- Patient Care & Health Information
- Diseases & Conditions
Dysarthria occurs when the muscles you use for speech are weak or you have difficulty controlling them. Dysarthria often causes slurred or slow speech that can be difficult to understand.
Common causes of dysarthria include nervous system disorders and conditions that cause facial paralysis or tongue or throat muscle weakness. Certain medications also can cause dysarthria.
Treating the underlying cause of your dysarthria may improve your speech. You may also need speech therapy. For dysarthria caused by prescription medications, changing or discontinuing the medications may help.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Signs and symptoms of dysarthria vary, depending on the underlying cause and the type of dysarthria. They may include:
- Slurred speech
- Slow speech
- Inability to speak louder than a whisper or speaking too loudly
- Rapid speech that is difficult to understand
- Nasal, raspy or strained voice
- Uneven or abnormal speech rhythm
- Uneven speech volume
- Monotone speech
- Difficulty moving your tongue or facial muscles
When to see a doctor
Dysarthria can be a sign of a serious condition. See your doctor if you have sudden or unexplained changes in your ability to speak.
In dysarthria, you may have difficulty moving the muscles in your mouth, face or upper respiratory system that control speech. Conditions that may lead to dysarthria include:
- Amyotrophic lateral sclerosis (ALS, or Lou Gehrig's disease)
- Brain injury
- Brain tumor
- Cerebral palsy
- Guillain-Barre syndrome
- Head injury
- Huntington's disease
- Lyme disease
- Multiple sclerosis
- Muscular dystrophy
- Myasthenia gravis
- Parkinson's disease
- Wilson's disease
Some medications, such as certain sedatives and seizure drugs, also can cause dysarthria.
Complications
Because of the communication problems dysarthria causes, complications can include:
- Social difficulty. Communication problems may affect your relationships with family and friends and make social situations challenging.
- Depression. In some people, dysarthria may lead to social isolation and depression.
- Daroff RB, et al., eds. Bradley's Neurology in Clinical Practice. 7th ed. Elsevier; 2016. https://www.clinicalkey.com. Accessed April 10, 2020.
- Dysarthria. American Speech-Language-Hearing Association. https://www.asha.org/public/speech/disorders/dysarthria/. Accessed April 6, 2020.
- Maitin IB, et al., eds. Current Diagnosis & Treatment: Physical Medicine & Rehabilitation. McGraw-Hill Education; 2020. https://accessmedicine.mhmedical.com. Accessed April 10, 2020.
- Dysarthria in adults. American Speech-Language-Hearing Association. https://www.asha.org/PRPPrintTemplate.aspx?folderid=8589943481. Accessed April 6, 2020.
- Drugs that cause dysarthria. IBM Micromedex. https://www.micromedexsolutions.com. Accessed April 10, 2020.
- Lirani-Silva C, et al. Dysarthria and quality of life in neurologically healthy elderly and patients with Parkinson's disease. CoDAS. 2015; doi:10.1590/2317-1782/20152014083.
- Signs and symptoms of untreated Lyme disease. Centers for Disease Control and Prevention. https://www.cdc.gov/lyme/signs_symptoms/index.html. Accessed April 6, 2020.
- Neurological diagnostic tests and procedures fact sheet. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Neurological-Diagnostic-Tests-and-Procedures-Fact. Accessed April 6, 2020.
Associated Procedures
- EEG (electroencephalogram)
- Electromyography (EMG)
- Lumbar puncture (spinal tap)
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Dilip Kumar Jayaraman ; Joe M. Das .
Affiliations
Last Update: June 5, 2023 .
- Continuing Education Activity
Dysarthria is a neuromotor disorder that results from abnormalities in speed, strength, accuracy, range, tone, or duration required for speech control. Decreased speech intelligibility characterizes the disorder. The content of the spoken language remains intact, so the patient can write and comprehend spoken and written language. Dysarthria is a motor speech disorder seen with many neurological causes. This activity reviews the main subtypes, evaluation, management of dysarthria, and the role of the interprofessional team in evaluating and improving patient care.
- Identify the different subtypes of dysarthria.
- Determine the etiology of dysarthria in common neurological disorders.
- Implement a comprehensive initial history, physical, and speech evaluation for patients with dysarthria.
- Apply best practices for the interprofessional team to achieve the overall goals of holistic individualized treatment to facilitate communication, decrease isolation, and improve patient outcomes.
- Introduction
Dysarthria is a neuromotor disorder that results from abnormalities in speed, strength, accuracy, range, tone, or duration required for speech control. [1] Decreased speech intelligibility characterizes the disorder. The content of the spoken language remains intact, so the patient can write and comprehend spoken and written language. Anarthria is the severe form in which there is a complete loss of motor speech production. [2]
Speech is a complex neuromuscular phenomenon achieved through the smooth coordination of 5 subsystems: respiration, phonation, resonance, articulation, and prosody. [3] Muscular dysfunction affecting any of these subsystems causes impairments in audibility, naturalness, intelligibility, and communication efficiency. Dysarthria profoundly affects the patient and their families, as communication is integrally related to expressing personality and social relationships. Since there is overlap in the functioning of the muscles, feeding and swallowing difficulty in patients with dysarthria is common.
Various neurological disorders can cause dysarthria. Dysarthria can arise from disorders at various locations of the neuroaxis, including the cerebral cortex, basal ganglia, cerebellum, cranial nerve nuclei, or peripheral nerves, and from a primary motor disorder of the tongue, larynx, and pharynx.
Mayo Clinic Classification (commonly used - groups dysarthria based on the location) [4]
Etiopathological Causes
- Infections: Creutzfeldt–Jakob disease, acquired immune deficiency disease.
- Vascular disorder: Ischemic and hemorrhagic strokes, arterio-venous malformations.
- Neoplasm: Primary and metastatic brain tumors.
- Demyelinating: Multiple sclerosis, Guillain–Barre disease.
- Degenerative: PD, progressive supra nuclear palsy, corticobasal degeneration, multiple system atrophy, Huntington disease (HD), ataxia telangiectasia.
- Trauma: TBI, chronic traumatic encephalopathy, cerebral palsy.
- Toxic: Heavy metal poisoning (Minamata disease due to methylmercury poisoning can cause dysarthria), alcohol, drugs
- Genetic: Sensory ataxic neuropathy, dysarthria, and ophthalmoparesis (SANDO) due to a mutation in the gene encoding the mitochondrial DNA polymerase gamma enzyme (POLG1) [5] [6]
In addition to the neurological causes, nonneurological causes, such as cleft lip or palate and laryngeal tumors, also cause difficulty with articulation. However, the condition is not termed dysarthria if it stems from nonneurological causes.
- Epidemiology
The exact incidence of dysarthria is not known, and incidence varies based on the underlying cause. About 90% of patients with PD develop dysarthria during the illness. In ALS patients, dysarthria may predate limb weakness by about 3 to 5 years; dysarthria affects about 70% of patients with limb weakness. [7] [8]
In one study evaluating stroke patients, 28% had both aphasia and dysarthria, and 24% had dysarthria only. In a study of children with neuromuscular diseases, the prevalence of dysarthria was 31.5%. [9] It is estimated that 10 to 60% of patients with TBI have dysarthria. [10]
- Pathophysiology
The motor control of speech occurs at multiple levels. The cranial nerve nuclei receive cortical supply through the corticobulbar tract. All other cranial nerves are innervated bilaterally except for the lower face, which receives contralateral innervation. The facial nerve terminates in 5 branches; the branches that contribute to the muscles of speech are the buccal, mandibular, and, to an extent, cervical. The glossopharyngeal nerve (IX), through the stylopharyngeal nerve, innervates the stylopharyngeus muscle and, through the pharyngeal branches, innervates the muscles of the pharynx. [11]
Through the pharyngeal branches, the vagus nerve innervates the pharyngeal muscles, which elevate the palate and cause pharyngeal constriction. The glossopharyngeal nerve provides a sensory supply to the stylopharyngeus, which elevates the pharynx during speech. The cricothyroid muscle supplied by the vagus’ superior laryngeal branch is the vocal cords’ chief tensor. The recurrent laryngeal nerve separates the vocal cords and opens the glottis through the posterior cricoarytenoids, closes the glottis through lateral cricoarytenoids, and relaxes the vocal cords through the vocalis.
Hypoglossal nerve nuclei originating in the medulla provide motor branches to the tongue, supplying the intrinsic and extrinsic muscles (except the palatoglossus).
Suprahyoid muscles: These influence tongue movements by altering the position of the hyoid bone.
- C1 fibers supply the geniohyoid muscle.
- The trigeminal nerve supplies the mylohyoid muscle and the anterior belly of the digastric muscle.
- The facial nerve supplies the stylohyoid muscle and posterior belly of the digastric muscle.
In the neuromuscular junction, acetylcholine produced in the presynaptic nerve terminal binds to receptors, ultimately creating an endplate potential strong enough to propagate action potential over the surface of the skeletal muscle membrane, resulting in muscle contraction. In myasthenia gravis, various autoantibodies interrupt these processes resulting in dysarthria and other symptoms. [12]
- History and Physical
Multiple neurological conditions cause dysarthria, so the natural course and clinical features can differ. The presentation can be acute in patients with acute ischemic stroke, whereas it can be delayed in neurodegenerative diseases like ALS.
Based on the Mayo classification, there are salient features of dysarthria [13] described below:
Flaccid: Speech is slow, with hypernasality and breathy vocal quality. One of the most common examples in clinical practice is idiopathic peripheral facial paralysis, in which the patient presents with facial paralysis and drooling. Another common cause is Guillain–Barre syndrome.
Spastic: Speech is harsh, with low pitch and constant errors. Speech evaluation shows hypernasality, reduced intelligibility, palatal elevation, and slow speech rate. Patients have signs of pseudobulbar palsy with dysphagia, hyperactive jaw jerk, and pseudobulbar affect. Patients with dysarthria-clumsy hand syndrome are noted to have facial weakness, dysarthria, and extremity dysmetria. [14]
Hypokinetic dysarthria: This is seen in PD due to the loss of dopaminergic neurons. Speech is monotone and poorly articulated and tends to be quiet. Delays in speech initiation mixed with rushing of words can be seen. Other characteristic signs, such as masked facial features, resting tremors, cogwheeling, and festinating gait, can be observed at the examination.
Hyperkinetic dysarthria: This is seen with basal ganglia lesions and associated hyperkinetic movement disorders, such as HD. Speech is harsh, with variation in loudness and rate of speech. There are occasional stoppages while speaking.
Ataxic dysarthria: This is commonly seen with disorders of the cerebellum or its connections. Speech has a “scanning” quality or irregular rhythm with the explosion of syllables. Prosody is impaired, with each syllable being pronounced slowly, and there is a pause after every syllable. There is decreased motor coordination manifested by axial and appendicular ataxia depending on the part of the cerebellum affected.
Mixed dysarthria: Two or more central nervous system components are affected in this type. This can be seen with ALS and multiple sclerosis. Speech is slow, prosody is disrupted, voice is strained, and there is marked hypernasality.
A thorough history and a detailed physical examination are crucial in evaluating patients presenting with dysarthria. A comprehensive initial speech evaluation is comprised of (1) history, (2) oral motor/speech mechanism exam, (3) screening of subsystems (respiration, phonation, articulation, resonance, and prosody), (4) perceptual assessment, and (5) intelligibility evaluation.
The water glass manometer test provides a gross assessment of pressure-generating capabilities for speech production. The patient must blow into a water-filled drinking glass with the straw secured at a certain depth inside the glass. If the patient can maintain a stream of bubbles for 5 seconds, breath support is adequate for most speech purposes. To be valid, the patient must maintain velopharyngeal closure and a tight lip seal around the straw. [15]
Perpetual assessment of speech helps observe the function of all speech subsets. This assessment provides insight into deficits and serves as a comparison tool. Passages such as "my grandfather" and "caterpillar passage" help assess perceptual speech. [16] [17] These passages help evaluate the speech repertoire, examine the subsystems of speech, contemporary vocabulary, and simple syntax, and assess polysyllabic word form.
The Caterpillar Passage
"Do you like amusement parks? Well, I sure do. To amuse myself, I went twice last spring. My most MEMORABLE moment was riding on the Caterpillar, which is a gigantic roller coaster high above the ground. When I saw how high the Caterpillar rose into the bright blue sky, I knew it was for me. After waiting in line for thirty minutes, I made it to the front, where the man measured my height to see if I was tall enough. I gave the man my coins, asked for change, and jumped on the cart. Tick, tick, tick, the Caterpillar climbed slowly up the tracks. It went SO high I could see the parking lot. Boy, was I SCARED! I thought to myself, "There's no turning back now." People were so scared they screamed as we zoomed fast and faster along the tracks. As quickly as it started, the Caterpillar came to a stop. Unfortunately, it was time to pack the car and drive home. That night I dreamt of the wild ride on the Caterpillar. Taking a trip to the amusement park and riding on the Caterpillar was my MOST memorable moment ever!"
Speech Intelligibility Evaluation
Assessment of intelligibility in dysarthric speakers (AIDS), sentence intelligibility test (SIT), and word intelligibility test are used to assess speech intelligibility. AIDS is the most commonly used and comprises word and sentence tasks. The patient reads or imitates 50 unsystematically chosen words from 12 phonetically similar words for each word. In the sentence task, the patient reads or imitates two sentences each for 220 words. The sentences are chosen from a collection of 100 sentences of each length. The judge derives an intelligibility score based on the percentage of words transcribed accurately.
SIT is an improved Windows version of the sentence portion of AIDS. It examines the intelligibility of words and sentences and estimates efficiency by examining the rate of intelligible words per minute in sentences.
The onset and progression of dysarthria and associated neurological complaints, such as tremors, dysphagia, and gait instability, can provide clues for the diagnosis. A medication list review should include potential overdoses and exposure to toxins, such as alcohol and cocaine. Having the patient count from 1 to 100 can bring out respiratory muscle fatigue in myasthenia gravis. Counting numbers without interruption (1–30) is another bedside tool to assess respiratory status. [18] Sustaining an "ah" sound is a functional bedside test to assess laryngeal function.
Imaging techniques, such as computed tomography (CT) of the head and magnetic resonance imaging (MRI) of the brain, are helpful initial tools in evaluation. In patients suspected of neuromuscular junction disorders, electromyography (EMG) and nerve conduction studies (NCS) are indicated. CBC (complete blood count), basic metabolic profile (BMP), and urine drug screening are indicated based on history and pretest probability. If GBS is suspected, evaluation of pulmonary function (vital capacity and negative inspiratory force) is indicated. [18]
Speech Assessment Tools
Frenchay Dysarthria Assessment is one of the most commonly used commercially available tools for dysarthria assessment. It was initially devised in 1980 and revised in 2008. It incorporates a series of tasks used to identify the dysarthria subtype. Speech pathologists rate the patient's speech employing a 5-point scoring system on the following (a) reflexes, (b) respiration, (c) lips, (d)palate, (e) laryngeal, (f) tongue, and (g) intelligibility, (h) influencing factors. [19]
For subjective assessment, self-report questionnaires such as Living with Neurologically Based Speech Difficulties (Living with Dysarthria - LwD) may be used. The severity of dysarthria may not always correspond to the extent of perceived communicative difficulties. [20]
- Treatment / Management
The overall goals of speech and language treatment are to facilitate the recovery of communication, to assist patients in developing strategies to compensate for communication disorders, and to counsel and educate people in the patient's environment on assistive communication supports to facilitate communication, decrease isolation, and meet the patient's wants and needs.
When developing the plan, it is essential to consider dysarthria's cause, severity, and underlying co-morbidities. Speech-language pathologists and physicians work together to formulate an individualized approach for the patient. Recent studies indicate that speech rehabilitation significantly improves speech in adults with stroke-related dysarthria and that interventions such as Lee Silverman Voice Treatment are effective for hypokinetic dysarthria in individuals with PD. [21] [22]
Broadly, types of therapy could be grouped as follows:
- Therapy targeting the speech-production subsystems
- Communication strategies
- Environmental adaptations
- Augmentative and alternative communication (AAC)
- Medical/surgical interventions.
Targeting the Speech-Production Subsystems
Speech pathologists can target the five individual subcomponents that produce speech.
Lee Silverman Voice Treatment and Pitch Limiting Voice Treatment target phonation; the former is a program that improves loudness and intelligibility and has been widely studied in PD, while the latter increases vocal loudness without increasing pitch. [23] [24] Articulation can be improved by increasing loudness, pausing, exaggerating articulation, and altering pitch variation. Respiratory muscle strength training supports breathing by altering posture to target respiration.
Communication Strategies
Providing feedback, clarifying, and encouraging are practical approaches for the partner. For the patient, setting up the conversation by gaining the partner's attention, slowing and repeating the phrases, and using nonverbal gestures, such as eye contact and facial expressions, are helpful strategies.
Speech supplementation, such as alphabet, syntactic, and topic, are helpful strategies. In alphabet supplementation, the speaker uses an alphabet board to identify the first letter of the spoken word. In topic supplementation, a phrase or cue word is uttered before speaking. Information about the grammar or word class is provided with each spoken word in the syntactic supplementation.
Behavioral communication intervention techniques such as biofeedback are shown to improve intelligibility. In stroke patients, biofeedback techniques increased the volume, decreased the speed, and improved the intelligibility. [25] [26]
Environmental Adaptations
Setting up optimal environmental conditions to increase understandability includes ensuring a quiet conversation background, intimate seating, and face-to-face interaction.
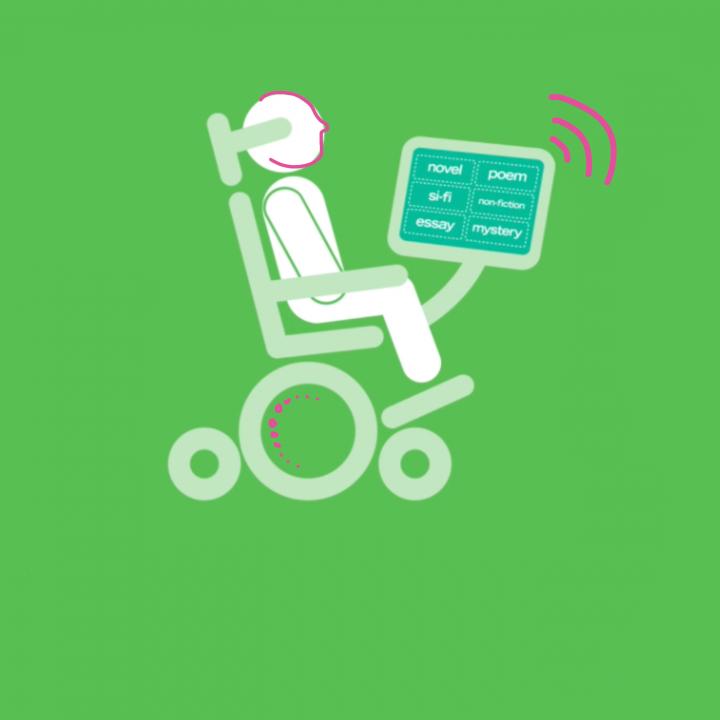
Augmentative and Alternative Communication (AAC)
AAC may include low-tech aids, such as picture boards or pen and paper, or high-tech aids, such as smartphones, voice synthesizers, digital records, and speech-generating devices. [27]
Computer-based interventions offer an exciting step toward dysarthria management. Some examples are:
- A mobile application for PD patients. It includes an assessment of the speech in addition to various other aspects of disease management [28]
- Feedback and individual practice using computers were as effective as traditional therapy in patients with stable dysarthria [29]
- Improvement in articulation and intelligibility was assessed in Virtual articulation therapy [30]
These small studies hold good promise for further expansion of computer-based interventions.
Medical/Surgical Interventions
Medical therapy should target the underlying neurological cause. In dysarthria arising from PD, therapy should focus on repleting dopaminergic therapy. The effects of PD drugs on dysarthria are variable. Subthalamic nucleus stimulation has some efficacy among surgical treatments, but speech intelligibility worsens, as with most surgical interventions in PD. [31] Improving spasticity in ALS with baclofen, tizanidine, and botulinum toxin type A has been tried. [8]
Laryngoplasty is an option if hoarseness is associated with recurrent laryngeal nerve palsy and does not improve with conservative management. Palatal lift improves resonance by surgically lifting the weak palate. Since the 2019 COVID pandemic, telehealth has become more relevant than ever. Telerehab (TR) is less expensive and equally effective in improving functional stroke outcomes, including speech, compared to traditional rehab. [32]
In another review of speech therapy administered via teletherapy in patients with PD, the patient reported overall increased satisfaction due to increased convenience and accessibility. Further research is needed, however, as the studies lacked double blinding, and there was heterogeneity in the protocol. [33]
- Differential Diagnosis
The differential diagnoses for dysarthria include aphasia, apraxia of speech, and aphemia.
Apraxia, in general, is a dysfunction of a learned motor task. Patients need help initiating speech and transitioning between sounds; they speak through trial and error, and their errors are inconsistent. When patients are asked to repeat a phrase exactly, especially a polysyllabic word (eg, television), different errors are noted in each attempt. Isolated apraxia of speech is rare; it is usually seen with aphasia. Imaging might show lesions in the dominant insula and Broca’s area. [34]
Aphasia is a language impairment. Depending on the location, language comprehension or production may be impaired. Patients also have difficulty writing and reading. [35]
Aphemia is a motor speech disorder resulting in near muteness. Patients have normal comprehension, reading, and writing.
Dysarthria is described as chronic if persistent for greater than 5 years. Dysarthia is considered stable in patients with nonprogressive etiologies.
Recovery also appears to be dependent on the etiology. One study evaluating dysarthria following stroke showed recovery in about half of the patients. [36] No estimates of the long-term prognosis of various diseases are available. However, from various anecdotal reports, it is evident that dysarthria is progressive in most neurodegenerative diseases.
Functional Communication Measures (FCMs) refer to rating scales used to define an individual’s functional abilities. They are seven-point rating scales, ranging from least functional (Level 1) to most functional (Level 7). They help measure a patient’s functional communication and swallowing abilities throughout speech-language pathology intervention.
- Complications
Speech difficulty can have a significant impact on the patient’s psychosocial life. Patients report stigmatization, changes in self-identity, and social and emotional disturbances due to post-stroke dysarthria. In children, behavioral problems and lack of access to education can lead to decreased future employment opportunities. Tools such as the Dysarthria Impact Profile (DIP) are available to assess the psychosocial impact of dysarthria. [37] Given the possibility of far-reaching effects, timely intervention should be the goal.
Dysarthria Impact Profile is used to assess the psychosocial impact of dysarthria. [38] Patients report how their condition hinders them in multiple circumstances, such as talking to people they do not know and ordering a meal in a restaurant. The tool is used for outcome measurement and for planning interventions. Communicative Participation Item Bank (CPIB) is a self-reported tool designed for adults with various communication disorders; this tool has clinical and research applications. [39] Patients report how their condition hinders them in multiple circumstances, such as talking to people they do not know and ordering a meal in a restaurant.
- Consultations
- Neurologist
- Speech and language pathologists
- Physiatrist (physical medicine and rehabilitation)
- Deterrence and Patient Education
When the patient or family first notices dysarthria, they should immediately bring it to the attention of an appropriate medical practitioner. Acute onset might be a symptom of stroke; hence, rapid evaluation in the hospital is warranted. If symptoms are progressive, patients are typically assessed by a primary care clinician and referred to specialists. Patient and caregiver strategies help during rehabilitation. [40]
Paying attention to the speaker, speaking in a quiet area with good lighting, repeating phrases that are not understood, and clarifying unclear statements by asking yes-or-no questions are some valuable strategies for caregivers. Patients should begin with one word or phrase before proceeding to complete sentences. Speaking slowly with frequent pauses helps ensure understanding. Frequently ensuring listeners understand and using pictures and writing are also helpful strategies. When tired and frustrated, dysarthria worsens. When necessary, using alternative methods of communication is warranted. Educating the listener about dysarthria improves recognition of the condition and their attitude toward the patients. [41]
- Pearls and Other Issues
The International Classification of Functioning, disability, and Health (ICF) is a classification system of health and health-related conditions developed by the World Health Organization (WHO) and published in 2001. It is a framework that addresses functioning and disability related to a health condition within the context of the individual’s activities and participation in everyday life.
The table below maps a patient with ataxic dysarthria due to a cerebellar stroke:
Activities and Participation Environmental and Personal Factors
- Enhancing Healthcare Team Outcomes
Dysarthria is among the most common neurological complaints and can arise from many primary neurological and nonneurological conditions. Collecting detailed history, including onset, progression, associated neurological symptoms, and collateral history from family and friends, is essential.
If dysarthria is a presenting symptom, extensive workup may be required to diagnose the underlying cause. Nurses are often the first to recognize speech difficulties in an inpatient who develops dysarthria and should inform the clinician and make recommendations for interventions. An interprofessional team, including a neurologist, physiatrist, nurses, and speech–language pathologist, must make the diagnosis and formulate a treatment plan. Social workers may assist in locating support groups and local resources for patients and families.
Conventional speech therapy and high-tech AAC devices can assist with functional communication when natural speech is not understandable. The Academy of Neurologic Communication Disorders and Sciences (ANCDS) and the American Speech–Language–Hearing Association (ASHA) published four practice guidelines between 2001–2004 to support the treatment of dysarthria. Various societies, such as the ANCDS, the National Parkinson’s Foundation, the Multiple Sclerosis Society, and the ALS Association, have practical guidelines for managing patients with dysarthria.
The Speech–Language Pathology Medical Review Guidelines published by ASHA focus on specific components of the speech production process, such as improving muscle strength and control, reducing consonant imprecision, and improving respiration for producing an adequate voice. [Level 5] ASHA has an evidence maps section highlighting the most recent evidence-based research in dysarthria. Emerging evidence suggests TR improves costs and patient satisfaction compared to traditional in-person therapy. The study evaluated post-stroke patients’ quality of life and motor, speech, and cognitive function. [32] [Level 1]
The prognosis of dysarthria depends on the cause. Proper consultation with specialists and education of family members and friends is required to optimize patient treatment and allow patients to regain their most significant level of independence. The treatment regimen is highly individualized and requires an extensive interprofessional team. Hence, prompt consultation with interprofessional specialists is recommended to improve outcomes.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Dilip Kumar Jayaraman declares no relevant financial relationships with ineligible companies.
Disclosure: Joe Das declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Jayaraman DK, Das JM. Dysarthria. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Disorders of communication: dysarthria. [Handb Clin Neurol. 2013] Review Disorders of communication: dysarthria. Enderby P. Handb Clin Neurol. 2013; 110:273-81.
- A phonation therapy approach for Mandarin-English bilingual clients with dysarthria. [Clin Linguist Phon. 2009] A phonation therapy approach for Mandarin-English bilingual clients with dysarthria. Lee T, McCann C. Clin Linguist Phon. 2009 Oct; 23(10):762-79.
- Validation and cross-linguistic adaptation of the Frenchay Dysarthria Assessment (FDA-2) speech intelligibility tests: Hebrew version. [Int J Lang Commun Disord. 2022] Validation and cross-linguistic adaptation of the Frenchay Dysarthria Assessment (FDA-2) speech intelligibility tests: Hebrew version. Icht M, Bergerzon-Bitton O, Ben-David BM. Int J Lang Commun Disord. 2022 Sep; 57(5):1023-1049. Epub 2022 Jun 17.
- Review Hypokinetic Dysarthria in Parkinson's Disease: A Narrative Review. [Sisli Etfal Hastan Tip Bul. 2023] Review Hypokinetic Dysarthria in Parkinson's Disease: A Narrative Review. Atalar MS, Oguz O, Genc G. Sisli Etfal Hastan Tip Bul. 2023; 57(2):163-170. Epub 2023 Jun 20.
- Speech treatment for Hebrew-speaking adolescents and young adults with developmental dysarthria: A comparison of mSIT and Beatalk. [Int J Lang Commun Disord. 2022] Speech treatment for Hebrew-speaking adolescents and young adults with developmental dysarthria: A comparison of mSIT and Beatalk. Carl M, Levy ES, Icht M. Int J Lang Commun Disord. 2022 May; 57(3):660-679. Epub 2022 Apr 1.
Recent Activity
- Dysarthria - StatPearls Dysarthria - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Types of Speech Impediments
Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
:max_bytes(150000):strip_icc():format(webp)/SanjanaGupta-d217a6bfa3094955b3361e021f77fcca.jpg)
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
Phynart Studio / Getty Images
Articulation Errors
Ankyloglossia, treating speech disorders.
A speech impediment, also known as a speech disorder , is a condition that can affect a person’s ability to form sounds and words, making their speech difficult to understand.
Speech disorders generally become evident in early childhood, as children start speaking and learning language. While many children initially have trouble with certain sounds and words, most are able to speak easily by the time they are five years old. However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders.
There are many different types of speech impediments, including:
- Articulation errors
This article explores the causes, symptoms, and treatment of the different types of speech disorders.
Speech impediments that break the flow of speech are known as disfluencies. Stuttering is the most common form of disfluency, however there are other types as well.
Symptoms and Characteristics of Disfluencies
These are some of the characteristics of disfluencies:
- Repeating certain phrases, words, or sounds after the age of 4 (For example: “O…orange,” “I like…like orange juice,” “I want…I want orange juice”)
- Adding in extra sounds or words into sentences (For example: “We…uh…went to buy…um…orange juice”)
- Elongating words (For example: Saying “orange joooose” instead of "orange juice")
- Replacing words (For example: “What…Where is the orange juice?”)
- Hesitating while speaking (For example: A long pause while thinking)
- Pausing mid-speech (For example: Stopping abruptly mid-speech, due to lack of airflow, causing no sounds to come out, leading to a tense pause)
In addition, someone with disfluencies may also experience the following symptoms while speaking:
- Vocal tension and strain
- Head jerking
- Eye blinking
- Lip trembling
Causes of Disfluencies
People with disfluencies tend to have neurological differences in areas of the brain that control language processing and coordinate speech, which may be caused by:
- Genetic factors
- Trauma or infection to the brain
- Environmental stressors that cause anxiety or emotional distress
- Neurodevelopmental conditions like attention-deficit hyperactivity disorder (ADHD)
Articulation disorders occur when a person has trouble placing their tongue in the correct position to form certain speech sounds. Lisping is the most common type of articulation disorder.
Symptoms and Characteristics of Articulation Errors
These are some of the characteristics of articulation disorders:
- Substituting one sound for another . People typically have trouble with ‘r’ and ‘l’ sounds. (For example: Being unable to say “rabbit” and saying “wabbit” instead)
- Lisping , which refers specifically to difficulty with ‘s’ and ‘z’ sounds. (For example: Saying “thugar” instead of “sugar” or producing a whistling sound while trying to pronounce these letters)
- Omitting sounds (For example: Saying “coo” instead of “school”)
- Adding sounds (For example: Saying “pinanio” instead of “piano”)
- Making other speech errors that can make it difficult to decipher what the person is saying. For instance, only family members may be able to understand what they’re trying to say.
Causes of Articulation Errors
Articulation errors may be caused by:
- Genetic factors, as it can run in families
- Hearing loss , as mishearing sounds can affect the person’s ability to reproduce the sound
- Changes in the bones or muscles that are needed for speech, including a cleft palate (a hole in the roof of the mouth) and tooth problems
- Damage to the nerves or parts of the brain that coordinate speech, caused by conditions such as cerebral palsy , for instance
Ankyloglossia, also known as tongue-tie, is a condition where the person’s tongue is attached to the bottom of their mouth. This can restrict the tongue’s movement and make it hard for the person to move their tongue.
Symptoms and Characteristics of Ankyloglossia
Ankyloglossia is characterized by difficulty pronouncing ‘d,’ ‘n,’ ‘s,’ ‘t,’ ‘th,’ and ‘z’ sounds that require the person’s tongue to touch the roof of their mouth or their upper teeth, as their tongue may not be able to reach there.
Apart from speech impediments, people with ankyloglossia may also experience other symptoms as a result of their tongue-tie. These symptoms include:
- Difficulty breastfeeding in newborns
- Trouble swallowing
- Limited ability to move the tongue from side to side or stick it out
- Difficulty with activities like playing wind instruments, licking ice cream, or kissing
- Mouth breathing
Causes of Ankyloglossia
Ankyloglossia is a congenital condition, which means it is present from birth. A tissue known as the lingual frenulum attaches the tongue to the base of the mouth. People with ankyloglossia have a shorter lingual frenulum, or it is attached further along their tongue than most people’s.
Dysarthria is a condition where people slur their words because they cannot control the muscles that are required for speech, due to brain, nerve, or organ damage.
Symptoms and Characteristics of Dysarthria
Dysarthria is characterized by:
- Slurred, choppy, or robotic speech
- Rapid, slow, or soft speech
- Breathy, hoarse, or nasal voice
Additionally, someone with dysarthria may also have other symptoms such as difficulty swallowing and inability to move their tongue, lips, or jaw easily.
Causes of Dysarthria
Dysarthria is caused by paralysis or weakness of the speech muscles. The causes of the weakness can vary depending on the type of dysarthria the person has:
- Central dysarthria is caused by brain damage. It may be the result of neuromuscular diseases, such as cerebral palsy, Huntington’s disease, multiple sclerosis, muscular dystrophy, Huntington’s disease, Parkinson’s disease, or Lou Gehrig’s disease. Central dysarthria may also be caused by injuries or illnesses that damage the brain, such as dementia, stroke, brain tumor, or traumatic brain injury .
- Peripheral dysarthria is caused by damage to the organs involved in speech. It may be caused by congenital structural problems, trauma to the mouth or face, or surgery to the tongue, mouth, head, neck, or voice box.
Apraxia, also known as dyspraxia, verbal apraxia, or apraxia of speech, is a neurological condition that can cause a person to have trouble moving the muscles they need to create sounds or words. The person’s brain knows what they want to say, but is unable to plan and sequence the words accordingly.
Symptoms and Characteristics of Apraxia
These are some of the characteristics of apraxia:
- Distorting sounds: The person may have trouble pronouncing certain sounds, particularly vowels, because they may be unable to move their tongue or jaw in the manner required to produce the right sound. Longer or more complex words may be especially harder to manage.
- Being inconsistent in their speech: For instance, the person may be able to pronounce a word correctly once, but may not be able to repeat it. Or, they may pronounce it correctly today and differently on another day.
- Grasping for words: The person may appear to be searching for the right word or sound, or attempt the pronunciation several times before getting it right.
- Making errors with the rhythm or tone of speech: The person may struggle with using tone and inflection to communicate meaning. For instance, they may not stress any of the words in a sentence, have trouble going from one syllable in a word to another, or pause at an inappropriate part of a sentence.
Causes of Apraxia
Apraxia occurs when nerve pathways in the brain are interrupted, which can make it difficult for the brain to send messages to the organs involved in speaking. The causes of these neurological disturbances can vary depending on the type of apraxia the person has:
- Childhood apraxia of speech (CAS): This condition is present from birth and is often hereditary. A person may be more likely to have it if a biological relative has a learning disability or communication disorder.
- Acquired apraxia of speech (AOS): This condition can occur in adults, due to brain damage as a result of a tumor, head injury , stroke, or other illness that affects the parts of the brain involved in speech.
If you have a speech impediment, or suspect your child might have one, it can be helpful to visit your healthcare provider. Your primary care physician can refer you to a speech-language pathologist, who can evaluate speech, diagnose speech disorders, and recommend treatment options.
The diagnostic process may involve a physical examination as well as psychological, neurological, or hearing tests, in order to confirm the diagnosis and rule out other causes.
Treatment for speech disorders often involves speech therapy, which can help you learn how to move your muscles and position your tongue correctly in order to create specific sounds. It can be quite effective in improving your speech.
Children often grow out of milder speech disorders; however, special education and speech therapy can help with more serious ones.
For ankyloglossia, or tongue-tie, a minor surgery known as a frenectomy can help detach the tongue from the bottom of the mouth.
A Word From Verywell
A speech impediment can make it difficult to pronounce certain sounds, speak clearly, or communicate fluently.
Living with a speech disorder can be frustrating because people may cut you off while you’re speaking, try to finish your sentences, or treat you differently. It can be helpful to talk to your healthcare providers about how to cope with these situations.
You may also benefit from joining a support group, where you can connect with others living with speech disorders.
National Library of Medicine. Speech disorders . Medline Plus.
Centers for Disease Control and Prevention. Language and speech disorders .
Cincinnati Children's Hospital. Stuttering .
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, and language .
Cleveland Clinic. Speech impediment .
Lee H, Sim H, Lee E, Choi D. Disfluency characteristics of children with attention-deficit/hyperactivity disorder symptoms . J Commun Disord . 2017;65:54-64. doi:10.1016/j.jcomdis.2016.12.001
Nemours Foundation. Speech problems .
Penn Medicine. Speech and language disorders .
Cleveland Clinic. Tongue-tie .
University of Rochester Medical Center. Ankyloglossia .
Cleveland Clinic. Dysarthria .
National Institute on Deafness and Other Communication Disorders. Apraxia of speech .
Cleveland Clinic. Childhood apraxia of speech .
Stanford Children’s Hospital. Speech sound disorders in children .
Abbastabar H, Alizadeh A, Darparesh M, Mohseni S, Roozbeh N. Spatial distribution and the prevalence of speech disorders in the provinces of Iran . J Med Life . 2015;8(Spec Iss 2):99-104.
By Sanjana Gupta Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
Dysarthria (difficulty speaking)
Dysarthria is where you have difficulty speaking because the muscles you use for speech are weak. It can be caused by conditions that damage your brain or nerves and some medicines. Speech and language therapy can help.
Immediate action required: Call 999 if:
- somebody's face droops on 1 side (the mouth or eye may have drooped)
- a person cannot lift up both arms and keep them there
- a person has difficulty speaking (speech may be slurred or garbled)
These can be signs of a stroke, which is a medical emergency. The symptoms of a stroke usually come on suddenly.
Check if it's dysarthria
The main symptom of dysarthria is unclear speech. This can make it difficult for you to make yourself understood.
Your speech may only be slightly unclear, or you may not be able to speak clearly at all.
Other symptoms include:
- difficulty moving your mouth, tongue or lips
- slurred or slow speech
- difficulty controlling the volume of your voice, making you talk too loudly or quietly
- a change in your voice, making it nasal, strained or monotone
- hesitating a lot when talking, or speaking in short bursts instead of full sentences
Being stressed or tired may make your symptoms worse.
Dysarthria is not the same as dysphasia, although you can have both conditions at the same time. Dysphasia, also known as aphasia , is where you have difficulty understanding words or putting them together in a sentence.
Non-urgent advice: See a GP if:
- you've noticed gradual changes to your or your child's speech and you're worried
They'll examine you and may refer you to a specialist for further tests.
Causes of dysarthria
Dysarthria is usually caused by damage to the brain or conditions that affect the nervous system. It can happen at any age.
Common causes include:
- stroke , severe head injury and brain tumours
- Parkinson's disease , multiple sclerosis and motor neurone disease
- cerebral palsy and Down's syndrome
It can also be a side effect of certain medicines, such as some medicines to treat epilepsy.
Treatment for dysarthria
If you have dysarthria, you'll usually be referred to a speech and language therapist. They'll offer therapy to help your speech and communication.
The therapy you're offered will be different depending on the cause of your dysarthria and how severe it is.
Some people may find therapy does not help their symptoms, or their speech may get worse as their condition progresses. Their therapy may focus on helping communication in other ways.
Speech and language therapy may include:
- exercises to strengthen the muscles used for speech
- strategies to make your speech easier to understand, such as slowing down when you're talking
- using communication aids, such as an alphabet board or a voice amplifier
Find out more
- Headway: communication problems after brain injury
- Stroke Association: communication tools
Page last reviewed: 17 February 2023 Next review due: 17 February 2026
- Understanding Your Brain & Body
Dysarthria and Cerebral Palsy Fact Sheet
What is dysarthria?
Dysarthria is a motor speech disorder that affects how clear and understandable a person’s speech is. Speaking involves many muscles in the body, including those used for breathing, vocal fold movement, and movement of the face and mouth. When control of these muscles is affected by a person’s CP, it can result in dysarthria. Between 50-90% of people with CP have dysarthria. Dysarthria can be mild and have minimal impact on communication, or it can be severe enough that a person may not be able to produce any understandable words.
How is dysarthria diagnosed in children with CP?
Speech-language pathologists (SLPs) diagnose dysarthria by listening to a child’s speech and observing different features. SLPs listen for characteristics like a slow rate of speech, strained voice quality, low volume, hypernasal speech, and imprecise production of consonant and vowel sounds to diagnose dysarthria. SLPs may ask the child to perform different speaking tasks so they can observe the child’s speech in single words, sentences, and at different rates of speech. They may also make observations of how the child’s mouth moves when they are talking. SLPs can also use different tools to judge the degree to which dysarthria is affecting the child’s ability to effectively communicate.
How does dysarthria change over time for children with CP?
All children learn to produce speech sounds and gradually improve their speech intelligibility (i.e., how much of their speech can be understood by other people) over the first several years of life. For many children with CP, dysarthria influences how their speech develops; however, speech intelligibility improves with development for most children with CP. Thanks to recent research, we have learned a lot about how speech develops in children with CP:
- Many children with CP start talking later than children with typical development, and symptoms of dysarthria can be hard to detect at young ages.
- Speech intelligibility increases the most rapidly between 3-5 years of age for most children with CP.
- Children with CP who have both dysarthria and language difficulties tend to have lower speech intelligibility long-term than children with typical language abilities.
What treatments are there for dysarthria in children with CP?
Augmentative/alternative communication (AAC) systems and devices are an important component of maximizing communication independence for many children with CP and dysarthria. However, the majority of children with CP communicate verbally or use a combination of speaking and AAC to communicate.
There are a few speech intervention approaches that have been shown to improve intelligibility for children with CP, including:
1. The Subsystems approach is an intensive treatment that focuses on each speech subsystem, starting with breath support.
2. Speech Intelligibility Treatment is an intensive treatment that focuses on having children use a “loud voice” and “big mouth.”
3. Lee Silverman Voice Treatment is also an intensive treatment, focused primarily on increasing loudness.
Overall, there is relatively little research on the effectiveness of speech interventions for children with CP, and a lot of variation in how well children respond to different strategies. More research is needed to learn how we can individualize speech treatment approaches to be most effective for individual children.

What are speech modification strategies for children with CP?
Speech modification strategies are techniques that speech-language pathologists use to help people with dysarthria improve their speech intelligibility. There are a few strategies that have been shown to be helpful for children and adolescents with cerebral palsy who have dysarthria and are components of the intervention strategies described above:
1. Using a slow rate of speech. Slowing down speaking rate can help speakers produce speech sounds more clearly and precisely and give their communication partners additional time to understand their speech.
2. Using a loud voice. It’s not good for anyone’s voice to scream; but, projecting their voice with healthy loudness can improve intelligibility for some children with dysarthria.
3. Emphasizing key words. Some words in a sentence are more important than others to getting your point across. By focusing on emphasizing key words in a sentence, speakers can draw attention to and focus their effort on clearly producing the words most important to helping listeners understand their message.
1. Nordberg A, Miniscalco C, Lohmander A, Himmelmann K. Speech problems affect more than one in two children with cerebral palsy: Swedish population-based study. Acta Paediatr [Internet]. 2013;102(2):161–6.
2. Mei C, Reilly S, Reddihough D, Mensah F, Morgan A. Motor speech impairment, activity, and participation in children with cerebral palsy. Int J Speech Lang Pathol. 2014;16(4):427–35.
3. Hustad KC, Allison K, McFadd E, Riehle K. Speech and language development in 2-year-old children with cerebral palsy. Developmental neurorehabilitation. 2014 Jun 1;17(3):167-75.
4. Schölderle T, Haas E, Ziegler W. Age norms for auditory-perceptual neurophonetic parameters: A prerequisite for the assessment of childhood dysarthria. J Speech, Lang Hear Res. 2020;63(4):1071–82.
5. Schölderle T, Haas E, Ziegler W. Dysarthria syndromes in children with cerebral palsy. Dev Med Child Neurol. 2021;63(4):444–9.
6. Hustad KC, Mahr T, Broman AT, Rathouz PJ. Longitudinal Growth in Single-Word Intelligibility Among Children With Cerebral Palsy From 24 to 96 Months of Age: Effects of Speech-Language Profile Group Membership on Outcomes. J Speech Lang Hear Res. 2020;63(January):32–48.
7. Mahr TJ, Rathouz PJ, Hustad KC. Longitudinal Growth in Intelligibility of Connected Speech From 2 to 8 Years in Children With Cerebral Palsy: A Novel Bayesian Approach. J Speech Lang Hear Res. 2017;63(September):2880–93.
8. Pennington L, Miller N, Robson S, Steen N. Intensive speech and language therapy for older children with cerebral palsy: a systems approach. Dev Med Child Neurol [Internet]. 2010;52(4):337–44.
9. Pennington L, Roelant E, Thompson V, Robson S, Steen N, Miller N. Intensive dysarthria therapy for younger children with cerebral palsy. Dev Med Child Neurol. 2013/02/28. 2013;55(5):464–71.
10. Levy ES, Chang YM, Hwang KH, McAuliffe MJ. Perceptual and acoustic effects of dual-focus speech treatment in children with dysarthria. J Speech, Lang Hear Res. 2021;
11. Levy ES, Chang YM, Ancelle JA, McAuliffe MJ. Acoustic and Perceptual Consequences of Speech Cues for Children With Dysarthria. J Speech, Lang Hear Res. 2017;60(6S):1766–79.
12. Boliek CA, Fox CM. Therapeutic effects of intensive voice treatment (LSVT LOUD®) for children with spastic cerebral palsy and dysarthria: A phase I treatment validation study. Int J Speech Lang Pathol [Internet]. 2017;19(6):601–15.
13. Fox CM, Boliek CA. Intensive Voice Treatment (LSVT LOUD) for Children with Spastic Cerebral Palsy and Dysarthria. J Speech Lang Hear Res [Internet]. 2012;
Dysarthria Speech Disorder Assessment Using Genetic Algorithm (GA)-Based Layered Recurrent Neural Network
- Conference paper
- First Online: 24 May 2024
- Cite this conference paper

- M. Usha 9
Part of the book series: Communications in Computer and Information Science ((CCIS,volume 2121))
Included in the following conference series:
- International Conference on Intelligent Computing for Sustainable Development
A speech issue known as dysarthria occurs because of muscular weakness and nerve damage following a stroke, an infection in the brain, or a brain injury. Many Speech Therapies are involved in assisting people with Dysarthria Speech Disorder. Dysarthria is also said to have an influence on the comprehensive potentiality, speech accessibility and a specific persons’ capability to unite and interconnect in day to day chores. The Purpose of this work is for the early detection of speech disorder hence would have a positive influence on the quality of life. An effective new approach for Dysarthria speech recognition requires optimization and learning patterns to get better accuracy measurements. In this, Cuckoo Search Optimization Technique is used for better accuracy results. Genetic Algorithm (GA)-based Layered Recurrent Neural Network Improved Cuckoo Search Optimization (GALRNN-ICSO) method is used for Dysarthria Speech Recognition. The suggested GALRNN-ICSO method's primary goal is to improve test-accuracy measurement via accuracy rate as well as the precision and RMSE rate while recognizing Dysarthria Speech. The objective is to increase the accuracy and cuts down the time required for Dysarthria Speech recognition. From the experimental result, proposed GALRNN-ICSO method ensures more accuracy with precise assessment of disorder compared to existing state-of-the-art methods.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Borrie, S.A., McAuliffe, M.J., Liss, J.M.: Perceptual learning of dysarthric speech: a review of experimental studies. J. Speech Langu. Hearing Res. 55 (1), 290–305 (2012)
Article Google Scholar
D. Rodrigues, L.A.M.P., Souza, A.N., Ramos, C.C., Yan, X.: Binary Cuckoo search: a binary cuckoo search algorithm for feature selection. In: IEEE International Symposium on Circuits and Systems (ISCAS), pp. 465–468 (2013)
Google Scholar
Kim, M., Cao, B., An, K., Wang, J.: Dysarthric speech recognition using convolutional LSTM neural network. Proc. Interspeech 2018 , 2948–2952 (2018)
Kadia, K.L., Selouani, S.A., Boudraa, B., Boudraa, M.: Fully automated speaker identification and intelligibility assessment in dysarthria disease using auditory knowledge. Biocybern. Biomed. Eng. 36 (1), 233–247 (2016)
Becerra, A., de la Rosa, J.I., Gonzalez, E.: Speech recognition in a dialog system: from conventional to deep processing. Multimedia Tools Appl. 77 , 15875–15911 (2018)
Gill, J., et al.: Adaptive neuro-fuzzy inference system (ANFIS) approach for the irreversibility analysis of a domestic refrigerator system using LPG/TiO2 nanolubricant. Energy Rep. 6 , 1405–1417 (2020)
Yakoub, M.S., Selouani, S., Zaidi, B.-F., Bouchair, A.: Improving dysarthric speech recognition using empirical mode decomposition and convolutional neural network. EURASIP J. Audio Speech Music Process. 2020 (1), 1–7 (2020)
Umapathy, S., Rachel, S., Thulasi, R.: Automated speech signal analysis based on feature extraction and classification of spasmodic dysphonia: a performance comparison of different classifiers. Int. J. Speech Technol. 21 , 9–18 (2018)
Rudzicz, F.: Articulatory knowledge in the recognition of dysarthric speech. IEEE Trans. Audio Speech Lang. Process. 19 (4), 947–960 (2011)
Copaci, D., Flores, A., Rueda, F., Alguacil, I., Blanco, D., Moreno, L.: Wearable elbow exoskeleton actuated with shape memory alloy. In: Ibáñez, J., González-Vargas, J., Azorín, J.M., Akay, M., Pons, J.L. (eds.) Converging Clinical and Engineering Research on Neurorehabilitation II. BB, vol. 15, pp. 477–481. Springer, Cham (2017). https://doi.org/10.1007/978-3-319-46669-9_79
Chapter Google Scholar
Chita-Tegmark, M., Scheutz, M.: Assistive robots for the social management of health: a framework for robot design and human–robot interaction research. Int. J. Soc. Robot. 1–21 (2020)
Nehaniv, C.L., Dautenhahn, K.: Imitation and Social Learning in ROBOTS, HUMANS and Animals: Behavioural, Social and Communicative Dimensions. Cambridge University Press, Cambridge (2007)
Book Google Scholar
Kennedy, J., Baxter, P., Belpaeme, T.: Nonverbal immediacy as a characterisation of social behaviour for human-robot interaction. Int. J. Soc. Robot. 9 , 109–128 (2017)
Takayanagi, K., Kirita, T., Shibata, T.: Comparison of verbal and emotional responses of elderly people with mild/moderate dementia and those with severe dementia in responses to seal robot, PARO. Front. Aging Neurosci. 6 , 257 (2014)
Bartlett, M.S., Littlewort, G., Frank, M., Lainscsek, C., Fasel, I., Movellan, J.: Recognizing facial expression: machine learning and application to spontaneous behavior. In: 2005 IEEE Computer Society Conference on Computer Vision and Pattern Recognition (CVPR'05), San Diego, CA, USA, pp. 568–573 (2005)
Sun, Y., Chen, Y., Wang, X., Tang, X.: Deep learning face representation by joint identification-verification. In: Proceedings of the 27th International Conference on Neural Information Processing Systems. NIPS’14, vol. 2, Cambridge, MA, USA, pp. 1988–1996, MIT Press (2014)
Altman, N.S.: An introduction to kernel and nearest-neighbor nonparametric regression. Am. Stat. 46 (3), 175–185 (1992)
Article MathSciNet Google Scholar
Download references
Author information
Authors and affiliations.
Department of Information Technology, KG College of Arts and Science College, Coimbatore, Tamil Nadu, India
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to M. Usha .
Editor information
Editors and affiliations.
Anurag University, Hyderabad, Telangana, India
S. Satheeskumaran
University of Leicester, Leicester, UK
Yudong Zhang
Aurel Vlaicu University of Arad, Arad, Romania
Valentina Emilia Balas
National University of Kaohsiung, Kaohsiung, Taiwan
Tzung-pei Hong
University of Teramo, Teramo, Italy
Danilo Pelusi
Rights and permissions
Reprints and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper.
Usha, M. (2024). Dysarthria Speech Disorder Assessment Using Genetic Algorithm (GA)-Based Layered Recurrent Neural Network. In: Satheeskumaran, S., Zhang, Y., Balas, V.E., Hong, Tp., Pelusi, D. (eds) Intelligent Computing for Sustainable Development. ICICSD 2023. Communications in Computer and Information Science, vol 2121. Springer, Cham. https://doi.org/10.1007/978-3-031-61287-9_22
Download citation
DOI : https://doi.org/10.1007/978-3-031-61287-9_22
Published : 24 May 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-61286-2
Online ISBN : 978-3-031-61287-9
eBook Packages : Computer Science Computer Science (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Caregiving Now Network
Communication Aids
Communication after a stroke.
Communication is often impacted after someone has a stroke. This is either due to damage to language centers in the brain, physical weakness or paralysis of muscles used for speech, or a combination. Below are some common communication impairments that can occur after a stroke, tips for effective communication, and alternative communication options.
Communication impairments
Aphasia is an acquired language disorder that impacts communication receptively and/or expressively. An individual may have difficulty comprehending spoken or written language and/or with expression of spoken or written language. Aphasia occurs as a result of damage to the brain, typically to the left hemisphere. It can be caused by a stroke, a traumatic brain injury, and neurodegenerative diseases. One of the key characteristics is anomia , or difficulty naming/word finding. There are many types of aphasia, but they are typically broken down by fluent and nonfluent aphasia types. Roughly 25-50% of strokes result in aphasia.
Fluent/receptive aphasia
This type of aphasia is characterized by someone being able to express themselves fluently, but has difficulty comprehending spoken or written language. A type of fluent aphasia that is commonly heard is Wernicke’s aphasia . Someone with this aphasia will speak fluently but it will often not make sense to the listener, and sentences include lexical-semantic disruptions. This language may include word or sound substitutions and a “roundabout” way of talking about things. People with this type of aphasia typically have little to no awareness that their language does not make sense to the listener, making therapy difficult.
Nonfluent/expressive aphasia
This type of aphasia is typically characterized by having difficulty with written and/or spoken language, with relatively intact comprehension. A type of nonfluent aphasia that is often talked about is called Broca’s aphasia. People with this type of aphasia will often have agrammatical and dysfluent speech. Speech often sounds halted, effortful, and stilted. The individual knows what they want to say, but has difficulty expressing it.
Global/severe aphasia
Someone with global aphasia will have impaired receptive and expressive language.
Motor speech disorders
A motor speech disorder is a disorder characterized by an impairment in the motor production or planning of speech, or an impairment in the neuromuscular execution of speech. The most common cause of motor speech disorders is vascular accidents, or strokes. They can also be caused by traumatic brain injuries, infections, and degenerative diseases.
Dysarthria is a type of neuromotor motor speech disorder that can be congenital or acquired. Dysarthria is a motor speech disorder that is caused by an impairment in the neuromuscular execution of speech, meaning there is an impairment in the musculature required for spoken language, caused by an impairment in the central or peripheral nervous system. There are various types of dysarthrias that are characterized by impairments such as weakness or paralysis, incoordination, variable muscle tone, and poor range of motion. Common dysarthria types caused by a stroke include flaccid dysarthria, spastic dysarthria, ataxic dysarthria, and mixed dysarthria. The type of dysarthria will depend on where the stroke occurs in the brain. It is estimated that 22-58% of people who have experienced an acute stroke present with dysarthria. An individual with dysarthria may have speech that sounds slurred, dysfluent, breathy, hypernasal, slow, strained, monopitch, rapid, irregular, and imprecise. The speech characteristics will depend on the type of dysarthria the individual has. Certain dysarthria types often have accompanying features. For example, someone who has weakness/paralysis may have facial drooping, contributing to their flaccid dysarthria.
Apraxia of speech
Apraxia of speech is a neuromotor motor speech disorder that is caused by an impairment of programming or planning the motor movements and positioning for speech. The individual has difficulty sequencing their motor movements. Unlike dysarthria, there is no weakness or incoordination of the speech musculature, there is a higher level impairment in the ability to plan the muscle movements required for speaking. Apraxia is most frequently caused by strokes, but can also be caused by traumatic brain injury, tumors, seizure disorder, and degenerative diseases. Speech will be characterized by inconsistent productions of words, slowed speech, speech sound errors and sound substitutions, difficulty at the beginning of words/sentences, monotone speech, difficulty initiating speech, and frequent revisions/restarts. Individuals may display articulatory groping where you can see the individual physically trying to make the sound.
Communication tips
- Acknowledge your communication partner. Recognize that their communication difficulties are not due to a lack of cognition and support them in contributing to the conversation, regardless of if it is verbal communication or not.
- Use clarifications: make sure they are understanding you and that you’re understanding what they are communicating.
- When working with individuals with aphasia, it can be helpful to use a slow rate and add in natural pauses.
Communication tools
Click on photos and links below to print communication tools for use.
- White boards : White boards can be useful, especially immediately after the stroke while the person is still recovering. If they can physically write and are able to express a meaningful written message, this can be a good short-term means of communication.

- written/verbal choices : if someone is severely impacted immediately following their stroke, writing down or saying a few choices and having them choose by pointing or blinking can be a way to allow them to express wants and needs.
- Customized Communication Flip Book
- A-E_Communincation_Passport_2013(1)
- Apps : There are many apps that can aid in communication.
- More downloadable handouts to aid in communication for healthcare
DON’T
- Treat them like they are not cognitively aware.
- Finish their sentences or cut them off.
- Start talking to someone else or change the topic while they are communicating.
- American Speech Language Hearing Association (ASHA) aphasia overview
- ASHA dysarthria overview
- Stroke Association communication aids

Aphasia vs. Dysarthria and More: A Look at Different Disorders and How They Affect Areas of the Brain
A lthough aging is a natural aspect of life, getting older can often accompany some scary diagnoses . When celebrity media personality Wendy Williams was first diagnosed with aphasia, many of her fans and followers were concerned about what that meant for the future of her health.
As it turns out, aphasia is only one of many speech-related disorders that affect the brain, typically as a symptom of a larger problem like stroke or brain injury. Keep reading to find out the differences between aphasia and dysarthria, plus other disorders that are similar and can affect the brain.
Aphasia is a type of frontotemporal dementia.
Frontotemporal dementia, according to the National Institute on Aging, is an umbrella term for a series of disorders (also known as frontotemporal disorder, or FTD) that is "the result of damage to neurons in the frontal and temporal lobes of the brain."
If you are diagnosed with FTD, you could also develop many different types of symptoms, including trouble walking, trouble communicating, difficulty regulating emotions, and unusual behaviors. Tragically, there is currently no cure for FTD, and it does worsen as it progresses.
According to the Cleveland Clinic, aphasia is specifically "a disorder where you have problems speaking or understanding what other people say." There are eight main kinds of aphasia, but the three most common types are Broca's aphasia, Global aphasia, and Wernicke's aphasia.
Aphasia affects two parts of the brain's communication centers. Symptoms can include struggling to form words, repeating phrases, or understanding what someone else is saying to them.
What is the difference between aphasia vs. dysarthria?
Per Connected Speech Pathology, aphasia and dysarthria have a lot in common, including that both are often caused by factors such as stroke and brain injuries.
The main difference between them is that aphasia is about damage to the areas of the brain that control language and dysarthria is about difficulty controlling the muscles used for speech.
Because dysarthria affects speech, it can also cause difficulty with breath control and articulation. There are six main types of dysarthria, which vary based on how the nervous system is affected. Symptoms can include things like slowed speech, slurred speech, jerky speech, sounding robotic or monotone, and speaking louder or more quietly than intended.
What are aphagia and dysphagia?
Similar to aphasia and dysarthria, aphagia concerns the mouth and nose, but instead of difficulty with speech, it causes the inability to swallow , according to the University of South Florida Health Sciences Center. Aphagia is similar to dysphagia, which, per the Cleveland Clinic, means "difficulty swallowing. "
There are three main types of dysphagia: oral (where the issue is with your mouth), oropharyngeal (where the issue is with your throat), or esophageal (where the problem is with your esophagus).
Like the other disorders on this list, dysphagia is a brain disorder. It can be caused by many issues, including dementia, ALS, brain tumors, Parkinson's disease, or multiple sclerosis. It has also been linked to muscle disorders and blockage issues.
What is apraxia?
According to the University of Washington, apraxia, sometimes known as apraxia of speech, is a speech disorder t hat impairs the ability to speak. Essentially, someone might know the word they want to say, but apraxia makes it difficult for them to communicate all the sounds.
Symptoms of apraxia might include slower speech, speech errors, difficulty imitating speech or sounds, or trying to use fingers to force the mouth and lips to move.

- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Expressive Aphasia: What to Know About Communication Disorders
- What Is It?
Expressive aphasia is a language disorder that makes it difficult for individuals to speak clearly and effectively. It is often the result of a stroke but can also be caused by other causes. This condition can range from mild, where a person may leave out small words in their speech, to severe, where many words are skipped.
People with expressive aphasia are usually aware of their difficulty in speaking, which can be emotionally taxing. Fortunately, speech therapy is a valuable resource that can greatly improve communication skills and alleviate the impact of expressive aphasia on daily life.
This article will cover expressive aphasia, other aphasia types, symptoms, causes, diagnosis, and treatments.
Thierry Dosogne / Getty Images
What Is Expressive Aphasia?
Expressive aphasia is a language problem in which it's hard for someone to say or write their thoughts. It's a type of "non-fluent aphasia," meaning that speaking is more challenging than understanding. People with this struggle might struggle to find the right words, form sentences correctly, or speak and write smoothly.
Broca's aphasia is a specific subtype of expressive aphasia. It is often caused by damage to the brain's left frontal lobe, impacting speech production but leaving comprehension intact.
A Word From Verywell
Expressive aphasia is one of the most frustrating language deficits a patient can have because they know what they want to say but struggle to convey it to those around them. Adapting to a deficit after speaking freely all your life can be a daunting task, but speech therapy and the patience and support of those around you can make a major difference.
Other Types of Aphasia
Aphasia can be divided into two main categories: fluent aphasia and non-fluent aphasia. The big difference between the two is how well they can speak compared to how well they understand.
- Fluent aphasia means people can talk smoothly but might use the wrong words and have trouble understanding.
- Non-fluent aphasia , such as Broca's, makes talking hard, but understanding is usually okay.
- Wernicke's aphasia , also known as "receptive" aphasia, is caused by damage to the left hemisphere of the brain, specifically in the area known as Wernicke's area. This condition leads to difficulties in understanding language, both spoken and written. People with Wernicke's aphasia often produce sentences that contain nonsensical or inappropriate words. They may also have trouble realizing their language errors and may not fully comprehend what others are saying to them.
- Global aphasia , the most severe form of aphasia, affects both expressive and receptive language skills. It affects all aspects of communication, making it challenging to express thoughts and comprehend language. This type of aphasia typically occurs following extensive damage to language areas of the brain.
- Anomic aphasia makes word retrieval and naming objects or concepts more difficult. People with anomic aphasia may struggle to find the right words, leading to pauses in speech as they search for vocabulary. However, their overall language fluency and comprehension remain relatively intact compared to other types of aphasia.
- Primary progressive aphasia (PPA) is a neurological condition where language abilities decline gradually, affecting speech, comprehension, and word finding. Unlike typical aphasia caused by stroke, PPA progresses slowly and is often associated with neurodegenerative disorders like Alzheimer's disease .
Expressive vs. Wernicke’s Aphasia
Expressive aphasia is when someone struggles to speak fluently, like in Broca's aphasia. They might speak in short, broken sentences with limited words.
Wernicke's aphasia makes it hard to understand and use words correctly. People with this type of aphasia might say things that don't make sense or have trouble understanding others.
Expressive vs. Global Aphasia
While expressive aphasia affects the ability to produce speech, global aphasia is a more severe form of language impairment that affects both speech production and understanding. Global aphasia leads to significant difficulties in communicating thoughts and understanding others.
Symptoms of Expressive Aphasia
People with expressive aphasia experience the following challenges:
- Struggling to create complete sentences
- Omitting common words like "is" or "the"
- Forming sentences that don't make sense
- Difficulty understanding spoken sentences
- Making errors in following instructions involving spatial concepts like "left" or "right"
- Using a similar word instead of the intended word, like saying "car" instead of "van"
People with expressive aphasia often find speaking and reading more challenging, but they generally have a good understanding of spoken language and can read effectively.
What Causes Expressive Aphasia?
Several factors can contribute to the development of expressive aphasia:
- Stroke : A stroke affecting the left hemisphere of the brain, particularly in the frontal lobe or "Broca's area"
- Traumatic brain injury (TBI) : Severe head injuries, such as those from accidents or falls, can lead to damage in the brain areas responsible for language production
- Brain tumors : Tumors located in or near the language centers of the brain can interfere with language processing and production
- Infections : Certain infections affecting the brain, such as encephalitis or meningitis, can result in expressive aphasia
- Neurodegenerative diseases : Conditions like dementia can gradually impair language abilities, including expressive language
Causes of expressive aphasia in children may include:
- Brain injury
- Developmental disorder
- Other medical conditions, such as brain tumors, traumatic brain injuries, or epilepsy (if the seizures affect the areas of the brain that process language)
How Is Expressive Aphasia Diagnosed?
Expressive aphasia is diagnosed through a comprehensive assessment process. Your healthcare providers typically follow these steps:
- They may ask questions, engage in conversation, and assess the person's ability to understand and respond appropriately.
- Conduct imaging scans such as magnetic resonance imaging (MRI) or computed tomography (CT) scans to identify brain injuries and determine the affected brain areas.
If imaging reveals signs of aphasia, a speech-language pathologist or speech therapist performs additional assessments. These assessments evaluate the extent of brain damage's impact on speech, reading, writing, and language comprehension. Based on the results, your healthcare provider can recommend a treatment plan.
How Expressive Aphasia Is Treated
When it comes to treating expressive aphasia, there are several approaches and strategies that can help improve communication skills and overall quality of life:
- Speech-language therapy to improve speaking and writing skills
- Communication aides like picture cards or electronic devices to help with communication
- Practicing memory, attention, and problem-solving to improve overall thinking skills
- Group sessions to practice talking and socializing with others who have aphasia
- Educate family members on how to help and provide ongoing support and encourage including the person with aphasia in conversations
Can a Person With Expressive Aphasia Fully Recover?
While recovery from expressive aphasia varies for each individual, some people can regain a significant amount of their language abilities through therapy and rehabilitation.
Consistent and dedicated speech-language therapy can improve speaking, understanding, and communication. It may take several months or years. However, complete recovery to pre-aphasia levels may not always be possible, and ongoing support and practice may be needed for long-term management.
Expressive aphasia is a language disorder ranging from mild to severe, affecting speech and writing production. This condition is caused by factors like stroke, traumatic brain injury, or neurodegenerative diseases, and diagnosis involves comprehensive assessments by a healthcare provider.
Treatment options such as speech therapy, communication aids, and family support can significantly improve communication skills and quality of life, although full recovery may vary.
MedlinePlus. Aphasia .
National Institute on Deafness and Other Communication Disorders. Aphasia .
National Aphasia Association. Aphasia therapy guide .
National Aphasia Association. Wernicke's (receptive) aphasia .
National Aphasia Association. Global aphasia .
The Aphasia Community. Anomic aphasia .
Stroke Association. Types of aphasia .
American Stroke Association. Types of aphasia .
Scottish Rite Foundation. What is aphasia disorder in children?
By Sarah Jividen, RN Jividen is a freelance healthcare journalist. She has over a decade of direct patient care experience working as a registered nurse specializing in neurotrauma, stroke, and the emergency room.

IMAGES
VIDEO
COMMENTS
Signs and symptoms of dysarthria vary, depending on the underlying cause and the type of dysarthria. They may include: Slurred speech. Slow speech. Inability to speak louder than a whisper or speaking too loudly. Rapid speech that is difficult to understand. Nasal, raspy or strained voice. Uneven or abnormal speech rhythm.
Dysarthria is a motor speech disorder. This happens when brain or nerve damage changes the way your muscles work. It can be mild to severe. Children and adults can have dysarthria. There are many reasons people have trouble talking. Dysarthria can happen with other speech and language problems.
Dysarthria (pronounced "dis-AR-three-uh") is a motor speech disorder that makes it difficult to form and pronounce words. Motor speech disorders occur when damage to your nervous system prevents you from fully controlling parts of your body that control speech, like your tongue, voice box (larynx) and jaw. Dysarthria makes it challenging to ...
Dysarthria is a condition in which the part of your brain that controls your lips, tongue, vocal cords, and diaphragm doesn't work well. It's hard for you to move those muscles the right way. This ...
Dysarthria is a speech sound disorder resulting from neurological injury of the motor component of the motor-speech system [1] and is characterized by poor articulation of phonemes. [2] In other words, it is a condition in which problems effectively occur with the muscles that help produce speech, often making it very difficult to pronounce ...
Incidence is the number of new cases of a disorder or condition identified in a specific time period.Prevalence is the number of individuals who are living with the disorder or condition in a given time period. Dysarthria is present in many neurologic diseases. As such, its incidence and prevalence vary based upon the nature and course of the underlying condition; condition severity; and ...
A speech impediment, or speech disorder, is a condition that makes it hard for you to communicate. There are many types of speech impediments, and anyone can develop one. In some cases, children are born with conditions that affect speech. Other times, people have conditions or injuries that affect speech. Speech therapy can help.
Symptoms. Involuntary movements, motor tics, myoclonus. Distorted vowels. Intermittent vocal quality changes, hypernasality. Excessive loudness variation. 6. Mixed Dysarthria. Possible Causes. Seen in Stroke or TBI with multiple areas of the brain affected.
Dysarthria is a neuromotor disorder that results from abnormalities in speed, strength, accuracy, range, tone, or duration required for speech control.[1] Decreased speech intelligibility characterizes the disorder. The content of the spoken language remains intact, so the patient can write and comprehend spoken and written language. Anarthria is the severe form in which there is a complete ...
Dysarthria is a motor speech disorder that happens because of weakness in the muscles necessary for producing speech or due to damage to the nervous system. It can affect a person's ability to produce and understand language. Many congenital and acquired conditions can lead to dysarthria. It might also be a side effect of some medications ...
Common causes of childhood speech impediments include: Autism spectrum disorder: A neurodevelopmental disorder that affects social and interactive development. Cerebral palsy: A congenital (from birth) disorder that affects learning and control of physical movement. Hearing loss: Can affect the way children hear and imitate speech.
Others may develop speech problems after a stroke or traumatic brain injury, or other trauma. To learn more about adult speech disorders, see apraxia of speech in adults, dysarthria, laryngeal cancer, and oral cancer. Seeing a Professional Testing for Speech Sound Disorders. A speech-language pathologist, or SLP, can test your child's speech.
Common causes of dysarthria include nervous system disorders and conditions that can cause facial paralysis, tongue or throat muscle weakness. An example of a nervous system disorder that typically causes dysarthria is amyotrophic lateral sclerosis (ALS), also referred to as Lou Gehrig disease. ALS is a progressive neurodegenerative disorder ...
Types of speech disorder include stuttering, apraxia, and dysarthria. There are many possible causes of speech disorders, including muscles weakness, brain injuries, degenerative diseases, autism ...
However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders. There are many different types of speech impediments, including: Disfluency. Articulation errors. Ankyloglossia. Dysarthria. Apraxia. This article explores the causes, symptoms, and treatment of the different ...
Dysarthria is a motor speech disorder caused by weakness of the speech muscles. Dysarthric speech may sound unclear, mumbled, or slurred. Common causes of dysarthria are stroke, ALS, and Parkinson's Disease. When deciding which dysarthria treatments to choose, focus on your patient's underlying impairment. To do this, ask yourself:
Dysarthria. Dysarthria results from impaired movement of the muscles used for speech production, including the lips, tongue, vocal folds, and/or diaphragm. The type and severity of dysarthria depend on which area of the nervous system is affected. A person with dysarthria may exhibit one or more of the following speech characteristics:
difficulty moving your mouth, tongue or lips. slurred or slow speech. difficulty controlling the volume of your voice, making you talk too loudly or quietly. a change in your voice, making it nasal, strained or monotone. hesitating a lot when talking, or speaking in short bursts instead of full sentences. Being stressed or tired may make your ...
Dysarthria is a motor speech disorder that affects how clear and understandable a person's speech is. Speaking involves many muscles in the body, including those used for breathing, vocal fold movement, and movement of the face and mouth. When control of these muscles is affected by a person's CP, it can result in dysarthria.
A speech issue known as dysarthria occurs because of muscular weakness and nerve damage following a stroke, an infection in the brain, or a brain injury. Many Speech Therapies are involved in assisting people with Dysarthria Speech Disorder. Dysarthria is also said...
Preliminary speech perception performance profiles of school-age children with childhood apraxia of speech, speech sound disorder, and typical development. Journal of Speech , Language, and ... Perceptual and acoustic effects of dual-focus speech treatment in children with dysarthria. Journal of Speech, Language, and Hearing Research, 64
Apraxia of speech (AOS), also called verbal apraxia, is a speech sound disorder affecting an individual's ability to translate conscious speech plans into motor plans, which results in limited and difficult speech ability. By the definition of apraxia, AOS affects volitional (willful or purposeful) movement pattern. However, AOS usually also affects automatic speech.
Dysarthria is a motor speech disorder that is caused by an impairment in the neuromuscular execution of speech, meaning there is an impairment in the musculature required for spoken language, caused by an impairment in the central or peripheral nervous system. There are various types of dysarthrias that are characterized by impairments such as ...
Because dysarthria affects speech, it can also cause difficulty with breath control and articulation. There are six main types of dysarthria, which vary based on how the nervous system is affected.
The field of speech-language pathology is practiced by a clinician known as a speech-language pathologist ( SLP) [1] or a speech and language therapist (SLT) [2]. SLPs also play an important role in the screening, diagnosis, and treatment of autism spectrum disorder (ASD), often in collaboration with pediatricians and psychologists.
Dysarthria is a motor speech disorder that impedes the physical production of speech. Speech in patients with dysarthria is generally characterized by poor articulation, breathy voice, and ...
Subtypes of dysarthria (e.g., flaccid, spastic, hypokinetic, etc.) are examined with focus on etiologies, oral mechanism and speech assessment findings, and evidence-based treatment with consideration for client-specific characteristics such as gender, culture, and health literacy. Apraxia of speech is covered with the same foci. Prerequisites ...
This study explores various approaches for the automated detection of dysarthria, integrating both traditional and emerging technologies, to develop a reliable and accessible dysarthria detection system that complements the expertise of healthcare professionals. Dysarthria, a motor speech disorder resulting from neurological impairments. This study explores various approaches for the automated ...
Expressive aphasia is a language disorder that makes it difficult for individuals to speak clearly and effectively. It is often the result of a stroke but can also be caused by other causes. This condition can range from mild, where a person may leave out small words in their speech, to severe, where many words are skipped.