

Browse all our research projects by topic We have funded more than 150 external research projects across a range of themes over the last five years
- Share on Twitter
- Share on LinkedIn
- Share on Facebook
- Share on WhatsApp
- Share by email
- Link Copy link
Please click below to see the research projects we've funded on the following topics.
- Analytics and data
- Children and young people
- Commissioning
- Community and voluntary
- Digital technology
- Efficiency and productivity
- Emergency medicine
- End of life care
- Funding and sustainability
- Improvement science
- Inequalities
- Integrated care
- Long-term conditions
- Mental health
- Older people
- Patient experience
- Patient safety
- Person-centred care
- Primary care
- Public health
- Quality improvement
- Quality of care
- Social care
- Social determinants of health
Share this page:
Health Foundation @HealthFdn
- Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
The Q community
Q is an initiative connecting people with improvement expertise across the UK.
Quick links
- News and media
- Events and webinars
Hear from us
Receive the latest news and updates from the Health Foundation
- 020 7257 8000
- [email protected]
- The Health Foundation Twitter account
- The Health Foundation LinkedIn account
- The Health Foundation Facebook account
Copyright The Health Foundation 2024. Registered charity number 286967.
- Accessibility
- Anti-slavery statement
- Terms and conditions
- Privacy policy

Research Topics & Ideas: Healthcare
100+ Healthcare Research Topic Ideas To Fast-Track Your Project

Finding and choosing a strong research topic is the critical first step when it comes to crafting a high-quality dissertation, thesis or research project. If you’ve landed on this post, chances are you’re looking for a healthcare-related research topic , but aren’t sure where to start. Here, we’ll explore a variety of healthcare-related research ideas and topic thought-starters across a range of healthcare fields, including allopathic and alternative medicine, dentistry, physical therapy, optometry, pharmacology and public health.
NB – This is just the start…
The topic ideation and evaluation process has multiple steps . In this post, we’ll kickstart the process by sharing some research topic ideas within the healthcare domain. This is the starting point, but to develop a well-defined research topic, you’ll need to identify a clear and convincing research gap , along with a well-justified plan of action to fill that gap.
If you’re new to the oftentimes perplexing world of research, or if this is your first time undertaking a formal academic research project, be sure to check out our free dissertation mini-course. In it, we cover the process of writing a dissertation or thesis from start to end. Be sure to also sign up for our free webinar that explores how to find a high-quality research topic.
Overview: Healthcare Research Topics
- Allopathic medicine
- Alternative /complementary medicine
- Veterinary medicine
- Physical therapy/ rehab
- Optometry and ophthalmology
- Pharmacy and pharmacology
- Public health
- Examples of healthcare-related dissertations
Allopathic (Conventional) Medicine
- The effectiveness of telemedicine in remote elderly patient care
- The impact of stress on the immune system of cancer patients
- The effects of a plant-based diet on chronic diseases such as diabetes
- The use of AI in early cancer diagnosis and treatment
- The role of the gut microbiome in mental health conditions such as depression and anxiety
- The efficacy of mindfulness meditation in reducing chronic pain: A systematic review
- The benefits and drawbacks of electronic health records in a developing country
- The effects of environmental pollution on breast milk quality
- The use of personalized medicine in treating genetic disorders
- The impact of social determinants of health on chronic diseases in Asia
- The role of high-intensity interval training in improving cardiovascular health
- The efficacy of using probiotics for gut health in pregnant women
- The impact of poor sleep on the treatment of chronic illnesses
- The role of inflammation in the development of chronic diseases such as lupus
- The effectiveness of physiotherapy in pain control post-surgery
Topics & Ideas: Alternative Medicine
- The benefits of herbal medicine in treating young asthma patients
- The use of acupuncture in treating infertility in women over 40 years of age
- The effectiveness of homoeopathy in treating mental health disorders: A systematic review
- The role of aromatherapy in reducing stress and anxiety post-surgery
- The impact of mindfulness meditation on reducing high blood pressure
- The use of chiropractic therapy in treating back pain of pregnant women
- The efficacy of traditional Chinese medicine such as Shun-Qi-Tong-Xie (SQTX) in treating digestive disorders in China
- The impact of yoga on physical and mental health in adolescents
- The benefits of hydrotherapy in treating musculoskeletal disorders such as tendinitis
- The role of Reiki in promoting healing and relaxation post birth
- The effectiveness of naturopathy in treating skin conditions such as eczema
- The use of deep tissue massage therapy in reducing chronic pain in amputees
- The impact of tai chi on the treatment of anxiety and depression
- The benefits of reflexology in treating stress, anxiety and chronic fatigue
- The role of acupuncture in the prophylactic management of headaches and migraines
Topics & Ideas: Dentistry
- The impact of sugar consumption on the oral health of infants
- The use of digital dentistry in improving patient care: A systematic review
- The efficacy of orthodontic treatments in correcting bite problems in adults
- The role of dental hygiene in preventing gum disease in patients with dental bridges
- The impact of smoking on oral health and tobacco cessation support from UK dentists
- The benefits of dental implants in restoring missing teeth in adolescents
- The use of lasers in dental procedures such as root canals
- The efficacy of root canal treatment using high-frequency electric pulses in saving infected teeth
- The role of fluoride in promoting remineralization and slowing down demineralization
- The impact of stress-induced reflux on oral health
- The benefits of dental crowns in restoring damaged teeth in elderly patients
- The use of sedation dentistry in managing dental anxiety in children
- The efficacy of teeth whitening treatments in improving dental aesthetics in patients with braces
- The role of orthodontic appliances in improving well-being
- The impact of periodontal disease on overall health and chronic illnesses
Tops & Ideas: Veterinary Medicine
- The impact of nutrition on broiler chicken production
- The role of vaccines in disease prevention in horses
- The importance of parasite control in animal health in piggeries
- The impact of animal behaviour on welfare in the dairy industry
- The effects of environmental pollution on the health of cattle
- The role of veterinary technology such as MRI in animal care
- The importance of pain management in post-surgery health outcomes
- The impact of genetics on animal health and disease in layer chickens
- The effectiveness of alternative therapies in veterinary medicine: A systematic review
- The role of veterinary medicine in public health: A case study of the COVID-19 pandemic
- The impact of climate change on animal health and infectious diseases in animals
- The importance of animal welfare in veterinary medicine and sustainable agriculture
- The effects of the human-animal bond on canine health
- The role of veterinary medicine in conservation efforts: A case study of Rhinoceros poaching in Africa
- The impact of veterinary research of new vaccines on animal health
Topics & Ideas: Physical Therapy/Rehab
- The efficacy of aquatic therapy in improving joint mobility and strength in polio patients
- The impact of telerehabilitation on patient outcomes in Germany
- The effect of kinesiotaping on reducing knee pain and improving function in individuals with chronic pain
- A comparison of manual therapy and yoga exercise therapy in the management of low back pain
- The use of wearable technology in physical rehabilitation and the impact on patient adherence to a rehabilitation plan
- The impact of mindfulness-based interventions in physical therapy in adolescents
- The effects of resistance training on individuals with Parkinson’s disease
- The role of hydrotherapy in the management of fibromyalgia
- The impact of cognitive-behavioural therapy in physical rehabilitation for individuals with chronic pain
- The use of virtual reality in physical rehabilitation of sports injuries
- The effects of electrical stimulation on muscle function and strength in athletes
- The role of physical therapy in the management of stroke recovery: A systematic review
- The impact of pilates on mental health in individuals with depression
- The use of thermal modalities in physical therapy and its effectiveness in reducing pain and inflammation
- The effect of strength training on balance and gait in elderly patients
Topics & Ideas: Optometry & Opthalmology
- The impact of screen time on the vision and ocular health of children under the age of 5
- The effects of blue light exposure from digital devices on ocular health
- The role of dietary interventions, such as the intake of whole grains, in the management of age-related macular degeneration
- The use of telemedicine in optometry and ophthalmology in the UK
- The impact of myopia control interventions on African American children’s vision
- The use of contact lenses in the management of dry eye syndrome: different treatment options
- The effects of visual rehabilitation in individuals with traumatic brain injury
- The role of low vision rehabilitation in individuals with age-related vision loss: challenges and solutions
- The impact of environmental air pollution on ocular health
- The effectiveness of orthokeratology in myopia control compared to contact lenses
- The role of dietary supplements, such as omega-3 fatty acids, in ocular health
- The effects of ultraviolet radiation exposure from tanning beds on ocular health
- The impact of computer vision syndrome on long-term visual function
- The use of novel diagnostic tools in optometry and ophthalmology in developing countries
- The effects of virtual reality on visual perception and ocular health: an examination of dry eye syndrome and neurologic symptoms
Topics & Ideas: Pharmacy & Pharmacology
- The impact of medication adherence on patient outcomes in cystic fibrosis
- The use of personalized medicine in the management of chronic diseases such as Alzheimer’s disease
- The effects of pharmacogenomics on drug response and toxicity in cancer patients
- The role of pharmacists in the management of chronic pain in primary care
- The impact of drug-drug interactions on patient mental health outcomes
- The use of telepharmacy in healthcare: Present status and future potential
- The effects of herbal and dietary supplements on drug efficacy and toxicity
- The role of pharmacists in the management of type 1 diabetes
- The impact of medication errors on patient outcomes and satisfaction
- The use of technology in medication management in the USA
- The effects of smoking on drug metabolism and pharmacokinetics: A case study of clozapine
- Leveraging the role of pharmacists in preventing and managing opioid use disorder
- The impact of the opioid epidemic on public health in a developing country
- The use of biosimilars in the management of the skin condition psoriasis
- The effects of the Affordable Care Act on medication utilization and patient outcomes in African Americans
Topics & Ideas: Public Health
- The impact of the built environment and urbanisation on physical activity and obesity
- The effects of food insecurity on health outcomes in Zimbabwe
- The role of community-based participatory research in addressing health disparities
- The impact of social determinants of health, such as racism, on population health
- The effects of heat waves on public health
- The role of telehealth in addressing healthcare access and equity in South America
- The impact of gun violence on public health in South Africa
- The effects of chlorofluorocarbons air pollution on respiratory health
- The role of public health interventions in reducing health disparities in the USA
- The impact of the United States Affordable Care Act on access to healthcare and health outcomes
- The effects of water insecurity on health outcomes in the Middle East
- The role of community health workers in addressing healthcare access and equity in low-income countries
- The impact of mass incarceration on public health and behavioural health of a community
- The effects of floods on public health and healthcare systems
- The role of social media in public health communication and behaviour change in adolescents
Examples: Healthcare Dissertation & Theses
While the ideas we’ve presented above are a decent starting point for finding a healthcare-related research topic, they are fairly generic and non-specific. So, it helps to look at actual dissertations and theses to see how this all comes together.
Below, we’ve included a selection of research projects from various healthcare-related degree programs to help refine your thinking. These are actual dissertations and theses, written as part of Master’s and PhD-level programs, so they can provide some useful insight as to what a research topic looks like in practice.
- Improving Follow-Up Care for Homeless Populations in North County San Diego (Sanchez, 2021)
- On the Incentives of Medicare’s Hospital Reimbursement and an Examination of Exchangeability (Elzinga, 2016)
- Managing the healthcare crisis: the career narratives of nurses (Krueger, 2021)
- Methods for preventing central line-associated bloodstream infection in pediatric haematology-oncology patients: A systematic literature review (Balkan, 2020)
- Farms in Healthcare: Enhancing Knowledge, Sharing, and Collaboration (Garramone, 2019)
- When machine learning meets healthcare: towards knowledge incorporation in multimodal healthcare analytics (Yuan, 2020)
- Integrated behavioural healthcare: The future of rural mental health (Fox, 2019)
- Healthcare service use patterns among autistic adults: A systematic review with narrative synthesis (Gilmore, 2021)
- Mindfulness-Based Interventions: Combatting Burnout and Compassionate Fatigue among Mental Health Caregivers (Lundquist, 2022)
- Transgender and gender-diverse people’s perceptions of gender-inclusive healthcare access and associated hope for the future (Wille, 2021)
- Efficient Neural Network Synthesis and Its Application in Smart Healthcare (Hassantabar, 2022)
- The Experience of Female Veterans and Health-Seeking Behaviors (Switzer, 2022)
- Machine learning applications towards risk prediction and cost forecasting in healthcare (Singh, 2022)
- Does Variation in the Nursing Home Inspection Process Explain Disparity in Regulatory Outcomes? (Fox, 2020)
Looking at these titles, you can probably pick up that the research topics here are quite specific and narrowly-focused , compared to the generic ones presented earlier. This is an important thing to keep in mind as you develop your own research topic. That is to say, to create a top-notch research topic, you must be precise and target a specific context with specific variables of interest . In other words, you need to identify a clear, well-justified research gap.
Need more help?
If you’re still feeling a bit unsure about how to find a research topic for your healthcare dissertation or thesis, check out Topic Kickstarter service below.

You Might Also Like:

15 Comments
I need topics that will match the Msc program am running in healthcare research please
Hello Mabel,
I can help you with a good topic, kindly provide your email let’s have a good discussion on this.
Can you provide some research topics and ideas on Immunology?
Thank you to create new knowledge on research problem verse research topic
Help on problem statement on teen pregnancy
This post might be useful: https://gradcoach.com/research-problem-statement/
can you provide me with a research topic on healthcare related topics to a qqi level 5 student
Please can someone help me with research topics in public health ?
Hello I have requirement of Health related latest research issue/topics for my social media speeches. If possible pls share health issues , diagnosis, treatment.
I would like a topic thought around first-line support for Gender-Based Violence for survivors or one related to prevention of Gender-Based Violence
Please can I be helped with a master’s research topic in either chemical pathology or hematology or immunology? thanks
Can u please provide me with a research topic on occupational health and safety at the health sector
Good day kindly help provide me with Ph.D. Public health topics on Reproductive and Maternal Health, interventional studies on Health Education
may you assist me with a good easy healthcare administration study topic
May you assist me in finding a research topic on nutrition,physical activity and obesity. On the impact on children
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Qualitative Research – a practical guide for health and social care researchers and practitioners
(0 reviews)
Darshini Ayton, Monash University
Tess Tsindos, Monash University
Danielle Berkovic, Monash University
Copyright Year: 2023
Last Update: 2024
ISBN 13: 9780645755404
Publisher: Monash University
Language: English
Formats Available
Conditions of use.
Table of Contents
- Acknowledgement of Country
- About the authors
- Accessibility statement
- Introduction to research
- Research design
- Data collection
- Data analysis
- Writing qualitative research
- Peer review statement
- Licensing and attribution information
- Version history
Ancillary Material
About the book.
This guide is designed to support health and social care researchers and practitioners to integrate qualitative research into the evidence base of health and social care research. Qualitative research designs are diverse and each design has a different focus that will inform the approach undertaken and the results that are generated. The aim is to move beyond the “what” of qualitative research to the “how”, by (1) outlining key qualitative research designs for health and social care research – descriptive, phenomenology, action research, case study, ethnography, and grounded theory; (2) a decision tool of how to select the appropriate design based on a guiding prompting question, the research question and available resources, time and expertise; (3) an overview of mixed methods research and qualitative research in evaluation studies; (4) a practical guide to data collection and analysis; (5) providing examples of qualitative research to illustrate the scope and opportunities; and (6) tips on communicating qualitative research.
About the Contributors
Associate Professor Darshini Ayton is the Deputy Head of the Health and Social Care Unit at Monash University in Melbourne, Australia. She is a transdisciplinary implementation researcher with a focus on improving health and social care for older Australians and operates at the nexus of implementation science, health and social care policies, public health and consumer engagement. She has led qualitative research studies in hospitals, aged care, not-for-profit organisations and for government and utilises a range of data collection methods. Associate Professor Ayton established and is the director of the highly successful Qualitative Research Methods for Public Health short course which has been running since 2014.
Dr Tess Tsindos is a Research Fellow with the Health and Social Care Unit at Monash University in Melbourne, Australia. She is a public health researcher and lecturer with strong qualitative and mixed methods research experience conducting research studies in hospital and community health settings, not-for-profit organisations and for government. Prior to working in academia, Dr Tsindos worked in community care for government and not-for-profit organisations for more than 25 years. Dr Tsindos has a strong evaluation background having conducted numerous evaluations for a range of health and social care organisations. Based on this experience she coordinated the Bachelor of Health Science/Public Health Evaluation unit and the Master of Public Health Evaluation unit and developed the Evaluating Public Health Programs short course in 2022. Dr Tsindos is the Unit Coordinator of the Master of Public Health Qualitative Research Methods Unit which was established in 2022.
Dr Danielle Berkovic is a Research Fellow in the School of Public Health and Preventive Medicine at Monash University in Melbourne, Australia. She is a public health and consumer-led researcher with strong qualitative and mixed-methods research experience focused on improving health services and clinical guidelines for people with arthritis and other musculoskeletal conditions. She has conducted qualitative research studies in hospitals and community health settings. Dr Berkovic currently provides qualitative input into Australia’s first Living Guideline for the pharmacological management of inflammatory arthritis. Dr Berkovic is passionate about incorporating qualitative research methods into traditionally clinical and quantitative spaces and enjoys teaching clinicians and up-and-coming researchers about the benefits of qualitative research.
Contribute to this Page
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 13, Issue 3
- Application of complexity theory in health and social care research: a scoping review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-4383-8650 Áine Carroll 1 , 2 ,
- Claire Collins 3 ,
- Jane McKenzie 3 ,
- Diarmuid Stokes 4 ,
- Andrew Darley 1
- 1 School of Medicine , University College Dublin , Dublin , Ireland
- 2 Academic Department , National Rehabilitation University Hospital , Dublin , Ireland
- 3 Henley Business School , University of Reading , Reading , UK
- 4 College of Health Sciences , University College Dublin , Dublin , Ireland
- Correspondence to Áine Carroll; aine.carroll{at}ucd.ie
Background Complexity theory has been chosen by many authors as a suitable lens through which to examine health and social care. Despite its potential value, many empirical investigations apply the theory in a tokenistic manner without engaging with its underlying concepts and underpinnings.
Objectives The aim of this scoping review is to synthesise the literature on empirical studies that have centred on the application of complexity theory to understand health and social care provision.
Methods This scoping review considered primary research using complexity theory-informed approaches, published in English between 2012 and 2021. Cochrane Database of Systematic Reviews, MEDLINE, CINAHL, EMBASE, Web of Science, PSYCHINFO, the NHS Economic Evaluation Database, and the Health Economic Evaluations Database were searched. In addition, a manual search of the reference lists of relevant articles was conducted. Data extraction was conducted using Covidence software and a data extraction form was created to produce a descriptive summary of the results, addressing the objectives and research question. The review used the revised Arksey and O’Malley framework and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-analysis Extension for Scoping Reviews (PRISMA-ScR).
Results 2021 studies were initially identified with a total of 61 articles included for extraction. Complexity theory in health and social care research is poorly defined and described and was most commonly applied as a theoretical and analytical framework. The full breadth of the health and social care continuum was not represented in the identified articles, with the majority being healthcare focused.
Discussion Complexity theory is being increasingly embraced in health and care research. The heterogeneity of the literature regarding the application of complexity theory made synthesis challenging. However, this scoping review has synthesised the most recent evidence and contributes to translational systems research by providing guidance for future studies.
Conclusion The study of complex health and care systems necessitates methods of interpreting dynamic prcesses which requires qualitative and longitudinal studies with abductive reasoning. The authors provide guidance on conducting complexity-informed primary research that seeks to promote rigor and transparency in the area.
Registration The scoping review protocol was registered at Open Science Framework, and the review protocol was published at BMJ Open ( https://bit.ly/3Ex1Inu ).
- QUALITATIVE RESEARCH
- International health services
- Quality in health care
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2022-069180
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
This study builds on previous evidence syntheses and synthesises the literature on empirical studies that have centred on the application of complexity theory to understand health and social care provision.
This review applies the latest guidance for the performance of scoping reviews.
The review covers the years 2012–2021 and includes English language papers only.
The review excluded educational settings.
Health and care systems around the globe are struggling to cope with the imbalance between increasing demands and system constraints. These challenges have been amplified with the advent of the COVID-19 pandemic. Traditional approaches to tackling these challenges have typically taken a positivistic approach using mechanistic linear reductionist methods more suited to physical systems than complex adaptive human systems and have failed to produce the necessary system transformation. These positivist views have been challenged as simplistic by various key complexity philosophers and scientists over the years. 1–5 Complexity theory and science have received increasing academic and health system attention in recent years as appreciation has grown that, to address increasingly complex and systemic issues, there is a need for collaborative, cross-sectoral, multidisciplinary working. However, how best to study complex social systems is unclear. What is acknowledged is that complex systems share certain characteristics; they consist of elements that interact dynamically in a non-linear manner with feedback loops in systems that are open and operate in conditions far from equilibrium. Each complex system has a history, which influences the behaviour of the system which is determined by the nature of the interactions between the elements. These interactions are adaptive and dynamic with unpredictable outcomes. 1 2 6 Preiser and colleagues in 2018 completed an evidence synthesis of prominent authors’ classifications of complex adaptive systems (CAS) features and characteristics and proposed a typology of six organising principles to inform practical implications and methods for studying and understanding complex systems. 6 These are the following: (1) it is constituted relationally; (2) it has adaptive capacities; (3) patterns of behaviour are a consequence of dynamic processes; (4) it is radically open; (5) it is determined contextually and (6) novel qualities emerge through complex causality. While there is an absence of a unifying theory of complexity, it is generally accepted that engaging with complex systems requires an entanglement of theories and methods.
While the increasing adoption of complexity-informed methods to empirically investigate health and social care settings is welcome, the literature to date has been critiqued for engaging with complexity in name only and lacking the required appreciation and engagement with the logic that underpins it. A scoping review performed by Thompson and colleagues in 2016 investigated complexity theory in health services research and found that, although complexity theory in healthcare was potentially useful, conceptual vagueness and variable theoretical application impeded its practical application. 7 In 2017, Rusoja and colleagues performed a systematic literature review examining health-related systems thinking and complexity ideas. 8 Similar to Thompson and colleagues, they also found that the literature was largely theoretical, suggesting the need for additional research involving practical application. These reviews are now somewhat outdated given the dynamic ever-changing flux of healthcare in the time that has passed since the reviews were published. In addition, these reviews focused on healthcare provision while omitting social care which is an integral component of the continuum of integrated care. Furthermore, the authors did not seek to characterise the components of complexity which were being used nor the theoretical underpinning of the research reviewed. Theory is important to research in that good theory informs the performance of high-quality research (qualitative or quantitative) about important issues that advance knowledge in the phenomenon of interest 9 and the Medical Research Council (MRC) guidance on the development and evaluation of complex interventions recommended that interventions should be developed systematically ‘using the best available evidence and appropriate theory’ 10 (p2). They also suggest that qualitative and mixed-methods approaches may be required to answer questions beyond effectiveness. When theory is used inappropriately, the benefit of using theory to inform high-quality research is negatively impacted. If used correctly, complexity theory offers a potentially useful perspective for the conceptualisation and resolution of problems in healthcare. Therefore, we identified a gap in the evidence regarding how complexity theory has been applied in health and social care research which warranted further examination and synthesis of the evidence to date. Evidence to date suggests limited description, features and attributes which may suggest a lack of appreciation of the underlying principles of a complex system when studying phenomena, which will be explored in this review.
The aim of this review is to map and describe the available research which has used complexity theory in health and social care settings. The authors seek to additionally expand on the previous evidence by providing a comprehensive understanding of the literature to date and offer guidance on how to apply complexity theory to research in health and social care in the future.
Ethical approval was not required, and this manuscript is an honest, accurate and transparent account of the study and no important aspects of the study have been omitted.
Guided by Munn and colleagues, 11 the authors determined that a scoping review was the most appropriate approach to systematically explore how complexity theory has been applied in health and social care research. The scoping review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) statement. 12 The initial exploratory search of the literature highlighted significant gaps in current knowledge regarding how and why complexity theory has been applied in health and social care settings. In accordance with best practice for scoping reviews, an a priori protocol was developed and published. 13 The framework for scoping reviews developed by Arksey and O’Malley (2005) and refinements made by subsequent authors 11 14–16 guided the methodology for the current review. This framework consists of six stages: specifying the research question; identifying relevant studies; study selection; charting the data and reporting the results; collating, summarising and reporting the findings; and consultation exercise.
Stage 1: specifying the research question
Following an initial search of the literature (MEDLINE, CINAHL) and consultation with authors of previously published systematic reviews in the area, 7 8 17 18 the scoping review research question was developed: ‘How has complexity theory been applied in health and social care research?’. The scoping review had the following objectives:
To map definitions and descriptions of complexity theory used in research regarding health and social care.
To describe the purpose of studies using the lens of complexity theory and phenomena of interest.
To investigate the methodologies used and the extent to which complexity theory has been employed in health and social care research.
To consider the settings and professions examined in these studies.
To assess the implications and outcomes of the application of complexity theory in health and social care research.
To identify gaps in the evidence base and make recommendations for future research.
To determine guidance for future researchers when applying complexity theory in research regarding health and social care.
Stage 2: identifying relevant studies
Relevant studies were identified according to the inclusion criteria and the Population, Concept and Context (PCC). 16
Population: Health and social care professionals.
Concept: Application of complexity theory in empirical research in health and/or social care.
Context: Health and social care settings.
Building on the evidence produced in the previous evidence syntheses, this scoping review considered qualitative and quantitative primary research using complexity theory–informed approaches, published in the English language between the years 2012 and 2021.
The following types of publications were excluded from the review: retrospective reviews, secondary analysis research, conference abstracts, book reviews, commentaries or editorial articles, opinion papers, letters and non-English articles.
Acknowledging that the review focused on the application of complexity theory regarding the provision of health and social care rather than the experience of receiving care, publications containing patient-only samples were excluded from the screening process.
An initial exploratory search strategy was developed in MEDLINE by three of the authors, including a university librarian experienced in the conduct of systematic reviews, using Medical Subjects Headings and text words ( online supplemental file 1 ). The search was adapted for each subsequent database and any additional key terms were added to all other database search strategies before conducting the searches within all included databases: Cochrane Database of Systematic Reviews, MEDLINE, CINAHL, EMBASE, Web of Science, PSYCHINFO, The NHS Economic Evaluation Database and The Health Economic Evaluations Database. In addition, a manual search of the reference lists of relevant articles was conducted. No quality appraisal was performed as the authors sought to describe, not evaluate, the available evidence on the topic.
Supplemental material
Stage 3: source of evidence selection.
Based on the inclusion and exclusion criteria, the authors independently screened titles, abstracts and full-text papers using the systematic review software tool, Covidence. 19 Each stage involved two reviewers who were independent and blinded to the fellow reviewer decision outcomes to reduce potential bias. Any disagreements were resolved through discussion and a third reviewer was not required. To ensure consistent application of the screening criteria, a pilot test of the screening process was undertaken by the two reviewers using a small, random sample (n=25) of the identified articles based on their titles and abstracts. Relevant articles were retrieved from each database separately and imported into the bibliographic manager, and EndNote and the Bramer method were used for deduplication. 20
Stage 4: data extraction
Data extraction was conducted using the Covidence software. The data extraction form ( Table 1 ) was tested on a small sample of studies (n=10) by two reviewers to ensure consistency and was modified to include further criteria to answer the research question and objections. The results of the data extraction were compared and discussed. No discrepancies occurred during this stage and did not require a third reviewer.
- View inline
Data extraction form for included studies
Stage 5: Collating, summarising and reporting the results
Using the information contained in the data extraction form, this step involved a descriptive and numerical summary of the information within the identified publications as they related to the objectives of the review. Full-text publications were referred to if further information was needed from a particular study. The terminology used to describe complex systems was extracted and synthesised using the features and attributes in the Preiser framework. 6 Research purpose(s) were extracted verbatim based on the verbs used in the purpose statement as described in the abstract and/or main body and the authors documented where more than one research purpose was mentioned. The implications were analysed regarding their relevance to practice, policy and research, whereas outcomes pertained to direct impact on the phenomena or tools developed as a result of the research which applied complexity theory.
Stage 6: Patient and public involvement
The hospital patient forum, a platform for dialogue and exchange of information relevant to patients regarding the hospital, participated in the design and interpretation of the results of the scoping review.
A total of 2021 articles were identified. Of these, 676 were duplicates. The titles and abstracts of 1345 articles were screened and 1108 did not meet the inclusion criteria and were therefore excluded. The remaining 237 articles were full-text screened. Full-text screening of the final 237 resulted in the final inclusion of 61 articles. There were 9 systematic reviews identified which were subsequently hand-searched for further relevant articles. The PRISMA flow chart is shown below in Figure 1 .
- Download figure
- Open in new tab
- Download powerpoint
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart.
Descriptive summary
The key characteristics of the included studies are described in online supplemental file 2 .
Year of publication
Figure 2 shows the distribution of the year of publication of the papers considered.
Year of publication.
The most publications were in 2018, 2019 and 2020 (eight publications). The fewest were in 2015 (2) followed by 2021 (3). The trendline is quite flat.
Journal of publication
As shown in Figure 3 , there were 43 different journals in which papers were published across a broad range of journal types. The most common journals for publication were Social Science and Medicine (n=7) and BMC Health Service Research (n=4). All other journals published between 1 and 2 papers.
Journal of publication.
Geographical location of study
Of the 61 publications, 17 studies were set in the USA and 11 in Canada and 8 in the UK. The complete geographical locations for the studies are shown in Figure 4 .
Geographical location of study.
Ethical considerations
Complexity studies present distinct ethical challenges for researchers, as unpredictability means research will be performed and decisions taken based on an imperfect understanding. Therefore, researchers need to be open and honest about the uncertainty and reflect critically on the decision-making processes. 21 In our scoping review, studies only reported standard research ethics committee approval procedures.
Objective 1: definitions and descriptions of complexity theory
36 papers (59%) provided a definition of complexity theory. In 23 (38%), no definition or description was given. 2 papers provided descriptions of complexity and 3 provided a definition of CAS. There was great variability in the definitions used.
Characteristics and features
Many different terms were used to describe complex systems. 10 papers used the term characteristics, 9 used concepts, 8 used the term principles and 20 papers were unclear. No papers cited Preiser’s typology. 6 The terms were mapped against the Preiser framework ( Table 2 ) with synonyms grouped against the most aligned principle.
Terms mapped against the features and attributes in the Preiser framework
The most reported terms were self-organisation (n=23), non-linearity (n=22) and emergence (n=18). The least reported features were radically open (n=3) and contextually determined (n=5).
Objective 2: research purpose and phenomenon of interest
Guided by Thompson and colleagues’ synthesis, the articles were analysed for their purpose and the phenomenon investigated. The majority of studies mentioned two or more research purposes (47.5%) across a variety of health and social care phenomena. These research purposes included assess, build, determine, develop, discuss, draw, elucidate, gain, generate, increase, inform, outline, present and unravel. The most common research phenomena with multiple purposes were working environment/context, implementation and change. Following studies with two or more research purposes, the most common research purposes sought to explore (9.8%) and describe (9.8%) the phenomenon. Research purposes aimed at exploring a wide variety of phenomena featured investigations of the role of physician assistants within a CAS, 22 the impact of workplace huddles in clinical practice, 23 the adoption of leadership at a microlevel through the influential acts of organising, 24 responses to intimate partner violence 25 and the naming or classification of physical assaults within relationship in the context of emergency departments. 26
Studies that sought to describe phenomena related to working environment/context included the processes and development of a dementia network, 27 decision-making processes within an intensive care setting [30] and the context of telenursing as a CAS [20]. Other studies sought to describe the clinical implications of non-linear dynamics within intimate partner violence, 28 physician leadership within healthcare organisations 29 and regional sustainability in healthcare improvement. 30
Thus, studies with two or more research purposes represent the most common application of complexity theory in health and social care research. Our analysis shows that the most common phenomena studied were implementation and working environment/context within health and social care respectively with 16 studies each within the identified articles.
Objective 3: research methodologies and application of complexity theory
28 studies (46%) had a qualitative research design. 17 studies (28%) were case studies and 9 studies (15%) used mixed methods. The most common application of complexity theory (52.5%) was as a theoretical framework to understand a phenomenon and conduct data analysis. A further 10 studies used complexity theory exclusively for the purpose of data analysis, whereas 8 studies primarily applied the theory as a theoretical framework. Where complexity theory was used as a theoretical underpinning, it was used to describe the setting or context they were studying as a CAS, to focus on a particular characteristic of complexity or to formulate research questions.
Complexity theory was frequently adopted in qualitative methods of inquiry. Qualitative methods or mixed-method studies (included a qualitative component) were based on case studies or studies which used grounded theory as an analytical method, content analysis and thematic analysis. These studies focused on particular characteristics of complexity theory to interpret their findings or as the foundation of a coding framework. However, some authors defined the exact characteristics of complexity that they were focusing on in their analysis, 29 31–41 whereas other studies broadly described conducting analysis with the lens of complexity theory 26 42–44 or not clearly stated. 45–47
A number of studies featured interventions or programmes that were founded on or informed by complexity theory. 48–50 Two studies featured an assessment framework or tool. 51 52 Tang and colleagues 53 applied complexity as a theoretical framework and data analysis, as well as to develop a model of policy implementation. In a similar fashion, Sawyer and colleagues 49 applied complexity in the development of a logic framework in the context of obesity prevention. One study used complexity theory to develop a conceptual model to help in the design and conduct of community-based health promotion evaluation. 54
Objective 4: settings, disciplines and professions
Of the 61 publications, 10 studies were hospital-based, 10 were based in a health system and 9 in a primary care setting. 2 studies were based in a rehabilitation setting.
A variety of disciplines and professions were reflected in the literature reviewed. We used the term multidisciplinary team (MDT) to describe a range of health service workers, both professionals and non-professionals described in the studies when more than two types of professionals were stated. Where patients were specifically mentioned as part of the MDT, we included that as a separate category, and also where non-traditional MDT members were specifically mentioned.
Of the 61 studies, 22 (34%) involved MDTs. Six (9%) involved nurses and 4 (6%) MDTs including patients. In 2 papers, there were no participants as the study involved documentary analysis and in 2, the participants were not specified.
Objective 5: Implications and outcomes of applying complexity theory
The most frequent implication was exclusively practice-related (44%). A full breakdown of imications and utcomes is provided in online supplemental file 2 . A significant proportion of studies had multiple implications. 21% of the studies contained implications for both practice and research, while 11.5% had implications in all three dimensions. Implications encompassed changes in clinical practice delivery such as huddles, 23 recommendations for motivational interviewing 45 and social work practice guidelines for dealing with families with complex needs. 55 From a policy perspective, recommendations included complexity-informed processes for the implementation of local drugs policy 35 and complexity-compatible policies regarding integrated healthcare. 37 Implications for future research were typically in relation to the phenomenon being investigated and reflection on their own methodological limitations, for example, Gear and colleagues 25 note the need for more diversity in the samples regarding intimate partner violence in a primary care setting while another study promoted the use of social network analysis and ethnographic approaches to explore the shifts in interactions following the implementation of a simulation tool within a healthcare CAS. 34 One study was unclear in their implications, while one study did not explicitly state any implications in the discussion of their findings.
Some studies contained pragmatic outcomes as a result of applying complexity theory. Reed and colleagues 43 developed 12 ‘Simple Rules’ intended to provide actionable guidance to support evidence translation and improvement in complex systems. Hodiamont et al 39 created a conceptual framework that can be used as a basis for the development of a classification of complexity in palliative care, with an understanding of the variance in patients according to their care needs. One study developed seven action recommendations to promote community resilience and population health. 56 Albers Mohrman et al 30 provided organising principles to facilitate change within a CAS, while Sawyer et al 49 developed a logic framework intended to inform sustainable systems change from a whole-systems approach. To identify the extent to which the identified publications were used in subsequent research, we assessed the number of citations of the 61 papers included in our review. As of 1 October 2022, the most cited papers were O’Sullivan et al (41) (219), Ssengooba et al (68) (171) and Tsasis et al (34) (151). Review objectives 6 and 7 will be addressed in the Discussion section.
To the best of the authors’ knowledge, this is the first scoping review to synthesise the literature on the application of complexity theory in health and social care research. Although earlier reviews examining complexity in healthcare literature are available, 7 8 the current review has identified that in the time since their publication, subsequent research has remained largely theoretical, with little progress in terms of the practical application of complexity theory. In addition, although research has occurred within what is described as health systems, none of the final papers had a social care context. Adult social care refers to services that provide support to people with physical disabilities, learning disabilities or physical and mental illnesses. Over a third of publications failed to provide a clear definition of complexity or provide the theoretical context for the research. What was meant by a complex system was ambiguous, heterogeneous and often ill-defined. The limited description, features and attributes used in many papers suggest a lack of appreciation for the principles of a complex system which the current authors believe is a basic requirement before appropriate methods and approaches can be selected for studying phenomena in a complex system. However, we acknowledge that as there is no unifying theory or agreed-upon definition of complexity, 57 58 it is unclear how many features and attributes of a complex system need to be considered when contemplating appropriate approaches, which may explain the lack of detail in the identified studies. Many studies referred to primary studies or discussion papers in the definition or description of complexity theory without citing the founding key theorists. This may be due to the complexities within the theory itself and later authors in the area present accessible literature to help researchers understand its underlying logic. Nonetheless, we would argue that an explicit explanation regarding the researchers’ understanding of and approach to complexity is vital to orientate the reader and highlight whether meaningful engagement with the phenomenon of interest has occurred.
Regarding methodologies employed, our findings indicate that since the Thompson and Rusoja reviews, empirical research has remained primarily qualitative and case study orientated, with most publications in the USA and Canada. Most studies applied complexity as both a theoretical framework and for data analysis. Several studies used complexity theory within qualitative research to analyse and code their data. The review also identified several case studies in which authors sought to understand a setting or service using a complexity-informed lens. This may be because the case study approach seeks to capture the richness of a phenomenon rather than simple cause and effect. To perform research into complex systems in which power law distributions are in operation, there is a need to interpret the processes of dynamicity and that requires qualitative and longitudinal studies. 59 There is also value in an abductive logic of inquiry, which allows for the weaving and entanglement of previous evidence into the greater understanding of the whole complex adaptive system. 60
Health and social care systems deal with many interconnected and entangled issues that require researchers in the field to take a participatory, inclusive, integrated and multidisciplinary approach to research and that requires theoretical and methodological pluralism. Researchers should embrace a rich tapestry of approaches to develop a deep understanding of the complex health and care systems in which we work and go forth with epistemic humility. In the application of complexity theory, there is great variance regarding the detail of how it is used. Some authors explicitly state the characteristics they focus on during data analysis, whereas other studies broadly stated they used the lens of complexity, and some did not clearly state what characteristics they used.
Complexity in health and social care empirical research remains predominantly hospital or health system focused and does not encompass the full continuum of care at this point. However, it does tend to be applied in contexts where multidisciplinary teams are involved, which has implications for managing the complexity of the context.
As nearly half of the studies contained implications for practice, it can be inferred that complexity theory has been empirically applied with the intention of improving health or social care practice. Limited evidence was found within the studies regarding how the knowledge from empirical findings was used to inform or improve the setting or phenomena being studied. However, a number of studies produced pragmatic tools or guides that were informed by complexity theory and for future engagement using a complexity lens. The heterogeneity of empirical studies is perhaps not unsurprising as it is still early days in the application of complexity theory to health and social care. Given Ashby’s law of requisite variety as operationalised in the Ashby space as described by Boisot and McKelvey, 59 this makes it hard to initially establish any consistency in the domain. We therefore propose guidance that could provide more comparability in evidence-based studies going forward.
Guidance for reporting complexity in health and social care research
As there is currently no definitive procedure for reporting such studies, we propose the following items for inclusion. These are not intended to be a rigid checklist but rather flexible guidance to be interpreted and adapted to support the reporting of theoretically and methodologically divergent research.
Provide a clear definition of complexity with an explanation of the theoretical underpinnings of your research so the reader can understand your ontological and epistemological stance. 61 62
Explain why complexity theory is relevant to the phenomenon being studied.
Identify the principles and characteristics of complexity theory that were explored.
Explicitly state how complexity is applied regarding the various stages of the research process, that is, theoretical underpinning, data collection and data analysis.
Describe the outcome or impact of the study in terms of direct change in health and social care setting, practice, policy or research.
Discuss ethical components of applying complexity theory and reflexivity to the specific phenomenon.
Include a statement on what the research is to inform or improve from the outset.
Limitations
The authors adapted their inclusion criteria to include articles from the past 10 years (2012–2021) due to project and time resources. Inclusion of previous years may have facilitated a fuller historical understanding. Health and social care educational settings were excluded and probably merit its own review in the future. Additionally, the search string and screening criteria focused on health and social care professionals and managers as the population in the study. Further evidence synthesis could be conducted in the future regarding patients and how complexity theory has been used to understand their experience. Additionally, future evidence synthesis could include publications that feature studies that include secondary analysis, as it was not the scope of the current study but may yield further insights into the application of complexity theory.
Complexity theory has been increasingly adopted to conduct research in the areas of health and social care. Despite ample application in the context, huge divergence exists in the evidence base regarding how it can be applied and what constitutes its application. For the field to progress and establish transparency in empirical findings, the output of this current review are principles that should be considered and applied, where necessary, in the conduct of research methodologies which involve the various versions of complexity theory. This scoping review builds on the growing field of ‘translational systems research’ 63 that seeks to translate the theoretical concepts of CAS science into practical applications. Although the guidance offered in the current review is based on the synthesis of studies in health and social care, the principles may be applied to other fields, such as business, technology or educational phenomenon. The principles resulting from this scoping review are intended to support the rigorous application of complexity theory in empirical research and contribute to future transparent evidence going forward. The authors believe that the findings and guidance detailed in this review will be of benefit to health and social care professionals, managers and researchers in their commitment to developing services for the people they intend to care for.
- Boulton JG ,
- Lichtenstein BM
- Prigogine I
- Preiser R ,
- De Vos A , et al
- Thompson DS ,
- Kustra E , et al
- Sievers J , et al
- Van de Ven AH
- Macintyre S , et al
- Peters MDJ ,
- Stern C , et al
- Tricco AC ,
- Zarin W , et al
- Carroll A ,
- Colquhoun H ,
- Godfrey C ,
- McInerney P , et al
- Tricco AC , et al
- Brainard J ,
- Churruca K ,
- Ellis LA , et al
- Kellermeyer L ,
- Bramer WM ,
- Giustini D ,
- de Jonge GB , et al
- Woermann M ,
- Burrows KE ,
- Abelson J ,
- Miller PA , et al
- Provost SM ,
- Lanham HJ ,
- Leykum LK , et al
- Ker J , et al
- Koziol-Mclain J
- Boustani MA ,
- Munger S , et al
- Ferrer RL , et al
- Albers Mohrman S ,
- (Rami) Shani AB
- Caffrey L ,
- Mertens F ,
- Helewaut F , et al
- Leykum LK ,
- McPherson E , et al
- Escrig-Pinol A ,
- Corazzini KN ,
- Blodgett MB , et al
- Grudniewicz A ,
- Tenbensel T ,
- Evans JM , et al
- Livingstone C
- Hodiamont F ,
- Leidl R , et al
- Trenholm S ,
- Fitzgerald K ,
- Price D , et al
- Doyle C , et al
- van Roode T ,
- Marcellus L
- Lawn S , et al
- Lévesque MC ,
- Jacquemin G , et al
- Sanford S ,
- Sider D , et al
- Colón-Emeric CS ,
- Corazzini K ,
- McConnell ES , et al
- den Hertog K ,
- Verhoeff AP , et al
- Kottke TE ,
- Huebsch JA ,
- Mcginnis P , et al
- Ferreira DMC ,
- Andersson Gäre B ,
- Greenhalgh T , et al
- O’Sullivan TL ,
- Kuziemsky CE ,
- Toal-Sullivan D , et al
- de Vos A , et al
- Shani AB (Rami ),
- Coghlan D ,
- Alexander BN
- O’Cathain A ,
- Duncan E , et al
- Rousseau N , et al
- Buckle Henning P ,
- Ciemins EL ,
- Kersten D , et al
- Björkman A ,
- Salzmann-Erikson M
- Stevenson J
- McDonald J , et al
- Amo-Adjei J ,
- Doku D , et al
- Augustinsson S ,
- Petersson P
- Barasa EW ,
- Molyneux S ,
- English M , et al
- Lindberg C ,
- Schneider M
- Bishai DM , et al
- McKechnie AC ,
- Johnson KA ,
- Baker MJ , et al
- de Bock BA ,
- Willems DL ,
- Weinstein HC
- Langer A , et al
- Ghazzawi A ,
- Kuziemsky C ,
- O’Sullivan T
- González MG ,
- Dozier AM , et al
- Filipovic J
- Ssengooba F ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
Twitter @AinemCarroll, @adarleyresearch
Contributors AC was responsible for study conceptualisation, study design, data collection, data analysis/synthesis and writing manuscript. AD was responsible for study design, data collection, data analysis/synthesis and writing manuscript. DS was responsible for study design and data collection. CC and JM were responsible for study conceptualisation and reviewing manuscript. AC is responsible for the overall content as guarantor. The guarantor accepts full responsibility for the finished work and/or the conduct of the study, had access to the data and controlled the decision to publish.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests None declared.
Patient and public involvement Patients and/or the public were involved in the design, conduct, reporting or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:

- Request new password
- Create a new account
Making Sense of Research in Nursing, Health and Social Care
Student resources, 6. approaches to and design of research in health and social care.
Reflective Exercise
Looking at the papers below, consider
- What is the research approach or design used?
- Does the design enable the researchers to answer the research hypothesis/aims/questions?
SUGGESTED SAGE ONLINE JOURNALS FOR USE
Qualitative design
Bartlett, R. (2012). Modifying the diary interview method to research the lives of people with dementia. Qualitative Health Research , 22 (12), 1717–26. Available at: http://journals.sagepub.com/doi/pdf/10.1177/1049732312462240
Quantitative design
Bainbridge, D. and Seow, H. (2017). Palliative care experience in the last 3 months of life: a quantitative comparison of care provided in residential, hospice, hospitals and the home form the perspectives of bereaved care givers. American Journal of Hospice and Palliative Medicine , 1–8. Available at: http://journals.sagepub.com/doi/pdf/10.1177/1049909117713497
ADDITIONAL MATERIALS
Further suggested resources to look at.
Journal of Mixed Methods Research : http://journals.sagepub.com/home/mmr

- Member Organisations
- Research, Implementation and Impact
- Social Care and Social Work
- Social Care - Kent, Surrey & Sussex Region
- Starting Well: Children's Mental Health
- Primary and Community Health Services
- Living Well with Dementia
- Co-production
- Public Health
- Digital Innovation
- Economics of Health and Social Care
- Implementation
- Public and Community Involvement
- What is PCIE?
- Getting Involved
- Support for researchers
- Introduction
- An overview of ARC KSS
- Who can help you with PCIE?
- Terminology and PCIE
- Why and When to do PCIE
- Why involve members of the public in research?
- Why do members of the public want to get involved in research?
- When to get members of the public involved?
- How to do PCIE
- Communication and Accessibility
- Planning for involvement and engagement
- How to recruit members of the public
- Equality, Diversity and Inclusion (EDI)
- Approaches – different options for undertaking PCIE
- Facilitating meetings and Group dynamics
- Impact and Evaluation
- Examples/Case Studies
- Appendix/Useful tools
- Learning and Development

- Learning and Development Finder
- Researchers Journeys

- Research Week
- Previous Research Weeks

- Resource Library
Your Health and Social Care Research Quick Guide
This guide is designed for those in practice to navigate the world of research.

In this section
Produced by Dr Diana Ramsey , ARC KSS Darzi Fellow (2021-2022) with insights and support from people working to deliver research in the Health and Social Care region, the Your Health and Social Care Research Quick Guide is a resource to help those working in health or social care to start or develop their research journey.
Packed with information, links and personal stories from people working across Kent, Surrey and Sussex, this guide has been designed to answer any questions you might have in regards to getting involved in research, building networks, research training and resources.
Whatever your research experience, this guide is for you.
View guide here

Subscribe to our newsletter
Sign up here
You can unsubscribe at any time by clicking the link in the footer of our emails. For information about our privacy practices, please visit this page . We use e-shot as our marketing platform. Learn more about e-shot's privacy practices here .
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Starting the research process
- 10 Research Question Examples to Guide Your Research Project
10 Research Question Examples to Guide your Research Project
Published on October 30, 2022 by Shona McCombes . Revised on October 19, 2023.
The research question is one of the most important parts of your research paper , thesis or dissertation . It’s important to spend some time assessing and refining your question before you get started.
The exact form of your question will depend on a few things, such as the length of your project, the type of research you’re conducting, the topic , and the research problem . However, all research questions should be focused, specific, and relevant to a timely social or scholarly issue.
Once you’ve read our guide on how to write a research question , you can use these examples to craft your own.
Note that the design of your research question can depend on what method you are pursuing. Here are a few options for qualitative, quantitative, and statistical research questions.
Other interesting articles
If you want to know more about the research process , methodology , research bias , or statistics , make sure to check out some of our other articles with explanations and examples.
Methodology
- Sampling methods
- Simple random sampling
- Stratified sampling
- Cluster sampling
- Likert scales
- Reproducibility
Statistics
- Null hypothesis
- Statistical power
- Probability distribution
- Effect size
- Poisson distribution
Research bias
- Optimism bias
- Cognitive bias
- Implicit bias
- Hawthorne effect
- Anchoring bias
- Explicit bias
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, October 19). 10 Research Question Examples to Guide your Research Project. Scribbr. Retrieved April 15, 2024, from https://www.scribbr.com/research-process/research-question-examples/
Is this article helpful?
Shona McCombes
Other students also liked, writing strong research questions | criteria & examples, how to choose a dissertation topic | 8 steps to follow, evaluating sources | methods & examples, unlimited academic ai-proofreading.
✔ Document error-free in 5minutes ✔ Unlimited document corrections ✔ Specialized in correcting academic texts
- Frontiers in Psychiatry
- Public Mental Health
- Research Topics
Burnout in the Health, Social Care and Beyond: Integrating Individuals and Systems
Total Downloads
Total Views and Downloads
About this Research Topic
Occupational burnout is a complex combination of emotional, cognitive, and behavioural factors that represents a mismatch between personal and professional responsibilities that results from a prolonged exposure to occupational stressors. Burnout contributes to poor mental wellbeing, which can lead ...
Keywords : Burnout, Healthcare, Societal Cost, Organizational Burnout
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
Internet Explorer is no longer supported by Microsoft. To browse the NIHR site please use a modern, secure browser like Google Chrome, Mozilla Firefox, or Microsoft Edge.

Suggest a research topic

This video is not supported by your browser.
Video transcript
Providing the most effective health and social care is a huge challenge. There are so many products and procedures in use, with more being developed all the time, but often there is little good evidence about what works and what doesn’t.
We commission and fund projects looking at the usefulness of new and existing tests, treatments and devices and at new and existing ways of doing things. We also look at how to improve public health to see what really works in practice.
To make good decisions about what research to fund we need a complete and balanced picture about which questions most urgently need answering. We ask patients, carers, clinicians, health care workers, service managers and researchers. Whoever you are, we need your voice too. Use the form below, with help from the examples, to make your research suggestions.
Your idea will be seen by our research funding programmes and, if suitable, taken to one of our decision-making committees that prioritises research for funding .
We receive a large number of valuable research suggestions each year. Not all of these can be funded. However, our research funding programmes work closely with patients, members of the public, users of social care services and carers as well as health and social care experts, to ensure our research will answer the most pressing questions. To find out if your question has reached a committee please contact [email protected]
Example: Birthplace
What should we test .
Where’s the best or safest place to have a baby?
Who is it for?
Pregnant women.
Help us understand what difference the evidence could make to patients and the public, the NHS or social care.
Although women are offered a choice where to have their baby; in hospital, in a birthing centre or at home, it doesn’t seem clear which is the best or safest. It is important to find this out because it would help women and healthcare professionals make an informed choice. It could also help to reduce the costs.
Example: Peanut allergy
What should we test.
Does oral immunotherapy help children with peanut allergy?
Children with peanut allergy.
Peanut allergy is very common in the UK and can be life threatening. Patients live in fear of accidentally eating peanuts, are restricted on their food choices and must carry epipens at all times. Due to lack of treatment, the only option is to avoid peanuts and many have accidental reactions. A treatment would be life changing for these patients.
Example: Street lighting, accidents and crime
Does reduced street lighting lead to more accidents and crime?
The general public.
Local Authorities are reducing levels of street lighting by using dimmer lights or turning lights off at a set time, often midnight. Some members of the public & media think that this could lead to increases in crime or road casualties. Research is needed to see if this is actually happening and to find out if there are other effects on public health and wellbeing.
Example: Chondroitin supplements
Does Chondroitin work for osteoarthritis in the hand?
Patients who have painful osteoarthritis in their hands.
A friend of mine takes chondroitin for osteoarthritis in her hands and says it helps with the pain and swelling. I have asked my doctor if I can get it on prescription, but she said that it isn’t a prescription drug. I have looked it up on the internet and there are some sites that says it works for some people. It is easy to get hold of online as a remedy for arthritis. Arthritis is a painful disease which affects a lot of people, and if it’s in your hands it really affects what you are able to do. I think we should test chondroitin properly to see if it helps in hand osteoarthritis and if it does, it should be made available on prescription.
The NIHR funds a wide range of research – see if the area you are interested in has been funded
A question which can be researched needs to be specific – tell us what existing product or procedure needs to be evaluated.
Is there a particular group for this test? Eg: Pregnant women, children with allergies, older men, the general public?
Is it about quality of life and/or length of life? Will it save time and/or money?
Providing contact information is optional, but enables our staff to clarify details of your research suggestion, should they need to.
If you selected 'Other' in the box above, please can you tell us a little more
Use of your personal information
By completing this form you are agreeing to your details being added to our databases.
Your personal information is held and used in compliance with the General Data Protection Regulation 2016 (GDPR) and the Data Protection Act (2018). The Department of Health and Social Care, NIHR is the Data Controller under GDPR. Under GDPR, we have a legal duty to protect any information we collect from you.
You should be aware that information given to us might be shared with other DHSC NIHR bodies for the purposes of statistical analysis and other DHSC NIHR management purposes. We also reserve the right to share details of research applications with other approved research funding organisations outside the NIHR in order to coordinate research activity in the UK. Information collected from you will not be passed to any third party outside the NIHR without your consent, except specifically as detailed above, or where we are under a statutory obligation or entitled to do so by law.
Applicants may be assured that DHSC NIHR is committed to protecting privacy and to processing all personal information in a manner that meets the requirements of GDPR.
View the NIHR Privacy Policy (opens in a new window)
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 06 April 2024
Healthcare on the brink: navigating the challenges of an aging society in the United States
- Charles H. Jones ORCID: orcid.org/0009-0004-0368-6463 1 &
- Mikael Dolsten 1
npj Aging volume 10 , Article number: 22 ( 2024 ) Cite this article
918 Accesses
4 Altmetric
Metrics details
- Epidemiology
- Health services
- Public health
The US healthcare system is at a crossroads. With an aging population requiring more care and a strained system facing workforce shortages, capacity issues, and fragmentation, innovative solutions and policy reforms are needed. This paper aims to spark dialogue and collaboration among healthcare stakeholders and inspire action to meet the needs of the aging population. Through a comprehensive analysis of the impact of an aging society, this work highlights the urgency of addressing this issue and the importance of restructuring the healthcare system to be more efficient, equitable, and responsive.
Similar content being viewed by others
The impact of healthcare reform on the dynamic changes in health service utilization and equity: a 10-year follow-up study
Wenqin Guo, Gangjun Liu, … Hui Qiao

Clustering of health, crime and social-welfare inequality in 4 million citizens from two nations
Leah S. Richmond-Rakerd, Stephanie D’Souza, … Terrie E. Moffitt

Harnessing big data for health equity through a comprehensive public database and data collection framework
Cameron Sabet, Alessandro Hammond, … Fatima Cody Stanford
Introduction
The United States is undergoing a demographic and health transformation that will have profound implications for its healthcare system and society. The population is aging at an unprecedented rate, with the baby boomer generation, defined as those born between 1946 and 1964, reaching retirement age and living longer than ever before. According to the U.S. Census Bureau, by 2030, all baby boomers will be older than 65, leading to about one in every five residents being retirement age 1 . This shift poses a dual challenge for the healthcare system: how to meet the increasing and complex healthcare needs of the elderly, and how to ensure that the system is prepared and equipped to provide quality and equitable care for this growing segment of the population.
The implications of this demographic shift are far-reaching. The healthcare system, as currently structured, is underprepared for the onslaught of demands this aging population will impose 2 . The system is also fragmented, inefficient, and costly, with gaps in coordination, quality, and access. Moreover, the system does not adequately address the social determinants of health, such as income, education, housing, transportation, and social support, that impact the health outcomes and health behaviors of the older adults 3 , 4 , 5 . Nor does it sufficiently engage the older adults and their caregivers in the planning and delivery of care or leverage the potential of community-based and home-based care models, which can improve the access, quality, and affordability of care for the elderly 6 .
However, the challenge does not end there. There is a growing shortage of healthcare providers, which means that the supply and availability of qualified and skilled healthcare professionals, such as physicians, nurses, pharmacists, clinical social workers and technicians, is insufficient and inadequate to meet the demand and need of the population. This phenomenon is even more pronounced in low- and middle-income countries, as well as in the rural and remote areas within the U.S. According to the World Health Organization (WHO), the global health workforce was 43.5 million in 2018, and is projected to grow to 53.9 million by 2030, but still falls short of the estimated demand of 80 million by 2030, resulting in a global shortfall of 18 million health workers, mostly in low- and middle-income countries 7 . In the U.S., a study by the Association of American Medical Colleges (AAMC) predicts a shortage of up to 139,000 physicians by 2033 8 . The shortage of healthcare providers has significant implications for the health sector, as it affects the access, quality, and cost of healthcare, as well as the health outcomes and satisfaction of the population.
As such, the U.S. is facing a healthcare paradox 9 . On one side, there is an aging population with increasing healthcare needs, and on the other, there is a strained healthcare system grappling with workforce shortages, capacity challenges, and fragmentation. Addressing this paradox requires innovative solutions, policy reforms, and a commitment to restructuring the healthcare system to be more efficient, equitable, and responsive to the needs of its aging citizens.
Although many of these issues may be front-of-mind for geriatrics specialists, many other stakeholders in the eldercare system likely do not understand the full scale of challenges brought on by a rapidly aging populace or may underestimate their preparedness for the resulting changes. This was seen in a recent survey of stakeholders in adult vaccine market, which represents a sector critical in the eldercare industry 10 . When presented with the projected rise of adult vaccines, a trend driven largely by the needs of the aging population, stakeholders across the market were unaware of the associated complexities and anticipated minimal challenges in adopting expanded vaccine schedules 10 . While vaccines represent only a portion of the eldercare market, it is reasonable to believe that this lack of a holistic understanding applies to all sectors in the eldercare industry.
This paper aims to stimulate dialogue and collaboration among the healthcare stakeholders, and to inspire action and innovation to address the needs and aspirations of the aging population. To accomplish this, this work will provide a comprehensive and critical analysis of the impact and implications of an aging society to highlight the importance and urgency of this issue.
Rising tide of healthcare needs: increasing demand and complexity of care
The U.S. population is aging rapidly because of two interrelated factors: the aging of the baby boomer generation, and the increase in life expectancy. The baby boomer generation constitutes the largest cohort in the U.S. history, with about 73 million members 11 . As this cohort reaches retirement age, the share of the population that is 65 and older will increase significantly, from 17% in 2022 to 21% in 2030, and to 23% in 2050 (Fig. 1A ) 12 . By 2050, the number of Americans aged 65 and older will increase by 40%, from 58 million in 2022 to 82 million in 2050.
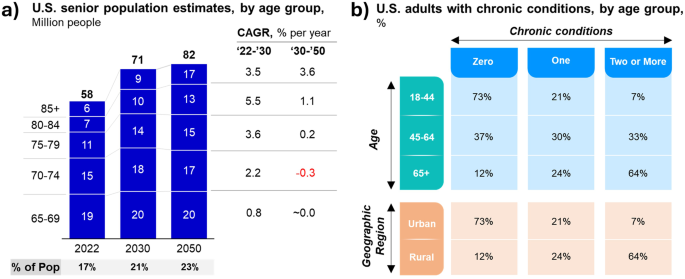
This figure illustrates the expected growth of the senior population and the associated increase in chronic disease burden. Raw data sourced from “2023 National Population Projections Tables: Main Series”, which utilizes official estimates of resident population on July 1, 2022 as the base for projecting the U.S. population from 2023 to 2100 (panel a ) and Boersma, et al., “Prevalence of Multiple Chronic Conditions Among U.S. Adults, 2018” (panel b ).
The aging population, particularly those over 85 years old, presents new challenges for the medical system. This will be the fastest growing segment, tripling in size from 6.5 million in 2022 to 17.3 million in 2050, a number comparable to the current population of New York state 13 . These elderly adults often suffer from multiple and complex health conditions, including age-related diseases that affect their heart, brain, and immune system. However, the medical system lacks the experience and expertise to effectively treat these diseases and provide specialized, personalized care for this vulnerable group. The increase in the share and size of the older population will have implications for the demand and supply of healthcare and social services, as well as for the economic and fiscal stability of the nation.
One of the main drivers of the increased healthcare demand and utilization among the elderly is the high prevalence of multiple chronic conditions (MCCs), which are defined as having two or more chronic diseases that last at least a year and require ongoing medical attention or limit activities of daily living 14 , 15 . According to the Centers for Disease Control and Prevention (CDC), 88% of older adults have at least one MCC, and 60% have at least two (Fig. 1B ). These include common conditions such as hypertension, arthritis, heart disease, cancer, diabetes, and chronic kidney disease. MCCs are associated with increased mortality, disability, functional decline, and reduced quality of life. Moreover, they pose significant challenges to healthcare provision and management, as they require complex and coordinated care across multiple settings and providers. A study by Machlin et al. (2019) found that among Medicare beneficiaries aged 65 and older, those with MCCs accounted for 94% of total healthcare expenditures in 2010, compared to 6% for those without MCCs 16 . The average annual expenditure per person was $21,342 for those with four or more MCCs, $13,272 for those with three MCCs, $9176 for those with two MCCs, and $5865 for those with one MCC. These figures contrast sharply with the $2025 spent for those without any MCC.
The high prevalence of MCCs among the elderly is expected to persist or even increase in the future, as it is closely linked to the increase in life expectancy. As people live longer, they are more likely to develop and accumulate chronic diseases over time, especially if they have risk factors such as age-related physiological changes, environmental exposures, lifestyle behaviors, genetic predispositions, and social determinants of health. For example, a study by Crimmins and Beltrán-Sánchez 17 found that the increase in life expectancy in the U.S. between 1998 and 2008 was accompanied by an increase in the number of years spent with MCCs, especially among the elderly 17 . The study estimated that the average number of years spent with MCCs increased from 7.2 to 8.6 for men aged 65 and older, and from 10.0 to 11.3 for women aged 65 and older. Therefore, the aging population will face a higher burden of chronic diseases and a lower quality of life in the coming decades. Making matters worse, the health and longevity of the next wave of aging people may also be affected by new external triggers, such as obesity, processed food intake, microbiome changes, climate change, pandemics, and pollution, which can have diverse and unpredictable impacts on different individuals. These triggers can also change the health behaviors and healthcare access of the elderly.
Another challenge that arises from the medication requirements of the aging population is polypharmacy, which is defined as the concurrent use of five or more medications 18 . Individuals aged 65 and over account for over a third of all prescribed medications in the U.S. 19 . However, polypharmacy can have negative consequences, such as increased risk of drug interactions, adverse drug events, medication non-adherence, and medication errors. These can lead to poor outcomes, such as reduced effectiveness, increased morbidity and mortality, and decreased quality of life. Therefore, polypharmacy necessitates careful medication management and monitoring, as well as regular medication reviews and deprescribing when appropriate. A study by Qato et al. 20 found that among U.S. adults aged 65 and older, the prevalence of polypharmacy increased from 31.4% in 1999-2000 to 35.8% in 2011-2012, and the prevalence of potentially inappropriate medication use increased from 8.7% to 10.0% 20 . The study also found that polypharmacy was associated with higher rates of emergency department visits and hospitalizations 20 .
The economic implications of the aging population for the healthcare sector are profound, as they affect not only the healthcare spending and resource utilization, but also the healthcare workforce, the healthcare quality, and the healthcare innovation. According to the Congressional Budget Office, the federal spending on major health programs for the elderly, such as Medicare and Medicaid, will increase from 6.6% of gross domestic product (GDP) in 2020 to 9.2% of GDP in 2050 21 . This projected growth is presumably driven by the older age segments differing healthcare utilization patterns and the increasing complexity of care. Specifically, it is estimated that adults aged 65+ visits doctors 20% more frequently than younger adults and experience a threefold increase in hospitalization rates 22 . This increased utilization and complexity of care drives increased spending as reported in a 2019 Kaiser Family Foundation study that found Medicare spending for beneficiaries aged 65 to 74 averages $7566, which nearly doubles to $16,145 for those aged 85 and older 23 .
The rising tide of healthcare needs due to an aging population is multifaceted, encompassing increased service utilization, higher prevalence of chronic diseases, escalated healthcare spending, and complex medication management. This scenario places unprecedented demands on the healthcare system, calling for innovative approaches in care delivery, financial planning, and resource allocation. Adapting to these changes requires a concerted effort from healthcare providers, policymakers, and stakeholders to ensure that the system is not only responsive but also sustainable in meeting the evolving needs of an aging society. Therefore, it is imperative to recognize and discuss the impact this evolution will have on the demand for healthcare professionals, such as physicians, nurses, pharmacists, and specialists in geriatrics, who will be the critical in providing adequate and appropriate care for the elderly with complex medical needs.
The overburdened healthcare landscape: healthcare delivery challenges
The demand for healthcare workers is expected to outpace the supply, resulting in a projected deficit of 1.2 million registered nurses and 121,900 physicians by 2030 8 , 21 . The healthcare workforce shortage is driven by several factors, such as the aging of the workforce itself, the insufficient supply of new entrants, the uneven distribution across regions and specialties, and the increased workload and stress of the workers. These factors are summarized in Table 1 , along with their implications and notable statistics.
The shortage of healthcare providers will have a ripple effect on the entire healthcare system, affecting the quality, accessibility, and affordability of care. Physician shortages lead to increased mortality, reduced preventive care, and higher healthcare spending 24 . Moreover, the shortage of physicians creates a competitive environment for talent, where healthcare providers vie for the limited pool of available professionals. This competition may result in sector consolidation, where larger and more affluent providers acquire or merge with smaller and less profitable ones, creating economies of scale and scope. However, this consolidation may also have negative consequences, such as reduced competition, increased market power, and higher prices 25 .
Appropriate staffing and labor supply are necessary for delivering care, but they are not sufficient without adequate resources and infrastructure. However, the current system is not well prepared to handle the increase in volume and complexity of care, resulting in overcrowding, wait times, delays, cancellations, and rationing of care. Some of the factors that contribute to this resource gap include:
The state and performance of care delivery. The U.S. healthcare infrastructure is in bad shape and needs more investment and improvement, as a 2017 report by the American Society of Civil Engineers gave it a D+ grade 26 . The system wastes about $750 billion, or 30% of its spending, every year on unnecessary or excessive costs, fraud, and other inefficiencies 27 . It also has high variation in the quality and results of care across different providers, places, and regions, which can lead to too much, too little, or improper use of services 28 . For instance, a report by the Dartmouth Atlas Project showed that Medicare spending per beneficiary ranged by more than three times across regions, and that more spending did not mean better quality or satisfaction 29 .
The lack and imbalance of beds. The U.S. has seen a decline in the number of hospital beds per person from 4.5 in 1980 to 2.4 in 2018, reflecting the move from inpatient to outpatient care and the attempts to save costs and enhance efficiency. However, this trend also implies that there is less excess capacity to cope with fluctuations in demand, such as during pandemics, disasters, or seasonal variations. Furthermore, the allocation of beds across states and regions is unequal, creating differences in access and quality of care for various populations 30 . For example, the states with the lowest number of beds per person are Nevada (1.8), Oregon (1.8), and Washington (1.9), while the states with the highest number of beds per person are South Dakota (4.1), North Dakota (4.0), and West Virginia (3.8) 31 .
The inadequacy and inefficiency of technology. The U.S. healthcare system is lagging behind in the adoption and use of information and communication technology (ICT), such as electronic health records (EHRs), telemedicine, and health information exchange (HIE), which can improve the quality, safety, and coordination of care, as well as reduce the costs and errors of care 32 . According to a 2023 report by the Organisation for Economic Co-operation and Development (OECD), the U.S. only hit the threshold of EHR use in 90% of physician offices, medical specialist offices, hospitals, and emergency rooms in 2021 33 . Although the U.S. joins 17-21 other countries that, depending on the setting, have achieved this milestone, it is one of the four countries that did not report having a mandated system in place 33 . As a result, access to records is inconsistent and may require use of multiple portals to view all of a patient’s medical data, impeding benefits that may be observed through shared medial data across practices 33 . For example, analysis of EHRs have supported efforts to predict risk of conditions such as gestational diabetes 34 and postpartum depression 35 as well as to evaluate medical trends during the COVID-19 pandemic 36 , 37 , 38 . The large volume of data used in such efforts has generated interest for the application of machine-learning, particularly deep learning, to parse through complex and multivariate relationships identifiable within patient records 39 , 40 , 41 . Despite the potential, there are various concerns that arise with the digitization and availability of such records, such as breaches through cyber-attacks 42 . Finding avenues to address such concerns regarding patient privacy will be an important step towards realizing the benefits from advances in EHRs and their analysis to identify health trends.
The resource gap in the U.S. healthcare system will have serious consequences for the health and well-being of the population, especially the elderly, who are more vulnerable and dependent on the availability and quality of care. A study by the Commonwealth Fund found that the U.S. ranked last among 11 high-income countries in the health outcomes and experiences of older adults, with the highest rates of mortality, disability, hospitalizations, and unmet needs 43 . Moreover, the resource gap will have implications for the innovation and competitiveness of the U.S. healthcare sector, as it will limit the ability and opportunity to develop and implement new and better ways of delivering and improving care, such as digital health, precision medicine, and artificial intelligence (AI) 44 .
The U.S. healthcare system is facing a supply crisis, as it is unable to meet the rising and complex needs of the aging population. The system is suffering from a shortage of labor and a constraint of resources, resulting in a capacity gap that affects the efficiency, equity, and quality of care. Addressing this crisis requires a strategic and comprehensive approach that involves increasing the quantity and quality of the healthcare workforce, enhancing the availability and accessibility of the healthcare resources, and improving the performance and productivity of the healthcare delivery. Achieving these goals requires collaboration and coordination among the healthcare providers, policymakers, and stakeholders, as well as a commitment and investment in the healthcare sector.
The fragmentation and disparity in healthcare provision: access challenges and the “rich-poor divide”
The U.S. healthcare system is facing a challenge not only in meeting the demand and supply of healthcare, but also in ensuring that the healthcare is accessible and affordable for all segments of the population, especially the elderly, who often face barriers and difficulties in obtaining and utilizing the care they need. The system is characterized by fragmentation and disparity, meaning that the healthcare provision is divided and disconnected across different providers, payers, and settings, and that the healthcare outcomes and experiences vary widely across different groups, regions, and conditions. These features of the system create inefficiencies, inequities, and inconsistencies in the access and quality of care, which can have negative impacts on the health and well-being of the population.
The fragmentation of the U.S. healthcare system stems from the lack of a universal and integrated system of healthcare coverage and delivery, which leads to gaps and overlaps in the coordination, continuity, and comprehensiveness of care 45 . The system is composed of multiple and competing payers, such as private insurers, public programs, and self-pay individuals, each with their own eligibility criteria, benefit packages, payment mechanisms, and administrative rules. This creates a complex and confusing landscape for the consumers and the providers, who have to navigate through different and often conflicting policies, procedures, and requirements. Moreover, the system is composed of multiple and independent providers, such as hospitals, clinics, physicians, nurses, pharmacists, and others, each with their own practice patterns, quality standards, and information systems. This creates a siloed and disjointed landscape for the delivery and management of care, which can result in duplication, fragmentation, and gaps in the care process.
The fragmentation of the U.S. healthcare system has significant implications for the access and quality of care, especially for the elderly, who often have multiple and complex needs that require coordinated and comprehensive care across different settings and providers. The fragmentation can lead to poor outcomes, such as increased errors, complications, readmissions, and costs, as well as reduced satisfaction, trust, and adherence 46 . For example, a study by Pham et al. 47 found that among Medicare beneficiaries aged 65 and older, those who had four or more chronic conditions and saw 10 or more physicians had twice the rate of preventable hospitalizations than those who saw two or fewer physicians 47 . Moreover, the fragmentation can lead to unmet needs, such as delayed or foregone care, as well as increased burden, such as out-of-pocket expenses, transportation difficulties, and caregiving responsibilities 48 . For example, among Medicare beneficiaries aged 65 and older, 15% reported having trouble getting timely appointments, 12% reported having trouble getting needed tests or treatments, and 9% reported having trouble getting needed medications 49 .
The disparity in the U.S. healthcare system stems from the unequal and unfair distribution of healthcare resources, opportunities, and outcomes across different groups, regions, and conditions, which leads to gaps and differences in the access, quality, and affordability of care 50 . The system is influenced by various factors, such as income, education, race, ethnicity, gender, age, geography, and disability, that affect the health status and health behaviors of the population, as well as the availability and utilization of healthcare services. These factors create a diverse and heterogeneous landscape for the consumers and the providers, who face different and often disproportionate challenges and barriers in obtaining and delivering care. Moreover, the system is influenced by various policies, programs, and practices, such as reimbursement rates, quality measures, and incentives, that affect the allocation and distribution of healthcare resources, such as workforce, facilities, equipment, and technology. These policies, programs, and practices create a dynamic and complex landscape for the payers and the policymakers, who must balance and align the competing and conflicting interests and objectives of the healthcare stakeholders.
As the demand for healthcare services increases due to the aging population, and the supply of healthcare workers and resources remains insufficient and inadequate, a new form of fragmentation and disparity is emerging in the U.S. healthcare system: the rich-poor divide. This refers to the phenomenon where the affluent and urban areas attract and retain more and better healthcare professionals and facilities, while the poor and rural areas are left with fewer and worse healthcare options. This creates a vicious cycle, where the rich areas have more access and quality of care, and the poor areas have less access and quality of care, leading to further widening of the health and economic gaps between them.
One of the factors that contributes to this new form of fragmentation and disparity is the market-driven and competitive nature of the U.S. healthcare sector, where healthcare providers are motivated by financial incentives and rewards to work in areas and specialties that offer higher compensation and recognition. This creates a situation where the supply of healthcare workers is skewed towards the areas and specialties that have more demand and resources, such as urban and affluent areas, and specialty and subspecialty care. Conversely, the supply of healthcare workers is scarce in the areas and specialties that have less demand and resources, such as rural and remote areas, and primary and geriatric care. This results in a mismatch between the needs and the availability of the healthcare workforce, which affects the access and quality of care for different populations.
One of the examples that illustrates this new form of fragmentation and disparity is the rise of travel nurses, who are registered nurses with advanced training and certification in various specialties, and work on a temporary or contract basis in different locations and settings. These nurses are in high demand, as they can fill the gaps and shortages of anesthesiologists (i.e., travel nurse anesthetist) or other nurse specialists, who are often concentrated in urban and academic centers. Moreover, these nurses are well compensated, as they can earn significantly higher salaries and benefits than regular nurses and have more flexibility and autonomy in choosing their assignments and schedules. However, these nurses also contribute to the fragmentation and disparity of the healthcare system, as they tend to work in areas and settings that offer more opportunities and rewards, such as affluent and urban areas, and private and specialty hospitals. This leaves the areas and settings that have less opportunities and rewards, such as poor and rural areas, and public and primary care facilities, with fewer and less qualified healthcare workers, which affects the access and quality of care for the populations they serve.
Addressing the challenge of fragmentation and disparity in the U.S. healthcare system requires a holistic and integrated approach that involves improving the coordination and continuity of care, enhancing the equity and inclusivity of care, and ensuring the affordability and sustainability of care. Achieving these goals requires collaboration and coordination among the healthcare providers, payers, policymakers, and stakeholders, as well as a commitment and investment in the healthcare sector.
Interventions, policy reform, and global comparison
As the number of individuals living into their 80s, 90s and beyond increases dramatically, focus has shifted from extending lifespan to enhancing the quality of these additional years. This approach, known as ‘delayed aging,’ has encompassed investments in technology and policies that increase the number of years lived without the accumulation of chronic conditions and other side effects of aging. Achieving this would result in the compression of morbidity, meaning that chronic illnesses would be concentrated into a shorter period towards the end of life. This shift would not only have an impact on the general health of the population, would also have a positive financial impact. For example, a 2013 study conducted by Goldman et al. estimated that wide-spread delayed aging would save the U.S. $7.1 trillion by 2060.
The emerging field of geroscience is central to increasing the number of healthy years in older populations. This discipline seeks to understand the relationship between aging and age-related diseases, aiming to mitigate the latter by targeting the biological processes of aging itself 51 . A key strategy involves identifying biomarkers and risk factors, such as socioeconomic and lifestyle choices, that predict disease development in later life (Table 2 ). Technological advancements have enabled the aggregation of large multi-Omics datasets and longitudinal medical records from diverse patient groups and different aging tissues 52 . These include blood, brain, muscle, heart, liver, joint, skeleton, fat, among others. For example, the Accelerating Medicines Partnership ® ’s (AMP ® ’s) Alzheimer’s Disease program has used a multi-omic analyses of molecular data from human brain samples to identify over 500 unique drug candidate targets 53 . This wealth of information offers an unprecedented opportunity to leverage AI methodologies to decipher unique patient markers and identify potential interventions.
Once these risk factors are identified, researchers can develop interventions that correct or mitigate them. These include addressing issues such as immune aging, chronic low-grade tissue inflammation, obesity, mitochondrial age-related insufficiency, and brain proteinopathies 54 . For instance, clinical studies with new targeted immune agents aim to rejuvenate the aging immune system using immune aging biomarkers as surrogate endpoints 55 . The hope is that restoring immune health could translate to beneficial downstream effects on the vascular, heart, brain, and kidney systems. The advent of the GLP-1 drug class (e.g., Semaglutide and Tirzepatide), which not only have the potential to prevent obesity-related diseases later in life, also offers a promising avenue for the reversal of metabolic aging and may even promote DNA repair in neurodegenerative diseases 56 . Maintaining muscle function is also crucial, particularly in the context of aging or chronic conditions like sarcopenia 57 . Insights into muscle augmenting factors and the ability to mobilize and differentiate muscle stem cells present critical areas for promoting healthy aging 58 . Bioengineering, including the development of exoskeletons for spinal injury patients, offers potential solutions for maintaining ambulation during aging 59 .
Future interventions may include longitudinal analyses of genome integrity and maintaining DNA fidelity systems. Reducing the accumulation of somatic mutations, which correlate with aging of bone marrow 60 , myeloid cell dysplasia (clonal hematopoiesis) 61 , vascular wall dysfunction 62 , and blood cancers 63 , could be possible. The first successful trials in gene therapy and gene editing have shed new light and promise on human disease, suggesting that restoring the integrity of the human genome and cell systems may increasingly be within our technological reach. This could expand to restore function in autoimmune and fibrotic diseases, further underscoring the transformative potential of geroscience and technology in improving healthcare for the elderly.
As the field of geroscience advances, there is a significant risk that these innovations may predominantly benefit those with substantial resources, further exacerbating the ‘rich-poor’ divide in eldercare and highlighting one type of inequity that tomorrow’s elderly may face. There is already evidence that compression of morbidity may be due more to socioeconomic factors than biological determinants 64 , 65 . However, we do not yet know what other challenges these future generations may face. New and emerging socioeconomic factors and factors associated with marginalized groups in younger populations will have a yet unknown impact on tomorrow’s elderly. The shifting healthcare requirements of younger demographics, characterized by factors such as the increase in gender-affirming care, escalating mental health issues, and substance misuse, including opioids, are likely to affect the future landscape of elderly care in ways that are currently unknown. The opioid crisis, as elaborated in Barbara Kingsolver’s Demon Copperhead , serves as an illustration of how prevalent health and societal challenges can have significant long-term impacts on public health and healthcare systems 66 . This narrative, which mirrors the broader societal problem of substance abuse, underscores the importance of incorporating equity as a fundamental factor in healthcare policy decisions. Ensuring that healthcare improvements, including those emerging from geroscience, are accessible to all, irrespective of their socioeconomic status, is vital to prevent further exacerbation of the economic disparity in eldercare.
To this end, the U.S. has launched policy reforms over the last two decades aimed at securing equitable healthcare for its senior citizens. These measures seek to confront salient challenges in the accessibility, quality, and financial viability of services catering to the elderly. The expansion of Medicaid under the Affordable Care Act (ACA), enacted in 2010, serves as a cornerstone of these initiatives, enhancing Medicaid’s scope to encompass superior benefits, cost reductions, and improved eldercare 67 . Significantly, the ACA reducing the Medicare Part D prescription drug “donut hole,” or drug coverage gaps, improving preventive care with no cost-sharing. Additional initiatives, such as Medicare Advantage, aim to improve eldercare coordination by allowing Medicare beneficiaries to enroll in managed care plans (Medicare Advantage). Medicare Advantage, for example, enrolled over 30.8 million individuals in 2023 alone, and now represent over 50% of all seniors on Medicare 68 .
As components of the patient protection models, accountable care organizations (ACOs) have also exhibited efficacy in enhancing care coordination, leading to improved patient outcomes and decreased costs. A 2021 report from the Centers for Medicare & Medicaid Services (CMS) asserts that ACOs yielded $17.7 billion in gross savings and $6.5 billion in net savings for Medicare between 2021 and 2022, while also improving the quality of care 69 . Alongside these models, enhancements in Long-Term Care and Support Services through the expansion of home and community-based services (HCBS) via Medicaid have substantially widened access to personalized long-term care 70 , 71 . These services are aimed at facilitating elderly individuals to ‘age in place’ 72 . In 2019 alone, Medicaid HCBS expenditures amounted to $162 billion, highlighting a sustained trend towards increased investment in services that promote autonomy and dignity for the elderly 73 . Additionally, this represents a cost-effective approach to long-term care by minimizing dependence on more costly institutional care settings.
Internationally, countries have adopted diverse strategies to address the healthcare needs of their aging populations. Japan and Germany, for example, both emphasize integrated care models and insurance-based solutions, like Germany’s statutory health insurance complemented by long-term care insurance 74 , 75 and Japan’s Long-Term Care Insurance 76 . However, Japan, as one of the world’s oldest populations, faces unique challenges in sustaining its healthcare workforce 77 . In an attempt to compensate for this, this country has positioned itself at the forefront of automating elder care including the development of technologies such as ‘care robots,’ to improve the quality of care in nursing homes 78 . Similar to Japan, Singapore has also implemented technological healthcare solutions for its aging population, investing in improving telemedicine, remote health monitoring apps, wearable wellness technology, and smart home solutions (e.g., fall detect sensors) to facilitate independent living and reduce the burden on the healthcare system 79 . This country is currently second in the word in terms of highest life expectancy, compared with the U.S. at 48 80 . Sweden, number 20 on that list 80 , is internationally recognized as a model for eldercare. It is another country that heavily focuses on ‘aging in place’ by providing heavily funded care through municipal taxes and government grants 81 .
It is often said that there is always tomorrow, implying that we can postpone our actions and decisions to a later date. However, this sentiment cannot hold true anymore when it comes to the care of the aging population. For us to have a prosperous tomorrow, we must begin planning and actioning today. The aging of the population is not a distant or hypothetical scenario, but a present and inevitable reality. We cannot afford to wait and see what happens. We must act and change what happens today. We have the potential and the responsibility to create a better and brighter future for the elderly and for ourselves. The question is: will we?
Data availability
No datasets were generated or analyzed for this manuscript.
Bureau, U. C. Older Population and Aging. United States Census Bureau https://www.census.gov/topics/population/older-aging.html (2023).
Chamie, J., Berkman, L., Hayutin, A. M., Smith, J. P. & Hoeksema, M. J. Why Population Ageing Matters: A Global Perspectives (Center for Migration Studies, 2007).
CDC. Equitably Addressing Social Determinants of Health and Chronic Diseases, CDC https://www.cdc.gov/chronicdisease/healthequity/social-determinants-of-health-and-chronic-disease.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fchronicdisease%2Fprograms-impact%2Fsdoh.htm (2022).
Lopes, L., Montero, A., Presiado, M., Liz H. Americans’ Challenges with Health Care Costs. KFF https://www.kff.org/health-costs/issue-brief/americans-challenges-with-health-care-costs/ (2023).
Chetty, R. et al. The association between income and life expectancy in the United States, 2001-2014. JAMA 315 , 1750–1766 (2016).
Article CAS PubMed PubMed Central Google Scholar
He, Y., Wei, B. & Li, Y. The impact of using community home-based elderly care services on older adults’ self-reported health: fresh evidence from China. Front. Public Health 11 , 1257463 (2023).
Article PubMed PubMed Central Google Scholar
WHO. Global Health Workforce statistics database. WHO https://www.who.int/data/gho/data/themes/topics/health-workforce (2023).
Dall, T. et al. The Complexities of Physician Supply and Demand: Projections From 2018 to 2033. AAMC https://www.aamc.org/system/files/2020-06/stratcomm-aamc-physician-workforce-projections-june-2020.pdf (2020).
Gurwitz, J. H. The paradoxical decline of geriatric medicine as a profession. JAMA 330 , 693–694 (2023).
Jones, C. H., Jenkins, M. P., Adam Williams, B., Welch, V. L. & True, J. M. Exploring the future adult vaccine landscape—crowded schedules and new dynamics. npj Vaccines 9 , 27 (2024).
Staff, A. C. 2020 Census Will Help Policymakers Prepare for the Incoming Wave of Aging Boomers. United States Census Bureau https://www.census.gov/library/stories/2019/12/by-2030-all-baby-boomers-will-be-age-65-or-older.html#:~:text=The%202020%20Census%20will%20provide,on%20America’s%20population%20age%20structure.%E2%80%9D&text=Born%20after%20World%20War%20II,will%20turn%2074%20next%20year (2019).
2023 National Population Projections Tables: Main Series. United States Census Bureau https://www.census.gov/data/tables/2023/demo/popproj/2023-summary-tables.html (2023).
QuickFacts: New York. United States Census Bureau https://www.census.gov/quickfacts/fact/table/NY/PST045223 (2023).
Davis-Ajami, M. L., Lu, Z. K. & Wu, J. Multiple chronic conditions and associated health care expenses in US adults with cancer: a 2010–2015 Medical Expenditure Panel Survey study. BMC Health Serv. Res. 19 , 1–10 (2019).
Article Google Scholar
Goodman, R. A., Posner, S. F., Huang, E. S., Parekh, A. K. & Koh, H. K. Peer reviewed: defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev. Chronic Dis. 10 , E66 (2013).
Machlin, S. R. & Soni, A. Health care expenditures for adults with multiple treated chronic conditions: estimates from the Medical Expenditure Panel Survey, 2009. Prev. Chronic Dis. 10 , E63 (2013).
Crimmins, E. M. & Beltrán-Sánchez, H. Mortality and morbidity trends: is there compression of morbidity? J. Gerontol. B: Psychol. Sci. Soc. Sci. 66 , 75–86 (2011).
Article PubMed Google Scholar
Masnoon, N., Shakib, S., Kalisch-Ellett, L. & Caughey, G. E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 17 , 1–10 (2017).
Cohen, R. A. & Boersma, P. Strategies used by adults aged 65 and over to reduce their prescription drug costs, 2016-2017. NCHS Data Brief 335 , 1–8 (2019).
Qato, D. M., Wilder, J., Schumm, L. P., Gillet, V. & Alexander, G. C. Changes in prescription and over-the-counter medication and dietary supplement use among older adults in the United States, 2005 vs 2011. JAMA Intern. Med. 176 , 473–482 (2016).
The 2020 Long-Term Budget Outlook. Congressional Budget Office https://www.cbo.gov/system/files/2020-09/56516-LTBO.pdf (2020).
Health, United States, 2014: With Special Feature on Adults Aged 55–64. National Center for Health Statistics https://www.cdc.gov/nchs/data/hus/hus14.pdf (2015).
Cubanski, J., Neuman T., Griffin, S., and Damico, A. Medicare Spending at the End of Life: A Snapshot of Beneficiaries Who Died in 2014 and the Cost of Their Care. KFF https://www.kff.org/medicare/issue-brief/medicare-spending-at-the-end-of-life/ (2016).
Zhang, X., Lin, D., Pforsich, H. & Lin, V. W. Physician workforce in the United States of America: forecasting nationwide shortages. Hum Resour Health 18 , 8 (2020).
Gaynor, M. & Town, R. the Impact of Hospital Consolidation—update (The Synthesis Project, Robert Wood Johnson Foundation, 2012).
2017 Infrastructure Report Card. ASCE https://www.infrastructurereportcard.org/wp-content/uploads/2016/10/2017-Infrastructure-Report-Card.pdf (2017).
McGinnis, J. M., Stuckhardt, L., Saunders, R. & Smith, M. Best care at lower cost: the path to continuously learning health care in America (National Academies Press, 2013).
Wennberg, J. E., Fisher, E. S. & Skinner, J. S. Geography and the debate over medicare reform: A reform proposal that addresses some underlying causes of Medicare funding woes: geographic variation and lack of incentive for efficient medical practices. Health Affairs 21 , W96–W112 (2002).
The Dartmouth Atlas of Health Care. Dartmouth Atlas Project https://www.dartmouthatlas.org/ (2024).
Hospital Beds per 1,000 Population by Ownership Type. KFF https://www.kff.org/other/state-indicator/beds-by-ownership/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D (2022).
Health Care Resources: Hospital Beds. OECD https://data.oecd.org/healtheqt/hospital-beds.htm (2020).
Adler-Milstein, J. & Jha, A. K. HITECH Act drove large gains in hospital electronic health record adoption. Health Aff 36 , 1416–1422 (2017).
Slawomirski, L. et al. Progress on implementing and using electronic health record systems. OECD https://www.oecd.org/publications/progress-on-implementing-and-using-electronic-health-record-systems-4f4ce846-en.htm (2023).
Artzi, N. S. et al. Prediction of gestational diabetes based on nationwide electronic health records. Nat. Med. 26 , 71–76 (2020).
Article CAS PubMed Google Scholar
Amit, G. et al. Estimation of postpartum depression risk from electronic health records using machine learning. BMC Pregnancy Childbirth 21 , 630 (2021).
Wood, A. et al. Linked electronic health records for research on a nationwide cohort of more than 54 million people in England: data resource. BMJ 373 (2021).
Wang, Q. Q., Kaelber, D. C., Xu, R. & Volkow, N. D. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol. Psychiatry 26 , 30–39 (2021).
Collaborative, O. et al. OpenSAFELY: factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients. MedRxiv https://doi.org/10.1101/2020.05.06.20092999 (2020).
Ayala Solares, J. R. et al. Deep learning for electronic health records: a comparative review of multiple deep neural architectures. J. Biomed. Inform. 101 , 103337 (2020).
Li, Y. et al. BEHRT: transformer for electronic health records. Sci. Rep. 10 , 7155 (2020).
Huang, S.-C., Pareek, A., Seyyedi, S., Banerjee, I. & Lungren, M. P. Fusion of medical imaging and electronic health records using deep learning: a systematic review and implementation guidelines. NPJ Digit Med. 3 , 136 (2020).
Keshta, I. & Odeh, A. Security and privacy of electronic health records: Concerns and challenges. Egypt Inform. J. 22 , 177–183 (2021).
Osborn, R., Doty, M. M., Moulds, D., Sarnak, D. O. & Shah, A. Older Americans were sicker and faced more financial barriers to health care than counterparts in other countries. Health Aff. 36 , 2123–2132 (2017).
Topol, E. J. High-performance medicine: the convergence of human and artificial intelligence. Nat. Med. 25 , 44–56 (2019).
Shortell, S. M. & McCurdy, R. K. Integrated health systems. IKMS 8 , 369–382 (2009).
Google Scholar
O’Malley, A. S. & Rich, E. C. Measuring comprehensiveness of primary care: challenges and opportunities. J. Gen. Intern. Med. 30 , 568–575 (2015).
Article PubMed Central Google Scholar
Pham, H. H., Schrag, D., O’Malley, A. S., Wu, B. & Bach, P. B. Care patterns in Medicare and their implications for pay for performance. NEJM 356 , 1130–1139 (2007).
Komisar, H. The Effects of Rising Health Care Costs on Middle-Class Economic Security , https://www.aarp.org/pri/topics/health/coverage-access/impacts-of-rising-healthcare-costs-AARP-ppi-sec.html (2013).
Shi, L., Regan, J., Politzer, R. M. & Luo, J. Community Health Centers and racial/ethnic disparities in healthy life. Int J Health Serv 31 , 567–582 (2001).
Braveman, P. & Gruskin, S. Defining equity in health. JECH 57 , 254 (2003).
CAS Google Scholar
Kennedy, B. K. et al. Geroscience: linking aging to chronic disease. Cell 159 , 709–713 (2014).
Babu, M. & Snyder, M. Multi-omics profiling for health. Mol Cell Proteomics 22 , 100561 (2023).
Alzheimer’s Disease. NIH https://www.nih.gov/research-training/accelerating-medicines-partnership-amp/alzheimers-disease (2021).
Tenchov, R., Sasso, J. M., Wang, X. & Zhou, Q. A. Aging Hallmarks and progression and age-related diseases: a landscape view of research advancement. ACS Chem Neurosci 15 , 1–30 (2024).
Tran Van Hoi, E. et al. Biomarkers of the ageing immune system and their association with frailty—a systematic review. Exp. Gerontol. 176 , 112163 (2023).
Wilbon, S. S. & Kolonin, M. G. GLP1 receptor Agonists—effects beyond obesity and diabetes. Cells 13 , 65 (2024).
Article CAS Google Scholar
Grevendonk, L. et al. Impact of aging and exercise on skeletal muscle mitochondrial capacity, energy metabolism, and physical function. Nat. Commun. 12 , 4773 (2021).
Sousa-Victor, P., García-Prat, L. & Muñoz-Cánoves, P. Control of satellite cell function in muscle regeneration and its disruption in ageing. Nat. Rev. Mol. Cell Biol. 23 , 204–226 (2022).
Kapsalyamov, A., Hussain, S. & Jamwal, P. K. State-of-the-art assistive powered upper limb exoskeletons for elderly. IEEE Access 8 , 178991–179001 (2020).
Patel, N., Dulau-Florea, A. & Calvo, K. R. Characteristic bone marrow findings in patients with UBA1 somatic mutations and VEXAS syndrome. Semin. Hematol. 58 , 204–211 (2021).
Park, S. J. & Bejar, R. Clonal hematopoiesis in cancer. Exp. Hematol. 83 , 105–112 (2020).
Revêchon, G., Merino, L. G., Machtel, P. & Eriksson, M. Somatic mutations in vascular wall function and age-associated disease. Eur. Heart J. 44 , 4208–4210 (2023).
Feusier, J. E. et al. Large-scale identification of clonal hematopoiesis and mutations recurrent in blood cancers. Blood Cancer Discov. 2 , 226–237 (2021).
House, J. S., Kessler, R. C. & Herzog, A. R. Age, socioeconomic status, and health. Milbank Q. 68 , 383–411 (1990).
Rowe, J. W. & Berkman, L. Decompression of morbidity and the workforce. Nat. Aging 2 , 3–4 (2022).
Kingsolver, B. Demon Copperhead (Harper, 2022).
The Affordable Care Act: A Stronger Medicare Program in 2012. CMS https://www.cms.gov/apps/files/medicarereport2012.pdf (2013).
Ochieng, N., Biniek, J. F., Freed, M., Damico, A., Neuman, T. Medicare Advantage in 2023: Enrollment Update and Key Trends. KFF https://www.kff.org/medicare/issue-brief/medicare-advantage-in-2023-enrollment-update-and-key-trends/ (2023).
ACOs & Cost Savings. NAACOS https://www.naacos.com/acos-and-cost-savings#:~:text=ACOs%20and%20Cost%20Savings,savings%2C%20according%20to%20CMS%20data . (2022).
Home- and Community-Based Services. CMS https://www.cms.gov/training-education/partner-outreach-resources/american-indian-alaska-native/ltss-ta-center/information/ltss-models/home-and-community-based-services (2023).
Chidambaram, P., Burns, A., Rudowitz, R. Who Uses Medicaid Long-Term Services and Supports? KFF https://www.kff.org/medicaid/issue-brief/who-uses-medicaid-long-term-services-and-supports/ (2023).
Aging in Place: Growing Older at Home. NIH https://www.nia.nih.gov/health/aging-place/aging-place-growing-older-home#resources (2023).
Burns, A., Mohamed, M., Watts, M. O. M. Pandemic-Era Changes to Medicaid Home- and Community-Based Services (HCBS): A Closer Look at Family Caregiver Policies. KFF https://www.kff.org/medicaid/issue-brief/pandemic-era-changes-to-medicaid-home-and-community-based-services-hcbs-a-closer-look-at-family-caregiver-policies/ (2023).
Wienecke, D. How does Germany care for the elderly? Medium https://dietrichwienecke.medium.com/how-does-germany-care-for-the-elderly-c394425a2e07 (2023).
Busse, R., Blümel, M., Knieps, F. & Bärnighausen, T. Statutory health insurance in Germany: a health system shaped by 135 years of solidarity, self-governance, and competition. Lancet 390 , 882–897 (2017).
Yamada, M. & Arai, H. Long-term care system in Japan. Ann. Geriatr. Med. Res. 24 , 174–180 (2020).
Okamoto, S. & Komamura, K. Towards universal health coverage in the context of population ageing: a narrative review on the implications from the long-term care system in Japan. Arch. Pub. Health 80 , 210 (2022).
Wright, J. Inside Japan’s long experiment in automating elder care. Technology Review https://www.technologyreview.com/2023/01/09/1065135/japan-automating-eldercare-robots/ (2023).
Koh, S. Tech-Assisted Healthcare: Revolutionizing Senior Care in Singapore. Medium https://medium.com/@koh.siag.lan/tech-assisted-healthcare-revolutionizing-senior-care-in-singapore-8fc53241d83a (2024).
Country Comparisons—Life expectancy at birth. CIA https://www.cia.gov/the-world-factbook/field/life-expectancy-at-birth/country-comparison/ (2024).
Lorenzoni, L. Case Study—Sweden. Organization for Economic Co-operation and Development https://extranet.who.int/kobe_centre/sites/default/files/pdf/Sweden_draft_rev-2.pdf (2021).
Auerbach, D. I. & Staiger, D. O. How fast will the registered nurse workforce grow through 2030? Projections in nine regions of the country. Nurs. Outlook 65 , 116–122 (2017).
Supply and Demand Projections of the Nursing Workforce: 2014-2030 . National Center for Health Workforce Analysis https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/projections/NCHWA_HRSA_Nursing_Report.pdf (2017).
State Physician Workforce Data Report. AAMC https://www.aamc.org/data-reports/workforce/report/state-physician-workforce-data-report (2019).
Nursing Shortage Fact Sheet. AACN https://www.aacnnursing.org/News-Information/Fact-Sheets/Nursing-Shortage (2022).
Health Workforce Shortage Areas. HRSA https://data.hrsa.gov/topics/health-workforce/shortage-areas (2024).
Geriatrics Workforce Enhancement Program. HRSA https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/funding/geriatrics-workforce-enhancement-programs-2019.pdf (2019).
American Nurses Association Well-Being Initiative. ANA https://www.nursingworld.org/practice-policy/work-environment/health-safety/disaster-preparedness/coronavirus/what-you-need-to-know/the-well-being-initiative/ (2019).
Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460 (2020).
Ferrucci, L. & Fabbri, E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 15 , 505–522 (2018).
Chia, C. W., Egan, J. M. & Ferrucci, L. Age-related changes in glucose metabolism, hyperglycemia, and cardiovascular risk. Circ. Res. 123 , 886–904 (2018).
Lena, A., Coats, A. J. S. & Anker, M. S. Metabolic disorders in heart failure and cancer. ESC Heart Fail 5 , 1092–1098 (2018).
Martin, L. et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J. Clin. Oncol. 31 , 1539–1547 (2013).
Tchkonia, T., Zhu, Y., Van Deursen, J., Campisi, J. & Kirkland, J. L. Cellular senescence and the senescent secretory phenotype: therapeutic opportunities. JCI 123 , 966–972 (2013).
Dominguez, L. J. & Barbagallo, M. The biology of the metabolic syndrome and aging. Curr. Opin. Clin. Nutr. Metab. Care 19 , 5–11 (2016).
Guo, Y. et al. Plasma proteomic profiles predict future dementia in healthy adults. Nat. Aging 4 , 247–260 (2024).
Rizvi, S., Raza, S. T. & Mahdi, F. Telomere length variations in aging and age-related diseases. Curr. Aging Sci. 7 , 161–167 (2014).
Liguori, I. et al. Oxidative stress, aging, and diseases. Clin. Interv. Aging 13 , 757–772 (2018).
Meehan, M. & Penckofer, S. The role of vitamin D in the aging adult. J. Aging Gerontol. 2 , 60–71 (2014).
Download references
Acknowledgements
The authors thank Andrew Hill and Marie Beitelshees (Bulmore Consulting, Lockport, NY, USA) for their strategic insights, editorial support, and review in preparing this article. This work was funded by Pfizer. We also thank Kristen Prentice for her strategic insight contributions. This work was funded by Pfizer.
Author information
Authors and affiliations.
Pfizer, 66 Hudson Boulevard, New York, New York, 10018, USA
Charles H. Jones & Mikael Dolsten
You can also search for this author in PubMed Google Scholar
Contributions
C.H.J. conceptualized the publication, developed the outline, researched sources, drafted and edited the manuscript, and provided strategic input. M.D. provided strategic insights, edited the manuscript, and provided research source material.
Corresponding authors
Correspondence to Charles H. Jones or Mikael Dolsten .
Ethics declarations
Competing interests.
The authors declare no competing non-financial but declare the following Competing Financial Interests: C.H.J. and D.M. report that they are employees of Pfizer Inc. and may hold stock or stock options in the company.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions

About this article
Cite this article.
Jones, C.H., Dolsten, M. Healthcare on the brink: navigating the challenges of an aging society in the United States. npj Aging 10 , 22 (2024). https://doi.org/10.1038/s41514-024-00148-2
Download citation
Received : 24 January 2024
Accepted : 21 March 2024
Published : 06 April 2024
DOI : https://doi.org/10.1038/s41514-024-00148-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Cookies on Be Part of Research
We use some essential cookies to make this service work.
We would like to use additional cookies to remember your settings, understand how you use Be Part of Research and improve the service.
We also use cookies set by other sites to help us deliver content via their services.
Keep up to date
Sign up for news and information about taking part and shaping research.
I'm looking for research about
- News and features
- Why take part?
- How to take part
- What happens on a study?
- Volunteering without a condition
- UK research registries
- Information for researchers
- Information for health and care professionals
- Web developer resources
What is health and care research?
- How are studies regulated, approved and funded?
- Frequently asked questions
Search for a study
You already conduct research in your day-to-day life. This research informs and broadens your understanding of things before you make a decision. Health and care research is the same. It seeks to find answers to questions about the best options available. It then uses these discoveries to make decisions about improvements or changes. This is so we can:
- diagnose diseases earlier or more accurately
- provide life-changing treatments
- prevent people from developing conditions
- improve health and care for generations to come
- ensure everyone has a better quality of life
Although health professionals already know a great deal, there are still so many questions that need answers. Sometimes, the outcome of research just confirms that what we have at the moment, is the best available to us right now.
How research contributes to our NHS
This short film explains the important role that research plays in the NHS and how important it is for the future that we all consider taking part ( video transcript ).
Good research is:
- Relevant – it answers questions that are important to the health and care of the public
- High quality – it has to follow strict legal standards
- Safe – it puts people’s safety and dignity first
The first clinical trial

The first clinical trial was conducted by James Lind. He was a Scottish doctor and a pioneer of naval hygiene in the Royal Navy. He conducted the first clinical trial in history in 1747.
James wanted to investigate whether citrus fruits cured scurvy. He selected twelve patients with scurvy on a ship, kept them together and gave them all different diets and monitored them. By the end of the week, the sailors whose daily diet included citrus fruits recovered, therefore proving that citrus fruit could cure scurvy.
We still celebrate this milestone each year on International Clinical Trials Day.
Myths about research
Understanding the facts is really important when deciding whether to take part in research. By clicking on the arrow next to each myth you can reveal the facts.
All health and care research is high risk
All health and social care research has to go through very strict ethical and regulatory checks before it can go ahead. There are lots of different ways to get involved with research . Some involve taking a new medicine or having a new form of treatment, others may be as simple as filling out a questionnaire or leaving a sample. People are very closely monitored while they are taking part in research, so although health and care research is not entirely risk-free, the chances of something going wrong are small.
My doctor will tell me about the research available
Not all health and care professionals will be fully informed about all of the research opportunities available to you. They might also not have the time to discuss it with you in your appointment. However, it is important to ask about opportunities to get involved in research as your healthcare professional will know how to find out what might be available. You can search for studies on this website by using the search bar at the very top of each page by typing in your town, postcode, body part, medicine or health condition. You can also find a condition by pressing the “ view conditions ” button.
Research can only take place in hospital
Health and care research can take place in many different places, from schools to care homes depending on the type of research. It is more common than ever before for research to take place in non-clinical settings. Digital technology provides a way of getting people involved from the comfort of their own homes.
Health and care research means taking lots of drugs
Not all health and care research involves taking drugs. The research may involve testing a new device to help monitor or administer a medicine for an illness. It could be about monitoring how certain changes in our diet and lifestyle could help the health of our nation in the future. Research might simply involve talking to someone, completing a short questionnaire or even using an app on a mobile device. There are also many different ways to be involved in research without being a participant in a research study .
People are treated like guinea pigs
Whatever the type of research, anyone who is involved should be treated with respect. The research is not being done to them but with them. People who participate in research often say that they feel well cared for as they have a dedicated contact within the research staff team. Research teams must follow ethical guidance and before the research can take place, they must seek approval for their plan from a Research Ethics Committee. Research that involves new medicines is not tested on people first. It will have gone through a process to ensure it is ready for use with people.
Health and care research is only about finding a cure
Research aims to prevent diseases as well as cure them. There are a range of factors which can contribute to your health, for example: where you live, what you eat and whether you have a good support network of family and friends. Public health research seeks to answer questions about some of these factors.
Research seeks to find ways for people to live well with long-term conditions. It can help to find out the best ways to care for people living with life-limiting illness and pain, which is known as ’palliative care’. Research can lead to improvements in end-of-life care across all diseases and to help patients to live in comfort and die with dignity.
Health and social care research only involves physical diseases, it cannot help with mental health
People’s health is not limited to physical disease, it includes their mental well being. Research therefore seeks to answer questions about mental health such as is medicine, counselling or a combination of both the best treatment for individuals living with depression? Members of the public can have a role in identifying and prioritising where health research is focused . Given increased awareness of the effects our mental health can have on our physical well being, this is likely to be a growing area of health and social care research. Read about all the research happening within the NIHR specialty for mental health .
Children are not allowed to participate in health and care research
Children can take part in health and care research with the permission of their legal guardian. The research team may meet with the child to make sure they understand what the research is about. They may use pictures to explain the study. Research in child health is vital to help find new and better ways to care for children. You can find studies for children by typing "Children" in the search box at the very top of this page.
Research only benefits the drug companies
Health research is funded by drug companies, charities and the government, although when the NHS undertakes research specifically for drug companies, the company pays the full cost. Everyone benefits from the development of new medicines, and without commercial drug companies there would be less research taking place.
Different types of research

Healthcare research
Sometimes health research studies may be referred to as ‘clinical trials’. They usually involve examining and observing people with different conditions and sometimes comparing them with people who don't have the condition. It can also involve research on samples of blood or other tissues, or tests such as scans or X-rays. Researchers can also analyse information in patient records, or the data from health and lifestyle surveys.

Public health research
Tackles some of the bigger health issues that affect society as a whole, for example, the impact of giving up smoking, how many steps a day for good health etc. It also looks at the benefits, costs, acceptability and the wider impact of treatments.

Social care research
Is about improving the lives of people who receive care and support from our social care sector. Research in social care could be about introducing new devices and technologies such as: lifting equipment to help with residents, exploring the impact of technology driven care environments or changing social care policies and practice.
Important research discoveries
.jpg)
Launched in 1961, the contraceptive pill was initially only prescribed to married women, but the law was relaxed in 1967. The pill works by suppressing fertility with either progesterone or oestrogen or, more commonly, a combination of both.

Penicillin was discovered in 1928 and developed into a drug in the early 1940s. Today it’s used to treat a broad range of bacterial infections accounting for around 45% of the antibiotics prescribed in the NHS in England.

Research in the 1980s and 1990s showed that low doses of blood-thinning drugs such as aspirin and warfarin significantly reduced the number of heart attacks and strokes in people at risk.
Before you go
Research is a team effort. We need members of the public, like you, to take part. Without volunteers, it would not be possible for research to happen.
- Reasons why people take part in research
- How to take part in research
- Learn about how studies are made safe
- Find My Rep
You are here
Making Sense of Research in Nursing, Health and Social Care
- Pam Moule - University of the West of England, UK
- Description
What is research and how does it work in the context of nursing, health and social care?
Now in its 7 th edition, this introductory guide provides you with a concise overview of the different research methods and terminology that you will come across when undertaking research in any course related to nursing, health and social care. The book’s easy-to-follow structure takes you from research novice to confident researcher, helping you to make sense of research and understand how it is implemented in healthcare practice.
The new edition includes:
- Updates in line with the 2018 NMC standards, with more information on the impact of GDPR, consent and vulnerable groups, Personal and Public Involvement (PPI), and work-based projects.
- Improved case examples of real research, with more on group work, poster presentations, research output and dissemination, literature reviews, and dissertations.
- Upgraded activities that include reflective exercises, critical appraisal tools, a dissemination plan, and a glossary, all in the book.
This is essential reading for undergraduate and postgraduate students within the health and therapy professions, nurses, midwives, physiotherapists, radiographers, occupational therapists, speech and language therapists, and paramedics.
Some books reach their silver anniversary and start to look dated and lose their relevancy. Making Sense of Research in Nursing, Health and Social Care however, has renewed and refreshed at each edition and maintains its applicability for today’s health and social care professionals.
One of the marks of a good textbook is its ability to appeal to readers across professional boundaries and with varying levels of experience in the topic at hand; Moule achieves this both engaging those new to research as well as providing different insights for those with more research knowledge and experience. One of the stated intentions of the book is to make research interesting and in so doing to help practitioners in their adoption of research and evidenced based practice within their work. Moule achieves this with the use of an accessible writing style which is at once both engaging and thought provoking. I would recommend this book as a must have on the shelf for any student of health and social care be they a first year undergraduate or a more experienced individual engaging in post graduate studies.
Evidence-based practice is crucial for the modern healthcare practitioner. Students can often shy away from the topic of research thinking that the subject is too complex for them. However, the benefits of this book in guiding them through the subject include: easy to read short sections with headings, clear key messages at the beginning and end of each chapter and links to current, credible sources of evidence to expand their reading further. Some students find it difficult to seek out credible secondary sources and this book gives them links to guidelines and reports which would be appropriate to inform their assignment work.
Books about the research process are not rare but few authors can clarify the basics with such ease like Pam Moule. This textbook is easy-to-read, speaks to the research novice in accessible language, and leaves the reader feeling well-initiated in research literacy. Without hesitation I would endorse this textbook for undergraduate health and social care students who will draw from it from the first term of study to the last. The chapters take the reader on a journey through critical reading right through to the fundamentals of research project design, and instill habits of systematic thought and process in all elements of research. Included are a number of helpful links and templates as well as examples to aid visualization of new concepts. This book is the perfect springboard to launch health and social care students into evidence-informed practice without overwhelming and scaring them off from what can undoubtedly become a more complex topic with further reading.
This is an informative and easy to read book, which introduces the students to research and directs them through the research process. I have used previous editions of this book and have it on the reading list for research modules I teach to both undergraduate and postgraduate students. The use of practice examples and scenarios clearly demonstrate research in action in health and social care. This new 7th edition will be a valuable addition to the reading list on my modules.
The previous editions of this book have been a steadfast resource and the ‘go to book’ for all levels of paramedic students studying at undergraduate level. The seventh edition of this book does not disappoint and will be the new ‘go to’ edition for current students who want to understand how to make sense of research in health and social care. The format of the book makes it easy to access the information making it a valuable and informative resource for all students in healthcare settings, and especially useful when undertaking a final project/dissertation.
This book is an excellent text that will provide an invaluable resource to health and social care practitioners who are new to research or those undertaking projects. The detailed discussion of the research process is written in an informative and authoritative way that informs the reader and makes the research process and terminology accessible.
Excellent - I will be directing students to this resource to support learning for enquiries into health and social care research.
Such a clear and easy to read text. A seminal volume!
Easy to understand for L5 students, applied examples and clear explanations.
this book is clearly written, easy to read and easy to understand
Preview this book
For instructors.
Please select a format:
Select a Purchasing Option
- Electronic Order Options VitalSource Amazon Kindle Google Play eBooks.com Kobo
Related Products

- Open access
- Published: 10 April 2024
Understanding social needs screening and demographic data collection in primary care practices serving Maryland Medicare patients
- Claire M. Starling 1 ,
- Marjanna Smith 1 ,
- Sadaf Kazi 2 , 3 ,
- Arianna Milicia 3 ,
- Rachel Grisham 4 ,
- Emily Gruber 4 ,
- Joseph Blumenthal 5 &
- Hannah Arem 1 , 6
BMC Health Services Research volume 24 , Article number: 448 ( 2024 ) Cite this article
93 Accesses
Metrics details
Health outcomes are strongly impacted by social determinants of health, including social risk factors and patient demographics, due to structural inequities and discrimination. Primary care is viewed as a potential medical setting to assess and address individual health-related social needs and to collect detailed patient demographics to assess and advance health equity, but limited literature evaluates such processes.
We conducted an analysis of cross-sectional survey data collected from n = 507 Maryland Primary Care Program (MDPCP) practices through Care Transformation Requirements (CTR) reporting in 2022. Descriptive statistics were used to summarize practice responses on social needs screening and demographic data collection. A stepwise regression analysis was conducted to determine factors predicting screening of all vs. a targeted subset of beneficiaries for unmet social needs.
Almost all practices (99%) reported conducting some form of social needs screening and demographic data collection. Practices reported variation in what screening tools or demographic questions were employed, frequency of screening, and how information was used. More than 75% of practices reported prioritizing transportation, food insecurity, housing instability, financial resource strain, and social isolation.
Conclusions
Within the MDPCP program there was widespread implementation of social needs screenings and demographic data collection. However, there was room for additional supports in addressing some challenging social needs and increasing detailed demographics. Further research is needed to understand any adjustments to clinical care in response to identified social needs or application of data for uses such as assessing progress towards health equity and the subsequent impact on clinical care and health outcomes .
Peer Review reports
There is increasing attention on the impact of factors such as economic stability, education, neighborhood, and built environment on healthcare outcomes and, in particular, how primary care settings can assess and address individual level health-related social needs (HRSN) [ 1 , 2 ]. In turn, the American Academy of Pediatrics (AAP) and the American Academy of Family Physicians (AAFP) both recommend that primary care providers screen and address social needs as part of routine primary care visits [ 3 ]. Patients with unmet social needs are at a higher risk of missing appointments, frequent emergency room visits, and hospitalization and rehospitalization [ 4 , 5 ]. Identifying social needs and collecting detailed patient demographics in primary care can be used to tailor care, allocate resources effectively, and advocate for equitable policies, making these workflows a critical step towards advancing health equity [ 1 , 2 , 3 ].
Despite acknowledgement of the importance of integrating social care in clinical settings including a recent mandate by the Centers for Medicare and Medicaid services for screening in inpatient settings, the implementation of social needs screening and demographic data collection is complex and resource intensive [ 6 , 7 ]. Furthermore, patients who screen positive for social needs may decline assistance to address those needs. These occurrences may prove frustrating to those conducting screening if they lack sufficient training on delivering screening or assisting individuals with addressing social needs [ 8 ]. Additionally, while many practices already collect basic demographic data such as age, ethnicity, and race, demographic information is not always collected in a culturally sensitive or inclusive manner. Demographic data collection processes are not standardized, and many demographic fields (e.g., education level, sexual orientation, and disability status) are sometimes not asked at all. As part of a contract to provide technical assistance to Maryland Primary Care Program (MDPCP) practices to support social needs screening and demographic data collection, we explored collected survey data to understand current practices around social needs screening and demographic data collection as well as potential areas for growth in screening delivery.
Study population
MDPCP is a voluntary program for eligible primary care practices that provides funding and support for the delivery of advanced primary care for Medicare beneficiaries throughout Maryland. MDPCP supports the overall health care transformation process and allows primary care providers to play an increased role in disease prevention, management of chronic disease, and prevention of unnecessary hospital utilization [ 9 ]. The primary goal of MDPCP is the sustainable transformation of primary care across Maryland to include all the elements of advanced primary care to support the health needs of state residents [ 9 ]. MDPCP is co-administered by teams at the Maryland Department of Health and the Center for Medicare and Medicaid Innovation (CMMI). At the time of the survey, the MDPCP network included n = 507 participating primary care practices representative of every county in Maryland.
MDPCP offers a combination of financial incentives and other supports tailored to primary care practices. These incentives encompass non-visit-based payments specifically designed for care coordination initiatives, as well as performance-based incentives, rewarding practices for achieving clinical quality, patient experience, and utilization benchmarks. In addition to financial incentives, MDPCP provides a variety of additional supports for care transformation MDPCP practices are paired with a Practice Transformation Coaches, who provide guidance, answer questions, and work directly with practices to improve processes that improve quality of care and decrease costs. In addition to Coaches, practices have access to the MDPCP Learning System encompassing a myriad of learning opportunities including User Groups, All-Practice Calls, and other collaborative forums for practices to learn from subject matter experts and fellow participants. Practices also have access to a handful of Guides including the Advancing Primary Care Guide, which provides information on MDPCP requirements, tactics for advancing the functions of primary care, and achieving care transformation. Additionally, practices have the option to partner with a Care Transformation Organization (CTO), who can assist with care management or other related patient services.
Data collection
Care transformation requirement (CTR) reporting questions ask MDPCP participants about progress on specific MDPCP requirements that span the five comprehensive primary care functions (Appendix 1 ). The five key functions of advanced primary care are care management, access and continuity, comprehensiveness, and coordination across the continuum of care, beneficiary and caregiver experience, and planned care for health outcomes. The questionnaire is developed by CMMI, and MDPCP participants respond in the online Centers for Medicare and Medicaid Services (CMS) program portal twice annually, as a requirement of program participation (Appendix 2 ). The survey used in this analysis was collected in the third quarter of 2022. This analysis was deemed exempt by the Georgetown/MedStar Institutional Review Board (Study 4698).
Statistical analysis
We used descriptive statistics to review social needs screening and demographic data collection responses from MDPCP practices . We conducted additional analysis to investigate responses by practice characteristics including practice size (small 1–2, medium 3–7, large 8 + providers) and hospital affiliation (yes or no). Further, a stepwise regression analysis was used to determine factors predicting the routine screening of beneficiaries for unmet social needs, comparing all beneficiaries to a specific targeted subsection. Variables used in the model were practice size, and hospital affiliation. 487 of the 507 records were used for regression analyses. We excluded practices if they did not report screening beneficiaries ( n = 4), practice size ( n = 1), or hospital affiliation status ( n = 15). SAS 9.4 (Cary, NC) was used in all analyses.
Practice responses on social needs screening and referral processes are presented in Table 1 . Among the MDPCP practices, nearly all reported some form of social needs screening for all (63%) or at least some (36%) beneficiaries. Many practices reported utilizing a social needs screening tool developed by the practice or affiliated health system (32%). Other practices reported screening using standardized screening tools, including, an unspecified standardized tool (21%); EHR-specific tool (19%); Accountable Health Communities (14%); and PRAPARE (5%). There was substantial variation in EHR vendors, with 23% of practices using EPIC, 17% using eClinicalWorks, 14% using Cerner, and 11% using Athenahealth. Approximately half (49.5%) of the practices reported conducting social needs screening annually, while 18% of practices reported conducting screenings at every visit and 15% when indicated based on reason for visit. Just over a quarter (27%) of practices reported linking responses to discrete ICD-10 or Social Determinants of Health (SDOH) Z codes.
Survey responses revealed variability regarding which patients receive social needs screening, screening frequency, EHR integration and use of Z-codes based on practice characteristics (Appendix 3 ). In an exploratory multivariate logistic regression we found that practices with a hospital affiliation were more likely to screen a targeted population than all patients (OR = 1.54, 95% CI = 1.05–2.27) and practices that were small- (1–2 providers) or medium-sized (3–7 providers) were more likely to screen all patients. (OR = 0.46, 95% CI = 0.26–0.80; OR = 0.46, 95% CI = 0.27–0.78, respectively; data shown in text only). Practices had the opportunity to describe which beneficiaries were targeted. Responses included individuals at high risk ( n = 67) or experiencing recent mental or clinical health events ( n = 18), participants in care management or care coordination programs ( n = 82), Health Equity Advancement Resource and Transformation (HEART) patients ( n = 25), and attendees of annual wellness visits ( n = 40).
When practices were asked to select social needs that they prioritize, common responses were transportation (93%), food insecurity (89%), housing instability (86%), financial resource strain (85%), and social isolation (84%) (Table 2 ). The least common needs prioritized were internet access (42%), phone access (46%), employment (48%), and language access (51%). Practices also reported which social needs were most challenging to support. The greatest challenges came with addressing housing instability (31%), internet access (31%), financial resource strain (30%), and medication affordability (30%).
Nearly all practices reported collecting patient demographics in some capacity (99%), with most practices reporting that demographic data are collected by a staff member (70%), collected at every visit (51%), annually (23%), or only at the patient’s initial visit (20%). Race and primary language were collected by nearly all practices (96%), gender identity was collected by 92%, relationship status by 87%, ethnicity by 87%, and employment status by 84% of practices. Other demographic factors were less commonly asked: only 49% of practices reported asking about sexual orientation, 48% asked about disability status, and 38% asked about highest level of education.
In this study we found that primary care practices participating in the MDPCP program overall had a high rate of social risk factor screening, with many using screeners that had been developed to meet individual practice needs. Commonly prioritized domains included transportation, food insecurity, housing instability, financial strain, and social isolation, the last being a commonly cited problem among older adults. Describing patterns of screening and demographics in this sample of practices across the state increase understanding of successes and challenges in real-world practice settings and informs potential future interventions.
Determining which patients should be screened and by whom in a busy primary care setting, as well as who can respond to identified needs, can be challenging. In our study there were differences both in which patients were screened and how often by practice [ 10 , 11 ]. Open ended responses suggested that among some MDPCP practices, screening was performed only for individuals who qualify for extra social assistance through the MDPCP program (i.e., those who qualify due to medical complexity and area deprivation index). Although we did not find other published literature focused specifically on Medicare patients at the state level, we found literature on programs focused on social needs screening among Medicaid populations in several states. Like Maryland practices, standardized measures and consistent approaches to measuring social needs have not been adopted or required in many states [ 12 , 13 , 14 ]. Further, a high percentage of the Maryland practices reported using home grown and standardized screening tools with additional questions to meet the practices’ needs. While the ability to aggregate social needs data across care settings can be challenging with different screeners, there is national movement to harmonize domains across various social risk factor screeners through the Gravity Project and the Office of the National Coordinator [ 12 , 15 ]. Notably, CMS has mandated social needs reporting in the inpatient setting beginning January 2024 for five specific domains, but has not specified a single tool or set of tools given that while there are some validated subsets of questions (e.g., Hunger Vital Signs), there is currently no gold standard tool [ 16 ]. Potential hurdles in requiring specific tools may include limitations on EHR technology, referral processes, and provider or staff level comfort and training in asking specific questions. Furthermore, implementing screening without supports for training the staff on trauma-informed approaches and how to respond to identified needs has the potential to cause more harm than benefit to patients. Thus, toolkits established by various professional societies and public health societies may be useful to determine which tools are most appropriate for a given practice and how to integrate them into care where practices have not yet started screening or encounter challenges [ 17 , 18 , 19 ].
Regarding practices with a hospital affiliation being more likely to screen a targeted population, one possibility is that practices affiliated with hospitals may have access to additional resources and supports that facilitate targeted screening efforts. Hospitals often have established practices including social risk factor screening for targeted subpopulations to address costly hospital readmissions, which may encourage affiliated practices to deliver more targeted screening practices. While it is unclear why small or medium-sized practices were more likely to screen all patients than a sub-population, it may have to do with more autonomy in workflow process, less customization of the EHR to target sub-populations, or differences in staffing and provider to patient ratios. While we cannot explain these differences from the survey alone, findings suggest that the size and affiliation of practices play a role in their screening practices, highlighting the importance of considering practice characteristics when designing specific supportive interventions or policies aimed at increasing screening rates.
It is important to highlight that MDPCP practices have achieved impressive levels of social needs screening and demographic data collection implementation. This success could be attributed largely to the program’s requirements and incentives to screen beneficiaries for social needs and collect demographic information. Additionally, the program provides technical support and resources to meet these requirements and to stand up social needs screening workflows if not already in place. By joining MDPCP, participating practices have demonstrated a commitment to advanced primary care, further indicating MDPCP participation may be associated with higher uptake of these workflows, as opposed to primary care practices who do not participate in similar value-based programs. Other states considering such programs may look to some of these supports when rolling out new requirements or incentives.
While the findings highlight the high level of social needs screening and demographic data collection, challenges in addressing identified needs may also be due to various factors including complexity of workflows and staffing, patients with social needs declining assistance, or limited local resource availability [ 20 ]. Previous research suggests patients may decline social needs assistance in healthcare settings if they do not feel like they need help, are confused about what is offered, are not confident that the assistance would be helpful, have experienced previous negative experiences, or feel fear and mistrust related to disclosing personal information [ 8 ]. In areas that posed the greatest referral challenges, policy efforts may be needed to deliver services and bridge the gaps to access. For example, the challenge of addressing housing needs is not newly identified; previous literature has shown increasing costs and declining supply have contributed to national housing availability and affordability challenges [ 21 , 22 ]. Medication cost continues to be a major problem cited in the literature, especially for older populations with a higher incidence of chronic diseases [ 23 , 24 ]. Financial strain among individuals often poses a challenge as financial needs fluctuate frequently, and changes can be dramatic; further, these changing needs over time are often not resolved by a one-time intervention and require long-term involvements [ 11 ]. Though research on the effects of internet access and health outcomes is still emerging, literature suggests investment in digital infrastructure by federal, state, and local governments is needed for further development of the internet as a means of addressing long-standing inequality in health [ 25 , 26 ]. While food insecurity and transportation were top needs prioritized within MDPCP practices, they did not present the same level of challenge to practices, perhaps due to wider availability of resources, partnerships, and supports such as transportation vouchers.
Although addressing connection to resources continues to be a challenge for practices, there are opportunities to leverage information from social needs screenings and demographic data collection in several other ways to improve care. Aggregate screening and demographic data can be used for quality improvement initiatives within primary care practices by analyzing trends and patterns in social needs data to help practices identify areas of unmet need, track outcomes, and update protocols for screening and referral processes. Additionally, data can be used to advocate for policy changes to address systemic issues affecting patients’ health outcomes. However, challenges in utilizing information from social needs screening and demographic data collection may still exist due to limited resources and capacity and lack of provider awareness and training availability.
Increased collection of detailed demographic data, particularly regarding sexual orientation, education level, and disability status presents an opportunity for improvement in primary care. Furthermore, collecting detailed demographic information can better allow practices to understand the need for targeted educational materials, track quality indicators, and address challenges faced by historically marginalized populations [ 26 , 27 ]. Still, even with good data collection approaches, some practices do not have the infrastructure or resources to analyze data to assess disparities in care or outcomes.
This study's strengths lie in its comprehensive analysis of a diverse range of primary care practices across Maryland. The inclusion of 507 practices with variations in size, location, and demographics enhances the representativeness of the findings and improves the generalizability of the results to a broader population. Consequently, the findings derived from studying a large population can contribute to a stronger evidence base for decision-making in healthcare and support the development of effective interventions and policies. A limitation of the study is the reliance on self-report, which may depend on the participants’ perspectives. Additionally, MDPCP practices meet eligibility criteria and voluntarily select to join the program, so these practices may be better equipped to join a value-based program that includes requirements or incentives to screen for social needs. Despite the limitations, our findings are novel in that few published studies highlight current practices at scale on social risk factor screening and referral in outpatient primary care settings for adults. Future research is warranted to show what strategies effectively increase uptake and drive meaningful change in social-needs responsive healthcare delivery.
MDPCP practices have demonstrated widespread adoption of social risk factor screenings and needs prioritization. While practices have implemented strategies to link patients to resources to address needs, challenges remain with providing social needs resources to beneficiaries from the primary care setting. Additionally, there is room for improvement in collecting certain demographic data fields within primary care practices. As the present analysis was based on cross-sectional data, future studies are needed to understand how to effect change in implementing or scaling social risk factor screening and detailed demographic data collection at the practice level. Additionally, future work is needed to understand how care is adjusted in response to identified social needs and how that impacts outcomes at the patient level.
Availability of data and materials
To access the datasets examined in this study, interested parties must follow the procedure outlined by the CMS. Requests should be submitted through the CMS website (cms.gov), and any queries can be directed to [email protected].
Abbreviations
Maryland Primary Care Program
Care Transformation Requirements
Center for Medicare and Medicaid Innovation
Centers for Medicare and Medicaid Services
Electronic Health Record
Social Determinants of Health
Social Determinants of Health. World Health Organization, 2023, at https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 . Accessed 9 Apr 2023.
DeVoe JE, Bazemore AW, Cottrell EK, et al. Perspectives in Primary Care: A Conceptual Framework and Path for Integrating Social Determinants of Health into Primary Care Practice. Ann Fam Med. 2016;14(2):104–8. https://doi.org/10.1370/afm.1917 .
Article PubMed PubMed Central Google Scholar
Lax Y, Bathory E, Braganza S. Pediatric primary care and subspecialist providers’ comfort, attitudes and practices screening and referring for social determinants of health. BMC Health Serv Res. 2021;21(1):956. https://doi.org/10.1186/s12913-021-06975-3 . PMID:34511119;PMCID:PMC8436516.
Andermann A; CLEAR Collaboration. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ. 2016;188(17–18):E474–83. https://doi.org/10.1503/cmaj.160177 .
Article Google Scholar
Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24(9):399–404. https://pubmed.ncbi.nlm.nih.gov/33989068/ . PMID: 30222918; PMCID: PMC6426124.
PubMed PubMed Central Google Scholar
McQueen A, Li L, Herrick CJ, Verdecias N, Brown DS, Broussard DJ, Smith RE, Kreuter M. Social Needs, Chronic Conditions, and Health Care Utilization among Medicaid Beneficiaries. Popul Health Manag. 2021;24(6):681–90. https://doi.org/10.1089/pop.2021.0065 . PMID: 33989068; PMCID: PMC8713253.
National Academies of Sciences, Engineering, and Medicine. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. Washington: The National Academies Press; 2019. https://doi.org/10.17226/25467 .
Book Google Scholar
Pfeiffer EJ, De Paula CL, Flores WO, Lavallee AJ. Barriers to Patients’ Acceptance of Social Care Interventions in Clinic Settings. Am J Prev Med. 2022;63(3 Suppl 2):S116–21. https://doi.org/10.1016/j.amepre.2022.03.035 . Epub 2022 Aug 17 PMID: 35987523.
Article PubMed Google Scholar
Centers for Medicare and Medicaid Services, Centers for Medicare and Medicaid Innovation Sate Innovations Group. https://innovation.cms.gov/files/x/mdtcocm-rfa.pdf . Accessed 9 Apr 2023.
Sandhu S, Xu J, Eisenson H, Prvu Bettger J. Workforce Models to Screen for and Address Patients’ Unmet Social Needs in the Clinic Setting: A Scoping Review. J Prim Care Community Health. 2021;12:21501327211021020. https://doi.org/10.1177/21501327211021021 . PMID: 34053370; PMCID: PMC8772357.
Kreuter MW, Thompson T, McQueen A, Garg R. Addressing Social Needs in Health Care Settings: Evidence, Challenges, and Opportunities for Public Health. Annu Rev Public Health. 2021;42:329–44. https://doi.org/10.1146/annurev-publhealth-090419-102204 . Epub 2021 Dec 16. PMID: 33326298; PMCID: PMC8240195.
Measuring Social Determinants of Health among Medicaid Beneficiaries: Early State Lessons. Center for Health Care Strategies, Inc. 2016. https://www.chcs.org/media/CHCS-SDOH-Measures-Brief_120716_FINAL.pdf . Accessed 21 June 2023.
States Reporting Social Determinants of Health Related Policies Required in Medicaid Managed Care. Kaiser Family Foundation. 2022. https://www.kff.org/other/state-indicator/states-reporting-social-determinant-of-health-related-policies-required-in-medicaid-managed-care-contracts/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D . Accessed 21 June 2023.
Social Determinants of Health Measurement Work Group: Final Report. Oregon Health Authority. 2021. https://www.oregon.gov/oha/HPA/ANALYTICS/SDOH%20Page%20Documents/SDOH%20final%20report%202_10_21.pdf . Accessed 21 June 2023.
The Gravity Project: Accelerating National Social Determinants of Health (SDOH) Data Standards. Gravity Project. 2022. https://confluence.hl7.org/download/attachments/46892727/Gravity%20Overview%20One%20Pager%2020220209.pdf?version=1&modificationDate=1644529823670&api=v2 . Accessed 21 June 2023.
Quality ID #487: Screening for Social Drivers of Health. Centers for Medicare & Medicaid Services. 2022. https://qpp.cms.gov/docs/QPP_quality_measure_specifications/CQM-Measures/2023_Measure_487_MIPSCQM.pdf . Accessed 21 June 2023.
Identifying and Addressing Social Needs in Primary Care Settings. Agency for Healthcare Research and Quality. 2021. https://www.ahrq.gov/sites/default/files/wysiwyg/evidencenow/tools-and-materials/social-needs-tool.pdf . Accessed 21 June 2023.
The Health Leads Social Health Data Toolkit. Health Leads. 2021. https://healthleadsusa.org/wp-content/uploads/2021/02/Health-Leads-Social-Health-Data-Toolkit.pdf . Accessed 21 June 2023.
A Guide to Using the Accountable Health Communities Health-Related Social Needs Screening Took: Promising Practices and Key Insights. Centers for Medicare & Medicaid Services. 2023. https://www.cms.gov/priorities/innovation/media/document/ahcm-screeningtool-companion . Accessed 21 June 2023.
Beidler LB, Razon N, Lang H, Fraze TK. “More than just giving them a piece of paper”: Interviews with Primary Care on Social Needs Referrals to Community-Based Organizations. J Gen Intern Med. 2022;37(16):4160–7. https://doi.org/10.1007/s11606-022-07531-3 . Epub 2022 Apr 14. PMID: 35426010; PMCID: PMC9708990.
Child Care and Housing: Big Expenses with Too Little Help Available. Center on Budget and Policy Priortities. 2019. https://www.cbpp.org/research/housing/child-care-and-housing-big-expenses-with-too-little-help-available . Accessed 13 July 2023.
Key facts about housing affordability in the U.S. Pew Research Center. 2022. https://www.pewresearch.org/short-reads/2022/03/23/key-facts-about-housing-affordability-in-the-u-s/ . Accessed 13 July 2023.
Soumerai SB, Pierre-Jacques M, Zhang F, et al. Cost-related medication nonadherence among elderly and disabled medicare beneficiaries: a national survey 1 year before the medicare drug benefit. Arch Intern Med. 2006;166(17):1829–35. https://doi.org/10.1001/archinte.166.17.1829 . PMID: 17000938.
Naci H, Soumerai SB, Ross-Degnan D, Zhang F, Briesacher BA, Gurwitz JH, Madden JM. Medication affordability gains following Medicare Part D are eroding among elderly with multiple chronic conditions. Health Aff (Millwood). 2014;33(8):1435–43. https://doi.org/10.1377/hlthaff.2013.1067 . PMID:25092846;PMCID:PMC4340076.
Studies and Data Analytics on Broadband and Health. Federal Communications Commision. 2022. https://www.fcc.gov/health/sdoh/studies-and-data-analytics . Accessed 13 July 2023.
Yu J, Meng S. Impacts of the Internet on Health Inequality and Healthcare Access: A Cross-Country Study. Front Public Health. 2022;9(10):935608. https://doi.org/10.3389/fpubh.2022.935608 . PMID:35757602;PMCID:PMC9218541.
Grasso C, McDowell MJ, Goldhammer H, Keuroghlian AS. Planning and implementing sexual orientation and gender identity data collection in electronic health records. J Am Med Inform Assoc. 2019;26(1):66–70. https://doi.org/10.1093/jamia/ocy137 . PMID:30445621;PMCID:PMC6657380.
Download references
Acknowledgements
Not applicable
This study was supported by the Centers for Disease Control and Prevention’s National Initiative to Address COVID-19 Health Disparities Among Populations at High-Risk and Underserved, Including Racial and Ethnic Minority Populations and Rural Communities grant number OT21-2103 through the Maryland Department of Health.
Author information
Authors and affiliations.
Implementation Science, Healthcare Delivery Research Program, MedStar Health Research Institute, 6525 Belcrest Road, Suite 700, Hyattsville, MD, 20782, USA
Claire M. Starling, Marjanna Smith & Hannah Arem
Department of Emergency Medicine, Georgetown University School of Medicine, 3900 Reservoir Road, Washington, NWDC, 20007, USA
National Center for Human Factors in Healthcare, MedStar Health Research Institute, 3007 Tilden St.Suite 6N, Washington, NWDC, 20008, USA
Sadaf Kazi & Arianna Milicia
Maryland Primary Care Program, Maryland Department of Health, 201 W. Preston Street, Baltimore, MD, 21201, USA
Rachel Grisham & Emily Gruber
MedStar Center for Biostatistics, Informatics and Data Science, MedStar Health Research Institute, 3007 Tilden St.Suite 6N, Washington, NWDC, 20008, USA
Joseph Blumenthal
Department of Oncology, Georgetown University School of Medicine, 3900 Reservoir Road, Washington, NWDC, 20007, USA
Hannah Arem
You can also search for this author in PubMed Google Scholar
Contributions
CMS and HA analyzed and interpreted the data and drafted the manuscript. MS, SK, AM, RG, EG, and JB contributed to revising the manuscript. All authors approved the version to be published and agreed to be accountable for the accuracy and integrity of the data.
Corresponding author
Correspondence to Claire M. Starling .
Ethics declarations
Ethics approval and consent to participate.
No consent was obtained to collect this data originally as it is mandated as part of CMS reporting. Using this data in the aggregate for publication was reviewed by the Georgetown University/Medstar Health IRB and deemed exempt (study 4698, modification approval date: December 15, 2022). CMS and the Maryland Department of Health approved the Georgetown/MedStar IRB decision.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Starling, C.M., Smith, M., Kazi, S. et al. Understanding social needs screening and demographic data collection in primary care practices serving Maryland Medicare patients. BMC Health Serv Res 24 , 448 (2024). https://doi.org/10.1186/s12913-024-10948-7
Download citation
Received : 22 January 2024
Accepted : 03 April 2024
Published : 10 April 2024
DOI : https://doi.org/10.1186/s12913-024-10948-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social needs screening
- Demographic data collection
- Primary care
- Community resources
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Sultan Qaboos Univ Med J
- v.8(1); 2008 Mar
Qualitative Research and its Uses in Health Care
Although relatively uncommon in health care research, qualitative research is now receiving recognition and is increasingly used in health care research with social and cultural dimensions. Unlike quantitative research, which is deductive and tends to analyze phenomena in terms of trends and frequencies, qualitative research seeks to determine the meaning of a phenomenon through description. It aims to develop concepts that aid in the understanding of natural phenomena with emphasis on the meaning, experiences and views of the participants. Differences among qualitative researchers exist on matters of ontology, epistemology, data collection methods and methods of evaluation. The aim of this article is not to act as a practical guide on how to conduct qualitative research, but is an attempt to give an introduction to qualitative research methods and their use in health-related research.
Q ualitative research is defined as an umbrella term covering an array of interpretative techniques which seek to describe, decode, translate and otherwise come to terms with the meaning, not the frequency, of certain more or less naturally occurring phenomena in the social world. 1 , 2
As a method of inquiry, it was first used by sociologists and anthropologists in the early twentieth century, although it existed much earlier than that in its non-structural form. Researchers studied cultures and groups in their own and foreign settings and told stories of their experience long before then. In the 1920s and 1930s, social anthropologists and sociologists implemented a more focused approach compared to the old unsystematic and journalistic style used in those days. Since the 1960s, qualitative research has experienced a steady growth starting with the development of grounded theory and new publications in ethnography. 3 , 4 The number of books, articles and papers related to qualitative research has increased tremendously during the past 20 years and more researchers, including health-related professionals, have moved to a more qualitative paradigm adapting and modifying these approaches to the study needs of their own areas. 4
Since qualitative research does not aim to enumerate, it is sometimes viewed as the exact opposite to quantitative methods and the two methods are frequently presented as antagonists. Quantitative research is based on structure and uses experiments and surveys as methods. In addition, it is deductive in nature and uses statistical sampling methods. In contrast, qualitative research is described as an action research using observation and interview methods. It is inductive in nature and depends on the purposeful selection of participants. Whereas quantitative researchers use reliability as a way of verification, qualitative researchers use validity. Recently, there has been a growing recognition that the quantitative-qualitative debate and distinction is unnecessary and that it would be more fruitful for the relation between the two methods to be complementary and overlapping rather than exclusive. 6 In fact, neither qualitative nor quantitative research is superior to the other; there are weaknesses and strengths in each method. Qualitative and quantitative research methods can indeed be seen as complementary and both are necessary to provide an understanding of a phenomenon.
Several researchers have argued that the research questions and the phenomenon under investigation should determine the methodology to used. 7 , 8 , 9 The crucial question, therefore, is not “what is the best research method?” but “what is the best research method for answering this question most effectively and efficiently?” 10 So, while qualitative and quantitative research may well investigate similar topics, each will address a different type of question. Holman sums up this position: “true understanding in medicine cannot be achieved without adding qualitative methods to the research arsenal”. 11
Traditional quantitative methods, such as randomised controlled trials, are the appropriate means of testing, for example, the effect of an intervention or a treatment, while a qualitative exploration of beliefs and understandings is needed to find out why the results of research are often not implemented in clinical practice. The aim of qualitative research is to develop concepts that can help us understand social phenomena in natural settings, giving emphasis on the meanings, experiences and views of the participants. 10
Qualitative research methods are the most suitable for this approach because of their emphasis on people’s lived experience. They are considered to be well suited for locating the meanings that people place on the events, processes, and structures of their lives and their perceptions, presuppositions and assumptions. 5 In his advice to graduate students, Patton lists a number of conditions that are suitable for a qualitative study. These include: questions about people’s experiences; inquiry into the meanings people make of their experiences; studying a person in the context of her or his social/interpersonal environment and research where it is difficult to develop a standardised instrument due to the lack of knowledge on the phenomenon. 12
ARGUMENTS FOR AND AGAINST QUALITATIVE METHODS
There are major differences of opinions among qualitative researchers on matters of ontology and epistemology as well as the methods to be used and criteria of evaluation. There are also disagreements about the nature, purpose, status and practice of its methods. A large number of authors take a predominantly method-based approach; authors such as Miles and Huberman 5 and Patton 12 put emphasis on data collection techniques. Another approach is to classify qualitative research according to research traditions, i.e. whether phenomenological, grounded theory or ethnography, amongst others. Authors such as Creswel 9 and Denzin and Lincolin 3 prefer this approach, which has the advantage of being based on systematisation of knowledge providing a sense of order and orientation. On the other hand, it has the disadvantage of oversimplification, ignoring the issues of the research question and conceptual frameworks used and the way these issues can shape the research process and the findings. 13 In addition, some researchers have decided to classify qualitative research according to the research question or the method of analysis.
Although the majority of qualitative researchers stress that qualitative research is inductive in nature, in contrast to quantitative research which is deductive, there are qualitative researchers who argue that both can be used for different purposes and at different times, and that qualitative research can be done in a deductive way where prior assumptions are tested on new cases. 14 Retroduction, which is defined as the movement backward and forward between theory and data or the combination of deduction and induction, is said to be a characteristic of qualitative research. 11 The degree of deduction or induction and which one follows the other depends on the research question. 12 .
Guba and Lincoln 15 used the term “emergent design” to describe a qualitative study design that emerges as the study progresses in response to the researcher’s early observations. There are also qualitative studies in health care that base their research questions on the results of prior literature of quantitative studies on the subject. 16 , 17 While the research questions in these studies were relatively precise, the method used was flexible.
Miles and Huberman 5 state that no study conforms exactly to a standard methodology and that the researcher bends the methodology to the peculiarities of the study. According to Creswell, 9 traditions of inquiry used “need not be pure, and one might mix procedures from several”. Mixing approaches and procedures is encouraged by some authors and regarded as a creative approach to qualitative research. 12
Studies using qualitative research in health care have been criticised for the misguided separation of method from theory and of technique from the conceptual underpinnings. 18 However, qualitative health researchers respond by stating that the choice of method and how it is used can perfectly well be matched to what is being studied rather than to the methodological leanings of the researcher. 10 It has been suggested that incorporating qualitative research method experts into health research teams enriches research and ensures that the right methodology is used for answering the right questions. Finally, using qualitative methods in health-related research has resulted in more insight into health professionals’ perceptions of lay participation in care and identification of barriers to changing healthcare practice.
QUALITATIVE RESEARCH APPROACHES
Grounded theory, phenomenology and ethnography are three approaches used in qualitative research. Grounded theory approach is a commonly used qualitative method in the social sciences to inductively generate or discover a theory out of the data. 9 Phenomenology and ethnography are more commonly used qualitative approaches in health care and will be highlighted below.
PHENOMENOLOGY
One of the major strengths of qualitative research is its emphasis upon understanding the phenomenon of interest holistically and in its context. The term phenomenology is popular and widely embraced, but its meaning has become confusing and faint. Different researchers refer to phenomenology differently. It can refer to an inquiry paradigm, an interpretive theory, a philosophy, an analytical perspective, a major qualitative research tradition or a research method framework. 12
In spite of the differences, all of these approaches share the focus of phenomenology, which is exploring how human beings make sense of experience and the meaning they give to these experiences. Phenomenology is being used in the social and human sciences including sociology, education, psychology, nursing and health sciences. 9
Phenomenologists are interested in how people put together the phenomena they experience in such a way as to make sense of the world and develop a worldview. They assume commonality in human experience and focus on meaning-making as the essence of human experience. The essence is the core meaning mutually understood through a phenomenon commonly experienced. 12 The phenomenon under study may be emotions, relationships, a programme, an organisation or a culture. 12 Bracketing is one of the central ideas in phenomenology. It means that the researcher has to set aside all of his prejudgments and his previous experience about the phenomena and approach the field with an open mind, imagination and intuition. Although important, bracketing is often said to be a difficult task. 9
Patton 12 describes the difference between conducting a phenomenological study and using a phenomenological perspective to a study. He argues that, “one can employ a general phenomenological perspective to elucidate the importance of using methods that capture people’s experience of the world without conducting a phenomenological study that focuses on the essence of shared experience”.
ETHNOGRAPHY
In ethnography, the researcher studies the structure and function of a group of people. An example of a structure or configuration is the kinship, while the function refers to patterns of relationships affecting and regulating behaviour. 9 The aim of ethnographic studies is to give a holistic picture of the social group studied, attempting to describe aspects of the cultural and social system of that particular group. These aspects could be the group history, religion, economy, politics or environment.
Data collection methods vary in ethnographic studies with observation and interviews being the most popular methods. Although some authors expressed concern that anthropological methods may be misused or applied superficially by the medical profession, 19 others, however, expressed the need for acknowledging and incorporating ethnographic methods in health care research. 20 Savage 19 explains that today the term ethnography can be applied to any small-scale social research carried out in everyday settings and uses several methods evolving in design and focusing on an individual’s meanings and explanations. In health care, ethnography has been used in topics related to health beliefs and practices, allowing these issues to be viewed in the context in which they occur and therefore helping broaden the understanding of behaviours related to health and illness. 20
In addition, there has been an increase in the amount of cross-cultural research and a change in the form of this research. Recently, more short-term ethnographic and cross-cultural studies have been undertaken, for example, studies sponsored by international development agencies or student exchange projects. 12
QUALITATIVE RESEARCH INSTRUMENTS
Qualitative research instruments used for data collection include interviews, observations, and analysis of documents. Interviews are the most common techniques used to gather research information. There are three types of interviews: structured, semi-structured and unstructured, described in some books as structured, informed and guided, respectively. 13
The semi-structured interview is more commonly used in health care-related qualitative research. Such an interview is characteristically based on a flexible topic guide that provides a loose structure of open-ended questions to explore experiences and attitudes. It has the advantage of great flexibility, enabling the researcher to enter new areas and produce richer data. In addition, it helps the researcher to develop a rapport with the informants. Semi-structured interviews elicit people’s own views and descriptions and have the benefit of uncovering issues or concerns that have not been anticipated by the researcher. 6 They are commonly used when the aim is to gain information on the perspectives, understandings and meanings constructed by people regarding the events and experiences of their lives. However, this type of interviewing is claimed to reduce the researcher’s control over the interview situation and take a longer time to conduct and analyse, in addition to the difficulties of the analysis process. 21
In health care, interviews are the appropriate tool to be used if the research is concerned with interpersonal aspects of care or if the available evidence is limited. 6
Another qualitative research instrument that can be used in health care research is the focus group. Focus group interviews have the advantage of being more time efficient as more people can be interviewed for the same amount of time. They also provide a richer source of data. On the other hand, focus group interviews tend to document the ‘public’ rather than the ‘private’ views of the individuals. In addition some people do not interview well in-group situations. 13
THE USE OF THE INTERVIEW GUIDE
Some qualitative researchers are reluctant to plan a design of their study in advance of the data collection. They argue that the phenomenon studied must first be discovered and they describe their design as emergent. However, increasingly more qualitative researchers appear ready to define a research question and develop an interview guide prior to starting the data collection. 11 Patton defines an interview guide as a series of topics or broad interview questions which the researcher is free to explore and probe with the interviewee. 12 The advantage of an interview guide is that it helps the interviewer pursue the same basic lines of inquiry with each person interviewed and manage the interviews in a more systematic and comprehensive way. The findings of earlier work are increasingly being used as a facilitator for further research. However, concepts drawn from earlier work are supposed to be held lightly and to be subject to reformulation or rejection by the researcher especially as the study goes on and the research progresses. 11 The extent to which such a flexibility of design is important will vary depending on the topic and the aim of the study.
Sampling strategies in qualitative research are largely determined by the purpose of the study. Statistical representativeness is not considered as a prime requirement in qualitative research and is not normally sought. Furthermore, qualitative data collection is more time consuming and expensive, which makes the use of a probability sample impractical. 6 The aim of sampling in qualitative research is to identify specific groups of people who hold characteristics or live in circumstances relevant to the phenomena being studied. In this way, identified informants are expected to enable enriched exploration of attitudes and aspects of behaviour relevant to the research. 10 Two types of samples used in qualitative research, maximum variation and homogenous samples, are explained below.
According to Patton, 12 maximum variation sampling is where the researcher attempts to study a phenomenon by seeking out settings or persons that represent the greatest differences in that phenomenon. A maximum variation sample documents diverse variations and identifies important common patterns by representing diverse cases to develop fully multiple perspectives about the cases. 9 This means that the participants are sampled based on particular predetermined criteria in order to cover a range of constituencies, such as different age, cultural background or class. 6
Similarly, the researcher can select the setting of the data collection on the basis that it is sufficiently similar to other settings in which generalisation is sought. This way the researcher is demonstrating the possibility that the setting studied is representative of the population studied. 2
In homogeneous sampling, the researcher chooses a small homogenous sample with the purpose of describing some particular subgroups in depth. 12
The sample size in qualitative research is not determined by fixed rules, but by factors such as the depth and duration of the interview and what is feasible for a single interviewer. 22 Although it is theoretically possible to carry out qualitative research on large samples, qualitative researchers find themselves obliged by time and resource limits to trade breadth for depth. 11 The sample size for interview studies is usually much smaller than those of a quantitative research, usually not exceeding 50 participants, although this can vary with the research question asked. 6 Patton 12 states, “there are no rules for sample size in qualitative inquiry”. In other words, sample size depends on the aim of the study and what is possible, given the time and resources available.
ANALYSING QUALITATIVE RESEARCH
Although there are plenty of guidelines for analysing qualitative research, applying these guidelines requires judgment and creativity because each qualitative study is unique. 12 A researcher might also be confused by the different terms used by qualitative researchers when describing analysis. Analysis might be described as interpretation, making sense of data, or transforming data. Analysis is sometimes presented to indicate different procedures based on language, theory or what is described as interpretive/descriptive analysis. 11 However, overlap can take place between these different methods and a researcher might decide to use a method of analysis that is based on language, such as symbolic interactionist, while using grounded theory to develop a theory at the same time. Most of the analytical approaches to qualitative research in health care are ‘generic’ and are not labelled within one of the specific traditions of qualitative research. A common approach in most of these studies is general and inductive in nature, but does not comply with the very systematic and rigorous inductive approach of grounded theory. In addition, it has been described that many researchers use a simple two-level analysis scheme followed by a more specific level. This means that the researcher can initiate the analysis based on the conceptual framework used in order to produce more inductive data, and the coding moves from the descriptive to the more interpretative and inferential codes. 5
COMPUTER USE IN QUALITATIVE DATA ANALYSIS
Qualitative research studies typically produce very large amount of data that needs to be managed efficiently. Computer packages can improve the efficiency of data management. 11 Computer programs provide a way of storing and retrieving material. They are therefore useful in locating cases, statements, phrases or even words, thereby replacing the tedious and time-consuming process of “cutting and pasting” and “colour coding”. The use of computer packages, however, is claimed to distance the analyst from the data, 11 and may take the place of a close and careful analysis. Using a computer programme can lead to quantitative analysis instead of qualitative, for example, counting occurrences, giving more weight to more frequent events, and ignoring isolated incidences. 23 In addition, computer programmes are said to fix and label categories during the analysis process and the researcher may be reluctant to change these categories. 9 Furthermore, the researcher is required to learn the computer programme, which may add to the time and effort he or she will need to spend on the research project. The researcher also has to be aware of the limitations of computer programmes. While computer packages can help with the intensive process of analysis and the management of large data sets, they are not a substitute for “immersion” in the data, and thorough knowledge that can enable the researcher to make comparisons, identify patterns and develop interpretations. 6 There are different packages available: Ethnograph, Atlas and NUD.IST are the mostly used. QSR NVivo is a new product developed by the makers of NUD.IST and is user-friendlier, more suitable for individual research projects and more visually attractive than previous packages.
THE ROLE OF THE RESEARCHER IN QUALITATIVE RESEARCH
Patton 12 states that, “the human element in qualitative research is both its strength and weakness”. It is considered a point of strength because it allows human insight and experience to develop new understandings of the world, and a point of weakness because it depends heavily on the researcher’s skills, creativity, training and intellect. Qualitative methods depend on both critical and creative thinking and the balance between the two in conducting the study and interpreting its results. The role of the researcher is approached differently according to the type of research tradition used. A phenomenologist researcher is required to bracket his/her own assumptions when collecting data. On the other hand, in an ethnographic study, the effect of the researcher on the interview and the interaction is seen as inevitable and important in shaping the results of the study.
Although practising clinicians routinely interview patients during their clinical work, interviewing is a well-established technique in sociology and related disciplines. One of the differences between clinical and research-aimed interviews lies in their different purposes. The usual aim of the clinical interview is to fit the patient’s problem into the appropriate medical category for diagnosis and management. On the other hand, the aim of a qualitative research interview is to discover the interviewee’s own meaning and avoid prior assumptions and preset categories. 22 Having said that, there are general skills in clinical interviewing that can be useful, such as listening and observation. A good level of self-awareness is necessary in the researcher in order to reduce possible biases.
Researchers in qualitative research need to consider how they are perceived by interviewees and the effect of features related to the researcher, such as class, race, and sex on the interview. This question is more important if the interviewee knows that the interviewer is a doctor. It has been described that a patient, or someone who is likely to be become one, may give what he or she thinks is a desirable response, thinking that the doctor will be pleased.
RIGOUR IN QUALITATIVE RESEARCH
Health field research is generally quantitative and based on biomedical traditions and experimental methods. In this field, qualitative research is criticized for being subject to researcher bias and for lacking reproducibility and generalisability. 10 Researchers presenting their qualitative work in health-related research are partly responsible for this view. Many qualitative researchers neglect the importance of giving an adequate description of their theoretical concepts and methods used in their research. A systematic research method is also essential when conducting qualitative research. Rigour in qualitative research includes procedures taken at different stages of the research process including during data collection and analysis. Several procedures have been described to increase rigour in qualitative research. For example, triangulation is commonly used as a way of validating of data.
TRIANGULATION
In triangulation, the researcher uses multiple methods, sources, researchers or theories to provide evidence that strengthens his or her study. Triangulation provides different ways of looking at the same phenomenon and adds credibility and confidence in the conclusions drawn from the study. There are two main types of triangulation, triangulation of sources and analyst triangulation. Patton 12 defines triangulation of sources as “checking out the consistency of different data sources within the same method”. When using this type of triangulation, the researcher compares the perspectives of people from different points of view. For example, studies in programme evaluation might compare the views of staff, clients or funding bodies. 12 Studies in health care have used this method of verification to study the accounts of doctors, patients, and managers in order to identify similarities and differences in views. An example is the study of patients’ versus doctors’ agendas in general practice. 23 Both similarities and differences from different sources, when given reasonable explanation, could contribute significantly to the credibility of the findings. Triangulation with multiple analysts can also be used as a method of verification. It is defined as “having two or more persons independently analyse the same qualitative data and compare their findings”. 12
QUALITATIVE RESEARCH IN HEALTH CARE MANAGEMENT
Recently, there has been a greater acceptance of the qualitative approach, even as a stand-alone method, in health care research. Institutions that control funding for medical research have developed ethical guidelines for assessing qualitative studies which indicates formal acceptance of this form of research within an area previously dominated by quantitative methods. 13 More qualitative research articles are published in health-related journals, in addition to a new qualitative research journal (Qualitative Health Research).
Quality of health care is one of the areas where qualitative methods can be used. The concept of quality in health care is multidimensional and multifaceted and some of the questions asked related to the quality of care or services may not be acquiescent to quantitative methods. 6 Qualitative research offers a variety of methods to be used for identifying what is really important to both patients and carers. It can also be used to identify and detect obstacles to change and the reasons why improvement does not occur. 6 It is therefore an essential component of health services research because it enables us to reach areas not amenable to quantitative research, for example, lay and professional health beliefs. In addition, qualitative description can be a prerequisite of quantitative research, particularly in areas that have received little previous investigation.
Qualitative research is widely used to study issues related to doctor-patient interaction especially in general practice. Studies concerning patients’ versus doctors’ agendas in general practice and general practitioners perceptions of effective health care are examples. 23 , 24 Recently there have been more studies concentrating on patients’ own perceptions and views regarding their health and health care services, for example a study on women’s views on the impact of operative delivery in the second stage of labour. 25 Another example is the study on middle-aged person’s experience of living with severe heart failure. 26
Another area where qualitative research is being used in health care is to identify obstacles and barriers to practice change by exploring the reasons behind certain behaviours. A good example of this is the study of patients’ decisions about whether or not to take anti-hypertensive drugs. 27 There are similar studies on issues such as the use of antibiotics in general practice and patient compliance.
In addition to issues related to the patients’ perception, some qualitative studies concentrated on factors fostering the doctor’s motivation and the effect of doctors’ social life and culture, in addition to issues related to the doctor’s own health. Examples are the study by Dumelow et al. 28 on the relation between a career and family life for English hospital consultants. Another example is a study aimed at exploring general practitioners’ perceptions of the effects of their profession and training on their attitudes to illness in themselves and colleagues. 29
Qualitative work can help in identifying cultural and social factors that affect health care positively or negatively. Such information can be helpful in improving service delivery. 6 Studies on patients from ethnic minorities have identified administrative and language barriers that affected health care and shed light on some of the beliefs and behaviours of these patients that might have affected help seeking and compliance. Good examples are the studies by Bush et al. 30 exploring the influences on smoking in Bangladeshi and Pakistani adults in the UK, and the multi-centre cross-cultural postnatal depression study. 31
There has been an increasing interest and use of qualitative research methods in primary health care and general practice articles. Britten 32 states that “the nature of general practice is such that a variety of research methods are needed to explore all its intricacies” He adds that qualitative methods can enrich research in general practice by opening up areas not amenable to quantitative methods, topics such as patient satisfaction, doctor-patient interaction, in addition to identifying and explaining attitudes, beliefs and behaviour. In addition, qualitative research has been used in the assessment of new technology methods used in health care. For example, the studies on the implementation of the National Health System information technology programme in the UK. 11 , 33
Qualitative research methods are receiving an increasing recognition in health care related research. The use of qualitative research in health care enables researchers to answer questions that may not be easily answered by quantitative methods. Moreover, it seeks to understand the phenomenon under study in the context of the culture or the setting in which it has been studied, therefore, aiding in the development of new research instruments, such as questionnaires that are more culturally acceptable. However, because health care related research has, for decades, been based on quantitative methods, the introduction of a new method requires researchers in health care who attempt to use it, to have a thorough understanding of its theoretical basis, methodology and evaluation techniques.
Acknowledgments
I would like to thank Sultan Qaboos University, Oman, for granting me a scholarship to do my PhD at the University of Nottingham, UK. I am also grateful to my PhD supervisor, Dr Margaret Oates, for her guidance and support.
- 44-207-097-1871
Dissertation Writing Tools
- 1. Complete Dissertation Writing Guide - eBook
- 2. Dissertation Templates Pack
- 3. Research Methodology Handbook
- 4. Academic Writing Checklist
- 5. Citation Style Guide
- 6. Time Management for Dissertation Writing
- 7. Literature Review Toolkit
- 8. Grammar and Style Guide
- 9. Dissertation Proposal Template
- 10.Five Pre-written Full Dissertation Papers

57+ Best Health and Social Care Dissertation Topics in 2023
Are you in the process of developing a health dissertation Topic? Have you already decided what you want to write about? Do you know how you will compile the paper? It is not as easy as it seems. In order to write a satisfying dissertation, you should gather sufficient information, organize the data, identify your […]

Table of Contents
Are you in the process of developing a health dissertation Topic?
Have you already decided what you want to write about, do you know how you will compile the paper.
It is not as easy as it seems. In order to write a satisfying dissertation, you should gather sufficient information, organize the data, identify your target audience, and determine the most appropriate topic for your research. Here are some tips that can help you with your decision.
A health dissertation topic should be something you really interested in. If your topic makes you curious and you’re eager to discover its solution, then you’re on the right track. But first, you need to absolutely know what you want to get from your research. For locating current research topics related to health, your best resource is usually medical journals.
You will choose the best health and social care dissertation topic, but great ideas can be taken through a renowned website. It will give you an edge over your friends and cut a niche for you in academic writing. The researchers usually dig deep into the subject with careful analysis.
The literature reviews are given balanced arguments and justification that demonstrate the logical and far-reaching ability of the aspirant. There are many health and social care dissertation topics that are unique enough to build a novelty for aspiring students. Here are some excellent examples for you.
Best Health and Social Care Dissertation Topics
If you are looking level 5 diploma in health and social care research project ideas below topics list give you the perfect idea for your required topics.
- Depression Health: Society is the biggest force that leads to the vehicle of depression among people of different age groups.
- Mitigation of diseases: How does society play the best role in the mitigation of diseases from the life of an orphan child by adopting them for medical expenditure?
- Health-Related Skills: Requirement of health-related skills for the people of society to show their social care towards the marginal sections of society.
- Health Problems and nurse role: How a nurse can aware of the people of society towards the different health problems and precautions related to them?
- Health Care Facilities: How people from lower-strata and marginal sections of society can be given the best health care facilities with the contribution of society?
- Depression Health Care: How to improve the condition of a person going through depression by providing him or her social support and care?
- Health Sector related to depression: What are the different aspects that fall under social care in the health sector related to depression?
- Health-related death: Improvement in the scenario of health-related death in developing countries through social care.
- Nurse role in providing health facilities: How nurses can play a significant role by providing health facilities to needy people free of cost?
- Nursing ethics suggest towards health: What does nursing ethics suggest towards the health and social care of people in society?
- Health Facilities for Old Age: Things that hinder the path of society in providing health-care facilities to needy people in old-age homes?
- Nursing care for old Age: How is the idea of part-time working in Orphanage-houses and old-age homes for nursing?
- Nursing profession: Social care is a vital part of the nursing profession as per its ethics.
- Care towards orphan children: Why it is important to make the adoption law easy to help society in showing their care towards orphan children?
- Social care importance in the health sector: Importance of social care in the health sector and how to enhance its level with law and policies?
- An analysis of the impact of the COVID-19 pandemic on the mental health of healthcare workers
- A comparative study of the effectiveness of different methods of managing chronic pain
- The role of community-based organizations in addressing health disparities
- An exploration of the use of telehealth in rural areas
- An analysis of the impact of social media on body image and disordered eating among young adults
- A comparative study of the effectiveness of different approaches to addiction treatment
- An exploration of the challenges and successes of implementing electronic health records in healthcare organizations
- An analysis of the impact of poverty on health outcomes
- A study of the effectiveness of interventions to reduce stigma surrounding mental illness
- An exploration of the challenges and successes of implementing health promotion programs in low-income communities
- A study of the relationship between social support and health outcomes in older adults
- An analysis of the impact of social determinants of health on cardiovascular disease risk
- A comparative study of the effectiveness of different approaches to managing obesity
- An exploration of the use of mindfulness-based therapies for anxiety and depression
- A study of the impact of workplace wellness programs on employee health and productivity
- An analysis of the role of cultural competence in healthcare delivery
- A comparative study of the effectiveness of different approaches to managing diabetes
- An exploration of the impact of social support on cancer outcomes
- A study of the effectiveness of interventions to reduce health disparities among racial and ethnic minorities
- An analysis of the impact of social media on the spread of misinformation about health
- A comparative study of the effectiveness of different approaches to managing hypertension
- An exploration of the challenges and successes of implementing palliative care in healthcare organizations
- A study of the impact of social support on the health of individuals with chronic illnesses
- An analysis of the impact of socioeconomic status on access to healthcare
- A comparative study of the effectiveness of different approaches to managing chronic fatigue syndrome
- An exploration of the impact of stigma on the mental health of LGBTQ+ individuals
- A study of the effectiveness of interventions to reduce health disparities among low-income communities
- An analysis of the role of community health workers in addressing health disparities
- A comparative study of the effectiveness of different approaches to managing rheumatoid arthritis
- An exploration of the impact of social support on the health of individuals with mental illnesses
- A study of the effectiveness of interventions to reduce health disparities among indigenous populations
- An analysis of the impact of social determinants of health on mental health outcomes
- A comparative study of the effectiveness of different approaches to managing asthma
- An exploration of the impact of stigma on the mental health of individuals with substance use disorders
- A study of the effectiveness of interventions to reduce health disparities among immigrants
- An analysis of the impact of social media on the spread of misinformation about vaccines
- A comparative study of the effectiveness of different approaches to managing multiple sclerosis
- An exploration of the impact of social support on the health of individuals with disabilities
- A study of the effectiveness of interventions to reduce health disparities among refugees
- An analysis of the impact of social determinants of health on infant mortality rates
Custom Dissertation Topics Brief Service on Health and social care from Experts
Paid topic mini proposal (500 words).
You will get the topics first and then the mini proposal which includes:
- An explanation why we choose this topic.
- 2-3 research questions.
- Key literature resources identification.
- Suitable methodology including raw sample size and data collection method
- View a Sample of Service
Note: After submiting your order please must check your email [inbox/spam] folders for order confirmation and login details.If email goes in spam please mark not as spam to avoid any communication gap between us.
Get An Expert Dissertation Writing Help To Achieve Good Grades
By placing an order with us, you can get;
- Writer consultation before payment to ensure your work is in safe hands.
- Free topic if you don't have one
- Draft submissions to check the quality of the work as per supervisor's feedback
- Free revisions
- Complete privacy
- Plagiarism Free work
- Guaranteed 2:1 (With help of your supervisor's feedback)
- 2 Instalments plan
- Special discounts
Other Related Posts
- Dissertation Topics in International Relations February 20, 2024 -->
- Unlock Your Academic Potential with the Right Topics for Dissertation October 12, 2023 -->
- 89+ Best Unique and Informative Speech Topics for Students January 6, 2023 -->
- Employment Law Dissertation Topics January 4, 2023 -->
- 59 Best Environmental Law Dissertation Topics & Examples January 4, 2023 -->
- 37 Monetary economics dissertation topics ideas March 20, 2022 -->
- 39 Economic geography dissertation topics examples March 19, 2022 -->
- 37 Public economics dissertation topics Ideas March 18, 2022 -->
- 39 Financial Economics Dissertation Topics Ideas March 17, 2022 -->
- 39 Experimental economics dissertation topics Ideas March 16, 2022 -->
- 39 Environmental Economics Dissertation Topics Ideas and Samples March 15, 2022 -->
- 39 Health economics dissertation topics Ideas and Examples March 14, 2022 -->
- 39 Business economics dissertation topics Ideas and Examples March 13, 2022 -->
- 39 Behavioral Economics Dissertation Topics Examples March 12, 2022 -->
- 39 Agricultural Economics Dissertation Topics Examples March 11, 2022 -->
WhatsApp and Get 35% off promo code now!
This paper is in the following e-collection/theme issue:
Published on 11.4.2024 in Vol 26 (2024)
Patients’ Experiences With Digitalization in the Health Care System: Qualitative Interview Study
Authors of this article:

Original Paper
- Christian Gybel Jensen 1 * , MA ;
- Frederik Gybel Jensen 1 * , MA ;
- Mia Ingerslev Loft 1, 2 * , MSc, PhD
1 Department of Neurology, Rigshospitalet, Copenhagen, Denmark
2 Institute for People and Technology, Roskilde University, Roskilde, Denmark
*all authors contributed equally
Corresponding Author:
Mia Ingerslev Loft, MSc, PhD
Department of Neurology
Rigshospitalet
Inge Lehmanns Vej 8
Phone: 45 35457076
Email: [email protected]
Background: The digitalization of public and health sectors worldwide is fundamentally changing health systems. With the implementation of digital health services in health institutions, a focus on digital health literacy and the use of digital health services have become more evident. In Denmark, public institutions use digital tools for different purposes, aiming to create a universal public digital sector for everyone. However, this digitalization risks reducing equity in health and further marginalizing citizens who are disadvantaged. Therefore, more knowledge is needed regarding patients’ digital practices and experiences with digital health services.
Objective: This study aims to examine digital practices and experiences with public digital health services and digital tools from the perspective of patients in the neurology field and address the following research questions: (1) How do patients use digital services and digital tools? (2) How do they experience them?
Methods: We used a qualitative design with a hermeneutic approach. We conducted 31 semistructured interviews with patients who were hospitalized or formerly hospitalized at the department of neurology in a hospital in Denmark. The interviews were audio recorded and subsequently transcribed. The text from each transcribed interview was analyzed using manifest content analysis.
Results: The analysis provided insights into 4 different categories regarding digital practices and experiences of using digital tools and services in health care systems: social resources as a digital lifeline, possessing the necessary capabilities, big feelings as facilitators or barriers, and life without digital tools. Our findings show that digital tools were experienced differently, and specific conditions were important for the possibility of engaging in digital practices, including having access to social resources; possessing physical, cognitive, and communicative capabilities; and feeling motivated, secure, and comfortable. These prerequisites were necessary for participants to have positive experiences using digital tools in the health care system. Those who did not have these prerequisites experienced challenges and, in some cases, felt left out.
Conclusions: Experiences with digital practices and digital health services are complex and multifaceted. Engagement in digital practices for the examined population requires access to continuous assistance from their social network. If patients do not meet requirements, digital health services can be experienced as exclusionary and a source of concern. Physical, cognitive, and communicative difficulties might make it impossible to use digital tools or create more challenges. To ensure that digitalization does not create inequities in health, it is necessary for developers and institutions to be aware of the differences in digital health literacy, focus on simplifying communication with patients and next of kin, and find flexible solutions for citizens who are disadvantaged.
Introduction
In 2022, the fourth most googled question in Denmark was, “Why does MitID not work?” [ 1 ]. MitID (My ID) is a digital access tool that Danes use to enter several different private and public digital services, from bank accounts to mail from their municipality or the state. MitID is a part of many Danish citizens’ everyday lives because the public sector in Denmark is digitalized in many areas. In recent decades, digitalization has changed how governments and people interact and has demonstrated the potential to change the core functions of public sectors and delivery of public policies and services [ 2 ]. When public sectors worldwide become increasingly digitalized, this transformation extends to the public health sectors as well, and some studies argue that we are moving toward a “digital public health era” that is already impacting the health systems and will fundamentally change the future of health systems [ 3 ]. While health systems are becoming more digitalized, it is important that both patients and digitalized systems adapt to changes in accordance with each other. Digital practices of people can be understood as what people do with and through digital technologies and how people relate to technology [ 4 ]. Therefore, it is relevant to investigate digital practices and how patients perceive and experience their own use of digital tools and services, especially in relation to existing digital health services. In our study, we highlight a broad perspective on experiences with digital practices and particularly add insight into the challenges with digital practices faced by patients who have acute or chronic illness, with some of them also experiencing physical, communicative, or cognitive difficulties.
An international Organization for Economic Cooperation and Development report indicates that countries are digitalized to different extents and in different ways; however, this does not mean that countries do not share common challenges and insights into the implementation of digital services [ 2 ].
In its global Digital Government Index, Denmark is presented as one of the leading countries when it comes to public digitalization [ 2 ]. Recent statistics indicate that approximately 97% of Danish families have access to the internet at home [ 5 ]. The Danish health sector already offers many different digital services, including web-based delivery of medicine, e-consultations, patient-related outcome questionnaires, and seeking one’s own health journal or getting test results through; “Sundhed” [ 6 ] (the national health portal) and “Sundhedsjournalen” (the electronic patient record); or the apps “Medicinkortet” (the shared medication record), “Minlæge” (My Doctor, consisting of, eg, communication with the general practitioner), or “MinSP” (My Health Platform, consisting of, eg, communication with health care staff in hospitals) [ 6 - 8 ].
The Danish Digital Health Strategy from 2018 aims to create a coherent and user-friendly digital public sector for everyone [ 9 ], but statistics indicate that certain groups in society are not as digitalized as others. In particular, the older population uses digital services the least, with 5% of people aged 65 to 75 years and 18% of those aged 75 to 89 years having never used the internet in 2020 [ 5 ]. In parts of the literature, it has been problematized how the digitalization of the welfare state is related to the marginalization of older citizens who are socially disadvantaged [ 10 ]. However, statistics also indicate that the probability of using digital tools increases significantly as a person’s experience of using digital tools increases, regardless of their age or education level [ 5 ].
Understanding the digital practices of patients is important because they can use digital tools to engage with the health system and follow their own health course. Researching experiences with digital practices can be a way to better understand potential possibilities and barriers when patients use digital health services. With patients becoming more involved in their own health course and treatment, the importance of patients’ health literacy is being increasingly recognized [ 11 ]. The World Health Organization defines health literacy as the “achievement of a level of knowledge, personal skills and confidence to take action to improve personal and community health by changing personal lifestyles and living conditions” [ 12 ]. Furthermore, health literacy can be described as “a person’s knowledge and competencies to meet complex demands of health in modern society, ” and it is viewed as a critical step toward patient empowerment [ 11 , 12 ]. In a digitalized health care system, this also includes the knowledge, capabilities, and resources that individuals require to use and benefit from eHealth services, that is, “digital health literacy (eHealth literacy)” [ 13 ]. An eHealth literacy framework created by Norgaard et al [ 13 ] identified that different aspects, for example, the ability to process information and actively engage with digital services, can be viewed as important facets of digital health literacy. This argument is supported by studies that demonstrate how patients with cognitive and communicative challenges experience barriers to the use of digital tools and require different approaches in the design of digital solutions in the health sector [ 14 , 15 ]. Access to digital services and digital literacy is becoming increasingly important determinants of health, as people with digital literacy and access to digital services can facilitate improvement of health and involvement in their own health course [ 16 ].
The need for a better understanding of eHealth literacy and patients’ capabilities to meet public digital services’ demands as well as engage in their own health calls for a deeper investigation into digital practices and the use of digital tools and services from the perspective of patients with varying digital capabilities. Important focus areas to better understand digital practices and related challenges have already been highlighted in various studies. They indicate that social support, assessment of value in digital services, and systemic assessment of digital capabilities are important in the use and implementation of digital tools, and they call for better insight into complex experiences with digital services [ 13 , 17 , 18 ]. Therefore, we aimed to examine digital practices and experiences with public digital health services and digital tools from the perspective of patients, addressing the following research questions: how do patients use digital services and digital tools, and how do they experience them?
We aimed to investigate digital practices and experiences with digital health services and digital tools; therefore, we used a qualitative design and adopted a hermeneutic approach as the point of departure, which means including preexisting knowledge of digital practices but also providing room for new comprehension [ 19 ]. Our interpretive approach is underpinned by the philosophical hermeneutic approach by Gadamer et al [ 19 ], in which they described the interpretation process as a “hermeneutic circle,” where the researcher enters the interpretation process with an open mind and historical awareness of a phenomenon (preknowledge). We conducted semistructured interviews using an interview guide. This study followed the COREQ (Consolidated Criteria for Reporting Qualitative Research) checklist [ 20 ].
Setting and Participants
To gain a broad understanding of experiences with public digital health services, a purposive sampling strategy was used. All 31 participants were hospitalized or formerly hospitalized patients in a large neurological department in the capital of Denmark ( Table 1 ). We assessed whether including patients from the neurological field would give us a broad insight into the experiences of digital practices from different perspectives. The department consisted of, among others, 8 inpatient units covering, for example, acute neurology and stroke units, from which the patients were recruited. Patients admitted to a neurological department can have both acute and transient neurological diseases, such as infections in the brain, stroke, or blood clot in the brain from which they can recover completely or have persistent physical and mental difficulties, or experience chronic neurological and progressive disorders such as Parkinson disease and dementia. Some patients hospitalized in neurological care will have communicative and cognitive difficulties because of their neurological disorders. Nursing staff from the respective units helped the researchers (CGJ, FGJ, and MIL) identify patients who differed in terms of gender, age, and severity of neurological illness. Some patients (6/31, 19%) had language difficulties; however, a speech therapist assessed them as suitable participants. We excluded patients with severe cognitive difficulties and those who were not able to speak the Danish language. Including patients from the field of neurology provided an opportunity to study the experience of digital health practice from various perspectives. Hence, the sampling strategy enabled the identification and selection of information-rich participants relevant to this study [ 21 ], which is the aim of qualitative research. The participants were invited to participate by either the first (CGJ) or last author (MIL), and all invited participants (31/31, 100%) chose to participate.
All 31 participants were aged between 40 to 99 years, with an average age of 71.75 years ( Table 1 ). Out of the 31 participants, 10 (32%) had physical disabilities or had cognitive or communicative difficulties due to sequela in relation to neurological illness or other physical conditions.
Data Collection
The 31 patient interviews were conducted over a 2-month period between September and November 2022. Of the 31 patients, 20 (65%) were interviewed face-to-face at the hospital in their patient room upon admission and 11 (35%) were interviewed on the phone after being discharged. The interviews had a mean length of 20.48 minutes.
We developed a semistructured interview guide ( Table 2 ). The interview questions were developed based on the research aim, findings from our preliminary covering of literature in the field presented in the Introduction section, and identified gaps that we needed to elaborate on to be able to answer our research question [ 22 ]. The semistructured interview guide was designed to support the development of a trusting relationship and ensure the relevance of the interviews’ content [ 22 ]. The questions served as a prompt for the participants and were further supported by questions such as “please tell me more” and “please elaborate” throughout the interview, both to heighten the level of detail and to verify our understanding of the issues at play. If the participant had cognitive or communicative difficulties, communication was supported using a method called Supported Communication for Adults with Aphasia [ 23 ] during the interview.
The interviews were performed by all authors (CGJ, FGJ, and MIL individually), who were skilled in conducting interviews and qualitative research. The interviewers are not part of daily clinical practice but are employed in the department of neurology from where the patients were recruited. All interviews were audio recorded and subsequently transcribed verbatim by all 3 authors individually.
a PRO: patient-related outcome.
Data Analysis
The text from each transcribed interview was analyzed using manifest content analysis, as described by Graneheim and Lundman [ 24 ]. Content analysis is a method of analyzing written, verbal, and visual communication in a systematic way [ 25 ]. Qualitative content analysis is a structured but nonlinear process that requires researchers to move back and forth between the original text and parts of the text during the analysis. Manifest analysis is the descriptive level at which the surface structure of the text central to the phenomenon and the research question is described. The analysis was conducted as a collaborative effort between the first (CGJ) and last authors (MIL); hence, in this inductive circular process, to achieve consistency in the interpretation of the text, there was continued discussion and reflection between the researchers. The transcriptions were initially read several times to gain a sense of the whole context, and we analyzed each interview. The text was initially divided into domains that reflected the lowest degree of interpretation, as a rough structure was created in which the text had a specific area in common. The structure roughly reflected the interview guide’s themes, as guided by Graneheim and Lundman [ 24 ]. Thereafter, the text was divided into meaning units, condensed into text-near descriptions, and then abstracted and labeled further with codes. The codes were categorized based on similarities and differences. During this process, we discussed the findings to reach a consensus on the content, resulting in the final 4 categories presented in this paper.
Ethical Considerations
The interviewees received oral and written information about the study and its voluntary nature before the interviews. Written informed consent was obtained from all participants. Participants were able to opt of the study at any time. Data were anonymized and stored electronically on locked and secured servers. The Ethics Committee of the Capitol Region in Denmark was contacted before the start of the study. This study was registered and approved by the ethics committee and registered under the Danish Data Protection Agency (number P2021-839). Furthermore, the ethical principles of the Declaration of Helsinki were followed for this study.
The analysis provided insights into 4 different categories regarding digital practices and experiences of using digital tools and services in health care systems: social resources as a digital lifeline, possessing the necessary capabilities, big feelings as facilitators or barriers, and life without digital tools.
Social Resources as a Digital Lifeline
Throughout the analysis, it became evident that access to both material and social resources was of great importance when using digital tools. Most participants already possessed and had easy access to a computer, smartphone, or tablet. The few participants who did not own the necessary digital tools told us that they did not have the skills needed to use these tools. For these participants, the lack of material resources was tied particularly to a lack of knowledge and know-how, as they expressed that they would not know where to start after buying a computer—how to set it up, connect it to the internet, and use its many systems.
However, possessing the necessary material resources did not mean that the participants possessed the knowledge and skill to use digital tools. Furthermore, access to material resources was also a question of having access to assistance when needed. Some participants who had access to a computer, smartphone, and tablet and knew how to use these tools still had to obtain help when setting up hardware, updating software, or getting a new device. These participants were confident in their own ability to use digital devices but also relied on family, friends, and neighbors in their everyday use of these tools. Certain participants were explicitly aware of their own use of social resources when expressing their thoughts on digital services in health care systems:
I think it is a blessing and a curse. I think it is both. I would say that if I did not have someone around me in my family who was almost born into the digital world, then I think I would be in trouble. But I feel sorry for those who do not have that opportunity, and I know quite a few who do not. They get upset, and it’s really frustrating. [Woman, age 82 years]
The participants’ use of social resources indicates that learning skills and using digital tools are not solely individual tasks but rather continuously involve engagement with other people, particularly whenever a new unforeseen problem arises or when the participants want a deeper understanding of the tools they are using:
If tomorrow I have to get a new ipad...and it was like that when I got this one, then I had to get XXX to come and help me move stuff and he was sweet to help with all the practical stuff. I think I would have cursed a couple of times (if he hadn’t been there), but he is always helpful, but at the same time he is also pedagogic so I hope that next time he showed me something I will be able to do it. [Man, age 71 years]
For some participants, obtaining assistance from a more experienced family member was experienced as an opportunity to learn, whereas for other participants, their use of public digital services was even tied directly to assistance from a spouse or family member:
My wife, she has access to mine, so if something comes up, she can just go in and read, and we can talk about it afterwards what (it is). [Man, age 85 years]
The participants used social resources to navigate digital systems and understand and interpret communication from the health care system through digital devices. Another example of this was the participants who needed assistance to find, answer, and understand questionnaires from the health care department. Furthermore, social resources were viewed as a support system that made participants feel more comfortable and safer when operating digital tools. The social resources were particularly important when overcoming unforeseen and new challenges and when learning new skills related to the use of digital tools. Participants with physical, cognitive, and communicative challenges also explained how social resources were of great importance in their ability to use digital tools.
Possessing the Necessary Capabilities
The findings indicated that possessing the desire and knowing how to use digital tools are not always enough to engage with digital services successfully. Different health issues can carry consequences for motor skills and mobility. Some of these consequences were visibly affecting how our participants interacted with digital devices, and these challenges were somewhat easy to discover. However, our participants revealed hidden challenges that posed difficulties. In some specific cases, cognitive and communicative inabilities can make it difficult to use digital tools, and this might not always be clear until the individual tries to use a device’s more complex functions. An example of this is that some participants found it easy to turn on a computer and use it to write but difficult to go through security measures on digital services or interpret and understand digital language. Remembering passwords and logging on to systems created challenges, particularly for those experiencing health issues that directly affect memory and cognitive abilities, who expressed concerns about what they were able to do through digital tools:
I think it is very challenging because I would like to use it how I used to before my stroke; (I) wish that everything (digital skills) was transferred, but it just isn’t. [Man, age 80 years]
Despite these challenges, the participants demonstrated great interest in using digital tools, particularly regarding health care services and their own well-being. However, sometimes, the challenges that they experienced could not be conquered merely by motivation and good intentions. Another aspect of these challenges was the amount of extra time and energy that the participants had to spend on digital services. A patient diagnosed with Parkinson disease described how her symptoms created challenges that changed her digital practices:
Well it could for example be something like following a line in the device. And right now it is very limited what I can do with this (iPhone). Now I am almost only using it as a phone, and that is a little sad because I also like to text and stuff, but I also find that difficult (...) I think it is difficult to get an overview. [Woman, age 62 years]
Some participants said that after they were discharged from the hospital, they did not use the computer anymore because it was too difficult and too exhausting , which contributed to them giving up . Using digital tools already demanded a certain amount of concentration and awareness, and some diseases and health conditions affected these abilities further.
Big Feelings as Facilitators or Barriers
The findings revealed a wide range of digital practices in which digital tools were used as a communication device, as an entertainment device, and as a practical and informative tool for ordering medicine, booking consultations, asking health-related questions, or receiving email from public institutions. Despite these different digital practices, repeating patterns and arguments appeared when the participants were asked why they learned to use digital tools or wanted to improve their skills. A repeating argument was that they wanted to “follow the times, ” or as a participant who was still not satisfied with her digital skills stated:
We should not go against the future. [Woman, age 89 years]
The participants expressed a positive view of the technological developments and possibilities that digital devices offered, and they wanted to improve their knowledge and skills related to digital practice. For some participants, this was challenging, and they expressed frustration over how technological developments “moved too fast ,” but some participants interpreted these challenges as a way to “keep their mind sharp. ”
Another recurring pattern was that the participants expressed great interest in using digital services related to the health care system and other public institutions. The importance of being able to navigate digital services was explicitly clear when talking about finding test answers, written electronic messages, and questionnaires from the hospital or other public institutions. Keeping up with developments, communicating with public institutions, and taking an interest in their own health and well-being were described as good reasons to learn to use digital tools.
However, other aspects also affected these learning facilitators. Some participants felt alienated while using digital tools and described the practice as something related to feelings of anxiety, fear, and stupidity as well as something that demanded “a certain amount of courage. ” Some participants felt frustrated with the digital challenges they experienced, especially when the challenges were difficult to overcome because of their physical conditions:
I get sad because of it (digital challenges) and I get very frustrated and it takes a lot of time because I have difficulty seeing when I look away from the computer and have to turn back again to find out where I was and continue there (...) It pains me that I have to use so much time on it. [Man, age 71 years]
Fear of making mistakes, particularly when communicating with public institutions, for example, the health care system, was a common pattern. Another pattern was the fear of misinterpreting the sender and the need to ensure that the written electronic messages were actually from the described sender. Some participants felt that they were forced to learn about digital tools because they cared a lot about the services. Furthermore, fears of digital services replacing human interaction were a recurring concern among the participants. Despite these initial and recurring feelings, some participants learned how to navigate the digital services that they deemed relevant. Another recurring pattern in this learning process was repetition, the practice of digital skills, and consistent assistance from other people. One participant expressed the need to use the services often to remember the necessary skills:
Now I can figure it out because now I’ve had it shown 10 times. But then three months still pass... and then I think...how was it now? Then I get sweat on my forehead (feel nervous) and think; I’m not an idiot. [Woman, age 82 years]
For some participants, learning how to use digital tools demanded time and patience, as challenges had to be overcome more than once because they reappeared until the use of digital tools was more automatized into their everyday lives. Using digital tools and health services was viewed as easier and less stressful when part of everyday routines.
Life Without Digital Tools: Not a Free Choice
Even though some participants used digital tools daily, other participants expressed that it was “too late for them.” These participants did not view it as a free choice but as something they had to accept that they could not do. They wished that they could have learned it earlier in life but did not view it as a possibility in the future. Furthermore, they saw potential in digital services, including digital health care services, but they did not know exactly what services they were missing out on. Despite this lack of knowledge, they still felt sad about the position they were in. One participant expressed what she thought regarding the use of digital tools in public institutions:
Well, I feel alright about it, but it is very, very difficult for those of us who do not have it. Sometimes you can feel left out—outside of society. And when you do not have one of those (computers)...A reference is always made to w and w (www.) and then you can read on. But you cannot do that. [Woman, age 94 years]
The feeling of being left out of society was consistent among the participants who did not use digital tools. To them, digital systems seemed to provide unfair treatment based on something outside of their own power. Participants who were heavily affected by their medical conditions and could not use digital services also felt left out because they saw the advantages of using digital tools. Furthermore, a participant described the feelings connected to the use of digital tools in public institutions:
It is more annoying that it does not seem to work out in my favour. [Woman, age 62 years]
These statements indicated that it is possible for individuals to want to use digital tools and simultaneously find them too challenging. These participants were aware that there are consequences of not using digital tools, and that saddens them, as they feel like they are not receiving the same treatment as other people in society and the health care system.
Principal Findings
The insights from our findings demonstrated that our participants had different digital practices and different experiences with digital tools and services; however, the analysis also highlighted patterns related to how digital services and tools were used. Specific conditions were important for the possibility of digital practice, including having access to social resources; possessing the necessary capabilities; and feeling motivated, secure, and comfortable . These prerequisites were necessary to have positive experiences using digital tools in the health care system, although some participants who lived up to these prerequisites were still skeptical toward digital solutions. Others who did not live up to these prerequisites experienced challenges and even though they were aware of opportunities, this awareness made them feel left out. A few participants even viewed the digital tools as a threat to their participation in society. This supports the notion of Norgaard et al [ 13 ] that the attention paid to digital capability demands from eHealth systems is very important. Furthermore, our findings supported the argument of Hjeltholt and Papazu [ 17 ] that it is important to better understand experiences related to digital services. In our study, we accommodate this request and bring forth a broad perspective on experiences with digital practices; we particularly add insight into the challenges with digital practices for patients who also have acute or chronic illness, with some of them also experiencing physical, communicative, and cognitive difficulties. To our knowledge, there is limited existing literature focusing on digital practices that do not have a limited scope, for example, a focus on perspectives on eHealth literacy in the use of apps [ 26 ] or intervention studies with a focus on experiences with digital solutions, for example, telemedicine during the COVID-19 pandemic [ 27 ]. As mentioned by Hjeltholt et al [ 10 ], certain citizens are dependent on their own social networks in the process of using and learning digital tools. Rasi et al [ 28 ] and Airola et al [ 29 ] argued that digital health literacy is situated and should include the capabilities of the individual’s social network. Our findings support these arguments that access to social resources is an important condition; however, the findings also highlight that these resources can be particularly crucial in the use of digital health services, for example, when interpreting and understanding digital and written electronic messages related to one’s own health course or when dealing with physical, cognitive, and communicative disadvantages. Therefore, we argue that the awareness of the disadvantages is important if we want to understand patients’ digital capabilities, and the inclusion of the next of kin can be evident in unveiling challenges that are unknown and not easily visible or when trying to reach patients with digital challenges through digital means.
Studies by Kayser et al [ 30 ] and Kanoe et al [ 31 ] indicated that patients’ abilities to interpret and understand digital health–related services and their benefits are important for the successful implementation of eHealth services—an argument that our findings support. Health literacy in both digital and physical contexts is important if we want to understand how to better design and implement services. Our participants’ statements support the argument that communication through digital means cannot be viewed as similar to face-to-face communication and that an emphasis on digital health literacy demonstrates how health systems are demanding different capabilities from the patients [ 13 ]. We argue that it is important to communicate the purposes of digital services so that both the patient and their next of kin know why they participate and how it can benefit them. Therefore, it is important to make it as clear as possible that digital health services can benefit the patient and that these services are developed to support information, communication, and dialogue between patients and health professionals. However, our findings suggest that even after interpreting and understanding the purposes of digital health services, some patients may still experience challenges when using digital tools.
Therefore, it is important to understand how and why patients learn digital skills, particularly because both experience with digital devices and estimation of the value of digital tools have been highlighted as key factors for digital practices [ 5 , 18 ]. Our findings indicate that a combination of these factors is important, as recognizing the value of digital tools was not enough to facilitate the necessary learning process for some of our participants. Instead, our participants described the use of digital tools as complex and continuous processes in which automation of skills, assistance from others, and time to relearn forgotten knowledge were necessary and important facilitators for learning and understanding digital tools as well as becoming more comfortable and confident in the use of digital health services. This was particularly important, as it was more encouraging for our participants to learn digital tools when they felt secure, instead of feeling afraid and anxious, a point that Bailey et al [ 18 ] also highlighted. The value of digital solutions and the will to learn were greater when challenges were viewed as something to overcome and learn from instead of something that created a feeling of being stupid. This calls for attention on how to simplify and explain digital tools and services so that users do not feel alienated. Our findings also support the argument that digital health literacy should take into account emotional well-being related to digital practice [ 32 ].
The various perspectives that our participants provided regarding the use of digital tools in the health care system indicate that patients are affected by the use of digital health services and their own capabilities to use digital tools. Murray et al [ 33 ] argued that the use of digital tools in health sectors has the potential to improve health and health delivery by improving efficacy, efficiency, accessibility, safety, and personalization, and our participants also highlighted these positive aspects. However, different studies found that some patients, particularly older adults considered socially vulnerable, have lower digital health literacy [ 10 , 34 , 35 ], which is an important determinant of health and may widen disparities and inequity in health care [ 16 ]. Studies on older adult populations’ adaptation to information and communication technology show that engaging with this technology can be limited by the usability of technology, feelings of anxiety and concern, self-perception of technology use, and the need for assistance and inclusive design [ 36 ]. Our participants’ experiences with digital practices support the importance of these focus areas, especially when primarily older patients are admitted to hospitals. Furthermore, our findings indicate that some older patients who used to view themselves as being engaged in their own health care felt more distanced from the health care system because of digital services, and some who did not have the capabilities to use digital tools felt that they were treated differently compared to the rest of society. They did not necessarily view themselves as vulnerable but felt vulnerable in the specific experience of trying to use digital services because they wished that they were more capable. Moreover, this was the case for patients with physical and cognitive difficulties, as they were not necessarily aware of the challenges before experiencing them. Drawing on the phenomenological and feministic approach by Ahmed [ 37 ], these challenges that make patients feel vulnerable are not necessarily visible to others but can instead be viewed as invisible institutional “walls” that do not present themselves before the patient runs into them. Some participants had to experience how their physical, cognitive, or communicative difficulties affected their digital practice to realize that they were not as digitally capable as they once were or as others in society. Furthermore, viewed from this perspective, our findings could be used to argue that digital capabilities should be viewed as a privilege tied to users’ physical bodies and that digital services in the health care system are indirectly making patients without this privilege vulnerable. This calls for more attention to the inequities that digital tools and services create in health care systems and awareness that those who do not use digital tools are not necessarily indifferent about the consequences. Particularly, in a context such as the Danish one, in which the digital strategy is to create an intertwined and user-friendly public digital sector for everyone, it needs to be understood that patients have different digital capabilities and needs. Although some have not yet had a challenging experience that made them feel vulnerable, others are very aware that they receive different treatment and feel that they are on their own or that the rest of the society does not care about them. Inequities in digital health care, such as these, can and should be mitigated or prevented, and our investigation into the experiences with digital practices can help to show that we are creating standards and infrastructures that deliberately exclude the perspectives of those who are most in need of the services offered by the digital health care system [ 8 ]. Therefore, our findings support the notions that flexibility is important in the implementation of universal public digital services [ 17 ]; that it is important to adjust systems in accordance with patients’ eHealth literacy and not only improve the capabilities of individuals [ 38 ]; and that the development and improvement of digital health literacy are not solely an individual responsibility but are also tied to ways in which institutions organize, design, and implement digital tools and services [ 39 ].
Limitations
This qualitative study provided novel insights into the experiences with public digital health services from the perspective of patients in the Danish context, enabling a deeper understanding of how digital health services and digital tools are experienced and used. This helps build a solid foundation for future interventions aimed at digital health literacy and digital health interventions. However, this study has some limitations. First, the study was conducted in a country where digitalization is progressing quickly, and people, therefore, are accustomed to this pace. Therefore, readers must be aware of this. Second, the study included patients with different neurological conditions; some of their digital challenges were caused or worsened by these neurological conditions and are, therefore, not applicable to all patients in the health system. However, the findings provided insights into the patients’ digital practices before their conditions and other challenges not connected to neurological conditions shared by patients. Third, the study was broad, and although a large number of informants was included, from a qualitative research perspective, we would recommend additional research in this field to develop interventions that target digital health literacy and the use of digital health services.
Conclusions
Experiences with digital tools and digital health services are complex and multifaceted. The advantages in communication, finding information, or navigating through one’s own health course work as facilitators for engaging with digital tools and digital health services. However, this is not enough on its own. Furthermore, feeling secure and motivated and having time to relearn and practice skills are important facilitators. Engagement in digital practices for the examined population requires access to continuous assistance from their social network. If patients do not meet requirements, digital health services can be experienced as exclusionary and a source of concern. Physical, cognitive, and communicative difficulties might make it impossible to use digital tools or create more challenges that require assistance. Digitalization of the health care system means that patients do not have the choice to opt out of using digital services without having consequences, resulting in them receiving a different treatment than others. To ensure digitalization does not create inequities in health, it is necessary for developers and the health institutions that create, design, and implement digital services to be aware of differences in digital health literacy and to focus on simplifying communication with patients and next of kin through and about digital services. It is important to focus on helping individuals meet the necessary conditions and finding flexible solutions for those who do not have the same privileges as others if the public digital sector is to work for everyone.
Acknowledgments
The authors would like to thank all the people who gave their time to be interviewed for the study, the clinical nurse specialists who facilitated interviewing patients, and the other nurses on shift who assisted in recruiting participants.
Conflicts of Interest
None declared.
- Year in search 2022. Google Trends. URL: https://trends.google.com/trends/yis/2022/DK/ [accessed 2024-04-02]
- Digital government index: 2019. Organisation for Economic Cooperation and Development. URL: https://www.oecd-ilibrary.org/content/paper/4de9f5bb-en [accessed 2024-04-02]
- Azzopardi-Muscat N, Sørensen K. Towards an equitable digital public health era: promoting equity through a health literacy perspective. Eur J Public Health. Oct 01, 2019;29(Supplement_3):13-17. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Digital practices. Umeå University. URL: https://www.umu.se/en/humlab/research/digital-practice/ [accessed 2024-04-02]
- It-anvendelse i befolkningen 2020. Danmarks Statistik. URL: https://www.dst.dk/da/Statistik/nyheder-analyser-publ/Publikationer/VisPub?cid=29450 [accessed 2024-04-02]
- Sundhed.dk homepage. Sundhed.dk. URL: https://www.sundhed.dk/borger/ [accessed 2024-04-02]
- Nøhr C, Bertelsen P, Vingtoft S, Andersen SK. Digitalisering af Det Danske Sundhedsvæsen. Odense, Denmark. Syddansk Universitetsforlag; 2019.
- Eriksen J, Ebbesen M, Eriksen KT, Hjermitslev C, Knudsen C, Bertelsen P, et al. Equity in digital healthcare - the case of Denmark. Front Public Health. Sep 6, 2023;11:1225222. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Digital health strategy. Sundhedsdatastyrelsen. URL: https://sundhedsdatastyrelsen.dk/da/english/digital_health_solutions/digital_health_strategy [accessed 2024-04-02]
- Hjelholt M, Schou J, Bojsen LB, Yndigegn SL. Digital marginalisering af udsatte ældre: arbejdsrapport 2. IT-Universitetet i København. 2018. URL: https://egv.dk/images/Projekter/Projekter_2018/EGV_arbejdsrapport_2.pdf [accessed 2024-04-02]
- Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. Jan 25, 2012;12(1):80. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Improving health literacy. World Health Organization. URL: https://www.who.int/activities/improving-health-literacy [accessed 2024-04-02]
- Norgaard O, Furstrand D, Klokker L, Karnoe KA, Batterham R, Kayser L, et al. The e-health literacy framework: a conceptual framework for characterizing e-health users and their interaction with e-health systems. Knowl Manag E Learn. 2015;7(4). [ CrossRef ]
- Kramer JM, Schwartz A. Reducing barriers to patient-reported outcome measures for people with cognitive impairments. Arch Phys Med Rehabil. Aug 2017;98(8):1705-1715. [ CrossRef ] [ Medline ]
- Menger F, Morris J, Salis C. Aphasia in an internet age: wider perspectives on digital inclusion. Aphasiology. 2016;30(2-3):112-132. [ CrossRef ]
- Richardson S, Lawrence K, Schoenthaler AM, Mann D. A framework for digital health equity. NPJ Digit Med. Aug 18, 2022;5(1):119. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hjelholt M, Papazu I. "De har fået NemID, men det er ikke nemt for mig” - Digital rum(me)lighed i den danske velfærdsstat. Social Kritik. 2021;2021-2(163). [ FREE Full text ]
- Bailey C, Sheehan C. Technology, older persons’ perspectives and the anthropological ethnographic lens. Alter. 2009;3(2):96-109. [ CrossRef ]
- Gadamer HG, Weinsheimer HG, Marshall DG. Truth and Method. New York, NY. Crossroad Publishing Company; 1991.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. Dec 16, 2007;19(6):349-357. [ CrossRef ] [ Medline ]
- Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. Philadelphia, PA. Lippincott Williams & Wilkins, Inc; 2012.
- Kvale S, Brinkmann S. InterViews: Learning the Craft of Qualitative Research Interviewing. Thousand Oaks, CA. SAGE Publications; 2009.
- Kagan A. Supported conversation for adults with aphasia: methods and resources for training conversation partners. Aphasiology. Sep 1998;12(9):816-830. [ CrossRef ]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. Feb 2004;24(2):105-112. [ CrossRef ] [ Medline ]
- Krippendorff K. Content Analysis: An Introduction to Its Methodology. Thousand Oaks, CA. SAGE Publications; 1980.
- Klösch M, Sari-Kundt F, Reibnitz C, Osterbrink J. Patients' attitudes toward their health literacy and the use of digital apps in health and disease management. Br J Nurs. Nov 25, 2021;30(21):1242-1249. [ CrossRef ] [ Medline ]
- Datta P, Eiland L, Samson K, Donovan A, Anzalone AJ, McAdam-Marx C. Telemedicine and health access inequalities during the COVID-19 pandemic. J Glob Health. Dec 03, 2022;12:05051. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rasi P, Lindberg J, Airola E. Older service users’ experiences of learning to use eHealth applications in sparsely populated healthcare settings in Northern Sweden and Finland. Educ Gerontol. Nov 24, 2020;47(1):25-35. [ CrossRef ]
- Airola E, Rasi P, Outila M. Older people as users and non-users of a video conferencing service for promoting social connectedness and well-being – a case study from Finnish Lapland. Educ Gerontol. Mar 29, 2020;46(5):258-269. [ CrossRef ]
- Kayser L, Kushniruk A, Osborne RH, Norgaard O, Turner P. Enhancing the effectiveness of consumer-focused health information technology systems through eHealth literacy: a framework for understanding users' needs. JMIR Hum Factors. May 20, 2015;2(1):e9. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Karnoe A, Furstrand D, Christensen KB, Norgaard O, Kayser L. Assessing competencies needed to engage with digital health services: development of the ehealth literacy assessment toolkit. J Med Internet Res. May 10, 2018;20(5):e178. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nielsen AS, Hanna L, Larsen BF, Appel CW, Osborne RH, Kayser L. Readiness, acceptance and use of digital patient reported outcome in an outpatient clinic. Health Informatics J. Jun 03, 2022;28(2):14604582221106000. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Murray E, Hekler EB, Andersson G, Collins LM, Doherty A, Hollis C, et al. Evaluating digital health interventions: key questions and approaches. Am J Prev Med. Nov 2016;51(5):843-851. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chesser A, Burke A, Reyes J, Rohrberg T. Navigating the digital divide: a systematic review of eHealth literacy in underserved populations in the United States. Inform Health Soc Care. Feb 24, 2016;41(1):1-19. [ CrossRef ] [ Medline ]
- Chesser AK, Keene Woods N, Smothers K, Rogers N. Health literacy and older adults: a systematic review. Gerontol Geriatr Med. Mar 15, 2016;2:2333721416630492. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mitra S, Singh A, Rajendran Deepam S, Asthana MK. Information and communication technology adoption among the older people: a qualitative approach. Health Soc Care Community. Nov 21, 2022;30(6):e6428-e6437. [ CrossRef ] [ Medline ]
- Ahmed S. How not to do things with words. Wagadu. 2016. URL: https://sites.cortland.edu/wagadu/wp-content/uploads/sites/3/2017/02/v16-how-not-to-do-ahmed.pdf [accessed 2024-04-02]
- Monkman H, Kushniruk AW. eHealth literacy issues, constructs, models, and methods for health information technology design and evaluation. Knowl Manag E Learn. 2015;7(4). [ CrossRef ]
- Brørs G, Norman CD, Norekvål TM. Accelerated importance of eHealth literacy in the COVID-19 outbreak and beyond. Eur J Cardiovasc Nurs. Aug 15, 2020;19(6):458-461. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by A Mavragani; submitted 14.03.23; peer-reviewed by G Myreteg, J Eriksen, M Siermann; comments to author 18.09.23; revised version received 09.10.23; accepted 27.02.24; published 11.04.24.
©Christian Gybel Jensen, Frederik Gybel Jensen, Mia Ingerslev Loft. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 11.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Unfavorable social factors may raise heart disease risk factors in Asian American adults
Having more unfavorable social determinants of health, such as being unemployed, uninsured or not having education beyond high school, was associated with an increased likelihood of having risk factors for cardiovascular disease among Asian American adults, according to new research published today in the Journal of the American Heart Association , an open access, peer-reviewed journal of the American Heart Association.
The investigation also noted that the link between these unfavorable social determinants of health variables and cardiovascular disease risk factors varied widely among people in different Asian American subgroups in this study. An association does not mean that social determinants of health directly caused the risk factor.
"Despite the perception that Asian Americans may be less impacted by social determinants of health compared to people in other racial/ethnic groups, our findings indicate unfavorable social factors are associated with higher prevalence of cardiovascular risk factors among Asian American adults," said lead study author Eugene Yang, M.D., a professor of medicine at the University of Washington School of Medicine in Seattle.
"The Asian American population is the fastest growing racial/ethnic group in the United States," Yang said. "People of South Asian heritage have higher rates of premature heart disease globally, and they recently have been found to have higher cardiovascular mortality than non-Hispanic white people. Better understanding of why differences in cardiovascular risk exist among Asian subgroups is vital to reducing risk and improving outcomes."
Researchers examined data from the National Health Interview Survey conducted in the U.S. from 2013 to 2018, which included 6,395 adults who self-identified as Asian.
Researchers rated 27 social determinants of health factors as favorable or unfavorable in six areas: economic stability (which included employment and income status); neighborhood and social cohesion (which gauged neighborhood trust and whether homes were owned or rented); psychological distress; food security; education; and health care utilization.
The analysis found a significant relationship between unfavorable social determinants of health and cardiovascular disease risk factors. This relationship varied among people in different Asian American subgroups. Among the findings:
- For all Asian groups included in the data, a higher unfavorable social determinants of health score by one standardized unit was associated with a 14% greater risk of high blood pressure; a 17% greater risk of poor sleep; and a 24% greater risk of Type 2 diabetes -- all of which increase the risk for developing cardiovascular disease.
- a 45% greater likelihood of Type 2 diabetes among Chinese adults and a 24% greater likelihood among Filipino adults;
- a 28% greater risk of high blood pressure among Filipino adults;
- a 42% increased likelihood of insufficient physical activity among Asian Indian adults, a 58% increased likelihood among Chinese adults and a 24% increased likelihood among Filipino adults;
- a 20% likelihood of suboptimal sleep among Asian Indian adults; and
- a 56% and 50% likelihood of nicotine exposure among Chinese adults and Filipino adults, respectively.
- Compared with other Asian American subgroups, adults who identified as Filipino reported the highest prevalence -- 4 out of 7 -- cardiovascular risk factors: poor sleep, high cholesterol, high blood pressure and obesity.
Yang said many social determinants of health are often interconnected, such as neighborhood cohesion, economic stability and use of the health care system.
"It is important to understand how different Asian subgroups are affected," he said. "When Asian people are lumped together, higher risk groups like South Asian people may not be treated aggressively enough, while groups with lower risk, like people of Korean and Japanese descent, may be overtreated for blood pressure or cholesterol."
Study background and details:
- The large, cross-sectional study reviewed data from 2013-2018 National Health Interview Surveys -- annual, nationally representative surveys of U.S. adults.
- Of the 6,395 Asian adults in the survey, about 22% self-identified as Filipino adults; 22% as Asian Indian adults; 21% as Chinese adults; and 36% as other Asian.
- The sample size of Asian American individuals in the national survey was too small to analyze several major Asian populations, including Japanese, Korean and Vietnamese people, as well as other smaller Asian subgroups.
- Nearly 56% of the group were women, and nearly 52% were between the ages of 18 and 44. About 77% of the participants were born outside the United States.
- Participants were assigned scores for social determinants of health by categorizing 27 variables as favorable or unfavorable.
- The cardiovascular risk factors were self-reported and were similar to the American Heart Association's Life's Essential 8 -- eight lifestyle metrics assessing ideal cardiovascular health. These eight metrics include: following a healthy diet, maintaining a healthy weight, getting regular exercise and enough quality sleep, avoiding nicotine exposure and maintaining healthy levels of blood pressure, glucose and cholesterol. However, healthy diet was not measured in this study. Reaching optimal levels of these eight metrics improves heart health and reduces the risk for heart disease and stroke.
Limitations of the study include that its small sample size did not allow for analysis of some Asian subgroups (Japanese, Korean, Vietnamese and other Asian people). In addition, it examined self-reported survey data on social factors and cardiovascular risk factors at a single point in time. Therefore, the analysis could not assess long-term social determinants of health patterns, and it could not prove that unfavorable social factors caused the development of cardiovascular disease risk factors. Furthermore, language barriers may have been a factor for some participants because the National Heath Interview Surveys were only conducted in English and Spanish.
Study authors noted that it is vital to include more Asian Americans in national surveys to reveal potential differences in optimal social determinants of health profiles and cardiovascular risk factor prevalence and outcomes.
- Heart Disease
- Cholesterol
- Mental Health Research
- Hypertension
- Diseases and Conditions
- Chronic Illness
- Health Policy
- Epidemiology
- Athletic training
- Public health
- Environmental impact assessment
- Personalized medicine
- Premature birth
Story Source:
Materials provided by American Heart Association . Note: Content may be edited for style and length.
Journal Reference :
- Alicia L. Zhu, Austin D. Le, Yuemeng Li, Latha P. Palaniappan, Malathi Srinivasan, Nilay S. Shah, Sally S. Wong, Javier Valero‐Elizondo, Tali Elfassy, Eugene Yang. Social Determinants of Cardiovascular Risk Factors Among Asian American Subgroups . Journal of the American Heart Association , 2024; DOI: 10.1161/JAHA.123.032509
Cite This Page :
Explore More
- No Two Worms Are Alike
- Quantum Effects in Electron Waves
- Star Trek's Holodeck Recreated Using ChatGPT
- Cloud Engineering to Mitigate Global Warming
- Detecting Delayed Concussion Recovery
- Bonobos: More Aggressive Than Thought
- Brightest Gamma-Ray Burst
- Stellar Winds of Three Sun-Like Stars Detected
- Fences Causing Genetic Problems for Mammals
- Ozone Impact On Fly Species
Trending Topics
Strange & offbeat.

IMAGES
VIDEO
COMMENTS
Browse all our research projects by topic We have funded more than 150 external research projects across a range of themes over the last five years. Browse all our research projects by topic. Copy link. Please click below to see the research projects we've funded on the following topics.
Topics & Ideas: Public Health. The impact of the built environment and urbanisation on physical activity and obesity; The effects of food insecurity on health outcomes in Zimbabwe; The role of community-based participatory research in addressing health disparities; The impact of social determinants of health, such as racism, on population health
Evidence from trials without randomisation or from single before-and-after studies, cohort, time series or matched case-controlled studies or observational studies. Evidence from well-designed descriptive studies or qualitative research. Opinions from expert committees or formal consensus methods. Expert opinion.
Significance of Qualitative Research. The qualitative method of inquiry examines the 'how' and 'why' of decision making, rather than the 'when,' 'what,' and 'where.'[] Unlike quantitative methods, the objective of qualitative inquiry is to explore, narrate, and explain the phenomena and make sense of the complex reality.Health interventions, explanatory health models, and medical-social ...
A long-time priority of health services research has been a focus on issues affecting access to care, including community factors, the availability of social services, and the social determinants of health. Social determinants of health have been defined by Healthy People 2020 as "conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a ...
1 INTRODUCTION. Over the past decade, an increased focus on the way that integrated health and social care (IHSC) services are delivered and a growing demand for improved service user experience have driven forward improvements in worldwide health and social care (HSC; World Health Organization, 2016a).Person-centred IHSC systems aim to follow principles of participatory care and governance ...
This guide is designed to support health and social care researchers and practitioners to integrate qualitative research into the evidence base of health and social care research. Qualitative research designs are diverse and each design has a different focus that will inform the approach undertaken and the results that are generated. The aim is to move beyond the "what" of qualitative ...
However, health and social care research, as with many other academic disciplines, is carried out within embedded hierarchies and structural inequalities in universities, public service ...
This chapter focuses on the use of online surveys and how these can aid research inquiry in health and social care. It draws on a case study to show how an online survey was used to research the contemporary issue of parental alienation (Morgan, Ahmad and Webster, 2020), a subject highly relevant to those working with children and families ...
Background Complexity theory has been chosen by many authors as a suitable lens through which to examine health and social care. Despite its potential value, many empirical investigations apply the theory in a tokenistic manner without engaging with its underlying concepts and underpinnings. Objectives The aim of this scoping review is to synthesise the literature on empirical studies that ...
International policies and legislation set a precedence of person-centred sustainable integrated Health and Social Care (HSC) that meets the health and wellbeing needs of service users through improved experiences. However, current research focuses on service models, with fewer studies investigating experiences and needs.
1. The Role of Research in the Health and Social Care Professions; 2. The Nature of Knowledge in Health and Social Care; 3. Overview of the Research Process; 4. Ethical Issues; 5. Searching and Reviewing the Literature; 6. Approaches to and Design of Research in Health and Social Care; 7. Research Problems, Aims, Questions and Hypotheses; 8 ...
Produced by Dr Diana Ramsey, ARC KSS Darzi Fellow (2021-2022) with insights and support from people working to deliver research in the Health and Social Care region, the Your Health and Social Care Research Quick Guide is a resource to help those working in health or social care to start or develop their research journey. Packed with ...
The first question asks for a ready-made solution, and is not focused or researchable. The second question is a clearer comparative question, but note that it may not be practically feasible. For a smaller research project or thesis, it could be narrowed down further to focus on the effectiveness of drunk driving laws in just one or two countries.
This is the first textbook to show how research using a range of qualitative and quantitative methods relates to improving health and social care practice. The book shows how different research approaches are undertaken in practice and the challenges and strengths of different methodologies, thus facilitating students to make informed decisions ...
This Research Topic will give a platform to investigators of various aspects of burnout to delineate how we can integrate individual and system approaches within health and social care. The topic will be of particular interest to policy makers, and human services staff and other professional groups that play a crucial role in the delivery of care.
However, our research funding programmes work closely with patients, members of the public, users of social care services and carers as well as health and social care experts, to ensure our research will answer the most pressing questions. To find out if your question has reached a committee please contact [email protected].
The US healthcare system is at a crossroads. With an aging population requiring more care and a strained system facing workforce shortages, capacity issues, and fragmentation, innovative solutions ...
Health and care research is the same. It seeks to find answers to questions about the best options available. It then uses these discoveries to make decisions about improvements or changes. This is so we can: diagnose diseases earlier or more accurately. provide life-changing treatments.
This handbook offers a comprehensive guide to action research as a strategy for inquiry and development in health and social care. It can be used by individuals or groups working independently on their own projects or as a basis for a tutor-led course. It features. * an introduction to the theories behind action research and other forms of ...
What is research and how does it work in the context of nursing, health and social care? Now in its 7 th edition, this introductory guide provides you with a concise overview of the different research methods and terminology that you will come across when undertaking research in any course related to nursing, health and social care. The book's easy-to-follow structure takes you from research ...
Health outcomes are strongly impacted by social determinants of health, including social risk factors and patient demographics, due to structural inequities and discrimination. Primary care is viewed as a potential medical setting to assess and address individual health-related social needs and to collect detailed patient demographics to assess and advance health equity, but limited literature ...
3 answers. Jan 29, 2018. I am interested to explore the following topics: · Women and care: the role of women in health and social care. · Women working with men patients: main issues and ...
For the past four years, I've had the privilege of leading the Division of Behavioral and Social Research (BSR). Every day, I work with a talented and dedicated team united by our passion for improving healthspan as we age through social, psychological, economic, and behavioral research at both the individual and population levels.
Grounded theory, phenomenology and ethnography are three approaches used in qualitative research. Grounded theory approach is a commonly used qualitative method in the social sciences to inductively generate or discover a theory out of the data. 9 Phenomenology and ethnography are more commonly used qualitative approaches in health care and ...
Best Health and Social Care Dissertation Topics. If you are looking level 5 diploma in health and social care research project ideas below topics list give you the perfect idea for your required topics. Depression Health: Society is the biggest force that leads to the vehicle of depression among people of different age groups.
Public Acceptability of Health and Social Care Funding Options: Funding Options for the NHS and Social Care in the UK. An assessment of how popular different funding approaches for the NHS and social care are among the general public, as part of a wider study on feasible options for the future funding of health and social care in the UK.
This paper is in the following e-collection/theme issue: eHealth Literacy / Digital Literacy (328) Focus Groups and Qualitative Research for Human Factors Research (700) Adoption and Change Management of eHealth Systems (639) Health Care Quality and Health Services Research (211) Health Literacy, Health Numeracy, and Numeracy (14) Demographics of Users, Social & Digital Divide (651)
Building community partnerships, having community specialists within a care team and using screening tools are all necessary steps to identifying and addressing social needs, according to experts ...
Asian American adults with more unfavorable factors related to income level, education, housing, access to health care and other social variables had a greater likelihood of having risk factors ...