- Search Menu
- Advance articles
- Author Guidelines
- Submission Site
- About Social Work
- About the National Association of Social Workers
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Mental Health Collection
Millions of Americans are affected by mental illnesses, and social workers are one of the largest providers of mental health and substance use services. The editors of the National Association of Social Workers publications have curated a special collection of mental health and social work-related articles from the four NASW journals. The articles are freely available for a limited time.
Social Work

Client Attitudes toward Integrating Religion and Spirituality in Mental Health Treatment: Scale Development and Client Responses Holly K. Oxhandler, James W. Ellor, and Matthew S. Stanford Volume 63, Issue 4, October 2018, Pages 337–346
The Power of Prevention and Youth Voice: A Strategy for Social Work to Ensure Youths’ Healthy Development Linda Sprague Martinez, Katie Richards-Schuster, et al. Volume 63, Issue 2, April 2018, Pages 135–143
Behavioral Mental Health: An Emerging Field of Service or an Oxymoron? Christopher G. Hudson Volume 63, Issue 1, January 2018, Pages 27–36
Trauma-Informed Social Work Practice Jill Levenson Volume 62, Issue 2, April 2017, Pages 105–113
Social Work Research

Multiple Disadvantage and Discrimination: Implications for Adolescent Health and Education Dana M. Prince, Anita Rocha, and Paula S. Nurius Volume 42, Issue 3, September 2018, Pages 169–179
Outcome Literature Review of Integrative Body–Mind–Spirit Practices for Mental Health Conditions Mo Yee Lee, Xiafei Wang, Chang Liu, et al. Volume 42, Issue 3, September 2018, Pages 251–266
An Analysis of Readmissions to a Mental Health Court David C. Kondrat, Donald M. Linhorst, P. Ann Dirks-Linhorst, et al. Volume 42, Issue 3, September 2018, Pages 237–250
Within-Group Effect Size Benchmarks for Cognitive–Behavioral Therapy in the Treatment of Adult Depression Allen Rubin and Miao Yu Volume 41, Issue 3, September 2017, Pages 135–144
Health & Social Work

Safety Fears Held by Caregivers about Relatives with Psychiatric Disorders Travis Labrum and Phyllis Solomon Volume 43, Issue 3, August 2018, Pages 165–174
The Mediating Role of Posttraumatic Stress Disorder with Tendency to Forgive, Social Support, and Psychosocial Functioning of Terror Survivors Michael Weinberg Volume 43, Issue 3, August 2018, Pages 147–154
Suicidal Ideation and Suicide Attempts among Women Seeking Treatment for Substance Use and Trauma Symptoms Stella M. Resko, Sarah Kruman Mountain, Suzanne Browne, et al. Volume 43, Issue 2, 1 May 2018, Pages 76–83
Providing Mental Health Care for the Complex Older Veteran: Implications for Social Work Practice Gayle Clark, Susan Rouse, Heather Spangler, et al. Volume 43, Issue 1, February 2018, Pages 7–14
Children & Schools

Teachers’ Perceptions of Student Mental Health: The Role of School-Based Mental Health Services Delivery Model Osayande Osagiede, Sheina Costa, Aaron Spaulding, et al. Volume 40, Issue 4, October 2018, Pages 240–248
School Shootings and the Need for More School-Based Mental Health Services Martell L. Teasley Volume 40, Issue 3, July 2018, Pages 131–134
Hope Squads: Peer-to-Peer Suicide Prevention in Schools Jennifer Wright-Berryman, Greg Hudnall, Rodney Hopkins, et al. Volume 40, Issue 2, April 2018, Pages 125–126
Efficient Wraparound Service Model for Students with Emotional and Behavioral Disorders: A Collaborative Model for School Social Workers and Teachers William C. Hunter, Susan Elizabeth Elswick, and Laura Baylot Casey Volume 40, Issue 1, January 2018, Pages 59–61
- Recommend to your Library
Affiliations

- Online ISSN 1545-6846
- Print ISSN 0037-8046
- Copyright © 2024 National Association of Social Workers
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- University Home
- Library Home
- SOPHIA Home
- < Previous
Home > MSW > MSW_PAPERS > 570
Master of Social Work Clinical Research Papers
Mental health social workers: the state of their well-being and support.
Laura Conway , St. Catherine University Follow
Date of Paper
Type of paper.
Clinical research paper
Degree Name
Master of Social Work (M.S.W.)
Social Work
First Advisor
Laurel Bidwell
Department/School
The mental health social worker experiences unique challenges on a daily basis. A social worker’s well-being affects not only the social worker at the individual level; but also directly affects agency and client outcomes, which in turn impacts the mental health system. Adequate support is crucial in maintaining social workers’ positive well-being (Graham & Shier, 2014).
Current rates of burnout among mental health professionals range from 21-61% (Morse, Salyers, Rollins, Monroe- DeVita & Pfahler, 2012). This suggests that there are gaps in adequate support for mental health social workers. A blend of systems theory, the strengths perspective and an empowerment model was used as the foundation from which to explore the individual, agency and community impacts of social worker well-being and adequate support.
Semi-structured qualitative interviews were used to explore the following questions: 1. What is the impact of working within the mental health field on social worker well-being?, 2. What types of supports do mental health social workers find to be the most helpful? and 3. What gaps do mental health social workers feel exist in level and type of support that they receive in their work? Seven interviews were conducted. A grounded theory approach was used to analyze the data to identify major emerging themes.
The findings suggest society’s dominant cultural values and attitudes stigmatize mental health care, which results in an inadequate mental health system. The stress associated with working within an ineffective system, as well as, lacking effective responses to self-care leads to both physical and mental impacts on personal well-being. Although mental health social workers have developed effective coping skills to positively maintain their well being, participants suggested the adoption of a systemic response to self-care and social change to influence mental health policy as primary ways of improving support for mental health social workers.
Recommended Citation
Conway, Laura. (2016). Mental Health Social Workers: The State of their Well-Being and Support. Retrieved from Sophia, the St. Catherine University repository website: https://sophia.stkate.edu/msw_papers/570
Email Author
Since June 29, 2016
Included in
Social Work Commons
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Author Corner
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
- Essay Editor
Mental Health Essay
Introduction
Mental health, often overshadowed by its physical counterpart, is an intricate and essential aspect of human existence. It envelops our emotions, psychological state, and social well-being, shaping our thoughts, behaviors, and interactions. With the complexities of modern life—constant connectivity, societal pressures, personal expectations, and the frenzied pace of technological advancements—mental well-being has become increasingly paramount. Historically, conversations around this topic have been hushed, shrouded in stigma and misunderstanding. However, as the curtains of misconception slowly lift, we find ourselves in an era where discussions about mental health are not only welcomed but are also seen as vital. Recognizing and addressing the nuances of our mental state is not merely about managing disorders; it's about understanding the essence of who we are, how we process the world around us, and how we navigate the myriad challenges thrown our way. This essay aims to delve deep into the realm of mental health, shedding light on its importance, the potential consequences of neglect, and the spectrum of mental disorders that many face in silence.
Importance of Mental Health
Mental health plays a pivotal role in determining how individuals think, feel, and act. It influences our decision-making processes, stress management techniques, interpersonal relationships, and even our physical health. A well-tuned mental state boosts productivity, creativity, and the intrinsic sense of self-worth, laying the groundwork for a fulfilling life.
Negative Impact of Mental Health
Neglecting mental health, on the other hand, can lead to severe consequences. Reduced productivity, strained relationships, substance abuse, physical health issues like heart diseases, and even reduced life expectancy are just some of the repercussions of poor mental health. It not only affects the individual in question but also has a ripple effect on their community, workplace, and family.
Mental Disorders: Types and Prevalence
Mental disorders are varied and can range from anxiety and mood disorders like depression and bipolar disorder to more severe conditions such as schizophrenia.
- Depression: Characterized by persistent sadness, lack of interest in activities, and fatigue.
- Anxiety Disorders: Encompass conditions like generalized anxiety disorder, panic attacks, and specific phobias.
- Schizophrenia: A complex disorder affecting a person's ability to think, feel, and behave clearly.
The prevalence of these disorders has been on the rise, underscoring the need for comprehensive mental health initiatives and awareness campaigns.
Understanding Mental Health and Its Importance
Mental health is not merely the absence of disorders but encompasses emotional, psychological, and social well-being. Recognizing the signs of deteriorating mental health, like prolonged sadness, extreme mood fluctuations, or social withdrawal, is crucial. Understanding stems from awareness and education. Societal stigmas surrounding mental health have often deterred individuals from seeking help. Breaking these barriers, fostering open conversations, and ensuring access to mental health care are imperative steps.
Conclusion: Mental Health
Mental health, undeniably, is as significant as physical health, if not more. In an era where the stressors are myriad, from societal pressures to personal challenges, mental resilience and well-being are essential. Investing time and resources into mental health initiatives, and more importantly, nurturing a society that understands, respects, and prioritizes mental health is the need of the hour.
- World Leaders: Several influential personalities, from celebrities to sports stars, have openly discussed their mental health challenges, shedding light on the universality of these issues and the importance of addressing them.
- Workplaces: Progressive organizations are now incorporating mental health programs, recognizing the tangible benefits of a mentally healthy workforce, from increased productivity to enhanced creativity.
- Educational Institutions: Schools and colleges, witnessing the effects of stress and other mental health issues on students, are increasingly integrating counseling services and mental health education in their curriculum.
In weaving through the intricate tapestry of mental health, it becomes evident that it's an area that requires collective attention, understanding, and action.
Short Essay about Mental Health
Mental health, an integral facet of human well-being, shapes our emotions, decisions, and daily interactions. Just as one would care for a sprained ankle or a fever, our minds too require attention and nurture. In today's bustling world, mental well-being is often put on the back burner, overshadowed by the immediate demands of life. Yet, its impact is pervasive, influencing our productivity, relationships, and overall quality of life.
Sadly, mental health issues have long been stigmatized, seen as a sign of weakness or dismissed as mere mood swings. However, they are as real and significant as any physical ailment. From anxiety to depression, these disorders have touched countless lives, often in silence due to societal taboos.
But change is on the horizon. As awareness grows, conversations are shifting from hushed whispers to open discussions, fostering understanding and support. Institutions, workplaces, and communities are increasingly acknowledging the importance of mental health, implementing programs, and offering resources.
In conclusion, mental health is not a peripheral concern but a central one, crucial to our holistic well-being. It's high time we prioritize it, eliminating stigma and fostering an environment where everyone feels supported in their mental health journey.
Frequently Asked Questions
- What is the primary focus of a mental health essay?
Answer: The primary focus of a mental health essay is to delve into the intricacies of mental well-being, its significance in our daily lives, the various challenges people face, and the broader societal implications. It aims to shed light on both the psychological and emotional aspects of mental health, often emphasizing the importance of understanding, empathy, and proactive care.
- How can writing an essay on mental health help raise awareness about its importance?
Answer: Writing an essay on mental health can effectively articulate the nuances and complexities of the topic, making it more accessible to a wider audience. By presenting facts, personal anecdotes, and research, the essay can demystify misconceptions, highlight the prevalence of mental health issues, and underscore the need for destigmatizing discussions around it. An impactful essay can ignite conversations, inspire action, and contribute to a more informed and empathetic society.
- What are some common topics covered in a mental health essay?
Answer: Common topics in a mental health essay might include the definition and importance of mental health, the connection between mental and physical well-being, various mental disorders and their symptoms, societal stigmas and misconceptions, the impact of modern life on mental health, and the significance of therapy and counseling. It may also delve into personal experiences, case studies, and the broader societal implications of neglecting mental health.
Related articles
What is chat gpt.
AI GPT chats have been getting a lot of attention over the last year. Not surprising since this new technology promises to change our future completely. The first and most well-known AI GPT chat software is ChatGPT officially released on November 30, 2022. In this article, we will answer the question “What is Chat GPT?”, explore how it works, and find out where to use the Chat GPT model. Chat GPT: definition As the name implies, ChatGPT is a chatbot that uses generative AI to process input p ...
How to Write an Essay in APA Format
There are a few styles of organizing and formatting material in an academic essay. To get high grades it is necessary to learn specific characteristics of each one. After reading this article students are certain to figure out how to write in APA format. What is APA format for an essay? It was the American Psychological Association who offered to use the APA style when formatting articles and academic papers. The specialists described all its aspects in a special Publication Manual, printed i ...
APA or MLA: Choosing the Right Citation Style for Your Paper
When it comes to academic writing, properly citing your sources is crucial. It not only helps you avoid plagiarism but also adds credibility to your work by showing that you've done your research. However, with various citation styles out there, it can be tricky to know which one to use. Two of the most common styles are APA (American Psychological Association) and MLA (Modern Language Association). In this article, we'll take a closer look at the APA vs MLA format to help you decide which is ri ...
How to Write Informative Essays
Informative essays are one of the main types of academic writing students must complete as part of the educational process. While this is a typical assignment in any curriculum, it can be hard to distinguish between different types of essays and how to write them. In this article, we’ll delve into the genre of this essay type, learn the definition of an informative essay, and how to write an informational essay. What is an informative essay? An informative essay is a piece of academic writin ...
MLA Format Essays: A Comprehensive Guide
Finishing an essay is one thing, but formatting it is a completely different affair. There are many style guides out there, so it can be hard to understand the differences between them. Today, you will learn about MLA format writing, what it is, when it’s used, and how to write MLA format essays. What is an MLA Style Essay? An MLA format essay is a piece of writing created in accordance with the MLA Style Handbook. This guide was developed by the Modern Language Association, the leading profe ...
How To Write Reflection Essays
How often do you contemplate how the tapestry of your experiences shapes your thoughts? A reflection paper lets you explore that. It's like deep diving into your life’s precious moments, examining how stories, books, events, or even lectures have influenced your views. This type of academic essay integrates a personal perspective, allowing you to openly express your opinions. In this guide, we will delve into the specifics of reflective writing, share some tips, and show some self-reflection es ...
Synthesis Essay Examples
A synthesis essay is another piece of academic discourse that students often find difficult to write. This assignment indeed requires a more nuanced approach to writing and performing research. It’s particularly relevant to students taking an AP English Language and Composition exam, so learning how to write a synthesis essay is crucial to getting a high score. This article will explore the definition of a synthesis essay, its functions, and objectives, and provide a tutorial on how to write a ...
Ace Your Graduation Speech with Aithor
Hello, Aithors! Can you feel it? That's the buzz of graduation season in the air:) And while we're all about the caps flying and the proud smiles, we also know that being asked to write a graduation speech can feel a bit like being handed a mountain to climb. Crafting a graduation speech is all about capturing the spirit of the journey you've been on, from the triumphs to the trials, and everything in between. It's a reflection of where you've been, and a beacon of light pointing towards where ...
Social Work in Mental Health Settings
Introduction, employment conditions, importance of social workers in mental health setting.
Social workers are regarded as highly trained individuals working closely to foster the standard of life and the well-being of other people through crisis intervention, policy changes, and educational programs. Social workers play a crucial role in ensuring that there is an improvement in general well-being and mental health among individuals. These professionals spend much of their time evaluating, identifying, nursing, and averting mental, emotional, and behavioral challenges. In addition, most social workers are dedicated to pursuing various social justice and striving to help the people affected by disabilities, poverty, unemployment, and other general and social problems. Mental health and social work are closely connected; they have been inseparable as their roots can be traced back to the 20 th century when the inaugural class was taught at Columbian University. Living with mental illness is often associated with severe challenges in society. Thus, the condition should be addressed effectively to ensure that individuals coexist comfortably. Therefore, social workers play a vital role in improving our society’s general well-being and mental health.
Over the recent years, the social work category has created a more comprehensive range of employment opportunities for individuals fascinated by studying mental health. It also helps in identifying the appropriate form of treatment and coming up with effective prevention measures. As a result, the stipulation and request for social workers specializing in psychiatry have increased significantly. According to Pilgrim (2019), employment in these two categories is anticipated to rise to approximately 18% between 2018 and 2028. This is because more individuals have begun to seek medication for their psychiatric challenges, behavioral complications, and, most critically, psychological challenges, hence illustrating the necessity for dilating the mental career. In the US, approximately one individual out of five is likely to experience or encounter mental illness yearly, which raises questions on the way and the role of social workers in diversifying the mental health sector and solving the existing challenges.
Typically, the mental healthcare sector’s social work has always been at the forefront of several economic, health, and other economic causes, such as lack or poor job, disability pay, and social security. Together with channeling for transparent and unbiased healthcare initiatives, the majority of the social care professionals also involve themselves in handling child abuse and negligence behaviors (Matthews, 2020). They also handle depression, anxiety, bipolar disorders, and significant life events such as divorce, terminal illness, and bereavement. In addition, they help individuals to cope with matters surrounding lack of jobs, residential homes, and the unending types of disabilities.
Nonetheless, psychiatric social workers play an important role in supporting various families, individuals, and, most importantly, communities as they tend to overcome the day-to-day challenges hindering their well-being. An illustration of this is the motive to address the patient’s substance abuse challenges and issues; mental and social workers play a crucial role in helping the addicts recover (Fazel & Betancourt, 2018). They also help them identify new employment opportunities, obtain an affordable form of housing, and most importantly, exploit the accessible mental health services. However, since different patients have different demands and needs, the social work professionals have to base their focal point on developing an indestructible connection based on transparency, empathy, and trust. This is essential to individuals with mental challenges as they might be more sensitive to specific communication models and experiences.
Psychiatric social workers use their strength, capability, knowledge, experience, and skills to assist patients with mental challenges to evaluate, detect and handle their pre-existing conditions. Contrary to the standard policies in the psychological field or category, psychiatric social works consider the environmental and societal elements that affect an individual’s emotional well-being and physical-mental (Golightley & Goemans, 2020). Therefore, this module primarily seeks to address the pre-existing hardship contributing to the human being’s general mental health complications. Furthermore, the clinical or psychiatric social workers also consider a variety of mental health challenges which enables them to work in various settings and assist and meet the needs and wants of the different patients.
Nevertheless, school social work is regarded as a unique section that primarily bases the focal point on the evolution, turn of events, and the mental health of the US students and the general education system. These well-trained, equipped, and educated individuals hence play a vital role in helping the children and younger adults experiencing mental illness and continuous behavioral challenges (Mwebe, 2017). Therefore, working closely or together with the teachers and parents enables the social workers offer academic support so as to help the students achieve their set goals and objectives. They also participate in offering individual and group counseling to enable the students to identify and recognize the signs of negligence and abuse and, most importantly, understand their home environments.
There are also substance abuse social workers facilitating the diagnosing process and treating drug addiction cases. They work closely with the patients to ensure that they have reduced or stopped drug and alcohol consumption. In addition, they are responsible for identifying the root causes of addiction, and most importantly, they have to come up with a detailed and effective treatment plan (Golightley & Goemans, 2020). Most of the substance and drug abuse social laborers are employed at various healthcare facilities, sudden and abrupt withdrawal centers, and even the mental clinics where drug addicts are trying to recover.
Nonetheless, for the patients undergoing acute crisis or are in a dangerous situation, they might hurt themselves. Therefore, the psychiatric social workers have to conduct a thorough evaluation, short-term crisis support, and, most crucially, care coordination as part of the crisis team. Furthermore, the mental illness social workers tend to work together with the crisis and emergency personnel to assess the needs and wants of their patients. They also play a crucial task in helping obtain the intensive and premium care they require and, most importantly, give recommendations regarding involuntary hospitalization (Fazel & Betancourt, 2018). However, the crisis service environment is regarded as short-term compared to the inpatient hospital mental illness settings. This is because the patients are directed to hospitals and intensive care facilities only when they receive long-term care.
In the outpatient psychiatric setting, the mental illness social workers offer effective therapy and care coordination to the individuals who do not require immediate hospitalization but still have a mental illness. However, most patients in this type of setup are at a higher risk of being hospitalized or discharged from an inpatient type of setting (Mwebe, 2017). The social workers in this setting also tend to work for longer hours to attend to their patients and even guide them through multiple systems compared to their counterparts in the inpatient setting. In addition, they have to offer therapy to patients with a wide range of mental health needs, including depression and anxiety.
The primary goal of psychiatric social workers is to stabilize and support individuals encountering intense and persistent psychological distress. They achieve this by combining diagnostic evaluations, individual and group therapies, and care coordination. In addition, they are responsible for conducting diagnostic assessments such as the mental treatment history, care management that entails monitoring the patient’s progress throughout the treatment period (Pilgrim, 2019). However, despite playing a pivotal role in transforming the mental illness setting, psychiatric social work also has several shortcomings. It is unpredictable and dangerous as there is a lack of insurance or coverage for mental health services. Furthermore, the setting also encounters a lack of an effective form of transportation and language barriers. However, this shortcoming may be curbed and mitigated by addressing the safety challenges and educating people.
In conclusion, social workers have significantly participated in transforming the mental illness sets. They have ensured that they diagnose and treat the existing mental health conditions. In addition, they have offered various individuals, parents, couples, and family therapies as well as helping them to overcome matters surrounding anxiety, depression, and other behavioral challenges. They have also ensured that overall human health and the well-being of individuals have improved in various societies. The social workers achieved this by connecting the patients to the needed services and facilitating communication between the relevant authorities and stakeholders to ensure the best care. Nonetheless, the social workers also work together with other organizations and clients to help them solve the challenges they encounter in their day-to-day lives.
Fazel, M., & Betancourt, T. S. (2018). Preventive mental health interventions for refugee children and adolescents in high-income settings. The Lancet Child & Adolescent Health , 2 (2), 121-132. Web.
Golightley, M., & Goemans, R. (2020). Social work and mental health . Sage.
Matthews, E. B. (2020). Both insider and outsider: On conducting social work research in mental health settings Beth Sapiro. Web.
Mwebe, H. (2017). Physical health monitoring in mental health settings: A study explores mental health nurses’ role views. Journal of Clinical Nursing , 26 (19-20), 3067-3078. Web.
Pilgrim, D. (2019). Critical concepts in mental health . Sage.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, November 4). Social Work in Mental Health Settings. https://studycorgi.com/social-work-in-mental-health-settings/
"Social Work in Mental Health Settings." StudyCorgi , 4 Nov. 2022, studycorgi.com/social-work-in-mental-health-settings/.
StudyCorgi . (2022) 'Social Work in Mental Health Settings'. 4 November.
1. StudyCorgi . "Social Work in Mental Health Settings." November 4, 2022. https://studycorgi.com/social-work-in-mental-health-settings/.
Bibliography
StudyCorgi . "Social Work in Mental Health Settings." November 4, 2022. https://studycorgi.com/social-work-in-mental-health-settings/.
StudyCorgi . 2022. "Social Work in Mental Health Settings." November 4, 2022. https://studycorgi.com/social-work-in-mental-health-settings/.
This paper, “Social Work in Mental Health Settings”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: December 28, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.

Home > College of Social and Behavioral Sciences > Social Work > Social Work Theses
Social Work Theses, Projects, and Dissertations
Theses/projects/dissertations from 2024 2024.
WHAT IS THE READINESS OF SOCIAL WORK STUDENTS TO WORK WITH AUTISTIC INDIVIDUALS? , Ignacio Aguilar Pelaez
EXAMINING EXPERIENCES AMONG SOCIAL WORKERS WORKING WITH PARENTS WHO SUFFER FROM SUBSTANCE USE DISORDER , Alicia Alvarado and Eleno Zepeda
COVID-19, SOCIAL ISOLATION, AND MSW STUDENTS’ MENTAL HEALTH , Cassandra Barajas
Through the Lens of Families and Staff in Emergency Shelters , Elizabeth Barcenas
MACHISMO: THE IMPACT IT HAS ON HISPANIC MALE COLLEGE STUDENTS RECEIVING MENTAL HEALTH SERVICES , Sara Barillas and Alexander Aguirre
THE DISPROPORTIONATE IMPACTS OF CERTAIN FACTORS THAT DIFFERENTIATE THE AMOUNT OF MENTAL HEALTH REFERRALS OF SCHOOL A COMPARED TO SCHOOL B , Jesus Barrientos
Correlation of Adverse Childhood Experiences and Somatic Symptoms in Adolescents , Shannon Beaumont
Caregivers of Dialysis Patients , Alyssa Bousquet and Amelia Murillo
Self-Care Habits and Burnout Among County Social Workers on the Central Coast of California , Jaclyn Boyd and Denise Ojeda
GENDER DYSPHORIA IN ADOLESCENCE AND THE MODELS OF CARE: A SYSTEMATIC LITERATURE REVIEW , Arnold Briseno
THE EFFECTS OF PARENTING STYLES ON COMMUNICATION AMONG ASIAN AMERICAN YOUNG ADULTS , Abigail Camarce
BARRIERS TO AND FACILITATORS OF CARE: EXPLORING HOW LOW-INCOME WOMEN ACCESS REPRODUCTIVE HEALTHCARE IN A RURAL COMMUNITY , Sydney Taylor Casey
CLIENT PERPETRATED VIOLENCE AND SAFETY CULTURE IN CHILD WELFARE: A SYSTEMATIC LITERATURE REVIEW , Amber Castro
ACCESSIBILITY OF SERVICES FOR TRANSGENDER ADOLESCENTS FROM A CHILD WELFARE PERSPECTIVE , Eduardo Cedeno
WHAT ARE THE BARRIERS TO SEEKING PSYCHOTHERAPY SERVICES ACROSS DIFFERENT RACIAL AND ETHNIC GROUPS? , Deysee Chavez and Elisa Rodarte
Homelessness In The Coachella Valley , Katrina Clarke
Challenges Veterans Encounter Receiving or Seeking Mental Health Services , Denise D. Contreras and Andrea Ramirez
EXAMINING THE EFFECTIVENESS OF PSYCHOSOCIAL INTERVENTIONS FOR OPIOID USE DISORDER: A SYSTEMATIC REVIEW , Elizabeth Ashley Contreras
IS A SOCIAL SUPPORT BASED MODEL BETTER FOR TREATING ALCOHOLISM? A SYSTEMATIC REVIEW , Jordan Anthony Contreras
SOCIAL WORKERS’ PREPAREDNESS FOR PRACTICE WITH PATIENTS EXPERIENCING PSYCHOTIC DISORDERS , Paula Crespin
INVESTIGATING THE LEVEL OF EVIDENCE OF ADVERSE CHILDHOOD EXPERIENCES AND PARENTING PRACTICES: A SYSTEMATIC REVIEW , Eloisa Deshazer
MENTAL HELP-SEEKING: BARRIERS AMONG AFRICAN AMERICANS: THE ROLE OF TECHNOLOGY IN ADDRESSING THOSE BARRIERS , Charneka Edwards
Treatment not Punishment: Youth Experiences of Psychiatric Hospitalizations , Maira Ferrer-Cabrera
THE BARRIERS TO NATURAL OUTDOOR SPACES: PERSPECTIVES FROM PEOPLE WITH MOBILITY DISABILITIES , Sierra Fields and Kailah Prince
IMPLEMENTATION OF MENTAL HEALTH SERVICES AND CURRICULUM FOR ELEMENTARY-AGED CHILDREN , Indra Flores Silva and Jason Kwan
POOR ACADEMICS FROM COLLEGE STUDENTS GRIEVING THROUGH COVID 19 , Sarah Frost
COMPASSION FATIGUE IN SHORT TERM RESIDENTIAL THERAPEUTIC PROGRAM SETTINGS , Sandra Gallegos
A SYSTEMATIC REVIEW ON THE EFFECTIVENESS OF THE GUN VIOLENCE RESTRAINING ORDER , Bonnie Galloway and Yasmeen Gonzalez-Ayala
STRESS AND HELP-SEEKING IN FARMWORKERS IN THE COACHELLA VALLEY , Alexis Garcia and Daniela Mejia
THE EFFECTIVNESS OF FEDERAL PELL GRANT PROGRAM , Maria Delcarmen Garcia Arias and Ashley Hernandez
PARENT INVOLVEMENT AND EDUCATIONAL OUTCOMES AMONG LATINO FAMILIES , Diana Garcia and Gabriela Munoz
IMPACT OF SCHOOL-BASED MENTAL HEALTH SERVICES ON STUDENT ATTENDANCE AT A SOUTHERN CALIFORNIA SCHOOL DISTRICT , Johanna Garcia-Fernandez and Morgan Stokes
BARRIERS TO GENDER-AFFIRMING CARE , Gloria Garcia
THE CONTRIBUTING FACTORS OF PLACEMENT INSTABILITY FOR PREGNANT FOSTER YOUTH , Amanda Garza and Shayneskgua Colen
PROGRESSION OF BLACK WOMEN IN TENURE RANKED POSITIONS , Unique Givens
Child Maltreatment Primary Prevention Methods in the U.S.: A Systematic Review of Recent Studies , Maria Godoy-Murillo
Assessing and Meeting the Needs of Homeless Populations , Mitchell Greenwald
Parity In Higher Education In Prison Programs: Does It Exist? , Michael Lee Griggs and Vianey Luna
SURROGACY AND IT'S EFFECTS ON THE MENTAL HEALTH OF THE GESTATIONAL CARRIER , DayJahne Haywood
SUBSTANCE USE TREATMENT WITHIN THE US PRISON SYSTEM , Timothy Hicks
LGBTQ+ College Students Hopeful Future Expectations , Savannah Hull
EFFECTS OF VOLUNTARY REMOVAL ON AN IMMIGRANT FAMILY , Miriam Jimenez
THE MOTIVATING FACTORS AFFECTING THE CONTINUANCE AND COMPLETION OF SUBSTANCE USE TREATMENT FOR MOTHERS , Jacquetta Johnson
FACTORS AFFECTING THE ENROLLMENT AND GRADUATION RATES AMONGST AFRICAN AMERICAN MALES IN THE UNITED STATES , Tracie Johnson
SUPPORTING FORMERLY INCARCERATED INDIVIDUALS IN HIGHER EDUCATION: A QUANTITATIVE STUDY , Lisa Marie Jones-Wiertz
PROTESTANT CHURCH WORKERS' KNOWLEDGE OF CHILD ABUSE REPORTING AND REPORTING BEHAVIOR , Rachel Juedes
Social Media Told Me I Have A Mental Illness , Kathleen Knarreborg
THE RELATIONSHIP BETWEEN ROLE MODELS, SOCIOECONOMIC MOBILITY BELIEFS, AND ACADEMIC OUTCOMES , Christian Koeu and Marisol Espinoza Garcia
CULTURAL AND STRUCTURAL BARRIERS OF UTILIZING MENTAL HEALTH SERVICES IN A SCHOOL-BASED SETTING FOR LATINX POPULATIONS , Silvia Lozano and Bridgette Guadalupe Calderon
EDUCATIONAL OUTCOMES FOR YOUTH THAT PARTICIPATED IN EXTENDED FOSTER CARE: A SYSTEMATIC REVIEW , Kassandra Mayorga and Roxana Sanchez
NON-BINARY IDENTITY WITHIN COMPETENCY TRAINING FOR MENTAL/BEHAVIORAL HEALTH PROVIDERS: A SYSTEMATIC REVIEW , Alexis McIntyre
Childhood Neglect and Incarceration as a Adult , Marissa Mejia and Diana Gallegos
IMPACT OF RESOURCE SCARCITY ON UNDOCUMENTED STUDENTS IN HIGHER EDUCATION , Sebastian Melendez Lopez
STUDY EXPLORING FEELINGS OF SELF-BLAME AND SHAME AMONG INDIVIDUALS RAISED BY SEVERELY MENTALLY ILL CAREGIVERS , Joanie Minion
THE OBSTACLES FACING HOMELESS VETERANS WITH MENTAL ILLNESS WHEN OBTAINING HOUSING , Melissa Miro
STUDENTS OF HIGHER EDUCATION RECEIVING SUPPLEMENTAL NUTRITION ASSISTANCE PROGRAM AND ITS IMPACT ON MENTAL HEALTH , Cristina Palacios Mosqueda
COMMERCIALLY SEXUALLY EXPLOITED CHILDREN TARGETED WITHIN SOCIAL SERVICES , Britny Ragland
ART THERAPY FOR BEREAVED SIBLINGS AFTER PEDIATRIC CANCER DEATH , Daniela Ramirez-Ibarra
HOW DID THE COVID-19 PANDEMIC IMPACT EXTENDED FOSTER CARE SOCIAL WORKERS WHILE PROVIDING SOCIAL SERVICES , Omar Ramirez and Victoria Lopez
A COMPARATIVE ANALYSIS OF BODY MODIFICATION BIASES IN THE MENTAL HEALTH FIELD , Lonese Ramsey
Bridging Training Gaps: Assessing Knowledge and Confidence of Mental Health Interns in Opioid Misuse Intervention for School-Aged Children and Adolescents , Carolina Rodriguez and Gabriela Guadalupe Gonzalez
PERCEPTIONS OF YOUTH ATHLETE SAFETY PARENTS VS DIRECTORS , Nicole Anais Rodriguez
SPIRITUALITY AND RECOVERY FROM ADDICTION: EXPERIENCES OF NARCOTICS ANONYMOUS MEMBERS , Elizabeth Romberger
ADVERSE CHILDHOOD EXPERIENCES AND ALTRUISM: THE IMPACT ON SOCIAL WORK AS A CAREER CHOICE , Nancy Salas and Brittany Altuna
MAJOR FACTORS OF SUSTAINING RECOVERY AFTER RELAPSE FROM A SUBSTANCE USE DISORDER , Amanda Tei Sandhurst
UNDERSTANDING THE PERSPECTIVES AND ATTITUDES OF 12-STEP PARTICIPANTS TOWARDS MEDICATION-ASSISTED TREATMENT , Christopher Scott
THE UTILIZATION OF MUSIC AND AUTONOMOUS SENSORY MERIDIAN RESPONSE IN REDUCING STRESS , Robert Scott
THE AFTERMATH OF THE PANDEMIC’S EFFECT ON COLLEGE STUDENT DEPRESSION , Lorena Sedano
Exploring the Experiences of Minority Former Foster Youths During and Post Care: A Qualitative Study , Caithlyn Snow
Factors that Contribute to Disparities in Access to Mental Health Services within Hispanic Adults , Jasmine Soriano
THE CHALLENGES TO THE IMPLEMENTATION OF ADMINISTRATION FOR CHILDREN AND FAMILIES MEMORANDUM: FOSTER CARE AS A SUPPORT TO FAMILIES , Rebecca Joan Sullivan-Oppenheim
RESILIENCE IN FATHERHOOD: EXPLORING THE IMPACT OF ABSENT FATHERS ON BLACK AMERICAN MEN'S PARENTING NARRATIVES AND PRACTICES , Ericah Thomas
FACTORS THAT IMPACT FOSTER YOUTHS’ HIGH SCHOOL GRADUATION , Esther Thomas
EXAMINING A RELATIONSHIP BETWEEN SEXUAL SATISFACTION AND CHILD MALTREATMENT , Amanda Titone
THE PRESENT STRUGGLES OF IMMIGRANT FARMWORKERS IN CALIFORNIA , Leslie Torres and Angelica Huerta
PROGRAM EVALUATION OF SCHOOL-BASED MENTAL HEALTH COUNSELING SERVICES , Yvette Torres and Emily Ann Rodriguez
Stressors, Caffeine Consumption, and Mental Health Concerns among College Students , Stacey Trejo
MENTAL HEALTH TREATMENT HELP SEEKING ATTITUDES AND BEHAVIORS AMONG LATINX COMMUNITY , Nancy Vieyra
JUSTICE-INVOLVED STUDENTS: EFFECTS OF USING SUPPORT SERVICES TO OVERCOME BARRIERS , Gabby Walker and Sofia Alvarenga
MANDATED REPORTERS’ KNOWLEDGE AND REPORTING OF CHILD ABUSE , Alexis Reilly Warye
THE COMMUNITY RESILIENCY MODEL (CRM) APPLIED TO TEACHER’S WELL-BEING , John Waterson
Addressing Rural Mental Health Crises: An Alternative to Police , Faith Ann Weatheral-block

Theses/Projects/Dissertations from 2023 2023
PROLONGED EXPOSURE TO CONGREGATE CARE AND FOSTER YOUTH OUTCOMES , Tiffany Acklin
YOU CALL US TREATMENT RESISTANT: THE EFFECTS OF BIASES ON WOMEN WITH BORDERLINE PERSONALITY DISORDER , Cassidy Acosta
EXAMINING SOCIAL DETERMINANTS OF HEALTH OF FORMERLY INCARCERATED CALIFORNIA STUDENTS WHO GRADUATED FROM PROJECT REBOUND , Ashley C. Adams
ALTERNATIVE APPROACHES TO POLICE INTERVENTIONS WHEN RESPONDING TO MENTAL HEALTH CRISES INCIDENTS , Karen Rivera Apolinar
Understanding Ethical Dilemmas in Social Work Practice , Arielle Arambula
IS THERE A RELATIONSHIP BETWEEN PROFESSORIAL-STUDENT RACIAL MATCH AND ACADEMIC SATISFACTION OF AFRICAN AMERICAN SOCIAL WORK STUDENTS , Ashlei Armstead
NON-SPANISH SPEAKING LATINOS' EXPERIENCES OF INTRAGROUP MARGINALIZATION AND THE IMPLICATIONS FOR ETHNIC IDENTITY , Marissa Ayala
SERVICES AVAILABLE IN THE MIXTEC COMMUNITY AND THE BARRIERS TO THOSE SERVICES , Currie Bailey Carmon
IMPACT OF OUTDOOR ADVENTURE ON THE SELF-ESTEEM, SELF-CONFIDENCE, AND COMFORT LEVEL OF BLACK AND BROWN GIRLS , Nathan Benham
THE ROLE UNDOCUMENTED STUDENT RESOURCE CENTERS PLAY IN SUPPORTING UNDOCUMENTED STUDENTS IN HIGHER EDUCATION , Cynthia Boyzo
Program Evaluation of Teen Parent Support Group , Brianne Yvonne Irene Brophy
THE IMPACT THE JOB STRESS OF A CHILD WELFARE SOCIAL WORKER HAS ON THE QUALITY OF THEIR RELATIONSHIP WITH THEIR INTIMATE PARTNER , Nadine Cazares
Adverse Effects for Siblings Who Witness Child Abuse , Leslie Chaires
ASIAN DISCRIMINATION: IN THE FIELD OF SOCIAL WORK , Sunghay Cho
PERCEIVED FINANCIAL STRAIN AND ITS EFFECTS ON COLLEGE STUDENTS’ WELFARE , Monica Contreras and Clarissa Adrianna Martinez
The Media and Eating Disorders , Diane Corey
INCREASING TEACHER AWARENESS OF MENTAL HEALTH IN CHILDREN , Sarah Alexis Cortes
The Investigation of Knowledge and Practice of Child Welfare Workers Providing Case Management to Children with Disabilities , Giselle Cruz
Page 1 of 17
Advanced Search
- Notify me via email or RSS
- Department, Program, or Office
- Disciplines
Author Corner
- School of Social Work homepage
A service of the John M. Pfau Library

Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright Acrobat Reader
Advertisement
Maslow and Mental Health Recovery: A Comparative Study of Homeless Programs for Adults with Serious Mental Illness
- Original Article
- Published: 12 February 2014
- Volume 42 , pages 220–228, ( 2015 )
Cite this article

- Benjamin F. Henwood 1 ,
- Katie-Sue Derejko 2 ,
- Julie Couture 1 &
- Deborah K. Padgett 2
12k Accesses
65 Citations
33 Altmetric
Explore all metrics
This mixed-methods study uses Maslow’s hierarchy as a theoretical lens to investigate the experiences of 63 newly enrolled clients of housing first and traditional programs for adults with serious mental illness who have experienced homelessness. Quantitative findings suggests that identifying self-actualization goals is associated with not having one’s basic needs met rather than from the fulfillment of basic needs. Qualitative findings suggest a more complex relationship between basic needs, goal setting, and the meaning of self-actualization. Transforming mental health care into a recovery-oriented system will require further consideration of person-centered care planning as well as the impact of limited resources especially for those living in poverty.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Dear Mental Health Practitioners, Take Care of Yourselves: a Literature Review on Self-Care

Person-Centred Approaches to Social Work Practice

The Biopsychosocial Approach: Towards Holistic, Person-Centred Psychiatric/Mental Health Nursing Practice
Charmaz, K. (2006). Constructing grounded theory: a practical guide through qualitative analysis . Los Angeles: Sage.
Google Scholar
Clarke, S., Oades, L. G., & Crowe, T. P. (2012). Recovery in mental health: A movement towards well-being and meaning in contrast to an avoidance of symptoms. Psychiatric Rehabilitation Journal, 35 , 297–304.
Article PubMed Google Scholar
Collins, S. E., Malone, D. K., & Clifasefi, S. L. (2013). Housing retention in single-site housing first for chronically homeless individuals with severe alcohol problems. American Journal of Public Health, 103 (S2), S269–S274.
Article PubMed Central PubMed Google Scholar
Culhane, D. (2008). The costs of homelessness: A perspective from the United States. European Journal of Homelessness, 2 , 97–114.
Dordick, G. A. (2002). Recovering from homelessness: Determining the “quality of sobriety” in a transitional housing program. Qualitative Sociology, 25 (1), 7–32.
Article Google Scholar
Draine, J., Salzer, M., Culhane, D., & Hadley, T. (2002a). Poverty, social problems, and serious mental illness. Psychiatric Services, 53 , 899.
Draine, J., Salzer, M. S., Culhane, D. P., & Hadley, T. R. (2002b). Role of social disadvantage in crime, joblessness, and homelessness among persons with serious mental illness. Psychiatric Services, 53 , 565–573.
Freund, K. S., & Lous, J. (2012). The effect of preventive consultations on young adults with psychosocial problems: a randomized trial. Health Education Research, 27 (5), 927–945.
Fukui, S., Starnino, V. R., Susana, M., Davidson, L. J., Cook, K., Rapp, C. A., et al. (2011). Effect of Wellness Recovery Action Plan (WRAP) participation on psychiatric symptoms, sense of hope, and recovery. Psychiatric Rehabilitation Journal, 34 (3), 214.
Gorman, D. (2010). Maslow’s hierarchy and social and emotional wellbeing. Aboriginal and Islander Health Worker Journal, 34 , 27–29.
Greenwood, R. M., Stefancic, A., & Tsemberis, S. (2013). Pathways housing first for homeless persons with psychiatric disabilities: Program innovation, research, and advocacy. Journal of Social Issues, 69 (4), 645–663.
Henwood, B. F., Stanhope, V., & Padgett, D. K. (2011). The role of housing: a comparison of front-line provider views in housing first and traditional programs. Administration and Policy in Mental Health, 38 , 77–85.
Hopper, K. (2007). Rethinking social recovery in schizophrenia: what a capabilities approach might offer. Social Science and Medicine, 65 (5), 868–879.
Hopper, K. (2012). Commentary: the counter-reformation that failed? A commentary on the mixed legacy of supported housing. Psychiatric Services, 63 (5), 461–463.
Hopper, K., Jost, J., Hay, T., & Welber, S. (1997). Homelessness, severe mental illness, and the institutional circuit. Psychiatric Services, 48 (5), 659–665.
Article CAS PubMed Google Scholar
Jacobson, N., & Greenley, D. (2001). What is recovery? A conceptual model and explication. Psychiatric Services, 52 , 482–485.
Kenrick, D. T., Griskevicius, V., Neuberg, S. L., & Schaller, M. (2010). Renovating the pyramid of needs. Perspectives on Psychological Science, 5 , 292–314.
Kertesz, S. G., Crouch, K., Milby, J. B., Cusimano, R. E., & Schumacher, J. E. (2009). Housing first for homeless persons with active addiction: are we overreaching? Milbank Quarterly, 87 (2), 495–534.
Kiel, J. M. (1999). Reshaping Maslow’s hierarchy of needs to reflect today’s educational and managerial philosophies. Journal of Instructional Psychology, 26 , 167.
Maslow, A. H. (1943). A theory of human motivation. Psychological Review, 50 , 370–396.
Maslow, A. H. (1970). Motivation and personality (2nd ed.). New York: Harper & Row.
Miles, M. B., & Huberman, A. M. (1994). Qualitative data analysis: An expanded sourcebook . Los Angeles: Sage.
Nelson, G., Lord, J., & Ochocka, J. (2001). Empowerment and mental health in community: Narratives of psychiatric consumer/survivors. Journal of Community & Applied Social Psychology, 11 , 125–142.
Nussbaum, M. C. (2006). Frontiers of justice: disability, nationality, species membership . Cambridge: Harvard University Press.
Ochocka, J., Nelson, G., & Janzen, R. (2005). Moving forward: Negotiating self and external circumstances in recovery. Psychiatric Rehabilitation Journal, 28 , 315–322.
Onken, S. J., Craig, C. M., Ridgway, P., Ralph, R. O., & Cook, J. A. (2007). An analysis of the definitions and elements of recovery: a review of the literature. Psychiatric Rehabilitation Journal, 31 , 9–22.
Padgett, D. K. (2007). There’s no place like (a) home: Ontological security among persons with serious mental illness in the United States. Social Science and Medicine, 64 (9), 1925–1936.
Padgett, D. K. (2008). Qualitative methods in social work research . Los Angeles: Sage.
Padgett, D. K., Smith, B., Henwood, B. F., & Tiderington, E. (2012). Life course adversity in the lives of formerly homeless persons with serious mental illness: context and meaning. American Journal of Orthopsychiatry, 82 , 421–430.
Palinkas, L. A., Horwitz, S. M., Chamberlain, P., Hurlburt, M. S., & Landsverk, J. (2011). Mixed-methods designs in mental health services research: A review. Psychiatric Services, 62 (3), 255–263.
Pearson, C., Montgomery, A. E., & Locke, G. (2009). Housing stability among homeless individuals with serious mental illness participating in Housing First programs. Journal of Community Psychology, 37 (3), 404–417.
Rawls, J. (1971). A theory of justice . Cambridge: Harvard University Press.
Ridgway, P. (2001). Restorying psychiatric disability: Learning from first person recovery narratives. Psychiatric Rehabilitation Journal, 24 , 335–343.
Roychowdhury, A. (2011). Bridging the gap between risk and recovery: a human needs approach. The Psychiatrist, 35 , 68–73.
SAMHSA (2011). SAMHSA announces a working definition of “recovery” from mental disorders and substance use disorders. Retrieved July 11, 2012, from http://www.samhsa.gov/newsroom/advisories/1112223420.aspx .
Sandelowski, M. (2001). Real qualitative researchers do not count: The use of numbers in qualitative research. Research in Nursing & Health, 24 , 230–240.
Article CAS Google Scholar
Stake, R. E. (1995). The art of case study research . Thousand Oaks: Sage.
Stefancic, A., & Tsemberis, S. (2007). Housing First for long-term shelter dwellers with psychiatric disabilities in a suburban county: A four-year study of housing access and retention. J Prim Prev, 28 (3–4), 265–279.
Tondora, J., Miller, R., & Davidson, L. (2012). The Top Ten Concerns about Person-Centered Care Planning in Mental Health Systems. International Journal of Person Centered Medicine, 2 (3), 410–420.
Trattner, W. I. (1998). From poor law to welfare state: A history of social welfare in America (6th ed.). New York: Free.
Tsemberis, S., & Eisenberg, R. F. (2000). Pathways to housing: Supported housing for street- dwelling homeless individuals with psychiatric disabilities. Psychiatric Services (Washington, D. C.), 51 (4), 487–493.
Tsemberis, S., Gulcur, L., & Nakae, M. (2004). Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. American Journal of Public Health, 94 , 651–656.
Viron, M., Bello, I., Freudenreich, O., & Shtasel, D. (2013). Characteristics of homeless adults with serious mental illness served by a state mental health transitional shelter. Community Mental Health Journal, 1–6. doi: 10.1007/s10597-013-9607-5 .
Wahba, M. A., & Bridwell, L. G. (1976). Maslow reconsidered: A review of research on the need hierarchy theory. Organizational Behavior and Human Performance, 15 , 212–240.
Download references
Acknowledgments
This research was supported by the National Institute of Mental Health (R01 69865).
Author information
Authors and affiliations.
School of Social Work, University of Southern California, 1150 S. Olive Street, #1429, Los Angeles, CA, 90015-2211, USA
Benjamin F. Henwood & Julie Couture
Silver School of Social Work, 838 Broadway, 3rd Floor, New York Recovery Study, New York, NY, 10003, USA
Katie-Sue Derejko & Deborah K. Padgett
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Benjamin F. Henwood .
Rights and permissions
Reprints and permissions
About this article
Henwood, B.F., Derejko, KS., Couture, J. et al. Maslow and Mental Health Recovery: A Comparative Study of Homeless Programs for Adults with Serious Mental Illness. Adm Policy Ment Health 42 , 220–228 (2015). https://doi.org/10.1007/s10488-014-0542-8
Download citation
Published : 12 February 2014
Issue Date : March 2015
DOI : https://doi.org/10.1007/s10488-014-0542-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health recovery
- Housing first
- Homelessness
- Serious mental illness
- Find a journal
- Publish with us
- Track your research
- Warning Signs and Symptoms
- Mental Health Conditions
- Common with Mental Illness
- Mental Health By the Numbers
- Individuals with Mental Illness
- Family Members and Caregivers
- Kids, Teens and Young Adults
- Maternal & New Parent Mental Health
- Veterans & Active Duty
- Identity and Cultural Dimensions
- Frontline Professionals
- Mental Health Education
- Support Groups
- NAMI HelpLine
- Publications & Reports
- Podcasts and Webinars
- Video Resource Library
- Justice Library
- Find Your Local NAMI
- Find a NAMIWalks
- Attend the NAMI National Convention
- Fundraise Your Way
- Create a Memorial Fundraiser
- Pledge to Be StigmaFree
- Awareness Events
- Share Your Story
- Partner with Us
- Advocate for Change
- Policy Priorities
- NAMI Advocacy Actions
- Policy Platform
- Crisis Intervention
- State Fact Sheets
- Public Policy Reports
- About Mental Illness
Complementary Health Approaches
Ect, tms and other brain stimulation therapies, getting treatment during a crisis, mental health medications, psychosocial treatments, psychotherapy, treatment settings, types of mental health professionals.
Innovations in the range of evidence based medications, therapy and psychosocial services such as psychiatric rehabilitation, housing, employment and peer supports have made wellness and recovery a reality for people living with mental health conditions.
Choosing the right mix of treatments and supports that work for you is an important step in the recovery process. Treatment choices for mental health conditions will vary from person to person. Even people with the same diagnosis will have different experiences, needs, goals and objectives for treatment. There is no “one size fits all” treatment.
When people are directly involved in designing their own treatment plan, including defining recovery and wellness goals, choosing services that support them and evaluating treatment decisions and progress , the experience of care and outcomes are improved.
There are many tools that can improve the experience on the road to wellness: medication, counseling (therapy), social support and education. Therapy, for example, can take many forms, from learning relaxation skills to intensively reworking your thinking patterns. Social support, acceptance and encouragement from friends, family and others can also make a difference. Education about how to manage a mental health condition along with other medical conditions can provide the skills and supports to enrich the unique journey toward overall recovery and wellness.
Together with a treatment team you can develop a well-rounded and integrated recovery plan that may include counseling, medications, support groups, education programs and other strategies that work for you.
Mental health professionals all have different roles. Understanding who can prescribe and monitor medication and provide therapy and counseling can offer can help you decide which is right for you.
Psychotherapy, also known as “talk therapy,” is when a person speaks with a trained therapist in a safe and confidential environment to explore and understand feelings and behaviours and gain coping skills.
Mental health crisis response services are a vital part of any mental health service system. A well-designed crisis response system can provide backup to community providers, perform outreach by connecting first-time users to appropriate services and improve community relations by providing reassurance that the person’s needs are met in a mental health crisis.
Treatment for mental health conditions is not a one size fits all approach. Treatment can include private doctors, community mental health centers, emergency rooms, hospitalization and substance abuse centers. Knowing where to look and what to expect can help reduce confusion and stress.
Some people find medications to be an important part of their treatment plan. Understanding their risks and benefits can help you make the right choice.
Psychosocial treatments look at someone’s psychological development and how it contributes to the way that they act in and respond to their social environment.
Complementary and alternative methods can help with recovery when traditional methods do not seem to be enough.
When treatments such as medication and therapy aren’t able to relieve the symptoms of depression or another mental health condition, brain stimulation therapies can be an option.

Know the warning signs of mental illness

Learn more about common mental health conditions
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264 , text “helpline” to 62640 , or chat online. In a crisis, call or text 988 (24/7).
The suicide crisis among young Black and Latino Chicagoans demands action
Black and latino youth and young adults ending their lives at younger ages points to the need for early intervention in schools and community-based clinics, two university of chicago researchers write..

From 2015 to 2021, there was a 19% increase in suicides by Black females and a 24% percent increase by Latino males, according to University of Chicago researchers.
stock.adobe.com
While many people in Chicago face challenges to their mental health, some groups have been impacted differently than others. Findings from our new study published in the American Journal of Public Health confirm that Black and Latino Chicagoans are dying by suicide earlier than white and Asian groups across the city.

We analyzed data from the Cook County Medical Examiner’s archive that tracked all suicide deaths in Cook County from 2015 to 2021. Earlier articles published in local outlets like the Chicago Sun-Times, WBEZ and the Chicago Tribune have highlighted racial differences in suicide among Cook County residents generally, though we designed our study to focus on suicide deaths in the city of Chicago. We felt that narrowing our analysis would allow us to target local policies that directly impact those living within city limits.
We found that between 2015 and 2021, suicide rates increased 12% among Asian females, 9% among Black males, 19% among Black females, and 24% among Latino males. White females (-4%) and white males (-2%) were the only groups to experience statistically significant decreases in suicide during this time. Still, the suicide rate for white males remains higher than all other groups at 18 per 100,000 in 2021.
There are also notable differences by age. Asian Chicagoans, with an average age of 42, and white Chicagoans, with an average age of 48, were often older when they died by suicide. Decedents who were Black and Latino typically skewed younger, as both groups had an average age of 38. A greater proportion of suicide deaths occurred among Black (10.4%) and Latino (7.8%) children and adolescents. Conversely, less than 3% of suicides among Asian and white individuals occurred among persons younger than 20.
Among adolescents aged 15 to 19, we saw a 21% increase in suicides in Black males and a 77% increase in Black females. Notably, the youngest person to die by suicide in Chicago across this time span was an 8-year-old Black boy.
Reopen mental health centers, address bias in social work licensing
Our results have direct implications for local policies on mental health care access. First, we must consider how the closure of half of the city’s 12 public mental health facilities may have had a disproportionate impact on communities already in need: Four of the six closed centers were located in predominantly Black and Latino neighborhoods. Local efforts like the Treatment Not Trauma campaign, led by the Collaborative for Community Wellness, have been instrumental in advocating for the reopening of city-run mental health centers to meet the increasing demand for treatment.
Second, with Black and Latino youth and young adults ending their lives at younger ages, there is a need for early intervention, through schools and community-based clinics, that is cost-effective and accessible to families. This includes equipping parents and family members with mental health resources and hiring more clinical staff in local schools.
Despite the city’s glaring need for more well-trained and culturally attuned mental health professionals, structural barriers like the licensed clinical social work exam have prevented social workers from receiving the licensure required to practice independently. A national report from 2022 found that less than half of Black applicants passed the exam on the first try, compared to more than 80% of white social workers who passed on their first attempt. Black social workers report facing racial bias throughout the examination process, which in turn limits the number of Black licensed clinical social workers available to provide therapeutic services both locally and nationally.
To close this gap, Chicago-based clinical social workers Cassandra Walker and Brit Holmberg developed a state bill proposing an alternative path to licensure that would allow persons who did not pass the exam on their first try to gain an additional 3,000 hours of clinical practice experience before obtaining their full license. This bill became law in January 2024.
Both of these local policy changes are helpful in reiterating the need for systems-level changes in the city’s approach to administering mental health services, particularly for Black and Latino residents. Further, intentional collaborations between clinicians, researchers, city leaders, community members and suicide survivors can help develop culturally grounded services that account for the unique mental health issues faced by Black and Latino Chicagoans. Together, these efforts have the potential to truly change lives while improving access to mental health treatment for all in need.
Janelle Goodwill, Ph.D., is a Neubauer Family Assistant Professor at the University of Chicago’s Crown Family School of Social Work, Policy, and Practice. Rachel Baccile is a senior research analyst at the University of Chicago’s Center for Health and the Social Sciences.
The Sun-Times welcomes letters to the editor and op-eds. See our guidelines .
Send letters to [email protected]


College of Social Work
Main navigation, behavioral health technician.
Behavioral Health Technicians (BHT) work under the supervision of licensed professionals, such as social workers, psychologists, or psychiatrists, to support the overall treatment and care of individuals with mental health or behavioral disorders. This 20-credit sequence of courses, open to enrolled undergraduate U students in any discipline, prepares students for state certification as a Behavioral Health Technician.
Undergraduate students interested in participating in the Behavioral Health Technician certification sequence should reach out to Prof Stephanie Bank for additional information and program details.
Behavioral Health Technicians:

- May work under the indirect supervision of licensed professionals, performing specific services within the approved scope of practice.
- May collect intake assessment information used to determine the well-being of a patient and the potential type of treatment options that might be appropriate.
- May support licensed clinical professionals in developing treatment plans and implementing interventions designed to address behavioral health issues.
- May conduct direct observation and monitoring of clients' behaviors, documenting significant observations, and reporting findings to the supervising professional.
- May facilitate therapeutic activities and recreational programs to enhance clients' social skills, emotional well-being, and overall functioning.
- May implement crisis intervention strategies in accordance with established protocols, ensuring the safety and well-being of clients during emergencies.
- May provide education and support to clients and their families on behavioral health issues, treatment options, and community resources.
- May implement behavioral management strategies including de-escalation techniques and crisis intervention as needed.
Learning outcomes include developing knowledge around:
- The role, function, and responsibilities of various mental health professions and community service agencies.
- The importance of whole health integration, strong support systems, and self-care habits for stress management and resiliency as a successful student and valued employee.
- Mental health and common mental health issues.
- Elements of positive psychology and whole health integration to enhance happiness and well-being.
- Ethical, legal, and professional responsibilities of helping professionals.
- Modes of non-verbal communication, as well as nuances of paraverbal and verbal communications and their implications.
- Effective conflict management and problem-solving strategies in a variety of interpersonal communication situations.
- The process of assessment and relevant interviewing skills in case management.
- Application of concepts of case management to the unique needs of multicultural clients and special populations.
- The legal and liability issues related to case management and report writing.
- The importance of the wraparound process and how it relates to child and family advocacy.
The College of Social Work is pleased to collaborate with other academic disciplines at the U that are interested in seeking course approval for the BHT sequence. Interdisciplinary coursework options will offer students a deeper understanding of the allied human services professionals with whom they are likely to interact. Academic programs interested in adding their courses can reach out to Prof Stephanie Bank .
COVID-19 Fear, Mental Health, and Substance Misuse Conditions Among University Social Work Students in Israel and Russia
Affiliations.
- 1 Regional Alcohol and Drug Abuse Research Center, Ben Gurion University of the Negev, 84105 Beer Sheva, Israel.
- 2 Department of Social Psychology, Moscow State University of Psychology and Education, Moscow, Russia.
- 3 Department of General Psychology, Penza State University, Penza, Russia.
- PMID: 32837438
- PMCID: PMC7338139
- DOI: 10.1007/s11469-020-00360-7
Publication types
- Case Reports
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Consort Psychiatr
- PMC10790731

Celebrating a Storied History: Moscow Preobrazhenskaya Mental Hospital Marks its 245 th Anniversary
Larisa a. burygina.
Mental-health Clinic No. 4 named after P. B. Gannushkin
Sergey A. Golubev
Oksana v. filipchenko, associated data.
- 1876. 217. 1. 76. [On the 100th anniversary of the Preobrazhenskaya hospital which takes place 13th of July 1877] Central State Archive of Moscow (Moscow)
Figure S2 . «About the centenary anniversary».
In 2022, Mental-health Clinic No. 4 named after P. B. Gannushkin, one of the oldest mental health institutions in Russia known as Preobrazhenskaya Hospital before the October Revolution of 1917, celebrated its 245 th anniversary. The history of the hospital reflects all stages of the evolution of the basic principles and aspects of mental health care in Russia. On many occasions, the institution served as a platform for eminent researchers and clinicians to achieve scientific breakthroughs and their application in practice. This article is a review of the major milestones in the history of the hospital. It highlights the great achievements of its psychiatrists and presents some previously unpublished archival documents that offer a new perspective on the history of Preobrazhenskaya Hospital.
INTRODUCTION
In 2022, Mental-health Clinic No. 4 named after P. B. Gannushkin, one of the oldest mental health institutions in Russia known as Preobrazhenskaya Hospital before the October Revolution, celebrated its 245 th anniversary. This represents the number of years since Catherine the Great signed a decree establishing the Moscow House of Invalids, where several dozen beds were set aside for the mentally ill. The document, issued in 1777 [1] , laid the foundation not only for Moscow’s first specialized institution that could accommodate patients with mental disorders, but also, without exaggeration, for the entire field of Russian psychiatry.
The implementation of the Pinel reform in Russia, the introduction of the concept of “moral treatment”, the first scientific conferences and open clinical discussions, all these stages in the evolution of the basic principles and aspects of mental health care have found their reflection in the history of Preobrazhenskaya Hospital over the past 245 years. This is why Vasily Gilyarovsky poetically referred to the Hospital as “the cradle of Russian psychiatry” [2] .
Each page in the history of Preobrazhenskaya Hospital is not only an impressive list of achievements and innovations, but also a unique gallery of distinguished names [3-7] . It served as a basis for the greatest medical luminaries of the time, such as V. F. Sabler, V. R. Butzke, V. A. Gilyarovsky, N. N. Bazhenov, A. V. Snezhnevsky, D. E. Melekhov, T. I. Yudin, S. G. Zhislin, and G. Y. Avrutsky, from which to make their scientific discoveries and validate them in practice; this was also the place where such luminaries of Russian psychiatry as S. S. Korsakov, A. U. Frese, E. K. Krasnushkin, P. E. Snesarev, A. S. Tiganov, and I. Y. Gurovich, and many others, began their medical careers.
It is a well-known and undisputed fact that Preobrazhenskaya Hospital was the first (and almost only one until the end of the 19 th century) psychiatric hospital to appear in Moscow. But historians and researchers in psychiatry have spent more than 100 years trying to dig up documents that could allow them to determine the exact year of its founding.
Starting in the second half of the 19 th century, the question has frustrated many eminent physicians of Preobrazhenskaya Hospital, including S. I. Steinberg [8] , I. V. Konstantinovsky [9] , N. N. Bazhenov [10] , M. A. Dzhagarov [11] , and A. B. Alexandrovsky [12] . Their work can now help us to form a fairly comprehensive view of how the State and society gradually, step by step, developed an awareness of what such an independent institution as a psychiatric hospital was all about. They painstakingly assembled scattered documents and facts to finally pinpoint with certainty the day it all began and the events that could be considered key milestones in the hospital’s history.
FROM FIRST MENTIONS TO 19th CENTURY REFORM
The first building that hosted Preobrazhenskaya Hospital, originally known as Moscow Dolgauz, opened its doors on June 15, 1808. In the 20 th century, it became routine to trace all anniversaries of the institution back to that date. But is that right? Could the mere fact that the hospital acquired its own building be considered the seminal event of the first inpatient psychiatric hospital in Moscow?
On July 13, 1777, Catherine the Great signed a decree mandating the opening of the House of Invalids in Moscow, with one of its “wards” dedicated to the care of the mentally ill. This is the date that, 100 years later, the doctors at Preobrazhenskaya Hospital referred to as the starting point in the history of their institution [8] . One of their main arguments was the fact that, on May 17, 1792, Catherine the Great issued a decree [1] establishing for the first time the position of Special Doctor at the mental health hospital. Hence, this decree confirms that this type of social institution for people with mental disorders already existed in 1792.
According to the decree signed by Catherine the Great, the primary role in the observation of patients was assigned to the warden, who was in charge not only of the guards (retired soldiers), but also of the doctor responsible for the professional supervision of patients. In reality, however, the staff physician had to juggle work at the mental health hospital with his duties in the nursing home, the hospice, and the almshouse. As a result, his attention was limited to those patients who had a chance of recovery [13] .
When assessing the efforts of the first doctors at the mental health hospital, such as F. Raschke, then C. Pouliard, A. Blimmer, J. Karas (and all this happened long before the hospital had its own building), N. N. Bazhenov wrote in his book about Preobrazhenskaya Hospital: “It is important to note that even then there was a firm belief that the insane person was a patient, with all that such a conclusion entailed, including examination by a physician, admission to the mental health hospital for treatment (no matter how crude and primitive that treatment might have been), and finally discharge when the physician was satisfied that the goal of admission (a cure) had been achieved” [10] .
Other doctors at Preobrazhenskaya Hospital also left their mark in the history of Russian psychiatry of the 19 th century. For example, Zinovy Ivanovich Kibalchich, Chief Doctor of the hospital in 1811–1828, left us a documented description of the prevailing realities in a mental hospital at the beginning of the 19 th century. In his 1821 article “Report on the House of the Insane in Moscow and the Methods of Treatment Used There” published in the Journal of the Imperial Philanthropic Society (issue No. 11, 1821), he not only described in detail Moscow Dolgauz and the methods of treatment used there, but he was also one of the first to point out the existence of mental disorders that are now referred to as “borderline conditions” [14] .
Vasily Fedorovich Sabler, chief doctor of Preobrazhenskaya Hospital in 1828–1871, was a true “revolutionary” in the early history of psychiatric care in Russia ( Figure 1 ).

A brilliant clinician and talented scientist, V. F. Sabler provided evidence for the nosological independence of progressive paralysis, described its accompanying mental and neurological disorders, and developed humanistic principles of individual approach to patients. He was one of the first to hypothesize that some forms of illness can evolve into others, and that severe somatic illness accompanied by high body temperature (fever) can contribute to the cure of psychosis.
In the history of Preobrazhenskaya Hospital, V. F. Sabler played an equally prominent role as an outstanding manager. With a radical reform of the hospital’s management system, he ensured that the Chief Doctor would become the actual head of the institution. He supervised all areas of the hospital’s activities and prepared reports on the clinic that were published in the press (including in Europe).
This administrative reform marked a dramatic shift in attitudes toward the mentally ill. V. F. Sabler was greatly influenced by Philippe Pinel’s concept, which led him to completely overhaul the patient management system, finally replacing the chains used on violent patients with straitjackets and restraint chairs with straps.
It was the first instance when treatment was given priority over charity. This included the first patient histories (known as “case sheets”, see Figure S1 in the Supplementary File 1 ) and prescription books. Depending on the course of their disease, patients were categorized as acute or chronic and treated using a different therapeutic approaches.
The new emphasis was not only on the medical observation of the patients, but also on their moral challenges and re-education. Patients were no longer seen as “dangerous madmen” but as “unreasonable children” who needed proper care and exercise. That is why occupational therapy was considered so important. According to the instruction “On the Exercises for the Sick People Placed at the Mental Health Hospital” published in 1834, each patient was assigned a strictly individual occupation. It was then that Preobrazhenskaya Hospital established a sewing shop, a tailor’s shop, a shoemaker’s shop, a dyer’s shop, a paint shop, a plasterer’s shop, and a vegetable garden. The women could also knit socks and embroider canvas.
V. F. Sabler initiated the effort to draft legislation on the mentally ill, which provided the impetus to address a long overdue problem in the patient examination process. For centuries, medical matters had been handled by officials with no expertise in diagnosing mental illness, and during the reign of Nicholas I, the authorities began committing patients to institutions “pending further orders” rather than “pending recovery”, as had always been the case. It was not until February 18, 1835, that a decree was issued establishing a procedure for forensic psychiatric examination that required convincing evidence of mental illness from credible medical experts.
In 1841, the so-called “special patient examination procedure” was introduced and implemented for the first time at Preobrazhenskaya Hospital. If in St. Petersburg the “lunatics” continued to be transported to the Provincial Board, in Moscow the “subjects” were now sent to Preobrazhenskaya Hospital for “expert examination” and placed in a ward specially purposed for such subjects in a section of St. Catherine’s Almshouse. Membership in the Patient Examination Committee was also established at that time and did not change until 1917. It included the hospital doctor, his/her assistant, the provincial marshal of the nobility, the chief of the district police or the head of the city. Patients were discharged only after a new examination, which could take place at the end of a two-year “observation” period, and this period could be shortened only by special decision of the Senate.
The hospital owes both its name, Preobrazhenskaya, and the confirmation of its new official status as a medical institution to V. F. Sabler. It was he who on May 31, 1838, petitioned Emperor Nicholas I to sign a decree renaming the Moscow Dolgauz as the Preobrazhenskaya Mental Hospital.
Assessing the changes that took place in the hospital during the first hundred years of its existence, historians of psychiatry are quite right to note that as early as the middle of the 19 th century Preobrazhenskaya Hospital had made the transition from a “charity house” to an in-patient psychiatric institution and had evolved into “the center of not only practical but also scientific psychiatry, which became the tradition of the Moscow psychiatric school, distinguishing it from the St. Petersburg psychiatric school” [7] .
These changes, most of which were introduced during V. F. Sabler’s leadership, allowed Samuil Ivanovich Shteinberg (the hospital’s chief doctor in 1872–1877) to begin work on the institution’s first collection of scientific papers in the run-up to the centennial of Preobrazhenskaya Hospital in 1877. The preserved documents (“Preobrazhenskaya Hospital Office File on the Centennial Anniversary...”) show that the preparations for this anniversary had begun well in advance. As early as in February 1876, the chief physician, S. I. Shteinberg, wrote a letter to the trustees of Preobrazhenskaya Hospital with a detailed plan of the celebration. A circular letter was sent to the staff instructing S. S. Korsakov, N. I. Derzhavin, and V. R. Butzke to begin preparing articles identifying the major milestones in the history and development of the hospital (Figure S2 in the Supplementary File 1 ).
In the 1870s and 1880s, the hospital attracted a cadre of brilliant and exceptionally gifted young physicians who introduced the most advanced methods of patient care into existing medical practice. First of all, this applies to Sergey Sergeyevich Korsakov, the founder of the nosological branch of psychiatry, the creator of the Moscow scientific school and the author of a classic course in psychiatry [4,5] . His name is closely connected with the history of the “therapeutic revolution” at Preobrazhenskaya Hospital. The energy and reputation of S. S. Korsakov helped to complete and irretrievably establish “moral treatment” at the hospital and the “open door” policy (from 1889), followed by out-of-hospital care, which radically changed the entire approach to patients.
20 th CENTURY: TRANSFORMATIONS AND ACHIEVEMENTS
Looking back, it is impossible to ignore one obvious fact: almost all the chief doctors of Preobrazhenskaya Hospital in the period before the Russian Revolution of 1917 acted as reformers of the entire Russian psychiatric care system. An honorable place in this gallery of illustrious figures is occupied by Nikolai Nikolaevich Bazhenov, chief doctor of the hospital in 1904–1917 ( Figure 2 ).

Preobrazhenskaya Hospital owes its vast expansion and the introduction of the then — revolutionary system of “advanced care” to this fascinating figure of Russian psychiatry, outstanding clinician, ingenious manager, and respected teacher.
In the new “advanced care” system, the uneducated wardens and nannies were replaced by young medical interns and sisters of mercy. The doors to the wards were unlocked, the bars on the windows were replaced with tempered glass, and the straitjackets were displayed as museum pieces [15-17] . To ensure that patients were under continuous and competent supervision, the interns were required to live in the hospital, rotate on round-the-clock duty, welcome new admissions, and complete patient histories and observation diaries. All direct patient care was assigned to mid-level medical staff. Thirty-two sisters of mercy washed and fed the patients, gave them baths, accompanied them on walks, etc. Each ward had a head nurse who distributed medications, served lunch and dinner, was in charge of laundry, and performed other household duties. Nannies and servants were assigned only janitorial duties. In the spirit of those times, the hospital widely applied a system of moral influence, a prototype of today’s psychosocial therapy that included respectful treatment and support of patients, their socialization, and involvement in various activities.
At the beginning of the 20 th century, with N. N. Bazhenov’s contribution, the hospital was transformed into a research and treatment institution, which became a center of advanced psychiatric knowledge. The scope of N. N. Bazhenov’s innovations is quite impressive: in just a few years the clinic, where at the turn of the century treatment of patients resembled more that in a prison than in a medical institution, was transformed into a modern hospital, on par with the best that Europe could offer [15-17] .
Preobrazhenskaya Hospital was also the place where the Law on the Mentally Ill, a revolutionary act for its time, was proposed 80 years before the adoption of the Russian Federal Law on Psychiatric Care in 1992. The legal principles outlined by N. N. Bazhenov at the first congress of the Russian Union of Neuropathologists and Psychiatrists in 1911 are still relevant today:
“The following issues need to be brought to the forefront of mental health care and legislated:
- The principle of extending state care to all mentally ill people in the country, and specifying the measures to implement this task and the central and local authorities responsible for these tasks.
- Conditions for allowing treatment at home in the patient’s own family.
- Sufficient safeguards must be in place to ensure that the principles of inviolability of the person and individual liberty can only be violated when the mental illness of the person in question makes this imperative” [18] .
N. Bazhenov is also connected with the first commemoration of the foundation of the hospital celebrated in the 20 th century. In December 1909 the 100 th anniversary of the opening of the first building hosting Preobrazhenskaya Hospital on Matrosskaya Tishina Street was commemorated in gushing but solemn fashion, with the participation of the general public.
By that time the clinic had already received a plot of 11 dessiatins of land with the two and three-story buildings of the former Kotov factory (known as “Kotov’s Half”) ( Figure 3 ).

The factory buildings were refurbished, and a dormitory for the staff was equipped with ventilation, plumbing, and even central heating, which allowed N. N. Bazhenov to write proudly that “now Preobrazhenskaya Hospital has such premises for the staff that few Russian or even Western European hospital institutions can boast of” [10] .
However, the problem of overcrowding could be solved only by the construction of new buildings on Kotov’s Half, which required additional funds. So, N. N. Bazhenov decided to organize a gala evening for the city’s dignitaries on the former Kotov estate.
The day of the anniversary celebration was packed with events, including a solemn liturgy and breakfast for 300 guests; in the afternoon, there was a large concert by professional musicians from Moscow; a festive tea ceremony for patients, distribution of anniversary souvenirs, such as cups with the hospital insignia; and in the evening a banquet for 200 guests was held at the Kotov’s cottage located in a picturesque setting on the border of the Preobrazhenskaya and Sokolnicheskaya groves.
In addition to the concert, the highlight of the “cultural program” was the exhibition, for which N. N. Bazhenov selected not only everyday objects from psychiatric hospitals of different centuries (straitjacket, restraint chair, and “case sheets”), but also the creative works of patients (paintings and caricatures, wood and paper crafts, embroidery, and knitting). The models of Preobrazhenskaya Hospital and the Eiffel Tower were particularly popular with the public, because of their size and resemblance to the originals.
In addition to the gala dinner, the guests were treated to a theatrical performance, which included an act from the play “The Marriage of Krechinsky”, with a reference to Preobrazhenskaya Hospital, and, at the end of the evening, fireworks from an area near the buildings in Kotov’s Half — N. N. Bazhenov did not miss a single opportunity to draw the attention of the patrons and city authorities to the matter of financing the future construction. In 1910–1914, his work culminated in the successful completion of three new buildings and repairs to the old factory facilities on Kotov’s Half.
But let’s take a closer look at the year of this anniversary: Why was it celebrated in 1909? For a long time, 1809 was mistakenly considered the year in which the first specialized hospital for the mentally ill was opened. It was mentioned both in the Historical Essay on the Imperial St. Catherine’s Almshouse by V. Molnar [13] and in the Historical Essay on Preobrazhenskaya Hospital by I. V. Konstantinovsky [9] . For this reason, the anniversary was celebrated in 1909 and the following plaque was installed on the facade of the building: “1809–1909: To the centenary of the Preobrazhenskaya Mental Hospital, the first in Moscow designed specifically for psychiatric purposes”.
Only later, while working on the manuscript of his book “The Moscow Dolgauz” or “Essays on the History of Preobrazhenskaya Hospital” did N. N. Bazhenov study the documents in the hospital archives and found out that the new mental health hospital in Preobrazhenskoye was opened earlier, in June 1808, when 53 patients from the house of the former Secret Expedition were transferred to the building on Matrosskaya Tishina 1 [10] .
By the beginning of the 20 th century, the records had cemented all three major milestones in the history of the establishment of Preobrazhenskaya Hospital: 1777, 1808, and 1838. One might think that this would have settled the question of the first dates for future celebrations once and for all.
However, the revolution of 1917 and the subsequent division of the hospitals sowed confusion into the “question of anniversaries”. In the spirit of Soviet traditions, Preobrazhenskaya Hospital was stripped of its former name in 1920 and became Moscow City Hospital No. 1. What’s more, in 1931, it was divided into two independent medical institutions with different goals and missions. The hospitals kept changing names, numbers, internal organizational structure, and overall scope of activities, and only relatively recently, in 2017, did the two hospitals return to their historical roots by merging under the name of P.B. Gannushkin Mental-health Clinic No. 4 ( Figure 4 ).

Over the next 100 years, Kotov’s half of Preobrazhenskaya Hospital acquired a different, but equally illustrious, name — Gannushkin Hospital. In the second half of the 20 th century, it maintained its position as an advanced center of research and practice, with many pioneering milestones in the history of Russian psychiatry:
- It developed the system of maintenance therapy, which is so important in preventing relapses.
- For the first time in the USSR, it began to use insulin shock therapy (under the direction of M. Y. Sereisky), as well as electroconvulsive therapy (with the contribution of G. A. Rotshtein).
- It also marked the beginning of the “psychopharmacological treatment era in psychiatry” with the trials of many medications that were subsequently integrated into mainstream clinical practice.
RECENT DEVELOPMENTS
Reflecting on the title of this article, “Celebrating a Storied History”, one may note that in 2022 the institution historically known as Preobrazhenskaya Hospital will celebrate its anniversary for the first time in more than a century since that memorable evening organized by N. N. Bazhenov at the former Kotov estate. How does Gannushkin Hospital, the illustrious heir to the great traditions established by Preobrazhenskaya Hospital, look at the new generation in the year of its 245 th anniversary?
More recently, just 3–4 years ago, it got a facelift after extensive repair and construction work to restore the buildings dating back to the early 20 th century. Most importantly, the reorganization allowed for more streamlined psychiatric care, created a common information space, rationalized territorial localization, and brought patient treatment and routing patterns into a consolidated format.
With four specialized clinics in operation since 2020, the hospital now has several new structural units, including a clinic for affective and suicidal disorders, a clinic for borderline conditions, a clinic for first psychotic episodes, a clinic for pharmacoresistant conditions, and a clinic for mental disorders that are compounded by substance abuse. The Mental Health Counseling Center, opened in 2021, provides outpatient care for individuals suffering from various mental disorders including somatoform, stress-related, and neurotic disorders.
Today Gannushkin Hospital boasts a center for complex diagnostics, a clinical and diagnostic department with specialized clinics (such as dentistry, ophthalmology, gynecology, ENT, ultrasound), an anesthesiology and intensive care unit, a clinical and diagnostic laboratory, a psychological and psychotherapeutic center, a social and legal assistance center, as well as a physiotherapy department (including a transcranial magnetic stimulation room and xenon therapy room), pharmacy, X-ray rooms, and a physiotherapy room.
At the moment, the hospital has 9 outpatient branches known as Psychoneurological Dispensaries (PNDs), some of which have a history spanning more than 100 years. 2 Three Memory Clinics were founded on the basis of PND. These medical and rehabilitation units are designed to help elderly patients with early signs of dementia and mild cognitive decline.
The staff of the oldest psychiatric hospital in Moscow has carefully passed down to younger generations traditions that combine the utmost sense of humanity and the highest level of professionalism in helping patients with mental disorders. These traditions are the cornerstone that enables the team at Mental-health Clinic No. 4 named after P. B. Gannushkin to live its mission every day by providing personalized and comprehensive mental health care based on the principles of partnership and trust, with the aim of restoring and maintaining a high quality of life for its patients.
Authors’ contribution
All the authors made a significant contribution to the article.
The research was carried out without additional funding.
Conflict of interest
The authors declare no conflicts of interest.
Supplementary data
Supplementary material related to this article can be found in the online version at doi: 10.17816/CP3704
Supplementary File 1
Figure S1 . «Case sheets».
1 The house on Myasnitskaya Street, formerly owned by the Secret Expedition, was transferred to the Public Charity Office in the early 19 th century. This is where the patients of the House of Invalids and the Madhouse were accommodated in 1801.
2 PND No. 8, for example, was founded in 1919 and made psychiatric history as the prototype of the emerging district-level psychiatric care in Soviet Russia.
- Digest of Laws of the Russian Empire. Saint Petersburg: Typography of the second division of the Emperor’s Chancellery; 1857. Vol.13. Laws on national welfare, public care and medicine [ Google Scholar ]
- Savenko U. S. 200 years of Preobrazhenskaya psychiatric hospital. Nezavisimii psychiatricheskii journal. 2008;(2):5. [ Google Scholar ]
- Aleksandrovsky U. A. History of Russian psychiatry. Moscow: GEOTAR-Media; 2013. Vol. 3. Psychiatry in persons [ Google Scholar ]
- Gilyarovskiy V. A. Memoirs. — Transcript of conversation from 16.09.1944. Museum of Psychiatric Hospital № 4 (Moscow); 1944. [ Google Scholar ]
- Cannabich U. V. History of psychiatry. Moscow: CTR MGP VOS; 1994. [ Google Scholar ]
- Tzetlin S. L. Memoirs. Transcript of conversation from 26.05.1944. Moscow: Museum of Psychiatric Hospital № 4; 1944. [ Google Scholar ]
- Yudin T. I. Essays on history of Russian psychiatry. Moscow: Miedgiz; 1951. [ Google Scholar ]
- Konstantinovsky I. V. Historical essay on Preobrazhenskaya hospital for insane people in Moscow. Moscow: G. Lissner and A. Gieshiel’s typography; 1897. [ Google Scholar ]
- Bazhenov N. N. History of Moscow Dolgauz, now Moscow city Preobrazhenskaya hospital for insanes. Moscow: Moscow city public government; 1909. [ Google Scholar ]
- Dzhagarov M. A. In: Report of the 1st Moscow psychiatric hospital from 1938. Dzhagarov M. A. , editor. Мoscow: The 1st Moscow psychiatric hospital; 1939. A brief historical essay [ Google Scholar ]
- Aleksandrovsky A. B. 140 ages of Moscow psychiatric hospital (former Preobrazhenskaya hospital) Forthcoming; 1950. [ Google Scholar ]
- Molnar V. Historical essay of the Emperor Ekaterinian asylum and the institutions of Public Care Government (Prikaz) which had its origins inside the asylum’s walls. Moscow: Moscow city typography; 1888. [ Google Scholar ]
- Kibalchich Z. I. Note on the Asylum for insane people in Moscow and on the methods of treatment used there Journal of the Emperor philanthropic society. 1821;(11) [ Google Scholar ]
- Gilyarovsky V. A. Personality and activity of N.N. Bazhenov (obituary) Journal of psychology. 1923;(3):5. [ Google Scholar ]
- Korkina M. V. Nikolai Nikolaievich Bazhenov: to the 150th anniversary S.S. Korsakov Journal of Neurology and Psychiatry. 2007; 107 (1):58. [ PubMed ] [ Google Scholar ]
- Voskresensky B. A., Ostapietz E. A. 150 year anniversary of Nikolai Nikolaevich Bazhenov Independent psychiatric journal. 2007;(4):8. [ Google Scholar ]
- Bazhenov N. N. Project of law on insane people and the explanatory note. Moscow: Moscow City typography; 1911. [ Google Scholar ]
Sitewide search

The UCLA Center for Health Policy Research (CHPR) is one of the nation's leading health policy research centers and the premier source of health policy information for California.
Browse Publications
Find an expert, view all projects.
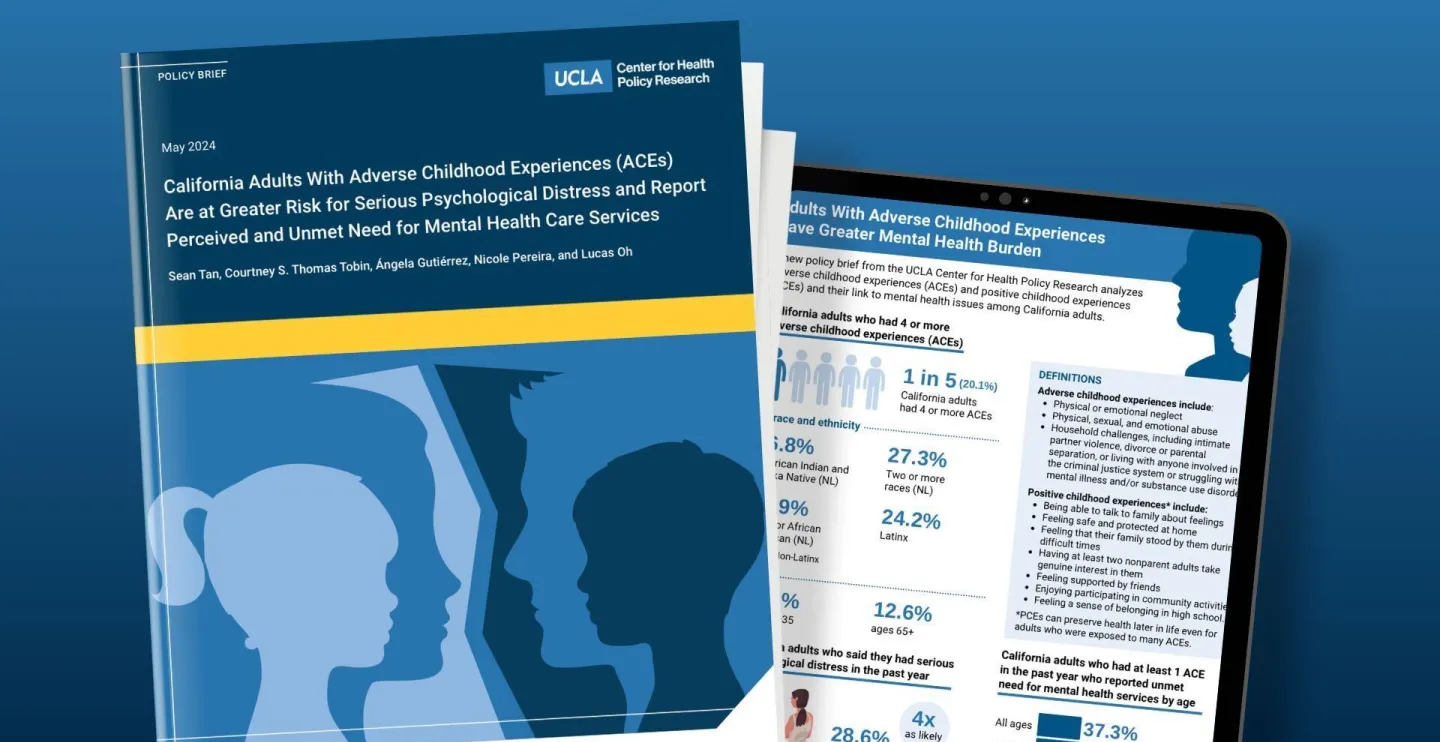
California Adults With Adverse Childhood Experiences (ACEs) Are at Greater Risk for Serious Psychological Distress and Report Perceived and Unmet Need for Mental Health Care Services
Summary: This policy brief uses data from the 2022 California Health Interview Survey to analyze the distribution of adverse childhood experiences (ACEs) and positive childhood experiences (PCEs) and their relationship to mental health issues such as serious psychological distress (SPD) and to perceived need and unmet need for mental health care among California adults.
Findings: About 1 in 5 California adults had high exposure to adverse childhood experiences (ACEs) in childhood (had four or more). Compared to adults ages 65 and older, greater proportions of young- (ages 18 to 35) and middle-aged adults (ages 36 to 49) had four or more ACEs. Adults who identified as Native American or Alaska Native, Latinx, Black or African American, or as belonging to two or more racial or ethnic groups, were more likely to have had high exposure to ACEs. Relative to California adults without any ACEs, a larger proportion of adults with four or more ACEs experienced SPD and had a perceived and unmet need for mental health services in the past year.
A larger proportion of older adults had four or more positive childhood experiences (PCEs) compared to young - and middle-aged adults. Compared to other racial and ethnic categories, adults identifying as Latinx, Black or African American, or as belonging to two or more racial and ethnic categories were more likely to report not having had any PCEs. Adults who did not have any PCEs were more likely to report experiencing SPD in the past year.
Read the Publication:
- Policy Brief: California Adults With Adverse Childhood Experiences (ACEs) Are at Greater Risk for Serious Psychological Distress and Report Perceived and Unmet Need for Mental Health Care Services
- Infographic
Social media links
Copied to clipboard

IMAGES
VIDEO
COMMENTS
The mental health crisis in the US underscores the invaluable role that social workers play. Their dedication, expertise, and community-focused approach are essential in providing support to individuals in need. Columbia School of Social Work plays a pivotal role in bolstering the impact and effectiveness of social workers in mental health care.
The role of social workers in community mental health is embedded in the broader relationship of people to social institutions. Social work's concern with the quality of life is sanctioned by the social system and involves, of necessity, some commitment to the institutions that organize and govern secular life.
Some common duties of a social worker include: Identifying and reaching out to those in need. Assessing people's needs and implementing a plan of action. Helping people adjust to major life ...
The title of books for social workers published more than 100 years ago such as Social Work in Hospitals: A Contribution to Progressive Medicine (Cannon, Citation 1913) or Social Work: Essays on the Meeting-Ground of Doctor and Social Worker (Cabot, Citation 1919), capture the essence of how the profession has connected social and environmental ...
Emotions are fundamental to human experience; they have numerous purposes and functions, from alerting people to danger to helping them build social relationships (Grant et al., 2014).Morrison (2007) has argued that social work needs to identify its claims to professional competence at a time of continuous change and that this requires social workers to handle both their own and others ...
The finding that social workers were involved in medication monitoring in a substantial minority of teams points to the need for training in this task to become a core part of mental health social work education (Bentley et al. 2005; Hughes & Cohen, 2010) and to the need for clarification of the social work role in this context. Finally, the ...
Mental Health And Social Work. Decent Essays. 1135 Words. 5 Pages. Open Document. Mental illness has become one of the most rapidly growing diagnoses to date ranging from clinical depression to Schizophrenia. It has become a worldwide epidemic and has created a shortage of specialized workers. As the shortage of veteran mental health workers ...
Introduction. Mental health and addiction concerns affect millions of individuals worldwide. They are the leading cause of the global burden of disease 1 2 and are among the primary causes of disability around the world. 3 In the USA, one in five adults (43.6 million) report a form of mental illness across a 1 year period, and there are >21.5 million individuals with substance use disorders. 4 ...
Mental health social workers remain a minority within a medically dominated workforce (Evans et al., 2012) meaning that when teams and services are faced with managing crises in an increasingly austere environment it might become more difficult for social workers to 'argue the importance of … a person's right to accommodation, building ...
from mental stress and strain encountered by workers in helping professions that include social workers. In helping professions such as nursing, social work, teaching, and ministry, there has been research on the concept of burnout and its effects on professionals. Maslach (2003) noted that the basic aspects of burnout are prevalent in research
Social work supports a holistic approach in mental health. The spirit dimension has emerged to be an important area in social work (Ow and Saparin 2014).Western-trained social workers have long been taught to avoid discussing spirituality (or religiosity) and its meaning for clients (Holloway 2007).This has resulted in failing to understand clients' knowledge and the meaning of spirituality ...
Client Attitudes toward Integrating Religion and Spirituality in Mental Health Treatment: Scale Development and Client Responses. Holly K. Oxhandler, James W. Ellor, and Matthew S. Stanford. Volume 63, Issue 4, October 2018, Pages 337-346. The Power of Prevention and Youth Voice: A Strategy for Social Work to Ensure Youths' Healthy Development.
Mental health social workers often occupy complex and contradictory spaces that are shaped by a range of legal, policy, and societal drivers. Although there are broad, commonly understood definitions of mental health social work in Australasia, the United Kingdom, and North America, practitioners often need to adjust their interventions to take ...
The mental health social worker experiences unique challenges on a daily basis. A social worker's well-being affects not only the social worker at the individual level; but also directly affects agency and client outcomes, which in turn impacts the mental health system. Adequate support is crucial in maintaining social workers' positive well-being (Graham & Shier, 2014). Current rates of ...
Advocacy is a very important role played by social workers especially as mental health service users are a group 'marginalised in some way by society' and it is 'about redressing the balance and helping voices to be heard, which otherwise would have gone unheard' (Beckett 2009:122). People with mental health problems experience ...
Mental health, an integral facet of human well-being, shapes our emotions, decisions, and daily interactions. Just as one would care for a sprained ankle or a fever, our minds too require attention and nurture. In today's bustling world, mental well-being is often put on the back burner, overshadowed by the immediate demands of life.
Mental health social workers contribute greatly to the community in undertaking a task that most people do not have the heart, disposition or courage to do. If more people were to delve into the profession, the community and the families dealing with mental illnesses would benefit significantly. NAME : Kerril Sommerville.
Importance of Social Workers in Mental Health Setting. Nonetheless, psychiatric social workers play an important role in supporting various families, individuals, and, most importantly, communities as they tend to overcome the day-to-day challenges hindering their well-being. An illustration of this is the motive to address the patient's ...
what is the readiness of social work students to work with autistic individuals?, ignacio aguilar pelaez. pdf. examining experiences among social workers working with parents who suffer from substance use disorder, alicia alvarado and eleno zepeda. pdf. covid-19, social isolation, and msw students' mental health, cassandra barajas. pdf
Transforming mental health care into a recovery-oriented system will require further consideration of person-centered care planning as well as the impact of limited resources especially for those living in poverty. ... School of Social Work, University of Southern California, 1150 S. Olive Street, #1429, Los Angeles, CA, 90015-2211, USA.
Social isolation and loneliness frequently co-occur but can also occur separately; both are associated with increased morbidity and mortality across all age groups, with worse health outcomes in mental, cardiovascular and neurological health. Perhaps most significantly, both are associated with an almost 30% higher rates of premature death ...
Innovations in the range of evidence based medications, therapy and psychosocial services such as psychiatric rehabilitation, housing, employment and peer supports have made wellness and recovery a reality for people living with mental health conditions. Choosing the right mix of treatments and supports that work for you is an important step in the recovery process. […]
A greater proportion of suicide deaths occurred among Black (10.4%) and Latino (7.8%) children and adolescents. Conversely, less than 3% of suicides among Asian and white individuals occurred ...
Behavioral Health Technician. Behavioral Health Technicians (BHT) work under the supervision of licensed professionals, such as social workers, psychologists, or psychiatrists, to support the overall treatment and care of individuals with mental health or behavioral disorders. This 20-credit sequence of courses, open to enrolled undergraduate U ...
Social Media Bans Alone Won't Improve Mental Health, Say Student Advocates. There is a significant perception gap between educators and students when it comes to the impact of social media on ...
COVID-19 Fear, Mental Health, and Substance Misuse Conditions Among University Social Work Students in Israel and Russia Int J Ment Health Addict . 2022;20(1):316-323. doi: 10.1007/s11469-020-00360-7.
In 2022, Mental-health Clinic No. 4 named after P. B. Gannushkin, one of the oldest mental health institutions in Russia known as Preobrazhenskaya Hospital before the October Revolution of 1917, celebrated its 245 th anniversary. The history of the hospital reflects all stages of the evolution of the basic principles and aspects of mental health care in Russia.
Promote Employee Mental Health and Wellbeing. The COVID-19 pandemic will affect the mental health and wellbeing of employees well beyond the immediacy of the initial crisis. Employers have a unique ability and responsibility to encourage and maintain a culture of wellbeing in the workplace. Employers can take action to identify, engage and ...
Care; and Human Rights in Mental Health. Keynote speeches delivered by experts and executives will be followed by panel discussions, forums, conferences, the Mental Health EXPO showcase, social & cultural events. Outstanding expertise and vast experience in the field of mental health, excellent accommodation facilities, cultural attractions of ...
Summary: This policy brief uses data from the 2022 California Health Interview Survey to analyze the distribution of adverse childhood experiences (ACEs) and positive childhood experiences (PCEs) and their relationship to mental health issues such as serious psychological distress (SPD) and to perceived need and unmet need for mental health care among California adults.