- Office of Clinical Trials
- Office of Research Integrity
- Office of Sponsored Programs
- Office of Undergraduate Research
- International Gaming Institute
- Nevada Institute of Personalized Medicine
- National Supercomputing Institute
- Science and Engineering Building
- Harry Reid Center
- Policies & Forms
- Faculty Awards
- Councils & Committees
- Faculty/Staff Directory
- Directories

Quick Links
- Directories Home
- Colleges, Schools, and Departments
- Administrative Units
- Research Centers and Institutes
- Resources and Services
- Employee Directory
- Contact UNLV
- Social Media Directory
- UNLV Mobile Apps
- Research Home
- Division Units
History of Research Ethics
This website is intended to give a brief description of the development of human subjects’ regulations and requirements in the United States. More in-depth coverage of this topic is available through Collaborative Institutional Training Initiative training.
- Info for Researchers
- Information for Research Subjects
- Institutional Review Boards
- Policies and Regulation
- Additional Resources
- Human Subjects Home
- Information For:
- Researchers
- Research Subjects
- Report a Concern/Provide Input
Nuremberg Code
A well-known chapter in the history of research with human subjects opened on Dec. 9, 1946, when an American military tribunal opened criminal proceedings against 23 leading German physicians and administrators for their willing participation in war crimes and crimes against humanity. Among the charges were that German physicians conducted medical experiments on thousands of concentration camp prisoners without their consent. Most of the subjects of these experiments died or were permanently crippled as a result. As a direct result of the trial, the Nuremberg Code was established in 1948, stating that “The voluntary consent of the human subject is absolutely essential,” making it clear that subjects should give consent and that the benefits of research must outweigh the risks. Although it did not carry the force of law, the Nuremberg Code was the first international document which advocated voluntary participation and informed consent.
Thalidomide
In the late 1950s, thalidomide was approved as a sedative in Europe; it was not approved in the United States by the FDA. The drug was prescribed to control sleep and nausea throughout pregnancy, but it was soon found that taking this drug during pregnancy caused severe deformities in the fetus. Many patients did not know they were taking a drug that was not approved for use by the FDA, nor did they give informed consent. Some 12,000 babies were born with severe deformities due to thalidomide. U.S. Senate hearings followed and in 1962 the so-called “Kefauver Amendments” to the Food, Drug, and Cosmetic Act were passed into law to ensure drug efficacy and greater drug safety. For the first time, drug manufacturers were required to prove to the FDA the effectiveness of their products before marketing them.
Tuskegee Syphilis Study (1932-1972)
An equally well-known chapter in history occurred during a research project conducted by the U.S. Public Health Service. Six hundred low-income African-American males, 400 of whom were infected with syphilis, were monitored for 40 years. Free medical examinations were given; however, subjects were not told about their disease. Even though a proven cure (penicillin) became available in the 1950s, the study continued until 1972 with participants being denied treatment. In some cases, when subjects were diagnosed as having syphilis by other physicians, researchers intervened to prevent treatment. Many subjects died of syphilis during the study. The study was stopped in 1973 by the U.S. Department of Health, Education, and Welfare only after its existence was publicized and it became a political embarrassment. In 1997, under mounting pressure, President Clinton apologized to the study subjects and their families.
Declaration of Helsinki
In 1964, the World Medical Association established the “Declaration of Helsinki,” which provides recommendations guiding medical doctors in biomedical research involving human subjects. The declaration governs international research ethics and defines rules for “research combined with clinical care” and “non-therapeutic research.” The Declaration of Helsinki was revised in 1975, 1983, 1989, and 1996 and is the basis for effective clinical practices used today.
- Research with humans should be based on the results from laboratory and animal experimentation
- Research protocols should be reviewed by an independent committee prior to initiation
- Informed consent from research participants is necessary
- Research should be conducted by medically/scientifically qualified individuals
- Risks should not exceed benefits
National Research Act (1974)
Because of the publicity from the Tuskegee Syphilis Study, the National Research Act of 1974 was passed. The National Research Act created the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. This commission was tasked with identifying the basic ethical principles that should underlie the conduct of biomedical and behavioral research involving human subjects. It was also tasked with developing guidelines that should be followed to assure that such research is conducted in accordance with these ethical principles. The commission drafted the Belmont Report, a foundational document in for the ethics of human subjects research in the United States.
Current Regulations
In 1981, the Department of Health and Human Services (DHHS) and the Food and Drug Administration (FDA) issued regulations based on the Belmont Report. The DHHS issued the Code of Federal Regulations (CFR) Title 45 (public welfare), Part 46 (protection of human subjects). The FDA issued CFR Title 21 (food and drugs), Parts 50 (protection of human subjects), and 56 (Institutional Review Boards). In 1991, the core DHHS regulations (45 CFR Part 46, Subpart A) were formally adopted by more than a dozen other departments and agencies that conduct or fund research involving human subjects as the Federal Policy for the Protection of Human Subjects, or the “Common Rule.” In 1991, the Department of Veterans Affairs promulgated this same rule at 38 CFR Part 16. Today, the 1991 version of the “Federal Policy,” as it is known, is widely shared by federal departments and agencies. The main elements of the Common Rule include the following:
- requirements for assuring compliance by research institutions;
- requirements for researchers obtaining and documenting informed consent;
- requirements for Institutional Review Board (IRB) membership, function, operations, review of research, and record keeping; and
- additional protections for certain vulnerable research subjects (pregnant women, prisoners, and children)
In addition, certain federally sponsored and much privately sponsored research is subject to the regulations of the Food and Drug Administration (FDA) at 21 CFR Parts 50 and 56. FDA regulations confer protections on human subjects in research when a drug, device, biologic, food additive, color additive, electronic product, or other test article subject to FDA regulation is involved. FDA regulations and the provisions of the Common Rule are largely congruent, although some significant differences exist. Both the Common Rule and the FDA regulations provide protections for human subjects in research.
- National Institutes of Health, Regulations and Ethical Guidelines
- History of Human Subjects Research and IRB Oversight
- Search Menu
Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- Ethnic Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Politics of Development
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

The Oxford Textbook of Clinical Research Ethics

- Cite Icon Cite
- Permissions Icon Permissions
The Oxford Textbook of Clinical Research Ethics is the first systematic and comprehensive reference on clinical research ethics. Under the editorship of experts from the National Institutes of Health of the United States, the book offers a wide-ranging and systematic examination of all aspects of research with human beings. Considering historical triumphs of research as well as tragedies, the textbook provides a framework for analysing the ethical aspects of research studies with human beings. Through both conceptual analysis and systematic reviews of empirical data, the textbook examines issues ranging from scientific validity, fair subject selection, risk benefit ratio, independent review, and informed consent as well as focused consideration of international research ethics, conflicts of interests and other aspects of responsible conduct of research. The editors of The Oxford Textbook of Clinical Research Ethics offer a work that critically assesses and advances scholarship in the field of human subjects research with human beings.
Signed in as
Institutional accounts.
- Google Scholar Indexing
- GoogleCrawler [DO NOT DELETE]
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

- Table of Contents
- Random Entry
- Chronological
- Editorial Information
- About the SEP
- Editorial Board
- How to Cite the SEP
- Special Characters
- Advanced Tools
- Support the SEP
- PDFs for SEP Friends
- Make a Donation
- SEPIA for Libraries
- Entry Contents
Bibliography
Academic tools.
- Friends PDF Preview
- Author and Citation Info
- Back to Top
The Ethics of Clinical Research
Clinical research attempts to address a relatively straightforward, and important challenge: how do we determine whether one medical intervention is better than another, whether it offers greater clinical benefit and/or poses fewer risks? Clinicians may one day be able to answer these questions by relying on computer models, thereby avoiding reliance on clinical research and the ethical concerns it raises. Until that day, clinical researchers begin by testing potential new medical interventions in the laboratory, and often in animals. While these methods can provide valuable information and, in the case of animal research, raise important ethical issues of their own, potential new interventions eventually must be tested in human beings. Interventions which work miracles in test tubes and in mice, often leave humans untouched, or worse off.
Testing medical interventions in humans typically poses some risks to the participants, no matter how many laboratory and animal tests precede it. In this way, the process of collecting data through clinical trials to improve health and well-being inevitably exposes research participants to some risks for the benefit of future patients. This brings us to the central ethical challenge posed by clinical research: When is it ethically permissible to expose research participants to risks of harm for the benefit of others? The present entry focuses on this concern, and canvasses the most prominent attempts to address it. The present entry largely brackets the range of interesting and important ethical challenges that arise in the course of conducting clinical research: How should it be reviewed? Who may conduct it? What must potential participants understand to give valid consent? May it be conducted in countries that will not be able to afford the intervention being tested? Do investigators have any obligations to treat unrelated medical conditions in participants that they uncover during the course of their research?
One might attempt to address the central ethical challenge by limiting clinical research to the medical setting, offering experimental interventions to patients who want to try them. This approach, which has the virtue of evaluating interventions in the process of trying to help individual patients, makes sense for comparisons of two or more interventions that are widely accepted and already in clinical use. In contrast, this approach poses enormous scientific and practical problems with respect to testing new interventions. On the practical side, who would be willing to manufacture a new intervention without knowing whether it works? What dose should be used? How often should the new drug be taken? More importantly, this approach might not yield reliable information as to whether the new treatment is useful or harmful until hundreds, perhaps thousands of people have received it. Clinical research is designed to address these concerns by systematically assessing potential new treatments in a small number of individuals, including very sick ones, before offering them more widely. As we go about our daily lives, driving cars, flushing our waste down the drain, exhaling, getting a dog, we inevitably expose others to risks of harm. Despite the fact that these practices pervade our lives, there has been surprisingly little philosophical analysis of the conditions under which they are acceptable (Hayenhjelm and Wolff 2012). In addition to being of value in its own right, evaluation of the central ethical challenge posed by clinical research thus provides an opportunity to consider one of the more fundamental concerns in moral theory: when is it acceptable to expose some individuals to risks of harm?
1. What is Clinical Research?
2. early clinical research, 3. abuses and guidelines, 4. clinical research and clinical care, 5. a libertarian analysis, 6. contract theory, 7. minimal risks, 8. goals and interests, 9. industry sponsored research, 10. learning health care, other internet resources, related entries.
Human subjects research is research which studies humans, as opposed to animals, atoms, or asteroids. Assessment of whether humans prefer 100 dollars or a 1% chance of 10,000 dollars constitutes human subjects research. Clinical research refers to the subset of human subjects research that evaluates the impact interventions have on human beings with the goal of assessing whether they might help to improve human health and well-being. The present analysis focuses on research that is designed to improve human health and well-being by identifying better methods to treat, cure or prevent illness or disease. This focus is intended to bracket the question of whether research on enhancements that might increase our well-being by making us better than normal, allowing us to remember more or worry less, without treating, curing, or preventing illness or disease qualifies as clinical research.
We shall also bracket the question of whether quality improvement and quality assurance projects qualify as clinical research. To briefly consider the type of research at the heart of this debate, consider a hospital which proposes to evaluate the impact of checklists on the quality of patient care. Half the nurses in the hospital are told to continue to provide care as usual; the other half are provided with a checklist and instructed to mechanically check off each item as they complete it when caring for their patients. The question of whether this activity constitutes clinical research is of theoretical interest as a means to clarifying the precise boundaries of the concept. Should we say that this is not clinical research because the checklist is used by the nurses, not administered to the patients? Or should we say this is clinical research because it involves the systematic testing of a hypothesis which is answered by collecting data on patient outcomes? The answer has significant practical implications, determining whether these activities must satisfy existing regulations for clinical research, including whether the clinicians need to obtain patients’ informed consent before the nurses taking care of them can use the checklist.
While clinical medicine is enormously better than it was 100 or even 50 years ago, there remain many diseases against which current clinical medicine offers an inadequate response. To name just a few, malaria kills over a million people, mostly children, every year; chronic diseases, chief among them heart disease and stroke, kill millions each year, and there still are no effective treatments for Alzheimer disease. The social value of clinical research lies in its ability to collect information that might be useful for identifying improved methods to address these conditions. Yet, it is the rare study which definitively establishes that a particular method is effective and safe for treating, curing or preventing some illness. The success of specific research studies more commonly lies in the gathering of information that, together with the results of many other studies, may yield these improvements. For example, prior to establishing the efficacy of a new treatment for a given condition, researchers typically need to identify the cause of the condition, possible mechanisms for treating it, a safe and effective dose, and ways of testing whether the drug alters the course of the disease.
The process of testing potential new treatments can take 10–15 years, and is standardly divided into phases. Formalized phase 0 studies are a relatively recent phenomenon involving the testing of interventions and methods which might be used in later phase studies. A phase 0 study might be designed to determine the mechanism of action of a particular drug and evaluate different ways to administer it. Phase 1 studies are the earliest tests of a new intervention and are conducted in small numbers of individuals. Phase 1 studies are designed to evaluate the pharmacokinetics and pharmacodynamics of new treatments, essentially evaluating how the drug influences the human body and how the human body influences the drug. Phase 1 studies also evaluate the risks of the treatment and attempt to identify an appropriate dose to be used in subsequent phase 2 studies. Phase 1 studies pose risks and frequently offer little if any potential for clinical benefit to participants. As a result, a significant amount of the ethical concern over clinical research focuses on phase 1 studies.
If phase 1 testing is successful, potential new treatments go on to larger phase 2 studies which are designed to further assess risks and also to evaluate whether there is any evidence that the treatment might be beneficial. Successful phase 2 studies are followed by phase 3 studies which involve hundreds, sometimes thousands of patients. Phase 3 studies are designed to provide a rigorous test of the efficacy of a treatment and frequently involve randomization of participants to the new treatment or a control, which might be the current treatment or a placebo. Finally, post-marketing or phase 4 studies evaluate the use of interventions in clinical practice.
The first three phases of clinical trials typically include purely research procedures, such as blood draws, imaging scans, or biopsies, that are included in the study to collect data regarding the treatment under study. Analysis of the central ethical challenge posed by clinical research thus focuses on three related risk-benefit profiles: (a) the risk-benefit profile of the interventions(s) under study; (b) the risk-benefit profile of the included research procedures; and (c) the risk-benefit profile of the study as a whole.
In some cases, receipt of potential new treatments is in the ex ante interests of research participants. For example, the risks posed by an experimental cancer treatment might be justified by the possibility that it will extend participants’ lives. Moreover, the risk/benefit profile of the treatment might be as favorable for participants as the risk/benefit profile of the available alternatives. In these cases, receipt of the experimental intervention ex ante promotes participants’ interests. In other cases, participation in research poses ‘net’ risks, that is, risks of harm which are not, or not entirely, justified by potential clinical benefits to individual participants. A first in human trial of an experimental treatment might involve a single dose to see whether humans can tolerate it. And it might occur in healthy individuals who have no need of treatment. These studies pose risks to participants and offer essentially no chance for clinical benefit. The qualifier to ‘essentially’ no chance of clinical benefit is intended to capture the fact that the research procedures included in clinical trials may inadvertently end up providing some clinical benefit to some participants. For example, a biopsy that is used to collect research data may disclose a previously unidentified and treatable condition. The chance for such benefit, albeit real, is typically so remote that it is not sufficient to compensate for the risks of the procedure. Whether a study as a whole poses net risks depends on whether the potential benefits of the experimental intervention compensate for its risks plus the net risks of the research procedures included in the study.
Clinical research which poses net risks raises important ethical concern. Net-risk studies raise concern that participants are being used as mere means to collect information to benefit future patients. Research procedures that pose net risks may seem to raise less concern when they are embedded within a study which offers a favorable risk-benefit profile overall. Yet, since these procedures pose net risks, and since the investigators could provide participants with the new potential treatment alone, they require justification. An investigator who is about to insert a needle into a research participant to obtain some blood purely for laboratory purposes faces the question of whether doing so is ethically justified, even when the procedure is included in a study that offers participants the potential for important medical benefit. The goal of ethical analyses of clinical research is to provide an answer.
Clinical research poses three types of net risks: absolute, relative, and indirect (Rid and Wendler 2011). Absolute net risks arise when the risks of an intervention or procedure are not justified by its potential clinical benefits. Most commentators focus on this possibility with respect to research procedures which pose some risks and offer (essentially) no chance of clinical benefit, such as blood draws to obtain cells for laboratory studies. Research with healthy volunteers is another example which frequently offers no chance for clinical benefit. Clinical research also poses absolute net risks when it offers a chance for clinical benefit which is not sufficient to justify the risks participants face. A kidney biopsy to obtain tissue from presumed healthy volunteers may offer some very low chance of identifying an unrecognized and treatable pathology. This intervention nonetheless poses net risks if the chance for clinical benefit for the participants is not sufficient to justify the risks of their undergoing the biopsy.
Relative net risks arise when the risks of a research intervention are justified by its potential clinical benefits, but the intervention’s risk-benefit profile is less favorable than the risk-benefit profile of one or more available alternatives. Imagine that investigators propose a randomized, controlled trial to compare an inexpensive drug against an expensive and somewhat more effective drug. Such trials make sense when, in the absence of a direct comparison, it is unclear whether the increased effectiveness of the more expensive drug justifies its costs. In this case, receipt of the cheaper drug would be contrary to participants’ interest in comparison to receiving the more expensive drug. The trial thus poses relative net risks to participants.
Indirect net risks arise when a research intervention has a favorable risk-benefit profile, but the intervention diminishes the risk-benefit profile of other interventions provided as part of or in parallel to the study. For example, an experimental drug for cancer might undermine the effectiveness of other drugs individuals are taking for their condition. The risks of research participation can be compounded if the indicated response to the harm in question poses additional risks. Kidney damage suffered as the result of research participation might lead to the need for short-term dialysis which poses additional risks to the individual; a participant who experiences a postlumbar puncture headache might need a ‘blood patch’ which poses some risk of blood entering the epidural space which would call for a further response which carries additional risks. While commentators tend to focus on the risks of physical harm, participation in clinical research can pose other types of risks as well, including psychological, economic, and social risks. Depending on the study and the circumstances, individuals who are injured as the result of participating in research might incur significant expenses. Most guidelines and regulations stipulate that evaluation of the acceptability of clinical research studies should take into account all the different risks to which participants are exposed.
To assess the ethics of exposing research participants to risks, one needs an account of why exposing others to risks raises ethical concern in the first place. Being exposed to risks obviously raises concern to the extent that the potential harm to which the risk refers is realized: the chance of a headache turns into an actual headache. Being exposed to risks also can lead to negative consequences as a result of the recognition that one is at risk of harm. Individuals who recognize that they face a risk may become frightened; they also may take costly or burdensome measures to protect themselves. In contrast, the literature on the ethics of clinical research implicitly assumes that being exposed to risks is not per se harmful. The mere fact that participants are exposed to risks is not regarded as necessarily contrary to their interests. It depends on whether the risk is realized in an actual harm.
It is one thing to expose a consenting adult to risks to save the health or life of an identified and present other, particularly when the two individuals are first degree relatives. It is another thing, or seems to many to be another thing, to expose consenting individuals to risks to help unknown and unidentified, and possibly future others. Almost no one objects to operating on a healthy, consenting adult to obtain a kidney that might save a present and ailing sibling, even though the operation poses some risk of serious harm and offers the donor no potential for clinical benefit. Attempts to obtain a kidney from a healthy, consenting adult and give it to an unidentified individual are met with greater ethical concern. The extent of the concern increases as the path from risk exposure to benefit becomes longer and more tenuous. Many clinical research studies expose participants to risks in order to collect generalizable information which, if combined with the results of other, as yet non-existent studies, may eventually benefit future patients through the identification of a new intervention, assuming the appropriate regulatory authorities approve it, some company or group chooses to manufacture it, and patients can afford to purchase it. The potential benefits of clinical research may thus be realized someday, but the risks and burdens are clear and present.
Increasingly, researchers obtain and store human biological samples for use in future research studies. These studies raise important questions regarding what might be called ‘contribution’ and ‘information’ risks. The former question concerns the conditions under which it is acceptable to ask individuals to contribute to answering the scientific question posed by a given study (Jonas 1969). The fact that this question has been ignored by many commentators and regulations may trace to an overly narrow understanding of individuals’ interests. Individuals undoubtedly have an interest in avoiding the kinds of physical harms, pain, infection, loss of organ function, that they face in clinical research. This leaves the question of whether individuals’ interests are implicated, and whether they can be set back, by contributing to particular projects, activities and goals?
Consider the routine practice of storing leftover samples of participants’ blood for use in future research projects. For the purposes of protecting participants’ interests, does it matter what goals these future studies attempt to advance? Can individuals be harmed if their samples are used to promote goals which conflict with their fundamental values? For example, are the interests of individuals who fundamentally oppose cloning set back if their samples are used in a study that successfully identifies improved methods to clone human beings?
The possibility of information risks garnered significant attention when investigators used DNA samples obtained from members of the Havasupai tribe in Arizona to study “theories of the tribe’s geographical origins.” The study’s conclusion that early members of the tribe had migrated from Asia across the Bering Strait contradicted the tribe’s own views that they originated in the Grand Canyon (Harmon 2010). Can learning the truth, in this case the origins of one’s tribal group, harm research participants?
Attempts to determine when it is acceptable to expose participant to risks for the benefit of others, including future others who do not yet exist, have been significantly influenced by its history, by how it has been conducted and, in particular, by how it has been misconducted (Lederer 1995; Beecher 1966). Thus, to understand the current state of the ethics of clinical research, it is useful to know something of its past.
Modern clinical research may have begun on the 20 th of May, 1747, aboard the HMS Salisbury. James Lind, the ship’s surgeon, was concerned with the costs scurvy was exacting on British sailors, and was skeptical of some of the interventions, cider, elixir of vitriol, vinegar, sea-water, being used at the time to treat it. Unlike other clinicians of his day, Lind did not simply assume that he was correct and treat his patients accordingly. He designed a study. He chose 12 sailors from among the 30 or so Salisbury’s crew members who were suffering from scurvy, and divided them into six groups of 2 sailors each. Lind assigned a different intervention to each of the groups, including two sailors turned research participants who received 2 oranges and 1 lemon each day. Within a week these two were sailors again; the others remained patients, and several were dying.
The ethics of clinical research begins by asking how we should think about the fate of these latter sailors. Did Lind treat them appropriately? Do they have a moral claim against Lind? It is widely assumed that physicians should do what they think is best for the patient in front of them. Lind, despite being a physician, did not follow this maxim. He felt strongly that giving sea water to individuals with scurvy was a bad idea, but he gave sea water to 2 of the sailors in his study to test whether he, or others, were right. To put the fundamental concern raised by clinical research in its simplest form: Did Lind sacrifice these two sailors, patients under his care, for the benefit of others?
Lind’s experiments represent perhaps the first modern clinical trial because he attempted to address one of the primary challenges facing those who set out to evaluate medical treatments. How does one show that any differences in the outcomes of the treatments under study are a result of the treatments themselves, and not a result of the patients who received them, or other differences in the patients’ environment or diet? How could Lind be confident that the improvements in the two sailors were the result of the oranges and lemons, and not a result of the fact that he happened to give them to the two patients who occupied the most salutary rooms on the ship? Lind tried to address the challenge of confounding variables by beginning with patients who were as similar as possible. He carefully chose the 12 subjects for his experiment from a much larger pool of ailing sailors; he also tried to ensure that all 12 received the same rations each day, apart from the treatments provided as part of his study. It is also worth noting that Lind’s dramatic results were largely ignored for decades, leading to uncounted and unnecessary deaths, and highlighting the importance of combining clinical research with effective promulgation and implementation. The Royal Navy did not adopt citrus rations for another 50 years (Sutton 2003), at which point scurvy essentially disappeared from the Royal Navy.
Lind’s experiments, despite controlling for a number of factors, did not exclude the possibility that his own choices of which sailors got which treatment influenced the results. More recent experiments, including the first modern randomized, placebo controlled trial of Streptomycin for TB in 1948 (D’Arcy Hart 1999), attempt to address this concern by assigning treatments to patients using a random selection process. By randomly assigning patients to treatment groups these studies ushered in the modern era of controlled, clinical trials. And, by taking the choice of which treatment a given patient receives out of the hands of the treating clinician, these trials underscore and, some argue, exacerbate the ethical concerns raised by clinical research (Hellman and Hellman 1991). A foundational principle of clinical medicine is the importance of individual judgment. A physician who decides which treatments her patients receive by flipping a coin is guilty of malpractice. A clinical investigator who relies on the same methods receives awards and gets published in elite journals. One might conclude that sacrifice of the interests of some, often sick patients, for the benefit of future patients, is essentially mandated by the scientific method (Miller & Weijer 2006; Rothman 2000). The history of clinical research seems to provide tragic support for this view.
The history of clinical research is littered with abuses. Indeed, one account maintains that the history of pediatric research is “largely one of child abuse” (Lederer and Grodin 1994, 19; also see Lederer 2003). This history has had a significant influence on how research ethicists understand the concerns raised by clinical research and on how policy makers attempt to address them. In particular, policy makers have responded to previous abuses by developing guidelines intended to prevent their recurrence.
The most influential abuses in this regard were the horrific experiments conducted by Nazi physicians during WW II (abuses perpetrated by Japanese physicians were also horrific, but have received significantly less attention). Response to these abuses led to the Nuremberg Code (Grodin & Annas 1996; Shuster 1997), which is frequently regarded as the first set of formal guidelines for clinical research, an ironic claim on two counts. First, there is some debate over whether the Nuremberg Code was intended to apply generally to clinical research or whether, as a legal ruling in a specific trial, it was intended to address only the cases before the court (Katz 1996). Second, the Germans themselves had developed systematic research guidelines as early as 1931 (Vollmann & Winau 1996). These guidelines were still legally in force at the time of the Nazi atrocities and clearly prohibited a great deal of what the Nazi doctors did.
Wide consensus developed by the end of the 1950s that the Nuremberg Code was inadequate to the ethics of clinical research. Specifically, the Nuremberg Code did not include a requirement that clinical research receive independent ethics review and approval. In addition, the first and longest principle in the Nuremberg Code states that informed consent is “essential” to ethical clinical research (Nuremberg Military Tribunal 1947). This requirement provides a powerful safeguard against the abuse of research participants. It also appears to preclude clinical research with individuals who cannot consent.
One could simply insist that the informed consent of participants is necessary to ethical clinical research and accept the opportunity costs thus incurred. Representatives of the World Medical Association, who hoped to avoid these costs, began meeting in the early 1960s to develop guidelines, which would become the Declaration of Helsinki, to address the perceived shortcomings of the Nuremberg Code (Goodyear, Krleza-Jeric, and Lemmens 2007). They recognized that insisting on informed consent as a necessary condition for clinical research would preclude a good deal of research designed to find better ways to treat dementia and conditions affecting children, as well as research in emergency situations. Regarding consent as necessary precludes such research even when it poses only minimal risks or offers participants a compensating potential for important clinical benefit. The challenge, still facing us today, is to identify protections for research participants which are sufficient to protect them without being so strict as to preclude appropriate research designed to benefit the groups to which they belong.
The Declaration of Helsinki (World Medical Organization 1996) allows individuals who cannot consent to be enrolled in clinical research based on the permission of the participant’s representative. The U.S. federal regulations governing clinical research take a similar approach. These regulations are not laws in the strict sense of being passed by Congress and applying to all research conducted on U.S. soil. Instead, the regulations represent administrative laws which effectively attach to clinical research at the beginning and the end. Research conducted using U.S. federal monies, for instance, research funded by the NIH, or research involving NIH researchers, must follow the U.S. regulations (Department of Health and Human Services 2005). Research that is included as part of an application for approval from the U.S. FDA also must have been conducted according to FDA regulations which, except for a few exceptions, are essentially the same. Although many countries now have their own national regulations (Brody 1998), the U.S. regulations continue to exert enormous influence around the world because so much clinical research is conducted using U.S. federal money and U.S. federal investigators, and the developers of medical treatments often want to obtain approval for the U.S. market.
The abuses perpetrated as part of the infamous Tuskegee syphilis study were made public in 1972, 40 years after the study was initiated. The resulting outcry led to the formation of the U.S. National Commission, which was charged with evaluating the ethics of clinical research with humans and developing recommendations for appropriate safeguards. These deliberations resulted in a series of recommendations for the conduct of clinical research, which became the framework for existing U.S. regulations. The U.S. regulations, like many regulations, place no clear limits on the risks to which competent and consenting adults may be exposed. In contrast, strict limits are placed on the level of research risks to which those unable to consent may be exposed, particularly children. In the case of pediatric research, the standard process for review and approval is limited to studies that offer a ‘prospect of direct’ benefit and research that poses minimal risk or a minor increase over minimal risk. Studies that cannot be approved in one of these categories must be reviewed by an expert panel and approved by a high government official. While this 4th category offers important flexibility, it implies that, at least in principle, U.S. regulations do not mandate a ceiling on the risks to which pediatric research participants may be exposed for the benefit of others. This reinforces the importance of considering how we might justify exposing participants to research risks, both minimal and greater than minimal, for the benefit of others.
Lind’s experiments on scurvy exemplify the fact that clinical research is often conducted by clinicians and often is conducted on patients. Many commentators have thus assumed that clinical research should be governed by the ethics of clinical care, and the methods of research should not diverge from the methods that are acceptable in clinical care. On this approach, participants should not be denied any beneficial treatments available in the clinical setting and they should not be exposed to any risks not present in the clinical setting.
Some proponents (Rothman 2000) argue that this approach is implied by the kind of treatment that patients, understood as individuals who have a condition or illness needing treatment, are owed. Such individuals are owed treatment that promotes, or at least is consistent with their medical interests. Others (Miller & Weijer 2006) argue that the norms of clinical research derive largely from the obligations that bear on clinicians. These commentators argue that it is unacceptable for a physician to participate in, or even support the participation of her patients in a clinical trial unless that trial is consistent with the patients’ medical interests. To do less is to provide substandard medical treatment and to violate one’s obligations as a clinician.
The claim that the treatment of research participants should be consistent with the norms which govern clinical care has been applied most prominently to the ethics of randomized clinical trials (Hellman & Hellman 1991). Randomized trials determine which treatment a given research participant receives based on a random process, not based on clinical judgment of which treatment would be best for that patient. Lind assigned the different existing treatments for scurvy to the sailors in his study based not on what he thought was best for them, but based on what he thought would yield an effective comparative test. Lind did not give each intervention to the same number of sailors because he thought that all the interventions had an equal chance of being effective. To the contrary, he did this because he was confident that several of the interventions were harmful and this design was the best way to show it. Contemporary clinical researchers go even further, assigning participants to treatments randomly. Because this aspect of clinical research represents a clear departure from the practice of clinical medicine it appears to sacrifice the interests of participants in order to collect valid data.
One of the most influential responses to this concern (Freedman 1987) argues that randomization is acceptable when the study in question satisfies what has come to be known as ‘clinical equipoise.’ Clinical equipoise obtains when, for the population of patients from which participants will be selected, the available clinical evidence does not favor one of the treatments being used over the others. In addition, it must be the case that there are no treatments available outside the trial that are better than those used in the trial. Satisfaction of these conditions seems to imply that the interests of research participants will not be undermined in the service of collecting scientific information. If the available data do not favor any of the treatments being used, randomizing participants seems as good a process as any other for choosing which treatment they receive.
Proponents of clinical equipoise as an ethical requirement for clinical research determine whether equipoise obtains not by appeal to the belief states of individual clinicians, but based on whether there is consensus among the community of experts regarding which treatment is best. Lind believed that sea water was ineffective for the treatment of scurvy. Yet, in the absence of agreement among the community of experts, this view essentially constituted an individual preference rather than a clinical norm. This suggests that it was acceptable for Lind to randomly assign sailors under his care to the prevailing treatments in order to test, in essence, whose preferred treatment was the best. In this way, the existence of uncertainty within the community of experts seems to offer a way to reconcile the methods of clinical research with the norms of clinical medicine.
Critics respond that even when clinical equipoise obtains for the population of patients, the specific circumstances of individual patients within that population might imply that one of the treatments under investigation is better for them (Gifford 2007). A specific patient may have reduced liver function which places her at greater risk of harm if she receives a treatment metabolized by the liver. And some patients may have personal preferences which incline them toward one treatment over another (e.g., they may prefer a one-time riskier procedure to multiple, lower risk procedures which pose the same collective risk). Current debate focuses on whether randomized clinical trials can take these possibilities into account in a way that is consistent with the norms of clinical medicine.
Even if the existence of clinical equipoise can justify some randomized trials, a significant problem remains, namely, many studies and procedures which are crucial to the identification and development of improved methods for protecting and advancing health and well-being are inconsistent with participants’ medical interests. This concern arises for many phase 1 studies which offer essentially no chance for medical benefit and pose at least some risks, and to that extent are inconsistent with the participants’ medical interests.
Phase 3 studies which randomize participants to a potential new treatment or existing standard treatment, and satisfy clinical equipoise, typically include purely research procedures, such as additional blood draws, to evaluate the drugs being tested. Enrollment in these studies may be consistent with participants’ medical interests in the sense that the overall risk-benefit ratio is at least as favorable as the available alternatives. Yet, evaluation of the overall risk-benefit profile of the study masks the fact that it includes individual procedures which are contrary to participants’ medical interests, and contrary to the norms of clinical medicine.
The attempt to protect research participants by appeal to the obligations clinicians have to promote the medical interests of their patients also seems to leave healthy volunteers unprotected. Alternatively, proponents might characterize this position in terms of clinicians’ obligations to others in general: clinicians should not perform procedures on others unless doing so promotes the individual’s clinical interests. This approach seems to preclude essentially all research with healthy volunteers. For example, many phase 1 studies are conducted in healthy volunteers to determine a safe dose of the drug under study. These studies, vital to drug development, are inconsistent with the principle that clinicians should expose individuals to risks only when doing so is consistent with their clinical interests. It follows that appeal to clinical equipoise alone cannot render clinical research consistent with the norms of clinical practice.
Commentators sometimes attempt to justify net-risk procedures that are included within studies, and studies that overall pose net risks by distinguishing between ‘therapeutic’ and ‘non-therapeutic’ research (Miller and Weijer 2006). The claim here is that the demand of consistency with participants’ medical interests applies only to therapeutic research; non-therapeutic research studies and procedures may diverge from these norms to a certain extent, provided participants’ medical interests are not significantly compromised. The distinction between therapeutic and non-therapeutic research is sometimes based on the design of the studies in question, and sometimes based on the intentions of the investigators. Studies designed to benefit participants, or investigators who intend to benefit participants are conducting therapeutic studies. Those designed to collect generalizable knowledge or in which the investigators intend to do so constitute non-therapeutic research.
The problem with the distinction between therapeutic and non-therapeutic research so defined is that research itself often is defined as a practice designed to collect generalizable knowledge and conducted by investigators who intend to achieve this end (Levine 1988). On this definition, all research qualifies as non-therapeutic. Conversely, most investigators intend to benefit their participants in some way or other. Perhaps they design the study in a way that provides participants with clinically useful findings, or they provide minor care not required for research purposes, or referrals to colleagues. Even if proponents can make good on the distinction between therapeutic and non-therapeutic research in theory, these practices appear to render it irrelevant to the practice of clinical research. More importantly, it is not clear why investigators’ responsibilities to patients, or patients’ claims on investigators, should vary as a function of this distinction. Why think that investigators are allowed to expose patients to some risks for the benefit of others, but only in the context of research that is not designed to benefit the participants? To apply this proposed resolution to pediatric research, why might it be acceptable to expose infants to risks for the benefit of others, but only in the context of studies which offer the infants no chance for personal benefit?
To take one possibility, it is not clear that this view can be defended by appeal to physicians’ role responsibilities. A prima facie plausible view holds that physicians’ role responsibilities apply to all encounters between physicians and patients who need medical treatment. This view would imply that physicians may not compromise patients’ medical interests when conducting therapeutic studies, but also seems to prohibit non-therapeutic research procedures with patients. Alternatively, one might argue that physicians’ role responsibilities apply only in the context of clinical care and so do not apply in the context of clinical research at all. This articulation yields a more plausible view, but does not support the use of the therapeutic/ non-therapeutic distinction. It provides no reason to think that physicians’ obligations differ based on the type of research in question.
Critics argue that these problems highlight the fundamental confusion that results when one attempts to evaluate clinical research based on norms appropriate to clinical medicine. They instead distinguish between the ethics of clinical research and the ethics of clinical care, arguing that it is inappropriate to assume that investigators are subject to the claims and obligations which apply to physicians, despite the fact that the individuals who conduct clinical research often are physicians (Miller and Brody 2007).
The claim that clinical research should satisfy the norms of clinical medicine has this strong virtue: it provides a clear method to protect individual research participants and reassure the public that they are being so protected. If research participants are treated consistent with their medical interests, we can be reasonably confident that improvements in clinical medicine will not be won at the expense of exploiting them. Most accounts of the ethics of clinical research now recognize the limitations of this approach and search for ways to ensure that research participants are not exposed to excessive risks without assuming that the claims of clinical medicine apply to clinical researchers (Emanuel, Wendler, and Grady 2000; CIOMS 2002). Dismissal of the distinction between therapeutic and non-therapeutic research thus yields an increase in both conceptual clarity and concern regarding the potential for abuse of research participants.
Clinicians, first trained as physicians taught to act in the best interests of the patient in front of them, often struggle with the process of exposing some patients to risky procedures for the benefit of others. It is one thing for philosophers to insist, no matter how accurately, that research participants are not patients and need not be treated according to the norms of clinical medicine. It is another thing for clinical researchers to regard research participants who are suffering from disease and illness as anything other than patients. These clinical instincts, while understandable and laudable, have the potential to obscure the true nature of clinical research, as investigators and participants alike try to convince themselves that clinical research involves nothing more than the provision of clinical care. One way to try to address this collective and often willful confusion would be to identify a justification for exposing research participants to net risks for the benefit of others.
It is often said that those working in bioethics are obsessed with the principle of respect for individual autonomy. Advocates of this view of bioethicists cite the high esteem accorded in the field to the requirement of obtaining individual informed consent and the frequent attempts to resolve bioethical challenges by citing its satisfaction. One might assume that this view within bioethics traces to implicit endorsement of a libertarian analysis according to which it is permissible for competent and informed individuals to do whatever they prefer, provided those with whom they interact are competent, informed and in agreement. In the words of Mill, investigators should be permitted to conduct research and expose participants to risks provided they obtain their “free, voluntary, and undeceived consent and participation” (On Liberty, page 11). Setting aside the question of whether this view accurately characterizes bioethics and bioethicists generally, it does not apply to the vast majority of work done on the ethics of clinical research. Almost no one in the field argues that it is permissible for investigators to conduct any research they want provided they obtain the free and informed consent of those they enroll.
Current research ethics does place significant weight on informed consent and many regulations and guidelines devote much of their length to articulating the requirement for informed consent. Yet, as exemplified by the response to the Nuremberg Code, almost no one regards informed consent as necessary and sufficient for ethical research. Most regulations and guidelines, beginning with the Declaration of Helsinki, first adopted in 1964 (World Medical Organization 1996), allow investigators to conduct research on humans only when it has been approved by an independent group charged with ensuring that the study is ethically acceptable. Most regulations further place limits on the types of research that independent ethics committees may approve. They must find that the research has important social value and the risks have been minimized, thereby restricting the types of research to which even competent adults may consent. Are these requirements justified, or are they inappropriate infringements on the free actions of competent individuals? The importance of answering this question goes beyond its relevance to debates over Libertarianism. Presumably, the requirements placed on clinical research have the effect of reducing to some extent the number of research studies that get conducted. The fact that at least some of the prohibited studies likely would have important social value, helping to identify better ways to promote health and well-being, provides a normative reason to eliminate the restrictions, unless there is some compelling reason to retain them.
The libertarian claim that valid informed consent is necessary and sufficient to justify exposing research participants to risks for the benefit of others seems to imply, consistent with the first principle of the Nuremberg Code, that research with individuals who cannot consent is unethical. This plausible and tempting claim commits one to the view that research with children, research in many emergency situations, and research with the demented elderly all are ethically impermissible. One could consistently maintain such a view but the social costs of adopting it would be great. It is estimated, for example, that approximately 70% of medications provided to children have not been tested in children, even for basic safety and efficacy (Roberts, Rodriquez, Murphy, Crescenzi 2003; Field & Behrman 2004; Caldwell, Murphy, Butow, and Craig 2004). Absent clinical research with children, pediatricians will be forced to continue to provide frequently inappropriate treatment, leading to significant harms that could have been avoided by pursuing clinical research to identify better approaches.
One response would be to argue that the Libertarian analysis is not intended as an analysis of the conditions under which clinical research is acceptable. Instead, the claim might be that it provides an analysis of the conditions under which it is acceptable to conduct clinical research with competent adults. Informed consent is necessary and sufficient for enrolling competent adults in research. While this view does not imply that research with participants who cannot consent is impermissible, it faces the not insignificant challenge of providing an account for why such research might be acceptable.
Bracketing the question of individuals who cannot consent, many of the limitations on clinical research apply to research with competent adults. How might these limitations be justified? One approach would be to essentially grant the Libertarian analysis on theoretical grounds, but then argue that the conditions for its implementation are rarely realized in practice. In particular, there are good reasons, and significant empirical data, to question how often clinical research actually involves participants who are sufficiently informed to provide valid consent. Even otherwise competent adults often fail to understand clinical research sufficiently to make their own informed decisions regarding whether to enroll (Flory and Emanuel 2004).
To consider an example which is much discussed in the research ethics literature, it is commonly assumed that valid consent for randomized clinical trials requires individuals to understand randomization. It requires individuals to understand that the treatment they will receive, if they enroll in the study, will be determined by a process which does not take into account which of the treatments is better for them (Kupst 2003). There is an impressive wealth of data which suggests that many, perhaps most individuals who participate in clinical research do not understand this (Snowden 1997; Featherstone and Donovan 2002; Appelbaum 2004). The data also suggest that these failures of understanding often are resistant to educational interventions.
With this in mind, one might regard the limitations on research with competent adults as betraying the paternalism embedded in most approaches to the ethics of clinical research (Miller and Wertheimer 2007). Although the charge of paternalism often carries with it some degree of condemnation, there is a strong history of what is regarded as appropriate paternalism in the context of clinical research. This too may have evolved from clinical medicine. Clinicians are charged with protecting and promoting the interests of the patient “in front of them”. Clinician researchers, who frequently begin their careers as clinicians, may regard themselves as similarly charged. Paternalism involves interfering with the liberty of agents for their own benefit (Feinberg 1986; see also entry on paternalism ). As the terms are used in the present debate, ‘soft’ paternalism involves interfering with the liberty of an individual in order to promote their interests on the grounds that the action being interfered with is the result of impaired decision-making: “A freedom-restricting intervention is based on soft paternalism only when the target’s decision-making is substantially impaired, when the agent lacks (or we have reason to suspect that he lacks) the information or capacity to protect his own interests—as when A prevents B from drinking the liquid in a glass because A knows it contains poison but B does not” (Miller & Wertheimer 2007). ‘Hard’ paternalism, in contrast, involves interfering with the liberty of an individual in order to promote their interests, despite the fact that the action being interfered with is the result of an informed and voluntary choice by a competent individual.
If the myriad restrictions on clinical research were justified on the basis of hard paternalism they would represent restrictions on individuals’ autonomous actions. However, the data on the extent to which otherwise competent adults fail to understand what they need to understand to provide valid consent suggests that the limitations can instead be justified on the grounds of soft paternalism. This suggests that while the restrictions may limit the liberty of adult research participants, they do not limit their autonomy. In this way, one may regard many of the regulations on clinical research not as inconsistent with the libertarian ideal, but instead as starting from that ideal and recognizing that otherwise competent adults often fail to attain it.
Even if most research participants had sufficient understanding to provide valid consent, it would not follow that there should be no limitations on research with competent adults. The conditions on what one individual may do to another are not exhausted by what the second individual consents to. Perhaps some individuals may choose for themselves to be treated with a lack of respect, even tortured. It does not follow that it is acceptable for me or you to treat them accordingly. As independent moral agents we need sufficient reason to believe that our actions, especially the ways in which we treat others, are appropriate, and this evaluation concerns, in typical cases, more than just the fact that the affected individuals consented to them.
Understood in this way, many of the limitations on the kinds of research to which competent adults may consent are not justified, or at least not solely justified, on paternalistic grounds. Instead, these limitations point to a crucial and often overlooked concern in research ethics. The regulations for clinical research often are characterized as protecting the participants of research from harm. Although this undoubtedly is an important and perhaps primary function of the regulations, they also have an important role in limiting the extent to which investigators harm research participants, and limiting the extent to which society supports and benefits from a process which inappropriately harms others. It is not just that research participants should not be exposed to risk of harm without compelling reason. Investigators should not expose them to such risks without compelling reason, and society should not support and benefit from their doing so.
This aspect of the ethics of clinical research has strong connections with the view that the obligations of clinicians restrict what sort of clinical research they may conduct. On that view, it is the fact that one is a physician and is obligated to promote the best interests of those with whom one interacts professionally which determines what one is allowed to do to participants. This connection highlights the pressing questions that arise once we attempt to move beyond the view that clinical research is subject to the norms of clinical medicine. There is a certain plausibility to the claim that a researcher is not acting as a clinician and so may not be subject to the obligations that bear on clinicians. Or perhaps we might say that the researcher/subject dyad is distinct from the physician/patient dyad and is not necessarily subject to the same norms. But, once we conclude that we need an account of the ethics of clinical research, distinct from the ethics of clinical care, one is left with the question of which limitations apply to what researchers may do to research participants.
It seems clear that researchers may not expose research participants to risks without sufficient justification, and also clear that this claim applies even to those who provide free and informed consent. The current challenge then is to develop an analysis of the conditions under which it is acceptable for investigators to expose participants to risks and determine to what extent current regulations need to be modified to reflect this analysis. To consider briefly the extent of this challenge, and to underscore and clarify the claim that the ethics of clinical research go beyond the protection of research participants to include the independent consideration of what constitutes appropriate behavior on the part of investigators, consider an example.
Physical and emotional abuse cause enormous suffering, and a good deal of research is designed to study various methods to reduce instances of abuse and also to help victims recover from being abused. Imagine that a team of investigators establishes a laboratory to promote the latter line of research. The investigators will enroll consenting adults and, to mimic the experience of extended periods of abuse in real life, they will abuse their participants emotionally and physically for a week. The abused participants will then be used in studies to evaluate the efficacy of different methods for helping victims to cope with the effects of abuse.
The proper response to this proposal is not to claim that the study is acceptable because the participants are competent and they gave informed consent. The proper response is to point out that, while these considerations are undoubtedly important, they do not establish that the study is ethically acceptable. One needs to consider many other things. Is the experiment sufficiently similar to real life abuse that its results will have external validity? Are there less risky ways to obtain the same results? Finally, even if these questions are answered in a way that supports the research, the question remains whether investigators may ethically treat their participants in this way. The fact that essentially everyone working in research ethics would hold that this study is unethical—investigators are not permitted to treat participants in this way—suggests that research ethics, both in terms of how it is practiced and possibly how it should be practiced, goes beyond respect for individual autonomy to include independent standards on investigator behavior. Defining those standards represents one of the more important challenges for research ethics.
As exemplified by Lind’s experiments on treatments for scurvy, clinical research studies were first conducted by clinicians wondering whether the methods they were using were effective. To answer this question, the clinicians altered the ways in which they treated their patients in order to yield information that would allow them to assess their methods. In this way, clinical research studies initially were part of, but an exception to standard clinical practice. As a result, clinical research came to be seen as an essentially unique activity. And widespread recognition of clinical research’s scandals and abuses led to the view that this activity needed its own extensive regulations.
More recently, some commentators have come to question the view that clinical research is a unique human activity, as well as the regulations and guidelines which result from this view. In particular, it has been argued that this view has led to overly restrictive requirements on clinical research, requirements that hinder scientists’ ability to improve medical care for future patients, and also fail to respect the liberty of potential research participants. This view is often described in terms of the claim that many regulations and guidelines for clinical research are based on an unjustified ‘research exceptionalism’ (Wertheimer 2010).
The central ethical concern raised by clinical research involves the practice of exposing participants to risks for the benefit of others. Yet, as noted previously, we are constantly exposing individuals to risks for our benefit and the benefit of others. When you drive to the store, you expose your neighbors to some increased risk of pollution for the benefits you derive from shopping; speeding ambulances expose pedestrians to risks for the benefit of the patients they carry; factories expose their workers to risks for the benefit of their customers; charities expose volunteers to risks for the benefit of recipients. Despite this similarity, clinical research is widely regarded as ethically problematic and is subject to significantly greater regulation, review, and oversight (Wilson and Hunter 2010). Almost no one regards driving, ambulances, charities, or factories as inherently problematic. Even those who are not great supporters of a given charity do not argue that it treats its volunteers as guinea pigs, despite exposing them to risks for the benefit of others. And no one argues that charitable activities should satisfy the requirements that are routinely applied to clinical research, such as the requirements for independent review and written consent based on an exhaustive description of the risks and potential benefits of the activity, its purpose, duration, scope, and procedures.
Given that many activities expose some to risks for the benefit of others, yet are not subject to such extensive regulation, some commentators conclude that many of the requirements for clinical research are unjustified (Sachs 2010, Stewart et al. 2008, and Sullivan 2008). This work is based on the assumption that, when it comes to regulation and ethical analysis, we should treat clinical research as we treat other activities in daily life which involve exposing some to risks for the benefit of others. This assumption leads to a straightforward solution to the central ethical problem posed by clinical research.
Exposing factory workers to risks for the benefit of others is deemed ethically acceptable when they agree to do the work and are paid a fair wage. The solution suggested for the ethical concern of non-beneficial research is to obtain consent and pay research participants a fair wage for their efforts. This view is much less restrictive than current regulations for clinical research, but seems to be less permissive than a Libertarian analysis. The latter difference is evident in claims that research studies should treat participants fairly and not exploit them, even if individuals consent to being so treated.
The gap between this approach and the traditional view of research ethics is evident in the fact that advocates of the traditional view tend to regard payment of research participants as exacerbating rather than resolving its ethical concerns, raising, among others, worries of undue inducement and commodification. Those who are concerned about research exceptionalism, in contrast, tend to regard payment as it is regarded in most other contexts in daily life: some is good and more is better.
The claims of research exceptionalism have led to valuable discussion of the extent to which clinical research differs from other activities which pose risks to participants for the benefit of others and whether any of the differences justify the extensive regulations and guidelines standardly applied to clinical research. Proponents of research exceptionalism who regard many of the existing regulations as unjustified face the challenge of articulating an appropriate set of regulations for clinical research. While comparisons to factory work provide a useful lens for thinking about the ethics of clinical research, it is not immediately obvious what positive recommendations follow from this perspective. After all, it is not as if there is general consensus regarding the regulations to which industry should be subject. Some endorse minimum wage laws; others oppose them. There are further arguments over whether workers should be able to unionize; whether governments should set safety standards for industry; whether there should be rules protecting workers against discrimination.
A few commentators (Caplan 1984; Harris 2005; Heyd 1996) try to justify exposing research participants to risks for the benefit of others by citing an obligation to participate in clinical research. At least all individuals who have access to medical care have benefited from the efforts of previous research participants in the form of effective vaccines and better medical treatments. One might try to argue that these benefits obligate us to participate in clinical research when its our turn.
Current participation in clinical research typically benefits future patients. However, if we incur an obligation for the benefits that are due to previous research studies, we presumably are obligated to the patients who participated in those studies, an obligation we cannot discharge by participating in current studies. This approach also does not provide a way to justify the very first clinical trials, such as Lind’s, which of necessity enrolled participants who had never benefited from previous clinical research.
Alternatively, one might argue that the obligation to participate does not trace to the benefits we receive from the efforts of previous research participants. Rather, the obligation is to the overall social system of which clinical research is a part (Brock 1994). For example, one might argue that individuals acquire this obligation as the result of being raised in the context of a cooperative scheme or society. We are obligated to do our part because of the many benefits we have enjoyed as a result of living within such a scheme.
The first challenge for this view is to explain why the mere enjoyment of benefits, without some prospective agreement to respond in kind, obligates individuals to help others. Presumably, your doing a nice thing for me yesterday, without my knowledge or invitation, does not obligate me to do you a good turn today. This concern seems even greater with respect to pediatric research. Children certainly benefit from previous research studies, but typically do so unknowingly and often with vigorous opposition. The example of pediatric research makes the further point that justification of clinical research on straightforward contractualist grounds will be difficult at best. Contract theories have difficulties with those groups, such as children, who do not accept in any meaningful way the benefits of the social system under which they live (Gauthier 1990).
In a Rawlsian vein, one might try to establish an obligation to participate in clinical research based on the choices individuals would make regarding the structure of society from a position of ignorance regarding their own place within that society, from behind a veil of ignorance (Rawls 1999). To make this argument, one would have to modify the Rawlsian argument in several respects. The knowledge that one is currently living could well bias one’s decision against the conduct of clinical research. Those who know they are alive at the time the decision is being made have already reaped many of the benefits they will receive from the conduct of clinical research.
To avoid these biases, we might stretch the veil of ignorance to obscure the generation to which one belongs—past, present or future (Brock 1994). Under a veil of ignorance so stretched, individuals might choose to participate in clinical research as long as the benefits of the practice exceed its overall burdens. One could then argue that justice as fairness gives all individuals an obligation to participate in clinical research when their turn comes. This approach seems to have the advantage of explaining why we can expose even children to some risks for the benefit of others, and why parents can give permission for their children to participate in such research. This argument also seems to imply not simply that clinical research is acceptable, but that, in a range of cases, individuals have an obligation to participate in it. It implies that adults whose turn has come are obligated to participate in clinical research, although for practical reasons we might refrain from forcing them to do so.
This justification for clinical research faces several challenges. First, Rawlsian arguments typically are used to determine the basic structure of society, that is, to determine a fair arrangement of the basic institutions within the society (Rawls 1999). If the structure of society meets these basic conditions, members of the society cannot argue that the resulting distribution of benefits and burdens is unfair. Yet, even when the structure of society meets the conditions for fairness, it does not follow that individuals are obligated to participate in the society so structured. Competent adults can decide to leave a society that meets these conditions rather than enjoy its benefits (whether they have any better places to go is another question). The right of exit suggests that the fairness of the system does not generate an obligation to participate, but rather defends the system against those who would argue that it is unfair to some of the participants over others. At most, then, the present argument can show that it is not unfair to enroll a given individual in a research study, that this is a reasonable thing for all individuals, including those who are unable to consent.
Second, it is important to ask on what grounds individuals behind the veil of ignorance make their decisions. In particular: are these decisions constrained or guided by moral considerations? (Dworkin 1989; Stark 2000). It seems plausible to think that they would be. After all, we are seeking the ethical approach or policy with respect to clinical research. The problem, then, is that the answer we get in this case may depend significantly on which ethical constraints are built into the system, rendering the approach question begging. Most importantly, we are considering whether it is ethical to expose individuals who cannot consent to risks for the benefit of others. If it isn’t, then it seems that this should be a limitation on the choices individuals can make from behind the veil of ignorance, in which case appeal to those choices will not be able to justify pediatric research, nor research with incompetent adults. And if this research is ethical it is unclear why we need this mechanism to justify it.
Proponents might avoid this dilemma by assuming that individuals behind the veil of ignorance will make decisions based purely on self-interest, unconstrained by moral limits or considerations. Presumably, many different systems would satisfy this requirement. In particular, the system that produces the greatest amount of benefits overall may well be one that we regard as unethical. Many endorse the view that clinical research studies which offer no potential benefit to participants and pose a high chance of serious risk, such as death, are unethical, independent of the magnitude of the social value to be gained. For example, almost all research ethicists would regard as unethical a study which intentionally infects a few participants with the HIV virus, even when the study offers the potential to identify a cure for AIDS. Yet, individuals behind the veil of ignorance who make decisions based solely on self-interest might well allow this study on the grounds that it offers a positive cost-benefit ratio overall: the high risks to a few participants are clearly outweighed by the potential to save the lives of millions.
The question here is not whether a reasonable person would choose to make those who are badly off even worse off in order to elevate the status of those more privileged. Rather, both options involve some individuals being in unfortunate circumstances, namely, infected with the HIV virus. The difference is that the one option (not conducting the study) involves many more individuals becoming infected over time, whereas the other option involves significantly fewer individuals being infected, but some as the result of being injected in the process of identifying a cure. Since the least desirable circumstances (being infected with HIV) are the same in both cases, the reasonable choice, even if one endorses the maximin strategy, seems to be whichever option reduces the total number of individuals who are in those circumstances, revealing that, in the present case at least, the Rawlsian approach seems not to take into account the way in which individuals end up in the positions they occupy.
Limits on risks are a central part of almost all current research regulations and guidelines. With respect to those who can consent, there is an essentially implicit agreement that the risks should not be too high (as noted earlier, some argue that there should not be any net risks to even competent adults in the context of so-called therapeutic research). However, there is no consensus regarding how to determine which risks are acceptable in this context. With respect to those who cannot consent, many commentators argue that clinical research is acceptable when the net risks are very low. The challenge, currently faced by many in clinical research, is to identify a standard, and find a reliable way to implement it, for what constitutes a sufficiently low risk in this context. An interesting and important question in this regard is whether the level of acceptable risks varies depending on the particular class of individuals who cannot consent. Is the level of acceptable risks the same for individuals who were once competent, such as previously competent adults with Alzheimer disease, individuals who are not now but are expected to become competent, such as healthy children, and individuals who are not now and likely never will be competent, such as individuals born with severe cognitive disabilities?
Some argue that the risks of clinical research qualify as sufficiently low when they are ‘negligible’, understood as risks that do not pose any chance of serious harm (Nicholson 1986). Researchers who ask children a few questions for research purposes may expose them to risks no more worrisome than that of being mildly upset for a few minutes. Exposing participants to a risk of minor harm for the benefit of others does not seem to raise ethical concern. Or one might argue that the ethical concerns it raises do not merit serious ethical concern. Despite the plausibility of these views, very few studies satisfy the negligible risk standard. Even routine procedures that are widely accepted in pediatric research, such as single blood draws, pose some, typically very low risk of more than negligible harm.
Others (Kopelman 2000; Resnik 2005) define risks as sufficiently low or ‘minimal’ when they do not exceed the risks individuals face during the performance of routine examinations. This standard provides a clear and quantifiable threshold for acceptable risks. Yet, the risks of routine medical procedures for healthy individuals are so low that this standard seems to prohibit intuitively acceptable research. This approach faces the additional problem that, as the techniques of clinical medicine become safer and less invasive, increasing numbers of procedures used in clinical research would move from acceptable to unacceptable. And, at a theoretical level, one might wonder why we should think that the risks we currently happen to accept in the context of clinical care for healthy children should define the level of risk that is acceptable in clinical research. Why think that the ethical acceptability of a blood draw in pediatric research depends on whether clinicians still use blood draws as part of clinical screening for healthy children?
Many guidelines (U.S. Department of Health and Human Services 2005; Australian National Health and Medical Research Council 1999) and commentators take the view that clinical research is ethically acceptable as long as the net risks do not exceed the risks individuals face in daily life. Many of those involved in clinical research implicitly assume that this minimal risk standard is essentially equivalent to the negligible risk standard. If the risks of research are no greater than the risks individuals face in daily life, then the research does not pose risk of any serious harm. As an attitude toward many of the risks we face in daily life, this view makes sense. We could not get through the day if we were conscious of all the risks we face. Crossing the street poses more risks than one can catalog, much less process readily. When these risks are sufficiently low, psychologically healthy individuals place them in the cognitive background, ignoring them unless the circumstances provide reason for special concern (e.g. one hears a siren, or sees a large gap in the sidewalk).
Paul Ramsey reports that members of the US National Commission often used the terms ‘minimal’ and ‘negligible’ in a way which seemed to imply that they were willing to allow minimal risk research, even with children, on the grounds that it poses no chance of serious harm (Ramsey 1978). The members then went on to argue that an additional ethical requirement for such research is a guarantee of compensation for any serious research injuries. This approach to minimal risk pediatric research highlights nicely the somewhat confused attitudes we often have toward risks, especially those of daily life.
We go about our daily lives as though harms with very low probability are not going to occur, effectively treating low probability harms as zero probability events. To this extent, we are not Bayesians about the risks of daily life. We treat some possible harms as impossible for the purposes of getting through the day. This attitude, crucial to living our lives, does not imply that there are no serious risks in daily life. The fact that our attitude toward the risks of everyday life is justified by its ability to help us to get through the day undermines its ability to provide an ethical justification for exposing research participants to the same risks in the context of non-beneficial research (Ross & Nelson 2006).
First, the extent to which we ignore the risks of daily life is not a fully rational process. In many cases, our attitude regarding risks is a function of features of the situation that are not correlated directly with the risk level, such as our perceived level of control and our familiarity with the activity (Tversky, Kahneman 1974; Tversky, Kahneman 1981; Slovic 1987; Weinstein 1989). Second, to the extent that the process of ignoring some risks is rational, we are involved in a process of determining which risks are worth paying attention to. Some risks are so low that they are not worth paying attention to. Consideration of them would be more harmful (would cost us more) than the expected value of being aware of them in the first place.
To some extent, then, our attitudes in this regard are based on a rational cost/benefit analysis. To that extent, these attitudes do not provide an ethical argument for exposing research participants to risks for the benefit of others. The fact that the costs to an individual of paying attention to a given risk in daily life are greater than the benefits to that individual does not seem to have any relevance for what risks we may expose them to for the benefit of others. Finally, there is a chance of serious harm from many of the activities of daily life. This reveals that the ‘risks of daily life’ standard does not preclude the chance of some participants experiencing serious harm. Indeed, one could put the point in a much stronger way. Probabilities being what they are, the risks of daily life standard implies that if we conduct enough minimal risk research eventually a few participants will die and scores will suffer permanent disability.
As suggested above, a more plausible line of argument would be to defend clinical research that poses minimal risk on the grounds that it does not increase the risks to which participants are exposed. It seems plausible to assume that at any given time an individual will either be participating in research or involved in the activities of daily life. But, by assumption, the risks of the two activities are essentially equivalent, implying that enrollment in the study, as opposed to allowing the participant to continue to participate in the activities of daily life does not increase the risks to which he is exposed.
The problem with this argument is that the risks of research often are additive rather than substitutive. For example, participation in a study might require the participant to drive to the clinic for a research visit. The present defense succeeds to the extent that this trip replaces another trip in the car, or some similarly risky activity in which the participant would have been otherwise involved. In practice, this often is not the case. The participant instead may simply put off the trip to the mall until after the research visit. In that case, the participant’s risk of serious injury from a car trip may be doubled as a result of her participation in research. Moreover, we accept many risks in daily life because the relevant activities offer those who pursue them a chance of personal benefit. We allow children to take the bus because we assume that the benefits of receiving an education justify the risks. The fact that we accept these risks given the potential benefits provides no reason to think that the same risks or even the same level of risk would be acceptable in the context of an activity which offers no chance of medical benefit. Finally, applied strictly, this justification seems to imply that investigators should evaluate what risks individuals would face if they did not enroll in the research, and enroll only those who would otherwise face similar or greater levels of risk.
In one of the most influential papers in the history of research ethics, Hans Jonas (1969) argues that the progress clinical research offers is normatively optional, whereas the need to protect individuals from the harms to which clinical research exposes them is mandatory. He writes:
… unless the present state is intolerable, the melioristic goal [of biomedical research] is in a sense gratuitous, and this is not only from the vantage point of the present. Our descendants have a right to be left an unplundered planet; they do not have a right to new miracle cures. We have sinned against them if by our doing, we have destroyed their inheritance not if by the time they come around arthritis has not yet been conquered (unless by sheer neglect). (Jonas 1969, 230–231)
Jonas’s view does not imply that clinical research is necessarily unethical, but the conditions on when it may be conducted are very strict. This argument may seem plausible to the extent that one regards, as Jonas does, the benefits of clinical research to be ones that make an acceptable state in life even better. The example of arthritis cited by Jonas characterizes this view. Curing arthritis, like curing dyspepsia, baldness, and the minor aches and pains of living and aging, may be nice, but may be thought to address no profound problem in our lives. If this were all that clinical research had to offer, we might be reluctant to accept many risks in order to achieve its goals. We should not, in particular, take much chance of wronging individuals, or exploiting them to realize these goals.
This argument makes sense to the extent that one regards the status quo as acceptable. Yet, without further argument, it is not clear why one should accept this view; it seems almost certain that those suffering from serious illness that might be addressed by future research will not accept it. Judgments regarding the present state of society concern very general level considerations and a determination that society overall is doing fairly well is consistent with many individuals suffering terrible diseases. Presumably, the suffering of these individuals provides some reason to conduct clinical research. In response, one might understand Jonas to be arguing that the present state of affairs involves sufficiently good medicine and adequately flourishing lives such that the needs which could now be addressed by additional clinical research are not of sufficient importance to justify the risks raised by conducting it. It might have been the case, at some point in the past, that life was sufficiently nasty, brutish and short to justify running the risk of exploiting research participants in the process of identifying ways to improve the human lot. But, we have advanced, in part thanks to clinical research, well beyond that point. This reading need not interpret Jonas as ignoring the fact that there remain serious ills to be cured. Instead, he might be arguing that these ills, while real and unfortunate, are not of sufficient gravity, or perhaps prevalence to justify the risks of conducting clinical research.
This view implicitly expands the ethical concerns raised by clinical research. We have been focusing on the importance of protecting individual research participants. However, Jonas assumes that clinical research also threatens society in some sense. There are at least two possibilities here. First, it might be thought that the conduct of unethical research reaches beyond individual investigators to taint society as a whole. This does not seem unreasonable given that clinical research typically is conducted in the name of and often for the benefit of society. Second, one might be concerned that allowing investigators to expose research participants to some risks for the benefit of others might put us on a slippery slope that ends with serious abuses throughout society.
An alternative reading would be to interpret Jonas as arguing from a version of the active-passive distinction. It is often claimed that there is a profound moral difference between actively causing harm versus merely allowing harm to occur, between killing someone versus allowing them to die, for example. Jonas often seems to appeal to this distinction when evaluating the ethics of clinical research. The idea is that conducting clinical research involves investigators actively exposing individuals to risks of harm and, when those harms are realized, it involves investigators actively harming them. The investigator who injects a participant with an experimental medication actively exposes the individual to risks for the benefit of others and actively harms, perhaps even kills those who suffer harm as a result. And, to the extent that clinical research is conducted in the name of and for the benefit of society in general, one can say without too much difficulty that society is complicit in these harms. Not conducting clinical research, in contrast, involves our allowing individuals to be subject to diseases that we might otherwise have been able to avoid or cure. And this situation, albeit tragic and unfortunate, has the virtue of not involving clear moral wrongdoing.
The problem with at least this version of the argument is that the benefits of clinical research often involve finding safer ways to treat disease. The benefits of this type of clinical research, to the extent they are realized, involve clinicians being able to provide less harmful, less toxic medications to patients. Put differently, many types of clinical research offer the potential to identify medical treatments which harm patients less than current ones. This not an idle goal. One study found that the incidence of serious adverse events from the appropriate use of clinical medications (i.e. excluding such things as errors in drug administration, noncompliance, overdose, and drug abuse) in hospitalized patients was 6.7%. The same study, using data from 1994, concludes that the approved and properly prescribed use of medications is likely the 5 th leading cause of death in the US (Lazarou, Pomeranz, and Corey 1998).
These data suggest that the normative calculus is significantly more complicated than the present reading of Jonas suggests. The question is not whether it is permissible to risk harming some individuals in order to make other individuals slightly better off. Instead, we have to decide how to trade off the possibility of clinicians exposing patients to greater risks of harm (albeit with a still favorable risk-benefit ratio) in the process of treating them versus clinical researchers exposing participants to risk of harm in the process of trying to identify improved methods to treat others. This is not to say that there is no normative difference between these two activities, only that that difference is not accurately described as the difference between harming individuals versus improving their lot beyond some already acceptable status quo. It is not even a difference between harming some individuals versus allowing other individuals to suffer harms. The argument that needs to be made is that harming individuals in the process of conducting clinical research potentially involves a significant moral wrong not present when clinicians harm patients in the process of treating them.
The primary concern here is that, by exposing participants to risks of harm, the process of conducting clinical research involves the threat of exploitation of a particular kind. It runs the risk of investigators treating persons as things, devoid of any interests of their own. The worry here is not so much that investigators and participants enter together into the shared activity of clinical research with different, perhaps even conflicting goals. The concern is rather that, in the process of conducting clinical research, investigators treat participants as if they had no goals at all or, perhaps, that any goals they might have are normatively irrelevant.
Jonas argues that this concern can be addressed, and the process of experimenting on some to benefit others made ethically acceptable, only when the research participants share the goals of the research study. Ethically appropriate research, on Jonas’s view, is marked by: “appropriation of the research purpose into the person’s own scheme of ends” (Jonas 1969, 236). And assuming that it is in one’s interests to achieve one’s, at least, proper goals, it follows that, by participating in research, participants will be acting in their own interests, despite the fact that they are thereby being exposed to risky procedures which are performed to collect information to benefit others.
Jonas claims in some passages that research participants, at least those with an illness, can share the goals of a clinical research study only when they have the condition or illness under study (Jonas 1969). These passages reveal something of the account of human interests on which Jonas’s arguments rely. On standard preference satisfaction accounts of human interests, what is in a given individual’s interests depends on what the individual happens to want or prefer, or the goals the individual happens to endorse, or the goals the individual would endorse in some idealized state scrubbed clean of the delusions, misconceptions and confusion which inform their actual preferences (Griffin 1986). On this view, participation in clinical research would promote an individual’s interests as long as she was well informed and wanted to participate. This would be so whether or not she had the condition being studied. Jonas’s view, in contrast, seems to be that there are objective conditions under which individuals can share the goals of a given research study. They can endorse the cause of curing or at least finding treatments for Alzheimer disease only if they suffer from the disease themselves.
One possible objection would be to argue that there are many reasons why an individual might endorse the goals of a given study, apart from having the disease themselves. One might have family members with the disease, or co-religionists, or have adopted improved treatment of the disease as an important personal goal. The larger question is whether participants endorsing the goals of a clinical research study is a necessary condition on its acceptability. Recent commentators and guidelines rarely, if ever, endorse this condition, although at least some of them might be assuming that the requirement to obtain free and informed consent will ensure its satisfaction. It might be assumed, that is, that competent, informed, and free individuals will enroll in research only when they share the goals of the study in question.
Jonas was cognizant of the extent to which the normative concerns raised by clinical research are not exhausted by the risks to which participants are exposed, but also include the extent to which investigators and by implication society are the agents of their exposure to risks. For this reason, he recognized that the libertarian response is inadequate, even with respect to competent adults who truly understand. Finally, to the extent Jonas’s claims rely on an objective account of human interests, one may wonder whether he adopts an overly restrictive one. Why should we think, on an objective account, that individuals will have an interest in contributing to the goals of a given study only when they have the disease it addresses? Moreover, although we will not pursue the point here, appeal to an objective account of human interests raises the possibility of justifying the process of exposing research participants to risks for the benefit of others on the grounds that contributing to valuable projects, including presumably some clinical research studies, promotes (most) individuals’ interests (Wendler 2010).
The fundamental ethical challenge posed by clinical research is whether it is acceptable to expose some to research risks for the benefit of others. In the standard formulation, the one we have been considering to this point, the benefits that others enjoy as the result of participants’ participation in clinical research are medical and health benefits, better treatments for disease, better methods to prevent disease.
Industry funded research introduces the potential for a very different sort of benefit and thereby potentially alters, in a fundamental way, the moral concerns raised by clinical research. Pharmaceutical companies typically focus on generating profit and increasing stock price and market share. Indeed, it is sometimes argued that corporations have an obligation to their shareholders to pursue increased market share and share price (Friedman 1970). This approach may well lead companies to pursue new medical treatments which have little or no potential to improve overall health and well-being (Huskamp 2006; Croghan and Pittman 2004). “Me-too” drugs are the classic example here. These are drugs identical in all clinically relevant respects to approved drugs already in use. The development of a me-too drug offers the potential to redistribute market share without increasing overall health and well-being.
There is considerable debate regarding how many me-too drugs there really are and what is required for a drug to qualify as effectively identical (Garattini 1997). For example, if the existing treatment needs to be taken with meals, but a new treatment need not, is that a clinically relevant advance? Bracketing these questions, a drug company may well be interested in a drug which clearly qualifies as a me-too drug. The company may be able, by relying on a savvy marketing department, to convince physicians to prescribe, and consumers to request the new one, thus increasing profit for the company without advancing health and well-being.
The majority of clinical research was once conducted by governmental agencies. For example, the US NIH is likely the largest governmental sponsor of clinical research in the world. However, its research budget has declined over the past 20 years (Mervis 2004, 2008), and it is estimated that a majority, perhaps a significant majority of clinical research studies are now conducted by industry: “as recently as 1991 eighty per cent of industry-sponsored trials were conducted in academic health centers…Impatient with the slow pace of academic bureaucracies, pharmaceutical companies have moved trials to the private sector, where more than seventy per cent of them are now conducted” (Elliott 2008, Angell 2008, Miller and Brody 2005).
In addition to transforming the fundamental ethical challenge posed by clinical research, industry sponsored research has the potential to transform the way that many of the specific ethical concerns are addressed within that context. For example, the possibility that investigators and funders may earn significant amounts of money from their participation in clinical research might, it is thought, warp their judgment in ways that conflict with appropriate protection of research participants (Fontanarosa, Flanagin, and DeAngelis 2005). When applied to investigators and funders this concern calls into question the very significant percentage of research funded by and often conducted by for-profit organizations. Skeptics might wonder whether the goal of making money has any greater potential to influence judgment inappropriately compared to many other motivations that are widely accepted, even esteemed in the context of clinical research, such as gaining tenure and fame, impressing one’s colleagues, or winning the Nobel Prize.
Financial conflicts of interest in clinical research point to a tension between relying on profits to motivate research versus insulating drug development and testing from the profit motive as a way of protecting research participants and future patients (Psaty and Kronmal 2008). Finally, if a company can make billions of dollars a year from a single drug, one wonders what constitutes an appropriate response to the participants who were vital to its development. On a standard definition, whether a given transaction is fair depends on the risks and burdens that each party to the transaction bears and the extent to which others benefit from the party’s participation in the transaction (see entry on exploitation ). A series of clinical research studies can result in a company earning tens of billions of dollars in profits. Recognizing that a fair level of benefit is a complex function of participants’ inputs compared to the inputs of others, and the extent to which third parties benefit from those inputs, it is difficult to see how one might fill in the details of this scenario to show that the typically minimal, or non-existent compensation offered to research participants is fair.
At the same time, addressing this potential for exploitation by offering substantial payments to research participants who contribute to especially lucrative studies would introduce its own set of ethical concerns: is payment an appropriate response to the kind of contribution made by research participants; might payment constitute an undue inducement to participate; will payment undermine other participants’ altruistic motivations; to what extent does payment encourage research participants to provide misleading or false information to investigators in order to enroll and remain in research studies?
Like most early clinical research, James Lind’s experiments on treatments for scurvy took place in the clinical setting, with a physician evaluating different possible treatments in his patients. This practice eventually led to concern that it did not offer sufficient protection for patients who were frequently unaware that they were involved in research. And this concern led to separating clinical research from clinical care and subjecting it to significantly more extensive regulations, including independent review and extensive consent. This approach offered greater protections for research participants and likely led to more sophisticated clinical trials as the result of being conducted by dedicated researchers rather than clinicians in their spare time.
This segregation of clinical research from clinical care has also had significant drawbacks. It makes clinical research much more expensive and much more difficult to conduct. Given that studies are conducted in specialized environments, this approach has also undermined to some extent the relevance that the findings of clinical trials have for clinical care. For example, clinical trials assessing possible new treatments for hypertension are conducted in individuals who are aware that the trials exist and take the time to find out what is required to enroll. These studies frequently have trouble enrolling sufficient numbers of participants and take years to complete. At the same time, on the other side of the clinical research/clinical care divide, millions of patients with hypertension who might be eligible for a clinical trial are obtaining care from their doctors. Moreover, the countless data points generated by these encounters, what dose did the patient receive, did they experience any side effects, how long did they last, end up gathering dust in the patients’ medical records rather than being systematically collected and used to inform future practice.
In response, commentators have called for developing learning health care systems. According to one definition, a learning health care system is one in which “science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with best practices seamlessly embedded in the care process, patients and families active participants in all elements, and new knowledge captured as an integral by-product of the care experience” (Committee on Learning 2013). The important point for present purposes is that these commentators are calling for the desegregation of clinical research and clinical care, with clinical research once again being conducted in the context of clinical care. This approach offers what seems a potentially appealing response to the central challenge of justifying the risks to which research participants are exposed. Put simply, this practice would be justified by the fact that the practice of exposing individuals to research risks is an essential component of a learning health care system which continuously evaluates methods of providing clinical care and passes the benefits of the improvements on to its members (Faden et al 2013).
The segregated model of clinical research was designed to protect research participants from exploitation. The primary drawbacks are that it is inefficient and it raises concerns over free riders, allowing patients to realize the benefits of improved clinical care without having to accept any of the risks associated with its generation. Learning health care systems are intended to address the problem of inefficiency. Given that all the members of learning health care systems are possible research participants and also beneficiaries of research, they may, in the process, address concerns over free riders.
The ethical challenge learning health care systems face is whether it is possible to do away with the segregated model, along with its regulations and practices, without reintroducing the potential for participant exploitation. For example, should individuals in a learning health care system be told that their data might be used for research purposes? Should they be notified when it is? To what extent can patients in learning health care systems be exposed to added risks for the purposes of research? Should they be permitted to decline being so exposed? In the end, then, on-going attempts to address the concerns raised by clinical research raise new ethical concerns and, thereby, offer opportunities for philosophers and others looking for interesting, not to mention practically important issues in need of analysis and resolution.
- Angell, M., 2008. “Industry sponsored clinical research: a broken system,” Journal of the American Medical Association , 80: 899–904.
- Appelbaum, P.S., with C.W. Lidz and T. Grisso, 2004. “Therapeutic misconception in clinical research: frequency and risk factors,” IRB: Ethics and Human Research , 26: 1–8.
- Australian Government, National Health and Medical Research Council, 1999. National statement on ethical conduct in research involving humans . Ch 2.1: 92. Commonwealth of Australia, 1999.
- Beecher, H. K., 1966. “Ethics and clinical research,” N Engl J Med , 274: 1354–60.
- Brock, D. W., 1994. “Ethical issues in exposing children to risks in research,” Chapter 3 (pp. 81–101) of Grodin and Glantz (eds.), Children as Research Subjects , New York: Oxford University Press.
- Brody, B.A., 1998. The Ethics of Biomedical Research: An International Perspective , Oxford: Oxford University Press.
- Caldwell, P.H.Y., with S.B. Murphy, P.H. Butow, and J.C. Craig, 2004. “Clinical trials in children,” Lancet , 364: 803–11.
- Caplan, A., 1984. “Is there a duty to serve as a subject in biomedical research?” IRB: Ethics and Human Research , 6: 1–5.
- Committee on the Learning Health Care System in America; Institute of Medicine; Smith M, Saunders R, Stuckhardt L, et al. (eds.), Best Care at Lower Cost: The Path to Continuously Learning Health Care in America , Washington, D.C.: National Academies Press; 2013 May 10.
- Council for International Organizations of Medical Sciences, 2002. International ethical guidelines for biomedical research involving human subjects . Geneva: CIOMS.
- Croghan, T.W., and P.M. Pittman, 2004. “The medicine cabinet: What’s in it, why, and can we change the contents?” Health Affairs , 23: 23–33.
- D’Arcy Hart, P., 1999. “A change in scientific approach: From alternation to randomised allocation in clinical trials in the 1940s,” BMJ , 319: 572–3.
- Department of Health and Human Services, 2005. Code of Federal Regulations : Title 45 (Public Welfare). Part 46: protection of human subjects (45 CFR 46). US Government Printing Office.
- Dworkin, R., 1989, “The original position,” in Reading Rawls , Norman Daniels (ed.), Stanford: Stanford University Press, 16–53.
- Dworkin, G., 2005. “Paternalism,” in Stanford Encyclopedia of Philosophy (Winter 2005 Edition), Edward N. Zalta (ed.), URL = < https://plato.stanford.edu/archives/win2005/entries/paternalism/ >.
- Elliott, C., 2008, “Guinea-pigging,” The New Yorker , January 7, 2008, p. 36.
- Emanuel, E.J., with D. Wendler and C. Grady 2000. “What makes clinical research ethical?,” Journal of the American Medical Association , 283: 2701–11.
- Faden, R.R., and T.L. Beauchamp, 1986. A History and Theory of Informed Consent , New York: Oxford University Press, pp. 200–232.
- Faden, R.R., N.E. Kass, S.N. Goodman, P. Pronovost, S. Tunis, and T.L Beauchamp. An ethics framework for a learning health care system: a departure from traditional research ethics and clinical ethics , Hastings Center Report 2013; Spec No: S16-27.
- Featherstone, K., and J.L. Donovan, 2002. “Why don’t they just tell me straight, why allocate it? The struggle to make sense of participating in a randomised controlled trial,” Social Science and Medicine , 55: 709–19.
- Feinberg, J., 1986. Harm to Self , Oxford: Oxford University Press, pp. 3–26.
- Field, M.J., and R.E. Behrman, 2004. The Ethical Conduct of Clinical Research Involving Children , Washington DC: National Academies Press, Ch. 2.
- Flory, J., and E. Emanuel, 2004. “Interventions to improve research participants’ understanding in informed consent for research: A systematic review,” Journal of the American Medical Association , 292: 1593–1601.
- Fontanarosa P.B., with A. Flanagin A. and C.D. DeAngelis, 2005. “Reporting conflicts of interest, financial aspects of research, and role of sponsors in funded studies,” Journal of the American Medical Association , 294: 110–11.
- Freedman, B., 1987. “Equipoise and the ethics of clinical research,” The New England Journal of Medicine , 317: 141–45.
- Friedman M., 1970, “The social responsibility of business is to increase its profits,” The New York Times Magazine , September 13, 1970.
- Garattini S., 1997. “Are me-too drugs justified?,” J Nephrol , 10: 283–94.
- Gauthier, D., 1990. Morals by Agreement , Oxford: Clarendon Press.
- Gifford, F., 2007. “Pulling the plug on clinical equipoise: A critique of Miller and Weijer,” Kennedy Institute of Ethics Journal , 17: 203–26.
- Goodyear, M.D., with K. Krleza-Jeric and T. Lemmens, 2007. “The Declaration of Helsinki,” BMJ , 335: 624–5.
- Grady, C., 2005. “Payment of clinical research subjects,” J Clin Invest , 115: 1681–7.
- Griffin, J., 1986. Well-being: Its Meaning, Measurement and Moral Importance , Oxford: Clarendon.
- Grodin, M.A., and G.J. Annas, 1996. “Legacies of Nuremberg: Medical ethics and human rights,” Journal of the American Medical Association , 276: 1682–83.
- Harmon, A., 2010. “Indian Tribe Wins Fight to Limit Research of Its DNA,” New York Times , 21 April 2010.
- Harris, J., 2005. “Scientific research is a moral duty,” Journal of Medical Ethics , 31: 242–48.
- Hayenhjelm, M., and J. Wolff, 2012. “The moral problem of risk impositions: A survey of the literature,” European Journal of Philosophy , 20 (Supplement S1): E26–E51.
- Hellman, S., and D.S. Hellman, 1991. “Of mice but not men: Problems of the randomized clinical trial,” The New England Journal of Medicine , 324: 1585–89.
- Heyd, D., 1996. “Experimentation on trial: Why should one take part in medical research?”, Jahrbuch fur Recht und Ethik [Annual Review of Law and Ethics] , 4: 189–204.
- Huskamp, H.A., 2006. “Prices, profits, and innovation: Examining criticisms of new psychotropic drugs’ value,” Health Affairs , 25: 635–46.
- Jonas, H., 1969. “Philosophical reflections on experimenting with human subjects”, Daedalus , 98: 219–247.
- Katz, J., 1996. “The Nuremberg Code and the Nuremberg trial. A reappraisal,” Journal of the American Medical Association 276: 1662–6.
- Kopelman, L.M., 2000. “Children as research subjects: A dilemma,” Journal of Medicine and Philosophy , 25: 745–64.
- Kupst, M.J., with A.F. Patenaude, G.A. Walco, and C. Sterling, 2003. “Clinical trials in pediatric cancer: Parental perspectives on informed consent,” Journal of Pediatric Hematology and Oncology , 25: 787–90.
- Lazarou, J., with B.H. Pomeranz and P.N. Corey, 1998. “Incidence of adverse drug reactions in hospitalized patients: A meta-analysis of prospective studies,” Journal of the American Medical Association ; 279: 1200–05.
- Lederer, S.E., 1995. Subjected to Science: Human Experimentation in America before the Second World War . Baltimore: Johns Hopkins University Press.
- –––, 2003, “Children as guinea pigs: Historical perspective,” Accountability in Research , 10(1): 1–16.
- Lederer, S.E., and M.A. Grodin, “Historical overview: Pediatric experimentation,” in M.A. Grodin and L.H. Glantz (eds.), Children as Research Subjects: Science, Ethics and Law , New York: Oxford University Press, 1994.
- Levine, R.J., 1988. Ethics and Regulation of Clinical Research . 2nd ed. New Haven, Conn: Yale University Press.
- Macklin, R., 1981. “Due and undue inducements: On paying money to research subjects,” IRB: A Review of Human Subjects Research , 3: 1–6.
- Mervis, J., 2004. “U.S. Science budget: Caught in a squeeze between tax cuts and military spending,” Science , 30: 587.
- –––, 2008. “U.S. Budget: Promising year ends badly after fiscal showdown squeezes science,” Science , 319: 18–9.
- Mill, John Stuart, 1869, On Liberty . Page reference to On Liberty and Other Writings , Stefan Collini (ed.), Cambridge, Cambridge University Press, 2005, 12th edition.
- Miller, F.G., and H. Brody, 2007. “Clinical equipoise and the incoherence of research ethics,” Journal of Medicine and Philosophy , 32: 151–65.
- Miller, F.G., and A. Wertheimer, 2007. “Facing up to paternalism in research ethics,” Hastings Center Report , 37: 24–34.
- Miller, P.B., and C. Weijer, 2006. “Trust based obligations of the state and physician-researchers to patient-subjects,” Journal of Medical Ethics , 32: 542–47.
- National Bioethics Advisory Commission (NBAC), 2001. Ethical and Policy Issues in Research Involving Human Participants . Washington, DC: NBAC.
- Nicholson, R.H., 1986. Medical Research with Children: Ethics, Law, Practice . Oxford: Oxford University Press. Pages 87–100.
- Nuremberg Code, 1947, in Trials of war criminals before the Nuremberg Military Tribunals under Control Council Law No. 10 , Vol. 2, Washington, D.C.: U.S. Government Printing Office, 1949, pp. 181–182. Reprinted in Journal of the American Medical Association , 276: 1961.
- Psaty, B.M., and R.A. Kronmal, 2008. “Reporting mortality findings in trials of rofecoxib for Alzheimer disease or cognitive impairment: A case study based on documents from rofecoxib litigation,” Journal of the American Medical Association , 299: 1813–7.
- Ramsey, P., 1978. “Ethical dimensions of experimental research on children”, in Research on Children: Medical Imperatives, Ethical Quandaries, and Legal Constraints , J. van Eys (ed.), Baltimore: University Park Press, p. 61.
- Rawls, J., 1999. A Theory of Justice . Cambridge, Mass: Belknap Press of Harvard University Press.
- Resnik, D.B., 2005. “Eliminating the daily life risks standard from the definition of minimal risk,” Journal of Medical Ethics , 31: 35–8.
- Rid, A., and D. Wendler, 2011. “A framework for risk-benefit evaluations in biomedical research,” Kennedy Institute of Ethics Journal , 21(2): 141–179.
- Roberts, R., with W. Rodriquez, D. Murphy, and T. Crescenzi, 2003. “Pediatric drug labeling: Improving the safety and efficacy of pediatric therapies,” Journal of the American Medical Association , 290: 905–11.
- Ross, L.F., and R.M. Nelson, 2006. “Pediatric research and the federal minimal risk standard,” Journal of the American Medical Association , 295: 759.
- Rothman, D.J., 2000. “The shame of medical research”, The New York Review of Books , 47 (19): 60–64.
- Sachs, Ben, 2010. “The exceptional ethics of the investigator-subject relationship,” Journal of Medicine and Philosophy , 35: 64–80.
- Shuster, E., 1997. “Fifty years later: The significance of the Nuremberg Code,” The New England Journal of Medicine , 337: 1436–40.
- Slovic, P., 1987. “Perception of risk,” Science , 236: 280–85.
- Snowdon, C., with J. Garcia, and D. Elbourne, 1997. “Making sense of randomization: Responses of parents of critically ill babies to random allocation of treatment in a clinical trial,” Social Science and Medicine , 45: 1337–55.
- Spilker, B., 1991. Guide to clinical trials , Philadelphia: Lippincott, Williams and Wilkins.
- Stark, C., 2000. “Hypothetical consent and justification,” Journal of Philosophy , 97: 313–34.
- Stewart, Paul M., with Anna Stears, Jeremy W. Tomlinson, and Morris J. Brown, 2008. “Regulation—the real threat to clinical research,” British Medical Journal , 337: 1085–1087.
- Sullivan, Richard, 2008. “The good, the bad and the ugly: Effect of regulation on cancer research,” Lancet Oncology , 9: 2–3.
- Sutton, G., 2003. “Putrid gums and ‘dead men’s cloaths’: James Lind aboard the Salisbury,” Journal of the Royal Society of Medicine , 96: 605–8.
- Tversky, A., and D. Kahneman, 1974. “Judgments under uncertainty: Heuristics and biases,” Science , 185: 1124–31.
- –––, 1981, “The framing of decisions and the rationality of choice,” Science , 211: 453–8.
- Vollmann J., and R. Winau, 1996. “Informed consent in human experimentation before the Nuremberg code,” British Medical Journal , 313: 1445–7.
- Weinstein, N., 1989. “Optimistic biases about personal risks,” Science , 246: 1232–3.
- Wenar, L., 2008. “John Rawls”, The Stanford Encyclopedia of Philosophy (Summer 2008 Edition) , Edward N. Zalta (ed.), URL = < https://plato.stanford.edu/archives/sum2008/entries/rawls/ >.
- Wendler, D., 2010, The Ethics of Pediatric Research , Oxford: Oxford University Press.
- Wertheimer, A., 2008. “Exploitation”, The Stanford Encyclopedia of Philosophy (Fall 2008 Edition), Edward N. Zalta (ed.), URL = < https://plato.stanford.edu/archives/fall2008/entries/exploitation/ >.
- –––, 2010, Rethinking the Ethics of Clinical Research: Widening the Lens , Oxford: Oxford University Press.
- Wilson, James, and David Hunter, 2010. “Research exceptionalism,” American Journal of Bioethics , 10: 45–54.
- World Medical Organization, 1996. Declaration of Helsinki , British Medical Journal, 313 (7070): 1448–1449.
How to cite this entry . Preview the PDF version of this entry at the Friends of the SEP Society . Look up topics and thinkers related to this entry at the Internet Philosophy Ontology Project (InPhO). Enhanced bibliography for this entry at PhilPapers , with links to its database.
- Bioethics.net , organized by the editors of the American Journal of Bioethics.
- Bioethics Literature Database , German site for conducting searches
- National Reference Center for Bioethics Literature , organized by the research library at the Kennedy Institute of Ethics
- Nuffield Council on Bioethics , organized by the Nuffield council, the preeminent organization on ethics in Britain
- Office for Human Research Protections (OHRP), Department of Health and Human Services, website of the office that oversees U.S. research regulations.
- PRIM&R , Public Responsibility in Medicine and Research
- SARETI , The South African Research Ethics Training Initiative
cloning | contract law, philosophy of | decision-making capacity | exploitation | health | informed consent | original position | paternalism | Rawls, John | risk
Copyright © 2021 by David Wendler < dwendler @ nih . gov >
- Accessibility
Support SEP
Mirror sites.
View this site from another server:
- Info about mirror sites
The Stanford Encyclopedia of Philosophy is copyright © 2023 by The Metaphysics Research Lab , Department of Philosophy, Stanford University
Library of Congress Catalog Data: ISSN 1095-5054
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- The revised...
The revised International Code of Medical Ethics unites doctors under one global medical ethos
- Related content
- Peer review
- Ramin W Parsa-Parsi , head 1 ,
- Raanan Gillon , emeritus professor of medical ethics 2 ,
- Urban Wiesing , director 3
- 1 Department for International Affairs, German Medical Association, Germany
- 2 Imperial College London, UK
- 3 Institute of Ethics and History of Medicine, University of Tübingen, Germany
The World Medical Association’s revised International Code of Medical Ethics offers a core set of ethical norms for all doctors worldwide to follow, write Ramin W Parsa-Parsi , Raanan Gillon , and Urban Wiesing
Increasing global mobility, and the growing plurality in society that comes with it, has an undeniable effect on medical practice. The likelihood of patients consulting doctors with different cultural backgrounds, religions, or secular values has increased substantially. This raises several essential questions for the medical profession around whether patients can expect a core set of ethical norms from all doctors regardless of their location, backgrounds, and beliefs or whether patients have to accept that ethical norms will differ depending on where they are in the world. We firmly believe that the medical profession across the world needs common answers to such questions and that there should be (and is) a core set of ethical norms for the world’s doctors.
The World Medical Association (WMA) was founded after the second world war largely to re-establish trust in the medical profession by re-affirming that there were some norms of medical practice that must apply to all doctors globally. The WMA Declaration of Geneva 1 —also known as the physician’s pledge and regarded as a modernised version of the Hippocratic oath—was adopted in 1948 and intended to prevent the horrific ethical failures of doctors during the war from being repeated. A year later, practical implications of that declaration for medical practice were agreed in the first International Code of Medical Ethics. 2 Then in 1964 the first code of ethics for medical research was published as the Declaration of Helsinki. 3
To re-establish trust in doctors and medicine, the medical organisations represented by the WMA clearly thought that their members, now more than 10 million doctors, were required to adhere to common norms of medical ethics no matter where they practised. But could that commitment survive the ever increasing challenges of globalisation? Yes; over a four year process, ending in October 2022, the WMA revised the International Code of Medical Ethics, with its own intrinsic international and intercultural input, augmented by a variety of international conferences at which drafts of the revised document were reviewed, and we have described this revision process in the Journal of Medical Ethics . 4 As the WMA regularly updates all its policies, and a substantive revision of the Declaration of Geneva had been concluded in 2017, it became even more important for the International Code of Medical Ethics to be reviewed and modernised.
The revised code provides a framework of ethical principles and values to which patients globally can expect doctors to adhere. The updated guidelines reflect consensus on certain globally acceptable and trust enhancing underlying ethical drivers and on important specific obligations that flow from these. The many “shoulds and musts” for doctors to adhere to in the revised code are underpinned by the four fundamental ethical principles of beneficence, non-maleficence, respect for autonomy, and justice/fairness, augmented by the two additional core ethical principles of respect for human life and respect for human dignity. 4 5
We acknowledge that the revision process would have benefited from even broader international participation, particularly from resource limited settings. 6 Nevertheless, it is reassuring that the international WMA workgroup tasked with leading the revision process agreed easily and rapidly on most parts of the code. After an extensive in-person and online international consultation process, the WMA General Assembly adopted the final version of the revised code unanimously. 4
When the international workgroup encountered conflict and tension on certain topics, most notably that of conscientious objection by doctors, it sought a balance between stating specific, detailed duties and providing more general accounts of duties that leave room for professional judgment and interpretation.
Potential conflicts between doctors’ duties and patient rights were considered in debates about the conscientious objection paragraph of the code, not only in the workgroup, but also in the WMA’s broader Medical Ethics Committee, in an online and worldwide public consultation, and in a conference dedicated to the subject of conscientious objection, where proponents of a broad spectrum of viewpoints were invited to speak and debate. Some of the most contentious moral issues that doctors encounter in their medical practice are not specifically included in the International Code of Medical Ethics—notably abortion and physician assisted suicide. However, the code focuses on laying down the basic ethical principles for doctors. Despite the existence of universal ethical principles, some genuine moral dilemmas arise, about which there will be deeply conflicting moral views, and a relatively short code of ethics cannot resolve them. 6
By adhering to these updated principles, the global medical community will reassure patients and populations and strengthen its own trustworthiness and professional standing. We advocate for the International Code of Medical Ethics to become standard reading for all medical students and doctors. One way to increase awareness of the code would be to include it in the curriculum of basic medical education.
With this comprehensive revision, the WMA once again shows that the physicians of the world are united by one global medical ethos.
Acknowledgments
The authors are grateful to Siobhan O’Leary for her assistance.
Competing interests: RWP-P has been a council member of the World Medical Association (WMA), a member of the WMA Medical Ethics Committee, and chair of the International Code of Medical Ethics revision workgroup. In this capacity, he received financial support for travel and accommodation for WMA International Code of Medical Ethics related conferences or meetings. RG was a member of the International Code of Medical Ethics revision workgroup. He is honorary president of the Institute of Medical Ethics and an elected member of BMA Council. UW is WMA ethics adviser and was a member of the International Code of Medical Ethics revision workgroup. In this capacity, he received financial support for travel and accommodation for WMA International Code of Medical Ethics related conferences or meetings. He also received grants or payments for lectures and presentations from the industry or organisations for other not directly related projects.
Provenance and peer review: Not commissioned; not externally peer reviewed.
- ↵ World Medical Association. WMA Declaration of Geneva. https://www.wma.net/policies-post/wma-declaration-of-geneva/
- ↵ World Medical Association. WMA International Code of Medical Ethics. https://www.wma.net/policies-post/wma-international-code-of-medical-ethics/
- ↵ World Medical Association. WMA Declaration of Helsinki—ethical principles for medical research involving human subjects. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
- Parsa-Parsi RW ,
- Beauchamp T ,
- Childress J
Groundbreaking Research Shows Ancient Egyptians Were Conducting Cancer Surgery Over 4,000 Years Ago
By putting an ancient skull under the microscope, scientists are proving that cancer research is about 1,000 years older than previously thought
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Julia_Binswanger.png)
Julia Binswanger
Daily Correspondent
:focal(564x322:565x323)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer_public/4b/ff/4bffec00-f9ae-42fd-9028-fe15eb5c4b21/skull_236.webp)
A new study published in the journal Frontiers in Medicine is radically changing ideas about early cancer studies.
Researchers examining an over 4,000-year-old Egyptian skull have found that ancient doctors may have used surgical intervention to treat brain cancer.
"What we found is the first evidence of a surgical intervention directly related to cancer," Edgard Camarós , paleopathologist at the University of Santiago de Compostela in Spain and co-author of the research paper, tells Live Science ’s Emily Cooke. "This is where modern medicine starts."
The skull, part of the University of Cambridge 's Duckworth Collection , dates from between 2687 and 2345 B.C.E. and belonged to a 30 to 35-year-old man. Since the mid-19th century, experts have been examining the Egyptian man’s cranial remains.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer_public/d4/a2/d4a2ef42-9e59-4240-a7bd-c96029846d59/still25_11__cut_marks_-min.webp)
Studying cancer in the ancient world can be tricky because the disease often presents in the soft tissue, and experts do not have access to a patient’s medical history. Previous research on the skull showed that the man had suffered from one large brain tumor and 30 small metastasized lesions.
Through microscope and microtomography scans, Camarós and his team found cut marks on the skull’s edges right where the cancerous lesions appeared. They concluded that a sharp metal tool was responsible for the incisions. Thus, ancient doctors were not only aware of the cancer, they were likely looking to learn more about it through surgical intervention.
“When we first observed the cut marks under the microscope, we could not believe what was in front of us,” says Tatiana Tondini , a researcher at the University of Tübingen and study co-author, in a statement.
“There was an uncomfortable silence in the room, because we knew what we had just discovered,” Camarós tells the New York Times ’ Jordan Pearson.
Before the study was published, researchers believed that the oldest description of cancer came from the Edwin Smith Papyrus , an ancient Egyptian medical text from around 1600 B.C.E. The new research changes the timeline on the first cancer treatments in human history, moving the date up about 1,000 years earlier.
Still, the researchers do not know whether doctors cut into the skull while the patient was still living or shortly after his death for a cancer-related autopsy.
“If those cut marks were done with that person alive, we’re talking about some kind of treatment directly related to the cancer,” Camarós tells CNN . He adds that either way, “it’s amazing to think that they performed a surgical intervention.”
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer_public/df/4d/df4deb53-a8e5-402c-b228-49046ae279e2/small_still25_11-_cut-marks_-_2.webp)
The researchers also found other evidence of ancient Egyptian medicine.
The team looked at the skull of a woman over 50 years old who lived between 664 and 343 B.C.E. The woman had two lesions related to a traumatic head injury that had healed. In turn, experts believe that someone attacked her with a sharp weapon and she likely survived with the help of medical treatment. Her skull also had a cancer-related lesion, but there weren’t signs she received treatment for it.
With this new evidence, Camarós and his team are wondering if other ancient societies studied cancer as well.
He tells Live Science , "If we know that more than 4,000 years ago, ancient Egyptians were trying to understand cancer at a surgical level, we are absolutely convinced that this is just the beginning of something that started many, many thousands of years ago."
Get the latest stories in your inbox every weekday.
/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/accounts/headshot/Julia_Binswanger.png)
Julia Binswanger | READ MORE
Julia Binswanger is a freelance arts and culture reporter based in Chicago. Her work has been featured in WBEZ, Chicago magazine, Rebellious magazine and PC magazine.
History and Development of Medical Ethics In the West
- First Online: 27 March 2019
Cite this chapter

- Georgina D. Campelia 2 &
- Denise M. Dudzinski 2
872 Accesses
This chapter will chart some of the history of medical ethics in the West, beginning before the term was coined in 1803 by Thomas Percival and ending with today’s notion of bioethics. This chapter will address some of the key conflicts and historical shifts that transformed medical ethics from an unnamed and amorphous idea to a distinctive field of study informing patient care. The path is complex with medical advances and pitfalls over the centuries that both compel and inhibit progress. With each historical shift, distinguishing features arise. Medical ethics first takes shape in oaths of faith and loyalty, where the virtues and moral obligations of physicians were grounded in the dictates of the gods, the state, the crown, and/or the church. Over the course of the sixteenth to the nineteenth centuries, these oaths come to be defined by an emerging practice of medicine. As such, the power of the oaths comes from the professional contract rather than those higher authorities. Even so, little has changed in the named virtues (fidelity, beneficence, compassion, integrity), and their moral standing continued to be founded on social consensus rather than moral argument. Finally, through the struggles and failures of scientific progress in the nineteenth and twentieth centuries, there is an urgent demand for the moral reasoning and rigorous justification that comes to define bioethics as we know it today.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Foucault, M. “Les Reportages d’Idees”, in Corriere Della Sera (Milan, 12 Nov. 1978; repr. In Dilder Eribon, Michel Foucault), 1989; Tr.1991.
Baker and McCullough [ 4 ].
See, e.g., Ellis [ 13 ], Gawande [ 16 ].
Here, and throughout, we use Allan Bloom’s translation of Plato’s Republic [ 42 ].
Here, and throughout, we use the Broadie and Rowe translation of Aristotle’s Nicomachean Ethics [ 2 ].
See Jahr [ 28 ].
Bibliography
1906: Richard Strong, MD, cholera. 2017. from Alliance for Human Research Protection. http://ahrp.org/1906-richard-strong-md-cholera /.
Aristotle. Nicomachean Ethics (trans: Broadie S and Rowe C, editors: Broadie S and Rowe C). Oxford: Oxford University Press; 2002.
Google Scholar
Baker R. Before bioethics: a history of American medical ethics from the colonial period to the bioethics revolution. New York, NY: Oxford University Press; 2013.
Book Google Scholar
Baker RB, McCullough LB. What is the history of medical ethics? In: Baker RB, McCullough LB, editors. The Cambridge world history of medical ethics. Cambridge, UK: Cambridge University Press; 2009.
Beauchamp TL, Childress JF. Principles of biomedical ethics. New York, NY: Oxford University Press; 2012.
Beecher H. Ethics and clinical research. N Engl J Med. 1966;274:1354–60.
Article CAS Google Scholar
Belli SR, Melvin M. The evolution of MEdical malpractice law. In: Vevaina JR, Bone RC, Kassoff E, editors. Legal aspects of medicine. New York, NY: Springer-Verlag; 1989.
Bonner BE. Mid wife’s Oath. In: Helm W, editors. Curious miscellaneous fragments of various subjects more particularly relative to english history from the year 1050, to the year 1701, compiled from British Writers during that period. London: Baldwin, Cradock and Joy; [1555] 1815.
Bruinius H. Better for all the world: the secret history of forced sterilization and America’s quest for racial purity. New York, NY: Alfred A. Knopf; 2006.
The Code of Hammurabi. (c. 1754 BC). Retrieved from http://avalon.law.yale.edu/ancient/hamframe.asp .
Code of Medical Ethics of the American Medical Association. Philadelphia: American Medical Association; 1847.
Daniel K. In the name of eugenics: genetics and the uses of human heredity. New York, NY: Alfred A. Knopf; 1985.
Ellis H. A history of surgery. London: Greenwich Medical Media; 2000.
Freedman B. Equipoise and the ethics of clinical research. N Engl J Med. 1987;317(3):141–5.
Garnet R. The book of oaths. In: Aughterson K, editor. Renaissance woman: a sourcebook: constructions of femininity in England. New York, NY: Routledge; [1649]1995. p. 212–214.
Gawande A. Two hundred years of surgery. N Engl J Med. 2012;366:1716–23.
Goldman D, Murray M. Studies on the use of refrigeration therapy in mental disease with report of sixteen cases. J Nerv Ment Dis. 1943;97(2):152–65.
Article Google Scholar
Gregory J. Observations on the duties and offices of a physician and on the method of promoting enquiry in philosophy. London: Strahan and Cadell; 1770.
Harvey JC. André Hellegers, the Kennedy institute, and the development of bioethics: the American–European connection. In: Garrett JR, Jotterand F, Ralston DC, editors. The development of bioethics in the United States. Dordrecht: Springer Science & Business Media; 2013. p. 37–54.
Chapter Google Scholar
Held V. Care and justice in the global context. Ratio Juris. 2004;17:141–55.
Highet MJ. Body Snatching & Grave Robbing: bodies for science. Hist Anthropol. 2006;16(4):415–40.
Hippocrates. The Hippocratic Oath (trans: North M): National Library of Medicine; 2002. Retrieved from https://www.nlm.nih.gov/hmd/greek/greek_oath.html .
History of the Medical Society of the State of New York. In: Walsh JJ, editor. New York, NY: Medical Society of the State of New York; 1907.
Hornblum AM. Acres of skin: human experiments at Holmesburg prison. New York, NY: Routledge; 1998.
Iniesta I. Hippocratic Corpus. Br Med J. 2011;342(7803):929.
Instruments of Association and Constitutions of the New Jersey Medical Society. In: Rogers FB, Sayre AR, editors. The healing art: a history of the medical Society of new Jersey. Trenton, NJ: The Medical Society of New Jersey; 1966.
Jahr F. Life sciences and the teaching of ethics. In: Miller IM, Sass H-M, editors. Essays in bioethics. Berlin: LIT Verlag Münster; 1926, 2013.
Jahr F. Bio-Ethik. Eine Umschau über die ethischen Beziehungen des Menschen zu Tier und Pflanze. Kosmos Handweiser für Naturfreunde. 1927;24(1):2–4.
Jonsen AR. The birth of bioethics. New York, NY: Oxford University Press; 1998.
Jonsen AR. A short history of medical ethics. New York, NY: Oxford University Press; 2000.
Jonsen AR. Celebrating Professor Al Jonsen: Hastings Center Beecher Award Ceremony. Paper presented at the The 19th Annual Meeting of the American Society for Bioethics and Humanities. Kansas City, MO; 2017.
Kalokairinou EM. Fritz Jahr’s bioethics imperative: its origin, point, and influence. JAHR. 2016;7/2(14):149–56.
Kristof N. Unmasking horror -- a special report.; Japan confronting gruesome war atrocity. The New York Times; 1995. Retrieved from http://www.nytimes.com/1995/03/17/world/unmasking-horror-a-special-report-japan-confronting-gruesome-war-atrocity.html?pagewanted=all .
Kuhse H, Singer P. What is bioethics? A historical introduction. In: Kuhse H, Singer P, editors. A Copanion to bioethics: second edition. Oxford: Blackwell Publishing Ltd; 2009.
Lovejoy B. Body Snatchers of Old New York. Lapham’s Quarterly; 2013.
Lovejoy B. The Gory New York City Riot that Shaped American Medicine. Smithsonian; 2014. Retrieved from http://www.smithsonianmag.com/history/gory-new-york-city-riot-shaped-american-medicine-180951766/ .
Mackenzie C, Stoljar N. Relational autonomy: feminist perspectives on autonomy, agency, and the social self. New York, NY: Oxford University Press; 2000.
The Manhattan Project: A New and Secret World of Human Experimentation. Retrieved 18 Sept 2017, from Georgetown University. https://bioethicsarchive.georgetown.edu/achre/final/intro_3.html .
Monro A. Presbyterian inquisition as it was lately Practised Against the Professors of the College of Edinburgh, Agust and September, 1690, in which the Spirit of Presbytery and their Present Method of Procedure is Plainly Discovered, Matter of Fact by Undeniable Instances Cleared, and Libels Against Particular Persons Discussed. London: J. Hindmarsh; 1691.
Ojanuaga D. The medical ethics of the "father of gynaecology", Dr J Marion Sims. J Med Ethics. 1993;19(1):28–31.
Pellegrino ED. Percival’s Medical Ethics : The moral philosophy of an 18th-century English gentleman. Arch Intern Med. 1986;146(11):2265–9.
Plato. The Republic of Plato. (trans: Bloom A, editor: Bloom A). United States of America: Basic Books; 1968.
Reilly P. Eugenics and involuntary sterilization. Annual Review Genomics and Human Genetics. 2015;16:351–68.
Richards EP. Advisory Committee on Human Radiation Experiments Report, Chapter 9; 1995. Retrieved from https://biotech.law.lsu.edu/research/reports/ACHRE/chap9_2.html .
Robinson F. Human rights and the global politics of resistance: feminist perspectives. Rev Int Stud. 2003;29(S1):161–80.
National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont report: ethical principles and guidelines for the protection of human subjects of research. United States of America: The Commission; 1979.
Ryan M. A manual of medical jurisprudence, compiled from the best medical and legal works; being an analysis of a course of lectures on forensic medicine, Annually delivered in London. 2nd ed. Philadelphia: Carrey and Lea; 1832.
Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;46(7):678–85.
Skloot R. The immortal life of Henrietta lacks. New York, NY: Crown Publishers; 2010.
Tietjens Meyers D, editor. Feminists rethink the self. Boulder: Westview Press; 1997.
Tronto J. Moral boundaries: a political argument for an ethic of care. New York, NY: Routledge; 1993.
The Tuskegee Timeline. Retrieved 18 Sept 2017, from Centers for Disease Control and Prevention; 2015. https://www.cdc.gov/tuskegee/timeline.htm
Urban Walker M. Moral understandings: feminist study in ethics. New York, NY: Routledge; 1998.
Wall LL. The medical ethics of Dr. J Marion Sims: a fresh look at the historical record. Journal of Medical Ethics. 2005;32(6):346–50.
Walter M. First, do harm. Nature. 2012;482:148–52.
World Medical Association. Declaration of Geneva; 1948. Retrieved September 2017, from World Medical Association: https://www.wma.net/policies-post/wma-declaration-of-geneva/ .
Suggested Literature
Eckenwiler LA, Cohn FG, editors. The ethics of Bioethis: mapping the moral landscape. Baltimore: Johns Hopkins University Press; 2007.
Download references
Author information
Authors and affiliations.
Department of Bioethics & Humanities, University of Washington School of Medicine, & UW Medicine Ethics Consultation Service, Seattle, WA, USA
Georgina D. Campelia & Denise M. Dudzinski
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Georgina D. Campelia .
Editor information
Editors and affiliations.
Department of Surgery, University of Buenos Aires, Buenos Aires, Argentina
Alberto R. Ferreres
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Campelia, G.D., Dudzinski, D.M. (2019). History and Development of Medical Ethics In the West. In: Ferreres, A. (eds) Surgical Ethics. Springer, Cham. https://doi.org/10.1007/978-3-030-05964-4_1
Download citation
DOI : https://doi.org/10.1007/978-3-030-05964-4_1
Published : 27 March 2019
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-05963-7
Online ISBN : 978-3-030-05964-4
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
This page uses technologies your browser does not support.
Many of our new website's features will not function and basic layout will appear broken.
Visit browsehappy.com to learn how to upgrade your browser.
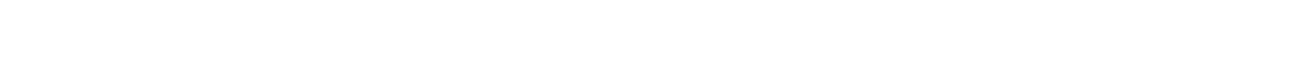
- university of new orleans
- campus news
- in memoriam: philosophy professor frank schalow
CAMPUS NEWS: MAY 30, 2024
In memoriam, in memoriam: philosophy professor frank schalow.
Share this article
Frank Schalow, a University of New Orleans philosophy faculty member, died May 25, 2024.
Frank Schalow, a University of New Orleans philosophy faculty member for nearly three decades and an internationally renowned authority on German philosopher Martin Heidegger, died on May 25 at the age of 68.
Schalow started his career at UNO in 1995 as an adjunct faculty member. In 2001, he was promoted to assistant professor and became a full professor in 2010. He taught classes including Introduction to Philosophy, Social Ethics, Ethics, The Philosophy of Kant and The Philosophy of Heidegger.
Schalow was a prolific author and researcher. He wrote 12 books on Heidegger and was the longtime co-editor of “Heidegger Studies,” an international journal published in four languages. Considered one of the most influential thinkers of the 20th century, Heidegger was best known for his philosophy of existentialism. Schalow’s other areas of research interest included ethics, medical ethics, phenomenology, and 19th and 20th century German thought.
“Dr. Schalow had the admiration of his students and the respect of his colleagues,” said Robert Stufflebeam, associate professor of philosophy. “He was the embodiment of the philosophy professor stereotype. He was brilliant, but quirky. He always wore a tie, even if it bore no stylistic relation to whatever shirt he was wearing. He always spoke thoughtfully and logically. He was never heard to raise his voice in anger. The philosophy program has suffered a great loss. Professor Schalow was one of a kind. He will be missed.”
In addition to the dozen books he authored on Heidegger, Schalow co-edited three books, wrote 16 chapters, and authored several dozen journal articles, review essays, critical discussions and book reviews, Stufflebeam said.
According to colleagues, Schalow’s commitment to his discipline was matched only by his devotion to the stray cats for which he cared for in his New Orleans neighborhood and his beloved New York Yankees.
Schalow earned a bachelor’s degree from the University of Denver, and both a master’s and doctorate in philosophy from Tulane University.

Student Access and Success Drives UNO’s New Enrollment VP
Uno-delgado partnership to enhance transfer student success in biology.
UNO and Innsbruck Students Create ‘History Exchange,’ An Oral History Podcast
- Patient Care & Health Information
- Diseases & Conditions
- Neurofibromatosis type 1
Neurofibromatosis type 1 (NF1) is a genetic condition that causes changes in skin pigment and tumors on nerve tissue. Skin changes include flat, light brown spots and freckles in the armpits and groin. Tumors can grow anywhere in the nervous system, including the brain, spinal cord and nerves. NF1 is rare. About 1 in 2,500 is affected by NF1.
The tumors often are not cancerous, known as benign tumors. But sometimes they can become cancerous. Symptoms often are mild. But complications can occur and may include trouble with learning, heart and blood vessel conditions, vision loss, and pain.
Treatment focuses on supporting healthy growth and development in children and early management of complications. If NF1 causes large tumors or tumors that press on a nerve, surgery can reduce symptoms. A newer medicine is available to treat tumors in children, and other new treatments are being developed.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Neurofibroma
Neurofibromatosis type 1 (NF1) usually is diagnosed during childhood. Symptoms are seen at birth or shortly afterward and almost always by age 10. Symptoms tend to be mild to moderate, but they can vary from person to person.
Symptoms include:
- Flat, light brown spots on the skin, known as cafe au lait spots. These harmless spots are common in many people. But having more than six cafe au lait spots suggests NF1. They often are present at birth or appear during the first years of life. After childhood, new spots stop appearing.
- Freckling in the armpits or groin area. Freckling often appears by ages 3 to 5. Freckles are smaller than cafe au lait spots and tend to occur in clusters in skin folds.
- Tiny bumps on the iris of the eye, known as Lisch nodules. These nodules can't easily be seen and don't affect vision.
- Soft, pea-sized bumps on or under the skin called neurofibromas. These benign tumors usually grow in or under the skin but can also grow inside the body. A growth that involves many nerves is called a plexiform neurofibroma. Plexiform neurofibromas, when located on the face, can cause disfigurement. Neurofibromas may increase in number with age.
- Bone changes. Changes in bone development and low bone mineral density can cause bones to form in an irregular way. People with NF1 may have a curved spine, known as scoliosis, or a bowed lower leg.
- Tumor on the nerve that connects the eye to the brain, called an optic pathway glioma. This tumor usually appears by age 3. The tumor rarely appears in late childhood and among teenagers, and almost never in adults.
- Learning disabilities. It's common for children with NF1 to have some trouble with learning. Often there is a specific learning disability, such as trouble with reading or math. Attention-deficit/hyperactivity disorder (ADHD) and speech delay also are common.
- Larger than average head size. Children with NF1 tend to have a larger than average head size due to increased brain volume.
- Short stature. Children who have NF1 often are below average in height.
When to see a doctor
See a healthcare professional if your child has symptoms of neurofibromatosis type 1. The tumors are often not cancerous and are slow growing, but complications can be managed. If your child has a plexiform neurofibroma, a medicine is available to treat it.
Neurofibromatosis type 1 is caused by an altered gene that either is passed down by a parent or occurs at conception.
The NF1 gene is located on chromosome 17. This gene produces a protein called neurofibromin that helps regulate cell growth. When the gene is altered, it causes a loss of neurofibromin. This allows cells to grow without control.
Risk factors
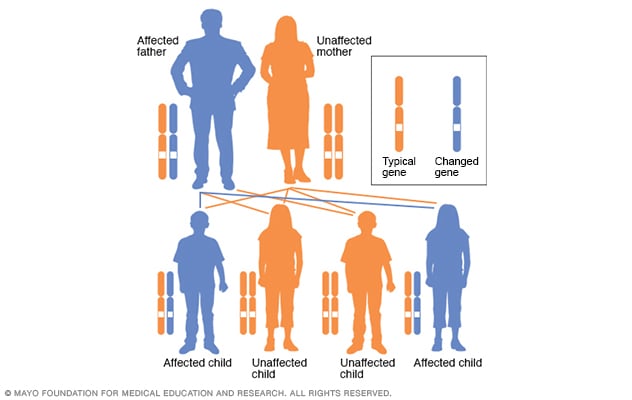
Autosomal dominant inheritance pattern
In an autosomal dominant disorder, the changed gene is a dominant gene. It's located on one of the nonsex chromosomes, called autosomes. Only one changed gene is needed for someone to be affected by this type of condition. A person with an autosomal dominant condition — in this example, the father — has a 50% chance of having an affected child with one changed gene and a 50% chance of having an unaffected child.
The biggest risk factor for neurofibromatosis type 1 (NF1) is a family history. For about half of people who have NF1, the disease was passed down from a parent. People who have NF1 and whose relatives aren't affected are likely to have a new change to a gene.
NF1 has an autosomal dominant inheritance pattern. This means that any child of a parent who is affected by the disease has a 50% chance of having the altered gene.
Complications
Complications of neurofibromatosis type 1 (NF1) vary, even within the same family. Generally, complications occur when tumors affect nerve tissue or press on internal organs.
Complications of NF1 include:
- Neurological symptoms. Trouble with learning and thinking are the most common neurological symptoms associated with NF1. Less common complications include epilepsy and the buildup of excess fluid in the brain.
- Concerns with appearance. Visible signs of NF1 can include widespread cafe au lait spots, many neurofibromas in the facial area or large neurofibromas. In some people this can cause anxiety and emotional distress, even if they're not medically serious.
- Skeletal symptoms. Some children have bones that didn't form as usual. This can cause bowing of the legs and fractures that sometimes don't heal. NF1 can cause curvature of the spine, known as scoliosis, that may need bracing or surgery. NF1 also is associated with lower bone mineral density, which increases the risk of weak bones, known as osteoporosis.
- Changes in vision. Sometimes a tumor called an optic pathway glioma develops on the optic nerve. When this happens, it can affect vision.
- Increase in symptoms during times of hormonal change. Hormonal changes associated with puberty or pregnancy might cause an increase in neurofibromas. Most people who have NF1 have healthy pregnancies but will likely need monitoring by an obstetrician who is familiar with NF1.
- Cardiovascular symptoms. People who have NF1 have an increased risk of high blood pressure and may develop blood vessel conditions.
- Trouble breathing. Rarely, plexiform neurofibromas can put pressure on the airway.
- Cancer. Some people who have NF1 develop cancerous tumors. These usually arise from neurofibromas under the skin or from plexiform neurofibromas. People who have NF1 also have a higher risk of other forms of cancer. They include breast cancer, leukemia, colorectal cancer, brain tumors and some types of soft tissue cancer. Screening for breast cancer should begin earlier, at age 30, for women with NF1 compared to the general population.
- Benign adrenal gland tumor, known as a pheochromocytoma. This noncancerous tumor produces hormones that raise your blood pressure. Surgery often is needed to remove it.
Neurofibromatosis type 1 care at Mayo Clinic
- Ferri FF. Neurofibromatosis. In: Ferri's Clinical Advisor 2024. Elsevier; 2024. https://www.clinicalkey.com. Accessed Feb. 21, 2024.
- Neurofibromatosis. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Neurofibromatosis-Fact-Sheet. Accessed Feb. 21, 2024.
- Korf BR, et al. Neurofibromatosis type 1 (NF1): Pathogenesis, clinical features, and diagnosis. https://www.uptodate.com/contents/search. Accessed Feb. 21, 2024.
- Saleh M, et al. Neurofibromatosis type 1 system-based manifestations and treatments: A review. Neurological Sciences. 2023; doi:10.1007/s10072-023-06680-5.
- Neurofibromatosis. American Association of Neurological Surgeons. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Neurofibromatosis. Accessed Feb. 21, 2024.
- Neurofibromatosis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/pediatrics/neurocutaneous-syndromes/neurofibromatosis. Accessed Feb. 21, 2024.
- Jankovic J, et al., eds. Neurocutaneous syndromes. In: Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Feb. 21, 2024.
- Armstrong AE, et al. Treatment decisions and the use of the MEK inhibitors for children with neurofibromatosis type 1-related plexiform neurofibromas. BMC Cancer. 2023; doi:10.1186/s12885-023-10996-y.
- Zitelli BJ, et al., eds. Neurology. In: Zitelli and Davis' Atlas of Pediatric Physical Diagnoses. 8th ed. Elsevier; 2023. https://www.clinicalkey.com. Accessed Feb. 21, 2024.
- Kellerman RD, et al. Neurofibromatosis (type 1). In: Conn's Current Therapy 2024. Elsevier; 2024. https://www.clinicalkey.com. Accessed Feb. 21, 2024.
- Babovic-Vuksanovic D (expert opinion). Mayo Clinic. March 26, 2024.
- Tamura R. Current understanding of neurofibromatosis type 1, 2 and schwannomatosis. International Journal of Molecular Sciences. 2021; doi:10.3390/ijms22115850.
- Legius E, et al. Revised diagnostic criteria for neurofibromatosis type 1 and Legius syndrome: An international consensus recommendation. Genetics in Medicine. 2021; doi:10.1038/s41436-021-01170-5.
- Find a doctor. Children's Tumor Foundation. https://www.ctf.org/understanding-nf/find-a-doctor/. Accessed Feb. 26, 2024.
- Ami TR. Allscripts EPSi. Mayo Clinic. April 18, 2024.
- Collecting Pennies Through the Pain
Associated Procedures
- Chemotherapy
- Cochlear implants
- Genetic testing
- Radiation therapy
- Stereotactic radiosurgery
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, have been ranked among the best Neurology & Neurosurgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Carrier testing for partners of MUTYH variant carriers: UK Cancer Genetics Group recommendations
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-9201-9216 Terri Patricia McVeigh 1 , 2 ,
- Fiona Lalloo 3 ,
- http://orcid.org/0000-0002-7918-4003 Kevin J Monahan 4 , 5 ,
- http://orcid.org/0000-0002-8626-188X Andrew Latchford 6 , 7 ,
- http://orcid.org/0000-0001-7071-7048 Miranda Durkie 8 ,
- Rachael Mein 9 ,
- http://orcid.org/0000-0002-6637-3411 Emma L Baple 10 , 11 ,
- http://orcid.org/0000-0002-3303-8713 Helen Hanson 11 , 12
- 1 Cancer Genetics Unit , Royal Marsden Hospital NHS Foundation Trust , London , UK
- 2 The Institute of Cancer Research , London , UK
- 3 Manchester Centre for Genomic Medicine , Manchester University Hospitals Foundation Trust , Manchester , UK
- 4 St Mark's the National Bowel Hospital and Academic Institute , London , UK
- 5 Imperial College London , London , UK
- 6 The Polyposis Registry , St Mark’s Centre for Familial Intestinal Cancer, St Mark's Hospital , London , UK
- 7 Surgery and Cancer , Imperial College London , London , UK
- 8 Sheffield Diagnostic Genetics Service , North East and Yorkshire Genomic Laboratory Hub, Sheffield Children’s NHS Foundation Trust , Sheffield , UK
- 9 NHS England , Redditch , UK
- 10 Medical Research (Level 4), RILD Wellcome Wolfson Centre , University of Exeter , Exeter , UK
- 11 Peninsula Clinical Genetics Service , Royal Devon University Healthcare NHS Foundation Trust , Exeter , UK
- 12 Faculty of Health and Life Sciences , University of Exeter Medical School , Exeter , UK
- Correspondence to Dr Terri Patricia McVeigh, Cancer Genetics Unit, Royal Marsden Hospital NHS Foundation Trust, London, UK; terri.mcveigh{at}gmail.com
https://doi.org/10.1136/jmg-2024-109910
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- Delivery of Health Care
- Digestive System Neoplasms
- Gastroenterology
- Genetic Carrier Screening
MUTYH -associated polyposis (MAP) is an autosomal recessive condition caused by biallelic constitutional pathogenic variants in the MUTYH gene. MAP is associated with colonic polyposis (typically adenomas, but less commonly hyperplastic, serrated or mixed) and increased cancer (colorectal, duodenal and others) risk. Variable expressivity has been noted; polyp burden has often been reported in the order of 100s and rarely greater than a thousand, 1 but colorectal cancer has also been reported in affected individuals in the absence of many, or any, preceding polyps. 2 MAP-associated penetrance is incomplete, but the risk of colorectal cancer in the absence of intervention is high. Although age at diagnosis of cancer is typically younger than sporadic cancers, at 47, phenotypic expression is usually adult in onset. 3 Recommended surveillance includes biannual colonoscopy from 18 to 20, and oesophagogastroduodenoscopy from 35. 4
The frequency of MAP is estimated to be at least 1 in 40 000, but the condition is likely underrecognised, given recessive inheritance pattern and variable phenotype. It is estimated that approximately 1%–2% of individuals of White European ancestry are heterozygous carriers of a pathogenic variant in MUTYH . 5–7 It is estimated that two pathogenic founder variants, c.536A>G (p.Y179C) and c.1187G>A (p.G396D), account for greater than 80% of pathogenic variants in this gene, with approximately 70% of affected individuals carrying at least one of these variants. 8 Several other recurrent variants have been identified in different groups ( table 1 ).
- View inline
Recurrent MUTYH variants in different populations
In the UK, MUTYH testing is currently offered as part of a panel of genes for investigation of individuals with a personal and/or family history of polyposis or early-onset colorectal cancer. 9 While the intention of testing of MUTYH is to identify individuals with MAP, testing frequently identifies heterozygous carriers of MUTYH variants, which, in isolation, would not account for the patient phenotype, as heterozygous carriers of this recessive trait do not have a significantly increased cancer risk. 10 Identification of a single MUTYH variant in an individual with a convincing MAP phenotype suggests another unidentified contributing risk allele. Outside NHS testing criteria, MUTYH is frequently included in commercial pan-cancer predisposition panels available in the private sector. Identification of a heterozygous MUTYH variant in an individual without a clinically relevant phenotype may represent an incidental finding. Such variants may also be ascertained through other routes, such as whole genome sequencing or tumour-based testing, depending on technology/filtering applied, research-based testing or direct-to-consumer testing, 11 although some companies/groups now recommend reporting only biallelic status. 12
The NHS England Genomic testing directory outlines indications for carrier testing in partners of individuals who carry recessive traits, to enable accurate and informed reproductive decision-making. Presently, criteria are reasonably broad, suggesting that such testing can be considered where the result would influence reproductive decision-making, if the carrier frequency of pathogenic variants in the associated gene is at least one in 70 (or if consanguinity is a consideration). While the carrier frequency of the common founder MUTYH variants in White Europeans is higher than this threshold, the frequency of these and other variants in MUTYH in non-European populations is not well established.
Although MAP is a high-risk heritable genetic disorder with a reported carrier frequency (at least in some populations) in excess of 1 in 70, the phenotype is adult in onset; and variants in this gene are much more likely to be ascertained incidentally compared with other recessive traits associated with highly penetrant disorders.
Previous work has demonstrated that testing of partners of patients with MAP is cost-effective. 13 However, ascertainment of heterozygous carriers of MUTYH variants is increasing, given associated growth in genetic testing using pan-cancer predisposition panels in patients with and without a MUTYH -related phenotype. Because of the relatively high carrier frequency of MUTYH variants in the general population, incidental detection of carrier status is not rare and represents a commonly encountered clinical challenge for genetics services, without a precedent in clinical guidelines to inform decision-making. 14 Cascade testing is associated with significant workload, particularly in countries with large family sizes. In England, Wales and Scotland, the average size of an extended three-generation family totals 19 individuals, and in Northern Ireland and Ireland, 64. 15 The potential workload is associated with testing of relatives and partners of heterozygous carriers, in the absence of proven cost-effectiveness needs due consideration. There are no specific guidelines related to testing of partners of carriers of recessive traits associated with later onset cancer risk. Considering this, we aimed to establish current practice (and variability thereof) in MUTYH cascade and partner/spousal carrier testing in the UK and Ireland, and to suggest MUTYH -specific modifications to existing criteria for testing for recessive traits.
To establish current practice, we surveyed lead genetic counsellors, cancer genetic consultant leads and clinical scientists in each regional genetics service in the four devolved nations in the UK, and in the Republic of Ireland, and clinicians in the specialist familial clinic in St Mark’s Polyposis Registry. Data collection was considered complete once at least one response (Microsoft form) was received from every relevant regional service (n=32). Variability was noted in practice of offering spousal testing and extent of testing (common variants or full gene sequencing) ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Survey of practice for MUTH carrier testing in UK Cancer Genetics/Specialist services. (A) Practice of carrier testing in partners of carriers of MUTYH variants. (B) Indications for carrier testing in partners of carriers of MUTYH variants. (C) Extent of testing in partners of carriers of MUTYH variants. MAP, MUTYH -associated polyposis.
In order to standardise practice, we discussed indications for, and extent of partner testing at a virtual meeting involving clinical and scientific leads from each genomic laboratory hub, in August 2023, facilitated by the UK Cancer Genetics Group. At this meeting, we agreed that clinical services were becoming increasingly inundated with requests to facilitate carrier testing for partners of heterozygous carriers of MUTYH variants ascertained via non-standard testing as well as extended cascade testing in families where the presence of MUTYH in the family was ascertained as an incidental finding, rather than in individuals with a matching polyposis phenotype.
Mindful of current pressures on NHS genomic laboratories and clinical genetics services, we agreed that:
Carrier testing for MUTYH should be prioritised for partners of patients with MAP (ie, biallelic carriers).
Testing should not be limited to recurrent variants (ie, full gene sequencing should be undertaken).
Testing should be offered irrespective of the ethnicity of the partner, given that the carrier frequency in populations outside of white Europeans is not well established.
Full MUTYH gene testing may be offered directly to children of patients with MAP in the event that their other parent is not available for carrier testing.
We agreed that carrier testing should not routinely be offered to partners of heterozygotes in the absence of consanguinity or a personal or family history of polyposis or colorectal cancer, particularly if reproductive decision-making will not be influenced (eg, in older individuals).
We believe that bespoke criteria for partner testing of MUTYH are required compared with other recessive traits and hope that these recommendations provide guidance to address the current inconsistencies in clinical practice.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
Acknowledgments.
The authors thank the clinicians and scientists who completed our survey, clinical leads and UK Cancer Genetics Group council members who participated in virtual meeting regarding NHS England Genomic Testing directory updates.
- Kastrinos F ,
- Steyerberg EW , et al
- Sieber OM ,
- Crabtree M , et al
- Poulsen MLM ,
- Bisgaard ML
- Monahan KJ ,
- Bradshaw N ,
- Dolwani S , et al
- Al-Tassan N ,
- Chmiel NH ,
- Maynard J , et al
- Cleary SP ,
- Cotterchio M ,
- Jenkins MA , et al
- Jenkins MA ,
- Dowty JG , et al
- Nielsen M ,
- Morreau H ,
- Vasen HFA , et al
- ↵ NHS National Genomic Test Directory Testing Criteria for Rare and Inherited Disease version 6 , 2024 . Available : https://www.england.nhs.uk/wp-content/uploads/2018/08/Rare-and-inherited-disease-eligibility-criteria-version-6-January-2024.pdf
- Theodoratou E ,
- Campbell H ,
- Tenesa A , et al
- Grody WW , et al
- Stoll J , et al
- McVeigh TP ,
- Donnelly D ,
- Al Shehhi M , et al
X @mcveighterri, @kevinjmonahan, @MirandaDurkie, @Helen_Hanson1
Contributors All authors conceived and contributed to writing of the commentary.
Funding HH is supported by the NIHR Exeter Biomedical Research Centre (NIHR203320). This study was supported by the National Institute for Health and Care Research Exeter Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. Funding for Open Access Fees was kindly provided by the UK Cancer Genetics Group.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer-reviewed.
Read the full text or download the PDF:
- Ethics & Leadership
- Fact-Checking
- Media Literacy
- The Craig Newmark Center
- Reporting & Editing
- Ethics & Trust
- Tech & Tools
- Business & Work
- Educators & Students
- Training Catalog
- Custom Teaching
- For ACES Members
- All Categories
- Broadcast & Visual Journalism
- Fact-Checking & Media Literacy
- In-newsroom
- Memphis, Tenn.
- Minneapolis, Minn.
- St. Petersburg, Fla.
- Washington, D.C.
- Poynter ACES Introductory Certificate in Editing
- Poynter ACES Intermediate Certificate in Editing
- Ethics & Trust Articles
- Get Ethics Advice
- Fact-Checking Articles
- IFCN Grants
- International Fact-Checking Day
- Teen Fact-Checking Network
- International
- Media Literacy Training
- MediaWise Resources
- Ambassadors
- MediaWise in the News
Support responsible news and fact-based information today!
- Newsletters
Opinion | Trump guilty on all counts: breaking down the media coverage of the historic trial
Despite the lack of cameras in the courtroom, the on-screen guilty counters and reports from the trial painted a vivid picture of a historic moment.

The headlines were stunning.
The New York Times: “TRUMP GUILTY ON ALL COUNTS.”
The Washington Post had the exact same, except without the all caps: “Trump guilty on all counts.”
The Wall Street Journal: “Trump Guilty on All Counts in Hush-Money Case.”
The cover of the upcoming issue of The New Yorker has an illustration of Donald Trump, the former and perhaps future president of the United States, being placed in handcuffs.
On Thursday, Trump was found guilty on all 34 charges in what became known as the “hush money trial.” In short, Trump was convicted of falsifying records to cover up money he paid to a porn actress to keep their sexual liaison quiet. Trump became the first former president to be convicted of a felony.
The six-week trial went to the jury on Wednesday, and many assumed it could take days, if not weeks, for the jury to reach a verdict. It ended up taking hours — about nine and a half.
New York Times contributing opinion writer Jonathan Alter was in the courtroom when it was announced that the jury had reached a verdict. “You could hear a collective gasp in the courtroom,” he wrote .
That was nothing compared to the reaction across television and the country when we learned that the jury found Trump guilty on all 34 charges. NBC News had a counter on the screen counting up as Laura Jarrett, the network’s senior legal correspondent, announced each count followed by the word “guilty.”
As the numbers rolled from 1 to 2 to 3 and so on, it looked like the pump at a gas station while filling up your car.
MSNBC’s Rachel Maddow said on air, “He became the first president ever convicted of a felony. And then seconds later, the first president ever convicted of two felonies. Then every few seconds for a few minutes thereafter, he kept breaking his own brand-new old record for the most crimes any American president had ever been convicted of.”
When the counting stopped, Alter wrote a sentence almost too stunning to believe: “Trump had become a felon.”
CBS News chief Washington correspondent Major Garrett said on air, “To hear that word ‘guilty,’ not just once, but 34 times about a former president of the United States in any context is completely uncharted territory. … This is not just a legal moment for this country. It is not just a political moment for this country. It is a moment where everything about politics and law and our orientation to both are convulsed as never before.”
The Washington Post’s Jeremy Barr noted , “The television coverage lacked some of the drama of other big court cases, since the courts did not allow the trial to be broadcast, part of a broader slate of restrictions on media access. Instead of hearing the ruling from the jury, television viewers had it relayed to them via correspondents in the courthouse.”
Still, reports from the courtroom painted a good picture.
CBS News’ Katrina Kaufman, who was in the courtroom when the verdict was announced, said, “I was watching (Trump) as the verdict came down and he just had this very blank look on his face, his eyes were so squinted that it was almost hard to tell if they were even open during part of the time that the foreman was reading that he was guilty on each of these 34 charges.”
NBC News’ Hallie Jackson summed it up well: “I think it’s worth taking a beat here and recognizing that whether you like this verdict or not, this is an historic moment.”
Why it mattered
On Sunday, MSNBC will air “Prosecuting Donald Trump: Witness to History.” The show had been in the works before Thursday’s verdict. The show will air at 9 p.m. Eastern on MSNBC and will be streamed on Peacock the next day. It will feature NBC/MSNBC reporters, analysts and hosts — including Rachel Maddow, Andrew Weissmann, Joy Reid, Chris Hayes, Lawrence O’Donnell and Katie Phang.
Phang is a former trial lawyer who hosts a show on MSNBC. She was in the courtroom for some of the trial, and I had a chance to trade emails with her on Thursday. Our exchange was before and after the verdict.
Tom Jones: Some of Trump’s legal issues include what happened on Jan. 6, election integrity in Georgia, taking classified documents out of the White House. What makes this particular case — the hush money trial — so important?
Katie Phang: On its face, this trial is so important because it’s the first criminal trial of a former president of the United States. But, I actually refer to this trial as Trump’s “New York election interference trial” (and not his “hush money” trial) because that’s really what this case is all about: the fact that Trump had business documents falsified so that he could conceal his violation of New York election law through hush money payments, fake invoices, etc.
Before this trial, there was a lot of focus and attention on Trump’s classified documents case in Florida and his D.C. election interference case as it wound its way to the U.S. Supreme Court. There was a lot of activity going on in Trump’s Fulton County election interference case, too. So I think some people forgot about this case because it was on the back-burner of media attention for a while.
But, lo and behold, it was Manhattan DA Alvin Bragg who indicted Trump first and it ended up being Bragg who took him to trial first. And when we redirected our attention to this trial, and the prosecution’s theory better crystalized, we were able to see that Trump very well could have lost the 2016 election if this negative information had been revealed. But for the conspiracy he entered into with David Pecker and Michael Cohen to hide this info from the voting public, Trump might not have been the 45th president of the United States. It’s a pretty heady thought and that’s why this case is so important.
Jones: You have followed the trial more closely than most, including being in the courtroom. What has stood out to you? And what, in particular, has struck you that you might not have noticed had you not been in the courtroom?
Phang: Being inside of the courtroom is a different energy because you can feel the tension, see the emotions, and be an eyewitness to history in the making. It’s tragic that there is no video or audio that is able to be transmitted from inside of the courtroom so that the American public can also be a witness to this moment in history. One thing that you don’t get to see if you’re not inside the courthouse (either inside the courtroom or inside the media/public overflow room) is the image of Donald Trump slumped in his chair with his eyes closed, perhaps asleep, perhaps thinking. That is an impression that lasts: to see the former president of the United States as a criminal defendant at his counsel’s table during a trial, looking like he’s taking a nap.
The immediate aftermath
Trump, reportedly, did not react visibly in the courtroom to the verdicts, but he was defiant afterward, telling reporters outside the courtroom that he was a “very innocent man” and calling the trial “rigged” and “disgraceful.”
He is scheduled to be sentenced on July 11, and most assuredly will appeal. Trump also is expected to have another news conference today in New York.
Conservatives, including conservative media, blasted the verdicts and the trial.
According to The New York Times” Michael M. Grynbaum and John Koblin , Fox News on-air personality Jeanine Pirro said, “There is something that is very wrong here; we have gone over a cliff in America. … God help America after what I’ve seen in the last few weeks.”
Fox News’ Laura Ingraham said it was “a disgraceful day for the United States, a day America may never recover from.”
Meanwhile, over on MSNBC, host Nicolle Wallace said, “For me, the Trump story has always been about asymmetry … and when we learned that a verdict was in, our coverage would have been totally the same if he’d been acquitted. It would have been respect and reverence for Judge Juan Merchan, that we’ve all been articulating over the last several hours. It would have been respect and reverence for the jurors who said, ‘Yeah, pick me, I’ll do it.’ I think if there was criticism, it might have been, you know, that the process didn’t yield a result that seemed plain to our eyes, right?”
The coverage I particularly found useful was what happens next. The networks were at their strongest when they asked — and more importantly, answered — questions such as, “Will Trump go to jail?” and, “Can Trump still run for president?” (By the way, here’s a good explainer from PolitiFact’s Louis Jacobson and Samantha Putterman: “Trump guilty in NY trial: Can he still run for president or vote as a convicted felon?” )
But the coverage then struggled when facts turned to punditry, and there were wild predictions on what it all means.
CNN’s Jake Tapper probably put it best when he said, “For those wondering about the political consequences of these 34 guilty verdicts, the short answer is, nobody has any idea. Period.”
Here are a few notable links and tidbits regarding the Trump verdict

“Today” show co-host Savannah Guthrie and “NBC Nightly News” anchor Lester Holt anchored NBC News’ breaking news coverage of the Trump verdict. (Courtesy: NBC News)
- All three of the major TV networks — ABC, CBS and NBC — brought in their evening news anchors for the breaking news coverage.
- ABC News’ Nathaniel Rakich with “How Trump’s guilty verdict will impact the 2024 presidential election.”
- The New York Times editorial board with “Donald Trump, Felon.”
- The Washington Post’s Isaac Stanley-Becker with “Challenges await Trump jurors after ‘surreal experience.’”
- The Atlantic’s David Frum with “Wrong Case, Right Verdict.”
- Axios’ Stef W. Kight, Juliegrace Brufke and Stephen Neukam with “Pro-Trump right erupts after guilty verdict.”
- Semafor’s David Weigel with “A taxonomy of Republican rage against the Trump verdict.”
Wall Street Journal executes yet another round of layoffs
For this item, I turn it over to my Poynter colleague Angela Fu.
The Wall Street Journal laid off at least eight people Thursday, prompting the paper’s union to stage a lunchtime walkout.
The cuts included reporters on the paper’s U.S. News and breaking news teams, according to the union. Editor-in-chief Emma Tucker told staff in an email Thursday that the paper will be “moving away from regional and local general news” as it restructures those teams. The Journal will eliminate certain positions and reassign reporters to other desks, including a new national affairs team that will cover “big topics” like abortion, guns, race, immigration and land use.
“These changes mean that U.S. News will no longer be a standalone coverage area and that we are closing the East Coast, Mid-U.S. and West Coast regional bureaus,” Tucker wrote. “But it does not mean that we are pulling back from the United States. Far from it: Our economics team is expanding into new regions; the National Affairs reporters will be based all around the country, looking to tell stories of national consequence wherever they arise.”
A spokesperson for the Journal wrote in an emailed statement that Tucker is “reshaping our newsroom with an eye towards digital growth, subscription growth and high-quality journalism.” They did not answer a question about whether staff could expect more cuts this year.
“While we recognize change can be difficult, it is necessary to ensure we have the right structure in place to support our objectives,” the spokesperson wrote.
The Journal has had at least six other rounds of layoffs this year, resulting in more than 60 job cuts. In February, the outlet restructured its Washington, D.C., bureau, laying off 30 journalists, and later made cuts to its world team and several noneditorial departments. In March, the Journal laid off five editors from its standards and ethics team and a foreign correspondent . In April, the outlet cut 11 people , most of whom worked on the Journal’s video and social teams, and in May, the paper laid off eight journalists as it restructured its Hong Kong and Singapore bureaus.
Though financial pressures have caused dozens of other news outlets — including NBC News, the Los Angeles Times and Vice — to cut staff this year, the Journal has been adamant that its layoffs are not cost-cutting measures. Tucker wrote in her email to staff Thursday that both subscriptions and engagement have been up in recent months. The Journal is also currently recruiting for 37 vacancies.
The Dow Jones segment — which includes The Wall Street Journal — of parent company News Corp. recently ended its third quarter with an EBITDA (earnings before interest, taxes, depreciation and amortization) of $118 million, up 8% from the same period last year. It was the highest third quarter on record.
The piecemeal cuts have angered the union representing Dow Jones employees in the U.S. and Canada. Union members have questioned why the company continues to cut jobs while it experiences record revenues and subscriptions. On Thursday, members covered Tucker’s office with sticky notes during their lunchtime walkout to protest the layoffs.
And now onto other media news, tidbits and interesting links …
- Peter Alexander will fill in as guest moderator of NBC’s “Meet the Press” for the next several weeks. Regular moderator Kristen Welker will be on maternity leave. Welker is expected to be back in the moderator’s chair by the party national conventions later this summer. People’s Virginia Chamlee wrote two weeks ago about Welker and her husband expecting a child via surrogate.
- Some really good points made in this column from Mediaite by Isaac Schorr: “Trump’s Trial Has the Media Falling Back Into All of Its Worst Habits.”
- Variety’s Brian Steinberg with “CNN Will Buck Tradition and Put Commercial Breaks in Biden-Trump Presidential Debate.”
- Axios’ Sara Fischer with “X and NewsNation plan live town halls with Trump, RFK Jr.”
- For Slate, Bill Pruitt with “The Donald Trump I Saw on ‘The Apprentice.’”
- CNN’s Hadas Gold with “A national network of local news sites is publishing AI-written articles under fake bylines. Experts are raising alarm.”
- Bilge Ebiri, a film critic for New York and Vulture, with “Here’s the Real Reason Why There’s Still No Oscar for Best Stunts.”
- GQ’s Alex Kirshner with “Stephen A. Smith on the State of Sports Journalism, Touching the ‘Third Rail,’ and Whether He’s Underpaid.”
- One of the best sports columns I’ve read in quite some time — The Washington Post’s Jerry Brewer with “How Grievance Splintered American Sports.”
- For The New York Times, Grayson Haver Currin with “Sarah McLachlan Is Resurfacing.”
More resources for journalists
- Reporting on the Rise of AI: A RAND-Poynter Masterclass
- Subscribe to Poynter’s Friday newsletter, Open Tabs with Poynter managing editor Ren LaForme, and get behind-the-scenes stories only available to subscribers.
- Manage big responsibilities without direct reports? Try Lead With Influence .
- Understand U.S. Immigration From the Border to the Heartland — Start any time.
Have feedback or a tip? Email Poynter senior media writer Tom Jones at [email protected] .
The Poynter Report is our daily media newsletter. To have it delivered to your inbox Monday-Friday, sign up here .

Opinion | Sally Buzbee steps down as executive editor of The Washington Post
Buzbee joined the Post in 2021 after a career at The Associated Press. She was the first female editor of the Post, which was founded in 1877.

What do horse race journalists think of ‘horse race journalism’?
As the 2024 presidential election approaches, breathless reporting of incremental polling has already begun.

Fact-check: Trump’s speech at Trump Tower after his New York felony conviction
Former President Donald Trump lashed out about his Manhattan trial and sought to defend his record and his character

IFCN announces new grant opportunity supported by Meta to combat AI-generated misinformation on WhatsApp
Grantees will have an opportunity to innovate with WhatsApp functionality
You must be logged in to post a comment.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Start your day informed and inspired.
Get the Poynter newsletter that's right for you.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Psychiatry
- v.55(1); Jan-Mar 2013
Ethics in medical research: General principles with special reference to psychiatry research
Ajit avasthi.
Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Abhishek Ghosh
Sidharth sarkar, sandeep grover.
Ethics is an understanding of the nature of conflicts arising from moral imperatives and how best we may deal with them. Ethics in medical research deals with the conflicts of interest across various levels. Guidelines have been proposed for standardized ethical practice throughout the globe. The four fundamental principles of ethics which are being underscored are autonomy, non-maleficence, beneficence, and justice. Some special ethical issues have particular relevance to psychiatric research arising primarily from the specific vulnerabilities of those with mental illness and the risks posed by some research methodologies. Accordingly, sensitivity is required in the design of psychiatric research. It is suggested that though the value of published guidelines and the help that may be available from research ethics committees is quite great, the primary responsibility for maintaining high standards of practice in research rests with research workers themselves.
INTRODUCTION
The word “ethics” is derived from the Greek word, ethos, which means custom or character. Ethics is an understanding of the nature of conflicts arising from moral imperatives and how best we may deal with them.[ 1 ] It deals with the choices we make and our actions in relation to those choices. It deals with the choices made by both clinicians and patients and the duties and obligations of clinicians to their patients. Medical ethics also deals with the choices made by society, the distribution of resources, and access to health care, and the dilemmas arising from them.[ 2 ] An issue, mainly for the developing countries, has been the extent to which ethical principles are considered universal or as culturally relative – the universalist versus the pluralist view. The challenge to international research ethics is to apply universal ethical principles to biomedical research in a multicultural world with a multiplicity of health-care systems and considerable variation in standards of health care.[ 3 ]
History is unfortunately peppered with stories of abuse carried out in the name of medical research. The most dreadful of all atrocities was possibly conducted by Nazi doctors who used convicts for human experimentation. The discovery of these experiments stunned the whole world which led to the formulation of Nuremberg code[ 4 ] to prevent recurrence of such episodes. It was the first international code for ethics in clinical research laying down the guidelines for research on human subjects. It laid down 10 clear principles to be followed by researchers and made voluntary consent essential, allowed subjects to withdraw from the experimentation at any time, banned experiments that could result in major injury or death of the subjects, and made mandatory to have preclinical data before experimenting on humans. Even Nuremberg code failed to terminate unethical research practices. Eventually a set of guidelines was adopted by the 18 th World Medical Association (WMA)[ 5 ] General Assembly, which was called the Declaration of Helsinki. It contained 32 principles, which stress on informed consent, confidentiality of data, vulnerable population, and requirement of a protocol, including the scientific reasons of the study, to be reviewed by the ethics committee. Though Declaration of Helsinki had created a stir in the medical community, medical atrocities continued. The malpractice in the Tuskegee Syphilis Study in the US was possibly the next eye opener which ushered the Belmont Report[ 6 ] in 1979 and laid the foundation for regulations regarding ethics and human subjects’ research in the US. With the increasing interest of pharmaceutical industries in carrying out research experiments in the developing and the underdeveloped countries, the Council for International Organizations of Medical Sciences (CIOMS)[ 3 ] in association with World Health Organization (WHO) developed “International Ethical Guidelines for Biomedical Research Involving Human Subjects” in 1982.
CARDINAL PRINCIPLES OF ETHICS IN RESEARCH
The four principles of Beauchamp and Childress – autonomy, non-maleficence, beneficence, and justice – have been extremely influential in the field of medical ethics, and are fundamental for understanding the current approach to ethical assessment in health care. Respect for autonomy stands for acting intentionally after being given sufficient information and time to understand the information. Beneficence is directed to promote the well-being of patients and society. On the other hand, non-maleficence implies first do no harm which can be achieved by careful decision making and having adequate training. Justice deals with the equitable distribution of social benefits.[ 7 , 8 ]
MEDICAL RESEARCH – DEFINITION, TYPES, AND ISSUES
The term “research” refers to a class of activity designed to develop or contribute to generalizable knowledge. Generalizable knowledge consists of theories, principles, or relationships, or the accumulation of information on which they are based, that can be corroborated by accepted scientific methods of observation and inference. In the present context, “research” includes both medical and behavioral studies pertaining to human health. Usually “research” is modified by the adjective “biomedical” to indicate its relation to health. Those who support the need for research argue that no new treatment should be offered outside the context of a controlled trial, so that treatments’ effectiveness and efficacy can be measured ab initio , not only for the sake of the patients currently receiving it but also for all future patients. Research involving human subjects includes:[ 1 , 9 ]
- Studies of a physiological, biochemical, or pathological process, or of the response to a specific intervention – whether physical, chemical, or psychological – in healthy subjects or patients;
- Controlled trials of diagnostic, preventive, or therapeutic measures in larger groups of persons, designed to demonstrate a specific generalizable response to these measures against a background of individual biological variation;
- Studies designed to determine the consequences for individuals and communities of specific preventive or therapeutic measures; and
- Studies concerning human health-related behavior in a variety of circumstances and environments.
Conflicts of interest are inherent to the majority of relationships among individuals and of those with companies and institutions and, certainly, research involving human beings is no exception. In relation to clinical research, conflicts of interest occur at different levels and usually permeate through various lines (e.g., in the pharmaceutical industry, about their decisions to invest and develop new products, especially vaccines and drugs, and also in relation to marketing of these products). Among the investigators, the conflicts may be related to the financial gains to participate in pharmacy sponsored trials, or to the expected academic career boost attained with the publication of the results of the trials and also to personal interests such as the financial support for trips to international conferences.[ 10 ]
Therefore, medical research which is absolutely necessary and fundamental for acquiring and propagating worthwhile novel knowledge is equally controversial because of the conflicts of interest of the researchers or the sponsors. Both universal and regional guidelines have been proposed to strike a balance between these two opposing interests and to ensure standardized ethical research.
PRINCIPLES OF ETHICS IN MEDICAL RESEARCH
Principles of essentiality.
Refers to whether the research is considered to be absolutely essential after a due consideration of the existing scientific knowledge in the proposed area of research. This should be scrutinized by an independent and responsible body of persons who, after careful consideration, come to the conclusion that the research is likely to benefit the humanity or environment.[ 11 ]
Principles of voluntariness, informed consent, and community agreement
Research participants should be fully apprised of the research and the associated risks and benefits. The participants should be informed of the right to abstain from the research or withdraw consent at any time. Where research entails treating any community, the principles of voluntariness and informed consent apply to the community as a whole and to each individual member. In case a person is incapable of giving consent, a legally acceptable guardian should give the informed consent.
Principles of non-exploitation
The participants should be fully apprised of all the possible dangers that may arise during the research so that they can appreciate all the physical and psychological risks. Each research should include an in-built mechanism for compensation for the human participants either through insurance cover or by any other appropriate means to cover foreseeable and unforeseeable risks, and provide remedial action and comprehensive aftercare.
Principles of privacy and confidentiality
The identity and records of the participants are as far as possible kept confidential (except when required for legal reasons). This is to avoid any form of hardship, discrimination or stigmatization as a consequence of having participated in the research.
Principles of precaution and risk minimization
Due care and caution should be taken at all stages of the research and experiment to ensure that the research participant and those affected by it including the community are put to the minimum risk, suffer from no known irreversible adverse effects, and generally, benefit from the research or experiment. There should be a plan for interim reviews to detect whether any intervention arm (active or control) is associated with increased risks, so that undue harms are avoided by stopping the research.
Principles of professional competence
Research should be conducted by competent and qualified persons who act with total integrity and impartiality and who have been made aware of the ethical considerations to be borne in mind in respect of such research or experiment.
Principles of accountability and transparency
The research or experiment should be conducted in a fair, honest, impartial, and transparent manner after full disclosure is made by those associated with the research or experiment of each aspect of their interest in the research, and any conflict of interest that may exist. Full and complete records of the research should be retained for such reasonable period as may be prescribed or considered necessary for the purposes of post-research monitoring, evaluation of the research, conducting further research, and scrutiny by the appropriate legal and administrative authority, if necessary.
Principles of the maximization of the public interest and of distributive justice
The research or experiment and its subsequent application should be conducted and used to benefit all human kind (and not just those who are socially better off), in particular, the research participants themselves and or the community from which they are drawn.
Principles of public domain
The research findings should be brought into the public domain so that its results are generally made known through scientific and other publications. This would help in consolidating the scientific knowledge base of the field being studied and would prevent the undue replication of studies which pose risks to some subjects.
Principles of totality of responsibility
Professional and moral responsibility should be observed, for the due observance of all the principles, guidelines, or prescriptions of those directly or indirectly connected with the medical research. This extends to the institutes where this research is carried out, as well as the sponsors of the research. The research should be duly monitored and constantly subject to review and remedial action at all stages.[ 11 ]
SPECIAL REFERENCE TO PSYCHIATRY RESEARCH
Neuropsychiatric disorders are highly prevalent conditions with significant morbidity, yet only modestly effective treatments are available. The suffering and loss caused by these diseases call for the development of truly innovative interventions. Testing such innovative approaches can carry risks of significant harm[ 12 ] even while raising hopes for future benefits.[ 13 ] Furthermore, the very nature of many neuropsychiatric disorders creates ethical complexity because many persons with such disorders have impaired cognition or emotion. If a patient's impairment is severe enough, he or she will be incompetent to give informed consent for research.[ 14 ] In our society, surrogate or proxy consent-based research remains an area of unsettled policy. Finally, at a more speculative level, interventions that alter behavior, or even knowledge that can predict or explain behaviors, can challenge traditional norms of social regulation and interaction.[ 15 ]
Methods for solving these dilemmas have included the development of more objective rules to guide the practitioner, such as utilitarianism and deontology. Deontological approaches possibly cannot resolve moral conflicts, and so the psychiatrist is “denied an available remedy.” Utilitarianism is seen by the authors as too difficult to calculate benefits and risks, and demands an impartiality that clinicians would find difficult to achieve. Both deontology and utilitarianism, a respect for patient autonomy, and utility, a measurement of consequences, are seen as theories that do not help clinicians in practice. This is particularly the case in conflict situations as in psychiatric research.[ 16 ] Therefore, research in psychiatry demands a special attention.
Issues in relation to competence and consent
Participation in research usually involves some degree of risk, discomfort, or sacrifice of the personal care that patients enjoy when they receive ordinary treatment.[ 17 ] Ordinarily, we allow research subjects to incur these discomforts or sacrifice personal care because we believe that people have the right to run certain risks for rewards that seem to them worthwhile. These rewards may include the pride that comes from altruistic behavior, the hope that they themselves might benefit from the results of the study at some point in the future, and the more immediate possibility that they may have access through the study to assessment techniques or therapeutic approaches that would not otherwise be available to them. But when subjects’ capacities to make decisions are impaired, they may materially misconstrue the situation into which they are entering.[ 18 ]
To resolve these conflicts, proposals have been made that range from banning certain types of research with psychiatric patients to requiring independent evaluation of the capacities of potential subjects, to appointing representatives to remove subjects from studies when the risk–benefit ratio appears to be swinging against them.[ 19 , 20 ]
As per WMA guidelines for ethical research, “In research involving subjects who are mentally incapable of giving consent, the physician should seek informed consent from the legally authorized representative. If no such representative is available and if the research cannot be delayed, the study may proceed without informed consent provided that the specific reasons for their inability to give informed consent have been stated in the research protocol and the study has been approved by a research ethics committee. Consent to remain in the research should be obtained as soon as possible from the subject or a legally authorized representative” (WMA 2008; clause 29). An additional caveat in clause 28 reads, “When a potential research subject who is deemed incompetent is able to give assent to decisions about participation in research, the physician must seek that assent in addition to the consent of the legally authorized representative. The potential subject's dissent should be respected.”[ 21 ] It should always be remembered that impairments exist on a spectrum, and some degree of dysfunction is not incompatible with competent decision making. Thus, although the presence of cognitive and related impairments in schizophrenia, for example, warrants concern about subjects’ abilities to decide whether to enter a research project, by no means does it call for the exclusion of all persons with schizophrenia from investigational studies. Individuals who have severe mental disorder and lack adequate decision-making capacity may improve significantly with educational remediation.[ 22 , 23 ] Patients can be given information through conversation, lectures, pamphlets, articles, medication groups, instruction sheets, books and videotapes, consent forms, and interactive videodiscs. Repeated disclosure of information is another technique which can be followed.[ 24 ]
However, systematic evaluation, even in non-psychiatric populations and in high-income countries, has shown that participants in randomized trials recall information poorly, are not often aware that placebos form one arm of treatment, demonstrate inadequate comprehension of the process of chance in treatment allocation, understand and use only a proportion of what is presented in consent forms, do not really understand the issue of equipoise, and participate not for altruistic reasons but because they expect some improvement by participation.[ 25 ] Cognitive dysfunction and the symptoms shown to be associated with impaired decisional capacity are not unique to schizophrenia and may occur with many other forms of illness.[ 26 ] Furthermore, studies have also shown that many people with schizophrenia are able to give informed consent and retain related information across time. So, diagnosis of mental illness itself does not disqualify a person to enter into a research as competence of decision making is case specific and variable across the time.
Issues in relation to confidentiality
Patients, health-care providers, and patient advocacy organizations have expressed increasing concern about the confidentiality of clinical information stored in large computerized databases.[ 27 – 30 ] The accumulation of ever-larger stockpiles of sensitive information raises reasonable concerns about inappropriate access and unauthorized disclosure. Given the stigma often attached to psychiatric disorders and psychiatric treatment, confidentiality of information on mental health and substance abuse treatment is especially critical. A few occurrences of inappropriate use or disclosure of clinical information have been well publicized.[ 28 , 30 ]
Firstly, continued research access to population-based records data is essential to protecting the rights and interests of people with psychiatric illness. Investigators conducting any such research should take all possible steps to limit access to confidential information, minimize risks of disclosure, and (when possible) obtain informed consent for research use of clinical data. The most effective strategy for preventing disclosure of confidential information is to remove all identifying information from medical records data before any research use.[ 31 ] Secondly, when potential research uses are anticipated at the time of data collection, those collecting clinical information should be obligated to advise patients regarding possible research use. However, obtaining individual informed consent for each specific research use is impossible or extremely impractical.[ 32 ] Lastly, research intended to increase public domain medical knowledge should be clearly differentiated from proprietary activities. If legitimate public domain research activities were clearly distinguished from other uses of large clinical databases, efforts to regulate storage and disclosure of clinical data could concentrate on the activities that are now largely unregulated.[ 33 ]
However, advances in mental health science promise great benefits for those who suffer, or will come to suffer, from mental illness and, in some cases, for research subjects themselves. While persons with mental illness may be vulnerable in several ways, research regulations that focus primarily on their vulnerabilities and deficits could encourage and possibly exacerbate the stigmatization already felt by this population.[ 34 , 35 ] Further, it may be unjust to exclude, by overly restrictive regulation, those people with mental illness who could benefit from research participation. An ethically appropriate framework for psychiatric research ethics balances rigorous protections for human subjects with recognition of the enormous social and individual benefits arising from well-designed and ethically conducted scientific research.[ 36 – 38 ] How this balance is struck has important implications for research ethics generally, particularly for research involving vulnerable persons.
Though a number of ethical guidelines have been formulated for clinical research, malpractice is still widely acknowledged. It could be understood by the fact that ethical guidelines in many countries like India are just the recommendations and not a law. For proper enforcement, guidelines should be made a part of the law as has been done in the US and some other countries of the world.[ 39 ] We need better research, and research done for the right reasons. The second intriguing issue is the cross-cultural applicability of ethical guidelines.[ 40 ] In this era of advanced globalization, the problems of medical ethics can no longer be viewed only from the perspective of wealthy countries. Global bioethics seeks to identify key ethical problems faced by the world's 6 billion inhabitants and envisages solutions that transcend national borders and cultures. The relevance of global bioethics is obvious with respect to international research ethics (as evidenced by the controversy over changes to the Declaration of Helsinki), global vaccine initiatives, or global health equity.[ 41 ] Last but not the least; doctors are specially trained to be good clinicians but are seldom taught even the fundamentals of ethical clinical research. The post-graduate dissertation or the PhD thesis is a precious opportunity to train tomorrow's investigators in the elements of ethical clinical research.[ 42 ] The attributes of a clinical researcher like truthfulness and accountability toward integrity are expected to propagate standardized ethical practice.
Source of Support: Nil
Conflict of Interest: None declared

IMAGES
VIDEO
COMMENTS
Our hope is that the Fundamentals of Medical Ethics series will suggest broad lessons to keep in mind as physicians, patients, research participants, families, and communities struggle with new ...
Modest Beginnings . The modern era of health care ethics is often traced to Henry Beecher's influential, 1966 article on ethical problems in clinical research, with particular attention (through a series of actual examples) to the failure to inform patients of the risks involved in experimental treatments (Beecher 1966).Beecher, a professor of anesthesiology at Harvard Medical School, soon ...
The Nuremberg Code is the most important document in the history of the ethics of medical research. 1-6 The Code was formulated 50 years ago, in August 1947, in Nuremberg, Germany, by American ...
The American medical ethics revolution: How the AMA's code of conduct has transformed physicians' relationships to patients, professionals, and society. Baltimore: Johns Hopkins University Press; 1999. pp. 17-51. [Google Scholar] Baker RB. Before bioethics: A history of American medical ethics from the colonial period to the bioethics ...
Abstract. Ethics are the moral values of human behavior and the principles which govern these values. The situation becomes challenging for a doctor when he assumes the role of researcher. The doctor-researcher has to serve both the roles and at times the zeal of an investigator has the potential to cloud the morality of the physician inside.
Histories have to begin somewhere. The expression "medical ethics" was not coined until 1803, when Thomas Percival (1740-1804), a physician from Manchester, England, introduced it in his eponymous book Medical Ethics (Percival 1803b) as a description of the professional duties of physicians and surgeons to their patients, to their fellow ...
apartheid, colonialism, Communism, health policy, imperialism, militarism, Nazi medicine, Nazi "medical ethics," and research ethics. Also included are the first global chronology of persons and texts; the first concise biographies of major figures in medical ethics; and the first comprehensive bibliography of the history of medical ethics.
1 Objectives. 1. To present an accessible but authoritative brief introductory history of the field of clinical ethics. 2. To present this history in the context of the broader history of clinical ethics dating to the Hippocratic Oath, evolving into professional medical ethics and, more recently, as bioethics. 3.
Respect for Autonomy (RFA) has been a mainstay of medical ethics since its enshrinement as one of the four principles of biomedical ethics by Beauchamp and Childress' in the late 1970s. This paper traces the development of this modern concept from Antiquity to the present day, paying attention to its Enlightenment origins in Kant and Rousseau. The rapid C20th developments of bioethics and ...
Founding chair of the History of Medical Ethics Affinity Group of the American Society of Bioethics and Humanities, Baker is the author and editor of numerous articles and books, including the award-winning American Medical Ethics Revolution (with Arthur L. Caplan, Linda L. Emanuel and Stephen R. Latham, 1999).
The term 'bioethics' was used for the first time by Potter in 1970 and has completed its first twenty-eight years of existence (Potter, 1970, 1971). This term is coming of age, which explains why it is beginning to have a sufficiently mature and systematic doctrine behind it. Download to read the full chapter text.
The declaration governs international research ethics and defines rules for "research combined with clinical care" and "non-therapeutic research.". The Declaration of Helsinki was revised in 1975, 1983, 1989, and 1996 and is the basis for effective clinical practices used today. Research with humans should be based on the results from ...
Abstract. The Oxford Textbook of Clinical Research Ethics is the first systematic and comprehensive reference on clinical research ethics. Under the editorship of experts from the National Institutes of Health of the United States, the book offers a wide-ranging and systematic examination of all aspects of research with human beings.
In one of the most influential papers in the history of research ethics, Hans Jonas (1969) argues that the progress clinical research offers is normatively optional, whereas the need to protect individuals from the harms to which clinical research exposes them is mandatory. ... Medical Research with Children: Ethics, Law, Practice. Oxford ...
A research ethics timeline from 1620 to present. ... This list is the authors' own interpretation of some important events in the history of research ethics and does not include every event that some people might regard as important. ... In the fall of 2001, Bruce Ivins, a biodefense researcher at the U.S. Army Medical Research Institute of ...
Medical ethics is an applied branch of ethics which analyzes the practice of clinical medicine and related scientific research. Medical ethics is based on a set of values that professionals can refer to in the case of any confusion or conflict. These values include the respect for autonomy, non-maleficence, beneficence, and justice. Such tenets may allow doctors, care providers, and families ...
Ethics are a guiding principle that shapes the conduct of researchers. It influences both the process of discovery and the implications and applications of scientific findings 1. Ethical considerations in research include, but are not limited to, the management of data, the responsible use of resources, respect for human rights, the treatment ...
The World Medical Association's revised International Code of Medical Ethics offers a core set of ethical norms for all doctors worldwide to follow, write Ramin W Parsa-Parsi , Raanan Gillon , and Urban Wiesing Increasing global mobility, and the growing plurality in society that comes with it, has an undeniable effect on medical practice. The likelihood of patients consulting doctors with ...
Most textbooks begin their coverage of research ethics with the Nuremburg Code. There is also early evidence that physicians used ethical considerations in research with humans when making decisions in the proper conduct of human experimentation. The idea of conducting medical research on animals before conducting it on humans was promoted by William Osler, a professor at Johns Hopkins.
Studying cancer in the ancient world can be tricky because the disease often presents in the soft tissue, and experts do not have access to a patient's medical history. Previous research on the ...
Today, "medical ethics" refers to the application of moral reasoning in the setting of clinical practice and medical research. This involves the use of moral theories (e.g., utilitarianism), moral principles (e.g., respect for autonomy), and virtues (e.g., trustworthiness) to help guide the medical field. With this in mind, our history ...
Research Ethics, v19 n2 p107-120 Apr 2023. As the burden of misconduct in medical research is increasingly recognised, questions have been raised about how best to address this problem. Whilst there are existing mechanisms for the investigation and management of misconduct in medical literature, they are inadequate to deal with the magnitude of ...
An independent medical effectiveness review organization, a "citizen's petition" to the FDA, and a number of media reports have alleged problems with study design, ethical lapses, a failure to ...
Bioethics and Clinical (Medical) Ethics. ... from one concerned about professional conduct and codes to its present status with an extensive scope that includes research ethics, public health ethics, organizational ethics, and clinical ethics. ... History of Present Illness, Past History, pertinent Family and Social History, Review of Systems ...
Considered one of the most influential thinkers of the 20th century, Heidegger was best known for his philosophy of existentialism. Schalow's other areas of research interest included ethics, medical ethics, phenomenology, and 19th and 20th century German thought. "Dr.
Neurofibromatosis type 1 (NF1) is a genetic condition that causes changes in skin pigment and tumors on nerve tissue. Skin changes include flat, light brown spots and freckles in the armpits and groin. Tumors can grow anywhere in the nervous system, including the brain, spinal cord and nerves. NF1 is rare. About 1 in 2,500 is affected by NF1.
In the UK, MUTYH testing is currently offered as part of a panel of genes for investigation of individuals with a personal and/or family history of polyposis or early-onset colorectal cancer.9 While the intention of testing of MUTYH is to identify individuals with MAP, testing frequently identifies heterozygous carriers of MUTYH variants, which, in isolation, would not account for the patient ...
The first International Guidance on the ethics of medical research involving subjects - the Nuremberg Code was formulated in 1947. ... Hence, one has to fall back on current history of medical research in India. The major historic milestones of the Indian Council of Medical Research reflect, in many ways, the growth and development of medical ...
The Wall Street Journal: "Trump Guilty on All Counts in Hush-Money Case.". The cover of the upcoming issue of The New Yorker has an illustration of Donald Trump, the former and perhaps future ...
Ethics in medical research deals with the conflicts of interest across various levels. Guidelines have been proposed for standardized ethical practice throughout the globe. The four fundamental principles of ethics which are being underscored are autonomy, non-maleficence, beneficence, and justice. ... History is unfortunately peppered with ...