2024 Best Online PhD in Health Services Research [Doctorate Guide]
A PhD in Health Services Research program could help you prepare for a career investigating complex issues that affect health services and public health.

Health services researchers study how economics, individual behavior, social structures, technology, and other factors influence the healthcare system. They analyze systemic problems like addiction, health disparities, and mental health disorders. Researchers in this field can also play a vital role in shaping public health policies.
Editorial Listing ShortCode:
If you enjoy data, medicine, and research, enrolling in an online PhD in Health Services Research program could be a strategic career move.

Universities Offering Online PhD in Health Services Research Degree Programs
Methodology: The following school list is in alphabetical order. To be included, a college or university must be regionally accredited and offer degree programs online or in a hybrid format.
Boston University
Boston University offers a PhD in Health Services Research. To graduate, students must complete about 42 credits of coursework and a dissertation. Potential courses include Research Theory and Design, Quantitative Methods for Health Services and Other Public Health Research, and Contemporary Structures of Health Services.
Boston University is accredited by the New England Commission of Higher Education.
Florida International University
Florida International University offers a PhD in Public Health with a concentration in Health Systems Research. This 70 credit program uses a hybrid format and is designed to help students finish their dissertations within 4 years. The curriculum focuses on applying systems thinking to improve population health.
Florida International University is accredited by the Southern Association of Colleges and Schools Commission on Colleges.
George Washington University
George Washington University offers a DHSc in Leadership in Clinical Practice and Education. This fully online program requires the completion of 48 credits and can potentially be completed in just 2.5 years. Potential courses include Interprofessional Collaboration in Practice, Practicum I and II, and Program Theory and Health Innovations.
GW is accredited by the Middle States Commission on Higher Education.
Loma Linda University
Loma Linda University offers an online program for a Doctor of Public Health that is open to applicants with little or no previous experience in the field of public health. Loma Linda’s online courses include synchronous meetings, and students are required to come to campus during the dissertation process. The program usually takes 3 to 5 years to complete.
Loma Linda University is accredited by the Western Association of Schools and Colleges.
University of South Florida
The University of South Florida offers a PhD in Public Health with a concentration in Health Services Research. The program requires the completion of at least 55 post-master’s credit hours, including a dissertation. Potential courses include History and Systems of Public Health, Introduction to Research Methods, and Applied Multivariate Statistical Methods.
The University of South Florida is accredited by the Southern Association of Colleges and Schools Commission on Colleges.
Online PhD in Health Services Research Programs

Health services research is a multidisciplinary field that uses qualitative and quantitative research methods to study and generate solutions for problems in the healthcare system.
Researchers examine how behavioral, cultural, economic, ethical, and political frameworks impact health services as well as people’s access to them. For example, a researcher could explore how economic inequalities in rural regions affect access to medical services, the cost of care, and patient outcomes.
Online health services doctoral programs prepare students to analyze and address the most urgent problems in healthcare today. Possible research areas include addiction, health disparities, immigrant health, maternal and child health policy, and population mental health.
Health services researchers draw on approaches and theories from many disciplines to investigate these complicated issues. Some of the topics that you may study during your PhD program include:
- Biostatistics
- Epidemiology
- Grant writing
- Health economics
- Health systems management
- Human rights
- Implementation science
- Medical technology
- Public health
- Quantitative research methods
- Research ethics
- Social and behavioral medicine
Throughout your doctoral studies, you’ll also have opportunities to hone your research skills inside and outside the online classroom. For instance, you may complete research-based course projects, applied research apprenticeships, and independent studies.
Most PhD in Health Services Research programs also require students to conduct original research and write a dissertation. Many doctorate holders remain in academia as instructors, postdoctoral fellows, and researchers. Other graduates secure positions in government agencies, private health-related corporations, or nonprofit organizations.
Possible job titles for professionals who hold a PhD in Health Services Research include:
- Core investigator
- Health policy consultant
- Program analyst
- Public health policy analyst
- Research director
- Health services researcher
- Senior policy manager
- University professor
If you have specific career goals, you could consider enrolling in an online health services research PhD program that offers relevant concentrations or graduate certificates. Possible areas of specialization in your online health services degree program may include bioinformatics, epidemiology, and health policy. Selecting a health services PhD program that allows you to pursue your research interests can help prepare you for your preferred career path.
Health Services Careers & Salaries
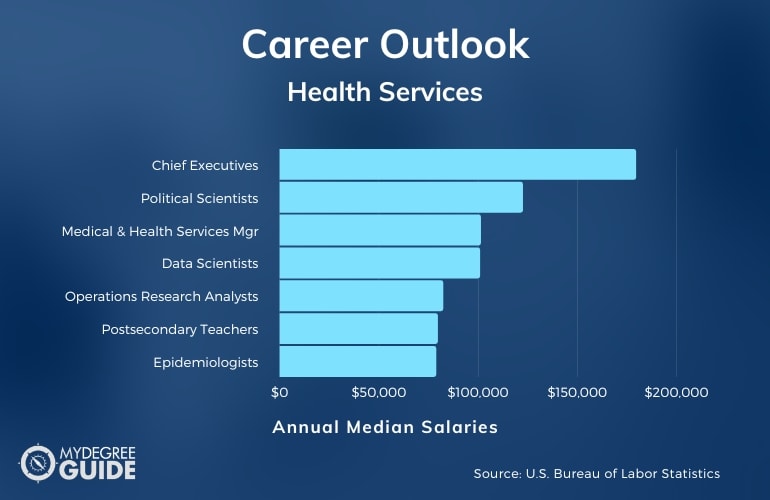
Demand for medical services has recently surged due to the aging population, public health crises like the COVID-19 pandemic, and other phenomena.
As a result, many organizations and political leaders have made it a priority to solve issues that impact healthcare access, equity, and policy. These groups often seek to hire skilled researchers who have graduated from healthcare PhD programs.
According to the Bureau of Labor Statistics , many careers associated with health services research pay above average wages and are projected to have faster than average job growth.
Your actual wage will depend on your employer, location, work experience, and other factors. The positions you can qualify for will also depend on your prior education, experience, and skill sets.
A doctorate in health services research can position you to take on a role in numerous industries and organizations. Potential work settings include hospitals, insurance companies, pharmaceutical companies, and other health systems.
Health services research professionals can also work for universities, research facilities, public health centers, nonprofit foundations, and federal and state government agencies.
Health Services Research PhD Curriculum & Courses

All online PhD programs in healthcare services research have unique curricula shaped by degree requirements, faculty expertise, and available concentrations. Here are some examples of courses you may be required to take:
- Clinical Outcomes Research: You’ll conduct clinical research using observational studies, randomized clinical trials, and other data-gathering methods.
- Cost Benefit Analysis for Health Services: This course explores the strengths and weaknesses of various approaches for conducting economic assessments of healthcare interventions and services.
- Foundations in Health Services Research: This course provides an overview of health services research scholarship.
- Grant Writing for Public Health Professionals: You can gain foundational grant writing skills and learn how to develop and evaluate budgets, organizational capacity, and partnerships.
- Health Decision Science: You’ll learn how to use quantitative methods like health economics and evidence-based medicine to make challenging decisions related to health services.
- Health and Human Rights: This class examines the intersections between human rights, public health policies, and political and social contexts.
- Legal Aspects of Public Health: You’ll study legal issues that influence the creation and management of public health initiatives.
- Methods in Health Services Research I: You’ll learn empirical techniques for health services research and best practices for implementing these methods.
- Methods in Health Services Research II: This course expands your knowledge of health services research by teaching econometric models and other advanced research methods.
- Policy Analysis for Population Health: You’ll develop strategies to advocate for policy changes, and you’ll conduct research on policy processes and outcomes related to population health.
Along with coursework, you may have the opportunity to complete research practicums or apprenticeships that allow you to develop hands-on research experience.
Admissions Requirements

All PhD in Health Research Services programs require a relevant bachelor’s or master’s degree. Other admissions criteria can vary among programs, but you may be required to submit these common materials:
- Curriculum vitae or resume
- GRE or GMAT test scores (not all programs require them)
- Letters of recommendation
- Personal statement
- Official transcripts
Many online healthcare PhD programs only admit a limited number of students, so competition can be fierce. Tailoring your application materials for each program is a strategic move that could help you stand out as a candidate.
Program Accreditation

As you research PhD programs, it’s beneficial to check each school’s accreditation status. Colleges with regional accreditation have undergone an external review process to verify that they provide students with a high-quality education.
Enrolling in an accredited doctoral program might make it possible to qualify for certain financial aid opportunities and transfer credits to another accredited school. Plus, many employers often prefer to hire candidates from accredited schools.
Many universities list their accreditation status on their website. You can also visit the US Department of Education ’s website to find accredited schools.
Financial Aid and Scholarships
When researching health services doctoral programs, you may also want to research financial aid opportunities. You might qualify for financial assistance that can decrease your upfront costs.
Many PhD programs provide graduate students with stipends, tuition waivers, and health insurance. In exchange for this funding package, students might be required to work as teaching assistants for undergraduate courses or to participate in research projects.
You can also complete the FAFSA application to determine your eligibility for federal aid. You may qualify for federal grants and work-study programs. Some PhD students also take out student loans from the federal government.
You may also qualify for scholarship opportunities. Your college might offer scholarships for incoming students who meet certain criteria. Some professional public health organizations also provide scholarships for graduate students studying health services.
What Is Health Services Research?

Health services research is an interdisciplinary field that uses diverse scientific methods and theoretical approaches to study pressing issues in healthcare.
These researchers investigate how complex frameworks—like cultural beliefs and economic systems—impact the accessibility, cost, and effectiveness of healthcare interventions. Many health services research professionals develop areas of expertise. For instance, a researcher may specialize in topics like:
- Health care inequalities
- Health policy and management
- Health outcomes measurement
- HIV and HCV
- Systems science methods
- Veteran health
Health services researchers can also play an essential role in guiding and reforming public health policy.
What Can You Do with a PhD in Health Services Research?

A PhD in Health Services Research helps prepare professionals for a range careers. Many PhD holders secure positions in academia as postsecondary teachers or researchers. Other graduates find employment with government agencies, where they can directly shape public health policies and laws.
Consulting firms, nonprofit organizations, and private corporations also hire professionals in this field. Potential roles in this area of expertise include research director, university professor, health services researcher, health policy consultant, policy analyst, and more.
How Long Does It Take to Get a Health Services Research PhD Online?

Most online PhD in Health Services Research programs take 3 to 5 years to complete if you enroll full-time. Most programs require 2 to 3 years of full-time coursework.
Some programs allow students to transfer credits from a master’s program, potentially reducing the time to finish the degree. After finishing your coursework, you’ll likely be required to write and defend a dissertation based on original research. Programs without a dissertation requirement can generally be completed in 3 years with full-time study.
Is a PhD in Health Services Research Worth It?

Yes, a PhD in Health Services Research is worth it for many students. This degree helps prepare you to tackle the issues affecting the healthcare system and public health today. As a researcher, you can play a direct role in developing innovative solutions to complicated healthcare problems, and you can help advocate for improved public health policies.
You may find a career in health services research particularly rewarding if you enjoy working with data and science. During your doctoral studies, you’ll have the opportunity to learn about analytical and scientific methods and theories from a range of disciplines.
Getting Your PhD in Health Services Research Online

Researching issues impacting health services often requires creativity, dedication, and a willingness to experiment with different methodologies.
You might consider earning a PhD in Health Services Research if you’re passionate about decreasing health disparities, improving access to medical services, and helping more people maintain healthy lifestyles. Many health services research PhD programs are available online to offer more flexibility for working professionals.
You can start this next step in your educational journey today by researching accredited colleges and universities that offer online doctoral programs in this field.

PhD, Health Services Research

Advance research, policy and practice to improve access, cost and quality of health services
The goal of this program is to provide interdisciplinary training in research, practice and policy analysis relevant to health programs.
- Request Info
Program Overview
The University of Maryland School of Public Health offers a Doctorate in Health Services Research (PhD). The program provides interdisciplinary training in research, practice, and policy relevant to the planning, management, and evaluation of clinical practice and public health programs. The program combines rigorous coursework with individual research mentoring.
See all Health Policy and Management graduate student resources .
For more information, see the Health Policy and Management flyer .
- To acquire a strong foundation of knowledge in the organizational, policy, economic and social factors which influence health and health services delivery;
- To acquire foundational and advanced research skills which result in the ability to develop an independent project in health services research;
- To demonstrate the ability to complete an independent project in health services research;
- To demonstrate oral and written communication skills appropriate for the dissemination of knowledge in health services research to both academic and professional/practitioner audiences
The Ph.D. in Health Services Research requires a minimum of 50 credits organized in four modules. Together with their advisor, students select 5 elective courses. After completing coursework, students must pass a written qualifying exam. All students then take an oral proposal defense before admission to candidacy. Once a candidate, students focus on their dissertation, culminating in an oral dissertation defense.
See the PhD program plan and competency checklist.
See the tentative schedule for HPM courses.
* The elective courses in the cognate area (track) are selected by the student and approved by the advisor.
PhD students are actively engaged in faculty research programs and their own independent scholarship. Participation in research activities ramps up in the first two years as students build and hone their skills. By the 3rd year, many students are formally employed as research assistants on faculty projects. Student scholarship is a critical component of the department’s research portfolio. Below are a few selected student-led journal manuscripts.
Andrew Andersen , Erin O’Rourke, Marshall Chin, et al. Promoting Health Equity and Eliminating Disparities Through Performance Measurement and Payment. Health Affairs 37(3); 2018.
Ivy Benejenk, Luisa Franzini, Dylan Roby, and Jie Chen . Disparities in Audio-only Telemedicine Use among Medicare Beneficiaries during the COVID-19 Pandemic. Medical Care 59(11); 2021.
Taehyun Kim , Daniel Marthey, and Michel Boudreaux. Contraceptive Access Reform and Abortion: Evidence from Delaware. Health Services Research 58(4); 2023.
Elle Pope and Neil Sehgal. Characterizing Industry Payments to US Teaching Hospitals and Affiliated Physicians: A Cross-Sectional Analysis of Open Payments Datasets from 2016 to 2022. Health Affairs Scholar 1(2); 2023.
Liyang Xie , Michel Boudreaux, and Luisa Franzini . Maryland’s Global Budget Revenue Program: Impact on Neonatal Intensive Care Unit Admissions and Infant Mortality. Medical Care. 59(8); 2021.
All admitted PhD students who enroll full-time and are not engaged in off-campus employment receive 2 years of full funding (stipend, tuition remission, and fringe benefits). After the 2nd year, students either join an externally funded project led by a faculty member or obtain their own independent support. Our students have obtained external support from AHRQ, RWJF, NQF, and other sources. Others have obtained internal support from competitive University of Maryland awards.
The department also offers competitive ad-hoc support for travel and for the purchase of dissertation materials (data, software, etc.). Many students obtain limited-time support through paid internships with federal agencies (e.g. AHRQ) that provide excellent opportunities to learn about non-academic research, policy and practice environments.
Below are organizations and agencies that provide funding opportunities to HSR PhD students before and during the dissertation phase.
- Agency for Healthcare Research and Quality
- SREB-State Doctoral Scholars Program – Dissertation Year Fellowship
- CDC Grants for Public Health Research Dissertation
- NSF Dissertation Improvement Grant
- Horowitz Foundation for Social Policy
- The Hewlett Foundation/IIE Dissertation Fellowship
- Russel Sage Foundation’s Dissertation Research Grant
- Aging Research Dissertation Awards To Increase Diversity
- Research Supplements To Promote Diversity In Health-Related Research
- Mental Health Dissertation Research Grants To Increase Diversity In The Mental Healt h Research Arena
- NIDA Substance Use/Substance Use Disorder Dissertation Research Award
- National Science Foundation East Asia And Pacific Summer Institutes For U.S. Graduate Students
- NSF Graduate Research Fellowships
- PhRMA Foundation Outcomes Research
- Susan G. Komen Breast Cancer Foundation Dissertation Research Program
- Many associations offer awards, e.g. Society of Family Planning.
The PhD program prepares students for careers in research and leadership in diverse settings. Graduates of the PhD program go on to careers in the public, private, and academic sectors. Recent placements include organizations such as PCORI, NIH, HRSA, CDC, VHA, Mathematica, NORC, Dartmouth College, Tulane University, Texas A&M University, University of Maryland, Baltimore County and the University of Pittsburg.
Alumni Spotlight

Suma Nair PhD, MS, RD obtained a PhD in Health Services Research from the University of Maryland in 2017. She currently serves as the Director of the Office of Quality Improvement (OQI) at the Health Resources and Services Administration. She leads and coordinates national and state technical assistance programs and activities, including those focused on special populations and the use of health information technology to drive clinical and operational quality improvements.

Andrew Anderson, Ph.D. began his studies at the University of Maryland in the Masters of Health Administration program (now, the MPH in Health Care Management). He moved on to the PhD program and graduated in 2019. He now serves as an assistant professor in the Department of Health Policy & Management at Johns Hopkins Bloomberg School of Public Health. His work aims to identify the social drivers of healthcare outcomes to inform the development of policy. During his time at UMD, he was a Robert Wood Johnson Foundation (RWJF) Health Policy Research Scholar.

Suited for...
- Individuals with a Master's Degree in Health Administration, Health Services, Public Health, Policy, Economics, Business Administration or a related field
- Individuals interested in the planning, administration, management and evaluation of health and public health programs

Program Highlights
- Flexible 50 credit program completed in 4-6 years
- Applied experiences in a variety of research settings
- Access to all the resources of a world-class University, located 15 miles from the nation's capital

Career Paths
- Health administration
- Federal, state, or local government policy analysis
- Research foundations (e.g., NORC, Think Tanks)
- Private sector research
Michel Boudreaux, PhD
Associate Professor Department of Health Policy and Management
[email protected] (301) 405-6118

PhD in Health Services Research and Health Policy
Doctoral program in health services research and health policy, rollins school of public health department of health policy and management.
The PhD in Health Services Research and Health Policy at the Rollins School of Public Health at Emory University is a full-time program that trains researchers in the fields of health policy, health economics, health management, and health services research.
Students take doctoral-level classes in the Department of Economics, the Department of Health Policy and Management, the Goizueta business school, and elsewhere throughout the university. Many students also collaborate with faculty on research.
Following the completion of their coursework, students work on their independent research for their dissertation.
What You’ll Learn
Students in our program take classes in one of two tracks: Economics or Organizations and Management .
Economics Track
Students in the Economics track take graduate-level classes in the Department of Economics, alongside students pursing a PhD in economics. The economics track prepares students to apply economic theory to evaluate topics in health and health policy.
Organizations and Management Track
Students in Organizations and Management take advanced and doctoral-level courses in Emory’s Goizueta School of Business. The track prepares students to examine questions pertaining to access, quality, cost of health care and health outcomes. Students in this track will learn how theories and concepts from fields such as organizational behavior and technology management can be applied to medicine and health care organizations.
Core Courses and More
All students in the program take classes in statistical methods, research design, and health policy seminar. Students have room to take electives, which could be any graduate-level class at Emory or nearby universities (Georgia State, Georgia Tech).
For more information, please see our program brochure and handbook .
What Can You Do With a Graduate Degree in Health Services Research and Health Policy?
The program prepares students for a variety of research-focused careers in academia, think tanks, foundations, government agencies, pharmaceutical firms, and consulting.
Our graduates are currently employed at:
- the American Cancer Society
- the Centers for Disease Control and Prevention
- the U.S. Department of Health and Human Services
- Emory University
- Weill Cornell Medical School
- Harvard Medical School
- IMPAQ International
- Johnson & Johnson
- MD Anderson
- National Taiwan University
- Northern Illinois University
- Northwestern University
- Taipei Medical University
- The Urban Institute
- Trilliant Health
- University of California at San Francisco
- Carnegie Mellon
- Washington University (St. Louis)
- The University of Virginia
We discourage applications from students who view a PhD as a credential or who want to focus exclusively on administration, management, or advocacy. There are other professional degrees that are better suited to those types of careers.
What Type of Research Will You Do in the Health Services Research and Health Policy PhD Program?
Students perform research on a wide variety of topics related to delivery of medical care, insurance, and the determinants of health. Some examples of the papers that students have published from their dissertations include:
The effect of Medicaid expansion on crime reduction: Evidence from HIFA-waiver expansions. Journal of Public Economics 2017. (Heifei Wen, Ph.D. 2015)
Heuristics in the delivery room. Science 2021. (Manasvini Singh, Ph.D. 2020)
Are two heads better than one or do too many cooks spoil the broth? The tradeoff between physician division of labor and patient continuity of care for older adults with complex chronic conditions. Health Services Research 2016. (Kenton Johnston, Ph.D. 2015).
Effect of Medicaid disenrollment on health care utilization among adults with mental health disorders. Medical Care 2019 (Xu Ji, Ph.D. 2017).
Patterns of use and survival outcomes of positron emission tomography for initial staging in elderly follicular lymphoma patients . Leukemia & Lymphoma 2017 (Ashish Rai, Ph.D. 2015)
Admissions Requirements
For detailed information about admissions, please see our program brochure .
Applicants should provide:
- a transcript,
- statement of purpose,
- resume/CV, and
- three letters of recommendation.
Please note:
- GRE scores are optional.
- Applicants do not need to have a master’s degree.
Visit Emory’s Laney Graduate School website to apply now .
You do not need to contact the program or faculty prior to applying. We give equal attention to all applications, regardless of whether applicants know faculty or have had prior contact with them. We do not routinely meet with applicants prior to the application deadline. However, if you have a specific question about the program that is not addressed in this document or would like to get a better sense if the program is a good fit for you, please send your question to the director, David Howard, [email protected] .
September 11, 2023
Application opens for Fall 2024
December 1, 2023
Application deadline
Late January-Early February, 2024
Offer letters sent to successful applicants

Program faculty
Students have wide leeway to work with faculty at any Emory school or department. Most students work with the faculty on the list below.
Department of Health Policy and Management
Kathleen Adams (Ph.D. Economics, University of Colorado) Risk behavior, maternal and child health, insurance coverage, Medicaid policy.
Sarah Blake (Ph.D. Public Policy, Georgia State/Georgia Institute of Technology) Maternal and child health, reproductive health, implementation science.
Puneet Chehal (Ph.D. Public Policy, Duke) Medicaid and chronic illness in underserved populations.
Janet Cummings (Ph.D. Health Policy, UCLA) Mental health and substance abuse policy.
Benjamin Druss (M.D., New York University) Mental health and substance abuse policy.
Maria Dieci (Ph.D. Health Policy, UC Berkeley) Health economics, global health and development economics.
Ilana Graetz (Ph.D. Health Policy, UC Berkeley) Health information technology, quality improvement.
David Howard (Ph.D. Health Policy, Harvard) Health economics, reimbursement policy, pharmaceutical markets.
Joseph Lipscomb (Ph.D. Economics, University of North Carolina) Health outcomes assessment and improvement.
Victoria Phillips (Ph.D. Economics, Oxford) Health economics, cost-effectiveness analysis.
Adam Wilk (Ph.D. Health Policy, University of Michigan) Access to care and Medicaid, coverage and payment for kidney failure treatment.
Courtney Yarborough (Ph.D. Public Policy, University of Georgia) Substance abuse policy, pharmaceutical markets.
Affiliated faculty in other departments at Emory
Michal Hórny (Ph.D. Health Services Research, Boston University) Department of Radiology. Health insurance benefit design, costs of care, price transparency, access to care.
Xu Ji (Ph.D. Health Policy, Emory) Department of Pediatrics. Health care quality, health outcomes, access to health care.
Dio Kavalieratos (Ph.D. Health Policy, University of North Carolina) Department of Family Medicine and Palliative Care. End-of-life care, implementation science.
Sara Markowitz (Ph.D. Economics, CUNY) Department of Economics. Health economics, labor economics, maternal and child health. Ian McCarthy (Ph.D. Economics, University of Indiana) Department of Economics. Health economics, industrial organization.
Evan Saltzman (Ph.D. Managerial Science and Applied Economics, University of Pennsylvania) Department of Economics. Health economics, industrial organization.
Current PhD Students
Lamont Sutton
Nada Boualam
Sonia Tetlow
Xinyue Zhang
Marissa Coloske
Martha Wetzel
Paul George
Jingxuan Zhao
Alex Soltoff
Elizabeth Staton
Zhuoqi Yang
Cristian Ramos
View the latest COVID-19 operational updates | Learn more
School of Public Health
A nationally top-ranked institution that offers a superior array of advanced degrees and is home to world-renowned research and training centers.
- Degrees & Programs
- Doctor of Philosophy (PhD)
Health Services Research, Policy & Administration PHD
- Community Engagement
- Student Resources
- Our PhD Students
- Recent Grads
- Cheré Williams [email protected]
- Director of Graduate Studies Karen Kuntz [email protected]
Transform healthcare with this multidisciplinary degree.
With a Health Services Research, Policy & Administration PhD you will engage in a multidisciplinary examination of the social, political, and economic forces that affect the organization, financing, and delivery of healthcare.
This program prepares students for a career in applied research as well as influencing policy that can have an impact on healthcare systems. Our graduates find meaningful and challenging positions at universities, government agencies, think tanks, health insurance providers, managed care organizations, and consulting firms.
- Program Brochure
Health Services Research, Policy & Administration PHD Profiles

Ben Weideman
I am working to build equitable outcomes for LGBTQIA+ people.
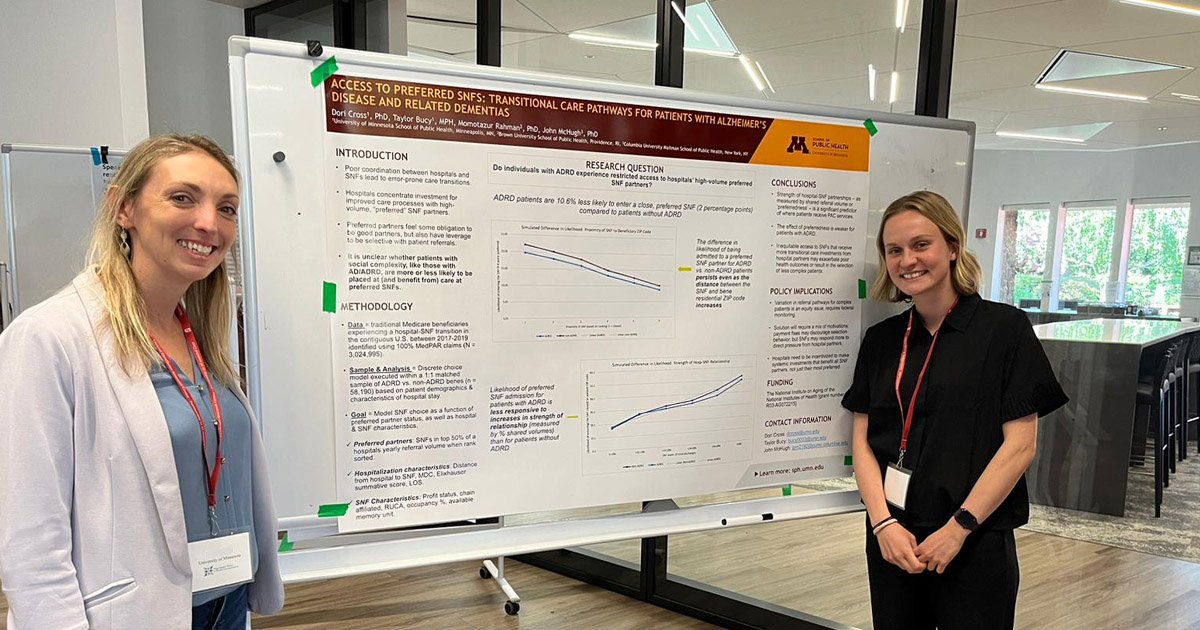
Taylor Bucy
I’m interested in the care experiences of older adults with serious mental illness.

Janet Porter
Janet Porter, PhD '94, is the 2018 recipient of the Gaylord Anderson Leadership Award.
Advantages of the Program
- Location. The School of Public Health is located within the Academic Health Center and a research university, allowing for collaboration and a multidisciplinary approach to learning.
- Tailored Options. Six areas of emphasis allow you to tailor your education to your interests. Our program also offers a joint degree in Law, Health and the Life Sciences (JD/PhD) with the Law School and an MD/PhD joint degree with medicine. More on joint and dual degrees.
- Collaborative Degree. Through a collaboration with the Division of Environmental Health Sciences, you can focus your studies on workplace injury policy with the Occupational Health Services Research and Policy PhD .
- Breadth. The Division of Health Policy and Management is home to five research centers that provide research opportunities to students and are rich sources for dissertation data.
Connect with Us
- Request More Information
- Prospective Students
- Current Students

Contact 420 Delaware St. S.E. Minneapolis, MN 55455
612-626-3500 [email protected]
- Degrees Offered
PhD in Health Services
Description.
The PhD Program in Health Services trains health services researchers and health policy analysts for careers in academic institutions, health delivery systems, public health departments, government agencies, and the private sector. The program prepares students to conduct high-quality independent, collaborative research and policy analysis by offering multidisciplinary, applied research opportunities on a wide variety of topics under the close mentorship of faculty. Students obtain advanced knowledge of the determinants of population health and of the health care system and they are exposed to several competing theoretical frameworks for conceptualizing both population health and the provision of health care. They develop research skills to identify and critically analyze the social, behavioral and health system effects on health and how organization, delivery, financing, and management of health services affect system performance.
Likely Careers
Health services researchers in academic institutions, health delivery systems, public health departments, government agencies, and the private sector, including insurance, pharmacy and biotechnology industries.
Applicants who have a bachelor, master, or professional degree in a field related to health services are given preference over applicants who do not have such experience.
Application Deadline: December 15
Application Deadline: Dec. 15, for Autumn Quarter entry
Competencies
Upon satisfactory completion of the PhD in Health Services, graduates will be able to:
- Meet the learning objectives of the MS program in Health Services ;
- Demonstrate comprehensive understanding of the determinants, trends and major issues confronting U.S. health care/policy and its effect on individual and population health and health inequalities;
- Critically appraise journal articles, evaluate the evidence, synthesize findings, draw inferences and apply alternative theoretical and conceptual models from a range of relevant disciplines to health services (HS);
- Use knowledge of the structures, process/quality, performance, policy, and environmental context to formulate solutions for health and health care problems;
- Explain how to collect primary health and health care data obtained by survey, abstracts of medical records (including electronic medical records), and qualitative or mixed methods;
- Assemble secondary data from existing public and private sources and apply various statistical techniques to answer HS questions;
- Develop in-depth substantive/disciplinary knowledge and method skills in an area of emphasis and apply to health services problems demonstrating application of AoE to dissertation work;
- Ensure the ethical and responsible conduct of research in the design, implementation and dissemination of HS research;
- Critically appraise grants, understand the grant writing and review process, write research proposals, and Final Dissertation Proposal approved by faculty as part of the general examination;
- Work collaboratively in multidisciplinary teams;
- Conduct an independent HS research study of publishable quality, characterized by conceptual and methodological rigor, as well as practical value;
- Effectively communicate issues, research findings, and implications of HS through multiple modalities to appropriate professional, scientific, policy, and lay audiences;
- Collaborate with policy makers, organizations, and communities to plan, conduct and translate research into health policy and practice; and
- Participate and assist in teaching or clinical practice while in the program.
Boston University Academics
Boston University
- Campus Life
- Schools & Colleges
- Degree Programs
- Search Academics
PhD in Health Services & Policy Research
For contact information, please visit the School of Public Health website .
The Doctor of Philosophy in Health Services & Policy Research (PhD) degree program offered by the Department of Health Law, Policy & Management is designed to provide individuals with excellent research skills for use in academic, industry, or government settings. Students have the opportunity to collaborate with senior faculty in innovative research crucial to the improvement of healthcare delivery, treatment outcomes, and government policies. Graduates are known for their excellent methodological skills and substantive knowledge of healthcare settings and policies, competencies that enable students to translate research findings into practical applications.
The doctoral program supports a focus on quantitative methods and qualitative methods, while fostering facility with mixed methods designs.
Learning Outcomes
Upon completion of the PhD in Health Services & Policy Research (HSPR), the graduate is able to:
- Analyze key factors that have the potential to influence health and provision and use of health services. These may include policy, organization, and financing of healthcare services. They may also include social, economic, cultural, political, and biological factors that influence population health, health equity, and the use of services.
- Critique, adapt, and develop theoretical analyses of health services and policies, including explanations of their structures and processes, the use of health services, the effectiveness and implementation of health policies, and the effects of health services and policies on individual and population health and health equity. This may be done by drawing upon the foundational fields of sociology, economics, anthropology, political science, psychology, demography, epidemiology, management, and/or organizational science.
- Develop original, relevant, and important research questions to pursue in HSPR that are grounded in both a critical analysis of prior HSPR literature and relevant theoretical perspectives.
- Identify and analyze the strengths and weaknesses of a variety of possible study designs that can appropriately address specific HSPR questions. Appropriate methods may employ experimental or observational approaches, qualitative or quantitative analytic techniques, and a variety of data types.
- Based on relevant theory and selected research question(s), develop an HSPR design, specifying study constructs, research objectives, hypotheses, and methods that reliably and validly measure outcomes of interest. Select optimal analytical approaches, in combination as necessary, to investigate hypotheses.
- Acquire and manage appropriate data to answer HSPR questions. Collect and manage primary health and healthcare utilization data and/or assemble and manage existing data from public and private data sources in accordance with an original research design.
- Apply appropriate analytical techniques to data in order to investigate HSPR questions. Utilize appropriate combinations of analytic techniques to enrich data analysis and interpretation.
- Develop, document, and employ procedures that ensure the reproducibility of the science, the responsible use of resources, mutual accountability with collaborators, and the ethical treatment of research subjects.
- Effectively communicate the process, findings, and implications of HSPR using multiple modes, including via peer-reviewed publications, oral presentations, and electronic media. Translate findings to multiple stakeholders and audiences including funders, research participants, colleagues, policymakers, news media, and managers.
Program Requirements
The doctoral program includes the coursework requirements outlined below, which typically total at least 42 credits. Students with an earned master’s degree may take fewer courses, if course waivers are granted based on previous relevant graduate coursework. However, in all cases, students are required to take no fewer than 32 credits of PhD coursework in residence at Boston University post-matriculation into the PhD program. A minimum grade of a B is required in all PhD coursework.
Foundations of Public Health
Effective public health requires expertise from many disciplines, and students need to have a broad foundation of knowledge across these diverse disciplines in order to collaborate effectively with other health professionals.
SPH PH 700 Foundations of Public Health (0 credits) is an online course designed to provide students with foundational knowledge in the profession and science of public health and factors related to public health. PH 700 meets the foundational knowledge criteria (as outlined by CEPH) for all SPH students.
Core PhD Courses
- SPH PH 842 Research Theory and Design (2 cr)
- SPH PH 843 Quantitative Methods for Health and Social Policy Research (2 cr)
- SPH PH 844 Introduction to Qualitative Methods for Health and Social Policy Research (2 cr)
- SPH PM 820 Introduction to Quality Measurement and Evaluation (2 cr)
- SPH PM 822 Advanced Quantitative Methods for Health and Social Policy Research (4 cr)
- SPH PM 828 Advanced Qualitative Methods (4 cr)
- SPH PM 842 Health Economics for Health and Social Policy Research or equivalent (4 cr)
- SPH PM 846 Advanced Quantitative Policy and Program Implementation and Evaluation (4 cr)
- SPH PM 864 Contemporary Structures of Health Services (2 cr)
- SPH PM 866 Theory in the Analysis of Health Services (2 cr)
Additional Course Requirements
- Healthcare Policy
- Implementation Science/Organizational Change
- Quality/Outcomes
Students are required to complete all the requirements for graduation within seven years of matriculation. PhD students are required to successfully complete the qualifying process, and complete and orally defend a dissertation.
Students who have completed the PhD coursework must register for SPH PM 980 Continuing Study each fall and spring semester until the dissertation is defended and accepted. PM 980 is ungraded and zero credits; it allows a student to be certified as full time and carries the equivalent of a 2-credit tuition charge plus the fee for student health insurance (unless waived). Students must adhere to dissertation submission deadlines and requirements.
All PhD students must adhere to the Doctoral Graduation Calendar in preparing and submitting the dissertation.
All SPH students will need a laptop or tablet for classes, purchased according to the recommendations of the Medical Campus Information Technology professionals.
Related Bulletin Pages
- Abbreviations and Symbols
Beyond the Bulletin
- School of Public Health
- SPH Admissions
- SPH Academic Calendar
- Master of Public Health
- Executive Master of Public Health
- Health Equity
- Dual Degree Programs
- Business Administration & Public Health
- Genetic Counseling & Public Health MS/MPH
- Medical Sciences & Public Health MS/MPH
- Medicine & Public Health MD/MPH
- Social Work & Public Health MSW/MPH
- Doctor of Public Health in Leadership, Management & Policy
- Applied Biostatistics
- Biostatistics
- Environmental Health
- Epidemiology
- Health Services & Policy Research
- Population Health Research
- Boston Consortium
- Departments
Terms of Use
Note that this information may change at any time. Read the full terms of use .
related websites
Accreditation.
Boston University is accredited by the New England Commission of Higher Education (NECHE).
- © Copyright
- Mobile Version
University of Washington
Health Systems and Population Health
School of public health.

- Health Services Doctor of Philosophy
- Academic Experience
- Academic Programs
Advance the Future of Public Health Research
3-5 years / full time / seattle, wa.
The University of Washington Health Services Doctor of Philosophy (Ph.D.) program trains the next generation of health services researchers and prepares them to become leaders in the field. Our graduates pursue research careers in top-tier universities, research and policy-making organizations, the health care industry, and government agencies. Recognizing the complex issues facing health services today and tomorrow, Health Services Ph.D. faculty and staff are committed to training students who will contribute to the health of diverse populations by producing high-quality, collaborative research on important topics and translating the results to practice and policy.
The Health Services Ph.D. program consistently ranks among the best in the United States. Our program offers exceptional instruction in research methods, evaluation, health care systems, health policy research, anti-racism, and the social determinants of health (the conditions of where people live, learn, work, worship and/or play).
Join our program and help make a difference in public health research.

Gain Unique Training
Our interdisciplinary Ph.D. program stands apart from others because of our team, curriculum, dedication to including anti-racist pedagogy in classrooms, and ongoing support for students and alumni.

Advance Public Health Research
All Ph.D. students are required to write a dissertation that significantly advances the state of knowledge in their chosen field, including having work published in academic journals.

Receive Expert Mentorship
Faculty are involved locally, nationally, and internationally in health services research and policy. They play an important role in improving health and shaping health care systems and policy worldwide.

Join Our Success
Our program attracts and welcomes strong scholars from unique and diverse backgrounds who have a passion for research. We aim to match each incoming student with funding and strong mentorship.
Application Dates
Application Opens September 1, 2024
Deadline December 15, 2024
Note: The program is no longer accepting applications for Autumn 2024 entry.
Information Sessions
Prospective Health Services Ph.D. students can register for and attend an information session to learn more about the program.
Stay Up-to-Date
Considering the Health Services PhD program? Sign up to receive email updates about upcoming application deadlines and more.
Alumni Connections
Health Services Ph.D. alumni can stay connected, learn about what their peers are doing, and support future public health professionals.
Our Social Media
Support students.
Help support future public health leaders today! Make a gift to a scholarship fund, such as the Health Systems Excellence, Equity, and Distinction (HSEED) Award.
MD/PhD Program
The Medical Scientist Training Program (MSTP) of the University of Pittsburgh and Carnegie Mellon University offers exceptionally talented individuals the opportunity to undertake a physician-scientist training program tailored to their specific research interests. During a period of 6–8 years, students meet the degree requirements of both a graduate school and the medical school, thus acquiring the knowledge, skills, and experience to begin careers in some of the most exciting areas of medical research.
The PhD Program in Health Services Research and Policy at the University of Pittsburgh’s Graduate School of Public Health, in the Department of Health Policy and Management, is one of 22 graduate programs participating in the MSTP that foster the development of future biomedical researchers by providing the highest quality of graduate medical training. The PhD program in Health Services Research and Policy was created to meet an ongoing need for public health researchers who focus on cost, access and quality of the health care system.
The graduate program provides students with the knowledge and skills to lead research programs in a range of institutional settings including...
- Not-for-profit research organizations and think-tanks
- State and federal government agencies
- Health systems
- Health plans and managed care organizations
The Institute of Medicine defines Health Services Research as a “Multi-disciplinary field of inquiry, both basic and applied, that examines the use, costs, quality, accessibility, delivery, organization, financing and outcomes of health care services to increase knowledge and understanding of the structures, processes and effects of health services for individuals and populations.”
The mission of the Doctoral Program in Health Policy and Management is to train students for excellence in conducting health services research and teaching health services research and policy.
Students undertake a rigorous program of study that encompasses research skills and quantitative analysis and provides a strong theoretical grounding in health policy, economics, statistics, health behavior, law and ethics. Students will develop an area of expertise, for example...
- Health economics
- Clinical decision sciences and modeling
- Policy and public programs
MD/PHD Curriculum Overview
MSTP students take a leave of absence from medical school courses to enroll in the Graduate School of Public Health between the second and third years of medical school and to complete the PhD coursework, conduct research, and defend their dissertation. All MSTP students in HSRP will have conducted three summer research rotations as medical students prior to beginning graduate training and therefore will have an identified HSRP faculty mentor at the point of entering graduate training.
Course and Examination Requirements
- Course requirements
- Program handbook (examination requirements are outlined under the Milestones section)
Program Faculty
View a list of faculty members.
Coronavirus (COVID-19): Latest Updates | Visitation Policies Visitation Policies Visitation Policies Visitation Policies Visitation Policies | COVID-19 Testing | Vaccine Information Vaccine Information Vaccine Information
Health Services Research and Policy

Our application for fall 2024 is now closed.
Health Services Research and Policy PhD Program
Since 1994, the PhD program in Health Services Research and Policy in the Department of Public Health Sciences has been highly successful in preparing students to become scholars for research, teaching, and public service careers in university, public policy, and governmental settings.
Our PhD program has also been designated as a STEM (Science, Technology, Engineering and Mathematics) program since 2010. Set within a large medical center with all its clinical research resources and collaborative faculty, our program focuses on interdisciplinary application of the social and behavioral science disciplines to real world health issues such as the organization, financing, and delivery of health care; the quality and safety of care; health outcomes; and the management of population health.
Read A Welcome Message from the Director
Program Highlights
- Our PhD program is designed to produce researchers who generate knowledge and strategies used in solving healthcare problems.
- Interdisciplinary courses, research and teaching, provide candidates with a broad range of skills.
- Our Ph.D. can be combined with other degrees such as the M.P.H. or M.D.
- Stipends, tuition grants, training and travel expenses are provided for doctoral study.
- The program prepares students for a career in academia, government or the private sector.
- Our PhD program exists within the Department of Public Health Sciences, which also houses MS programs in Epidemiology, Public Health, Health Services Research, and Clinical Investigations, and a PhD program in Epidemiology.
Current PhD Students
PhD Graduates
Primary Faculty
Publications per year
What Sets Us Apart

Information on core courses, electives, lab rotations to guide you through our program

We support and guide trainees in several areas of research. Browse research by current program trainees

Mentor Relationships
Our program faculty offer a wide range of research experience to mentor you towards your Ph.D.
Discover Public Health Sciences
Latest News
May 10, 2024 Dr. Melissa Kah Poh Loh has been recognized as a recipient of the 40 Under 40 in Cancer Award
April 4, 2024 March Health Equity Update
March 28, 2024 Air Quality in Schools: Shielding Kids with Intellectual and Developmental Disabilities from COVID
Upcoming Events
There is no upcoming seminar scheduled.
All Events »
What Our Students Say...

"I chose the University of Rochester's Health Services Research and Policy program because the faculty and staff provide students with a supportive environment to develop their research ideas. The program also has a flexible curriculum. Students can take classes offered by other departments- i.e., data science, psychology."
Hometown: Zhejiang, China
Undergraduate Degree: Finance
Areas of Interest: Health Economics; Price Transparency in Healthcare; Quality and Cost; Econometric Modeling
For information related to the doctoral degree program in Health Services Research and Policy, please contact:
Yue Li, PhD , Director
Health Services Research and Policy Doctoral Program Department of Public Health Sciences University of Rochester Medical Center
Office: (585) 275-3276 Fax: (585) 461-4532
Connect With Us On Social Media

Beyond Education. Experience.
Graduate programs.
- Professional Doctorate
- Certificate
- Professional Doctorate Programs
- Master’s Programs
- Certificate Programs
- Financial Aid
- Event Calendar
Experiential Learning

Should I Go To Grad School: 4 Questions to Consider
Global Reach
Experience our network..
Campus Locations
Career outcome.

- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Concentration in Health Services Research and Policy
Offered By: Department of Health Policy and Management
Onsite | Full-Time | 4 - 5 years
- MAS Application Fee Waiver Requirements
- Master of Arts (MA) in Geography and Environmental Engineering
- Master of Arts and Master of Science in Public Health (MA/MSPH)
- Master of Arts in Public Health Biology (MAPHB)
- Master of Bioethics (MBE)
- Mission, Vision, and Values
- Student Experience
- Program Outcomes
- For Hopkins Undergraduate Students
- Master of Health Science (MHS) - Department of Biochemistry and Molecular Biology
- Master of Health Science (MHS) - Department of Epidemiology
- Alumni Update
- MHS Combined with a Certificate Program
- Master of Health Science (MHS) - Department of Molecular Microbiology and Immunology
- Alumni Highlights
- Post-Baccalaureate Program in Environmental Health for Pre-Medicine Students
- Bachelor's/MHS in Health Economics and Outcomes Research
- MHS HEOR Careers
- Frequently Asked Questions
- Master of Health Science (MHS)
- Concurrent School-Wide Master of Health Science Program in Biostatistics
- Master of Health Science - Department of Population, Family and Reproductive Health
- Master of Health Science Online (MHS) - Department of Population, Family and Reproductive Health
- Careers in Health Economics
- Core Competencies
- Meet the Director
- What is Health Economics
- MPH Capstone Schedule
- Concentrations
- Online/Part-Time Format
- Requirements
Tuition and Funding
- Executive Board Faculty
- Master of Science (MS) in Geography and Environmental Engineering
- Independent Professional Project and Final Essay
- Program Objectives and Outcomes
- Internships
- Master of Science (ScM) - Department of Biochemistry and Molecular Biology
- Master of Science (ScM) - Department of Biostatistics
- Master of Science (ScM) - Department of Epidemiology
- Master of Science (ScM) - Department of Molecular Microbiology and Immunology
- ScM Faculty Advisers
- Master of Science in Engineering (MSE) in Geography and Environmental Engineering
- Bachelor's/MSPH in Health Policy
- FAQ for MSPH in Health Policy
- Field Placement Experience
- MSPH Capstone
- MSPH Practicum
- Required and Elective Courses
- Student Timeline
- Career Opportunities
- 38-Week Dietetics Practicum
- Completion Requirements
- MSPH/RD Program FAQ
- Program Goals
- Master's Essay Titles
- Application Fee Waiver Requirements
- Doctor of Philosophy (PhD) - Department of Biostatistics
- Doctor of Philosophy (PhD) - Department of Epidemiology
- Program Goals and Expectations
- Doctor of Philosophy (PhD) - Department of Molecular Microbiology and Immunology
- Doctor of Philosophy (PhD) - Department of Population, Family and Reproductive Health
- Doctor of Philosophy (PhD) in Clinical Investigation
- Track in Environmental Sustainability, Resilience, and Health
- Track in Exposure Sciences and Environmental Epidemiology
- Track in Health Security
- Track in Toxicology, Physiology and Molecular Mechanisms
- PhD in Geography and Environmental Engineering Faculty Advisers
- Recent Graduates and Dissertation Titles
- PhD Funding
- PhD TA Requirement
- Recent Dissertation Titles
- JHU-Tsinghua Doctor of Public Health
- Core Course Requirements
- Concentration in Women’s and Reproductive Health
- Custom Track
- Concentration in Environmental Health
- Concentration in Global Health: Policy and Evaluation
- Concentration in Health Equity and Social Justice
- Concentration in Health Policy and Management
- Concentration in Implementation Science
- Meet Current Students
- Combined Bachelor's / Master's Programs
- Concurrent MHS Option for BSPH Doctoral Students
- Concurrent MSPH Option for JHSPH Doctoral students
- Doctor of Medicine and Doctor of Philosophy (MD/PhD)
- Adolescent Health Certificate Program
- Bioethics Certificate Program
- Climate and Health Certificate Program
- Clinical Trials Certificate Program
- Community- Based Public Health Certificate Program
- Demographic Methods Certificate Program
- Environmental and Occupational Health Certificate Program
- Epidemiology for Public Health Professionals Certificate Program
- Evaluation: International Health Programs Certificate Program
- Food Systems, the Environment and Public Health Certificate Program
- Frequently Asked Questions for Certificate Programs
- Gender and Health Certificate Program
- Gerontology Certificate Program
- Global Digital Health Certificate Program
- Global Health Certificate Program
- Global Health Practice Certificate Program
- Health Communication Certificate Program
- Health Disparities and Health Inequality Certificate Program
- Health Education Certificate Program
- Health Finance and Management Certificate Program
- Health and Human Rights Certificate Program
- Healthcare Epidemiology and Infection Prevention and Control Certificate Program
- Humane Sciences and Toxicology Policy Certificate Program
- Humanitarian Health Certificate Program
- Implementation Science and Research Practice Certificate Program
- Injury and Violence Prevention Certificate Program
- International Healthcare Management and Leadership Certificate Program
- Leadership for Public Health and Healthcare Certificate Program
- Lesbian, Gay, Bisexual, Transgender, and Queer (LGBTQ) Public Health Certificate Program
- Maternal and Child Health Certificate Program
- Mental Health Policy, Economics and Services Certificate Program
- Non-Degree Students General Admissions Info
- Pharmacoepidemiology and Drug Safety Certificate Program
- Population Health Management Certificate Program
- Population and Health Certificate Program
- Product Stewardship for Sustainability Certificate Program
- Public Health Advocacy Certificate Program
- Public Health Economics Certificate Program
- Public Health Informatics Certificate Program
- Public Health Practice Certificate Program
- Declaration of Intent - Public Health Preparedness
- Public Health Training Certificate for American Indian Health Professionals
- Public Mental Health Research Certificate Program
- Quality, Patient Safety and Outcomes Research Certificate Program
- Quantitative Methods in Public Health Certificate Program
- Requirements for Successful Completion of a Certificate Program
- Rigor, Reproducibility, and Responsibility in Scientific Practice Certificate Program
- Risk Sciences and Public Policy Certificate Program
- Spatial Analysis for Public Health Certificate Program
- Training Certificate in Public Health
- Tropical Medicine Certificate Program
- Tuition for Certificate Programs
- Vaccine Science and Policy Certificate Program
- Online Student Experience
- Online Programs for Applied Learning
- Barcelona Information
- Fall Institute Housing Accommodations
- Participating Centers
- Registration, Tuition, and Fees
- Agency Scholarship Application
- General Scholarship Application
- UPF Scholarship Application
- Course Evaluations
- Online Courses
- Registration
- General Institute Tuition Information
- International Students
- Directions to the Bloomberg School
- All Courses
- Important Guidance for ONSITE Students
- D.C. Courses
- Registration and Fees
- Cancellation and Closure Policies
- Application Procedures
- Career Search
- Current Activities
- Current Trainees
- Related Links
- Process for Appointing Postdoctoral Fellows
- Message from the Director
- Program Details
- Admissions FAQ
- Current Residents
- Elective Opportunities for Visiting Trainees
- What is Occupational and Environmental Medicine?
- Admissions Info
- Graduates by Year
- Compensation and Benefits
- How to Apply
- Academic Committee
- Course Details and Registration
- Tuition and Fees
- ONLINE SOCI PROGRAM
- Principal Faculty
- Johns Hopkins RAPID Psychological First Aid
- General Application
- JHHS Application
- Areas of Study
- Important Dates
- Our Faculty
- Welcome Letter
- Descripción los Cursos
- Programa en Epidemiología para Gestores de Salud, Basado en Internet
- Consultants
- Britt Dahlberg, PhD
- Joke Bradt, PhD, MT-BC
- Mark R. Luborsky, PhD
- Marsha Wittink, PhD
- Rebekka Lee, ScD
- Su Yeon Lee-Tauler, PhD
- Theresa Hoeft, PhD
- Vicki L. Plano Clark, PhD
- Program Retreat
- Mixed Methods Applications: Illustrations
- Announcements
- 2023 Call for Applications
- Jennifer I Manuel, PhD, MSW
- Joke Bradt, PhD
- Josiemer Mattei, PhD, MPH
- Justin Sanders, MD, MSc
- Linda Charmaran, PhD
- Nao Hagiwara, PhD
- Nynikka R. A. Palmer, DrPH, MPH
- Olayinka O. Shiyanbola, BPharm, PhD
- Sarah Ronis, MD, MPH
- Susan D. Brown, PhD
- Tara Lagu, MD, MPH
- Theresa Hoft, PhD
- Wynne E. Norton, PhD
- Yvonne Mensa-Wilmot, PhD, MPH
- A. Susana Ramírez, PhD, MPH
- Animesh Sabnis, MD, MSHS
- Autumn Kieber-Emmons, MD, MPH
- Benjamin Han, MD, MPH
- Brooke A. Levandowski, PhD, MPA
- Camille R. Quinn, PhD, AM, LCSW
- Justine Wu, MD, MPH
- Kelly Aschbrenner, PhD
- Kim N. Danforth, ScD, MPH
- Loreto Leiva, PhD
- Marie Brault, PhD
- Mary E. Cooley, PhD, RN, FAAN
- Meganne K. Masko, PhD, MT-BC/L
- PhuongThao D. Le, PhD, MPH
- Rebecca Lobb, ScD, MPH
- Allegra R. Gordon, ScD MPH
- Anita Misra-Hebert, MD MPH FACP
- Arden M. Morris, MD, MPH
- Caroline Silva, PhD
- Danielle Davidov, PhD
- Hans Oh, PhD
- J. Nicholas Dionne-Odom, PhD RN ACHPN
- Jacqueline Mogle, PhD
- Jammie Hopkins, DrPH, MS
- Joe Glass, PhD MSW
- Karen Whiteman, PhD MSW
- Katie Schultz, PhD MSW
- Rose Molina, MD
- Uriyoán Colón-Ramos, ScD MPA
- Andrew Riley, PhD
- Byron J. Powell, PhD, LCSW
- Carrie Nieman MD, MPH
- Charles R. Rogers, PhD, MPH, MS, CHES®
- Emily E. Haroz, PhD
- Jennifer Tsui, Ph.D., M.P.H.
- Jessica Magidson, PhD
- Katherine Sanchez, PhD, LCSW
- Kelly Doran, MD, MHS
- Kiara Alvarez, PhD
- LaPrincess C. Brewer, MD, MPH
- Melissa Radey, PhD, MA, MSSW
- Sophia L. Johnson, PharmD, MPH, PhD
- Supriya Gupta Mohile, MD, MS
- Virginia McKay, PhD
- Andrew Cohen, MD, PhD
- Angela Chen, PhD, PMHNP-BC, RN
- Christopher Salas-Wright, PhD, MSW
- Eliza Park MD, MS
- Jaime M. Hughes, PhD, MPH, MSW
- Johanne Eliacin, PhD, HSPP
- Lingrui Liu ScD MS
- Meaghan Kennedy, MD
- Nicole Stadnick, PhD, MPH
- Paula Aristizabal, MD
- Radhika Sundararajan, MD
- Sara Mamo, AuD, PhD
- Tullika Garg, MD MPH FACS
- Allison Magnuson, DO
- Ariel Williamson PhD, DBSM
- Benita Bamgbade, PharmD, PhD
- Christopher Woodrell MD
- Hung-Jui (Ray) Tan, MD, MSHPM
- Jasmine Abrams, PhD
- Jose Alejandro Rauh-Hain, MD
- Karen Flórez, DrPH, MPH
- Lavanya Vasudevan, PhD, MPH, CPH
- Maria Garcia, MD, MPH
- Robert Brady, PhD
- Saria Hassan, MD
- Scherezade Mama, DrPH
- Yuan Lu, ScD
- 2021 Scholars
- Sign Up for Our Email List
- Workforce Training
- Cells-to-Society Courses
- Course/Section Numbers Explained
- Pathway Program with Goucher College
- The George G. Graham Lecture
About the Concentration in Health Services Research and Policy
The PhD concentration in Health Services Research and Policy provides a firm grounding in public health principles, research and evaluation methods, policy analysis and numerous content areas related to health and health services delivery and population health. The program at Johns Hopkins is one of the oldest and most respected of its type in the nation.
In this concentration, students acquire the conceptual and methodological tools needed to conduct research, program evaluation, and policy analysis and synthesis to advance the state of knowledge. The curriculum emphasizes the following areas: public and private sector health insurance and financing, organization and delivery of health care, methods for measuring and improving quality and safety of medical care, methods to measure personal and population health status, methods for assessing the impact of government health care policy on individuals and populations, and patient-centered outcomes research and comparative effectiveness research methods for assessing the impact of technology and treatments on patient outcomes. Emphasis is placed on special need populations, such as older adults, minorities, persons with mental illness and substance abuse, high burden diseases, and disabilities.
The development of research and analysis methods, as well as content knowledge is also stressed. In addition to careers in academia, the program prepares students for leadership careers as health services researchers and health care policy analysts working in public or private agencies or organizations. There are many research opportunities within research centers of the Department and elsewhere within the Johns Hopkins University and Health System. Also the Baltimore-Washington area is the home to the largest concentration of public and private health services research and health care policy analysis organizations in the world. Formal and informal relationship with these agencies, including research practicas, thesis collaborations and part-time employment are encouraged and facilitated.
What Can You Do With a Graduate Degree In Health Services Research And Policy?
The program prepares students for successful research careers in health services and outcomes. Former students have gone onto careers in academia, government, research-oriented non-profits, and the private sector. Visit the Graduate Employment Outcomes Dashboard to learn about Bloomberg School graduates' employment status, sector, and salaries.
View a list of selected recent graduates and dissertation titles for the PhD Concentration in Health Services Research and Policy.
Curriculum for the Concentration in Health Services Research and Policy
Browse an overview of the requirements for this PhD program in the JHU Academic Catalogue , explore all course offerings in the Bloomberg School Course Directory , and find many more details in the program's Student Handbook.
Admissions Requirements
For general admissions requirements, please visit the How to Apply page.
Standardized Test Scores
Standardized test scores are not required and not reviewed for this program. If you have taken a standardized test such as the GRE, GMAT, or MCAT and want to submit your scores, please note that they will not be used as a metric during the application review. Applications will be reviewed holistically based on all required application components.
Jennifer L. Wolff, PhD ’03, MHS '95,
Jennifer L. Wolff, PhD ’03, MHS '95, advances policies and programs that improve quality of care and life of older adults with complex health needs and their caregivers.

All accepted PhD students receive a standard funding package. As of September 1, 2023 this package includes full tuition support, a $30,000 per year stipend, individual health, dental, and vision insurance and the University Health Services clinic fee for four years.
For funding sources, please see PhD funding page .
Need-Based Relocation Grants Students who are admitted to PhD programs at JHU starting in Fall 2023 or beyond can apply to receive a $1500 need-based grant to offset the costs of relocating to be able to attend JHU. These grants provide funding to a portion of incoming students who, without this money, may otherwise not be able to afford to relocate to JHU for their PhD program. This is not a merit-based grant. Applications will be evaluated solely based on financial need. View more information about the need-based relocation grants for PhD students .
Questions about the program? We're happy to help. [email protected] 410-955-2488
Health Sciences Library
- Library Resources
Research Databases
- ClinicalKey
- Global Health
- Google Scholar
Connect with HSL
Health sciences library hours.
- Today closed
- Sunday closed
- Monday 8am - 5pm
- Tuesday 8am - 5pm
- Wednesday 8am - 5pm
- Thursday 8am - 5pm
- Friday 8am - 5pm
- May 25 closed
- May 26 closed
- May 27 closed
- May 28 8am - 5pm
- May 29 8am - 5pm
- May 30 8am - 5pm
- May 31 8am - 5pm
- Jun 1 closed
- Jun 2 closed
- Jun 3 8am - 5pm
- Jun 4 8am - 5pm
- Jun 5 8am - 5pm
- Jun 6 8am - 5pm
- Jun 7 8am - 5pm
- Jun 8 closed
- Jun 9 closed
- Jun 10 8am - 5pm
- Jun 11 8am - 5pm
- Jun 12 8am - 5pm
- Jun 13 8am - 5pm
- Jun 14 8am - 5pm
- Jun 15 closed
Explore Health Sciences Topics
- Clinical Support
- Systematic Reviews
- Research Impact and Data Visualization
- AHEC Digital Library
- Evidence-Based Practice
- Course Reserves
- Citing & Writing Tools
- Health Literacy
Featured Guides
- (Allied) Health Sciences
- Bioinformatics
- Health Data & Statistics
- Health Literacy and Patient Education
- Medicine/Clinical
- Open Access and Scholarly Communications
- Public Health
- NIH Data Management and Sharing Policy
Popular Guides
Health sciences library spaces.

Health Sciences Library – Basement

Health Sciences Library – Floor 1

Health Sciences Library – Floor 2
Upcoming health sciences library events, monday, june 10, 2024.
10am - 11am
Wednesday, June 12, 2024
Wednesday, june 19, 2024, health sciences library projects.


Exploring UNC Research Networks and Impact Metrics with VOSViewer
Interactive network graphics of publication output, areas of research focus, and collaboration patterns offer a technological advance over static, flat images. VOSviewer Online allows users such as prospective faculty and students to explore data up close that show faculty research strengths and how a particular unit or school collaborates with other researchers and institutions around the world.

COVID-19 Research Output and Collaboration Analysis
Bibliometric analysis of UNC-Chapel Hill research output related to COVID-19 through April 2021. Includes author, institution, collaboration, and topic analyses.

Gillings School of Global Public Health 10-Year Research Analysis
The Health Sciences Library (HSL) has partnered with administration at UNC-Chapel Hill’s Gillings School of Global Public Health (SPH) on a series of projects to reveal collaboration patterns of research faculty, illustrate evolution in research foci over time, and demonstrate SPH impact.
Health Sciences Library News

Appointment: Liaison to Dentistry and Systematic Review Coordinator

A new website for the Health Sciences Library

Carolina librarians edit “Perspectives on Justice, Equity, Diversity and Inclusion in Libraries”
Health sciences library partners.
HSL provides direct support to health affairs schools and UNC Medical Center :
- Adams School of Dentistry
- Eshelman School of Pharmacy
- Gillings School of Global Public Health
- UNC School of Medicine , including the Department of Health Sciences
- UNC School of Nursing
Our partners located at HSL include:
- Carolina Health Informatics Program
- Office of Interprofessional Education and Practice
- UNC Global Women’s Health
Health Sciences Library Staff
Hsl administration.
- Michelle Cawley - Interim AUL for Health Sciences and Director, Health Sciences Library
- Fei Yu - Health Technology and Informatics Librarian
HSL Clinical and Statewide Engagement
- Hannah Burrows - Community Outreach and Global Health Librarian
- Jamie Conklin - Health Sciences Librarian and Liaison to Nursing
- Beth Moreton - Nursing Liaison Librarian
- Terri Ottosen - Community Engagement and Health Literacy Librarian
- Lauren Tomola - AHEC Knowledge Management Librarian
- Sarah Wright - Head, Clinical and Statewide Engagement
HSL Clinical, Academic, and Research Engagement
- Carrie Baldwin-SoRelle - Health Sciences Librarian and Liaison to School of Public Health
- Rebecca Carlson - HSL Librarian & Liaison to School of Pharmacy
- Adam Dodd - Applications Analyst
- Karen Grigg - Health Sciences Librarian for Collections & Instruction
- Barrie Hayes - Bioinformatics & Research Data Librarian
- Emily Jones - Liaison to Dentistry & Systematic Review Coordinator
- Barbara Renner - Liaison Librarian, Allied Health Sciences/Evaluation Specialist
HSL Information Access and Discovery
- Michael Campbell - Interlibrary Lending Specialist
- Chip GrawOzburn - Borrowing and Billing Specialist, Interlibrary Lending
- Antonio Gross - Information Associate and HSL Student Supervisor
- Lee Haney - Information Associate and Reserves Manager
- Stefanie Nutting - Information Associate & User Services Support Specialist
- Liza Philbeck - Information & Access Services Supervisor
No staff members found

QUICK LINKS
Degrees and programs powered by experience
Undergraduate
NEWS, DISCOVERY, AND ANALYSIS FROM AROUND THE WORLD

Explore our global campuses
Find unique opportunities for experience-powered learning and discovery.

Our hub for research and graduate education at the intersection of technology, security, and policy
Explore Arlington

Massachusetts
Established in 1898, our first campus is a comprehensive hub for learning, discovery, and urban engagement
Explore Boston
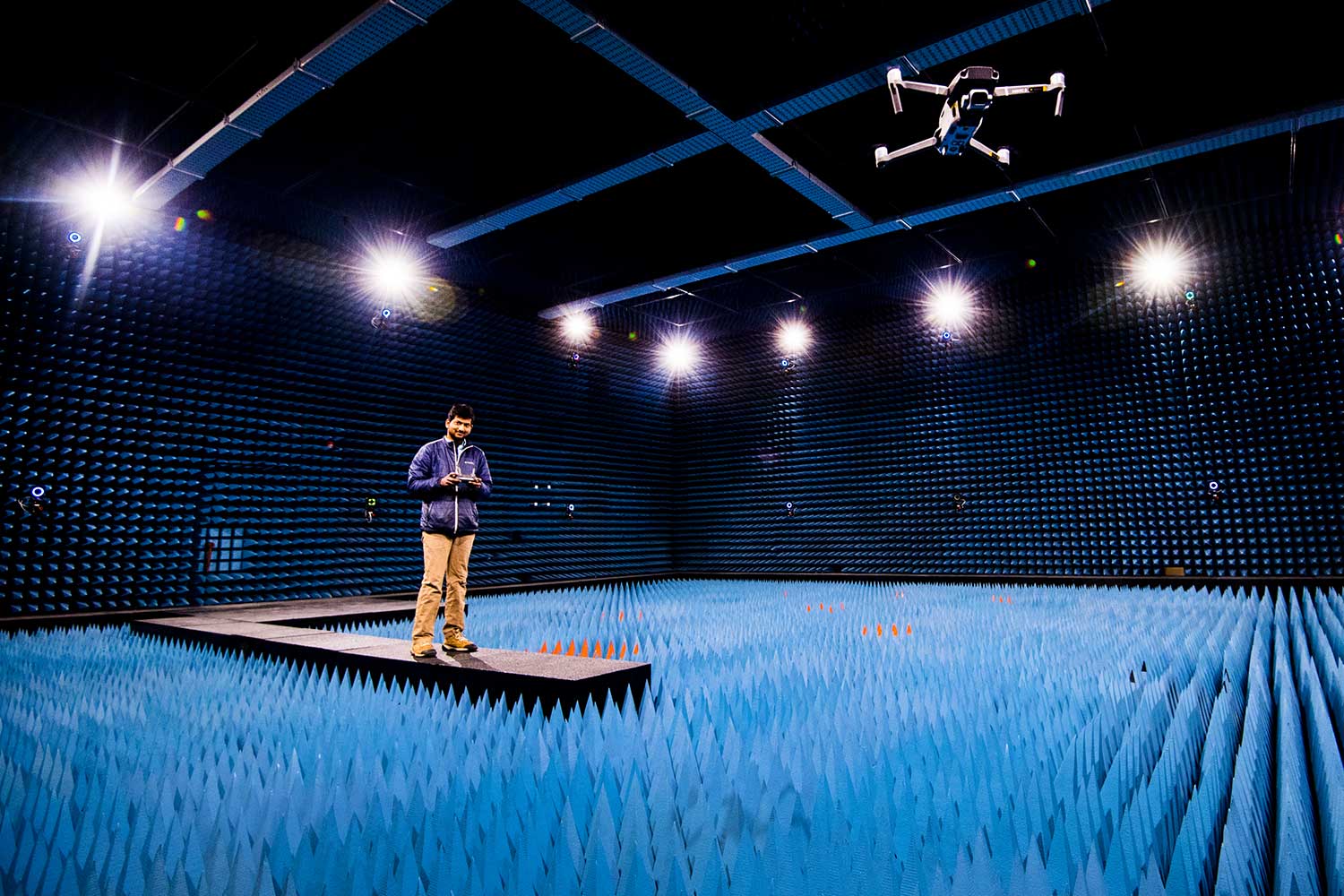
Home to world-class national security and defense research and a magnet for science-based startups
Explore Burlington

North Carolina
An engine for professional education in the life and health sciences
Explore Charlotte

Our hub in Europe, with undergraduate and postgraduate degrees—including a U.S./U.K. double degree—and world-leading network science research
Explore London

Graduate education and entrepreneurship programming to support the rapidly transforming finance and tech economies
Explore Miami

A vibrant center for coastal sustainability research and innovation
Explore Nahant

Our West Coast undergraduate campus offering unique entrepreneurship and social impact programming, and home to the Mills Institute
Explore Oakland

An engine for economic development with graduate degrees and research in technology, and home to the Roux Institute
Explore Portland

Graduate degrees and research focused on the region’s booming tech industry, and undergraduate summer programs
Explore Seattle
Graduate education for high-tech fields in the heart of California’s Big Tech region
Explore Silicon Valley

Preparing professionals to thrive in high-demand fields in North America’s third-largest tech market
Explore Toronto

Professional education aligned with British Columbia’s rising startup and high-tech ecosystem
Explore Vancouver

#LikeAHusky
Plenty of room to do your own thing. Many ways to feel like a Husky.

17 Division I teams, including varsity esports. 55 intramural sports, and 64 club teams. And a packed DogHouse on game nights. Go, Huskies!
Take Action
Quick Links
Campus Locations

Today, a vanguard of donors is driving Northeastern’s historic $1.3 billion fundraising campaign. With initiatives that span the globe, accelerating outcomes, we’re creating a better world right now. Learn more about our mission
Copyright 2024 Northeastern University
Online introductory R courses for environmental health data science skills
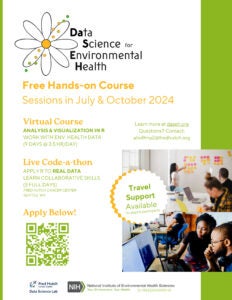
- Practitioners, professionals, or researchers in the environmental health space who want programming and data science skills.
- Educators who want programming and data science skills with a focus on environmental health
- Practitioners, professionals, researchers, or advanced students from Minority Serving Institutions or institutions without training opportunities like DaSEH.
News from the School

From public servant to public health student

Exploring the intersection of health, mindfulness, and climate change

Conference aims to help experts foster health equity

Building solidarity to face global injustice
This paper is in the following e-collection/theme issue:
Published on 16.5.2024 in Vol 26 (2024)
Person-Generated Health Data in Women’s Health: Scoping Review
Authors of this article:

- Jalisa Lynn Karim 1 , BA, BMath ;
- Rachel Wan 1 , BSc, BSN, RN ;
- Rhea S Tabet 2 , BSc ;
- Derek S Chiu 3 , BSc, MSc ;
- Aline Talhouk 1 , BA, MSc, PhD
1 Department of Obstetrics and Gynaecology, University of British Columbia, Vancouver, BC, Canada
2 Department of Pharmacology and Therapeutics, McGill University, Montréal, QC, Canada
3 Department of Molecular Oncology, University of British Columbia, Vancouver, BC, Canada
Corresponding Author:
Aline Talhouk, BA, MSc, PhD
Department of Obstetrics and Gynaecology
University of British Columbia
593 - 828 West 10th Ave
Vancouver, BC, V5Z 1M9
Phone: 1 604 875 3111
Email: [email protected]
Background: The increased pervasiveness of digital health technology is producing large amounts of person-generated health data (PGHD). These data can empower people to monitor their health to promote prevention and management of disease. Women make up one of the largest groups of consumers of digital self-tracking technology.
Objective: In this scoping review, we aimed to (1) identify the different areas of women’s health monitored using PGHD from connected health devices, (2) explore personal metrics collected through these technologies, and (3) synthesize facilitators of and barriers to women’s adoption and use of connected health devices.
Methods: Following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for scoping reviews, we searched 5 databases for articles published between January 1, 2015, and February 29, 2020. Papers were included if they targeted women or female individuals and incorporated digital health tools that collected PGHD outside a clinical setting.
Results: We included a total of 406 papers in this review. Articles on the use of PGHD for women steadily increased from 2015 to 2020. The health areas that the articles focused on spanned several topics, with pregnancy and the postpartum period being the most prevalent followed by cancer. Types of digital health used to collect PGHD included mobile apps, wearables, websites, the Internet of Things or smart devices, 2-way messaging, interactive voice response, and implantable devices. A thematic analysis of 41.4% (168/406) of the papers revealed 6 themes regarding facilitators of and barriers to women’s use of digital health technology for collecting PGHD: (1) accessibility and connectivity, (2) design and functionality, (3) accuracy and credibility, (4) audience and adoption, (5) impact on community and health service, and (6) impact on health and behavior.
Conclusions: Leading up to the COVID-19 pandemic, the adoption of digital health tools to address women’s health concerns was on a steady rise. The prominence of tools related to pregnancy and the postpartum period reflects the strong focus on reproductive health in women’s health research and highlights opportunities for digital technology development in other women’s health topics. Digital health technology was most acceptable when it was relevant to the target audience, was seen as user-friendly, and considered women’s personalization preferences while also ensuring accuracy of measurements and credibility of information. The integration of digital technologies into clinical care will continue to evolve, and factors such as liability and health care provider workload need to be considered. While acknowledging the diversity of individual needs, the use of PGHD can positively impact the self-care management of numerous women’s health journeys. The COVID-19 pandemic has ushered in increased adoption and acceptance of digital health technology. This study could serve as a baseline comparison for how this field has evolved as a result.
International Registered Report Identifier (IRRID): RR2-10.2196/26110
Introduction
The practice of keeping notes to monitor one’s health is not a recent phenomenon. Individuals have long recognized the benefits of tracking various health aspects, including the ability to be more active participants in managing their health, gaining a more complete picture of their health, and reducing the frequency of in-person appointments; however, this tracking was previously done through paper logs [ 1 ]. Today, with the proliferation of digital tools, self-tracking has significantly evolved and become more prevalent. The increasing pervasiveness of technology, particularly mobile phones, has seamlessly integrated it into our daily lives, making self-tracking more accessible and convenient than ever before [ 2 ]. Connected digital health technologies such as smartphones, wearables (eg, smartwatches), sensors, the Internet of Things (eg, internet-enabled weight scales), and web-based applications have permeated society and are increasingly adopted to collect and track health data. In 2021, a total of 87% of Canadians owned a smartphone, up by 73% from 2009 [ 3 ]. With >350,000 digital health apps accessible via these smartphones [ 4 ], approximately two-thirds of Canadians digitally track at least one aspect of their health [ 5 ]; similar statistics have been reported in the United States [ 6 ]. Moreover, since the introduction and popularization of fitness trackers in 2010, sensors and wearable devices have increasingly become part of daily life [ 2 ]. During the global COVID-19 pandemic, self-tracking took on even greater significance [ 7 , 8 ]. With the heightened awareness of health and the need for proactive measures, individuals have turned to self-tracking to monitor their well-being and make informed decisions. With this transformation, self-tracking has transcended its previous boundaries, offering individuals new opportunities to optimize their well-being and ushering in a new era of personalized health care [ 9 - 11 ].
Digital health tools have revolutionized the active and passive collection of health data through various applications and wearable devices. These various digital health tools collect and generate an unprecedented amount of data that can be used to glean insights into one’s health. Person-generated health data (PGHD), which are clinically relevant data captured outside traditional care settings [ 12 ], provide valuable insights that empower users to self-monitor and reflect on their health. PGHD can refer to any data collected from wearable and smart devices as well as self-input information into platforms such as mobile apps and websites. By leveraging digital technologies, individuals can collect and store their health data, enabling them to actively manage their own health and monitor chronic conditions. Furthermore, the integration of these data with research presents an opportunity to improve the patients’ experience and enhance personalized medicine. The recognition of this opportunity has started to take shape with patient-reported outcome measures and patient-reported experience measures being increasingly recognized as essential information to assess quality of care and prioritize patient-centered approaches and with mandatory assessment as part of clinical trials [ 13 ]. Seamlessly linking PGHD that are captured outside traditional care settings with clinical data and disease models can unlock new possibilities for tailored treatments and predictive informatics. The integration of digital health tools not only facilitates patient-provider communication but also offers opportunities for education, increased awareness, self-tracking, and self-monitoring without burdening health care resources. By focusing on the individual’s experience, personalization, and prevention, digital health tools contribute to a patient-centered care paradigm that aims to optimize health care outcomes and improve overall well-being while empowering patients to take charge of their health.
In recent years, the emergence of femtech, defined as technology-driven solutions specifically designed to address women’s health needs and concerns, has revolutionized the landscape of self-tracking and health care for women [ 14 ]. Femtech encompasses a wide range of digital tools, such as period-tracking apps, fertility monitors, pregnancy trackers, and menopause management platforms. These innovative solutions empower women to track and manage their reproductive health, menstrual cycles, and overall well-being with greater accuracy and ease. Femtech has not only provided women with personalized insights into their bodies but has also helped break taboos and encouraged open conversations about topics that were once stigmatized or ignored. The rapid growth of femtech has promoted access to women’s health information, greater autonomy in decision-making, and enhanced overall health care experiences for women worldwide. It has become an integral part of the self-tracking movement, demonstrating the transformative power of technology in promoting women’s health and well-being.
In this study, we reviewed the use of digital tools and PGHD in women’s health research, focusing on articles published between January 1, 2015, and February 29, 2020, before the COVID-19 pandemic. Our review encompassed various connected health devices, which included both passive data collection devices such as wearable sensors and active input devices such as smartphone apps and websites. This review sought to accomplish the following:
- Identify the different areas of women’s health and health-related behaviors monitored using PGHD from connected health devices.
- Explore personal metrics collected through these technologies.
- Synthesize facilitators and barriers that impact women’s adoption and use of connected health devices in managing their health.
This scoping review was conducted based on our previously published protocol [ 15 ]. We adopted the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) guidelines [ 16 ]. The completed checklist is provided in Multimedia Appendix 1 [ 16 ].
Search Strategy
The search strategy was designed in close collaboration with a reference librarian with input from the authors (JLK and AT). We searched a total of 5 databases: MEDLINE, Embase, APA PsycINFO, CINAHL Complete, and Web of Science Core Collection. Initial searches were completed in early March 2020. Searches were limited to articles published in 2015 or later because publications with the keyword “digital health” started to emerge in the literature around that time [ 17 ], and with the fast evolution of the field, previous articles may not be relevant to the current landscape. Keywords and subject headings were designed to search the literature for the intersection of the following 4 topics: women, health, digital devices, and tracking. The full search strategy, including a full list of search terms, was published with the protocol [ 15 ] and is available in Multimedia Appendix 2 .
Eligibility Criteria
We were interested in digital technologies and interventions targeting women and people assigned female at birth. To be included in the review, studies needed to specifically target women, focus on female-only health topics (eg, menstruation), or only include female participants. We included a variety of publication types but excluded conference abstracts and conference reviews, editorials, letters, and comments due to the limited details in such literature.
We excluded articles that presented digital health tools designed for health care providers as we were primarily interested in devices and apps that women can engage with outside a clinical setting. Articles only discussing the use of real-time consultations, whether through video, phone, or web-based chat, were excluded. We excluded articles that described digital health tools used solely for educational purposes; to maintain the focus of the review on tracking or monitoring one’s data for health, devices must have allowed users to input personal health data.
The complete inclusion and exclusion criteria are presented in Textbox 1 . We decided to retain the original inclusion end date of February 29, 2020, to maintain a focus on the literature before the COVID-19 pandemic and avoid potential complexities caused by pandemic-related disruptions in research and health care practices. Concentrating on prepandemic literature also established a clear baseline for future comparisons and allowed us to maintain feasibility of completion without compromising quality given the broad scope of the review.
Inclusion criteria
- Published between January 1, 2015, and February 29, 2020
- Refers to a health issue that pertains only to women or comprises only female participants of any age
- Includes the use of connected health tools for tracking or monitoring some aspect of health, which could include smartphone apps, wearable devices, the Internet of Things (eg, Bluetooth- or internet-enabled glucometers, blood pressure cuffs, and weight scales), and implantable devices
- Involves data collection from the user of the connected health tool (ie, the user either manually inputs data into the device or they are automatically uploaded)
- The user must be able to interact with the app or device on her own at home (outside a clinical setting)
- Available in English
Exclusion criteria
- Not available in English
- Conference abstracts, conference reviews, editorials, letters, or comments
- Study media releases and user reviews of specific applications
- Research conducted on animals
- Research involving male participants
- Tracking of infants and children unless tracking breastfeeding (because breastfeeding is directly related to the mother’s health and body)
- Devices or apps that are meant for health care provider use or use in a clinical setting only or cannot be used independently without a health care provider present
- Digital health tools that are only for educational or informational purposes and do not allow the user to enter or track her own data (ie, no information exchange)
- Telemedicine services (eg, live video consultations with health care providers)
Study Selection
We imported the results from the database searches to the Covidence systematic review software (Veritas Health Innovation). Covidence detected records believed to be duplicates, and these were manually checked before removing them. In addition, some articles were manually recognized as duplicates during the screening process and were subsequently tagged as duplicates and removed. Screening was conducted independently by at least 2 reviewers (JLK, RST, and AT) at both the abstract screening stage and the full-text screening stage. We attempted to contact the corresponding authors of articles that passed abstract screening when we were unable to locate the full text. Conflicts at either stage were discussed and agreed upon among the 3 authors involved in the screening process.
Data Charting and Deviations From the Protocol
The final list of data charting elements is provided in Textbox 2 . Data charting for all elements except for usability and acceptability was conducted using Google Sheets created by the study team. The categories for different data charting options were initially created based on a small subset of articles and were discussed among the authors involved in the charting process. The team met regularly throughout the data charting process to discuss and refine coding categories that best summarized the data. Starting with more granular categories and later combining them into broader concepts was necessary to summarize the number of articles included in this review. For each article included, data were charted by one reviewer (RW or RST) and verified for accuracy by a second reviewer (JLK). Data were summarized in bar graphs, maps, and tables (JLK, RST, and DSC), as presented in the following sections. For the locations, we recorded the countries from which the participants were recruited (if applicable). If an article did not describe recruiting participants, then the countries of the authors were recorded based on the authors’ affiliations.
Article information
- Year of first publication
Study characteristics
- Country or countries in which the research was conducted
- Research study type
Contexts for women’s connected health
- Health areas of focus
Digital device details
- Types of digital health
- Metrics collected by the devices
Usability and acceptability
- Facilitators of and barriers to the use of the technologies (coded into themes)
For the thematic analysis, articles that mentioned any aspect of usability, acceptability, facilitators, or barriers to the use of digital health tools were imported into NVivo (R1 2020; QSR International). Coding was done independently by 2 reviewers (JLK and RW) and then combined through discussions. As with the data charting process, we initially coded more granularly and then grouped the detailed codes together later in the analytic process. Decisions on how to group the codes into themes and subthemes were made through group consensus (JLK, RW, and AT).
In our protocol, we indicated that we would extract the name of the device or app used in each study. While we did complete this step in our data charting, we have not presented the results in this paper. Several articles either did not specify the brand name (eg, only specified that it was a mobile app) or had digital health tools named after the study, so we did not find this information useful to showcase in our results. There were no other deviations from the published protocol.
The searches identified 14,629 records that were imported into the Covidence software for deduplication and screening. After deduplication, a total of 9102 articles were screened for relevance, and 8545 (93.88%) were excluded based on title and abstract. From reading the full texts of the remaining 557 records, an additional 151 (27.1%) were excluded. The most common reasons for exclusion were the inability of study participants to enter or track their own data (58/151, 38.4%) or because the digital health technology was designed to be used by or with a health care provider (48/151, 31.8%). The remaining 406 publications were included in the scoping review. Some of the included publications reported on the same research project; in those cases, all of them were included. Our search did not encounter any articles that directly addressed or mentioned the inclusion of intersex, transgender, or nonbinary participants. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram detailing the full study selection process is shown in Figure 1 . The list of included articles sorted by health areas of focus can be found in Multimedia Appendix 3 [ 18 - 58 ].

Year and Country
There was an increasing trend in number of publications per year, with 10.1% (41/406) of the articles published in 2015, a total of 13.3% (54/406) of the articles published in 2016, a total of 18% (73/406) of the articles published in 2017, a total of 26.4% (107/406) of the articles published in 2018, and 29.6% (120/406) of the articles published in 2019. Only 2.7% (11/406) of the publications were from 2020 because our cutoff date for inclusion was February 29, 2020.
Articles included in the review covered worldwide research, including every continent except Antarctica ( Figure 2 ). As we only considered articles written in English, most of the articles were published in Western, English-speaking countries, primarily the United States (169/406, 41.6% of the articles), the United Kingdom (34/406, 8.4% of the articles), Australia (33/406, 8.1% of the articles), and Canada (19/406, 4.7% of the articles). Other countries where several included articles were published were China (13/406, 3.2% of the articles), the Netherlands (13/406, 3.2% of the articles), Spain (13/406, 3.2% of the articles), and Sweden (10/406, 2.5% of the articles).
Interestingly, of the 169 articles from the United States, 26 (15.4%) specifically focused on African American or Black, ethnic minority, or low-income women. One study from Singapore specifically included multiethnic women [ 18 ], and a study from Australia included Indigenous Australian women as their participants [ 19 ]. In addition, one review conducted by researchers in Australia looked specifically at studies with women from culturally and linguistically diverse backgrounds [ 20 ].

Study Types
The types of studies that used digital health tools in women’s health research are reported in Figure 3 by year of publication (note that the articles could fall into more than one study category). The most common study type encountered was feasibility or acceptability studies (197/406, 48.5% of the articles, including 9/197, 4.6% protocols), followed by effectiveness studies (146/406, 36% of the articles, including 36/146, 24.7% protocols) and publications reporting on digital tool prototypes (73/406, 18% of the articles). Effectiveness studies reported on outcome measures of an intervention, including randomized and nonrandomized trials with one or more study arms. Reviews (of published literature, apps, or wearables), viewpoints, manuals, case studies, or analytical methods (56/406, 13.8% of the articles combined) were also encountered. Observational or correlative studies (44/406, 10.8% of the articles, including 3/44, 7% protocols) were studies that observed the health behaviors of individuals through digital health technologies without assessing the effectiveness of an intervention or analyzed associations between variables (eg, associations between heart rate and loss-of-control eating) [ 21 ]. Finally, measurement studies (23/406, 5.7% of the articles) reported on the validity, reliability, or accuracy of a digital health tool.

Health Areas of Focus
The analysis of the reviewed articles highlighted research in several recurring women’s health areas of focus. A full breakdown of the health areas is reported in Table 1 (articles could fall into more than one health area). Pregnancy and the postpartum period emerged as the most prominent health area with 42.6% (173/406) of the articles. Within this category, there was a specific emphasis on general care and monitoring (45/173, 26% of the articles), physical activity and diet (34/173, 19.7% of the articles), and glucose monitoring (31/173, 17.9% of the articles). Cancer was identified as the second most common health area, with 19.5% (79/406) of the articles dedicated to its exploration. Specifically, a significant focus was observed on the relationship between cancer and cardiovascular health, with 47% (37/79) of the articles addressing this aspect. The impact of lifestyle on overall health and well-being was also addressed, with 14.3% (58/406) of the articles delving into physical activity, sedentary behavior, diet, weight, and obesity. Menstrual, sexual, and reproductive health were explored in 12.1% (49/406) of the articles to shed light on various aspects of women’s reproductive health and associated concerns, with 76% (37/49) focusing on menstrual cycle tracking or fertility monitoring. Furthermore, 9.9% (40/406) of the articles were dedicated to chronic conditions (such as urinary incontinence, osteoporosis, and diabetes) with the aim of enhancing understanding and developing interventions for individuals living with chronic health conditions. To accommodate articles that did not fit within the primary health areas, an Other category comprising 6.4% (26/406) of the articles was established. This category included articles on athlete monitoring (10/26, 38% of the articles), such as heart rate monitoring during sports tournaments; mental health and quality of life (9/26, 35% of the articles); gender-based violence (3/26, 12% of the articles); and more. Finally, a small subset of 0.5% (2/406) of the articles did not align with any specific health area; these included a publication reporting results from a survey on African American women’s willingness to participate in eHealth research [ 22 ] and a publication analyzing women’s interactions with digital health technologies [ 23 ]. These articles were included because, although they did not discuss a specific health area, they still focused on women’s use of digital health tools in general.
a PCOS: polycystic ovary syndrome.
b CVD: cardiovascular disease.
c COPD: chronic obstructive pulmonary disease.
d SLE: systemic lupus erythematosus.
e IC: interstitial cystitis.
f BPS: bladder pain syndrome.
g ABL: accidental bowel leakage.
Figure 4 shows how the health areas of focus for women’s use of digital health changed over the years that were included in the review (2015-2019 plus January 2020-February 2020). There was an increasing trend from 2015 to 2020 in the number of publications focusing on pregnancy and the postpartum period, as well as cancer and menstrual, sexual, and reproductive health. However, articles focused on women’s use of digital health for lifestyle-related topics and chronic conditions did not see a notable increase over those years.

Type of Digital Health and Metrics Collected
Within the articles reviewed, smartphone, mobile, or tablet apps emerged as the most prevalent type of digital health (295/406, 72.7% of the articles), followed by wearable devices (165/406, 40.6% of the articles) and websites or patient portals (93/406, 22.9% of the articles). Other types of technology were not investigated as much. For example, 13.5% (55/406) of the articles addressed smart devices or the Internet of Things (referring to objects with sensors that connect to a network, such as Bluetooth-enabled glucometers and blood pressure machines). Finally, 7.4% (30/406) of the articles reported on 2-way messaging, 1% (4/406) of the articles reported on interactive voice response telephone calls, and only 0.5% (2/406) of the articles reported on implantable devices. With respect to the metrics collected, we found >250 metrics, such as heart rate, number of steps, mood, ovulation test results, and days of menstruation. A full list of the metrics is reported in Multimedia Appendix 4 .
Thematic Analysis
Of the 406 articles included in this scoping review, 168 (41.4%) mentioned usability, acceptability, facilitators, or barriers to the use of digital health tools at least once. Our thematic analysis identified 6 themes: (1) accessibility and connectivity, (2) design and functionality, (3) accuracy and credibility, (4) audience and adoption, (5) impact on community and health service, and (6) impact on health and behavior. The themes are described in further detail in the following sections.
The thematic analysis detailed in the following sections is primarily based on the views of the participants in the studies we reviewed to provide a user perspective; however, one subsection in theme 5 focuses on the health care provider perspective.
Theme 1: Accessibility and Connectivity
The accessibility and connectivity of digital technologies emerged as an important theme with two subthemes: (1) cost and convenience and (2) connectivity, compatibility, and software issues.
Cost and Convenience
Our analysis revealed that the cost and convenience of digital tools collecting PGHD are important factors that can impact their adoption and use. On the one hand, digital health technologies can be seen as more affordable compared to traditional health care visits and more accessible to a wider range of people, including those of a lower socioeconomic status. On the other hand, they can also be perceived as too expensive and novelty items, and associated extra costs such as data plans can also be a barrier for some people. Because PGHD can be collected and entered throughout the day in real time, and because most people carry a phone around with them every day, these technologies offer greater convenience than traditional in-person health care encounters by providing anytime, anywhere virtual access and putting information at people’s fingertips through smartphones and web platforms. One user spoke about an in-app treatment program:
That was what was so good about this, I can do this at home myself, no need to book an appointment, find the time and suit others, and you know, that process of booking a time. [ 24 ]
Some inconvenient aspects of digital health technologies include uncomfortable wearables that are too bulky, difficulty of use, or not fitting into the users’ lifestyles, as noted in one article:
Women also mentioned that the comfort of the wearable sensors was a barrier. Comfort became a barrier for some women during exercise and hot weather. [ 25 ]
Devices with a short battery life and wearables that are not water resistant are also considered inconvenient as they require the user to frequently remember to charge the device or put the wearable back on after water-based activities. Certain restrictions, such as not being able to wear a device in a workplace, can also create inconvenient barriers for some users.
Connectivity, Compatibility, and Software Issues
Factors related to connectivity and other issues such as device synchronization, freezing, or disconnection can significantly impact the user experience and engagement with digital health tools. For example, the dependence on mobile and internet access can be a disadvantage. Cellphone and network coverage limitations can pose an important barrier in rural areas or during travel. Where mobile data or Wi-Fi connection are limited, people may struggle to use digital health tools that require internet connection; this can create disparities in access to health care resources, particularly for those of a lower socioeconomic status or living in remote communities with limited infrastructure. Incompatibility between operating systems such as Android and iOS, iPhone and iPad, or various browsers can also be an important barrier to accessing digital health technology.
Software issues can significantly impact the user experience of digital health technologies. Broken links can prevent users from accessing valuable information or features within apps or websites. App crashes can discourage users from engaging with the digital health tool altogether. In addition, slow loading times can negatively impact the user experience, making it challenging for users to access information or features quickly and efficiently.
Theme 2: Design and Functionality
The second theme centered on design and functionality and included four subthemes: (1) appearance and design; (2) functionality and features; (3) personalization; and (4) safety, privacy, and security.
Appearance and Design
Appearance and design play important roles in the success of connected health devices. In terms of app design, the color scheme and layout facilitate user-friendliness. Bad formatting can make it difficult for users to read or understand the content of an app or website. Font size that is too small can be challenging for those with visual impairments, and some color combinations can be difficult to read. The quality of the images used in digital health interventions can also impact user experience, with low-quality images potentially making it difficult for users to interpret the information being presented.
Apps that are visually appealing and easy to use are more likely to be successful. When it comes to wearables, women tend to prefer sleek, understated designs that are esthetically pleasing without being bulky. A sleek design can encourage use of the wearable. For example, some women consider their wearable to be a fashion item that sparks conversation, which encourages their continued use of the device, as illustrated in a participant quote:
Um, that it’s, like, kind of stylish, like, I feel, like, cool that I wear one. A lot of people ask me, they’re like, oh, which one is that, like, is that a Fitbit, is that an Apple watch? It has the interchangeable bands and stuff like that, so, you can, like, change the color of it and everything. It’s like a conversation piece. [ 26 ]
Other women prefer more discretion in the design of wearables and their size or in the app icon on their mobile device because they do not want to reveal the purpose of the device to others. People may feel self-conscious when wearing the device or using the app, especially if it reveals their medical condition. For example, the following quote is from a study that incorporated a sensor band worn on the wrist to help female undergraduate students with problematic drinking:
P310 noted that while in class, “my professor commented on it which made me feel awkward.” [ 27 ]
Functionality and Features
In terms of functionality, the availability of clinical interpretation of user data is deemed essential, and health warnings based on recorded PGHD are noted to be helpful. Moreover, notifications and reminders are also useful for improving adherence to self-tracking and maintaining goals, and users appreciate receiving automated SMS text messages and feedback on progress. Actionable advice is seen as very important, and women expressed a desire for more interaction and the ability to integrate with other apps. For example, users want the ability to access information from their health record and to be able to see graphical summaries of their data over time. Regarding the presentation of information, users appreciate concise information written in simple language. Choice of words is also perceived as especially important to ensure that the information is easy to understand. People enjoy the gamification of content, and the graphical presentation of results is found to be informative.
The ability to upload multimedia and the ability to customize the application’s displays and notifications are noted as features that improve user engagement and satisfaction. The ability to record voice notes and consultations within apps is noted as a desirable feature, as well as having the option to book appointments directly through apps. Women also want the option to sync their desktop or phone calendar with apps to remind them of medical appointments and prescription requests, as some researchers noted:
Women could see the potential usefulness of being reminded to order their next prescription through the electronic alerts system. They found managing the monthly prescription requests challenging long-term and found setting up the reminder easy with the alert popping up on their phone or tablet. [ 28 ]
The application also allows women to set appointment reminders to ensure she is not missing her appointments and developing gaps in her care [...] “It allows me to remain organized for my visits to my OB with concerns, questions, symptoms I have experienced since my last visit.” [ 29 ]
Issues that negatively impact user engagement and outcomes are the inability to edit information or unsubscribe from notifications, which are sometimes thought to be either inconvenient or intrusive, as well as the presence of advertisements within the app. Ease of use is essential as apps or websites that are difficult to navigate can discourage users from engaging with them. For example, a study including the use of a mobile phone app reported the following:
A hindrance and disliked aspect was the difficulty in navigating through the app (eg, no back button, clunkiness, and the inability of participants to edit their inputted daily goals) as well as a lack of color and visuals within the app, giving it a clinical appearance. [ 30 ]
Some women are not comfortable answering questions that they consider intrusive, such as those related to sexual health. They rely on applications to provide trusted information about their condition and want suggestions for additional resources such as website links and local information.
Personalization
Women generally expressed a desire for greater personalization across several features within digital health tools. Messages and notifications that are personalized to the user’s health and self-tracking history and goals are more motivational and less likely to be ignored or perceived as irritating. Even factors such as using a first name in messages from the app make women feel like the messages are more personal and supportive.
Users have individual preferences when it comes to the frequency and timing of notifications, and it is important for digital health apps to allow for the customization of these settings as they can greatly impact user engagement and adherence. Moreover, users expressed a desire for the ability to customize their goals and the metrics they tracked. For example, they may want to change their goals in an app when their life circumstances change (eg, moving, starting a new job, becoming pregnant, or sustaining an injury). The ability to customize the dashboard of an app or website according to the user’s goals was also expressed as a desired feature. The ability to make these customizations will improve their adherence in the long run as their goals evolve.
When it comes to wearables, their placement on the body influences users’ preference and adherence to their use. For example, some women may prefer a wrist-worn device, whereas others may prefer a chest strap, a ring, or a device worn on the waist or ankle. The type of activity being monitored may also influence placement preference. A wrist-worn device may be more appropriate for monitoring steps, whereas a chest strap may be better suited for monitoring heart rate during exercise. Furthermore, placement preference may also be influenced by factors such as comfort, convenience, and visibility. A user may prefer a wrist-worn device because it is more visible and easier to access, whereas another user may prefer a device worn on the waist because it is less obtrusive and more comfortable during exercise or sleep. For instance, one study found the following:
Eight of the participants (40%) reported at some point of the long study period that the smart wristbands were uncomfortable to wear, especially at night. The wristbands irritated the skin, possibly due to pregnancy-related swelling. [ 31 ]
Finally, users have different preferences for how they want information to be presented in an app or website. Some people prefer to read content that is written out with citations and links to external websites. Others enjoy learning content from videos or audio recordings. When looking at their trends and progress, some users like to look at detailed graphs showing their daily progress, whereas others prefer to look at the data occasionally and only receive high-level information. The challenges concerning personalization were articulated by several authors:
It’s a difficult one. Some women want the full picture to fully understand what they are taking. Others want a black and white sketch, but not the details. They just want to know enough. Others do not want to see the picture, they just want to get on with it without knowing too much. Catering for all is a challenge. [ 28 ]
Safety, Privacy, and Security
Women are sometimes concerned about the physical safety of certain devices. For example, some mothers worried about their wearable wristbands scratching their babies [ 31 ]. Others worried about the effects of wearable devices on their skin, as expressed by a participant:
It’s weird because it does have a little laser thing on it, and I wonder if that’s, like, harming my skin (laughing). Like, I’ll sleep in it, and when I wake up I’ll have a red spot on my arm, it’s itchy sometime or sensitive, and I think it’s because of the laser thing, but I don’t really know. [ 26 ]
Some women are concerned about the privacy and security of digital health technologies and expect appropriate safeguards to be implemented in the tools they use. However, privacy and data security are not a concern for all women:
As I said, I’m very critical about patient data in general, especially in terms of data security...If you have a free app, it really depends on what happens to the private data. As a matter of fact, usually the information is stored on the app itself, and so other apps might gain access to the data easily. [ 32 ]
The survey revealed a low level of concern about issues relating to privacy or security of personal data. This suggests that privacy concerns were secondary to the benefits offered by uploading personal details into apps to provide the type of customisation they seek. [ 33 ]
Researchers also shared that some users perceived there to be more privacy when using an app as compared to traditional ways of communicating:
Some participants perceived the storage of their glucose levels on the smartphone as more secure than their current registration in a booklet. [ 34 ]
Women, particularly those who worked outside of the home, also commented that they appreciated the added convenience and privacy of this [text-based] communication method over phone-based communication. [ 34 ]
Theme 3: Accuracy and Credibility
In theme 3, we identified accuracy and credibility as important factors for acceptability considerations in digital health technologies.
The accuracy of digital health can impact user trust and adoption. Digital health tools enable users to keep track of their health, symptoms, and behaviors over time without relying on memory recall, which can be inaccurate or incomplete. Many studies reported that digital tracking can lead to more accurate data collection compared to paper-based methods. For example, at-home measurements of blood pressure and other vital signs have been found to be more accurate than those taken in a hospital or clinic setting. In some cases, apps are even able to accurately predict users’ menstrual cycles and mood changes. In addition, food diaries and activity trackers are often found to be more accurate when tracked within the app compared to using traditional paper-based methods. As the following participant conveyed, digital health may also make it easier for patients to tell the truth about their habits or health concerns:
I like this principle because...I know exactly, that via tablet one would admit things you wouldn’t necessarily tell the doctor or nurse. So, for starters, you can state it in the application. Of course, a conversation shouldn’t be missed afterwards, but this might make it easier for you to overcome yourself. [ 32 ]
However, accuracy can still be an issue in digital health. Different devices can produce different measurements, and some devices may miscount steps, the intensity of workouts, or the quantity and quality of sleep. For example, some women reported devices not tracking their steps while pushing a grocery cart or stroller, whereas others found that their steps were overcounted due to arm movements while they were seated. In addition, some users reported that food tracking options in apps were limited and did not include foods from their culture. Therefore, users may perceive digital health tools as not being representative of their true activity, which may lead them to discontinue the use of the devices. The following participant quote refers to a wrist-worn activity tracker:
Out paddling and we’re huffing and puffing and barely breathing and this isn’t even triggering anything. So it shows [...] that our 150 minute goal is like 60 or half of that. But we’ve actually put in the effort and then you just give up after a while. Like there’s no way I can make this. [ 35 ]
Women often prefer evidence-based health information (eg, explanations of conditions and symptoms and health advice) from a trustworthy source, such as an app curated from up-to-date and evidence-based research, over general internet searches. Users reported that the information provided in some apps was incomplete or inaccurate, with gaps in content or contradictory information that diminished their trustworthiness. In such cases, users may still prefer to talk to a health professional for more trustworthy information. Some women may also find it challenging to trust information that does not disclose sources as they are unsure of its reliability. Devices that are endorsed by, cite, and link to trustworthy health sources are more appealing to users. When sharing results from a web-based survey, the authors of one study reported the following:
Some respondents were specific about from where such advice should come, stating that they wanted expert, credible and up-to-date advice while others noted that they would like to see more Australian-specific or locally-based information in apps or apps that were not linked to the manufacturers of pregnancy or baby products. [ 33 ]
Theme 4: Audience and Adoption
Our fourth theme concerns audience and adoption, which includes two subthemes: (1) demographics and inclusivity and (2) timing and circumstances.
Demographics and Inclusivity
One of the challenges with digital health is to avoid one-size-fits-all interventions and to strive to tailor interventions to address the specific needs of different populations. Digital health that targets specific demographic groups or specific health conditions may increase the adoption of digital tools in those populations. That said, even when targeting people with specific health conditions as the audience, attention must be paid to the language and content in apps and websites. Some researchers noted that women did not want to participate or continue in their study because they did not want to constantly be confronted with their disease. Too much of a focus on disease and ill health can deter women from engaging with the tools, as commented on by some authors:
All but one participant preferred text content that focused on health and physical activity rather than content explicit to cancer. [ 36 ]
The women emphasized that less attention should be paid to chronic disease management and medication as the only treatment option. [...] it was important to explain the implications of the result of the scan and the risk of fractures in a way that will not place the women in a sickness role unnecessarily. [...] The knowledge base of osteoporosis should focus on osteoporosis as a common condition instead of a chronic bone disease. [ 37 ]
Younger women are often more familiar with and more comfortable using digital technology and, therefore, are more likely to use and adhere to a digital health protocol. Users with low technology skills want more training on how to use the digital health tools properly. Little provision is made for those for whom English is not their primary language, which can limit the accessibility and usefulness of digital health interventions. Factors such as language barriers, cultural beliefs, or lack of access to technology may lead to less adoption by some people belonging to ethnic minority groups. The relevance and usefulness of digital health may also vary based on geographic location.
Digital health tools are negatively perceived by some users if not designed to be inclusive of attributes such as body type or gender. For example, users prefer applications that use pictures or models that represent a diverse range of body sizes. Digital health technologies may not be gender inclusive and can conflate sex and gender. It is important to consider the unique health needs and experiences of individuals across the gender spectrum, as several researchers reported:
Participants commented on an exercise demonstration video and recommended that the model should have an “everyday-look” (e.g. plain clothes, jewellery). Also a choice of models of different ages to engage a wider range of patients and help them to relate or identify with the model was proposed. [ 38 ]
[Participant quote]: Maybe the body image it presents...like on a lot of apps, the people doing it looked like they were athletes already. And maybe they should have more people that look normal. [ 39 ]
Two women commented on the gendered design of most FTAs. FTA092 commented that “I chose Clue because it’s the only app that wasn’t pink.” FTA051 also found the gendered design of her previous app insulting; “my last app had a pink flower and was called MyDays or something ...I felt like they were trying to lure me in with this kind of ‘women’s’ approach” (FTA051). She subsequently stopped using that app and downloaded Clue. [ 40 ]
Timing and Circumstances
Individuals are more motivated to use digital health tools during times of illness or when they have a specific health goal in mind. The introduction of technology at the appropriate time impacts the utility and effectiveness of digital health interventions, especially when they are integrated into existing health care systems and routines. Digital health apps need to account for existing medical conditions or medical history to ensure accurate and complete information. For example, technologies that do not provide an option to indicate current pregnancy are perceived as frustrating to users as the in-app goals or notifications can be irrelevant and inconsiderate of their current limitations. In a focus group, one mother shared the following:
I get frustrated with the Garmin [smartwatch] because I wear my watch during the night so it tracks my sleeping as well. Then it gives you like an insight—so a little note will pop up and you know whether your sleep has been really regular or you’ve had irregular sleep. I wish that there was a thing that during pregnancy where that I could put in and say I’m pregnant, because I got those notes that your sleep is really irregular, and I was like, “Because I’m pregnant!” [ 23 ]
Users who are not experiencing symptoms or who perceive their health to be good are less likely to adopt digital health tools as they may not perceive any benefit from using them. Moreover, those who are already tracking their health using other methods (eg, paper-based tracking) are less interested in trying a new digital health tool. Similarly, regarding wearables, some people may already have a wearable and be less interested in having an additional wearable device.
Theme 5: Impact on Community and Health Service
This theme considers the impact of PGHD on community and health service, with three subthemes: (1) communication and community support, (2) clinical integration, and (3) health care provider perspective.
Communication and Community Support
One of the many perceived benefits by users of digital health interventions is the sense of community that these platforms enable. Even though some women reported feeling uncomfortable sharing personal information with strangers in a virtual group, most found that the ability to connect with others who shared similar experiences provided a sense of belonging and support that was motivating and reassuring, as shared by one woman:
What I did love about the apps is the forums. So if you have a weird pain or, you know, you have cramp in your legs at three a.m., you can get on your phone straight away, and you can get support by the women who are going through the same thing. [ 41 ]
Discussion forums and social media platforms associated with digital health interventions are perceived as helpful for connecting with others, sharing personal stories, and receiving support. Digital health interventions can also help women elicit support from friends and family to stay motivated and achieve health goals. For example, researchers who reported on women’s experiences of an app for stress urinary incontinence shared that some participants found it easier to talk to friends about an app for pelvic floor muscle training rather than talk about incontinence [ 24 ]. This can enable increased accountability and further encourage adherence to the intervention. One woman spoke about how her family supported her engagement with a digital health intervention for physical activity maintenance among female cancer survivors:
My husband’s a good motivator. When I say I’m going for a walk, he’ll go with me...with my sister-in-law and her kids, it’s they want to go with me; so it’s how many steps have you got today? Or, are we going to go for a walk. That kind of thing. And with my husband and my daughter it’s, “how many steps did you get today, did you do your workout, let us get it going.” [ 36 ]
In addition to support from family, friends, and community members, these digital platforms can provide an alternative to speaking with a health care provider in person. Asynchronous communication with health care providers is helpful especially for those who may not have easy access to in-person visits or for those who are uncomfortable discussing sensitive information face-to-face. Records of PGHD can also improve the ability to gather and share details with health care providers about symptoms that are difficult to remember during an in-person visit.
Clinical Integration
Women are more willing to participate in digital health interventions if they perceive that they have a direct impact on their clinical care. They appreciate the idea that their health is being monitored and that someone is keeping an eye on their data. Furthermore, women want to see more integration of their clinical test results within their digital health apps and websites. This increases their motivation to adhere to the interventions prescribed through the digital health application.
It was noted that physicians and other health care providers play a crucial role in promoting the use of digital health interventions among patients. As noted in the following participant quote, women enjoy being able to communicate with a health care provider through digital health:
I like it because you can tell the doctor what’s going on and submit it to your doctor, that is the main reason I like it because you can talk directly to your doctor and tell them what is going on without going in or calling. [ 42 ]
Women are more likely to adopt and use technology if it is recommended by their health care providers, family members, or friends. Women reported that digital health interventions were more effective when they were supported by a health care team. For example, having access to a health coach or counselor or receiving feedback from a health care provider on their progress increases their motivation to adhere to the interventions. This support also provides reassurance that they are on the right track toward achieving their health goals. However, some patients become frustrated when they receive conflicting advice from the digital health tool and their health care provider.
Health Care Provider Perspective
Some articles included thoughts from health care providers on digital health tools collecting PGHD [ 20 , 37 , 43 - 55 ]. From the health care provider perspective, digital health can offer several benefits, including the ability to monitor patients’ adherence to treatment and interventions. This can be particularly helpful for patients with chronic conditions that require ongoing management. Providers can use digital health tools to track patients’ progress and identify any potential issues that may require further attention, which can lead to improved clinical outcomes and reduce unnecessary consultations. For instance, one provider learned about their patient’s anxiousness through a mobile health intervention:
I didn’t know my patient was feeling anxious...But when she wrote it down, we could talk about it... [ 43 ]
Some health care providers expressed that digital health tracking could give them a more accurate picture of their patients’ activities and adherence to treatments. In a study about perspectives on a sensor attached to pills that can send data such as date and time of ingestion, a provider commented the following:
A positive would be data and getting a better grip on compliance. (...) I’m making sure the patient is adhering - assuming that the patient is taking everything inside of that blister, you can have confirmation of that. [ 44 ]
In addition, digital health can improve the efficiency of care delivery by providing education and resources directly to patients. This can help patients better understand their condition, treatment options, and self-management strategies, which can lead to better health outcomes.
However, it was also noted that digital health interventions should not replace in-person visits but rather complement them. Some health care providers are concerned about overreliance on digital health tools as well as the potential for misinterpretation of the data they provide. There may be a lack of feedback on the correct use of interventions, such as interpretations of medical advice provided, and health care providers have raised concerns about the safety and trustworthiness of the medical advice generated by the digital health tools. Health care providers especially worry about medico-legal effects of having information from digital health tools taken out of context or without considering the full picture of the user’s history and health, as demonstrated in the following quotes:
As a health care professional, I’m just mindful that if there was a video of me up there talking, if that was taken out of context or shared with another person where that information was not appropriate, that’s a concern to me. [ 45 ]
One anesthesiologist raised, “Who has access to the responses that I provide? Because if a patient receives information from me which they hold onto and is taken out of context, in a medical–legal situation, then that’s a big issue as well.” [ 46 ]
Providers may also find that the abundance of information generated by digital health tools can be overwhelming and time-consuming to manage, adding to an already hectic workflow and blurring professional boundaries. Large volumes of alerts and notifications from digital health tools can be disruptive to health care providers, who expressed the need to set boundaries regarding how and when they engaged with digital health tools. In a study reporting on perspectives about digital health from key informants (health care providers and researchers), one participant shared their thoughts on the potential for digital health to increase workload and liability:
Sometimes the more information that we provide for them (doctors), the more work and liability we give them, right? So if they get so much information that becomes actionable but they are overwhelmed, now they would be obligated to do something with this patient, they are in a chain of distribution, a chain of liability. [ 44 ]
Theme 6: Impact on Health and Behavior
Finally, our sixth theme describes the impact of PGHD on health and health behaviors.
Several studies reported that digital health interventions helped users stay motivated and, in turn, improved their health habits and behaviors, such as adherence to medication, physical activity, and healthy eating. The ability of users to look back at their data helps them identify patterns in their health and behaviors, which increases their awareness of their health and habits. The awareness then allows them to be more mindful of their habits and encourages self-reflection, thus promoting a deeper understanding of their health and well-being. The tracking of patterns in their health, combined with the educational component of some digital health tools, helps users come up with better self-management strategies and feel more confident in their ability to reach their health goals, giving them a greater sense of self-efficacy and control over their health. In a digital health intervention aimed at treating lymphedema following breast cancer treatment, a participant spoke of changes in her awareness of symptoms and improvements:
It helped me realize that I had excess fluid. My arms got lighter each time I did the exercises. My arms began to feel less heavy. It noticed it in my clothes as well. [ 56 ]
Digital health interventions are often reported to positively impact the mental health and well-being of individuals. Women reported improvements in their mood, emotional state, and coping abilities. They also reported a reduction in stress and anxiety levels, which can lead to improvements in overall health outcomes. The digital health tools provide users with a sense of support and accountability as well as feelings of accomplishment when meeting their goals.
However, it is important to note that, while digital health interventions can have many benefits, they may not be suitable for everyone and may even have negative effects on some individuals. For example, some users reported increased anxiety due to excessive monitoring or notifications, and others reported negative effects on their thoughts or worsening of symptoms related to health conditions. Some users found that self-tracking made them more attached to their phones, less likely to engage in social activities, and more isolated overall. Care should be taken to ensure that users do not become obsessive about self-tracking as this can be counterproductive or even harmful. Being hyperfocused on their symptoms or health condition could be distressing and even detrimental to their overall well-being. Therefore, it is important to carefully monitor the use of digital health interventions and adjust them as needed to ensure the best possible outcomes for each individual. One woman spoke about her overreliance on an app used to track breastfeeding:
I stopped using it because um I thought I’m being too anal about this...being too concerned about it, I just need to stress less, and just go with the flow and just be a bit more relaxed about it...so, that’s why I stopped using it completely, and then I think the breastfeeding improved from there ’cause I was worrying about it less. [ 57 ]
Table 2 provides a summary of the thematic analysis grouped into barriers and facilitators. It is worth noting that many things are both a barrier and a facilitator (eg, cost) depending on the individual. In addition, the presence of a specific feature may be a facilitator, whereas the absence of it may be a barrier.
Principal Findings
In this scoping review, we summarized information from 406 articles on digital technologies collecting PGHD and how they have been used in women’s health research. We found a steady increase in articles meeting our inclusion criteria from 2015 to 2020, indicating an increasing trend in the uptake and use of digital health tools in women’s health research before the COVID-19 pandemic. Most included studies (310/406, 76.4%) were feasibility or acceptability studies, effectiveness studies, or reports of digital tool prototypes. Most studies (299/406, 73.6%) focused on tracking conditions related to pregnancy or the postpartum period, cancer survivorship, or menstrual, sexual, and reproductive health. Several types of digital health were represented, with the most common being apps, wearable devices, and websites or patient portals. Through our thematic analysis, we found several considerations of facilitators of and barriers to using digital health tools, including the accessibility and convenience of the tools, visual appearance, device functionality and ability to personalize the user experience, and accuracy of the algorithms and information provided. It is also important to consider the target audience to optimize the adoption of the tools. Engagement with digital health tools may help users improve their health and health-related behaviors and gather support from friends, family, and other digital health users. Women are more likely to use digital health if it is recommended by a health care provider, but there are both benefits and challenges that health care providers may face if considering integrating digital health technology into clinical practice.
A previously published scoping review focused on information and communications technologies as a tool for women’s empowerment [ 59 ]. They reported that the concept of empowerment appeared in various ways with no clear consensus on the definition, with some studies mentioning terms such as self-concept, self-esteem, self-worth, and self-efficacy. Our thematic analysis also found that some women’s use of digital health tools increases their self-efficacy in managing their health. Another systematic review of 13 digital health interventions for midlife women found that many interventions did not use a specific behavior change theory [ 60 ]. Our scoping review did not examine the effectiveness of the interventions described, but those designing digital health tools and interventions may want to carefully consider behavioral theories in the design to increase adoption and retention rates and adherence to interventions.
Overall, digital health technology to collect PGHD has gained popularity over the past several years. The integration of wearables, smartphones, and digital health technologies has enabled the integration of passive data collection. This wealth of data provides valuable insights into various aspects of health, enabling informed decisions and the adoption of proactive measures to improve well-being. The uptake of this technology will usher in a new era in how we manage our health and well-being. This transformation has changed how we engage with our health and shifted our perception of health and the approach we take toward maintaining it.
Femtech, as a subset of digital health technology, has grown in popularity. This was evidenced by the large increase in the number of articles published between 2015 and 2020 that used digital health tools to track metrics during pregnancy and the postpartum period as well as metrics related to menstrual, sexual, and reproductive health. These technologies empower women and people assigned female at birth to take charge of their health. This is particularly relevant for people with conditions that are not diseases or health concerns per se but are nevertheless part of managing their overall health and well-being. In this way, femtech can provide a greater sense of control over reproductive health and choices, which can be precarious in many settings worldwide. However, in a previous scoping review, researchers reported that many mobile health apps do not follow data privacy, sharing, and security standards [ 61 ]. Issues related to the privacy and security of personal health data may be especially important when it comes to tracking reproductive health in settings where sexual and reproductive health rights are not guaranteed. This focus on pregnancy and reproductive health is consistent with the fact that women’s health research has largely focused on reproductive health topics [ 62 ]. Researchers and digital health developers must address gaps in women’s health regarding areas that are not strictly related to reproductive health. Women’s health encompasses much more than obstetrics and gynecology; even for health conditions that affect men and women, there may be sex or gender differences in disease presentation, personal experiences, and treatment plans. While using gendered language and design in femtech has the potential to reinforce stereotypes regarding femininity that could cause harm [ 63 ], there is a need for apps to provide content relevant to female populations while being gender inclusive and conscious of biases in the language and advice presented.
When analyzing themes related to acceptability, personalization emerged as a key aspect influencing the adoption and sustained use of digital health tools. People respond positively and want to engage with tools that cater to their unique needs and preferences. The ability to customize elements such as the frequency of notifications, specific health measures tracked and displayed, goal-setting options, and the amount of health information provided enhanced user engagement and motivation. However, offering too many personalization options might overwhelm users, making apps or devices cumbersome to use and navigate. Simplicity and ease of use should not be compromised in the pursuit of personalization. Creating personalized experiences that are intuitive and user-friendly while integrating multiple functionalities into a given device is an important consideration. Recognizing that a “one-size-fits-all” approach is inadequate, digital intervention designers need to define their target audience clearly. Apps that cater to specific groups, such as those with certain chronic health conditions, may inherently provide a sense of personalization by addressing their unique requirements. We have also learned the importance of ensuring that the design is inclusive and accessible to everyone within the target audience. Our findings that some tools are not sensitive to certain circumstances such as pregnancy are consistent with those of a systematic review of digital health interventions for postpartum women, in which the authors reported that barriers related to postpartum status could make it more difficult to engage with the interventions [ 58 ]. Tools designed with these circumstances in mind may be more engaging for women during pregnancy and the postpartum period, leading to greater adoption and quality of the technologies. Attrition can be high among users of digital health interventions [ 64 , 65 ], but most participants were willing to self-track when motivated by a specific health condition.
An important finding of this review was the growing demand and expectation that PGHD are integrated with clinical care. As digital health continues evolving, patients seek more seamless interactions between digital health data and health care providers. Moreover, services delivered through digital health technologies were not expected to replace the role of health care professionals but rather to be a useful tool to support health care management. Maintaining the human touch during communication for health care delivery was seen as important, with technology complementing clinical care to enhance the overall experience for patients and providers.
One of the critical considerations in clinical integration is the accuracy of PGHD collected from digital health tools. Ensuring the reliability and validity of the data is essential for effective clinical decision-making. Striking a balance between patient empowerment and health care provider oversight is crucial to achieving the best possible outcomes. In general, it is important for health care providers to actively propose digital health during patient visits and encourage its use. While challenges and concerns associated with the use of digital health are noted from health care providers’ perspective, such as concerns about medico-legal effects, maintaining professional boundaries, and not adding an abundance of work, the benefits of these tools in supporting patient care and improving outcomes are perceived as important.
Strengths, Limitations, and Future Directions
There are some limitations to this scoping review. Our inclusion criteria did not cover conference abstracts, conference reviews, editorials, letters, comments, or gray literature. Our review also did not include articles written in languages other than English. Therefore, there may be other uses of PGHD in women’s health that were not captured in this review. The assessments of the quality of included articles, the effectiveness of the interventions, or the accuracy in validating PGHD were outside this review’s scope and were not performed. Our aim was to provide a broad overview of PGHD in published women’s health research literature rather than evaluating the quality of the digital technologies or intervention effectiveness. Another limitation is the rapid growth of digital health and femtech, especially during the COVID-19 pandemic. It is important to note that this scoping review only captures the use of PGHD in women’s health before the emergence of the pandemic. We suggest that this review may provide a baseline for comparison in a future scoping review that captures articles published in March 2020 or later. The strengths of this review include the large number of publications analyzed and the data charting process conducted in duplicate by 2 reviewers. The broad scope of this review also helps provide an overall picture of digital health for women and highlights gaps in the research literature.
Future endeavors in this space should consider digital health tools for women for nonreproductive topics such as chronic health conditions that primarily affect women or conditions that have sex or gender differences in presentation and treatment. Within reproductive health, there was a large focus on pregnancy, but there is an unmet need for research and digital health tools appropriate for women in perimenopause and menopause. A previous literature review found <5 articles published between 2010 and 2020 about digital health technologies that meet the psychosocial needs of women experiencing menopause [ 66 ]. There may also be further opportunities for digital health tools geared toward specific racial or ethnic groups that are culturally sensitive and available in multiple languages. A systematic review found that barriers to the use of digital health among culturally and linguistically diverse populations include lower literacy levels and the use of complex medical terminology in some apps, lack of recognition of cultural concerns, stereotypes, and inaccurate portrayals of cultural groups [ 67 ]. Previous scoping reviews in the space of women’s digital health have identified the need for femtech to pay more attention to cultural appropriateness and consider cultural contexts in their design [ 68 , 69 ].
Conclusions
In conclusion, the integration of wearables, smartphones, and other forms of digital health has revolutionized how we approach and engage with our health. Personalization, inclusivity, and integration with clinical care are vital aspects of developing effective digital health solutions. By understanding the needs of the target audience, providing meaningful personalization, and ensuring data accuracy, digital health can truly transform health care and empower individuals to take charge of their well-being while maintaining a collaborative relationship with health care professionals.
Acknowledgments
Thank you to Shannon Cheng, reference librarian, for her work in developing the search strategy and conducting the database searches. A big thank you to Dr Beth Payne for reviewing the manuscript draft and providing helpful feedback. AT is funded by a Michael Smith Health Research British Columbia Scholar award.
Data Availability
The data sets generated during this study are available in the OSF repository [ 70 ].
Authors' Contributions
JLK and AT conceived the study and designed the study protocol. JLK, RST, and AT conducted the article screening. JLK, RW, and RST conducted the data charting. JLK, RST, and DSC created the visualizations and tables of the charted data. The thematic analysis coding was conducted by JLK and RW, with additional discussions with AT in refining the themes. JLK, RST, and AT wrote the draft of the manuscript. All authors reviewed the manuscript before submission.
Conflicts of Interest
None declared.
PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) checklist.
Full search strategy.
List of included articles by health area.
Metrics collected in the included studies.
- Conceptualizing a data infrastructure for the capture, use, and sharing of patient-generated health data in care delivery and research through 2024. The Office of the National Coordinator for Health Information Technology. Jan 2018. URL: https://www.healthit.gov/sites/default/files/onc_pghd_final_white_paper.pdf [accessed 2024-05-03]
- DeSilva J, Prensky-Pomeranz R, Zweig M. Digital health consumer adoption report 2020. RockHealth. Feb 26, 2021. URL: https://rockhealth.com/insights/digital-health-consumer-adoption-report-2020 [accessed 2024-05-03]
- Taylor P. Penetration of mobile devices in Canada as share of the population from 2009 to 2021. Statista. URL: https://www.statista.com/statistics/462386/mobile-device-penetration-canada [accessed 2024-05-03]
- Olsen E. Digital health apps balloon to more than 350,000 available on the market, according to IQVIA report. MobiHealthNews. Aug 4, 2021. URL: https://www.mobihealthnews.com/news/digital-health-apps-balloon-more-350000-available-market-according-iqvia-report [accessed 2024-05-03]
- Paré G, Leaver C, Bourget C. Diffusion of the digital health self-tracking movement in Canada: results of a national survey. J Med Internet Res. May 02, 2018;20(5):e177. [ CrossRef ] [ Medline ]
- Fox S, Duggan M. Tracking for health. Pew Research Center. Jan 28, 2013. URL: https://www.pewresearch.org/internet/wp-content/uploads/sites/9/media/Files/Reports/2013/PIP_TrackingforHealth-with-appendix.pdf [accessed 2024-05-03]
- Peek N, Sujan M, Scott P. Digital health and care in pandemic times: impact of COVID-19. BMJ Health Care Inform. Jun 2020;27(1):e100166. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Budd J, Miller BS, Manning EM, Lampos V, Zhuang M, Edelstein M, et al. Digital technologies in the public-health response to COVID-19. Nat Med. Aug 2020;26(8):1183-1192. [ CrossRef ] [ Medline ]
- Bruining N. The post-pandemic legacy: the breakthrough of digital health and telemedicine. Cardiovasc Res. Jul 27, 2021;117(9):e118-e119. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Meskó B. COVID-19's impact on digital health adoption: the growing gap between a technological and a cultural transformation. JMIR Hum Factors. Sep 19, 2022;9(3):e38926. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kim KK, Jalil S, Ngo V. Improving self-management and care coordination with person-generated health data and mobile health. In: Edmunds M, Hass C, Holve E, editors. Consumer Informatics and Digital Health. Cham, Switzerland. Springer; Jan 18, 2019.
- Shapiro M, Johnston D, Wald J, Mon D. Patient-generated health data. White paper. RTI International. 2012. URL: https://www.rti.org/publication/patient-generated-health-data-white-paper [accessed 2024-05-03]
- Vodicka E, Kim K, Devine EB, Gnanasakthy A, Scoggins JF, Patrick DL. Inclusion of patient-reported outcome measures in registered clinical trials: evidence from ClinicalTrials.gov (2007-2013). Contemp Clin Trials. Jul 2015;43:1-9. [ CrossRef ] [ Medline ]
- Femtech—time for a digital revolution in the women’s health market. Frost & Sullivan. Jan 31, 2018. URL: https://www.frost.com/frost-perspectives/femtechtime-digital-revolution-womens-health-market [accessed 2024-05-03]
- Karim JL, Talhouk A. Person-generated health data in women's health: protocol for a scoping review. JMIR Res Protoc. May 28, 2021;10(5):e26110. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. Oct 02, 2018;169(7):467-473. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ahmadvand A, Kavanagh D, Clark M, Drennan J, Nissen L. Trends and visibility of "digital health" as a keyword in articles by JMIR publications in the new millennium: bibliographic-bibliometric analysis. J Med Internet Res. Dec 19, 2019;21(12):e10477. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lau Y, Cheng LJ, Chi C, Tsai C, Ong KW, Ho-Lim SS, et al. Development of a healthy lifestyle mobile app for overweight pregnant women: qualitative study. JMIR Mhealth Uhealth. Apr 23, 2018;6(4):e91. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Maxwell H, O’Shea M, Stronach M, Pearce S. Empowerment through digital health trackers: an exploration of Indigenous Australian women and physical activity in leisure settings. Ann Leis Res. Oct 04, 2019;24(1):150-167. [ CrossRef ]
- Hughson JP, Daly JO, Woodward-Kron R, Hajek J, Story D. The rise of pregnancy apps and the implications for culturally and linguistically diverse women: narrative review. JMIR Mhealth Uhealth. Nov 16, 2018;6(11):e189. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ranzenhofer LM, Engel SG, Crosby RD, Haigney M, Anderson M, McCaffery JM, et al. Real-time assessment of heart rate variability and loss of control eating in adolescent girls: a pilot study. Int J Eat Disord. Feb 2016;49(2):197-201. [ FREE Full text ] [ CrossRef ] [ Medline ]
- James DC, Harville C2, Whitehead N, Stellefson M, Dodani S, Sears C. Willingness of African American women to participate in e-Health/m-Health research. Telemed J E Health. Mar 2016;22(3):191-197. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lupton D, Maslen S. The more-than-human sensorium: sensory engagements with digital self-tracking technologies. Senses Soc. Jul 25, 2018;13(2):190-202. [ CrossRef ]
- Asklund I, Samuelsson E, Hamberg K, Umefjord G, Sjöström M. User experience of an app-based treatment for stress urinary incontinence: qualitative interview study. J Med Internet Res. Mar 14, 2019;21(3):e11296. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Huberty J, Ehlers DK, Kurka J, Ainsworth B, Buman M. Feasibility of three wearable sensors for 24 hour monitoring in middle-aged women. BMC Womens Health. Jul 30, 2015;15:55. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Haney AC. Young female college millennials' intent for behavior change with wearable fitness technology. Walden University. 2018. URL: https://scholarworks.waldenu.edu/dissertations/5197/ [accessed 2020-04-11]
- Leonard NR, Silverman M, Sherpa DP, Naegle MA, Kim H, Coffman DL, et al. Mobile health technology using a wearable sensorband for female college students with problem drinking: an acceptability and feasibility study. JMIR Mhealth Uhealth. Jul 07, 2017;5(7):e90. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Brett J, Boulton M, Watson E. Development of an e-health app to support women prescribed adjuvant endocrine therapy after treatment for breast cancer. Patient Prefer Adherence. Dec 11, 2018;12:2639-2647. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chaudhry BM. Expecting great expectations when expecting. Mhealth. Jan 10, 2018;4:2. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mann D, Riddell L, Lim K, Byrne LK, Nowson C, Rigo M, et al. Mobile phone app aimed at improving iron intake and bioavailability in premenopausal women: a qualitative evaluation. JMIR Mhealth Uhealth. Sep 28, 2015;3(3):e92. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Grym K, Niela-Vilén H, Ekholm E, Hamari L, Azimi I, Rahmani A, et al. Feasibility of smart wristbands for continuous monitoring during pregnancy and one month after birth. BMC Pregnancy Childbirth. Jan 17, 2019;19(1):34. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Goetz M, Müller M, Matthies LM, Hansen J, Doster A, Szabo A, et al. Perceptions of patient engagement applications during pregnancy: a qualitative assessment of the patient's perspective. JMIR Mhealth Uhealth. May 26, 2017;5(5):e73. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lupton D, Pedersen S. An Australian survey of women's use of pregnancy and parenting apps. Women Birth. Aug 2016;29(4):368-375. [ CrossRef ] [ Medline ]
- de Mooij MJ, Hodny RL, O'Neil DA, Gardner MR, Beaver M, Brown AT, et al. OB nest: reimagining low-risk prenatal care. Mayo Clin Proc. Apr 2018;93(4):458-466. [ CrossRef ] [ Medline ]
- Kokts-Porietis RL, Stone CR, Friedenreich CM, Froese A, McDonough M, McNeil J. Breast cancer survivors' perspectives on a home-based physical activity intervention utilizing wearable technology. Support Care Cancer. Aug 2019;27(8):2885-2892. [ CrossRef ] [ Medline ]
- Gell NM, Tursi A, Grover KW, Dittus K. Female cancer survivor perspectives on remote intervention components to support physical activity maintenance. Support Care Cancer. May 2020;28(5):2185-2194. [ CrossRef ] [ Medline ]
- Ravn Jakobsen P, Hermann AP, Søndergaard J, Wiil UK, Clemensen J. Development of an mHealth application for women newly diagnosed with osteoporosis without preceding fractures: a participatory design approach. Int J Environ Res Public Health. Feb 13, 2018;15(2):330. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Harder H, Holroyd P, Burkinshaw L, Watten P, Zammit C, Harris PR, et al. A user-centred approach to developing bWell, a mobile app for arm and shoulder exercises after breast cancer treatment. J Cancer Surviv. Dec 2017;11(6):732-742. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Depper A, Howe PD. Are we fit yet? English adolescent girls’ experiences of health and fitness apps. Health Sociol Rev. Jul 04, 2016;26(1):98-112. [ CrossRef ]
- Gambier-Ross K, McLernon DJ, Morgan HM. A mixed methods exploratory study of women's relationships with and uses of fertility tracking apps. Digit Health. Jul 25, 2018;4:2055207618785077. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lupton D. ‘It just gives me a bit of peace of mind’: Australian women’s use of digital media for pregnancy and early motherhood. Societies. Sep 15, 2017;7(3):25. [ CrossRef ]
- Logsdon MC, Lauf A, Stikes R, Revels A, Vickers-Smith R. Partnering with new mothers to develop a smart phone app to prevent maternal mortality after hospital discharge: a pilot study. J Adv Nurs. Jan 2020;76(1):324-327. [ CrossRef ] [ Medline ]
- Wright AA, Raman N, Staples P, Schonholz S, Cronin A, Carlson K, et al. The HOPE pilot study: harnessing patient-reported outcomes and biometric data to enhance cancer care. JCO Clin Cancer Inform. Dec 2018;2:1-12. [ FREE Full text ] [ CrossRef ] [ Medline ]
- de Mendoza AH, Cabling ML, Dilawari A, Turner JW, Fernández N, Henderson A, et al. Providers' perspectives on adherence to hormonal therapy in breast cancer survivors. Is there a role for the digital health feedback system? Health Technol (Berl). Mar 2019;9(2):175-184. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Willcox JC, van der Pligt P, Ball K, Wilkinson SA, Lappas M, McCarthy EA, et al. Views of women and health professionals on mHealth lifestyle interventions in pregnancy: a qualitative investigation. JMIR Mhealth Uhealth. Oct 28, 2015;3(4):e99. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ke JX, George RB, Wozney L, Chorney JL. Patient-centred perioperative mobile application in Cesarean delivery: needs assessment and development. Can J Anaesth. Oct 2019;66(10):1194-1201. [ CrossRef ] [ Medline ]
- Firet L, de Bree C, Verhoeks CM, Teunissen DA, Lagro-Janssen AL. Mixed feelings: general practitioners' attitudes towards eHealth for stress urinary incontinence - a qualitative study. BMC Fam Pract. Jan 26, 2019;20(1):21. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Garnweidner-Holme LM, Borgen I, Garitano I, Noll J, Lukasse M. Designing and developing a mobile smartphone application for women with gestational diabetes mellitus followed-up at diabetes outpatient clinics in Norway. Healthcare (Basel). May 21, 2015;3(2):310-323. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Grassl N, Nees J, Schramm K, Spratte J, Sohn C, Schott TC, et al. A web-based survey assessing the attitudes of health care professionals in Germany toward the use of telemedicine in pregnancy monitoring: cross-sectional study. JMIR Mhealth Uhealth. Aug 08, 2018;6(8):e10063. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pais S, Parry D, Petrova K, Rowan J. Acceptance of using an ecosystem of mobile apps for use in diabetes clinic for self-management of gestational diabetes mellitus. Stud Health Technol Inform. 2017;245:188-192. [ Medline ]
- Ragavan MI, Ferre V, Bair-Merritt M. Thrive: a novel health education mobile application for mothers who have experienced intimate partner violence. Health Promot Pract. Mar 2020;21(2):160-164. [ CrossRef ] [ Medline ]
- Runkle J, Sugg M, Boase D, Galvin SL, C Coulson C. Use of wearable sensors for pregnancy health and environmental monitoring: descriptive findings from the perspective of patients and providers. Digit Health. Feb 06, 2019;5:2055207619828220. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sadigursky A. Move my mood: development and evaluation of a mobile mental health self-help app using behavioral activation for women with postpartum depression. Alliant International University. 2018. URL: https://books.google.co.in/books/about/Move_My_Mood.html?id=dYtP0AEACAAJ&redir_esc=y [accessed 2020-03-30]
- Scherr CL, Feuston JL, Nixon DM, Cohen SA. A two-phase approach to developing SNAP: an iPhone application to support appointment scheduling and management for women with a BRCA mutation. J Genet Couns. Apr 2018;27(2):439-445. [ CrossRef ] [ Medline ]
- Tommasone G, Bazzani M, Solinas V, Serafini P. Midwifery e-health: from design to validation of “mammastyle — Gravidanza Fisiologica”. In: Proceedings of the IEEE 18th International Conference on e-Health Networking, Applications and Services (Healthcom). 2016. Presented at: Healthcom 2016; September 14-16, 2016; Munich, Germany. [ CrossRef ]
- Fu MR, Axelrod D, Guth AA, Wang Y, Scagliola J, Hiotis K, et al. Usability and feasibility of health IT interventions to enhance Self-Care for Lymphedema Symptom Management in breast cancer survivors. Internet Interv. Sep 2016;5:56-64. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dienelt K, Moores CJ, Miller J, Mehta K. An investigation into the use of infant feeding tracker apps by breastfeeding mothers. Health Informatics J. Sep 2020;26(3):1672-1683. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lim S, Tan A, Madden S, Hill B. Health professionals' and postpartum women's perspectives on digital health interventions for lifestyle management in the postpartum period: a systematic review of qualitative studies. Front Endocrinol (Lausanne). Nov 8, 2019;10:767. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mackey A, Petrucka P. Technology as the key to women's empowerment: a scoping review. BMC Womens Health. Feb 23, 2021;21(1):78. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sediva H, Cartwright T, Robertson C, Deb SK. Behavior change techniques in digital health interventions for midlife women: systematic review. JMIR Mhealth Uhealth. Nov 09, 2022;10(11):e37234. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Alfawzan N, Christen M, Spitale G, Biller-Andorno N. Privacy, data sharing, and data security policies of women's mHealth apps: scoping review and content analysis. JMIR Mhealth Uhealth. May 06, 2022;10(5):e33735. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hallam L, Vassallo A, Pinho-Gomes AC, Carcel C, Woodward M. Does journal content in the field of women's health represent women's burden of disease? A review of publications in 2010 and 2020. J Womens Health (Larchmt). May 2022;31(5):611-619. [ CrossRef ] [ Medline ]
- Figueroa CA, Luo T, Aguilera A, Lyles CR. The need for feminist intersectionality in digital health. Lancet Digit Health. Aug 2021;3(8):e526-e533. [ CrossRef ]
- Jabir AI, Lin X, Martinengo L, Sharp G, Theng YL, Tudor Car L. Attrition in conversational agent-delivered mental health interventions: systematic review and meta-analysis. J Med Internet Res. Feb 27, 2024;26:e48168. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Meyerowitz-Katz G, Ravi S, Arnolda L, Feng X, Maberly G, Astell-Burt T. Rates of attrition and dropout in app-based interventions for chronic disease: systematic review and meta-analysis. J Med Internet Res. Sep 29, 2020;22(9):e20283. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cronin C, Hungerford C, Wilson RL. Using digital health technologies to manage the psychosocial symptoms of menopause in the workplace: a narrative literature review. Issues Ment Health Nurs. Jun 2021;42(6):541-548. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Whitehead L, Talevski J, Fatehi F, Beauchamp A. Barriers to and facilitators of digital health among culturally and linguistically diverse populations: qualitative systematic review. J Med Internet Res. Feb 28, 2023;25:e42719. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Birati Y, Yefet E, Perlitz Y, Shehadeh N, Spitzer S. Cultural and digital health literacy appropriateness of app- and web-based systems designed for pregnant women with gestational diabetes mellitus: scoping review. J Med Internet Res. Oct 14, 2022;24(10):e37844. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Woodley SJ, Moller B, Clark AR, Bussey MD, Sangelaji B, Perry M, et al. Digital technologies for women's pelvic floor muscle training to manage urinary incontinence across their life course: scoping review. JMIR Mhealth Uhealth. Jul 05, 2023;11:e44929. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Person-generated health data in women’s health: scoping review. OSF Home. Mar 7, 2024. URL: https://osf.io/3eync/ [accessed 2024-05-07]
Abbreviations
Edited by T de Azevedo Cardoso; submitted 04.10.23; peer-reviewed by D Liu, M Herron; comments to author 23.02.24; revised version received 15.03.24; accepted 26.03.24; published 16.05.24.
©Jalisa Lynn Karim, Rachel Wan, Rhea S Tabet, Derek S Chiu, Aline Talhouk. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 16.05.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Researchers say future is bright for treating substance abuse through mobile health technologies
Despite the high prevalence of substance abuse and its often devastating outcomes, especially among disadvantaged populations, few Americans receive treatment for substance use disorders. However, the rise of mobile health technologies can make treatments more accessible.
Researchers at the University of Oklahoma are creating and studying health interventions delivered via smartphones to make effective, evidence-based treatments available to those who cannot or don't want to enter traditional in-person treatment. Michael Businelle, Ph.D., co-director of the TSET Health Promotion Center, a program of OU Health Stephenson Cancer Center, recently published a paper in the Annual Review of Clinical Psychology that details the current landscape of mobile health technology for substance use disorders and suggests a roadmap for the future.
The Health Promotion Research Center (HPRC) is at the forefront of mobile health technologies worldwide, having attracted $65 million in grants and supporting nearly 100 mobile health studies. Within HPRC, Businelle leads the mHealth Shared Resource, which launched the Insight™ mHealth Platform in 2015 to create and test technology-based interventions. A multitude of health apps are available commercially, but few have undergone the research necessary to determine if they are effective. Businelle sees the promise of rigorously tested smartphone apps to fill gaps in substance abuse treatment.
"According to the Substance Abuse and Mental Health Services Administration, only 6% of people with substance use disorders receive any form of treatment," Businelle said. "There are many reasons -- we have a shortage of care providers, people may not have reliable transportation, may not be able to get away from work, or they may not be able to afford treatment. However, 90% of all U.S. adults own smartphones, and technology now allows us to create highly tailored interventions delivered at the time that people need them."
Businelle and his team have many mobile health studies underway for substance abuse, and the Insight™ mHealth Platform is used by other research institutions across the United States. The mobile health field is large and growing, not only for substance abuse but for mental health disorders like depression and anxiety. In his publication, Businelle makes several recommendations for research going forward.
Re-randomize clinical trial participants
Thus far, most clinical trials for mobile health interventions have mirrored traditional clinical trials studying new drugs, in which participants are randomly assigned to receive a new drug or a placebo and stay in those groups for the duration of the trial. But that approach doesn't work well for substance abuse trials, Businelle said. For example, if people don't quit smoking on their targeted quit date, they are unlikely to quit during the trial. Unlike traditional trials, mobile health apps can be programmed to re-randomize participants, or move them to a different intervention that might work better for them, he said.
"Instead of being stuck receiving a treatment that we know isn't likely to be effective for an individual, the app can easily re-randomize participants to different treatments," he said. "Just because they weren't successful with one type of intervention doesn't mean that another one won't work."
Objectively verify self-reports
Most substance abuse interventions have historically relied on people to report their own relapses. Unfortunately, because of stigma, people don't always report their usage truthfully, Businelle said. However, technology can now be used to biochemically verify self-reported substance use. In six of his smoking cessation trials, Businelle verifies whether participants have smoked by asking them to blow into a small device connected to a smartphone that detects the presence of carbon monoxide. Facial recognition software confirms the participant is the one testing.
"It is really important for the accuracy of our studies to objectively verify what people report," he said. "We are also developing similar noninvasive technologies that can detect the use of other types of substances without collecting urine or blood samples."
What is a successful outcome?
In mobile health substance abuse trials, success is often measured by whether a person is still using a substance at the end of the trial. But reality isn't usually so straightforward. Businelle said people may stop and start using a substance several times during a six-month trial. Instead of emphasizing the end result, he recommends using technology to assess the effectiveness of an intervention at daily, weekly and monthly intervals. By understanding the number of days of abstinence or number of days until a relapse, for example, the intervention can be more accurately assessed and improved.
Mobile health technology has disadvantages, such as the potential lack of a therapeutic relationship that can develop between patient and therapist, and because some people may need more intensive treatments than mobile health can provide. However, mobile health is still in its infancy.
"Mobile health interventions may reduce stigma because people do not have to attend treatment in person," Businelle said. "Because there is a severe shortage of qualified therapists, always-available behavior change apps could become a first line of treatment for substance abuse, with traditional counseling being reserved for those who do not respond to mobile health interventions."
- Mental Health Research
- Public Health Education
- Health Policy
- Mental Health
- Mobile Computing
- Educational Technology
- Information Technology
- Public Health
- World Development
- Social Issues
- Substance abuse
- Sleep disorder
- Psychoactive drug
- Mobile phone radiation and health
- Illusion of control
- Stem cell treatments
- Air pollution
Story Source:
Materials provided by University of Oklahoma . Note: Content may be edited for style and length.
Journal Reference :
- Michael S. Businelle, Olga Perski, Emily T. Hébert, Darla E. Kendzor. Mobile Health Interventions for Substance Use Disorders . Annual Review of Clinical Psychology , 2024; 20 (1) DOI: 10.1146/annurev-clinpsy-080822-042337
Cite This Page :
Explore More
- Life Expectancy May Increase by 5 Years by 2050
- Toward a Successful Vaccine for HIV
- Highly Efficient Thermoelectric Materials
- Toward Human Brain Gene Therapy
- Whale Families Learn Each Other's Vocal Style
- AI Can Answer Complex Physics Questions
- Otters Use Tools to Survive a Changing World
- Monogamy in Mice: Newly Evolved Type of Cell
- Sustainable Electronics, Doped With Air
- Male Vs Female Brain Structure
Trending Topics
Strange & offbeat.
Sanatorium Valuyevo

View prices for your travel dates
- Excellent 13
- Very Good 22
- All languages ( 65 )
- Russian ( 65 )
- English ( 0 )

Own or manage this property? Claim your listing for free to respond to reviews, update your profile and much more.
SANATORIUM VALUYEVO

40 Facts About Elektrostal
Written by Lanette Mayes
Modified & Updated: 17 May 2024
Reviewed by Jessica Corbett

Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to captivate you.
This article will provide you with 40 fascinating facts about Elektrostal, giving you a better understanding of why this city is worth exploring. From its origins as an industrial hub to its modern-day charm, we will delve into the various aspects that make Elektrostal a unique and must-visit destination.
So, join us as we uncover the hidden treasures of Elektrostal and discover what makes this city a true gem in the heart of Russia.
Key Takeaways:
- Elektrostal, known as the “Motor City of Russia,” is a vibrant and growing city with a rich industrial history, offering diverse cultural experiences and a strong commitment to environmental sustainability.
- With its convenient location near Moscow, Elektrostal provides a picturesque landscape, vibrant nightlife, and a range of recreational activities, making it an ideal destination for residents and visitors alike.
Known as the “Motor City of Russia.”
Elektrostal, a city located in the Moscow Oblast region of Russia, earned the nickname “Motor City” due to its significant involvement in the automotive industry.
Home to the Elektrostal Metallurgical Plant.
Elektrostal is renowned for its metallurgical plant, which has been producing high-quality steel and alloys since its establishment in 1916.
Boasts a rich industrial heritage.
Elektrostal has a long history of industrial development, contributing to the growth and progress of the region.
Founded in 1916.
The city of Elektrostal was founded in 1916 as a result of the construction of the Elektrostal Metallurgical Plant.
Located approximately 50 kilometers east of Moscow.
Elektrostal is situated in close proximity to the Russian capital, making it easily accessible for both residents and visitors.
Known for its vibrant cultural scene.
Elektrostal is home to several cultural institutions, including museums, theaters, and art galleries that showcase the city’s rich artistic heritage.
A popular destination for nature lovers.
Surrounded by picturesque landscapes and forests, Elektrostal offers ample opportunities for outdoor activities such as hiking, camping, and birdwatching.
Hosts the annual Elektrostal City Day celebrations.
Every year, Elektrostal organizes festive events and activities to celebrate its founding, bringing together residents and visitors in a spirit of unity and joy.
Has a population of approximately 160,000 people.
Elektrostal is home to a diverse and vibrant community of around 160,000 residents, contributing to its dynamic atmosphere.
Boasts excellent education facilities.
The city is known for its well-established educational institutions, providing quality education to students of all ages.
A center for scientific research and innovation.
Elektrostal serves as an important hub for scientific research, particularly in the fields of metallurgy, materials science, and engineering.
Surrounded by picturesque lakes.
The city is blessed with numerous beautiful lakes, offering scenic views and recreational opportunities for locals and visitors alike.
Well-connected transportation system.
Elektrostal benefits from an efficient transportation network, including highways, railways, and public transportation options, ensuring convenient travel within and beyond the city.
Famous for its traditional Russian cuisine.
Food enthusiasts can indulge in authentic Russian dishes at numerous restaurants and cafes scattered throughout Elektrostal.
Home to notable architectural landmarks.
Elektrostal boasts impressive architecture, including the Church of the Transfiguration of the Lord and the Elektrostal Palace of Culture.
Offers a wide range of recreational facilities.
Residents and visitors can enjoy various recreational activities, such as sports complexes, swimming pools, and fitness centers, enhancing the overall quality of life.
Provides a high standard of healthcare.
Elektrostal is equipped with modern medical facilities, ensuring residents have access to quality healthcare services.
Home to the Elektrostal History Museum.
The Elektrostal History Museum showcases the city’s fascinating past through exhibitions and displays.
A hub for sports enthusiasts.
Elektrostal is passionate about sports, with numerous stadiums, arenas, and sports clubs offering opportunities for athletes and spectators.
Celebrates diverse cultural festivals.
Throughout the year, Elektrostal hosts a variety of cultural festivals, celebrating different ethnicities, traditions, and art forms.
Electric power played a significant role in its early development.
Elektrostal owes its name and initial growth to the establishment of electric power stations and the utilization of electricity in the industrial sector.
Boasts a thriving economy.
The city’s strong industrial base, coupled with its strategic location near Moscow, has contributed to Elektrostal’s prosperous economic status.
Houses the Elektrostal Drama Theater.
The Elektrostal Drama Theater is a cultural centerpiece, attracting theater enthusiasts from far and wide.
Popular destination for winter sports.
Elektrostal’s proximity to ski resorts and winter sport facilities makes it a favorite destination for skiing, snowboarding, and other winter activities.
Promotes environmental sustainability.
Elektrostal prioritizes environmental protection and sustainability, implementing initiatives to reduce pollution and preserve natural resources.
Home to renowned educational institutions.
Elektrostal is known for its prestigious schools and universities, offering a wide range of academic programs to students.
Committed to cultural preservation.
The city values its cultural heritage and takes active steps to preserve and promote traditional customs, crafts, and arts.
Hosts an annual International Film Festival.
The Elektrostal International Film Festival attracts filmmakers and cinema enthusiasts from around the world, showcasing a diverse range of films.
Encourages entrepreneurship and innovation.
Elektrostal supports aspiring entrepreneurs and fosters a culture of innovation, providing opportunities for startups and business development.
Offers a range of housing options.
Elektrostal provides diverse housing options, including apartments, houses, and residential complexes, catering to different lifestyles and budgets.
Home to notable sports teams.
Elektrostal is proud of its sports legacy, with several successful sports teams competing at regional and national levels.
Boasts a vibrant nightlife scene.
Residents and visitors can enjoy a lively nightlife in Elektrostal, with numerous bars, clubs, and entertainment venues.
Promotes cultural exchange and international relations.
Elektrostal actively engages in international partnerships, cultural exchanges, and diplomatic collaborations to foster global connections.
Surrounded by beautiful nature reserves.
Nearby nature reserves, such as the Barybino Forest and Luchinskoye Lake, offer opportunities for nature enthusiasts to explore and appreciate the region’s biodiversity.
Commemorates historical events.
The city pays tribute to significant historical events through memorials, monuments, and exhibitions, ensuring the preservation of collective memory.
Promotes sports and youth development.
Elektrostal invests in sports infrastructure and programs to encourage youth participation, health, and physical fitness.
Hosts annual cultural and artistic festivals.
Throughout the year, Elektrostal celebrates its cultural diversity through festivals dedicated to music, dance, art, and theater.
Provides a picturesque landscape for photography enthusiasts.
The city’s scenic beauty, architectural landmarks, and natural surroundings make it a paradise for photographers.
Connects to Moscow via a direct train line.
The convenient train connection between Elektrostal and Moscow makes commuting between the two cities effortless.
A city with a bright future.
Elektrostal continues to grow and develop, aiming to become a model city in terms of infrastructure, sustainability, and quality of life for its residents.
In conclusion, Elektrostal is a fascinating city with a rich history and a vibrant present. From its origins as a center of steel production to its modern-day status as a hub for education and industry, Elektrostal has plenty to offer both residents and visitors. With its beautiful parks, cultural attractions, and proximity to Moscow, there is no shortage of things to see and do in this dynamic city. Whether you’re interested in exploring its historical landmarks, enjoying outdoor activities, or immersing yourself in the local culture, Elektrostal has something for everyone. So, next time you find yourself in the Moscow region, don’t miss the opportunity to discover the hidden gems of Elektrostal.
Q: What is the population of Elektrostal?
A: As of the latest data, the population of Elektrostal is approximately XXXX.
Q: How far is Elektrostal from Moscow?
A: Elektrostal is located approximately XX kilometers away from Moscow.
Q: Are there any famous landmarks in Elektrostal?
A: Yes, Elektrostal is home to several notable landmarks, including XXXX and XXXX.
Q: What industries are prominent in Elektrostal?
A: Elektrostal is known for its steel production industry and is also a center for engineering and manufacturing.
Q: Are there any universities or educational institutions in Elektrostal?
A: Yes, Elektrostal is home to XXXX University and several other educational institutions.
Q: What are some popular outdoor activities in Elektrostal?
A: Elektrostal offers several outdoor activities, such as hiking, cycling, and picnicking in its beautiful parks.
Q: Is Elektrostal well-connected in terms of transportation?
A: Yes, Elektrostal has good transportation links, including trains and buses, making it easily accessible from nearby cities.
Q: Are there any annual events or festivals in Elektrostal?
A: Yes, Elektrostal hosts various events and festivals throughout the year, including XXXX and XXXX.
Elektrostal's fascinating history, vibrant culture, and promising future make it a city worth exploring. For more captivating facts about cities around the world, discover the unique characteristics that define each city . Uncover the hidden gems of Moscow Oblast through our in-depth look at Kolomna. Lastly, dive into the rich industrial heritage of Teesside, a thriving industrial center with its own story to tell.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
Share this Fact:

COMMENTS
Best Online Graduate Certificates In Nursing ... The remainder of the curriculum focuses on research, leadership and health services delivery. Though USD delivers coursework remotely for this ...
Most online PhD in Health Services Research programs take 3 to 5 years to complete if you enroll full-time. Most programs require 2 to 3 years of full-time coursework. Some programs allow students to transfer credits from a master's program, potentially reducing the time to finish the degree.
With Walden University's online PhD in Health Services degree, students will prepare to meet the challenges and issues of today's healthcare system. ... You will find 24/7 tech support, writing services, online research tools, tutorials, webinars, help identifying research funding, and much more.
4301 West Markham, Mail Slot 820. Little Rock, AR 72205. Email: [email protected]. Overview The Fay W. Boozman College of Public Health offers a program of instruction leading to the Doctor of Philosophy (Ph.D.) degree in Health Systems and Services Research (HSSR). The program provides students with the theoretical and methodological ...
Program Overview. The University of Maryland School of Public Health offers a Doctorate in Health Services Research (PhD). The program provides interdisciplinary training in research, practice, and policy relevant to the planning, management, and evaluation of clinical practice and public health programs.
The PhD in Health Services Research and Health Policy at the Rollins School of Public Health at Emory University is a full-time program that trains researchers in the fields of health policy, health economics, health management, and health services research. Students take doctoral-level classes in the Department of Economics, the Department of ...
The PhD in Health Policy and Management is a full-time doctoral program that trains its students to conduct original investigator-initiated research through a combination of coursework and research mentoring. The curriculum includes core coursework that is common across the four concentrations and courses specific to each individual concentration.
Transform healthcare with this multidisciplinary degree. With a Health Services Research, Policy & Administration PhD you will engage in a multidisciplinary examination of the social, political, and economic forces that affect the organization, financing, and delivery of healthcare.
Description. The PhD Program in Health Services trains health services researchers and health policy analysts for careers in academic institutions, health delivery systems, public health departments, government agencies, and the private sector. The program prepares students to conduct high-quality independent, collaborative research and policy ...
The mission of the PhD Program in Health Services and Policy Research is to develop research scientists/scholars who are equipped to frame and answer important questions about health services, drawing upon a diverse array of theoretical and methodological approaches. The program is particularly focused on developing graduates who can generate ...
The Doctor of Philosophy in Health Services & Policy Research (PhD) degree program offered by the Department of Health Law, Policy & Management is designed to provide individuals with excellent research skills for use in academic, industry, or government settings. Students have the opportunity to collaborate with senior faculty in innovative ...
Advance the Future of Public Health Research 3-5 Years / Full Time / Seattle, WA. The University of Washington Health Services Doctor of Philosophy (Ph.D.) program trains the next generation of health services researchers and prepares them to become leaders in the field. Our graduates pursue research careers in top-tier universities, research and policy-making organizations, the health care ...
The PhD in Health Services Research and Policy prepares researchers and scholars for careers in universities and other organizations, such as state and local governmental agencies and private health-related industries (insurers, pharmaceuticals, philanthropic foundations, etc.), where health services research is conducted.
Mission and Purpose The Ph.D. program in Public Health - Health Services Research concentration prepares individuals to help inform government officials, corporate leaders, clinicians, health plan managers and others making choices about complex health-related problems and issues. Students in the Ph.D. Program learn to apply research methods and scientific knowledge to the study of health…
The PhD in Health Services Research consists of a common core curriculum, concentration, and elective courses in either Health Systems and Policy or Knowledge Discovery and Health Informatics, and dissertation sequence courses. The coursework is intended to ensure that students have sufficient knowledge, background and skills needed to conduct ...
Drexel Dornsife's Doctor of Philosophy (PhD) in Health Services Research and Policy program is designed to train doctoral students to pursue original quantitative, qualitative, and/or mixed methods research in the broad areas of health policy and health services research in the United States and abroad, with an emphasis on research that can be translated into policy, programs, and/or practice.
The PhD program in Health Services Research and Policy was created to meet an ongoing need for public health researchers who focus on cost, access and quality of the health care system. The graduate program provides students with the knowledge and skills to lead research programs in a range of institutional settings including...
Through our PhD program in Health Services Research, you will engage in a multidisciplinary examination of the economic, social, and political forces that affect the organization, financing, and delivery of health care. This training will enable you to choose a career where you can apply research skills to influence policy and impact health ...
Since 1994, the PhD program in Health Services Research and Policy in the Department of Public Health Sciences has been highly successful in preparing students to become scholars for research, teaching, and public service careers in university, public policy, and governmental settings.. Our PhD program has also been designated as a STEM (Science, Technology, Engineering and Mathematics ...
The Real Meaning of 'Working Knowledge'. Northeastern is the world leader in experiential learning. Here, graduate students—from the master's through the doctorate, and in professional and certificate programs—put knowledge to work at Fortune 500 and startup companies, universities, government agencies, nonprofits, and global ...
The PhD concentration in Health Services Research and Policy provides a firm grounding in public health principles, research and evaluation methods, policy analysis and numerous content areas related to health and health services delivery and population health. The program at Johns Hopkins is one of the oldest and most respected of its type in ...
The cost of earning a D.N.P. depends on the individual program and your status as an in-state or out-of-state student. Tuition for the programs ranked on this page ranges between $327 and $955 per ...
Gillings School of Global Public Health 10-Year Research Analysis. The Health Sciences Library (HSL) has partnered with administration at UNC-Chapel Hill's Gillings School of Global Public Health (SPH) on a series of projects to reveal collaboration patterns of research faculty, illustrate evolution in research foci over time, and demonstrate SPH impact.
Explore our global campuses. Find unique opportunities for experience-powered learning and discovery. Founded in 1898, Northeastern is a global, experiential, research university built on a tradition of engagement with the world.
Dr. Ava Hoffman at Fred Hutchinson Cancer Center is leading an NIEHS R25 grant program entitled Data Science for Environmental Health (DaSEH). DaSEH is a short course that combines online learning and an in-person project-focused intensive to provide short introductory R courses geared towards these intended audiences:
Background: The increased pervasiveness of digital health technology is producing large amounts of person-generated health data (PGHD). These data can empower people to monitor their health to promote prevention and management of disease. Women make up one of the largest groups of consumers of digital self-tracking technology. Objective: In this scoping review, we aimed to (1) identify the ...
Elektrostal , lit: Electric and Сталь , lit: Steel) is a city in Moscow Oblast, Russia, located 58 kilometers east of Moscow. Population: 155,196 ; 146,294 ...
The Health Promotion Research Center (HPRC) is at the forefront of mobile health technologies worldwide, having attracted $65 million in grants and supporting nearly 100 mobile health studies.
3.5. Very good. 64 reviews. Location 4.2. Cleanliness 3.5. Service 3.7. Value 3.6. The sanatorium "Valuevo" is a historical health resort located in a unique location of the New Moscow on the territory of 30 hectares of the ancient noble estate of Count Musin-Pushkin with a perfectly preserved architectural ensemble and a landscape park, in an ...
40 Facts About Elektrostal. Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to ...