Narrative therapy with an emotional approach for people with depression: Improved symptom and cognitive-emotional outcomes
Affiliations.
- 1 Department of Counseling, Dankook University, Seoul, Korea.
- 2 Red Cross College of Nursing, Chung-Ang University, Seoul, Korea.
- 3 Department of Nursing, Daegu Health College, Daegu, Korea.
- 4 College of Nursing, Seoul National University, Seoul, Korea.
- PMID: 25753316
- DOI: 10.1111/jpm.12200
Accessible summary: Narrative therapy is a useful approach in the treatment of depression that allows that person to 're-author' his/her life stories by focusing on positive interpretations, and such focus on positive emotions is a crucial component of treatment for depression. This paper evaluates narrative therapy with an emotional approach (NTEA) as a therapeutic modality that could be used by nurses for persons with depression. A nurse-administered NTEA intervention for people with depression appears effective in increasing cognitive-emotional outcomes, such as hope, positive emotions and decreasing symptoms of depression. Thus, NTEA can be a useful nursing intervention strategy for people with depression.
Abstract: Narrative therapy, which allows a person to 're-author' his/her life stories by focusing on positive interpretations, and emotion-focused therapy, which enables the person to realize his/her emotions, are useful approaches in the treatment of depression. Narrative therapy with an emotional approach (NTEA) aims to create new positive life narratives that focus on alternative stories instead of negative stories. The purpose of this study was to evaluate the effects of the NTEA programme on people with depression utilizing a quasi-experimental design. A total of 50 patients (experimental 24, control 26) participated in the study. The experimental group completed eight sessions of the NTEA programme. The effects of the programme were measured using a self-awareness scale, the Nowotny Hope Scale, the Positive Affect and Negative Affect Scale, and the Center for Epidemiological Studies-Depression Scale. The two groups were homogeneous. There were significant differences in hope, positive and negative emotions, and depression between the experimental and control group. The results established that NTEA can be a useful nursing intervention strategy for people with depression by focusing on positive experiences and by helping depressed patients develop a positive identity through authoring affirmative life stories.
Keywords: depression; emotional approach; hope; narrative therapy; self-awareness.
© 2015 John Wiley & Sons Ltd.
- Cognition / physiology*
- Depression / therapy*
- Emotions / physiology*
- Middle Aged
- Narrative Therapy / methods*
- Outcome Assessment, Health Care*

Collection: Evidence for the effectiveness of narrative therapy
Evidence for the effectiveness of narrative therapy.
Francoise Karibwendea, Japhet Niyonsengaa, Serge Nyirinkwayac, Innocent Hitayezud, Celestin Sebuhoroa,Gitimbwa Simeon Sebatukuraa, Jeanne Marie Nteteaand Jean Mutabaruka
Background: Narrative Therapy is an efficacious treatment approach widely practiced for various psychological conditions. However, few studies have examined its effectiveness on resilience, a robust determinant of one’s mental health, and there has been no randomized controlled trial in sub-Saharan Africa.
Objective: This study sought to evaluate the efficacy of narrative therapy for the resilience oforphaned and abandoned children in Rwanda.
Method: This study was a‘parallel randomized controlled trial in which participants (n= 72) were recruited from SOS Children’s Village. Half of the participants (n= 36) were randomly allocated to the intervention group and the rest to the delayed narrative therapy group. For the intervention group, children attended ten sessions (55 min each) over 2.5 months. Data were collected using the Child and Youth Resilience Measure (CYRM) and analyzed using mixed ANOVA within SPSS version 28.
Result: The results from ANOVA indicated a significant main effect of time and group for resilience total scores. Of interest, there was a significant time by group interaction effect for resilience. Pairwise comparison analyses within-group showed a significant increase in resilience in the intervention group, and the effect size was relatively large in this group.
Conclusion: Our findings highlight the notable efficacy of narrative therapy for children’s resilience in the intervention group. Therefore, health professionals and organizations working with orphaned and abandoned children will apply narrative therapy to strengthen their resilience and improve mental health.
Link: https://www.tandfonline.com/doi/epdf/10.1080/20008066.2022.2152111?needAccess=true&role=button
Carlos A. Chimpén-López, Meritxell Pascheco, Teresa Pretel-Luque, Rebeca Bastón and Daniel Chimpén-Sagrado
We present The Couple’s Tree of Life (CTOL) as a new col- lective narrative methodology to strengthen couple rela- tionships and prevent conflicts. The CTOL, based on the tree of life methodology (Ncube & Denborough, Tree of Life, mainstreaming psychosocial care and support: a man- ual for facilitators, REPSSI, 2007), aims to reinforce the identity and strengths of the couple. We explain the CTOL implementation process and illustrate it step by step with a group of 14 adult heterosexual Caucasian couples who belonged to Protestant churches in Madrid (Spain). As a way to assess its usefulness before applying the CTOL to other groups of couples, we conducted a pre-post evalua- tion using the Dyadic Adjustment Scale of Spanier(1976). We found an improvement in dyadic adjustment, quality, understanding of, and satisfaction with, the relationship. The results, though not generalizable at this stage, suggest that the CTOL could reinforce the couple’s identity while maintaining individual identities. We also discuss the pos- sible applications of couples therapy. Link
The purpose of this study was to explore women’s experiences in a narrative therapy-based group conducted to help participants re-author their stories. Seven women who were either patients or individuals enrolled in Transition Support for Employment at a psychiatric clinic participated in the meetings, one every fortnight. Each session explored a theme based on narrative therapy techniques such as externalization. The participants wrote their reflections during each session, and completed the Beck Depression Inventory-Second Edition (BDI-II) during the initial and final sessions. An affinity diagram was developed to classify their written reflections into 22 lower categories (e.g., new understanding of self , forward-looking-understanding of life ) and 4 upper categories (“Insight,” “Sharing with others,” “Changes with understanding of lives,” “Higher motivation”). The relationship among five lower categories comprising “Insight” was explored, and it became apparent that clarification of participants’ own thoughts about social problems functioned as a mediator promoting the process. The largest portion of depressed feelings emerged during the initial session, and four participants had lower scores for BDI-II items such as self-criticism in the final session. The results suggest that the group’s purpose was realized. However, future studies should examine participants’ feelings more closely, especially during the initial session.
https://onlinelibrary.wiley.com/doi/full/10.1111/jpr.12326
Esther Oi Wah Chow, MSW, RSW, PhD, *, and Sai-Fu Fung, BSocSc, MA, PhD
*Address correspondence to: Esther O. W. Chow, MSW, MNTCW, PhD, RSW, Department of Social and Behavioural Sciences, City University of Hong Kong, Tat Chee Avenue, Kowloon, Hong Kong. [email protected]
Background and Objectives: We developed a new group practice using strength- and meaning-based Narrative Therapy (NT) for older Chinese living in Hong Kong (HK), to enhance their life wisdom. This paper reports on the intervention and its short- and longer-term effectiveness. Research Design and Methods A randomized waitlist-controlled trial (RCT) was conducted. A total of 157 older adults were randomly recruited, of whom 75 were randomly assigned to the intervention group which received four two-hour bi-weekly NT sessions using the ‘Tree of Life’ (ToL) metaphor. The others were placed on a waitlist. Perceived wisdom was assessed using the Brief Self-Assessed Wisdom Scale (BSAWS). Assessment occurred at baseline (T0), end of treatment (T1), and four (T2) and eight months later (T3). Over-time effects of NT on wisdom scores were assessed using latent growth curve models with time-invariant covariates for impact. Results The intervention (NT) group showed significant, sustainable over-time within-group improvement in perceived wisdom. Moreover, compared with the control group, the NT group showed significant immediate improvements in perceived wisdom [F(2.726, p = 0.041)], which were maintained at all follow-up points. This effect remained after controlling for age, gender and educational level [TML(11) = 17.306, p = 0.098, RMSEA = 0.079, CFI = 0.960]. No adverse reaction was recorded. Discussion and Implications NT underpinned by a ToL methodology offers a new theory to understand, promote and appreciate perceived wisdom in older Chinese living in HK. It contributes to psychotherapy and professional social work practice for older Chinese.
Mustafa Kemal Yöntem, Ömer Özer, Yeliz Kan
The purpose of this study was to adapt the Tree of Life application, which was developed based on narrative approach and used for trauma interventions frequently, into career counseling and evaluate its effectiveness on secondary schoolers’ career decision-making self-efficacy. Within the scope of the study, the effectiveness of career counseling program based on narrative therapy was investigated. This study is a quasi-experimental research which was carried out in Turkey. In this research, a 2X2 quasi-experimental design with pre-test and post-test measurements was used. First, two groups were formed, one as experimental and one as a control group. The career story development program based on the narrative therapy which was developed by the researchers was applied on the participants in the experimental group. All of the participants in the study were seventh grade students in the secondary school and 14 years old. The experiment group had 13 participants (6 male, 7 female), and the control group consisted of 12 participants (5 male, 7 female). Demographic Form and Career Decision-Making Self-Efficacy (CDMSES) Scale were used as the data collection tools. In order to examine the research questions, Mann Whitney U-test was conducted between the pre-test and post-test scores of the experimental and control groups. According to the findings, while there was no significant difference between the pre-test scores for all sub-dimensions and total scores of the experimental group and the control group (p>, 05), significant differences were observed in the post-test scores in favor of the experimental group (p <, 05).
Effat Ghavibazou, Simin Hosseinian and Abbas Abdollahi The current study was designed as quasi‐experimental with a pretest and post‐test evaluating the efficacy of narrative therapy on communication patterns for women experiencing low marital satisfaction. Thirty women experiencing low marital satisfaction were chosen using convenience sampling and were randomly assigned to an intervention and waiting list group. The intervention group was treated individually by narrative therapy in eight 45‐minute sessions. Results from repeated measurement ANOVA revealed significant differences between and within the groups and interaction between and within groups. Independent and paired t‐test results showed significant improvement in the intervention group in their marital satisfaction, male‐demand/female‐withdraw, and total demand/withdraw with maintenance at eight weeks follow‐up. Results included increased marital satisfaction, reduced male‐demand/female‐withdraw, and reduced total demand/withdraw. Thus, results show that narrative therapy is effective in increasing the marital satisfaction indicators of male‐demand/female‐withdraw, total demand/withdraw, and marital satisfaction. Link.
Esther Oi Wah Chow and Doris Yuen Hung Fok
Chow, E. O. W., & Fok, D. Y. H. (2020). Recipe of Life: A Relational Narrative Approach in Therapy With Persons Living With Chronic Pain. Research on Social Work Practice , 30 (3), 320-329.
This paper reports on the use of a culturally resonant adaptation to a narrative therapy methodology with older adults in Hong Kong diagnosed with chronic pain. The metaphor of ‘spiritual seasoning of life’ was applied throughout six group-based sessions that followed narrative therapy maps. Three themes illuminating significant life enhancements were generated from subsequent participant interviews: Rediscovery of Personal Capabilities, Validation of Preferred Identity and Fusion of Spiritual Seasoning of Life. The authors conclude that narrative therapy was shown to be an applicable and effective approach for people living with chronic pain.
De-Hui Ruth Zhou, Yu-Lung Marcus Chiu, Tak-Lam William Lo, Wai-Fan Alison Lo, Siu-Sing Wong, Chi Hoi Tom Leung, Chui-Kam Yu, Yuk Sing Geoffrey Chang & Kwok-Leung Luk
Journal of Mental Health, published online 15 Jul 2020
DOI: 10.1080/09638237.2020.1793123
https://www.tandfonline.com/doi/abs/10.1080/09638237.2020.1793123?journalCode=ijmh20
Situated in the Hong Kong context, this study utilises a methodology commonly associated with evidence-based practice to determine the helpfulness of collective narrative therapy groups for family members of someone living with schizophrenia. Until now, local programs to support family members have largely focussed on imparting skills and knowledge in caregiving. By way of an alternative, this article provides in replicable detail an account of steps taken to engage with creative metaphors and culturally-specific adaptations to narrative practice that centre the skills and knowledge family members already have. The authors conclude that the practice implications of their study point to the helpfulness of a narrative stance for eliciting stories about existing knowledge, the significance of attending to the uniqueness of culture and context, and the benefits of exploring preferred identity stories for family members with caring responsibilities.
Esther OW Chow
Chow, E. O. (2018). Narrative Group Intervention to reconstruct Meaning of Life among Stroke Survivors: A Randomized Clinical Trial Study. Neuropsychiatry , 08(04). doi:10.4172/neuropsychiatry.1000450
This study evaluated a narrative therapy meaning-making approach in relation to stroke survival. Following a series of conversations that focussed on deconstructing dominant life stories, externalising problem-saturated experience, and re-authoring identity, participants reported sustained improvements across a range of outcome measures. Stroke knowledge, mastery, self-esteem, hope, meaning in life, and life satisfaction were all demonstrated to have increased, whereas experiences of depression had decreased. The authors conclude that the indicated effects for self-concepts and improved meaning in life were sufficiently encouraging to suggest narrative therapy may be a viable option for facilitating stroke recovery.
Sarah Penwarden (2018) [ PhD thesis, University of Waikato ]
A key concern for therapists is how therapeutic change occurs, and what particular elements of therapy lead towards change. This project investigated how one approach in narrative therapy—rescued speech poetry—might enhance another therapeutic approach, re-membering conversations. Re-membering conversations nurture connections between a bereaved person and a loved person who has died. These conversations actively weave the stories of the lost loved one back into the life of the bereaved person, so that the loved one’s values and legacies continue to resound. This research explored how a literary approach—rescued speech poetry—potentially enhanced the nearness and contribution of a loved one, through capturing stories in a poetic form.
Marie-Nathalie Beaudoin, Meredith Moersch and Benjamin S. Evare
Journal of Systemic Therapies, Vol. 35, No. 3, 2016, pp. 42–59
This article examines the effectiveness of narrative therapy in boosting 8- to 10-year-old children’s social and emotional skills in school. Data were collected from 353 children over two years, and two research assistants independently coded 813 stories. Children’s personal accounts of their attempts at solving conflicts in their daily lives were collected before and after a series of narrative conversations, and compared to stories collected during the same time interval with a control group. The control data included a set of stories from waitlisted participants and those from students assigned to only a control group. The results of the study show that children receiving narrative therapy intervention showed a significant improvement in self-awareness, self-management, social awareness/empathy, and responsible decision making when compared to their own first stories and the stories from children in the control group. Improvement in relationship skills was present in both cohorts but was significant only for the second year. There was no significant gender difference. Narrative therapy practices such as externalizing and re-authoring can significantly contribute to the development of children’s social and emotional skills. Implications of these results are discussed for all forms of therapeutic interventions, regardless of theoretical orientation.
M. Seo, H. S. Kang, Y. J. Lee, S. M. Chae. Journal of Psychiatric and Mental Health Nursing Volume 22, Issue 6, pages 379–389, August 2015 : http://onlinelibrary.wiley.com/resolve/doi?DOI=10.1111/jpm.12200
Narrative therapy, which allows a person to ‘re-author’ his/her life stories by focusing on positive interpretations, and emotion-focused therapy, which enables the person to realize his/her emotions, are useful approaches in the treatment of depression. Narrative therapy with an emotional approach (NTEA) aims to create new positive life narratives that focus on alternative stories instead of negative stories. The purpose of this study was to evaluate the effects of the NTEA programme on people with depression utilizing a quasi-experimental design. A total of 50 patients (experimental 24, control 26) participated in the study. The experimental group completed eight sessions of the NTEA programme. The effects of the programme were measured using a self-awareness scale, the Nowotny Hope Scale, the Positive Affect and Negative Affect Scale, and the Center for Epidemiological Studies-Depression Scale. The two groups were homogeneous. There were significant differences in hope, positive and negative emotions, and depression between the experimental and control group. The results established that NTEA can be a useful nursing intervention strategy for people with depression by focusing on positive experiences and by helping depressed patients develop a positive identity through authoring affirmative life stories.
Erbes CR, Stillman JR, Wieling E, Bera W, Leskela J. J Trauma Stress. 2014 Dec;27(6):730-3. doi: 10.1002/jts.21966 . Epub 2014 Nov 10.
Narrative therapy is a postmodern, collaborative therapy approach based on the elaboration of personal narratives for lived experiences. Many aspects of narrative therapy suggest it may have great potential for helping people who are negatively affected by traumatic experiences, including those diagnosed with posttraumatic stress disorder (PTSD). The potential notwithstanding, narrative therapy is relatively untested in any population, and has yet to receive empirical support for treatment among survivors of trauma. A pilot investigation of the use of narrative therapy with 14 veterans with a diagnosis of PTSD (11 treatment completers) is described. Participants completed structured diagnostic interviews and self-report assessments of symptoms prior to and following 11 to 12 sessions of narrative therapy. After treatment, 3 of 11 treatment completers no longer met criteria for PTSD and 7 of 11 had clinically significant decreases in PTSD symptoms as measured by the Clinician Administered PTSD Scale. Pre- to posttreatment effect sizes on outcomes ranged from 0.57 to 0.88. These preliminary results, in conjunction with low rates of treatment dropout (21.4%) and a high level of reported satisfaction with the treatment, suggest that further study of narrative therapy is warranted as a potential alternative to existing treatments for PTSD.
Majid Yoosefi Looyeh, Khosrow Kamali, Amin Ghasemi, Phuangphet Tonawanik The Arts in Psychotherapy, 2014, 41: 1: 16-20 DOI: 10.1016/j.aip.2013.11.005
This study applied group narrative therapy to treating symptoms of social phobia among 10–11 year old boys. The treatment group received fourteen 90-min sessions of narrative therapy twice a week. Group narrative therapy was effective in reducing symptoms of social phobia at home and school as reported by parents and teachers.
Lopes, Rodrigo T.: Gonçalves, Miguel M.; Machado, Paulo; Sinai, Dana; Bento, Tiago & Salgado, João. Psychotherapy Research . Nov 2014, Vol. 24 Issue 6, p.662-674.
Systematic studies of the efficacy of Narrative Therapy (NT) for depression are sparse. Objective: To evaluate the efficacy of individual NT for moderate depression in adults compared to Cognitive-Behavioral Therapy (CBT). Method: Sixty-three depressed clients were assigned to either NT or CBT. The Beck Depression Inventory-II (BDI-II) and Outcome Questionnaire-45.2 (OQ-45.2) were used as outcome measures. Results: We found a significant symptomatic reduction in both treatments. Group differences favoring CBT were found on the BDI-II, but not on the OQ-45.2. Conclusions: Pre- to post-treatment effect sizes for completers in both groups were superior to benchmarked waiting-list control groups.
Lambie, I., Murray, C., Krynen, A., Price, M., & Johnston, E. (2013). The Evaluation of Undercover Anti-Bullying Teams. (Report). Auckland: Ministry of Education, Te Tāhuhu o Te Mātauranga.
https://www.dulwichcentre.com.au/UABT-Final-Report.pdf
Bullying is a significant societal problem in schools, having serious implications for both victims and perpetrators. While there have been many interventions developed to try and combat bullying in schools, many of these interventions are not formally evaluated. The current study evaluated an anti-bullying intervention that adopts a restorative approach that uses peer-led Undercover Anti-bullying Teams (UABTs) to combat bullying in the classroom. To evaluate this approach, the current study implemented the use of a pre- test/post-test experimental design in additional to qualitative interview data. The results suggest that following the intervention, there was a significant reduction in victimisation and a significant increase in students’ perceptions of personal support from other students in the class. Additionally, a number of themes emerged to suggest feelings of “inclusion” and “social support” were helpful to reduce distress for victims, and to help them feel more confident in the classroom. Additionally, the central elements of “autonomy” and “teamwork” that are inherent in the UABT intervention were helpful for team members in supporting the bullying victim and reducing bullying in the classroom.
Cashin, A, Browne, G, Bradbury, J & Mulder, AM 2013 Journal of Child and Adolescent Mental Health Nursing, vol. 26, no. 1, pp. 32-41. http://dx.doi.org/10.1111/jcap.12020
The aim of this pilot study was to be the first step toward empirically determining whether narrative therapy is effective in helping young people with autism who present with emotional and behavioral problems. Autism is increasingly being recognized in young people with average and above intelligence. Because of the nature of autism, these young people have difficulty navigating the challenges of school and adolescence. Narrative therapy can help them with their current difficulties and also help them develop skills to address future challenges. Narrative therapy involves working with a person to examine and edit the stories the person tells himself or herself about the world. It is designed to promote social adaptation while working on specific problems of living. This pilot intervention study used a convenience sample of 10 young people with autism (10–16 years) to evaluate the effectiveness of five 1 hr sessions of narrative therapy conducted over 10 weeks. The study used the parent-rated Strengths and Difficulties Questionnaire (SDQ) as the primary outcome measure. Secondary outcome measures were the Kessler-10 Scale of Psychological Distress (K-10), the Beck Hopelessness Scale, and a stress biomarker, the salivary cortisol to dehydroepiandrosterone (DHEA) ratio.
Significant improvement in psychological distress identified through the K-10 was demonstrated. Significant improvement was identified on the Emotional Symptoms Scale of the SDQ. The cortisol:DHEA ratio was responsive and a power analysis indicated that further study is indicated with a larger sample. Narrative therapy has merit as an intervention with young people with autism. Further research is indicated.
Mala German Educational & Child Psychology . Dec2013, Vol. 30 Issue 4, p75-99
This paper evaluates the use of the ‘Tree of Life’ (ToL) intervention with a class of 29 Year 5 pupils (aged 9 and 10-years-old) in a primary school in North London. This was an exploratory study to see if ToL could be adapted to a mainstream education setting and could be used as a whole class intervention. This paper examines the effectiveness of ToL in enhancing the pupils’ self-esteem and in developing their understanding of their own culture and that of their peers. Findings from semi-structured interviews, preand post-intervention, were used to explore the pupils’ baseline knowledge of their own family and cultural background and in their understanding of key concepts such as ‘culture’, ‘ethnicity’, and ‘racism.’ Qualitative analysis was applied to identify key themes emerging from these interviews. Results from quantitative analysis found a significant improvement in the pupil’s self-concept post-intervention. The pupils also reported positive improvements in cultural understanding of themselves and other class members whilst some reported a reduction in racist behaviour. This paper concludes with a discussion of the limitations of the study and advocates that EPs become more involved in utilising strength-based interventions in developing cultural understanding and community cohesion.
Looyeh MY, Kamali K, Shafieian R
Family Research and Development Centre, Faculty of Education, University of Malaya, Kuala Lumpur, Malaysia. [email protected] This study explored the effectiveness of group narrative therapy for improving the school behavior of a small sample of girls with attention-deficit/hyperactivity disorder (ADHD). Fourteen clinics referred 9- to 11-year-old girls with a clinical diagnosis of ADHD were randomly assigned to treatment and wait-list control groups. Posttreatment ratings by teachers showed that narrative therapy had a significant effect on reducing ADHD symptoms 1 week after completion of treatment and sustained after 30 days. Arch Psychiatr Nurs. 2012 Oct;26(5):404-10. doi: 10.1016/j.apnu.2012.01.001. Epub 2012 Mar 28. http://www.ncbi.nlm.nih.gov/pubmed/22999036
Elaine Hannen, Kevin Woods
Educational Psychology in Practice 01/2012; 28(2):187-214. DOI:10.1080/02667363.2012.669362 https://www.tandfonline.com/doi/abs/10.1080/02667363.2012.669362?journalCode=cepp20#preview The National Institute for Clinical Excellence identifies educational psychologists as appropriate specialists to deliver interventions to promote the emotional well-being of children and families. A role for practitioner educational psychologists in providing specific therapeutic interventions has also been proposed by commentators. The present study reports an evaluative case study of a narrative therapy intervention with a young person who self-harms. The analysis of data suggests that the narrative therapy intervention was effectively implemented and resulted in attributable gains in emotional well-being, resilience and behaviour for the young person. The authors discuss the role of the educational psychologist in delivering specific therapeutic interventions within a local authority context and school-based setting. Consideration is also made of the development of the evidence base for the effectiveness of narrative therapy intervention with young people who self-harm.
Everett McGuinty, MA, David Armstrong, PhD, John Nelson, MA, and Stephanie Sheeler, BA Journal of Child and Adolescent Psychiatric Nursing ISSN 1073-6077 http://onlinelibrary.wiley.com/doi/10.1111/j.1744-6171.2011.00305.x/abstract Author contact: [email protected] The intent of this article is to explore the efficacy of both the literal and concrete externalization aspects within narrative therapy, and the implementation of interactive metaphors as a combined psychotherapeutic approach for decreasing anxiety with people who present with high-functioning autism. The purpose of this exploratory article is to propose the use of externalizing metaphors as a treatment modality as a potentially useful way to engage clients. Specifically, a three-step process of change is described, which allows for concretizing affective states and experiences, and makes use of visual strengths of people presenting with an autism spectrum disorder. A selective review was conducted of significant works regarding the process of change in narrative therapy, with particular emphasis on metaphors. Works were selected based on their relevance to the current paper and included both published works (searched via Psyc-INFO) and materials from narrative training sessions. Further research is needed to address the testable hypotheses resulting from the current model. This line of research would not only establish best practices in a population for which there is no broadly accepted treatment paradigm, but would also contribute to the larger fields of abnormal psychology, emotion regulation, and cognitive psychology by further elucidating the complex ways these systems interact.
Lynette P. Vromans & Robert D. Schweitzer (2010)
Psychotherapy Research , 19 March 2010, doi: 10.1080/10503301003591792 http://www.ncbi.nlm.nih.gov/pubmed/20306354
This study investigated depressive symptom and interpersonal relatedness outcomes from eight sessions of manualized narrative therapy for 47 adults with major depressive disorder. Post-therapy, depressive symptom improvement (d=1.36) and proportions of clients achieving reliable improvement (74%), movement to the functional population (61%), and clinically significant improvement (53%) were comparable to benchmark research outcomes. Post-therapy interpersonal relatedness improvement (d=.62) was less substantial than for symptoms. Three-month follow-up found maintenance of symptom, but not interpersonal gains. Benchmarking and clinical significance analyses mitigated repeated measure design limitations, providing empirical evidence to support narrative therapy for adults with major depressive disorder.
Sommayeh Sadat MacKean *, Hossein Eskandari, Ahmad Borjali , Delaram Ghodsi
* Msc in General Psychology, Faculty of Psychology and Educational Sciences, Allameh Tabatabaii University, Tehran, Iran – Faculty of Psychology and Educational Sciences, Allameh Tabatabaii University, Tehran, Iran. Tel: +98- 912- 1868311 , [email protected]
This study was carried out according to importance of body image in overweight women, and in order to compare the effect of diet therapy and narrative therapy on the body image improvement. Materials and Methods: This was a quasi experimental-interventional study. 30 overweight women were selected through randomized sampling method within women who referred to professional clinic of nutrition and diet therapy and they randomly divided to two interventions and one control group. Group 1 only received diet therapy (for 5weeks), group 2 received narrative therapy in addition to diet therapy and control group received no intervention.
Narrative therapy was a group therapy that consisted of 12 sessions and each session last 50 minutes that performed twice a week. Control group received no intervention. Weight of subjects was measured with light cloths by a Seca balance scale to the nearest 0.5 kg and their height was measured by stadio-meter to 0.5 cm. Body Mass Index was calculated by dividing weight (in kg) to squared height (in m2). Data of Body Image were gathered through Multidimensional Body-Self Relation Questionnaire. Data were analyzed by covariance analysis, Tukey and paired t test using SPSS 16 software.
Results: The mean of body image at the beginning of the study in the control group, was 135.20 and it was134.60 after the intervention. In group 1, at the beginning of the study the mean was 148.1 and after the intervention was 147.50. In group 2, at the beginning of the study the mean was 150.80 and after the intervention the result was 163.90. Data analysis showed that at the end of the study diet therapy had no significant effect on developing of body image (P>0.05). But narrative therapy was more effective than diet therapy in developing of body image in overweight women (P<0.001). Conclusion: According to effect of narrative therapy on body image development, this method is more suitable than the other methods which have greater results in weight loss. Pajoohandeh Journal. 2010; 15 (5) :225-232 http://pajoohande.sbmu.ac.ir/browse.php?a_code=A-10-1-655&sid=1&slc_lang=en
Jennifer Poolea, Paula Gardner, Margaret C. Flower & Carolynne Cooper Social Work With Groups, Volume 32, Issue 4, 2009 https://www.tandfonline.com/doi/abs/10.1080/01609510902895086#.Uk-lShBKiSo In this article, the authors report on a qualitative study that explored the use of narrative therapy with a diverse group of older adults dealing with mental health and substance misuse issues. Narrative therapy supports individuals to critically assess their lives and develop alternative and empowering life stories that aim to keep the problem in its place. Although the literature suggests this is a promising intervention for individuals, there is a lack of research on narrative therapy and group work. Aiming to address this gap, the authors developed and researched a narrative therapy group for older adults coping with mental health and substance misuse issues in Toronto, Canada. Taking an ethnographic approach, field notes and interviews provided rich data on how, when, and for whom, such a group could be beneficial. Findings contribute to the literature on group work, older adults, and narrative therapy.
Karen Young and Scot Cooper (2008) Journal of Systemic Therapies, Vol. 27, No. 1, 2008, pp. 67–83
Link to full article.
In this article, we will report on the Narrative Therapy Re-Visiting Project. Narrative ways of thinking shape research in ways that strive to center the voice of the therapy participant. We will present qualitative research findings that bring to the forefront the personal thoughts of the participants about what was meaningful and useful in therapeutic conversations. This contribution moves away from solely interpreted understandings of professionals and toward co-composed understandings between professionals and therapy participants. In a follow-up meeting, persons who have come to us for single session therapy/consultation, return to re-visit videotape of the earlier session.
All of the sessions took place in a walk-in clinic and in single session consultations; therefore the feedback is about narrative practice in a single session encounter. The authors systematically document the participants’ accounts and descriptions of meaningful moments and experiences of the therapeutic process using qualitative methodology and attempt to discern from them themes and implications for therapeutic practice.
Lynette Vromans (2008) [PhD thesis, Queensland University of Technology]
The research aim, to investigate the process and outcome of narrative therapy, comprised theoretical and empirical objectives. The first objective was to articulate a theoretical synthesis of narrative theory, research, and practice. The process of narrative reflexivity was identified as a theoretical construct linking narrative theory with narrative research and practice. The second objective was to substantiate this synthesis empirically by examining narrative therapy processes, specifically narrative reflexivity and the therapeutic alliance, and their relation to therapy outcomes. The third objective was to support the proposed synthesis of theory, research, and practice and provide quantitative evidence for the utility of narrative therapy, by evaluating depressive symptom and inter-personal relatedness outcomes through analyses of statistical significance, clinical significance, and benchmarking …
To support this theoretical synthesis, a process-outcome trial evaluated eight-sessions of narrative therapy for 47 adults with major depressive disorder. Dependent process variables were narrative reflexivity (assessed at Sessions 1 and 8) and therapeutic alliance (assessed at Sessions 1, 3, and 8). Primary dependent outcome variables were depressive symptoms and inter-personal relatedness. Primary analyses assessed therapy outcome at pre-therapy, post-therapy, and three-month follow-up and utilized a benchmarking strategy to the evaluate pre-therapy to post-therapy and post-therapy to follow-up gains, effect size and pre-therapy to post-therapy clinical significance … The clinical trial provided empirical support for the utility of narrative therapy in improving depressive symptoms and inter-personal relatedness from pre-therapy to post-therapy: the magnitude of change indicating large effect sizes (d = 1.10 to 1.36) for depressive symptoms and medium effect sizes (d = .52 to .62) for inter-personal relatedness.
Therapy was effective in reducing depressive symptoms in clients with moderate and severe pre-therapy depressive symptom severity. Improvements in depressive symptoms, but not inter-personal relatedness, were maintained three-months following therapy. The reduction in depressive symptoms and the proportion of clients who achieved clinically significant improvement (53%) in depressive symptoms at post-therapy were comparable to improvements from standard psychotherapies, reported in benchmark research. This research has implications for assisting our understanding of narrative approaches, refining strategies that will facilitate recovery from psychological disorder and providing clinicians with a broader evidence base for narrative practice … This thesis was awarded the Outstanding Doctoral Thesis award across the Queensland University of Technology Faculty of Health. Read the complete thesis here .
Read examiner comments here: Examiner number 1 (pdf, 47 KB), Examiner number 2 (pdf, 15 KB).
Lewis Mehl-Madrona, MD, PhD
The Permanente Journal/ Fall 2007/ Volume 11 No. 4
Narrative approaches to psychotherapy are becoming more prevalent throughout the world. We wondered if a narrative-oriented psychotherapy group on a locked, inpatient unit, where most of the patients were present involuntarily, could be useful. The goal would be to help involuntary patients develop a coherent story about how they got to the hospital and what happened that led to their being admitted and link that to a story about what they would do after discharge that would prevent their returning to hospital in the next year.
Sonja Berthold (June 2006)
Funded by Relationships Australia Northern Territory
This is an independent evaluation of a narrative therapy/collective narrative practice project conducted in two Aboriginal communities in Arnhem Land – Yirrkala & Gunyangara. The project aimed to:
- reduce suicidal thinking/behaviour/injury, self-harm and death by suicide
- enhance resilience, respect, resourcefulness, interconnectedness, and mental health of individuals, families, and communities and to reduce prevalence of risk conditions
- increase support available to individuals, families, and communities who have been affected by suicidal behaviours.
The project was conducted in partnership between Dulwich Centre and Relationships Australia Northern Territory. For more information about the project, read: ‘Linking stories and initiatives: A narrative approach to working with the skills and knowledge of communities’ by David Denborough, Carolyn Koolmatrie, Djapirri Mununggirritj, Djuwalpi Marika, Wayne Dhurrkay, & Margaret Yunupingu.
The independent evaluation found:
Did this project work? Yes, this project worked because it:
- reminded people of their strength and of their dreams
- increased the self-esteem and confidence of individual and groups, and reinforced their ability to deal with suicide and suicidal thinking
- created an opportunity for these communities to forge links with another Indigenous community, a link which strengthens and comforts both
- provided an audience for the stories and passed on the responses
- people see that their knowledge and experience is of value to others
- the community came together to celebrate their strengths and abilities
- ensured that local workers were linked into and supporting this process
- left a resource that is still being used.
What was done well?
- Good, thorough consultation with resulted in changes
- Professional and respectful approach
- Project tried to link in outside workers to help the project continue
- The narrative approach was very successful and well accepted
- Connected very strongly with key leaders in each community
- Delivered relevant, interesting, and useful training
- Provided learning opportunity for Yolgnu people through ensuring local people were involved in the narrative approach
- The team were flexible and able to respond to what was needed and have maintained a connection with the communities
- Made sure that they left a resource for the community to use.
To read the entire evaluation, click here (pdf, 307 KB).
Mim Weber, Kierrynn Davis, & Lisa McPhie (2006) Australian Social Work, 59 (4), 391–405. doi: 10.1080/03124070600985970
This paper reports on a study conducted with seven women who identified themselves as experiencing depression as well as an eating disorder and who live in a rural region of northern New South Wales. Self-referred, the women participated in a weekly group for 10 weeks, with a mixture of topics, conducted within a narrative therapy framework. A comparison of pre- and post-group tests demonstrated a reduction in depression scores and eating disorder risk. All women reported a change in daily practices, together with less self-criticism. These findings were supported by a post-group evaluation survey that revealed that externalisation of, and disengagement from, the eating disorder strongly assisted the women to make changes in their daily practices. Although preliminary and short-term, the outcomes of the present study indicate that group work conducted within a narrative therapy framework may result in positive changes for women entangled with depression and an eating disorder.
Margaret L. Keeling, L. Reece Nielson Contemporary Family Therapy , September 2005, Volume 27, Issue 3, pp 435-452
International and minority populations tend to underutilize mental health services, including marriage and family therapy. Models of marriage and family therapy developed in the West may reflect Western values and norms inappropriate for diverse cultural contexts. This article presents an exploratory, qualitative study of a narrative therapy approach with Asian Indian women. This study adds to the small body of narrative-based empirical studies, and has a unique focus on intercultural applications and the experience of participants. Participant experience was examined along four phenomenological dimensions. Findings indicate the suitability of narrative interventions and nontraditional treatment delivery for this population.
Evril Silver, Alison Williams, Fiona Worthington, and Nicola Phillips (1998) Journal of Family Therapy, 20, 413–422.
This is a retrospective audit of the therapy outcome of 108 children with soiling and their families. Fifty-four children were treated by externalizing and 54 comparison children and families were treated by the usual methods in the same clinic. The results from the externalizing group were better and compared favourably with standards derived from previous studies of soiling. Externalizing was rated as much more helpful by parents at follow-up.
David Besa, California Graduate School of Family Psychology (1994) Research on Social Work Practice, 4 (3), 309–325. doi: 10.1177/104973159400400303
This study assessed the effectiveness of Narrative Therapy in reducing parent/child conflicts. Parents measured their child’s progress by counting the frequency of specific behaviours during baseline and intervention phases. The practitioner-researcher used single-case methodology with a treatment package strategy, and the results were evaluated using three multiple baseline designs. Six families were treated using several Narrative Therapy techniques including externalisation, relative influence questioning, identifying unique outcomes and unique accounts, bringing forth unique re-descriptions, facilitating unique circulation, and assigning between-session tasks. Compared to baseline rates, five of six families showed improvements in parent/child conflict, ranging from an 88% to a 98% decrease in conflict. Improvements occurred only when Narrative Therapy was applied and were not observed in its absence.
Fred W. Seymour & David Epston (1989) Australian & New Zealand Journal of Family Therapy, 10 (3).
Childhood stealing is a distressing problem for families and may have wider community costs since childhood stealers often become adult criminals. This paper describes a therapeutic ‘map’ that emphasises direct engagement of the child, along with his/her family, in regarding the child from ‘stealer’ to ‘honest person’. Analysis of therapy with 45 children revealed a high level of family engagement and initial behaviour change. Furthermore, a follow-up telephone call made 6–12 months after completion of therapy sessions revealed that 80% of the children had not been stealing at all or had substantially reduced rates of stealing. This community practice, which was in part researched by Seymour and Epston, has recently been written up in some detail in ‘ Community approaches – real and virtual – to stealing ’ (pdf, 68 KB) [Epston, D., & Seymour, F. (2008). In Epston, D., Down under and up over: Travels with narrative therapy , Warrington, England: AFT Publishing Limited, pp. 139–156.]
Report by Linzi Rabinowitz. Researchers: Linzi Rabinowitz and Rebecca Goldberg
Hero Books are a psychosocial support intervention developed by Jonathan Morgan (REPSSI) which are informed by narrative therapy ideas. This study presents preliminary evidence to support the contention that the mainstreaming of PSS (psychosocial support) in the South African school curriculum by means of the Hero Book is likely to produce two significant outcomes:
- learners who have undergone the Hero Book process are more likely to perform better in the learning areas of Life Orientation and Language (Home Language and first additional Language) than learners whose educators did not use Hero Books as measured by the same learning outcomes and assessment standards
- learners whose educators used the Hero Book methodology to pursue academic outcomes are more likely to exhibit an improvement in their psychosocial wellbeing than learners whose educators do not use the Hero Book methodology.
A mix of quantitative and qualitative data collection and analysis supports these findings. While none of the findings are conclusive, and the study admittedly has limitations, the strongest quantitative finding is this one: 77% of learner’s academic performance as measured by an average mark for all three learning areas (Home Language, First Additional Language, and Life Orientation) improved overall for the Hero book group, as opposed to 55% in the control groups. This finding suggests that the hero book intervention might be pursued purely on its potential as a methodology to enhance academic learning outcomes, and where any improvements in the psychosocial wellbeing of learners is an added bonus of the intervention. The sample size consisted of four control groups and four intervention groups across two research sites, the Western Cape and KwaZulu Natal. There was a total of 172 learners in the control groups and 113 in the intervention groups. For full report, contact Jonathan Morgan: [email protected]
Social media
Subscribe to email news, acknowledgements.

- Open access
- Published: 12 September 2022
Paper 2: a systematic review of narrative therapy treatment outcomes for eating disorders—bridging the divide between practice-based evidence and evidence-based practice
- Janet Conti 1 , 2 ,
- Lauren Heywood 1 ,
- Phillipa Hay 2 , 3 ,
- Rebecca Makaju Shrestha 1 &
- Tania Perich 1 , 2
Journal of Eating Disorders volume 10 , Article number: 138 ( 2022 ) Cite this article
6894 Accesses
2 Citations
30 Altmetric
Metrics details
Narrative therapy has been proposed to have practice-based evidence however little is known about its research evidence-base in the treatment of eating disorders. The aim of this study was to conduct a systematic review of the outcome literature of narrative therapy for eating disorders.
Treatment outcome data were extracted from 33 eligible included studies following systematic search of five data bases. The study is reported according to Preferred Reporting items for Systematic Reviews and Meta-Analyses guidelines.
Of the identified 33 studies, 3 reported positive outcomes using psychometric instruments, albeit some were outdated. Otherwise, reported outcomes were based on therapy transcript material and therapist reports. The most commonly reported treatment outcome was in relation to shifts in identity narratives and improved personal agency with a trend towards under-reporting shifts in ED symptoms. Some improvements were reported in interpersonal and occupational engagement, reduced ED symptoms, and improved quality of life, however, there was an absence of standardized measures to support these reports.
Conclusions
This systematic review found limited support for narrative therapy in the treatment of eating disorders through practice-based evidence in clinician reports and transcripts of therapy sessions. Less is known about systematic treatment outcomes of narrative therapy. There is a need to fill this gap to understand the effectiveness of narrative therapy in the treatment of EDs through systematic (1) Deliveries of this intervention; and (2) Reporting of outcomes. In doing so, the research arm of narrative therapy evidence base will become more comprehensively known.
Plain English summary
Narrative therapy has been proposed as a promising intervention for the treatment of eating disorders. However, the treatment outcomes of narrative therapy for eating disorders are under-researched. This systematic review of the literature has demonstrated limited support for narrative therapy through practice-based evidence in clinician reports and transcripts of therapy sessions. These reports demonstrated how narrative therapy was associated with identity shifts, some symptom reduction, reduced hospitalisations, improved agency over the problem and improvements in quality of life. There is a need for future research to systematically report treatment outcomes. This will fill a gap in research evidence-base for narrative therapy in the treatment of eating disorders.
Eating disorders (EDs) such as anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder (BED) and other specified feeding and eating disorders [ 1 ] are prevalent in the community and have implications for physical, psychological and social wellbeing. Around 8.4% of women and 2.2% of men are diagnosed in their lifetimes [ 2 ] and, due to the nature of these conditions, EDs may be difficult to treat and often involve complex, ongoing care and multiple forms of treatment in both inpatient and outpatient settings [ 3 ].
Despite the prevalence and potential to run a chronic course that is associated with adverse impacts on quality of life [ 4 ], the effectiveness of the current evidence-based ED treatments is incomplete. Cochrane and other systematic reviews have shown that family therapies for AN, including Family-Based Therapy [ 5 ] and psychosocial treatments for BN, including cognitive behavioural therapy (CBT) and interpersonal psychotherapy [ 6 ] to be most efficacious treatments for these eating disorders, respectively. For example, systematic reviews have found that CBT for BN had moderate to large treatment outcome effects that were maintained over time [ 7 ] and benefits have been reported for adult AN [ 8 ]. There is less data to support the long term benefits of psychological therapies in the treatment of BED, however moderate support has been found for CBT and guided self-help [ 9 ]. Futhermore, a range of rates of relapse in EDs have been reported, as wide as from 9 to 52% [ 10 ], and definitions of relapse and remission rates may vary greatly within the literature.
There has also been increased research into the perspectives of those with a lived experience that goes some way in understanding how and why first line ED treatment do not work for all [ 11 , 12 , 13 ]. This has led many to suggest that there may be some sub-types of EDs, ‘severe and enduring’ in nature, that may require more specialised and targeted treatment over a longer period of time [ 14 ]. Others have suggested that treatments need to expand beyond a primary focus on eating behaviour change, for example to the rebuilding of identity outside the ED identity [ 12 ]. Furthermore, expanding the range of ED treatments that may be tailored to the experiencing person may go some way in preventing EDs running a chronic course and reduce the current rates of treatment attrition [ 12 , 15 , 16 ].
For those with severe and enduring EDs, there have been three randomised controlled trials to assess the effectiveness of treatment interventions [ 3 ]. Authors noted that although inpatient programs were found to be potentially effective in the shorter term, no evidence was found for longer term treatment gains for this group [ 3 ]. Types of treatments and settings may not necessarily be more effective than others, with insufficient evidence being found on one review for the superiority of either inpatient or outpatient settings [ 17 ].
Qualitative research of women who have recovered from eating disorders have noted that women experienced a fragmented sense of self when recovering, including rebuilding a more durable sense of identity with reclaiming relationships and self-acceptance also featuring as important [ 18 ]. Narrative therapy is a form of therapy developed by Michael White and David Epston [ 19 , 20 , 21 ] that provides an alternative therapeutic intervention that positions the person as the expert of their life and the problem (including an ED) as external to them. Focusing on identity and its performance, narrative therapy is a process-orientated therapy that focuses on externalizing and unpacking the meaning of problem stories to find and reconstruct hidden identity narratives that have been obscured by the dominant problem narrative [ 19 ]. This form of therapy is based on the philosophies of post-structuralism and social constructivism [ 21 ] and therefore understands that the language used in therapy matters in how identity narratives are constructed. In narrative therapy, therapists prioritise the language used by the person, including the metaphors to depicted their lived ED experience [ 20 , 22 ], and proposes that language shapes identity narratives whose meaning are performed in a person’s life [ 19 , 23 ].
In sum, narrative therapy may hold specific benefits in that it may address elements less considered in other therapies, such as the narrative metaphor to understand identity negotiation and its performance, which may fit the needs and preferences for the treatment of EDs as noted by those with a lived experience [ 12 ]. Narrative therapists have proposed that narrative therapy has “practice-based evidence” [ 24 ] for its effectiveness, however, to our knowledge there is no systematic review evaluating the research evidence for its efficacy in the treatment of EDs.
The current study
The aim of this study was to conduct a systematic review of the literature to assess the reported therapeutic outcomes of narrative therapy in the treatment of ED. This review aims to determine the efficacy of narrative therapy interventions in the treatment of ED and to assess symptom measures and other reported treatment outcomes. A further aim of this review is to describe the range of treatment outcome variables, which have used in the systematically reviewed studies.
This systematic review was carried out as per the guidelines set by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 25 ].
The protocol is registered with PROSPERO and is available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020175507 .
Identification and selection of studies
The databases searched included PsychINFO, MEDLINE, EMBASE, SocIndex and ProQuest Dissertations and Theses (grey literature) between 1979 and 4th July 2021. Key words used were (anorexi* OR anore*) OR (bulimi* or bulim*) OR (eat* or eating) OR (binge eat*) AND (intervention* OR treatment* OR therapy OR counsel*) AND (narrative).
The inclusion criteria were papers that met the following criteria: (a) published in English, (b) focused on the content of narrative therapy interventions (including specific details of said content); (c) included a sample of individuals in treatment for any ED, with the exception of books that describe narrative therapy interventions and case studies that use illustrative examples. Articles were excluded if they were (a) review papers, (b) not published in English, (c) if full text was unavailable, or (d) did not describe therapy outcomes. Therapy outcomes included scales measuring symptom severity and those described in case studies.
Study selection
One reviewer (LH) ran the identified search terms across all electronic databases, including grey literature. Another reviewer (JC) identified relevant articles from their personal library of narrative therapy resources. All texts were then combined and duplicates removed. The title and abstract of each paper were individually evaluated by two reviewers (LH and JC) for their adherence to inclusion criteria and any discrepancies were resolved by a third reviewer (PH). The full text of publications were obtained if they met criteria and any unavailable full texts were excluded. The first reviewer (LH) assessed eligibility of full-text references for inclusion, with assistance from the second reviewer (JC) regarding any uncertainties.
Articles included were assessed at (i) Title screening, (ii) Abstract screening and (iii) Full text screening. Title, and abstract screening was independently undertaken by two reviewers (LH and JC). A third reviewer (PH) resolved any discrepancies. Full text screening was undertaken initially independently by two reviewers (LH and JC) and any discrepancies were resolved between them through discussion.
Articles that were selected for data extraction post full text screening included (i) An eating disorder (ii) Narrative therapy as a treatment of an eating disorder (iii) Full text available in English. Articles were excluded during full text screening included those that (i) Severely lacked any qualitative case study or quantitative data and; (ii) Theoretical papers. Data extraction was completed by LH.
Quality assessment
All included publications were assessed independently by two reviewers (LH and JC) as outlined in paper 1 [ 26 ] using independent quality appraisal assessment tools adapted from the Downs & Black Checklist [ 27 ] and the Joanna Briggs Institute’s Checklist for Text and Opinion [ 28 ].
The preliminary search from the combined databases yielded the results outlined in paper 1 [ 26 ] with 1434 results and an additional 11 articles from JC’s library. The same process was followed as outlined in flowchart for the search results in paper 1 [ 26 ] resulting in the same 33 texts included for this systematic review (Fig. 1 ). Fourteen of the 33 (42%) papers consisted of case study designs ( n = 1), 10 (30%) case studies of between two to four clients, and six (18%) of the papers reported on five or more client cases. Three studies did not report the number of clients from which their data was obtained. Additional study characteristics are reported in paper 1 [ 26 ].
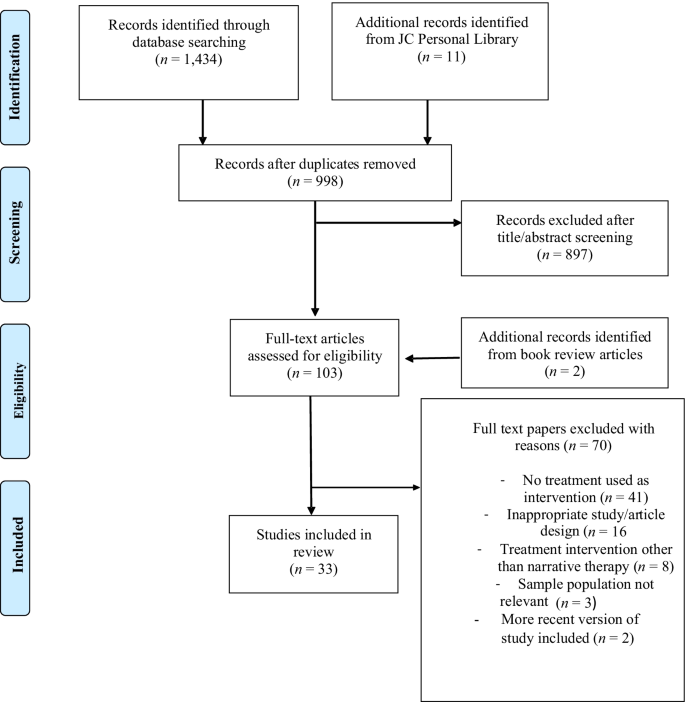
Flow chart of search strategy
Quality appraisal findings–outcome quality ratings
Table S1 and Table S2 (see Additional file 1 ) display the quality appraisal ratings for each of the included references. In relation to outcome data, seven (21%) articles clearly described the main outcomes of the intervention. Treatment outcomes were not reported in 8 (24%) papers and were unclear in 17 (52%) papers. The main findings were clearly reported in 14 (42%) papers and were unclear or not reported in the remaining papers. Overall, the quality ratings for the reporting of treatment outcomes indicated that these were insufficiently reported in the papers.
Synthesis of narrative therapy outcomes
Three papers included quantitative outcome measures and two studies reporting ethics approval. All but one of the 32 papers reported qualitative outcomes, including participant experiences, therapy transcripts and therapist reflections (see Table S3 for data extraction summary, Additional file 1 ).
Quantitative outcomes
Of the three studies reporting quantitative outcomes, one was a group narrative therapy intervention for seven participants with the dual presentations of eating concerns and depression [ 29 ]. The authors outlined that after a 10 week intervention, participants reported a reduction in ED symptoms as measured by the Eating Disorder Inventory (EDI) [ 30 ] and depressive symptoms as measured by the Depression, Anxiety and Stress Scale (DASS) [ 31 ]. They also reported results of a post-treatment survey that through externalisation and disengagement from the ED, participants reported a change in everyday living practices and less self-criticism.
A larger study with 645 participants in Israel reported that an intervention that integrated narrative therapy with motivational interviewing found that the dropout rate was < 10% during the first two months of treatment [ 32 ]. They also reported remission rates using the ED Global Clinical Score [ 33 ] of an average outcome score based on (i) Weight maintenance at least 15% ideal body weight; (ii) Menstruation in women for at least 12 months; (iii) Absence of purging behaviours; (iv) Normalization of eating habits; and (v) Social adjustment based on resumption of school or work. Reported remission rates at the end of treatment [15 months to 4 years]/4 year follow up were 69%/68% (AN) and 81%/83% (BN) respectively. Remission was defined as fully recovered or much improved, where much improved was defined as partial remission with infrequent occurrence of symptoms and return to social and occupational functioning.
A final study reported outcomes for a case study where a 28 year old woman had 10 sessions of narrative therapy over 12 weeks and reported a significant decrease on one of the scales of the EDI-3 (ascetism) [ 34 ] in addition to other qualitative therapist reported improvements.
Qualitative outcomes
There were a range of qualitative outcomes that were cited by the papers as being reported by individuals who experienced narrative therapy for eating problems and some therapist reflections on what they learnt from those with a lived experience. This highlighted to two-way nature of the therapeutic relationship as highlighted by Michael White [ 35 ].
Client outcomes
A range of client outcomes were reported by authors of the included papers. Outcomes most frequently cited related to identity shifts and turning points over the course of therapy. Seventeen of the 33 papers outlined a range of ways that persons with a lived ED experience reclaimed and strengthened a sense of identity outside of the dominant ED identity [ 29 , 36 , 37 , 38 ], including remembering who I am [ 39 ]; visualization of future without ED [ 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ], improved confidence and self-esteem [ 48 ], self-expression [ 49 ], alongside reclaiming identity from abuse narratives [ 50 , 51 ], and thickening preferred identity through values [ 52 ].
A number of narrative therapy practices were identified as key in the reclaiming of identities hidden by the problem saturated ED identity. A frequently cited practice was externalisation of the problem [ 29 , 45 , 47 , 53 , 54 , 55 , 56 ] with the use of the person’s language forms or experience-near naming [ 45 ], including metaphor and personification of the problem [ 53 , 54 ]. Other narrative practices that were associated with revealing identities concealed by the ED identity included: the tree of life metaphor [ 46 ] and the deconstruction of dominant discourses (or dismantling of taken-for-granted assumptions) that supported problematic identities [ 42 , 47 , 49 , 55 , 57 ].
Other outcomes reported included: reconnecting individuals with a sense of hope [ 36 , 42 , 46 , 58 , 59 ] and improvements in self-care and self-compassion [ 36 , 39 , 40 , 44 , 50 , 51 ]. Furthermore, narrative therapy was also noted as facilitating individuals in the claiming of their voice [ 40 , 58 ], including through their own speaking positions [ 60 ], and increased assertiveness [ 59 , 61 ].
An increased sense of personal agency, including over the ED, was also noted as an outcome of the narrative therapy therapeutic process [ 29 , 36 , 38 , 41 , 43 , 58 , 61 , 62 ] with two papers talking about how narrative therapy outcomes included increased readiness to change [ 58 , 63 ]. Nine papers outlined a range of ways that individuals' eating practices were reported to have changed including reduced ED symptoms [ 29 , 36 , 40 , 61 ], reduced hospital admissions [ 51 , 59 ]; reduced fear about gaining weight [ 62 ], and discernment of body sensations related to eating [ 36 ] Three articles also reported improvements in associated mood and anxiety symptoms were evident over the course of the narrative therapy intervention [ 48 , 51 , 56 ].
Other treatment outcomes that were reported as having positive impacts on individuals’ relationships included emotional closeness [ 64 ], negotiating clearer boundaries in relationships [ 53 , 65 ], connection with family and friends [ 39 , 43 , 51 , 56 , 59 , 61 ] and others in the treatment [ 46 ]. Four papers also reported that the individuals resumed work and/or study after the narrative therapy treatment intervention [ 51 , 56 , 61 , 65 ].
Therapist reflections–two way impacts of therapeutic intervention
Authors also outlined a range of ways that they were changed through their work as narrative therapists with those with a lived ED experience. This included a connection with their own creativity [ 39 ] and a recognition of the power imbued in professional contexts and the impacts of these on clients [ 60 ] and how therapy can also take the stance as political action to address injustices in society. Therapeutic letter writing was also seen as an opportunity for further reflection by both clients and therapists and also an opportunity for therapists to be open to being corrected by the client [ 64 ].
Narrative therapy outcomes to date are predominantly reported in the form of case studies with transcripts from therapy sessions and therapist reflections to exemplify some of the reported shifts in the context of therapy sessions. Three studies reported outcomes using standardized measures, including the EDI and DASS, with the largest study that included integrated narrative therapy with MI [ 32 ] measuring clinical outcome using the ED Global Clinical Score [ 33 ] that is currently outdated and infrequently used in current ED literature. These studies reported significant improvement in ED symptoms as measured by these instruments; however two of the studies had sample sizes of seven [ 29 ] and one respectively [ 34 ].
Given that identity shifts in the recovering of lost identities are a focus of narrative therapy, the most frequently cited treatment outcomes were stated on these terms. Examples of identity shifts were most frequently linked to the practice of externalisation of the problem with the use of the person’s own experience-near terms. Deconstruction or the unpacking of taken for granted assumptions supporting the ED identity was also cited as a narrative practice that facilitated the finding lost identities. Identity shifts, and addressing these in treatment, has been found to be an important component of ED treatment experiences and/or inadequately addressed in ED treatment interventions from the perspectives of those with a lived ED experience [ 12 ]. Narrative therapy has scope to comprehensively engage individuals (and their families) in finding hidden identity narratives that have been obscured by problem-saturated narratives or the ED identity. The papers included in this systematic review provided a range of exemplars of how narrative therapy practices engaged individuals in finding and strengthening hidden identity narratives.
Identity shifts in narrative therapy are understood as significant because they are not merely descriptive but also performative. For example, in the words of Jerome Bruner [ 23 ] “In the end, we become the autobiographical narratives by which we “tell about” our lives” (p. 694). Michael White & David Epston [ 21 ] have termed this enactment of identity narratives as performance of the meaning. Performing new meanings was noted in the therapy transcripts and therapist reports and included the areas of improved social and occupational functioning, some improvements in ED symptoms, and a reduction in need for hospital admissions. There was significant variability across the studies in the meaning performances that were reported. This may reflect the spirit of narrative therapy that is, the person is the expert of their life and the expert of what outcomes are significant to them. Nevertheless, the absence of consistency in the reporting of outcomes, including ED symptoms, means that the effectiveness of narrative therapy based on the research evidence is largely inconclusive.
The paucity of high quality quantitative research into narrative therapy is not unique to the treatment of EDs. Some of the broader challenges in researching the effectiveness of narrative therapy arise in the context of divergent philosophical paradigms. Psychotherapy research has traditionally assumed positivist epistemologies that require manualisation and replication of therapies [ 66 ]. These traditional research paradigms may be perceived to be at variance with the focus of narrative therapy on personal narratives, social and relational processes with a prioritization of the language and personal agency of the person with a lived experience [ 66 , 67 ]. Nevertheless, narrative therapy research is gradually bridging the divide between positivist and social/relational approaches for example, in outcome research in depression [ 68 ] and post-traumatic stress disorder [ 69 ]. However, studies that focus on both outcomes and therapeutic process have continued to be predominantly exploratory [ 67 ].
Evidence-based practice has three arms: the research evidence and evidence from the clinician and the client’s experiences [ 70 ]. This review has found that there is limited support for narrative therapy for EDs from the practice-based evidence of clinician reports and therapy transcripts. However, in the absence of research that systematically analyses treatment outcomes, including in relation to ED symptoms, it is difficult if not impossible to know whether the narrative therapy intervention widely reported in a case study form will be translate to a broader group of individuals who experience EDs.
Implications
This systematic review highlights how the outcomes of narrative therapy for EDs are currently under-reported and incomplete. However, this does not mean that narrative therapy interventions are ineffective in the treatment of EDs. Rather, it means that [ 1 ] there is an absence of systematic collection and analysis of treatment outcomes in terms of symptom improvement and quality of life, including social, relational and occupational engagement; and [ 2 ] further research is needed to document these and other outcomes that narrative therapists are witnesses to in their therapeutic practices.
In the absence of systematic reporting of outcomes, including relation to ED symptom reduction and improved quality of life, it is not possible at this point to conclude that narrative therapy is effective in the treatment of EDs. Narrative therapy continues to be positioned as having a “fringe role” [ 71 ] (p.77), including in the treatment of EDs. Being unrecognised as an “evidence-based practice” for eating disorders continues to limit narrative therapy practice in the treatment of EDs. This has implications for the breadth of treatment choices available to those with a lived ED experience.
There is a need for narrative therapists and researchers to engage in more systematic outcome research to substantiate what clinicians witness in the therapy room. Greater engagement is needed with the available tools being used to measure the outcome and effectiveness of treatments for EDs. If the existing tools are insufficient to measure the identity shifts and meaning performances that are central to narrative therapy, then new and more comprehensive tools need to be developed the prioritise the voice and personal agency for the experiencing person. Further research is also needed into ways that identity shifts mediate other changes, such as ED symptom reduction. Greater clarity is also needed as to the essential versus desirable components of narrative therapy and how outcome variables might be aligned and mapped onto these therapeutic components. Exploring outcomes through mixed methods design would provide scope to research narrative therapy outcomes in terms of both ED symptom reduction whilst also privileging the voice of the experiencing person in defining what recovery means to them. Given the understanding in narrative therapy that identity is constituted in socio-cultural discourses, identity shifts pre-, post, and within- therapy sessions would be well suited to analysis through critical discourse [ 72 ] and discursive [ 73 ] qualitative methodologies.
Study strengths and limitations
In addition to the study’s strengths and limitations outlined in paper 1 [ 26 ], few of the papers in this review systematically reported on treatment outcome data, including ED symptoms. The majority of articles consisted of a clinician’s overall description of a treatment process with one to five clients. These papers included exemplar transcripts; however, this data was not analysed with qualitative methods. Likewise, very few of the papers used standardized medical or psychological measurements and when these were included, they tended to be outdated.
These omissions from papers on narrative therapy for EDs may be because narrative therapists position the experiencing person, rather than the therapist or researcher, as the expert on their life. This includes what therapeutic shifts are meaningful to the person and what constitutes recovery. Therefore the papers included these types of descriptions of outcomes of narrative therapy. This can be seen as both a strength of the papers and a limitation. A strength in that the papers gave voice to the person with a lived experience to determine what was significant for them in terms of treatment and shifts through therapy. A weakness in that there was an absence of consistency in the reporting of outcomes and an inability to draw conclusions about the effectiveness of narrative therapy in symptom reduction and improvements in quality of life.
Furthermore, there were no papers that reported a control group to compare outcomes between narrative therapy and another therapy or a control group. Because of the characteristics of the papers that met the study selection criteria, the quality assessment was based on text and opinion, and therefore descriptive. There was insufficient data in the papers to do a more comprehensive systematic review of treatment outcomes. Given the few papers that met selection criteria, we included all papers. This led to a bias towards greater inclusion of lower quality case studies by therapists that included their impressions of treatment outcome and selected exemplar transcripts to illustrate these.
Concluding remarks
There are presently insufficient reports in the current literature to be able to make any conclusions or recommendations about the effectiveness of narrative therapy in the treatment of EDs. There is a need for researchers and practitioners to creatively engage in bridging the epistemological gap between positivist psychotherapy research and the practice-based evidence of clinicians who engage clients with narrative therapy. Consideration needs to be given to ways that narrative therapy interventions for EDs may be delivered, and their outcomes systematically measured, with a focus on social and emotional processes and without losing the spirit of narrative therapy where the person is positioned as not the problem and the expert of their life. This research has scope to be influential, not only in systematically researching outcomes for narrative therapy, but more broadly in the field of EDs where the experiencing person is at the centre of discerning what outcomes are significant for them and why, rather than this being decided primarily by researchers.
Abbreviations
Anorexia nervosa
Bulimia nervosa
Cognitive behavioural therapy
Eating disorder inventory
Depression, anxiety and stress scale
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, D.C.: American Psychiatric Association; 2013.
Book Google Scholar
Galmiche M, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr. 2019;109(5):1402–13.
Article PubMed Google Scholar
Kotilahti E, West M, Isomaa R, Karhunen L, Rocks T, Ruusunen A. Treatment interventions for severe and enduring eating disorders: systematic review. Int J Eat Disord. 2020;53(8):1280–302.
Touyz SW, Hay P. Severe and enduring anorexia nervosa (SE-AN): in search of a new paradigm. J Eat Disord. 2015;3(26):1–3.
Google Scholar
Fisher CA, Skocic S, Rutherford KA, Hetrick SE. Family therapy approaches for anorexia nervosa. Cochrane Database Syst Rev. 2019. https://doi.org/10.1002/14651858.CD004780.pub4 .
Article PubMed PubMed Central Google Scholar
Hay P, Bacaltchuk J, Stefano S, Kashyap P. Psychological treatments for bulimia nervosa and binging. Cochrane Database Syst Rev. 2009. https://doi.org/10.1002/14651858.CD000562.pub3 .
Svaldi J, Schmitz F, Baur J, Hartmann AS, Legenbauer T, Thaler C, et al. Efficacy of psychotherapies and pharmacotherapies for Bulimia nervosa. Psychol Med. 2019;49(6):898–910.
Galsworthy-Francis L, Allan S. Cognitive behavioural therapy for anorexia nervosa: a systematic review. Clin Psychol Rev. 2014;34(1):54–72.
Ghaderi A, Odeberg J, Gustafsson S, Råstam M, Brolund A, Pettersson A, et al. Psychological, pharmacological, and combined treatments for binge eating disorder: a systematic review and meta-analysis. PeerJ. 2018;6: e5113.
Khalsa SS, Portnoff LC, McCurdy-McKinnon D, Feusner JD. What happens after treatment? A systematic review of relapse, remission, and recovery in anorexia nervosa. J Eat Disord. 2017;5(1):20.
Conti JE, Joyce C, Natoli S, Skeoch K, Hay P. “I’m still here, but no one hears you”: a qualitative study of young women’s experiences of persistent distress post family-based treatment for adolescent anorexia nervosa. J Eat Disord. 2021. https://doi.org/10.1186/s40337-021-00496-4 .
Conti JE, Joyce C, Hay P, Meade T. “Finding my own identity”: a qualitative metasynthesis of adult anorexia nervosa treatment experiences. BMC Psychol. 2020;8:110.
Rance N, Moller NP, Clarke V. “Eating disorders are not about food, they’re about life”: client perspectives on anorexia nervosa treatment. J Health Psychol. 2015. https://doi.org/10.1177/1359105315609088 .
Hay PJ, Touyz S, Sud R. Treatment for severe and enduring anorexia nervosa: a review. Aust N Z J Psychiatry. 2012;46(12):1136–44.
DeJong H, Broadbent H, Schmidt U. A systematic review of dropout from treatment in outpatients with anorexia nervosa. Int J Eat Disord. 2012;45(5):635–47.
Shapiro JR, Berkman ND, Brownley KA, Sedway JA, Lohr KN, Bulik C. Bulimia nervosa treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40(4):321–36.
Hay PJ, Touyz S, Claudino AM, Lujic S, Smith CA, Madden S. Inpatient versus outpatient care, partial hospitalisation and waiting list for people with eating disorders. Cochrane Database Syst Rev. 2019. https://doi.org/10.1002/14651858.CD010827.pub2 .
Stockford C, Stenfert Kroese B, Beesley A, Leung N. Women’s recovery from anorexia nervosa: a systematic review and meta-synthesis of qualitative research. Eat Disord. 2019;27(4):343–68.
White M. Maps of narrative practice. New York: Norton; 2007.
White M. Narrative practice: continuing the conversations. New York: W.W. Norton; 2011.
White M, Epston D. Narrative means to therapeutic ends. New York: Norton; 1990.
Conti JE. “I don’t think anorexia is the way out”. Reconstruction of meaning in women’s narratives of anorexia nervosa over ten years. J Constr Psychol. 2016;29:165–83.
Bruner J. Life as narrative. Soc Res. 1987;54:11–32.
Epston D. Experience, contradiction, narrative & imagination: selected papers of David Epston & Michael White, 1989-1991. Adelaide: Dulwich Centre; 1992.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009. https://doi.org/10.1371/journal.pmed.1000097 .
Heywood L, Conti JE, Hay P. Paper 1: a systematic synthesis of narrative therapy treatment components for eating disorders. J Eat Disord. 2022. https://doi.org/10.1186/s40337-022-00635-5 .
Downs SH, Black N. Checklist for measuring study quality. J Epidemiol Commun Health. 1998;56(6):377–84.
Article Google Scholar
Joanna Briggs Institute. The Joanna Briggs institute critical appraisal tools for use in JBI systematic reviews; 2017 [Available from: file:///Users/janetconti1/Downloads/169-joanna-briggs-institute-2017-critical-appraisal%20(2).pdf.
Weber M, Davis K, McPhie L. Narrative therapy, eating disorders and groups: enhancing outcomes in rural NSW. Aust Soc Work. 2006;59(4):391–405.
Garner DM, Olmsted MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int J Eat Disord. 1983;2(2):15–34.
Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. Sydney: Psychology Foundation of Australia; 1995.
Golan M. The journey from opposition to recovery from eating disorders: multidisciplinary model integrating narrative counseling and motivational interviewing in traditional approaches. J Eat Disord. 2013. https://doi.org/10.1186/2050-2974-1-19 .
Garfinkel PE, Moldofsky H, Garner DM. The outcome of anorexia nervosa: significance of clinical features, body image and behavior modification. In: Vigersky RA, editor. Anorexia nervosa. New York: Raven Press; 1977. p. 315–29.
Garner DM. EDI-3, eating disorder inventory-3 professional manual. Lutz: Psychological Assessment Resources; 2004.
White M. Narratives of therapists’ lives. Adelaide: Dulwich Centre Publications; 1997. p. 242.
Beaudoin M. Affective double listening: 16 dimensions to facilitate the exploration of affect, emotions, and embodiment in narrative therapy. J Syst Ther. 2020;39(1):1–18.
Lainson KJ. From ‘disorder’ to political action: conversations that invite collective considerations to individual experiences of women who express concerns about eating and their bodies. Int J Narrat Ther Commun Work. 2016;2:1–15.
Tsun On-Kee A. Overeating as a serious problem and foods as real good friends: revising the relationship with food and self in narrative conversations. Int J Narrat Ther Commun Work. 2011;2:3–15.
Nylund D. Poetic means to anti-anorexic ends. J Syst Ther. 2002;21(4):18–34.
Scott N, Hanstock TL, Patterson-Kane L. Using narrative therapy to treat eating disorder not otherwise specified. Clin Case Stud. 2013;12(4):307–21.
Epston D, Morris F, Maisel R. A narrative approach to so-called anorexia/bulimia. In: Weingarten K, editor. Cultural resistances: Challenging beliefs about men, women and therapy. New York: Harrington Park Press; 1995. p. 69–101.
Russell S. Deconstructing perfectionism: narrative conversations with those suffering from eating issues. Int J Narrat Ther Commun Work. 2007;3:21–9.
White M. Deconstruction and therapy. Dulwich Cent Newsl. 1991;3:21–40.
Borden A. Every conversation is an opportunity. Int J Narrat Ther Commun Work. 2007;4:38–53.
Weber M. Narrative therapy, ‘eating disorders’, and assessment. Int J Narrat Ther Commun Work. 2007;2:63–70.
Ibrahim J, Tchanturia K. Patients’ experience of a narrative group therapy approach informed by the “tree of life” model for individuals with anorexia nervosa. Int J Group Psychother. 2018;68(1):80–91.
Lundby G. Creating different versions of life: talking about problems with children and their parents. Int J Narrat Ther Commun Work. 2014;1:18–26.
Ingamells KM. Wilbur the worrier becomes Wilbur the warrior: a teaching story for narrative family therapists. J Syst Ther. 2016;35(4):43–57.
Brown C, Weber S, Ali S. Women’s body talk: a feminist narrative approach. J Syst Ther. 2008;27(2):92–104.
Brown C. The dangers of trauma talk: counterstorying co-occurring strategies for coping with trauma. J Syst Ther. 2018;37(3):42–60.
Maisel R, Epston D, Borden A. Biting the hand that starves you. Inspiring resistance to anorexia/bulimia. New York: Norton; 2004.
Dennstedt C. The interplay of substance misuse and disordered eating practices in the lives of young women. Int J Narrat Ther Commun Work. 2010;3:52–63.
Howells K. Narrative work and the metaphor of ‘home.’ Int J Narrat Ther Commun Work. 2009;4:32–42.
Lock A, Epston D, Maisel R, de Faria N. Resisting anorexia/bulimia: Foucauldian perspectives in narrative therapy. Br J Guid Couns. 2005;33(3):315–32.
Lock A, Epston D, Maisel R. Countering that which is called anorexia. Narrat Inq. 2004;14(2):275–301.
Kantor A. Narrative therapy with adolescent females with eating disturbed behavior [Masters]. Canada: The University of Manitoba; 2000.
Lainson KJ. Narrative therapy, neuroscience and anorexia. A reflection on practices, problems and possibilities. Int J Narrat Ther Commun Work. 2019;3:80–95.
Robbins JM, Pehrsson D. Anorexia nervosa: a synthesis of poetic and narrative therapies in the outpatient treatment of young adult women. J Creat Ment Health. 2009;4(1):42–56.
Kraner M, Ingram K. Bursting out–breaking free. A group program for young womsn wanting to reclaim their lives from anorexia nervosa. Gecko. 1997;3:31–57.
Craggs T, Reed A. A service-user and therapist reflect on context, difference, and dialogue in a therapy for anorexia. Int J Narrat Ther Commun Work. 2007;3:30–8.
Zimmerman JL, Dickerson VC. Tales of the body thief. Externalising and deconstructing eating problems. In: Hoyt M, editor. Constructive therapies. London: Guilford Press; 1994. p. 295–318.
Pederson K. Uncovering bulimia’s demanding voice: challenges from a narrative therapist’s perspective. Int J Narrat Ther Commun Work. 2016;4:1–12.
White M. Anorexia nervosa: a cybernetic perspective selected papers. Dulwich Centre: Adelaide; 1986. p. 65–75.
Davidson H, Birmingham CL. Letter writing as a therapeutic tool. Eat Weight Disord. 2000. https://doi.org/10.1007/BF03339750 .
Dallos R. Attachment narrative therapy: integrating ideas from narrative and attachment theory in systemic family therapy with eating disorders. J Fam Ther. 2004;26:40–65.
Larner G. Family therapy and the politics of evidence. J Fam Ther. 2004;26:17–39.
Wallis J, Burns J, Capdevila R. What Is narrative therapy and what is it not? The usefulness of q methodology to explore accounts of white and Epston’s (1990) approach to narrative therapy. Clin Psychol Psychother. 2011;18:486–97.
Lopes RT, Goncalves MM, Fassnacht DB, Machado PP, Sousa I. Long-term effects of psychotherapy on moderate depression: a comparative study of narrative therapy and cognitive-behavioral therapy. J Affect Disord. 2014;167:64–73.
Erbes CR, Stillman JR, Wieling E, Bera W, Leskela J. Examination and use of narrative therapy with individuals diagnosed with PTSD. J Trauma Stress. 2014;27:730–3.
Sackett DL, Rosenberg AMC, Muir Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71–2.
Stillman JR, Erbes CR. Speaking two languages: A conversation between narrative therapy and scientific practices. J Syst Ther. 2012;31(1):74–88.
de Fina A, Schiffrin D, Bamberg M. Discourse and identity. Cambridge: Cambridge University Press; 2006.
Wetherell M. A step too far: discursive psychology, linguistic ethnography and questions of identity. J Socioling. 2007;11(5):661–81.
Download references
Acknowledgements
The authors would like to acknowledge Daphne Hewson, formerly Macquarie University, for her contributions to the narrative therapy framework that has guided this systematic review.
Not Applicable.
Author information
Authors and affiliations.
School of Psychology, Western Sydney University, Sydney, Australia
Janet Conti, Lauren Heywood, Rebecca Makaju Shrestha & Tania Perich
Translational Health Research Institute, Western Sydney University, Sydney, Australia
Janet Conti, Phillipa Hay & Tania Perich
School of Medicine, Western Sydney University, Sydney, Australia
Phillipa Hay
You can also search for this author in PubMed Google Scholar
Contributions
Each of the authors have made substantive contributions to this paper; this included conception of this research (JC and TP), the selection of search terms and systematic review of the databases (LH (final) and RMS (draft)), screening of papers for eligibility for inclusion in this review (LH & JC), systematic review of outcomes reported in papers (JC, LH & PH), and all authors contributed to sections of the draft paper and review of the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Janet Conti .
Ethics declarations
Ethics approval and consent to participate, consent for publication, availability of data and materials, competing interests.
The author(s) declare(s) that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Narrative Therapy components and outcomes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Conti, J., Heywood, L., Hay, P. et al. Paper 2: a systematic review of narrative therapy treatment outcomes for eating disorders—bridging the divide between practice-based evidence and evidence-based practice. J Eat Disord 10 , 138 (2022). https://doi.org/10.1186/s40337-022-00636-4
Download citation
Received : 08 May 2022
Accepted : 14 July 2022
Published : 12 September 2022
DOI : https://doi.org/10.1186/s40337-022-00636-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Eating disorders
- Narrative therapy
- Treatment outcomes
- Systematic review
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- CORRESPONDENCE
- 14 May 2024
Interpersonal therapy can be an effective tool against the devastating effects of loneliness
- Myrna M. Weissman 0 &
- Jennifer J. Mootz 1
Columbia University Vagelos College of Physicians and Surgeons, New York, USA.
You can also search for this author in PubMed Google Scholar
Your News feature ‘Why loneliness is bad for your health’ ( Nature 628 , 22–24; 2024 ) accurately notes the serious health consequences of loneliness, as well as emerging research on its underlying neural mechanisms. But there are potential solutions beyond those mentioned in the article.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 629 , 531 (2024)
doi: https://doi.org/10.1038/d41586-024-01420-x
Competing Interests
The authors declare no competing interests.
Related Articles
See more letters to the editor
- Public health

Neglecting sex and gender in research is a public-health risk
Comment 15 MAY 24

Is the Internet bad for you? Huge study reveals surprise effect on well-being
News 12 MAY 24

How ignorance and gender inequality thwart treatment of a widespread illness
Outlook 09 MAY 24
Inequality is bad — but that doesn’t mean the rich are
Correspondence 14 MAY 24
Use fines from EU social-media act to fund research on adolescent mental health
Correspondence 09 APR 24

Circulating myeloid-derived MMP8 in stress susceptibility and depression
Article 07 FEB 24

Only 0.5% of neuroscience studies look at women’s health. Here’s how to change that
World View 21 NOV 23
Research Associate - Metabolism
Houston, Texas (US)
Baylor College of Medicine (BCM)
Postdoc Fellowships
Train with world-renowned cancer researchers at NIH? Consider joining the Center for Cancer Research (CCR) at the National Cancer Institute
Bethesda, Maryland
NIH National Cancer Institute (NCI)
Faculty Recruitment, Westlake University School of Medicine
Faculty positions are open at four distinct ranks: Assistant Professor, Associate Professor, Full Professor, and Chair Professor.
Hangzhou, Zhejiang, China
Westlake University
PhD/master's Candidate
PhD/master's Candidate Graduate School of Frontier Science Initiative, Kanazawa University is seeking candidates for PhD and master's students i...
Kanazawa University
Senior Research Assistant in Human Immunology (wet lab)
Senior Research Scientist in Human Immunology, high-dimensional (40+) cytometry, ICS and automated robotic platforms.
Boston, Massachusetts (US)
Boston University Atomic Lab
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
The Use of Narrative Therapy on Paranoid Schizophrenia
- Research in progress
- Published: 10 May 2023
- Volume 68 , pages 273–280, ( 2023 )
Cite this article

- Karina Therese G. Fernandez 1 ,
- Anne Therese Marie B. Martin 1 &
- Dana Angelica S. Ledesma 1
Research suggests that a clinical diagnosis of schizophrenia is strongly linked with experiencing negative stereotypes and an inability to recover. In challenging the scientific-logical practice of diagnostic labeling, which totalizes the person’s experience around the illness, Narrative therapy offers a unique approach to treating schizophrenia by putting the spotlight on the client’s values, strengths, and beliefs. This allows the client to discover an alternative life narrative beyond their diagnosis. This study presents a case of a 40-year-old woman with paranoid schizophrenia. She felt that the people in her workplace were out to harm her so she would never work in her field again. At home, she had also begun to question herself as a mother. Narrative therapy techniques such as externalization, thickening the landscape of action and identity, and re-membering were used to aid the client’s recovery and helped her to shift from a problematic view of her identity. The present case focuses on providing steps to guide practitioners in using Narrative therapy for a case where the client has internalized their diagnosis as their identity.
This is a preview of subscription content, log in via an institution to check access.

Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

Conflicted Stories: A Case of Expanded Reality

Narrative enhancement and cognitive therapy (NECT) to improve social functioning in people with serious mental illness: study protocol for a stepped-wedge cluster randomized controlled trial

Dissociative Identity Disorder and Narrative
Data availability.
The authors have no data or materials to declare that are relevant to the content of this article.
Code Availability
The authors did not use any software application and thus do not have a code.
Abbreviations
Diagnostic and Statistical Manual V
American Psychiatric Association (APA). (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington DC: American Psychiatric Association.
American Psychiatric Association (APA). (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787
Beaudoin, M. (2005). Agency and choice in the face of trauma: A narrative therapy map. Journal of Systemic Therapies, 24 (4), 32–50. https://doi.org/10.1521/jsyt.2005.24.4.32
Article Google Scholar
Bullimore, P. (2003). Altering the balance of power: Working with voices. International Journal of Narrative Therapy and Community Work, 3 , 22–28.
Google Scholar
Carey, M., & Russell, S. (2002). Externalising: Commonly asked questions. International Journal of Narrative Therapy & Community Work, 2 , 76–84.
Carr, A. (1998). Michael White’s Narrative Therapy. Contemporary Family Therapy, 20 (4), 485–503.
Chae, Y., & Kim, J. (2015). Case study on narrative therapy for schizophrenic adolescents. Procedia—Social and Behavioral Science, 205 , 53–55.
Corrigan, P. W., Watson, A. C., & Barr, L. (2006). The self-stigma of mental illness: Implications for self-esteem and self-efficacy. Journal of Social and Clinical Psychology, 25 (8), 875–884. https://doi.org/10.1521/jscp.2006.25.8.875
Denborough, D. (2014). Retelling the stories of our lives: Everyday narrative therapy to draw inspiration and transform experience . W W Norton & Co.
Fung, K. M. T., Tsang, H. W. H., & Corrigan, P. W. (2008). Self-stigma of people with schizophrenia as predictor of their adherence to psychosocial treatment. Psychiatric Rehabilitation Journal, 32 (2), 95–104. https://doi.org/10.2975/32.2.2008.95.104
Article PubMed Google Scholar
Hasan, A. A. -H., & Musleh, M. (2018). Self-stigma by people diagnosed with schizophrenia, depression and anxiety: Cross-sectional survey design. Perspectives in Psychiatric Care, 54 (2), 142–148. https://doi.org/10.1111/ppc.12213
Kinjo, T., & Morioka, M. (2011). Narrative responsibility and moral dilemma: A case study of a family’s decision about a brain-dead daughter. Theoretical Medicine and Bioethics, 32 (2), 91–99. https://doi.org/10.1007/s11017-010-9160-y
Kondrat, D. C., & Teater, B. (2009). An anti-stigma approach to working with persons with severe mental disability: Seeking real change through narrative change. Journal of Social Work Practice, 23 (1), 35–47. https://doi.org/10.1080/02650530902723308
Lloyd, H., Lloyd, J., Fitzpatrick, R., & Peters, M. (2017). The role of life context and self-defined well-being in the outcomes that matter to people with a diagnosis of schizophrenia. Health Expectations: An International Journal of Public Participation in Health Care and Health Policy, 20 (5), 1061–1072. https://doi.org/10.1111/hex.12548
MacLeod, M. (2019). Using the narrative approach with adolescents at risk for suicide. Canadian Journal of Counselling and Psychotherapy, 53 (1). Retrieved from https://cjc-rcc.ucalgary.ca/article/view/61213
Morgan, A. (2000). What is Narrative Therapy: An Easy to Read Introduction . Dulwich Center Publication.
Ngazimbi, E. E., Lambie, G. W., & Shillingford, M. A. (2008). The use of narrative therapy with clients diagnosed with bipolar disorder. Journal of Creativity in Mental Health, 3 (2), 157–174. https://doi.org/10.1080/15401380802226661
Özçelik, E. K., & Yıldırım, A. (2018). Schizophrenia patients’ family environment, internalized stigma and quality of life. Journal of Psychiatric Nursing / Psikiyatri Hemsireleri Dernegi, 9 (2), 80–87. https://doi.org/10.14744/phd.2017.07088
Sugawara, H., & Mori, C. (2018). The self-concept of person with chronic schizophrenia in Japan. Neuropsychopharmacology Reports, 38 (3), 124–132. https://doi.org/10.1002/npr2.12016
Article PubMed PubMed Central Google Scholar
White, M. (2005). Michael White workshop notes . Dulwich Centre. https://dulwichcentre.com.au/product/michael-whites-workshop-notes-michael-white/
White, M. (2007). Maps of narrative practice . W. W. Norton
White, M. (2011). Narrative practice: Continuing the conversations . (D. Denborough, Ed.). W W Norton & Co.
White, M. (2016). Chapter 1: Deconstruction and therapy. In Narrative Therapy Classics (pp. 11–54). Adelaide: Dulwich Centre Pty Ltd.
White, M., & Epston, D. (1990). Narrative means to therapeutic ends . W. W. Norton, New York
Download references
Acknowledgements
The authors would like to acknowledge the Ateneo Bulatao Center for its constant encouragement and support to advance academic research alongside clinical practice.
The authors did not receive support from any organization for the submitted work.
Author information
Authors and affiliations.
Department of Psychology, Ateneo de Manila University, Katipunan Avenue, 1108, Quezon City, Metro Manila, Philippines
Karina Therese G. Fernandez, Anne Therese Marie B. Martin & Dana Angelica S. Ledesma
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study. Material preparation, data collection, and analysis were performed by Karina Therese G. Fernandez. The first draft of the manuscript was written by Karina Therese G. Fernandez, Anne Therese Marie B. Martin, and Dana Angelica S. Ledesma. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Karina Therese G. Fernandez .
Ethics declarations
Conflicts of interest.
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics Approval
This study received ethical approval from the University Research Ethics Office of the Ateneo de Manila University. This research study was conducted retrospectively from data obtained for clinical purposes. A copy of the approval letter has been provided in Appendix A.
Consent to Participate and Publication
In the informed consent given by the Ateneo Bulatao Center for Psychological Services to its therapy clients, there is a very detailed checklist of the extent of how their information can be used. One specific item is “session notes for the purposes of research (paper publications and paper presentations). We have attached a copy of an unsigned informed consent form for reference (see Appendix B).
Informed Consent
By signing an informed consent form, we obtained permission from the client to share her story. Furthermore, her identifying information was changed to ensure confidentiality. Though the informed consent form already covers the consent for data in the therapy sessions to be published, as recommended by informal discussions with members of the University Research Ethics Committee of the Ateneo de Manila University, a second request for informed consent to publish was made after therapy.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Fernandez, K.T.G., Martin, A.T.M.B. & Ledesma, D.A.S. The Use of Narrative Therapy on Paranoid Schizophrenia. Psychol Stud 68 , 273–280 (2023). https://doi.org/10.1007/s12646-022-00709-z
Download citation
Received : 12 July 2021
Accepted : 15 December 2022
Published : 10 May 2023
Issue Date : September 2023
DOI : https://doi.org/10.1007/s12646-022-00709-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Paranoid schizophrenia
- Internalized stigma
- Narrative therapy
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Addict Health
- v.10(1); 2018 Jan
Effectiveness of Narrative Therapy in Groups on Psychological Well-being and Distress of Iranian Women with Addicted Husbands
Mohammad khodayarifard.
1 Professor, Department of Educational Psychology and Counseling, School of Psychology and Education, University of Tehran, Tehran, Iran
Gholamreza Sohrabpour
2 Department of Educational Psychology and Counseling, School of Psychology and Education, University of Tehran, Tehran, Iran
This paper investigated the effectiveness of narrative therapy in groups on psychological well-being and distress among Iranian women with addicted husbands.
The research was an experimental study with pretest-posttest control group design along with follow-ups of one month and three months. The statistical population consisted of all the women with addicted husbands who referred to welfare and social service houses of district 10 in Tehran, Iran. Participants were forty-four persons who had mental health score lower than the mean of statistical society. They were selected using the voluntary sampling method, and were also randomly assigned to two groups, experimental and control. After the early loss, each group included twenty persons and was evaluated by Mental Health Inventory (MHI-28). The experimental group received 10 sessions of the group counseling. Data were analyzed with repeated measure ANOVA and Bonferroni post-hoc test.
The results showed that psychological well-being of women who received the sessions of group counseling "narrative therapy" was improved significantly rather than those who did not received that (P < 0.001), and psychological distress of them was reduced significantly in comparison to the women who did not participated in the sessions (P < 0.001).
Based on these findings, it seems that narrative therapy in groups is effective in the promotion of psychological well-being of women with addicted husbands, and also could be effective in reducing their psychological distress. Therefore, it can be concluded that narrative therapy group interventions improve mental health of women with addicted husbands.
Introduction
Cultural identity has a profound impact on our sense of well-being within our society and on our mental health as well. Our cultural background refers to our ethnicity, but it is also profoundly influenced by social class, religion, migration, geography, gender oppression, racism, and sexual orientation, as well as family dynamics. All these factors influence people's social location in our society, their access to resources, their inclusion in dominant definitions of “belonging”, and the extent to which they will be privileged or oppressed within the larger society. These factors also influence how family members relate to their cultural heritage, to others of their cultural group, and to preserving cultural traditions. Having a sense of belonging, historical continuity, and identity with one's own people is a basic psychological need. 1
It is possible to consider two distinct vectors in Iranian culture: nationalist and Islamist. The nationalist aspect of Iranian culture is related to ancient Persian civilization and Zoroastrianism heritage which date 2000-3000 BC, but are still prevalent in different aspects of Iranian society such as calendar, New Year Festivals (Nowrooz) and Persian literature. On the other hand, Islamist and subsequently Shiism aspects are relatively younger and date back to the 7th and 16th centuries, respectively. It has been suggested that besides Persian and Islamist influences, the effects of Western culture on Iranian society should be taken into consideration. In collectivistic societies, private life is invaded by group’s interests, whereas in individualistic societies identity is based on the individuals. Like many other collectivist societies, Iran tends to operate on the basis of personal relationships among individuals, rather than on the basis of impersonal institutions. 2
Friedman et al. 3 declared that research on psychology and counseling within the family's context is very important. From a system’s perspective, family's central status should be considered as far as any dysfunction or illness of family member influence the other members. Families both affect and are affected by a mentally ill member through a dynamic process impacting patterns of communication, interactional styles, family responsibilities, and family roles as the family adapts to the physical and psychological demands of managing the illness and disorder. 4
Addiction is a disorder in self-regulation. Individuals who become dependent on addictive substances cannot regulate their emotions, self-care, self-esteem, and relationships. 5 Several women with drug-using husbands eventually got divorced, compared to women with non-drug using husbands. Women who were living with drug-using husbands had more opportunities to use drugs such as heroin. 6
Studies have generally shown that higher levels of alcohol and drug use and higher levels of substance-related problems increase risk for partner aggression. With regard to relationship factors among couples with addiction, violent couples are shown to exhibit poorer behaviorally-coded communication strategies versus those who are not violent. These results were consistent with the pattern of findings from clinical samples that suggest that partner discordance in addiction-related behaviors is related to a range of couple-related problems, including partner violence. 7 One of the indicators of mental health is psychological well-being. Deci and Ryan 8 noticed that psychological well-being is a concept with some combination of positive effectiveness such as happiness and functioning in individual and social life. Other indicator of mental health is psychological distress. In this regard, Drapeau et al. 9 indicated that psychological distress, as measured by the Mental Health Inventory (MHI-28), is presented by symptoms of depression, anxiety, and stress which are related to concerns, and is known to arise a lot of severity.
Shallcross declared that although traditional forms of therapy, like talk therapy, can be successful in facilitating achievement of improving individual's moods, traditional techniques are not always successful, so there is a need for creative techniques. 10
Viv notified that Bruner, who was a psychologist, has argued that we have two different ways of knowing the world: paradigmatic or logico-scientific knowing, which is based on the way in which we organize and communicate experience through stories. According to Bruner, our capacity to narrate develops almost as soon as we acquire language; and from an early age, we are intuitively aware of how to tell stories. While paradigmatic approaches to knowledge, which emphasize conceptual and abstract models of reality, have long had greater status than stories in academic discourse, both are necessary means of making sense of human experience. Our understanding of the world involves interplay between these two modes of thinking. 11 Duba et al. 12 notified that although there is little research about the effectiveness of narrative therapy in groups, recent studies are doing support for that. In fact, narrative therapy has been displayed useful in the group context. Ricks et al. 13 believed that counselors and psychologists in narrative therapy approach in groups are encouraged to use innovative techniques for reframing of individual's narrations. Vromans and Schweitzer 14 declared in their research that narrative therapy could be effective on mental health of individuals. That is to say that narrative therapy could reduce symptoms and sings of depression in adults and make their mental health promote. Morgan et al. 15 showed in their research about narrative therapy with elderly persons presenting with substance abuse concerns that participating in this group counseling gives a safe place to participants to share painful elements. They learned how to overcome their difficulties. Results from this study indicated how group counseling, "narrative therapy", creates a safe venue for individuals who suffer from problems related to substance abuse. Cloitre et al. 16 demonstrated that narrative therapy approach affected mental health of women suffering from post-traumatic stress disorder more than other approaches. In addition, they viewed that this approach could be effective in the promotion of emotions regulation, relationships, and the general functioning of women.
There are differences between men and women about having psychological distress. Deasy et al. 17 declared that women report depression, anxiety, and stress more than men. Regarding this factor that women play important roles in the family base, and also women with addicted husbands are exposed to psychological vulnerability more than normal women, considering this group seems essential. In addition, regarding the fact that people with lower mental health made the stories full of problems, necessity of intervention through narrative therapy in groups, and following this, reducing the rate of official and emotional divorce is presented more clearly. Therefore, the present research is the study about effectiveness of narrative therapy in groups on mental health among women with addicted husbands.
The present study as an experimental one included pretest-posttest control group design as well as follow up; and sampling is done voluntarily. In order to analyze the data, repeated measure ANOVA using SPSS software (version 24, IBM Corporation, Armonk, NY, USA) was applied. The statistical population consisted of all the women with addicted husbands who referred to welfare and social service houses of district 10 in Tehran, Iran. Considering the ethics fundamentals of research for this specific group and in order for them to take part more eagerly, the sampling method was of voluntary type, so that all the women with addicted husbands referring to all the welfare and social service houses of district 10 in Tehran City, all of which residing at the district, were invited to attend the sessions of narrative therapy in groups. Then, those who attended were registered. Before presenting the independent variable (narrative therapy in groups), necessary investigations were conducted in individual sessions by the researcher in order to recognize the appropriate conditions of the research participants (for instance: being interested in participating in the sessions, having the mental health score less than the average of the mental health score of the entire group). From among those who registered, forty-four persons with lower scores who had appropriate conditions and the required motivation for attending the group sessions were selected. Then, they were randomly assigned to the two experimental and control groups. After the initial drop out, each group included 20 persons. For the control group, it was explained that they will not be trained and it was agreed that after the end of sessions, 1-month and 3-months follow-ups and upon the approval of the related authorities of district 10, group consultation in the method of narrative therapy may be applied for them and also for all the persons who had made positive answers to the call and had been registered, in the case of their agreement. Demographic data were collected by applying a self-report questionnaire. The inclusion criteria of persons were: 1) women with addicted husbands, 2) being at least 25-year-old, and 3) being literate.
The exclusion criteria of persons were: 1) not cooperating in the research. 2) not being sure about honest answer to the questions, and 3) being addicted before marriage.
The women did not understand about cleaving to two groups "experimental and control" until doing the treatment protocol completely. In order to control the Hawthorne Effect, attention to the control group was as much as the experimental group as far as the treatment protocol applied for the control group during 2 weeks.
The MHI-28 questionnaire has 28 items which was codified by Veit and Ware, 18 and translated and validated in Iran by Besharat. 19 This instrument has two subscales; psychological well-being (14 items) and psychological distress (14 items). Answering in Likert scale is from completely agree (5 points) to completely disagree (1 point). The reliability of this instrument in the method of retest for normal subjects in the subscales of psychological well-being and psychological distress was reported 0.89 and 0.87, respectively, and for the subjects with disorders, was reported 0.77 and 0.82, respectively. Internal consistency for normal subjects in subscales of psychological well-being and psychological distress was reported 0.91 and 0.88, respectively, and for the subjects with disorders, 0.85 and 0.89, respectively. The correlation of this instrument with general health questionnaire (GHQ) in the subscales of psychological well-being and psychological distress was -0.85 and 0.86, respectively that indicates the concurrent validity of this instrument. 19
According to Dryden, 20 number of sessions and the intervals between the sessions are different according to the quality of the subjects brought to the group sessions. Generally, group narrative therapy has fewer sessions than many traditional group consultations. Payne 21 declared that there is no fixed contract regarding the duration of group narrative therapy sessions. Techniques and practices applied in narrative therapy in groups shortened the duration of this method rather than many other methods. In fact, group narrative therapy is not short-term, but generally, narrative techniques and works applied in this group method can make the duration of consultation shorter than many other intervention methods. Moreover, there is no hypothesis regarding weekly sessions or any pre-determined interval between sessions.
The general plan of the sessions, excerpted from intervention plan of White et al., 22 was as follows:
First session (introducing the rules): Participants introduced themselves; who they are and what their goals are. The laws related to the group were explained. Regular attendance, having activity in the group, doing weekly duties, and having open communications in the group were considered. Group narrative therapy was explained and the purpose of forming this group was clearly stated. The persons were encouraged to discuss about any question about the approach of group narrative therapy. Group relaxation as well as visualization of self in the best possible status was done. In addition, the persons were encouraged to narrate the troubled story dominating their lives. Finally, homework was assigned for the members, so that they write and expand their life stories.
Second session (checking narrations and starting externalizing): The previous session was reviewed and the homework assigned in the previous session was brought up. The goals, values, the content of intervention, and what is supposed to be done were expressed and explained. A common situation was formed and the clients were directed. The troublesome narratives of the subjects were investigated and the details of what the clients expressed were listened carefully. The session was concluded. In order for the clients to understand their metaphors (beginning of externalization), they were assigned to write their metaphors of the environment, surroundings, and generally, the trouble.
Third session (naming the problem and its metaphor): The problems related to the homework were examined. Then, the program of that session was clearly expressed and the persons' metaphors were investigated. The members rewrote about the first time they got sensitive to their trouble. After investigating the narratives of the members, they were named common problems by giving priority to the clients' words, languages, and their metaphors. The subjects of the session were concluded and practice was assigned for the members to consider their problems separated from themselves and to externalize them.
Fourth session (continuing to do naming the problem and its metaphors and strategies): After investigating the problems related to homework and reviewing the previous session, the problem was metaphorized (giving a tangible name to the problem). It was talked about the ways through which the problem distresses the members, and discussed about the impact of problem on the members. The members were assigned to practice in group and consider the problem as a foreign enemy. Regarding the attitudes to problem, group discussion was formed. Finally, the subjects were concluded and homework was assigned for the members to find and write the tricks of the problem causing that impact on them.
Fifth session (beginning of the problem intrusion on persons and their communication, and beginning of the influential questions): Firstly, the previous session was reviewed and the problems of the homework were investigated. Then, regarding the members' cognition of the problem, group discussion was formed. The members were informed about the fact that how the problem declares itself to the members, overcomes them, and impacts on them through the family members, the people around them, and their surrounding environment. How the problem can dominate persons through dreams, beliefs, values, etc. was explained. Group practice was formed in order for tackling the problem as a foreign enemy and recognizing the techniques used by the problem for impacting on the persons. The subjects were concluded and the members were asked to collect their favorite subjects, memories, photos, etc., related to the subject of the sessions, as homework.
Sixth session (completing the intrusion of the problem on persons and their communication and using the deconstruction technique): After reviewing the previous session and investigating the problems of homework, the progress of the members was evaluated and the persons made their feedbacks about the sessions. Goals and wishes of the problem regarding the lives of persons were explained and expanded, and the assistants of the problem and their confederates were discussed in group with the goal of empowering the problem. Roles were played in the group and sentence completion practice was done by the persons. The persons were assigned to complete their incomplete sentences.
Seventh session (the intrusion of persons on the problem and their abilities as well as writing to the problem): Firstly, the problems of homework were investigated. Then, techniques for confronting the problem were discussed in the group. The abilities and positive attributes of the persons were presented in the form of group practice. Group discussion about focusing on the peoples' goals, and their assistants for overcoming the problem was formed, and the group practice of role playing technique was applied. Finally, the persons were assigned to write a letter to the problem and to mention their pros and cons in that letter.
Eighth session (unique consequences): The problems of homework were investigated. It was focused on unique consequences by asking questions such as: Has the problem ever tried to overcome you but you have not let it? What was your feeling? In what environment were you? What were you doing? Explain the details, etc. The feelings of persons were considered and investigated. The persons discussed in group about the fact that a person is in no way the problem and the problem is the problem, and in fact, it is the person who has problem. Group relaxation as well as visualization of the self in the best possible status was done. The persons were assigned to rewrite the narrative of their lives from the past to the present as homework.
Ninth session (rewriting the narration of life): After reviewing and investigating the problems of homework, group discussion was formed about the self, surroundings, relations, attitudes, behaviors, etc. in the situations wherein the persons were able to overcome their problems. Theoretical and practical parts of life narratives were explained as well as how to do the new narrative theoretically and practically. We were able to make new narratives for any happening, and from among different narratives we could attain the best one. Group relaxation and visualization of the self in the best possible way was formed. The members were assigned to rewrite the narrative of their lives from the present to the future and to give a new title to their life narrative.
Tenth session (summarizing and evaluating): Firstly, homework as well as all the sessions was reviewed and feedback of the members about the sessions and their viewpoints about the group were presented. Then, the persons talked about their feelings. Group discussion was formed about what they had learned from the group and generally any change having been occurred as a result of taking part in this group. The members mentioned their evidence about changes as a result of taking part in these sessions. Group discussion was formed about the reaction of the members when confronting other problems in their lives and they were asked to present their criticisms regarding the group, the process of the sessions, etc. Finally, a memorial was presented to the group members.
The members were asked to attend within one week after this session so as to take part in the posttest. In order for conducting the posttest for the control group, they were informed that they must be present at the time of conducting the posttest. According to the design of the present research, it was agreed that the experimental and control groups should attend for reimplementation of the questionnaires in one-month and three-month duration.
Findings related to demographic characteristics of women are provided in table 1 . The findings show that the groups "experimental and control" have not significant differences in domains such as age, education, number of children, the duration of living with their husbands, having a job for themselves and their husbands.
Demographic findings related to the groups of experimental and control
SD: Standard deviation
Descriptive findings of pretest, posttest, one month and three months follow-ups and the signification of within and between group effects are provided in table 2 . According to the table, the posttest mean of experimental group has a significant difference with pretest mean of that, but the posttest mean of control group has not a significant difference with pretest mean of this group. In addition, there is no significant difference about two follow-ups with posttest in the experimental group. These findings declared that group counseling "narrative therapy" has been effective significantly on psychological well-being and distress, and also its effect has been durable.
Summary of descriptive findings about subscales of mental health inventory (MHI) and the signification of within and between group effects
For doing assumptions of repeated measure ANOVA, Shapiro-Wilk test for normality of data, Levene's test for homogeneity of variances, Box's M test for equality of covariance-matrices of dependent variables among the groups, and Mauchly's test for sphericity of data and showing equality of error covariance among dependent variables in the groups were employed.
About psychological well-being, findings of Shapiro-Wilk test (0.96) with signification (P = 0.160), Levene's test (f = 0.14, P = 0.700), Box's M test (20.30) with signification (α < 0.05 = 0.001), and Mauchly's test (0.79) with signification (P = 0.120) were found.
Findings of repeated measure ANOVA about psychological well-being and distress show that interaction of two variables "time and group" is significant. Because index "F" obtained of interaction of these two variables is significant for psychological well-being (147.30) with signification of (P < 0.001, P = 0.001), interaction of two variables "time and group" is significant. It means that independent variable has been effective on dependent variable. In the other words, narrative therapy in groups has been effective significantly on mental health of women with addicted husbands.
Findings of Bonferroni post-hoc test show that mean difference of pretest-posttest for the psychological well-being variable (P < 0.001) and for the psychological distress variable (P < 0.001) is significant, but that of posttest-follow-up "1" for each variable (P = 0.090, P = 0.730, respectively) and posttest-follow-up "2" for each variable (P = 0.190, P = 0.110, respectively) is not significant. It means that narrative therapy in groups has affected on the variables and its effects approach is durable on mental health of women with addicted husbands.
Because women play important roles in the family and women with addicted husbands are exposed to psychological vulnerability more than normal women, it seems that considering this group is essential. Many of them have to take responsibility of financial issues and patronage of family in addition to the home affairs and children upbringing. This fact creates unfavorable consequences such as: severe conflicts, emotional separation, divorce, and dissolution. Therefore, doing consultative interventions for the women could be so effective. The present research is done in order to investigate the effects of narrative therapy in groups on psychological well-being and distress among women with addicted husbands.
One of the results of the research shows that the psychological well-being's score of the women who participated in group counseling is increased significantly in comparison to the women who did not participated in the group. In the other words, the group counseling could improve psychological well-being of the women, and its effects maintained in the follow-ups (one month and three months). Studies have examined distal risk factors for partner violence, including individual and couple-based characteristics among those seeking treatment for alcohol or drug addiction. In addition, according to Payne,21 who acclaimed that personal narratives of individuals are presented in group counseling to understand how they play roles in various social and personal positions, and their relationships with themselves and others, this finding is explained obviously.
Other finding shows that the score of psychological distress among the women who received the sessions of the group counseling is reduced significantly rather than those who did not receive that. In the other words, this group counseling could be effective on psychological distress of the women, and also its effects maintained during the follow-ups of "1 and 3 months". On the one hand, psychological distress is presented by symptoms of depression, anxiety, and stress; on the other hand, Morgan et al. 15 declared that the use of group counseling "narrative therapy" with individuals with substance abuse concerns creates suitable conditions without any prejudgment in which the participants obtain a good status to share painful and upset feelings in the life. Results indicated that learning of the participants about overcoming their problems and having better feeling is increased, this finding is presented clearly. Furthermore, one way to develop one’s own theoretical approach is to consider questions of how people change; what motivates people to behave, think, and feel in the ways that they do; and how someone grows and develops. These elements are foundational and must be considered when developing a theoretical orientation. In addition, one’s view of human nature will influence which type of theoretical orientation the counselor decides on and subsequently selects 23 that group narrative therapy approach focusing on the elements.
Generally, the findings of the present research show that narrative therapy in groups affects the mental health of women with addicted husbands. A woman with a drug-using husband has to overcome not only her own addiction but the impact of her husband’s addiction as well; 6 these women challenge more with familial situations. If the counselor believes that one’s internal state (e.g., thoughts) leads to the clients’ emotional distress, then the counselor will select a theory that specifically focuses on the role of changing thoughts in order to increase mental health and well-being. If one believes that the clients’ narratives or stories have impact on their mental health, then the counselor will more likely select a theory that focuses on the stories that clients create. The techniques used with this theory will focus on how the stories one creates can actually be modified if the client is taught how to reconstruct the story line. 23 In this regard, Hibel and Polanco 24 represented that a fundamental element to success in the narrative therapy approach is listening to the clients’ stories instead of to symptoms and/or information needed to gain insight. They suggested that group members and group facilitators listen carefully for how clients view themselves in the process of group counseling. Therefore, focus should be on the clients’ intentions and goals as opposed to focus on causes that have influenced the clients’ behaviors and challenges.
It could be said that non-assistance of/access to the other family members in the sessions of group counseling is a limitation of this research. It is offered that this research would do more with cooperation of all of the family members, especially husbands. The paper suggests further investigation of narrative therapy in groups in regard to mental health of women with addicted husbands in the other cultural and social contexts, and demographic variables.
The results of this research showed that narrative therapy in groups is effective in increasing mental health of women with addicted husbands. Although the women in Iran had to tolerate husband’s addiction, and challenge more with their familial situations, several women with addicted husbands got divorced. This research demonstrated that narrative therapy approach affected mental health of women with addicted husbands, and its effects were significant during the time.
In the Iranian society, any malfunction of men in the family influences the other members. Women with addicted husbands in this country have a more important role in controlling life affairs than normal women. They have to take responsibility of financial issues; hence, they confront with many life problems and make the stories full of problems. It seems that in the collectivist religious society of Iran, what is fundamental to the psychological interpretation is recognizing the problems and the ways of penetration of them as a factor which plays many important roles in the life, and thinking of the women as tolerating the bad situation where their husbands are usually without job or have jobs that do not make enough income; so that the women are forced to provide life incomes. The techniques of narrative therapy in groups focus on what the life problems are and how the women create the stories in their life and how they can modify these stories for penetrating them and having a better life.
Acknowledgments
It is gratitude for all of the organizers who occupied Municipality of district 10, Shobeiri-G sector, located at 16 Metri of this district, Tehran, Iran, and for all of the participants in this research.
Conflicts of Interest
The Authors have no conflict of interest.
- Review article
- Open access
- Published: 10 May 2024
Metformin mitigates dementia risk among individuals with type 2 diabetes
- Nicholas Aderinto 1 ,
- Gbolahan Olatunji 2 ,
- Emmanuel Kokori 2 ,
- Praise Fawehinmi 3 ,
- Abdulrahmon Moradeyo 1 ,
- Stephen Igwe 2 ,
- Rebecca Ojabo 4 ,
- Badrudeen Olalekan Alabi 2 ,
- Emmanuel Chuka Okafor 4 ,
- Damilola Ologbe 5 ,
- Ayobami Olafimihan 6 &
- David B. Olawade 7
Clinical Diabetes and Endocrinology volume 10 , Article number: 10 ( 2024 ) Cite this article
292 Accesses
Metrics details
This mini-narrative review explores the relationship between diabetes and dementia, focusing on the potential mitigating role of metformin in reducing cognitive decline among individuals with type 2 diabetes. The interplay of factors such as glycemic control, diabetic complications, and lifestyle influences characterises diabetes-related dementia. This review emphasises the significance of comprehensive diabetes management in addressing the heightened risk of dementia in this population. Methodologically, the review synthesises evidence from 23 studies retrieved through searches on PubMed, Embase, Google Scholar, and Scopus. Current evidence suggests a predominantly positive association between metformin use and a reduced risk of dementia in individuals with diabetes. However, the review shows the complex nature of these outcomes, revealing variations in results in some studies. These discrepancies show the importance of exploring dose–response relationships, long-term effects, and demographic diversity to unravel the complexities of metformin's impact on cognitive health. Limitations in the existing body of research, including methodological disparities and confounding variables, necessitate refined approaches in future studies. Large-scale prospective longitudinal studies and randomised controlled trials focusing specifically on cognitive effects are recommended. Propensity score matching and exploration of molecular mechanisms can enhance the validity of findings in clinical practice. From a clinical perspective, metformin can serve as a potential adjunctive therapy for individuals with diabetes at risk of cognitive decline.
Introduction
Diabetes-related dementia is a significant concern due to the increased risk of dementia in individuals with type 2 diabetes [ 1 ]. The relationship between diabetes and dementia is complex and multifaceted [ 1 ]. Studies have shown that both low and high HbA1C levels are associated with an increased risk of dementia in individuals with diabetes, indicating a non-linear relationship [ 1 , 2 ]. Additionally, uncontrolled diabetes has been linked to an elevated risk of Alzheimer's disease, highlighting the importance of glycemic control in mitigating dementia risk [ 3 ]. Furthermore, severe diabetic retinal disease has been identified as a potential risk factor for dementia in individuals with type 2 diabetes, emphasising the need for comprehensive management of diabetic complications to reduce the likelihood of developing dementia [ 4 ].
The impact of lifestyle factors on diabetes-related dementia has also been investigated, with studies suggesting that a combination of healthy lifestyle factors is associated with a reduced risk of dementia in patients with type 2 diabetes [ 5 ]. However, the aetiology of diabetes-related dementia remains unclear, and it has been proposed that dementia in diabetic patients should be regarded as an independent disease, distinct from Alzheimer's disease and vascular dementia, due to its unique pathophysiological characteristics related to diabetes [ 6 , 7 , 8 ].
The investigation into metformin as a potential mitigating agent for dementia risk among individuals with diabetes is grounded in the expanding body of evidence highlighting its plausible neuroprotective role [ 9 ]. Metformin's potential as a neuroprotective agent has been linked to its ability to lower mortality and age-related diseases independently of its impact on diabetes control [ 10 , 11 , 12 , 13 , 14 ]. Empirical evidence suggests that metformin might mitigate dementia risk by reducing oxidative stress, inflammation, and apoptosis and countering the deleterious effects of advanced glycosylation end products produced during hyperglycemia [ 10 , 11 ]. These collective findings show metformin's potential not only in diabetes management but also in addressing neurological disorders. This study aims to review the current evidence for metformin as a mitigating agent for dementia risk among individuals with diabetes.
Methodology
We searched PubMed, Embase, Google Scholar and Scopus to conduct this narrative review see Table 1 . We formulated a database search strategy based on keywords such as "diabetes," "diabetes mellitus," "diabetes mellitus, Type 2", "metformin," "biguanides," "metformin benefits," "anti-diabetic medications," "memory," "cognition," "cognitive-impairment," "amnestic mild cognitive impairment," "Alzheimer's disease," "Parkinson's disease," and "dementia." We also used other texts selected based on the existing literature and/or obtained from related bibliographies, combined using Boolean operators as follows: ((dementia) OR (cognitive-impairment) OR (cognitive function) OR (neurodegenerative diseases)) AND ((metformin) OR (anti-diabetic drugs)). Furthermore, we manually searched relevant articles cited within the retrieved studies to avoid omitting important research articles.
We only considered articles that a) presented results in English, b) had full text available, and c) specifically assessed dementia risk in patients with diabetes who were on metformin therapy. On the other hand, we excluded studies with a) missing data, b) articles that did not focus on metformin use in type 2 diabetes mellitus, c) studies performed on patients with significant neurological, psychiatric disease or cancer, and d) studies performed in vitro or animal models. We limited the study scope to randomised controlled trials, retrospective cohort studies, prospective observational studies, comparator studies, and case–control studies but excluded books, letters, editorials, conferences, and commentaries.
During the data extraction process, we evaluated the study characteristics such as the publication type, year, study design, study focus, sample size, and the number of positive and negative outcomes. It is important to note that we focused on the probable benefit of metformin in mitigating dementia risk among individuals with diabetes despite the controversial nature of the topic.
Current evidence in existing literature
Our review identified 23 studies, including sample sizes ranging from 305 to 446,105 participants see Table 2 . A majority of these studies, 17 out of the 23 [ 10 , 11 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 ], reported positive outcomes regarding the relationship between metformin use and dementia risk in individuals with diabetes. Metformin is the preferred first-line drug for the treatment of type 2 diabetes mellitus [ 9 ]. It can be safely administered with other antidiabetic drugs and has been demonstrated to reduce insulin resistance and improve glycaemic control [ 9 ]. However, a review of clinical trials paints a mixed picture of the connection between the use of metformin and the incidence of dementia among patients with diabetes.
The findings of observational studies examining the possible link between metformin and dementia risk have been inconclusive. Eleven (57.9%) of the 19 analysed publications had positive results, proving that metformin may help lower the risk of dementia [ 10 , 11 , 13 , 14 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 27 ]. Five articles (26.3%) had an elevated risk [ 25 , 26 , 28 , 29 , 30 ], whereas three (15.8%) provided a condition for decreased risk [ 15 , 16 , 17 ]. A retrospective cohort study by Chin-Hsiao Tseng indicated a lower risk when metformin was used with other medications, such as acarbose and pioglitazone [ 18 ]. At the end of a 6-month follow-up study, a significant difference in cognitive performance compared to baseline in frail women treated with extended-release metformin (p: 0.007) was observed [ 27 ]. Huang et al. highlighted the protective benefits of metformin when used at a low dose [ 16 ]. At the same time, Huang et al. reported higher doses of metformin with a higher intensity showed no protective role against dementia [ 16 ]. However, cohort studies by Yi-Chun Kuan showed mixed results. They raised questions because they linked long-term metformin use to a higher risk of dementia from all causes, including vascular disease and Alzheimer's disease [ 28 , 32 ]. Scherrer et al. showed that the effects of metformin vary in different subpopulations, indicating a lower risk in some individuals (> 50 years) [ 21 ].
Furthermore, the results from I-Shiang Tzeng raise questions about the possibility that metformin and DPP-4 inhibitor combination therapy alleviated the risk of dementia [ 26 ]. These varied results highlight the complex nature of the connection between dementia and metformin use and highlight the need for additional studies, especially examining dose–response interactions, long-term effects, and demographic diversity to offer a more thorough understanding. Among the notable findings is a study conducted by Chin-Hsiao Tseng in 2019, which indicated a reduction in the risk of dementia associated with metformin, particularly in the female population [ 18 ]. Furthermore, the use of a combination of three drugs (Metformin, acarbose, pioglitazone) was associated with the lowest risk of dementia, as highlighted in the same study [ 18 ]. Additionally, a study by Yonghwan Kim et al. demonstrated a dose–response relationship, revealing that Metformin use in an elderly population with diabetes mellitus contributed to a reduction in dementia risk [ 19 ]. However, a retrospective cohort study by Ariela R. Orkaby et al. in 2017 suggested that metformin was associated with a lower risk of subsequent dementia compared to sulfonylurea use in veterans aged 75 years and older [ 13 ]. Notably, a lower risk was also observed in a subset of younger veterans who maintained an HbA1C value of 7% and exhibited good renal function [ 13 ]. In the 2015 study by Kwang-pil Ko et al., a comprehensive evaluation of metformin's efficacy in modulating physical and mental profiles was undertaken, revealing favourable outcomes [ 22 ]. Specifically, within the age group of 65 to 74 years, metformin demonstrated a statistically significant association with a reduced risk of dementia across various racial categories. However, a distinctive pattern emerged among patients aged 75 years and older, as metformin exhibited no statistically significant association with dementia within this older demographic [ 23 ].
Theoretically, antidiabetic drugs designed to ameliorate insulin resistance within the brain hold promise in preventing Alzheimer's disease or dementia [ 18 , 31 ]. In a study involving 17,200 new users of metformin, a lower risk of dementia was reported in a subset of younger veterans exhibiting HbA1C values ≥ 7%, those with good renal function, and individuals of white ethnicity [ 13 ]. In a study conducted, T2DM compared with no medication, sulfonylureas alone reduced the HR from 1 to 0.85 (0.71–1.01), metformin alone to 0.76 (0.58–0.98), while with combined oral therapy, the HR was 0.65 (0.56–0.74) [ 20 ]. Adjustments included cerebrovascular diseases so that non-stroke-related dementias were found to be decreased in DM with sulfonylurea and metformin therapy. T2DM increases the risk of dementia more than 2-fold.
Elevated blood glucose levels pose a potential threat to cerebral function, contributing to an elevated risk of dementia in individuals with diabetes [ 19 , 31 ]. The link between diabetes and dementia is likely multifactorial, involving mechanisms such as inflammation, oxidative stress, atherosclerosis, amyloid-β deposition, brain insulin resistance accompanied by hyperinsulinemia, advanced glycation end-products (AGEs), and dysregulation of lipid metabolism [ 20 , 33 ]. Metformin, recognised as the primary first-line therapy for type 2 diabetes mellitus, operates by curbing hepatic gluconeogenesis and augmenting muscular glucose uptake by activating 5'-adenosine monophosphate-activated protein kinase (AMPK) [ 21 ]. Beyond its glucose-lowering effects, metformin has demonstrated additional benefits in individuals with type 2 diabetes, including reducing the risk of atherosclerotic events, protection against certain cancers, and an anti-ageing effect [ 20 ].
The potential neuroprotective effects of metformin are suggested to stem from its capacity to inhibit inflammatory responses and enhance cognitive function [ 16 ]. Apolipoprotein E (APOE), a crucial protein in lipid transport and brain injury repair, is implicated in Alzheimer's disease risk [ 21 ]. Specific APOE gene polymorphisms, particularly the ε4 allele, elevate the risk of AD, while the ε2 allele is associated with reduced risk [ 10 ]. The APOE ε4 allele is also linked to an increased risk of cerebral amyloid angiopathy and age-related cognitive decline. A recent study hinted at an association between metformin use and a faster decline in delayed memory among carriers of the APOE ε4 allele, prompting the need for further research to elucidate the potential influence of APOE ε4 genotype on the therapeutic effects of metformin [ 29 ].
Limitations and future directions
Existing studies on metformin’s involvement in reducing dementia risk in patients with diabetes have significant limitations that should be considered. First, many studies have methodological variances, such as differences in study design, sample size, and outcome measures. This variation makes obtaining standardised results difficult and direct comparisons between investigations difficult. Furthermore, the heterogeneity within the examined groups, which includes age and diabetes duration, complicates interpretation and restricts the generalizability of the findings. Most observational studies failed to address bias or did not address it clearly, making the evidence less efficient. Another significant issue is the possibility of confounding variables influencing the outcomes. Factors such as genetic predisposition, lifestyle decisions, and concurrent pharmaceutical use may all impact cognitive performance independent of metformin, making it difficult to assign observed effects to medication alone. Furthermore, contradictions in studies are exacerbated by differences in the definitions of dementia and cognitive decline between studies.
Future studies should target certain areas to address these constraints and to increase understanding. Large-scale, well-designed, prospective longitudinal studies with long follow-up periods can provide stronger data and aid in determining causation. In addition, randomised controlled trials (RCTs) focusing only on the cognitive effects of metformin would provide more control over confounding factors. Subgroup analyses within the diabetic population, considering variables such as age, sex, and diabetes management details, would help better understand the influence of metformin on various patient groups. Applying propensity score matching, or at the very least, a match for age, sex, and health status, will improve data validity by lowering baseline variability and, if possible, investigate the relationship between metformin usage, B-12 vitamin levels, and dementia. To inform clinical practice, it is critical to investigate dose–response relationships and optimal dosages for potential cognitive benefits.
Furthermore, a thorough examination of the molecular mechanisms underlying the influence of metformin on cognitive performance is required. This knowledge can guide focused therapies and identify individuals most benefit from metformin therapy. Future research should prioritise uniform study designs, investigate specific demographic subgroups, and explore molecular causes to improve the reliability and usefulness of the findings in clinical practice.
Implications for clinical practice
Clinically, the favourable results observed in multiple studies imply that metformin may be a feasible alternative for people with diabetes, particularly for those at risk of cognitive loss see Fig. 1 .
Metformin in dementia risk in type 2 diabetes
Healthcare practitioners should inform patients about the potential cognitive benefits in addition to glycemic control. However, care is advised owing to inconsistent findings and potential issues, such as the variation in the metformin outcome, increased risk of vitamin B-12 insufficiency, and identified risk with certain combinations, emphasising the importance of tailored treatment programs and regular cognitive monitoring. A multidisciplinary approach that combines endocrinologists, neurologists, and senior experts is required to address the complicated connection between diabetes control and cognitive health. Senior experts such as diabetologists are key in tailoring diabetes treatment plans to achieve optimal glycemic control [ 34 ]. In addition, it is essential also to involve psychologists and occupational therapists. These professionals play pivotal roles in the identification, comprehensive assessment, and rehabilitation processes associated with dementia [ 35 ]. They collaborate closely to develop tailored interventions that address cognitive deficits and consider the individual's emotional and functional aspects [ 36 ]. This collaborative effort ensures a more personalised approach to patient care.
At the public health level, awareness programs should be launched to educate diabetic patients about the potential cognitive consequences of metformin and the significance of making informed decisions. Comprehensive studies investigating dose–response connections, long-term consequences, and population-specific effects should receive research funding. Public health guidelines must be revised to reflect increasing evidence, giving healthcare practitioners clear advice on using metformin in diabetes management taking both glycaemic control and cognitive outcomes into account. Policymakers should consider these findings when developing diabetes management policies and public health initiatives to ensure that possible cognitive effects are integrated into broader healthcare programs.
Limitations and strengths of review
The review provides clear implications for clinical practice, suggesting that metformin may be a feasible adjunctive therapy for individuals with diabetes at risk of cognitive decline. The multidisciplinary approach recommended for navigating the complex relationship between diabetes control and cognitive health enhances the practicality of the review's recommendations. Also, the review identifies varied outcomes across studies, emphasising the complexity of the relationship between metformin use and dementia risk. This acknowledgement of diverse findings encourages a more cautious interpretation and highlights the need for further research. However, the included studies exhibit methodological disparities, including differences in study design, sample size, and outcome measures. This variation makes it challenging to obtain standardised results and directly compare findings between investigations.
The body of evidence exploring metformin's role in mitigating dementia risk among individuals with diabetes presents a complex yet promising landscape. The interplay between diabetes and dementia shows the importance of glycemic control and comprehensive management of diabetic complications in reducing the likelihood of cognitive decline. This mini-narrative review reveals a spectrum of outcomes regarding the potential connection between metformin use and dementia risk in patients with diabetes. While a majority of studies suggest a positive association between metformin use and a reduced risk of dementia, the complex nature of these findings prompts a cautious interpretation. Dose–response interactions, long-term effects, and demographic diversity emerge as critical factors requiring further investigation to understand metformin's impact on cognitive health. Noteworthy variations in outcomes across studies highlight the need for standardised methodologies and robust study designs in future research endeavours.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
Advanced Glycosylation End Products
Alzheimer's Disease
5'-Adenosine Monophosphate-Activated Protein Kinase
Apolipoprotein E
Vitamin B-12
Epsilon 2 (APOE gene polymorphism)
Epsilon 4 (APOE gene polymorphism)
Hemoglobin A1c
Hazard Ratio
Randomized Controlled Trials
Type 2 Diabetes Mellitus
Crane PK, Walker R, Hubbard RA, Li G, Nathan DM, Zheng H, et al. Glucose levels and risk of dementia. N Engl J Med. 2013;369:540–8. https://doi.org/10.1056/NEJMoa1215740 .
Article CAS PubMed PubMed Central Google Scholar
Geijselaers SLC, Sep SJS, Stehouwer CDA, Biessels GJ. Glucose regulation, cognition, and brain MRI in type 2 diabetes: a systematic review. Lancet Diabetes Endocrinol. 2015;3:75–89. https://doi.org/10.1016/S2213-8587(14)70148-2 .
Article CAS PubMed Google Scholar
Xu WL, von Strauss E, Qiu CX, Winblad B, Fratiglioni L. Uncontrolled diabetes increases the risk of Alzheimer’s disease: a population-based cohort study. Diabetologia. 2009;52:1031–9. https://doi.org/10.1007/s00125-009-1323-x .
Exalto LG, Biessels GJ, Karter AJ, Huang ES, Quesenberry CP, Whitmer RA. Severe Diabetic retinal disease and dementia risk in type 2 diabetes. J Alzheimer’s Dis. 2014;42:S109–17. https://doi.org/10.3233/JAD-132570 .
Article Google Scholar
Wang B, Wang N, Sun Y, Tan X, Zhang J, Lu Y. Association of combined healthy lifestyle factors with incident dementia in patients with type 2 diabetes. Neurology. 2022;99:E2336–45. https://doi.org/10.1212/WNL.0000000000201231 .
Tsugawa A, Ogawa Y, Takenoshita N, Kaneko Y, Hatanaka H, Jaime E, et al. Decreased muscle strength and quality in diabetes-related dementia. Dement Geriatr Cogn Dis Extra. 2017;7:454–62. https://doi.org/10.1159/000485177 .
Article PubMed PubMed Central Google Scholar
Hanyu H, Hirose D, Fukasawa R, Hatanaka H, Namioka N, Sakurai H. Guidelines for the clinical diagnosis of diabetes mellitus-related dementia. J Am Geriatr Soc. 2015;63:1721–3. https://doi.org/10.1111/jgs.13581 .
Article PubMed Google Scholar
Mayeda ER, Karter AJ, Huang ES, Moffet HH, Haan MN, Whitmer RA. Racial/ethnic differences in dementia risk among older type 2 diabetic patients: the diabetes and aging study. Diabetes Care. 2014;37:1009–15. https://doi.org/10.2337/dc13-0215 .
Campbell JM, Stephenson MD, de Courten B, Chapman I, Bellman SM, Aromataris E. Metformin use associated with reduced risk of dementia in patients with diabetes: a systematic review and meta-analysis. J Alzheimer’s Dis. 2018;65:1225–36. https://doi.org/10.3233/JAD-180263 .
Wium-Andersen IK, Osler M, Jørgensen MB, Rungby J, Wium-Andersen MK. Antidiabetic medication and risk of dementia in patients with type 2 diabetes: a nested case–control study. Eur J Endocrinol. 2019;181:499–507. https://doi.org/10.1530/EJE-19-0259 .
Hsu CC, Wahlqvist ML, Lee MS, Tsai HN. Incidence of dementia is increased in type 2 diabetes and reduced by the use of sulfonylureas and metformin. J Alzheimers Dis. 2011;24(3):485–93. https://doi.org/10.3233/JAD-2011-101524 .
Article CAS Google Scholar
Campbell JM, Bellman SM, Stephenson MD, Lisy K. Metformin reduces all-cause mortality and diseases of ageing independent of its effect on diabetes control: a systematic review and meta-analysis. Ageing Res Rev. 2017;40:31–44. https://doi.org/10.1016/j.arr.2017.08.003 .
Orkaby AR, Cho K, Cormack J, Gagnon DR, Driver JA. Metformin vs sulfonylurea use and risk of dementia in US veterans aged ≥65 years with diabetes. Neurology. 2017;89:1877–85. https://doi.org/10.1212/WNL.0000000000004586 .
Samaras K, Makkar S, Crawford JD, Kochan NA, Wen W, Draper B, et al. Metformin use is associated with slowed cognitive decline and reduced incident dementia in older adults with type 2 diabetes: the sydney memory and ageing study. Diabetes Care. 2020;43:2691–701. https://doi.org/10.2337/DC20-0892 .
Ng TP, Feng L, Yap KB, Lee TS, Tan CH, Winblad B. Long-term metformin usage and cognitive function among older adults with diabetes. J Alzheimer’s Dis. 2014;41:61–8. https://doi.org/10.3233/JAD-131901 .
Huang K-H, Tsai Y-F, Lee CB, Gau S-Y, Tsai T-H, Chung N-J, et al. The correlation between metformin use and incident dementia in patients with new-onset diabetes mellitus: a population-based study. J Pers Med. 2023;13:738. https://doi.org/10.3390/jpm13050738 .
Luchsinger JA, Perez T, Chang H, Mehta P, Steffener J, Pradabhan G, et al. Metformin in amnestic mild cognitive impairment: results of a pilot randomized placebo controlled clinical trial. J Alzheimer’s Dis. 2016;51:501–14. https://doi.org/10.3233/JAD-150493 .
Tseng C-H. Dementia risk in type 2 diabetes patients: acarbose use and its joint effects with metformin and pioglitazone. Aging Dis. 2020;11:658.
Kim Y, Kim H-S, Lee J, Kim Y-S, You H-S, Bae Y-J, et al. Metformin use in elderly population with diabetes reduced the risk of dementia in a dose-dependent manner, based on the Korean NHIS-HEALS cohort. Diabetes Res Clin Pract. 2020;170:108496. https://doi.org/10.1016/j.diabres.2020.108496 .
Chin-Hsiao T. Metformin and the Risk of Dementia in Type 2 Diabetes Patients. Aging Dis. 2019;10(1):37–48. https://doi.org/10.14336/AD.2017.1202 .
Scherrer JF, Salas J, Floyd JS, Farr SA, Morley JE, Dublin S. Metformin and sulfonylurea use and risk of incident dementia. Mayo Clin Proc. 2019;94:1444–56. https://doi.org/10.1016/j.mayocp.2019.01.004 .
Ko K-P, Ma SH, Yang J-J, Hwang Y, Ahn C, Cho Y-M, et al. Metformin intervention in obese non-diabetic patients with breast cancer: phase II randomized, double-blind, placebo-controlled trial. Breast Cancer Res Treat. 2015;153:361–70. https://doi.org/10.1007/s10549-015-3519-8 .
Scherrer JF, Morley JE, Salas J, Floyd JS, Farr SA, Dublin S. Association between metformin initiation and incident dementia among African American and white veterans health administration patients. Ann Fam Med. 2019;17:352–62. https://doi.org/10.1370/afm.2415 .
Newby D, Linden AB, Fernandes M, Molero Y, Winchester L, Sproviero W, Ghose U, Li QS, Launer LJ, Duijn CMV, Nevado-Holgado AJ. Comparative effect of metformin versus sulfonylureas with dementia and Parkinson's disease risk in US patients over 50 with type 2 diabetes mellitus. BMJ Open Diabetes Res Care. 2022;10(5):e003036. https://doi.org/10.1136/bmjdrc-2022-003036 .
de Jager J, Kooy A, Lehert P, Wulffele MG, van der Kolk J, Bets D, et al. Long term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: randomised placebo controlled trial. BMJ. 2010;340:c2181–c2181. https://doi.org/10.1136/bmj.c2181 .
Tzeng I-S, Hsieh T-H. Collocation of metformin and dipeptidyl peptidase-4 inhibitor is associated with increased risk of diabetes-related vascular dementia: a single hospital study in Northern Taiwan. Expert Opin Investig Drugs. 2023;32:171–6. https://doi.org/10.1080/13543784.2023.2178417 .
Mone P, Martinelli G, Lucariello A, Leo AL, Marro A, De Gennaro S, Marzocco S, Moriello D, Frullone S, Cobellis L, Santulli G. Extended-release metformin improves cognitive impairment in frail older women with hypertension and diabetes: preliminary results from the LEOPARDESS Study. Cardiovasc Diabetol. 2023;22(1):94. https://doi.org/10.1186/s12933-023-01817-4 .
Kuan Y-C, Huang K-W, Lin C-L, Hu C-J, Kao C-H. Effects of metformin exposure on neurodegenerative diseases in elderly patients with type 2 diabetes mellitus. Prog Neuro-Psychopharmacol Biol Psychiatry. 2017;79:77–83. https://doi.org/10.1016/j.pnpbp.2017.06.002 .
Xue Y, Xie X. The association between metformin use and risk of developing severe dementia among ad patients with type 2 diabetes. Biomedicines. 2023;11:2935. https://doi.org/10.3390/biomedicines11112935 .
Luchsinger JA, Ma Y, Christophi CA, Florez H, Golden SH, Hazuda H, et al. Metformin, lifestyle intervention, and cognition in the diabetes prevention program outcomes study. Diabetes Care. 2017;40:958–65. https://doi.org/10.2337/dc16-2376 .
Zhou C, Peng B, Qin Z, Zhu W, Guo C. Metformin attenuates LPS-induced neuronal injury and cognitive impairments by blocking NF-κB pathway. BMC Neurosci. 2021;22(1):73. https://doi.org/10.1186/s12868-021-00678-5 .
Rabieipoor S, Zare M, Ettcheto M, Camins A, Javan M. Metformin restores cognitive dysfunction and histopathological deficits in an animal model of sporadic Alzheimer’s disease. Heliyon. 2023;9(7):e17873. https://doi.org/10.1016/j.heliyon.2023.e17873 .
Ji S, Wang L, Li L. Effect of metformin on short-term high-fat diet-induced weight gain and anxiety-like behavior and the gut microbiota. Front Endocrinol. 2019;10:704. https://doi.org/10.3389/fendo.2019.00704 .
Tong PC, Chan SC, Chan WB, Ho KK, Leung GT, Lo SH, Mak GY, Tse TS. Consensus statements from the diabetologists & endocrinologists alliance for the management of people with hypertension and type 2 diabetes mellitus. J Clin Med. 2023;12(10):3403. https://doi.org/10.3390/jcm12103403 .
Sridhar GR. On psychology and psychiatry in diabetes. Indian J Endocrinol Metab. 2020;24(5):387–95. https://doi.org/10.4103/ijem.IJEM_188_20 .
Aderinto N, Olatunji G, Abdulbasit M, Ashinze P, Faturoti O, Ajagbe A, Ukoaka B, Aboderin G. The impact of diabetes in cognitive impairment: a review of current evidence and prospects for future investigations. Medicine. 2023;102(43):e35557. https://doi.org/10.1097/MD.0000000000035557 .
Download references
Acknowledgements
No funding was received for this study.
Author information
Authors and affiliations.
Department of Medicine and Surgery, Ladoke Akintola University of Technology, Ogbomoso, Nigeria
Nicholas Aderinto & Abdulrahmon Moradeyo
Department of Medicine and Surgery, University of Ilorin, Ilorin, Nigeria
Gbolahan Olatunji, Emmanuel Kokori, Stephen Igwe & Badrudeen Olalekan Alabi
Southern Illinois University Edwardsville, Edwardsville, IL, USA
Praise Fawehinmi
Afe Babalola University, Ado-Ekiti, Ado, Nigeria
Rebecca Ojabo & Emmanuel Chuka Okafor
William Harvey Hospital, Ashford, UK
Damilola Ologbe
John H. Stroger Jr Hospital of Cook County, Chicago, IL, USA
Ayobami Olafimihan
Department of Allied and Public Health, School of Health, Sport and Bioscience, University of East London, London, UK
David B. Olawade
You can also search for this author in PubMed Google Scholar
Contributions
NA conceptualised the study; All authors were involved in the literature review; GO & EK extracted the data from the reviewed studies; All authors wrote the final and first drafts. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Nicholas Aderinto .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Aderinto, N., Olatunji, G., Kokori, E. et al. Metformin mitigates dementia risk among individuals with type 2 diabetes. Clin Diabetes Endocrinol 10 , 10 (2024). https://doi.org/10.1186/s40842-024-00168-7
Download citation
Received : 26 December 2023
Accepted : 18 January 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s40842-024-00168-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Diabetes Mellitus
- Cognitive impairment
Clinical Diabetes and Endocrinology
ISSN: 2055-8260
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Introduction: Narrative therapy (NT) has a post-modern approach and assumes people as experts that construct. their narratives. Aim: This study aims to provide a review of relevant literature from ...
To be included, articles had to present the results of research on narrative therapy or a psychotherapeutic approach incorporating either the original narrative therapy model or another narrative approach to psychotherapy, for adults with mood disorders. Articles could report on any study design and any sample size.
The main objective of narrative therapy is the well-being and happiness of children; therefore, the factors that lead to the superior compliance of individuals with the requirements and threats of life are the components of this approach. Narrative therapy methods also comprise the 'telling, listening, re-telling, and re-listening of stories.'
Revie w of Narrativ e Therapy: Research and Utility. Mary Etchison. David M. Kleist. Idaho State University. Narrative therapy has captured the attention of many in the family. counseling field ...
Background: Narrative exposure therapy (NET) is a short-term psychological treatment for post-traumatic stress disorder (PTSD) that has been investigated in various contexts among traumatized refugees and other trauma survivors.Sustained treatment results have been reported, but the methodological quality of the trials needs a more thorough examination.
In other words, "the how" of narrative therapy was emphasised in addition to "the what" of the practice components of narrative therapy. Within the articles, this worldview was located within the philosophical traditions of social constructionism and poststructuralism , including an emphasis of therapy unpacking or deconstructing social ...
Narrative therapy is a process of co-authoring life narratives that transforms literature into a practice which helps and heals clients. In a sense, the therapist serves as the client's writing coach, equipping the client to work through his or her "problems" by means of life writing. Narrative therapy, emerging from a post-modern, social constructive background, constitutes a unique ...
Narrative therapy is seldom the subject of quantitative research , perhaps because narrative therapy avoids using diagnostic classifications in order to privilege "the voice of those who consult with us … working with their truth and their version of reality" . For some, this makes it unsuitable for quantitative research methods.
Abstract. Introduction: Narrative therapy (NT) has a post-modern approach and assumes people as experts that construct their narratives. Aim: This study aims to provide a review of relevant literature from 1995 to 2021 on studies using narrative therapy, considering how to use it, the application of this approach, and its outcomes.
In this article, the authors will describe a creative writing therapeutic group program they developed based on narrative therapy and narrative medicine principles. This was a Social Science and Humanities Research Council—Partnership Engagement Grant funded project, the aim of which was to develop a facilitator's manual for people interested in offering this group, titled "Journey ...
Despite the importance of narrative, emotional and meaning-making processes in psychotherapy, there has been no review of studies using the main instruments developed to address these processes. The objective is to review the studies about client narrative and narrative-emotional processes in psychotherapy that used the Narrative Process Coding System or the Narrative-Emotion Process Coding ...
The research on narrative therapy is at the beginning. Published research involves qualitative and case studies. O'Connor et al. found that in a qualitative study of eight clients, narrative therapy significantly reduced the presenting problem.Smith et al. and Sells et al. using qualitative research found reflecting teams used in narrative therapy for the most part to be effective.
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on NARRATIVE THERAPY. Find methods information, sources, references or conduct a literature review on ...
Accessible summary: Narrative therapy is a useful approach in the treatment of depression that allows that person to 're-author' his/her life stories by focusing on positive interpretations, and such focus on positive emotions is a crucial component of treatment for depression. This paper evaluates narrative therapy with an emotional approach (NTEA) as a therapeutic modality that could be used ...
Abstract. Narrative therapy has captured the attention of many in the family counseling field. Despite the apparent appeal of narrative therapy as a therapeutic modality, research on its effectiveness is in its in-fancy. This article will review current research on narrative therapy and discuss why a broader research base has yet to be developed.
Research article. First published online December 13, 2019. ... 2015), which aligns with many strengths of narrative therapy. This article discusses how narrative therapy (White & Epston, 1990) can be used in IBHC settings to reduce the stigma of treating mental health and empower patients as experts of their lives (Geertz, ...
Externalizing the problem, a contribution of narrative therapy (White & Epston, 1990), is already utilized in this stage by way of reframing problems in terms of attachment needs (Johnson, 2004), but therapists using narrative-informed EFT can extend externalization to other factors contributing to relationship stress. While attachment needs ...
This article presents a case study using a combined narrative psychological and experiential art therapy approach. We address the clinical application, explore the psychotherapeutic process of reconstructing a person's life story, and consider its implications for personal recovery and psychological wellbeing.
Narrative worldview. Aspects of the narrative worldview were expressed in 28 of the identified articles. Pedersen [] defined narrative therapy as a belief system or philosophy, rather than being limited to a collection of psychological techniques.This idea was mirrored across many of the articles identified in the search, with 18 references describing how narrative therapy encapsulates core ...
The effectiveness of narrative therapy with young people with autism (2013) Developing our cultural strengths: Using the 'Tree of Life' strength-based, narrative therapy intervention in schools, to enhance self-esteem, cultural understanding and to challenge racism (2013) An exploratory study of the effectiveness of group narrative therapy on ...
Nevertheless, narrative therapy research is gradually bridging the divide between positivist and social/relational approaches for example, in outcome research in depression and post-traumatic stress disorder . However, studies that focus on both outcomes and therapeutic process have continued to be predominantly exploratory .
Narrative therapy has been proposed to have practice-based evidence however little is known about its research evidence-base in the treatment of eating disorders. The aim of this study was to conduct a systematic review of the outcome literature of narrative therapy for eating disorders. Treatment outcome data were extracted from 33 eligible included studies following systematic search of five ...
Columbia University Vagelos College of Physicians and Surgeons, New York, USA. Your News feature 'Why loneliness is bad for your health' (Nature 628, 22-24; 2024) accurately notes the ...
Research suggests that a clinical diagnosis of schizophrenia is strongly linked with experiencing negative stereotypes and an inability to recover. In challenging the scientific-logical practice of diagnostic labeling, which totalizes the person's experience around the illness, Narrative therapy offers a unique approach to treating schizophrenia by putting the spotlight on the client's ...
The present research is done in order to investigate the effects of narrative therapy in groups on psychological well-being and distress among women with addicted husbands. One of the results of the research shows that the psychological well-being's score of the women who participated in group counseling is increased significantly in comparison ...
This mini-narrative review explores the relationship between diabetes and dementia, focusing on the potential mitigating role of metformin in reducing cognitive decline among individuals with type 2 diabetes. The interplay of factors such as glycemic control, diabetic complications, and lifestyle influences characterises diabetes-related dementia. This review emphasises the significance of ...
1. Introduction. One in six adults in England were found to have a common mental health disorder in a 2014 National Statistics report, and one third of them reported current use of a mental health treatment, with medication being the most common form of treatment reported ().However, health care services including GPs, inpatient, outpatient, and community services were all utilized for mental ...