- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- How to present patient...
How to present patient cases
- Related content
- Peer review
- Mary Ni Lochlainn , foundation year 2 doctor 1 ,
- Ibrahim Balogun , healthcare of older people/stroke medicine consultant 1
- 1 East Kent Foundation Trust, UK
A guide on how to structure a case presentation
This article contains...
-History of presenting problem
-Medical and surgical history
-Drugs, including allergies to drugs
-Family history
-Social history
-Review of systems
-Findings on examination, including vital signs and observations
-Differential diagnosis/impression
-Investigations
-Management
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1
The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the patient’s condition and further management can be planned accordingly. 2 To give a high quality presentation you need to take a thorough history. Consultants make decisions about patient care based on information presented to them by junior members of the team, so the importance of accurately presenting your patient cannot be overemphasised.
As a medical student, you are likely to be asked to present in numerous settings. A formal case presentation may take place at a teaching session or even at a conference or scientific meeting. These presentations are usually thorough and have an accompanying PowerPoint presentation or poster. More often, case presentations take place on the wards or over the phone and tend to be brief, using only memory or short, handwritten notes as an aid.
Everyone has their own presenting style, and the context of the presentation will determine how much detail you need to put in. You should anticipate what information your senior colleagues will need to know about the patient’s history and the care he or she has received since admission, to enable them to make further management decisions. In this article, I use a fictitious case to show how you can structure case presentations, which can be adapted to different clinical and teaching settings (box 1).
Box 1: Structure for presenting patient cases
Presenting problem, history of presenting problem, medical and surgical history.
Drugs, including allergies to drugs
Family history
Social history, review of systems.
Findings on examination, including vital signs and observations
Differential diagnosis/impression
Investigations
Case: tom murphy.
You should start with a sentence that includes the patient’s name, sex (Mr/Ms), age, and presenting symptoms. In your presentation, you may want to include the patient’s main diagnosis if known—for example, “admitted with shortness of breath on a background of COPD [chronic obstructive pulmonary disease].” You should include any additional information that might give the presentation of symptoms further context, such as the patient’s profession, ethnic origin, recent travel, or chronic conditions.
“ Mr Tom Murphy is a 56 year old ex-smoker admitted with sudden onset central crushing chest pain that radiated down his left arm.”
In this section you should expand on the presenting problem. Use the SOCRATES mnemonic to help describe the pain (see box 2). If the patient has multiple problems, describe each in turn, covering one system at a time.
Box 2: SOCRATES—mnemonic for pain
Associations
Time course
Exacerbating/relieving factors
“ The pain started suddenly at 1 pm, when Mr Murphy was at his desk. The pain was dull in nature, and radiated down his left arm. He experienced shortness of breath and felt sweaty and clammy. His colleague phoned an ambulance. He rated the pain 9/10 in severity. In the ambulance he was given GTN [glyceryl trinitrate] spray under the tongue, which relieved the pain to 5/10. The pain lasted 30 minutes in total. No exacerbating factors were noted. Of note: Mr Murphy is an ex-smoker with a 20 pack year history”
Some patients have multiple comorbidities, and the most life threatening conditions should be mentioned first. They can also be categorised by organ system—for example, “has a long history of cardiovascular disease, having had a stroke, two TIAs [transient ischaemic attacks], and previous ACS [acute coronary syndrome].” For some conditions it can be worth stating whether a general practitioner or a specialist manages it, as this gives an indication of its severity.
In a surgical case, colleagues will be interested in exercise tolerance and any comorbidity that could affect the patient’s fitness for surgery and anaesthesia. If the patient has had any previous surgical procedures, mention whether there were any complications or reactions to anaesthesia.
“Mr Murphy has a history of type 2 diabetes, well controlled on metformin. He also has hypertension, managed with ramipril, and gout. Of note: he has no history of ischaemic heart disease (relevant negative) (see box 3).”
Box 3: Relevant negatives
Mention any relevant negatives that will help narrow down the differential diagnosis or could be important in the management of the patient, 3 such as any risk factors you know for the condition and any associations that you are aware of. For example, if the differential diagnosis includes a condition that you know can be hereditary, a relevant negative could be the lack of a family history. If the differential diagnosis includes cardiovascular disease, mention the cardiovascular risk factors such as body mass index, smoking, and high cholesterol.
Highlight any recent changes to the patient’s drugs because these could be a factor in the presenting problem. Mention any allergies to drugs or the patient’s non-compliance to a previously prescribed drug regimen.
To link the medical history and the drugs you might comment on them together, either here or in the medical history. “Mrs Walsh’s drugs include regular azathioprine for her rheumatoid arthritis.”Or, “His regular drugs are ramipril 5 mg once a day, metformin 1g three times a day, and allopurinol 200 mg once a day. He has no known drug allergies.”
If the family history is unrelated to the presenting problem, it is sufficient to say “no relevant family history noted.” For hereditary conditions more detail is needed.
“ Mr Murphy’s father experienced a fatal myocardial infarction aged 50.”
Social history should include the patient’s occupation; their smoking, alcohol, and illicit drug status; who they live with; their relationship status; and their sexual history, baseline mobility, and travel history. In an older patient, more detail is usually required, including whether or not they have carers, how often the carers help, and if they need to use walking aids.
“He works as an accountant and is an ex-smoker since five years ago with a 20 pack year history. He drinks about 14 units of alcohol a week. He denies any illicit drug use. He lives with his wife in a two storey house and is independent in all activities of daily living.”
Do not dwell on this section. If something comes up that is relevant to the presenting problem, it should be mentioned in the history of the presenting problem rather than here.
“Systems review showed long standing occasional lower back pain, responsive to paracetamol.”
Findings on examination
Initially, it can be useful to practise presenting the full examination to make sure you don’t leave anything out, but it is rare that you would need to present all the normal findings. Instead, focus on the most important main findings and any abnormalities.
“On examination the patient was comfortable at rest, heart sounds one and two were heard with no additional murmurs, heaves, or thrills. Jugular venous pressure was not raised. No peripheral oedema was noted and calves were soft and non-tender. Chest was clear on auscultation. Abdomen was soft and non-tender and normal bowel sounds were heard. GCS [Glasgow coma scale] was 15, pupils were equal and reactive to light [PEARL], cranial nerves 1-12 were intact, and he was moving all four limbs. Observations showed an early warning score of 1 for a tachycardia of 105 beats/ min. Blood pressure was 150/90 mm Hg, respiratory rate 18 breaths/min, saturations were 98% on room air, and he was apyrexial with a temperature of 36.8 ºC.”
Differential diagnoses
Mentioning one or two of the most likely diagnoses is sufficient. A useful phrase you can use is, “I would like to rule out,” especially when you suspect a more serious cause is in the differential diagnosis. “History and examination were in keeping with diverticular disease; however, I would like to rule out colorectal cancer in this patient.”
Remember common things are common, so try not to mention rare conditions first. Sometimes it is acceptable to report investigations you would do first, and then base your differential diagnosis on what the history and investigation findings tell you.
“My impression is acute coronary syndrome. The differential diagnosis includes other cardiovascular causes such as acute pericarditis, myocarditis, aortic stenosis, aortic dissection, and pulmonary embolism. Possible respiratory causes include pneumonia or pneumothorax. Gastrointestinal causes include oesophageal spasm, oesophagitis, gastro-oesophageal reflux disease, gastritis, cholecystitis, and acute pancreatitis. I would also consider a musculoskeletal cause for the pain.”
This section can include a summary of the investigations already performed and further investigations that you would like to request. “On the basis of these differentials, I would like to carry out the following investigations: 12 lead electrocardiography and blood tests, including full blood count, urea and electrolytes, clotting screen, troponin levels, lipid profile, and glycated haemoglobin levels. I would also book a chest radiograph and check the patient’s point of care blood glucose level.”
You should consider recommending investigations in a structured way, prioritising them by how long they take to perform and how easy it is to get them done and how long it takes for the results to come back. Put the quickest and easiest first: so bedside tests, electrocardiography, followed by blood tests, plain radiology, then special tests. You should always be able to explain why you would like to request a test. Mention the patient’s baseline test values if they are available, especially if the patient has a chronic condition—for example, give the patient’s creatinine levels if he or she has chronic kidney disease This shows the change over time and indicates the severity of the patient’s current condition.
“To further investigate these differentials, 12 lead electrocardiography was carried out, which showed ST segment depression in the anterior leads. Results of laboratory tests showed an initial troponin level of 85 µg/L, which increased to 1250 µg/L when repeated at six hours. Blood test results showed raised total cholesterol at 7.6 mmol /L and nil else. A chest radiograph showed clear lung fields. Blood glucose level was 6.3 mmol/L; a glycated haemoglobin test result is pending.”
Dependent on the case, you may need to describe the management plan so far or what further management you would recommend.“My management plan for this patient includes ACS [acute coronary syndrome] protocol, echocardiography, cardiology review, and treatment with high dose statins. If you are unsure what the management should be, you should say that you would discuss further with senior colleagues and the patient. At this point, check to see if there is a treatment escalation plan or a “do not attempt to resuscitate” order in place.
“Mr Murphy was given ACS protocol in the emergency department. An echocardiogram has been requested and he has been discussed with cardiology, who are going to come and see him. He has also been started on atorvastatin 80 mg nightly. Mr Murphy and his family are happy with this plan.”
The summary can be a concise recap of what you have presented beforehand or it can sometimes form a standalone presentation. Pick out salient points, such as positive findings—but also draw conclusions from what you highlight. Finish with a brief synopsis of the current situation (“currently pain free”) and next step (“awaiting cardiology review”). Do not trail off at the end, and state the diagnosis if you are confident you know what it is. If you are not sure what the diagnosis is then communicate this uncertainty and do not pretend to be more confident than you are. When possible, you should include the patient’s thoughts about the diagnosis, how they are feeling generally, and if they are happy with the management plan.
“In summary, Mr Murphy is a 56 year old man admitted with central crushing chest pain, radiating down his left arm, of 30 minutes’ duration. His cardiac risk factors include 20 pack year smoking history, positive family history, type 2 diabetes, and hypertension. Examination was normal other than tachycardia. However, 12 lead electrocardiography showed ST segment depression in the anterior leads and troponin rise from 85 to 250 µg/L. Acute coronary syndrome protocol was initiated and a diagnosis of NSTEMI [non-ST elevation myocardial infarction] was made. Mr Murphy is currently pain free and awaiting cardiology review.”
Originally published as: Student BMJ 2017;25:i4406
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed
- ↵ Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: opinions of internal medicine clerkship directors. J Gen Intern Med 2009 ; 24 : 370 - 3 . doi:10.1007/s11606-008-0900-x pmid:19139965 . OpenUrl CrossRef PubMed Web of Science
- ↵ Olaitan A, Okunade O, Corne J. How to present clinical cases. Student BMJ 2010;18:c1539.
- ↵ Gaillard F. The secret art of relevant negatives, Radiopedia 2016; http://radiopaedia.org/blog/the-secret-art-of-relevant-negatives .
Clinical Radiology Case Presentation: Do's and Don'ts
Affiliations.
- 1 Division of Clinical Radiology, Department of Radiodiagnosis, Christian Medical College, Vellore, Tamil Nadu, India.
- 2 Division of Clinical Radiology, Department of Interventional Radiology, Christian Medical College, Vellore, Tamil Nadu, India.
- PMID: 34316108
- PMCID: PMC8299493
- DOI: 10.1055/s-0041-1729489
Clinical case presentation is part of daily routine for doctors to communicate with each other to facilitate learning, and ultimately patient management. Hence, the art of good clinical case presentation is a skill that needs to be mastered. Case presentations are a part of most undergraduate and postgraduate training programs aimed at nurturing oratory and presentation design skills. This article is an attempt at providing a trainee in radiology a guideline to good case presentation skills.
Keywords: clinical case presentation; clinical radiology case presentation; presentation skills; resident training.
Indian Radiological Association. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Publication types
- Bioimaging Sciences
- Bioimaging Sciences Division
- Clinical Trials Office
- TIMC & Imaging Support Services
- Interventional Oncology Research Lab
- Health Care Research
- Publications
- Imaging Informatics
- Abdominal Imaging
- Breast Imaging
- Cardiac Imaging
- Emergency Radiology
- Interventional Radiology
- Medical Physics
- Musculoskeletal Radiology
- Neuroradiology
- Nuclear Cardiology
- Nuclear Medicine
- Pediatric Radiology
- Thoracic Imaging
- VA Services
- Clinical Locations
- CDS Presentation
- EPIC Decision Support FAQ
- Non-EPIC users FAQ
- CMS - CDS – Appropriate Use Criteria
- To Reach Radiology
- Contact for Various Services
- Questions about Contrast
- Difficult to Order Studies
- Protocolling
- Yale Health
- Further Resources
- Official Interpretations on Outside Imaging Exams
- Practice Guidelines
- For Patients
- Premedication Policy
- Oral Contrast Policies
- CT Policy Regarding a Patient with a Single Kidney
- CT Policy Regarding Contrast-Associated Acute Kidney Injury
- For Diabetic Patients on Glucophage
- Gadolinium Based Contrast Agents
- Gonadal shielding policy for and X-ray/CT
- Policy for Power Injection
- Breastfeeding Policies
- Low-Osmolar Iodinated Contrast and Myasthenia Gravis
- CT intraosseous needle iodinated contrast injection
- Policy Regarding Testing for Pregnancy
- YDR Oral Contrast Policy for Abdominal CT in ED Patients
- YDR Policy for Suspected Pulmonary Embolism in Pregnancy
- Insulin Pumps and Glucose Monitors
- Critical Result Guidelines
- Q & A on "Change order" button for CT and MRI protocols
- EpiPen How to & Safety
- Thoracic Radiology
- West Haven VA
- Emeritus Faculty
- Secondary Faculty Listing
- Voluntary Faculty Listing
- Guidelines for Appointment
- Voluntary Guidelines Clarification
- Application Requirements & Process
- Vol. Faculty Contact Info & Conference Scheduling
- Visiting IR Scholarships for Women and URiM
- Neuroimaging Sciences Training Program
- Why Yale Radiology?
- Applicant Information
- Selection Procedure
- EEO Statement
- Interview Information
- Resident Schedule
- Clinical Curriculum
- Being Well @Yale
- Contact Information & Useful Links
- IR Integrated Application Info
- IR Independent Application Info
- Meet the IR Faculty
- Meet the IR Trainees
- YDMPR Program Overview
- Program Statistics
- Applying to the Program
- YDMPR Eligibility
- Current Physics Residents
- Graduated Residents
- Meet the Faculty
- Residents Wellbeing Policy
- Breast Imaging Fellowship
- Body Imaging Fellowship
- Cardiothoracic Imaging Fellowship
- The ED Fellow Experience
- How to Apply
- Virtual Tour for Applicants
- Current ED Fellows
- Meet the ED Faculty
- Applying to the Fellowship
- Fellowship Origins
- Program Director
- Current Fellows
- Howie's OpEd
- Musculoskeletal Imaging Fellowship
- Neuroradiology Fellowship
- Nuclear Radiology Fellowship
- Pediatric Radiology Fellowship
- Tanzania IR Initiative
- Opportunities for Yale Residents
- Medical School Curriculum
- Elective in Diagnostic Radiology
Elective Case Presentations
- Visiting Students
- Physician Assistant (PA) Radiology Course
- Radiology Educational Videos
- Anatomy Presentations
- Visiting IR Scholarships
- Information Technology
- Graduate Students
- Yale-New Haven Hospital School of Diagnostic Ultrasound
- Radiologic Technology Opportunities
- Educational Resources
- CME & Conferences
- The Boroff-Forman Lecture Series
- Grand Rounds Schedule
- Yale Radiology & Biomedical Imaging Global Outreach Program Tanzania
- Contrast Policies
- MRI Safety Policies and Procedures
- Pregnancy related guidelines
- Radiation safety policies
- COVID19 related SBARS
- Other policies
- Peer Learning and Fellow recheck Program
- Attending Radiologists Resources and SOPs
- Related News and Articles
INFORMATION FOR
- Residents & Fellows
- Researchers
Cardiothoracic
- Skip List Items
- Aberrant Right Subclavian artery
- Anterior_Superior Mediastinal Mass
- Aortic Transection
- Assymetric Pulmnary Edema
- Dermatomyositis ILD
- Post Operative Mediastinal Infections
- Posterior Mediastinal Mass
Gastrointestinal
- Aberrant Left Subclavian
- Colonic Rupture
- Colovesicular Fistula
- Diverticulitis
- Esophagram Complications
- Gallstone Illeus
- Pancreatic Adenocarcinoma
- Portal Venous Gas
- Toxic Megacolon
Genitourinary
- Autosomal Domminant Polycystic Kidney Disease
- Bladder Pheochromocytoma
- Urachal Adenocarcinoma
Musculoskeletal
- Multiple Myeloma
- Osteosarcoma Humerus
- Rheumatoid Arthritis
Miscellaneous
- Retroperitoneal Hemorrhage
- Retropharyngeal Abscess
- Splenic Laceration
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cardiovasc Dis
- v.2(3); 1975
RADIOLOGIC CASE PRESENTATION
L. paul gerson.
Department of Radiology, St. Luke's Episcopal and Texas Children's Hospitals, Houston, Texas 77025.
Edward B. Singleton
2 Texas Heart Institute, Houston, Texas 77025.
Full text is available as a scanned copy of the original print version. Get a printable copy (PDF file) of the complete article (453K), or click on a page image below to browse page by page.
Images in this article
Image on p.257
Click on the image to see a larger version.
- UTHealth Houston
- UTHealth TMC IR Residents
- Recent Alumni
- TMC IR Faculty
- How to Apply
- Welcome from the Chiefs
- Curriculum and Education
- Benefits, Moonlighting, and Wellness
- Clinician-Educator Track & Teaching
- Resident Research
- Resident Leadership & Accomplishments
- Dual Certification in DR and Nuclear Radiology
- Interviews and Open House
- Class of 2024
- Class of 2025
- Class of 2026
- Class of 2027
- Application Process
- Salary and Benefits
- Program Personnel
- Body Imaging
- Training Program
- Neuroradiology Faculty
- Previous Fellows
- Equipment List
- Research and Publications
- Program Contact
- PET/CT Imaging Mini-Fellowship with hands-on training
- Sports, Orthopedic and Emergency Imaging Fellowship
- Cardiothoracic Fellowship
- Current Fellows
- Course Overview & Electives
- Relevant Links
- Radiology Research Opportunities
- Visiting Student
Case Presentations
- Meet the Officers
- Monthly Meeting Calendar
- Educational Resources
- Conference Schedules
CASE PRESENTATIONS 2021 – 2022
Acute ACL Tear_Andrew Wang, MS4_Kumaravel, MD_June 2021
Tibial Plateau Fractures, Joseph Wilder, MS4, Kumaravel, MD_June 2021
Anoxic Brain Injury_Parth Patel, MS3_Lee, MD_Patel_June 2021
Uterine Scar Endometriosis_KarenPereira, MS3_Sanhaji, MD_June 2021
Acute splenic laceration_Bryan Hoang, MD_Pomfret, MD_Tapnio, MD_June 2021
Pediatric Omental Infarction_Emma Holmes, MS4_Hester, MD_Tapnio, MD_June 2021
Aortic Dissection_Joseph Kim, MS4_Kumaraval, MD_Awdeh, MD_May 2021
Desmoid Tumor_Ava Mirtsching, MS4_Bande, MD_Awdeh, MD_May 2021
Nonspecific Interstital Pnemonia (NSIP)-Interstital Lund Disease (ILD)_Ashley Tom, MS4_Su, MD_Awdeh, MD_May 2021
CASE PRESENTATIONS 2020 – 2021
ARDS Shelley Burge, MS4_Kumaravel, MD_Awdeh, MD_Apr 2021
Acute Appendicitis_John Jackson, MS4, Awdeh, MD_Apr 2021
Cervical Spine Facture_Anamaria Dragan, MS4, Pomfret, MD, Awdeh, MD_Apr 2021
Back pain following a fall, Jesse Degani, MS4, Awdeh, MD, Mar 2021
COVID Pneumonia with ARDS, Jessilyn Laney, MS4, Awdeh, MD, Mar 2021
Dens Type II, Aashini Patel, MS4, Kumaravel, MD, Awdeh, MD, Mar 2021
Extubated Pediatric Patient with Worsening Respiratory Status, Kayla Walter, MS4, Schwartz, MD, Awdeh, MD, Mar 2021
Mesenteric Ischemia Presentation, William Morris, MS4, Su, MD, Awdeh, MD, Mar 2021
Methotrexate Leukoencephalopathy, Sungita Kumar, MS4, Bonfante-Mejia, MD, Awdeh, MD, Mar 2021
Necrotizing Pancreatitis, Frances Howard, MS4, Wang, MD, Awdeh, MD, Mar 2021
Pneumoperitoneum, Chad Zhao, MS4, Awdeh, MD, Mar 2021
Acute Pancreatitis, Sarah Linson MS4, Lambert, MD, Wang, MD, Foss,MD, Awdeh, MD, Feb 2021
Advanced Neurodegeneration, Nicloe Thomason MS4, Khanpara, MD, Awdeh, MD, Feb 2021
Ankle Pain, Angie Aceves MS4, Awdeh, MD, Feb 2021
Appendiceal Rupture, Alexander Yin MS4, Awdeh, MD, Feb 2021
Bisphosphonate Fracture, Eric Tom MS4, Awdeh, MD, Feb 2021
Incidental Cardiac Finding, John Krapf MS4, Awdeh, MD_Feb 2021
Lateral Epicondylitis, Annika Medhus MS4, Kumaravel, MD_Awdeh, MD, Feb 2021
Mature Cystic Ovarian Teratoma, Olivia Ortiz MS4, Foss, MD, Awdeh, MD, Feb 2021
Pulmonary Embolism, Kyle Meissner MS4, Awdeh, MD, Feb 2021
Pyelonephritis, Eric Fris MS4, Awdeh, MD, Feb 2021
Vacterl, Tori Waters MS4, McCarty, MD, Awdeh, MD, Feb 2021
Abscess_Thomas Rogers, MS4_B.Wand, MD_Awdeh, MD_Jan 2021
Acute Triquetral Fracture _ Radiocarpal Subluxation_Jason Fuller, MS4_Bilow, MD_Awdeh, MD_Jan 2021AD 4013
Distal Femur Fracture Due to Trauma_Maryam Haider, MS4_Bilow, MD_Awdeh, MD_Jan 2021
Filum Terminale Lipoma_Zachary DeZeeuw, MS4_Samant, MD_Awdeh, MD_Jan 2021
Ground Level Fall in a patient w_ Cerebral Palsy_Jacqueline Dickey, MS4_Bilow, MD_Awdeh, MD_Jan 2021
Malrotation_Keziah Thomas, MS4_Qiao, MD_Awdeh, MD_Jan 2021
Renal Abscess _ Pyelonephritis_Weston Grove, MS4_Green, MD_Awdeh, MD_Jan 2021
Traumatic Pneumothorax_Stephen Palasi, MS4_Kumaraval, MD_Bawa, MD_Awdeh, MD_Jan 2021
ACL Tears_Adam Lazarus MS4_Spence, MD_Awdeh, MD_Dec 2020
Acute Scrotum in Children_John McCarthy, MS4_Tavernier, MD_Awdeh, MD_Dec 2020
Diabetic Foot Osteomyelitis_Min Yi Dong, MS4_Pomfret, MD_Awdeh, MD_Dec 2020
Fracture w_ Ankylosing Spondylitis_Frederick Lemaistre, MS4_ Hester, MD, Awdeh, MD_Dec 2020
MVA Fractures and Pneumothorax_Bert Ma, MS4_Greenfield, MD_Awdeh, MD_Dec 2020
Pulmonary Abscess_Marina Ibraheim, MS4_Conners, MD_Awdeh, MD_Dec 2020
Shoulder Dislocation with Bony Defects_Sahira Farooq, MS4_Bilow, MD_Awdeh, MD_Dec 2020
Tibial Avulsion Fractures_Nicolas Merutka, MS4_Bilow, MD_Awdeh, MD_Dec 2020
Traumatic Splenic Laceration_Kyle Lauck, MS4_Bilow, MD_Awdeh, MD_Dec 2020
Abdominal Pain_Ge Yan MS4_R. Hlis, MD_H. Awdeh, MD_Nov 2020
Aortic Dissection_Kyle Sheppard MS4_F. Celii, MD_H. Awdeh, MD_Nov 2020
Blunt Chest Truama_Michelle Ghebranious MS4_L. Ellerbrook, MD_H. Awdeh, MD_Nov 2020
Cervical Spine Truama_Justin Carranza MS4_C. Desai, MD_H. Awdeh, MD_Nov 2020
Extrahepathatic Cholangiocinoma_Angela Sheng MS4_W. Floss,MD_H. Awdeh,MD_Nov 2020
Femur Fracture _ Fat Emboli_Margeaux Epner MS4_E. Friedman, MD_H. Awdeh, MD_Nov 2020
Fracture of the Right Hip_Keziah Thomas MS4_W. Green, MD_H. Awdeh, MD_Nov 2020
Horseshoe Kidney_Shannon Swisher MS4_S. Neville, MD_H. Awdeh, MD_Nov 2020
Left Intraparenchymal Hemorrhage_Angela Murira MS4_R. Hills, MD_Awdeh, MD_Nov 2020
Seatbelt Syndrome_Devonne Harris MS4_N Chinapuvvala, MD_C. Desai, MD_H. Awdeh_Nov 2020
Subdural Hematoma_Jacqueline Woloski MS4_C. Sitton, MD_H. Awdeh, MD_Nov 2020
Translational Injury_Priscila Olague MS4_Y. Munir, MD_H. Awdeh, MD_Nov 2020
Abdominal Wall Abscesses_Jessica Williams MS4_Talley, MD_Awdeh, MD_Oct 2020
Acute Appendicitis_Tracy Nwanna MS4_Kumaravel, MD_Awdeh, MD_Oct 2020
Blunt Trauma-Spine_Amy Mulikin MS4_Bosserman, MD_Awdeh, MD_Oct 2020
Colonic Pseudo-Obstruction-Ogilvie Syndrome_Andrei Loghin MS4_Doyle, MD_Jarolimek, MD_Awdeh, MD_Oct 2020
Hepatic Encephalopathy_Frank Cai MS4_Pasciak, MD_Awdeh, MD_Oct 2020
Necrotizing Enterocolitis_Jocelyn Ursua MS4_John, MD_Awdeh, MD_Oct 2020
Ovarian Cysts-Dysmenorrhea_Jamie Haro-Silerio MS4_Bande, MD_Awdeh, MD_Oct 2020
Sarcomatoid Renal Cell Carcinoma_Ayana Taylor MS4_Talley, MD_Hasapes,MD_Awdeh, MD_Oct 2020
Trauma-Pneumothorax_Fauniel Self MS4_Bosserman, MD_Awdeh, MD_Oct 2020
Traumatic Bowel Injury_Rachel Carson MS4_Bilow MD, Awdeh MD_Oct 2020
Uterine Anomalies_Danielle Wilson MS4_Bilow, MD_Awdeh, MD_Oct 2020
ACL tear, Jordon Price MS4, A Bosserman MD Sep 2020
Anoxic brain Injury, Daniel Abramson MS4, M Patino MD Sep 2020
Gallstone Ileus Sally Choi MS4, M Lambert MD Sep 2020
Imaging in Sickle Cell disease, Maria Hernandez MS4, Thupili MD Sep 2020
Perilunate dislocation, Kevin Sok MS4, M Kumaravel MD Sep 2020
Rotator Cuff Repair, John Howell MS4, Kumaravel MD Sep 2020
Cystic Peritoneal Mass, Alexa Janda MS4, Kramer MD Aug 2020
Distal Femoral Fracture, Joaquin Santoy MS4, Scott MD Aug 2020
Hip Fracture, Ashley Notzon MS4, M Kumaravel MD MSK Aug 2020
Ocular Trauma Alex Villarreal MS4, S Scott MD, Aug 2020
Brain death, Kehan Vohra MS4, Bilow MD, ER July 2020
Comminuted Distal Femoral Fracture, Kevin Sok MS4, Kumaravel MD, MSK July 2020
Distal Tibial Fracture, Sally Choi MS4, Kumaravel MD, MSK July 2020
Peritonsillar Abscess, Austin Pickrell MS4, Patino MD, Clark MD July 2020
Rapunzel Syndrome Aashini Patel MS4, Greenfield MD, Pedi July 2020
Subcutaneous Emphysema, Annika Medhus MS4, Bande MD, thoracic July 2020
Traumatic Arm injury, Justin Tran MS4, Bilow MD, ER July 2020
CASE PRESENTATIONS 2019-2020
Womens’ Imaging
Ruptured Ectopic Pregnancy, Trinh Tammy MS4, P Bawa MD
Ductal Carcinoma of the Breast, Janda Alexandra MS3, M Kumaravel MD
Malignant Phyllodes Tumor, Vu Alan MS4, M Kumaravel MD
Body Imaging
Cirrhosis, Jessica Sanders MS3, Nathan Doyle MD, P Bawa MD
Vesicoureteral Reflux Cross Fused Ectopy, Joshua Rosengarten MS4, M. Kumaravel MD
Xanthogranulomatous Pyelonephritis, Davis Joy MS3, S. Narayanan MD
Abdominal Gun Shot Wound, Dugger Samuel MS4, P Bawa MD
Adenosquamous Carcinoma, Leonid Khokhlov MS4 Visiting Student, Dr. P.Bawa
Bladder Wall Injury, Dunlop Catherine MS4, P Bawa MD
Boerhaave Syndrome and Esophageal Stricture, Gaglani Tanmay MS4, Dr. Thosani, Dr. Thupili
Cervical Ectopic Pregnancy, David Wideman MS4, M. Kumaravel MD
Chronic Pancreatitis, Ontiveros Diana MS4, Dr. J. Talley PGY2
Gluteal Abscess, Maryam Alam MS3, P Bawa MD
Hepatocellular Carcinoma, Desai Ami MS4, N. Doyle MD, S. Burke MD
Metastatic Cholangiocarcinoma, Chernis Julia MS4, P Bawa MD, A Wolfe MD, C Costelleo MD
Mucinous Adenocarcinoma, lliana Chapa MS4, Wan MD, Shin MD
Ovarian Cancer with Large Bowel Obstruction, Bareis Alexander MS4,M. Kumaravel MD
Pancreatic Ductal Adenocarcinoma, Wright Kaylor MS4,S Burke MD, V. Tammisetti MD
Renal Cell Carcinoma, John Howell MS3, M Hanna MD
Sigmoid Volvulus, Sorkin Johnathan MS4, M. Redwine MD, S. Balabhadra MD
Testicular Seminoma, Haqqani Fatima MS4, R. Vikram MD
ER Radiology
Aortic Injury , Steven Ajluni C., Dr. P. Bawa, Dr. M. Kumaravel
Avulsion with Liver Laceration and Hemoperitoneum, Wood Roland MS4, Dr. R. Bilow
Blunt Aortic Injury_ Aortic Transection of Proximal Descending Aorta with Pseudoaneurysm, Drummond, Olivia MS4, L. Sanhaji MD
Brain Hemorrhage GSW, Rose Kevelyn MS4, R.Bilow
Cervical Spine Trauma, Ellis Ryan C MS4, C. Carney MD
Eye Trauma, Howard James J MS4, M. Tran MD
Facial Trauma, Wythe Stephanie MS4, M. Kumaravel MD
Pelvic Fracture and Extraperitoneal Bladder Rupture, Cooper Quiroz MS4, Dr. Chinapuvvula
Splenic Injury with Subcapsular Hematoma and Pseudoaneurysms , Alford Yakira MS4, Dr. R. Bilow
Traumatic Thoracic Aortic Pseudoaneurysm , Sullivan Kirbi MS4, N. Chinapuvvula MD
MSK – Radiology
Multiple Myeloma, Chopra Maneera MS4, Dr. P. Bawa, Dr. B. Wang
Anterior Bundle Ulnar Collateral Ligament Tear, Tran Justin MS3, M. Kumaravel MD
Biceps Tendon Injury, Carter Dalton MS4, P. Bawa MD
Chondroblastoma of the Knee, Milhoan Madison MS4, Dr. R. Kumar
Distal Femur Fracture, Andrews Reid MS4, Dr. P.Bawa
Osteoarthritis-Osteoarthrosis of the Knees, Patrick Conner MS4, Dr. H. Awdeh
Patella Tendon Tear, Rabinovich A. MS4, Dr. K. Bande, Dr. N. Beckmann
Pelvic Ring Injury, Hays Matthew MS4, Dr. P.Bawa
Segond Fracture, Choi Sally MS3, Dr. M. Kumaravel
Sickle Cell Crisis, Gaskey Gregory MS4, M. Kumaravel MD
Vertebral Osteomyelitis , Lam Brian MS4, S. Belchuk MD, K. Bande MD
Pedi Radiology
Acute Disseminated Encephalomyelitis, Martin Amanda MS4, H.Awdeh
Grade 3 Vesicoureteral Reflux, Lin Amanda MS4, M. Kumaravel MD
Hirschsprung Disease , Amber Garza MS4, M. Kumaravel MD
Hirschsprung Disease_, Hicks Kelsey MS4, M. Kumaravel MD
Hodgkin’s Lymphoma, Alexandria Lawrence MS4, Dr. P. Bawa. pdf
Intussusception, Abeysekera Radhini MS4, Dr. Wang PGY-2, Dr. H. Awdeh
Sepsis/Hydronephrosis 2/2 Obstructive Infected Nephrolithiasis, Rozean Colby MS4,P. Bawa MD
Acute Appendicitis, Chen Vanessa MS4, C. Yalniz MD
Brainstem Pilocytic Astrocytoma , Arca Makenna MS3, E. Bonfante- Mejia MD
Left Lung Pneumatocele , Jacob Dangerfield MS4, K. Hughes MD
RSV with Acute Hypoxemic Respiratory Failure, Air leak Syndrome with Spontaneous Pneumothorax, Pneumomediastinum and Pneumoperitoneum, Steward Sydne MS3, Dr. J. Hester, Dr. S. Greenfield
Salter Harris II Tibial Fracture, Kyra Frost MS4, Dr.M. Kumaravel
Salter-Harris III (Tillaux) Fracture, Dillion William MS4, Dr. Johnathan D Hester
Thoracic Imaging
Anterior Mediastinal Mass, Omar Alnatour MS4, Dr. P. Bawa
Pulmonary Embolism with Right Heart Strain, Hancock Saxon MS4, M. Kumaravel MD
Cardiac Tamponade Non-inflammatory Pericardial Effusion, Sandra Coker MS4, Dr. P.Bawa
Interstitial Lung Disease-Head Cheese Sign, Isabella Alamo-Ciufetelli MS3, B. Wang MD, Dr. P.Bawa
Pulmonary Embolism, Marc St Cyr MS4, Dr. P. Bawa
Pulmonary Nodule, Ashley Notzon MS3, E. Odisio MD, M. Lambert MD
VASC/IR – Radiology
Angiography Pre-Embolization with Internal Iliac Artery Selection, Viranmontes Jose MS4, J. Guccione MD
Bronchial Artery Embolization, Zacharia Grami MS4, Dr. K. Bande MS2
Clear Cell RCC, Srinivasan Aditya MS4, K. BlairMD
Mesenteric Angiography with Intervention for Chronic Portal Vein Occlusion, Korf Janelle MS3, Dr. Z. Bhatti
MSSA Endocarditis, Andrew Gulde MS4, Dr. P.Bawa
Positional Plagiocephaly, Coburn Ryan MS4, R Patel MD
- McGovern Medical School Facebook Page
- McGovern Medical School X Page
- McGovern Medical School Instagram Page
- McGovern Medical School YouTube Page
- McGovern Medical School LinkedIn Page
- Medical School IT (MSIT)
- Campus Carry
- Emergency Info
- How to report sexual misconduct
- University Website Policies

Case report
- Report problem with article
- View revision history
Citation, DOI, disclosures and article data
At the time the article was created Matt A. Morgan had no recorded disclosures.
At the time the article was last revised Matt A. Morgan had no recorded disclosures.
- Case reports
Case reports are a type of radiology research literature. They belong to the class of descriptive studies .
On this page:
- Related articles
The purpose of a radiology case report is to describe the patient history, clinical course, and imaging for a notable or unusual case. The case may be intended to aid other practitioners in interpretation, but frequently the oddity, rarity, and non-generalisibility of cases are meant more to amuse or entertain the reader.
A case report typically contains:
- a short introduction
- patient history and presentation
- a discussion of the imaging and other relevant interventions
- patient course
- summary/discussion
In radiology case reports, images from multiple imaging modalities are usually included, and gross pathology or histology is considered an excellent addition.
Case reports are generally considered the easiest and fastest radiology research paper to assemble.
Although debatable, the lack of "generalisibility" of case reports causes them to be regarded as lesser vehicles within research. Many journals will no longer accept case reports, for various reasons.
One disadvantage of case reports is that it may contribute to a type of recall bias in the reader. The attention the reader gives to a vanishingly rare case is held by the mind in a disproportionate regard compared with more common cases. The well-known maxim "an atypical presentation of a common disease is more likely than a typical presentation of a rare disease", is an effort to combat this type of bias.
Other disadvantages of case reports include:
- large numbers of case reports introduce an element of "noise" when searching the literature
- case reports claiming the first presentation of a case often find that they are actually not the first
- journals find that case reports do not get accessed as much as original research (it lowers their "impact factor")
That said, there are some advantages to case reports as well:
- the easier format allows junior researchers a chance to contribute to the literature, and helps them develop their skills
- a few case reports may develop into larger contributions to original research (for instance, in interventional radiology)
- they can be entertaining
- 1. Buckley O, Torreggiani WC. The demise of the case report. AJR Am J Roentgenol. 2007;189 (2): W54-5. doi:10.2214/AJR.07.2203 - Pubmed citation
- 2. Branstetter BF. Case reports: a premature demise. AJR Am J Roentgenol. 2008;190 (1): W80. doi:10.2214/AJR.07.2953 - Pubmed citation
Incoming Links
- BJR|case reports
- Case series
Related articles: Research
- case report
- case series
- Bayes' theorem
- Bayes' factor
- sensitivity
- specificity
- sensitivity and specificity of multiple tests
- positive predictive value (PPV)
- negative predictive value (NPV)
- incidence
- likelihood ratio (LR)
- standard error of the mean
- confidence interval (CI)
- retrospective studies
- prospective studies
- student t-test
- paired t-test
- one-way ANOVA
- factorial ANOVA
- repeated measures ANOVA
- multivariate ANOVA (MANOVA)
- single linear regression
- multiple linear regression analysis
- multiple logistic regression analysis
- chi-squared test
- automation bias
- length time bias
- lead time bias
- recall bias
- selection bias
Promoted articles (advertising)
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers


Case of pediatric cerebellar, hippocampal, and basal nuclei transient edema with restricted diffusion (CHANTER) syndrome in a 2-year-old girl
- Case Report
- Open access
- Published: 17 April 2024
Cite this article
You have full access to this open access article

- Robert A. Koenigsberg 1 , 2 ,
- Luke Ross ORCID: orcid.org/0009-0000-0884-8362 1 ,
- Jason Timmerman 1 ,
- Rithika Surineni 1 ,
- Kara Breznak 2 &
- Tina C. Loven 2
157 Accesses
Explore all metrics
Cerebellar, hippocampal, and basal nuclei transient edema with restricted diffusion (CHANTER) syndrome is a recently described entity that refers to a specific pattern of cerebellar edema with restricted diffusion and crowding of the fourth ventricle among other findings. The syndrome is commonly associated with toxic opioid exposure. While most commonly seen in adults, we present a case of a 2-year-old girl who survived characteristic history and imaging findings of CHANTER syndrome.
Similar content being viewed by others
Bilateral lesions of the basal ganglia and thalami (central grey matter)—pictorial review

Autoimmune encephalitis: what the radiologist needs to know

Comprehensive review of Wernicke encephalopathy: pathophysiology, clinical symptoms and imaging findings
Avoid common mistakes on your manuscript.
Introduction
Cerebellar, hippocampal, and basal nuclei transient edema with restricted diffusion (CHANTER) syndrome represents a rare disorder with a constellation of imaging findings in patients with opioid neurotoxicity. Clinically, patients present with altered mental status in the context of substance intoxication. The recently described pattern of imaging findings includes cytotoxic edema in bilateral hippocampi, cerebellar cortices, and the basal ganglia [ 1 ]. Patients also frequently develop early obstructive hydrocephalus from fourth ventricular compression [ 2 ]. Although these findings are usually associated with irreversible neuronal death and poor overall outcomes, patients with CHANTER syndrome can show significant clinical and radiographic improvement over time [ 1 ]. The disease has almost exclusively been observed and reported in adults, but we present the case of a 2-year-old girl who was found unconscious after consuming fentanyl. Her clinical presentation, history, and subsequent imaging findings are all consistent with a diagnosis of CHANTER syndrome.
Case description
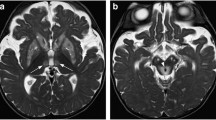
A 2-year-old female was found unconscious in her home for an unknown length of time. Urine drug screen was positive for fentanyl and a respiratory panel was positive for influenza. Noncontrast head computed tomography (CT) performed at day of presentation showed diffuse hypodensity in the bilateral cerebellar hemispheres and early ventriculomegaly (Fig. 1 a, ab).
Two-year-old girl found unresponsive after fentanyl ingestion. a Axial noncontrast CT head at the level of the posterior fossa shows bilateral diffuse cerebellar hypodensity suggestive of diffuse edema or infarction. b Mild ventriculomegaly is noted at the level of the lateral ventricles
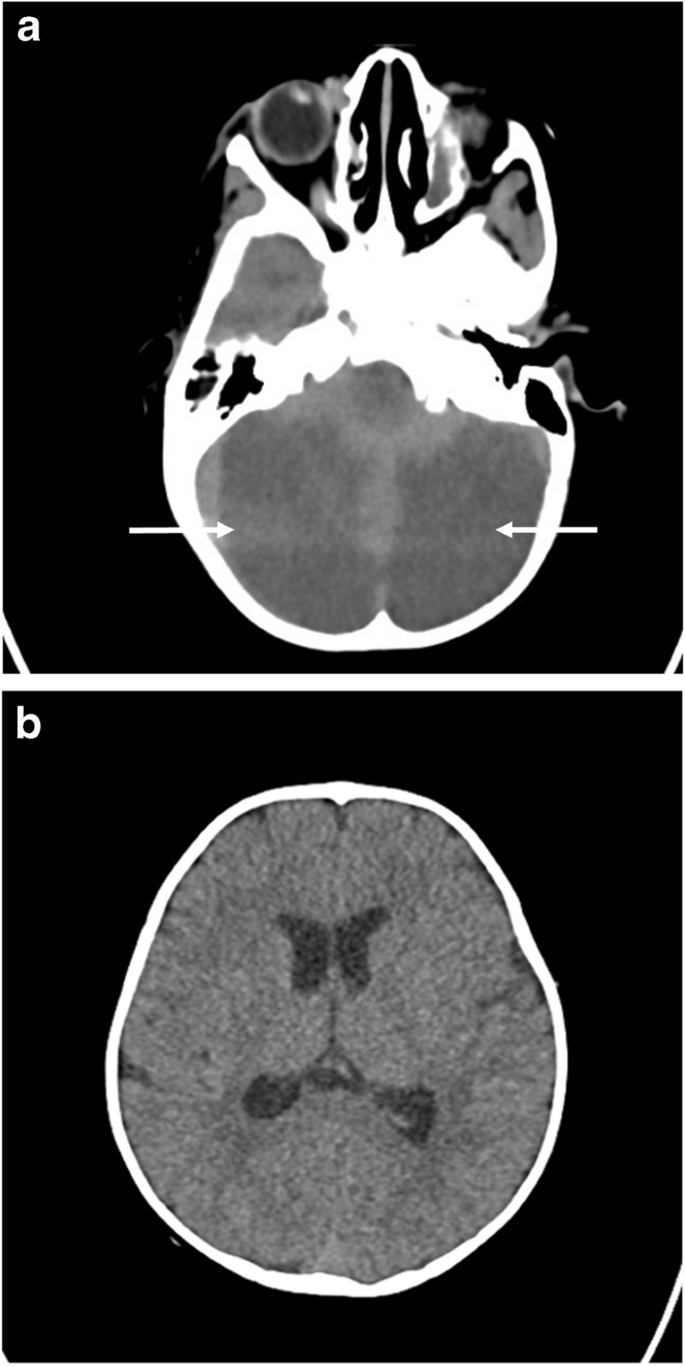
Subsequent brain magnetic resonance imaging (MRI) showed worsening of cerebellar edema, mass effect, and cerebellar herniation. There was bilateral restricted diffusion involving the cerebellum confirmed on apparent diffusion coefficient ADC map (Fig. 2 a and b). Bilateral restricted diffusion was also demonstrated separately within the hippocampus bilaterally (Fig. 2 c). Coronal T2 imaging demonstrated diffuse cerebellar edema with superior transtentorial herniation and downward tonsillar herniation at the level of the foramen magnum (Fig. 2 d). Magnetic resonance angiography (MRA) of the brain was performed which showed normal caliber of the intracranial arteries, including the vertebral arteries at the skull base (not shown). However, there was proximal dural venous sinus distention due to bilateral sigmoid sinus compression from bilateral cerebellar edema (Fig. 2 e and f).
a Axial diffusion-weighted image (DWI) b1,000 s/mm 2 showing diffuse cerebellar restricted diffusion confirmed as profound decreased signal on ADC map ( b ). c Axial DWI shows symmetric hippocampal restricted diffusion (curved arrows). Superior transtentorial herniation with cerebellar cortical restricted diffusion (straight arrow). d T2-weighted coronal image shows diffuse cortical cerebellar hemispheric edema with superior transtentorial herniation and bilateral downward cerebellar tonsillar herniation (straight arrows). Notice relative sparing of edema in cerebellar vermis (curved arrow). e Sagittal contrast T1 midline image demonstrating severe brainstem compression. Notice severely dilated sagittal (arrow) and straight (*) dural sinuses and compression of fourth ventricle (curved arrow). f Axial contrast T1 image at the level of the medulla confirming symmetric bilateral sigmoid sinus compression (arrows). g Follow-up T2 axial image obtained 2 months after initial presentation shows bilateral cerebellar encephalomalacia
Following MRI, the patient was emergently taken to the operating room for suboccipital decompressive craniectomy including C1 laminectomy. Postoperatively, the patient’s neurological exam gradually improved as she awoke and became progressively more alert. One month after presentation, the patient was discharged to rehabilitation moving both upper extremities without difficulty but had decreased movement of the bilateral lower extremities. Follow-up imaging at 2 months demonstrated resolution of cerebellar edema, with resultant bilateral cerebellar encephalomalacia (Fig. 2 g). At 10 months after initial presentation, the patient was able to ambulate independently and had neurologically recovered.
The Centers for Disease Control (CDC) reports that in 2021 alone, more than 80,000 people died of an opioid overdose [ 3 ]. It is reported that thousands of infants are born each year with opioid withdrawal. Furthermore, toddlers are ingesting caregiver’s medications and children and adolescents are prescribed opioids leading to addictions [ 4 ]. The most common place for a pediatric opioid death is in the household and most of these deaths are unintentional. The most common drugs implicated in pediatric overdose deaths were prescription opioids [ 4 ]. While the increasing toll of opioid addiction is often discussed among adults, the pediatric population has become a significant victim of the epidemic.
A spectrum of opioid toxicity–related syndromes has been described in the literature. These include CHANTER syndrome, pediatric opioid use-associated neurotoxicity with cerebellar edema (POUNCE) syndrome, heroin-associated spongiform leukoencephalopathy (also known as “chasing the dragon leukoencephalopathy”), and opioid-associated amnestic syndrome (OAA). While all these toxidromes share many similarities, they can be distinguished from one another by differences on imaging.
POUNCE syndrome has previously been described in children accidentally exposed to opioids who presented with altered mental status [ 5 ]. On imaging, malignant cerebellar edema is a prominent finding which often results in obstructive hydrocephalus similar to CHANTER syndrome. POUNCE syndrome is not associated with involvement of the hippocampi and basal ganglia, unlike CHANTER syndrome (as seen in our case). POUNCE syndrome is characterized by its predilection for white matter with areas of hypoattenuation on CT, and T2 hyperintense lesions on MRI [ 1 ]. Similar cases of accidental pediatric overdoses with subsequent cerebral edema have also shown a pattern of leukoencephalopathy rather than hippocampal and basal ganglia injury [ 6 , 7 ]. This is hypothesized to be due to differing distribution and predominance of opiate receptors between adults and children [ 8 ].
Clinically, pediatric opioid intoxication manifests similarly to adults. The most common presenting symptoms include drowsiness, vomiting, respiratory depression, miosis, agitation, and tachycardia [ 9 ]. Opioid overdose in children differs from the adult population in that there can be a delayed onset of toxicity, unexpectedly severe poisoning, and prolonged toxic effects. These can be attributed to the fact that children have differing rates of drug absorption and differing metabolisms, and drugs may distribute more easily into the central nervous system of children [ 10 ]. Furthermore, children often ingest higher doses than adults per kilogram of body weight and are less likely to have any opioid tolerance [ 11 ].
Diffuse cerebellar edema with restricted diffusion and crowding of the fourth ventricle are hallmark imaging findings of CHANTER syndrome [ 12 ]. This pattern of restricted diffusion was found in our 2-year-old patient after a fentanyl overdose, who presented with cerebellar edema and fourth ventricular compression. Vascular imaging ruled out arterial occlusion as the etiology of cerebellar edema and the patient’s history of fentanyl consumption made CHANTER syndrome the likely diagnosis. Fortunately, the patient did not further suffer from venous infarction, although there was imaging evidence of venous hypertension. Yet, we postulate that the deep ganglionic and hippocampal signal changes encountered in these patients are perhaps related to venous hypertension, which was potentially present in our case.
Conclusions
This case report presents a young child who was diagnosed with CHANTER syndrome and ultimately survived. With the use of opioids evermore increasing, identifying, diagnosing, and treating the various opioid toxidromes, especially in children, are of paramount importance. We hope that our case increases the awareness of this entity.
Atac MF, Vilanilam GK, Damalcheruvu PR et al (2023) Cerebellar, hippocampal, and basal nuclei transient edema with restricted diffusion (CHANTER) syndrome in the setting of opioid and phencyclidine use. Radiol Case Rep 18:3496–3500. https://doi.org/10.1016/j.radcr.2023.07.015
Article PubMed PubMed Central Google Scholar
Jasne AS, Alsherbini KH, Smith MS et al (2019) Cerebellar hippocampal and basal nuclei transient edema with restricted diffusion (CHANTER) syndrome. Neurocrit Care 31:288–296. https://doi.org/10.1007/s12028-018-00666-4
(2023) Opioid overdose. https://www.cdc.gov/drugoverdose/deaths/opioid-overdose.html . Accessed 26 Feb 2024
Gaither JR, Shabanova V, Leventhal JM (2018) US national trends in pediatric deaths from prescription and illicit opioids, 1999–2016. JAMA Netw Open 1:e186558. https://doi.org/10.1001/jamanetworkopen.2018.6558
Kim DD, Prasad AN (2020) Clinical and radiologic features of pediatric opioid use-associated neurotoxicity with cerebellar edema (POUNCE) syndrome. Neurology 94:710–712. https://doi.org/10.1212/WNL.0000000000009293
Article PubMed Google Scholar
Jasne AS, Alsherbini KA, Smith MS et al (2020) Response to “Malignant cerebella edema in three-year-old girl following accidental opioid ingestion and fentanyl administration.” Neuroradiol J 33:158. https://doi.org/10.1177/1971400920903106
Shrot S, Poretti A, Tucker EW et al (2017) Acute brain injury following illicit drug abuse in adolescent and young adult patients: spectrum of neuroimaging findings. Neuroradiol J 30:144–115. https://doi.org/10.1177/1971400917691994
Zagon IS, Gibo DM, McLaughlin PJ (1990) Adult and developing human cerebella exhibit different profiles of opioid binding sites. Brain Res 523:62–68. https://doi.org/10.1016/0006-8993(90)91635-t
Article CAS PubMed Google Scholar
Lavonas EJ, Banner W, Bradt P et al (2013) Root causes, clinical effects, and outcomes of unintentional exposures to buprenorphine by young children. J Pediatr 163:1377–1383. https://doi.org/10.1016/j.jpeds.2013.06.058 . e1–3
Boyer EW (2012) Management of opioid analgesic overdose. N Engl J Med 367:146–155. https://doi.org/10.1056/NEJMra1202561
Article CAS PubMed PubMed Central Google Scholar
Stoecker WV, Madsen DE, Cole JG, Woolsey Z (2016) Boys at risk: fatal accidental fentanyl ingestions in children: analysis of cases reported to the FDA 2004–2013. Mo Med 113:476–479
PubMed PubMed Central Google Scholar
Mallikarjun KS, Parsons MS, Nigogosyan Z et al (2022) Neuroimaging findings in CHANTER syndrome: a case series. AJNR Am J Neuroradiol 43:1136–1141. https://doi.org/10.3174/ajnr.A7569
Download references
Author information
Authors and affiliations.
Department of Radiology, Temple University Hospital, Philadelphia, PA, USA
Robert A. Koenigsberg, Luke Ross, Jason Timmerman & Rithika Surineni
Saint Christopher’s Hospital for Children, Philadelphia, PA, USA
Robert A. Koenigsberg, Kara Breznak & Tina C. Loven
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Luke Ross .
Ethics declarations
Conflicts of interest, additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Koenigsberg, R.A., Ross, L., Timmerman, J. et al. Case of pediatric cerebellar, hippocampal, and basal nuclei transient edema with restricted diffusion (CHANTER) syndrome in a 2-year-old girl. Pediatr Radiol (2024). https://doi.org/10.1007/s00247-024-05928-2
Download citation
Received : 02 October 2023
Revised : 05 April 2024
Accepted : 08 April 2024
Published : 17 April 2024
DOI : https://doi.org/10.1007/s00247-024-05928-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cerebellar infarction
- Find a journal
- Publish with us
- Track your research
ACR President William T. Herrington, MD, FACR, Calls on Leaders to Mentor, Nominate Next Generation
The page you recommended will be added to the "what others are reading" feed on "My ACR".
The page you bookmarked will be added to the "my reading list" feed on "My ACR".
Please enter at least 3 characters

Derailing Case Blue
Stiff Soviet resistance thwarted Hitler’s plan in the south along the Eastern Front in the summer of 1942.
This article appears in: April 2020
By Pat McTaggart
After the brutal defensive fighting during the winter of 1941-1942, Adolf Hitler was ready for another round with the Russians. This time, his armies would strike south with the twin goals of conquering the Caucasus and its rich oil fields and taking the city of Stalingrad. As far back as July 1940, when the planning for the invasion of the Soviet Union began, those two objectives had been part of the overall plan.
The unexpected Soviet resistance in late 1941 put a hold on those plans, but they were still on Hitler’s mind even after his failure to take Moscow and Leningrad earlier in the year. The Germans needed oil, and the Caucasus would provide it. He also knew that controlling Stalingrad would mean the loss of a major industrial city and would also cut traffic on the southern portion of the Volga River.
It would be a massive operation, code-named Fall Blau (Case Blue), that involved two panzer armies, three infantry armies, and the 2nd Hungarian Army. The plan was to advance on a broad front stretching from the Sea of Azov to Kursk. In his Führer Directive 41 promulgated on April 12, 1942, Hitler laid out his goals for the southern part of the Soviet Union: “All available forces will be concentrated on the main operations in the southern sector, with the aim of destroying the enemy before the Don [River], in order to secure the Caucasian oil fields and the passes through the Caucasus Mountains themselves.”
Hitler also detailed how this was to be accomplished. “The purpose is, as already stated, to occupy the Caucasus Front by decisively attacking and destroying the Russian forces stationed in the Voronezh area to the south, west or north of the Don … individual breaches of the front should take the form of close pincer movements. We must avoid closing the pincers too late, thus giving the enemy the possibility of avoiding destruction.”
In general, Hitler planned to take the city of Voronezh with a combined panzer-infantry assault and destroy Soviet forces there, giving him a bridgehead on the eastern bank of the Voronezh River, a tributary of the Don. The Führer Directive continued: “Armored and motorized formations are to continue the attack south from Voronezh, with their left flank on the Don River in support of a second breakthrough to take place from the general area east of Kharkov. Here too, the objective is not simply to break the Russian front, but in cooperation with the motorized forces thrusting down the Don, to destroy the enemy armies.”
It sounded simple. Voronezh would be taken quickly, and with that accomplished, the armored and mechanized forces would form the anvil behind the Soviet forces defending the approaches to the Volga River and Stalingrad. The German forces attacking from the east would be the hammer, and the Soviet armies caught between the two would be eliminated, depriving the Russians of vital troops needed to defend Stalingrad and the Caucasus.
The force tasked with taking Voronezh was Army Group von Weichs under the command of General Maximilian Freiherr von Weichs an dem Glon, who was also the commander of the 2nd German Army. The 2nd Army consisted of General Erwin Vierow’s LV Army Corps (45th, 95th, and 299th Infantry Divisions, and the 1st SS Brigade). Army Group von Weichs’ armored fist was General Hermann Hoth’s 4th Panzer Army. Hoth had three corps: General Erich Straube’s XIII (82nd and 385th Infantry and 11th Panzer Divisions), General Willibald Freiherr von Langermann und Erlankamp’s XXIV Panzer (377th Infantry, 9th Panzer, and 3rd Motorized Divisions), and General Werner Kempf’s XLVIII Panzer (24th Panzer and the Gross Deutschland, or Motorized Division).
During the coming operation, some of these divisions would be transferred back and forth between corps as needed. Other divisions would be added to the attack as it continued.
General Gustav Jany’s 2nd Hungarian Army, consisting of two corps, was also under von Weichs’ command. As a reserve force, von Weichs could count on four infantry divisions. General Wolfram von Richthofen (a cousin of the Red Baron of World War I fame) would provide air support with his VIII Air Corps.
Facing von Weichs was Lt. Gen. Filipp Ivanovich Golikov’s Briansk Front. Golikov had an impressive force under his command consisting of three infantry armies and one tank army with 19 rifle divisions, seven rifle brigades, six mechanized brigades, and 30 tank brigades. Air support for the front would be under the control of Maj. Gen. Konstantin Nikolaevich Smirnov’s 2nd Air Army.
In conjunction with the planning of Case Blue, the Germans began an intelligence operation designed to keep Soviet eyes off the southern area of the front. The German offensive in 1941 had come dangerously close to taking its objective of Moscow, and the 2nd and 3rd Panzer Armies of Army Group Center were in almost the exact same positions they had occupied since mid-November. A German salient at Rzhev pointed like a dagger toward Moscow, and the Russians knew it would make a perfect jump-off point for another try at the Soviet capital.

Fall Kreml (Case Kremlin) was set up to play on Stalin’s fears about another assault on Moscow. A top-secret directive from Army Group Center sent out on May 29 stated, “The OHK [Oberkommando des Heeres, or German Army High Command] has ordered the earliest possible resumption of the attack on Moscow.”
Reconnaissance flights in the Moscow area were increased, and sealed maps of the Moscow sector were sent to the army group with orders that they would remain sealed until June 10. When they were opened, corps and divisional staffs began planning for the offensive, unaware that the entire operation was a ruse. Russian spies reported all this activity to Stavka (the Soviet high command), which began making plans to meet the attack that was expected to begin on August 1.
Stalin believed that the Germans, even after the losses they had taken in 1941, could possibly launch two simultaneous operations, one aimed at Moscow and the other directed at the Caucasus. Soviet reports state that he was more concerned about the one directed at Moscow and considered the other extremely unlikely. As late as June 26, Stalin still believed that Case Blue was mostly nonsense. In a telephone call to Golikov, he said that it “was something concocted by intelligence people.”
He must have had some doubts about his own convictions, however, as he ordered Golikov to plan an attack in the Orel area as a preemptive move, just in case the Germans were planning a southern offensive. The Soviet general was still fine-tuning his attack when the Germans struck.
The generals in Berlin were confident that Army Group von Weichs would accomplish its goals quickly and with little difficulty. Golikov’s forward troops defended an area crisscrossed by the Sosna River and its tributaries, as well as by ravines known as balkas. German planning had taken that into account, and if bridges were blown or fords were too heavily defended, engineers stationed just behind the front could be rushed forward to repair or build new bridges over which the advance could continue.
Dawn came early during the summer in southern Russia. The soldiers in forward Soviet positions noticed a thin mist rising from the ravines and hollows as the sky began to lighten at 2 am on June 28. Behind that mist, German reconnaissance units were already on the move, headed for the Russian line.
Suddenly, the western sky lit up as army, corps, and divisional artillery opened fire on Soviet positions. Shells whined over the heads of the attacking Germans, smashing enemy trenches and strongpoints before continuing eastward in a rolling barrage. Close behind the barrage, elements of von Richtofen’s VIII Air Corps rained down bombs on specific fortified strongpoints before heading east to strafe and bomb targets of opportunity and identified supply dumps and communications hubs.
The results were devastating. As the men of Brig. Gen. Walter Hörnlein’s Gross Deutschland Division advanced toward their first objective, the supposedly strongly fortified village of Dubrovka, they found nothing but carnage. The divisional history reported, “Dubrovka itself has been flattened—wreckage and ruins—not a house was left standing, not a fence, only smoking timbers and smoldering rubble.”
The men moved on. A key objective was the capture of bridges crossing the Tim River. Infantrymen of Lt. Col. Ludwig Kohlhaas’s 3rd Battalion, 2nd Infantry Regiment, Gross Deutschland Division sliced through the battered Soviet defenses and reached the narrow river by 6 am. Although the road bridge crossing the river had been destroyed, a rail bridge still stood. Men of Kohlhaas’s 11th Company speedily crossed the bridge and drove defending Russians on the eastern bank out of their positions.
At the height of its success, the 11th was mistakenly attacked by the Luftwaffe, causing several casualties. Kohlhaas was wounded in the attack and had to turn command of the battalion over to a subordinate. He was awarded the Knight’s Cross on November 22 for his actions, just nine days before he was killed in combat.

It was the same all along von Weichs’ front. The speedy advance of the German forward units captured several crossings that were needed for the armored onslaught that would soon follow. The engineers that followed in the wake of the first wave strengthened bridges to support the panzers and built crossing points across the numerous balkas in the area.
As news of the successes of the forward elements reached higher headquarters, Hoth prepared to launch his armored fist. Von Langermann’s XXIV Panzer Corps had approximately 350 tanks, while Kempf’s XLVIII Panzer Corps had about 325. Together, the two corps were to strike the boundary of Lt. Gen. Mikhail Artemevich Pasegov’s 40th Army and Maj. Gen. Nikolai Pavlovich Pukhov’s 13th Army.
The forward positions of Pasegov’s army were defended by five infantry divisions (45th, 62nd, 121st, 160th, and 212th), with the 6th Rifle Division and three rifle brigades farther to the rear. His armor included the 14th and 170th Tank Brigades with a total of about 70 tanks and Maj. Gen. Mikhail Ivanovich Pavelkin’s 16th Tank Corps with about 180 tanks.
Pukhov had four rifle divisions (15th, 132nd, 143rd, and 148th) at the front and the 307th Rifle Division and a rifle brigade in reserve. The 13th Army’s armored force consisted of the 129th Tank Brigade with some 40 tanks and Maj. Gen. Mikhail Efimovich Katukov’s 1st Tank Corps, which was also the front reserve, containing about 170 tanks.
At 10 am, the order came: “Panzer Marsch.” Von Langermann and Kempf rolled forward toward the crossings that had been built or captured. The Russians facing them were in disarray for the most part. Having been pummeled by artillery and bombed and strafed by the Luftwaffe, many defensive positions had simply disappeared. Communications lines had been severed, leaving higher headquarters out of contact with subordinate units, and even company commanders had a hard time communicating with their sub-units.
“We were confident of victory,” wrote Colonel Maximilian Reichsfreiherr von Edelsheim, commander of the 24th Panzer’s 26th Rifle Regiment. In a 1986 letter to the author, he described the scene: “My unit followed close behind the panzers of the 24th Panzer Regiment. Great clouds of dust arose as we pushed forward. To our left and right, similar clouds were raised by other panzer or mechanized units. It seemed like nothing could stop us. We were to find out differently later on, but this day was ours.”
Lieutenant Georg Köhler was in von Edelsheim’s 3rd Company. Ten years before his death in 2006, he wrote to the author concerning the advance: “My men were in a fine mood. Our morale was high. The engineers and other forward elements of the division had done their work well, and we had few problems in crossing the ravines and streams in front of us. As we advanced, we could see clouds of dust rising on our left. It was the bulk of the Gross Deutschland Division moving forward.”
Kempf’s two divisions headed at full speed toward the Tim River, where they slammed into Colonel Mikhail Borisovich Anashkin’s 160th Rifle Division and the neighboring 212th Rifle Division, which were stationed along the western bank north and south of the city of Tim. Not yet recovered from the morning barrage, the Russian defenders were easily overcome, and the panzers continued to race to the southwest.
North of Kempf, von Langermann’s corps also had great success. Brig. Gen. Hermann Balck’s 11th Panzer Division, after crossing the Tim, smashed into Colonel Afanasii Nikitovich Slyshkin’s 15th Rifle Division, shattering its defenses and sending survivors fleeing toward the rear. To Balck’s right, Maj. Gen. Petr Maksimovich Zykov’s 121st Rifle Division met the same fate at the hands of Brig. Gen. Johannes Baessler’s 9th Panzer Division. The first day had lived up to expectations: the panzers were headed to Voronezh, and it seemed that the great envelopment intended to destroy Russian forces west of the Don would proceed as scheduled.
Parsegov reported by radio to Briansk Front headquarters. He told Golikov that the 40th Army had sustained “significant losses,” but, he reported, the army was still capable of combat. He also asked for tank reinforcements to counter the German panzers.

Golikov relayed the request to Stavka. In response, Maj. Gen. Pavelkin’s 16th Tank Corps (107th, 109th, and 164th Tank Brigades) and Maj. Gen. Nikolai Vladimirovich Feklenko’s 17th Tank Corps (66th, 67th, and 174th Tank Brigades and the 31st Mechanized Brigade) were ordered forward to the Kshen River. The 115th and 116th Tank Brigades were also pulled from the Briansk Front reserve and sent forward to bolster Parsegov’s forces.
In addition to those forces, Stavka ordered the Southern Front’s 4th Tank Corps (45th, 47th, and 102nd Tank Brigades and 4th Mechanized Brigade), commanded by Lt. Gen. Vasilii Aleksandrovich Mishulin, and Maj. Gen. Vasilii Mikhailovich Badanov’s 24th Tank Corps (54th and 130th Tank Brigades, 24th Mechanized Brigade, and 4th Guards) north to the Stary Oskol area. When they arrived at their destination, they were to prepare for a counterattack against an expected German attempt to capture the river crossing points near the town.
During the early hours of June 29, it began to rain. It soon turned into a downpour with lightning illuminating the steppe. Throughout the morning, Hoth’s panzers and motorized troops struggled to advance on dirt roads and paths that had suddenly turned to mud. Wachtmeister Siegfried Freyer was in 4th Battalion, Panzer Regiment 24. “We could get little traction for the panzers, because the mud clung to our tracks,” he remembered. “The panzer would slide this way and that way, and it was hard to keep any kind of formation. The engines were also overworked as we tried to move forward in that slime.”
At around 11 am, the rain stopped and the sun came out, its fiery heat quickly drying the sodden ground. By 1 pm, Hoth’s troops were moving forward again at full speed. With Junkers Ju-87 Stuka dive bombers swarming overhead and German artillery blasting Soviet defenses, the 11th Panzer reached the banks of the Kshen River about 10 kilometers west of Volavo. Farther north, German infantry was pushing the Russians back toward Livny.
Upon reaching the Kshen, the 11th Panzer ran into Pavelkin’s 16th Tank Corps, which was arriving piecemeal in the area. Since the Soviets did not yet have a force strong enough to counter the Germans, they retreated to await reinforcements. South of Balck, the 9th Panzer was probing 40th Army defenses situated on the eastern bank of the Kshen.
Kempf’s XLVIII Panzer Corps was also making good progress. The Gross Deutschland and 24th Panzer crossed the Kshen and established bridgeheads about 40 kilometers south of the 11th Panzer, with the Gross Deutschland advancing 47 kilometers for the day.
To the Gross Deutschland’s right, Brig. Gen. Bruno Hauenschild had pushed elements of his 24th Panzer across the Kshen bridgehead and hit Maj. Gen. Mikhail Danilovich Grishin’s 6th Rifle Division, which was scattered after a short, sharp fight. As night fell, an advance unit of the division entered the village of Bykovo.
A cluster of trucks was near one of the houses, and upon entering the building, the Germans found maps and documents relating to the Soviet defenses. The Germans had just missed capturing the headquarters staff of the 40th Army. Although the staff had escaped, the material left behind was an intelligence boon. Furthermore, Pasegov had lost command and control over his army, which would be of great help to the Germans in the coming days.
While German forces were battering the 40th Army, General Jany was having a more difficult time as the 2nd Hungarian Army tried to push its way through the Soviet defenses south of the town of Tim. Colonel Vasilii Pavlovich Sokolov’s 45th Rifle Division resisted all attempts by the Hungarians to breach its line. On Sokolov’s flanks, the 212th and 62nd Rifle Divisions also held their own. Soviet resistance also increased on Parsegov’s right flank as Maj. Gen. Nikolai Pavlovich Pukhov’s 13th Army, reinforced by Katukov’s 1st Tank Corps, occupied positions on von Langermann’s left flank.
Late on the 29th, the 1st and 16th Tank Corps launched an attack on the 11th Panzer Division. Although supported by infantry, the attack was poorly coordinated, and the 11th easily repulsed it. The failure showed that the Russians still had quite a way to go when it came to using combined forces and armor en masse.
Undeterred, Stalin directed Golikov to plan another armored attack for the next day. The operation was to use the 1st, 4th, 16th, 17th, and 24th Tank Corps in an effort to halt the German advance and restore a proper defensive line. Soviet forces would have an approximate 2-to-1 advantage in tanks over their German opponents for the attack. Instead of a decisive action, however, it turned into another debacle during the next few days.

Katukov’s 1st Tank Corps hit Balck’s 11th Panzer once again, and once again the assault was plagued by poor command and control between the corps’ subordinate brigades. The same could be said for Pavelkin’s 16th Tank Corps, which attacked the lead elements of Balck’s division. Ultimately, Pavelkin’s surviving tanks were forced to retreat across the Olym River, where they tried to regroup with the remnants of Katukov’s corps.
The 4th and 17th Tank Corps went up against the Gross Deutschland and 24th Panzer Divisions. Mishulin’s 4th Tank Corps met the 14th Panzer 10 kilometers south of Gorshechnoye, about 62 kilometers southwest of Voronezh. With his corps strung out, Mishulin had only two of his four brigades at his immediate disposal. They were easily defeated by Hauenschild’s panzers.
“Tank after tank exploded under our shells,” Wachmeister Freyer recalled. “To us it seemed suicidal, but the Ivans still came. It was almost like practice on the firing range as we destroyed the enemy armor.”
To make things worse, Badanov’s 24th Tank Corps was nowhere to be found on the field of battle. His forces were still assembling at Stary Oskol, about 12 kilometers southwest of Gorshechnoye. Although he must have heard the sounds of battle, he did not have sufficient forces in the area to commit them to the fight.
Meanwhile, Feklenko proved to be an utter failure. He could have joined the battle if he had attacked from Kastornoye, about 16 kilometers away. Instead, he moved his units to and fro, effectively scattering his brigades. With communication between himself and his brigades disintegrating, the 17th proved easy pickings for German combat groups. The 17th was decimated, losing more than three-quarters of its 179 tanks. Feklenko was relieved of his command on July 1.
While the armored battle in the north ran its course, General Paulus launched his 6th Army’s assault against Marshal Semen Konstantinovich Timoshenko’s Southwest Front. This was the southern pincer of the opening phase of Case Blue. Although the attack had to be postponed a day because of heavy rain, Paulus’s troops made good progress in most places on June 30. Swinging his corps to the northeast, he was well on his way to link up with von Weichs’ forces. When the connection was made, it would effectively surround Soviet forces south of Voronezh and deprive the Russians of much needed troops to defend the eastern bank of the Don.
The combination of the defeat of Golikov’s tank corps and the opening of Paulus’s offensive convinced Stavka to order Parsegov’s 40th Army and two of Timoshenko’s armies, the 21st (Maj. Gen. Alexi Ilyich Danilov) and the 28th (Lt. Gen. Dmitrii Ivanovich Riabyshev) to retreat from their perilous positions to a new defensive line along the Olym and Oskol Rivers. Beginning at dawn on July 2, the Soviet armies attempted to pull back under a hail of German artillery fire. The VIII Air Corps, now commanded by Maj. Gen. Martin Fiebig, added to the chaotic retreat as it strafed and bombed the Russian columns.
The Germans kept up their pursuit. At Gorshechnoye, the Gross Deutschland captured the village after a fight that left 51 Soviet tanks destroyed. On Hörnlein’s right flank, the 24th Panzer also kept up the pressure. It seemed that the first phase of Case Blue would be a success.
Stavka’s hope of establishing its new defensive line was shattered as German troops crossed the Oskol River. It was now evident that the paramount Soviet objective should be to get as many troops as possible across the Don River.
While things seemed to be going well for the Germans in von Weichs’ southern sector, Pushkov’s 13th Army was putting up a tougher fight north of Voronezh. Golikov now had his headquarters inside the city, and he was determined to hold it. To bolster Pushkov’s defenses, he had Colonel Sarkis Sogomanovich Martirosian’s 340th Rifle Division, the 1st Guards Rifle Division, two tank brigades, and Colonel Ivan Fedorovich Lunev’s 8th Cavalry Corps (21st and 112th Cavalry Divisions) move forward to reinforce him.
Stalin was also determined to hold Voronezh. With his armies south of the city crumbling, the city’s rail hub and the railway lines east of the city running to the southeast became increasingly important. If a new line could be formed behind the Don or the Voronezh Rivers, those tracks would be vital in moving supplies and troops to endangered areas in the south.

On July 3, the situation south of Voronezh continued to deteriorate for the Soviets. The 40th Army was now in total disarray. Hoth ordered Kempf to release Maj. Gen. Sigfrid Henrici’s 16th Motorized Division from his corps reserve and send it racing toward Stary Oskol, where it linked up with the advance elements of the 6th Army. Although the 40th Army was now encircled, there were still gaps in the German lines due to the panzer divisions’ involvement in the fighting around Voronezh, and many Red Army soldiers were still able to continue their retreat to the Don.
The 28th and 21st Armies were also reeling under combined German armor and infantry attacks. Novy Oskol fell on the evening of July 3, and an attempt to form a new defensive line was only partially successful. During the past few days, the 21st and 40th Armies had lost more than half their fighting strength, and the 28th was not in much better shape.
On the map, it looked like the Russians were facing a tremendous disaster. With two armies effectively destroyed and another barely hanging on, an immense gap was opening between the Briansk and Southwest Fronts. As a remedy Stalin ordered two reserve armies to move forward. The 5th Reserve (Lt. Gen. Vasilii Ivanovich Kuznetsov) and the 7th (Maj. Gen. Vladimir Iakolevich Kolpakchi), each with six rifle divisions, were sent to the front to prevent Paulus from exploiting the gap.
Furthermore, Moscow ordered Lt. Gen. Maksim Antonovich Antoniuk’s 3rd Reserve Army (six rifle divisions) to take up positions along the Don River north of Voronezh and Maj. Gen. Fedor Mikhailovich Kharitonov’s 6th Reserve Army (seven rifle divisions) to river positions south of the city.
Things were still going well for Paulus south of Voronezh, but the units advancing toward Voronezh started to notice a turn in enemy tactics. North of Krassyana Polyana, about 90 kilometers southwest of the city, the 1st Infantry Regiment of the Gross Deutschland set out to take an objective known as Hill 204. Advance elements of the regiment found manned field positions that spewed out deadly fire as reconnaissance forces pushed ahead. The Germans were somewhat taken aback after the past few days of pursuit. Ivan was finally standing and fighting.
The regiment commander, Colonel Otto Kohler, deployed his 2nd Battalion and then ordered his men to attack. The marshy area in front of the hill made it extremely difficult for armored vehicles to operate, so it was up to the infantry to take the hill in a frontal assault. German artillery was met by Soviet artillery as the men moved forward at 8 pm.
It was a bloody fight. The Soviets manned strongly fortified bunkers and positions that had to be taken in hand-to-hand combat. Flamethrowers were called forward to burn out the Russians, who refused to retreat a step. As men shot each other at close range or hacked away at each other with knives and entrenching tools, it seemed that the battalion might fail to take its objective.
With the issue in doubt, 1st Lt. Fritz Schulz, a company commander in the battalion, took matters into his own hands. Commandeering some assault guns, he led them and his company through the marshy area and around a stream. Attacking the Russians from the unexpected direction, Schulz was in their positions before they could fully react. With the Soviet fire divided, the rest of the battalion was able to take the hill after a costly fight during which Schulz was severely wounded.
The 24th Panzer and troops of the other divisions facing Voronezh were also finding an enemy that refused to retreat until threatened by annihilation. With most of the 40th, 21st, and 28th Armies still retreating toward the Don crossing, these suicidal rearguard actions were vital to their survival. As they noticed the Russians slipping away, it became even more vital that Hoth’s armor push south along the Don to form a line behind them.
The situation was apparent in Berlin. If the Soviet units west of the Don were not destroyed, the first phase of Case Blue would be a failure. Although he was pleased with the advance of the 6th Army, Hitler saw the danger of Hoth’s panzer divisions getting bogged down in the fight for the approaches to Voronezh. He now concluded that his original plan to take Voronezh by a lightning armored thrust might not be best for the overall operation.

Making a quick flight to von Bock’s headquarters, Hitler and his field marshal held a brief meeting. According to historian Paul Carell, Hitler told von Bock, “I no longer insist upon the capture of the city. I also no longer consider it necessary, and I leave it up to you to move Hoth’s armored forces south immediately.”
Hitler’s comment was a remarkable one for the usually decisive Führer. He did not directly order von Bock to forget about taking Voronezh. Instead, his vague statement left things hanging in the air. Taking the city was supposed to be one of his major objectives, but now it seemed to be of secondary importance. Still, the possession of Voronezh would free up all of Hoth’s 4th Panzer Army to swing south in force. The more von Bock thought about his options, the more he wavered.
The situation in the Voronezh sector at the end of July 3 seemed to favor the Germans, even with the increasing Soviet resistance. Straube’s XIII Army Corps had advanced almost halfway between the Oskol and Don Rivers in the north, while in the center, von Langermann’s XXIV Panzer Corps had advanced east of Kastornoye. On von Langermann’s right flank, Kempf’s XLVIII Panzer Crops was also halfway between the Oskol and the Don.
As von Bock vacillated, the 4th Panzer Army and 2nd Army continued with their original orders on July 4. The arrival of Soviet reinforcements along Army Group von Weichs’ northern flank forced some changes to the original plan. With Straube’s XIII Army Corps reporting increased resistance and local counterattacks, von Langermann was ordered to shift his advance toward the northeast to strengthen the infantry. The shift left Kempf to carry on the drive to Voronezh from the west.
Lead elements of the Gross Deutschland reached the village of Devitsa, named for the river it sat next to. Soviet engineers had already blown the bridge that crossed the river, and the advance was halted while a new bridge was hastily constructed. The Gross Deutschland was now only nine kilometers from the Don.
While the bridge was being constructed, the rain stopped and the sun came out. Early in the afternoon, the lead elements of Infantry Regiment 2, Gross Deutschland crossed the Devitsa and continued westward on the drying roads. With the rest of the division following, the spearhead had the Don in sight by mid-afternoon.
Reconnaissance units reported that the enemy was moving troops across the river to the east bank with several ferries. The regimental commander, Colonel Eugen Garski, immediately issued a series of orders to his units. Since the steep approaches to the ferry crossings were unsuitable for building a bridge, he had the crossings brought under artillery fire as soon as the guns could be positioned.
Maps showed that a railroad bridge was located north of the crossings. Garski sent two companies to capture it while the rest of the regiment assembled. As they approached the bridge, the Germans realized that the Russians were unaware of their presence. They noticed that reinforced defensive positions had been erected on the eastern bank, and that a primitive armored train sat on the railway tracks.
An attempt to take the bridge by surprise ran into trouble when Soviet sentries finally noticed the dust raised by the hastily advancing Germans. Mortar and artillery fire began to fall among the Germans, and the armored train soon joined in. Although the train was soon set ablaze by German artillery, the heavy fire prevented the capture of the bridge. Meanwhile, the burning train had also set the bridge on fire, turning it into an inferno that would make it useless.
While the Gross Deutschland was engaged with the Soviets, von Hauenschild was having better luck. About 20 kilometers south of Gorski’s men, the 24th was able to establish bridgeheads across the Don south of the village of Ustye. These were soon reinforced, allowing the troops on the eastern bank to beat off several disorganized Soviet attacks.
Faced with the threat from the south, Golikov sought to strengthen Voronezh’s defenses. With his front stretched out along the Don, there were few forces readily available. The 13th Army was still holding out north of the city, but it could spare no men. Parsegov had been relieved on July 3, and his replacement, Lt. Gen. Markian Mikhailovich Popov, was in the process of trying to redeploy the 40th Army south of the city. He too had no troops to spare. West of Voronezh, defending the area between the Don and Voronezh Rivers, were the 53rd and 75th Fortified Regions.

A fortified region was planned for defense. It consisted of obstacles and strongpoints that would provide mutual assistance to one another. Troops belonging to fortified regions were largely immobile and were expected to defend their positions to the last man.
In the city proper, there were several undermanned NKVD units that were armed with only light weapons. The city’s defenses also included elements of the 3rd Air Defense Division, which contributed antiaircraft weapons that could also be used for ground fire.
The defenses directly north of the city were occupied by Colonel Ivan Illich Ulitin’s 232nd Rifle Division. Colonel Aleksandr Nikolaevich Afanasov’s Siberian 309th Rifle Division was still arriving by rail. As elements of the division detrained, they were immediately sent to occupy positions south of the city.
With the 24th Panzer assembled for an advance to its south, the Gross Deutschland finally encountered some luck. Foiled in the attempt to take the railroad bridge, Hörnlein spread his division out to search for a new crossing. At 7 pm, elements of Köhler’s 1st Infantry Regiment reached the village of Semiluki, about nine kilometers west of Voronezh. To the Germans’ surprise, they found a lightly guarded road bridge intact.
The commander of the 7th Company, 1st Lt. Carl-Ludwig Blumenthal, gathered his men and set up a plan of attack. Under the covering fire of a heavy machine-gun section, Blumenthal led his men forward, scattering the Russians on the western side of the bridge while coming under fire from bunkers on the opposite bank.
The river was fairly shallow where the bridge lay, and a Sergeant Hempel jumped into the water. Although up to his neck, Hempel made it across the 75 meters that separated the east and west banks, removing demolition charges with his bare hands. Although the bridge had been damaged, the Germans were able to force a crossing by the end of the day and establish a bridgehead that would be reinforced by troops crossing in inflatable boats.
Considerable time was spent during the night with the crossing and assembly of troops from Kempf’s panzer corps for a concentrated attack on Voronezh. Hoth, it seems, was hesitant about committing armored forces to the attack without the absolute certainty that it would succeed. He did not know how weakly defended his objective actually was, so instead of taking Voronezh with the forces at hand, he wasted precious time with the buildup.
While the assault on Voronezh was taking more time than had been contemplated, Paulus’s 6th Army was still advancing eastward. His troops were making good progress, but the Russians had the advantage of trading land for time as they pulled back toward the Don. The armored forces of the 4th Panzer Army tied down around Voronezh made the retreat easier by allowing the Soviets on the Southwest Front to concentrate on saving themselves without the fear of a massive encirclement.
As the 24th Panzer and Gross Deutschland prepared to continue their assault on July 5, Stavka ordered Golikov to prepare an armored counterattack northwest of Voronezh. Maj. Gen. Aleksandr Ilyich Liziukov’s 5th Tank Army would spearhead the assault.
The 5th Tank Army was spread out, and it took most of July 5 to reach its designated assembly area. German fighters and bombers roamed the sky, with the Red Air Force noticeably absent. With constant harassment from the air, movement was extremely difficult for Soviet armor. Furthermore, Golikov was unable to keep in constant contact with Liziukov’s headquarters, which further hampered the operation.

Meanwhile, Kempf’s panzer corps was finally advancing toward Voronezh. Overcoming stiffening resistance from recently arrived infantry units, the Germans found themselves fighting in the western outskirts of the city by the end of the day. In Berlin, the Army general staff was getting increasingly nervous about the XLVIII Panzer Corps tied down at Voronezh.
In his diary, Halder wrote, “The Don has been reached on a wide front west and south of Voronezh, but any attempt now to rush fortified Voronezh might result in total dissipation of the attacking power of the 24th Panzer Division and the Gross Deutschland Division…. To me, the situation looks this way: Hoth had the mission to strike for Voronezh but didn’t relish the idea, and so approached the operation with reluctance…. Von Bock has become completely dependent on Hoth’s initiative and has oriented the offensive toward Voronezh to a greater degree than he could answer for.”
July 6 saw several developments in the Voronezh area. The 24th Panzer moved into the western section of the city proper and found itself engaged in house-to-house fighting. Narrow streets hampered the panzers’ mobility, and the division’s motorized infantry were put in the lead, slowly overcoming Soviet defenses.
On the left and right flanks of the 24th, the Gross Deutschland and 16th Motorized Division also found themselves heavily engaged. Gross Deutschland’s forward elements, consisting of two rifle companies riding atop assault guns, reached the city’s railroad station before being forced back by a Russian counterattack. Units of Brig. Gen. Helmuth Schlömer’s 3rd Motorized Division, which had been transferred from von Langermann’s panzer corps, eventually relieved the exhausted division and continued the drive. By the end of the day, the Germans had established a large bridgehead in the eastern half of the city.
To the north, Liziukov was still getting his armor ready for the counterattack on the 24th Panzer Corps. Despite his assembly and communications problems, he ordered Maj. Gen. Pavel Alekseevich Rotmistrov, commander of the 7th Tank Corps, to attack Balck’s 11th Panzer at 6 am. Using his 67th and 87th Tank Brigades, which had massed north of the village of Bolshaya Polyana, Rotmistrov struck a German battle group composed of about 50 panzers in the area around the village of Krasnaya Polyana, about 55 kilometers northwest of Voronezh.
The two Soviet brigades consisted of 96 T-34 medium tanks armed with 76.2mm main guns and a scattering of T-60 light tanks, which carried 20mm cannons. Most of the German panzers were Panzer IIIs mounting 50mm guns, which had great difficulty penetrating the T-34’s frontal armor.
Rotmistrov’s attack caught the Germans off guard, and the panzers began a hasty retreat to the south. Crossing the shallow Kobylia Snova River some four kilometers south of Krasnaya Polyana, the Germans slowed their retreat, stopping to fire before pulling back again. The Russians kept close to the Germans, resulting in the negation of most Luftwaffe support (in the dust and confusion of battle, the German pilots had a difficult time distinguishing friend from foe).
The battle continued throughout the day, ending only as darkness fell. If the initial two attacking Soviet brigades had been reinforced, the Russian attack might have had serious consequences for the German forces around Voronezh. However, Maj. Gen. Aleksei Fedorovich Popov’s 11th Tank Corps, equipped with more than 180 tanks, was still detraining as the fighting died down, and Colonel Andrei Grigorovich Kravchenko’s 2nd Tank Corps, also with more than 180 tanks, was hours from its designated assembly area.
As the sun rose on July 7, Liziukov ordered Rotmistrov to continue his attack, promising reinforcements. However, only a battalion of the 12th Motorized Regiment and the 59th Tank Battalion (50 tanks) were available to join the fight. As the Soviets pressed their attack, Baessler’s 9th Panzer Division arrived on the scene with about 120 tanks, mostly Panzer IIIs. Baessler’s timely arrival stopped Rotmistrov along the Kobylia Snova for the time being.
In Voronezh, Kempf’s corps worked at rooting out the Russian pockets of resistance remaining in the city. By nightfall, the city had been all but cleared, but the German troops were exhausted and in need of rest. Infantry units were moving up to relieve the mechanized forces within Voronezh, but for the moment Kempf’s men would still be on the front line to defend against any Soviet attempts to retake the city.

Stalin’s decision to fight for the city had been costly. Maj. Gen. Ivan Danilovich Cherniakhovskii’s 18th Tank Corps, which was committed to the battle piecemeal as it arrived, was particularly bloodied in the savage street fighting, having lost the 189th and 181st Tank Brigades with 116 tanks.
The Briansk Front was now almost split in half, and Stavka realized that it was much too unwieldy for one commander. Therefore, on the night of the 7th, Stalin ordered the front to be split in two. Golikov would command the new Voronezh Front, which was charged with defending the area west of the Don north and south of the city itself. Lt. Gen. Nikandr Evlampievich Chibisov would temporarily command the revamped Briansk Front, which would defend the area northwest of the city.
On July 8, Rotmistrov finally had his combined forces in place for an all-out attack on von Langermann’s corps. The remaining units of the 11th Tank Corps were now in place, as were the tank brigades of the 2nd Tank Corps. With a numerically superior enemy facing them, the Germans were once again forced to conduct a fighting withdrawal.
The Soviets pressed their attack, forcing the Germans back some six kilometers. When the panzers reached the Sukhaia River in the vicinity of Malaya Pokrovka, they dug in and called for Luftwaffe support. With a static defensive line that could be clearly marked, Stukas and low-level fighters shot up several of the advancing Soviet tanks while German artillery added its deadly thunder to the battle. The swampy terrain in the area also hindered the Russian advance and tactical movement.
For the next few days, Liziukov threw his forces against von Langermann’s corps. Some minor penetrations were made, but they were quickly stopped by aggressive German counterattacks. With the arrival of Colonel Otto Butze’s 340th Infantry Division, the 11th Panzer was gradually taken out of the line to be used as a mobile “fire brigade.” By July 15, the front northwest of Voronezh had stabilized with both sides thoroughly worn out from more than a week of heavy fighting. As more infantry came into the line, both sides worked at establishing strong positions to counter any enemy attack.
In Voronezh itself, Kempf’s corps, which was now being replaced by arriving infantry divisions, was still warding off Soviet counterattacks in some areas. Together with the 57th and 168th Infantry Divisions from General Hans von Obstfelder’s XXIX Army Corps, Kempf’s troops stopped a concerted attack by Lt. Gen. Antionuk’s 60th Army (the former 3rd Reserve Army).
After Antionuk’s failure to break the German line, the fighting at Voronezh also died down for a time. Although the Germans had managed to secure a bridgehead across the Don and Voronezh Rivers, the strong Soviet defenses facing them prevented any further eastward movement in the area. The 24th and Gross Deutschland finally came off the line, but their surviving panzers were badly in need of repair, and there was also a shortage of fuel, which made immediate deployment to the south impossible.
Stalin’s decision to hold the Voronezh sector effectively unhinged an important part of the opening phase of Case Blue. Although poorly coordinated, the Soviet armored attacks northwest of the city forced the 9th and 11th Panzer Divisions to remain in place to prevent an enemy breakthrough. The street fighting and von Bock’s hesitation, coupled with Hitler’s vague orders to von Bock on July 3, kept the proposed armored gallop along the Don from happening.
There would be no grand encirclement to trap the Soviet forces west of the Don. Even though Paulus’s 6th Army was still advancing in its drive toward Stalingrad, the Don crossings in the southeast would remain open for the retreating Russians.
Although battered, those divisions would receive reinforcements to flesh out their ranks and would be used in and around Stalingrad to thwart the German attempt to totally dominate the city. Together with new divisions that were being sent to the area, the divisions saved from the German trap would be part of the Soviet force that would sound the death knell of the 6th Army in the coming year.
Author Pat McTaggart is an expert on the Eastern Front World War II. He writes from his home in Elkader, Iowa.
Back to the issue this appears in
Share This Article
- via= " class="share-btn twitter">
Related Articles

European Theater
Marek Edelman, a leader of the 1943 Warsaw Ghetto Uprising, kept alive through the years the memory of those who perished.

Conspicuous Gallantry at Tarawa: Alexander “Sandy” Bonnyman’s Medal of Honor

Operations Titanic’s Paradummies

Blunder or Deception? Stilwell at Myitkyina
From around the network.
Action off Santa Cruz: Last Stand of the USS Hornet
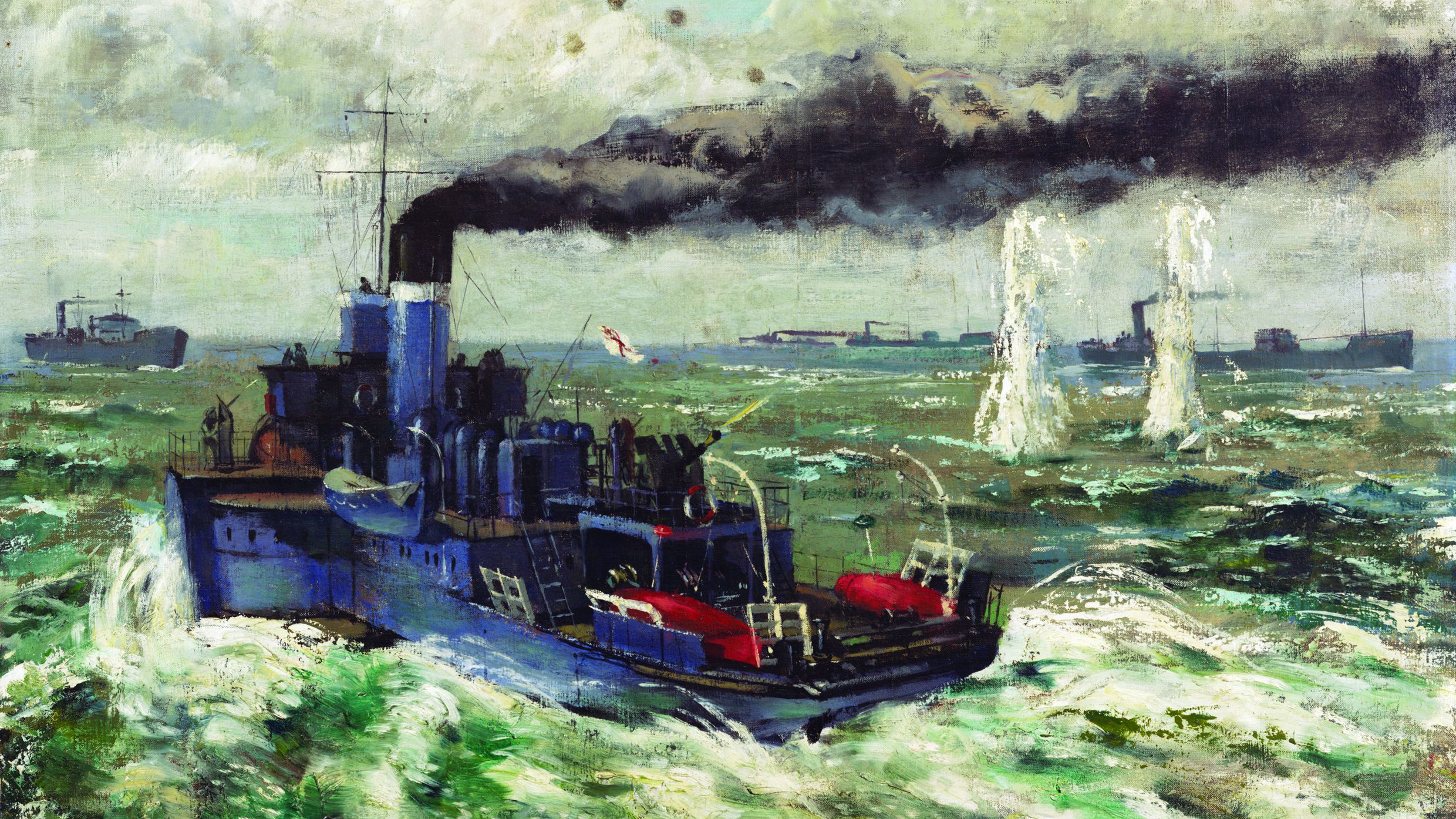
Heroes of the Red Duster: The British Royal Merchant Navy

Patton: from Gafsa to El Guettar

Yanks in the RAF
- Yekaterinburg
- Novosibirsk
- Vladivostok

- Tours to Russia
- Practicalities
- Russia in Lists
Rusmania • Deep into Russia
- Voronezh Region

The major city of Voronezh, with a population of over one million, was originally founded to protect Russia’s southern borders. By the end of the 17th Century Peter the Great had made the city the centre of Russian shipbuilding and the flagship Goto Predestinatsia was built here, which has now become one of the symbols of the city. During the Second World War much of the city was destroyed, meaning the city’s architecture is now predominantly Soviet. The city is also the unofficial capital of Russia's Black Earth Region.
Plan your next trip to Russia
Ready-to-book tours.
Your holiday in Russia starts here. Choose and book your tour to Russia.
REQUEST A CUSTOMISED TRIP
Looking for something unique? Create the trip of your dreams with the help of our experts.

IMAGES
VIDEO
COMMENTS
Hence, the art of good clinical case presentation is a skill that needs to be mastered. Case presentations are a part of most undergraduate and postgraduate training programs aimed at nurturing oratory and presentation design skills. This article is an attempt at providing a trainee in radiology a guideline to good case presentation skills.
Citation, DOI, disclosures and article data. Presentation refers to the clinical details that need to be included as part of Radiopaedia case s and can include symptoms, signs, physical examination findings, relevant past history and/or laboratory studies. Complications, if part of the initial disease process (e.g. hemorrhage as a complication ...
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence.1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Clinical Radiology Case Presentation Punnen et al. 25 Indian Journal of Radiology and ImagingVol. 31 No. 1/2021 2021. Indian Radiological Association. A simple "step by step" guide to formulating a comprehen - sive case presentation is as follows: Step 1: Finding the Right Case to Present Any case with a learning point is a good case to ...
RSNA Case Collection is a collection of peer-reviewed radiology cases. Home | RSNA Case Collection To help offer the best experience possible, RSNA uses cookies on its site.
Hence, the art of good clinical case presentation is a skill that needs to be mastered. Case presentations are a part of most undergraduate and postgraduate training programs aimed at nurturing oratory and presentation design skills. This article is an attempt at providing a trainee in radiology a guideline to good case presentation skills.
Clinical case presentation is part of daily routine for doctors to communicate with. each other to facilitate le arning, and ultimately patient management. Hence, the art. of good clinical case ...
Discussion. The case series has many of the same advantages and disadvantages of the case report. The presentation of multiple cases lends more weight to an underlying hypothesis (stated or unstated) than does a single case report. The case series has less power in defending a hypothesis than other retrospective or prospective studies, however.
Radiology Case Presentation Peggy Wu, MS3 7/13/2018. S L I D E 1 ML • HPI - 54 yo male who presented with 2 months of L ptosis, bilateral upper extremity weakness, and fatigue with chewing in 9/2016 - Subsequently diagnosed with myasthenia gravis
A. Aberrant Right Subclavian artery. Anterior_Superior Mediastinal Mass. Aortic Transection. Assymetric Pulmnary Edema.
Cases. By sharing our collective experience through interesting and classic patient cases, we can make a real difference in how people are imaged and diagnosed. Each case belongs to a contributing member and all cases are reviewed by our dedicated editors to ensure they reach quality standards and abide by privacy guidelines. Cases can public ...
1. 2. Interactive Radiology Case Presentation Gamal Rabie Agmy, MD, FCCP Professor of chest Diseases, Assiut university. 3. Spot Diagnosis. 4. 5. S Curve of Golden When there is a mass adjacent to a fissure, the fissure takes the shape of an "S". The proximal convexity is due to a mass, and the distal concavity is due to atelectasis.
Date of Presentation: Topic of Presentation: Grading Rubric: There was an adequate discussion of the case presentation including (but not limited to): -age -presenting symptoms -past medical and/or surgical history High quality imaging of the relevant organ systems was provided, including
Full text. Full text is available as a scanned copy of the original print version. Get a printable copy (PDF file) of the complete article (453K), or click on a page image below to browse page by page.
Case reports are not currently accepted within Radiography, ending in 2021, with Radiology Case Reports suggested as an alternative. Other options include the Journal of Medical Imaging and Radiation Sciences, Radiologic Technology and The South African Radiographer.A search of all previously published case reports within Radiography generated 38 articles between 2013 and 2021, with a total of ...
Case Presentations; Radiology Interest Group. ... Case Presentations. CASE PRESENTATIONS 2021 - 2022. June. Acute ACL Tear_Andrew Wang, MS4_Kumaravel, MD_June 2021. Tibial Plateau Fractures, Joseph Wilder, MS4, Kumaravel, MD_June 2021. Anoxic Brain Injury_Parth Patel, MS3_Lee, MD_Patel_June 2021.
Radiology Case Reports is an open-access journal publishing exclusively case reports that feature diagnostic imaging. Categories in which case reports can be placed include the musculoskeletal system, spine, central …. View full aims & scope. $550.
Radiology Case Presentation (no spoilers) Horseshoe Kidney Anna Gilman, MS4 West Penn Clinical Campus Temple University School of Medicine Case Background USPSTF Guidelines for AAA Screening The USPSTF recommends one-time screening for abdominal aortic aneurysm (AAA) with. Get started for FREE Continue.
A case report typically contains: a short introduction; patient history and presentation; a discussion of the imaging and other relevant interventions; patient course; summary/discussion; In radiology case reports, images from multiple imaging modalities are usually included, and gross pathology or histology is considered an excellent addition.
Cerebellar, hippocampal, and basal nuclei transient edema with restricted diffusion (CHANTER) syndrome is a recently described entity that refers to a specific pattern of cerebellar edema with restricted diffusion and crowding of the fourth ventricle among other findings. The syndrome is commonly associated with toxic opioid exposure. While most commonly seen in adults, we present a case of a ...
In his Presidential Address at ACR 2024, outgoing American College of Radiology® (ACR®) President William T. Herrington, MD, FACR, discussed change management and called on leaders to enlist those who can identify disruptive change or technology. "We need many and varied brains to participate, anticipate, recognize and predict change," said Herrington, who cited numerous industry ...
(2016). The Provisioning Crisis during the First World War. Russian Studies in History: Vol. 55, Provincial Life in Russia during the First World War, pp. 209-233.
Voronezh UFO incident. The Voronezh UFO incident was an alleged UFO and extra-terrestrial alien sighting reported by a group of children in Voronezh, Soviet Union, on September 27, 1989. [1] [2] The area has been popular with UFO-hunting tourists. [3]
A Soviet tank, destroyed in a futile attempt to stem the Nazi tide during the early days of Case Blue, billows smoke on the Russian steppe. Katukov's 1st Tank Corps hit Balck's 11th Panzer once again, and once again the assault was plagued by poor command and control between the corps' subordinate brigades.
Voronezh. The major city of Voronezh, with a population of over one million, was originally founded to protect Russia's southern borders. By the end of the 17th Century Peter the Great had made the city the centre of Russian shipbuilding and the flagship Goto Predestinatsia was built here, which has now become one of the symbols of the city ...