useful, to subdivide further the volitional group into those who perform and those who only intend to perform. In the postintentional preactional stage, individuals are labeled “intenders,” whereas in the actional stage they are labeled “actors.” Thus, a suitable subdivision within the health behavior change process yields three groups: preintenders, intenders, and actors. The term “stage” in this context was chosen to allude to the stage theories, but not in the strict definition that includes irreversibility and invariance. The terms “phase” or “mindset” may be equally suitable for this distinction. The basic idea is that individuals pass through different mindsets on their way to behavior change. Thus, interventions may be most efficient when tailored to these particular mindsets. For example, preintenders are supposed to benefit from confrontation with outcome expectancies and some level of risk communication. They need to learn that the new behavior (e.g., becoming physically active) has positive outcomes (e.g., well-being, weight loss, fun) as opposed to the negative outcomes that accompany the current (sedentary) behavior (such as developing an illness or being unattractive). Moreover, it has been found that preintenders benefit more from gain-framed than from loss-framed outcome expectancies (Detweiler et al., 1999 ).
In contrast, intenders should not benefit much from such health messages in the form of outcome expectancies because, after setting a goal, they have already moved beyond this mindset. Rather, they should benefit from planning to translate their intentions into action. Finally, actors do not need any treatment at all unless one wants to improve their relapse prevention skills. Then, they should be prepared for particular high-risk situations in which lapses are imminent.
The HAPA is designed as an open architecture based on a collection of various principles, rather than on specific testable assumptions. It was developed in 1988 (Schwarzer, 1992 ) as an attempt to integrate the model of action phases (Heckhausen, 1980 ) with social-cognitive theory (Bandura, 1986 ). It has five major principles that make it distinct from other models.
Principle 1: Motivation and volition . The first principle suggests that one should divide the health behavior change process into two phases. A switch of mindsets occurs when people move from deliberation to action. First comes the motivation phase in which people develop their intentions. Afterward, they enter the volition phase.
Principle 2: Two volitional phases . In the volition phase, there are two groups of individuals: those who have not yet translated their intentions into action, and those who have. There are inactive as well as active persons in this phase. In other words, in the volitional phase, one finds intenders as well as actors, who are characterized by different psychological states. Thus, in addition to health behavior change as a continuous process, one can also create three categories of people with different mindsets depending on their current point of residence within the course of health behavior change: Preintenders, intenders, and actors.
Principle 3: Postintentional planning . Intenders who are in the volitional preactional stage are motivated to change, but do not act because they might lack the right skills to translate their intention into action. Planning is a key strategy at this point. Planning serves as an operative mediator between intentions and behavior.
Principle 4: Two kinds of mental simulation . Planning can be divided into action planning and coping planning. Action planning pertains to the when, where, and how of intended action. Coping planning includes the anticipation of barriers and the design of alternative actions that help to attain one’s goals in spite of the impediments.
Principle 5: Phase-specific self-efficacy . Perceived self-efficacy is required throughout the entire process. However, the nature of self-efficacy differs from phase to phase, because there are different challenges as people progress from one phase to the next one. Goal setting, planning, initiative, action, and maintenance pose challenges that are not of the same nature. Therefore, one should distinguish between preactional self-efficacy, coping self-efficacy, and recovery self-efficacy. Sometimes the terms task self-efficacy instead of preaction self-efficacy, and maintenance self-efficacy instead of coping and recovery self-efficacy are preferred.
In sum, HAPA is a health-behavior change framework with an open architecture. The HAPA has two layers, a continuum layer and a phase (or stage) layer. Depending on the research question, one might choose the one or the other. The HAPA is designed as a sequence of two continuous self-regulatory processes, a goal setting phase (motivation) and a goal pursuit phase (volition). The second phase is subdivided into a preaction phase and an action phase. One can superimpose these three phases on the continuum model as a second layer and regard phase as a moderator. This two-layer architecture allows a switch between the continuum model and the stage model, depending on the given research question. The stage layer is useful when designing stage-matched interventions. For preintenders, one needs risk and resource communication, for example by addressing the pros and cons of the critical behavior. For intenders, planning treatments are helpful to support people who lack the necessary skills to translate their intentions into behavior. And for actors, one needs to stabilize their newly adopted health behaviors through relapse prevention strategies.
The HAPA allows both the researcher and the practitioner to make a number of choices. Although it was initially inspired by distinguishing between a motivational and a volitional stage, and later extended to the distinction between preintenders, intenders, and actors, one need not necessarily group individuals according to such stages. If the purpose is to predict behavior change, one would specify a mediator model that includes postintentional constructs (such as planning and volitional self-efficacy) as proximal predictors of performance (Scholz, Nagy, Göhner, Luszczynska, & Kliegel, 2009 ).
For the purpose of stage-tailored interventions, however, usually three stage groups are established. This does not exclude the possibility of generating more than three stages. For example, for some research questions, one might want to subdivide the preintenders into precontemplators and contemplators, according to the TTM (Velicer & Prochaska, 2008 ), or opt for a distinction between preintenders who are either (a) unaware of an issue, (b) aware but unengaged, or (c) deciding (Weinstein, Lyon, Sandman, & Cuite, 1998 . Thus, the HAPA is not a puristic stage model, but a versatile theoretical framework that allows for a variety of approaches.
General Issues in Health Behavior Change
Goal conflict, goal hierarchies, and priority management in health self-regulation.
Studies are usually limited to one behavior and a corresponding behavioral goal (intention). This is a deliberate choice because the more complex the research question, the less likely it becomes to find the evidence. But we need to acknowledge the fact that people do have multiple goals that are often in conflict. For example, the intention to work out every day might serve the goal to become slim, which, in turn, may serve the broader goal to become attractive for a potential partner, and so on. Depending on the value placed on the superordinate goal, the subordinate goal might have a certain chance to be pursued while competing goals (enjoying dinner parties) are being downgraded. A variety of action-control components operate in the volition phase that help a person adhere to a chosen regimen. Relapse prevention and harm reduction strategies are needed to stabilize intentions and behaviors in times of conflict. Such strategies need to be part of interventions designed to preclude people from regressing from action to earlier stages.
Goal setting, intention formation, effort investment, planning, action control, and disengagement are self-regulatory constructs. Health self-regulation encompasses a broad range of cognitions and behaviors. Studies could benefit from work in other fields, for example from relapse prevention theory (Marlatt, 2002 ; Marlatt et al., 1995 ) and self-regulation theories (Baumeister & Vohs, 2004 ; Carver & Scheier, 1998 ; Cervone, Shadel, Smith, & Fiori, 2006 ; Kuhl, 2001 ; Maes & Karoly, 2005 ).
Self-regulatory constructs other than self-efficacy might help to further explain postintentional processes of health behavior change. Theories of volition emphasize that self-regulation refers to an individual’s ability to focus attention on the task at hand and to keep a favorable emotional balance. Self-competencies that refer to regulation of attentional and emotional components of goal-directed behavior might play a crucial role across all phases of health behavior change. In different stages of goal pursuit, people need to pay attention and stay with the task at hand. They need to concentrate even when an interfering task emerges. Moreover, controlling interfering emotions such as boredom, anger, distress, exhaustion, anxiety, or reluctance requires a number of cognitive skills. Self-regulation of attention and emotion might also be seen as a stable personal disposition, an individual difference characteristic that enables habitual control over recurrent actions, as well as in the process of behavior change (see Cervone et al., 2006 ; Kuhl, 2001 ).
From the perspective of modeling health behavior change, the question arises how many and which volitional factors should be included to bridge the intention–behavior gap. After the inclusion of planning and volitional self-efficacy, action control would be a third promising candidate. Future research needs to find out to which degree an accumulation of further volitional factors would account for substantial variance of health behaviors, or whether this would rather violate the postulate of parsimony. In some studies, we have added the construct of action control to the model (Schüz, Sniehotta, Mallach, Wiedemann, & Schwarzer, 2009 ; Sniehotta, Nagy, Scholz, & Schwarzer, 2006 ). Although planning is a prospective strategy—that is, behavioral plans are made before the situation is encountered—action control is a concurrent self-regulatory strategy, in which the ongoing behavior is continuously evaluated with regard to a behavioral standard. A study on dental flossing (Schüz et al., 2009 ) has investigated stage-specific effects of an action control treatment (a dental flossing calendar). The intervention led to higher action control levels at follow-up, thus indicating volitional effects. However, the action control intervention did not improve intention formation, and, thus, had no motivational effect, as hypothesized. Action control facilitated flossing behavior in volitional individuals only. In other words, a beneficial effect emerged only in the stage-matched condition. This result suggests that only intenders and actors benefit from self-regulatory treatments. A very parsimonious intervention, such as the provision of dental calendars for self-monitoring, may bring forth notable effects if correctly addressed to individuals who are in a volitional phase.
A further question is whether we should judge the quality and usefulness of a model only in terms of explained behavioral variance. Gaining insight into mediating processes upgrades the importance of such mediators as secondary outcomes. The mediators are relevant criteria by themselves. Even if we cannot immediately change a certain refractory behavior, we might move a crucial step further by changing one of the proximal mediators into the right direction.
The Debate About Continuum Versus Stage Models
When identifying individuals with different mindsets and separating them for particular analyses or treatments, we are dealing with a stage model. By this, we go beyond the quest for mediating factors. Stage is supposed to operate as a moderator with two or more levels (e.g., preintenders, intenders, actors). The assumption is that the mean values of social-cognitive variables and behavior differ between these subgroups. Moreover, the mediating mechanism may differ as well. Technically, the analysis reflects a moderated mediation (Lippke, Wiedemann, et al., 2009 ). How exactly individuals with different mindsets differ in terms of the causal mechanisms of health behavior change remains a research agenda for the future. Evidence in favor of moderated mediation would support the discontinuity hypothesis, which means that change does not reflect a continuum, but rather a process that involves two or more qualitative stages (mindsets). This notion of discontinuity has been demonstrated in a number of contributions (Armitage, Povey, & Arden, 2003 ; Lippke, Ziegelmann, et al., 2009 ). There are also studies that attempt to combine a continuum model (TPB) with the stages approach (Courneya, Nigg, & Estabrooks, 1998 ).
A better way of demonstrating the usefulness of a stage distinction is documented by experimental effects when manipulating one or more of the proposed mediators. Improving self-efficacy in women who were motivated to practice breast self-examination has resulted in higher levels of this behavior (Luszczynska, 2004 ). Improving action planning and coping planning in patients motivated to increase their physical activity has also been successful (Luszczynska, 2006 ; Sniehotta, Scholz, & Schwarzer, 2006 ; Ziegelmann, Lippke & Schwarzer, 2006 ). If a proposed mediator is effective at a particular stage, but not at the other, then we need to identify which individuals reside at which stage and tailor the treatment (e.g., planning, self-efficacy interventions) to one group.
The usefulness of stages also depends on the validity of their assessment. Stages are based upon discontinuity, thus the assessment tool must identify individuals who belong to a relatively homogeneous group that is clearly distinct from the previous and/or subsequent group. The stage algorithm, thus, must produce such homogeneous groups on the basis of relevant criteria. This, however, poses a major problem. In the TTM, the main criterion for grouping is the passage of time. For example, someone is judged to be a preparer when she or he intends to change within a month, or someone is promoted from actor to maintainer after adhering to the desired behavior for 6 months. Obviously, this is based upon average clinical experience. Therefore, we rather avoid time as a criterion and use psychological variables, in particular intention and behavior, to build a staging algorithm (Lippke, Ziegelmann, Schwarzer, & Velicer, 2009 ). Nevertheless, all criteria suffer from some arbitrariness.
Indistinct boundaries exist between stages, and these make misclassification likely. Even the best set of social-cognitive variables cannot attain perfect validity because personal characteristics are often instable. Intentions may change within a day, rendering the staging outcome unreliable. However, intention instability is not a problem germane to stage theories. It causes trouble in continuum theories as well. Predicting Time 2 performance by Time 1 intention may be biased due to changes in intention during the observation period. Instability of predictors is a general problem in all approaches that deal with change. Misclassification of individuals would, however, be a serious matter if these persons were treated with an adverse intervention. So far, there is not much evidence of harm created by stage mismatch (except for selective dropout from treatment). All treatments appear to be more or less beneficial or are, at worst, ineffective (Dijkstra, Conijn, & De Vries, 2006 ). A stage assessment procedure of poor validity may underestimate the usefulness of stages and lead to unsuccessful health-promotion efforts. But if stage-matched individuals, on average, gain more than mismatched or unmatched individuals, they do have an advantage.
The debate about stages of change as opposed to a continuum of change resembles a debate on the scientific truth about the objective world. The quest for the existence of stages assumes that the nature of health behavior change is either one or the other, and that the only task is to “discover” whether stages truly exist. However, stage is a construct, not nature. We invent the notion of stages to help us understand how people change and to provide better treatment to those who have difficulties in changing their behaviors. We construct stages to open another window that allows for a different view on the change process. Thus, the question is not whether stages truly exist, but whether stage is a useful construct.
Moreover, there is no difference between stages and “pseudostages.” The latter term refers to a categorization of a “truly existing continuum” into stages. However, continuum is also a construct. A continuum is frequently subdivided into categories, although this is accompanied by the loss of some information because it is regarded as useful to illustrate unique characteristics of a variable’s distribution or its relationship to others. Then, the question remains: When does the assumption of stages appear to be more useful than the continuum hypothesis?
If we find that certain groups of individuals undergoing a change process share common features and have similar mindsets that are distinct from those in a different group at a different point in the change process, then we might want to label them as residents of a particular stage, such as preintenders, intenders, or actors. This is useful because we obtain a fresh view on the features of individuals within a hypothetical change process. Whether this process is truly a series of qualitative steps or an underlying action-readiness continuum remains a matter of judgment. We do not discover the existence of one or the other; we rather choose a construct that provides a convenient template for subsequent research efforts. If, for example, scientists regard some individuals as “inclined abstainers,” they have deliberately chosen a category and created a label that improves communication about the phenomenon in question. Due to its biological connotations, the choice of the stage label may have been unfortunate, but, meanwhile, it has proven useful and has led to a success history in health psychology. The focus is not on the illusion of scientific truth, but on practicability, and one important aspect of the latter is therapeutic effectiveness. If stage-tailored interventions turn out to be more effective than untailored ones, the construct of stage has proven useful.
Understanding the Mechanisms of Health Behavior Change
To understand better the mechanisms of health behavior change, we need to identify mediator effects as well as moderator effects. The HAPA, for example, as a parsimonious mediator model does not explicitly include moderators, except of stage. Stage as a moderator indicates that a prediction model within one stage group operates in a different way than a prediction model within an adjacent stage group. This is similar to the assumption that one set of social-cognitive variables can move people from stage A to B, whereas a different set of variables can move people from stage B to C.
Although action planning has been found to mediate the intention–behavior relation (Gollwitzer & Sheeran, 2006 ), some studies have failed to find such mediation effects (Norman & Conner, 2005 ). This suggests that the relationships among intentions, planning, and behavior might also depend on other factors. For example, the degree to which planning mediates between intentions and behavior has been found to be higher in older than in younger individuals (Renner, Spivak, Kwon, & Schwarzer, 2007 ; Scholz, Sniehotta, Burkert, & Schwarzer, 2007 ). This represents a case of moderated mediation. Perceived self-efficacy is one potential moderator for the degree to which planning has an effect on subsequent behaviors. It is expected to moderate the planning-behavior relation because people harboring self-doubts might fail to act upon their plans. For persons with a high level of self-efficacy, planning might be more likely to facilitate goal achievement. Self-efficacious people feel more confident about translating their plans into actual behavior. In other words, whether planning interventions (independent variable) actually affect behavior (dependent variable) might depend on the individual’s level of self-efficacy (moderator). In a study on physical activity, longitudinal data from an online survey were used to examine similar interrelationships (Lippke, Wiedemann, et al., 2009 ). Only those persons who had a sufficiently high level of exercise self-efficacy acted upon their plans. Conversely, participants who were harboring self-doubts failed to act upon their plans (see also Gutiérrez-Doña, Lippke, Renner, Kwon, & Schwarzer, 2009 ).
Mediator models work well in some groups, but not in others. By comparing men and women, younger and older individuals, and those from different cultures, we identify relevant moderators (Renner, Spivak, Kwon, & Schwarzer, 2007 ; Reuter, Ziegelmann, Wiedemann, Lippke, Schüz, & Aiken, 2009 ; Ziegelmann, Lippke, & Schwarzer, 2006 ). When a mediator model (be it a simple three-variable model, or a more complex one) has strong interrelations within one category of people, but weak associations within a different category of people, then this is a case of moderated mediation. The amount to which the mediator translates the effect of the independent variable on the dependent variable depends on the levels of a moderator variable. Such moderators can be sex, age, culture, and the like, but also can be psychological variables that are closely related to the constructs used in health behavior models (Hankonen, Absetz, Ghisletta, Renner, & Uutela, 2010 ). Temporal stability of intention, for example, may be a moderator (Conner, 2008 ). Moderated mediation is also possible with psychosocial variables, such as intention or planning. For example, the intention–behavior link is mediated by planning, and this mediator effect can be moderated by level of intention (Wiedemann, Schüz, Sniehotta, Scholz, & Schwarzer, 2009 ). Here, we have a special case in which the independent variable (intention) of a mediator model serves the function of a moderator in addition. In other words, only in highly motivated persons does the intention operate via planning on the improvement of adherence, whereas in poorly motivated persons no such mediator effect is visible.
The best way to demonstrate the mechanisms of health behavior change is the experimental manipulation of those variables that are supposed to produce behaviors or to move people from one stage to another (Michie, Rothman, & Sheeran, 2007 ; Reuter, Ziegelmann, Wiedemann, & Lippke, 2008 ; Weinstein, 1993 ). Various experimental studies have shown that self-efficacy interventions do make a difference, which attests to the fact that self-efficacy is indeed an operative construct that facilitates volitional processes, such as effort and persistence (Luszczynska, Tryburcy, & Schwarzer, 2007 ).
The finding that a model fits the data does not prove that the chosen model is the only one or the best one that fits. The question is whether this model appears to be empirically superior to alternative models. Finding the best model for a particular research context requires consideration of several questions: Which model accounts for most of the criterion variance? Which one provides the best insight into the causal mechanism of health behavior change? Is the model that makes the best prediction also the best one for the design of interventions? Which is the most parsimonious one?
To test the validity of a model in comparison with other theories of health behavior change, experimental studies are required (Weinstein, Lyon, Sandman, & Cuite, 1998 ). So far, most of the studies that aim at comparing determinants from different theories are mainly correlational ones. A minority of studies includes experimental manipulations and examines the maintenance of behavior change by means of follow-up assessment. Future research should include the manipulation of constructs from one theory in one sample, and manipulation of the constructs from a different theory (such as TPB) in another sample. For example, at the stage of intention development, one group could be treated by improving positive attitudes and subjective norms (TPB), whereas the other group could be treated by improving self-efficacy, outcome expectancies, and risk perception (HAPA). At the stage of goal pursuit, on the other hand, one group could be treated by improving perceived behavioral control (TPB), whereas the other could be treated by enhancing a combination of self-efficacy, action planning, and relapse prevention (HAPA). It is unlikely that one will ever find an acid test to compare all models with each other since they are partly incompatible—as are, for example, stage models versus continuum models. Researchers tend to prefer eclectic approaches, such as selecting attractive elements from one model and implanting them into another, which also can be seen as a means of theory evolution (Lippke & Ziegelmann, 2008 ; Sniehotta, 2009a , 2009 b).
Health behavior change is a major challenge to health psychology and public health research. The key question is how to predict and modify the adoption and maintenance of health behaviors such as physical exercise, weight control, preventive nutrition, dental hygiene, condom use, and accident prevention, as well as the modification of problem drinking, substance use, smoking, reckless driving, overeating, or unprotected sexual intercourse. Public health efforts aim at changing environments, for example, when imposing a ban on smoking in certain places. Such policy decisions must be based upon sound research that identifies causes and effects and also predicts the likelihood of compliance with such measures. On the other hand, most lifestyle changes are based on individual health self-regulation that includes the motivational, volitional, and actional processes of abandoning health-compromising behaviors in favor of health-enhancing behaviors. We have described various psychological constructs such as intention, risk perception, outcome expectancies, perceived self-efficacy, and planning. None of them constitutes a “magic bullet.” They need to operate in concert, and that is why theories and models are needed to better understand the mechanisms of diverse health behavior change processes. The distinction between continuum models and stage models is helpful to grasp the general philosophy of certain approaches. To illustrate very different viewpoints, we have provided one example of a continuum model (theory of planned behavior) and one example of a stage model (transtheoretical model). Then, a two-layer hybrid framework was introduced (health action process approach). All models are meaningful and justified to serve as starting points for research. Depending on context and research questions, one might see a particular model as being more reasonable than others. All currently discussed models have limitations and cannot account fully for the complexity of behavior change mechanisms. As an example for such a mechanism that is not included in any theory, we have chosen moderated mediation. This method refers to why change takes place, as well as in whom change takes place. There are populations for whom a particular mediator model might make the best predictions, whereas another mediator model might work superiorly in a different population. Whatever mechanism is studied in the adoption and maintenance of health behaviors, it is most important to make our implicit theories explicit, because insight does emerge from data without theory (Rothman, 2000 ; Weinstein et al., 1998 ).
Abraham, C. ( 2008 ). Beyond stages of change: Multi-determinant continuum models of action readiness and menu-based interventions. Applied Psychology: An International Review, 57, 30–41.
Abraham, C., & Sheeran, P. ( 2000 ). Understanding and changing health behaviour : From health beliefs to self-regulation. In P. Norman, C. Abraham, & M. Conner (Eds.), Understanding and changing health behaviour (pp. 3–24). Amsterdam: Harwood.
Google Scholar
Google Preview
Abraham, C., & Sheeran, P. ( 2003 ). Acting on intentions: The role of anticipated regret. British Journal of Social Psychology, 42, 495–511.
Abraham, C., & Sheeran, P. ( 2005 ). The health belief model. In M. Conner, & P. Norman (Eds.), Predicting health behavior (pp. 28–80). Maidenhead: Open University Press.
Abraham, C., Sheeran, P., & Johnston, M. ( 1998 ). From health beliefs to self-regulation: Theoretical advances in the psychology of action control. Psychology & Health, 13, 569–591.
Adams, J., & White, M. ( 2003 ). Are activity promotion interventions based on the transtheoretical model effective? A critical review. British Journal of Sports Medicine, 37, 106–114.
Ajzen, I. ( 1991 ). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211.
Araújo-Soares, V., McIntyre, T., & Sniehotta, F.F. ( 2009 ). Predicting changes in physical activity amongst adolescents: The role of self-efficacy, intention, action planning and coping planning. Health Education Research, 24, 128–139.
Armitage, C.J. ( 2008 ). A volitional help sheet to encourage smoking cessation: A randomized exploratory trial. Health Psychology, 27, 557–566.
Armitage, C.J. ( 2009 ). Is there utility in the transtheoretical model? British Journal of Health Psychology, 14, 195–210.
Armitage, C.J., & Arden, M.A. ( 2002 ). Exploring discontinuity pattern in the transtheoretical model: An application of the theory of planned behavior. British Journal of Health Psychology, 7, 89–103.
Armitage, C.J., & Arden, M.A. ( 2008 ). How useful are the stages of change for targeting interventions? Randomized test of a brief intervention to reduce smoking. Health Psychology, 27, 789–798 .
Armitage, C.J., & Conner, M. ( 2001 ). Efficacy of the theory of planned behaviour: A meta-analytic review. British Journal of Social Psychology, 40, 471–499.
Armitage, J.C., Povey, R., & Arden, M.A. ( 2003 ). Evidence for discontinuity patterns across the stages of change: A role for attitudinal ambivalence. Psychology & Health, 18, 373–386.
Bandura, A. ( 1986 ). Social foundations of thought and action . Englewood Cliffs, NJ: Prentice Hall.
Bandura, A. ( 1997 ). Self-efficacy: The exercise of control . New York: Freeman.
Bandura, A. ( 2000 ). Cultivate self-efficacy for personal and organizational effectiveness. In E.A. Locke (Ed), The Blackwell handbook of principles of organizational behavior (pp. 120–136). Oxford, England: Blackwell.
Baumeister, R.F., Heatherton, T.F., & Tice, D.M. ( 1994 ). Losing control: How and why people fail at self-regulation . San Diego, CA: Academic Press.
Baumeister, R.F., & Vohs, K.D. (Eds.). ( 2004 ). Handbook of self-regulation: Research, theory, and applications. New York: Guilford Press.
Biddle, S.J.H., & Fuchs, R. ( 2009 ). Exercise psychology: A view from Europe. Psychology of Sport and Exercise, 10, 410–419.
Brewer, N.T., Weinstein, N.D., Cuite, C.L., & Herrington, J.E. ( 2004 ). Risk perceptions and their relation to risk behavior. Annals of Behavioral Medicine, 27, 125–130.
Carver, C.S., & Scheier, M.F. ( 1998 ). On the self-regulation of behavior . New York: Cambridge University Press.
Cervone, D., Shadel, W.G., Smith, R.E., & Fiori, M. ( 2006 ). Self-regulation: Reminders and suggestions from personality science. Applied Psychology: An International Review, 55, 333–385.
Chapman, J., Armitage, C.J., & Norman, P. ( 2009 ). Comparing implementation intention interventions in relation to young adults’ intake of fruit and vegetables. Psychology & Health, 24, 317–332.
Conner, M. ( 2008 ). Initiation and maintenance of health behaviors. Applied Psychology: An International Review, 57, 42–50.
Conner, M., & Norman, P. (Eds.). ( 2005 ). Predicting health behavior: Research and practice with social cognition models (2nd ed.). Buckingham, England: Open University Press.
Conner, M., Sandberg, T., McMillan, B., & Higgins, A. ( 2006 ). Role of anticipated regret in adolescent smoking initiation. British Journal of Health Psychology, 11, 85–101.
Conner, M., & Sparks, P. ( 2005 ). The theory of planned behaviour and health behaviours. In M. Conner, & P. Norman (Eds.), Predicting health behaviour: Research and practice with social cognition models (2nd ed., pp. 170–222). Maidenhead, UK: Open University Press.
Courneya, K.S., Nigg, C.R., & Estabrooks, P.A. ( 1998 ). Relationships among the theory of planned behavior, stages of change, and exercise behavior in older persons over a three year period. Psychology and Health, 13, 355–367.
Croyle, R.T., Sun, Y., & Louie, D. ( 1993 ). Psychological minimization of cholesterol test results: Moderators of appraisal in college students and community residents. Health Psychology, 12, 503–507.
Detweiler, J.B., Bedell, B.T., Salovey, P., Pronin, E., & Rothman, A.J. ( 1999 ). Message framing and sunscreen use: Gain-framed messages motivate beach-goers. Health Psychology, 18, 189–196.
de Vet, E., de Nooijer, J., de Vries, N.K., & Brug, J. ( 2008 ). Testing the transtheoretical model for fruit intake: Comparing web-based tailored stage-matched and stage-mismatched feedback. Health Education Research, 23, 218–227.
DiClemente, C.C., & Prochaska, J.O. ( 1982 ). Self-change and therapy change of smoking behavior: A comparison of processes of change in cessation and maintenance. Addictive Behaviors, 7, 133–142.
Dijkstra, A., Conijn, B., & De Vries, H. ( 2006 ). A match-mismatch test of a stage model of behaviour change in tobacco smoking. Addiction, 101, 1035–1043.
Dunton, G.F., & Vaughan, E. ( 2008 ). Anticipated affective consequences of physical activity adoption and maintenance. Health Psychology, 27, 703–710.
Eyal, T., Liberman, N., Trope, Y., & Walther, E. ( 2004 ). The pros and cons of temporally near and distant action. Journal of Personality and Social Psychology, 86(6), 781–795.
Fishbein, M., & Ajzen, I. ( 1975 ). Belief, attitude, intention, and behavior: An introduction to theory and research . Reading, MA: Addison-Wesley.
Gibbons, F.X., & Gerrard, M. ( 1997 ). Health images and their effects on health behavior. In B.P. Buunk, & F.X. Gibbons (Eds.), Health, coping, and well-being: Perspectives from social comparison theory (pp. 63–94). Mahwah, NJ: Erlbaum.
Gibbons F.X., Gerrard, M., & Lane, D.J. ( 2003 ). A social-reaction model of adolescent health risk. In J.J. Suls, & K.A. Wallston (Eds.), Social psychological foundations of health and illness (pp. 107–136). Oxford, England: Blackwell.
Godin, G., & Kok, G. ( 1996 ). The theory of planned behavior: A review of its applications to health-related behaviors. American Journal of Health Promotion, 11, 87–97.
Göhner, W., Seelig, H., & Fuchs, R. ( 2009 ). Intervention effects on cognitive antecedents of physical exercise: A 1-year follow-up study . Applied Psychology: Health and Well-being, 1, 233–256.
Gollwitzer, P.M. ( 1999 ). Implementation intentions: Strong effects of simple plans. American Psychologist, 54, 493–503.
Gollwitzer, P.M., & Sheeran, P. ( 2006 ). Implementation intentions and goal achievement: A meta-analysis of effects and processes. Advances in Experimental Social Psychology, 38, 69–119.
Gutiérrez-Doña, B., Lippke, S., Renner, B., Kwon, S., & Schwarzer, R. ( 2009 ). How self-efficacy and planning predict dietary behaviors in Costa Rican and South Korean women: A moderated mediation analysis. Applied Psychology: Health & Well-Being, 1, 91–104.
Hahn, A., & Renner, B. ( 1998 ). Perception of health risks: How smoker status affects defensive optimism. Anxiety, Stress, and Coping, 11, 93–112.
Hankonen, N., Absetz, P., Ghisletta, P., Renner, B., & Uutela, A. ( 2010 ). Gender differences in social cognitive determinants of exercise adoption. Psychology & Health, 25(1), 55–69. doi:10.1080/08870440902736972.
Heckhausen, H. ( 1980 ). Motivation und handeln. Lehrbuch der motivationspsychologie [Motivation and action. Textbook of motivation psychology]. Berlin: Springer-Verlag.
Heckhausen, H. ( 1991 ). Motivation and action. Berlin: Springer.
Heckhausen, H., & Gollwitzer, P.M. ( 1987 ). Thought contents and cognitive functioning in motivational vs. volitional states of mind. Motivation and Emotion, 11 , 101–120.
Herzog, T.A., & Blagg, C.O. ( 2007 ). Are most precontemplators contemplating smoking cessation? Assessing the validity of the stages of change. Health Psychology, 26, 222–231.
Janis, I.L., & Mann, L. ( 1977 ). Decision making: A psychological analysis of conflict, choice, and commitment . London: Cassel & Collier Macmillan.
Jeffery, R.W., French, S.A., & Rothman, A.J. ( 1999 ). Stage of change as a predictor of success in weight control in adult women. Health Psychology, 18, 543–546.
Klein, W.M.P., & Cerully, J.L. ( 2007 ). Risk appraisal. In R.F. Baumeister, & K.D. Vohs (Eds.), Encyclopedia of social psychology Vol. 2 (pp. 756–758). Thousand Oaks, CA: Sage.
Kraft, P., Sutton, S.R., & McCreath Reynolds, H. ( 1999 ). The transtheoretical model of behaviour change: Are the stages qualitatively different? Psychology & Health, 14(3), 433–450.
Kuhl, J. ( 1983 ). Motivation, konflikt und handlungskontrolle. [Motivation, conflict, and action control]. Berlin: Springer.
Kuhl, J. ( 2001 ). Motivation und persönlichkeit. Interaktionen psychischer systeme [Motivation and personality: Interactions of mental systems]. Göttingen, Germany: Hogrefe.
Lawton, R., Conner, M., & McEachan, R. ( 2009 ). Desire or reason: Predicting health behaviors from affective and cognitive attitudes. Health Psychology, 28, 56–65.
Leventhal, H., Singer, R., & Jones, S. ( 1965 ). Effects of fear and specificity of recommendation upon attitudes and behavior. Journal of Personality and Social Psychology, 2, 20–29.
Leventhal, H., Weinman, J., Leventhal, E., & Phillips, L.A. ( 2008 ). Health psychology: The search for pathways between behavior and health. Annual Review of Psychology, 59, 477–505.
Lewin, K. ( 1947 ). Group decision and social change. In T.M. Newcomb, & E.L. Hartley (Eds.), Readings in social psychology (pp. 330–344). New York: Holt.
Lewin, K., Dembo, T., Festinger, L.A., & Sears, P.S. ( 1944 ). Level of aspiration. In J. McV. Hunt (Ed.), Personality and the behavior disorders Vol. 1 (pp. 333–378). New York: Ronald.
Lippke, S., Wiedemann, A.U., Ziegelmann, J.P., Reuter, T., & Schwarzer, R. ( 2009 ). Self-efficacy moderates the mediation of intentions into behavior via plans. American Journal of Health Behavior, 33, 521–529.
Lippke, S., & Ziegelmann, J.P. ( 2008 ). Theory-based health behavior change: Developing, testing and applying theories for evidence-based interventions. Applied Psychology: International Review, 57, 698–716.
Lippke, S., Ziegelmann, J.P., & Schwarzer, R. ( 2004 ). Initiation and maintenance of physical exercise: Stage-specific effects of a planning intervention. Research in Sports Medicine, 12, 221–240.
Lippke, S., Ziegelmann, J.P., & Schwarzer, R. ( 2005 ). Stage-specific adoption and maintenance of physical activity: Testing a three-stage model. Psychology of Sport & Exercise, 6, 585–603.
Lippke, S., Ziegelmann, J.P., Schwarzer, R., & Velicer, W.F. ( 2009 ). Validity of stage assessment in the adoption and maintenance of physical activity and fruit and vegetable consumption. Health Psychology, 28, 183–193.
Luszczynska, A. ( 2004 ). Change in breast self-examination behavior: Effects of intervention on enhancing self-efficacy. International Journal of Behavioral Medicine, 11, 95–103.
Luszczynska, A. ( 2006 ). An implementation intentions intervention, the use of planning strategy, and physical activity after myocardial infarction. Social Science and Medicine, 62, 900–908.
Luszczynska, A., Mazurkiewicz, M., Ziegelmann J.P., & Schwarzer, R. ( 2007 ). Recovery self-efficacy and intention as predictors of running or jogging behavior: A cross-lagged panel analysis over a two-year period. Psychology of Sport and Exercise, 8, 247–260.
Luszczynska, A., & Schwarzer, R. ( 2003 ). Planning and self-efficacy in the adoption and maintenance of breast self-examination: A longitudinal study on self-regulatory cognitions. Psychology and Health, 18, 93–108.
Luszczynska, A., & Schwarzer, R. ( 2005 ). Social cognitive theory. In M. Conner, & P. Norman (Eds.), Predicting health behaviour (2nd ed. rev., pp. 127–169). Buckingham, UK: Open University Press.
Luszczynska, A., Sobczyk, A., & Abraham, C. ( 2007 ). Planning to reduce weight: Implementation intentions intervention helps to reduce body weight among overweight or obese women by prompting action planning. Health Psychology, 26, 507–512.
Luszczynska, A., Tryburcy, M., & Schwarzer, R. ( 2007 ). Improving fruit and vegetable consumption: A self-efficacy intervention compared to a combined self-efficacy and planning intervention. Health Education Research, 22, 630–638.
Maes, S., & Karoly, P. ( 2005 ). Self-regulation assessment and intervention in physical health and illness: A review. Applied Psychology: An International Review, 54, 267–299.
Marlatt, G.A. ( 2002 ). Harm reduction: Pragmatic strategies for managing high-risk behaviours . New York: Guilford.
Marlatt, G.A., Baer, J.S., & Quigley, L.A. ( 1995 ). Self-efficacy and addictive behavior. In A. Bandura (Ed), Self-efficacy in changing societies (pp. 289–315). New York: Cambridge University Press.
Michie, S., Rothman, A.J., & Sheeran, P. ( 2007 ). Advancing the science of behaviour change. Psychology and Health, 22, 249–253.
Noar, S.M., Benac, C.N., & Harris, M.S. ( 2007 ). Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin, 133, 673–693.
Norman, P., & Conner, M. ( 2005 ). The theory of planned behavior and exercise: Evidence for the mediating and moderating roles of planning on intention-behavior relationships. Journal of Sport & Exercise Psychology, 27, 488–504.
Norman, P., Boer, H., & Seydel, E.R. ( 2005 ). Protection motivation theory. In M. Conner, & P. Norman (Eds.), Predicting health behavior (pp. 81–126). Maidenhead, UK: Open University Press.
Panzer, M., & Renner, B. ( 2008 ). To be or not to be at risk: Spontaneous reactions to risk information. Psychology & Health, 23, 617–627.
Prochaska, J.O., & DiClemente, C.C. ( 1983 ). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51, 390–395.
Prochaska, J.O., DiClemente, C.C., & Norcross, J.C. ( 1992 ). In search of how people change: Applications to addictive behaviors. American Psychologist, 47, 1102–1114.
Prochaska, J.O., & Velicer, W.F. ( 1997 ). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12, 38–48.
Quinlan, K.B., & McCaul, K.D. ( 2000 ). Matched and mismatched interventions with young adult smokers: Testing a stage theory. Health Psychology, 19, 165–171.
Radcliffe, N.M., & Klein, W.M.P. ( 2002 ). Dispositional, unrealistic, and comparative optimism: Differential relations with knowledge and processing of risk information and beliefs about personal risk. Personality and Social Psychology Bulletin, 28, 836–846.
Renner, B. ( 2004 ). Biased reasoning: Adaptive responses to health risk feedback. Personality and Social Psychology Bulletin, 30, 384–396.
Renner, B., Kwon, S., Yang, B.-H., Paik, K.-C., Kim, S.H., Roh, S., et al. ( 2008 ). Social-cognitive predictors of dietary behaviors in South Korean men and women. International Journal of Behavioral Medicine, 15, 4–13.
Renner, B., & Schwarzer, R. ( 2005 ). The motivation to eat a healthy diet: How intenders and nonintenders differ in terms of risk perception, outcome expectancies, self-efficacy, and nutrition behavior. Polish Psychological Bulletin, 36(1), 7–15.
Renner, B., Spivak, Y., Kwon, S., & Schwarzer, R. ( 2007 ). Does age make a difference? Predicting physical activity of South Koreans. Psychology and Aging, 22, 482–493.
Reuter, T., Ziegelmann, J.P., Wiedemann, A.U., & Lippke, S. ( 2008 ). Dietary planning as a mediator of the intention-behavior relation: An experimental-causal-chain design. Applied Psychology: An International Review. Special Issue: Health and Well-Being, 57, 194–207.
Reuter, T., Ziegelmann, J.P., Wiedemann, A.U., Lippke, S., Schüz, B., & Aiken, L.S. (2009). Planning bridges the intention-behavior gap: Age makes a difference and strategy use explains why. Psychology & Health (in press). http://dx.doi.org/10.1080/08870440902939857.
Richert, J., Reuter, T., Wiedemann, A.U., Lippke, S., Ziegelmann, J., & Schwarzer, R. ( 2010 ). Differential effects of planning and self-efficacy on fruit and vegetable consumption. Appetite, 54, 611–614. doi: 10.1016/j.appet.2010.03.006.
Rodgers, W.M., Hall, C.R., Blanchard, C.M., McAuley, E., & Munroe, K.J. ( 2002 ). Task and scheduling self-efficacy as predictors of exercise behaviour. Psychology and Health, 27, 405–416.
Rodgers, W.M., Murray, T.C., Courneya, K.S., Bell, G.J., & Harber, V.J. ( 2009 ). The specificity of self-efficacy over the course of a progressive exercise program. Applied Psychology: Health and Well-Being, 1, 211–232.
Rodgers, W., & Sullivan, M.J.L. ( 2001 ). Task, coping and scheduling self-efficacy in relation to frequency of physical activity. Journal of Applied Social Psychology, 31, 741–753.
Rothman, A.J. ( 2000 ). Toward a theory-based analysis of behavioral maintenance. Health Psychology, 19, 64–69.
Scholz, U., Nagy, G., Göhner, W., Luszczynska, A., & Kliegel, M. ( 2009 ). Changes in self-regulatory cognitions as predictors of changes in smoking and nutrition behaviour. Psychology & Health, 24, 545–561.
Scholz, U., Schüz, B., Ziegelmann, J.P., Lippke, S., & Schwarzer, R. ( 2008 ). Beyond behavioural intentions: Planning mediates between intentions and physical activity. British Journal of Health Psychology, 13, 479–494.
Scholz, U., Sniehotta, F.F., Burkert, S., & Schwarzer, R. ( 2007 ). Increasing physical exercise levels: Age-specific benefits of planning. Journal of Aging and Health, 19, 851–866.
Scholz, U., Sniehotta, F.F., & Schwarzer, R. ( 2005 ). Predicting physical exercise in cardiac rehabilitation: The role of phase-specific self-efficacy beliefs. Journal of Sport & Exercise Psychology, 27, 135–151.
Schüz, B., Sniehotta, F.F., Mallach, N., Wiedemann, A., & Schwarzer, R. ( 2009 ). Predicting transitions from preintentional, intentional and actional stages of change: Adherence to oral self-care recommendations. Health Education Research, 24, 64–75.
Schwarzer, R. ( 1992 ). Self-efficacy in the adoption and maintenance of health behaviors: Theoretical approaches and a new model. In R. Schwarzer (Ed.), Self-efficacy: Thought control of action (pp. 217–243). Washington, DC: Hemisphere.
Schwarzer, R. ( 1994 ). Optimism, vulnerability, and self-beliefs as health-related cognitions: A systematic overview. Psychology and Health, 9, 161–180.
Schwarzer, R. ( 2008 ). Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Applied Psychology: An International Review, 57, 1–29.
Schwarzer, R., & Renner, B. ( 2000 ). Social-cognitive predictors of health behavior: Action self-efficacy and coping self-efficacy. Health Psychology, 19, 487–495.
Schwarzer, R., Richert, J., Kreausukon, P., Remme, L., Wiedemann, A.U., & Reuter, T. ( 2010 ). Translating intentions into nutrition behaviors via planning requires self-efficacy: Evidence from Thailand and Germany. International Journal of Psychology, 54, 260–268.
Schwarzer, R., Schüz, B., Ziegelmann, J.P., Lippke, S., Luszczynska, A., & Scholz, U. ( 2007 ). Adoption and maintenance of four health behaviors: Theory-guided longitudinal studies on dental flossing, seat belt use, dietary behavior, and physical activity. Annals of Behavioral Medicine, 33, 156–166.
Sheeran, P. ( 2002 ). Intention-behavior relations: A conceptual and empirical review. European Review of Social Psychology, 12, 1–36.
Sheeran, P., Milne, S., Webb, T.L., & Gollwitzer, P.M. ( 2005 ). Implementation intentions and health behaviours. In M. Conner, & P. Norman (Eds.), Predicting health behaviour: Research and practice with social cognition models (2nd ed., pp. 276–323). Maidenhead, England: Open University Press.
Sniehotta, F.F. ( 2009 a). Towards a theory of intentional behaviour change: Plans, planning, and self-regulation. British Journal of Health Psychology, 14, 261–273.
Sniehotta, F.F. ( 2009 b). An experimental test of the theory of planned behavior. Applied Psychology: Health and Well-Being, 1, 257–270.
Sniehotta, F.F., Nagy, G., Scholz, U., & Schwarzer, R. ( 2006 ). The role of action control in implementing intentions during the first weeks of behaviour change. British Journal of Social Psychology, 45(1), 87–106.
Sniehotta, F.F., Scholz, U., & Schwarzer, R. ( 2005 ). Bridging the intention-behaviour gap: Planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychology & Health, 20, 143–160.
Sniehotta, F.F., Scholz, U., & Schwarzer, R. ( 2006 ). Action plans and coping plans for physical exercise: A longitudinal intervention study in cardiac rehabilitation. British Journal of Health Psychology, 11, 23–37.
Sniehotta, F.F., Schwarzer, R., Scholz, U., & Schüz, B. ( 2005 ). Action planning and coping planning for long-term lifestyle change: Theory and assessment. European Journal of Social Psychology, 35, 565–576.
Suls, J. ( 2011 ). Social comparison processes: Implications for physical health. In H.S. Friedman (Ed.), The Oxford handbook of health psychology . New York: Oxford University Press.
Sutton, S. ( 2005 ). Stage models of health behaviour. In M. Conner, & P. Norman (Eds.), Predicting health behaviour: Research and practice with social cognition models (2nd ed., pp. 223–275). Maidenhead, UK: Open University Press.
Taylor, S.E., & Brown, J.D. ( 1994 ). Positive illusions and well-being revisited: Separating fact from fiction. Psychological Bulletin, 116, 21–27.
Trafimow, D., & Fishbein, M. ( 1995 ). Do people really distinguish between behavioral and normative beliefs? British Journal of Social Psychology, 34, 257–266.
Trafimow, D., & Sheeran, P. ( 1998 ). Some tests of the distinction between cognitive and affective beliefs. Journal of Experimental Social Psychology, 34, 378–397.
Trafimow, D., Sheeran, P., Lombardo, B., Finlay. K.A., Brown, J., & Armitage, C.J. ( 2004 ). Affective and cognitive control of persons and Behaviours. British Journal of Social Psychology, 43, 207–224.
Van Osch, L., Lechner, L., Reubsaet, A., Wigger, S., & de Vries, H. ( 2008 ). Relapse prevention in a national smoking cessation contest: Effects of coping planning. British Journal of Health Psychology, 13, 525–535.
Velicer, W.F., & Prochaska, J.O. ( 2008 ). Stage and non-stage theories of behavior and behavior change: A comment on Schwarzer. Applied Psychology: An International Review, 57(1), 75–83.
Velicer, W.F., Prochaska, J.O., & Redding, C.A. ( 2006 ). Tailored communications for smoking cessation: Past successes and future directions. Drug and Alcohol Review, 25, 47–55.
Velicer, W.F., Redding, C.A., Sun, X., & Prochaska, J.O. ( 2007 ). Demographic variables, smoking variables, and outcome across five studies. Health Psychology, 26, 278–287.
Webb, M.S., Hendricks, P.S., & Brandon, T.H. ( 2007 ). Expectancy priming of smoking cessation messages enhances the placebo effect of tailored interventions. Health Psychology, 26, 598–609.
Weinstein, N.D. ( 1980 ). Unrealistic optimism about future life events. Journal of Personality and Social Psychology, 39, 806–820.
Weinstein, N.D. ( 1988 ). The precaution adoption process. Health Psychology, 7, 355–386.
Weinstein, N.D. ( 1993 ). Testing four competing theories of health-protective behavior. Health Psychology, 12, 324–333.
Weinstein, N.D., Lyon, J.E., Sandman, P.M., & Cuite, C.L. ( 1998 ). Experimental evidence for stages of health behavior change: The precaution adoption process model applied to home radon testing. Health Psychology, 17, 445–453.
Weinstein, N.D., Rothman, A.J., & Sutton, S.R. ( 1998 ). Stage theories of health behavior: Conceptual and methodological issues. Health Psychology, 17, 290–299.
Wiedemann, A.U., Schüz, B., Sniehotta, F.F., Scholz, U., & Schwarzer, R. ( 2009 ). Disentangling the relation between intentions, planning, and behaviour: A moderated mediation analysis. Psychology & Health, 24, 67–79.
Ziegelmann, J.P., Lippke, S. & Schwarzer, R. ( 2006 ). Adoption and maintenance of physical activity: Planning interventions in young, middle-aged, and older adults. Psychology & Health, 21, 145–163.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 10 May 2021
Sustained behavior change is key to preventing and tackling future pandemics
- Susan Michie ORCID: orcid.org/0000-0003-0063-6378 1 &
- Robert West ORCID: orcid.org/0000-0001-6398-0921 2
Nature Medicine volume 27 , pages 749–752 ( 2021 ) Cite this article
20k Accesses
51 Citations
445 Altmetric
Metrics details
- Health care
- Health policy
Investment in research and programs to discover and apply the principles that underpin sustained behavior change is needed to address the continuing threat from COVID-19 and future pandemics and will require collaboration among behavioral, social, biomedical, public-health and clinical scientists.
Human behavior was instrumental in causing COVID-19, and changing it has been vital to tackling this pandemic. The countries that have done best in mitigating COVID-19’s harms to health and to their economies have rapidly and successfully persuaded their populations to enact large-scale behavior change. Some of these interventions have been highly effective, others have been less so, and some have produced substantial social and financial harm. In particular, national ‘lockdowns’ have been effective in keeping people from interacting, to reduce the spread of disease 1 , but they have been very damaging to people’s lives and to national economies. Therefore, lockdowns should ideally be used only to bring transmission levels low enough to be controllable by other policies. These policies include adequate ‘find, test, trace, isolate and support’ systems 2 ; border controls and quarantine to prevent reseeding of infections; the creation of safe working, domestic and transport spaces; and the promotion of personal protective behaviors such as the use of face coverings 3 .
Capability, opportunity and motivation
Large-scale, sustained behavior change is needed to reduce the risk of, and to prepare for, future pandemics 4 . The COVID-19 pandemic has shown that populations will adopt at least some of the required behaviors under certain conditions 5 . However, adoption has been variable across countries, over time and across social groups 5 .
Achieving sustained behavior change requires a sound understanding by policymakers and intervention designers of what underpins the behaviors concerned. For example, what does it take in all cultures to ensure that, where appropriate, people keep safe physical distances from each other, wear face coverings masks and disinfect their hands? What is needed to ensure that adequate ventilation is provided in enclosed spaces, and that people in high-risk settings use personal protective equipment effectively?
We provide here important behavioral targets for the prevention and mitigation of pandemics such as COVID-19 (Table 1 ). The behaviors vary in what is needed to enact them and the contextual influences on them.
A simple, comprehensive way of understanding behavior is through the ‘capability–opportunity–motivation–behavior’ (COM-B) model 6 , 7 (Fig. 1 ). This model takes as its premise that for any behavior to occur, people must have the following: the relevant physical and psychological capabilities; the opportunity; and greater motivation to perform that behavior than anything else they could be doing at the time. Capability and opportunity feed into motivation, so that having greater capability and opportunity can increase motivation (Fig. 1 ). Behavior then feeds back, and so changing behavior can, in turn, influence capability, opportunity and/or motivation. Thus, behavior is part of an evolving and interacting system. Creating sustained behavior change requires changes to capability, opportunity and motivation that are mutually reinforcing.

Capability, opportunity and motivation are all essential for any behavior to occur. Capability and opportunity influence motivation. Behavior feeds back to influence capability, opportunity and motivation.
Physical capabilities include strength, stamina, and physical and psychomotor skills, whereas psychological capabilities include knowledge, resilience, and mental skills. Motivation comprises both reflective processes, such as self-conscious decision-making, and automatic processes that involve emotions and habits. Opportunity involves having the resources, time and physical space to enact a behavior. It also involves having social structures, norms and cues that make the behavior possible or promote it. The World Health Organization has used the COM-B model to make recommendations for improving adherence to rules and guidance on behaviors that are protective against COVID-19 8 .
Requirements for behavior change
The development of effective interventions requires an understanding of what changes in capability, motivation or opportunity, or their combination, will drive behavior change. Getting the balance wrong can be disastrous. For example, in 2020, the UK government largely failed in its attempts to get people with COVID-19 to self-isolate when needed, in part because it did not heed this lesson. Survey data showed that fewer than 50% of people with COVID-19 symptoms reported staying at home for the required isolation period 9 . Failure to self-isolate appeared to be driven largely by financial need or domestic or caring responsibilities—i.e., a lack of opportunity 9 . People on low incomes were just as motivated to self-isolate when needed as were those with more financial resources, but did so less 10 . Those who found it easiest to isolate were those who could work from large homes and had the funds to order in meals and other services. Adequate financial and practical support should have been a key part of the solution, and it has been a cornerstone of effective pandemic control in many countries, with up to 100% of lost wages being reimbursed, and with the provision of free alternative accommodation and daily visits. In the USA, introduction in some jurisdictions of emergency statutory entitlement to sick leave for people with symptoms or who had to quarantine was found to be effective in reducing cases 11 .
The UK government appeared to have erroneously assumed that the main reason people did not isolate was a lack of motivation, whereas it was instead a lack of opportunity. It threatened a fine of £10,000 for failure to comply with isolation mandates. An evaluation of free, mass testing in the city of Liverpool found that the take up of diagnostic tests among disadvantaged groups was as low as 4% in some areas 12 , and a £36 billion ‘test, trace and isolate system’ was estimated to have reached as little as 3% of contacts of people who had tested positive for COVID-19 13 . It seems that the threat of a large monetary fine did have a motivational influence, but it was opposite to that intended, with the best way of avoiding a fine being to avoid a test.
The behavior change wheel
The UK case study described above illustrates the fact that for mass behavioral changes to achieve their intended outcome, systematic approaches need to move from an understanding of behavior in its context to identifying interventions and policies that can change the behavior. One such framework is the behavior change wheel, developed through the integration of 19 frameworks identified in a literature review 7 , 14 , 15 (Fig. 2 ). This wheel can be used to link the COM-B model with nine possible types of intervention and seven policy options for implementation. Intervention designers can use the wheel to identify the intervention types most likely to achieve the desired change and can then choose the most appropriate mixture of implementation options, given whatever constraints may be operating.
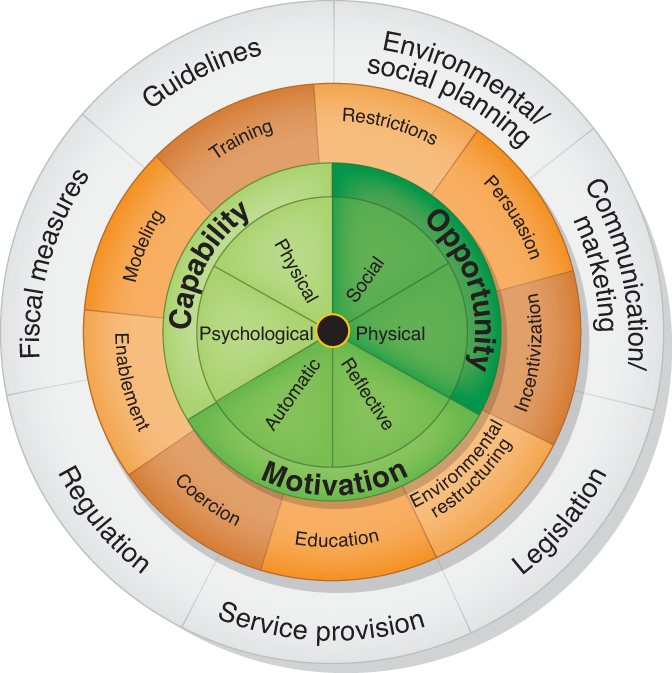
The layers in the wheel are not intended to line up with each other. Two publications 7 , 14 have provided tables showing how a COM-B analysis points to intervention types and policy options most likely to be effective in a given context.
Use of the behavior change wheel framework can be illustrated by the challenge of getting healthcare staff to adhere to infection prevention and control guidelines. A published study identified a range of interventions that could be effective 16 , but it was important to go further and consider the capability, opportunity and motivation issues that needed to be addressed in a given context. First, in terms of capability, there was the nature of the guidelines, how they were communicated and what training was needed for this. Second, in the context of opportunity, it was essential to consider the physical spaces the staff worked in and the support they received from managers 16 . Third, for motivation, it was important that staff had trust in their personal protective equipment and that it was comfortable to use as required. Finally, to fully address the capability, opportunity and motivational issues, it was essential to include all staff, including support staff, in the process of intervention development and implementation 15 . The findings of this study further illustrated the need to treat all the actors and behaviors in a given scenario as part of an interconnected system, and pointed to workplace culture as an important influence, specifically managerial and peer support, social-norms solidarity and a focus on safety rather than complacency 16 .
Leadership, trust and solidarity
When it comes to motivation to adhere to stringent pandemic control regulations, variation in practices across different countries has highlighted the importance of good leadership fostering public trust in government and experts, and a sense of solidarity 17 . Trust derives from people seeing authorities as part of and serving the community 18 , and this in turn derives from these authorities treating the public as a respected partner rather than as a problem 19 .
The importance of fostering trust and solidarity has informed much of the advice provided by behavioral scientists participating in the UK government’s Scientific Advisory Group for Emergencies. This group has urged the government to understand the diversity of communities that make up the UK population, and to engage with, consult, listen to and learn from them. In addition, the government was urged to support and enable the population to adhere; to avoid blame and punishment; to recognize, reward and celebrate achievements, often in challenging circumstances; and to communicate clearly, consistently and concisely, in line with evidence. Finally, the government was advised to be transparent, honest and open in written and verbal communication; to engender trust; and to avoid socially divisive language, policies and behavior.
Sustaining behavior change involves taking these principles and applying them to create a mutually reinforcing system in which capability, opportunity and motivation support each other (Table 2 ). For example, sustained improvements in knowledge will need education about viral transmission and its prevention to be built into educational programs at all levels. Improved opportunity will require structural changes to inhabited spaces to make it easier to achieve social distancing when required. Sustained changes to motivation will involve the development of social identities that place greater value on behaviors that mitigate infection risk and the development of habits and routines that embed these behaviors into everyday life.
The principles noted above are generic. Detailed scientific investigation is needed to develop and successfully apply them to create interventions suited to different scenarios. Such interventions have been called ‘behavioral, environmental, social and systems interventions’ (BESSIs) 4 . Despite the importance of these kinds of intervention, research investment in all BESSIs collectively has been estimated to be less than 4% of the $3.3 billion in global spending on COVID-19 research 20 . In a comparison of BESSI versus pharmacological trials, the contrast is stark: as of December 2020, there were 1,725 registered pharmacological trials and 213 conducted pharmacological trials, but only 11 registered BESSI trials and 3 conducted BESSI trials 21 .
Tackling inequalities
An important lesson from the COVID-19 pandemic is that no person or community or country can protect themselves or itself on their or its own: humans are all interconnected, and solutions must be global. Building pandemic-resilient societies for the future must include changing population-wide behaviors, as well as reducing inequalities. Embedding behaviors into societies requires changes to physical and social environments, such as fostering safe workplaces and norms around hygiene behaviors. These need to be underpinned by community activation, organization regulation and national legislation.
Societies that are already unequal have been made more so by the COVID-19 pandemic, with the virus spreading most aggressively in overcrowded, multigenerational housing and poorly regulated workplaces. Furthermore, those with pre-existing health problems and those from specific ethnic backgrounds, both linked to poverty, were hit harder by the virus. Structural racism in many countries meant that those who were already more vulnerable were made doubly so due to low incomes and poor working conditions. On top of these increased inequalities came government policies that exacerbated inequalities further in many countries. In the UK, workers on regular salaries were more financially protected than those working in the precarious economy, and mortgage-holders were better protected than renters.
Testing for the virus, as well as medicines and vaccines, will continue to be vital to the strategy for tackling COVID-19 and future pandemics. But a substantial rebalancing of funding on research and programs needed to embed behavioral changes across society and address inequality will also be critical in the long run.
Flaxman, S. et al. Nature 584 , 257–261 (2020).
Article CAS Google Scholar
Rajan, S., Cylus, J. & McKee, M. Eurohealth 26 , 34–39 (2020).
Google Scholar
West, R., Michie, S., Rubin, G. J. & Amlôt, R. Nature Human Behaviour 4 , 451–459 (2020).
Article Google Scholar
Michie, S. & West, R. Br. Med. J. 370 , m2982 (2020).
Becher, M., Stegmueller, D., Brouard, S. & Kerrouche, E. Preprint at https://doi.org/10.2139/ssrn.3652543 (2020).
West, R. & Michie, S. Qeios https://doi.org/10.32388/WW04E6.2 (2020).
Michie, S., van Stralen, M. M. & West, R. Implement. Sci. 6 , 42 (2011).
World Health Organization. Regional Office for Europe. https://apps.who.int/iris/handle/10665/337574 (November 2020).
Smith, L. E. et al. Brit. Med. J. 372 , n608 (2021).
Atchison, C. J. et al. BMJ Open 11 , e043577 (2021).
Pichler, S., Wen, K. & Ziebarth, N. R. Health Aff. 39 , 2197–2204 (2020).
University of Liverpool. https://www.liverpool.ac.uk/research/news/articles/covid-19-liverpool-community-testing-pilot-interim-findings-published/ (23 December 2020)
Wood, P. CityAM https://www.cityam.com/dido-harding-slammed-for-three-per-cent-test-and-trace-success-rate/ (10 November 2020).
West, R., Michie, S., Chadwick, P., Atkins, L. & Lorencatto, F. Public Health England https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/933328/UFG_National_Guide_v04.00__1___1_.pdf (2020).
Michie, S., Atkins, L. & West, R. The Behaviour Change Wheel: A Guide To Designing Interventions (Silverback Publishing, 2014).
Houghton, C. et al. Cochrane Database Syst. Rev . https://doi.org/10.1002/14651858.CD013582 (2020).
Wright, L., Steptoe, A. & Fancourt, D. Preprint at medRxiv https://doi.org/10.1101/2020.10.19.20215376 (2020).
Brewer, M.B. in Rationality and Social Responsibility: Essays in Honor of Robyn Mason Dawes 215–232 (Psychology Press, 2008).
Tyler, T. R. & Blader, S. L. Pers. Soc. Psychol. Rev. 7 , 349–361 (2003).
Head, M. G. et al. Lancet Glob. Health 8 , e1295–e1304 (2020).
BESSI. https://www.bessi-collab.net (accessed 23 April 2021).
Download references
Author information
Authors and affiliations.
Centre for Behaviour Change, University College London, London, UK
Susan Michie
Department of Behavioural Science and Health, Institute of Epidemiology and Healthcare, University College London, London, UK
Robert West
You can also search for this author in PubMed Google Scholar
Contributions
S.M. and R.W. contributed to the concept for this Comment, and to the initial drafting and to revisions.
Corresponding authors
Correspondence to Susan Michie or Robert West .
Ethics declarations
Competing interests.
S.M. and R.W. are unpaid directors of the Unlocking Behavior Change community interest company, and are participants in the Independent Scientific Pandemic Insights Group on Behaviours of the UK Scientific Advisory Group for Emergencies, and in the Independent Scientific Advisory Group for Emergencies.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Michie, S., West, R. Sustained behavior change is key to preventing and tackling future pandemics. Nat Med 27 , 749–752 (2021). https://doi.org/10.1038/s41591-021-01345-2
Download citation
Published : 10 May 2021
Issue Date : May 2021
DOI : https://doi.org/10.1038/s41591-021-01345-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The environmental awareness of nurses as environmentally sustainable health care leaders: a mixed method analysis.
- Olga María Luque-Alcaraz
- Pilar Aparicio-Martínez
- Manuel Vaquero-Abellán
BMC Nursing (2024)
Infection prevention and control programme priorities for sustainable health and environmental systems
- Gemma L. Saravanos
- Md Saiful Islam
BMC Global and Public Health (2024)
Rethinking the city resilience: COM-B model-based analysis of healthcare accessing behaviour changes affected by COVID-19
- Zigeng Fang
Journal of Housing and the Built Environment (2024)
The Covid-19 resilience journey of vulnerable young South Africans
- Ansie Fouché
- Kate Cockcroft
- Linda Theron
Current Psychology (2024)
Factors influencing staff attitudes to COVID-19 vaccination in care homes in England: a qualitative study
- Bettina Friedrich
- Gillian Forbes
- Vivi Antonopoulou
BMC Health Services Research (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Health Communication and Behavior Change
- First Online: 14 September 2022
Cite this chapter

- Neetu Purohit 2
556 Accesses
The impetus of public health is on promotive and preventive approaches. Since efforts to promote and prevent are communicative, health communication is being increasingly recognized as a pertinent discipline to bring in desired change in health behavior. The epidemics and pandemics of last decade have further emphasized role of behavior and behavior change to keep oneself and others safe. Health communication aims at informing people about health programs and policies, empowering them to adopt healthy behaviors, attracting attention of policy-makers to unattended health issues and for framing health issues for public debate, regulation, and resolution. Health communication apprises about systematic and scientific ways to use communication processes for bringing in desired change in human behavior by combining theory and practice and involving multiple stakeholders. The present chapter will attempt to provide insights on emergence of biopsychosocial model, theories of behavior change, health communication, types of communication and steps in planning health communication intervention for behavior change. Though, health communication primarily revolves around social communication, its scope is wide and therefore the chapter also throws light on use of interpersonal communication in counselling during patient–provider communication or counselling sessions at facility or during household visits. The chapter also delves into use of mass and social media in designing health communication interventions for reach and coverage. Lastly, it stresses on the importance of scientific planning, robust implementation, continuous monitoring and evaluation in the management of health communication interventions to ensure designing of evidence-based behavior change communication interventions with opportunity for timely corrections for bringing in desired change and also learning lessons for expansion and future replication.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Ajzen, I., & Fishbein, M. (1980). Understanding attitudes and predicting social behavior . Prentice-Hall.
Google Scholar
Andrade, E. L., Evans, W. D., Barrett, N. D., Cleary, S. D., Edberg, M. C., & Alvayero, R. D. (2018). Development of the place-based Adelante social marketing campaign for prevention of substance use, sexual risk and violence among Latino immigrant youth. Health Education Research, 33 (2), 125–144.
Article CAS Google Scholar
Backer, T. E., Rogers, E. M., & Sopory, P. (1992). Designing health communication Campaign: What works? Sage Publications, Inc. https://doi.org/10.4135/9781483325521
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory . Printice-Hall
Bandura, A. (1977). Social learning theory . Prentice-Hall.
Barokas, J. (1995). Lessons learned from public health campaigns and applied to anti-DWI norms development (DOT HS 808 273) . U.S. Department of Transportation, National Highway Traffic Safety Administration.
Becker, M. H. (1974). The health belief model and personal health behavior. Health Education Monographs , 2 (Entire Issue)
Bernhardt, J. (2004). Communication at the core of public health. American Journal of Public Health, 94 (12), 2051–2052.
Article Google Scholar
Butland, B., et al. (2007). Tackling obesities: Future choices—project report (2nd ed.). Foresight Programme of the Government Office for Science.
Central Office of Information (COI). (2009). Communications and behaviour change . COI.
Chamberlain, M. A. (1996). Health communication: Making the most of new media technologies-An international overview. Journal of Health Communication, 1 (1), 43–50.
DeJong, W., & Atkin, C. K. (1995). A review of national television PSA campaigns for preventing alcohol-impaired driving, 1987–1992. Journal of Public Health Policy, 16 (1), 59–80.
Dias, D., & Paulo Silva Cunha, J. (2018). Wearable health devices-vital sign monitoring, systems and technologies. Sensors (Basel, Switzerland) , 18 (8), 2414. https://doi.org/10.3390/s18082414
Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science, 96 , 129–136.
Fishbein, D. B., Dowson, J. E., & Robinson, L. E. (1994a). Human ehrlichiosis in the United states, 1985 to 1990. Annals of Internal Medicine, 120 , 736–743.
Fishbein, M., Middlestadt, S., & Hitchcock, P. (1994b). Using information to change sexually transmitted disease-related behaviors: An analysis based on the theory of reasoned action. In R. DiClemente & J. Peterson (Eds.), Preventing AIDS: Theories of methods of behavioral interventions (pp. 61–78). Plenum Press.
Chapter Google Scholar
Freimuth, V., & Quinn, S. C. (2004). The contributions of health communication to eliminating health disparities. American Journal of Public Health, 94 (12), 2053–2054.
Gillispie, M. A., & Ellis, L. B. M. (1993). Computer-based education revisited. Journal of Medical Systems, 17 , 119–125
Gittell & Vidal. (1998). Community organizing: Social capital as a development strategy . Sage.
Book Google Scholar
Glanz, K., Lewis, F. M., & Rimer, B. K. (1997). Linking theory, research and practice. In K. Glanz, F. M. Lewis, & B. K. Rimer (Eds.), Health behavior and health education: Theory, research and practice (2nd ed., pp. 19–35). Jossey-Bass.
Gupta, P., & Purohit, N. (2020). Promoting health behaviour in young people in India: Learning for use of Social Media. International Journal of Behavioral Sciences, 14 (3), 122–130. https://doi.org/10.30491/ijbs.2020.210704.1178
Haines-Saah, R. J., Kelly, M. T., Oliffe, J. L., Bottorff, J. L. (2015). Picture me smoke free: A qualitative study using social media and digital photography to engage young adults in tobacco reduction and cessation. Journal of Medical Internet Research , 17(1):e27.
Health Development Agency. (2003). Understanding changes in behaviour and attitudes towards health services: The contribution of research from health promotion and public health . Health Development Agency.
Heldman, A., Schindelar, J., & Weaver, J. B. (2013). Social Media engagement and public health communication: implications for public health organizations being truly “Social.” Public Health Review, 35 (1), 1–18.
Homer, J. B., & Hirsch, G. B. (2006). System dynamics modeling for public health: Background and opportunities. American Journal of Public Health, 96 (3), 452–458. https://doi.org/10.2105/AJPH.2005.062059
Article PubMed PubMed Central Google Scholar
Jacobs, M. A., Cha, S., Villanti, A. C., & Graham, A. L. (2016). Using Tumblr to reach and engage young adult smokers: A proof of concept in context. American Journal of Health Behavior, 40 (1), 48–54.
Kaplan, A. M., & Haenlein, M. (2010). Users of the world, unite! The challenges and opportunities of social media. Business Horizons, 53 (1), 59–68.
Leventhal, H. (1973). Changing attitudes and habits to reduce risk factors in chronic disease. American Journal of Cardiology, 31 , 571–580.
Looyestyn, J., Kernot, J., Boshoff, K., & Maher, C. (2018). A web-based, social networking beginners’ running intervention for adults aged 18 to 50 years delivered via a facebook group: Randomized controlled trial. Journal of Medical Internet Research, 20 (2), 1–13.
Ogden, J. (2004). Health psychology : A textbook. Open University Press.
Pechmann, C., Pan, L., Delucchi, K,, Lakon, C. M., Prochaska, J. J. (2015). Development of a Twitter-based intervention for smoking cessation that encourages high-quality social media interactions via auto messages. Journal of Medical Internet Research, 17 (2).
Prochaska, J, O., Di Clemente, C. C., & Norcross, J. C. (1992). In search of how people change—Applications to addictive behaviors. American Psychologist, 47 , 1102–1114.
Prochaska, J. O., & DiClemente, C. C. (1983). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51 (3), 390–395.
Rimal, R. N., & Lapinski, M. K. (2009). Why health communication is important in public health. Bulletin of the World Health Organization, 87 (4), 247–247a. https://doi.org/10.2471/blt.08.056713
Rimer, B. & Glanz, K. (2005). Theory at a glance. A guide for health promotion practice , 2nd ed. US Department of Health and Human Services. http://www.cancer.gov/cancertopics/cancerlibrary/theory pdf.
Rogers, E. M. (1996). The field of health communication today: An up-to-date report. Journal of Health Communication, 1 (1), 15–23.
Rogers, E. M., & Storey, J. D. (1987). Communication campaigns. In C. R. Berger & S. H. Chaffee (Eds.), Handbook of communication science (pp. 817–846). Sage Publications Inc.
Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1994). The health belief model and HIV risk behavior change. In R. J. DiClemente & J. L. Peterson (Eds.), Preventing AIDS: Theories and methods of behavioral interventions (pp. 5–24). Plenum.
Sampson, R. J., Raudenbush, S. W., & Earls, F. (1997). Neighborhoods and violent crime: A multilevel study of collective efficacy. Science, 277 , 918–924.
Smith, M. J. (1982). Persuasion and human action: A review and critique of social influence theories . Wadsworth.
Struik, L. L., Baskerville, N. B. (2014). The role of facebook in crush the crave, a mobile-and social media-based smoking cessation intervention: Qualitative framework analysis of posts. Journal of Medical Internet Research, 16 (7).
Wallack, L. (1981). Mass media Campaigns: The odds against finding behavior change. Health Education Quarterly., 8 (3), 209–260.
World Health Organization (WHO). (2008). Behavior change strategies and health: The role of health systems. EUR/RC58/10. WHO.
Download references
Author information
Authors and affiliations.
IIHMR University, Jaipur, India
Neetu Purohit
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Neetu Purohit .
Editor information
Editors and affiliations.
S. D. Gupta
Rights and permissions
Reprints and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Purohit, N. (2022). Health Communication and Behavior Change. In: Gupta, S.D. (eds) Healthcare System Management. Springer, Singapore. https://doi.org/10.1007/978-981-19-3076-8_12
Download citation
DOI : https://doi.org/10.1007/978-981-19-3076-8_12
Published : 14 September 2022
Publisher Name : Springer, Singapore
Print ISBN : 978-981-19-3075-1
Online ISBN : 978-981-19-3076-8
eBook Packages : Social Sciences Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Diet & Nutrition
Changing Your Habits for Better Health
- Español
On this page:

What stage of change are you in?
Contemplation: are you thinking of making changes, preparation: have you made up your mind, action: have you started to make changes, maintenance: have you created a new routine, clinical trials.
Are you thinking about being more active? Have you been trying to cut back on less healthy foods? Are you starting to eat better and move more but having a hard time sticking with these changes?
Old habits die hard. Changing your habits is a process that involves several stages. Sometimes it takes a while before changes become new habits. And, you may face roadblocks along the way.
Adopting new, healthier habits may protect you from serious health problems like obesity and diabetes . New habits, like healthy eating and regular physical activity, may also help you manage your weight and have more energy. After a while, if you stick with these changes, they may become part of your daily routine.

The information below outlines four stages you may go through when changing your health habits or behavior. You will also find tips to help you improve your eating, physical activity habits, and overall health. The four stages of changing a health behavior are
- contemplation
- preparation
- maintenance
Contemplation: “I’m thinking about it.”
In this first stage, you are thinking about change and becoming motivated to get started.
You might be in this stage if you
- have been considering change but are not quite ready to start
- believe that your health, energy level, or overall well-being will improve if you develop new habits
- are not sure how you will overcome the roadblocks that may keep you from starting to change
Preparation: “I have made up my mind to take action.”
In this next stage, you are making plans and thinking of specific ideas that will work for you.
- have decided that you are going to change and are ready to take action
- have set some specific goals that you would like to meet
- are getting ready to put your plan into action
Action: “I have started to make changes.”
In this third stage, you are acting on your plan and making the changes you set out to achieve.
- have been making eating, physical activity, and other behavior changes in the last 6 months or so
- are adjusting to how it feels to eat healthier, be more active, and make other changes such as getting more sleep or reducing screen time
- have been trying to overcome things that sometimes block your success
Maintenance: “I have a new routine.”
In this final stage, you have become used to your changes and have kept them up for more than 6 months.
You might be in this stage if
- your changes have become a normal part of your routine
- you have found creative ways to stick with your routine
- you have had slip-ups and setbacks but have been able to get past them and make progress
Did you find your stage of change? Read on for ideas about what you can do next.
Making the leap from thinking about change to taking action can be hard and may take time. Asking yourself about the pros (benefits) and cons (things that get in the way) of changing your habits may be helpful. How would life be better if you made some changes?
Think about how the benefits of healthy eating or regular physical activity might relate to your overall health. For example, suppose your blood glucose, also called blood sugar, is a bit high and you have a parent, brother, or sister who has type 2 diabetes . This means you also may develop type 2 diabetes. You may find that it is easier to be physically active and eat healthy knowing that it may help control blood glucose and protect you from a serious disease.

You may learn more about the benefits of changing your eating and physical activity habits from a health care professional. This knowledge may help you take action.
Look at the lists of pros and cons below. Find the items you believe are true for you. Think about factors that are important to you.
Healthy Eating
Physical activity.
If you are in the preparation stage, you are about to take action. To get started, look at your list of pros and cons. How can you make a plan and act on it?
The chart below lists common roadblocks you may face and possible solutions to overcome roadblocks as you begin to change your habits. Think about these things as you make your plan.
Once you have made up your mind to change your habits, make a plan and set goals for taking action. Here are some ideas for making your plan:
- learn more about healthy eating and food portions
- learn more about being physically active
- healthy foods that you like or may need to eat more of—or more often
- foods you love that you may need to eat less often
- things you could do to be more physically active
- fun activities you like and could do more often, such as dancing
After making your plan, start setting goals for putting your plan into action. Start with small changes. For example, “I’m going to walk for 10 minutes, three times a week.” What is the one step you can take right away?
You are making real changes to your lifestyle, which is fantastic! To stick with your new habits
- review your plan
- look at the goals you set and how well you are meeting them
- overcome roadblocks by planning ahead for setbacks
- reward yourself for your hard work
Track your progress
- Tracking your progress helps you spot your strengths, find areas where you can improve, and stay on course. Record not only what you did, but how you felt while doing it—your feelings can play a role in making your new habits stick.
- Recording your progress may help you stay focused and catch setbacks in meeting your goals. Remember that a setback does not mean you have failed. All of us experience setbacks. The key is to get back on track as soon as you can.
- You can track your progress with online tools such as the NIH Body Weight Planner . The NIH Body Weight Planner lets you tailor your calorie and physical activity plans to reach your personal goals within a specific time period.
Overcome roadblocks
- Remind yourself why you want to be healthier. Perhaps you want the energy to play with your nieces and nephews or to be able to carry your own grocery bags. Recall your reasons for making changes when slip-ups occur. Decide to take the first step to get back on track.
- Problem-solve to “outsmart” roadblocks. For example, plan to walk indoors, such as at a mall, on days when bad weather keeps you from walking outside.
- Ask a friend or family member for help when you need it, and always try to plan ahead. For example, if you know that you will not have time to be physically active after work, go walking with a coworker at lunch or start your day with an exercise video.
Reward yourself
- After reaching a goal or milestone, allow for a nonfood reward such as new workout gear or a new workout device. Also consider posting a message on social media to share your success with friends and family.
- Choose rewards carefully. Although you should be proud of your progress, keep in mind that a high-calorie treat or a day off from your activity routine are not the best rewards to keep you healthy.
- Pat yourself on the back. When negative thoughts creep in, remind yourself how much good you are doing for your health by moving more and eating healthier.
Make your future a healthy one. Remember that eating healthy, getting regular physical activity, and other healthy habits are lifelong behaviors, not one-time events. Always keep an eye on your efforts and seek ways to deal with the planned and unplanned changes in life.

Now that healthy eating and regular physical activity are part of your routine, keep things interesting, avoid slip-ups, and find ways to cope with what life throws at you.
Add variety and stay motivated
- Mix up your routine with new physical activities and goals, physical activity buddies, foods, recipes, and rewards.
Deal with unexpected setbacks
- Plan ahead to avoid setbacks. For example, find other ways to be active in case of bad weather, injury, or other issues that arise. Think of ways to eat healthy when traveling or dining out, like packing healthy snacks while on the road or sharing an entrée with a friend in a restaurant.
- If you do have a setback, don’t give up. Setbacks happen to everyone. Regroup and focus on meeting your goals again as soon as you can.
Challenge yourself!
- Revisit your goals and think of ways to expand them. For example, if you are comfortable walking 5 days a week, consider adding strength training twice a week. If you have limited your saturated fat intake by eating less fried foods, try cutting back on added sugars, too. Small changes can lead to healthy habits worth keeping.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at www.ClinicalTrials.gov .
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank: Dr. Carla Miller, Associate Professor, Ohio State University
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Social Determinants and Health Behaviors: Conceptual Frames and Empirical Advances
Susan e. short.
a Department of Sociology, Brown University, Box 1916, Providence, RI 02912, USA
Stefanie Mollborn
b Institute of Behavioral Science and Department of Sociology, University of Colorado Boulder, UCB 483, Boulder, CO 80309-0483, USA
Health behaviors shape health and well-being in individuals and populations. Drawing on recent research, we review applications of the widely applied “social determinants” approach to health behaviors. This approach shifts the lens from individual attribution and responsibility to societal organization and the myriad institutions, structures, inequalities, and ideologies undergirding health behaviors. Recent scholarship integrates a social determinants perspective with biosocial approaches to health behavior dynamics. Empirical advances model feedback among social, psychological and biological factors. Health behaviors are increasingly recognized as multidimensional and embedded in health lifestyles, varying over the life course and across place and reflecting dialectic between structure and agency that necessitates situating individuals in context. Advances in measuring and modeling health behaviors promise to enhance representations of this complexity.
Introduction
At any given point, an individual’s health and health behaviors reflect physical endowments in combination with a cumulated set of experiences and circumstances that have unfolded over time, in distinct social and physical contexts. This perspective, a blend of medical sociology, social demography, and social epidemiology, emphasizes the social milieu of health, or what is more commonly known as the social determinants of health . Over the past decade, scientific and policy interest in the social determinants of health has grown markedly, reflecting increasing consensus that overall health and health disparities are shaped significantly by nonmedical factors [ 1 , 2 ]. While these nonmedical factors include individual characteristics, such as education, income, and health beliefs, many others derive from an individual’s social and physical contexts – families, schools, workplaces, neighborhoods, and the larger politicaleconomic organization of society – “upstream” factors that further enable or constrain health[ 3 ]. Other nonmedical factors include the institutional and ideational contexts that shape normative environments and contribute to ideas and identities [ 3 – 5 ].
This emphasis on ‘extra-individual’ social factors is reflected in the recent 2020 Healthy People framework, published by the U.S. Department of Health and Human Services, which states:
“health and health behaviors are determined by influences at multiple levels, including personal (i.e., biological, psychological), organizational/institutional, environmental (i.e., both social and physical), and policy levels…Historically, many health fields have focused on individual-level health determinants and interventions.”
Below we review recent research on social determinants with a focus on health behaviors. Health behaviors are conceptually and practically pivotal in research on health. Conceptually, they are recognized as key mediating mechanisms between more distal structural and ideological environments and individual health outcomes. Practically, health behaviors are estimated to account for about 40% of deaths in the U.S. annually [ 7 ]. We organize this review thematically, highlighting selected conceptual frames and empirical advances in sociology and related fields, with emphasis on research published since 2013.
1. Health Behaviors – Definitions and Emerging Concepts
Health behaviors, sometimes called health-related behaviors, are actions taken by individuals that affect health or mortality. These actions may be intentional or unintentional, and can promote or detract from the health of the actor or others. Actions that can be classified as health behaviors are many; examples include smoking, substance use, diet, physical activity, sleep, risky sexual activities, health care seeking behaviors, and adherence to prescribed medical treatments. Health behaviors are frequently discussed as individual-level behaviors, but they can be measured and summarized for individuals, groups, or populations. Health behaviors are dynamic, varying over the lifespan, across cohorts, across settings, and over time. With smoking in the U.S, for example, the likelihood of initiation varies with age. Recent cohorts of adults are less likely to smoke than those in the mid-1900s, smoking prevalence is higher in the south than in the west, and smoking became less common after the Surgeon General’s Report of 1964 [ 8 – 11].
Focused interest in health behaviors, and efforts aimed at changing them, emerged in the midtwentieth century [ 12 ]. Narrowly defined biomedical approaches to health behavior research and interventions have been critiqued in recent years for an overemphasis on individual choice and personal responsibility; this individual focus is reflected in theories built around educating individuals to change health beliefs and actions [ 4 ]. A sociological approach expands the bounds of inquiry by emphasizing the need to examine individual actions in context, recognizing a role for structure as well as agency. Such an approach considers the place of constraints that limit choice, and the role of normative structures that shape the social values attached to activities, identities, and choices. It also engages themes of inequality and power in society.
Conceptual and methodological advances in defining health behaviors emphasize integrative and dynamic measurement. An important theoretical advance in the last decade is the concept of “health lifestyles” [ 4 , 13 ]. Policies targeting health behaviors tend to focus on a single behavior, often finding that these behaviors are resistant to change. A health lifestyle approach instead views behaviors as occurring in sets and influencing each other, developing from deeply rooted identities arising from membership in social groups [ 14 ]. Thus, health lifestyles are enacted at the individual level but are shaped by the meso and macro levels. Understanding the interplay between health behaviors is seen as fundamental for successfully changing those behaviors [ 15 ]. Most of the limited empirical work has focused on adults [ 16 , 17 ], but research and policy is now targeting the early life course as well [ 5 , 18 ]. For example, Mollborn et al . modeled U.S. preschoolers’ predominant health lifestyles and the intergenerational processes that give rise to them, finding that they predicted school readiness in kindergarten [ 5 ].
A significant methodological advance has been the collection of more refined data on health behaviors through intensive longitudinal data collection [ 19 ]. Innovations in technology allow for simultaneous and frequent data collection on social and spatial dimensions of activities in real time, creating enhanced opportunities to learn how individuals practice health behaviors as they unfold in usual social and spatial settings [ 20 – 22 ]. In the Human Mobility Project, Palmer and colleagues tested the feasibility of administering dynamic, location-based surveys by asking participants to download an app and install it on their phones, thereby gathering data on the phone’s positioning as participants moved through their daily routines and completed the surveys [ 23 ]. Others highlight the promise of health behavior interventions that provide frequent consistent reminders, monitoring, and rewards, through wearable devices, including monitors, [ 24 , 25 ], such as a pilot study that suggested that personally tailored text messaging about diabetes self-care to adolescents with type I diabetes was associated with greater glycemic control after three months [ 26 ].
2. A “Social Determinants” Approach to Health Behaviors
The interdisciplinary approach labeled “social determinants” seeks to understand how the social world shapes people’s health. One major pathway is through health behaviors. Health scholars distinguish between “downstream” (individual, in the body) and “upstream” (social structural, macro-level) causes of health behaviors [ 27 ]. Examples of the latter include institutions such as the health care system – which is changing rapidly in the U.S. due to the Affordable Care Act and is a target of ongoing research [ 28 ] – and the labor market – recession-based changes in this institution have spurred recent research on health implications [ 29 – 31 ]. For example, Kalousova and Burgard examined subjective and objective recessionary hardships, finding that they predicted problematic substance use in distinct ways [ 31 ]. Medical and psychological research focuses largely on downstream causes, while political, economic, and sociological research focuses more on the upstream [ 3 ]. The “meso” level between these two extremes is also fundamental for understanding health behaviors [ 32 ]. This level focuses on the proximate settings in which people live their lives – neighborhoods, workplaces, families, and the like – as well as the interpersonal interactions that take place within these settings. For example, examinations of women’s HIV risk in sub-Saharan Africa has traditionally focused on dynamics within sexual relationships, but more recent work recognizes the need to situate these relationships within the larger context of women’s lives, including their kinship, caregiving, and family responsibilities, as it is the family and kinship system in which gender, economic vulnerability and HIV risk are embedded [ 33 ].
Cutting-edge research into social determinants is taking place at the meso level. The importance of place for people’s health is increasingly acknowledged [ 34 ]. For example, the effects of neighborhoods on health behaviors [ 35 – 38 ], a longstanding focus of research, are becoming better understood by modeling neighborhoods dynamically, accounting for selection, and modeling spatial features of neighborhood environments [ 39 , 40 ]. Wodtke measured neighborhood poverty across childhood, finding that long-term exposure was positively associated with the likelihood of becoming a teen parent [ 41 ]. The spread of health behaviors in people’s social networks can now be modeled statistically [ 42 ], and scholars are working to disentangle causality from selection in understanding these processes of social contagion [ 43 – 45 ]. The benefits of social support are being further elaborated, but a nuanced view that also highlights the dark side of social relationships is emerging [ 42 , 43 ]. Examining peer influences on adolescent smoking behavior, Haas and colleagues conducted a dynamic social network analysis that distinguishes between increases and decreases in smoking, and explicitly incorporates endogenous network change, to show that while peer behavior influences smoking initiation, it is less related to smoking cessation [ 42 ].
Important concepts related to social determinants of health, like discrimination and stress, transcend the macro, meso, and micro levels [ 46 ]. For instance, discrimination is encoded in institutional practices, plays out in interaction at conscious and unconscious levels through processes involving bias and stigma [ 47 – 50 ], and affects individuals through health-damaging self-perceptions [ 32 ] and stereotype threat [ 51 ].
Similarly, key demographic factors, like social class, race/ethnicity, gender, and sexual orientation, influence health through all of these levels [ 52 – 54 ]. For example, gender is conceptualized not only as an individual level characteristic, but also as embedded in and constitutive of social structure, with implications for health behaviors, and even the expression of biological variation ([ 53 , 55 , 56 ]).Viewing social class as a fundamental cause of health disparities [ 57 ], many researchers illustrate how higher social class enables greater access to knowledge and resources, often yielding health advantages at the institutional, interactional, and individual levels and leading to altered behaviors [ 13 , 58 – 60 ]. The concept of intersectionality [ 61 – 63 ] further complicates this perspective by acknowledging that people experience multiple social statuses simultaneously, and their effects on health behaviors are not simply additive. These nuanced multilevel approaches to understanding health behaviors are increasingly common and may yield multipronged policy strategies [ 52 , 64 ].
3. Biosocial Processes: Situating Individuals in Social and Physical Contexts
As conceptual and empirical attention to social and ecological factors grows, so, too, do efforts to expand understanding of biological factors. These advances intersect in biosocial approaches that include concepts such as embodiment, biological embedding, social genomics, and systems approaches [ 65 – 67 ]. Embodiment is the process of the biological incorporation of societal and ecological context from the physical and social worlds in which we live [ 68 ]. Embedding emphasizes the developmental aspects of embodiment by focusing on timing of environmental exposures, with an emphasis on exposures that occur early in the life course, perhaps coincidental with critical periods of brain or biological development, and with potential to shape life-long outcomes through a variety social and biological mechanisms, some of which span generations [ 65 ]. For example, Bygren reviews possible mechanisms that could contribute to the intergenerational transmission of alcoholism, including changes to sperm that result from paternal alcohol exposure [ 69 ]. Social genomics focuses on identifying the ways social experiences regulate genetic activity [ 67 , 70 ]. Finally, systems approaches emphasize dynamic interplay, or feedback, between and within “environments” and often “biological” processes. Ip and colleagues, for example, inform interventions related to childhood obesity by developing dynamic models that incorporate feedback between health behaviors (food intake, activity levels) and physiology (mood, genetic factors), and include inputs such as poverty and local food environment, by blending agent-based modeling approaches and frequentist statistical approaches [ 71 ]. Focusing on policy, Zhang and colleagues develop agent-based simulations to model processes of dietary decision-making to find polices that emphasize healthy eating norms may be more effective than those regulating food prices or local food outlets [ 72 ].
Conceptually, interaction approaches emphasize that while social environments shape health behaviors, not all individuals respond in the same way to the same environments [ 73 ]. Mitchell and colleagues illustrate this with an analysis of post-partum depression, making the case that some women are genetically more reactive to stress environments. Among women with the polymorphisms associated with reactivity, those in poor environments experience worse outcomes, and those in rich environments experience better outcomes. In contrast, embodiment or social genomics emphasizes how health behaviors, such as smoking or diet, shape genomic activity or other measured biology. Such approaches might, for example, illustrate how smoking or physical activity is associated with telomere length or allostatic load [ 74 , 75 ]. In practice these approaches overlap. Complexity is evident in real world examples. Cultural norms, including gender norms, regarding diet or play can be embodied in bone development or body size, and these physical characteristics can in turn shape health behaviors [ 53 , 76 ]. Institutional and cultural racism, associated conscious or unconscious bias, and discrimination,can be associated with psychosocial stress, health behaviors, and health outcomes [ 77 ] but these relationships will vary across individuals.
Detailing biosocial processes linking social environment and health behaviors is challenging. Example investigations include discrimination and social resistance [ 78 , 79 ], emotions and stress [ 80 , 81 ], and cognitive processes such as decision-making and framing [ 82 ]. Attempts to incorporate feedback processes conceptually and methodologically are growing [ 83 , 84 ], as are efforts to address the challenges of causality [ 85 ]. For example, in an analysis of exercise and alcohol consumption, Wagner and colleagues use the random assignment of roommates in the first year of college to disentangle the selection of peer environments from peer and genetic effects on health behaviors [ 85 ].
4. Elaborating Life Course and Intergenerational Processes
Health behaviors change over an individual’s life course. Some behaviors – like riding in a car seat – are only important early in life, while others – like drinking alcohol – emerge later. Yet people with similar social locations exhibit similar health behaviors throughout life, even though those behaviors change with age [ 86 ]. The key principles of the interdisciplinary life course theoretical perspective [ 87 , 88 ] help explain individuals’ health behaviors over time.
First, human lives are shaped by historical times [ 88 , 89 ]. For example, social acceptance of smoking in the U.S. has varied tremendously from decade to decade, influencing both people’s likelihood of smoking and the degree to which genetic susceptibility to smoking is associated with smoking behavior [ 90 ]. Second, the nature and timing of life events is consequential in a person’s later life course [ 91 ]. Pregnancy is seen as a risky sexual behavior for teens, but not for married adults [ 92 ]. Teen pregnancy is tied to other risky health behaviors in adolescence such as drug use [ 93 ] [ 94 ] and later-life outcomes such as educational attainment [ 95 ]. Third, people’s lives are linked within and across generations. Across generations, parents’ health behaviors shape their children’s health and vice versa [ 96 , 97 ]. Within generations, young people’s behaviors are influenced by those of their friends [ 44 ]. Fourth, people are agentic, making active choices among the options that their structural locations provide [ 4 , 13 ]. Thus, integrating social structural processes with psychological constructs such as planful competence and risk aversion is fundamental for more accurately predicting people’s health behaviors. Overall, the life course perspective emphasizes the dynamic nature of social circumstances and health, which is reflected in emerging research [ 88 , 98 – 101 ]. For example, research on migration emphasizes dynamic processes of “acculturation” after arriving in a new place [ 102 ].
Methodological challenges in this area are abundant. Reverse causality between health behaviors and structural location is a concern, as is selection bias [ 95 ]. Recent work on health behaviors from a life course perspective emphasizes dynamic processes such as developmental timing, cooccurrence, fluctuation, and nonlinear relationships [ 41 , 103 – 107 ]. For instance, Boynton-Jarrett and colleagues found that frequent life disruptions in adolescence across several domains predicted cumulative violence exposure and risky health behaviors [ 103 ]. Modeling theoretical ideas that follow from life course frames is methodologically challenging. Statistical techniques such as multilevel growth curve and trajectory modeling, age-period-cohort models, and latent class analyses are helping empirical tests catch up to theoretical innovations [ 5 , 64 , 95 , 108 – 110 ]. For example, Wang and colleagues modeled six distinct trajectories of engagement in risk behaviors such as delinquency, substance use, and sex, following Bahamian youth from grades 6–9, demonstrating the importance of early social risk factors for high risk trajectories [ 110 ].
Conclusions
Health behaviors are associated with a multitude of health and well-being outcomes at the individual and population levels. Drawing on recent research in sociology and related fields, we draw attention in this review to the application of a “social determinants” approach – now widely applied to health – to the specific topic of health behaviors. Such an approach shifts the lens from individual attribution and responsibility for health behaviors – to societal organization and the myriad institutions, structures, inequalities, and ideologies that undergird observed variation in health behaviors. We emphasize that a social determinants approach is not at odds with the incorporation of biological and psychological processes; rather, it recognizes the interplay between them in complex, dynamic systems, embracing a population approach that situates individuals in context. Life course frames that emphasize interdisciplinarity, history, time, context, and linked lives guide much recent investigation. And notably, through the conceptual refocus around social determinants and societal organization, a growing emphasis on links among health behaviors is emerging, upending the more usual single-disease, or single-health behavior, orientation to research and research specialization.
Future directions in “social determinants” research on health behaviors will be guided by this foundational thinking. The abundance of new data – including but not limited to administrative, geographic, social network, social media, medical, and genomic data – will provide ample opportunity for creative exploration. Our knowledge about health behavior dynamics is context-dependent. Changing societal factors, such as the legalization of marijuana use in some settings, or the implementation of the Affordable Care Act in the U.S., render understanding about individual health behaviors incomplete, as these understandings are contingent on context. The very populations that use marijuana or seek health care will change, as will the dynamics, determinants, and consequences of their health behaviors. Innovative science on the social determinants of health behaviors will continue to elaborate this complexity and expand the frames that guide health behavior research.
- Health behaviors reflect interplay between people and contextual factors.
- “Social determinants” include societal institutions, ideologies, and inequalities.
- Health behaviors contribute to and reflect embodiment and other biosocial processes.
- Recent work engages health lifestyles, agency, and multilevel life course dynamics.
- Empirical advances model feedback among social, psychological and biological factors.
Acknowledgements
We thank Leah Pierson for research assistance. We also acknowledge support from the Population Studies and Training Center at Brown University, which receives core support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development through grants R24HD041020 and T32HD007338, and the Institute of Behavioral Science at the University of Colorado Boulder, which receives core support through grant R24HD066613.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References and Recommended Reading
- Tools and Resources
- Customer Services
- Affective Science
- Biological Foundations of Psychology
- Clinical Psychology: Disorders and Therapies
- Cognitive Psychology/Neuroscience
- Developmental Psychology
- Educational/School Psychology
- Forensic Psychology
- Health Psychology
- History and Systems of Psychology
- Individual Differences
- Methods and Approaches in Psychology
- Neuropsychology
- Organizational and Institutional Psychology
- Personality
- Psychology and Other Disciplines
- Social Psychology
- Sports Psychology
- Share This Facebook LinkedIn Twitter
Article contents
Habit formation and behavior change.
- Benjamin Gardner Benjamin Gardner Department of Psychology, King's College London
- and Amanda L. Rebar Amanda L. Rebar Department of Human, Health, and Social Sciences, Central Queensland University
- https://doi.org/10.1093/acrefore/9780190236557.013.129
- Published online: 26 April 2019
Within psychology, the term habit refers to a process whereby contexts prompt action automatically, through activation of mental context–action associations learned through prior performances. Habitual behavior is regulated by an impulsive process, and so can be elicited with minimal cognitive effort, awareness, control, or intention. When an initially goal-directed behavior becomes habitual, action initiation transfers from conscious motivational processes to context-cued impulse-driven mechanisms. Regulation of action becomes detached from motivational or volitional control. Upon encountering the associated context, the urge to enact the habitual behavior is spontaneously triggered and alternative behavioral responses become less cognitively accessible.
By virtue of its cue-dependent automatic nature, theory proposes that habit strength will predict the likelihood of enactment of habitual behavior, and that strong habitual tendencies will tend to dominate over motivational tendencies. Support for these effects has been found for many health-related behaviors, such as healthy eating, physical activity, and medication adherence. This has stimulated interest in habit formation as a behavior change mechanism: It has been argued that adding habit formation components into behavior change interventions should shield new behaviors against motivational lapses, making them more sustainable in the long-term. Interventions based on the habit-formation model differ from non-habit-based interventions in that they include elements that promote reliable context-dependent repetition of the target behavior, with the aim of establishing learned context–action associations that manifest in automatically cued behavioral responses. Interventions may also seek to harness these processes to displace an existing “bad” habit with a “good” habit.
Research around the application of habit formation to health behavior change interventions is reviewed, drawn from two sources: extant theory and evidence regarding how habit forms, and previous interventions that have used habit formation principles and techniques to change behavior. Behavior change techniques that may facilitate movement through discrete phases in the habit formation trajectory are highlighted, and techniques that have been used in previous interventions are explored based on a habit formation framework. Although these interventions have mostly shown promising effects on behavior, the unique impact on behavior of habit-focused components and the longevity of such effects are not yet known. As an intervention strategy, habit formation has been shown to be acceptable to intervention recipients, who report that through repetition, behaviors gradually become routinized. Whether habit formation interventions truly offer a route to long-lasting behavior change, however, remains unclear.
- automaticity
- behavior change
- dual process
What Are Habits and Habitual Behaviors ?
Everyday behaviors shape human health. Many of the dominant causes of death, including heart disease, diabetes, cancer, chronic lower respiratory diseases, and stroke, are preventable (World Health Organization, 2017 ). Adopting health-promoting behaviors such as eating more healthily or increasing physical activity may improve quality of life, physical and mental health, and extend lives (Aune et al., 2017 ; Centers for Disease Control and Prevention, 2014 ; Rebar et al., 2015 ; World Health Organization, 2015 ). For some behaviors, one performance is sufficient to attain desired health outcomes; a single vaccination, for example, can yield immunity to disease (e.g., Harper et al., 2004 ). For many behaviors, however, achieving meaningful health outcomes depends on repeated performance: Going for a run once, for example, will not achieve the same health benefits as regular activity over a prolonged period (Erikssen et al., 1998 ). In such instances, behavior change must be viewed as a long-term process, which can be conceptually separated into stages of initiation and maintenance (Prochaska & DiClemente, 1986 ; Rothman, 2000 ). This distinction is important from a practical perspective because while people may possess the capability, opportunity, and motivation to initiate behavior change (Michie, van Stralen, & West, 2011 ), they often fail to maintain it over time, lapsing back into old patterns of behavior (Dombrowski, Knittle, Avenell, Araujo-Soares, & Sniehotta, 2014 ). Some have attributed this to changes in motivation after initial experiences of action (Armitage, 2005 ; Rothman, 2000 ). People may overestimate the likelihood of positive outcomes or the valence of such outcomes, or they may fail to anticipate negative outcomes (Rothman, 2000 ). Alternatively, a newly adopted behavior may lose value and so become deprioritized over time. Motivation losses threaten to derail initially successful behavior change attempts.
Habit formation has attracted special attention as a potential mechanism for behavior change maintenance (Rothman, Sheeran, & Wood, 2009 ; Verplanken & Wood, 2006 ) because habitual behaviors are thought to be protected against any dips in conscious motivation. Viewing habit as a means to maintenance may seem truistic; in everyday discourse, a habit is an action done repetitively and frequently, and so making action habitual will necessarily entail maintenance. Within psychology, however, the term habit denotes a process whereby exposure to a cue automatically triggers a non-conscious impulse to act due to the activation of a learned association between the cue and the action (Gardner, 2015 ). Habit is learned through “context-dependent repetition” (Lally, van Jaarsveld, Potts, & Wardle, 2010 ): Repeated performance following exposure to a reliably co-occurring cue reinforces mental cue-action associations. As these associations develop, the habitual response gradually becomes the default, with alternative actions becoming less cognitively accessible (Danner, Aarts, & de Vries, 2008 ). Habit is formed when exposure to the cue is sufficient to arouse the impulse to enact the associated behavior without conscious oversight (Gardner, 2015 ; Neal, Wood, Labrecque, & Lally, 2012 ; Wood, Labrecque, Lin, & Rünger, 2014 ). In the absence of stronger influences favoring alternative actions, the habit impulse will translate smoothly and non-consciously into action, and the actor will experience behavior as directly cued by the context (Wood & Neal, 2007 ).
Defining habit as a process that generates behavior breaks with earlier definitions, which depicted habit as a form of behavior (see Gardner, 2015 ). This definition of habit as a process resolves a logical inconsistency that arises from portraying habit as a determinant of behavior (e.g., Hall & Fong, 2007 ; Triandis, 1980 ); as Maddux ( 1997 , pp. 335–336) noted, “a habit cannot be both the behavior and the cause of the behavior.” It also allows for the habit process to manifest in multiple ways for any behavior. A distinction has been drawn between habitually instigated and habitually executed behavior (Gardner, Phillips, & Judah, 2016 ; Phillips & Gardner, 2016 ). Habitual instigation refers to habitual triggering of the selection of an action and a non-conscious commitment to performing it upon encountering a cue that has consistently been paired with the action in the past. Habitual execution refers to habit facilitating completion of the sub-actions that comprise any given action such that the cessation of one action in a sequence automatically triggers the next. Take, for example, “eating a bag of chips.” While people typically mentally represent this activity as a single unit of action (Wegner, Connally, Shearer, & Vallacher, 1983 , cited in Vallacher & Wegner, 1987 ), it can be deconstructed into a series of discrete sub-actions (e.g., “opening bag,” “putting hand in bag,” “putting food in mouth,” “chewing,” “swallowing”; Cooper & Shallice, 2000 ). “Eating a bag of chips” is habitually instigated to the extent that the actor is automatically cued to select “eating chips” from available behavioral options. This may also activate the first sub-action in the sequence (“opening bag”). “Eating a bag of chips” is habitually executed to the extent that the cessation of, for example, “putting my hand in the bag” habitually cues “putting food in mouth,” the cessation of which habitually cues “chewing,” and so on, until the perceptually unitary action (“eating a bag of chips”) is complete. 1 The term habitual behavior describes any action that is either instigated or executed habitually. This includes actions that are habitually instigated but non-habitually executed (e.g., habitually triggered to begin eating a bag of chips, but deliberates about how many chips to put in mouth), non-habitually instigated but habitually executed (e.g., consciously decides to eat a bag of chips, but habitually puts the chips in mouth, chews, and swallows), or both habitually instigated and habitually executed (e.g., habitually starts eating chips, and habitually puts them in mouth, chews, and swallows; Gardner, 2015 ). This description allows for a behavior to be habitual, yet not fully automated (see Aarts, Paulussen, & Schaalma, 1997 ; Marien, Custers, & Aarts, 2019 ) and better resonates with everyday experiences of complex health behaviors such as physical activity, which may be partly habit-driven, yet also require conscious oversight to be successfully completed (Rhodes & Rebar, 2019 ).
Habit has been implicated in behaviors across a range of domains, including media consumption (LaRose, 2010 ), purchasing patterns (Ji & Wood, 2007 ), environmentally relevant actions (Kurz, Gardner, Verplanken, & Abraham, 2014 ), and health behaviors. Studies have pointed to a multitude of health-related actions that may potentially be performed habitually, including dietary consumption (Adriaanse, Kroese, Gillebaart, & De Ridder, 2014 ), physical activity (Rebar, Elavsky, Maher, Doerksen, & Conroy, 2014 ), medication adherence (Hoo, Boote, Wildman, Campbell, & Gardner, 2017 ), handwashing (Aunger et al., 2010 ), and dental hygiene (Wind, Kremers, Thijs, & Brug, 2005 ). Habit strength is consistently found to correlate positively with behavioral frequency (Gardner, de Bruijn, & Lally, 2011 ; Rebar et al., 2016 ) and may bridge the “gap” between intention and behavior, though there are varying accounts regarding interplay between habits and intentions in regulating behavior. Some have argued that people are more likely to act on intentions when they have habits for doing so (Rhodes & de Bruijn, 2013 ). When motivation is momentarily low upon encountering associated contexts, habit may translate into performance despite motivational lapses. In this way, habit has been proposed to represent a form of self-control, protecting regularly performed behaviors that are desired in the longer-term against shorter-term motivation losses (Galla & Duckworth, 2015 ). Other studies have suggested that habit can direct action despite intentions not to act (Neal, Wood, Wu, & Kurlander, 2011 ; Orbell & Verplanken, 2010 ; but see Rebar et al., 2014 ). For example, one study showed that United Kingdom smokers with habits for smoking while drinking alcohol reported “action slips” after the introduction of a smoking ban in public houses; despite intending to adhere to the ban, several reporting “finding themselves” beginning to light up cigarettes while consuming alcohol (Orbell & Verplanken, 2010 ). These two perspectives concur in highlighting the potential for habit to override conscious motivational tendencies. Such effects may be attributable to habitual instigation rather than execution (Gardner et al., 2016 ); someone who is habitually prompted to act is more likely to frequently perform those actions and to do so without relying on intention.
The effects of habit—or more specifically, instigation habit (Gardner et al., 2016 )—have important implications for behavior maintenance. By virtue of their cue-dependent, automatic nature (Orbell & Verplanken, 2010 ), habitually instigated behaviors should, in theory, persist even when they no longer serve the goal that initially motivated performance, or where motivation has eroded (Wood & Neal, 2007 ). For example, a person starting a new job out of town may consistently decide to commute by bicycle, which will likely create a habit for bicycle commuting whereby the workday morning context automatically prompts bicycle use without any deliberation over available alternatives (Verplanken, Aarts, Knippenberg, & Moonen, 1998 ). This may, however, lead to instances whereby the commuter “accidentally” uses the bicycle out of habit, despite, for example, knowing of road closures that will slow the journey and which would render alternative transport modes preferable (see Verplanken, Aarts, & Van Knippenberg, 1997 ). This example demonstrates several key features of habitual responses: learning via consistent pairing of cues (e.g., 8 a.m. on a workday) and action (selecting the bicycle); cue-dependent automaticity (using the bicycle at 8 a.m. on a workday without deliberation); and goal-independence, persisting even where an actor no longer has the motivation to act or is motivated to act in another way (e.g., when roads are closed). It also demonstrates how habit formation can maintain behavior by “locking in” new behaviors, protecting them against losses in conscious motivation. Habit development may also play a useful role in cessation of unwanted behaviors. Many ingrained behaviors—for example, eating high-calorie snacks—persist because they have become habitual and so are difficult to change. The lack of reliance on conscious intentions that is characteristic of habitual behavior, and which is thought to protect new behaviors against motivation losses, makes it difficult to break unwanted habits despite strong intentions to do so (Webb & Sheeran, 2006 ). While habit formation per se is not a sufficient strategy for “giving up” an unwanted behavior, behavior change can be made easier by seeking to form a new (“good”) habit in place of the old (“bad”) habit, rather than attempting only to inhibit the unwanted action (Adriaanse, van Oosten, de Ridder, de Wit, & Evers, 2011 ). Indeed, in the real world, habit development often involves displacing existing actions with more desirable alternatives such as eating healthy snacks in place of higher-calorie foods (Lally, Wardle, & Gardner, 2011 ; McGowan et al., 2013 ). Such “habit substitution” can take one of two basic forms, involving either avoidance of cues to the unwanted action or the development of new responses that compete with the unwanted habitual response. The “habit discontinuity hypothesis” speaks to the former of these, arguing that naturally occurring disruption of contexts—such as a residential relocation, for example—discontinues exposure to old habit cues (Walker, Thomas, & Verplanken, 2015 ). This represents an opportunity for people to act on their conscious motivation in response to newly encountered cues, and so to develop new, potentially more desirable habitual responses such as using active travel modes in place of more sedentary travel options like driving (Verplanken & Roy, 2016 ). Bad habits offer established cue-response structures that can hasten learning of new, good habits. Thus, where discontinued cue exposure is not feasible, people may seek to develop new cue-behavior associations to compete with and ultimately override old associations (Bouton, 2000 ; Walker et al., 2015 ). For example, people wishing to reduce habitual unhealthy snacking may form plans that dictate that when they are watching television and wish to snack (cue), they will eat fruit (new, desired behavior) instead of high-calorie foods (undesired, habitual behavior; e.g., Adriaanse, Gollwitzer, De Ridder, De Wit, & Kroese, 2011 ). In both instances of discontinued cue exposure and the adoption of competing responses to existing cues, the development of new habit associations and the decaying (or deprioritizing) of old habit associations are thought to occur concurrently (Adriaanse et al., 2011 ; Walker et al., 2015 ; Wood & Neal, 2007 ).
How Does Habit Form?
There have been calls for habit formation, whether focused solely on establishing new actions or displacing unwanted actions, to be adopted as an explicit goal for behavior change interventions (Rothman et al., 2009 ; Verplanken & Wood, 2006 ). Developing effective habit formation interventions requires an understanding of how habit forms.
The concept of behavior as an automatic response to covarying contextual cues, directed by learned cue-action associations, is rooted in behaviorist principles and studies of animal learning (e.g., Hull, 1943 ; Skinner, 1938 ; Thorndike, 1911 ). For example, in his maze-learning studies, Tolman ( 1932 ) noted that his rats, having repeatedly run down the route at the end of which was a food reward, continued to pursue that route even when the reward was removed. Adams ( 1982 ) trained rats to press a lever in a cage so as to receive intermittently delivered sucrose pellets. After receiving a lithium chloride injection that caused ingestion of the sucrose to induce nausea, those rats that were more highly trained (i.e., had pressed and received the sucrose reward a greater number of times in the training phase) were likely to persist longer in pressing the lever. Of course, unlike rats, humans possess the cognitive capacity to anticipate and reflect on their actions, and health-related behaviors among humans are inherently more complex than selecting maze routes or pressing levers. Yet, homologous neural processes are implicated in the acquisition and practice of habitual responses in rats and humans (Balleine & O’Doherty, 2010 ), and, like rats, people can acquire habitual behavioral responses despite a lack of insight into those behaviors or the associations that govern their performance (Bayley, Frascino, & Squire, 2005 ).
The route to human habit formation is conceptually simple: A behavior must be repeatedly performed in the presence of a cue or set of cues (i.e., context) so that cue-behavior associations may develop. For behaviors that are initially purposeful and goal-directed, the habit-formation process represents a period of transition whereby behavioral regulation transfers from a reflective and deliberative processing system to an impulsive system, which generates action rapidly and automatically based solely on activation of associative stores of knowledge (Strack & Deutsch, 2004 ). While there has been much lab-based research into the learning of relatively simple habitual responses in humans (e.g., button pressing; Webb, Sheeran, & Luszczynska, 2009 ), only relatively recently have studies focused on formation of real-world health-related habits (Fournier et al., 2017 ; Judah, Gardner, & Aunger, 2013 ; Lally et al., 2010 ). This work has largely been facilitated by the development of the Self-Report Habit Index (SRHI; Verplanken & Orbell, 2003 ), which affords reflections on the “symptoms” of habit, such as repetitive performance, mental efficiency, and lack of awareness.
Lally et al.’s ( 2010 ) seminal habit formation study used an SRHI sub-scale to assess the trajectory of the relationship between repetition and habit development among 96 participants for a 12-week period. They were instructed to perform a self-chosen physical activity or diet-related behavior (e.g., “going for a walk”) in response to a naturally occurring once-daily cue (e.g., “after breakfast”). Each day, they reported whether they had performed the action on the previous day, and if so, rated the experienced automaticity of its performance. Habit development within individuals was found to be most accurately depicted by an asymptotic curve, with early repetitions achieving sharpest habit gains, which later slowed to a plateau. The level at which habit peaked differed across participants, with some reportedly attaining scores at the high end of the automaticity index and others peaking below the scale mean. This plateau was reached at a median of 66 days post-baseline, though there was considerable between-person variation in the time taken to reach the plateau (18–254 days, the latter a statistical forecast assuming continued performance beyond the study period). These findings were echoed in a study of adoption of a novel stretching behavior (Fournier et al., 2017 ). Once-daily performance was found to yield asymptotic increases in self-reported habit strength. Habit plateaued at a median of 106 days for a group that performed the stretch every morning upon waking, and 154 days for those who stretched in the evening before bed, which the authors interpreted as evidence of the role of cortisol (which naturally peaks in the morning) in habit learning.
These studies reveal that habit development is not linear; if this were so, the fourth repetition of a behavior would have the same reinforcing impact on habit as would, say, the 444th. Rather, the asymptotic growth curve demonstrates that initial repetitions have the greatest impact on habit development. This in turn demands that the habit formation process be broken down into discrete phases and that the early phase, characterized by the sharpest gains in automaticity, may be a critical period during which people require most support to sustain motivation before the action becomes automatic (Gardner, Lally, & Wardle, 2012 ). Lally and Gardner ( 2013 ) have proposed a framework that organizes habit formation (and substitution) into four interlinked phases (see also Gardner & Lally, 2019 ). It argues that, for new behaviors initially driven by conscious motivation, habit forms when a person (1) makes a decision to act and (2) acts on his or her decision (3) repeatedly, (4) in a manner conducive to the development of cue-behavior associations. Phases 1 and 2 may be taken together to represent pre-initiation, occurring before the first enactment of the new behavior, whereas phases 3 and 4 are post-initiation phases, addressing the motivational and volitional elements needed to sustain behavior after initial performance (phase 3) and the effect of repetition on habit associations (phase 4) (see also Kuhl, 1984 ; Rhodes & de Bruijn, 2013 ; Rothman, 2000 ). Phase 3 captures the critical period after initiation but before habit strength has peaked (Fournier et al., 2017 ; Lally et al., 2010 ).
The framework is not intended as a theory or model of the habit formation process, but rather as a means to conceptually organize the processes and mechanisms that underpin habit development. According to the framework, any variable can promote habit formation in one or more of four ways: It may enhance motivation (phase 1) or action control (i.e., the enactment of intentions into behavior; Kuhl, 1984 ; Rhodes & de Bruijn, 2013 ) (phase 2) so as to initiate the behavior; it may modify motivation and other action control processes to continue to perform the behavior (phase 3); or it may strengthen cue-behavior associations (phase 4). One variable may operate through multiple processes: For example, anticipating pleasure from action can motivate people to perform it for the first time (phase 1) and to continue to perform it (phase 3) (Radel, Pelletier, Pjevac, & Cheval, 2017 ; Rothman et al., 2009 ). The experience of pleasure can also quicken learning of cue-behavior associations (phase 4) (de Wit & Dickinson, 2009 ). By extension, Lally and Gardner’s ( 2013 ) framework categorizes techniques that promote habit formation according to their likely mechanism (or mechanisms) of action; techniques may enhance motivation (phase 1) or action control (phase 2) to initiate change, sustain motivation and action control over time (phase 3), or reinforce cue-behavior associations (phase 4).
Which Behavior Change Techniques Should Be Used to Form Habit?
The most comprehensive taxonomy of behavior change techniques currently available defines habit formation as a discrete technique, which it defines as any effort to “prompt rehearsal and repetition of the behavior in the same context repeatedly so that the context elicits the behaviour” (Michie et al., 2013 , Suppl. Table 3 , p. 10). Yet, this definition incorporates only context-dependent repetition and not any other technique that may promote habit by increasing the likelihood of context-dependent repetition (i.e., promoting motivation or action control; phases 1–3 of Lally and Gardner’s framework) or enhancing the contribution of each repetition to the learning of habit associations (phase 4). Although context-dependent repetition is necessary for habit to form, it realistically requires supplementation with techniques targeting pre- and post-initiation phases en route to habit formation (Gardner Lally, & Wardle, 2012 ). While Michie et al. ( 2013 ) treat habit formation as a unitary technique, habit formation may perhaps be more realistically seen as an intervention approach that comprises a broader suite of techniques, which marry context-dependent repetition with strategies that: reinforce motivation; boost action control capacity, opportunity, or skills; facilitate post-initiation repetition; or quicken the learning of associations arising from repetition.
Theory points to techniques that may facilitate progression through these phases. Intention formation (phase 1 of Lally & Gardner’s [ 2013 ] framework) is likely when people anticipate that the action or its likely consequences will be positive and believe that they have a realistic opportunity and capability to perform the behavior (Ajzen, 1991 ; Bandura, 2001 ; Michie et al., 2011 ; Rogers, 1983 ; Schwarzer, Lippke, & Luszczynska, 2011 ). Providing information on the likely positive consequences of action, or choosing to pursue actions that are already most highly valued, may therefore aid habit development by enhancing motivation. Action control skills are required to initiate intention enactment (phase 2) and to maintain the behavior by consistently prioritizing the intention over competing alternatives (phase 3). This will likely be facilitated by self-regulatory techniques such as planning, setting reminders, self-monitoring, and reviewing goals to ensure they remain realistic and attractive, and receiving (intrinsic) rewards contingent on successful performance (Gardner et al., 2012 ; Lally & Gardner, 2013 ). People are most likely to engage in context-dependent repetition in response to highly salient cues (e.g., event- rather than time-based cues, which likely require conscious monitoring; McDaniel & Einstein, 1993 ). Pairing the action with more frequently and consistently encountered cues may quicken habit learning at phase 4 (Gardner & Lally, 2019 ). Highly specific action plans detailing exactly what will be done and in exactly which situation (i.e., implementation intentions; Gollwitzer, 1999 ) should therefore be conducive to the acquisition of associations (but see Webb et al., 2009 ). Implementation intentions can also facilitate habit substitution: By consistently enacting new, pre-specified cue responses that directly compete with existing habitual responses, such as feeding children water instead of sugary drinks (McGowan et al., 2013 ), new responses may acquire the potential to override and erode old habitual responses (Adriaanse et al., 2011 ). The reinforcing value of repetition may also be strengthened where intrinsic reward is delivered or attention is drawn to an undervalued intrinsic reward arising from action (Radel et al., 2017 ).
Which Behavior Change Techniques Have Been Used to Form Habit, and with What Effect?
While theory can recommend techniques that should be used to promote habit formation, evaluations of habit-based interventions are needed to show which techniques have been used, and with what effect, in real-world behavior change contexts. To this end, a systematic literature search was run to identify habit-based health-promotion interventions and to document the behavior change methods used.
Four psychology and health databases (Embase, Medline, PsycInfo, Web of Science) were searched in March 2018 to identify sources that had cited one of nine key papers about habit and health. These sources were selected to capture topics of habit measurement (Gardner, Abraham, Lally, & de Bruijn, 2012 ; Ouellette & Wood, 1998 ; Verplanken & Orbell, 2003 ), principles and processes of habit formation (Gardner, Lally, & Wardle, 2012 ; Lally & Gardner, 2013 ; Lally et al., 2010 ; Lally et al., 2011 ), and conceptual commentaries (Gardner, 2015 ; Wood & Rünger, 2016 ). Papers were eligible for review if they (a) were published in English, (b) were peer-reviewed, (c) reported primary quantitative or qualitative data, (d) had tested efficacy or effectiveness for changing behavior or habit, (e) used interventions designed to promote habit formation for health behaviors, (f) targeted context-dependent repetition, and (g) were informed by theory or evidence around habit, operationalized as a learned automatic response to contextual cues or a process that generates such responses. Interventions adopted primarily to elucidate the habit formation process (rather than to develop or assess intervention effectiveness; e.g., Judah et al., 2013 ; Lally et al., 2010 ) and any that focused exclusively on breaking existing habits (e.g., Armitage, 2016 ) were excluded. For each eligible intervention, all available material was coded, including linked publications (e.g., protocols), to identify component techniques using the Behavior Change Technique Taxonomy v1 (Michie et al, 2013 ).
Twenty papers, reporting evaluations of 19 interventions, were identified. Four of the 19 interventions represented variants of interventions used elsewhere in the 20 papers. For example, one trial evaluated the same habit-based intervention component in two conditions, which varied only in the frequency of supplementary motivational interviews and booster phone calls (Simpson et al., 2015 ). Thus, the 19 could be reduced to 15 unique habit-based interventions, of which four focused on both dietary and physical activity habits, six on physical activity (or sedentary behavior) only, two on dietary consumption only, two on dental hygiene, and one on food safety. In all of the studies, habit measures were self-reported.
Diet and Physical Activity Interventions
One randomized controlled trial (RCT) compared, in overweight and obese adults, an intervention that included advice on forming and substituting healthy for unhealthy habits, with a non-habit-based intervention that emphasized relationships with food, body image, and weight biases (Carels et al., 2014 ; see also Carels et al., 2011 ). Those in the habit-based intervention received training on changing old routines and developing new ones, including advice on using cues and forming implementation intentions. Both intervention groups received weekly weight assessments and monitored their physical activity, calorie intake, and output. At a 6-month follow-up, both the habit-based ( n = 30) and non-habit intervention groups ( n = 29) were eating a healthier diet, exercising more regularly, and had lost weight. Physical activity habit strengthened and sitting habit weakened in both groups, though no between-group differences were found in weight loss or habit strength.
Lally et al.’s ( 2008 ) “Ten Top Tips” weight loss intervention centered on a leaflet outlining recommendations for forming healthy eating and physical activity habits, as supplemented by a daily adherence monitoring diary. The leaflet included advice on routinization, identifying effective cues, and habit substitution. A small non-randomized trial compared the intervention, augmented with monthly ( n = 35) or weekly weighing ( n = 34), against a no-treatment control. The intervention group lost more weight than the control group at 8 weeks and maintained weight loss at 32 weeks. Scores at 32 weeks suggested the tips had become habitual, and habit change correlated positively with weight loss (Lally et al., 2008 ; see also Lally et al., 2011 ). In a subsequent RCT (Beeken et al., 2012 , 2017 ), intervention recipients ( n = 267) lost more weight at 3 months than did a usual-care group ( n = 270). At 24 months, the intervention group had maintained weight loss, though the usual care group had lost a similar amount of weight. Habit strength, measured only at baseline and 3 months, increased more in the intervention than in the control group (Beeken et al., 2017 ). Weight loss at 3 months was attributable to gains in both habit and self-regulatory skill (Kliemann et al., 2017 ).
Simpson et al.’s ( 2015 ) weight-loss intervention provided participants with motivational advice designed to prompt intention formation, with information about how to form dietary and activity habits, and social support. Two intervention variants, differing according to the frequency of sessions, were evaluated against a minimal-treatment control, which did not feature habit-based advice, in a feasibility RCT among obese patients. Recipients of the more intensive intervention variant ( n = 55) showed greater BMI reduction at a 12-month follow-up than did the less intensive intervention ( n = 55) or control groups ( n = 60). There were no between-group differences at 12 months in physical activity or overall healthy eating, nor were there differences in activity or diet habit scores.
One RCT compared an 8-week computer-tailored intervention designed to reduce cardiovascular risk against a no-treatment control among cardiac and diabetes rehabilitation patients who already intended to increase their activity and fruit and vegetable consumption (Storm et al., 2016 ). The intervention provided information about health risks of inactivity and unhealthy diet and enhancing self-regulatory skills. Immediately following intervention cessation, fruit and vegetable consumption and physical activity habit and behavior scores were greater among the intervention ( n = 403) than control group ( n = 387), but no differences were observed 3 months post-baseline.
Physical Activity and Sedentary Behavior Interventions
An intervention for new gym members promoted habits for both physical activity and preparatory actions for gym attendance (e.g., packing a gym bag; Kaushal, Rhodes, Meldrum, & Spence, 2017 ). Members received advice on how to form habits, including selecting time cues, setting action plans, and using accessories to increase enjoyment and so support cue-consistent performance and foster intrinsic motivation, which theory suggests can strengthen the impact of repetition on habit development (Lally & Gardner, 2013 ). Moderate-to-vigorous physical activity gains, objectively observed at an 8-week follow-up, were greater among intervention recipients ( n = 47) than the no-treatment control group ( n = 47). Habit strength was not assessed.
All 49 participants in Fournier et al.’s ( 2017 ) RCT were given access to twice-weekly, 1-hour tailored physical activity sessions for 28 weeks, with one group ( n = 23) also sent SMS reminders targeting intrinsic motivation and consistent performance to the intervention group to foster habitual attendance. Although physical activity habit strength (assessed using a subscale of the SRHI) increased for both groups immediately post-intervention, the SMS group experienced quicker habit gains. Marginally greater activity was observed in the SMS group at 12 months.
One 4-month intervention for middle- to older-aged adults comprised seven 2-hour group sessions and sought to create new balance and strength exercise habits by recommending small modifications to everyday routines (e.g., placing frequently used items on high shelves to promote stretching to reach them) (Fleig et al., 2016 ; see also Clemson et al., 2012 ). An uncontrolled trial among 13 participants showed that, while there were no apparent changes in objectively measured physical performance, there were considerable habit strength gains for the recommended actions over 6 months. Notably, participants reported in interviews that the exercises had become automatically triggered, yet they performed them consciously, suggesting that the intervention promoted habitual instigation rather than execution.
Another intervention promoting small activity changes in older adulthood was evaluated in two papers (Matei et al., 2015 ; White et al., 2017 ). Drawing on Lally et al.’s ( 2008 ) “Ten Top Tips,” it comprised a leaflet offering recommendations for integrating and substituting light-intensity physical activities into everyday routines, with supplementary self-monitoring record sheets (Gardner, Thune-Boyle, et al., 2014 ). An 8-week uncontrolled trial was undertaken among two discrete samples (Matei et al., 2015 ). No changes were found in sitting time, physical activity, or sitting or physical activity habit among one sample ( n = 16), but a second sample ( n = 27) reported decreased sitting time and increased walking. Qualitative data suggested both groups experienced automaticity gains and some health benefits. A subsequent pilot RCT showed that intervention recipients ( n = 45) experienced no greater change than did a control group ( n = 46) who received a pre-existing fact sheet promoting activity and reducing sitting, but with no habit-based advice (White et al., 2017 ). Both groups reduced sitting time and sitting habit and increased activity and activity habit.
Using an experience sampling design, Luo et al. ( 2018 ) tracked change in standing or moving breaks from sedentary behavior in office workers given 3 weeks of access to automated computer-based reminders to break up sitting, timed to occur based on daily self-selected work and break durations. Although sitting behavior was not monitored, habit strength and self-regulation for taking “moving breaks” during work hours both increased significantly across the study.
Similarly, Pedersen et al. ( 2014 ) evaluated a software package that automatically deactivated desk-based employees’ computer screens every 45 minutes to substitute new physical activity habits for existing prolonged sitting habits. Although all participants received information on the detrimental health impact of sitting and benefits of activity, self-report activity data suggested that those who used the software for 13 weeks ( n = 17) expended greater energy per day than did those not given the software ( n = 17).
Dietary Interventions
One intervention promoted habitual healthy child-feeding practices among parents of children aged 2–6 years (McGowan et al., 2013 ). On each of four occasions over 8 weeks, parents chose to pursue one of four families of habit formation targets (increased feeding of fruit, vegetables, water, and healthy snacks). They received advice on the importance of child dietary consumption and on self-regulatory strategies, including action planning, goal setting, and context-dependent repetition. An RCT showed that intervention parents ( n = 58) reported greater child intake of vegetables, water, and healthy snacks but a waiting-list control group ( n = 68) did not. Habit strength increased for all three behaviors, and a habit score averaged across behaviors correlated with behavior change (McGowan et al., 2013 ; see also Gardner, Sheals, Wardle, & McGowan, 2014 ).
In one RCT, fruit and vegetable consumption changes were compared between participants who received habit-based messages, and those receiving general, non-habit-based tips for increasing consumption or messages about healthy eating more broadly (Rompotis et al., 2014 ). Notably, habit-based messages focused on anticipating stimulus control and environmental modification and on eating the same fruits and vegetables at the same time each day, so targeting both habitual instigation and execution (see Phillips & Gardner, 2016 ). The intervention was delivered via SMS in one set of conditions and email in the other. At 8-weeks post-intervention, both intervention groups (SMS n = 26, email n = 30) had increased fruit consumption and fruit habit strength, but those in all other conditions had not (SMS fruit and vegetable tips, n = 24, SMS healthy eating tips, n = 23; email fruit and vegetable tips, n = 29, email healthy eating n = 29). No effects were found on vegetable consumption or habit.
Oral Hygiene
Two school-based interventions aimed to increase tooth brushing in primary school children. One involved weekly dental hygiene lessons and daily tooth brushing practice time (Gaeta, Cavazos, Cabrera, & Rosário, 2018 ). School visits were also made by health promoters, and a seminar was held for teachers. One control group ( n = 52) received the visits and seminar only, and a second control group ( n = 52) received the seminar only. A quasi-experiment showed that children in the habit-based intervention ( n = 106) and visits-and-seminar control group had less dental plaque, and a stronger tooth brushing habit at 12-week follow-up than did the seminar-only control group. The habit-based intervention group had the lowest plaque.
Wind et al.’s ( 2005 ) intervention also involved allocation of a designated tooth brushing time during the school day and encouragement from teachers. Tooth brushing rates increased in the intervention group ( n = 141) during treatment but not in the control group (the nature of which could not be identified from the published report; n = 155). There were no differences in behavior at 12-months post-intervention nor in habit at any follow-up.
Food Safety
An intervention promoted the microwaving of dishcloths or sponges, for hygiene reasons (Mullan, Allom, Fayn, & Johnston, 2014 ). Recipients received emails and a poster providing instructions on how and why to microwave the dishcloths and sponges, designed to be placed in kitchens to act as a cue to the action. In an RCT, one intervention group was instructed to self-monitor their action, for intervention purposes, every 3 days ( n = 15) and another every 5 days ( n = 17). Relative to those who received an unrelated control treatment ( n = 13), frequency and habit strength increased in the two intervention groups at 3 weeks and was sustained to the final 6-week follow-up.
Behavior Change Techniques Used in Previous Interventions
A total of 32 discrete behavior change techniques were each identified in at least one of the 15 interventions (see Table 1 and Table 2 ). Aside from context-dependent repetition itself—which, as an inclusion criterion, was necessarily present in all interventions—the most commonly used were “use prompts and cues” (present in 11 interventions; 73%), “action planning” (8 interventions; 53%), “provide instruction on how to perform the behavior” (8 interventions; 53%), “set behavioral goals” (8 interventions; 53%), and “self-monitor behavior” (7 interventions; 47%). Also common were “behavioral practice or rehearsal” (6 interventions; 40%), “provide information on health consequences” (6 interventions; 40%), and “problem solving” (5 interventions; 33%). “Behavioral substitution” and habit substitution (labeled “habit reversal” in the taxonomy) were each used in 4 interventions (27%).
Table 1. Behavior Change Techniques Identified in 15 Habit Formation Interventions
Note . With the exception of “context-dependent repetition,” all technique labels are taken from the BCT Taxonomy v1 (Michie et al., 2013 ).
* This technique is labeled “habit formation” in the BCT Taxonomy v1 (Michie et al., 2013 ). Rephrasing this as “context-dependent repetition” more clearly delineates the underlying technique (i.e., to consistently repeat behavior in an unvarying context) from the outcome that it is designed to serve (i.e., to form habit). It also better acknowledges the possibility that such repetition may not lead to the formation of habit. For example, Lally et al. ( 2010 ) observed some participants who failed to attain peak habit strength in an 84-day study period, and some who experienced gains that peaked at low levels, suggesting that while repetition had rendered the behavior more habitual, the action remained predominantly regulated by conscious motivation rather than habit.
Table 2. Behavior Change Techniques Documented in 15 Habit Formation Interventions
Note . All technique labels are taken from the BCT Taxonomy v1 (Michie et al., 2013 ).
While all 15 interventions were based on the principle of habit formation, none used context-dependent repetition as a standalone technique. 2 The use of techniques additional to repetition echoes the view that in the real world, habit is best promoted by embedding context-dependent repetition into a broader package of techniques that also target motivation and action control, which are prerequisites for repetition (Lally & Gardner, 2013 ). Techniques most commonly adopted in past interventions have focused predominantly on action control (e.g., planning, goal-setting, identifying cues, rehearsing action, problem solving). The relative paucity of techniques targeting motivation may reflect an assumption that, for most of the behaviors targeted, intervention recipients generally recognize the value of behavior change, but lack the volitional skills, opportunities, or resources to change. Whether motivation should be targeted as part of a habit-formation intervention will depend on whether target populations understand the need for change and prioritize the target behavior above alternatives.
Fewer than half of the 15 interventions appear to have addressed factors that may moderate the relationship between repetition and habit development. Theory and evidence suggest that the mental associations that underlie habit will develop most strongly or quickly where actions are more simple or intrinsically rewarding and in response to cues that are salient and consistently encountered (Lally & Gardner, 2013 ; McDaniel & Einstein, 1993 ; Radel et al., 2017 ). Several of the reviewed interventions purposively promoted habit formation for simple behaviors (Beeken et al., 2017 ; Fleig et al., 2016 ; Lally et al., 2010 , 2011 ; Matei et al., 2015 ; Mullan et al., 2014 ; White et al., 2017 ). Kaushal et al. ( 2017 ) emphasized the importance of intrinsic reward in their physical activity promotion intervention, and Fournier et al. ( 2017 ) targeted intrinsic motivation. These studies highlight how interventions may move beyond simply promoting repetition toward targeting factors that may reduce the number of repetitions required for a target behavior to become habitual.
How Should Habit-Based Interventions Be Evaluated?
Previous interventions attest to the potential for habit-based approaches to change behavior. Although many intervention studies were not designed to test effectiveness, 13 of the 15 interventions were associated with positive change on at least one index of behavior or behavior-contingent outcomes (e.g., weight loss) at one or more follow-ups. Process evaluations pointed to the strengthening of habit as a key mechanism underpinning behavioral change based on increases in self-reported automaticity scores or qualitative reflections on the subjective experience of automaticity (Fleig et al., 2016 ; Gardner, Sheals, et al., 2014 ; Kliemann et al., 2017 ; Lally et al., 2011 ; Matei et al., 2015 ). Additionally, acceptability studies have suggested that recipients find the concept of context-dependent repetition—which distinguishes habit-based and non-habit-based interventions—easy to understand and follow (Fleig et al., 2016 ; Gardner, Sheals, et al., 2014 ; Lally et al., 2011 ; Matei et al., 2015 ).
Limitations of evaluation methods preclude understanding of how best to support habit formation. It is not yet clear whether promotion of context-dependent repetition is necessary for habit to develop or, indeed, whether it represents the most “active” ingredient of a habit formation intervention. One study found that a control group that did not receive habit-based advice reported similar physical activity habit gains to those among a group that received habit guidance (White et al., 2017 ). Conversely, another study showed that intervention recipients deviated from habit-based advice (e.g., by setting goals that were not specific, measurable, or achievable), yet habit strengthened (Gardner, Sheals, et al., 2014 ). Habit formation may therefore arise as a byproduct of interventions that do not explicitly target habit development. The unique contribution of context-dependent repetition to behavior change remains unclear because none of the reviewed studies compared a habit-based intervention with an otherwise identical non-habit-based equivalent. Indeed, most studies have evaluated habit formation interventions against minimal-treatment control groups or used uncontrolled designs. Future research should seek to compare matched habit- and non-habit-based interventions or otherwise use factorial designs, which allow testing for isolated effects within a multicomponent intervention, or mediation analyses, which can assess whether habit change underpins intervention effects.
Intervention evaluations have also been limited by short follow-up periods, which is ironic given that the key purported benefit of incorporating habit formation into interventions is the potential to increase longevity of behavior change. Few studies evaluated outcomes over 12 months or longer, with the longest observed follow-up being 24 months (Beeken et al., 2017 ). Beeken et al.’s ( 2017 ) “Ten Top Tips” intervention showed greater impact than did a non-habit-based usual-care treatment on dietary and physical activity habits, and weight loss, at the 3-month follow-up, which the authors found to be due in part to habit development (Kliemann et al., 2017 ). Yet, while weight loss was maintained at 24 months, the advantage conferred by the habit-based intervention over usual care was lost, suggesting that any habit gains may have dissipated, or alternatively, that for those who were successful in maintaining the behaviors over the 2-year period, habit formation had occurred regardless of condition. These possibilities cannot be investigated because habit strength was not evaluated at 24 months. Elsewhere, however, a small exploratory (non-intervention) study suggested that habit gains may erode over time: Among a group of participants forming dental flossing habits over 8 weeks, habit strength had considerably eroded in the subgroup of participants who provided data at a 6-month follow-up (Judah et al., 2013 ). Until more is done to assess the longevity of habit-based intervention effects, the hypothesis that habit persists over time, and so supports behavior maintenance, remains insufficiently tested.
Theory proposes that, through consistent performance, behaviors become habitual such that they are initiated automatically upon encountering cues via the activation of learned context-behavior associations. Habitual behaviors are thought to be self-sustaining, and so forming a habit has been proposed as a means to promote long-term maintenance of behavior. Interventions that seek to promote habit formation should include not only advice on context-dependent repetition, but also techniques that support the motivation and action control needed to repeat the action and that may enhance the reinforcing value of repetition on habit development. Fifteen interventions were found to have used habit formation principles to encourage engagement in health-promoting behaviors, and these have tended to supplement advice on repetition with action control techniques. Previous research suggests a habit-based approach has much to offer to behavior change initiatives; habit formation offers an acceptable, easily understood intervention strategy, with the potential to change behavior and yield favorable health outcomes. Yet, the unique effects of habit-specific techniques, and the longevity of effects, have not been adequately explored. The central assumption of the habit-based approach—that habit gains translate into long-term behavior maintenance—remains largely untested.
- Aarts, H. , Paulussen, T. , & Schaalma, H. (1997). Physical exercise habit: On the conceptualization and formation of habitual health behaviors. Health Education Research , 12 (3), 363–374.
- Adriaanse, M. A. , Gollwitzer, P. M. , De Ridder, D. T. D. , De Wit, J. B. F. , & Kroese, F. M. (2011). Breaking habits with implementation intentions: A test of underlying processes . Personality and Social Psychology Bulletin , 37 (4), 502–513.
- Adams, C. D. (1982). Variations in the sensitivity of instrumental responding to reinforcer devaluation . Quarterly Journal of Experimental Psychology B: Comparative and Physiological Psychology , 34B (2), 77–98.
- Adriaanse, M. A. , Kroese, F. M. , Gillebaart, M. , & De Ridder, D. T. (2014). Effortless inhibition: Habit mediates the relation between self-control and unhealthy snack consumption. Frontiers in Psychology , 5 , 444.
- Adriaanse, M. A. , van Oosten, J. M. F. , de Ridder, D. T. D. , de Wit, J. B. F. , & Evers, C. (2011). Planning what not to eat: Ironic effects of implementation intentions negating unhealthy habits. Personality and Social Psychology Bulletin , 37 , 69–81.
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes , 50 (2), 179–211.
- Armitage, C. J. (2005). Can the theory of planned behavior predict the maintenance of physical activity? Health Psychology , 24 (3), 235–245.
- Armitage, C. J. (2016). Evidence that implementation intentions can overcome the effects of smoking habits . Health Psychology , 35 (9), 935–943.
- Aune, D. , Giovannucci, E. , Boffetta, P. , Fadnes, L. T. , Keum, N. , Norat, T. , . . . Tonstad, S. (2017). Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality: A systematic review and dose-response meta-analysis of prospective studies . International Journal of Epidemiology , 46 (3), 1029–1056.
- Aunger, R. , Schmidt, W.-P. , Ranpura, A. , Coombes, Y. , Maina, P. M. , Matiko, C. N. , & Curtis, V. (2010). Three kinds of psychological determinants for hand-washing behavior in Kenya . Social Science & Medicine , 70 (3), 383–391.
- Balleine, B. W. , & O’Doherty, J. (2010). Human and rodent homologies in action control: Corticostriatal determinants of goal-directed and habitual action . Neuropsychopharmacology Reviews , 35 , 48–69.
- Bandura, A. (2001). Social cognitive theory: An agentic perspective. Annual Review of Psychology , 52 (1), 1–26.
- Bayley, P. J. , Frascino, J. C. , & Squire, L. R. (2005). Robust habit learning in the absence of awareness and independent of the medial temporal lobe . Nature , 436 (7050), 550–553.
- Beeken, R. J. , Croker, H. , Morris, S. , Leurent, B. , Omar, R. , Nazareth, I. , & Wardle, J. (2012). Study protocol for the 10 Top Tips (10TT) trial: Randomised controlled trial of habit-based advice for weight control in general practice . BMC Public Health , 12 (1), 667.
- Beeken, R. J. , Leurent, B. , Vickerstaff, V. , Wilson, R. , Croker, H. , Morris, S. , . . . Wardle, J. (2017). A brief intervention for weight control based on habit-formation theory delivered through primary care: Results from a randomised controlled trial . International Journal of Obesity , 41 (2), 246–254.
- Bouton, M. E. (2000). A learning theory perspective on lapse, relapse, and the maintenance of behavior change. Health Psychology , 19 (1S), 57–63.
- Carels, R. A. , Burmeister, J. M. , Koball, A. M. , Oehlhof, M. W. , Hinman, N. , LeRoy, M. , . . . Darby, L. A. (2014). A randomized trial comparing two approaches to weight loss: Differences in weight loss maintenance. Journal of Health Psychology , 19 (2), 296–311.
- Carels, R. A. , Young, K. M. , Koball, A. M. , Gumble, A. , Darby, L.A. , . . . Hinman, N. (2011). Transforming your life: An environmental modification approach to weight loss . Journal of Health Psychology , 16 , 430–438.
- Centers for Disease Control and Prevention . (2014). Physical activity . Atlanta, GA: U.S. Department of Health & Human Services.
- Clemson, L. , Singh, M. A. F. , Bundy, A. , Cumming, R. G. , Manollaras, K. , O’Loughlin, P. , & Black, D. (2012). Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): Randomised parallel trial . BMJ , 345 , e4547.
- Cooper, R. , & Shallice, T. (2000). Contention scheduling and the control of routine activities . Cognitive Neuropsychology , 17 (4), 297–338.
- Danner, U. N. , Aarts, H. , & de Vries, N. K. (2008). Habit vs. intention in the prediction of future behavior: The role of frequency, context stability and mental accessibility of past behavior . British Journal of Social Psychology , 47 (2), 245–265.
- de Wit, S. , & Dickinson, A. (2009). Associative theories of goal-directed behavior: A case for animal–human translational models. Psychological Research , 73 (4), 463–476.
- Dombrowski, S. U. , Knittle, K. , Avenell, A. , Araujo-Soares, V. , & Sniehotta, F. F. (2014). Long-term maintenance of weight loss with non-surgical interventions in obese adults: Systematic review and meta-analyses of randomised controlled trials . BMJ , 348 , g2646.
- Erikssen, G. , Liestøl, K. , Bjørnholt, J. , Thaulow, E. , Sandvik, L. , & Erikssen, J. (1998). Changes in physical fitness and changes in mortality . The Lancet , 352 (9130), 759–762.
- Fleig, L. , McAllister, M. M. , Chen, P. , Iverson, J. , Milne, K. , McKay, H. A. , . . . Ashe, M. C. (2016). Health behavior change theory meets falls prevention: Feasibility of a habit-based balance and strength exercise intervention for older adults . Psychology of Sport and Exercise , 22 , 114–122.
- Fournier, M. , d’Arripe-Longueville, F. , Rovere, C. , Easthope, C. S. , Schwabe, L. , El Methni, J. , & Radel, R. (2017). Effects of circadian cortisol on the development of a health habit. Health Psychology , 36 (11), 1059–1064.
- Gaeta, M. L. , Cavazos, J. , Cabrera, M. del R. , & Rosário, P. (2018). Fostering oral hygiene habits and self-regulation skills: An intervention with preschool children . Family & Community Health , 41 (1), 47–54.
- Galla, B. M. , & Duckworth, A. L. (2015). More than resisting temptation: Beneficial habits mediate the relationship between self-control and positive life outcomes . Journal of Personality and Social Psychology , 109 (3), 508–525.
- Gardner, B. (2015). A review and analysis of the use of “habit” in understanding, predicting and influencing health-related behavior . Health Psychology Review , 9 (3), 277–295.
- Gardner, B. , Abraham, C. , Lally, P. , & de Bruijn, G.-J. (2012). Towards parsimony in habit measurement: Testing the convergent and predictive validity of an automaticity subscale of the self-report habit index . International Journal of Behavioral Nutrition and Physical Activity , 9 (1), 102–113.
- Gardner, B. , de Bruijn, G.-J. , & Lally, P. (2011). A systematic review and meta-analysis of applications of the self-report habit index to nutrition and physical activity behaviors. Annals of Behavioral Medicine , 42 (2), 174–187.
- Gardner, B. , & Lally, P. (2019). Modeling habit formation and its determinants. In B. Verplanken (Ed.), The psychology of habit (pp. 207–229). New York, NY: Springer.
- Gardner, B. , Lally, P. , & Wardle, J. (2012). Making health habitual: The psychology of “habit-formation” and general practice . British Journal of General Practice , 62 (605), 664–666.
- Gardner, B. , Phillips, L. A. , & Judah, G. (2016). Habitual instigation and habitual execution: Definition, measurement, and effects on behavior frequency . British Journal of Health Psychology , 21 (3), 613–630.
- Gardner, B. , Sheals, K. , Wardle, J. , & McGowan, L. (2014). Putting habit into practice, and practice into habit: A process evaluation and exploration of the acceptability of a habit-based dietary behavior change intervention . International Journal of Behavioral Nutrition and Physical Activity , 11 (1), 135.
- Gardner, B. , Thune-Boyle, I. , Iliffe, S. , Fox, K. R. , Jefferis, B. J. , Hamer, M. , . . . Wardle, J. (2014). “On Your Feet to Earn Your Seat,” a habit-based intervention to reduce sedentary behavior in older adults: Study protocol for a randomized controlled trial . Trials , 15 , 368.
- Gollwitzer, P. M. (1999). Implementation intentions: Strong effects of simple plans. American Psychologist , 54 (7), 493.
- Hall, P. A. , & Fong, G. T. (2007). Temporal self-regulation theory: A model for individual health behavior . Health Psychology Review , 1 (1), 6–52.
- Harper, D. M. , Franco, E. L. , Wheeler, C. , Ferris, D. G. , Jenkins, D. , Schuind, A. , . . . De Carvalho, N. S. (2004). Efficacy of a bivalent L1 virus-like particle vaccine in prevention of infection with human papillomavirus types 16 and 18 in young women: A randomised controlled trial . The Lancet , 364 (9447), 1757–1765.
- Hoo, Z. H. , Boote, J. , Wildman, M. J. , Campbell, M. J. , & Gardner, B. (2017). Determinants of objective adherence to nebulised medications among adults with cystic fibrosis: An exploratory mixed methods study comparing low and high adherers . Health Psychology and Behavioral Medicine , 5 (1), 299–316.
- Hull, C. L. (1943). Principles of behavior: An introduction to behavior theory . New York, NY: Appleton-Century-Crofts.
- Ji, M. F. , & Wood, W. (2007). Purchase and consumption habits: Not necessarily what you intend . Journal of Consumer Psychology , 17 (4), 261–276.
- Judah, G. , Gardner, B. , & Aunger, R. (2013). Forming a flossing habit: An exploratory study of the psychological determinants of habit formation. British Journal of Health Psychology , 18 (2), 338–353.
- Kaushal, N. , Rhodes, R. E. , Meldrum, J. T. , & Spence, J. C. (2017). The role of habit in different phases of exercise . British Journal of Health Psychology , 22 (3), 429–448.
- Kliemann, N. , Vickerstaff, V. , Croker, H. , Johnson, F. , Nazareth, I. , & Beeken, R. J. (2017). The role of self-regulatory skills and automaticity on the effectiveness of a brief weight loss habit-based intervention: Secondary analysis of the 10 top tips randomised trial . International Journal of Behavioral Nutrition and Physical Activity , 14 , 119.
- Kuhl, J. (1984). Volitional aspects of achievement motivation and learned helplessness: Toward a comprehensive theory of action control. In B. A. Maher & W. A. Maher (Eds.), Progress in experimental personality research (Vol. 13, pp. 99–171). New York, NY: Academic Press.
- Kurz, T. , Gardner, B. , Verplanken, B. , & Abraham, C. (2014). Habitual behaviors or patterns of practice? Explaining and changing repetitive climate-relevant actions . WIRES Climate Change , 6 , 113–128.
- Lally, P. , Chipperfield, A. , & Wardle, J. (2008). Healthy habits: Efficacy of simple advice on weight control based on a habit-formation model . International Journal of Obesity , 32 (4), 700–707.
- Lally, P. , & Gardner, B. (2013). Promoting habit formation. Health Psychology Review , 7 (Suppl. 1), S137–S158.
- Lally, P. , Van Jaarsveld, C. H. , Potts, H. W. , & Wardle, J. (2010). How are habits formed: Modelling habit formation in the real world . European Journal of Social Psychology , 40 (6), 998–1009.
- Lally, P. , Wardle, J. , & Gardner, B. (2011). Experiences of habit formation: A qualitative study. Psychology, Health & Medicine , 16 (4), 484–489.
- LaRose, R. (2010). The problem of media habits . Communication Theory , 20 , 194–222.
- Luo, Y. , Lee, B. , Wohn, D. Y. , Rebar, A. L. , Conroy, D. E. , & Choe, E. K. (2018, April). Time for break: Understanding information workers’ behavior through a break prompting system . Paper presented at the 2018 CHI Conference on Human Factors in Computing Systems, Montreal, Canada.
- Maddux, J. E. (1997). Habit, health and happiness. Journal of Sport & Exercise Psychology , 19 (4), 331–346.
- Marien, H. , Custers, R. , & Aarts, H. (2019). Understanding the formation of human habits: An analysis of mechanisms of habitual behavior. In B. Verplanken (Ed.), The psychology of habit (pp. 51–69), New York, NY: Springer.
- Matei, R. , Thuné-Boyle, I. , Hamer, M. , Iliffe, S. , Fox, K. R. , Jefferis, B. J. , & Gardner, B. (2015). Acceptability of a theory-based sedentary behavior reduction intervention for older adults (“On Your Feet to Earn Your Seat”) . BMC Public Health , 15 (1), 606.
- McDaniel, M. A. , & Einstein, G. O. (1993). The importance of cue familiarity and cue distinctiveness in prospective memory . Memory , 1 (1), 23–41.
- McGowan, L. , Cooke, L. J. , Gardner, B. , Beeken, R. J. , Croker, H. , & Wardle, J. (2013). Healthy feeding habits: Efficacy results from a cluster-randomized, controlled exploratory trial of a novel, habit-based intervention with parents . The American Journal of Clinical Nutrition , 98 (3), 769–777.
- Michie, S. , Richardson, M. , Johnston, M. , Abraham, C. , Francis, J. , Hardeman, W. , . . . Wood, C. E. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine , 46 (1), 81–95.
- Michie, S. , Van Stralen, M. M. , & West, R. (2011). The behavior change wheel: A new method for characterising and designing behavior change interventions . Implementation Science , 6 (1), 42–53.
- Mullan, B. , Allom, V. , Fayn, K. , & Johnston, I. (2014). Building habit strength: A pilot intervention designed to improve food-safety behavior . Food Research International , 66 , 274–278.
- Neal, D. T. , Wood, W. , Labrecque, J. S. , & Lally, P. (2012). How do habits guide behavior? Perceived and actual triggers of habits in daily life . Journal of Experimental Social Psychology , 48 (2), 492–498.
- Neal, D. T. , Wood, W. , Wu, M. , & Kurlander, D. (2011). The pull of the past: When do habits persist despite conflict with motives? Personality and Social Psychology Bulletin , 37 (11), 1428–1437.
- Orbell, S. , & Verplanken, B. (2010). The automatic component of habit in health behavior: Habit as cue-contingent automaticity. Health Psychology , 29 (4), 374–383.
- Ouellette, J. A. , & Wood, W. (1998). Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychological Bulletin , 124 (1), 54–74.
- Pedersen, S. J. , Cooley, P. D. , & Mainsbridge, C. (2014). An e-health intervention designed to increase workday energy expenditure by reducing prolonged occupational sitting habits . Work , 49 (2), 289–295.
- Phillips, L. A. , & Gardner, B. (2016). Habitual exercise instigation (vs. execution) predicts healthy adults’ exercise frequency . Health Psychology , 35 (1), 69–77.
- Prochaska, J. O. , & DiClemente, C. C. (1986). Toward a comprehensive model of change. In W. Miller & N. Heather (Eds.), Treating addictive behavior (pp. 3–27). New York, NY: Plenum.
- Quinn, J. M. , Pascoe, A. , Wood, W. , & Neal, D. T. (2010). Can’t control yourself? Monitor those bad habits. Personality and Social Psychology Bulletin , 36 (4), 499–511.
- Radel, R. , Pelletier, L. , Pjevac, D. , & Cheval, B. (2017). The links between self-determined motivations and behavioral automaticity in a variety of real-life behaviors. Motivation and Emotion , 41 (4), 443–454.
- Rebar, A. L. , Dimmock, J. A. , Jackson, B. , Rhodes, R. E. , Kates, A. , Starling, J. , & Vandelanotte, C. (2016). A systematic review of the effects of non-conscious regulatory processes in physical activity . Health Psychology Review , 10 (4), 395–407.
- Rebar, A. L. , Elavsky, S. , Maher, J. P. , Doerksen, S. E. , & Conroy, D. E. (2014). Habits predict physical activity on days when intentions are weak. Journal of Sport and Exercise Psychology , 36 (2), 157–165.
- Rebar, A. L. , Stanton, R. , Geard, D. , Short, C. , Duncan, M. J. , & Vandelanotte, C. (2015). A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations . Health Psychology Review , 9 (3), 366–378.
- Rhodes, R. E. , & de Bruijn, G.-J. (2013). What predicts intention-behavior discordance? A review of the action control framework. Exercise and Sport Sciences Reviews , 41 (4), 201–207.
- Rhodes, R. E. , & Rebar, A. L. (2019). Physical activity habit: Complexities and controversies. In B. Verplanken (Ed.), The psychology of habit (pp. 91–109). New York, NY: Springer.
- Rogers, R. W. (1983). Cognitive and physiological processes in fear appeals and attitude change: A revised theory of protection motivation. In B. L. Cacioppo & L. L. Petty (Eds.), Social psychophysiology: A sourcebook . London, U.K.: Guilford Press.
- Rompotis, C. J. , Grove, J. R. , & Byrne, S. M. (2014). Benefits of habit-based informational interventions: A randomised controlled trial of fruit and vegetable consumption . Australian and New Zealand Journal of Public Health , 38 (3), 247–252.
- Rothman, A. J. (2000). Toward a theory-based analysis of behavioral maintenance . Health Psychology , 19 (1S), S64–S69.
- Rothman, A. J. , Sheeran, P. , & Wood, W. (2009). Reflective and automatic processes in the initiation and maintenance of dietary change. Annals of Behavioral Medicine , 38 (Suppl. 1), s4–s17.
- Schwarzer, R. , Lippke, S. , & Luszczynska, A. (2011). Mechanisms of health behavior change in persons with chronic illness or disability: The Health Action Process Approach (HAPA) . Rehabilitation Psychology , 56 (3), 161–170.
- Simpson, S. A. , McNamara, R. , Shaw, C. , Kelson, M. , Moriarty, Y. , Randell, E. , . . . Duncan, D. (2015). A feasibility randomised controlled trial of a motivational interviewing-based intervention for weight loss maintenance in adults . Health Technology Assessment , 19 (50).
- Skinner, B. F. (1938). The behavior of organisms: An experimental analysis . New York, NY: Appleton-Century-Crofts.
- Storm, V. , Dörenkämper, J. , Reinwand, D. A. , Wienert, J. , De Vries, H. , & Lippke, S. (2016). Effectiveness of a web-based computer-tailored multiple-lifestyle intervention for people interested in reducing their cardiovascular risk: A randomized controlled trial . Journal of Medical Internet Research , 18 (4), e78.
- Strack, F. , & Deutsch, R. (2004). Reflective and impulsive determinants of social behavior . Personality and Social Psychology Review , 8 (3), 220–247.
- Thorndike, E. L. (1911). Animal intelligence (2nd ed.). New York, NY: Hafner.
- Tolman, E. C. (1932). Purposive behavior in animals and men . New York, NY: Appleton-Century-Crofts.
- Triandis, H. C. (1980). Values, attitudes, and interpersonal behavior. In Nebraska symposium on motivation (Vol. 27, pp. 195–259). Lincoln: University of Nebraska Press.
- Vallacher, R. R. , & Wegner, D. M. (1987). What do people think they’re doing? Action identification and human behavior. Psychological Review , 94 (1), 3–15.
- Verplanken, B. , Aarts, H. , Knippenberg, A. , & Moonen, A. (1998). Habit versus planned behavior: A field experiment. British Journal of Social Psychology , 37 (1), 111–128.
- Verplanken, B. , Aarts, H. , & Van Knippenberg, A. (1997). Habit, information acquisition, and the process of making travel mode choices. European Journal of Social Psychology , 27 (5), 539–560.
- Verplanken, B. , & Orbell, S. (2003). Reflections on past behavior: A self-report index of habit strength . Journal of Applied Social Psychology , 33 (6), 1313–1330.
- Verplanken, B. , & Roy, D. (2016). Empowering interventions to promote sustained lifestyles: Testing the habit discontinuity hypothesis in a field experiment . Journal of Environmental Psychology , 45 , 127–134.
- Verplanken, B. , & Wood, W. (2006). Interventions to break and create consumer habits . Journal of Public Policy & Marketing , 25 (1), 90–103.
- Walker, I. , Thomas, G. O. , & Verplanken, B. (2015). Old habits die hard: Travel habit formation and decay during an office relocation. Environment and Behavior , 47 (10), 1089–1106.
- Webb, T. L. , & Sheeran, P. (2006). Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin , 132 , 249–268.
- Webb, T. L. , Sheeran, P. , & Luszczynska, A. (2009). Planning to break unwanted habits: Habit strength moderates implementation intention effects on behavior change. British Journal of Social Psychology , 48 (3), 507–523.
- White, I. , Smith, L. , Aggio, D. , Shankar, S. , Begum, S. , Matei, R. , . . . Jefferis, B. J. (2017). On Your Feet to Earn Your Seat: Pilot RCT of a theory-based sedentary behavior reduction intervention for older adults . Pilot and Feasibility Studies , 3 (1), 23.
- Wind, M. , Kremers, S. , Thijs, C. , & Brug, J. (2005). Toothbrushing at school: Effects on toothbrushing behavior, cognitions and habit strength . Health Education , 105 (1), 53–61.
- Wood, W. , Labrecque, J. S. , Lin, P.-Y. , & Rünger, D. (2014). Habits in dual process models. In J. W. Sherman , B. Gawronski , & Y. Trope (Eds.), Dual process theories of the social mind (pp. 371–385). New York, NY: Guilford Press.
- Wood, W. , & Neal, D. T. (2007). A new look at habits and the habit-goal interface . Psychological Review , 114 (4), 843–863.
- Wood, W. , & Rünger, D. (2016). Psychology of habit. Annual Review of Psychology , 67 , 289–314.
- World Health Organization . (2015). Global status report on road safety 2015 . Geneva, Switzerland: World Health Organization.
- World Health Organization . (2017). Global health observatory data . Geneva, Switzerland: World Health Organization.
1. Rhodes and colleagues have extended this line of thinking by incorporating preparatory actions into the process, showing that habitual preparation for an activity (e.g., packing a gym bag) can influence frequency of engagement in the focal behavior (in this case, exercise; Kaushal, Rhodes, Meldrum, & Spence, 2017 ). However, this differs from the instigation–execution distinction in that it focuses on the role of habit in different behaviors (preparatory actions vs. focal actions) rather than different roles of habit in the same behavior.
2. This is perhaps inevitable given the present review criteria, which excluded studies that used context-dependent repetition to study the habit formation process itself. However, real-world studies of the formation of health habits have not been based on context-dependent repetition alone; both Lally et al. ( 2010 ) and Fournier et al. ( 2017 ) instructed participants to use prompts and cues and set action plans or implementation intentions (see also Judah et al., 2013 ).
Related Articles
- Methods of Health Behavior Change
- Theoretical Approaches to Physical Activity Promotion
- Use of Wearable Activity Trackers for Physical Activity Promotion
Printed from Oxford Research Encyclopedias, Psychology. Under the terms of the licence agreement, an individual user may print out a single article for personal use (for details see Privacy Policy and Legal Notice).
date: 17 May 2024
- Cookie Policy
- Privacy Policy
- Legal Notice
- Accessibility
- [66.249.64.20|81.177.182.159]
- 81.177.182.159
Character limit 500 /500
Search Icon
Events See all →
Hands on history.

10:00 a.m. - 2:30 p.m.
Penn Museum, 3260 South St.
268th Commencement

Franklin Field
Vahe Sarkissian

World Cafe Live, 3025 Walnut St.
Wawa Welcome America Day
10:00 a.m. - 5:00 p.m.
Arts, Humanities, & Social Sciences
What predicts human behavior and how to change it
In the largest quantitative synthesis to date, dolores albarracín and her team dig through years of research on the science behind behavior change to determine the best ways to promote changes in behavior..
Pandemics, global warming, and rampant gun violence are all clear lessons in the need to move large groups of people to change their behavior. When a crisis hits, researchers, policymakers, health officials, and community leaders have to know how best to encourage people to change en masse and quickly. Each crisis leads to rehashing the same strategies, even those that have not worked in the past, due to the lack of definitive science of what interventions work across the board combined with well intended but erroneous intuitions.

To produce evidence on what determines and changes behavior, Dolores Albarracín and her colleagues from Penn’s Social Action Lab undertook a review of all of the available meta-analyses—a synthesis of the results from multiple studies—to determine what interventions work best when trying to change people’s behavior. What results is a new classification of predictors of behavior and a novel, empirical model for understanding the different ways to change behavior by targeting either individual or social/structural factors.
A new paper published in Nature Reviews Psychology reports that the strategies that people assume will work—like giving people accurate information or trying to change their beliefs—do not. At the same time, others like providing social support and tapping into individuals’ behavioral skills and habits as well as removing practical obstacles to behavior (e.g., providing health insurance to encourage health behaviors) can have more sizable impacts.
“Interventions targeting knowledge, general attitudes, beliefs, administrative and legal sanctions, and trustworthiness—these factors researchers and policymakers put so much weight on—are actually quite ineffective,” says Albarracín, the Alexandra Heyman Nash University Professor in the Annenberg School for Communication and director of the Science of Science Communication Division of the Annenberg Public Policy Center, who also has an appointment in Penn’s School of Arts & Sciences. “They have negligible effects.”
Unfortunately, many policies and reports are centered around goals like increasing vaccine confidence (an attitude) or curbing misinformation. Policymakers must look at evidence to determine what factors will return the investment, Albarracín says.
Co-author Javier Granados Samayoa, the Vartan Gregorian Postdoctoral Fellow at the Annenberg Public Policy Center , has noticed researchers’ tendency to target knowledge and beliefs when creating behavior change interventions.
“There’s something about it that seems so straightforward—you think and therefore you do. But what the literature suggests is that there are a lot of intervening processes that have to line up for people to actually act on those beliefs, so it’s not that easy,” he says.
Read more at Annenberg School for Communication.
Class of 2025 relishes time together at Hey Day

Picturing artistic pursuits
Hundreds of undergraduates take classes in the fine arts each semester, among them painting and drawing, ceramics and sculpture, printmaking and animation, photography and videography. The courses, through the School of Arts & Sciences and the Stuart Weitzman School of Design, give students the opportunity to immerse themselves in an art form in a collaborative way.

Campus & Community
Penn celebrates operation and benefits of largest solar power project in Pennsylvania
Solar production has begun at the Great Cove I and II facilities in central Pennsylvania, the equivalent of powering 70% of the electricity demand from Penn’s academic campus and health system in the Philadelphia area.

Education, Business, & Law
Investing in future teachers and educational leaders
The Empowerment Through Education Scholarship Program at Penn’s Graduate School of Education is helping to prepare and retain teachers and educational leaders.

‘The Illuminated Body’ fuses color, light, and sound
A new Arthur Ross Gallery exhibition of work by artist Barbara Earl Thomas features cut-paper portraits reminiscent of stained glass and an immersive installation constructed with intricately cut material lit from behind.

IMAGES
VIDEO
COMMENTS
Personal hygiene and social participation have traditionally fostered health in diverse ways. Keeping one's body clean to thwart illnesses and avoid infections is imperative. Cleaning hands, brushing teeth, cleaning cutlery helps in preventing infections. One should strive to avoid the appearance of microbes in the body.
The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46 (1), 81-95. doi: 10.1007/s12160-013-9486-6 [Google Scholar] Miller AL, Lo S, Bauer KW, & Fredericks EM (2020).
The local, state and national, government has many roles and responsibilities in health and behavior change (Altman, 2001). An effective public health system that can assure the nation's health requires the collaborative efforts of a complex network of people and organizations in the public and private sectors, as well as an alignment of policy and practice of governmental public health ...
Effectively encouraging patients to change their health behavior is a critical skill for primary care physicians. Modifiable health behaviors contribute to an estimated 40 percent of deaths in the ...
Health behavior change is among the top recommendations for improving health and strengthening empowerment of patients with lifestyle-related chronic diseases, which constitute the largest part of the disease burden. An array of behavior change techniques (BCTs) have been developed to support behavior change initiation and maintenance.
The handbook incorporates theory- and evidence-based approaches to behavior change with chapters from leading theorists, researchers, and practitioners from multiple disciplines, including psychology, sociology, behavioral science, economics, and implementation science. Chapters are organized into three parts: (1) Theory and Behavior Change; (2 ...
Many health-promoting behaviours must be repeated over the long-term to have a meaningful impact on health. For example, successful management of long-term conditions relies on sustained medication adherence (Ho et al., Citation 2009).Conversely, lasting health effects of discontinuing previously ingrained, repetitive health-risk behaviours arise from maintaining cessation (Hill et al ...
INTRODUCTION. The primary practical purpose of research into behavior change is the development of interventions that will be effective, subject to other constraints such as affordability [1, 2].In doing so, one wants to be able to draw on research findings that identify behavior change techniques (BCTs) that, if enacted appropriately, are most likely to effect the desired change.
Abstract. An overview of theoretical constructs and mechanisms of health behavior change is provided, based on a self-regulation framework that makes a distinction between goal setting and goal pursuit. Risk perception, outcome expectancies, and task self-efficacy are seen as predisposing factors in the goal setting phase (motivational phase ...
Large-scale, sustained behavior change is needed to reduce the risk of, and to prepare for, future pandemics 4. The COVID-19 pandemic has shown that populations will adopt at least some of the ...
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers. ... Policy and practice of behavior change in health contexts; Behavior change technique development; Mechanisms of action of behavior change interventions;
In general, behavioral interventions use different ways of thinking, feeling, acting, or relating with others to stimulate a change in a person's behavior to promote their health and well-being. For example, a behavioral intervention could be aimed at modifying something about a person's living environment or diet, with the goal of ...
The present chapter will attempt to provide insights on emergence of biopsychosocial model, theories of behavior change, health communication, types of communication and steps in planning health communication intervention for behavior change. Though, health communication primarily revolves around social communication, its scope is wide and ...
There are many different models and theories which are developed and used to encourage people to change their health behaviour such as: 'The biopsychosocial model is the view that health and illness are produced by a combination of physical, psychological, and cultural factors'. (ENGEL, 1977). The biopsychosocial model indicates that there ...
New habits may help you look better and have more energy. The information below outlines four stages you may go through when changing your health habits or behavior. You will also find tips to help you improve your eating, physical activity habits, and overall health. The four stages of changing a health behavior are. contemplation. preparation.
'Setting a goal for health behavior change, however, is seldom sufficient for behavior change to actually occur.' Goals are mental representations of desired outcomes, 1 and goal setting is the process by which one identifies specific goals and determines how they will be achieved. 2 Because there are many ways in which one's health can be improved, identifying specific and actionable ...
Behavior change is our best hope in reducing problems such as preventable diseases, chronic illnesses, health disparities, violence, and death around the world. In this Age of Information, where society has shifted to an economy based on information computerization, gamification has become a prevalent force in promoting such changes.
753 Words. 4 Pages. Open Document. Behavior Change Plan Regina Martin This is a health behavioral change plan where I will prioritize the Seven Dimensions of Wellness as they rank in my current life and includes a rationale and details on why each category fell in particular spot when I rate it. The first dimension of health on my list is ...
Policies targeting health behaviors tend to focus on a single behavior, often finding that these behaviors are resistant to change. A health lifestyle approach instead views behaviors as occurring in sets and influencing each other, developing from deeply rooted identities arising from membership in social groups [ 14 ].
Research around the application of habit formation to health behavior change interventions is reviewed, drawn from two sources: extant theory and evidence regarding how habit forms, and previous interventions that have used habit formation principles and techniques to change behavior. ... Papers were eligible for review if they (a) were ...
To produce evidence on what determines and changes behavior, Dolores Albarracín and her colleagues from Penn's Social Action Lab undertook a review of all of the available meta-analyses—a synthesis of the results from multiple studies—to determine what interventions work best when trying to change people's behavior. What results is a new classification of predictors of behavior and a ...