- Research article
- Open access
- Published: 18 March 2022

Experiences of new diagnoses among HIV-positive persons: implications for public health
- Adobea Yaa Owusu ORCID: orcid.org/0000-0003-2223-7896 1
BMC Public Health volume 22 , Article number: 538 ( 2022 ) Cite this article
2763 Accesses
4 Citations
Metrics details
Ready acceptance of experiences of new diagnoses among HIV-positive persons is a known personal and public health safety-net. Its beneficial effects include prompt commencement and sustenance of HIV-positive treatment and care, better management of transmission risk, and disclosure of the HIV-positive status to significant others. Yet, no known study has explored this topic in Ghana; despite Ghana’s generalised HIV/AIDS infection rate. Existing studies have illuminated the effects of such reactions on affected significant others; not the infected.
This paper studied qualitatively the experiences of new diagnoses among 26 persons living with HIV/AIDS. Sample selection was random, from two hospitals in a district in Ghana heavily affected by HIV/AIDS. The paper applied the Hopelessness Theory of Depression.
As expected, the vast majority of respondents experienced the new diagnoses of their HIV-positive infection with a myriad of negative psychosocial reactions, including thoughts of committing suicide. Yet, few of them received the news with resignation. For the vast majority of respondents, having comorbidities from AIDS prior to the diagnosis primarily shaped their initial reactions to their diagnosis. The respondents’ transitioning to self-acceptance of their HIV-positive status was mostly facilitated by receiving counselling from healthcare workers.
Conclusions
Although the new HIV-positive diagnosis was immobilising to most respondents, the trauma faded, paving the way for beneficial public health actions. The results imply the critical need for continuous education on HIV/AIDS by public health advocates, using mass media, particularly, TV. Healthcare workers in VCTs should empathise with persons who experience new diagnoses of their HIV-positive status.
Peer Review reports
News of a newly-diagnosed HIV-positive status has the tendency to lead to negative psychosocial outcomes for persons living with HIV/AIDS (PLWHAs) [ 1 , 2 , 3 ]. In this paper, the concept of newly-diagnosed refers to the first time a respondent was informed of his/her HIV-positive status. Implications of this operational definition are discussed later on in the paper. Humans depict cognitive, emotional, and motivational deficits on hearing bad news and experiencing what is deemed uncontrollable events [ 4 ]. This is very likely to apply to PLWHAs particularly, when confronted with the news of being HIV-positive for the first time. Particularly, PLWHAs are known to mostly experience neurocognitive disorders associated with the infection [ 5 ], and often experience common mental disorders [ 6 , 7 ]. This is especially the case when PLWHAs fairly expect or self-perceive negative social reactions such as spousal abuse, dismissal from employment, stigma and discrimination, among others [ 8 ]. Peterson and Seligman ([ 4 ], p. 347) christened these series of responses on such occasions as “learned helplessness phenomenon.”
There are numerous news reports of persons who have committed suicide shortly after an HIV-positive diagnosis. This includes even the case of a female physician from the Eket local government area of Akwa Ibom, Nigeria [ 9 ]. Previous researchers note that after the initial diagnosis of a disease believed to be life-threatening, and particularly incurable, patients are known to experience an immediate descent into several distressing psychological and emotional states of mind [ 1 , 2 , 10 ]. These range from disbelief to denial to being utterly scared and shocked. Some even think that their life is not worth living anymore and imagine that indeed, the disease has already taken a final toll on them [ 2 , 3 ]. This brings to the fore the need to study the reactions of PLWHAs right after their initial diagnosis. Research and programme interventions on adaptation to a new HIV diagnosis provide personal and public health safety-nets and are thus needed [ 2 , 11 ]. Such research and interventions are helpful in educating newly-diagnosed PLWHAs on HIV [ 1 , 10 ] and promoting their health [ 1 , 8 , 12 ].
Acceptance of the news of an HIV-positive diagnosis is critical for several reasons [ 2 ]. Engagement in and sustenance of HIV treatment and care [ 1 , 2 ], viral load (VL), CD4 counts [ 2 , 13 ], and transmission risk [ 2 , 11 , 14 ] are affected by the reaction to the news of diagnosis. Reactions also affect perceptions of stigma and disclosure activity [ 2 , 11 ]. Conversely, difficulties with accepting diagnosed HIV-positive status has serious potential negative consequences for individuals and the general public [ 15 , 16 ]. From the angle of healthcare practitioners, better handling of new diagnosis of an HIV-positive status and related disclosure could greatly buffer the psychosocial and mental health of the newly-diagnosed PLWHAs, and help facilitate healthcare seeking and retention. These include the management of less traumatised disclosure, reduction of self-stigmatisation, and better management of romantic and family relationships [ 2 , 14 ]. Others are the reduction of viral transmission [ 14 , 17 ], and improvement in general public health and well-being of populations [ 1 , 14 ]. Knowing the experiences of new diagnoses among HIV-positive persons is, therefore, likely to facilitate successful linkage and retention of such persons in healthcare for HIV [ 1 , 2 ]. This is critical and is also known to be a significant gap in the HIV care continuum in some parts of the world, even the U.S. with all its known medical advancement [ 11 ].
Based on previous related literature, this paper primarily examines qualitatively the experiences of new diagnoses of 26 Ghanaian PLWHAs to the first news of their HIV-positive status. Second, it attempts to untangle the situations surrounding these experiences to determine what might have influenced such reactions. Third, the paper delineates the processes that particularly helped the PLWHAs transition from negative psychological reactions to showing positive reactions and seeking HIV treatment. Fourth, it adds to the core literature on managing experiences of new diagnoses of an HIV-positive status, and illuminates their importance to public health. It is hoped that this paper will facilitate a better acceptance of an HIV-positive sense of self which is known to aid PLWHAs to accept, adjust, and more effectively cope with their diagnosis. This will aid them to better manage the complexities of living with the infection [ 2 , 18 ]. This paper specifies the knowledge to Ghana and more importantly, Ghana’s most HIV/AIDS-affected district [ 19 , 20 ]. A thorough search on the experiences of PLWHAs’ new diagnoses in Ghana yielded no known results despite the fact that Ghana has a generalised HIV/AIDS epidemic: more than 1% of the residents have the infection [ 21 ]. This paper aims to fill that gap.
Immediate reactions to news of HIV positive status in Africa
The literature on the immediate reactions to the initial diagnosis of HIV-positive status is also sparse, and a majority of what research there is comes from South Africa. Such findings overwhelmingly corroborate each other: immediately after being diagnosed HIV-positive, PLWHAs studied depict deep negative emotions. Visser et al. [ 22 ] studied the phenomenon in South Africa, using a semi-structured interview of 293 pregnant women who were undergoing HIV test during antenatal care. On hearing the news, those who tested positive were shocked, and got frightened that they would be abandoned and discriminated against.
Fabianova [ 23 ] undertook a longitudinal study in Nairobi, Kenya, on the psychosocial aspects of being PLWHA. When the respondents who visited VCTs were first informed of their HIV-positive status, 89% of them felt sad due to their HIV-positive status, 60% had feelings of fear and anxiety, 30% felt angry, 25% felt distressed, and 15% cried. Additional psychosocial behaviours exhibited by the respondents included grief, guilt, hopelessness, helplessness, anger, disbelief, self-blame or blamed others, and aggression towards a counsellor. Their sadness was mostly in reference to close relatives who had died of AIDS. Their fears related mostly to the loss of their social position. Other fears surrounded loss of life, ambition, sexual relations, independence, physical performance, and financial stability [ 23 ]. While Fabianova [ 23 ] observed from the extant literature that suicide is a common reaction for persons who are first informed of their HIV/AIDS status, her study found that less than 1% of participants attempted suicide on hearing of their confirmed HIV-positive status. Most of Fabianova’s ([ 23 ], p. 201) respondents already considered themselves to be “walking corpses” and even visualised their funeral and grave.
Fabianova [ 23 ] enumerated several explanatory factors that unpacked her respondents’ reactions to their initial diagnoses of being HIV-positive. These included gender, level of preparedness of a client in the pre-testing session, and type of sexual relationship(s) they were in. Others included levels of general knowledge of HIV/AIDS, and HIV/AIDS-related stigma in their community. Fabianova ([ 23 ], p. 199) discovered that males responded to the initial HIV/AIDS diagnosis with anger, disbelief, and aggression. The females cried, got shocked, “swallowed big lumps of air, saliva subconsciously, shook both their hands in refusal and blame [sic] the others almost immediately.”
Other key explanatory factors for Fabianova’s ([ 23 ], p. 199) respondents’ immediate reactions included concerns about “lack of immediate elaborate support structures”, extent of level of awareness about HIV/AIDS, level of HIV/AIDS-related stigma, availability of antiretroviral therapy (ART), and support groups to enable them move on with their lives. Feelings of guilt for the infection were explained by whether the individual felt his/her lifestyle exposed him/her to it, and type of sexual involvement they were engaged in. They felt guilty that they would infect a spouse if they were married. If they were in an unstable/non-married relationship, they did not feel guilty, and shared the blame with the casual sexual partner. Sixty-two percent blamed their partners or the environment with the excuse that they stayed loyal to their partners. Fabianova’s ([ 23 ], p. 200) respondents who tested on their own volition did so based on their own or a partner’s “failure”, poor health or “accidental happening”, or work commitments.
The theoretical framework adopted for this paper, the Hopelessness Theory of Depression, is grounded on depression. Depression is currently one of the five leading causes of the disease burden internationally, except in sub-Saharan Africa (SSA) [ 24 ]. Researchers note that depressive disorders and other common mental health disorders (CMDs--depression, anxiety and somatization) were critically linked to the Millennium Development Goals, particularly gender equity, poverty, HIV/AIDS, and maternal and child health [ 24 , 25 ]. Importantly, depression is the most diagnosed psychiatric disorder among PLWHAs. Depression also serves as a risk factor for the progression of HIV/AIDS. In African settings, a growing appreciation of an important link between CMDs and HIV/AIDS has been established [ 7 , 23 ] as well. HIV has unleashed “a significant strain” on mental health in Africa ([ 24 ], p. 61; [ 26 ]). The huge burden of HIV/AIDS in SSA accounts for 16% of depression in the sub-region [ 24 ]. Alternatively, a neurobiological association exists between HIV and CMDs: “the HIV virus has quite specific detrimental effects on neuronal function” ([ 24 ], pp. 61 & 65). Evidence-based reports in African settings and other developing nations (studies conducted in Sao Paulo, Bangkok, Kinshasa, Nairobi, and Ethiopia), found both more symptoms and a higher prevalence of depression among symptomatic PLWHAs than among non-symptomatic or HIV-negative persons [ 24 ].
Theoretical framework: the hopelessness theory of depression
The Hopelessness Theory of Depression is applied to this paper. It is a diathesis-stress theory which posits that organisms express some form of cognitive and emotional deficits after experiencing a bad event. The theory argues that three depressogenic inferential styles serve as risk factors of depression [ 27 , 28 ]. These are the tendency to attribute a bad event to a global or stable cause; the tendency to perceive bad events as having many disastrous consequences; and the propensity to view oneself as flawed or inefficient [ 28 , 29 ]. Making negative inference upsurges the possibility of hopelessness while feeling hopeless makes depression inevitable. With this explanation, the theory assumes hopelessness as a critical underlying factor to depression. Adding to the causal explanation, Seligman [ 30 ] stated that the symptoms, cure and prevention of a bad event also model depression. In societies like Ghana, where HIV is associated with nonconformity to societal expectations and/or sexual promiscuity, PLWHAs may be more exposed to adverse emotional and cognitive symptoms after receiving an HIV-positive report.
The application of the thesis of the Hopelessness Theory of Depression to HIV-positive populations in SSA is not new. Govender and Schlebusch’s [ 31 ] study in Kwa-Zulu Natal, South Africa, applied Beck’s Hopelessness Scale and Beck’s Depression Inventory [ 32 ] to their assessment of the correlation between depression, hopelessness, and suicidal thoughts in PLWHAs. Schlebusch and Govender [ 33 ] used the same inventories to study PLWHAs in a University-affiliated hospital in South Africa. Primarily, they studied the prevalence of risk of suicidal ideation in PLWHAs immediately after their first diagnosis. Kylmä et al. [ 34 ] also studied the full gamut/dynamics of the concept of hope (hope, despair, hopelessness) among PLWHAs. Their study yielded information on how PLWHAs’ perceptions of hope could facilitate their clinical care. The Hopelessness Theory of Depression is applied to the discussion of the findings.
Study setting and cultural context of LMKM
The LMKM, the catchment area for the study, is situated in the Eastern Region of Ghana. The region, one of ten at the time of data collection, had 2,633,154 residents by Ghana’s last Population and Housing census of 2010, making it the third most-populated region. The Eastern Region is mostly semi-urban [ 35 ]. The LMKM, one of 26 administrative municipalities/districts in the Eastern Region by the time of data collection, covers 12.4% of the region, with total land mass of 304.4 km 2 . The 2010 Population and Housing Census recorded 89,246 residents of the Municipality comprising 46.5% males and 53.5% females. Christians were 92.8%; other religious groups include Muslims and traditionalists [ 36 ]. The indigenes are ethnic Dangmes and speak Krobo. They are a patrilineal descent group, which means they inherit property through their father’s lineage.
Sampling and data collection
This study used a “descriptive, multiple case study approach” ([ 2 ], p. 2; [ 37 ]). This method generates interviewees’ in-depth descriptions of their situations, views and realities regarding issues. This provides deep insights of their actions and choices [ 38 ]. In this study, the pool of cases of the individual respondents is considered a “multiple case study approach” ([ 2 , p. 2; 37 ]). Additionally, the findings from the study municipality forms a case study. As Kutnick et al. [ 2 ] note, case studies are exceptionally useful in eliciting contextual situations, when they are important to a particular study. Examples are cultural, social and structural impediments (such as stigma, and fear) to post-diagnosis HIV care [ 37 ].
This paper analysed data from 26 (13 each from two hospitals studied) out of 38 PLWHAs interviewed qualitatively through personal interviews from June to July 2015. The data used for this study formed part of a large data set from a project which primarily studied the linkages between housing conditions and the reported health status of PLWHAs (see [ 39 , 40 , 41 , 42 ]). The implications of recruiting individuals further away from their diagnosis for this paper are addressed in the section on limitations. The interviews were conducted with the aid of a pretested semi-structured question guide. Table 1 has the key questions asked. Some of these key questions in Table 1 were probing questions that emanated from the main/initial interview guide, because it is open ended, as is the norm with data collection tools for qualitative studies. The initial sample of 38 comprised both males and females who were selected using random sampling [ 2 ] as part of a research project which primarily studied the nexus between the health status of PLWHAs in the LMKM and their housing conditions.
The project comprised both qualitative and quantitative data collection. The qualitative interview guide has been submitted as Additional file 1 . First, the study district, LMKM, was conveniently selected based on its lead, by the time of developing the project proposal, in having persons with HIV/AIDS in Ghana, due to which the government had focused on strengthening healthcare institutions and personnel in the district for the fight against HIV/AIDS. Second, two out of three health facilities in the study district were also conveniently selected—a government and quasi-government hospitals. These had been specially equipped by the Government since 2002, to manage HIV/AIDS cases, thus conveniently leaving out the other government hospital [ 39 , 40 , 41 , 42 ]. Respondents had come to HIV/AIDS Voluntary Counseling and Testing (VCT) Centres in the two hospitals--St. Martins de Porres Hospital in Agormanya and Atua Government Hospital in Atua, near Agormanya, for care. Third, respondents were initially selected conveniently for having been medically diagnosed of being HIV-positive prior to the study, after which they had to verbally self-confirm their status to the PIs of the study.
Interviewing took place in these VCTs. The VCTs operated only on weekdays. For each day during the weekdays, based on prior reconnaissance survey, 40 respondents were targeted for both qualitative and quantitative interviews from the daily list of attendees in each hospital. One-third of these were selected randomly and interviewed. If there were less than 40 people in a day, half of them were randomly selected for interviews. For each day fewer than one-fourth of our initial sample were males, we increased the chances of having males in the sample, by including every fourth male from the initial list of persons who did not make it to the list from which final sampling was done [see [ 20 , 40 , 42 ]. This is justified based on a preponderance of female PLWHAs in the study district [ 20 , 40 , 42 ], Ghana, and also, sub-Sahara Africa generally [ 40 , 42 , 43 , 44 ]. Respondents were given unique codes to prevent being re-interviewed during the course of the study. Five male and female graduate student interviewers were assigned to each study hospital, including one qualitative interviewer.
Qualitative or otherwise, a respondent got randomly selected for an interview when a prior interview had ended, beginning with a random start from the list of assigned codes, till the selected list was exhausted in a day. Similar sampling arrangements were made for each VCT used. The random selection of the respondents was necessary to spread their selection over the designated one month of study, for purposes of having a variety of cases/stories over the study period, for richer analysis. Out of the estimated average of about 40 PLWHAs who would visit each VCT per day, it was necessary to randomly select some and leave others out, to facilitate spreading respondent selection over time as said already. Additionally, it was expedient to randomly distribute the respondents between the qualitative study and survey data collection approaches for the larger project, to avoid possible biases in the responses from these two approaches.
Respondents were males and females, 18 years or older, and confirmed their HIV-positive status to the principal investigators (PIs). The interviewing time for a respondent in the qualitative study ranged between 35 and 50 min. The language used for the interview was left to the respondent’s choice between Krobo, the indigenous language in the LMKM, Twi, the indigenous language spoken the most in Ghana, and English, Ghana’s official language due to its colonial past. With prior permission from the respondents, the interviews were audio recorded.
This paper uses the qualitative data from the project. The original sample of 38 for the initial qualitative data was primarily informed by previous literature on the need to reach saturation in qualitative interviews [ 20 , 42 , 45 , 46 ] which was achieved subjectively after interviewing about 10 respondents in each of the two study sites [ 20 ]. Although thematic saturation is usually achieved with 30 qualitative participants [ 20 , 45 , 46 ], 10 respondents gave us thematic saturation at each VCT, because they were quite homogenous [ 20 ]. Previous studies [ 20 , 38 , 42 , 45 , 47 ] have defined thematic saturation as recurrence or repetitiveness of responses from qualitative respondents. Despite reaching saturation with a combined 20 respondents from both VCT centres, we continued interviewing up to 38 of them to meet an initial objective of spreading respondent selection over a month [ 40 , 42 ], with the hope of having some variety of responses due to the case study nature. The sample of 26 for this paper were selected from the 38 because the rest did not respond to the primary question on how they experienced the new diagnoses of their HIV-positive status (see [ 2 ]).
Ethical clearance and data quality approaches
Ethical clearance was sought from the Ethical Committee for Humanities at the University of Ghana, Legon ( ECH 017/14–15 ) , and the Ethical Review Board of the Memorial University at St. Johns, Newfoundland, Canada. Permissions were also sought from the Ethical Review Committee of the Ghana Health Service (GHS-ERC: 02/11/14) for using institutions under its jurisdiction for the study, as well as from the Eastern Regional Directorate of the Ghana Health Service. The District Health Management Directorate of the LMKM and the administrators of the study hospitals responded to the written permissions with verbal permissions to undertake the study. The respondents were informed of the objectives of the study, assured of confidentiality, and their informed consent was sought. They were also informed that their participation was voluntary and they would not be penalised if they opted to turn down the interview at any time during the process.
One person declined to be interviewed, citing time constraints. No identifiable markers were used for the respondents (see [ 20 , 39 , 40 , 42 ]).
Data analysis
The data were transcribed verbatim, and reviewed by the author and team of transcribers to ensure accuracy. The adequacy of translation from the local languages to English was ascertained by holding several meetings between the author and the transcribers to interrogate the correct translations forth and back till a mutual agreement was reached on the correct translations.
Based on the deductive approach, the data analysis was done focusing on the objectives of the study [ 40 ]. Qualitative thematic content analysis, which enables interrogating narratives from all cases studied for a combined result [ 20 , 40 , 42 , 48 ], guided generating themes and subthemes for this paper. In this paper, the qualitative thematic content analysis used also qualifies to be called a discourse or conversation analysis [ 49 , 50 ]. It used a qualitative thematic coding [ 50 , 51 ] of the different interviews/conversations with the respondents and observed the three key features of qualitative content analysis described by Schreier [ 50 ]. These are reducing the data, systematically analysing them, and applying flexibility in the analysis. The systematic analysis meant carefully examining every single aspect of the transcribed data and systematically describing their meaning [ 50 , 52 ], as well as comparing and relating different parts of the data to one another [ 50 ]. NVivo version 11 professional software [ 53 ] was used to identify themes and sub-themes relevant to the objectives of the study and other relevant information. Again, back and forth meetings were held between the author and the team of two coding assistants, who coded the data independently, to mutually agree on their meaning and context.
These repeated processes of reviewing the data enhance intercoder reliability subjectively and improve the credibility/validity and reliability of qualitative data [ 40 , 42 , 54 ].
Based on previous research [ 2 , 11 , 34 ] respondents’ experiences of the new diagnoses of their HIV-positive status were adjudged as negative if the respondent either expressed shock, disbelief, worry, fear/panic, felt the HIV infection would kill him/her, or immediately contemplated suicide. Respondents’ experiences of their new diagnoses were classified as resigned acceptance if they readily accepted the new diagnoses and/or showed some optimism instantly that they could survive the infection. Finally, their experiences of the new diagnoses were considered resigned neutral when the respondent indicated he/she showed no emotion upon receiving the first news of his/her HIV-positive status (Fig. 1 & Table 2 ).
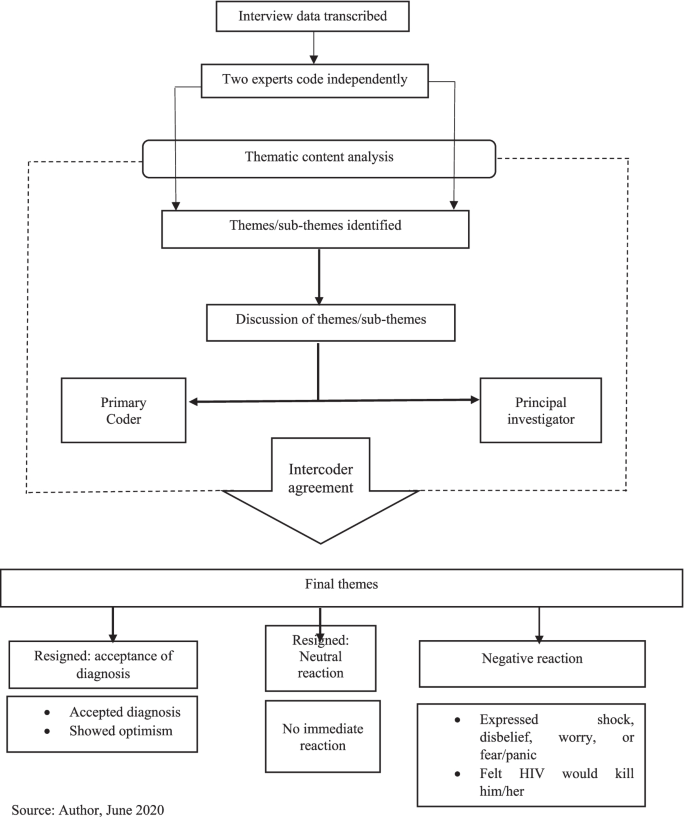
Data analysis workflow
Reflexivity
Reflexively, the author’s cultural and theoretical population health orientation admittedly had some influence on aspects of the research process, although these were minimal. These included the choice of the title. Being fully aware of the extent of stigmatisation culturally associated with HIV/AIDS in Ghana [ 20 , 40 , 42 ], the PIs of the project from which data for this paper emanates were curious about how respondents would experience the new diagnoses with the infection.
Nevertheless, given the author’s extensive training in the dogma and ethics of scientific research, particularly regarding the need for value-neutrality and objectivity [ 54 ], the author’s cultural and theoretical backgrounds did not otherwise influence the data analysis and interpretation. This was applicable to most of the research process as well.
Socio-demographic characteristics of respondents
The respondents’ ages ranged from 25 to 68 years old. They were mostly females (80.77%, n = 21), primarily indigenous Dangmes (84.62%, n = 22), and generally had low socio-economic status. Also, they were mostly single (separated/widowed after cohabiting/never married/widowed), and they had been officially diagnosed HIV-positive for a range of six months to 12 years (Table 3 ).
Thematic findings
Experiences of new diagnoses of hiv/aids.
Table 2 summarises the experiences of new diagnoses among the respondents, upon hearing of their HIV seropositive status. There were negative and resigned reactions. Verbatim responses are identified with the type of hospital the respondent used: government or quasi-government.
Negative reactions
The data showed that the vast majority of the respondents seemed to have been very hard hit and traumatised by the news of HIV-positive test result, and expressed very negative sentiments. For these, the experiences of new diagnoses ranged from disbelief, to being very disturbed. Few mentioned the thought of killing themselves, incessant crying, and feeling that they would die from AIDS. Other reactions included being very frustrated, very surprised, very frightened, deep shock, deep worry, being heartbroken/devastated, self-blame, and avoiding going to hospital till conversion to AIDS (Table 2 ):
“ It was very hard for me when I first heard it; in fact, I cried and cried.” ( Government hospital).
“In fact I was very frustrated. I even decided to take poison so that I will die before the sickness [HIV] becomes worse.” (Government hospital).
“I was very surprised and shocked when I was first told I had this disease. It was very heart-breaking.” (Government hospital).
Resigned reactions
On the contrary, few respondents showed resignation towards the bad news. These comprised three who readily accepted the diagnosis and two who seemed neutral to it. From their responses, respondents who accepted their diagnosis seemed to have readily and consciously accepted/embraced the diagnosis of HIV-positive and encoded it rather smoothly as part of their identity.
“When I was told I was not perturbed because I knew people who were also taking the drug” [ARVs]. (Quasi-government hospital).
The very few respondents who seemed to have been neutral to their new diagnosis of HIV/AIDS seemed to have continued with their lives seamlessly on the spare of the moment they received the news, and did not take a break to react to the news of being HIV-positive.
“I was ill for long time so when I was told about it I only continued to take medications.” (Government hospital) .
Further analysis indicated that these experiences of the new diagnoses were influenced by certain background situations. These are discussed in the next section.
Factors influencing experiences of the new diagnoses
For the very few respondents whose new diagnoses experiences were neutral, being ill for a long time before the HIV-positive diagnosis, and accepting that sickness is inevitable and could happen anytime, were what influenced their experiences of the new HIV-positive diagnoses:
“ … as for sickness, it’s sickness; you have less control over sickness, so I didn’t really do anything.” (Quasi-government hospital).
Two of the few respondents who readily accepted their new diagnosed HIV-positive status said they experienced persistent comorbidities from the HIV infection. Resultantly, they voluntarily went to the VCTs to test for their HIV status:
“I started falling sick and strange rashes kept appearing on my skin, so when I took it to the hospital, I was told it was the virus.” (Government hospital).
“I frequently fell sick … and it was not getting better so I came to the hospital myself … I came (willingly) to them to be tested when I realised I have changed. So they were even happy I walked to them myself to be tested.” (Quasi-government hospital).
Including two multiple responses, the vast majority who responded negatively to the experiences of new diagnoses of HIV-positive status, mentioned four main situations that informed their experiences of the new diagnoses. Mostly, they suffered comorbidities from their infection.
“For about seven months I was not feeling well. It even got to a point I lost consciousness. All forms of tests were ran on me … but they could not find exactly what was wrong...My boss advised me … so I went to the hospital for the test and the nurses said I was HIV-positive.” (Government hospital).
Next, nearly half of the respondents who reacted negatively said a spouse/partner was HIV-positive and thus knew they had contracted the infection from them, and/or due to that, health personnel tested them also for the infection. Importantly, half of these PLWHAs did not know their partners’ HIV status prior to respondent’s diagnosis.
“ I was staying with my husband by then but he died so it was after he died that the doctors realised that it was this disease he died of … afterwards I was tested and diagnosed with this disease.” (Government hospital).
Similar to those who readily embraced their diagnosis, a few of those whose new diagnoses experiences were negative were tested voluntarily based on their sexual partner’s infection. Likewise, several participants whose new diagnoses experiences were triggered by the onset of comorbidities said they voluntarily went for the testing. Additionally, for a slim minority of the latter, their conviction to go for the VCT was based on mass media (often television) announcements and discussions on the signs and symptoms of HIV/AIDS.
“Already I suspected that my husband had all the symptoms that are discussed on TV and radio about this disease. He fell sick often and also coughed most of the time.” (Government hospital).
“Even though I wasn’t falling sick, I came to be tested willingly after they announced everybody should get tested … .” (Government hospital).
“… I used to fall sick frequently and that was when a lot of noise and adverts were made about this disease on television and radio...I went to the St. Martin’s hospital and told the doctors about my situation and he asked me go for an HIV test and that was when I got to know I had this disease.” (Quasi-government hospital ).
Finally, few (including two who gave multiple responses—primarily that a spouse/partner was HIV-positive) mentioned that they got tested when they were pregnant.
“I was about to give birth to my second born … my husband is also HIV-positive.” (Government hospital ).
“I was diagnosed when I was pregnant when my second born and I visited the hospital … Yes, [my husband is HIV-positive].” (Government hospital).
Factors that facilitated transitioning to accept HIV-positive self
For the few respondents who showed resignation towards the experiences of their new HIV-positive diagnoses, there was no need for transitioning to accepting an HIV-positive self. Two of these respondents who readily embraced the new HIV-positive diagnoses said they already knew persons who were HIV-positive and were taking antiretroviral medications (ARVs):
“I realised I was not the only victim; many people are also victims …” (Quasi-government hospital ).
Two others said they already had comorbidities from AIDS and started treatment right after diagnoses:
“ I was ill for a long time so when I was told about it I only continued to take medications.”
(Government hospital ).
Another participant thought sickness is inevitable and thus did not need to worry about such diagnosis.
Nearly one-third of the respondents whose experiences of the new HIV-positive diagnoses were negative gave no response regarding what influenced their transitioning to accepting their new HIV-positive diagnoses. They mostly felt uncomfortable/reluctant talking about it. The rest mentioned what facilitated their transitioning more spontaneously and/or more readily after some amount of probing. The vast majority of the rest who experienced negative reactions said the most important help with their transitioning was counselling from health workers who encouraged them to initiate and continue treatment, with the assurance that if they did so, they would survive the infection.
“… After I came here [VCT] and was advised and encouraged to see something to live for, I have been okay. They [health personnel] have been very friendly and encouraging. In fact, they have helped me a lot .” (Government hospital).
“ They [health personnel] counsel us and tell us the fact that we have this virus does not mean our world has come to an end.” (Government hospital).
“… After being put on medication, going through counselling and tests, and being told what to do, I was hopeful that if you adhered to the medication you could live long.” ( Quasi-government hospital).
For one of these, her mother-in-law was the main person who empathised with her:
“I was really worried and disturbed but the encouragement and advice from the nurses and my mother-in-law … has helped me. After I told her [mother-in-law] I had been diagnosed … she brought me here [VCT] to introduce me [to a nurse] , so she has been helpful.” (Government hospital).
The second main issue that facilitated the transitioning for few of the respondents was their awareness of the current medical advancement in the treatment of HIV infection, due to which “you would live long” ( Quasi-government hospital) despite the infection:
“… because they have drugs to treat it, I was OK. Provided it will not cut short my life span I am happy.” ( Quasi-government hospital).
“In the olden days when there were no drugs you thought you would die … after being told, so you become afraid, but now we know there are drugs available so if you are able to take your drugs you don’t have any problem.” ( Quasi-government hospital).
Three respondents alluded to accepting medical diagnoses, facing reality, and living by Biblical principles as facilitating their acceptance of their new diagnoses.
“ I accepted it because you can’t deny what a doctor says” ( Quasi-government hospital).
“I was disturbed but I thought to myself that it had already happened ” ( Quasi-government hospital) .
“I didn’t kill myself because I am a Christian and the Bible speaks against that. I forgot about everything and decided to keep coming for the medications and now by the grace of God I have lived for over twelve years .” ( Government hospital).
There was, however, a lone-voice who said she had still not settled down to the reality of being HIV-positive after having been diagnosed three years prior and seeking treatment for one-year post diagnosis. Thus, she has not been consistent in getting treatment and is already feed up with seeking treatment:
“It seemed to be untrue. From time to time I stopped taking the medication … I am fed up with coming to seek treatment. I have been treating the sickness for over a year but the symptoms recur after I see the doctor.” ( Quasi-government hospital).
This lone-voice mentioned having severe comorbidities which were probably due to starting healthcare for HIV two years after diagnosis. She also mentioned experiencing extreme discrimination and ostracisation both at home and in public, which no doubt, are linked to her comorbidities.
This section discusses the findings of the study, with a bearing on the tenets of the Hopelessness Theory of Depression. Fear has been associated with HIV since its discovery in the 1980s. Fear is mostly fueled by misconceptions associated with the virus which is mostly linked to death and stigmatisation [ 55 ]. Grounded on fear of death and a feeling of helplessness, a wide range of reactions are exhibited upon diagnosis or disclosure of an individual’s HIV-positive status. Although these reactions are both from the individual in question and significant others of this individual, the literature has mostly focused on the reactions of the persons affiliated with these individuals after disclosure [ 56 , 57 ]. Indeed, very few studies explore the individual’s reactions upon diagnosis or testing positive for the virus [ 55 , 58 ]. Based on this drawback and the known public health significance of such immediate reactions to HIV-positive diagnosis, this paper examined the experiences of new diagnoses of Ghanaian PLWHAs after hearing the “bad news.”
Importantly, a critical examination of differences between participants from each of the two hospitals studied shows that 11 respondents from the government hospital had negative reactions to the new experience of their HIV/AIDS diagnosis while ten in the quasi-government hospital did so. On the other hand, the experiences of two respondents from the quasi-government hospital was adjudged as “Resigned: accepted diagnosis” while one participant from the government hospital showed a ‘Resigned: accepted diagnosis.” There were no other differences in the participants’ reactions between the two study sites (Table 2 ). Rather, the difference between the respondents basically stemmed from the influences on their experiences of the new HIV-positive diagnoses discussed earlier (Table 2 ), which did not have a relationship with the particular hospital they received healthcare from. While previous researchers have articulated the lack of major differences in the findings from the respondents used for the qualitative study in the project [ 39 , 41 ], they have further clarified that the respondents’ similar socio-bio-demographic background is mostly responsible for the lack of major differences in the findings [ 20 , 39 , 41 ].
The findings from this study have corroborated those of previous authors that receiving the news of newly-diagnosed HIV-positive status is often met with reactions that are “complex and multi-faceted” ([ 2 ], p. 12). Additionally, the findings that respondents had varied responses and a myriad of experiences to the new diagnoses of their HIV-positive status is in line with reports from several studies (example: [ 2 , 58 ]). Most of the initial reactions of respondents in this study were very traumatising and discouraging. These included a few who contemplated suicide upon hearing the news; supporting Fabianova’s [ 23 ] findings in Nairobi.
Similar to previous research [ 55 , 58 ], findings from this study indicate that though negative emotional and psychological reactions may occur upon learning of an HIV-positive status, respondents may also resign themselves to their fate—to accept or numb their feelings about the new disclosure of their HIV+ diagnoses. Likewise, this study found that respondents who were already exposed to HIV/AIDS needed no transitioning to self-acceptance of their HIV-positive status. This corroborates previous findings [ 55 ]. Nearly all the respondents settled down later, after experiencing the new diagnoses, initiated and continued with their healthcare for HIV/AIDS. This affirms previous assertions that such initial feelings regarding information on a newly-diagnosed HIV-positive status mostly fade away eventually [ 3 , 23 ].
Again, the paper corroborates previous findings and highlights the buffering role of healthcare providers in moderating the experiences of new diagnoses of HIV-positive persons [ 1 , 11 ]: the vast majority of the respondents who adapted to their HIV-positive status attributed it to counselling and support from healthcare personnel. This role of the healthcare workers in aiding respondents’ transition to accepting their HIV-positive selves affirms the documented importance of social support in ameliorating the otherwise negative effects of experiencing a health trauma [ 23 , 59 ]. Research has identified HIV counsellors’ or health providers’ choice of words and emotions as crucial in determining peoples’ reaction to the initial diagnosis of HIV infection [ 55 , 58 ]. When these emotions were hopeful and assuaging, patients were more likely to be calm and comforted, and vice versa [ 58 ].
The findings of this study underscore the fact that PLWHAs who experience new HIV-positive diagnosis will need to receive such interventions early [ 12 ]. These interventions are needed to give them hope in life to abate extreme psychosocial trauma that can be associated with experiences of new HIV-positive status [ 11 , 60 ]. Per the findings of this paper, such interventions should include educating PLWHAs experiencing new HIV-positive diagnosis that new medical advances for HIV-positive infection make it possible for PLWHAs experiencing new HIV-positive diagnosis to lead normal lives and live long, if they seek early treatment and adhere to prescribed healthcare.
A fair number of the respondents mentioned being infected by their spouses/partners who were alive or deceased (also see [ 40 ]), implying that they probably were not using condoms and other modes to prevent HIV transmission from their sexual partners. This finding is not unlikely considering that Owusu [ 42 ] found that the PLWHAs studied were hardly using any form of protection against HIV with their sexual partners, whether in stable or unstable relationships. Two respondents were exceptions--they used condoms, but inconsistently [ 40 ]. Furthermore, Owusu [ 40 ] found that the unmarried or non-co-habiting PLWHAs had not disclosed their HIV-positive status to their sexual partners, with the exception of one respondent. PLWHAs who fail to disclose their status to their partners may have been living in a state of denial and or may fear/have feared the ramifications of disclosing their status. They may thus refuse to disclose as a way of attenuating the anticipated effect of disclosing, as previous authors have attested to [ 12 , 15 , 23 ].
Additionally, findings from this paper illuminate the importance of voluntary counseling and testing. Majority of the respondents mentioned having had comorbidities before they tested for their HIV-positive status. Other researchers have indicated that anticipated reaction influences decisions on voluntary testing for HIV [ 55 , 58 ]. Previous research clearly notes potential barriers to voluntary testing for HIV in Ghana. These include the fear of stigma, discrimination and abuse, and possible dissolution of romantic relationships associated with being a PLWHA. Importantly, there is fear of the perception that an HIV-positive diagnosis is a death warrant [ 16 , 61 ]. Antenatal-linked VCT is a policy strategy in Ghana for HIV control through a nationwide integration of VCT and antenatal care [ 62 ]. However, clients may disagree to it.
The findings from this paper mostly tally with the Hopelessness Theory of Depression’s core proposition; the respondents overwhelmingly perceived the experiences of their new HIV-positive status as translating into unwelcome consequences and negative inferences, as did respondents in other SSA settings [ 12 , 23 ]. This plausibly led to depression and feelings of hopelessness among them. Also, this perspective may have underlain the self-blame by a few of them for being HIV-positive [ 28 , 29 ]. Furthermore, this paper confirms the Hopelessness Theory of Depression’s propositions that underlying perceived bad situations and experiences which are attributed to internal factors lead to depression. Conversely, those ascribed to presumed external factors/influences give comfort/are reassuring [ 4 ]. In this study, the experiences of new HIV-positive diagnoses were mostly negative for respondents with internal factors such as having comorbidities and having a spouse/partner with HIV/AIDS.
In consonance with Peterson’s and Seligman’s [ 4 ] Hopelessness Theory of Depression’s propositions, respondents of this study said that external factors motivated them to take commendable actions such as going for VCT. These included the influence of health education through mass media, counselling by healthcare practitioners, and information regarding modern medical advancements which can help PLWHAs live without comorbidities, and possibly survive the infection. Furthermore, these factors facilitated their adaptation to their HIV-positive selves.
Nevertheless, this paper does not substantiate Peterson and Seligman’s [ 4 ] Hopelessness Theory of Depression fully. Contrary to their proposition, in this study, fewer respondents mentioned that a series of external factors such as knowing someone who has HIV/AIDS, and being given a near-mandatory HIV test at an antenatal clinic were what influenced their negative reactions. Conversely, other internal factors such as having comorbidities and having an HIV-positive romantic partner influenced few of the respondents to positively adapt to their HIV-positive diagnoses. In this study, therefore, the clear diathesis of external factors giving psychosocial comfort and internal factors unleashing mental discomfort in response to hearing the often unwelcome first news of being HIV-positive was not fully supported. This was also true of Assen et al.’s [ 12 ] study in Ethiopia.
Hence, this paper corroborates Govender and Schlebusch’s [ 31 ] synthesis of the Hopelessness Theory of Depression. These authors emphasise that the numerous internal and external challenges that face PLWHAs such as discrimination, stigmatisation, abuse, financial, marital, and healthcare challenges, among others, may [also combine to] have connotations for the loss of control over one’s life, fear of the future, and feeling of helplessness. As well, they may underlie the negative inferences which exacerbate the feeling of hopelessness and increase the likelihood of depressive symptoms stemming from experiencing new diagnosis of HIV/AIDS.
This paper adds to the knowledge on the personal and public health effects of experiencing new HIV-positive diagnosis. Particularly, it highlights the commendable public health effects of receiving new diagnosis for HIV-positive status and illuminates the role of social support in seeking and continuing healthcare for the diagnosis. Also, it attests to the role of healthcare workers and behaviour change communication, using mass media, in fighting the menace of HIV/AIDS. Furthermore, as articulated above, this paper did not fully support the conclusions of Peterson’s and Seligman’s [ 4 ] Hopelessness Theory of Depression’s framework. Rather, the paper contributes additional information to it in the form of an anti-thesis. Additionally, unlike Fabianova’s [ 23 ] study in Nairobi, this study did not find that the respondents acted with aggression towards counsellors who first broke the news of their HIV-positive status to them.
More importantly, this paper has navigated new frontiers in the body of knowledge in its thematic area of study. First, contrary to Fabianova’s [ 23 ] findings that some of her respondents attempted suicide, non-of the respondents in this study mentioned having attempted to take their lives, although a few of them revealed they had suicidal ideation. This may be due to the fewer respondents this study engaged as well as its cross-sectional design, compared to Fabianova’s [ 23 ] respondents, and the longitudinal approach to her study. Second, this study has newly articulated outstanding information on factors which facilitate PLWHAs’ transitioning to accepting and settling down to their experiences of new HIV-positive status. Third, unlike previous literature, this study has uniquely found that having comorbidities from HIV/AIDS was the primary reason that influenced the respondents to voluntarily test for their HIV-positive status. The uniqueness of this finding may be linked to the awareness that VCT of HIV/AIDS status is very rare in Ghana [ 63 , 64 ].
Limitations
The qualitative nature of this study better facilitates unearthing the complexities associated with experiences of new diagnoses among HIV-positive persons and learning about the adaptation process [ 2 ]. Also, the repeated data analyses this paper employed strengthens its reliability and validity. However, when interpreting these findings, some limitations should be considered. With HIV-positive status being a very sensitive issue, and highly stigmatised in Ghana [ 16 , 65 , 66 ], social desirability of responses may have influenced the findings [ 2 ]. Being a retrospective study, recall bias may also affect the reliability of the responses [ 2 , 20 ]. This is with particular reference to the time lapse between the moment a respondent was newly-diagnosed with HIV/AIDS, as operationalised above, and the time of the study. Recruiting individuals further away from their diagnosis is a limitation; it could lead to recall bias. Furthermore, the study is cross-sectional and does not permit inference of causality [ 67 ]. Additionally, being a qualitative study with a fairly small sample size, the findings are not generalisable to non-respondents in the LMKM and also, Ghana as a whole [ 67 ].
Omona ([ 68 ], p. 181) posits that although random sampling is rare in qualitative studies, they are not out of place as they facilitate sampling the “desired number of individuals …” from a generated sampling frame, which he asserts improves the credibility of the sample (also see [ 69 ], p. 28). Yet, as hinted previously in this paper, random sampling in qualitative studies could pose some limitations. A careful search of the literature does not specify such limitations. However, the author guesstimates that random sampling in qualitative studies may rob the data of the quality of focusing on some key persons/texts of interest to the study which convenience sampling will provide. Lastly, based on the primary focus of the project, this paper did not undertake a diagnostic assessment for depression among the respondents. The paper is thus unable to ascertain if depression contributed to experiences of the new diagnoses of HIV-positive status among the PLWHAs studied.
Evidence elsewhere suggests that upon receiving the initial news of an HIV-positive diagnosis, most people have strong psychosocial reactions [ 23 , 55 , 70 ]. Such reactions are also known to have very critical public health implication [ 1 , 2 , 14 ]. Yet little research has focused on the initial reactions of newly-diagnosed PLWHAs in SSA, particularly Ghana. Neither has the implications of their reactions for personal and public health been extensively studied [ 2 , 11 ]]. This makes this study of the experiences of new HIV-positive diagnoses very timely. The personal and public health implications of one’s experience of new diagnosis of HIV-positive status is critically important for Ghana, which has a generalised HIV-positive infection [ 21 ].
Consistent with the literature, the vast majority of the respondents became extremely traumatised and immobilised when they experienced new diagnoses of their HIV-positive status. A few, however, more readily resigned to their HIV-positive identity. Regardless of their experiences of new diagnoses of HIV/AIDS, having comorbidities prior to diagnosis influenced their experiences the most. This was followed by having/having had a spouse/partner especially, and/or knowing someone who was HIV-positive, prior to their diagnoses. Next, respondents mentioned being influenced by health education through mass media, TV particularly, on signs and symptoms of HIV/AIDS. Importantly, health education, counselling, reassurance and empathy from healthcare workers provided hope. Furthermore, these facilitated their transitioning to settling down to self-acceptance of an HIV-positive status and continuing with healthcare. Finally, this paper concludes that to a large extent, the findings are applicable to the tenets of the Hopelessness Theory of Depression used as a framework for this study. Consequently, this paper found hopelessness as an important driving force to negative reactions towards one’s experience of his/her new HIV-positive diagnosis.
Conclusions from this paper have several public health significances. It highlights the continuous need for and strengthening of behaviour change communication on HIV/AIDS by the Ghana AIDS Commission and Ghana Health Service. This should emphasise its signs and symptoms, the need to seek early treatment, and adherence to prescribed ARVs. Strengthening the use of mass media, small groups, schools, churches/mosques and person-to-person channels in such endeavours is important. HIV/AIDS-related health promotion and education should also continue to emphasise prevention, but importantly, state that once infected, HIV/AIDS can be controlled; the infected person can live without comorbidities and need not succumb to the infection. Stakeholders should work harder towards educating residents in the LMKM, and for that matter, Ghanaians generally, about voluntary testing of HIV status. Most of the respondents in this study mentioned having had comorbidities from HIV/AIDS prior to their new diagnoses. Onset of comorbidities for HIV/AIDS prior to diagnosis and treatment can make the treatment expensive; it can also diminish the chances of surviving the infection severely [ 71 , 72 ].
Given the high rates of HIV/AIDS in the study district and Region, the health education should also emphasise the need for persons whose sexual partners are HIV-positive—particularly those who show signs and symptoms of the infection, and all who engage in at-risk sex, to practice safer sex. Finally, the paper recommends increased social support and empathy for PLWHAs in LMKM particularly and in Ghana generally, from family, friends, neighbors, community leaders, healthcare professionals, and organised groups such as members of their religious affiliation, if any [ 20 , 40 , 42 ]. This study has unearthed social support as a critical moderating element in the transitioning of PLWHAs to integrating their HIV-positive self-concept, initiating, and adhering to prescribed healthcare. Families, social groups, and healthcare professionals should empathise with PLWHAs.
Availability of data and materials
The datasets used and/or analysed during this study are available from the author on reasonable request. The key questions for the study have been provided in the paper, in Table 1 . The complete question guide used to collect the data has also been provided online as Additional file 1 .
Abbreviations
Acquired immune deficiency syndrome
Anti-retroviral therapy
Antiretroviral medications
Common mental health disorders
Ethics Committee on Humanities
Ethical Review Committee
Ghana AIDS Commission
Ghana Health Service
Ghana Statistical Service
Human immunodeficiency virus
Lower Manya Krobo Municipality
Principal Investigator
Persons living with HIV/AIDS
Research Assistants
Sub-Saharan Africa
University of California San Francisco
Voluntary counselling and testing
Chu C, Selwyn PA. Diagnosis and initial management of acute HIV infection. Am Fam Physician. 2010;81(10):1239–44.
PubMed Google Scholar
Kutnick AH, Gwadz MV, Cleland CM, Leonard NR, Freeman R, Ritchie AS, et al. It’s a process: reactions to HIV diagnosis and engagement in HIV care among high-risk heterosexuals. Front Public Health. 2017;10(5):100. https://doi.org/10.3389/fpubh.2017.00100 .
Article Google Scholar
University of California San Franscisco. Coping with HIV/AIDS: Mental Health. HIV in Site Project: the UCSF Center for HIV Information. 2018. http://hivinsite.ucsf.edu/insite?page=pb-daily-mental . Accessed 2 May 2018.
Google Scholar
Peterson C, Seligman ME. Causal explanations as a risk factor for depression: theory and evidence. Psychol Rev. 1984;91(3):347. https://doi.org/10.1037/0033-295X.91.3.347 .
Article CAS PubMed Google Scholar
Alford K, Banerjee S, Nixon E, O’Brien C, Pounds O, Butler A, et al. Assessment and management of HIV-associated cognitive impairment: experience from a multidisciplinary memory service for people living with HIV. Brain Sci. 2019;9(2):37. https://doi.org/10.3390/brainsci9020037 .
Article PubMed Central Google Scholar
Stein DJ, Seedat S, Emsley RA, Olley BO. HIV/AIDS in Africa—a role for the mental health practitioner? S Afr J Psychiatry. 2005;95(3):167–8.
Rivera-Rivera Y, García Y, Toro V, Cappas N, López P, Yamamura Y, et al. Depression correlates with increased plasma levels of inflammatory cytokines and a dysregulated oxidant/antioxidant balance in HIV-1-infected subjects undergoing antiretroviral therapy. J Clin Cell Immunol. 2014;5(6). https://doi.org/10.4172/2155-9899.1000276 .
Wanyenze RK, Kamya MR, Fatch R, Mayanja-Kizza H, Baveewo S, Sawires S, et al. Missed opportunities for HIV testing and late-stage diagnosis among HIV-infected patients in Uganda. PLoS One. 2011;6(7). https://doi.org/10.1371/journal.pone.0021794 .
Nairaland Forum. A female doctor commits suicide after testing positive to HIV. 2011. http://www.nairaland.com/720421/female-doctor-commits-suicide-after . Accessed 25 May 2018.
Hosek SG, Lemos D, Harper GW, Telander K. Evaluating the acceptability and feasibility of project ACCEPT: An intervention for youth newly diagnosed with HIV. AIDS Educ Prev. 2011;23(2):128–44. https://doi.org/10.1521/aeap.2011.23.2.128 .
Article PubMed PubMed Central Google Scholar
Moitra E, Chan PA, Stein MD. Open trial of an acceptance-based behavior therapy intervention to engage newly diagnosed HIV patients in care: rationale and evidence of feasibility and acceptability. Behav Modif. 2015;39(5):670–90. https://doi.org/10.1177/0145445515590977 .
Assen A, Molla F, Wondimu A, Abrha S, Melkam W, Tadesse E, et al. Late presentation for diagnosis of HIV infection among HIV positive patients in South Tigray zone, Ethiopia. BMC Public Health. 2016;16(1):558. https://doi.org/10.1186/s12889-016-3263-y .
Dodd PJ, Garnett GP, Hallett TB. Examining the promise of HIV elimination by ‘test and treat’ in hyper-endemic settings. AIDS (London, England). 2010;24(5):729–35. https://doi.org/10.1097/QAD.0b013e32833433fe .
Pettifor A, MacPhail C, Corneli A, Sibeko J, Kamanga G, Rosenberg N, et al. NIAID center for HIV/AIDS vaccine immunology. Continued high risk sexual behavior following diagnosis with acute HIV infection in South Africa and Malawi: implications for prevention. AIDS Behav. 2011;15(6):1243–50. https://doi.org/10.1007/s10461-010-9839-0 .
Skinner D, Mfecane S. Stigma, discrimination and the implications for people living with HIV/AIDS in South Africa. SAHARA J. 2004;1(3):157–64.
Article CAS Google Scholar
Koka E, Ahorlu CK, Agyeman DK. Social death through HIV and AIDS stigmatization and discrimination in Ghana: a case study of the central regional hospital, Cape Coast, Ghana. Advanc Appl Sociol. 2013;3(06):231–6.
Miller WC, Rosenberg NE, Rutstein SE, Powers KA. The role of acute and early HIV infection in the sexual transmission of HIV. Curr Opin HIV AIDS. 2010;5(4):277–82. https://doi.org/10.1097/COH.0b013e32833a0d3a .
Gwadz M, de Guzman R, Freeman R, Kutnick A, Silverman E, Leonard NR, et al. Exploring how substance use impedes engagement along the HIV care continuum: a qualitative study. Front Public Health. 2016;4:62. https://doi.org/10.3389/fpubh.2016.00062 .
Lund R, Agyei-Mensah S. Queens as mothers: the role of the traditional safety net of care and support for HIV/AIDS orphans and vulnerable children in Ghana. Geo J. 2008;71(2–3):93–106. https://doi.org/10.1007/s10708-008-9145-9 .
Owusu AY, Laar A. Managing HIV-positive sero-status in Ghana’s most HIV concentrated district: self-perceived explanations and theoretical discourse. Afr J AIDS Res. 2018;17(1):82–90. https://doi.org/10.2989/16085906.2017.1419268 .
Article PubMed Google Scholar
GAC. Summary of the 2016 sentinel survey report. Accra: GAC; 2017. http://www.ghanaids.gov.gh/gac1/aids_info.php . Accessed 10 Jan 2018
Visser MJ, Makin JD, Vandormael A, Sikkema KJ, Forsyth BW. HIV/AIDS stigma in a south African community. AIDS Care. 2009;21(2):197–206.
Fabianova L. Psychosocial aspects of people living with HIV/AIDS. In Social and psychological aspects of HIV/AIDS and their ramifications 2011. IntechOpen. doi: https://doi.org/10.5772/21148 . https://www.intechopen.com/books/social-and-psychological-aspects-of-hiv-aids-and-their-ramifications/psychosocial-aspects-of-people-living-with-hiv-aids . Accessed 14 Oct 2019.
Patel V, Stein DJ. Common mental disorders in sub-Saharan Africa: the triad of depression, anxiety and somatization. In: Akyeampong E, Hill A, Kleinman A, editors. The culture of mental illness and psychiatric practice in Africa. Bloomington: Indiana University Press; 2015. p. 50–72. http://www.jstor.org/stable/j.ctt16gz69f.6 . Accessed 26 Jun 2019.
Miranda JJ, Patel V. Achieving the Millennium Development Goals: does mental health play a role? PLoS Med. 2005;2(10):e291.
Collins PY, Holman AR, Freeman MC, Patel V. What is the relevance of mental health to HIV/AIDS care and treatment programs in developing countries? A systematic review. AIDS (London, England). 2006;20(12):1571–82.
Abela JR. The hopelessness theory of depression: a test of the diathesis–stress and causal mediation components in third and seventh grade children. J Abnorm Child Psychol. 2001;29(3):241–54.
Abela JR, Payne AV. A test of the integration of the hopelessness and self-esteem theories of depression in schoolchildren. Cogn Ther Res. 2003;27(5):519–35. https://doi.org/10.1023/A:1026303020478 .
Waszczuk MA, Coulson AE, Gregory AM, Eley TC. A longitudinal twin and sibling study of the hopelessness theory of depression in adolescence and young adulthood. Psychol Med. 2016;46(9):1935–49. https://doi.org/10.1017/S0033291716000489 .
Seligman ME. Helplessness. On depression, development and death. San Francisco: Freeman; 1975.
Govender RD, Schlebusch L. Hopelessness, depression and suicidal ideation in HIV-positive persons. S Afr J Psychiatry. 2012;18(1):16–21. https://doi.org/10.4102/sajpsychiatry.v18i1.302 .
Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42(6):861 52. GSS. Population and Housing census 2010. Final results. Accra: GSS.2012.
Schlebusch L, Govender RD. Elevated risk of suicidal ideation in HIV-positive persons. Depress Res Treat. 2015;2015. https://doi.org/10.1155/2015/609172 .
Kylmä J, Vehviläinen-Julkunen K, Lähdevirta J. Hope, despair and hopelessness in living with HIV/AIDS: a grounded theory study. J Adv Nurs. 2001;33(6):764–75. https://doi.org/10.1046/j.1365-2648.2001.01712.x .
GSS. Population and Housing census 2010. Final results. Accra: GSS; 2012.
GSS. Population and Housing Report: District Analytical Report 2010, Lower Manya Krobo Municipal. 2014. http://www.statsghana.gov.gh/docfiles/2010_District_Report/Eastern/LOWER%20 MANYA%20KROBO.pdf. Accessed 14 Jul 2019.
Yin RK. Case study research: design and methods. Thousand Oaks, SAGE 2013;14(1):69–71.
Baxter P, Jack S. Qualitative case study methodology: study design and implementation for novice researchers. Qual Rep. 2008;13(4):544–59.
Tenkorang EY, Owusu AY, Laar AK. Housing and health outcomes of persons living with HIV/AIDS (PLWHAs) in the lower Manya Krobo district, Ghana. J Health Care Poor Underserved. 2017;28(1):191–215. https://doi.org/10.1353/hpu.2017.0017 .
Owusu AY. A gendered analysis of living with HIV/aids in the eastern region of Ghana. BMC Public Health. 2020;20:751. https://doi.org/10.1186/s12889-020-08702-9 .
Tenkorang EY, Owusu AY, Laar AK, Yeboah EH. Housing, psychosocial and adherence counseling among HIV+ persons in Ghana. Health Promot Int. 2019;34(2):204–14. https://doi.org/10.1093/heapro/dax072 .
Owusu AY. Social contexts of living with HIV/AIDS in the eastern region of Ghana. Istanbul Univ J Sociol. 2019;39(2):425–54. https://doi.org/10.26650/SJ.2019.39.2.0109 .
NACP. HIV sentinel survey report. Accra: Ghana Health Service/Ministry of Health; 2018. p. 2019.
Owusu, A. Y. Gender, Adolescents, and Achieving Sustainable Development Goals in Ghana. In A. Williams & I. Luginaah (Eds.). Gender Matters Globally: Geography, Health and Sustainability (Chapter 4). Routledge. Forthcoming. ISBNS: Hardback: 9780367743901; Ebook: 9780367743918; Future paperback: 9780367743925.
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82.
Mason M. Sample size and saturation in PhD studies using qualitative interviews. In Forum qualitative Sozialforschung/Forum: qualitative social research 2010;11(3).
Sedziafa AP, Tenkorang EY, Owusu AY. “… he always slaps me on my ears”: the health consequences of intimate partner violence among a group of patrilineal women in Ghana. Culture Health Sexual. 2016;18(12):1379–92. https://doi.org/10.1080/13691058.2016.1187291 .
Lieblich A, Tuval-Mashiach R, Zilber T. Narrative research: reading, analysis, and interpretation, vol. 27: Thousand Oaks, Sage; 1998.
Book Google Scholar
Krippendorff K. Content analysis: an introduction to its methodology. Thousand Oaks: Sage; 2004.
Schreier M. Qualitative content analysis in practice. Thousand Oaks: Sage; 2012.
Boyatzis RE. Transforming qualitative information: thematic analysis and code development. Thousand Oaks: Sage; 1998.
Mayring P. Qualitative content analysis. Forum Qualitative Sozialforschung/ Forum. Qual Soc Res. 2000;1(2):20. https://doi.org/10.17169/fqs-1.2.1089 https://www.qualitative-research.net/index.php/fqs/article/view/1089 . Accessed 20 Apr 2021.
QSR International. NVivo professional version 11. Boston: QSR International; 2015.
Babbie ER. The practice of social research. 13th ed. Scarborough: Wadsworth/Cengage Learning; 2013.
Anderson M, Elam G, Gerver S, Solarin I, Fenton K, Easterbrook P. “It took a piece of me”: initial responses to a positive HIV diagnosis by Caribbean people in the UK. AIDS Care. 2010;22(12):1493–8. https://doi.org/10.1080/09540121.2010.482125 .
Greeff M, Phetlhu R, Makoae LN, Dlamini PS, Holzemer WL, Naidoo JR, et al. Disclosure of HIV status: experiences and perceptions of persons living with HIV/AIDS and nurses involved in their care in Africa. Qual Health Res. 2008;18(3):311–24. https://doi.org/10.1177/1049732307311118 .
Simbayi LC, Kalichman SC, Strebel A, Cloete A, Henda N, Mqeketo A. Disclosure of HIV status to sex partners and sexual risk behaviours among HIV-positive men and women, Cape Town, South Africa. Sex Transm Infect. 2007;83(1):29–34.
Hult JR, Maurer SA, Moskowitz JT. “I'm sorry, you're positive”: a qualitative study of individual experiences of testing positive for HIV. AIDS Care. 2009;21(2):185–8. https://doi.org/10.1080/09540120802017602 .
de-Graft Aikins A. Mental illness and destitution in Ghana: A Social-psychological perspective. In: Akyeampong E, Hill AG, Kleinman AM, editors. The Culture of Mental Illness and Psychiatric Practice in Africa. Bloomington: Indiana university press; 2015. p. 112–43. http://www.jstor.org/stable/j.ctt16gz69f.6 Accessed 26 Jun 2019.
Baumgartner LM, David KN. Accepting being poz: the incorporation of the HIV identity into the self. Qual Health Res. 2009;19(12):1730–43. https://doi.org/10.1177/1049732309352907 .
NAP+, GAC and UNAIDS. Persons living with HIV Stigma Index Study, Ghana. Accra: NAP+, GAC and UNAIDS; 2014. http://www.stigmaindex.org/sites/default/files/reports/GHANA%20Stigma%20Index%20report%202014.pdf . Accessed 4 Apr 2016. Revised report
Baiden F, Baiden R, Williams J, Akweongo P, Clerk C, Debpuur C, et al. Review of antenatal-linked voluntary counseling and HIV testing in sub-Saharan Africa: lessons and options for Ghana. Ghana Med J. 2005;39(1):8–13. https://doi.org/10.4314/gmj.v39i1.35974 .
Article CAS PubMed PubMed Central Google Scholar
Gadegbeku C, Saka R, Mensah B. Attitude of the Youth towards Voluntary Counselling and Testing (VCT) of HIV/AIDS in Accra, Ghana. J Biol Agri Healthcare. 2013;3(11):133 www.iiste.org .
Oppong AK. HIV/AIDS knowledge and uptake of HIV counselling and testing among undergraduate private university students in Accra, Ghana. Reprod Health. 2013;10:17. https://doi.org/10.1186/1742-4755-10-17 .
Tenkorang EY, Owusu AY. Examining HIV-related stigma and discrimination in Ghana: what are the major contributors? Sex Health. 2013;10(3):253–62. https://doi.org/10.1071/SH12153 .
Dapaah JM, Spronk R. When the clinic becomes a home. Successful VCT and ART services in a stressful environment. J Soc Aspects HIV/AIDS. 2016;13(1):142–51. https://doi.org/10.1080/17290376 .
Badaru UM, Ogwumike OO, Adeniyi AF, Nelson EE. Determinants of caregiving burden and quality of life of informal caregivers of African stroke survivors: literature review. Int J Disabil Human Dev. 2017;16(3):249–58. https://doi.org/10.1515/ijdhd-2016-0041 .
Omona J. Sampling in qualitative research: improving the quality of research outcomes in higher education. Makerere J Higher Educ. 2013;4(2):169–85. https://doi.org/10.4314/majohe.v4i2.4 .
Miles M, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2nd ed. Thousand oaks: Sage; 1994.
Peirce A. The emotional impact of an HIV diagnosis. 2017. https://www.everydayhealth.com/hiv-aids/hiv-diagnosis-emotional-impact.aspx . Accessed 2 May 2018.
GAC. National HIV & AIDS Strategic Plan 2016-2020. 2016. http://www.ghanaids.gov.gh/gac1/pubs/COMPREHENSIVE%20NSP%202016-2020.pdf . Accessed 17 May 2020.
Owusu AY, Asante KT. Current HIV/AIDS status, access to antiretroviral treatment, and HIV related stigma in Ghana. Policy Brief. 2020. Accra: ISSER.
Download references
Acknowledgements
Professor Eric Y. Tenkorang of the Department of Sociology, Memorial University of Newfoundland and Labrador in Canada, was the PI for the project and participated in the data collection. Professor Tenkorang also principally solicited for the funds for this study from the IDRC. The Author is grateful to him. Dr. Kofi Takyi Asante of ISSER, University of Ghana, Legon, is also acknowledged for proofreading an earlier version of this paper.
Funding for data collection for this research was provided by the International Development Research Centre (IDRC), through the Canadian-African Research Grant. Matching grants were provided by the Department of Sociology, Memorial University of Newfoundland and Labrador, Canada. IDRC and the Memorial University played no role in the design of the study, data collection, analysis, and interpretation, as well as the writing of the manuscript.
Author information
Authors and affiliations.
Institute of Statistical, Social and Economic Research (ISSER), University of Ghana, P. O. Box LG 74, Legon, Ghana
Adobea Yaa Owusu
You can also search for this author in PubMed Google Scholar
Contributions
AYO contributed to conceptualising the study and served as a co-Principal Investigator (co-PI). AYO mostly focused on the qualitative aspect of the project from which the data for this paper emanates. AYO also developed the in-depth interview guide, helped to liaise with technical staff of the Ghana Health Service and Ghana AIDS Commission for explanations to some HIV/AIDS technical and policy-related issues in Ghana. Furthermore, AYO led in the acquisition of ethical clearance from the University of Ghana. Additionally, AYO co-supervised field staff during the data collection, and handled the quality control, and analysis of the qualitative data. AYO wrote and finalised this paper single-handedly. Since this paper is sole-authored, the final version of the manuscript does not require the approval of any other person prior to being submitted and published.
Author’s information
AYO is an Associate Professor at the Institute of Statistical, Social and Economic Research, College of Humanities, University of Ghana, Legon, Ghana. AYO is a Medical Sociologist, Public Health, and behavioural health specialist.
Corresponding author
Correspondence to Adobea Yaa Owusu .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval were sought from the following: 1) Ethical Review Board of the Memorial University at St. Johns, Newfoundland, Canada, 2) the Ethics Committee for Humanities at the University of Ghana, Legon (ECH 017/14–15), and 3) the Ghana Health Service’s Ethical Review Board (GHS-ERC: 02/11/14). The Protocol Submission form which was filled to seek ethical permission from the Ghana-based ethical committees included five options for types of consent to be sought from the respondents, under the section on “consent process”, with instructions to “circle all that applies.” We chose all of "written”, “oral”, “English language”, and "local language” options. These were approved by the ethics committees, as part of the general approval we received. The need to approve non-written consent as well as the use of the local languages is informed by the fact that not everyone in the study’s catchment area, which is applicable to the rest of Ghana, can read and write. Respondents who consented to participate in the study by writing had to append their signature or initials to a written form provided by the Ethical Committee for Humanities at the University of Ghana. Field enumerators recorded verbal consent on the said form for respondents who could not read and write. Permission to conduct the study were also received from 1) the Ghana Health Service’s Eastern Regional Directorate, 2) The LMKM Directorate of the Ghana Health Service, and 3) the Administrators of the Atua Government, and St. Martins De Pores hospitals. Each participant gave a written or verbal informed consent to participate before they were interviewed.
Consent for publication
Not applicable.
Competing interests
The author declares that there are no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Qualitative/Indepth Interview Guide. Housing and Health Needs of Persons Living with HIV/AIDS Project. Open-ended qualitative indepth interview guide with sections A to G and ending with demographic/background data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Owusu, A.Y. Experiences of new diagnoses among HIV-positive persons: implications for public health. BMC Public Health 22 , 538 (2022). https://doi.org/10.1186/s12889-022-12809-6
Download citation
Received : 04 July 2020
Accepted : 21 February 2022
Published : 18 March 2022
DOI : https://doi.org/10.1186/s12889-022-12809-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Comorbidities
- Psychosocial outcomes
- Qualitative research
- Experiences of new HIV-positive diagnoses
- Hopelessness theory of depression
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Clinical Ethics Services
- Ethical AI Services
- Custom Workshops
- Medical Student Education
- In the News
- Impact Videos and Stories
- Frequently Asked Questions
- Policies, Disclosures and Reports

Confidentiality in the Age of AIDS: A Case Study in Clinical Ethics
Print this case study here: Case Study – Confidentiality in the Age of AIDS
The Journal of Clinical Ethics, Fall 1993
Martin L Smith, STD, is an Associated in the Department of Bioethics, Cleveland Clinic Foundation, Cleveland, Ohio.
Kevin P Martin, MD is a Child and Adolescent Psychiatrist in the Department of Mental Health, Kaiser Permanente, Cleveland.
INTRODUCTION
AIDS (acquired immunodeficiency syndrome), now in pandemic proportions, presents formidable challenges to health-care professionals. The human immunodeficiency virus (HIV) infection and its related diseases have also raised a number of thorny ethical questions about government and social policy, health-care delivery systems, and the very nature of the physician-patient relationship. This article presents the case of an HIV-positive patient who presented the treating physician, a psychiatrist, with an ethical dilemma. We provide the details of the case, identify the ethical issues it raises, and examine the ethical principles involved. Finally, we present a case analysis that supports the physician’s decision. Our process of ethical analysis and decision making is a type of casuistry,1 which involves examining the circumstances and details of the case, considering analogous cases, determining which maxim(s) should rule the case and to what extent, and weighing accumulated arguments and considerations for the options that have been identified. The goal of this method is to arrive at a reasonable, prudent moral judgement leading to action.
The patient, Seth, is a 32-year-old, HIV-positive, gay, white male whose psychiatric social worker had referred him to a community-mental-health-center psychiatrist for evaluation. He had a history of paranoid schizophrenia that went back several years. He had been functioning well for the last two years as an outpatient on antipsychotic medications and was working full time, socializing actively, and sharing an apartment with a female roommate.
The social worker described a gradual deterioration over several months. Seth had become less compliant with his medication and with his appointments at the mental-health center, had lost his job, had been asked to leave his apartment, and was living on the streets. He was described as increasingly disorganized and paranoid. His behavior was increasingly inappropriate, and he had only limited insight into his condition.
On examination, Seth was thin, casually dressed, slightly disheveled, and with poor hygiene. His speech was spontaneous, not pressured, and loose with occasional blocking. [That is, he spoke spontaneously, he could be interrupted, and his speech was unfocused with occasional interruption of thought sequence.] His psychomotor activity was labile [unstable]. His affect was cheerful and inappropriately seductive, and he described his mood as ”mellow.” He denied having hallucinations, systematized delusions and suicidal or homicidal ideation. He admitted having ideas of reference [incorrect interpretation of casual incidents and external events as having direct reference to himself], was clearly paranoid, and at times appeared to be internally stimulated. He made statements such as: “They’re blaming me for everything,” and “I’m scared all the time,” although he was too guarded or disorganized to provide more detail. His cognitive functioning was impaired, and testing was difficult given his distracted, disorganized state. His judgement was significantly impaired, and his insight was quite limited.
At the time of the evaluation, Seth indiscriminately revealed his HIV-positive status to the staff and other patients. He claimed he had been HIV positive for five years, and he denied that he had developed any symptoms of disease or taken any HIV-related medications. He was not considered reliable, and the staff sought confirmation. After he provided the location and approximate date of his most recent HIV test, the physician confirmed that the patient had been HIV positive at least since the test, about a year earlier.
When asked, Seth stated that the was not currently in a relationship. He appeared to be disorganized and could not name his most recent sexual partner(s). He could not remember whether he had been practicing safer sex and whether he had informed his partners of his HIV positive status.
In addition to the information he obtained during the evaluation, the psychiatrist, by chance, had limited personal knowledge of the patient. Through his own involvement as a member of the local gay community, the psychiatrist had briefly met the patient twice – once while attending an open discussion at the lesbian-gay community center, and later, at a worship service in a predominantly lesbian-gay church. The physician recalled that Seth had seemed to be functioning quite adequately, at least superficially. He was somewhat indiscriminately flirtatious, his behavior was otherwise appropriate, and he did not appear to be psychotic or disorganized in his thinking. He was not overtly paranoid and did not publicly reveal his HIV-positive status.
Through the church, the psychiatrist had also become acquainted with Maxwell and Philip, who were partners in a primary sexual relationship. Before Seth’s decompensation [deterioration of existing defenses, leading to an exacerbation of pathologic behavior], but after he was known to have tested HIV positive, Seth and Maxwell had been lovers. Maxwell left Philip and moved in with Seth for about two months, but then left Seth and returned to Philip around the time of Seth’s decompensation.
The psychiatrist was not privy to details of Maxwell and Seth’s or Maxwell and Philip’s sexual practices. He did not know of the HIV status of Maxwell or Philip, or whether either had ever been tested. In addition, he was unaware of whether Maxwell or Philip know of Seth’s HIVpositive status at the time of Maxwell’s relationship with Seth, or at any time thereafter. During the evaluation, Seth did not recall having met the psychiatrist, nor did he mention his relationship with Maxwell.
Seth agreed to enter a crisis stabilization unit and to resume treatment with antipsychotic medications. Free to come and go at will during daylight hours, he left the unit on day two, failed to return, and was lost to follow-up. His mental status had not changed significantly before he left the crisis unit.
In this case, the physician’s duty to maintain physician-patient confidentiality conflicts with his duty as a psychiatrist to warn third parties at risk. Clearly, a patient’s status as HIV positive is a matter of confidentiality between doctor and patient. Just as clear is the risk for third parties to whom the patient may pass the virus via sexual intercourse. It is unknown whether everyone infected with HIV will develop AIDS, or how many months or years may intervene between infection and the appearance of full-blown AIDS. However, once AIDS develops it is always fatal.2 Therefore, there is a potentially lethal risk to a person having intercourse, particularly without employing safer sex-practices, with another infected with the HIV virus.
This ethical conflict raises two questions. Is it permissible to violate confidentiality to warn a third party at risk? Is there a duty to violate confidentiality to warn a third party at risk? The potential benefit to the third parties must be considered, as well as the strength of the principle of confidentiality in the patient-physician relationship. There is also wider societal consideration as to how breaches of confidentiality, even for good reasons, will affect voluntary testing and seeking of prophylactic treatment by HIV-positive persons. This societal consideration must be weighed against the benefit to the individual third party of knowing the risk and then choosing to be tested and treated and choosing to be tested and treated and choosing to take precautions against infecting others.
In this case, another issue arises from the fact that the physicians of at least one third party who may have been placed at risk possibly without his knowledge, was obtained through personal knowledge, outside the professional relationship. Is it appropriate to bring this information into the clinical setting, particularly because it is so central to the primary ethical issue? Does the physician have an obligation to act on this information?
Finally, two additional sets of issues complicate this case. First, the patient’s decompensation and disappearance necessitate the physician’s choosing a course of action without patient consent or cooperation, and with patient-supplied information that is incomplete and probably unreliable. Second, a breach of confidentiality could greatly damage the physician’s position as a psychiatrist and a trusted member of the gay community, offering assistance directly to some and referral to many others. Given these issues, what should the physician do?
BACKGROUND DISCUSSION
Some background information will be useful in analyzing the ethical issues of the case. This information includes basic ethical values and norms, and legal mandates and opinions about confidentiality, the duty to warn, and HIV/AIDS reporting.
Whether privacy is viewed as a derivative value from the principle of autonomy or as a fundamental universal need with its own nature and importance,3 privacy, and the associated issue of confidentiality, is generally accepted as essential to the relationship between physician and patient. The purpose of confidentiality is to prevent unauthorized persons from learning information shared in confidence.4 Stated more positively, confidentiality promotes the free flow of communication between doctor and patient, thereby encouraging patient disclosure, which in turn should lead to more accurate diagnosis, better patient education, and more effective treatment.
The Hippocratic Oath is evidence of the long-standing tradition of confidentiality in Western though: “What I may see or hear in the course of treatment… I will keep to myself, holding such things shameful to be spoken about.” More recently, the American Medical Association,6 the American Psychiatric Association,7 the American College of Physicians, and the Infectious Diseases Society of America8 have reaffirmed the right of privacy and confidentiality, specifically for HIV-positive patients. Without the informed consent of the patient, physicians should not disclose information about their patient. The Center for Disease Control also recommends that patient confidentiality be maintained, because the organization believes that a successful response to the HIV epidemic depend on research and on the voluntary cooperation of infected persons.9That is, the interests of society seem best served if the trust and cooperation of those at greatest risk can be obtained and maintained.10
Within the complexities of clinical care, should patient confidentiality be regarded as absolute, never to be breached under any circumstances (as claimed by the World Medical Association in its 1949 International Code of Medical Ethics11)? Or should confidentiality be regarded as a prima facie duty? (That is, should it be binding on all occasions unless it is in conflict with equal or higher duties?12)
Most commentators and codes conclude that patient confidentiality is not absolute and, therefore, it could – and even should – be overridden under come conditions.13 In other words, in a specific situation in which patient confidentiality is one value at stake, the health-care provider’s actual duty is determined by weighing the various competing prima facie duties and corresponding values, including confidentiality. (As might be expected, not all authors accept this conditional view of confidentiality and argue for its absolute quality.14) There is less unanimity about the circumstances under which patient confidentiality can be justifiably breached. More specifically for HIV-positive patients, the controversy revolves around the premise that some circumstances might create a duty to warn endangered third parties, even at the expense of confidentiality. The potential for harm to HIV-positive patients through breaches of confidentiality is great. Discrimination, isolation, hospitality, and stigmatization are all too real for these patients when their HIV-positive status has become known to others.15 Further, societal harm is possible if these patients – who might ordinarily seek medical attention voluntarily – refrain from doing so, knowing that professional breaches of confidentiality may ensue. Without ignoring this potential societal harm, the majority opinion of professional codes and of ethical and legal experts16 foresee the possibility of a duty to warn through discrete disclosure, especially if others are in clear and imminent danger if the patient cannot be persuaded to change hi behaviors or to notify those at risk of exposure.
Public health regulations often reflect the same conclusion – that confidentiality can be compromised under certain circumstances – and therefore mandate reporting HIV-positive and AIDS patients to public health authorities. Patient confidentiality is not to be upheld so strictly that it obviates an ethically justified (and usually legally mandated) duty to report such cases to authorized health agencies. Those who support such public policies view society’s right to promote its health and safety, and the need for accurate epidemiological information, to be at least as important as an individual’s right to privacy and confidentiality.
In trying to balance patient confidentiality with other professional values, the California Supreme Court decision in Tarasoff v. Regents of the University of California17 has become a guideline for other courts and health-care professionals (although technically this decision applies to only one state and specifically addresses a unique set of circumstances). In this famous and controversial case heard before the California Supreme Court in 1976, the majority opinion held that the duty of confidentiality in psychotherapy is outweighed by the duty to protect an intended victim from a serious danger of violence. The court explained the legal obligation to protect and the potential duty to warn as follows:
When a therapist determines, or pursuant to the standards of his profession should determine that his patient presents a serious danger of violence to another, he incurs an obligation to use reasonable care to protect the intended victim against such danger. The discharge of this duty may require the therapist to take one or more various steps, depending upon the nature of the case. Thus, it may call for him to warn the intended victim or others likely to apprise the victim of the danger, to notify the police, or to take whatever steps are reasonably necessary under the circumstances.18
Regarding the limits placed on confidentiality under these conditions, the court stated: “The protective privilege ends where the public peril begins.” This “Tarasoff Tightrope” identifies for the professional the dual duties of promoting the well-being and interests of the patient and protecting public and private safety.
Given the general jurisdictional autonomy of each state, the duty to protect and the potential duty to warn as adopted in California has been applied differently in different states.20 Although most commentators assume that Tarasoff is relevant for sorting out the issue of confidentiality relative to HIV-positive patients, this assumption is not universally accepted.21
Without a state statute or court case that specifically addresses the tension between patient confidentiality and the right of others to know whether they may have been exposed to HIV infection, and given the conundrum of legal principles relating to AIDS confidentiality, it is unclear as to who must be warned and under what circumstances.22 This lack of clarity is in indication that, in practice, the professional duty to warn is not absolute but always conditioned by the circumstances of the case (that is, the duty to warn is a prima facie value).
The above paragraphs describe an emerging consensus among health-care professionals who face confidentiality dilemmas, although universal agreement has not been fully achieved. Further, this emerging consensus and its contributing principles by no means provide easy answers to ethical quandaries. Each case, with its own specific set of relevant circumstances, must be analyzed and judged individually. Such an analysis of the presented case now follows.
AN ANALYSIS
Seth’s case, perceived as a dilemma by the psychiatrist, could be brushed aside easily if the information obtained outside the therapeutic relationship was simply ignored. But the lethality of HIV infection makes it difficult to dismiss the information either as irrelevant or inadmissible for serious consideration. Had the information been obtained by unethical means (for example, by coercion or deception), a stronger justification for not using the information might be made. Such is not the situation. Without reason to ignore this information, the psychiatrist must incorporate this “data of happenstance” into his decision. To do so, of course, places him precisely at the crossroads of the dilemma: to uphold confidentiality, to warn the third party, or to create an option that supports the values behind these apparently conflicting duties.
Several factors ethically support both a breach of confidentiality and the physician’s duty to warn and protect the third party: the emerging professional consensus that confidentiality is not absolute; the known identity of a third party who stands in harm’s way; the risk to unknown and unidentified sexual partners of the third party; and the deadliness of AIDS. Such a combination of factors is what the professional statements noted above23 have tried to address in their allowance for limits to patient confidentiality. In this case, the risk to the known third party has already been established, but other people may be at risk, including sexual partners of the patient and those of the third party. Individuals infected and unaware will not benefit from prophylactic therapies.
An additional reason for the psychiatrist to warn the third part is the patient’s mental status, which probably renders him incapable of informing his sexual partner(s) or of consenting to the physician’s informing them. On admission, he was not able to name his partner(s), and he was lost to follow-up without significant change in his mental status. Without the decision-making capacity of the likelihood of action on the part of the patient, any warning to the third party would have to come from the physician or through public health officials notified by the physician.
But the duty to warn, incidental information, and mental status are not the only factors that need to be considered here. Patients are subject to the risks of discrimination when their HIV status is disclosed. But for a patient who has indiscriminately revealed his own HIV-positive status, the physician’s contribution to this risk of discrimination through discreet disclosure to one person may be minimal.
Also, to be considered is the societal risk that testing and prophylactic treatment of HIV-positive persons will decrease if confidentiality is not upheld. Members of the lesbian and gay community are often mistrusting of medical and mental health professionals,24 perhaps with valid reason. Mistrust, fear, and nonparticipation in voluntary programs may increase if confidentiality cannot be assured. Persons will be less likely to come forward voluntarily for education, testing, or other assistance if their well-being is threatened as a result. In Tarasoff, the court declared that protective privilege ends where social peril begins. In this case, overriding the protective privilege of the individual could lead to greater societal peril. Trust in this physician by members of the lesbian and gay community benefits individuals and the community as a whole, by improving access to medical and mental health services. A breach of confidentiality, if it became known, could damage this trust, as well as the physician’s reputation, reducing his professional contributions to the community. This professional loss would be significant.
Also, to be considered is the general knowledge of the higher risk among gay and bisexual men for HIV infection, as well as the information in the gay community as to what constitutes high risk behavior and what precautions can decrease risk of infection. Thus, we can reasonably assume that a gay or bisexual male is already aware of his risk and that of his sexual partner(s) for carrying the HIV virus. Warning a probably knowledgeable third party about the HIV-positive status may be of little benefit to the third party, while it risks the greater individual, societal, and professional harms discussed above. Regarding the risk to unknown sexual partners of the patient, whatever their number, the physician is powerless to change their fate precisely because they are unknown to him.
The duty to maintain patient confidentiality and the duty to warn third parties at risk can both be viewed as prima facie duties. In clinical situations such as the one described here, when one duty must be weighed against another to arrive at an ethically supportable solution, the weighing should take place only in the context of the given case. In this case, we found no solution that upholds all the duties; thus, a choice must be made between the two duties.
We submit that, although there is support for the physician to warn the third party, there is greater support for upholding confidentiality in this case. The individual risk of discriminatory harm from disclosure is possible, although admittedly small. Further, it is reasonable to presume the third party’s awareness of his risk and of the risk to his sexual partner(s) of carrying the HIV virus, and thus, his awareness of the need for appropriate precautions.
Even more persuasive is the peril to the local gay community and the wider society if a breach of confidentiality increases mistrust of the healthcare system and decreases the effectiveness of this particular psychiatrist to provide quality professional care. In this case, the confidentiality of the physician-patient relationship should be maintained.
What has been presented here can serve as a model for ethical decision making within the complexities of clinical care. As cases and their accompanying ethical questions arise, the details of each case should be gathered. Any tendency to label the case prematurely as a particular type (for example, a duty-to-warn case) should be resisted. Such a label can divert attention from relevant details that make each case unique. In examining the facts of the case and judging their significance, the values and duties at stake can be identified. If necessary and practical, background material and analogous cases should be researched. Ethical dilemmas present persons with hard choices. While several solutions may have some ethical support, few can be labeled as perfect solutions. Often, choosing one solution over another leaves behind an ethically significant value and regrettably may even produce harm. The circumstances described here presented the psychiatrist with a hard choice and no easy answer. We have suggested an ethically supported solution, but we found no perfect solution for the dilemma.
1. A.R. Jonsen, “Casuistry as Methodology in Clinical Ethics,” Theoretical Medicine 12 (1991): 295-307. 2. J.W. Curran, H.W. Jaffee, A.M. Hardy, et al., “Epidemiology of HIV Infection and AIDS in the United States,” Science 239 (1988): 610-16. 3. T.L. Beauchamp and J.F. Childress, Principles of Biomedical Ethics (New York: Oxford University Press, 1983). 4. W.J. Winslade, “Confidentiality,” in Encyclopedia of Bioethics, ed. W.T. Reich (New York: Free Press, 1978). 5. L. Walters, “Ethical Aspects of Medical Confidentiality,” in Contemporary Issues in Bioethics,3rd edition, ed. T.L. Beauchamp and L. Walters (Belmont, Calif.: Wadsworth, 1989). 6. Council on Ethical and Judicial Affairs of the American Medical Association, “Ethical Issues Involved in the Growing AIDS Crisis,” Journal of the American Medical Association 259 (1988): 1360-61. 7. American Psychiatry Association, “AIDS Policy: Confidentiality and Disclosure,” American Journal of Psychiatry 145 (1988): 541-42. 8. Health and Public Policy Committee of the American College of Physicians, and lnfectious Diseases Society of America, “A quired Immunodeficiency Syndrome,” Annals of Internal Medicine 104 (1986): 575-81. 9. Centers for Disease Control, “Additional Recommendations to Reduce Sexual and Drug-Related Transmission of Human T-Lymphotropic Virus Type I I1/L y mph adenopathy-Associated Virus,” Morbidity and Mortality Weekly Report 35 (1986a): 152-55. 10. R. Gillan, “AIDS and Medical Confidentiality,” in Contemporary lssues in Bioethics. Code of Ethics, 1949 World Medical Association,” in Encyclopedia of Bioethics. 11. W.O. Ross, The Foundations of Ethics (Oxford, England: Clarendon Press, 1939). 12. Beauchamp and Childress, Principles of Biomedical Ethics; Winslade, “Confidentiality”; Walters, “Ethical Aspects of Medical Confidentiality”; AMA, “Report on Ethical Issues”; APA, “AIDS Policy”; American College of Physicians and Infectious Diseases Society of America, “Acquired Immunodeficiency Syndrome”; S. Bok, “The Limits of Confidentiality,” Hastings Center Re port 13 (February 1983): 24- 31; H.E. Emson, “Confidentiality: A Modified Value,” Journal of Medical Ethics 14 (1988): 87-90. 13. M.H. Kottow, “Medical Confidentiality: An Intransigent and Absolute Obligation,” Journal of Medical Ethics 12 (1986):117-22. 14. R.J. Blendon and K. Donelan, “Discrimination against People with AIDS,” New England Journal of Medicine 319 (1988): 1022-26; L.O. Gostin, “The AIDS Litigation Project: A National Review of Court and Human Rights Commission Decisions, Part II: Dis crimination,” Journal of American Medical Association 263 (1990): 2086-93. 15. G.J. Annas, “Medicolegal Di lemma: The HIV-Positive Patient Who Won’t Tell the Spouse,” Medical Aspects of Human Sexuality 21 (1987):16; T.A. Brennan, “AIDS and the Limits of Confidentiality: The Physician’s Duty to Warn. Contacts of Seropositive Individuals,” Journal of General Internal Medicine 4 (1989): 242-46: B.M. Dickens, “Legal Limits of AIDS, Confidentiality,” Journal of the American Medical Assoclarion 259 (1988):3449-?1; S.L. Lentz. ”Confidentiality and lnformed Consent and the Acquired Immunodeficiency. Syndro111e. Epidemic,” . Archives of Pathology, & Laboratory Medicine 114 (1990):304 8; D. Seiden, “HIV ·Seropositive Patients and Confidentiality,” Clinical Ethics Report (1987): 1-8H.Zomina, “Warning Third 16. Tarasoff v. Regents of the University of California, 11Cat.3d 425,551 P 2d ht (1,976) 17. Ibid. 18. R.D. Mackay, “Dangerous. Patients: Third Party Safety and Psychiatrists’ Duties: Walking the Tarasoff Tightrope,” Medicine, Science & the Law 3Q (1990): 52-56, 19. LA. Gray and A.R. Harding, “Confidentiality Limits with Clients Who Have the AIDS Virus,” Journal of Counseling and Development 6 (1988):219-23. 20. S. Perry, “Warning Third ‘Parties at Risk of AIDS: APA’s Policy is a Barrier to Treatment,” Hospital and Community Psychiatry 40 {1989):’ i5.8-6I. 21. L.O Gostin, The AIDS Litigation Project: A National Review of Court and Human Rights Commission Decisions. Part 1: The Social Impact of AIDS,” Journal of the American Medical Association 263 (1990), ‘961-7Q 22. AMA; “Report on Ethical Issues”; APA, “AIDS Policy”; American College of Physics and Infectious Diseases Society of America” Acquired lmmunodeficiency Syndrome.” 23. L. Dardick and KE Grady, “Openness between·:Gay Persons and Health Professionals,” Annals of Internal Medicine 93 -(1 80): 115-.19; T.A. DeCrescenzo, Homophobia: A Study of the Attitudes of Mental Health Professionals toward Homosexuality. Journal of Social Work and Homosexuality 2 (198):.84): 115-36.
Print this case study here: Case Study – Gathering Information and Casuistic Analysis
Gathering Information and Casuistic Analysis
Journal of Clinical Ethics By Athena Beldecos and Robert M. Arnold
Athena Beldecos is a graduate student in medical ethics in the Department of History and Philosophy of Science, University of Pittsburgh.
Robert M. Arnold, MD is an Assistant Professor of Medicine, and the Associate Director for Education, Center for Medical Ethics, University of Pittsburgh.
In their article, “Confidentiality in the Age of AIDS,” Martin L. Smith and Kevin P. Martin present a complex case in clinical ethics. Their analysis examines a physician’s quandary when treating a mentally incompetent HIV-positive patient: whether to uphold physician-patient confidentiality or to violate this confidentiality by warning a third party. Out critique focuses on the way the problem is conceptualized and the analytic methods used to resolve the case, rather than on the solution itself. We believe that several problems in the authors’ analysis arise from a misinterpretation of the casuistic method. Furthermore, we argue that Smith and Martin present a case that is insufficiently detailed, thereby precluding the identification of all of the moral problems in the case and the development of creature solutions to the problem(s) identified. We note several reasons why there is a need to gather more information prior to determining the appropriate ethical response. Finally, we suggest ways in which similar problems in clinical ethics might be avoided in the future.
IS THIS CASUISTRY?
The authors conceive of their “process of ethical analysis and decision making” as a “type of casuistry.” Although we agree that casuistry, as outlined by A.R. Josen,1 is a potentially fruitful technique for practical ethical decision making, we believe that certain essential features of such casuistic reasoning are not clearly present in Smith and Martin’s analysis.
The power and scope of casuistry are derived not only from attention to details and careful identification of circumstances in the presentation of individual cases, but – more importantly – from the process of case comparison. Using this method, a case under moral consideration is situated in a family of related cases, whereby the casuist examines the similarities and differences between the cases at hand. The context of an individual case and how its conflicting maxims appear within that particular context are the raw materials of the case-comparison method. The relative weight of conflicting maxims in an individual case is ascertained by comparison to analogous cases. With casuistry, moral judgement does not involve a more traditional retreat to the weighing of conflicting duties or general principles. Rather, moral guidance is provided by an ever-growing body of paradigm cases that represent unambiguous instances in which moral consensus is easily obtained. It is crucial that the casuist place the case under consideration in its proper taxonomic context(s) and that she or he identify the most appropriate paradigm, whether it be real or hypothetical.
The authors do identify a paradigm case, but their analysis departs from casuistry on several interrelated points. The authors do not proceed by analogical reasoning. Had they done so, they might have discovered that their chosen paradigm is inappropriate, due to significant dissimilarities with Seth’s case. Finally, their insufficiently detailed case precludes a thorough measurement of the similarities and differences between the cases at hand. For it is in the details that an individual case may differ from a paradigm case.
The authors’ analytic method has more in common with principle-based ethics2 than casuistry. They do not use a variety of similarly situated cases to point out and balance the relevant moral maxims instead, they extract the conflicting duties and principles from their paradigm, the Tarasoff case,3 and apply them directly to Seth’s case. The authors weigh one prima facie duty “against another to arrive at an ethically supportable solution.” Furthermore, the weighing takes place “only in the context of the given case.” Thus, case comparison, an intrinsic element of casuistry, is not performed. Instead, the authors’ major goal seems to be finding and applying a sufficiently modified principle regarding confidentiality to resolve the case at hand.
WHY TARASOFF IS PROBLEMATIC AS A PARADIGM CASE
By using Tarasoff as a paradigm case in their analysis, Smith and Martin situate their case in the family of “duty-to-warn” (prevention-of-harm) cases. It is reasonable that they identify this particular taxonomy as a starting point for their analysis. However, they do not test the appropriateness of the paradigm by systematically comparing and contrasting it with Seth’s case. The authors note the uniqueness of the circumstances of the Tarasoff case and its limited applicability but nonetheless proceed to use it as a paradigm. Casuistry, however, seeks closest-match paradigms. The use of analogical reasoning would have illuminated the similarities and differences between the two cases and would have helped the authors to determine which morally relevant features a paradigm case should minimally share with its analogous cases.
In the Tarasoff case, the court held that a psychotherapist, to whom a patient had confided a murderous intent, had a duty to protect the intended victim from harm.4 This duty includes warning the third party at risk, among other interventions. The unique circumstances of Tarasoff include the imminence of fatal harm to an identified, yet unsuspecting, individual. Although the authors are correct in noting the precedent-setting value of Tarasoff, the dissimilarities between Tarasoff and Seth’s case are so numerous as to suggest the selection of another paradigm.
First, a critical aspect in Tarasoff is the prevention of future fatal harm. Based on the circumstances of the case, there is no evidence of preventable fatal harm to Maxwell. For this condition to be satisfied, the psychiatrist would have to be assured of Maxwell’s seronegativity and have evidence of a current or an intended sexual relationship between Maxwell and Seth. The preventable harm to Maxwell consists of not allowing him the opportunity to institute early anti-viral therapy or to reconsider his life goals in the face of a fatal disease. A casuist would need to assess, using a series of cases, the moral difference between the fatal harm in Tarasoff and the lesser harms in the case of Seth.
Second, Tarasoff involves a person maliciously intending to harm another person. However, there is no evidence suggesting that Seth intended to harm Maxwell. Here, a casuist might begin the analysis using a paradigm case in which a physician is aware of his HIV-positive patient’s malicious intention to infect a third party from that point, one could progressively change the variables of the case to approach the degree of moral ambiguity and complexity shown in Seth’s case. This process would culminate in a case involving sexual relationship between a patient and his partner.
Third, the notion of harm with respect to HIV transmission is quite different from the harm to be prevented in Tarasoff . One might argue that fatal harm to others is averted by informing Maxwell of his risk for HIV positivity. He can subsequently alter his sexual practices and, thus, prevent the future spread of the virus. Herein lies the problem. In Tarasoff the person warned of the harm is also the person at risk of being harmed. In the case under discussion, however, warning Maxwell might prevent harm to other, yet unnamed individuals. A case analogous to Seth’s should describe a situation in which the possible harm has already occurred and the future harm to be avoided consists of preventing future transmission. An analogous case might involve issues of confidentiality in regard to the (vertical) transmission of a fatal genetic disease that manifests itself after sexual maturity. Imagine, for example, a young man afflicted with a severe and incurable genetic disease who has proceeded to start a family without disclosing his genetic status to his wife. Does his personal physician have a duty to uphold confidentiality in this case, or should he notify the spouse so that she can make informed reproductive decisions?
Fourth, in Tarasoff , the victim was presumably unaware of the intended harm. In Seth’s case, one can argue that Maxwell knows (or can be reasonably expected to know) the potential risk of having sexual relations with a homosexual. The authors mention this factor but do not provide a way to assess its importance. To test the importance of this morally relevant fact, a series of cases in which the third party is more (or less) responsible for knowing about the possibility of risk could be used for comparison. For example, how would our intuitions about physician disclosure in this case differ if Seth were a bisexual male who did not inform his wife of his unprotected extramarital affairs with gay and bisexual men?
Fifth, Seth was reported to have publicly announced his HIV-positive status, whereas the patient in Tarasoff disclosed his intent to kill within a protected doctor-patient relationship. Does the fact that “Seth indiscriminately revealed his HIV-positive status to the staff and other patients” at a community-mental-health-center make it easier for the psychiatrist to justify a violation of confidentiality in the name of protecting potential victims? Unfortunately, there is insufficient information to determine whether Seth’s public disclosure qualifies as a fair warning to potential victims and sanctions a violation of confidentiality. This point is potentially an important difference between Tarasoff and Seth’s case. The authors, however, would need to gather additional information concerning the circumstances of Seth’s public disclosures (when they began, to whom they were addressed, and so forth) before evaluating the weight of this morally relevant feature by comparison to a similar case.
Sixth, Tarasoff does not address the issue of how the duty to uphold confidentiality might be affected when a patient’s mental competence is in question. Seth’s case involves a mentally incompetent patient presumed to be “incapable of informing his sexual partner(s) [of his HIV positivity] or of consenting to the physician’s informing them.” The circumstances of this case raise the question: Does Seth’s physician have the same obligation to respect his patient’s confidences as he would have if Seth were a mentally competent adult patient? Central to this analysis is an understanding of how the underlying justifications for respecting the confidences of incompetent patients might differ from those of competent patients. Although the authors briefly discuss the implications of Seth’s impaired mental status, they could have profitably expanded their analysis of the ethical significance of a patient’s competency in regard to the physician’s duty to maintain confidentiality. The authors neglect to discuss, for example, how the selection of a surrogate to speak on Seth’s behalf might influence the case’s resolution.
Identifying which should be the determining factor(s) in deciding Seth’s case is a difficult moral problem. However, the first step is any casuistic analysis is to determine where the case fits in relation to other cases. Without this basic first step, it is too easy to neglect factors that may be critical in determining the proper course of action or to reply upon ad hoc, intuitive decisions.
THE NEED FOR A RICHLY DETAILED CASE
The casuistic method to which Smith and Martin supposedly subscribe, demands attention to the context of the particular case at hand, so that it may be compared to and contrasted with paradigm cases in which the ethical analysis is clear. A casuist needs sufficiently detailed information to be able to identify all of the moral issues and, thereby, situate an individual case in its appropriate taxonomy.
In Seth’s case, the authors seem to decide prematurely on the ethical issue, inappropriately hindering the search for future data. In the rush to identify and resolve the presumed ethical conflict, the ethicist may neglect to collect critical information.5 Without adequate information, the ethicist is unable to determine accurately what kind of case it is. While obtaining more information might be less interesting than theoretical analysis, often the most prudent course of action is to gather more information from the sources available in order to clarify and embellish the initial facts. Prior to leading the psychiatrist through a philosophical analysis of how to resolve the conflict between the duty to warn and the duty to uphold confidentiality, the authors should have urged the psychiatrist to obtain more information.
It is difficult, for example, to weigh the impact of Seth’s mental incompetency against the duty to maintain confidentiality because of a lack of sufficient information. Information regarding the severity of Seth’s mental illness and the chances of its reversibility would be useful in determining whether Seth should be viewed as only temporarily or permanently incompetent. If Seth is incompetent, it is not clear who should assess the harm done to Seth by a breach of confidentiality. We know too little about Seth’s life to determine who would most appropriately serve as his surrogate. Furthermore, it is not clear that violating Seth’s confidentiality would result in the social harms the authors forecast. In order to make this point, the authors would need to identify a case analogous to Seth’s, in which violating an incompetent person’s confidences is ill-advised because it might lead competent patients to mistrust or fear the health-care system.
In the previous section, we identified a variety of morally relevant factors in Seth’s case and suggested how they might affect one’s analysis. Determining the importance of the various factors in this case, however, requires the ethicist to obtain information concerning the following: the efficacy of antiviral treatment in HIV-positive persons, Seth and Maxwell’s sexual practices, the probability that Maxwell knows of Seth’s seropositivity, the degree to which Maxwell can reasonably be expected to know the risk of homosexual encounters, Seth’s previous comments regarding confidentiality, who is best situated to serve as Seth’s surrogate, and the degree to which violating an incompetent patient’s confidentiality will lead other patients to lose trust in physicians and thus avoid the health-care system. Some of this information might be obtained from Seth’s social worker. Other data, however, can be obtained only by reviewing the empirical literature. We admit that much of this information may be unobtainable. Knowing the limits of one’s knowledge, however, will allow an honest appraisal of how uncertainty regarding various factors affects one’s moral decision making. This is preferable to not attempting to ascertain the information at all.
CREATIVE SOLUTIONS
The failure to gather sufficient information often leads to an impoverished understanding of the ethical issues that a case raises. In Seth’s case, the authors present the case as though there were one question: Is it permissible/obligatory to violate Seth’s confidentiality to warn Maxwell? Asked this way, there appears to be only two resolutions to the case: either a physician protects Seth’s confidentiality by failing to warn Maxwell o the risk, or he violates Seth’s confidentiality by warning Maxwell. Upon collection of sufficient data, one might discover ways to resolve the case that would allow all relevant values to be promoted. In some cases, additional information may provide the ethicist with an “end run” around the presumed ethical problem. For instance, if the ethicist learns that Maxwell is already aware of Seth’s seropositivity, then the ethical quandary vanishes. There is strong pedagogical justification for the authors to provide us with sufficient information to conclude that the quandary could have been resolved by seeking additional information and to help us develop innovative solutions that might promote the competing values.
Even if more information does not allow one to avoid the ethical conflict, it may prove useful in determining how best to resolve the case. It is simplistic to view the outcome of ethical analysis as a hierarchical ranking of two competing values or principles. Intermediate solutions often exist, which allow one to respect both competing values. Even in those cases where it is justified to promote one value over another, one is nevertheless obligated to consider alternative courses of action that respect, as much as possible, the other value. The authors neglect an important step in ethical problem solving – attempting to develop creative solutions that, if they cannot perfectly respect all values, at least cause as little damage as possible. This approach, known in American law as “the least restrictive alternative,”6 recognizes that solutions can be more or less respectful of ethical principles. Thus, for example, one might decide that the risk to Maxwell is sufficiently high so that some violation of Seth’s confidentiality is permissible. A variety of options would still be open. (1) The psychiatrist could call Maxwell (or have the public health department do so) and inform him that he may have been exposed to the HIV virus and thus, he should be tested. (2) The psychiatrist could call Maxwell, identify himself as Seth’s physician, and attempt to ascertain what Maxwell knows about Seth’s serostatus and what the nature of their sexual relationship was. That evidence could then be used to determine whether further actions are in order. (3) The psychiatrist could call Maxwell and tell him that he is Seth’s physician, hat he knows of Maxwell and Seth’s sexual relationship, and that Seth is HIV positive. He could then urge Maxwell to be tested. A similar range of alternatives could be developed if one decides that respecting Seth’s confidentiality is the most important value.
PREVENTIVE ETHICS
A final question is simply why this problem arose. If we assume, as the authors do, that “choosing one solution [in an ethical dilemma] over another leaves behind an ethically significant value and regrettably may even produce harm,” we should attempt to prevent ethical dilemmas from occurring.7 However, typically, case discussions focus on how to “solve” the problem at hand without determining how and why the problem arose, and how it might be avoided in the future. As E. Haavi Morreim points out: “Our moral lives are comprised, not of terrible hypotheticals from which there are no escapes, but of complex situations whose constituent elements are often amenable to considerable alterations.”8 The psychiatrist in this case may not have been able to anticipate Seth’s disappearance, but perhaps he could have asked additional questions on his initial encounter to prevent the resulting ethical quandary. For instance, it would have been useful if the psychiatrist had gathered information about Seth’s values and desires prior to his decompensation. Furthermore, if the physician had asked Seth for permission to talk to his friends, whether others knew of his seropositivity, whether the doctor could release this information to Seth’s sexual partners. or to identify his moral surrogate, this additional information could have ameliorated the quandary that subsequently arose.
In the final analysis, we may well agree with Smith and Martin about how the psychiatrist should handle this case. In this article we have tried to criticize not the answer, but the process by which the answer was reached. We urge ethicists who are dealing with a challenging case to use the process of case comparison in their analysis, examining a variety of analogous cases; to seek sufficient information to be able to identify all the moral issues in a case and situate the case in its proper taxonomic family; to attempt to develop creative, “least-restrictive” alternatives to ethical dilemmas; and to determine if there are ways that the ethical problem can be prevented in the future. Close attention to these points is likely to improve ethical decision making in the clinical setting and ethical analyses of cases presented in the bioethics literature.
ACKNOWLEDGMENTS
We would like to thank our friends and colleagues for their helpful comments on this paper: Lisa Parker, PhD; Joel Frader, MD; Peter Ubel, MD; and Shawn Wright. JD, MPH.
1. A.R. Jonsen, “Casuistry as Methodology in Clinical Ethics,” Theoretical Medicine 12 (1991): 295-307.
2. T.L Beauchamp and J.F. Childress, Principles of Biomedical Ethics (New York: Oxford University Press, 1989).
3. 3c. Tarasoff v. Regents of the University of California, 17 Cal. 3d 425. 551 P.2d 334 (1976}.
5. N. Whitman, Creative Medical Teaching (SaIt Lake City: University of Utah School of Medicine, 1990).
6. Lake v. Cameron. 364 F. 2d 657 (D.C. Cir. 1966).
7. L. Forrow R.M. Arnold and L.S. Parker, “Preventive Ethics: Expanding the Horizons of Clinical Ethics:· The Journal of Clinical Ethics (forthcoming).
8. E.H. Morreim, “Philosophy Lessons from the Clinical Sening.” Theoretical Medicine 7 (1986): 47-63.
TARASOFF: Discussion Questions
1. Traditionally, the Tarasoff case pits two goods or values against each other: confidentiality between therapist and patient vs. protection of an intended victim. Why is each a value?
2. Confidentiality is not only a value, but it has been called a duty which is incumbent on health care professionals to maintain secrecy about information gained in the course of interaction with a patient or client. Confidentiality derives from the more fundamental value of autonomy, the right each person has to be one’s own self-decider, one’s own intentional agent.
Protection of an intended victim likewise becomes a duty. To discharge that duty, the court argued, the therapist is obliged to warn the intended victim or others, to notify the police, or to take steps which are reasonably necessary to guard the intended victim.
Formulate an argument that supports the duty of confidentiality over the duty to warn an intended victim. Then formulate an argument which supports the duty to warn over the duty to protect confidentiality. (Being able to make good cases for each of the values shows the ambiguity involved here. Bring into your arguments the issue of the foreseeability of violence (is violence clearly foreseeable, probably foreseeable or unforseeable?) and the element of control over the patient by the therapist.)
3. One can easily use the Tarasoff decision to show the two principal ways of argument, consequentialist and non-consequentialist. Formulate an argument from a utilitarian (consequentialist) perspective, i.e., emphasize risk over benefit in arguing for safety and again, in arguing for confidentiality.
Next, consider confidentiality and the right to be protected as goods in themselves, regardless of consequences. Show how each value is tied to the meaning of being human and indicate how such a value can be argued for without consideration of consequences.
4. Notice how the arguments being proposed by the committee deny the absolute nature of either value. Rather, the committee is attempting to justify an action that is indicated in favor of one value over another, while acknowledging that both values are human goods. How would one attempt to argue when faced with the position that confidentiality or protection were absolute values?
Further Readings
Beauchamp, Tom and LeRoy Walters (eds.) 1994. “The Management of Medical Information” in Contemporary Issues in Bioethics. Fourth Edition. Belmont, CA: Wadsworth:123-186.
Kleinman, Irwin. 1993. “Confidentiality and the Duty to Warn.” Canadian Medical Association Journal 149: 1783-1785.
Perlin, Michael L. 1992. “Tarasoff and the Dilemma of the Dangerous Patient: New Directions for the 1990’s.” Law and Psychology Review 16: 29-63.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 09 April 2024
Late presentations and missed opportunities among newly diagnosed HIV patients presenting to a specialty clinic in Lebanon
- Maya Mahmoud 1 ,
- Tala Ballouz 2 ,
- Chloe Lahoud 3 ,
- Jana Adnan 3 ,
- Paola Abi Habib 3 ,
- Reem Saab 3 ,
- Haya Farhat 3 na1 ,
- Mohammad El Hussein 3 na1 &
- Nesrine Rizk 4
Scientific Reports volume 14 , Article number: 8296 ( 2024 ) Cite this article
174 Accesses
5 Altmetric
Metrics details
- HIV infections
Late presentation to medical care of individuals infected with the human immunodeficiency virus (HIV) is linked to poor outcomes and increased morbidity and mortality. Missed opportunities for a prompt diagnosis are frequently reported among late presenters. We aimed to estimate the proportion of late presenters and missed opportunities in diagnosis among newly diagnosed HIV-positive subjects presenting to a specialty clinic in Lebanon. This is a retrospective chart review of all newly diagnosed adult HIV-positive subjects presenting to clinic from 2012 to 2022. Demographic, laboratory, and clinical data were collected at initial HIV diagnosis or presentation to medical care. We defined late presentation as having a CD4 count < 350 or AIDS-defining event regardless of CD4 count. Advanced disease is defined as having a CD4 count below 200 cells/μL or the presence of an AIDS-defining illness, regardless of the CD4 count. A missed opportunity was defined as the presence of an indicator condition (IC) that suggests infection with HIV/AIDS during 3 years preceding the actual HIV diagnosis and not followed by a recommendation for HIV testing. The proportions for demographic, epidemiological, and clinical characteristics are calculated by excluding cases with missing information from the denominator. Our cohort included 150 subjects (92.7% males; 63.6% men who have sex with men (MSM); 33.3% heterosexuals; median age 30.5 years at diagnosis). 77 (51.3%) were late presenters and 53 (35.3% of all subjects, 68.8% of late presenters) had advanced HIV on presentation. Up to 76.5% of late presenters had a presentation with an HIV-related condition at a healthcare provider without getting HIV test within the previous 3 years. The most frequent ICs were weight loss, generalized lymphadenopathy, constitutional symptoms, and chronic idiopathic diarrhea. Overall mortality rate was 4% (6/150 individuals). All-cause mortality among those who presented with AIDS was 15.4% (6/39 subjects). In our setting, late presentations and missed opportunities for HIV diagnosis are common. In the Middle East, AIDS mortality remains high with a large gap in HIV testing. To effectively influence policies, comprehensive analyses should focus on estimating the preventable health and financial burdens of late HIV presentations. Another concern pertains to healthcare providers’ attitudes and competencies.
Similar content being viewed by others

Long COVID: major findings, mechanisms and recommendations
Hannah E. Davis, Lisa McCorkell, … Eric J. Topol
Long-term risk of psychiatric disorder and psychotropic prescription after SARS-CoV-2 infection among UK general population
Yunhe Wang, Binbin Su, … Daniel Prieto-Alhambra

Persistence in risk and effect of COVID-19 vaccination on long-term health consequences after SARS-CoV-2 infection
Ivan Chun Hang Lam, Ran Zhang, … Eric Yuk Fai Wan
Introduction
Antiretroviral therapy (ART) remains one of the most important medical advancements in the twentieth century. There is ample evidence that effective ART improves cellular immunity and subsequently reduces AIDS-related morbidity and mortality. However, achieving the full benefits of ART is dependent on early HIV detection and initiation of treatment 1 . Late diagnosis of HIV has been associated with poorer health outcomes 2 , increased healthcare costs, and risk of onward transmission 3 , 4 , 5 , 6 , 7 . Yet, even in countries with adequate HIV testing recommendations and healthcare resources, late presenters (defined as those with a CD4 count less than 350 cells/mm 3 or the presence of an AIDS-related illness at presentation) still constitute at least half of people living with HIV (PLWH) 8 , 9 , 10 , 11 and continue to be a hurdle to HIV eradication efforts globally 12 .
Several sociodemographic, psychosocial, and structural risk factors—at the patient, provider, and policy level—have been identified to be associated with late presentation. Fear of HIV-related stigma and discrimination, poor social support, and low risk perception are among some of the common patient-related factors preventing people from seeking timely testing. Providers have described insufficient time and resources, the laborious process of counseling and consent, as well as low provider-perceived risk of transmission as barriers to offering an HIV test 13 , 14 . Studies of missed opportunities for earlier diagnoses have shown that individuals with late presentations had often presented to healthcare settings several times, sometimes with indicator conditions (ICs) before an HIV test was eventually made 15 . Meanwhile, the presence of punitive laws and policies, such as the criminalization of sex work and same-sex sexual acts, in some countries deter individuals from seeking HIV testing 16 .
While several studies have been conducted worldwide to investigate late presentations and missed opportunities, only a few have been conducted in the Middle East and North Africa (MENA) region 15 , 17 , 18 , 19 . Although the region has seen significant improvements in HIV services, early HIV diagnosis remains a challenge 7 . Recent numbers from the region show that only 67% of PLWH are aware of their status, and a considerable proportion of individuals newly diagnosed with HIV present with an advanced stage 20 . In Lebanon, the first HIV case was reported in 1984 21 , which has evolved to reach approximately 3000 cases in 2021 22 . The prevalence rate of HIV in Lebanon is less than 0.1%, with indications of a concentrated epidemic among marginalized populations, especially MSM. The prevalence of missed diagnoses and late presentations in Lebanon is unknown.
In this study, we aimed to (1) assess the epidemiologic characteristics of subjects presenting to an HIV clinic in an academic medical center in Lebanon, (2) examine the rate and risk factors of late presentations, and (3) quantify missed opportunities among late presenters.
Materials and methods
Our study is a retrospective chart review of all newly diagnosed, treatment-naïve HIV-positive individuals, aged more than 18 years old, who presented to the American University of Beirut Medical Center (AUBMC) between January 1, 2012 and December 31, 2022. The AUBMC is an academic medical center in Lebanon with over 365 beds and a large outpatient department. The HIV-centered services started in 1984 and includes outpatient and inpatient services. The study was approved by the ethics committee, the Institutional Review Board (IRB) of the American University of Beirut Medical Center (AUBMC). The requirement for informed consent was waived by the Institutional Review Board at AUBMC due to the retrospective nature of the study. All research activities and methods were performed in accordance with the guidelines stated in the declaration of Helsinki and Belmont Report for research involving human subjects.
The subjects’ medical records were reviewed to collect demographic and clinical data including age at diagnosis, gender, nationality, sexual orientation, HIV transmission route, CD4 cell count, AIDS-defining conditions, and clinical indicator diseases at the time of diagnosis of HIV infection. MSM were defined as male participants reporting a homosexual or bisexual HIV-transmission mode and/or a sexual preference at the time of visit.
Outcome definitions
The primary outcome of interest was the proportion of individuals with a late presentation, defined as presenting for care with a CD4 cell count below 350 cells/μL at HIV diagnosis, or presenting with an AIDS-defining event regardless of the CD4 cell count 23 . Secondary outcomes included (1) factors associated with late presentation, (2) the proportion of individuals presenting with advanced HIV disease (AHD), defined as a CD4 count below 200 cells/μL or the presence of an AIDS-defining illness regardless of CD4 count 24 , and (3) missed opportunities for diagnoses, defined as failure to diagnose HIV in the presence of an IC that should have triggered testing for HIV as per guidelines 25 . Indicator conditions (IC) are classified as “AIDS defining illnesses” events and “other events” that are known to be associated with advanced HIV but not categorized as AIDS-defining 26 . Any IC that was present in the 3 years preceding HIV diagnosis, and not followed by a recommendation for HIV testing was considered a missed opportunity for earlier HIV diagnosis. ICs documented within 1 month of HIV diagnosis were considered related to the newly diagnosed disease and therefore not considered as a missed opportunity.
Statistical methods
We used descriptive statistics to analyze participant characteristics and outcomes of interest. Continuous variables are reported as median with interquartile range (IQR); categorical or ordinal variables as frequencies (N) and percentages (%). We explored the associations of several predictor variables with the outcome of late presentation using univariate and multivariable logistic regression model. Model selection was based on findings from other studies and age at diagnosis, gender, mode of transmission, and nationality were included. The calculated proportions for demographic, epidemiological, and clinical characteristics are derived after excluding cases with missing information from the denominator. We reported odds ratio (OR) with 95% confidence intervals (CI). All analyses were conducted in R (version 4.1, May 2021).
Participant characteristics at diagnosis
A total of 150 individuals newly diagnosed with HIV presented to our clinic between 2012 and 2022. The median age was 30.5 years (IQR 26–42 years), and the majority identified as men (N = 139, 92.7%) and Lebanese (N = 119, 79.3%) (Table 1 ). Most of the non-Lebanese individuals were Arab nationals (primarily originating from Iraq, Syria and Saudi Arabia) presenting to Lebanon for medical care. Overall, 82 (63.6%) individuals acquired HIV through MSM contact and 43 (33.3%) through heterosexual contact. Only 3.1% (N = 4) of patients reported IV drug use as the mode of HIV transmission.
Twenty-four (16%) of our newly diagnosed patients were aged more than 50 years old. Among them, 23 were males, and 1 was female. Within this sub-group, the median age at diagnosis was 58 years old. The median CD4 count was 197 cells/mm 3 , compared to 353 in our patients aged less than 50 years, with 13 (54.2%) patients presenting with a CD4 count less than 200. Fifteen were heterosexuals, and nine were men who have sex with men (Supplementary Table 1 ).
Late presentation
Overall, 77 individuals (51.3%) were late presenters and had a CD4 cell count of < 350 cells/mm 3 at the time of HIV diagnosis. Among those, 43 (55.8%) had a CD4 cell count of < 200 cells/mm 3 and 39 (50.6%) presented with AIDS-related conditions. A total of six individuals out of 150 died (15.4% of those presenting with an AIDS defining illness, 4.0% of all participants). The median CD4 cell count at HIV diagnosis was 506.5 (436.2–638.8) and 191.0 (67.0–258.0) cells/mm3 in non-late presenters and late presenters, respectively.
Late presentation was significantly associated with older age (OR 1.05, 95% CI 1.02–1.09, p = 0.003). Although an association with MSM transmission was observed, it did not reach statistical significance (OR 2.47, 95% CI 0.98–6.66, p = 0.062) (Supplementary Table 2 ).
Missed opportunities for earlier HIV testing
To identify indicator conditions, we reviewed medical records before the presentation and HIV diagnosis. Comprehensive data on indicator conditions were present in 51 of 77 charts of late presenters (66.2%). In total, there were 68 ICs among 39 participants (76.5%) in the preceding 3 years prior to HIV testing. Of the 39 participants with a missed opportunity for HIV diagnosis, 27 (69.2%) subjects had one or more AIDS-defining conditions and 9 (23.1%) subjects had ICs consistent with AIDS defining conditions. The most frequent ICs were unexplained weight loss (18/68, 26.5%), unexplained lymphadenopathy (9/68, 13.2%) unexplained fatigue and malaise (7/68, 10.3%), unexplained chronic diarrhea (6/68, 8.8%) and unexplained fever with no apparent etiology (6/68, 8.8%). Seven AIDS-defining ICs were identified. Those included recurrent pneumonia in five cases, four of which were confirmed to be pneumocystis jirovecii pneumonia (PCP) (Table 2 ).
Late presenters with advanced HIV
Among the 77 late presenters, 53 (68.8% of late presenters and 35.3% of all newly diagnosed) presented with an advanced HIV stage. Of these 53 participants, 39 (73.6%) had at least one AIDS defining illness at the time of diagnosis (44 conditions in total). The most frequent presentations were HIV wasting (16/44, 36.4%), PCP (9/44, 20.5%), candida esophagitis (4/44, 9.1%), cerebral toxoplasmosis (3/44, 6.8%), mycobacterium tuberculosis infection (2/44, 4.5%), Kaposi sarcoma (2/44, 4.5%), and Burkitt lymphoma (2/44, 4.5%) (Table 3 ).
Key findings
To the best of our knowledge, this is one of few studies in the MENA region assessing late presentations of HIV and missed opportunities for earlier diagnosis 17 , 18 , 19 , 27 , 28 . We found that more than half of the newly diagnosed subjects in our cohort (51.3%) were late presenters and 35.3% had advanced HIV disease on presentation. Mortality from HIV-related death was around 5% among our cohort while mortality from HIV in the world is approximately 2% 29 . Mortality among those presenting with AIDS in our cohort was approximately 16%. Almost three in four of late presenters had attended a medical facility for an IC in the 3 years preceding diagnosis; of these, almost one in four presented with an AIDS defining conditions without getting tested for HIV.
Evidence in context
As of December 2022, Lebanon had an estimated 2600 PLWH, with an incidence rate below 0.03% 30 . It is important to note that reported numbers likely underestimate the true count of PLWH in Lebanon, primarily due to reliance on passive reporting. Our findings correspond with those presented in the national report. In fact, the 2018 UNAIDS report revealed that 26% of individuals newly diagnosed with HIV in Lebanon presented at an advanced stage, characterized by an initial CD4 count below 200 cells/mm 3 31 . Few studies have described late presentations in the MENA region 32 , 33 . Our results are in line with data from Turkey and Iran. Studies conducted in Turkey found that 50–69% of the PLWH presented late to medical care, and 25–40% of subjects had advanced HIV at the time of diagnosis 26 , 34 , 35 , 36 , 37 . Similarly, a large retrospective cohort study conducted in Iran revealed a prevalence of late diagnosis in around 58.2% of subjects 17 . Surveillance studies from Yemen and Saudi Arabia showed higher prevalence of late HIV. The cohort study from Yemen showed that 83% of PLWH presented with a CD4 less than 350 and 52% with CD4 count less than 200 18 . The study from Saudi Arabia included 977 subjects and revealed that 20% of HIV positive subjects had a CD4 < 350 at diagnosis, and 50% presented with AIDS at diagnosis 19 . Late diagnosis indicates a gap in HIV testing 38 , 39 , which is a notable observation from the countries of the MENA region. In fact, according to the UNAIDS, by the end of 2018, more than half of PLWH in the MENA region were not aware of their seropositivity status 40 .
In our study, subjects who presented late were older and were men who had sex with men. Interestingly, women only represented 7.3% of our population (11 out of 150), indicating potential additional social obstacles that women encounter when seeking HIV care. This aligns with national data from Lebanon, indicating that the country faces a concentrated HIV epidemic among MSM, comprising 12% of cases 41 . While our study did not specifically address barriers to testing, the increased prevalence of late presenters among individuals aged more than 50 years and MSM in our cohort may be attributed to persistent barriers to adequate HIV testing 39 . This phenomenon could be linked to lower testing rates in these demographics, potentially influenced by social, cultural and legal barriers such as criminalization of homosexuality, stigma preventing adequate sexual education, lack of access to HIV testing and poor comprehensive sexual and reproductive health provision 42 . Around six out of ten people with HIV are from marginalized groups, including MSM, transgender individuals, IV drug users, sex workers, and their clients 43 . However, it is precisely these marginalized communities who encounter significant challenges in accessing HIV prevention, testing, treatment, and care services due to stigma and discrimination. We performed subgroup analyses for the subgroups late presenters with and without advanced disease (presented in Supplemental Table 3 ). As expected, the only difference was the CD4 count, 281 and 89 cells/mml for the without and with advanced disease, respectively.
PLWH in Lebanon continue to face social stigmatization and discrimination impacting different aspects of their lives. Particularly, the MSM population experiences homophobia and legal consequences, given that the Lebanese penal code prohibits sexual relations deemed "contradicting the laws of nature", punishable by up to a year in prison. Nevertheless, Lebanon is relatively more accepting of sexual rights compared to other countries in the MENA region, making it a favorable location for getting tested and treated for HIV 44 . HIV testing is available at medical laboratories, hospitals, or free of charge at Voluntary Counseling and Testing (VCT) centers in Lebanon. These centers are spread throughout the country, ensuring accessibility for the entire population, including refugees. Lebanon follows a comprehensive "treatment for all" strategy in addressing HIV/AIDS 45 . The Ministry of Public Health (MOPH) provides free treatment to over 60% of individuals aware of their HIV status including Syrian and Palestinian refugees.
There is a paucity of published data on missed opportunities in the MENA region. Similar to our findings, a study from Morocco reported that 69% of their 650-subject cohort had missed opportunities for HIV testing 15 . In contrast, studies from countries outside the MENA region such as Italy, Sweden, Germany and UK showed that 21–27% of newly diagnosed HIV subjects who sought medical care for ICs were not offered HIV testing 46 , 47 , 48 , 49 , 50 . The missed opportunity proportion is higher in our cohort. Limited awareness or knowledge among healthcare workers, along with negative perceptions and stigma associated with HIV within this group, may account for missed opportunities. Risk factors for HIV infection might not be adequately addressed by the treating physician. Firstly, subjects may not have disclosed their sexual activity, sexual orientation, and gender identity because of fear of discrimination and stigma. Secondly, healthcare workers with negative perceptions towards specific populations—sex workers, IV drug users, LGBTQ + community- and lack of adequate training regarding sexual health matters often fail to properly address the behaviors and sexual orientations of their subjects 51 .
Missed opportunities can lead to late detection and diagnosis of HIV with consequent associated complications including higher morbidity and mortality, altered response to antiretroviral therapy (ART) , increased cost of medical care, and HIV transmission within the community 46 , 52 , 53 . More efforts are needed to provide HIV-specific training and to eliminate stigma and discrimination related to HIV among healthcare providers.
Limitations
Our study has several limitations that may have influenced our findings. Firstly, being a single-center study could restrict the generalizability of our results to the broader Lebanese population or other populations. The retrospective nature of our study also posed limitations on data collection, particularly regarding socioeconomic aspects such as housing situation, poverty, and risky sexual practices, which could have offered additional insights into factors associated with late presentation and missed opportunities.
Moreover, there is a potential underestimation of the proportion of missed opportunities in our population. Our results rely on data collected from medical records, and other opportunities may have been present but not documented. Conversely, we cannot guarantee that verbal recommendations for HIV testing by healthcare providers were documented or, if refused by the subject, leading to a possible overestimation of missed opportunities.
The collected data also lacked crucial clinical details on management and follow-up. Notably, some subjects were discharged to home with hospice care, despite their initial diagnosis being conducted at our center. The initiation of Antiretroviral Therapy (ART) presents an intriguing aspect; however, our data collection did not encompass this specific information for all subjects. Similarly, details regarding the time to death and potential Immune Reconstitution Inflammatory Syndrome (IRIS) were not included in our data collection.
Unforeseen circumstances significantly impacted our study, especially after 2019, affecting clinic follow-up, detailed history, and thorough evaluation and diagnostic investigation. Lebanon faced political turmoil and economic failure starting in 2019, resulting in disruptions to clinical operations and ongoing follow-up. The subsequent COVID-19 pandemic further compounded the situation by imposing additional movement restrictions through lockdowns, leading to several subjects either being lost to follow-up or conducting virtual visits.
In our cohort, and likely in the MENA region, late presentation with HIV and missed opportunities for HIV diagnosis are common, even in instances where HIV testing is clearly indicated. To effectively influence policies, it is imperative to expand research efforts and conduct comprehensive analyses to quantify the proportion of late presenters and missed opportunities in the region, and to explore the factors contributing to these findings. Future studies should prioritize the estimation of the preventable financial burden associated with late HIV presentation resulting from diminished productivity and increased healthcare expenditure. Another concern pertaining to healthcare providers’ attitudes and competencies should trigger a serious reform in the healthcare provider curricula regarding sexual health and reproductive health issues.
Data availability
De-identified participant data that underlie the results reported in this article can be shared upon reasonable requests to the corresponding author. Data requestors will need to sign a data access agreement form.
Xie, Y., Zhu, J., Lan, G. & Ruan, Y. Benefits of early ART initiation on mortality among people with HIV. Lancet HIV 9 (6), e377 (2022).
Article CAS PubMed Google Scholar
Croxford, S. et al. Mortality and causes of death in people diagnosed with HIV in the era of highly active antiretroviral therapy compared with the general population: An analysis of a national observational cohort. Lancet Public Health 2 (1), e35–e46 (2017).
Article PubMed Google Scholar
Ellis, S., Curtis, H. & Ong, E. L. HIV diagnoses and missed opportunities. Results of the British HIV Association (BHIVA) National Audit 2010. Clin. Med. 12 (5), 430 (2012).
Article Google Scholar
Belay, H., Alemseged, F., Angesom, T., Hintsa, S. & Abay, M. Effect of late HIV diagnosis on HIV-related mortality among adults in general hospitals of Central Zone Tigray, northern Ethiopia: A retrospective cohort study. HIV AIDS-Res. Palliat. Care 20 , 187–192 (2017).
Fleishman, J. A., Yehia, B. R., Moore, R. D., Gebo, K. A. & Network, H. R. The economic burden of late entry into medical care for patients with HIV infection. Med. Care 48 (12), 1071 (2010).
Article PubMed PubMed Central Google Scholar
UNAIDS. Global HIV & AIDS statistics—Fact sheet. 2022.
Shakiba, E. et al. Epidemiological features of HIV/AIDS in the Middle East and North Africa from 1990 to 2017. Int. J. STD AIDS 32 (3), 257–265 (2021).
Op de Coul, E. L. et al. Factors associated with presenting late or with advanced HIV disease in the Netherlands, 1996–2014: Results from a national observational cohort. BMJ Open 6 (1), 009688 (2016).
Petrakis, V. et al. Late presenters of HIV infection in an HIV unit of a tertiary university hospital in a rural region of Greece. AIDS Res. Hum. Retroviruses 36 (7), 601–605 (2020).
Belaunzaran-Zamudio, P. F. et al. The population impact of late presentation with advanced HIV disease and delayed antiretroviral therapy in adults receiving HIV care in Latin America. Am. J. Epidemiol. 189 (6), 564–572 (2020).
Shen, Y., Wang, J., Qi, T., Wang, Z. & Lu, H. Trends in clinical characteristics of HIV-infected patients initiating antiretroviral therapy in Shanghai from 2006 to 2011. Int. J. STD AIDS. 25 (7), 504–510 (2014).
Organization, W. H. Consolidated Guidelines on HIV Prevention, Testing, Treatment, Service Delivery and Monitoring: Recommendations for a Public Health Approach (World Health Organization, 2021).
Google Scholar
Tan, K. R. Perceived barriers and facilitators to routine HIV screening/testing in primary care settings among healthcare providers in the Southeastern United States: A systematic review of the literature; 2016.
Leblanc, N. M. Providers' Perceptions of Couples HIV Testing and Counseling in South Florida: A Qualitative Study (University of Miami, 2016).
Marih, L. et al. Missed opportunities for HIV testing in patients newly diagnosed with HIV in Morocco. BMC Infect. Dis. 21 (1), 48 (2021).
Kavanagh, M. M. et al. Law, criminalisation and HIV in the world: Have countries that criminalise achieved more or less successful pandemic response?. BMJ Glob. Health 6 (8), e006315 (2021).
Mohammadi, Y., Mirzaei, M., Shirmohammadi-Khorram, N. & Farhadian, M. Identifying risk factors for late HIV diagnosis and survival analysis of people living with HIV/AIDS in Iran (1987–2016). BMC Infect. Dis. 21 (1), 390 (2021).
Nabih, M. F., Puteh, S. E. W. & Nur, A. M. Evaluation of selected outcomes of combination antiretroviral therapy: Yemen cohort retrospective descriptive studies. Sci. Rep. 9 (1), 19923 (2019).
Article ADS CAS PubMed PubMed Central Google Scholar
Memish, Z. A. et al. Antiretroviral therapy, CD4, viral load, and disease stage in HIV patients in Saudi Arabia: A 2001–2013 cross-sectional study. J. Infect. Dev. Ctries 9 (7), 765–769 (2015).
UNAIDS. The Path that Ends AIDS; 2023.
Mokhbat, J. E. I. N., Abdulkarim, F., Kulaylat-Shatila, M. & Salem, Z. The acquired immunodeficiency syndrome: Report of the first cases in Lebanon and review of the literature. J. Med. Liban. 35 , 295–311 (1985).
UNAIDS. Lebanon Fact Sheet; 2022.
Antinori, A. et al. Late presentation of HIV infection: A consensus definition. HIV Med. 12 (1), 61–64 (2011).
Boyd, A. T. et al. Addressing advanced HIV disease and mortality in global HIV programming. AIDS Res. Ther. 17 (1), 40 (2020).
HIV in Europe. HIV indicator conditions: Guidance for implementing HIV testing in adults in health care settings. Copenhagen: Copenhagen University; 2012. http://www.eurotest.org/Portals/0/Documents/Guidance.pdf.pdf?ver=2014-01-29-113626-000 . Accessed Jan 2024.
Karaosmanoğlu, H. K. M. B. et al. Late presentation among patients with human immunodeficiency virus infection in Turkey. Cent. Eur. J. Public Health 27 (3), 229–234. https://doi.org/10.21101/cejph.a5416 (2019).
Shokoohi, M. et al. Remaining gap in HIV testing uptake among female sex workers in Iran. AIDS Behav. 21 (8), 2401–2411 (2017).
Elgalib, A. et al. Predictors of late presentation and advanced HIV disease among people living with HIV in Oman (2000–2019). BMC Public Health 21 (1), 2029 (2021).
Article CAS PubMed PubMed Central Google Scholar
Global HIV & AIDS statistics—Fact sheet. https://www.unaids.org/en/resources/fact-sheet .
. UNAIDS Country factsheets LEBANON 2022.
UNAIDS Country Progress Report—Lebanon; 2019.
Shokoohi, M. et al. Remaining gap in HIV testing uptake among female sex workers in Iran. AIDS Behav. 21 , 2401–2411 (2017).
Elgalib, A. et al. Predictors of late presentation and advanced HIV disease among people living with HIV in Oman (2000–2019). BMC Public Health 21 (1), 1–8 (2021).
Aydin, O. A., Karaosmanoglu, H. K., Korkusuz, R. & Nazlican, O. Toxoplasma gondii IgG seroprevalence in HIV/AIDS patients. Turk. Parazitol. Derg. 35 (2), 65–67 (2011).
Karaosmanoglu, H. K., Aydin, O. A. & Nazlican, O. Profile of HIV/AIDS patients in a tertiary hospital in Istanbul, Turkey. HIV Clin. Trials 12 (2), 104–108 (2011).
Aydin, ÖA. K. H., Korkusuz, R., Özeren, M. & Özcan, N. Mucocutaneous manifestations and the relationship to CD4 lymphocyte counts among Turkish HIV/AIDS patients in Istanbul, Turkey. Turk. J. Med. Sci. 45 (1), 89–92 (2015).
Yemisen, M. A. O. et al. Epidemiological profile of naive HIV-1/AIDS patients in Istanbul: The largest case series from Turkey. Curr. HIV Res. 12 (1), 60–64 (2014).
Jeong, S. J. et al. Late presentation into care of HIV disease and its associated factors in Asia: Results of TAHOD. AIDS Res. Hum. Retroviruses 32 (3), 255–261 (2016).
Late Presentation Working Groups in Euro S, Cohere. Estimating the burden of HIV late presentation and its attributable morbidity and mortality across Europe 2010–2016. BMC Infect. Dis. 20 (1), 728 (2020).
https://www.middleeastmedicalportal.com/hiv-and-aids-in-the-middle-east-north-africa-mena-by-avert-org/ .
UNAIDS Country Progress Report-Lebanon; 2020.
Assi, A. et al. Prevalence of HIV and other sexually transmitted infections and their association with sexual practices and substance use among 2238 MSM in Lebanon. Sci. Rep. 9 (1), 15142 (2019).
Article ADS PubMed PubMed Central Google Scholar
https://www.unaids.org/sites/default/files/media_asset/JC3032_AIDS_Data_book_2021_En.pdf . UNAIDS data 2021.
Wilson Dib, R. et al. HIV in Lebanon: Reasons for testing, engagement in care, and outcomes in Patients with Newly diagnosed HIV infections. AIDS Behav. 24 (8), 2290–2298 (2020).
UNAIDS Country Progress Report; 2014. https://www.unaidsorg/sites/default/files/country/documents/LBN_narrative_report_2014pdf .
Ellis, S., Curtis, H., Ong, E. L., British, H. I. V. A., Audit BC, Standards s-c. HIV diagnoses and missed opportunities. Results of the British HIV Association (BHIVA) National Audit 2010. Clin. Med. (Lond.) 12 (5), 430–434 (2012).
Scognamiglio, P. et al. The potential impact of routine testing of individuals with HIV indicator diseases in order to prevent late HIV diagnosis. BMC Infect. Dis. 13 , 473 (2013).
Brannstrom, J. et al. Deficiencies in the health care system contribute to a high rate of late HIV diagnosis in Sweden. HIV Med. 17 (6), 425–435 (2016).
Tominski, D. et al. The late-presenting HIV-infected patient 30 years after the introduction of HIV testing: Spectrum of opportunistic diseases and missed opportunities for early diagnosis. HIV Med. 18 (2), 125–132 (2017).
van den Bogaart, L. et al. Overlooked cases of HIV infection: An Italian tale of missed diagnostic opportunities. Eur. J. Intern. Med. 73 , 30–35 (2020).
Ballouz, T. G. N. & Rizk, N. HIV-related stigma among health-care workers in the MENA region. Lancet HIV 7 (5), e311–e313. https://doi.org/10.1016/S2352-3018(19)30401-1 (2020) ( Epub 2020 Jan 9 ).
Belay, H., Alemseged, F., Angesom, T., Hintsa, S. & Abay, M. Effect of late HIV diagnosis on HIV-related mortality among adults in general hospitals of Central Zone Tigray, northern Ethiopia: A retrospective cohort study. HIV AIDS (Auckl). 9 , 187–192 (2017).
PubMed PubMed Central Google Scholar
Fleishman, J. A. Y. B., Moore, R. D. & Gebo, K. A. HIV research network. The economic burden of late entry into medical care for patients with HIV infection. Med. Care 48 (12), 1071–1079. https://doi.org/10.1097/MLR0b013e3181f81c4a (2010).
Download references
Author information
These authors contributed equally: Haya Farhat and Mohammad El Hussein.
Authors and Affiliations
Department of Internal Medicine, American University of Beirut Medical Center, Beirut, Lebanon
Maya Mahmoud
Epidemiology, Biostatistics and Prevention Institute (EBPI), University of Zurich (UZH), Zurich, Switzerland
Tala Ballouz
Faculty of Medicine, American University of Beirut Medical Center, Beirut, Lebanon
Chloe Lahoud, Jana Adnan, Paola Abi Habib, Reem Saab, Haya Farhat & Mohammad El Hussein
Division of Infectious Diseases, Department of Internal Medicine, American University of Beirut Medical Center, Riad El Solh, Beirut, 1107 2020, Lebanon
Nesrine Rizk
You can also search for this author in PubMed Google Scholar
Contributions
M.M: data collection, data interpretation, manuscript writing, manuscript review and editing. T.B: manuscript writing and conceptualization, data analysis and interpretation. C.L: data collection, manuscript review and editing. J.A: data collection, manuscript review and editing. P.A.H: data collection, manuscript review and editing. R.S: data collection, manuscript review and editing. H.F: data collection, manuscript review and editing. M.E.H: data collection. N.R: manuscript writing, manuscript review and editing, and conceptualization.
Corresponding author
Correspondence to Nesrine Rizk .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary tables., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Mahmoud, M., Ballouz, T., Lahoud, C. et al. Late presentations and missed opportunities among newly diagnosed HIV patients presenting to a specialty clinic in Lebanon. Sci Rep 14 , 8296 (2024). https://doi.org/10.1038/s41598-024-55277-1
Download citation
Received : 04 September 2023
Accepted : 22 February 2024
Published : 09 April 2024
DOI : https://doi.org/10.1038/s41598-024-55277-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Late presenters
- Missed opportunities
- AIDS-defining conditions
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.

Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Case study of a patient who has been diagnosed HIV positive
14 Case study of a patient who has been diagnosed HIV positive Brian Thornton Chapter aims • To provide you with a case study of a patient who is living with a diagnosis of HIV together with the rationale for care • To encourage you to research and deepen your knowledge of HIV/AIDS Introduction This chapter provides you with an example of the nursing care that a patient with HIV might require. The case study has been written by an HIV nurse specialist and provides you with a patient profile to enable you to understand the context of the patient. The case study aims to guide you through the assessment, nursing action and evaluation of a patient with HIV together with the rationale for care. Patient profile Ms Jessie Chitalwa is a 27-year-old Nigerian lady who has lived in the UK since the age of 22. She is doing a business studies degree at a local university. She attended accident and emergency (A&E) with a 2-week history of increasing shortness of breath and lethargy. She tested HIV positive on a point of care test in A&E. Her working diagnosis is pneumocystis pneumonia and she has been prescribed intravenous co-trimoxazole to treat this. She arrived on the ward overnight, at 11 p.m., and you are her nurse for the morning shift, starting at 7.15 a.m. Activity A definition of HIV was given in Chapter 1 and asked you to revise your anatomy and physiology (see Montague et al 2005 ). Before reading the case study, try to find out how HIV affects the immune system. What key issues did you discover for how HIV affects the immune system? This comprehensive article may help you to research this: Flannigan J (2008). HIV and AIDS: transmission, testing and treatment. Nursing Standard 22(34):48–56. Online. Available at: http://nursingstandard.rcnpublishing.co.uk/archive/article-hiv-and-aids-transmission-testing-and-treatment (accessed July 2011). Assessment on admission When greeting and introducing yourself to Ms Chitalwa, you notice she is very anxious and visibly upset. Her vital signs are: pulse 118 regular, respiratory rate 28, temperature 37.3°C tympanic, oxygen saturation 94% (receiving 2-L oxygen via nasal specs). She is in a bay with five other patients on your medical ward. During your assessment discussion with Ms Chitalwa, using the Roper, Logan and Tierney ( Roper et al 2000 ) model of activities of daily living, you note that she is normally totally independent in all activities of daily living (see Table 14.1 ). Table 14.1 Assessment of Ms Chitalwa using the Roper, Logan and Tierney model Maintaining a safe environment She requires assistance due to reduced mobility and lethargy. Local hazards include the oxygen tubing for her nasal specs and the drip stand and tubes for her intravenous co-trimoxazole Communicating She is fluent in English, which is her second language. Shortness of breath is reducing her sentence length. Recent HIV diagnosis has been a shock to her and she appears to be upset and withdrawn. She is very worried that her HIV status will be discovered by the other patients in her bay, as well as by her flatmates when they come to visit her. She seems reluctant to communicate about her HIV diagnosis. She has spent a lot of her time reading her bible. She is happy to be called Jessie Breathing Jessie becomes short of breath easily. She is receiving oxygen therapy via a humidification system and nasal specs. She finds it difficult to have a deep breath, and starts coughing Eating and drinking Her appetite has been reduced for the last week. She is a vegetarian. She feels nauseous when she tries to eat Eliminating She is too weak to walk to the bathroom, even with assistance Personal cleansing and dressing She is able to wash herself with a bowl at the bedside. She has been unable to bathe or shower for the last 3 days due to her lethargy and shortness of breath Controlling body temperature Currently no problems Mobility Severely reduced. Can barely manage five steps without becoming distressed. Oxygen and IV therapy are continuous so her range is already restricted due to the length of the tubes and IV lines Working and playing Does not want to discuss this right now Expressing sexuality Does not want to discuss this right now Sleeping Feels tired but has had a very unsettled night. Has not slept properly for several days, cannot remember how long Dying She is convinced that she is dying. The recent HIV diagnosis has made her resign herself to this fact. She has seen people die of HIV in Nigeria when she was younger and remembers the pain and suffering they went through, as well as the stigma for them and their families Ms Chitalwa’s problems Based on your assessment of Ms Chitalwa, the following problems should form the basis of your care plan: • Jessie is unable to independently maintain a safe environment. Activity See Appendix 4 in Holland et al (2008) for possible questions to consider during the assessment stage of care planning. • Jessie has reduced communication ability, partly due to shortness of breath and partly due to her current psychological state and fear of her HIV diagnosis being discovered. • Jessie has pneumonia. • Jessie has reduced blood oxygen saturation levels and is short of breath. • Jessie has reduced appetite and is at risk of inadequate nutritional intake. • Jessie has reduced mobility and is at risk of deep vein thrombosis and other hazards of prolonged immobility. • Jessie is unable to walk to the bathroom. • Jessie is tired but unable to sleep. • Jessie is worried that she is going to die. • Jessie has an intravenous cannula in situ, and is receiving intravenous therapy. Jessie’s nursing care plans 1. Problem: Jessie is unable to independently maintain a safe environment. Goal: To ensure a safe environment. Nursing action Rationale Ensure the call buzzer is within reach at all times So Jessie is able to summon assistance as required and not attempt to do things beyond her current level of capability, potentially causing her condition to deteriorate or for her to fall Ensure Jessie is aware that she should summon assistance and not try to push herself to do things which she is not currently capable of To re-enforce to Jessie that she is unwell and that it is OK for her to ask for assistance Evaluation: Jessie’s environment remained safe throughout her hospital stay and recovery. 2. Problem: Jessie has reduced communication ability, partly due to shortness of breath and partly due to her current psychological state and fear of her HIV diagnosis being discovered. Goal: To ensure optimum communication with Jessie. Goal: To support Jessie psychologically with her recent HIV diagnosis. Nursing action Rationale Try to ask closed questions, if possible To reduce the need for Jessie to feel she has to respond with long answers Ensure privacy for discussions, taking Jessie to a private room as soon as this is feasible Jessie will hopefully be more able to have conversations about HIV infection in a private setting, when she is aware that the rest of the patients will not be able to overhear Make Jessie aware of the good prognosis and longevity for people with HIV infection To reduce her fears of death or pain because of her HIV infection To enable Jessie to realise that she should recover and lead a normal life, but will have to take medicines every day Refer to psychology service To ensure an appropriately trained health professional is able to assess and support Jessie with her concerns and worries Ensure all healthcare professionals are aware of Jessie’s concerns over confidentiality of her HIV infection To reduce the risk of her HIV status being mentioned or discussed either in front of her, therefore disclosing to the other patients in her bay, or in public areas where the discussions could be overheard by other patients or visitors Evaluation:
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Medical placements
- Revision and future learning
- The end of the journey
- Medicines management
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

- Case report
- Open access
- Published: 07 December 2018
Extensive dental caries in a HIV positive adult patient on ART; case report and literature review
- Dunstan Kalanzi ORCID: orcid.org/0000-0003-0076-8573 1 ,
- Harriet Mayanja-Kizza 2 ,
- Damalie Nakanjako 2 &
- Nelson K. Sewankambo 2
BMC Oral Health volume 18 , Article number: 205 ( 2018 ) Cite this article
5226 Accesses
7 Citations
Metrics details
The estimated number of people living with human immunodeficiency virus (HIV) (PLHIV) in Uganda is 1.5 million (7.3%). As of June 2016, 60% (898,197) of PLHIV were enrolled and receiving antiretroviral therapy (ART). In scientific literature, the effect of HIV and ART on dental caries remains equivocal. At the Prosthetics Clinic of the Department of Dentistry, Makerere University College of Health Sciences, we have seen a number of PLHIV who require replacement of missing teeth with partial or complete dentures as a result of extensive caries. Here we report a case of an HIV positive female patient with extensive dental caries resulting in complete edentulous jaws, associated with psychological stress and stigmatization.
Case presentation
A 52-year-old patient, HIV positive for fourteen (14) years and receiving antiretroviral therapy (ART) for the last four years wanted to replace her missing teeth for effective feeding and cosmetic reasons. A diagnosis of partially edentulous maxillary and mandibular arches, cervical caries of tooth # 12, 15, 25, 34 and retained roots of tooth # 11, 13, 22 and 35 was made. Following oral health education and mouth preparation, this patient received a set of removable acrylic full upper and lower dentures.
This case may represent the long-term effects of HIV and ART on oral health status especially tooth surfaces in some PLHIV. Further evaluation is required to ascertain if this was an isolated case or it is a common finding among HIV positive adult patients receiving long-term ART in sub-Saharan Africa. Information emerging from these studies would establish the magnitude of dental caries among PLHIV and guide the development of appropriate oral health care guidelines in the management of people living with HIV.
Peer Review reports
The HIV epidemic in Uganda continues to be generalized with the national HIV prevalence reported at 7.3%, which approximates to 1.5 million PLHIV. As of June 2016, about 60% (898,197) of HIV positive individuals were enrolled in HIV treatment programs and receiving antiretroviral therapy (ART), which is the gold standard in the treatment and prevention of HIV [ 1 ]. Until 2017 when the test and treat approach was adopted [ 2 ], the national guideline for ART initiation was a CD4 count of 250 cells/μl and below [ 3 ]. The use of ART has profound impact on the pattern of oral disease including a decreased prevalence of HIV-related oral lesions ranging from 10 to 50% [ 4 , 5 ]. Dental caries is a dynamic pathological process that is primarily dependent on the development of virulent bio-films (plaque) formed on tooth surfaces from interactions of oral microbes (and their products), host salivary constituents, and dietary carbohydrates [ 6 ]. Saliva plays a significant role in oral and systemic health and its absence affects the quality of life. Individuals who suffer from salivary gland dysfunction are at risk of developing dental caries, periodontal diseases, and oral fungal infections [ 7 ]. Xerostomia and salivary gland hypofunction have been shown to be associated with HIV infection [ 8 , 9 ]. This case report presents a unique clinical presentation of severe caries and missing teeth in a 52-year-old adult requiring replacement with complete dentures, for improved feeding and cosmetic reasons.
A 52-year-old HIV positive patient presented to the Prosthetics Clinic of the Department of Dentistry at Makerere University College of Health Sciences in March 2017 with a desire to replace her missing teeth and remove the broken ones so that she could look aesthetically pleasing as well as improve her nutrition. She had been taking Tenofovir, Lamivudine and Efavirenz since 2014; and cotrimoxazole prophylaxis since 2004. She was generally in good health with no other chronic systemic illnesses. She reported having lost her first three teeth as a young girl resulting from tooth decay in the early 1980s’. Between that time and 2008, she lost two more teeth as a result of tooth decay. In 2008, she reported suffering from a severe febrile illness that left her bed ridden for two weeks, during which time she was unable to perform proper oral hygiene measures. Upon recovery, she noticed that her gums were bleeding and some of her teeth were loose and a number were lost (See Table 1 below).
Between 2014, when ART was initiated until she presented to our clinic, she reported suffering from extensive tooth decay that caused more loss of teeth leaving her with just four teeth and four retained roots (Figs. 1 & 2 ). There is no history of smoking or alcohol consumption and a diet rich in refined sugars. Table 2 shows her CD4 and viral load measurements, as shown in her records at the HIV treatment centre.
A and B, show inflamed upper labial marginal gingiva, cervical caries of the remaining teeth and retained roots secondary to caries. C and D, show diffuse blackish-purple pigmentation on the hard palatal surface and dorsum of the tongue probably secondary to ART or Kaposi’s sarcoma
Orthopantogram showing the remaining teeth and retained roots
Her diet consisted of predominantly high fiber carbohydrates including plantain, cassava, potatoes, rice, maize flour bread (posho) with fish, meat, beans, groundnut paste sauce and vegetables. As regards oral hygiene, she reported brushing twice a day using warm salt rinses.
On general examination, she was in fairly good general health condition without pallor of the mucous membranes, yellowing of the sclera or palpable cervical lymphadenopathy. The face was symmetrical with prominence of the zygomatic bones, sunken cheeks and mandibular prognathism, features associated with tooth loss. Temporomandibular joint (TMJ) examination showed no signs and symptoms of dysfunction.
Intraorally, there were light to moderate plaque deposits on the remaining dentition with diffuse blackish-purple pigmentation on the hard palatal surface and dorsum of the tongue probably secondary to ART or Kaposi’s sarcoma (Fig. 1 ). In the maxillary arch, tooth # 12, 15 and 25 were present with a peculiar type of cervical caries (caries affecting a significant portion of the cervix/neck of the tooth). There were also retained roots of tooth # 11, 13, and 22. In the mandibular arch, only tooth # 34 with the same peculiar cervical caries and retained root of tooth # 35 were present.
A diagnosis of partially edentulous maxillary and mandibular arches, retained roots of tooth # 11, 13, 22 and 35, as well as cervical caries of 12, 15, 25 and 34 was made. Following oral health education and mouth preparation, this patient received a set of removable acrylic full upper and lower dentures, which has significantly improved her feeding abilities and cosmetic concerns. (Fig. 3 ).

Before and after complete dentures to restore feeding and cosmesis
In this report we present the case of a female adult HIV positive patient receiving ART for two years and cotrimoxazole prophylaxis 13 years. She presented with severe dental caries and was rehabilitated with removable acrylic full upper and lower dentures. She desired to have her teeth replaced as a result of masticatory inability and social stigmatization due to her facial profile. It is well established that people with dentofacial abnormalities experience social consequences including greater degrees of social avoidance and being perceived as possessing negative personality characteristics [ 10 ]. Even minor facial abnormalities and hidden impairments such as total tooth loss can result in social stigma [ 11 ] and psychological stress comparable to visible facial disfigurements that have a profound effect on individuals [ 12 ], hence the need for replacement of missing teeth. The overarching need for replacement of the missing teeth was to improve aesthetics as a result of personal and societal pressure.
In this particular case, the patient reported that she suffered from a “severe caries” from the time she started her regimen of reverse transcriptase inhibitors although she had lost some teeth before that. In the literature, only two cases of severe caries associated with the use protease inhibitors and nucleoside reverse transcriptase inhibitors have been reported in HIV infected people [ 13 , 14 ]. Dental caries is a dynamic pathological process that is primarily dependent on the development of virulent bio-films formed on tooth surfaces from interactions of oral microbes, host salivary constituents, and dietary carbohydrates [ 6 , 15 ]. Documented studies from literature have shown that HIV infection is associated with xerostomia and salivary gland hypofunction [ 8 , 9 ]. The infiltration of HIV and proliferation of CD8 lymphocytes in salivary glands along with the use of antiretroviral therapy (ART) decrease the salivary flow rate and change the normal microbial flora of the oral cavity [ 16 ]. It is also worth noting that this patient is on an ART regimen that includes tenofovir, which has been associated with loss of bone mineral density [ 17 , 18 , 19 , 20 ]. Whether what is seen in the long bones, joints and spine occurs in alveolar bone resulting in periodontal disease is an area that warrants research. Noteworthy is the fact that this patient’s dental caries dated back before ART initiation, hence the need for well-characterised studies to understand HIV-and ART-related and un-related risk of dental caries to inform targeted prevention and care interventions.
The limitation regarding this report is the quality of the orthopantogram (OPG). The x-ray machine accessed by our patients requires calibration for better results.
Conclusions
This case demonstrates that people living with HIV may be susceptible to extensive caries that may be related to HIV and ART, and complete loss of teeth compounds the stigma associated with HIV/AIDS. Further studies are needed to investigate the mechanisms of increased risk of caries among PLHIV to inform development of appropriate oral health care guidelines.
Abbreviations
Antiretroviral therapy
Human immunodeficiency virus
Orthopantogram
People living with HIV
Tenofovir disoproxil fumarate
Temporomandibular joint
Uganda AIDS Commission: The Uganda HIV and AIDS country progress reports July 2015–June 2016. 2016.
Google Scholar
UNAIDS. 2018. http://www.unaids.org/en/resources/presscentre/featurestories/2018/april/test-and-treat-showing-results-in-uganda-and-zambia . Accessed 17 Oct 2018.
Ministry of Health Uganda: National Antiretroviral Treatment Guidelines for adults, adolescents , and children. 2009.
Ceballos-Salobrena A, Gaitan-Cepeda LA, Ceballos-Garcia L, Lezama-Del Valle D. Oral lesions in HIV/AIDS patients undergoing highly active antiretroviral treatment including protease inhibitors: a new face of oral AIDS? AIDS Patient Care STDs. 2000;14(12):627–35.
Article PubMed Google Scholar
Patton LL, McKaig R, Strauss R, Rogers D, Eron JJ Jr. Changing prevalence of oral manifestations of human immuno-deficiency virus in the era of protease inhibitor therapy. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 2000;89(3):299–304.
Hajishengallis E, Parsaei Y, Klein MI, Koo H. Advances in the microbial etiology and pathogenesis of early childhood caries. Mol Oral Microbiol. 2017;32(1):24–34. https://doi.org/10.1111/omi.12152 . Epub 2016 Feb 4.
Nittayananta W, Talungchit S, Jaruratanasirikul S, Silpapojakul K, Chayakul P, Nilmanat A, Pruphetkaew N. Effects of long-term use of HAART on oral health status of HIV-infected subjects. Journal of oral pathology & medicine. 2010;39(5):397–406.
Navazesh M, Mulligan R, Karim R, Mack WJ, Ram S, Seirawan H, Greenspan J, Greenspan D, Phelan J, Alves M. Effect of HAART on salivary gland function in the Women's interagency HIV study (WIHS). Oral Dis. 2009;15(1):52–60.
Nittayananta W, Chanowanna N, Jealae S, Nauntofte B, Stoltze K. Hyposalivation, xerostomia and oral health status of HIV-infected subjects in Thailand before HAART era. Journal of oral pathology & medicine. 2010;39(1):28–34.
Article Google Scholar
Newton JT, Fiske J, Foote O, Frances C, Loh IM, Radford DR. Preliminary study of the impact of loss of part of the face and its prosthetic restoration. J Prosthet Dent. 1999;82(5):585–90.
McGrouther DA. Facial disfigurement. Br Med J. 1997;314(7086):991.
Davis DM, Fiske J, Scott B, Radford DR. Prosthetics: the emotional effects of tooth loss: a preliminary quantitative study. Br Dent J. 2000;188(9):503–6.
PubMed Google Scholar
Glick MBP, Danik J. Severe caries and use of protease inhibitors. J Dent Res. 1998;77(Supplement):84.
Nedwick-Castro KA, Vieira AR. Failure to control caries in an AIDS-affected individual: a case report. Case reports in dentistry. 2012;2012:643436.
Article PubMed PubMed Central Google Scholar
Guo L, Shi W. Salivary biomarkers for caries risk assessment. Journal of the California Dental Association. 2013;41(2):107–9 112-108.
PubMed PubMed Central Google Scholar
Rezaei-Soufi L, Davoodi P, Abdolsamadi HR, Jazaeri M, Malekzadeh H. Dental caries prevalence in human immunodeficiency virus infected patients receiving highly active anti-retroviral therapy in Kermanshah Iran. Cell journal . 2014;16(1):73–8.
Carr A, Hoy J. Low bone mineral density with tenofovir: does statistically significant mean clinically significant? Clinical infectious diseases. 2010;51(8):973–5.
Iwen F, Grigsby LP, Mansky LM, Gopalakrishnan R, Mansky KC. Tenofovir-associated bone density loss. Ther Clin Risk Manag. 2010;6:41–7.
Post FA, Hamzah L, Fox J. Tenofovir disoproxil fumarate–associated bone loss: does vitamin D–binding protein play a role? AIDS. 2017;31(1):178–9.
Guerri-Fernandez R, Villar-Garcia J, Diez-Perez A, Prieto-Alhambra D. HIV infection, bone metabolism, and fractures. Arquivos brasileiros de endocrinologia e metabologia. 2014;58(5):478–83.
Download references
Acknowledgements
This case report was part of a research fellowship training supported by Grant Number D43TW010132 supported by Office of The Director, National Institutes of Health (OD), National Institute of Dental & Craniofacial Research (NIDCR), National Institute of Neurological Disorders and Stroke (NINDS), National Heart, Lung, And Blood Institute (NHLBI), Fogarty International Center (FIC), National Institute on Minority Health and Health Disparities (NIMHD). The authors also acknowledge Damalie Nakanjako’s group leader award from MUII-plus with funding from Wellcome Trust grant number 107743/z/15/z and THRiVE 2 project Grant number DEL-15-011 (Nelson Sewankambo) with funding from Wellcome Trust grant 107742/Z/15/z. The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS)’s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust and the UK government. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the supporting offices.
Author information
Authors and affiliations.
Department of Dentistry, School of Health Sciences, Makerere University College of Health Sciences, P.O. Box 7072, Kampala, Uganda
Dunstan Kalanzi
Department of Medicine, School of Medicine, Makerere University College of Health Sciences, Kampala, Uganda
Harriet Mayanja-Kizza, Damalie Nakanjako & Nelson K. Sewankambo
You can also search for this author in PubMed Google Scholar
Contributions
DK conceptualized this case report and drafted the manuscript, HMK, DN and NKS reviewed the case report and provided technical input. All authors approved the final manuscript for publication.
Corresponding author
Correspondence to Dunstan Kalanzi .
Ethics declarations
Consent for publication.
Written and signed consent to publish the images in this case report was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Kalanzi, D., Mayanja-Kizza, H., Nakanjako, D. et al. Extensive dental caries in a HIV positive adult patient on ART; case report and literature review. BMC Oral Health 18 , 205 (2018). https://doi.org/10.1186/s12903-018-0675-3
Download citation
Received : 15 July 2018
Accepted : 22 November 2018
Published : 07 December 2018
DOI : https://doi.org/10.1186/s12903-018-0675-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychological stress
BMC Oral Health
ISSN: 1472-6831
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Cardiovascular risk evaluation of HIV-positive patients in a case-control study: comparison of the D:A:D and Framingham equations
Affiliation.
- 1 Infectious Diseases, CHU Saint-Pierre, Brussels, Belgium.
- PMID: 25394024
- PMCID: PMC4224912
- DOI: 10.7448/IAS.17.4.19515
Introduction: Patients with HIV infection are at increased risk of developing cardiovascular disease (CVD) due to complex interactions between traditional CVD risk factors, antiretroviral therapy (ART) and HIV infection itself (1). Prevention of CVD is essential as it remains the most common serious non-AIDS event and contributes significantly to all-cause mortality. A cardiovascular risk-assessment model tailored to HIV population is thus essential.
Materials and methods: We conducted a retrospective case-control study within the HIV cohort of the Saint-Pierre Hospital, Brussels. Cases (n=73) presented a first CVD (ischemic heart disease or stroke) between January 2002 and December 2012. Controls (n=142) were patients without any CVD and were matched for age, race, sex and follow-up duration. We used Wilcoxon test to identify predictors of cardiovascular risk among the data collected. We compared Framingham (2) and DAD (Data Collection on Adverse Events of anti-HIV drugs) (3) equations calculated in all patients at time of event, two, four and six years before. We then simulated the impact on the DAD scores if different therapeutic interventions had been introduced when patient cardiovascular risk at ten years exceeded 20%.
Results: Comparison of cases and controls showed that C-reactive protein (CRP) >3 mg/L (p=0.008) and HIV viral load >50 copies/ml (p=0.007) at time of event, as well as slower increase in CD4 cell count (p=0.035), were significantly more frequent in cases. DAD and Framingham median scores in cases and controls are shown in Figure 1 and Table 1. Smoking cessation lowered the DAD score of cases at time of event from 21.6% to 18.3%, modification of ART (discontinuation of indinavir, lopinavir and abacavir) lowered it from 21.6% to 17%, while both interventions with control of blood pressure and cholesterol lowered it from 21.6% to 12.4%.
Conclusions: Increased CRP levels, uncontrolled HIV viral load at time of event and slower immunologic response were found to be associated with increased CVD risk. DAD score in cases increased more and faster over time than the Framingham score and seems therefore to be more accurate in identifying HIV-positive patients at high risk of CVD. Different therapeutic interventions could have led to a significant reduction of the DAD score in these patients and should remain a priority in patient management.
- Case Report
- Open access
- Published: 05 April 2024
Missed opportunities for HIV testing and sexual health-related challenges in an individual with intellectual disability: a case report
- Lina Martina Würfel 1 , 2 ,
- Anja Potthoff 1 , 2 ,
- Sandeep Nambiar 1 &
- Adriane Skaletz-Rorowski 1 , 2
AIDS Research and Therapy volume 21 , Article number: 20 ( 2024 ) Cite this article
174 Accesses
1 Altmetric
Metrics details
HIV testing remains an important tool in identifying people living with HIV/AIDS (PLWHA). An early diagnosis of HIV can lead to a prolonged life expectancy if treatment is initiated promptly. Indicator conditions can be the first sign of an HIV infection and should therefore be recognised and consequently a HIV test should be carried out. Testing should occur in all individuals as sexuality can be experienced by everyone, and stigma can lead to the exclusion of vulnerable groups, leading to a gap in diagnosis and treatment [ 1 , 2 ].
Case presentation
A 63-year-old man, who identifies as bisexual and has had an intellectual disability since birth, presented at our health care centre for HIV testing. A decade ago, the patient was diagnosed with Stage III Diffuse Large B-cell Non-Hodgkin Lymphoma, an AIDS defining cancer. The patient presented at a Haematology and Oncology department 3 months prior, due to a weight loss of 10 kg over the past 5 months. Oral thrush, an HIV-indicator condition, had been diagnosed by the otolaryngologists shortly before. During this medical evaluation, pancytopenia was identified. Despite the presence of indicator conditions, the patient was never tested for HIV in the past. Staff members from the care facility for intellectually disabled suggested conducting a HIV test in our clinic through the public health department, where HIV positivity was revealed. The AIDS-defining diagnosis, along with a CD4 + cell count of 41/µl, suggests a prolonged period of HIV positivity.
Due to the presence of existing indicator conditions, an earlier HIV diagnosis was possible. We contend that most of the recent illnesses could have been prevented if earlier testing had been carried out. Therefore, patients presenting with AIDS indicator conditions, including those with mental disabilities, should be given the opportunity to be tested for HIV. HIV/AIDS trainings should be made available to health care professionals as well as to personnel interacting with vulnerable groups.
HIV testing continues to be a crucial method for identifying people living with HIV/AIDS (PLWHA) [ 3 ]. An early detection of HIV, followed by prompt initiation of treatment, can contribute to an extended life expectancy. Recognizing indicator conditions as potential early signs of HIV infection is essential, underscoring the importance of promptly conducting an HIV test. HIV-indicator conditions are those associated with or as a result of immunodeficiency and include AIDS-defining conditions [ 2 , 4 ]. Testing should be inclusive, as everyone, regardless of their sexual orientation and their mental capacity, can be vulnerable to HIV.
A 63-year-old bisexual man, with an intellectual disability since birth, presented at our center for HIV testing. Ten years prior, he had been diagnosed with Diffuse Large B-cell Non-Hodgkin Lymphoma in Stage III, an AIDS-defining cancer that requires an HIV Test [ 5 ]. Subsequently, he underwent therapy with Rituximab (8x) and CHOP (cyclophosphamide, doxorubicin hydrochloride (hydroxydaunomycin), vincristine sulfate (Oncovin) and prednisone) (6x). Three months before attending our center, he presented at a department of Hematology, Oncology, and Palliative Medicine for further investigation due to pancytopenia and a weight loss of 10 kg over the last 5 months (BMI: 17.6 kg/m2). At that time, the patient also reported experiencing heartburn. The patient denied having fever, chills, and night sweats. Additionally, there were recurrent middle ear infections, with the most recent one resulting in a perforated eardrum. Furthermore, there was an increase in episodes of panic attacks and the possibility of epilepsy was evaluated. The otolaryngologists had diagnosed oral thrush, a HIV-indicator condition, and the patient had already been receiving treatment with Amphotericin B suspension.
Amongst the diagnostics that were carried out to further investigate the symptoms the patient was presenting were, a CT scan, an esophagogastroduodenoscopy, and a bone marrow biopsy. The CT scan of the neck and thorax revealed a persistently stable lymphadenopathy, with some additional regression; a recurrence of Diffuse Large B-cell Non-Hodgkin Lymphoma could therefore be excluded. The CT scan showed an incidental finding of a hepatosplenomegaly and 4 small nodules up to 8 mm in the right lung. The esophagogastroduodenoscopy only revealed scars and transverse furrows of unclear etiology, with no evidence of a sustained fungal infection. Amphotericin B suspension was subsequently discontinued. A bone marrow biopsy was also performed but yielded no significant findings. The patient was subsequently released from the hospital. An HIV test was not carried out.
Following a training session on HIV, employees from the care facility for disabled individuals suggested carrying out an HIV test in our patient. Testing was carried out in our clinic in collaboration with the public health department, which led to the identification of HIV positivity.
The highest viral load was 73,763 copies/ml with a CD4 + helper cell count of 41/µl. The reduced CD4 + helper cell count, and the history of AIDS-defining and HIV-associated diseases imply that the diagnosis of HIV had been delayed for an extended period.
At the time of presentation at our medical center, there were no indications for other sexually transmitted infections.
Upon conversation with the patient, it emerged that he has resided in a residential facility for individuals with intellectual disabilities since 1996, with his legal caregiver being his brother. In terms of his sexual history, he was in a heterosexual relationship for eight years in the past. In 2011, the patient established a stable relationship with a homosexual man. Following this, he engaged in regular sexual encounters with different partners both inside and outside the facility. There is no record of drug use, and condom usage was infrequent.
Given the patient’s HIV-indicator conditions among the medical history such as oral thrush, pancytopenia, and wasting syndrome, as well as Diffuse Large B-cell Non-Hodgkin Lymphoma, an AIDS-defining cancer diagnosed in 2013, the question now arises as to when the HIV infection may have occurred and whether an earlier diagnosis would have been possible if HIV testing had been carried out, since indicator conditions were present.
Possible barriers hindering a timely diagnosis may have been: Stigma among physicians, which could entail erroneous assumptions regarding the sexuality of individuals with mental disabilities, failure to identify indicator conditions and test for HIV, lack of awareness among affected individuals with mental disabilities, resulting in a limited understanding of HIV and potential omission of crucial information during medical consultations, the failure to acknowledge sexuality and inadequate collection of sexual history, and insufficient inclusivity in HIV testing for all individuals.
The estimated median time for seroconversion to a CD4 + cell count below 200 cells/mm3 lies at 7,93 years [ 6 ], although not definitive, there is a strong likelihood that HIV would have been detected if HIV testing had been conducted at the onset of an indicator condition, a decade earlier. Furthermore, early HIV treatment initiation would likely have mitigated a significant part, if not all, of the more recent illness and probable HIV-related complications. This highlights the significance of HIV testing.
Assumptions and stereotyping may lead a physician to wrongly believe that a mentally disabled person is incapable of engaging in sexual relations [ 7 ].
Consequently, this stereotyping could undermine the patient’s diagnosis, impede treatment, and hinder the attainment of positive health outcomes [ 8 ]. It is crucial to diagnose HIV early in order to initiate treatment promptly, as PLWHA who start highly active antiretroviral therapy (HAART) at a later stage, with a lower CD4 + cell count, seem to exhibit a higher propensity for AIDS-related complications at advanced ages, in contrast to those who initiated treatment earlier [ 9 ].
Provider-initiated testing for indicator conditions may hold particular significance for individuals with intellectual disabilities, as it could hinder their comprehension of HIV, their ability to disclose risky behavior, and/or their capacity to seek testing independently.
On the other hand, individuals at risk of acquiring HIV and PLWHA frequently experience elevated rates of mental health issues in comparison to the general population. Therefore, it is of great importance to integrate diagnostic methods such as HIV tests among the routine checkups to reduce the impact of stigma. HIV Testing should be inclusive for everyone, regardless of the social status, disabilities, and living conditions, sexuality should be addressed openly and assumptions should be avoided [ 10 , 11 ].
Providing HIV/AIDS training through workshops and trainings for healthcare workers and related personnel who interact with vulnerable groups has proven to be highly significant, as demonstrated in this instance. If the center for disabled individuals had not proposed an HIV test for our patient, the diagnosis might not have been uncovered [ 12 ].
Additionally, sexuality needs to be acknowledged and addressed in individuals with disabilities, including those with learning disabilities, to provide education on safer sex practices and to facilitate HIV testing.
Overall, medical teams failed to recommend HIV testing in this patient multiple times, initially during the 2013 lymphoma diagnosis and at subsequent presentations with symptoms suggestive of AIDS. However, care facility staff deserve credit for recognizing the necessity of HIV testing after training and ensuring its arrangement.
Conclusions
Patients presenting with indicator conditions, including those with mental disabilities, should be tested for HIV to ensure an early diagnosis, and all patients should be asked about their sexuality as everyone can be vulnerable to HIV. Furthermore, more trainings should be made available to health care professionals and related personnel regarding sexual health.
Data availability
No datasets were generated or analysed during the current study.
Jordans CCE, Vasylyev M, Rae C, Jakobsen ML, Vassilenko A, Dauby N et al. National medical specialty guidelines of HIV indicator conditions in Europe lack adequate HIV testing recommendations: a systematic guideline review. Euro Surveill. 2022;27(48).
UN Targets [Available from. https://www.unaids.org/en/topics/2025_target_setting .
Vaz-Pinto I, Gorgulho A, Esteves C, Guimarães M, Castro V, Carrodeguas A, Medina D. Increasing HIV early diagnosis by implementing an automated screening strategy in emergency departments. HIV Med. 2022;23(11):1153–62.
Article PubMed PubMed Central Google Scholar
Bull L, Rayment M. HIV-indicator-condition-driven HIV testing: clinically effective but still rarely implemented. Clin Med (Lond). 2016;16(2):175–9.
Article PubMed Google Scholar
Lodi S, Phillips A, Touloumi G, Geskus R, Meyer L, Thiébaut R, et al. Time from human immunodeficiency virus seroconversion to reaching CD4 + cell count thresholds < 200, <350, and < 500 Cells/mm³: assessment of need following changes in treatment guidelines. Clin Infect Dis. 2011;53(8):817–25.
Article CAS PubMed Google Scholar
Deffew A, Coughlan B, Burke T, Rogers E. Staff member’s views and attitudes to supporting people with an intellectual disability: a multi-method investigation of intimate relationships and sexuality. J Appl Res Intellect Disabil. 2022;35(4):1049–58.
Nyblade L, Stockton MA, Giger K, Bond V, Ekstrand ML, Lean RM, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. 2019;17(1):25.
Wada N, Jacobson LP, Cohen M, French A, Phair J, Muñoz A. Cause-specific mortality among HIV-infected individuals, by CD4(+) cell count at HAART initiation, compared with HIV-uninfected individuals. Aids. 2014;28(2):257–65.
Remien RH, Stirratt MJ, Nguyen N, Robbins RN, Pala AN, Mellins CA. Mental health and HIV/AIDS: the need for an integrated response. Aids. 2019;33(9):1411–20.
Deblonde J, De Koker P, Hamers FF, Fontaine J, Luchters S, Temmerman M. Barriers to HIV testing in Europe: a systematic review. Eur J Public Health. 2010;20(4):422–32.
Mangurian C, Cournos F, Schillinger D, Vittinghoff E, Creasman JM, Lee B, et al. Low rates of HIV Testing among adults with severe Mental illness receiving care in Community Mental Health settings. Psychiatr Serv. 2017;68(5):443–8.
Download references
No external funding was obtained for the research and preparation of this manuscript. All aspects of this work were conducted using resources available within the authors’ affiliated institutions.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
WIR-Walk In Ruhr – Center for Sexual Health and Medicine, Große Beckstraße 12, 44787, Bochum, Germany
Lina Martina Würfel, Anja Potthoff, Sandeep Nambiar & Adriane Skaletz-Rorowski
Interdisciplinary Immunological Outpatient Clinic, Center for Sexual Health and Medicine, Department of Dermatology, Venereology and Allergology, Ruhr-Universität Bochum, Bochum, Germany
Lina Martina Würfel, Anja Potthoff & Adriane Skaletz-Rorowski
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, A.P. and A.S.R.; writing—original draft preparation, L.M.W.; writing—review and editing, L.M.W., A.P., A.S.R., S.N.; supervision, A.P.; project administration, A.P.; All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Adriane Skaletz-Rorowski .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Informed consent Statement
Written informed consent has been obtained from the legal caregiver of the patient.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Würfel, L.M., Potthoff, A., Nambiar, S. et al. Missed opportunities for HIV testing and sexual health-related challenges in an individual with intellectual disability: a case report. AIDS Res Ther 21 , 20 (2024). https://doi.org/10.1186/s12981-024-00606-7
Download citation
Received : 26 February 2024
Accepted : 19 March 2024
Published : 05 April 2024
DOI : https://doi.org/10.1186/s12981-024-00606-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Intellectual disability
- HIV testing
- Public health
AIDS Research and Therapy
ISSN: 1742-6405
- Submission enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Iran Red Crescent Med J
- v.17(6); 2015 Jun
Perception of Patients With HIV/AIDS From Stigma and Discrimination
Mandana saki.
1 Department of Nursing, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, IR Iran
Sima Mohammad Khan Kermanshahi
Eesa mohammadi, minoo mohraz.
2 Iranian Research Center for HIV/AIDS, Iranian Institute for Reduction of High Risk Behavior, Tehran University of Medial Sciences, Tehran, IR Iran
Background:
Stigma and discrimination among patients with HIV/AIDS cause various problems for the patients and their health systems.
Objectives:
The purpose of this study was to explain the perceived experiences of the patients from stigma and discrimination and their roles on health-seeking services among patients.
Patients and Methods:
This was a qualitative research using content analysis approach and semi-structured interviews, conducted on patients living with HIV/ADS, during 2013 - 2014 in Iran. Sampling started purposefully and continued in a snowball.
The experiences of patients with HIV/AIDS from stigma and discrimination led to exploring three main themes and nine subthemes. The main themes were multidimensional stigma, rejection, and insult and discrimination in receiving health services.
Conclusions:
Stigma and discrimination play an important role in patients' lives and hinder them from accessing the treatment. The patients' responses to this event by secrecy strategy can be an important factor in the disease prevalence.
1. Background
AIDS is regarded as one of the greatest human challenges and risk factors for health ( 1 ). Based on the facts and figures issued by World Health Organization (WHO) and Joint United Nations Program on HIV/AIDS, of 35.3 million people living with HIV/AIDS, about six million live in Asia ( 2 ). According to the latest figures issued by Iran Ministry of Health, 26120 people have been diagnosed as HIV/AIDS patients ( 3 ).
The first patients with AIDS in America were homosexual young men. It is believed worldly that HIV is mainly transmitted through sexual intercourse. AIDS also occurs mostly to people who participate in unusual sexual activities ( 4 , 5 ). HIV infection is not socially acceptable in most countries and women living with HIV/AIDS are labeled as adultery ( 6 , 7 ). These people are stigmatized and pushed out of the community. Stigmatization from the disease deeply degrades the person's personality from a whole to an ordinary and finally to a stigmatized human being ( 8 ). Therefore, this person loses social status and gets labels ( 9 ). Stigma is created within the society and attached to cultural, social, spatial and historical factors ( 10 , 11 ). Although it is important to realize where and how stigma has formed in special cultural and political statuses, cultural differences and discrimination should be identified since socio-cultural beliefs, values and morals have structured in cultural backgrounds, which form stigma and discrimination ( 12 ).
Stigma and discrimination associated with HIV/AIDS are viewed as one of the greatest challenges mentioned for HIV infection ( 13 ). HIV-infected people are considered socially unusual. They are unpleasantly different from the public and threatening to the public ( 6 , 12 , 14 ).
Health-related stigma is a social process which appears as isolation, rejection, blame or devaluation ( 11 ). It occurs when the person is treated unequally and unfairly ( 6 ). Stigma and discrimination are world events which seriously affect the lives of people with HIV. HIV prevention ( 15 ), access to treatment and care ( 16 ), disclosure ( 17 ), seeking support ( 18 ), social interaction ( 19 ), identity ( 18 ), and people living with HIV/AIDS-infected individuals and their human rights ( 16 ) are all influenced by the stigma and discrimination caused by HIV/AIDS. The negative consequences connected to HIV stigma may force the infected people to delay or refuse treatment or hide their disease from others. The fear from stigma causes denial, secrecy, depression and shame. The disclosure of HIV status faces the person with the feelings of shame and self-suspicion ( 19 ). Therefore, HIV-infected people who fear from the disclosure of their status because of stigma and discrimination are willing to hide their status. They think disclosing their status may not only create a complicated and stressful situation, but also causes the person to lose family support and health care provision ( 19 , 20 ). Findings from a study conducted on HIV-positive people in South Africa indicated that 57% of the sample reported their status secretly, 73% had the feeling of guilt due to their positive status, and 43% had the feeling of shame ( 4 ). In a study in Botswana, 94% of patients with AIDS kept their status as a secret in the community, 69% hid the situation from the family, and 12% were not satisfied to disclose their situation at all ( 21 ). Secrecy and disease denial due to HIV/AIDS stigma may lead to the continuity of risky sexual behaviors ( 22 ). The results of some studies indicated that fear can influence the access to treatment and care services and it has been seen as a barrier to help seeking ( 23 , 24 ). They state that their reluctance to AIDS services is a strategy for protection of the patient and the family from stigma and social isolation ( 23 , 25 ).
HIV/AIDS stigma and discrimination have a crucial impact on the life of people living with HIV/AIDS and can be an important barrier for voluntary test and consultation ( 5 , 26 ). In a study on 482 males who had sexual intercourse with males, it was found that 82% of the participants never preferred to do HIV tests. The feeling of shame, fear and embarrassment were the barriers for reluctance to health care seeking of risky people and their stigma ( 25 ).
In Iran, HIV/AIDS is regarded not only as a medical but also a social problem. This can delay the treatment and cause a lot of troubles for patients and their families. Reduction of stigma and discrimination has been emphasized in the health system as an emergency preference because of the increase of AIDS in the Iranian population and its opposition with support, treatment and prevention. The importance and the impact of stigma and discrimination related to the disease in Iranian culture on one hand and the impact of cultural differences on patients' health-seeking attitudes and support services given by the health care system on the other hand composed the framework of this qualitative study. The interrelatedness of stigma and discrimination with the socio-cultural context led the researchers to outline this study.
2. Objectives
The aim of the study was to explain the perceived experiences of patients from stigma and discrimination and their roles on health-seeking services among patients during 2013 - 2014 in Iran.
3. Patients and Methods
The present study was a qualitative research using conventional content analysis. All qualitative studies consider a whole view of human phenomenon; so, this can be one of the most appropriate methods for studying people's experiences as a social phenomenon. Qualitative conventional content analysis is a method that can clarify the concealed patterns from the inside of data content ( 27 ).
In this study, the criteria focused on the participants' ability to speak and understand Farsi, have a good physical, mental and cognitional condition, and intend to take part in the study. The domain of the study included the Clinics of Education Hospital and AIDS Research Center affiliated to Tehran University of Medial Sciences. Sampling started purposefully and continued in a snowball. Thereafter, to make the concepts and categories more abstract, we applied theoretical sampling with inclusion of the patients' families and health professionals. All the participants were highly satisfied with participation when the aim of the study was described to them. For collecting the data, deep interviews and semi–structured interviews in a face-to-face manner were conducted. The interviews started with an open–ended question, like: "What were your challenges in your social interactions with others?" Afterwards, considering the participant's answer, the researcher formed probing questions to be asked. All the interviews were performed in Farsi by the first writer. Each interview lasted 45 - 90 minutes. The setting for each interview was the participant's choice. Finally, 18 personal interviews with 13 patients, three family members and two health professionals were completed ( Table 1 ). Data collection continued till data saturation. At the data saturation point, no new data could be obtained by the interviews ( 28 ). With the participant's agreement, the interview was recorded on a tape. For data analysis, the following eight steps were used: preparing the data; determining on the conceptual units; coding the units; coding the whole text and matching the codes to the text; developing the generated codes and categories based on similarities, revising categories and recomparing with the data for solidity of the codes; creating themes and comparing the categories and reporting the findings ( 27 ). MAXQDA 2007 software was used for data analysis ( Table 2 ).
Lincoln and Guba’s 4-item criterion was used for assessing the accuracy of this study. Prolonged engagement and member check were used for creditability. To assure the researcher's perception from the data, a brief version of the participants’ interviews were returned to the participants. Peer check was applied for confirmability of the data. In this way, the whole coded data and categories were reviewed by supervisors and peer advisors. The audit trail was applied for dependability of the data. In this study, the researcher kept the original data, categories and subthemes till the end of the research process. In this study, sampling was accomplished with the highest variance in age, gender, level of education, and the duration of infection. This can help the transferability and stability of the data ( 29 ).
For this study, a legal permit was received from the Tarbiat Modares University Research Ethical Committee with the number D- 52/3535. In addition, written agreements were taken from the participants after full description of the research aim, data collection method, data record, safety and comfort at the time of interview, their right to leave the program, and keeping their names and the data as a secret.
Interviews with 13 patients, three family members and two health professionals helped us to access the complete information, repetition and saturation of data. From the researched data, after removing the overlapping items, 224 codes were obtained. The main extracted concepts in this study involved three basic themes and nine subthemes. The main themes were multidimensional stigma, rejection, and discrimination and insults in health services ( Table 2 ).
4.1. Multidimensional Stigma
The participants mentioned many painful experiences resulted from being labeled as HIV/AIDS-positive patients. This category included such subthemes as social stigma, self-stigma and treatment system stigma.
4.1.1. Social Stigma
The participants claimed that social stigma caused them to be judged wrongly in their social relations. They felt the insulting and humiliating looks by the society. The female patients felt it much more. "People as well as health professionals look at us in an unusual manner. I tried a lot to ignore their behavior and looks. This problem annoyed me so much. In spite of all these misbehaviors, I attempted very hard to bear a healthy child by receiving pregnancy health care on time" (a 24-year-old woman).
Labeling as prostitutes and sexual stigma is important and agonizing for the participants. They understood that most of the people in the society think that AIDS originates from sexual deviances and matches immorality. "The society regards HIV-positive women as prostitutes. Being seen in hospital by an acquaintance or a relative is really painful since they think of me as a street woman who betrays her husband. I gave up the treatment process for this reason" (a 52-year-old woman).
4.1.2. Self-Stigma
Participants reported the feelings of shame and embarrassment because of HIV/AIDS. To be away from stigma, they put mask on their faces when referring to treatment centers. "When I decided to follow treatment, I wore big sunglasses, since I felt shameful of being cured in an AIDS center" (a 32-year-old woman).
4.1.3. Health Professionals
Patients' experiences from stigma indicated that some physicians and health professionals labeled positive patients with HIV with stigma and discrimination. They pushed the patients away from themselves and deprived them from treatment services. "Some of the physicians treated us impolitely. As they knew about our infection, they refused to visit us. The lab professionals misbehaved us" (a 24-year-old woman).
4.2. Rejection
The participants claimed that as they were identified as patients with HIV/AIDS in the community, they faced isolation from family members, relatives and friends, and even social separation, loneliness, hopelessness, social rejection and home-leave. The rejection category had the subthemes as self-isolation, family and relative rejection, and friend and community rejection.
4.2.1. Self-Isolation
The participants reduced and cut their social relations and kept away from the community. They ran away from stigma and concealed their illness. "After finding out my HIV/AIDS infection, I cut my friends not to let them know about my condition and have wrong judgment about me. I like to receive services from AIDS patients’ club, but I am afraid of being known by students or colleagues; so, I do not take part in club programs" (a 32-year-old man).
4.2.2. Family and Relative Rejection
The participants' experiences suggested the family's unwillingness in having relations with them. When people around knew about the patients' HIV infection, they forced the patients to leave the house and let them alone.
"My father is a physician. When he got informed of my positive HIV status, he forced me to leave the house and did not let me live with the family again. He explained that I was a threatening being for the family members, especially for my sisters. This kind of behavior led me to depression and caused me to delay my treatment" (a 30-year-old man).
4.2.3. Friends and Community Rejection
The participants mentioned friends and community awareness as one of the most humiliating experiences. "I was pushed away by the community since I was five years old. My classmates humiliated and mistreated me. My chair was taken away from others. None of my classmates were allowed to get in touch or even have a talk with me. The teacher would punish them" (a 17-year-old man).
4.3. Discrimination and Insult in Receiving Services
Almost all the participants encountered challenges while receiving health and medical services. Most of the patients mentioned such problems as discriminatory behaviors offered by physicians, health professionals' unwillingness in giving services to them, lack of cooperation in acceptance of patients with HIV in hospitals. The "discrimination and insult in receiving services" category had subthemes as: "discrimination in giving services", "insult and humiliation by health professionals", and "ignorance in giving services".
4.3.1. Discrimination in Receiving Services
Most of the participants mentioned the experience of discrimination in receiving temporary and clinical services.
"One month ago, the doctor ordered to hospitalize me in the Psychiatric Ward, but they did not take the actions due to my positive HIV status" (a 17-year-old man).
"One day, I visited a gynecologist for my internal infection. As she found out about my disease, she did not examine me and left for a reason. I went to another one. This time I did not say anything about my disease. She prescribed some medications. I did not dare to ask about the contradictory side effects of HIV medications with the newly given ones" (a 32-year-old woman).
4.3.2. Insult and Humiliation by Health Professionals
Most of the participants experienced receiving the services along with insult, humiliation, devaluation, mistreatment and wrong pre-judgment.
"I referred to a dentist for my tooth pain. He refused to provide any services to me. In the presence of other patients, he tore out my record file and put it in the trash" (a 32-year-old woman).
4.3.3. Ignorance in Giving Services
The participants experienced lack of attention in care and treatment needs and long-time waiting. "After my cesarean section in hospital, they put the label "positive HIV" on my bed. No one came to check me for some time. I felt my rights are ignored as a human" (a 24-year-old woman).
5. Discussion
After passing of three decades from HIV/AIDS epidemic, HIV stigma is still the main issue for HIV-infected patients ( 30 ). Although United Nation (UN) AIDS emphasized on stigma reduction programs for prevention and control of HIV/AIDS in public health areas, rare studies have been conducted in this field ( 31 ).
The purpose of this study was to clarify the HIV/AIDS patients' perception and experiences from discrimination and its role on health service reception. The ideas obtained from this research involved three main themes and nine subthemes. The main themes were multilateral stigma, rejection, and insult and discrimination in receiving services.
Lekganyane et al. ( 32 ) believed that stigma inevitably led to discrimination. It started from a nonsense cycle through which people talked about the fear of their disease and infection disclosure. Gaudine et al. ( 8 ) described four themes about stigma: separation from others, the experience of rejection, anger of being viewed as a social patient, and disease concealment. These stigma themes included three important aspects, as shame and shyness, different behaviors, and stigma due to the fear of transmission and recall. Deacon et al. ( 33 ) identified four kinds of stigma including discrimination, expected stigma, self-stigma, and secondary stigma. Stigma is often multidimensional ( 33 ). Liamputtong et al. ( 34 ) described three kinds of stigma associated with AIDS: self-stigma, perceived stigma and enacted stigma.
AIDS is a health and medical phenomenon with broad economic, cultural and social aspects. Its stigma targets the social status of infected people. An HIV/AIDS-infected person lives a life full of fear, pain, hopelessness and indecision. He/she also has a disappointing image of the disease and near-death image. In spite of all those mentioned, he/she receives discrimination, devaluation, rejection and preconception from the community. In this study, however, stigma was associated with cultural backgrounds. This means that, in addition to the patient, his/her family is influenced by the community negative attitudes. This social reaction results from the idea that HIV/AIDS-infected people have got infected as a result of immoral sexual behaviors. As homosexual behaviors contradict Islamic beliefs, they are not confirmed by our society. Therefore, this can intensify the complexity of HIV/AIDS stigma in the community. Since homosexual behaviors oppose Islamic socio-cultural rules, they have a religiously stigma base which creates assertive judgments and thus, they are not socially accepted.
VanLandingham et al. (2005) claimed that there were different reactions toward HIV/AIDS-infected people and their families ( 35 ). Their reactions were more positive compared to the past. Stigma alters during the time. The past stigma may not be the today stigma. It was found that Thai people have got more positive attitudes toward HIV/AIDS-infected females ( 34 , 35 ).
We found out that by taking cultural backgrounds into account, women are exposed to more stigmas. Women living with HIV are blamed of sexual deviances and adultery. Several studies have implied that women have been more vulnerable to stigma, especially when HIV/AIDS is mentioned as a transmittable sexual disease ( 14 , 35 ). HIV/AIDS is under negative judgement due to immoral behaviors of prostitutes. Stigma may appear because of sexual misuses or adultery. It may cause rejection and degradation ( 9 ).
Discrimination in rendering the services to patients with HIV/AIDS is one of the critical outcomes of stigma. This can negatively affect care and treatment fields and act as a major barrier for infected patients to receive services. Discrimination itself has many effects on the society. It cannot weaken the HIV stigma. It can cause other problems. Nondisclosure of HIV/AIDS and concealment of HIV/AIDS is a strategy used in response to this discrimination ( 36 ). Concealment of the disease from health professionals may lead to a rise in the number of infected people and the disease prevalence. The bad looks of the community to patients with HIV have caused the patients not to introduce themselves to health professionals and physicians while referring to treatment centers. They have found out that they will face rejection or discrimination while receiving services if their disease is disclosed. Discrimination means to distinguish between HIV-positive people and other patients. Not tracing the treatment process by patients is the result of discrimination and rejection. This can create a cycle of health and social issues.
Participants of the study explained their experiences associated with giving services and insult and degradation from health professionals. They also mentioned their experience about bad behaviors of most general practitioners or dentists and gynecologist. Most participants stated that not being accepted by the physician caused them to ignore or delay the treatment process. Some claimed that they concealed their disease to receive services in subsequent visits with physicians. Multisocial prejudices toward people with HIV/AIDS not only have reduced the social supports offered by health professionals but have also created various types of discriminations such as judgment attitudes, avoidance from patient, rejected treatment, health care services and unwanted disclosure in health care centers. Along with the present study and the discrimination problem in offering medical and dental services, a study in Nigeria was conducted. The results of the study focused on the discriminatory attitudes towards HIV-infected patients, given by dentists ( 37 ). A study in Kenya highlighted the fear of being infected among midwifery caregivers, which concluded social stigma and discrimination for patients ( 5 ).
As it was noted, stigma and discrimination can appear as big barriers for HIV/AIDS-infected people, which hinder them from accessing health, medical and care services. The results of this research can inform patients, families and health givers of practical aspects of HIV/AIDS stigma and discrimination. They may assist them to reduce the outcomes and complication of their disease by planning and support.
As HIV/AIDS infection is increasing in Iran, it is necessary to plan and practice proper strategies for eliminating wrong conception among public, families and medical teams, by which stigma and discrimination could be reduced to the least extend. According to the findings obtained, HIV/AIDS stigma has had an unpleasant impact on the society and it has been a barrier for the participants to access and gain equal social and medical rights. Studies have indicated that insufficient knowledge, misconceptions about the transmission ways, and the fear of being infected may lead to inappropriate social behaviors towards these patients. Showing sympathy and empathy with patients and creating a cultural background for the public as well as a general knowledge about HIV/AIDS can create positive attitudes for patients' health care. In this way, their social difficulties can be lessened.
Acknowledgments
The researchers appreciate the full cooperation of Tarbiat Modares University. Their special thanks go to the participants referring to AIDS and Behavioral Disease Counseling Center as well as the positive companions of the club. Surely, without their help and support, conducting this study would not be easy.
Authors’ Contributions: Mandana Saki was involved in the study interviews, extracting and encoding the data, data analysis and drafting the article. Sima Mohammad Khan Kermanshahi and Eesa Mohammadi were involved in revising the codes and data analysis and reviewing the content critically. Minoo Mohraz was involved in final revisions and critical reading.
Funding/Support: This study was a part of a Ph.D. of nursing thesis, financially supported by the Research Administration of Tarbiat Modares University, Iran.

IMAGES
VIDEO
COMMENTS
A 35-year-old HIV-positive man was admitted to our hospital with intermittent fever for several months (Figure 1) and chronic diarrhea. He was diagnosed HIV-positive 4 years earlier and had subsequently developed several AIDS-defining diseases such as Pneumocystis carinii pneumonia and CMV retinitis. Three months before admission the patient began complaining of watery diarrhea and recurrent ...
One study found that the overall rate of infections up to four months after the insertion of an intrauterine device was the same among HIV-negative women as among HIV-positive women. 29 Therefore ...
Case study methods involve an in-depth, longitudinal (over a long period of time) examination of a single instance or event, a case. This case study is about Anamika (name changed), a 35-year-old female who is an empowered HIV-positive and presently works as Community Co-ordinator at an anti-retroviral treatment (ART) centre.
Indeed, in a recent study involving 482 persons with HIV infection who had received a diagnosis of lymphoma, 12% had lymphoma IRIS. 28 The brisk growth of this patient's mass was most likely ...
Dr. Anne M. Neilan: This 16-year-old, sexually active male adolescent was referred for an evaluation for HIV PrEP. An estimated 1 in 2 Black men who have sex with men in the United States will ...
In 2011, the patient presented disseminated cutaneous lesions caused by Leishmania, as assessed by histopathological analysis of skin biopsy samples. In July 2012, the patient was readmitted for presenting febrile disease with splenomegaly and pancytopenia, in addition to showing positive results for laboratory tests for leishmaniasis (Table 1 ...
AIDS as a human crisis may lead to devastating psychological trauma and stress for patients. Therefore, it is necessary to study different aspects of their lives for better support and care. Accordingly, this study aimed to explain the lived experience of HIV-infected patients in the face of a positive diagnosis of the disease. This qualitative study is a descriptive phenomenological study.
Abstract. This case study demonstrates a 36-year-old ex-intravenous drug user (IVDU) who had been initially tested positive for human immunodeficiency virus (HIV) twice using Enzyme Immunoassay (EIA) method (Particle agglutination, PA done), but a year later he was tested HIV-negative. The patient was asymptomatic for HIV and T helper cells ...
However, few international HIV studies capture the experiences of PLHIV beyond viral suppression. The Positives Perspectives study, Wave 2 (Positive Perspectives 2) is one of the largest, global, HIV patient-reported outcomes studies to date. Staying true to the goal of meaningful involvement of PLHIV in HIV care from the Denver
COVID-19 status among HIV-positive patients.15,16 Thirty-six case series have so far been conducted on HIV patients co-infected with COVID-19. In these studies, most of the participants have been on ART, have had a CD4 T-cell count ranging from 63 to 1,441 cells/ mm3, and have had a mild-to-moderate COVID-19 disease, with
Ready acceptance of experiences of new diagnoses among HIV-positive persons is a known personal and public health safety-net. Its beneficial effects include prompt commencement and sustenance of HIV-positive treatment and care, better management of transmission risk, and disclosure of the HIV-positive status to significant others. Yet, no known study has explored this topic in Ghana; despite ...
This article presents the case of an HIV-positive patient who presented the treating physician, a psychiatrist, with an ethical dilemma. We provide the details of the case, identify the ethical issues it raises, and examine the ethical principles involved. In their article, "Confidentiality in the Age of AIDS," Martin L. Smith and Kevin P. Martin present a complex case in clinical ethics.
Our study is a retrospective chart review of all newly diagnosed, treatment-naïve HIV-positive individuals, aged more than 18 years old, who presented to the American University of Beirut Medical ...
He is HIV positive and is managed by an ID provider who referred him for follow-up with a primary care provider to manage his non-HIV conditions. According to the ID provider, his blood pressure has been elevated >130/80 mm Hg ×3. ... The patient in this case study presents with an elevated blood pressure. The most common diagnosis seen in the ...
A 25-year-old previously healthy woman is found to have a positive test for human immunodeficiency virus type 1 (HIV-1) antibody as part of a routine examination for insurance coverage.
Ms Jessie Chitalwa is a 27-year-old Nigerian lady who has lived in the UK since the age of 22. She is doing a business studies degree at a local university. She attended accident and emergency (A&E) with a 2-week history of increasing shortness of breath and lethargy. She tested HIV positive on a point of care test in A&E.
Based on the lived experience of these patients, it was found that after facing a positive diagnosis, HIV-infected tend to deny that they are infected. In this regard, various studies have shown that AIDS/HIV patients in different stages of the disease and their lives try to deny it in different ways [37-39]. The HIV-infected also stated that ...
Research suggests patient navigators and case management may help mitigate such barriers. 14,18 However, prior interventions have focused on newly diagnosed PLWH in the general population or PLWH transitioning from incarceration to the community. 19-21 Little is known about the effect of case management services on HIV treatment engagement ...
Symptoms of HIV patients with COVID-19 included coughing (81.3%), fever (62.8%), and dyspnea (60%). Hydroxychloroquine (39.34%) and azithromycin (36.58%) were the common treatment options for COVID-19. The total death rate in HIV-positive patients with COVID-19 was about 9%. Conclusion: In the current systematic review, we demonstrated that HIV ...
Background The estimated number of people living with human immunodeficiency virus (HIV) (PLHIV) in Uganda is 1.5 million (7.3%). As of June 2016, 60% (898,197) of PLHIV were enrolled and receiving antiretroviral therapy (ART). In scientific literature, the effect of HIV and ART on dental caries remains equivocal. At the Prosthetics Clinic of the Department of Dentistry, Makerere University ...
Introduction: Patients with HIV infection are at increased risk of developing cardiovascular disease (CVD) due to complex interactions between traditional CVD risk factors, antiretroviral therapy (ART) and HIV infection itself (1). Prevention of CVD is essential as it remains the most common serious non-AIDS event and contributes significantly to all-cause mortality.
HIV-positive individuals engaged in care are more likely to be virally suppressed, improving clinical outcomes and decreasing chances of HIV transmission. ... Overall, the average median duration of TCM enrollment from the start of the study period to TCM case closure was 224 days. We also compared TCM members to all Amida Care members not ...
Given the patient's HIV-indicator conditions among the medical history such as oral thrush, pancytopenia, and wasting syndrome, as well as Diffuse Large B-cell Non-Hodgkin Lymphoma, an AIDS-defining cancer diagnosed in 2013, the question now arises as to when the HIV infection may have occurred and whether an earlier diagnosis would have been possible if HIV testing had been carried out ...
Abstract. The aim of this article was to explore the experiences and attitudes of people with HIV/AIDS. A systematic review of qualitative studies was carried out. Twenty-seven articles were included, with sample sizes ranging from 3 to 78. Articles from North America, South America, Central America, Europe, and Africa were included.
When they told me about my HIV-positive status, they labeled "high-risk HIV-positive" on my bed. I asked about the label. They told "it is a drug abuse label" Marginalized patient in the hospital: Health system stigma: In some cases, I prefer not to disclose my positive HIV status when I am in a group. My problem becomes all family's problem.