How To Write a Critical Appraisal

A critical appraisal is an academic approach that refers to the systematic identification of strengths and weakness of a research article with the intent of evaluating the usefulness and validity of the work’s research findings. As with all essays, you need to be clear, concise, and logical in your presentation of arguments, analysis, and evaluation. However, in a critical appraisal there are some specific sections which need to be considered which will form the main basis of your work.

Structure of a Critical Appraisal
Introduction.
Your introduction should introduce the work to be appraised, and how you intend to proceed. In other words, you set out how you will be assessing the article and the criteria you will use. Focusing your introduction on these areas will ensure that your readers understand your purpose and are interested to read on. It needs to be clear that you are undertaking a scientific and literary dissection and examination of the indicated work to assess its validity and credibility, expressed in an interesting and motivational way.
Body of the Work
The body of the work should be separated into clear paragraphs that cover each section of the work and sub-sections for each point that is being covered. In all paragraphs your perspectives should be backed up with hard evidence from credible sources (fully cited and referenced at the end), and not be expressed as an opinion or your own personal point of view. Remember this is a critical appraisal and not a presentation of negative parts of the work.
When appraising the introduction of the article, you should ask yourself whether the article answers the main question it poses. Alongside this look at the date of publication, generally you want works to be within the past 5 years, unless they are seminal works which have strongly influenced subsequent developments in the field. Identify whether the journal in which the article was published is peer reviewed and importantly whether a hypothesis has been presented. Be objective, concise, and coherent in your presentation of this information.
Once you have appraised the introduction you can move onto the methods (or the body of the text if the work is not of a scientific or experimental nature). To effectively appraise the methods, you need to examine whether the approaches used to draw conclusions (i.e., the methodology) is appropriate for the research question, or overall topic. If not, indicate why not, in your appraisal, with evidence to back up your reasoning. Examine the sample population (if there is one), or the data gathered and evaluate whether it is appropriate, sufficient, and viable, before considering the data collection methods and survey instruments used. Are they fit for purpose? Do they meet the needs of the paper? Again, your arguments should be backed up by strong, viable sources that have credible foundations and origins.
One of the most significant areas of appraisal is the results and conclusions presented by the authors of the work. In the case of the results, you need to identify whether there are facts and figures presented to confirm findings, assess whether any statistical tests used are viable, reliable, and appropriate to the work conducted. In addition, whether they have been clearly explained and introduced during the work. In regard to the results presented by the authors you need to present evidence that they have been unbiased and objective, and if not, present evidence of how they have been biased. In this section you should also dissect the results and identify whether any statistical significance reported is accurate and whether the results presented and discussed align with any tables or figures presented.
The final element of the body text is the appraisal of the discussion and conclusion sections. In this case there is a need to identify whether the authors have drawn realistic conclusions from their available data, whether they have identified any clear limitations to their work and whether the conclusions they have drawn are the same as those you would have done had you been presented with the findings.
The conclusion of the appraisal should not introduce any new information but should be a concise summing up of the key points identified in the body text. The conclusion should be a condensation (or precis) of all that you have already written. The aim is bringing together the whole paper and state an opinion (based on evaluated evidence) of how valid and reliable the paper being appraised can be considered to be in the subject area. In all cases, you should reference and cite all sources used. To help you achieve a first class critical appraisal we have put together some key phrases that can help lift you work above that of others.
Key Phrases for a Critical Appraisal
- Whilst the title might suggest
- The focus of the work appears to be…
- The author challenges the notion that…
- The author makes the claim that…
- The article makes a strong contribution through…
- The approach provides the opportunity to…
- The authors consider…
- The argument is not entirely convincing because…
- However, whilst it can be agreed that… it should also be noted that…
- Several crucial questions are left unanswered…
- It would have been more appropriate to have stated that…
- This framework extends and increases…
- The authors correctly conclude that…
- The authors efforts can be considered as…
- Less convincing is the generalisation that…
- This appears to mislead readers indicating that…
- This research proves to be timely and particularly significant in the light of…
You may also like

- En español – ExME
- Em português – EME
Critical Appraisal: A Checklist
Posted on 6th September 2016 by Robert Will

Critical appraisal of scientific literature is a necessary skill for healthcare students. Students can be overwhelmed by the vastness of search results. Database searching is a skill in itself, but will not be covered in this blog. This blog assumes that you have found a relevant journal article to answer a clinical question. After selecting an article, you must be able to sit with the article and critically appraise it. Critical appraisal of a journal article is a literary and scientific systematic dissection in an attempt to assign merit to the conclusions of an article. Ideally, an article will be able to undergo scrutiny and retain its findings as valid.
The specific questions used to assess validity change slightly with different study designs and article types. However, in an attempt to provide a generalized checklist, no specific subtype of article has been chosen. Rather, the 20 questions below should be used as a quick reference to appraise any journal article. The first four checklist questions should be answered “Yes.” If any of the four questions are answered “no,” then you should return to your search and attempt to find an article that will meet these criteria.
Critical appraisal of…the Introduction
- Does the article attempt to answer the same question as your clinical question?
- Is the article recently published (within 5 years) or is it seminal (i.e. an earlier article but which has strongly influenced later developments)?
- Is the journal peer-reviewed?
- Do the authors present a hypothesis?
Critical appraisal of…the Methods
- Is the study design valid for your question?
- Are both inclusion and exclusion criteria described?
- Is there an attempt to limit bias in the selection of participant groups?
- Are there methodological protocols (i.e. blinding) used to limit other possible bias?
- Do the research methods limit the influence of confounding variables?
- Are the outcome measures valid for the health condition you are researching?
Critical appraisal of…the Results
- Is there a table that describes the subjects’ demographics?
- Are the baseline demographics between groups similar?
- Are the subjects generalizable to your patient?
- Are the statistical tests appropriate for the study design and clinical question?
- Are the results presented within the paper?
- Are the results statistically significant and how large is the difference between groups?
- Is there evidence of significance fishing (i.e. changing statistical tests to ensure significance)?
Critical appraisal of…the Discussion/Conclusion
- Do the authors attempt to contextualise non-significant data in an attempt to portray significance? (e.g. talking about findings which had a trend towards significance as if they were significant).
- Do the authors acknowledge limitations in the article?
- Are there any conflicts of interests noted?
This is by no means a comprehensive checklist of how to critically appraise a scientific journal article. However, by answering the previous 20 questions based on a detailed reading of an article, you can appraise most articles for their merit, and thus determine whether the results are valid. I have attempted to list the questions based on the sections most commonly present in a journal article, starting at the introduction and progressing to the conclusion. I believe some of these items are weighted heavier than others (i.e. methodological questions vs journal reputation). However, without taking this list through rigorous testing, I cannot assign a weight to them. Maybe one day, you will be able to critically appraise my future paper: How Online Checklists Influence Healthcare Students’ Ability to Critically Appraise Journal Articles.
Feature Image by Arek Socha from Pixabay
Robert Will
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
No Comments on Critical Appraisal: A Checklist
Hi Ella, I have found a checklist here for before and after study design: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools and you may also find a checklist from this blog, which has a huge number of tools listed: https://s4be.cochrane.org/blog/2018/01/12/appraising-the-appraisal/
What kind of critical appraisal tool can be used for before and after study design article? Thanks
Hello, I am currently writing a book chapter on critical appraisal skills. This chapter is limited to 1000 words so your simple 20 questions framework would be the perfect format to cite within this text. May I please have your permission to use your checklist with full acknowledgement given to you as author? Many thanks
Thank you Robert, I came across your checklist via the Royal College of Surgeons of England website; https://www.rcseng.ac.uk/library-and-publications/library/blog/dissecting-the-literature-the-importance-of-critical-appraisal/ . I really liked it and I have made reference to it for our students. I really appreciate your checklist and it is still current, thank you.
Hi Kirsten. Thank you so much for letting us know that Robert’s checklist has been used in that article – that’s so good to see. If any of your students have any comments about the blog, then do let us know. If you also note any topics that you would like to see on the website, then we can add this to the list of suggested blogs for students to write about. Thank you again. Emma.
i am really happy with it. thank you very much
A really useful guide for helping you ask questions about the studies you are reviewing BRAVO
Dr.Suryanujella,
Thank you for the comment. I’m glad you find it helpful.
Feel free to use the checklist. S4BE asks that you cite the page when you use it.
I have read your article and found it very useful , crisp with all relevant information.I would like to use it in my presentation with your permission
That’s great thank you very much. I will definitely give that a go.
I find the MEAL writing approach very versatile. You can use it to plan the entire paper and each paragraph within the paper. There are a lot of helpful MEAL resources online. But understanding the acronym can get you started.
M-Main Idea (What are you arguing?) E-Evidence (What does the literature say?) A-Analysis (Why does the literature matter to your argument?) L-Link (Transition to next paragraph or section)
I hope that is somewhat helpful. -Robert
Hi, I am a university student at Portsmouth University, UK. I understand the premise of a critical appraisal however I am unsure how to structure an essay critically appraising a paper. Do you have any pointers to help me get started?
Thank you. I’m glad that you find this helpful.
Very informative & to the point for all medical students
How can I know what is the name of this checklist or tool?
This is a checklist that the author, Robert Will, has designed himself.
Thank you for asking. I am glad you found it helpful. As Emma said, please cite the source when you use it.
Greetings Robert, I am a postgraduate student at QMUL in the UK and I have just read this comprehensive critical appraisal checklist of your. I really appreciate you. if I may ask, can I have it downloaded?
Please feel free to use the information from this blog – if you could please cite the source then that would be much appreciated.
Robert Thank you for your comptrehensive account of critical appraisal. I have just completed a teaching module on critical appraisal as part of a four module Evidence Based Medicine programme for undergraduate Meducal students at RCSI Perdana medical school in Malaysia. If you are agreeable I would like to cite it as a reference in our module.
Anthony, Please feel free to cite my checklist. Thank you for asking. I hope that your students find it helpful. They should also browse around S4BE. There are numerous other helpful articles on this site.
Subscribe to our newsletter
You will receive our monthly newsletter and free access to Trip Premium.
Related Articles

Risk Communication in Public Health
Learn why effective risk communication in public health matters and where you can get started in learning how to better communicate research evidence.

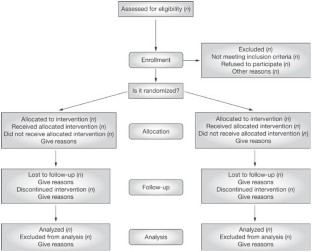
Why was the CONSORT Statement introduced?
The CONSORT statement aims at comprehensive and complete reporting of randomized controlled trials. This blog introduces you to the statement and why it is an important tool in the research world.

Measures of central tendency in clinical research papers: what we should know whilst analysing them
Learn more about the measures of central tendency (mean, mode, median) and how these need to be critically appraised when reading a paper.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Perspect Clin Res
- v.12(2); Apr-Jun 2021
Critical appraisal of published research papers – A reinforcing tool for research methodology: Questionnaire-based study
Snehalata gajbhiye.
Department of Pharmacology and Therapeutics, Seth GS Medical College and KEM Hospital, Mumbai, Maharashtra, India
Raakhi Tripathi
Urwashi parmar, nishtha khatri, anirudha potey.
1 Department of Clinical Trials, Serum Institute of India, Pune, Maharashtra, India
Background and Objectives:
Critical appraisal of published research papers is routinely conducted as a journal club (JC) activity in pharmacology departments of various medical colleges across Maharashtra, and it forms an important part of their postgraduate curriculum. The objective of this study was to evaluate the perception of pharmacology postgraduate students and teachers toward use of critical appraisal as a reinforcing tool for research methodology. Evaluation of performance of the in-house pharmacology postgraduate students in the critical appraisal activity constituted secondary objective of the study.
Materials and Methods:
The study was conducted in two parts. In Part I, a cross-sectional questionnaire-based evaluation on perception toward critical appraisal activity was carried out among pharmacology postgraduate students and teachers. In Part II of the study, JC score sheets of 2 nd - and 3 rd -year pharmacology students over the past 4 years were evaluated.
One hundred and twenty-seven postgraduate students and 32 teachers participated in Part I of the study. About 118 (92.9%) students and 28 (87.5%) faculties considered the critical appraisal activity to be beneficial for the students. JC score sheet assessments suggested that there was a statistically significant improvement in overall scores obtained by postgraduate students ( n = 25) in their last JC as compared to the first JC.
Conclusion:
Journal article criticism is a crucial tool to develop a research attitude among postgraduate students. Participation in the JC activity led to the improvement in the skill of critical appraisal of published research articles, but this improvement was not educationally relevant.
INTRODUCTION
Critical appraisal of a research paper is defined as “The process of carefully and systematically examining research to judge its trustworthiness, value and relevance in a particular context.”[ 1 ] Since scientific literature is rapidly expanding with more than 12,000 articles being added to the MEDLINE database per week,[ 2 ] critical appraisal is very important to distinguish scientifically useful and well-written articles from imprecise articles.
Educational authorities like the Medical Council of India (MCI) and Maharashtra University of Health Sciences (MUHS) have stated in pharmacology postgraduate curriculum that students must critically appraise research papers. To impart training toward these skills, MCI and MUHS have emphasized on the introduction of journal club (JC) activity for postgraduate (PG) students, wherein students review a published original research paper and state the merits and demerits of the paper. Abiding by this, pharmacology departments across various medical colleges in Maharashtra organize JC at frequent intervals[ 3 , 4 ] and students discuss varied aspects of the article with teaching faculty of the department.[ 5 ] Moreover, this activity carries a significant weightage of marks in the pharmacology university examination. As postgraduate students attend this activity throughout their 3-year tenure, it was perceived by the authors that this activity of critical appraisal of research papers could emerge as a tool for reinforcing the knowledge of research methodology. Hence, a questionnaire-based study was designed to find out the perceptions from PG students and teachers.
There have been studies that have laid emphasis on the procedure of conducting critical appraisal of research papers and its application into clinical practice.[ 6 , 7 ] However, there are no studies that have evaluated how well students are able to critically appraise a research paper. The Department of Pharmacology and Therapeutics at Seth GS Medical College has developed an evaluation method to score the PG students on this skill and this tool has been implemented for the last 5 years. Since there are no research data available on the performance of PG Pharmacology students in JC, capturing the critical appraisal activity evaluation scores of in-house PG students was chosen as another objective of the study.
MATERIALS AND METHODS
Description of the journal club activity.
JC is conducted in the Department of Pharmacology and Therapeutics at Seth GS Medical College once in every 2 weeks. During the JC activity, postgraduate students critically appraise published original research articles on their completeness and aptness in terms of the following: study title, rationale, objectives, study design, methodology-study population, inclusion/exclusion criteria, duration, intervention and safety/efficacy variables, randomization, blinding, statistical analysis, results, discussion, conclusion, references, and abstract. All postgraduate students attend this activity, while one of them critically appraises the article (who has received the research paper given by one of the faculty members 5 days before the day of JC). Other faculties also attend these sessions and facilitate the discussions. As the student comments on various sections of the paper, the same predecided faculty who gave the article (single assessor) evaluates the student on a total score of 100 which is split per section as follows: Introduction –20 marks, Methodology –20 marks, Discussion – 20 marks, Results and Conclusion –20 marks, References –10 marks, and Title, Abstract, and Keywords – 10 marks. However, there are no standard operating procedures to assess the performance of students at JC.
Methodology
After seeking permission from the Institutional Ethics Committee, the study was conducted in two parts. Part I consisted of a cross-sectional questionnaire-based survey that was conducted from October 2016 to September 2017. A questionnaire to evaluate perception towards the activity of critical appraisal of published papers as research methodology reinforcing tool was developed by the study investigators. The questionnaire consisted of 20 questions: 14 questions [refer Figure 1 ] graded on a 3-point Likert scale (agree, neutral, and disagree), 1 multiple choice selection question, 2 dichotomous questions, 1 semi-open-ended questions, and 2 open-ended questions. Content validation for this questionnaire was carried out with the help of eight pharmacology teachers. The content validity ratio per item was calculated and each item in the questionnaire had a CVR ratio (CVR) of >0.75.[ 8 ] The perception questionnaire was either E-mailed or sent through WhatsApp to PG pharmacology students and teaching faculty in pharmacology departments at various medical colleges across Maharashtra. Informed consent was obtained on E-mail from all the participants.

Graphical representation of the percentage of students/teachers who agreed that critical appraisal of research helped them improve their knowledge on various aspects of research, perceived that faculty participation is important in this activity, and considered critical appraisal activity beneficial for students. The numbers adjacent to the bar diagrams indicate the raw number of students/faculty who agreed, while brackets indicate %
Part II of the study consisted of evaluating the performance of postgraduate students toward skills of critical appraisal of published papers. For this purpose, marks obtained by 2 nd - and 3 rd -year residents during JC sessions conducted over a period of 4 years from October 2013 to September 2017 were recorded and analyzed. No data on personal identifiers of the students were captured.
Statistical analysis
Marks obtained by postgraduate students in their first and last JC were compared using Wilcoxon signed-rank test, while marks obtained by 2 nd - and 3 rd -year postgraduate students were compared using Mann–Whitney test since the data were nonparametric. These statistical analyses were performed using GraphPad Prism statistical software, San Diego, Calfornia, USA, Version 7.0d. Data obtained from the perception questionnaire were entered in Microsoft Excel sheet and were expressed as frequencies (percentages) using descriptive statistics.
Participants who answered all items of the questionnaire were considered as complete responders and only completed questionnaires were analyzed. The questionnaire was sent through an E-mail to 100 students and through WhatsApp to 68 students. Out of the 100 students who received the questionnaire through E-mail, 79 responded completely and 8 were incomplete responders, while 13 students did not revert back. Out of the 68 students who received the questionnaire through WhatsApp, 48 responded completely, 6 gave an incomplete response, and 14 students did not revert back. Hence, of the 168 postgraduate students who received the questionnaire, 127 responded completely (student response rate for analysis = 75.6%). The questionnaire was E-mailed to 33 faculties and was sent through WhatsApp to 25 faculties. Out of the 33 faculties who received the questionnaire through E-mail, 19 responded completely, 5 responded incompletely, and 9 did not respond at all. Out of the 25 faculties who received the questionnaire through WhatsApp, 13 responded completely, 3 were incomplete responders, and 9 did not respond at all. Hence, of a total of 58 faculties who were contacted, 32 responded completely (faculty response rate for analysis = 55%). For Part I of the study, responses on the perception questionnaire from 127 postgraduate students and 32 postgraduate teachers were recorded and analyzed. None of the faculty who participated in the validation of the questionnaire participated in the survey. Number of responses obtained region wise (Mumbai region and rest of Maharashtra region) have been depicted in Table 1 .
Region-wise distribution of responses
Number of responses obtained from students/faculty belonging to Mumbai colleges and rest of Maharashtra colleges. Brackets indicate percentages
As per the data obtained on the Likert scale questions, 102 (80.3%) students and 29 (90.6%) teachers agreed that critical appraisal trains the students in doing a review of literature before selecting a particular research topic. Majority of the participants, i.e., 104 (81.9%) students and 29 (90.6%) teachers also believed that the activity increases student's knowledge regarding various experimental evaluation techniques. Moreover, 112 (88.2%) students and 27 (84.4%) faculty considered that critical appraisal activity results in improved skills of writing and understanding methodology section of research articles in terms of inclusion/exclusion criteria, endpoints, and safety/efficacy variables. About 103 (81.1%) students and 24 (75%) teachers perceived that this activity results in refinement of the student's research work. About 118 (92.9%) students and 28 (87.5%) faculty considered the critical appraisal activity to be beneficial for the students. Responses to 14 individual Likert scale items of the questionnaire have been depicted in Figure 1 .
With respect to the multiple choice selection question, 66 (52%) students and 16 (50%) teachers opined that faculty should select the paper, 53 (41.7%) students and 9 (28.1%) teachers stated that the papers should be selected by the presenting student himself/herself, while 8 (6.3%) students and 7 (21.9%) teachers expressed that some other student should select the paper to be presented at the JC.
The responses to dichotomous questions were as follows: majority of the students, that is, 109 (85.8%) and 23 (71.9%) teachers perceived that a standard checklist for article review should be given to the students before critical appraisal of journal article. Open-ended questions of the questionnaire invited suggestions from the participants regarding ways of getting trained on critical appraisal skills and of improving JC activity. Some of the suggestions given by faculty were as follows: increasing the frequency of JC activity, discussion of cited articles and new guidelines related to it, selecting all types of articles for criticism rather than only randomized controlled trials, and regular yearly exams on article criticism. Students stated that regular and frequent article criticism activity, practice of writing letter to the editor after criticism, active participation by peers and faculty, increasing weightage of marks for critical appraisal of papers in university examinations (at present marks are 50 out of 400), and a formal training for research criticism from 1 st year of postgraduation could improve critical appraisal program.
In Part II of this study, performance of the students on the skill of critical appraisal of papers was evaluated. Complete data of the first and last JC scores of a total of 25 students of the department were available, and when these scores were compared, it was seen that there was a statistically significant improvement in the overall scores ( P = 0.04), as well as in the scores obtained in methodology ( P = 0.03) and results section ( P = 0.02). This is depicted in Table 2 . Although statistically significant, the differences in scores in the methodology section, results section, and overall scores were 1.28/20, 1.28/20, and 4.36/100, respectively, amounting to 5.4%, 5.4%, and 4.36% higher scores in the last JC, which may not be considered educationally relevant (practically significant). The quantum of difference that would be considered practically significant was not decided a priori .
Comparison of marks obtained by pharmacology residents in their first and last journal club
Marks have been represented as mean±SD. The maximum marks that can be obtained in each section have been stated as maximum. *Indicates statistically significant ( P <0.05). IQR=Interquartile range, SD=Standard deviation
Scores of two groups, one group consisting of 2 nd -year postgraduate students ( n = 44) and second group consisting of 3 rd -year postgraduate students ( n = 32) were compared and revealed no statistically significant difference in overall score ( P = 0.84). This is depicted in Table 3 . Since the quantum of difference in the overall scores was meager 0.84/100 (0.84%), it cannot be considered practically significant.
Comparison of marks obtained by 2 nd - and 3 rd -year pharmacology residents in the activity of critical appraisal of research articles
Marks have been represented as mean±SD. The maximum marks that can be obtained in each section have been stated as maximum. P <0.05 was considered to be statistically significant. IQR=Interquartile range, SD=Standard deviation
The present study gauged the perception of the pharmacology postgraduate students and teachers toward the use of critical appraisal activity as a reinforcing tool for research methodology. Both students and faculties (>50%) believed that critical appraisal activity increases student's knowledge on principles of ethics, experimental evaluation techniques, CONSORT guidelines, statistical analysis, concept of conflict of interest, current trends and recent advances in Pharmacology and trains on doing a review of literature, and improves skills on protocol writing and referencing. In the study conducted by Crank-Patton et al ., a survey on 278 general surgery program directors was carried out and more than 50% indicated that JC was important to their training program.[ 9 ]
The grading template used in Part II of the study was based on the IMRaD structure. Hence, equal weightage was given to the Introduction, Methodology, Results, and Discussion sections and lesser weightage was given to the references and title, abstract, and keywords sections.[ 10 ] While evaluating the scores obtained by 25 students in their first and last JC, it was seen that there was a statistically significant improvement in the overall scores of the students in their last JC. However, the meager improvement in scores cannot be considered educationally relevant, as the authors expected the students to score >90% for the upgrade to be considered educationally impactful. The above findings suggest that even though participation in the JC activity led to a steady increase in student's performance (~4%), the increment was not as expected. In addition, the students did not portray an excellent performance (>90%), with average scores being around 72% even in the last JC. This can be probably explained by the fact that students perform this activity in a routine setting and not in an examination setting. Unlike the scenario in an examination, students were aware that even if they performed at a mediocre level, there would be no repercussions.
A separate comparison of scores obtained by 44 students in their 2 nd year and 32 students in their 3 rd year of postgraduation students was also done. The number of student evaluation sheets reviewed for this analysis was greater than the number of student evaluation sheets reviewed to compare first and last JC scores. This can be spelled out by the fact that many students were still in 2 nd year when this analysis was done and the score data for their last JC, which would take place in 3 rd year, was not available. In addition, few students were asked to present at JC multiple times during the 2 nd /3 rd year of their postgraduation.
While evaluating the critical appraisal scores obtained by 2 nd - and 3 rd -year postgraduate students, it was found that although the 3 rd -year students had a mean overall score greater than the 2 nd -year students, this difference was not statistically significant. During the 1 st year of MD Pharmacology course, students at the study center attend JC once in every 2 weeks. Even though the 1 st -year students do not themselves present in JC, they listen and observe the criticism points stated by senior peers presenting at the JC, and thereby, incur substantial amount of knowledge required to critically appraise papers. By the time, they become 2 nd -year students, they are already well versed with the program and this could have led to similar overall mean scores between the 2 nd -year students (71.50 ± 10.71) and 3 rd -year students (72.34 ± 10.85). This finding suggests that attentive listening is as important as active participation in the JC. Moreover, although students are well acquainted with the process of criticism when they are in their 3 rd year, there is certainly a scope for improvement in terms of the mean overall scores.
Similar results were obtained in a study conducted by Stern et al ., in which 62 students in the internal medicine program at the New England Medical Center were asked to respond to a questionnaire, evaluate a sample article, and complete a self-assessment of competence in evaluation of research. Twenty-eight residents returned the questionnaire and the composite score for the resident's objective assessment was not significantly correlated with the postgraduate year or self-assessed critical appraisal skill.[ 11 ]
Article criticism activity provides the students with practical experience of techniques taught in research methodology workshop. However, this should be supplemented with activities that assess the improvement of designing and presenting studies, such as protocol and paper writing. Thus, critical appraisal plays a significant role in reinforcing good research practices among the new generation of physicians. Moreover, critical appraisal is an integral part of PG assessment, and although the current format of conducting JCs did not portray a clinically meaningful improvement, the authors believe that it is important to continue this activity with certain modifications suggested by students who participated in this study. Students suggested that an increase in the frequency of critical appraisal activity accompanied by the display of active participation by peers and faculty could help in the betterment of this activity. This should be brought to attention of the faculty, as students seem to be interested to learn. Critical appraisal should be a two-way teaching–learning process between the students and faculty and not a dire need for satisfying the students' eligibility criteria for postgraduate university examinations. This activity is not only for the trainee doctors but also a part of the overall faculty development program.[ 12 ]
In the present era, JCs have been used as a tool to not only teach critical appraisal skills but also to teach other necessary aspects such as research design, medical statistics, clinical epidemiology, and clinical decision-making.[ 13 , 14 ] A study conducted by Khan in 2013 suggested that success of JC program can be ensured if institutes develop a defined JC objective for the development of learning capability of students and also if they cultivate more skilled faculties.[ 15 ] A good JC is believed to facilitate relevant, meaningful scientific discussion, and evaluation of the research updates that will eventually benefit the patient care.[ 12 ]
Although there is a lot of literature emphasizing the importance of JC, there is a lack of studies that have evaluated the outcome of such activity. One such study conducted by Ibrahim et al . assessed the importance of critical appraisal as an activity in surgical trainees in Nigeria. They reported that 92.42% trainees considered the activity to be important or very important and 48% trainees stated that the activity helped in improving literature search.[ 16 ]
This study is unique since it is the first of its kind to evaluate how well students are able to critically appraise a research paper. Moreover, the study has taken into consideration the due opinions of the students as well as faculties, unlike the previous literature which has laid emphasis on only student's perception. A limitation of this study is that sample size for faculties was smaller than the students, as it was not possible to convince the distant faculty in other cities to fill the survey. Besides, there may be a variation in the manner of conduct of the critical appraisal activity in pharmacology departments across the various medical colleges in the country. Another limitation of this study was that a single assessor graded a single student during one particular JC. Nevertheless, each student presented at multiple JC and thereby came across multiple assessors. Since the articles addressed at different JC were disparate, interobserver variability was not taken into account in this study. Furthermore, the authors did not make an a priori decision on the quantum of increase in scores that would be considered educationally meaningful.
Pharmacology students and teachers acknowledge the role of critical appraisal in improving the ability to understand the crucial concepts of research methodology and research conduct. In our institute, participation in the JC activity led to an improvement in the skill of critical appraisal of published research articles among the pharmacology postgraduate students. However, this improvement was not educationally relevant. The scores obtained by final-year postgraduate students in this activity were nearly 72% indicating that there is still scope of betterment in this skill.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge the support rendered by the entire Department of Pharmacology and Therapeutics at Seth GS Medical College.

Writing a Critical Analysis
What is in this guide, definitions, putting it together, tips and examples of critques.
- Background Information
- Cite Sources
Library Links
- Ask a Librarian
- Library Tutorials
- The Research Process
- Library Hours
- Online Databases (A-Z)
- Interlibrary Loan (ILL)
- Reserve a Study Room
- Report a Problem
This guide is meant to help you understand the basics of writing a critical analysis. A critical analysis is an argument about a particular piece of media. There are typically two parts: (1) identify and explain the argument the author is making, and (2), provide your own argument about that argument. Your instructor may have very specific requirements on how you are to write your critical analysis, so make sure you read your assignment carefully.

Critical Analysis
A deep approach to your understanding of a piece of media by relating new knowledge to what you already know.
Part 1: Introduction
- Identify the work being criticized.
- Present thesis - argument about the work.
- Preview your argument - what are the steps you will take to prove your argument.
Part 2: Summarize
- Provide a short summary of the work.
- Present only what is needed to know to understand your argument.
Part 3: Your Argument
- This is the bulk of your paper.
- Provide "sub-arguments" to prove your main argument.
- Use scholarly articles to back up your argument(s).
Part 4: Conclusion
- Reflect on how you have proven your argument.
- Point out the importance of your argument.
- Comment on the potential for further research or analysis.
- Cornell University Library Tips for writing a critical appraisal and analysis of a scholarly article.
- Queen's University Library How to Critique an Article (Psychology)
- University of Illinois, Springfield An example of a summary and an evaluation of a research article. This extended example shows the different ways a student can critique and write about an article
- Next: Background Information >>
- Last Updated: Feb 14, 2024 4:33 PM
- URL: https://libguides.pittcc.edu/critical_analysis
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 20 January 2009
How to critically appraise an article
- Jane M Young 1 &
- Michael J Solomon 2
Nature Clinical Practice Gastroenterology & Hepatology volume 6 , pages 82–91 ( 2009 ) Cite this article
52k Accesses
100 Citations
431 Altmetric
Metrics details
Critical appraisal is a systematic process used to identify the strengths and weaknesses of a research article in order to assess the usefulness and validity of research findings. The most important components of a critical appraisal are an evaluation of the appropriateness of the study design for the research question and a careful assessment of the key methodological features of this design. Other factors that also should be considered include the suitability of the statistical methods used and their subsequent interpretation, potential conflicts of interest and the relevance of the research to one's own practice. This Review presents a 10-step guide to critical appraisal that aims to assist clinicians to identify the most relevant high-quality studies available to guide their clinical practice.
Critical appraisal is a systematic process used to identify the strengths and weaknesses of a research article
Critical appraisal provides a basis for decisions on whether to use the results of a study in clinical practice
Different study designs are prone to various sources of systematic bias
Design-specific, critical-appraisal checklists are useful tools to help assess study quality
Assessments of other factors, including the importance of the research question, the appropriateness of statistical analysis, the legitimacy of conclusions and potential conflicts of interest are an important part of the critical appraisal process
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Making sense of the literature: an introduction to critical appraisal for the primary care practitioner

How to appraise the literature: basic principles for the busy clinician - part 2: systematic reviews and meta-analyses

How to appraise the literature: basic principles for the busy clinician - part 1: randomised controlled trials
Druss BG and Marcus SC (2005) Growth and decentralisation of the medical literature: implications for evidence-based medicine. J Med Libr Assoc 93 : 499–501
PubMed PubMed Central Google Scholar
Glasziou PP (2008) Information overload: what's behind it, what's beyond it? Med J Aust 189 : 84–85
PubMed Google Scholar
Last JE (Ed.; 2001) A Dictionary of Epidemiology (4th Edn). New York: Oxford University Press
Google Scholar
Sackett DL et al . (2000). Evidence-based Medicine. How to Practice and Teach EBM . London: Churchill Livingstone
Guyatt G and Rennie D (Eds; 2002). Users' Guides to the Medical Literature: a Manual for Evidence-based Clinical Practice . Chicago: American Medical Association
Greenhalgh T (2000) How to Read a Paper: the Basics of Evidence-based Medicine . London: Blackwell Medicine Books
MacAuley D (1994) READER: an acronym to aid critical reading by general practitioners. Br J Gen Pract 44 : 83–85
CAS PubMed PubMed Central Google Scholar
Hill A and Spittlehouse C (2001) What is critical appraisal. Evidence-based Medicine 3 : 1–8 [ http://www.evidence-based-medicine.co.uk ] (accessed 25 November 2008)
Public Health Resource Unit (2008) Critical Appraisal Skills Programme (CASP) . [ http://www.phru.nhs.uk/Pages/PHD/CASP.htm ] (accessed 8 August 2008)
National Health and Medical Research Council (2000) How to Review the Evidence: Systematic Identification and Review of the Scientific Literature . Canberra: NHMRC
Elwood JM (1998) Critical Appraisal of Epidemiological Studies and Clinical Trials (2nd Edn). Oxford: Oxford University Press
Agency for Healthcare Research and Quality (2002) Systems to rate the strength of scientific evidence? Evidence Report/Technology Assessment No 47, Publication No 02-E019 Rockville: Agency for Healthcare Research and Quality
Crombie IK (1996) The Pocket Guide to Critical Appraisal: a Handbook for Health Care Professionals . London: Blackwell Medicine Publishing Group
Heller RF et al . (2008) Critical appraisal for public health: a new checklist. Public Health 122 : 92–98
Article Google Scholar
MacAuley D et al . (1998) Randomised controlled trial of the READER method of critical appraisal in general practice. BMJ 316 : 1134–37
Article CAS Google Scholar
Parkes J et al . Teaching critical appraisal skills in health care settings (Review). Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No.: cd001270. 10.1002/14651858.cd001270
Mays N and Pope C (2000) Assessing quality in qualitative research. BMJ 320 : 50–52
Hawking SW (2003) On the Shoulders of Giants: the Great Works of Physics and Astronomy . Philadelphia, PN: Penguin
National Health and Medical Research Council (1999) A Guide to the Development, Implementation and Evaluation of Clinical Practice Guidelines . Canberra: National Health and Medical Research Council
US Preventive Services Taskforce (1996) Guide to clinical preventive services (2nd Edn). Baltimore, MD: Williams & Wilkins
Solomon MJ and McLeod RS (1995) Should we be performing more randomized controlled trials evaluating surgical operations? Surgery 118 : 456–467
Rothman KJ (2002) Epidemiology: an Introduction . Oxford: Oxford University Press
Young JM and Solomon MJ (2003) Improving the evidence-base in surgery: sources of bias in surgical studies. ANZ J Surg 73 : 504–506
Margitic SE et al . (1995) Lessons learned from a prospective meta-analysis. J Am Geriatr Soc 43 : 435–439
Shea B et al . (2001) Assessing the quality of reports of systematic reviews: the QUORUM statement compared to other tools. In Systematic Reviews in Health Care: Meta-analysis in Context 2nd Edition, 122–139 (Eds Egger M. et al .) London: BMJ Books
Chapter Google Scholar
Easterbrook PH et al . (1991) Publication bias in clinical research. Lancet 337 : 867–872
Begg CB and Berlin JA (1989) Publication bias and dissemination of clinical research. J Natl Cancer Inst 81 : 107–115
Moher D et al . (2000) Improving the quality of reports of meta-analyses of randomised controlled trials: the QUORUM statement. Br J Surg 87 : 1448–1454
Shea BJ et al . (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology 7 : 10 [10.1186/1471-2288-7-10]
Stroup DF et al . (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283 : 2008–2012
Young JM and Solomon MJ (2003) Improving the evidence-base in surgery: evaluating surgical effectiveness. ANZ J Surg 73 : 507–510
Schulz KF (1995) Subverting randomization in controlled trials. JAMA 274 : 1456–1458
Schulz KF et al . (1995) Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 273 : 408–412
Moher D et al . (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Medical Research Methodology 1 : 2 [ http://www.biomedcentral.com/ 1471-2288/1/2 ] (accessed 25 November 2008)
Rochon PA et al . (2005) Reader's guide to critical appraisal of cohort studies: 1. Role and design. BMJ 330 : 895–897
Mamdani M et al . (2005) Reader's guide to critical appraisal of cohort studies: 2. Assessing potential for confounding. BMJ 330 : 960–962
Normand S et al . (2005) Reader's guide to critical appraisal of cohort studies: 3. Analytical strategies to reduce confounding. BMJ 330 : 1021–1023
von Elm E et al . (2007) Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335 : 806–808
Sutton-Tyrrell K (1991) Assessing bias in case-control studies: proper selection of cases and controls. Stroke 22 : 938–942
Knottnerus J (2003) Assessment of the accuracy of diagnostic tests: the cross-sectional study. J Clin Epidemiol 56 : 1118–1128
Furukawa TA and Guyatt GH (2006) Sources of bias in diagnostic accuracy studies and the diagnostic process. CMAJ 174 : 481–482
Bossyut PM et al . (2003)The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. Ann Intern Med 138 : W1–W12
STARD statement (Standards for the Reporting of Diagnostic Accuracy Studies). [ http://www.stard-statement.org/ ] (accessed 10 September 2008)
Raftery J (1998) Economic evaluation: an introduction. BMJ 316 : 1013–1014
Palmer S et al . (1999) Economics notes: types of economic evaluation. BMJ 318 : 1349
Russ S et al . (1999) Barriers to participation in randomized controlled trials: a systematic review. J Clin Epidemiol 52 : 1143–1156
Tinmouth JM et al . (2004) Are claims of equivalency in digestive diseases trials supported by the evidence? Gastroentrology 126 : 1700–1710
Kaul S and Diamond GA (2006) Good enough: a primer on the analysis and interpretation of noninferiority trials. Ann Intern Med 145 : 62–69
Piaggio G et al . (2006) Reporting of noninferiority and equivalence randomized trials: an extension of the CONSORT statement. JAMA 295 : 1152–1160
Heritier SR et al . (2007) Inclusion of patients in clinical trial analysis: the intention to treat principle. In Interpreting and Reporting Clinical Trials: a Guide to the CONSORT Statement and the Principles of Randomized Controlled Trials , 92–98 (Eds Keech A. et al .) Strawberry Hills, NSW: Australian Medical Publishing Company
National Health and Medical Research Council (2007) National Statement on Ethical Conduct in Human Research 89–90 Canberra: NHMRC
Lo B et al . (2000) Conflict-of-interest policies for investigators in clinical trials. N Engl J Med 343 : 1616–1620
Kim SYH et al . (2004) Potential research participants' views regarding researcher and institutional financial conflicts of interests. J Med Ethics 30 : 73–79
Komesaroff PA and Kerridge IH (2002) Ethical issues concerning the relationships between medical practitioners and the pharmaceutical industry. Med J Aust 176 : 118–121
Little M (1999) Research, ethics and conflicts of interest. J Med Ethics 25 : 259–262
Lemmens T and Singer PA (1998) Bioethics for clinicians: 17. Conflict of interest in research, education and patient care. CMAJ 159 : 960–965
Download references
Author information
Authors and affiliations.
JM Young is an Associate Professor of Public Health and the Executive Director of the Surgical Outcomes Research Centre at the University of Sydney and Sydney South-West Area Health Service, Sydney,
Jane M Young
MJ Solomon is Head of the Surgical Outcomes Research Centre and Director of Colorectal Research at the University of Sydney and Sydney South-West Area Health Service, Sydney, Australia.,
Michael J Solomon
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jane M Young .
Ethics declarations
Competing interests.
The authors declare no competing financial interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Young, J., Solomon, M. How to critically appraise an article. Nat Rev Gastroenterol Hepatol 6 , 82–91 (2009). https://doi.org/10.1038/ncpgasthep1331
Download citation
Received : 10 August 2008
Accepted : 03 November 2008
Published : 20 January 2009
Issue Date : February 2009
DOI : https://doi.org/10.1038/ncpgasthep1331
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Emergency physicians’ perceptions of critical appraisal skills: a qualitative study.
- Sumintra Wood
- Jacqueline Paulis
- Angela Chen
BMC Medical Education (2022)
An integrative review on individual determinants of enrolment in National Health Insurance Scheme among older adults in Ghana
- Anthony Kwame Morgan
- Anthony Acquah Mensah
BMC Primary Care (2022)
Autopsy findings of COVID-19 in children: a systematic review and meta-analysis
- Anju Khairwa
- Kana Ram Jat
Forensic Science, Medicine and Pathology (2022)
The use of a modified Delphi technique to develop a critical appraisal tool for clinical pharmacokinetic studies
- Alaa Bahaa Eldeen Soliman
- Shane Ashley Pawluk
- Ousama Rachid
International Journal of Clinical Pharmacy (2022)
Critical Appraisal: Analysis of a Prospective Comparative Study Published in IJS
- Ramakrishna Ramakrishna HK
- Swarnalatha MC
Indian Journal of Surgery (2021)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
How to critically appraise an article
Affiliation.
- 1 Surgical Outcomes Research Centre, Royal Prince Alfred Hospital, Missenden Road, Sydney, NSW 2050, Australia. [email protected]
- PMID: 19153565
- DOI: 10.1038/ncpgasthep1331
Critical appraisal is a systematic process used to identify the strengths and weaknesses of a research article in order to assess the usefulness and validity of research findings. The most important components of a critical appraisal are an evaluation of the appropriateness of the study design for the research question and a careful assessment of the key methodological features of this design. Other factors that also should be considered include the suitability of the statistical methods used and their subsequent interpretation, potential conflicts of interest and the relevance of the research to one's own practice. This Review presents a 10-step guide to critical appraisal that aims to assist clinicians to identify the most relevant high-quality studies available to guide their clinical practice.
Publication types
- Decision Making*
- Evidence-Based Medicine*
Medicine: A Brief Guide to Critical Appraisal
- Quick Start
- First Year Library Essentials
- Literature Reviews and Data Management
- Systematic Search for Health This link opens in a new window
- Guide to Using EndNote This link opens in a new window
- A Brief Guide to Critical Appraisal
- Manage Research Data This link opens in a new window
- Articles & Databases
- Anatomy & Radiology
- Medicines Information
- Diagnostic Tests & Calculators
- Health Statistics
- Multimedia Sources
- News & Public Opinion
- Aboriginal and Torres Strait Islander Health Guide This link opens in a new window
- Medical Ethics Guide This link opens in a new window
Have you ever seen a news piece about a scientific breakthrough and wondered how accurate the reporting is? Or wondered about the research behind the headlines? This is the beginning of critical appraisal: thinking critically about what you see and hear, and asking questions to determine how much of a 'breakthrough' something really is.
The article " Is this study legit? 5 questions to ask when reading news stories of medical research " is a succinct introduction to the sorts of questions you should ask in these situations, but there's more than that when it comes to critical appraisal. Read on to learn more about this practical and crucial aspect of evidence-based practice.
What is Critical Appraisal?
Critical appraisal forms part of the process of evidence-based practice. “ Evidence-based practice across the health professions ” outlines the fives steps of this process. Critical appraisal is step three:
- Ask a question
- Access the information
- Appraise the articles found
- Apply the information
Critical appraisal is the examination of evidence to determine applicability to clinical practice. It considers (1) :
- Are the results of the study believable?
- Was the study methodologically sound?
- What is the clinical importance of the study’s results?
- Are the findings sufficiently important? That is, are they practice-changing?
- Are the results of the study applicable to your patient?
- Is your patient comparable to the population in the study?
Why Critically Appraise?
If practitioners hope to ‘stand on the shoulders of giants’, practicing in a manner that is responsive to the discoveries of the research community, then it makes sense for the responsible, critically thinking practitioner to consider the reliability, influence, and relevance of the evidence presented to them.
While critical thinking is valuable, it is also important to avoid treading too much into cynicism; in the words of Hoffman et al. (1):
… keep in mind that no research is perfect and that it is important not to be overly critical of research articles. An article just needs to be good enough to assist you to make a clinical decision.
How do I Critically Appraise?
Evidence-based practice is intended to be practical . To enable this, critical appraisal checklists have been developed to guide practitioners through the process in an efficient yet comprehensive manner.
Critical appraisal checklists guide the reader through the appraisal process by prompting the reader to ask certain questions of the paper they are appraising. There are many different critical appraisal checklists but the best apply certain questions based on what type of study the paper is describing. This allows for a more nuanced and appropriate appraisal. Wherever possible, choose the appraisal tool that best fits the study you are appraising.
Like many things in life, repetition builds confidence and the more you apply critical appraisal tools (like checklists) to the literature the more the process will become second nature for you and the more effective you will be.
How do I Identify Study Types?
Identifying the study type described in the paper is sometimes a harder job than it should be. Helpful papers spell out the study type in the title or abstract, but not all papers are helpful in this way. As such, the critical appraiser may need to do a little work to identify what type of study they are about to critique. Again, experience builds confidence but having an understanding of the typical features of common study types certainly helps.
To assist with this, the Library has produced a guide to study designs in health research .
The following selected references will help also with understanding study types but there are also other resources in the Library’s collection and freely available online:
- The “ How to read a paper ” article series from The BMJ is a well-known source for establishing an understanding of the features of different study types; this series was subsequently adapted into a book (“ How to read a paper: the basics of evidence-based medicine ”) which offers more depth and currency than that found in the articles. (2)
- Chapter two of “ Evidence-based practice across the health professions ” briefly outlines some study types and their application; subsequent chapters go into more detail about different study types depending on what type of question they are exploring (intervention, diagnosis, prognosis, qualitative) along with systematic reviews.
- “ Clinical evidence made easy ” contains several chapters on different study designs and also includes critical appraisal tools. (3)
- “ Translational research and clinical practice: basic tools for medical decision making and self-learning ” unpacks the components of a paper, explaining their purpose along with key features of different study designs. (4)
- The BMJ website contains the contents of the fourth edition of the book “ Epidemiology for the uninitiated ”. This eBook contains chapters exploring ecological studies, longitudinal studies, case-control and cross-sectional studies, and experimental studies.
Reporting Guidelines
In order to encourage consistency and quality, authors of reports on research should follow reporting guidelines when writing their papers. The EQUATOR Network is a good source of reporting guidelines for the main study types.
While these guidelines aren't critical appraisal tools as such, they can assist by prompting you to consider whether the reporting of the research is missing important elements.
Once you've identified the study type at hand, visit EQUATOR to find the associated reporting guidelines and ask yourself: does this paper meet the guideline for its study type?
Which Checklist Should I Use?
Determining which checklist to use ultimately comes down to finding an appraisal tool that:
- Fits best with the study you are appraising
- Is reliable, well-known or otherwise validated
- You understand and are comfortable using
Below are some sources of critical appraisal tools. These have been selected as they are known to be widely accepted, easily applicable, and relevant to appraisal of a typical journal article. You may find another tool that you prefer, which is acceptable as long as it is defensible:
- CASP (Critical Appraisal Skills Programme)
- JBI (Joanna Briggs Institute)
- CEBM (Centre for Evidence-Based Medicine)
- SIGN (Scottish Intercollegiate Guidelines Network)
- STROBE (Strengthing the Reporting of Observational Studies in Epidemiology)
- BMJ Best Practice
The information on this page has been compiled by the Medical Librarian. Please contact the Library's Health Team ( [email protected] ) for further assistance.
Reference list
1. Hoffmann T, Bennett S, Del Mar C. Evidence-based practice across the health professions. 2nd ed. Chatswood, N.S.W., Australia: Elsevier Churchill Livingston; 2013.
2. Greenhalgh T. How to read a paper : the basics of evidence-based medicine. 5th ed. Chichester, West Sussex: Wiley; 2014.
3. Harris M, Jackson D, Taylor G. Clinical evidence made easy. Oxfordshire, England: Scion Publishing; 2014.
4. Aronoff SC. Translational research and clinical practice: basic tools for medical decision making and self-learning. New York: Oxford University Press; 2011.
- << Previous: Guide to Using EndNote
- Next: Manage Research Data >>
- Last Updated: Mar 27, 2024 9:22 AM
- URL: https://deakin.libguides.com/medicine
Please enter both an email address and a password.
Account login
- Show/Hide Password Show password Hide password
- Reset Password
Need to reset your password? Enter the email address which you used to register on this site (or your membership/contact number) and we'll email you a link to reset it. You must complete the process within 2hrs of receiving the link.
We've sent you an email.
An email has been sent to Simply follow the link provided in the email to reset your password. If you can't find the email please check your junk or spam folder and add [email protected] to your address book.
- About RCS England

MRCS Part A
- Dissecting the literature: the importance of critical appraisal
08 Dec 2017
Kirsty Morrison
This post was updated in 2023.
Critical appraisal is the process of carefully and systematically examining research to judge its trustworthiness, and its value and relevance in a particular context.
Amanda Burls, What is Critical Appraisal?

Why is critical appraisal needed?
Literature searches using databases like Medline or EMBASE often result in an overwhelming volume of results which can vary in quality. Similarly, those who browse medical literature for the purposes of CPD or in response to a clinical query will know that there are vast amounts of content available. Critical appraisal helps to reduce the burden and allow you to focus on articles that are relevant to the research question, and that can reliably support or refute its claims with high-quality evidence, or identify high-level research relevant to your practice.

Critical appraisal allows us to:
- reduce information overload by eliminating irrelevant or weak studies
- identify the most relevant papers
- distinguish evidence from opinion, assumptions, misreporting, and belief
- assess the validity of the study
- assess the usefulness and clinical applicability of the study
- recognise any potential for bias.
Critical appraisal helps to separate what is significant from what is not. One way we use critical appraisal in the Library is to prioritise the most clinically relevant content for our Current Awareness Updates .
How to critically appraise a paper
There are some general rules to help you, including a range of checklists highlighted at the end of this blog. Some key questions to consider when critically appraising a paper:
- Is the study question relevant to my field?
- Does the study add anything new to the evidence in my field?
- What type of research question is being asked? A well-developed research question usually identifies three components: the group or population of patients, the studied parameter (e.g. a therapy or clinical intervention) and outcomes of interest.
- Was the study design appropriate for the research question? You can learn more about different study types and the hierarchy of evidence here .
- Did the methodology address important potential sources of bias? Bias can be attributed to chance (e.g. random error) or to the study methods (systematic bias).
- Was the study performed according to the original protocol? Deviations from the planned protocol can affect the validity or relevance of a study, e.g. a decrease in the studied population over the course of a randomised controlled trial .
- Does the study test a stated hypothesis? Is there a clear statement of what the investigators expect the study to find which can be tested, and confirmed or refuted.
- Were the statistical analyses performed correctly? The approach to dealing with missing data, and the statistical techniques that have been applied should be specified. Original data should be presented clearly so that readers can check the statistical accuracy of the paper.
- Do the data justify the conclusions? Watch out for definite conclusions based on statistically insignificant results, generalised findings from a small sample size, and statistically significant associations being misinterpreted to imply a cause and effect.
- Are there any conflicts of interest? Who has funded the study and can we trust their objectivity? Do the authors have any potential conflicts of interest, and have these been declared?
And an important consideration for surgeons:
- Will the results help me manage my patients?
At the end of the appraisal process you should have a better appreciation of how strong the evidence is, and ultimately whether or not you should apply it to your patients.
Further resources:
- How to Read a Paper by Trisha Greenhalgh
- The Doctor’s Guide to Critical Appraisal by Narinder Kaur Gosall
- CASP checklists
- CEBM Critical Appraisal Tools
- Critical Appraisal: a checklist
- Critical Appraisal of a Journal Article (PDF)
- Introduction to...Critical appraisal of literature
- Reporting guidelines for the main study types
Kirsty Morrison, Information Specialist
Share this page:
- Library Blog
Critically Analyzing Information Sources: Critical Appraisal and Analysis
- Critical Appraisal and Analysis
Initial Appraisal : Reviewing the source
- What are the author's credentials--institutional affiliation (where he or she works), educational background, past writings, or experience? Is the book or article written on a topic in the author's area of expertise? You can use the various Who's Who publications for the U.S. and other countries and for specific subjects and the biographical information located in the publication itself to help determine the author's affiliation and credentials.
- Has your instructor mentioned this author? Have you seen the author's name cited in other sources or bibliographies? Respected authors are cited frequently by other scholars. For this reason, always note those names that appear in many different sources.
- Is the author associated with a reputable institution or organization? What are the basic values or goals of the organization or institution?
B. Date of Publication
- When was the source published? This date is often located on the face of the title page below the name of the publisher. If it is not there, look for the copyright date on the reverse of the title page. On Web pages, the date of the last revision is usually at the bottom of the home page, sometimes every page.
- Is the source current or out-of-date for your topic? Topic areas of continuing and rapid development, such as the sciences, demand more current information. On the other hand, topics in the humanities often require material that was written many years ago. At the other extreme, some news sources on the Web now note the hour and minute that articles are posted on their site.
C. Edition or Revision
Is this a first edition of this publication or not? Further editions indicate a source has been revised and updated to reflect changes in knowledge, include omissions, and harmonize with its intended reader's needs. Also, many printings or editions may indicate that the work has become a standard source in the area and is reliable. If you are using a Web source, do the pages indicate revision dates?
D. Publisher
Note the publisher. If the source is published by a university press, it is likely to be scholarly. Although the fact that the publisher is reputable does not necessarily guarantee quality, it does show that the publisher may have high regard for the source being published.
E. Title of Journal
Is this a scholarly or a popular journal? This distinction is important because it indicates different levels of complexity in conveying ideas. If you need help in determining the type of journal, see Distinguishing Scholarly from Non-Scholarly Periodicals . Or you may wish to check your journal title in the latest edition of Katz's Magazines for Libraries (Olin Reference Z 6941 .K21, shelved at the reference desk) for a brief evaluative description.
Critical Analysis of the Content
Having made an initial appraisal, you should now examine the body of the source. Read the preface to determine the author's intentions for the book. Scan the table of contents and the index to get a broad overview of the material it covers. Note whether bibliographies are included. Read the chapters that specifically address your topic. Reading the article abstract and scanning the table of contents of a journal or magazine issue is also useful. As with books, the presence and quality of a bibliography at the end of the article may reflect the care with which the authors have prepared their work.
A. Intended Audience
What type of audience is the author addressing? Is the publication aimed at a specialized or a general audience? Is this source too elementary, too technical, too advanced, or just right for your needs?
B. Objective Reasoning
- Is the information covered fact, opinion, or propaganda? It is not always easy to separate fact from opinion. Facts can usually be verified; opinions, though they may be based on factual information, evolve from the interpretation of facts. Skilled writers can make you think their interpretations are facts.
- Does the information appear to be valid and well-researched, or is it questionable and unsupported by evidence? Assumptions should be reasonable. Note errors or omissions.
- Are the ideas and arguments advanced more or less in line with other works you have read on the same topic? The more radically an author departs from the views of others in the same field, the more carefully and critically you should scrutinize his or her ideas.
- Is the author's point of view objective and impartial? Is the language free of emotion-arousing words and bias?
C. Coverage
- Does the work update other sources, substantiate other materials you have read, or add new information? Does it extensively or marginally cover your topic? You should explore enough sources to obtain a variety of viewpoints.
- Is the material primary or secondary in nature? Primary sources are the raw material of the research process. Secondary sources are based on primary sources. For example, if you were researching Konrad Adenauer's role in rebuilding West Germany after World War II, Adenauer's own writings would be one of many primary sources available on this topic. Others might include relevant government documents and contemporary German newspaper articles. Scholars use this primary material to help generate historical interpretations--a secondary source. Books, encyclopedia articles, and scholarly journal articles about Adenauer's role are considered secondary sources. In the sciences, journal articles and conference proceedings written by experimenters reporting the results of their research are primary documents. Choose both primary and secondary sources when you have the opportunity.
D. Writing Style
Is the publication organized logically? Are the main points clearly presented? Do you find the text easy to read, or is it stilted or choppy? Is the author's argument repetitive?
E. Evaluative Reviews
- Locate critical reviews of books in a reviewing source , such as the Articles & Full Text , Book Review Index , Book Review Digest, and ProQuest Research Library . Is the review positive? Is the book under review considered a valuable contribution to the field? Does the reviewer mention other books that might be better? If so, locate these sources for more information on your topic.
- Do the various reviewers agree on the value or attributes of the book or has it aroused controversy among the critics?
- For Web sites, consider consulting this evaluation source from UC Berkeley .
Permissions Information
If you wish to use or adapt any or all of the content of this Guide go to Cornell Library's Research Guides Use Conditions to review our use permissions and our Creative Commons license.
- Next: Tips >>
- Last Updated: Apr 18, 2022 1:43 PM
- URL: https://guides.library.cornell.edu/critically_analyzing
Writing Academically
Proofreading, other editing & coaching for highly successful academic writing
- Editing & coaching pricing
- Academic coaching
- How to conduct a targeted literature search
How to write a successful critical analysis
- How to write a strong literature review
- Cautious in tone
- Formal English
- Precise and concise English
- Impartial and objective English
- Substantiate your claims
- The academic team

For further queries or assistance in writing a critical analysis email Bill Wrigley .
What do you critically analyse?
In a critical analysis you do not express your own opinion or views on the topic. You need to develop your thesis, position or stance on the topic from the views and research of others . In academic writing you critically analyse other researchers’:
- concepts, terms
- viewpoints, arguments, positions
- methodologies, approaches
- research results and conclusions
This means weighing up the strength of the arguments or research support on the topic, and deciding who or what has the more or stronger weight of evidence or support.
Therefore, your thesis argues, with evidence, why a particular theory, concept, viewpoint, methodology, or research result(s) is/are stronger, more sound, or more advantageous than others.
What does ‘analysis’ mean?
A critical analysis means analysing or breaking down the parts of the literature and grouping these into themes, patterns or trends.
In an analysis you need to:
1. Identify and separate out the parts of the topic by grouping the various key theories, main concepts, the main arguments or ideas, and the key research results and conclusions on the topic into themes, patterns or trends of agreement , dispute and omission .
2. Discuss each of these parts by explaining:
i. the areas of agreement/consensus, or similarity
ii. the issues or controversies: in dispute or debate, areas of difference
ii. the omissions, gaps, or areas that are under-researched
3. Discuss the relationship between these parts
4. Examine how each contributes to the whole topic
5. Make conclusions about their significance or importance in the topic
What does ‘critical’ mean?
A critical analysis does not mean writing angry, rude or disrespectful comments, or expressing your views in judgmental terms of black and white, good and bad, or right and wrong.
To be critical, or to critique, means to evaluate . Therefore, to write critically in an academic analysis means to:
- judge the quality, significance or worth of the theories, concepts, viewpoints, methodologies, and research results
- evaluate in a fair and balanced manner
- avoid extreme or emotional language

- strengths, advantages, benefits, gains, or improvements
- disadvantages, weaknesses, shortcomings, limitations, or drawbacks
How to critically analyse a theory, model or framework
The evaluative words used most often to refer to theory, model or framework are a sound theory or a strong theory.
The table below summarizes the criteria for judging the strengths and weaknesses of a theory:
- comprehensive
- empirically supported
- parsimonious
Evaluating a Theory, Model or Framework
The table below lists the criteria for the strengths and their corresponding weaknesses that are usually considered in a theory.
Critical analysis examples of theories
The following sentences are examples of the phrases used to explain strengths and weaknesses.
Smith’s (2005) theory appears up to date, practical and applicable across many divergent settings.
Brown’s (2010) theory, although parsimonious and logical, lacks a sufficient body of evidence to support its propositions and predictions
Little scientific evidence has been presented to support the premises of this theory.
One of the limitations with this theory is that it does not explain why…
A significant strength of this model is that it takes into account …
The propositions of this model appear unambiguous and logical.
A key problem with this framework is the conceptual inconsistency between ….
How to critically analyse a concept
The table below summarizes the criteria for judging the strengths and weaknesses of a concept:
- key variables identified
- clear and well-defined
Evaluating Concepts
Critical analysis examples of concepts
Many researchers have used the concept of control in different ways.
There is little consensus about what constitutes automaticity.
Putting forth a very general definition of motivation means that it is possible that any behaviour could be included.
The concept of global education lacks clarity, is imprecisely defined and is overly complex.
Some have questioned the usefulness of resilience as a concept because it has been used so often and in so many contexts.
Research suggests that the concept of preoperative fasting is an outdated clinical approach.
How to critically analyse arguments, viewpoints or ideas
The table below summarizes the criteria for judging the strengths and weaknesses of an argument, viewpoint or idea:
- reasons support the argument
- argument is substantiated by evidence
- evidence for the argument is relevant
- evidence for the argument is unbiased, sufficient and important
- evidence is reputable
Evaluating Arguments, Views or Ideas
Critical analysis examples of arguments, viewpoints or ideas
The validity of this argument is questionable as there is insufficient evidence to support it.
Many writers have challenged Jones’ claim on the grounds that …….
This argument fails to draw on the evidence of others in the field.
This explanation is incomplete because it does not explain why…
The key problem with this explanation is that ……
The existing accounts fail to resolve the contradiction between …
However, there is an inconsistency with this argument. The inconsistency lies in…
Although this argument has been proposed by some, it lacks justification.
However, the body of evidence showing that… contradicts this argument.
How to critically analyse a methodology
The table below provides the criteria for judging the strengths and weaknesses of methodology.
An evaluation of a methodology usually involves a critical analysis of its main sections:
design; sampling (participants); measurement tools and materials; procedure
- design tests the hypotheses or research questions
- method valid and reliable
- potential bias or measurement error, and confounding variables addressed
- method allows results to be generalized
- representative sampling of cohort and phenomena; sufficient response rate
- valid and reliable measurement tools
- valid and reliable procedure
- method clear and detailed to allow replication
Evaluating a Methodology
Critical analysis examples of a methodology
The unrepresentativeness of the sample makes these results misleading.
The presence of unmeasured variables in this study limits the interpretation of the results.
Other, unmeasured confounding variables may be influencing this association.
The interpretation of the data requires caution because the effect of confounding variables was not taken into account.
The insufficient control of several response biases in this study means the results are likely to be unreliable.
Although this correlational study shows association between the variables, it does not establish a causal relationship.
Taken together, the methodological shortcomings of this study suggest the need for serious caution in the meaningful interpretation of the study’s results.
How to critically analyse research results and conclusions
The table below provides the criteria for judging the strengths and weaknesses of research results and conclusions:
- appropriate choice and use of statistics
- correct interpretation of results
- all results explained
- alternative explanations considered
- significance of all results discussed
- consistency of results with previous research discussed
- results add to existing understanding or knowledge
- limitations discussed
- results clearly explained
- conclusions consistent with results
Evaluating the Results and Conclusions
Leave a Reply
Click here to cancel reply.
You must be logged in to post a comment.
WRITING FORMATS FOR EDITING OR COACHING
- Essay or assignment
- Thesis or dissertation
- Proposal for PhD or Masters research
- Literature review
- Journal article or book chapter
- IELTS writing tasks 1 & 2 for general and academic writing
- Resumes & cover letters
- Presentations
- Applications & submissions
Do you have a question?
- Academic writing skills
- Academic English skills
- The Academic team
- Privacy policy
- Terms and conditions
- ABN: 15796080518
- 66 Mungarie Street, Keperra, Qld 4054 Australia
- Email: [email protected]
Website design and development by Caboodle Web

- Subject Guides
Academic writing: a practical guide
Criticality in academic writing.
- Academic writing
- The writing process
- Academic writing style
- Structure & cohesion
- Working with evidence
- Referencing
- Assessment & feedback
- Dissertations
- Reflective writing
- Examination writing
- Academic posters
- Feedback on Structure and Organisation
- Feedback on Argument, Analysis, and Critical Thinking
- Feedback on Writing Style and Clarity
- Feedback on Referencing and Research
- Feedback on Presentation and Proofreading
Being critical is at the heart of academic writing, but what is it and how can you incorporate it into your work?
What is criticality?
What is critical thinking.
Have you ever received feedback in a piece of work saying 'be more critical' or 'not enough critical analysis' but found yourself scratching your head, wondering what that means? Dive into this bitesize workshop to discover what it is and how to do it:
Critical Thinking: What it is and how to do it (bitesize workshop)[YouTube]
University-level work requires both descriptive and critical elements. But what's the difference?
Descriptive
Being descriptive shows what you know about a topic and provides the evidence to support your arguments. It uses simpler processes like remembering , understanding and applying . You might summarise previous research, explain concepts or describe processes.
Being critical pulls evidence together to build your arguments; what does it all mean together? It uses more complex processes: analysing , evaluating and creating . You might make comparisons, consider reasons and implications, justify choices or consider strengths and weaknesses.
Bloom's Taxonomy is a useful tool to consider descriptive and critical processes:
Bloom's Taxonomy [YouTube] | Bloom's Taxonomy [Google Doc]
Find out more about critical thinking:

What is critical writing?
Academic writing requires criticality; it's not enough to just describe or summarise evidence, you also need to analyse and evaluate information and use it to build your own arguments. This is where you show your own thoughts based on the evidence available, so critical writing is really important for higher grades.
Explore the key features of critical writing and see it in practice in some examples:
Introduction to critical writing [Google Slides]
While we need criticality in our writing, it's definitely possible to go further than needed. We’re aiming for that Goldilocks ‘just right’ point between not critical enough and too critical. Find out more:

Critical reading
Criticality isn't just for writing, it is also important to read critically. Reading critically helps you:
- evaluative whether sources are suitable for your assignments.
- know what you're looking for when reading.
- find the information you need quickly.
Critical reading [Interactive tutorial] | Critical reading [Google Doc]
Find out more on our dedicated guides:

Using evidence critically
Academic writing integrates evidence from sources to create your own critical arguments.
We're not looking for a list of summaries of individual sources; ideally, the important evidence should be integrated into a cohesive whole. What does the evidence mean altogether? Of course, a critical argument also needs some critical analysis of this evidence. What does it all mean in terms of your argument?
Find out more about using evidence to build critical arguments in our guide to working with evidence:

Critical language
Critical writing is going to require critical language. Different terms will give different nuance to your argument. Others will just keep things interesting! In the document below we go through some examples to help you out:

Assignment titles: critical or descriptive?
Assignment titles contain various words that show where you need to be descriptive and where you need to be critical. Explore some of the most common instructional words:
Descriptive instructional words
define : give the precise meaning
examine : look at carefully; consider different aspects
explain : clearly describe how a process works, why a decision was made, or give other information needed to understand the topic
illustrate : explain and describe using examples
outline : give an overview of the key information, leaving out minor details
Critical instructional words
analyse : break down the information into parts, consider how parts work together
discuss : explain a topic, make comparisons, consider strengths & weaknesses, give reasons, consider implications
evaluate : assess something's worth, value or suitability for a purpose - this often leads to making a choice afterwards
justify : show the reasoning behind a choice, argument or standpoint
synthesise : bring together evidence and information to create a cohesive whole, integrate ideas or issues
CC BY-NC-SA Learnhigher
More guidance on breaking down assignment titles:
- << Previous: Structure & cohesion
- Next: Working with evidence >>
- Last Updated: Jun 4, 2024 10:44 AM
- URL: https://subjectguides.york.ac.uk/academic-writing

Study Toolbox: Critically Evaluating Articles
- General Study Tips
- Note Taking
- Mind Mapping
- Searching Online Databases
- Searching Business Source Complete
- Searching CINAHL Ultimate
- Searching ProQuest Central
- Searching Science Direct
- Critically Evaluating Articles
- Critically Evaluating Websites
- Using Ebook Central
- Assignment Process
- Structure of an Academic Essay
- Understanding Instructional Words in Essays, Assignments & Exams
- Essay Checklist
- Literature Review
- APA Referencing
- Studying for Exams and Tests
- Tips for taking Exams
Why should I critically evaluate an article?
Just because information has been printed in a journal or magazine it does not mean that it is accurate or appropriate to use in assignments.
An article may represent the views or opinions of the author that are not based on evidence, so it is essential to develop skills to evaluate what you read.
Before using information you find in an article it is important to judge its accuracy, objectivity and establish that the information comes from a reliable and appropriate source.
Consider the following criteria before using and citing an article in an assignment:
- Authorship & Authority
- Type of periodical publication
- Primary or Secondary Source
- Objectivity & Bias
When evaluating an article it is important to consider why the article was written and what impact this has on the objectivity of the article.
To identify the purpose of an article ask yourself:
- Is the article trying to persuade the reader?
- Is the article informing the reader?
- Is the article trying to prove something?
Investigating who the author is and their qualifications can help verify the quality of the information and the credibility of the article.
To judge the author’s credibility find out:
- Who is the author?
- What are the author’s qualifications?
- Is the author an expert in the topic presented in the article?
- What else has the author written?
- Has the author been referenced by other authors?
- Is the author affiliated to an organisation or institution that promotes a particular point of view?
- Is the tone and style of writing factual?
- Are there any grammar and/or spelling errors?
To investigate the author’s credibility search for the author online and check academic databases to locate other articles by the author or if the author has been cited by other authors.
Make sure to investigate the author’s area of expertise because if the author is writing on a subject in their field of study the article is more authoritative than an article written on a subject outside of the author’s expertise.
Consider the tone, style and quality of the writing. Inappropriate style and incorrect spelling/grammar may indicate the author’s poor credibility.
Articles are found in periodical publications and are published on a regular basis e.g. weekly, monthly or quarterly. Periodical publications include newspapers, popular magazines, trade magazines and scholarly/academic journals. It is important to identify which type of periodical publication an article comes from.
What does peer reviewed mean?
Video credited to McMaster Libraries.
McMaster Libraries. (2014, June 19). How library stuff works: Peer review [Video]. YouTube. https://www.youtube.com/watch?v=Z4JJbkpLPQI
How to read a scholarly article...
McMaster Libraries. (2015, August 25). How library stuff works: How to read scholarly articles [Video]. YouTube. https://www.youtube.com/watch?v=Oq6RiJLlzlk
It is essential to identify if an article is a primary or secondary source because they offer different types of information and perspectives.
Currency asks the question ‘is the information current’? It is important to know when an article was published. Determining an article’s currency allows you to judge if it is up to date with current facts and opinions of a topic or if the information is out of date which may mean it is inaccurate and/or misleading.
When judging the currency of an article it is important to take the topic into consideration. Some topics such as those in the sciences require current information. Whereas, other subjects such as history value older material as well as current material.
To discover an article’s currency consider the following questions:
- When was the article published?
- Is the information up to date, out of date or timeless?
- Is the article sufficiently up to date for your purpose?
When evaluating an article, it is important to investigate if the article is objective or if there is some form of bias. Bias occurs when an author allows personal opinions, beliefs and/or values to influence how information is presented. Bias inhibits impartial judgement leading to information being presented in a misleading and/or inaccurate way.
To investigate if an article is objective or biased ask the following questions:
- What is the purpose of this article? Is it to persuade, to inform or to prove?
- Does the author present objective arguments or is the author expressing their biased opinion without evidence to back up this opinion?
- Is the author affiliated to an organisation or institution that promotes a particular viewpoint? Is the author promoting this viewpoint in the article?
- Are alternative sides of the issue or topic presented?
- Are there any political, ideological, cultural, religious, institutional or personal biases?
- Is the article in a journal or magazine that is political, an alternative press or sponsored by a company or an industry lobby group? If yes, the publication may have an inherent bias towards a particular point of view that will impact articles printed in it.
- What is the objective of those involved in the publishing of the journal or magazine? Does the article show a bias towards the publisher’s particular point of view?
When evaluating an article for objectivity and bias check for a sound argument, supporting facts and references that include sources representing more than one point of view.
Video credited to LIBCSU: North Carolina State University Libraries.
LIBCSU. (2015, June 10). Evaluating sources for credibility [Video]. YouTube. https://www.youtube.com/watch?v=PLTOVoHbH5c
One of the critical steps in evaluating an article is questioning if the information is accurate.
To evaluate an article’s accuracy consider the following questions:
- Is the author affiliated with a known, respectable institution?
- Are references included to identify where any factual information and/or data comes from?
- Are the references used real, credible and relevant?
- Can you verify the information in another source?
- Is the information consistent with other authors’ findings on the same topic?
- Does the text follow basic rules of grammar, spelling and composition?
- Is a bibliography and/or reference list included?
Check the accuracy of information found in articles by checking the sources and references used and research the topic to compare the information with other reliable sources. If you find factual errors, you may want to question the quality and accuracy of the article.
How do I evaluate information?
Video credited to University of South Australia.
University of South Australia. (2017, October 23). Study help: Evaluating information [Video]. YouTube. https://www.youtube.com/watch?v=2U3dkTLjuvE
Popular vs Scholarly Sources
University of South Australia. (2017, October 20). Study help: Scholarly sources explained [Video]. YouTube. https://www.youtube.com/watch?v=IRCHdhdS_aU
Checklist for evaluating articles
- Checklist for evaluating articles This checklist is to help you evaluate articles and decide if the information is accurate and reliable.
- << Previous: Searching Science Direct
- Next: Critically Evaluating Websites >>
- Last Updated: Jun 6, 2024 12:05 PM
- URL: https://sitacnz.libguides.com/Study_Toolbox

- Teesside University Student & Library Services
- Learning Hub Group
Critical Appraisal for Health Students
- Critical Appraisal of a qualitative paper
- Critical Appraisal: Help
- Critical Appraisal of a quantitative paper
- Useful resources
Appraisal of a Qualitative paper : Top tips

- Introduction
Critical appraisal of a qualitative paper
This guide aimed at health students, provides basic level support for appraising qualitative research papers. It's designed for students who have already attended lectures on critical appraisal. One framework for appraising qualitative research (based on 4 aspects of trustworthiness) is provided and there is an opportunity to practise the technique on a sample article.
Support Materials
- Framework for reading qualitative papers
- Critical appraisal of a qualitative paper PowerPoint
To practise following this framework for critically appraising a qualitative article, please look at the following article:
Schellekens, M.P.J. et al (2016) 'A qualitative study on mindfulness-based stress reduction for breast cancer patients: how women experience participating with fellow patients', Support Care Cancer , 24(4), pp. 1813-1820.
Critical appraisal of a qualitative paper: practical example.
- Credibility
- Transferability
- Dependability
- Confirmability
How to use this practical example
Using the framework, you can have a go at appraising a qualitative paper - we are going to look at the following article:
Step 1. take a quick look at the article, step 2. click on the credibility tab above - there are questions to help you appraise the trustworthiness of the article, read the questions and look for the answers in the article. , step 3. click on each question and our answers will appear., step 4. repeat with the other aspects of trustworthiness: transferability, dependability and confirmability ., questioning the credibility:, who is the researcher what has been their experience how well do they know this research area, was the best method chosen what method did they use was there any justification was the method scrutinised by peers is it a recognisable method was there triangulation ( more than one method used), how was the data collected was data collected from the participants at more than one time point how long were the interviews were questions asked to the participants in different ways, is the research reporting what the participants actually said were the participants shown transcripts / notes of the interviews / observations to ‘check’ for accuracy are direct quotes used from a variety of participants, how would you rate the overall credibility, questioning the transferability, was a meaningful sample obtained how many people were included is the sample diverse how were they selected, are the demographics given, does the research cover diverse viewpoints do the results include negative cases was data saturation reached, what is the overall transferability can the research be transferred to other settings , questioning the dependability :, how transparent is the audit trail can you follow the research steps are the decisions made transparent is the whole process explained in enough detail did the researcher keep a field diary is there a clear limitations section, was there peer scrutiny of the researchwas the research plan shown to peers / colleagues for approval and/or feedback did two or more researchers independently judge data, how would you rate the overall dependability would the results be similar if the study was repeated how consistent are the data and findings, questioning the confirmability :, is the process of analysis described in detail is a method of analysis named or described is there sufficient detail, have any checks taken place was there cross-checking of themes was there a team of researchers, has the researcher reflected on possible bias is there a reflexive diary, giving a detailed log of thoughts, ideas and assumptions, how do you rate the overall confirmability has the researcher attempted to limit bias, questioning the overall trustworthiness :, overall how trustworthy is the research, further information.
See Useful resources for links, books and LibGuides to help with Critical appraisal.
- << Previous: Critical Appraisal: Help
- Next: Critical Appraisal of a quantitative paper >>
- Last Updated: May 29, 2024 10:15 AM
- URL: https://libguides.tees.ac.uk/critical_appraisal
7 Steps for How to Write an Evaluation Essay (Example & Template)
In this ultimate guide, I will explain to you exactly how to write an evaluation essay.
1. What is an Evaluation Essay?
An evaluation essay should provide a critical analysis of something.
You’re literally ‘evaluating’ the thing you’re looking up.
Here’s a couple of quick definitions of what we mean by ‘evaluate’:
- Merriam-Webster defines evaluation as: “to determine the significance, worth, or condition of usually by careful appraisal and study”
- Collins Dictionary says: “If you evaluate something or someone, you consider them in order to make a judgment about them, for example about how good or bad they are.”
Here’s some synonyms for ‘evaluate’:
So, we could say that an evaluation essay should carefully examine the ‘thing’ and provide an overall judgement of it.
Here’s some common things you may be asked to write an evaluation essay on:
This is by no means an exhaustive list. Really, you can evaluate just about anything!
Get a Pdf of this article for class
Enjoy subscriber-only access to this article’s pdf
2. How to write an Evaluation Essay
There are two secrets to writing a strong evaluation essay. The first is to aim for objective analysis before forming an opinion. The second is to use an evaluation criteria.
Aim to Appear Objective before giving an Evaluation Argument
Your evaluation will eventually need an argument.
The evaluation argument will show your reader what you have decided is the final value of the ‘thing’ you’re evaluating.
But in order to convince your reader that your evaluative argument is sound, you need to do some leg work.
The aim will be to show that you have provided a balanced and fair assessment before coming to your conclusion.
In order to appear balanced you should:
- Discuss both the pros and cons of the thing
- Discuss both the strengths and weaknesses of the thing
- Look at the thing from multiple different perspectives
- Be both positive and critical. Don’t make it look like you’re biased towards one perspective.
In other words, give every perspective a fair hearing.
You don’t want to sound like a propagandist. You want to be seen as a fair and balanced adjudicator.
Use an Evaluation Criteria
One way to appear balanced is to use an evaluation criteria.
An evaluation criteria helps to show that you have assessed the ‘thing’ based on an objective measure.
Here’s some examples of evaluation criteria:
- Strength under pressure
- Longevity (ability to survive for a long time)
- Ease of use
- Ability to get the job done
- Friendliness
- Punctuality
- Ability to predict my needs
- Calmness under pressure
- Attentiveness
A Bed and Breakfast
- Breakfast options
- Taste of food
- Comfort of bed
- Local attractions
- Service from owner
- Cleanliness
We can use evaluation criteria to frame out ability to conduct the analysis fairly.
This is especially true for if you have to evaluate multiple different ‘things’. For example, if you’re evaluating three novels, you want to be able to show that you applied the same ‘test’ on all three books!
This will show that you gave each ‘thing’ a fair chance and looked at the same elements for each.
3. How to come up with an Evaluation Argument
After you have:
- Looked at both good and bad elements of the ‘thing’, and
- Used an evaluation criteria
You’ll then need to develop an evaluative argument. This argument shows your own overall perspective on the ‘thing’.
Remember, you will need to show your final evaluative argument is backed by objective analysis. You need to do it in order!
Analyze first. Evaluate second.
Here’s an example.
Let’s say you’re evaluating the quality of a meal.
You might say:
- A strength of the meal was its presentation. It was well presented and looked enticing to eat.
- A weakness of the meal was that it was overcooked. This decreased its flavor.
- The meal was given a low rating on ‘cost’ because it was more expensive than the other comparative meals on the menu.
- The meal was given a high rating on ‘creativity’. It was a meal that involved a thoughtful and inventive mix of ingredients.
Now that you’ve looked at some pros and cons and measured the meal based on a few criteria points (like cost and creativity), you’ll be able to come up with a final argument:
- Overall, the meal was good enough for a middle-tier restaurant but would not be considered a high-class meal. There is a lot of room for improvement if the chef wants to win any local cooking awards.
Evaluative terms that you might want to use for this final evaluation argument might include:
- All things considered
- With all key points in mind
4. Evaluation Essay Outline (with Examples)
Okay, so now you know what to do, let’s have a go at creating an outline for your evaluation essay!
Here’s what I recommend:
4.1 How to Write your Introduction
In the introduction, feel free to use my 5-Step INTRO method . It’ll be an introduction just like any other essay introduction .
And yes, feel free to explain what the final evaluation will be.
So, here it is laid out nice and simple.
Write one sentence for each point to make a 5-sentence introduction:
- Interest: Make a statement about the ‘thing’ you’re evaluating that you think will be of interest to the reader. Make it a catchy, engaging point that draws the reader in!
- Notify: Notify the reader of any background info on the thing you’re evaluating. This is your chance to show your depth of knowledge. What is a historical fact about the ‘thing’?
- Translate: Re-state the essay question. For an evaluative essay, you can re-state it something like: “This essay evaluates the book/ product/ article/ etc. by looking at its strengths and weaknesses and compares it against a marking criteria”.
- Report: Say what your final evaluation will be. For example you can say “While there are some weaknesses in this book, overall this evaluative essay will show that it helps progress knowledge about Dinosaurs.”
- Outline: Simply give a clear overview of what will be discussed. For example, you can say: “Firstly, the essay will evaluate the product based on an objective criteria. This criteria will include its value for money, fit for purpose and ease of use. Next, the essay will show the main strengths and weaknesses of the product. Lastly, the essay will provide a final evaluative statement about the product’s overall value and worth.”
If you want more depth on how to use the INTRO method, you’ll need to go and check out our blog post on writing quality introductions.
4.2 Example Introduction
This example introduction is for the essay question: Write an Evaluation Essay on Facebook’s Impact on Society.
“Facebook is the third most visited website in the world. It was founded in 2004 by Mark Zuckerberg in his college dorm. This essay evaluates the impact of Facebook on society and makes an objective judgement on its value. The essay will argue that Facebook has changed the world both for the better and worse. Firstly, it will give an overview of what Facebook is and its history. Then, it will examine Facebook on the criteria of: impact on social interactions, impact on the media landscape, and impact on politics.”
You’ll notice that each sentence in this introduction follows my 5-Step INTRO formula to create a clear, coherent 5-Step introduction.
4.3 How to Write your Body Paragraphs
The first body paragraph should give an overview of the ‘thing’ being evaluated.
Then, you should evaluate the pros and cons of the ‘thing’ being evaluated based upon the criteria you have developed for evaluating it.
Let’s take a look below.
4.4 First Body Paragraph: Overview of your Subject
This first paragraph should provide objective overview of your subject’s properties and history. You should not be doing any evaluating just yet.
The goal for this first paragraph is to ensure your reader knows what it is you’re evaluating. Secondarily, it should show your marker that you have developed some good knowledge about it.
If you need to use more than one paragraph to give an overview of the subject, that’s fine.
Similarly, if your essay word length needs to be quite long, feel free to spend several paragraphs exploring the subject’s background and objective details to show off your depth of knowledge for the marker.
4.5 First Body Paragraph Example
Sticking with the essay question: Write an Evaluation Essay on Facebook’s Impact on Society , this might be your paragraph:
“Facebook has been one of the most successful websites of all time. It is the website that dominated the ‘Web 2.0’ revolution, which was characterized by user two-way interaction with the web. Facebook allowed users to create their own personal profiles and invite their friends to follow along. Since 2004, Facebook has attracted more than one billion people to create profiles in order to share their opinions and keep in touch with their friends.”
Notice here that I haven’t yet made any evaluations of Facebook’s merits?
This first paragraph (or, if need be, several of them) should be all about showing the reader exactly what your subject is – no more, no less.
4.6 Evaluation Paragraphs: Second, Third, Forth and Fifth Body Paragraphs
Once you’re confident your reader will know what the subject that you’re evaluating is, you’ll need to move on to the actual evaluation.
For this step, you’ll need to dig up that evaluation criteria we talked about in Point 2.
For example, let’s say you’re evaluating a President of the United States.
Your evaluation criteria might be:
- Impact on world history
- Ability to pass legislation
- Popularity with voters
- Morals and ethics
- Ability to change lives for the better
Really, you could make up any evaluation criteria you want!
Once you’ve made up the evaluation criteria, you’ve got your evaluation paragraph ideas!
Simply turn each point in your evaluation criteria into a full paragraph.
How do you do this?
Well, start with a topic sentence.
For the criteria point ‘Impact on world history’ you can say something like: “Barack Obama’s impact on world history is mixed.”
This topic sentence will show that you’ll evaluate both pros and cons of Obama’s impact on world history in the paragraph.
Then, follow it up with explanations.
“While Obama campaigned to withdraw troops from Iraq and Afghanistan, he was unable to completely achieve this objective. This is an obvious negative for his impact on the world. However, as the first black man to lead the most powerful nation on earth, he will forever be remembered as a living milestone for civil rights and progress.”
Keep going, turning each evaluation criteria into a full paragraph.
4.7 Evaluation Paragraph Example
Let’s go back to our essay question: Write an Evaluation Essay on Facebook’s Impact on Society .
I’ve decided to use the evaluation criteria below:
- impact on social interactions;
- impact on the media landscape;
- impact on politics
Naturally, I’m going to write one paragraph for each point.
If you’re expected to write a longer piece, you could write two paragraphs on each point (one for pros and one for cons).
Here’s what my first evaluation paragraph might look like:
“Facebook has had a profound impact on social interactions. It has helped people to stay in touch with one another from long distances and after they have left school and college. This is obviously a great positive. However, it can also be seen as having a negative impact. For example, people may be less likely to interact face-to-face because they are ‘hanging out’ online instead. This can have negative impact on genuine one-to-one relationships.”
You might notice that this paragraph has a topic sentence, explanations and examples. It follows my perfect paragraph formula which you’re more than welcome to check out!
4.8 How to write your Conclusion
To conclude, you’ll need to come up with one final evaluative argument.
This evaluation argument provides an overall assessment. You can start with “Overall, Facebook has been…” and continue by saying that (all things considered) he was a good or bad president!
Remember, you can only come up with an overall evaluation after you’ve looked at the subject’s pros and cons based upon your evaluation criteria.
In the example below, I’m going to use my 5 C’s conclusion paragraph method . This will make sure my conclusion covers all the things a good conclusion should cover!
Like the INTRO method, the 5 C’s conclusion method should have one sentence for each point to create a 5 sentence conclusion paragraph.
The 5 C’s conclusion method is:
- Close the loop: Return to a statement you made in the introduction.
- Conclude: Show what your final position is.
- Clarify: Clarify how your final position is relevant to the Essay Question.
- Concern: Explain who should be concerned by your findings.
- Consequences: End by noting in one final, engaging sentence why this topic is of such importance. The ‘concern’ and ‘consequences’ sentences can be combined
4.9 Concluding Argument Example Paragraph
Here’s a possible concluding argument for our essay question: Write an Evaluation Essay on Facebook’s Impact on Society .
“The introduction of this essay highlighted that Facebook has had a profound impact on society. This evaluation essay has shown that this impact has been both positive and negative. Thus, it is too soon to say whether Facebook has been an overall positive or negative for society. However, people should pay close attention to this issue because it is possible that Facebook is contributing to the undermining of truth in media and positive interpersonal relationships.”
Note here that I’ve followed the 5 C’s conclusion method for my concluding evaluative argument paragraph.
5. Evaluation Essay Example Template
Below is a template you can use for your evaluation essay , based upon the advice I gave in Section 4:
6. 23+ Good Evaluation Essay Topics
Okay now that you know how to write an evaluation essay, let’s look at a few examples.
For each example I’m going to give you an evaluation essay title idea, plus a list of criteria you might want to use in your evaluation essay.
6.1 Evaluation of Impact
- Evaluate the impact of global warming on the great barrier reef. Recommended evaluation criteria: Level of bleaching; Impact on tourism; Economic impact; Impact on lifestyles; Impact on sealife
- Evaluate the impact of the Global Financial Crisis on poverty. Recommended evaluation criteria: Impact on jobs; Impact on childhood poverty; Impact on mental health rates; Impact on economic growth; Impact on the wealthy; Global impact
- Evaluate the impact of having children on your lifestyle. Recommended evaluation criteria: Impact on spare time; Impact on finances; Impact on happiness; Impact on sense of wellbeing
- Evaluate the impact of the internet on the world. Recommended evaluation criteria: Impact on connectedness; Impact on dating; Impact on business integration; Impact on globalization; Impact on media
- Evaluate the impact of public transportation on cities. Recommended evaluation criteria: Impact on cost of living; Impact on congestion; Impact on quality of life; Impact on health; Impact on economy
- Evaluate the impact of universal healthcare on quality of life. Recommended evaluation criteria: Impact on reducing disease rates; Impact on the poorest in society; Impact on life expectancy; Impact on happiness
- Evaluate the impact of getting a college degree on a person’s life. Recommended evaluation criteria: Impact on debt levels; Impact on career prospects; Impact on life perspectives; Impact on relationships
6.2 Evaluation of a Scholarly Text or Theory
- Evaluate a Textbook. Recommended evaluation criteria: clarity of explanations; relevance to a course; value for money; practical advice; depth and detail; breadth of information
- Evaluate a Lecture Series, Podcast or Guest Lecture. Recommended evaluation criteria: clarity of speaker; engagement of attendees; appropriateness of content; value for monet
- Evaluate a journal article. Recommended evaluation criteria: length; clarity; quality of methodology; quality of literature review ; relevance of findings for real life
- Evaluate a Famous Scientists. Recommended evaluation criteria: contribution to scientific knowledge; impact on health and prosperity of humankind; controversies and disagreements with other scientists.
- Evaluate a Theory. Recommended evaluation criteria: contribution to knowledge; reliability or accuracy; impact on the lives of ordinary people; controversies and contradictions with other theories.
6.3 Evaluation of Art and Literature
- Evaluate a Novel. Recommended evaluation criteria: plot complexity; moral or social value of the message; character development; relevance to modern life
- Evaluate a Play. Recommended evaluation criteria: plot complexity; quality of acting; moral or social value of the message; character development; relevance to modern life
- Evaluate a Film. Recommended evaluation criteria: plot complexity; quality of acting; moral or social value of the message; character development; relevance to modern life
- Evaluate an Artwork. Recommended evaluation criteria: impact on art theory; moral or social message; complexity or quality of composition
6.4 Evaluation of a Product or Service
- Evaluate a Hotel or Bed and Breakfast. Recommended evaluation criteria: quality of service; flexibility of check-in and check-out times; cleanliness; location; value for money; wi-fi strength; noise levels at night; quality of meals; value for money
- Evaluate a Restaurant. Recommended evaluation criteria: quality of service; menu choices; cleanliness; atmosphere; taste; value for money.
- Evaluate a Car. Recommended evaluation criteria: fuel efficiency; value for money; build quality; likelihood to break down; comfort.
- Evaluate a House. Recommended evaluation criteria: value for money; build quality; roominess; location; access to public transport; quality of neighbourhood
- Evaluate a Doctor. Recommended evaluation criteria: Quality of service; knowledge; quality of equipment; reputation; value for money.
- Evaluate a Course. Recommended evaluation criteria: value for money; practical advice; quality of teaching; quality of resources provided.
7. Concluding Advice

Evaluation essays are common in high school, college and university.
The trick for getting good marks in an evaluation essay is to show you have looked at both the pros and cons before making a final evaluation analysis statement.
You don’t want to look biased.
That’s why it’s a good idea to use an objective evaluation criteria, and to be generous in looking at both positives and negatives of your subject.
Read Also: 39 Better Ways to Write ‘In Conclusion’ in an Essay
I recommend you use the evaluation template provided in this post to write your evaluation essay. However, if your teacher has given you a template, of course use theirs instead! You always want to follow your teacher’s advice because they’re the person who will be marking your work.
Good luck with your evaluation essay!

Chris Drew (PhD)
Dr. Chris Drew is the founder of the Helpful Professor. He holds a PhD in education and has published over 20 articles in scholarly journals. He is the former editor of the Journal of Learning Development in Higher Education. [Image Descriptor: Photo of Chris]
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ 15 Self-Actualization Examples (Maslow's Hierarchy)
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ Forest Schools Philosophy & Curriculum, Explained!
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ Montessori's 4 Planes of Development, Explained!
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ Montessori vs Reggio Emilia vs Steiner-Waldorf vs Froebel
2 thoughts on “7 Steps for How to Write an Evaluation Essay (Example & Template)”
What an amazing article. I am returning to studying after several years and was struggling with how to present an evaluative essay. This article has simplified the process and provided me with the confidence to tackle my subject (theoretical approaches to development and management of teams).
I just wanted to ask whether the evaluation criteria has to be supported by evidence or can it just be a list of criteria that you think of yourself to objectively measure?
Many many thanks for writing this!

Usually we would want to see evidence, but ask your teacher for what they’re looking for as they may allow you, depending on the situation.
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
- Share full article
Advertisement
Subscriber-only Newsletter
The Ethicist
Can i use a.i. to grade my students’ papers.
The magazine’s Ethicist columnist on artificial intelligence platforms, and whether it’s hypocritical for teachers to use these tools while forbidding students from doing the same.

By Kwame Anthony Appiah
I am a junior-high-school English teacher. In the past school year, there has been a significant increase in students’ cheating on writing assignments by using artificial intelligence. Our department feels that 13-year-old students will only become better writers if they practice and learn from the successes and challenges that come with that.
Recently our department tasked students with writing an argumentative essay, an assignment we supported by breaking down the process into multiple steps. The exercise took several days of class time and homework to complete. All of our students signed a contract agreeing not to use A.I. assistance, and parents promised to support the agreement by monitoring their children when they worked at home. Yet many students still used A.I.
Some of our staff members uploaded their grading rubric into an A.I.-assisted platform, and students uploaded their essays for assessment. The program admittedly has some strengths. Most notable, it gives students writing feedback and the opportunity to edit their work before final submission. The papers are graded within minutes, and the teachers are able to transfer the A.I. grade into their roll book.
I find this to be hypocritical. I spend many hours grading my students’ essays. It’s tedious work, but I feel that it’s my responsibility — if a student makes an effort to complete the task, they should have my undivided attention during the assessment process.
Here’s where I struggle: Should I embrace new technology and use A.I.-assisted grading to save time and my sanity even though I forbid my students from using it? Is it unethical for teachers to ask students not to use A.I. to assist their writing but then allow an A.I. platform to grade their work? — Name Withheld
From the Ethicist:
You have a sound rationale for discouraging your students from using A.I. to draft their essays. As with many other skills, writing well and thinking clearly will improve through practice. By contrast, you already know how to grade papers; you don’t need the practice.
What matters is whether an A.I.-assisted platform can reliably appraise and diagnose your students’ writing, providing the explanation and guidance these students need to improve. In theory, such tools — and I see that there are several on the market, including from major educational publishers — have certain advantages. The hope is that they can grade without inconsistency, without getting tired, without being affected by the expectations that surely affect those of us who hand-grade student work.
I notice you haven’t raised concerns about whether the platform provides reliable assessments; you’ll have to decide if it does. (If it isn’t quite up to snuff, it might become so in a year or two, so your question will persist.) Provided the platform does a decent job of assessment, though, I don’t see why you must do it all yourself. You should review the A.I.-annotated versions of your students’ writing, check that you agree with the output, and make notes of issues to bring up in class. But time saved in evaluating the papers might be better spent on other things — and by “better,” I mean better for the students. There are pedagogical functions, after all, that only you can perform.
In sum: It’s not hypocritical to use A.I. yourself in a way that serves your students well, even as you insist that they don’t use it in a way that serves them badly.
Readers Respond
The previous question was from a reader who asked about professional boundaries. He wrote: “I am a retired, married male psychiatrist. A divorced female former patient of mine contacted me recently, 45 years after her treatment ended. Would it be OK to correspond with her by email? Or is this a case of ‘once a patient, always a patient?’”
In his response, the Ethicist noted: “The relevant professional associations tend to have strictures that are specifically about sexual relationships with former patients. … In light of the potential for exploitation within the therapist-patient relationship, these rules are meant to maintain clear boundaries, protect patient welfare, uphold the integrity of the profession and eliminate any gray areas that could lead to ethical breaches. But though you do mention her marital status, and yours, you’re just asking about emailing her — about establishing friendly relations. The question for you is whether she might be harmed by this, whether whatever knowledge or trust gained from your professional relationship would shadow a personal one. Yes, almost half a century has elapsed since your professional relationship, but you still have to be confident that a correspondence with her clears this bar. If it does, you may email with a clear conscience.” ( Reread the full question and answer here. )
As always, I agree with the Ethicist. I would add that the letter writer’s former patient doesn’t realize that the therapist is actually two different people — the professional and the regular person underneath. Therapists portray their professional selves to their clients. The former client may be disappointed upon meeting the therapist outside of the professional context. Additionally, the feelings she has toward the therapist may be based on transference, and they would need to address that. — Annemarie
I am a clinical psychologist. While the Ethicist’s description of professional ethical boundaries is correct, there is more to the story, and I disagree with his conclusion. A very big question here is why this former patient contacted him after 45 years. That is a question that is best explored and answered within the context of a therapeutic relationship. He would be well- advised to respond in a kind and thoughtful way to convey the clear message that he is not available for ongoing communication, and he should suggest that she consult with another therapist if she feels that would be helpful. — Margaret
In my case, it was the therapist who reached out to me, seeking to establish a friendship several years after our sessions ended. I was surprised, but he shared that he had since experienced a similar personal tragedy to one I had explored with him in sessions. Since it had been several years since we saw each other professionally, I responded. There was never any hint of romantic or sexual interest. Still, as he continued to reach out to me, clearly desiring a friendship, it never felt right to me. It did feel unprofessional, as his knowledge of me was borne out of a relationship meant to be professional, never personal, as warmly as we might have felt during our sessions. I ended up being disappointed in him for seeking out my friendship. — Liam
I am a (semi)retired psychiatrist who has been practicing since 1974. In my opinion, “once a patient, always a patient” is correct. Establishing any type of personal relationship with a former patient could undo progress the patient may have made in treatment, and is a slippery slope toward blatantly unethical behavior. As psychiatrists, our responsibility is to work with patients in confronting and resolving issues that are preventing them from having a reality-based perception of their life. With such an outlook, they are more capable of establishing satisfying relationships with others. An ethical psychiatrist is not in the business of providing such satisfaction to his or her patients. — Roger
I think there is a difference between being friendly and being friends with a former client. As someone who used to attend therapy with a therapist I think dearly of, she made it clear to me that it was OK to send her emails with life updates after our therapeutic relationship ended. But beyond that, I think it would be inappropriate and uncomfortable to pursue a friendship with her, and vice versa, because of the patient-provider relationship that we previously had and the power dynamic that existed between us. The letter writer didn’t share the content of the email his former patient sent to him, but if it’s just a friendly life update, I think it’s fine to write back and thank her for sharing. Beyond that, I feel like it would be unprofessional to meet or pursue a deeper relationship. — Meghan
Kwame Anthony Appiah is The New York Times Magazine’s Ethicist columnist and teaches philosophy at N.Y.U. His books include “Cosmopolitanism,” “The Honor Code” and “The Lies That Bind: Rethinking Identity.” To submit a query: Send an email to [email protected]. More about Kwame Anthony Appiah
- Open access
- Published: 01 June 2024
A model of contributors to a trusting patient-physician relationship: a critical review using a systematic search strategy
- Seraina Petra Lerch 1 , 2 , 3 ,
- Rahel Hänggi 4 ,
- Yara Bussmann 4 &
- Andrea Lörwald 4
BMC Primary Care volume 25 , Article number: 194 ( 2024 ) Cite this article
99 Accesses
Metrics details
The lack of trust between patients and physicians has a variety of negative consequences. There are several theories concerning how interpersonal trust is built, and different studies have investigated trust between patients and physicians that have identified single factors as contributors to trust. However, all possible contributors to a trusting patient-physician relationship remain unclear. This review synthesizes current knowledge regarding patient-physician trust and integrates contributors to trust into a model.
A systematic search was conducted using the databases MEDLINE (Ovid), Embase (Ovid), PsycINFO (Ovid), and Eric (Ovid). We ran simultaneous searches for a combination of the phrases: patient-physician relationship (or synonyms) and trust or psychological safety. Six-hundred and twenty-five abstracts were identified and screened using pre-defined criteria and later underwent full-text article screening. We identified contributors to trust in the eligible articles and critically assessed whether they were modifiable.
Forty-five articles were included in the review. Patient-centered factors that contributed modifiable promoters of trust included psychological factors, levels of health education and literacy, and the social environment. Physician-centered factors that added to a trusting patient-physician relationship included competence, communication, interest in the patient, caring, the provisioning of health education, and professionalism. The patient-physician alliance, time spent together, and shared decision-making also contributed to trusting relationships between patients and physicians. External contributors included institutional factors, how payments are made, and additional healthcare services.
Our model summarized modifiable contributors to a trusting patient-physician relationship. We found that providing sufficient time during patient-physician encounters, ensuring continuity of care, and fostering health education are promising starting points for improving trust between patients and physicians. Future research should evaluate the effectiveness of interventions that address multiple modifiable contributors to a trusting patient-physician relationship.
Peer Review reports
Introduction
Trust, as a cornerstone of human relationships, applies to the patient-physician relationship. Relationship building is a basic skill for the medical professional [ 1 , 2 ]. There is evidence that trust between patients and doctors has a positive effect and, if trust is missing, leads to potentially negative consequences. A meta-analysis confirmed that trust was positively associated with improved health outcomes [ 3 ] in, for example, diabetes [ 4 ], cancer [ 5 ], and human immunodeficiency virus infections (HIV infections) [ 6 ]. Trust also increases positive behavioral outcomes in patients [ 7 ], such as treatment adherence [ 8 , 9 ]. In contrast, low trust in physicians has been shown to negatively affect various patient health outcomes [ 4 , 6 , 10 , 11 , 12 , 13 , 14 ]. Economically, if trust in physicians is missing, it has adverse financial effects on healthcare systems [ 15 ]. Furthermore, a physician may be more likely to incur complaints when trusting relationships with patients are lacking [ 16 ].
In medicine, trust can be understood as being social or interpersonal [ 17 , 18 ]. Social trust refers to individuals’ trust in institutions or systems, such as the healthcare system or physicians in general, while interpersonal trust refers to the trust between two individuals [ 18 , 19 ]. Social trust is believed to affect interpersonal trust in medical settings [ 17 , 18 ]. There are various theories of trust from different disciplines [ 20 , 21 , 22 , 23 ]. However, the most prominent interpersonal trust theory in psychology (and applied in medical settings) is from Mayer et al., who defined trust as the willingness of an individual to be vulnerable to the actions of another based on the expectation that the other will perform a particular action important to the trustor, irrespective of the ability to monitor or control the other party [ 24 ]. Their theory of interpersonal trust suggests that benevolence, integrity, ability, propensity to trust, and perceived risk are components of a trust relationship [ 24 ]. When applied to the patient-physician relationship, the physician’s ability, integrity, and benevolence act as contributors. At the same time, a patient’s propensity to trust—their willingness to trust others—and the perceived risk they take when trusting a physician are also important factors. However, the reality is likely more complex, and there are probably more contributors to a trusting patient-physician relationship than the theory proposes. While different evidence-based studies have investigated the patient-physician trust relationship, to our knowledge, there has been no synthesis of all the evidence-based contributors to the relationship. In 2000, there was a call for an empirical conceptualization of trust. Rather than single theories used to explain interpersonal patient-physician trust or studies investigating isolated contributors of trust, the idea was to synthesize empirical evidence concerning how patient-physician trust can evolve into a model [ 19 ]. A recent review on trust in the medical field has renewed the need for such an empirical conceptualization of patient-physician trust [ 25 ]. Therefore, this study aimed to summarize the empirical evidence, identify the contributors to a trusting patient-physician relationship, and integrate them into a model. This model can then be used to identify potential approaches and leverage points to improve patient-physician trust. The two main research questions were:
Which factors contribute to a trusting patient-physician relationship?
Which of these factors can act as potential leverage points to improve the patient-physician relationship?
In addition, we critically assessed contributors based on how they are already implemented in healthcare systems and medical education.
As the research questions were too broad for a systematic or scoping review, a critical review with a systematic search approach was used to answer the first research question. Critical reviews focus on empirical research [ 26 ] to evaluate what is known about a specific topic and integrate it into a framework [ 26 , 27 ]. They may use a systematic search strategy to integrate the strengths of systematic and critical reviews [ 27 ], including all relevant literature, to avoid biases.
Search strategy
We searched the databases MEDLINE (Ovid), Embase (Ovid), PsycINFO (Ovid), and ERIC (Ovid) for a combination of terms (or synonyms) referring to the patient-physician relationship and trust or psychological safety. Database searches were run simultaneously as multifile searches in Ovid. For the results, Ovid’s de-duplicator was used. No study or clinical trial registries or online resources were searched. No experts were contacted, nor was a citation search conducted. A reproducible search for all of the databases is as follows:
Embase (1974 to January 13, 2022), ERIC (1965 to May 2021), Ovid MEDLINE(R) ALL (1946 to January 13, 2022), APA PsycInfo (1806 to January Week 1, 2022).
(patient* adj2 physician* adj2 (relation* or alliance or rapport)).ti, ab.
(trust* or psychological safety).ti, ab.
remove duplicates from 3.
We did not use any language, time period, study design, or other restrictions for the searches, and no search filters were used. The comprehensive literature search was run on January 13, 2022 and 630 articles were retrieved. An information specialist assisted in framing the research questions and provided information on the different types of reviews. Once a first draft of the search strategy was developed, multiple feedback rounds with the information specialist were conducted until the search strategy was finalized.
Screening process
Fifty-three records were retrieved from Ovid MEDLINER ALL, 509 from Embase, 1 from ERIC, and 67 from APA PsycInfo. In total, 630 records were found. As OVID’s de-duplication process did not identify all duplicates, any remaining duplicates were removed by SPL using EndNote’s duplicate identification strategy and a manual approach. After de-duplication, 613 articles remained, which were screened in two rounds. The first round was screened according to title and abstract. In the second round, 116 articles were evaluated for inclusion based on the full texts. SPL and RH did the screening, and AL decided when there were disagreements between SPL and RH. A study selection flowchart is shown in Fig. 1 .
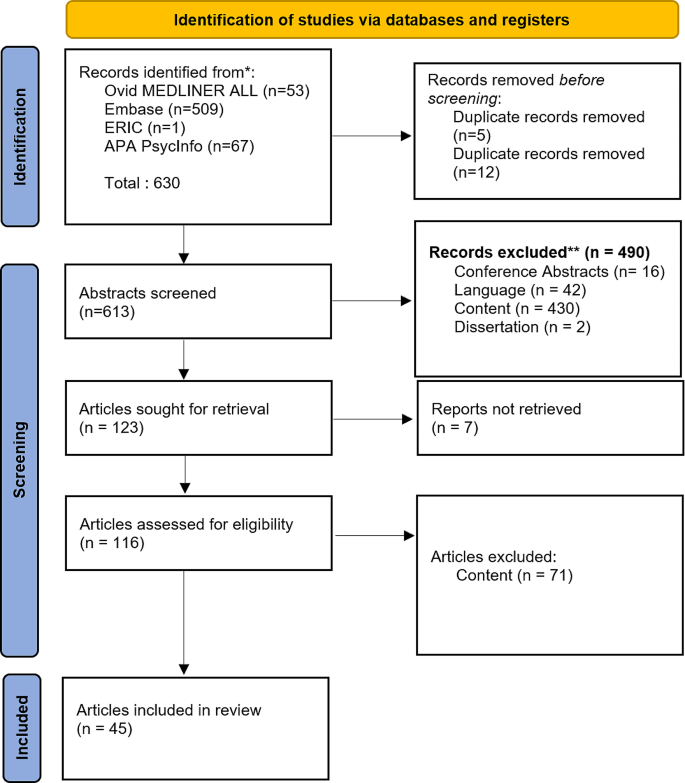
PRISMA study flowchart
We included studies that reported factors contributing to a trusting relationship between patients and physicians and excluded those that only reported contributing factors between patients and health professionals other than physicians (or no contributors). We also included studies that explicitly measured trust between a patient and physician either quantitatively or qualitatively and excluded those with no measure of patient trust in physicians (e.g., only generalized patient trust or trust in other health professionals). We included quantitative, qualitative, and mixed methods papers and excluded dissertations and conference abstracts. Only articles in English and German were included.
Data synthesis and categorization
We first extracted the contributors mentioned in the studies as this review focused on integrating contributors to a trusting patient-physician relationship into an overall model. Extracted data included information on the setting, patients, physicians, how trust was operationalized, and which factors had a positive, negative, or no effect on the relationship. Contributors were then categorized into patient-related, physician-related, context-related, or patient- and physician-related factors. Study sizes and methods of measurement were highlighted. The factors were then synthesized, and the modifiable ones were extracted and displayed in a model.
Forty-five heterogeneous studies reported factors contributing to a trusting patient-physician relationship. An overview of these studies, including the contributors to trust for each study, can be found in Appendix 1 .
Patient-related factors
Several patient-related contributors to a trusting relationship were investigated, sometimes with contrasting results from different studies. These included demographic characteristics (gender, marital status, age, ethnicity, birthplace, and country of residence), health condition, health education and literacy, socioeconomic status, religious beliefs, social environment, psychological factors, and the patient’s health condition and status.
Studies found better mental and physical health status tended to positively affect the relationship—although this result was mixed. In several studies, a good general health condition and better self-reported health status were associated with increased trust towards the physician [ 28 , 29 , 30 , 31 , 32 ]. However, other studies found no correlation between self-reported health status and trust. For specific health conditions, low-risk adults without chronic illnesses had higher trust in their physicians than adults with risk factors such as diabetes or high lipid levels [ 33 , 34 , 35 , 36 , 37 ]. Disease progression, including relapses and lack of improvement of a medical condition, was negatively associated with trust [ 38 , 39 ], whereas a shorter duration of illness increased trust in the physician [ 29 ]. However, two studies found no connection between trust, disease duration [ 40 ], and healing [ 36 ].
Patient health education and literacy levels were found to promote a trusting patient-physician relationship, with higher health education [ 41 ] and literacy [ 42 ] levels contributing to trust and low health literacy [ 43 ] hindering it.
Patient socioeconomic status, including occupation, employment, educational and income levels, and the presence or type of health insurance, were all potential contributors, with high (household) income and educational levels, having health insurance, and being employed positively related to trust; although, these findings were ambiguous. Religious belief was also associated with trust in physicians [ 31 ].
The social environment, including social support and the care experiences of family members, further contributed to a trusting patient-physician relationship. In particular, poor social support negatively influenced trust [ 43 ], as did dissatisfaction with the care of family members [ 44 , 45 ].
The health locus of control was also associated with trust. This describes how a person views control of their health. An internal health locus of control suggests that the person sees oneself as controlling their health, whereas an external locus means that the person perceives external factors influencing their health.
Several patient psychological factors, including a propensity to trust, their coping mechanisms and attachment style, the health locus of control, and general trust in caregivers contributed to a trusting patient-physician relationship. Individuals who see powerful others as their health locus of control (i.e., believing other people, such as health professionals, can control their health) exhibited higher trust in physicians [ 46 ]. Poor coping styles hindered trust [ 43 ], while the willingness to reframe situations (a healthy coping style) added to a trusting patient-physician relationship [ 44 ]. For the most part, a general trust in doctors, caregivers, the healthcare system, or online health communities was associated with higher trust [ 47 , 48 , 49 ]. However, these findings were ambiguous regarding the propensity to trust. One study found that a patient’s propensity to trust predicted trust in their physician [ 50 ], although other studies did not find this connection [ 31 , 36 ]. Table 1 summarizes all of the evidence concerning patient-related factors.
Physician-related factors
Demographic characteristics, competence, communication, exploring, caring, provisioning health education, reputation, professionalism, and availability were investigated as potential contributors to a trusting patient-physician relationship.
Demographic characteristics of the physician, such as age and gender, did not contribute to a trusting relationship, although these findings were ambiguous.
Physician competency, including the perceived competence of the physician by the patient [ 41 , 44 , 51 , 55 , 68 , 69 , 70 ], the physician being up-to-date in their specialization [ 71 ], and having more years of experience [ 71 ] helped to build a trusting relationship with patients. Communication skills, including general communication skills [ 29 , 38 , 44 , 52 , 70 , 72 , 73 ], compassion, listening to the patient [ 41 , 44 , 52 ], as well as nonverbal behavior such as good eye contact, providing undivided attention, open body language, and smiling [ 41 , 44 , 52 , 73 ] also enhanced the trust relationship as did patient-centered [ 63 , 74 , 75 ], comprehensive care [ 30 ].
Physicians exploring a patient’s disease and problems [ 69 ], illness experiences [ 28 ], and the context of the patient [ 44 , 68 ] promoted a trusting relationship along with caring behavior [ 52 , 70 , 75 ] such as empathy [ 50 , 76 ] and compassion [ 41 , 44 , 69 ].
Provisioning health education to the patient contributed to a trusting relationship [ 38 , 41 , 64 , 68 , 69 ]; however, one study did not find any association between these factors [ 71 ].
We did identify physician reputation [ 71 ] and the reputation of their medical specialty [ 28 , 34 , 39 ] as contributing to a trusting relationship. Moreover, different aspects of professionalism [ 71 , 73 ], such as honesty [ 51 , 55 , 69 ] and availability [ 41 ], contributed to a trusting patient-physician relationship, while being disrespectful, arrogant, or cynical were negatively associated with trust [ 41 , 73 , 75 ]. These results are summarized in Table 2 .
Physician- and patient-related factors
Contributors related to the physician and patient were concordance, time spent together, the patient-physician alliance, and shared decision-making.
In relation to concordance, both gender and race were tested as promoters of trust; however, only gender concordance was identified as being a contributor [ 35 , 41 ].
Time spent together included time spent in a single session, the overall time spent together, and the continuity of care. Most results indicated that more time spent together in a single session [ 28 , 71 , 73 ] (with the physician giving the patient enough time to explain the reason for the visit [ 77 ]) promoted trust, whereas physicians appearing rushed was a barrier to a trusting relationship [ 44 ]. If the duration of the relationship with the doctor was long-term [ 28 , 36 , 77 ], the patient had higher rates of follow-up visits [ 51 ] and more physician visits in general [ 37 , 57 ]. Nevertheless, those findings were mixed, and not all studies found an association between the duration of a relationship with the doctor [ 40 , 45 ] and the number of team visits [ 47 , 48 ]. However, continuity of care [ 51 ] and continuity with one physician added to a trusting relationship [ 30 ].
Within the patient-physician alliance, alliances in shared decision-making [ 65 ] and having a good rapport [ 71 ] were found to enhance trust, while a patient’s perception of a physician’s distrust was a barrier [ 41 ]. Finding common ground [ 28 ] and shared identity [ 52 ] were tested but did not show any association with trust. In contrast, shared decision-making contributed to a trusting relationship that promoted trust in most studies [ 41 , 42 , 44 ]. These findings are summarized in Table 3 .
Context-related factors
Context-related factors such as practice/institution, physician payments, and additional healthcare services were investigated as potential contributors to trusting relationships.
Most aspects of the practice or the institution were found to contribute to a trusting relationship, with easy accessibility [ 30 ] to the practice and a good reputation [ 71 ] promoting trust, while institutional betrayal [ 65 ] hindered it. The atmosphere of the practice also mattered. A good practice or organizational climate added to a trusting relationship [ 35 ], whereas perceived chaos hampered it [ 29 ]. Patients having enough physician choice also added to a trusting relationship [ 48 ], while managed care settings contributed to mistrust [ 41 ]. Inpatient settings enhanced trust compared to outpatient settings [ 59 ]. Regarding payments, situations where patients do not know how the physician is paid or the physician is paid by the number of office visits rather than a fixed salary [ 30 ] contributed to a trusting relationship. In contrast, public disclosure of payments was negatively associated with trust [ 78 ]. Additional health services such as addiction consultations [ 79 ], preventive services [ 77 ], and the coordination of specialty care [ 30 ] also contributed to patient-physician trust. These findings are summarized in Table 4 .
Potential leverage points to improve a trusting relationship
We integrated the modifiable contributors to a trusting patient-physician relationship from each conceptual group into a model and identified potential leverage points for improving the relationship (Fig. 2 ).
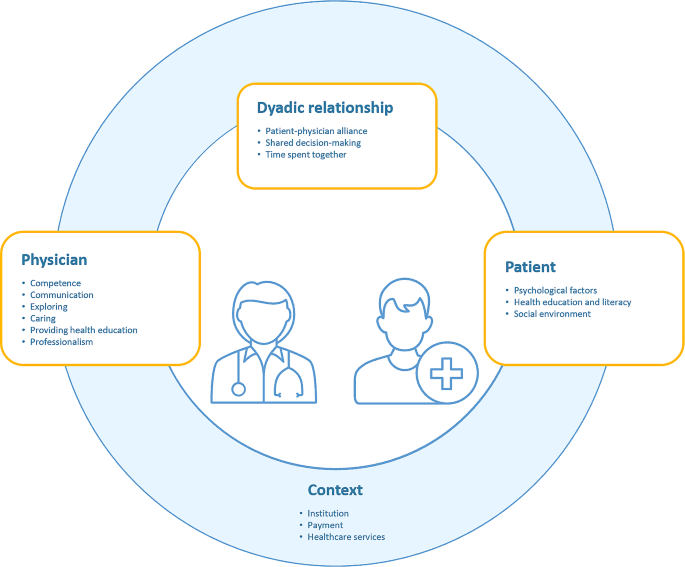
Model of contributors to a trusting patient-physician relationship
Patient-centered leverage points
Within patient-centered factors, health education and literacy, the social environment, and psychological factors were modifiable. A patient who is better educated about health and can understand and use this education for themselves (health literacy) may form better trusting relationships with their physicians; thus, interventions should focus on improving health education and literacy. Patient psychological factors such as coping styles and health locus of control are other potential leverage points to increase trust within the relationship. The social environment, specifically receiving sufficient social support, was a further modifiable contributor to trust, indicating that targeted interventions should aim to improve patients’ social support systems.
Physician-centered leverage points
We identified physicians’ competence, communication skills, exploring, caring, the provisioning of health education, and professionalism as modifiable contributors to a trusting patient-physician relationship. For competence, being up-to-date in the specialization and perceived as competent are leverage points that could increase trust. Communication skills, including verbal and nonverbal behavior, exploring patient health, and professionalism, can also be learned and are, hence, modifiable. Caring, including empathy and compassion, is a skill that can be increased through interventions and also used to increase trust. In addition, physicians can be taught how to provide health education, and specific material can be provided to them for health education, which is another potential leverage point.
Patient and physician-centered leverage points
We identified shared decision-making, the patient-physician alliance, and time spent together as contributors that can be modified. Although time spent together and the continuity of care is context-dependent, awareness can be raised among physicians, and specific training can help the physician allow patients to explain the reason for their visit. Alliances and shared decision-making are skills taught during medical school: therefore, potential interventions already exist. Shared decision-making also includes healthcare professionals other than physicians. Therefore, one possible intervention strategy would be to foster interprofessional education and teamwork to support shared decision-making between patients and healthcare professionals.
Context-dependent leverage points
The healthcare system, provisioning of additional healthcare services, transparency regarding physician payment, and characteristics of the practice or institution (e.g., keeping a good institutional climate and having mechanisms to prevent institutional betrayal) are modifiable contributors; however, these strongly depend on the specific country. Furthermore, only a few studies have investigated contributors to a trusting relationship within this conceptual group. Therefore, the list of context-dependent contributors may be limited.
We conducted a critical review with a systematic search strategy to identify evidence-based contributors to a trusting patient-physician relationship and integrated the modifiable contributors into a model. Our results confirm the existing theory of interpersonal trust [ 24 ], and, in line with this theory, we found that the physician’s caring (benevolence), competence and communication (ability), and professionalism (integrity) were contributors to a trusting patient-physician relationship. In addition, the physician’s exploring and provisioning of health education also contributed to a trusting relationship. We confirmed the importance of a patient’s propensity to trust as a psychological contributor and were able to add more psychological factors, including coping style and health locus of control. We further added the patient’s level of health education and literacy, and social environment as contributing factors and confirmed that, as the risk a patient must take concerning their health decreases, the easier it is for them to trust the physician. Our model further adds physician- and patient-related factors and the institutional context. The latter indicates the importance of including social trust in understanding interpersonal trust in medicine, as suggested by Mechanic [ 18 ]. One highly prominent factor was health education, which can be addressed by the physician, patient, and the context, which suggests that fostering health education is a promising intervention to increase trust.
Patient psychological factors such as coping styles and health locus of control are modifiable contributors to a trusting relationship. Previous studies have shown that coping styles can be improved for chronically ill patients [ 80 ], while other interventions can address a patient’s health locus of control and improve their social support systems. Furthermore, social support interventions have been shown to be effective in patients with different diseases [ 81 , 82 , 83 ]. Health education could be addressed through e-learning and by provisioning self-help groups that exchange ideas about diseases [ 84 ] with educational tools and teaching materials [ 85 ]. However, these interventions are system-related as the healthcare system must offer those interventions.
Medical education
Most physician-centered modifiable contributors to a trusting relationship fall under the scope of medical education. Competence is acquired and addressed through university education, graduate school, and continuing education. Communication skills are taught in medical education courses, and professionalism is addressed as a CanMED role [ 86 ]. Exploration is an important skill that is already part of communication curriculums [ 87 ] and is based on the common-sense model of illness [ 88 ]. Physicians can be taught to provide health education [ 89 ]; however, it is a skill that medical students find difficult to achieve [ 90 ]. Further intervention possibilities could address a physician’s ability to express compassion and empathy. A recent review summarized educational methods used to address medical student empathy [ 91 ], with simulation training shown to be an effective tool [ 92 ].
A practical example that implements the described practices can be found in the Presence 5 project, which teaches physicians to better listen to patients, explore their story and emotions, and connect with them. These teachings have had positive effects on the physicians’ attitude, compassion, communication, and exploring behavior [ 93 , 94 ].
Patient- and physician-related factors
As with physician-related contributors to trust, patient- and physician-related promoters of trust could be addressed through medical education. Building an alliance with patients and learning about shared decision-making are skills taught in medical school [ 95 ]. The physician can also be made aware that spending sufficient time with a patient is relevant to building trust; however, the ability to modify this contributor is dependent on the healthcare and billing system.
Context-dependent contributors
We found that a transparent billing system and institution-related contributors such as reputation, medical practice atmosphere, accessibility, and additional healthcare services contributed to a trusting patient-physician relationship. A recent discussion on making health care more accessible can be found in Gupta et al. [ 96 ].
One healthcare system that addresses many of these factors is Canada’s patient-centered model: ‘the patient’s medical home.’ Under this model, patients can choose a physician they feel comfortable with and who will continuously manage their health care over their lifespan. Each physician is surrounded by a team that considers the patient’s situation and may provide additional healthcare services when needed. This model ensures that each patient receives comprehensive and accessible care that provides sufficient time with the physician and guarantees continuity of care [ https://patientsmedicalhome.ca/ , 97 ]. Over the long term, patient medical homes have led to better care, decreased costs, and more satisfaction for providers and patients [ https://patientsmedicalhome.ca/ , 97 ]. Other positive aspects of the patient’s medical home, aside from increased continuity of care and the availability of additional health care services, may lie within the aspect of time spent together [ 98 ] or improved disease progression [ 99 ], which is also addressed within the patient’s medical homes.
Strengths and limitations
The strength of this critical review lies in the systematic search approach, which only included papers that operationalized or specifically described trust. Despite this approach, we cannot ensure that we have included all empirical contributors to patient-physician trust that have been researched. While the systematic search did limit bias in the identified contributors within the critical assessment of what could be modifiable or not, the critical assessment could be biased through the author’s background. However, we discussed the process in depth as a team.
Our search strategy included psychological safety as a synonym for trust, as well as the terms rapport, alliance, and relationship. We checked indexed search terms to ensure the inclusion of relevant synonyms. In the past, trust was more conceptualized as rapport or alliance, whereas today, it is associated with a newer term: “psychological safety.” While we tried to include relevant search terms, we might have missed some, limiting the results.
While our search was not limited to patients trusting their physicians, most papers focused on this and excluded physicians’ trust in their patients. Dyadic analyses of patient-physician trust are scarce. However, Petrocchi et al. (2019) have begun investigating patient-physician trust as a dyad [ 100 ]. Some papers only reported correlations of trust with unmodifiable, less relevant, but easy-to-gather factors, such as sex or age. Thus, more contributors to trust may have yet to be investigated.
Implications for future research
Interestingly, many non-modifiable or insignificant contributors, such as physician or patient demographics, were investigated in almost every study we reviewed. However, the most promising contributors, such as health education, were barely explored. Future research should investigate modifiable and promising contributors to a trusting relationship that have, as yet, been barely researched, including patient psychological factors and additional healthcare services. Additionally, factors that have not been investigated should be addressed, including digitized healthcare settings and how telemedicine, chatbots, and video consultations affect patients’ trust in physicians. Further research should also focus on measuring how successful physician interventions are, as previous research and interventions have not increased patient trust [ 101 , 102 ]. Future interventions should also consider multiple contributors to trust, as they are all related. For such interventions, the outcomes for each contributor should be evaluated first, with trust as a secondary outcome.
As the present review aimed to create a model of patient-physician trust, only studies that included trust between patients and physicians were included, with other healthcare professionals excluded. However, research has already acknowledged the importance of trusting relationships for all healthcare professionals [ 103 ], which should be further expanded. Thus, shared contributors to trust between healthcare professionals, their differences, and potential leverage points should also be identified.
Implications for practice
Our critical review has demonstrated that there are more contributors to a trusting patient-physician relationship than the theory of interpersonal trust proposes, and the context in which the patient-physician relationship takes place is highly relevant. One way to increase trust within the patient-physician relationship is to implement healthcare systems that are organized similarly to the Canadian ‘patient’s medical homes’ model. Changing the healthcare system is also an effective tool to simultaneously address multiple contributors to trust.
At the level of the institution, enhancing trust should focus on health education, which can be addressed through the implementation of self-help and support groups, providing high-quality health educational material, and training healthcare professionals.
At the physician level, we recommend taking as much time as possible for each patient to explore their perspective and current situation, organize (as much as possible) continuity of care, and ensure patient health education.
Using a systematic search, our model summarizes identified modifiable contributors to a trusting patient-physician relationship. Providing sufficient time during patient-physician encounters, ensuring continuity of care, and fostering health education are promising leverage points for improving trust between patients and physicians. Future research should evaluate the effectiveness of interventions that address multiple modifiable contributors to a trusting patient-physician relationship.
Data availability
The data (review search) of the current review are available from the corresponding author on reasonable request.
von Gunten CF, Ferris FD, Emanuel LL. The patient-physician relationship. Ensuring competency in end-of-life care: communication and relational skills. JAMA. 2000;284(23):3051–7.
Article Google Scholar
Mahmud A. Doctor-patient relationship. Pulse. 1970;3(1):12–4.
Birkhauer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, Gerger H. Trust in the health care professional and health outcome: a meta-analysis. PLoS ONE. 2017;12(2):e0170988.
Article PubMed PubMed Central Google Scholar
Alazri M, Neal R. The association between satisfaction with services provided in primary care and outcomes in type 2 diabetes mellitus. Diabet Med. 2003;20(6):486–90.
Article CAS PubMed Google Scholar
Mainous AG 3rd, Kern D, Hainer B, Kneuper-Hall R, Stephens J, Geesey ME. The relationship between continuity of care and trust with stage of cancer at diagnosis. Fam Med. 2004;36(1):35–9.
Preau M, Leport C, Salmon-Ceron D, Carrieri P, Portier H, Chene G, Spire B, Choutet P, Raffi F, Morin M. Health-related quality of life and patient-provider relationships in HIV-infected patients during the first three years after starting PI-containing antiretroviral treatment. AIDS Care. 2004;16(5):649–61.
Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE. 2014;9(4):e94207.
Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. 1998;47(3):213–20.
CAS PubMed Google Scholar
Trachtenberg F, Dugan E, Hall MA. How patients’ trust relates to their involvement in medical care. J Fam Pract. 2005;54(4):344–52.
PubMed Google Scholar
Thom DH, Kravitz RL, Bell RA, Krupat E, Azari R. Patient trust in the physician: relationship to patient requests. Fam Pract. 2002;19(5):476–83.
Article PubMed Google Scholar
Kao AC, Green DC, Zaslavsky AM, Koplan JP, Cleary PD. The relationship between method of physician payment and patient trust. JAMA. 1998;280(19):1708–14.
Balkrishnan R, Dugan E, Camacho FT, Hall MA. Trust and satisfaction with physicians, insurers, and the medical profession. Med Care. 2003;41(9):1058–64.
Mainous AG 3rd, Kern D, Hainer B. The relationship between continuity of care and trust with stage of cancer at diagnosis. 2004.
Tarn DM, Meredith LS, Kagawa-Singer M, Matsumura S, Bito S, Oye RK, Liu H, Kahn KL, Fukuhara S, Wenger NS. Trust in one’s physician: the role of ethnic match, autonomy, acculturation, and religiosity among Japanese and Japanese Americans. Ann Fam Med. 2005;3(4):339–47.
Quigley DD, Reynolds K, Dellva S, Price RA. Examining the business case for patient experience: a systematic review. J Healthc Manag. 2021;66(3):200–24.
PubMed PubMed Central Google Scholar
Levinson W. Physician-patient communication. JAMA. 1994;272(20).
Goold SD. Money and trust: relationships between patients, physicians, and health plans. J Health Polit Policy Law. 1998;23(4):687–95.
Mechanic D. Changing medical organization and the erosion of trust. Milbank Q. 1996;74(2):171–89.
Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med. 2000;15(7):509–13.
Article CAS PubMed PubMed Central Google Scholar
Sisk B, Baker JN. A model of interpersonal trust, credibility, and relationship maintenance. Pediatrics. 2019;144(6).
Hardin R. Trust: Polity; 2006.
Garrett L. Betrayal of Trust - the collapse of global public health. Oxford University Press; 2003.
Siegrist M, Gutscher H, Earle TC. Perception of risk: the influence of general trust, and general confidence. J Risk Res. 2006;8(2):145–56.
Mayer RC, Davis JH, Schoorman FD. An integrative model of organizational trust. Acad Manage Rev. 1995;20(3).
Taylor LA, Nong P, Platt J. Fifty years of trust research in health care: a synthetic review. Milbank Q. 2023;101(1):126–78.
Sutton A, Clowes M, Preston L, Booth A. Meeting the review family: exploring review types and associated information retrieval requirements. Health Info Libr J. 2019;36(3):202–22.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108.
Fiscella K, Meldrum S, Franks P, Shields CG, Duberstein P, McDaniel SH, Epstein RM. Patient trust: is it related to patient-centered behavior of primary care physicians? Med Care. 2004;42(11):1049–55.
Kowalski C, Nitzsche A, Scheibler F, Steffen P, Albert U-S, Pfaff H. Breast cancer patients’ trust in physicians: The impact of patients’ perception of physicians’ communication behaviors and hospital organizational climate. [References]: Patient Education and Counseling. Vol.77(3), 2009, pp. 344–348.; 2009.
O’Malley AS, Forrest CB. Beyond the examination room: primary care performance and the patient-physician relationship for low-income women. J Gen Intern Med. 2002;17(1):66–74.
Benjamins MR. Religious influences on trust in physicians and the health care system. Int J Psychiatry Med. 2006;36(1):69–83.
Nelms E, Wang L, Pennell M, Wewers ME, Seiber E, Adolph MD, Paskett ED, Ferketich AK. Trust in physicians among rural medicaid-enrolled smokers. JRural Health. 2014;30(2):214–20.
Google Scholar
Bachinger SM, Kolk AM, Smets EM. Patients’ trust in their physician–psychometric properties of the Dutch version of the wake forest physician trust scale. Patient Educ Couns. 2009;76(1):126–31.
Marcinowicz L, Jamiolkowski J, Gugnowski Z, Strandberg EL, Fagerstrom C, Pawlikowska T. Evaluation of the trust in physician scale (TIPS) of primary health care patients in north-east Poland: a preliminary study. Family Med Prim Care Rev. 2017;19(1):39–43.
Bonds DE, Foley KL, Dugan E, Hall MA, Extrom P. An exploration of patients’ trust in physicians in training. J Health Care Poor Underserved. 2004;15(2):294–306.
Ruch W, Heintz S. Experimentally manipulating items informs on the (Limited) construct and criterion validity of the humor styles Questionnaire. Front Psychol. 2017;8:616.
Becker ER, Roblin DW. Translating primary care practice climate into patient activation: the role of patient trust in physician. Med Care. 2008;46(8):795–805.
Mack JW, Kang TI. Care experiences that foster trust between parents and physicians of children with cancer. Pediatr Blood Cancer. 2020;67(11):(no pagination).
Yang J, Lu Y, Liao X, Chang MP. Examining patient trust towards physicians between clinical departments in a Chinese hospital. PLoS ONE. 2021;16(11 November):(no pagination).
Aloba O, Mapayi B, Akinsulore S, Ukpong D, Fatoye O. Trust in physician scale: factor structure, reliability, validity and correlates of trust in a sample of Nigerian psychiatric outpatients. Asian J Psychiatry. 2014;11:20–7.
Cook KS, Kramer RM, Thom DH, Stepanikova I, Mollborn SB, Cooper RM. Trust and Distrust in Patient-Physician Relationships: Perceived Determinants of High- and Low-Trust Relationships in Managed-Care Settings. [References]: Kramer, Roderick M, editor; Cook, Karen S, editor. (2004). Trust and distrust in organizations: Dilemmas and approaches. (pp. 65–98). xii, 381 pp. New York, NY, US: Russell Sage Foundation; US.; 2004.
Dehghan H, Keshtkaran A, Ahmadloo N, Bagheri Z, Hatam N. Patient involvement in care and breast cancer patients’ quality of Life- a structural equation modeling (SEM) approach. Asian Pac J cancer Prevention: APJCP. 2018;19(9):2511–7.
Gupta C, Bell SP, Goggins K, Cawthon C, Nwosu SK, Schildcrout JS, Kripalani S. Health literacy is an independent predictor of physician distrust. Circulation Conference: American Heart Association. 2013;128(22 Suppl. 1).
Canavera K. Rebuilding trust. Patient Educ Couns. 2021;104(5):996–7.
Oguro N, Suzuki R, Yajima N, Sakurai K, Wakita T, Hall MA, Kurita N. The impact that family members’ health care experiences have on patients’ trust in physicians. BMC Health Serv Res. 2021;21(1):1122.
Brincks AM, Feaster DJ, Burns MJ, Mitrani VB. The influence of health locus of control on the patient-provider relationship. Psychol Health Med. 2010;15(6):720–8.
Bonds DE, Camacho F, Bell RA, Duren-Winfield VT, Anderson RT, Goff DC. The association of patient trust and self-care among patients with diabetes mellitus. BMC Fam Pract. 2004;5:26.
Kao AC. Trust and agency: the patient-physician relationship in the era of managed care: dissertation abstracts international section A: humanities and social sciences. Vol.59(5-A),1998, pp. 1790.; 1998.
Audrain-Pontevia AF, Menvielle L. Effects of interpersonal trust among users of online health communities on patient trust in and satisfaction with their physician. Int J Technol Assess Health Care. 2018;34(1):56–62.
Wu Q, Jin Z, Wang P. The Relationship between the physician-patient relationship, physician empathy, and patient trust. J Gen Intern Med. 2021.
Hillen MA, de Haes HC, Smets EM. Cancer patients’ trust in their physician-a review. Psychooncology. 2011;20(3):227–41.
Gopichandran V, Chetlapalli SK. Trust in the physician-patient relationship in developing healthcare settings: a quantitative exploration. Indian J Med Ethics. 2015;12(3):141–8.
Wang W, Zhang H, Washburn DJ, Shi H, Chen Y, Lee S, Du Y, Maddock JE. Factors influencing trust towards physicians among patients from 12 hospitals in China. Am J Health Behav. 2018;42(6):19–30.
Baidya M, Gopichandran V, Kosalram K. Patient-physician trust among adults of rural Tamil Nadu: a community-based survey. J Postgrad Med. 2014;60(1):21–6.
Hamelin ND, Nikolis A, Armano J, Harris PG, Brutus JP. Evaluation of factors influencing confidence and trust in the patient-physician relationship: a survey of patient in a hand clinic. Chirurgie De La main. 2012;31(2):83–90.
Zhao DH, Rao KQ, Zhang ZR. Patient trust in physicians: empirical evidence from Shanghai, China. Chin Med J. 2016;129(7):814–8.
Dong E, Liang Y, Liu W, Du X, Bao Y, Du Z, Jin M. Construction and validation of a preliminary Chinese version of the wake forest physician trust scale. Med Sci Monit. 2014;20:1142–50.
Gupta C, Bell SP, Schildcrout JS, Fletcher S, Goggins KM, Kripalani S. Predictors of health care system and physician distrust in hospitalized cardiac patients. J Health Communication. 2014;19(Supplement 2):44–60.
Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians: effects of choice, continuity, and payment method. J Gen Intern Med. 1998;13(10):681–6.
Blanch-Hartigan D, van Eeden M, Verdam MGE, Han PKJ, Smets EMA, Hillen MA. Effects of communication about uncertainty and oncologist gender on the physician-patient relationship. Patient Educ Couns. 2019;102(9):1613–20.
Mainous AG 3rd, Baker R, Love MM, Gray DP, Gill JM. Continuity of care and trust in one’s physician: evidence from primary care in the United States and the United Kingdom. Fam Med. 2001;33(1):22–7.
Gopichandran V, Wouters E, Chetlapalli SK. Development and validation of a socioculturally competent trust in physician scale for a developing country setting. BMJ Open. 2015;5(4):e007305.
Kushnir T, Bachner YG, Carmel S, Flusser H, Galil A. Pediatricians’ communication styles as correlates of global trust among jewish and bedouin parents of disabled children. J Dev Behav Pediatr. 2008;29(1):18–25.
Rawaf MM, Kressin NR. Exploring racial and sociodemographic trends in physician behavior, physician trust and their association with blood pressure control. J Natl Med Assoc. 2007;99(11):1248–54.
Shoemaker K, Smith CP. The impact of patient-physician alliance on trust following an adverse event. Patient Educ Couns. 2019;102(7):1342–9.
Holwerda N, Sanderman R, Pool G, Hinnen C, Langendijk JA, Bemelman WA, Hagedoorn M, Sprangers MAG. Do patients trust their physician? The role of attachment style in the patient-physician relationship within one year after a cancer diagnosis. Acta Oncol. 2013;52(1):110–7.
Aaraas IJ, Jones B, Gupta TS. [Norwegian and Australian physicians’ attitudes to adverse events]. Tidsskr nor Laegeforen. 2005;125(16):2204–6.
Berry LL, Parish JT, Janakiraman R, Ogburn-Russell L, Couchman GR, Rayburn WL, Grisel J. Patients’ commitment to their primary physician and why it matters. Ann Fam Med. 2008;6(1):6–13.
Thom DH, Campbell B. Patient-physician trust: an exploratory study. J Fam Pract. 1997;44(2):169–76.
Wolfson DB, Lynch TJ. Increasing trust in health care. Am J Manag Care. 2021;27(12):520–2.
Shaya B, Al Homsi N, Eid K, Haidar Z, Khalil A, Merheb K, Honein-Abou Haidar G, Akl EA. Factors associated with the public’s trust in physicians in the context of the Lebanese healthcare system: a qualitative study. BMC Health Serv Res. 2019;19(1):525.
Thom DH. Physicians’ trust in patients. JAMA - J Am Med Association. 2019;322(8):780–2.
Hendren EM, Kumagai AK. A matter of trust. Acad Medicine: J Association Am Med Colleges. 2019;94(9):1270–2.
Hillen MA, de Haes H, Stalpers LJA, Klinkenbijl JHG, Eddes EH, Butow PN, van der Vloodt J, van Laarhoven HWM, Smets EMA. How can communication by oncologists enhance patients’ trust? An experimental study. Ann Oncol. 2014;25(4):896–901.
El Malla H, Kreicbergs U, Steineck G, Wilderang U, El Sayed Elborai Y, Ylitalo N. Parental trust in health care - a prospective study from the children’s cancer hospital in Egypt. Psychooncology. 2013;22(3):548–54.
Weng HC. Does the physician’s emotional intelligence matter? Impacts of the physician’s emotional intelligence on the trust, patient-physician relationship, and satisfaction. Health Care Manage Rev. 2008;33(4):280–8.
Parchman ML, Burge SK. The patient-physician relationship, primary care attributes, and preventive services. Fam Med. 2004;36(1):22–7.
Kanter GP, Carpenter D, Lehmann LS, Mello MM. US nationwide disclosure of industry payments and public trust in physicians. JAMA netw. 2019;2(4):e191947.
King C, Collins D, Patten A, Nicolaidis C, Englander H. Trust in hospital physicians among patients with substance use disorder referred to an addiction consult service: a mixed-methods study. J Addict Med. 2021;09.
de Ridder D, Schreurs K. Developing interventions for chronically ill patients: is coping a helpful concept? Clin Psychol Rev. 2001;21(2):205–40.
van Dam HA, van der Horst FG, Knoops L, Ryckman RM, Crebolder HF, van den Borne BH. Social support in diabetes: a systematic review of controlled intervention studies. Patient Educ Couns. 2005;59(1):1–12.
Lian OS, Rottingen JA. [The physicians–homo economicus or homo sociologicus?]. Tidsskr nor Laegeforen. 2002;122(17):1682–5.
Guillory J, Chang P, Henderson CR Jr., Shengelia R, Lama S, Warmington M, Jowza M, Waldman S, Gay G, Reid MC. Piloting a text message-based social support intervention for patients with chronic pain: establishing feasibility and preliminary efficacy. Clin J Pain. 2015;31(6):548–56.
Ghasemi M, Hosseini H, Sabouhi F. Effect of peer group education on the quality of life of elderly individuals with diabetes: a randomized clinical trial. Iran J Nurs Midwifery Res. 2019;24(1):44–9.
Delmas A, Clement B, Oudeyer P-Y, Sauzéon H. Fostering health education with a serious game in children with asthma: pilot studies for assessing learning efficacy and automatized learning personalization. Front Educ. 2018;3.
Verkerk MA, de Bree MJ, Mourits MJ. Reflective professionalism: interpreting CanMEDS’ professionalism. J Med Ethics. 2007;33(11):663–6.
Wissenschaften SAM. Kommunikation im medizinischen alltag. Ein Leitfaden für die Praxis. In.: Schweizerische Akademie der Medizinischen Wissenschaften (SAMW); 2019.
Diefenbach MA, Leventhal H. The common-sense model of illness representation: theoretical and practical considerations. J Social Distress Homeless. 2016;5(1):11–38.
Tresolini CP, Stritter FT. An analysis of learning experiences contributing to medical students’ self-efficacy in conducting patient education for health promotion. Teach Learn Med. 1994;6(4):247–54.
Benbassat J. Undesirable features of the Medical Learning Environment: a narrative review of the literature. Adv Health Sci Educ. 2013;18(3):527–36.
Sinclair S, Kondejewski J, Jaggi P, Dennett L, Roze des Ordons AL, Hack TF. What is the state of compassion education? A systematic review of compassion training in health care. Acad Med. 2021;96(7):1057–70.
Karvelyte M, Rogers J, Gormley GJ. Walking in the shoes of our patients’: a scoping review of healthcare professionals learning from the simulation of patient illness experiences. Adv Simul (Lond). 2021;6(1):43.
Shankar M, Henderson K, Garcia R, Li G, Titer K, Acholonu RG, Essien UR, Brown-Johnson C, Cox J, Shaw JG et al. Presence 5 for racial justice workshop: fostering dialogue across medical education to disrupt anti-black racism in clinical encounters. MedEdPORTAL. 2022;18:11227.
Brown-Johnson C, Cox J, Shankar M, Baratta J, De Leon G, Garcia R, Hollis T, Verano M, Henderson K, Upchurch M, et al. The Presence 5 for racial justice framework for anti-racist communication with black patients. Health Serv Res. 2022;57(Suppl 2):263–78.
Durand MA, DiMilia PR, Song J, Yen RW, Barr PJ. Shared decision making embedded in the undergraduate medical curriculum: a scoping review. PLoS ONE. 2018;13(11):e0207012.
Gupta R, Binder L, Moriates C. Rebuilding trust and relationships in medical centers: a focus on health care affordability. JAMA. 2020;324(23):2361–2.
Jackson GL, Powers BJ, Chatterjee R, Bettger JP, Kemper AR, Hasselblad V, Dolor RJ, Irvine RJ, Heidenfelder BL, Kendrick AS, et al. The patient centered medical home. A systematic review. Ann Intern Med. 2013;158(3):169–78.
Takach M. Reinventing Medicaid: state innovations to qualify and pay for patient-centered medical homes show promising results. Health Aff (Millwood). 2011;30(7):1325–34.
Klitzner TS, Rabbitt LA, Chang RR. Benefits of care coordination for children with complex disease: a pilot medical home project in a resident teaching clinic. J Pediatr. 2010;156(6):1006–10.
Petrocchi S, Iannello P, Lecciso F, Levante A, Antonietti A, Schulz PJ. Interpersonal trust in doctor-patient relation: evidence from dyadic analysis and association with quality of dyadic communication. Soc Sci Med. 2019;235:112391.
Thom DH. Training physicians to increase patient trust. J Eval Clin Pract. 2000;6(3):245–53.
Thom DH, Bloch DA, Segal ES. An intervention to increase patients’ trust in their physicians. Acad Med. 1999;74(2):195–8.
Rasiah S, Jaafar S, Yusof S, Ponnudurai G, Chung KPY, Amirthalingam SD. A study of the nature and level of trust between patients and healthcare providers, its dimensions and determinants: a scoping review protocol. BMJ Open. 2020;10(1):e028061.
Download references
Acknowledgements
We would like to thank the information specialist team at the library of the medical faculty of Bern. They supported the development of our research question and a search strategy. We also thank Adrian Michel (mediamatician) for the model illustration. The preliminary results of this review were presented at the European Health Psychology Conference on August 27, 2022 in Bratislava.
Not applicable.
Author information
Authors and affiliations.
Faculty of Behavioural and Cultural Studies, Ruprecht Karls-University, Heidelberg, Germany
Seraina Petra Lerch
University Hospital of Old Age Psychiatry and Psychotherapy, University of Bern, Bern, Switzerland
Institute of Medical Psychology, Heidelberg University Hospital, Bergheimer Str. 20, DE-69115, Heidelberg, Germany
Institute for Medical Education, Department for Assessment and Evaluation, University of Bern, Bern, Switzerland
Rahel Hänggi, Yara Bussmann & Andrea Lörwald
You can also search for this author in PubMed Google Scholar
Contributions
S. P. L. conzeptualization, methodology, formal Analysis, writing original draft, visualization, supervisionR. H. formal Analysis, visualizationY. B. formal Analysis, visualization. A.L. conzeptualization, methodology, formal Analysis, writing review & editing, visualization, supervision. All authors reviewed and approved the manuscript.
Corresponding author
Correspondence to Seraina Petra Lerch .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lerch, S.P., Hänggi, R., Bussmann, Y. et al. A model of contributors to a trusting patient-physician relationship: a critical review using a systematic search strategy. BMC Prim. Care 25 , 194 (2024). https://doi.org/10.1186/s12875-024-02435-z
Download citation
Received : 03 October 2023
Accepted : 17 May 2024
Published : 01 June 2024
DOI : https://doi.org/10.1186/s12875-024-02435-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient trust
- Patient-physician relationship
- Communication
- Health education
- Theory of trust
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
- Open access
- Published: 31 May 2024
Freely available, online videos to support neurological physiotherapists and students in task-specific training skill acquisition: a scoping review
- Nicola C.M. Towersey 1 ,
- Kelvin Sasse 1 ,
- Verna Stavric 1 ,
- Gemma Alder 1 &
- Nicola L. Saywell 1
BMC Medical Education volume 24 , Article number: 603 ( 2024 ) Cite this article
121 Accesses
Metrics details
Videos to support learning of clinical skills are effective; however, little is known about the scope and educational quality of the content of freely available online videos demonstrating task-specific training (TST). This review aimed to determine the extent, characteristics of freely available online videos, and whether the content is suitable to guide skill acquisition of task-specific training for neurological physiotherapists and students.
A scoping review was conducted. Google video and YouTube were searched in December 2022. Videos that met our eligibility criteria and were explicitly designed for (TST) skill acquisition were included in the report.
Ten videos met the inclusion criteria and were difficult to find amongst the range of videos available. Most were presented by physiotherapists or occupational therapists, originated from the USA, featured stroke as the condition of the person being treated, and involved a range of interventions (upper limb, constraint induced movement therapy, balance, bicycling). Most videos were created by universities or private practices and only two used people with a neurological condition as the participant. When the content of videos and their presentation (instruction and/or demonstration), was assessed against each key component of TST (practice structure, specificity, repetition, modification, progression, feedback), five of the videos were rated very suitable and five moderately suitable to guide skill acquisition. Most videos failed to demonstrate and provide instruction on each key component of TST and were missing at least one component, with feedback most frequently omitted.
Conclusions
There are many freely available online videos which could be described as demonstrating TST; very few are suitable to guide skill acquisition. The development of a standardised and validated assessment tool, that is easy to use and assesses the content of TST videos is required to support learners to critically evaluate the educational quality of video content. Guidelines based on sound teaching theory and practice are required to assist creators of online videos to provide suitable resources that meet the learning needs of neurological physiotherapists and students.
Peer Review reports
Task-specific training (TST) is a common rehabilitation strategy used and taught by a wide range of allied health professionals including physiotherapists, occupational therapists, speech language therapists and academic institutions. It involves goal directed practice, repetition, progressive challenge, and positive reinforcement to optimise motor learning [ 1 ]. TST has been shown to be effective at inducing cortical reorganization, decreasing disability and improving functional outcomes for people with neurological conditions such as stroke, Parkinson’s disease, spinal cord injury and cerebral palsy [ 2 , 3 , 4 , 5 , 6 , 7 , 8 ]. TST is referred to in the literature by a range of terms, including ‘repetitive functional task practice’, ‘repetitive task practice’ [ 3 ], ‘task-orientated therapy’ [ 1 ] and ‘task-related training’ [ 9 ]. For this review, it will be referred to as task-specific training (TST).
The widespread use of the internet has extended traditional education by enabling users to search for, watch, and share a large variety of freely available online videos to supplement their learning. The use of online videos has grown in popularity over the past decade with ease of access and low cost making them one of the most frequently used self-learning resources for health professionals and students [ 10 , 11 , 12 ]. Videos have been shown to significantly improve learning outcomes [ 13 ], however, mechanisms for controlling the content within online videos are limited. The results of internet searches are determined by an algorithm using likes, views, and popularity rather than an assessment of whether the content is suitable to guide skill acquisition [ 14 , 15 ] and previous studies have found online videos often omit key learning points and are of variable educational quality [ 14 , 16 , 17 , 18 ].
Freely available online videos may be useful to guide skill acquisition and reinforce learning for neurological physiotherapists and students. However, there is a need to evaluate the quality of the content of these videos to ensure that they are based on best practice. To our knowledge, there has been no research exploring the extent, characteristics, and educational quality of freely available online videos for the skill acquisition of TST. In this scoping review, our aim was to determine the extent, characteristics, and whether the content of freely available online videos is suitable to guide skill acquisition of TST.
A scoping review was conducted and carried out according to the Preferred Reporting Items for Systematic Review and meta-analysis for scoping reviews (PRISMA- ScR), adapting the five stages suggested by Arksey and O’Malley and the Joanna Briggs Institute (JBI) for evidence synthesis [ 21 , 22 , 23 ]. An a priori protocol was developed to guide this review prior to undertaking it.
Identifying relevant videos
A detailed search plan outlining the search terms, sources, eligibility criteria, and delimiters was established based on suggestions by Godin et al. [ 24 ], and in consultation with a senior librarian. The JBI; Population, Concept and Context (PCC) elements were used to formulate a combination of search terms to maintain transparency, ensure organised search methods, and reduce the risk of bias [ 23 ]. The population included neurological physiotherapy, the condition of interest or intended audience, were left open. The concept was the demonstration and instruction of TST that a novice could use for skill acquisition. The context included rehabilitation. Refer to Table 1 for the initial search terms.
The inclusion criteria included videos with the stated purpose to teach TST and included an element of physical skill demonstration and instruction. Videos had to be freely available online via a device with internet capabilities, in English, without subscription requirements to access, and within the scope of neurological physiotherapy practice [ 25 ]. There were no restrictions on the rehabilitation setting, date of upload, duration of video, or country of origin (Table 2 ).
A pilot search was carried out as suggested by the JBI guidelines [ 23 ] and following discussion between authors; search terms and the eligibility criteria were refined to reduce ambiguity regarding the definition of TST, and the level of instruction required for the video. For this review, TST included practice of meaningful tasks. Tasks were considered part-task if they were linked to a whole-task reconstruction; virtual reality involving the upper limb was considered part-task as it lacked the manipulation of physical objects and were included. Instructions needed to be provided during TST with sufficient detail to allow a novice to apply it. These could have been in the form of subtitles, voice-over, or directly to the camera.
Google video search engine and YouTube were searched due to their high use, free access and relevancy ordered results [ 26 ]. YouTube has 2,562 million active users, while Google is the dominant global search engine, with an 84.08% worldwide market share [ 26 , 27 ]. Internet Protocol (IP) addresses and being logged into Google accounts have been found to contribute 11.7% to variation in results [ 19 ]. Therefore, searches were performed with personalised search off, in Google Chrome incognito browser, with relevancy sorting on, to improve the consistency of the search results. To reduce the effect of algorithmic searching, all preliminary searches were conducted on the Firefox search engine, with official searches performed in Google incognito, from the same IP address, on a single day in Auckland, New Zealand.
The searches were conducted from Auckland, New Zealand (NZ), on the 16th of December 2022 by KS. The complete search strategy used in Google video search engine and YouTube is in Appendix 1 . Ten searches were conducted on each search engine with the first 10 pages of each search (representing 100 results) screened for relevance. This number was chosen to capture a wide range of the most relevant results, while still being feasible to screen [ 24 ]. Potentially relevant videos were bookmarked in a folder named after the search engine and in a subfolder with the search terms used [ 24 ]. If a video was embedded within a website, it was followed to its source and then bookmarked, to reduce duplicates.
Finally, a series of YouTube channels were hand searched to identify missed videos. Consistency was maintained by the same reviewer (KS), using the same IP address, applying the same method as the primary searches, on a single day (22nd December 2022).
Video selection
Videos were selected using the following process. Duplicates were removed and KS screened all the videos against the eligibility criteria. A second reviewer (NT) independently cross-checked 20% of videos, to check for consistency and appropriate application of the selection criteria. Any discrepancies were referred to NLS to be resolved by consensus.
Data charting
Data charting was used to synthesise and interpret the data [ 21 ]. KS and NT independently viewed the selected videos and summarised the data in a Microsoft (MS) Excel spreadsheet, based on the JBI guidelines [ 22 , 23 ]. The data extracted for this review were the video title, upload date, duration, number of views, likes/ dislikes, the presenter(s), the participant(s), source, country of origin, intervention, the key components of TST (practice structure, specificity, repetition, modification, progression, feedback) and how they were presented (instruction and/or demonstration).
Summarising and reporting results
To address the extent and characteristics of the selected videos, we identified trends using data analysing tools and pivot tables in MS Excel and presented the data descriptively.
Scoring of videos
The suitability of videos to guide skill acquisition was assessed using a pragmatic scoring system developed for this scoping review. Although previous studies have developed scoring systems to evaluate online material [ 28 , 29 ], none were appropriate for the purpose of this study. The scoring system was developed after reviewing pertinent literature [ 30 , 31 ] and seeking expert opinion. It evaluated video content against the agreed key components of TST for motor learning (practice structure, specificity, repetition, modification, progression, feedback) and whether demonstration and instruction were provided on each component. Videos were scored from 0 to 2 for each of the six TST components for a total possible score of 12. Components scored 2 if both demonstration and instruction were provided, 1 if they provided either one, or 0 for a missing component. Those videos scoring 0–4 were considered unsuitable, 5–8 moderately suitable and 9–12 very suitable to guide skill acquisition. Data analysis was conducted by KS, and NT and NSW, physiotherapists with extensive clinical and teaching experience in neurological physiotherapy.
Identification and selection of material
Google Video and YouTube searches resulted in 2,000 videos. After initial screening of titles and thumbnails, 179 were bookmarked as potentially relevant. Hand-searching YouTube channels identified an additional 12 videos, resulting in 191 videos being manually inputted into a MS Excel spreadsheet.
All 191 videos were screened against the eligibility criteria by KS, with NT cross-checking 20% between January 11th, 2023, and January 13th, 2023. The agreement between reviewers was high (95%), exceeding the PRISMA-ScR guidelines requirements of 70–80% agreement [ 22 ]. A third reviewer (NLS) adjudicated any discrepancies (7%) with reference to the definition of TST and the inclusion criteria. Of the181 rejected videos, seven were duplicates, four were unavailable in English, 74 did not meet our definition for TST, 47 did not explicitly state that the purpose of the video was to teach TST, six had no skills demonstration in the video and 43 did not have sufficient instruction to allow a novice to repeat. Only ten videos fulfilled the eligibility criteria (0.4% of videos identified, 5% of videos bookmarked) and were included in the review, as represented in Fig. 1 .
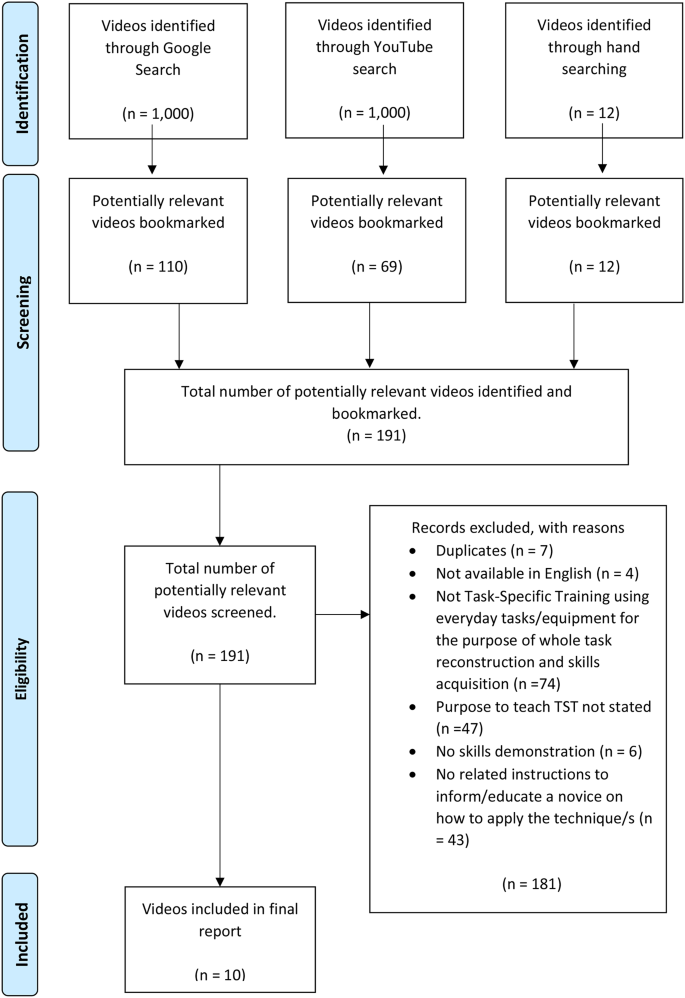
PRISMA flow diagram
Description of included videos
Videos had been uploaded to the platform a median of 30 months prior to our search date (range: 7–79 months). The median length of videos was 5.32 min (range: 3–20 min), with a median of 1386.5 views (range: 181–21950). The median number of likes for a video was 11.5 (range: 2–581), and the number of dislikes for all videos was 0. Occupational therapists were presenters in five of the videos, physiotherapists in two and the professional status of the presenter was unidentified in three videos. The focus of most videos was stroke rehabilitation (9) with cerebral palsy rehabilitation presented in one. Only two of the videos included people with the selected condition as participants. Seven videos were uploaded by universities, two by clinicians in a private practice and one by an unidentified contributor. Most videos were created in the United States of America (USA) with one each from Australia and India. A range of interventions were presented including upper limb training (7), bicycle training (1), constraint induced movement therapy (1), and balance training (1). A summary of the characteristics of the included videos is provided in Table 3 .
Only 10 videos explicitly stated that the purpose of the video was to teach TST and therefore had their content assessed for its suitability to guide skill acquisition. The videos were assessed in relation to the key components of TST (practice structure, specificity, repetition, modification, progression, feedback) and how they were presented (with instruction and/or demonstration). All videos included demonstration and instruction about manipulating practice structure to promote motor learning. Specificity was demonstrated in all videos using physical objects relevant to the task, while only three videos provided instruction in addition to demonstration. Nine of the videos provided demonstration and instruction on the use of repetition, with one video providing instruction only. Five videos provided demonstration and instruction on how to modify the activity, three provided instructions only and two failed to provide modification. Seven videos provided demonstration and instruction on progressions, with two videos providing instruction only, and one failing to demonstrate or provide instruction on any form of progression. None of the videos demonstrated the provision of feedback to promote motor learning and only one video provided instruction on how to provide feedback. The scores for videos ranged from 6 to 9/12 with five videos being considered moderately suitable and five very suitable to guide skill acquisition. Only one video included all the key components of TST and none of the videos provided demonstration and instruction on each component. A breakdown of the TST components and suitability scores is detailed in Table 4 .
This review was the first, to our knowledge, to examine the extent, characteristics, and suitability of freely available online videos that guide skill acquisition of TST for neurological physiotherapists and students. Despite a wide and comprehensive search strategy, only ten videos met the eligibility criteria. This suggests that despite over 2000 videos being available, there is a lack of suitable material to address the skill acquisition of TST for neurological physiotherapists and students.
This review highlights a fundamental problem when searching for educational videos online. Namely, it is difficult to find the few suitable videos amongst the array of videos of variable educational quality. It is unlikely that everyday internet users would be prepared to screen so many videos to find those ones related to TST which provide adequate information for training skill acquisition. Several authors have suggested mechanisms to improve the identification of educational videos. The use of a domain based ranking system, that ranks videos from trusted sources (universities or health organisations) higher up in the search results may make identification easier [ 32 ]. The use of inbuilt educational filters, with a strict criterion for labelling content as educational, might also improve identification [ 32 , 33 ]. In addition, organisations with an interest in educating physiotherapists could identify and disseminate existing online videos that are suitable to guide skill acquisition.
During our review of the characteristics of videos, we noticed that physiotherapists and occupational therapists created the majority of TST videos using a range of interventions, mainly featuring the upper limb, and the condition of stroke. None of the videos demonstrated the use of TST during walking, which would be particularly useful for neurological physiotherapists and students, as this is often their focus in rehabilitation. People with a neurological condition used as participants were found in only two of the videos. One of the strengths of video is that it can depict authentic, real-world experiences of people with neurological conditions during rehabilitation sessions. The lack of involvement of people who have real impairments means subtleties in using TST skills for people with a neurological condition will be overlooked. Time constraints and ethical considerations may have been factors in the reduced involvement of people with neurological conditions, however, overcoming these issues to include people with real impairments would enhance the learning experience.
The suitability of videos to guide skill acquisition was assessed in relation to the key components of TST and how they were presented (with demonstration and/ or instructions) and were found to be variable. None of the videos provided demonstration and instruction for each component of TST, and only one video included all the key components. The use of instruction and demonstration has been found to optimise skill acquisition [ 34 , 35 ], therefore, its omission would impact users’ understanding of the components and their ability to perform TST effectively. Feedback was omitted in all but one video, which was concerning as feedback is essential for motor learning and an integral component of TST [ 36 , 37 ]. These results support the findings of previous studies, which found videos created for health professions to be of low educational quality and missing key information. Videos on surface anatomy omitted key aspects related to upper and lower limb anatomy, such as vessels, nerves, cubital fossa, wrists, and hands [ 28 ]. Videos by physiotherapists on shoulder joint mobilisation techniques failed to describe or illustrate vital aspects of techniques such as patient and therapist position, force of application and dosage [ 17 ]. Online videos have also frequently been found to contain inaccurate, contradictory, or misleading information [ 28 , 32 , 38 , 39 ] with no reference to sources or evidence; this is in part due to the lack of peer review processes to monitor quality [ 38 ]. This highlights, that users need to critically evaluate the content of videos, and that improvements need to be made before they can be recommended as a valuable learning resource.
It has been suggested that the quality of video content for education can be filtered by evaluating variables such as the uploading source, video duration or the subjective estimation by viewers, expressed as likes/dislikes. The uploading source in particular has been found to be valuable for discriminating and predicting the quality of video content. Those uploaded by professionals, professional associations, and credible health care organisations are often of higher quality and are more suitable for education than those uploaded by individuals [ 38 , 40 , 41 , 42 , 43 ]. In contrast, video duration and the likes/dislikes ratio were found to be unreliable as a predictor of quality [ 14 , 40 , 42 , 43 ]. These results are consistent with the findings from our study which found that the videos sourced from educational institutions or private clinics were more suitable to guide skill acquisition. Neurological physiotherapists and students should consider the source of online videos to assist them to assess the educational quality of video resources.
This review highlights the importance of evaluating the content within freely available online videos. There are several tools available for assessing the quality, flow, and user friendliness of websites [ 44 ], evaluating health information on the internet, and the credibility of websites [ 45 ]. Although these tools are somewhat useful, they do not assess the content of the video in sufficient detail to help users determine if they are a suitable learning resource to guide skill acquisition. The development of content specific quality tools is required to assist learners to critically evaluate the quality of video content. In addition, guidelines based on sound teaching theory and practice are required to assist creators of online videos to create high quality resources that meet the needs of neurological physiotherapists and students.
This study was the first, to our knowledge, to examine the extent, characteristics of freely available online videos, and whether the content is suitable to guide skill acquisition of TST for neurological physiotherapists and students. Previous studies [ 38 , 39 ] have evaluated the quality of online videos using various gross assessment tools [ 44 , 45 , 46 ]. However, these tools do not evaluate the video content; our study assessed whether the content of freely available online TST videos is suitable to guide skill acquisition. This review has identified difficulties neurological physiotherapists and students face in sourcing relevant videos of good educational quality without subscriptions to specialised domains. Attempts were made throughout the searches to reduce the impacts of search engine personalisation; and consistent reporting of the search strategy and methods, maintained rigour and transparency.
Limitations
The criteria used to evaluate the suitability of the video content for skill acquisition was developed by the authors, was subjective, and may have been affected by observer bias. To reduce the risk of bias, two authors (KS, NT) assessed each video independently. The use of American spelling was used as it resulted in the most search results however, it may have influenced the identification of videos and resulted in the higher prevalence of videos from the USA. Forty-seven videos were excluded as they did not fit our inclusion criteria of explicitly stating that the purpose was the teach. It is acknowledged that some of these videos may have been videos teaching TST.
There are very few suitable online videos that are freely available and specifically designed to support neurological physiotherapists and students in the skill acquisition of TST. The development of a standardised and validated assessment tool, that is easy to use and assesses the content of TST videos is required to support learners to critically evaluate the educational quality of video content. Guidelines based on sound teaching theory and practice are required to assist creators of online videos to provide suitable resources that meet the needs of neurological physiotherapists and students.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Task-specific training
United States of America
Constraint Induced Movement Therapy
Joanna Briggs Institute
New Zealand
Internet protocol
Population, Concept, Context
Winstein CJ, Wolf SL, Dromerick AW, Lane CJ, Nelsen MA, Lewthwaite R, et al. Effect of a Task-oriented Rehabilitation Program on Upper Extremity Recovery following Motor Stroke: the ICARE Randomized Clinical Trial. JAMA. 2016;315(6):571–81.
Article Google Scholar
English C, Hillier SL, Lynch EA. Circuit class therapy for improving mobility after stroke. Cochrane Database Syst Rev. 2017;6(6):Cd007513.
Google Scholar
French B, Thomas LH, Coupe J, McMahon NE, Connell L, Harrison J, et al. Repetitive task training for improving functional ability after stroke. Cochrane Database Syst Rev. 2016;11(11):Cd006073.
Hornby TG, Reisman DS, Ward IG, Scheets PL, Miller A, Haddad D, et al. Clinical Practice Guideline to improve locomotor function following chronic stroke, incomplete spinal cord Injury, and Brain Injury. J Neurol Phys Ther. 2020;44(1):49–100.
Kwakkel G, Veerbeek JM, van Wegen EE, Wolf SL. Constraint-induced movement therapy after stroke. Lancet Neurol. 2015;14(2):224–34.
Lin SH, Dionne TP. Interventions to Improve Movement and Functional outcomes in Adult Stroke Rehabilitation: review and evidence Summary. J Participat Med. 2018;10(1).
Ni M, Hazzard JB, Signorile JF, Luca C. Exercise guidelines for Gait function in Parkinson’s Disease: a systematic review and Meta-analysis. Neurorehabil Neural Repair. 2018;32(10):872–86.
Sakzewski L, Gordon A, Eliasson A-C. The state of the evidence for intensive Upper Limb Therapy approaches for Children with Unilateral Cerebral Palsy. J Child Neurol. 2014;29(8):1077–90.
Bayona NA, Bitensky J, Salter K, Teasell R. The role of task-specific training in rehabilitation therapies. Top Stroke Rehabil. 2005;12(3):58–65.
Pearson Education. Beyond Millennials: The Next Generation of Learners. 2018.
Rapp AK, Healy MG, Charlton ME, Keith JN, Rosenbaum ME, Kapadia MR. YouTube is the most frequently used Educational Video Source for Surgical Preparation. J Surg Educ. 2016;73(6):1072–6.
Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P t. 2014;39(7):491–520.
Noetel M, Griffith S, Delaney O, Sanders T, Parker P, del Pozo Cruz B, et al. Video improves learning in higher education: a systematic review. Rev Educ Res. 2021;91(2):204–36.
Frongia G, Mehrabi A, Fonouni H, Rennert H, Golriz M, Günther P. YouTube as a potential training resource for laparoscopic fundoplication. J Surg Educ. 2016;73(6):1066–71.
Srinivasa K, Chen Y, Henning MA. The role of online videos in teaching procedural skills to post-graduate medical learners: a systematic narrative review. Med Teach. 2020;42(6):689–97.
Derakhshan A, Lee L, Bhama P, Barbarite E, Shaye D. Assessing the educational quality of ‘YouTube’ videos for facelifts. Am J Otolaryngol. 2019;40(2):156–9.
Shah S, Patel R, Patel N, Patel I. Low educational quality and trustworthiness of YouTube videos by physiotherapists on shoulder joint mobilization techniques: a descriptive study. J Man Manip Ther. 2022;30(6):334–41.
Küçükakkaş O, İnce B. Can YouTube be used as an educational tool in lymphedema rehabilitation? Arch Physiother. 2022;12(1):5.
Hannák A, Sapiezynski P, Kakhki AM, Krishnamurthy B, Lazer D, Mislove A et al. Measuring personalization of web search. Proceedings of the 22nd international conference on World Wide Web. 2013.
Bianchi T. Worldwide desktop market share of leading search engines from January 2015 to December 2022: Statista; 2023 January 6 Available from: https://www.statista.com/statistics/216573/worldwide-market-share-of-search-engines/ .
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–26.
Godin K, Stapleton J, Kirkpatrick SI, Hanning RM, Leatherdale ST. Applying systematic review search methods to the grey literature: a case study examining guidelines for school-based breakfast programs in Canada. Syst Reviews. 2015;4(1):138.
Lennon S. Physical Management in Neurological Rehabilitation. 2 ed2004.
Bianchi T. Global search engine desktop market share 2022: Statista; 2023, January 6 Available from: https://www.statista.com/statistics/216573/worldwide-market-share-of-search-engines/ .
Kemp SD. 2022: Global Overview Report: Data Reportal - Global Digital Insights; 2022, May 4 Available from: https://datareportal.com/reports/digital-2022-global-overview-report .
Azer SA. Can “YouTube” help students in learning surface anatomy? Surg Radiol Anat. 2012;34(5):465–8.
Murugiah K, Vallakati A, Rajput K, Sood A, Challa NR. YouTube as a source of information on cardiopulmonary resuscitation. Resuscitation. 2011;82(3):332–4.
Hubbard IJ, Parsons MW, Neilson C, Carey LM. Task-specific training: evidence for and translation to clinical practice. Occup Ther Int. 2009;16(3–4):175–89.
Kleim JA, Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008;51(1):S225–39.
Sunderland N, Camm CF, Glover K, Watts A, Warwick G. A quality assessment of respiratory auscultation material on YouTube. Clin Med (Lond). 2014;14(4):391–5.
Camm CF, Sunderland N, Camm AJ. A quality assessment of cardiac auscultation material on YouTube. Clin Cardiol. 2013;36(2):77–81.
Preston E, Ada L, Dean CM, Stanton R, Waddington G, Canning C. The Physiotherapy eSkills Training Online resource improves performance of practical skills: a controlled trial. BMC Med Educ. 2012;12:119.
Dong C, Goh PS. Twelve tips for the effective use of videos in medical education. Med Teach. 2015;37(2):140–5.
Levin MF, Demers M. Motor learning in neurological rehabilitation. Disabil Rehabil. 2021;43(24):3445–53.
Maier M, Ballester BR, Verschure P. Principles of Neurorehabilitation after Stroke based on Motor Learning and Brain plasticity mechanisms. Front Syst Neurosci. 2019;13:74.
Madathil KC, Rivera-Rodriguez AJ, Greenstein JS, Gramopadhye AK. Healthcare information on YouTube: a systematic review. Health Inf J. 2015;21(3):173–94.
Erdem MN, Karaca S. Evaluating the Accuracy and Quality of the information in kyphosis videos Shared on YouTube. Spine (Phila Pa 1976). 2018;43(22):E1334–9.
Lee JS, Seo HS, Hong TH. YouTube as a potential training method for laparoscopic cholecystectomy. Ann Surg Treat Res. 2015;89(2):92–7.
Lee H, Choi A, Jang Y, Lee JI. YouTube as a learning tool for four shoulder tests. Prim Health Care Res Dev. 2018;20:e70.
Ajumobi AB, Malakouti M, Bullen A, Ahaneku H, Lunsford TN. YouTube™ as a source of Instructional Videos on Bowel Preparation: a content analysis. J Cancer Educ. 2016;31(4):755–9.
Desai T, Shariff A, Dhingra V, Minhas D, Eure M, Kats M. Is content really king? An objective analysis of the public’s response to medical videos on YouTube. PLoS ONE. 2013;8(12):e82469.
Bernard A, Langille M, Hughes S, Rose C, Leddin D, Veldhuyzen van Zanten S. A systematic review of patient inflammatory bowel disease information resources on the world wide web. Am J Gastroenterol. 2007;102(9):2070–7.
Silberg WM, Lundberg GD, Musacchio RA. Assessing, controlling, and assuring the quality of medical information on the internet: Caveant Lector et viewor–let the reader and viewer beware. JAMA. 1997;277(15):1244–5.
Team HON. Health On the Net 2020 updated March 2020; cited 2023 May 13. Available from: https://www.hon.ch/en/ .
Download references
Acknowledgements
Melanie Grant (Senior librarian) contributed to the design of the search strategy.
Kelvin Sasse was funded as part of a student summer scholarship funded by the School of Clinical Sciences, Physiotherapy Department, Auckland University of Technology. Auckland, New Zealand.
Author information
Authors and affiliations.
School of Clinical Sciences, Department of Physiotherapy, Health and Rehabilitation Research Institute, Auckland University of Technology, Northshore Campus, Private Bag 92006, Auckland, 1142, New Zealand
Nicola C.M. Towersey, Kelvin Sasse, Verna Stavric, Gemma Alder & Nicola L. Saywell
You can also search for this author in PubMed Google Scholar
Contributions
NT, NLS, GA and VS conceived and designed the study and contributed to manuscript preparation. KS collected, collated, analysed the data, and contributed to the writing of the manuscript. NT, NLS, GA and VS also contributed to data collection and analysis. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Nicola C.M. Towersey .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Towersey, N., Sasse, K., Stavric, V. et al. Freely available, online videos to support neurological physiotherapists and students in task-specific training skill acquisition: a scoping review. BMC Med Educ 24 , 603 (2024). https://doi.org/10.1186/s12909-024-05545-5
Download citation
Received : 21 June 2023
Accepted : 09 May 2024
Published : 31 May 2024
DOI : https://doi.org/10.1186/s12909-024-05545-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Search engine
- Neurological rehabilitation
- Physiotherapy
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Find a Program
- Find A Contractor

- 2024 Announcements
- 2023 Announcements
- 2022 Announcements
- 2021 Announcements
- Social Media
- Press Release Email List
$39.6 Million Is Now Available To Low Income New Yorkers For Home Energy Efficiency and Electrification Upgrades
New york becomes first state to offer u.s. department of energy home energy rebate funding; funds now available through state’s empower+ program.
May 30, 2024
Governor Kathy Hochul today joined U.S. Department of Energy (DOE) Secretary Granholm and White House Senior Advisor John Podesta at the Andromeda Community Initiative in Queens to celebrate New York State becoming the first state in the nation to offer the first phase of Inflation Reduction Act (IRA) Home Electrification and Appliance Rebates (HEAR) Program funding to consumers. The initial $39.6 million formula grant will expand the reach of New York’s EmPower+ program by allowing more low-income families to improve their homes with energy efficiency and electrification upgrades that will reduce energy costs and transition away from burning fossil fuels in their homes. Today's announcement supports the State’s nation-leading Climate Leadership and Community Protection Act (Climate Act) goal to reduce greenhouse gas emissions by 85 percent by 2050 and requirement for at least 35 percent, with a goal of 40 percent of the benefits of clean energy investments supporting disadvantaged communities.
“As the first state in the nation to offer these Inflation Reduction Act rebates, we are expanding access to home improvements that will save New Yorkers money on their energy bills and reduce our reliance on fossil fuels,” Governor Hochul said . “Thanks to our strong partnership between New York State, the Biden Administration, and U.S. Department of Energy, we are making important progress to make the clean energy transition affordable for all New Yorkers.”
U.S. Secretary of Energy Jennifer M. Granholm said , “From tax credits to rebates, the Biden-Harris Administration is determined to lower costs for American families and change the economics of home energy bill. New York is leading the charge as states across the country gear up to launch their Home Energy Rebates program— delivering jobs, savings, and healthier homes.”
Today’s announcement represents the first step in New York State deploying these IRA rebates to residents. Funding for the full portfolio of IRA Home Energy Rebate programs and deployment of additional rebates is expected later this year. The State is eligible to receive a total of $317.7 million through the DOE’s IRA Home Energy Rebate programs: $159.3 million for the Home Efficiency Rebates program and $158.4 million for HEAR program.
In April 2024, the U.S DOE approved the New York State Energy Research and Development Authority’s (NYSERDA) partial-scope application for this initial funding, which allows NYSERDA’s low income EmPower+ program to expand its current reach by providing funding for additional energy efficiency and beneficial electrification improvements, such as insulation and air sealing, heat pumps for space and water heating, and any necessary electrical upgrades to support those improvements. Beginning today, eligible owners of one- to four-family households that have a household income below 80 percent of the Area Median Income or participate in a utility payment assistance program will automatically be enrolled to benefit from IRA HEAR incentives when they apply to the EmPower+ program. Incentives are provided to residents through EmPower+ contractors to reduce the cost of installing energy efficiency and electrification upgrades in a home or apartment, making them more affordable for New Yorkers. For more information including the application process and eligibility requirements, please visit NYSERDA’s website .
NYSERDA is currently working towards developing and submitting the full HEAR application to enable rebate offers to moderate-income residents, up to 150 percent of area median income, and to owners of larger low- and moderate-income multifamily buildings, including high-efficiency electric appliance rebates.
NYSERDA President and CEO Doreen M. Harris said , “The Inflation Reduction Act will be critical in helping New Yorkers make affordable home efficiency upgrades while also leveraging the state’s strong commitment to reduce emissions and confront the global challenge of climate change. With this funding, the State’s expanded EmPower+ program will focus on those who need assistance the most by providing the opportunity to reap the benefits of high-performance, energy-saving measures throughout their homes.”
Senate Majority Leader Charles Schumer said , “The Home Electrification and Appliance Rebates/HEAR program is the secret sauce of our groundbreaking Inflation Reduction Act: it saves consumers money on energy costs while reducing the polluting greenhouse gasses driving global warming. With this $40 million federal boost, the HEAR program will reduce the cost of installing energy efficiency and electrification upgrades in a home or apartment, making them more affordable for New Yorkers while radically reducing carbon pollution. I am proud to stand with Secretary Granholm and the Biden administration to announce this major investment in clean energy and environmental justice and thank Governor Hochul for helping New York achieve a healthier and brighter future.”
House Minority Leader Hakeem Jeffries said , “This $39.6 million in Inflation Reduction Act rebate funding will allow New Yorkers to breathe cleaner, safer air, put money back in the pockets of families and help bring this nation-leading climate plan to life. In the last Congress, House Democrats, in partnership with President Biden and Senate Democrats, passed the transformational Inflation Reduction Act to create the largest investment in combating the climate crisis in the history of the world. I am grateful to President Biden, the U.S. Department of Energy and Governor Hochul for their partnership in securing this important funding for New York.”
Representative Grace Meng said , “Thank you to Governor Hochul, Secretary Granholm and Senior Advisor Podesta for coming to Queens to commemorate these millions of dollars for home energy efficiency and electrification upgrades. As New York’s representative on the House of Representatives’ Regional Leadership Council – which works to promote and implement legislation signed by President Biden – I’m thrilled that our state will be the first in the nation to offer this rebate funding. It will go a long way toward reducing energy costs and ensuring a cleaner, healthier future for New Yorkers. I’m so proud that I helped to pass the Bipartisan Infrastructure Law which continues to deliver needed resources across our state.”
Representative Adriano Espaillat said , “As we enter the summer months, I commend Governor Hochul on today's announcement expanding New York's EmPower+program, making it more accessible for low-income families who rely on this funding to ensure energy efficiency for their homes. New York is once again leading the way in innovation and implementation of the IRA Home Electrification and Appliance Rebates (HEAR) Program to put families first and make energy efficiency more affordable for all.”
Representative Joe Morelle said , “Too many families continue to feel the pressure of rising costs. From healthcare to prescription drugs to heating and cooling their homes and other basic necessities, I’ve heard horrific stories of people cutting corners to make ends meet, something we cannot allow to continue. Thanks to federal funds I secured as a part of the Inflation Reduction Act, this Department of Energy program will help ensure people’s homes are updated with energy-saving and cost-saving technologies, all at a reduced cost. I’m grateful to Governor Hochul for her leadership, and I look forward to continuing our work together to uplift families in Monroe County and across New York State.”
Representative Jamaal Bowman said , “We need to make bold investments in renewable energy everywhere—from our schools to our homes. Heating our houses in the winter, keeping them cool in the summer, and using our stoves and other appliances should not contribute to the climate catastrophe we are facing. I am so excited to join Governor Hochul and Secretary Granholm in announcing nearly $40 million in funding now available to New Yorkers for home energy efficiency and electrification upgrades and rebates—with even more to come. I am especially proud that these investments focus on low-income New Yorkers and marginalized groups who are most impacted by the harms of the climate crisis and the burden of high electricity bills. The Home Energy Rebate Programs are a direct result of our transformational Inflation Reduction Act, which is consistently putting money back in people’s pockets. This new funding will lower costs for hardworking New Yorkers and support New York in reaching its climate goals.”
Representative Ritchie Torres said , “I am proud to join Governor Hochul in announcing a massive $39.6 million investment in energy rebate funding for low-income New Yorkers. This money is the direct result of the unprecedented green energy investments in President Joe Biden and Congressional Democrats’ landmark Infrastructure Reduction Act (IRA). The increased energy efficiency brought by the HEAR Program’s retrofits will save low-income Bronxites money. It will also reduce carbon emissions – especially important in a borough with the highest rates of asthma and other respiratory illnesses in the city. This program is an excellent example of how Democratic policy is working to impact the daily lives of those in our district and beyond. It is often a privilege to think about energy efficiency when considering housing, due to the limited access of resources, but with the IRA it is feasible. For a community that already struggles with accessibility, this is a step in the right direction.”
Representative Dan Goldman said , “As we transition into a cleaner, greener economy, it is vital that no one – regardless of their circumstance – is left behind. Through President Biden and House Democrats' Inflation Reduction Act, we can finally ensure that everyone has access to the energy and efficiency upgrades that have revolutionized our nation's green infrastructure. I'm proud that under Governor Kathy Hochul's leadership, New York is the first in the nation to roll out these rebates, allowing low-income families across the state to participate in our nation's green transition.”
Building Performance Contractors Association President Hal Smith said , “On behalf of New York’s Building Performance contractors, hats off to everyone who has helped to lead the way for the whole country. It is a great time to be a New Yorker!”
Rewiring America CEO Ari Matusiak said , “Today marks a landmark moment in the implementation of the largest climate bill in history. We congratulate New York for becoming the first state in the nation to roll out the Home Electrification and Appliance Rebates and applaud the Department of Energy for prioritizing getting these dollars out the door and into communities. By crafting a program that meets the needs of its communities and directing this first tranche of funding exclusively to low-income households that stand to benefit the most from lower energy bills and healthier homes, New York is taking an important step in ensuring that the transition to an all-electric future is an equitable one. We’re eager to see the next batch of rebate programs roll out in the coming months and to see states follow New York’s lead in thoughtfully designing effective programs that make the most of this historic opportunity.”
Climate & Energy at Natural Resources Defense Council New York Policy Director Samantha Wilt said , “New York is the first state to leverage the IRA's Home Electrification and Appliance Rebates Program to invest in the homes of the state's most vulnerable families while cutting climate pollution. These funds are being invested in a way that drives benefits to the New Yorkers who need them most and ensures that the harms from burning fossil fuels are reduced in disadvantaged communities. With this investment, New York will be delivering more all-electric appliances, insulation, and wiring upgrades for seriously improved, zero-emission homes.”
Buildings are one of the most significant sources of greenhouse gas emissions in New York State and through NYSERDA and utility programs over $6.8 billion is being invested to decarbonize buildings. By improving energy efficiency in buildings and advancing statewide installations of onsite storage, renewables and electric vehicle charging equipment, the State will reduce its carbon pollution and advance toward the ambitious target of reducing on-site energy consumption by 185 TBtu by 2025, the equivalent of powering 1.8 million homes.
New York State's Nation-Leading Climate Plan
New York State's climate agenda calls for an orderly and just transition that creates family-sustaining jobs, continues to foster a green economy across all sectors and ensures that at least 35 percent, with a goal of 40 percent, of the benefits of clean energy investments are directed to disadvantaged communities. Guided by some of the nation’s most aggressive climate and clean energy initiatives, New York is advancing a suite of efforts – including the New York Cap-and-Invest program (NYCI) and other complementary policies – to reduce greenhouse gas emissions 40 percent by 2030 and 85 percent by 2050 from 1990 levels. New York is also on a path to achieving a zero-emission electricity sector by 2040, including 70 percent renewable energy generation by 2030, and economywide carbon neutrality by mid-century. A cornerstone of this transition is New York's unprecedented clean energy investments, including more than $28 billion in 61 large-scale renewable and transmission projects across the State, $6.8 billion to reduce building emissions, $3.3 billion to scale up solar, nearly $3 billion for clean transportation initiatives and over $2 billion in NY Green Bank commitments. These and other investments are supporting more than 170,000 jobs in New York’s clean energy sector as of 2022 and over 3,000 percent growth in the distributed solar sector since 2011. To reduce greenhouse gas emissions and improve air quality, New York also adopted zero-emission vehicle regulations, including requiring all new passenger cars and light-duty trucks sold in the State be zero emission by 2035. Partnerships are continuing to advance New York’s climate action with more than 400 registered and more than 130 certified Climate Smart Communities, nearly 500 Clean Energy Communities, and the State’s largest community air monitoring initiative in 10 disadvantaged communities across the State to help target air pollution and combat climate change.
Media Inquiries
- Executive Chamber, Phone: 518-474-8418, Ext. n/a Email: [email protected]

IMAGES
VIDEO
COMMENTS
A critical appraisal is an academic approach that refers to the systematic identification of strengths and weakness of a research article with the intent of evaluating the usefulness and validity of the work's research findings. As with all essays, you need to be clear, concise, and logical in your presentation of arguments, analysis, and ...
5. finally, you evaluate your new or amended practice. ces ol: n n n e l Critical appraisal is essential to: combat information overload; identify papers that are clinically relevant; Continuing Professional Development (CPD) - critical appraisal is a requirement for the evidence based medicine component of many membership exams.
After selecting an article, you must be able to sit with the article and critically appraise it. Critical appraisal of a journal article is a literary and scientific systematic dissection in an attempt to assign merit to the conclusions of an article. Ideally, an article will be able to undergo scrutiny and retain its findings as valid.
Here are some of the tools and basic considerations you might find useful when critically appraising an article. In a nutshell when appraising an article, you are assessing: 1. Its relevance ...
Whilst critical appraisal can be a whole course for students, this article aims to provide an introduction to help students to get started with the right questions, and make
critically about each section before you evaluate the article as a whole. You do not have to be an expert in the field to start to critically evaluate a research article. As you gain experience, you will become more critical, but it is still possible to question and evaluate a text in the early stages of your studies. The abstract
INTRODUCTION. Critical appraisal of a research paper is defined as "The process of carefully and systematically examining research to judge its trustworthiness, value and relevance in a particular context."[] Since scientific literature is rapidly expanding with more than 12,000 articles being added to the MEDLINE database per week,[] critical appraisal is very important to distinguish ...
This guide is meant to help you understand the basics of writing a critical analysis. A critical analysis is an argument about a particular piece of media. There are typically two parts: (1) identify and explain the argument the author is making, and (2), provide your own argument about that argument.
Critical appraisal is a systematic process through which the strengths and weaknesses of a research study can be identified. This process enables the reader to assess the study's usefulness and ...
Appraising the body of research. The critical appraisal of individual studies occurs within the broader goal of exploring how a body of work contributes to knowledge, policy, and practice. Methods exist to help reviewers assess how the research they have examined can contribute to practice and real world impact.
SuMMarY. Critical appraisal is a systematic process used to identify the strengths. and weaknesse s of a res earch article in order t o assess the usefulness and. validity of r esearch findings ...
Abstract. Critical appraisal is a systematic process used to identify the strengths and weaknesses of a research article in order to assess the usefulness and validity of research findings. The most important components of a critical appraisal are an evaluation of the appropriateness of the study design for the research question and a careful ...
Critical appraisal forms part of the process of evidence-based practice. " Evidence-based practice across the health professions " outlines the fives steps of this process. Critical appraisal is step three: Ask a question. Access the information. Appraise the articles found.
Critical appraisal allows us to: reduce information overload by eliminating irrelevant or weak studies. identify the most relevant papers. distinguish evidence from opinion, assumptions, misreporting, and belief. assess the validity of the study. assess the usefulness and clinical applicability of the study. recognise any potential for bias.
Books, encyclopedia articles, and scholarly journal articles about Adenauer's role are considered secondary sources. In the sciences, journal articles and conference proceedings written by experimenters reporting the results of their research are primary documents. Choose both primary and secondary sources when you have the opportunity.
To be critical, or to critique, means to evaluate. Therefore, to write critically in an academic analysis means to: judge the quality, significance or worth of the theories, concepts, viewpoints, methodologies, and research results. evaluate in a fair and balanced manner. avoid extreme or emotional language. You evaluate or judge the quality ...
analyse: break down the information into parts, consider how parts work together. discuss: explain a topic, make comparisons, consider strengths & weaknesses, give reasons, consider implications. evaluate: assess something's worth, value or suitability for a purpose - this often leads to making a choice afterwards. justify: show the reasoning behind a choice, argument or standpoint
An article may represent the views or opinions of the author that are not based on evidence, so it is essential to develop skills to evaluate what you read. Before using information you find in an article it is important to judge its accuracy, objectivity and establish that the information comes from a reliable and appropriate source.
Take a quick look at the article Step 2. Click on the Credibility tab above - there are questions to help you appraise the trustworthiness of the article, read the questions and look for the answers in the article. Step 3. Click on each question and our answers will appear. Step 4.
Typically, the word "critical" has a negative connotation. Think of words like "critique" and "criticise" and you see why. However, with essay writing, being asked to write "critically" does not necessarily mean you need to be negative. Instead, you are voicing your opinion in a logical and coherent way that is based upon ...
ment for critical appraisal exists. The criteria used to assess the validity and relevance of scientific SuMMarY Critical appraisal is a systematic process used to identify the strengths and weaknesses of a research article in order to assess the usefulness and validity of research findings. The most important components of a critical
Study power! The power of the trial will depend on: - outcome of interest (binary or continuous), - minimum treatment effect felt to be clinically important
How to write an Evaluation Essay. There are two secrets to writing a strong evaluation essay. The first is to aim for objective analysis before forming an opinion. The second is to use an evaluation criteria. Aim to Appear Objective before giving an Evaluation Argument. Your evaluation will eventually need an argument.
On this note, the article recognizes and welcomes the creation of several complementary measures by the government. At the same time, the article cautions that substantively addressing the problem requires a generational change that moves Australian culture away from an ideological privileging of the private sector.
Based on our research questions, we performed iterative literature searches (detailed below) followed by critical appraisal by the authors, and transformed the resulting insights into the critical discussion presented in the main section of the present article by applying the 6 quality criteria of the SANRA scale : 1.
What matters is whether an A.I.-assisted platform can reliably appraise and diagnose your students' writing, providing the explanation and guidance these students need to improve.
Critical reviews focus on empirical research to evaluate what is known about a specific topic and integrate it into a framework [26, 27]. They may use a systematic search strategy to integrate the strengths of systematic and critical reviews [ 27 ], including all relevant literature, to avoid biases.
It also comes nearly a month after the election of three new members on appraisal district's board of directors. The board can appoint people to the citizen review board. The board can appoint ...
The development of content specific quality tools is required to assist learners to critically evaluate the quality of video content. In addition, guidelines based on sound teaching theory and practice are required to assist creators of online videos to create high quality resources that meet the needs of neurological physiotherapists and ...
NYSERDA President and CEO Doreen M. Harris said, "The Inflation Reduction Act will be critical in helping New Yorkers make affordable home efficiency upgrades while also leveraging the state's strong commitment to reduce emissions and confront the global challenge of climate change. With this funding, the State's expanded EmPower+ program ...