Case Studies of Challenges in Emergency Care for Children With Autism Spectrum Disorder
Affiliations.
- 1 From the Division of Emergency Medicine, Cincinnati Children's Hospital Medical Center, Cincinnati, OH.
- 2 Department of Pediatrics, University of Colorado School of Medicine, Aurora, CO.
- PMID: 32205797
- DOI: 10.1097/PEC.0000000000002074
Autism spectrum disorder (ASD) affects more than 1% of children in the United States, with the rate of new diagnoses climbing significantly in the last 15 years. Emergent conditions and subsequent visits to the emergency department (ED) can be particularly challenging for children with ASD, most of whom also have comorbidities in addition to their deficits in social communication and interaction. In the emergency setting, these conditions can cause a range of behaviors that result in challenges for health care providers and may result in suboptimal experiences for children with ASD and their families. We present the ED course of 3 children with ASD to illustrate these challenges, emphasize successful strategies, and highlight opportunities for improvement.
Copyright © 2020 Wolters Kluwer Health, Inc. All rights reserved.
- Autism Spectrum Disorder* / epidemiology
- Autism Spectrum Disorder* / therapy
- Comorbidity
- Emergency Medical Services*
- Emergency Service, Hospital
- Emergency Treatment
- United States

Case Reports in Autism
Loading... Editorial 23 January 2024 Editorial: Case reports in autism Marco Colizzi and Fengyu Zhang 516 views 0 citations
Case Report 05 January 2024 Successful perioperative preparation of a child with autism spectrum disorder in collaboration with his school for special needs education: a case report Yuto Arai , 2 more and Yoshihiro Maegaki 1,180 views 0 citations
Community Case Study 02 November 2023 An individual-supported program to enhance placement in a sheltered work environment of autistic individuals mostly with intellectual disability: a prospective observational case series in an Italian community service Roberta Maggio , 7 more and Francesca Cucinotta 1,119 views 0 citations
Case Report 29 September 2023 Case Report: A playful digital-analogical rehabilitative intervention to enhance working memory capacity and executive functions in a pre-school child with autism Sabrina Panesi , 1 more and Lucia Ferlino 1,443 views 0 citations
Case Report 24 August 2023 Autism spectrum disorder and Coffin–Siris syndrome—Case report Luka Milutinovic , 4 more and Milica Pejovic Milovancevic 1,705 views 1 citations
Case Report 21 August 2023 Case report: A novel frameshift mutation in BRSK2 causes autism in a 16-year old Chinese boy Yu Hu , 7 more and Lixin Yang 1,308 views 1 citations
Case Report 18 August 2023 Case report: Substantial improvement of autism spectrum disorder in a child with learning disabilities in conjunction with treatment for poly-microbial vector borne infections Amy Offutt and Edward B. Breitschwerdt 7,782 views 0 citations
Case Report 17 August 2023 Fecal microbiota transplantation in a child with severe ASD comorbidities of gastrointestinal dysfunctions—a case report Cong Hu , 8 more and Yan Hao 1,304 views 0 citations
Case Report 28 July 2023 Autism spectrum disorder, very-early onset schizophrenia, and child disintegrative disorder: the challenge of diagnosis. A case-report study Michelangelo Di Luzio , 5 more and Stefano Vicari 2,339 views 1 citations
Case Report 19 June 2023 Case report: An evaluation of early motor skills in an infant later diagnosed with autism Lauren G. Malachowski , 1 more and Amy Work Needham 1,646 views 0 citations
Case Report 03 May 2023 Case report: Preemptive intervention for an infant with early signs of autism spectrum disorder during the first year of life Costanza Colombi , 7 more and Annarita Contaldo 4,235 views 2 citations
Case Report 26 April 2023 Case report: Treatment-resistant depression, multiple trauma exposure and suicidality in an adolescent female with previously undiagnosed Autism Spectrum Disorder Ilaria Secci , 5 more and Marco Armando 4,080 views 2 citations
Loading... Community Case Study 30 November 2022 A case study on the effect of light and colors in the built environment on autistic children’s behavior Ashwini Sunil Nair , 7 more and Xiaowei Zuo 10,972 views 7 citations
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 29 May 2024
A case–control study on pre-, peri-, and neonatal risk factors associated with autism spectrum disorder among Armenian children
- Meri Mkhitaryan 1 ,
- Tamara Avetisyan 2 , 3 ,
- Anna Mkhoyan 4 ,
- Larisa Avetisyan 2 , 5 &
- Konstantin Yenkoyan 1
Scientific Reports volume 14 , Article number: 12308 ( 2024 ) Cite this article
Metrics details
- Autism spectrum disorders
- Public health
- Risk factors
We aimed to investigate the role of pre-, peri- and neonatal risk factors in the development of autism spectrum disorder (ASD) among Armenian children with the goal of detecting and addressing modifiable risk factors to reduce ASD incidence. For this purpose a retrospective case–control study using a random proportional sample of Armenian children with ASD to assess associations between various factors and ASD was conducted. The study was approved by the local ethical committee, and parental written consent was obtained. A total of 168 children with ASD and 329 controls were included in the analysis. Multivariable logistic regression analysis revealed that male gender, maternal weight gain, use of MgB6, self-reported stress during the pregnancy, pregnancy with complications, as well as use of labor-inducing drugs were associated with a significant increase in the odds of ASD, whereas Duphaston use during pregnancy, the longer interpregnancy interval and birth height were associated with decreased odds of ASD. These findings are pertinent as many identified factors may be preventable or modifiable, underscoring the importance of timely and appropriate public health strategies aimed at disease prevention in pregnant women to reduce ASD incidence.
Introduction
Autism spectrum disorder is a neurodevelopmental disorder by the Diagnostic and Statistical Manual of Mental Disorders, the 5th Edition (DSM-5). It is identified by limited repeating patterns of behavior, activities, and interests, as well as impaired social interaction and communication 1 . A systematic review of research articles spanning from 2012 to 2021 indicates that the worldwide median prevalence of ASD in children stands at 1% 2 . Nevertheless, this reported percentage may not fully capture the actual prevalence of ASD in low- and middle-income nations, potentially leading to underestimations. In 2016, data compiled by the CDC's Autism and Developmental Disabilities Monitoring (ADDM) Network revealed that approximately one out of 54 children in the United States (one out of 34 boys and one out of 144 girls) received a diagnosis of ASD. This marks a ten percent increase from the reported rate of one out of 59 in 2014, a 105 percent increase from one out of 110 in 2006, and a 176 percent increase from one out of 150 in 2000 3 . According to the most recent update from the CDC’s ADDM Network, one out of 36 (2.8%) 8-year-old children has been diagnosed with ASD. These latest statistics exceed the 2018 findings, which indicated a rate of 1 in 44 (2.3%) 4 . To our understanding, there is no existing registry for ASD in the Republic of Armenia (RA). Additionally, there is no available data concerning the incidence and prevalence of ASD in the country.
The etiology of ASD remains unclear despite substantial research on the disorder; yet, important advances have been made in identifying some of the disorder's genetic and neurobiological underpinnings. It has been discovered that ASD is heritable, with environmental variables also being involved 5 , 6 , 7 . According to certain research, ASD is associated with both hereditary and environmental factors 5 , 8 , 9 . It is especially important to identify environmental risk factors because, unlike genetic risk factors, they can be prevented.
There are more than 20 pre-, peri- and neonatal risk factors associated with ASD 10 , 11 , 12 . Prenatal risk factors that have been associated with ASD involve parental age 13 , interpregnancy interval 14 , 15 , immune factors (such as autoimmune diseases, both viral and bacterial infections during pregnancy) 16 , 17 , medication use (especially antidepressants, anti-asthmatics, and anti-epileptics) 18 , 19 , 20 , maternal metabolic conditions (such as diabetes, gestational weight gain, and hypertension) 21 , 22 , 23 , and maternal dietary factors (such as folic acid and other supplement use, maternal iron (Fe) intake, as well as maternal vitamin D levels) 24 , 25 , 26 , 27 , 28 , 29 .
Numerous studies indicate that an increased risk of ASD is linked to several perinatal and neonatal factors. These factors include small gestational age or preterm birth, gestational small or large size, the use of labor and delivery drugs 30 , 31 , 32 , 33 . The risk of ASD associated with cesarean delivery is also a subject of continuous discussion 34 , 35 , 36 . Overall, there is no apparent link between assisted conception and a notably higher risk of ASD, however some particular therapies might make ASD more likely.
This study aimed to determine main pre-, peri- and neonatal risk factors linked to ASD among Armenian children. The following research questions were derived to address the objectives of the study:
What are the primary prenatal risk factors associated with the development of ASD among Armenian children?
How do perinatal factors such as maternal complications during childbirth, labor mode, labor interventions, use of labor-inducing drugs, contribute to the risk of ASD in Armenian children?
What neonatal factors, such as birth weight and gestational age, are linked to the likelihood of ASD diagnosis among Armenian children?
How do socio-demographic factors, such as parental education, gender of the child, number of kids in the family, sequence of the kid, influence the relationship between pre-, peri-, and neonatal risk factors and risk of ASD among Armenian children?
To the best of our knowledge, this was the first study of its kind conducted in Armenia that focused on a variety of factors linked to ASD.
The analysis encompassed a total sample of 497 participants, consisting of 168 children diagnosed with ASD and 329 children without ASD. The descriptive analysis revealed significant differences between the cases and controls on several socio demographic variables as well as prenatal, peri- and neonatal risk factors (see Tables 1 , 2 , 3 and 4 ).
The summary of socio demographic characteristics (Table 1 ). Among the cases (the ASD group), the distribution of gender of the child was significantly different to that in the control group. More specifically, while the distribution of male and female were balanced in the control group (52.89% and 47.11% respectively), the proportion of male children was significantly higher in the ASD group (82.14% and 17.86% respectively, p < 0.01). Furthermore, the number of children in the families of cases and controls were slightly different. While the proportion of cases and controls who had two children were similar, families with one child were slightly higher in the ASD group compared to the control group (29.94% and 17.02% respectively, p < 0.01). This picture is reversed with respect to the number of families with more than two children (16.17% and 29.79% respectively). A higher percentage of ASD cases are the first child in the family compared to controls (67.86% vs. 49.54%, p < 0.01). The proportion of non-married families (those that reported to be single, widowed, divorced etc.) were higher in the ASD group compared to the control group (10.24% and 4.28% respectively, p < 0.05). The distribution of the level of educational attainment of the parents were also different between the groups. More specifically, the prevalence of university degree among the cases were somewhat lower compared to that in the control group.
The summary of prenatal risk factors (Table 2 ). With respect to prenatal risk factors, there were significant differences between the cases and controls in interpregnancy intervals, self-reported complications and diseases, medication use, vitamin D levels, maternal weight gain, and the self-reported stress during pregnancy. More specifically, the cases had on average lower interpregnancy intervals compared to the controls (M = 12.9 and M = 23.7 months respectively, p < 0.01). The cases more frequently reported to have had complications during the pregnancy compared to the controls (42.86% and 8.54% respectively, p < 0.01). The prevalence of reported infectious diseases, other diseases and anemia during the pregnancy were also somewhat higher among the cases compared to the control group. The use of medications was higher among the cases compared to the control group (41.67% and 17.74% respectively, p < 0.01). Various medications including vitamins, anticoagulants, Paracetamol, MgB6, Duphaston, iron preparation, No-spa, calcium preparation, antibiotics, and Utrogestan showed significant differences in usage between cases and controls (all p < 0.05) (Table 3 ). The maternal weight gain among the cases was on average higher among the cases compared to the control group (M = 15.4 and M = 13.9 kg respectively, p < 0.05). The self-reported stress was also more frequent among the cases compared to the controls (56.02 and 10.98% respectively, p < 0.01). Specifically, comparing data on self-reported stress during different pregnancy periods, it was obvious that 47.06% of mothers of cases and 91.25% of mothers in the control group reported no stress experienced during pregnancy. During the first trimester, 14.38% of mothers with cases of autism reported stress, whereas only 0.94% of mothers in the control group reported stress. In the second trimester, 11.11% of mothers with cases of autism reported stress, compared to 4.06% of mothers in the control group. During the third trimester, 8.50% of mothers with cases of autism reported stress, while 1.88% of mothers in the control group reported stress. Across the entire pregnancy, 18.95% of mothers with cases of autism reported stress, compared to 1.88% of mothers in the control group. The differences in stress levels between the two groups were statistically significant, indicating a potential link between maternal stress during pregnancy and the odds of autism spectrum disorder in offspring.
The summary of perinatal and neonatal risk factors (Table 4 ). The interpretation of the data comparing various peri- and neonatal risk factors between cases (individuals with ASD) and controls (individuals without ASD) are shown below. 83.33% of cases and 91.77% of controls were born within 37–42 weeks of gestation, with a statistically significant difference ( p < 0.05), whereas 16.67% of cases and 8.23% of controls were born either preterm (before 37 weeks) or post-term (after 42 weeks), also showing a significant difference. There was no statistically significant difference in birth weight between cases and controls (M = 3137.8 and M = 3176.9 g respectively, p > 0.05). The mean birth height was slightly lower for cases compared to controls (M = 50.4 and M = 50.9 cm), with a statistically significant difference ( p < 0.05). No statistically significant difference was reported regarding mode of labor. According to the data interventions during labor were reported more in ASD group compared to controls (39.76% and 17.23% respectively, p < 0.01). Also, labor-inducing drugs were administered more in cases compared to the controls (39.76% and 21.04%, p < 0.01).
The results of multivariable logistic regression
The multivariable logistic regression analysis indicated significant associations between sociodemographic, prenatal, perinatal and neonatal risk factors. More specifically, male children have 4 times higher odds of having ASD compared to female children (OR = 4.21, CI 2.33–7.63). Among prenatal factors, the maternal weight gain, use of MgB6, the self-reported stress during the pregnancy, as well as pregnancy with complications were associated with a significant increase in the odds of ASD, whereas use of Duphaston was associated with decreased odds of ASD (see Table 5 ). Additionally, the longer interpregnancy interval was associated with decreased odds of ASD diagnosis (OR = 0.708, CI 0.52–0.97). Among peri- and neonatal factors, use of labor-inducing drugs was associated with increase in the odds of ASD diagnosis (OR = 2.295, CI 1.3–4.1), while birth height showed association with decrease in odds (OR = 0.788, CI 0.6–1.0).
Our study provides comprehensive insights into the multifaceted nature of ASD, elucidating the intricate relationships between sociodemographic, prenatal, perinatal, and neonatal factors and ASD risk.
Our findings highlight significant gender disparities in ASD prevalence, with a notably higher proportion (4:1) of male children in the ASD group. This aligns with existing literature demonstrating a male predominance in ASD diagnosis 37 . Meanwhile, Loomes et al. reported 3:1 male-to-female ratio referring to a diagnostic gender bias, where girls meeting the criteria for ASD are at an elevated risk of not receiving a clinical diagnosis 38 . Furthermore, our study highlights the potential impact of family structure on the likelihood of ASD occurrence, indicating higher ASD rates among first-born children and in households where the parents are non-married (divorced, widowed, separated, etc.). A study conducted by Ugur et al. yielded comparable findings, suggesting that the prevalence of being the eldest child was higher in the ASD group compared to the control group 39 . Contrary to this, research conducted in the United States found no evidence to suggest that children diagnosed with ASD are more likely to live in households not composed of both their biological or adoptive parents compared to children without ASD 40 .
The association between prenatal risk factors and ASD risk underscores the importance of maternal health during pregnancy. Our findings suggest that factors such as lower IPIs, maternal complications and diseases during pregnancy, medication use, vitamin D levels, maternal weight gain and maternal self-reported stress during pregnancy may increase the odds of ASD in offspring. It is crucial to note that the higher number of firstborn children among cases compared to the control group could introduce bias when accurately estimating the association between IPI and ASD. Therefore, the coefficients of IPI should be interpreted cautiously. Despite this, we opted not to remove this variable from the model, as IPI is recognized as an important factor in existing literature. Several studies report different results regarding long and short IPIs and ASD risk 14 , 15 , 41 , 42 . The underlying reasons for the link between ASD and short and long IPIs may differ. Short IPIs could be associated with maternal nutrient depletion, stress, infertility, and inflammation, whereas long IPIs may be linked to infertility and related complications. According to our results the frequency of self-reported complications during pregnancy was notably higher among children with ASD compared to the controls. Additionally, there was a somewhat higher prevalence of reported infectious diseases, other illnesses, and anemia during pregnancy among the cases compared to the control group. Several previous investigations have associated maternal hospitalization resulting from infection during pregnancy with an elevated risk of ASD. This includes a substantial study involving over two million individuals, which indicated an increased risk associated with viral and bacterial infections during the prenatal period 12 , 17 . Furthermore, our study results indicate that medication usage during pregnancy was more common among the mothers of cases than the controls. Notably, various medications, including vitamins, anticoagulants, Paracetamol, MgB6, Duphaston, iron preparation, No-spa, calcium preparation, antibiotics, and Utrogestan (micronized progesterone), exhibited significant differences in usage between the cases and controls. According to the results of multiple logistic regression analysis use of MgB6 was associated with a significant increase in the odds of ASD, whereas use of Duphaston (Dydrogesterone), a progestin medication, was associated with decreased odds of ASD. Emphasizing the potential impact of additional variables in evaluating the link between Duphaston and ASD is essential. There is a possibility of factors overlooked in our study. However, after analyzing the included variables, no significant confounding effects were detected. This assessment involved scrutinizing the Cramer’s V value between Duphaston and other variables, and sequentially introducing new variables into the model to evaluate changes in the coefficients of Duphaston. In both cases, no significant confounding effects emerged. In contrast to our results certain researchers have shown that the use of supplements during pregnancy is linked to a decreased risk of ASD in offsprings compared to those whose mothers did not take supplements during pregnancy 43 , 44 . The results of an epidemiology study conducted by Li et al. have showed that prenatal progestin exposure was strongly associated with ASD prevalence, and the experiments in rats showed that prenatal consumption of progestin-contaminated seafood induced autism-like behavior 45 . On the other hand other authors suggest that insufficient maternal progesterone levels might contribute to both obstetrical complications and ASD development 46 . The observed association regarding MgB6 use could potentially be influenced by an unmeasured confounding variable in our study. This warrants further investigation and consideration in future research. Additionally, our study highlighted another modifiable risk factor for ASD that was significantly associated with higher odds of ASD: maternal gestational weight gain. This factor retained its significance even in the multivariable analysis. This finding is consistent with the results of several studies which have shown that maternal metabolic conditions like diabetes, gestational weight gain, and hypertension have been associated with mechanisms pertinent to ASD, such as oxidative stress, fetal hypoxia, and chronic inflammation 23 , 47 . These conditions can induce prolonged or acute hypoxia in the fetus, which might pose a substantial risk factor for neurodevelopmental disturbances.
Furthermore, our findings suggest that the self-reported stress during pregnancy was associated with a significant increase in the odds of ASD. When comparing self-reported stress levels during different pregnancy periods, a notable disparity emerged. The statistically significant differences in stress levels between the two groups were reported in all trimesters of pregnancy suggesting a potential correlation between maternal stress during pregnancy and the odds of autism spectrum disorder in offspring. Several authors report comparable findings suggesting that prenatal maternal stress show significant association with both autistic traits and Attention Deficit Hyperactivity Disorder (ADHD) behaviors 48 , 49 , 50 , 51 . Various mechanisms could be suggested to explain the link between prenatal stress and likelihood of ASD. For instance, stress during pregnancy can trigger physiological changes in the mother's body, such as increased cortisol levels and alterations in immune function, which may impact fetal development and contribute to the risk of ASD. Also, stress may affect placental function, leading to adverse changes in the transfer of nutrients and oxygen to the fetus. Furthermore, prenatal stress can influence gene expression in both the mother and the developing fetus. Certain genes involved in brain development and the stress response system may be affected, potentially increasing the risk of ASD. Additionally, maternal stress may influence parenting behaviors and interactions with the child after birth. High levels of maternal stress may affect the quality of caregiving, which in turn can impact the child's social and emotional development, potentially contributing to ASD risk. Lastly, stress during pregnancy could induce epigenetic modifications, which are alterations in gene expression that occur without changes in DNA sequence. These modifications might affect neurodevelopmental processes, making individuals more susceptible to ASD.
Our study reports notable statistical difference among cases and controls regarding gestational age. According to the results 16.67% of cases were born either preterm (before 37 weeks) or post-term (after 42 weeks), highlighting another significant distinction. Early gestational age is linked with unfavorable health consequences, such as developmental delays and subsequent intellectual impairments throughout childhood and adolescence. Similar results are reported by several authors as well 30 , 31 , 52 . According to our study results birth height was associated with decrease in odds of ASD, however there was no statistically significant difference in birth weight between cases and controls. Some authors demonstrated that infants with birth weights of < 2.5 kg were associated with ADHD and ASD 53 , 54 .
Other than the previously mentioned factors the results of our study have demonstrated that use of labor-inducing drugs was associated with increase in the odds of ASD. The study participants did not report or specify the type of used labor-inducing drugs. Recent investigations have indicated a potential correlation between the utilization of drugs during labor and delivery and the emergence of ASD 55 , 56 , especially given the increased usage of epidurals and labor-inducing medications in the past 30 years. However, conflicting findings exist, with some studies suggesting no link between the administration of labor-inducing drugs and the risk of ASD development 57 , 58 . Recent findings from Qiu et al. propose a potential link between maternal labor epidural analgesia and the risk of ASD in children, particularly when oxytocin was concurrently administered. However, oxytocin exposure in the absence of labor epidural analgesia did not show an association with ASD risk in children 59 . The potential link between the use of labor-inducing drugs and the risk of ASD is complex and not yet fully understood. However, several mechanisms have been proposed to explain this association: for example, labor-inducing drugs, such as oxytocin and prostaglandins, can affect hormonal levels in both the mother and the fetus. These hormonal changes may impact brain development and neural connectivity, potentially increasing the risk of ASD. In addition, labor induction may increase the risk of oxygen deprivation (hypoxia) during labor. Prolonged hypoxia during birth has been linked to adverse neurological outcomes, including an increased risk of neurodevelopmental disorders like ASD. Furthermore, labor induction can lead to an inflammatory response in both the mother and the fetus. This immune system activation may affect neurodevelopmental processes and contribute to the development of ASD. Overall, the relationship between labor-inducing drugs and ASD risk is multifactorial and likely involves interactions between genetic, environmental, and biological factors. Further research is needed to elucidate the specific mechanisms underlying this association.
To our knowledge this is the first study identifying potential pre-, peri- and neonatal risk factors associated with ASD in Armenia.
Limitations and strength
While our study possesses a retrospective design, a notable limitation, it depended on parental recall for details dating back several years. Additionally, the sample was not balanced in terms of gender, with more male children included, potentially introducing selection bias. Despite the relatively small sample size multivariable analysis using the presence or absence of ASD as the dependent variable was implemented to address potential confounding factors.
Nevertheless, our study included a representative sample of the Armenian ASD population, evaluating various factors in comparison with a randomly selected control group matched for age. All ASD diagnoses were made according to DSM-5 by professionals (psychiatrists, pediatricians, neurologists, speech therapists and developmental psychologists), and face-to-face interviews with parents at the time of the interview minimized the risk of information bias.
Our findings indicated that male gender, maternal weight gain, MgB6 usage, self-reported stress during pregnancy, pregnancy complications, and labor-inducing drugs were linked to a significant rise in ASD odds (Fig. 1 ). Conversely, the use of Duphaston during pregnancy, longer interpregnancy intervals, and higher birth height were associated with reduced odds of ASD (Fig. 1 ). These observations underpin the significance of regional investigations to uncover the unique environmental factors contributing to ASD. The implications are profound, as several identified factors may be preventable or adjustable, highlighting the urgency of implementing evidence-based practices and public health interventions. Emphasizing a culture of health promotion, screenings, timely diagnosis, and disease prevention strategies, particularly among pregnant women, holds promise for reducing ASD and related disorders. Moreover, further prospective and focused research is imperative to discern the interplay between various factors and gene-environment interactions that may serve as potential ASD risk factors. Enhanced understanding in this area could lead to earlier detection and improved ASD management. Future studies incorporating analyses of biological samples for genetic, epigenetic, and inflammatory markers will be pivotal in elucidating underlying mechanisms and ushering in a new phase of research focusing on modifiable risk factors for developmental disorders.
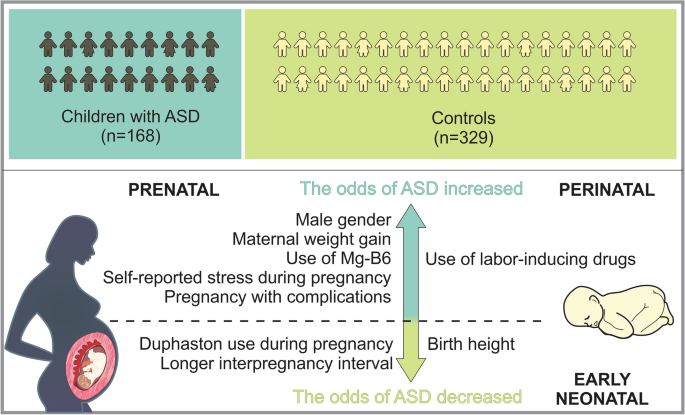
Sum up scheme showing prenatal, perinatal and neonatal factors which increase, as well as decrease the odds of ASD.
The study population comprised of 497 participants, of which 168 were children with ASD and 329 were typical development controls. The subject recruitment was done during 2021 to 2022. The controls and children with ASD were age matched (3–18 years). The subjects were formally diagnosed with ASD according to DSM-5 by professionals (pediatricians, neurologists, speech therapists and developmental psychologists). The children with ASD were recruited at MY WAY Educational and Rehabilitation Center in Yerevan. Inclusion criteria for cases were age between 3 and 18 years with ASD with diagnosis confirmed using DSM-V. Exclusion criteria for cases were other neurodevelopment disorders other than ASD. The control participants were randomly selected in the same period at Muratsan Hospital Complex. They were not known to have any neurodevelopmental or behavioral disruptions that might be related to ASD. The control group consisted exclusively of individuals diagnosed with simple conditions like flu or a simple routine physical examination.
Questionnaire and data collection
The self-reported questionnaire was completed via a face-to-face interview with the child’s parent. The questionnaire comprised three sections: various aspects of sociodemographic characteristics, prenatal risk factors, and perinatal/neonatal risk factors. Each section addressed specific questions related to these factors for comprehensive data collection. On average, the questionnaire was completed in about 15 to 20 min. The parent had the choice of accepting or refusing to complete the questionnaire. At the end of the process, the completed questionnaires were collected and sent for data entry by using SPSS 21 statistical software. The questionnaire was designed to acquire the information regarding risk factors of ASD. It consisted of different sections: sociodemographic characteristics (e.g., age, sex, family history of ASD, etc.), data on prenatal risk factors (e.g., pregnancy process, complications during pregnancy, infections during pregnancy, other diseases, stress, medication and supplement use during pregnancy, vitamin D level, etc.), questions related to maternal lifestyle risk factors (e.g., smoking, alcohol consumption, gestational weight gain). Respondents were also asked about peri- and neonatal risk factors, including gestational age, gestational size, the use of labor and delivery drugs, mode of delivery, etc.
Ethics disclosure
The study protocol was approved by the Ethics Committee (N 8–2/20; 27.11.2020) of Yerevan State Medical University in line with the principles set forth in the Declaration of Helsinki. Written informed consent was obtained from all the parents of the participants prior to data collection.
Statistical analysis
The data was processed and modelled in Python (version 3.11.6), an open- source software often used for data processing and modelling. The statistical analysis was performed by using the Statsmodels package (version 0.14.1) 60 .
Descriptive statistics were employed to summarize the characteristics of the study variables. Continuous variables were described using means and standard deviations, while categorical variables were presented as proportions. Prior to statistical analysis, numeric variables underwent standardization through the computation of z scores. To evaluate potential multicollinearity among predictor variables, the Variable Inflation Index (VIF) was computed. A predetermined threshold of 5 was established, and variables exceeding this threshold were considered indicative of multicollinearity. Bivariate analyses were conducted to explore associations between predictor variables and the outcome variable (presence or absence of autism diagnosis). T-tests were employed for continuous variables, while chi-squared tests were utilized for nominal and categorical variables. A multivariable logistic regression model was constructed to estimate the relationship between predictor variables and the outcome variable (autism diagnosis). Initially, a comprehensive strategy was employed by first fitting a null model and then iteratively introducing blocks of variables (e.g., socio demographic factors prenatal, peri- and neonatal factors). After introducing the new block of factors, a likelihood ratio test was conducted to evaluate the contribution of the added variables. If the p -value associated with the likelihood ratio test was insignificant ( p > 0.05), the preference was given to a less complex model. In our analysis all added blocks had significant contribution to the overall fit of the model.
Subsequently, the significance of each variable was systematically assessed by applying a stepwise elimination technique whereby insignificant variables were progressively removed from the model. Similar to the above-mentioned process, at each step, a likelihood ratio test to evaluate the significance of the excluded variable was conducted. If the p -value associated with this test was found to be insignificant ( p > 0.05), the adoption of a simpler model was favored. This iterative process allowed us to identify the most parsimonious model that retained statistically significant predictors while minimizing unnecessary complexity. Odds ratios (ORs) were computed, accompanied by 95% confidence intervals (CIs), to quantify the strength and direction of these associations.
Data availability
Data can be made available by the corresponding author upon reasonable request.
Diagnostic and Statistical Manual of Mental Disorders: DSM-5 TM , 5th Ed . xliv, 947 (American Psychiatric Publishing, Inc., Arlington, VA, US, 2013). https://doi.org/10.1176/appi.books.9780890425596 .
Zeidan, J. et al. Global prevalence of autism: A systematic review update. Autism Res. 15 , 778–790 (2022).
Article PubMed PubMed Central Google Scholar
CDC. Autism and Developmental Disabilities Monitoring (ADDM) Network. Centers for Disease Control and Prevention https://www.cdc.gov/ncbddd/autism/addm.html (2023).
CDC. Data and Statistics on Autism Spectrum Disorder | CDC. Centers for Disease Control and Prevention https://www.cdc.gov/ncbddd/autism/data.html (2024).
Tick, B., Bolton, P., Happé, F., Rutter, M. & Rijsdijk, F. Heritability of autism spectrum disorders: A meta-analysis of twin studies. J. Child Psychol. Psychiatry 57 , 585–595 (2016).
Article PubMed Google Scholar
Lord, C., Elsabbagh, M., Baird, G. & Veenstra-Vanderweele, J. Autism spectrum disorder. Lancet 392 , 508–520 (2018).
Muhle, R. A., Reed, H. E., Stratigos, K. A. & Veenstra-VanderWeele, J. The emerging clinical neuroscience of autism spectrum disorder: A review. JAMA Psychiatry 75 , 514–523 (2018).
Bai, D. et al. Association of genetic and environmental factors with autism in a 5-country cohort. JAMA Psychiatry 76 , 1035–1043 (2019).
Jutla, A., Reed, H. & Veenstra-VanderWeele, J. The architecture of autism spectrum disorder risk: What do we know, and where do we go from here?. JAMA Psychiatry 76 , 1005–1006 (2019).
Gardener, H., Spiegelman, D. & Buka, S. L. Perinatal and neonatal risk factors for autism: A comprehensive meta-analysis. Pediatrics 128 , 344–355 (2011).
Guinchat, V. et al. Pre-, peri- and neonatal risk factors for autism. Acta Obstet. Gynecol. Scand. 91 , 287–300 (2012).
Yenkoyan, K., Mkhitaryan, M. & Bjørklund, G. Environmental risk factors in autism spectrum disorder: A narrative review. Curr. Med. Chem. https://doi.org/10.2174/0109298673252471231121045529 (2024).
Lyall, K. et al. The association between parental age and autism-related outcomes in children at high familial risk for autism. Autism. Res. 13 , 998–1010 (2020).
Cheslack-Postava, K. et al. Increased risk of autism spectrum disorders at short and long interpregnancy intervals in Finland. J. Am. Acad. Child Adolesc. Psychiatry 53 , 1074-1081.e4 (2014).
Zerbo, O., Yoshida, C., Gunderson, E. P., Dorward, K. & Croen, L. A. Interpregnancy interval and risk of autism spectrum disorders. Pediatrics 136 , 651–657 (2015).
Lee, B. K. et al. Maternal hospitalization with infection during pregnancy and risk of autism spectrum disorders. Brain Behav. Immun. 44 , 100–105 (2015).
Zerbo, O. et al. Maternal infection during pregnancy and autism spectrum disorders. J. Autism Dev. Disord. 45 , 4015–4025 (2015).
Christensen, J. et al. Prenatal valproate exposure and risk of autism spectrum disorders and childhood autism. JAMA 309 , 1696–1703 (2013).
Article CAS PubMed PubMed Central Google Scholar
Bromley, R. L. et al. The prevalence of neurodevelopmental disorders in children prenatally exposed to antiepileptic drugs. J. Neurol. Neurosurg. Psychiatry 84 , 637–643 (2013).
Gidaya, N. B. et al. In utero exposure to β-2-adrenergic receptor agonist drugs and risk for autism spectrum disorders. Pediatrics 137 , e20151316 (2016).
Walker, C. K. et al. Preeclampsia, placental insufficiency, and autism spectrum disorder or developmental delay. JAMA Pediatr 169 , 154–162 (2015).
Krakowiak, P. et al. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics 129 , e1121-1128 (2012).
Li, M. et al. The association of maternal obesity and diabetes with autism and other developmental disabilities. Pediatrics 137 , e20152206 (2016).
Black, M. M. Effects of vitamin B12 and folate deficiency on brain development in children. Food Nutr. Bull. 29 , S126-131 (2008).
Surén, P. et al. Association between maternal use of folic acid supplements and risk of autism spectrum disorders in children. JAMA 309 , 570–577 (2013).
Skalny, A. V. et al. Magnesium status in children with attention-deficit/hyperactivity disorder and/or autism spectrum disorder. Soa Chongsonyon Chongsin Uihak 31 , 41–45 (2020).
PubMed PubMed Central Google Scholar
Virk, J. et al. Preconceptional and prenatal supplementary folic acid and multivitamin intake and autism spectrum disorders. Autism 20 , 710–718 (2016).
Whitehouse, A. J. O. et al. Maternal vitamin D levels and the autism phenotype among offspring. J. Autism Dev. Disord. 43 , 1495–1504 (2013).
Zhong, C., Tessing, J., Lee, B. & Lyall, K. Maternal dietary factors and the risk of autism spectrum disorders: A systematic review of existing evidence. Autism Res. 13 , 1634–1658 (2020).
Moore, G. S., Kneitel, A. W., Walker, C. K., Gilbert, W. M. & Xing, G. Autism risk in small- and large-for-gestational-age infants. Am. J. Obstet. Gynecol. 206 (314), e1-9 (2012).
Google Scholar
Leavey, A., Zwaigenbaum, L., Heavner, K. & Burstyn, I. Gestational age at birth and risk of autism spectrum disorders in Alberta, Canada. J. Pediatr. 162 , 361–368 (2013).
Smallwood, M. et al. Increased risk of autism development in children whose mothers experienced birth complications or received labor and delivery drugs. ASN Neuro. 8 , 1759091416659742 (2016).
Qiu, C. et al. Association between epidural analgesia during labor and risk of autism spectrum disorders in offspring. JAMA Pediatr. 174 , 1168–1175 (2020).
Curran, E. A. et al. Association between obstetric mode of delivery and autism spectrum disorder: A population-based sibling design study. JAMA Psychiatry 72 , 935–942 (2015).
Curran, E. A. et al. Research review: Birth by caesarean section and development of autism spectrum disorder and attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. J. Child Psychol. Psychiatry 56 , 500–508 (2015).
Nagano, M. et al. Cesarean section delivery is a risk factor of autism-related behaviors in mice. Sci. Rep. 11 , 8883 (2021).
Article ADS CAS PubMed PubMed Central Google Scholar
Werling, D. M. & Geschwind, D. H. Sex differences in autism spectrum disorders. Curr. Opin. Neurol. 26 , 146–153 (2013).
Loomes, R., Hull, L. & Mandy, W. P. L. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry 56 , 466–474 (2017).
Ugur, C., Tonyali, A., Goker, Z. & Uneri, O. S. Birth order and reproductive stoppage in families of children with autism spectrum disorder. Psychiatry Clin. Psychopharmacol. 29 , 509–514 (2019).
Article Google Scholar
Freedman, B. H., Kalb, L. G., Zablotsky, B. & Stuart, E. A. Relationship status among parents of children with autism spectrum disorders: A population-based study. J. Autism. Dev. Disord. 42 , 539–548 (2012).
Gunnes, N. et al. Interpregnancy interval and risk of autistic disorder. Epidemiology 24 , 906–912 (2013).
Durkin, M. S., Allerton, L. & Maenner, M. J. Inter-pregnancy intervals and the risk of autism spectrum disorder: Results of a population-based study. J. Autism. Dev. Disord. 45 , 2056–2066 (2015).
Levine, S. Z. et al. Association of maternal use of folic acid and multivitamin supplements in the periods before and during pregnancy with the risk of autism spectrum disorder in offspring. JAMA Psychiatry 75 , 176–184 (2018).
Article ADS PubMed PubMed Central Google Scholar
Schmidt, R. J., Iosif, A.-M., Guerrero Angel, E. & Ozonoff, S. Association of maternal prenatal vitamin use with risk for autism spectrum disorder recurrence in young siblings. JAMA Psychiatry 76 , 391–398 (2019).
Li, L. et al. Prenatal progestin exposure is associated with autism spectrum disorders. Front Psychiatry 9 , 611 (2018).
Whitaker-Azmitia, P. M., Lobel, M. & Moyer, A. Low maternal progesterone may contribute to both obstetrical complications and autism. Med Hypotheses 82 , 313–318 (2014).
Article CAS PubMed Google Scholar
Vecchione, R. et al. Maternal dietary patterns during pregnancy and child autism-related traits: Results from two US cohorts. Nutrients 14 , 2729 (2022).
Ronald, A., Pennell, C. & Whitehouse, A. Prenatal maternal stress associated with ADHD and autistic traits in early childhood. Front. Psychol. https://doi.org/10.3389/fpsyg.2010.00223 (2011).
Caparros-Gonzalez, R. A. et al. Stress during pregnancy and the development of diseases in the offspring: A systematic-review and meta-analysis. Midwifery 97 , 102939 (2021).
Manzari, N., Matvienko-Sikar, K., Baldoni, F., O’Keeffe, G. W. & Khashan, A. S. Prenatal maternal stress and risk of neurodevelopmental disorders in the offspring: A systematic review and meta-analysis. Soc. Psychiatry Psychiatr. Epidemiol. 54 , 1299–1309 (2019).
Say, G. N., Karabekiroğlu, K., Babadağı, Z. & Yüce, M. Maternal stress and perinatal features in autism and attention deficit/hyperactivity disorder. Pediatr. Int. 58 , 265–269 (2016).
Abel, K. M. et al. Deviance in fetal growth and risk of autism spectrum disorder. Am. J. Psychiatry 170 , 391–398 (2013).
Song, I. G. et al. Association between birth weight and neurodevelopmental disorders assessed using the Korean National Health Insurance Service claims data. Sci. Rep. 12 , 2080 (2022).
Lampi, K. M. et al. Risk of autism spectrum disorders in low birth weight and small for gestational age infants. J. Pediatr. 161 , 830–836 (2012).
Bashirian, S., Seyedi, M., Razjouyan, K. & Jenabi, E. The association between labor induction and autism spectrum disorders among children: A meta-analysis. Curr. Pediatr. Rev. 17 , 238–243 (2021).
Oberg, A. S. et al. Association of labor induction with offspring risk of autism spectrum disorders. JAMA Pediatr. 170 , e160965 (2016).
Karim, J. L. et al. Exogenous oxytocin administration during labor and autism spectrum disorder. Am. J. Obstet. Gynecol. MFM 5 , 101010 (2023).
Qiu, C. et al. Association of labor epidural analgesia, oxytocin exposure, and risk of autism spectrum disorders in children. JAMA Netw. Open 6 , e2324630 (2023).
Seabold, S. & Perktold, J. Statsmodels: Econometric and Statistical Modeling with Python. Proceedings of the 9th Python in Science Conference 92–96 (2010) https://doi.org/10.25080/Majora-92bf1922-011 .
Download references
Acknowledgements
We express our gratitude to all parents participated in the study.
This work was supported by Higher Education and Science Committee, Ministry of Education, Science, Culture and Sports of RA (24YSMU-CON-I-3AN and 23LCG-3A020), and YSMU.
Author information
Authors and affiliations.
Neuroscience Laboratory, Cobrain Center, Yerevan State Medical University Named After M. Heratsi, 0025, Yerevan, Armenia
Meri Mkhitaryan & Konstantin Yenkoyan
Cobrain Center, Yerevan State Medical University Named After M. Heratsi, 0025, Yerevan, Armenia
Tamara Avetisyan & Larisa Avetisyan
Muratsan University Hospital Complex, Yerevan State Medical University Named After M. Heratsi, 0075, Yerevan, Armenia
Tamara Avetisyan
Department of Infectious Diseases, Yerevan State Medical University Named After M. Heratsi, 0025, Yerevan, Armenia
Anna Mkhoyan
Department of Hygiene, Yerevan State Medical University Named After M. Heratsi, 0025, Yerevan, Armenia
Larisa Avetisyan
You can also search for this author in PubMed Google Scholar
Contributions
M.M. and K.Y. conceived the project; M.M., T.A., A.M., L.A. and K.Y. designed experiments, collected and analyzed data; M.M., T.A., A.M., L.A., and K.Y. wrote the draft; M.M., A.M., and K.Y. edited the manuscript. K.Y. obtained funding and supervised the study. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Konstantin Yenkoyan .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Mkhitaryan, M., Avetisyan, T., Mkhoyan, A. et al. A case–control study on pre-, peri-, and neonatal risk factors associated with autism spectrum disorder among Armenian children. Sci Rep 14 , 12308 (2024). https://doi.org/10.1038/s41598-024-63240-3
Download citation
Received : 02 March 2024
Accepted : 27 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1038/s41598-024-63240-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Autism spectrum disorder
- Case–control study
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
COVID-19 Pandemic Experiences of Families in Which a Child/Youth Has Autism and Their Service Providers: Perspectives and Lessons Learned
- Original Article
- Open access
- Published: 20 May 2024
Cite this article
You have full access to this open access article

- David B. Nicholas ORCID: orcid.org/0000-0003-4480-322X 1 ,
- Rosslynn T. Zulla ORCID: orcid.org/0000-0001-9881-830X 1 ,
- Jill Cielsielski 1 ,
- Lonnie Zwaigenbaum ORCID: orcid.org/0000-0001-9607-0799 2 &
- Olivia Conlon 1
191 Accesses
1 Altmetric
Explore all metrics
The impacts of the COVID-19 pandemic on autistic children/youth and their families and on service providers are not yet well-understood. This study explored the lived experiences of families with an autistic child and service providers who support them regarding the impacts of the pandemic on service delivery and well-being.
In this qualitative study, families and service providers (e.g., early intervention staff, service providers, school personnel) supporting autistic children/youth were interviewed. Participants were recruited from a diagnostic site and two service organizations that support autistic children/youth.
Thirteen parents and 18 service providers participated in either an individual or group interview. Findings indicate challenges associated with pandemic restrictions and resulting service shifts. These challenges generally imposed negative experiences on the daily lives of autistic children/youth and their families, as well as on service providers. While many were adversely affected by service delivery changes, families and service agencies/providers pivoted and managed challenges. Shifts have had varied impacts, with implications to consider in pandemic planning and post-pandemic recovery.
Results highlight the need for autism-focused supports, as well as technology and pandemic preparedness capacity building within health, therapeutic and educational sectors in order to better manage shifts in daily routines during emergencies such as a pandemic. Findings also offer instructive consideration in service delivery post-pandemic.
Similar content being viewed by others

COVID-19 Pandemic and Impact on Patients with Autism Spectrum Disorder
Brief report: impact of the covid-19 pandemic on asian american families with children with developmental disabilities.

The COVID-19 Pandemic Experience for Families of Young Children with Autism
Avoid common mistakes on your manuscript.
The COVID-19 pandemic was associated with service disruptions that substantially affected autistic individuals and their families, resulting in shifts in daily life. As efforts were made to limit COVID-19 risk, individual and family routines and resources shifted. Public health measures have now largely been lifted, yet some pandemic shifts and impacts remain. This study elicited the experiences of families of autistic children and youth as they navigated the pandemic, from the perspective of both families and service providers.
Children and youth with autism were deeply affected by the COVID-19 pandemic (Colizzi et al., 2020 ; Shorey et al., 2021 ). In terms of daily life, daily routines were interrupted, with early outcomes such as behavioural difficulties and social and communication challenges (Mutluer et al., 2020 ). School closures limited many supports that autistic children/youth typically access (Colizzi et al., 2020 ). In one study, over 70% of families of children with special needs experienced decreased educational/therapeutic services (e.g., reduced number of sessions, changes to therapy modality) during the pandemic (Jeste et al., 2020 ). Virtual delivery of educational and therapeutic services was attempted to sustain services while reducing in-person contact (Assenza et al., 2021 ; Shorey et al., 2021 ), with mixed responses to these shifts. Family caregivers expressed concern about the loss of direct involvement of professionals in service delivery, and worried about their child’s skill regression (Latzer et al., 2021 ; Stankovic et al., 2022 ).
The implementation of social distancing and infection control protocols in daily life was noted to create substantial confusion for some children/youth. Many autistic children did not fully comprehend the pandemic, as well as related requirements for physical isolation and hygiene/safety precautions. These children/youth variably struggled with adhering to safety protocols (e.g., wearing masks) due to autism-related challenges such as sensory sensitivities (Mutluer et al., 2020 ). It was perceived that autistic children/youth who understood the pandemic and its implications had better outcomes (Asbury et al., 2021 ).
Pandemic Impacts on Families
Changes in therapeutic services and education required many parents to independently support their child’s schooling and support needs (Shorey et al., 2021 ). The struggle to organize activities amidst a lack of supports (Assenza et al., 2021 ; Colizzi et al., 2020 ) reportedly resulted in feelings of inadequacy and anxiety among parents (Assenza et al., 2021 ; Colizzi et al., 2020 ; Mutluer et al., 2020 ). Among families in which the child experienced challenges such as complex behavioral issues, parents reported higher levels of stress related to caregiving, thus seeking respite services (Manning et al., 2020 ). In comparison to parents of typically developing peers, parents of autistic children reported lower resiliency and poorer coping as well as greater anxiety and depression (Wang et al., 2021 ).
Impacts on Service Providers
Similar to what was reported by families, substantial pandemic impacts also were described by service providers. Teachers working with special needs populations indicated that online school platforms impeded their ability to provide multi-sensory curricula (Kim et al., 2021 ), teach using multiple prompts (e.g., verbal, visual, tactile) (Kim et al., 2021 ), and support students to self-regulate as they learn (Lambert & Schuck, 2021 ). Teachers also reported that the delivery of lessons in online school platforms was difficult for children with focus/attention and self-regulation challenges (Lambert & Schuck, 2021 ). Autism service providers reported concerns related to certain interventions not being as effective over technology platforms, and online platforms not being effective or appropriate with some children, such as those who were minimally verbal (Fell et al., 2023 ). A lack of technology including devices and internet, and low technology literacy impeded online teaching and assessments (Kellom et al., 2023 ; Steed & Leech, 2021 ). Additional challenges included a lack of collaboration with parents in online education (Steed & Leech, 2021 ), and concerns over the accessibility of online platforms related to English proficiency (Kellom et al., 2023 ).
The service landscape was drastically modified or decreased (Colizzi et al., 2020 ), resulting in long-standing impacts that are not yet fully realized. There further has been relatively little examination of how the pandemic was experienced by autism service providers and its impact on their practice. This is a critical gap given that service providers are often relied upon by parents to support and devise strategies to help autistic children. There is need to better understand family and service provider experiences and perspectives relative to gaps and opportunities that have unfolded as a result of the COVID-19 pandemic. To address this gap, this study explored the lived experiences of families with an autistic child and service providers who support them. Research questions were: (1) How was the COVID-19 pandemic experienced by families in which a child/youth has autism, and their service providers?, (2) What were the barriers to, and facilitators of, service delivery in the pandemic?, and (3) What recommendations are offered to improve service delivery?
Parents of autistic children (to 18 years) and their service providers were recruited from a regional diagnostic/specialty care center and two service delivery centers offering educational, therapeutic and developmental supports within a large city in western Canada. These organizations delivered direct support to autistic children/youth and their families during the pandemic.
Data collection occurred from August 2020 to May 2021. During this period, the jurisdiction underwent several transitions, moving back and forth from restrictions to re-openings in public spaces. Recruitment was undertaken with the support of intermediaries in the above organizations who informed both families and service providers via word-of-mouth and email. Potential participants were provided with information about the study, and if study participation was desired, they were invited to engage in an interview.
Semi-structured interview guides for families and service providers were developed by team members who bring experience in qualitative autism-focused research as well as in service provision, and the team included a parent with first-person family experience of autism. For parents, questions focused on the perceived impacts of the COVID-19 pandemic relative to service access and experience, daily life and well-being. Questions to service providers elicited perceived impacts of the pandemic on service delivery and child, family and service provider well-being. Examples of questions are outlined in Table 1 .
Conducted via Zoom technology or telephone, interviews lasted 0.5 to 1 h. All interviews were audio recorded and transcribed verbatim for subsequent analysis. Families and community service providers who support autistic children/youth and their families were involved in study design, as well as reflecting on findings and manuscript development (e.g., reviewing and providing feedback on the manuscript).
A qualitative content analysis approach guided data management and analysis (Elo & Kyngas, 2008 ; Graneheim & Lundman, 2004 ). This approach grounded codes in participants’ perspectives, and delineated experiences, impacts and recommendations. Transcripts were analyzed using a three-step process: (1) reviewing the transcripts to gain an understanding of the data, (2) conducting an inductive analysis, and (3) mapping the data to generate themes (Elo & Kyngas, 2008 ; Graneheim & Lundman, 2004 ). The inductive analysis approach comprised three steps: coding data to develop units of meaning (line-by-line coding) , grouping these units into a logical schema (creating categories) , and interpreting and organizing these units (determining themes) . Analysis was undertaken by one team member (JC), with other team members (RTZ, DBN) reviewing a portion of the coding, thus supporting the categorization of codes and generation of themes (Elo & Kyngas, 2008 ; Graneheim & Lundman, 2004 ). Reviews of codes, categories and emergent themes occurred on a regular basis amongst team members. NVivo 12 data management and analysis software was used to support the data analysis.
Trustworthiness (qualitative research rigor) was demonstrated via peer debriefing, member checking, referential adequacy and team memoing to document and justify analytic decision making (Lincoln & Guba, 2005 ). These measures demonstrate thematic resonance with the data and suggest rigor in the analytic process. Institutional research ethics board review and approval were obtained from host university sites prior to study commencement (University of Calgary Conjoint Faculties Research Ethics Board #REB20-0367). Psychosocial support was available and offered to participants if needed, but was not requested. All identifying information was removed from transcripts prior to data analysis.
In total, 33 individuals participated in this study, comprising 13 parents (12 mothers and 1 father) and 18 service providers. The autistic children of participating parents ranged in age from 8 to 18 years of age, and included 12 males and 1 female. Demographic information about represented families are outlined in Table 2 . Service providers comprised healthcare and community service professionals from multiple disciplines (e.g., physicians, psychologists, speech language pathologists, behavior analysts, occupational therapists, social workers, nurses), school-based providers (e.g., educational consultants, teachers) and program administrators/leaders (e.g., program coordinators, program/agency directors). All healthcare/service providers worked in autism-related services and practiced during the pandemic.
Overall, participants stated that autistic children and their families experienced significant challenges and adjustments on a daily basis during the COVID-19 pandemic. Parents navigated various services in seeking to help their child—some with perceived benefits and others not. Service providers described seeking to accommodate children’s needs while adhering to shifting safety management protocols. Themes emerged in each group (families and service providers), as follows: (a) pivoting quickly and on an ongoing basis, (b) accommodating changes and addressing needs, (c) impacts on health and well-being, and (d) holding onto hope yet concern for the future. The themes include sub-themes, as outlined below.
(a) Pivoting Quickly and on an Ongoing Basis
The onset of the COVID-19 pandemic elicited rapid shifts in services, with deleterious impacts on families and service providers. Emerging sub-themes within this experience were ‘Service Shifts and Uncertainties’ and ‘Family Fears and Strains’; each sub-theme is outlined below.
Service Shifts and Uncertainties
Services that were deemed ‘non-essential’ (e.g., schools, accessible transportation services) were closed or substantially decreased or modified, resulting in limited resources and support for autistic children/youth and their families, notably with some services shifting to virtual modalities. Service providers needed to rapidly seek to understand and then navigate resources to address child/family needs. As one service provider recalled,
Non-essential services were closed and essential services were open, and we felt like we fit in a middle ground there. We really needed to figure out how to continue to provide services to our families. We knew the families were going to be really struggling with kids out of school and out of routine. But we weren’t necessarily designated as an essential service in an obvious way. So we had to establish a connection… so that we were able to continue to provide services, and that gave us that opportunity to do a critical support needs assessment so we could focus our attention on those [children/families] with the highest level of need.
Service providers felt that the lack of clarity about what constituted an ‘essential’ service in the pandemic, left families unclear about what they could access which further left them under-served. Service insufficiency and vagueness in guidelines heightened the demands of family caregiving, as observed by a service provider:
It was so unclear to families [whether] they were [or were not] allowed to have respite [care]. Of our families, at least 50% of them stopped having anyone come into their home so now they have twenty-four hours a day [caring for] their child with huge needs, and they’re in charge twenty-four hours which made them burn out.
Due to public health protocols, in-person supports were transitioned to an array of remote/electronic formats (e.g., telephone, text, email, online synchronous platform). For many service providers and families, this change required rapid learning about how to use various online platforms and navigate shifting services. A service provider recalled,
We shifted gears… overnight. We went from having no video conference capacity to here’s your Zoom login and ID, and then we all had to figure out how to do a Zoom meeting.
Service providers described trying to prioritize support needs such as addressing behavioral struggles and emotional strain due to the loss of school and diminished autism-related supports. They recalled seeking to implement service flexibility to better accommodate family needs and schedules. Yet, they also described uncertainty and worry as they adjusted quickly amidst unknown health risks associated with these shifts.
Making changes in service delivery was described to be especially difficult early in the pandemic. For service providers, modifying services to align with safety protocols was rendered more challenging due to a lack of knowledge about COVID-19, uncertainty about the effectiveness of safety protocols, and unknown impacts of these shifts and service gaps on autistic children and their families. A service provider recalled,
I never said, “It’s going to be okay” because I didn’t know. But I would say, “We’re going to figure this out.” And then I’d wait for direction, but the communication was not there…. No one knew what the heck was going on… so that fear of the unknown was very, very present with the team.
Shifting services became particularly difficult in cases in which children/youth required assistive and/or medical support. For instance, one service provider recalled significant challenges coordinating and sending communication devices to families in distant rural regions during service and school closures. Seeking to offer support in these circumstances, staff improvised and sought to remain in relatively close contact with families, as possible, as reflected on by a service provider:
When COVID-19 first started, we gathered information from the families and then prepared documents of a whole bunch of things to share with families. As a coordinator, I went to every single family’s home and whether I stood outside or at their kitchen table, whatever they were comfortable with and had conversations about COVID-19, about impact, [and] about what our services were to look like.
Family Fears and Strains
For families, the pandemic ushered in fears about COVID-19 transmissibility as well as decreased services to address anxiety and support well-being. An array of services (e.g., in-home support, recreation, social skills, healthcare, public transportation) were either shut down, modified, or delayed. For instance, alterations to public transportation meant that some families had to delay appointments. The sudden shutdown of schools and after-school resources was described as ‘ terrible ’, ‘ so stressful ’ and ‘ very confusing ’ by families. Parents sought to help their autistic child accommodate to sudden transitions in school and after-school activities, yet children/youth had significant difficulty, as illustrated by a parent who reflected on the difficulty with school transitions:
School was quite difficult. It was really difficult to get [autistic child] to do the school [work]…. He was supposed to have… two hours of work, but… it was taking him like four hours…. It was a big stress on our relationship too because… I was trying to get him to do the work and he didn’t want to.
Changes in daily routines such as requisites to stay home, were difficult for some children/youth to understand and accept. In response, parents trialed various strategies to help their child cope. For instance, some parents created a schedule for their child in an attempt to heighten predictability in the day and week.
(b) Accommodating Changes and Addressing Needs
As the pandemic continued over time, families experienced ongoing changes in service delivery and in daily routines. Sub-themes in this overall theme were, ‘Prioritizing Safety, but at a Cost’, ‘Reliance on Virtual Services’, and ‘Family Adjustment’, as described below.
Prioritizing Safety, but at a Cost
As the COVID-19 pandemic lingered, the need for adherence to safety and adjustment to ongoing changes remained a priority for agency leaders as they sought to support families relative to child development and well-being. Service providers described extensive measures such as the use of personal protective equipment and social distancing, while simultaneously monitoring and attending to child/youth and family needs. With a focus on safety, service providers felt hindered in their ability to effectively engage children/youth as they were accustomed to, and thus provide optimal support, as described by a service provider:
We can’t really do our jobs [when we’re] six feet from our kids [service recipients] because in order to actively engage them and get them interested in what we’re doing, I can’t be across the room right, because often times, they thrive upon like facial expression. We’re interacting with something and we are modelling what to do with it. Well, if I’m sitting on the other side of the room…, they’re not going to be engaged with me.
In terms of economic sufficiency and stability, both service providers and families variably faced vulnerability. Compensation for some service providers and parents were viewed as inadequate and difficult to access. Reflecting on required employment absence due to illness or quarantine, a service provider commented:
The funding to cover you when you are sick or you have to isolate which is a government mandate, only covers you one time a year…. In this global pandemic, they’re saying people are going to go on multiple bouts of isolation…, but we provide support [only] once. How are businesses supposed to keep up with that? They can’t. But how are people supposed to go on isolation multiple times without getting paid?
Negative pandemic impacts on financial stability both for families and services providers were deemed to be under-addressed. Further, inflationary pressures later in the pandemic resulted in lingering financial strain, with potentially heightened and continuing effects on families and service providers.
Reliance on Virtual Services
As the pandemic persisted, service providers modified supports through a combination of in-person and virtual formats (e.g., email, online, telephone, synchronous platforms). In choosing approaches, families’ needs and preferences, to a degree, guided services, as noted by a service provider:
The families became the driver… because they were in it twenty-four hours a day and they could see, ‘here’s what we need to work on’. It was less ‘cookie cutter’ service and more family-focused.
Virtual service delivery was seen to have benefited service providers through eliminating the need to travel to and from appointments, providing a venue for quick check-ins with families, and offering an efficient means for coworkers to meet and engage in peer support. For several families (but not for all), virtual support emerged as a vicarious silver lining of the pandemic in advancing an alternative platform for service delivery to children/youth and families. A service provider noted,
[Technology] opened up the way we communicate. Now our staff is asking our participants, “What is your preferred way of communicating? Should I text you? Should I FaceTime you? Are we emailing? Do you like phone calls?” So we’ve learned to actually expand the way we communicate with our participants, and it’s been extremely positive. Moving forward, we are trying to find ways to continue that because our participants are even wanting to communicate with each other which has never come up before, but now they are looking. It’s almost like they’ve found a new way that’s acceptable to communicate.
While identifying benefits of online communication, the adjustment to the use of virtual platforms was viewed both positively and negatively. Service providers contended that success in transitioning to and using online support platforms with families seemed to depend on both the age of the child and the quality of relationship between the child/youth and service provider. Service providers indicated that younger children tended to have more difficulty transitioning to online social support groups relative to older children/youth who, in many cases, were more comfortable engaging in online dialogue. Transitioning from in-person to virtual support was deemed to be easier for families with whom service providers had a pre-existing relationship and strong rapport, as opposed to families that accessed service provision after the introduction of restrictions to face-to-face contact.
Along with benefits, service providers noted challenges with using online support platforms. These included communication barriers, individual/family lack of access to or comfort with technology, overuse of technology by children/youth, lower levels of interest/participation among families, and online fatigue. Such challenges created uncertainty among service providers about the utility of virtual support for all families and circumstances. In such instances of suboptimal or negative impacts of technology for support provision, service providers doubted their capacity to do their job as well as they could have in person. As an example, a service provider described a sense of helplessness intervening via virtual engagement:
Sometimes you would be watching a kid literally slamming their head on a wall and you can’t do anything because you’re on this side of the computer. Sometimes it was just about sitting with the parents and saying, “I see everything, [and] you’re [doing] a very good job…. You’re being everything your child needs you to be right now. This is hard and I see you and I hear you”. It was really hard to not be that person that could be in the home with them. Our service model is to be in there, doing the ‘nitty gritty’ with the parents, and working through it together.
Another service provider lamented about the shift from face-to-face to virtual programming:
Every [identified evening each week] was this party that everybody went to. I have been doing this for fifteen years and I always look forward to [that] night, and I would just love going around the recreation center, and seeing all the social skills groups and the parents looking so happy. Here’s all this range of parents meeting in their very normal environment, and having coffee and tea and it’s all support. I think that was a big loss for me personally as a clinician.
Family Adjustment
Adjustment to the pandemic was experienced in varying ways by individuals and families. Most parents indicated that their child adjusted to required protocols such as masking, social distancing and washing hands, though some indicated the need for prompting and/or assistance. In a few cases, parents reported needing to continually provide guidance and/or reinforcement to ensure their child’s compliance with safety protocols. Several parents further stated that their child’s difficulty adhering to protocols resulted in decreased outings and in turn, greater social isolation:
We don’t take [the autistic child out of the home] anymore. He doesn’t do really well with masks. I don’t want to risk tak[ing] him out and then he will have a meltdown.
The prolonged duration of the pandemic was reported to require ingenuity and persistence by parents in seeking strategies to meet their child’s pressing, and in some cases, shifting needs. Some parents described organizing “safe” social gatherings (e.g., socially distanced activities), and strategically setting up occasions for social connection, as needed, to support child/youth wellness. One parent utilized increased time at home during the pandemic to teach her child household skills such as cooking, dishwashing, house cleaning and laundry.
To help manage and cope with additional family caregiver tasks and strains, parents variably relied on government resources (as available), and in some cases, used these resources to fund needed supports. While such resource availability differed among families, support sometimes was provided by relatives, neighbours, privately-funded services and/or other resources in the community. Learning to be independently resourceful and a sole (or predominantly sole) caregiver during the pandemic was consistently described as difficult, and was especially so for those who had previously relied heavily on formal supports (e.g., therapeutic services, respite care) to address the daily care needs of their child and, in particular, those whose child had complex care needs.
Periodic shifting from in-person to online school (and vice-versa) created substantial difficulty for some children/youth and families. Despite these challenges, additional support was described by several parents as largely unavailable. Parents described a range of responses including both appreciation and frustration/dissatisfaction with modified services and schooling. As an example, a parent conveyed appreciation; however, this reflected challenge with online schooling:
He (the child) would get up and once he saw her (the school attendant’s) face, she (the school attendant) would get him out of bed. [Otherwise] he wouldn’t get out of bed [so] I’d have the phone right there. She was amazing. Now I don’t know if that was something that the school had told her to do. I really believe it was something that she had done all herself. I really believe it was an individual thing, same with all of [her support with] the curriculum…. I’m pretty sure she modified everything herself, with no support or guidance from any professional from the school.
When online schooling transitioned to in-person delivery, some parents chose to continue online often to avoid heightened risk of their child acquiring COVID-19. In other cases, parents sent their child to school in-person; however, with concern about risk of exposure to COVID-19, as recalled by a parent:
People started testing positive in the schools and then the unknown. So then I had to take him out of it, and keep him home because he was getting anxious and frustrated.
(c) Impacts on Health and Well-being
Health and mental health impacts were experienced by both family members and service providers as a result of the extended existence of pandemic conditions and the rapid, multiple and ongoing changes in daily routines and service provision. The sub-theme, ‘mental distress of service providers’ highlights professional and personal tensions for service providers particularly as they navigated pandemic restrictions and the sub-theme, ‘psychosocial and behavioral impacts on families’ reflects challenges experienced by autistic children/youth and their families. A final sub-theme, ‘positive adaptation’ identifies areas of growth or positive experiences associated with the pandemic, as well as resources for moving forward. Each subtheme is described below.
Mental Distress of Service Providers
Service providers conveyed professional and personal tensions such as worry and feelings of disconnectedness from family, friends and co-workers while ‘putting on a brave face’ and supporting families. A service provider reflected on her ongoing adjustment and struggle with shifting public health guidelines:
The changing of the guidelines [was tough]. One week we think we have got it, we’ve got everything laid out, we have a plan. And then we come back on the Monday and the guidelines have shifted again…. The fatigue of new kinds of policies and procedures always crop up. Then you are trying to remember what the latest one was, and hope that you are ticking off all of the boxes, you are doing things correctly…, not forgetting something or being negligent.
Perceived burden from these shifts and tensions increased at key junctures of the pandemic. For instance, when schools closed, educational assistants experienced fear of financial insecurity and job loss. Once schools opened, educational assistants experienced concern as they returned to work yet had to quarantine on a frequent basis and were worried that COVID-19 sick leave benefits would not cover living expenses.
Over time, service providers reportedly became more familiar with, and adept at adapting to, a changing environment. Administrators variably sought to develop organizational or team strategies to support their employees. Strategies included mental health/wellness checks and support to staff in an attempt to create safe spaces to debrief and provide emotional support, exchange strategies, trade work tasks, facilitate peer support and cover shifts for fellow employees.
The ambiguity of what constituted “essential” services was reported to be stressful and problematic for parents and service providers. Of particular concern, unclear understanding about ‘vulnerable’ communities created misperceptions and under-recognition of the unique daily challenges that families of autistic children/youth experienced. For several parents, pandemic-related challenges were conflated with other struggles, as described by a parent:
I think they should realize that the special needs population, kind of like the elderly population, isn’t going to have the same issues that the general population has. Everything is like more emotional, more exacerbated when you have this cognitive gap in understanding, you have a gap in physical support because you can’t be around people. Life is very isolating when life is normal, right? We can’t go to the same places and do the same things that other families do when life is normal. But then you add a pandemic on top of that so now you’re even more isolated, and it’s very difficult. I mean I’m sure this happens to all the parents, but you burn out and [elements of this circumstance aren’t] going to get better over time.
Psychosocial and Behavioral Impacts on Families
Parents observed heightened child/youth anxiety, loneliness and challenging/problematic behaviors (e.g., meltdowns, chewing, picking, aggression) during the pandemic. The loss of in-person educational, recreational and social activities (e.g., school, music lessons, swimming instruction, summer camps) meant a lack of opportunities to socialize with peers and engage in desired activities, as reflected by a concerned parent:
Our son has been struggling with aggression…. At the beginning of the COVID [pandemic], it was… bad and then it… got a bit better…. We fell into a bit more of a routine and stuff. And then the last couple of months,… he’s been very aggressive. So my anxiety is really bad now because every time he moves towards me, I’m worried that he’s going to hurt me.
Parents reported substantial stress from the disruptions in services, and the resultant pressure to find alternative resources to support their child’s pre-existing, emerging or heightened needs. Some described worry about preserving their existing supports, and were uncertain about how to navigate autism service funding during the pandemic, with further concern that if their funding allotment (from government-provided autism supports) wasn’t spent, it would be lost. Learning to support their child in multiple areas and managing personal/family pressures (e.g., managing schooling, supporting their child’ adjustment, behaviors, emotions and socialization, dealing with strained finances and family pressures) grew increasingly difficult, and yielded emotional burden on parents. This was ascribed as an intense pressure and sense of personal failure by a parent:
I felt like I was failing as mom, I’m probably going to get emotional, I felt awful. I was so stressed out and my husband’s hours at that point, still hadn’t been cut, he was still working regular hours and so it was like this is bogus. Like I can’t do this. Me having [a learning disability] and having to teach my kids. My son’s teacher and I weren’t getting along so some of her emails [that were] coming back at me were [critical of me]. I had to send them an email saying, “For my mental health right now, I cannot have to feel the pressure of having my kid’s school work done, because these marks that you are giving them are reflecting me. It is making me very depressed right now. I can’t handle this, no!” They’re sitting there telling my kids they’re doing their stuff wrong. Well, it’s not them doing it wrong, obviously it’s me teaching them wrong because I don’t know what you’re really asking.
Along with care-related transitions and struggles, some parents identified relational challenges within family life. Relational challenges included marital conflict and difficulty coping with strain that was exacerbated by reduced supports.
Positive Adaptation
In contrast to these challenges, positive experiences were also described by some participants. For several parents, the changes in service delivery did not have as drastic and negative an impact on their children as they had anticipated. Several parents reported not experiencing medical support disruptions or adverse health impacts, and some perceived improved well-being in their family. Similarly, some parents identified no or few deleterious impacts on their child’s social skills or mental health. Two parents felt that online school enabled their child to maintain helpful connections with teachers and peers.
Supporting adaptation and coping during the pandemic, parents described the buffering effect of optimism, skill development (e.g., navigation), and supportive relationships. Prior to the pandemic, several parents had an established network of support which they felt had continued and ultimately contributed to their own and their family’s well-being in the pandemic. These resources were viewed to be helpful, as illustrated by a parent:
As soon as the school stopped running, everybody lost their occupational therapist, physical therapist, behavioural therapist, their sensory rooms—everything. Families were struggling and I was very lucky… because I’ve been doing this for a little while and reaching out and building up my toolbox.
Several parents described appreciation for dedicated and compassionate service providers (e.g., teachers’ aides, community service providers, government resource workers) with whom they worked. For instance, several parents recalled teaching assistants providing extra time and support to their child, which was deeply valued.
(d) Hope Yet Caution for the Future
Support for families and service providers was noted to positively impact their expectations for the future. Such beneficial support was categorized in sub-themes of, ‘targeted supports’ and ‘ongoing supports’, with each sub-theme briefly summarized below.
Targeted Supports
Both parents and service providers recommended targeted pandemic-related supports to families. Parents suggested resources for children/youth such as explanatory social narratives or focused conversations to help autistic children/youth better understand appropriate detail about a given disaster (e.g., a pandemic) and resulting protocols. They suggested that service providers need to be empathic toward parents and families, and parents need to be patient with themselves and their children. Service providers emphasized their need to incorporate self-care, and they suggested that policy/program-based decision making in community care should better address and reflect the needs of workers, as illustrated by a service provider:
I think one of the main pieces of work that really helped us and really drove us forward and has held us steadfast today, six months later, and I would recommend that any organization going through anything similar do this in the future, is to develop a set of principles by which to make decisions and spend time on that. We were able to develop about five principles and we have gone back to that several times. We had a lot of input from the staff, it’s very much a shared development of those principles so that is a recommendation because I think that really helps to figure out what’s most important for you as an organization and how to make decisions.
Recommendations for policy and decision makers focused on clearer messaging and enhanced capacity to support families of autistic children/youth. Parents emphasized the need for timely and tailored communication regarding required service delivery changes. They further advocated for additional funding and the availability of respite services and after-school activities for children/youth. These changes were thought to more likely result in ensuring needed resources in constrained conditions such as a pandemic. Service providers suggested revisiting and widening the definition of ‘essential’ services to incorporate autism services. All participant groups emphasized the need for heightened pandemic planning and capacity building among education and service organizations in supporting autistic children/youth.
Ongoing Supports
In moving forward, several parents and service providers hoped for continuing online supports during and beyond the pandemic. One parent desired access to online communication resources within daily school routines. Several service providers recommended an expansion of virtual service delivery during and after the pandemic in the aim of minimizing the need for travel to services by families or, in the case of home visits, time required of services providers for travel. Yet for other service providers and families, the return to face-to-face services was strongly welcomed; hence, ongoing flexibility of service delivery modalities has emerged as important.
This study elicited the experiences of families with an autistic child and their service providers as they navigated the pandemic. Findings demonstrated substantial shifts including a protracted reduction and modification of therapeutic and educational supports during the pandemic. Findings amplify important areas for consideration that are both specific to pandemic conditions and extend beyond this historical ‘moment’ of pandemic constraint.
Decreased and modified services in the pandemic left parents pressured to independently fend for themselves in accessing support for their child and family. Such a shift and challenge corroborate earlier studies reporting deleterious impacts on autistic children/youth and their families as a result of service shutdowns and reductions (Colizzi et al., 2020 ; Garcia et al., 2021 ; Mutluer et al., 2020 ; Wang et al., 2021 ).
Coping mechanisms via personal assets (e.g., acquiring multiple skills, knowledge of resources) and networks of support were integral to navigating the pandemic. This finding is aligned with studies that convey the tenacity and proactivity of parents in: (i) educating their children on the emerging daily realities of COVID-19 (Majoko & Dudu, 2020 ), (ii) creating home-based child/youth learning (Majoko & Dudu, 2020 ), and (iii) building a network to support caregiving and wellness (Majoko & Dudu, 2020 ). Study findings indicate the need to develop educational interventions to enhance family caregivers’ skills (e.g., wayfinding, advocacy), and to ensure service sufficiency (e.g., respite care).
Studies further document multiple challenges among service providers such as moving from in-person to virtual services (Sheehan et al., 2022 ; Spain et al., 2021 ), shifting service delivery options (e.g., forgoing lengthy diagnostic assessments; Spain et al., 2021 ), adhering to infection control protocols (Sheehan et al., 2022 ), and configuring care spaces (e.g., adhering to public health protocols; Sheehan et al., 2022 ; Spain et al., 2021 ). For service providers, stress emerged due to perceived risk to personal and family safety (Sheehan et al., 2022 ), which invites human resource policy and practice planning within the disability sector. Other priorities include support for work-life balance and capacity building in the optimal use of virtual technology (Sheehan et al., 2022 ).
Similar to existing literature, this study illuminated stretched workloads of community and educational service providers due to the extensive support needs of children/youth and families amidst heightened stress and constrained resources. Pre-existing system gaps (e.g., funding cuts, insufficient services) and new pandemic-related challenges (e.g., insufficient financial compensation for quarantine leave, lack of time to adjust to new operational protocols), coupled with ongoing uncertainty (e.g., unknown health risk, unpredictable shifts in public health guidelines) culminated in extraordinary burden, with physical and mental health impacts. Ongoing shifts over the course of pandemic, changes in daily work life and deleterious impacts on worker well-being, have required agencies to pivot over the course of the pandemic, yet with limited alternative staffing options. This in turn is purported to have resulted in continuing strain among service providers. This strain on the well-being of services providers post-pandemic and in future emergencies, warrants further inquiry and consideration of human resource support needs.
Study findings illuminate the need for technology capacity building in autism services. Transitioning from in-person to virtual services and education requires re-configuring complex content, with relational and environmental considerations that may not easily translate across these diverse service delivery/teaching modalities. Best practices are needed to optimally support children in their development at difficult times and contexts such as pandemics or other disasters. In moving forward, changing norms regarding flexibility in service delivery approaches and the viability of virtual options for some children and families may provide ongoing opportunities to enhance care, given the positive experiences described by some of the participants in the current study.
In terms of schooling within a pandemic, collaboration between parents and teachers seems integral to supporting children/youth (Kim et al., 2021 ; Schuck et al., 2023 ). While the literature does not highlight the extent or role of collaboration prior to or during the COVID-19 pandemic, collaborative relationships appear pivotal in helping to address children’s challenges within and beyond a pandemic, and in proactive planning for a possible future widespread emergency/disaster.
Experiences from the literature and this study inform virtual support development for children/youth and their families. Although virtual modalities to support families emerged in the 2000s (Kane & DeBar, 2023 ), such remote services exponentially increased in the COVID-19 pandemic, as exemplified in this literature (Fell et al., 2023 ) and our study. Building a strong technology infrastructure (e.g., accessibility, effectiveness metrics) is needed. Studies addressing virtual interventions for autistic children/youth have highlighted the importance of providing training to implementers (Fell et al., 2023 ; Kane & DeBar, 2023 ), tailoring the intervention to the individual (Bundy et al., 2023 ; Fell et al., 2023 ), ensuring access and capacity to use online platforms (Fell et al., 2023 ; Kane & Debar, 2023 ), and infusing infrastructural and administrative supports to sustain the intervention (Fell et al., 2023 ). Additional considerations highlighted in this study include the importance of wrap-around technological support particularly in the early stages of one’s use of an online platform and incorporating diverse methods to engage families. Attention to the social determinants of health and upholding an equity and inclusion framework are critical in equitably supporting the range of population needs and addressing variability in technology access (Zwaigenbaum et al., 2021 ). Further, integrating an equity lens in the distribution of resources is critical to moving forward in a socially just manner.
Preparedness for a pandemic or other disaster is integral to supporting autistic children and youth and their families. In this study, accessible information tailored to the specific needs of children, youth and families was strongly recommended. Organizational and systemic strategies are needed to ensure such information and service coordination are available (Dai & Hu, 2021 ; Kusumi et al., 2023 ). As an example of such an approach, crisis emergency teams were created within a special needs school in Japan to provide ongoing guidance throughout the COVID-19 pandemic. These teams comprised school staff and health authority personnel (Kusumi et al., 2023 ). Such innovation illustrates important collaboration across sectors to develop responsive strategy. This is particularly important given that specific communities (e.g., the autistic community in a rural and remote region) may have particular logistical, informational and support challenges (e.g., impeded information and resource access).
Targeted COVID-19 information and supports for the autism community likely would have assisted autistic individuals and their families to better navigate the pandemic. Systemic vagueness in determining ‘essential’ services and the determination of some key services as ‘non-essential’ rendered it challenging for therapeutic and educational personnel to work with autistic children/youth and their families as they otherwise likely would have. These findings amplify the importance of clear messaging focused on pressing issues, with attention on the needs of autistic children and their families.
The literature is beginning to document disability-led initiatives and innovation that addressed informational gaps in the pandemic. For instance, in China, a disability-led initiative emerged from growing concerns that families of children with developmental disabilities required appropriate and updated information on COVID-19 risk, strategies to mitigate COVID-19 exposure, and supports for children. This initiative comprised international and local volunteers who (i) tailored and disseminated comprehensive and inclusive web-based COVID-19 information (e.g., health risk and prevention strategies) to disability communities, and (ii) coordinated the delivery of tangible resources (e.g., medication, PPE) to families (Dai & Hu, 2021 ). In Canada, AIDE Canada ( www.aidecanada.ca ) offered a devoted website with COVID-19 resources specific to autistic individuals and their families. Strategies and resources addressing pressing issues for autistic individuals and their families emerge as priorities in the event of a potential future disaster such as a pandemic.
Overall, these findings offer important considerations for critical reflection and service advancement that go beyond the COVID-19 pandemic (Zwaigenbaum et al., 2021 ). For instance, service insufficiency and systemic challenges have persisted, and warrant critical reflection and targeted action. Post-pandemic mental health concerns, financial challenges among families, and deep resource and service gaps, are examples of continuing areas of challenge to be addressed.
Study Limitations
While addressing the experiences of families and service providers, this study did not specifically gather perspectives from school staff and residential care workers who supported autistic children/youth during the pandemic. The sample lacked extensive first-person experience from autistic children/youth, and disproportionately included families in which the autistic child/youth was male; hence, further study is needed based on a broader sample representation. The sample further reflected lived experience in only one region in Canada which highlights the need for future studies within broader regional and sociodemographic contexts in ascertaining how regional and other demographic factors may nuance service delivery experiences.
Study data were collected relatively early in the pandemic; hence, emergent or longer-term impacts of the pandemic (and beyond) are needed, as are future interventional studies that examine proactive approaches fostering preparedness, pandemic support and post-pandemic recovery. Notably, such additional research is underway by members of this research team.
This study strongly asserts the need for pandemic and post-pandemic planning and support, with specific focus on the needs of autistic children and their families. To that end, collaboration amongst those with lived experience in the autistic community, service providers and program/policy decision makers is integral in the important aim of ensuring sufficiently-resourced supports and services both within and beyond a pandemic.
Asbury, K., Fox, L., Deniz, E., Code, A., & Toseeb, U. (2021). How is COVID-19 affecting the mental health of children with special educational needs and disabilities and their families? Journal of Autism and Developmental Disorders , 51 (5), 1772–1780. https://doi.org/10.1007/s10803-020-04577-2 .
Article PubMed Google Scholar
Assenza, C., Catania, H., Antenore, C., Gobbetti, T., Gentili, P., Paolucci, S., & Morelli, D. (2021). Continuity of care during COVID-19 lockdown: A survey on stakeholders’ experience with telerehabilitation. Frontiers in Neurology , 11 , 1813. https://doi.org/10.3389/fneur.2020.617276 .
Article Google Scholar
Bundy, R., Mandy, W., Kenny, L., & Ali, D. (2023). Autistic people and telehealth practiceduring the COVID-19 pandemic: A scoping review. Review Journal of Autism and Developmental Disorders , 1–19. https://doi.org/10.1007/s40489-023-00387-1 .
Colizzi, M., Sironi, E., Antonini, F., Ciceri, M. L., Bovo, C., & Zoccante, L. (2020). Psychosocial and behavioral impact of COVID-19 in Autism Spectrum Disorder: An online parent survey. Brain Sciences , 10 (6), 341. https://doi.org/10.3390/brainsci10060341 .
Article PubMed PubMed Central Google Scholar
Dai, R., & Hu, L. (2021). Inclusive communications in COVID-19: A virtual ethnographic study of disability support network in China. Disability & Society , 37 (1), 3–21.
Elo, S., & Kyngäs, H. (2008). The qualitative content analysis. Journal of Advanced Nursing , 62 , 107–115.
Fell, L. A., Albright, C. M., Kryszak, E. M., Butter, E., & Kuhlthau, K. A. (2023). Provider perspectives on telehealth services for children with autism spectrum disorder during the coronavirus disease 2019 pandemic. Academic Pediatrics , 23 (6), 1196–1203.
Garcia, J. M., Lawrence, S., Brazendale, K., Leahy, N., & Fakuda, D. (2021). Brief report: The impact of the COVID-19 pandemic on health behaviors in adolescents with Autism Spectrum Disorder. Disability and Health Journal , 14 (2). https://doi.org/10.1016/j.dhjo.2020.101021 .
Graneheim, U. H., & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today , 24 , 105–112.
Jeste, S., Hyde, C., Distefano, C., Halladay, A., Ray, S., Porath, M., & Thurm, A. (2020). Changes in access to educational and healthcare services for individuals with intellectual and developmental disabilities during COVID-19 restrictions. Journal of Intellectual Disability Research , 64 (11), 825–833. https://doi.org/10.1111/jir.12776 .
Kane, C. L., & DeBar, R. M. (2023). A descriptive review of telehealth for individuals with autism spectrum disorder. Behavior Modification , 47 (2), 504–546.
Kellom, K. S., Flaherty, C. M., Cacia, J., Christiansen, A., Cordero, L., Hah, J., Kennelly, A., Ortiz, P., Stefanski, K., Wozniak, S. N., & Wallis, K. E. (2023). Provider and caregiver perspectives on telehealth assessments for autism spectrum disorder in young children: A multimethod DBPNet study exploring equity. Journal of Developmental and Behavioral Pediatrics , 44 (6), e397–e411. https://doi.org/10.1097/DBP.0000000000001198 .
Kim, M., Santiago, J. A., Park, C. W., & Kim, M. J. (2021). Adapted physical teaching online during COVID-19: Experiences from the South of the United States. International Journal of Disability Development and Education , 69 (1), 239–252.
Kusumi, Y., Tominaga, M., Nagasawa, H., & Fujii, A. (2023). One school’s management of students with intellectual disabilities during the COVID-19 outbreak in Japan: A study based on interviews with teachers. Journal of Intellectual Disabilities , 27 (2), 354–369. https://doi.org/10.1177/17446295221082731 .
Lambert, R., & Schuck, R. (2021). The Wall now between us: Teaching math to students with disabilities during the COVID-19 spring of 2020. The Asia-Pacific Education Researcher , 30 , 289–298.
Article PubMed Central Google Scholar
Latzer, I. T., Leitner, Y., & Karnieli-Miller, O. (2021). Core experiences of parents of children with autism during the COVID-19 pandemic lockdown. Autism , 25 (4), 1047–1059. https://doi.org/10.1177%2F1362361320984317.
Lincoln, Y. S., & Guba, E. G. (2005). Paradigmatic controversies, contradictions, and emerging confluences. In N. K. Denzin & Y. S. Lincoln (Eds.), The Sage handbook of qualitative research (pp. 191–215) Sage.
Majoko, T., & Dudu, A. (2020). Parents’ strategies for home educating their children with Autism Spectrum disorder during the COVID-19 period in Zimbabwe. International Journal of Developmental Disabilities , 1–6.
Manning, J., Billian, J., Matson, J., Allen, C., & Soares, N. (2020). Perceptions of families of individuals with Autism Spectrum disorder during the COVID-19 crisis. Journal of Autism and Developmental Disorders , 51 (8), 2920–2928. https://doi.org/10.1007/s10803-020-04760-5 .
Mutluer, T., Doenyas, C., & Genc, H. A. (2020). Behavioral implications of the Covid-19 process for Autism Spectrum Disorder, and individuals’ comprehension of and reactions to the pandemic conditions. Frontiers in Psychiatry , 11 . https://doi.org/10.3389/fpsyt.2020.561882 .
Schuck, R. K., Lambert, R., & Wang, M. (2023). Collaborating with parents during COVID-19 online teaching: Special educator perspectives. Education 3–13: International Journal of Primary Elementary and Early Years Education , 51 (2), 292–305.
Google Scholar
Sheehan, R., Dalton-Locke, C., Ali, A., San Juan, N. V., Totsika, V., & Hassiotis, A. (2022). Effects of the COVID-19 pandemic on mental healthcare and services: Results of a UK survey of front-line staff working with people with intellectual disability and/or autism. BJPsych Bulletin , 46 , 201–207. https://doi.org/10.1192/bjb.2021.52 .
Shorey, S., Lau, L. S. T., Tan, J. X., Ng, E. D., & Ramkumar, A. (2021). Families with children with neurodevelopmental disorders during COVID-19: A scoping review. Journal of Pediatric Psychology , 46 (5), 514–525. https://doi.org/10.1093/jpepsy/jsab029 .
Spain, D., Mason, D., Capp, S. J., Stoppelbein, L., White, S. W., & Happe, F. (2021). This may be a really good opportunity to make the world a more autism friendly place’: Professionals’ perspectives on the effects of COVID-19 on autistic individuals. Research in Autism Spectrum Disorders , 83 , 1–13.
Stankovic, M., Stojanovic, A., Jelena, S., Stankovic, M., Shih, A., & Stankovic, S. (2022). The Serbian experience of challenges of parenting children with autism spectrum disorders during the COVID-19 pandemic and the state of emergency with lockdown. European Child & Adolescent Psychiatry , 31 (4), 693–693. https://doi.org/10.1007/s00787-021-01917-0 .
Steed, E. A., & Leech, M. (2021). Shifting to remote learning during COVID-19: Differences for early childhood and early childhood special education teachers. Early Childhood Education Journal , 49 , 789–798.
Wang, L., Li, D., Pan, S., Zhai, J., Xia, W., Sun, C., & Zou, M. (2021). The relationship between 2019-nCoV and psychological distress among parents of children with autism spectrum disorder. Globalization and Health , 17 (1), 1–14. https://doi.org/10.1186/s12992-021-00674-8 .
Zwaigenbaum, L., Bishop, S., Stone, W. L., Ibanez, L., Halladay, A., Goldman, S., Kelly, A., Klaiman, C., Lai, M., Miller, M., Saulnier, C., Siper, P., Sohl, K., Warren, Z., & Wetherby, A. (2021). Rethinking autism spectrum disorder assessment for children during COVID-19 and beyond. Autism Research , 14 (11), 2251–2259. https://doi.org/10.1002/aur.2615 .
Download references
This study has been funded by the Canadian Institutes of Health Research, Grant #OV7-170376.
Author information
Authors and affiliations.
Faculty of Social Work, Central and Northern Alberta Region, University of Calgary, Edmonton, AB, Canada
David B. Nicholas, Rosslynn T. Zulla, Jill Cielsielski & Olivia Conlon
Department of Pediatrics, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, AB, Canada
Lonnie Zwaigenbaum
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to David B. Nicholas .
Ethics declarations
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Nicholas, D.B., Zulla, R.T., Cielsielski, J. et al. COVID-19 Pandemic Experiences of Families in Which a Child/Youth Has Autism and Their Service Providers: Perspectives and Lessons Learned. J Autism Dev Disord (2024). https://doi.org/10.1007/s10803-024-06402-6
Download citation
Accepted : 08 May 2024
Published : 20 May 2024
DOI : https://doi.org/10.1007/s10803-024-06402-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychosocial impacts
- Service providers
- Service delivery
- Find a journal
- Publish with us
- Track your research
Book Appointment
- Autism Treatment
- Behavior Problems
- Mental Retardation
- Parental Guidance
- Cerebral Palsy
- Learning Disabilities
- Poor Memory
- Down Syndrome
- Sensory Processing Disorder
- Testimonials
A Case Study of Autism: Paul, 3 Years Old
- Autism Blog
- A Case Study of Autism:…
Arun was brought for consultation with Dr. A M Reddy by his parents. He was about 4 years old, the second child to the parents. Even while he was being brought into the room, we could hear his loud wailing. It took some time for the child to calm down and later we could observe that the child was very restless. He was running around the room, pulling down cushions and generally creating chaos in the room and mother was quite harried in trying to control him. He was diagnosed with ASD (Autism Spectrum Disorder).
What is ASD?
Autism or Mutinism as it was earlier known was thought primarily to affect communication skills but with more studies, it was understood that autistic children display a wide range of symptoms, hence the word “spectrum” was added to Autism disorder. Autism is a complex neurodevelopmental disorder which affects a person’s social behavior and communication skills.
Why it occurs?
The exact reason why ASD occurs is not known but many risk factors have been identified like age of the parents, poor ovulation, infections or exposures to harmful chemicals or radiation during pregnancy, thyroid, diabetes type of hormonal disorders, birth injuries, infections in childhood, vaccinations, etc.
What are its symptoms?
As its name suggests, ASD displays a myriad of symptoms but some of the common symptoms of ASD is lack of speech. While some children have no speech, in some children speech that was developed before may regress. Many of them do not prefer to mingle with children of their age group. Repetitive action, physical restlessness, inability to understand emotions, mood swings like sudden bouts of excitement, crying without any reason, are few symptoms displayed by many autistic children.
Aggressive behaviors like self-harming, head-banging, tantrum-throwing, biting/pushing others, destructiveness, can be displayed by few. Response to name call, having sustained eye contact, unable to understand commands, stereotypical actions and stimming are some of the common symptoms exhibited by many.
Coming back to the case of Arun, a detailed case history was noted down by our doctors, a summary of which is given below.
He is the second child and the age difference between both the siblings is seven years. After the first child was born, the mother developed hypothyroidism for which she was on thyroxine 50 mcg daily tablets. No history of abortions or contraceptive use was reported. Father was apparently healthy. The age of the parents was 35 and 38 years respectively during conception. She conceived naturally and pregnancy was apparently uneventful. But on deeper probing few differences were found out between both the pregnancies.
While during the first pregnancy the parents were in India, but during second there were in the United States. She was advised to continue with the same dosage of thyroxine and during 6-7 months of the pregnancy, she was given flu and T Dap vaccine. The child was born of emergency C – section as the water broke early. The birth cry was normal and seemingly the child was progressing well but after his first birthday, the child had a bout of severe gastrointestinal infection when they visited India where he was hospitalized for three days and given medicines.

Parents were worried that he seems to put everything in his mouth and his favorite items were paper, cloth, wall plaster. His demands have to be met, else he used to become very upset. Emotional connectivity towards parents was less. He would not follow simple commands and it was becoming increasingly difficult for the parents to manage him. With therapies, his eye contact improved a little and was able to follow a few simple commands but the progress was slow.
He was a picky eater and liked crunchy foods. His bowels were constipated and he was not yet toilet trained. He was given Cuprum Sulph 10 M and was kept on regular follow up.
On the next visit to Dr. A M Reddy Autism Center , the parents complained that their child developed itching on the skin but his restlessness reduced slightly. The medication was continued for about three months during which the child’s anger reduced by 30%, his eye contact improved and he was no longer constipated. His itching too reduced in the meanwhile. A second dose was repeated and about six to seven months of treatment, he started saying few words, tantrum-throwing reduced and his habit of putting everything in the mouth was gone.
The dose was repeated in 50M potency. After about a year and half of treatment, he started interactive communication, giving relevant answers to questions and was doing much better. On the advice of Dr. A M Reddy, they placed him in normal school and he is doing well.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Post comment
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Yonago Acta Med
- v.67(2); 2024 May
- PMC11128085

Long-Term Outcomes for a Student with Severely Challenging Behavior in a Special Needs School for Intellectual Disabilities: A School Consultation Case Study
Masahiko inoue.
* Department of Clinical Psychology, Graduate School of Medical Sciences, Tottori University, Yonago 683-8503, Japan
Self-injurious, stereotyped, and aggressive/destructive behaviors exhibited by individuals with intellectual disabilities and autism spectrum disorders are called challenging behaviors (CBs). Severe CBs often require long-term treatment involving psychosocial approaches based on behavioral interventions and/or medication. A boy with severe CB enrolled in a special needs school, with diagnoses of autism and intellectual disability, was the client of the study. This case report describes the long-term outcomes of eight years of continuous school consultation. The student’s severe CB improved with environmental adjustments in the classroom, unified teacher involvement, instruction of leisure and communication skills, and medication. Long-term research on changes in CBs through school consultation is limited, and this case report provides important insights into the development of effective educational programs and curricula for severe CBs in school-aged children.
Recently, the term Challenging Behavior (CB) has been used in studies examining problematic behaviors associated with developmental disabilities such as autism spectrum disorder (ASD), attention deficit hyperactivity disorder, and intellectual developmental disorders (IDD). CB is not a diagnosis; rather, it is a term that emphasizes the issues arising from the interactions between individual and social factors. 1 Recent research has focused on persistence and long-term outcomes for CB in people with IDD and ASD, with several studies noting that severe CB, in particular, can persist for more than 10 years. 2 , 3 It has been shown that without an appropriate teaching environment, instructional system, and curriculum for CB, CB can become more severe throughout a child’s school years, even in special needs schools. 4 However, in the Japanese special needs education system, standard educational guidelines and functional assessments for severe CBs have not been institutionalized. School consultations with outside professional organizations for serious CB are important, 5 but many studies on this subject are short-lived and of limited effectiveness. 6 Long-term findings on school-age interventions and prognoses for severe CBs are useful for developing appropriate educational programs and curricula in schools. This case report presents the long-term outcome of one boy in a functional assessment-based school consultation for severe CB by Inoue and Oda. 6
PATIENT REPORT
The client in this case study was an 11-year-old boy diagnosed with IDD and ASD at age three, enrolled in the primary fifth grade at a special needs school for IDD. He was unable to take an intelligence test owing to CB. However, he could understand simple instructions, express himself using four-word sentences, and read some Kanji characters.
He lived with his parents and had been attending a special needs class at a local elementary school. However, by the third grade, the child continued to engage in aggressive behaviors such as biting, grabbing hair, and kicking at school and after-school facilities. Finally, partly owing to physical abuse by his parents, he was placed in a facility for IDD and transferred to a special needs school in that school district. In the Japanese education system, when a child has an IDD, and CB is severe, they are often educated in a special needs school for children with IDD in the school district rather than in a special needs class, and this was the case for this boy.
His parents regularly visited him at the facility and brought him sweets. He did not resist these visits, looked forward to the presents, and made no comments about wanting to go home. The consultant (author) was unable to assess the impact of the parental physical abuse because the school did not have detailed information about it. Upon admission to the facility, he showed strong resistance to new people and environments and demonstrated aggressive behaviors (hitting, kicking, biting, grabbing hair, and spitting). He also frequently engaged in self-injurious behaviors (hitting his head, biting his hand, and crying, among others). He also exhibited behavior such as defecating in places other than toilets, overturning school lunches, and throwing objects. At the facility, he wandered around at night, strangled children in other rooms, and engaged in various dangerous and aggressive behaviors.
School consultation
The author served as a consultant by visiting schools five to 11 times a year. Three to six consultations regarding students with CB were conducted during each visit to the school, including the student in this report. Each consultation lasted 15 to 20 minutes. The consultees were homeroom teachers, grade-level teachers, and facility staff. The school consultations were based on the functional assessment with applied behavior analysis approach, which is well-supported as an approach to CBs in individuals with IDD and ASD. 7 The consultation procedure was based on Inoue and Oda’s study. 6 The consultant (author) worked with the consultees (teachers/facility staff) using a strategy sheet 8 to determine antecedent control to prevent CB from occurring and teach appropriate alternative behaviors.
Antecedent control in the classroom environment
Owing to the severity of the CB, the teaching team was rotated so that there were two teachers. Group education was not possible, and individual education was provided. The following environmental adjustments were made as antecedent control procedures. A “private classroom” with cushioned walls was used as the classroom because of the student’s self-injurious behavior of hitting his head against the wall. The structure of the room is shown in Figure 1 . Classroom postings and educational materials were removed from classrooms to prevent disruptive behavior. Educational materials and leisure items were stored in the observation room across the hallway and only placed in the classroom as needed. The student’s desk and chair legs were fixed in place with thick plywood. Windows, on which he might bump his head, were boarded up in the lower half of the room. The room was partitioned to provide a cool-down space. A video camera was installed in the room so that if the student became unstable, the teacher could leave the classroom to allow him a cool-down period and monitor him from the observation room. A handover system was established at the end of each school year to ensure a consistent support policy based on the consultation with the author. The system ensured that at least one teacher familiar with the case would be included in the following year’s team.

Environment around the classroom.
Appropriate alternative behaviors
School consultations focused on functional assessment for CB and teaching appropriate alternative behaviors. A functional assessment of the student’s CB was conducted through behavioral observation using the ABC chart. The ABC chart is a tool used to estimate the function of a behavior through direct observation, in the form of a sheet that records antecedents (A), behaviors (B), and consequences (C). As a result, there were different topographies of his CB, which included aggression, destruction, and self-injury; multiple functions, including communication (such as demands and avoidance) were inferred depending on the context; and sensory functions were estimated. Therefore, we taught leisure and communication skills, such as study time and recess, as appropriate alternative behaviors for each situation.
Leisure skills: For leisure skills, we initially introduced activities such as looking at advertisements and magazines, playing with a train toy, and using coloring books, which were considered to be the student’s favorite activities. However, he was unable to sustain performing these activities on his own. Also, regarding coloring books, he sometimes chewed, broke, and ate crayons and magic markers, which sometimes led to new CB.
For this reason, leisure activities were initially integrated into the assignment schedule with the goal of achieving independence in performing leisure skills. As a result, the student was able to work independently on several leisure activities. By the end of his junior year, he was able to engage in leisure activities alone for 10–30 minutes, including doing puzzles depicting his favorite characters, playing with building blocks, and coloring. In upper secondary school, he was able to request his teachers to use leisure activity picture cards. Additionally, he could go to the library to check out a DVD of his choice and return it after watching it.
Communication skills: When the student was in elementary school, several words in the teacher’s instructions triggered self-injurious behavior. And it was presumed that this behavior is a function of the escape. To address this, a list of these negative words was created, and the teachers were unified in their efforts to avoid using them. It became clear that the aggressive behaviors occurred when the child was crying, throwing things, or hitting his head against the floor or a wall, and when a teacher was nearby. When he began exhibiting these behaviors, the teacher did not forcibly stop him, but instead moved away and watched him.
The skill of requesting a particular choice among the leisure activity cards was taught as a target behavior. We also taught him the communication skill of refusal by introducing “I will not do it” cards. As a result, the student was less likely to act out during study time and was able to stay calm during recess.
Japanese version of the Aberrant Behavior Checklist score and medication
The Aberrant Behavior Checklist (ABC) 9 consists of 58 items, each scored on a 4-point Likert scale. It has five domains: irritability, lethargy/withdrawal, stereotypy, hyperactivity, and inappropriate speech. The Japanese version of the ABC (ABC-J) has been shown by Ono 10 to be as reliable and valid as the original. Figure 2 shows the ABC-J score trends and medication changes over eight years. The vertical axis shows scores, and the horizontal axis shows the evaluation time. The evaluation occurred twice every academic year, once in May and again 10 months later in March. May of the second year of high school was excluded owing to missing data.

ABC-J score trends and medication changes over eight years. T1 (primary 5th grade, May), T2 (primary 5th grade, March), T3 (primary 6th grade, May), T4 (primary 6th grade, March), T5 (secondary 1st grade, May), T6 (secondary 1st grade, March), T7 (secondary 2nd grade, May), T8 (secondary 2nd grade, March), T9 (secondary 3rd grade, May), T10 (secondary 3rd grade, March), T11 (high school 1st grade, May), T12 (high school 1st grade, March), T13 (high school 2nd grade, March), T14 (high school 3rd grade, May).
The ABC-J score was 69 at T1, the beginning of the intervention (primary 5th grade, May), peaked at 155 at T3 (primary 6th grade, May), and remained between 64 and 108 until T9 (secondary 3rd grade, May). Scores then decreased to 46 points at T10 (secondary 3rd grade, March) and continued to decline progressively to 4 points at T14 (high school 3rd grade, May).
Medication was prescribed by medical providers independently of the school consultation and did not involve the authors. Initially, risperidone was prescribed. Biperiden hydrochloride and fluvoxamine maleate were started in junior high school. In upper secondary school, the patient began to feel unsteady while walking. Risperidone and fluvoxamine maleate were reduced.
Figure 3 shows the ABC-J sub-domain scores at T1 (primary 5th grade, May), when the support started, and at T11 (high school 1st grade, May) and T14 (high school 3rd grade, May) when CB improved significantly. At T1, lethargy and irritability were high (26 and 20 points, respectively). Hyperactivity scored 12 points, inappropriate speech 7 points, and stereotypy scored 4 points. The ratios of these scores remained similar until T10. Scores other than irritability decreased at T11. At T14, irritability also decreased to 2 points.

Difference in ABC-J subscale and total scores by time. T1 (primary 5th grade, May), T11 (high school 1st grade, May), T14 (high school 3rd grade, May).
This case report describes the long-term outcome of school counseling based on functional assessment for a boy with ASD and IDD who was admitted to an institution owing to reported abuse at home and severe CB. For non-drug treatment of intense CB, elimination of excitatory stimuli and structuring of the classroom environment to provide the child with predictability are effective antecedent controls, making CB less likely to occur. 11
The consultant suggested to the school administration and teachers the creation of an instructional system and antecedent control for the prevention of CB. The consultant then advised the teachers regarding conducting functional assessments using ABC chart, selecting appropriate alternative behaviors, and choosing effective teaching methods.
The classroom environment and teacher assignments were developed through cooperation between school administrators and teachers. The teachers shared their ideas during the ongoing consultations. The ability to conduct consultations across academic years also played a critical role in effectively transitioning between grades and departments. The result of this long-term consultation case was the student’s acquisition of leisure and communication skills that substituted for CB functions in different situations that arose during his school life.
Long-term data on severe CB is limited. Few case reports describe specific approaches and improvements. The long-term changes in ABC-J scores in this report indicate that even as CBs decrease, they still show significant long-term fluctuation. Inoue et al. 4 analyzed long-term changes in severity of CB. This previous study suggested that changes in school age students were more likely to be observed for behavior groups such as hyperactivity. This case study supported this result, although the scale used was different.
In particular, in this case, a maximum dose of 5.7 mg of risperidone was administered at the peak severity of CB. The dosage of risperidone in childhood is not to exceed 3 mg (3 mL) for patients weighing 45 kg or more, and it is possible that the patient was oversedated at one point. In the UK, the national project STOMP is being promoted to stop over medication involving psychotropic medicines for people with IDD, ASD or both. 12 To successfully implement STOMP, stakeholders were required to be engaged in the process. 13 This case demonstrates the need for long-term collaboration with a patient’s healthcare provider to adjust the patient’s medication to accommodate changes as well as to consider side effects.
Both risperidone, an atypical antipsychotic drug, and function-based behavior-analytic interventions are widely used and empirically validated treatments for reducing CB in children with autism. 14 However, little is known about the interactions between the medication’s pharmacodynamics and behavioral function. 15 In this case, we did not control for the timing of the introduction of the behavioral interventions and pharmacotherapy, nor were we able to demonstrate functional changes in CB at each time point. Future research is needed to elucidate the long-term effects of both behavioral interventions and pharmacotherapy on aspects of behavioral topography and function.
Ethics statement
Written informed consent for the study and publication was obtained from the parents, school, and facility.
Acknowledgments
Acknowledgments: We thank the student, parents, school teachers, and facility staff. This work was supported by Grant-in-Aid for Scientific Research (B) Grant Number (JP17H02716) and Health and Labor Sciences Research Grant (22GC1019).
The authors declare no conflict of interest.
Groundbreaking study connects genetic risk for autism to changes observed in the brain
A groundbreaking study led by UCLA Health has unveiled the most detailed view of the complex biological mechanisms underlying autism, showing the first link between genetic risk of the disorder to observed cellular and genetic activity across different layers of the brain.
The study is part of the second package of studies from the National Institutes of Health consortium, PsychENCODE. Launched in 2015, the initiative, chaired by UCLA neurogeneticist Dr. Daniel Geschwind, is working to create maps of gene regulation across different regions of the brain and different stages of brain development. The consortium aims to bridge the gap between studies on the genetic risk for various psychiatric disorders and the potential causal mechanisms at the molecular level.
"This collection of manuscripts from PsychENCODE, both individually and as a package, provides an unprecedented resource for understanding the relationship of disease risk to genetic mechanisms in the brain," Geschwind said.
Geschwind's study on autism, one of nine published in the May 24 issue of Science , builds on decades of his group's research profiling the genes that increase the susceptibility to autism spectrum disorder and defining the convergent molecular changes observed in the brains of individuals with autism. However, what drives these molecular changes and how they relate to genetic susceptibility in this complex condition at the cellular and circuit level are not well understood.
Gene profiling for autism spectrum disorder, with a few exceptions in smaller studies, has long been limited to using bulk tissue from brains from autistic individuals after death. These tissue studies are unable to provide detailed information such as the differences in brain layer, circuit level and cell type-specific pathways associated with autism as well as mechanisms for gene regulation.
To address this, Geschwind used advances in single-cell assays, a technique that makes it possible to extract and identify the genetic information in the nuclei of individual cells. This technique provides researchers the ability to navigate the brain's complex network of different cell types.
More than 800,000 nuclei were isolated from post-mortem brain tissue of 66 individuals from ages 2 to 60, including 33 individuals with autism spectrum disorder and 30 neurotypical individuals who acted as controls. The individuals with autism included five with a defined genetic form called 15q duplication syndrome. Each sample was matched by age, sex, and cause of death balanced across cases and controls.
Through this, Geschwind and his team were able to identify the major cortical cell types affected in autism spectrum disorder, which included both neurons and their support cells, known as glial cells. In particular, the study found the most profound changes in the neurons that connect the two hemispheres and provide long range connectivity between different brain regions and a group of interneurons, called somatostatin interneurons that are important for maturation and refinement of brain circuits.
A critical aspect of this study was the identification of specific transcription factor networks -- the web of interactions whereby proteins control when a gene is expressed or inhibited -- that drive these changes that were observed. Remarkably, these drivers were enriched in known high-confidence autism spectrum disorder risk genes and influenced large changes in differential expression across specific cell subtypes. This is the first time that a potential mechanism connects changes occurring in brain in ASD directly to the underlying genetic causes.
Identifying these complex molecular mechanisms underlying autism and other psychiatric disorders studied could work to develop new therapeutics to treat these disorders.
"These findings provide a robust and refined framework for understanding the molecular changes that occur in brains in people with ASD -- which cell types they occur in and how they relate to brain circuits," Geschwind said. "They suggest that the changes observed are downstream of known genetic causes of autism, providing insight into potential causal mechanisms of the disease."
- Birth Defects
- Brain Tumor
- Nervous System
- Disorders and Syndromes
- Learning Disorders
- Brain Injury
- Neural development
- Alzheimer's disease
- Homosexuality
- Haemophilia
Story Source:
Materials provided by University of California - Los Angeles Health Sciences . Note: Content may be edited for style and length.
Journal Reference :
- Brie Wamsley, Lucy Bicks, Yuyan Cheng, Riki Kawaguchi, Diana Quintero, Michael Margolis, Jennifer Grundman, Jianyin Liu, Shaohua Xiao, Natalie Hawken, Samantha Mazariegos, Daniel H. Geschwind. Molecular cascades and cell type–specific signatures in ASD revealed by single-cell genomics . Science , 2024; 384 (6698) DOI: 10.1126/science.adh2602
Cite This Page :
Explore More
- Brain Network Responsible for Stuttering
- When Should You Neuter or Spay Your Dog?
- Why Do Dyeing Poison Frogs Tap Dance?
- Cold Supply Chains for Food: Huge Savings
- Genetic Mosaicism More Common Than Thought
- How Killifish Embryos Survive 8 Month Drought
- Simple Food Swaps to Cut Greenhouse Gases
- Fossil Porcupine in a Prickly Dilemma
- Future Climate Impacts Put Whale Diet at Risk
- Charge Your Laptop in a Minute?
Trending Topics
Strange & offbeat.

Special Education and Inclusive Learning
Therapeutic Play: Unlocking Emotional and Mental Wellbeing in Children
The therapeutic nature of play.
Play is a fundamental aspect of childhood, inspiring awe and wonder as children explore and problem-solve, learning about the world around them each step of the way. While the benefits of play for physical development are clear— enhancing motor skills and coordination through the manipulation of resources—its therapeutic value has come into sharper focus, particularly during the pandemic. This article looks at the therapeutic benefits of play, exploring how it supports emotional and mental wellbeing, and how teachers and parents can harness this power to raise healthier, happier children.
Building Trust and Connection
Play is inherently a social activity that teaches trust and forms connections. Through shared experiences and sustained engagement, children develop a sense of safety and belonging. It provides a unique environment where thoughts and feelings – worries, concerns, excitement, or happiness—can be expressed without words. This non-verbal expression is crucial for emotional release and stress reduction, offering moments of calm and focus amidst busy lives.
Making Sense of the World
Children use play to make sense of their surroundings. It helps build self-confidence and resilience as they navigate challenges and learn to deal with setbacks. Play also offers a sense of control and freedom, essential for developing a sense of calm and enjoyment. By initiating play, children experience autonomy, which is vital for their emotional development.
Emotional Regulation and Self-Reflection
Therapeutic play encourages children to make choices and solve problems, teaching them self-reflection and self-regulation. These skills are crucial for emotional development, enabling children to manage their thoughts and feelings effectively. According to child psychologist Bruno Bettelheim, play acts as a bridge between a child’s experiences and the real world, allowing them to process and resolve their concerns.
Creating a Safe and Trusting Environment
For play to be therapeutic, providing a safe and trusting environment where children feel secure to explore and express themselves is essential. This environment should be free from fear, allowing children to experiment and communicate openly. Such conditions have a lifelong impact, as children apply new abilities like self-expression and emotional regulation to other areas of their lives.
The Role of Educators in Therapeutic Play
Facilitating engagement and ownership.
Educators play a pivotal role in enabling the therapeutic value of play. By understanding each child’s unique interests, educators can create engaging activities that resonate with them. Children must take ownership of their play. Adults should act as observers, intervening only when necessary or invited, and respecting the child’s choices and individuality. This is where a highly skilled teaching assistant knows when to step back.
Nurturing Imagination and Cultural Capital
Our role in therapeutic play is to provide time, space, and opportunity to explore freely, nurturing their ideas and imaginations. Every child brings their own experiences and cultural capital to play, and it is important to enhance this through exposure to new and enriching experiences. As American psychologist Charles Schaefer noted, “We are never more fully alive, more completely ourselves, or more deeply engrossed in anything than when we are playing.”
Supporting Emotional and Social Development
Therapeutic play supports emotional and social development by allowing children to express their feelings and learn social skills. Expressive arts like drawing, clay modelling, and finger painting can help children articulate their emotions and reflect on their inner selves. Imaginative pretend play and puppet play allow children to practise socially accepted behaviours in a safe environment.

Play Therapy: A Structured Approach
“In play therapy, toys are like the child’s words, and play is their language.” — Association for Play Therapy
Understanding Play Therapy
Play therapy is a structured approach where play is used as a medium for children to express their thoughts and feelings. According to the Association for Play Therapy (APT), play therapy helps children relieve stress, connect with others, stimulate creative thinking, regulate emotions, and boost self-esteem. In play therapy, toys are like the child’s words, and play is their language.
How Play Therapy Works
Children often communicate emotional distress through their behaviour, as they may not have the verbal language to express their feelings. For instance, a child experiencing parental divorce may act out to communicate their anxiety. In play therapy, children use toys to express what troubles them, allowing them to cope with difficult emotions and find solutions to problems.
Role of the Therapist
In play therapy, therapists provide a playroom with a range of toys that help children express their feelings and problems. Children choose the toys and how they want to play with them. Therapists observe and sometimes engage in imaginary play, setting limits if the child’s behaviour becomes problematic. This natural expression through play helps bring out the child’s issues, facilitating healing and understanding.
The Importance of Parental Involvement
Ideally, parents are their children’s first and best playmates. When parents are involved in play, children tend to be more creative and engaged. The best play occurs when adults play alongside children, listening and responding to them, rather than just providing toys or supervision. Parental involvement in play therapy can enhance its effectiveness by providing emotional support and continuity at home.
Practical Applications of Therapeutic Play
“Play is not only our creative drive; it’s a fundamental mode of learning.” — David Elkind
- Creating a Play-Friendly Environment: Schools can create dedicated spaces for play, ensuring they are safe and stocked with a variety of materials that encourage creativity and expression. This could include art supplies , building blocks, costumes for role-play, and outdoor play equipment.
- Integrating Play into the Curriculum: Play should be woven into the daily curriculum , not just relegated to playtimes. Teachers can incorporate play-based learning in subjects like maths, science, and communication to make learning more engaging and less stressful.
- Training Educators: Professional development for teachers should include training on the therapeutic benefits of play and how to facilitate it effectively. This training can help teachers recognise signs of emotional distress and use play as a tool for intervention.
- Peer Play Programs: Schools can implement peer play programs where older students are paired with younger ones to mentor through play. This not only benefits the younger children but also fosters leadership and empathy in older students.
- Creating a Play-Rich Environment: Parents can create a play-rich environment at home by providing a variety of toys and materials that stimulate imagination and creativity. It’s important to have both structured and unstructured playtime.
- Engaging in Play: Parental involvement in play is crucial. Parents should actively engage in play with their children, following the child’s lead and allowing them to direct the play.
- Balancing Screen Time: While digital play has its benefits, it’s important to balance screen time with physical and imaginative play . Parents can set limits on screen time and encourage activities like outdoor play, arts and crafts, and board games.
- Observing and Understanding: By observing their children at play, parents can gain insights into their emotional states and any underlying issues. This observation can guide parents in providing the emotional support their children need.
- Setting Up a Play Therapy Room: A play therapy room should be a safe, welcoming space equipped with a variety of toys, art supplies, and other materials that allow children to express themselves. This may include dolls, action figures, sandboxes, puppets, and dress-up clothes.
- Building a Therapeutic Relationship: The therapist’s role is to build a trusting relationship with the child. This involves being empathetic, nonjudgmental, and supportive, allowing the child to feel safe and understood.
- Using Specific Toys and Techniques: Therapists use specific toys and techniques tailored to the child’s needs. For example, a sandbox can be used for a child to create scenes that represent their inner world, while art therapy can help another child express emotions through drawing.
- Involving the Family: Family involvement can enhance the effectiveness of play therapy. Therapists may conduct sessions with parents to help them understand their child’s needs and learn how to support therapeutic play at home.
- Monitoring Progress: Therapists continuously monitor the child’s progress, adjusting the therapeutic approach as needed. This might include changing the types of play activities or incorporating new techniques to address emerging issues.
Case Studies
Case study 1: overcoming anxiety.
Emma (7) was experiencing severe anxiety due to her parents’ recent divorce . She began acting out at school and withdrawing from friends. During play therapy, Emma used a dollhouse to recreate her family dynamics, expressing her fears and confusion about the changes in her life. Through guided play, Emma articulated her feelings and developed coping strategies. Over time, her anxiety reduced , and she became more engaged and happier at school and home.
Case Study 2: Building Social Skills
Liam (5) struggled with social interactions and often felt isolated. His teachers introduced structured play activities encouraging cooperation and communication, such as building projects, Lego and team games. Liam gradually developed better social skills, learning to share, take turns, and express his thoughts. His confidence grew, and he began forming friendships with his peers.
Therapeutic play is profoundly powerful, offering children a natural and effective way to process their emotions, build social skills, and develop resilience. Educators, parents, and therapists can significantly enhance children’s emotional and mental wellbeing by creating environments that support and encourage play . Embracing play as a fundamental aspect of childhood nurtures happier and healthier children and lays the foundation for lifelong emotional health and personal growth.
References Used
Fiss, A. L., Håkstad, R. B., Looper, J., Pereira, S. A., Sargent, B., Silveira, J., Willett, S., & Dusing, S. C. (2023). Embedding Play to Enrich Physical Therapy . Behavioral Sciences , 13 (6), 440. https://doi.org/10.3390/bs13060440
Håkstad, R. B., Øberg, G. K., Girolami, G. L., & Dusing, S. C. (2022). Enactive explorations of children’s sensory-motor play and therapeutic handling in physical therapy . Frontiers in Rehabilitation Sciences , 3 , 994804. https://doi.org/10.3389/fresc.2022.994804
Senko, K., & Bethany, H. (2019). PLAY THERAPY: An Illustrative Case. Innovations in Clinical Neuroscience , 16 (5-6), 38-40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6659989/
Please share if you enjoyed this post.
Similar posts.

Teacher Blogging: 100 Reasons to blog in 2023
Why Education Blogging is worthwhile This is my 100th blog post. So to celebrate I tried to come up…

How School Leaders Can Implement Lessons from Thinking, Fast and Slow
How School Leaders Can Implement Lessons from Thinking, Fast and Slow By Daniel Kahneman In his bestselling book, Thinking,…

A PESTLE Analysis of AI in UK Education
As part of my MSc I had to produce a business report on the UK education system. I couldn’t do…

A Quick Guide to Completing a School Leadership Application & Personal Statement
Writing a School Leadership Application that will get you an Interview Completing a school leadership personal statement and application…

The Ultimate Guide to Transitions.
A Guide to supporting transitions and changes with Autistic students within school.
Transition is a challenge that our students face on a daily basis. These transitions take place on a range of scales. From the micro transition of switching thoughts between tasks to major physical transitions between environments. The number of individual transitions an individual will undertake throughout the day is huge. Each one may well be a source of stress and anxiety for each student. The level of this anxiety and how it is communicated to us will vary dramatically. As with all the actions of our students this stress may not be easy for us to interpret. The quotes are from Autistic people I asked but are anonymised. I know I do not include enough Autistic voice, I will strive to expand this in future posts (I would welcome your comments.)

School Leadership: developing a Vision for your School
Creating a School Vision This is part of a series of posts based on my NPQH learning. A strong,…
One Comment
- Pingback: Unlock the Potential of Play: Maximising Joy and Learning
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Discover more from Special Education and Inclusive Learning
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading
You must be logged in to post a comment.


IMAGES
COMMENTS
The following case studies present three different children with ASD and describe the SLP's strategies to enhance communication and quality of life. The three case studies demonstrate various options in AAC intervention that can be used by children of different ages. —Ann-Mari Pierotti, MS, CCC-SLP. Case Study 1: Anderson | Case Study 2 ...
Conditions and needs of autistic children have impacts on both the children and the family members who have crucial roles in raising the child. The prevalence of autism is increasing, and this fact makes it necessary to focus more on experiences of parents who have children with autism spectrum disorder (ASD). Hence, this study aimed to reflect ...
Participants. The six children (three girls and three boys) participating in the present case study were recruited from a large longitudinal population-based study, performed at the Child Neuropsychiatric Clinic (CNC) in Gothenburg (Kantzer et al., Citation 2013, Citation 2018).The children were initially identified by a general ASD screening at age 2.5 years at the public child health-care ...
Spending time in nature has benefits for wellbeing in children, but relatively little is known about how autistic children experience nature. Framed by self-determination theory, this case study addresses this gap by exploring the experiences of 25 autistic children participating in a Forest School at their specialist school in the East of ...
Keywords: outdoor learning, nature-based learning, special education, case study, autism. Citation: Friedman S and Morrison SA (2021) "I just want to stay out there all day": A Case Study of Two Special Educators and Five Autistic Children Learning Outside at School. Front. Educ. 6:668991. doi: 10.3389/feduc.2021.668991
Although autism studies worldwide have recently gained significant recognition, the experience of raising a child with autism in Greece is seriously underrepresented and unexplored. ... A Case Study of Parent-Child Interaction Therapy for a Young Child with Autism Spectrum Disorder: Behavioral and Developmental Considerations. Psychology. 2020 ...
McDaniel J., Brady N. C., Warren S. F. (2022). Effectiveness of responsivity intervention strategies on prelinguistic and language outcomes for children with autism spectrum disorder: A systematic review and meta-analysis of group and single case studies. Journal of Autism and Developmental Disorders, 52, 4783-4816.
In 1980 the American Psychiatric Association was finalizing diagnostic criteria that would shape the face of autism 1 in the future, and public schools in the United States (U.S.) had been offering educational services to children and youth with disabilities, as mandated by a federal law, for about four years. At that time, autism was a very low-prevalence disorder, occurring in only 2-5 ...
In previous studies, at least three profiles based on these skills have been suggested; autism with language and non-verbal cognitive skills within the average/normal range (ALN), autism with ...
Most studies of social robot interventions for children with autism spectrum disorder have been laboratory experiments focusing on component skills. ... Ismail LI, et al. (2012) Initial response in HRI-a case study on evaluation of child with autism spectrum disorders interacting with a humanoid robot Nao. Procedia Engineering 41: 1448-1455 ...
Case Studies: sharing real-life outcomes and positive experiences. Getting it right for Early Intervention by Grandparent of a former pupil "Our grandson went to a small, local playschool where the kind staff tried valiantly to help him, but it was quite disastrous for him, the staff assigned to him and also the other children.
Focus of the case study Strategies to support the inclusion of an 8-year old autistic pupil with significant anxiety Principles illustrated 1. Understanding the strengths, interests and challenges of the autistic child and young person 2. Enabling the voice of the autistic child and young person to contribute to and influence decisions 3.
CASE STUDY EXAMPLE effective instructional strategy and parents of children with ASD have used this strategy to successfully teach requesting. Additionally, naturalistic intervention is designed to be conducted within natural routines. Next, Mrs. Dell creates a data collection system that is succinct and easy to implement
Abstract. This article aims to observe all the manifestations of the behavior of a child with Autism Spectrum Disorder (ASD), which shows deficits mainly in the communication sector. Also, the ...
The following case studies present three different children with ASD and describe the SLP's strategies to enhance communication and quality of life. The three case studies demonstrate various options in AAC intervention that can be used by children of different ages. —Ann-Mari Pierotti, MS, CCC-SLP Anderson: Excitement and Joy Through ...
This case study of an inclusive classroom provides a comprehensive description of writing processes allowing for demonstration of an assessment procedure and goal development. The case studied is a 6th grade inclusion classroom whereby 2 students were included and diagnosed with an ASD, their typically developing classmates served as a control ...
Abstract. Autism spectrum disorder (ASD) affects more than 1% of children in the United States, with the rate of new diagnoses climbing significantly in the last 15 years. Emergent conditions and subsequent visits to the emergency department (ED) can be particularly challenging for children with ASD, most of whom also have comorbidities in ...
Frontiers in Psychiatry is proud to present our Case Reports series. Our case reports aim to highlight unique cases of patients that present with an unexpected/unusual diagnosis, treatment outcome, or clinical course. Case reports provide insight into the differential diagnosis, decision-making, and clinical management of unusual cases and are a valuable educational tool.<br/><br/>This ...
This case study shows how an 8-year-old boy with autism and mild intellectual disability underwent positive psychological development in terms of play, social communication, and mentalization during a year and a half of group-based therapy using COMSI®-(COMmunication and Social Interaction). This eclectic treatment has a relational approach and is based on developmental psychology, knowledge ...
A case-control study on pre-, peri-, and neonatal risk factors associated with autism spectrum disorder among Armenian children Meri Mkhitaryan 1 , Tamara Avetisyan 2 , 3 ,
Clinical case scenarios: Autism: recognition, referral and diagnosis. September 2011 Page 5 of 60 Clinical case scenarios for professionals working with children and young people Case scenario 1: Howard - recognition, referral and diagnosis Presentation Howard is 7 years old and presents at his GP with his mother as she is
from Integra wrote the case studies and Dr. Glenys Jones was project manager. She also supported the team in writing the guidelines and the case studies. About the Autism Education Trust (AET) The AET partnership focuses on enhancing the knowledge, understanding, skills and practice of staff in Early Years provision, Schools and Post-16 settings.
The present case-control study established effect sizes of change in autistic symptoms, comorbid behavioral problems as well as IQ after one year. Methodology: An intervention group ( N = 20; age: 3.4-7.9 years) and a treatment-as-usual control group ( N = 20; age: 3.2-7.3 years) of children with ASD were matched for developmental and ...
April 25, 202 1. Autism spectrum disorder is considered in broad neurodevelopmen tal. disorder, experience in roughly 1 in 68 children globally ( Autism and. Developmental Disabilities Monitoring ...
Purpose The impacts of the COVID-19 pandemic on autistic children/youth and their families and on service providers are not yet well-understood. This study explored the lived experiences of families with an autistic child and service providers who support them regarding the impacts of the pandemic on service delivery and well-being. Methods In this qualitative study, families and service ...
These measures were shown to be reliable and valid. For Study 2, ELSA was adapted for younger children (ELSA‐Toddler [ELSA‐T]) with samples averaging 29 min from 19 toddlers (2;8-4;10 years) with ASD. Again, measures of frequency of utterances and conversational turns derived from ELSA‐T were shown to have strong psychometric properties.
A Case Study of Autism:…. Arun was brought for consultation with Dr. A M Reddy by his parents. He was about 4 years old, the second child to the parents. Even while he was being brought into the room, we could hear his loud wailing. It took some time for the child to calm down and later we could observe that the child was very restless.
This case study supported this result, although the scale used was different. In particular, in this case, a maximum dose of 5.7 mg of risperidone was administered at the peak severity of CB. ... function-based behavior-analytic interventions are widely used and empirically validated treatments for reducing CB in children with autism. 14 ...
A groundbreaking study has unveiled the most detailed view of the complex biological mechanisms underlying autism, showing the first link between genetic risk of the disorder to observed cellular ...
Case Studies Case Study 1: Overcoming Anxiety. Emma (7) was experiencing severe anxiety due to her parents' recent divorce. She began acting out at school and withdrawing from friends. During play therapy, Emma used a dollhouse to recreate her family dynamics, expressing her fears and confusion about the changes in her life.