Please sign in to continue
Processing payment, please wait...
- children & families
- Create account
- open the search modal
- open the menu

- Case studies
These case studies, developed with carers, address different situations where social work can offer input to carers. Each has information about the situation and case records, and highlights important topics that relate to that situation with questions for practice.
- Open access learning resources
- Social work with carers
We have always said we would stay together till the very end. That is all I want, to be together in our own home.
Anne has been married to Arthur for over 70 years. Arthur has end-stage Chronic Pulmonary Disease and is nearing the end of his life.
Read more about Anne's story below.
Download the About Anne case study (PDF)
Read Anne’s story
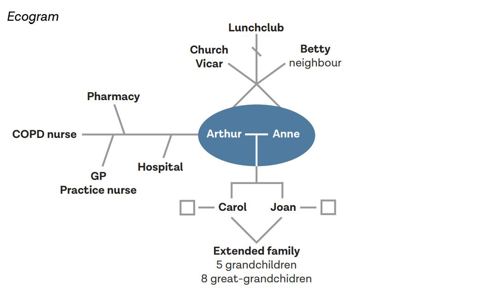
Anne Woolsey is married to Arthur, 94. They have been married for over 70 years and live in their own bungalow in a village. Anne and Arthur have two daughters, five grandchildren and eight great-grandchildren. The family are quite dispersed across the country. Their nearest daughter Carol, who lives 40 miles away, visits twice a month. Daughter Jean visits every other month. Both daughters phone regularly. Their neighbour Betty calls in most days.
Arthur has end-stage Chronic Pulmonary Disease (COPD) and is nearing the end of his life. Arthur is currently housebound, using oxygen at home. He has support from a Community COPD nurse. Anne has provided care for Arthur for eight years, and the support that he needs is increasing. The COPD affects Arthur’s mobility and he is unable to get to the toilet in time at night. Most mornings he awakens with soiled sheets which distresses him. Anne continues to look after the home and has started to manage the finances, which previously Arthur did. Anne and Arthur find it difficult to talk with each other about Arthur’s death. They would both like Arthur to die at home, with his wife and daughters.
Anne’s health is generally good, though she has mild arthritis and takes tablets for angina. However, she is becoming less strong and more tired. Anne has some hearing impairment and finds it difficult to read small print. Anne devotes her time to caring for Arthur and no longer goes to church. Both were previously active in the community and attended a local lunch club. Anne is determined to be there for Arthur and does not like to leave him, even with someone else. Her main concern is that she will not be able to support Arthur till the end. Anne is beginning to find it difficult to look after the home and garden, and to feel quite isolated. She is not confident in managing the family finances and is not sure how she will manage when Arthur is gone.
Carol is concerned about her mother not sleeping well and looking tired. She rings the local authority.
You are the social worker, and go out to see Anne and Arthur.
One-page profile and ecogram

- What potential is there in the Care Act 2014 to support Anne flexibly as things change?
How can you develop integrated support for the family in this end-of-life phase?
How can social work’s therapeutic role support Anne and Arthur?
It’s my choice to care for my family and I want to keep on doing that, and be a good mum and a good daughter.
Eve is a carer for her father, who has early-stage vascular dementia and numerous health problems. She has two children: a son, Matt, who is 17 and has Crohn’s disease, and a daughter, Joanne, who is 15.
Read more about Eve's story below.
Download the About Eve case study (PDF)
Read Eve's story
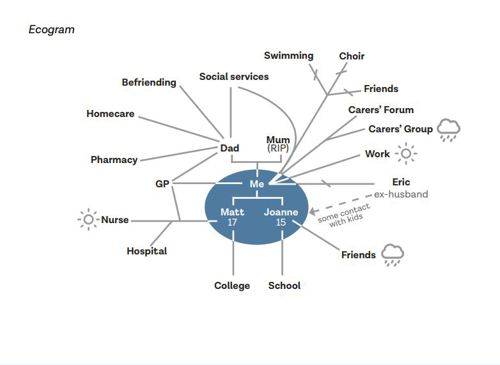
Eve Davies lives in a town. She has two children, a son, Matt, who is 17 and has Crohn’s disease, and a daughter, Joanne, who is 15. Eve’s mother died four years ago, and her father, Geoff, lives close by. Geoff is living with early stage vascular dementia and numerous health problems relating to a heart attack he had two years ago. Eve works part time in an administration role at a local college. She has lost contact with her friends and lost touch with her hobbies (swimming and singing in a choir) because she has prioritised her family.
Matt is at college studying for his A levels. He is frustrated that his illness is interfering with all aspects of his life. Joanne is becoming more withdrawn and resentful as an increasing amount of Eve’s time is taken up with other family members. Geoff often forgets to eat or wash, and is finding it more difficult to carry out daily tasks. Following a social care assessment, he has a befriending service stop by every week and a homecare team each morning to check he’s ok and supervise his medication, which Eve sets up for them. The care agency have reported that there’s a possibility Geoff has been accessing his medication and taking it. Geoff remains adamant that he is fine, and with Eve’s support he can manage.
Eve is feeling stressed and isolated. She wants to increase her working hours for financial reasons, but is unable to as she needs to be available for Geoff. Eve is having problems with sleeping and feels generally run down, and recently has been suffering from stomach pain and nausea. She says that she feels ‘withdrawn from normal life.’ She tried attending a carers’ group but found that listening to other carers’ problems highlighted her own. Instead, she sometimes uses an online forum at night when everyone else is asleep.
Eve was recently referred by her GP for a carer’s assessment.
You are the social worker and go to see Eve.

How can the Care Act 2014 duty to assess how far a carer is willing and able to care empower Eve?
How can a whole family approach help everyone to understand and respond to this situation?
What does a strengths-based approach look like for someone living with dementia?

About George
Just tell me what help is out there and I will get it sorted.
George helps out their friend David who lives 150 miles away across the Welsh border. David has depression and has been in and out of hospital.
Read more about George's story below.
Download the About George case study (PDF)
Read George’s story
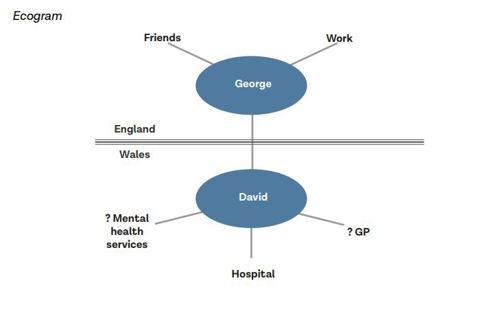
George Cook and David Taylor grew up in the same small border town and went to the same all-boy’s school in Wales. George moved away to London and became a lawyer. They are nonbinary (pronouns they, them), and have a busy work and social life. David was diagnosed with depression when he was in his late 30s. He lives alone and is often unemployed, and is a regular drug user. David’s parents are both dead and his friends have drifted away, apart from George.
George loves their childhood friend and wants to make sure he is ok. They go back to visit David every 4-6 weeks, whenever work allows. It is a 3 hour trip each way, and George usually stays overnight, tidies up, encourages David to go out for a walk, and brings shopping and anything David needs. George usually gives David some money, though they worry what David might spend it on.
George is finding the physical toll of the visits is getting too much. The greatest impact, though, is emotional. David sends frequent messages, including through the night, and George doesn’t feel able not to respond. At times, the messages are very low and George will call and be on the phone for hours. One time, David did not answer and George drove to see him, missing an important work meeting.
George has no idea what would help. They have called the council and said they need to talk to someone who knows about social services. The person they spoke to said that they could talk to a social worker to get some advice but it is complex because David lives in Wales.
You are the social worker and arrange a video call with George.

How can you ensure that borders are not a barrier to good social work?
How can you support George to have the relationship that they want with their friend?
How can you help people to balance risk enablement and risk management?
It’s lonely and I could do with somewhere to let off steam.
Jake supports his second wife Deborah, who has Parkinson’s. He does not see himself as a carer.
Read more about Jake's story below.
Download the About Jake case study (PDF)
Read Jake's story
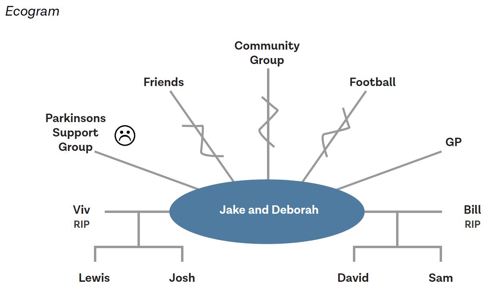
Jake Adler is 63 and looks after his wife Deborah. Deborah was diagnosed with Parkinson’s two years after they got married. They were both widowed and met through the Jewish community group. They each have two sons, who visit regularly, as well as friends and neighbours that they see often.
Over the last year, Deborah has found it increasingly difficult to leave the house and is reluctant to have visitors. Jake has gradually given up his social activities and has not renewed his season ticket for the football.
Jake was an engineer so he has done some DIY in their home to make things easier for Deborah. He provides all the physical help that she needs and manages everything in the home. Jake has taken pride in not asking anyone for help. A few months ago, a friend suggested that he went along to a support group for family of people with Parkinson’s. Jake found that most people there were women and that he didn’t want to talk about Deborah’s illness. He just wanted someone to talk to about the things he was interested in.
Deborah has become more withdrawn and Jake misses her even though she is there. The social network had been maintained by Deborah and so they are now falling out of touch with people.
One of the neighbours suggested that Jake ask the council about a ramp to get in and out of the house, and so he phoned up and agreed to a carer’s assessment.
You are the social worker and arrange to meet Jake in a café to talk.

- How can social work empower people as carers if they do not see themselves as having this role?
- How do gender differences and socially configured roles affect the experiences of caring?
- What is the social work role in tackling loneliness?
About Josef
I’d like some free time on my own to have time to myself or go out with friends. I need someone to talk to about mum.
Josef is 16 and lives with his mother, Dorota, who was diagnosed with Bipolar disorder seven years ago. Josef was born in England. His parents are Polish and his father sees him infrequently.
Read more about Josef's story below.
Download the About Josef case study (PDF)
Read Josef's story
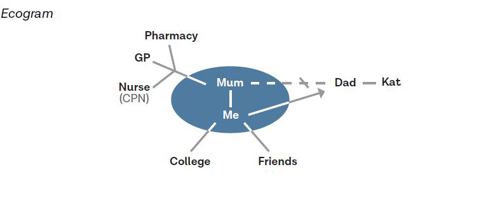
Josef Mazur lives in a small town with his mother Dorota who is 39. Dorota was diagnosed with Bi-polar disorder seven years ago after she was admitted to hospital. She is currently unable to work. Josef’s father, Stefan, lives in the same town and he sees him every few weeks. Josef was born in England. His parents are Polish and he speaks Polish at home.
Josef is doing a foundation art course at college. Dorota is quite isolated because she often finds it difficult to leave the house. Dorota takes medication and had regular visits from the Community Psychiatric Nurse when she was diagnosed and support from the Community Mental Health team to sort out her finances. Josef does the shopping and collects prescriptions. He also helps with letters and forms because Dorota doesn’t understand all the English. Dorota gets worried when Josef is out. When Dorota is feeling depressed, Josef stays at home with her. When Dorota is heading for a high, she tries to take Josef to do ‘exciting stuff’ as she calls it. She also spends a lot of money and is very restless.
Josef worries about his mother’s moods. He is worried about her not being happy and concerned at the money she spends when she is in a high mood state. Josef struggles to manage his day around his mother’s demands and to sleep when she is high. Josef has not told anyone about the support he gives to his mother. He is embarrassed by some of the things she does and is teased by his friends, and he does not think of himself as a carer. Josef has recently had trouble keeping up with course work and attendance. He has been invited to a meeting with his tutor to formally review attendance and is worried he will get kicked out. Josef has some friends but he doesn’t have anyone he can confide in. His father doesn’t speak to his mother.
Josef sees some information online about having a parent with a mental health problem. He sends a contact form to ask for information. Someone rings him and he agrees to come into the young carers’ team and talk to a social worker.
You are the social worker and have a meeting with Josef.

- How can a human-rights approach empower Josef?
- What social work capabilities are needed to build a relationship with Josef?
- What considerations are there around capacity, confidentiality and consent?
About Michelle and Joel
We need to know what will happen when we can’t look after Daniel.
Michelle and Joel have been married for 45 years and have two sons, Clinton in Scotland and Daniel, who is 34 and lives with them. Daniel has a learning disability.
Read more about Michelle and Joel's story below.
Download the Michelle and Joel case study (PDF)
Read Michelle and Joel's story
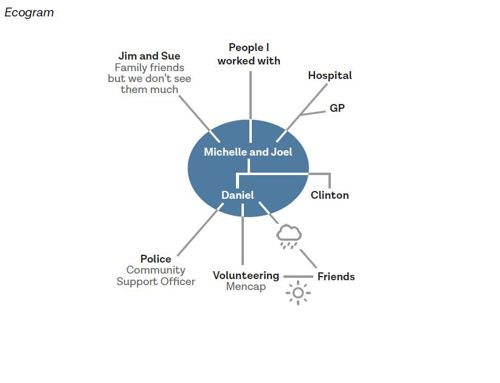
Michelle and Joel Tyndell live in a city. They were both born in Kingston, Jamaica, and moved to the United Kingdom in the 1970s just after they were married. They have been married for 45 years and have two sons, Clinton in Scotland and Daniel, who is 34 and lives with them. Daniel has a learning disability. Michelle gave up work when Daniel was 16 to support him. Joel retired three years ago. Over the years they have sought support through the council but it has never worked very well.
Daniel volunteers at a local charity a few days a week, helping with teas and coffees. He would like to live independently. Joel and Michelle are worried this won’t work. Daniel is well known in the local community. He is also known to the police due to a few incidents where he has been violent. Daniel is often misunderstood as it is not immediately clear that he has a learning disability, and people who don’t know him can react to his behaviour. This is made worse by racist stereotyping also affecting how people react to him. Daniel has some friends from volunteering and some other friends from the local area.
Joel and Michelle support Daniel to ensure he is washed and dressed appropriately, has had his medication and knows where he needs to be. Sometimes Daniel refuses his medication. Daniel has a mobile phone which he is able to make and receive calls on. Sometimes Michelle drives Daniel and sometimes they take him to the bus. Daniel has his own money but it is not clear what he is spending it on. Michelle and Joel are concerned that Daniel may be giving money to his friends.
Joel and Michelle love their son, however they are exhausted and feel undervalued by providing his care. They have had to make choices to put Daniel first, have few friends and rely on each other. Joel had a heart attack last year and they are fearful about what will happen with Daniel in the future. Before children, Michelle and Joel were keen music fans.
Michelle and Joel recently rang the council and asked for someone to talk to them about their situation.
You are the social worker go out to see Michelle and Joel.

- How does the Care Act 2014’s duties around preventing needs help you to plan for the future?
- How can you balance the needs of the different family members involved?
- How can you ensure your practice is sensitive to any cultural difference?
About Muhammed and Maryam
I want to fulfill my responsibility to my daughter.
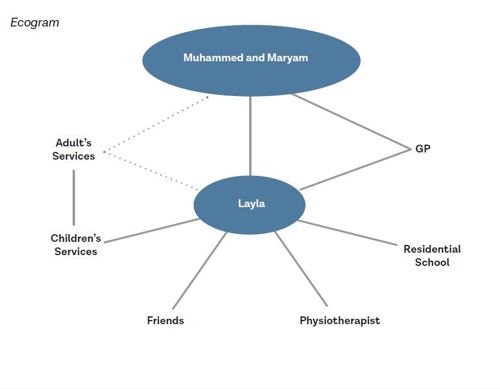
Muhammed and Maryam have one child Layla who is 17 years old. Layla was born with Spina Bifida and has been attending a residential college.
Read more about Muhammed and Maryam's story below.
Download the About Muhammed and Maryam case study (PDF)
Read Muhammed and Maryam's story
Muhammed and Maryam Hossain live on the edge of a large city. Muhammed’s parents came to the UK from Bangladesh in the 70s and he was born here. He married Maryam from Bangladesh 25 years ago and she came to live in the UK then. They have one child Layla who is 17 year’s old. Layla was born with Spina Bifida. She uses a walking aid and has an electric wheelchair. Layla has been attending a residential college where she has made good friends. She hopes to keep studying and to move in with friends.
Muhammed and Maryam want to support Layla and also to ensure that she is safe and her religion (Islam) is respected.
Muhammed and Maryam are conscious that people they know through the college had a difficult experience when their children turned 18. They want to ensure that Layla has the right support and opportunities, and to start planning for that now. They don’t have any savings themselves. Muhammed’s job is not well paid and they don’t have a house of their own. Recent increases in bills have made it difficult for them to manage when Layla comes home as the house needs to be warmer and they use more electricity.
Muhammed rang the council and asked to speak to a social worker.
You are the social worker and go out to visit them with an interpreter as Maryam finds complex topics in English difficult.

- How does the Care Act 2014’s duties around transition help you to empower this family?
- How can you ensure that both carers are fully involved and their needs are considered?
- What is the social work role in promoting economic wellbeing?
About Susan
I’d like someone to discuss my concerns with and talk things through, so I feel reassured I am making the right choices, for both of us. I must get it right.
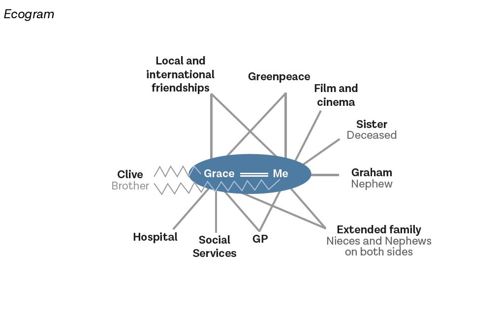
Susan is the carer for her partner Grace who is 82. Grace has become increasingly frail and, following hospital admission and rehabilitation, has agreed to a trial for three months in a care home.
Read more about Susan's story below.
Download the About Susan case study (PDF)
Read Susan's story
Susan Reinfeld is 70 years old. She is primary carer for her partner, Grace Wilson, who is 82. In their younger days Susan and Grace travelled widely, they had a large network of friends and although they don’t have any children of their own, they have nieces and nephews. Susan is particularly close to her nephew Graham. Grace has generally taken the lead in decisions and in the relationship. Sometimes now she gets angry with Susan if she doesn’t do things the way Grace expects or if Susan makes a suggestion that Grace sees as ‘stupid.’ Grace’s family has at times struggled with her sexuality and while her relationship with her nieces and nephews is good, her relationship with her brother Clive has been more difficult.
Over recent years Grace has become increasingly frail and has relied on Susan to get washed and dressed, and use the toilet, as well as maintain the home and cook meals. Two months ago, Grace had a fall and was admitted to the hospital. She was discharged to a rehabilitation bed in a care home. Before the hospital admission Susan and Grace were not in contact with services. Whilst in hospital and the care home, Susan has visited every day and helped Grace with personal care. Grace frequently phones and texts Susan. After six weeks of rehabilitation, Grace continues to need support to walk and with all her personal care, including support at night. You have been involved in a multi-disciplinary assessment which has recommended that Grace needs 24-hour care. As part of this assessment, Susan talked about how exhausted she is, and said that she no longer feels able to support Grace at home because of the impact on her health. Grace has agreed to a trial three months in a care home.
Susan and Grace are not legal partners, as they have not entered into a civil partnership nor are they married. Susan has no power of attorney for Grace. Susan is worried about the costs of a home and how this will be paid for. She feels guilty about ‘letting Grace down’ and sad about the future she will no longer have with Grace. Susan is also worried about Clive’s reaction.
Susan has asked to speak to someone about her concerns.
You are the social worker and go to meet Susan.

- How can a human rights perspective help you to empower Susan and Grace?
- How can you act as a navigator to make the systems around Susan and Grace transparent and understandable?
- How does an intersectional view of Susan’s and Grace’s identities (seeing the overlapping aspects of identity) help you to understand how they respond to social care?
< Back to 'Social work with carers' homepage .
Social Work Practice with Carers

Case Study 5: Michelle and Joel
Download the whole case study as a PDF file
Michelle and Joel
Michelle and Joel live in a city. They have been married for 45 years and have two sons, Clinton in Scotland and Daniel, who is 34 and lives with them. Daniel has a learning disability. Michelle gave up work when Daniel was 16 to support him. Joel retired three years ago. Over the years they have sought support through the council but it has never worked very well.
When you have looked at the materials for the case study and considered these topics, you can use the critical reflection tool and the action planning tool to consider your own practice.
- One-page profile
- Support plan
Transcript (.pdf, 31KB)
Name: Michelle Tyndell Joel Tyndell
Gender: Female Male
Age: 65, 68
Ethnicity: Black British
Download resource as a PDF file
First language: English
Religion: Christian
Daniel volunteers at a local charity a few days a week, helping with teas and coffees. He would like to live independently. Joel and Michelle are worried this won’t work. Daniel is well known in the local community. He is also known to the police due to a few incidents where he has been violent. Daniel is often misunderstood as it is not immediately clear that he has a learning disability, and people who don’t know him can react to his behaviour. Daniel has some friends from volunteering and some other friends from the local area.
Joel and Michelle support Daniel to ensure he is washed and dressed appropriately, has had his medication and knows where he needs to be. Sometimes Daniel refuses his medication. Daniel has a mobile phone which he is able to make and receive calls on. Sometimes Michelle drives Daniel and sometimes they take him to the bus. Daniel has his own money but it is not clear what he is spending it on. Michelle and Joel are concerned that Daniel may be giving money to his friends.
Joel and Michelle love their son, however they are exhausted and feel undervalued by providing his care. They have had to make choices to put Daniel first, have few friends and rely on each other. Joel had a heart attack last year and they are fearful about what will happen with Daniel in the future. Before children, Michelle and Joel were keen music fans.
Michelle and Joel recently rang the council and asked for someone to talk to them about their situation. You have been out to visit them and met Daniel briefly. You have completed the assessment and the support plan. Daniel has agreed to an assessment which will happen soon.
Name : Michelle Tyndell Joel Tyndell
Ethnicity: Black British Black British
First language: English English
Religion: Christian Christian
Date chronology completed 6 March 2016
Date shared with person 6 March 2016
Michelle Tyndell
What others like and admire about me
I care for my family
I have a great sense of humour
I am determined
I moved to England and I made a life for myself and my family
I brought up my boys to be good people
What is important to me
My children
My husband – I want him to be with me for a long time
To know that Daniel will be looked after when we are gone
Daniel and Clinton not getting into any trouble
How best to support me
Someone to know about us
To know who will look after Daniel when we are gone
To have help that works, not that makes things more difficult
Make sure Joel is well
Make sure Daniel doesn’t get into fights
Let me know if I am doing things right

Joel Tyndell
I provide for my family
I was a good worker and I worked hard
People in the neighbourhood respect us I moved to England and I made a life for myself and my family
My sons – I want them to do well in life
My wife should have some help
I want Daniel to be looked after when we are gone
I don’t want Daniel to get into trouble with the Police
Talking to my friends about the world
To know what will happen to Daniel when we are gone
To have some help for Michelle that gives her a rest
Make sure Daniel doesn’t get into trouble
Don’t tell us what to do, suggest things
Let me know what you can do, I don’t know what help there is
Provide advice on support for parents in this situation
Michelle and Joel’s Ecogram
Name : Michelle and Joel
Date completed : 6 March 2016

Carers Assessment
Address 1 Railway Terrace, Hamton, City ZZ1 Z11
Telephone 012345 123456
Date of birth 3.12.50 1.09.47
GP Dr Fish, Station Surgery
How would you like us to contact you?
Do you need any support with communication?
About the person/ people I care for
My relationship to this person Mother and father
Name Daniel Tyndall
Telephone 012345 234567
Email [email protected]
Gender Male
Date of birth 29.7.81 Age 34
Ethnicity Black British
First language English
Religion None
GP Dr Cox, Station Surgery
Please tell us about any existing support the person you care for already has in place. This could be home care, visits or support from a community, district or community psychiatric nurse, attending any community groups or day centres, attending any training or adult learning courses, or support from friends and neighbours.
Daniel goes to Mencap twice a week as a volunteer at a centre a short bus ride or drive away – he helps out with the refreshments and also he takes part in activities. Daniel likes photography and computer games, but he doesn’t like making things.
The GP surgery arranged an epilepsy nurse to see Daniel sometimes. They send his prescription to the pharmacy for us to collect.
Daniel has two friends he has met through volunteering – Chris and Joline (Jo). They go out sometimes to the cinema or to the pub.
Daniel also has some friends in town that we don’t know that well. He met them when he was in his early 20s and he still sees them. They tend to hang round in town and we think he goes out to meet them. We are concerned that they are taking or borrowing money from him. ‘They are a bad influence and will get him into trouble’ (Joel).
Daniel gets Personal Independence Payment and also Employment and Support Allowance but this has just changed and we don’t really understand it.
Daniel used to go to day centre before it closed and he started volunteering. We had a direct payment for a while but it was very complicated. We couldn’t find personal assistants so we used the agency but then there were lots of different people and we all (Daniel too) agreed it was better not to have the direct payment.
Daniel recently said that he would like to live independently.
The things I do as a carer to give support
Please use the space below to tell us about the things you do as a carer (including the emotional and practical support you provide such as personal care, preparing meals, supporting the person you care for to stay safe, motivating and re-assuring them, dealing with their medication and / or their finances).
Daniel has a learning disability but nobody has ever been able to tell us what exactly it is. He also has epilepsy and has to take medication for that. Daniel seems fine when you meet him. He struggles to follow conversations and he doesn’t remember instructions unless you write them down. He can read big print and simple words but he can’t manage official letters. Daniel doesn’t ‘do dates and times’ so you need to remind him about things. We have a calendar and a list for him, and we have a list for what he needs to take when he goes out (phone, money, keys). Daniel can be a bit clumsy and we try to keep the house tidy and make sure there isn’t anything breakable. He doesn’t like fiddly tasks because he gets annoyed that he can’t do them well. Daniel looks after himself mostly’ (Michelle)
Daniel doesn’t have seizures often and he usually knows if he is starting to get one. This tends to happen when he is stressed or overexcited. We make sure that there aren’t things that he can hurt himself with if he has a seizure. The epilepsy nurse advised us about this. We don’t leave the house when Daniel is having a shower.
Sometimes Daniel gets frustrated and then it is best to just tell him it’s ok and leave him alone. When you push things he shouts and he has hit people in the past but he has never hurt us.
Daniel can be taken advantage of because he doesn’t remember if he has paid for things and he will try to help you if you ask. Also he can’t tell money apart easily so he might give you the wrong note or coin. Daniel thinks the best of people and likes to do things for them. We think some of the people that he thinks are his friends might ask him for money.
Daniel spends a lot of time in his room playing on his phone.
We remind Daniel to have a shower and brush his teeth each morning. We make sure he has clean clothes on.
Michelle does the washing and cleaning in the house and cooks all the meals.
Joel collects Daniel’s medication and makes sure he takes it every day – sometimes he doesn’t want to and then Joel has to persuade him.
Joel checks Daniel’s bag and pockets before he goes out to make sure he has what he needs for the day.
We call Daniel if he isn’t back for lunch or tea.
Joel helped Daniel get his benefits and set up a bank account, and helps him look at the statements and any other letters.
Michelle puts appointments in the calendar and drives Daniel to them and goes with him. She drives him to the centre or we walk him to the bus stop.
How my caring role impacts on my life
Please use the space below to tell us about the impact your caring role has on your life.
It was difficult for us to have children and we thank God for them.
When Daniel was little we didn’t understand why he was different and we didn’t get any help until he was at school. We were told by a doctor that he had ‘development delay’ but we never understood why. Daniel always needed more help than Clinton and didn’t do well at school. We got some advice particularly from the speech and language therapist and also from the epilepsy nurse, but we mostly got on with it ourselves.
When Daniel was 16, he left school and Michelle gave up work. Daniel got into trouble with the Police after a fight. We got some support from social services for him to go to Mencap and they have helped with him going there and then being a volunteer.
The main impact is the worry. We have been worried about Daniel getting into trouble with fighting. We are worried about his friends and we wonder if we should check his phone and his social media to see who he is in contact with. Daniel has his own money but sometimes it disappears really quickly and he doesn’t have anything to show for it – we worry that he is being taken advantage of.
Also it is quite stressful if we are asking Daniel to do something like take medication or have a shower and he doesn’t want to.
‘ We are exhausted’. We have had to put Daniel first, and we have given up a lot – all our friends except for a few, and going out in the evenings. We really only have each other. We don’t feel appreciated sometimes and that makes us feel guilty.
Joel had a heart attack last year and we are both fearful about what will happen with Daniel in the future. Daniel recently said he wants to live on his own but we don’t see how that will work. We don’t see how someone else would be able to look after him as we have.
What supports me as a carer?
Please use the space below to tell us about what helps you in your caring role.
Chris and Jo at the Mencap centre help Daniel and go out with him sometimes in the evening.
The epilepsy nurse gave us lots of advice.
The GP helps Joel with his medication and makes sure the pharmacy gets his prescription.
Jim and Sue who are friends from when we arrived in England see us a few times a year and that is lovely. Our son Clinton visits a few times a year.
My feelings and choices about caring
Please use the space below to tell us about how you are feeling and if you would like to change anything about your caring role and your life.
We don’t mind helping Daniel, he is our son and we love him and we want to look after him.
We want Daniel to be ok and not to get into trouble. We need to know what will happen when we can’t look after Daniel.
We want to not have to worry so much.
We need to stay healthy as long as we can to look after him.
It would be nice to see friends more and have someone to talk to other than just us. And to know that we are doing the right thing.
Information, advice and support
Let us know what advice or information you feel would help you and what sort of support you think would be beneficial to you in your caring role.
We don’t really know what is out there so we need someone to advise us but it has to work for us. Some of the help in the past didn’t work for us.
Maybe it would help to have:
Some more time for us
Advice about how to keep Daniel out of trouble
Some help with knowing what to do if Daniel doesn’t want to take his medication
Advice about benefits
A plan in place for the future
It would be good for Daniel to have some advice and support from people who know what it is like to have a learning disability and epilepsy. We understand that he wants to be more independent but he does need to know how to be safe.
To be used by social care assessors to consider and record measures which can be taken to assist the carer with their caring role to reduce the significant impact of any needs. This should include networks of support, community services and the persons own strengths. To be eligible the carer must have significant difficulty achieving 1 or more outcomes without support; it is the assessors’ professional judgement that unless this need is met there will be a significant impact on the carer’s wellbeing. Social care funding will only be made available to meet eligible outcomes that cannot be met in any other way, i.e. social care funding is only available to meet unmet eligible needs
Date assessment completed 6 March 2016
Social care assessor conclusion
Michelle and Joel have provided support to Daniel since he was born as carers as well as parents. They provide daily support to Daniel. The only other support is from Mencap where Daniel volunteers and from community health services. Joel, Michelle and Daniel have a few family friends.
Joel and Michelle love their son greatly and want to continue to support him. They identify that there is a risk of them becoming unwell and Daniel getting into trouble without further support. In particular, Joel had a heart attack last year and Daniel may be at risk from his friends. Joel and Michelle are experiencing stress and it is important to support them now to avoid potential breakdown of the situation through ill-health or inability to support Daniel as he needs.
Daniel has told his parents that he wants to live independently. This causes them concern and they are worried about what will happen when they are gone. This area needs to be explored more with Daniel in his own assessment, and then with him and his parents together. There needs to be a plan in place for the future.
As part of this assessment we talked about Joel and Michelle getting in touch with their friends and building support through the carers’ centre. Advice, support and planning would help to promote Michelle and Joel’s wellbeing and help them to continue as carers which is what they want.
Eligibility decision Eligible for support
What’s happening next Create support plan for Joel and Michelle
Carry out assessment for Daniel
Completed by
Organisation Signing this form (for carer)
Please ensure you read the statement below in bold, then sign and date the form.
I understand that completing this form will lead to a computer record being made which will be treated confidentially. The council will hold this information for the purpose of providing information, advice and support to meet my needs. To be able to do this the information may be shared with relevant NHS Agencies and providers of carers’ services. This will also help reduce the number of times I am asked for the same information.
If I have given details about someone else, I will make sure that they know about this.
I understand that the information I provide on this form will only be shared as allowed by the Data Protection Act.
Support plan completed by
Organisation
Date of support plan: 6 March 2016
This plan will be reviewed on: 6 July 2017
Joel and Michelle are happy for their assessment and support plan to be considered as part of Daniel’s assessment, however they do not want them to be shared with Daniel.
Signing this form
Learning disability
Research highlights that community learning disability teams are effective when they put the individual and their surrounding family or carers at the heart of a service (National LD Professional Senate 2015). The manual on social work with people with autism (DH 2015) highlights issues of carer identity, carers networks, parental/care identity, stigma, recognition and validation plus advice around self-help and having a life.
- Department of Health (2015) A manual for good social work practice: Supporting adults who have autism , The College of Social Work
- Challenging Behaviour Foundation (2016) Stopping Over-Medication of People with a Learning Disability, Autism or Both (STOMP): a family carer perspective
- SCIE (2011) Improving access to social care for adults with autism
- SCIE (2011) At a glance 21: Personalisation briefing: Implications for people with autistic spectrum conditions and their family carers
- NICE quality standard on Autism
- Justice for LB, The Tale of Laughing Boy
Tool 1: Involving parents of people with a learning disability
Recent interest has centred on attachment theory – a stalwart in child and family social work (Shemmings 2016) – having application to relationship based social work with adults and their carers (RiPfA 2015, Bennett 2011), and promoting positive change (Baim and Morrison 2011) across the life course (Howe 2011). A good practice project (DH 2013) with people with learning disability included a case study with an organisational model based on Attachment, Object Relations, Developmental, Systemic and Trauma theories – essentially a psychotherapy based service rather than social work but with transferable practice lessons.
- The College of Social Work (2011) The Business Case for Social Work with Adults: A Discussion Paper
- Baim and Morrison (2011) Attachment-based practice with adults
- Carers Trust (2015) Dads care too: A survey of the experiences of fathers who are carers
Tool 2: Social Work capabilities for attachment-aware practice
Practice example
- Blog (2013) In Carers Week I’m resisting the term “older parent”
Risk enablement and independence
The literature review uncovered an interesting document that concerned people with learning disabilities and challenging behaviour going into hospital (NHS England 2014). Written for family carers, it offered the description of the social worker’s role as to: assess your loved one’s whole situation and what life was like before their admission – their history, their relationships, their home life, their occupation, their wishes. Called Getting It Right, it said all people with learning disabilities will have a named worker (social worker or nurse) and that the social worker may be the responsible clinician. Within these processes direct payments has attracted attention with suggestions of social worker reluctance and lack of imagination. There are, in theory, few restrictions to the use of payments to support carer’s or to curtail innovation (Dittrich 2013).
- RiPfA Frontline: Risk enablement (Chart)
- SCIE (2011) At a glance 37: Challenging behaviour: a guide for family carers on getting the right support for adults
- SCIE (2011) At a glance 39: Challenging behaviour: a guide for family carers on getting the right support for teenagers
- SCIE (2011) At a glance 38: Challenging behaviour: a guide for family carers on getting the right support for children
- SCIE (2010) SCIE Report 36: Enabling risk, ensuring safety: Self-directed support and personal budgets
- NICE quality standards on Learning disabilities and challenging behaviour
- NIHR (2014) Risk, Safeguarding and Personal Budgets: exploring relationships and identifying good practice
- SCIE Challenging behaviour and learning disabilities: independent living (video)
- SCIE (2014) Care Act: a strengths-based approach
- Tool 3: Risk enablement chart – RiPfA (2015) Frontline chart: Risk enablement
- Tool 4: Risk Principles (RiPfA Good decision making handbook)
Older family carers
Research flags life change awareness as an important element of work with people with learning disabilities (RCGP/RCP 2012). Understanding transition theory remains an essential in using life course development knowledge in social work practice with adults (Crawford and Walker 2010).
- SCIE (2015) Adult carer transition in practice under the Care Act 2014
- Carers UK and Age UK (2015) Caring into later life
- Carers Trust (2015) Caring About Older Carers Providing Support for People Caring Later in Life
- Princess Royal Trust for Carers (2011) Always On Call, Always Concerned A Survey of the Experiences of Older Carers
- Mencap (2013) Short breaks support is failing family carers: reviewing progress 10 years on from Mencap’s first Breaking Point report
- UCL (2015) The emotional wellbeing of older carers
- Fitzroy (2015) Who will care after I’m gone? An insight into the pressures facing parents of people with learning disabilities
- SCIE (2010) Supporting carers: the social worker
- SCIE Action for Carers, Surrey video – respite service co-production
- SCIE Innovation: Living together
- Tool 5: Planning for people with learning disabilities – Foundation for people with learning disabilities (2010) Supporting you and your family as you grow older together A booklet for people with learning disabilities who live at home with an older family carer
- Tool 6: Planning for older family carers – Foundation for people with learning disabilities (2010) Supporting you as an older family carer A booklet to support older family carers of people with learning disabilities to get the right support now and to plan for emergencies and the long term
Ethnicity and culture and language
Common factors identified in the research for social work practitioners working with adults and their carers included information, advice and guidance – having the specialist knowledge or knowing where to signpost people – assessment and the processes of carer-directed self-support, and using knowledge and skills to work with the whole network of relevant people.
- Carers UK (2012) Half a Million Voices: improving support for BAME carers
- Foundation for people with learning disabilities (2012) Reaching out to people with learning disabilities and their families from black and minority ethnic communities
- Race Equality Foundation (2010) Improving health and social care support for carers from black and minority ethnic communities
- SCIE (2010) SCIE Report 31: Good practice in social care for refugees and asylum seekers
- Care Council for Wales (2010) Different words, different worlds?: the concept of language choice in social work and social care
- Race Equality Foundation (2018) Dementia and Minority Ethnic Carers
- Tool 7: Culturally Competent Planning – Foundation for people with learning disabilities (2012) Guidance for Families of People with Learning Disabilities and Practitioners in Developing Culturally Competent Planning
Download the tool as a PDF file
This tool sets out a parent’s view of their sons growing up. You can use it to reflect on how you respect the thoughts and feelings of parents who care for their children as they grow up and grow older.
‘Respect the thoughts and feelings of me as a parent, I really want my sons to move on and have a great life as independent as possible, but I have spent all their life so far caring for them and protecting them and that next step is a huge step!
Remember in your eyes and the law according to the Care Act 2014 and the Children and Families Act 2014 when my son reached 18 he was an adult, but nothing has changed on a day to day basis, he still wakes me up at 5am demanding to know what the day will bring!
Plan with us as a family ensure we are part of all the conversations, we are pretty resilient – we will have good ideas of our own.’
Please think outside the box and help us find activities and experiences for our sons that to other young people without additional support needs are pretty ordinary. Our sons should be able to access all activities that other young people do, they just may need a little support to enable this to happen, this is where we need your help.
It’s not rocket science! – we want for our sons what everyone else would want for their sons and daughters we want them to be happy and to lead a fulfilled life – we don’t want extraordinary we just want ordinary!’
How will I work with people with learning disabilities alongside their parents to enable them to ‘have a great life?’
You can use this tool to consider a transition point in someone’s life.
Back to Summary
This tool sets out the social work capabilities in the Professional Capabilities Framework that relate to attachment-aware practice. You can use this to consider your own practice and learning needs.
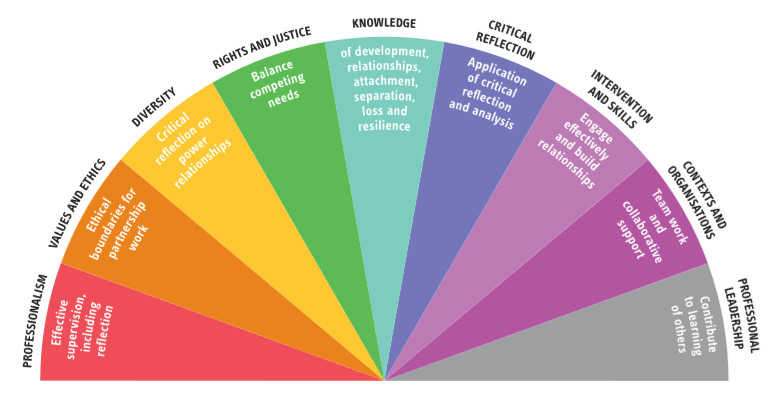
What are my strengths in relationship-based working?
Where do I need to develop my practice?
How will I do this?
What support do I need?
This tool is taken from RiPFA’s Adult attachment – Implications for adult social care practice: Frontline Briefing (2015)
This tool sets out the stages of a mediation process. You can use it to plan and deliver a mediation session.
Tool 3: Risk enablement
Risk enablement is a key skill for practitioners in promoting wellbeing and achieving outcomes.
As an approach, risk enablement identifies a link between risk and enablement. Risk enablement recognises that taking carefully considered risks can enable individuals and help improve their wellbeing.
Positive risk-taking is a way of working with risk that promotes enablement. It is important to remember that the ‘positive’ in positive risk-taking refers to the outcome not the risk.
Too 4: Risk Principles
The aim of this tool is to help ensure the culture you work in supports good decisions about risk.
Research shows that the environment in which people operate affects how they make decisions.
You can use this tool to identify how your organisational or team culture supports you to make good decisions about risk. Consider each principle in turn and identify how far this is embedded and what needs to happen to improve things.
A booklet to support older family carers of people with learning disabilities to get the right support now and to plan for emergencies and the long term
Tool 6: Planning for people with learning disabilities
Supporting you and your family as you grow older together A booklet for people with learning disabilities who live at home with an older family carer.
This booklet tells you more about:
- Good questions to ask
- Things that can help you now and in the future
- Some of the people who can help you.
Tool 7: Culturally competent planning
Reaching Out to people with learning disabilities and their families from Black and Minority Ethnic communities Guidance for Families of People with Learning Disabilities and Practitioners in Developing Culturally Competent Planning
The Foundation for People with Learning Disabilities
This guide is written in response to the Reaching out to families project’s conclusion that practitioners need to demonstrate more cultural competence in planning.
- Equal opportunities
- Complaints procedure
- Terms and conditions
- Privacy policy
- Cookie policy
- Accessibility

