An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Endocrinol
- v.2015; 2015


An Overview of Diabetes Management in Schizophrenia Patients: Office Based Strategies for Primary Care Practitioners and Endocrinologists
Aniyizhai annamalai.
1 Departments of Psychiatry and Internal Medicine, Yale School of Medicine, 34 Park Street, New Haven, CT 06519, USA
2 Department of Psychiatry, Yale School of Medicine, 34 Park Street, New Haven, CT 06519, USA
Diabetes is common and seen in one in five patients with schizophrenia. It is more prevalent than in the general population and contributes to the increased morbidity and shortened lifespan seen in this population. However, screening and treatment for diabetes and other metabolic conditions remain poor for these patients. Multiple factors including genetic risk, neurobiologic mechanisms, psychotropic medications, and environmental factors contribute to the increased prevalence of diabetes. Primary care physicians should be aware of adverse effects of psychotropic medications that can cause or exacerbate diabetes and its complications. Management of diabetes requires physicians to tailor treatment recommendations to address special needs of this population. In addition to behavioral interventions, medications such as metformin have shown promise in attenuating weight loss and preventing hyperglycemia in those patients being treated with antipsychotic medications. Targeted diabetes prevention and treatment is critical in patients with schizophrenia and evidence-based interventions should be considered early in the course of treatment. This paper reviews the prevalence, etiology, and treatment of diabetes in schizophrenia and outlines office based interventions for physicians treating this vulnerable population.
1. Introduction
People with schizophrenia have an increased risk of diabetes and other metabolic abnormalities. A renewed interest in this phenomenon has been sparked by the adverse metabolic effects of antipsychotic medications used in the treatment of schizophrenia. It is now well established that people with serious mental illness (SMI), including schizophrenia, have excess morbidity and mortality leading to a reduced lifespan of 20–25 years compared with the rest of the population [ 1 , 2 ]. The increased mortality is largely attributable to physical illness, including metabolic abnormalities and cardiovascular disease, rather than factors that are directly associated with psychiatric illness such as suicide or homicide. Metabolic syndrome occurs in one in three patients and diabetes in one in five patients [ 3 ]. These abnormalities not only confer an elevated cardiovascular risk and increased mortality in those with schizophrenia and other mental illness [ 4 ], but also are associated with poor psychiatric and functional outcomes [ 5 ].
For many people with schizophrenia and other serious mental illness, the mental health center is the primary point of contact with the health care system [ 6 ]. But there are multiple barriers to adequate screening and treatment at the mental health centers [ 7 ]. Referrals to community medical providers are challenging, in part due to administrative barriers, lack of communication between mental health and primary care practitioners and clinics, and also poor patient experience in medical settings. For patients with schizophrenia, psychiatric symptoms and cognitive deficits limit their social functioning and a fast paced medical health care environment is difficult to navigate. In one survey, these patients cited continuity of care and listening skills as qualities important in medical practitioners [ 8 , 9 ].
Patients with SMI are usually on treatments that include psychopharmacologic agents, psychotherapy, and other social interventions. Antipsychotics are a cornerstone of treatment in those with schizophrenia. A category of agents, known as second-generation antipsychotics, have been used since the early 1990s and in the last two decades there has been a tremendous increase in use of these medications [ 9 ]. These agents are now known to contribute significantly to obesity and metabolic syndrome, though there are variations in magnitude of risk between individual agents [ 10 ]. This, along with the increased smoking rates seen in people with schizophrenia, results in an increased cardiovascular risk and ultimately leads to worsened mortality rates [ 4 , 11 ].
In spite of increased awareness among mental health providers of the increased prevalence of metabolic syndrome in SMI, rates of screening and treatment remain poor [ 12 ]. The mortality gap between this patient group and the rest of the population, largely due to medical illnesses, has not narrowed [ 13 ]. Primary care providers already have the specialized medical knowledge necessary to treat medical conditions in those with schizophrenia. Increased awareness among medical providers of the high medical morbidity and mortality in schizophrenia is critical. Skills of primary care such as empathic listening, targeted education, continuity of care, and care coordination with mental health providers all have the potential to significantly improve the health of patients with schizophrenia.
2. Prevalence of Diabetes Diagnosis and Treatment in Schizophrenia
The rate of metabolic syndrome and diabetes in patients with schizophrenia is higher than the general population. A meta-analysis of several studies comprising over 25,000 patients with schizophrenia and related disorders showed an overall rate of metabolic syndrome at 32.5% and hyperglycemia at 19% [ 3 ].
A large multisite study, the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE), examined the effectiveness of different antipsychotic medications in over 1400 patients with schizophrenia. In addition to psychiatric outcomes, the study also examined physical health indicators. Metabolic syndrome was seen in more than 40% of patients. Diabetes was seen in 11% of patients and fasting glucose levels >100 mg/dl were seen in more than 25% of patients in this study. Rates of treatment for metabolic syndrome were low with more than 30% of patients with diabetes not receiving treatment [ 12 ].
The prevalence of diabetes in schizophrenia has been estimated to be 2-3-fold higher than in the general population and estimates of prevalence range from 10 to 15% [ 14 ]. In a study of over 400 patients with schizophrenia, the prevalence of diabetes and impaired glucose tolerance was 6.3% and 23.4%, respectively, in the total sample [ 15 ]. Diabetes prevalence was 4-5 times higher within each age group. The difference in diabetes prevalence between those with schizophrenia and the general population rose linearly with age from 1.6% in the 15–25 age group to 19.2% in the 55–65 age group. Interestingly, while the prevalence of metabolic syndrome is higher in those with schizophrenia, the increase in prevalence with age is the same as the general population. This suggests that the development of diabetes in schizophrenia is not solely secondary to metabolic syndrome but there may also be an inherent vulnerability to diabetes, possibly aggravated by pharmacological effects of some antipsychotics [ 16 ].
A large number of patients with schizophrenia and other SMI receive their psychiatric care at specialized mental health settings. A national screening program of 10,084 patients over several of these centers showed 37% of patients with schizophrenia had an elevated fasting glucose (>100 mg/dl) [ 17 ]. The rates of treatment were low, even among those with known diabetes. Approximately 40% of patients with schizophrenia and diagnosed diabetes reported not receiving any antihyperglycemics. This corroborates with the low rates of treatment seen in the CATIE study.
3. Etiology of Development of Diabetes in Schizophrenia
A link between schizophrenia and diabetes has been known for over a century, long before the use of antipsychotic medications. There is debate about the degree of contribution of genetics and environmental factors to development of diabetes.
Epidemiological studies show an increased risk of developing diabetes in people with schizophrenia with and without antipsychotics [ 18 ]. Some studies of people with antipsychotic naïve, first episode schizophrenia show impaired glucose tolerance and higher insulin resistance compared to healthy cohorts [ 19 ].
There is also evidence that antipsychotics increase metabolic risks, with second-generation agents showing differentially higher risk over time compared to first generation agents [ 20 ]. A recent comparative meta-analysis of metabolic abnormalities among unmedicated and first episode patients with schizophrenia showed a comparable rate with the general population [ 21 ]. These rates were much lower when compared with people with chronic schizophrenia established on medications. This would imply that most, if not all, the metabolic risk in schizophrenia patients is conferred by antipsychotic agents.
As can be seen, the data on the extent to which antipsychotics confer metabolic risk are conflicting. The relative contributions of genetic susceptibility and antipsychotic treatment to increased prevalence of diabetes are uncertain. The following sections review briefly some mechanisms postulated to explain the association of diabetes with schizophrenia.
3.1. Genetic Susceptibility to Diabetes
A common inherited susceptibility to both diabetes and schizophrenia has been postulated based on the observation that diabetes is more common in family members of those with schizophrenia [ 22 ]. A common genetic linkage between the two diseases has been suggested. Some authors report abnormal glucose metabolism and insulin signaling in the brain of those with schizophrenia [ 19 , 23 ]. Genes involved in both glucose metabolism and cognitive function may increase the risk of diabetes in schizophrenia patients. There is also a suggestion of a common molecular mechanism underlying both cognitive deficits such as working memory and glucose metabolism [ 23 ].
3.2. Neuroendocrine Pathways Increasing Diabetes Risk
Some studies have reported dysregulation of the hypothalamic pituitary axis and high serum cortisol levels in people with schizophrenia. Elevated serum cortisol increases gluconeogenesis, insulin resistance, and symptoms of metabolic syndrome. It is hypothesized that the elevated cortisol also increases serum leptin levels with a resultant increase in appetite [ 24 ]. Some authors have also implicated nutritional factors in a common pathway for development of both diabetes and schizophrenia [ 25 ]. For example, a low level of vitamin D during childhood may be associated with schizophrenia and vitamin D may affect insulin response to glucose stimulation [ 26 ]. Gestational zinc deficiency has also been proposed as a possible mediator of a common etiologic pathway [ 27 ].
3.3. Antipsychotics and Risk of Diabetes
Antipsychotics lead to weight gain and a higher risk of obesity related complications including diabetes [ 20 ]. The metabolic effects on glucose and insulin metabolism between agents within each class of antipsychotics are different [ 28 ]. Second-generation or atypical antipsychotics had three times the rate of new onset metabolic syndrome compared to first generation or typical or conventional antipsychotics after three years on medications [ 20 ]. At the three-year follow-up, impaired fasting glucose was more frequent in those treated with the second-generation agents. But the difference between the two groups of agents was not significant when clozapine and olanzapine were excluded from the analysis. Both clozapine and olanzapine are second-generation antipsychotics.
In a large meta-analysis comprising 25,992 patients, one in five patients with schizophrenia had hyperglycemia; the rate of metabolic syndrome was 51.9% for clozapine, 28.2% for olanzapine, and 27.9% for risperidone [ 3 ]. Risperidone is also a second-generation agent.
These medications cause weight gain by multiple mechanisms mediated by their effect on hypothalamic regulation and action on dopaminergic, serotoninergic, and histaminergic receptors [ 29 ]. The resulting obesity is a risk for hyperglycemia but antipsychotics can also directly cause diabetes. One postulated mechanism is the ability of antipsychotics to block the pancreatic muscarinic (M3) receptor. Leptin resistance is another proposed mechanism.
3.4. Nonmedication Environmental Factors
It is well known that patients with schizophrenia and other serious mental illnesses have unhealthy lifestyles with poor diets and inadequate physical activity [ 30 – 33 ]. This places them at higher risk of obesity and other metabolic complications. Factors that contribute to poor access to healthy lifestyle choices in individuals with schizophrenia are lower socioeconomic status, lower educational level, living situation (residential settings and living in areas with abundance of fast food facilities), and social isolation. Symptoms of schizophrenia such as low motivation, apathy, and cognitive deficits also could play a role in preventing access to healthy lifestyles. Patients with schizophrenia are also much more likely to be dependent on tobacco [ 34 ] and this further increases risk for cardiovascular disease. The following is a summary of the proposed common pathways between the two disease conditions.
Relationship between Diabetes and Schizophrenia
- higher occurrence of diabetes in family members of schizophrenia patients [ 22 ],
- abnormal glucose metabolism in schizophrenia patients [ 19 , 23 ],
- common mechanism proposed for cognitive deficit and glucose metabolism [ 23 ].
- hypothalamic axis dysregulation and elevated cortisol in schizophrenia [ 24 ],
- nutritional deficiencies proposed as common pathway for both diseases [ 25 – 27 ].
- effect on hypothalamic regulation, dopaminergic, serotonergic, and histaminergic receptors [ 29 ],
- other proposed mechanisms: action on pancreatic muscarinic receptor and leptin resistance [ 29 ].
- poor diet and lack of access to quality foods [ 30 – 32 ],
- inadequate physical activity due to symptoms and social isolation [ 30 , 31 , 33 ].
4. Treatment of Diabetes in Schizophrenia
Developing effective treatment programs for diabetes care is imperative for people with schizophrenia. See Table 1 for a summary of recommendations for diabetes management in these patients. As seen above, they are at risk not simply for diabetes but also for other metabolic conditions that lead to increased cardiovascular risk and mortality. The first step in diabetes management is prevention.
Special considerations for diabetes treatment in schizophrenia patients.
Prevention of obesity is an important part of preventing diabetes in schizophrenia patients as in the general population. Comprehensive programs to improve diet and physical activity of people with schizophrenia and other mental illnesses have been shown to be effective for clinically significant weight loss [ 35 ] as well as metabolic parameters. One program showed a greater decline in fasting blood sugars compared to controls [ 36 ]. Evidence has shown that for these programs to be effective they have to be of longer duration, include both education and activity within group settings, and include both nutrition and physical activity components. Manualized programs may be more successful than unstructured interventions. Individual clinicians can also provide office based counseling with specific targets for behavior change and periodic monitoring of weights and metabolic parameters [ 37 ]. This should happen at both the primary care site and the psychiatrist's office.
Another key strategy in preventing diabetes is periodic monitoring of patients. Most expert recommendations argue for frequent monitoring of metabolic parameters in those with schizophrenia [ 38 ]. These patients should be considered high risk regardless of age and presence of other risk factors. A targeted approach to screening should be employed in all patients, but frequency of screening will need to be higher in those on antipsychotics. In this particular patient population, adherence and follow-up may be an issue and so glycosylated hemoglobin (HbA1c) may be preferable to a fasting glucose level as a screening test. For those on antipsychotics, screening should be done at baseline and then at 3-month intervals. If the HbA1c levels remain stable, screening can be reduced to 6-month or 1-year intervals.
Primary care physicians should also confer with the treating psychiatrist when a patient with schizophrenia gains excessive weight or develops glucose intolerance. The treating psychiatrist may not be aware of the development of glucose intolerance and other metabolic abnormalities. Also, the psychiatrist may be able to change the antipsychotic medication if the patient is on an agent that has a high risk of causing obesity and diabetes. Among antipsychotic agents, ziprasidone has shown to be the least likely to cause significant weight gain and should be considered in all patients [ 39 ]. Aripiprazole and other antipsychotics such as perphenazine, fluphenazine, and haloperidol can be considered as second line agents to switch to for attenuation of weight gain. As described above, clozapine and olanzapine are the antipsychotics most likely to cause weight gain as well as hyperglycemia and other metabolic complications. Risperidone and quetiapine are next in line in terms of likelihood of causing obesity and diabetes. While every attempt should be made to switch to an antipsychotic agent with lower metabolic risks, it should be remembered that the metabolic abnormalities are not always reversible with cessation of the offending agent. Also clozapine represents a special case since its use is limited to patients who failed other antipsychotics; thus a switch out of clozapine may not be possible.
Many pharmacologic agents have been studied in patients with schizophrenia and other psychotic disorders to prevent or reverse the weight gain and metabolic abnormalities found in patients treated with antipsychotic medications [ 40 ]. Metformin is a promising agent as it has the potential for modest weight loss and improves insulin sensitivity and glucose regulation. The Diabetes Prevention Study showed that, in the general population, metformin is effective in preventing conversion to diabetes in those with impaired glucose tolerance but less effective than lifestyle interventions aimed at improving eating and physical activity behavior [ 41 ].
In people on antipsychotics, metformin has been studied for both prevention and treatment of antipsychotic-induced weight gain. It has been shown to be effective in attenuating weight gain on antipsychotics and improving glucose regulation [ 42 , 43 ]. Olanzapine is the most commonly studied antipsychotic in the metformin trials. In a sample of patients with chronic schizophrenia on olanzapine, metformin was effective in reducing both weight and HbA1c levels [ 44 ]. The weight loss compared to placebo was modest at 2 kg, which is similar to weight loss observed with metformin in the general population. In another cohort of patients who were early in the course of schizophrenia, metformin was superior to lifestyle interventions but combined intervention was superior to either intervention alone [ 45 ]. Mean reduction in body mass index (BMI) was about 1.8 in the group that received both metformin and lifestyle interventions compared to an increase in BMI of 1.2 in the placebo group. The fasting glucose decreased by a mean of 7.2 mg/dl in the metformin and lifestyle interventions group while it increased by 1.2 mg/dl in the placebo group. Metformin has also shown efficacy in improving weight and metabolic profile in patients on clozapine [ 46 ].
Thus, metformin has shown efficacy in improving glucose regulation in those with schizophrenia, though the effect sizes are small as in the general population. It should be considered early in the course of illness in all patients with schizophrenia who are obese and have evidence of glucose dysregulation, even if they are not on antipsychotics. However, given that the reductions in weight and glucose are small, metformin is only one step in the treatment of those with glucose intolerance.
The bulk of the data on metabolic abnormalities and antipsychotics is on weight gain related to these agents. Besides metformin, topiramate, an anticonvulsant, has shown some success in treating antipsychotic related weight gain [ 47 ]. Some prominent side effects such as cognitive impairment may be a deterrent for its use in schizophrenia. Other available weight loss agents such as orlistat, lorcaserin, and naltrexone/bupropion combination have not been adequately studied in the schizophrenia population. None of these agents affect glucose metabolism. Thus it is not clear if they can prevent conversion to diabetes. Other novel agents used for treatment of diabetes are being studied for diabetes prevention in prediabetic patients. However, the potential benefits both in the general population and in those with schizophrenia are unknown at this time.
Diabetes care in those with schizophrenia should be intensive and started early. As in all patients, the primary goal is to prevent long-term complications. Patients with schizophrenia have multiple other cardiovascular risk factors. Other conditions such as tobacco dependence and hypertension should be aggressively treated. Obstructive sleep apnea is another cardiovascular risk factor that is highly prevalent in this population [ 48 ]. As outlined above, diet and exercise measures can be effective and patients should be referred to a structured treatment program, if available. At a minimum, they should be referred to a nutritionist for specific recommendations on dietary modifications for managing diabetes.
At all stages of prevention and treatment, providers should communicate with family members or other caregivers. In patients with schizophrenia, issues of adherence and follow-up may be even more problematic than in the general population. Due to psychiatric symptoms and cognitive deficits, longer visits and simplified explanation of recommendations may be necessary. The long-term risks of poorly treated diabetes, including increased mortality, should be clearly delineated. Providers should also recognize that symptoms such as paranoia or delusions might interfere with adherence to recommendations. For this reason, providers should arrange for frequent follow-up visits, especially in initial stages of treatment. Providers will also need to coordinate care with specialists for routine diabetes care such as visits for a fundoscopic eye exam.
Adequate hygiene may be a problem in some patients and so special attention should be paid to foot care. They may not report neuropathic symptoms readily and a foot exam should be done at every visit. In the event of vascular complications with development of a diabetic ulcer, wound care should be aggressive with close follow-up. Poor dentition is frequently seen in these patients and efforts should be made to obtain dental evaluation and treatment to prevent gingivitis and other infectious complications. Sexual dysfunction, which can result from diabetes, can also be due to antipsychotic treatment. These medications affect sexual function through multiple mechanisms including elevated prolactin levels. Similarly, gastroparesis, a complication of diabetes, can also result from anticholinergic medications that are often used to combat adverse effects of antipsychotics.
Attention should also be paid to psychotropic medications that can cause chronic kidney disease. Lithium is a mood stabilizer used in patients with schizophrenia and coexisting mood disorder. Long-term treatment with lithium is associated with a range of glomerular and tubular disorders resulting in chronic kidney disease and rarely renal failure [ 49 ]. Potential interactions between psychotropics and agents used to treat diabetes and comorbid hypertension and hyperlipidemia should also be taken into consideration [ 50 ].
It is worthwhile to note that some antipsychotic medications, especially quetiapine and olanzapine, have been associated with acute onset of hyperglycemia and ketoacidosis [ 51 ]. Cognitive dysfunction associated with elevated glucose levels may be mistaken for the patient's baseline cognitive deficit resulting in delay in detection of hyperglycemia.
Other measures to prevent and treat comorbidities, such as use of aspirin and preventive immunizations, should be based on current evidence-based guidelines, as with any diabetic patient.
Antidiabetic agents with lesser likelihood of weight gain should be used whenever possible, since these patients are already on psychotropic medications that cause weight gain. If they are on medications that can cause hypoglycemia, very specific recommendations on immediate management should be provided to both patients and caregivers. Similarly, if self-monitoring with finger stick glucose measurements is necessary, caregivers may have to be involved for those patients with significant impairments. The frequency of glucose self-monitoring should also be tailored to the patient's capabilities. Target HbA1c goals should be individualized. The cardiovascular benefits of intensive glucose control should be balanced against the risks of hypoglycemia and the capacity of the patient to self-manage this complication of treatment. Providers should be flexible in tailoring treatment goals to each individual patient.
If aggressive lifestyle interventions and pharmacotherapy are inadequate to achieve target glucose levels and insulin administration becomes necessary, the insulin regimen should be kept as simple as possible. A basal insulin regimen offers the benefit of lesser risk of hypoglycemia. But in those whose level of hyperglycemia warrants additional prandial insulin, a premixed insulin regimen may be simpler to administer. Tight glucose control may not be possible in all patients. For any insulin regimen, patients should receive specialized nursing education and this may have to be delivered over multiple sessions. Home nursing services can be arranged in areas where such resources are available. Family members and caretakers can be trained in supervising or administering finger-stick glucose measurements and insulin injections. Depending on the practice setting, the treating psychiatrist may be able to assist with arranging for specialized services in the community, such as additional case management or nursing services. Coordination of care with the psychiatrist is of paramount importance.
Finally, bariatric surgery should be considered in patients with severe obesity with or without diabetes. It has been shown to improve diabetes measures beyond what is expected with weight loss in the general population [ 52 ]. Studies of bariatric surgery in patients with schizophrenia are lacking. However, bariatric surgery is effective in patients with bipolar disorder and psychiatric outcomes are not worse [ 53 , 54 ]. Therefore, patients with serious mental illness, if selected and managed appropriately, can be good candidates for bariatric surgery. Patients with schizophrenia should not be denied the procedure solely on account of their mental illness. In those who have failed other measures, it may be the only treatment option, especially in severely obese patients with coexisting diabetes.
5. Conclusion
Patients with schizophrenia represent a high-risk population for developing diabetes. The etiology is multifactorial and is a combination of genetic susceptibility, common biologic pathways, environmental factors, and treatment with antipsychotic medications. In spite of increased awareness of the high cardiovascular morbidity and early mortality in this population, rates of screening and treatment remain low. These patients often do not engage adequately in treatment with their primary care providers. An appropriate treatment milieu should be provided to better engage patients in treatment. A key strategy in preventing and treating diabetes and other components of metabolic syndrome should be prevention. Patients with schizophrenia should be seen and evaluated periodically to screen for diabetes and other cardiovascular risk factors. Aggressive lifestyle interventions should be employed for those with obesity and prediabetes or diabetes. Metformin has potential for attenuating weight gain and preventing diabetes and should be considered early in at-risk patients. Pharmacologic measures and bariatric surgery can be as effective in the schizophrenia population as in the general population. However, psychiatric symptoms or cognitive deficits often interfere with optimal diabetes care in these patients and primary care providers should pay special attention to their individualized needs. Providers should collaborate with treating psychiatrists to optimize both medical and psychiatric treatment to prevent the early mortality seen in this vulnerable population.
Conflict of Interests
The authors declare that there is no conflict of interests to declare in the publication of this paper.
- Research article
- Open access
- Published: 23 March 2012
Effective lifestyle interventions to improve type II diabetes self-management for those with schizophrenia or schizoaffective disorder: a systematic review
- Adriana Cimo 1 ,
- Erene Stergiopoulos 1 ,
- Chiachen Cheng 1 , 2 ,
- Sarah Bonato 3 &
- Carolyn S Dewa 1 , 4
BMC Psychiatry volume 12 , Article number: 24 ( 2012 ) Cite this article
16k Accesses
53 Citations
3 Altmetric
Metrics details
The prevalence of type II diabetes among individuals suffering from schizophrenia or schizoaffective disorders is more than double that of the general population. By 2005, North American professional medical associations of Psychiatry, Diabetes, and Endocrinology responded by recommending continuous metabolic monitoring for this population to control complications from obesity and diabetes. However, these recommendations do not identify the types of effective treatment for people with schizophrenia who have type II diabetes. To fill this gap, this systematic evidence review identifies effective lifestyle interventions that enhance quality care in individuals who are suffering from type II diabetes and schizophrenia or other schizoaffective disorders.
A systematic search from Medline, CINAHL, PsycINFO, and ISI Web of Science was conducted. Of the 1810 unique papers that were retrieved, four met the inclusion/exclusion criteria and were analyzed.
The results indicate that diabetes education is effective when it incorporates diet and exercise components, while using a design that addresses challenges such as cognition, motivation, and weight gain that may result from antipsychotics.
Conclusions
This paper begins to point to effective interventions that will improve type II diabetes management for people with schizophrenia or other schizoaffective disorders.
Peer Review reports
In 2005, the World Health Organization (WHO) predicted that the prevalence of type II diabetes will double by 2030, to affect 366 million people globally [ 1 ]. Consequently WHO developed an action plan to increase access to type II diabetes healthcare by 2013 [ 2 ]. The increasing rate of this chronic illness is a concern because when glucose (sugar) cannot be absorbed by vital organs, glucose remains in the bloodstream. This leads to persistently high blood glucose levels, which is used as an indicator in diabetes management. Consistently high blood glucose is linked to complications such as cardiovascular disease, blindness, neuropathy, kidney failure, and poor wound healing resulting in infection that may lead to amputation [ 3 ].
Not everyone is at equal risk for the development of this chronic illness. Individuals suffering from schizophrenia and schizoaffective disorders are at a greater risk of type II diabetes, with prevalence rates reaching more than two times those of the general population [ 4 – 6 ]. While it has been reported that people with schizophrenia may be genetically predisposed to type II diabetes, several other risk factors could contribute to the development of type II diabetes among people with schizophrenia [ 7 ]. Some antipsychotic medications such as olanzapine and clozapine, can cause side effects that promote the onset of type II diabetes [ 8 – 10 ]. These side effects include weight gain, dyslipidemia, hypertension, cardiovascular disease and decreased glucose tolerance [ 4 , 6 , 11 ]. Furthermore, El-Mallakh [ 6 ] observed that poorer health is exacerbated due to high rates of unemployment and reliance on social support, often leaving patients without financial resources to follow dietary guidelines.
Between 2004 and 2005, the debilitating health challenges associated with schizophrenia were recognized by the American Psychiatric Association (APA), American Diabetes Association (ADA), Canadian Diabetes Association (CDA), American Association of Clinical Endocrinologists (AACE), and the North American Association for the Study of Obesity (NAASO) [ 4 , 12 ]. These professional associations recommended continuous metabolic monitoring as a strategy to both prevent and diagnose type II diabetes [ 4 ]. Additionally, the need for interdisciplinary care incorporating psychiatrists, psychiatric nurses, family physicians, and diabetes specialists was recognized in response to the complexity of these combined illnesses [ 12 ]. However, effective treatment was not included for people with schizophrenia who have type II diabetes.
Given the risk of diabetes-related complications, the ADA and the CDA recommend that all individuals with type II diabetes be provided with Diabetes Self-Management Education (DSME) to successfully control their blood sugar [ 13 , 14 ]. Although DSME that incorporates lifestyle interventions are employed for the general population with type II diabetes, such programs are rarely offered to people who experience schizophrenia and who have type II diabetes. This is reflective of the fact that this population receives poorer diabetes care compared to those without severe mental illness [ 15 , 16 ]. Goldberg et al. [ 15 ] found that the frequency of screening and monitoring exams, such as tests for glycated hemoglobin (HbA1c), eye examinations, and identifying serum fat levels, were not meeting the ADA's and CDA's recommendations. Individuals with schizophrenia were also less likely to receive diabetes education. Dickerson et al. [ 17 ] found that 48% of participants with severe mental illness had not received diabetes education within the last 6 months. As a result, this population experiences higher rates of hospitalization for hyper or hypoglycaemic episodes, and for infections [ 18 ].
Taken together, suboptimal diabetes care quality and the absence of effective treatment recommendations for people who have type II diabetes and schizophrenia or schizoaffective disorders is contributing to a life expectancy that is 20% lower than the general population [ 18 , 19 ]. In response to the need for evidence on this topic, this systematic evidence review (SER) will identify effective lifestyle interventions that enhance quality care in individuals who have type II diabetes and schizophrenia or schizoaffective disorders. Thus, the results from this review can be used to improve type II diabetes management, thereby reducing the burden on the healthcare system from the complications associated with chronically high blood glucose.
Literature search
Electronic searches using Medline, PsycINFO, CINAHL, and ISI Web of Science databases were conducted on June 15, 2011. The search strategies, which are presented in Table 1 , were developed in consultation with SB, a librarian scientist. The literature search yielded the identification of 1810 possibly eligible studies. From these, 920 abstracts were retrieved from Medline, 411 from PsycINFO, 88 from CINAHL and 391 from ISI Web of Science.
Eligibility assessment
Each title and abstract was independently screened by AC and ES in accordance with the following inclusion criteria that was developed a priori: i) study participants must have a medical diagnosis of both type II diabetes and schizophrenia or schizoaffective disorder, ii) the intervention must target a lifestyle factor associated with diabetes self-care, such as problem-solving skills, education classes, diet or exercise, iii) the outcome measures that determine the success of the intervention must either consider HbA1c, fasting blood glucose (FBG), body mass index (BMI) or weight lost (measured in pounds or kilograms). Interventions that did not exclusively recruit individuals with schizophrenia or schizoaffective disorder were considered. Studies were excluded if they were in a language other than English, French, Italian or Greek; focused on metabolic syndrome, genetics or screening; or considered risk factors for developing type II diabetes without testing an intervention. Abstracts were also read if a title did not provide sufficient information for exclusion. After considering abstracts for eligibility, full text articles were rated for eligibility. In accordance with an inter-rater reliability of 0.40, disagreements between AC and ES were discussed with a third rater, CSD, and a collective consensus was reached. The eligible articles were subsequently rated for quality, and relevant references were considered.
Quality assessment
A 13-item quality assessment checklist was adapted from Lagerveld et al. [ 20 , 21 ]. Items assessed study design, intervention measurements, outcome measurements, and the presentation of data and analysis. Additional file 1 contains a complete list of items. Each study that met the inclusion/exclusion criteria was independently screened by AC and ES for quality assessment criteria adapted and developed a priori. The inter-rater reliability was 0.62. All disagreements in scoring were discussed and quality rating was reached through consensus between the two independent raters.
Articles that met all quality items were considered excellent. Papers were rated fair and excluded if they had any of the following exclusion criteria: i) does not state the main features of the population which was defined as stating the recruitment location, geographic location, age, gender and eligibility criteria; ii) no account for lifestyle factors during data collection and analysis; iii) follow-up measurements do not include HbA1c, BMI, weight loss, and/or FBG. Therefore, a study was considered good if it did not meet the criteria to be considered fair, but lost other quality points, such as not discussing initial participation rates, and not using appropriate statistical methods or calculating statistical significance.
Determining relevant literature
The systematic search of four databases (Medline, PsycINFO, CINAHL, and Web of Science) yielded a total of 1810 unique studies. Raters AC and ES independently screened titles and eliminated those that met the exclusion criteria. A total of 304 abstracts were reviewed in accordance with the inclusion/exclusion criteria. Of these, 49 full-text articles were retrieved. Four articles met the final inclusion criteria. This process of inclusions and exclusions is depicted in Figure 1 .
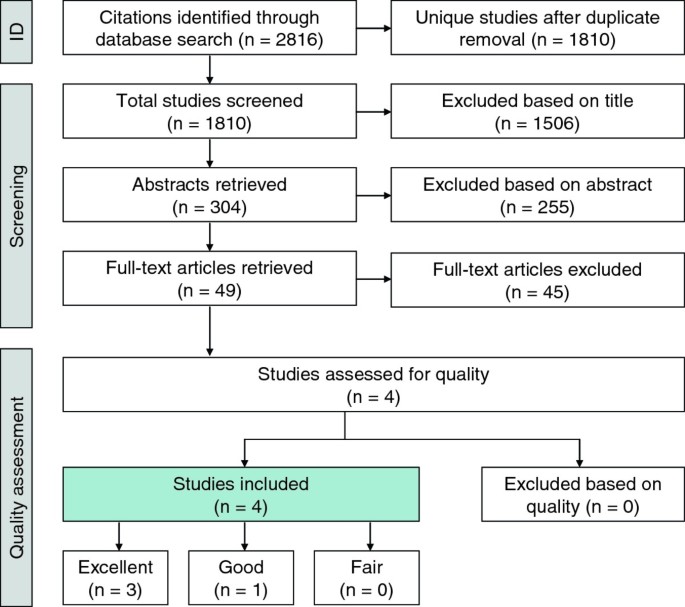
Flowchart of literature search results and inclusions/exclusions .
The following is a list of reasons for excluding the 45 full text articles: i) A total of 2.2% (n = 1) was a textbook chapter that elaborated on a study already included; ii) Another 2.2% (n = 1) proposed an intervention that would hypothetically be effective without testing its effectiveness; iii) 4.4% of articles (n = 2) were interventions where outcome measurements did not include blood glucose or weight assessment; iv) A total of 15.6% (n = 7) did not include both type II diabetes and schizophrenia in the study population; v) Another 22.2% of the articles (n = 10) focused on increasing glycaemic control through changing medication, without addressing lifestyle factors; vi) The remaining 53.3% of papers (n = 24) did not assess the effectiveness of an intervention.
Methodological quality
The four articles that met all inclusion criteria were assessed using the methodological quality assessment checklist that categorized articles as being excellent, good or fair. Of these, three were assessed to be excellent, and the remaining study was rated good. Thus, no articles were excluded at this step, because all met quality criteria good or better.
Characteristics of included studies
The significant characteristics of each paper are presented in Table 2 . Major findings of each intervention analyzed are presented in Table 3 . The included articles also shared common elements: each study recruited participants from different US states; they all considered the older-adult population, as indicated by the mean participant age ranging between 44-53 years; interventions each included exercise promotion and nutrition education; they also incorporated components that addressed the challenges associated with this particular population, such as decreased cognitive ability and reduced motivation [ 22 , 23 ]. For example, inpatient modules in Lindenmayer's et al. [ 24 ] study were taught for four months before initiating a new level. Some of McKibbin et al.'s [ 23 ] strategies involved gradually introducing new topics, utilizing memory aids, and providing minimal text so as to simplify messages. One important difference to note is the variation in study locations: two programs recruited from a psychiatric hospital inpatient setting [ 24 , 25 ]. The remaining two articles addressed health needs of individuals in out-patient mental health settings, such as board-and-care accommodations and community clubhouses [ 23 , 26 ].
Results of in-patient interventions
Both in-patient programs provided information regarding the importance of exercise, and provided strategies for making this lifestyle change [ 24 , 25 ]. After enhancing patient motivation through classes, achieving physical activity recommendations in both studies were promoted by providing exercise facilities. Lindenmayer et al.'s [ 24 ] knowledge assessment of the four month fitness and exercise module demonstrated an improvement in scores, as they increased from 56.6% to 67.6% ( P < 0.001). Participants in Teachout et al.'s [ 25 ] intervention were given additional resources: pedometers, encouragement to walk, and yoga classes. Fitness knowledge was not assessed following the intervention.
In both studies, nutrition lessons were aimed at improving dietary habits. In Lindenmayer et al.'s [ 24 ] program, workshops provided dietary tips and a weekly 25 dollars was given to enable the purchase of healthy foods. This strategy was successful as the knowledge assessment scale for the four month section on nutrition and healthy lifestyle increased from 57% to 69.4% ( P < 0.001). Teachout et al.'s [ 25 ] method involved modules on healthy meal planning, shopping and food preparation over a period of six months. However, participant knowledge gained from this approach was not measured.
Overall, the psychiatric in-patient interventions had a positive impact on weight, BMI and blood glucose measurements, thus indicating the effectiveness of combining diet and exercise. After 12 months, participants with type II diabetes and severe mental illness in Lindenmayer et al.'s [ 24 ] trial lost a mean total of 5.98 lb. BMI was also reduced from 33.94 kg/m2 to 30.55 kg/m2 (statistical significance was not calculated for BMI or weight loss). Furthermore, blood glucose also decreased significantly, from an average of 115.85 mg/DL to 98.05 mg/DL ( P < 0.001). This reduction was significantly related to the nutrition module that was completed during the beginning of the intervention. Similarly, all of Teachout et al.'s [ 25 ] participants reduced their weight, with an average loss of 20.35 lb, and 40% of fasting glucose levels met the recommended value as outlined by the ADA (statistical significance was not calculated).
Results of out-patient interventions
In McKibbin et al.'s [ 23 ] six month Diabetes Awareness and Rehabilitation Training (DART), participants received 90-min weekly sessions providing diet, exercise and other diabetes self-care strategies such as monitoring blood glucose levels. Physical activity modules involved learning about the different types of exercise, how being active can impact blood glucose, and how to keep track of daily exercise. Participants were also given pedometers, encouraged to walk, and tracked weekly weight changes to increase motivation.
Participants additionally received simplified nutrition education that provided knowledge of the different food groups, adequate portion sizes, healthy meal planning and label reading, as well as substituting sugar consumption with fat and fibre.
Comparing the outcome measurements of the DART program with a Usual Care (UC) group that received pamphlets from the ADA and continued seeing their family physician indicated the effectiveness of the DART intervention. While the control group gained a total of 6.8 lbs during the study period, intervention participants lost an average of 5.1 lbs ( P < 0.001). Correspondingly, DART participants' BMI was reduced on average from 33.6 kg/m2 to 32.9 kg/m2, whereas the UC increased from 32.9 kg/m2 to 33.9 kg/m2 ( P < 0.001). Study participants also enhanced their diabetes knowledge from 0.5 to 0.7, while there was no change in the scores for the control group ( P < 0.001). Although there was a reduction in fasting blood glucose and HbA1c in both the experimental and control group, findings were not statistically significant.
The effectiveness of this intervention was measured six months after the end of the study [ 26 ]. The DART group maintained their average BMI of 32.9 kg/m2, while the control group continued to gain weight, totaling an average of 34 kg/m2. Although diabetes knowledge dropped at 12 months from 0.7 to 0.6, it was still higher than the baseline value of 0.5. Therefore, the follow-up study revealed that sustainable skills were gained from the DART intervention.
The current literature assessing the management of type II diabetes for individuals with schizophrenia and schizoaffective disorders has indicated that there are a number of tactics used to manage blood glucose levels. One that has drawn attention involves changing the antipsychotics prescribed. Antipsychotics have been the focus because of the weight gain and glucose intolerance that is associated with use of these medications [ 4 , 5 , 11 ]. A meta-analysis conducted by Barnett et al. [ 10 ] reported that patients treated with clozapine and olanzapine have higher rates of weight gain and therefore increased diagnosis of type II diabetes compared to other antipsychotics. Consistent with these findings are case studies that changed antipsychotic medications as an intervention to manage blood glucose in type II diabetes. Lerner et al. [ 27 ] lowered the dose of olanzapine for two patients and noted a reduction in blood glucose levels. Furthermore, a total of four case studies observed a remission of type II diabetes upon the replacement of olanzapine with risperidone, as HbA1c levels normalized [ 28 – 31 ]. Given the impact of antipsychotic medications in the development of this disease, recommendations are often made to change prescriptions if persistent weight gain and onset of type II diabetes occurs [ 10 , 12 , 32 ]. However, this treatment approach poses challenges because individuals with schizophrenia may experience a relapse of psychotic or depressive symptoms during the transition period between medications [ 33 , 34 ]. Moreover, not every individual has a therapeutic response to all antipsychotics [ 35 ].
Considering the challenges with changing antipsychotic medication, our SER aimed at determining effective delivery of diet and lifestyle interventions to enable management of type II diabetes in individuals with schizophrenia or schizoaffective disorders. The success of diet and lifestyle interventions to prevent or manage type II diabetes in individuals with and without schizophrenia or schizoaffective disorders has been documented in the literature. Menza et al. [ 36 ] conducted a 12-month lifestyle intervention that combined diet and physical activity in patients with schizophrenia and schizoaffective disorders. Findings included reduced weight and BMI, increased nutritional knowledge, and improved HbA1c levels, thus minimizing risk of type II diabetes development. Torgerson et al. [ 37 ] was successful in preventing the onset of type II diabetes in obese individuals by combining weight loss with the inhibition of an enzyme that breaks down fats. Additionally, Lim et al.'s [ 38 ] paper suggests that weight loss enabled by restricting calories to 600 kcal/day is an effective method to decrease BMI within the general type II diabetes population ( P < 0.05). Calorie restriction also corresponded to greater blood glucose control, as glycated hemoglobin decreased to normal levels in 8 weeks ( P < 0.05).
While the relationship between lifestyle interventions with weight loss and improved glycated hemoglobin is well documented, the most effective way of delivering DSME is not always clear for individuals with schizophrenia or schizoaffective disorders. Therefore, our paper makes an important contribution to the literature by highlighting effective DSME strategies to support the integration of healthy habits into lifestyle. Each DSME lifestyle intervention reviewed in our paper observed reduced weight and BMI in the presence of intervention strategies that addressed the challenges associated with schizophrenia, such as decreased cognitive ability, reduced motivation and limited access to resources [ 6 , 22 , 23 ]. Additionally, Lindenmayer et al. [ 24 ] and Teachout et al. [ 25 ] observed that diet can reduce fasting blood glucose.
One drawback consistent in all interventions was the absence of finding statistical significance when HbA1c levels were reduced. One likely explanation is the fact that interventions were not long enough to observe changes in HbA1c levels [ 23 , 39 ]. This is because retrieving an accurate measure may require blood glucose to be controlled for more than three months. If lifestyle changes were not fully adopted, it would be more difficult to see a reduction in HbA1c, even if some changes occurred. In contrast, blood glucose measures depict blood glucose at one point in time and this value can fluctuate hourly. Thus, HbA1c is considered a more reliable measure of overall blood glucose control. Additionally, HbA1c has been correlated with diabetes complications, while blood glucose has not [ 39 ].
Because all quality ratings of the analyzed studies resulted in excellent and good assessments, there is a strong level of evidence to support our conclusion made in this SER [ 40 ]. However, while the findings of this paper indicate that lifestyle interventions positively impact type II diabetes management, there were limitations associated with the heterogeneity of the study settings included in the analysis. In the psychiatric inpatient setting, participation in the interventions was structured in the individual's daily routine. Conversely, in McKibbin et al.'s [ 23 ] study, recruitment from community clubhouses and board-and-care facilities indicates that participant involvement required a greater level of self-motivation. Therefore, care needs to be taken if inpatient interventions are adapted in outpatient settings, because individuals within the community may have limited access to fitness resources, such as gym equipment and safe areas to exercise.
As a result of limiting searches to four databases containing primarily peer-reviewed material, a potential publication bias is an additional limitation of this SER. However, the databases searched covered an extensive scope of clinical disciplines that were relevant for the nature of the research question: PsycINFO captures psychological literature, CINAHL retrieves the nursing and allied health, Medline contains medical literature, while ISI Web of Science is multidisciplinary. Additionally, while grey literature was not searched for directly, PsycINFO includes doctoral theses available in Dissertations Abstracts International. Additionally, due to a lack of fluency in languages other than English, French, Italian and Greek, papers in other languages were not considered.
While the analyzed studies indicate the short-term effectiveness of lifestyle interventions in individuals with type II diabetes and schizophrenia, the long-term sustainability of treatment outcomes has not been explored. Additionally, it has been observed that such lifestyle interventions are effective for older adults with type II diabetes and schizophrenia. However, the success of such approaches within the first episode population is unknown. Although adults over 40 years of age are an important population to consider due to the increased risk factors of diabetes from long-term use of antipsychotics and being over the age of 45, the onset of type II diabetes in individuals aged 20 to 49 years is increasing [ 12 , 41 , 42 ]. Therefore, an additional recommendation for future research involves determining the effectiveness of such programs for youth and young adults experiencing early-onset psychosis who also have type II diabetes.
Overall, the current state of the literature suggests promise within this line of inquiry. However, our review also indicates that there are gaps in the current literature. Of additional significance is the need for interdisciplinary teams when addressing the complex health concerns associated with both schizophrenia and type II diabetes [ 12 ].
Findings of this SER suggest that lifestyle interventions can be effective in managing type II diabetes in patients that concurrently have schizophrenia or schizoaffective disorders. However, they should be sensitive to the unique challenges associated with type II diabetes and schizophrenia. These challenges include decreased cognition and motivation, limited resources, as well as negative side effects (i.e. loss of energy and weight gain) that may result from antipsychotics. Successful strategies involved positive encouragement to make changes, gradual introduction of new concepts and skills relating to diet and exercise, conveying simple messages for complex topics such as food skills relating to cooking and planning meals, and incorporating memory aids [ 23 , 24 ].
The findings of this review indicate a strong level of evidence; there are effective interventions for people with schizophrenia and type II diabetes. However, there is a need for continued research to fill gaps. These include exploration of the long-term sustainability of DSME lifestyle interventions, and addressing the young adult population suffering from schizophrenia or schizoaffective disorders with type II diabetes. Furthermore, the need for interdisciplinary interventions should be kept in mind, as the collective expertise of psychiatrists, psychiatric nurses, family physicians and diabetes educators such as dietitians are all needed. Taking these factors into account will enable policies and interventions to be developed that improve the healthcare and quality of life of individuals with type II diabetes and schizophrenia or schizoaffective disorders.
World Health Organization: Diabetes Fact sheet N°312. [ http://www.who.int/mediacentre/factsheets/fs312/en/ ]
World Health Organization: 2008-2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases. [ http://www.who.int/nmh/Actionplan-PC-NCD-2008.pdf ]
Nelms M, Sucher KP, Lacey K, Long Roth S: Nutrition Therapy and Pathophysiology. 2010, Belmont, CA: Wadsworth Cengage Learning, 2
Google Scholar
American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity: Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. 2004, 27: 596-601.
Article Google Scholar
Heald A: Physical health in schizophrenia: a challenge for antipsychotic therapy. Eur Psychiatry. 2010, 25: S6-S11.
Article PubMed Google Scholar
El-Mallakh P: Doing my best: Poverty and self-care among individuals with schizophrenia and diabetes mellitus. Arch Psychiatr Nurs. 2007, 21: 49-60. 10.1016/j.apnu.2006.10.004.
Gough SCL, O'Donovan MC: Clustering of metabolic comorbidity in schizophrenia: a genetic contribution?. J Psychopharmacol. 2005, 19: 47-55. 10.1177/0269881105058380.
Krosnick A, Wilson MG: A retrospective chart review of the clinical effects of atypical antipsychotic drugs on glycemic control in institutionalized patients with schizophrenia and comorbid diabetes mellitus. Clin Ther. 2005, 27: 320-326. 10.1016/j.clinthera.2005.02.017.
Article CAS PubMed Google Scholar
Melkersson K, Dahl ML: Adverse metabolic effects associated with atypical antipsychotics - Literature review and clinical implications. Drugs. 2004, 64: 701-723. 10.2165/00003495-200464070-00003.
Barnett AH, Mackin P, Chaudhry I, Farooqi A, Gadsby R, Heald A, Hill J, Millar H, Peveler R, Rees A, et al: Minimising metabolic and cardiovascular risk in schizophrenia: diabetes, obesity and dyslipidaemia. J Psychopharmacol. 2007, 21: 357-373.
Cohn TA, Sernyak MJ: Metabolic monitoring for patients treated with antipsychotic medications. Can J Psychiatry-Revue Canadienne De Psychiatrie. 2006, 51: 492-501.
Woo V, Harris SB, Houlden RL: Canadian Diabetes Association Position Paper: Antipsychotic Medications and Associated Risks of Weight Gain and Diabetes. Can J Diabetes. 2005, 29: 111-112.
Canadian Diabetes Association: Clinical practice guidelines for the prevention and management of diabetes in Canada. Canadian Journal of Diabetes. 2008, 32 (Supplement 1): S1-S201.
American Diabetes Association: Standards of medical care in diabetes - 2012. Diabetes Care. 2012, 35 (Sup): S11-S63.
Goldberg RW, Kreyenbuhl JA, Medoff DR, Dickerson FB, Wohlheiter K, Fang J, Brown CH, Dixon LB: Quality of diabetes care among adults with serious mental illness. Psychiatr Serv. 2007, 58: 536-543. 10.1176/appi.ps.58.4.536.
Frayne SM, Halanych JH, Miller DR, Wang F, Lin H, Pogach L, Sharkansky EJ, Keane TM, Skinner KM, Rosen CS, Berlowitz DR: Disparities in Diabetes Care. Arch Intern Med. 2005, 165: 2631-2638. 10.1001/archinte.165.22.2631.
Dickerson FB, Goldberg RW, Brown CH, Kreyenbuhl JA, Wohlheiter K, Fang L, Medoff D, Dixon LB: Diabetes knowledge among persons with serious mental illness and type 2 diabetes. Psychosomatics. 2005, 46: 418-424. 10.1176/appi.psy.46.5.418.
Becker T, Hux J: Risk of acute complications of diabetes among people with schizophrenia in Ontario, Canada. Diabetes Care. 2011, 34: 398-402. 10.2337/dc10-1139.
Article PubMed PubMed Central Google Scholar
Newman SC, Bland RC: Mortality in a cohort of patients with schizophrenia: a record linkage study. Can j psychiatry Revue canadienne de psychiatrie. 1991, 36: 239-245.
CAS PubMed Google Scholar
Lagerveld SE, Bultmann U, Franche RL, van Dijk FJ, Vlasveld MC, van der Feltz-Cornelis CM, Bruinvels DJ, Huijs JJ, Blonk RW, van der Klink JJ, Nieuwenhuijsen K: Factors associated with work participation and work functioning in depressed workers: a systematic review. J Occup Rehabil. 2010, 20: 275-292. 10.1007/s10926-009-9224-x.
Article CAS PubMed PubMed Central Google Scholar
Mallen C, Peat G, Croft P: Quality assessment of observational studies is not commonplace in systematic reviews. J Clin Epidemiol. 2006, 59: 765-769. 10.1016/j.jclinepi.2005.12.010.
Dickinson D, Gold JM, Dickerson FB, Medoff D, Dixon LB: Evidence of exacerbated cognitive deficits in schizophrenia patients with comorbid diabetes. Psychosomatics. 2008, 49: 123-131. 10.1176/appi.psy.49.2.123.
McKibbin CL, Patterson TL, Norman G, Patrick K, Jin H, Roesch S, Mudaliar S, Barrio C, O'Hanlon K, Griver K, et al: A lifestyle intervention for older schizophrenia patients with diabetes mellitus: A randomized controlled trial. Schizophr Res. 2006, 86: 36-44. 10.1016/j.schres.2006.05.010.
Lindenmayer JP, Khan A, Wance D, Maccabee N, Kaushik S: Outcome Evaluation of a Structured Educational Wellness Program in Patients With Severe Mental Illness. J Clin Psychiatry. 2009, 70: 1385-1396. 10.4088/JCP.08m04740yel.
Teachout A, Kaiser SM, Wilkniss SM, Moore H: Paxton House: Integrating Mental Health and Diabetes Care for People with Serious Mental Illnesses in a Residential Setting. Psychiatric Rehabil J. 2011, 34: 324-327. 10.2975/34.4.2011.324.327.
McKibbin CL, Golshan S, Griver K, Kitchen K, Wykes TL: A healthy lifestyle intervention for middle-aged and older schizophrenia patients with diabetes mellitus: A 6-month follow-up analysis. Schizophr Res. 2010, 121: 203-206. 10.1016/j.schres.2009.09.039.
Lerner V, Libov I, Kanevsky M: High-dose olanzapine-induced improvement of preexisting type 2 diabetes mellitus in schizophrenic patients. Int J Psychiatry Med. 2003, 33: 403-410. 10.2190/8J17-J4PB-F2KX-05YY.
Wu P-L, Lane H-Y, Su K-P: Risperidone alternative for a schizophrenic patient with olanzapine-exacerbated diabetic mellitus. Psychiatry Clin Neurosci. 2006, 60: 115-116. 10.1111/j.1440-1819.2006.01469.x.
Melkersson K, Hulting A-L: Recovery from new-onset diabetes in a schizophrenic man after withdrawal of olanzapine. Psychosomatics: J Consult Liaison Psychiatry. 2002, 43: 67-70. 10.1176/appi.psy.43.1.67.
Waldman JC, Yaren S: Atypical antipsychotics and glycemia: a case report. The Can J Psychiatry/La Revue canadienne de psychiatrie. 2002, 47: 686-687.
Ashim S, Warrington S, Anderson IM: Management of diabetes mellitus occurring during treatment with olanzapine: report of six cases and clinical implications. J Psychopharmacol. 2004, 18: 128-132. 10.1177/0269881104040253.
Gothefors D, Adolfsson R, Attvall S, Erlinge D, Jarbin H, Lindstrom K, von Hausswolff-Juhlin YL, Morgell R, Toft E, Osby U: Swedish clinical guidelines-Prevention and management of metabolic risk in patients with severe psychiatric disorders. Nordic J Psychiatry. 2010, 64: 294-302. 10.3109/08039488.2010.500397.
Ganguli R, Brar JS, Mahmoud R, Berry SA, Pandina GJ: Assessment of strategies for switching patients from olanzapine to risperidone: a randomized, open-label, rater-blinded study. Bmc Med. 2008, 6: 17-10.1186/1741-7015-6-17.
Weiden PJ: Switching in the era of atypical antipsychotics. An updated review. Postgrad Med. 2006, Spec No: 27-44.
PubMed Google Scholar
Kane JM, Marder SR: Psychopharmacologic treatment of schizophrenia. Schizophr Bull. 1993, 19: 287-302.
Menza M, Vreeland B, Minsky S, Gara M, Radler DR, Sakowitz M: Managing Atypical antipsychotic-associated weight gain: 12-month data on a multimodal weight control program. J Clin Psychiatry. 2004, 65: 471-477.
Torgerson JS, Hauptman J, Boldrin MN, Sjostrom L: XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004, 27: 155-161. 10.2337/diacare.27.1.155.
Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R: Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. 2011,
Landgraf R: HbA1c-the gold standard in the assessment of diabetes treatment?. Dtsch Med Wochenschr. 2006, 131 (Suppl 8): S243-246.
Ariens GA, van Mechelen W, Bongers PM, Bouter LM, van der Wal G: Physical risk factors for neck pain. Scand J Work Environ Health. 2000, 26: 7-19. 10.5271/sjweh.504.
American Diabetes Association: Diabetes Statistics. [ http://www.diabetes.org/diabetes-%20basics/diabetes-statistics/ ]
Lipscombe LL, Hux JE: Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995-2005: a population-based study. Lancet. 2007, 369: 750-756. 10.1016/S0140-6736(07)60361-4.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-244X/12/24/prepub
Download references
Acknowledgements
Dr. Dewa and the practicum students, AC and ES, gratefully acknowledge the support of Dr. Dewa's CIHR/PHAC Applied Public Health Chair. The Centre for Addiction and Mental Health receives funding from the Ontario Ministry of Health and Long-Term Care to support research infrastructure.
Author information
Authors and affiliations.
Centre for Research on Employment and Workplace Health, Centre for Addition and Mental Health, 455 Spadina, Suite 300, Toronto, Ontario, M5S 2G8, Canada
Adriana Cimo, Erene Stergiopoulos, Chiachen Cheng & Carolyn S Dewa
Canadian Mental Health Association, Clinic & Resource Centre, 272 Park Avenue, Thunder Bay, P7B 1C5, Canada
Chiachen Cheng
Library Services, Centre for Addiction and Mental Health, 33 Russell Street, Toronto, M5S 2S1, Canada
Sarah Bonato
Department of Psychiatry, University of Toronto, 250 College Street, Toronto, M5T 1R8, Canada
Carolyn S Dewa
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Carolyn S Dewa .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
AC led the conception, design, data acquisition, analysis and interpretation of the data. ES collaborated on the design, data acquisition and analysis. CC collaborated on the design and acquisition of data. SB collaborated on the design and data acquisition. CSD collaborated on the conception, design and acquisition of data, and supervised the data analysis and interpretation. All authors read and approved the final manuscript.
Electronic supplementary material
12888_2011_966_moesm1_esm.doc.
Additional file 1: Quality assessment checklist; The additional file contains the quality checklist criterion that was used to determine the quality of the papers being analyzed for the systematic review . Scores of each article are displayed as well as the quality checklist items that were adapted from Lagerveld et al. [ 20 ]. (DOC 35 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Cimo, A., Stergiopoulos, E., Cheng, C. et al. Effective lifestyle interventions to improve type II diabetes self-management for those with schizophrenia or schizoaffective disorder: a systematic review. BMC Psychiatry 12 , 24 (2012). https://doi.org/10.1186/1471-244X-12-24
Download citation
Received : 12 August 2011
Accepted : 23 March 2012
Published : 23 March 2012
DOI : https://doi.org/10.1186/1471-244X-12-24
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Schizophrenia
- Lifestyle Intervention
- Severe Mental Illness
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
The Strong Link Between Schizophrenia and Diabetes

That there is a strong link between schizophrenia and diabetes is not a new discovery. The relationship between diabetes and schizophrenia has been known for more than 100 years. While after a century much about the connection is still not well understood, medical and mental health professionals are building knowledge about the connection and using it to develop better prevention and treatment for people who live with both schizophrenia and diabetes.
The number of people with both illnesses is significant. People with schizophrenia are three times more likely than the general population to develop type 2 diabetes (Toich, 2017). Further, 20-30 percent of people with schizophrenia will develop diabetes type 2 (Cohn, 2012). These numbers are too high to dismiss as coincidence. What is it that influences the connection between these drastically different medical and psychiatric conditions? Here’s a look at what researchers are discovering.
Schizophrenia, Antipsychotic Medication, and Diabetes
One culprit for the development of diabetes in people with schizophrenia is antipsychotic medication . Antipsychotics are an essential component of schizophrenia treatment. They’re necessary to reduce the hallucinations, delusions, and many other symptoms of schizophrenia. Antipsychotics, however, have dangerous side effects, including weight gain (" Are There Any Safe Antipsychotics in Diabetes Treatment? ").
Weight gain from antipsychotic medications is often significant. Antipsychotic medications can cause obesity, high cholesterol, and an increase in triglycerides, or fats found in the blood. These conditions can cause type 2 diabetes.
Many different types of antipsychotics and atypical antipsychotics are available. Ideally, people with schizophrenia take medications that cause the least amount of weight gain, such as aripiprazole (Abilify) or ziprasidone (Geodon); however, this isn’t always the case. Multiple classic and atypical antipsychotics are available and widely used to treat schizophrenia. Chlorpromazine (Thorazine), clozapine (Clozaril), and olanzapine (Zyprexa) are among those that cause the biggest amount of weight gain.
Attributing diabetes to weight gain from medication has proven to be too simplistic. Sometimes, diabetes develops very rapidly after someone is newly diagnosed with schizophrenia. Researchers have found that some people who experience their first episode of psychosis already have indications of type 2 diabetes:
- Decreased glucose tolerance
- High fasting plasma glucose levels
- High fasting plasma insulin levels
- Increased insulin resistance
This happens either before or shortly after medication treatment begins, before weight gain and other side-effects have begun; therefore, the link between schizophrenia and diabetes isn’t merely from medication. There is something about schizophrenia itself that contributes to the development of diabetes.
Factors Contributing to the Schizophrenia and Diabetes Link
Without a doubt, medication-induced weight gain is part of the reason these two serious conditions co-occur. It’s just not the only factor. Knowing what else contributes to the development of diabetes in people with schizophrenia can lead to better treatment and management strategies.
These factors solidify the link between diabetes and schizophrenia:
- Genetics . There is a genetic component not yet fully understood that makes some people more prone than others to develop these illnesses.
- Developmental risk factors . Premature birth, low birth weight, and other pregnancy and delivery complications can contribute to both schizophrenia and diabetes.
- Lifestyle . Often, schizophrenia is associated with cigarette smoking, poor diet, and lack of exercise, all things that are detrimental to health.
- Social health problems . Low income, poor housing circumstances, and difficulty meeting basic needs are risk factors for serious health problems like the combination of diabetes and schizophrenia.
Living with both schizophrenia and diabetes presents numerous challenges (" Schizophrenia Makes Diabetes Management Challenging "). Understanding the unbreakable link can help lead to a treatment approach that incorporates the management of both illnesses together. This can improve the quality of life for people with combined type 2 diabetes and schizophrenia.
article references
APA Reference Peterson, T. (2022, January 4). The Strong Link Between Schizophrenia and Diabetes, HealthyPlace. Retrieved on 2024, May 30 from https://www.healthyplace.com/diabetes/mental-health/the-strong-link-between-schizophrenia-and-diabetes
Medically reviewed by Harry Croft, MD
Related Articles

Complete List of Diabetes Medications for Type 1 and Type 2
Starlix for treatment of diabetes - starlix full prescribing information, four ways to prevent diabetes when you live with a mental illness, glucagen for diabetics - glucagen full prescribing information, diabetes and the mental health connection sitemap, precose for treatment of diabetes - precose full prescribing information, challenges of treating diabetes when you have adhd.
2024 HealthyPlace Inc. All Rights Reserved. Site last updated May 30, 2024
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 February 2022
Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics
- Christoph U. Correll ORCID: orcid.org/0000-0002-7254-5646 1 , 2 , 3 ,
- Amber Martin 4 ,
- Charmi Patel 5 ,
- Carmela Benson 5 ,
- Rebecca Goulding 6 ,
- Jennifer Kern-Sliwa 5 ,
- Kruti Joshi 5 ,
- Emma Schiller 4 &
- Edward Kim ORCID: orcid.org/0000-0001-8247-6675 7
Schizophrenia volume 8 , Article number: 5 ( 2022 ) Cite this article
15k Accesses
51 Citations
14 Altmetric
Metrics details
- Schizophrenia
Clinical practice guidelines (CPGs) translate evidence into recommendations to improve patient care and outcomes. To provide an overview of schizophrenia CPGs, we conducted a systematic literature review of English-language CPGs and synthesized current recommendations for the acute and maintenance management with antipsychotics. Searches for schizophrenia CPGs were conducted in MEDLINE/Embase from 1/1/2004–12/19/2019 and in guideline websites until 06/01/2020. Of 19 CPGs, 17 (89.5%) commented on first-episode schizophrenia (FES), with all recommending antipsychotic monotherapy, but without agreement on preferred antipsychotic. Of 18 CPGs commenting on maintenance therapy, 10 (55.6%) made no recommendations on the appropriate maximum duration of maintenance therapy, noting instead individualization of care. Eighteen (94.7%) CPGs commented on long-acting injectable antipsychotics (LAIs), mainly in cases of nonadherence (77.8%), maintenance care (72.2%), or patient preference (66.7%), with 5 (27.8%) CPGs recommending LAIs for FES. For treatment-resistant schizophrenia, 15/15 CPGs recommended clozapine. Only 7/19 (38.8%) CPGs included a treatment algorithm.
Similar content being viewed by others

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers

Long COVID: major findings, mechanisms and recommendations

Psilocybin microdosers demonstrate greater observed improvements in mood and mental health at one month relative to non-microdosing controls
Introduction.
Schizophrenia is an often debilitating, chronic, and relapsing mental disorder with complex symptomology that manifests as a combination of positive, negative, and/or cognitive features 1 , 2 , 3 . Standard management of schizophrenia includes the use of antipsychotic medications to help control acute psychotic episodes 4 and prevent relapses 5 , 6 , whereas maintenance therapy is used in the long term after patients have been stabilized 7 , 8 , 9 . Two main classes of drugs—first- and second-generation antipsychotics (FGA and SGA)—are used to treat schizophrenia 10 . SGAs are favored due to the lower rates of adverse effects, such as extrapyramidal effects, tardive dyskinesia, and relapse 11 . However, pharmacologic treatment for schizophrenia is complicated because nonadherence is prevalent, and is a major risk factor for relapse 9 and poor overall outcomes 12 . The use of long-acting injectable (LAI) versions of antipsychotics aims to limit nonadherence-related relapses and poor outcomes 13 .
Patient treatment pathways and treatment choices are determined based on illness acuity/severity, past treatment response and tolerability, as well as balancing medication efficacy and adverse effect profiles in the context of patient preferences and adherence patterns 14 , 15 . Clinical practice guidelines (CPG) serve to inform clinicians with recommendations that reflect current evidence from meta-analyses of randomized controlled trials (RCTs), individual RCTs and, less so, epidemiologic studies, as well as clinical experience, with the goal of providing a framework and road-map for treatment decisions that will improve quality of care and achieve better patients outcomes. The use of clinical algorithms or other decision trees in CPGs may improve the ease of implementation of the evidence in clinical practice 16 . While CPGs are an important tool for mental health professionals, they have not been updated on a regular basis like they have been in other areas of medicine, such as in oncology. In the absence of current information, other governing bodies, healthcare systems, and hospitals have developed their own CPGs regarding the treatment of schizophrenia, and many of these have been recently updated 17 , 18 , 19 . As such, it is important to assess the latest guidelines to be aware of the changes resulting from consideration of updated evidence that informed the treatment recommendations. Since CPGs are comprehensive and include the diagnosis as well as the pharmacological and non-pharmacological management of individuals with schizophrenia, a detailed comparative review of all aspects of CPGs for schizophrenia would have been too broad a review topic. Further, despite ongoing efforts to broaden the pharmacologic tools for the treatment of schizophrenia 20 , antipsychotics remain the cornerstone of schizophrenia management 8 , 21 . Therefore, a focused review of guideline recommendations for the management of schizophrenia with antipsychotics would serve to provide clinicians with relevant information for treatment decisions.
To provide an updated overview of United States (US) national and English language international guidelines for the management of schizophrenia, we conducted a systematic literature review (SLR) to identify CPGs and synthesize current recommendations for pharmacological management with antipsychotics in the acute and maintenance phases of schizophrenia.
Systematic searches for the SLR yielded 1253 hits from the electronic literature databases. After removal of duplicate references, 1127 individual articles were screened at the title and abstract level. Of these, 58 publications were deemed eligible for screening at the full-text level, from which 19 were ultimately included in the SLR. Website searches of relevant organizations yielded 10 additional records, and an additional three records were identified by the state-by-state searches. Altogether, this process resulted in 32 records identified for inclusion in the SLR. Of the 32 sources, 19 primary CPGs, published/issued between 2004 and 2020, were selected for extraction, as illustrated in the PRISMA diagram (Fig. 1 ). While the most recent APA guideline was identified and available for download in 2020, the reference to cite in the document indicates a publication date of 2021.
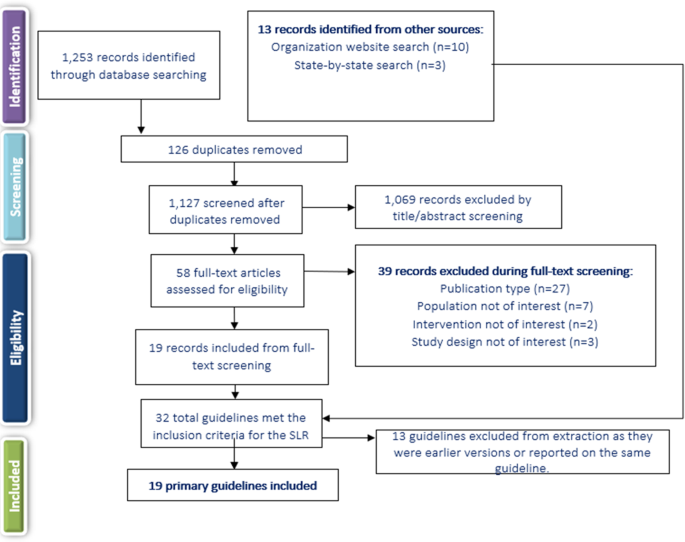
SLR systematic literature review.
Of the 19 included CPGs (Table 1 ), three had an international focus (from the following organizations: International College of Neuropsychopharmacology [CINP] 22 , United Nations High Commissioner for Refugees [UNHCR] 23 , and World Federation of Societies of Biological Psychiatry [WFSBP] 24 , 25 , 26 ); seven originated from the US; 17 , 18 , 19 , 27 , 28 , 29 , 30 , 31 , 32 three were from the United Kingdom (British Association for Psychopharmacology [BAP] 33 , the National Institute for Health and Care Excellence [NICE] 34 , and the Scottish Intercollegiate Guidelines Network [SIGN] 35 ); and one guideline each was from Singapore 36 , the Polish Psychiatric Association (PPA) 37 , 38 , the Canadian Psychiatric Association (CPA) 14 , the Royal Australia/New Zealand College of Psychiatrists (RANZCP) 39 , the Association Française de Psychiatrie Biologique et de Neuropsychopharmacologie (AFPBN) from France 40 , and Italy 41 . Fourteen CPGs (74%) recommended treatment with specific antipsychotics and 18 (95%) included recommendations for the use of LAIs, while just seven included a treatment algorithm Table 2 ). The AGREE II assessment resulted in the highest score across the CPGs domains for NICE 34 followed by the American Psychiatric Association (APA) guidelines 17 . The CPA 14 , BAP 33 , and SIGN 35 CPGs also scored well across domains.
Acute therapy
Seventeen CPGs (89.5%) provided treatment recommendations for patients experiencing a first schizophrenia episode 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 40 , 41 , but the depth and focus of the information varied greatly (Supplementary Table 1 ). In some CPGs, information on treatment of a first schizophrenia episode was limited or grouped with information on treating any acute episode, such as in the CPGs from CINP 22 , AFPBN 40 , New Jersey Division of Mental Health Services (NJDMHS) 32 , the APA 17 , and the PPA 37 , 38 , while the others provided more detailed information specific to patients experiencing a first schizophrenia episode 14 , 18 , 19 , 23 , 24 , 28 , 33 , 34 , 35 , 36 , 39 , 41 . The American Association of Community Psychiatrists (AACP) Clinical Tips did not provide any information on the treatment of schizophrenia patients with a first episode 29 .
There was little agreement among CPGs regarding the preferred antipsychotic for a first schizophrenia episode. However, there was strong consensus on antipsychotic monotherapy and that lower doses are generally recommended due to better treatment response and greater adverse effect sensitivity. Some guidelines recommended SGAs over FGAs when treating a first-episode schizophrenia patient (RANZCP 39 , Texas Medication Algorithm Project [TMAP] 28 , Oregon Health Authority 19 ), one recommended starting patients on an FGA (UNHCR 23 ), and others stated specifically that there was no evidence of any difference in efficacy between FGAs and SGAs (WFSBP 24 , CPA 14 , SIGN 35 , APA 17 , Singapore guidelines 36 ), or did not make any recommendation (CINP 22 , Italian guidelines 41 , NICE 34 , NJDMHS 32 , Schizophrenia Patient Outcomes Research Team [PORT] 30 , 31 ). The BAP 33 and WFBSP 24 noted that while there was probably no difference between FGAs and SGAs in efficacy, some SGAs (olanzapine, amisulpride, and risperidone) may perform better than some FGAs. The Schizophrenia PORT recommendations noted that while there seemed to be no differences between SGAs and FGAs in short-term studies (≤12 weeks), longer studies (one to two years) suggested that SGAs may provide benefits in terms of longer times to relapse and discontinuation rates 30 , 31 . The AFPBN guidelines 40 and Florida Medicaid Program guidelines 18 , which both focus on use of LAI antipsychotics, both recommended an SGA-LAI for patients experiencing a first schizophrenia episode. A caveat in most CPGs was that physicians and their patients should discuss decisions about the choice of antipsychotic and that the choice should consider individual patient factors/preferences, risk of adverse and metabolic effects, and symptom patterns 17 , 18 , 19 , 22 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 41 .
Most CPGs recommended switching to a different monotherapy if the initial antipsychotic was not effective or not well tolerated after an adequate antipsychotic trial at an appropriate dose 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 32 , 33 , 35 , 36 , 39 . For patients initially treated with an FGA, the UNHCR recommended switching to an SGA (olanzapine or risperidone) 23 . Guidance on response to treatment varied in the measures used but typically required at least a 20% improvement in symptoms (i.e. reduction in Positive and Negative Syndrome Scale or Brief Psychiatric Rating Scale scores) from pre-treatment levels.
Several CPGs contained recommendations on the duration of antipsychotic therapy after a first schizophrenia episode. The NJDMHS guidelines 32 recommended nine to 12 months; CINP 22 recommended at least one year; CPA 14 recommended at least 18 months; WFSBP 25 , the Italian guidelines 41 , and NICE 34 recommended 1 to 2 years; and the RANZCP 39 , BAP 33 , and SIGN 35 recommended at least 2 years. The APA 17 and TMAP 28 recommended continuing antipsychotic treatment after resolution of first-episode symptoms but did not recommend a specific length of therapy.
Twelve guidelines 14 , 18 , 22 , 24 , 28 , 30 , 31 , 33 , 34 , 35 , 36 , 39 , 40 (63.2%) discussed the treatment of subsequent/multiple episodes of schizophrenia (i.e., following relapse). These CPGs noted that the considerations guiding the choice of antipsychotic for subsequent/multiple episodes were similar to those for a first episode, factoring in prior patient treatment response, adverse effect patterns and adherence. The CPGs also noted that response to treatment may be lower and require higher doses to achieve a response than for first-episode schizophrenia, that a different antipsychotic than used to treat the first episode may be needed, and that a switch to an LAI is an option.
Several CPGs provided recommendations for patients with specific clinical features (Supplementary Table 1 ). The most frequently discussed group of clinical features was negative symptoms, with recommendations provided in the CINP 22 , UNHCR 23 , WFSBP 24 , AFPBN 40 , SIGN 35 , BAP 33 , APA 17 , and NJDMHS guidelines; 32 negative symptoms were the sole focus of the guidelines from the PPA 37 , 38 . The guidelines noted that due to limited evidence in patients with predominantly negative symptoms, there was no clear benefit for any strategy, but that options included SGAs (especially amisulpride) rather than FGAs (WFSBP 24 , CINP 22 , AFPBN 40 , SIGN 35 , NJDMHS 32 , PPA 37 , 38 ), and addition of an antidepressant (WFSBP 24 , UNHCR 23 , SIGN 35 , NJDMHS 32 ) or lamotrigine (SIGN 35 ), or switching to another SGA (NJDMHS 32 ) or clozapine (NJDMHS 32 ). The PPA guidelines 37 , 38 stated that the use of clozapine or adding an antidepressant or other medication class was not supported by evidence, but recommended the SGA cariprazine for patients with predominant and persistent negative symptoms, and other SGAs for those with full-spectrum negative symptoms. However, the BAP 33 stated that no recommendations can be made for any of these strategies because of the quality and paucity of the available evidence.
Some of the CPGs also discussed treatment of other clinical features to a limited degree, including depressive symptoms (CINP 22 , UNHCR 23 , CPA 14 , APA 17 , and NJDMHS 32 ), cognitive dysfunction (CINP 22 , UNHCR 23 , WFSBP 24 , AFPBN 40 , SIGN 35 , BAP 33 , and NJDMHS 32 ), persistent aggression (CINP 22 , WFSBP 24 , CPA 14 , AFPBN 40 , NICE 34 , SIGN 35 , BAP 33 , and NJDMHS 32 ), and comorbid psychiatric diagnoses (CINP 22 , RANZCP 39 , BAP 33 , APA 17 , and NJDMHS 32 ).
Fifteen CPGs (78.9%) discussed treatment-resistant schizophrenia (TRS); all defined it as persistent, predominantly positive symptoms after two adequate antipsychotic trials; clozapine was the unanimous first choice 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 . However, the UNHCR guidelines 23 , which included recommendations for treatment of refugees, noted that clozapine is only a reasonable choice in regions where white blood cell monitoring and specialist supervision are available, otherwise, risperidone or olanzapine are alternatives if they had not been used in the previous treatment regimen.
There were few options for patients who are resistant to clozapine therapy, and evidence supporting these options was limited. The CPA guidelines 14 therefore stated that no recommendation can be given due to inadequate evidence. Other CPGs discussed options (but noted there was limited supporting evidence), such as switching to olanzapine or risperidone (WFSBP 24 , TMAP 28 ), adding a second antipsychotic to clozapine (CINP 22 , NICE 34 , TMAP 28 , BAP 33 , Florida Medicaid Program 18 , Oregon Health Authority 19 , RANZCP 39 ), adding lamotrigine or topiramate to clozapine (CINP 22 , Florida Medicaid Program 18 ), combination therapy with two non-clozapine antipsychotics (Florida Medicaid Program 18 , NJDMHS 32 ), and high-dose non-clozapine antipsychotic therapy (BAP 33 , SIGN 35 ). Electroconvulsive therapy was noted as a last resort for patients who did not respond to any pharmacologic therapy, including clozapine, by 10 CPGs 17 , 18 , 19 , 22 , 24 , 28 , 32 , 35 , 36 , 39 .
Maintenance therapy
Fifteen CPGs (78.9%) discussed maintenance therapy to various degrees via dedicated sections or statements, while three others referred only to maintenance doses by antipsychotic agent 18 , 23 , 29 without accompanying recommendations (Supplementary Table 2 ). Only the Italian guideline provided no reference or comments on maintenance treatment. The CINP 22 , WFSBP 25 , RANZCP 39 , and Schizophrenia PORT 30 , 31 recommended keeping patients on the same antipsychotic and at the same dose on which they had achieved remission. Several CPGs recommended maintenance therapy at the lowest effective dose (NJDMHS 32 , APA 17 , Singapore guidelines 36 , and TMAP 28 ). The CPA 14 and SIGN 35 defined the lower dose as 300–400 mg chlorpromazine equivalents or 4–6 mg risperidone equivalents, and the Singapore guidelines 36 stated that the lower dose should not be less than half the original dose. TMAP 28 stated that given the relapsing nature of schizophrenia, the maintenance dose should often be close to the original dose. While SIGN 35 recommended that patients remain on the same antipsychotic that provided remission, these guidelines also stated that maintenance with amisulpride, olanzapine, or risperidone was preferred, and that chlorpromazine and other low-potency FGAs were also suitable. The BAP 33 recommended that the current regimen be optimized before any dose reduction or switch to another antipsychotic occurs. Several CPGs recommended LAIs as an option for maintenance therapy (see next section).
Altogether, 10/18 (55.5%) CPGs made no recommendations on the appropriate duration of maintenance therapy, noting instead that each patient should be considered individually. Other CPGs made specific recommendations: Both the Both BAP 33 and SIGN 35 guidelines suggested a minimum of 2 years, the NJDMHS guidelines 32 recommended 2–3 years; the WFSBP 25 recommended 2–5 years for patients who have had one relapse and more than 5 years for those who have had multiple relapses; the RANZCP 39 and the CPA 14 recommended 2–5 years; and the CINP 22 recommended that maintenance therapy last at least 6 years for patients who have had multiple episodes. The TMAP was the only CPG to recommend that maintenance therapy be continued indefinitely 28 .
Recommendations on the use of LAIs
All CPGs except the one from Italy (94.7%) discussed the use of LAIs for patients with schizophrenia to some extent. As shown in Table 3 , among the 18 CPGs, LAIs were primarily recommended in 14 CPGs (77.8%) for patients who are non-adherent to other antipsychotic administration routes (CINP 22 , UNHCR 23 , RANZCP 39 , PPA 37 , 38 , Singapore guidelines 36 , NICE 34 , SIGN 35 , BAP 33 , APA 17 , TMAP 28 , NJDMHS 32 , AACP 29 , Oregon Health Authority 19 , Florida Medicaid Program 18 ). Twelve CPGs (66.7%) also noted that LAIs should be prescribed based on patient preference (RANZCP 39 , CPA 14 , AFPBN 40 , Singapore guidelines 36 , NICE 34 , SIGN 35 , BAP 33 , APA 17 , Schizophrenia PORT 30 , 31 , AACP 29 , Oregon Health Authority 19 , Florida Medicaid Program 18 ).
Thirteen CPGs (72.2%) recommended LAIs as maintenance therapy 18 , 19 , 24 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 40 . While five CPGs (27.8%), i.e., AFPBN 40 , RANZCP 39 , TMAP 28 , NJDMHS 32 , and the Florida Medicaid Program 18 recommended LAIs specifically for patients experiencing a first episode. While the CPA 14 did not make any recommendations regarding when LAIs should be used, they discussed recent evidence supporting their use earlier in treatment. Five guidelines (27.8%, i.e., Singapore 36 , NICE 34 , SIGN 35 , BAP 33 , and Schizophrenia PORT 30 , 31 ) noted that evidence around LAIs was not sufficient to support recommending their use for first-episode patients. The AFPBN guidelines 40 also stated that LAIs (SGAs as first-line and FGAs as second-line treatment) should be more frequently considered for maintenance treatment of schizophrenia. Four CPGs (22.2%, i.e., CINP 22 , UNHCR 23 , Italian guidelines 41 , PPA guidelines 37 , 38 ) did not specify when LAIs should be used. The AACP guidelines 29 , which evaluated only LAIs, recommended expanding their use beyond treatment for nonadherence, suggesting that LAIs may offer a more convenient mode of administration or potentially address other clinical and social challenges, as well as provide more consistent plasma levels.
Treatment algorithms
Only Seven CPGs (36.8%) included an algorithm as part of the treatment recommendations. These included decision trees or flow diagrams that map out initial therapy, durations for assessing response, and treatment options in cases of non-response. However, none of these guidelines defined how to measure response, a theme that also extended to guidelines that did not include treatment algorithms. Four of the seven guidelines with algorithms recommended specific antipsychotic agents, while the remaining three referred only to the antipsychotic class.
LAIs were not consistently incorporated in treatment algorithms and in six CPGs were treated as a separate category of medicine reserved for patients with adherence issues or a preference for the route of administration. The only exception was the Florida Medicaid Program 18 , which recommended offering LAIs after oral antipsychotic stabilization even to patients who are at that point adherent to oral antipsychotics.
Benefits and harms
The need to balance the efficacy and safety of antipsychotics was mentioned by all CPGs as a basic treatment paradigm.
Ten CPGs provided conclusions on benefits of antipsychotic therapy. The APA 17 and the BAP 33 guidelines stated that antipsychotic treatment can improve the positive and negative symptoms of psychosis and leads to remission of symptoms. These CPGs 17 , 33 as well as those from NICE 34 and CPA 14 stated that these treatment effects can also lead to improvements in quality of life (including quality-adjusted life years), improved functioning, and reduction in disability. The CPA 14 and APA 17 guidelines noted decreases in hospitalizations with antipsychotic therapy, and the APA guidelines 17 stated that long-term antipsychotic treatment can also reduce mortality. The UNHCR 23 and the Italian 41 guidelines noted that early intervention increased positive outcomes. The WFSBP 24 , AFPBN 40 , CPA 14 , BAP 33 , APA 17 , and NJDMHS 32 affirmed that relapse prevention is a benefit of continued/maintenance treatment.
Some CPGs (WFSBP 24 , Italian 41 , CPA 14 , and SIGN 35 ) noted that reduced risk for extrapyramidal adverse effects and treatment discontinuation were potential benefits of SGAs vs. FGAs.
The risk of adverse effects (e.g., extrapyramidal, metabolic, cardiovascular, and hormonal adverse effects, sedation, and neuroleptic malignant syndrome) was noted by all CPGs as the major potential harm of antipsychotic therapy 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 29 , 30 , 31 , 32 , 34 , 35 , 36 , 37 , 39 , 40 , 41 , 42 . These adverse effects are known to limit long-term treatment and adherence 24 .
This SLR of CPGs for the treatment of schizophrenia yielded 19 most updated versions of individual CPGs, published/issued between 2004 and 2020. Structuring our comparative review according to illness phase, antipsychotic type and formulation, response to antipsychotic treatment as well as benefits and harms, several areas of consistent recommendations emerged from this review (e.g., balancing risk and benefits of antipsychotics, preferring antipsychotic monotherapy; using clozapine for treatment-resistant schizophrenia). On the other hand, other recommendations regarding other areas of antipsychotic treatment were mostly consistent (e.g., maintenance antipsychotic treatment for some time), somewhat inconsistent (e.g., differences in the management of first- vs multi-episode patients, type of antipsychotic, dose of antipsychotic maintenance treatment), or even contradictory (e.g., role of LAIs in first-episode schizophrenia patients).
Consistent with RCT evidence 43 , 44 , antipsychotic monotherapy was the treatment of choice for patients with first-episode schizophrenia in all CPGs, and all guidelines stated that a different single antipsychotic should be tried if the first is ineffective or intolerable. Recommendations were similar for multi-episode patients, but factored in prior patient treatment response, adverse effect patterns, and adherence. There was also broad consensus that the side-effect profile of antipsychotics is the most important consideration when making a decision on pharmacologic treatment, also reflecting meta-analytic evidence 4 , 5 , 10 . The risk of extrapyramidal symptoms (especially with FGAs) and metabolic effects (especially with SGAs) were noted as key considerations, which are also reflected in the literature as relevant concerns 4 , 45 , 46 , including for quality of life and treatment nonadherence 47 , 48 , 49 , 50 .
Largely consistent with the comparative meta-analytic evidence regarding the acute 4 , 51 , 52 and maintenance antipsychotic treatment 5 effects of schizophrenia, the majority of CPGs stated there was no difference in efficacy between SGAs and FGAs (WFSBP 24 , CPA 14 , SIGN 35 , APA 17 , and Singapore guidelines 36 ), or did not make any recommendations (CINP 22 , Italian guidelines 41 , NICE 34 , NJDMHS 32 , and Schizophrenia PORT 30 , 31 ); three CPGs (BAP 33 , WFBSP 24 , and Schizophrenia PORT 30 , 31 ) noted that SGAs may perform better than FGAs over the long term, consistent with a meta-analysis on this topic 53 .
The 12 CPGs that discussed treatment of subsequent/multiple episodes generally agreed on the factors guiding the choices of an antipsychotic, including that the decision may be more complicated and response may be lower than with a first episode, as described before 7 , 54 , 55 , 56 .
There was little consensus regarding maintenance therapy. Some CPGs recommended the same antipsychotic and dose that achieved remission (CINP 22 , WFSBP 25 , RANZCP 39 , and Schizophrenia PORT 30 , 31 ) and others recommended the lowest effective dose (NJDMHS 32 , APA 17 , Singapore guidelines 36 , TMAP 28 , CPA 14 , and SIGN 35 ). This inconsistency is likely based on insufficient data as well as conflicting results in existing meta-analyses on this topic 57 , 58 , 59 .
The 15 CPGs that discussed TRS all used the same definition for this condition, consistent with recent commendations 60 , and agreed that clozapine is the primary evidence-based treatment choice 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , reflecting the evidence base 61 , 62 , 63 . These CPGs also agreed that there are few options well supported by evidence for patients who do not respond to clozapine, with a recent meta-analysis of RCTs showing that electroconvulsive therapy augmentation may be the most evidence-based treatment option 64 .
One key gap in the treatment recommendations was how long patients should remain on antipsychotic therapy after a first episode or during maintenance therapy. While nine of the 17 CPGs discussing treatment of a first episode provided a recommended timeframe (varying from 1 to 2 years) 14 , 22 , 24 , 32 , 33 , 34 , 35 , 39 , 41 , the APA 17 and TMAP 28 recommended continuing antipsychotic treatment after resolution of first-episode symptoms but did not recommend a specific length of therapy. Similarly, six of the 18 CPGs discussing maintenance treatment recommended a specific duration of therapy (ranging from two to six years) 14 , 22 , 25 , 32 , 39 , while as many as 10 CPGs did not point to a firm end of the maintenance treatment, instead recommending individualized decisions. The CPGs not stating a definite endpoint or period of maintenance treatment after repeated schizophrenia episodes or even after a first episode of schizophrenia, reflects the different evidence types on which the recommendation is based. The RCT evidence ends after several years of maintenance treatment vs. discontinuation supporting ongoing antipsychotic treatment; however, naturalistic database studies do not indicate any time period after which one can safely discontinue maintenance antipsychotic care, even after a first schizophrenia episode 8 , 65 . In fact, stopping antipsychotics is associated not only with a substantially increased risk of hospitalization but also mortality 65 , 66 , 67 . In this sense, not stating an endpoint for antipsychotic maintenance therapy should not be taken as an implicit statement that antipsychotics should be discontinued at any time; data suggest the contrary.
A further gap exists regarding the most appropriate treatment of negative symptoms, such as anhedonia, amotivation, asociality, affective flattening, and alogia 1 , a long-standing challenge in the management of patients with schizophrenia. Negative symptoms often persist in patients after positive symptoms have resolved, or are the presenting feature in a substantial minority of patients 22 , 35 . Negative symptoms can also be secondary to pharmacotherapy 22 , 68 . Antipsychotics have been most successful in treating positive symptoms, and while eight of the CPGs provided some information on treatment of negative symptoms, the recommendations were generally limited 17 , 22 , 23 , 24 , 32 , 33 , 35 , 40 . Negative symptom management was a focus of the PPA guidelines, but the guidelines acknowledged that supporting evidence was limited, often due to the low number of patients with predominantly negative symptoms in clinical trials 37 , 38 . The Polish guidelines are also one of the more recently developed and included the newer antipsychotic cariprazine as a first-line option, which although being a point of differentiation from the other guidelines, this recommendation was based on RCT data 69 .
Another area in which more direction is needed is on the use of LAIs. While all but one of the 19 CPGs discussed this topic, the extent of information and recommendations for LAI use varied considerably. All CPGs categorized LAIs as an option to improve adherence to therapy or based on patient preference. However, 5/18 CPGs (27.8%) recommended the use of LAI early in treatment (at first episode: AFPBN 40 , RANZCP 39 , TMAP 28 , NJDMHS 32 , and Florida Medicaid Program 18 ) or across the entire illness course, while five others stated there was not sufficient evidence to recommend LAIs for these patients (Singapore 36 , NICE 34 , SIGN 35 , BAP 33 , and Schizophrenia PORT 30 , 31 ). The role of LAIs in first-episode schizophrenia was the only point where opposing recommendations were found across CPGs. This contradictory stance was not due to the incorporation of newer data suggesting benefits of LAIs in first episode and early-phase patients with schizophrenia 70 , 71 , 72 , 73 , 74 in the CPGs recommending LAI use in first-episode patients, as CPGs recommending LAI use were published between 2005 and 2020, while those opposing LAI use were published between 2011 and 2020. Only the Florida Medicaid CPG recommended LAIs as a first step equivalent to oral antipsychotics (OAP) after initial OAP response and tolerability, independent of nonadherence or other clinical variables. This guideline was also the only CPG to fully integrate LAI use in their clinical algorithm. The remaining six CPGs that included decision tress or treatment algorithms regarded LAIs as a separate paradigm of treatment reserved for nonadherence or patients preference rather than a routine treatment option to consider. While some CPGs provided fairly detailed information on the use of LAIs (AFPBN 40 , AACP 29 , Oregon Health Authority 19 , and Florida Medicaid Program 18 ), others mentioned them only in the context of adherence issues or patient preference. Notably, definitions of and means to determine nonadherence were not reported. One reason for this wide range of recommendations regarding the placement of LAIs in the treatment algorithm and clinical situations that prompt LAI use might be due to the fact that CPGs generally favor RCT evidence over evidence from other study designs. In the case of LAIs, there was a notable dissociation between consistent meta-analytic evidence of statistically significant superiority of LAIs vs OAPs in mirror-image 75 and cohort study designs 76 and non-significant advantages in RCTs 77 . Although patients in RCTs comparing LAIs vs OAPs were less severely ill and more adherent to OAPs 77 than in clinical care and although mirror-image and cohort studies arguably have greater external validity than RCTs 78 , CPGs generally disregard evidence from other study designs when RCT evidence exits. This narrow focus can lead to disregarding important additional data. Nevertheless, a most updated meta-analysis of all 3 study designs comparing LAIs with OAPs demonstrated consistent superiority of LAIs vs OAPs for hospitalization or relapse across all 3 designs 79 , which should lead to more uniform recommendations across CPGs in the future.
Only seven CPGs included treatment algorithms or flow charts to guide LAI treatment selection for patients with schizophrenia 17 , 18 , 19 , 24 , 29 , 35 , 40 . However, there was little commonality across algorithms beyond the guidance on LAIs mentioned above, as some listed specific treatments and conditions for antipsychotic switches, while others indicated that medication choice should be based on a patient’s preferences and responses, side effects, and in some cases, cost effectiveness. Since algorithms and flow charts facilitate the reception, adoption and implementation of guidelines, future CPGs should include them as dissemination tools, but they need to reflect the data and detailed text and be sufficiently specific to be actionable.
The systematic nature in the identification, summarization, and assessment of the CPGs is a strength of this review. This process removed any potential bias associated with subjective selection of evidence, which is not reproducible. However, only CPGs published in English were included and regardless of their quality and differing timeframes of development and publication, complicating a direct comparison of consensus and disagreement. Finally, based on the focus of this SLR, we only reviewed pharmacologic management with antipsychotics. Clearly, the assessment, other pharmacologic and, especially, psychosocial interventions are important in the management of individuals with schizophrenia, but these topics that were covered to varying degrees by the evaluated CPGs were outside of the scope of this review.
Numerous guidelines have recently updated their recommendations on the pharmacological treatment of patients with schizophrenia, which we have summarized in this review. Consistent recommendations were observed across CPGs in the areas of balancing risk and benefits of antipsychotics when selecting treatment, a preference for antipsychotic monotherapy, especially for patients with a first episode of schizophrenia, and the use of clozapine for treatment-resistant schizophrenia. By contrast, there were inconsistencies with regards to recommendations on maintenance antipsychotic treatment, with differences existing on type and dose of antipsychotic, as well as the duration of therapy. However, LAIs were consistently recommended, but mainly suggested in cases of nonadherence or patient preference, despite their established efficacy in broader patient populations and clinical scenarios in clinical trials. Guidelines were sometimes contradictory, with some recommending LAI use earlier in the disease course (e.g., first episode) and others suggesting they only be reserved for later in the disease. This inconsistency was not due to lack of evidence on the efficacy of LAIs in first-episode schizophrenia or the timing of the CPG, so that other reasons might be responsible, including possibly bias and stigma associated with this route of treatment administration. Lastly, gaps existed in the guidelines for recommendations on the duration of maintenance treatment, treatment of negative symptoms, and the development/use of treatment algorithms whenever evidence is sufficient to provide a simplified summary of the data and indicate their relevance for clinical decision making, all of which should be considered in future guideline development/revisions.
The SLR followed established best methods used in systematic review research to identify and assess the available CPGs for pharmacologic treatment of schizophrenia with antipsychotics in the acute and maintenance phases 80 , 81 . The SLR was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, including use of a prespecified protocol to outline methods for conducting the review. The protocol for this review was approved by all authors prior to implementation but was not submitted to an external registry.
Data sources and search algorithms
Searches were conducted by two independent investigators in the MEDLINE and Embase databases via OvidSP to identify CPGs published in English. Articles were identified using search algorithms that paired terms for schizophrenia with keywords for CPGs. Articles indexed as case reports, reviews, letters, or news were excluded from the searches. The database search was limited to CPGs published from January 1, 2004, through December 19, 2019, without limit to geographic location. In addition to the database sources, guideline body websites and state-level health departments from the US were also searched for relevant CPGs published through June 2020. A manual check of the references of recent (i.e., published in the past three years), relevant SLRs and relevant practice CPGs was conducted to supplement the above searches and ensure and the most complete CPG retrieval.
This study did not involve human subjects as only published evidence was included in the review; ethical approval from an institution was therefore not required.
Selection of CPGs for inclusion
Each title and abstract identified from the database searches was screened and selected for inclusion or exclusion in the SLR by two independent investigators based on the populations, interventions/comparators, outcomes, study design, time period, language, and geographic criteria shown in Table 4 . During both rounds of the screening process, discrepancies between the two independent reviewers were resolved through discussion, and a third investigator resolved any disagreement. Articles/documents identified by the manual search of organizational websites were screened using the same criteria. All accepted studies were required to meet all inclusion criteria and none of the exclusion criteria. Only the most recent version of organizational CPGs was included for data extraction.
Data extraction and synthesis
Information on the recommendations regarding the antipsychotic management in the acute and maintenance phases of schizophrenia and related benefits and harms was captured from the included CPGs. Each guideline was reviewed and extracted by a single researcher and the data were validated by a senior team member to ensure accuracy and completeness. Additionally, each included CPG was assessed using the Appraisal of Guidelines for Research and Evaluation II (AGREE II) tool. Following extraction and validation, results were qualitatively summarized across CPGs.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data that support the findings of the SLR are available from the corresponding author upon request.
Correll, C. U. & Schooler, N. R. Negative symptoms in schizophrenia: a review and clinical guide for recognition, assessment, and treatment. Neuropsychiatr. Dis. Treat. 16 , 519–534 (2020).
Article PubMed PubMed Central Google Scholar
Kahn, R. S. et al. Schizophrenia. Nat. Rev. Dis. Prim. 1 , 15067 (2015).
Article PubMed Google Scholar
Millan, M. J. et al. Altering the course of schizophrenia: progress and perspectives. Nat. Rev. Drug Discov. 15 , 485–515 (2016).
Article CAS PubMed Google Scholar
Huhn, M. et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet 394 , 939–951 (2019).
Article CAS PubMed PubMed Central Google Scholar
Kishimoto, T., Hagi, K., Nitta, M., Kane, J. M. & Correll, C. U. Long-term effectiveness of oral second-generation antipsychotics in patients with schizophrenia and related disorders: a systematic review and meta-analysis of direct head-to-head comparisons. World Psychiatry 18 , 208–224 (2019).
Leucht, S. et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet 379 , 2063–2071 (2012).
Carbon, M. & Correll, C. U. Clinical predictors of therapeutic response to antipsychotics in schizophrenia. Dialogues Clin. Neurosci. 16 , 505–524 (2014).
Correll, C. U., Rubio, J. M. & Kane, J. M. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry 17 , 149–160 (2018).
Emsley, R., Chiliza, B., Asmal, L. & Harvey, B. H. The nature of relapse in schizophrenia. BMC Psychiatry 13 , 50 (2013).
Correll, C. U. & Kane, J. M. Ranking antipsychotics for efficacy and safety in schizophrenia. JAMA Psychiatry 77 , 225–226 (2020).
Kane, J. M. & Correll, C. U. Pharmacologic treatment of schizophrenia. Dialogues Clin. Neurosci. 12 , 345–357 (2010).
Kane, J. M., Kishimoto, T. & Correll, C. U. Non-adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry 12 , 216–226 (2013).
Correll, C. U. et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J. Clin. Psychiatry 77 , 1–24 (2016).
Remington, G. et al. Guidelines for the pharmacotherapy of schizophrenia in adults. Can. J. Psychiatry 62 , 604–616 (2017).
American Psychiatric Association. Treatment recommendations for patients with schizophrenia. Am. J. Psychiatry 161 , 1–56 (2004).
Institute of Medicine (US) Committee to Advise the Public Health Service on Clinical Practice Guidelines, Field, M. J., & Lohr, K. N. (Eds.). Clinical Practice Guidelines: Directions for a New Program. (National Academies Press (US), 1990).
American Psychiatric Association. Practice Guideline for the Treatment of Patients With Schizophrenia , 3rd edn. (2021). https://doi.org/10.1176/appi.books.9780890424841 .
Florida Medicaid Drug Therapy Management Program. 2019–2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults . (2020). Available at: https://floridabhcenter.org/wp-content/uploads/2021/04/2019-Psychotherapeutic-Medication-Guidelines-for-Adults-with-References_06-04-20.pdf .
Mental Health Clinical Advisory Group, Oregon Health Authority. Mental Health Care Guide for Licensed Practitioners and Mental Health Professionals. (2019). Available at: https://sharedsystems.dhsoha.state.or.us/DHSForms/Served/le7548.pdf .
Krogmann, A. et al. Keeping up with the therapeutic advances in schizophrenia: a review of novel and emerging pharmacological entities. CNS Spectr. 24 , 38–69 (2019).
Fountoulakis, K. N. et al. The report of the joint WPA/CINP workgroup on the use and usefulness of antipsychotic medication in the treatment of schizophrenia. CNS Spectr . https://doi.org/10.1017/S1092852920001546 (2020).
Leucht, S. et al. CINP Schizophrenia Guidelines . (CINP, 2013). Available at: https://www.cinp.org/resources/Documents/CINP-schizophrenia-guideline-24.5.2013-A-C-method.pdf .
Ostuzzi, G. et al. Mapping the evidence on pharmacological interventions for non-affective psychosis in humanitarian non-specialised settings: A UNHCR clinical guidance. BMC Med. 15 , 197 (2017).
Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, Part 1: Update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J. Biol. Psychiatry 13 , 318–378 (2012).
Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, Part 2: Update 2012 on the long-term treatment of schizophrenia and management of antipsychotic-induced side effects. World J. Biol. Psychiatry 14 , 2–44 (2013).
Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia - a short version for primary care. Int. J. Psychiatry Clin. Pract. 21 , 82–90 (2017).
Moore, T. A. et al. The Texas Medication Algorithm Project antipsychotic algorithm for schizophrenia: 2006 update. J. Clin. Psychiatry 68 , 1751–1762 (2007).
Texas Medication Algorithm Project (TMAP). Texas Medication Algorithm Project (TMAP) Procedural Manual . (2008). Available at: https://jpshealthnet.org/sites/default/files/inline-files/tmapalgorithmforschizophrenia.pdf .
American Association of Community Psychiatrists (AACP). Clinical Tips Series, Long Acting Antipsychotic Medications. (2017). Accessed at: https://drive.google.com/file/d/1unigjmjFJkqZMbaZ_ftdj8oqog49awZs/view .
Buchanan, R. W. et al. The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr. Bull. 36 , 71–93 (2010).
Kreyenbuhl, J. et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr. Bull. 36 , 94–103 (2010).
New Jersey Division of Mental Health Services. Pharmacological Practice Guidelines for the Treatment of Schizophrenia . (2005). Available at: https://www.state.nj.us/humanservices/dmhs_delete/consumer/NJDMHS_Pharmacological_Practice_Guidelines762005.pdf .
Barnes, T. R. et al. Evidence-based guidelines for the pharmacological treatment of schizophrenia: updated recommendations from the British Association for Psychopharmacology. J. Psychopharmacol. 34 , 3–78 (2020).
National Institute for Health and Care Excellence (NICE). Psychosis and schizophrenia in adults: prevention and management. (2014). Available at: http://www.nice.org.uk/guidance/cg178 .
Scottish Intercollegiate Guidelines Network (SIGN). Management of Schizophrenia: A National Clinical Guideline . (2013). Available at: https://www.sign.ac.uk/assets/sign131.pdf .
Verma, S. et al. Ministry of Health Clinical Practice Guidelines: Schizophrenia. Singap. Med. J. 52 , 521–526 (2011).
CAS Google Scholar
Szulc, A. et al. Recommendations for the treatment of schizophrenia with negative symptoms. Standards of pharmacotherapy by the Polish Psychiatric Association (Polskie Towarzystwo Psychiatryczne), part 1. Rekomendacje dotyczace leczenia schizofrenii z. objawami negatywnymi. Stand. farmakoterapii Polskiego Tow. Psychiatrycznego, czesc 1. 53 , 497–524 (2019).
Google Scholar
Szulc, A. et al. Recommendations for the treatment of schizophrenia with negative symptoms. Standards of pharmacotherapy by the Polish Psychiatric Association (Polskie Towarzystwo Psychiatryczne), part 2. Rekomendacje dotyczace leczenia schizofrenii z. objawami negatywnymi. Stand. farmakoterapii Polskiego Tow. Psychiatrycznego, czesc 2. 53 , 525–540 (2019).
Galletly, C. et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the management of schizophrenia and related disorders. Aust. N. Z. J. Psychiatry 50 , 410–472 (2016).
Llorca, P. M. et al. Guidelines for the use and management of long-acting injectable antipsychotics in serious mental illness. BMC Psychiatry 13 , 340 (2013).
De Masi, S. et al. The Italian guidelines for early intervention in schizophrenia: development and conclusions. Early Intervention Psychiatry 2 , 291–302 (2008).
Article Google Scholar
Barnes, T. R. Evidence-based guidelines for the pharmacological treatment of schizophrenia: recommendations from the British Association for Psychopharmacology. J. Psychopharmacol. 25 , 567–620 (2011).
Correll, C. U. et al. Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiatry 74 , 675–684 (2017).
Galling, B. et al. Antipsychotic augmentation vs. monotherapy in schizophrenia: systematic review, meta-analysis and meta-regression analysis. World Psychiatry 16 , 77–89 (2017).
Pillinger, T. et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry 7 , 64–77 (2020).
Rummel-Kluge, C. et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr. Bull. 38 , 167–177 (2012).
Angermeyer, M. C. & Matschinger, H. Attitude of family to neuroleptics. Psychiatr. Prax. 26 , 171–174 (1999).
CAS PubMed Google Scholar
Dibonaventura, M., Gabriel, S., Dupclay, L., Gupta, S. & Kim, E. A patient perspective of the impact of medication side effects on adherence: results of a cross-sectional nationwide survey of patients with schizophrenia. BMC Psychiatry 12 , 20 (2012).
McIntyre, R. S. Understanding needs, interactions, treatment, and expectations among individuals affected by bipolar disorder or schizophrenia: the UNITE global survey. J. Clin. Psychiatry 70 (Suppl 3), 5–11 (2009).
Tandon, R. et al. The impact on functioning of second-generation antipsychotic medication side effects for patients with schizophrenia: a worldwide, cross-sectional, web-based survey. Ann. Gen. Psychiatry 19 , 42 (2020).
Zhang, J. P. et al. Efficacy and safety of individual second-generation vs. first-generation antipsychotics in first-episode psychosis: a systematic review and meta-analysis. Int. J. Neuropsychopharmacol. 16 , 1205–1218 (2013).
Zhu, Y. et al. Antipsychotic drugs for the acute treatment of patients with a first episode of schizophrenia: a systematic review with pairwise and network meta-analyses. Lancet Psychiatry 4 , 694–705 (2017).
Kishimoto, T. et al. Relapse prevention in schizophrenia: a systematic review and meta-analysis of second-generation antipsychotics versus first-generation antipsychotics. Mol. Psychiatry 18 , 53–66 (2013).
Leucht, S. et al. Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: systematic review, Bayesian meta-analysis, and meta-regression of efficacy predictors. Am. J. Psychiatry 174 , 927–942 (2017).
Samara, M. T., Nikolakopoulou, A., Salanti, G. & Leucht, S. How many patients with schizophrenia do not respond to antipsychotic drugs in the short term? An analysis based on individual patient data from randomized controlled trials. Schizophr. Bull. 45 , 639–646 (2019).
Zhu, Y. et al. How well do patients with a first episode of schizophrenia respond to antipsychotics: a systematic review and meta-analysis. Eur. Neuropsychopharmacol. 27 , 835–844 (2017).
Bogers, J. P. A. M., Hambarian, G., Michiels, M., Vermeulen, J. & de Haan, L. Risk factors for psychotic relapse after dose reduction or discontinuation of antipsychotics in patients with chronic schizophrenia. A systematic review and meta-analysis. Schizophr. Bull. Open 46 , Suppl 1 S326 (2020).
Tani, H. et al. Factors associated with successful antipsychotic dose reduction in schizophrenia: a systematic review of prospective clinical trials and meta-analysis of randomized controlled trials. Neuropsychopharmacology 45 , 887–901 (2020).
Uchida, H., Suzuki, T., Takeuchi, H., Arenovich, T. & Mamo, D. C. Low dose vs standard dose of antipsychotics for relapse prevention in schizophrenia: meta-analysis. Schizophr. Bull. 37 , 788–799 (2011).
Howes, O. D. et al. Treatment-resistant schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am. J. Psychiatry 174 , 216–229 (2017).
Masuda, T., Misawa, F., Takase, M., Kane, J. M. & Correll, C. U. Association with hospitalization and all-cause discontinuation among patients with schizophrenia on clozapine vs other oral second-generation antipsychotics: a systematic review and meta-analysis of cohort studies. JAMA Psychiatry 76 , 1052–1062 (2019).
Siskind, D., McCartney, L., Goldschlager, R. & Kisely, S. Clozapine v. first- and second-generation antipsychotics in treatment-refractory schizophrenia: systematic review and meta-analysis. Br. J. Psychiatry 209 , 385–392 (2016).
Siskind, D., Siskind, V. & Kisely, S. Clozapine response rates among people with treatment-resistant schizophrenia: data from a systematic review and meta-analysis. Can. J. Psychiatry 62 , 772–777 (2017).
Wang, G. et al. ECT augmentation of clozapine for clozapine-resistant schizophrenia: a meta-analysis of randomized controlled trials. J. Psychiatr. Res. 105 , 23–32 (2018).
Tiihonen, J., Tanskanen, A. & Taipale, H. 20-year nationwide follow-up study on discontinuation of antipsychotic treatment in first-episode schizophrenia. Am. J. Psychiatry 175 , 765–773 (2018).
Taipale, H. et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia. Schizophr. Res . 197 , 274–280 (2018).
Taipale, H. et al. 20-year follow-up study of physical morbidity and mortality in relationship to antipsychotic treatment in a nationwide cohort of 62,250 patients with schizophrenia (FIN20). World Psychiatry 19 , 61–68 (2020).
Carbon, M. & Correll, C. U. Thinking and acting beyond the positive: the role of the cognitive and negative symptoms in schizophrenia. CNS Spectr. 19 (Suppl 1), 38–52 (2014).
PubMed Google Scholar
Krause, M. et al. Antipsychotic drugs for patients with schizophrenia and predominant or prominent negative symptoms: a systematic review and meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 268 , 625–639 (2018).
Kane, J. M. et al. Effect of long-acting injectable antipsychotics vs usual care on time to first hospitalization in early-phase schizophrenia: a randomized clinical trial. JAMA Psychiatry 77 , 1217–1224 (2020).
Schreiner, A. et al. Paliperidone palmitate versus oral antipsychotics in recently diagnosed schizophrenia. Schizophr. Res. 169 , 393–399 (2015).
Subotnik, K. L. et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia. A randomized clinical trial. JAMA Psychiatry 72 , 822–829 (2015).
Tiihonen, J. et al. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am. J. Psychiatry 168 , 603–609 (2011).
Zhang, F. et al. Efficacy, safety, and impact on hospitalizations of paliperidone palmitate in recent-onset schizophrenia. Neuropsychiatr. Dis. Treat. 11 , 657–668 (2015).
Kishimoto, T., Nitta, M., Borenstein, M., Kane, J. M. & Correll, C. U. Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. J. Clin. Psychiatry 74 , 957–965 (2013).
Kishimoto, T. et al. Effectiveness of long-acting injectable vs oral antipsychotics in patients with schizophrenia: a meta-analysis of prospective and retrospective cohort studies. Schizophr. Bull. 44 , 603–619 (2018).
Kishimoto, T. et al. Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of randomized trials. Schizophr. Bull. 40 , 192–213 (2014).
Kane, J. M., Kishimoto, T. & Correll, C. U. Assessing the comparative effectiveness of long-acting injectable vs. oral antipsychotic medications in the prevention of relapse provides a case study in comparative effectiveness research in psychiatry. J. Clin. Epidemiol. 66 , S37–41 (2013).
Kishimoto, T., Hagi, K., Kurokawa, S., Kane, J. M. & Correll, C. U. Long-acting injectable versus oral antipsychotics for the maintenance treatment of schizophrenia: a systematic review and comparative meta-analysis of randomised, cohort, and pre-post studies. Lancet Psychiatry 8 , 387–404 (2021).
Cook, D. J., Mulrow, C. D. & Haynes, R. B. Systematic reviews: synthesis of best evidence for clinical decisions. Ann. Intern. Med. 126 , 376–380 (1997).
Higgins, J. P. T. & Green, S. Cochrane Collaboration Handbook for Systematic Reviews of Interventions . (The Cochrane Collaboration and John Wiley & Sons, Ltd, 2008).
Download references
Acknowledgements
This study received financial funding from Janssen Scientific Affairs.
Open Access funding enabled and organized by Projekt DEAL.

Author information
Authors and affiliations.
The Zucker Hillside Hospital, Department of Psychiatry, Northwell Health, Glen Oaks, NY, USA
- Christoph U. Correll
Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Department of Psychiatry and Molecular Medicine, Hempstead, NY, USA
Charité Universitätsmedizin Berlin, Department of Child and Adolescent Psychiatry, Berlin, Germany
Evidera, Waltham, MA, USA
Amber Martin & Emma Schiller
Janssen Scientific Affairs, LLC, Titusville, NJ, USA
Charmi Patel, Carmela Benson, Jennifer Kern-Sliwa & Kruti Joshi
Goulding HEOR Consulting Inc., Vancouver, BC, Canada
Rebecca Goulding
Biohaven Pharmaceuticals, New Haven, CT, USA
You can also search for this author in PubMed Google Scholar
Contributions
C.C., A.M., R.G., C.P., C.B., K.J., J.K.S., E.S. and E.K. contributed to the conception and the design of the study. A.M., R.G. and E.S. conducted the literature review, including screening, and extraction of the included guidelines. All authors contributed to the interpretations of the results for the review; A.M. and C.C. drafted the manuscript and all authors revised it critically for intellectual content. All authors gave their final approval of the completed manuscript.
Corresponding author
Correspondence to Christoph U. Correll .
Ethics declarations
Competing interests.
C.C. has received personal fees from Alkermes plc, Allergan plc, Angelini Pharma, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Inc, Janssen Pharmaceutica/Johnson & Johnson, LB Pharma International BV, H Lundbeck A/S, MedAvante-ProPhase, Medscape, Neurocrine Biosciences, Noven Pharmaceuticals, Inc, Otsuka Pharmaceutical Co, Inc, Pfizer, Inc, Recordati, Rovi, Sumitomo Dainippon Pharma, Sunovion Pharmaceuticals, Inc, Supernus Pharmaceuticals, Inc, Takeda Pharmaceutical Company Limited, Teva Pharmaceuticals, Acadia Pharmaceuticals, Inc, Axsome Therapeutics, Inc, Indivior, Merck & Co, Mylan NV, MedInCell, and Karuna Therapeutics and grants from Janssen Pharmaceutica, Takeda Pharmaceutical Company Limited, Berlin Institute of Health, the National Institute of Mental Health, Patient Centered Outcomes Research Institute, and the Thrasher Foundation outside the submitted work; receiving royalties from UpToDate; and holding stock options in LB Pharma. A.M., R.G., and E.S. were all employees of Evidera at the time the study was conducted on which the manuscript was based. C.P., C.B., K.J., J.K.S., and E.K. were all employees of Janssen Scientific Affairs, who hold stock/shares, at the time the study was conducted.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Correll, C.U., Martin, A., Patel, C. et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. Schizophr 8 , 5 (2022). https://doi.org/10.1038/s41537-021-00192-x
Download citation
Received : 26 February 2021
Accepted : 02 November 2021
Published : 24 February 2022
DOI : https://doi.org/10.1038/s41537-021-00192-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Psychosis superspectrum ii: neurobiology, treatment, and implications.
- Roman Kotov
- William T. Carpenter
- Katherine G. Jonas
Molecular Psychiatry (2024)
Sex Differences Between Female and Male Individuals in Antipsychotic Efficacy and Adverse Effects in the Treatment of Schizophrenia
- Megan Galbally
- Karen Wynter
- Susanna Every-Palmer
CNS Drugs (2024)
Antipsychotic Discontinuation through the Lens of Epistemic Injustice
- Helene Speyer
- Lene Falgaard Eplov
Community Mental Health Journal (2024)
Delphi panel to obtain clinical consensus about using long-acting injectable antipsychotics to treat first-episode and early-phase schizophrenia: treatment goals and approaches to functional recovery
- Celso Arango
- Andrea Fagiolini
BMC Psychiatry (2023)
Machine learning methods to predict outcomes of pharmacological treatment in psychosis
- Lorenzo Del Fabro
- Elena Bondi
- Paolo Brambilla
Translational Psychiatry (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Exploring sensory processing and sensory experience in everyday life for adults with schizophrenia: A collaborative approach
Add to collection, downloadable content.
- Affiliation: School of Medicine, Department of Allied Health Sciences, Division of Occupational Science and Occupational Therapy
- Occupational scientists are interested in studying the relationship between sensations people experience in daily life and the knowledge of the things they do (Hocking, 2009). People living with serious mental illness such as schizophrenia experience barriers in both aforementioned areas. They spend on average more time than the general population doing “nothing” (i.e., remaining idle or sleeping) (Cella et al., 2016), and also have biomarkers of atypical sensory processing (Javitt, 2009). However, the relationship between sensory processing biomarkers and people’s lived sensory experiences remains unclear. In response, this dissertation adopts an epistemologically pluralist (Kinsella, 2012) approach to put research on sensory processing and sensory experience in dialogue. This is done through an occupational perspective, which thinks about everyday doing and its health and well-being implications (Njelesani et al., 2014; Wilcock, 1998, 2007; Yerxa et al., 1990). More specifically, this dissertation asks the following questions in two areas: 1) How do people living with schizophrenia or other serious mental illness(es) understand and describe their sensory experiences through the things they do in everyday life, as well as language from sensory processing measures? and 2) What can health researchers learn from using an instrument development approach influenced by collaborative ethnography (Lassiter, 2005)? How did this collaborative approach influence both my and the participants’ understanding of research in general? The first study is a scoping review on research about sensory processing and participation for adults living with schizophrenia spectrum disorders (SSD). The second study explored the ways in which study participants – referred to as consultants (Lassiter, 2005) – verbalized their sensory experiences, focusing on the form and content (i.e., how and what people described using words) and the paradigms (technical or interpretive) in which those experiences are communicated (Kinsella, 2012). The third study examined the transformative potential of research participation as a collective occupation, drawing upon Mertens’ (2007) transformative paradigm, Anderson and Braud’s (2011) work on transpersonal research, critical occupational science, and mental health service user-led research. Findings from the three studies were synthesized in the concluding section of the dissertation and connected to implications for occupational science and the broader health sciences.
- occupational therapy
- sensory processing
- occupational science
- sensory experience
- Mental health
- schizophrenia
- Occupational therapy
- https://doi.org/10.17615/1pyd-st42
- Dissertation
- In Copyright - Educational Use Permitted
- Bailliard, Antoine
- Bagatell, Nancy
- Park, Melissa
- Womack, Jenny
- Zhang, Wanqing
- Doctor of Philosophy
- University of North Carolina at Chapel Hill Graduate School
This work has no parents.
Select type of work
Master's papers.
Deposit your masters paper, project or other capstone work. Theses will be sent to the CDR automatically via ProQuest and do not need to be deposited.
Scholarly Articles and Book Chapters
Deposit a peer-reviewed article or book chapter. If you would like to deposit a poster, presentation, conference paper or white paper, use the “Scholarly Works” deposit form.
Undergraduate Honors Theses
Deposit your senior honors thesis.
Scholarly Journal, Newsletter or Book
Deposit a complete issue of a scholarly journal, newsletter or book. If you would like to deposit an article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
Deposit your dataset. Datasets may be associated with an article or deposited separately.
Deposit your 3D objects, audio, images or video.
Poster, Presentation, Protocol or Paper
Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 29, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Grief in aged care: Guidance needed to assist families
by Flinders University

There is an urgent need for government, researchers and aged care staff to come together to establish a formal approach to the grief and loss experienced by families in the residential aged care system, a Flinders University-led review has found.
"Families whose relatives enter the aged care system often start grieving from the moment their family member is placed into residential care and it grows from there," says study lead author Dr. Priyanka Vandersman, a Senior Research Fellow at Flinders University's Research Center for Palliative Care, Death and Dying.
"Our research shows that right from the start, how families are treated and assisted throughout this complex process has a profound impact on how they experience this grief ."
The study , published in Archives of Gerontology and Geriatrics , reviewed 35 papers examining the grief, loss, and bereavement experience of family caregivers of those entering, living and dying in residential aged care, as well as related interventions.
Findings showed the quality of care provided to the resident at the end of their life and after death strongly influenced a family's grief reaction. Furthermore, the study highlighted how support, including from social workers , as well as educational interventions also impacted their experience.
"We already knew that good quality care provided to a dying person can lead to a good grief experience for their family, but our review went further and showed it's only one piece of a much larger jigsaw puzzle," says Dr. Vandersman.
"Involving families in the older person's care, having open conversations about their loved ones' health decline and deterioration, care options and choices, as well as helping them prepare for death, were the other key elements that influenced the family caregivers' grief."
The authors say this demonstrates there is a need for a greater focus from the residential aged care sector, government agencies and research entities to work together in developing and implementing a comprehensive approach to grief, loss, and bereavement care.
This should include service policies, staff training and support, as well as family resources to support everyday care practices.
"Recognizing the emotional experiences and support needs of families and caregivers can enhance our understanding of the aging, caring, dying, grieving pathway for older people and their families," suggests co-author, Professor Jennifer Tieman, Director of the Research Center for Palliative Care, Death and Dying.
"We need to invest in leadership within the sector, along with service initiatives and staff education, if we are to facilitate timely and meaningful discussions around end-of-life care needs.
"Communication and discussions can help residents and families by providing support and guidance around administrative and logistical decisions, while also ensuring they receive responsive and proactive care throughout the person's final months, weeks, and days of life."
Explore further
Feedback to editors

Study shows effectiveness of updated COVID-19 vaccines wanes moderately over time, is lower against current variants
1 minute ago

Scientists discover a novel modulator of human regulatory T cells

Engineered DNA 'warhead' targets a common cancer mutation
2 minutes ago

Pulling out the stops: Deletion of regnase-1 promotes anti-tumor activity in NK cells
12 minutes ago

Study finds people living with dementia who had surgery for hip fractures lived longer than those treated non-surgically

Survey on trust and equity in emergency departments aims to improve system for all patients
22 minutes ago

Too much or too little: The impact of protein dosage on fetal development
48 minutes ago

New research platform assesses brain cancer mutations during surgery

Study shows phone use boosts mood of teenagers

How anti-Asian hate is worsening older San Franciscans' health
Related stories.

Study finds caregiving can affect quality of life for up to a year after loss
Oct 30, 2019

Death doulas: Helping people at the end of their life
Mar 6, 2024

What is palliative care? And how is it different to end-of-life care?
Aug 4, 2023

Researchers call for greater investment in bereavement care
Mar 16, 2024

Need for formal bereavement support in dementia care is largely underestimated
Jun 9, 2023

Family members can share grief during the holidays, but how each person grieves is different
Dec 11, 2018
Recommended for you

Study suggests vocal exploration in babies is important for speech development
21 hours ago

A protein-based risk score for hip-fracture using an aptamer-based proteomic platform

Study shows more than just social media use may be causing depression in young adults
18 hours ago

The mind after midnight: Study shows disrupted sleep increases risk for suicide and homicide
22 hours ago
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
The Landmark Decision: Understanding Roe V. Wade
This essay about Roe v. Wade explores the landmark Supreme Court decision of 1973, which affirmed a woman’s constitutional right to choose whether to terminate her pregnancy. It discusses the case’s origins, the Court’s ruling on the right to privacy, and the framework established for regulating abortion. Highlighting the societal impact and ongoing debate surrounding the decision, the essay emphasizes its significance in shaping reproductive rights, political discourse, and American culture. Roe v. Wade remains a polarizing issue, symbolizing the tension between individual autonomy and state interests in matters of personal morality and medical ethics.
How it works
In the realm of American jurisprudence, few cases have had as profound an impact as Roe v. Wade. This landmark decision, handed down by the United States Supreme Court in 1973, fundamentally altered the landscape of reproductive rights in the country. At its core, Roe v. Wade addressed the constitutionality of laws that criminalized or restricted access to abortion, sparking a national dialogue that continues to resonate to this day.
The case originated in Texas, where a woman identified as “Jane Roe” challenged the state’s abortion laws, which prohibited the procedure except to save the life of the mother.
Roe argued that these restrictions violated her constitutional right to privacy. The Supreme Court, in a 7-2 decision, agreed with Roe, asserting that the right to privacy encompassed a woman’s right to choose whether to terminate her pregnancy.
Central to the Court’s ruling was the concept of viability, referring to the point at which a fetus could potentially survive outside the womb. The Court established a framework that divided pregnancy into three trimesters, with different levels of state interest and regulation permitted at each stage. During the first trimester, the decision to terminate a pregnancy was deemed solely within the realm of the woman and her physician. As the pregnancy progressed, the state’s interest in regulating abortion became more substantial, but could not override the woman’s right to choose until the point of viability.
Roe v. Wade ignited a firestorm of debate and controversy that continues to shape American politics and culture. Proponents hailed the decision as a victory for women’s rights and reproductive freedom, while opponents decried it as an assault on the sanctity of life and the traditional family unit. In the decades since the ruling, Roe v. Wade has faced numerous legal challenges and attempts to undermine or overturn it, yet it remains the law of the land.
Beyond its immediate legal implications, Roe v. Wade has had far-reaching societal effects. It has fueled ongoing debates over the role of government in regulating personal medical decisions, the intersection of morality and law, and the definition of personhood. The case has also become a rallying cry for activists on both sides of the abortion issue, shaping electoral politics, judicial appointments, and public policy at all levels of government.
Despite its significance, Roe v. Wade remains a contentious and divisive issue in American society. Public opinion on abortion rights fluctuates, reflecting shifting cultural attitudes, religious beliefs, and political ideologies. Yet, the decision’s enduring legacy lies in its recognition of a woman’s autonomy over her own body and the recognition of reproductive rights as fundamental to gender equality and individual liberty.
In conclusion, Roe v. Wade stands as a pivotal moment in American legal history, reshaping the landscape of reproductive rights and sparking a national conversation that endures to this day. Whether viewed as a triumph of individual freedom or a challenge to traditional values, the decision continues to shape the contours of American society and inspire passionate advocacy on all sides of the issue.
Cite this page
The Landmark Decision: Understanding Roe v. Wade. (2024, May 28). Retrieved from https://papersowl.com/examples/the-landmark-decision-understanding-roe-v-wade/
"The Landmark Decision: Understanding Roe v. Wade." PapersOwl.com , 28 May 2024, https://papersowl.com/examples/the-landmark-decision-understanding-roe-v-wade/
PapersOwl.com. (2024). The Landmark Decision: Understanding Roe v. Wade . [Online]. Available at: https://papersowl.com/examples/the-landmark-decision-understanding-roe-v-wade/ [Accessed: 30 May. 2024]
"The Landmark Decision: Understanding Roe v. Wade." PapersOwl.com, May 28, 2024. Accessed May 30, 2024. https://papersowl.com/examples/the-landmark-decision-understanding-roe-v-wade/
"The Landmark Decision: Understanding Roe v. Wade," PapersOwl.com , 28-May-2024. [Online]. Available: https://papersowl.com/examples/the-landmark-decision-understanding-roe-v-wade/. [Accessed: 30-May-2024]
PapersOwl.com. (2024). The Landmark Decision: Understanding Roe v. Wade . [Online]. Available at: https://papersowl.com/examples/the-landmark-decision-understanding-roe-v-wade/ [Accessed: 30-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
- Share full article
Advertisement
Supported by
For Some Families of Color, a Painful Fight for a Cystic Fibrosis Diagnosis
Universal screenings for the inherited disease promised to get babies diagnosed and treated sooner. But they still miss some children of color.

By Liz Szabo
By the time Rena Barrow-Wells gave birth to her fourth baby in 2020, she was well-versed in caring for a child with cystic fibrosis. She was also experienced in fighting for a diagnosis of the disease, which runs in families and can severely damage the lungs and digestive system.
Nineteen years earlier, her first son, Jarrod, displayed classic symptoms of cystic fibrosis as a newborn — failure to gain weight; a stubborn, phlegmy cough; and frequent, oily stools. But instead of identifying the cause of her son’s illness, doctors at the New Orleans emergency room where she took Jarrod blamed his poor growth on his mother, who is Black and was a teenager at the time. Ms. Barrow-Wells said that doctors had accused her of starving her son, placed the two of them in a room with video surveillance and reported her to child protective services.
Doctors discharged Jarrod two weeks later without a diagnosis. It would take four years — and dozens of additional visits to doctors and emergency rooms — for Jarrod to be diagnosed with cystic fibrosis. By then, she said, the disease had interfered with his body’s ability to absorb nutrients for so long that he was profoundly malnourished. Children who are diagnosed after they are 2 months old are also at greater risk of serious lung problems and death.
People from minority communities have struggled to receive lifesaving care for cystic fibrosis for decades, in large part because many doctors were traditionally taught that the disease almost exclusively affects white people , said Dr. Jennifer Taylor-Cousar, a professor of medicine and pediatrics at the University of Colorado Anschutz Medical Campus. Several factors have fueled that misconception, she said, including limited testing and scientific research that focused on white patients and failed to identify the full range of affected populations, as well as bias against patients of color, some of whom were blamed for their symptoms, as happened with Ms. Barrow-Wells and Jarrod.
Still, Ms. Barrow-Wells had reason to hope in 2020 that things would be easier for her newborn son, Jahsir. The way cystic fibrosis was diagnosed had changed dramatically since Jarrod was born. Since 2010 , all states have screened newborns for the disease, an effort that promised to help all babies with cystic fibrosis receive a diagnosis and treatment in the critical first weeks of life, before the disease causes serious organ damage.
A newborn screening should have quickly confirmed what Ms. Barrow-Wells soon recognized — that Jahsir’s salty skin and foul-smelling diapers were signs that he, too, had cystic fibrosis.
But her baby’s screening came back negative. Ms. Barrow-Wells, who now lives in Lawrenceville, Georgia, begged doctors to test her baby’s sweat to see if it had the high levels of salt that are a hallmark of the disease. She reminded them that her older son’s diagnosis meant the baby was at high risk.
But Jahsir’s pediatrician pointed to the negative test result as proof that her son was fine, she said, and told her to stop worrying.
Experts say that universal testing has given some doctors a false sense of security: While early detection has undoubtedly transformed diagnosis for the disease, state screening programs still miss children with cystic fibrosis, particularly those who aren’t white.
Jahsir was diagnosed with cystic fibrosis at 3 months old. “A person shouldn’t have to go through so much,” Ms. Barrow-Wells said.
A New Genomic Era, But Lingering Disparities
Cystic fibrosis is a progressive disease caused by defects in a single gene. It makes the mucus that coats the inside of the body thick and sticky. Instead of protecting the airways, the digestive tract and other organs and tissues, the mucus in people with cystic fibrosis causes blockages, damage and infections .
Nearly 40,000 Americans have cystic fibrosis, about 15 percent of whom are people of color, according to data from a Cystic Fibrosis Foundation patient registry .
The disease occurs when people inherit two defective copies of the gene, called CFTR — one from the mother and one from the father. People who inherit a single defective copy don’t develop the disease but can pass on the mutation.
Only a few decades ago, people with cystic fibrosis often died in childhood or adolescence. Scientific advances and public health initiatives, including newborn screening, have transformed the prognosis and quality of life for people living with it. Half of the babies born with cystic fibrosis in 2021 can expect to live to age 65 or older, according to the C.F.F.
Universal screening has helped doctors diagnose babies an average of three months sooner, said Dr. Clement Ren, the director of the Cystic Fibrosis Center at Children’s Hospital of Philadelphia. It has also provided a clearer picture of who actually has cystic fibrosis: The share of newly diagnosed patients who are Black or Hispanic increased from 9 percent in 2000 to 14 percent in 2020 . (This includes newborns as well as people who aren’t diagnosed until later in life.)
Dr. Ren said he recently diagnosed a Hispanic baby born in New Jersey who came to his hospital in Philadelphia, the closest cystic fibrosis center. “She was two weeks old,” Dr. Ren said. “That is the goal: to diagnose babies within the first month of life.”
The screening process starts before newborns leave the hospital, with a blood test for a protein that is commonly elevated in babies with cystic fibrosis. If a sample shows high levels, the newborn is then tested for genetic mutations. Scientists have identified hundreds of mutations that can drive the disease.
But the genetic tests now used are largely based on older clinical trials that enrolled mostly white children , focusing primarily on genetic mutations found in people of European ancestry, said Dr. Meghan McGarry, a pediatric pulmonologist at Seattle Children’s Hospital. As a result, they can miss babies with less common mutations that originated in Africa, Asia and Latin America.
One study examined nine screening panels commonly used across the United States and found that although they accurately identified an estimated 95 percent of white babies with cystic fibrosis, they missed, on average, 44 percent of Asian babies , 22 percent of Black infants and 14 percent of Hispanic, Native American and Alaskan Native babies.
Some states screen for more mutations than others. Wisconsin’s screening program is so robust — it tests for 689 mutations — that Montana, Kansas and Connecticut now send their newborn samples to the state.
New Jersey, which for years only screened for one mutation, now tests for 139 ; Pennsylvania and Florida have also expanded their screenings.
But in Mississippi, where nearly 38 percent of the population in 2020 was Black, newborns are still tested for only a single genetic variant that is primarily found in white people.
For many states, the biggest barrier is cost. The more mutations included in a screening panel, the greater the expense, said Dr. Rachel Linnemann, the director of the Children’s Healthcare of Atlanta and Emory University Cystic Fibrosis Care Center.
In Georgia, where Ms. Barrow-Wells lives, the cystic fibrosis screening program only tests for 39 variants. She is working with state officials to increase that number. Although Jahsir, now 3, is receiving therapy to protect his lungs and improve his nutrition, her older son has significant scarring on his lungs and pancreas. Five years ago, he needed emergency surgery for a collapsed lung caused by years of damage. Ms. Barrow-Wells said she felt fortunate that Jarrod, now 23, was able to take a new type of cystic fibrosis drug that is prolonging life for many patients.
The Shortfalls of Screening
Even states with robust screening programs can miss babies with rare genetic mutations. Cambrey Vasconez White, 34, requested genetic testing when she was pregnant. Her husband had a cousin with cystic fibrosis, meaning that he might carry one of the genetic mutations that causes the disease. Ms. White, who is Hispanic, wanted to know if she did, too.
In California, where Ms. White lives, the screening program tests for 75 mutations, including ones more commonly found among Hispanic people. Ms. White’s test came back negative , as did the newborn screening for her son, Rowland, born in 2021.
Ms. White didn’t believe the result: Rowland screamed and cried after breastfeeding, a common symptom of cystic fibrosis, which interferes with digestion and can cause stomach pain . Rowland also failed to gain weight. When he began to fall off his growth curve, Ms. White said, she pushed for more testing.
Some pediatricians are reluctant to order additional testing for babies who screen negative, even if they have signs of the disease, Dr. McGarry said, because they don’t realize that the screenings can be inaccurate or that nonwhite babies can inherit the disease.
“Parents are told, ‘Your child had a normal newborn screen. You are crazy.’ It’s becoming a barrier to care. That’s the opposite of what it was meant to be,” she said.
Doctors eventually agreed to further testing, and Rowland was diagnosed with cystic fibrosis at 6 months old. Rowland and both of his parents had rare mutations not included in California’s panel.
Rowland’s experience underscores why doctors can’t rely on screening alone, said Dr. Susanna McColley, a professor of pediatrics in pulmonary and sleep medicine at the Northwestern University Feinberg School of Medicine. She said that children who have symptoms or a sibling with the disease should be referred to a cystic fibrosis center for a definitive diagnostic test, called a sweat test, regardless of their screening results.
Before universal screening, doctors “used to do a lot more sweat tests for kids with poor growth, recurrent respiratory symptoms or both,” Dr. McColley said.
To better educate doctors and patients, the Cystic Fibrosis Foundation plans to release new screening guidelines this fall that promote racial equity. And both the foundation and the Centers for Disease Control and Prevention are funding efforts to improve screening — work Dr. McGarry said is sorely needed for families like Ms. Barrow’s.
“It can take a lot of persistence, determination and knowledge from the person with cystic fibrosis or the parent to get that diagnosis,” Dr. McGarry said. “Not every family has that.”
The Mysteries and Wonders of Our DNA
Women are much more likely than men to have an array of so-called autoimmune diseases, like lupus and multiple sclerosis. A new study offers an explanation rooted in the X chromosome .
DNA fragments from thousands of years ago are providing insights into multiple sclerosis, diabetes, schizophrenia and other illnesses. Is this the future of medicine ?
A study of DNA from half a million volunteers found hundreds of mutations that could boost a young person’s fertility and that were linked to bodily damage later in life.
In the first effort of its kind, researchers now have linked DNA from 27 African Americans buried in the cemetery to nearly 42,000 living relatives .
Environmental DNA research has aided conservation, but scientists say its ability to glean information about humans poses dangers .
That person who looks just like you is not your twin. But if scientists compared your genomes, they might find a lot in common .

IMAGES
VIDEO
COMMENTS
The prevalence of diabetes in schizophrenia has been estimated to be 2-3-fold higher than in the general population and estimates of prevalence range from 10 to 15% . In a study of over 400 patients with schizophrenia, the prevalence of diabetes and impaired glucose tolerance was 6.3% and 23.4%, respectively, in the total sample . Diabetes ...
T2D tended to be less intrusive than schizophrenia, and the mental surplus reflected the individual's current ability to deal with and manage disease-related changes. Schizophrenia symptoms fluctuated over time, impacting the prioritization of diabetes self-care.
Schizophrenia is directly and indirectly linked to diabetes. Research also suggests genetic and developmental risk factors can increase the risk for both conditions. Schizophrenia is a complex ...
Background Patients with schizophrenia are at least twice as likely to develop diabetes mellitus compared to the general population. This is of significance in Qatar given the high prevalence of obesity and diabetes. Furthermore, the lifespan of people with schizophrenia is shortened by approximately 15 years, partly due to long-term microvascular and macrovascular complications. High quality ...
Diabetes in people with schizophrenia is typically associated with an earlier age of onset than in the general population, and more diabetes-related complications; Treatment of type 2 diabetes in people with schizophrenia is generally the same as for those without schizophrenia. Lifestyle factors should be addressed and metformin used first line.
As in the general population, the prevalence of type 2 diabetes. in people with schizophrenia rises with age [ 5], and the risk of. type 2 diabetes in people with schizophrenia is 2- to 5-fold ...
Although a higher prevalence of diabetes has also been previously reported in schizophrenia (8, 9), disentangling the secondary and primary (endogenous) relationships has been difficult. Rajkumar et al. ( 3 ) used the large Danish registries to demonstrate that diabetes is associated with schizophrenia independently of antipsychotic drug treatment.
INTRODUCTION. People with severe mental illness, including schizophrenia, have two to three times higher mortality rates than the background population (Nielsen et al., 2013; Walker et al., 2015).Living with severe mental illness is associated with lifestyle behaviours that increase the risk of chronic physical illness such as type 2 diabetes (Stubbs et al., 2015; Vancampfort et al., 2017).
Type 2 diabetes mellitus (T2DM) is common among people with schizophrenia, with meta-analyses suggesting a prevalence rate of around 11%. 1, 2 Similarly, pre-diabetes (PD), defined as having impaired fasting glucose and/or impaired glucose tolerance, is prevalent among people with schizophrenia, with more than a quarter of the patients meeting ...
managing diabetes or its risk factors? DePaul University School of Nursing . Angelica Leon. Diabetes Management Interventions in Patients with Schizophrenia: An Integrative Review of the Literature . Methods. Diabetes and Schizophrenia thus would directly influence the patient intervention as it shifts the focus of the initiative to a diabetes
Individuals with psychotic disorders experience substantial health disparities with respect to diabetes, including increased risk of incident diabetes and of poor diabetes outcomes (eg, diabetes complications and mortality). Low-quality medical care for diabetes is a significant contributor to these poor health outcomes. A thoughtful approach to both diabetes pharmacotherapy and drug ...
The prevalence of type II diabetes among individuals suffering from schizophrenia or schizoaffective disorders is more than double that of the general population. By 2005, North American professional medical associations of Psychiatry, Diabetes, and Endocrinology responded by recommending continuous metabolic monitoring for this population to control complications from obesity and diabetes.
1. We have presented a detailed clinical report of a case of schizophrenia associated with a true diabetes mellitus. 2. Analysis of the literature and clinical experience reveals such a combination to be extremely rare, our case being but the second definitive one recorded. 3. We have commented briefly on the psychosomatic and constitutional significance of this clinical combination of diseases.
Background People with severe mental illnesses (SMIs) have reduced life expectancy compared with the general population. Diabetes is a contributor to this disparity, with higher prevalence and poorer outcomes in people with SMI. Aim To determine the impact of SMI on healthcare processes and outcomes for people with type 2 diabetes (T2DM). Design and setting Retrospective, observational ...
The mental health state dominates in relation to diabetes self-care and individuals experience challenges balancing between the two conditions. However, there exists a general acknowledgement for diabetes and its long-term complications as a serious medical condition demanding careful attention and treatment. Conclusion
The number of people with both illnesses is significant. People with schizophrenia are three times more likely than the general population to develop type 2 diabetes (Toich, 2017). Further, 20-30 percent of people with schizophrenia will develop diabetes type 2 (Cohn, 2012). These numbers are too high to dismiss as coincidence.
Searches for schizophrenia CPGs were conducted in MEDLINE/Embase from 1/1/2004-12/19/2019 and in guideline websites until 06/01/2020. Of 19 CPGs, 17 (89.5%) commented on first-episode ...
Much research has been done regarding the symptoms and treatment of schizophrenia and this essay will emphasize on the symptoms, physiology and treatment of schizophrenia ... avolition, and alogia) and medical morbidities (e.g. inflammation and diabetes) (Oishi, 2017). Cognitive damage is a major factor of schizophrenia and is not secondary to ...
Essay Example: Schizophrenia, a convoluted and frequently misconstrued psychological ailment, intricately alters an individual's cognition, emotions, and conduct. The fifth iteration of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), issued by the American Psychiatric Association.
Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book chapter, use the "Scholarly Articles and Book Chapters" deposit option.
Exploring sensory processing and sensory experience in everyday life for adults with schizophrenia: A collaborative approach Skip to Content. Carolina Digital Repository ... Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book ...
Schizophrenia; Skin cancer; Stroke; Type 2 diabetes; ... The study, published in Archives of Gerontology and Geriatrics, reviewed 35 papers examining the grief, loss, ...
This essay about Roe v. Wade explores the landmark Supreme Court decision of 1973, which affirmed a woman's constitutional right to choose whether to terminate her pregnancy. ... Diabetes Dementia Alcoholism Schizophrenia Epilepsy Alternative Medicine Anxiety Bipolar Disorder Ebola Virus Teenage Pregnancy. Leave your email and we will send a ...
Universal screenings for the inherited disease promised to get babies diagnosed and treated sooner. But they still miss some children of color.