An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Rep Pract Oncol Radiother
- v.19(5); 2014 Sep


Case presentation – A five-year survival of the patient with glioblastoma brain tumor
Hubert urbańczyk.
a Centrum Onkologii, Instytut im. Marii Skłodowskiej-Curie, Oddział w Gliwicach, Zakład Radioterapii, Poland
Anita Strączyńska-Niemiec
b Centrum Onkologii, Instytut im. Marii Skłodowskiej-Curie, Oddział w Gliwicach, Zakład Patologii Nowotworów, Poland
Grzegorz Głowacki
Dariusz lange, leszek miszczyk.
This paper presents an atypical case of a patient with brain tumor of the glioblastoma multiforme (GBM) type who achieved a 5-year survival. Some general information is provided including epidemiology, diagnostic and treatment procedures (surgery and radio-chemo-therapy), and prognosis of survival related to GBM. The course of the disease, including its main symptoms, individual reasons for the delay of adjuvant treatment, after the primary surgical treatment, 37-month period of the decease free survival, as well as comprehensive management after the tumor recurrence are also presented. Histopathology confirming the clinical diagnosis is discussed in a separate chapter.
1. Background
Primary brain tumors account for about 2% of all malignant neoplasms in adults. Approximately a half of them represent gliomas, derived from neuroepithelial cells, among which glioblastoma (GBM) is the most common type.
GBM cases represent about 20% of all primary brain tumors in the adult population, and about 75% of all the anaplastic gliomas. 1 The prevalence of GBM is about 2–4 cases per 100,000. It is more common in men than in women, and its incidence increases with age. 2 Only sporadically, GBM can be found in individuals younger than 20 years of age, and its frequency rapidly increases, starting from the 5-th decade of life.
The treatment results of patients diagnosed with GBM are often unsatisfactory, and the outcome is usually poor. Currently, the main standard therapeutic methods include a radical surgical procedure, combined with radio-chemo-therapy. Some innovative methods of radiotherapy based on the application of novel radiosensitizers of corpuscular irradiation or radio-immune-therapy are now being investigated. A median survival time of patients diagnosed with GBM, treated only with the use of neurosurgical procedures are 3–5 months. The application of conventional adjuvant radiotherapy prolongs this average time about 3-fold, with a three-year survival for only about 6% of patients.
The post-treatment survival time depends on many clinical factors, such as general patient condition, age, and histopathological type of the tumor. Simson et al. demonstrated statistically significant longer survival periods among patients in whom the primary tumor location was in the frontal lobe, in comparison to the ones in whom it was located in the parietal or temporal cerebral region (11.4 months vs. 9.6 months vs. 9.1 months, respectively; p = 0.01). 3 Severity of neurological symptoms, limits of the performed surgical procedures, and response to the applied therapy, based on imaging tests, also represent prognostic factors.
Etiology of malignant neoplasms of the central nervous system (CNS) is still unknown. The most common of many probable carcinogens include: nitrosamines, pesticides, herbicides, petrochemical substances, polyvinyl chloride, and electromagnetic irradiation. However, the role of these pro-carcinogenic factors has not been unequivocally proven. 4,5 In contrast, it has been documented that patients exposed to ionizing irradiation have an increased risk of the CNS malignant gliomas. According to the current state of knowledge in the field of molecular biology and genetics of these malignancies, two main hypotheses related to their development have been proposed. The first one includes de novo creation which is related to the loss of heterozygotic properties in chromosomes 9p, 10, 17p, and with the amplification of genes for the EGFR and CDK4 (this type of malignant growth occurs more often in older patients). The second one involves the creation of anaplastic gliomas, through the progression of gliomas with a lower malignancy grade (encountered more often in younger patients). 6,7
Currently, a required standard of therapy for patients with GBM is a combined treatment, including tumor resection, with following concomitant radio-chemo-therapy, and adjuvant chemo-therapy, based on Temozolomide. In patients who undergo non-radical surgery, or who are not treated surgically, the palliative whole brain radiotherapy (WBRT), stereotactic radiation surgery (SRS), or combination of both of these therapeutic methods are used. Also, the application of palliative chemotherapy and symptomatic treatment remain important. In addition, alternatively fractionated radiotherapy, brachytherapy, targeted molecular therapy, radio-immune-therapy, hadrone therapy, or radio-sensitizers can be considered in individual cases.
In 2005, Stupp et al. presented results of a randomized study conducted by EORTC ( European Organization for Research and Treatment of Cancer ) and NCIC ( National Cancer Institute of Canada ), comparing the application of combined radio-chemo-therapy based on Temozolomide and radical radiotherapy alone. The combined management in a statistically significant manner prolonged the total survival time from 12.1 to 14.6 months, and the rate of 2-year survival was 26.5%, compared to 10.4% for radiotherapy alone. 8 The follow-up results, after a longer period of observation, confirmed the previous reports. The 2-, 3-, and 4-year survival rates were 27.3%, 16.7%, and 12.9%, respectively ( p < 0.0001) in the patients’ group treated with a combined therapy, and 11.2%, 4.3%, and 3.8%, in the patients’ group treated with radiotherapy only. 9
Unfortunately, despite the use of Temozolomide, the results are unsatisfactory. The reason for this therapeutic failure is the GBM resistance to most chemotherapeutic agents or rapid development of the GBM as a result of genetic transformations within the tumor cells. The main mechanism of the GBM resistance to alkylating agents, such as temozolomide, procarbazine, or nitrogen mustard derivatives, is the repair of damages caused by these drugs with involvement of protein coded by MGMT ( O 6 -methyl-guanine-DNA methyl-transferase ) gene.
A degree of methylation of the promoter's region of MGMT gene appears to be closely correlated with a therapeutic response of the glioma cells. Hypermethylation of this part of the gene significantly increases treatment efficacy among patients treated with Temozolomide, 10 influencing their survival period, as well. 9
2. Case presentation
The patient is a 38 year old Caucasian male, smoker (about 10–15 cigarettes per day for 20 years), without other relevant family or personal risk factors for neoplasic disease who had suffered from severe headaches and nausea (his first disease symptoms) since August of 2005. He did not seek any medical help until November of 2005, when he presented to his doctor, due to exacerbation of those symptoms. No abnormalities on both physical and neurological examinations were detected at that time.
On December 30th of 2005, the CT scan of his brain was remarkable for the following findings: “An expansive lesion of approximately 5 cm × 3 cm in size, located in the right temporal lobe, with nonhomogenic, post-contrast signal amplification. A large edema surrounding the lesion. A compression of the occipital corner of the right lateral ventricle. A slight enlargement of the supratentorial ventricular system, shifting to the left.”
On January 25th of 2006, the patient underwent surgical therapy, including right temporal craniotomy, with total resection of the tumor. On February 7th of 2006, a histopathology examination (identification number 475,958; Info-Pat, Poznań, Poland), confirmed a diagnosis of the GBM IV stage (according to WHO classification). Microscopic images of the tumor are presented ( Figs. 1–5 ).

Microscopic image of patient's tumor.

After the surgery, the patient was referred to the Institute of Radiation Oncology in Gliwice, Poland, for the post-operative radiotherapy. Although the patient was qualified for this treatment, he did not arrive to the Institute of Radiation Oncology on the day of the scheduled preparatory procedures. The reason for his absence was a simultaneous diagnostic finding of the left lung's tumor, for which the patient underwent a thoracotomy with the wedge tumor resection (for diagnostic purposes). On June 12th of 2006, based on the histopathological examination results, which showed post-tuberculosis lesions, the patient's pulmonary treatment was completed.
In February 2007, approximately 13 months after his brain tumor surgery, the patient again presented to the Institute of Oncology, and according to the follow-up diagnostic work-up, no brain tumor recurrence was found. Due to the absence of tumor, no radiotherapy was considered, and “watchful waiting” was recommended including brain imaging studies (CT or MRI) to be repeated every 3 months. In the face of the atypical disease course, an additional verification of the histopathological diagnosis was also performed, confirming the original findings of the GBM. The patient had remained under close control until February 2009 (37 months from his initial brain tumor surgery), and at that time the brain tumor recurrence was found. His recurrent tumor was located in the primary tumor's bed, and its size was 4 cm × 5.3 cm × 3.5 cm ( Fig. 6 ). However, those findings were not associated with any particular symptoms or abnormalities on subsequent physical or neurological examinations of the patient. On March 16th 2009, the patient underwent another craniotomy with the subtotal tumor resection. (MRI scans after the second craniotomy are shown in Figs. 7 and 8 .) The histopathology examination was again consistent with GBM. During the period from May 11th to June 19th of 2009, the patient received the radiotherapy dose of 60 Gy/30 fractions to the tumor lodge, including the residual tumor, with 2.5 cm of tissue margin. Due to the lack of the patient's consent, no chemotherapy was implemented. During the irradiation period, he had the first seizure episode, and was started on antiepileptic therapy (Depakine 200 mg a day). He continued this therapy for the rest of his life. After the radiotherapy, diagnostic follow-up examinations were conducted every 3 months. At the beginning of March 2010, another recurrence was found, and the tumor was localized in an upper part of the tumor bed, within the previously irradiated area (its size was 3.7 cm × 2.6 cm × 2.3 cm). Surprisingly, the patient had not experienced any symptoms, and his physical and neurological examinations were unremarkable. On March 13th of 2010, the stereotactic radiotherapy, using a single dose of 8 Gy applied to the area of recurrent tumor was performed. Unfortunately, on the control examination, on July 6th of 2010, further progression of the GBM was found. The patient expired on November 15th of 2010, in the local hospital (Zawiercie, Poland), due to the tumor expansion, resulting in cerebral edema, herniation, and multi-organ failure.

CT scan of recurrence tumor.

MRI scan after the second craniotomy.

3. Histopathology examination
On a histopathology specimen, the large areas of thrombotic necrosis, most probably caused by a large tumor size (5 cm × 3 cm) were found. In contrast, no “palisade” necrosis (with the characteristic palisade-like cell arrangements), typical for this type of tumor, was found.
Within vital tumor structures, a high cellular polymorphism was found. Besides some small calls (with hyperchromatic nucleus and scarce amount of cytoplasm), mostly atypical cells (giant, multisided or oval, with numerous nuclei with abnormal shapes, and visible nucleoli) were present. The cells revealed a strongly positive GFAP reaction that can be indicative of their glioma-type origin. Also, some distinctive GBM features, including proliferation of vascular endothelium (focal areas of numerous mitotic figures, in high power field – HPF), were visible. The described microscopic images are presented in Figs. 1–5 (the images of primary and recurrent tumors appear identical).
In this paper, we presented a remarkably long survival period (63 months since the initial onset of symptoms, and 58 months since the primary surgical treatment) of the GBM patient. An important message from our case study that could be useful in the management of many other GBM cases is that the initial complete resection suggests a beneficial role of radical neurosurgery in the early GBM treatment and potential survival period.
Unfortunately, we are unable to indicate the specific reasons for such a long survival of our relatively asymptomatic patient who experienced some disadvantages, including the second malignancy, which caused the delay in the application of his radiotherapy.
Nevertheless, it should be emphasized that personalized, patient-centered approach, using comprehensive diagnostic and therapeutic strategies, as well as vigilant, multi-level follow-up care, should be helpful in explaining different factors, contributing to overall survival. In addition, our single case presentation illustrates several challenges that are common to many GBM patients, and merit further, more individualized research on this devastating disease.
Conflict of interest
None declared.
Financial disclosure

- Weill Cornell Medicine

- Case Studies: Patients With Brain Tumors
- Symptoms of a Brain Tumor
- Diagnosing and Treating a Brain Tumor
- Surgery for Brain Tumors in Adults
- Doctors Who Treat Brain Tumors in Adults
- Cognitive Remediation After Brain Tumor Surgery
What our Patients Say

Our Care Team

- Chair and Neurosurgeon-in-Chief
- Margaret and Robert J. Hariri, MD ’87, PhD ’87 Professor of Neurological Surgery
- Vice Provost of Business Affairs and Integration

- Vice Chair for Clinical Research
- David and Ursel Barnes Professor of Minimally Invasive Brain Surgery
- Professor of Neurosurgery, Neurology, and Otolaryngology
- Director, Center for Epilepsy and Pituitary Surgery
- Co-Director, Surgical Neuro-oncology

- Assistant Professor of Neurological Surgery
- Leon Levy Research Fellow
- Feil Family Brain and Mind Research Institute

- Professor of Radiology in Neurological Surgery

- Associate Professor, Neurological Surgery

- Director, Neurosurgical Radiosurgery
- Professor of Clinical Neurological Surgery
- Robert G. Schwager, MD ’67 Education Scholar, Cornell University

- Chief of Neurological Surgery, NewYork-Presbyterian Queens
- Co-director, Weill Cornell Medicine CSF Leak Program

- Chief of Neurological Surgery, NewYork-Presbyterian Brooklyn Methodist
- Professor, Neurological Surgery
- Director, Brain Metastases Program
- Co-director, William Rhodes and Louise Tilzer-Rhodes Center for Glioblastoma

- Director of Neuro-oncology
- Director, Brain Tumor Center, Sandra and Edward Meyer Cancer Center

- Hematologist/oncologist (Brooklyn)
- Assistant Attending Neurologist, NewYork-Presbyterian Hospital
- Assistant Professor of Neuro-Oncologist
Weill Cornell Medicine Neurological Surgery 525 East 68 Street, Box 99 New York, NY 10065 Phone: 866-426-7787

Clinical Presentation
Statement of ethics, disclosure statement, a 58-year-old woman with left-sided weakness and a history of a pediatric brain tumor: a case report.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Shaakir Hasan , Michael J. Gigliotti , Melvin Deutsch , Stacey L. Reed , Rodney E. Wegner; A 58-Year-Old Woman with Left-Sided Weakness and a History of a Pediatric Brain Tumor: A Case Report. Case Rep Oncol 7 May 2018; 11 (1): 131–137. https://doi.org/10.1159/000487430
Download citation file:
- Ris (Zotero)
- Reference Manager
Background: An uncommon but well-established complication of cranial irradiation is secondary neoplasm. This case presentation documents a radiation-induced malignant glioma 55 years after being diagnosed with “cerebral sarcoma,” now defined as atypical meningioma. This not only represents the longest reported latency period for a patient initially receiving over 30 Gy, but also provides a valuable historical perspective of neuro-oncology. Clinical Presentation: A 58-year-old female presenting with progressive left-sided upper and lower extremity weakness with a past medical history significant for “cerebral sarcoma” was diagnosed with glioblastoma multiforme. This patient had previously been treated with resection and adjuvant radiation therapy via a 280-kVP orthovoltage machine and received 3,390 rad to the posterior three-quarters of the skull for “cerebral sarcoma.” Conclusion: A comprehensive investigation of the past medical history helped uncover a mysterious pediatric diagnosis, helped drive the management 5 decades later, and serves as a reminder that seemingly safe interventions may still cause harm.
“Cerebral sarcoma” was defined in the literature as a neoplasm of the meninges prior to 1979, when the World Health Organization classified several subtypes of typical (grade I), atypical (grade II), and anaplastic (grade III) meningioma [ 1 ]. Given long-term toxicity risks, the utilization of radiotherapy in meningiomas remains controversial while postoperative radiotherapy is no longer indicated in pediatric populations [ 2 ].
This is largely because an uncommon but well-established complication of cranial irradiation is a secondary neoplasm [ 3, 4 ]. Notably, 1.3% of glioblastoma cases are associated with a previous exposure to radiation, with a median latency period of 9 years [ 5, 6 ]. Some studies suggest that doses greater than 30 Gy puts the patient at higher risk for malignancy compared to lower doses (less than 18 Gy), although others suggest that there is no threshold dose [ 3, 5 ].
We present the case of a radiation-induced glioblastoma multiforme (GBM) in a 58-year-old female who was treated for a “cerebral sarcoma” 55 years earlier, for which the original records were obtained.
Past Medical History
An otherwise healthy 58-year-old female revealed that in 1962 as a 3-year-old child she had been treated for a “cerebral sarcoma” with surgery and radiation. At the time, she presented with a headache and was diagnosed with an intracranial tumor via a ventriculogram. Excision of the lesion was described as “completely or nearly completely resected,” and per the pathology report was described as a “cerebral sarcoma or meningiosarcoma.” Adjuvant radiotherapy was requested by the neurosurgeon and the administering radiologist reluctantly agreed, noting that “meningiomas are not ordinarily treated with radiotherapy although some may respond, and sarcomas are certainly not radioresponsive. However, careful radiation therapy cannot do any harm and probably may do some good” (Fig. 1 ).

Assessment and plan of the treating radiologist from 1962.
The patient was treated with a 280-kVP orthovoltage machine with 2 lateral fields, prescribed to 14 cm depth on the right and 6 cm depth on the left. She ultimately received 3,390 of a planned 4,000 rad for 39 days in 1962 to the posterior three-fourths of the entire skull. Treatment was discontinued due to an intensely erythematous scalp, although no other toxicities or neurologic deficits were noted.
Examination
The patient presented with a 1-week history of progressively worsening left-sided upper and lower extremity weakness, described as an inability to hold objects in her left hand and frequent falls secondary to a left foot drop. The weakness eventually culminated in an episode where the patient fell out of bed and could not get up. Physical examination demonstrated stable vital signs, diffuse 3/5 strength in the left upper and lower extremities, and a right frontal craniotomy scar with surrounding soft tissue fibrosis (Karnofsky performance status 70).
Pathological Findings
A contrast-enhanced brain MRI demonstrated a 3 × 3 cm right frontoparietal resection cavity surrounded by a 5 × 4 cm area of heterogeneous contrast enhancement extending to the right corona radiata and periventricular white matter with associated cerebral edema (Fig. 2 ). The mass was not technically resectable due to location and biopsy was consistent with GBM, wild-type isocitrate dehydrogenase and unmethylated O 6 -methylguanine DNA methyltransferase (MGMT), with an MIB-1 index of 50% (Fig. 3 ).

T1-weighted brain MRI with contrast at the time of diagnosis of radiation-induced glioblastoma multiforme.

Radiation-induced glioblastoma multiforme demonstrating increased cellularity with marked nuclear atypia, necrosis, and vascular endothelialization.
It was determined that further maximal safe resection would not provide a beneficial therapeutic value, therefore definitive full-dose chemoradiation was recommended. Citing a declining performance status and discontent with the role radiation played in causing her malignancy, the patient ultimately declined treatment. Since identifying information was not used in the context of this case, informed consent for this case presentation was not required.
“Meningiosarcoma” or “cerebral sarcoma” are no longer considered histopathological diagnoses, but our patient likely had a variant of meningioma, which would have an approximately 90% chance of local control in such a scenario [ 7 ]. To this day, the role of radiotherapy in the management of typical and atypical meningiomas remains controversial, although several treatment paradigms have been established since the patient originally presented in 1962 [ 8 ]. For instance, there is virtually no indication for postoperative radiotherapy for meningioma in the pediatric population given the long-term toxicity risks [ 2 ]. As was the case for most radiation therapy in that era, the dose was limited by developing erythema of the scalp, an acute toxicity of little consequence, unlike the late and at that time unknown effect of secondary malignancy.
Cahan et al. [ 9 ] defined parameters of radiation-induced malignant gliomas (RIGMs) as follows: tumors localizing to where radiotherapy was applied, an adequate latency period measured in years, a histology different than that of the original tumor, and the patient should not have an underlying pathology favoring the growth of tumors. In this case, all four parameters were met. Although 80% of patients have a typical latency period within 15 years prior to the development of a secondary malignancy, the longest reported latency period includes a female who was treated for tinea capitis, presumably at a small dose, 61 years preceding the onset of a secondary malignancy [ 5, 10 ]. Prior to this case, the longest latency period between exposure of at least 30 Gy and induction of high-grade glioma was 37 years [ 11 ].
Histologically, radiation-induced GBMs are no different than de novo GBMs; however, there have been conflicting reports of whether RIMGs have greater homogeneity of gene expression [ 3, 12, 13 ]. With a median survival of 11 months, the prognosis for radiation-induced glioblastomas is comparable to that of GBMs with the unmethylated MGMT promoter gene, suggesting that perhaps they are associated with less favorable tumor biology [ 14, 15 ]. It should be noted that the vast majority of reported RIMGs were published before MGMT status testing became commonplace and before adjuvant temozolamide was established as the standard of care [ 16 ]. However, the median survival of RIMGs since 2007 was still 11.5 months [ 5 ].
The ideal management for de novo or secondary GBM in a medically fit patient includes gross total resection followed by adjuvant chemoradiation at a total dose of 6,000 cGy in 30 fractions with concurrent and adjuvant temozolomide [ 16 ]. The risk of neurotoxicity such as brain necrosis theoretically increases in the setting of reirradiation, which may be why only approximately 40% of patients with radiation-induced GBMs received reirradiation as part of their treatment [ 15 ]. Nevertheless, the risk of radionecrosis is minimal with reirradiation to the brain so long as the cumulative dose is less than 100 Gy at 2 Gy per fraction [ 17-19 ]. Furthermore, Paulino et al. [ 15 ] demonstrated that among 85 cases of RIMGs, the 35 patients who underwent reirradiation at a median dose of 50 Gy (range 30–76 Gy) had a median survival of 13 months compared to 8 months of those who were not reirradiated, without additional toxicity. It should be mentioned that potential long-term toxicity of reirradiation to the brain may not have been observed because most patients do not survive long enough to develop it.
This case illustrates how past medical history, going back even 50 years, is instrumental to workup and management. Two uncommon and valuable pieces of information include the patient’s knowledge of her pathology as a 3-year-old and medical records dating back to 1962, both of which helped determine the diagnosis and treatment. The medical records also provide a rare window as to how medicine was practiced 5 decades ago and how it has evolved since then. Importantly, they serve as a humble reminder that there are many aspects of medicine still unknown to clinicians, including the possibility that a seemingly safe therapeutic intervention can still cause harm.
We ensure the accuracy, quality, and integrity of this case report. No identifying patient information was disclosed.
The authors of this paper would like to disclose that they have no financial or other conflicts of interest in relation to this case study and publication.

Email alerts
Citing articles via, related articles.
- Online ISSN 1662-6575
INFORMATION
- Contact & Support
- Information & Downloads
- Rights & Permissions
- Terms & Conditions
- Catalogue & Pricing
- Policies & Information
- People & Organization
- Stay Up-to-Date
- Regional Offices
- Community Voice
SERVICES FOR
- Researchers
- Healthcare Professionals
- Patients & Supporters
- Health Sciences Industry
- Medical Societies
- Agents & Booksellers
Karger International
- S. Karger AG
- P.O Box, CH-4009 Basel (Switzerland)
- Allschwilerstrasse 10, CH-4055 Basel
- Tel: +41 61 306 11 11
- Fax: +41 61 306 12 34
- Email: [email protected]
- Experience Blog
- Privacy Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
PERSPECTIVE article
Case report: end-stage recurrent glioblastoma treated with a new noninvasive non-contact oncomagnetic device.

- 1 Kenneth R. Peak Brain and Pituitary Tumor Treatment Center, Department of Neurosurgery, Houston Methodist Neurological Institute, Houston, TX, United States
- 2 Department of Neurosurgery, Houston Methodist Research Institute, Houston, TX, United States
- 3 Department of Neurosurgery, Weill Cornell Medical College, New York, NY, United States
Alternating electric field therapy has been approved for glioblastoma (GBM). We have preclinical evidence for anticancer effects in GBM cell cultures and mouse xenografts with an oscillating magnetic field (OMF) generating device. Here we report OMF treatment of end-stage recurrent glioblastoma in a 53-year-old man who had undergone radical surgical excision and chemoradiotherapy, and experimental gene therapy for a left frontal tumor. He experienced tumor recurrence and progressive enlargement with leptomeningeal involvement. OMF for 5 weeks was well tolerated, with 31% reduction of contrast-enhanced tumor volume and reduction in abnormal T2-weighted Fluid-Attenuated Inversion Recovery volume. Tumor shrinkage appeared to correlate with treatment dose. These findings suggest a powerful new noninvasive therapy for glioblastoma.
Introduction
For glioblastoma (GBM), the most common malignant tumor of the brain in adults, treatment outcome remains dismal. In over 40 years median survival has only shown modest improvement ( 1 ), and standard of care treatment often has negative impact on quality of life ( 2 ). Treatment including radiation and chemotherapy takes a heavy toll. Frequently patients cannot tolerate the completion of the prescribed chemotherapy cycles. Thus, there is a great unmet need for a completely different therapeutic approach with better outcome and less toxicity.
A new FDA-approved treatment involving electric fields alternating at 200 kHz called Optune™ therapy is now available for recurrent GBM as monotherapy and in combination with temozolomide for newly diagnosed GBM ( 3 , 4 ). It is also being tested in clinical trials for other cancers. Its hypothesized mechanism of action involves disruption of tubulin dimers, mitotic spindles, and cell division by electric field-induced dipole alignment and dielectrophoresis ( 5 ). It has a modest effect on survival, increasing median overall survival by 0.6 month in recurrent GBM ( 3 ), and in newly diagnosed GBM by 31% ( 4 ). Even this modest effect is encouraging for patients.
It has been shown that electromagnetic fields (EMF) produce anticancer effects in vitro ( 6 , 7 ). We have conducted preclinical experiments with a new noninvasive wearable device known as an Oncomagnetic device that generates oscillating magnetic fields (OMF) by rotating strong permanent magnets ( 8 , 9 ). The OMF generating components (oncoscillators) of the device can be attached to a helmet and treatment with the device does not require shaving the head. Using the oncoscillators of the device and specially devised patterns of magnet rotations we have produced strong selective anticancer effects in patient derived GBM and xenografted mouse models without causing adverse effects on cultured normal cells and normal mice ( 10 – 12 ). The mechanism of action of OMF differs from Optune™ and involves disruption of the electron transport in the mitochondrial respiratory chain causing elevation of reactive oxygen species and caspase-dependent cancer cell death ( 10 – 12 ).
Here we report evidence of treatment response in the first patient to ever receive this therapy with an untreatable left frontal GBM, treated with a wearable Oncomagnetic device in an FDA-approved Expanded Access Program.
Case Description
The patient is a 53-year-old man who first presented with altered mental status in May 2018. Imaging studies documented a large tumor in the left frontal lobe extending across the midline into the right frontal lobe, with diffuse and extensive infiltration through the corpus callosum. There was mass effect and severe edema. He was taken to the operating room on June 4, 2018, where he underwent left frontal craniotomy and radical excision of the tumor. The tumor was histopathologically confirmed as GBM. At the time of the surgery, the excision extended across the midline into the right frontal lobe. He was enrolled in a herpes simplex virus-thymidine kinase gene therapy program and received viral injection during surgery per protocol. In addition, per protocol, and as standard of care, he received concomitant radiation therapy and chemotherapy with temozolomide.
In August 2019, the patient presented with an area of contrast enhancement on MRI scan along the left ventricle. At first this was thought to be a treatment effect. This area progressively enlarged. Evaluations done before OMF treatment initiation on January 16, March 3, and April 15, 2020, demonstrated a clear recurrence. The tumor abutted the ventricle and there was evidence of leptomeningeal spread. The patient had already had radiation therapy and chemotherapy and the tumor was now progressing. The presence of leptomeningeal disease portends poor outcome, with median survival of 3.5 to 3.9 months ( 13 ).
Because of inadequacy of any standard of care options he was enrolled in an FDA-approved Expanded Access Program (EAP) for compassionate use treatment with the Oncomagnetic device. He signed an informed consent on April 15, 2020. The EAP study was carried out under a protocol approved by the Houston Methodist Research Institute Institutional Review Board.
Oncomagnetic Device
The Oncomagnetic device consists of 3 oncoscillators securely attached to an acrylonitrile butadiene styrene helmet and connected to a microprocessor-based electronic controller operated by a rechargeable battery ( Figure 1 ). Further details regarding the device are given in the Supplementary Appendix . Based on a finite element model-based calculation of the spread of the field and the size and magnetization of the rotated diametrically magnetized neodymium magnets, we estimated that the combined effective field (at least 1 mT in strength) of the 3 oncoscillators covered the entire brain, including the upper part of the brain stem.
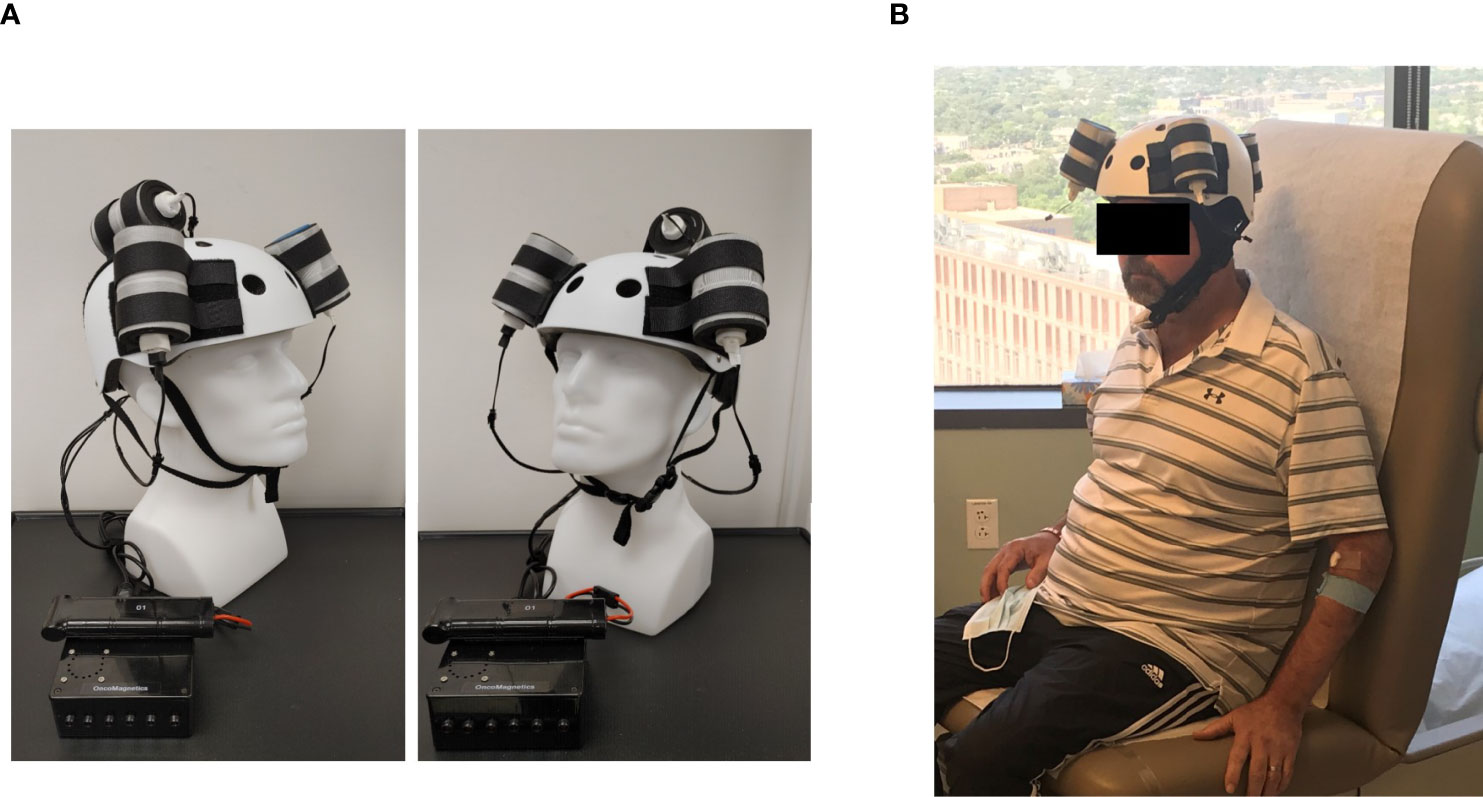
Figure 1 Oncomagnetic Device. (A) Device helmet with 3 oncoscillators securely attached to it. The oncoscillators are connected to a controller box powered by a rechargeable battery. (B) The patient wearing the device helmet with three oncoscillators attached.
Oscillating Magnetic Field Treatment
The treatment consists of intermittent application of an OMF that needs to be generated by rotating permanent magnets in a specific frequency profile and timing pattern to be effective. The patient received this treatment initially in the Peak Center clinic under the supervision of the treating physician and the Principal Investigator (DSB) of this study for the first 3 days. The dose was escalated over this period as follows. On the first day, the treatment was for 2 hours with a 5-min break between the first and the second hour. On the second and third days, it was increased to 2 and 3 2-hour sessions, respectively, with 1-hour breaks between the sessions. The patient’s spouse was trained in the use and care of the device on these days. After this initial supervised phase, the treatment was continued at home unsupervised with the same regimen as on the third day, above. The spouse was instructed to maintain a daily log of the conduct and progress of treatment, and any observed treatment and adverse effects.
Clinical Evaluations and Neuroimaging
The patient was evaluated clinically by the treating physician on each of the 3 days that he received treatment in the clinic and 7, 16, 30 and 44 days after initiation of treatment. Magnetic Resonance Imaging (MRI) scans were done on Days 1, 3, 7, 16, 30 and 44. The Day 1 scan was done before initiation of treatment. All other scans were done after treatment initiation. The treatment was paused on Day 37 because of an unfortunate but unrelated severe closed head injury (CHI). MRI scans were done on a Siemens Magnetom Terra 7T scanner. MRI scans included T1 magnetization prepared rapid gradient echo scans with and without gadolinium contrast, and T2-weighted Fluid-Attenuated Inversion Recovery (FLAIR), T2-weighted Turbo Spin Echo, Diffusion Weighted Imaging, Susceptibility Weighted Imaging, proton Magnetic Resonance spectroscopy and Diffusion Tensor Imaging scans. Treatment effect on contrast-enhanced tumor (CET) was evaluated according to the response assessment in neuro-oncology (RANO) criteria for clinical trials ( 14 ). In addition, an automated software-based method developed in house was used to objectively calculate the CET volume (see below and Supplementary Appendix ).
Data Analysis
Post-contrast T1 anatomical and T2-FLAIR MRI scans at each of the 6 time points were used to determine changes in contrast-enhanced tumor (CET) volume and non-enhanced tumor infiltration, respectively, before and after initiation of treatment. Information on image processing, data normalization and plotting are given in the Supplementary Appendix . Values obtained from pre-treatment clinical scans taken at 2 time points over 3 months before enrollment of the patient were also plotted on the same graph. Because this is a single patient case report, we could not perform any meaningful statistical analysis. However, to obtain a semi-quantitative assessment of the significance of the trend seen with treatment, we analyzed the changes in CET volume using Bayesian logic, given the observed increasing trend at two pre-treatment time points. Accordingly, we assumed that the chance of increase, decrease and no change in the rate of tumor growth was the same at each time point after treatment initiation to calculate the probability of a decrease at each post-treatment initiation time point.
The patient received OMF treatment with the Oncomagnetic device for 36 days. The treatment regimen was changed at various times during this period based on the caregiver reports and clinical findings, as described below.
Clinical Findings
After the initial 3 days of supervised treatment, the patient was seen again by the treating physician in the outpatient clinic on Day 7 from the start of treatment. Because of inattention at baseline, the patient was having difficulty with the length of treatment sessions. They were reduced to 2 hours/day Monday through Friday with Saturday and Sunday off. The Day 16 clinical examination revealed that he was tolerating the treatment sessions well, so they were increased to a total of 3 hours/day (in one-hour increments with 5 min breaks) Monday through Friday and the weekends off. On Day 30 visit, the patient reported headaches related to transient hypertension for which he was taking medication. The treating physician increased blood pressure medication (Valsartan) with improvement. The treatment was paused on Day 36 because of a closed head injury from a fall. Whether the fall was related to the treatment in any way is uncertain. It is worth noting, however, that the patient had experienced several falls before initiation of treatment. At the last follow-up on Day 44 the patient was admitted to the inpatient unit for evaluation of closed head injury and underwent detailed assessment. There were no serious adverse events reported during treatment. The patient’s caregivers reported subjective improvement in speech and cognitive function.
MRI Findings
Evaluation of the T1 post-contrast clinical MRI scans obtained before initiation of treatment showed progression in accordance with the RANO criteria ( Figure 2A ). All scans acquired during treatment showed stable disease, according to these criteria ( Figure 2A ). To obtain an objective quantitative assessment of the CET volume we used an automated MATLAB software-based script. This analysis showed marked changes in CET volume with treatment. Figure 2B shows a plot of the CET volume as a function of time before and after initiation of treatment. It reveals that there was substantial growth of the tumor volume over the 3 months before the treatment. Within the first 3 days of treatment the trend is reversed with the volume steeply decreasing by ~10% on Day 7 and then less steeply by 31% on Day 30. Based on a Bayesian-type assessment of the probability of a decrease in CET volume at each post-treatment initiation time point, the decrease at Day 30 is statistically significant at P = 0.036. The treatment was paused on Day 37. After the pause we see another trend reversal and an increase in CET volume on Day 44.
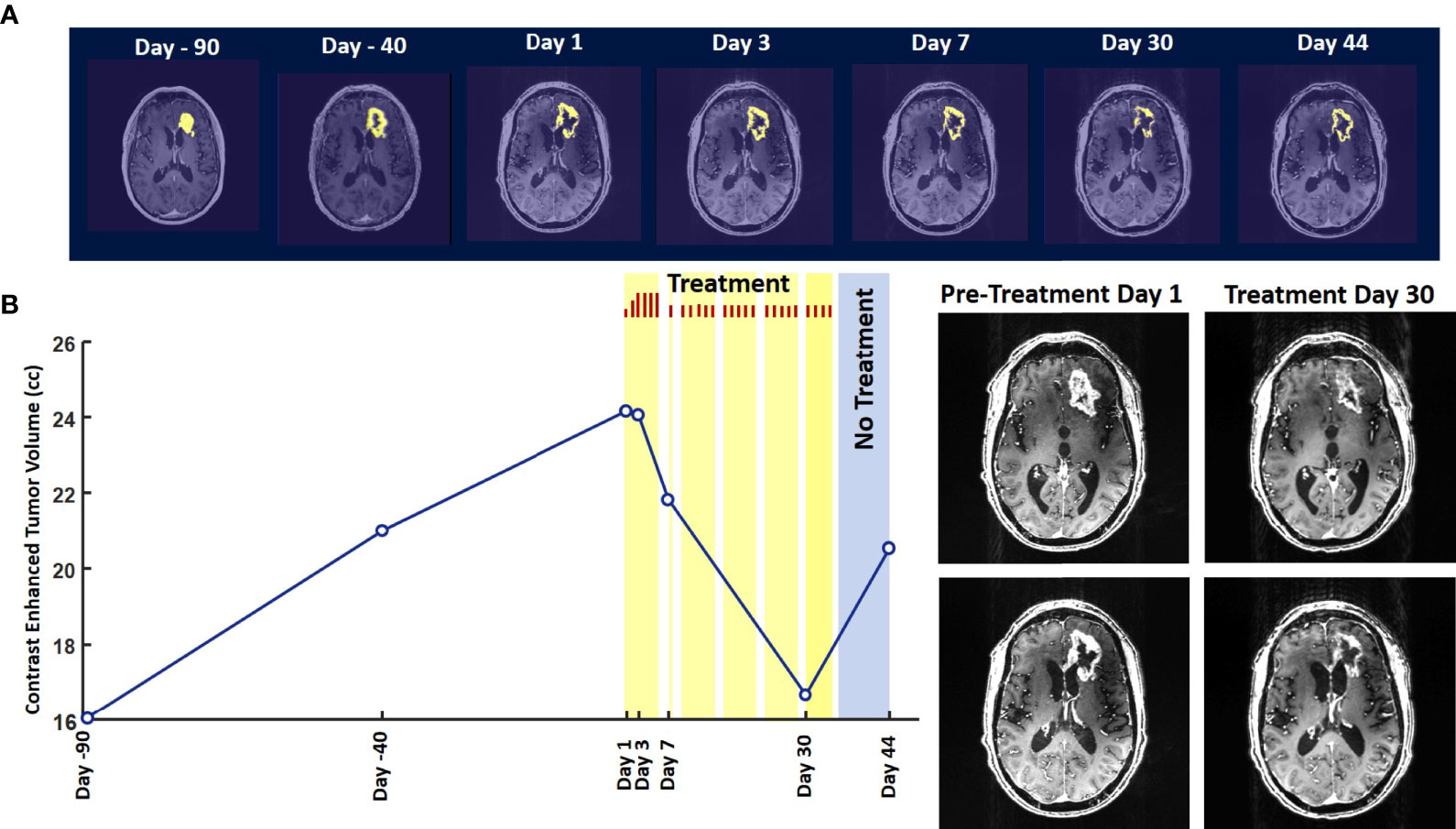
Figure 2 Change in Contrast-Enhanced Tumor Volume. (A) T1-weighted axial post-contrast scans showing the contrast-enhanced tumor (CET) highlighted with an overlayed automated computer program-generated light-yellow mask at different time points (B) Left – A graph showing the change in CET volume over time. The treatment times and durations are shown as red bars and light-yellow highlights. The long pause in treatment is shown as a light-blue highlight. Right – T1-weighted axial post-contrast scans showing CET at two levels along the dorso-ventral axis at Day 1 before treatment and Day 30 of treatment.
The T2-FLAIR data in Figure 3A show changes in enhanced intensity volume of 1 – 11% over time. The decreases in volume are greater after a 3-day pause in treatment on Day 7 and after an 8-day pause on Day 44. These decreases are likely due to reduction in treatment-related cerebral edema and/or reduction in non-contrast enhancing tumor infiltration. The patient died ~3 months after cessation of treatment from the CHI. A brain only autopsy showed a resection cavity in the left frontal lobe (6.0 x 5.0 x 3.5 cm) and recurrent/residual glioblastoma with associated treatment effect (see Figures 3B–E ). Residual/recurrent high-grade glioma was present, including foci of densely cellular tumor, focal microvascular proliferation, and necrosis ( Figure 3C ). In addition, there was prominent treatment effect with pallor and rarefaction of white matter ( Figure 3D ), reactive astrocytosis, infarct-like necrosis ( Figure 3E ) and bizarre nuclear atypia within residual tumor cells. Additional features of treatment effect included dystrophic calcifications ( Figure 3E ).
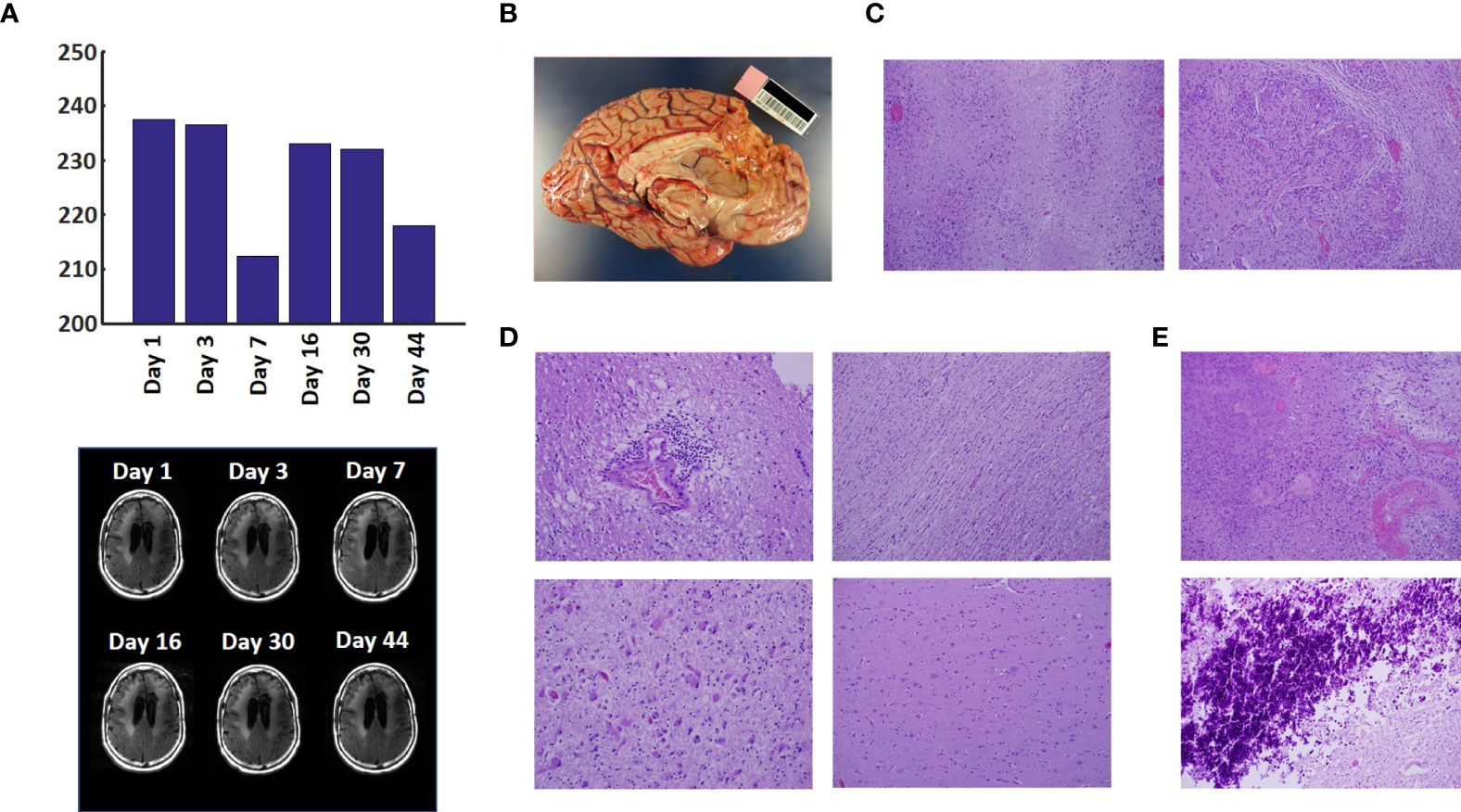
Figure 3 Variation in Enhanced Intensity Volumes in T2-FLAIR MRI Scans and Autopsy Findings. (A) Top – Bar plots of the volumes of T2-FLAIR intensity enhancement in the whole brain at different time points. Overall, there was up to 11% decrease in T2 FLAIR volume over the course of treatment. Bottom – Representative T2-FLAIR images are shown. (B) Left hemisphere of the brain, examined grossly, showing no tumor mass. (C) Photomicrographs of the left cortex showing bland necrosis, residual tumor, and microvascular proliferation with thick-walled vessels. (D) Top left – Microscopic field of the left cingulate cortex showing a focus of rarefied, perivascular inflammation. Bottom left – Cortical field showing rarefied parenchyma and residual tumor cells, enlarged with treatment-type effect that can be seen in GBM. Top right – Micrographic field of the corpus callosum showing thinned, rarefied white matter tract. Bottom right – Field showing relatively uninvolved contralateral (right) cortex. (E) Top – Micrographic field in the left cortex showing infarct-like necrosis (left), tumor (right), and fibrin thrombus (lower right). Bottom – Left cortical field showing necrotic tissue with dystrophic calcification.
The findings of this study indicate that Oncomagnetic device-based OMF therapy is well tolerated by a patient who has end-stage recurrent GBM with leptomeningeal involvement and has no other available effective treatment options. They also demonstrate a clinically significant reduction in CET volume with reductions in non-enhanced tumor volume and/or edema in T2-FLAIR scans. The temporal profile of changes in CET volume also suggests a correlation with the treatment dose and the presence or absence of treatment. When the treatment dose was higher (6 hours/day for 4 days) we see a tumor volume reduction rate of 2.32 cm 3 /day. When it was lower (2 hours/day for 9 days and 3 hours/day for 18 days) the reduction is 1.03 cm 3 /day. Moreover, when the treatment was paused for 8 days the decreasing trend reversed and the CET volume increased, instead. Assuming that the ~1.03 cm 3 /day decreasing trend had continued until the treatment was paused, we can estimate that the CET volume grew at the rate of 1.26 cm 3 /day during the pause. Despite the apparent correlation it is possible that the treatment response is independent of the short-term changes in the treatment dose.
To our knowledge, there is no report in the literature of a noninvasive treatment-related shrinkage of CET volume of GBM at a rate comparable to that seen in this study. One published report on Optune™ therapy has reported that the time course of change in tumor volume in MRI scans shows a ~15% reduction over ~3 months ( 15 ). Besides Optune™, the other type of treatment approved by the FDA and recommended as a standard in National Comprehensive Cancer Network guidelines for recurrent GBM is the anti-vascular endothelial growth factor (VEGF) monoclonal antibody, Bevacizumab ( 16 , 17 ). Bevacizumab treatment response of reduction in tumor volume on MRI scans has been reported to be lower than is observed in the present study ( 18 ). Furthermore, while anti-VEGF drugs in general have mild toxicity profiles and two Phase II trials have shown anti-tumor efficacy ( 19 , 20 ), a subsequent Phase III trial did not show a significant increase in overall survival ( 21 – 23 ).
Noninvasive Oncomagnetic device based OMF therapy appears to be a safe and efficacious new modality of treatment against GBM that potentially has many advantages over existing treatments. The present report has the limitation of the treatment being conducted in only a single patient so far. Extending it to more patients in research studies would provide additional information regarding safety and efficacy.
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Houston Methodist Research Institute Institutional Review Board. The patient/participant provided their written informed consent to participate in this study. Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
Author Contributions
SH and DB designed the study and drafted the manuscript. SH designed the device used in the study, supervised its construction and testing and quantitively analyzed the imaging data. DB provided medical care to the study subject, supervised the delivery of device treatment, and conducted his clinical assessments. SH, MS, and DB designed the device treatment protocol and interpreted the findings. LN constructed and tested the device and provided device treatment to the study subject. All authors contributed to the article and approved the submitted version.
This work was supported by a grant from the Translational Research Initiative of the Houston Methodist Research Institute to SH and DB, and by Donna and Kenneth Peak, the Kenneth R. Peak Foundation, the John S. Dunn Foundation, the Taub Foundation, the Blanche Green Fund of the Pauline Sterne Wolff Memorial Foundation, the Kelly Kicking Cancer Foundation, the Gary and Marlee Swarz Foundation, the Methodist Hospital Foundation, and the Veralan Foundation. The John S. Dunn Foundation also supports the Distinguished Professorship of MS.
Conflict of Interest
SH, MS, and DB are listed as inventors on a U.S. patent application filed by Houston Methodist Hospital for the device used in this report.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank the patient for graciously volunteering to be a research subject in this study and the rest of his family for supporting him. We appreciate the assistance of Dr. Matthew Cykowski, MD, Department of Pathology and Genomic Medicine, who provided pathologic description and images. We thank Blessy S. John and Alvin Saldon for aiding in device construction.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2021.708017/full#supplementary-material
1. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy Plus Concomitant and Adjuvant Temozolomide for Glioblastoma. N Engl J Med (2005) 352:987–96. doi: 10.1056/NEJMoa043330
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Henriksson R, Asklund T, Poulsen HS. Impact of Therapy on Quality of Life, Neurocognitive Function and Their Correlates in Glioblastoma Multiforme: A Review. J Neurooncol (2011) 104:639–46. doi: 10.1007/s11060-011-0565-x
3. Stupp R, Wong ET, Kanner AA, Steinberg D, Engelhard H, Heidecke V, et al. NovoTTF-100A Versus Physician’s Choice Chemotherapy in Recurrent Glioblastoma: A Randomised Phase III Trial of a Novel Treatment Modality. Eur J Cancer (2012) 48:2192–202. doi: 10.1016/j.ejca.2012.04.011
4. Stupp R, Taillibert S, Kanner A, Read W, Steinberg D, Lhermitte B, et al. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs Maintenance Temozolomide Alone on Survival in Patients With Glioblastoma: A Randomized Clinical Trial. JAMA (2017) 318:2306–16. doi: 10.1001/jama.2017.18718
5. Tuszynski JA, Wenger C, Friesen DE, Preto J. An Overview of Sub-Cellular Mechanisms Involved in the Action of TTFields. Int J Environ Res Public Health 13 (2016) 13:1–23. doi: 10.3390/ijerph13111128
CrossRef Full Text | Google Scholar
6. Saliev T, Begimbetova D, Masoud AR, Matkarimov B. Biological Effects of non-Ionizing Electromagnetic Fields: Two Sides of a Coin. Prog Biophys Mol Biol (2019) 141:25–36. doi: 10.1016/j.pbiomolbio.2018.07.009
7. Jimenez H, Blackman C, Lesser G, Debinski W, Chan M, Sharma S, et al. Use of non-Ionizing Electromagnetic Fields for the Treatment of Cancer. Front Biosci (Landmark Ed) (2018) 23:284–97. doi: 10.2741/4591
8. Helekar SA, Convento S, Nguyen L, John BS, Patel A, Yau JM, et al. The Strength and Spread of the Electric Field Induced by Transcranial Rotating Permanent Magnet Stimulation in Comparison With Conventional Transcranial Magnetic Stimulation. J Neurosci Methods (2018) 309:153–60. doi: 10.1016/j.jneumeth.2018.09.002
9. Helekar SA, Voss HU. Transcranial Brain Stimulation With Rapidly Spinning High-Field Permanent Magnets. IEEE Access (2016) 4:2520–8. doi: 10.1109/ACCESS.2016.2568739
10. Helekar S, Sharpe M, Pichumani K, Ijare O, Nguyen L, Baskin D. CTNI-48. Novel Treatment of End Stage Recurrent Glioblastoma Treated With a Noninvasive Oncomagnetic Device Using Oscillating Magnetic Fields – a New and Powerful Noninvasive Therapy. Neuro-Oncol (2020) 22:ii53–3. doi: 10.1093/neuonc/noaa215.214
11. Helekar S, Hambarde S, Baskin D, Sharpe M. EXTH-13. Potent Anticancer Effects of a New Wearable Noninvasive Oncomagnetic Device: Cellular Mechanisms of Action. Neuro-Oncol (2020) 22:ii89–9. doi: 10.1093/neuonc/noaa215.367
12. Hambarde S, Sharpe M, Baskin D, Helekar S. CBIO-07. Cell Death Induced by an Oscillating Magnetic Field in Patient Derived Glioblastoma Cells is Mediated by Reactive Oxygen Species. Neuro-Oncol (2020) 22:ii17–7. doi: 10.1093/neuonc/noaa215.067
13. Andersen BM, Miranda C, Hatzoglou V, DeAngelis LM, Miller AM. Leptomeningeal Metastases in Glioma: The Memorial Sloan Kettering Cancer Center Experience. Neurology (2019) 92:e2483–91. doi: 10.1212/WNL.0000000000007529
14. Wen PY, Chang SM, Van den Bent MJ, Vogelbaum MA, Macdonald DR, Lee EQ. Response Assessment in Neuro-Oncology Clinical Trials. J Clin Oncol (2017) 35:2439–49. doi: 10.1200/JCO.2017.72.7511
15. Robins HI, Nguyen HN, Field A, Howard S, Salamat S, Deming DA. Molecular Evolution of a Glioblastoma Controlled With Tumor Treating Fields and Concomitant Temozolomide. Front Oncol (2018) 8:451. doi: 10.3389/fonc.2018.00451
16. Kreisl TN, Zhang W, Odia Y, Shih JH, Butman JA, Hammoud D, et al. A Phase II Trial of Single-Agent Bevacizumab in Patients With Recurrent Anaplastic Glioma. Neuro Oncol (2011) 13:1143–50. doi: 10.1093/neuonc/nor091
17. Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, et al. Bevacizumab Alone and in Combination With Irinotecan in Recurrent Glioblastoma. J Clin Oncol (2009) 27:4733–40. doi: 10.1200/JCO.2008.19.8721
18. Daniels D, Guez D, Last D, Hoffmann C, Nass D, Talianski A, et al. Early Biomarkers From Conventional and Delayed-Contrast Mri to Predict the Response to Bevacizumab in Recurrent High-Grade Gliomas. AJNR Am J Neuroradiol (2016) 37:2003–9. doi: 10.3174/ajnr.A4866
19. Vredenburgh JJ, Desjardins A, Herndon JE 2nd, Marcello J, Reardon DA, Quinn JA, et al. Bevacizumab Plus Irinotecan in Recurrent Glioblastoma Multiforme. J Clin Oncol (2007) 25:4722–9. doi: 10.1200/JCO.2007.12.2440
20. Vredenburgh JJ, Desjardins A, Herndon JE 2nd, Dowell JM, Reardon DA, Quinn JA, et al. Phase II Trial of Bevacizumab and Irinotecan in Recurrent Malignant Glioma. Clin Cancer Res (2007) 13:1253–9. doi: 10.1158/1078-0432.CCR-06-2309
21. Chinot OL, Wick W, Mason W, Henriksson R, Saran F, Nishikawa R, et al. Bevacizumab Plus Radiotherapy-Temozolomide for Newly Diagnosed Glioblastoma. N Engl J Med (2014) 370:709–22. doi: 10.1056/NEJMoa1308345
22. Wick W, Gorlia T, Bendszus M, Taphoorn M, Sahm F, Harting I, et al. Lomustine and Bevacizumab in Progressive Glioblastoma. N Engl J Med (2017) 377:1954–63. doi: 10.1056/NEJMoa1707358
23. Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, et al. A Randomized Trial of Bevacizumab for Newly Diagnosed Glioblastoma. N Engl J Med (2014) 370:699–708. doi: 10.1056/NEJMoa1308573
Keywords: magnetic resonance imaging, contrast enhanced tumor, compassionate use treatment, radiation-type tumor necrosis 2, oscillating magnetic fields
Citation: Baskin DS, Sharpe MA, Nguyen L and Helekar SA (2021) Case Report: End-Stage Recurrent Glioblastoma Treated With a New Noninvasive Non-Contact Oncomagnetic Device. Front. Oncol. 11:708017. doi: 10.3389/fonc.2021.708017
Received: 11 May 2021; Accepted: 21 June 2021; Published: 22 July 2021.
Reviewed by:
Copyright © 2021 Baskin, Sharpe, Nguyen and Helekar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: David S. Baskin, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Progress to Advance Care, Treatments, and Outcomes for Brain Tumor Patients
April 25, 2022 , by Brittany Cordeiro, NCI-CONNECT Program Manager

Neuro-Oncologist Dr. Jing Wu reviews brain tumor scans
Read about our advances in care, treatments, and patient outcomes for brain and other central nervous systems tumors in honor of Brain Tumor Awareness Month.
An estimated 700,000 people in the United States are living with a brain tumor. Over 25,000 more will be diagnosed with a cancerous brain or other central nervous system (CNS) tumor this year. The causes are not known. And, while males are slightly more likely to develop brain cancer than females, brain tumors do not discriminate.
In May, the brain tumor community joins together to raise awareness about brain tumors through education. By sharing the rarity and uniqueness of brain and other CNS tumors— 1.3 percent of all new cancers cases and over 130 different types—we can inspire research and clinical studies to improve diagnosis and standardize care.
We also hope to champion progress by sharing the work that NCI-CONNECT and the NCI Center for Cancer Research's Neuro-Oncology Branch (NOB) have completed over the last year to advance care, treatments, and patient outcomes.
Investigating New Therapies and Methods to Improve Outcomes
Nci-connect clinical studies expansion.
In 2021, NCI-CONNECT expanded two clinical studies—an immunotherapy drug trial and a tumor tissue repository study—to its national network of collaborative institutions to reach more people with rare brain and spine tumors and help researchers advance their knowledge of the diseases faster.
The first-of-its-kind immunotherapy drug trial is designed to test whether stimulating the immune system using nivolumab is effective and can shrink (or control the growth or spread of) specific types of recurrent rare brain and spine tumors. The trial first launched in 2017 at the NOB. Now, the trial is being led by NOB Associate Research Physician Marta Penas-Prado, M.D. It is also testing the changes that nivolumab induces in immune cells in peripheral blood during treatment—and whether nivolumab can improve the symptoms of people with these tumors.
The new multi-institutional Tissue Outcomes Study collects tumor tissue and comprehensive clinical data from deceased patients with rare brain and spine tumors, and people who were pregnant at diagnosis (or became pregnant after diagnosis). The study is breaking silos by working across the NCI-CONNECT national network. It is led by Dr. Penas-Prado.
NCI-CONNECT First-in-Human Study
In other firsts, NCI-CONNECT launched a first-in-human phase 1 clinical trial for people with recurrent rare brain and spine tumors. Led by Brett Theeler, M.D., neurologist and neuro-oncologist in the United States Army Medical Corps and NCI-CONNECT clinical collaborator, the trial is studying ONC206, an oral cancer therapy. The trial tests the dosing and safety in adult patients.
NOB Immunotherapy and Glioblastoma Trial
Glioblastoma is the most common type of primary brain cancer. People with this disease or a variant called gliosarcoma have poor long-term outcomes. NOB Chief and NCI-CONNECT Co-Leader Mark Gilbert, M.D., is leading a new clinical trial testing an immunotherapy treatment to slow or stop the spread of cancer cells in people with glioblastoma and gliosarcoma. The trial will also evaluate a test that may help determine who is likely to get an immune response.
We designed the study based on quality science and built-in cutting-edge techniques. The study results should be a very important contribution to the field.
Mark Gilbert, M.D., NOB Chief and NCI-CONNECT Co-Leader
Outcomes Intervention Studies
Under the leadership of NOB Deputy Chief and NCI-CONNECT Co-Leader Terri Armstrong, Ph.D., NCI-CONNECT also launched three studies in 2021 to measure if an intervention helps improve outcomes. Led by Amanda King, Ph.D., an iCURE postdoctoral fellow in the Patient Outcomes Program, a virtual reality study for patients with brain cancer investigates if using a virtual reality headset to deliver relaxation techniques helps to reduce the distress and anxiety that people experience ahead of their magnetic resonance imaging (MRI) scans and clinical appointments.
Led by assistant investigator Dorela Shuboni-Mulligan, Ph.D., CRTA postdoctoral fellow in the Patient Outcomes Program, a sleep observation study measures daytime sleepiness and activity patterns using a smart wearable device. This will provide insight into the impact of sleep disturbance on those with brain cancers.
Led by assistant investigator Alvina Acquaye, psychosocial behavioral specialist for NCI-CONNECT, the CALM therapy intervention study uses individualized therapy to address negative feelings and improve a person’s mood and the way they feel. This study will determine if using the CALM intervention helps to reduce depressive symptoms in people with brain cancer.
Bringing the Community Together to Advance Science and Patient Care
Virtual educational webinars were held to join experts across disciplines with advocates—and provide forums for thoughtful discussion about challenges and solutions.
Targeting CNS Tumor Metabolism
To advance the field of CNS tumor metabolism, NOB Investigator Mioara Larion, Ph.D., and Dr. Gilbert co-led a virtual symposium with the Society for Neuro-Oncology (SNO) on April 6-7, 2021. It was the first conference entirely dedicated to education and research on brain tumor metabolism . Over 500 people registered to attend. The conference brought together clinicians, researchers, trainees, patients, and experts in the field of metabolism.
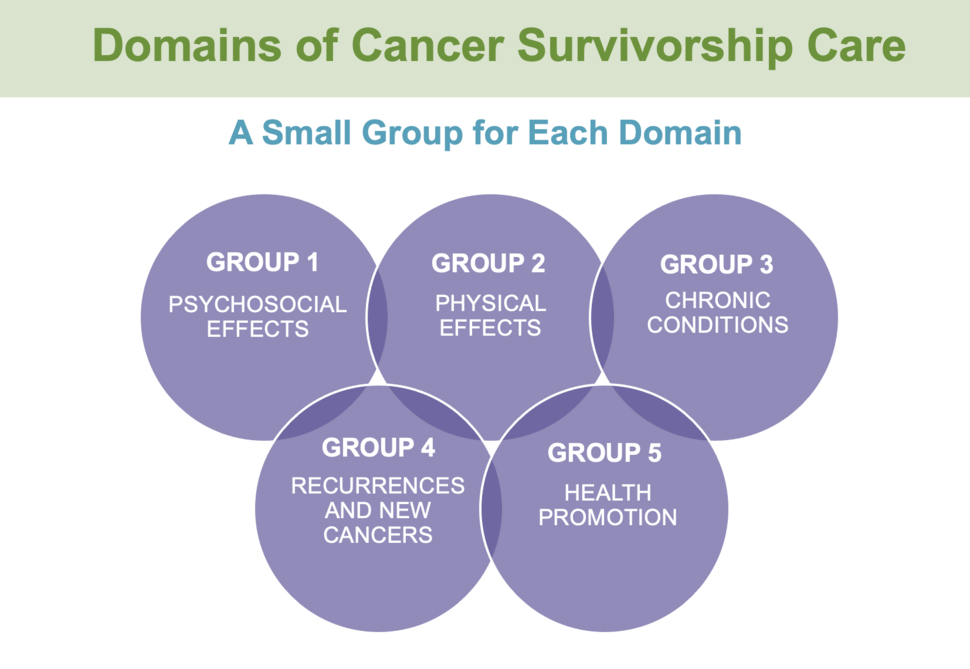
Survivorship Care in Neuro-Oncology Symposium
NOB Assistant Research Physician Heather Leeper, M.D., and Dr. Armstrong co-led the Survivorship Care in Neuro-Oncology Symposium on June 21-22, 2021. The symposium brought together neuro-oncology providers, researchers, advocates, patients, and care partners virtually to learn, discuss the challenges experienced by people living with brain and spine tumors, and develop survivorship care guidelines. Over 250 people attended the symposium.
Introduction to Career Pathways in Neuro-Oncology
On January 11, 2022, the NOB partnered with SNO to offer trainees of all disciplines the opportunity to learn about neuro-oncology careers in basic science, clinical care, and research. The free virtual event offered insights, opportunities, and strategies shared by world-renowned neuro-oncology professionals to expand a neuro-oncology career. There was also a post-session panel discussion for attendees to share their thoughts with experts.
NIH Tumor Boards and Journal Clubs
To encourage referrals and further collaboration, in 2020 we expanded our virtual journal club and weekly multidisciplinary NIH Neuro-Oncology Tumor Board live sessions to include investigators and cases from participating NCI-CONNECT consortium sites. As of November 2021, 28 providers had presented 41 cases at 24 tumor board meetings with 60 to 70 participants.
Awarding and Recognizing Pioneering Work
National research awards.
In 2021, Lasker Clinical Research Scholar and NOB Investigator Jing Wu, M.D., Ph.D., was accepted into the NExT (NCI Experimental Therapeutics) Program , which provides resources for projects focused on developing therapies for unmet needs. Dr. Wu leads the NOB Translational Research Program, which is dedicated to developing clinical trials for people living with brain and spine tumors. Her work combines both clinical and laboratory research and is making a difference in the field.
Dr. Penas-Prado received an Award for Excellence in Rare CNS Disease at the 2021 SNO Annual Meeting for her abstract on the interim analysis of the immune checkpoint inhibitor nivolumab for people with rare CNS cancers trial. As of March 10, 2021, the interim analysis of the clinical trial determined that the disease control rate exceeded the minimum required to pass the interim analysis in the heavily pretreated cohort and continue the trial.
Ultimately, this multicenter study should advance our understanding of these tumors, set the foundation for future trials, and provide better treatment options.
Marta Penas-Prado, M.D., NOB Associate Research Physician
Dr. Penas-Prado also received the 2022 Center for Cancer Research Staff Clinician Leadership Merit Award for leading our rare CNS tumor clinic and clinical trials, a national tumor board, and an international symposium.
Dr. Leeper received an Award for Excellence in Survivorship at the 2021 SNO Annual Meeting for her abstract with the NOB Patient Outcomes Program on whether economic strain and mood disturbance during the COVID-19 pandemic may have additional impacts on patients’ symptoms and function. Dr. Leeper concluded that worse financial toxicity scores were strongly associated with worse overall symptom burden, worse anxiety and depression scores, and worse overall health-related quality of life scores.
Trainee and Mentor Awards
Postbaccalaureate Research Fellow Yeonju Kim was selected as the Outstanding Post-Graduate Trainee at the 22nd Annual Center for Cancer Research Fellows and Young Investigators Colloquium, where she gave an oral presentation. Kim is mentored by NOB Staff Scientist Orieta Celiku, Ph.D., Dr. Gilbert, and Dr. Armstrong. Her colloquium abstract was titled, "ACROSS: Accrual and Access to Neuro-Oncology trials in the United States. "
Dr. Celiku received the 2022 NCI Staff Scientists and Staff Clinicians Outstanding Mentor Award for her exemplary mentorship in developing the next generation of cancer researchers.
Sharing Progress to Raise Awareness
The NOB and NCI-CONNECT published over 80 abstracts that were presented at national meetings, one journal supplement, and 10 manuscripts. Our work modified two National Comprehensive Cancer Network (NCCN) guidelines for rare CNS tumors in 2020 and 2021. Our progress is made possible by the participation of patients and their care partners in our programs.
To continue our efforts in brain and spine tumor care, treatment, and research—and to improve survival and quality of life for people living with the disease—we encourage you to join us for Brain Tumor Awareness Month in May and share these advances. Educating those living with (or not yet diagnosed with) a brain or spine tumor can make an impact.
- Dermatology
- Gastroenterology
- Geriatric Medicine and Gerontology
- Gynecology and Obstetrics
- Heart and Vascular
- Neurology and Neurosurgery
- Ophthalmology
- Orthopaedics
- Otolaryngology–Head and Neck Surgery
- Physical Medicine and Rehabilitation
- Plastic and Reconstructive Surgery
- Psychiatry and Behavioral Sciences
- Pediatric Specialties
- Pediatric Diabetes and Endocrinology
- Pediatrics Florida
- Pediatric Gastroenterology and GI Surgery
- Pediatric Heart
- Pediatrics Maryland/DC
- Pediatric Neurology & Neurosurgery
- Pediatric Orthopaedics
- Physician Affiliations
- Health Care Technology
- High-Value Health Care
- Clinical Research Advancements
- Precision Medicine Excellence
- Patient Safety
Case Presentation: Ganglioglioma Brain Tumor
Alan Cohen, director of Johns Hopkins pediatric neurosurgery, shares the case of a 12-year-old boy who had a generalized seizure that led him to the emergency room. An MRI showed a tumor in the left parietal lobe of the brain. Using frameless stereotactic guidance and intraoperative MRI, Cohen and his team carefully removed the tumor, which had scalloped the overlying skull with pressure since it arose from the cerebral cortex. Pathology identified the tumor as a rare benign ganglioglioma, WHO grade 1.

Related Presenters

Alan Cohen, MD
Director of the Johns Hopkins Division of Pediatric Neurosurgery
View full profile
- About Johns Hopkins Medicine
- Contact Johns Hopkins Medicine
- Centers & Departments
- Maps & Directions
- Find a Doctor
- Patient Care
- Terms & Conditions of Use
- Privacy Statement
Connect with Johns Hopkins Medicine
Join Our Social Media Communities >
Clinical Connection
- Otolaryngology—Head and Neck Surgery
- Contact Johns Hopkins
© The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System. All rights reserved.
Privacy Policy and Disclaimer
Clinical Trials
Brain tumor.
Displaying 155 studies
The purpose of this study is to compare how well single fraction stereotactic radiosurgery works versus fractionated stereotactic radiosurgery in treating patients with cancer that has spread to the brain from other parts of the body and has been removed by surgery. Single fraction stereotactic radiosurgery is a specialized radiation therapy that delivers a single, high dose of radiation directly to the tumor and may cause less damage to normal tissue. Fractionated stereotactic radiosurgery delivers multiple, smaller doses of radiation therapy over time.
The purpose of this study is to determine whether there is an increase in the time of a first occurrence of either: local recurrence, leptomeningeal disease, or symptomatic radiation brain necrosis in patients with brain metastases who receive SRS prior to surgery as compared to patients who receive surgery prior to SRS.
The purpose of this study is to compare the effect of adding whole brain radiotherapy with hippocampal avoidance and memantine to stereotactic radiosurgery versus stereotactic radiosurgery alone in treating patients with cancer that has spread to the brain and come back in other areas of the brain after earlier stereotactic radiosurgery. Hippocampus avoidance during whole-brain radiation therapy decreases the amount of radiation that is delivered to the hippocampus, which is a brain structure that is important for memory.
The medicine memantine is also often given with whole brain radiation therapy because it may decrease the risk of side effects of radiation on ...
The purpose of this study is to evauate how well genetic testing works in guiding treatment for patients with solid tumors that have spread to the brain. Several genes have been found to be altered or mutated in brain metastases such as NTRK, ROS1, CDK or PI3K. Medications that target these genes such as abemaciclib, GDC-0084, and entrectinib may stop the growth of tumor cells by blocking some of the enzymes needed for cell growth. Genetic testing may help doctors tailor treatment for each mutation.
The purpose of this study is to compare local and general anesthesia (Awake vs. Asleep Craniotomy) in the removal of brain tumors that are in areas of the brain that do not directly control bodily functions (non-eloquent gliomas).
The purpose of this research is to compare two different standard-of-care pre-surgical imaging methods.
The goal of this study is to investigate the feasibility of successfully obtaining intra-operative OCT imaging and data during standard brain surgery.
The purpose of this study is to evaluate whether radiation therapy with adjuvant PCV is more effective in treating anaplastic glioma or low grade glioma.
This phase II trial studies how well vemurafenib and cobimetinib work in treating patients with BRAF V600E mutation positive craniopharyngioma. Vemurafenib and cobimetinib may stop the growth of tumor cells by blocking some of the enzymes needed for cell growth.
The purpose of this study is to demonstrate improved planning for meningioma and similar brain tumor surgery.
The purpose of this study is to validate the effectiveness and clinical use of array and next generation sequencing tests in hopes of adopting these tests as standard of care and advancing glioma patient care and clinical practice at Mayo Clinic and beyond.
The purpose of this project is to provide expanded access to ONC201 for patients with previously-treated H3 K27M-mutant and/or midline high grade gliomas who cannot access ONC201 through clinical trials.
The purpose of this study is to explore the translational abilities of desorption electrospray ionization mass spectrometry (DESI-MS) as intraoperative diagnostic tool to identify cancerous versus noncancerous tissue and estimate the percentage of tumor infiltration in tissue biopsies, by monitoring depletion of N-acetylaspartate (NAA) and aberrations of the phospholipid signature of neurological tissue; and to identify the presence of IDH mutations by monitoring the 2-hydroxyglutarate (2HG) and, therefore, differentiate between IDH-mutant and wild-type gliomas.
The purpose of this study is to establish a prospective repository of detailed patient-specific information regarding the structure and function of human brain tissue impacted by disease and therapeutic interventions, detailing the neurologic and cognitive performance during the course of disease management.
This study aims to demonstrate that the efficacy of treatment with selumetinib as measured by event-free survival (EFS) is non-inferior compared to treatment with carboplatin/vincristine (CV) in previously-untreated low-grade glioma (LGG) not associated with BRAFV600E mutations or systemic neurofibromatosis type 1 (NF1).
The purpose of this study is to determine whether neurologic examination in the outpatient setting is sufficient to predict suitability to drive in order to make recommendations of driving safety for patients with brain metastases.
The purpose of this study is to compare stereotactic radiosurgery (SRS) to whole brain radiotherapy (WBRT) in patients with 5 or more brain metastases.
All lesions 4.0 cm to 6.0 cm will receive 32.5 Gy/5 fractions and will be analyzed separately. The portion of the trial is written as a phase II study without randomization noting the rarity of unresected brain metastasis of this size and the lack of comfort of treating radiation oncologist and neurosurgeons with single fraction SRS for tumors this large. However, noting the paucity of prospective data for this patient population enrolling patients on a clinical trial will provide a more accurate historical control for future trials. Although this cohort was enrolled on the prospective phase I trial from ...
The purpose of this study is to determine the safety and feasibility of intra-operative Ommaya Reservoir placement during a clinically indicated tumor surgery in order to facilitate a longitudinal access to cerebrospinal fluid (CSF) for analysis of exploratory and future tumor biomarkers for individualized monitoring.
The purpose of this study is to use stored glioma specimens stored by the Tissue Registry under the oversight of the Neuro-Oncology program.
The purpose of this study is to evaluate the clinical outcomes of hypofractionation with planned courses of re-irradiation for patients with diffuse midline gliomas of the pons.
Subjects will be screened by neurosurgery, radiation oncology, or pediatric oncology at outpatient clinic or by the multidisciplinary pediatric central nervous system tumor conference. Interested qualified patients and their families will be consented and offered participation in this study
The purpose of this study is to utilize a novel approach of combining advanced radiation delivery with proton beam therapy with advanced tumor visualization with 18F-DOPA PET and MRI imaging. We will study the effectiveness and safety of this technique delivering the entire treatment over 1-2 weeks.
The purpose of this study is to determine the presence of immunosuppressive molecules and immunosuppressive leukocytes in brain tumor patients’ blood.
This trial studies the natural history of brain function, quality of life, and seizure control in patients with brain tumor who have undergone surgery. Learning about brain function, quality of life, and seizure control in patients with brain tumor who have undergone surgery may help doctors learn more about the disease and find better methods of treatment and on-going care.
RATIONALE: Vaccines made from a gene-modified virus may help the body build an effective immune response to kill tumor cells.
PURPOSE: This phase I trial is studying the side effects and best dose of viral therapy in treating patients with recurrent glioblastoma multiforme.
The purpose of this study is to investigate the safety, diagnostic performance, and clinical usefulness of the imaging agent Gleolan™ (Aminolevulinic Acid Hydrochloride, ALA HCl, ALA, 5-ALA), an orally administered imaging agent for the real-time detection and visualization of meningiomas during tumor resection surgery. ALA is a prodrug that is metabolized intracellularly to form the fluorescent molecule Protoporphyrin IX (PpIX).
The purpose of this study is to evaluate the use of fluorine F 18 fluorodopa-labeled PET scanning for the planning of surgery and radiation therapy to treat patients who have newly diagnosed high- or low-grade glioma brain tumors. New imaging procedures, such as fluorine F 18 fluorodopa-labeled PET scans, may help in guiding surgery and radiation therapy and allow doctors to plan better treatment.
This pilot clinical trial studies fluorine F 18 fluorodopa (18F-DOPA)-positron emission tomography (PET) in planning surgery in patients with gliomas. New imaging procedures, such as 18F-DOPA-PET scan, may help find gliomas and may help in planning surgery.
The purpose of this study is to use a nutrient called 18F-FDOPA and PET/CT scan to help determine where and how big the tumor is, as well as how aggressive the tumor is. This will help treating physicians to target diseased areas with higher than standard doses of radiation, in order to improve the effectiveness of radiation in this tumor.
This randomized phase III trial studies armodafinil to see how well it works in reducing cancer-related fatigue in patients with high grade glioma. Armodafinil may help relieve fatigue in patients with high grade glioma.
Biospecimen banks are a modern attempt to centralize collections of human blood and tissue samples along with health information and personal history. The Neuro-Oncology Program Registry and Biobank will be used for research purposes to increase our understanding of nervous system tumors.
The purpose of this study is to determine the feasibility of hippocampal-avoidance (HA) with proton therapy in suprasellar or midline low-grade gliomas (LGGs).
This phase II trial studies how well vismodegib and focal adhesion kinase (FAK) inhibitor GSK2256098 work in treating patients with meningiomas that may have gotten bigger or grew back after treatment. Vismodegib and FAK inhibitor GSK2256098 may stop the growth of tumor cells by blocking some of the enzymes needed for cell growth.
The purpose of this study is to improve patient care by optimizing and measuring magnetic resonance imaging methods for the early detection of brain cancer response to therapy.
The purpose of this study is to develop an MRS-based measurement of 2-HG that is reliable, and to assess the reproducibility of the method(s) above on a cohort of patients with IDH mutant low grade gliomas.
RATIONALE: Stereotactic radiosurgery may be able to send x-rays directly to the tumor and cause less damage to normal tissue. Radiation therapy uses high-energy x rays to kill tumor cells. It is not yet known whether stereotactic radiosurgery is more effective than whole-brain radiation therapy in treating patients with brain metastases that have been removed by surgery.
PURPOSE: This randomized phase III trial studies how well stereotactic radiosurgery works compared to whole-brain radiation therapy in treating patients with brain metastases that have been removed by surgery.
This randomized phase III trial studies how well radiation therapy works compared with observation in treating patients with newly diagnosed grade II meningioma that has been completely removed by surgery. Radiation therapy uses high energy x-rays to kill tumor cells and shrink tumors.
The purpose of this study is to verify the gene array data by examining the protein expression in brain tissue of diffuse intrinsic pontine glioma (DIPG) patients compared to normal healthy subjects using western blot.
This pilot research trial studies blood brain barrier differences in patients with brain tumors undergoing surgery. Studying samples of tissue and blood from patients with brain tumors in the laboratory may help doctors to understand how well drugs get into different parts of a brain tumor. This may help them to determine which types of drugs may be best for treating brain tumors.
This is a prospective, observational registry in patients who have been prescribed Gliadel Wafer by the physician as part of usual care.
The purpose of this study is to collect minimal risk normal samples, both prospectively collected and those stored at the patient's home institution and any outside institutions, along with clinical data. For this same end, the study provides for a wide scope of research, including detailed genetic analysis, and provides mechanisms for reporting of results back to participants and/or their treating physicians.
This study aims to evaluate the safety of preoperative radiosurgery in the treatment of patients with biopsy-proven high grade glioma prior to conventional therapy. Safety is defined as any acute grade 3 (CTCAE v5.0) or greater unplanned adverse event from the time of enrollment until 4 weeks following postoperative radiotherapy.
The purpose of this study is to test the effectiveness and safety of Optune® given concomitantly with radiation therapy (RT) and temozolomide (TMZ) in newly diagnosed GBM patients, compared to radiation therapy and temozolomide alone. In both arms, Optune® and maintenance temozolomide are continued following radiation therapy.
RATIONALE: Radiation therapy uses high-energy x-rays to kill tumor cells. Drugs used in chemotherapy, such as temozolomide, work in different ways to stop the growth of tumor cells, either by killing the cells or by stopping them from dividing. Giving radiation therapy together with temozolomide may kill more tumor cells. It is not yet known whether giving temozolomide during and/or after radiation therapy is more effective than radiation therapy alone in treating anaplastic glioma.
PURPOSE: This randomized phase III trial is studying giving temozolomide during and/or after radiation therapy to see how well it works compared to radiation therapy ...
The purpose of this study is to develop and pilot a novel early intervention program for children undergoing proton radiation thereapy (PRT) for brain tumors.
Survivors of childhood brain cancers who undergo radiation therapy can have damage to normal brain tissue. Activities such as attention training and physical exercise can improve mental function in children with brain injury that is caused by the radiation therapy. Improvements in children’s ability to learn, behavior and fitness will lead to a better developmental outcome and quality of life in the longer term.
The purpose of this study is to generate preliminary data on the impact of standard, first line treatment on the plasma metabolome of patients with a new diagnosis of glioma.
The purpose of this study is to investigate the effectiveness and safety of REC-2282 in patients with progressive NF2 mutated meningiomas who have either NF2 disease-related meningioma or sporadic meningiomas that have NF2 mutations.
This randomized phase II clinical trial studies the side effects and how well proton beam or intensity-modulated radiation therapy works in preserving brain function in patients with IDH mutant grade II or III glioma. Proton beam radiation therapy uses tiny charged particles to deliver radiation directly to the tumor and may cause less damage to normal tissue. Intensity-modulated or photon beam radiation therapy uses high-energy x-ray beams shaped to treat the tumor and may also cause less damage to normal tissue. Patients will be more likely to be randomized to proton beam radiation therapy. It is not yet known if ...
This randomized phase III trial is studying maintenance chemotherapy to see how well it works compared to observation following induction chemotherapy and radiation therapy in treating young patients with newly diagnosed ependymoma. Drugs used in chemotherapy, such as vincristine sulfate, carboplatin, cyclophosphamide, etoposide, and cisplatin, work in different ways to stop the growth of tumor cells, either by killing the cells or by stopping them from dividing. Giving more than one drug (combination chemotherapy) may kill more tumor cells. Radiation therapy uses high-energy x-rays to kill tumor cells. Specialized radiation therapy that delivers a high dose of radiation directly to ...
The purpose of this study is to tailor treatment for medulloblastoma based on molecular distinctions between tumors in order to improve cure rates for molecularly aggressive medulloblastoma, while reducing treatment-related morbidities in survivors of less aggressive medulloblastoma. It is possible that subjects in this study will benefit from a reduction in treatment complications, more effective therapy, and higher rates of survival.
The purpose of this study is to utilize fresh tumor tissue to aid the development of future therapies for brain cancer.
This research study is studying several investigational drugs as a possible treatment for Glioblastoma (GBM). The drugs involved in this study are : - Abemaciclib - Temozolomide (temodar) - Neratinib - CC115
The purpose of this study is to collect and store brain tissue samples and blood from children with brain cancer that will be tested in the laboratory. Collecting and storing samples of tumor tissue and blood from patients to test in the laboratory may help the study of cancer in the future.
The purpose of this study is to learn more about the changes in levels of Spexin, leptin and other biomarkers such as adiponectin and resting energy expenditure before and after hypothalamic surgery.
The purpose of this study is to assess whether there is superiority of overall survival (OS) when enzastaurin rather than placebo is added to the regimen of temozolomide with radiation therapy followed by temozolomide for the treatment of patients with newly diagnosed glioblastoma in Denovo Genomic Marker 1 (DGM1) biomarker-positive patients.
The overall goal of this project is to survey parents of children who have undergone proton radiation for brain tumors and collect key information that will improve the feasibility of our proposed intervention. The survey will include questions on experience with proton treatment and opinion regarding a proposed early intervention.
The purpose of this study is to evaluate the safety and feasibility of surgical resection for pre-recurrent brain tumors. Eligible patients with surgically accessible latent tumors desiring surgical resection will be enrolled to prospectively track short- and long-term outcomes. Safety will be evaluated by quantifying rates of surgical morbidity as compared to patients undergoing RT after surgery, or no surgery for similar latent disease. Variables evaluated will include postoperative complications including death within 30 days, wound infection, length of hospital stay, and readmission rates.
This randomized phase II/III trial studies how well temozolomide and veliparib work and compare them to temozolomide alone in treating patients with newly diagnosed glioblastoma multiforme. Drugs used in chemotherapy, such as temozolomide, work in different ways to stop the growth of tumor cells, either by killing the cells, by stopping them from dividing, or by stopping them from spreading. Veliparib may stop the growth of tumor cells by blocking some of the enzymes needed for cell growth. It is not yet known whether temozolomide is more effective with or without veliparib in treating glioblastoma multiforme.
This phase II trial studies how well combination chemotherapy works in treating younger patients with newly diagnosed, non-metastatic desmoplastic medulloblastoma. Drugs used in chemotherapy, such as vincristine sulfate, cyclophosphamide, methotrexate, etoposide, and carboplatin, work in different ways to stop the growth of tumor cells, either by killing the cells or by stopping them from dividing.
The purpose of this study is to evaluate cognitive function and to determine neurocognitive assessment using a select CogState test battery in patients with primary intracranial malignancies receiving photon- or proton-based cranial irradiation with curative intent.
The purpose of this study is to examine the pharmacological effects of the compound BI 907828 on patient tumors at an early stage of drug development.
The purpose of this study is to evaluate the side effects and best dose of CB-839 hydrochloride (CB-839) in combination with radiation therapy and temozolomide in treating participants with IDH-mutated diffuse or anaplastic astrocytoma. CB-839 may stop the growth of tumor cells by blocking some of the enzymes needed for cell growth. Radiation therapy uses high energy x-rays to kill tumor cells and shrink tumors. Drugs used in chemotherapy, such as temozolomide, work in different ways to stop the growth of tumor cells, either by killing the cells, by stopping them from dividing, or stopping them from spreading. Giving CB-839 with ...
The purpose of this study is to combine MRI images with histologic and genetic analysis of cancer (from blood and tissue samples) to improve the overall accuracy of diagnosis and effectiveness of cancer treatment.
The purpose of this study is to confirm detection of the H3K27M mutation in patient biofluids (CSF, blood, urine, saliva) and uncover the molecular histone (alkaline protein) profile of H3K trimethylation and H3S phosphorylation in the circulating nucleosomes isolated from the biofluids of patients with H3K27M tumors.
The goal of this study is to further evaluate the ability of fluciclovine PET to discriminate between radiation necrosis and tumor progression in patients with previously irradiated intracranial metastatic disease.
This research trial studies neuropsychological (learning, remembering or thinking) and behavioral testing in younger patients with cancer. Collecting information over time from a series of tests may help doctors develop effective tests to measure neuropsychological and behavioral function of patients with cancer.
The purpose of this registry called Every Child, is to collect data and biospecimens from multiple body sources for younger patients with cancer over time. Gathering health information over time from younger patients with cancer may help doctors find better methods of treatment and on-going care.
This study is collecting and storing malignant, borderline malignant neoplasms, and related biological samples from young patients with cancer. Collecting and storing samples of tumor tissue, blood, and bone marrow from patients with cancer to study in the laboratory may help the study of cancer in the future.
The purpose of this study is to analyze the effect of sacituzumab govitecan in treating patients with HER2-negative breast cancer that has spread to the brain (brain metastases). Sacituzumab govitecan is a monoclonal antibody, called sacituzumab, linked to a chemotherapy drug, called govitecan. Sacituzumab is a form of targeted therapy because it attaches to specific molecules on the surface of cancer cells, known as Trop-2 receptors, and delivers govitecan to kill them. Giving sacituzumab govitecan may shrink the cancer in the brain and/or extend the time until the cancer gets worse.
The purpose of this study is to estimate the event-free survival (EFS) distribution for newly-diagnosed patients with BRAFV600-mutant high-grade glioma (HGG) without H3 K27M mutations excluding anaplastic pleomorphic xanthoastrocytoma (aPXA) and anaplastic ganglioglioma (aGG) treated with radiation therapy followed by a maintenance combination of dabrafenib and trametinib and to compare this EFS to contemporary historical controls.
The purpose of the Pediatric Proton Consortium Registry (PPCR) is to enroll children who have been treated with proton radiation in the United States in order to describe the population that currently receives protons and better evaluate its benefits over other therapies. The data collected from this study will help facilitate research on proton beam radiation therapy and allow for collaborative research. The PPCR will collect demographic and clinical data which many centers that deliver proton radiation therapy already collect in routine operations.
The purpose of the study is to compare the efficacy and safety of nivolumab administered alone versus bevacizumab in patients diagnosed with recurrent glioblastoma (a type of brain cancer, also known as GBM), and to evaluate the safety and tolerability of nivolumab administered alone or in combination with ipilimumab in patients with different lines of GBM therapy.
The purpose of this study is to evaluate the benefit of using intravenous fluorescein sodium (FS) and YELLOW 560 nm microscope filter (YE560) during surgery for vestibular schwannomas (VS), Meningioma, Head and Neck Paraganglioma, or Head and Neck Schwannoma and to determine the optimum FS dose and timing to be used with the YE560 device.
The purpose of this study is to evaluate the safety and effectiveness of using Exablate Model 4000 Type-2.0/2.1 in adults with Glioblastoma brain tumors to increase temporarily the permeability of the blood brain barrier, allowing increased passage of circulating free DNA (cfDNA) for sampling and analysis.
The purpose of this study is to evaluate the safety and tolerability of marizomib in combination with Temozolomide-based radiochemotherapy versus standard Temozolomide-based radiochemotherapy alone in newly diagnosed glioblastoma patients.
This randomized phase II trial studies how well dose-escalated photon intensity-modulated radiation therapy (IMRT) or proton beam radiation therapy works compared with standard-dose radiation therapy when given with temozolomide in patients with newly diagnosed glioblastoma. Radiation therapy uses high-energy x-rays and other types of radiation to kill tumor cells and shrink tumors. Specialized radiation therapy that delivers a high dose of radiation directly to the tumor may kill more tumor cells and cause less damage to normal tissue. Drugs, such as temozolomide, may make tumor cells more sensitive to radiation therapy. It is not yet known whether dose-escalated photon IMRT ...
The purpose of this study is to create a new Magnetic resonance imaging (MRI) technique with true contrast to the background reference points in functional MR images of individual patients. Functional MRI has been widely used in staging, grading and treatment response monitoring of glioblastoma. MRI has great soft tissue and tumor tissue contrast and can assist in outlining the target. It has proven able to offer functional information such as cell density, permeability of the micro-blood vessels, and the oxygen level of the tumor.
The purpose of this study is to demonstrate non-inferior 12-month overall survival of patients with GlioblastomA (GBM) treated with dose escalated hypofractionated radiotherapy compared to standard of care. Also, to demonstrate the safety and favorable quality of life via physician-reported G3+ toxicitycompare if SBRT is non-inferior to standard of care on the proportion of overall survival of patients with glioblastoma 12 months after randomization.
This phase II trial studies how well pazopanib hydrochloride works in treating patients with advanced or progressive malignant pheochromocytoma or paraganglioma. Pazopanib hydrochloride may stop the growth of tumor cells by blocking some of the enzymes needed for cell growth and by blocking blood flow to the tumor.
The purpose of this study is to assess 177Lu-DTPA-omburtamab, which is a radioactive labelling of a murine monoclonal antibody targeting B7-H3, to treat children and adolescents diagnosed with medullablastoma and with recurrent or refractory to frontline therapy.
RATIONALE: Modafinil may help improve memory, attention, and fatigue caused by cancer treatment.
PURPOSE: This phase II randomized trial studies how well modafinil works in treating children with memory and attention problems caused by cancer treatment for a brain tumor.
Drugs used as chemotherapy, such as carboplatin, etoposide, and ifosfamide work in different ways to stop the growth of tumor cells, either by killing the cells or by stopping them from dividing. Radiation therapy uses high-energy x rays to kill tumor cells. Giving chemotherapy with radiation therapy may kill more tumor cells. This phase II trial studies how well chemotherapy and radiation therapy work in treating younger patients with newly diagnosed central nervous system germ cell tumors.
The purpose of this study is to evaluate LET-based modeling as an early and accurate predictor for white-matter changes as identified on MRI and DTI in pediatric patients with primary central nervous system and skull base malignancies following proton beam therapy
This is an adaptive design, randomized controlled, Phase 3 clinical trial in patients with glioblastoma multiforme (GBM) or gliosarcoma (GS), previously treated with surgery (if appropriate), standard of care chemo-radiation with temozolomide, +/- adjuvant temozolomide, and bevacizumab and now has progressive disease during or after bevacizumab. A total of up to 180 eligible patients with recurrent/progressive GBM or GS will be randomized to receive either the investigational drug (VAL-083) or "Investigator's choice of salvage therapy" as a contemporaneous control, in a 2:1 fashion. Up to 120 eligible patients will be randomized to receive VAL-083 at 40 mg/m2 IV on days ...
The primary purposes of this study are to identify experimental therapies that improve OS for GBM patients in the Screening stage (Stage 1), determining if predefined patient subtypes or associated biomarkers uniquely benefit from the treatment and to confirm identified effective experimental therapies and associated biomarker signatures in an expansion stage (Stage 2) designed to support a new drug application.
The purpose of this study is to assess the safety and technical feasibility of TheraSphere GBM in patients with recurrent glioblastoma (GBM).
The primary objectives of this study are to determine the maximum tolerated dose/recommended phase 2 dose (MTD/RP2D) of selumetinib + vinblastine for children with progressive or recurrent LGGs, and to determine if selumetinib + vinblastine will lead to improved event-free survival (EFS) outcome compared with selumetinib alone for children with progressive or recurrent LGGs.
The purpose of this study is to evaluate the side effects of vaccine therapy in treating patients with glioblastoma that has come back. Vaccines made from a person's white blood cells mixed with tumor proteins from another person's glioblastoma tumors may help the body build an effective immune response to kill tumor cells. Giving vaccine therapy may work better in treating patients with glioblastoma.
The objectives of this study are to determine the impact of omega-3 supplementation on promoting facial nerve function recovery, and to determine the impact of omega-3 supplementation on Vestibular schwannoma (VS) tumor control.
The purpose of this study is to compare the efficacy and safety of eflornithine in combination with lomustine, compared to lomustine taken alone, in treating patients whose anaplastic astrocytoma has recurred/progressed after radiation and temozolomide chemotherapy.
The purpose of this study is to evaluate how well veliparib, radiation therapy, and temozolomide work in treating participants with newly diagnosed malignant glioma without H3 K27M or BRAFV600E mutations. Veliparib may stop the growth of tumor cells by blocking some of the enzymes needed for cell growth. Radiation therapy uses high energy x-rays to kill tumor cells and shrink tumors. Drugs used in chemotherapy, such as temozolomide, work in different ways to stop the growth of tumor cells, either by killing the cells, by stopping them from dividing, or by stopping them from spreading. Giving veliparib, radiation therapy, and temozolomide ...
The purpose of this study is to assess the safety, effectiveness and pharmacokinetic (PK) of 2 dosing regimens of encorafenib + binimetinib combination in patients with BRAFV600-mutant melanoma with brain metastasis.
This randomized phase II trial studies how well giving vaccine therapy with or without bevacizumab works in treating patients with recurrent glioblastoma multiforme that can be removed by surgery. Vaccines consisting of heat shock protein-peptide complexes made from a person's own tumor tissue may help the body build an effective immune response to kill tumor cells that may remain after surgery. Monoclonal antibodies, such as bevacizumab, can block tumor growth in different ways. Some block the ability of tumor cells to grow and spread. Others find tumor cells and help kill them. It is not yet known whether giving vaccine ...
The purpose of this Phase 1/2, open-label, single-arm study is to determine the safety and the maximal tolerated dose (MTD) of VAL-083 in patients with recurrent malignant glioma. Pharmacokinetic (PK) properties will be explored and tumor responses to treatment will be evaluated.
The purpose of this study is to determine the response rate to the combination of pembrolizumab and NT-I7 in patients with recurrent glioblastoma.
The primary objective of this study is to assess the effect of berubicin compared with lomustine on overall survival (OS) in adult patients with Glioblastoma Multiforme (GBM) (WHO Grade IV) that has recurred after standard initial therapy.
This partially randomized phase I/II trial studies the side effects and the best dose of anti-endoglin monoclonal antibody TRC105 when given together with bevacizumab and to see how well they work in treating patients with glioblastoma multiforme that has come back. Monoclonal antibodies, such as anti-endoglin monoclonal antibody TRC105 and bevacizumab, may find tumor cells and help kill them. Giving anti-endoglin monoclonal antibody TRC105 together with bevacizumab may be an effective treatment for glioblastoma multiforme.
This phase II trial studies the side effects and how well pembrolizumab works in combination with standard therapy in treating patients with glioblastoma. Drugs used in the chemotherapy, such as pembrolizumab and temozolomide, work in different ways to stop the growth of tumor cells, either by killing the cells, by stopping them from dividing, or by stopping them from spreading. Radiation therapy uses high energy beams to kill tumor cells and shrink tumors. Giving pembrolizumab and standard therapy comprising of temozolomide and radiation therapy may kill tumor cells.
The purpose of this study is to compare the effectiveness of AG-881 to placebo in participants with residual or recurrent Grade 2 glioma with an IDH1 or IDH2 mutation who have undergone surgery as their only treatment. Participants will be required to have central confirmation of IDH mutation status prior to randomization.
This proposal is for a pilot study comparing volumes of 18F-DOPA-PET avidity with contrast enhancement and T2 FLAIR on MRI. We then plan to compare patterns of failure with target volumes, pre-treatment MRI changes and pre-treatment 18F-DOPA-PET.
The pupose of this study is to evaluate whether or not selumetinib works just as well as the standard treatment with carboplatine/vincristine (CV) for subjects with NF1-associated low grade glioma (LGG), and to see if selumetinib is better than CV in improving vision in subjects with LGG of the optic pathway (vision nerves). Selumetinib is a drug that works by blocking some enzymes that low grade glioma tumor cells need for their growth. This results in killing tumor cells. Drugs used as chemotherapy, such as carboplatin and vincristine, work in different ways to stop the growth of tumor cells, either by ...
This randomized phase II trial studies how well low-dose lenalidomide works compared with high-dose lenalidomide in treating children with juvenile pilocytic astrocytomas or optic nerve pathway gliomas that have come back (recurrent), have not responded to treatment (refractory), or are growing, spreading, or getting worse (progressive). Lenalidomide may stop the growth of tumor cells by blocking blood flow to the tumor. It is not yet known whether low-dose lenalidomide is more or less effective than high-dose lenalidomide in treating patients with juvenile pilocytic astrocytomas or optic nerve pathway gliomas.
This phase II trial studies how well reduced doses of radiation therapy to the brain and spine (craniospinal) and chemotherapy work in treating patients with newly diagnosed type of brain tumor called WNT)/Wingless (WNT)-driven medulloblastoma. Recent studies using chemotherapy and radiation therapy have been shown to be effective in treating patients with WNT-driven medulloblastoma. However, there is a concern about the late side effects of treatment, such as learning difficulties, lower amounts of hormones, or other problems in performing daily activities. Radiotherapy uses high-energy radiation from x-rays to kill cancer cells and shrink tumors. Drugs used in chemotherapy, such as ...
This randomized phase III trial is studying two different combination chemotherapy regimens to compare how well they work when given before a peripheral stem cell transplant in treating young patients with newly diagnosed supratentorial primitive neuroectodermal tumors or high-risk medulloblastoma. Drugs used in chemotherapy work in different ways to stop the growth of tumor cells, either by killing the cells or by stopping them from dividing. Giving more than one drug (combination chemotherapy) together with a peripheral stem cell transplant may allow more chemotherapy to be given so that more tumor cells are killed. It is not yet known which ...
The goal of this study is to correlate protein content in vestibular schwannomas and cerebrospinal fluid to patient outcomes, imaging findings, and other relevant clinical endpoints in patients who presented with both this tumor type and hydrocephalus.
This phase II trial studies how well dynamic susceptibility contrast-enhanced magnetic resonance imaging (DSC-MRI) works in measuring relative cerebral blood volume (rCBV) for early response to bevacizumab in patients with glioblastoma that has come back. DSC-MRI may help evaluate changes in the blood vessels within the cancer to determine a patient?s response to treatment.
This phase III trial compares memantine to usual treatment in treating patients with brain tumors that are newly diagnosed or has come back (recurrent). Memantine may block receptors (parts of nerve cells) in the brain known to contribute to a decline in cognitive function. Giving memantine may make a difference in cognitive function (attention, memory, or other thought processes) in children and adolescents receiving brain radiation therapy to treat a primary brain tumor.
The purpose of this study is to estimate the efficacy of LUTATHERA treatment in patients with recurrent grade 1 meningioma as measured by 6-month PFS rate, and to estimate the efficacy of LUTATHERA treatment in patients with recurrent grade 2 or 3 meningioma as measured by 6-month PFS rate.
The purpose of this study is to evaluate the effectiveness and safety of pemigatinib in participants with previously-treated, locally advanced/metastatic or surgically unresectable solid tumor malignancies harboring activating FGFR mutations or translocations.
The purpose of this study is to evaluate the effectiveness of Perampanel on seizure frequency in adult patients with brain-tumor with and without seizures associated with glioma.
The main objective of the Brain Tumor Repository is to allow access to coded patient data by researchers both inside and outside of the Mayo Clinic system so that important research questions can be answered.
The purpose of this study is to evaluate the effect of immunotherapy drugs (ipilimumab and nivolumab) in treating patients with glioblastoma that has come back (recurrent) and carries a high number of mutations. Cancer is caused by changes (mutations) to genes that control the way cells function. Tumors with high number of mutations may respond well to immunotherapy. Immunotherapy with monoclonal antibodies such as ipilimumab and nivolumab may help the body's immune system attack the cancer and may interfere with the ability of tumor cells to grow and spread. Giving ipilimumab and nivolumab may lower the chance of recurrent glioblastoma ...
The purpose of this study is to evaluate the feasibility of twice daily memantine started before radiation therapy (RT) and continued one month after radiation therapy (RT), and to evaluate the feasibility of twice daily (BID) memantine started before RT and continued 3 and 6 months after RT.
This is a Phase 1, open-label, first-in-human (FIH) dose-escalation study designed to evaluate the safety, tolerability, pharmacokinetics (PK), pharmacodynamics (PD) and preliminary antitumor activity of DCC-2618, administered orally (PO), in adult patients with advanced malignancies. The study consists of 2 parts, a dose-escalation phase and an expansion phase.
This randomized phase II trial studies how well giving temozolomide and irinotecan hydrochloride together with or without bevacizumab works in treating young patients with recurrent or refractory medulloblastoma or central nervous system (CNS) primitive neuroectodermal tumors. Drugs used in chemotherapy, such as temozolomide and irinotecan hydrochloride, work in different ways to stop the growth of tumor cells, either by killing the cells, by stopping them from dividing, or by stopping them from spreading. Monoclonal antibodies, such as bevacizumab, can block tumor growth in different ways. Some block the ability of tumor cells to grow and spread. Others find tumor cells ...
This is a peripheral blood Collection Protocol to study the T-cell immune responses of patients with malignancies displaying one of three different patterns of antigen expression: (1) Cohort 1 focuses on cancers displaying a high (80-90%) frequency of MUC1 expression and variably high (unreported to 50%) HER2/neu (“HER2”) expression; (2) Cohort 2 focuses on primary or secondary myelofibrosis (MF) displaying mutated calreticulin (muCALR); (3) Cohort 3 focuses on glioblastoma multiforme (GBM) which often displays the cytomegalovirus tegument protein CMVpp65. Cohort 1 includes blood collections for in vitro studies which are a component of NIH-funded Project 3 within the Mayo Clinic ...
The purpose of this study is to collect adult human blood, cerebrospinal fluid, brain, and spine tissues/fluids at time of surgery in order to conduct future studies of the cellular mechanisms of tissue invasion utilized by brain and spine tumors of the central nervous system (CNS).
The purpose of this study is to assess the feasibility, and the strengths and weaknesses of using an innovative chaplain-led spiritual interview with participants who have progressive neurologic conditions, end stage renal disease, and other advanced diseases with the purpose of creating a Spiritual Legacy Document (SLD) for them; to identify spiritual themes expressed in the interviews; to describe the spiritual well-being, spiritual coping strategies, and QOL of the primary participants and their designated support persons with validated questionnaires at enrollment and after two weeks after being interviewed and two weeks after receiving their SLD; to describe the investigators’ growth in understanding the spirituality of ...
The purpose of this research study is to understand the natural history of vision in patients with OPG and determine if there are factors (e.g. age at diagnosis, male/female, tumor location, features of the MRI exam, etc) that predict future vision loss or change in tumor size.
Another purpose of the study is to collect and store blood and tissue samples to use for future research to evaluate if there are certain variations in DNA, RNA, or proteins that predict the likelihood of an OPG to grow or cause vision loss.
This randomized phase IIb trial studies how well low-dose carvedilol works in preventing heart failure in cancer survivors exposed to high dose anthracyclines for management of childhood cancer. Patients who received high-dose anthracycline chemotherapy are at a much greater risk for developing heart failure compared to survivors who didn't get any anthracycline chemotherapy. Heart failure happens when the heart muscle has been weakened and can't pump blood as well as it should. Carvedilol may help lower the risk of cardiovascular complications.
The purpose of this study is to evaluate the side effects and best dose of nivolumab when given together with multi-fraction stereotactic radiosurgery and to see how well they work with or without ipilimumab in treating participants with grade II-III meningioma that has come back. Monoclonal antibodies, such as nivolumab and ipilimumab, may interfere with the ability of tumor cells to grow and spread. Stereotactic radiosurgery is a specialized radiation therapy that delivers a single, high dose of radiation directly to the tumor and may cause less damage to normal tissue. It is not yet known whether giving nivolumab and multi-fraction ...
The purpose of the study is to assess the efficacy of rozanolixizumab as measured by seizure freedom, change in cognitive function, use of rescue medication, onset of seizure freedom and to assess safety and tolerability.
The study aims to characterize patient factors, such as pre-existing comorbidities, cancer type and treatment, and demographic factors, associated with short- and long-term outcomes of COVID-19, including severity and fatality, in cancer patients undergoing treatment. The study also is aimed to describe cancer treatment modifications made in response to COVID-19, including dose adjustments, changes in symptom management, or temporary or permanent cessation. Lastely, evaluate the association of COVID-19 with cancer outcomes in patient subgroups defined by clinico-pathologic characteristics.
The objectives of this study are to determine the Maximum Tolerated Dose (MTD) and the Recommended Phase 2 Dose (RP2D) of NMS-03305293 in combination with temozolomide (TMZ) in patients with diffuse gliomas at first relapse (Phase I), and to determine the antitumor effectiveness of the combination of NMS-03305293 and TMZ in patients with isocitrate dehydrogenase (IDH) wild type glioblastoma at first relapse as measured by the 6-month Progression Free Survival (PFS) rate (Phase II).
The purpose of this study is to identify common genetic variants contributing to the risk of glioma. Evaluate gene-gene and gene-environmental interactions with strong biologic relevance to identify gene-gene and gene-environment interactions for glioma risk.
The purpose of this study is to evaluate brigatinib alone for patients with brain metastases from anaplastic lymphoma kinase (ALK) positive non-small cell lung cancer (NSCLC), who have either not been treated previously with a tyrosine kinase inhibitor (TKI) targeting ALK or who have had prior exposure to crizotinib.
The primary objective of this study is to determine whether stereotactic radiosurgery (SRS) relative to whole brain radiotherapy with hippocampal avoidance (HA-WBRT) plus memantine for brain metastases from small cell lung cancer (SCLC) prevents cognitive function failure as measured by cognitive decline on a battery of tests: the Hopkins Verbal Learning Test – Revised (HVLT-R), Controled Oral Word Association (COWA) test, and the Trail Making Test (TMT).
The purpose of this study is to comparatively evaluate the use of the GLOW800 visualization tool for ICG-VA versus the standard of care visualization tool FL800.
The purpose of this research study is to determine how well neratinib works in treating breast cancer that has spread to the brain. Neratinib is a recently discovered oral drug that may stop breast cancer cells from growing abnormally by inhibiting (or blocking) members of a family of proteins that include Human Epidermal Growth Factor Receptor 2 (HER2).
In this research study, the investigators are looking to see how well neratinib works to decrease the size of or stabilize breast cancer that has spread to the brain. The investigators are also looking at how previous treatments have affected your ...
The purpose of this study is to assess the safety and effectiveness of combined Toca 511 and Toca FC, versus a standard of care single agent chemotherapy, for patients who are having surgery to remove a first or second recurrence of glioblastoma or anaplastic astrocytoma.
The purpose of this study is to assess the combination of INCMGA00012 with radiation therapy (RT) and bevacizumab with or without epacadostat in the treatment of recurrent glioblastoma (GBM). Regimen A of this study has been completed and Mayo Clinic will only be participating in the Regimen B portion.
The purpose of this study is to determine whether dose-intensive tandem Consolidation, in a randomized comparison with single cycle Consolidation, provides an event-free survival (EFS) and overall survival (OS). The study population will be high-risk patients (non-Wnt and non-Shh sub-groups) with medulloblastoma, and for all patients with central nervous system (CNS) embryonal tumors completing "Head Start 4" Induction. This study will further determine whether the additional labor intensity (duration of hospitalizations and short-term and long-term morbidities) associated with the tandem treatment is justified by the improvement in outcome. It is expected that the tandem (3 cycles) Consolidation regimen will produce a ...
The purpose of this Pediatric MATCH screening and multi-sub-study phase II trial studies how well treatment that is directed by genetic testing works in pediatric patients with solid tumors, non-Hodgkin lymphomas, or histiocytic disorders that have progressed following at least one line of standard systemic therapy and/or for which no standard treatment exists that has been shown to prolong survival. Genetic tests look at the unique genetic material (genes) of patients' tumor cells. Patients with genetic changes or abnormalities (mutations) may benefit more from treatment which targets their tumor's particular genetic mutation, and may help doctors plan better treatment for ...
This randomized phase II study aims to investigate whether the addition of bevacizumab to standard corticosteroid therapy results in greater improvement in symptoms and less treatment-induced symptoms compared with standard corticosteroid therapy for patients with symptomatic brain radionecrosis following radiosurgery. It is hypothesized that the addition of bevacizumab to standard care corticosteroids will reduce treatment-induced toxicities and improve neurologic impairments in patients with brain radionecrosis following radiosurgery for brain metastases.
RATIONALE: Dasatinib may stop the growth of tumor cells by blocking some of the enzymes needed for cell growth. Monoclonal antibodies, such as bevacizumab, can block tumor growth in different ways. Some block the ability of tumor cells to grow and spread. Others find tumor cells and help kill them or carry tumor-killing substances to them. Bevacizumab may also block the growth of the tumor by blocking blood flow to the tumor. It is not yet known whether bevacizumab together with dasatinib are more effective than a placebo in treating patients with recurrent or progressive high-grade glioma or glioblastoma multiforme. ...
The purpose of this study is to assess the side effects and best dose of ATR kinase inhibitor VX-970 when given together with whole brain radiation therapy for the treatment of patients who have non-small cell lung cancer that has spread from the original (primary) tumor to the brain. VX-970 may stop the growth of tumor cells by blocking some of the enzymes needed for cell growth. Radiation therapy uses high energy x-rays to kill tumor cells and shrink tumors. Giving VX-970 together with radiation therapy may be a better treatment for non-small cell lung cancer.
The study is a prospective, randomized controlled phase III trial, to test the efficacy, safety and neurocognitive outcomes of advanced NSCLC patients, following stereotactic radiosurgery (SRS) for 1-10 brain metastases, treated with NovoTTF-100M compared to supportive treatment alone. The device is an experimental, portable, battery operated device for chronic administration of alternating electric fields (termed TTFields or TTF) to the region of the malignant tumor, by means of surface, insulated electrode arrays.
This clinical trial is studying long-term follow-up in patients who are or have participated in Children's Oncology Group studies. Developing a way to track patients enrolled in Children's Oncology Group studies will help doctors gather long-term follow-up information and may help the study of cancer in the future.
This phase I trial studies the side effects and the best dose of wild-type reovirus (viral therapy) when given with sargramostim in treating younger patients with high grade brain tumors that have come back or that have not responded to standard therapy. A virus, called wild-type reovirus, which has been changed in a certain way, may be able to kill tumor cells without damaging normal cells. Sargramostim may increase the production of blood cells and may promote the tumor cell killing effects of wild-type reovirus. Giving wild-type reovirus together with sargramostim may kill more tumor cells.
The purpose of this study is to determine the maximum tolerated dose (MTD) and/or the recommended Phase 2 dose (RP2D) of WSD0922-FU in subjects with recurrent glioblastoma, IDH wildtype (GBM), anaplastic astrocytoma, IDH wildtype (AA) and CNS metastases of non-small cell lung cancer (NSCLC).
This study proposes to develop and maintain a biorepository of blood samples collected from patients receiving definitive chemoradiotherapy for locally advanced rectal cancer, locally advanced pancreatic cancer, non-small cell lung cancer, or cervical cancer. The ultimate goal of this biorepository will be to provide the resource to initiate an exploration of ctDNA as a potential liquid biopsy for GI and Thoracic malignancy detection and surveillance.
The purpose of this is to evaluate the safety, effectivess, pharmacokinetics, and pharmacodynamics of FT-2102 as a single agent and in combination with other anti-cancer drugs in patients with advanced solid tumors and gliomas. The study is divided into two parts: single agent FT-2102 followed by combination therapy. Part 1: A single agent, open-label study in up to five cohorts (glioma, hepatobiliary tumors, chondrosarcoma, intrahepatic cholangiocarcinoma, and other IDH1 mutant solid tumors) that will include a Phase 1 dose confirmation followed by a Phase 2 investigation of clinical activity in up to 4 cohorts. During the dose confirmation, additional doses or ...
The objectives of this study are to:
- Measure the short and long-term overall and nasal-specific quality of life (QOL) impact of patients undergoing Endoscopic Endonasal Skull Base Surgery (EESBS) for pituitary and sellar lesions.
- Determine the relative difference in QOL impact of EESBS for patients undergoing surgery for functional and nonfunctional pituitary adenomas.
- Generate baseline data to development and validate a site-specific endoscopic-specific comprehensive QOL for EESBS.
- Particular tumors of interest include pituitary tumors, Rathke’s cleft cysts, craniopharyngiomas, clival chordomas and chondrosarcomas.
- Specific QOL aims focus on olfaction (sense of smell), gustation (sense of taste) and nasal function.
Intraoperative Microdialysis During Neurosurgery for Central Nervous System Malignancies
The purpose of this study is to assess the safety and tolerability of ADI-PEG 20 combined with pemetrexed and cisplatin in patients with tumors requiring arginine such as advanced malignant pleural mesothelioma, advanced peritoneal mesothelioma (for dose escalation cohort only), non squamous non-small cell lung cancer (stage IIIB/IV), metastatic uveal melanoma, advanced liver cell cancer or recurrent high-grade glioma.
The purpose of this study is to evaluate SV-BR-1-GM in metastatic or locally recurrent breast cancer patients, in combination with the PD-1 inhibitor INCMGA00012 and the IDO inhibitor epacadostat. Patients who with advanced breast cancer who have failed prior therapies will be eligible to enroll in this study. The study will evaluate SV-BR-1-GM in combination with INCMGA00012 and epacadostat. Treatment cycles will be every 3 weeks with evaluations for tumor progression or response every 6-12 weeks.
THe purpose of this study is to examine the current and (potential) future therapeutic relevance of pharmacogenomics (PGx) testing for a cohort of cancer patients in order to improve quality of life (QOL) in patients receiving clinical care at Mayo Clinic.
The purpose of this study is to find out more about the side effects of rovalpituzumab tesirine (SC16LD6.5) and what doses of rovalpituzumab tesirine (SC16LD6.5) are safe for people with specific delta-like protein 3-expressing cancers.
The purpose of this study is to develop a biorepository of blood samples from cancer patients participating in the Gemini (IRB 19-006717) protocol. These samples will be used for future biomarker discovery and other translational studies.
The goal of the study is to create a database of clinical information and a repository of biological specimens for genetic, molecular and microbiological research to better understand hereditary cancer and help develop new therapies and preventive strategies.
The purpose of this multicenter prospective observational case-control study is to train and validate Adela’s cfMeDIP-seq based methylome profiling platform to detect and differentiate multiple cancer subtypes. In addition, this study includes longitudinal follow-up for a subset of participants to train and validate the methylome profiling platform to detect minimal residual disease and recurrence.
The purpose of this study is to determine the prevalence of genetic mutations in cancer patients from various ethnic populations seeking care at Mayo Clinic cancer clinics.
The purpose of this study is to evaluate the challenges, behavioral patterns, and preferences of minority patient participation in clinical trials. Also, to develop and validate a personalized clinical trial educational platform to boost participation among underserved cancer patients.
Falls are common and catastrophic in cancer patients. Cancer patients are vulnerable to falls due to muscle loss. In prescribing exercise in a data driven manner to cancer patients, our hypothesis is this "prescription" for exercise will eventually be demonstrated to reduce the occurrence of injurious falls.
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
A case study of a long-term glioblastoma survivor with unmethylated MGMT and hypermutated genotype
Affiliations.
- 1 Cure Brain Cancer Biomarkers and Translational Research Group, Prince of Wales Clinical School, University of New South Wales, Sydney, New South Wales 2052, Australia.
- 2 Neurospine Clinic, Prince of Wales Hospital, Randwick, New South Wales 2031, Australia.
- 3 University of New South Wales, Sydney, New South Wales 2031, Australia.
- 4 Department of Medical Oncology, Nelune Comprehensive Cancer Centre, Prince of Wales, Hospital, Randwick, New South Wales 2031, Australia.
- PMID: 31160353
- PMCID: PMC6549560
- DOI: 10.1101/mcs.a003251
Effective treatments that extend survival of malignant brain tumor glioblastoma (GBM) have not changed in more than a decade; however, there exists a minority patient group (<5%) whose survival is longer than 3 yr. We herein present a case report of a long-term surviving 51-yr-old female diagnosed with a MGMT unmethylated GBM. The patient was progression-free for 23 mo. Fresh primary and recurrent tumor samples were collected and processed for patient-derived model development. Whole-genome sequencing (WGS) was performed concurrently with additional standard of care diagnostics. WGS revealed a hypermutated genotype in the germline tissue and in both the primary and recurrent tumor samples. Specific to the matched tumors, an average of 30 cancer driver genes were mutated. Noteworthy was the identification of a nonsynonymous mutation in the POLE gene. As a possible instigator of the hypermutational genotype observed in the tumors, we identified nonsynonymous germline mutations within the mismatch repair genes, MLH1 and PMS2 Mutations within these genes are often indicative of the pan-cancer phenotype known as Lynch syndrome; however, their pathogenicity remains unreported. We performed a drug screen of 165 compounds, which identified one compound, YM155, an experimental survivin inhibitor, that showed effectivity to the patient-derived cell lines of both tumors. Treatment selection based on a patient's genome to individualize treatment for GBM patients could potentially be useful in the clinic. This is a promising avenue for further translational research, with larger databases and integrated platforms to increase the efficiency of analyzing and interpreting the individual genomic data of GBM.
Keywords: glioblastoma; glioma.
© 2019 Jue et al.; Published by Cold Spring Harbor Laboratory Press.
Publication types
- Case Reports
- Research Support, Non-U.S. Gov't
- Brain Neoplasms / diagnostic imaging
- Brain Neoplasms / drug therapy
- Brain Neoplasms / genetics*
- DNA Mismatch Repair / genetics
- Drug Screening Assays, Antitumor
- Gene Regulatory Networks
- Germ-Line Mutation
- Glioblastoma / diagnostic imaging
- Glioblastoma / drug therapy
- Glioblastoma / genetics*
- Imidazoles / pharmacology*
- Middle Aged
- Naphthoquinones / pharmacology*
- Neoplasm Recurrence, Local
- Whole Genome Sequencing
- Naphthoquinones
- sepantronium
- Search Menu
- Advance articles
- Editor's Choice
- Supplements
- Author Guidelines
- Submission Site
- Why Publish With Us?
- Open Access
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Branded Books
- Journals Career Network
- About Neuro-Oncology Practice
- About the Society for Neuro-Oncology
- About the European Association of Neuro-Oncology
- Editorial Board
- Dispatch Dates
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Clinical case presentation, initial supportive care, initial diagnostic imaging, epidemiology, standard-of-care treatment, follow-up imaging, prognosis and survivorship.
- < Previous
Case-Based Review : newly diagnosed glioblastoma
- Article contents
- Figures & tables
- Supplementary Data
Derek R. Johnson, Shannon E. Fogh, Caterina Giannini, Timothy J. Kaufmann, Aditya Raghunathan, Philip V. Theodosopoulos, Jennifer L. Clarke, Case-Based Review : newly diagnosed glioblastoma, Neuro-Oncology Practice , Volume 2, Issue 3, September 2015, Pages 106–121, https://doi.org/10.1093/nop/npv020
- Permissions Icon Permissions
Glioblastoma (WHO grade IV astrocytoma) is the most common and most aggressive primary brain tumor in adults. Optimal treatment of a patient with glioblastoma requires collaborative care across numerous specialties. The diagnosis of glioblastoma may be suggested by the symptomatic presentation and imaging, but it must be pathologically confirmed via surgery, which can have dual diagnostic and therapeutic roles. Standard of care postsurgical treatment for newly diagnosed patients involves radiation therapy and oral temozolomide chemotherapy. Despite numerous recent trials of novel therapeutic approaches, this standard of care has not changed in over a decade. Treatment options under active investigation include molecularly targeted therapies, immunotherapeutic approaches, and the use of alternating electrical field to disrupt tumor cell division. These trials may be aided by new insights into glioblastoma heterogeneity, allowing for focused evaluation of new treatments in the patient subpopulations most likely to benefit from them. Because glioblastoma is incurable by current therapies, frequent clinical and radiographic assessment is needed after initial treatment to allow for early intervention upon progressive tumor when it occurs.
A 73-year-old man presented to his local emergency department after experiencing a generalized seizure. He had moderate left-sided weakness in the initial postictal period which quickly resolved. In retrospect, the patient had noted subjective left-hand “clumsiness” for a month prior to the seizure, but had not reported it to his family or physician. A CT scan was obtained in the emergency room and was followed shortly by an MRI (Fig. 1 ). The patient was then referred to our institution for further care.

(A) Unenhanced CT, (B) T2-weighted FLAIR, (C) gradient echo T1-weighted, and (D) post-gadolinium spin echo T1-weighted images depict a relatively circumscribed mass in the left superior temporal lobe with both solid, enhancing components and some cystic or necrotic areas. Moderate edema signal surrounds a portion of the mass.
The presentation of high-grade glioma is variable, depending on the location of the lesion within the brain. Headaches, seizures, and subacutely progressive neurological deficits are all common presenting symptoms.
Antiepileptic Therapy
Patients who present with seizure should be treated with antiepileptic drug (AED) therapy. An optimum AED choice would have rapid efficacy, few side effects, and no drug–drug interactions. In clinical practice, levetiracetam is often chosen as the first-line agent in this setting. 1 Studies have suggested that some AEDs may have direct antitumor effects. For example, valproic acid is a histone deacetylase (HDAC) inhibitor, 2 while levetiracetam is an MGMT inhibitor. 3 However, no impact of AED choice on survival has been proven, so AED choice should be based on efficacy and tolerability.
In patients with high-grade glioma who have not had a seizure, there is no proven role for long-term prophylactic AED therapy, and the American Academy of Neurology recommends against the routine use of prophylactic AEDs outside of the immediate perioperative period. 4 As previous studies of prophylactic AED therapy evaluated older agents in mixed patient populations, some experts question their applicability to current practice. A large trial of lacosamide vs placebo for seizure prophylaxis in patients with high-grade gliomas is ongoing to address this issue. 5
Corticosteroid Therapy
In patients presenting with headaches or focal neurological deficits, symptoms may be due to peritumoral vasogenic edema, which may respond to corticosteroid therapy. Dexamethasone is often started at 16 mg daily in 4 divided doses, and tapered down to the lowest effective dose or discontinued altogether. While this dosing schedule is widely used based on the short pharmacologic half-life of dexamethasone, the biological half-life is in excess of 36 hours, and daily or twice-daily dosing is effective and more convenient for maintenance therapy in most patients. Gastrointestinal prophylaxis and pneumocystis prophylaxis should be considered in patients in whom long-term corticosteroid treatment is anticipated.
Clinical Case Relevance
The patient was started on antiepileptic therapy at the time of his original emergency department visit. He had no further seizures. His exam was pertinent for a Karnofsky Performance Score of 90, and subtle left-sided pronator drift and slowing of rapid hand and foot movements on the left side were his only findings on physical exam. Dexamethasone was not initiated as he did not have symptoms of elevated intracranial pressure, such as headache or papilledema.
Because the symptomatic presentation of brain tumors is nonspecific, the presumptive diagnosis of brain tumor is often made only after imaging. Glioblastoma may be initially imaged with CT, particularly in the emergency department setting, but MRI provides more diagnostic information.
The typical CT appearance of glioblastoma is a mass lesion, often iso- to hyperattenuating (bright) in comparison to normal gray matter, with surrounding hypoattenuation due to infiltrating tumor and vasogenic edema. Contrast-enhanced CT classically reveals a centrally necrotic enhancing mass. Given that vascular proliferation is a hallmark of glioblastoma, intratumoral hemorrhage is common and may be visualized on CT, though it is more frequently identified as microhemorrhages on MR susceptibility-weighted imaging (SWI). Calcification is uncommon in glioblastoma, but can occasionally be seen.
On MRI, nearly all glioblastomas enhance with gadolinium contrast, usually showing a thick, irregular rind of tumor surrounding a necrotic cavity. Heterogeneity of signal intensity and contrast enhancement within glioblastomas and irregularity in shape are expected. Vascular hyperpermeability contributes to surrounding vasogenic edema visible as high signal intensity on T2-weighted images. Hemorrhage may complicate the appearance of glioblastoma, with acute and early subacute hemorrhage appearing hypointense on T2-weighted images and iso- to hyperintense on T1-weighted images. This intrinsic T1 hyperintensity of blood is similar in appearance to gadolinium enhancement, so it is crucial to always compare T1-weighted postcontrast images with T1-weighted precontrast images to ensure accurate judgment of enhancement.
The infiltrative nature of glioblastoma is generally more apparent on MRI than on CT. Mass-like signal abnormality infiltrating along white matter tracts is suggestive of glioma as opposed to other entities. However, distinguishing between nonenhancing infiltrative glial tumor with edema and vasogenic edema from any other etiology can be difficult or impossible. Frequently, glial infiltration and thickening of the cerebral cortex can be appreciated on T2-weighted and T2-weighted FLAIR images, which may help to distinguish gliomas from other neoplasms. Multifocality, distant, or diffuse disease may be seen initially in approximately 13% of glioblastoma cases, with some areas sometimes looking less aggressive than the primary mass. 6 It is also well established that microscopic glial tumor cell infiltration is expected to extend beyond visualized signal abnormality on MRI.
The differential diagnosis of glioblastoma often includes metastasis and CNS lymphoma. Generally speaking, glioblastoma tends to be more irregularly shaped than metastases because of its predilection for spread along white matter tracts, 7 but there is overlap at least in qualitative analysis. Primary CNS lymphoma (PCNSL) in the immunocompetent patient is most often homogeneous in signal intensity and enhancement, though exceptions do occur; while heterogeneity and central necrosis are more common in CNS lymphoma in the immunocompromised.
Advanced MRI techniques including perfusion imaging techniques such as dynamic susceptibility contrast (DSC) imaging, diffusion-weighted imaging (DWI), diffusion tensor imaging (DTI), SWI, and MR spectroscopy may help to distinguish glioblastoma from other tumors. Given the histological hallmark of neovascularity in glioblastoma, increased blood volume (often expressed as rCBV, or relative cerebral blood volume) is expected within at least portions of a glioblastoma. 8–10 On MR spectroscopy, glioblastoma typically has the nonspecific findings of elevated choline and decreased N-acetylaspartate (NAA) and may have elevated lipid and lactate resonances. Generally speaking, the choline:NAA ratio increases with astrocytoma grade. 11 Due to the infiltrative nature of glioblastoma relative to metastases, one may expect greater CBV 12 , 13 and greater choline:creatine 14 , 15 in the peritumoral areas of glioblastoma relative to metastases. rCBV also tends to be greater in enhancing tumor and peritumoral areas of glioblastoma than in CNS lymphoma. 12 Apparent diffusion coefficient tends to be lower in CNS lymphoma than in glioblastoma, given the great hypercellularity of lymphoma. 12 Microhemorrhages on SWI are found in most glioblastomas but rarely in CNS lymphoma. 16 , 17 Differentiation of glioblastoma and lymphoma using multiparametric advanced MRI has also been suggested. 18 Imaging genomic mapping is a burgeoning area of research that has begun to discover associations between MRI features and glioblastoma genotypes and clinical phenotypes. 19
Many published reports using advanced MRI techniques have relied on quantitative analyses, which are currently difficult to standardize across imaging platforms and institutions. For example, with perfusion imaging, there exists great variability in all steps from IV gadolinium bolus injection to scanner platforms used to MRI scan parameters chosen to post-processing software and analysis techniques used. 20 Given the technical variabilities of advanced MR techniques and expected glioblastoma heterogeneity, there are limits to the sensitivity and specificity of these techniques. The standardization of advanced MRI is well recognized as a pressing clinical and research need.
The initial imaging obtained for this patient included a CT and contrast-enhanced MRI, shown in Fig. 1 . Both of these images, and the MRI in particular, were concerning for glioblastoma, and metastasis and non-neuroplastic entities such as infection or demyelination were thought to be significantly less likely.
Surgical resection is the primary treatment for glioblastomas. The goals of surgery are tissue diagnosis, including molecular and genetic tumor analysis, as well as cytoreduction for alleviation of presenting symptoms and improved tumor control. As previously discussed, in the appropriate context imaging can be very suggestive of glioblastoma. However, tissue diagnosis is the standard of care and only in cases of truly inaccessible tumors (such as brainstem lesions) or grave infirmity of the patient, precluding surgical candidacy, should treatment be undertaken without pathological confirmation of disease.
The surgical approach of choice is maximal safe resection. Over the past several years, significant data have accumulated supporting the idea that maximizing the extent of tumor resection positively impacts survival for patients with newly diagnosed glioblastoma. 21 , 22 In a single institution study of 949 patients with high-grade gliomas, more than half of whom were operated on for the first time, the extent of resection was shown to be an independent predictor (gross total resection [GTR] vs near total resection [NTR], NTR vs subtotal resection [STR]) of prolonged survival (median OS 11 months GTR, 9 months NTR, and 5 months STR). 23
The association between extent of resection and survival benefit holds true even for tumors that are difficult to resect. In a study of multicentric high-grade glioma, resection of a dominant lesion was strongly predictive of improved overall survival when compared with biopsy only (12 months vs 4 months). 24 In the setting of insular high-grade gliomas, one of the most technically difficult eloquent cortical areas to access surgically, extent of resection ≥90% of the tumor provided 2-year overall survival of 91% compared with 75% for volumetric resection <90% of the tumor, in addition to improved progression-free survival. 25 The beneficial effect of maximal resection has also been suggested to extend to elderly patients without an increase in mortality or complications. 26
Several technical intraoperative adjuncts have been developed in an effort to maximize the extent of safe resection. 27 , 28 Use of frameless stereotactic guidance, which allows for optimal patient positioning, accurate tailoring of the craniotomy, and safe access trajectory to the tumor, has become standard for resection of glioblastomas. Recent advances have made it possible for intraoperative guidance to integrate imaging tools such as tractography, which allows for identification of motor, speech, and visual pathways, as well as MR spectroscopy to facilitate accurate targeting of presumed higher-grade areas within a heterogeneous tumor. 29 In cases where only a biopsy is planned, such imaging integration allows targeting of regions likely to optimize diagnostic yield and accuracy.
Direct cortical mapping allows identification of motor pathways and, when combined with awake craniotomy used for mapping of language areas, is an important adjunct to surgical resection of lesions in eloquent cortex. 25 , 30 A systematic review of the literature showed that direct cortical mapping decreases late severe neurological deficits from 8.25% to 3.4% and increases the rate of GTR from 58% to 75%. 31
Intraoperative MRI has been used in an attempt to maximize extent of surgical resection and identification of residual resectable tumor. 32 In a study including both high-grade and low-grade tumors, use of intraoperative MRI increased the volumetric extent of resection from 76% to 96%. 33 However, the high installation cost of an intraoperative magnet as well as the complexities involved in its intraoperative use have led to research into alternate ways to identify residual tumor during surgical resection. The utilization of fluorescence guidance has been recently advocated. The use of fluorophores such as 5-aminolevulenic acid (5-ALA) or fluorescein, which accumulate in areas of blood brain disruption, can be a powerful adjunct that allows for the accurate identification of tumor borders and possible residual disease at the time of resection. 34–36 In a systematic review of 10 studies, patients who underwent surgery utilizing 5-ALA for maximizing resection had improved 6-month progression-free survival and overall survival. 37 A multicenter, randomized, phase III trial of 5-ALA-guided surgery found higher rates of gross total resection and 6-month progression-free survival in the 5-ALA group without any increase in adverse events. 38
Following the initial multicenter, randomized trial of implantable carmustine polymer wafers in the treatment of recurrent high-grade glioma, Attenello et al reported their experience with their use during surgery for newly diagnosed high-grade gliomas and found an overall median survival of 13.5 months without any increased incidence of complications. 39 , 40 Although the use of chemotherapy implants appears to be safe in the setting of primary glioblastoma, the relative lack of improved survival and the fact that much of the data regarding the use of chemotherapy wafer implants predates the use of temozolomide (TMZ), has limited enthusiasm for this approach.
Surgery for high-grade gliomas is in general associated with relatively low rates of major complications. In an analysis of the patients in the Glioma Outcomes Project, an overall complication rate of 24% was reported for surgical treatment of newly diagnosed high-grade gliomas. In decreasing frequency, major complications included: depression (11%), worsened neurological status (8.1%), seizures (7.5%), adverse drug reaction (5.2%), DVT (4.2%), intracranial bleeding (1.6%), and pulmonary embolism and wound infection (0.5% each). Perioperative mortality was reported as 1.5%. 41 These results were similar to an earlier study that reported 13% major complications and 1.7% mortality in patient undergoing craniotomy for intraparenchymal tumors. 42 In an analysis of the California Inpatient Database, Marcus et al reported a 30-day readmission rate of 13.2% for patients who underwent surgical treatment for a glioma who were originally discharged home. The most common presentations at readmission were seizures (20.9%) and surgical infection (14.5%). 43
In summary, surgery remains the first and very important treatment modality for a newly diagnosed glioblastoma. Its effectiveness for optimizing overall survival is related to the extent of resection and its safety is dependent on various intraoperative adjuncts that allow for accurate localization of the tumor as well as eloquent cortical areas.
The patient underwent resection of his tumor without use of awake craniotomy or intraoperative MRI. Following surgery, his left-sided weakness was transiently worse but it then improved back to the presurgical baseline. His extensive resection placed him in a more favorable prognostic group than biopsy alone would have. Preoperative and postoperative MRI images are displayed in Fig. 2 .

Post-gadolinium spin echo T1-weighted images (A) before and (B) after surgery.
The histological diagnosis in this case was WHO grade IV astrocytoma (glioblastoma). It was an infiltrative astrocytoma showing areas of high cellularity and brisk mitotic activity (Fig. 3 A), tumor necrosis (Fig. 3 B), and microvascular proliferation (Fig. 3 C). The diagnostic criteria from the WHO (2007) include presence of cytological atypia, mitotic activity, microvascular proliferation, and/or tumor necrosis. 44 Briefly, an infiltrative astrocytoma exhibiting cytological atypia alone, including elongated, irregular and hyperchromatic nuclei, is considered WHO grade II (diffuse astrocytoma). The presence of increased cellularity, nuclear atypia, and mitotic activity warrant a WHO grade III (anaplastic astrocytoma) designation. Tumors that additionally show microvascular proliferation and/or necrosis are WHO grade IV (glioblastoma). Classic microvascular proliferation has the appearance of “glomeruloid tufts,” consisting of multilayered, mitotically active endothelial cells admixed with smooth muscle cells/pericytes (as represented in Fig. 3 C). Although necrosis surrounded by pseudopalisading tumor cells is most characteristic of glioblastoma (Fig. 3 B), both geographic and pseudopalisading tumor necrosis can be present and are associated with similarly dismal prognoses. Astrocytoma grading is based on the highest histological grade. Since infiltrative astrocytomas can have considerable regional heterogeneity, especially toward their infiltrative border into surrounding parenchyma, it is important to assess whether a biopsy sample is representative of the entire tumor by correlating histological, clinical, and radiological findings. A biopsy taken at the periphery of a ring-enhancing mass could well show a low to moderately cellular tumor (as seen in Fig. 3 D) with/without mitoses, prompting an inaccurate diagnosis of diffuse or anaplastic astrocytoma (WHO grade II or III) rather than glioblastoma (WHO grade IV).

The biopsies demonstrated an infiltrating population of atypical astrocytic cells, showing (A) brisk mitotic activity, (B) tumor necrosis, and (C) microvascular proliferation, consistent with a diagnosis of glioblastoma. A biopsy from the periphery of this mass may show (D) a low-to-moderately cellular tumor, with or without mitoses, corresponding to a lower histological grade. In images (A) and (C), photographed at 400× magnification, the scale bars on the bottom right represent 20 µm. In images (B) and (D), photographed at 200× magnification, the scale bars represent 50 µm.

(A) The first MRI following chemoradiotherapy and (B) MRI evidence of tumor progression approximately 2 years later. Both are post-gadolinium spin echo T1-weighted images.
Historically, glioblastomas have been distinguished based on their clinical presentation as primary (de novo) or secondary glioblastomas that develop in progression from a lower grade astrocytoma. Primary glioblastomas, the most common (>90%), develop with a short clinical history without clinical or pathological evidence of a lower grade precursor, and are typically seen in older patients. There are no definite histological features to distinguish primary and secondary glioblastomas. With advancing molecular information, however, it is clear that primary and secondary glioblastoma are two different diseases.
Mutation of isocitrate dehydrogenase (IDH) is frequently seen in low-grade glioma, and is also found in approximately 12% of glioblastomas. 45 The presence of IDH mutation within a glioblastoma is suggestive of secondary glioblastoma, regardless of any previous history of low-grade glioma. 46–50 In glioblastoma, mutations almost exclusively involve residue 132 (R132) of IDH1 resulting in the substitution of arginine. 46 , 51 The presence of IDH1 mutation in glioblastoma has been associated with younger age and relatively longer survival. 52–56 Alterations in receptor tyrosine kinase pathways have also been frequently identified in glioblastomas. 57 Epidermal growth factor receptor (EGFR) activation, either by amplification of wild-type EGFR or by deletion of exons 2–7 that encode the extracellular domain (the variant III mutation) resulting in ligand-independent constitutive activation of EGFR, 47–49 is more commonly seen among primary glioblastomas. Mutations of the TP53 gene are frequent in, but not exclusive of, secondary glioblastomas. 50 , 58 , 59 On the other hand, mutations in the promoter region of the telomerase reverse transcriptase ( TERT ) gene are predominantly found in primary glioblastomas that lack IDH1 mutations, and appear to be associated with worse prognosis. 49 ,60–62
The gene for the DNA-repair enzyme O(6)-methylguanine-DNA methyltransferase ( MGMT ) has a promoter region that is rich in CG dinucleotide (CpG) sites that are normally unmethylated. However, in glioblastomas, the cytosine in these CpG sites may become methylated, resulting in transcriptional silencing of MGMT and subsequent impairment of the DNA-repair process. 63–65 Glioblastomas with MGMT -promoter hypermethylation are unable to repair the DNA damage caused by alkylating agents (such as TMZ), and carry a more favorable prognosis than tumors without methylation of MGMT . 66–69 Tumors with IDH mutation frequently have MGMT promoter methylation. 70
Integrated genomic analysis has revealed subsets of high-grade astrocytomas based on the differential expression of prognostic markers. 71 , 72 Three to four major subgroups are generally well recognized, and their distinction appears to be relatively robust on meta-analysis. 73 At one end of the spectrum is the proneural subgroup, characterized by alterations in markers associated with neurogenesis, strongly associated with IDH1 mutations, and tending to have more favorable outcomes. The mesenchymal subgroup is at the other end of the spectrum, expressing markers usually associated with mesenchymal tissue and increased angiogenesis, associated with loss and/or mutation of the NF1 gene, and tending to have relatively worse outcomes. These expression-based subgroups were also distinguished by their CpG island methylation status. 74 Glioblastomas in the proneural subgroup were more frequently found to show widespread CpG island hypermethylation, termed a glioma CpG island methylator phenotype (G-CIMP), which was not usually seen in tumors of the mesenchymal subgroup.
At present, the diagnosis of glioblastomas per the 2007 WHO guidelines is based on well-established histological features. However, testing for MGMT status is becoming accepted as a standard of care for newly diagnosed glioblastomas, as is screening for IDH1 mutations. As newer therapeutic modalities emerge, there is increasing recognition for the need to communicate the status of prognostically and therapeutically relevant genomic markers to help guide clinical decisions for patient management. In a preliminary attempt to address this, consensus guidelines suggested at an international meeting of neuropathologists recommended that pathologists to provide an integrated diagnosis that incorporates the histological diagnosis and relevant molecular information. 75 For example, the diagnosis of glioblastoma, WHO grade IV, might also include the results of the IDH1 mutation status, MGMT status, and other relevant markers.
Pathology revealed glioblastoma, MGMT methylated. The MGMT methylation status is prognostic of better survival, relative to patients with unmethylated MGMT , and it also may predict response to treatment in some situations, to be discussed later.
Glioblastoma is the most common primary brain tumor in adults. In the United States, the age-adjusted incidence rate is 3.19 (95% confidence interval 3.16–3.21) per 100 000 persons. 76 The lifetime risk of being diagnosed with an invasive cancer of the nervous system, most of which are either glioblastoma or glioblastoma precursors, is approximately 1 in 161, with the risk of dying from an invasive cancer of the nervous system being approximately 1 in 222. 77 Thus, while glioblastoma remains a relatively rare tumor, many patients will be aware of one or more acquaintances or relatives with this condition purely by chance, sometimes raising concern of clustering of tumors by geography or within a family.
Glioblastoma is more common in men than women, as are all infiltrating gliomas. Incidence rises with age, peaking in the 75–84 age range. Thus, though the overall age-adjusted incidence rate of glioblastoma does not appear to be rising, the raw number of tumors diagnosed each year is expected to climb in coming decades due to aging of the population at large. In the United States, glioblastoma is more common amongst non-Hispanic whites than in black, Asian/Pacific Islander, or American Indian/Alaskan native groups.
Ionizing radiation remains the only proven exposure risk factor for glioblastoma. Typically, radiation-induced glioblastoma is seen years after therapeutic radiation for another tumor or medical condition. Diagnostic radiation, for example from CT scanning or even dental X-rays may theoretically confer increased risk of glioma, but this has not yet been confirmed in large-scale epidemiological studies. Nonionizing radiation, specifically related to the use of cellular telephones, has not been convincingly linked to glioma incidence, but this is an area of active investigation. Asthma and atopic disease are associated with lower risk of glioblastoma in multiple studies, with one meta-analysis showing a reduction in glioma risk of 40% in patients with allergies. 78
Many patients with glioblastoma are concerned about possible genetic risk factors, and ask about the advisability of screening for relatives. A heritable component to glioblastoma risk has long been demonstrated by the association between glioblastoma and Mendelian cancer syndromes including the Lynch and Li-Fraumeni syndromes. Recently, genome-wide association studies have revealed single nucleotide polymorphisms (SNPs) associated with glioblastoma risk. These SNPs have been identified within the candidate genes TERT (chromosome 5p15.33), EGFR (7p11.2), CDKN2B (9p21.3), TP53 (17p13.1), and RTEL1 (20q13.33). 79 Other SNP associations such as those within CCDC26 (8q24.21) and PHLDB1 (11q23.3) are mainly associated with IDH-mutant tumors and thus risk of secondary glioblastoma. Most of the currently identified risk SNPs confer only a modest increase in risk of glioma, and thus the absolute risk of glioma remains low even in individuals carrying the risk SNPs.
The patient came from a large family with a history of a number of different tumor types, but no first or second degree relatives with primary brain tumors. He was reassured that his family members were at low risk of primary brain tumor, and no screening studies were recommended.
Glioblastoma is an infiltrative tumor, with residual disease present after surgery, even in cases of radiographic gross total resection. Additional treatment to address this residual tumor is thus necessary as soon as the operative site has healed appropriately. This additional treatment may take the form radiation therapy (RT), chemotherapy, or both, depending on the clinical scenario.
Current Standard-of-Care Therapy
The current standard-of-care treatment for newly diagnosed glioblastoma was established by a landmark trial conducted by the European Organization for Research and Treatment of Cancer (EORTC) and the National Cancer Institute of Canada Trials Group (NCIC). 80 In this trial patients were randomized to RT alone (the previous standard of care) vs RT with concurrent and adjuvant oral TMZ chemotherapy. In this trial, median survival was 12.1 months in the radiation-only arm and 14.6 months in the TMZ arm. More importantly, combined chemoradiotherapy significantly increased the proportion of relatively long-term survivors from 10.9% to 27.2% at two years and from 1.9% to 9.8% at five years. Patients whose tumors had methylation of the promoter for the MGMT gene ( MGMT methylated) had greater benefit from the addition of TMZ (46% 2-year survival vs 27% for the MGMT unmethylated patients), but MGMT unmethylated patients still had incremental benefit from the addition of TMZ (14% 2-year survival vs <2%). 69
Numerous studies have indicated a benefit to using RT in the treatment of gliomas. 81 , 82 A dose of 60 Gy in 2 Gy fractions is the recommended dose based on prior studies indicating that doses up to but not exceeding 60 Gy impact survival. 83 , 84 Despite agreement of a standard dose recommended in both clinical trials and practice, there is tremendous variability in the volume of tissue irradiated. A common approach endorsed by the Radiation Therapy Oncology Group and other cooperative groups is to target the tumor edema with a 2.5-cm margin to a dose of 46 Gy followed by a cone down to the resection cavity and contrast-enhancing tumor with similar margin to a dose of 60 Gy. 85 Other cooperative groups also recommend a staged approach initially including tumor edema with a cone down to the enhancing tumor, but only add a 1-cm margin. Additional strategies include treating the enhancing tumor and resection cavity with a 2–3-cm margin to a total dose of 60 Gy without a staged volume reduction. 80 The volume of brain irradiated in each of these scenarios is substantially different. While studies have demonstrated comparable outcomes comparing conformal radiation to whole brain irradiation, similar comparisons have not been made between these varied radiation approaches. 86
Typically, TMZ is given daily during RT at a dose of 75 mg per square meter of surface area each day, followed by a rest period of approximately a month at the end of radiation. TMZ is then resumed at the dose of 150 mg per square meter on days 1–5 of a single 28-day cycle, and subsequent 28-day cycles are dosed at 200 mg per square meter on days 1–5 if the first adjuvant cycle was well tolerated. In the clinical trial that proved the efficacy of this approach, a total of 6 adjuvant cycles were given. 80 In practice, some physicians recommend more than 6 cycles, though there is currently no definitive data demonstrating that more prolonged regimens are associated with superior survival.
Side Effect Management
The most common symptomatic side effects of treatment are mild fatigue, nausea, and constipation. All patients receiving TMZ should be provided with antiemetic therapy, both to take prior to each TMZ dose to prevent nausea and also for as-needed use. Antiemetics of the serotonin 5-HT3 receptor antagonist class, such as ondansetron and granisetron, are often used for this purpose. TMZ often causes mild thrombocytopenia, but severe thrombocytopenia, neutropenia, and anemia are much less common. Asymptomatic leukopenia is very common in patients on TMZ. Prophylaxis against Pneumocystis jiroveci pneumonia with trimethoprim/sulfamethoxazole or an alternative agent is recommended for the full duration of TMZ therapy.
Common acute radiation side effects include headaches, nausea, exacerbation of presenting symptoms, hair loss, skin reaction at the site of radiation, and fatigue. Less common acute side effects can include dry mouth or altered taste, hearing impairment or seizures. Possible late side effects of radiation include decreased pituitary hormonal production, cataract formation, secondary cancers, and nerve damage. Radiation necrosis can occur and cause symptoms similar to tumor recurrence or stroke. Necrosis is initially managed with steroids but may require more intensive options such as surgery or bevacizumab therapy. 87
Neurocognition can be altered during initial therapy secondary to inflammation, anxiety, and medications, but radiation can also cause cognitive impairment months to years after it is completed, even in the absence of tumor progression. Learning and memory are the most commonly impaired cognitive domains. The extent of impairment may be related to patient-specific factors, but also related to volume of tissue irradiated and location of the radiation field. For example, dose to hippocampal structures has been found to influence extent of neurocognitive dysfunction. 88–90
Elderly Patients and Patients with Poor Performance Status
The pivotal trial that demonstrated the efficacy of TMZ for newly diagnosed glioblastoma did not include patients over the age of 70, leaving unanswered the question of whether this regimen is effective and well tolerated in elderly patients. 80 Moreover, a number of trials have been conducted that suggest, at least in some circumstances, abbreviated or less intensive treatments may be effective in older patients. In a randomized, phase III trial conducted by the Nordic Clinical Brain Tumor Study Group, patients age 60 or older with glioblastoma were randomized to the typical 6 weeks of RT, 2 weeks of hypofractionated RT, or TMZ without RT. 91 The trial demonstrated that both the hypofractionated RT and TMZ monotherapy were superior to 6 weeks of RT with respect to overall survival. Similarly, in the German NOA-08 trial, patients over 65 years of age were randomized to dose-dense TMZ or standard 6-week RT, with similar outcomes in each group. 92 Both the Nordic and NOA-08 trials demonstrated that MGMT methylation was predictive of response to TMZ therapy. Patients whose tumors demonstrated methylation of MGMT had better survival when treated with regimens that contained TMZ, whereas patients with unmethylated MGMT did better when treated with RT. Although both these studies were randomized phase III studies, there are significant limitations in interpreting the data. Notably, 6 weeks of RT with concurrent and adjuvant TMZ was not an arm in either study, so direct comparisons of these alternative approaches to the current standard of care are not possible. In addition, the definition of elderly varied across these trials and across other, retrospective analyses.
Currently, as no therapy has been proven superior or equivalent to standard combined chemoradiotherapy in elderly patients, this therapy is a reasonable option for patients of any age with good performance status who are felt likely to tolerate intensive treatment. In patients with poor performance status or those in whom treatment tolerability is a concern, treatment choice should be informed by MGMT methylation testing. In patients with MGMT methylation, TMZ monotherapy is reasonable, whereas RT monotherapy is an option for patients without MGMT methylation. Given the results of the Nordic trial, as well as a previous trial that demonstrated that abbreviated RT was not inferior to 6-week RT, hypofractionated RT is preferable to the standard six-week schedule in this patient group if not combined with chemotherapy. 93
Optune (NovoTTF-100A)
Recently released information, in the form of a press release and a presentation at a neuro-oncology specialty meeting, suggests that the addition of therapy with alternating electric fields via the Optune device (NovoCure) may prolong both progression-free and overall survival by several months when combined with standard chemoradiotherapy for newly diagnosed glioblastoma. 94 In the trial for which data were presented, Optune therapy was initiated at the time of initiation of adjuvant TMZ therapy and continued until tumor progression. While this result is cause for optimism, the results presented were from an interim data analysis, and publication of the full trial data in a peer-reviewed journal will be necessary before Optune therapy can be critically evaluated for possible inclusion in a new standard of care for glioblastoma.
Recent Clinical Trial Results
After combined chemoradiotherapy became the standard of care, more aggressive dosing of TMZ was tested in hopes that it might provide additional efficacy. RTOG 0525, a large phase III study, compared a dose-dense schedule of TMZ after RT with the standard 5-day schedule. No difference in survival was noted in either MGMT methylated or MGMT unmethylated patients. 85 Cilengitide, a targeted drug that inhibits integrins, was added to standard RT and TMZ in two separate clinical trials, a phase III study in MGMT methylated patients 95 and a phase II study in MGMT unmethylated patients, 96 but did not show improvement in survival in either case. The addition of the antiangiogenic agent bevacizumab, an antibody against VEGF, to standard RT and TMZ was tested in two large phase III trials. While there was some improvement in progression-free survival, no improvement in overall survival was noted in either of these trials. 97 , 98 As such, bevacizumab has not at this time been approved for use in initial treatment of glioblastoma.
Important Ongoing Clinical Trials
There are numerous phase I and II trials around the world testing the addition of other drugs to standard therapy, including targeted agents, cytotoxic agents, and a variety of immune-targeting approaches. In addition, there are trials in progress testing alternative radiation techniques such as proton therapy or imaging-guided radiation dose escalation, and trials testing metabolic approaches against cancer such as variations on the ketogenic diet.
With regard to phase III trials, a randomized, placebo-controlled trial is currently ongoing that tests the addition of an autologous vaccine made from a patient's own tumor and their own dendritic cells (DCVax-L) to initial adjuvant TMZ. 99 Another glioblastoma immunotherapy approach, using the EGFRvIII-targeted experimental cancer vaccine rindopepimut (CDX-110), is being evaluated in the ACT IV trial. 100 Within the elderly population specifically, a randomized, phase III trial comparing hypofractionated RT alone or in combination with TMZ has completed accrual in Canada, Europe, and Japan 101 ; the results are eagerly awaited to further inform whether combination therapy is effective in this patient population.
The patient had excellent performance status and was felt to be a candidate for standard chemoradiotherapy, despite his age of 73. He developed mild nausea and moderate fatigue during chemoradiotherapy, but no life-threatening toxicities. He likewise tolerated adjuvant TMZ well from a symptomatic standpoint, though several cycles had to be briefly delayed due to mild thrombocytopenia. He discontinued TMZ therapy and moved to an observational phase following the sixth adjuvant cycle. Had he not been judged a good candidate for standard therapy, a TMZ-only approach, sparing radiation, would have been an acceptable alternative for an elderly man with an MGMT -methylated tumor.
Initial Postoperative Imaging
Postoperative imaging is strongly recommended within the first 48 hours following surgical resection in order to establish a postoperative baseline. If MRI is obtained, it is important to compare precontrast T1-weighted images with post-contrast T1-weighted images in order to detect true residual enhancement, as blood products in or around the surgical bed are usually present and may cause T1 shortening on both pre-gadolinium and post-gadolinium images. It is also crucial to perform DWI in order to detect any perioperative infarction, which may subsequently gain enhancement in the subacute phase, lose restricted diffusion, and present as a troubling, new enhancing lesion on subsequent MRI follow-ups. 102
Long-term Follow-up
Generally, patients undergo monthly clinical evaluation and blood work during adjuvant TMZ, with MRI every other month. After the completion of TMZ, imaging is recommended every 2 to 3 months until 2 years from the end of treatment. After this time, MRI can be performed less often, provided the patient and physician are comfortable with this approach. Regardless of duration of disease-free survival, clinical evaluation and imaging should take place on at least an annual basis.
It is expected that the imaging appearance of a treated glioblastoma will evolve over time. One hopes for tumor regression after chemoradiation, but a temporary worsening of imaging findings, including increased contrast enhancement and edema signal with mass effect, is very common as a reaction to treated and dying tumor. This phenomenon is known as pseudoprogression, named so because the MRI appearance may be identical to tumor progression when, in fact, subsequent follow-up examinations with no change in therapy show regression of these imaging findings. 103 There is, unfortunately, often no basis on which to discriminate post-treatment related enhancement from enhancement related to viable tumor using standard morphological MRI.
Pseudoprogression may be more common with the combined use of TMZ with RT, it is more common in those with MGMT promoter methylation, and it has been associated with an improved clinical outcome in some cohorts. 104 , 105 The incidence of pseudoprogression is on the order of 30%, 106 depending on how it is judged, and most pseudoprogression occurs within 3 months of the end of RT. However, pseudoprogression occurring after this 3-month period but within the first year is not uncommon, particularly in those with MGMT promoter methylation. 107
The Macdonald criteria has been used as a framework for judging glioblastoma progression or regression, relying mainly upon 2-dimensional maximal diameters of contrast-enhancing lesions. 108 In 2010, the Response Assessment in Neurooncology (RANO) criteria were published, updating the Macdonald criteria in several important ways, while maintaining a reliance upon the product of perpendicular diameters of contrast-enhancing lesions as an indicator of tumor size and status. 109 One very important caveat in the RANO criteria is that, because of the common occurrence of pseudoprogression with modern chemoradiation therapy, a radiographic diagnosis of tumor progression cannot be made within the first 3 months of the end of chemoradiation if an enlarging, enhancing lesion is within the high-dose field of RT. Any apparent tumor progression within the first 3 months after radiation must be closely followed to differentiate early tumor progression from pseudoprogression. Because pseudoprogression occasionally occurs beyond 3 months from the end of radiotherapy, some would advocate early follow-up scans to confirm or deny pseudoprogression if there is apparent radiographic progression occurring even beyond the 3-month window after radiotherapy. RANO also allows for the determination of progression when there is nonenhancing tumoral progression, as nonenhancing tumor progression is not uncommon. 6 New, discrete, masslike abnormalities or new cortical expansion with T2 lengthening suggest nonenhancing tumor progression per RANO criteria. Unfortunately, distinguishing nonenhancing tumor from other treatment-related effects and edema is often difficult or impossible.
Given the complexity of MRI interpretation, other means of glioblastoma treatment response assessment are needed. Estimates of tumor cell proliferation rates and invasion have been made through the analysis of MRI coupled with computational modeling as a means to monitor treated glioblastomas over time. 110 , 111 Physiologic or mechanistic imaging techniques such as dynamic susceptibility contrast (DSC) perfusion imaging, dynamic contrast enhanced perfusion imaging (DCE), DWI, spectroscopy, and PET with various tracers also may aid in distinguishing progressing tumor from treatment-related changes such as pseudoprogression and radiation necrosis, but their implementation has to date been so variable site-to-site that these techniques have not been included in the RANO criteria.
Generally speaking, it is expected that CBV will be elevated with viable high-grade glioma but not radiation necrosis, and possibly not elevated with pseudoprogression, though data for pseudoprogression are as yet less clear. 112–119 However, the variability in perfusion imaging has already been mentioned, there is often overlap between CBV in viable glioblastoma and radiation-induced changes, there is frequently an admixture of viable tumor and radiation-induced changes, and leakage of gadolinium into the interstitium breaks tracer-kinetic modeling assumptions and presents a challenge to accurate determination of CBV. In order to optimize CBV measurement, the use of a leakage-correction option is advised during image postprocessing. Many experts also recommend the use of a gadolinium preload prior to the acquisition of DSC images. Histogram and voxel-wise analyses of perfusion data hold promise for improving the differentiation between viable tumor and treatment-related changes, but they are postprocessing intensive. 120 , 121 Given the frequent admixture of residual glioma and radiation-related changes, determination of a residual/recurrent tumor fraction would be desirable and such a metric using CBV has been shown to correlate with overall survival. 122 Importantly, the relative change in lesion CBV over time may be crucial in judging tumoral stability or progression, 123 though it bears stating explicitly that uniformity in perfusion technique between time points is mandatory for the best chance at fair comparisons.
DCE perfusion imaging, which is generally more technically demanding than DSC perfusion imaging, also holds promise for differentiating recurrent glioblastoma from treatment-related changes, using metrics such as the volume transfer coefficient k trans and initial area under the curve. 118 ,124–126 MR spectroscopy can be technically challenging to perform well and interpret, but after therapy choline and lipid and lactate levels have been shown to correlate with glioma outcomes. 119 , 127 More data on the value of MR spectroscopy in the glioblastoma post-treatment setting is needed. ADC values from DWI imaging, particularly when using advanced analysis techniques such as histogram analysis and functional diffusion maps (fDMs), 128–133 may also help to differentiate recurrent tumor from treatment-related changes. Amino acid PET may also aid in this discrimination better than with FDG PET but these techniques need further evaluation. 134–138 Finally, it is likely that multiparametric approaches with advanced MRI techniques will add to assessment of glioblastoma treatment response. 119
The first MRI following the completion of chemoradiotherapy, shown in Fig. 4 A, demonstrated a rim of contrast enhancement around the resection cavity that had not been visible on the initial postoperative imaging (Fig. 2 B). The patient was asymptomatic, the changes were suspected to be treatment-related, and no change of plan was recommended. He remained clinically and radiographically stable for nearly 2 years until he had tumor progression along the medial margin of his resection cavity, as shown in Fig. 4 B. His KPS at the time of progression was 80, due to increased left-sided weakness, but he was still able to live independently with his wife. After discussing options including continuing to focus on aggressive tumor treatment, potentially at the cost of short-term quality of life, vs prioritizing quality of life and supportive care with hospice, he chose to pursue salvage chemotherapy, the details of which are beyond the scope of this review.
Overall Survival
Survival after diagnosis of glioblastoma has been steadily improving over the course of the last decade, for reasons both known and unknown. The widespread adoption of TMZ for newly diagnosed glioblastoma in and after 2005 was associated with in an increase in population-level survival. 139 Likewise, though a survival benefit has yet to be demonstrated in a randomized prospective trial, population-based data suggest that survival also improved after the FDA approval of bevacizumab for recurrent glioblastoma. 140 Additional improvements in the survival of patients with glioblastoma may be due to incremental improvement in surgery, radiation, and supportive care.
The median survival figure of 14.6 months from the pivotal TMZ trial is often shared with patients with newly diagnosed glioblastoma, but clinical trial median survival numbers have little relevance when predicting the specific prognosis of an individual patient. Many factors can significantly impact survival, including but not limited to age at diagnosis, performance status, extent of resection, MGMT methylation status, and IDH mutation status. Median survival by MGMT methylation status in recent phase III trials is shown in Table 1 . A number of survival prognostication systems have been published, but again these are more relevant to cohorts than patients as individuals. In the long-term follow-up of the pivotal phase III TMZ trial, among patients treated with radiation and TMZ, 27.2% were still alive at 2 years, 16.0% at 3 years, 12.1% at 4 years, and 9.8% at 5 years. 141 Survival to 10 years or longer is very rare.
Survival by MGMT methylation status in recent phase III trials for newly diagnosed glioblastoma
a OS statistics from Stupp Lancet Oncology 2009; PFS statistics from Hegi NEJM 2005. All statistics regard the RT + TMZ trial arm.
Abbreviations: MGMT, O(6)-methylguanine-DNA methyltransferase; OS, overall survival; PFS, progression-free survival; EORTC, European Organisation for Research and Treatment of Cancer; NCIC, National Cancer Institute of Canada; RTOG, Radiation Therapy Oncology Group.
Because glioblastoma is an intrinsically fatal diagnosis, and treatment can cause significant side effects, most tumor treatment plans require the sacrifice of some quality of life in the short term in the hope of gaining duration of life in the longer term. Early in the course of disease, this is a trade-off that most patients readily accept, though some choose to forgo aggressive therapy. With each successive treatment, the expected duration of benefit tends to decrease and toxicity may increase, so the merits of focusing purely on quality of life should be readdressed regularly, for example at the time of clinical or radiographic progression. When the service is available, patients may benefit from speaking with a palliative care physician early in the course of their disease, and maintaining the relationship until the end of their lives. While death may occur precipitously as the result of a pulmonary embolism or intracerebral hemorrhage, most patients die after weeks or rarely months of progressive decline following the decision to discontinue aggressive tumor therapy, and hospice services can be extremely valuable to patients and their families in this situation.
Supportive Care (Long-term)
Most patients with glioblastoma who have experienced a seizure require lifelong AED therapy, particularly if seizures occur during or after initial tumor therapy. There is variability in practice regarding patients who experienced seizure at initial presentation and are seizure-free on anti-epileptic therapy following tumor treatment. Many neuro-oncologists recommend lifelong AED therapy in this situation as well, whereas others will consider tapering patients off of antiepileptic therapy after 1 to 2 years if he patient is interested in doing so and electroencephalogram (EEG) at that time does not demonstrate epileptiform discharges. Of course, freedom from seizures cannot be guaranteed, with or without continuation of antiepileptic therapy. Patients electing to attempt to discontinue AEDs should be counseled about seizure safety and avoiding high-risk activities.
Anticoagulation
Patients with glioblastoma are at significant risk of venous thromboembolism and related complications. There is no proven role for prophylactic anticoagulant therapy to prevent deep venous thrombosis (DVT). 142 Instead, patients should be educated about the symptoms of DVT and pulmonary embolism (PE), and physicians should have a low threshold for obtaining confirmatory testing if these symptoms occur. The diagnosis of glioblastoma is not a contraindication for treatment with systemic anticoagulation if a DVT/PE occurs, even in the setting of antiangiogenic therapy. 143 Treatment with low molecular weight heparin products has been shown to be more effective that oral anticoagulation with warfarin in patients with cancer. 144
Psychological and Emotional Well-being
Symptoms of depression and anxiety are common and undertreated in patients with glioblastoma. Many factors may contribute to depression in patients with glioblastoma, including loss of independence and function, the adjustment to the idea of a significantly shortened life, and possibly a direct biological effect of the tumor on neurotransmitter signaling. 145 Many patients and their families find cancer support groups, or ideally brain-tumor-specific support groups, very beneficial both for practical advice and the knowledge that they are not alone in facing this diagnosis. Antidepressant therapy and/or referral to a mental health professional should be considered for patients with symptoms that extend beyond the range of normal adjustment and negatively impact the quality of their lives.
Despite recent progress, glioblastoma remains an incurable tumor with survival under a year and a half for most patients. Multidisciplinary care is necessary to maximize survival time and preserve quality of life. In appropriately selected patients, aggressive surgery may relieve symptoms and prolong survival. Medical oncologists, radiation oncologists, and neurologists work as a team to design and deliver the initial treatment plan, typically involving the combination of RT and TMZ chemotherapy. Radiologists with expertise in the complexities of glioblastoma imaging help make the initial diagnosis and monitor response to therapy.
For glioblastoma survival to continue to improve, advances in each of these specialties and collaboration between specialties will be required. Advances in neurosurgical technique aided by advanced imaging modalities will allow for more extensive safe tumor resection at time of diagnosis and at time of recurrence. Ongoing clinical trials may help refine the long-recognized role of RT for the treatment of newly diagnosed glioblastoma in general and also define its role relative to that of TMZ in elderly patients. Novel therapeutic strategies, recently with an emphasis on molecularly targeted therapies and immunotherapeutic approaches, also hold the potential to significantly change the care of glioblastoma.
Conflict of interest statement . No conflicts of interest are reported for any author.
Rosati A , Buttolo L , Stefini R et al. . Efficacy and safety of levetiracetam in patients with glioma: a clinical prospective study . Arch Neurol . 2010 ; 67 (3) : 343 – 346 .
Google Scholar
Barker CA , Bishop AJ , Chang M et al. . Valproic acid use during radiation therapy for glioblastoma associated with improved survival . Int J Radiat Oncol Biol Phys . 2013 ; 86 (3) : 504 – 509 .
Bobustuc GC , Baker CH , Limaye A et al. . Levetiracetam enhances p53-mediated MGMT inhibition and sensitizes glioblastoma cells to temozolomide . Neuro Oncol . 2010 ; 12 (9) : 917 – 927 .
Glantz MJ , Cole BF , Forsyth PA et al. . Practice parameter: anticonvulsant prophylaxis in patients with newly diagnosed brain tumors. Report of the Quality Standards Subcommittee of the American Academy of Neurology . Neurology . 2000 ; 54 (10) : 1886 – 1893 .
Health USNIo . Lacosamide for Seizure Prophylaxis in High-Grade Gliomas . https://clinicaltrials.gov/ct2/show/NCT01432171 . Accessed February 1, 2015 .
Chamberlain MC . Radiographic patterns of relapse in glioblastoma . J Neurooncol . 2011 ; 101 (2) : 319 – 323 .
Blanchet L , Krooshof PW , Postma GJ et al. . Discrimination between metastasis and glioblastoma multiforme based on morphometric analysis of MR images . AJNR Am J Neuroradiol . 2011 ; 32 (1) : 67 – 73 .
Jackson A , Kassner A , Annesley-Williams D et al. . Abnormalities in the recirculation phase of contrast agent bolus passage in cerebral gliomas: comparison with relative blood volume and tumor grade . AJNR Am J Neuroradiol . 2002 ; 23 (1) : 7 – 14 .
Law M , Yang S , Babb JS et al. . Comparison of cerebral blood volume and vascular permeability from dynamic susceptibility contrast-enhanced perfusion MR imaging with glioma grade . AJNR Am J Neuroradiol . 2004 ; 25 (5) : 746 – 755 .
Boxerman JL , Schmainda KM , Weisskoff RM . Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not . AJNR Am J Neuroradiol . 2006 ; 27 (4) : 859 – 867 .
Liu ZL , Zhou Q , Zeng QS et al. . Noninvasive evaluation of cerebral glioma grade by using diffusion-weighted imaging-guided single-voxel proton magnetic resonance spectroscopy . J Int Med Res . 2012 ; 40 (1) : 76 – 84 .
Wang S , Kim S , Chawla S et al. . Differentiation between glioblastomas, solitary brain metastases, and primary cerebral lymphomas using diffusion tensor and dynamic susceptibility contrast-enhanced MR imaging . AJNR Am J Neuroradiol . 2011 ; 32 (3) : 507 – 514 .
Cha S , Lupo JM , Chen MH et al. . Differentiation of glioblastoma multiforme and single brain metastasis by peak height and percentage of signal intensity recovery derived from dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging . AJNR Am J Neuroradiol . 2007 ; 28 (6) : 1078 – 1084 .
Chawla S , Zhang Y , Wang S et al. . Proton magnetic resonance spectroscopy in differentiating glioblastomas from primary cerebral lymphomas and brain metastases . J Comput Assist Tomogr . 2010 ; 34 (6) : 836 – 841 .
Server A , Josefsen R , Kulle B et al. . Proton magnetic resonance spectroscopy in the distinction of high-grade cerebral gliomas from single metastatic brain tumors . Acta Radiol . 2010 ; 51 (3) : 316 – 325 .
Radbruch A , Wiestler B , Kramp L et al. . Differentiation of glioblastoma and primary CNS lymphomas using susceptibility weighted imaging . Eur J Radiol . 2013 ; 82 (3) : 552 – 556 .
Deistung A , Schweser F , Wiestler B et al. . Quantitative susceptibility mapping differentiates between blood depositions and calcifications in patients with glioblastoma . PloS One . 2013 ; 8 (3) : e57924 .
Kickingereder P , Wiestler B , Sahm F et al. . Primary central nervous system lymphoma and atypical glioblastoma: multiparametric differentiation by using diffusion-, perfusion-, and susceptibility-weighted MR imaging . Radiology . 2014 ; 272 (3) : 843 – 850 .
Pope WB . Genomics of brain tumor imaging . Neuroimaging Clin N Am . 2015 ; 25 (1) : 105 – 119 .
Willats L , Calamante F . The 39 steps: evading error and deciphering the secrets for accurate dynamic susceptibility contrast MRI . NMR Biomed . 2013 ; 26 (8) : 913 – 931 .
Laws ER , Parney IF , Huang W et al. . Survival following surgery and prognostic factors for recently diagnosed malignant glioma: data from the Glioma Outcomes Project . J Neurosurg . 2003 ; 99 (3) : 467 – 473 .
Sanai N , Berger MS . Glioma extent of resection and its impact on patient outcome . Neurosurgery . 2008 ; 62 (4) : 753 – 764 ; discussion 264–756 .
McGirt MJ , Chaichana KL , Gathinji M et al. . Independent association of extent of resection with survival in patients with malignant brain astrocytoma . J Neurosurg . 2009 ; 110 (1) : 156 – 162 .
di Russo P , Perrini P , Pasqualetti F et al. . Management and outcome of high-grade multicentric gliomas: a contemporary single-institution series and review of the literature . Acta Neurochir (Wien) . 2013 ; 155 (12) : 2245 – 2251 .
Sanai N , Polley MY , Berger MS . Insular glioma resection: assessment of patient morbidity, survival, and tumor progression . J Neurosurg . 2010 ; 112 (1) : 1 – 9 .
Holdhoff M , Rosner GL , Alcorn S et al. . ‘Elderly’ patients with newly diagnosed glioblastoma deserve optimal care . J Neurooncol . 2013 ; 113 (2) : 343 – 344 .
Chang SM , Nelson S , Vandenberg S et al. . Integration of preoperative anatomic and metabolic physiologic imaging of newly diagnosed glioma . J Neurooncol . 2009 ; 92 (3) : 401 – 415 .
Farshidfar Z , Faeghi F , Mohseni M et al. . Diffusion tensor tractography in the presurgical assessment of cerebral gliomas . Neuroradiol J . 2014 ; 27 (1) : 75 – 84 .
Gempt J , Soehngen E , Forster S et al. . Multimodal imaging in cerebral gliomas and its neuropathological correlation . Eur J Radiol . 2014 ; 83 (5) : 829 – 834 .
Sanai N , Mirzadeh Z , Berger MS . Functional outcome after language mapping for glioma resection . N Engl J Med . 2008 ; 358 (1) : 18 – 27 .
De Witt Hamer PC , Robles SG , Zwinderman AH et al. . Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis . J Clin Oncol . 2012 ; 30 (20) : 2559 – 2565 .
Maldaun MV , Khawja SN , Levine NB et al. . Awake craniotomy for gliomas in a high-field intraoperative magnetic resonance imaging suite: analysis of 42 cases . J Neurosurg . 2014 ; 121 (4) : 810 – 817 .
Hatiboglu MA , Weinberg JS , Suki D et al. . Impact of intraoperative high-field magnetic resonance imaging guidance on glioma surgery: a prospective volumetric analysis . Neurosurgery . 2009 ; 64 (6) : 1073 – 1081 ; discussion 1081 .
Acerbi F , Broggi M , Eoli M et al. . Fluorescein-guided surgery for grade IV gliomas with a dedicated filter on the surgical microscope: preliminary results in 12 cases . Acta Neurochir (Wien) . 2013 ; 155 (7) : 1277 – 1286 .
Bi WL , Laws ER Jr . Searching for the light: fluorescence guidance in glioma resection . World Neurosurg . 2014 ; 82 (1–2) : 54 – 55 .
Li Y , Rey-Dios R , Roberts DW et al. . Intraoperative fluorescence-guided resection of high-grade gliomas: a comparison of the present techniques and evolution of future strategies . World Neurosurg . 2014 ; 82 (1–2) : 175 – 185 .
Zhao S , Wu J , Wang C et al. . Intraoperative fluorescence-guided resection of high-grade malignant gliomas using 5-aminolevulinic acid-induced porphyrins: a systematic review and meta-analysis of prospective studies . PloS One . 2013 ; 8 (5) : e63682 .
Stummer W , Pichlmeier U , Meinel T et al. . Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial . Lancet Oncol . 2006 ; 7 (5) : 392 – 401 .
Attenello FJ , Mukherjee D , Datoo G et al. . Use of Gliadel (BCNU) wafer in the surgical treatment of malignant glioma: a 10-year institutional experience . Ann Surg Oncol . 2008 ; 15 (10) : 2887 – 2893 .
Brem H , Piantadosi S , Burger PC et al. . Placebo-controlled trial of safety and efficacy of intraoperative controlled delivery by biodegradable polymers of chemotherapy for recurrent gliomas. The Polymer-brain Tumor Treatment Group . Lancet . 1995 ; 345 (8956) : 1008 – 1012 .
Chang SM , Parney IF , McDermott M et al. . Perioperative complications and neurological outcomes of first and second craniotomies among patients enrolled in the Glioma Outcome Project . J Neurosurg . 2003 ; 98 (6) : 1175 – 1181 .
Sawaya R , Hammoud M , Schoppa D et al. . Neurosurgical outcomes in a modern series of 400 craniotomies for treatment of parenchymal tumors . Neurosurgery . 1998 ; 42 (5) : 1044 – 1055 ; discussion 1055–1046 .
Marcus LP , McCutcheon BA , Noorbakhsh A et al. . Incidence and predictors of 30-day readmission for patients discharged home after craniotomy for malignant supratentorial tumors in California (1995–2010) . J Neurosurg . 2014 ; 120 (5) : 1201 – 1211 .
Louis DN , Ohgaki H , Wiestler OD et al. . The 2007 WHO classification of tumours of the central nervous system . Vol 114 . 2007/07/10 ed2007 .
Google Preview
Parsons DW , Jones S , Zhang X et al. . An integrated genomic analysis of human glioblastoma multiforme . Science. 2008 ; 321 (5897) : 1807 – 1812 .
Hartmann C , Meyer J , Balss J et al. . Type and frequency of IDH1 and IDH2 mutations are related to astrocytic and oligodendroglial differentiation and age: a study of 1,010 diffuse gliomas . Acta Neuropathol . 2009 ; 118 (4) : 469 – 474 .
Sugawa N , Ekstrand AJ , James CD et al. . Identical splicing of aberrant epidermal growth factor receptor transcripts from amplified rearranged genes in human glioblastomas . Proc Natl Acad Sci USA . 1990 ; 87 (21) : 8602 – 8606 .
Ohgaki H , Dessen P , Jourde B et al. . Genetic pathways to glioblastoma: a population-based study . Cancer Res . 2004 ; 64 (19) : 6892 – 6899 .
Brennan CW , Verhaak RG , McKenna A et al. . The somatic genomic landscape of glioblastoma . Cell. 2013 ; 155 (2) : 462 – 477 .
Louis DN , von Deimling A , Chung RY et al. . Comparative study of p53 gene and protein alterations in human astrocytic tumors . J Neuropathol Exp Neurol . 1993 ; 52 (1) : 31 – 38 .
Yan H , Parsons DW , Jin G et al. . IDH1 and IDH2 mutations in gliomas . N Engl J Med . 2009 ; 360 (8) : 765 – 773 .
SongTao Q , Lei Y , Si G et al. . IDH mutations predict longer survival and response to temozolomide in secondary glioblastoma . Cancer Sci . 2012 ; 103 (2) : 269 – 273 .
Hartmann C , Hentschel B , Wick W et al. . Patients with IDH1 wild type anaplastic astrocytomas exhibit worse prognosis than IDH1-mutated glioblastomas, and IDH1 mutation status accounts for the unfavorable prognostic effect of higher age: implications for classification of gliomas . Acta Neuropathol . 2010 ; 120 (6) : 707 – 718 .
Bujko M , Kober P , Matyja E et al. . Prognostic value of IDH1 mutations identified with PCR-RFLP assay in glioblastoma patients . Mol Diagn Ther . 2010 ; 14 (3) : 163 – 169 .
Yan W , Zhang W , You G et al. . Correlation of IDH1 mutation with clinicopathologic factors and prognosis in primary glioblastoma: a report of 118 patients from China . PloS One . 2012 ; 7 (1) : e30339 .
Metellus P , Coulibaly B , Colin C et al. . Absence of IDH mutation identifies a novel radiologic and molecular subtype of WHO grade II gliomas with dismal prognosis . Acta Neuropathol . 2010 ; 120 (6) : 719 – 729 .
Comprehensive genomic characterization defines human glioblastoma genes and core pathways . Nature . 2008 ; 455 (7216) : 1061 – 1068 .
von Deimling A , Eibl RH , Ohgaki H et al. . p53 mutations are associated with 17p allelic loss in grade II and grade III astrocytoma . Cancer Res . 1992 ; 52 (10) : 2987 – 2990 .
Newcomb EW , Cohen H , Lee SR et al. . Survival of patients with glioblastoma multiforme is not influenced by altered expression of p16, p53, EGFR, MDM2 or Bcl-2 genes . Brain Pathol . 1998 ; 8 (4) : 655 – 667 .
Simon M , Hosen I , Gousias K et al. . TERT promoter mutations: a novel independent prognostic factor in primary glioblastomas . Neuro Oncol . 2015 ; 17 (1) : 45 – 52 .
Nonoguchi N , Ohta T , Oh JE et al. . TERT promoter mutations in primary and secondary glioblastomas . Acta Neuropathol . 2013 ; 126 (6) : 931 – 937 .
Labussiere M , Boisselier B , Mokhtari K et al. . Combined analysis of TERT, EGFR, and IDH status defines distinct prognostic glioblastoma classes . Neurology . 2014 ; 83 (13) : 1200 – 1206 .
Bello MJ , Alonso ME , Aminoso C et al. . Hypermethylation of the DNA repair gene MGMT: association with TP53 G:C to A:T transitions in a series of 469 nervous system tumors . Mutat Res . 2004 ; 554 (1–2) : 23 – 32 .
Nakagawachi T , Soejima H , Urano T et al. . Silencing effect of CpG island hypermethylation and histone modifications on O6-methylguanine-DNA methyltransferase (MGMT) gene expression in human cancer . Oncogene . 2003 ; 22 (55) : 8835 – 8844 .
Esteller M , Garcia-Foncillas J , Andion E et al. . Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents . N Engl J Med . 2000 ; 343 (19) : 1350 – 1354 .
Thon N , Eigenbrod S , Grasbon-Frodl EM et al. . Predominant influence of MGMT methylation in non-resectable glioblastoma after radiotherapy plus temozolomide . J Neurol Neurosurg Psychiatry . 2011 ; 82 (4) : 441 – 446 .
Rivera AL , Pelloski CE , Gilbert MR et al. . MGMT promoter methylation is predictive of response to radiotherapy and prognostic in the absence of adjuvant alkylating chemotherapy for glioblastoma . Neuro Oncol . 2010 ; 12 (2) : 116 – 121 .
Ishii D , Natsume A , Wakabayashi T et al. . Efficacy of temozolomide is correlated with 1p loss and methylation of the deoxyribonucleic acid repair gene MGMT in malignant gliomas . Neurol Med Chir (Tokyo) . 2007 ; 47 (8) : 341 – 349 ; discussion 350 .
Hegi ME , Diserens AC , Gorlia T et al. . MGMT gene silencing and benefit from temozolomide in glioblastoma . N Engl J Med . 2005 ; 352 (10) : 997 – 1003 .
Mulholland S , Pearson DM , Hamoudi RA et al. . MGMT CpG island is invariably methylated in adult astrocytic and oligodendroglial tumors with IDH1 or IDH2 mutations . Int J Cancer . 2012 ; 131 5 : 1104 – 1113 .
Phillips HS , Kharbanda S , Chen R et al. . Molecular subclasses of high-grade glioma predict prognosis, delineate a pattern of disease progression, and resemble stages in neurogenesis . Cancer Cell . 2006 ; 9 (3) : 157 – 173 .
Verhaak RG , Hoadley KA , Purdom E et al. . Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1 . Cancer Cell . 2010 ; 17 (1) : 98 – 110 .
Huse JT , Phillips HS , Brennan CW . Molecular subclassification of diffuse gliomas: seeing order in the chaos . Glia . 2011 ; 59 (8) : 1190 – 1199 .
Noushmehr H , Weisenberger DJ , Diefes K et al. . Identification of a CpG island methylator phenotype that defines a distinct subgroup of glioma . Cancer Cell . 2010 ; 17 (5) : 510 – 522 .
Louis DN , Perry A , Burger P et al. . International Society Of Neuropathology–Haarlem consensus guidelines for nervous system tumor classification and grading . Brain Pathol . 2014 ; 24 (5) : 429 – 435 .
Ostrom QT , Gittleman H , Farah P et al. . CBTRUS statistical report: Primary brain and central nervous system tumors diagnosed in the United States in 2006–2010 . Neuro Oncol . 2013 ; 15 (Suppl 2) : ii1 – i56 .
Howlader N , Noone AM , Krapcho M et al. . (eds). SEER Cancer Statistics Review, 1975–2011 . Bethesda, MD : National Cancer Institute . http://seer.cancer.gov/csr/1975_2011/ , based on November 2013 SEER data submission, posted to the SEER web site, April 2014 .
Linos E , Raine T , Alonso A , Michaud D . Atopy and risk of brain tumors: a meta-analysis . J Natl Cancer Inst . 2007 ; 99 (20) : 1544 – 1550 .
Ostrom QT , Bauchet L , Davis FG et al. . The epidemiology of glioma in adults: a “state of the science” review . Neuro Oncol . 2014 ; 16 (7) : 896 – 913 .
Stupp RR , Mason WPWP , van den Bent MJMJ et al. . Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma . N Engl J Med . 2005 ; 352 (10) : 987 – 996 .
Shapiro WR , Young DF . Treatment of malignant glioma. A controlled study of chemotherapy and irradiation . Arch Neurol . 1976 ; 33 (7) : 494 – 450 .
Walker MD , Alexander E Jr , Hunt WE et al. . Evaluation of BCNU and/or radiotherapy in the treatment of anaplastic gliomas. A cooperative clinical trial . J Neurosurg . 1978 ; 49 (3) : 333 – 343 .
Salazar OM , Rubin P , Feldstein ML et al. . High dose radiation therapy in the treatment of malignant gliomas: final report . Int J Radiat Oncol Biol Phys . 1979 ; 5 (10) : 1733 – 1740 .
Walker MD , Strike TA , Sheline GE . An analysis of dose-effect relationship in the radiotherapy of malignant gliomas . Int J Radiat Oncol Biol Phys . 1979 ; 5 (10) : 1725 – 1731 .
Gilbert MR , Wang M , Aldape KD et al. . Dose-Dense Temozolomide for Newly Diagnosed Glioblastoma: A Randomized Phase III Clinical Trial . J Clin Oncol . 2013 ; 31 (32) : 4085 – 4091 .
Kita M , Okawa T , Tanaka M et al. . [Radiotherapy of malignant glioma--prospective randomized clinical study of whole brain vs local irradiation] . Gan No Rinsho . 1989 ; 35 (11) : 1289 – 1294 .
Levin VA , Bidaut L , Hou P et al. . Randomized double-blind placebo-controlled trial of bevacizumab therapy for radiation necrosis of the central nervous system . Int J Radiat Oncol Biol Phys . 2011 ; 79 (5) : 1487 – 1495 .
Crossen JR , Garwood D , Glatstein E et al. . Neurobehavioral sequelae of cranial irradiation in adults: a review of radiation-induced encephalopathy . J Clin Oncol . 1994 ; 12 (3) : 627 – 642 .
Gondi V , Hermann BP , Mehta MP et al. . Hippocampal dosimetry predicts neurocognitive function impairment after fractionated stereotactic radiotherapy for benign or low-grade adult brain tumors . Int J Radiat Oncol Biol Phys . 2013 ; 85 (2) : 348 – 354 .
Roman DD , Sperduto PW . Neuropsychological effects of cranial radiation: current knowledge and future directions . Int J Radiat Oncol Biol Phys . 1995 ; 31 (4) : 983 – 998 .
Malmström A , Grønberg BH , Marosi C et al. . Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial . Lancet Oncol . 2012 ; 13 (9) : 916 – 926 .
Wick W , Platten M , Meisner C et al. . Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial . Lancet Oncol . 2012 ; 13 (7) : 707 – 715 .
Ferguson M , Rodrigues G , Cao J et al. . Management of high-grade gliomas in the elderly . Semin Radiat Oncol . 2014 ; 24 (4) : 279 – 288 .
Novocure . Novocure Announces the EF-14 Phase III Clinical Trial of Tumor Treating Fields in Patients with Newly Diagnosed Glioblastoma has been Terminated at the Interim Analysis due to Early Success . http://www.novocure.com/~/media/Files/N/Novocure/press-release/2014/201408-EF14-Trial-Results-Press-Release.pdf . Accessed February 1, 2015 .
Stupp R , Hegi ME , Gorlia T et al. . Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma with methylated MGMT promoter (CENTRIC EORTC 26071–22072 study): a multicentre, randomised, open-label, phase 3 trial . Lancet Oncol . 2014 ; 15 (10) : 1100 – 1108 .
Nabors LB , Fink KL , Mikkelsen T et al. . Two cilengitide regimens in combination with standard treatment for patients with newly diagnosed glioblastoma and unmethylated MGMT gene promoter: results of the open-label, controlled, randomized phase II CORE study . Neuro Oncol . 2015 ; 17 5 : 708 – 717 .
Chinot OL , Wick W , Mason W et al. . Bevacizumab plus radiotherapy–temozolomide for newly diagnosed glioblastoma . N Engl J Med . 2014 ; 370 (8) : 709 – 722 .
Gilbert MR , Dignam JJ , Armstrong TS et al. . A randomized trial of bevacizumab for newly diagnosed glioblastoma . N Engl J Med . 2014 ; 370 (8) : 699 – 708 .
Health USNIo . Study of a Drug [DCVax®-L] to Treat Newly Diagnosed GBM Brain Cancer . https://clinicaltrials.gov/ct2/show/NCT00045968 . Accessed February 1, 2015 .
Swartz AM , Li QJ , Sampson JH . Rindopepimut: a promising immunotherapeutic for the treatment of glioblastoma multiforme . Immunotherapy . 2014 ; 6 (6) : 679 – 690 .
Health USNIo . Radiation Therapy With or Without Temozolomide in Treating Older Patients With Newly Diagnosed Glioblastoma Multiforme . https://www.clinicaltrials.gov/ct2/show/NCT00045968 . Accessed February 1, 2015 .
Smith JS , Cha S , Mayo MC et al. . Serial diffusion-weighted magnetic resonance imaging in cases of glioma: distinguishing tumor recurrence from postresection injury . J Neurosurg . 2005 ; 103 (3) : 428 – 438 .
Hygino da Cruz LC Jr , Rodriguez I , Domingues RC et al. . Pseudoprogression and pseudoresponse: imaging challenges in the assessment of posttreatment glioma . AJNR Am J Neuroradiol . 2011 ; 32 (11) : 1978 – 1985 .
Brandes AA , Franceschi E , Tosoni A et al. . MGMT promoter methylation status can predict the incidence and outcome of pseudoprogression after concomitant radiochemotherapy in newly diagnosed glioblastoma patients . J Clin Oncol . 2008 ; 26 (13) : 2192 – 2197 .
Gerstner ER , McNamara MB , Norden AD et al. . Effect of adding temozolomide to radiation therapy on the incidence of pseudo-progression . J Neurooncol . 2009 ; 94 (1) : 97 – 101 .
Brandsma D , Stalpers L , Taal W et al. . Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas . Lancet Oncol . 2008 ; 9 (5) : 453 – 461 .
Stuplich M , Hadizadeh DR , Kuchelmeister K et al. . Late and prolonged pseudoprogression in glioblastoma after treatment with lomustine and temozolomide . J Clin Oncol . 2012 ; 30 (21) : e180 – e183 .
Macdonald DR , Cascino TL , Schold SC Jr et al. . Response criteria for phase II studies of supratentorial malignant glioma . J Clin Oncol . 1990 ; 8 (7) : 1277 – 1280 .
Wen PY , Macdonald DR , Reardon DA et al. . Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group . J Clin Oncol . 2010 ; 28 (11) : 1963 – 1972 .
Zaw TM , Pope WB , Cloughesy TF , Lai A et al. . Short-interval estimation of proliferation rate using serial diffusion MRI predicts progression-free survival in newly diagnosed glioblastoma treated with radiochemotherapy . J Neurooncol . 2014 ; 116 (3) : 601 – 608 .
Neal ML , Trister AD , Cloke T et al. . Discriminating survival outcomes in patients with glioblastoma using a simulation-based, patient-specific response metric . PloS One . 2013 ; 8 (1) : e51951 .
Barajas RF Jr , Chang JS , Segal MR et al. . Differentiation of recurrent glioblastoma multiforme from radiation necrosis after external beam radiation therapy with dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging . Radiology . 2009 ; 253 (2) : 486 – 496 .
Kim YH , Oh SW , Lim YJ et al. . Differentiating radiation necrosis from tumor recurrence in high-grade gliomas: assessing the efficacy of 18F-FDG PET, 11C-methionine PET and perfusion MRI . Clin Neurol Neurosurg . 2010 ; 112 (9) : 758 – 765 .
Sugahara T , Korogi Y , Tomiguchi S et al. . Posttherapeutic intraaxial brain tumor: the value of perfusion-sensitive contrast-enhanced MR imaging for differentiating tumor recurrence from nonneoplastic contrast-enhancing tissue . AJNR Am J Neuroradiol . 2000 ; 21 (5) : 901 – 909 .
Hu LS , Baxter LC , Smith KA et al. . Relative cerebral blood volume values to differentiate high-grade glioma recurrence from posttreatment radiation effect: direct correlation between image-guided tissue histopathology and localized dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging measurements . AJNR Am J Neuroradiol . 2009 ; 30 (3) : 552 – 558 .
Mangla R , Singh G , Ziegelitz D et al. . Changes in relative cerebral blood volume 1 month after radiation-temozolomide therapy can help predict overall survival in patients with glioblastoma . Radiology . 2010 ; 256 (2) : 575 – 584 .
Gahramanov S , Raslan AM , Muldoon LL et al. . Potential for differentiation of pseudoprogression from true tumor progression with dynamic susceptibility-weighted contrast-enhanced magnetic resonance imaging using ferumoxytol vs. gadoteridol: a pilot study . Int J Radiat Oncol Biol Phys . 2011 ; 79 (2) : 514 – 523 .
Kim HS , Goh MJ , Kim N et al. . Which combination of MR imaging modalities is best for predicting recurrent glioblastoma? Study of diagnostic accuracy and reproducibility . Radiology . 2014 ; 273 (3) : 831 – 843 .
Seeger A , Braun C , Skardelly M et al. . Comparison of three different MR perfusion techniques and MR spectroscopy for multiparametric assessment in distinguishing recurrent high-grade gliomas from stable disease . Acad Radiol . 2013 ; 20 (12) : 1557 – 1565 .
Kim HS , Kim JH , Kim SH et al. . Posttreatment high-grade glioma: usefulness of peak height position with semiquantitative MR perfusion histogram analysis in an entire contrast-enhanced lesion for predicting volume fraction of recurrence . Radiology . 2010 ; 256 (3) : 906 – 915 .
Tsien C , Galban CJ , Chenevert TL et al. . Parametric response map as an imaging biomarker to distinguish progression from pseudoprogression in high-grade glioma . J Clin Oncol . 2010 ; 28 (13) : 2293 – 2299 .
Hu LS , Eschbacher JM , Heiserman JE et al. . Reevaluating the imaging definition of tumor progression: perfusion MRI quantifies recurrent glioblastoma tumor fraction, pseudoprogression, and radiation necrosis to predict survival . Neuro Oncol . 2012 ; 14 (7) : 919 – 930 .
Boxerman JL , Ellingson BM , Jeyapalan S et al. . Longitudinal DSC-MRI for Distinguishing Tumor Recurrence From Pseudoprogression in Patients With a High-grade Glioma . Am J Clin Oncol . 2014 . [Epub ahead of print] .
Suh CH , Kim HS , Choi YJ et al. . Prediction of pseudoprogression in patients with glioblastomas using the initial and final area under the curves ratio derived from dynamic contrast-enhanced T1-weighted perfusion MR imaging . AJNR Am J Neuroradiol . 2013 ; 34 (12) : 2278 – 2286 .
Yun TJ , Park CK , Kim TM et al. . Glioblastoma Treated with Concurrent Radiation Therapy and Temozolomide Chemotherapy: Differentiation of True Progression from Pseudoprogression with Quantitative Dynamic Contrast-enhanced MR Imaging . Radiology . 2015 ; 274 3 : 830 – 840 .
Shin KE , Ahn KJ , Choi HS et al. . DCE and DSC MR perfusion imaging in the differentiation of recurrent tumour from treatment-related changes in patients with glioma . Clin Radiol . 2014 ; 69 (6) : e264 – e272 .
Li Y , Lupo JM , Parvataneni R et al. . Survival analysis in patients with newly diagnosed glioblastoma using pre- and postradiotherapy MR spectroscopic imaging . Neuro Oncol . 2013 ; 15 (5) : 607 – 617 .
Ellingson BM , Malkin MG , Rand SD et al. . Validation of functional diffusion maps (fDMs) as a biomarker for human glioma cellularity . J Magn Reson Imaging . 2010 ; 31 (3) : 538 – 548 .
Ellingson BM , Malkin MG , Rand SD et al. . Volumetric analysis of functional diffusion maps is a predictive imaging biomarker for cytotoxic and anti-angiogenic treatments in malignant gliomas . J Neurooncol . 2011 ; 102 (1) : 95 – 103 .
Moffat BA , Chenevert TL , Lawrence TS et al. . Functional diffusion map: a noninvasive MRI biomarker for early stratification of clinical brain tumor response . Proc Natl Acad Sci USA 2005 ; 102 (15) : 5524 – 5529 .
Ellingson BM , Cloughesy TF , Lai A et al. . Quantitative probabilistic functional diffusion mapping in newly diagnosed glioblastoma treated with radiochemotherapy . Neuro Oncol . 2013 ; 15 (3) : 382 – 390 .
Pope WB , Qiao XJ , Kim HJ et al. . Apparent diffusion coefficient histogram analysis stratifies progression-free and overall survival in patients with recurrent GBM treated with bevacizumab: a multi-center study . J Neurooncol . 2012 ; 108 (3) : 491 – 498 .
Lutz K , Wiestler B , Graf M et al. . Infiltrative patterns of glioblastoma: Identification of tumor progress using apparent diffusion coefficient histograms . J Magn Reson Imaging . 2014 ; 39 (5) : 1096 – 1103 .
Terakawa Y , Tsuyuguchi N , Iwai Y et al. . Diagnostic accuracy of 11C-methionine PET for differentiation of recurrent brain tumors from radiation necrosis after radiotherapy . J Nucl Med . 2008 ; 49 (5) : 694 – 699 .
Rachinger W , Goetz C , Popperl G et al. . Positron emission tomography with O-(2-[18F]fluoroethyl)-l-tyrosine versus magnetic resonance imaging in the diagnosis of recurrent gliomas . Neurosurgery . 2005 ; 57 (3) : 505 – 511 ; discussion 505–511 .
Mehrkens JH , Popperl G , Rachinger W et al. . The positive predictive value of O-(2-[18F]fluoroethyl)-L-tyrosine (FET) PET in the diagnosis of a glioma recurrence after multimodal treatment . J Neurooncol . 2008 ; 88 (1) : 27 – 35 .
Chen W , Silverman DH , Delaloye S et al. . 18F-FDOPA PET imaging of brain tumors: comparison study with 18F-FDG PET and evaluation of diagnostic accuracy . J Nucl Med . 2006 ; 47 (6) : 904 – 911 .
Ledezma CJ , Chen W , Sai V et al. . 18F-FDOPA PET/MRI fusion in patients with primary/recurrent gliomas: initial experience . Eur J Radiol . 2009 ; 71 (2) : 242 – 248 .
Darefsky AS , King JT Jr , Dubrow R . Adult glioblastoma multiforme survival in the temozolomide era: a population-based analysis of Surveillance, Epidemiology, and End Results registries . Cancer . 2012 ; 118 (8) : 2163 – 2172 .
Johnson DR , Leeper HE , Uhm JH . Glioblastoma survival in the United States improved after Food and Drug Administration approval of bevacizumab: a population-based analysis . Cancer . 2013 ; 119 (19) : 3489 – 3495 .
Stupp R , Hegi ME , Mason WP et al. . Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial . Lancet Oncol . 2009 ; 10 (5) : 459 – 466 .
Jo JT , Schiff D , Perry JR . Thrombosis in brain tumors . Semin Thromb Hemost . 2014 ; 40 (3) : 325 – 331 .
Norden AD , Bartolomeo J , Tanaka S et al. . Safety of concurrent bevacizumab therapy and anticoagulation in glioma patients . J Neurooncol . 2012 ; 106 (1) : 121 – 125 .
Lee AY , Levine MN , Baker RI et al. . Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer . N Engl J Med . 2003 ; 349 (2) : 146 – 153 .
Liu R , Page M , Solheim K et al. . Quality of life in adults with brain tumors: current knowledge and future directions . Neuro Oncol . 2009 ; 11 (3) : 330 – 339 .
- chemotherapy regimen
- glioblastoma
- surgical procedures, operative
- diagnostic imaging
- temozolomide
- standard of care
Email alerts
Related articles in pubmed, citing articles via.
- SNO Twitter
- Recommend to your Library
Affiliations
- Online ISSN 2054-2585
- Print ISSN 2054-2577
- Copyright © 2024 Society for Neuro-Oncology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Brain Tumor and Neuro-Oncology Research
Innovations in brain tumor and neuro-oncology.
- Laser Interstitial Thermotherapy with real-time MRI using the Monteris AutoLitt System
- Brain mapping with functional MRI (fMRI), Diffusion Tensor Imaging (DTI) and/or magnetoencephalography (MEG) to optimize identification of brain tumors and surrounding normal tissues
- Intraoperative MRI to maximize safety and completeness of tumor removal
- New techniques for optical and fluorescence imaging to better identify infiltrating tumor
- Convection Enhanced Delivery (CED): A technology to improve delivery of small anti-tumor molecules and chemotherapy to brain tumors
- Stereotactic Radiosurgery using Gamma Knife or CyberKnife®
Current Clinical Trials
UH provides both standard and advanced nonoperative treatments for patients with brain tumors through our advanced and extensive clinical trials. Many of these are offered in collaboration with the NCI-funded Adult Brain Tumor Consortium (ABTC), a group of 15 elite “Brain Tumor Centers of Excellence” which collaborate to offer the most innovative treatments to patients with brain tumors. Clinical trial offers change frequently, but current offers include:
- Tumor vaccines (immunotherapy) to teach the patient’s own immune system to fight their tumor
- New drugs specifically targeting brain tumor “stem cells” which are resistant to current therapies
- Gene therapy for brain tumors
- New agents targeting “angio-genesis,” the need for tumors to acquire a new blood supply
- Convection Enhanced Deliver (CED). New ways to deliver drugs and immunotoxins specifically to the tumor while avoiding toxicity from the normal brain.
- Innovative combinations of chemotherapeutic agents which are more powerful together than apart
Specific trials include:
- ABTC 0603 – A Phase I/II Trial of Hydroxychloroquine in conjunction with Radiation therapy and concurrent and Adjuvant Temozolomide in Patients with Newly diagnosed Glioblastoma Multiforme (Version 01/08/09)
- ABTC 0703 – Phase I/II study of the poly (ADP-ribose) polymerase-1(PARP-1) inhibitor BSI-201 in patients with newly diagnosed malignant glioma (version 02/06/09)
- ABTC 0904 – A Biomarker and Phase II Study of GDC-0449 in Patients with Recurrent Glioblastoma Multiforme
- ABTC 0901 – An Open Label, Phase 2 Study Evaluating the Safety and Efficacy of IMC-3G3 or IMC-1121B in Patients with Recurrent Glioblastoma Multiforme
- Patient Care & Health Information
- Diseases & Conditions
- Brain tumor
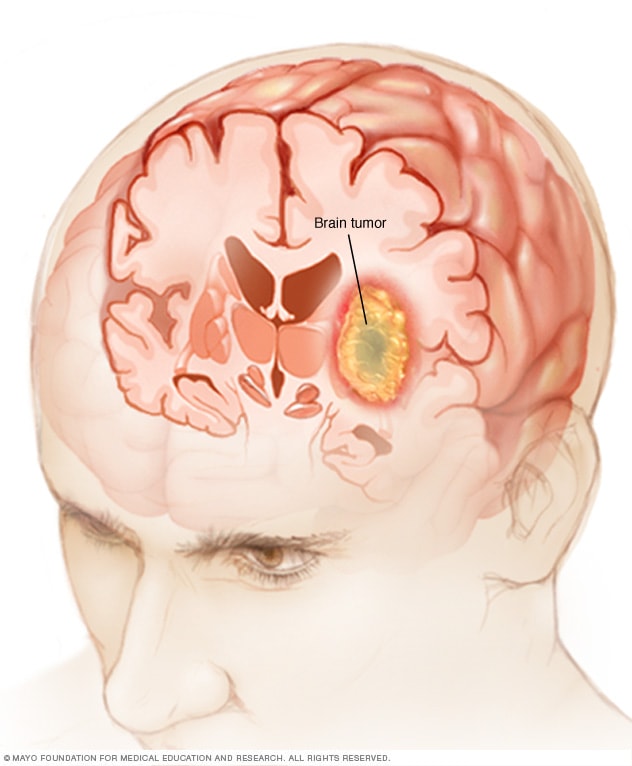
A brain tumor can form in the brain cells (as shown), or it can begin elsewhere and spread to the brain. As the tumor grows, it creates pressure on and changes the function of surrounding brain tissue, which causes signs and symptoms such as headaches, nausea and balance problems.
A brain tumor is a growth of cells in the brain or near it. Brain tumors can happen in the brain tissue. Brain tumors also can happen near the brain tissue. Nearby locations include nerves, the pituitary gland, the pineal gland, and the membranes that cover the surface of the brain.
Brain tumors can begin in the brain. These are called primary brain tumors. Sometimes, cancer spreads to the brain from other parts of the body. These tumors are secondary brain tumors, also called metastatic brain tumors.
Many different types of primary brain tumors exist. Some brain tumors aren't cancerous. These are called noncancerous brain tumors or benign brain tumors. Noncancerous brain tumors may grow over time and press on the brain tissue. Other brain tumors are brain cancers, also called malignant brain tumors. Brain cancers may grow quickly. The cancer cells can invade and destroy the brain tissue.
Brain tumors range in size from very small to very large. Some brain tumors are found when they are very small because they cause symptoms that you notice right away. Other brain tumors grow very large before they're found. Some parts of the brain are less active than others. If a brain tumor starts in a part of the brain that's less active, it might not cause symptoms right away. The brain tumor size could become quite large before the tumor is detected.
Brain tumor treatment options depend on the type of brain tumor you have, as well as its size and location. Common treatments include surgery and radiation therapy.
There are many types of brain tumors. The type of brain tumor is based on the kind of cells that make up the tumor. Special lab tests on the tumor cells can give information about the cells. Your health care team uses this information to figure out the type of brain tumor.
Some types of brain tumors usually aren't cancerous. These are called noncancerous brain tumors or benign brain tumors. Some types of brain tumors usually are cancerous. These types are called brain cancers or malignant brain tumors. Some brain tumor types can be benign or malignant.
Benign brain tumors tend to be slow-growing brain tumors. Malignant brain tumors tend to be fast-growing brain tumors.
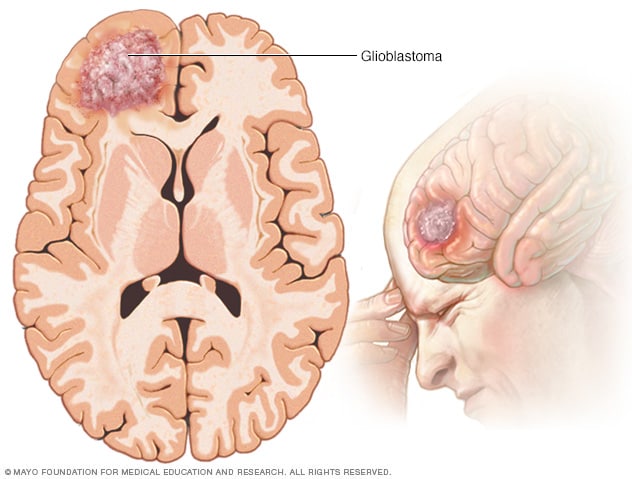
Glioblastoma
Glioblastoma is a type of cancer that starts in cells called astrocytes that support nerve cells. It can form in the brain or spinal cord.
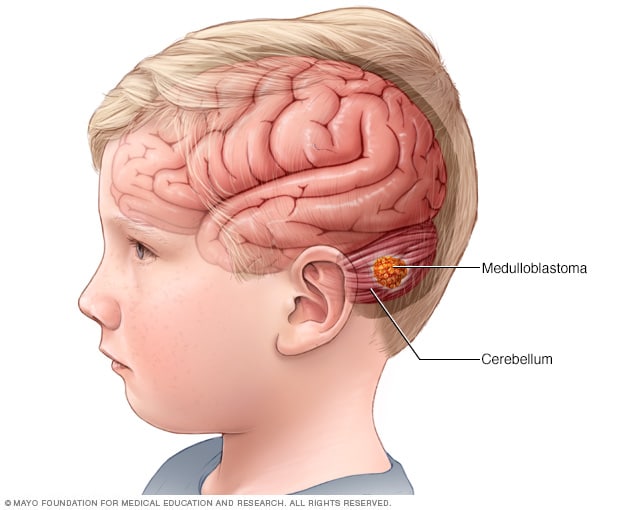
Medulloblastoma
Medulloblastoma is a type of brain cancer that starts in the part of the brain called the cerebellum. Medulloblastoma is the most common type of cancerous brain tumor in children.
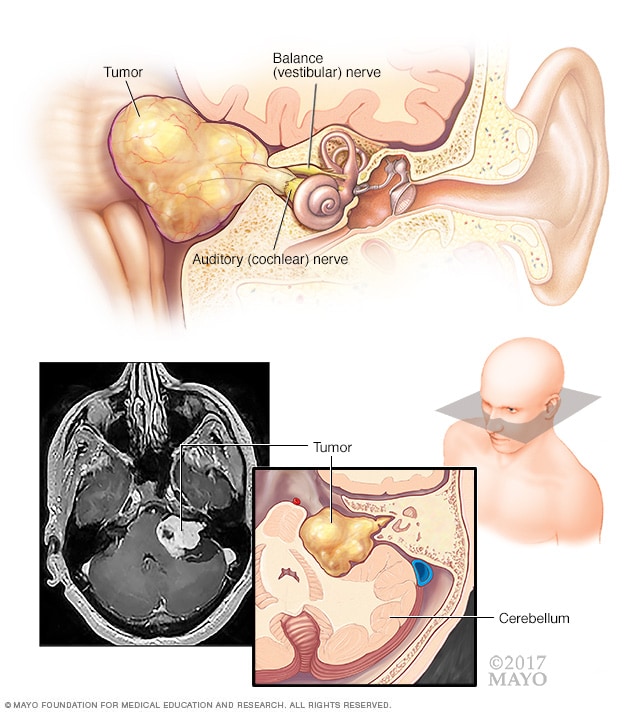
Acoustic neuroma (vestibular schwannoma)
An acoustic neuroma (vestibular schwannoma) is a benign tumor that develops on the balance and hearing nerves leading from the inner ear to the brain. These nerves are twined together to form the vestibulocochlear nerve (eighth cranial nerve). The pressure on the nerve from the tumor may cause hearing loss and imbalance.
Types of brain tumors include:
- Gliomas and related brain tumors. Gliomas are growths of cells that look like glial cells. The glial cells surround and support nerve cells in the brain tissue. Types of gliomas and related brain tumors include astrocytoma , glioblastoma , oligodendroglioma and ependymoma . Gliomas can be benign, but most are malignant. Glioblastoma is the most common type of malignant brain tumor.
- Choroid plexus tumors. Choroid plexus tumors start in cells that make the fluid that surrounds the brain and spinal cord. This fluid is called cerebrospinal fluid. Choroid plexus tumors are located in the fluid-filled cavities in the brain, called the ventricles. Choroid plexus tumors can be benign or malignant. Choroid plexus carcinoma is the malignant form of this type of brain tumor. It's more common in children.
- Embryonal tumors. Embryonal tumors begin in cells that are left over from fetal development. The cells, called embryonal cells, stay in the brain after birth. Embryonal tumors are malignant brain tumors that happen most often in babies and young children. The most common type of embryonal tumor is medulloblastoma . It's usually located in the lower back part of the brain, called the cerebellum.
- Germ cell tumors. Germ cell tumors start in reproductive cells, called germ cells, that go on to become the sperm and egg cells. Germ cells are mostly in the ovaries and testicles. But sometimes they're in other parts of the body, including the brain. When germ cell tumors happen in the brain, they're often located near the pineal gland or the pituitary gland. Germ cell tumors are mostly benign. They're more common in children.
- Pineal tumors. Pineal tumors start in and around the brain's pineal gland. The pineal gland is located in the center of the brain. It makes a hormone called melatonin that helps with sleep. Pineal tumors can be benign or malignant. Pineoblastoma is a malignant type of pineal tumor that's most common in children.
- Meningiomas. Meningiomas are brain tumors that start in the membranes around the brain and spinal cord. Meningiomas are usually benign, but sometimes they can be malignant. Meningiomas are the most common type of benign brain tumor.
- Nerve tumors. Nerve tumors are growths that happen in and around nerves. The most common type that happens in the head is acoustic neuroma , also called schwannoma. This benign tumor is located on the main nerve that connects the inner ear to the brain.
- Pituitary tumors. Brain tumors can begin in and around the pituitary gland. This small gland is located near the base of the brain. Most tumors that happen in and around the pituitary gland are benign. Pituitary tumors happen in the pituitary gland itself. Craniopharyngioma is a type of brain tumor that happens near the pituitary gland.
- Other brain tumors. Many other types of rare tumors can happen in and around the brain. Tumors can start in the muscles, blood vessels and connective tissue around the brain. Tumors can form in the bones of the skull. Malignant brain tumors can start from the germ-fighting immune system cells in the brain. This type of brain cancer is called primary central nervous system lymphoma.

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
The signs and symptoms of a brain tumor depend on the brain tumor's size and location. Symptoms also might depend on how fast the brain tumor is growing, which is also called the tumor grade.
General signs and symptoms caused by brain tumors may include:
- Headache or pressure in the head that is worse in the morning.
- Headaches that happen more often and seem more severe.
- Headaches that are sometimes described as tension headaches or migraines.
- Nausea or vomiting.
- Eye problems, such as blurry vision, seeing double or losing sight on the sides of your vision.
- Losing feeling or movement in an arm or a leg.
- Trouble with balance.
- Speech problems.
- Feeling very tired.
- Confusion in everyday matters.
- Memory problems.
- Having trouble following simple commands.
- Personality or behavior changes.
- Seizures, especially if there is no history of seizures.
- Hearing problems.
- Dizziness or a sense that the world is spinning, also called vertigo.
- Feeling very hungry and gaining weight.
Brain tumors that aren't cancerous tend to cause symptoms that develop slowly. Noncancerous brain tumors also are called benign brain tumors. They might cause subtle symptoms that you don't notice at first. The symptoms might get worse over months or years.
Cancerous brain tumors cause symptoms that get worse quickly. Cancerous brain tumors also are called brain cancers or malignant brain tumors. They cause symptoms that come on suddenly. They get worse in a matter of days or weeks.
Brain tumor headaches
Headaches are the most common symptom of brain tumors. Headaches happen in about half of people with brain tumors. Headaches can happen if a growing brain tumor presses on healthy cells around it. Or a brain tumor can cause swelling in the brain that increases pressure in the head and leads to a headache.
Headache pain caused by brain tumors is often worse when you wake up in the morning. But it can happen at any time. Some people have headaches that wake them from sleep. Brain tumor headaches tend to cause pain that's worse when coughing or straining. People with brain tumors most often report that the headache feels like a tension headache. Some people say the headache feels like a migraine.
Brain tumors in the back of the head might cause a headache with neck pain. If the brain tumor happens in the front of the head, the headache might feel like eye pain or sinus pain.
Brain tumor symptoms by location
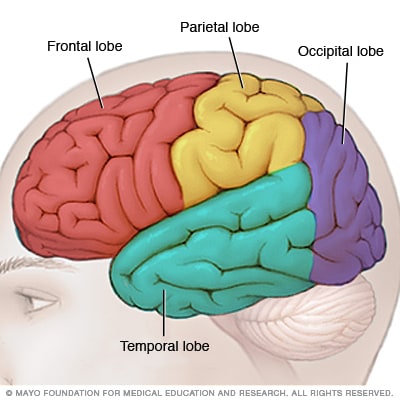
Brain lobes
Each side of your brain contains four lobes. The frontal lobe is important for cognitive functions and control of voluntary movement or activity. The parietal lobe processes information about temperature, taste, touch and movement, while the occipital lobe is primarily responsible for vision. The temporal lobe processes memories, integrating them with sensations of taste, sound, sight and touch.
The main part of the brain is called the cerebrum. Brain tumors in different parts of the cerebrum might cause different symptoms.
- Brain tumors in the front of the brain. The frontal lobes are in the front of the brain. They control thinking and movement. Frontal lobe brain tumors might cause balance problems and trouble walking. There might be personality changes, such as forgetfulness and lack of interest in usual activities. Sometimes family members notice that the person with the brain tumor seems different.
- Brain tumors in the middle of the brain. The parietal lobes are in the upper middle part of the brain. They help process information about touch, taste, smell, vision and hearing. Parietal lobe brain tumors can cause problems related to the senses. Examples include vision problems and hearing problems.
- Brain tumors in the back of the brain. The occipital lobes are in the back of the brain. They control vision. Occipital lobe brain tumors can cause vision loss.
- Brain tumors in the lower part of the brain. The temporal lobes are on the sides of the brain. They process memories and senses. Temporal lobe brain tumors can cause memory problems. They might cause someone to see, taste or smell something that isn't there. Sometimes the taste or smell is unpleasant or unusual.
When to see a doctor
Make an appointment with your health care provider if you have persistent signs and symptoms that worry you.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get the latest brain tumor advice from Mayo Clinic delivered in your inbox.
Sign up for free and receive the latest on brain tumor treatment, diagnosis and surgery.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
You will receive the first brain tumor email in your inbox shortly, which will include information on treatment, diagnosis, surgery and how brain cancer teams at Mayo Clinic approach personalized care.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Brain tumors that begin in the brain
Brain tumors that start as a growth of cells in the brain are called primary brain tumors. They might start right in the brain or in the tissue nearby. Nearby tissue might include the membranes that cover the brain, called meninges. Brain tumors also can happen in nerves, the pituitary gland and the pineal gland.
Brain tumors happen when cells in or near the brain get changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. The changes tell the cells to grow quickly and continue living when healthy cells would die as part of their natural life cycle. This makes a lot of extra cells in the brain. The cells can form a growth called a tumor.
It's not clear what causes the DNA changes that lead to brain tumors. For many people with brain tumors, the cause is never known. Sometimes parents pass DNA changes to their children. The changes can increase the risk of having a brain tumor. These hereditary brain tumors are rare. If you have a family history of brain tumors, talk about it with your health care provider. You might consider meeting with a health care provider trained in genetics to understand whether your family history increases your risk of having a brain tumor.
When brain tumors happen in children, they're likely to be primary brain tumors. In adults, brain tumors are more likely to be cancer that started somewhere else and spread to the brain.
Cancer that spreads to the brain
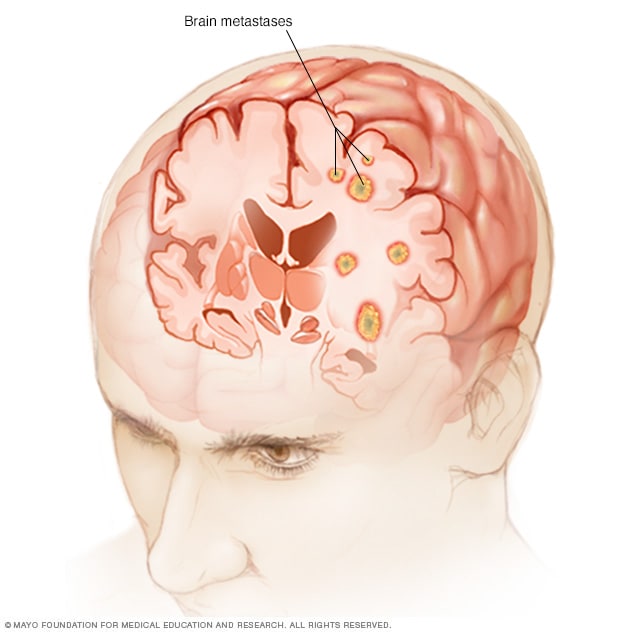
Brain metastases
Brain metastases happen when cancer begins elsewhere in the body and spreads (metastasizes) to the brain.
Secondary brain tumors happen when cancer starts somewhere else and spreads to the brain. When cancer spreads, it's called metastatic cancer.
Any cancer can spread to the brain, but common types include:
- Breast cancer.
- Colon cancer.
- Kidney cancer.
- Lung cancer.
It's not clear why some cancers spread to the brain and others are more likely to spread to other places.
Secondary brain tumors most often happen in people who have a history of cancer. Rarely, a brain tumor may be the first sign of cancer that began somewhere else in the body.
In adults, secondary brain tumors are far more common than are primary brain tumors.
Risk factors
In most people with primary brain tumors, the cause isn't clear. But doctors have identified some factors that may raise the risk.
Risk factors include:
- Age. Brain tumors can happen at any age, but they happen most often in older adults. Some brain tumors mostly affect adults. Some brain tumors happen most often in children.
- Race. Anyone can get a brain tumor. But some types of brain tumors are more common in people of certain races. For example, gliomas are more common in white people. Meningiomas are more common in Black people.
Exposure to radiation. People who have been exposed to a strong type of radiation have an increased risk of brain tumor. This strong radiation is called ionizing radiation. The radiation is strong enough to cause DNA changes in the body's cells. The DNA changes can lead to tumors and cancers. Examples of ionizing radiation include radiation therapy used to treat cancer and radiation exposure caused by atomic bombs.
Low-level radiation from everyday objects isn't linked to brain tumors. Low levels of radiation include the energy that comes from cellphones and radio waves. There is no convincing evidence that using cellphones causes brain tumors. But more studies are happening to make sure.
- Inherited syndromes that increase the risk of brain tumor. Some DNA changes that increase the risk of brain tumor run in families. Examples include the DNA changes that cause neurofibromatosis 1 and 2, tuberous sclerosis, Lynch syndrome, Li-Fraumeni syndrome, Von Hippel-Lindau disease, familial adenomatous polyposis, Cowden syndrome, and Gorlin syndrome.
There's no way to prevent brain tumors. If you get a brain tumor, you didn't do anything to cause it.
People with an increased risk of brain tumor might consider screening tests. Screening isn't brain tumor prevention. But screening might help find a brain tumor when it's small and treatment is more likely to be successful.
If you have a family history of brain tumor or inherited syndromes that increase the risk of brain tumor, talk about it with your health care provider. You might consider meeting with a genetic counselor or other health care provider trained in genetics. This person can help you understand your risk and ways to manage it. For example, you might consider brain tumor screening tests. Testing might include an imaging test or a neurological exam to test your vision, hearing, balance, coordination and reflexes.
Brain tumor care at Mayo Clinic
- Niederhuber JE, et al., eds. Cancer of the central nervous system. In: Abeloff's Clinical Oncology. 6th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Sept. 27, 2022.
- Adult central nervous system tumors treatment (PDQ) — Patient version. National Cancer Institute. https://www.cancer.gov/types/brain/patient/adult-brain-treatment-pdq. Accessed Sept. 27, 2022.
- Brain tumor. Cancer.Net. https://www.cancer.net/cancer-types/brain-tumor/view-all. Accessed Nov. 1, 2022.
- Louis DN, et al. The 2021 WHO classification of tumors of the central nervous system: A summary. Neuro-Oncology. 2021; doi:10.1093/neuonc/noab106.
- Chheda MG, et al. Uncommon brain tumors. https://www.uptodate.com/contents/search. Accessed Nov. 10, 2022.
- Childhood medulloblastoma and other central nervous system embryonal tumors treatment (PDQ) — Patient version. National Cancer Institute. https://www.cancer.gov/types/brain/patient/child-cns-embryonal-treatment-pdq. Accessed Nov. 15, 2022.
- Childhood central nervous system germ cell tumors treatment (PDQ) — Patient version. National Cancer Institute. https://www.cancer.gov/types/brain/patient/child-cns-germ-cell-treatment-pdq. Accessed Nov. 15, 2022.
- Ostrom QT, et al. CBTRUS statistical report: Primary brain and other central nervous system tumors diagnosed in the United States in 2015-2019. Neuro-Oncology. 2022; doi:10.1093/neuonc/noac202.
- Winn HR, ed. Youmans and Winn Neurological Surgery. 8th ed. Elsevier; 2023. https://www.clinicalkey.com. Accessed Sept. 27, 2022.
- Wong ET, et al. Overview of the clinical features and diagnosis of brain tumors in adults. https://www.uptodate.com/contents/search. Accessed Sept. 27, 2022.
- Edlow JA, et al. Medical and nonstroke neurological causes of acute, continuous vestibular symptoms. Neurology Clinics. 2015; doi:10.1016/j.ncl.2015.04.002.
- Cellphones and cancer risk. National Cancer Institute. https://www.cancer.gov/about-cancer/causes-prevention/risk/radiation/cell-phones-fact-sheet. Accessed Oct. 21, 2022.
- Central nervous system cancers. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1425. Oct. 28, 2022.
- Stereotactic radiosurgery (SRS) and stereotactic body radiotherapy (SBRT). RadiologyInfo.org. https://www.radiologyinfo.org/en/info/stereotactic. Nov. 4, 2022.
- Distress management. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1431. Accessed Sept. 27, 2022.
- Muthupillai R, et al. Magnetic resonance elastography. Nature Medicine. 1996; doi:10.1038/nm0596-601.
- Murphy MC, et al. MR elastography of the brain and its application in neurological diseases. NeuroImage. 2019l doi:10.1016/j.neuroimage.2017.10.008.
- Warner KJ. Allscripts EPSi. Mayo Clinic. Jan. 7, 2021.
- Member institutions. Alliance for Clinical Trials in Oncology. https://www.allianceforclinicaltrialsinoncology.org/main/public/standard.xhtml?path=/Public/Institutions. Accessed Nov. 30, 2022.
- Genetic/familial high-risk assessment: Breast, ovarian and pancreatic. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1503. Accessed Nov. 30, 2022.
- Lynch syndrome management. AskMayoExpert. 2021.
- Brain tumor FAQs
- Living with Brain Tumors
- Long Term Brain Cancer Survivor
- Punk Guitarist Survives Brain Tumor
- What is a brain tumor? A Mayo Clinic expert explains
Associated Procedures
- Ablation therapy
- Acupuncture
- Brain stereotactic radiosurgery
- Chemotherapy
- Needle biopsy
- Positron emission tomography scan
- Radiation therapy
- Stereotactic radiosurgery
News from Mayo Clinic
- Mayo Clinic Minute: Learn about meningioma and glioblastoma brain tumors Aug. 07, 2023, 02:00 p.m. CDT
- Against the odds Sept. 29, 2022, 11:00 a.m. CDT
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, have been ranked among the best Neurology & Neurosurgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

A Guide to Applied Machine Learning for Biologists pp 243–255 Cite as
Case Study 2: Brain Tumor Classification
- Mohammad “Sufian” Badar 2 , 3 ,
- Hussam Bin Mehare 4 ,
- Jishnu Pillai Anilkumar 5 ,
- Khairol Amali bin Ahmad 6 &
- Mohammad Rehan Badar 7
- First Online: 22 June 2023
474 Accesses
- The original version of this chapter was revised. The correction to this chapter is available at https://doi.org/10.1007/978-3-031-22206-1_11
Brain tumor classification is a very important area in medical image analysis as it has the potential to improve the diagnosis and treatment of brain tumors. In order to properly plan therapy and manage patients, it is essential to accurately classify brain tumors, which are one of the major causes of cancer-related fatalities globally.
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Change history
03 august 2023.
A correction has been published.
Author information
Authors and affiliations.
Department of Computer Science and Engineering, School of Engineering Sciences and Technology (SEST), Jamia Hamdard University, New Delhi, India
Mohammad “Sufian” Badar
Senior Teaching Faculty, Department of Bioengineering, University of California, Riverside, CA, USA
Department of Mechanical Engineering, Z.H. College of Engineering and Technology, Aligarh Muslim University, Aligarh, Uttar Pradesh, India
Hussam Bin Mehare
Department of Computer Science & Engineering, Presidency University, Bengaluru, Karnataka, India
Jishnu Pillai Anilkumar
National Defence University of Malaysia, Sungai Besi, Kuala Lumpur, Malaysia
Khairol Amali bin Ahmad
Consultant Physician, Apollo Hospital, Director, Badar Medical Centre (BMC), Shaheen Bagh, New Delhi, India
Mohammad Rehan Badar
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Mohammad “Sufian” Badar .
Editor information
Editors and affiliations.
Department of Computer Science and Engineering, School of Engineering Sciences and Technology (SEST) Jamia Hamdard University, New Delhi, India, Senior Teaching Faculty (Former), Department of Bioengineering, University of California, Riverside, Riverside, CA, USA
Mohammad "Sufian" Badar
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter.
Badar, M.“., Mehare, H.B., Anilkumar, J.P., Amali bin Ahmad, K., Badar, M.R. (2023). Case Study 2: Brain Tumor Classification. In: Badar, M.". (eds) A Guide to Applied Machine Learning for Biologists. Springer, Cham. https://doi.org/10.1007/978-3-031-22206-1_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-22206-1_10
Published : 22 June 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-22205-4
Online ISBN : 978-3-031-22206-1
eBook Packages : Biomedical and Life Sciences Biomedical and Life Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 16 January 2024
Intra-tumoral T cells in pediatric brain tumors display clonal expansion and effector properties
- Aditi Upadhye 1 na1 ,
- Kevin E. Meza Landeros ORCID: orcid.org/0009-0004-4496-6824 1 , 2 na1 ,
- Ciro Ramírez-Suástegui 1 ,
- Benjamin J. Schmiedel ORCID: orcid.org/0000-0002-9103-9378 1 ,
- Edwin Woo 3 ,
- Serena J. Chee 4 , 5 ,
- Denise Malicki 6 , 7 ,
- Nicole G. Coufal ORCID: orcid.org/0000-0001-6547-1733 7 , 8 ,
- David Gonda 7 , 9 ,
- Michael L. Levy 7 , 9 ,
- Jason A. Greenbaum ORCID: orcid.org/0000-0002-1381-0390 1 ,
- Grégory Seumois ORCID: orcid.org/0000-0002-8164-6852 1 ,
- John Crawford 7 , 10 , 11 , 12 ,
- William D. Roberts 7 , 8 ,
- Stephen P. Schoenberger 1 ,
- Hilde Cheroutre 1 ,
- Christian H. Ottensmeier 1 , 5 , 13 ,
- Pandurangan Vijayanand ORCID: orcid.org/0000-0001-7067-9723 1 , 5 , 14 na2 &
- Anusha-Preethi Ganesan ORCID: orcid.org/0000-0003-3775-9996 1 , 7 , 8 na2
Nature Cancer ( 2024 ) Cite this article
1692 Accesses
15 Altmetric
Metrics details
- Immunosurveillance
- Neuroimmunology
- Paediatric cancer
Brain tumors in children are a devastating disease in a high proportion of patients. Owing to inconsistent results in clinical trials in unstratified patients, the role of immunotherapy remains unclear. We performed an in-depth survey of the single-cell transcriptomes and clonal relationship of intra-tumoral T cells from children with brain tumors. Our results demonstrate that a large fraction of T cells in the tumor tissue are clonally expanded with the potential to recognize tumor antigens. Such clonally expanded T cells display enrichment of transcripts linked to effector function, tissue residency, immune checkpoints and signatures of neoantigen-specific T cells and immunotherapy response. We identify neoantigens in pediatric brain tumors and show that neoantigen-specific T cell gene signatures are linked to better survival outcomes. Notably, among the patients in our cohort, we observe substantial heterogeneity in the degree of clonal expansion and magnitude of T cell response. Our findings suggest that characterization of intra-tumoral T cell responses may enable selection of patients for immunotherapy, an approach that requires prospective validation in clinical trials.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
111,21 € per year
only 9,27 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Phenotypic diversity of T cells in human primary and metastatic brain tumors revealed by multiomic interrogation
Vladimir Wischnewski, Roeltje R. Maas, … Johanna A. Joyce

CD103+ regulatory T cells underlie resistance to radio-immunotherapy and impair CD8+ T cell activation in glioblastoma
Luuk van Hooren, Shanna M. Handgraaf, … Leila Akkari

Large T cell clones expressing immune checkpoints increase during multiple myeloma evolution and predict treatment resistance
Cirino Botta, Cristina Perez, … the iMMunocell study group
Data availability
Processed scRNA-seq and TCR-seq data generated from pediatric brain tumors and NSCLC can be accessed in GEO under accession number GSE221776 . Previously published scRNA-seq data that were reanalyzed here are available under accession codes GSE163108 (ref. 40 ) and GSE123813 (ref. 30 ). Public pediatric brain tumor datasets used for survival analysis, and expression analysis of MHCI, MHCII , KEGG pathway enrichment and CLEC2D can be accessed from the Gabriella Miller Kids First Data Resource Portal ( https://portal.kidsfirstdrc.org/login ) through the CAVATICA ( https://www.cavatica.org ) cloud-based platform, and clinical data can be accessed using PedcBioPortal ( https://pedcbioportal.kidsfirstdrc.org ). Source data for all main and extended data figures are provided as Source Data files. All other data supporting the findings of this study are available from the corresponding author on reasonable request. Source data are provided with this paper.
Code availability
All codes for bioinformatic analysis were deposited in our GitHub repository ( https://github.com/vijaybioinfo/PBT_2023 ).
Pollack, I. F. Brain tumors in children. N. Engl. J. Med. 331 , 1500–1507 (1994).
Article CAS PubMed Google Scholar
Jones, C. & Baker, S.J. Unique genetic and epigenetic mechanisms driving paediatric diffuse high-grade glioma. Nat. Rev. Cancer 14 , 651–661 (2014).
Article CAS Google Scholar
Chevignard, M., Câmara-Costa, H., Doz, F. & Dellatolas, G. Core deficits and quality of survival after childhood medulloblastoma: a review. Neurooncol. Pract. 4 , 82–97 (2017).
PubMed Google Scholar
Makale, M. T., McDonald, C. R., Hattangadi-Gluth, J. A. & Kesari, S. Mechanisms of radiotherapy-associated cognitive disability in patients with brain tumours. Nat. Rev. Neurol. 13 , 52–64 (2017).
Hwang, E. I. et al. The current landscape of immunotherapy for pediatric brain tumors. Nat. Cancer 3 , 11–24 (2022).
Article PubMed Google Scholar
Dunkel, I. J. et al. Nivolumab with or without ipilimumab in pediatric patients with high-grade CNS malignancies: safety, efficacy, biomarker, and pharmacokinetics: checkMate 908. Neuro. Oncol. 25 , 1530–1545 (2023).
Article PubMed PubMed Central Google Scholar
Bouffet, E. et al. Immune checkpoint inhibition for hypermutant glioblastoma multiforme resulting from germline biallelic mismatch repair deficiency. J. Clin. Oncol. 34 , 2206–2211 (2016).
Fried, I. et al. Preliminary results of immune modulating antibody MDV9300 (pidilizumab) treatment in children with diffuse intrinsic pontine glioma. J. Neurooncol . 136 , 189–195 (2018).
Binnewies, M. et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat. Med. 24 , 541–550 (2018).
Article CAS PubMed PubMed Central Google Scholar
Bruni, D., Angell, H. K. & Galon, J. The immune contexture and Immunoscore in cancer prognosis and therapeutic efficacy. Nat. Rev. Cancer 20 , 662–680 (2020).
Tumeh, P. C. et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 515 , 568–571 (2014).
Patel, R. R., Ramkissoon, S. H., Ross, J. & Weintraub, L. Tumor mutational burden and driver mutations: characterizing the genomic landscape of pediatric brain tumors. Pediatr. Blood Cancer 67 , e28338 (2020).
Mok, T. S. K. et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet 393 , 1819–1830 (2019).
Schumacher, T. N. & Schreiber, R. D. Neoantigens in cancer immunotherapy. Science 348 , 69–74 (2015).
Gubin, M. M. et al. Checkpoint blockade cancer immunotherapy targets tumour-specific mutant antigens. Nature 515 , 577–581 (2014).
Robbins, P. F. et al. Mining exomic sequencing data to identify mutated antigens recognized by adoptively transferred tumor-reactive T cells. Nat. Med. 19 , 747–752 (2013).
Tran, E. et al. T-cell transfer therapy targeting mutant KRAS in cancer. N. Engl. J. Med. 375 , 2255–2262 (2016).
Carreno, B. M. et al. Cancer immunotherapy. A dendritic cell vaccine increases the breadth and diversity of melanoma neoantigen-specific T cells. Science 348 , 803–808 (2015).
Ott, P. A. et al. An immunogenic personal neoantigen vaccine for patients with melanoma. Nature 547 , 217–221 (2017).
Lowery, F. J. et al. Molecular signatures of antitumor neoantigen-reactive T cells from metastatic human cancers. Science 375 , 877–884 (2022).
Kvistborg, P. & Yewdell, J. W. Enhancing responses to cancer immunotherapy. Science 359 , 516–517 (2018).
Chiou, S. H. et al. Global analysis of shared T cell specificities in human non-small cell lung cancer enables HLA inference and antigen discovery. Immunity 54 , 586–602.e8 (2021).
Ganesan, A. P. et al. Tissue-resident memory features are linked to the magnitude of cytotoxic T cell responses in human lung cancer. Nat. Immunol. 18 , 940–950 (2017).
Clarke, J. et al. Single-cell transcriptomic analysis of tissue-resident memory T cells in human lung cancer. J. Exp. Med. 216 , 2128–2149 (2019).
Savas, P. et al. Single-cell profiling of breast cancer T cells reveals a tissue-resident memory subset associated with improved prognosis. Nat. Med. 24 , 986–993 (2018).
Han, J. et al. Resident and circulating memory T cells persist for years in melanoma patients with durable responses to immunotherapy. Nat. Cancer 2 , 300–311 (2021).
Liu, B. et al. Temporal single-cell tracing reveals clonal revival and expansion of precursor exhausted T cells during anti-PD-1 therapy in lung cancer. Nature Cancer 3 , 108–121 (2022).
Li, H. et al. Dysfunctional CD8 T cells form a proliferative, dynamically regulated compartment within human melanoma. Cell 176 , 775–789.e18 (2019).
Sade-Feldman, M. et al. Defining T cell states associated with response to checkpoint immunotherapy in melanoma. Cell 175 , 998–1013.e20 (2018).
Yost, K. E. et al. Clonal replacement of tumor-specific T cells following PD-1 blockade. Nat. Med. 25 , 1251–1259 (2019).
Gide, T. N. et al. Distinct immune cell populations define response to anti-PD-1 monotherapy and anti-PD-1/anti-CTLA-4 combined therapy. Cancer Cell 35 , 238–255.e6 (2019).
Kurtulus, S. et al. Checkpoint blockade immunotherapy induces dynamic changes in PD-1 − CD8 + tumor-Infiltrating T cells. Immunity 50 , 181–194.e6 (2019).
Siddiqui, I. et al. Intratumoral Tcf1 + PD-1 + CD8 + T cells with stem-like properties promote tumor control in response to vaccination and checkpoint blockade immunotherapy. Immunity 50 , 195–211.e10 (2019).
Castellino, F. et al. Chemokines enhance immunity by guiding naive CD8 + T cells to sites of CD4 + T cell-dendritic cell interaction. Nature 440 , 890–895 (2006).
Brewitz, A. et al. CD8 + T cells orchestrate pDC-XCR1 + dendritic cell spatial and functional cooperativity to optimize priming. Immunity 46 , 205–219 (2017).
Mackay, L. K. et al. Hobit and Blimp1 instruct a universal transcriptional program of tissue residency in lymphocytes. Science 352 , 459–463 (2016).
Mackay, L. K. et al. The developmental pathway for CD103 + CD8 + tissue-resident memory T cells of skin. Nat. Immunol. 14 , 1294–1301 (2013).
Lim, M. et al. Phase III trial of chemoradiotherapy with temozolomide plus nivolumab or placebo for newly diagnosed glioblastoma with methylated MGMT promoter. Neuro. Oncol . 24 , 1935–1949 (2022).
Omuro, A. et al. Radiotherapy combined with nivolumab or temozolomide for newly diagnosed glioblastoma with unmethylated MGMT promoter: an international randomized phase III trial. Neuro. Oncol. 25 , 123–134 (2022).
Article PubMed Central Google Scholar
Mathewson, N. D. et al. Inhibitory CD161 receptor identified in glioma-infiltrating T cells by single-cell analysis. Cell 184 , 1281–1298.e26 (2021).
Corridoni, D. et al. Single-cell atlas of colonic CD8 + T cells in ulcerative colitis. Nat. Med. 26 , 1480–1490 (2020).
Jonsson, A. H. et al. Granzyme K + CD8 T cells form a core population in inflamed human tissue. Sci. Transl. Med. 14 , eabo0686 (2022).
Xu, T. et al. Single-cell profiling reveals pathogenic role and differentiation trajectory of granzyme K + CD8 + T cells in primary Sjögren’s syndrome. JCI Insight 8 , e167490 (2023).
Trapnell, C. et al. The dynamics and regulators of cell fate decisions are revealed by pseudotemporal ordering of single cells. Nat. Biotechnol. 32 , 381–386 (2014).
Baitsch, L. et al. Exhaustion of tumor-specific CD8 + T cells in metastases from melanoma patients. J. Clin. Invest. 121 , 2350–2360 (2011).
Gros, A. et al. PD-1 identifies the patient-specific CD8 + tumor-reactive repertoire infiltrating human tumors. J. Clin. Invest. 124 , 2246–2259 (2014).
Thommen, D. S. et al. A transcriptionally and functionally distinct PD-1 + CD8 + T cell pool with predictive potential in non-small-cell lung cancer treated with PD-1 blockade. Nat. Med. 24 , 994–1004 (2018).
Chen, R. et al. Antigen presentation machinery signature-derived CALR mediates migration, polarization of macrophages in glioma and predicts immunotherapy response. Front. Immunol. 13 , 833792 (2022).
Sledzinska, A. et al. Regulatory T cells restrain Interleukin-2- and Blimp-1-dependent acquisition of cytotoxic function by CD4 + T cells. Immunity 52 , 151–166.e6 (2020).
Eschweiler, S. et al. Intratumoral follicular regulatory T cells curtail anti-PD-1 treatment efficacy. Nat. Immunol. 22 , 1052–1063 (2021).
Awad, M. M. et al. Personalized neoantigen vaccine NEO-PV-01 with chemotherapy and anti-PD-1 as first-line treatment for non-squamous non-small cell lung cancer. Cancer Cell 40 , 1010–1026.e11 (2022).
Ott, P. A. et al. A phase Ib trial of personalized neoantigen therapy plus Anti-PD-1 in patients with advanced melanoma, non-small cell lung cancer, or bladder cancer. Cell 183 , 347–362.e24 (2020).
Pittet, M. J. et al. High frequencies of naive Melan-A/MART-1-specific CD8 + T cells in a large proportion of human histocompatibility leukocyte antigen (HLA)-A2 individuals. J. Exp. Med. 190 , 705–715 (1999).
Schmidt, N., Flecken, T. & Thimme, R. Tumor-associated antigen specific CD8 + T cells in hepatocellular carcinoma—a promising target for immunotherapy. Oncoimmunology 3 , e954919 (2014).
Moustaki, A. et al. Antigen cross-presentation in young tumor-bearing hosts promotes CD8 + T cell terminal differentiation. Sci. Immunol. 7 , eabf6136 (2022).
Sekine, T. et al. TOX is expressed by exhausted and polyfunctional human effector memory CD8 + T cells. Sci. Immunol. 5 , eaba7918 (2020).
Alfei, F. et al. TOX reinforces the phenotype and longevity of exhausted T cells in chronic viral infection. Nature 571 , 265–269 (2019).
Alspach, E. et al. MHC-II neoantigens shape tumour immunity and response to immunotherapy. Nature 574 , 696–701 (2019).
Gorsi, H. S. et al. Nivolumab in the treatment of recurrent or refractory pediatric brain tumors: a single institutional experience. J. Pediatr. Hematol. Oncol. 41 , e235–e241 (2019).
Mascarenhas, L. et al. Phase 1 clinical trial of durvalumab in children with solid and central nervous system tumors. J. Clin. Oncol. 40 , 10029 (2022).
Article Google Scholar
Meckiff, B. J. et al. Imbalance of regulatory and cytotoxic SARS-CoV-2-reactive CD4 + T cells in COVID-19. Cell 183 , 1340–1353.e16 (2020).
Wolock, S. L., Lopez, R. & Klein, A. M. Scrublet: computational identification of cell doublets in single-cell transcriptomic data. Cell Syst . 8 , 281–291.e89 (2019).
Stuart, T. et al. Comprehensive integration of single-cell data. Cell 177 , 1888–1902.e21 (2019).
Tran, H. T. N. et al. A benchmark of batch-effect correction methods for single-cell RNA sequencing data. Genome Biol. 21 , 12 (2020).
Korsunsky, I. et al. Fast, sensitive and accurate integration of single-cell data with Harmony. Nat. Methods. 16 , 1289–1296 (2019).
Denisenko, E. et al. Systematic assessment of tissue dissociation and storage biases in single-cell and single-nucleus RNA-seq workflows. Genome Biol. 21 , 130 (2020).
van den Brink, S. C. et al. Single-cell sequencing reveals dissociation-induced gene expression in tissue subpopulations. Nat. Methods 14 , 935–936 (2017).
Behr, F. M. et al. Blimp-1 rather than Hobit drives the formation of tissue-resident memory CD8 + T cells in the lungs. Front. Immunol. 10 , 400 (2019).
Hänzelmann, S., Castelo, R. & Guinney, J. GSVA: gene set variation analysis for microarray and RNA-seq data. BMC Bioinf. 14 , 7 (2013).
Conway, J. R., Lex, A. & Gehlenborg, N. UpSetR: an R package for the visualization of intersecting sets and their properties. Bioinformatics 33 , 2938–2940 (2017).
Shugay, M. et al. VDJtools: unifying post-analysis of T cell receptor repertoires. PLoS Comput. Biol. 11 , e1004503 (2015).
Csárdi, G. & Nepusz, T. The igraph software package for complex network research. InterJ. Complex Syst. 1695 , 1–9 (2006).
Google Scholar
McCann, K. et al. Targeting the tumor mutanome for personalized vaccination in a TMB low non-small cell lung cancer. J. Immunother. Cancer 10 , e003821 (2022).
Therneau, T. M. & Grambsch, P. M. in Modeling Survival Data: Extending the Cox Model (eds Therneau T. M. & Grambsch P. M.) 39–77 (Springer, 2000).
Download references
Acknowledgements
We thank J. D. Elster and M. Paul (Department of Pediatrics, University of California San Diego and Rady Children’s Hospital) for supporting patient recruitment, and we thank R. Newbury, K. Shayan, J. Mo, N. Ellington, D. Wang and S. Tucker (Department of Pathology, University of California San Diego and Rady Children’s Hospital) for providing fresh brain tumor tissue for research from the material that is surplus beyond clinical testing needs. We thank H. Simon and M. Mondal for support with sequencing. This work was supported by Hyundai Hope On Wheels, Peacock Foundation and Curebound (Pedal The Cause) for research into pediatric brain tumors; the funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. Support is also acknowledged from the Whitaker Fund (C.H.O.), William K. Bowes Jr Foundation (P.V.) and National Institutes of Health K08 CA230164 (A.P.G.).
Author information
These authors contributed equally: Aditi Upadhye, Kevin E. Meza Landeros.
These authors jointly supervised this work: Pandurangan Vijayanand, Anusha-Preethi Ganesan.
Authors and Affiliations
La Jolla Institute for Immunology, La Jolla, CA, USA
Aditi Upadhye, Kevin E. Meza Landeros, Ciro Ramírez-Suástegui, Benjamin J. Schmiedel, Jason A. Greenbaum, Grégory Seumois, Stephen P. Schoenberger, Hilde Cheroutre, Christian H. Ottensmeier, Pandurangan Vijayanand & Anusha-Preethi Ganesan
Center for Genomic Sciences, National Autonomous University of Mexico, Cuernavaca, Mexico
Kevin E. Meza Landeros
Southampton University Hospitals NHS Trust, Southampton, UK
Department of Respiratory Medicine, Liverpool Heart and Chest Hospital NHS Foundation Trust, Liverpool, UK
Serena J. Chee
Department of Molecular and Clinical Cancer Medicine, Institute of Systems, Molecular and Integrative Biology, University of Liverpool, Liverpool, UK
Serena J. Chee, Christian H. Ottensmeier & Pandurangan Vijayanand
Department of Pathology, University of California San Diego, La Jolla, CA, USA
Denise Malicki
Rady Children’s Hospital, San Diego, CA, USA
Denise Malicki, Nicole G. Coufal, David Gonda, Michael L. Levy, John Crawford, William D. Roberts & Anusha-Preethi Ganesan
Department of Pediatrics, University of California San Diego, La Jolla, CA, USA
Nicole G. Coufal, William D. Roberts & Anusha-Preethi Ganesan
Department of Neurological Surgery, University of California San Diego, La Jolla, CA, USA
David Gonda & Michael L. Levy
Department of Neurosciences, University of California San Diego, La Jolla, CA, USA
John Crawford
Department of Pediatrics, University of California Irvine, Irvine, CA, USA
Children’s Hospital Orange County, Irvine, CA, USA
Clatterbridge Cancer Center NHS Foundation Trust, Liverpool, UK
Christian H. Ottensmeier
Department of Medicine, University of California San Diego, La Jolla, CA, USA
Pandurangan Vijayanand
You can also search for this author in PubMed Google Scholar
Contributions
A.U. performed the experimental work, along with data generation, analysis and interpretation, and manuscript review. K.E.M.L. performed bioinformatic evaluation and data analysis. C.R.S. performed bioinformatic evaluation, data analysis and manuscript review. B.J.S. conducted experimental work related to NSCLC. E.W. and S.J.C. recruited patients with NSCLC and performed sample collection. A.P.G., D.M., N.G.C., D.G. and M.L.L. recruited patients with pediatric brain tumors and performed sample collection. J.A.G. performed mutanome analysis. G.S. supervised the sequencing work. J.C. and W.D.R. were involved with study development, patient recruitment and manuscript review. S.P.S. performed mutanome analysis and paper review. H.C. interpreted the data and reviewed the manuscript. C.H.O. was involved with study development, patient recruitment and manuscript review. P.V. was involved with study design, data generation and review, and manuscript writing and review. A.P.G. was involved with study design, patient recruitment, data generation and review, and manuscript writing and review. P.V. and A.P.G. conceived, supervised and led the work.
Corresponding authors
Correspondence to Pandurangan Vijayanand or Anusha-Preethi Ganesan .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Cancer thanks Vassiliki Boussiotis and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended data fig. 1 clinical parameters do not correlate with t cell clonal expansion..
Correlation of CD4 + (left panel) or CD8 + (right panel) T cell clonal expansion with clinical and pathological characteristics of PBT patients (CD4 + , n = 26; CD8 + , n = 32). Patients with <50 CD8 + or CD4 + T cells with TCR data were excluded. Error bars represent mean ± s.e.m.
Source data
Extended data fig. 2 mutanome analysis of pediatric brain tumors..
a , Schema of mutanome analysis and neoantigen profiling in pediatric brain tumors. b , Number of genomic tumor-specific variants in pediatric brain tumors ( n = 9) (top); table shows top 10 high-confidence tumor-specific variants detected in two index patients (MBL, medulloblastoma; HGG, high-grade glioma) (bottom). c , Kaplan-Meier survival curve based on T cell gene signature in pediatric high-grade glioma from the Pediatric Brain Tumor Atlas (PBTA); n = 36 per signature group; n.s . denotes P = 0.078 by multivariate Cox regression; HR, hazard ratio; CI, confidence interval.
Extended Data Fig. 3 CD8+ T cell subsets within pediatric brain tumors.
a , Violin plots show the per-cell distribution of unique genes, unique molecular identifiers (UMI), and percentage of UMI mapped to mitochondrial genome in 26,332 single CD8 + T cells across clusters in PBT ( n = 38). Box plots extend from the 25 th to 75 th percentile and the center line represents the median. Whiskers are bounded by 25 th percentile - 1.5*interquartile range or 75 th percentile + 1.5*interquartile range. b , UMAP shows Seurat clustering of 26,332 CD8 + T cell transcriptomes in PBT ( n = 38). c , Heatmap shows top 50 differentially-expressed genes using MAST across CD8 + T cell clusters. d , GSEA plot shows enrichment of the indicated gene signatures in the indicated CD8 + T cell clusters. e , Gene set enrichment analysis (GSEA) plot showing enrichment of the ICB response signature 31 in clonally-expanded versus non-expanded T cells from PBT patients (CD8 + , n = 38; CD4 + , n = 35). In d and e , FDR-adjusted P value ( q ) and normalized enrichment score (NES) determined using fgsea package on R. f , Pie charts show TRAV, TRAJ and TRBV gene usage by T cells in MAIT cell clusters (below, key).
Extended Data Fig. 4 Composition and phenotype of tumor-infiltrating CD8+ T cells.
a , Subset composition of tumor-infiltrating CD8 + T cells (stacked to 100%) across PBT patients ( n = 38); numbers above bars represent total number of CD8 + T cells per patient and when <50, numbers are highlighted in red. b , Proportion of CD8 + T cell subsets among total CD8 + T cells in newly diagnosed (n = 34) versus recurrent (n = 4) tumors (above, key); all comparisons are non-significant by nonparametric two-tailed Mann-Whitney test. Error bars represent mean ± s.e.m. c , Analysis of canonical pathways from the Ingenuity Pathway Analysis database (horizontal axis; bars in plot) for which clonally-expanded CD8 + T cells from PBT show enrichment, presented as the frequency of differentially-expressed genes encoding components of each pathway that are upregulated or downregulated (key) in clonally-expanded CD8 + T cells relative to their expression in non-expanded cells (left vertical axis), and adjusted P values (right vertical axis; line; Fisher’s exact test); numbers above bars indicate total genes in each pathway. d , Crater plot displays genes differentially-expressed between clonally-expanded (clone size > 1) versus non-expanded (clone size = 1) CD8 + T cells from PBT ( n = 38) (X axis) or pre-ICB tumors from ICB responders 30 ( n = 6) (Y axis). Top right quadrant displays genes upregulated in clonally-expanded CD8 + T cells that are shared between PBT and tumors from ICB responders. Size of dots represents significance (Benjamini-Hochberg FDR-corrected P -value < 0.05 and log2 fold change > 0.35 or < −0.35 using MAST) and color of dots represents mean expression of displayed genes.
Extended Data Fig. 5 T cell responses in pediatric brain tumors versus adult brain tumors.
a , UMAP (left) and violin (right) displays TCF7 expression across subsets in tumor-infiltrating CD8 + T cells from PBT ( n = 38). Inset (above left) shows proportion of TCF7 -expressing cells per subset. b , UMAP (left) and violin (right) displays KLRB1 expression across subsets in tumor-infiltrating CD8 + T cells from PBT ( n = 38). Inset (above left) shows proportion of KLRB1 -expressing cells per subset. c , Expression of CLEC2D transcripts in adult glioblastoma (GBM, n = 96), pediatric high-grade glioma (pHGG, n = 25) or pediatric low-grade glioma (pLGG, n = 93) from PedcBioPortal datasets. In a-c , box plots extend from the 25 th to 75 th percentile and the center line represents the median. Whiskers represent minimum and maximum values. d , Single-cell trajectory analysis showing relationship between cells in different CD8 + T cell subsets (line) in pediatric brain tumors, constructed using Monocle 3.
Extended Data Fig. 6 Tumor-infiltrating PD-1 + CD8+ T cells display clonal expansion and cytokine production.
a , Proportion of clonally-expanded CD8 + T cells in PDCD1 -non-expressing versus PDCD1 -expressing CD8 + T cells ( n = 32) (top); **** P = 1.6×10 −5 . Proportion of PDCD1 -expressing CD8 + T cells in non-expanded versus clonally-expanded CD8 + T cells in PBT ( n = 32) (bottom); **** P = 1.8×10 −5 . P value determined by nonparametric two-tailed Wilcoxon matched-pairs signed rank test in both analyses. Patients with <50 CD8 + T cells with TCR data were excluded. b , Representative flow-cytometric gating strategy for the assessment of CD103, cytotoxic molecule, and cytokine expression in total CD8 + T cells and in PD-1 neg CD8 + T cells versus PD-1 + CD8 + T cells from PBT (also related to Fig. 4b,c ). c , Proportion (left plot) of cells expressing IL2 in PDCD1 -non-expressing versus PDCD1 -expressing CD8 + T cells in PBT ( n = 38). Flow-cytometric analysis (right) of the expression and proportion of IL-2 + cells in PD-1 neg CD8 + T cells versus PD-1 + CD8 + T cells from PBT patients ( n = 7); n.s . denotes P = 0.16 by non-parametric two-tailed Wilcoxon matched-pairs signed rank test. d , Bar chart shows polyfunctionality based on the production of multiple cytokines in PD-1 neg CD8 + T cells versus PD-1 + CD8 + T cells from PBT ( n = 7). e , GSEA plot shows enrichment of cell cycle gene signature in PDCD1 -expressing versus PDCD1 -non-expressing CD8 + T cells in PBT ( n = 38). P value and NES as in Fig. 2a .
Extended Data Fig. 7 Expression of transcripts encoding HLA molecules and features of LAG3 -expressing CD8+ T cells in pediatric brain tumors.
Expression of ( a ) HLA-A, HLA-B, HLA-C, HLA-DRB1, HLA-DPB1 ,and HLA-DQB1 transcripts and ( b ) antigen processing and presentation signature genes across six diagnoses in the PBTA; error bars represent mean ± s.e.m. CPP, choroid plexus papilloma ( n = 16); CrPh, craniopharyngioma ( n = 36); LGG, low-grade glioma ( n = 302); HGG, high-grade glioma ( n = 148); MBL, medulloblastoma ( n = 119); AE, anaplastic ependymoma ( n = 93). c , Volcano plot shows differentially-expressed genes between LAG3 -non-expressing versus LAG3 -expressing CD8 + T cells from PBT patients with low expression of PDCD1 in CD8 + T cells ( n = 10) (Benjamini-Hochberg FDR-corrected P value < 0.05, log2 fold change > 0.35 or < −0.35 using MAST); dot size and color as in Fig. 6b .
Extended Data Fig. 8 CD4+ T cell subsets within pediatric brain tumors.
a , Violin plots show the per-cell distribution of unique genes, unique molecular identifiers (UMI), and percentage of UMI mapped to mitochondrial genome in 14,994 single CD4 + T cells across clusters in PBT ( n = 35). Box plots extend from the 25 th to 75 th percentile and the center line represents the median. Whiskers are bounded by 25 th percentile - 1.5*interquartile range or 75 th percentile + 1.5*interquartile range. b , UMAP shows Seurat clustering of 14,994 CD4 + T cell transcriptomes in PBT ( n = 35). c , Heatmap shows top 50 differentially-expressed genes using MAST across CD4 + T cell clusters. d , GSEA plot shows enrichment of the indicated gene signatures in the indicated CD4 + T cell clusters. e , GSEA plot shows enrichment of CD4-CTL gene signature in clonally-expanded versus non-expanded non-T REG CD4 + T cells. In d and e , P value and NES determined as in Fig. 2a . f , Proportion of clonally-expanded CD4 + T cells in PDCD1 -non-expressing versus PDCD1 -expressing non-T REG CD4 + T cells ( n = 24); Patients with <50 CD4 + T cells with TCR data or patients with 0 PDCD1 + CD4 + T cells were excluded; ** P = 0.0018 by nonparametric two-tailed Wilcoxon matched-pairs signed rank test. g , Flow-cytometric analysis of IL-2 expression and proportion of IL-2 + cells in PD-1 neg CD4 + T cells versus PD-1 + CD4 + T cells from PBT patients ( n = 10); n.s . denotes P = 0.37 by non-parametric two-tailed Wilcoxon matched-pairs signed rank test.
Supplementary information
Reporting summary, supplementary table 1.
All supplementary tables in one Excel spreadsheet with multiple tabs.
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Source data fig. 3, source data fig. 4, source data fig. 5, source data fig. 6, source data fig. 7, source data fig. 8, source data extended data fig./table 1, source data extended data fig./table 2, source data extended data fig./table 3, source data extended data fig./table 4, source data extended data fig./table 5, source data extended data fig./table 6, source data extended data fig./table 7, source data extended data fig./table 8, rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Upadhye, A., Meza Landeros, K.E., Ramírez-Suástegui, C. et al. Intra-tumoral T cells in pediatric brain tumors display clonal expansion and effector properties. Nat Cancer (2024). https://doi.org/10.1038/s43018-023-00706-9
Download citation
Received : 31 May 2023
Accepted : 11 December 2023
Published : 16 January 2024
DOI : https://doi.org/10.1038/s43018-023-00706-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Cancer newsletter — what matters in cancer research, free to your inbox weekly.
- Study Protocol
- Open access
- Published: 08 April 2024
Rational and design of prophylactic cranial irradiation (PCI) and brain MRI surveillance versus brain MRI surveillance alone in patients with limited-stage small cell lung cancer achieving complete remission (CR) of tumor after chemoradiotherapy: a multicenter prospective randomized study
- Mengyuan Chen 1 ,
- Runhua Li 1 ,
- Yue Kong 1 ,
- Lei Shi 1 ,
- Jing Wang 1 ,
- Yuezhen Wang 1 ,
- Yujin Xu 1 ,
- Yongling Ji 1 &
- Xiao Hu 1
BMC Cancer volume 24 , Article number: 429 ( 2024 ) Cite this article
139 Accesses
Metrics details
Prophylactic cranial irradiation (PCI) is part of standard care in limited-stage small cell lung cancer (SCLC) at present. As evidence from retrospective studies increases, the benefits of PCI for limited-stage SCLC are being challenged.
A multicenter, prospective, randomized controlled study was designed. The key inclusion criteria were: histologically or cytologically confirmed small cell carcinoma, age ≥ 18 years, KPS ≥ 80, limited-stage is defined as tumor confined to one side of the chest including ipsilateral hilar, bilateral mediastinum and supraclavicular lymph nodes, patients have received definitive thoracic radiotherapy (regardless of the dose-fractionation of radiotherapy used) and chemotherapy, evaluated as complete remission (CR) of tumor 4–6 weeks after the completion of chemo-radiotherapy. Eligible patients will be randomly assigned to two arms: (1) PCI and brain MRI surveillance arm, receiving PCI (2.5 Gy qd to a total dose of 25 Gy in two weeks) followed by brain MRI surveillance once every three months for two years; (2) brain MRI surveillance alone arm, undergoing brain MRI surveillance once every three months for two years. The primary objective is to compare the 2-year brain metastasis-free survival (BMFS) rates between the two arms. Secondary objectives include 2-year overall survival (OS) rates, intra-cranial failure patterns, 2-year progression-free survival rates and neurotoxicity. In case of brain metastasis (BM) detect during follow-up, stereotactic radiosurgery (SRS) will be recommended if patients meet the eligibility criteria.
Based on our post-hoc analysis of a prospective study, we hypothesize that in limited-stage SCLC patients with CR after definitive chemoradiotherapy, and ruling out of BM by MRI, it would be feasible to use brain MRI surveillance and omit PCI in these patients. If BM is detected during follow-up, treatment with SRS or whole brain radiotherapy does not appear to have a detrimental effect on OS. Additionally, this approach may reduce potential neurotoxicity associated with PCI.
Peer Review reports
Small cell lung cancer (SCLC) accounts for approximately 15-20% of all cases of bronchopulmonary carcinoma. It is characterized by high malignancy, a tendency to early metastasis. At the time of diagnosis, about one-third of cases are of limited-stage [ 1 ]. The standard treatment is chemoradiotherapy for the majority of limited-stage SCLC patients [ 2 ].
A meta-analysis showed that prophylactic cranial irradiation (PCI) significantly reduce the incidence of BM by 25.3% compared to the control group (33.3% vs. 58.6%, P < 0.001), in patients who achieved complete remission (CR) after chemoradiotherapy, and it also improved the 3-year overall survival (OS) rate by 5.4% (20.7% vs. 15.3%, P = 0.01) [ 3 ]. Based on this study, PCI has been recommended for patients with limited-stage SCLC who have achieved a good response to chemoradiotherapy [ 2 , 4 ].
However, the meta-analysis [ 3 ] has several limitations. The most important one is that no routine brain MRI was performed before PCI. A study conducted in the era of MRI demonstrated that 25% of newly diagnosed SCLC patients had brain metastasis (BM), and the cumulative incidence of BM after initial treatment could exceed 50% [ 5 ]. Our retrospective study showed that among all limited-stage SCLC patients who did not receive PCI and developed BM, 30.2% of them were detected before planned PCI with brain MRI [ 6 ]. Therefore, it can be speculated that some of the patients included in this meta-analysis actually received “treatment” rather than “prophylaxis”.
We have completed a prospective randomized study on the target volume of thoracic radiotherapy in limited-stage SCLC [ 7 ]. Our post-hoc analysis showed that, among 300 patients who received definitive chemoradiotherapy in this study, 134 (44.7%) achieved CR, 105 patients received PCI. All patients underwent baseline brain MRI, and 85.6% of them received brain MRI before PCI. The median follow-up time for the entire group was 22.3 months. Although PCI significantly reduced the incidence of BM (16.2% vs. 37.9%, P = 0.02), the median survival time for the PCI and the non-PCI arm were 30.2 months and 30.5 months, respectively, with 3-year OS rates of 39.9% and 43.0% ( P = 0.93). PCI did not significantly improve the OS of patients who achieved CR after chemoradiotherapy. Among the 300 patients, 143 (47.7%) patients achieved partial remission (PR), of whom, 90 patients received PCI. Before PCI, 90.9% of patients received brain MRI. The median survival time for the PCI and the non-PCI arm were 27.4 months and 18.6 months, respectively, with 3-year OS rates of 42.6% and 17.4% ( P <0.0001). PCI significantly improved the OS of patients who achieved PR after chemoradiotherapy (unpublished data).
Therefore, in the era of routine brain MRI surveillance, the role of PCI in limited-stage SCLC warrants further study. Based on above preliminary results, we speculate that PCI could be spared in patients who achieve CR after definitive chemoradiotherapy and instead, receive brain MRI surveillance. Even if BM is detected during follow-up, subsequent salvage treatment with SRS or whole-brain radiotherapy (WBRT) would not have a detrimental effect on OS.
Study design and objective
This is a prospective, randomized controlled study that includes patients with limited-stage SCLC who achieve CR after definitive chemoradiotherapy. Eligible patients will be randomly assigned to two arms:
Control arm: Patients receive PCI and regular brain MRI surveillance.
Study arm: Patients receive regular brain MRI surveillance alone.
If BM is detected during follow-up, SRS is recommended when appropriate.
The primary endpoint is to compare the 2-year brain metastasis -free survival (BMFS) rates between the two arms. Secondary endpoints include 2-year OS, intra-cranial failure patterns, 2-year progression-free survival (PFS), cognitive functions(Hopkins Verbal Learning Test will be used to assess cognitive function).
Key eligibility criteria
Inclusion criteria:
Histologically or cytologically confirmed small cell carcinoma.
Age ≥ 18 years.
Karnofsky Performance Status (KPS) ≥ 80.
Limited-stage disease, defined as tumor confined to one side of the chest including ipsilateral lung, bilateral mediastinal lymph nodes, and bilateral supraclavicular lymph nodes (metastatic lymph nodes defined as short-axis diameter ≥ 1 cm or showing increased metabolic activity on PET-CT, or confirmed by mediastinoscopy / EBUS / TBNA biopsy). Pleural effusion thickness on chest CT is less than 1 cm (unless cytologically confirmed as malignant pleural effusion). Staging is determined according to the 8th edition of the AJCC staging system (2017), specifically stages I-IIIC without intrapulmonary metastasis.
Have received curative-intent thoracic radiotherapy and chemotherapy.
Assessment of treatment response within 4–6 weeks after completion of curative-intent thoracic chemoradiotherapy shows CR (evaluation includes contrast-enhanced chest and abdominal CT, contrast-enhanced brain MRI, whole-body bone scan, and lung cancer biomarkers such as NSE and ProGRP).
Willingness and ability to comply with the follow-up schedule.
Full understanding of the study and voluntary signing of an informed consent form.
Exclusion criteria:
History of malignant tumors in other parts of the body (previous or concurrent), excluding non-malignant melanoma, papillary carcinoma of the thyroid and cervical carcinoma in situ.
Patients who have undergone curative surgery (excluding biopsy).
Patients with a history of mental illness, in pregnancy or lactation.
Uncontrolled diabetes, hypertension, or severe active infections.
Manifested chronic central nervous system disorders.
Contraindications for brain MRI examination.
Other situations deemed unsuitable for enrollment by doctors in charge.
Pre-treatment evaluation
Baseline staging include enhanced MRI of the brain, enhanced CT of the chest and upper abdomen, ultrasonography of the supraclavicular lymph nodes and bone scan. PET-CT is recommended, bone scan could be omitted if PET-CT is available. Laboratory tests include routine blood tests, routine liver and kidney function tests, lung cancer biomarker tests, electrocardiogram, echocardiography and pulmonary function test.
Statistical analysis & sample size considerations
The study is designed as a prospective, randomized controlled non-inferiority trial. Based on previous study results, we hypothesize that the 2-year BMFS rate in the control group is 83%, and the 2-year BMFS in the study group is 68%, which is deemed acceptable as non-inferior. With a power of 80% and a one-sided significance level of 0.025, considering a shedding rate of 10%, 110 patients will be required in each group.
Radiotherapy
Positioning and ct/mri simulation.
All patients will be placed in supine position with thermoplastic mask for whole-brain immobilization. Contrast-enhanced CT simulations are recommended. The slice thickness of the scan should be ≤ 5 mm, and the scanning range should extend from 2 cm above the skull to the lower margin of the 7th cervical vertebra, including the entire cranial and neck. When PCI with hippocampal avoidance is required, a MRI simulation of the brain is strongly recommended and the thickness of the brain MRI scanning should be 1 mm.
Definition of radiation target volume
The entire brain is contoured as the clinical target volume (CTV), and the CTV is expanded by 0.3 cm to create the planning target volume (PTV) which is named PTV-Brain. The PTV of hippocampal avoidance PCI is named PTV-HA. PTV-HA is PTV-Brain minus hippocampi. Critical organs at risk (OAR) include the bilateral lenses and eyeballs. For patients who are eligible for brain MRI simulation, bilateral hippocampi should be contoured.
Radiation dose and planning evaluation
The prescribed dose for PTV is 2.5 Gy per fraction, once daily, 5 days a week for two weeks. The minimum requirement for the radiation technique is three-dimensional conformal radiotherapy. If PCI with hippocampal avoidance is required, the minimum requirement for irradiation method is stated to be IMRT. Helical tomotherapy is recommended if available.After completing the radiation treatment planning, the dose distribution in the target volume and the dose to OAR are evaluated. The dose-volume histogram (DVH) is used as a fundamental tool, and the dose distribution in the PTV and OAR is assessed based on the distribution of dose curves in three-dimensional space. The prescribed dose is determined based on the dose received by 95% of the PTV, with dose uniformity ranging from 94 to 106%. The dose constraints for OAR are as follows: lenses: Dmax < 9 Gy, Dmean < 5 Gy; hippocampi: Dmax < 16 Gy, Dmean < 9 Gy.
Toxicity evaluation
Treatment related toxicities will be evaluated in accordance with Common Terminology Criteria for Adverse Events (CTCAE) 5.0 criteria. (1) Complete blood counts and physical examinations will be performed at least once a week during radiation therapy. (2) Adverse events related to the nervous system will be documented at least once a week during radiation therapy and during follow-up. Hopkins Verbal Learning Test will be used to assess cognitive function.
Tumor response evaluation criteria and definition of survival time
Tumor response will be evaluated according to Response Evaluation Criteria in Solid Tumors (RECIST) 1.1 criteria.
Brain metastasis-free survival (BMFS) is defined as the time from the start of treatment to BM or death from any cause. Progression-free survival (PFS) is defined as the time from the start of treatment to disease progression or death from any cause. Overall survival (OS) is defined as the time from the start of treatment to death from any cause.
All enrolled patients will be followed up starting from the start of PCI and continuing for 2 years or until death. Follow-up will be conducted once every three months. At each follow-up, patients routinely received examination of brain enhanced MRI, chest and abdomen enhanced CT, and lung tumor markers. After two years, the frequency of follow-up is left to the discretion of the doctor in charge.
Radiotherapy for brain metastasis
For patients with ≤ 5 intracranial metastases and a maximum diameter of ≤ 3 cm for a single metastasis, SRS or Cyber Knife radiotherapy will be recommended. Otherwise, WBRT will be administered, especially for patients who have not yet received PCI. For patients who have received PCI and developed BM, SRS or Cyber Knife will be recommended.
SCLC tends to develop early distant metastasis. Brain is a common site of metastasis in SCLC patients, with approximately 25% of patients present with brain metastases at the time of initial diagnosis [ 5 ]. Due to the presence of the blood-brain barrier, conventional chemotherapy drugs have limited efficacy in penetrating brain tissue, making it a potential “sanctuary” for small brain metastatic lesions. Therefore, PCI does not truly “prevent” the development of BM, it plays a role of eliminating potentially but undetectable small metastasis in brain.
With the advances in comprehensive treatment, the prognosis of limited-stage SCLC patients has improved, the probability of BM has also increased correspondingly. Among patients who achieved CR after treatment, the incidence of BM within 2 years was 67%, with the brain being the first site of metastasis in 45% of cases [ 8 ].
A meta-analysis demonstrated that in patients who achieved a complete response (CR) after chemoradiotherapy, PCI could significantly reduce the incidence of BM by 25.3% ( P < 0.001) compared to the control group. Additionally, it was associated with a 5.4% improvement in 3-year overall survival rate ( P = 0.01) [ 3 ].
However, due to the limitations of the meta-analysis, and with the availability of MRI for regular surveillance of BM, the role of PCI in improving OS in SCLC patients is being challenged.
A prospective randomized study conducted by EORTC demonstrated that extensive-stage SCLC patients who received PCI had significantly better outcomes compared to the observation group (1-year incidence of symptomatic BM: 14.6% vs. 40.4%; median survival time: 6.7 months vs. 5.4 months; 1-year overall survival rate: 27.1% vs. 13.3%) [ 9 ]. However, one of the major limitations of this study was the absence of pre-PCI brain MRI. In contrast, a phase III randomized study showed that in extensive-stage SCLC patients who have ruled out BM with MRI, PCI did not have a positive impact on OS, compared to the observation group [ 10 ].
Traditionally, WBRT is recommended for SCLC patients with BM. A recent large cohort study [ 11 ] compared the outcomes of SCLC patients with BM who received SRS or WBRT. The results showed that those treated with SRS had a median survival time of 8.5 months and a time to central nervous system progression (TTCP) of 8.1 months, while patients with a solitary BM treated with SRS had a median survival time of 11.0 months, and those treated with WBRT had a median survival time of 5.2 months. Although WBRT improved TTCP, it did not improve OS. Furthermore, after adjusting for prognostic factors, the OS results favored SRS.
Another study showed that in limited-stage SCLC patients who underwent MRI surveillance after definitive chemoradiotherapy, the occurrence of BM and survival rates did not significantly differ between patients who received SRS for detected BM and those who received PCI [ 12 ]. The survival benefit was attributed at least partially to SRS, reducing the contribution of PCI to survival. Although PCI is still recommended based on previous studies, these benefits may be diminished if MRI and SRS are available for diagnosis and treatment.
These findings challenge the traditional approach of using WBRT or PCI for all SCLC patients with BM and suggest that SRS guided by MRI surveillance could be a viable alternative in selected cases. However, it is important to consider individual patient factors, tumor characteristics, and treatment goals when determining the most appropriate management strategy.
Pezzi et al. [ 13 ] reported that in patients with limited-stage SCLC who had BM excluded by MRI were matched using a propensity score, although the 3-year incidence of BM was higher in the non-PCI group than in the PCI group, the difference was not statistically significant (20.4% vs. 11.2%, P = 0.10). Also, whether PCI was performed or not did not affect the overall survival (HR: 0.84, 95% CI: 0.604–1.180, P = 0.32).
Similarly, Qi et al. [ 14 ] conducted a retrospective matched analysis of 150 patients with limited-stage SCLC. The results showed a significantly lower 3-year cumulative incidence of BM in the PCI group compared to the non-PCI group (14.7% vs. 22.7%, P = 0.007), but there was no significant difference in median survival time between the two groups (35 months vs. 28 months, P = 0.128).
Of note, PCI potentially leads to acute and late neuro-toxicities. A pooled analysis of the RTOG 0212 and 0214 showed that patients who received PCI had reduced cognitive function as measured by the Hopkins Verbal Learning Test at the 6-month and 12-month follow-up, compared to baseline ( P = 0.002). Patient-reported cognitive decline was even three times higher ( P < 0.0001) [ 15 ]. A survey indicated that 38% of limited-stage SCLC patients who did not receive PCI had concerns about the side effects [ 16 ].
At present, there is no prospective randomized controlled study on PCI versus regular MRI follow-up after definitive radio-chemotherapy for limited-stage SCLC available. However, several similar studies are underway. SWOG S1827 [ 17 ] is a phase III prospective randomized controlled study that aims to enroll patients with limited-stage SCLC who have received radical therapy and patients with extensive-stage SCLC who have responded to systemic therapy. The study will randomize patients into two groups: one group will receive PCI plus regular brain MRI follow-up, while the other group will receive only regular brain MRI follow-up. The primary objective of the study is to compare the two-year survival rates between the two groups. The PRIMA Lung Study [ 18 ] is conducted by EORTC, has similar study design, aims to investigate whether brain MRI surveillance alone is non-inferior in terms of OS compare to PCI followed by brain MRI surveillance in both limited and extensive-stage SCLC patients. Another Chinese study [ 19 ] recruits and randomize limited-stage SCLC patients who achieve remission after first-line chemoradiotherapy to PCI or MRI surveillance. The primary end point is OS at two years.
In conclusion, with the widespread use of brain MRI, the favorable prognosis of SRS for treating SCLC BM, and the insights gained from the Japanese prospective study on PCI in extensive-stage SCLC, as well as the emphasis on the quality of life of long-term survivors, it is worthwhile to conduct a prospective randomized study comparing active brain MRI surveillance alone with PCI after chemoradiotherapy for limited-stage SCLC. The results of this study are highly likely to change current clinical practices.
Data availability
Not applicable.
Govindan R, Page N, Morgensztern D, William R, Ryan T, Anna V, et al. Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol. 2006;24(28):4539–44.
Article PubMed Google Scholar
https:// www.nccn.org/professionals/physician_gls/pdf/sclc.pdf .
Aupérin A, Arriagada R, Pignon JP, Le PC, Gregor A, Stephenset RJ. Prophylactic cranial irradiation for patients with small cell lung cancer in complete remission. N Engl J Med. 1999;341:476–84.
Clinical practice guideline for. Radiation therapy in small cell lung cancer (2020 version) Chinese Journal of Radiation Oncology|. Chin J Radiat Oncol. 2020;29(8):608–14.
Google Scholar
Seute T, Leffers P, ten Velde GP, Twijnstra A. Detection of brain metastases from small cell lung cancer: consequences of changing imaging techniques (CT versus MRI). Cancer. 2008;112(8):1827–34.
Wu Q, Chen M, Peng F, et al. A study of the prognosis of patients with limited-stage small cell lung cancer who did or did not receive prophylactic cranial irradiation after effective chemoradiotherapy. Front Oncol. 2023;13:1118371.
Article PubMed PubMed Central Google Scholar
Hu X, Bao Y, Xu YJ, Zhu H, Chen M, et al. Final report of a prospective randomized study on thoracic radiotherapy target volume for limited-stage small cell lung cancer with radiation dosimetric analyses. Cancer. 2020;126(4):840–9.
Article CAS PubMed Google Scholar
Arriagada R, Le Chevalier T, Borie F, Santos-Miranda JA, Bardec E, Laplanche A, et al. Prophylactic cranial irradiation for patients with small–cell lung cancer in complete remission. J Natl Cancer Inst. 1995;87(3):183–90.
Slotman B, Faivre-Finn C, Kramer G, Rankin E, Snee M, Hatton M, et al. Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med. 2007;357(7):664–72.
Takahashi T, Yamanaka T, Seto T, Nokihara H, Saka H, Nishio M, Kaneda H, et al. Prophylactic cranial irradiation versus observation in patients with extensive-disease small-cell lung cancer: a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2017;18(5):663–71.
Rusthoven CG, Yamamoto M, Bernhardt D, Smith DE, Robin TP. Evaluation of first-line radiosurgery vs whole-brain radiotherapy for small cell lung cancer brain metastases: the FIRE-SCLC Cohort Study. JAMA Oncol. 2020;6(7):1028–37.
Ozawa Y, Omae M, Fujii M, Takashi M, Masato K, Shinyaet S, et al. Management of brain metastasis with magnetic resonance imaging and stereotactic irradiation attenuated benefits of prophylactic cranial irradiation in patients with limited-stage small cell lung cancer. BMC Cancer. 2015;15:15:589.
Pezzi TA, Fang P, Gjyshi O, Feng L, Liu S, Komaki R, et al. Rates of overall survival and Intracranial Control in the magnetic resonance imaging era for patients with Limited-Stage Small Cell Lung Cancer with and without prophylactic cranial irradiation. JAMA Netw Open. 2020;3(4):e201929.
Qi C, Li W, Li H, Patel A, Beriwal S, et al. Benefits of prophylactic cranial irradiation in the MRI era for patients with Limited Stage Small Cell Lung Cancer. Front Oncol. 2022;12:833478.
Gondi V, Paulus R, Bruner DW, Christina A, Elizabeth M, Aaron W, et al. Decline in tested and self-reported cognitive functioning after prophylactic cranial irradiation for lung cancer: pooled secondary analysis of Radiation Therapy Oncology Group randomized trials 0212 and 0214. Int J Radiat Oncol Biol Phys. 2013;86(4):656–64.
Lok BH, Ma J, Foster A, Perez A, Abraham J. Factors influencing the utilization of prophylactic cranial irradiation in patients with limited-stage small cell lung cancer. Adv Radiat Oncol. 2017;2(4):548–54.
SWOG S1827 (MAVERICK). Testing whether the use of brain scans alone instead of brain scans plus preventive brain radiation affects lifespan in patients with small cell lung cancer. https://clinicaltrials.gov/ct2/show/NCT04155034 .
PRophylactic Cerebral Irradiation or Active MAgnetic. Resonance imaging surveillance in small-cell lung Cancer patients (PRIMALung Study). https://clinicaltrials.gov/study/NCT04790253?cond=NCT04790253&rank=1
Efficacy and Safety of Prophylactic Cranial Irradiation Versus MRI Surveillance in Patients. With limited-stage small cell Lung Cancer who Achieved Remission after First-line Chemoradiotherapy: a Multicenter Randomized Controlled Phase III Clinical Trial. https://clinicaltrials.gov/study/NCT04829708?cond=NCT04829708&rank=1
Download references
Acknowledgements
All authors have read and approved the manuscript.
This work was funded by the National Natural Science Foundation of China (grant numbers 81402540), Zhejiang Science and Technology Plan on Medicine and Health (grant number 2019KY046, 2022KY618 and 2023KY610), Science and Technology Project of Wenling City (2019S0180018) and Zhejiang Cancer Hospital Special Program of Investigator-Initiated Clinical Trial (IIT2022ZA005).
Author information
Authors and affiliations.
Zhejiang Cancer Hospital, Hangzhou Institute of Medicine (HIM), Chinese Academy of Sciences, Hangzhou, Zhejiang, 310022, China
Mengyuan Chen, Runhua Li, Yue Kong, Lei Shi, Jing Wang, Yuezhen Wang, Yujin Xu, Yongling Ji & Xiao Hu
You can also search for this author in PubMed Google Scholar
Contributions
Mengyuan Chen wrote the main manuscript text, Runhua Li counted the sample size, Lei Shi, Yuezhen Wang and Jin Wang Yue Kong participated in the design of the research scheme,and Xiao Hu, Yongling Ji and Yujin Xu examined and revised the manuscript, other authors participated in reviewing and revising the language.
Corresponding author
Correspondence to Xiao Hu .
Ethics declarations
Ethics approval and consent to participate.
All experimental protocols were approved by the Medical Ethics Committee of Zhejiang Cancer Hospital(The Ethics is IRB-2022-758, the work will be obtained from all subjects and/or their legal guardian(s). The corresponding author has read the journal policies and submit this manuscript in accordance with those policies, we confirmed that informed consent will be obtained from all subjects and/or their legal guardian(s).
Consent to publication
Conflict of interest.
The authors have no competing interests as defined by BMC, or other interests that might be perceived to influence the results and/or discussion reported in this paper. The manuscript had not been published elsewhere, nor are they under consideration by another publisher.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chen, M., Li, R., Kong, Y. et al. Rational and design of prophylactic cranial irradiation (PCI) and brain MRI surveillance versus brain MRI surveillance alone in patients with limited-stage small cell lung cancer achieving complete remission (CR) of tumor after chemoradiotherapy: a multicenter prospective randomized study. BMC Cancer 24 , 429 (2024). https://doi.org/10.1186/s12885-024-12123-x
Download citation
Received : 06 September 2023
Accepted : 14 March 2024
Published : 08 April 2024
DOI : https://doi.org/10.1186/s12885-024-12123-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Small cell lung cancer
- Limited-stage
- Prophylactic cranial irradiation
- MRI surveillance
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Abstract. This paper presents an atypical case of a patient with brain tumor of the glioblastoma multiforme (GBM) type who achieved a 5-year survival. Some general information is provided including epidemiology, diagnostic and treatment procedures (surgery and radio-chemo-therapy), and prognosis of survival related to GBM.
A Blackout, A Brain Tumor, and Brain Surgery. Fortunately for Stephanie her tumor was low grade, with a much better prognosis than many other types of gliomas. "When treating brain tumors, we often deal with glioblastoma, which is a more serious matter," says Dr. Ramakrishna.
Abstract. Background: An uncommon but well-established complication of cranial irradiation is secondary neoplasm. This case presentation documents a radiation-induced malignant glioma 55 years after being diagnosed with "cerebral sarcoma," now defined as atypical meningioma. This not only represents the longest reported latency period for a patient initially receiving over 30 Gy, but also ...
J.O. Blakeley and K. ShannonN Engl J Med 2023;389:179-181. Papillary craniopharyngiomas are ultra-rare tumors of the central nervous system (CNS), with fewer than 600 new cases per year in the ...
1 Kenneth R. Peak Brain and Pituitary Tumor Treatment Center, Department of Neurosurgery, ... Imaging studies documented a large tumor in the left frontal lobe extending across the midline into the right frontal lobe, with diffuse and extensive infiltration through the corpus callosum. ... Because this is a single patient case report, we could ...
Discussion. Glioblastoma multiforme (GBM) tumors are aggressive and fast-growing stage IV brain tumors. Glioblastoma multiforme is a subtype of gliomas, which are tumors affecting the glial cells ...
Nature Reviews Cancer 20 , 1 ( 2020) Cite this article. This Focus issue highlights current research into the unique biology of brain tumours and brain metastasis and how this research might ...
In May, the brain tumor community joins together to raise awareness about brain tumors through education. By sharing the rarity and uniqueness of brain and other CNS tumors—1.3 percent of all new cancers cases and over 130 different types—we can inspire research and clinical studies to improve diagnosis and standardize care.
Case Presentation: Ganglioglioma Brain Tumor. Alan Cohen, director of Johns Hopkins pediatric neurosurgery, shares the case of a 12-year-old boy who had a generalized seizure that led him to the emergency room. An MRI showed a tumor in the left parietal lobe of the brain. Using frameless stereotactic guidance and intraoperative MRI, Cohen and ...
The purpose of this study is to demonstrate improved planning for meningioma and similar brain tumor surgery. A Study of Genetic Testing in the Care of Glioma ... The purpose of this multicenter prospective observational case-control study is to train and validate Adela's cfMeDIP-seq based methylome profiling platform to detect and ...
Abstract. Effective treatments that extend survival of malignant brain tumor glioblastoma (GBM) have not changed in more than a decade; however, there exists a minority patient group (<5%) whose survival is longer than 3 yr. We herein present a case report of a long-term surviving 51-yr-old female diagnosed with a MGMT unmethylated GBM.
In a randomized, phase III trial conducted by the Nordic Clinical Brain Tumor Study Group, patients age 60 or older with glioblastoma were randomized to the typical 6 weeks of RT, 2 weeks of hypofractionated RT, or TMZ without RT. 91 The trial demonstrated that both the hypofractionated RT and TMZ monotherapy were superior to 6 weeks of RT with ...
Many of these are offered in collaboration with the NCI-funded Adult Brain Tumor Consortium (ABTC), a group of 15 elite "Brain Tumor Centers of Excellence" which collaborate to offer the most innovative treatments to patients with brain tumors. ... Phase I/II study of the poly (ADP-ribose) polymerase-1(PARP-1) inhibitor BSI-201 in patients ...
Stereotactic radiosurgery for patients with multiple brain metastases: A case-matched study comparing treatment results for patients with 2-9 versus 10 or more tumors. J Neurosurg. 2014; 121: 16-25. Crossref; ... guidelines are intended to serve as an accessible and comprehensive guide to brain SRS for patients with metastatic brain tumors ...
The signs and symptoms of a brain tumor depend on the brain tumor's size and location. Symptoms also might depend on how fast the brain tumor is growing, which is also called the tumor grade. General signs and symptoms caused by brain tumors may include: Headache or pressure in the head that is worse in the morning.
This case study will show how deep learning techniques work in medical image analysis and how they may be used to improve patient outcomes in the detection and treatment of brain tumors. CNN-based models are improving in accuracy and dependability due to their expanding popularity and deep learning developments, which open the door for new ...
A case involving a patient diagnosed with a brain tumor late in her pregnancy highlights strategies for managing such challenging situations. Presentation. A 34-year-old patient, 27 weeks into her first pregnancy, was admitted to the obstetric unit of Hillcrest Hospital, a Cleveland Clinic hospital, for observation. She reported experiencing ...
A British man who rejected the standard of care to treat his brain cancer has lived with the typically fatal glioblastoma tumor growing very slowly after adopting a ketogenic diet, providing a case study that researchers say reflects the benefits of using the body's own metabolism to fight this particularly aggressive cancer instead of chemo and radiation therapy.
a, Study overview.ETMR, embryonal tumor with multilayered rosettes. b, TCR clone size distribution among tumor-infiltrating CD4 + and CD8 + T cells across pediatric patients with brain tumors (PBT ...
Presented new case studies demonstrating clinical responses in two patients with B cell malignancies, chronic lymphocytic leukemia (CLL) and primary central nervous system lymphoma (PCNSL), each ...
Prophylactic cranial irradiation (PCI) is part of standard care in limited-stage small cell lung cancer (SCLC) at present. As evidence from retrospective studies increases, the benefits of PCI for limited-stage SCLC are being challenged. A multicenter, prospective, randomized controlled study was designed. The key inclusion criteria were: histologically or cytologically confirmed small cell ...
Medulloblastoma and pilocytic astrocytoma are the two most common pediatric brain tumors with overlapping imaging features. In this proof-of-concept study, we investigated using a deep learning classifier trained on a multicenter data set to differentiate these tumor types. We developed a patch-based 3D-DenseNet classifier, utilizing automated tumor segmentation. Given the heterogeneity of ...