An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(1); 2023 Jan


The Role of Social Determinants of Health in Promoting Health Equality: A Narrative Review
Khushbu chelak.
1 Public Health and Epidemiology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
Swarupa Chakole
2 Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
Significant health disparities exist locally and even throughout the nation. Dipping health inequalities necessitates a focus on the inadequate spread of power, money, and resources, as well as the situations of daily living, which may be addressed through social determinants of health. This study aimed to review the role of health-related social factors in overcoming health disparities. We conducted a search of English-language literature, including studies published on health and health equalities or inequalities. Most reports show that social determinants of health have a higher effect on health. The elimination process of these health inequities occurs through well-designed economic and social policies. Every aspect of social determinants influences the health aspects of people; hence, some areas to focus on include employment, education, socioeconomic status, social support networks, health policies, and healthcare access. Launching interventions to reduce health disparities can help improve the community’s health and health equality.
Introduction and background
According to the World Health Organization (WHO), social determinants of health (SDH) are defined as the circumstances in which humans are born, develop, live, earn, and age. At the international, regional, and state or local levels, the distribution of money, power, and resources shapes these circumstances [ 1 ]. The WHO Commission on Social determinants of Health (CSDH) has stated that progress on SDH is the most successful means of enhancing all people’s well-being and raising disparities [ 2 ]. The WHO established the CSDH based on SDH intervention, which is the most effective strategy to improve well-being and reduce inequality [ 2 ]. Important aspects include governmental, financial, and traditional organizations, based on factors such as manageable healthcare and learning organizations; safe ecological conditions; aesthetically pleasant neighborhoods; and the availability of nutritious food [ 3 ]. Nowadays, health challenges such as being overweight, cardiovascular diseases, diabetes, and depression are prominent, wreaking havoc upon people because of the increasing demands of a high lifestyle. This leads to people suffering from non-communicable diseases. These socioeconomic variables contribute to societal stratification and health disparities among persons of different social and economic classes, genders, and ethnicity.
History of social determinants of health inequality
In the 19th century, people started becoming aware of the factors that had an impact on the health of the population [ 4 ]. Rudolf Virchow, a pioneer in this field, testified on the role of poverty in generating a disease that led to a plague outbreak in Prussia [ 4 ]. Friedrich Engels also studied to find out about the increased mortality. After that, Salvador Allende tried in Chile to demonstrate the importance of political and social variables in people’s health inequities [ 4 ]. All of them tried to frame how factors influence health and what role they play. Marmot emphasized that the workplace may be an important location for addressing disparities. Similarly, changing housing might have an impact on physical and mental health [ 5 ]. Cutting across the structural inequalities, health inequality is a more contemporary challenge and possibly a consequence of the imbalances in development planning and economic design [ 6 ]. Interventions on health and its disparities help overcome further problems [ 7 ]. There is a long history of housing evidence from several reviews [ 8 ]. People suffering from the financial crisis and economic disparities were also among the many who were deeply affected by the growing socioeconomic demands in the early days.
Methodology
This article presents a narrative review of SDH in promoting health equality. PubMed and Google Scholar were used to find all original and review articles with original reports. A set of keywords and Medical Subject Headings (MeSH) terms related to health inequalities and SDH were used. Keywords used were social inequalities, social inequities, poverty, health determinants, behavior, economic status, and social movement. The following MeSH terms were used interchangeably and in combination to find all relevant articles: social determinants, health inequities, and social movement. All free full-text PubMed Central articles were searched using Pubmed and Google Scholar. Studies that discussed the relationship between health inequities, the importance of social determinants, health inequities, health policies, social factors, health equality, and social movement were included. Articles that reviewed SDH in a more general way and whose main focus was not health inequalities and equalities were excluded (Figure (Figure1 1 ).

Social determinants of health
A subcategory of health factors is SDH, as shown in Figure Figure2 2 .

Source: Open access journal under a CC-BY license contributed by social determinants of health. Available at: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 [ 9 ].
The most significant health factors include government policy, medical availability, individual behavioral choices, and biological and genetic features [ 3 ]. Examples of SDH include occupation, job status, workplace safety, level of income, opportunities for education, job and place of work protection, inequity between men and women, and segregation based on race. The various health aspects of SDH include food poverty and limitations of access to nutritious food options, housing, and helpful facilities available; early childhood growth and experiences; inclusion in the community and social assistance; the prevalence of crime and exposure to violent behavior; neighborhood circumstances and physical environment; and possibilities for recreation and leisure, as shown in Table Table1 1 .
Source: Open access journal under a CC-BY license contributed by social determinants of health (2018). Available at: https://www.christenseninstitute.org/wp-content/uploads/2018/10/Social-Determinants-of-Health-Table.png [ 10 ].
Social determinants of health indicators
Social determinants determine how health is affected, how they play a significant role in influencing health, and how we can improve health for all. Some of the effects of social determinants affect health in the long term. For example, a less educated person might have less knowledge about how to utilize resources which may affect their ability to use resources to the fullest. Thus, social determinants play a role which must be recognized and improved.
Socioeconomic Status
Financial stress and socioeconomic status are a combination of a family’s or ordinary citizen’s profession, academic performance, wealth, and economic standing. Wealth and power are characteristics that influence a person’s socioeconomic status. The total amount earned in earnings or compensation over a year is income. Income limits a family’s overall lifestyle and influences their consumption habits [ 11 ]. Discrimination based on caste, creed, and gender makes a person vulnerable, enabling them to stop asking for more. They are subjugated to extreme pressure, which only worsens their mental status and health. Health education and programs must be used to educate people about how beneficial it is to count everyone as a whole. The promotion of health equality and equity remains the most significant goal of balancing financial stress.
Equality Education
Education is a means of improving one’s socioeconomic standing. A wealthy family’s socioeconomic status suggests a higher chance of enrolling and graduating from college. Family background, rather than other factors, such as supplemental educational services, significantly influence how much and what kind of education people get and what kind of employment they obtain [ 11 ]. The goal of improving income equality and eradicating poverty through education has not been met. Higher wages and social policies that support low-income families are needed to enhance students’ social and economic conditions [ 11 ]. Educational perspectives allow us to take a comprehensive and clearer view of the causes of health and disease in a population and must be paid attention to [ 4 ].
Gender Inequality and Age Inequality
Women earn less and are more likely to be poor. Institutional discrimination in a patriarchal society, where women were supposed to be mothers and spouses rather than part of the formal workforce, is to blame for gender inequality [ 11 ]. Poverty is more prevalent among the youngest and oldest population groups. Children are more likely to be poor than other age groups. School attainment, high school graduation rates, and reading skills are all impacted by poverty [ 11 ]. Health inequality does not mean just some kind of health difference but the differences in health like that of a pregnant woman who has fewer resources and is deficient and the newborn child who might be underweight leading to problems such as stunting and growth retardation. This adversely affects the opportunities and performances of those afflicted by it and can be corrected by successfully evaluating the determinants affecting health [ 6 ].
Economic Inequality
The United States has the least poverty rates and the most restrictive social policies regarding escaping poverty. Except for Mexico and Turkey, all other developed countries have more significant income disparity than the United States. Young people, full-time workers in low-status jobs, people of color, illiterate people, and women are most likely to be poor [ 11 ]. In influenced market knowledge and customer needs individualized society, incomes or wealth are alternate socioeconomic indicators [ 3 ].
Economic Power
Economic power is the ability to improve the standard of living of a country or business. Economic power represents the status of people with higher socioeconomic status wielding more power than those with lower socioeconomic status. For example, employment provides income that shapes choices about housing, child care, education, medical care, and food, among others. Influence is a factor of being able to produce, buy, and sell. Power is the primary force in today’s era. Because the curriculum is governed by teachers, school board members, and national standards, teachers and students have power connections [ 11 ].
Implications of a System Approach
In a systems approach, the current state of affairs and its factors are both causes and outcomes. Rather than a linear path of socioeconomic variables leading to various health outcomes, they are interconnected in a causal web. The feedback loops result in outcomes that influence the causes. Low income and deprivation, for example, lead to inferior health outcomes, exacerbating the group’s poor and worsening health. A more advanced model, such as the system dynamic model, is necessary to operationalize [ 12 ]. Early events and life cycle, occupational considerations, social ties (social networks and support, discrimination, neighborhood characteristics), and healthcare are all identified as social risk factors [ 13 ]. Eliminating these health inequities indicates that well-designed economic and social policies can promote health and health equity. It outlines 10 guidelines to keep in mind while launching interventions to reduce health disparities [ 14 ]. The circumstances increase their impact on life [ 15 ]. The physical atmosphere, opportunities for learning, suitable housing, occupation, and wealth are examples of these circumstances, known as SDH [ 16 ]. Recommendations such as improving living conditions and inequalities among people are justified in their own right but the way these are linked to health is problematic [ 17 ]. The magnitude of inequalities should be viewed with caution because the study does not take caste into account, potentially exaggerating socioeconomic inequalities [ 18 ].
Policies for Improving Health Equality
While numerous public policies contribute to public health and equality, enhancing public health is not the society’s or the government’s only goal. Although these initiatives have been effective at commencing actions addressing SDH, continuing inequities, and diverse social, economic, and cultural differences across India, more cooperation is required across the current programs of different ministries [ 18 ], resulting in policy incoherence may develop. Due to a lack of policy coherence throughout the government, one branch of the government may ensure the introduction of a national development plan of action, for example, TB free response to the change of the WHO [ 19 ]. At the same time, other parts promote exports, industrialization, and proposals that are dangerous to human life. The single cause for these discrepancies is a lack of knowledge among areas of the connections between health and quality of life, on the one hand, and more significant health determinants, such as productivity expansion, on the other. Another cause is that unrelated initiatives may have unexpected consequences that are not monitored or addressed. In its preamble, the Indian Constitution provides core values for establishing a social order in the country. An orderly society is built on these core values. Equality, various freedoms, socioeconomic justice, and individual dignity are fundamental principles for governing a democratic country like India. The policy approach will protect the social rights of people [ 20 ].
The healthcare system must comprehend the obligations of other parts and establish mutual consideration of health, its consequences, and great social welfare or life characteristics to contribute to policy coherence across government. It needs novel solutions and institutions that create avenues for debate and decision-making that cut across typical policy silos in government. In practice, this entails taking a variety of acts, such as facilitating seminars of government policymakers, program leaders, and healthcare provider organizations, to promote policy, service, and program coherence in response to the needs of disadvantaged groups, such as via conferences conducted at numerous organizational stages and with private and government providers. For evaluation of policy progress and pitfalls, from a theoretical perspective, several policy-making frameworks can be used to describe how programs are developed and executed [ 21 ].
The policy windows model by Kingdom (1995) is crucial as it illustrates how and why issues become part of the policy agenda before implementation [ 22 ]. Three streams are coupled or decoupled problem, policy, and politics; according to Kingdom, open and close strategy opportunities. The gathering of proof regarding health inequality is essential but not enough for policy change. Problems must be viewed or identified as problems that can be addressed by legislation. Complicated by the fact that general populace initiatives in largely unrelated domains may have population health implications [ 23 ]. The collection of facts, particularly the Acheson Report, has aided in the designation of health disparities as a political issue. Similar inquiries have formed the issue in other places [ 24 ].
Socioeconomic Determinants and Health Inequities
SDH must all be incorporated into public health services to reduce health disparities. Health services must be adapted to the demands of distinct population groups. Due to the build-up of difficulty through several areas and over the life course, different social groups in the population differ in their empowerment to participate in health interventions. Many public health programs have not met or are not meeting their health equity targets due to a lack of healthcare-specific interventions and a failure to reach out to vulnerable people and address significant social variables that affect public health. Disparities exist between public and private health systems [ 25 ]. Policy efforts at the health system level are required to monitor and improve these disparities [ 25 ]. The coronavirus disease 2019 (COVID-19) pandemic has had the greatest impact on groups that have faced discrimination and historical injustices [ 26 ]. Poor living conditions and exploitative labor have become more prevalent, allowing for inequitable income distribution and health risks [ 26 ]. Governments have exploited the pandemic to further erode civil and human rights and promote extractives [ 26 ]. A post-COVID-19 world must ensure equity, social justice, solidarity, and a shift in the balance of power and resources for poor and marginalized people [ 26 ].
Lower-income societies with lower smoking rates have a lower incidence of lung cancer [ 27 ]. Individual smoking patterns or different rates of illness prevalence and incidence among social groups, i.e., inequalities, are caused by balances or imbalances in community norms and social structures. Sick people are diametrically opposed to the overall healthy population [ 27 ]. The term health inequalities in SDH (SDHI) has recently been taken to refer to settings, social structures, social norms, and some determinants. Three primary paths have been proposed to describe how the social environment causes fitness inequities [ 28 ]. Social choice, or mobility of community, suggests that health, relatively more than the other way around, determines socioeconomic status. As a result, healthier people will be happier. They move toward a higher socioeconomic status than others who were less beneficial, resulting in inequities. Social causation claims that discrepancies in health outcomes are caused by a variety of unequally distributed material, psychosocial, and behavioral factors [ 29 , 30 ].
A life path viewpoint indicates various features throughout life (e.g., malnutrition in the maternal prenatal period, low learning services in infancy, physically hazardous employment, influence, and manifest illness trends across time). The eco-social method tries to assimilate these organic, communal, and natural variables in illness through a vigorous process of incorporation which means we accurately integrate natural effects from the substantial and the social world [ 7 , 31 ]. Over the last 40 years, research on health inequalities and growth has shed light on the income well-being trend [ 32 ]. Measuring the disparity between subgroups requires using different health data based on the relevant dimension of inequality (i.e., demographic, socioeconomic, or geographic factors) [ 33 ]. Monitoring health inequality at the national level assists in assessing the impact of policies, programs, and practices on the disadvantaged subgroup [ 33 ]. This priority will be given to the proposed Sustainable Development Goals. which ask countries to increase the income, gender, geographical location, race, age, ethnicity, disability, migrant status, and other relevant characteristics at the national level [ 34 ].
Conceptual Limitations of Inequalities
SDHI covertly and overtly embraces substantial parts of a Newtonian view of reality (i.e., reductionism, linearity, and hierarchy), as do most notions connected to health outcomes [ 35 ]. This reductive approach is represented by a factor influencing health outcomes, for example, socioeconomic stratification of mortality due to asthma and the selection of interventions that focus on a single determinant, for example, improving thermal comfort in homes with insufficient heat [ 36 ]. Another common assumption in this debate is linearity, which argues that determinants of inequalities can be used in a variety of situations [ 30 ]. Differential access to healthcare or education is presumed to be health disparities in results [ 37 ], essentially in a linear pattern, whether overtly or implicitly [ 38 ]. In the case of what works in terms of tackling health inequalities, disappointingly very less relevant reviews have been conducted [ 39 ].
Conclusions
After reviewing the current literature on SDH and health inequalities, we conclude that economic and social factors such as poverty, social exclusion, and others are usually regarded as SDH. Interventions are the most effective strategies to improve everyone’s well-being and reduce inequalities. The severity of employment, geography, and education imply that better healthcare management and expanded education and work prospects are required. Additional efforts in this area will likely help overcome social health inequalities in communities and achieve health equality. Policies that reduce social disadvantage can reduce health inequalities. The current state of the health sector, for which the union and state governments are equally responsible, and the right to health is not equally distributed can only be corrected if the union and state governments start practicing and introducing more efforts to achieve health equality. Health rights should be given to all people, encouraging them to use more services. Hence, making them healthier, more productive, and fit.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.

How to write an Essay Applying Social Determinants of Health

As governments worldwide struggle to find solutions to health disparities, it is becoming clear that medicine alone is not the solution. Social determinants of health (SDOH) greatly influence the health and well-being of individuals and the community. Factors like economic stability, neighborhoods, access to health care, etc., affect and shape the health of everyone within a community. Understanding these determinants and addressing them is one way of ensuring health equity.
Writing a social determinants of health essay requires a comprehensive understanding of all the determinants, their intricate relationships, and their implications. This essay should also illuminate all issues affecting health and the importance of addressing such issues to achieve health equity.
In this guide, our nursing writers will help you understand SDOH and how to write social determinants of health essay.
What are the Social Determinants of Health?
Social determinants of health, also known as SDOH, refer to the environmental conditions that influence a person’s health. The World Health Organization (WHO) defines SDOH as all non-medical factors that influence the health outcomes of individuals. They are conditions in which people are born, grow, work, interact, age, and other wider forces that affect their daily lives.
SDOH significantly influences health inequalities compared to any other issue, including access to healthcare services. For instance, unemployment or job insecurity leads to poor health by increasing stress and reducing access to healthcare and healthy living conditions due to financial difficulties. Moreover, prolonged unemployment exacerbates mental health issues like depression, further worsening health problems.
According to the Centers for Disease Control and Prevention (CDC), addressing SDOH issues accelerates the progress needed to establish a world where people attain the highest level of health.
What are the five Social Determinants of Health?
The SDOH can be grouped into five different categories:
Economic Stability
Social and community context.
- Health and Healthcare
Neighbourhood and Built Environment
Addressing all social determinants of health is key to improving people's health.
Economic stability is the absence of factors that result in major fluctuations in a nation's smooth running and growth. It is characterized by fluctuating income, high debt, job insecurity, lack of support, lack of employment, unpredictable market conditions, etc.
People with steady jobs and finances are more likely to live healthy lives because they can afford nutritious foods. Money allows people to meet all their basic needs, including good food, proper housing, and quality healthcare. Meeting these needs is essential for personal and community well-being.
According to a recent report by the U.S. Census Bureau , the national poverty rate is at 11.5% or 37.9
A country that is facing economic instability will have its people suffering from high-stress levels, anxiety, depression, and an increased risk of suicide cases. This instability results in increased access to healthy foods, good healthcare, and safe housing, thus worsening overall health.
What's more, economically stable individuals generally experience better health outcomes than those from poor backgrounds. This is because they can afford resources such as medications, affordable health coverage, etc, that protect and improve their health.
Education is a significant social determinant of health. It shapes and changes people's lives by equipping them with the right skills necessary to lift them out of poverty. People who can access high-quality education have the power to change their lives by eating healthy and accessing quality healthcare.
According to an analysis by the U.S. Department of Education, 130 million people in America lack basic literacy skills. This means they are not able to read and understand simple text. This makes it harder to complete hospital tests, follow written instructions or identify expiration dates of prescription medication.
Older people, those with low cognitive abilities, low socioeconomic status, and those with limited English proficiency have low health literacy.
For example, a person who has gone to school and acquired quality education can read about issues affecting their health and make the right choices. Alternatively, a person with less formal education cannot distinguish between trustworthy and untrustworthy information.
Lack of education or the lowest level of education is linked to lower income, which is, in turn, linked to poor health. By adopting education interventions, governments can help improve inequalities and individuals' health outcomes.
Improving health literacy helps eliminate barriers to understanding crucial information about
Social and community context refers to the environments in which people live, work, worship, and interact. It includes relationships among people and the networks they create within institutions.
The social and community context is divided into two parts: social networks and social support. Social networks encompass interpersonal social relationships, while social support is about the assistance that a person can receive from their social networks.
Understanding social and community context is essential to solving health disparities.
The social and community context includes essential issues such as civic participation, community cohesion, discrimination, incarceration, etc. These issues make it challenging for people to prepare for or respond to health emergencies.
Positive social and community relationships result in positive living and health outcomes. On the other hand, negative social relationships result in
So, how does social and community context affect health? For starters, connecting with other people in the community means access to emotional support. Connecting with others helps build a safety net for physical and mental health, reducing the risk of mental health issues such as depression and anxiety.
Additionally, communities that have strong social cohesion can come together in times of trouble and find solutions to contribute to healthier living.
When writing an SDOH essay, you must show how social and community context affects health to write an effective paper.
Healthcare Access and Quality
One in 10 people in the U.S. does not have health insurance. This means that when they fall sick, many will not seek health care or be denied services. Additionally, they could lack the resources needed to acquire medications or pay for medical tests.
Healthcare access and quality are determined by these components: availability, accessibility, affordability, and quality of healthcare services.
Availability of healthcare services
if a community lacks clinics, hospitals or any other facilities or healthcare providers such as nurses and doctors to offer healthcare services to its people, then it is detrimental to the people's health.
Access to healthcare is key to managing chronic health conditions. Primary care is essential for efficient and patient-centered care.
Accessibility
If a community has healthcare facilities but accessing them is difficult, then it is an issue. People living mostly in rural areas often face the biggest challenge of accessing healthcare facilities, mainly due to bad roads and greater distances.
According to research , 75% of people living in Colorado identified transportation as the biggest issue preventing them from accessing healthcare. It causes late hospital arrivals, missed appointments, and hesitancy to make follow-up appointments.
Transportation affects people’s ability to reach their doctor's offices on time for their appointments and to stay for the duration of the appointments. Missing an appointment also means that one has to go back to the hospital; otherwise, it will be incomplete care.
Quality of care
Quality of care refers to how effectively, safely, and timely healthcare services are provided to those in need. It also means ensuring that those in need receive patient-centered care.
A society will be said to have achieved quality health care when there is reduced mortality and morbidity, improved quality of life, and patient satisfaction.
Some of the barriers to quality care in society include income, racial bias, distance transportation, etc., and overcoming these barriers will help improve the health of the population.
Built environments include walkways, buildings, apartments, urban spaces, roads, parks, cities, etc. Neighborhood and built environment is characterized by factors such as quality housing, access to healthy foods and recreational spaces,
The neighborhood and environments a person lives in have a major impact on their health and health outcomes. For starters, the built environment influences a person's level of physical activity. For instance, if there are no parks, gyms, walkways, or other spaces people can use to exercise, their physical health will be greatly affected.
Additionally, access to highly nutritious foods is essential for maintaining good health. For instance, if a community lacks grocery stores, supermarkets, and farmers markets with health foods and is only surrounded by fast food outlets, there will be more cases of lifestyle diseases such as diabetes, high cholesterol levels, and hypertension.
Nurse's Role in Addressing Social Determinants of Health
Nurses play a crucial role in addressing social determinants of health to promote equality and healing for all. Here are some of the nurse's roles:
- Nurses help enhance health literacy, improving the quality and safety of all patients. Some of the ways they do this are by asking their patients' preferred language, being compassionate, and using methods of learning verification, such as utilizing language interpreters.
- Nurses also advocate for all patients within a healthcare system, helping them navigate the hospital and access the needed resources. They ensure that patients' voices, especially those in vulnerable positions, are heard and needs are met.
- Nurses are also instrumental in advocating for policies that promote health equity and address SDOH at all levels. Some nurses are also primary participants in policy development that helps bridge the gap between the delivery of care and social needs within the community.
- Nurses collaborate with other healthcare providers, such as social workers and public health experts, to promote a multifaceted approach to health that considers all aspects of a patient’s life. Additionally, nurses help in supporting services that address SDOH to enhance the overall health of the community.
- Nurses have the role of assuring that the voice of everyone, including patients and families, is incorporated into the clinical and community health systems.
- Nurses can also conduct extensive research to identify how SDOH affects individuals and community health outcomes and devise interventions to help mitigate these issues. Additionally, the study's results can be useful in informing policy developments.
- Nurses can also apply what they have learned in clinical practice, ensuring strategies for addressing SDOH are grounded in scientific evidence, which improves the chances of success.
Steps for Writing a Social Determinants of Health Essay
Now that you understand what SDOH means and the different determinants, you can begin writing your essay.
Understand the Prompt
An essay writing prompt explains how your instructor expects you to write the essay, the writing style to use, the information to include, and the sources to use.
So read the prompt given and highlight all the keywords. The words that are considered 'buzz words' will help you know how to structure and write your essay well.
If a topic is highlighted, ensure you understand it. Identify the reasoning you need to use, e.g., why, what, who, etc., to write an effective essay.
If there is no topic provided, you will need to come up with one. Some of the topics you can consider for your social determinants of health are:
- Rediscovering the social determinants of health.
- Examine how access to nutritious food affects health outcomes
- The role of food policies in ensuring food security and preventing diseases.
- Importance of social and community support in promoting health and preventing illnesses.
- Analyze how job insecurity is a significant roadblock to promoting health equity.
- Discuss the role of public policy in addressing social determinants of health.
- Social determinants of mental health issues and the significance of addressing them.
Select a topic that you will have an easy time writing about. Also, consider the topics that you are puzzled by or something that you would like to learn more about.
The next step is locating the right information to help you write an effective essay.
You can use academic databases such as PubMed, JSTOR, Google Scholar, etc., to find peer-reviewed articles on SDOH.
Additionally, consider using reputable health organizations and government agencies such as the U.N., WHO, and CDC to gather relevant reports and data about SDOH.
In addition, books and academic publications should be used to provide an in-depth analysis of different social determinants of health.
Ensure you evaluate your sources for credibility, accuracy, and relevance
Structure Your Social Determinant of Health Essay
Before writing, you must understand how to structure a social determinants essay. An SDOH essay has the same structure as another academic essay. This means it is divided into an introduction, body paragraphs, and conclusion.
Introduction
Hook, e.g., a shocking statistic about the impact of social determinants on health.
- Meaning of SDOH.
- Importance of SDOH
- Thesis statement (state the purpose of the essay and what you
Body Paragraphs
The body part of your essay should discuss all five social determinants of health. Address all these in different determinants in each paragraph.
Here is how you should organize the body paragraphs:
Determinant 1
- Topic sentence
- Evidence and examples supporting your topic sentence
- Impact each determinant has on health
Follow this format for all the other paragraphs.
The last part of your social determinant of health essay is the conclusion. This part summarizes what you have discussed in the body part and provides recommendations for change.
Related: How to write an essay for a nursing class.
Write Your Essay
Begin your essay with a captivating introduction that grabs readers' attention and makes them want to read the rest of your essay. This is key in ensuring your message is read by people who can make changes happen.
Next, write the body of your essay, ensuring that each paragraph addresses one idea. For every point you share, ensure you provide relevant data, research findings, and real-world examples to support it.
Ensure that you address every determinant and show how patients, their families, and the community in general are affected.
Finish your SDOH essay with a great conclusion that summarizes everything you have discussed in throughout your paper. Make sure you mention the importance of addressing SDOH to ensure health equity.
Revise and Proofread Your Essay
Before submitting your essay, ensure you accomplish the goals and objectives you set in the beginning. It is also about checking the focus and the organization of the paper. So check all the ideas shared while thinking about the big picture. Check whether all the ideas complement your thesis statements.
Additionally, check for grammar, spelling, and formatting errors. To simplify the process, use appropriate software such as Grammarly.
Understanding the social determinants of health ( SDOH ) is key to finding solutions to the root causes of health inequalities within a community and ensuring health equity. Each SDOH plays a crucial role in shaping the health outcomes of the population and can either enhance people's well-being or contribute to health disparities. Tackling these determinants one by one can help ensure health equity.
When tasked to write a social determinants of health essay, you must address all the determinants, explore their relationships, and come up with actionable solutions to address them.
If you are having a hard time writing this type of essay, our online nursing essay experts can help. Reach out to us today for more information.
Struggling with
Related Articles

Best Topics and Ideas for Social Media and Nursing
Nursing Student's Ultimate Guide to Writing a Nursing Care Plan
AMA Citation and Formatting Style for Medical Paper
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
Social Determinants of Health
What are social determinants of health.
Social determinants of health (SDOH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.
SDOH can be grouped into 5 domains:
Suggested citation
Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Retrieved [date graphic was accessed], from https://health.gov/healthypeople/objectives-and-data/social-determinants-health
Social determinants of health (SDOH) have a major impact on people’s health, well-being, and quality of life. Examples of SDOH include:
- Safe housing, transportation, and neighborhoods
- Racism, discrimination, and violence
- Education, job opportunities, and income
- Access to nutritious foods and physical activity opportunities
- Polluted air and water
- Language and literacy skills
SDOH also contribute to wide health disparities and inequities. For example, people who don't have access to grocery stores with healthy foods are less likely to have good nutrition. That raises their risk of health conditions like heart disease, diabetes, and obesity — and even lowers life expectancy relative to people who do have access to healthy foods.
Just promoting healthy choices won't eliminate these and other health disparities. Instead, public health organizations and their partners in sectors like education, transportation, and housing need to take action to improve the conditions in people's environments.
That's why Healthy People 2030 has an increased and overarching focus on SDOH.
How Does Healthy People 2030 Address SDOH?
One of Healthy People 2030’s 5 overarching goals is specifically related to SDOH: “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.”
In line with this goal, Healthy People 2030 features many objectives related to SDOH. These objectives highlight the importance of "upstream" factors — usually unrelated to health care delivery — in improving health and reducing health disparities.
More than a dozen workgroups made up of subject matter experts with different backgrounds and areas of expertise developed these objectives. One of these groups, the Social Determinants of Health Workgroup , focuses solely on SDOH.
Explore Research Related to SDOH
Social determinants of health affect nearly everyone in one way or another. Our literature summaries provide a snapshot of the latest research related to specific SDOH.
View SDOH Infographics
Each SDOH infographic represents a single example from each of the 5 domains of the social determinants of health. You can download them, print them, and share them with your networks.
Learn How SDOH Affect Older Adults
SDOH have a big impact on our chances of staying healthy as we age. Healthy People’s actionable scenarios highlight ways professionals can support older adults’ health and well-being.
The Office of Disease Prevention and Health Promotion (ODPHP) cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
The Social Determinants of Health Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
The social determinants of health are the conditions in the environment in which people live, learn, work, play, worship, and age. I agree that the social environment in which people live can affect their health status. Health outcomes are not determined solely by biological factors or access to quality health care (Centers for Disease Control and Prevention, n.d.). Resources that improve the quality of life can significantly impact the health of a population.
Examples of these resources include safe and affordable housing, access to education, public safety, availability of healthy food, local emergency services, and an environment free of life-threatening toxins (Office of Disease Prevention and Health Promotion, n.d.). I also support the recent shift in the view that it is solely up to the individual to influence their health in favor of recognizing the significant impact of external influences on it. In the modern world, very little depends on the individual. At first glance, he can choose what to eat, whether to exercise, and whether to seek medical care in a timely manner.
In fact, most of the choices that affect health are made by the marketing machine, the government, and life circumstances. For example, modern advertising presses from all sides, forcing one to choose specific products that are often not conducive to a healthy lifestyle. The need to work hard to earn money for these products pushes people to sacrifice a healthy sleep schedule and exercise. This chain has many links, but the result is always the same: people’s health is largely not up to them. External factors also indirectly affect health, such as health inequalities. When I read the CDC (2022) report on these inequalities, I was most surprised by the racial and ethnic inequalities. In an era of globalization and liberalization of society, a phenomenon like racism must be eradicated. The field of health care is one in which treating people equally is sometimes vital. That is why I believe that racial and ethnic discrimination in this area must be eradicated in the first place.
Centers for Disease Control and Prevention. (2022). Health equity considerations and racial and ethnic minority groups . Centers for Disease Control and Prevention. Web.
Centers for Disease Control and Prevention. (n.d.). Frequently asked questions . Web.
Office of Disease Prevention and Health Promotion. (n.d.). Social determinants of health . Web.
- CDC Employment Opportunities
- Process of Pharmaceutical Manufacture of Tablets
- Bullying: Violence in Children and Adolescents
- Reasonable Accommodation for the People with Disability
- How the Pandemic Affects the US Healthcare System
- Community Outreach Program for Veterans’ Mental Health Outcomes
- Health Promotion and Interdisciplinary Approach
- Organizational Culture for Safety in Healthcare
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, January 8). The Social Determinants of Health. https://ivypanda.com/essays/the-social-determinants-of-health/
"The Social Determinants of Health." IvyPanda , 8 Jan. 2023, ivypanda.com/essays/the-social-determinants-of-health/.
IvyPanda . (2023) 'The Social Determinants of Health'. 8 January.
IvyPanda . 2023. "The Social Determinants of Health." January 8, 2023. https://ivypanda.com/essays/the-social-determinants-of-health/.
1. IvyPanda . "The Social Determinants of Health." January 8, 2023. https://ivypanda.com/essays/the-social-determinants-of-health/.
Bibliography
IvyPanda . "The Social Determinants of Health." January 8, 2023. https://ivypanda.com/essays/the-social-determinants-of-health/.

115 Health Disparities and Social Determinants Nursing Topics and Examples
James colson dnp, rn.
- May 15, 2024
- Nursing Topics and Ideas
Health disparities, or inequalities in health status and healthcare access among different population groups, persist as a significant challenge in healthcare systems worldwide. These disparities are often rooted in social determinants of health, encompassing factors like socioeconomic status, education, employment, and access to healthcare.
Health Disparities and Social Determinants Nursing Topics
This article is a collection of Health Disparities and Social Determinants Nursing Topics and Nursing Research Paper Examples. We’ll explore PICOT questions examples on Health Disparities and Social Determinants of Health, nursing research questions, EBP &, capstone project ideas, research paper topics and nursing essay topic ideas to deepen our understanding and commitment to mitigating health disparities.
PICOT Questions Examples on Health Disparities and Social Determinants of Health
- In low-income urban communities (P), how does the implementation of nutrition education and healthy food access (I) compared to the absence of such interventions (C) affect childhood obesity rates (O) within a 2-year period (T)?
- Among pregnant women from disadvantaged backgrounds (P), what is the effect of comprehensive prenatal care and education (I) on birth outcomes and neonatal health (O) compared to minimal or no prenatal care (C) within 9 months (T)?
- In marginalized rural populations (P), how does the introduction of telehealth services (I) compared to traditional in-person healthcare (C) impact the management of chronic diseases (O) over a 12-month period (T)?
- Among elderly residents in underserved communities (P), what is the impact of social isolation interventions (I) on mental health and overall well-being (O) compared to those without such interventions (C) within 6 months (T)?
- In disadvantaged urban neighborhoods (P), how does access to safe recreational spaces (I) compared to limited or no access (C) influence physical activity levels (O) within a 1-year period (T)?
- In homeless populations (P), what is the effect of access to housing assistance programs (I) on healthcare utilization and overall health (O) compared to those without housing support (C) within a 3-year period (T)?
- Among individuals with low educational attainment (P), how does participation in adult education programs (I) compared to no participation (C) affect health literacy and healthcare decision-making (O) over a 2-year period (T)?
- In immigrant communities (P), what is the impact of culturally tailored health promotion programs (I) on the prevalence of chronic diseases (O) compared to non-tailored programs (C) within a 5-year period (T)?
- In underserved rural areas (P), how does the availability of transportation services (I) compared to limited transportation options (C) influence healthcare access and preventive care utilization (O) within a 2-year period (T)?
- Among individuals with low income (P), what is the effect of job training and employment assistance programs (I) on overall well-being and healthcare access (O) compared to unemployment (C) over a 3-year period (T)?
Working on a Nursing Paper?
Get Nursing Writing Services for your nursing papers, presentations and capstone projects. ZERO AI, ZERO Plagiarism, and 💯 Timely Delivery.
You can also check out PICOT Questions Examples on Gastrointestinal Nursing
Evidence-Based Practice (EBP) Project Ideas on Health Disparities and Social Determinants of Health
- Implementing community-based educational programs targeting social determinants of health in underserved neighborhoods.
- Developing a program to address food deserts and improve healthy food access in disadvantaged communities.
- Evaluating the impact of telehealth services on healthcare access and outcomes in rural populations.
- Creating interventions to combat social isolation and improve mental health in elderly, isolated individuals.
- Designing a community-wide initiative to increase access to safe recreational spaces and promote physical activity.
- Implementing housing assistance programs to improve the health and well-being of homeless individuals.
- Developing adult education programs to enhance health literacy and healthcare decision-making.
- Creating culturally tailored health promotion programs for immigrant communities.
- Designing transportation services to enhance healthcare access in underserved rural areas.
- Establishing job training and employment assistance programs for individuals with low income to improve overall well-being and healthcare access.
- Assessing the impact of income inequality on health disparities and exploring potential policy interventions.
- Evaluating the effectiveness of targeted interventions to reduce health disparities in maternal and child health.
- Investigating the role of education and health literacy in addressing disparities in preventive care utilization.
- Assessing the impact of access to safe housing on overall health outcomes and healthcare utilization.
- Developing and evaluating interventions to address the digital divide and improve telehealth access in underserved communities.
- Exploring the relationship between neighborhood characteristics, such as crime rates and safety, and healthcare access in disadvantaged areas.
- Assessing the role of transportation infrastructure in reducing healthcare disparities in rural populations.
- Investigating the impact of employment stability and job security on healthcare access and utilization.
- Exploring the connection between environmental factors, such as air quality and access to green spaces, and health disparities.
- Assessing the effectiveness of community health worker programs in addressing disparities in chronic disease management.
Nursing Capstone Project Ideas on Health Disparities and Social Determinants of Health
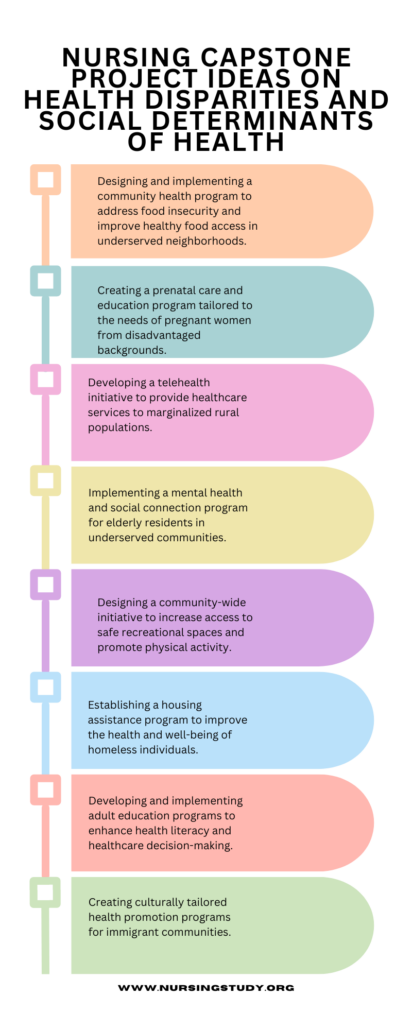
- Designing and implementing a community health program to address food insecurity and improve healthy food access in underserved neighborhoods.
- Creating a prenatal care and education program tailored to the needs of pregnant women from disadvantaged backgrounds.
- Developing a telehealth initiative to provide healthcare services to marginalized rural populations.
- Implementing a mental health and social connection program for elderly residents in underserved communities.
- Establishing a housing assistance program to improve the health and well-being of homeless individuals.
- Developing and implementing adult education programs to enhance health literacy and healthcare decision-making.
- Designing a transportation services program to enhance healthcare access in underserved rural areas.
- Establishing job training and employment assistance programs to improve overall well-being and healthcare access for individuals with low income.
- Investigating the impact of policy interventions on reducing health disparities in maternal and child health.
- Evaluating the effectiveness of targeted educational interventions in reducing disparities in preventive care utilization.
- Assessing the impact of supportive housing programs on overall health outcomes and healthcare utilization among homeless populations.
- Developing and evaluating strategies to bridge the digital divide and improve telehealth access in underserved communities.
- Investigating the role of community policing and safety measures in improving healthcare access in disadvantaged neighborhoods.
- Developing transportation infrastructure improvements to reduce healthcare disparities in rural populations.
- Exploring the impact of employee wellness programs on healthcare access and utilization for low-income workers.
- Investigating the influence of environmental justice initiatives on reducing health disparities related to environmental factors.
- Assessing the effectiveness of community health worker programs in addressing disparities in chronic disease management and health education.
- Designing and implementing a program to address social determinants of health within specific underserved communities.
You can also check out Nursing Research Paper Topics on Interprofessional Collaboration in Healthcare
Nursing Research Paper Topics on Health Disparities and Social Determinants of Health
- The Role of Social Determinants of Health in Shaping Health Disparities: A Comprehensive Review.
- Community-Based Interventions to Improve Healthy Food Access and Reduce Food Deserts.
- Telehealth Services in Rural Healthcare: Bridging the Gap in Healthcare Access.
- The Impact of Social Isolation on Mental Health in the Elderly Population.
- Safe Recreational Spaces and Physical Activity: Strategies for Addressing Health Disparities.
- The Health and Well-being of Homeless Populations: The Role of Housing Assistance Programs.
- Health Literacy and Healthcare Decision-Making: A Path to Reducing Disparities.
- Culturally Tailored Health Promotion Programs for Immigrant Communities: A Systematic Review.
- Transportation Services and Healthcare Access in Underserved Rural Areas.
- Job Training and Employment Assistance: An Avenue to Reducing Health Disparities.
- Income Inequality and Its Impact on Health Disparities: An Examination of the Evidence.
- Maternal and Child Health Disparities: Addressing Inequities in Prenatal and Postnatal Care.
- Education and Health Literacy: Exploring Their Role in Preventive Care Disparities.
- The Impact of Access to Safe Housing on Overall Health and Healthcare Utilization.
- The Digital Divide and Telehealth Access: A Barrier to Health Equity.
- Neighborhood Characteristics and Healthcare Access in Disadvantaged Areas.
- Transportation Infrastructure and Healthcare Access: An Examination of Rural Communities.
- Employment Stability and Healthcare Access: The Connection between Job Security and Health Equity.
- Environmental Factors and Health Disparities: Addressing Air Quality, Green Spaces, and Health Outcomes.
- Community Health Workers in Reducing Disparities: Evidence and Implications for Practice.
Nursing Research Questions on Health Disparities and Social Determinants of Health
- How do social determinants of health influence the prevalence and persistence of health disparities among various population groups?
- What are the most effective strategies for addressing food deserts and improving healthy food access in disadvantaged communities?
- What is the impact of telehealth services in increasing healthcare access and improving health outcomes for marginalized rural populations?
- How does social isolation among elderly individuals in underserved communities affect their mental health and overall well-being?
- What are the key factors influencing physical activity levels in communities with limited access to safe recreational spaces?
- What is the impact of housing assistance programs on the health and well-being of homeless individuals, and how do these programs affect healthcare utilization?
- How do adult education programs enhance health literacy and healthcare decision-making among individuals with limited educational attainment?
- What are the outcomes of culturally tailored health promotion programs in addressing health disparities among immigrant communities?
- How do transportation services improve healthcare access and preventive care utilization in underserved rural areas?
- What is the relationship between job training and employment assistance programs, employment stability, and overall well-being, and how do these factors affect healthcare access?
- What role do policy interventions play in reducing health disparities related to maternal and child health outcomes?
- How do targeted educational interventions impact disparities in preventive care utilization among different population groups?
- What are the outcomes of supportive housing programs in improving overall health outcomes and healthcare utilization among homeless populations?
- What strategies effectively bridge the digital divide and enhance telehealth access in underserved communities?
- How does community policing and safety measures influence healthcare access in disadvantaged neighborhoods?
- What impact do transportation infrastructure improvements have on healthcare disparities in rural communities?
- How do employee wellness programs affect healthcare access and utilization for low-income workers?
- What role do environmental justice initiatives play in reducing health disparities related to environmental factors such as air quality and access to green spaces?
- What is the effectiveness of community health worker programs in addressing disparities in chronic disease management and health education?
- How can healthcare providers and policymakers address social determinants of health within specific underserved communities to reduce health disparities?
Nursing Essay Topic Ideas on Health Disparities and Social Determinants of Health

- Health Disparities and Social Determinants of Health.
- Food Deserts and Their Impact on Community Health
- Telehealth and Rural Healthcare for Underserved Populations.
- Understanding Social Isolation in the Elderly.
- Recreational Spaces and Physical Activity.
- The Role of Housing Assistance Programs.
- Health Literacy and Informed Decision-Making for Equity in Healthcare.
- Cultural Sensitivity in Health Promotion Programs for Immigrant Communities.
- Transportation Barriers to Healthcare Access.
- Employment Assistance Programs and Health Equity.
- The Economics of Health Disparities.
- Maternal and Child Health Disparities.
- Education as a Determinant of Health.
- Safe Housing and Health Outcomes.
- Telehealth in the Digital Divide to Expand Access to Care.
- Neighborhood Safety and Healthcare Access.
- Transportation Infrastructure and Health Equity.
- Job Security and Employee Well-being and its Implications for Health.
- Breathing Clean Air: Environmental Justice and Health Disparities.
- Community Health Workers as Champions of Health Equity.
- The Role of Social Determinants of Health in Shaping Health Disparities
- The Digital Divide and Telehealth Access.
- Culturally Tailored Health Promotion Programs for Immigrant Communities.
- Income Inequality and Its Impact on Health Disparities.
- Housing Assistance Programs and the Health and Well-being of Homeless Populations.
- Health Literacy and Healthcare Decision-Making.
You can also check out Nursing Essay Topic Ideas on Psychosocial Nursing
Health Disparities and Social Determinants Nursing Research Paper Examples
- Health Disparities Discussion
- Disparities And Determinants Of Health
- Social Determinants Of Health
- How address these four social determinants of health
- What are social determinants of health?
Health disparities rooted in social determinants of health continue to be a formidable challenge for healthcare systems globally. Understanding the complex interplay between these determinants and health outcomes is crucial for addressing disparities and achieving health equity.
The PICOT questions examples, evidence-based practice project ideas, capstone project ideas, research paper topics, and research questions in this article are valuable resources for nursing students and professionals seeking to expand their knowledge and contribute to the field of health disparities and social determinants of health.
1. What are the 5 social determinants of health?
Healthy People 2030 sets data-driven national objectives in five key areas of SDOH: healthcare access and quality, education access and quality, social and community context, economic stability, and neighborhood and built environment.
2. What are health disparities?
Health disparities are preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations.
3. What is the relationship between determinants of health and health disparities that exist in different populations?
Social Determinants of Health (SDOH), Social Risk Factors, and Social Needs are all separate concepts that often are conflated. All three contribute to health disparities, and addressing all three is critical to advancing health equity.
4. What are the main determinants in health disparities?
Social determinants of health such as poverty, unequal access to health care, lack of education, stigma, and racism are underlying, contributing factors of health inequities.
- Social Determinants of Health: A Comparative Approach by Alan Davidson and Kevin J. Denny.
- Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare by Institute of Medicine.
- Health Disparities in the United States: Social Class, Race, Ethnicity, and the Social Determinants of Health by Donald A. Barr.
- Public Health: Social Determinants, Health Promotion, and Disease Prevention by Bernice L. Hausman.
- The Color of Health: Racial and Ethnic Disparities in the U.S. Health Care System by Leonard S. Pechter.
- Health Equity, Social Justice and Human Rights edited by Michael Marmot, Rachel Gisselquist, and David B. Taylor.
- The Social Determinants of Health: Coming of Age edited by Donald J. Lee and Michael W. Botsis.
- Health and Social Justice: Politics, Ideology, and Inequity in the Distribution of Disease by Richard Hofrichter.
- Beyond Health Insurance: Public Policy to Improve Health edited by James A. Morone and Lawrence R. Jacobs.
Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, what you'll learn.
- Nursing Careers
- Nursing Paper Solutions
- Nursing Theories
- Nursing Writing Guides
Related Posts
- How to Write a DNP Project Proposal with Examples
- Capstone vs Thesis vs Dissertation in Nursing
- 266+ Nursing Capstone Project Ideas and Topics for BSN, MSN – DNP [With Examples – updated]
Important Links
Knowledge base, paper examples, nursing writing services.
Nursingstudy.org helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Phone: +1 628 261 0844
Mail: [email protected]

We Accept:

@2015-2024, Nursingstudy.org
We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essays Examples >
- Essay Topics
Essays on Social Determinants Of Health
13 samples on this topic
To many college goers, crafting Social Determinants Of Health papers comes easy; others need the help of various types. The WowEssays.com collection includes expertly crafted sample essays on Social Determinants Of Health and related issues. Most definitely, among all those Social Determinants Of Health essay examples, you will find a piece that get in line with what you imagine as a decent paper. You can be sure that literally every Social Determinants Of Health work showcased here can be used as a vivid example to follow in terms of general structure and writing different chapters of a paper – introduction, main body, or conclusion.
If, however, you have a hard time coming up with a solid Social Determinants Of Health essay or don't have even a minute of extra time to explore our sample database, our free essay writer company can still be of great assistance to you. The matter is, our authors can craft a model Social Determinants Of Health paper to your individual needs and specific requirements within the defined timespan. Buy college essays today!
News Stories: A Sample Essay For Inspiration & Mimicking
Introduction
Essay On Social Determinants Of Health
Free social determinants of health essay example.
Question 1: What are the Social Determinants of Health?
Health Care Essay
{Author Name [first-name middle-name-initials last-name]} {Institution Affiliation [name of Author’s institute]}
“Social determinants of health”
Addiction: Exemplar Essay To Follow
Social Determinants of Health (SDH) affecting various forms of Addiction:

Perfect Model Research Paper On Social Determinants Of Health
Example of cost, quality and access in health sector essay, social determinants of health essay samples, example of research paper on relationship between race and health inequalities, reasons health professional teams can ensure environmental sustainability critical thinking example.
Description Globalisation is often regarded as a process that leads people from around the world to share a common economic, emotional, social and cultural space from wherever they are in the world (Guidotti, 2015). Nowadays everybody is affected either directly or indirectly. As the world continues to integrate on this front, it emerges that there arises benefits and problems in equal measure because in the long run there will be a sharing of economic, cultural, political and environmental powers among many nations of the world (McMichael & Butler, 2006).
275 words = 1 page double-spaced

Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline

Essay on Social Determinants Of Health
Students are often asked to write an essay on Social Determinants Of Health in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Social Determinants Of Health
Social determinants: a vital role in our health.
Our health is affected by factors beyond medical care. These are called social determinants of health. They include our income, education, housing, and access to healthy food and safe environments. These factors can influence our health in many ways. For example, people with low incomes are more likely to live in neighborhoods with high crime rates and poor air quality. They may also have less access to healthy food and medical care. As a result, they are more likely to experience health problems.
Impact on Health
The social determinants of health can have a significant impact on our health. For example, people who live in poverty are more likely to experience chronic diseases such as heart disease, stroke, and diabetes. They are also more likely to die prematurely. People who have low levels of education are also more likely to experience health problems. They may have difficulty understanding health information or accessing health care services.
Addressing Social Determinants: A Path to Better Health
There are many ways to address the social determinants of health and improve the health of our communities. One important step is to increase access to affordable housing, healthy food, and safe environments. We also need to invest in education and job training programs to help people get good-paying jobs. Additionally, we need to make sure that everyone has access to affordable health care.
By addressing the social determinants of health, we can create a healthier future for all.
250 Words Essay on Social Determinants Of Health
What are social determinants of health.
Social determinants of health are factors in the places where people live, learn, work, and play that affect a wide range of health risks and outcomes. These factors are like the soil in which plants grow. If the soil is healthy, the plants will likely be healthy too. But if the soil is not good, the plants might not grow well.
Money and Education
One big factor is how much money people have and how much education they get. People with more money and education often have better health. This is because they can afford better food, live in safer homes, and get better medical care. Education helps people learn about healthy ways to live and can lead to better jobs.
Neighborhood and Environment
Where a person lives also matters. Some neighborhoods have clean air and water, safe parks, and good schools. Others might have pollution, violence, and no safe places to play or exercise. These conditions can affect people’s health a lot.
Access to Health Care
Being able to get medical help when it’s needed is very important. But not everyone can get to a doctor or hospital easily. Sometimes, there aren’t enough doctors in an area. Other times, people might not have insurance to pay for the doctor.
In short, many things outside of our bodies influence our health. By understanding and improving these social determinants, we can help everyone have a better chance at a healthy life.
500 Words Essay on Social Determinants Of Health
The social determinants of health are the factors in our environment that can affect our health. These factors include things like where we live, our education, our job, our income, and our access to healthcare. They can also include things like our social support, our relationships with others, and our exposure to violence or discrimination.
Where We Live
Where we live can have a big impact on our health. For example, people who live in poverty are more likely to experience health problems than people who live in affluence. This is because poverty can make it difficult for people to access healthy food, safe housing, and quality healthcare. It can also lead to stress, which can take a toll on our physical and mental health.
Our Education
Our education can also affect our health. People with higher levels of education are more likely to be healthy than people with lower levels of education. This is because education can help us learn about healthy behaviors, such as eating healthy foods, getting regular exercise, and avoiding tobacco and alcohol. Education can also help us get better jobs, which can lead to better housing, better healthcare, and better overall health.
Our job can also affect our health. People who work in hazardous jobs, such as construction or mining, are more likely to experience health problems than people who work in less hazardous jobs. This is because hazardous jobs can expose workers to dangerous chemicals, dust, and fumes. They can also lead to stress, which can take a toll on our physical and mental health.
Our income can also affect our health. People with higher incomes are more likely to be healthy than people with lower incomes. This is because higher incomes can allow people to afford healthier food, better housing, and better healthcare. Higher incomes can also reduce stress, which can improve our physical and mental health.
Our Access to Healthcare
Our access to healthcare can also affect our health. People who have health insurance are more likely to get regular checkups and preventive care than people who do not have health insurance. This is because health insurance can make it more affordable for people to see a doctor.
The social determinants of health are complex and interconnected. They can affect our health in many ways, both positive and negative. By understanding the social determinants of health, we can work to create policies and programs that promote health and well-being for all.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Why I Chose Accounting
- Essay on Social Class Inequality
- Essay on Social Class And Education
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

Essay On Social Determinants Of Health
There are many social determinants of health. Some of these include income, occupation, education, race, and gender. Each of these factors play a role in how healthy a person is.
Income is one of the most important social determinants of health. People who earn more money are generally healthier than those who earn less. This is because they can afford to buy better food and have better access to health care. They can also afford to live in safer neighborhoods with better schools and parks.
Occupation is another important social determinant of health. People who work in dangerous or unhealthy jobs are more likely to get sick than those who work in safe environments. This is because their jobs expose them to harmful chemicals or other hazards.
Education is another important social determinant of health. People who have more education are generally healthier than those who have less education. This is because they know more about how to stay healthy and prevent diseases. They also tend to have better jobs with higher incomes.
Race is another important social determinant of health. People of color are generally not as healthy as white people. This is partly because they often live in neighborhoods with fewer resources and worse schools and parks. They also face discrimination in the workplace and in the health care system.
Gender is another important social determinant of health. Women are not as healthy as men, on average, partly because they often earn less money and have fewer opportunities for good jobs. They also face discrimination in the workplace and in the health care system.
There are many other social determinants of health, including housing, food, transportation, and social support. All of these factors play a role in how healthy a person is.
It is important to remember that social determinants of health are not the only things that affect our health. Personal choices also play a role. People who eat unhealthy foods and don’t exercise are more likely to get sick than those who eat healthy foods and exercise regularly. But it is clear that social determinants of health play a major role in our overall well-being.
An explanation of the phrase “social determinants of health” The social determinants of health include settings, as well as organizational effects on them. Furthermore, they are influenced by currency distribution, influence, and resources at both local and global levels. They assess a person’s accurate social, personal, and physical assets in order to achieve his or her objectives, fulfill his or her requirements, and cope with changes in his or her circumstances.
The social determinants of health are significant because they reveal why some people are healthier than others and also help in understanding the health disparities that exist among different social groups. It is important to study the social determinants of health because they provide information on how different policies can be implemented in order to improve the overall health of the population.
Health is determined by a number of factors, including biology, environment, lifestyle and socioeconomic status. The social determinants of health are those factors that influence an individual’s health status within society.
There are a variety of social determinants of health, but some of the most important include:
– Income and Wealth: Low income and wealth are associated with poorer health outcomes. This is due to a variety of factors, including lack of access to health care, poor living conditions, and stress from economic insecurity.
– Education: Studies have shown that people with more education tend to have better health outcomes than those with less education. This is likely due to the fact that people with more education are more likely to have higher incomes and better jobs, and they are also more likely to have access to health information and resources.
– Employment Status: Unemployed people are more likely to have poorer health outcomes than those who are employed. This is likely due to the fact that unemployed people often have lower incomes and fewer resources, which can lead to stress and poorer living conditions.
– Race/Ethnicity: Health disparities exist among different racial and ethnic groups in the United States. Studies have shown that minority groups, such as African Americans and Hispanics, tend to have worse health outcomes than whites. This is likely due to a variety of factors, including socioeconomic status, access to health care, and exposure to stressors such as racism and discrimination.
– Gender: Women tend to have worse health outcomes than men. This is likely due to a number of factors, including biological differences, social roles, and access to health care.
– Sexual Orientation: Health disparities exist among different sexual orientations. Studies have shown that lesbian, gay, bisexual, and transgender (LGBT) individuals tend to have worse health outcomes than heterosexuals. This is likely due to a number of factors, including discrimination, lack of access to health care, and stress from hiding one’s sexual orientation.
Each of these social determinants of health can influence an individual’s health status in a variety of ways. For example, low income can lead to poor living conditions, which can in turn lead to health problems. Additionally, minority groups may have less access to health care and resources, which can also lead to poorer health outcomes.
The social determinants of health are important because they reveal why some people are healthier than others and also help in understanding the health disparities that exist among different social groups. By understanding the social determinants of health, we can develop policies and programs that aim to improve the overall health of the population.
Social determinants of health, as defined by the World Health Organization (WHO), are complex, interconnected, and comparable social and economic systems that account for most health disparities. Such social and economic structures include not just the social situation but also people’s physical surroundings, medical services, structural aspects as well as societal elements (WHO n.d.). The phrase “social determinants of health” refers to events such as where individuals are conceived, reared, lived their lives, worked, and sought oldness.
Health, in other words, is not merely a matter of personal responsibility; it is also shaped by the social and economic environments within which people live their lives. Health is determined by a complex interaction between people and their physical and social environment.
Health disparities among different social groups are shaped by the distribution of money, power, and resources in society. Health is not only about access to health services; it is also about the quality of the environment, education, employment, food, housing, and social support. The conditions in which people live their lives determine their health status.
More Essays
- Social Determinants Of Health Essay
- Advantages And Disadvantages Of The Biomedical Model Of Health Essay
- Disparity In Health Essay
- Seeking Health Care Case Study Essay
- Public Health Approach To Mental Health
- Public Health In The 19th Century Essay
- The Importance Of Health Promotion Essay
- Public Health Case Study Essay
- Health In The Elizabethan Era
Leave a Comment Cancel reply
Save my name, email, and website in this browser for the next time I comment.

The Social Determinants Of Health (SDOH) Essay
Throughout the course of their life, individuals will experience varying degrees of health and well being. An individual’s health is measured based on the different types of conditions and resources that they are exposed to. These conditions and resources can be identified through what is called The Social Determinants of Health (SDOH). SDOH are used to identify the health status of an individual, community and population. The SDOH covers a broad range of measures that include income, housing and environmental factors .
According to the World Health Organisation (WHO), the SDOH are defined as “the conditions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels” (WHO, 2015) Without apt income, housing and environmental factors to assist in achieving and maintain ideal health, the health status of an individual will gradually decrease. Overtime, this decrease can trigger a series of unfavourable circumstances that will result in the downward spiral of health resulting in negative outcomes.
In order to maintain the ideal health status, an individual is to have a stable source of income. Income is considered one of the most important SDOH as it is one of the main factors in order survive in our modern monetary based society . Individuals or populations who have access to a high or stable source of income are generally associated with better health (WHO, 2015). Furthermore have a greater advantage on the socioeconomic status ladder in regards to work, education and housing. Lower down the status ladder, individuals or populations that have low or no income , have a lower socioeconomic status.
Therefore, are at a greater risk of negative health impacts through implications such as lack of education and poverty. Education is an important element that an individual requires in order to succeed in gaining stability. Without education, an individual lacks competency in attaining a career of which they can further develop their health status and resources. The career rewards them with the ability to achieve a steady income. Without a steady income, an individual is at risk of losing access to a variety of amenities such as; medical services, safe housing and nutrition.
This loss of income due to not gaining an education can lead to the individual descending into poverty. Poverty is one of the top leading issues in the world that increases the likelihood of incurring a wide range of serious health associated issues. Poverty occurs when an individual or population have little or no income in a difficult environment. This results in the individual becoming unable to access basic human requirements such as clean water , food, medical services, education and shelter (CDC, 2014).
When these basic human needs aren’t met a wide range of health issues and diseases are introduced to the individual or population such as diarrhoea, tuberculosis, malaria, pneumonia and general poor hygiene. These diseases are easily preventable, but are usually caused by a lack of resources such as a secure home or shelter that has access to suitable facilities such as; water, food and sanitary amenities. This leads into the next SDOH, which is housing. Housing is regarded as an important SDOH as poor housing or lack of access to housing can lead to a wide range of health issues that can impact on an individual or family.
The definition of housing is “the provision of accommodation”. (Oxford Dictionary, 1884). Having access to a house, or a secure shelter to live is considered one of the most fundamental necessities to a stable lifestyle (Queensland Government, 2015) Without the presence of a home or shelter, an individual is more susceptible to poorer health as opposed to those with adequate housing. There are varieties of different housing related issues that can negatively impact on the health of an individual or community.
A few examples of these issues are affordability and housing conditions. The affordability of housing poses as a major issue for many individuals, families or communities as the cost of owning or renting a home continues to rise rapidly in price compared to the rate in which income is being earned. (Australian Government, 2008). The continuous increase in cost can introduce many negative factors on an individual’s health such as stress, mental health issues and social isolation that can trigger premature death.
Many individuals discover they are unable to keep up with the rising cost of housing, which results in the individual finding accommodation in housing in poorly designed buildings with unsavoury living conditions . The design of a house or shelter is critical to individuals, communities or populations as those who are exposed to poor housing conditions are considered to be more susceptible to suffer from physical and mental health problems (Queensland Government).
Examples of what diseases an individual can contract due to poor housing conditions are diseases such as tuberculosis, cardiovascular disease , asthma or housing related injuries. These disease or injuries are due to poor ventilation, indoor air pollution and unstable infrastructure ( WHO, 2015). The environment in which an individual’s housing is located is also considered crucial as they can be exposed to various environmental factors that can cause serious health problems .
Environment is considered a SDOH as an individual’s health can be affected by the location in which they live and the environmental factors they are exposed to. These environmental factors can negatively impact the health of an individual or community through various situations such as location and work. The location in which an individual lives impacts health in a number of different ways. This includes living in rural areas as opposed to living in suburban/ metropolitan areas.
Individuals based in rural areas lack access to quality health care services, housing and jobs. Limited access to these amenities can cause negative indirect impacts on an individual’s health status such as mental health issues, social isolation and shorter lifespan’s. Metropolitan areas also provide many negative health impacts even though it provides better resources and support compared to rural areas. Individuals that reside in these areas are more inclined to develop diseases such as diabetes, obesity, heart disease and respiratory diseases (Friel, 2010).
These diseases are trigger through various lifestyle influences such as poor diet, lack of exercise, air pollution, smoking, excessive consumption of alcohol and substance abuse . In terms of work, individuals in metropolitan areas are more likely to have exposure to more job opportunities, which boosts their chances of income compared to rural areas. In rural area’s, work is a major issue as there is not enough job opportunities to account for the number of people living in the rural communities. With lack of job opportunities or skills gained hrough education, individuals are unable to source income, thus falling lower on the socioeconomic ladder.
This can lead to a number of issues such as depression, alcoholism, suicide and homelessness (National Rural Health Alliance INC. , 2015). Individuals that have gained a job in rural areas are more susceptible to diseases such as respiratory disease, skin disease and cardiovascular disease due to working in jobs involving mining, building or chemicals in order to gain income (National Rural Health Alliance INC, 2015) In the end, these factors all contribute to attaining an ideal level of health.
It is apparent that income, housing and environment are directly linked to one another. Without the stability of income, an individual is exposed to a lack of education. This, in turn, assists the individual to gain access to a career. Without the presence of an income, the individual is deprived of their basic human needs such as housing. Without income, the individual is unable to afford adequate housing, which forces them to descend into unfavourable living conditions. Unfavourable living conditions links into the environment in which the individual is exposed to, such as location.
Location is not only limited to the area, but includes the nation as a whole. Remote and suburban areas offer different lifestyles but it is the nation that defines the resources of the area. When linked together, these factors all contribute, define and measure the health conditions of individuals, communities and populations in an appropriate and reliable extent through the use of the SDOH. This confirms that the SDOH play an important factor in the health status of individuals and action must be taken in order to help individuals affected by these determinants.
To export a reference to this essay please select a referencing style below:
Related essays:
- History of Mental Health by Mind
- Determinants Of Health Essay
- How to improve Homelessness
- Medical Savings Accounts
- Tele Education Essay Examples
- Solutions for Homelessness
- The Bubble Economy of Japan
- Entering American Business In a Foreign Country
- High School Dropout Rate Among Low-Income Students
- Disparities in Health of Children
- History of Education
The Influence of Educational Determinants on Children’s Health: A Scoping Review of Reviews

- 1 University of Bordeaux, Institut National de la Santé et de la Recherche Médicale (NSERM), Bordeaux Population Health (BPH), U1219, Méthodes de Recherche Interventionnelle pour la Santé des Populations (MéRISP), Population Health Translational Research (PHARES)/Equipe Labellisée Ligue Contre le Cancer, Centre d’Investigation Clinique 1401/Centre Hospitalier Universitaire de Bordeaux, Service de Prévention, Institut de Santé Publique, d’Épidémiologie et de Développement (ISPED)/Chaire Prévention, Bordeaux, France
- 2 INVEST Flagship Research Center, Department of Psychology and Speech-Language Pathology, University of Turku, Turku, Finland
- 3 Fédération Promotion Santé, Auberviliers, France
- 4 University of Bordeaux, INSERM, BPH, U1219/PHARES, Bordeaux, France
- 5 Santé Publique France, Paris, France
Objectives: Education is one of the most important social determinants shaping the development and wellbeing of children. The purpose of this review of reviews is to inform policymakers, practitioners and public health stakeholder involved in developing child-friendly policies outside of the healthcare system.
Methods: We carried out a scoping review of reviews. It included 32 reviews.
Results: We identified four main categories of educational determinants in relation to children’s health: 1) the organization and structure of educational activities, 2) the interpersonal relations in the educational facilities and structures, 3) the spatial environment of educational facilities and structures, 4) social inequalities in the educational facilities and structures. This last category highlighted the capacity of education system to act on inequalities derived from the way social structures are organized.
Conclusion: We suggest a conceptual framework for action which distinguishes structural determinant (gender, race, social class, etc.) and structuring determinant (public policy, systems of governance, organization of cultures/values consideration). Finally, we discuss on how these social structures and structuring determinants influence the intermediary educational determinants collated in the review.
Introduction
The first few years of life have a crucial impact on the health of children, and their future wellbeing as adults. Investment in children’s health is not only a matter of social justice [ 1 ], it is also sound economic and societal strategy since investing in children actually delivers economic benefits throughout the rest of their life cycle (health expenditure, employability, productivity, etc.) [ 2 ].
Education, in particular, is one of the most important social determinants shaping the development and wellbeing of children [ 3 ]. Education can be defined as a process, formal or informal, which intentionally targets children’s capacities to absorb knowledge, skills and values, and to manage their emotions and social relations. These capacities enable children to become autonomous, engaged, accomplished members of society [ 4 ]. Education has a direct impact on health indicators such as life expectancy, as well as certain health-related behaviors (e.g., smoking, diet, sexual health) and medical problems (e.g., depression, obesity, chronic illnesses) [ 5 ]. For example, high-quality early childhood education and care (ECEC) settings (for children aged 0–6) can help children to improve their self-regulation skills, their capacity to form relationships, knowledge acquisition and the development of specific social, motor and cognitive skills [ 6 ], with long-term consequences for their physical health and life skills [ 7 , 8 ]. Through its holistic approach to child development, high-quality ECEC can promote child school readiness, and is reported particularly beneficial from children from low-income households [ 9 – 11 ]. It is important that educational facilities and structures are staffed with competent professionals, capable of fostering affectionate and reassuring interactions in surroundings which are safe, hygienic and accessible to parents. Groups size should allow good interaction among children and between children and adults, with effective and caring supervision to ensure educational cohesion [ 12 ].
There is no clear consensus regarding the form of educational interventions and policies required to create conditions conducive to good health in children. Despite the growing corpus of public health research aimed at developing models and frameworks to improve and strengthen the positive links between education and health, these studies are often largely overlooked or misunderstood by public policymakers. The purpose of this review is thus to provide an overview of the current state of knowledge regarding the determinants of education and their consequences on child health. This overview aims to inform policymakers, practitioners and public health stakeholders involved in developing child-friendly policies outside the healthcare system. In other words, the objective of this review is to identify the documented determinants within educational facilities and structures that is associated with the amelioration of children’s health.
Study Design
A scoping review of reviews can help providing a broad overview of the existing corpus of research into a topic. We adopted the methodology proposed by Arksey and O’Malley [ 13 ]. We used the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines (PRISMA 2020) [ 14 ].
Identifying the Research Question
This scoping review of reviews aimed at identifying the way educational determinants can improve children’s physical, cognitive, mental, and social health. To specify and focus our research questions, we used the PICoS (population-phenomena of interest-context-study design) framework, an adaptation of the PICO (population-intervention-comparison-outcomes) framework for reviews including qualitative reviews [ 15 , 16 ].
P—Population
This review focuses on children from birth up to the end of elementary school (12 years old), without any diagnosed health conditions. There are two main categories of educational establishments associated with this age range: ECEC settings (ages 0–6) and primary schools (ages 6–12).
I—Phenomena of Interest
Our phenomena of interest are educational determinants and child health. Education can be defined either as a context or a process. It is associated with institutions which provide explicit and deliberate learning and activities which are aimed to develop social, physical, emotional or cognitive development. Education is also present in parent-child interactions, but we chose not to include these aspects since this review is part of a broader project which includes a review focusing specifically on parenting determinants. We adopted the definition of health proffered by the World Health Organization (WHO): “a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity” [ 17 ].
C—Context
We chose to focus on structural educational determinants, rather than individual and biological determinants. By structural determinant, we mean the various systems that generate health inequities. Structural determinants are defined as “those that generate stratification and social class divisions in the society and that define individual socioeconomic position within hierarchies of power, prestige and access to resources.” [ 8 ] They include processes of governance, economic and social policies, cultural context and social structures that affect income, working conditions, housing, and education [ 18 ].
S—Study Design
We included all articles using a review method. As systematic methods are not used in all academic disciplines, we chose to also include all studies described as reviews by the authors or by the electronic databases.
Research Paradigm and Research Question
Our research has been thought in the pragmatic paradigm. This paradigm aims at utilizing the best methods to investigate real-world problems and to provide an action-oriented framework for research [ 19 , 20 ]. This review is the first part of a scientific program which support decision-making by making an analytical approach to public policy on children’s health easier. Thus, our main research question is: what are the determinants providing good health in education facilities and structures?
Identifying Relevant Studies
The search strategy was developed by the two first authors (AF, LW) with regular meetings with the other authors (M-PL, CD, LC). The final strategy was approved by a specialized librarian at the School of Public Health of the blind for review. The search was performed from July to September 2022. Search strategy included terms related to:
i) Institutions and activities explicitly concerned with learning (e.g., schools and child care facilities) and development (e.g., physical activities, music, creative activities).
ii) children’s health and development.
iii) review articles.
To capture as many relevant publications as possible, the list of terms was iteratively revised after searching the databases. The strategy was thus narrowed down by date of publication (between 2010 and 2022), language (French or English) and type of publication (peer-review) ( Supplementary Additional File S1 ).
We searched the following electronic databases ( Supplementary Additional File S2 ): PROQUEST (ERIC, International Bibliography of the Social Sciences (IBSS), Linguistics and Language Behavior Abstracts (LLBA), Political Science Database, Sociological abstract), EBSCOHOST (APA PsycInfo, APA PsycArticles, Psychology and Behavioral Sciences Collection, SocINDEX with Full Text, CINAHL Complete), Web of sciences, Pubmed. Reference lists of key publications were also manually searched by the review team. Covidence (a review software program) was then used to identify and screen the studies. The search also encompassed grey literature: OECD, the British Education Index, the Center for the Developing Child (Harvard), UNESCO, EURYCIDE, WHO.
Study Selection
The study selection process consisted of three stages: 1) title screening, 2) title and abstract screening, 3) full-text screening. The full-text screening was performed by two reviewers (AF and LW). The inclusion and exclusion criteria are detailed in the table below ( Table 1 ).
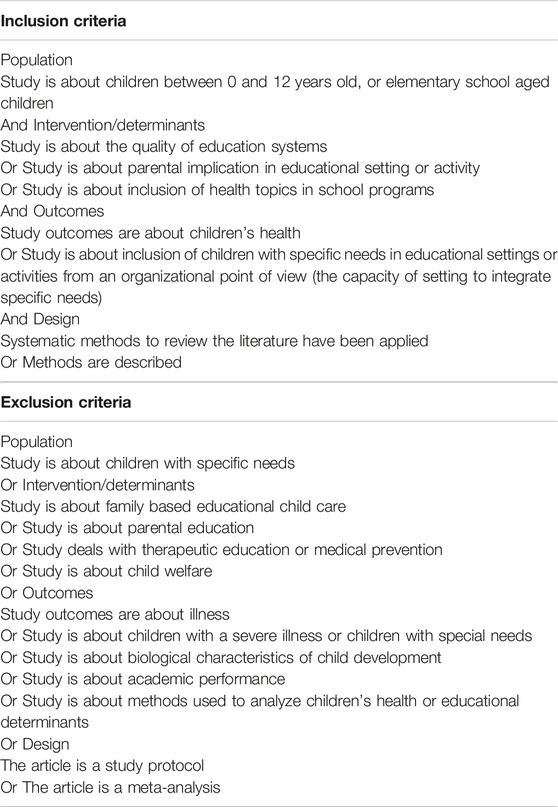
Table 1 . Inclusion and exclusion criteria (APPIE study, Bordeaux, France, 2024).
Charting the Data
Synthesis and interpretation of data were performed by two reviewers (AF and LW) using a data extraction tool ( Supplementary Additional File S3 ).
The first author (AF) utilized a three-stage process to analyze the results: 1) description of the reviews included in the sample, 2) thematic analysis of the reviews with reference to outcomes, research question and the main purpose of the scoping review of reviews. For the second step, an inductive analysis was used.
Collating, Summarizing and Reporting the Results
We include an introductory section aiming at describing the reviews included in our selection. It includes a flowchart, as recommended in the PRISMA guidelines. In a second sub-section, we tackle our research question (association between determinants within educational facilities and structures and children’s health).
Description of the Selected Sample of Reviews
The original search conducted from June to September 2022 yielded 5,067 potentially relevant articles. After duplication and relevance screening, 316 citations met the eligibility criteria based on title and abstract. The corresponding full-text articles were obtained for review: 36 were related to a patient population outside the scope of the review, 84 had a study design which did not meet the reviewing method criteria, 20 were centered on interventions which were not in the education sector, 18 had outcomes referring to another definition of health incompatible with the own from the WHO, 6 were not translated into French or English, 9 were unobtainable and 111 were not relevant. Thirty-two (32) articles were thus included in the final review ( Figure 1 ).
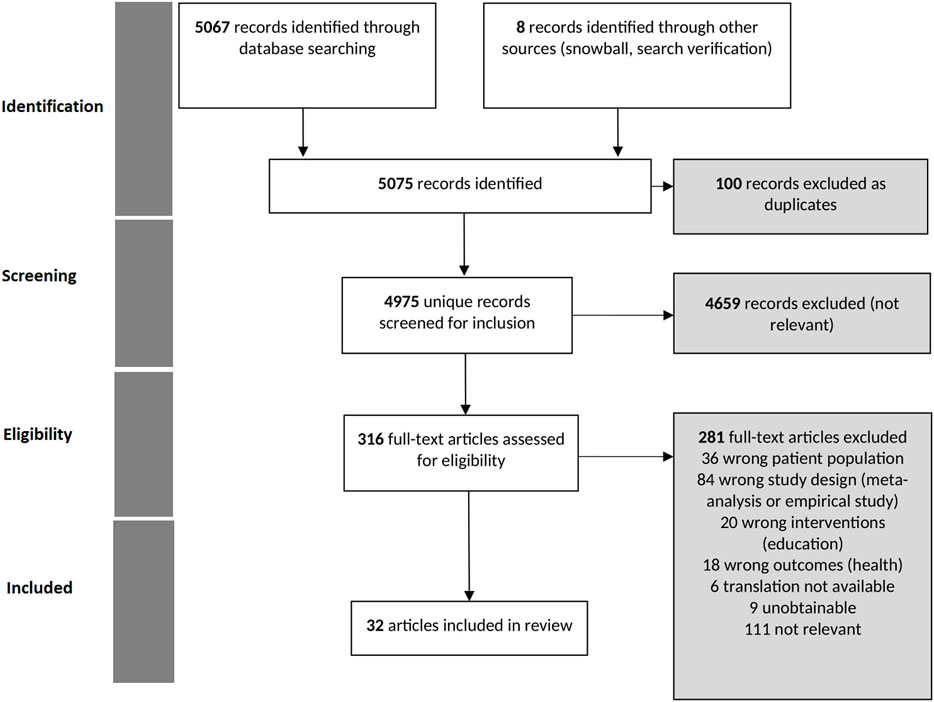
Figure 1 . PRISMA flowchart of study selection process (APPIE study, Bordeaux, France, 2024).
We divided educational facilities and structures into several categories based on the study setting ( Table 2 ), and their denomination in French and English. The full description of the articles is presented in Supplementary Additional File S4 .
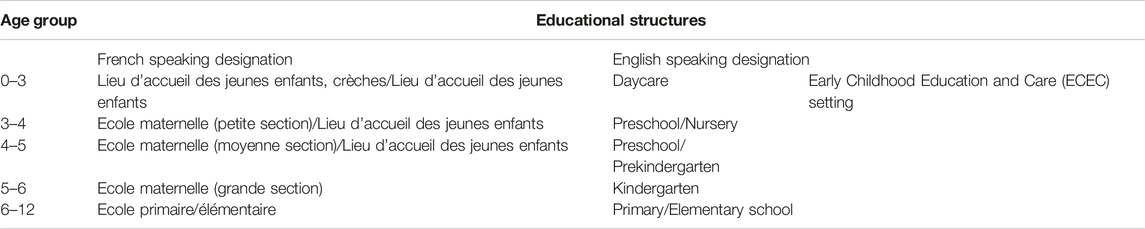
Table 2 . Different types of educational structures (APPIE study, Bordeaux, France, 2024).
Almost half of the reviews identified were conducted between 2020 and 2022 ( n = 16/32), with the clear majority published by lead authors attached to an American or European institution ( n = 25/32). Half of the reviews focused on ECEC settings (ages 0–6) ( n = 14/32). The majority of the reviews identified focused on the organization of educational activities ( n = 15/32), with the least-discussed subject being the spatial environment of educational facilities and structures ( n = 7/32) ( Table 3 ).
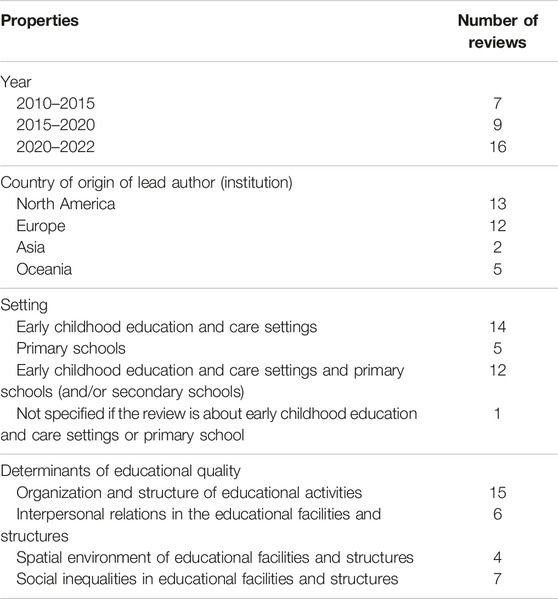
Table 3 . Properties of the reviews included in our scoping review (APPIE study, Bordeaux, France, 2024).
Association Between Educational Facilities and Structures and Children’s Health
Thematic analysis of these reviews revealed four major subjects of interest: 1) Organization and structuring of educational activities; 2) the interpersonal relations in the educational facilities and structures; 3) Spatial environment of educational facilities and structures; 4) Social inequalities in educational facilities and structures.
Organization and Structure of Educational Activities
The teaching program or curriculum.
Different educational innovations are described in the reviews:
• Social-emotional learning interventions: the acquisition of cognitive and non-cognitive skills, sometimes referred to as “socio-emotional skills” or “general skills” conducive to healthy development (interpersonal skills, responsible decision-making, self-awareness, social awareness and self-control) [ 21 – 24 ]);
• Mindfulness interventions: the capacity to “ intentional self-regulation of attention from moment to moment, and other definitions have since emerged centering on focal awareness of experience in the present moment ” (28: 1221) [ 25 – 27 ];
• Innovative educational formats such as learning-through-play and outdoor learning, the use of stories or brief interludes of physical activity during traditional sessions [ 21 , 28 – 31 ].
In both ECEC settings and primary schools, the social-emotional learning interventions tend to focus on the regulation of emotions, problem-solving and coping skills, empathy, self-esteem, wellbeing, positive emotion, social capacities, building better relationships between teachers and pupils, satisfaction with one’s life and overall fulfilment, while helping to protect against depression, anxiety, stress, emotional problems and negative emotions, particularly among children exhibiting symptoms of psychological disorders [ 22 , 23 ]. Studies analyzing mindfulness interventions have shown that such program can have beneficial effects for children, particularly by helping them to overcome emotional problems and negative emotions, and by boosting social and emotional skills, wellbeing and self-esteem, particularly in children with emotional problems or stress issues [ 22 , 25 ]. Yoga , regarded as encompassing aspects of mindfulness and meditation as well as physical postures, breathing and relaxation techniques, may also have positive effects in terms of reducing anxiety, depression and inhibition, while encouraging feelings of physical and psychological wellbeing, self-esteem, resilience, attention and even educational performance [ 26 ]. Broadly speaking, such interventions appear to have a greater impact on emotional and behavioral problems and hyperactivity between the end of pre-school and the onset of adolescence [ 25 ]. For both social emotional learning interventions and mindfulness interventions, the reviews suggest that there is no clear consensus on the impact of these interventions on child health and that the existing research is in need of consolidation [ 24 , 25 , 27 ].
In primary schools, innovative teaching methods such as outdoor learning and learning through play, integrated with more traditional lessons, may boost children’s social involvement [ 22 ]. Outdoor learning may take many forms: outdoor adventure play, the creation of school gardens, excursions or the teaching of traditional subjects in natural surroundings [ 28 ]. Review conclude that these forms of learning can increase the level of engagement shown by pupils, conducive to better appropriation of lessons, stronger exam results and improved social and emotional skills, collaboration and self-esteem [ 21 , 28 ] and dietary health [ 30 ]. However, the authors highlight the lack of established evidence for the connection between such activities and their expected health benefits. Innovative teaching methods like the use of stories by teachers can improve pupils’ language skills and create a friendly, respectful environment. Storytelling can also be a means of conveying messages about healthy behavior, lifestyle habits, dependency and psychosomatic troubles [ 31 ]. Innovative teaching methods like brief interludes of physical activity during traditional sessions can have a positive impact on the self-efficacy of children, improving the children’s physical conditions, fundamental movement skills, their quality of life and self-confidence, as well as the pleasure they take in physical activity [ 32 – 35 ].
Extra-Curricular Activities
Including physical activity among extra-curricular activities has been shown to have a positive impact on children’s depression, anxiety, stress and psychological distress. Participation in a variety of activities such as sport, dance and martial arts can boost self-efficacy, self-esteem, wellbeing and mental health, while reducing emotional problems, anxiety, negative emotions and symptoms of depression [ 22 ]. Team sport activities appear to have greater beneficial effects than individual sports. Other forms of organized activity such as youth organizations and arts groups have a positive impact on self-esteem, self-confidence, satisfaction in life and optimism [ 22 ]. Studies focusing on the practice of yoga and artistic activities outside of teaching hours have yielded contradictory results [ 25 – 27 ]. Interventions involving the creation of after-school clubs have been shown to improve social and emotional skills, with lasting effects when monitored over a period of 12 months [ 22 ].
Furthermore, informal learning activities may also be developed outside of school hours. For example, one review focusing on informal learning of STEM subjects (sciences, technology, engineering and mathematics) looked at the use of STEM skills to resolve everyday social problems, making for a more concrete and contextualized learning experience [ 36 ]. The review suggests that this learning approach shows great promise, particularly within family or community contexts, but there is still a lack of research into the potential effects of this form of learning on the socio-emotional capacities of pre-school children.
The Interpersonal Relations in the Educational Facilities and Structures
In primary school, when pupils feel they receive a higher level of support from their teachers, and when pupil-teacher relations are perceived as being strong, there is a notable increase in wellbeing, self-esteem, a sense of effectiveness, general life satisfaction, positive emotions, executive functions and self-regulation in children [ 37 , 38 ].
The majority of interventions seeking to improve teacher-pupil interactions by means of educational resources, emotional support resources, specific organizational arrangements in the classroom yielded positive, but modest returns [ 22 , 38 ]. Organizational support appears to be the most promising component [ 38 ]. Furthermore, teachers’ emotional skills and their efforts to manage emotions have received little attention [ 37 ]. Teachers perform numerous actions which can be regarded as forms of “care,” and spent large amounts of time with pupils outside of activities strictly related to cognitive learning, particularly in pre-school facilities [ 37 ]. Teachers’ capacities for their own emotional management have a positive impact on their sense of self-efficacy and their capacity to recognize children’s emotions, which in turn influences the emotional capabilities of the children.
With regard to relationships among peers (pupil-pupil interactions), positive relations in this sphere are a protective factor against internalizing and externalizing problems, self-harm and suicide, and are conducive to positive emotions, improving feelings of happiness, self-efficacy, optimism and wellbeing. As with pupil-teacher relations, interventions intended to strengthen relations among peers are beneficial when they succeed in developing social skills. Compared with working individually, getting children to work in collaboration have a positive impact on certain forms of cognitive development such as visual discrimination, visual perception and problem-solving, although it does not appear to have any impact on other capacities such as spatial awareness or reading [ 39 ].
Regarding relationships among family and ECEC settings, participatory techniques, with activities suggested by parents, or even family activities involving parents and children, may further boost the sense of engagement for family. One review also highlights the reciprocal connections between the environment in ECEC settings and the home environment [ 40 ]. It has also been noted that differentiation between the play materials at hand in the home and nursery environments was positively correlated with greater autonomy and the capacity to express positive emotions [ 40 ]. Moreover, it has been shown that parents and families are of the utmost importance during the transition to primary school [ 41 ].
Spatial Environment of Educational Facilities and Structures
The spatial component of educational structures is sometimes described as a “third educator”. Moving away from its former “passive” definition, it is now considered a complex and dynamic reality.
In ECEC settings, the “homely” atmosphere which prevails in facilities for very young children—including the presence of cozy spaces, outdoor spaces, spaces for family interactions and a general attention to aesthetic details—may help to prevent the development of social and emotional problems in children [ 40 ]. In one study cited in the same review [ 40 ], three-year-old children declare their preference for “soft” colors and elements in cozy spaces, whereas five-year-old children express a preference for “smooth” spaces with lively colors and harder surfaces. A review has also noted the beneficial effects of reading areas, books and writing materials on voluntary learning through play, and the acquisition of cognitive skills [ 40 ].
With regard to the outdoor play areas, children of pre-school age are more inclined to engage in functional and dramatic play (more complex forms of play) outdoors than they are indoors [ 40 ]. Natural materials and outdoor play areas may boost physical activity and functional, dramatic, independent play, as well as the overall quality of social behaviors. The physical diversity of outdoor facilities helps children to develop motor skills such as balance and coordination. Play areas specifically designed to bring children into contact with the natural environment may encourage independent exploration, autonomous constructive play, dramatic play and scientific experimentation through play, i.e., observing nature [ 40 ]. Introducing natural materials to manufactured play areas encourages decision-making, problem-solving, engagement and self-regulation, particularly in open play structures which enable children to test their courage [ 40 ]. Mobile physical activity equipment and avoiding overcrowding in play areas allows children to be more physically active [ 42 ], to have more complex play interactions and to exhibit less aggressive behavior [ 40 ].
In terms of the impact of facility organization, in ECEC settings, striking a balance between the simplicity and complexity of facilities or games may be important when it comes to nurturing interaction and cooperation. For example, a dollhouse can be regarded as a complex toy whereas a push-along toy is simple. Painting walls different colors (complex characteristics) may also encourage cooperation [ 40 ]. The balance between opened and closed spaces is also important to modulate interactions and promote engagement with learning activities. While complexity is important to stimulate children, it is also important to clarify the spatial organization of play areas, particularly by creating thematic zones which reinforce the continuity of play for the children, encouraging exploration, interaction and cooperation. Providing healthy food and ready access to water and sanitation facilities in schools can improve the health-related behaviors of children, particularly in terms of reducing the incidence of illness resulting from poor hygiene [ 42 – 44 ].
In conclusion, the co-construction of play areas, where children and teachers collaborate in the design process, has been shown to be essential to better reflect the perceptions and representations of both parties. Indeed, co-construction appear to be a fundamental priority when designing complex systems which define the physical environment of educational facilities [ 40 ].
Social Inequalities in Educational Facilities and Structures
The educational careers of children between the ages of 0 and 12 often involve changing institutions, particularly if the employment circumstances of their parents change [ 11 ]. The consequences of social inequalities may be mitigated by the capacity of educational facilities to provide a counterpoint to “chaotic environments” by establishing routines, imposing regular sleep patterns (nap time) and improving self-regulation through activities tailored to children’s needs [ 11 , 45 ]. The educational facilities and structures can also reinforce social inequalities [ 9 ]: gender and ethnic inequalities are specifically addressed in some reviews included in our scoping of the literature. First, we define how institutions influence gender inequalities, and second, we examine how they influence ethnic inequalities.
Gender inequalities have been explicitly reported in three reviews [ 39 , 46 , 47 ]. For example, discussion and cognitive development are greater for boys with low learning ability when they are in a collaborative task with a girl with high learning ability. Whereas for girls with low learning ability, collaborating with a boy with high learning ability shows no additional advantage over independent work, which may be linked to power imbalances in collaboration [ 39 ]. On the other hand, socio-emotional learning is found to have a greater beneficial effect on the mental health of girls than boys, and girl pupils are more sensitive to potential conflicts at the start of the year between students and teachers, and revealed more anxiety about these events [ 47 ]. They are also more at risk of developing mental health difficulties than boys, such difficulties being strongly linked to the pressure to achieve good grades at school [ 47 ]. Parental involvement in children’s school results, and fear for the future based on school results, have a strong negative influence on girls’ mental health [ 46 ]. However, there are still questions about the relationship between mental health and the pressure to get good grades, and about the role of other determinants in this relationship [ 47 ]. The fact that educational settings can reinforce gender inequalities is raised in a review that mentions that this element is often posited as a hypothesis but not always analyzed in depth [ 46 ].
Ethnic inequalities have been reported in one review [ 48 ]. In the United States, it has also been observed that African-Americans suffer from the highest rates of educational exclusion and that boys are at the greatest risk of exclusion [ 48 ]. The problem is that exclusion makes pupils miss out on teaching time, as well as relationships and interactions within the establishment, leading to disaffection, negative consequences on the school environment and long-term complications for the excluded pupils, compromising their chances of successfully completing their education and multiplying the risk of failure, dropping out, absenteeism, problematic social behaviors and even, in some cases, hastening their entanglement with the juvenile justice system [ 48 ].
A Conceptual Framework for Action: From Structural to Structuring Determinants of Education
The last section on social inequalities highlights that the educational determinants like education activities, the interpersonal relation within educational institution and? Spatial environment can reproduce social inequalities if social structures are not considered. But the education system also has the capacity to transform the inequalities generated by the structures [ 48 ]. For example, modifying the school environment may modify the roles children take on in play. One study observed that, after changing the outdoor play environment, children who had been dominant in the previous playground configuration did not always maintain this dominance following the introduction of greenery and trampolines to the playground [ 40 ]. Moreover, the perceived manifestation of diversity policies improves psychological adjustment to school among immigrant youths [ 48 ]. A review shows that culturally sensitive mentoring programs for ethnic minority and socially disadvantaged young people can lead to improved mental health [ 48 ]. School values must incorporate a degree of sensitivity to other social characteristics and adopt an intersectional perspective to encourage behavior conducive to a productive learning environment, good relations within the school and an all-round positive school environment. Educational systems have the power to transform societies from the inside, creating fairer systems and instilling the values of social justice from early on.
Based on the results contained in this review, our ambition is to develop an active approach to the notion of structural determinants. We thus propose the concept of “structuring determinants” referring to those determinants which shape the effects of social structures (race, gender, social class, etc.) on the health of children in different environments (including educational facilities and structures). The structuring determinants may take the form of policies, cultural influences or systems of governance. In the long term, these structuring determinants may also have a conditioning effect on lived environments, empowering them to alter social structures. Structuring determinants are therefore determinants which serve to mitigate the impact of social structures on social systems (like educational systems). Moreover, the focus on structuring determinants may mitigate the impact of exceptional situations like the COVID-19 successive lockdowns that considerably affected children’s health [ 49 ]. By integrating the results identified in our literature review, as well as the contribution made by the concept of structuring determinants, we can construct a more comprehensive framework for understanding the ways in which social structures, lived environments like educational systems and structuring determinants can influence children’s health ( Figure 2 ).
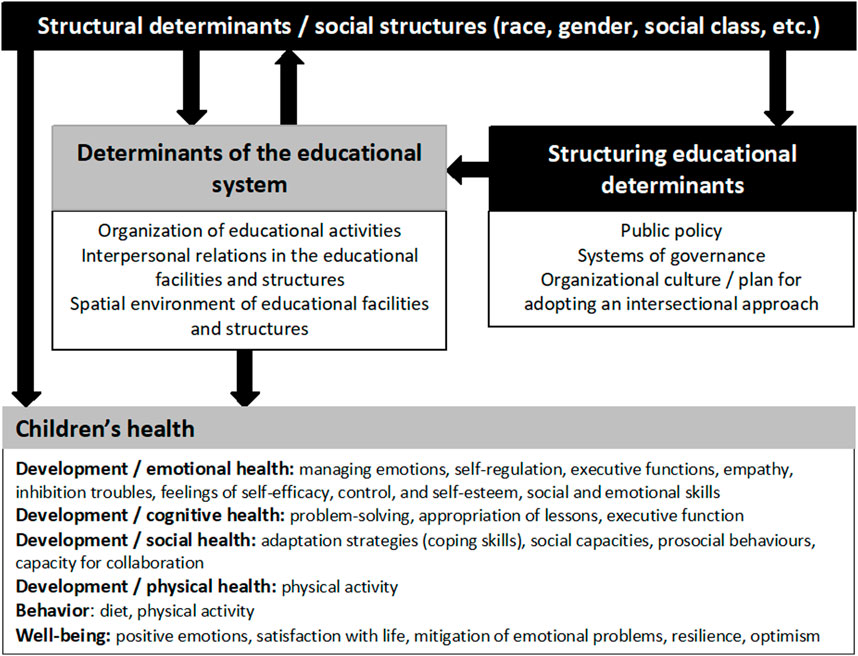
Figure 2 . Conceptual framework for action (APPIE study, Bordeaux, France, 2024).
Limitations and Avenues for Further Research
As with any review, we had certain hypotheses for the type of reviews which would be pertinent to our analysis. We expected to find more reviews dealing with parental involvement and the home environment. However, a large proportion of reviews matching this description were in fact excluded from our selection because they were interventional in their focus but did not consider the effect of such interventions on children’s health. We intentionally excluded meta-analyses, because the aim of this review was to offer a scope of the different educational determinant.
We also excluded a large number of reviews focusing on the inclusion of children on the autism spectrum. We were surprised to find that this subject was approached exclusively from the angle of the inclusive capacities of pupils, rather than the inclusive capacities of schools, which could have been a way of addressing structural determinants. We thus decided to exclude the articles in question because they dealt with a population with special needs. In addition, the design of our study is a scoping review of reviews, which might also explain that we found less publications on this issue. Nevertheless, published studies dealing with autism, public policies and the right to education show that this issue is particularly important [ 50 – 52 ]. Moreover, children with special education needs benefit from inclusive education and schools, as institutions, also benefit from such inclusive approach. The council of Europe reminds that “Inclusive education benefits all learners. It is not limited to integrating children with specific needs into mainstream education, but has a positive impact on all children, the school institutions and the community at large” [ 53 ]. A scoping review focused on inclusive education as a whole education approach (with respect to disability, gender, ethnicity, etc.) and its impact on children health could shed further light on this relevant topic.
We also had to exclude some reviews about school workforce because the link with children health was not explicitly addressed. This is the reason why this issue only appears in the section about the interpersonal relations at school. However, it remains a crucial issue. Structuring determinants like public policies may focus on the importance of the quality of teachers’ initial and continuing education training. Furthermore, a greater attention should be placed on teachers’ working conditions as well as that of the entire education community, because such conditions may have an impact both on teachers and students. For example, it has been demonstrated that pupils taught by teachers who feel that their working conditions are unfair are more likely to be dissatisfied at school, to play truant, to experience psychosomatic troubles and depression, and to receive lower grades than those taught by teachers not burdened by this feeling of injustice [ 54 ].
As noted above, it would be pertinent to build upon this initial review with a follow-up focusing on structuring determinants within educational systems which are conducive to the wellbeing of children.
We observed four main categories of determinants (the organization of educational activities, the interpersonal relations in the education facilities and structures and spatial environment in the educational facilities and structures) which influence children’s health. The section on social inequalities has allowed us to make a distinction between structural and structuring determinant and to propose a comprehensive framework addressing structural inequalities in educational systems.
Author Contributions
AF, LW, M-PL, and LC conceived the study. AF and LW conducted the literature search. AF and LW extracted the data from the retrieved studies. AF, M-PL, CF, AR-S, SV, and JB-W categorized the results and interpreted them. AF developed the initial draft of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/phrs.2024.1606372/full#supplementary-material
1. Spencer, N, Raman, S, O’Hare, B, and Tamburlini, G. Addressing Inequities in Child Health and Development: Towards Social justice. BMJ Paediatr Open (2019) 3(1):e000503. doi:10.1136/bmjpo-2019-000503
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Irwin, LG, Siddiqi, A, and Hertzman, G Early Child Development: A Powerful Equalizer . Vancouver (BC): Human Early Learning Partnership (2007).
Google Scholar
3. World health organization (WHO) Closing the Gap in a Generation. Health Equity Through Action on the Social Determinants of Health . Geneva: WHO (2008).
4. Hahn, RA, and Truman, BI. Education Improves Public Health and Promotes Health Equity. Int J Health Serv Plan Adm Eval (2015) 45(4):657–78. doi:10.1177/0020731415585986
5. Feinstein, L, Sabates, R, Anderson, TM, Sorhaindo, A, and Hammond, C What Are the Effects of Education on Health? (2006). p. 185.
6. Anderson, LM, Shinn, C, Fullilove, MT, Scrimshaw, SC, Fielding, JE, Normand, J, et al. The Effectiveness of Early Childhood Development Programs: A Systematic Review. Am J Prev Med (2003) 24(3, Suppl. ment):32–46. doi:10.1016/s0749-3797(02)00655-4
7. UNICEF Worlds of Influence Understanding What Shapes Child Well-Being in Rich Countries . Florence: Innocenti (2020). (Innocenti Report Card) Report No: 16.
8. Solar, O, and Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health. Social Determinants of Health Discussion Paper 2 (Policy and Practice) . Manila: WHO Regional Office for the Western Pacific (2015). Available from: https://apps.who.int/iris/handle/10665/249161 (Accessed December 14, 2021).
9. Barnett, W. Effectiveness of Early Educational Intervention. Science (2011) 333(6045):975–8. doi:10.1126/science.1204534
10. Larose, MP Adversité Socioéconomique, Fréquentation d’un Service d’éducation Préscolaire, et Développement de l’enfant: Investigations Expérimentales et Longitudinales Populationnelles . Montréal: Université de Montréal (2021).
11. Phillips, D, and Lowenstein, A. Early Care, Education, and Child Development. Annu Rev Psychol (2011) 62(1):483–500. doi:10.1146/annurev.psych.031809.130707
12. Melhuish, E, Ereky-Stevens, K, Petrogiannis, K, Ariescu, A, Penderi, E, Rentzou, K, et al. A Review of Research on the Effects of Early Childhood Education and Care (ECEC) on Child Development. (CARE Project; Curriculum Quality Analysis and Impact Review of European Early Childhood Education and Care (ECEC)) . Geneva: Utrecht University (2015). p. 100.
13. Arksey, H, and O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int J Soc Res Methodol (2005) 8(1):19–32. doi:10.1080/1364557032000119616
CrossRef Full Text | Google Scholar
14. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ (2021) 372:n71. doi:10.1136/bmj.n71
15. Aromataris, E, Fernandez, R, Godfrey, CM, Holly, C, Khalil, H, and Tungpunkom, P. Summarizing Systematic Reviews: Methodological Development, Conduct and Reporting of an Umbrella Review Approach. JBI Evid Implement (2015) 13(3):132–40. doi:10.1097/XEB.0000000000000055
16. Methley, AM, Campbell, S, Chew-Graham, C, McNally, R, and Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A Comparison Study of Specificity and Sensitivity in Three Search Tools for Qualitative Systematic Reviews. BMC Health Serv Res (2014) 14:579. doi:10.1186/s12913-014-0579-0
17. World Health Organization (WHO). Constitution of the World Health Organization. Am J Public Health Nations Health (1946) 36(11):1315–23.
18. Commission on Social Determinants of Health. Combler le Fossé en une Génération: Instaurer l’équité en Santé en Agissant sur les Déterminants Sociaux de la Santé: Rapport Final de la Commission des Déterminants Sociaux de la Santé . Strasbourg: Organisation mondiale de la Santé (2009). Available from: https://apps.who.int/iris/handle/10665/44083 (Accessed January 26, 2022).
19. Miller, FG, Fins, JJ, and Bacchetta, MD. Clinical Pragmatism: John Dewey and Clinical Ethics. J Contemp Health L Pol (1996) 13(1):27–51.
PubMed Abstract | Google Scholar
20. Yvonne Feilzer, M. Doing Mixed Methods Research Pragmatically: Implications for the Rediscovery of Pragmatism as a Research Paradigm. J Mix Methods Res (2010) 4(1):6–16. doi:10.1177/1558689809349691
21. Lohr, A, Krause, K, McClelland, D, Van Gorden, N, Gerald, L, Del Casino, V, et al. The Impact of School Gardens on Youth Social and Emotional Learning: A Scoping Review. J Adventure Educ Outdoor Learn (2021) 21(4):371–84. doi:10.1080/14729679.2020.1838935
22. Yu, T, Xu, J, Jiang, Y, Hua, H, Zhou, Y, and Guo, X. School Educational Models and Child Mental Health Among K-12 Students: A Scoping Review. CHILD Adolesc Psychiatry Ment Health (2022) 16(1):32. doi:10.1186/s13034-022-00469-8
23. McLeod, BD, Sutherland, KS, Martinez, RG, Conroy, MA, Snyder, PA, and Southam-Gerow, MA. Identifying Common Practice Elements to Improve Social, Emotional, and Behavioral Outcomes of Young Children in Early Childhood Classrooms. Prev Sci (2017) 18:204–13. doi:10.1007/s11121-016-0703-y
24. Djamnezhad, D, Koltcheva, N, Dizdarevic, A, Mujezinovic, A, Peixoto, C, Coelho, V, et al. Social and Emotional Learning in Preschool Settings: A Systematic Map of Systematic Reviews. Front Educ (2021) 6. doi:10.3389/feduc.2021.691670
25. Sun, Y, Lamoreau, R, O’Connell, S, Horlick, R, and Bazzano, AN. Yoga and Mindfulness Interventions for Preschool-Aged Children in Educational Settings: A Systematic Review. Int J Environ Res Public Health (2021) 18(11):6091. doi:10.3390/ijerph18116091
26. Hart, N, Fawkner, S, Niven, A, and Booth, JN. Scoping Review of Yoga in Schools: Mental Health and Cognitive Outcomes in Both Neurotypical and Neurodiverse Youth Populations. Children (2022) 9(6):849. doi:10.3390/children9060849
27. Jansen, P, Schulze, A, and Nottberg, C. Influence of Mindfulness-Based Interventions on Executive Functions in Childhood: A Systematic Review. Z Entwicklungspsychologie Padagogische Psychol (2016) 48(4):206–16. doi:10.1007/s12671-023-02084-w
28. Mann, J, Gray, T, Truong, S, Brymer, E, Passy, R, Ho, S, et al. Getting Out of the Classroom and Into Nature: A Systematic Review of Nature-Specific Outdoor Learning on School Children’s Learning and Development. Front Public Health (2022) 10:877058. doi:10.3389/fpubh.2022.877058
29. Schneider, S, Pharr, J, and Bungum, T. Impact of School Garden Participation on the Health Behaviors of Children. Health Behav Pol Rev (2017) 4(1):46–52. doi:10.14485/hbpr.4.1.5
30. Skelton, KR, Lowe, C, Zaltz, DA, and Benjamin-Neelon, SE. Garden-Based Interventions and Early Childhood Health: An Umbrella Review. Int J Behav Nutr Phys Act (2020) 17(1):121. doi:10.1186/s12966-020-01023-5
31. Pulimeno, M, Piscitelli, P, and Colazzo, S. Children’s Literature to Promote Students’ Global Development and Wellbeing. Health Promot Perspect (2020) 10(1):13–23. doi:10.15171/hpp.2020.05
32. Papadopoulos, N, Mantilla, A, Bussey, K, Emonson, C, Olive, L, McGillivray, J, et al. Understanding the Benefits of Brief Classroom-Based Physical Activity Interventions on Primary School-Aged Children’s Enjoyment and Subjective Wellbeing: A Systematic Review. J Sch Health (2022) 92:916–32. doi:10.1111/josh.13196
33. Kuzik, N, da Costa, BGG, Hwang, Y, Verswijveren, SJJM, Rollo, S, Tremblay, MS, et al. School-Related Sedentary Behaviours and Indicators of Health and Well-Being Among Children and Youth: A Systematic Review. Int J Behav Nutr Phys Act (2022) 19(1):40–32. doi:10.1186/s12966-022-01258-4
34. Lai, S, Costigan, S, Morgan, P, Lubans, D, Stodden, D, Salmon, J, et al. Do School-Based Interventions Focusing on Physical Activity, Fitness, or Fundamental Movement Skill Competency Produce a Sustained Impact in These Outcomes in Children and Adolescents? A Systematic Review of Follow-Up Studies. Sports Med (2014) 44(1):67–79. doi:10.1007/s40279-013-0099-9
35. Kuzik, N, Poitras, VJ, Tremblay, MS, Lee, EY, Hunter, S, and Carson, V. Systematic Review of the Relationships Between Combinations of Movement Behaviours and Health Indicators in the Early Years (0-4 Years). BMC Public Health (2017) 17(Suppl. 5):849. doi:10.1186/s12889-017-4851-1
36. Alexandre, S, Xu, Y, Washington-Nortey, M, and Chen, C. Informal STEM Learning for Young Children: A Systematic Literature Review. Int J Environ Res Public Health (2022) 19(14):8299. doi:10.3390/ijerph19148299
37. Denham, S, Bassett, H, and Zinsser, K. Early Childhood Teachers as Socializers of Young Children’s Emotional Competence. Early Child Educ J (2012) 40(3):137–43. doi:10.1007/s10643-012-0504-2
38. Sankalaite, S, Huizinga, M, Dewandeleer, J, Xu, C, de Vries, N, Hens, E, et al. Strengthening Executive Function and Self-Regulation through Teacher-Student Interaction in Preschool and Primary School Children: A Systematic Review. Front Psychol (2021) 12:718262. doi:10.3389/fpsyg.2021.718262
39. Sills, J, Rowse, G, and Emerson, L. The Role of Collaboration in the Cognitive Development of Young Children: A Systematic Review. Child Care Health Dev (2016) 42(3):313–24. doi:10.1111/cch.12330
40. Berti, S, Cigala, A, and Sharmahd, N. Early Childhood Education and Care Physical Environment and Child Development: State of the Art and Reflections on Future Orientations and Methodologies. Educ Psychol Rev (2019) 31(4):991–1021. doi:10.1007/s10648-019-09486-0
41. Fane, J, MacDougall, C, Redmond, G, Jovanovic, J, and Ward, P. Young Children’s Health and Wellbeing Across the Transition to School: A Critical Interpretive Synthesis. Child Aust (2016) 41(2):126–40. doi:10.1017/cha.2016.4
42. Herr, RM, Diehl, K, Schneider, S, Osenbruegge, N, Memmer, N, Sachse, S, et al. Which Meso-Level Characteristics of Early Childhood Education and Care Centers Are Associated With Health, Health Behavior, and Well-Being of Young Children? Findings of a Scoping Review. Int J Environ Res Public Health (2021) 18(9):4973. doi:10.3390/ijerph18094973
43. Colley, P, Myer, B, Seabrook, J, and Gilliland, J. The Impact of Canadian School Food Programs on Children’s Nutrition and Health: A Systematic Review. Can J Diet Pract Res Publ Dietit Can Rev Can Prat Rech En Diet Une Publ Diet Can (2019) 80(2):79–86. doi:10.3148/cjdpr-2018-037
44. Jasper, C, Le, TT, and Bartram, J. Water and Sanitation in Schools: A Systematic Review of the Health and Educational Outcomes. Int J Environ Res Public Health (2012) 9(8):2772–87. doi:10.3390/ijerph9082772
45. Martin, A, Johnson, AD, and Castle, S. Reframing High-Quality Public Preschool as a Vehicle for Narrowing Child Health Disparities Based on Family Income. Acad Pediatr (2021) 21(3):408–13. doi:10.1016/j.acap.2020.07.004
46. Troy, D, Anderson, J, Jessiman, PE, Albers, PN, Williams, JG, Sheard, S, et al. What Is the Impact of Structural and Cultural Factors and Interventions Within Educational Settings on Promoting Positive Mental Health and Preventing Poor Mental Health: A Systematic Review. BMC Public Health (2022) 22(1):524. doi:10.1186/s12889-022-12894-7
47. Stentiford, L, Koutsouris, G, and Allan, A. Girls, Mental Health and Academic Achievement: A Qualitative Systematic Review. Educ Rev (2021) 75:1224–54. doi:10.1080/00131911.2021.2007052
48. Welsh, R, and Little, S. Caste and Control in Schools: A Systematic Review of the Pathways, Rates and Correlates of Exclusion Due to School Discipline. Child Youth Serv Rev (2018) 94:315–39. doi:10.1016/j.childyouth.2018.09.031
49. Rajmil, L, Hjern, A, Boran, P, Gunnlaugsson, G, de Camargo, O, Raman, S, et al. Impact of Lockdown and School Closure on Children’s Health and Well-Being During the First Wave of COVID-19: A Narrative Review. BMJ Paediatr Open (2021) 5(1):e001043. doi:10.1136/bmjpo-2021-001043
50. van Kessel, R, Roman-Urrestarazu, A, Ruigrok, A, Holt, R, Commers, M, Hoekstra, RA, et al. Autism and Family Involvement in the Right to Education in the EU: Policy Mapping in the Netherlands, Belgium and Germany. Mol Autism (2019) 10(1):43. doi:10.1186/s13229-019-0297-x
51. van Kessel, R, Walsh, S, Ruigrok, ANV, Holt, R, Yliherva, A, Kärnä, E, et al. Autism and the Right to Education in the EU: Policy Mapping and Scoping Review of Nordic Countries Denmark, Finland, and Sweden. Mol Autism (2019) 10(1):44. doi:10.1186/s13229-019-0290-4
52. van Kessel, R, Hrzic, R, Cassidy, S, Brayne, C, Baron-Cohen, S, Czabanowska, K, et al. Inclusive Education in the European Union: A Fuzzy-Set Qualitative Comparative Analysis of Education Policy for Autism. Soc Work Public Health (2021) 36(2):286–99. doi:10.1080/19371918.2021.1877590
53. Commissaire aux droits de l’homme L’éducation Inclusive, un facteur Essentiel de la Cohésion Sociale des Sociétés Plurielles . London: Commissaire aux droits de l’homme (2015). Available from: https://www.coe.int/fr/web/commissioner/blog/-/asset_publisher/xZ32OPEoxOkq/content/id/10024340 (Accessed November 16, 2023).
54. Elovainio, M, Pietikäinen, M, Luopa, P, Kivimäki, M, Ferrie, JE, Jokela, J, et al. Organizational Justice at School and Its Associations With Pupils’ Psychosocial School Environment, Health, and Wellbeing. Soc Sci Med (2011) 73:1675–82. doi:10.1016/j.socscimed.2011.09.025
Keywords: children, social determinansts of health, education, scoping review, health in all policies
Citation: Fillol A, Wallerich L, Larose M-P, Ferron C, Rivadeneyra-Sicilia A, Vandentorren S, Brandler-Weinreb J and Cambon L (2024) The Influence of Educational Determinants on Children’s Health: A Scoping Review of Reviews. Public Health Rev 45:1606372. doi: 10.3389/phrs.2024.1606372
Received: 04 July 2023; Accepted: 24 April 2024; Published: 05 June 2024.
Reviewed by:
Copyright © 2024 Fillol, Wallerich, Larose, Ferron, Rivadeneyra-Sicilia, Vandentorren, Brandler-Weinreb and Cambon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
PHR is edited by the Swiss School of Public Health (SSPH+) in a partnership with the Association of Schools of Public Health of the European Region (ASPHER)+
*Correspondence: Amandine Fillol, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
Register to vote Register by 18 June to vote in the General Election on 4 July.
- Health and social care
- Public health
Wider Determinants of Health: June 2024 update
Update of data on the individual, social and environmental factors which influence the health of the population and impact on inequalities in health.
Applies to England
Wider determinants of health.
https://fingertips.phe.org.uk/profile/wider-determinants
This tool brings together available indicators at England and local authority levels on the wider determinants of health.
The Wider Determinants of Health tool is designed to:
- draw attention to the broad range of individual, social and environmental factors which influence our health
- provide the public health system with intelligence on the wider determinants of health, to help improve population health and reduce health inequalities
This release contains new data for the following indicators:
- average weekly earnings
- gender pay gap
- long term claimants of Jobseeker’s Allowance
- rate of economic inactivity
- food insecurity
- individuals not reaching the Minimum Income Standard
- unemployment (model based)
- affordability of home ownership
- rate of work-related illness
- air pollution: fine particulate matter
If you would like to send us feedback on the tool contact [email protected] .
Is this page useful?
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. Please fill in this survey (opens in a new tab) .

IMAGES
VIDEO
COMMENTS
The social determinants of health (SDH) are the non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social ...
Introduction and background. According to the World Health Organization (WHO), social determinants of health (SDH) are defined as the circumstances in which humans are born, develop, live, earn, and age. At the international, regional, and state or local levels, the distribution of money, power, and resources shapes these circumstances [ 1 ].
The objective of this essay is to clarify the understanding and use of Social Determinants of Health (SDOH) by exploring basic characteristics of 'determinants' and 'fundamental causes,' the 'social,' 'structure,' and 'modifiability,' and to consider theoretical and practical implications of this reconceptualization for public health.
Social determinants of health (SDOH) greatly influence the health and well-being of individuals and the community. Factors like economic stability, neighborhoods, access to health care, etc., affect and shape the health of everyone within a community. Understanding these determinants and addressing them is one way of ensuring health equity.
Social determinants of health (SDOH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. SDOH can be grouped into 5 domains: Economic Stability. Education Access and Quality. Health Care Access and Quality.
The social determinants of health that typically make up this field of study are social class, sex, age, race, and ethnicity. In this essay I focus mainly on social class but note that there is a ...
The disease development directly results from SDoH since they are to blame for health disparities. Various social determinants increase the likelihood of sickness, including poverty, substandard housing, social isolation, lack of uncontaminated water, restricted availability of health care, and insufficient medical systems (Maani & Galea, 2020).
CDC Strategies for Reducing Health Disparities 2016. HHS Action Plan to reduce racial and ethnic health disparities. 2020 Update to HHS Action Plan. Healthy People 2030 Objectives. Information on health conditions, health behaviors, populations, settings and systems, and social determinants of health. Last Updated: Jan 22, 2024 3:25 PM.
Papers are all peer-reviewed. Background: ... Commission on Social Determinants of Health made it perfectly clear that policies for health equity ... Having health framed as a social phenomenon emphasizes health as a topic of social justice more broadly. Consequently, health equity (described by the absence of unfair and avoidable or remediable ...
The Declaration expresses a global commitment to addressing the social determinants of health for advancing equity and to building the political momentum for reducing health inequities. Resolution WHA65.8 (2012) endorsed the Political Declaration, and a subsequent resolution recognized the importance of the focus on social determinants.2.
Through this essay, we have delved into the complex relationship between these social determinants and health outcomes, highlighting the need for targeted interventions to address health disparities and promote equity in healthcare. By understanding the root causes of poor health outcomes and working towards creating a more just and equitable ...
Evaluating intersectoral processes for action on the social determinants of health: learning from key informants. (Discussion Paper Series on Social Determinants of Health, 5) 1.Socioeconomic factors. 2.Health care rationing. 3.Interinstitutional relations. 4.National health programs. 5.Health policy. I.Loewenson, Rene.
Social determinants of health (SDOH) are non-medical factors that affect health outcomes. They include the conditions in which people are born, grow, work, live, and age. SDOH also include the broader forces and systems that shape everyday life conditions. These forces and systems encompass economic policies, development agendas, social norms ...
Social determinants of health are the factors that impact the health and well-being of individuals, families, and communities within a broader social and economic context. These include certain characteristics like social and economic status, education, employment, housing, access to healthcare, environmental factors, and social support networks.
The Social Determinants of Health Essay. The social determinants of health are the conditions in the environment in which people live, learn, work, play, worship, and age. I agree that the social environment in which people live can affect their health status. Health outcomes are not determined solely by biological factors or access to quality ...
This article is a collection of Health Disparities and Social Determinants Nursing Topics and Nursing Research Paper Examples. We'll explore PICOT questions examples on Health Disparities and Social Determinants of Health, nursing research questions, EBP &, capstone project ideas, research paper topics and nursing essay topic ideas to deepen our understanding and commitment to mitigating ...
Social determinants of health The analysis of social determinants and health equity aims to understand the biopsychosocial genesis of the health - disease process, understanding the determinants and social conditions in which a person is born, it grows, live, work , and age (WHO, 2005) this includes political , cultural , economic aspects and aspects related to health systems.
Introduction A person's health can be affected by many factors such as housing, income and environment. This essay will define and explain the term 'social determinants of health', discuss why housing, income and environment are considered social determinants of health and how these determinants can have a negative affect on one's health. The World Health Organisation posits that the ...
The WowEssays.com collection includes expertly crafted sample essays on Social Determinants Of Health and related issues. Most definitely, among all those Social Determinants Of Health essay examples, you will find a piece that get in line with what you imagine as a decent paper.
396 Words. 2 Pages. Open Document. Determinants of health are many factors combined to affect the health of individuals and communities. Health Starts within the environment we live in, the kind of work we do, the schools we attend, our neighborhood and surrendering communities. "HealthyPeople.gov" (2017), defines social determinants as ...
And if you're also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic. Let's take a look… 100 Words Essay on Social Determinants Of Health Social Determinants: A Vital Role in Our Health. Our health is affected by factors beyond medical care. These are called social determinants of health.
The social determinants of health are those factors that influence an individual's health status within society. There are a variety of social determinants of health, but some of the most important include: - Income and Wealth: Low income and wealth are associated with poorer health outcomes. This is due to a variety of factors, including ...
More recently, leading public health and medical journals have dedicated special issues to these topics. 19 - 21 The growing body of robust, empirical research strongly links spiritual beliefs ...
Health—Getting Further Faster. Year 2 Brief Evaluation Report. May 2023. Public Health Opportunity. Healthy People 2030 includes a national goal to improve social determinants of health (SDOH): "Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all." 1 We have a ...
These conditions and resources can be identified through what is called The Social Determinants of Health (SDOH). SDOH are used to identify the health status of an individual, community and population. The SDOH covers a broad range of measures that include income, housing and environmental factors. According to the World Health Organisation ...
The first of the papers in this issue, titled "Caring for the older transgender adults: social, nursing, and medical challenges" by Milionis and colleagues, introduces a conceptual model for the care of older transgender adults, with particular attention to challenges in the provision of healthcare as well as in the social environment.
Objectives: Education is one of the most important social determinants shaping the development and wellbeing of children. The purpose of this review of reviews is to inform policymakers, practitioners and public health stakeholder involved in developing child-friendly policies outside of the healthcare system.
Life expectancy at birth is considered a parameter of the social development, health system, or economic development of a country. We aimed to investigate the effects of GDP per capita (as the economic factor), health care expenditure, the number of medical doctors (as social factors), and CO2 emissions (as the environmental factor) on life expectancy. We used panel data analysis for 13 ...
1 PROBLEM. In November 2023, the World Health Organization (WHO) produced a report 1 entitled "Integrating the social determinants of health into health workforce education and training." It urged academic institutions and educators to reform curricula and make "action on the social determinants of health a key part of the role and responsibilities" of all health workers.
The Wider Determinants of Health tool is designed to: draw attention to the broad range of individual, social and environmental factors which influence our health. provide the public health system ...