An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Recent Advances and Clinical Outcomes of Kidney Transplantation
Charat thongprayoon.
1 Division of Nephrology, Department of Medicine, Mayo Clinic, Rochester, MN 55905, USA; [email protected]
Panupong Hansrivijit
2 Department of Internal Medicine, University of Pittsburgh Medical Center Pinnacle, Harrisburg, PA 17105, USA; ude.cmpu@ptijivirsnah
Napat Leeaphorn
3 Department of Nephrology, Department of Medicine, Saint Luke’s Health System, Kansas City, MO 64111, USA; [email protected]
Prakrati Acharya
4 Division of Nephrology, Department of Medicine, Texas Tech University Health Sciences Center, El Paso, TX 79905, USA; [email protected]
Aldo Torres-Ortiz
5 Department of Medicine, Ochsner Medical Center, New Orleans, LA 70121, USA; moc.liamtoh@68t_odlA
Wisit Kaewput
6 Department of Military and Community Medicine, Phramongkutklao College of Medicine, Bangkok 10400, Thailand; moc.liamg@orhpentisiw
Karthik Kovvuru
7 Division of Nephrology, Department of Medicine, University of Mississippi Medical Center, Jackson, MS 39216, USA; ude.cmu@uruvvokk (K.K.); ude.cmu@irudnaks (S.R.K.)
Swetha R. Kanduri
Tarun bathini.
8 Department of Internal Medicine, University of Arizona, Tucson, AZ 85724, USA; moc.liamg@bbocajnurat
Wisit Cheungpasitporn
Recent advances in surgical, immunosuppressive and monitoring protocols have led to the significant improvement of overall one-year kidney allograft outcomes. Nonetheless, there has not been a significant change in long-term kidney allograft outcomes. In fact, chronic and acute antibody-mediated rejection (ABMR) and non-immunological complications following kidney transplantation, including multiple incidences of primary kidney disease, as well as complications such as cardiovascular diseases, infections, and malignancy are the major factors that have contributed to the failure of kidney allografts. The use of molecular techniques to enhance histological diagnostics and noninvasive surveillance are what the latest studies in the field of clinical kidney transplant seem to mainly focus upon. Increasingly innovative approaches are being used to discover immunosuppressive methods to overcome critical sensitization, prevent the development of anti-human leukocyte antigen (HLA) antibodies, treat chronic active ABMR, and reduce non-immunological complications following kidney transplantation, such as the recurrence of primary kidney disease and other complications, such as cardiovascular diseases, infections, and malignancy. In the present era of utilizing electronic health records (EHRs), it is strongly believed that big data and artificial intelligence will reshape the research done on kidney transplantation in the near future. In addition, the utilization of telemedicine is increasing, providing benefits such as reaching out to kidney transplant patients in remote areas and helping to make scarce healthcare resources more accessible for kidney transplantation. In this article, we discuss the recent research developments in kidney transplants that may affect long-term allografts, as well as the survival of the patient. The latest developments in living kidney donation are also explored.
1. Introduction
Kidney transplantation is the optimal treatment for improving survival and quality of life for patients with end-stage kidney disease (ESKD) [ 1 ]. Advances in surgical, immunosuppressive and monitoring protocols have led to a significant improvement in overall one-year kidney allograft survival of >95% [ 2 ]. Nonetheless, there has not been a significant change in long-term kidney allograft outcomes. In fact, chronic and acute antibody-mediated rejection (ABMR) has continued to cause kidney allograft failures [ 3 ]. In addition, non-immunological complications following kidney transplantation, such as the recurrence of primary kidney disease and other complications, such as cardiovascular diseases, infections, and malignancy also play important roles in poor long-term allografts and patient survival [ 4 , 5 , 6 ].
In their research into immunologic monitoring and diagnostics in kidney transplants [ 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 ], a number of groups have made attempts in the recent past towards determining the peripheral molecular fingerprints of ongoing rejection [ 7 , 8 ] and predicting acute rejection [ 7 ]. Contemporary researchers have measured the levels of donor-derived cell-free DNA (dd-cfDNA) and showed higher predictive abilities for acute rejection [ 9 , 10 , 11 , 12 ], especially antibody-mediated rejection (ABMR) diagnostics in cases with a combination of donor specific antibodies (DSA) and dd-cfDNA [ 13 , 14 ]. In addition, a molecular microscope diagnostic system for the evaluation of allograft biopsies has been recently introduced within transplant practice, particularly in complex cases. This has mainly been introduced for the purpose of enhancing histological diagnostics [ 15 ].
Recent studies have been conducted aimed at preventing or treating ABMR [ 16 , 17 ]. In 2017, imlifidase (IdeS), an endopeptidase derived from Streptococcus pyogenes, was utilized in a desensitization regimen in an open-label phase 1–2 trial [ 16 ]. An instant impact was observed by a significant decline in plasma IgG levels. Another single-center phase 2 study that focused mainly on the pharmacokinetics, effectiveness and safety of IdeS treatment was conducted and proved a reduction in anti-human leukocyte antigen (HLA) antibodies using a complement-dependent cytotoxicity test [ 17 ].
In recent years, there has been significant progress in research into kidney transplantation and kidney donation [ 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 ], including articles [ 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ] published in our current Special Issue "Recent Advances and Clinical Outcomes of Kidney Transplantation" ( https://www.mdpi.com/journal/jcm/special_issues/outcomes_kidney_transplantation ).
In this article, we discuss the recent research developments in kidney transplantation that may impact long-term allografts and patient survival, as well as the latest developments in living kidney donation.
2. Non-HLA Antibodies in Transplantation
When it comes to solid organ transplantation, one major immunological obstacle is the detection the non-self structures that exist in the donor cells. Human leukocyte antigens (HLA) are considered the most important non-self allo-antigens in organ transplantation. In addition, patients can form antibodies against targets other than HLA [ 85 ]. Multiple targets for these non-HLA antibodies have been studied in kidney transplantation over the last decade ( Figure 1 ). Recent studies have provided findings that suggest the an importance of non-HLA mismatches between donors and recipients in the development of acute rejection and long-term kidney allograft outcomes [ 68 , 78 , 86 , 87 , 88 , 89 , 90 , 91 , 92 ].

Post-transplant antibodies against human leukocyte antigen (HLA) and non-HLA antigens [ 68 , 78 , 86 , 87 , 88 , 89 , 90 , 91 , 92 ]. Abbreviations: human leukocyte antigen (HLA), major histocompatibility complex class I related chain A antigen (MICA); angiotensin type 1 receptor (AT1R); endothelin-1 type A receptor (Anti-ETAR); FMS-like tyrosine kinase 3 (FLT3); Epidermal growth factor-like repeats and discoidin I-like domain 3 (EDIL3); Intercellular adhesion molecule 4 (ICAM4).
3. Active AMR
Chronic active ABMR is one of the major causes of long-term allograft loss [ 93 , 94 , 95 ]. Tocilizumab, a humanized monoclonal antibody targeting the interleukin (IL)-6 receptor, has been assessed in patients with acute and chronic active ABMR [ 96 , 97 , 98 ], given that IL-6 mediates various inflammatory and immunomodulatory pathways, including the expansion and activation of T cells and B cells [ 98 ]. Furthermore, there is a genetically engineered humanized Immunoglobulin (Ig)G1 monoclonal antibody that binds to IL-6, inhibiting its interaction with IL-6R. Direct inactivation of IL-6 may limit a rebound induced by the accumulation of IL-6 [ 99 , 100 ]. Preliminary investigations from phase 1–2 trials demonstrated the efficacy of the C1q inhibitor for the prevention of a delayed graft function (DGF) and to lessen the occurrence of chronic active ABMR [ 101 , 102 ]. Although the inhibition of the first step in both the classical and lectin pathways of complement activation may serve as another tool to overcome critical sensitization, such data need to be validated in larger cohorts. Several trials are currently being conducted, and new developments will conceivably provide us with practical ways to counteract the deleterious consequences of ABMR [ 103 ].
4. Cardiovascular Diseases in Kidney Transplant Recipients
The burden of cardiovascular diseases on ESKD is improved after kidney transplantation [ 104 ]. However, it remains the leading cause of reduced early renal graft loss and mortality, as it is associated with significant morbidity and healthcare costs [ 104 ]. Major phenotypes of cardiovascular diseases among kidney transplant recipients include ischemic heart disease, congestive heart failure, valvular heart disease, arrhythmias and pulmonary hypertension ( Figure 2 ).

Incidence (%) of cardiovascular disease in kidney transplant recipients.
Reported risk factors for cardiovascular disease in kidney transplant recipients include inflammatory and immunosuppressive agents, episodes of allograft rejection, as well as traditional cardiovascular risk factors, such as hypertension, hyperlipidemia, smoking, obesity, chronic kidney disease, proteinuria, and diabetes mellitus, all of which add to a transplant recipient’s cardiovascular risk profile [ 104 ]. Hypertension is common among kidney transplant recipients and uncontrolled hypertension in kidney transplant recipients is associated with increased cardiovascular mortality and morbidity, and reduced allograft survival [ 105 ]. Furthermore, weight gain is also a significant problem in post-kidney transplant patients. Weight gain after transplantation can unfavorably affect patient outcomes [ 106 ]. Identifying these risk factors and adopting strategies to abolish these risk factors may potentially prevent, and help manage, post-transplant obesity. The underlying mechanisms for the increased occurrence of dyslipidemia post-transplant are due to immunosuppressive medications, proteinuria, and post-transplant diabetes [ 107 , 108 ].
The medical management of risk factors includes strategies employed in the chronic kidney disease (CKD) population, with credence given to approaches specific for kidney transplant recipients, such as the choice of maintenance immunosuppression, steroid tapering or withdrawal, and particular anti-hypertensive regimens ( Table 1 ). Overall, cardiovascular morbidity and mortality in kidney transplant recipients has decreased over the last few decades, likely due to improved detection and the timely management of risk factors. Recognition of these complications is important in assessing cardiovascular disease risk in kidney transplant recipients, and optimizing screening and therapeutic approaches. These include lifestyle and immunosuppressive regimen modification, as well as the best feasible regimen for glycemic and lipid controls according to an individual’s metabolic profile and medical history.
Cardiovascular risk factors among kidney transplant recipients and suggested management.
American College of Cardiology (ACC); angiotensin-converting enzyme inhibitor (ACEI); American Heart Association (AHA); angiotensin-II receptor blocker (ARB); aspirin (ASA); body mass index (BMI); blood pressure (BP); complete blood count (CBC); calcium-channel blockers (CCB); chronic kidney disease (CKD); cardiovascular disease (CVD); diabetes mellitus (DM); electrocardiography (ECG); estimated glomerular filtration rate (eGFR); Kidney Diseases Improving Global Outcomes (KDIGO); kidney transplant (KTx).
5. Preexisting Diabetes and Post-Transplantation Diabetes
Preexisting diabetes and post-transplantation diabetes confer reduced patient and graft survival in kidney transplant recipients [ 71 , 73 , 125 ]. Hyperglycemia is present in nearly 90% of kidney transplant recipients in the immediate postoperative period, but it is not sustained in the majority [ 126 ]. In addition to the general risk factors for diabetes, there are also certain transplantation-related factors (e.g., specific immunosuppressive agents, surgical stress and inflammation, nutritional interventions) placing kidney transplant recipients at elevated risk of hyperglycemia [ 126 ]. Some transplant immunosuppressive medications, including corticosteroids, calcineurin Inhibitors (CNIs), and mammalian target of rapamycin (mTOR) inhibitors, are associated with a higher incidence of metabolic complications such as post-transplantation diabetes. CNIs impair insulin secretion and sensitivity and directly damage pancreatic islet cells [ 127 ].
A robust evidence base guiding precise glycemic goals is currently lacking in kidney transplant recipients. Management is largely guided by evidence from the general diabetes population [ 71 , 73 , 125 ]. Hospital management of hyperglycemia is primarily achieved through an insulin regimen that takes into account rapid changes in glucocorticoid doses, nutritional modalities and renal function during the immediate post-transplantation period. There is an opportunity to use oral or non-insulin injectable agents in a considerable number of patients by the time they are discharged from the hospital, or in the long run. The use of specific oral or non-insulin injectable agents is guided by patient specifics and the pharmacologic properties of medications. Although several studies have suggested the safe use of sodium glucose transport 2 (SGLT2) inhibitors in kidney transplant recipients [ 128 ], future studies assessing their efficacy and safety are needed, since SGLT2 inhibitor treatment also carries an increased risk of genital tract infections and, possibly, of urinary tract infections [ 129 ]; kidney transplant recipients are particularly susceptible to infections due to immunosuppressive regimens.
6. Posttransplant Malignancy
Cancer is one of the three major causes of death after kidney transplantation [ 130 , 131 ]. Posttransplant malignancy occurrence is widely recognized ( Table 2 ). The effect of viral infections, induction and immunosuppressive maintenance regimens have been proposed as important risk factors for posttransplant malignancy. The increased risk of cancer may be due to viral reactivation induced by immunosuppressive agents or impaired immune surveillance leading to faster tumor growth [ 132 ]. A higher degree of immunosuppression is associated with an increased risk of malignancy, and calcineurin inhibitors can promote carcinogenesis [ 132 ].
Standardized incidence ratio of cancers in kidney transplant recipients [ 133 ].
Confidence Interval (CI).
7. Infection
Solid organ transplant recipients are at greater risk of infection than the non-immunosuppressed population ( Table 3 ) [ 134 ]. Infections are the most common non-cardiovascular causes of mortality following kidney transplantation, accounting for 15%–20% of mortality [ 131 , 135 ]. The first six months post-transplant is the time of greatest infection risk. There are also times when patients encounter adverse reactions to immunosuppressive agents [ 136 , 137 ]. Among all infectious complications, viruses are considered to be the most common agents [ 138 ]. Herpes simplex virus, varicella zoster virus, BK polyomavirus, cytomegalovirus, Epstein–Barr virus, hepatitis B virus, and adenovirus are well-known etiologic agents of viral infections in kidney transplant patients worldwide [ 138 ]. In order to prevent opportunistic infections in kidney transplant recipients, antimicrobial prophylaxis is recommended after kidney transplantation. The recommended prophylactic method after transplant differs based on the organism, as well as individual patient characteristics.
Infection post kidney transplantation.
* Center-dependent multidrug resistant bacteria like Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant Enterococcus (VRE), extended-spectrum beta-lactamases (ESBLs); ** With prophylaxis – with Bactrim and Gancyclovir/Valganciclovir; Abbreviations: cytomegalovirus (CMV), lymphocytic choriomeningitis virus (LCM), Epstein-Barr Virus (EBV), hepatitis B virus (HBV), hepatitis C virus (HCV), Trypanosoma cruzi (T. cruzi), Varicella Zoster virus (VZV), human herpes virus 8 (HHV-8).
8. Latest Developments in Living Kidney Donation
Living donor kidney transplants are the best option for many patients with ESKD for several reasons, including (1) better long-term graft survival, (2) no need to wait on the transplant waiting list for a kidney from a deceased donor, (3) transplant surgery can be planned and (4) lower risks of rejection and DGF [ 139 ]. Living donor kidney transplantation is the optimal treatment for patients with ESKD [ 139 ]. The expansion of living donor programs was made possible by new modes of living donation and by the extension of the living donor pool [ 139 ].
To expand the donor pool, a well-developed paired kidney donation program and the adequate reimbursement of costs associated with donation are fundamental elements [ 140 ]. Paired kidney donation provides living kidney donation for noncompatible donor/recipient pairs that otherwise would not be feasible or need desensitization [ 141 ]. Other possible approaches for increasing the donor pool include ABO-incompatible transplantation [ 142 ], the utilization of higher risk donors, advanced donation with a voucher system, and providing donors with financial incentives [ 141 , 143 , 144 ].
Over the past decade, the long-term risks of kidney donation have been described. Living donors seem to have a higher risk of ESKD, particularly in obese donors and also for African American donors with an apolipoprotein L1 (APOL1) high-risk genotype. In African American living kidney donors, those with the APOL1 high-risk genotype (prevalent in about 13% of African Americans in the United States) had an almost three times more accelerated decline in estimated glomerular filtration rate (eGFR) after adjusting for pre-donation eGFR than those with a low-risk genotype [ 145 ].
9. Post-Transplant Hyperparathyroidism and Bone Disease
Successful renal transplantation results in a reduction in parathyroid hormone (PTH), especially during the first 3 months after transplantation [ 146 ]. However, elevated PTH levels can still be found in 30% to 60% of patients 1 year after transplantation. Persistent hyperparathyroidism following kidney transplantation can result in notable complications, such as fracture/bone diseases, cardiovascular disease, vascular calcification, and allograft dysfunction ( Figure 3 ). Associated factors for persistent hyperparathyroidism are long dialysis duration, high PTH levels prior to transplantation, lower eGFR post-transplant, post-transplant hypercalcemia, and post-transplant high alkaline phosphatase.

Effects and risk factors of post-transplant hyperparathyroidism.
10. Potential Directions and Future Scope
Researchers need to instantly shift their focus on the unaddressed concerns with respect to kidney transplants. Because of the limited supply of organs, numerous potential recipients still have to spend more time in dialysis, waiting for a transplant. Sensitization to HLA antigens inhibits the recipients’ access to transplants, compromising the survival of the graft due to chronic and acute AMR. The publication of complete data from a multi-center second-phase test that explores how IdeS is useful in desensitization is underway ( {"type":"clinical-trial","attrs":{"text":"NCT02790437","term_id":"NCT02790437"}} NCT02790437 ). The phase 3 trial, uncovering the impact of clazakizumab following transplantation, was launched recently, with the outcomes of the phase 2 trial to be released soon.
Moreover, the lack of experienced and skilled professionals could hinder the diagnostic correctness of complications following transplantation. Furthermore, medication non-adherence among patients could increase the alloimune reaction. Notably, medical research on the costimulation blockade during kidney transplantation is underway. A randomized sixty-month multi-center study (CIRRUS, {"type":"clinical-trial","attrs":{"text":"NCT03663335","term_id":"NCT03663335"}} NCT03663335 ) in kidney transplant is also underway, with the aim of defining the range of dosage and assessing the tolerability, safety, and effectiveness of some newly developed anti-CD40 monoclonal antibodies in two distinct cohorts in comparison to a tacrolimus-based regimen. Recently, a phase 2a clinical trial, with the purpose of assessing how effective the dual costimulation blockade with anti-CD40 (VIB4920) is when combined with belatacept in kidney transplantation patients ( {"type":"clinical-trial","attrs":{"text":"NCT04046549","term_id":"NCT04046549"}} NCT04046549 ), was registered.
Big data is increasingly being utilized, with the establishment of a large collection of cohorts and the usage of electronic health records (EHRs) in kidney transplantation and artificial intelligence, which might be useful in solving problems related to the survival analysis of patients who have gone through kidney transplantation [ 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 ]. In the present era, it is strongly believed that big data and artificial intelligence will greatly reshape the research done on kidney disease and, consequently, improve the general clinical practice of nephrology [ 156 ].
The benefits of telemedicine include reaching out to patients in remote areas and helping to make scarce healthcare resources more accessible. As telemedicine applications continue to proliferate, studies have demonstrated that telehealth for transplant care may be associated with a reduction in cost and time, and may also improve access to transplantation for ESKD patients [ 157 , 158 ].
11. Conclusions
The most recent endeavors in kidney transplantation tend to mainly focus on noninvasive monitoring, as well as the improvement of histological diagnostics with the aid of molecular techniques. Such studies offer creative means that can be used to find immunosuppressive agents, which can effectively overcome critical sensitization, prevent the creation of anti-HLA antibodies, treat chronic active ABMR, and reduce non-immunological complications following kidney transplantation, such as the recurrence of primary kidney disease and other complications, such as cardiovascular diseases, infections, and malignancy. In the present era of utilizing EHRs, it is strongly believed that big data and artificial intelligence will reshape the research done on kidney transplantation in the near future. In addition, the utilization of telemedicine is increasing, providing benefits such as reaching out to kidney transplant patients in remote areas and helping to make scarce healthcare resources more accessible for kidney transplantation.
This research received no external funding.
Conflicts of Interest
We do not have any potential financial or non-financial conflicts of interest.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Collection 01 April 2017
Kidney Transplantation
Kidney transplantation is the preferred therapeutic approach for patients with end-stage renal disease. Many challenges remain, however, including a shortage of donor organs, immunological barriers, and the need for long-term immunosuppression, which is associated with an increased risk of infections and malignancies. This collection of articles from Nature Reviews Nephrology discusses a wide range of important topics in kidney transplantation, including long-term risks to living kidney donors, desensitization strategies to enable ABO-incompatible transplantation, antibody-mediated rejection, mechanisms of allograft inflammation, long-term outcomes in paediatric recipients, and the impact of hepatitis C virus infection in transplantation.
- Collection content
- Opinion and comment
- Research Highlights
Renal and cardiac assessment of living kidney donor candidates
To ensure suitability for living kidney donation, donor candidates must be thoroughly evaluated. This Review describes current approaches to the assessment of renal function, haematuria, and cardiac risk in living kidney donor candidates as well as strategies to improve efficiency in the evaluation process, focusing on additional investigations that are commonly ordered by transplant centres rather than the minimum initial screening requirements.
- Ngan N. Lam
- Krista L. Lentine
- Amit X. Garg
Roles of mTOR complexes in the kidney: implications for renal disease and transplantation
The mTOR pathway has a role in the development of renal disease, kidney transplant rejection and malignancies. Here, the authors discuss the mechanisms by which mTOR complexes drive the pathogenesis of these diseases as well as the therapeutic potential of mTOR inhibitors.
- Daniel Fantus
- Natasha M. Rogers
- Angus W. Thomson
The importance of non-HLA antibodies in transplantation
Antibodies directed against non-HLA antigens such as angiotensin type 1 receptor, perlecan and collagen have been implicated in antibody-mediated rejection. Here, Elaine Reed and Qiuheng Zhang discuss the clinical relevance and pathogenesis of these non-HLA antibodies in renal, heart and lung transplantation.
- Qiuheng Zhang
- Elaine F. Reed
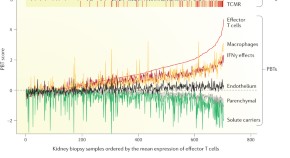
Molecular assessment of disease states in kidney transplant biopsy samples
Molecular phenotyping of renal biopsy samples from transplant recipients has the potential to improve diagnostic precision and understanding of disease processes. In this Review, Philip Halloran et al . describe their strategy to develop a system that enables the molecular assessment of transplant biopsy samples. They discuss the molecular phenotypes of rejection and injury, and how these studies have improved understanding of the processes that occur in renal transplants over time.
- Philip F. Halloran
- Konrad S. Famulski

Complement in disease: a defence system turning offensive
The functions of the complement system are diverse and extend beyond its role in host defence; complement activation is now known to contribute to numerous immunological, inflammatory and age-related conditions, including kidney disorders. Here, John Lambris and colleagues discuss the key activating, regulatory, and effector mechanisms of the complement system. They highlight important crosstalk connections with other regulatory systems, and, with a focus on kidney disease and transplantation, describe the involvement of complement in clinical conditions as well as promising therapeutic approaches.
- Daniel Ricklin
- Edimara S. Reis
- John D. Lambris

Role of TLRs and DAMPs in allograft inflammation and transplant outcomes
Graft necrosis resulting from ischaemia–reperfusion injury leads to the release of endogenous molecules — damage-associated molecular patterns (DAMPs) — which trigger a sterile inflammatory reaction. The resulting immune response can impair transplant tolerance or result in acute or chronic graft rejection. In this Review, Braza et al . discuss the nature of DAMPs and their downstream signalling pathways, with a focus on Toll-like receptors. They outline various strategies to inhibit DAMP-induced inflammation with the aim of improving the outcomes of solid organ transplantation, and discuss the challenge of inhibiting the innate immune response within the graft without compromising the patient's response to pathogens.
- Faouzi Braza
- Sophie Brouard
- Daniel R. Goldstein

Memory T cells in organ transplantation: progress and challenges
Memory T cells and their ability to generate an anamnestic response are vital for protective immunity, but have a potentially detrimental impact on allograft survival. Here, Allan Kirk and colleagues discuss the generation of memory T cells, their role in allograft rejection and therapeutic strategies that target allospecific memory T-cell responses and might improve outcomes in organ transplantation.
- Jaclyn R. Espinosa
- Kannan P. Samy
- Allan D. Kirk

Mesenchymal stromal cells in renal transplantation: opportunities and challenges
The unique immunomodulatory properties of multipotent mesenchymal stromal cells (MSCs) make them a promising candidate for cell therapy in organ transplantation. Here, the authors review preclinical data that support the potential tolerance-inducing effects of MSCs in transplant models and the results of initial clinical studies in kidney transplantation.
- Federica Casiraghi
- Norberto Perico
- Giuseppe Remuzzi
Long-term effects of paediatric kidney transplantation
Renal transplantation can be successfully performed in patients of all ages, and the short-term and medium-term outcomes have improved over the past decades. In this Review, Christer Holmberg and Hannu Jalanko discuss the long-term effects of kidney transplantation on paediatric recipients. They outline the adverse effects that can occur with regard to growth, bone health, metabolic and cardiovascular complications, and malignancies, and highlight the challenges that remain in managing the care of paediatric renal transplant recipients.
- Christer Holmberg
- Hannu Jalanko

Phosphate and FGF-23 homeostasis after kidney transplantation
Dysregulated phosphate metabolism is a common consequence of kidney disease and renal transplantation. In this Review, Martin H. de Borst and colleagues outline the pathophysiology of dysregulated phosphate metabolism in renal transplant recipients and discuss the effect of this dysregulation on the cardiovascular system, bone, and the kidney graft. They also propose possible strategies to correct phosphate abnormalities in these patients.
- Leandro C. Baia
- Ita Pfeferman Heilberg
- for the NIGRAM investigators

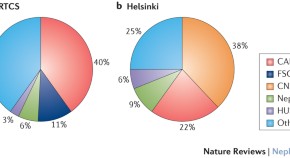
Strategies to overcome the ABO barrier in kidney transplantation
The development of effective desensitization strategies has enabled ABO incompatible (ABOi) kidney transplantation to become an established treatment option for patients with end-stage renal disease. Here, the authors review the mechanisms that underlie acceptance and rejection of ABOi grafts, recipient desensitization strategies, patient outcomes and novel treatment strategies that might promote graft acceptance and enable minimization of immunosuppression.
- Georg A. Böhmig
- Andreas M. Farkas
- Thomas Wekerle

Microbiota—implications for immunity and transplantation
Resident microorganisms in the human body vastly outnumber host cells and have an important role in human physiology. In this Review, Bromberg and colleagues discuss the basic principles that guide analyses of the microbiota, including the challenges of measuring and quantifying microbiota. They also discuss the influence of the microbiota on the immune system and the implications of these effects on organ failure and transplantation.
- Jonathan S. Bromberg
- W. Florian Fricke
- Emmanuel F. Mongodin
Long-term medical risks to the living kidney donor
Transplantation of kidneys from living donors benefits patients with end-stage renal disease, but living donation is associated with short-term and long-term risks. In this Review, the authors summarize studies that have examined the long-term medical outcomes for living kidney donors, focusing on the first 10 years after donation. They also consider the need to further assess risk in specific populations of donors.
Primary disease recurrence—effects on paediatric renal transplantation outcomes
Renal transplantation is the optimal form of renal replacement therapy for children with end-stage renal disease; however, disease recurrence can lead to graft loss, morbidity and death. In this Review, Justine Bacchetta and Pierre Cochat provide an update on the epidemiology, pathophysiology, effects and management of disease recurrence after paediatric renal transplantation. They also describe pretransplantation and post-transplantation risk-reduction strategies that aim to minimize the possibility of disease recurrence, and thus improve both graft and patient outcomes.
- Justine Bacchetta
- Pierre Cochat
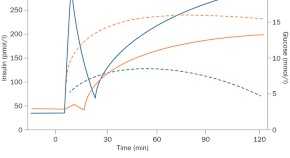
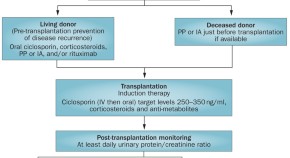
Emerging treatments for post-transplantation diabetes mellitus
Post-transplantation diabetes mellitus (PTDM) is a frequent complication among renal transplant recipients, and is associated with cardiovascular disease and reduced lifespan. In this Review, Jenssen and Hartmann discuss the diagnostic criteria for PTDM and evaluate available and emerging treatment options, highlighting the considerations that should be made when selecting an appropriate therapeutic regimen.
- Trond Jenssen
- Anders Hartmann

Hepatitis C and its impact on renal transplantation
Hepatitis C virus (HCV) infection imposes a substantial economic, clinical, and societal burden worldwide. In this Review, Morales and Fabrizi compare the treatment options that are available to patients with HCV infection, before and after renal transplantation. The development of novel therapeutic strategies and the clinical complications associated with HCV infection are discussed. The authors conclude with an assessment of the safe use of organs donated from individuals with active HCV infection.
- Jose M. Morales
- Fabrizio Fabrizi
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
A systematic review of kidney transplantation outcomes in patients with end-stage renal disease due to childhood lower urinary tract malformations
- Urology – Review
- Published: 21 May 2024
Cite this article

- Hakan Bahadir Haberal 1 na1 ,
- Muhammet Irfan Donmez 2 na1 ,
- Alberto Piana 3 ,
- Alessio Pecoraro 4 ,
- Thomas Prudhomme 5 ,
- Beatriz Bañuelos Marco 6 ,
- Alicia López-Abad 7 ,
- Riccardo Campi 4 , 8 ,
- Romain Boissier 9 ,
- Alberto Breda 10 ,
- Angelo Territo 10 on behalf of
EAU Young Academic Urologists (YAU) Kidney Transplantation Working Group
66 Accesses
4 Altmetric
Explore all metrics
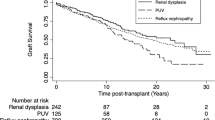
Patients with lower urinary tract malformations (LUTM) were suspended from kidney transplantation (KT) programs in the past due to various concerns. Consequently, only a limited number of studies have explored this topic at hand. In this study, our objective was to perform a systematic review (SR) to evaluate the current evidence regarding KT outcomes as well as patient survival (PS), postoperative complications and urinary tract infections (UTI) in individuals with childhood LUTM.
The search encompassed databases of Web of Science, Medline (via PubMed), and Embase (via Scopus) to identify all studies reporting outcomes on KT for patients with LUTM. The research included articles published in English from January 1995 till September 2023.
Of the 2634 yielded articles, 15 met the inclusion criteria, enrolling a total of 284,866 KT patients. There was significantly better 5-year graft survival (GS) in recipients with LUTM compared to the control group (RR, 1.04; 95% CI 1.02–1.06); while GS at 1-year and 10-year, and PS at 1-year, 5-year and 10-year were similar between groups. On the other hand, the postoperative UTI rate was significantly higher in the LUTM group (RR: 4.46; 95% CI 1.89–10.51). However, data on serum creatinine and estimated glomerular filtration rate on follow-up were insufficient.
GS and PS rates appear to be similar in patients with childhood LUTM and those with normal lower urinary tract functions. Despite a higher postoperative UTI rate within this patient group, it appears that this has no effect on GS rates.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others
Long-term outcome of kidney transplantation in patients with congenital anomalies of the kidney and urinary tract

Endourological Management of Urological Complications Following Renal Transplantation
Renal transplantation in children weighing <15 kg: does concomitant lower urinary tract dysfunction influence the outcome, data availability.
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Stonebrook E, Hoff M, Spencer JD (2019) Congenital anomalies of the kidney and urinary tract: a clinical review. Curr Treat Options Pediatr 5(3):223–235. https://doi.org/10.1007/s40746-019-00166-3
Article PubMed PubMed Central Google Scholar
Harada R, Hamasaki Y, Okuda Y, Hamada R, Ishikura K (2022) Epidemiology of pediatric chronic kidney disease/kidney failure: learning from registries and cohort studies. Pediatr Nephrol 37(6):1215–1229. https://doi.org/10.1007/s00467-021-05145-1
Article PubMed Google Scholar
Czyzewski L, Sanko-Resmer J, Wyzgal J, Kurowski A (2014) Assessment of health-related quality of life of patients after kidney transplantation in comparison with hemodialysis and peritoneal dialysis. Ann Transplant 19:576–585
Article CAS PubMed Google Scholar
Guha C, van Zwieten A, Khalid R, Kim S, Walker A, Francis A, Didsbury M, Teixeira-Pinto A, Barton B, Prestidge C, Lancsar E, Mackie F, Kwon J, Howard K, Mallitt KA, Howell M, Jaure A, Hayes A, Raghunandan R, Petrou S, Lah S, McTaggart S, Craig JC, Wong G (2023) Longitudinal assessment of the health-related quality of life of children and adolescents with chronic kidney disease. Kidney Int 103(2):357–364. https://doi.org/10.1016/j.kint.2022.09.026
Purnell TS, Auguste P, Crews DC, Lamprea-Montealegre J, Olufade T, Greer R, Ephraim P, Sheu J, Kostecki D, Powe NR, Rabb H, Jaar B, Boulware LE (2013) Comparison of life participation activities among adults treated by hemodialysis, peritoneal dialysis, and kidney transplantation: a systematic review. Am J Kidney Dis 62(5):953–973. https://doi.org/10.1053/j.ajkd.2013.03.022
Riley P, Marks SD, Desai DY, Mushtaq I, Koffman G, Mamode N (2010) Challenges facing renal transplantation in pediatric patients with lower urinary tract dysfunction. Transplantation 89(11):1299–1307. https://doi.org/10.1097/tp.0b013e3181de5b8c
Marchal S, Kalfa N, Iborra F, Badet L, Karam G, Broudeur L, Branchereau J, Abdo N, Thuret R (2020) Long-term outcome of renal transplantation in patients with congenital lower urinary tract malformations: a multicenter study. Transplantation 104(1):165–171. https://doi.org/10.1097/TP.0000000000002746
Cornwell LB, Ingulli EG, Mason MD, Ewing E, Riddell JV (2021) Renal transplants due to congenital anomalies of the kidney and urinary tract (CAKUT) have better graft survival than non-CAKUT controls: analysis of over 10,000 patients. Urology 154:255–262. https://doi.org/10.1016/j.urology.2021.01.005
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Article Google Scholar
First MR (1992) Renal transplantation for the nephrologist: new immunosuppressive drugs. Am J Kidney Dis 19(1):3–9. https://doi.org/10.1016/s0272-6386(12)70195-6
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hrobjartsson A, Kirkham J, Juni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schunemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. https://doi.org/10.1136/bmj.i4919
Artiles A, Dominguez A, Subiela JD, Boissier R, Campi R, Prudhomme T, Pecoraro A, Breda A, Burgos FJ, Territo A, Hevia V, Group E-YKTW (2023) Kidney transplant outcomes in elderly population: a systematic review and meta-analysis. Eur Urol Open Sci 51:13–25. https://doi.org/10.1016/j.euros.2023.02.011
Mesnard B, Territo A, Campi R, Hevia V, Andras I, Piana A, Pecoraro A, Boissier R, Prudhomme T, Transplantation EA-YAUgoK (2023) Kidney transplantation from elderly donors (> 70 years): a systematic review. World J Urol 41(3):695–707. https://doi.org/10.1007/s00345-023-04311-4
Prudhomme T, Mesnard B, Abbo O, Banuelos B, Territo A, Transplantation EAUYAUgoK, the EAUYAUgoPU (2023) Postoperative surgical complications after pediatric kidney transplantation in low weight recipients (<15 kg) a systematic review. Curr Opin Organ Transplant 28(4):297–308
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Haberal HB, Zakri R, Olsburgh J (2022) Medium and long-term clinical outcomes of kidney transplantation in patients with prune belly syndrome: a single-centre experience. Urology 169:245–249. https://doi.org/10.1016/j.urology.2022.08.023
Rickard M, Chua ME, Zu’bi F, Dos Santos J, Koyle MA, Lorenzo AJ, Farhat WA (2020) Comparative outcome analysis of pediatric kidney transplant in posterior urethral valves children with or without pretransplant Mitrofanoff procedure. Pediatr Transplant 24(8):e13798. https://doi.org/10.1111/petr.13798
Al-Khudairi N, Riley P, Desai DY, Reid C, Marks SD, Mamode N (2013) Interventions for impaired bladders in paediatric renal transplant recipients with lower urinary tract dysfunction. Transpl Int 26(4):428–434. https://doi.org/10.1111/tri.12063
Kaya Aksoy G, Koyun M, Dinckan A, Aliosmanoglu I, Gemici A, Gultekin E, Comak E, Akman S (2021) Graft survival in patients with lower urinary tract dysfunction. Exp Clin Transplant 19(2):125–130. https://doi.org/10.6002/ect.2018.0029
Christman MS, Canning DA, Schast AP, Baluarte HJ, Kaplan BS (2013) Renal transplantation into a diverted urinary system-is it safe in children? J Urol 190(2):678–682. https://doi.org/10.1016/j.juro.2013.02.019
Figueiredo R, Meireles D, Costa T, Mota C, Caldas Afonso A (2021) Renal transplant in pediatric patients with congenital abnormalities of the lower urinary tract. Exp Clin Transplant 19(4):310–315. https://doi.org/10.6002/ect.2020.0325
Aki FT, Aydin AM, Dogan HS, Donmez MI, Erkan I, Duzova A, Topaloglu R, Tekgul S (2015) Does lower urinary tract status affect renal transplantation outcomes in children? Transplant Proc 47(4):1114–1116. https://doi.org/10.1016/j.transproceed.2014.10.069
Luke PP, Herz DB, Bellinger MF, Chakrabarti P, Vivas CA, Scantlebury VP, Hakala TR, Jevnikar AM, Jain A, Shapiro R, Jordan ML (2003) Long-term results of pediatric renal transplantation into a dysfunctional lower urinary tract. Transplantation 76(11):1578–1582. https://doi.org/10.1097/01.TP.0000090866.00241.0C
Saad IR, Habib E, ElSheemy MS, Abdel-Hakim M, Sheba M, Mosleh A, Salah DM, Bazaraa H, Fadel FI, Morsi HA, Badawy H (2016) Outcomes of living donor renal transplantation in children with lower urinary tract dysfunction: a comparative retrospective study. BJU Int 118(2):320–326. https://doi.org/10.1111/bju.13347
Hebenstreit D, Csaicsich D, Hebenstreit K, Muller-Sacherer T, Berlakovich G, Springer A (2018) Long-term outcome of pediatric renal transplantation in boys with posterior urethral valves. J Pediatr Surg 53(11):2256–2260. https://doi.org/10.1016/j.jpedsurg.2018.07.003
Kara E, Sakaci T, Ahbap E, Sahutoglu T, Koc Y, Basturk T, Sevinc M, Akgol C, Kayalar AO, Ucar ZA, Unsal A, Seyahi N (2016) Posttransplant urinary tract infection rates and graft outcome in kidney transplantation for end-stage renal disease due to reflux nephropathy versus chronic glomerulonephritis. Transplant Proc 48(6):2065–2071. https://doi.org/10.1016/j.transproceed.2016.05.009
Lopez Pereira P, Ortiz R, Espinosa L, Martinez Urrutia MJ, Lobato R, Alonso A, Jaureguizar E (2014) Does bladder augmentation negatively affect renal transplant outcome in posterior urethral valve patients? J Pediatr Urol 10(5):892–897. https://doi.org/10.1016/j.jpurol.2014.01.011
Traxel E, DeFoor W, Minevich E, Reddy P, Alam S, Reeves D, Sheldon C (2011) Low incidence of urinary tract infections following renal transplantation in children with bladder augmentation. J Urol 186(2):667–671. https://doi.org/10.1016/j.juro.2011.03.155
Territo A, Bajeot AS, Mesnard B, Campi R, Pecoraro A, Hevia V, Piana A, Doumerc N, Breda A, Boissier R, Prudhomme T (2023) Open versus robotic-assisted kidney transplantation: a systematic review by the European Association of Urology (EAU)—Young Academic Urologists (YAU) Kidney Transplant Working Group. Actas Urol Esp (Engl Ed) 47(8):474–487. https://doi.org/10.1016/j.acuroe.2023.03.003
Salomon L, Fontaine E, Gagnadoux MF, Broyer M, Beurton D (1997) Posterior urethral valves: long-term renal function consequences after transplantation. J Urol 157(3):992–995. https://doi.org/10.1016/s0022-5347(01)65128-0
Oomen L, de Wall LL, Cornelissen EAM, Feitz WFJ, Bootsma-Robroeks C (2021) Prognostic factors on graft function in pediatric kidney recipients. Transplant Proc 53(3):889–896. https://doi.org/10.1016/j.transproceed.2020.10.017
Amesty MV, Garcia-Vaz C, Espinosa L, Martinez-Urrutia MJ, Lopez-Pereira P (2021) Long-term renal transplant outcome in patients with posterior urethral valves. prognostic factors related to bladder dysfunction management. Front Pediatr 9:646923. https://doi.org/10.3389/fped.2021.646923
Colgan R, Jaffe GA, Nicolle LE (2020) Asymptomatic bacteriuria. Am Fam Physician 102(2):99–104
PubMed Google Scholar
Banuelos Marco B, Donmez MI, Geppert T, Prudhomme T, Campi R, Mesnard B, Hevia V, Boissier R, Pecoraro A, Territo A, Eau - Yau Kidney Transplant PWG, (2023) Renal transplantation in pediatric recipients: considerations and preoperative assessment strategies. Actas Urol Esp (Engl Ed) 47(6):351–359. https://doi.org/10.1016/j.acuroe.2023.03.002
Sager C, Burek C, Duran V, Corbetta JP, Weller S, Paz E, Lopez JC (2011) Outcome of renal transplant in patients with abnormal urinary tract. Pediatr Surg Int 27(4):423–430. https://doi.org/10.1007/s00383-010-2704-4
Jesus LE, Pippi Salle JL (2015) Pre-transplant management of valve bladder: a critical literature review. J Pediatr Urol 11(1):5–11. https://doi.org/10.1016/j.jpurol.2014.12.001
Basiri A, Otookesh H, Hosseini R, Simforoosh N, Moghaddam SM (2009) Kidney transplantation before or after augmentation cystoplasty in children with high-pressure neurogenic bladder. BJU Int 103(1):86–88. https://doi.org/10.1111/j.1464-410X.2008.08081.x
Salman B, Hassan A, Selim M, Abdelbaky T, Sultan S, Halawa A (2018) Renal transplant in abnormal bladder: treatment options and their effects on graft outcome. Exp Clin Transplant 16(6):660–664. https://doi.org/10.6002/ect.2016.0360
Nahas WC, Antonopoulos IM, Piovesan AC, Pereira LM, Kanashiro H, David-Neto E, Ianhez LE, Srougi M (2008) Comparison of renal transplantation outcomes in children with and without bladder dysfunction. a customized approach equals the difference. J Urol 179(2):712–716. https://doi.org/10.1016/j.juro.2007.09.094
Neild GH, Dakmish A, Wood S, Nauth-Misir R, Woodhouse CR (2004) Renal transplantation in adults with abnormal bladders. Transplantation 77(7):1123–1127. https://doi.org/10.1097/01.tp.0000116712.56265.78
McKay AM, Kim S, Kennedy SE (2019) Long-term outcome of kidney transplantation in patients with congenital anomalies of the kidney and urinary tract. Pediatr Nephrol 34(11):2409–2415. https://doi.org/10.1007/s00467-019-04300-z
Adams J, Mehls O, Wiesel M (2004) Pediatric renal transplantation and the dysfunctional bladder. Transpl Int 17(10):596–602. https://doi.org/10.1007/s00147-004-0784-6
Download references
Acknowledgements
None declared.
Author information
Hakan Bahadir Haberal and Muhammet Irfan Donmez have contributed equally to this article.
Authors and Affiliations
Department of Urology, Ankara Ataturk Sanatorium Training and Research Hospital, Ministry of Health, University of Health Sciences, 06290, Ankara, Turkey
Hakan Bahadir Haberal
Department of Urology, Division of Pediatric Urology, Istanbul University Istanbul Faculty of Medicine, Istanbul, Turkey
Muhammet Irfan Donmez
Department of Urology, San Luigi Gonzaga Hospital, University of Turin, Orbassano, Turin, Italy
Alberto Piana
Unit of Urological Robotic Surgery and Renal Transplantation, Careggi Hospital, University of Florence, Florence, Italy
Alessio Pecoraro & Riccardo Campi
Department of Urology and Kidney Transplantation, Rangueil University Hospital, Toulouse, France
Thomas Prudhomme
Department of Urology, Renal Transplant Division, University Hospital Clínico San Carlos, Madrid, Spain
Beatriz Bañuelos Marco
Department of Urology, Virgen de La Arrixaca University Hospital, Murcia, Spain
Alicia López-Abad
Department of Experimental and Clinical Medicine, University of Florence, Florence, Italy
Riccardo Campi
Department of Urology and Renal Transplantation, La Conception University Hospital, Marseille, France
Romain Boissier
Uro-Oncology and Kidney Transplant Unit, Department of Urology at “Fundació Puigvert” Hospital, Autonoma University of Barcelona, Barcelona, Spain
Alberto Breda & Angelo Territo
You can also search for this author in PubMed Google Scholar
Contributions
Study concept and design: H.B.H., M.I.D., A.P., A.P., T.P., B.B.M., A.B., and A.T.; analysis and interpretation of data: H.B.H., M.I.D., and A.T.; drafting of the manuscript: H.B.H., M.I.D., A.P., A.P., T.P., B.B.M., A.L., R.C., R.B., A.B., and A.T.; statistical analysis: H.B.H. and M.I.D.; supervision: R.C., R.B., and A.B. All authors reviewed the manuscript.
Corresponding author
Correspondence to Hakan Bahadir Haberal .
Ethics declarations
Conflict of interest, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Haberal, H.B., Donmez, M.I., Piana, A. et al. A systematic review of kidney transplantation outcomes in patients with end-stage renal disease due to childhood lower urinary tract malformations. Int Urol Nephrol (2024). https://doi.org/10.1007/s11255-024-04079-5
Download citation
Received : 12 April 2024
Accepted : 11 May 2024
Published : 21 May 2024
DOI : https://doi.org/10.1007/s11255-024-04079-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Congenital abnormalities
- End-stage renal disease
- Graft survival
- Kidney transplantation
- Urinary tract
- Find a journal
- Publish with us
- Track your research
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Cover Archive
- Author videos
- Supplements
- Cover Images
- Author Guidelines
- Submission Site
- Open Access Options
- Why publish with NDT?
- About the ERA
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Terms and Conditions
- Editorial Fellowship
- The ERA Journals
- Journals on Oxford Academic
- Books on Oxford Academic

Browse issues

Cover image

Volume 39, Issue 5, May 2024
Eular 2023 recommendations for sle treatment: synopsis for the management of lupus nephritis: the european renal association–immunonephrology working group (era-iwg) perspective.
- View article
- Supplementary data
Using genomics to understand severe COVID-19
Maintaining kidney replacement therapy during armed conflicts, does it matter how we measure urinary creatinine in patients taking sglt2 inhibitors, shared decision making in elderly patients with kidney failure, endothelial to mesenchymal transition in kidney fibrosis, cell–cell communication in kidney fibrosis, treatment standard, anaemia in ckd—treatment standard, original article, how obesity and metabolic syndrome affect cardiovascular events, progression to kidney failure and all-cause mortality in chronic kidney disease.


Twenty-four-hour urine oxalate and risk of chronic kidney disease

Chronic kidney disease increases the susceptibility to negative effects of low and high potassium intake

Early progression of chronic histologic lesions in kidney transplant biopsies is not associated with HLA histocompatibility

Statin therapy and the incidence of atherosclerotic cardiovascular events after kidney transplantation
Insomnia in patients on incident maintenance dialysis and the risk of major acute cardio-cerebrovascular events and all-cause mortality.

Higher beta-hydroxybutyrate ketone levels associated with a slower kidney function decline in ADPKD

A new approach for cognitive impairment pattern in chronic kidney disease

Intraindividual difference in estimated GFR by creatinine and cystatin C, cognitive trajectories and motoric cognitive risk syndrome

Urinary peptide analysis to predict the response to blood pressure medication
Research letter, utility of 2-year kidney failure risk equation for advanced chronic kidney disease: analysis from the stop-acei trial, proliferative glomerulonephritis with monoclonal immunoglobulin deposits in the native or posttransplant kidney, initial rituximab monotherapy for adult indiopathic nephrotic syndrome with minimal change lesion pattern, email alerts.
- ndt Twitter
- ERA Twitter
- ERA Facebook
- ERA Instagram
- ERA LinkedIn
- Recommend to Your Librarian
Affiliations

- Online ISSN 1460-2385
- Print ISSN 0931-0509
- Copyright © 2024 European Renal Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Transplant Research Center
Kidney and pancreas transplant research program.
The Kidney and Pancreas Transplant Research Program within the Mayo Clinic Transplant Research Center focuses its research efforts on overcoming the challenges that limit the success of kidney and pancreas transplantation.
Research focus areas
Research focus areas in the Kidney and Pancreas Transplant Research Program include:
Overcoming antibody barriers
Reducing disease recurrence, improving long-term success, expanding living-donor transplants, pre-emptive transplantation, immunosuppression characteristics and new treatments, managing cardiovascular complications.
Here's a closer look at the focus areas.
Researchers in the Kidney and Pancreas Transplant Research Program have led the way in developing treatment strategies that reduce antibody levels, which allowed for successful living-donor kidney transplants even with incompatible blood types.
Antibodies are proteins produced by the body to protect it against substances, cells or organs that are foreign. These antibodies are essential for health. However, at times these antibodies can prevent a patient from receiving a transplant, because they can quickly destroy the transplanted kidney or pancreas. Antibodies can be directed against blood groups or against donor cells (called a positive crossmatch).
Researchers have developed several strategies to allow transplantation even in the presence of antibodies.
- At Mayo Clinic, investigators apply sophisticated techniques to differentiate which antibodies pose a problem for transplantation and which don't.
- Researchers also apply techniques to remove these antibodies from blood before transplant and to control negative effects of these antibodies on the kidney with medications.
- Patients with kidney failure and high levels of antibodies can receive kidneys from a larger pool of living donors and may be able to participate in Mayo Clinic's paired donation program . As a result, qualified patients with kidney failure are able to avoid lengthy or indefinite waiting periods for deceased-donor transplants.
Ongoing research in the area of antibody resistance includes:
- The effect of antibody development on the transplanted kidney and pancreas
- Laboratory investigations of the cells responsible for producing damaging antibodies
- Clinical testing of new treatments for reducing or preventing the production of donor-specific antibodies
Researchers in the Kidney and Pancreas Transplant Research Program are studying ways to identify treatments that reduce the risk of recurrent disease after a kidney transplant.
Several of the diseases that can cause kidney failure can come back and attack a newly transplanted kidney. In fact, approximately 20% to 25% of kidney transplants are lost because of disease recurrence.
To address this problem, Mayo Clinic researchers have taken several steps.
- First, researchers identified diseases that are most likely to recur in the transplanted kidney.
- Second, with the use of protocol biopsies, researchers identified the earliest signs of disease recurrence in the transplanted kidney, with the intent of improving outcomes by treating patients when disease recurrence is detected.
- Third, researchers developed new treatments that can be given to the patient to prevent disease recurrence or to treat it when it occurs.
Researchers have made significant advances in the prevention and treatment of some of the most dangerous diseases for the transplanted kidney, including focal segmental glomerulosclerosis , membranous nephropathy and membranoproliferative glomerulonephritis.
Research in this area continues to further refine disease classification and identify optimal treatment options to prevent disease recurrence because each of these diseases seems to require specific management strategies.
The premature loss of transplanted organs traditionally has been attributed to poorly characterized diseases that are frequently lumped together under the term "chronic rejection."
Researchers in the Kidney and Pancreas Transplant Research Program have taken a different approach to this problem by first questioning what precisely causes the loss of kidney and pancreas transplants.
Using kidney biopsies and careful examination of laboratory and clinical parameters, the Mayo Clinic researchers determined that kidney transplants can be lost for multiple reasons. In most cases, the cause of the kidney loss was because of known diseases that could potentially be prevented and treated.
These investigations also make it abundantly clear that a comprehensive approach addressing all the threats that can harm the transplanted organ is needed for transplant success.
Researchers developed a series of tools that allow them to monitor outcomes-particular management strategies.
These tools include:
- A continually updated database to gather information about a multitude of clinical, laboratory and biopsy parameters in thousands of patients over time
- Protocol biopsies for pathology review of kidney transplants at specific time points during the first 10 years after transplant
- Microarray studies examining the expression of thousands of genes within kidney transplant tissues, helping researchers understand how the kidney reacts in response to injury
- Screening tests for potentially damaging viral infections and immune responses in kidney transplant recipients
- Monitoring of the production of antibodies against the transplanted kidney or pancreas, thus allowing researchers to determine whether immunosuppressive medications that the patient receives after the transplant are effective
Mayo Clinic has performed living-donor kidney transplants since 1963 and has the largest single-living-donor program in the United States.
In order for the practice of living-donor transplant to remain successful and safe for both donor and recipient, researchers in the Kidney and Pancreas Transplant Research Program have placed a high priority on research into the short- and long-term outcomes for kidney donation.
Ongoing clinical investigations include:
- Effect of kidney donation on blood pressure
- Impact of obesity on kidney donation
- Long-term outcomes of kidney donation
- Impact of donor age on transplant success
Researchers in the Kidney and Pancreas Transplant Research Program also have a strong commitment to expand pre-emptive transplantation — transplantation of a kidney in patients who have never received dialysis.
Investigators have shown in the past that dialysis prior to transplantation limits the life span of the recipient. Avoiding dialysis, particularly for more than one year, has beneficial consequences for the patient and perhaps the transplanted organ. In addition, pre-emptive transplantation reduces medical costs.
At times, patients are told that a period of dialysis is required before receiving a transplant. Researchers at Mayo Clinic believe that patients should be encouraged to consider transplantation as their kidneys start to fail.
The success of this program is closely tied to the success of living-donor kidney transplantation in the Kidney and Pancreas Transplant Research Program. However, it's possible to achieve pre-emptive transplantation with deceased-donor kidneys if patients are placed on the waiting list soon enough.
Ongoing investigations include:
- Evaluation of medical, psychological, quality of life and financial implications of pre-emptive transplantation
- Evaluation on how collaborative efforts with referring physicians and even insurance companies can facilitate pre-emptive transplantation
The Kidney and Pancreas Transplant Research Program has conducted and participated in many clinical studies designed to examine the benefits associated with new immunosuppressive medications and combinations of medications compared with established regimens.
Because most organ transplants require the use of two or more medications combined over time, the design of optimal immunosuppression regimens for individual organs and patient groups has grown more complex.
Mayo Clinic researchers have examined changes in the structure of transplanted kidneys using protocol biopsies and determined that prolongation of kidney survival likely will require re-examination of the approach to immunosuppression after the first year post-transplant.
By understanding what is happening inside the transplanted organ, researchers can design new strategies to achieve long-term success. Protocol biopsies are essential tools to achieve this goal.
Mayo Clinic researchers and physicians are conducting research to identify the causes of cardiovascular disease in kidney transplant recipients and the benefits of different treatment and prevention strategies.
Certain kidney transplant recipients are at higher risk of developing cardiovascular complications, such as heart attack, stroke and loss of blood supply to the limbs, typically from underlying medical diseases and medication-related toxicities.
Research studies using database information and measuring heart biomarkers in thousands of kidney transplant recipients at Mayo Clinic have improved the ability to identify patients who are at risk of heart problems after transplant
Investigators have found that the biomarker troponin levels can provide a more accurate measure of cardiac risk than can traditional cardiac measurements, such as a cardiac stress test, and can indicate whether surgical intervention is needed prior to kidney transplant.
The goals of this research are to achieve lower risk for patients and to conduct cardiac studies for patients who can benefit the most.
Ongoing studies include:
- Determining whether troponin can also be used to assess heart status after kidney or pancreas transplant
- Assessing how modifications in the treatment of patients before the transplant can reduce levels of troponin and perhaps reduce risk
Program faculty
Here's a list of faculty in the Kidney and Pancreas Transplant Research Program by campus location.
- Chakkera, Harini, M.D.
- Heilman, Raymond L., M.D.
- Huskey, Janna L. M.D.
- Kaplan, Bruce, M.D.
- Khamash, Hasan A, M.D.
- Mathur, Amit K., M.D.
- Morales, Alejandro, M.D.
- Moss, Adyr A., M.D.
- Petrides, Savas, M.D.
- Reddy, Kunam S., M.B.B.S.
- Singer, Andrew L., M.D., Ph.D.
- Sukumaran, Sumi Nair, M.B.B.S.
- Croome, Kristopher (Kris) P., M.D.
- Gonwa, Thomas A., M.D.
- Lee, David D., M.D.
- Mai, Martin L., M.D.
- Oshel, Katherine, M.D.
- Perry, Dana K., M.D.
- Prendergast, Mary B., M.D.
- Taner, Burcin C., M.D.
- Wadei, Hani M., M.D.
- Amer, Hatem, M.D.
- Cosio, Fernando G., M.D.
- Cramer, Carl H. II., M.D.
- Dean, Patrick G., M.D.
- Heimbach, Julie K., M.D.
- Hickson, LaTonya J., M.D.
- Issa, Naim S., M.D.
- Kudva, Yogish C., M.B.B.S.
- Kukla, Aleksandra M.D.
- Larsen, Brandon T., M.D., Ph.D.
- Lorenz, Elizabeth C., M.D.
- Norby, Suzanne M., M.D.
- Nyberg, Scott M.D., Ph.D.
- Prieto, Mikel, M.D.
- Schinstock, Carrie A., M.D.
- Stegall, Mark D., M.D.
- Taler, Sandra J., M.D.
More about research at Mayo Clinic
- Research Faculty
- Laboratories
- Core Facilities
- Centers & Programs
- Departments & Divisions
- Clinical Trials
- Institutional Review Board
- Postdoctoral Fellowships
- Training Grant Programs
- Publications
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.

American Association of Kidney Patients
Kidney Transplantation

There is a national transplant waiting list for people who are waiting for all types of transplants. Every 10 minutes, a new person is added to the list. Most of the people on the list are waiting for a kidney transplant. How long one has to wait is different for each person. The average time to wait for a kidney is 3-5 years. For some it might be shorter and for others it might be longer. You should ask your kidney care team to tell you about kidney transplantation as a treatment option for your kidney disease.
Most people on Hemodialysis or Peritoneal Dialysis can consider getting a kidney transplant. Some in CKD Stage 4 or 5 may be able to get a transplant and not have to go on any type of dialysis – this is called a pre-emptive transplant.
What are the Types of Kidney Transplants?
Living Donation is when a person donates a kidney to a friend or someone related to them. Living donated kidneys take away the long wait for a transplant. These kidneys usually function longer than a kidney from someone who has died.
A donor will be told about any risks related to donating a kidney. Living donors can live a healthy life with one kidney. They can apply for money to help cover travel and lodging. There are living donor assistance program such as, www.livingdonorassistance.org and www.transplantfoundation.org where the donor may find help. Help for a donor might include:
- Travel expenses
- Food and lodging
- Medications
- Hospital and physician charges
Paired/Exchange Donation may be an option for those who know someone who wants to donate a kidney. Sometimes the donor is cleared to donate but is not a good match for the patient. If this happens, the patient and donor may be able to enter into a paired kidney donation program. These programs pair the kidney and the patient with the best kidney match. This can start a “chain” of kidney donations. Ask the transplant team if they have a program like this. If they don't, they can tell you about transplant centers who do.
Deceased Donation is the most common form of kidney donation. These kidneys come from people who have died and donated their organs for transplant. These kidneys need to be transplanted soon after the donor has died. It is important for their family to know that they want to be a donor. If not, the family may decide not to donate their organs. Anyone can sign up to be an organ donor. Go to the link DonateLife America www.donatelife.net to find out more.
Altruistic Donation is when someone donates a kidney to any patient on the wait list. These kidneys might be given to a patient on the waitlist at a transplant center. They might used for a paired kidney transplant chain. These donors usually do not know the person they are giving a kidney to.
Pre-emptive Transplant is when a patient gets a transplant before they have to go on dialysis. Studies show this can result in better kidney and health outcomes. This type of transplant is more likely if a person has a living donor. The sooner you learn about your treatment choices, the better. This will give you time to decide if a transplant is best for you.
Find a Transplant Center
To find a transplant center in your area visit the Organ Procurement and Transplantation Network (OPTN) website . Then follow these steps:
- Select "Transplant Centers by Organ" under Member Type
- Select "Kidney" for Organ Type
- Select your state or region
donor-seeker program*
The Donor Seeker® is the only 15-minute video course that will help you "talk up" your search for a living kidney donor. This fast-tracked program includes confidence-building conversation examples, and key talking points on how to share your story and ask others to help you spread the word. You’ll also find a robust resource section full of informative links, downloadable forms, and a course completion certificate. Whether listening in English or Spanish—the universal language is sure to increase your odds for attracting interested individuals who can advance your path to transplant. *If you prefer to use your mobile device, you can now access the "Donor Seeker" app from the Apple App Store or Google Play Store .
Learn how to apply these powerful communication tips—and start attracting interested donors today! Click here to start.
*AAKP is a Simon Says Seminars, inc. | TransplantStrong Community Partner.
AAKP's Top Resources on Kidney Transplantation education
For more information on this topic, check out the following resources!
- Understanding Kidney Transplantation brochure
- Kidney Transplant Today e-newsletter*
- AAKP HealthLine webinars
- aakpRENALIFE magazine*
- AAKP Delicious! kidney-friendly recipes
- VIDEO, Northwestern Medicine -Inside the OR: Kidney Transplant Surgery
- CDC Fact Sheet on Kidney Disease (2023)
*Benefit of membership, join today!
iChoose Kidney Risk Calculator*
The iChoose Kidney risk calculator is a tool that educates patients about the risk of available treatment options for kidney disease. This tool shows estimated risks of patient survival (probability of staying alive) and mortality (probability of dying) with different treatment options (dialysis or transplant) given the patient's demographic and clinical history at dialysis start.
My Dialysis Choice* If you kidneys fail, dialysis can save your life. But, dialysis is not just a medical treatment. It can also affect every aspect of your lifestyle. This online tool will help you choose the right treatment for you, so you feel your best and live the way you want to.
*iChoose Kidney Risk Calculator is an online application tool created by a team of researchers at Emory University, funded by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number ULl TR000454 and KL2TR000455, and further supported through a grant from the Carlos and Marguerite Mason Trust Foundation (Emory University).
*My Dialysis Choice is an online application tool created by the non-profit Medical Education Institute.
Visit our Post-Kidney Transplant Care and Your Health web page!
Proper care of your kidney transplant is a lifelong process. You will need to take care of yourself and actively monitor your health. You will also need to be aware of signs and symptoms that should be reported to your transplant team immediately. The more you know, the more power you have to keep you and your donor kidney healthy. Visit our post-kidney transplant care and your health web page for more information on post-transplant care.

Please enter your contact information here:
Your Name (required)
Your Email (required)
Your Message ...
Hot Topics in Kidney Health
Join us as we highlight the latest in kidney research, dispel myths, bring you up-to-date news in kidney care, and answer questions from patients to help them live well with kidney disease or a transplant.
Subscribe on Apple Podcasts
Subscribe on spotify.
Power lifechanging research, education and advocacy to ensure that every person facing kidney disease gets the chance to thrive—not simply survive. Give today and help us provide FREE resources, support, and hope for patients, loved ones and healthcare heroes.
Unfiltered Story: Next steps after losing a transplant
Losing a kidney transplant can feel very overwhelming. Today we're here with Anthony Tuggle, a former NKF board member, to hear how he's coping with losing a transplant and learn what's next for him.
Coping with losing a transplant
Everyone loves to talk about kidney transplant success stories but rarely do we talk about what happens if a transplant fails. On today's episode Dori Muench, a post transplant social worker, and Sue George, a kidney warrior with experience losing a transplant, are here to discuss the impact of losing a kidney and how to cope.
Artificial Kidneys
When will the artificial kidney be ready for human use? Learn more about the progress of the artificial kidney and how it will affect someone's quality of life from expert Shuvo Roy, Ph.D.
What is a high KDPI kidney?
When a kidney from a deceased donor becomes available, it is scored on a system called the Kidney Donor Profile Index (KDPI). How accurate is it at predicting possible transplant survival? On this episode, we speak with experts to get the facts
Fad diets and kidney diets
It’s hard to keep up with all the new fad diets out there. Do you know which ones are right for you and your kidney health? On this episode, you will hear from experts on finding the diet that's right for you and how to stick to it.
Superfoods for people with kidney disease
You may have heard the buzzword superfoods but what are they and do they have special qualities? Board-certified renal dietitian, Jen Hernadez is here to break it down.
What do clinical end points and trials mean for CKD research?
Clinical trials exist to help prevent, screen for, diagnose, or treat diseases and other health problems. Without them, we would not have new treatments or other advances in health and medicine. But how are the clinical trial endpoints, or the preferred outcomes of these trials determined? Today, Anthony Gucciardo NKF’s Senior Vice President of Strategic Partnerships, Dr. Joseph Vassalotti, NKF’s Chief Medical Officer, and Kent Bressler, a Patient advocate and FSGS patient, discuss this and more.
Mindfulness meditation for kidney patients
You may have heard the term mindfulness before but what does it mean, what are the benefits, and how can you integrate mindfulness into your life? On today’s episode Gary Petingola a Social Worker certified to teach Mindfulness-Based Stress Reductionexplains all this and more.
Transplants for All
At the National Kidney Foundation, we believe that everyone who needs a kidney should get a kidney. To make this dream a reality, we’ve launched the Transplants for All Initiative. What is this initiative and how will it make a difference in the lives of people with kidney disease? In today’s episode special guests Morgan Reid, NKF’s Transplant Policy & Strategy Director and Haley Jenson, NKF’s Transplant Programs Director explain this and more.
BONUS: Sexuality and kidney disease
Sexual dysfunction is incredibly common in patients with kidney disease. In today's bonus episode, you'll learn about why it is so prevalent, the different treatment options, and how to improve communication around this important but often neglected aspect of health.
LGBTQ+ advocacy in healthcare
Over 50% of LGBTQIA-plus people have experienced some form of healthcare discrimination and over 25% of transgender people reported being denied care due to their transgender status. Not having proper health care or avoiding health care due to discrimination, can result in dire consequences, including an increased risk of health problems like kidney disease. What is this discrimination, and how can you advocate for yourself and LGBTQIA+ rights? In today’s episode Dr. Joshua Wilder, a podiatrist, and Representative Jeff Currey, two kidney transplant recipients and members of the LGBTQIA+ community, discuss this and more.
NKF Innovation Fund: developing new treatments for kidney patients
For far too long treatments for CKD haven’t changed. Launched in 2021, the NKF Innovation Fund works to accelerate funding, and development of therapies that kidney patients deserve. On this episode, you will hear from NKF CEO Kevin Longino interviews Kathleen St. Jean, Chief Commercial Officer of 34 Lives, one of the first recipients of a significant investment from NKF’s Innovation Fund to help further develop a new technology to rehabilitate donated kidneys for transplantation.
Living donors and mental health
Donating a kidney is one of the most selfless gifts one person can give to another. But what is that experience like for the donor before and after the transplant surgery? Today, we'll hear from Jessica Kolansky, a living kidney donor, and Alexandra Catalyst, a transplant coordinator, about the post transplant experience and what resources are available to donors after the surgery.
Laughter therapy for kidney patients
Is laughter really the best medicine? On today’s episode we’ll discuss an exciting new coping strategy for dialysis patients called guided group laughing therapy. What is it and how does it help? Dr. Paul Bennet who ran a study on the benefits of laughing therapy and Kimberly Super-Harrigan, a dialysis patient, are here to break it down.
BMI and weight management for kidney patients and living donors
Obesity is one of the major risk factors for developing kidney disease, which is measured through the body mass index or BMI. This measurement factors into the process for both living donors and transplant recipients. On today’s episode, you’ll learn how to measure your BMI and hear from both kidney patients on how managing their weight affected their kidney health.
Access to reproductive care for kidney patients
In 2022, the US Supreme Court overturned precedent established by Roe v Wade, eliminating the constitutional right to abortion. Family planning decisions can be difficult and complex for kidney patients. On today’s episode, we’ll discuss how this impacts kidney patients and disadvantaged patients with limited access to healthcare.
Game Changers: Treating CKD earlier
Did you know that 40% of chronic kidney disease progression may be preventable with earlier diagnosis and treatment? On this episode, you will hear the facts around treating CKD earlier from Dr. Joe Vassalotti, NKF’s Chief Medical Officer. You will also hear from Jane DeMeis on her journey with kidney disease.
Exercise and bone health: what CKD patients should know
Keeping your body and bones strong are important when you have kidney disease. Do you know what types of exercise are good for kidney patients? What about for transplant recipients or people on dialysis? In this episode, we sat down with experts to discuss the benefits and recommendations of managing an exercise routine.
Managing fluid intake as a CKD patient
It is important that certain individuals with CKD limit their fluid intake, but many don’t understand why or where to begin. On today’s episode, we sat down with experts to discuss fluid restriction, such as why it’s important, the negative effects of consuming too much, and ways to manage a fluid-restricted diet.
Treatment options for undocumented people with kidney disease
Undocumented people face increased barriers to accessing health coverage and care, including treatment for kidney disease. In this episode, our guest experts discuss what treatment options are currently available for undocumented people and what kind of advocacy efforts are being made to improve their access to health care.
Breaking Down New Medicare Coverage for Immunosuppressant Drugs
The Medicare coverage for immunosuppressive drugs for kidney transplant patients has recently been expanded. But what does this new benefit cover and who is eligible? in this podcast, Cynthia Nichols-Jackson, a registered nurse and a program coordinator for the National Kidney Foundation, and Troy Zimmerman, a special projects director for the National Kidney Foundation, discuss how this new policy will affect the future for kidney transplants.
Should You Follow A Special Diet After Transplant?
How potassium affects kidney patients
One of the jobs your kidneys is to manage your body’s levels of potassium, which keeps your heartbeat regular and your muscles working right. Many kidney patients need to watch what they eat to ensure that their potassium levels don’t become too high and cause dangerous health risks. On today’s episode, you’ll hear how to best manage your potassium levels to protect yourself.
How kidney patients should protect themselves from COVID-19 in 2022
While many people feel like the world is headed back to normal, many kidney patients can feel left behind. COVID-19 is still top of mind for those who are immunocompromised and we're here to offer resources and support. On today's episode, our guests will answer your questions about how COVID-19 affects transplant, dialysis, and early stage CKD patients.
What is basic science research and why is it important?
When we hear the word research, most of us think of innovative breakthrough treatments and technologies. But applied clinical research could not be possible without another type of research called basic science research in which scientists study the fundamental processes of the human body. In this episode, we’ll learn what basic science research is and how it applies to the area of kidneys and kidney disease.
Working with your clinician to make shared decisions for your care
Shared decision making can play a vital role in the treatment of kidney disease. When physicians involve patients in their care, they may be able to help slow progression and improve outcomes. In this episode, we discussed how patients and their physicians can achieve this and hear stories from patients who have been there.
How kidney disease affects your mental health
People with chronic conditions like kidney disease face mental health struggles such as depression or anxiety. In many kidney patients those challenges often go overlooked or undertreated. In this episode, we sat down with a mentor and mentee from NKF Peers to discuss their experiences and the importance of talking to someone who knows what you've been through.
Tips for finding a living donor
If you are in need of a kidney transplant, finding a living donor can sound scary and overwhelming. Where should you start and what’s the best way to share your story with the world? In this episode, you will hear from transplant recipients who once stood in your shoes.
Pig kidneys in humans? Xenotransplantation explained.
From the invention of the dialysis machine to the first successful kidney transplant, science has come a long way in extending life for kidney patients. Is transplantation between humans and animals the next step? In this episode, you will hear from a doctor behind the first successful transplant of a human receiving a pig kidney and where the science can take us from here.
Deciding to become a living donor
Pregnancy and kidney disease
Pregnancy can be an exciting time for most people, but what does it look like if you are a kidney patient? What does pregnancy look like if they have kidney disease, are on dialysis, or have received a transplant? In this episode, we’ll hear useful facts and tips from transplant nephrologist Dr. Mariana Markell, as well as personal stories from Cari Maxwell and Katie Reed, two mothers living with kidney disease.
What are SGLT2 Inhibitors and are they the right drug for you?
You might have heard about drugs called SGLT2 inhibitors used in treatment of kidney disease, but, just like many other kidney patients, you might not know if they’re right for you. On this episode, we explain how different SGLT2 inhibitors are from other kidney disease medications, discuss side effects, cost, and the ongoing research around this category of drugs.
How much sodium is safe for kidney patients?
Most patients on dialysis need to limit the amount of sodium in their diets. But how much sodium is safe and what are some ways to add flavor to your diet? On today‘s episode, our experts cover examples of high sodium foods, recommendations for low sodium substitutes, and how much sodium people with kidney disease should have as a part of a healthy diet.
What do changes to eGFR calculation mean for patients?
Tips for overcoming financial hardship for kidney patients
Many kidney disease patients often face financial hardships, such as having to leave a job or struggling to pay for medications. We sat down with physician and a postdoctoral research fellow Dr. Issac Acquah to talk about his recent research into the financial impact on people with chronic kidney disease.
How to become an advocate for kidney health
Over the past year, NKF advocates have won a number of policy campaigns both in Congress and state capitals across the country - but we're not done yet. In this episode, we discussed some recent wins and our upcoming challenges for the kidney advocate community with Jeff Currey, a Connecticut State Representative and kidney transplant recipient, and Armand Halter, an NKF patient advocate who helped lead NKF’s efforts to pass the Connecticut version of the Living Donor Protection Act.
A major worry for many people right now is the Delta variant, a highly contagious strain of COVID-19 which is making headlines across the United States. The FDA has just authorized a third dose of the COVID-19 vaccine so that immune compromised patients can better protecting themselves from the virus. What does this mean for CKD, dialysis, and transplant patients? We spoke with Dr. Joseph Vassalotti, NKF Chief Medical Officer, in a recent Facebook Live to share the facts about the Delta variant, COVID-19 booster shots, and other concerns facing kidney patients.
Coping with depression & anxiety during a global pandemic
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
New Research Supports Expansion of Kidney Donation to Include Organs from Deceased Patients Who Once Had Dialysis

New @hopkinsneph study investigates potential remedy for kidney donor shortage. @KidneydrChirag ›
Researchers from Johns Hopkins Medicine propose a novel approach to addressing the pressing issue of a kidney donor shortage through findings that suggest a promising method to expand the pool of available kidney donors by utilizing deceased donors on dialysis for kidney transplants.
The findings, published in the May 23rd issue of JAMA , identifies that while those who received such kidneys experienced a “significant delay” in the function of the transplanted organ compared to those whose donors did not have dialysis, there was no significant difference in rates of transplant failure or death.
According to the United Network for Organ Sharing , (UNOS) approximately 100,000 patients are on the waiting list for kidney transplants in the United States. Some 25,000 successful kidney transplants were performed in 2022, the latest year for which complete data are available, and it is estimated that fewer than 20,000 of those on the list will receive transplants from deceased donors.
Historically, according to UNOS, more than 20% of deceased donor kidneys are not used each year, largely several of them are not utilized due to concerns that acute kidney injury (AKI) in the kidneys and dialysis used to treat the donors renders the kidneys too damaged for transplantation.
However, recent studies suggest there might not be much long-term difference between how the organ recipient’s body responds to a deceased donor kidney exposed to dialysis prior to transplant surgery and a diseased donor kidney not exposed to dialysis before transplant surgery.
These deceased donors are receiving dialysis treatment because they have severe AKI around the time of their death. It is known that kidneys with AKI are at a higher risk of delayed graft function (DGF) in recipients—a term for when the transplanted kidney does not work right away. What has been unclear, is whether DGF predicts shortened life expectancy and organ function over the long term.
Suppose studies prove that the risks associated with the transplantation of kidneys from deceased donors on dialysis are minimal in regard to long term life expectancy of the graft and quality of life of the recipient. In that case, this will go a long way toward increasing the number of available kidney donors.
“With patients waiting many years to receive a kidney, and a significant portion of them deteriorate or succumb to their condition while on the waiting list, we need to rapidly increase the pool of available kidneys,” says Chirag Parikh, M.D., Ph.D. , professor of medicine and the director of the division of Nephrology at Johns Hopkins Medicine and key investigator for the study.
For the study, researchers analyzed medical records for 1,944 kidney transplant patients gathered from 58 U.S. organ transplant organizations from the years 2010 and 2018 with 954 receiving kidneys from deceased donors who underwent dialysis and matched them to 990 receiving kidneys from deceased donors who had not undergone dialysis.
Results showed there was higher incidence of DGF in patients who received kidneys from donors who were deceased and who underwent dialysis than there was for patients with kidneys from donors who were deceased and who did not receive dialysis. However, the kidney recipients with higher DGF did not show any significant differences in long-term graft failure (permanent loss of function of the transplanted organ).
“There is significant variability in the utilization of kidneys from high risk deceased donors across the country,” Parikh says. “The findings from this study should encourage organ procurement organizations and transplant professionals to cautiously bring kidneys with severe AKI, from deceased donors who received dialysis, into the allocation pool.”
Along with Dr. Parikh, members of the study team from Johns Hopkins Medicine are Yumeng Wen, MD, PhD; Nitya Srialluri, MD, MS, MHS, and Heather Thiessen Philbrook, M, Math.
Funding for the study was provided by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant T32DK007732-27, grant U01DK-116097, grant U01DK-116066, grant R01DK-126739, and grant U01DK130058, the National Institute on Minority Health and Health Disparities grant R01MD-014161, the National Institute of Biomedical Imaging and Bioengineering grant R01EB-032910; grants R01DK-123041, U01DK-126654, and U01DK-110961, the National Institute of Allergy and Infectious Diseases grant K24AI-146137; the NIDDK and grant P30DK079310 from the George M. O’Brien Kidney Center at Yale University grants R01DK-93770, K24DK090203 and grant P30DK079310.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 27, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
reputable news agency
Research indicates kidneys from deceased donors who were on dialysis are suboptimal
by Elana Gotkine
Receipt of a kidney from a deceased donor who underwent dialysis is associated with an increased incidence of delayed graft function, according to a study published online May 23 in JAMA .
Yumeng Wen, M.D., Ph.D., from Johns Hopkins University in Baltimore, and colleagues compared outcomes of transplant recipients who received kidneys from deceased donors who underwent dialysis prior to kidney donation versus recipients of kidneys from deceased donors who did not undergo dialysis in a retrospective cohort study using data from 58 U.S. organ procurement organizations.
Among the donors with kidneys transplanted, 514 underwent dialysis prior to transplantation and were matched to 514 who did not undergo dialysis. The researchers found that compared with kidney transplants from donors who did not receive dialysis, kidney transplants from donors who received dialysis prior to donation had an increased risk for delayed graft function (59.2 versus 24.6%; adjusted odds ratio, 4.17).
At a median follow-up of 34.1 months, the incidence rates did not differ significantly for all-cause graft failure, death-censured graft failure, or death for transplants from donors who received dialysis prior to donation versus donors who did not receive dialysis.
"Future research should investigate whether the higher procurement and acceptance rates of kidneys from deceased donors who received dialysis are associated with shorter waiting times and better outcomes for patients," the authors write.
Xingxing S. Cheng et al, Expanding the Overton Window in Deceased Kidney Donor Eligibility—Enough to Make a Difference?, JAMA (2024). DOI: 10.1001/jama.2024.8734
Copyright © 2024 HealthDay . All rights reserved.
Explore further
Feedback to editors

Scientists identify key protein that preserves motor ability during aging

Study reveals brain mechanisms behind speech impairment in Parkinson's
2 hours ago

Researchers discover vaccine originally created for HIV may also combat cancer

Hitting the target with non-invasive deep brain stimulation: Potential therapy for addiction, depression and OCD
5 hours ago

New study launches following the discovery of a second case of avian influenza spreading from cows to humans
10 hours ago

Neuroscientists use AI to simulate how the brain makes sense of the visual world
17 hours ago

The light or the content? What we know about screens and sleep disruption
18 hours ago

For some endometriosis-related ovarian cancers, timing is everything

Researchers genetically modify E. coli bacteria with part of HIV virus in bid for successful vaccine

Researchers develop 3D model to better treat neurological disorders
Related stories.

Pediatric kidney transplant patients fare better when kidney is from live donor
Aug 16, 2022

Donated kidneys from deceased COVID-19 patients are safe to transplant, according to study
Jun 12, 2023

When a kidney transplant fails, retransplantation may offer better survival over dialysis
Dec 28, 2021

Kidney transplants from, to extreme elderly feasible in ESRD
Apr 14, 2020

Graft survival similar for kidneys from octogenarians
Aug 15, 2017

Kidney transplantation between people with HIV is safe, study finds
Jul 23, 2020
Recommended for you

Researchers identify promising protein candidate for metabolic disease treatment
May 28, 2024

Next-gen knee training model heads for global markets

New therapy proven effective against rejection in kidney transplantation

Study demonstrates how gut microbes process steroids—using flatulence

New surgical tool moves tiny bioparticles with robotics and acoustic energy
May 24, 2024

Study further illuminates ability of cancer drug to lower blood sugar
May 23, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Advertisement
Supported by
Ozempic Cuts Risk of Chronic Kidney Disease Complications, Study Finds
A major clinical trial showed such promising results that the drug’s maker halted it early.
- Share full article

By Dani Blum
Dani Blum has reported on Ozempic and similar drugs since 2022.
Semaglutide, the compound in the blockbuster drugs Ozempic and Wegovy , dramatically reduced the risk of kidney complications, heart issues and death in people with Type 2 diabetes and chronic kidney disease in a major clinical trial, the results of which were published on Friday. The findings could transform how doctors treat some of the sickest patients with chronic kidney disease, which affects more than one in seven adults in the United States but has no cure.
“Those of us who really care about kidney patients spent our whole careers wanting something better,” said Dr. Katherine Tuttle, a professor of medicine at the University of Washington School of Medicine and an author of the study. “And this is as good as it gets.” The research was presented at a European Renal Association meeting in Stockholm on Friday and simultaneously published in The New England Journal of Medicine .
The trial, funded by Ozempic maker Novo Nordisk, was so successful that the company stopped it early . Dr. Martin Holst Lange, Novo Nordisk’s executive vice president of development, said that the company would ask the Food and Drug Administration to update Ozempic’s label to say it can also be used to reduce the progression of chronic kidney disease or complications in people with Type 2 diabetes.
Diabetes is a leading cause of chronic kidney disease, which occurs when the kidneys don’t function as well as they should. In advanced stages, the kidneys are so damaged that they cannot properly filter blood. This can cause fluid and waste to build up in the blood, which can exacerbate high blood pressure and raise the risk of heart disease and stroke, said Dr. Subramaniam Pennathur, the chief of the nephrology division at Michigan Medicine.
The study included 3,533 people with kidney disease and Type 2 diabetes, about half of whom took a weekly injection of semaglutide, and half of whom took a weekly placebo shot.
Researchers followed up with participants after a median period of around three and a half years and found that those who took semaglutide had a 24 percent lower likelihood of having a major kidney disease event, like losing at least half of their kidney function, or needing dialysis or a kidney transplant. There were 331 such events among the semaglutide group, compared with 410 in the placebo group.
People who received semaglutide were much less likely to die from cardiovascular issues, or from any cause at all, and had slower rates of kidney decline.
Kidney damage often occurs gradually, and people typically do not show symptoms until the disease is in advanced stages. Doctors try to slow the decline of kidney function with existing medications and lifestyle modifications, said Dr. Melanie Hoenig, a nephrologist at Beth Israel Deaconess Medical Center who was not involved with the study. But even with treatment, the disease can progress to the point that patients need dialysis, a treatment that removes waste and excess fluids from the blood, or kidney transplants.
The participants in the study were extremely sick — the severe complications seen in some study participants are more likely to occur in people the later stages of chronic kidney disease, said Dr. George Bakris, a professor of medicine at the University of Chicago Medicine and an author of the study. Most participants in the trial were already taking medication for chronic kidney disease.
For people with advanced kidney disease, in particular, the findings are promising. “We can help people live longer,” said Dr. Vlado Perkovic, a nephrologist and renal researcher at the University of New South Wales, Sydney, and another author of the study.
While the data shows clear benefits, even the researchers studying drugs like Ozempic aren’t sure how, exactly, they help the kidneys. One leading theory is that semaglutide may reduce inflammation, which exacerbates kidney disease.
And the results come with several caveats: Roughly two-thirds of the participants were men and around two-thirds were white — a limitation of the study, the authors noted, because chronic kidney disease disproportionately affects Black and Indigenous patients. The trial participants taking semaglutide were more likely to stop the drug because of gastrointestinal issues, which are common side effects of Ozempic.
Doctors said they wanted to know whether the drug might benefit patients who have kidney disease but not diabetes, and some also had questions about the potential long-term risks of taking semaglutide.
Still, the results are the latest data to show that semaglutide can do more than treat diabetes or drive weight loss. In March, the F.D.A. authorized Wegovy for reducing the risk of cardiovascular issues in some patients. And scientists are examining semaglutide and tirzepatide, the compound in the rival drugs Mounjaro and Zepbound, for a range of other conditions , including sleep apnea and liver disease.
If the F.D.A. approves the new use, it could drive even more demand for Ozempic, which has faced recurrent shortages .
“I think it’s a game changer,” Dr. Hoenig said, “if I can get it for my patients.”
Dani Blum is a health reporter for The Times. More about Dani Blum
A Close Look at Weight-Loss Drugs
Reduced Disease Complications: Semaglutide, the compound in Ozempic and Wegovy, dramatically reduced the risk of kidney complications , heart issues and death in people with Type 2 diabetes and chronic kidney disease in a major clinical trial.
Supplement Stores: GNC and the Vitamin Shoppe are redesigning displays and taking other steps to appeal to people who are taking or are interested in drugs like Ozempic and Wegovy.
Senate Investigation: A Senate committee is investigating the prices that Novo Nordisk charges for Ozempic and Wegovy, which are highly effective at treating diabetes and obesity but carry steep price tags.
A Company Remakes Itself: Novo Nordisk’s factories work nonstop turning out Ozempic and Wegovy , but the Danish company has far bigger ambitions.
Transforming a Small Danish Town: In Kalundborg, population under 17,000, Novo Nordisk is making huge investments to increase production of Ozempic and Wegovy.

COMMENTS
Abstract. Recent advances in surgical, immunosuppressive and monitoring protocols have led to the significant improvement of overall one-year kidney allograft outcomes. Nonetheless, there has not been a significant change in long-term kidney allograft outcomes. In fact, chronic and acute antibody-mediated rejection (ABMR) and non-immunological ...
R.A. Montgomery and OthersN Engl J Med 2022;386:1889-1898. Genetically modified pig kidney xenografts were transplanted into two brain-dead human recipients. The xenografts functioned immediately ...
The New England Journal of Medicine has published the most manuscripts on kidney transplantation (n = 26) and is the most cited journal (n = 15,642). The United States has the highest number of publications (n = 61). Kashika is the corresponding author with the most published papers (n = 5; 2892 citations).
Research Topics. See all (4) Learn more about Research Topics. Transplant-related clinical and translational research, reflecting the dynamic field of kidney transplantation from immunobiology to noninvasive genomic biomarkers in the diagnosis of acute rejection.
Kidney transplantation is limited by graft rejection, complications owing to long-term immunosuppression and a shortage of donor organs. ... Kidney Research Institute, New York City, NY, USA.
Kidney Transplantation. Kidney transplantation is the preferred therapeutic approach for patients with end-stage renal disease. Many challenges remain, however, including a shortage of donor ...
Over the past 65 years, kidney transplantation has evolved into the optimal treatment for patients with kidney failure, dramatically reducing suffering through improved survival and quality of life. However, access to transplant is still limited by organ supply, opportunities for transplant are inequitably distributed, and lifelong transplant survival remains elusive. To address these ...
This Research Topic aims to publish manuscripts on how to improve long-term outcomes after kidney transplantation. These include ex-vivo studies, immunosuppressive strategies, and treating acute and chronic cellular and humoral rejection. Welcome Topics include, but are not limited to the following:• Ex-vivo strategies to improve outcome ...
All other transplant papers in Volume 35 of NDT are also highly recommended and acknowledged. In the January 2020 issue of NDT, the research group from the Westmead Hospital and University of Sydney investigated a potential obesity and gender bias in access to deceased donor kidney transplantation . This is an important clinical issue and all ...
Purpose Patients with lower urinary tract malformations (LUTM) were suspended from kidney transplantation (KT) programs in the past due to various concerns. Consequently, only a limited number of studies have explored this topic at hand. In this study, our objective was to perform a systematic review (SR) to evaluate the current evidence regarding KT outcomes as well as patient survival (PS ...
Renal transplantation is a life-saving strategy for patients with end-stage renal disease that generally offers a favorable quality of life. However, immune-related post-transplant allograft dysfunctions have been demonstrated to be the principal reason for unfavorable short-term and long-term outcomes. <br/>The immune system, which involves the complement system, immune cells, antibodies, and ...
Topics. NephJC Editorials; Images in Kidney Medicine; About. Society About NKF ... Health Services Research Center, Department of Medicine and Department of Surgery, Emory University School of Medicine, Atlanta, GA ... The top 5 barriers to kidney transplantation as reported by transplant staff were transportation (63.7%), low health literacy ...
The purpose of this trial is to evaluate the reduction in incidence and severity of delayed graft function when using QPI-1002 with kidney transplants from donors older than 45 years who have brain death. J&J Vaccine Booster in Transplant Recipients Scottsdale/Phoenix, AZ; Jacksonville, FL; Rochester, MN.
An official journal of the European Renal Association - European Dialysis and Transplant Association. Publishes peer-reviewed original clinical and laboratory research across the full range of nephrology, dialysis, and transplantation.
The author who published the most kidney transplantation papers was Cooper (n = 114), followed by Sanchs (n = 44) and Hara ... Early research topics included natural antibodies, HR, antibodies, acute vascular rejection, endothelial cells, complement activation, and in vitro studies. With the evolution of time and the development of medical ...
In fact, approximately 20% to 25% of kidney transplants are lost because of disease recurrence. To address this problem, Mayo Clinic researchers have taken several steps. First, researchers identified diseases that are most likely to recur in the transplanted kidney. Second, with the use of protocol biopsies, researchers identified the earliest ...
The research involved 22 patients who were diagnosed with antibody-mediated rejection (AMR) following a kidney transplant at the University Hospital Vienna and Charité-Universitätsmedizin ...
Kidney Transplantation - AAKP. read more. read more. AAKP offers a bi-monthly magazine as well as five e-newsletters. Check out our recent issues and subscribe. read more. The AAKP HealthLine is a webinar-based program educates patients and their family members on a variety of important health care topics from the comfort of their home or office.
The impact of renal allograft rejection treatment on infection development has not been formally defined in the literature. Methods . We conducted a retrospective cohort study of 185 rejection (case) and 185 nonrejection (control) kidney transplant patients treated at our institution from 2014 to 2020 to understand the impact of rejection on ...
Hot Topics in Kidney Health. Join us as we highlight the latest in kidney research, dispel myths, bring you up-to-date news in kidney care, and answer questions from patients to help them live well with kidney disease or a transplant.
We research many topics dealing with kidney transplant rejection, including diagnostic criteria, infection risk and incompatibility factors. Our lab also has a longstanding interest in pancreas transplants and has conducted research to establish guidelines for diagnosing antibody-mediated rejection of pancreas allografts-updated Banff grading ...
Background: HCMV causes severe clinical complications in transplant recipients and may lead to graft rejection. Successful renal transplantation heavily relies on the early prevention and diagnosis of CMV infections, followed by prompt prophylactic treatment before transplantation. Despite the majority of renal rejection cases with acute HCMV infections being asymptomatic and occurring one to ...
Keywords: renal transplantation, graft function, nephrotoxicity, kidney rejection, malignancy . Important Note: All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements.Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer ...
For the study, researchers analyzed medical records for 1,944 kidney transplant patients gathered from 58 U.S. organ transplant organizations from the years 2010 and 2018 with 954 receiving kidneys from deceased donors who underwent dialysis and matched them to 990 receiving kidneys from deceased donors who had not undergone dialysis.
Receipt of a kidney from a deceased donor who underwent dialysis is associated with an increased incidence of delayed graft function, according to a study published online May 23 in JAMA. Yumeng ...
The research was presented at a European Renal Association meeting in Stockholm on Friday and simultaneously published in The New England Journal of ... or needing dialysis or a kidney transplant ...