An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection


Medical Technologies Past and Present: How History Helps to Understand the Digital Era
Vanessa rampton.
1 Institute for Health and Social Policy and Department of Philosophy, McGill University, Montréal, Canada
Maria Böhmer
2 Center for Medical Humanities, History of Medicine Section, University of Zurich, Zürich, Switzerland
Anita Winkler
This article explores the relationship between medicine’s history and its digital present through the lens of the physician-patient relationship. Today the rhetoric surrounding the introduction of new technologies into medicine tends to emphasize that technologies are disturbing relationships, and that the doctor-patient bond reflects a more ‘human’ era of medicine that should be preserved. Using historical studies of pre-modern and modern Western European medicine, this article shows that patient-physician relationships have always been shaped by material cultures. We discuss three activities – recording, examining, and treating – in the light of their historical antecedents, and suggest that the notion of ‘human medicine’ is ever-changing: it consists of social attributions of skills to physicians that played out very differently over the course of history.
Human beings have their own goals and intentions, and products should help them to realize them in an optimal way. In many cases, though, these goals and intentions do not exist independently from the technologies that are used. [Technologies] do much more than merely function – they help to shape human existence. Peter-Paul Verbeek (2015, 28)
Introduction
A wide range of novel digital technologies related to medicine and health seem poised to change medical practice and to challenge traditional notions of the patient-physician relationship (Boeldt et al. 2015; Loder 2017; Fagherazzi 2020). A number of recent pieces have explored the ethical implications of this, asking, for example, whether new means of delivering ‘greater efficiency, consistency and reliability might do so at the expense of meaningful human interaction in the care context’ (Topol Review 2019, 22). Various contributions from patients, physicians, bioethicists, and social scientists have warned that computer technologies somehow stand between the physician and the patient and that there is a fundamentally human aspect of medicine that coexists uneasily with machines (e.g. Gawande 2018; Verghese 2017). As a remedy, recent contributions call for ‘clinical empathy’ not only as a desirable characteristic trait of future physicians, but even as a selection criterion for medical students (Bartens 2019). The role history plays in these discussions is striking. Commentators often assume that current concerns about how technologies may lead to the ‘de-humanisation of care’ (Topol Review 2019, 22) are the unprecedented products of technological, social, and cultural transformations in the late twentieth-/early twenty-first centuries. When the history of medicine is referenced, it is largely in one of the following ways: first, to emphasize that today ‘[w]e are at a unique juncture […] with the convergence of genomics, biosensors, the electronic patient record[,] smartphone apps, [and AI]’ (Ibid., 6), whereby the singularity of the digital era makes historical comparisons with antique predecessors seemingly irrelevant. Second, the history of medicine is used in a nostalgic manner to refer to past medical practices, seemingly grounded in the ability of a doctor to ‘liste[n] well and sho[w] empathy,’ as having a fundamentally human element that is threatened by the digital era (Liu, Keane and Denniston 2018, 113; see also Johnston 2018). With some notable exceptions (e.g. Greene 2016, Kassell 2016, Timmermann and Anderson 2006), historians of medicine have largely refrained from attempting to interpret recent digital developments within their broader historical contexts. The historicity of digital medicine in its various forms and the insights of the history of medicine for contextualising the patient-physician relationship in the digital era have yet to be fully fleshed out.
In this contribution, we draw on historical examples and the work of historians of medicine to highlight how all technological devices are ‘expressions of medical change’ (Timmermann and Anderson 2006, 1), and to show how past analogue objects shaped physician-patient relationships in ways that remain relevant today. Our focus is on Western European medicine since the early modern period. While acknowledging the profound differences between medicines in particular historical times and places, we argue, first, that patients and doctors have always interacted in complex relationships mediated by objects. Medical objects and technologies are not only aids for performing certain human tasks, but themselves have a mediating function and impact how physicians and patients alike perceive illness and treatment. We then contend, second, that history helps inform current discussions because it highlights the plurality of ways in which the physician-patient relationship has been conceived in different eras. In particular, the ability of the physician to listen well and show empathy seems to be not so much a historical constant but rather a social attribution of certain skills to physicians that played out very differently over the course of history. Both points help us to show that some of the hopes and fears related to digital technologies are not so entirely new after all.
We work through these hypotheses in relation to three activities in the clinical encounter that have been significantly affected by digital medical technologies, namely i) recording (Electronic Health Records), ii) examining (Telemedicine), and iii) treating (Do-It-Yourself medical devices). In each case, we begin with a specific contemporary technology and the debates around it before showing how a historical perspective can contribute to our understanding of them. First, we discuss electronic health records in the light of current criticisms which maintain that this technology cuts valuable time the doctor should be spending with the patient, thereby threatening an assumed core responsibility of the physician, namely listening empathetically to the patient. History shows that physicians have not always seen administrative record-keeping as foreign to their main work with patients; rather, it has been a formative part of their professional identity at different times. Moreover, the value that both physicians and patients ascribed to empathic listening has varied substantially over time. Second, in the case of examining, we start from the observation that current debates about telemedicine focus on the greater distance between patients and physicians this technology brings about. The historical perspective demonstrates that these debates are but one example of how changing examination technologies affect both physical distance and reciprocal understanding in the patient-physician relationship. Our examples illuminate that physical proximity in the medical encounter is a modern phenomenon, and that it did not always imply a meeting of the minds between physician and patient and vice versa. Finally, our third section on self-treatment demonstrates that Do-It-Yourself devices have the potential to challenge medical authority and, by giving patients more power, alter those power balances between physician and patient that are constitutive of an idealised view of the patient-physician relationship. Yet here too there are significant historical precedents for thinking of doctors and patients as but two players within complex networks of people and technologies, in which patients ascribe value to a multiplicity of relationships.
Record-keeping: computers and the administered patient
Electronic health records (EHRs), that is computer-based patient records, have transformed the way contemporary medicine is practiced (see, for example, Topol, Steinhubl and Torkamani 2015, 353). While the electronic recording of patient files by individual health care providers has become common practice since the 1990s, a central virtual collection and storage of all health data relating to an individual patient is a rather new development which is currently being debated and technically introduced in various states. This virtual patient file is of secondary order because it is fed with original electronic files derived from various primary recording systems (GP, clinic etc.), and it follows a population health surveillance logic rather than the logic of the treatment of individual cases. The main idea is that both patients and health care providers have access to a corpus of health documents, which is as complete as possible, to make diagnosis and treatment more efficient, more precise and safer for patients, and less costly for the health system. While patients may make use of this possibility on a voluntary basis and are asked to distribute access rights to providers, healthcare providers are obliged to cooperate and feed the system with relevant data (for a local example see current implementation efforts in Switzerland and its pitfalls as described in Wüstholz and Stolle 2020). One of the main premises of supporters is that EHRs will facilitate not only networking and interprofessional cooperation but also enhance communication between doctors and patients: they ‘provide health care teams with a more complete picture of their patients’ health [and] improve communication among members of the care team, as well as between them and their patients’ (Canada Health Infoway; see also Porsdam, Savulescu and Sahakian 2016).
Yet critical discussions surrounding the introduction of EHRs doubt exactly that. They suggest that the increasing documentation, virtual storage and sharing of sensitive patient data threatens an assumed historical core value of the doctor-patient relationship, namely the possibility of physicians establishing an intimate and ‘deeper connection’ with their patients (Ratanawongsa et al. 2016, 127). From the perspective of healthcare providers, professionals criticise the time-consuming nature of EHRs, arguing that this technology supplants the time the doctor has for direct communication and time spent ‘in meaningful interactions with patients’ (Sinsky et al. 2016, 753). That screens are coming ‘in between doctors and patients’ is a widespread notion (Gawande 2018). In addition, medicine’s increasing dependence on screens is perceived as undermining important social rituals, such as exchanges between physicians and other healthcare colleagues who used to discuss their cases in more informal ways (Verghese 2017). Last but not least, EHRs are seen as a major factor contributing to declining physician health and professional satisfaction because of their time-consuming data entry that reduces face-to-face patient care (Friedberg et al. 2013). This last point seems to be crucial as the digital interfaces of EHRs indeed require a maximum of standardisation, homogenisation and formalisation of recording styles that necessarily conflicts with more informal, individual recording techniques. On the one hand, doctors are forced to fill in fields and checkboxes that do not correspond to their own knowledge priorities, that is the things they would want to highlight in a certain case from the perspective of their specialty. On the other hand, they have difficulties in identifying relevant information when too much data on an individual patient has been entered by too many people. The desired interprofessional collaboration thus runs the risk of complicating instead of facilitating the making of a diagnosis. Surgeon Atul Gawande maintains that in the past, analogue documentation forced physicians to bring essential points into focus: ‘[d]octors’ handwritten notes were brief and to the point. With computers, however, the shortcut is to paste in whole blocks of information […] rather than selecting the relevant details. The next doctor must hunt through several pages to find what really matters’ (2018). Together, these points of critique suggest not only a certain fear that the increasing digitisation of patient records might disturb relationships that in the pre-digital era were based on professional intuition and meaningful, trust-building face-to-face communication. The critique also suggests that what is threatened is the meaning and satisfaction a physician takes from his/her recording work.
From the perspective of patients, other concerns related to EHRs are more relevant, among them the safety of personal health data. But while notions of privacy – who has control over the data, who owns the patient history – are important for patients, a number of studies also show that patients perceive the careful digital documentation of their case as something positive (Assis-Hassid et al. 2015; Sobral, Rosenbaum and Figueiredo-Braga 2015). ‘Forced to choose between having the right technical answer and a more human interaction, [patients] picked having the right technical answer,’ reports Gawande (2018; see also Hammack-Aviran et al., 2020). It thus seems that as long as patients think EHRs are providing them with a higher quality of care, they readily accept EHRs and their doctors’ dependence on screens – hence adapting their expectations to technological change.
In order to scrutinize these purported threats and attitudes towards EHRs, the rich history of patient records provides a relevant historical backdrop. In studying patient records, historians have addressed exactly these issues: they have examined how the patient-physician relationship has changed over time and have used medical records to gain insights into how past physicians documented medical knowledge, how this influenced their perceptions of their professional identity, and their obligations vis-à-vis patients (Risse and Warner 1992). As a first step, it is important to see that even though EHRs pose new challenges because of their digital form, recording individual patients’ histories as part of medical practice and ‘thinking in cases’ as a form of epistemic reasoning are a historical continuum (Forrester 1996; Hess and Mendelsohn 2010). The patient history dates to ancient Hippocratic medicine when detailed medical records were written on clay tablets and handed down for centuries to preserve the esteemed knowledge of antiquity (Pomata 2010). Yet the content and form of medical records, as well as the practices producing them have changed remarkably over time (Behrens, Bischoff, and Zelle 2012). In Western Europe, physicians in sixteenth-century Italy re-appropriated the ancient practice and typically recorded their cases in paper notebooks, as part of a larger trend to systematize and record information (Kassell 2016; see also Pomata 2010). As Lauren Kassell notes, the records of early modern practitioners ‘took the form of diaries, registers or testimonials, often they were later ordered, through indexing or commonplacing, by patient, disease or cure, providing the basis for medical observations, sometimes printed as a testimony to a doctor’s expertise as well as his contribution to the advancement of science’ (2016, 122). The historical perspective reveals that the rationale for a particular type of medical record-keeping always developed in tandem with the technical capabilities for its enactment, changing ideas of how diseases should be recorded, as well as with the preferences of individual physicians (ibid. 120). Crucially, as the organization of these collections of patient histories changed, so too did medical knowing and normative ideas about the physician-patient relationship (Hess and Mendelsohn 2010; Dinges et al. 2016).
As shown above, current critical discussions about EHRs tend to evoke a medical past in which patients were given time to talk about their illness, doctors listened and engaged in meaningful interactions, and record-keeping did not interfere with these processes. Allegedly, there were few concerns over misuse of data as there was less data produced and fewer players in the game. How does this popular nostalgic view correspond to research findings in the history of medicine? To some extent, the context of ‘bedside medicine’ comes close to these ideas. This model of care remained dominant in Western Europe until the nineteenth-century. One of the main ways in which physicians generated medical knowledge at the bedside of patients was to conduct ‘verbal analysis of subjectively defined sensations and feelings’ by patients (Jewson 1976, 229-230), and these patient testimonials provided the details recounted in physicians’ notes (Fissell 1991, 92). This is partly because the early modern doctor-patient relationship was based on a ‘horizontal’ model of healing (Pomata 1998, 126-27, 135) and a legally binding ‘agreement for a cure’ (ibid., 25 passim), which gave considerable power to patients, placing them on ‘near-equal hermeneutic footing’ with doctors (Fissell 1991, 92). Physician and patron (patient) made a contract in which the mostly upper class-patient would only pay fees after ‘successful’ treatment; vice versa, doctors were not obliged to treat a patient but would rather take on patients whose potential cure, and ability to pay fees, could be foreseen. Patients’ verbal satisfaction and willingness to conduct word-of-mouth publicity for a practicing physician were key to his reputation at that time and influenced physicians’ relationships with their clients.
However, it is problematic to project today’s vision of a desirable empathic relation between doctors and patients back into the past. Although upper-class patients clearly had some power in their relationship with physicians, the dominance of patients’ speech in medical records as such should not be interpreted as proof that doctors cared about their patients in the modern sense of showing understanding. With respect to nineteenth-century bourgeois medicine, Roy Porter noted that flattery and attention in the medical encounter were calculated practices of physicians concerned to secure clients and that ‘solemn bedside palaver[,] a grave demeanour, an air of benign and unflappable authority’ were all part of the prized ‘art of never leaving without a favourable prognosis’ (1999, 672). In a similar vein, Iris Ritzmann has emphasized that eighteenth-century doctors were eager to adhere to a certain ‘savoir faire,’ that is rules of conduct that would allow them to obscure the fact that in many cases, their abilities to heal were very limited (1999). And in Paul Weindling’s assessment of German medical routines, physicians’ desires to satisfy the patient subjectively were even purely instrumental: ‘[s]ympathy with the feelings of the sick was an economic necessity owing to the competition between practitioners’ (1987, 409). In all these cases, the value ascribed to direct physician-patient dialogue was very different from today’s ideas about an empathic encounter between physicians and patients; an engaged bedside manner often had more to do with calculated support for an upper class and sometimes hypochondriac clientele.
Similarly, as concerns the careful documentation of a patient’s medical condition and history, historical evidence shows that doctors did not do it primarily for their patients’ needs but for purposes of professional standing. This was important at a time when physicians’ scientific authority still needed to be established. The fact that in many cases there were several physicians involved in the treatment of the same case made documentation and communication between physicians (and sometimes for the public) especially relevant – and especially conflictual. Eighteenth-century case histories reflecting the context of bedside medicine indeed suggest that doctors were sometimes eager to publish case histories of patients that would bespeak their ability to heal by highlighting the misfortune of their competitors in order to enhance their own reputation. This shows how misleading the popular nostalgic view of a past intimate and unbroken bond between physicians and patients is, and that analogue paper technology did not necessarily strengthen this bond but could also be used in ways that were not beneficial for patients. Unlike today, this was an era in which practices of record-keeping mirror multiple, local and highly individual ways of documentation; the formalisation and standardisation of patient files which 19 th -century hospital medicine would trigger was yet to come.
As hospitals and laboratories became important institutions for medicine in the century roughly between 1770 and 1870, they also changed the practices of record-keeping, as the customary interrogation of patients’ accounts of the course of their disease did not coincide with changing understandings of disease, scientific interests and cultural expectations (see Granshaw 1992). For instance, French anatomist and pathologist Xavier Bichat (1771-1802) dismissed note-keeping based on patients’ narratives as an obsolete method for knowledge-making. He observed in his Anatomie générale (1801), ‘you will have taken notes for twenty years from morning to night at the bedside of the sick [and] it will all seem to you but confusion stemming from symptoms that fail to coalesce, and therefore provide a sequence of incoherent phenomena’ (1801, xcix, our translation). The kind of medicine favoured by Bichat and like-minded physicians focused on gaining anatomical and physiological insights directly from the body, using both physical examination and remote techniques in the laboratory. One way in which record-keeping changed to accommodate these interests was in the use of a more technical language to describe the experiences and expressions of patients. Mary Fissell argues that with the rise of hospital medicine, ‘doctors begin to sound like doctors, and patients’ voices disappear’ because doctors interpret patients’ words and replace them with medical equivalents (1991, 99). More generally, historians have shown that during the nineteenth century, medical culture changed in a way that gradually diminished the importance of patient narratives in medical writing (Nolte 2009).
How did these changes in recording practices play out for patients in the medical encounter ? From the historical perspective, the fact that physicians adopted a more technical language in their interactions and records should not be taken as evidence for a loss of human interaction or as something that patients necessarily disliked. On the contrary, the more systematised and formalised type of record-keeping was considered state of the art and was in accordance with a rapidly growing belief in the natural sciences among both patients and the general public (Huerkamp 1989, 64). This is related to the emergence of a specific concept of scientific reasoning that, in turn, fostered a sense of ‘scientific objectivity’ that called for dispassionate observation and accurate recording (Daston and Gallison 2010; Kennedy 2017). By the end of the nineteenth century, academic physicians had managed to create such professional authority that the ‘horizontal model of healing,’ in which the physician courted his upper-class clients, was replaced by a vertical model, in which the patient subjected himself to the authority of the physician. A Berlin doctor advised his fellow colleagues in 1896 that they should communicate their medical prescriptions to patients in a way that ‘prevents any misunderstandings and so that no further question can be addressed to him’ (cited in Huerkamp 1989, 66, our translation). For patients, this growing scientific authority and paternalism meant very different things, depending on class and social status. While medical services became accessible to more people, in particular thanks to the introduction of obligatory health insurance for workers, lower classes often experienced medicine as an instrument of power rather than benevolence (Huerkamp 1989). But even for the well-to-do, who undoubtedly benefitted from newly developed medical techniques, in particular in the realm of surgery, the acceptance of medical paternalism, male rhetoric and heroic cures came with high costs. This is suggested, for instance, in a famous letter by the court lady and writer Frances (Fanny) Burney who underwent a mastectomy in 1811, a rare document offering a patient’s perspective on these matters (Epstein, 1986).
From the perspective of doctors at the turn of the nineteenth century, record-keeping was associated not only with professional obligations but also with personal fulfilment. In many European countries, physicians were asked to provide expert opinion for juridical and administrative regulations as the state was increasingly interested in tracking its population’s health (Ruckstuhl and Ryter 2017; Schmiedebach 2018). In her study of Swiss physician Caesar Adolf Bloesch’s private practice (1804-1863), Lina Gafner shows the extent to which he perceived medical practice documentation as constitutive of his professional role and self-understanding as a medical expert. Bloesch’s patient journal ‘constitutes one single gigantic research report’ (2016, 265) because it was key for allowing him to generalize from the experiences gained in his practice in order to produce knowledge to contribute to contemporary scientific discussions. Gafner notes that the ‘format he gave his journals [leads] us to assume that scientific or public health-related ambitions were part of Bloesch’s professional self-image’ (263). In contrast to this historical example, where patient care and journal keeping were combined in the light of professional ambition, it stands out that healthcare providers of today tend to see their administrative work as opposed to patient care, even as separate and conflicting tasks; it is assumed that for physicians ‘seeing patients doesn't feel like work in the way that data entry feels like work’ (Amenta 2017). This is probably related to the fact that many physicians experience the requirement of working with a given software as a limiting restraint, which they are not really able to control, while they experience working with patients as something they have learned to master. As Gawande admits: ‘a system that promised to increase my mastery over my work has, instead, increased my work’s mastery over me’ (2018). It thus seems that it is primarily the question of ownership that distinguishes past recording styles from today’s recording systems: it is difficult to individually appropriate something which is designed to harmonize if not eliminate individual recording styles.
Yet even as Bloesch and contemporaries embraced the administrative tasks associated with medical note-taking as an opportunity to become a medical expert, other nineteenth-century physicians had different views of its value. But their criticisms of record-keeping were not motivated by the inherent value they saw in interactions with patients. Rather, their critiques were linked to a notable shift during the nineteenth century as scientific interest, triggered by administrative requirements as well as different disease conceptions and methods (e.g. in epidemiology research), changed its focus from the individual case study to population studies (see Hess and Mendelsohn 2010). In Nikolas Rose’s words, ‘the regularity and predictability of illness, accidents and other misfortunes within a population’ became ‘central vectors in the administration of the biopolitical agendas of the emerging nation states’ (2001, 7). Bound up with a new emphasis on tabulation, as well as ‘precision and reliability,’ various German-speaking hospitals instigated a new tabular format designed to enable physicians to compile their observations of patients into ward journals organized into columns and, eventually, generate an annual account of the course of disease (Hess and Mendelsohn 2010, 294). Yet in response some physicians rejected what they saw as excessively confining recording requirements. Volker Hess and J. Andrew Mendelsohn describe how the chief physician at a Berlin clinic ranted about the ‘inadequacy of our [tabular] journals’ and their inability to produce medical knowledge (295). While Mendelsohn and Hess themselves remark that such tabular ward journals were very ‘far from the patient history as observation, as prose narrative’ (293), the physicians’ rejection of the use of columns to record cases was not motivated by a concern to recover patients’ own narrations of their ailments or the feeling that record-keeping prevented them from properly attending to their patients’ needs. On the contrary, these physicians were concerned with producing an annual disease history and were frustrated that ‘the ultimately administrative format’s own rigid divisions blocked the writing of a synoptic history’ (296). Rather than recovering a face-to-face encounter with patients, they were interested in finding a recording format that would allow them to present a more compelling and sophisticated general description of disease, relying on mass information.
The current consensus among historians of medicine is that we should neither conceive medical records as ‘unmediated records of experiences of illness and healing’ (Kassell 2016, 126) nor as disentangled from the medical encounter itself. Rather, ‘processes of record-keeping were integral to medical consultations’ because ‘as ritualised displays and embodied knowledge, case books shaped the medical encounters that they recorded’ (122; see also Warner 1999). In relation to how ‘computerization’ is shaping contemporary medical encounters, three main points are of note. First, physicians have not always seen time spent writing and recording patient histories as in competition with interacting with patients themselves. At various times in history, the careful documentation of individual cases was perceived as a fundamental resource for generating medical knowledge and time spent doing so as part of the self-identity of physicians. Against the repudiation of digital record-keeping by today’s physicians, historical evidence shows that to the extent that physicians saw record-keeping as coinciding with their overall knowledge objectives, they accepted and even embraced it. This is linked to a second point, namely that prolonged time spent listening to the patient talk was not historically seen as evidence of good medical practice. For example, in an era when listening at length to patients was associated with the obsequious physician catering to the ego of the upper-class patient, the sober inscription in a nineteenth-century casebook noted that ‘too much talking showed that little was wrong’ with the patient (Weindling 1987, 395). Finally, patients too accepted administrative work by doctors as a sign of expertise and not necessarily as something that reduced the doctor’s attention to them. While the power balance changed in favour of doctors and ascribed less epistemic value to patients’ words, this was not necessarily negatively received by patients. History therefore shows that we should not view technological changes as isolated from the broader medical culture surrounding them but rather as shaping and co-constructing this culture. Today’s fear that the introduction of EHRs might change the communication and relation between physicians and patients for the worse tends to blame technology for a broader cultural and medical change of which it is just one tiny aspect, that is the growing belief in data and the logic of gaining stratified knowledge to provide relevant information about any one patients’ condition. Given that patients’ expectations exist in a dynamic relationship with how physicians learn, make decisions and interact with them, EHRs are themselves bound up with creating new conditions for the physician-patient relationship.
Examining: telemedicine and the distant patient
A further way in which digitalization has influenced the medical encounter is that it has emerged as the new virtual consulting room, thereby radically transforming the settings and procedures of physical examination. Although most people still go to ‘see the doctor,’ medical encounters today no longer have to take place in physical spaces but can occur via telephone or internet – what is broadly referred to as telemedicine, literally healing at a distance (from the Greek ‘tele’ and Latin ‘medicus’) (Strehle and Shabde 2006, 956). According to the World Health Organization, as a global phenomenon, telemedicine is more widespread than EHRs with more than half of responding member states having a telehealth component in their national health policy (WHO 2016). In the context of the COVID-19 pandemic, telemedicine has been overwhelmingly seen as ‘[a]n opportunity in a crisis’ and has further gained in popularity (Greenhalgh et al., 2020; see also Chauhan et al., 2020). A senior NHS official cited by The Economist called the widespread adoption of remote care (viz. telemedicine) a ‘move away from the dominant mode of medicine for the last 5,000 years’ (2020, 55). In the virtual examination room, patients can ask a physician for a diagnosis, a prescription and a treatment plan and send information about diseased body parts via digital media. When inquiring about the health conditions of their patients from a virtual consultation room, physicians sometimes need to ask their patients for certain practices of self-examination and self-treatment (Mathar 2010, section III). Advocates of telemedicine emphasize that there is no risk of mutual infection, advantages of cost savings, convenience, and better accessibility to medical care generally and for people living in rural and remote areas in particular. In Switzerland, for instance, the Medgate Tele Clinic promises to ‘bring the doctor to you, wherever needed’ (2019) while the U.S. Doctor on Demand characterizes itself as ‘[a] doctor who is always with you’ (2019). Patients, meanwhile, appreciate the greater availability of physicians, less travel time and better overall experience (Abrams and Korba 2018). However, telemedicine also raises various critical questions about the effects of physical distance on the physician-patient relationship. In particular, can the quality of the examination and diagnosis be high enough if a physician only sees his/her patient via screen but cannot smell, palpate and auscultate him/her? Furthermore, how can a trusting doctor-patient relationship be established virtually and at a distance? (see Mathar 2010, 13). While some of these critiques are based on the assumption that a fitting medical encounter between physician and patient should be a ‘good, old-fashioned, technology-free, dialogue between physician and patient’ (Sanders 2003, 2), we show below that all encounters inevitably ‘pass through a cultural sieve’ (Mitchell and Georges 2000, 387). Not only has the perceived need for the physical proximity of physician and patient varied substantially over history, but historical physicians and patients have not seen physical distance as preventing them from achieving emotional understanding. Whether physical examinations took place in-person or remotely, at each point in history doctors relied on their knowledge and its applications, that is a cultural lens through which s/he gazes on, over or into the human body. Regardless if examined remotely or closely, changes in examination procedures always challenge the established sense of the emotional bond between patient and physician, which therefore needs to be defined anew.
The standard physical examination as we know it today was considered less important in Europe up to roughly 1800 because of the conventions governing the relationship between physician and patient/patron, and also because of the conventions governing the relationship between male doctor and female patients. Many physicians considered physical examination morally inappropriate and saw it as dispensable for making a diagnosis. Physicians of upper-class patients generally considered their task more to advise than to examine and treat (Ritzmann 1999, 203). From his close analysis of a casebook by a seventeenth-century English physician, Stanley Joel Reiser concludes that the ‘maintenance of human dignity and physical privacy placed limits on human interaction through touch’ (1978, 4). Given the desirability of maintaining physical distance, physicians relied on and developed other sources of knowledge than their own sense of touch. The physical examination was ‘the method least used’ by the seventeenth-century physician who rather favoured ‘the patient’s narrative and [his] own visual [outward] observations’ of the patient’s body. In her study of a manuscript authored by a surgeon-apothecary of the same historical period, Fissell singles out blood-letting as one ‘of the few occasions on which a professional […] might routinely touch a patient’ and notes that it was necessarily ‘transformed into a careful ritual, one which attempted to compensate for the transgressive nature of the encounter. The blood-letter's courteous attention to returning the patient to his or her un-touched status underlines the mixture of courtesy and technique which made good medical practice’ (1993, 23). In ways now unfamiliar to us, manners and morals interacted to make physical examination and touching patients an ancillary part of the desirable patient-doctor encounter at that time.
Regular in-person physical examination as a routine practice and diagnostic technology is a rather recent development that came along with a new anatomical understanding of disease during the course of the nineteenth century, namely that diseases can be traced to individual body parts such as organs, tissues and cells, rather than unbalanced bodily humours (Reiser 1978, 29). It was at this time that the doctor’s examination skills no longer depended on the patient’s word and the surface of the (possibly distant) body, but started relying on what the doctor could glean from the patient’s organic interior (Kennedy 2017). In order to ‘get’ to the physical conditions of the body’s interior, a number of instruments were developed to facilitate the new credo of examination. The most famous example of such a nineteenth-century examination technology is the stethoscope, invented by French physician René Laennec (1781-1826). ‘By giving access to body noises – the sounds of breathing, the blood gurgling around the heart – the stethoscope changed approaches to internal disease,’ wrote Roy Porter, ‘the living body was no longer a closed book: pathology could now be done on the living’ (1999, 208). Crucially, technologies like the stethoscope brought the physician and patient into the examination room together but by providing physicians with privileged access to the seat of disease did not necessarily bring them closer in terms of understanding. Doctors now heard things that remained unheard to the patient, and this provoked a distancing in terms of illness perceptions. In Reiser’s account, the stethoscope ‘liberated doctors from patients and, by doing so, paradoxically enabled doctors to think they helped them better. […] Listening to the body seemed to get one further diagnostically than did listening to the patient’ (2009, 26).
The result is visible in the resistance surrounding some examination technologies that allowed physicians to delve into the body’s interior in order to gain new anatomical and pathological insights but that proved too transgressive for some existing physician-patient contacts. The vaginal speculum, introduced into examination procedures in Paris in the early-nineteenth century, may have fitted well with physicians’ new commitments to empiricism and observation. But at the time of the speculum’s introduction, female genital organs, in contrast to other organs, were regarded ‘as so mysterious and so sacred that no matter how serious the disease that afflicted them might be, it was no justification for an examination either by sight or touch’ (Murphy 1891, cited in Moscucci 1990, 110). Although the speculum was in line with pathological disease concepts and close, interior observation, moral considerations continued to undermine its suitability in the clinical context. At a meeting of the Royal Medical and Chirurgical Society, chronicled in the Lancet , commentators associated the speculum with both female and physician corruption, and the loss of moral virginity and innocence caused by its insertion into the body (Anon. 1850). In Margarete Sandelowski’s estimation, the vaginal speculum ‘required physicians not only to touch women’s genitals, but also to look at them, and thus imperiled the relationship male physicians wanted to establish with female patients’ (2000, 75). Here was a case in which technology challenged the socially accepted relationship between (male) physicians and (female) patients of a particular class because its application demanded increased physical closeness, and therefore was seen as undesirable and transgressive. As Claudia Huerkamp notes, it took a long time to establish a specific ‘medical culture’ in which the physical examination of female parts by a male physician was not perceived as breaking a taboo (1989, 67).
In other instances, the use of the speculum and the unprecedented access it provided to women’s anatomy mirrored existing power structures. The first uses of the speculum were justified in reference to and tested on the most vulnerable members of society. Deirdre Cooper Owens (2017) has demonstrated that in the U.S., racist arguments helped to defend the speculum’s application and experimentation on black, enslaved women as they were deemed to have a particularly ‘robust’ constitution, high tolerance of pain, and so on. Medical men such as James Marion Sims, who by his own account was the inventor of the speculum, combined his privileged access to enslaved women’s bodies with intrusive forms of examination in order to gain new knowledge crucial for the emerging field of gynaecology. This was also true for Irish immigrants in the U.S. (Owens 2017) and in the case of prostitutes in France and Germany, where the speculum was used as an instrument of the medical police (Moscucci 1990, 112). Prostitutes were screened using this new instrumentation as supposed carriers of venereal disease, whereas male clients did not need to undergo any screening. This highlights how intrusion into the body in the name of more accurate examination was frequently bound up with power and control, especially of marginalized groups.
Even as the seat of disease became increasingly associated with specific locations inside the body, this coexisted with the notion that medicine could still be conducted ‘at a distance.’ The example of the telephone demonstrates how tele-instruments worked alongside close examination devices that adhered to the principle of disease as located in particular interior body parts. In fact, the potentiality of the telephone for the medical profession was apparent from its invention in 1876; 4 as Michael Kay notes, the first inter-connected users were doctors, pharmacists, hospitals and infirmaries (2012). Practitioners used the technology, which enabled the clear transmission and reproduction of complex sounds for the first time, to improve existing instruments, or to devise entirely new examination methods. For instance, in November 1879, the Lancet published the case of an American doctor who, when phoned in the middle of the night by a woman anxious about her granddaughter’s cough, asked for the child to be held up to the telephone so that he could hear it (Anon. 1879). A group of physicians predicted in 1880 that home telephones would allow a new specialty of long-distance practitioners to ‘each settle themselves down at the centre of a web of wires and auscult at indefinite distances from the patients,’ potentially replacing the traditional stethoscope (cited in Greene 2016, 306). The telephone was also lauded for its potential to uncover foreign objects lodged in patients’ bodies, for example by acting as a metal detector (see Kay 2012). In line with the belief that a ‘good examination’ required a physician having access to the body’s interior in order to discover the seat of disease according to the localisation principle, the telephone was seen as an extension of the doctor’s ear that could improve examination and diagnosis.
In this context, reactions to the increased physical distance between physician and patient varied. The benefits of using a telephone instead of the more traditional speaking tube, which allowed breath to pass from one speaker to another, when communicating with patients with contagious diseases were recognised very early (Aronson 1977, 73). A testimonial letter, written by the Lady Superintendent at the Manchester Hospital for Sick Children in 1879, stated: ‘[The recently installed telephone] is of the greatest value in connection with the Fever Ward, enabling me to always be in communication without risk of infection’ (cited in Kay 2012). Yet some physicians worried that telephone technology had effectively ‘shrunk’ perceived social distance between them and the working classes, making them liable to be overly contacted by the general public. As one doctor complained in the Lancet in 1883: ‘[a]s if the Telegraph and the Post Office did not sufficiently invade and molest our leisure, it is now proposed to medical men that they should become subscribers to the Telephone Company, and so lay themselves open to communications from all quarters and at all times. […] The only fear we have is that when people can open up a conversation with us for a penny, they will be apt to abuse the privilege […] ’ (cited in Kay 2012) . Not only were doctors concerned about the telephone invading their ‘leisure,’ they worried that they might be overrun by the public, and their medical expertise would be needlessly exploited. Because of the inherent fear of doctors that an excessively frequent use of the telephone could flatten the social order and their standing within society, it is not surprising that the public use of the telephone came under critical medical scrutiny. This is visible in the way that telephones themselves came to be seen as seats of infection. At the end of the nineteenth century when most telephones were for public use (Fischer 1992), the British Medical Journal cautioned there was a need to curtail ‘the promiscuous use of the mouth-pieces of public telephones’ (Anon. 1887, 166). In general, the use of the telephone was informed by insights from bacteriology, which transformed individual disease ‘into a public health event affecting communities and nations’ (Koch 2011, 2), and placed new emphasis on the need to keep potentially infectious bodies as well as social classes at clear distance from one another (see Peckham 2015).
In relation to the pitfalls of today’s telemedicine and the fundamental questions of physical distance and emotional rapprochement in the medical encounter, these historical findings demonstrate that what was perceived as the ‘normal’ setting and procedure of medical examination could change remarkably within a rather short time. Before the nineteenth century, close physical examination generally played a less prominent role while patients’ illness accounts had a greater weight in the medical encounter. Indeed, in some contexts physical distance was seen as the prerogative of good medical practice. Post-1800, by contrast, is characterized by the standardisation of physical close examination, but also by the introduction of new technologies into the patient-physician relationship that themselves challenged socially-accepted degrees of physical closeness. However, this does not necessarily mean that such technologies disturbed a former unbroken bond, rather, various technologies became players in the game and could (or not) be appropriated by patients and doctors alike. Technology did not simply affect the physician-patient relationship, rather, existing societal and moral understandings influenced how technologies came into being and how they were used (Peckham 2015, 153). Our historical examples suggest that rather than seeing telemedicine as something fundamentally new and potentially threatening because it seemingly undermines a personal relationship, it may be more useful to acknowledge that technologies and cultural understandings always govern the degree of physical closeness and distance in medical encounters, and that this has had manifold implications for the emotional doctor-patient bond. The success of telepsychotherapy during the Covid-19 pandemic is perhaps a case in point. Even as it is unique among medical specialities because of the extent to which it considers the human relationship as fundamental for healing, psychotherapy via phone or video link has increased dramatically during the public health crisis, and also had good results (Békés and Aafjes-van Doorn 2020). This points not only to how physician-patient closeness and emotional understanding can exist in times of physical distance, but also to the constantly variable ways in which both the cultural imagination and experience of distance manifest themselves (Kolkenbrock 2020).
Self-treatment: do-it-yourself medical devices and the expert patient
The third field of digital medicine that we would like to put into historical perspective is one of the fastest growing fields of eHealth, namely do-it-yourself (DIY) health technologies. Such technologies broadly refer to the mobile devices that ‘now allow consumers to diagnose and treat their own medical conditions without the presence of a health professional’ (Greene 2016, 306). Silicon Valley firms sell ‘disintermediation,’ that is the possibility of cutting out middlemen – physicians – and allowing consumers to better control their health via their devices (Eysenbach 2007). Significant private investments have been driving these changes which, in the forms of smart devices and wearable technologies, often imply purchasing a product (e.g. a smartphone) and related applications and tools (see Greene 2016; Matshazi 2019). The website Digital Trends 2019 ranking of ‘the 10 best health apps’ range from Fitocracy, a running app that allows you to track your progress and that promises a fitness experience with a ‘robust community of like-minded individuals’, to Carbs that transfers the meals you have eaten into charts of calories, to Fitbit Coach that promises you the experience of having a personal trainer on your smartphone (de Looper 2019). 5 Health systems have bought on and increasingly ask patients to observe and monitor themselves with the help of these technologies, and in some cases, the use of apps to measure blood pressure, pulse and body weight such as Amicomed and Beurer HealthManager are closely connected to the possibilities of sharing one’s data remotely with a physician. In terms of reception, the delegation of tasks to digital devices is associated with patients having new options and new knowledge of their own health. In the estimation of one hospital CEO, this dramatic ‘democratization’ of technology and of knowledge signals ‘a true coming of age of the patient at the centre of the healthcare universe’ (Rosenberg 2019). In the words of chronic patient and patients’ rights advocate Michael Mittleman, while there may be benefits for patients when technologies take over certain tasks that were previously the prerogative of physicians, such technologies nevertheless pose a fundamental challenge to the ‘golden bond’ that previously characterized the patient physician-relationship, for example in the age of the house call (conversation with the author, 2019). It is clear from these statements that DIY devices – because they suggest that the more beneficial relationship is that between the patient/consumer and his/her devices – challenge previous assumptions about the inherent value of the physician-patient relationship as well as the balance of power between those two actors (see Obermeyer and Emmanuel 2016).
Both the notion that patients inherently benefit from circumventing physicians and taking their health into their own hands, as well as the idea of a close, almost familial bond that characterized the physician-patient relationship prior to contemporary DIY practices can be nuanced if we acknowledge that do-it-yourself medical practices have a long and varied history. As Roy Porter has noted, in the eighteenth-century, ‘ordinary people mainly treated themselves, at least in the first instance[,] “medicine without doctors” [was] a necessity for many and a preference for some’ (1999, 281). Only in the nineteenth-century did the medical profession establish a monopoly in health care and have the official power to determine what was ‘health’ and ‘sickness’. In the previous centuries, local and pluralistic ‘medical markets’ embraced far more providers of health services and their varied tools, including barbers, surgeons, quacks and charlatans, so that patients chose among the options that most convinced them or that were affordable to them (Ritzmann 2013, 418). But patients also had the option to help and treat themselves using the means at their disposal – Fissell argues that a person who fell ill in 1500 and still in 1800 almost always first sought medical treatment in a domestic context: ‘[h]e or she relied upon his or her own medical knowledge of healing plants and procedures, consulted manuscript or printed health guides, and asked family, neighbors, and friends for advice’ (2012, 533). As Fissell points out, the enormous diffusion and importance of self-therapy at the time meant that the ‘boundary between patients and practitioners was hard to pin down’ (534). While current depictions of an idealised interaction between physician and patient assume a physician who through his/her knowledge examines, advises and treats the non-knowing patient, history shows that the presumed boundaries between the expert and lay person are far more blurred than is usually assumed.
The presumed novelty of a de-centralised market for DIY devices that potentially threatens the dual relationship between physicians and patients can be put into perspective when considering historical examples. Due to a fairly unregulated medical market in the early modern period, competition was high and the business of medicinal recipes lucrative. In this context, profit-motivated apothecaries benefited from offering new recipes made from exotic products: as of the fifteenth century European pharmacies stocked many wares with medicinal properties – including spices, elements such as sulphur, and plants, for examplemastic and sundew – and these were bought by people who gathered and dealt in medicinal plants (or ‘simples’) and other apothecaries, who made them into medicines. In the wake of the European voyages of discovery, the range of products became ever wider and more expensive, and apothecaries were a very profitable business branch for a long time (Ehrlich 2007, 51-55). King and Weaver have used evidence from remedy books in eighteenth-century England to show how families purchased recipes for remedies, and resold both the recipes and the medicines they brewed to other local people (2000, 195). Until the nineteenth century the medical market flourished and was accessible and lucrative for many participants, while the demand for ‘medical’ services was high, particularly in towns and cities. Access to the technologies of healing – whether domestic medical guides or healing herbs – allowed patients to control their health and treatments according to a wide range of scientific explanations. In contrast to other European countries that meanwhile had developed some restrictions for apothecaries and their suppliers, in Britain the market-place was remarkably varied in the light of the free-market principle caveat emptor (let the buyer beware). ‘In English conditions,’ wrote Porter, ‘irregulars, quacks and nostrum-mongers seized the opportunities a hungry market offered’ (1995, 460). In these conditions of market-oriented healing, both patients and healers alike believed, sometimes fervently, in the effectiveness of the remedies on offer. Moreover, the network of relationships in which such transactions took place was remarkably fluid, with patients using the services of several health professionals in succession or simultaneously.
In the following centuries, medical practice and science would change dramatically due to the rise of academic training as a prerequisite to enter the medical profession, a development seen across Europe, as well as the integration of physicians into national health agendas. A growing belief in science and a paternalistic ideal of the academic physician attributed to him the sole power over medical practice and technologies. It became more difficult for other healers to participate in the health market, and the knowledge of the self-treating patient was diminished as well. As part of the attempt to counteract competition from non-educated or apprenticed healers, in the United Kingdom only registered doctors could hold various public posts, such as public vaccinator, medical officer and the like (Bynum 2006, 214). Yet ‘alternative’ medicine, a term that contained all those healers not licenced and accepted by the respective medical registers, continued to satisfy patients’ needs, although to a lesser extent. In Weindling’s assessment of the prospects of university-educated physicians to attract clients in nineteenth-century Berlin, ‘[f]ierce competition from a range of unorthodox practitioners must be assumed’ (1987, 398). The popularity of hydropathic doctors and water cures, mud-bathing and vegetarianism are but some examples of how alternative medicines co-existed alongside official ones and were increasingly popular treatments even though they did not meet the contemporary academic criteria of standards regarding safety and efficacy (Ko 2016). Thus patients often looked beyond qualified physicians to other practitioners, and their own sensibilities played a considerable role in which relationships they chose to develop.
A look into twentieth-century history shows that DIY practices were integrated into official medicine as well (Timmermann 2010; Falk 2018). The significant rise of chronic diseases and life-long treatment, for instance, required the co-operation of patients in the form of self-tracking and observation of their bodies since it could not be done by medical experts alone. In the first decades of the twentieth century, DIY methods and technologies for measuring blood pressure or sugar became particularly vital, transforming the roles of ‘patient’ and ‘doctor’ and relationship between them. Examining the history of self-measuring blood pressure, Eberhard Wolff notes that patients doing so in the 1930s required both patience and training, and also were pushed into a more active and participatory role during medical treatment: it was not the doctor anymore but the patient who produced and controlled relevant data that were decisive for further medical decisions and treatment (2014, 2018). With the rise of the risk factor model in mid-twentieth century – the identification of factors in patient’s behaviour and habits that were suspected of contributing to the development of a chronic disease – DIY practices grew ever more important and so did its technologies. From this moment, the idea of preventing disease shifted towards individual, possibly damaging behaviours such as smoking and diet that could trigger a number of different diseases. As a consequence, the patient received more responsibility in order to live up to the new credo of maintaining his or her personal health (Lengwiler and Madarász 2010). Optimizing a personal healthy life style hence did not necessarily occur in direct consultation with a doctor but rather in conjunction with health products available on the market. In the words of sociologist Nikolas Rose, in the course of the twentieth century:
[t]he very idea of health was re-figured – the will to health would not merely seek the avoidance of sickness or premature death, but would encode an optimization of one’s corporeality to embrace a kind of overall “well-being” … It was this enlarged will to health that was amplified and instrumentalized by new strategies of advertising and marketing in the rapidly growing consumer market for health (2001, 17-18).
According to Rose, by such developments, ‘selfhood has become intrinsically somatic – ethical practices increasingly take the body as a key site for work on the self’ (18). But he also argues that by linking our well-being to the quality of our individual biology we have not become passive in the face of our biological fate. On the contrary, biological identity has become ‘bound up with more general norms of enterprising, self actualizing, responsible personhood’ (18-19). By considering ourselves responsible for our own biology as key to our health, we have come to depend on ‘professionals of vitality’ (22) whether they be purveyors of DIY devices, genetic counsellors, drug companies or doctors.
With respect to contemporary debates over DIY practices, some have argued that they allow both doctors and patients to be ‘experts’ and call for ‘a relationship of interactive partnership,’ not only because patients today are often informed but also because ideally they know best their own bodies and ailments (Kennedy 2003). Against this idealising assessment, the historical perspective makes us aware that while self-help and self-treatment have been an important dimension of past medical cultures, it appears that historically, patients have not relied as much on a face-to-face empathetic encounter with any one physician as today’s debates suggest. Moreover, today as in the past, the mere existence of markets for medical devices influences how consumers/patients decide whether to resist or embrace the various possibilities of self-treatment as well as their relationships with those who provide it. As Porter has argued, purveyors of ‘alternative’ medicines rationalised their therapeutic effects in ways that differed from official scientific methods and using arguments that likewise changed over time. Depending on the perspective of whose model of evidence users deemed most credible, the co-existence of diverse models for practicing medicine must be assumed throughout history and despite nineteenth-centuries attempts to eliminate unorthodox medicines (Timmermann 2010). The result was a diverse network of fast-changing relationships in which no single one was ascribed the ultimate power to heal. Reflecting on this history, historian of medicine and physician Jeremy Greene has stated that contemporary DIY devices therefore appear ‘neither wholly new nor wholly liberating’ (2016, 308). Our analysis corroborates Greene’s, in that it shows how those who use new DIY technologies may free themselves from their traditional relationship of dependence on physicians, while also creating new relationships with those actors who produce apps or conduct marketing. Yet our study also suggests that there is no one ethical conclusion about whether DIY or physician-dominated care is a better way of living up to a more humane medicine. Ethical arguments and the grounds on which we are supposed to resolve them are complex and variable. As seen in these historical examples, they have changed profoundly over time with each technology and medical concept challenging and refashioning the doctor-patient bond anew. Furthermore, there is no such thing as a ‘timeless’ doctor’s healing presence, or even medical expertise, or an ill person/patient. As shown above, as health and illness are defined, redefined and challenged throughout history, this process creates both expert and patient, as well as shapes the relationship between them.
An oft-heard concern about ‘computerization’ in medicine is that digital objects are changing human interactions. While various representatives from the tech side are optimistic about the effects of increasingly dynamic and intelligent objects in the medical encounter, some patients and physicians are more skeptical and see their social relationships as disturbed by new technologies. ‘Doctors don’t talk to patients’ is the most common complaint the CEO at a Montreal hospital recounted hearing from current patients (conversation between the author and Lawrence Rosenberg, 2019). Fears that increasing digitization of medicine will disturb the relationship that can potentially make the patient ‘whole’ again are not without foundation (King 2020). However, without a clear baseline for assessing changes we have limited scope for drawing conclusions about present day realities or long-term trends. Given the appeal of using the past to suggest a more ‘human’ but lost era of medical practice, a less nostalgic but more sophisticated understanding of the past as provided by historical research would serve us well. In this sense, history can counteract a characteristically modern myopia, namely, as intellectual historian Teresa Bejan has put it, our ‘endearing but frustrating tendency to view every development in public life as if it were happening for the first time’ (2017, 19).
As we saw in the examples dealing with record keeping, examining and self-treatment, trends that consider the patient as an object – a diseased lung, or a malfunctioning heart valve – and the concomitant use of technologies to record, examine and treat physical symptoms were necessarily in tension with patients’ own accounts of how they became ill and of the symptoms they experienced. In fact, concerns about the loss of meaningful personal contact in the medical encounter are incomprehensible without reference to a historical trend dating back to the beginning of the nineteenth century which seems to undermine the patient’s perspective by focusing on increasingly specialised processes within the body. Yet neither before nor after that time is there an unmediated patient’s voice that we are able to recover: the medical record as historical source has its own distinct material history, and patients’ expectations were always bound up with broader societal views about acceptable standards of healing. The historical perspective also shows that we should not take for granted the linear narrative of the technological as adverse to human relations and reducing empathetic understanding in the medical encounter – to paraphrase Lauren Kassell, the digital is not just the enemy of the human (2016, 128). Rather, it makes us aware that our understanding of the doctor-patient relationship and of its role in healing are themselves historically contingent. The idea of ‘a friendly, family doctor “being there”’ and the association of medicine with a ‘desirable clinical relationship’ (as opposed to e.g. perfect health) is an idea that has played out very differently in the course of history (Porter 1999, 670). There were times in which listening to patients was bound up with completely different expectations from both sides, and there were times in which physical examination was not seen as an indispensable part of medical practice. Moreover, while the monopoly of the physician in matters of health care and the focus on the (exclusive) healing potential of the clinical relationship is of relatively recent origin, we have seen that the popularity and economy of DIY devices has a much longer history, one that resists a linear account of DIY devices as something purely liberating. Hence, in contrast to idealised and simplified historical narratives that lament the loss of human relationships, more sophisticated accounts should acknowledge that medical objects and technologies are not the strange and disturbing ‘other’ in the medical encounter but rather integral players therein. As Frank Trentmann has put it, ‘things and humans are inseparably interwoven in mutually constitutive relationships’ (2009, 307). While the authors of a recent study suggest that ‘the traditional dyadic dynamics of the medical encounter has been altered into a triadic relationship by introducing the computer into the examination room’ (Assis-Hassid et al. 2015, 1), it seems more likely that the dyadic relationship has never existed.
Vanessa Rampton received funding from the Branco Weiss Fellowship – Society in Science.
1 We rely on a definition used by science and technology scholars whereby the term ‘technology’ operates on three levels (see Bijker, Hughes and Pinch 2012, xlii). First, there is the physical level, referring to tangible objects such as a smartphone, wellness band, or stethoscope. The second level of meaning concerns activities or processes, such as 3D printing or creating X-rays. The third level refers to knowledge people have in addition to what they do, for example the knowledge that underpins the conduct of a surgical procedure. This approach shows the extent to which specific tools and techniques, knowledge, and rationales for intervention are intricately bound together. Our use of the term ‘digital,’ that is involving computer technology, in relation to medicine ‘includes categories such as mobile health (mHealth), health information technology (IT), wearable devices, telehealth and telemedicine, and personalized medicine’ (U.S. Food and Drug Administration).
2 As a rule, while systematic reviews of telemedicine generally portray it as effective as in-person consultation or promising, evidence is limited and fast-evolving (Ekeland, Bowes and Flottorp 2010; Kruse et al. 2017; Lee et al. 2017).
3 In Germany, legislators have reacted to these concerns by limiting video consultation to cases in which physician and patient have physically met before, and primarily using it for monitoring the course of disease, including chronic ones, or the healing of an injury (Heinrich 2017).
4 Scottish-born US inventor Alexander Graham Bell was the first to be awarded the U.S. patent for the invention of the telephone in 1876 (Fischer 1992).
5 Interestingly, and probably most important for their users, nine out of ten among the ranked apps are available as free downloads ( https://www.digitaltrends.com/mobile/best-health-apps/ , June 16, 2019).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Abrams, Ken and Casey Korba. 2018. "Consumers are on Board with Virtual Health Options. Can the Health Care System Deliver?” https://www2.deloitte.com/insights/us/en/industry/health-care/virtual-health-care-consumer-experience-survey.html .
- Amenta, Conrad. 2017. “What’s Digitization Doing to Health Care?” Vice . https://motherboard.vice.com/en_us/article/785v3z/whats-digitization-doing-to-health-care.
- Amicomed. 2018-2019. San Francisco, CA. https://www.amicomed.us/ .
- Anon. Practice by Telephone. The Lancet. 1879; 2 :819. [ Google Scholar ]
- Anon. Proceedings of a Meeting of the Royal Medical and Chirurgical Society on the Use of the Speculum, 28 May 1850, and Relevant Correspondence. The Lancet. 1850; 1 :701–06. [ Google Scholar ]
- Anon. 1887. “The Telephone as a Source of Infection.” British Medical Journal : 166.
- Aronson SH. The Lancet on the Telephone 1876-1975. Medical History. 1977; 21 :69–87. doi: 10.1017/S0025727300037182. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Assis-Hassid S, et al. Enhancing Patient-Doctor-Computer Communication in Primary Care: Towards Measurement Construction. Israel Journal of Health Policy Research. 2015; 4 (4):1–11. doi: 10.1186/2045-4015-4-4. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bartens, Werner. 2019. ”Angehende Ärzte müssen Empathie Zeigen.“ Süddeutsche Zeitung . 31 July. https://www.sueddeutsche.de/gesundheit/medizinstudium-empathie-auswahlverfahren-1.4546284 .
- Behrens R., N. Bischoff and C. Zelle, eds. 2012. Der ärztliche Fallbericht. Epistemische Grundlagen und textuelle Strukturen dargestellter Beobachtung . Wiesbaden: Harrassowitz.
- Bejan TM. Mere Civility: Disagreement and the Limits of Toleration . Harvard: Harvard University Press; 2017. [ Google Scholar ]
- Békés V, Aafjes-van Doorn K. Psychotherapists’ Attitudes toward Online Therapy during the COVID-19 Pandemic. Journal of Psychotherapy Integration. 2020; 30 (2):238–247. doi: 10.1037/int0000214. [ CrossRef ] [ Google Scholar ]
- Beurer HealthManager. 2018-2019. Ulm: Beurer GmbH. https://www.beurer.com/web/gb/ .
- Bichat X. Anatomie générale, appliquée à la physiologie et à la médecine . Paris: Brosson; 1801. [ Google Scholar ]
- Bijker, Wiebe E., Thomas P. Hughes and Trevor Pinch, eds. 2012 [1987]. The Social Construction of Technological Systems: New Directions in the Sociology and History of Technology . Cambridge: The MIT Press.
- Boeldt, D. L. et al. 2015. “How Consumers and Physicians View New Medical Technology: Comparative Survey.” Journal of Medical Internet Research 17 (9): e215. doi: 10.2196/jmir.4456: 10.2196/jmir.4456 . [ PMC free article ] [ PubMed ]
- Bynum WF, et al. The Rise of Science in Medicine, 1850-1913. In: Bynum WF, et al., editors. The Western Medical Tradition, 1800-2000 . Cambridge: Cambridge University Press; 2006. pp. 111–239. [ Google Scholar ]
- Canada Health Infoway. 2001-2019. Toronto: Canada Health Infoway. https://www.infoway-inforoute.ca/en/solutions/digital-health-foundation/electronic-medical-records/benefits-of-emrs .
- Chauhan V, et al. Novel Coronavirus (COVID-19): Leveraging Telemedicine to Optimize Care While Minimizing Exposures and Viral Transmission. J Emerg Trauma Shock. 2020; 13 (1):20–24. doi: 10.4103/JETS.JETS_32_20. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Colombat, de l’Isère, Marc . Traité des maladies des femmes et de l’hygiène spéciale de leur sexe . Paris: Libraire médicale de labé; 1838. [ Google Scholar ]
- Cooper Owens D. Medical Bondage: Race, Gender, and the Origins of American Gynecology . Atlanta: University of Georgia Press; 2017. [ Google Scholar ]
- Daston LJ, Galison P. Objectivity . New York: Zone; 2010. [ Google Scholar ]
- de Looper, Christian. 2019. “The 10 Best Health Apps.” Digital Trends , 5 January. https://www.digitaltrends.com/mobile/best-health-apps/ .
- Dinges, Martin, Kay Peter Jankrift, Sabine Schlegelmilch, and Michael Stolberg, eds. 2016. Medical Practice, 1600-1900: Physicians and their Patients . Translated by Margot Saar. Clio Medica, volume 96. Leiden: Brill Rodopi.
- Doctor On Demand. 2012-2019. San Francisco, CA. https://www.doctorondemand.com/ .
- Ehrlich, Anna. 2007. Ärzte, Bader, Scharlatane. Die Geschichte der österreichischen Medizin . Wien: Amalthea.
- Economist, The . “How Covid-19 Unleashed the National Health Service.” 3 December 2020: 55-56. https://www.economist.com/britain/2020/12/03/how-covid-19-unleashed-the-nhs .
- Ekeland AG, Bowes A, Flottorp S. Effectiveness of Telemedicine: A Systematic Review of Reviews. Int J Med Inform. 2010; 79 :736–771. doi: 10.1016/j.ijmedinf.2010.08.006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Epstein JL. Writing the Unspeakable: Fanny Burney's Mastectomy and the Fictive Body. Representations. 1986; 16 :131–166. doi: 10.2307/2928516. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eysenbach G. From Intermediation to Disintermediation and Apomediation: New Models for Consumers to Access and Assess the Credibility of Health Information in the Age of Web 2.0. Stud Health Technol Inform. 2007; 129 (Pt 1):162–6. [ PubMed ] [ Google Scholar ]
- Fagherazzi, Guy. 2020. “Digital Health Strategies to Fight COVID-19 Worldwide: Challenges, Recommendations, and a Call for Papers.” Journal of Medical Internet Research 22 (6): e19284. [ PMC free article ] [ PubMed ]
- Falk O. Der Patient als epistemische Größe. Praktisches Wissen und Selbsttechniken in der Diabetestherapie 1922-1960. Medizinhistorisches Journal. 2018; 53 (1):36–58. doi: 10.25162/medhist-2018-0002. [ CrossRef ] [ Google Scholar ]
- Fischer CS. America Calling: A Social History of the Telephone to 1940 . Berkley: University of California Press; 1992. [ Google Scholar ]
- Fissell ME. The Disappearance of the Patient’s Narrative and the Invention of Hospital Medicine. In: Wear A, French R, editors. British Medicine in an Age of Reform . London: Routledge; 1991. pp. 92–109. [ Google Scholar ]
- ---- 1993. “Innocent and Honorable Bribes: Medical Manners in Eighteenth-Century Britain.” In The Codification of Medical Morality: Historical and Philosophical Studies of the Formalization of Western Medical Morality in the Eighteenth and Nineteenth Centuries . Volume 1: Medical Ethics and Etiquette in the Eighteenth Century , edited by Robert Baker, Dorothy Porter and Roy Porter, 19-46. Dordrect: Springer Science + Business Media.
- ---- 2012. “The Medical Marketplace, the Patient, and the Absence of Medical Ethics in Early Modern Europe and North America.” In The Cambridge History of World Medical Ethics , edited by Robert Baker and Laurence McCullough, 533-39. Cambridge: Cambridge University Press.
- Forrester J. If p, then what? Thinking in Cases. History of the Human Sciences. 1996; 9 (3):1–25. doi: 10.1177/095269519600900301. [ CrossRef ] [ Google Scholar ]
- Friedberg MW, et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. Santa Monica, CA: RAND Corporation; 2013. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gafner L, et al. Administrative and Epistemic Aspects of Medical Practice: Caesar Adolf Bloesch (1804-1863) In: Dinges M, et al., editors. Medical Practice, 1600-1900: Physicians and their Patients . Leiden: Brill Rodopi; 2016. pp. 253–70. [ PubMed ] [ Google Scholar ]
- Gawande, Atul. 2018. “Why Doctors Hate Their Computers.” The New Yorker . 12 November. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers .
- Granshaw L. The Rise of the Modern Hospital in Britain. In: Wear A, editor. Medicine in Society . Cambridge: Cambridge University Press; 1992. pp. 197–218. [ Google Scholar ]
- Greene J. Do-it-Yourself Medical Devices: Technology and Empowerment in American Health Care. New England Journal of Medicine. 2016; 374 :305–9. doi: 10.1056/NEJMp1511363. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Greenhalgh T, et al. Video Consultations for Covid-19: An Opportunity in a Crisis? BMJ. 2020; 368 :m998. doi: 10.1136/bmj.m998. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hammack-Aviran CM, et al. Research Use of Electronic Health Records: Patients’ Views on Alternative Approaches to Permission. AJOB Empirical Bioethics. 2020; 11 (3):172–186. doi: 10.1080/23294515.2020.1755383. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heinrich, Christian. 2017. “Treffen im virtuellen Sprechzimmer.“ Die Zeit 22 (24 May): 33. https://www.zeit.de/2017/22/telemedizin-sprechstunde-arzt-krankenkasse-erstattung-video .
- Hess V, Andrew Mendelsohn J. Case and Series: Medical Knowledge and Paper Technology, 1600–1900. History of Science. 2010; 48 (3-4):287–314. doi: 10.1177/007327531004800302. [ CrossRef ] [ Google Scholar ]
- Huerkamp, Claudia. 1989. “Ärzte und Patienten. Zum strukturellen Wandel der Arzt-Patient-Beziehung vom ausgehenden 18. bis zum frühen 20. Jahrhundert.“ In Medizinische Deutungsmacht im sozialen Wandel des 19. und frühen 20. Jahrhunderts , edited by Alfons Labisch und Reinhard Spree, 57-73. Bonn: Psychiatrie-Verlag.
- Jewson ND. The Disappearance of the Sick-Man from Medical Cosmology, 1770-1870. Sociology. 1976; 10 :225–44. doi: 10.1177/003803857601000202. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnston SC. Anticipating and Training the Physician of the Future: The Importance of Caring in an Age of Artificial Intelligence. Acad Med. 2018; 93 (8):1105–1106. doi: 10.1097/ACM.0000000000002175. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kassell, Lauren, 2016. “Paper Technologies, Digital Technologies: Working with Early Modern Medical Records.” In The Edinburgh Companion to the Critical Medical Humanities , edited by S. Atkinson, J. Macnaughton and J. Richards, 120-135. Edinburgh: Edinburgh University Press. http://www.jstor.org/stable/10.3366/j.ctt1bgzddd . [ PubMed ]
- Kay, Michael. 2012. “Give the Doc a Phone: A Historical long-view of Telephone Use and Public Health in Britain.” https://michaelakay.wordpress.com/2012/02/14/give-the-doc-a-phone-a-historical-long-view-of-telephone-use-and-public-health-in-britain/ .
- Kennedy I. Patients are Experts in their own Field. BMJ. 2003; 326 (7402):1276–7. doi: 10.1136/bmj.326.7402.1276. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kennedy M. Technology. In: The Routledge, editor. Research Companion to Nineteenth-Century British Literature and Science , edited by John Holms and Sharon Ruston. London: Routledge; 2017. pp. 3011–328. [ Google Scholar ]
- King S, Weaver A. Lives in Many Hands: The Medical Landscape in Lancashire, 1700-1820. Medical History. 2000; 44 (2):173–200. doi: 10.1017/S0025727300000016. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- King, Martina. 2020. “"Nach Aufnahme arterielle Hypotonie": Personenkonzept und Kommunikationsformen in der Experten-Medizin.” Gesnerus 77 (2): 411-37.
- Ko, Y. 2016. “Sebastian Kneipp and the Natural Cure Movement of Germany: Between Naturalism and Modern Medicine.” Uisahak 25(3): 557-590. doi: 10.13081/kjmh.2016.25.557. [ PMC free article ] [ PubMed ]
- Koch T. Disease Maps: Epidemics on the Ground . Chicago: University of Chicago Press; 2011. [ Google Scholar ]
- Kolkenbrock, Marie. 2020. “The Dance of the Porcupines. On Finding the Balance between Proximity and Distance in Times of Pandemic.” The Hedgehog Review Blog: Critical Reflections on Contemporary Culture . 21 April. https://hedgehogreview.com/blog/thr/posts/the-dance-of-the-porcupines .
- Kruse CS, et al. The Effectiveness of Telemedicine in the Management of Chronic Heart Disease: A Systematic Review. J R Soc Med Open. 2017; 8 (3):1–7. doi: 10.1177/2054270416681747. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee SWH, et al. Comparative Effectiveness of Telemedicine Strategies on Type 2 Diabetes Management: A Systematic Review and Network Meta-analysis. Scientific Reports. 2017; 7 :12680. doi: 10.1038/s41598-017-12987-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lengwiler M, Madarász J. Präventionsgeschichte als Kulturgeschichte der Gesundheitspolitik. In: Lengwiler M, Madarász J, editors. Das präventive Selbst: Eine Kulturgeschichte moderner Gesundheitspolitik . Bielefeld: Transcript; 2010. pp. 11–28. [ Google Scholar ]
- Liu X, Keane PA, Denniston AK. Time to Regenerate: The Doctor in the Age of Artificial Intelligence. Journal of the Royal Society of Medicine. 2018; 11 (4):113–116. doi: 10.1177/0141076818762648. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Loder, Natasha. 2017. “Is There a Doctor in my Pocket?” 1843 Magazine, The Economist . https://www.1843magazine.com/technology/is-there-a-doctor-in-my-pocket .
- Mathar, Thomas. 2010. Der digitale Patient. Zu den Konsequenzen eines technowissenschaftlichen Gesundheitssystems . Bielefeld: Transcript.
- Matshazi N. Digital Health Funding Breaks New Record in 2018. 2019. [ Google Scholar ]
- Medgate Tele Clinic. 2000-2019. Basel: Medgate AG. https://www.medgate.ch/ .
- Mitchell L, Georges E. Cross-Cultural Cyborgs: Greek and Canadian Women’s Discourses on Fetal Ultrasound. In: Saetnan AR, Oudshoorn N, Kirejczyk M, editors. Bodies of Technology: Women’s Involvement with Reproductive Medicine . Columbus: Ohio State University Press; 2000. pp. 384–409. [ Google Scholar ]
- Moscucci O. The Science of Woman: Gynaecology and Gender in England, 1800–1929 . Cambridge: Cambridge University Press; 1990. [ Google Scholar ]
- Nolte K. Vom Verschwinden der Laienperspektive aus der Krankengeschichte: Medizinische Fallberichte im 19. Jahrhundert. In: Brändli-Blumenbach S, Lüthi B, Spuhler G, editors. Zum Fall machen, zum Fall werden. Wissensproduktion und Patientenerfahrung in Medizin und Psychiatrie des 19. und 20. Jahrhunderts . Frankfurt, New York: Campus; 2009. pp. 33–61. [ Google Scholar ]
- Obermeyer Z, Emanuel EJ. Predicting the Future – Big Data, Machine Learning, and Clinical Medicine. NEJM. 2016; 375 :1216–19. doi: 10.1056/NEJMp1606181. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peckham R. Panic Encabled: Epidemics and the Telegraphic World. In: Peckham R, editor. Empires of Panic: Epidemics and Colonial Anxieties . Hong Kong: Hong Kong University Press; 2015. pp. 131–54. [ Google Scholar ]
- Pomata G. Patients, Healers and the Law in Early Modern Bologna . Baltimore: Johns Hopkins University Press; 1998. Contracting a Cure . [ Google Scholar ]
- ---- 2010. “Sharing Cases: The Observationes in Early Modern Medicine.” Early Science and Medicine 15:193-236. [ PubMed ]
- ---- 2014. “The Medical Case Narrative: Distant Reading of an Epistemic Genre.” Literature and Medicine 32 (1): 1-23. [ PubMed ]
- Porsdam SM, Savulescu J, Sahakian BJ. Facilitating the Ethical Use of Health Data for the Benefit of Society: Electronic Health Records, Consent and the Duty of Easy Rescue. Phil Trans R Soc A. 2016; 374 :20160130. doi: 10.1098/rsta.2016.0130. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Porter R. The Eighteenth Century. In: The Western Medical Tradition, editor. 800 BC to AD 1800 , 10th edition, edited by Conrad Lawrence, Michael Neve, Vivian Nutton, Roy Porter, and Andrew Wear. Cambridge: Cambridge University Press; 2011. pp. 371–475. [ Google Scholar ]
- ---- 1999. The Greatest Benefit to Mankind. A Medical History of Humanity from Antiquity to the Present . Fontana Press.
- Ratanawongsa N, et al. Association between Clinician Computer Use and Communication with Patients in Safety-Net Clinics. JAMA Intern Med. 2016; 176 (1):125–128. doi: 10.1001/jamainternmed.2015.6186. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reiser SJ. Medicine and the Reign of Technology . Cambridge: Cambridge University Press; 1978. [ Google Scholar ]
- ---- 2009. Technological Medicine: The Changing World of Doctors and Patients . Cambridge: Cambridge University Press.
- Risse GB, Warner JH. Reconstructing Clinical Activities: Patient Records in Medical History. Social History of Medicine. 1992; 5 (2):183–205. doi: 10.1093/shm/5.2.183. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rose N. The Politics of Life Itself. Theory, Culture & Society. 2001; 18 (6):1–30. doi: 10.1177/02632760122052020. [ CrossRef ] [ Google Scholar ]
- Rosenberg, Lawrence. 8 May 2019. “Disintermediation.” Presentation given at Workshop: Medicine without Doctors? Disintermediation and Patient Agency . 4 th Workshop in the series on the Impact of Technological Change on the Surgical Profession. Jewish General Hospital, Montreal.
- Ruckstuhl B, Ryter E. Öffentliche Gesundheit in der Schweiz seit 1750 . Chronos: Zurich; 2017. Von der Seuchenpolizei zu Public Health . [ Google Scholar ]
- Ritzmann I. Vom gemessenen zum angemessenen Körper. Human Enhancement als historischer Prozess. Schweizerische Ärztezeitung. 2013; 94 (11):410–22. [ Google Scholar ]
- ---- 1999. “Der Verhaltenskodex des “Savoir faire” als Deckmantel ärztlicher Hilflosigkeit? Ein Beitrag zur Arzt-Patient-Beziehung im 18. Jahrhundert.” Gesnerus 56:197-219.
- Russey, Cathy. 2019. “Healthcare Wearables are Becoming Important for Staying Alive.” 15 January. https://www.wearable-technologies.com/2019/01/healthcare-wearables-are-becoming-important-for-staying-alive/ .
- Sandelowski M. This Most Dangerous Instrument: Propriety, Power, and the Vaginal Speculum. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2000; 29 (1):73–82. doi: 10.1111/j.1552-6909.2000.tb02759.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sanders R. Medical Technology: A Critical Perspective. The Internet Journal of Medical Technology. 2003; 2 (1):1–7. [ Google Scholar ]
- Schmiedebach H-P, editor. Medizin und öffentliche Gesundheit: Konzepte, Akteure, Perspektiven . Oldenbourg: De Gruyter; 2018. [ Google Scholar ]
- Sinsky C, et al. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Annals of Internal Medicine. 2016; 165 (11):753–760. doi: 10.7326/M16-0961. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sobral D, Rosenbaum M, Figueiredo-Braga M. Computer Use in Primary Care and Patient-Physician Communication. Patient Education and Counseling. 2015; 98 (12):1568–76. doi: 10.1016/j.pec.2015.07.002. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Strehle EM, Shabde N. One Hundred Years of Telemedicine: Does this new Technology have a place in Paediatrics? Archives of Disease in Childhood. 2006; 91 :956–959. doi: 10.1136/adc.2006.099622. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- “The Topol Review: Preparing the Healthcare Workforce to Deliver the Digital Future. An Independent Report on Behalf of the Secretary of State for Health and Social Care.” 2019. Published by Health Education England. https://topol.hee.nhs.uk/ .
- Timmermann C. Risikofaktoren: Der scheinbar unaufhaltsame Erfolg eines Ansatzes aus der amerikanischen Epidemiologie in der deutschen Nachkriegszeit. In: Lengwiler M, Madarász J, editors. Das präventive Selbst: Eine Kulturgeschichte moderner Gesundheitspolitik . Bielefeld: Transcript; 2010. pp. 251–277. [ Google Scholar ]
- Timmermann C, Anderson J, editors. Devices and Designs. Medical Technologies in Historical Perspective . London: Palgrave MacMillan; 2006. [ Google Scholar ]
- Toombs SK. The Meaning of Illness: A Phenomenological Account of the Different Perspectives of Physician and Patient . Dordrecht: Springer-Science+Busniess Media; 1992. [ Google Scholar ]
- Topol EJ, Steinhubl SR, Torkamani A. Digital Medical Tools and Sensors. JAMA. 2015; 313 (4):353–354. doi: 10.1001/jama.2014.17125. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Trentmann F. Materiality in the Future of History: Things, Practices, and Politics. Journal of British Studies. 2009; 48 (29):283–307. doi: 10.1086/596123. [ CrossRef ] [ Google Scholar ]
- U.S. Food and Drug Administration. ca. 1995-2019. Silver Spring: U.S. Food and Drug Administration; U.S. Department of Health and Human Services. https://www.fda.gov/medical-devices/digital-health#mobileapp .
- Verbeek P-P. Beyond Interaction: A Short Introduction to Mediation Theory. Interactions. 2015; 22 (3):26–31. doi: 10.1145/2751314. [ CrossRef ] [ Google Scholar ]
- Verghese A. What this Computer needs is a Physician: Humanism and Artificial Intelligence. JAMA. 2017; 319 (1):19–20. doi: 10.1001/jama.2017.19198. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Warner JH. The Uses of Patient Records by Historians: Patterns, Possibilities and Perplexities. Health and History. 1999; 1 (2/3):101–11. doi: 10.2307/40111336. [ CrossRef ] [ Google Scholar ]
- Weindling P. Medical Practice in Imperial Berlin: The Casebook of Alfred Grotjahn. Bulletin of the History of Medicine. 1987; 61 (3):391–410. [ PubMed ] [ Google Scholar ]
- Wolff E. Über das Blutdruckmessen, einen Selbstversuch und ärztliches Alltagshandeln. Schweizerische Ärztezeitung. 2014; 95 (11):460. [ Google Scholar ]
- ---- 2018. “Das ʻQuantified Selfʼ als historischer Prozess. Die Blutdruck-Selbstmessung seit dem frühen 20. Jahrhundert zwischen Fremdführung und Selbstverortung.” Medizin, Gesellschaft und Geschichte 36:43-83.
- World Health Organization . Report of the third global survey on eHealth. Geneva: WHO Document Production Services; 2016. Global Diffusion of eHealth: Making Universal Health Coverage Achievable. [ Google Scholar ]
- Wüstholz, Florian, and Daniel Stolle. 2020. “Das kranke Dossier.” Republik . 27 July. https://www.republik.ch/2020/07/27/das-kranke-dossier .
Latest Issue
Psychiatry’s new frontiers
Hope amid crisis
Recent Issues
- AI explodes Taking the pulse of artificial intelligence in medicine
- Health on a planet in crisis
- Real-world health How social factors make or break us
- Molecules of life Understanding the world within us
- The most mysterious organ Unlocking the secrets of the brain
- All Articles
- The spice sellers’ secret
- ‘And yet, you try’
- Making sense of smell
- Before I go
- My favorite molecule
- View all Editors’ Picks
- Diversity, Equity & Inclusion
- Infectious Diseases
- View All Articles
High-tech health
How digital medicine is improving patient care
By Tracie White
Illustration by Bryan Christie
Photography by Timothy Archibald
As digital technology has become more portable, easy to use and affordable, it has begun to capture the minds of medical researchers. From new imaging tools to mobile devices, Stanford researchers are exploring how to use technologically advanced tools to fill gaps in patient care. And it’s begun to make a difference.
The following four stories show ways researchers at Stanford are exploring the use of new technologies to solve old problems. An emergency room physician uses tablet computers to train community health care workers in underserved rural areas of Haiti and India. Radiologists transform holograms to assist in breast tumor removal. Heart doctors are dovetailing on society’s obsession with smartphones to try “pinging” people off the couch and onto their feet. And researchers are using Google Glass to provide at-home therapy for children with autism.
“There is a revolution in health care that is in large parts driven by technology,” said Michael Halaas , associate dean for industry relations and digital health. “There are a lot of great ideas emerging about how to transform health care that are digitally driven, but they need to be validated and thoughtfully introduced. We remain focused on developing digital health tools that can improve health while keeping the human element that is vital to care delivery.”
E-curriculum
Years ago, Ayesha Khan ’s grandfather was hit by a semitruck as he rode a bicycle along a road in rural Pakistan. With no emergency response system in place — no 911, no ambulance service — he lay severely injured by the side of the road until someone eventually drove by and delivered him to the hospital. After 30 more minutes, he died in the waiting room without receiving care.
Now Khan, MD, a Stanford emergency medicine physician, uses digital devices to address these kinds of voids in care in the developing world. Working first in Haiti and now in rural India, Khan and her team have developed an app-based curriculum to train community members in basic health care delivery — from half a world away at Stanford.
“My grandfather, he died in this sort of unceremonious way,” said Khan, Stanford Medicine clinical assistant professor of emergency medicine, who immigrated to the United States from Pakistan when she was 3. “Where my family comes from has somewhat inspired me. I’m passionate about health equity.”

By studying animated, spoken lesson plans accessed on digital tablets, completing a work book and passing the tests provided on the tablet, health care workers with limited education have been successfully trained in first-line treatment for acute complaints. These providers are now controlling bleeding, and stabilizing airway obstructions and seizures.
They diagnose and treat urinary tract infections, sexually transmitted diseases, broken limbs, skin infections, fever, upper respiratory infections, diarrhea and high blood pressure. They care for severe wounds. And they triage patients toward more intense levels of care when necessary.
“My desire was that the program we created not rely heavily on people flying back and forth; that’s just not sustainable,” Khan said. “We developed an e-curriculum so that the program was not dependent on live trainers.”
Currently, five health care workers ages 19 to 21 who grew up as orphans are providing first-line care for patients within their community of 28,000 in Haiti. In rural India, 54 women from the states of Uttar Pradesh and Bihar provide care to patients in the 54 villages where they live and now work. Four local facilitators in India used the app to train the women, who are considered past childbearing age and are seen as a burden in their communities.
“This project has a twofold advantage,” Khan said. “It provides health care to communities without it, and it employs people marginalized within their own communities.” The workers are paid through the community where they work, and a Stanford grant helped fund their training. “Now that we see the program working, I’m so eager for the chance to grow,” said Khan, adding that she’s exploring opportunities to expand into Kenya. “There is so much scope for it to help around the world.”
Reading minds
Nine-year-old Alex, who has a high-functioning form of autism, has always had difficulty making eye contact and understanding social cues, traits that are typical of someone with his disorder. Making friends has been a challenge, particularly on the playground.
“In preschool, he was hit with a mallet and kicked in the face by children. They were upset with him, and he couldn’t see it coming,” said his mother, Donji Cullenbine. “Children were very scary for him.”
About a year and a half ago, Stanford researchers hooked Alex up with a Google Glass visual headset, which he thought was really cool. It helped teach him how to read other people’s emotions through their facial expressions.
The new form of behavioral therapy uses a Stanford-designed app paired with Google Glass to help children distinguish between eight classical facial expressions indicating happiness, sadness, anger, disgust, surprise, fear, contempt or neutral. The wearable computer links to the smartphone app through the local wireless network. The device has a glasses-like frame with a camera to record the view of the person wearing it, a small screen and a speaker for verbal cues.
“Within a couple of weeks, he started to flick glances at me. I had tried for years to get him to engage with my face, but he never stayed for more than a second.”
Researchers designed three different formats to help engage kids. The first is “free play,” which gives auditory clues about the emotions of others. The other two are games — “Guess My Emotion,” in which parents act out emotions for the child to guess what they are, and “Capture the Smile,” in which the child tries to elicit a certain emotion from the parent or other caregiver. Alex particularly liked the “Guess My Emotion” game and free play. The app seemed to his mother to make a difference.

“Within a couple of weeks, he started to flick glances at me,” said Cullenbine, who agreed to have Alex participate in a clinical trial in 2017 to test the new home-based therapy. “I had tried for years to get him to engage with my face, but he never stayed for more than a second.”
The clinical trial included 14 families, each with a child who had been clinically diagnosed with autism. The children used the Google Glass setup over a 10-week period, according to the study, which was published in Digital Medicine in August.
One-on-one treatment with a trained therapist has been shown to be effective in treating autism, but a shortage of therapists means many children aren’t being treated early enough, said Dennis Wall , PhD, the study’s senior author and Stanford Medicine associate professor of pediatrics and of biomedical data science.
A window of opportunity is being missed, and that’s where Wall hopes this new digital health-based therapy can step in.
“The only way to break through the problem is to create reliable, home-based treatment systems,” he said. “It’s a really important unmet need.”
Results from early clinical trials have been overwhelmingly positive, Wall said.
“We’re seeing improved eye contact, emotional awareness, an ability to understand and appreciate emotions,” he said. And comments from parents have reflected this early success. “Parents said things like, ‘A switch has been flipped; my child is looking at me.’ Or, ‘Suddenly the teacher is telling me that my child is engaging in the classroom.’”
By the trial’s end, Alex recognized emotions so well in others that one day at home he exclaimed: “Mommy, I can read minds!”
“I thought, ‘He got it!’” his mother said. “He understands there is information on people’s faces that he can interpret.”
Couch potatoes
Doctors know exercise helps prevent heart disease, but trying to motivate people to get off the couch is no easy task. MyHeart Counts, an iPhone app developed by Stanford researchers, not only collects massive amounts of research data from smartphone users to study cardiovascular health, it also pings them when it’s time to stand up.
“We are giving them customized prompts to encourage them to exercise,” said Anna Shcherbina , a graduate student in biomedical informatics on the MyHeart Counts team. “We’re trying to determine which prompts work the best to encourage exercise.”
If a user sits for more than an hour, for example, the Stanford MyHeart Counts app sends a reminder to get up even if just for a moment. Users who set daily goals of 10,000 steps will get a friendly prompt on the days they fall short, such as, “You are at 115 steps now, and you need 9,885 more to reach your goal. Walking to your next appointment will help you reach your step goal.”
The app also presents users with graphs that show how they compare with other users in terms of daily step counts, how happy they are, how much they sleep and even how many vegetables they are eating.
“Consumer adoption of smartphones really has opened up this whole new world,” said Steve Hershman , PhD, a member of the MyHeart Counts team and director of mHealth in cardiovascular medicine at Stanford Medicine. “It’s amazing the volume of information researchers can get from these apps. And they’re also just sort of fun to use. They help make research more human.”
The app, which now collects such data as daily activity levels, blood pressure, cholesterol and cardiovascular health from 50,000 users in the United States, Hong Kong and the United Kingdom, was designed in 2015. It was one of the inaugural mobile health apps launched on Apple’s ResearchKit platform.
“It’s amazing the volume of information researchers can get from these apps. And they’re also just sort of fun to use. They help make research more human.”
Researchers published their first study based on data collected from 49,000 MyHeart Counts app users in JAMA Cardiology in December 2016. The study found that use of apps for collecting large amounts of health care data could transform cardiovascular research. Results also showed that among groups of subjects with similar activity levels, those who were active throughout the day, rather than in a single, relatively short interval, reported better levels of cardiovascular health with lower rates of chest pain, heart attacks and atrial fibrillation. The next research study is expected to be ready for publication soon, Hershman said.
Today’s 2.0 version of the app also includes an added consent module that allows users who have a 23andMe account to securely share their genetic information with Stanford researchers. “At first it was just a way to collect data for medical research,” Hershman said. “Now we’re really hoping to change people’s health.”
Holograms in surgery
Looking to increase precision during the surgical removal of breast tumors, a Stanford research team developed a technique that brings holographic images into the operating room.
Surgeons refer to MRI images on computer displays to help guide their incisions, but there is still quite a bit of guesswork because tumors come in various three-dimensional shapes and sizes.
As a result, either too much tissue gets removed or too little, said Bruce Daniel , MD, professor of radiology and director of IMMERS , the incubator for medical mixed and extended reality at Stanford.
“The surgeon can’t always tell what’s what,” Daniel said. The team developed a mixed-reality system using Microsoft’s HoloLens headsets to reflect a three-dimensional image of a patient’s tumor, based on MRI scans, directly on the diseased breast. The surgeon looks through the headset, which includes a holographic computer, and aligns a floating holographic image of the tumor onto the surgical site. The goal is to use the tools to increase the precision of the removal of the entire tumor, leaving as much of the healthy breast tissue as intact as possible, said Brian Hargreaves , PhD, Stanford Medicine professor of radiology and of electrical engineering and co-director of IMMERS.
“It gives me X-ray vision,” said Amanda Wheeler , MD, clinical associate professor of surgery who is participating in a pilot clinical research study of 10 patients that uses the new system. Prior to surgery, Wheeler puts on the headset, then uses markers to sketch the reflection of the hologram onto the patient’s breast. “It helps me plan the surgical site, making sure I’m getting as much accuracy as possible. I love it.”
Among the 300,000 women who are diagnosed yearly with breast cancer, about half are eligible for radiation and a lumpectomy that removes the tumor and leaves the remainder of the breast intact, the American Cancer Society reported. But deciding whether to have a lumpectomy rather than a mastectomy — total breast removal — is often difficult. It’s further hampered by the fact that 20 percent of women who have lumpectomies require a second surgery because the surgeon didn’t remove all the cancerous tissue the first time.
“Because this new method helps surgeons determine exactly where to cut out the cancerous breast tumor, it should reduce the number of second surgeries,” Daniel said.
Tracie White
Tracie White is a science writer in the Office of Communications. Email her at [email protected] .
Email the author
The Information Technology in Medicine Essay
Modern healthcare, being primarily focused on providing quality patient care, cannot exist apart from information technology. For this reason, medical employees are now obliged to learn how to beneficially use technology as well as practice proper communication with patients on the subject of its use in the process of treatment. The discipline, which will be analyzed in the course of the paper, is aimed at defining major tools necessary for providing quality healthcare to the community. Thus, the most significant insight acquired during the course is the high necessity of learning how to convey the importance of information technology to the patients in the simplest way possible.
To begin with, it is necessary to dwell upon the notions that should be processed by the students throughout the course. The subject’s primary goal was to introduce the most common technologies now used in healthcare and their significance to the sphere. Another part of the course was dedicated to the nuance of proper communication with patients using both technology and interpersonal communication.
Before the course enrollment, I considered information technology to be more of an arbitrary helping tool rather than part and parcel of medical practice. However, by the end of the course, I have discovered that the proper use of technology tools can potentially help save hundreds of human lives. Researchers claim that such tools as the Clinical Decision Support System (CDSS) prevent doctors from making false diagnoses due to cognitive overload (Ancker et al., 2017). Besides helping medicals focus more on the treatment process, it is also a key tool for the precise statistical data, crucial for the further development of healthcare across the state.
Another crucial aspect obtained during the course is the ability to assess personal strengths and weaknesses when it comes to cooperation with information systems. As a result, I have discovered that my major strength is the ability to adapt to technology use quite quickly. This benefit also concerns almost all young specialists who are used to information technology from an early age. Such knowledge puts more adolescent specialists at a serious advantage in terms of healthcare system development. However, the skills of fast learning do not concern some patients who are to be educated on the use of technology tools during their treatment process.
According to the researchers, effective patient education is the key to successful treatment due to the patient’s willingness to collaborate (Jimenez & Lewis, 2018). Hence, I believe my major weakness to be the ability to communicate with patients in a way beneficial for their desire to be educated. Despite various already existing methods on patient education, there is still a strong need to develop further research on the topic in order to make it more productive.
In my opinion, the development of healthcare informatics is now rapidly moving towards its zenith due to the beneficial environment. The strategies of further researches are now being planned for the next decades. However, automatized systems of clinical history have introduced the issue of privacy for both patients and medical employees (Iyengar et al., 2018). For this reason, I believe sustaining privacy while maintaining technological advancements in the medical sphere to be one of the most significant topics for further investigation. Moreover, the field of healthcare informatics develops too fast for educators to adapt to the process.
As a result, many specialized educational establishments fail to provide proper students’ preparation on the subject (Ashrafi et al., 2019). Hence, another subject of further investigation should be the methods in which students could be informed of the information technologies used in the field.
Speaking of my personal evaluation of the competencies aligned to the course, the progress is definitely visible by the end of the course, but there are still a lot of details requiring reconsideration. My understanding of the outlines introduced in the course syllabus, including the ability to analyze major programs and methods of computer-human interaction critically is clear and exhaustive. However, in order to maintain the obtained knowledge and skills, there should be more practical tasks, which may help build on the progress. The most valuable output I realized throughout the course is the fact that subjects concerning medicine and technology require constant and comprehensive learning in order to remain relevant in the field.
Taking everything into consideration, it may be concluded that the course of healthcare informatics is an integral part of medical education in the context of the 21st century. In the following reflection of the course, some of its major constituents and outputs were introduced and analyzed. When it comes to personal knowledge and skills gained, the most significant discoveries are the necessity to continually improve on the subject in order to realize how to convey the information to the patients. Even the most advanced technology may be of no help if the patients are not willing to collaborate. Further research on the subject includes more methods for patient education and examination of privacy maintenance.
Ancker, J. S., Edwards, A., Nosal, S., Hauser, D., Mauer, E., & Kaushal, R. (2017). Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC medical informatics and decision making , 17 (1), 36.
Ashrafi, N., Kuilboer, J. P., Joshi, C., Ran, I., & Pande, P. (2019). Health informatics in the classroom: An empirical study to investigate higher education’s response to healthcare transformation. Journal of Information Systems Education , 25 (4), 5.
Iyengar, A., Kundu, A., & Pallis, G. (2018). Healthcare informatics and privacy. IEEE Internet Computing , 22 (2), 29-31.
Jimenez, Y. A., & Lewis, S. J. (2018). Radiation therapy patient education using VERT: a combination of technology with human care. Journal of medical radiation sciences , 65 (2), 158-162.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, February 12). The Information Technology in Medicine. https://ivypanda.com/essays/the-information-technology-in-medicine/
"The Information Technology in Medicine." IvyPanda , 12 Feb. 2022, ivypanda.com/essays/the-information-technology-in-medicine/.
IvyPanda . (2022) 'The Information Technology in Medicine'. 12 February.
IvyPanda . 2022. "The Information Technology in Medicine." February 12, 2022. https://ivypanda.com/essays/the-information-technology-in-medicine/.
1. IvyPanda . "The Information Technology in Medicine." February 12, 2022. https://ivypanda.com/essays/the-information-technology-in-medicine/.
Bibliography
IvyPanda . "The Information Technology in Medicine." February 12, 2022. https://ivypanda.com/essays/the-information-technology-in-medicine/.
- Nursing Informatics: Definition and Development
- Health Informatics in the United States
- Public Health Informatics
- Cerner Application Information System in Specialized Dental Centers Evaluation
- Leadership in Nursing: CASNET System
- Electronic Health Records System in Med Organization
- Healthcare It Governance: Information Management in the Hospital Setting
- Centers for Disease Control and Prevention Website Tools
Essay on the Impact of Technology on Health Care
Technology has grown to become an integral part of health. Healthcare organizations in different parts of the world are using technology to monitor their patients’ progress while others are using technology to store patients’ data (Bonato 37). Patient outcomes have improved due to technology, and health organizations that sought profits have significantly increased their income because of technology. It is no doubt that technology has influenced medical services in varied ways. Therefore, it would be fair to conclude that technology has positively affected healthcare.
First, technology has improved access to medical information and data (Mettler 33). One of the most significant advantages triggered by technology is the ability to store and access patient data. Medical professionals can now track patients’ progress by retrieving data from anywhere. At the same time, the internet has allowed doctors to share medical information rapidly amongst themselves, an instance that leads to more efficient patient care.
Second, technology has allowed clinicians to gather big data in a limited time (Chen et al. 72). Digital technology allows instant data collection for professionals engaged in epidemiological studies, clinical trials, and those in research. The collection of data, in this case, allows for meta-analysis and permits healthcare organizations to stay on top of cutting edge technological trends.
In addition to allowing quick access to medical data and big data technology has improved medical communication (Free et al. 54). Communication is a critical part of healthcare; nurses and doctors must communicate in real-time, and technology allows this instance to happen. Also, healthcare professionals can today make their videos, webinars and use online platforms to communicate with other professionals in different parts of the globe.
Technology has revolutionized how health care services are rendered. But apart from improving healthcare, critics argue that technology has increased or added extra jobs for medical professionals (de Belvis et al. 11). Physicians need to have excellent clinical skills and knowledge of the human body. Today, they are forced to have knowledge of both the human body and technology, which makes it challenging for others. Technology has also improved access to data, and this has allowed physicians to study and understand patients’ medical history. Nevertheless, these instances have opened doors to unethical activities such as computer hacking (de Belvis et al. 13). Today patients risk losing their medical information, including their social security numbers, address and other critical information.
Despite the improvements that have come with adopting technology, there is always the possibility that digital technological gadgets might fail. If makers of a given technology do not have a sustainable business process or a good track record, their technologies might fail. Many people, including patients and doctors who solely rely on technology, might be affected when it does. Apart from equipment failure, technology has created the space for laziness within hospitals.
Doctors and patients heavily rely on medical technology for problem-solving. In like manner, medical technologies that use machine learning have removed decision-making in different hospitals; today, medical tools are solving people’s problems. Technology has been great for our hospitals, but the speed at which different hospitals are adapting to technological processes is alarming. Technology often fails, and when it does, health care may be significantly affected. Doctors and patients who use technology may be forced to go back to traditional methods of health care services.
Bonato, P. “Advances in Wearable Technology and Its Medical Applications.” 2010 Annual International Conference of The IEEE Engineering in Medicine and Biology , 2010, pp. 33-45.
Chen, Min et al. “Disease Prediction by Machine Learning Over Big Data from Healthcare Communities.” IEEE Access , vol. 5, 2017, pp. 69-79.
De Belvis, Antonio Giulio et al. “The Financial Crisis in Italy: Implications for The Healthcare Sector.” Health Policy , vol. 106, no. 1, 2012, pp. 10-16.
Free, Caroline et al. “The Effectiveness of M-Health Technologies for Improving Health and Health Services: A Systematic Review Protocol.” BMC Research Notes , vol. 3, no. 1, 2010, pp. 42-78.
Mettler, Matthias. “Blockchain Technology in Healthcare: The Revolution Starts Here.” 2016 IEEE 18Th International Conference On E-Health Networking, Applications and Services (Healthcom) , 2016, pp. 23-78.
Cite this page
Similar essay samples.
- Company Financial Analysis, Tomkins plc.
- Essay on the Difference Between the Fordist and Flexible Systems of Pr...
- Women´s experiences of initiation of breastfeeding on the labour ward
- Essay on the Chronology of a Terrorist Attack
- Essay on Human Resources Performance Analysis
- Essay on Is This the End of Diabetes and Obesity?
Advertisement
Medical Technologies Past and Present: How History Helps to Understand the Digital Era
- Published: 07 July 2021
- Volume 43 , pages 343–364, ( 2022 )
Cite this article

- Vanessa Rampton ORCID: orcid.org/0000-0003-4445-8024 1 ,
- Maria Böhmer 2 &
- Anita Winkler 2
31k Accesses
4 Citations
2 Altmetric
Explore all metrics
This article explores the relationship between medicine’s history and its digital present through the lens of the physician-patient relationship. Today the rhetoric surrounding the introduction of new technologies into medicine tends to emphasize that technologies are disturbing relationships, and that the doctor-patient bond reflects a more ‘human’ era of medicine that should be preserved. Using historical studies of pre-modern and modern Western European medicine, this article shows that patient-physician relationships have always been shaped by material cultures. We discuss three activities – recording, examining, and treating – in the light of their historical antecedents, and suggest that the notion of ‘human medicine’ is ever-changing: it consists of social attributions of skills to physicians that played out very differently over the course of history.
Similar content being viewed by others

ChatGPT: towards AI subjectivity
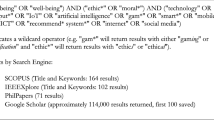
The Ethics of Digital Well-Being: A Thematic Review

The Emergence of the Digital Nomad: A Review and Analysis of the Opportunities and Risks of Digital Nomadism
Avoid common mistakes on your manuscript.
Human beings have their own goals and intentions, and products should help them to realize them in an optimal way. In many cases, though, these goals and intentions do not exist independently from the technologies that are used. [Technologies] do much more than merely function – they help to shape human existence. Peter-Paul Verbeek (2015, 28)
Introduction
A wide range of novel digital technologies related to medicine and health seem poised to change medical practice and to challenge traditional notions of the patient-physician relationship (Boeldt et al. 2015; Loder 2017; Fagherazzi 2020). A number of recent pieces have explored the ethical implications of this, asking, for example, whether new means of delivering ‘greater efficiency, consistency and reliability might do so at the expense of meaningful human interaction in the care context’ (Topol Review 2019, 22). Various contributions from patients, physicians, bioethicists, and social scientists have warned that computer technologies somehow stand between the physician and the patient and that there is a fundamentally human aspect of medicine that coexists uneasily with machines (e.g. Gawande 2018; Verghese 2017). As a remedy, recent contributions call for ‘clinical empathy’ not only as a desirable characteristic trait of future physicians, but even as a selection criterion for medical students (Bartens 2019). The role history plays in these discussions is striking. Commentators often assume that current concerns about how technologies may lead to the ‘de-humanisation of care’ (Topol Review 2019, 22) are the unprecedented products of technological, social, and cultural transformations in the late twentieth-/early twenty-first centuries. When the history of medicine is referenced, it is largely in one of the following ways: first, to emphasize that today ‘[w]e are at a unique juncture […] with the convergence of genomics, biosensors, the electronic patient record[,] smartphone apps, [and AI]’ (Ibid., 6), whereby the singularity of the digital era makes historical comparisons with antique predecessors seemingly irrelevant. Second, the history of medicine is used in a nostalgic manner to refer to past medical practices, seemingly grounded in the ability of a doctor to ‘liste[n] well and sho[w] empathy,’ as having a fundamentally human element that is threatened by the digital era (Liu, Keane and Denniston 2018, 113; see also Johnston 2018). With some notable exceptions (e.g. Greene 2016, Kassell 2016, Timmermann and Anderson 2006), historians of medicine have largely refrained from attempting to interpret recent digital developments within their broader historical contexts. The historicity of digital medicine in its various forms and the insights of the history of medicine for contextualising the patient-physician relationship in the digital era have yet to be fully fleshed out.
In this contribution, we draw on historical examples and the work of historians of medicine to highlight how all technological devices are ‘expressions of medical change’ (Timmermann and Anderson 2006, 1), and to show how past analogue objects shaped physician-patient relationships in ways that remain relevant today. Our focus is on Western European medicine since the early modern period. While acknowledging the profound differences between medicines in particular historical times and places, we argue, first, that patients and doctors have always interacted in complex relationships mediated by objects. Medical objects and technologies are not only aids for performing certain human tasks, but themselves have a mediating function and impact how physicians and patients alike perceive illness and treatment. We then contend, second, that history helps inform current discussions because it highlights the plurality of ways in which the physician-patient relationship has been conceived in different eras. In particular, the ability of the physician to listen well and show empathy seems to be not so much a historical constant but rather a social attribution of certain skills to physicians that played out very differently over the course of history. Both points help us to show that some of the hopes and fears related to digital technologies are not so entirely new after all.
We work through these hypotheses in relation to three activities in the clinical encounter that have been significantly affected by digital medical technologies, namely i) recording (Electronic Health Records), ii) examining (Telemedicine), and iii) treating (Do-It-Yourself medical devices). In each case, we begin with a specific contemporary technology and the debates around it before showing how a historical perspective can contribute to our understanding of them. First, we discuss electronic health records in the light of current criticisms which maintain that this technology cuts valuable time the doctor should be spending with the patient, thereby threatening an assumed core responsibility of the physician, namely listening empathetically to the patient. History shows that physicians have not always seen administrative record-keeping as foreign to their main work with patients; rather, it has been a formative part of their professional identity at different times. Moreover, the value that both physicians and patients ascribed to empathic listening has varied substantially over time. Second, in the case of examining, we start from the observation that current debates about telemedicine focus on the greater distance between patients and physicians this technology brings about. The historical perspective demonstrates that these debates are but one example of how changing examination technologies affect both physical distance and reciprocal understanding in the patient-physician relationship. Our examples illuminate that physical proximity in the medical encounter is a modern phenomenon, and that it did not always imply a meeting of the minds between physician and patient and vice versa. Finally, our third section on self-treatment demonstrates that Do-It-Yourself devices have the potential to challenge medical authority and, by giving patients more power, alter those power balances between physician and patient that are constitutive of an idealised view of the patient-physician relationship. Yet here too there are significant historical precedents for thinking of doctors and patients as but two players within complex networks of people and technologies, in which patients ascribe value to a multiplicity of relationships.
Record-keeping: computers and the administered patient
Electronic health records (EHRs), that is computer-based patient records, have transformed the way contemporary medicine is practiced (see, for example, Topol, Steinhubl and Torkamani 2015, 353). While the electronic recording of patient files by individual health care providers has become common practice since the 1990s, a central virtual collection and storage of all health data relating to an individual patient is a rather new development which is currently being debated and technically introduced in various states. This virtual patient file is of secondary order because it is fed with original electronic files derived from various primary recording systems (GP, clinic etc.), and it follows a population health surveillance logic rather than the logic of the treatment of individual cases. The main idea is that both patients and health care providers have access to a corpus of health documents, which is as complete as possible, to make diagnosis and treatment more efficient, more precise and safer for patients, and less costly for the health system. While patients may make use of this possibility on a voluntary basis and are asked to distribute access rights to providers, healthcare providers are obliged to cooperate and feed the system with relevant data (for a local example see current implementation efforts in Switzerland and its pitfalls as described in Wüstholz and Stolle 2020). One of the main premises of supporters is that EHRs will facilitate not only networking and interprofessional cooperation but also enhance communication between doctors and patients: they ‘provide health care teams with a more complete picture of their patients’ health [and] improve communication among members of the care team, as well as between them and their patients’ (Canada Health Infoway; see also Porsdam, Savulescu and Sahakian 2016).
Yet critical discussions surrounding the introduction of EHRs doubt exactly that. They suggest that the increasing documentation, virtual storage and sharing of sensitive patient data threatens an assumed historical core value of the doctor-patient relationship, namely the possibility of physicians establishing an intimate and ‘deeper connection’ with their patients (Ratanawongsa et al. 2016, 127). From the perspective of healthcare providers, professionals criticise the time-consuming nature of EHRs, arguing that this technology supplants the time the doctor has for direct communication and time spent ‘in meaningful interactions with patients’ (Sinsky et al. 2016, 753). That screens are coming ‘in between doctors and patients’ is a widespread notion (Gawande 2018). In addition, medicine’s increasing dependence on screens is perceived as undermining important social rituals, such as exchanges between physicians and other healthcare colleagues who used to discuss their cases in more informal ways (Verghese 2017). Last but not least, EHRs are seen as a major factor contributing to declining physician health and professional satisfaction because of their time-consuming data entry that reduces face-to-face patient care (Friedberg et al. 2013). This last point seems to be crucial as the digital interfaces of EHRs indeed require a maximum of standardisation, homogenisation and formalisation of recording styles that necessarily conflicts with more informal, individual recording techniques. On the one hand, doctors are forced to fill in fields and checkboxes that do not correspond to their own knowledge priorities, that is the things they would want to highlight in a certain case from the perspective of their specialty. On the other hand, they have difficulties in identifying relevant information when too much data on an individual patient has been entered by too many people. The desired interprofessional collaboration thus runs the risk of complicating instead of facilitating the making of a diagnosis. Surgeon Atul Gawande maintains that in the past, analogue documentation forced physicians to bring essential points into focus: ‘[d]octors’ handwritten notes were brief and to the point. With computers, however, the shortcut is to paste in whole blocks of information […] rather than selecting the relevant details. The next doctor must hunt through several pages to find what really matters’ (2018). Together, these points of critique suggest not only a certain fear that the increasing digitisation of patient records might disturb relationships that in the pre-digital era were based on professional intuition and meaningful, trust-building face-to-face communication. The critique also suggests that what is threatened is the meaning and satisfaction a physician takes from his/her recording work.
From the perspective of patients, other concerns related to EHRs are more relevant, among them the safety of personal health data. But while notions of privacy – who has control over the data, who owns the patient history – are important for patients, a number of studies also show that patients perceive the careful digital documentation of their case as something positive (Assis-Hassid et al. 2015; Sobral, Rosenbaum and Figueiredo-Braga 2015). ‘Forced to choose between having the right technical answer and a more human interaction, [patients] picked having the right technical answer,’ reports Gawande (2018; see also Hammack-Aviran et al., 2020). It thus seems that as long as patients think EHRs are providing them with a higher quality of care, they readily accept EHRs and their doctors’ dependence on screens – hence adapting their expectations to technological change.
In order to scrutinize these purported threats and attitudes towards EHRs, the rich history of patient records provides a relevant historical backdrop. In studying patient records, historians have addressed exactly these issues: they have examined how the patient-physician relationship has changed over time and have used medical records to gain insights into how past physicians documented medical knowledge, how this influenced their perceptions of their professional identity, and their obligations vis-à-vis patients (Risse and Warner 1992). As a first step, it is important to see that even though EHRs pose new challenges because of their digital form, recording individual patients’ histories as part of medical practice and ‘thinking in cases’ as a form of epistemic reasoning are a historical continuum (Forrester 1996; Hess and Mendelsohn 2010). The patient history dates to ancient Hippocratic medicine when detailed medical records were written on clay tablets and handed down for centuries to preserve the esteemed knowledge of antiquity (Pomata 2010). Yet the content and form of medical records, as well as the practices producing them have changed remarkably over time (Behrens, Bischoff, and Zelle 2012). In Western Europe, physicians in sixteenth-century Italy re-appropriated the ancient practice and typically recorded their cases in paper notebooks, as part of a larger trend to systematize and record information (Kassell 2016; see also Pomata 2010). As Lauren Kassell notes, the records of early modern practitioners ‘took the form of diaries, registers or testimonials, often they were later ordered, through indexing or commonplacing, by patient, disease or cure, providing the basis for medical observations, sometimes printed as a testimony to a doctor’s expertise as well as his contribution to the advancement of science’ (2016, 122). The historical perspective reveals that the rationale for a particular type of medical record-keeping always developed in tandem with the technical capabilities for its enactment, changing ideas of how diseases should be recorded, as well as with the preferences of individual physicians (ibid. 120). Crucially, as the organization of these collections of patient histories changed, so too did medical knowing and normative ideas about the physician-patient relationship (Hess and Mendelsohn 2010; Dinges et al. 2016).
As shown above, current critical discussions about EHRs tend to evoke a medical past in which patients were given time to talk about their illness, doctors listened and engaged in meaningful interactions, and record-keeping did not interfere with these processes. Allegedly, there were few concerns over misuse of data as there was less data produced and fewer players in the game. How does this popular nostalgic view correspond to research findings in the history of medicine? To some extent, the context of ‘bedside medicine’ comes close to these ideas. This model of care remained dominant in Western Europe until the nineteenth-century. One of the main ways in which physicians generated medical knowledge at the bedside of patients was to conduct ‘verbal analysis of subjectively defined sensations and feelings’ by patients (Jewson 1976, 229-230), and these patient testimonials provided the details recounted in physicians’ notes (Fissell 1991, 92). This is partly because the early modern doctor-patient relationship was based on a ‘horizontal’ model of healing (Pomata 1998, 126-27, 135) and a legally binding ‘agreement for a cure’ (ibid., 25 passim), which gave considerable power to patients, placing them on ‘near-equal hermeneutic footing’ with doctors (Fissell 1991, 92). Physician and patron (patient) made a contract in which the mostly upper class-patient would only pay fees after ‘successful’ treatment; vice versa, doctors were not obliged to treat a patient but would rather take on patients whose potential cure, and ability to pay fees, could be foreseen. Patients’ verbal satisfaction and willingness to conduct word-of-mouth publicity for a practicing physician were key to his reputation at that time and influenced physicians’ relationships with their clients.
However, it is problematic to project today’s vision of a desirable empathic relation between doctors and patients back into the past. Although upper-class patients clearly had some power in their relationship with physicians, the dominance of patients’ speech in medical records as such should not be interpreted as proof that doctors cared about their patients in the modern sense of showing understanding. With respect to nineteenth-century bourgeois medicine, Roy Porter noted that flattery and attention in the medical encounter were calculated practices of physicians concerned to secure clients and that ‘solemn bedside palaver[,] a grave demeanour, an air of benign and unflappable authority’ were all part of the prized ‘art of never leaving without a favourable prognosis’ (1999, 672). In a similar vein, Iris Ritzmann has emphasized that eighteenth-century doctors were eager to adhere to a certain ‘savoir faire,’ that is rules of conduct that would allow them to obscure the fact that in many cases, their abilities to heal were very limited (1999). And in Paul Weindling’s assessment of German medical routines, physicians’ desires to satisfy the patient subjectively were even purely instrumental: ‘[s]ympathy with the feelings of the sick was an economic necessity owing to the competition between practitioners’ (1987, 409). In all these cases, the value ascribed to direct physician-patient dialogue was very different from today’s ideas about an empathic encounter between physicians and patients; an engaged bedside manner often had more to do with calculated support for an upper class and sometimes hypochondriac clientele.
Similarly, as concerns the careful documentation of a patient’s medical condition and history, historical evidence shows that doctors did not do it primarily for their patients’ needs but for purposes of professional standing. This was important at a time when physicians’ scientific authority still needed to be established. The fact that in many cases there were several physicians involved in the treatment of the same case made documentation and communication between physicians (and sometimes for the public) especially relevant – and especially conflictual. Eighteenth-century case histories reflecting the context of bedside medicine indeed suggest that doctors were sometimes eager to publish case histories of patients that would bespeak their ability to heal by highlighting the misfortune of their competitors in order to enhance their own reputation. This shows how misleading the popular nostalgic view of a past intimate and unbroken bond between physicians and patients is, and that analogue paper technology did not necessarily strengthen this bond but could also be used in ways that were not beneficial for patients. Unlike today, this was an era in which practices of record-keeping mirror multiple, local and highly individual ways of documentation; the formalisation and standardisation of patient files which 19 th -century hospital medicine would trigger was yet to come.
As hospitals and laboratories became important institutions for medicine in the century roughly between 1770 and 1870, they also changed the practices of record-keeping, as the customary interrogation of patients’ accounts of the course of their disease did not coincide with changing understandings of disease, scientific interests and cultural expectations (see Granshaw 1992). For instance, French anatomist and pathologist Xavier Bichat (1771-1802) dismissed note-keeping based on patients’ narratives as an obsolete method for knowledge-making. He observed in his Anatomie générale (1801), ‘you will have taken notes for twenty years from morning to night at the bedside of the sick [and] it will all seem to you but confusion stemming from symptoms that fail to coalesce, and therefore provide a sequence of incoherent phenomena’ (1801, xcix, our translation). The kind of medicine favoured by Bichat and like-minded physicians focused on gaining anatomical and physiological insights directly from the body, using both physical examination and remote techniques in the laboratory. One way in which record-keeping changed to accommodate these interests was in the use of a more technical language to describe the experiences and expressions of patients. Mary Fissell argues that with the rise of hospital medicine, ‘doctors begin to sound like doctors, and patients’ voices disappear’ because doctors interpret patients’ words and replace them with medical equivalents (1991, 99). More generally, historians have shown that during the nineteenth century, medical culture changed in a way that gradually diminished the importance of patient narratives in medical writing (Nolte 2009).
How did these changes in recording practices play out for patients in the medical encounter ? From the historical perspective, the fact that physicians adopted a more technical language in their interactions and records should not be taken as evidence for a loss of human interaction or as something that patients necessarily disliked. On the contrary, the more systematised and formalised type of record-keeping was considered state of the art and was in accordance with a rapidly growing belief in the natural sciences among both patients and the general public (Huerkamp 1989, 64). This is related to the emergence of a specific concept of scientific reasoning that, in turn, fostered a sense of ‘scientific objectivity’ that called for dispassionate observation and accurate recording (Daston and Gallison 2010; Kennedy 2017). By the end of the nineteenth century, academic physicians had managed to create such professional authority that the ‘horizontal model of healing,’ in which the physician courted his upper-class clients, was replaced by a vertical model, in which the patient subjected himself to the authority of the physician. A Berlin doctor advised his fellow colleagues in 1896 that they should communicate their medical prescriptions to patients in a way that ‘prevents any misunderstandings and so that no further question can be addressed to him’ (cited in Huerkamp 1989, 66, our translation). For patients, this growing scientific authority and paternalism meant very different things, depending on class and social status. While medical services became accessible to more people, in particular thanks to the introduction of obligatory health insurance for workers, lower classes often experienced medicine as an instrument of power rather than benevolence (Huerkamp 1989). But even for the well-to-do, who undoubtedly benefitted from newly developed medical techniques, in particular in the realm of surgery, the acceptance of medical paternalism, male rhetoric and heroic cures came with high costs. This is suggested, for instance, in a famous letter by the court lady and writer Frances (Fanny) Burney who underwent a mastectomy in 1811, a rare document offering a patient’s perspective on these matters (Epstein, 1986).
From the perspective of doctors at the turn of the nineteenth century, record-keeping was associated not only with professional obligations but also with personal fulfilment. In many European countries, physicians were asked to provide expert opinion for juridical and administrative regulations as the state was increasingly interested in tracking its population’s health (Ruckstuhl and Ryter 2017; Schmiedebach 2018). In her study of Swiss physician Caesar Adolf Bloesch’s private practice (1804-1863), Lina Gafner shows the extent to which he perceived medical practice documentation as constitutive of his professional role and self-understanding as a medical expert. Bloesch’s patient journal ‘constitutes one single gigantic research report’ (2016, 265) because it was key for allowing him to generalize from the experiences gained in his practice in order to produce knowledge to contribute to contemporary scientific discussions. Gafner notes that the ‘format he gave his journals [leads] us to assume that scientific or public health-related ambitions were part of Bloesch’s professional self-image’ (263). In contrast to this historical example, where patient care and journal keeping were combined in the light of professional ambition, it stands out that healthcare providers of today tend to see their administrative work as opposed to patient care, even as separate and conflicting tasks; it is assumed that for physicians ‘seeing patients doesn't feel like work in the way that data entry feels like work’ (Amenta 2017). This is probably related to the fact that many physicians experience the requirement of working with a given software as a limiting restraint, which they are not really able to control, while they experience working with patients as something they have learned to master. As Gawande admits: ‘a system that promised to increase my mastery over my work has, instead, increased my work’s mastery over me’ (2018). It thus seems that it is primarily the question of ownership that distinguishes past recording styles from today’s recording systems: it is difficult to individually appropriate something which is designed to harmonize if not eliminate individual recording styles.
Yet even as Bloesch and contemporaries embraced the administrative tasks associated with medical note-taking as an opportunity to become a medical expert, other nineteenth-century physicians had different views of its value. But their criticisms of record-keeping were not motivated by the inherent value they saw in interactions with patients. Rather, their critiques were linked to a notable shift during the nineteenth century as scientific interest, triggered by administrative requirements as well as different disease conceptions and methods (e.g. in epidemiology research), changed its focus from the individual case study to population studies (see Hess and Mendelsohn 2010). In Nikolas Rose’s words, ‘the regularity and predictability of illness, accidents and other misfortunes within a population’ became ‘central vectors in the administration of the biopolitical agendas of the emerging nation states’ (2001, 7). Bound up with a new emphasis on tabulation, as well as ‘precision and reliability,’ various German-speaking hospitals instigated a new tabular format designed to enable physicians to compile their observations of patients into ward journals organized into columns and, eventually, generate an annual account of the course of disease (Hess and Mendelsohn 2010, 294). Yet in response some physicians rejected what they saw as excessively confining recording requirements. Volker Hess and J. Andrew Mendelsohn describe how the chief physician at a Berlin clinic ranted about the ‘inadequacy of our [tabular] journals’ and their inability to produce medical knowledge (295). While Mendelsohn and Hess themselves remark that such tabular ward journals were very ‘far from the patient history as observation, as prose narrative’ (293), the physicians’ rejection of the use of columns to record cases was not motivated by a concern to recover patients’ own narrations of their ailments or the feeling that record-keeping prevented them from properly attending to their patients’ needs. On the contrary, these physicians were concerned with producing an annual disease history and were frustrated that ‘the ultimately administrative format’s own rigid divisions blocked the writing of a synoptic history’ (296). Rather than recovering a face-to-face encounter with patients, they were interested in finding a recording format that would allow them to present a more compelling and sophisticated general description of disease, relying on mass information.
The current consensus among historians of medicine is that we should neither conceive medical records as ‘unmediated records of experiences of illness and healing’ (Kassell 2016, 126) nor as disentangled from the medical encounter itself. Rather, ‘processes of record-keeping were integral to medical consultations’ because ‘as ritualised displays and embodied knowledge, case books shaped the medical encounters that they recorded’ (122; see also Warner 1999). In relation to how ‘computerization’ is shaping contemporary medical encounters, three main points are of note. First, physicians have not always seen time spent writing and recording patient histories as in competition with interacting with patients themselves. At various times in history, the careful documentation of individual cases was perceived as a fundamental resource for generating medical knowledge and time spent doing so as part of the self-identity of physicians. Against the repudiation of digital record-keeping by today’s physicians, historical evidence shows that to the extent that physicians saw record-keeping as coinciding with their overall knowledge objectives, they accepted and even embraced it. This is linked to a second point, namely that prolonged time spent listening to the patient talk was not historically seen as evidence of good medical practice. For example, in an era when listening at length to patients was associated with the obsequious physician catering to the ego of the upper-class patient, the sober inscription in a nineteenth-century casebook noted that ‘too much talking showed that little was wrong’ with the patient (Weindling 1987, 395). Finally, patients too accepted administrative work by doctors as a sign of expertise and not necessarily as something that reduced the doctor’s attention to them. While the power balance changed in favour of doctors and ascribed less epistemic value to patients’ words, this was not necessarily negatively received by patients. History therefore shows that we should not view technological changes as isolated from the broader medical culture surrounding them but rather as shaping and co-constructing this culture. Today’s fear that the introduction of EHRs might change the communication and relation between physicians and patients for the worse tends to blame technology for a broader cultural and medical change of which it is just one tiny aspect, that is the growing belief in data and the logic of gaining stratified knowledge to provide relevant information about any one patients’ condition. Given that patients’ expectations exist in a dynamic relationship with how physicians learn, make decisions and interact with them, EHRs are themselves bound up with creating new conditions for the physician-patient relationship.
Examining: telemedicine and the distant patient
A further way in which digitalization has influenced the medical encounter is that it has emerged as the new virtual consulting room, thereby radically transforming the settings and procedures of physical examination. Although most people still go to ‘see the doctor,’ medical encounters today no longer have to take place in physical spaces but can occur via telephone or internet – what is broadly referred to as telemedicine, literally healing at a distance (from the Greek ‘tele’ and Latin ‘medicus’) (Strehle and Shabde 2006, 956). According to the World Health Organization, as a global phenomenon, telemedicine is more widespread than EHRs with more than half of responding member states having a telehealth component in their national health policy (WHO 2016). In the context of the COVID-19 pandemic, telemedicine has been overwhelmingly seen as ‘[a]n opportunity in a crisis’ and has further gained in popularity (Greenhalgh et al., 2020; see also Chauhan et al., 2020). A senior NHS official cited by The Economist called the widespread adoption of remote care (viz. telemedicine) a ‘move away from the dominant mode of medicine for the last 5,000 years’ (2020, 55). In the virtual examination room, patients can ask a physician for a diagnosis, a prescription and a treatment plan and send information about diseased body parts via digital media. When inquiring about the health conditions of their patients from a virtual consultation room, physicians sometimes need to ask their patients for certain practices of self-examination and self-treatment (Mathar 2010, section III). Advocates of telemedicine emphasize that there is no risk of mutual infection, advantages of cost savings, convenience, and better accessibility to medical care generally and for people living in rural and remote areas in particular. In Switzerland, for instance, the Medgate Tele Clinic promises to ‘bring the doctor to you, wherever needed’ (2019) while the U.S. Doctor on Demand characterizes itself as ‘[a] doctor who is always with you’ (2019). Patients, meanwhile, appreciate the greater availability of physicians, less travel time and better overall experience (Abrams and Korba 2018). However, telemedicine also raises various critical questions about the effects of physical distance on the physician-patient relationship. In particular, can the quality of the examination and diagnosis be high enough if a physician only sees his/her patient via screen but cannot smell, palpate and auscultate him/her? Furthermore, how can a trusting doctor-patient relationship be established virtually and at a distance? (see Mathar 2010, 13). While some of these critiques are based on the assumption that a fitting medical encounter between physician and patient should be a ‘good, old-fashioned, technology-free, dialogue between physician and patient’ (Sanders 2003, 2), we show below that all encounters inevitably ‘pass through a cultural sieve’ (Mitchell and Georges 2000, 387). Not only has the perceived need for the physical proximity of physician and patient varied substantially over history, but historical physicians and patients have not seen physical distance as preventing them from achieving emotional understanding. Whether physical examinations took place in-person or remotely, at each point in history doctors relied on their knowledge and its applications, that is a cultural lens through which s/he gazes on, over or into the human body. Regardless if examined remotely or closely, changes in examination procedures always challenge the established sense of the emotional bond between patient and physician, which therefore needs to be defined anew.
The standard physical examination as we know it today was considered less important in Europe up to roughly 1800 because of the conventions governing the relationship between physician and patient/patron, and also because of the conventions governing the relationship between male doctor and female patients. Many physicians considered physical examination morally inappropriate and saw it as dispensable for making a diagnosis. Physicians of upper-class patients generally considered their task more to advise than to examine and treat (Ritzmann 1999, 203). From his close analysis of a casebook by a seventeenth-century English physician, Stanley Joel Reiser concludes that the ‘maintenance of human dignity and physical privacy placed limits on human interaction through touch’ (1978, 4). Given the desirability of maintaining physical distance, physicians relied on and developed other sources of knowledge than their own sense of touch. The physical examination was ‘the method least used’ by the seventeenth-century physician who rather favoured ‘the patient’s narrative and [his] own visual [outward] observations’ of the patient’s body. In her study of a manuscript authored by a surgeon-apothecary of the same historical period, Fissell singles out blood-letting as one ‘of the few occasions on which a professional […] might routinely touch a patient’ and notes that it was necessarily ‘transformed into a careful ritual, one which attempted to compensate for the transgressive nature of the encounter. The blood-letter's courteous attention to returning the patient to his or her un-touched status underlines the mixture of courtesy and technique which made good medical practice’ (1993, 23). In ways now unfamiliar to us, manners and morals interacted to make physical examination and touching patients an ancillary part of the desirable patient-doctor encounter at that time.
Regular in-person physical examination as a routine practice and diagnostic technology is a rather recent development that came along with a new anatomical understanding of disease during the course of the nineteenth century, namely that diseases can be traced to individual body parts such as organs, tissues and cells, rather than unbalanced bodily humours (Reiser 1978, 29). It was at this time that the doctor’s examination skills no longer depended on the patient’s word and the surface of the (possibly distant) body, but started relying on what the doctor could glean from the patient’s organic interior (Kennedy 2017). In order to ‘get’ to the physical conditions of the body’s interior, a number of instruments were developed to facilitate the new credo of examination. The most famous example of such a nineteenth-century examination technology is the stethoscope, invented by French physician René Laennec (1781-1826). ‘By giving access to body noises – the sounds of breathing, the blood gurgling around the heart – the stethoscope changed approaches to internal disease,’ wrote Roy Porter, ‘the living body was no longer a closed book: pathology could now be done on the living’ (1999, 208). Crucially, technologies like the stethoscope brought the physician and patient into the examination room together but by providing physicians with privileged access to the seat of disease did not necessarily bring them closer in terms of understanding. Doctors now heard things that remained unheard to the patient, and this provoked a distancing in terms of illness perceptions. In Reiser’s account, the stethoscope ‘liberated doctors from patients and, by doing so, paradoxically enabled doctors to think they helped them better. […] Listening to the body seemed to get one further diagnostically than did listening to the patient’ (2009, 26).
The result is visible in the resistance surrounding some examination technologies that allowed physicians to delve into the body’s interior in order to gain new anatomical and pathological insights but that proved too transgressive for some existing physician-patient contacts. The vaginal speculum, introduced into examination procedures in Paris in the early-nineteenth century, may have fitted well with physicians’ new commitments to empiricism and observation. But at the time of the speculum’s introduction, female genital organs, in contrast to other organs, were regarded ‘as so mysterious and so sacred that no matter how serious the disease that afflicted them might be, it was no justification for an examination either by sight or touch’ (Murphy 1891, cited in Moscucci 1990, 110). Although the speculum was in line with pathological disease concepts and close, interior observation, moral considerations continued to undermine its suitability in the clinical context. At a meeting of the Royal Medical and Chirurgical Society, chronicled in the Lancet , commentators associated the speculum with both female and physician corruption, and the loss of moral virginity and innocence caused by its insertion into the body (Anon. 1850). In Margarete Sandelowski’s estimation, the vaginal speculum ‘required physicians not only to touch women’s genitals, but also to look at them, and thus imperiled the relationship male physicians wanted to establish with female patients’ (2000, 75). Here was a case in which technology challenged the socially accepted relationship between (male) physicians and (female) patients of a particular class because its application demanded increased physical closeness, and therefore was seen as undesirable and transgressive. As Claudia Huerkamp notes, it took a long time to establish a specific ‘medical culture’ in which the physical examination of female parts by a male physician was not perceived as breaking a taboo (1989, 67).
In other instances, the use of the speculum and the unprecedented access it provided to women’s anatomy mirrored existing power structures. The first uses of the speculum were justified in reference to and tested on the most vulnerable members of society. Deirdre Cooper Owens (2017) has demonstrated that in the U.S., racist arguments helped to defend the speculum’s application and experimentation on black, enslaved women as they were deemed to have a particularly ‘robust’ constitution, high tolerance of pain, and so on. Medical men such as James Marion Sims, who by his own account was the inventor of the speculum, combined his privileged access to enslaved women’s bodies with intrusive forms of examination in order to gain new knowledge crucial for the emerging field of gynaecology. This was also true for Irish immigrants in the U.S. (Owens 2017) and in the case of prostitutes in France and Germany, where the speculum was used as an instrument of the medical police (Moscucci 1990, 112). Prostitutes were screened using this new instrumentation as supposed carriers of venereal disease, whereas male clients did not need to undergo any screening. This highlights how intrusion into the body in the name of more accurate examination was frequently bound up with power and control, especially of marginalized groups.
Even as the seat of disease became increasingly associated with specific locations inside the body, this coexisted with the notion that medicine could still be conducted ‘at a distance.’ The example of the telephone demonstrates how tele-instruments worked alongside close examination devices that adhered to the principle of disease as located in particular interior body parts. In fact, the potentiality of the telephone for the medical profession was apparent from its invention in 1876; 4 as Michael Kay notes, the first inter-connected users were doctors, pharmacists, hospitals and infirmaries (2012). Practitioners used the technology, which enabled the clear transmission and reproduction of complex sounds for the first time, to improve existing instruments, or to devise entirely new examination methods. For instance, in November 1879, the Lancet published the case of an American doctor who, when phoned in the middle of the night by a woman anxious about her granddaughter’s cough, asked for the child to be held up to the telephone so that he could hear it (Anon. 1879). A group of physicians predicted in 1880 that home telephones would allow a new specialty of long-distance practitioners to ‘each settle themselves down at the centre of a web of wires and auscult at indefinite distances from the patients,’ potentially replacing the traditional stethoscope (cited in Greene 2016, 306). The telephone was also lauded for its potential to uncover foreign objects lodged in patients’ bodies, for example by acting as a metal detector (see Kay 2012). In line with the belief that a ‘good examination’ required a physician having access to the body’s interior in order to discover the seat of disease according to the localisation principle, the telephone was seen as an extension of the doctor’s ear that could improve examination and diagnosis.
In this context, reactions to the increased physical distance between physician and patient varied. The benefits of using a telephone instead of the more traditional speaking tube, which allowed breath to pass from one speaker to another, when communicating with patients with contagious diseases were recognised very early (Aronson 1977, 73). A testimonial letter, written by the Lady Superintendent at the Manchester Hospital for Sick Children in 1879, stated: ‘[The recently installed telephone] is of the greatest value in connection with the Fever Ward, enabling me to always be in communication without risk of infection’ (cited in Kay 2012). Yet some physicians worried that telephone technology had effectively ‘shrunk’ perceived social distance between them and the working classes, making them liable to be overly contacted by the general public. As one doctor complained in the Lancet in 1883: ‘[a]s if the Telegraph and the Post Office did not sufficiently invade and molest our leisure, it is now proposed to medical men that they should become subscribers to the Telephone Company, and so lay themselves open to communications from all quarters and at all times. […] The only fear we have is that when people can open up a conversation with us for a penny, they will be apt to abuse the privilege […] ’ (cited in Kay 2012) . Not only were doctors concerned about the telephone invading their ‘leisure,’ they worried that they might be overrun by the public, and their medical expertise would be needlessly exploited. Because of the inherent fear of doctors that an excessively frequent use of the telephone could flatten the social order and their standing within society, it is not surprising that the public use of the telephone came under critical medical scrutiny. This is visible in the way that telephones themselves came to be seen as seats of infection. At the end of the nineteenth century when most telephones were for public use (Fischer 1992), the British Medical Journal cautioned there was a need to curtail ‘the promiscuous use of the mouth-pieces of public telephones’ (Anon. 1887, 166). In general, the use of the telephone was informed by insights from bacteriology, which transformed individual disease ‘into a public health event affecting communities and nations’ (Koch 2011, 2), and placed new emphasis on the need to keep potentially infectious bodies as well as social classes at clear distance from one another (see Peckham 2015).
In relation to the pitfalls of today’s telemedicine and the fundamental questions of physical distance and emotional rapprochement in the medical encounter, these historical findings demonstrate that what was perceived as the ‘normal’ setting and procedure of medical examination could change remarkably within a rather short time. Before the nineteenth century, close physical examination generally played a less prominent role while patients’ illness accounts had a greater weight in the medical encounter. Indeed, in some contexts physical distance was seen as the prerogative of good medical practice. Post-1800, by contrast, is characterized by the standardisation of physical close examination, but also by the introduction of new technologies into the patient-physician relationship that themselves challenged socially-accepted degrees of physical closeness. However, this does not necessarily mean that such technologies disturbed a former unbroken bond, rather, various technologies became players in the game and could (or not) be appropriated by patients and doctors alike. Technology did not simply affect the physician-patient relationship, rather, existing societal and moral understandings influenced how technologies came into being and how they were used (Peckham 2015, 153). Our historical examples suggest that rather than seeing telemedicine as something fundamentally new and potentially threatening because it seemingly undermines a personal relationship, it may be more useful to acknowledge that technologies and cultural understandings always govern the degree of physical closeness and distance in medical encounters, and that this has had manifold implications for the emotional doctor-patient bond. The success of telepsychotherapy during the Covid-19 pandemic is perhaps a case in point. Even as it is unique among medical specialities because of the extent to which it considers the human relationship as fundamental for healing, psychotherapy via phone or video link has increased dramatically during the public health crisis, and also had good results (Békés and Aafjes-van Doorn 2020). This points not only to how physician-patient closeness and emotional understanding can exist in times of physical distance, but also to the constantly variable ways in which both the cultural imagination and experience of distance manifest themselves (Kolkenbrock 2020).
Self-treatment: do-it-yourself medical devices and the expert patient
The third field of digital medicine that we would like to put into historical perspective is one of the fastest growing fields of eHealth, namely do-it-yourself (DIY) health technologies. Such technologies broadly refer to the mobile devices that ‘now allow consumers to diagnose and treat their own medical conditions without the presence of a health professional’ (Greene 2016, 306). Silicon Valley firms sell ‘disintermediation,’ that is the possibility of cutting out middlemen – physicians – and allowing consumers to better control their health via their devices (Eysenbach 2007). Significant private investments have been driving these changes which, in the forms of smart devices and wearable technologies, often imply purchasing a product (e.g. a smartphone) and related applications and tools (see Greene 2016; Matshazi 2019). The website Digital Trends 2019 ranking of ‘the 10 best health apps’ range from Fitocracy, a running app that allows you to track your progress and that promises a fitness experience with a ‘robust community of like-minded individuals’, to Carbs that transfers the meals you have eaten into charts of calories, to Fitbit Coach that promises you the experience of having a personal trainer on your smartphone (de Looper 2019). 5 Health systems have bought on and increasingly ask patients to observe and monitor themselves with the help of these technologies, and in some cases, the use of apps to measure blood pressure, pulse and body weight such as Amicomed and Beurer HealthManager are closely connected to the possibilities of sharing one’s data remotely with a physician. In terms of reception, the delegation of tasks to digital devices is associated with patients having new options and new knowledge of their own health. In the estimation of one hospital CEO, this dramatic ‘democratization’ of technology and of knowledge signals ‘a true coming of age of the patient at the centre of the healthcare universe’ (Rosenberg 2019). In the words of chronic patient and patients’ rights advocate Michael Mittleman, while there may be benefits for patients when technologies take over certain tasks that were previously the prerogative of physicians, such technologies nevertheless pose a fundamental challenge to the ‘golden bond’ that previously characterized the patient physician-relationship, for example in the age of the house call (conversation with the author, 2019). It is clear from these statements that DIY devices – because they suggest that the more beneficial relationship is that between the patient/consumer and his/her devices – challenge previous assumptions about the inherent value of the physician-patient relationship as well as the balance of power between those two actors (see Obermeyer and Emmanuel 2016).
Both the notion that patients inherently benefit from circumventing physicians and taking their health into their own hands, as well as the idea of a close, almost familial bond that characterized the physician-patient relationship prior to contemporary DIY practices can be nuanced if we acknowledge that do-it-yourself medical practices have a long and varied history. As Roy Porter has noted, in the eighteenth-century, ‘ordinary people mainly treated themselves, at least in the first instance[,] “medicine without doctors” [was] a necessity for many and a preference for some’ (1999, 281). Only in the nineteenth-century did the medical profession establish a monopoly in health care and have the official power to determine what was ‘health’ and ‘sickness’. In the previous centuries, local and pluralistic ‘medical markets’ embraced far more providers of health services and their varied tools, including barbers, surgeons, quacks and charlatans, so that patients chose among the options that most convinced them or that were affordable to them (Ritzmann 2013, 418). But patients also had the option to help and treat themselves using the means at their disposal – Fissell argues that a person who fell ill in 1500 and still in 1800 almost always first sought medical treatment in a domestic context: ‘[h]e or she relied upon his or her own medical knowledge of healing plants and procedures, consulted manuscript or printed health guides, and asked family, neighbors, and friends for advice’ (2012, 533). As Fissell points out, the enormous diffusion and importance of self-therapy at the time meant that the ‘boundary between patients and practitioners was hard to pin down’ (534). While current depictions of an idealised interaction between physician and patient assume a physician who through his/her knowledge examines, advises and treats the non-knowing patient, history shows that the presumed boundaries between the expert and lay person are far more blurred than is usually assumed.
The presumed novelty of a de-centralised market for DIY devices that potentially threatens the dual relationship between physicians and patients can be put into perspective when considering historical examples. Due to a fairly unregulated medical market in the early modern period, competition was high and the business of medicinal recipes lucrative. In this context, profit-motivated apothecaries benefited from offering new recipes made from exotic products: as of the fifteenth century European pharmacies stocked many wares with medicinal properties – including spices, elements such as sulphur, and plants, for examplemastic and sundew – and these were bought by people who gathered and dealt in medicinal plants (or ‘simples’) and other apothecaries, who made them into medicines. In the wake of the European voyages of discovery, the range of products became ever wider and more expensive, and apothecaries were a very profitable business branch for a long time (Ehrlich 2007, 51-55). King and Weaver have used evidence from remedy books in eighteenth-century England to show how families purchased recipes for remedies, and resold both the recipes and the medicines they brewed to other local people (2000, 195). Until the nineteenth century the medical market flourished and was accessible and lucrative for many participants, while the demand for ‘medical’ services was high, particularly in towns and cities. Access to the technologies of healing – whether domestic medical guides or healing herbs – allowed patients to control their health and treatments according to a wide range of scientific explanations. In contrast to other European countries that meanwhile had developed some restrictions for apothecaries and their suppliers, in Britain the market-place was remarkably varied in the light of the free-market principle caveat emptor (let the buyer beware). ‘In English conditions,’ wrote Porter, ‘irregulars, quacks and nostrum-mongers seized the opportunities a hungry market offered’ (1995, 460). In these conditions of market-oriented healing, both patients and healers alike believed, sometimes fervently, in the effectiveness of the remedies on offer. Moreover, the network of relationships in which such transactions took place was remarkably fluid, with patients using the services of several health professionals in succession or simultaneously.
In the following centuries, medical practice and science would change dramatically due to the rise of academic training as a prerequisite to enter the medical profession, a development seen across Europe, as well as the integration of physicians into national health agendas. A growing belief in science and a paternalistic ideal of the academic physician attributed to him the sole power over medical practice and technologies. It became more difficult for other healers to participate in the health market, and the knowledge of the self-treating patient was diminished as well. As part of the attempt to counteract competition from non-educated or apprenticed healers, in the United Kingdom only registered doctors could hold various public posts, such as public vaccinator, medical officer and the like (Bynum 2006, 214). Yet ‘alternative’ medicine, a term that contained all those healers not licenced and accepted by the respective medical registers, continued to satisfy patients’ needs, although to a lesser extent. In Weindling’s assessment of the prospects of university-educated physicians to attract clients in nineteenth-century Berlin, ‘[f]ierce competition from a range of unorthodox practitioners must be assumed’ (1987, 398). The popularity of hydropathic doctors and water cures, mud-bathing and vegetarianism are but some examples of how alternative medicines co-existed alongside official ones and were increasingly popular treatments even though they did not meet the contemporary academic criteria of standards regarding safety and efficacy (Ko 2016). Thus patients often looked beyond qualified physicians to other practitioners, and their own sensibilities played a considerable role in which relationships they chose to develop.
A look into twentieth-century history shows that DIY practices were integrated into official medicine as well (Timmermann 2010; Falk 2018). The significant rise of chronic diseases and life-long treatment, for instance, required the co-operation of patients in the form of self-tracking and observation of their bodies since it could not be done by medical experts alone. In the first decades of the twentieth century, DIY methods and technologies for measuring blood pressure or sugar became particularly vital, transforming the roles of ‘patient’ and ‘doctor’ and relationship between them. Examining the history of self-measuring blood pressure, Eberhard Wolff notes that patients doing so in the 1930s required both patience and training, and also were pushed into a more active and participatory role during medical treatment: it was not the doctor anymore but the patient who produced and controlled relevant data that were decisive for further medical decisions and treatment (2014, 2018). With the rise of the risk factor model in mid-twentieth century – the identification of factors in patient’s behaviour and habits that were suspected of contributing to the development of a chronic disease – DIY practices grew ever more important and so did its technologies. From this moment, the idea of preventing disease shifted towards individual, possibly damaging behaviours such as smoking and diet that could trigger a number of different diseases. As a consequence, the patient received more responsibility in order to live up to the new credo of maintaining his or her personal health (Lengwiler and Madarász 2010). Optimizing a personal healthy life style hence did not necessarily occur in direct consultation with a doctor but rather in conjunction with health products available on the market. In the words of sociologist Nikolas Rose, in the course of the twentieth century:
[t]he very idea of health was re-figured – the will to health would not merely seek the avoidance of sickness or premature death, but would encode an optimization of one’s corporeality to embrace a kind of overall “well-being” … It was this enlarged will to health that was amplified and instrumentalized by new strategies of advertising and marketing in the rapidly growing consumer market for health (2001, 17-18).
According to Rose, by such developments, ‘selfhood has become intrinsically somatic – ethical practices increasingly take the body as a key site for work on the self’ (18). But he also argues that by linking our well-being to the quality of our individual biology we have not become passive in the face of our biological fate. On the contrary, biological identity has become ‘bound up with more general norms of enterprising, self actualizing, responsible personhood’ (18-19). By considering ourselves responsible for our own biology as key to our health, we have come to depend on ‘professionals of vitality’ (22) whether they be purveyors of DIY devices, genetic counsellors, drug companies or doctors.
With respect to contemporary debates over DIY practices, some have argued that they allow both doctors and patients to be ‘experts’ and call for ‘a relationship of interactive partnership,’ not only because patients today are often informed but also because ideally they know best their own bodies and ailments (Kennedy 2003). Against this idealising assessment, the historical perspective makes us aware that while self-help and self-treatment have been an important dimension of past medical cultures, it appears that historically, patients have not relied as much on a face-to-face empathetic encounter with any one physician as today’s debates suggest. Moreover, today as in the past, the mere existence of markets for medical devices influences how consumers/patients decide whether to resist or embrace the various possibilities of self-treatment as well as their relationships with those who provide it. As Porter has argued, purveyors of ‘alternative’ medicines rationalised their therapeutic effects in ways that differed from official scientific methods and using arguments that likewise changed over time. Depending on the perspective of whose model of evidence users deemed most credible, the co-existence of diverse models for practicing medicine must be assumed throughout history and despite nineteenth-centuries attempts to eliminate unorthodox medicines (Timmermann 2010). The result was a diverse network of fast-changing relationships in which no single one was ascribed the ultimate power to heal. Reflecting on this history, historian of medicine and physician Jeremy Greene has stated that contemporary DIY devices therefore appear ‘neither wholly new nor wholly liberating’ (2016, 308). Our analysis corroborates Greene’s, in that it shows how those who use new DIY technologies may free themselves from their traditional relationship of dependence on physicians, while also creating new relationships with those actors who produce apps or conduct marketing. Yet our study also suggests that there is no one ethical conclusion about whether DIY or physician-dominated care is a better way of living up to a more humane medicine. Ethical arguments and the grounds on which we are supposed to resolve them are complex and variable. As seen in these historical examples, they have changed profoundly over time with each technology and medical concept challenging and refashioning the doctor-patient bond anew. Furthermore, there is no such thing as a ‘timeless’ doctor’s healing presence, or even medical expertise, or an ill person/patient. As shown above, as health and illness are defined, redefined and challenged throughout history, this process creates both expert and patient, as well as shapes the relationship between them.
An oft-heard concern about ‘computerization’ in medicine is that digital objects are changing human interactions. While various representatives from the tech side are optimistic about the effects of increasingly dynamic and intelligent objects in the medical encounter, some patients and physicians are more skeptical and see their social relationships as disturbed by new technologies. ‘Doctors don’t talk to patients’ is the most common complaint the CEO at a Montreal hospital recounted hearing from current patients (conversation between the author and Lawrence Rosenberg, 2019). Fears that increasing digitization of medicine will disturb the relationship that can potentially make the patient ‘whole’ again are not without foundation (King 2020). However, without a clear baseline for assessing changes we have limited scope for drawing conclusions about present day realities or long-term trends. Given the appeal of using the past to suggest a more ‘human’ but lost era of medical practice, a less nostalgic but more sophisticated understanding of the past as provided by historical research would serve us well. In this sense, history can counteract a characteristically modern myopia, namely, as intellectual historian Teresa Bejan has put it, our ‘endearing but frustrating tendency to view every development in public life as if it were happening for the first time’ (2017, 19).
As we saw in the examples dealing with record keeping, examining and self-treatment, trends that consider the patient as an object – a diseased lung, or a malfunctioning heart valve – and the concomitant use of technologies to record, examine and treat physical symptoms were necessarily in tension with patients’ own accounts of how they became ill and of the symptoms they experienced. In fact, concerns about the loss of meaningful personal contact in the medical encounter are incomprehensible without reference to a historical trend dating back to the beginning of the nineteenth century which seems to undermine the patient’s perspective by focusing on increasingly specialised processes within the body. Yet neither before nor after that time is there an unmediated patient’s voice that we are able to recover: the medical record as historical source has its own distinct material history, and patients’ expectations were always bound up with broader societal views about acceptable standards of healing. The historical perspective also shows that we should not take for granted the linear narrative of the technological as adverse to human relations and reducing empathetic understanding in the medical encounter – to paraphrase Lauren Kassell, the digital is not just the enemy of the human (2016, 128). Rather, it makes us aware that our understanding of the doctor-patient relationship and of its role in healing are themselves historically contingent. The idea of ‘a friendly, family doctor “being there”’ and the association of medicine with a ‘desirable clinical relationship’ (as opposed to e.g. perfect health) is an idea that has played out very differently in the course of history (Porter 1999, 670). There were times in which listening to patients was bound up with completely different expectations from both sides, and there were times in which physical examination was not seen as an indispensable part of medical practice. Moreover, while the monopoly of the physician in matters of health care and the focus on the (exclusive) healing potential of the clinical relationship is of relatively recent origin, we have seen that the popularity and economy of DIY devices has a much longer history, one that resists a linear account of DIY devices as something purely liberating. Hence, in contrast to idealised and simplified historical narratives that lament the loss of human relationships, more sophisticated accounts should acknowledge that medical objects and technologies are not the strange and disturbing ‘other’ in the medical encounter but rather integral players therein. As Frank Trentmann has put it, ‘things and humans are inseparably interwoven in mutually constitutive relationships’ (2009, 307). While the authors of a recent study suggest that ‘the traditional dyadic dynamics of the medical encounter has been altered into a triadic relationship by introducing the computer into the examination room’ (Assis-Hassid et al. 2015, 1), it seems more likely that the dyadic relationship has never existed.
Abrams, Ken and Casey Korba. 2018. "Consumers are on Board with Virtual Health Options. Can the Health Care System Deliver?” https://www2.deloitte.com/insights/us/en/industry/health-care/virtual-health-care-consumer-experience-survey.html .
Amenta, Conrad. 2017. “What’s Digitization Doing to Health Care?” Vice . https://motherboard.vice.com/en_us/article/785v3z/whats-digitization-doing-to-health-care.
Amicomed. 2018-2019. San Francisco, CA. https://www.amicomed.us/ .
Anon. 1879. “Practice by Telephone.” The Lancet 2: 819.
Google Scholar
Anon. 1850. “Proceedings of a Meeting of the Royal Medical and Chirurgical Society on the Use of the Speculum, 28 May 1850, and Relevant Correspondence.” The Lancet 1: 701-06.
Anon. 1887. “The Telephone as a Source of Infection.” British Medical Journal : 166.
Aronson, Sidney H. 1977. “The Lancet on the Telephone 1876-1975.” Medical History 21: 69-87.
Article Google Scholar
Assis-Hassid, Shiri, et al. 2015. “Enhancing Patient-Doctor-Computer Communication in Primary Care: Towards Measurement Construction.” Israel Journal of Health Policy Research 4 (4): 1-11. https://doi.org/10.1186/2045-4015-4-4 .
Bartens, Werner. 2019. ”Angehende Ärzte müssen Empathie Zeigen.“ Süddeutsche Zeitung . 31 July. https://www.sueddeutsche.de/gesundheit/medizinstudium-empathie-auswahlverfahren-1.4546284 .
Behrens R., N. Bischoff and C. Zelle, eds. 2012. Der ärztliche Fallbericht. Epistemische Grundlagen und textuelle Strukturen dargestellter Beobachtung . Wiesbaden: Harrassowitz.
Bejan, Teresa M. 2017. Mere Civility: Disagreement and the Limits of Toleration . Harvard: Harvard University Press.
Book Google Scholar
Békés, V. and K. Aafjes-van Doorn. 2020. “Psychotherapists’ Attitudes toward Online Therapy during the COVID-19 Pandemic.” Journal of Psychotherapy Integration 30 (2): 238-247. https://doi.org/10.1037/int0000214 .
Beurer HealthManager. 2018-2019. Ulm: Beurer GmbH. https://www.beurer.com/web/gb/ .
Bichat, Xavier. 1801. Anatomie générale, appliquée à la physiologie et à la médecine. Paris: Brosson.
Bijker, Wiebe E., Thomas P. Hughes and Trevor Pinch, eds. 2012 [1987]. The Social Construction of Technological Systems: New Directions in the Sociology and History of Technology . Cambridge: The MIT Press.
Boeldt, D. L. et al. 2015. “How Consumers and Physicians View New Medical Technology: Comparative Survey.” Journal of Medical Internet Research 17 (9): e215. doi: 10.2196/jmir.4456: https://doi.org/10.2196/jmir.4456 .
Bynum, W. F. 2006. “The Rise of Science in Medicine, 1850-1913.” In The Western Medical Tradition, 1800-2000 , edited by W. F. Bynum et al., 111-239. Cambridge: Cambridge University Press.
Canada Health Infoway. 2001-2019. Toronto: Canada Health Infoway. https://www.infoway-inforoute.ca/en/solutions/digital-health-foundation/electronic-medical-records/benefits-of-emrs .
Chauhan, Vivek et al. 2020. “Novel Coronavirus (COVID-19): Leveraging Telemedicine to Optimize Care While Minimizing Exposures and Viral Transmission.” J Emerg Trauma Shock 13 (1): 20–24.
Colombat, de l’Isère, Marc. 1838. Traité des maladies des femmes et de l’hygiène spéciale de leur sexe , vol. 1 Paris: Libraire médicale de labé.
Cooper Owens, Deirdre. 2017. Medical Bondage: Race, Gender, and the Origins of American Gynecology . Atlanta: University of Georgia Press.
Daston, Lorraine J., and Peter Galison. 2010. Objectivity . New York: Zone.
de Looper, Christian. 2019. “The 10 Best Health Apps.” Digital Trends , 5 January. https://www.digitaltrends.com/mobile/best-health-apps/ .
Dinges, Martin, Kay Peter Jankrift, Sabine Schlegelmilch, and Michael Stolberg, eds. 2016. Medical Practice, 1600-1900: Physicians and their Patients . Translated by Margot Saar. Clio Medica, volume 96. Leiden: Brill Rodopi.
Doctor On Demand. 2012-2019. San Francisco, CA. https://www.doctorondemand.com/ .
Ehrlich, Anna. 2007. Ärzte, Bader, Scharlatane. Die Geschichte der österreichischen Medizin . Wien: Amalthea.
Economist, The . “How Covid-19 Unleashed the National Health Service.” 3 December 2020: 55-56. https://www.economist.com/britain/2020/12/03/how-covid-19-unleashed-the-nhs .
Ekeland, Anne G., Alison Bowes, and Signe Flottorp. 2010. “Effectiveness of Telemedicine: A Systematic Review of Reviews.” Int J Med Inform 79:736–771.
Epstein, Julia L. 1986. “Writing the Unspeakable: Fanny Burney's Mastectomy and the Fictive Body.” Representations 16:131–166.
Eysenbach, G. 2007. “From Intermediation to Disintermediation and Apomediation: New Models for Consumers to Access and Assess the Credibility of Health Information in the Age of Web 2.0.” Stud Health Technol Inform 129 (Pt 1): 162-6.
Fagherazzi, Guy. 2020. “Digital Health Strategies to Fight COVID-19 Worldwide: Challenges, Recommendations, and a Call for Papers.” Journal of Medical Internet Research 22 (6): e19284.
Falk, Oliver. 2018. “Der Patient als epistemische Größe. Praktisches Wissen und Selbsttechniken in der Diabetestherapie 1922-1960." Medizinhistorisches Journal 53 (1): 36-58.
Fischer, Claude S. 1992. America Calling: A Social History of the Telephone to 1940 . Berkley: University of California Press.
Fissell, Mary E. 1991. “The Disappearance of the Patient’s Narrative and the Invention of Hospital Medicine.” In British Medicine in an Age of Reform , edited by A. Wear and R. French, 92-109. London: Routledge.
---- 1993. “Innocent and Honorable Bribes: Medical Manners in Eighteenth-Century Britain.” In The Codification of Medical Morality: Historical and Philosophical Studies of the Formalization of Western Medical Morality in the Eighteenth and Nineteenth Centuries . Volume 1: Medical Ethics and Etiquette in the Eighteenth Century , edited by Robert Baker, Dorothy Porter and Roy Porter, 19-46. Dordrect: Springer Science + Business Media.
---- 2012. “The Medical Marketplace, the Patient, and the Absence of Medical Ethics in Early Modern Europe and North America.” In The Cambridge History of World Medical Ethics , edited by Robert Baker and Laurence McCullough, 533-39. Cambridge: Cambridge University Press.
Forrester, John. 1996. “If p, then what? Thinking in Cases.” History of the Human Sciences 9 (3): 1-25.
Friedberg, Mark W. et al. 2013. “Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy.” Santa Monica, CA: RAND Corporation. https://www.rand.org/pubs/research_reports/RR439.html .
Gafner, Lina. 2016. “Administrative and Epistemic Aspects of Medical Practice: Caesar Adolf Bloesch (1804-1863).” In Medical Practice, 1600-1900: Physicians and their Patients , edited by Martin Dinges et al., 253-70. Leiden: Brill Rodopi.
Gawande, Atul. 2018. “Why Doctors Hate Their Computers.” The New Yorker . 12 November. https://www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers .
Granshaw, Linda. 1992. “The Rise of the Modern Hospital in Britain.” In Medicine in Society , edited by Andrew Wear, 197-218. Cambridge: Cambridge University Press.
Chapter Google Scholar
Greene, Jeremy. 2016. “Do-it-Yourself Medical Devices: Technology and Empowerment in American Health Care.” New England Journal of Medicine 374:305-9.
Greenhalgh, Trisha et al. 2020. “Video Consultations for Covid-19: An Opportunity in a Crisis?” BMJ , 368: m998. doi: https://doi.org/10.1136/bmj.m998 .
Hammack-Aviran, Catherine M. et al. 2020. “Research Use of Electronic Health Records: Patients’ Views on Alternative Approaches to Permission.” AJOB Empirical Bioethics 11 (3): 172-186. doi: https://doi.org/10.1080/23294515.2020.1755383 .
Heinrich, Christian. 2017. “Treffen im virtuellen Sprechzimmer.“ Die Zeit 22 (24 May): 33. https://www.zeit.de/2017/22/telemedizin-sprechstunde-arzt-krankenkasse-erstattung-video .
Hess, V. and J. Andrew Mendelsohn. 2010. “Case and Series: Medical Knowledge and Paper Technology, 1600–1900.” History of Science 48 (3-4): 287–314. https://doi.org/10.1177/007327531004800302 .
Huerkamp, Claudia. 1989. “Ärzte und Patienten. Zum strukturellen Wandel der Arzt-Patient-Beziehung vom ausgehenden 18. bis zum frühen 20. Jahrhundert.“ In Medizinische Deutungsmacht im sozialen Wandel des 19. und frühen 20. Jahrhunderts , edited by Alfons Labisch und Reinhard Spree, 57-73. Bonn: Psychiatrie-Verlag.
Jewson, Nicholas D. 1976. “The Disappearance of the Sick-Man from Medical Cosmology, 1770-1870.” Sociology 10: 225-44.
Johnston, S. C. 2018. “Anticipating and Training the Physician of the Future: The Importance of Caring in an Age of Artificial Intelligence.” Acad Med 93 (8): 1105-1106. doi: https://doi.org/10.1097/ACM.0000000000002175 .
Kassell, Lauren, 2016. “Paper Technologies, Digital Technologies: Working with Early Modern Medical Records.” In The Edinburgh Companion to the Critical Medical Humanities , edited by S. Atkinson, J. Macnaughton and J. Richards, 120-135. Edinburgh: Edinburgh University Press. http://www.jstor.org/stable/10.3366/j.ctt1bgzddd .
Kay, Michael. 2012. “Give the Doc a Phone: A Historical long-view of Telephone Use and Public Health in Britain.” https://michaelakay.wordpress.com/2012/02/14/give-the-doc-a-phone-a-historical-long-view-of-telephone-use-and-public-health-in-britain/ .
Kennedy, I. 2003. “Patients are Experts in their own Field.” BMJ 326 (7402): 1276-7.
Kennedy, Meegan. 2017. “Technology.” In The Routledge Research Companion to Nineteenth-Century British Literature and Science , edited by John Holms and Sharon Ruston, 3011-328. London: Routledge.
King, Steven and Alan Weaver. 2000. “Lives in Many Hands: The Medical Landscape in Lancashire, 1700-1820.” Medical History 44 (2): 173-200.
King, Martina. 2020. “"Nach Aufnahme arterielle Hypotonie": Personenkonzept und Kommunikationsformen in der Experten-Medizin.” Gesnerus 77 (2): 411-37.
Ko, Y. 2016. “Sebastian Kneipp and the Natural Cure Movement of Germany: Between Naturalism and Modern Medicine.” Uisahak 25(3): 557-590. doi: 10.13081/kjmh.2016.25.557.
Koch, Tom. 2011. Disease Maps: Epidemics on the Ground . Chicago: University of Chicago Press.
Kolkenbrock, Marie. 2020. “The Dance of the Porcupines. On Finding the Balance between Proximity and Distance in Times of Pandemic.” The Hedgehog Review Blog: Critical Reflections on Contemporary Culture . 21 April. https://hedgehogreview.com/blog/thr/posts/the-dance-of-the-porcupines .
Kruse, Clemens S. et al. 2017. “The Effectiveness of Telemedicine in the Management of Chronic Heart Disease: A Systematic Review.” J R Soc Med Open 8 (3): 1–7. doi: https://doi.org/10.1177/2054270416681747 .
Lee, Shaun Wen Huey et al. 2017. “Comparative Effectiveness of Telemedicine Strategies on Type 2 Diabetes Management: A Systematic Review and Network Meta-analysis.” Scientific Reports 7:12680. doi: https://doi.org/10.1038/s41598-017-12987-z .
Lengwiler, Martin, and Jeannette Madarász. 2010. “Präventionsgeschichte als Kulturgeschichte der Gesundheitspolitik.” In Das präventive Selbst: Eine Kulturgeschichte moderner Gesundheitspolitik , edited by Martin Lengwiler and Jeannette Madarász, 11-28. Bielefeld: Transcript.
Liu, Xiaoxuan, Pearse A. Keane and Alastair K Denniston. 2018. “Time to Regenerate: The Doctor in the Age of Artificial Intelligence.” Journal of the Royal Society of Medicine 11 (4): 113-116.
Loder, Natasha. 2017. “Is There a Doctor in my Pocket?” 1843 Magazine, The Economist . https://www.1843magazine.com/technology/is-there-a-doctor-in-my-pocket .
Mathar, Thomas. 2010. Der digitale Patient. Zu den Konsequenzen eines technowissenschaftlichen Gesundheitssystems . Bielefeld: Transcript.
Matshazi, Nqaba. 2019. “Digital Health Funding Breaks New Record in 2018.” 24 January. https://healthcareweekly.com/digital-health-funding/ .
Medgate Tele Clinic. 2000-2019. Basel: Medgate AG. https://www.medgate.ch/ .
Mitchell, Lisa and Eugenia Georges. 2000. “Cross-Cultural Cyborgs: Greek and Canadian Women’s Discourses on Fetal Ultrasound.” In Bodies of Technology: Women’s Involvement with Reproductive Medicine , edited by Ann Rudinow Saetnan, Nelly Oudshoorn, and Marta Kirejczyk, 384-409. Columbus: Ohio State University Press.
Moscucci, Ornella. 1990. The Science of Woman: Gynaecology and Gender in England, 1800–1929 . Cambridge: Cambridge University Press.
Nolte, Karen. 2009. “Vom Verschwinden der Laienperspektive aus der Krankengeschichte: Medizinische Fallberichte im 19. Jahrhundert.” In Zum Fall machen, zum Fall werden. Wissensproduktion und Patientenerfahrung in Medizin und Psychiatrie des 19. und 20. Jahrhunderts , edited by S. Brändli-Blumenbach, B. Lüthi, and G. Spuhler, 33-61. Frankfurt, New York: Campus.
Obermeyer, Ziad, and Ezekiel J. Emanuel. 2016. “Predicting the Future – Big Data, Machine Learning, and Clinical Medicine.” NEJM 375:1216-19.
Peckham, Robert. 2015. “Panic Encabled: Epidemics and the Telegraphic World.” In Empires of Panic: Epidemics and Colonial Anxieties , edited by Robert Peckham, 131-54. Hong Kong: Hong Kong University Press.
Pomata, Gianna. 1998. Contracting a Cure. Patients, Healers and the Law in Early Modern Bologna . Baltimore: Johns Hopkins University Press.
---- 2010. “Sharing Cases: The Observationes in Early Modern Medicine.” Early Science and Medicine 15:193-236.
---- 2014. “The Medical Case Narrative: Distant Reading of an Epistemic Genre.” Literature and Medicine 32 (1): 1-23.
Porsdam, Sebastian Mann, Julian Savulescu, and Barbara J. Sahakian. 2016. “Facilitating the Ethical Use of Health Data for the Benefit of Society: Electronic Health Records, Consent and the Duty of Easy Rescue.” Phil Trans R Soc A 374:20160130. https://doi.org/10.1098/rsta.2016.0130 .
Porter, Roy. 2011 [1995]. “The Eighteenth Century.” In The Western Medical Tradition, 800 BC to AD 1800 , 10th edition, edited by Conrad Lawrence, Michael Neve, Vivian Nutton, Roy Porter, and Andrew Wear, 371-475. Cambridge: Cambridge University Press.
---- 1999. The Greatest Benefit to Mankind. A Medical History of Humanity from Antiquity to the Present . Fontana Press.
Ratanawongsa, Neda et al. 2016. “Association between Clinician Computer Use and Communication with Patients in Safety-Net Clinics.” JAMA Intern Med 176 (1): 125-128. doi: https://doi.org/10.1001/jamainternmed.2015.6186 .
Reiser, Stanley Joel. 1978. Medicine and the Reign of Technology . Cambridge: Cambridge University Press.
---- 2009. Technological Medicine: The Changing World of Doctors and Patients . Cambridge: Cambridge University Press.
Risse, Guenter B. and John Harley Warner. 1992. “Reconstructing Clinical Activities: Patient Records in Medical History.” Social History of Medicine 5 (2): 183-205.
Rose, Nikolas. 2001. “The Politics of Life Itself.” Theory, Culture & Society 18 (6): 1-30.
Rosenberg, Lawrence. 8 May 2019. “Disintermediation.” Presentation given at Workshop: Medicine without Doctors? Disintermediation and Patient Agency . 4 th Workshop in the series on the Impact of Technological Change on the Surgical Profession. Jewish General Hospital, Montreal.
Ruckstuhl, Brigitte and Elisabeth Ryter. 2017. Von der Seuchenpolizei zu Public Health. Öffentliche Gesundheit in der Schweiz seit 1750 . Chronos: Zurich.
Ritzmann, Iris. 2013. “Vom gemessenen zum angemessenen Körper. Human Enhancement als historischer Prozess.” Schweizerische Ärztezeitung 94 (11): 410-22.
---- 1999. “Der Verhaltenskodex des “Savoir faire” als Deckmantel ärztlicher Hilflosigkeit? Ein Beitrag zur Arzt-Patient-Beziehung im 18. Jahrhundert.” Gesnerus 56:197-219.
Russey, Cathy. 2019. “Healthcare Wearables are Becoming Important for Staying Alive.” 15 January. https://www.wearable-technologies.com/2019/01/healthcare-wearables-are-becoming-important-for-staying-alive/ .
Sandelowski, Margarete. 2000. “This Most Dangerous Instrument: Propriety, Power, and the Vaginal Speculum”. Journal of Obstetric, Gynecologic & Neonatal Nursing 29 (1): 73-82.
Sanders, R. 2003. “Medical Technology: A Critical Perspective.” The Internet Journal of Medical Technology 2 (1): 1-7. https://print.ispub.com/api/0/ispub-article/4943 .
Schmiedebach, Heinz-Peter, ed. 2018. Medizin und öffentliche Gesundheit: Konzepte, Akteure, Perspektiven . Oldenbourg: De Gruyter.
Sinsky, Christine et al. 2016. “Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties.” Annals of Internal Medicine 165 (11): 753-760.
Sobral, Dilermando, Marcy Rosenbaum, and Margarida Figueiredo-Braga. 2015. “Computer Use in Primary Care and Patient-Physician Communication.” Patient Education and Counseling 98 (12): 1568-76.
Strehle, E. M. and N. Shabde. 2006. “One Hundred Years of Telemedicine: Does this new Technology have a place in Paediatrics?” Archives of Disease in Childhood 91:956-959.
“The Topol Review: Preparing the Healthcare Workforce to Deliver the Digital Future. An Independent Report on Behalf of the Secretary of State for Health and Social Care.” 2019. Published by Health Education England. https://topol.hee.nhs.uk/ .
Timmermann, Carsten. 2010. “Risikofaktoren: Der scheinbar unaufhaltsame Erfolg eines Ansatzes aus der amerikanischen Epidemiologie in der deutschen Nachkriegszeit.” In Das präventive Selbst: Eine Kulturgeschichte moderner Gesundheitspolitik , edited by Martin Lengwiler and Jeannette Madarász, 251-277. Bielefeld: Transcript.
Timmermann, Carsten, and Julie Anderson, eds. 2006. Devices and Designs. Medical Technologies in Historical Perspective . London: Palgrave MacMillan.
Toombs, S. Kay. 1992. The Meaning of Illness: A Phenomenological Account of the Different Perspectives of Physician and Patient . Dordrecht: Springer-Science+Busniess Media.
Topol, Eric J., Steven R. Steinhubl, and Ali Torkamani. 2015. “Digital Medical Tools and Sensors.” JAMA 313 (4): 353-354.
Trentmann, Frank. 2009. “Materiality in the Future of History: Things, Practices, and Politics.” Journal of British Studies 48 (29): 283-307.
U.S. Food and Drug Administration. ca. 1995-2019. Silver Spring: U.S. Food and Drug Administration; U.S. Department of Health and Human Services. https://www.fda.gov/medical-devices/digital-health#mobileapp .
Verbeek, Peter-Paul. 2015. “Beyond Interaction: A Short Introduction to Mediation Theory.” Interactions 22 (3): 26-31.
Verghese, Abraham. 2017. “What this Computer needs is a Physician: Humanism and Artificial Intelligence.” JAMA 319 (1): 19-20.
Warner, John Harley. 1999. “The Uses of Patient Records by Historians: Patterns, Possibilities and Perplexities.” Health and History 1 (2/3): 101-11
Weindling, Paul. 1987. “Medical Practice in Imperial Berlin: The Casebook of Alfred Grotjahn.” Bulletin of the History of Medicine 61 (3): 391-410.
Wolff, Eberhard. 2014. “Über das Blutdruckmessen, einen Selbstversuch und ärztliches Alltagshandeln.” Schweizerische Ärztezeitung 95(11): 460. https://www.zora.uzh.ch/id/eprint/107023/1/saez-02492.pdf .
---- 2018. “Das ʻQuantified Selfʼ als historischer Prozess. Die Blutdruck-Selbstmessung seit dem frühen 20. Jahrhundert zwischen Fremdführung und Selbstverortung.” Medizin, Gesellschaft und Geschichte 36:43-83.
World Health Organization. 2016. “Global Diffusion of eHealth: Making Universal Health Coverage Achievable.” Report of the third global survey on eHealth. Geneva: WHO Document Production Services. https://apps.who.int/iris/handle/10665/252529 .
Wüstholz, Florian, and Daniel Stolle. 2020. “Das kranke Dossier.” Republik . 27 July. https://www.republik.ch/2020/07/27/das-kranke-dossier .
Download references
Vanessa Rampton received funding from the Branco Weiss Fellowship – Society in Science.
Author information
Authors and affiliations.
Institute for Health and Social Policy and Department of Philosophy, McGill University, Montréal, Canada
Vanessa Rampton
Center for Medical Humanities, History of Medicine Section, University of Zurich, Zürich, Switzerland
Maria Böhmer & Anita Winkler
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Vanessa Rampton .
Ethics declarations
1 We rely on a definition used by science and technology scholars whereby the term ‘technology’ operates on three levels (see Bijker, Hughes and Pinch 2012, xlii). First, there is the physical level, referring to tangible objects such as a smartphone, wellness band, or stethoscope. The second level of meaning concerns activities or processes, such as 3D printing or creating X-rays. The third level refers to knowledge people have in addition to what they do, for example the knowledge that underpins the conduct of a surgical procedure. This approach shows the extent to which specific tools and techniques, knowledge, and rationales for intervention are intricately bound together. Our use of the term ‘digital,’ that is involving computer technology, in relation to medicine ‘includes categories such as mobile health (mHealth), health information technology (IT), wearable devices, telehealth and telemedicine, and personalized medicine’ (U.S. Food and Drug Administration).
2 As a rule, while systematic reviews of telemedicine generally portray it as effective as in-person consultation or promising, evidence is limited and fast-evolving (Ekeland, Bowes and Flottorp 2010; Kruse et al. 2017; Lee et al. 2017).
3 In Germany, legislators have reacted to these concerns by limiting video consultation to cases in which physician and patient have physically met before, and primarily using it for monitoring the course of disease, including chronic ones, or the healing of an injury (Heinrich 2017).
4 Scottish-born US inventor Alexander Graham Bell was the first to be awarded the U.S. patent for the invention of the telephone in 1876 (Fischer 1992).
5 Interestingly, and probably most important for their users, nine out of ten among the ranked apps are available as free downloads ( https://www.digitaltrends.com/mobile/best-health-apps/ , June 16, 2019).
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Rampton, V., Böhmer, M. & Winkler, A. Medical Technologies Past and Present: How History Helps to Understand the Digital Era. J Med Humanit 43 , 343–364 (2022). https://doi.org/10.1007/s10912-021-09699-x
Download citation
Accepted : 12 May 2021
Published : 07 July 2021
Issue Date : June 2022
DOI : https://doi.org/10.1007/s10912-021-09699-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Digital technologies
- Telemedicine
- Do-it-yourself
- Find a journal
- Publish with us
- Track your research
Essay About Medical Technology
Medical digitized records, powerful imaging devices, small sophisticated tools – medical technology plays an important role in modern healthcare system and significantly alter the provision of care.
The world of medical technology is vast. It includes all the medicines, instruments, procedures, and support systems necessary to provide care. Recognized medical experts indicate that medicine become increasingly dependent on the technology. They already became a part of hospitals and even invade our homes.
According to the experts, the technologies are used in all medical fields.
Doctors and specialists use them both for the prevention, diagnosis, and treatment as well as for the rehabilitation or home care. For example, doctors use vaccines to prevent disease outbreaks, medical imaging for early detection, or laboratory tests and screening for diagnoses. In addition, there are supporting technologies, such as sterilization, and those relating to infrastructure of hospitals, particularly for ensuring the power supply in case of failure. Without this technology, about 80% of care could not be provided.
Technology Term Paper
Medical technology is often associated with big expensive devices such as scanners, the magnetic resonance imaging, and nuclear medicine imaging systems. However, these devices represent only a small part of the medical arsenal of a health facility. The park equipment also includes thousands of small instruments and medical devices. It is in this area where there is the largest number of innovations.
In many other sectors there are important technological advances, including laboratory analysis. For example, development in genetic testing allows to predict the risk of certain cancer types.

Proficient in: Disease
“ Thank you so much for accepting my assignment the night before it was due. I look forward to working with you moving forward ”
Drug technologies also demonstrate considerable progress. Today, drugs are used not only to treat patients, but also to prevent diseases, reduce symptoms, and improve quality of life for people with chronic disease. This change affects spending on drugs. According to the Canadian Institute for Health Information, the cost of drugs has increased from 288 million in 1975 to six billion thirty years later, which represents 22% of health spending in Quebec.
In short, if medical technologies improve the quality of health care and health care delivery, they also pose many challenges to be faced.
As it was mentioned above, medical technology plays today a very important role in healthcare system. Students, who want to write their research project on medical technology, have to thoroughly study the origins and evolution of the phenomenon. They will have to find and process a great deal of information from reliable and verified sources and present clearly their own ideas on the matter.
If you want to write a good research proposal, you have to take advantage of free sample research papers on medical technology. These free papers can guide you through the complex process of scientific text writing and show you how to structure your paper.
Are you looking for a top-notch custom written research paper on Medical Technology topics? Is confidentiality as important to you as the high quality of the product?
Try our writing service at EssayLib.com! We can offer you professional assistance at affordable rates. Our experienced PhD and Master’s writers are ready to take into account your smallest demands. We guarantee you 100% authenticity of your paper and assure you of dead on time delivery. Proceed with the order form:
Please, feel free to visit us at EssayLib.com and learn more about our service!
Cite this page
Essay About Medical Technology. (2019, Dec 05). Retrieved from https://paperap.com/paper-on-research-paper-on-medical-technology/
"Essay About Medical Technology." PaperAp.com , 5 Dec 2019, https://paperap.com/paper-on-research-paper-on-medical-technology/
PaperAp.com. (2019). Essay About Medical Technology . [Online]. Available at: https://paperap.com/paper-on-research-paper-on-medical-technology/ [Accessed: 17 May. 2024]
"Essay About Medical Technology." PaperAp.com, Dec 05, 2019. Accessed May 17, 2024. https://paperap.com/paper-on-research-paper-on-medical-technology/
"Essay About Medical Technology," PaperAp.com , 05-Dec-2019. [Online]. Available: https://paperap.com/paper-on-research-paper-on-medical-technology/. [Accessed: 17-May-2024]
PaperAp.com. (2019). Essay About Medical Technology . [Online]. Available at: https://paperap.com/paper-on-research-paper-on-medical-technology/ [Accessed: 17-May-2024]
- Why I Would Be An Asset To The Medical School And The Medical Profession Pages: 3 (648 words)
- Medical Malpractice: Medical Service Pages: 2 (429 words)
- The Critical Application of 3D Printing in the Medical and Non-Medical Fields Pages: 4 (991 words)
- How Medical Personnel Support the Patient's Right to Refuse Medical Care Pages: 2 (552 words)
- Anesthesia, Medical Research and Electronic Medical Records Pages: 2 (462 words)
- The Benefits of Information Technology: The Benefits of Information Technology Pages: 1 (297 words)
- Medical Billing and Coding Pages: 1 (300 words)
- Medical Billing and Coding(Certified Nursing Assistant) Pages: 4 (1052 words)
- Computerization of the Medical Records Pages: 36 (10602 words)
- American Association of Medical Assistants Pages: 11 (3195 words)
10 Successful Medical School Essays
Sponsored by.

-- Accepted to: Harvard Medical School GPA: 4.0 MCAT: 522
Sponsored by A ccepted.com : Great stats don’t assure acceptance to elite medical schools. The personal statement, most meaningful activities, activity descriptions, secondaries and interviews can determine acceptance or rejection. Since 1994, Accepted.com has guided medical applicants just like you to present compelling medical school applications. Get Accepted !
I started writing in 8th grade when a friend showed me her poetry about self-discovery and finding a voice. I was captivated by the way she used language to bring her experiences to life. We began writing together in our free time, trying to better understand ourselves by putting a pen to paper and attempting to paint a picture with words. I felt my style shift over time as I grappled with challenges that seemed to defy language. My poems became unstructured narratives, where I would use stories of events happening around me to convey my thoughts and emotions. In one of my earliest pieces, I wrote about a local boy’s suicide to try to better understand my visceral response. I discussed my frustration with the teenage social hierarchy, reflecting upon my social interactions while exploring the harms of peer pressure.
In college, as I continued to experiment with this narrative form, I discovered medical narratives. I have read everything from Manheimer’s Bellevue to Gawande’s Checklist and from Nuland’s observations about the way we die, to Kalanithi’s struggle with his own decline. I even experimented with this approach recently, writing a piece about my grandfather’s emphysema. Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love. I have augmented these narrative excursions with a clinical bioethics internship. In working with an interdisciplinary team of ethics consultants, I have learned by doing by participating in care team meetings, synthesizing discussions and paths forward in patient charts, and contributing to an ongoing legislative debate addressing the challenges of end of life care. I have also seen the ways ineffective intra-team communication and inter-personal conflicts of beliefs can compromise patient care.
Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love.
By assessing these difficult situations from all relevant perspectives and working to integrate the knowledge I’ve gained from exploring narratives, I have begun to reflect upon the impact the humanities can have on medical care. In a world that has become increasingly data driven, where patients can so easily devolve into lists of numbers and be forced into algorithmic boxes in search of an exact diagnosis, my synergistic narrative and bioethical backgrounds have taught me the importance of considering the many dimensions of the human condition. I am driven to become a physician who deeply considers a patient’s goal of care and goals of life. I want to learn to build and lead patient care teams that are oriented toward fulfilling these goals, creating an environment where family and clinician conflict can be addressed efficiently and respectfully. Above all, I look forward to using these approaches to keep the person beneath my patients in focus at each stage of my medical training, as I begin the task of translating complex basic science into excellent clinical care.
In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better understand her patients. Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient’s humanity at the center of her approach to clinical care.
This narrative distinguishes Morgan as a candidate for medical school effectively, as she provides specific examples of how her passions intersect with medicine. She first discusses how she used poetry to process her emotional response to a local boy’s suicide and ties in concern about teenage mental health. Then, she discusses more philosophical questions she encountered through reading medical narratives, which demonstrates her direct interest in applying writing and the humanities to medicine. By making the connection from this larger theme to her own reflections on her grandfather, Morgan provides a personal insight that will give an admissions officer a window into her character. This demonstrates her empathy for her future patients and commitment to their care.
Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient's humanity at the center of her approach to clinical care.
Furthermore, it is important to note that Morgan’s essay does not repeat anything in-depth that would otherwise be on her resume. She makes a reference to her work in care team meetings through a clinical bioethics internship, but does not focus on this because there are other places on her application where this internship can be discussed. Instead, she offers a more reflection-based perspective on the internship that goes more in-depth than a resume or CV could. This enables her to explain the reasons for interdisciplinary approach to medicine with tangible examples that range from personal to professional experiences — an approach that presents her as a well-rounded candidate for medical school.
Disclaimer: With exception of the removal of identifying details, essays are reproduced as originally submitted in applications; any errors in submissions are maintained to preserve the integrity of the piece. The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this article.
-- Accepted To: A medical school in New Jersey with a 3% acceptance rate. GPA: 3.80 MCAT: 502 and 504
Sponsored by E fiie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
"To know even one life has breathed easier because you have lived. This is to have succeeded." – Ralph Waldo Emerson.
The tribulations I've overcome in my life have manifested in the compassion, curiosity, and courage that is embedded in my personality. Even a horrific mishap in my life has not changed my core beliefs and has only added fuel to my intense desire to become a doctor. My extensive service at an animal hospital, a harrowing personal experience, and volunteering as an EMT have increased my appreciation and admiration for the medical field.
At thirteen, I accompanied my father to the Park Home Animal Hospital with our eleven-year-old dog, Brendan. He was experiencing severe pain due to an osteosarcoma, which ultimately led to the difficult decision to put him to sleep. That experience brought to light many questions regarding the idea of what constitutes a "quality of life" for an animal and what importance "dignity" plays to an animal and how that differs from owner to owner and pet to pet. Noting my curiosity and my relative maturity in the matter, the owner of the animal hospital invited me to shadow the professional staff. Ten years later, I am still part of the team, having made the transition from volunteer to veterinarian technician. Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
As my appreciation for medical professionals continued to grow, a horrible accident created an indelible moment in my life. It was a warm summer day as I jumped onto a small boat captained by my grandfather. He was on his way to refill the boat's gas tank at the local marina, and as he pulled into the dock, I proceeded to make a dire mistake. As the line was thrown from the dock, I attempted to cleat the bowline prematurely, and some of the most intense pain I've ever felt in my life ensued.
Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
"Call 911!" I screamed, half-dazed as I witnessed blood gushing out of my open wounds, splashing onto the white fiberglass deck of the boat, forming a small puddle beneath my feet. I was instructed to raise my hand to reduce the bleeding, while someone wrapped an icy towel around the wound. The EMTs arrived shortly after and quickly drove me to an open field a short distance away, where a helicopter seemed to instantaneously appear.
The medevac landed on the roof of Stony Brook Hospital before I was expeditiously wheeled into the operating room for a seven-hour surgery to reattach my severed fingers. The distal phalanges of my 3rd and 4th fingers on my left hand had been torn off by the rope tightening on the cleat. I distinctly remember the chill from the cold metal table, the bright lights of the OR, and multiple doctors and nurses scurrying around. The skill and knowledge required to execute multiple skin graft surgeries were impressive and eye-opening. My shortened fingers often raise questions by others; however, they do not impair my self-confidence or physical abilities. The positive outcome of this trial was the realization of my intense desire to become a medical professional.
Despite being the patient, I was extremely impressed with the dedication, competence, and cohesiveness of the medical team. I felt proud to be a critical member of such a skilled group. To this day, I still cannot explain the dichotomy of experiencing being the patient, and concurrently one on the professional team, committed to saving the patient. Certainly, this experience was a defining part of my life and one of the key contributors to why I became an EMT and a volunteer member of the Sample Volunteer Ambulance Corps. The startling ring of the pager, whether it is to respond to an inebriated alcoholic who is emotionally distraught or to help bring breath to a pulseless person who has been pulled from the family swimming pool, I am committed to EMS. All of these events engender the same call to action and must be reacted to with the same seriousness, intensity, and magnanimity. It may be some routine matter or a dire emergency; this is a role filled with uncertainty and ambiguity, but that is how I choose to spend my days. My motives to become a physician are deeply seeded. They permeate my personality and emanate from my desire to respond to the needs of others. Through a traumatic personal event and my experiences as both a professional and volunteer, I have witnessed firsthand the power to heal the wounded and offer hope. Each person defines success in different ways. To know even one life has been improved by my actions affords me immense gratification and meaning. That is success to me and why I want to be a doctor.
This review is provided by EFIIE Consulting Group’s Pre-Health Senior Consultant Jude Chan
This student was a joy to work with — she was also the lowest MCAT profile I ever accepted onto my roster. At 504 on the second attempt (502 on her first) it would seem impossible and unlikely to most that she would be accepted into an allopathic medical school. Even for an osteopathic medical school this score could be too low. Additionally, the student’s GPA was considered competitive at 3.80, but it was from a lower ranked, less known college, so naturally most advisors would tell this student to go on and complete a master’s or postbaccalaureate program to show that she could manage upper level science classes. Further, she needed to retake the MCAT a third time.
However, I saw many other facets to this student’s history and life that spoke volumes about the type of student she was, and this was the positioning strategy I used for her file. Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA. Although many students have greater MCAT scores than 504 and higher GPAs than 3.80, I have helped students with lower scores and still maintained our 100% match rate. You are competing with thousands of candidates. Not every student out there requires our services and we are actually grateful that we can focus on a limited amount out of the tens of thousands that do. We are also here for the students who wish to focus on learning well the organic chemistry courses and physics courses and who want to focus on their research and shadowing opportunities rather than waste time deciphering the next step in this complex process. We tailor a pathway for each student dependent on their health care career goals, and our partnerships with non-profit organizations, hospitals, physicians and research labs allow our students to focus on what matters most — the building up of their basic science knowledge and their exposure to patients and patient care.
Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA.
Even students who believe that their struggle somehow disqualifies them from their dream career in health care can be redeemed if they are willing to work for it, just like this student with 502 and 504 MCAT scores. After our first consult, I saw a way to position her to still be accepted into an MD school in the US — I would not have recommended she register to our roster if I did not believe we could make a difference. Our rosters have a waitlist each semester, and it is in our best interest to be transparent with our students and protect our 100% record — something I consider a win-win. It is unethical to ever guarantee acceptance in admissions as we simply do not control these decisions. However, we respect it, play by the rules, and help our students stay one step ahead by creating an applicant profile that would be hard for the schools to ignore.
This may be the doctor I go to one day. Or the nurse or dentist my children or my grandchildren goes to one day. That is why it is much more than gaining acceptance — it is about properly matching the student to the best options for their education. Gaining an acceptance and being incapable of getting through the next 4 or 8 years (for my MD/PhD-MSTP students) is nonsensical.
-- Accepted To: Imperial College London UCAT Score: 2740 BMAT Score: 3.9, 5.4, 3.5A
My motivation to study Medicine stems from wishing to be a cog in the remarkable machine that is universal healthcare: a system which I saw first-hand when observing surgery in both the UK and Sri Lanka. Despite the differences in sanitation and technology, the universality of compassion became evident. When volunteering at OSCE training days, I spoke to many medical students, who emphasised the importance of a genuine interest in the sciences when studying Medicine. As such, I have kept myself informed of promising developments, such as the use of monoclonal antibodies in cancer therapy. After learning about the role of HeLa cells in the development of the polio vaccine in Biology, I read 'The Immortal Life of Henrietta Lacks' to find out more. Furthermore, I read that surface protein CD4 can be added to HeLa cells, allowing them to be infected with HIV, opening the possibility of these cells being used in HIV research to produce more life-changing drugs, such as pre-exposure prophylaxis (PreP). Following my BioGrad laboratory experience in HIV testing, and time collating data for research into inflammatory markers in lung cancer, I am also interested in pursuing a career in medical research. However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude. As the surgeon explained that the cancer had metastasised to her liver, I watched him empathetically tailor his language for the patient - he avoided medical jargon and instead gave her time to come to terms with this. I have been developing my communication skills by volunteering weekly at care homes for 3 years, which has improved my ability to read body language and structure conversations to engage with the residents, most of whom have dementia.
However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude.
Jude’s essay provides a very matter-of-fact account of their experience as a pre-medical student. However, they deepen this narrative by merging two distinct cultures through some common ground: a universality of compassion. Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
From their OSCE training days to their school’s Science society, Jude connects their analytical perspective — learning about HeLa cells — to something that is relatable and human, such as a poor farmer’s notable contribution to science. This approach provides a gateway into their moral compass without having to explicitly state it, highlighting their fervent desire to learn how to interact and communicate with others when in a position of authority.
Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
Jude’s closing paragraph reminds the reader of the similarities between two countries like the UK and Sri Lanka, and the importance of having a universal healthcare system that centers around the just and “world-class” treatment of patients. Overall, this essay showcases Jude’s personal initiative to continue to learn more and do better for the people they serve.
While the essay could have benefited from better transitions to weave Jude’s experiences into a personal story, its strong grounding in Jude’s motivation makes for a compelling application essay.
-- Accepted to: Weill Cornell Medical College GPA: 3.98 MCAT: 521
Sponsored by E fie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
Following the physician’s unexpected request, we waited outside, anxiously waiting to hear the latest update on my father’s condition. It was early on in my father’s cancer progression – a change that had shaken our entire way of life overnight. During those 18 months, while my mother spent countless nights at the hospital, I took on the responsibility of caring for my brother. My social life became of minimal concern, and the majority of my studying for upcoming 12th- grade exams was done at the hospital. We were allowed back into the room as the physician walked out, and my parents updated us on the situation. Though we were a tight-knit family and my father wanted us to be present throughout his treatment, what this physician did was give my father a choice. Without making assumptions about who my father wanted in the room, he empowered him to make that choice independently in private. It was this respect directed towards my father, the subsequent efforts at caring for him, and the personal relationship of understanding they formed, that made the largest impact on him. Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
It was during this period that I became curious about the human body, as we began to learn physiology in more depth at school. In previous years, the problem-based approach I could take while learning math and chemistry were primarily what sparked my interest. However, I became intrigued by how molecular interactions translated into large-scale organ function, and how these organ systems integrated together to generate the extraordinary physiological functions we tend to under-appreciate. I began my undergraduate studies with the goal of pursuing these interests, whilst leaning towards a career in medicine. While I was surprised to find that there were upwards of 40 programs within the life sciences that I could pursue, it broadened my perspective and challenged me to explore my options within science and healthcare. I chose to study pathobiology and explore my interests through hospital volunteering and research at the end of my first year.
Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
While conducting research at St. Michael’s Hospital, I began to understand methods of data collection and analysis, and the thought process of scientific inquiry. I became acquainted with the scientific literature, and the experience transformed how I thought about the concepts I was learning in lecture. However, what stood out to me that summer was the time spent shadowing my supervisor in the neurosurgery clinic. It was where I began to fully understand what life would be like as a physician, and where the career began to truly appeal to me. What appealed to me most was the patient-oriented collaboration and discussions between my supervisor and his fellow; the physician-patient relationship that went far beyond diagnoses and treatments; and the problem solving that I experienced first-hand while being questioned on disease cases.
The day spent shadowing in the clinic was also the first time I developed a relationship with a patient. We were instructed to administer the Montreal cognitive assessment (MoCA) test to patients as they awaited the neurosurgeon. My task was to convey the instructions as clearly as possible and score each section. I did this as best I could, adapting my explanation to each patient, and paying close attention to their responses to ensure I was understood. The last patient was a challenging case, given a language barrier combined with his severe hydrocephalus. It was an emotional time for his family, seeing their father/husband struggle to complete simple tasks and subsequently give up. I encouraged him to continue trying. But I also knew my words would not remedy the condition underlying his struggles. All I could do was make attempts at lightening the atmosphere as I got to know him and his family better. Hours later, as I saw his remarkable improvement following a lumbar puncture, and the joy on his and his family’s faces at his renewed ability to walk independently, I got a glimpse of how rewarding it would be to have the ability and privilege to care for such patients. By this point, I knew I wanted to commit to a life in medicine. Two years of weekly hospital volunteering have allowed me to make a small difference in patients’ lives by keeping them company through difficult times, and listening to their concerns while striving to help in the limited way that I could. I want to have the ability to provide care and treatment on a daily basis as a physician. Moreover, my hope is that the breadth of medicine will provide me with the opportunity to make an impact on a larger scale. Whilst attending conferences on neuroscience and surgical technology, I became aware of the potential to make a difference through healthcare, and I look forward to developing the skills necessary to do so through a Master’s in Global Health. Whether through research, health innovation, or public health, I hope not only to care for patients with the same compassion with which physicians cared for my father, but to add to the daily impact I can have by tackling large-scale issues in health.
Taylor’s essay offers both a straightforward, in-depth narrative and a deep analysis of his experiences, which effectively reveals his passion and willingness to learn in the medical field. The anecdote of Taylor’s father gives the reader insight into an original instance of learning through experience and clearly articulates Taylor’s motivations for becoming a compassionate and respectful physician.
Taylor strikes an impeccable balance between discussing his accomplishments and his character. All of his life experiences — and the difficult challenges he overcame — introduce the reader to an important aspect of Taylor’s personality: his compassion, care for his family, and power of observation in reflecting on the decisions his father’s doctor makes. His description of his time volunteering at St. Michael’s Hospital is indicative of Taylor’s curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship. Moreover, he shows how his volunteer work enabled him to see how medicine goes “beyond diagnoses and treatments” — an observation that also speaks to his compassion.
His description of his time volunteering at St. Michael's Hospital is indicative of Taylor's curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship.
Finally, Taylor also tells the reader about his ambition and purpose, which is important when thinking about applying to medical school. He discusses his hope of tackling larger scale problems through any means possible in medicine. This notion of using self interest to better the world is imperative to a successful college essay, and it is nicely done here.
-- Accepted to: Washington University
Sponsored by A dmitRx : We are a group of Chicago-based medical students who realize how challenging medical school admissions can be, so we want to provide our future classmates with resources we wish we had. Our mission at AdmitRx is to provide pre-medical students with affordable, personalized, high-quality guidance towards becoming an admitted medical student.
Running has always been one of my greatest passions whether it be with friends or alone with my thoughts. My dad has always been my biggest role model and was the first to introduce me to the world of running. We entered races around the country, and one day he invited me on a run that changed my life forever. The St. Jude Run is an annual event that raises millions of dollars for St. Jude Children’s Research Hospital. My dad has led or our local team for as long as I can remember, and I had the privilege to join when I was 16. From the first step I knew this was the environment for me – people from all walks of life united with one goal of ending childhood cancer. I had an interest in medicine before the run, and with these experiences I began to consider oncology as a career. When this came up in conversations, I would invariably be faced with the question “Do you really think you could get used to working with dying kids?” My 16-year-old self responded with something noble but naïve like “It’s important work, so I’ll have to handle it”. I was 16 years young with my plan to become an oncologist at St. Jude.
As I transitioned into college my plans for oncology were alive and well. I began working in a biochemistry lab researching new anti-cancer drugs. It was a small start, but I was overjoyed to be a part of the process. I applied to work at a number of places for the summer, but the Pediatric Oncology Education program (POE) at St. Jude was my goal. One afternoon, I had just returned from class and there it was: an email listed as ‘POE Offer’. I was ecstatic and accepted the offer immediately. Finally, I could get a glimpse at what my future holds. My future PI, Dr. Q, specialized in solid tumor translational research and I couldn’t wait to get started.
I was 16 years young with my plan to become an oncologist at St. Jude.
Summer finally came, I moved to Memphis, and I was welcomed by the X lab. I loved translational research because the results are just around the corner from helping patients. We began a pre-clinical trial of a new chemotherapy regimen and the results were looking terrific. I was also able to accompany Dr. Q whenever she saw patients in the solid tumor division. Things started simple with rounds each morning before focusing on the higher risk cases. I was fortunate enough to get to know some of the patients quite well, and I could sometimes help them pass the time with a game or two on a slow afternoon between treatments. These experiences shined a very human light on a field I had previously seen only through a microscope in a lab.
I arrived one morning as usual, but Dr. Q pulled me aside before rounds. She said one of the patients we had been seeing passed away in the night. I held my composure in the moment, but I felt as though an anvil was crushing down on me. It was tragic but I knew loss was part of the job, so I told myself to push forward. A few days later, I had mostly come to terms with what happened, but then the anvil came crashing back down with the passing of another patient. I could scarcely hold back the tears this time. That moment, it didn’t matter how many miraculous successes were happening a few doors down. Nothing overshadowed the loss, and there was no way I could ‘get used to it’ as my younger self had hoped.
I was still carrying the weight of what had happened and it was showing, so I asked Dr. Q for help. How do you keep smiling each day? How do you get used to it? The questions in my head went on. What I heard next changed my perspective forever. She said you keep smiling because no matter what happened, you’re still hope for the next patient. It’s not about getting used to it. You never get used to it and you shouldn’t. Beating cancer takes lifetimes, and you can’t look passed a life’s worth of hardships. I realized that moving passed the loss of patients would never suffice, but I need to move forward with them. Through the successes and shortcomings, we constantly make progress. I like to imagine that in all our future endeavors, it is the hands of those who have gone before us that guide the way. That is why I want to attend medical school and become a physician. We may never end the sting of loss, but physicians are the bridge between the past and the future. No where else is there the chance to learn from tragedy and use that to shape a better future. If I can learn something from one loss, keep moving forward, and use that knowledge to help even a single person – save one life, bring a moment of joy, avoid a moment of pain—then that is how I want to spend my life.
The change wasn’t overnight. The next loss still brought pain, but I took solace in moving forward so that we might learn something to give hope to a future patient. I returned to campus in a new lab doing cancer research, and my passion for medicine continues to flourish. I still think about all the people I encountered at St. Jude, especially those we lost. It might be a stretch, but during the long hours at the lab bench I still picture their hands moving through mine each step of the way. I could never have foreseen where the first steps of the St. Jude Run would bring me. I’m not sure where the road to becoming a physician may lead, but with helping hands guiding the way, I won’t be running it alone.
This essay, a description of the applicant’s intellectual challenges, displays the hardships of tending to cancer patients as a milestone of experience and realization of what it takes to be a physician. The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional. In this way, the applicant gives the reader some insight into the applicant’s mindset, and their ability to think beyond the surface for ways to become better at what they do.
However, the essay fails to zero in on the applicant’s character, instead elaborating on life events that weakly illustrate the applicant’s growth as a physician. The writer’s mantra (“keep moving forward”) is feebly projected, and seems unoriginal due to the lack of a personalized connection between the experience at St. Jude and how that led to the applicant’s growth and mindset changes.
The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional.
The writer, by only focusing on grief brought from patient deaths at St. Jude, misses out on the opportunity to further describe his or her experience at the hospital and portray an original, well-rounded image of his or her strengths, weaknesses, and work ethic.
The applicant ends the essay by attempting to highlight the things they learned at St. Jude, but fails to organize the ideas into a cohesive, comprehensible section. These ideas are also too abstract, and are vague indicators of the applicant’s character that are difficult to grasp.
-- Accepted to: New York University School of Medicine
Sponsored by MedEdits : MedEdits Medical Admissions has been helping applicants get into medical schools like Harvard for more than ten years. Structured like an academic medical department, MedEdits has experts in admissions, writing, editing, medicine, and interview prep working with you collaboratively so you can earn the best admissions results possible.
“Is this the movie you were talking about Alice?” I said as I showed her the movie poster on my iPhone. “Oh my God, I haven’t seen that poster in over 70 years,” she said with her arms trembling in front of her. Immediately, I sat up straight and started to question further. We were talking for about 40 minutes, and the most exciting thing she brought up in that time was the new flavor of pudding she had for lunch. All of sudden, she’s back in 1940 talking about what it was like to see this movie after school for only 5¢ a ticket! After an engaging discussion about life in the 40’s, I knew I had to indulge her. Armed with a plethora of movie streaming sights, I went to work scouring the web. No luck. The movie, “My Son My Son,” was apparently not in high demand amongst torrenting teens. I had to entreat my older brother for his Amazon Prime account to get a working stream. However, breaking up the monotony and isolation felt at the nursing home with a simple movie was worth the pandering.
While I was glad to help a resident have some fun, I was partly motivated by how much Alice reminded me of my own grandfather. In accordance with custom, my grandfather was to stay in our house once my grandmother passed away. More specifically, he stayed in my room and my bed. Just like grandma’s passing, my sudden roommate was a rough transition. In 8th grade at the time, I considered myself to be a generally good guy. Maybe even good enough to be a doctor one day. I volunteered at the hospital, shadowed regularly, and had a genuine interest for science. However, my interest in medicine was mostly restricted to academia. To be honest, I never had a sustained exposure to the palliative side of medicine until the arrival of my new roommate.
The two years I slept on that creaky wooden bed with him was the first time my metal was tested. Sharing that room, I was the one to take care of him. I was the one to rub ointment on his back, to feed him when I came back from school, and to empty out his spittoon when it got full. It was far from glamorous, and frustrating most of the time. With 75 years separating us, and senile dementia setting in, he would often forget who I was or where he was. Having to remind him that I was his grandson threatened to erode at my resolve. Assured by my Syrian Orthodox faith, I even prayed about it; asking God for comfort and firmness on my end. Over time, I grew slow to speak and eager to listen as he started to ramble more and more about bits and pieces of the past. If I was lucky, I would be able to stich together a narrative that may or may have not been true. In any case, my patience started to bud beyond my age group.
Having to remind him that I was his grandson threatened to erode at my resolve.
Although I grew more patient with his disease, my curiosity never really quelled. Conversely, it developed further alongside my rapidly growing interest in the clinical side of medicine. Naturally, I became drawn to a neurology lab in college where I got to study pathologies ranging from atrophy associated with schizophrenia, and necrotic lesions post stroke. However, unlike my intro biology courses, my work at the neurology lab was rooted beyond the academics. Instead, I found myself driven by real people who could potentially benefit from our research. In particular, my shadowing experience with Dr. Dominger in the Veteran’s home made the patient more relevant in our research as I got to encounter geriatric patients with age related diseases, such as Alzhimer’s and Parkinson’s. Furthermore, I had the privilege of of talking to the families of a few of these patients to get an idea of the impact that these diseases had on the family structure. For me, the scut work in the lab meant a lot more with these families in mind than the tritium tracer we were using in the lab.
Despite my achievements in the lab and the classroom, my time with my grandfather still holds a special place in my life story. The more I think about him, the more confident I am in my decision to pursue a career where caring for people is just as important, if not more important, than excelling at academics. Although it was a lot of work, the years spent with him was critical in expanding my horizons both in my personal life and in the context of medicine. While I grew to be more patient around others, I also grew to appreciate medicine beyond the science. This more holistic understanding of medicine had a synergistic effect in my work as I gained a purpose behind the extra hours in the lab, sleepless nights in the library, and longer hours volunteering. I had a reason for what I was doing that may one day help me have long conversations with my own grandchildren about the price of popcorn in the 2000’s.
The most important thing to highlight in Avery’s essay is how he is able to create a duality between his interest in not only the clinical, more academic-based side of medicine, but also the field’s personal side.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather. These two experiences build up the “synergistic” relationship between caring for people and studying the science behind medicine. In this way, he is able to clearly state his passions for medicine and explain his exact motives for entering the field. Furthermore, in his discussion of her grandfather, he effectively employs imagery (“rub ointment on his back,” “feed him when I came back from school,” etc.) to describe the actual work that he does, calling it initially as “far from glamorous, and frustrating most of the time.” By first mentioning his initial impression, then transitioning into how he grew to appreciate the experience, Avery is able to demonstrate a strength of character, sense of enormous responsibility and capability, and open-minded attitude.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather.
Later in the essay, Avery is also able to relate his time caring for his grandfather to his work with Alzheimer’s and Parkinson’s patients, showcasing the social impact of his work, as the reader is likely already familiar with the biological impact of the work. This takes Avery’s essay full circle, bringing it back to how a discussion with an elderly patient about the movies reminds him of why he chose to pursue medicine.
That said, the essay does feel rushed near the end, as the writer was likely trying to remain within the word count. There could be a more developed transition before Avery introduces the last sentence about “conversations with my own grandchildren,” especially as a strong essay ending is always recommended.
-- Accepted To: Saint Louis University Medical School Direct Admission Medical Program
Sponsored by Atlas Admissions : Atlas Admissions provides expert medical school admissions consulting and test preparation services. Their experienced, physician-driven team consistently delivers top results by designing comprehensive, personalized strategies to optimize applications. Atlas Admissions is based in Boston, MA and is trusted by clients worldwide.
The tension in the office was tangible. The entire team sat silently sifting through papers as Dr. L introduced Adam, a 60-year-old morbidly obese man recently admitted for a large open wound along his chest. As Dr. L reviewed the details of the case, his prognosis became even bleaker: hypertension, diabetes, chronic kidney disease, cardiomyopathy, hyperlipidemia; the list went on and on. As the humdrum of the side-conversations came to a halt, and the shuffle of papers softened, the reality of Adam’s situation became apparent. Adam had a few months to live at best, a few days at worst. To make matters worse, Adam’s insurance would not cover his treatment costs. With no job, family, or friends, he was dying poor and alone.
I followed Dr. L out of the conference room, unsure what would happen next. “Well,” she muttered hesitantly, “We need to make sure that Adam is on the same page as us.” It’s one thing to hear bad news, and another to hear it utterly alone. Dr. L frantically reviewed all of Adam’s paperwork desperately looking for someone to console him, someone to be at his side. As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy. That empathy is exactly what I saw in Dr. L as she went out of her way to comfort a patient she met hardly 20 minutes prior.
Since high school, I’ve been fascinated by technology’s potential to improve healthcare. As a volunteer in [the] Student Ambassador program, I was fortunate enough to watch an open-heart surgery. Intrigued by the confluence of technology and medicine, I chose to study biomedical engineering. At [school], I wanted to help expand this interface, so I became involved with research through Dr. P’s lab by studying the applications of electrospun scaffolds for dermal wound healing. While still in the preliminary stages of research, I learned about the Disability Service Club (DSC) and decided to try something new by volunteering at a bowling outing.
As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy.
The DSC promotes awareness of cognitive disabilities in the community and seeks to alleviate difficulties for the disabled. During one outing, I collaborated with Arc, a local organization with a similar mission. Walking in, I was told that my role was to support the participants by providing encouragement. I decided to help a relatively quiet group of individuals assisted by only one volunteer, Mary. Mary informed me that many individuals with whom I was working were diagnosed with ASD. Suddenly, she started cheering, as one of the members of the group bowled a strike. The group went wild. Everyone was dancing, singing, and rejoicing. Then I noticed one gentleman sitting at our table, solemn-faced. I tried to start a conversation with him, but he remained unresponsive. I sat with him for the rest of the game, trying my hardest to think of questions that would elicit more than a monosyllabic response, but to no avail. As the game ended, I stood up to say bye when he mumbled, “Thanks for talking.” Then he quickly turned his head away. I walked away beaming. Although I was unable to draw out a smile or even sustain a conversation, at the end of the day, the fact that this gentleman appreciated my mere effort completely overshadowed the awkwardness of our time together. Later that day, I realized that as much as I enjoyed the thrill of research and its applications, helping other people was what I was most passionate about.
When it finally came time to tell Adam about his deteriorating condition, I was not sure how he would react. Dr. L gently greeted him and slowly let reality take its toll. He stoically turned towards Dr. L and groaned, “I don’t really care. Just leave me alone.” Dr. L gave him a concerned nod and gradually left the room. We walked to the next room where we met with a pastor from Adam’s church.
“Adam’s always been like that,” remarked the pastor, “he’s never been one to express emotion.” We sat with his pastor for over an hour discussing how we could console Adam. It turned out that Adam was part of a motorcycle club, but recently quit because of his health. So, Dr. L arranged for motorcycle pictures and other small bike trinkets to be brought to his room as a reminder of better times.
Dr. L’s simple gesture reminded me of why I want to pursue medicine. There is something sacred, empowering, about providing support when people need it the most; whether it be simple as starting a conversation, or providing support during the most trying of times. My time spent conducting research kindled my interest in the science of medicine, and my service as a volunteer allowed me to realize how much I valued human interaction. Science and technology form the foundation of medicine, but to me, empathy is the essence. It is my combined interest in science and service that inspires me to pursue medicine. It is that combined interest that makes me aspire to be a physician.
Parker’s essay focuses on one central narrative with a governing theme of compassionate and attentive care for patients, which is the key motivator for her application to medical school. Parker’s story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field. This effectively demonstrates to the reader what kind of doctor Parker wants to be in the future.
Parker’s narrative has a clear beginning, middle, and end, making it easy for the reader to follow. She intersperses the main narrative about Adam with experiences she has with other patients and reflects upon her values as she contemplates pursuing medicine as a career. Her anecdote about bowling with the patients diagnosed with ASD is another instance where she uses a story to tell the reader why she values helping people through medicine and attentive patient care, especially as she focuses on the impact her work made on one man at the event.
Parker's story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field.
All throughout the essay, the writing is engaging and Parker incorporates excellent imagery, which goes well with her varied sentence structure. The essay is also strong because it comes back full circle at its conclusion, tying the overall narrative back to the story of Dr. L and Adam, which speaks to Parker’s motives for going to medical school.
-- Accepted To: Emory School of Medicine
Growing up, I enjoyed visiting my grandparents. My grandfather was an established doctor, helping the sick and elderly in rural Taiwan until two weeks before he died at 91 years old. His clinic was located on the first floor of the residency with an exam room, treatment room, X-ray room, and small pharmacy. Curious about his work, I would follow him to see his patients. Grandpa often asked me if I want to be a doctor just like him. I always smiled, but was more interested in how to beat the latest Pokémon game. I was in 8th grade when my grandfather passed away. I flew back to Taiwan to attend his funeral. It was a gloomy day and the only street in the small village became a mourning place for the villagers. Flowers filled the streets and people came to pay their respects. An old man told me a story: 60 years ago, a village woman was in a difficult labor. My grandfather rushed into the house and delivered a baby boy. That boy was the old man and he was forever grateful. Stories of grandpa saving lives and bringing happiness to families were told during the ceremony. At that moment, I realized why my grandfather worked so tirelessly up until his death as a physician. He did it for the reward of knowing that he kept a family together and saved a life. The ability for a doctor to heal and bring happiness is the reason why I want to study medicine. Medical school is the first step on a lifelong journey of learning, but I feel that my journey leading up to now has taught me some things of what it means to be an effective physician.
With a newfound purpose, I began volunteering and shadowing at my local hospital. One situation stood out when I was a volunteer in the cardiac stress lab. As I attached EKG leads onto a patient, suddenly the patient collapsed and started gasping for air. His face turned pale, then slightly blue. The charge nurse triggered “Code Blue” and started CPR. A team of doctors and nurses came, rushing in with a defibrillator to treat and stabilize the patient. What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care. I want to be a leader as well as part of a team that can make a difference in a person’s life. I have refined these lessons about teamwork and leadership to my activities. In high school I was an 8 time varsity letter winner for swimming and tennis and captain of both of those teams. In college I have participated in many activities, but notably serving as assistant principle cellist in my school symphony as well as being a co-founding member of a quartet. From both my athletic experiences and my music experiences I learned what it was like to not only assert my position as a leader and to effectively communicate my views, but equally as important I learned how to compromise and listen to the opinions of others. Many physicians that I have observed show a unique blend of confidence and humility.
What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care.
College opened me up to new perspectives on what makes a complete physician. A concept that was preached in the Guaranteed Professional Program Admissions in Medicine (GPPA) was that medicine is both an art and a science. The art of medicine deals with a variety of aspects including patient relationships as well as ethics. Besides my strong affinity for the sciences and mathematics, I always have had interest in history. I took courses in both German literature and history, which influenced me to take a class focusing on Nazi neuroscientists. It was the ideology of seeing the disabled and different races as test subjects rather than people that led to devastating lapses in medical ethics. The most surprising fact for me was that doctors who were respected and leaders in their field disregarded the humanity of patient and rather focused on getting results from their research. Speaking with Dr. Zeidman, the professor for this course, influenced me to start my research which deals with the ethical qualms of using data derived from unethical Nazi experimentation such as the brains derived from the adult and child euthanasia programs. Today, science is so result driven, it is important to keep in mind the ethics behind research and clinical practice. Also the development of personalized genomic medicine brings into question about potential privacy violations and on the extreme end discrimination. The study of ethics no matter the time period is paramount in the medical field. The end goal should always be to put the patient first.
Teaching experiences in college inspired me to become a physician educator if I become a doctor. Post-MCAT, I was offered a job by Next Step Test Prep as a tutor to help students one on one for the MCAT. I had a student who stated he was doing well during practice, but couldn’t get the correct answer during practice tests. Working with the student, I pointed out his lack of understanding concepts and this realization helped him and improves his MCAT score. Having the ability to educate the next generation of doctors is not only necessary, but also a rewarding experience.
My experiences volunteering and shadowing doctors in the hospital as well as my understanding of what it means to be a complete physician will make me a good candidate as a medical school student. It is my goal to provide the best care to patients and to put a smile on a family’s face just as my grandfather once had. Achieving this goal does not take a special miracle, but rather hard work, dedication, and an understanding of what it means to be an effective physician.
Through reflecting on various stages of life, Quinn expresses how they found purpose in pursuing medicine. Starting as a child more interested in Pokemon than their grandfather’s patients, Quinn exhibits personal growth through recognizing the importance of their grandfather’s work saving lives and eventually gaining the maturity to work towards this goal as part of a team.
This essay opens with abundant imagery — of the grandfather’s clinic, flowers filling the streets, and the village woman’s difficult labor — which grounds Quinn’s story in their family roots. Yet, the transition from shadowing in hospitals to pursuing leadership positions in high schools is jarring, and the list of athletic and musical accomplishments reads like a laundry list of accomplishments until Quinn neatly wraps them up as evidence of leadership and teamwork skills. Similarly, the section about tutoring, while intended to demonstrate Quinn’s desire to educate future physicians, lacks the emotional resonance necessary to elevate it from another line lifted from their resume.
This essay opens with abundant imagery — of the grandfather's clinic, flowers filling the streets, and the village woman's difficult labor — which grounds Quinn's story in their family roots.
The strongest point of Quinn’s essay is the focus on their unique arts and humanities background. This equips them with a unique perspective necessary to consider issues in medicine in a new light. Through detailing how history and literature coursework informed their unique research, Quinn sets their application apart from the multitude of STEM-focused narratives. Closing the essay with the desire to help others just as their grandfather had, Quinn ties the narrative back to their personal roots.
-- Accepted To: Edinburgh University UCAT Score: 2810 BMAT Score: 4.6, 4.2, 3.5A
Exposure to the medical career from an early age by my father, who would explain diseases of the human body, sparked my interest for Medicine and drove me to seek out work experience. I witnessed the contrast between use of bone saws and drills to gain access to the brain, with subsequent use of delicate instruments and microscopes in neurosurgery. The surgeon's care to remove the tumour, ensuring minimal damage to surrounding healthy brain and his commitment to achieve the best outcome for the patient was inspiring. The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Whilst shadowing a surgical team in Texas, carrying out laparoscopic bariatric procedures, I appreciated the surgeon's dedication to continual professional development and research. I was inspired to carry out an Extended Project Qualification on whether bariatric surgery should be funded by the NHS. By researching current literature beyond my school curriculum, I learnt to assess papers for bias and use reliable sources to make a conclusion on a difficult ethical situation. I know that doctors are required to carry out research and make ethical decisions and so, I want to continue developing these skills during my time at medical school.
The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Attending an Oncology multi-disciplinary team meeting showed me the importance of teamwork in medicine. I saw each team member, with specific areas of expertise, contributing to the discussion and actively listening, and together they formed a holistic plan of action for patients. During my Young Enterprise Award, I facilitated a brainstorm where everyone pitched a product idea. Each member offered a different perspective on the idea and then voted on a product to carry forward in the competition. As a result, we came runners up in the Regional Finals. Furthermore, I started developing my leadership skills, which I improved by doing Duke of Edinburgh Silver and attending a St. John Ambulance Leadership course. In one workshop, similar to the bariatric surgeon I shadowed, I communicated instructions and delegated roles to my team to successfully solve a puzzle. These experiences highlighted the crucial need for teamwork and leadership as a doctor.
Observing a GP, I identified the importance of compassion and empathy. During a consultation with a severely depressed patient, the GP came to the patient's eye level and used a calm, non-judgmental tone of voice, easing her anxieties and allowing her to disclose more information. While volunteering at a care home weekly for two years, I adapted my communication for a resident suffering with dementia who was disconnected from others. I would take her to a quiet environment, speak slowly and in a non-threatening manner, as such, she became talkative, engaged and happier. I recognised that communication and compassion allows doctors to build rapport, gain patients' trust and improve compliance. For two weeks, I shadowed a surgeon performing multiple craniotomies a day. I appreciated the challenges facing doctors including time and stress management needed to deliver high quality care. Organisation, by prioritising patients based on urgency and creating a timetable on the ward round, was key to running the theatre effectively. Similarly, I create to-do-lists and prioritise my academics and extra-curricular activities to maintain a good work-life balance: I am currently preparing for my Grade 8 in Singing, alongside my A-level exams. I also play tennis for the 1st team to relax and enable me to refocus. I wish to continue my hobbies at university, as ways to manage stress.
Through my work experiences and voluntary work, I have gained a realistic understanding of Medicine and its challenges. I have begun to display the necessary skills that I witnessed, such as empathy, leadership and teamwork. The combination of these skills with my fascination for the human body drives me to pursue a place at medical school and a career as a doctor.
This essay traces Alex's personal exploration of medicine through different stages of life, taking a fairly traditional path to the medical school application essay. From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
Alex details how experiences conducting research and working with medical teams have confirmed his interest in medicine. Although the breadth of experiences speaks to the applicant’s interest in medicine, the essay verges on being a regurgitation of the Alex's resume, which does not provide the admissions officer with any new insights or information and ultimately takes away from the essay as a whole. As such, the writing’s lack of voice or unique perspective puts the applicant at risk of sounding middle-of-the-road.
From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
The essay’s organization, however, is one of its strengths — each paragraph provides an example of personal growth through a new experience in medicine. Further, Alex demonstrates his compassion and diligence through detailed stories, which give a reader a glimpse into his values. Through recognizing important skills necessary to be a doctor, Alex demonstrates that he has the mature perspective necessary to embark upon this journey.
What this essay lacks in a unique voice, it makes up for in professionalism and organization. Alex's earnest desire to attend medical school is what makes this essay shine.
-- Accepted To: University of Toronto MCAT Scores: Chemical and Physical Foundations of Biological Systems - 128, Critical Analysis and Reading Skills - 127, Biological and Biochemical Foundations of Living Systems - 127, Psychological, Social, and Biological Foundations of Behavior - 130, Total - 512
Moment of brilliance.
Revelation.
These are all words one would use to describe their motivation by a higher calling to achieve something great. Such an experience is often cited as the reason for students to become physicians; I was not one of these students. Instead of waiting for an event like this, I chose to get involved in the activities that I found most invigorating. Slowly but surely, my interests, hobbies, and experiences inspired me to pursue medicine.
As a medical student, one must possess a solid academic foundation to facilitate an understanding of physical health and illness. Since high school, I found science courses the most appealing and tended to devote most of my time to their exploration. I also enjoyed learning about the music, food, literature, and language of other cultures through Latin and French class. I chose the Medical Sciences program because it allowed for flexibility in course selection. I have studied several scientific disciplines in depth like physiology and pathology while taking classes in sociology, psychology, and classical studies. Such a diverse academic portfolio has strengthened my ability to consider multiple viewpoints and attack problems from several angles. I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
I was motivated to travel as much as possible by learning about other cultures in school. Exposing myself to different environments offered me perspective on universal traits that render us human. I want to pursue medicine because I believe that this principle of commonality relates to medical practice in providing objective and compassionate care for all. Combined with my love for travel, this realization took me to Nepal with Volunteer Abroad (VA) to build a school for a local orphanage (4). The project’s demands required a group of us to work closely as a team to accomplish the task. Rooted in different backgrounds, we often had conflicting perspectives; even a simple task such as bricklaying could stir up an argument because each person had their own approach. However, we discussed why we came to Nepal and reached the conclusion that all we wanted was to build a place of education for the children. Our unifying goal allowed us to reach compromises and truly appreciate the value of teamwork. These skills are vital in a clinical setting, where physicians and other health care professionals need to collaborate as a multidisciplinary team to tackle patients’ physical, emotional, social, and psychological problems.
I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
The insight I gained from my Nepal excursion encouraged me to undertake and develop the role of VA campus representative (4). Unfortunately, many students are not equipped with the resources to volunteer abroad; I raised awareness about local initiatives so everyone had a chance to do their part. I tried to avoid pushing solely for international volunteerism for this reason and also because it can undermine the work of local skilled workers and foster dependency. Nevertheless, I took on this position with VA because I felt that the potential benefits were more significant than the disadvantages. Likewise, doctors must constantly weigh out the pros and cons of a situation to help a patient make the best choice. I tried to dispel fears of traveling abroad by sharing first-hand experiences so that students could make an informed decision. When people approached me regarding unfamiliar placements, I researched their questions and provided them with both answers and a sense of security. I found great fulfillment in addressing the concerns of individuals, and I believe that similar processes could prove invaluable in the practice of medicine.
As part of the Sickkids Summer Research Program, I began to appreciate the value of experimental investigation and evidence-based medicine (23). Responsible for initiating an infant nutrition study at a downtown clinic, I was required to explain the project’s implications and daily protocol to physicians, nurses and phlebotomists. I took anthropometric measurements and blood pressure of children aged 1-10 and asked parents about their and their child’s diet, television habits, physical exercise regimen, and sunlight exposure. On a few occasions, I analyzed and presented a small set of data to my superiors through oral presentations and written documents.
With continuous medical developments, physicians must participate in lifelong learning. More importantly, they can engage in research to further improve the lives of their patients. I encountered a young mother one day at the clinic struggling to complete the study’s questionnaires. After I asked her some questions, she began to open up to me as her anxiety subsided; she then told me that her child suffered from low iron. By talking with the physician and reading a few articles, I recommended a few supplements and iron-rich foods to help her child. This experience in particular helped me realize that I enjoy clinical research and strive to address the concerns of people with whom I interact.
Research is often impeded by a lack of government and private funding. My clinical placement motivated me to become more adept in budgeting, culminating in my role as founding Co-President of the UWO Commerce Club (ICCC) (9). Together, fellow club executives and I worked diligently to get the club ratified, a process that made me aware of the bureaucratic challenges facing new organizations. Although we had a small budget, we found ways of minimizing expenditure on advertising so that we were able to host more speakers who lectured about entrepreneurship and overcoming challenges. Considering the limited space available in hospitals and the rising cost of health care, physicians, too, are often forced to prioritize and manage the needs of their patients.
No one needs a grand revelation to pursue medicine. Although passion is vital, it is irrelevant whether this comes suddenly from a life-altering event or builds up progressively through experience. I enjoyed working in Nepal, managing resources, and being a part of clinical and research teams; medicine will allow me to combine all of these aspects into one wholesome career.
I know with certainty that this is the profession for me.
Jimmy opens this essay hinting that his essay will follow a well-worn path, describing the “big moment” that made him realize why he needed to become a physician. But Jimmy quickly turns the reader’s expectation on its head by stating that he did not have one of those moments. By doing this, Jimmy commands attention and has the reader waiting for an explanation. He soon provides the explanation that doubles as the “thesis” of his essay: Jimmy thinks passion can be built progressively, and Jimmy’s life progression has led him to the medical field.
Jimmy did not make the decision to pursue a career in medicine lightly. Instead he displays through anecdotes that his separate passions — helping others, exploring different walks of life, personal responsibility, and learning constantly, among others — helped Jimmy realize that being a physician was the career for him. By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously. The ability to evaluate multiple options and make an informed, well-reasoned decision is one that bodes well for Jimmy’s medical career.
While in some cases this essay does a lot of “telling,” the comprehensive and decisive walkthrough indicates what Jimmy’s idea of a doctor is. To him, a doctor is someone who is genuinely interested in his work, someone who can empathize and related to his patients, someone who can make important decisions with a clear head, and someone who is always trying to learn more. Just like his decision to work at the VA, Jimmy has broken down the “problem” (what his career should be) and reached a sound conclusion.
By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously.
Additionally, this essay communicates Jimmy’s care for others. While it is not always advisable to list one’s volunteer efforts, each activity Jimmy lists has a direct application to his essay. Further, the sheer amount of philanthropic work that Jimmy does speaks for itself: Jimmy would not have worked at VA, spent a summer with Sickkids, or founded the UWO finance club if he were not passionate about helping others through medicine. Like the VA story, the details of Jimmy’s participation in Sickkids and the UWO continue to show how he has thought about and embodied the principles that a physician needs to be successful.
Jimmy’s essay both breaks common tropes and lives up to them. By framing his “list” of activities with his passion-happens-slowly mindset, Jimmy injects purpose and interest into what could have been a boring and braggadocious essay if it were written differently. Overall, this essay lets the reader know that Jimmy is seriously dedicated to becoming a physician, and both his thoughts and his actions inspire confidence that he will give medical school his all.
The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this content.
- Contributors
- Mission and Values
- Submissions
- The Regulatory Review In Depth

The Future of Technology in Health Care
Alyson diaz , julia englebert , and carson turner.

Scholars discuss the need for federal regulations to combat risks associated with technology in health care.
Most U.S. adults use technology to improve their health—nearly 60 percent browse the Internet for medical information, and over 40 percent obtain care through telemedicine . Despite technology’s health care potential, however, six out of ten Americans are uncomfortable with their health care provider relying on AI to diagnose diseases and recommend treatments.
AI can enhance quality of care by helping physicians verify their diagnoses and detect diseases earlier. For example, researchers have found that AI technology can help predict a patient’s risk of breast cancer. Similarly, a combination of physician expertise and AI algorithms can increase the accuracy of diagnoses.
Yet, AI systems can fail, and if humans rely too much on software, an underlying problem in one algorithm can injure more patients than a single physician’s error. In addition, AI algorithms incorporate biases from available data. For example, Black patients receive , on average, less pain medication than white patients. An algorithm trained to recommend pain treatment from these health records could suggest lower doses of painkillers for Black patients, irrespective of biological needs.
At the same time, technology can help underserved communities gain access to health care. These communities often experience shortages of trained practitioners and standard health care facilities, resulting in higher risk of disease and misdiagnoses. Telehealth, as one example, increases access to quality care by allowing patients to meet with doctors online or have their vitals monitored remotely.
Currently, no federal law regulates the use of AI in health care. Although the U.S. Food and Drug Administration (FDA) reviews most products using technology or AI software on patients, it does not currently make determinations as to whether uses of AI in health care are safe for patients. Instead, FDA approves AI-enabled devices through a process known as 510(k) review . During a 510(k) review, a manufacturer must show that its technology is “substantially equivalent” to a product already available in the market. The process allows AI-enabled devices to be approved without clinical trials proving their safety or accuracy.
Last year, the Biden Administration pledged to oversee the responsible development of AI, including in health-related fields. President Joseph R. Biden’s executive order on the subject includes requirements for health care providers to inform users when the content they provide is AI-generated and not reviewed by a physician. In addition, providers are responsible for mitigating potential risks posed by the technology and ensuring that it expands access to care.
Health professionals have also expressed concern about adolescents self-diagnosing medical conditions discussed by influencers who promote telemedicine on social media. Currently, FDA does not require telemedicine companies to disclose information about potential risks of services, and companies receive free speech protections as “advertisers.”
Advocates for stricter regulation of technology in health care point out that telehealth providers escape regulation by classifying themselves as communication platforms that connect patients with doctors, and not as providers of medical services. Telehealth companies maintain their independence from medical providers, allowing them to avoid legal liability for those providers’ actions.
In this week’s Saturday Seminar, scholars offer varying suggestions on regulating the use of technology in health care.
- AI algorithms are inherently biased, yet no federal regulation addresses the risk of biased diagnostics when AI is used in health care, recent Seattle University School of Law graduate Natalie Shen argues in an article in the Seattle Journal of Technology, Environmental & Innovation Law . Shen explains that in the absence of federal action, states have taken the lead in passing laws to address automated decision systems such as AI in health care. By analyzing New Jersey’s and California’s approaches, Shen recommends improvements to future state legislation, including extending any future law’s coverage to the private health insurance sector, and imposing continuous assessment requirements as AI technology evolves.
- In an article for the Virginia Law Review , Berkeley Law Schools Khiara M. Bridges argues that educating patients about the risk of race-based algorithmic bias should be a prerequisite before using AI in health care. Bridges explains that people of color are more likely to distrust physicians and health care institutions and thus, are likely to be skeptical of medical AI. Furthermore, medical algorithms are developed based on a primarily white “general population,” reducing their predictive accuracy for communities of color, Bridges notes . She argues that disclosure of AI-related risks would foster patient-physician dialogue in communities of color, encouraging more patients of color to use the technology and ultimately remedying existing algorithmic biases.
- Regulation of AI-enabled health tools must include pre-market authorization and continued performance monitoring processes, urge Joana Gonçalves-Sá of Complexity Science Hub and Flávio Pinheiro of NOVA Information Management School in an chapter in Multidisciplinary Perspectives on Artificial Intelligence and the Law . Gonçalves-Sá and Pinheiro propose improvements to FDA’s pilot program, Total Product Lifecycle , which tracks the safety risks of AI. Under the program, an AI company can achieve “precertified status” if it can demonstrate that it develops high quality algorithms and continues to monitor their effectiveness after market entry, Gonçalves-Sá and Pinheiro explain . FDA should also investigate the reliability of datasets and engineers that train AI tools, Gonçalves-Sá and Pinheiro recommend .
- Regulators should lower legal barriers that prevent community organizations such as Black churches from helping poor and marginalized people to gain access to telehealth services, argues Meighan Parker of the University of Chicago Law School in a recent article in the Columbia Science and Technology Law Review . Parker notes that although community organizations such as Black churches could help some people to overcome mistrust of health care providers, involving them could cause conflicts between the churches’ beliefs and patients’ medical needs, or open the churches to malpractice liability. In response, Parker proposes softening or adjusting regulatory barriers to ensure that churches will not face ethical conflict or legal liability for connecting people with needed telehealth services.
- In a note in the Washington Journal of Law, Technology & Arts , Kaitlin Campanini , a student at Pace University Elisabeth Haub School of Law , argues that the U.S. Drug Enforcement Administration’s lax regulation of telehealth providers has worsened inadequate mental health treatment and increased excessive drug prescriptions. Although telehealth providers’ business models can render treatment more convenient and affordable, the expedited treatment model they offer “blurs the line between offering health care to patients and selling controlled substances to customers.” This is because such companies fall into a regulatory gray area. They disclaim providing medical services by maintaining that they are independent from providers. Yet they aggressively market stimulants to consumers and facilitate questionable prescriptions after short, virtual evaluations.
- In a recent note in the Belmont Law Review , J.D. candidate Nora Klein argues that regulators should close legal loopholes that allow direct-to-consumer (DTC) pharmaceutical companies to unfairly influence social media users. Klein notes that DTC pharmaceutical companies have avoided FDA advertising regulations in part by labeling themselves as entities over which FDA has no regulatory authority. Accordingly, these entities are only subject to FTC advertising regulations, which are difficult to enforce, Klein observes . She argues that the DTC model is harmful because it leads to misdiagnoses and patient complications more often than traditional health care services. To address the problem, Klein proposes that FDA require DTC pharmaceutical companies to disclose important drug information to consumers.
The Saturday Seminar is a weekly feature that aims to put into written form the kind of content that would be conveyed in a live seminar involving regulatory experts. Each week, The Regulatory Review publishes a brief overview of a selected regulatory topic and then distills recent research and scholarly writing on that topic.
Related Essays

The Troubled Teen Industry’s Troubling Lack of Oversight
The federal government must step in to regulate an industry fraught with youth abuse.

Reforming Accountable Care Organizations
Experts explore opportunities to reduce costs and promote health equity.

A Review of Health Care in the Court
Several U.S. Supreme Court cases from this past term have significant implications for the provision of medical care.
This paper is in the following e-collection/theme issue:
Published on 16.5.2024 in Vol 26 (2024)
Person-Generated Health Data in Women’s Health: Scoping Review
Authors of this article:

- Jalisa Lynn Karim 1 , BA, BMath ;
- Rachel Wan 1 , BSc, BSN, RN ;
- Rhea S Tabet 2 , BSc ;
- Derek S Chiu 3 , BSc, MSc ;
- Aline Talhouk 1 , BA, MSc, PhD
1 Department of Obstetrics and Gynaecology, University of British Columbia, Vancouver, BC, Canada
2 Department of Pharmacology and Therapeutics, McGill University, Montréal, QC, Canada
3 Department of Molecular Oncology, University of British Columbia, Vancouver, BC, Canada
Corresponding Author:
Aline Talhouk, BA, MSc, PhD
Department of Obstetrics and Gynaecology
University of British Columbia
593 - 828 West 10th Ave
Vancouver, BC, V5Z 1M9
Phone: 1 604 875 3111
Email: [email protected]
Background: The increased pervasiveness of digital health technology is producing large amounts of person-generated health data (PGHD). These data can empower people to monitor their health to promote prevention and management of disease. Women make up one of the largest groups of consumers of digital self-tracking technology.
Objective: In this scoping review, we aimed to (1) identify the different areas of women’s health monitored using PGHD from connected health devices, (2) explore personal metrics collected through these technologies, and (3) synthesize facilitators of and barriers to women’s adoption and use of connected health devices.
Methods: Following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for scoping reviews, we searched 5 databases for articles published between January 1, 2015, and February 29, 2020. Papers were included if they targeted women or female individuals and incorporated digital health tools that collected PGHD outside a clinical setting.
Results: We included a total of 406 papers in this review. Articles on the use of PGHD for women steadily increased from 2015 to 2020. The health areas that the articles focused on spanned several topics, with pregnancy and the postpartum period being the most prevalent followed by cancer. Types of digital health used to collect PGHD included mobile apps, wearables, websites, the Internet of Things or smart devices, 2-way messaging, interactive voice response, and implantable devices. A thematic analysis of 41.4% (168/406) of the papers revealed 6 themes regarding facilitators of and barriers to women’s use of digital health technology for collecting PGHD: (1) accessibility and connectivity, (2) design and functionality, (3) accuracy and credibility, (4) audience and adoption, (5) impact on community and health service, and (6) impact on health and behavior.
Conclusions: Leading up to the COVID-19 pandemic, the adoption of digital health tools to address women’s health concerns was on a steady rise. The prominence of tools related to pregnancy and the postpartum period reflects the strong focus on reproductive health in women’s health research and highlights opportunities for digital technology development in other women’s health topics. Digital health technology was most acceptable when it was relevant to the target audience, was seen as user-friendly, and considered women’s personalization preferences while also ensuring accuracy of measurements and credibility of information. The integration of digital technologies into clinical care will continue to evolve, and factors such as liability and health care provider workload need to be considered. While acknowledging the diversity of individual needs, the use of PGHD can positively impact the self-care management of numerous women’s health journeys. The COVID-19 pandemic has ushered in increased adoption and acceptance of digital health technology. This study could serve as a baseline comparison for how this field has evolved as a result.
International Registered Report Identifier (IRRID): RR2-10.2196/26110
Introduction
The practice of keeping notes to monitor one’s health is not a recent phenomenon. Individuals have long recognized the benefits of tracking various health aspects, including the ability to be more active participants in managing their health, gaining a more complete picture of their health, and reducing the frequency of in-person appointments; however, this tracking was previously done through paper logs [ 1 ]. Today, with the proliferation of digital tools, self-tracking has significantly evolved and become more prevalent. The increasing pervasiveness of technology, particularly mobile phones, has seamlessly integrated it into our daily lives, making self-tracking more accessible and convenient than ever before [ 2 ]. Connected digital health technologies such as smartphones, wearables (eg, smartwatches), sensors, the Internet of Things (eg, internet-enabled weight scales), and web-based applications have permeated society and are increasingly adopted to collect and track health data. In 2021, a total of 87% of Canadians owned a smartphone, up by 73% from 2009 [ 3 ]. With >350,000 digital health apps accessible via these smartphones [ 4 ], approximately two-thirds of Canadians digitally track at least one aspect of their health [ 5 ]; similar statistics have been reported in the United States [ 6 ]. Moreover, since the introduction and popularization of fitness trackers in 2010, sensors and wearable devices have increasingly become part of daily life [ 2 ]. During the global COVID-19 pandemic, self-tracking took on even greater significance [ 7 , 8 ]. With the heightened awareness of health and the need for proactive measures, individuals have turned to self-tracking to monitor their well-being and make informed decisions. With this transformation, self-tracking has transcended its previous boundaries, offering individuals new opportunities to optimize their well-being and ushering in a new era of personalized health care [ 9 - 11 ].
Digital health tools have revolutionized the active and passive collection of health data through various applications and wearable devices. These various digital health tools collect and generate an unprecedented amount of data that can be used to glean insights into one’s health. Person-generated health data (PGHD), which are clinically relevant data captured outside traditional care settings [ 12 ], provide valuable insights that empower users to self-monitor and reflect on their health. PGHD can refer to any data collected from wearable and smart devices as well as self-input information into platforms such as mobile apps and websites. By leveraging digital technologies, individuals can collect and store their health data, enabling them to actively manage their own health and monitor chronic conditions. Furthermore, the integration of these data with research presents an opportunity to improve the patients’ experience and enhance personalized medicine. The recognition of this opportunity has started to take shape with patient-reported outcome measures and patient-reported experience measures being increasingly recognized as essential information to assess quality of care and prioritize patient-centered approaches and with mandatory assessment as part of clinical trials [ 13 ]. Seamlessly linking PGHD that are captured outside traditional care settings with clinical data and disease models can unlock new possibilities for tailored treatments and predictive informatics. The integration of digital health tools not only facilitates patient-provider communication but also offers opportunities for education, increased awareness, self-tracking, and self-monitoring without burdening health care resources. By focusing on the individual’s experience, personalization, and prevention, digital health tools contribute to a patient-centered care paradigm that aims to optimize health care outcomes and improve overall well-being while empowering patients to take charge of their health.
In recent years, the emergence of femtech, defined as technology-driven solutions specifically designed to address women’s health needs and concerns, has revolutionized the landscape of self-tracking and health care for women [ 14 ]. Femtech encompasses a wide range of digital tools, such as period-tracking apps, fertility monitors, pregnancy trackers, and menopause management platforms. These innovative solutions empower women to track and manage their reproductive health, menstrual cycles, and overall well-being with greater accuracy and ease. Femtech has not only provided women with personalized insights into their bodies but has also helped break taboos and encouraged open conversations about topics that were once stigmatized or ignored. The rapid growth of femtech has promoted access to women’s health information, greater autonomy in decision-making, and enhanced overall health care experiences for women worldwide. It has become an integral part of the self-tracking movement, demonstrating the transformative power of technology in promoting women’s health and well-being.
In this study, we reviewed the use of digital tools and PGHD in women’s health research, focusing on articles published between January 1, 2015, and February 29, 2020, before the COVID-19 pandemic. Our review encompassed various connected health devices, which included both passive data collection devices such as wearable sensors and active input devices such as smartphone apps and websites. This review sought to accomplish the following:
- Identify the different areas of women’s health and health-related behaviors monitored using PGHD from connected health devices.
- Explore personal metrics collected through these technologies.
- Synthesize facilitators and barriers that impact women’s adoption and use of connected health devices in managing their health.
This scoping review was conducted based on our previously published protocol [ 15 ]. We adopted the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) guidelines [ 16 ]. The completed checklist is provided in Multimedia Appendix 1 [ 16 ].
Search Strategy
The search strategy was designed in close collaboration with a reference librarian with input from the authors (JLK and AT). We searched a total of 5 databases: MEDLINE, Embase, APA PsycINFO, CINAHL Complete, and Web of Science Core Collection. Initial searches were completed in early March 2020. Searches were limited to articles published in 2015 or later because publications with the keyword “digital health” started to emerge in the literature around that time [ 17 ], and with the fast evolution of the field, previous articles may not be relevant to the current landscape. Keywords and subject headings were designed to search the literature for the intersection of the following 4 topics: women, health, digital devices, and tracking. The full search strategy, including a full list of search terms, was published with the protocol [ 15 ] and is available in Multimedia Appendix 2 .
Eligibility Criteria
We were interested in digital technologies and interventions targeting women and people assigned female at birth. To be included in the review, studies needed to specifically target women, focus on female-only health topics (eg, menstruation), or only include female participants. We included a variety of publication types but excluded conference abstracts and conference reviews, editorials, letters, and comments due to the limited details in such literature.
We excluded articles that presented digital health tools designed for health care providers as we were primarily interested in devices and apps that women can engage with outside a clinical setting. Articles only discussing the use of real-time consultations, whether through video, phone, or web-based chat, were excluded. We excluded articles that described digital health tools used solely for educational purposes; to maintain the focus of the review on tracking or monitoring one’s data for health, devices must have allowed users to input personal health data.
The complete inclusion and exclusion criteria are presented in Textbox 1 . We decided to retain the original inclusion end date of February 29, 2020, to maintain a focus on the literature before the COVID-19 pandemic and avoid potential complexities caused by pandemic-related disruptions in research and health care practices. Concentrating on prepandemic literature also established a clear baseline for future comparisons and allowed us to maintain feasibility of completion without compromising quality given the broad scope of the review.
Inclusion criteria
- Published between January 1, 2015, and February 29, 2020
- Refers to a health issue that pertains only to women or comprises only female participants of any age
- Includes the use of connected health tools for tracking or monitoring some aspect of health, which could include smartphone apps, wearable devices, the Internet of Things (eg, Bluetooth- or internet-enabled glucometers, blood pressure cuffs, and weight scales), and implantable devices
- Involves data collection from the user of the connected health tool (ie, the user either manually inputs data into the device or they are automatically uploaded)
- The user must be able to interact with the app or device on her own at home (outside a clinical setting)
- Available in English
Exclusion criteria
- Not available in English
- Conference abstracts, conference reviews, editorials, letters, or comments
- Study media releases and user reviews of specific applications
- Research conducted on animals
- Research involving male participants
- Tracking of infants and children unless tracking breastfeeding (because breastfeeding is directly related to the mother’s health and body)
- Devices or apps that are meant for health care provider use or use in a clinical setting only or cannot be used independently without a health care provider present
- Digital health tools that are only for educational or informational purposes and do not allow the user to enter or track her own data (ie, no information exchange)
- Telemedicine services (eg, live video consultations with health care providers)
Study Selection
We imported the results from the database searches to the Covidence systematic review software (Veritas Health Innovation). Covidence detected records believed to be duplicates, and these were manually checked before removing them. In addition, some articles were manually recognized as duplicates during the screening process and were subsequently tagged as duplicates and removed. Screening was conducted independently by at least 2 reviewers (JLK, RST, and AT) at both the abstract screening stage and the full-text screening stage. We attempted to contact the corresponding authors of articles that passed abstract screening when we were unable to locate the full text. Conflicts at either stage were discussed and agreed upon among the 3 authors involved in the screening process.
Data Charting and Deviations From the Protocol
The final list of data charting elements is provided in Textbox 2 . Data charting for all elements except for usability and acceptability was conducted using Google Sheets created by the study team. The categories for different data charting options were initially created based on a small subset of articles and were discussed among the authors involved in the charting process. The team met regularly throughout the data charting process to discuss and refine coding categories that best summarized the data. Starting with more granular categories and later combining them into broader concepts was necessary to summarize the number of articles included in this review. For each article included, data were charted by one reviewer (RW or RST) and verified for accuracy by a second reviewer (JLK). Data were summarized in bar graphs, maps, and tables (JLK, RST, and DSC), as presented in the following sections. For the locations, we recorded the countries from which the participants were recruited (if applicable). If an article did not describe recruiting participants, then the countries of the authors were recorded based on the authors’ affiliations.
Article information
- Year of first publication
Study characteristics
- Country or countries in which the research was conducted
- Research study type
Contexts for women’s connected health
- Health areas of focus
Digital device details
- Types of digital health
- Metrics collected by the devices
Usability and acceptability
- Facilitators of and barriers to the use of the technologies (coded into themes)
For the thematic analysis, articles that mentioned any aspect of usability, acceptability, facilitators, or barriers to the use of digital health tools were imported into NVivo (R1 2020; QSR International). Coding was done independently by 2 reviewers (JLK and RW) and then combined through discussions. As with the data charting process, we initially coded more granularly and then grouped the detailed codes together later in the analytic process. Decisions on how to group the codes into themes and subthemes were made through group consensus (JLK, RW, and AT).
In our protocol, we indicated that we would extract the name of the device or app used in each study. While we did complete this step in our data charting, we have not presented the results in this paper. Several articles either did not specify the brand name (eg, only specified that it was a mobile app) or had digital health tools named after the study, so we did not find this information useful to showcase in our results. There were no other deviations from the published protocol.
The searches identified 14,629 records that were imported into the Covidence software for deduplication and screening. After deduplication, a total of 9102 articles were screened for relevance, and 8545 (93.88%) were excluded based on title and abstract. From reading the full texts of the remaining 557 records, an additional 151 (27.1%) were excluded. The most common reasons for exclusion were the inability of study participants to enter or track their own data (58/151, 38.4%) or because the digital health technology was designed to be used by or with a health care provider (48/151, 31.8%). The remaining 406 publications were included in the scoping review. Some of the included publications reported on the same research project; in those cases, all of them were included. Our search did not encounter any articles that directly addressed or mentioned the inclusion of intersex, transgender, or nonbinary participants. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram detailing the full study selection process is shown in Figure 1 . The list of included articles sorted by health areas of focus can be found in Multimedia Appendix 3 [ 18 - 58 ].

Year and Country
There was an increasing trend in number of publications per year, with 10.1% (41/406) of the articles published in 2015, a total of 13.3% (54/406) of the articles published in 2016, a total of 18% (73/406) of the articles published in 2017, a total of 26.4% (107/406) of the articles published in 2018, and 29.6% (120/406) of the articles published in 2019. Only 2.7% (11/406) of the publications were from 2020 because our cutoff date for inclusion was February 29, 2020.
Articles included in the review covered worldwide research, including every continent except Antarctica ( Figure 2 ). As we only considered articles written in English, most of the articles were published in Western, English-speaking countries, primarily the United States (169/406, 41.6% of the articles), the United Kingdom (34/406, 8.4% of the articles), Australia (33/406, 8.1% of the articles), and Canada (19/406, 4.7% of the articles). Other countries where several included articles were published were China (13/406, 3.2% of the articles), the Netherlands (13/406, 3.2% of the articles), Spain (13/406, 3.2% of the articles), and Sweden (10/406, 2.5% of the articles).
Interestingly, of the 169 articles from the United States, 26 (15.4%) specifically focused on African American or Black, ethnic minority, or low-income women. One study from Singapore specifically included multiethnic women [ 18 ], and a study from Australia included Indigenous Australian women as their participants [ 19 ]. In addition, one review conducted by researchers in Australia looked specifically at studies with women from culturally and linguistically diverse backgrounds [ 20 ].

Study Types
The types of studies that used digital health tools in women’s health research are reported in Figure 3 by year of publication (note that the articles could fall into more than one study category). The most common study type encountered was feasibility or acceptability studies (197/406, 48.5% of the articles, including 9/197, 4.6% protocols), followed by effectiveness studies (146/406, 36% of the articles, including 36/146, 24.7% protocols) and publications reporting on digital tool prototypes (73/406, 18% of the articles). Effectiveness studies reported on outcome measures of an intervention, including randomized and nonrandomized trials with one or more study arms. Reviews (of published literature, apps, or wearables), viewpoints, manuals, case studies, or analytical methods (56/406, 13.8% of the articles combined) were also encountered. Observational or correlative studies (44/406, 10.8% of the articles, including 3/44, 7% protocols) were studies that observed the health behaviors of individuals through digital health technologies without assessing the effectiveness of an intervention or analyzed associations between variables (eg, associations between heart rate and loss-of-control eating) [ 21 ]. Finally, measurement studies (23/406, 5.7% of the articles) reported on the validity, reliability, or accuracy of a digital health tool.

Health Areas of Focus
The analysis of the reviewed articles highlighted research in several recurring women’s health areas of focus. A full breakdown of the health areas is reported in Table 1 (articles could fall into more than one health area). Pregnancy and the postpartum period emerged as the most prominent health area with 42.6% (173/406) of the articles. Within this category, there was a specific emphasis on general care and monitoring (45/173, 26% of the articles), physical activity and diet (34/173, 19.7% of the articles), and glucose monitoring (31/173, 17.9% of the articles). Cancer was identified as the second most common health area, with 19.5% (79/406) of the articles dedicated to its exploration. Specifically, a significant focus was observed on the relationship between cancer and cardiovascular health, with 47% (37/79) of the articles addressing this aspect. The impact of lifestyle on overall health and well-being was also addressed, with 14.3% (58/406) of the articles delving into physical activity, sedentary behavior, diet, weight, and obesity. Menstrual, sexual, and reproductive health were explored in 12.1% (49/406) of the articles to shed light on various aspects of women’s reproductive health and associated concerns, with 76% (37/49) focusing on menstrual cycle tracking or fertility monitoring. Furthermore, 9.9% (40/406) of the articles were dedicated to chronic conditions (such as urinary incontinence, osteoporosis, and diabetes) with the aim of enhancing understanding and developing interventions for individuals living with chronic health conditions. To accommodate articles that did not fit within the primary health areas, an Other category comprising 6.4% (26/406) of the articles was established. This category included articles on athlete monitoring (10/26, 38% of the articles), such as heart rate monitoring during sports tournaments; mental health and quality of life (9/26, 35% of the articles); gender-based violence (3/26, 12% of the articles); and more. Finally, a small subset of 0.5% (2/406) of the articles did not align with any specific health area; these included a publication reporting results from a survey on African American women’s willingness to participate in eHealth research [ 22 ] and a publication analyzing women’s interactions with digital health technologies [ 23 ]. These articles were included because, although they did not discuss a specific health area, they still focused on women’s use of digital health tools in general.
a PCOS: polycystic ovary syndrome.
b CVD: cardiovascular disease.
c COPD: chronic obstructive pulmonary disease.
d SLE: systemic lupus erythematosus.
e IC: interstitial cystitis.
f BPS: bladder pain syndrome.
g ABL: accidental bowel leakage.
Figure 4 shows how the health areas of focus for women’s use of digital health changed over the years that were included in the review (2015-2019 plus January 2020-February 2020). There was an increasing trend from 2015 to 2020 in the number of publications focusing on pregnancy and the postpartum period, as well as cancer and menstrual, sexual, and reproductive health. However, articles focused on women’s use of digital health for lifestyle-related topics and chronic conditions did not see a notable increase over those years.

Type of Digital Health and Metrics Collected
Within the articles reviewed, smartphone, mobile, or tablet apps emerged as the most prevalent type of digital health (295/406, 72.7% of the articles), followed by wearable devices (165/406, 40.6% of the articles) and websites or patient portals (93/406, 22.9% of the articles). Other types of technology were not investigated as much. For example, 13.5% (55/406) of the articles addressed smart devices or the Internet of Things (referring to objects with sensors that connect to a network, such as Bluetooth-enabled glucometers and blood pressure machines). Finally, 7.4% (30/406) of the articles reported on 2-way messaging, 1% (4/406) of the articles reported on interactive voice response telephone calls, and only 0.5% (2/406) of the articles reported on implantable devices. With respect to the metrics collected, we found >250 metrics, such as heart rate, number of steps, mood, ovulation test results, and days of menstruation. A full list of the metrics is reported in Multimedia Appendix 4 .
Thematic Analysis
Of the 406 articles included in this scoping review, 168 (41.4%) mentioned usability, acceptability, facilitators, or barriers to the use of digital health tools at least once. Our thematic analysis identified 6 themes: (1) accessibility and connectivity, (2) design and functionality, (3) accuracy and credibility, (4) audience and adoption, (5) impact on community and health service, and (6) impact on health and behavior. The themes are described in further detail in the following sections.
The thematic analysis detailed in the following sections is primarily based on the views of the participants in the studies we reviewed to provide a user perspective; however, one subsection in theme 5 focuses on the health care provider perspective.
Theme 1: Accessibility and Connectivity
The accessibility and connectivity of digital technologies emerged as an important theme with two subthemes: (1) cost and convenience and (2) connectivity, compatibility, and software issues.
Cost and Convenience
Our analysis revealed that the cost and convenience of digital tools collecting PGHD are important factors that can impact their adoption and use. On the one hand, digital health technologies can be seen as more affordable compared to traditional health care visits and more accessible to a wider range of people, including those of a lower socioeconomic status. On the other hand, they can also be perceived as too expensive and novelty items, and associated extra costs such as data plans can also be a barrier for some people. Because PGHD can be collected and entered throughout the day in real time, and because most people carry a phone around with them every day, these technologies offer greater convenience than traditional in-person health care encounters by providing anytime, anywhere virtual access and putting information at people’s fingertips through smartphones and web platforms. One user spoke about an in-app treatment program:
That was what was so good about this, I can do this at home myself, no need to book an appointment, find the time and suit others, and you know, that process of booking a time. [ 24 ]
Some inconvenient aspects of digital health technologies include uncomfortable wearables that are too bulky, difficulty of use, or not fitting into the users’ lifestyles, as noted in one article:
Women also mentioned that the comfort of the wearable sensors was a barrier. Comfort became a barrier for some women during exercise and hot weather. [ 25 ]
Devices with a short battery life and wearables that are not water resistant are also considered inconvenient as they require the user to frequently remember to charge the device or put the wearable back on after water-based activities. Certain restrictions, such as not being able to wear a device in a workplace, can also create inconvenient barriers for some users.
Connectivity, Compatibility, and Software Issues
Factors related to connectivity and other issues such as device synchronization, freezing, or disconnection can significantly impact the user experience and engagement with digital health tools. For example, the dependence on mobile and internet access can be a disadvantage. Cellphone and network coverage limitations can pose an important barrier in rural areas or during travel. Where mobile data or Wi-Fi connection are limited, people may struggle to use digital health tools that require internet connection; this can create disparities in access to health care resources, particularly for those of a lower socioeconomic status or living in remote communities with limited infrastructure. Incompatibility between operating systems such as Android and iOS, iPhone and iPad, or various browsers can also be an important barrier to accessing digital health technology.
Software issues can significantly impact the user experience of digital health technologies. Broken links can prevent users from accessing valuable information or features within apps or websites. App crashes can discourage users from engaging with the digital health tool altogether. In addition, slow loading times can negatively impact the user experience, making it challenging for users to access information or features quickly and efficiently.
Theme 2: Design and Functionality
The second theme centered on design and functionality and included four subthemes: (1) appearance and design; (2) functionality and features; (3) personalization; and (4) safety, privacy, and security.
Appearance and Design
Appearance and design play important roles in the success of connected health devices. In terms of app design, the color scheme and layout facilitate user-friendliness. Bad formatting can make it difficult for users to read or understand the content of an app or website. Font size that is too small can be challenging for those with visual impairments, and some color combinations can be difficult to read. The quality of the images used in digital health interventions can also impact user experience, with low-quality images potentially making it difficult for users to interpret the information being presented.
Apps that are visually appealing and easy to use are more likely to be successful. When it comes to wearables, women tend to prefer sleek, understated designs that are esthetically pleasing without being bulky. A sleek design can encourage use of the wearable. For example, some women consider their wearable to be a fashion item that sparks conversation, which encourages their continued use of the device, as illustrated in a participant quote:
Um, that it’s, like, kind of stylish, like, I feel, like, cool that I wear one. A lot of people ask me, they’re like, oh, which one is that, like, is that a Fitbit, is that an Apple watch? It has the interchangeable bands and stuff like that, so, you can, like, change the color of it and everything. It’s like a conversation piece. [ 26 ]
Other women prefer more discretion in the design of wearables and their size or in the app icon on their mobile device because they do not want to reveal the purpose of the device to others. People may feel self-conscious when wearing the device or using the app, especially if it reveals their medical condition. For example, the following quote is from a study that incorporated a sensor band worn on the wrist to help female undergraduate students with problematic drinking:
P310 noted that while in class, “my professor commented on it which made me feel awkward.” [ 27 ]
Functionality and Features
In terms of functionality, the availability of clinical interpretation of user data is deemed essential, and health warnings based on recorded PGHD are noted to be helpful. Moreover, notifications and reminders are also useful for improving adherence to self-tracking and maintaining goals, and users appreciate receiving automated SMS text messages and feedback on progress. Actionable advice is seen as very important, and women expressed a desire for more interaction and the ability to integrate with other apps. For example, users want the ability to access information from their health record and to be able to see graphical summaries of their data over time. Regarding the presentation of information, users appreciate concise information written in simple language. Choice of words is also perceived as especially important to ensure that the information is easy to understand. People enjoy the gamification of content, and the graphical presentation of results is found to be informative.
The ability to upload multimedia and the ability to customize the application’s displays and notifications are noted as features that improve user engagement and satisfaction. The ability to record voice notes and consultations within apps is noted as a desirable feature, as well as having the option to book appointments directly through apps. Women also want the option to sync their desktop or phone calendar with apps to remind them of medical appointments and prescription requests, as some researchers noted:
Women could see the potential usefulness of being reminded to order their next prescription through the electronic alerts system. They found managing the monthly prescription requests challenging long-term and found setting up the reminder easy with the alert popping up on their phone or tablet. [ 28 ]
The application also allows women to set appointment reminders to ensure she is not missing her appointments and developing gaps in her care [...] “It allows me to remain organized for my visits to my OB with concerns, questions, symptoms I have experienced since my last visit.” [ 29 ]
Issues that negatively impact user engagement and outcomes are the inability to edit information or unsubscribe from notifications, which are sometimes thought to be either inconvenient or intrusive, as well as the presence of advertisements within the app. Ease of use is essential as apps or websites that are difficult to navigate can discourage users from engaging with them. For example, a study including the use of a mobile phone app reported the following:
A hindrance and disliked aspect was the difficulty in navigating through the app (eg, no back button, clunkiness, and the inability of participants to edit their inputted daily goals) as well as a lack of color and visuals within the app, giving it a clinical appearance. [ 30 ]
Some women are not comfortable answering questions that they consider intrusive, such as those related to sexual health. They rely on applications to provide trusted information about their condition and want suggestions for additional resources such as website links and local information.
Personalization
Women generally expressed a desire for greater personalization across several features within digital health tools. Messages and notifications that are personalized to the user’s health and self-tracking history and goals are more motivational and less likely to be ignored or perceived as irritating. Even factors such as using a first name in messages from the app make women feel like the messages are more personal and supportive.
Users have individual preferences when it comes to the frequency and timing of notifications, and it is important for digital health apps to allow for the customization of these settings as they can greatly impact user engagement and adherence. Moreover, users expressed a desire for the ability to customize their goals and the metrics they tracked. For example, they may want to change their goals in an app when their life circumstances change (eg, moving, starting a new job, becoming pregnant, or sustaining an injury). The ability to customize the dashboard of an app or website according to the user’s goals was also expressed as a desired feature. The ability to make these customizations will improve their adherence in the long run as their goals evolve.
When it comes to wearables, their placement on the body influences users’ preference and adherence to their use. For example, some women may prefer a wrist-worn device, whereas others may prefer a chest strap, a ring, or a device worn on the waist or ankle. The type of activity being monitored may also influence placement preference. A wrist-worn device may be more appropriate for monitoring steps, whereas a chest strap may be better suited for monitoring heart rate during exercise. Furthermore, placement preference may also be influenced by factors such as comfort, convenience, and visibility. A user may prefer a wrist-worn device because it is more visible and easier to access, whereas another user may prefer a device worn on the waist because it is less obtrusive and more comfortable during exercise or sleep. For instance, one study found the following:
Eight of the participants (40%) reported at some point of the long study period that the smart wristbands were uncomfortable to wear, especially at night. The wristbands irritated the skin, possibly due to pregnancy-related swelling. [ 31 ]
Finally, users have different preferences for how they want information to be presented in an app or website. Some people prefer to read content that is written out with citations and links to external websites. Others enjoy learning content from videos or audio recordings. When looking at their trends and progress, some users like to look at detailed graphs showing their daily progress, whereas others prefer to look at the data occasionally and only receive high-level information. The challenges concerning personalization were articulated by several authors:
It’s a difficult one. Some women want the full picture to fully understand what they are taking. Others want a black and white sketch, but not the details. They just want to know enough. Others do not want to see the picture, they just want to get on with it without knowing too much. Catering for all is a challenge. [ 28 ]
Safety, Privacy, and Security
Women are sometimes concerned about the physical safety of certain devices. For example, some mothers worried about their wearable wristbands scratching their babies [ 31 ]. Others worried about the effects of wearable devices on their skin, as expressed by a participant:
It’s weird because it does have a little laser thing on it, and I wonder if that’s, like, harming my skin (laughing). Like, I’ll sleep in it, and when I wake up I’ll have a red spot on my arm, it’s itchy sometime or sensitive, and I think it’s because of the laser thing, but I don’t really know. [ 26 ]
Some women are concerned about the privacy and security of digital health technologies and expect appropriate safeguards to be implemented in the tools they use. However, privacy and data security are not a concern for all women:
As I said, I’m very critical about patient data in general, especially in terms of data security...If you have a free app, it really depends on what happens to the private data. As a matter of fact, usually the information is stored on the app itself, and so other apps might gain access to the data easily. [ 32 ]
The survey revealed a low level of concern about issues relating to privacy or security of personal data. This suggests that privacy concerns were secondary to the benefits offered by uploading personal details into apps to provide the type of customisation they seek. [ 33 ]
Researchers also shared that some users perceived there to be more privacy when using an app as compared to traditional ways of communicating:
Some participants perceived the storage of their glucose levels on the smartphone as more secure than their current registration in a booklet. [ 34 ]
Women, particularly those who worked outside of the home, also commented that they appreciated the added convenience and privacy of this [text-based] communication method over phone-based communication. [ 34 ]
Theme 3: Accuracy and Credibility
In theme 3, we identified accuracy and credibility as important factors for acceptability considerations in digital health technologies.
The accuracy of digital health can impact user trust and adoption. Digital health tools enable users to keep track of their health, symptoms, and behaviors over time without relying on memory recall, which can be inaccurate or incomplete. Many studies reported that digital tracking can lead to more accurate data collection compared to paper-based methods. For example, at-home measurements of blood pressure and other vital signs have been found to be more accurate than those taken in a hospital or clinic setting. In some cases, apps are even able to accurately predict users’ menstrual cycles and mood changes. In addition, food diaries and activity trackers are often found to be more accurate when tracked within the app compared to using traditional paper-based methods. As the following participant conveyed, digital health may also make it easier for patients to tell the truth about their habits or health concerns:
I like this principle because...I know exactly, that via tablet one would admit things you wouldn’t necessarily tell the doctor or nurse. So, for starters, you can state it in the application. Of course, a conversation shouldn’t be missed afterwards, but this might make it easier for you to overcome yourself. [ 32 ]
However, accuracy can still be an issue in digital health. Different devices can produce different measurements, and some devices may miscount steps, the intensity of workouts, or the quantity and quality of sleep. For example, some women reported devices not tracking their steps while pushing a grocery cart or stroller, whereas others found that their steps were overcounted due to arm movements while they were seated. In addition, some users reported that food tracking options in apps were limited and did not include foods from their culture. Therefore, users may perceive digital health tools as not being representative of their true activity, which may lead them to discontinue the use of the devices. The following participant quote refers to a wrist-worn activity tracker:
Out paddling and we’re huffing and puffing and barely breathing and this isn’t even triggering anything. So it shows [...] that our 150 minute goal is like 60 or half of that. But we’ve actually put in the effort and then you just give up after a while. Like there’s no way I can make this. [ 35 ]
Women often prefer evidence-based health information (eg, explanations of conditions and symptoms and health advice) from a trustworthy source, such as an app curated from up-to-date and evidence-based research, over general internet searches. Users reported that the information provided in some apps was incomplete or inaccurate, with gaps in content or contradictory information that diminished their trustworthiness. In such cases, users may still prefer to talk to a health professional for more trustworthy information. Some women may also find it challenging to trust information that does not disclose sources as they are unsure of its reliability. Devices that are endorsed by, cite, and link to trustworthy health sources are more appealing to users. When sharing results from a web-based survey, the authors of one study reported the following:
Some respondents were specific about from where such advice should come, stating that they wanted expert, credible and up-to-date advice while others noted that they would like to see more Australian-specific or locally-based information in apps or apps that were not linked to the manufacturers of pregnancy or baby products. [ 33 ]
Theme 4: Audience and Adoption
Our fourth theme concerns audience and adoption, which includes two subthemes: (1) demographics and inclusivity and (2) timing and circumstances.
Demographics and Inclusivity
One of the challenges with digital health is to avoid one-size-fits-all interventions and to strive to tailor interventions to address the specific needs of different populations. Digital health that targets specific demographic groups or specific health conditions may increase the adoption of digital tools in those populations. That said, even when targeting people with specific health conditions as the audience, attention must be paid to the language and content in apps and websites. Some researchers noted that women did not want to participate or continue in their study because they did not want to constantly be confronted with their disease. Too much of a focus on disease and ill health can deter women from engaging with the tools, as commented on by some authors:
All but one participant preferred text content that focused on health and physical activity rather than content explicit to cancer. [ 36 ]
The women emphasized that less attention should be paid to chronic disease management and medication as the only treatment option. [...] it was important to explain the implications of the result of the scan and the risk of fractures in a way that will not place the women in a sickness role unnecessarily. [...] The knowledge base of osteoporosis should focus on osteoporosis as a common condition instead of a chronic bone disease. [ 37 ]
Younger women are often more familiar with and more comfortable using digital technology and, therefore, are more likely to use and adhere to a digital health protocol. Users with low technology skills want more training on how to use the digital health tools properly. Little provision is made for those for whom English is not their primary language, which can limit the accessibility and usefulness of digital health interventions. Factors such as language barriers, cultural beliefs, or lack of access to technology may lead to less adoption by some people belonging to ethnic minority groups. The relevance and usefulness of digital health may also vary based on geographic location.
Digital health tools are negatively perceived by some users if not designed to be inclusive of attributes such as body type or gender. For example, users prefer applications that use pictures or models that represent a diverse range of body sizes. Digital health technologies may not be gender inclusive and can conflate sex and gender. It is important to consider the unique health needs and experiences of individuals across the gender spectrum, as several researchers reported:
Participants commented on an exercise demonstration video and recommended that the model should have an “everyday-look” (e.g. plain clothes, jewellery). Also a choice of models of different ages to engage a wider range of patients and help them to relate or identify with the model was proposed. [ 38 ]
[Participant quote]: Maybe the body image it presents...like on a lot of apps, the people doing it looked like they were athletes already. And maybe they should have more people that look normal. [ 39 ]
Two women commented on the gendered design of most FTAs. FTA092 commented that “I chose Clue because it’s the only app that wasn’t pink.” FTA051 also found the gendered design of her previous app insulting; “my last app had a pink flower and was called MyDays or something ...I felt like they were trying to lure me in with this kind of ‘women’s’ approach” (FTA051). She subsequently stopped using that app and downloaded Clue. [ 40 ]
Timing and Circumstances
Individuals are more motivated to use digital health tools during times of illness or when they have a specific health goal in mind. The introduction of technology at the appropriate time impacts the utility and effectiveness of digital health interventions, especially when they are integrated into existing health care systems and routines. Digital health apps need to account for existing medical conditions or medical history to ensure accurate and complete information. For example, technologies that do not provide an option to indicate current pregnancy are perceived as frustrating to users as the in-app goals or notifications can be irrelevant and inconsiderate of their current limitations. In a focus group, one mother shared the following:
I get frustrated with the Garmin [smartwatch] because I wear my watch during the night so it tracks my sleeping as well. Then it gives you like an insight—so a little note will pop up and you know whether your sleep has been really regular or you’ve had irregular sleep. I wish that there was a thing that during pregnancy where that I could put in and say I’m pregnant, because I got those notes that your sleep is really irregular, and I was like, “Because I’m pregnant!” [ 23 ]
Users who are not experiencing symptoms or who perceive their health to be good are less likely to adopt digital health tools as they may not perceive any benefit from using them. Moreover, those who are already tracking their health using other methods (eg, paper-based tracking) are less interested in trying a new digital health tool. Similarly, regarding wearables, some people may already have a wearable and be less interested in having an additional wearable device.

Theme 5: Impact on Community and Health Service
This theme considers the impact of PGHD on community and health service, with three subthemes: (1) communication and community support, (2) clinical integration, and (3) health care provider perspective.
Communication and Community Support
One of the many perceived benefits by users of digital health interventions is the sense of community that these platforms enable. Even though some women reported feeling uncomfortable sharing personal information with strangers in a virtual group, most found that the ability to connect with others who shared similar experiences provided a sense of belonging and support that was motivating and reassuring, as shared by one woman:
What I did love about the apps is the forums. So if you have a weird pain or, you know, you have cramp in your legs at three a.m., you can get on your phone straight away, and you can get support by the women who are going through the same thing. [ 41 ]
Discussion forums and social media platforms associated with digital health interventions are perceived as helpful for connecting with others, sharing personal stories, and receiving support. Digital health interventions can also help women elicit support from friends and family to stay motivated and achieve health goals. For example, researchers who reported on women’s experiences of an app for stress urinary incontinence shared that some participants found it easier to talk to friends about an app for pelvic floor muscle training rather than talk about incontinence [ 24 ]. This can enable increased accountability and further encourage adherence to the intervention. One woman spoke about how her family supported her engagement with a digital health intervention for physical activity maintenance among female cancer survivors:
My husband’s a good motivator. When I say I’m going for a walk, he’ll go with me...with my sister-in-law and her kids, it’s they want to go with me; so it’s how many steps have you got today? Or, are we going to go for a walk. That kind of thing. And with my husband and my daughter it’s, “how many steps did you get today, did you do your workout, let us get it going.” [ 36 ]
In addition to support from family, friends, and community members, these digital platforms can provide an alternative to speaking with a health care provider in person. Asynchronous communication with health care providers is helpful especially for those who may not have easy access to in-person visits or for those who are uncomfortable discussing sensitive information face-to-face. Records of PGHD can also improve the ability to gather and share details with health care providers about symptoms that are difficult to remember during an in-person visit.
Clinical Integration
Women are more willing to participate in digital health interventions if they perceive that they have a direct impact on their clinical care. They appreciate the idea that their health is being monitored and that someone is keeping an eye on their data. Furthermore, women want to see more integration of their clinical test results within their digital health apps and websites. This increases their motivation to adhere to the interventions prescribed through the digital health application.
It was noted that physicians and other health care providers play a crucial role in promoting the use of digital health interventions among patients. As noted in the following participant quote, women enjoy being able to communicate with a health care provider through digital health:
I like it because you can tell the doctor what’s going on and submit it to your doctor, that is the main reason I like it because you can talk directly to your doctor and tell them what is going on without going in or calling. [ 42 ]
Women are more likely to adopt and use technology if it is recommended by their health care providers, family members, or friends. Women reported that digital health interventions were more effective when they were supported by a health care team. For example, having access to a health coach or counselor or receiving feedback from a health care provider on their progress increases their motivation to adhere to the interventions. This support also provides reassurance that they are on the right track toward achieving their health goals. However, some patients become frustrated when they receive conflicting advice from the digital health tool and their health care provider.
Health Care Provider Perspective
Some articles included thoughts from health care providers on digital health tools collecting PGHD [ 20 , 37 , 43 - 55 ]. From the health care provider perspective, digital health can offer several benefits, including the ability to monitor patients’ adherence to treatment and interventions. This can be particularly helpful for patients with chronic conditions that require ongoing management. Providers can use digital health tools to track patients’ progress and identify any potential issues that may require further attention, which can lead to improved clinical outcomes and reduce unnecessary consultations. For instance, one provider learned about their patient’s anxiousness through a mobile health intervention:
I didn’t know my patient was feeling anxious...But when she wrote it down, we could talk about it... [ 43 ]
Some health care providers expressed that digital health tracking could give them a more accurate picture of their patients’ activities and adherence to treatments. In a study about perspectives on a sensor attached to pills that can send data such as date and time of ingestion, a provider commented the following:
A positive would be data and getting a better grip on compliance. (...) I’m making sure the patient is adhering - assuming that the patient is taking everything inside of that blister, you can have confirmation of that. [ 44 ]
In addition, digital health can improve the efficiency of care delivery by providing education and resources directly to patients. This can help patients better understand their condition, treatment options, and self-management strategies, which can lead to better health outcomes.
However, it was also noted that digital health interventions should not replace in-person visits but rather complement them. Some health care providers are concerned about overreliance on digital health tools as well as the potential for misinterpretation of the data they provide. There may be a lack of feedback on the correct use of interventions, such as interpretations of medical advice provided, and health care providers have raised concerns about the safety and trustworthiness of the medical advice generated by the digital health tools. Health care providers especially worry about medico-legal effects of having information from digital health tools taken out of context or without considering the full picture of the user’s history and health, as demonstrated in the following quotes:
As a health care professional, I’m just mindful that if there was a video of me up there talking, if that was taken out of context or shared with another person where that information was not appropriate, that’s a concern to me. [ 45 ]
One anesthesiologist raised, “Who has access to the responses that I provide? Because if a patient receives information from me which they hold onto and is taken out of context, in a medical–legal situation, then that’s a big issue as well.” [ 46 ]
Providers may also find that the abundance of information generated by digital health tools can be overwhelming and time-consuming to manage, adding to an already hectic workflow and blurring professional boundaries. Large volumes of alerts and notifications from digital health tools can be disruptive to health care providers, who expressed the need to set boundaries regarding how and when they engaged with digital health tools. In a study reporting on perspectives about digital health from key informants (health care providers and researchers), one participant shared their thoughts on the potential for digital health to increase workload and liability:
Sometimes the more information that we provide for them (doctors), the more work and liability we give them, right? So if they get so much information that becomes actionable but they are overwhelmed, now they would be obligated to do something with this patient, they are in a chain of distribution, a chain of liability. [ 44 ]
Theme 6: Impact on Health and Behavior
Finally, our sixth theme describes the impact of PGHD on health and health behaviors.
Several studies reported that digital health interventions helped users stay motivated and, in turn, improved their health habits and behaviors, such as adherence to medication, physical activity, and healthy eating. The ability of users to look back at their data helps them identify patterns in their health and behaviors, which increases their awareness of their health and habits. The awareness then allows them to be more mindful of their habits and encourages self-reflection, thus promoting a deeper understanding of their health and well-being. The tracking of patterns in their health, combined with the educational component of some digital health tools, helps users come up with better self-management strategies and feel more confident in their ability to reach their health goals, giving them a greater sense of self-efficacy and control over their health. In a digital health intervention aimed at treating lymphedema following breast cancer treatment, a participant spoke of changes in her awareness of symptoms and improvements:
It helped me realize that I had excess fluid. My arms got lighter each time I did the exercises. My arms began to feel less heavy. It noticed it in my clothes as well. [ 56 ]
Digital health interventions are often reported to positively impact the mental health and well-being of individuals. Women reported improvements in their mood, emotional state, and coping abilities. They also reported a reduction in stress and anxiety levels, which can lead to improvements in overall health outcomes. The digital health tools provide users with a sense of support and accountability as well as feelings of accomplishment when meeting their goals.
However, it is important to note that, while digital health interventions can have many benefits, they may not be suitable for everyone and may even have negative effects on some individuals. For example, some users reported increased anxiety due to excessive monitoring or notifications, and others reported negative effects on their thoughts or worsening of symptoms related to health conditions. Some users found that self-tracking made them more attached to their phones, less likely to engage in social activities, and more isolated overall. Care should be taken to ensure that users do not become obsessive about self-tracking as this can be counterproductive or even harmful. Being hyperfocused on their symptoms or health condition could be distressing and even detrimental to their overall well-being. Therefore, it is important to carefully monitor the use of digital health interventions and adjust them as needed to ensure the best possible outcomes for each individual. One woman spoke about her overreliance on an app used to track breastfeeding:
I stopped using it because um I thought I’m being too anal about this...being too concerned about it, I just need to stress less, and just go with the flow and just be a bit more relaxed about it...so, that’s why I stopped using it completely, and then I think the breastfeeding improved from there ’cause I was worrying about it less. [ 57 ]
Table 2 provides a summary of the thematic analysis grouped into barriers and facilitators. It is worth noting that many things are both a barrier and a facilitator (eg, cost) depending on the individual. In addition, the presence of a specific feature may be a facilitator, whereas the absence of it may be a barrier.
Principal Findings
In this scoping review, we summarized information from 406 articles on digital technologies collecting PGHD and how they have been used in women’s health research. We found a steady increase in articles meeting our inclusion criteria from 2015 to 2020, indicating an increasing trend in the uptake and use of digital health tools in women’s health research before the COVID-19 pandemic. Most included studies (310/406, 76.4%) were feasibility or acceptability studies, effectiveness studies, or reports of digital tool prototypes. Most studies (299/406, 73.6%) focused on tracking conditions related to pregnancy or the postpartum period, cancer survivorship, or menstrual, sexual, and reproductive health. Several types of digital health were represented, with the most common being apps, wearable devices, and websites or patient portals. Through our thematic analysis, we found several considerations of facilitators of and barriers to using digital health tools, including the accessibility and convenience of the tools, visual appearance, device functionality and ability to personalize the user experience, and accuracy of the algorithms and information provided. It is also important to consider the target audience to optimize the adoption of the tools. Engagement with digital health tools may help users improve their health and health-related behaviors and gather support from friends, family, and other digital health users. Women are more likely to use digital health if it is recommended by a health care provider, but there are both benefits and challenges that health care providers may face if considering integrating digital health technology into clinical practice.
A previously published scoping review focused on information and communications technologies as a tool for women’s empowerment [ 59 ]. They reported that the concept of empowerment appeared in various ways with no clear consensus on the definition, with some studies mentioning terms such as self-concept, self-esteem, self-worth, and self-efficacy. Our thematic analysis also found that some women’s use of digital health tools increases their self-efficacy in managing their health. Another systematic review of 13 digital health interventions for midlife women found that many interventions did not use a specific behavior change theory [ 60 ]. Our scoping review did not examine the effectiveness of the interventions described, but those designing digital health tools and interventions may want to carefully consider behavioral theories in the design to increase adoption and retention rates and adherence to interventions.
Overall, digital health technology to collect PGHD has gained popularity over the past several years. The integration of wearables, smartphones, and digital health technologies has enabled the integration of passive data collection. This wealth of data provides valuable insights into various aspects of health, enabling informed decisions and the adoption of proactive measures to improve well-being. The uptake of this technology will usher in a new era in how we manage our health and well-being. This transformation has changed how we engage with our health and shifted our perception of health and the approach we take toward maintaining it.
Femtech, as a subset of digital health technology, has grown in popularity. This was evidenced by the large increase in the number of articles published between 2015 and 2020 that used digital health tools to track metrics during pregnancy and the postpartum period as well as metrics related to menstrual, sexual, and reproductive health. These technologies empower women and people assigned female at birth to take charge of their health. This is particularly relevant for people with conditions that are not diseases or health concerns per se but are nevertheless part of managing their overall health and well-being. In this way, femtech can provide a greater sense of control over reproductive health and choices, which can be precarious in many settings worldwide. However, in a previous scoping review, researchers reported that many mobile health apps do not follow data privacy, sharing, and security standards [ 61 ]. Issues related to the privacy and security of personal health data may be especially important when it comes to tracking reproductive health in settings where sexual and reproductive health rights are not guaranteed. This focus on pregnancy and reproductive health is consistent with the fact that women’s health research has largely focused on reproductive health topics [ 62 ]. Researchers and digital health developers must address gaps in women’s health regarding areas that are not strictly related to reproductive health. Women’s health encompasses much more than obstetrics and gynecology; even for health conditions that affect men and women, there may be sex or gender differences in disease presentation, personal experiences, and treatment plans. While using gendered language and design in femtech has the potential to reinforce stereotypes regarding femininity that could cause harm [ 63 ], there is a need for apps to provide content relevant to female populations while being gender inclusive and conscious of biases in the language and advice presented.
When analyzing themes related to acceptability, personalization emerged as a key aspect influencing the adoption and sustained use of digital health tools. People respond positively and want to engage with tools that cater to their unique needs and preferences. The ability to customize elements such as the frequency of notifications, specific health measures tracked and displayed, goal-setting options, and the amount of health information provided enhanced user engagement and motivation. However, offering too many personalization options might overwhelm users, making apps or devices cumbersome to use and navigate. Simplicity and ease of use should not be compromised in the pursuit of personalization. Creating personalized experiences that are intuitive and user-friendly while integrating multiple functionalities into a given device is an important consideration. Recognizing that a “one-size-fits-all” approach is inadequate, digital intervention designers need to define their target audience clearly. Apps that cater to specific groups, such as those with certain chronic health conditions, may inherently provide a sense of personalization by addressing their unique requirements. We have also learned the importance of ensuring that the design is inclusive and accessible to everyone within the target audience. Our findings that some tools are not sensitive to certain circumstances such as pregnancy are consistent with those of a systematic review of digital health interventions for postpartum women, in which the authors reported that barriers related to postpartum status could make it more difficult to engage with the interventions [ 58 ]. Tools designed with these circumstances in mind may be more engaging for women during pregnancy and the postpartum period, leading to greater adoption and quality of the technologies. Attrition can be high among users of digital health interventions [ 64 , 65 ], but most participants were willing to self-track when motivated by a specific health condition.
An important finding of this review was the growing demand and expectation that PGHD are integrated with clinical care. As digital health continues evolving, patients seek more seamless interactions between digital health data and health care providers. Moreover, services delivered through digital health technologies were not expected to replace the role of health care professionals but rather to be a useful tool to support health care management. Maintaining the human touch during communication for health care delivery was seen as important, with technology complementing clinical care to enhance the overall experience for patients and providers.
One of the critical considerations in clinical integration is the accuracy of PGHD collected from digital health tools. Ensuring the reliability and validity of the data is essential for effective clinical decision-making. Striking a balance between patient empowerment and health care provider oversight is crucial to achieving the best possible outcomes. In general, it is important for health care providers to actively propose digital health during patient visits and encourage its use. While challenges and concerns associated with the use of digital health are noted from health care providers’ perspective, such as concerns about medico-legal effects, maintaining professional boundaries, and not adding an abundance of work, the benefits of these tools in supporting patient care and improving outcomes are perceived as important.
Strengths, Limitations, and Future Directions
There are some limitations to this scoping review. Our inclusion criteria did not cover conference abstracts, conference reviews, editorials, letters, comments, or gray literature. Our review also did not include articles written in languages other than English. Therefore, there may be other uses of PGHD in women’s health that were not captured in this review. The assessments of the quality of included articles, the effectiveness of the interventions, or the accuracy in validating PGHD were outside this review’s scope and were not performed. Our aim was to provide a broad overview of PGHD in published women’s health research literature rather than evaluating the quality of the digital technologies or intervention effectiveness. Another limitation is the rapid growth of digital health and femtech, especially during the COVID-19 pandemic. It is important to note that this scoping review only captures the use of PGHD in women’s health before the emergence of the pandemic. We suggest that this review may provide a baseline for comparison in a future scoping review that captures articles published in March 2020 or later. The strengths of this review include the large number of publications analyzed and the data charting process conducted in duplicate by 2 reviewers. The broad scope of this review also helps provide an overall picture of digital health for women and highlights gaps in the research literature.
Future endeavors in this space should consider digital health tools for women for nonreproductive topics such as chronic health conditions that primarily affect women or conditions that have sex or gender differences in presentation and treatment. Within reproductive health, there was a large focus on pregnancy, but there is an unmet need for research and digital health tools appropriate for women in perimenopause and menopause. A previous literature review found <5 articles published between 2010 and 2020 about digital health technologies that meet the psychosocial needs of women experiencing menopause [ 66 ]. There may also be further opportunities for digital health tools geared toward specific racial or ethnic groups that are culturally sensitive and available in multiple languages. A systematic review found that barriers to the use of digital health among culturally and linguistically diverse populations include lower literacy levels and the use of complex medical terminology in some apps, lack of recognition of cultural concerns, stereotypes, and inaccurate portrayals of cultural groups [ 67 ]. Previous scoping reviews in the space of women’s digital health have identified the need for femtech to pay more attention to cultural appropriateness and consider cultural contexts in their design [ 68 , 69 ].
Conclusions
In conclusion, the integration of wearables, smartphones, and other forms of digital health has revolutionized how we approach and engage with our health. Personalization, inclusivity, and integration with clinical care are vital aspects of developing effective digital health solutions. By understanding the needs of the target audience, providing meaningful personalization, and ensuring data accuracy, digital health can truly transform health care and empower individuals to take charge of their well-being while maintaining a collaborative relationship with health care professionals.
Acknowledgments
Thank you to Shannon Cheng, reference librarian, for her work in developing the search strategy and conducting the database searches. A big thank you to Dr Beth Payne for reviewing the manuscript draft and providing helpful feedback. AT is funded by a Michael Smith Health Research British Columbia Scholar award.
Data Availability
The data sets generated during this study are available in the OSF repository [ 70 ].
Authors' Contributions
JLK and AT conceived the study and designed the study protocol. JLK, RST, and AT conducted the article screening. JLK, RW, and RST conducted the data charting. JLK, RST, and DSC created the visualizations and tables of the charted data. The thematic analysis coding was conducted by JLK and RW, with additional discussions with AT in refining the themes. JLK, RST, and AT wrote the draft of the manuscript. All authors reviewed the manuscript before submission.
Conflicts of Interest
None declared.
PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) checklist.
Full search strategy.
List of included articles by health area.
Metrics collected in the included studies.
- Conceptualizing a data infrastructure for the capture, use, and sharing of patient-generated health data in care delivery and research through 2024. The Office of the National Coordinator for Health Information Technology. Jan 2018. URL: https://www.healthit.gov/sites/default/files/onc_pghd_final_white_paper.pdf [accessed 2024-05-03]
- DeSilva J, Prensky-Pomeranz R, Zweig M. Digital health consumer adoption report 2020. RockHealth. Feb 26, 2021. URL: https://rockhealth.com/insights/digital-health-consumer-adoption-report-2020 [accessed 2024-05-03]
- Taylor P. Penetration of mobile devices in Canada as share of the population from 2009 to 2021. Statista. URL: https://www.statista.com/statistics/462386/mobile-device-penetration-canada [accessed 2024-05-03]
- Olsen E. Digital health apps balloon to more than 350,000 available on the market, according to IQVIA report. MobiHealthNews. Aug 4, 2021. URL: https://www.mobihealthnews.com/news/digital-health-apps-balloon-more-350000-available-market-according-iqvia-report [accessed 2024-05-03]
- Paré G, Leaver C, Bourget C. Diffusion of the digital health self-tracking movement in Canada: results of a national survey. J Med Internet Res. May 02, 2018;20(5):e177. [ CrossRef ] [ Medline ]
- Fox S, Duggan M. Tracking for health. Pew Research Center. Jan 28, 2013. URL: https://www.pewresearch.org/internet/wp-content/uploads/sites/9/media/Files/Reports/2013/PIP_TrackingforHealth-with-appendix.pdf [accessed 2024-05-03]
- Peek N, Sujan M, Scott P. Digital health and care in pandemic times: impact of COVID-19. BMJ Health Care Inform. Jun 2020;27(1):e100166. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Budd J, Miller BS, Manning EM, Lampos V, Zhuang M, Edelstein M, et al. Digital technologies in the public-health response to COVID-19. Nat Med. Aug 2020;26(8):1183-1192. [ CrossRef ] [ Medline ]
- Bruining N. The post-pandemic legacy: the breakthrough of digital health and telemedicine. Cardiovasc Res. Jul 27, 2021;117(9):e118-e119. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Meskó B. COVID-19's impact on digital health adoption: the growing gap between a technological and a cultural transformation. JMIR Hum Factors. Sep 19, 2022;9(3):e38926. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kim KK, Jalil S, Ngo V. Improving self-management and care coordination with person-generated health data and mobile health. In: Edmunds M, Hass C, Holve E, editors. Consumer Informatics and Digital Health. Cham, Switzerland. Springer; Jan 18, 2019.
- Shapiro M, Johnston D, Wald J, Mon D. Patient-generated health data. White paper. RTI International. 2012. URL: https://www.rti.org/publication/patient-generated-health-data-white-paper [accessed 2024-05-03]
- Vodicka E, Kim K, Devine EB, Gnanasakthy A, Scoggins JF, Patrick DL. Inclusion of patient-reported outcome measures in registered clinical trials: evidence from ClinicalTrials.gov (2007-2013). Contemp Clin Trials. Jul 2015;43:1-9. [ CrossRef ] [ Medline ]
- Femtech—time for a digital revolution in the women’s health market. Frost & Sullivan. Jan 31, 2018. URL: https://www.frost.com/frost-perspectives/femtechtime-digital-revolution-womens-health-market [accessed 2024-05-03]
- Karim JL, Talhouk A. Person-generated health data in women's health: protocol for a scoping review. JMIR Res Protoc. May 28, 2021;10(5):e26110. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. Oct 02, 2018;169(7):467-473. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ahmadvand A, Kavanagh D, Clark M, Drennan J, Nissen L. Trends and visibility of "digital health" as a keyword in articles by JMIR publications in the new millennium: bibliographic-bibliometric analysis. J Med Internet Res. Dec 19, 2019;21(12):e10477. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lau Y, Cheng LJ, Chi C, Tsai C, Ong KW, Ho-Lim SS, et al. Development of a healthy lifestyle mobile app for overweight pregnant women: qualitative study. JMIR Mhealth Uhealth. Apr 23, 2018;6(4):e91. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Maxwell H, O’Shea M, Stronach M, Pearce S. Empowerment through digital health trackers: an exploration of Indigenous Australian women and physical activity in leisure settings. Ann Leis Res. Oct 04, 2019;24(1):150-167. [ CrossRef ]
- Hughson JP, Daly JO, Woodward-Kron R, Hajek J, Story D. The rise of pregnancy apps and the implications for culturally and linguistically diverse women: narrative review. JMIR Mhealth Uhealth. Nov 16, 2018;6(11):e189. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ranzenhofer LM, Engel SG, Crosby RD, Haigney M, Anderson M, McCaffery JM, et al. Real-time assessment of heart rate variability and loss of control eating in adolescent girls: a pilot study. Int J Eat Disord. Feb 2016;49(2):197-201. [ FREE Full text ] [ CrossRef ] [ Medline ]
- James DC, Harville C2, Whitehead N, Stellefson M, Dodani S, Sears C. Willingness of African American women to participate in e-Health/m-Health research. Telemed J E Health. Mar 2016;22(3):191-197. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lupton D, Maslen S. The more-than-human sensorium: sensory engagements with digital self-tracking technologies. Senses Soc. Jul 25, 2018;13(2):190-202. [ CrossRef ]
- Asklund I, Samuelsson E, Hamberg K, Umefjord G, Sjöström M. User experience of an app-based treatment for stress urinary incontinence: qualitative interview study. J Med Internet Res. Mar 14, 2019;21(3):e11296. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Huberty J, Ehlers DK, Kurka J, Ainsworth B, Buman M. Feasibility of three wearable sensors for 24 hour monitoring in middle-aged women. BMC Womens Health. Jul 30, 2015;15:55. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Haney AC. Young female college millennials' intent for behavior change with wearable fitness technology. Walden University. 2018. URL: https://scholarworks.waldenu.edu/dissertations/5197/ [accessed 2020-04-11]
- Leonard NR, Silverman M, Sherpa DP, Naegle MA, Kim H, Coffman DL, et al. Mobile health technology using a wearable sensorband for female college students with problem drinking: an acceptability and feasibility study. JMIR Mhealth Uhealth. Jul 07, 2017;5(7):e90. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Brett J, Boulton M, Watson E. Development of an e-health app to support women prescribed adjuvant endocrine therapy after treatment for breast cancer. Patient Prefer Adherence. Dec 11, 2018;12:2639-2647. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chaudhry BM. Expecting great expectations when expecting. Mhealth. Jan 10, 2018;4:2. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mann D, Riddell L, Lim K, Byrne LK, Nowson C, Rigo M, et al. Mobile phone app aimed at improving iron intake and bioavailability in premenopausal women: a qualitative evaluation. JMIR Mhealth Uhealth. Sep 28, 2015;3(3):e92. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Grym K, Niela-Vilén H, Ekholm E, Hamari L, Azimi I, Rahmani A, et al. Feasibility of smart wristbands for continuous monitoring during pregnancy and one month after birth. BMC Pregnancy Childbirth. Jan 17, 2019;19(1):34. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Goetz M, Müller M, Matthies LM, Hansen J, Doster A, Szabo A, et al. Perceptions of patient engagement applications during pregnancy: a qualitative assessment of the patient's perspective. JMIR Mhealth Uhealth. May 26, 2017;5(5):e73. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lupton D, Pedersen S. An Australian survey of women's use of pregnancy and parenting apps. Women Birth. Aug 2016;29(4):368-375. [ CrossRef ] [ Medline ]
- de Mooij MJ, Hodny RL, O'Neil DA, Gardner MR, Beaver M, Brown AT, et al. OB nest: reimagining low-risk prenatal care. Mayo Clin Proc. Apr 2018;93(4):458-466. [ CrossRef ] [ Medline ]
- Kokts-Porietis RL, Stone CR, Friedenreich CM, Froese A, McDonough M, McNeil J. Breast cancer survivors' perspectives on a home-based physical activity intervention utilizing wearable technology. Support Care Cancer. Aug 2019;27(8):2885-2892. [ CrossRef ] [ Medline ]
- Gell NM, Tursi A, Grover KW, Dittus K. Female cancer survivor perspectives on remote intervention components to support physical activity maintenance. Support Care Cancer. May 2020;28(5):2185-2194. [ CrossRef ] [ Medline ]
- Ravn Jakobsen P, Hermann AP, Søndergaard J, Wiil UK, Clemensen J. Development of an mHealth application for women newly diagnosed with osteoporosis without preceding fractures: a participatory design approach. Int J Environ Res Public Health. Feb 13, 2018;15(2):330. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Harder H, Holroyd P, Burkinshaw L, Watten P, Zammit C, Harris PR, et al. A user-centred approach to developing bWell, a mobile app for arm and shoulder exercises after breast cancer treatment. J Cancer Surviv. Dec 2017;11(6):732-742. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Depper A, Howe PD. Are we fit yet? English adolescent girls’ experiences of health and fitness apps. Health Sociol Rev. Jul 04, 2016;26(1):98-112. [ CrossRef ]
- Gambier-Ross K, McLernon DJ, Morgan HM. A mixed methods exploratory study of women's relationships with and uses of fertility tracking apps. Digit Health. Jul 25, 2018;4:2055207618785077. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lupton D. ‘It just gives me a bit of peace of mind’: Australian women’s use of digital media for pregnancy and early motherhood. Societies. Sep 15, 2017;7(3):25. [ CrossRef ]
- Logsdon MC, Lauf A, Stikes R, Revels A, Vickers-Smith R. Partnering with new mothers to develop a smart phone app to prevent maternal mortality after hospital discharge: a pilot study. J Adv Nurs. Jan 2020;76(1):324-327. [ CrossRef ] [ Medline ]
- Wright AA, Raman N, Staples P, Schonholz S, Cronin A, Carlson K, et al. The HOPE pilot study: harnessing patient-reported outcomes and biometric data to enhance cancer care. JCO Clin Cancer Inform. Dec 2018;2:1-12. [ FREE Full text ] [ CrossRef ] [ Medline ]
- de Mendoza AH, Cabling ML, Dilawari A, Turner JW, Fernández N, Henderson A, et al. Providers' perspectives on adherence to hormonal therapy in breast cancer survivors. Is there a role for the digital health feedback system? Health Technol (Berl). Mar 2019;9(2):175-184. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Willcox JC, van der Pligt P, Ball K, Wilkinson SA, Lappas M, McCarthy EA, et al. Views of women and health professionals on mHealth lifestyle interventions in pregnancy: a qualitative investigation. JMIR Mhealth Uhealth. Oct 28, 2015;3(4):e99. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ke JX, George RB, Wozney L, Chorney JL. Patient-centred perioperative mobile application in Cesarean delivery: needs assessment and development. Can J Anaesth. Oct 2019;66(10):1194-1201. [ CrossRef ] [ Medline ]
- Firet L, de Bree C, Verhoeks CM, Teunissen DA, Lagro-Janssen AL. Mixed feelings: general practitioners' attitudes towards eHealth for stress urinary incontinence - a qualitative study. BMC Fam Pract. Jan 26, 2019;20(1):21. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Garnweidner-Holme LM, Borgen I, Garitano I, Noll J, Lukasse M. Designing and developing a mobile smartphone application for women with gestational diabetes mellitus followed-up at diabetes outpatient clinics in Norway. Healthcare (Basel). May 21, 2015;3(2):310-323. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Grassl N, Nees J, Schramm K, Spratte J, Sohn C, Schott TC, et al. A web-based survey assessing the attitudes of health care professionals in Germany toward the use of telemedicine in pregnancy monitoring: cross-sectional study. JMIR Mhealth Uhealth. Aug 08, 2018;6(8):e10063. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pais S, Parry D, Petrova K, Rowan J. Acceptance of using an ecosystem of mobile apps for use in diabetes clinic for self-management of gestational diabetes mellitus. Stud Health Technol Inform. 2017;245:188-192. [ Medline ]
- Ragavan MI, Ferre V, Bair-Merritt M. Thrive: a novel health education mobile application for mothers who have experienced intimate partner violence. Health Promot Pract. Mar 2020;21(2):160-164. [ CrossRef ] [ Medline ]
- Runkle J, Sugg M, Boase D, Galvin SL, C Coulson C. Use of wearable sensors for pregnancy health and environmental monitoring: descriptive findings from the perspective of patients and providers. Digit Health. Feb 06, 2019;5:2055207619828220. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sadigursky A. Move my mood: development and evaluation of a mobile mental health self-help app using behavioral activation for women with postpartum depression. Alliant International University. 2018. URL: https://books.google.co.in/books/about/Move_My_Mood.html?id=dYtP0AEACAAJ&redir_esc=y [accessed 2020-03-30]
- Scherr CL, Feuston JL, Nixon DM, Cohen SA. A two-phase approach to developing SNAP: an iPhone application to support appointment scheduling and management for women with a BRCA mutation. J Genet Couns. Apr 2018;27(2):439-445. [ CrossRef ] [ Medline ]
- Tommasone G, Bazzani M, Solinas V, Serafini P. Midwifery e-health: from design to validation of “mammastyle — Gravidanza Fisiologica”. In: Proceedings of the IEEE 18th International Conference on e-Health Networking, Applications and Services (Healthcom). 2016. Presented at: Healthcom 2016; September 14-16, 2016; Munich, Germany. [ CrossRef ]
- Fu MR, Axelrod D, Guth AA, Wang Y, Scagliola J, Hiotis K, et al. Usability and feasibility of health IT interventions to enhance Self-Care for Lymphedema Symptom Management in breast cancer survivors. Internet Interv. Sep 2016;5:56-64. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dienelt K, Moores CJ, Miller J, Mehta K. An investigation into the use of infant feeding tracker apps by breastfeeding mothers. Health Informatics J. Sep 2020;26(3):1672-1683. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lim S, Tan A, Madden S, Hill B. Health professionals' and postpartum women's perspectives on digital health interventions for lifestyle management in the postpartum period: a systematic review of qualitative studies. Front Endocrinol (Lausanne). Nov 8, 2019;10:767. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mackey A, Petrucka P. Technology as the key to women's empowerment: a scoping review. BMC Womens Health. Feb 23, 2021;21(1):78. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sediva H, Cartwright T, Robertson C, Deb SK. Behavior change techniques in digital health interventions for midlife women: systematic review. JMIR Mhealth Uhealth. Nov 09, 2022;10(11):e37234. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Alfawzan N, Christen M, Spitale G, Biller-Andorno N. Privacy, data sharing, and data security policies of women's mHealth apps: scoping review and content analysis. JMIR Mhealth Uhealth. May 06, 2022;10(5):e33735. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hallam L, Vassallo A, Pinho-Gomes AC, Carcel C, Woodward M. Does journal content in the field of women's health represent women's burden of disease? A review of publications in 2010 and 2020. J Womens Health (Larchmt). May 2022;31(5):611-619. [ CrossRef ] [ Medline ]
- Figueroa CA, Luo T, Aguilera A, Lyles CR. The need for feminist intersectionality in digital health. Lancet Digit Health. Aug 2021;3(8):e526-e533. [ CrossRef ]
- Jabir AI, Lin X, Martinengo L, Sharp G, Theng YL, Tudor Car L. Attrition in conversational agent-delivered mental health interventions: systematic review and meta-analysis. J Med Internet Res. Feb 27, 2024;26:e48168. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Meyerowitz-Katz G, Ravi S, Arnolda L, Feng X, Maberly G, Astell-Burt T. Rates of attrition and dropout in app-based interventions for chronic disease: systematic review and meta-analysis. J Med Internet Res. Sep 29, 2020;22(9):e20283. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cronin C, Hungerford C, Wilson RL. Using digital health technologies to manage the psychosocial symptoms of menopause in the workplace: a narrative literature review. Issues Ment Health Nurs. Jun 2021;42(6):541-548. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Whitehead L, Talevski J, Fatehi F, Beauchamp A. Barriers to and facilitators of digital health among culturally and linguistically diverse populations: qualitative systematic review. J Med Internet Res. Feb 28, 2023;25:e42719. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Birati Y, Yefet E, Perlitz Y, Shehadeh N, Spitzer S. Cultural and digital health literacy appropriateness of app- and web-based systems designed for pregnant women with gestational diabetes mellitus: scoping review. J Med Internet Res. Oct 14, 2022;24(10):e37844. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Woodley SJ, Moller B, Clark AR, Bussey MD, Sangelaji B, Perry M, et al. Digital technologies for women's pelvic floor muscle training to manage urinary incontinence across their life course: scoping review. JMIR Mhealth Uhealth. Jul 05, 2023;11:e44929. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Person-generated health data in women’s health: scoping review. OSF Home. Mar 7, 2024. URL: https://osf.io/3eync/ [accessed 2024-05-07]
Abbreviations
Edited by T de Azevedo Cardoso; submitted 04.10.23; peer-reviewed by D Liu, M Herron; comments to author 23.02.24; revised version received 15.03.24; accepted 26.03.24; published 16.05.24.
©Jalisa Lynn Karim, Rachel Wan, Rhea S Tabet, Derek S Chiu, Aline Talhouk. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 16.05.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Announcement
Tele manas- a toll-free helpline for students, ssp account creation link: https://ssp.postmatric.karnataka.gov.in/ca/.
- BTech Aeronautical Engineering: Course & Admission 2024 | MIT
- “Bad practice in Medicine must be rooted out,” World Medical Education President Prof David Gordon tells graduating students
- KMC Manipal moves up, MCOPS retains place in QS World Ranking by Subject 2018.
- Research Advisory Council
- List of Student Clubs | Manipal Academy of Higher Education (formerly, Manipal University)
- Vision and Mission
- Institute of Eminence (IoE)
- Ombudsman Details
- Administration
- Gender Sensitization
- Anti Ragging Policy
- Corporate Relations
- Caution notice
- Mandatory Disclosure
- Back to Campus AV
- Fee Notifications - Seniors
- Around Campus
- Around Manipal
- Student Affairs
- Campus Tour
- Student Feedback on Services at MAHE
- Sports and Fitness
- International Collaborations (OIAC)
- Centres Established under MAHE
- Innovation & Entrepreneurship
- Ranking & Recognition
- Destination Manipal
- Industry Partnership
- Green Manipal
- Research Groups
- Social Impact
- 31st Convocation
- W20-MAHE-Knowledge Partnership
- NEP 2020 implementation at MAHE
- Conferences etc
- MAHE Annual Reports
- MAHE Convocation Reports
- MAHE Silver Jubilee Newsletter
- Manipal Matters
- e-Content Development Facilities
- Grievance Redressal
- International Faculty Members
- Undergraduate (UG)
- Postgraduate (PG)
- Post Master's
- Super Speciality (SS)
- Integrated Programme
- Lateral Entry Admissions
- Post Graduate (PG) Diploma
- Advanced PG Diploma
- Certificate
- PG Certificate
- Executive Diploma
- Programs Offered
- Indian / Domestic
- International
- Eligibility & Admission Process
- Entrance Exams
- Dates To Remember
- Fees & Refunds
- Scholarships & Financial Aid
- Study In India (SII)
- Spot Admissions
- New Programs 2024
- MAHE Online Programs
- MAHE Webinars
- Admissions 2024
- Download Prospectus
- Public Advisory
- CoVid 19 Circulars
- Admissions Webpages Help
- Kasturba Medical College (KMC) Manipal
- Kasturba Medical College (KMC) Mangalore
- Centre for Integrative Medicine & Research (CIMR) Manipal
- Manipal College of Dental Sciences (MCODS) Manipal
- Manipal College of Dental Sciences (MCODS) Mangalore
- Melaka Manipal Medical College (MMMC) Manipal
- Manipal Institute of Regenerative Medicine (MIRM) Bengaluru
- Department of Basic Medical Sciences (DBMS) Manipal
- Manipal College of Pharmaceutical Sciences (MCOPS) Manipal
- Manipal College of Health Professions (MCHP) Manipal
- Manipal School of Life Sciences (MSLS) Manipal
- Manipal College of Nursing (MCON) Manipal
- Prasanna School of Public Health (PSPH) Manipal
- Manipal Institute of Virology (MIV) Manipal
- Manipal Tata Medical College (MTMC) Jamshedpur
- Manipal Centre for Biotherapeutics Research (MCBR) Manipal
- International Centre for Health Sciences (ICHS)
- Manipal Institute of Technology (MIT) Manipal
- Manipal School of Information Sciences (MSIS) Manipal
- Department of Sciences (DSc) Manipal
- Manipal School of Architecture & Planning (MSAP) Manipal
- Department of Design (DOD) Manipal
- Department of Atomic & Molecular Physics (DAMP) Manipal
- Manipal Institute of Management (MIM) Manipal
- Dept of Commerce (DOC) Manipal
- Welcomgroup Graduate School of Hotel Administration (WGSHA) Manipal
- Manipal Centre for Natural Sciences (MCNS) Manipal
- International Centre for Applied Sciences (ICAS) Manipal
- Manipal Institute of Technology (MIT) Bengaluru
- Srishti Manipal Institute of Art, Design and Technology (SMI) Bengaluru
- Manipal Institute of Communication (MIC) Manipal
- Manipal Centre for Humanities (MCH) Manipal
- Manipal Centre for European Studies (MCES) Manipal
- Gandhian Centre for Philosophical Arts & Sciences (GCPAS) Manipal
- Department of Library & Information Science (DLIS) Manipal
- Department of Philosophy (DoP) Manipal
- Department of Languages (DoL) Manipal
- Dept of Geopolitics & International Relations (DGIR) Manipal
- Directorate of Online Education
- Certificate Courses
- Certificate course in Restorative Dentistry
- Certificate in Fashion Design: Course, Admission 2022 | MSAP
- Certificate Course in Panchakarma Technician & Massage Therapist
- Certificate Course - Animation Technology
- Clinical and Diagnostic Virology
- Allied Health Sciences
- B.Sc. (Physician Assistant)
- B.Sc. Cardiovascular Technology
- B.Sc. Cardiovascular Technology - Get complete Details of B.Sc. Cardiovascular Technology...
- B.Sc. Exercise and Sports Sciences
- B.Sc. Health Information Management
- B.Sc. Medical Imaging Technology
- B.Sc. Medical Laboratory Technology
- B.Sc. Renal Replacement Therapy & Dialysis Technology
- Bachelor in Prosthetics and Orthotics
- Bachelor of Occupational Therapy: Course, Admission | MCHP
- Bachelor of Optometry
- Bachelor of Optometry: Course, Fees, Admission | MCHP
- Bachelor of Physiotherapy (Mangalore): Admission | MCHP
- Bachelor of Physiotherapy: Course, Admission | MCHP
- BASLP (Mangalore): Course, Eligibility, Admission 2022-23 | MCHP
- BASLP: Course, Eligibility, Fees, Admission | MCHP
- BSc Anaesthesia & Operation Theatre: Course, Admission | MCHP
- BSc Clinical Nutrition & Dietetics: Course, Admission | MCHP
- BSc CVT (Mangalore): Course, Eligibility, Admission | MCHP
- BSc Emergency Medicine Technology: Course, Admission | MCHP
- BSc Exercise and Sports Science: Course, Admission | MCHP
- BSc Health Information Management: Course, Admission | MCHP
- BSc Medical Laboratory Technology: Course, Admission | MCHP
- BSc MIT (Mangalore): Course, Eligibility, Admission | MCHP
- BSc MIT - B.Sc. Medical Imaging Technology
- BSc Nuclear Medicine Technology: Course, Admission | MCHP
- BSc Perfusion Technology: Course, Admission | MCHP
- BSc Psychology: Course, Eligibility, Fees, Admission | MCHP
- BSc Radiotherapy Technology: Course, Admission | MCHP
- BSc Respiratory Therapy (Mangalore): Course, Admission | MCHP
- BSc Respiratory Therapy: Course, Fees, Admission | MCHP
- BSc RRT & DT (Mangalore): Course, Fees, Admission | MCHP
- BSc RRT & DT: Course, Eligibility, Fees, Admission | MCHP
- BSc RTT (Mangalore): Course, Eligibility, Admission | MCHP
- B. Arch: Course, Eligibility, Fees, Admission | MSAP
- B.Sc Physics: Course, Fees, Admission | DAMP Manipal
- B.Com (Business Process Services): Admission | DOC Manipal
- B.Com (Hons.) - Banking & Finance
- B.Com (Hons.) - Business Analytics
- B.Com (Hons.) - Corporate Accounting
- B.Com (Professional): Course, Admission | DOC Manipal
- BDS (Bachelor of Dental Surgery): Course, Admission 2022 | MMMC
- BDS - Bachelor of Dental Surgery
- B. Des Fashion Design: Course, Fees, Admission | MSAP
- B. Des Interior Design: Course, Fees, Admission | MSAP
- B.Des Fashion Design
- B.Des Interior Design
- B. Tech (Cyber Physical systems)
- B.Sc. Applied Science (International Transfer Program in Engineering): Course, Fees,...
- BTech (Computer Science & Engineering - Cyber Security)
- BTech (Computer Science & Engineering - Data Science)
- BTech (Computer Science & Engineering - Artificial Intelligence)
- BTech Aeronautical Engineering: Course & Admission | MIT
- BTech Artificial Intelligence & Machine Learning: Admission | MIT
- BTech Automobile Engineering: Admission Process, Eligibility, Fees
- BTech Biomedical Engineering: Course & Admission | MIT
- BTech Biotechnology: Course & Admission | MIT
- BTech Chemical Engineering: Course & Admission | MIT
- BTech Civil Engineering: Course & Admission | MIT
- BTech Computer & Communication Engineering: Admission | MIT
- BTech Computer Science & Engineering
- BTech Computer Science Engineering: Course & Admission | MIT
- BTech Data Science Engineering: Course & Admission | MIT
- BTech Electrical and Electronics Engineering (EEE): Admission | MIT
- BTech Electronics & Communication Engineering
- BTech Electronics and Communication Engineering: | MIT
- BTech Electronics and Instrumentation Engineering: Admission | MIT
- BTech Industrial Engineering : Course & Admission | MIT
- BTech Information Technology
- BTech IT (Information Technology): Course & Admission | MIT
- BTech Mechanical Engineering: Course & Admission | MIT
- BTech Mechatronics Engineering: Course & Admission | MIT
- BA Culinary Arts: Course, Fees, Admission | WGSHA
- BHM: Course, Eligibility, Fees, Admission | WGSHA
- B.A. (Hons.) English
- B.A. (Hons.) History & Economics
- B.A. (Hons.) History & Political Science
- B.A. (Hons.) History & Sociology
- B.A. (Hons.) Political Science & Economics
- B.A. (Hons.) Political Science & Sociology
- B.A. (Hons.) Psychology
- B.A. (Hons.) Psychology - Course Structure
- B.A. (Hons.) Sociology & Economics
- BA Humanities
- Undergraduate Program (B.Des.)
- Undergraduate Program (BFA)
- Undergraduate Skill-Based Vocational Program (B.Voc)
- BA (Hons.) European Languages and Intercultural Studies
- B.Com LLB (Hons)
- BA LLB (Hons)
- BBA LLB (Hons)
- BSc Biotechnology
- BSc Biotechnology Honors
- BBA: Course, Eligibility, Fees, Admission | DOC Manipal
- B.A. (Hons.) Journalism and Mass Communication
- BA Honours - Media & Communication
- BSc Animation Course
- BVoc in Graphics and Digital Media
- MBBS - Bachelor of Medicine & Bachelor of Surgery
- MBBS: Course, Eligibility, Fees, Admission 2022 | MMMC
- Student Mobility Center
- UG - Electives
- BSc Nursing
- Post Basic B.Sc. in Nursing
- BPharm (Bachelor of Pharmacy): Course, Admission | MCOPS
- PharmD (Doctor of Pharmacy): Course, Admission | MCOPS
- BA in Aesthetics and Peace Studies
- BA Public Policy and Administration
- Diploma in Dental Hygienist
- Diploma in Dental Mechanic
- Diploma in Dental Operating Room Assistant
- DPharm: Course, Eligibility, Fees, Admission | MCOPS
- MSc Applied Mathematics & Computing: Admission | DSc Manipal
- MSc Chemistry: Course, Admission | DSc Manipal
- MSc Geology: Course, Admission | DSc Manipal
- MSc Physics: Course, Admission | DSc Manipal
- M.Optom (Master of Optometry): Course, Admission | MCHP
- M.Sc Renal Replacement Therapy & Dialysis Technology
- M.Sc. (Anaesthesia & Operation Theatre Technology)
- M.Sc. (Emergency Medical Technology)
- Master of Physiotherapy (MPT) (Manipal)
- M.Sc. Clinical Psychology (at Mangalore)
- M.Sc. Echocardiography
- Master of Occupational Therapy: Course, Admission | MCHP
- MSc Audiology (Mangalore): Course, Admission | MCHP
- MSc Audiology: Course, Eligibility, Fees, Admission | MCHP
- MSc CCIT - M.Sc. Cardiac Catheterization & Intervention Technology
- MSc CCIT: Course, Eligibility, Fees, Admission | MCHP
- MSc Clinical Psychology: Course, Fees, Admission MCHP
- MSc Echocardiography: Course, Fees, Admission | MCHP
- MSc Exercise and Sports Science: Course, Admission | MCHP
- MSc Health informatics: Course, Fees, Admission | MCHP
- MSc Health Information Management: Course, Admission | MCHP
- MSc Medical Imaging Technology: Course, Admission | MCHP
- MSc Medical Laboratory Technology: Course, Admission | MCHP
- MSc Medical Radiation Physics: Course, Admission | MCHP
- MSc Nuclear Medicine Technology: Course, Admission | MCHP
- MSc Perfusion Technology: Course, Admission | MCHP
- MSc Respiratory Therapy: Course, Fees, Admission | MCHP
- MSc RRT & DT: Course, Eligibility, Fees, Admission| MCHP
- MSc SLP (Mangalore): Course, Eligibility, Admission | MCHP
- MSc Speech Language Pathology: Course, Admission | MCHP
- M. Des Sustainable Design: Course, Admission | MSAP
- MArch Urban Design Development Course
- Atomic & Molecular Physics
- MSc - Biostatistics
- MSc Biophysics
- M.Sc by Research in Biotherapeutics
- M.Com (Professional): Course, Admission | DOC Manipal
- M.Com Banking Technology: Course, Admission | DOC Manipal
- M.Com Logistics & Supply Chain: Admission | DOC Manipal
- MA Digital & Creative Marketing: Admission | DOC Manipal
- MSc Business Analytics: Course, Admission | DOC Manipal
- MSc Financial Economics: Course, Admission | DOC Manipal
- MSc Health Economics: Course, Admission | DOC Manipal
- MSc in Biostatistics
- MSc in Data Science
- MSc in Digital Epidemiology
- MDS - Master of Dental Surgery
- M. Des Interior Design: Course, Fees, Admission | MSAP
- M.Des Interior Design
- MA Fashion Management
- M.Tech (Data Science)
- M.Tech (Machine Intelligence & Decision Science)
- M.Tech (Medical Informatics)
- M.Tech Defence Technology
- MSc Courses
- MTech (Electric Vehicle Technology)
- MTech (Internet of Things)
- MTech - Master of Technology
- MTech - Wireless and Mobile Communications
- MTech Automobile Engineering
- MTech Avionics
- MTech Biomedical Engineering
- MTech Chemical Engineering
- MTech Computer Aided Analysis & Design
- MTech Computer Networking and Engineering
- MTech Computer Science & Engineering
- MTech Computer Science & Information Security
- MTech Digital Electronics and Communication Engineering
- MTech Embedded Control and Automation
- MTech Engineering Management
- MTech Environmental Engineering
- MTech in Construction Engineering Management
- MTech Industrial Automation & Robotics
- MTech Industrial Biotechnology
- MTech Manufacturing Engineering
- MTech Microelectronics
- MTech Power Electronic & Drives
- MTech Software Engineering
- MTech Structural Engineering
- MTech Thermal Sciences & Energy Systems
- Doctoral Studies and Research
- MA European Studies
- MA Geopolitics and International Relations
- M.Sc Dietetics and Applied Nutrition
- MA Indian Cuisine & Food Culture: Course, Admission | WGSHA
- MHM: Course, Eligibility, Fees, Admission | WGSHA
- MA English Language and Literature
- MA European Literature and Culture
- MA Sociology
- Postgraduate Arts Program: Professional Practices
- Postgraduate Professional Program
- Postgraduate Professional Program in Fine Arts (MFA)
- Postgraduate Professional Program in Planning (M.Plan)
- Specialization Courses - Eligibility, Fees, Facilities & Admission
- Master of Computer Application (MCA)
- Master of Engineering (ME): Course, Admission | MSIS
- MSc Yoga Therapy
- LL.M. Programs
- Work Integrated Learning Program (WILP)
- Master of Library & Information Science
- M.Sc Genome Engineering
- M.Sc. Tissue Engineering
- MSc Bioinformatics
- MSc by Research in Life Sciences
- MSc Medical Biotechnology
- MSc Molecular Biology and Human Genetics
- MSc Systems Biology
- MSc Biomolecular Physics
- MA Film Art & Film Making
- MA Media & Communication
- MA Multimedia and Communication
- M.Sc (Reproductive Genetics)
- M.Sc. Genetic Counseling
- M.Sc. Reproductive and Developmental Biology
- Master of Surgery
- MD - Doctor of Medicine
- MD-PhD; MS-PhD Program
- MS - Master of Surgery
- MSc Forensic Science
- MSc Clinical Embryology
- MSc Medical Course
- MSc Medical Courses
- Integrated Ph.D
- MSc Nursing
- Nurse Practitioner Critical Care Postgraduate Residency Programme
- MPharm: Course, Eligibility, Fees, Admission | MCOPS
- PharmD (Post Baccalaureate): Course, Admission | MCOPS
- MA Ecosophical Aesthetics
- MA in Art and Peace Studies
- MA Indian Philosophy
- MA Sanskrit Studies
- M.Sc. (Health Technology Assessment)
- MHA (Master of Hospital Administration)
- MPH (Master of Public Health)
- MSW (Master of Social Work)
- MA Public Policy
- M.Sc. by Research in Translational Neuroscience : Admission | MIRM
- MSc Stem Cell Technology & Regenerative Biology: Admission | MIRM
- MSc Clinical Virology: Course, Fees, Admission | MIV
- MPhil Clinical Psychology: Course, Admission | MCHP
- MPhil Psychiatric Social Work
- Certificate Course in Cone Beam Computed Tomography
- Certificate course in Forensic Odontology
- Certificate Course in Forensic Odontology - Online Module
- Certificate Course in Microimplant Anchorage
- Certificate course in Minor Oral Surgery
- Certificate course in Modern Endodontic Practice
- Integrated Dental Photography
- Certificate Course in Yoga
- Certificate Course in Bioinformatics
- Certificate Course in Sports Communication
- Observership in Surgical Oncology
- Certificate Course on Introduction to Medical Writing Program in Pharmaceutical Science:...
- Certificate in Translational Research: Admission 2022 | MCOPS
- Certificate Course in Biostatistics, Epidemiology and Research Methodology
- Certificate Course in Qualitative Research Methods
- Certificate Course on Evidence Synthesis
- Leadership in Public Health - Certificate Course
- Basic virological techniques
- Cell culture and virus isolation techniques
- Diagnostic Virology
- Laboratory biosafety and biosecurity
- Medical entomology
- Molecular Diagnostic techniques
- Fellowship in Head and Neck Oncology
- Fellowship in Infectious Diseases
- Fellowship in Neonatology
- Fellowship in Neuroanaesthesia
- Fellowship in Onco - Surgery
- Fellowship in Oncopathology
- Fellowship in Pediatric Anesthesia
- Fellowship in Pediatric Hematology and Oncology
- Fellowship in Urogynecology
- B. Des Interior Design (Lateral): Course, Admission | MSAP
- B.Des - Fashion Design (Lateral)
- B.Des Interior Design (Lateral)
- PG Diploma in Sports Communication
- PGDCC - PG Diploma in Corporate Communication
- BSc MIT (Lateral): Course, Eligibility, Admission | MCHP
- BSc MLT (Lateral): Course, Eligibility, Admission | MCHP
- BSc Respiratory Therapy (Lateral): Course, Admission | MCHP
- B. Des Fashion Design (Lateral): Course, Admission | MSAP
- BTech Lateral Entry: Course & Admission 2023 | MIT
- BPharm (Lateral): Course, Eligibility, Admission 2023 | MCOPS
- BSc MIT (Lateral): Course, Eligibility, Admission 2023 | MCHP
- BSc MLT (Lateral): Course, Eligibility, Admission 2023 | MCHP
- BSc Respiratory Therapy (Lateral): Course, Admission 2023 | MCHP
- B. Des Fashion Design (Lateral): Course, Admission 2023 | MSAP
- B. Des Interior Design (Lateral): Course, Admission 2023 | MSAP
- BTech Lateral Entry: Course & Admission 2022 | MIT
- PhD | Doctor of Philosophy
- DM - Doctor of Medicine
- MCh - Master of Chirurgiae
- PG Diploma in Health Communications
- News & Events
- Established Centres
- In-house Publications
- Find Researcher
- Policies & Forms
- Technologies available for licensing
- Student Research Forum
- Conferences

Explore Our Campuses!
Offering an outstanding experience that redefines campus tours at mahe and its constituent institutes..

That Ignites your Dreams
2024 admissions open.


Experience online programmes

300+ programs. 30+ disciplines. One Manipal
MAHE Manipal is one of India's leading academic and research institutions. It has been granted Institution of Eminence status by the Ministry of Education, Government of India.

Faculty of Health Sciences

Faculty of Science and Technology

Management, Liberal Arts, Humanities, Social Science & Law
Research is in our nature.
Ever since the foundation in 1953, we have applied our research efforts to develop scientific knowledge with an emphasis on interdisciplinary research and engagement with wider research community.
Crores of Research Grant for the FY 2018-19
international collaborations
IPRs filed in the last two years

International Collaborations
Manipal Academy of Higher Education is a globally engaged institution with active partnership with more than 250+ leading universities around the globe. Our relations with institutions, government agencies and organisations in study, research and service provide faculty and students access to world-class institutions, experiences and resources.

MAHE celebrates Founder's Day to mark Dr T M A Pai's 126th birth anniversary

MAHE Celebrates Special Convocation for Conferment of Honorary Doctorate to Shri K. V. Kamath

Fatty Liver Disease Linked to Elevated Heart Disease Risk

MAHE Shines Bright in QS World University Rankings 2024

MIT, MAHE launches “HBSF-MAHE EduEmpower Scholarship” for B. Tech Aspirants: an initiative anchored by an alumnus of MIT

KMC Manipal sets new benchmark in medical training with Virtual Dissection Lab inauguration

WGSHA Celebrates Culinary Milestone with Inauguration of Food Pod

MAHE & KOREAMMR Join Forces to Lead the Way in 3D Bioprinted Medical Solutions
Quality Control Mechanisms of the Cell: From E.coli to Humans

21st Control Instrumentation Systems Conference

International Conference on Data Science & Exploration in AI
National Student Energy Summit 2024

State-of-the-Art Facility Opens Doors
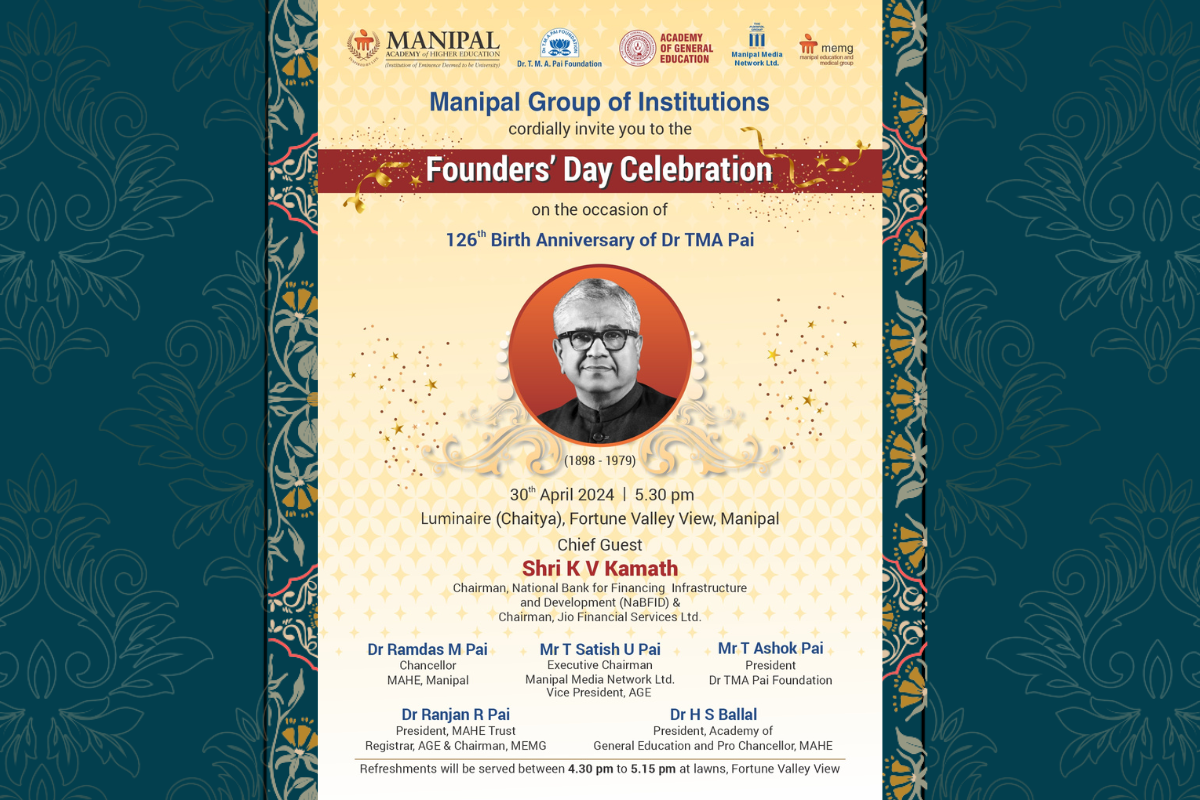
Founders' Day Celebration
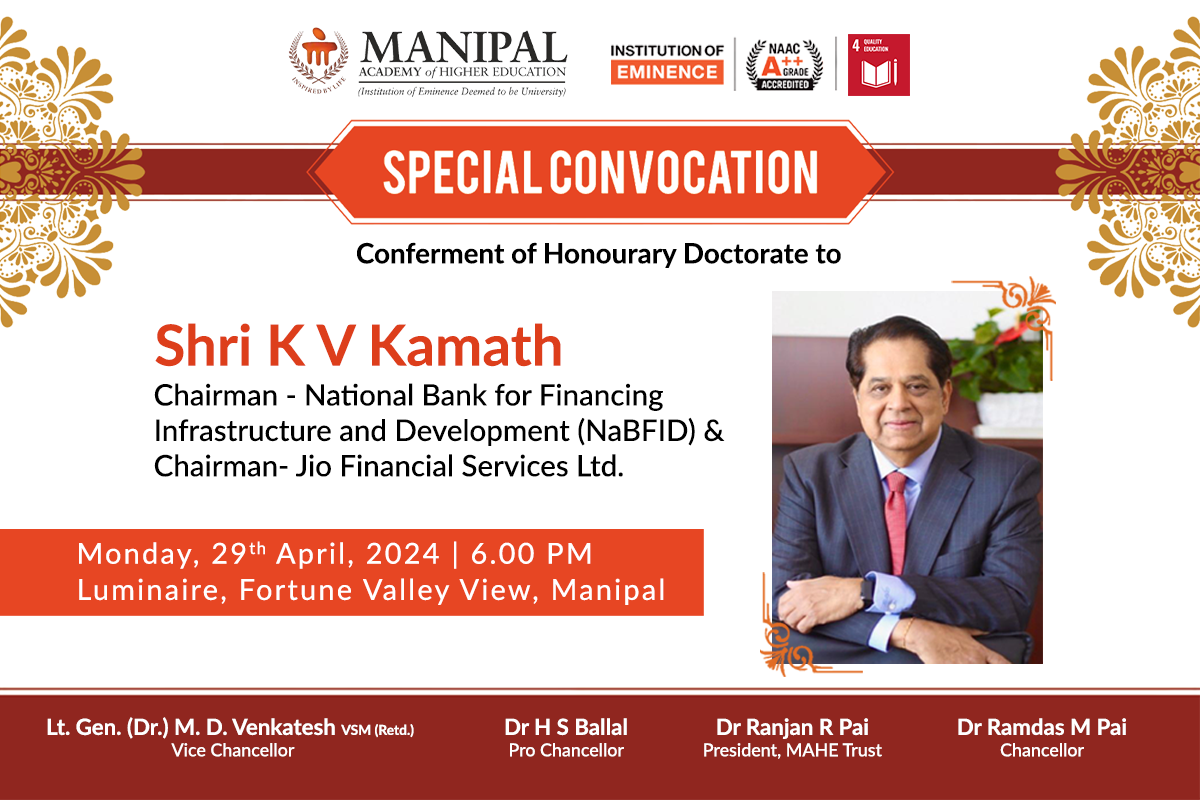
Shri K V Kamath to Receive Honorary Doctorate from MAHE
Global Health Symposium 2024
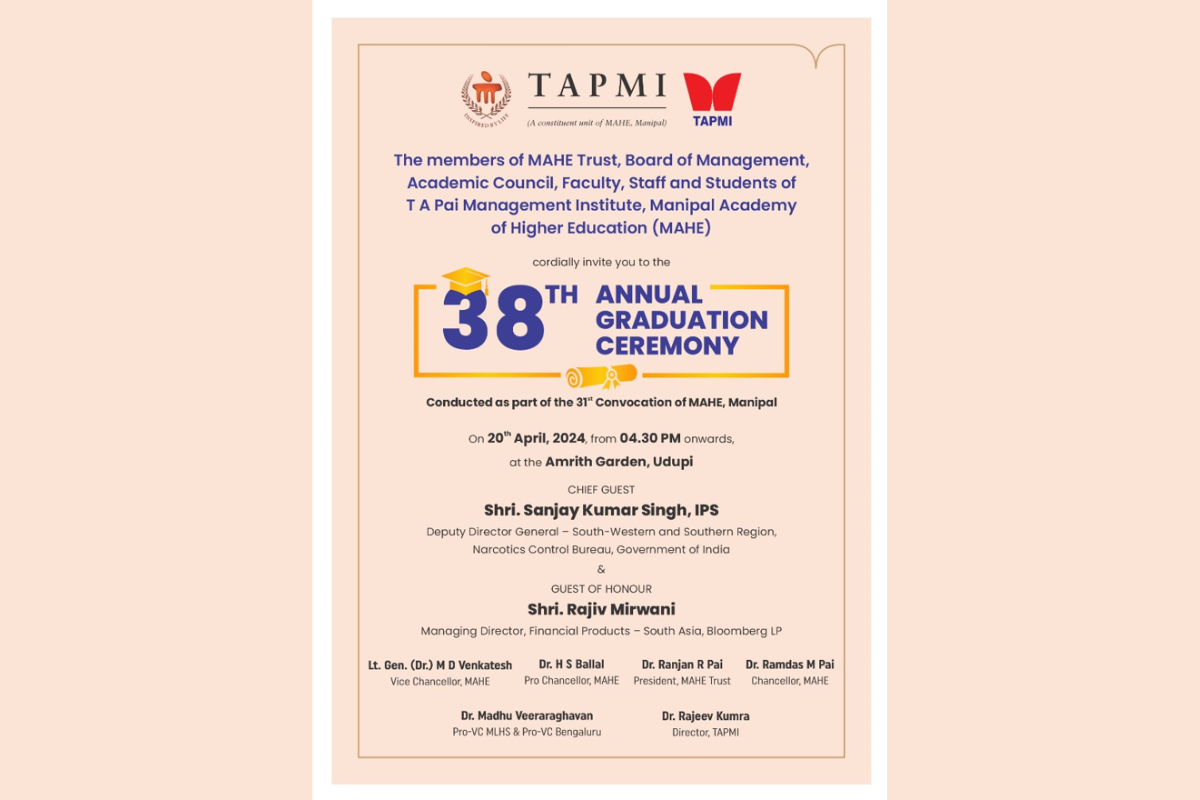
Annual Graduation Ceremony
Alumni Stories
Our alumni are making their mark in the world as decision-makers, innovators, change agents, thought-leaders, and creators, each in their own original way. Please visit our Alumni page to know more.

Satya Nadella
Ceo microsoft.

Vikas Khanna
Renowned chef.

Rajeev Suri
Ceo inmarsat.

Ishita Malviya
Professional surfer.
We use cookies on this website to make your browsing experience better. By continuing to use this website, you agree to our Privacy & Cookie Policy .
share this!
May 7, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
The quantum theory of gravitation, effective field theories and strings: Past and present
by Clare Sansom, SciencePOD

Gravity is one of four fundamental interactions. The most precise description of this force is still provided by Einstein's General Theory of Relativity, published in 1915, an entirely classical theory. This description sets gravity apart from the other three forces—strong, weak, and electromagnetism—all described by quantum fields. Therefore, any attempt to unify the four forces must depend on a description of gravity that uses the principles of quantum mechanics.
This has been an active area of theoretical physics since the 1930s. A historian and a physicist, Alessio Rocci from VUB in Brussels and Thomas Van Riet from KU Leuven in Belgium have set out a historical overview of the development of quantum theories of gravity to explain our current view on a future unified theory of the four forces. This work has been published in The European Physical Journal H .
Physicists began to investigate the quantum theory of gravitation in the 1930s, taking a perturbative approach, convinced that there should be no fundamental difference between the gravitational force and the other interactions. However, finding a description of the gravitational interaction according to the laws of quantum mechanics is still a very complex task.
Later in the century, Steven Weinberg, a pioneer of both effective field theory and the standard model of particle physics , began a process of cross-fertilization between these areas and the research area of quantum gravity that produced our current view on Einstein's theory. From the mid-1980s, string theory set up a possible framework to approach quantum gravity using a 'top-down' approach. The effective field theory approach to strong forces drove the development of the 'bottom-up' perspective, culminating in the mid-1990s.
Recently, physicists have started a new program called Swampland to overcome the criticism of string theory that arose in the 2000s. Van Riet says, "The ultimate hope is that the Swampland program can lead to general patterns with observational consequences."
Provided by SciencePOD
Explore further
Feedback to editors

Airborne technology brings new hope to map shallow aquifers in Earth's most arid deserts
5 hours ago

First-generation medical students face unique challenges and need more targeted support, say researchers
6 hours ago

Thermoelectric materials approach boosts band convergence to avoid time-consuming trial-and-error approach

Ion swap dramatically improves performance of CO₂-defeating catalyst

Military rank affects medical care, offering societal insights: Study

Mystery CRISPR unlocked: A new ally against antibiotic resistance?
7 hours ago

Researchers develop a detector for continuously monitoring toxic gases
8 hours ago

Sea otter study finds tool use allows access to larger prey, reduces tooth damage

Accelerated discovery research unveils 21 novel materials for advanced organic solid-state laser technology

Breaking bonds to form bonds: New chemical reaction with potential applications in medicinal chemistry
Relevant physicsforums posts, planck's constant times the speed of light.
3 hours ago
What drives osmosis? (Statistics or Dynamics?)
May 15, 2024
Calculating vacuum -- These numbers do not make sense
How is a magnetic field formed in a space surrounded by one pole, why is my homemade cloud chamber not working.
May 13, 2024
Relation between Rosenbluth Potentials and Spitzer Resistivity
May 12, 2024
More from Other Physics Topics
Related Stories

The strangest coincidence in physics: The AdS/CFT correspondence
Dec 21, 2023

Explaining gravity without string theory
Nov 6, 2020

New work reveals the 'quantumness' of gravity
May 1, 2024

Scientists closer to finding quantum gravity theory after measuring gravity on microscopic level
Feb 23, 2024

Why quantum mechanics defies physics
Dec 29, 2023

Effective Field Theories and the nature of the universe
Mar 24, 2021
Recommended for you

Scientists demonstrate the survival of quantum coherence in a chemical reaction involving ultracold molecules

Scientists use generative AI to answer complex questions in physics
12 hours ago

Quantum experts review major techniques for isolating Majoranas
11 hours ago

Researchers call for a new measurement of time for tunneling particles

Method milestone for quantum physics: Rapid test for topological 2D materials

Physicists demonstrate first metro-area quantum computer network in Boston
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Phys.org in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
Technology is an imperative aspect of society since the advent of the industrial revolution. One of the areas which have immensely benefited from the arrival of advanced technologies is the healthcare industry. For example, state-of-the-art equipment is available for improving patient care with the goal of enhancing the quality of life.
By analysing a wide range of examples, we have aimed to understand and systematize how medical technologies shape illness. We have identified six ways that technology can have such impact. First, technology may create awareness of disease by revealing asymptomatic signs or markers (imaging techniques, blood tests).
This article explores the relationship between medicine's history and its digital present through the lens of the physician-patient relationship. Today the rhetoric surrounding the introduction of new technologies into medicine tends to emphasize that technologies are disturbing relationships, and that the doctor-patient bond reflects a more ...
As digital technology has become more portable, easy to use and affordable, it has begun to capture the minds of medical researchers. From new imaging tools to mobile devices, Stanford researchers are exploring how to use technologically advanced tools to fill gaps in patient care. ... "There is a revolution in health care that is in large ...
Technology-Associated Medical Errors Medical Technology and Patient Safety Advances in medical technology can be a double-edged sword, according to the numerous research findings discussed by Powell-Cope and colleagues (2008). On the one hand improved technology can prevent adverse events from happening, thereby reducing the prevalence of medical errors, but the introduction of new technology ...
Medtronic is a well-known medical technology development company established in Fridley, Minnesota. This company was founded in 1949 by Earl Bakken. The medical device company has two headquarters of which one is located outside of the United States in Dublin, Ireland and another one here in the United States located in Fridley, Minnesota.
The World Health Organization (WHO) defines health technology as the application of organised knowledge and skills in the form of medicines, medical devices, vaccines, procedures and systems developed to solve a health problem and improve quality of life (World Health Organization, Health technology assessment).The Organisation for Economic Co-operation and Development (OECD) defines health ...
This essay examines the state of Artificial Intelligence (AI) based technology applications in healthcare and the impact they have on the industry. This study comprised a detailed review of the ...
Genomics, cancer blood tests, MRIs, sleep analysis and many other innovations now allow patients to gain the most comprehensive picture of their health ever available. As a result, these ...
Essay On Medical Technology. 948 Words4 Pages. Heads or tails Medical technology is a broad field where innovations plays a crucial role in the delivery of healthcare. These technologies are evolving at an immensely fast rate, with creating new technologies and updating old technologies. Medical technology is used for Pharmaceutical, equipment ...
The history of medical robots, though short, has required much creativity. Since their launch just over 20 years ago, the robotic systems that have been used clinically have evolved substantially. The basic rules and approaches to the use of robots in medicine had to be invented. For example, industrial robots were not intended for use near people, so the whole strategy to ensure the safety of ...
The Information Technology in Medicine Essay. Exclusively available on IvyPanda. Modern healthcare, being primarily focused on providing quality patient care, cannot exist apart from information technology. For this reason, medical employees are now obliged to learn how to beneficially use technology as well as practice proper communication ...
Essay, Pages 52 (12921 words) Views. 5818. ABSTRACT. The current medical innovations around the world have led to increased concerns about their role in the increasing of medical costs and the burdens on the healthcare systems. On the other hand, medical technology is one of the booming industries of the world, which promises much growth and ...
The first essay is a long essay on Advancements In Medical Technology of 400-500 words. This long essay about Advancements In Medical Technology is suitable for students of class 7, 8, 9 and 10, and also for competitive exam aspirants. The second essay is a short essay on Advancements In Medical Technology of 150-200 words.
Browse essays about Medical Technology and find inspiration. Learn by example and become a better writer with Kibin's suite of essay help services. Essay Examples
Therefore, it would be fair to conclude that technology has positively affected healthcare. First, technology has improved access to medical information and data (Mettler 33). One of the most significant advantages triggered by technology is the ability to store and access patient data. Medical professionals can now track patients' progress ...
This article explores the relationship between medicine's history and its digital present through the lens of the physician-patient relationship. Today the rhetoric surrounding the introduction of new technologies into medicine tends to emphasize that technologies are disturbing relationships, and that the doctor-patient bond reflects a more 'human' era of medicine that should be ...
856. Medical digitized records, powerful imaging devices, small sophisticated tools - medical technology plays an important role in modern healthcare system and significantly alter the provision of care. The world of medical technology is vast. It includes all the medicines, instruments, procedures, and support systems necessary to provide care.
975 Words. 4 Pages. 4 Works Cited. Open Document. In today's medical field technology plays a big role when it comes to patient care. Technology is huge when it comes to giving the patient the best type of quality care when they are in the hospital. In the old days people would just write it down on a sheet of paper and record it by hand ...
Pages: 1 (610 words) Views: 1603. Grade: 5. Download. The use impact technology in the medical field can go from the use of EMR's (Electronic Medical Records), blood pressure machines, thermometers, EKG's and many more things. Without technology it would make working in the medical field just that much harder.
REVIEW. In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better ...
Scholars discuss the need for federal regulations to combat risks associated with technology in health care. Most U.S. adults use technology to improve their health—nearly 60 percent browse the Internet for medical information, and over 40 percent obtain care through telemedicine. Despite technology's health care potential, however, six out ...
Background: The increased pervasiveness of digital health technology is producing large amounts of person-generated health data (PGHD). These data can empower people to monitor their health to promote prevention and management of disease. Women make up one of the largest groups of consumers of digital self-tracking technology. Objective: In this scoping review, we aimed to (1) identify the ...
The Medical Physics publishes papers helping health professionals perform their responsibilities more effectively and efficiently. Abstract Background In recent years, genetic algorithms have been applied in the field of nuclear technology design, producing superior optimization results compared to traditional methods.
MAHE is India's Top Ranked Private University For Engineering, Medical, MBA, Pharmacy, Fashion Design and Architecture courses. Apply now for Admission 2024 at MAHE (formerly, Manipal University)
Medical research advances and health news. Tech Xplore. The latest engineering, electronics and technology advances. Science X. The most comprehensive sci-tech news coverage on the web.