- U.S. Department of Health & Human Services
- National Institutes of Health
En Español | Site Map | Staff Directory | Contact Us
- Science Education
- Science Topics

What is medical ultrasound?
How does it work, what is ultrasound used for, are there risks, what are examples of nibib-funded projects using ultrasound.
Medical ultrasound falls into two distinct categories: diagnostic and therapeutic.
Diagnostic ultrasound can be further sub-divided into anatomical and functional ultrasound. Anatomical ultrasound produces images of internal organs or other structures. Functional ultrasound combines information such as the movement and velocity of tissue or blood, softness or hardness of tissue, and other physical characteristics, with anatomical images to create “information maps.” These maps help doctors visualize changes/differences in function within a structure or organ.
Therapeutic ultrasound also uses sound waves above the range of human hearing but does not produce images. Its purpose is to interact with tissues in the body such that they are either modified or destroyed. Among the modifications possible are: moving or pushing tissue, heating tissue, dissolving blood clots, or delivering drugs to specific locations in the body. These destructive, or ablative, functions are made possible by use of very high-intensity beams that can destroy diseased or abnormal tissues such as tumors. The advantage of using ultrasound therapies is that, in most cases, they are non-invasive. No incisions or cuts need to be made to the skin, leaving no wounds or scars.
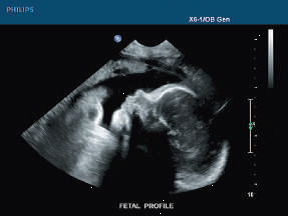
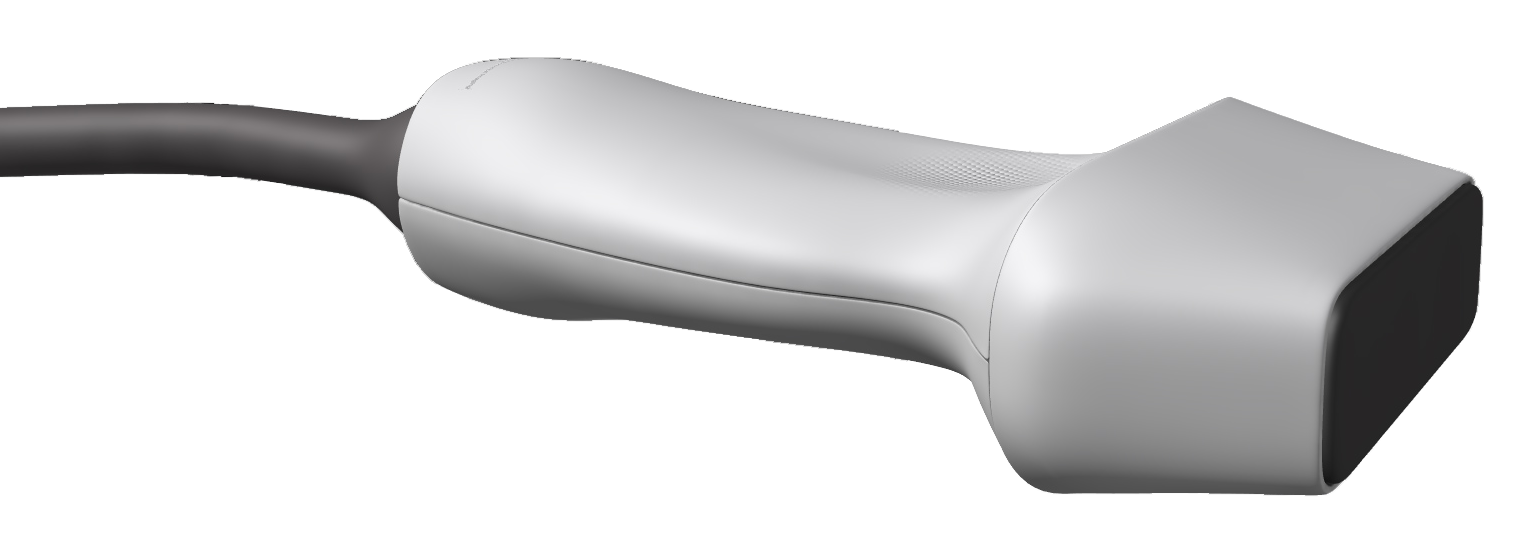
Ultrasound waves are produced by a transducer, which can both emit ultrasound waves, as well as detect the ultrasound echoes reflected back. In most cases, the active elements in ultrasound transducers are made of special ceramic crystal materials called piezoelectrics. These materials are able to produce sound waves when an electric field is applied to them, but can also work in reverse, producing an electric field when a sound wave hits them. When used in an ultrasound scanner, the transducer sends out a beam of sound waves into the body. The sound waves are reflected back to the transducer by boundaries between tissues in the path of the beam (e.g. the boundary between fluid and soft tissue or tissue and bone). When these echoes hit the transducer, they generate electrical signals that are sent to the ultrasound scanner. Using the speed of sound and the time of each echo’s return, the scanner calculates the distance from the transducer to the tissue boundary. These distances are then used to generate two-dimensional images of tissues and organs.
During an ultrasound exam, the technician will apply a gel to the skin. This keeps air pockets from forming between the transducer and the skin, which can block ultrasound waves from passing into the body.
Click here to watch a short video about how ultrasound works.
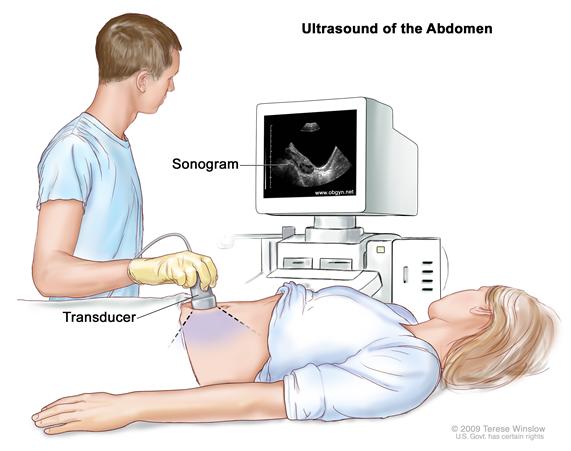
Diagnostic ultrasound. Diagnostic ultrasound is able to non-invasively image internal organs within the body. However, it is not good for imaging bones or any tissues that contain air, like the lungs. Under some conditions, ultrasound can image bones (such as in a fetus or in small babies) or the lungs and lining around the lungs, when they are filled or partially filled with fluid. One of the most common uses of ultrasound is during pregnancy, to monitor the growth and development of the fetus, but there are many other uses, including imaging the heart, blood vessels, eyes, thyroid, brain, breast, abdominal organs, skin, and muscles. Ultrasound images are displayed in either 2D, 3D, or 4D (which is 3D in motion).
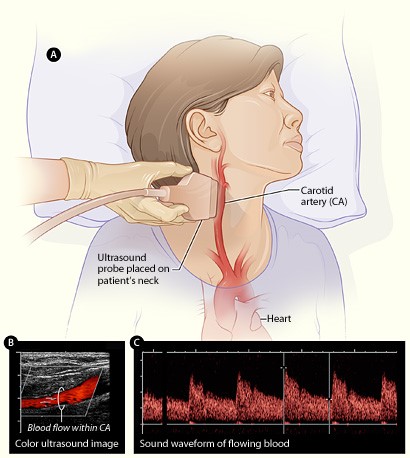
Functional ultrasound. Functional ultrasound applications include Doppler and color Doppler ultrasound for measuring and visualizing blood flow in vessels within the body or in the heart. It can also measure the speed of the blood flow and direction of movement. This is done using color-coded maps called color Doppler imaging. Doppler ultrasound is commonly used to determine whether plaque build-up inside the carotid arteries is blocking blood flow to the brain.
Another functional form of ultrasound is elastography, a method for measuring and displaying the relative stiffness of tissues, which can be used to differentiate tumors from healthy tissue. This information can be displayed as either color-coded maps of the relative stiffness; black-and white maps that display high-contrast images of tumors compared with anatomical images; or color-coded maps that are overlayed on the anatomical image. Elastography can be used to test for liver fibrosis, a condition in which excessive scar tissue builds up in the liver due to inflammation.
Ultrasound is also an important method for imaging interventions in the body. For example, ultrasound-guided needle biopsy helps physicians see the position of a needle while it is being guided to a selected target, such as a mass or a tumor in the breast. Also, ultrasound is used for real-time imaging of the location of the tip of a catheter as it is inserted in a blood vessel and guided along the length of the vessel. It can also be used for minimally invasive surgery to guide the surgeon with real-time images of the inside of the body.
Therapeutic or interventional ultrasound. Therapeutic ultrasound produces high levels of acoustic output that can be focused on specific targets for the purpose of heating, ablating, or breaking up tissue. One type of therapeutic ultrasound uses high-intensity beams of sound that are highly targeted, and is called High Intensity Focused Ultrasound (HIFU). HIFU is being investigated as a method for modifying or destroying diseased or abnormal tissues inside the body (e.g. tumors) without having to open or tear the skin or cause damage to the surrounding tissue. Either ultrasound or MRI is used to identify and target the tissue to be treated, guide and control the treatment in real time, and confirm the effectiveness of the treatment. HIFU is currently FDA approved for the treatment of uterine fibroids, to alleviate pain from bone metastases, and most recently for the ablation of prostate tissue. HIFU is also being investigated as a way to close wounds and stop bleeding, to break up clots in blood vessels, and to temporarily open the blood brain barrier so that medications can pass through.
Diagnostic ultrasound is generally regarded as safe and does not produce ionizing radiation like that produced by x-rays. Still, ultrasound is capable of producing some biological effects in the body under specific settings and conditions. For this reason, the FDA requires that diagnostic ultrasound devices operate within acceptable limits. The FDA, as well as many professional societies, discourage the casual use of ultrasound (e.g. for keepsake videos) and recommend that it be used only when there is a true medical need.
The following are examples of current research projects funded by NIBIB that are developing new applications of ultrasound that are already in use or that will be in use in the future:
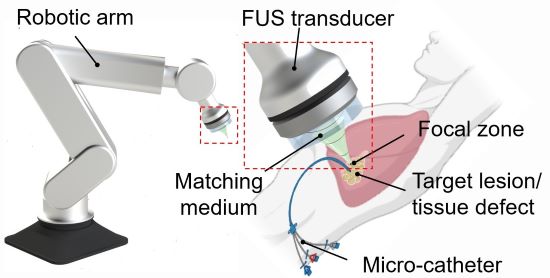
3D printing through the skin : Researchers at Duke University have developed a method to 3D print biocompatible structures through thick, multi-layered tissues. The approach entails using focused ultrasound to solidify a special ink that has been injected into the body to repair bone or repair soft tissues, for example. Initial experiments in animal tissue suggest the method could turn highly invasive surgical procedures into safer, less invasive ones. (Image on left courtesy of Junjie Yao (Duke University) and Yu Shrike Zhang (Harvard Medical School and Brigham and Women’s Hospital)).
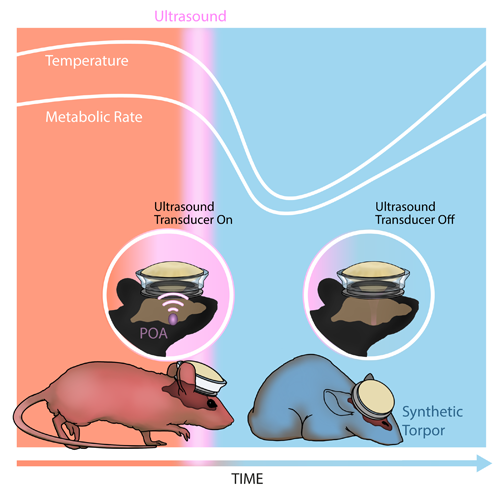
Inducing a hibernation-like state : Researchers at Washington University in St. Louis used ultrasound waves directed into the brain to lower the body temperature and metabolic rates of mice, inducing a hibernation-like state, called torpor. The researchers replicated some of these results in rats, which, like humans, don’t naturally enter torpor. Inducing torpor could help minimize damage from stroke or heart attack and buy precious time for patients in critical care. (Image on right courtesy of Yang et al./Washington University in St. Louis).
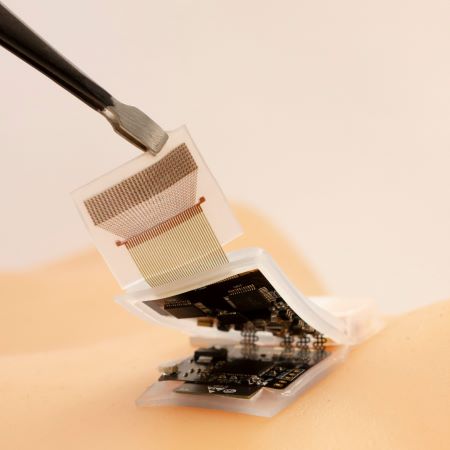
High-quality imaging at home : Brigham and Women’s Hospital researchers compared ultrasound scans acquired by experts with those taken by inexperienced volunteers, finding little difference in the image quality of the two groups. The unconventional approach of having patients take ultrasound images of themselves at home and share them with healthcare professionals could allow for remote monitoring and reduce the need for hospitalization. (Image on right courtesy of Duggan et al./Brigham and Women's Hospital).
Reviewed December 2023
Explore More
Heath Topics
- Breast Cancer
- Cardiovascular Disease
- Digestive Diseases
- Heart Disease
- Musculoskeletal Disease
- Reproductive Health
- Women's Health
Research Topics
- Optical Imaging
- Ultrasound (US) diagnostic
- Ultrasound (US) therapy
PROGRAM AREAS
- Ultrasound: Diagnostic and Interventional
Inside NIBIB
- Director's Corner
- Funding Policies
- NIBIB Fact Sheets
- Press Releases

Ultrasound (introduction)
- Report problem with article
- View revision history
Citation, DOI, disclosures and article data
At the time the article was created Matt A. Morgan had no recorded disclosures.
At the time the article was last revised Joachim Feger had no financial relationships to ineligible companies to disclose.
- USG (ultrasonography)
- Ultrasonography
- USS (ultrasound scanning)
Ultrasound ( US ) is an imaging technology that uses high-frequency sound waves to characterize tissue. It is a useful and flexible modality in medical imaging and often provides an additional or unique characterization of tissues when compared to other modalities such as conventional radiography or CT .
On this page:
Terminology, clinical applications.
- Related articles
Ultrasound is the most common term used for this modality however occasionally ultrasonography (USG), or just sonography are used. When abbreviated, USS, short for ultrasound scanning, may be used as an alternative. Echography is a rare synonym but is seen especially concerning ultrasound of the eye 3 .
For historical reasons, ultrasound of the heart tends to be called echocardiography , or often just echo.
Ultrasound is used in a wide variety of clinical settings to depict pathology and features and has several advantages but also disadvantages compared to other imaging modalities.
ultrasound uses non-ionizing sound waves and has not been associated with carcinogenesis - this is particularly important for the evaluation of the fetal and gonads
in most centers, ultrasound is more readily available than more advanced cross-sectional modalities such as CT or MRI
ultrasound examination is less expensive to perform than CT or MRI
ultrasound is straightforward to perform portably, unlike CT/MRI
there are few (if any) contraindications to the use of ultrasound, compared with MRI or contrast-enhanced CT
the real-time nature of ultrasound imaging is useful for the evaluation of physiology as well as anatomy (e.g. fetal heart rate )
Doppler evaluation of organs and vessels adds a dimension of physiologic data, not available on other modalities (except some MRI sequences)
ultrasound images may not be as adversely affected by metallic objects, as opposed to CT or MRI
an ultrasound exam can easily be extended to cover another organ system or evaluate the contralateral extremity
Disadvantages
training is required to accurately and efficiently conduct an ultrasound exam and there is non-uniformity in the quality of examinations ("operator dependence")
ultrasound is not capable of evaluating the internal structure of tissue types with high acoustical impedance (e.g. bone, air). It is also limited in evaluating structures encased in bone (e.g. cerebral parenchyma inside the calvaria)
the high frequencies of ultrasound result in a potential risk of thermal heating or mechanical injury to tissue at a microscopic level, this is of most concern in fetal imaging
ultrasound has its own set of unique artifacts ( US artifacts ), which can potentially degrade image quality or lead to misinterpretation
some ultrasound exams may be limited by abnormally large body habitus
Physical principles
A sound wave is transmitted through liquids as a longitudinal wave, in which the movements of particles in a medium are parallel to the direction of propagation of the sound wave 2 . Sound wave transmits their energy mechanically, through pressure variations on the particles. Regions of high pressure and density are called "compressions" while regions of low pressure and density are called "rarefactions" 1 .
The frequency of the sound waves used in medical ultrasound is in the range of millions of cycles per second (megahertz, MHz) . In contrast, the upper range of audible frequencies for humans is around 20 thousand cycles per second (20 kHz) 2 .
Ultrasound images are produced by relying on properties of acoustic physics (reflection, refraction, absorption 2 , and scattering). These properties cause attenuation of ultrasound that is used to localize and characterize different tissue types 2 . The amount of attenuation of ultrasound is described by the attenuation coefficient . Acoustic impedance is a physical property of a tissue in which how much resistance it offers to stop the transmission of an ultrasound beam 2 . Differences between the acoustic impedance of the two mediums govern the proportions of reflected and transmitted sound waves 2 .
The angle of the transmitted sound waves (refracted waves) is governed by Snell's law 2 . The velocity of the transmitted wave can be either be higher or slower than the incident wave depending on the type of material it passes through 2 . During the change in velocity, the wavelength changes while the frequency remains constant 2 . The compressibility (or stiffness) of the material and density of the material affects the velocity of the ultrasound wave. The lower the compressibility (or higher the stiffness), or the lower the density, the higher the velocity of ultrasound because the frequency remains constant while the wavelength increases 2 .
The intensity/loudness/amplitude of ultrasound is measured as milliwatts cm -2 or watts cm -2 . Diagnostic and low-intensity ultrasound range from 0.1 to 1 watts cm -2 , while high-intensity ultrasound is more than 10 watts cm -2 4 . Power is energy generated per unit time, measured in joules per second or watts 5 . The intensity or power of the ultrasound is directly proportional to the square of the amplitude 5 . Meanwhile, relative sound intensity is measured by decibels, which compares the relative intensity of two sound beams 2 . The loss of 3 decibels will reduce the sound intensity by half 2 .
Device function
An ultrasound transducer , also known as a probe , operates based on the physical principles of ultrasound . It sends an ultrasound pulse into tissue and then receives echoes back. The echoes contain spatial and contrast information. The concept is analogous to sonar used in nautical applications, but the technique in medical ultrasound is more sophisticated, gathering enough data to form a rapidly moving two-dimensional grayscale image.
Some characteristics of returning echoes from tissue can be selected out to provide additional information beyond a grayscale image. Doppler ultrasound , for instance, can detect a frequency shift in echoes, and determine whether the tissue is moving toward or away from the transducer. This is invaluable for the evaluation of some structures such as blood vessels or the heart ( echocardiography ).
Ultrasound continues to evolve additional functions, including 3D ultrasound imaging , elastography , and contrast-enhanced ultrasound using microbubbles .
Signals from the transducer are fed into a digital scan converter to display them as image on a monitor screen 6 .
Quiz questions
- 1. Frederick W. Kremkau. Sonography Principles and Instruments. (2015) ISBN: 9780323322713 - Google Books
- 2. Dowdey, James E., Murry, Robert C., Christensen, Edward E., 1929-. Christensen's Physics of Diagnostic Radiology. (1990). Pages 323-327. ISBN: 9780812113105 - Google Books
- 3. Graziano M, Biondino D, Fioretto I. Carotid-Cavernous Fistulas: The Utility of Ocular Echography in Their Differentiation [Letter]. Clin Ophthalmol. 2023;17:1421-2. doi:10.2147/OPTH.S420582 - Pubmed
- 4. Uddin S, Komatsu D, Motyka T, Petterson S. Low-Intensity Continuous Ultrasound Therapies—A Systematic Review of Current State-Of-The-Art and Future Perspectives. JCM. 2021;10(12):2698. doi:10.3390/jcm10122698 - Pubmed
- 5. Shriki J. Ultrasound Physics. Crit Care Clin. 2014;30(1):1-24. doi:10.1016/j.ccc.2013.08.004 - Pubmed
- 6. Ophir J & Maklad N. Digital Scan Converters in Diagnostic Ultrasound Imaging. Proc IEEE. 1979;67(4):654-64. doi:10.1109/proc.1979.11289
Incoming Links
- Radiologist
- Thermal index
- Male reproductive system
- Ionising radiation
- Interstitial line sign
- Abdominal radiography
- Point-of-care ultrasound (curriculum)
- Arthrogram (anaesthetic)
- Cross-sectional imaging
- Attenuation coefficient
- Pulse repetition frequency
- Noise power spectrum
- Echocardiography
- M-mode (ultrasound)
- Attenuation (ultrasound)
- Vocal cord paralysis
- Photoacoustic imaging
- Reverberation artifact
- Basilic vein cannulation (ultrasound)
- Parasternal short axis view - normal (transthoracic echocardiography)
- Parasternal long axis view - normal (transthoracic echocardiography)
- Giant cell tumour of the tendon sheath
- Question 2823
Related articles: Imaging technology
- imaging technology
- electronvolt
- nuclear shell model
- photoluminescence
- K-absorption edge
- electron binding energy
- linear attenuation coefficient
- mass attenuation coefficient
- imaging in practice
- x-ray physics
- radiation risk factor
- thermionic emission
- filament circuit
- space charge effect
- anode angle
- heel effect
- off focus radiation
- line focus principle
- radiographic distortion
- kilovoltage peak
- milliampere-seconds (mAs)
- rotating envelope x-ray tube
- tube rating
- compensating filter
- automatic exposure control (AEC)
- beam collimators
- bucky factor
- virtual grid
- air gap technique
- intensifying screen
- developer solution
- fixing solution
- silver recovery
- entrance phosphor
- photocathode
- output phosphor
- computed radiography
- flat panel detector (FPD)
- charge-coupled device (CCD)
- radiographic contrast
- signal to noise ratio
- mammography
- clothing artifact
- hair artifact
- jewelry artifact
- grid cut off
- tissue weighting factor
- entrance skin dose
- coulomb per kilogram
- as low as reasonably achievable (ALARA)
- radiation protection
- background radiation
- background radiation equivalent time
- deterministic effect
- dose limits
- inverse square law
- radiation damage (biomolecular)
- radiation damage (skin injury)
- radiation-induced lung cancer
- ionization chambers
- thermoluminescent dosimeter
- film dosimeter
- fluoroscopy vs fluorography
- automatic brightness control (ABC)
- recursive filtration
- CT in practice
- helical CT scanning
- step and shoot scanning
- ultra-high-resolution CT (UHRCT)
- CT x-ray tube
- CT fluoroscopy
- cone-beam CT
- virtual non-contrast imaging
- urinary system
- musculoskeletal
- neuroimaging
- cinematic rendering
- filtered back projection
- Hounsfield unit
- iterative reconstruction
- maximum intensity projection (MIP)
- minimum intensity projection (MinIP)
- metal artifact reduction algorithm
- volume rendering
- CT spatial resolution
- CT contrast discrimination
- noise in CT
- CT dose index (CTDI)
- dose length product (DLP)
- size-specific dose estimate (SSDE)
- tube current modulation
- diatrizoate (Gastrografin)
- iothalamate (Conray)
- ioxaglate (Isopaque 370)
- meglumine iotroxate (Biliscopin)
- iodixanol (Visipaque)
- iohexol (Omnipaque)
- iopamidol (Isovue)
- iopromide (Ultravist)
- ioversol (Optiray)
- ioxilan (Oxilan)
- ethiodized poppy seed oil (Lipiodol)
- iophendylate (Pantopaque/Myodil)
- vicarious contrast material excretion
- iodide mumps
- contrast media extravasation
- iodinated contrast-induced thyrotoxicosis
- contrast media and breastfeeding
- barium sulfate
- motion artifact
- transient interruption of contrast
- motion blur
- beam hardening
- partial volume averaging
- quantum mottle (noise)
- photon starvation
- aliasing in CT
- truncation artifact
- ring artifact
- tube arcing
- out of field artifact
- air bubble artifact
- windmill artifact
- cone beam effect
- zebra artifact
- stair-step artifact
- Godfrey N Hounsfield
- MRI physics
- MRI in practice
- gradient coil
- phased array coil
- radiofrequency coil
- volume coil
- surface coil
- electronics and data processing
- magnetic field
- radiofrequency receiver
- radiofrequency transmitter
- 1.5 T vs 3 T
- ultrahigh field MRI
- acquisition time
- Fourier transformation
- motion compensation
- signal-to-noise ratio (SNR)
- spatial resolution
- zero filling interpolation
- T1 weighted image
- T2 weighted image
- proton density weighted image
- chemical exchange saturation transfer
- CSF flow studies
- apparent diffusion coefficient (ADC)
- diffusion tensor imaging and fiber tractography
- echo-planar pulse sequences
- fat-suppressed imaging sequences
- in-phase and out-of-phase
- spoiled gradient echo MRI
- steady-state free precession
- short tau inversion recovery (STIR)
- fluid attenuation inversion recovery (FLAIR)
- turbo inversion recovery magnitude (TIRM)
- double inversion recovery (DIR)
- metal artifact reduction sequence (MARS)
- dynamic susceptibility contrast (DSC) MR perfusion
- dynamic contrast enhanced (DCE) MR perfusion
- arterial spin labeling (ASL) MR perfusion
- cerebral blood flow (CBF)
- cerebral blood volume (CBV)
- mean transit time (MTT)
- negative enhancement integral (NEI)
- time to peak (TTP)
- saturation recovery sequences
- fast spin echo (FSE)
- 3d fast spin echo
- spiral pulse sequences
- susceptibility-weighted imaging (SWI)
- contrast-enhanced MRA
- phase contrast imaging
- time of flight angiography
- 2-hydroxyglutarate peak : resonates at 2.25 ppm
- alanine peak : resonates at 1.48 ppm
- choline peak : resonates at 3.2 ppm
- citrate peak : resonates at 2.6 ppm
- creatine peak : resonates at 3.0 ppm
- BOLD imaging
- gamma-aminobutyric acid (GABA) peak : resonates at 2.2-2.4 ppm
- glutamine-glutamate peak : resonates at 2.2-2.4 ppm
- Hunter's angle
- lactate peak : resonates at 1.3 ppm
- lipids peak : resonates at 1.3 ppm
- myoinositol peak : resonates at 3.5 ppm
- MR fingerprinting
- N-acetylaspartate (NAA) peak : resonates at 2.0 ppm
- propylene glycol peak : resonates at 1.13 ppm
- central point artifact
- herringbone artifact
- inhomogeneity artifact
- moiré fringes
- RF overflow artifact
- zebra stripes
- zipper artifact
- cross-excitation
- fat-water swapping
- slice-overlap artifact a.k.a. cross-talk artifact
- phase-encoded motion artifact
- entry slice phenomenon
- black boundary artifact
- chemical shift artifact
- dielectric effect artifact
- magic angle effect
- blooming artifact
- aliasing (wrap around) artifact
- Gibbs (truncation) artifact
- zero-fill artifact
- gadolinium contrast agents
- gastrointestinal MRI contrast agents
- reticuloendothelial MRI contrast agents
- tumor-specific MRI contrast agents
- chromium-labeled red blood cells
- Gd-DTPA-labeled dextran
- Gd-DTPA-labeled albumin
- gadofosveset trisodium
- gadoxetate disodium
- gadobenate dimeglumine
- gadodiamide
- gadopentetate dimeglumine
- gadoterate meglumine
- gadoteridol
- gadoversetamide
- nephrogenic systemic fibrosis (NSF)
- magnetic shielding
- specific absorption rate
- ultrasound physics
- linear array
- convex array
- phased array
- frame averaging (frame persistence)
- axial resolution
- lateral resolution
- elevational (azimuthal) resolution
- temporal resolution
- grey-scale imaging
- time-gain compensation
- harmonic imaging
- real-time imaging
- Doppler effect
- color Doppler
- power Doppler
- Doppler angle
- pulse repetition frequency and scale
- wall filter
- color write priority
- packet size (dwell time)
- peak systolic velocity
- end-diastolic velocity
- resistive index
- pulsatility index
- Reynolds number
- panoramic imaging
- compound imaging
- transient elastography
- shear wave elastography
- strain elastography
- Young's modulus
- 2D ultrasound
- 3D ultrasound
- 4D ultrasound
- acoustic shadowing
- acoustic enhancement
- beam width artifact
- color comet tail artifact
- ring down artifact
- mirror image artifact
- side lobe artifact
- speckle artifact
- speed displacement artifact
- refraction artifact
- multipath artifact
- electrical interference artifact
- tissue vibration
- spectral broadening
- motion (flash) artifact
- twinkling artifact
- acoustic streaming
- mechanical index
- thermal index
- history of ultrasound
- atomic structure
- metastable state
- alpha decay
- electron capture
- gamma decay
- photomultiplier tube
- pulse height analyzer
- single photon emission computed tomography (SPECT)
- positron emission tomography (PET)
- tissue to background ratio
- fundamentals of radiopharmaceuticals
- radiopharmaceutical labeling
- nuclear reactor produced radionuclides
- cyclotron produced radionuclides
- chromium-51
- F-18 fluorodeoxyglucose (FDG)
- F-18 sodium fluoride (NaF)
- F-18 2-(1-{6-[(2-[fluorine-18]fluoroethyl)(methyl)amino]-2-naphthyl}-ethylidene)malononitrile
- Ga-67 citrate
- Ga-68 DOTATATE
- I-123 iodide
- I-123 ioflupane (DaTSCAN)
- I-123 ortho -iodohippurate
- In-111 Octreoscan
- In-111 OncoScint
- In-111 Prostascint
- In-111 oxine labeled WBC
- krypton-81m
- nitrogen-13
- phosphorus-32
- Tc-99m DMSA
- Tc-99m DTPA
- Tc-99m DTPA aerosol
- Tc-99m HMPAO
- Tc-99m HMPAO labeled WBC
- Tc-99m MAG3
- Tc-99m mercaptoacetyltriglycine
- Tc-99m pertechnetate
- Tc-99m labeled RBC
- Tc-99m sestamibi
- Tc-99m sulfur colloid
- Tc-99m sulfur colloid (oral)
- thallium-201 chloride
- samarium-153
- strontium-89
- pharmaceuticals used in nuclear medicine
- phase-contrast imaging
- deep-learning reconstruction
- photon counting CT
- virtual non-contrast imaging
- magnetomotive ultrasound (MMUS)
- superb microvascular imaging
- ultrafast Doppler imaging
- ultrasound localization microscopy
- compressed sensing
- chemical exchange saturation transfer (CEST)
- electron paramagnetic resonance imaging (EPR)
- hyperpolarized carbon-13 MRI
- low-field MRI
- total body PET system
- magnetic particle imaging (MPI)
- photoacoustic imaging
- terahertz imaging
Promoted articles (advertising)
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers


Fetal Ultrasound
- • An imaging study in which high-frequency sound waves create pictures of a fetus inside the uterus
- • For viewing the fetus during pregnancy
- • It is also utilized to guide procedures such as amniocentesis or chorionic villus sampling
- • Involves Ob/Gyn and Maternal-Fetal Medicine
- Prenatal Ultrasound Scan
- Transvaginal Ultrasound
- 3D/4D Ultrasound
- Pelvic Ultrasound
What is ultrasound?
Who performs an ultrasound, how do ultrasounds assist pregnancy, in what other ways is ultrasound used, how do you prepare for an ultrasound, how is yale medicine's use of ultrasound technology unique.
Since the mid-20th century, ultrasound has been used extensively to create a "picture" of what's happening inside our bodies. For pregnant women, it is an indispensable aspect to care.
At Yale Medicine Maternal-Fetal Medicine , our physicians and sonographers perform more than 16,000 ultrasounds a year.
"Experience counts. This is the only way we can approach the fetus like a patient. With sophisticated ultrasound, we now have ways to identify fetal problems and guide treatment," says Joshua Copel, MD , a Yale Medicine expert in prenatal diagnosis and fetal therapy. "If a baby has an abnormal amount of fluid in the chest, we can use an ultrasound-guided needle to drain it out. Or we can deliver blood to the umbilical cord. The first of these types of transfusions were done here at Yale in 1984."
Think of ultrasound—sometimes called a sonogram—as sonar for the body. A small instrument called a “transducer” transmits high-frequency sound waves, bouncing them off structures in the body and using the reflected sound waves to paint a picture.
The sound waves can determine the distance, size, shape and consistency of an object. A computer compiles these results to create an image of the object, be it a fetus, an adult heart, or a tumor in the kidney.
Specially trained physicians and sonographers perform ultrasounds by spreading gel on the skin adjacent to the body part to be imaged. (The gel helps to conduct the sound waves and makes it easier to move the transducer over the skin.) Most ultrasound procedures are painless and non-invasive.
Ultrasound imaging has been used for decades and has an excellent safety record. It’s important to remember that ultrasound uses sound waves; it does not use ionizing radiation, like X-rays, which can cause harm after prolonged exposure
Ultrasound is the most widely used medical imaging method for viewing a fetus during pregnancy. It is also utilized to guide procedures such as amniocentesis or chorionic villus sampling .
An ultrasound may be done at almost any time during a pregnancy, even as early as about five weeks after conception. During the first trimester, it can confirm a viable pregnancy and heartbeat, measure the distance from the head to the rear end in order to confirm gestational age, and identify problems such as molar or ectopic pregnancies. It can also identify some uterine or pelvic problems in the mother.
In the second trimester, ultrasound can pinpoint fetal malformations, confirm multiple pregnancies (though this is ideally done in the first trimester), monitor levels of amniotic fluid and evaluate how well the fetus is doing.
In the third trimester, ultrasound can show the placenta's placement, how the fetus is moving and presented for birth, and measure how well the baby is growing.
- Abdominal ultrasound can create images of abdominal tissues and organs.
- Ultrasound may guide surgeons as they perform biopsies and other procedures.
- Ultrasound may map brain structures.
- Ultrasound can visualize the interior of the ear or the eye.
- Ultrasound can find clots in veins in the leg.
- It can find bleeding in the abdomen or chest after a motor vehicle accident.
There is no special preparation for a routine ultrasound, though it may make sense to wear loose clothes for comfort. Ultrasounds are painless. Saline used in sonohysterography (a procedure in which saline is injected through the cervix into the uterus, in order to produce a more detailed ultrasound image) occasionally causes mild cramping, but over-the-counter medication is usually enough to manage this pain.
At Yale Medicine, we are skilled at using ultrasound to guide care.
"Three percent of babies are born with major birth defects, many of which can be identified with ultrasound," says Dr. Copel. "But it's critical to have experienced eyes and hands do the scans. At Yale, we have both the experience and premium-level equipment with better technology than typically found in other settings."
We have pioneered the use of transvaginal ultrasound early in pregnancy, as well as the use of ultrasound to diagnose pelvic pain, breast cancer and ectopic pregnancy. Yale physicians continue to explore the use of ultrasound to map the brain and track the vascular behavior of cancerous tumors.
We are also exploring the use of Doppler ultrasound to monitor cardiovascular conditions.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Sonography 2nd trimester assessment, protocols, and interpretation.
Doaa Jabaz ; Suzanne M. Jenkins .
Affiliations
Last Update: November 12, 2023 .
- Continuing Education Activity
The mid-trimester obstetric ultrasound (also known as the second-trimester anatomy scan or anomaly scan) is a routine examination in many countries. It plays a pivotal role in ensuring the well-being of both the pregnant patient and the developing fetus. A cornerstone of modern prenatal care, this non-invasive imaging technique, typically performed between weeks 18 and 22 of gestation, is aimed primarily at assessing fetal anatomy and detecting any fetal anomalies. A 2-dimensional grayscale ultrasound with a curvilinear transabdominal probe is routinely used to evaluate the fetal number, viability, gestational age, anatomical survey, placental location, amniotic fluid, and maternal pelvic organs. A transvaginal probe, color Doppler, and 3-dimensional ultrasound are not routinely used. Still, they may be implemented in certain clinical scenarios, especially when placenta previa or a fetal anomaly is suspected, or to provide accurate cervical length measurement. This activity outlines the indication, safety, and technique of second-trimester ultrasound and highlights the role of the interprofessional team in conducting and interpreting the study to improve the antenatal care provided.
- Apply principles of the scanning protocol used systematically in the anatomy scan.
- Screen for common fetal abnormalities and genetic syndromes using second-trimester obstetric sonography, ensuring early detection and appropriate referral for further evaluation.
- Select appropriate transducer frequencies and imaging planes to optimize image quality and diagnostic accuracy during second-trimester obstetric sonography.
- Collaborate with an interprofessional team on strategies to optimize patient outcomes when using ultrasound for pregnancy evaluation.
- Introduction
Antenatal ultrasonography is widely used in pregnancy to assess fetal growth and anatomy. Although ultrasound screening is now an integral part of routine antenatal care, recommendations for the delivery of obstetric ultrasound vary from country to country. [1] [2] The history of sonography in obstetrics dates from the classic 1958 Lancet paper of Ian Donald and his team from Glasgow. Clinical researchers have seized technological developments such as real-time imaging, color and power Doppler, transvaginal sonography, and 3D and 4D imaging to enhance the investigation and management of patients in areas as diverse as assessment of fetal growth and well-being, screening for fetal anomalies, and ultrasound-guided procedures as an essential component of fetal therapy. [3]
Diagnosing a fetal anomaly significantly reduces perinatal mortality and morbidity and maternal morbidity. Prenatal diagnosis enables a psychologically less traumatic and early medical termination of pregnancy. It also decreases the probable complications associated with the continuation of pregnancy and labor, prevents an unnecessary cesarean section for a fetus with lethal anomalies diagnosed too late for medical termination of pregnancy, allows for delivery to be planned at the optimal time in a well-equipped tertiary center with necessary neonatal care facilities, and allows for in utero therapy in selected cases. Performed systematically, high-resolution ultrasound can now accurately diagnose more than 200 abnormalities. A normal scan is often obtained, but there is tremendous relief of psychological distress, anxiety, and somatic symptoms after the report. [4] The literature includes descriptions of anatomical surveys performed before 18 weeks, but other studies have repeatedly shown that more anomalies are diagnosed if the scan is performed after 18 weeks. [5] [6]
The detection rate of the screening second-trimester ultrasound scan is good in high-risk patients examined by a well-trained sonographer. On the other hand, the scan can also be sensitive in anomaly detection if a systemic searching pattern is followed in low-risk pregnant women. [7]
- Indications
An ultrasound scan performed between 18 and 22 weeks of gestation is appropriate in all pregnancies as a part of routine antenatal evaluation and screening because it provides the pregnant woman and her care provider with information about multiple aspects of her pregnancy. The obstetrical ultrasound will inform and/or confirm the number of fetuses present, the gestational age, and the location of the placenta. It will present an opportunity to diagnose congenital anomalies, detect soft markers of aneuploidy, and identify maternal pelvic pathology. [8]
- Contraindications
Based on current evidence, routine clinical scanning of every woman during pregnancy using real-time B-mode imaging is not contraindicated. The American Institute of Ultrasound in Medicine (AIUM) and the National Electrical Manufacturers Association (NEMA) regulated that the ultrasound device has to display the emitted energy through the thermal index (TI) and the mechanical index (MI). Both indexes are not perfect indicators of the risks of thermal and non-thermal bioeffects, but currently, they should be accepted as the most practical and understandable methods of estimating the potential for such risks.
Acoustic outputs in B-mode and M-mode are generally not high enough to produce deleterious effects. The significant temperature increase may be generated by spectral Doppler mode, particularly near a bone. This should not prevent using this mode when clinically indicated, provided the user has adequate knowledge of the instrument's acoustic output or access to the relevant TI. Exposure time and acoustic output should be kept to the lowest levels consistent with obtaining diagnostic information and limited to medically indicated procedures rather than purely for entertainment purposes. The "as low as reasonably achievable" (ALARA) principle best expresses this unequivocal demand for safety. [9] [10]
The examination is mainly performed with gray-scale 2D ultrasound. Harmonic imaging may enhance the visualization of subtle anatomic details, particularly in patients who scan poorly. High-frequency ultrasound transducers increase the spatial resolution but decrease the penetration of the sound beam. Several factors influence the optimal transducer and operating frequency choice, including maternal habitus, fetal position, and the approach used. Most basic examinations are satisfactorily performed with 3 to 5 MHz transabdominal transducers. [11]
The scan should be performed according to international standards and by accredited sonographers who have completed appropriate training programs supported by scientific societies. [11]
A sonologist, a physician with training and experience in this field, supervises and interprets the exams. It is the physician's responsibility to write a report based on the sonographer's data and, if necessary, personally scan the patient to validate or change the differential diagnosis. [12]
- Preparation
Reason for examination : the sonographer should validate the indication for the ultrasound examination. The last menstrual period (or the estimated delivery date) should be documented. This information is critical in correctly targeting specific structures, choosing a transvaginal and/or transabdominal technique, and determining whether additional studies may be helpful (eg, Doppler velocimetry).
Patient positioning : a semirecumbent position is most commonly used in obstetrics and gynecology. A padded table and pillow are used to ensure maximal comfort. It is preferable to elevate the head of the bed as some pregnant women cannot lie flat, especially in late pregnancy. For the transvaginal exam, a lithotomy position is used.
Special consideration for obese patients : in obese individuals, imaging can be improved by placing the transducer on the side rather than on the midline while the patient is lying on her side. The transvaginal probe is also helpful in these patients. [13]
Bladder filling : this is useful when the lower uterine segment is of interest. It is often of little benefit in obstetric ultrasound examination as it can falsely diagnose placenta previa or an elongated cervix. Transvaginal sonography is usually performed with an empty bladder.
- Technique or Treatment
A. Fetal Biometry and Well-being: The following sonographic parameters can help to estimate gestational age and fetal size:
- Biparietal diameter (BPD)/head circumference (HC): measured at a cross-sectional view of the fetal head at the level of the thalami and cavum septi pellucidi without visualization of the cerebellum. BPD is commonly measured from the leading edge (outer edge of the proximal skull) to the leading edge (inner edge of the distal skull), while HC is measured around the outside of the skull bone echoes. When the head shape is flattened (dolichocephaly) or round (brachycephaly), HC is more reliable than BPD.
- Abdominal circumference (AC) or diameter: can be measured using the ellipse function at the outer surface of the skin on a transverse section of the fetal abdomen at the junction of the umbilical vein, portal sinus, and stomach.
- Femur length (FL): measured along the longest axis of the ossified diaphysis but excluding distal femoral epiphysis. [14] [15] [16]
Measurements should be performed in a standardized manner based on strict quality criteria. [17] Reference standards appropriate for the local population should be used to interpret the measurement results. BPD and/or HC are preferable to other growth parameters in estimating gestational age. [18] [19]
B. Anatomical Survey: This comprehensive assessment encompasses the evaluation of various fetal structures and organs to ensure their normal development and functionality. To facilitate a clear understanding of the intricacies involved in this critical diagnostic procedure, the following table offers a systematic overview of the key anatomical elements typically examined during an anatomic survey (see Table. Minimal Requirements and Optional Views for the Routine Mid-Trimester Anomaly Scan). [16]
Table. Minimal Requirements and Optional Views for the Routine Mid-Trimester Anomaly Scan.
Head, including skull and brain:
- Skull: size, shape, integrity, and bone density require routine evaluation. All these characteristics can be visualized at the time of the head measurements. Size measurements are performed as mentioned in the biometry section. The skull normally has an oval shape without focal protrusions. Alterations of shape (eg, lemon, strawberry, cloverleaf) should be documented and investigated. [20] Normal skull density is manifested as a continuous echogenic structure interrupted only by cranial sutures in specific anatomical locations. The absence of this whiteness or extreme visibility of the fetal brain should raise suspicion of poor mineralization (eg, osteogenesis imperfecta, hypophosphatasia). Poor mineralization is also suggested when the skull becomes easily depressed due to manual pressure from transducer placement against the maternal abdominal wall. [21]
- Transventricular plane: demonstrates the anterior and posterior portion of the lateral ventricles. The frontal horns (anterior portion) appear as 2 comma-shaped fluid-filled structures separated medially by the cavum septi pellucidi (CSP), a fluid-filled cavity. The CSP becomes visible around 16 weeks and undergoes obliteration near term or in the early neonatal period. It should always be visualized between 18 and 37 weeks. The value of visualizing the CSP for identifying cerebral anomalies has been debated. However, this structure is altered with many cerebral lesions such as holoprosencephaly, agenesis of the corpus callosum, severe hydrocephaly, and septo-optic dysplasia. The posterior portion of the lateral ventricles is a complex formed by the atrium that continues posteriorly into the occipital horn. In a normal fetus, each atrium is usually measured up to 10 mm in transverse diameter; otherwise, it is generally followed to rule out early ventriculomegaly. [11] [22] [11]
- Transcerebellar plane: This plane is inferior to the BPD plane, with the probe tilted backward into the posterior fossa. The plane is correct when one can visualize the thalami and cavum septum pellucidum in the same plane as the cerebellum. The cerebellum is a dumbbell-shaped structure with symmetrical lobes. The central vermis is slightly more echogenic than the lateral lobes. The transcerebellar diameter (the widest measurement across the cerebellum perpendicular to the falx) in millimeters correlates with the gestational age up to 20 weeks and is larger than the gestational age after this time. A cerebellum measuring 2 mm less than gestational age is a concerning finding. The cisterna magna can be measured from the posterior margin of the cerebellar vermis to the inside of the occipital bone in the midline. A measurement of 2 mm to 10 mm is normal in the second and third trimesters. The nuchal fold is a measurement taken from the outer skin line to the outer bone in the midline. Less than 6 mm is considered normal up to 22 weeks. [23]
- Transthalamic plane: The anatomic landmarks include, from anterior to posterior, the frontal horns of the lateral ventricles, the CSP, the thalami, and the hippocampal gyruses. [24]
Examples of fetal head abnormalities: [25]
- Thickened nuchal skin fold: Assessment of the nuchal fold is typically made using a transcerebellar plane. A nuchal fold thickness of >6 mm is considered abnormal and is seen in 80% of newborns with Down syndrome.
- Cystic hygroma: a localized, single, or loculated, fluid-filled cavity usually occurs in the neck. It is seen in fetuses with nonimmune fetal hydrops, Turner syndrome, and trisomy syndromes 13, 18, and 21. Detection of a cystic hygroma should prompt an amniocentesis since the prevalence of cytogenetic abnormalities has been reported as high as 73%.
- Meningoceles are seen as fluid-filled cystic structures, and encephaloceles as brain-filled cystic structures that extend through a bony calvarial defect, usually in the occipital or frontal region. The entity most commonly mistaken for a small meningocele is a cystic hygroma. Careful scanning, however, will reveal no calvarial defect with a cystic hygroma. The absence of brain tissue within the sac is the single most favorable prognostic feature. Associated anomalies include Arnold-Chiari malformation, Dandy-Walker syndrome, and Meckel-Gruber syndrome (encephalocele, microcephaly, polydactyly, and cystic dysplastic kidneys). [26]
Face/neck: early detection of facial abnormalities may lead to the diagnosis of multiple syndromes, which allows counseling of the parents and optimal care of the fetus. A coronal view is usually used to assess the nose and lips. The biorbital and interorbital distances are measured by obtaining a transverse view at the level of the orbits, while a sagittal view is used to assess the facial profile and the cervical spine. [27]
Examples of face/neck abnormalities:
- Nasal bone absence/ hypoplasia: in the second trimester, hypoplastic nasal bone must be considered as important as an absence. Trisomy 21 is associated with nasal bone absence/hypoplasia in approximately 40% to 80% of cases. [28]
- Hypertelorism and hypotelorism: the distance between the 2 inner canthi, known as interocular distance (IOD), approximates the ocular diameter (specific charts are used). The distance between the 2 outer canthi is known as binocular distance (BOD). Hypertelorism (increase in IOD and BOD) may be associated with frontal encephaloceles, craniosynostoses, exposure to phenytoin, and cleft lip and palate. Hypotelorism (reduced IOD and BOD ) is usually associated with holoprosencephaly and other brain malformations. [25]
- Cleft lip and palate are the most common face malformations. Other congenital anomalies are seen in about half of the cases [25]
- Neck masses include teratoma, lymphangioma, enlarged thyroid, branchial cleft cyst, and rarely a sarcoma. [25]
Thorax: The shape of the thorax, ribs, and homogeneous echogenicity of both lungs can be examined in axial views. The integrity of the diaphragm can be examined through the sagittal or coronal view. For the basic cardiac screening, a proper 4-chamber view of the fetal heart should be obtained with the assessment of the following: the heart rate (from 120 to 160 beats per minute), location (in the left chest), axis (about 45° toward the left side of the fetus), and size (not larger than one-third the area of the chest), 2 atria, 2 ventricles, 2 atrioventricular valves. Abnormalities like mediastinal shift, lung masses, pleural effusions, diaphragmatic hernia, tachycardia, dextrocardia, cardiomegaly, pericardial effusion, ventricular septal defect, and abnormal chamber size can be detected. Cardiomegaly can be due to congenital heart disease, severe fetal anemia, or a small chest. [16]
Abdomen: organ situs should be determined. The fetal stomach should be identified in its normal position on the left side. The fetal umbilical cord insertion site should be examined for evidence of a ventral wall defect. Normal kidneys, along with the adrenal glands, are seen on either side of the spine just below the level of the fetal stomach. [21] The kidneys appear echogenic in the early weeks and gradually become hypoechoic compared with the adjacent bowel and liver. Fetal ureters are not usually visible antenatally unless they are dilated. Persistent absence of the bladder should be considered abnormal from 15 weeks. [29]
Examples of fetal abdomen abnormalities:
- Echogenic bowel: defined as bowel with an echogenicity ≥ that of surrounding bone; the differential diagnosis for this finding is broad and includes normal variant, congenital viral infection, cystic fibrosis, aneuploidy, and intra-amniotic bleeding. Previous reports have also suggested an increased incidence of intrauterine growth restriction (IUGR) and intrauterine fetal demise in fetuses with echogenic bowel. [30]
- Fetal bowel dilatation: characterized by fluid-filled intestinal loops that measure at least 15 mm in length or 7 mm in diameter. Dilated fetal bowel is a sign of intestinal mechanical or functional obstruction. Its prevalence will depend on the underlying condition: bowel atresia or stenosis, malrotation with volvulus, meconium ileus, total colonic aganglionosis, and meconium plug syndrome. [31]
- Dysplastic kidneys: result from abnormal development of the glomeruli and nephrons along with a disproportionately increased stroma. They appear large and bright, usually with cystic spaces. Typically, the cysts are multiple, thin-walled with no connections, randomly placed in the renal parenchyma, and form an irregularly outlined kidney. Rarely, dysplastic kidneys appear uniformly echogenic on ultrasound without cysts and can be difficult to differentiate from normal kidneys. The renal pelvis and ureters are not seen. Dysplastic kidneys are often associated with other syndromes such as VACTERL association, Meckel–Gruber syndrome, Fraser syndrome, and CHARGE syndrome. Most babies with isolated unilateral multicystic renal disease tend to have a good outcome. The size and number of cysts in unilateral multicystic disease do not influence the outcome. Bilateral involvement is generally associated with severe oligohydramnios and has a poor prognosis owing to the resultant pulmonary hypoplasia. [29]
- Infantile polycystic kidney disease (Potter type I): has an autosomal recessive inheritance. It carries a 25% risk in subsequent pregnancies. The age of onset of this condition is varied and is subdivided into perinatal, neonatal, infantile, and juvenile. The perinatal onset type is the most common and characterized by bilaterally enlarged and homogenously hyperechogenic kidneys, with or without oligohydramnios, renal failure occurring in utero, and 40% to 50% affected with hepatic fibrosis. Kidneys are affected earlier, and hepatic fibrosis is common in late-onset polycystic kidney disease. Perinatal mortality is usually caused by pulmonary hypoplasia after severe oligo- or anhydramnios. [29]
- When evaluating urinary bladder distention and pyelectasis in the male fetus, severe or progressive oligohydramnios, progressive bladder wall thickening, and a persistently dilated posterior urethra are most consistent with posterior urethral valves. Although oligohydramnios, dilated posterior urethra, and bladder wall thickening can be seen in prune belly syndrome, these findings are likely transient. Vesicoureteral reflux, ureterovesical junction obstruction, and non-refluxing, nonobstructive megacystis–megaureter should be considered when pyelectasis and megacystis are present without additional bladder, urethral, or renal abnormalities. [32]
- The 2 most common congenital abdominal wall defects are omphalocele and gastroschisis. Omphalocele appears as an outpouching of the abdominal wall recovered by an inner membrane of the parietal peritoneum and an outer layer of amnion and Wharton jelly. It usually occurs at the base of the umbilical cord, the cord insertion being located at the apex of the herniated sac, which contains variable amounts of different visceral organs, usually, bowel or liver or both; concurrent malformations are described in up to 74% of fetuses. It is considered the consequence of a failure of bowel loops to return to the body cavity after their normal physiological herniation into the umbilical cord during the sixth to tenth week of development. Gastroschisis is characterized by a full-thickness abdominal wall closure defect, which permits evisceration of the fetal abdominal contents, specifically bowel herniation. The orifice of the defect is usually small and, nearly always, is right-sided to umbilicus insertion. There is no surrounding membrane or sac, and these free-floating loops of the intestine may become edematous due to direct exposure to the amniotic fluid. Children of young mothers are more susceptible. It is not usually associated with other anomalies, but sometimes it may occur combined with congenital heart disease, ectopia, cordis, neural tube, and diaphragmatic defects. Survival rates are good (85% to 97%). [33]
Spine: The choice of the scanning planes used to evaluate the spine's integrity depends upon the fetal position. However, a longitudinal view should always be obtained because it may reveal other spinal malformations, including vertebral abnormalities and sacral agenesis. In sagittal planes, the ossification centers of the vertebral body and posterior arches form 2 parallel lines that converge in the sacrum. In the second and third trimesters of gestation, the conus medullaris is usually found at the level of L2 to L3. The integrity of the neural canal is inferred by the regular disposition of the ossification centers of the spine and the presence of soft tissue covering the spine. [11]
Extremities: assessment of all limbs, including the hands and feet, should be done to evaluate the bone shape, size, and integrity. Most prenatal-onset skeletal dysplasias present with a relative disproportion of the skeletal measurements compared with those of the cranium. One of the most critical determinations that ultrasound must make is neonatal or infantile lethality. Lethality occurs in most skeletal dysplasias due to a small chest circumference and resultant pulmonary hypoplasia. Using ultrasound criteria for lethality, a chest-to-abdominal circumference ratio of <0.6 and a femur length-to-abdominal circumference ratio of <0.16 strongly suggest lethality. [34]
Examples of fetal skeletal dysplasia:
- Thanatophoric Dysplasia: is the most common lethal skeletal dysplasia. Inheritance is generally autosomal dominant. It is characterized by disproportionate dwarfism with very short extremities, which are bowed in type 1 and maybe straight in type 2. The trunk length is normal, but the thorax is narrow. There is a distinct flattening of vertebral ossification centers (platyspondyly) and a large head, depressed nasal bridge, prominent forehead, and protruding eyes. Skull deformity is often present due to the premature closure of cranial sutures. Cloverleaf skull deformity is generally seen in type 2. Polyhydramnios is present in almost 50% of cases. [35]
- Achondroplasia: is the most common nonlethal skeletal dysplasia without mental impairment. At about 20 weeks of gestation, fetuses with achondroplasia had normal biometric parameters, including FL, which became abnormally short only in the third trimester. The micromelia is rhizomelic, and the head tends to be large. Typical facial features include a prominent forehead, depressed nasal bridge, and mid-face hypoplasia. The phalanges are short; typical gaps are seen between the fingers, and digital deviation leads to the appearance of a " trident'’ hand. [36]
- Osteogenesis Imperfe ista: a heterogeneous group of disorders caused by gene mutations that encode type I collagen, increasing bone fragility. The major features are collapsed vertebral bodies, rib fractures, and, in more severe cases, thin shafts with fractures and bowing deformities. Fetal movements may be reduced. The skull may be thinner than usual, and the weight of the US probe may deform the head quite easily. [35]
Gender: If the external genitalia is to be visualized for gender determination, imaging in both mid-sagittal and axial planes is recommended to minimize error. A mid-sagittal image of the lower abdomen below the cord insertion demonstrates the penis and scrotum caudally to the cord insertion in a male fetus and the flat mons pubis caudal to the cord insertion in a female fetus. A transverse image, just below the level of the bladder, best taken with the knees separated, demonstrates the penis and scrotum between the thighs in males and 3 lines representing the labia in females. Testes are undescended at this gestation and usually descend later in the third trimester. [23]
C. Placenta and Amniotic Fluid Volume: assessing the placental location, appearance, and its relation with the internal cervical os is essential. Amniotic fluid volume can be estimated subjectively or by measuring the deepest vertical pocket. A vertical pocket of ≤2 cm and ≥8 cm are regarded as oligohydramnios and polyhydramnios, respectively. [16] [37] [16]
D. Cervix, Uterine Morphology, and Adnexa: There is insufficient evidence to recommend routine screening of asymptomatic and symptomatic pregnant women with transvaginal ultrasound cervical length. [38] Maternal adnexal or uterine pathologies like masses that may interfere with fetal growth or labor should be documented.
- Clinical Significance
The mid-trimester ultrasound scan should be performed according to international standards and preferably by accredited sonographers.
When a structural abnormality is detected, the obstetrician wants to know: How severe is the anomaly? Is it lethal? Does the fetus have a chromosomal abnormality? What is the cause? How can the fetus be best salvaged? A fetal karyotype is indicated when there are multiple structural malformations, associated fetal growth retardation, certain anomalies like cystic hygroma, non-immune hydrops, and cardiovascular defects. It is better to know the fetal karyotype during pregnancy rather than wait until after delivery, as the baby may not often survive, the chromosomal cultures might fail, and valuable information might be lost, which could be vital for future counseling.
Management guidelines for a lethal anomaly like anencephaly and bilateral renal agenesis indicate termination of the pregnancy. If the defect is nonprogressive and correctable at birth, as in mild hydronephrosis with good renal function, the decision would be to wait until term delivery followed by neonatal treatment. Fetal therapy of a structurally malformed fetus requires a multidisciplinary team comprised of the obstetrician, geneticist, neonatologist, and pediatric surgeon. Malformations that require correction in utero are those that would cause deterioration of the fetal organs if left alone. [4]
- Enhancing Healthcare Team Outcomes
The optimal obstetric outcome can be expected by the early initiation of prenatal care. An essential element of prenatal care is the early detection of possible malformations, which is the primary goal of the mid-trimester anomaly scan. This cannot be achieved without optimized coordination among interprofessional team members, including well-trained sonographers, specialists-referral and parent counseling systems, nurses, obstetricians, fetal medicine specialists, surgeons, and others.
Health professionals involved in second-trimester obstetric sonography must possess specific technical skills, including proficiency in operating ultrasound equipment, identifying fetal structures, and interpreting sonographic images accurately. Continuous training and skill development are essential to maintain competency in this rapidly evolving field.
A well-defined strategy involves establishing standardized protocols and guidelines for conducting second-trimester obstetric sonography. This ensures consistency in care delivery and reduces variations in practice. It also includes setting objectives for the scan, such as screening for fetal anomalies or assessing fetal growth based on the patient's specific clinical indications.
Effective interprofessional communication is vital for the success of obstetric sonography. Physicians, nurses, and sonographers must collaborate closely to ensure that the scan is performed correctly, that findings are communicated accurately, and that patients receive clear explanations. Open and respectful communication among team members fosters trust and enhances patient care.
Ultimately, the interprofessional team can enhance patient-centered care in second-trimester obstetric sonography by fostering a collaborative approach that emphasizes skills development, shared responsibilities, effective communication, and care coordination. This leads to improved patient outcomes, safety, and team performance while respecting the unique challenges and complexities of obstetric care.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Doaa Jabaz declares no relevant financial relationships with ineligible companies.
Disclosure: Suzanne Jenkins declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Jabaz D, Jenkins SM. Sonography 2nd Trimester Assessment, Protocols, and Interpretation. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- A short history of sonography in obstetrics and gynaecology. [Facts Views Vis Obgyn. 2013] A short history of sonography in obstetrics and gynaecology. Campbell S. Facts Views Vis Obgyn. 2013; 5(3):213-29.
- Review Routine ultrasound for fetal assessment before 24 weeks' gestation. [Cochrane Database Syst Rev. 2021] Review Routine ultrasound for fetal assessment before 24 weeks' gestation. Kaelin Agten A, Xia J, Servante JA, Thornton JG, Jones NW. Cochrane Database Syst Rev. 2021 Aug 26; 8(8):CD014698. Epub 2021 Aug 26.
- Prenatal screening for fetal aneuploidy in singleton pregnancies. [J Obstet Gynaecol Can. 2011] Prenatal screening for fetal aneuploidy in singleton pregnancies. Chitayat D, Langlois S, Douglas Wilson R, SOGC GENETICS COMMITTEE, CCMG PRENATAL DIAGNOSIS COMMITTEE. J Obstet Gynaecol Can. 2011 Jul; 33(7):736-750.
- Guidelines for the Management of a Pregnant Trauma Patient. [J Obstet Gynaecol Can. 2015] Guidelines for the Management of a Pregnant Trauma Patient. Jain V, Chari R, Maslovitz S, Farine D, Maternal Fetal Medicine Committee, Bujold E, Gagnon R, Basso M, Bos H, Brown R, et al. J Obstet Gynaecol Can. 2015 Jun; 37(6):553-74.
- Review Evaluation of prenatally diagnosed structural congenital anomalies. [J Obstet Gynaecol Can. 2009] Review Evaluation of prenatally diagnosed structural congenital anomalies. Gagnon A, GENETICS COMMITTEE. J Obstet Gynaecol Can. 2009 Sep; 31(9):875-881.
Recent Activity
- Sonography 2nd Trimester Assessment, Protocols, and Interpretation - StatPearls Sonography 2nd Trimester Assessment, Protocols, and Interpretation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

15 templates

26 templates
49 templates
american history
76 templates
great barrier reef
17 templates
39 templates
Basics of Ultrasound - Science Lesson for High School
It seems that you like this template, basics of ultrasound - science lesson for high school presentation, free google slides theme, powerpoint template, and canva presentation template.
****It's hard to believe that ultrasound has only been around since the 1940s! Back then an independent scientist named Karl Dussik probably had no idea his invention would be so important in medicine. Ultrasound works by using sound waves to create an image of organs and structures inside the body without having to open it up. It can be hard to understand for high school students, but not if you use this creative presentation design full of graphs, charts, illustrations and infographics!
Features of this template
- 100% editable and easy to modify
- 35 different slides to impress your audience
- Available in different colors
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Available colors.
Original Color
Related posts on our blog

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access


Register for free and start editing online
UC San Diego Team Wins Entrepreneurship Challenge for Third Year in a Row
Startup aims to provide life-saving technology for stroke victims.
- Mika Ono - [email protected]
- Xochitl Rojas-Rocha - [email protected]
Published Date
Topics covered:.
- Nanotechnology
- Entrepreneurship
Share This:
Article content.
When paramedics arrive at the scene, they confront a woman experiencing classic signs of a stroke. She is confused, slurring her words and having difficulty moving one arm. The first responders know that time is of the essence. For every minute that a stroke patient goes untreated, the more brain cells die and the worse the patient’s prognosis.
But treatment depends on what type of stroke it is—whether it is caused by a blockage of vessels or bleeding inside the brain. Administering the wrong treatment makes the patient’s condition worse. So there is little the paramedics can do except transport the patient to the hospital to be examined by medical staff there.
A team of students from the University of California San Diego hopes to rewrite the ending to stories like this one, which represent an all-too-common scenario; stroke is the second-leading cause of death worldwide, according to the World Health Organization . The UC San Diego team wants to create a company to give first responders and emergency room personnel a new, portable and cost-effective tool to rapidly diagnose stroke patients and speed treatment.
The team’s pitch was awarded first place in the National Nanotechnology Entrepreneurship Challenge (NTEC), which also drew competitors from Stanford University, Virginia Tech and others of the National Nanotechnology Coordinated Infrastructure network. This is the third year in a row that a team from UC San Diego mentored by Yves Theriault, program manager for education and outreach at the UC San Diego Qualcomm Institute (QI), has won the competition.
This year’s group is composed of Freddy Garcia, a nanoengineering Ph.D. student in the UC San Diego Jacobs School of Engineering; Beeta Zamani ’24, an undergraduate nanoengineering major in the Jacobs School; and Laura Charria ’24, an undergraduate cognitive science major in the UC San Diego School of Social Sciences.
“It is a great team,” said Theriault, who was joined as a mentor this year by Oscar Vazquez Mena, who is Garcia’s Ph.D. advisor and an associate professor in the Aiiso Yufeng Li Family Department of Chemical and Nano Engineering at the UC San Diego Jacobs School of Engineering. “It’s a winning technology.”
‘Novel Advantages’
The group’s proposal grew out of Garcia’s interest in metamaterials — materials engineered to have properties rarely observed in nature. Garcia realized that metamaterials could be used in conjunction with existing ultrasound technology to surmount current barriers to imaging the brain.
“The novelty of it all comes down to the metamaterials that we’re creating,” said Garcia. “Ultrasound waves propagate through skin — there’s no problem there — but when it comes to a bone like the skull, waves can’t get through. You just get a lot of diffraction. But with the metamaterials between the skull and the ultrasound waves, you can allow waves to go through by matching the impedance of the skull.”
As part of the NTEC program, the students sought out and interviewed potential customers to explore the market for products that could be created from this technology.
After completing 21 interviews, the students chose to focus on imaging for rapid diagnosis of strokes. While the competition in this space included portable CT scanners, these machines were expensive, bulky and energy- and staff-intensive compared to the ultrasound device the students wanted to offer.
“We can essentially have a headgear that you put on [a patient],” Zamani said. “You’re able to leave that on and have imaging of the brain and extended blood flow monitoring, which are really novel advantages. Making that portable and accessible is really the niche that we’re trying to target.”
The Winning Formula
The NTEC competition culminated in a virtual showcase event in which each team presented a two-minute video about its work to a panel of judges.
“The competition was intense, very tough,” said Garcia. “And there was more competition than last year, because there were 15 groups instead of 10.”
Ultimately, though, the UC San Diego team prevailed.
Garcia credits his teammates. “Beeta and Laura really transformed this idea we had into something that was easy to digest and fun to look at with the presentation,” he said. “Everyone had great technology; it was interesting, cutting-edge. But, in the end, if you can’t really translate that to two minutes, you lose a lot of people. So the creativity, ideas, technology, innovation, and putting that all together into a two-minute video set us apart. I’m really proud to have these people on my team.”
“Being able to work with your team — especially when it’s getting down to the deadlines — and to effectively communicate to your audience, your investors and your end-users is really so fundamental,” added Zamani.
Charria not only praised her teammates, but also called out the group’s origins in the Qualcomm Institute’s cleanroom facility, Nano3. “I feel it’s important to trace our group back to Nano3 and the Qualcomm Institute,” she said. “Without them, I wouldn’t have been able to meet everyone on the team, including Freddy, Beeta and Yves.”
Bringing It Forward
While the team is at somewhat of a crossroads—Charria and Zamani are graduating as Garcia continues his Ph.D. studies—the startup continues to evolve.
Garcia notes that, in addition to the NTEC program, the business idea is being honed through two other entrepreneurship programs: the National Science Foundation’s Innovation Corps (I-Corps), which they just finished, and the MedTech Acceleration Program in the UC San Diego Institute for the Global Entrepreneur .
“The MedTech accelerator covers the foundations for entrepreneurs and what we have to look into,” said Garcia. “They go very deep into it, including FDA regulations, so that’s been helping a lot.”
In the meantime, as they look toward graduation, Charria and Zamani appreciate how much they learned from the NTEC competition.
“[NTEC] is an opportunity that I wish every student had the opportunity to experience at least once in their life,” said Charria. “It’s not only about working on our own startup, but also listening and learning from what the other teams are doing all around the nation.”
“A lot of the engineering curriculum is focused on teaching you the theories, how to be an engineer, all the technical details,” said Zamani. “Being more involved in the entrepreneurship aspects allowed me to see how technical knowledge can be used in conjunction with business strategies to make powerful technologies that can really change the world.”
Learn more about the UC San Diego Qualcomm Institute’s nanotechnology facilities and internships .
You May Also Like
Design lab alumnus perspective, a change of direction, study: surgical intervention improves quality of life for patients with acoustic neuroma, stay in the know.
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.
You have been successfully subscribed to the UC San Diego Today Newsletter.
Campus & Community
Arts & culture, visual storytelling.
- Media Resources & Contacts
Signup to get the latest UC San Diego newsletters delivered to your inbox.
Award-winning publication highlighting the distinction, prestige and global impact of UC San Diego.
Popular Searches: Covid-19 Ukraine Campus & Community Arts & Culture Voices
Ultrasound in gynaecology
Dec 19, 2019
670 likes | 1.94k Views
Ultrasound in gynaecology. Dr S hruthi A G Senior Resident Dept of OBG YMCH. Ultrasound use in gynaecology has become a standard and valuable tool for the clinician in many aspects of daily practice Ease of use and relatively low cost
Share Presentation

Presentation Transcript
Ultrasound in gynaecology Dr Shruthi A G Senior Resident Dept of OBG YMCH
Ultrasound use in gynaecology has become a standard and valuable tool for the clinician in many aspects of daily practice • Ease of use and relatively low cost • Adjunct to clinical practice for everyday decision making
Ultrasound brings light into the female pelvis visualizing the uterus and adnexa • This imaging modality can help in diagnosis and management of many uterine and ovarian or adnexal disorders • Clinical information is obtained about morphology, hormonal status, sensation, pelvic organ mobility and vascular anatomy • Most of the pelvic masses can be characterised by B-mode and Doppler ultrasound.
Noninvasive procedure utilizes high frequency sound waves. Soft tissue imaging possible. No ionizing radiation. • 2 modes: • Transabdominal • Trasvaginal TAB- requires distended bladder, • Best used for large masses like fibroid / ovarian T. TVS – Does not require full bladder • Avoids the difficulties due to obesity • Better image
List of indications American Institute of Ultrasound in Medicine(AIUM) • Pelvic pain • Menstual abnormalities: • Dysmenorrhea • Menorrhagia • Metrorrhagia • Menometrorrhagia • Delayed menses or precocious puberty • Postmenopausal bleeding
Follow up of previously detected abnormality • Evaluation and /or monitoring of infertile patients • Abnormal pelvic examination • Evaluation of congenital anomalies • Excessive bleeding,pain or fever after delivery • Early pregnancy failures or pregnancy of uncertain outcome including ectopic pregnancies • Localization of a IUCD • Screening for malignancy in patients with increased risk • Further characterization of a pelvic abnormality detected on another imaging study
Normal findings UTERUS • It is important to note the timing of a woman’s cycle for the proper interpretation of the normal and its variants • Note if the woman is premenopausal or post menopausal • Can be Performed transabdominally , which requires atleast a partialy distended bladder that displaces the small bowel and gaseous intestines from th area being viewed • Or more precisely transvaginally with the bladder emptied • Rarely both modalities are used in cases of a large uterus or a large pelvic mass
Uterine size: • Length- long axis from fundus to cervix; 5-8cms • Depth- anteropoeterior measurement perpendicular to length; 1.5-3cms • Width- coronal view; 2.5-5cms. • Volume: length*depth*width*0.53= normal is <100cm3 • Postmenopausal uterus is smaller than the premenopausal uterus and endometrium has maximum thickness of <5mm
Endometrium • Depends on the timing of the menstrual cycle; • 1-4 mm thick during menstruation • Folicular phase: 8-15mm, trilaminar appearance- two proliferating bands &a central canal echo. • Secretory phase: thickness remains same but the proliferating bands and the central echo blend to form a single hyperechoic band. • Myometrium • Hypoechogenic & homogenous • Cervix
Ovary • Moderately echogenic, well demarcated • Location : just above the iliac vesselsand lateral to the edge of the broad ligament • Other sites: pod, lower abdomen • Folicular phase: a group of antral follicles(Mid proliferative phase) 4-8 antral follicles, 3-5mm • Ovulation : one dominant follicle maximum of 18-24mm, rest of the follicles reaches maximum to 10mm. • Corpus luteum- more solid, echogenic, disappears within a day or two of menstruation
Uterine abnormalities FIBROIDS • Most common uterine pathology • Uterine contour irregularity and enlargement • Hypoechoic or heterogenous uterine mass • Degenerative changes: irregular, anechoic areas in cystic degeneration; bright and highly echogenic area in calcified degeneration • Location • Pedunculatedmyomas- Mimic adnexal masses, vascular bridge connecting the mass to the uterus • Submucous fibroid: SIS with excellent ultrasound technique
Adenomyosis • A condition where the endometrial glands and stroma are present deep in the myometrium with surrounding myometrial hypertrophy • Usg findings: • Rainy pattern of acoustic shadowing • Normal vessels • Enlarged uterus(AP diameter) • Asymmetry • Myometrial cysts: cystic spaces ranging from 2-7 mm located within the myometrium
More common diagnostic feature • Diffuse heterogenous echo texture of myometrium • Asymmetric thickening of either the anterior or posterior wall of the uterus • Subendometrial myometrial cysts- causes endometrial myometrial junction to be poorly defined • Subendometrial echogenic linear striations • Globular enlarged uterus without a definitive mass.
Endometrial pathology • Submucous leiomyoma • Endometrial polyp • SIS
Saline infusion sonography • Saline infusion sonography : (Sonohysterography) • 20-40ml of salin, it is performed within first 10day of menstrual cycle. • Complications are minimal • Single dose of doxycycline 20mg • Contraindication: Pregnancy, active pelvic infection
Post menopausal bleeding • A thin stripe of <4 mm on TVS can exclude endometrial disease • Localization of IUCD • TVS can detect both the proximal and distal ends of the vertical arm • 3D TVS using multiplanar views has proven to superior.
Ovarian/ adnexal abnormalities • Safe, quick, inexpensive and in skilled hands a reliable method to help distinguish between most benign and malignant condition sof the adnexa • Morphological characteristic swhich increase the risk of malignancy • Solid components ( excrescences or papillary projections) • Irregularities • Decreased resistance index • Neovascularization • Ascitis • Doppler ultrasound gives a better information about neovascularization
Ectopic pregnancy • βHCG ≥ 1500 without a intra uterine sac, ectopic pregnancy should be suspected. • Intrauterine gestation sac is seen by TVS with βHCG levels between 1000-2000mIU/ml • Most telling usg finding: • a live embryo n the adnexa followed by a tubal ring ( doughnut or bagel sign ) with or without haemorrhage • Intrauterine pseudo sac along with complex adnexal mass • Free fluid in the POD and thickened endometrium with no viable intra uterine pregnancy • Rule out early gestation and heterotrophic pregnancy.
Pelvic pain • Ovarian torsion • Endometriosis • Pelvic inflammatory disease/tubo-ovarian abscess • TVS and Doppler helps in sorting out the differential diagnosis
Ovarian torsion • Is a surgical emergency • USG features: • enlarged ovary that appears oedematous • Heterogenousechotexture • Small cystic areas towards the periphery • Some free fluid • comparision with the morphological appearance and the blood flow patterns by Doppler.
Endometriosis • Most common eitiology of chronic pelvic pain • Endometriotic cysts : • Multilocular • Low level internal echoes • Hyperechoic • Thickened cyst wall • TVS is poor in detecting the presence of adhesions and mild endometriotic implants • In deep infiltrating disease where it involves the POD, hypoechoic linear thickening or nodules/masses is seen; POD can also be obliterated with or without free fluid
Pelvic inflammatory disease • Can cause acute or chronic pelvic pain • Hydrosalphinx is seen by USG as tubular adnexal structure with septations or nodules in its wall
Therapeutic application : • Oocyte retrieval in IVF • Draining of chocolate cyst • draining of pelvic abscess • In evacuation of molar pregnancy • Transcervial cannulation and sperm injection into fallopian tube • Retrieval of missing IUCD • Injection of methotrexate into an ectopic sac. • Focused ultrasound therapy
ROLE OF DOPPLER
DOPPLER EFFECT • Observed changes in the frequency of transmitted waves when relative motion exists between the source and an observer • Frequency of waves increases when source and observer move closer and vice versa
PRINCIPLES • Sound is a form of mechanical energy that travels through media as pressure waves generated when an object vibrates • Audible sound frequency ranges from 20Hz to 20 kHz • Frequency range of obstetric transducer is 2-5 MHz • To produce vibrations at the rate of millions of cycles per second, special materials with piezoelectric properties are used
DOPPLER SIGNAL PROCESSING
DOPPLER ULTRASOUND IN GYNECOLOGY • OVARIAN MASS • To differentiate between benign and malignant ovarian tumours • Neovascularization causes decrease in impedance to flow in malignant lesions • High level of colour content and high blood velocity indicates malignancy • Vascularization of solid nodules is predictive
2) OVARIAN TORSION Abnormal flow pattern in affected ovary : - Reduced overall vascularity - Greater impedance in supplying vessels - Absence of blood flow - Whirlpool sign: vessels spiralling round each other or ovary (clockwise or counterclock wise wrapping of vessels in the twisted vascular pedicle)
3) INFERTILITY • Some studies have demonstrated relationship between perifollicular vascularity and pregnancy rates, (higher if embryo from highly vascularized follicle)- controversial • Loss of subendometrial blood flow is indicative of tubal blockage PERIFOLLICULAR VASCULARITY
4) ENDOMETRIAL CANCER • Vascularity of endometrium (low impedance in myometrial and endometrial vessels) along with thickness • Greater depth of myometrial invasion by tumour associated with greater vascularity and lower impedance • Other characteristics are: - Higher colour score - greater number of feeding vessels
5) TROPHOBLASTIC DISEASE Non invasive mole: - High velocity and low resistance flow in uterine arterial circulation - Less intra tumoral flow in trophoblastic tissue Invasive mole and choriocarcinoma: - Increase in uterine vascularity - Increase in tumour vascularity
Doppler has been used to differentiate between adenomyosis and fibroid uterus Adenomyosis: Diffuse hypervascularity throughout the lesion Fibroid : Typical peripheral flow
ARTERIOVENOUS MALFORMATION • Multiple communication between arterial and venous system without an intervening capillary network • Can be iatrogenic secondary to dilatation and curettage and caesarean • Vascular tangle of blood vessels with high velocity low resistance flow
PSEUDOANEURYSM • Can occur as a complication secondary to dilation and curettage • Appears as blood filled cystic structure with swirling arterial flow • Also called Yin Yang sign
BIOSAFETY • Ultrasound beams transmit energy into tissue so possibility of hazard has to be considered • Likely mechanisms for harmful effects: - Tissue heating as ultrasound energy is absorbed - Cavitation: Gas bubbles in the tissue react under the influence of pressure fluctuations
There is a considerable amount of literature on the safety of diagnostic ultrasound • There are several organizations that actively scrutinize the literature and monitor the safety of ultrasound • Such as : British Medical Ultrasound Society • World Federation for Ultrasound in Medicine and Biology (WFUMB)
Approach now is to use the ALARA principle (As Low as Reasonably Achievable) • More caution has to be used with pulsed doppler especially during early pregnancy • Many systems now display the output in terms of Thermal Index (TI) and Mechanical Index (MI)
GUIDELINES FOR SAFE USE • Use the lowest possible transmit power which will give a diagnostic result (TI and MI <1) • Use minimum scan time possible • Check that transducer ceases to transmit when the image is frozen
- More by User
The Role of Ultrasound in Obstetric and Gynaecology
The Role of Ultrasound in Obstetric and Gynaecology. Max Brinsmead PhD FRANZCOG May 2006. Potential uses for ultrasound in obstetrics 1 :. Locate the pregnancy – exclude ectopic Assess viability – assessment of threatened miscarriage Determining gestation & dates Crown rump length
943 views • 9 slides
Ultrasound in Medicine
Ultrasound in Medicine. This presentation will explain what ultrasound is and how it is used in medicine.. What is Ultrasound?. Ultrasound is simply sound that has a very high frequency.Humans are not able to hear ultrasound, though some animals can hear them.Sounds with frequencies above 20 000 h
994 views • 26 slides
Ultrasound in Perineology
The Perineologist. Architect of the perineum.Perfect knowledge of the 3 axis anatomy.Holistic view of the woman.Needs good eyes and good fingersLearn with ULTRASOUND . Aim of the lecture. To show how ultrasound could study all the aspectsof the perineum.It should become a teaching t
459 views • 27 slides
Electro surgery in Gynaecology
Electro surgery in Gynaecology. Prof.Surendra Nath Panda. Dept. of OBGYN M.K.C.G.Medical College Berhampur, Orissa, India. History. Heat therapy known since antiquity “Heat cures when everything fails” …Hipocrates. Albucasis (980BC) used hot iron to stop bleeding.
670 views • 38 slides
LITIGATION IN GYNAECOLOGY 2012
LITIGATION IN GYNAECOLOGY 2012. Litigation. Impact of law in O&G far outweighs other medical fields Substantially more interaction with the health care system: Pregnancy Avoidance of pregnancy Childbirth Menopause. NHS: £400m paid out for malpractice
304 views • 15 slides
ULTRASOUND In MEDICINE
ULTRASOUND In MEDICINE. Dr/Aida Radwan. Chapter (1) ULTRASOUND WAVES. Most of the information about our physical surroundings comes to us through our senses of hearing and sight المشاهده .
522 views • 32 slides
Ultrasound In Medicine
Ultrasound In Medicine. Chapter- 3. Ultrasound instrumentation. Modes of ultrasound imaging. 0. 2. 4. 6. 8. 10. A- Scan (Pulsed Scan). Echoes are shown in screen as pulses Give us information about the diameter of structures Is one dimensional Transducer is fixed. f. initial
741 views • 22 slides
Paediatric gynaecology
Paediatric gynaecology. Special patients: need special approach! Selected topics for this presentation: Examination of the prepubertal child and adolescent Paediatric vulvovaginal conditions Lower abdominal mass Contraception for adolescents. Examination of the prepubertal child 2.
361 views • 10 slides
Gynaecology Oncology
Gynaecology Oncology. Ram Athavale Consultant Gynaecological Oncology University Hospitals Coventry & Warwickshire NHS Trust. Aims. A framework for main gynaecological cancers To provide a foundation for further study. Gynaecological malignancies. Gynaecological malignancies.
1.22k views • 77 slides
Ultrasound in gynaecology. By Dr. Khattab KAEO Assis. Prof. of Obstetrics and Gynaecology Faculty of Medicine, Al-Azhar University, Damietta. Introduction. Ultrasound has a frequency >20 000 Hz (20kHz). However, ultrasound machines have frequencies of 2-10 mega Hz (MHz).
535 views • 21 slides
Community Gynaecology
Community Gynaecology. User Satisfaction Survey June 2012. Community Gynaecology. User Satisfaction Survey June 2012. Why do the user surveys?. Community Gynaecology Service. The service :
416 views • 25 slides

Gynaecology
Gynaecology is the medical practice dealing with the health of the female reproductive system. Aware yourself about the female health conditions and get brief information related to it.
321 views • 10 slides
Walk in Ultrasound
Walk-in Ultrasound It is very common for clients to walk in our ultrasound clinic in Canada and get best service especially from professional doctors. Our clinic is located in the heart of Canada.
67 views • 6 slides
Ultrasound Course in Obstetrics and Gynaecology
Ultrasound is a growing career field (a lucrative one too) and is becoming an increasingly attractive alternative to radiologic procedure. The promising career is one reason to consider ultrasound courses in Obstetrics and Gynaecology. To gain a proper highlight on our respected courses & programs, do stop by at http://lifewaytrainingcenter.com.
56 views • 3 slides
Ultrasound in Gurgaon
https://dranmolsethi.com Searching for the best ultrasound clinic? If yes, then you have come to right place. Avail cost-effective Ultrasound in Gurgaon fromDr. Anmolu2019s Ultrasound Clinicwhich is done by the experienced radiologist Dr. AnmolSethi. We have the advanced ultrasound machine that capture good images during the test.
132 views • 12 slides
Ultrasound in Medicine. عنوان درس : اولتراسوند در پزشکی. References:. Physical Principles of Medical Ultrasonics C.R.Hill, J.C.Bamber, G. R. ter Haar John Wiley &Sons, 2004 Diagnostic Ultrasound Imaging and Blood Flow Measurements K. Kirk Shung Taylor & Francis 2006
214 views • 16 slides
GYNAECOLOGY RADIOTHERAPY AND CHEMOTHERAPY IN GYNAECOLOGY د. اسراء المعيني
GYNAECOLOGY RADIOTHERAPY AND CHEMOTHERAPY IN GYNAECOLOGY د. اسراء المعيني. PRINCIPLES OF RADIATION THERAPY
647 views • 19 slides
Gynaecology Assignment Help in Australia
Gynecologists are specialized doctors in womenu2019s health to improve the health of reproductive systems.
85 views • 7 slides

Gynaecology in Meerut
Prem Hospital has the best gynaecologist in Meerut, Delhi to assist in female infertility treatment issues and offers expert ivf counselling & support to infertile couples.
84 views • 6 slides
Cosmetic Gynaecology
At Institute of Laser and Aesthetic Medicine(ILAMED), Cosmetic Gynaecology is a relatively new field that focuses on improving the aesthetic appearance of the female genitalia. This field of medicine addresses the concerns of women who may be dissatisfied with the appearance of their genitalia due to childbirth, aging, or other factors. Hereu2019s what you need to know about Cosmetic Gynaecology. For more information visit our site:- https://www.ilamed.org/courses/cosmetic-gynecology/
139 views • 11 slides

best gynaecology doctor in Chennai
22 views • 2 slides
Gynaecology Clinic In Dubai
The Gynaecology Clinic in Dubai at Medstar Speciality Hospital is a leading destination for women's health, offering expert medical care, compassionate consultations, and cutting-edge treatments to address a wide range of gynecological concerns with precision and sensitivity.
7 views • 3 slides
Brittney Bernardoni and Hani Kuttab receive 2024 UW Health Physician Excellence Awards

Two BerbeeWalsh Department of Emergency Medicine faculty were among those honored at this year’s UW Health Physician Excellence Awards ceremony, held May 15, 2024, in Madison. The prestigious, peer-nominated awards recognize physicians who demonstrate exceptional skills in clinical practice, education, leadership or regional services and a commitment to the institution’s mission, vision and values.
Brittney Bernardoni, MD – Rising Star Leadership Excellence Award
Dr. Brittney Bernardoni’s visionary leadership has advanced patient care and has grown UW Health’s reputation as a recognized destination for multidisciplinary critical care providers. She joined UW Health in 2021 as an emergency intensivist and not long after, she was promoted to Assistant Medical Director for Quality for Med Flight.
Dr. Bernardoni has built a nationally respected quality improvement program for Med Flight that includes formal peer review—something that is quite rare. And, she has catapulted UW Health’s reputation as a national center for ECMO life-support technology – saving some of UW Health’s sickest patients.
A strong fellowship program is essential for recruiting outstanding intensivists, and Dr. Bernardoni led a herculean effort to launch a two-year Emergency Medicine–Anesthesia Critical Care fellowship and now serves as Associate Program Director.
As Dr. Andrew Cathers shared: “I have not met another physician who has a comparable combination of clinical excellence as well as administrative and leadership skill.”
Hani Kuttab, MD – Rising Star Clinical Practice Excellence Award
Dr. Hani Kuttab was a standout clinician from the early stages of his emergency ultrasound fellowship with the Department of Emergency Medicine. He joined the faculty as an Assistant Professor and Assistant Ultrasound Director in 2020 and became Medical Director of East Madison Hospital Emergency Department three years later.
Dr. Kuttab has transformed the clinical experience for patients living with sickle cell disease. The inherited blood disorder affects 8-10% of African Americans and causes intense flare-ups of pain that often require emergency care.
To address delays in care, Dr. Kuttab led a multidisciplinary team in creating individual pain management plans easily accessed in each patient’s electronic health record and launched a Rapid ED Pain Management Plan. To reduce bias and stigma, he coordinated the grand round presentation “Humanizing Medicine: Learning from Patients with Sickle Cell Disease.” His gift for making people feel seen and supported has made him an extraordinary agent for change.
This year marks the 14th annual Physician Excellence Awards at UW Health.
- Facebook Logo
- Twitter Logo
- Linkedin Logo

IMAGES
VIDEO
COMMENTS
Possible fetal positions can include: Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left.
Fetal ultrasonography is an essential element in the evaluation of anomalies and fetal well-being throughout pregnancy. The increasing incidence of morbid obesity, hypertension, and gestational diabetes within the reproductive age group places this high-risk population at increased adverse fetal events such as stillbirth and fetal anomalies. In every trimester, there are specific maternal and ...
I. Basic Ultrasound Physics. Sound is a series of pressure waves propagating through a medium. One cycle of the acoustic wave is composed of a complete positive and negative pressure change. The wavelength is the distance traveled during one cycle. The frequency of the wave is measured in cycles per second or Hertz (cycles/s, Hz) (Illustration ...
breech presentation: fetal rump presenting towards the internal cervical os, this has three main types. frank breech presentation (50-70% of all breech presentation): hips flexed, knees extended (pike position) complete breech presentation (5-10%): hips flexed, knees flexed (cannonball position) footling presentation or incomplete (10-30%): one ...
Ultrasound imaging. Ultrasound uses high frequency sound waves to visualize internal structures. It works by transmitting sound waves into the body using a transducer probe, which detects the echoes as they bounce off tissues and organs. The echoes are processed to form images on the ultrasound machine screen in real-time.
Clean the ultrasound probe. 4. Apply a tourniquet. 5. Apply gel to the ultrasound probe. 6. Identify the target vein in the transverse plane: note the depth of the anterior wall of the vein and pay attention to any adjacent structures. 7. Once identified, rotate the probe into the longitudinal plane.
Basic Training. Sound/Ultrasound. • Longitudinal mechanical wave • Transmitted through medium by local displacement of particles within medium - compression & rarefaction • Frequency (Hertz) = cycles/sec • Human audible range = 20Hz - 20,000Hz (20kHz) • Ultrasound = frequencies above audible range.
Diagnostic ultrasound is a non-invasive diagnostic technique used to image inside the body. Ultrasound probes, called transducers, produce sound waves that have frequencies above the threshold of human hearing (above 20KHz), but most transducers in current use operate at much higher frequencies (in the megahertz (MHz) range).
Case Study Clinical presentation: An 82-year-old female experiencing a "knocking" sensation and shooting pain in her left preauricular region for 4 weeks presented with a referral from her general practitioner requesting an ultrasound of the temporal arteries. No history of blunt head trauma or a pulsatile mass in the left preauricular ...
Lecture 25b: The basics of gynecological ultrasound. This lecture was delivered by Dr. Shabnam Bobdiwala at ISUOG's Basic Training Course in gynecology in partnership with Erasmus Medical Center, in Rotterdam in 2018. The basics of gynecological ultrasound. Feel free to download this presentation to support your learning.
Citation, DOI, disclosures and article data. Ultrasound ( US) is an imaging technology that uses high-frequency sound waves to characterize tissue. It is a useful and flexible modality in medical imaging and often provides an additional or unique characterization of tissues when compared to other modalities such as conventional radiography or CT.
Ultrasound is the most widely used medical imaging method for viewing a fetus during pregnancy. It is also utilized to guide procedures such as amniocentesis or chorionic villus sampling . An ultrasound may be done at almost any time during a pregnancy, even as early as about five weeks after conception. During the first trimester, it can ...
Ultrasound Etiquette. Introduce yourself to your patient and ask permission to scan. Only expose the area of the body being scanned. Wipe the patient off after the exam is completed. Clean off the probe and cord. Soap and water.
Basics of Ultrasound. Sep 25, 2012 •. 458 likes • 233,219 views. Dr. Sreedhar Rao. Business Technology. 1 of 43. Download now. Download to read offline. Basics of Ultrasound - Download as a PDF or view online for free.
Antenatal ultrasonography is widely used in pregnancy to assess fetal growth and anatomy. Although ultrasound screening is now an integral part of routine antenatal care, recommendations for the delivery of obstetric ultrasound vary from country to country.[1][2] The history of sonography in obstetrics dates from the classic 1958 Lancet paper of Ian Donald and his team from Glasgow. Clinical ...
Ultrasound works by using sound waves to create an image of organs and structures inside the body without having to open it up. It can be hard to understand for high school students, but not if you use this creative presentation design full of graphs, charts, illustrations and infographics!
Health & Medicine. 1 of 50. Download now. Presentation1, basic principle of ultrasound. - Download as a PDF or view online for free.
Presentation Transcript. Ultrasound • Sound waves above 20 KHz are usually called as ultrasound waves. • Sound waves propagate mechanical energy causing periodic vibration of particles in a continuous, elastic medium. • Sound waves cannot propagate in a vacuum since there are no particles of matter in the vacuum.
Physics • Diagnostic ultrasound uses sound waves in the frequency range 2-20 MHz • Key properties of sound waves: • Frequency is number of times per second the sound wave is repeated • Wavelength is the distance traveled in 1 cycle • Amplitude is distance between peak and trough. Physics - Parallel Concepts • Conceptually ...
An ultrasound image displays the magnitude (absolute value of amplitude) of ultrasound echoes , so a physical understanding of acoustic wave reflection is valuable for interpreting the images θι angle of incidence θr angle of reflection θt angle of transmission at a planar interface between a material with sound speed c 1and a
Presentation Transcript. Physics of Ultrasound Krystal Kerney Kyle Fontaine Ryan O'Flaherty. Basics of Ultrasound • Ultrasound is sound with frequencies higher than about 20 kHz • For medical ultrasound, systems operate at much higher frequencies, typically 1 - 10 MHz • Propagation of ultrasound waves are defined by the theory of ...
Ultrasound Technologists get images of internal organs using sound waves. History :) All started with Doctor Karl Theodore Dussik and Professor Ian Donald. ... What are AI writing tools and how can they help with making presentations? May 22, 2024. Brainstorm using mind map ideas and examples; May 21, 2024. Overcome presentation deadlines with ...
The presentation will outline the transthoracic echocardiogram features that will be seen in a normal heart during pregnancy as well as the findings expected in patients with known cardiac disease. In addition, the presentation will also outline the echocardiographic features of decompensation. ... Ultrasound enhancing agents significantly ...
Relative Q̇DIA measurements have valid physiological underpinnings, are reliable day-to-day, and reproducible analyzer-to-analyzer. Contrast-enhanced ultrasound is a viable, minimally invasive method for assessing costal Q̇DIA in humans and may provide a tool to monitor diaphragm hemodynamics in clinical settings.
The thoracic outlet is a narrow space in the lower neck bound by the clavicle anteriorly and first rib posteriorly wherein the neurovascular bundle consisting of the subclavian vein, subclavian artery, and brachial plexus travels through. 1 Venous thoracic outlet syndrome refers specifically to the compression and thrombosis of the subclavian vein. . The compression of the subclavian vein is a ...
Garcia realized that metamaterials could be used in conjunction with existing ultrasound technology to surmount current barriers to imaging the brain. ... Beeta and Laura really transformed this idea we had into something that was easy to digest and fun to look at with the presentation," he said. "Everyone had great technology; it was ...
For the ultrasound radiomics features, a similar feature selection procedure was also executed as that for breath-omics with the correlation analysis-based feature selection was removed. Therefore, 29 multi-omics features(10 breath-omics, 10 ultrasound raidomics, and 9 clinic-omics) were used for the breast cancer diagnosis mode construction.
Presentation Transcript. Ultrasound in gynaecology Dr Shruthi A G Senior Resident Dept of OBG YMCH. Ultrasound use in gynaecology has become a standard and valuable tool for the clinician in many aspects of daily practice • Ease of use and relatively low cost • Adjunct to clinical practice for everyday decision making.
Poster, Presentation, Protocol or Paper. Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book chapter, use the "Scholarly Articles and Book Chapters" deposit option.
He joined the faculty as an Assistant Professor and Assistant Ultrasound Director in 2020 and became Medical Director of East Madison Hospital Emergency Department three years later. ... To reduce bias and stigma, he coordinated the grand round presentation "Humanizing Medicine: Learning from Patients with Sickle Cell Disease." His gift for ...