
- Request new password
- Create a new account

Essentials of Mental Health Nursing
Student resources, chapter 25: mental health risk assessment: a personalised approach, case study: high risk indicators.
Jenny is 35 and lives with her husband and 9-year-old son. Though employed as a welfare officer, she has felt unable to work for over three months. A new manager joined her team six months ago, and has criticised her work performance on several occasions. Jenny has felt low since her mother died a year ago, to whom she was very close. She has been finding it difficult to motivate herself, is struggling to sleep properly, has begun to think that everything is pointless and is going wrong, and has again begun to think about taking an overdose. She believes that her husband has had enough of her ‘moods’ and irritability, and fears he may leave her.
Jenny has had two in-patient admissions in the last four years, each precipitated by her taking a significant overdose of prescribed antidepressant and anxiolytic medication, with alcohol. On each occasion, she had felt highly stressed for a prolonged period: moving accommodation; trying to complete a college course; trying to look after her young son; missing her husband whilst he is away working as a lorry driver.
Jenny has again been feeling very stressed, particularly when trying to respond to the demands of her 77-year-old, proud and independent father, who lives nearby – becoming increasingly infirm, he has had a couple of recent falls. Jenny has always had a difficult relationship with her father, who is often critical of her and always favoured her brother. Though close to her only brother, he lives over 200 miles away.
- What are some relevant examples of static and dynamic risk factors?
- Which would merit special attention as ‘high’ risk indicators?
- What are some relevant protective factors?
- Which structured assessment tools might be helpful in complementing the assessment process?
- What might be some limitations of these tools?
- Sketch out a formulation using the 5Ps framework.
- What ideas would this give you about the specific focus for treatment and care?
› Possible answer
- e.g. sensitive to criticism, history of overdoses, loss (of mother), prolonged stress, limited supports, sense of isolation, hopelessness, suicidal ideation.
- e.g. previous significant risk behaviour, prolonged stress (given her previous experiences), active suicidal intent (planning and preparation).
- e.g. strong family values/relationships, support from husband and brother, having a job, positive and active engagement with the mental health service, previous response to treatment and recovery.
- e.g. START, Beck Hopelessness Scale, Beck Suicide Intent Scale, a Depression Inventory, mood diary/thought record, baseline activity monitoring schedule, sleep chart, and a simple mood scaling record.
- e.g. level of subjectivity, potential bias in completion (both for self and observer/practitioner rated tools), over-focus upon symptoms, potential for increasing distress, poor use/completion as a consequence of features of the illness (e.g. low motivation).
- Compare your sketch with the following example formulation diagram
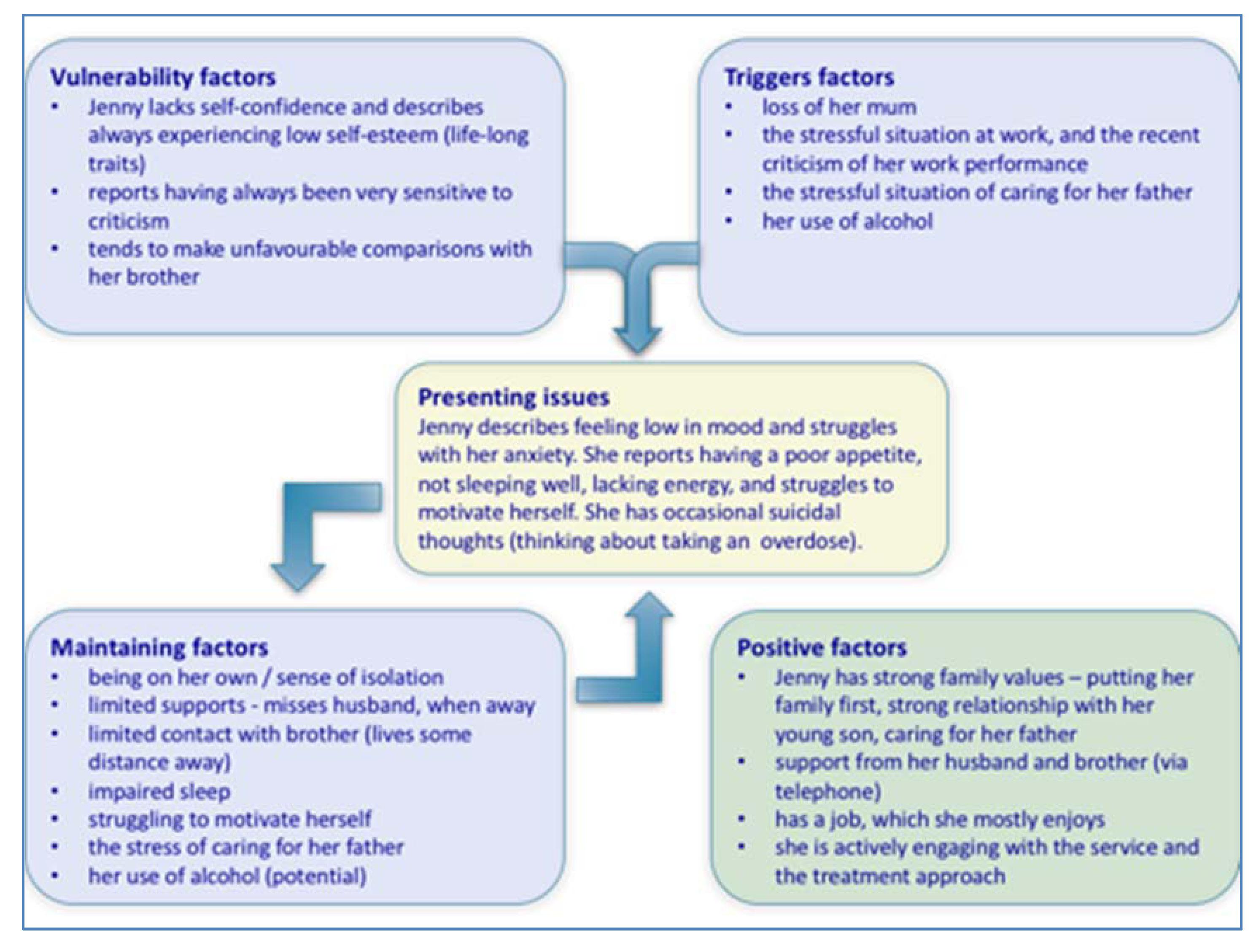
7. What ideas would this give you about the specific focus for treatment and care?
Compare your response with the following – you may have considered assisting Jenny to:
form an illness timeline. set and work towards personal goals – incorporating opportunities for positive risk taking. form a rationale and engage in the following interventions – as examples : sleep promoting strategies. building confidence and cultivating self-esteem. activity planning and self-monitoring. developing skills in structured problem-solving. recognising and responding to unhelpful thoughts. practising methods of relaxation and stress management. mobilising her support network . staying well planning (relapse prevention planning). pharmacological option (as part of a combined pharmacological and psychosocial approach): anti-depressant medication.
- Research article
- Open access
- Published: 25 November 2021
Mental health professionals’ perceived barriers and enablers to shared decision-making in risk assessment and risk management: a qualitative systematic review
- Nafiso Ahmed ORCID: orcid.org/0000-0001-6732-1317 1 ,
- Sally Barlow 1 ,
- Lisa Reynolds 2 ,
- Nicholas Drey 3 ,
- Fareha Begum 1 ,
- Elizabeth Tuudah 4 &
- Alan Simpson 4 , 5 , 6
BMC Psychiatry volume 21 , Article number: 594 ( 2021 ) Cite this article
25k Accesses
9 Citations
36 Altmetric
Metrics details
Risk assessment and risk management are fundamental processes in the delivery of safe and effective mental health care, yet studies have shown that service users are often not directly involved or are unaware that an assessment has taken place. Shared decision-making in mental health systems is supported by research and advocated in policy. This systematic review (PROSPERO: CRD42016050457) aimed to explore the perceived barriers and enablers to implementing shared decision-making in risk assessment and risk management from mental health professionals’ perspectives.
PRISMA guidelines were followed in the conduct and reporting of this review. Medline, CINAHL, EMBASE, PsycINFO, AMED and Internurse were systematically searched from inception to December 2019. Data were mapped directly into the Theoretical Domains Framework (TDF), a psychological framework that includes 14 domains relevant to behaviour change. Thematic synthesis was used to identify potential barriers and enablers within each domain. Data were then matched to the three components of the COM-B model: Capability, Opportunity, and Motivation.
Twenty studies met the eligibility criteria. The findings of this review indicate that shared decision-making is not a concept commonly used in mental health services when exploring processes of risk assessment and risk management. The key barriers identified were ‘power and best interest’ (social influences) and ‘my professional role and responsibility’ (social/professional role and identity). Key enablers were ‘therapeutic relationship’ (social influences) and ‘value collaboration’ (reinforcement). The salient barriers, enablers and linked TDF domains matched COM-B components ‘opportunity’ and ‘motivation’.
The review highlights the need for further empirical research to better understand current practice and mental health professionals’ experiences and attitudes towards shared decision-making in risk assessment and risk management.
Peer Review reports
In mental health services, Shared Decision Making (SDM) is a means of delivering recovery orientated care through involving individuals in decisions about their care. For a decision to be ‘shared’ it must involve: at least two participants, the sharing of information, and a decision that is made and agreed upon by all parties [ 1 ]. These criteria are reflected in a shared decision model [ 2 ], which proposes that SDM occurs when all participants are informed, involved, and influential in the decision-making process. It is, however, emphasised that the three SDM components are on a sliding scale of influence that is dependent on context, capacity and desire to influence [ 2 ].
In shared decision-making, the aim is to recognise and utilise the unique expertise of healthcare professionals and services users to produce better decisions, and potentially better outcomes. While healthcare professionals may be experts in diagnosis, aetiology, prognosis, treatment options, and outcome probabilities [ 3 ]; service users are experts about the impact of the condition on their lives, their preferences, their personal attitudes towards risks, and often know what works best for them regarding their condition and treatment [ 4 ].
Studies report positive effects of SDM interventions on patient outcomes within different mental health populations. A randomised control trial (RCT) for people with depression reported a positive impact on patient participation in treatment decision-making and patient satisfaction [ 5 ]. Another RCT of an intervention for people with schizophrenia found SDM improved social recovery [ 6 ]. A pilot trial of a SDM intervention with veterans with post-traumatic stress disorder (PTSD) found positive impacts on patients’ receptivity to evidence-based treatment [ 7 ]. In contrast, some studies report no significant effect of SDM on clinical outcomes for people with severe mental illness [ 8 ] and depression [ 9 ], although they acknowledge that further long-term work may be needed to detect an effect.
Shared decision-making is endorsed and advocated in international healthcare policy [ 10 , 11 ]. Research has found that both service users and professionals support SDM. A qualitative research synthesis examining stakeholders’ attitudes towards SDM in mental health reported that service users valued their voice being heard, listened to, and supported to express themselves in encounters with professionals [ 12 ]. Several barriers to SDM were identified from the service user’s perspective, including feelings of perceived inadequacy, fear of being judged and a lack of trust. Barriers to SDM for professionals included: the service user lacking cognitive capacity or insight; where stigma negatively influenced the service user’s attitude towards SDM; and the professional’s own attitudes, motivation, willingness, empathy, and ability to engage and implement SDM. Professionals also highlighted challenges surrounding the competing priorities of their role, mainly them being accountable and responsible for managing risk.
Implementing SDM may pose challenges when there are concerns about the potential risks to self or others [ 13 , 14 ]. In these circumstances, mental health professionals (MHP) may not feel able to engage service users in decisions about their care. Potential barriers cited in the literature include inadequate training in suicide prevention [ 15 ]; fears about negative adverse reaction from individuals who pose a risk to other [ 16 ] and the ‘blame culture’ observed in mental health care [ 17 ], whereby MHPs are increasingly fearful of culpability and litigation. It has been suggested that this has resulted in more defensive or risk-averse practice intended to prevent harm [ 18 , 19 ].
Risk in mental health care is often used to refer to the possibility of an adverse event, outcome or behaviour arising from the unwanted actions of the service user [ 20 , 21 ]: notably risk of harm to self, others, or both, and may include self-harm, suicide, or violence. Risk also signifies the vulnerabilities that a person with mental illness may be exposed to, such as side effects from medication, exploitation, victimisation, bullying, and discrimination [ 22 , 23 ]. These risks occur frequently but are considered less in the assessment and management of risks [ 24 ].
Risk Assessment (RA) and Risk Management (RM) are the mechanisms used by MHPs to identify and minimise risk. There are three main approaches to assessing risk in mental health care: unstructured clinical judgement, actuarial methods and structured clinical judgement [ 25 ]. Unstructured clinical judgement typically involves professionals making judgements based on their clinical experience, opinion, intuition or ‘gut feeling’. Actuarial methods provide the assessor with a statistical means to combine information and calculate risk [ 26 ]. The subjective nature and poor predictive accuracy of these approaches have resulted in recommendations for them not to be used on their own in clinical practice [ 27 ]. Structured clinical judgement is considered the best approach to assessing risk [ 28 ]; this involves the use of a standardised RA tool to aid a professional in their clinical judgement [ 25 ].
Nonetheless, studies have found wide variability in the methods used to assess risk in UK mental health services [ 29 ] and forensic services in Australia and New Zealand [ 30 ]. These studies agree that a more consistent approach to RA is needed in mental health services. A multitude of evidence-based guidance is available to help standardise the process and support professionals in their assessment of risk [ 28 , 31 , 32 , 33 ]. A model for assessing suicidality, for example, provides guidance on the importance of language, the structure of the clinical interview, questioning, actuarial tools and risk categorisation [ 31 ].
Risk management is informed by the RA and includes the key actions or strategies that are designed to prevent or limit undesirable outcomes. Strategies may include treatment, supervision (i.e. help with planning daily activities), or monitoring (i.e. identifying and looking out for early warning signs) [ 28 ]. Several RM and safety planning interventions have been developed that can be used to mitigate, contain or improve RM [ 34 , 35 , 36 ].
The need to involve service users in the RA and RM process has been advocated in current professional guidance, policy, and research [ 28 , 33 , 37 ]. Involving service users is a means of minimising the gap between professionals and service users’ perspectives of risk [ 38 , 39 ] and thus, ensuring that the plan developed meets the individual’s needs [ 33 ]. This can lead to more accurate prediction and management of risk. Another potential benefit of involvement is that the individual is empowered to take responsibility for their choices, which can be a motivator for change [ 40 ]. It has been suggested that service user involvement can improve confidence and self-management skills, which may have long term impacts on reducing dependency on services, thereby increasing cost-effectiveness [ 37 ].
The UK Department of Health (DH) best practice guideline, specifically recommends SDM. Studies have shown, however, that service users are often unaware that a RA has taken place [ 41 , 42 ].
Although Higgins, Doyle [ 24 ] found that more than three-quarters of MHPs reported ‘always’ involving service users in risk assessment (77.8%) and safety planning (78.4%), only 50% of the respondents reported that they ‘always’ informed service users about their risk level, while only 43% of the respondents reported that they ‘always’ developed a shared responsibility with the service user for safety. Despite professionals reporting a high rate of service user involvement, these findings suggest that SDM is not routinely nor fully implemented.
A recent systematic review of mixed methods studies explored the service users’ perspective of helpful RM practices within mental health services [ 43 ]. Two categories of beneficial RM practices were identified: interpersonal relationships and communication; and agency and autonomy. A key finding was that trust fosters openness in relationships and enables discussion of risks, especially when service users felt that their distress was understood or their accounts were validated by professionals. Service users preferred professionals to maintain responsibility for RM initially but that eventually (at their own pace) they wished to regain control.
Other systematic reviews in this field have focused on interventions that promote SDM in RA and RM in forensic mental health settings [ 36 , 44 ]. A qualitative synthesis of research examining professionals attitudes towards SDM in the broader field of mental health exists [ 12 ], however, the authors acknowledge that the rigour of a full systematic review was not adopted. There is currently no systematic review of MHPs’ experiences and attitudes towards implementing SDM in the assessment and management of risk. A synthesis of studies will improve our understanding of the discrepancies in reported practice and identify factors that may help or hinder its implementation. The specific review question was:
What do mental health professionals perceive as the barriers and enablers to SDM in RA and RM?
This review was conducted in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 45 ]. The protocol is registered on PROSPERO (CRD42016050457).
Eligibility criteria
The SPIDER framework (sample, phenomenon of interest, design, evaluation, research type) was used to specify eligibility criteria [ 46 ]. An additional S was added to capture the ‘setting’ criterion of adult mental health services. The SPIDER framework is a tool for developing a search strategy that has been designed from the PICO tool, specifically for reviews that aim to synthesise qualitative and mixed-method research studies. Due to limited resources, only studies written in English were included in the review. Table 1 lists the inclusion and exclusion criteria.
Search strategy
The EBSCOhost and Ovid Online platforms were used to search six electronic bibliographic databases: MEDLINE; EMBASE; PsycINFO; CINAHL; AMED and Internurse. Databases were searched from inception. The last search was completed on the 4th December 2019.
The search strategy used a combination of medical subject headings (MeSH) and free text key terms related to concepts of ‘mental health’, ‘health professionals’, ‘experiences’, ‘shared decision making’, ‘risk assessment’ and ‘risk management’. A full electronic search strategy is presented in Additional file 1 .
Two grey literature databases were also searched for relevant unpublished empirical research studies; Bielefeld Academic Search Engine (BASE) and Open Grey. Citation chaining was performed on all articles selected for inclusion to identify further studies of interest, and this involved searching the reference lists (backward chaining) and using Google Scholar to identify and review papers that had cited the included articles (forward chaining).
Study selection
Search results were imported into a systematic review management software EPPI-reviewer 4 [ 47 ] and duplicates removed. Two-stage screening was undertaken: stage 1 screened the titles and abstracts of studies against the eligibility criteria; stage 2, further assessed full-text of potential studies against the eligibility criteria. Study authors were contacted if more information was needed.
To minimise risk of bias, two authors (NA and FB) independently assessed titles and abstracts, and subsequently, full-text articles. A full-text review was carried out if at least one of the reviewers believed that the study met the inclusion criteria at the title and abstract screening stage. At full-text review, any discrepancies regarding eligibility were resolved by consensus and in consultation with a third author (AS/LR). Also, studies were included only once if they had multiple articles. The original or most relevant to the review question was used as the primary article for the study’s results.
The ‘Three I’s Scale of Influence Model’ [ 2 ] was used as a framework for study selection. Studies that reported on a least one of the three components (informed, involved and influential) of SDM in RA and RM were included. Stacey, Felton [ 2 ] definitions of the SDM components can be found in Additional file 2 .
Data extraction
An electronic data extraction form was devised and piloted on two of the included studies. The following data items were extracted: author(s), publication year, research question/aim, geographical location, sample size, setting, data collection, and method of analysis. The entire results sections, including direct quotations and author interpretations were imported directly into NVivo 11 software [ 48 ]. For studies with multiple publications, results were extracted and collated from all the linked reports but only one publication was used as the source of study results. Data extraction was carried out by the first author (NA) and cross-checked by a second author (SB): disagreements were resolved through discussion.
Quality appraisal
Dixon-Woods, Shaw [ 49 ] prompts were used to assess the quality and relevance of individual studies within this review. These prompts focus on the universal features of qualitative research and have been devised to ‘sensitise appraisers to the various dimensions of articles that require evaluation’ (p224). Two reviewers (NA and AJ or UF – see acknowledgements) read the papers independently and answered a series of questions on the quality appraisal checklist (e.g., Are the research questions clear?). They recorded their response as Yes (Y), No (N), Can’t tell (−). A rating system was then used to categorise the papers: Key paper (meets all quality criteria and clearly fits with review question); Satisfactory (meets most quality criteria and fits well to review question); Unsure (mixed responses to quality criteria and lack of clarity regarding relevance to review question); and Poor (does not meet quality criteria) [ 50 ]. No studies were excluded based on methodological quality; however, a sensitivity analysis (described below) was conducted to see the impact of removing lower-rated studies on the review findings. Any disagreements were discussed in full, and a rating was agreed (Additional file 3 ).
Data synthesis
The Theoretical Domains Framework (TDF) was used to explore the factors that influence the implementation of SDM in RA and RM with individuals with mental illness. The TDF is a behaviour change framework developed by a group of experts to simplify and integrate the large number of psychological theories relevant to behaviour change [ 51 ]. The TDF has been used by researchers across a range of healthcare settings to identify determinants of behaviour, namely the barriers and enablers to implementation, and to inform intervention design [ 52 ]. The original TDF has 12 domains derived from 33 health and social psychology theories and 128 key theoretical constructs. The framework was later validated and refined by Cane, O’Connor [ 52 ] to include 14 theoretical domains. The revised version of the framework was used in this review, Cane et al. (2012) definition of each domain is presented in (Additional file 2 ).
The Capability, Opportunity, and Motivation (COM-B) model was then used to condense the relevant TDF domains into three components that interact to predict behaviour. The model was developed as part of the broader framework of the behaviour change wheel [ 53 ] and provides a basis for intervention design. Each component of the COM-B model is divided into sub-components that capture important distinctions. Capability can be physical (e.g. skills) or psychological (e.g. interpersonal skills and knowledge) and represents an individual’s capacity to carry out the behaviour. Opportunity can be physical (e.g. environmental factors) and social (e.g. social influences) and is defined as all the factors that lie outside the individual that influence the behaviour. Motivation can be reflective (e.g. beliefs, intentions) or automatic (e.g. emotions) and characterises the brain processes that drive behaviour [ 53 ]. The most relevant TDF domains and linked components that are likely important to changing behaviour were identified [ 52 ].
The data synthesis process drew on established analysis methods recommended in the TDF guidelines [ 54 ], and used in previous studies applying the TDF [ 55 , 56 , 57 ]. Data synthesis involved the following six stages:
Step 1: developing a coding manual
A coding guide was developed based on the definitions of the three components of SDM [ 2 ], and the 14 domains and 84 constructs from Cane, O’Connor [ 52 ]. To provide guidance and confidence that a piece of text represents a domain, statements of how the domain applies to the research context were also included in the coding guide.
Step 2: pilot coding exercise
To ensure consistency between coders and refine the coding guideline, two coders (NA and ET) jointly coded the extracted findings from two randomly selected included papers. Any disagreements were discussed until consensus was reached; where consensus could not be reached a third researcher was consulted. The final version of the coding guide is included in Additional file 2 .
Step 3: coding papers and assessing reliability
Two researchers (NA and ET) independently coded the extracted findings from the remaining included papers using the coding guideline and via NVivo 11 software [ 48 ]. Findings relating to the target behaviour were coded to the SDM components [ 2 ], whereas potential barriers and enablers identified within the included papers were coded to the 14 domains of the TDF [ 52 ]. For example, the statement ‘“[the risk assessment is] one thing … you never discuss with service users just in case it alarms them”’ was coded to the ‘informed’ component and the ‘beliefs about consequences’ domain. If the participant’s response or the author’s interpretation represented more than one TDF domain, the text was coded to multiple domains. For example, “You know that you’re going to have suicide risk but you think well, the psychologists will deal with that bit … so to want to deal with it, even as part of the overall care, I think you’d want some type of supervision” was coded to both “social professionals’ role and identity” and “social influences”.
Inter-coder reliability was assessed by calculating the percentage agreement/disagreement (prior to consensus being reached), to measure consistency in coding within and across domains [ 58 ]. Reliability between two coders is considered acceptable if percentage agreement > 60% is achieved [ 54 ]. Discrepancies in coding were addressed by NA and ET with a consensus reached by discussion. AS was available to resolve any disputes over discrepancies; however, this was not required.
Step 4: developing overarching themes
Data within the domains were further analysed by the lead researcher (NA) using thematic synthesis [ 59 ]. Text coded into each domain were compared across papers, and findings representing similar ideas were grouped together. An overarching theme was then generated to categorise the initial themes. The overarching themes represent the specific factor perceived to influence SDM in RA and RM. For example, findings that suggest rapport, alliance or connection facilitate discussion about risk with service users were categorised as ‘therapeutic relationship’.
Step 5: mapping the COM-B model to the TDF domains
The relevant TDF domains were matched to the COM-B components [ 53 ]. The lead researcher (NA) drew on the links between the TDF domains and COM-B components identified by a group of experts in a consensus exercise reported in Cane, O’Connor [ 52 ]. The most relevant TDF domains (and themes within) were identified based on a frequency count of studies by domain. The TDF domains (and themes within) identified in at least 60% ( n = 11) of the included studies were considered salient in understanding the target behaviour.
Step 6: sensitivity analysis
A sensitivity analysis was carried out to determine whether the methodological quality of studies impacted on the findings of the review. The results from the lowest-rated studies were removed from the synthesis to see if this influenced the key themes originally identified. No studies were excluded based on methodological quality.
A total of 8211 papers were yielded in the databases searches; and 1420 additional papers were included from other sources. After the removal of duplicates, a total of 8652 papers were eligible for screening. Following title and abstract screening, 8491 papers were excluded, and 161 full text papers were reviewed; 134 papers were excluded at full-text, and 20 studies (reported in 27 papers) met the inclusion criteria for this review. The PRISMA diagram of study selection can be seen in Fig. 1 .
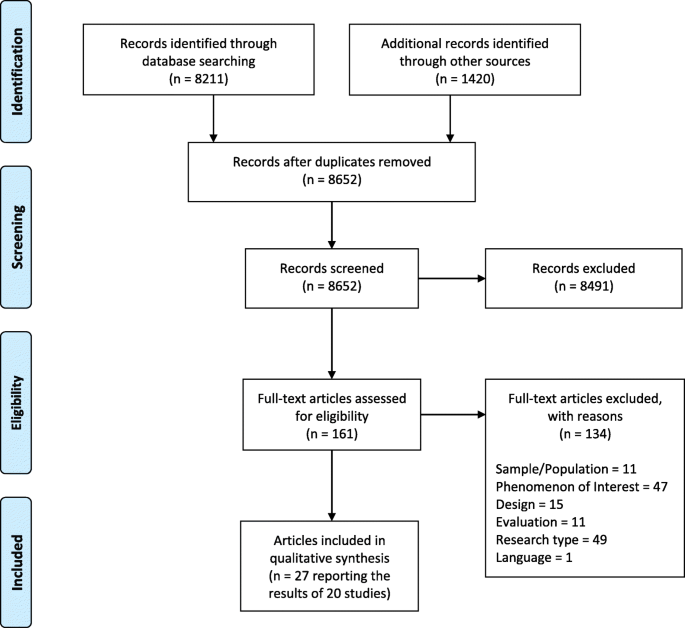
A PRISMA flow diagram detailing the search strategy and results (Moher et al., 2009) [ 45 ]
All papers gained the rating of either key paper ( n = 9) or satisfactory ( n = 11). Papers were rated satisfactory if they did not meet all of the quality criteria and/or did not clearly fit with the review question. For example, papers that reported on specific risk decisions i.e. decision-making regarding neuroleptic medication [ 60 ]; specific RM practices i.e. clinician-patient alliance during mechanical restraint [ 61 ]; or contained very limited findings relevant to the review question [ 62 ] were rated satisfactory. Quality appraisal of the included studies can be seen in Additional file 3 .
Study characteristics
Over half of the included studies were conducted in the UK ( n = 11), two in Belgium and the remaining studies in Australia, Canada, Taiwan, Denmark, Sweden, Italy, and Norway. The papers were published between 1999 and 2019 and were predominantly qualitative in design ( n = 18). Semi-structured interviews were the most common data collection method ( n = 15); four studies utilised focus groups [ 61 , 63 , 64 , 65 ]; and one used in-depth interviews [ 60 ]. Three studies used unstructured observation in addition to semi-structured interviews [ 66 , 67 , 68 ]. One study surveyed participants before conducting the qualitative interviews [ 69 ], and one described using a mixed-methods approach [ 65 ] comprising of focus groups and a quantitative analysis technique (i.e., inductive content analysis). Their findings, however, included several illustrative quotes that were deemed relevant to the review question.
Over half of the studies gathered data from adult psychiatric/forensic inpatient settings. ( n = 12). Other settings included adult community mental health teams ( n = 4) or both inpatient and community mental health settings ( n = 4).
The included studies focused on a range of risk issues including suicidality ( n = 7); risk to others [ 16 ]; self-neglect [ 70 ] and violence [ 64 ]. Two of the studies explored safety and risk within the broader topic of care-planning [ 20 , 62 ]. Other studies explored specific RM practices [ 61 , 65 , 68 , 71 ]; the tension between promoting recovery and managing risk [ 66 , 72 ]; and risk-minimisation and risk-taking [ 73 ]. One study examined clinicians’ perspectives of supporting service users who wished to discontinue from medication, which is a form of risk-taking [ 60 ]. Several of the included studies [ 16 , 20 , 66 , 71 , 74 ] had multiple publications from the same study [ 42 , 75 , 76 , 77 , 78 , 79 , 80 ]. The characteristics of the included studies are summarised in Table 2 .
Coder reliability and sensitivity analysis
Interrater agreement between the two coders across the three SDM components and 14 TDF domains ranged from 83.1 to 100%. For the sensitivity analysis, removing all the studies that gained an overall ‘satisfactory’ rating [ 60 , 61 , 62 , 63 , 64 , 67 , 68 , 69 , 70 , 73 , 74 ] resulted in one domain (knowledge) no longer being relevant. The same salient TDF domains were identified, with the addition of ‘beliefs about consequences’ and ‘emotions’. The findings of the sensitivity analysis demonstrated that the exclusion of these studies would have had a small impact on the overall findings.
The following section begins by summarising study findings relating to the components of SDM. Then, the key barriers and enablers within each of the TDF domains and COM-B components are summarised.
SDM components
None of the included studies directly referred to the term SDM in RA and RM with individuals with mental illness. However, all studies reported on at least one component of the ‘Three Is of Influence’ SDM model [ 2 ].
The ‘informed’ component was identified in several of the included studies. Professionals spoke openly about not discussing risk with service users; that RA was undertaken without the service user’s knowledge; and that the content of the RA was not always shared with the individual [ 16 , 20 , 62 , 63 , 66 , 81 ]. Conversely, in describing RM practices, professionals emphasised the importance of providing information to service users during observation and mechanical restraint [ 61 , 71 , 82 ]. In a study about forensic mental health services, professionals believed that keeping the service user informed and prepared before meetings, as well as discussing risk factors contributed to forming a trusting relationship [ 64 ].
In other studies, professionals acknowledged that they do not generally involve service users in the RA process [ 16 , 20 , 63 , 64 ], some reported involving service users for obligatory, and information gathering purposes [ 20 , 67 , 70 , 82 ]. Others believed it was important to involve and collaborate with service users in RM planning [ 64 , 65 , 83 ] for reasons discussed later.
The ‘influence’ component was also mapped to findings within this review. Some professionals described the need to make decisions on behalf of the service user [ 66 , 70 , 72 , 83 ], thus inhibiting the service user’s influence in the RA and RM process. Other professionals valued collaborating with service users and supporting their choice in decisions that involved risk [ 60 , 64 ]. Positive risk-taking was encouraged to support service users’ influence in decision-making [ 66 , 71 , 72 , 73 ].
Barriers and enablers
Through the use of the TDF [ 52 ], potential barriers and enablers to the SDM components in RA and RM were identified. Barriers and enablers ranged across twelve domains: knowledge, skills; social/professional role and identity; beliefs about capabilities; beliefs about consequences; reinforcement; intentions; goals; memory, attention and decision processes; environmental context and resources; social influences; and emotions . Relevant domains, and the how they relate to barriers and enablers are presented in Table 3 .
TDF domains (and the themes within) were then mapped to COM-B components and sub-components (Fig. 2 ). Based on a frequency count of studies by domain (Table 3 ), the most relevant domains were: social influences ( n = 18); social/professional role and identity ( n = 16); reinforcement ( n = 14); goal ( n = 13); environmental context and resources ( n = 12) and beliefs about capabilities ( n = 11). The key barriers were ‘power and best interest’ ( n = 11) and ‘my professional role and responsibility’ ( n = 12). The key enablers were ‘therapeutic relationship’ ( n = 12), and ‘value collaboration’ ( n = 11). The key barriers and enablers linked with TDF domains: ‘social influences’, ‘social/professional role and identity’ and ‘reinforcement’. The salient TDF domains (and barriers and enablers within) matched COM-B components: ‘opportunity’ and ‘motivation’.
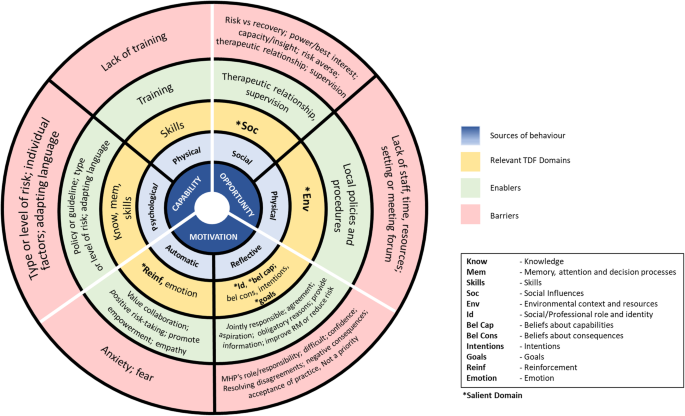
TDF domains mapped to COM-B components and sub-components
Below, is a summary of the review findings of the barriers and enablers matched to TDF domain and COM-B component. Both first-order (direct quotations) and second-order (authors interpretation) themes are presented using illustrative quotations. Direct quotes have been presented in italics.
Professionals referred to policy and legislation in guiding them in supporting service users’ influence in decision-making or risk-taking [ 73 ]. In a study about service users who wish to discontinue taking neuroleptic medication [ 60 ], professionals working in early intervention services demonstrated openness towards supporting discontinuation and said that this was guided by their understanding of the National Institute for Health and Care Excellence (NICE) guidelines and research:
“The evidence we have is that it is worth giving most people a trial off the medication in order to see if their illness would be a relapsing recurring one” [ 60 ] p244)
Memory, attention and decision processes
Professionals’ implementation behaviours may have been influenced by the type of risk identified. In Langan [ 16 ], professionals believed that service users were less involved in a discussion about risk to others than risk to self:
“I think risk to other people tends to be thought of as being...You know, look at it historically and see what has happened before. Whereas, risk of suicide, although that’s important as well, tends to be more on how the patient feels, in terms of harming themselves, at that time. So, probably, risk to self is more centred on the patient” [ 16 ] p476)
In other studies, individual factors were key in determining service users’ readiness to be released from mechanical restraint [ 61 ]; and if risk-taking could be supported [ 60 , 73 ].
Some professionals attributed their reluctance to discussing suicide with service users to lack of formal training [ 69 , 74 , 81 , 83 ] . Limited training was also considered a barrier to engaging service users in RM:
“I have never done any training on this topic. I know that I may change my attitude towards the patients, but I don’t know how to do it” [ 65 ] p7)
Some professionals’ believed that additional training in risk would enhance their practice in caring for suicidal service users [ 69 ]. In a study about risk to others [ 16 ], a psychiatrist explained how training in RA and RM enabled him to discuss risk openly with a service user:
Professionals described adapting the language of risk to aid them in communicating with service users. In Langan and Lindow [ 42 ], professionals questioned the helpfulness in using the term risk: “I mean, I don’t like to use terms like ‘risk’ in that sense, but I mean I think he does accept that there are concerns about his behaviour” [ 42 ] p16). Instead, they reported using terms such as “early warning signs” or “relapse indicators” to facilitate discussion about risk with service users.
In a study about suicidal ideation, nurses reported adapting their communication to align with the service user’s communication preferences [ 82 ]:
“I ask patients how they feel about it when I talk to them about suicidality and how they prefer to have these interactions” [ 82 ] p2870)
Professionals also reported adapting their communication style with individuals who wished to discontinue taking neuroleptic medication [ 60 ]. The communication style that they adopted, i.e. collaborative or coercive, was based on their judgement of the risk factors and perceived outcome. Other professionals were reported to have used euphemistic language to avoid open dialogue about suicide with service users, : “oh, well, you know, if you’re not feeling right” [ 81 ] p105)).
Opportunity
Social influences.
The tension between managing risk and promoting recovery resulted in professionals experiencing role conflict [ 20 , 64 , 72 , 73 , 74 , 83 ]. Findings indicate that RM practices influence other aspects of care including therapeutic relationships, decision-making, and recovery [ 64 , 65 , 72 , 74 , 78 ]. In a study about continuous observation [ 71 , 77 ], a professional explained that while developing a therapeutic relationship with the service user was important, the utmost priority was maintaining safety:
“Every encounter with a patient should be made therapeutic … but it isn’t the primary purpose. The primary purpose is safety. I think the policy makes it very clear that safety trumps everything else” [ 77 ] p553)
Findings suggest that the pressure of managing risk could lead to power imbalances that inhibit service users’ involvement or influence in the decision-making process:
‘ … risk dominated the decision-making of professionals to such an extent that it defined how service users were understood and treated with limited evidence of power-sharing and involvement of service users in decisions’ [ 66 ] p1142).
Some professionals reported using coercion [ 68 ] to maintain the service users safety:
“If we indicate to patients that we are going to the seclusion room, then few patients say they’d “rather not”. But even when they say they’d “rather not”, we do it anyway, and then we emphasise, “Look, we want to protect you against your thoughts” [ 83 ] p1129)
Decisions about risk are sometimes made by professionals in what they believe to be the service user’s best interest [ 16 , 20 , 60 , 65 , 66 , 70 , 71 , 72 , 74 ]:
“Of course it can get difficult if the service user says no, “I want, I want to do it my way now,“ Um, and then you have to have a very different conversation and you need to say that we feel collectively as a team that at this stage it’s still a risk” [ 72 ] p4)
Factors relating directly to the service user, such as insight or mental capacity impede on the SDM components in RA and RM [ 42 , 60 , 61 , 65 , 70 , 71 , 72 , 73 , 83 ]:
“We can share the responsibility with the patient only when he has totally understood and accepted what is happening to himself, otherwise it is very difficult … ” [ 65 ] p7)
A risk-averse team culture was highlighted as a barrier to positive risk-taking [ 72 , 73 ] and the sharing of risk information with service users:
“To my shame, there are cases that I follow that culture, that I hide that risk assessment or secret. Why? Because I want to protect the individual from the knowledge of that.., their illness that they have can be a risk to themselves or to the others. It’s a practice that I’m not very comfortable but nevertheless, I raise my hand and say I have” [ 20 ] p6)
Some professionals’ reluctance to talk openly about suicide or trauma was reinforced in team culture [ 81 , 83 ]. In a study about service users who wished to discontinue from neuroleptic medication, professionals spoke about the change in service culture [ 60 ]. With the ‘old’ culture described as less acceptant of discontinuation and service users influence in the decision-making process.
Developing a therapeutic relationship and trust enabled professionals to facilitate discussion about risk with service users [ 16 , 69 , 82 ], as well to collaborate in RM [ 71 ] and gather information for RA purposes [ 67 ]:
“Rapport is key . .. it means I can get the information I need and that they’re more likely to actually tell me whether they’re still suicidal or not, and then from there we can work out what they need together” [ 69 ] p310)
Others felt that knowing the service user enabled them to support positive risk-taking:
“If you’re beginning to know a bit more about who they are, you might feel able to take greater therapeutic risks, in the hope of encouraging them to take responsibility” [ 71 ] p478)
A good therapeutic relationship was reported to be beneficial in challenging situation, for example, communicating negative decisions to service users [ 64 ]. Therapeutic trust and alliance were also viewed as critical strategies in engaging service users in RM [ 61 , 65 ].
Conversely, where the quality of the therapeutic relationship was less than ideal, it was considered a barrier to involving service users in RA and RM. Staff acknowledged that they were more likely to err on the side of caution with RM with service users that were less well known [ 71 ]. In other studies, professionals recognised that the therapeutic relationship may be better with one professional compared to another and that this could impact on the service user’s openness about risk and engagement in RM [ 61 , 77 ]. Authors concluded that professionals lack of interaction with service users and distance from their subjective experience suggest a relational distance [ 66 ]. In a study about the risk to others, professional’s tentativeness in language, for example, “I try to discuss risk with him” , was attributed to the quality of therapeutic relationship [ 42 ].
Supervision was considered essential and beneficial to support discussing risk, such as suicidality, with service users [ 69 , 81 , 83 ]; and perceived as an enabler to engaging service users in RM [ 71 , 77 ]:
Environmental context and resources
Professionals reported that they did not have the time or opportunity to get to know or directly relate to service users [ 65 , 66 , 71 ]. High caseloads, staff shortages, lack of training and resources were highlighted as factors that impede practice [ 63 , 66 , 69 ]. For example, in Forsberg, Tai [ 60 ], the pressure of increased caseloads, administration and service targets were reported as barriers to supporting service users to discontinue from medication. In a study about suicidal ideation, a nurse reported:
“Sometimes I spend more time reporting than being present with the person. That is a shame! I sometimes wonder what is most important, “What I write down or what I really do with that person?”. Of course, I believe it is important that you write down things in case something happens, but I also believe that there are too many administrative tasks” [ 83 ] p1130)
In Felton, Repper [ 66 ], professionals recognised that most of their time was spent in an office and that this caused a spatial distance between themselves and service users. Professionals were critical of organisational requirements to persistently document risks [ 82 ] and the amount of screening and assessments they needed to do for service users at risk of suicide. Instead, they questioned the value of these tasks as they believed it limited their time to meaningfully engage with service users.
Findings indicate that the setting or meeting structure used to discuss and make decisions about risk may impede on the service user’s involvement or influence in the process [ 62 , 66 ].
“Formal ward round-based review meetings were named as a place for risks to be discussed although not necessarily in the presence of service users” [ 62 ] p12).
Nurses reported the difficulty in communicating risk with service users when they were not invited to the RA meeting or not directly involved in developing the RA [ 64 ], and they believed that this hindered their ability to promote the service users participation in decisions. Professionals also highlighted that if the environment or setting was inappropriate, for example unsafe, noisy and distracting, this could impact on the service users’ involvement in RM [ 65 , 77 ].
Local policies and procedures were considered an aid to communication about risk with service users. In Langan [ 16 ], a voluntary sector organisation reported that their local policies encourage openness between professionals and service users about risk. Specifically, it was a requirement for professionals to complete RA forms jointly with service users, or the voluntary organisation operated an open access policy where individuals could freely access any information about their risks.
Social/professional role and identity
Findings indicate that professionals retain responsibility for managing risk [ 16 , 20 , 63 , 65 , 66 , 70 , 71 , 72 , 74 ], which may be influencing the service users involvement in the RA and RM process.
Findings mapped to this domain were associated with data within the ‘social influences’ domain, for example, professionals making decisions in the best interest of the service user or conforming to their teams’ risk averse culture. In Holley, Chambers [ 72 ], professionals described making decisions on behalf of service users by drawing on their professional knowledge and expertise for managing risk.
In many of the included studies, decision-making regarding risk was described as a team responsibility with little mention of the service user’s input [ 66 , 67 , 70 , 72 ]. In a study about service users who self-neglect, the author concluded that:
“it was not clear how often the teams made decisions based on what they thought was appropriate for the client, rather than on the client’s personal and informed choice” [ 70 ].
Professionals’ responsibility for reducing risk of harm to the individual and others conflicted with their intention to work collaboratively with the service user:
“You know they [meaning colleagues] have a duty to protect the populous from risk. Sometimes that may not chime with the personal interest of the patient ...” [ 60 ] p243)
Findings indicate that therapeutic engagement with individuals at risk of suicide was not always prioritised by nurses or realised by other MHP’s as part of their role [ 69 , 81 ]. For some, facilitating discussion about suicidality or trauma was considered the responsibility of the psychologist or psychiatrist [ 81 , 83 ] . For others, the service user was responsible for initiating discussion about suicidality:
“Basically, it’s down to them to tell us … we’ve no other way really unless they already told their relative so they’re gonna have to be speaking about it” [ 81 ] p105)
Beliefs about capabilities
Conversations with service users about risk and therapeutic risk-taking were described as difficult [ 16 , 66 , 81 ]. Some professionals lacked confidence in approaching the topic of ‘risk to others’ with service users [ 16 ], whereas others expressed a lack of confidence about how to talk with service users about suicide [ 81 ]. Professionals highlighted the need for more training on suicidality in their education:
‘ … although all participants are specialized in mental health nursing, one of them stated that she does not feel educated or confident enough to talk with patients about suicide, and another informant stated that there should be much more focus on caring for suicidal persons in the education’ [ 80 ] p33).
They acknowledged that risk information might not be shared with service users because of potential disagreements [ 20 ]. In a study about the risk to others, reaching a mutual agreement with an individual who disagreed with their identified risks was described as challenging:
“Very difficult. Very difficult. He’ll deny many of the incidents that I’ve told you about. He’ll say that the police are wrong, that they were harassing him. That he didn’t do these things. That he’s not a risk to other people …. So it’s very, very difficult, yeah, to find any middle ground there really” [ 42 ] p18)
When the service user and professional had conflicting viewpoints about discontinuation from medication, this impeded on the service user’s influence in the process [ 60 ]. The professional, instead, attempted to increase the service user’s agreement with their perspective.
On the other hand, the level of agreement about risk was highlighted as an enabler to involving service users in RM:
“Obviously, if they can acknowledge that there is a problem then we’re in a much better position to ensure that they put something in place which works” [ 42 ] p17)
Beliefs about consequences
Professionals expressed a range of views about the potential consequences of involving service users in the RA and RM process. Many were concerned that discussing risk with a service user or involving them in RM would cause the individual distress or harm [ 16 , 20 , 81 , 82 ]:
“Sometimes we avoid involving patients in order to preserve his saneness. In the psychiatric field is difficult to evaluate how much information the patient may tolerate” [ 65 ] p7)
Some professionals believed that discussing risk with others could be damaging to their therapeutic relationship with the service user and lead to disengagement [ 16 ] . Others were worried that involving service users in RA would reinforce stigma:
“the stigma of the mental health is still very prevalent in our society so by doing a risk assessment you more or less emphasise that stigma. .. You are a very risky person, you’re dangerous to yourself, and you’re dangerous to society, whereas this doesn’t go well with the recovery that we try to achieve for that person” [ 20 ] p8)
Professionals also feared negative consequences for themselves by discussing risk with service users. In Awenat, Peters [ 81 ], following a suicide, professionals were worried about being blamed for negligence. This resulted in them recording detailed information to clear themselves of blame should a suicide occur, as well as cautious discussions with service users in case they disclosed suicidal ideation. Similarly, in other studies, professionals highlighted the need to document decisions accurately and follow protocol to protect themselves from blame should their decision be questioned [ 74 , 83 ]. Professionals who encouraged risk-taking [ 73 ] or supported a service user’s wish to discontinue from medication [ 60 ] were also fearful of being blamed if negative outcomes occurred as a result of their decision.
“Risk-taking and promoting an individual’s freedom is encouraged but you’re conscious of the fact that if someone gets hurt, it’s not just them. .. criticism will be levelled at each level within the authority” [ 73 ] p180)
In other studies, fear of being blamed influenced the decision-making process and resulted in professionals adopting defensive or restrictive approaches [ 71 , 83 ].
Professionals’ concern for their personal safety acted as a barrier to both discussing ‘risk to others’ with service users [ 16 ] and involving service users in RM [ 65 ].
Some professionals were resigned to their current practice of not involving service users in the RA and RM process [ 20 ]. Others were willing to move towards involving service user more in the process:
“I’m quite open to change and including the person more in it, rather than it just being professionals talking about the risks” [ 16 ] p477)
Nonetheless, professionals’ aspirations for greater service user involvement in RA and RM did not necessarily reflect practice [ 72 ]:
‘Whilst everyone considered openness a good idea in principle, practice had not always caught up with aspirations’ [ 16 ].
The extent to which professionals consider the SDM components important in the RA and RM process influenced their implementation behaviour. For example, involving service users in RA and RM was not considered a priority for some professionals:
‘… they had given little consideration to how they could directly and actively involve clients in the assessment and management of risk’ [ 63 ] p810).
For others, interpersonal engagement with service users at risk of suicide was not prioritised [ 69 ] and discussion about suicidal ideation was considered counterproductive [ 68 ]. Obligatory reasons for involving service users in RA and RM practices, i.e. for assessment and information gathering purposes, were provided by professionals in several studies [ 20 , 61 , 63 , 65 , 67 , 70 , 74 , 82 , 83 ]:
“In order to take care of these suicidal patients, I try to build a trusting relationship with them. If I can build a good trusting relationship with them, they will trust me. They will give me the information I need and then we can explore their problems and try to help them to prevent future suicide attempts” [ 67 ] p687)
Forming agreements with service users (or a shared-decision) was considered an important step in the RM process [ 61 , 82 , 83 ]. In several studies, professionals emphasised the importance in openly communicating about risk, as well as providing the service user with knowledge and information about their risk [ 16 , 65 , 71 , 83 ]:
‘These nurses avoid imposing instant protection and instead engage in dialogue with patients that facilitates understanding of risks and potentially risky situations (e.g. taking a bath), the meaning that patients attach to risks and potentially risky situations, and what can be done to address risks’ [ 83 ] p1126).
Professionals acknowledged that RM was more likely to be helpful or effective if the service user was involved in the RA process [ 16 , 61 , 65 , 67 , 69 , 71 , 82 , 83 ]:
“I think it’s more of a risk if it’s other people talking about them behind their back. I think the more that things can be out in the open, the less of a risk it is” [ 42 ] p14)
Reinforcement
Professionals emphasised the importance in communicating to service users about their risk [ 72 ], as well as encouraging service users to talk about their distress or suicidality [ 81 , 82 , 83 ].
“The opportunity to interact is the ultimate. .. it’s a really important interaction.. . It can be the difference between life and death” [ 69 ] p309)
Some believed that RM was more likely helpful if service users were involved in decision-making [ 71 ]. Others valued supporting choice and collaboration, and this guided their interaction with service users who wished to discontinue from medication [ 60 ]. Positive risk-taking encouraged some professionals to support the service user’s choice or influence [ 61 , 62 , 71 , 72 , 73 ].
Professionals were motivated to support service users’ influence and positive risk-taking as this favoured autonomy, empowerment, and recovery [ 65 , 66 , 72 , 73 , 82 ]:
“if it is her wish to look after her finances then actually she is entitled and that needs to be explored very slowly with her [. . .] You can give her advice whether it’s a good decision or a bad decision but it’s her decision to take control of it” [ 72 ] p3)
Professionals stressed the importance in demonstrating empathy, compassion and instilling hope [ 67 , 69 , 77 , 82 , 83 ]. They believed that empathy supported service user to work through their distress and talk about suicidal feelings:
“I feel it’s important to feel and show empathy. If you don’t have empathy, you have no way of realising the patients’ torment and discomfort, or how serious or how strongly they feel about attempting suicide” [ 67 ] p687)
Professionals expressed negative emotions that impact on the assessment and management of risk with individuals with mental illness. In Barnicot, Insua-Summerhayes [ 71 ], anxiety in preventing harm and about being blamed may have influenced decision-making around continuous observation and led to restrictive practices. The possibility of a negative outcome from supporting a service user to discontinue from medication triggered anxiety in professionals [ 60 ]. While approaching the issue of risk created anxiety for some professionals [ 20 , 66 , 80 ], others expressed fear in approaching sensitive topics such as risk to others [ 16 ] or suicidal risk [ 69 , 80 , 81 ]. For example, a professional described their concern about possibly being the last person to have spoken to someone who takes their own life:
“I think it’s scary because you don’t want to be the last person having that conversation and they do something. You don’t want to think you’ve done anything that could have erm, actually aggravated them or tipped them over the edge or you’ve said something that has made them think about something” [ 81 ] p106)
The findings of this review indicate that SDM is not a term commonly used in mental health services when exploring processes of RA and RM. The components of SDM (i.e. informed, involved and influential) are referred to but are not being implemented consistently in the RA and RM process. MHPs spoke openly about not discussing risk with service users, involving service users in the process, or supporting their influence in decision-making about risk. This is in line with studies of service user accounts of RA and RM [ 20 , 38 , 42 ], where it was found that service users were often unaware of the RA and RM plan.
Through the use of the TDF [ 52 ], this systematic review has provided a comprehensive understanding of the perceived barriers and enablers to the SDM components in RA and RM from the literature. The salient COM-B components (and linked TDF domains) identified from the findings of this review were social and physical opportunity (i.e. ‘social influences’ and ‘environmental context and resources’), which refer to the social, cultural, and environmental influences on behaviour; and reflective and automatic motivation (i.e. ‘social/professional role and identity’, ‘beliefs about capabilities’, ‘goals’ and ‘reinforcement’), which characterise the cognitive processes that drive behaviour.
Mental health policy at an international level recommends that the processes of RA and RM are collaborative, person-centered and based on SDM [ 28 , 33 , 84 ]; however, there were many factors identified in this review that potentially impede on practice.
Managing risk and delivering recovery-orientated care were experienced as competing priorities that led to practice dilemma. The tension was believed to arise from organisational expectations, legal responsibilities, and contradictory frameworks of practice. Policy guidelines emphasise protection, harm minimisation, public safety, and duty of care. At the same time, they recommend recovery-orientated care based upon the components of SDM, positive risk-taking, therapeutic relationships, and empowerment. Our findings show professionals acknowledged the primacy of RM and the impact this had on other aspects of care including therapeutic relationships, and positive risk-taking. Boardman and Roberts [ 37 ] argue that it is possible to strike a balance between managing risk and delivering recovery-orientated care. They propose shifting towards a ‘person-centred’ approach to assessing and managing risk, based on SDM and collaborative safety planning.
Reluctance to talk about suicidality with service users or to support positive risk-taking were believed to be reinforced in a risk-averse team culture. Simpson [ 85 ] reported similar findings and highlighted the need for a ‘safe’ environment for professionals to openly discuss and disclose uncertainties, challenges, and alternative treatment options within the team. In addition, the findings of this review suggest that professionals tried to make decisions about risk with the service users’ best interests in mind, but at times this was the professionals’ interpretation of best interests and not necessarily the service users’. This is problematic as a capacitous service user is the expert on their own best interests, and even when not capacitous their wishes and views ought to be taken into account. Factors relating directly to the service user, such as capacity and insight, were considered barriers to discussing risk and collaborating with the service user in RM planning, thus impeding best interest decisions. It has been argued that paternalistic approaches to decision-making can cause practice conflicts between the ethical principles of autonomy on the one hand, and beneficence and non-maleficence on the other [ 86 ]. In mental health care, decision-making can be justified in terms of respecting the service user’s choice (autonomy), the professional’s duty to promote good (beneficence) or to prevent harm (non-maleficence) [ 86 ]. Paternalistic approaches may conflict with the autonomy of a non-capacitous service user, when decisions are made based on the professional’s interpretation of the best interests of the service user [ 87 ]. Experiencing a mental health crisis can lead to diminished capacity and competency to make a decision and in these circumstances, paternalistic interventions have been justified on the basis of the requirements of beneficence or non-maleficence [ 88 ]. Breeze [ 87 ] argues that the assessment of rationality or competency has the potential to be subjective and value-laden and although paternalism maybe justified in some situations, it should be exercised with caution. For example, where there is a disagreement between the professional and service user about what is considered ‘best interest’, it should not be assumed that the service user’s view is irrational or wrong, indeed S. 1 [ 4 ] Mental Capacity Act (2005) states that ‘A person is not to be treated as unable to make a decision merely because he makes an unwise decision’ [ 89 ].
Developing a therapeutic relationship and gaining trust enabled professionals to engage service users in a discussion about suicidality, as well as promote positive risk-taking and collaboration in RM. A recent review of service users’ perspectives of helpful RM practices [ 43 ] found that interpersonal relationship and communication aided RM to be inclusive for service users, and trust was considered to nurture open discussion about risk. In a study about risk-taking and recovery [ 90 ], service users also reported that therapeutic relationships developed trust, and this led to more collaborative discussion and decision-making.
Study findings suggest that professionals may be retaining responsibility for assessing and managing risk and thus limiting the extent to which service users are genuinely informed, involved or influential in the process. Negative beliefs about consequences inhibited professionals from implementing SDM in RA and RM. On the one hand, professionals were concerned that discussing risk could cause the service user distress, to disengage from services or to feel stigmatised. On the other hand, professionals were fearful of being blamed or investigated for negative outcomes from supporting risk-taking, i.e. service user who wished to discontinue taking medication, or discussing suicidality. Fear of blame led professionals to accurately document decision-making to protect themselves should their decision later be questioned, as well as cautious discussion with service users about suicidal thoughts. A culture of blame and risk aversion continues to pervade mental health services [ 91 ] that is said to derive from bureaucratic management styles, perception of failure, political pressures and media influences [ 17 , 92 ]. In a qualitative study, professionals expressed concern about restrictive practices potentially being eliminated as they felt that this would make it difficult to maintain safety [ 93 ], they were also concerned about being blamed when a negative event occurred.
Beliefs about consequences provoked negative emotions for some professionals who expressed fear and anxiety about preventing harm. Supervision was highlighted as a potential aid in discussing suicidal thoughts with service users. Tragic incidents can occur even after careful decision-making and thus professionals can expect to be accountable for decision-making and its implementation but not outcomes that they have no control over [ 94 ]. For MHPs to move away from paternalism and towards promoting SDM, change needs to occur at an organisational level [ 37 ]. Professionals need to know that they have managerial and institutional support, especially in situations where negative beliefs about consequences occur. It has been suggested that developing therapeutic risk-taking in practice requires organisations to support professionals by creating safe spaces to hold uncertainty, multidisciplinary working, shared responsibility, and supervision [ 88 ]. Institutional fear of things ‘going wrong’ is perhaps not helped by anxieties over the hyperbolic media coverage that can emerge when tragedies do occur [ 95 ]. The media’s negative portrayal of mental illness and misleading association with violence [ 96 , 97 ] may contribute to the continuing stigma of mental illness; the preoccupation with RM in mental health care; and misconstrued perceptions of the actual risk posed towards others by individuals with mental illness. In reality, 11% of all homicide convictions in the UK, during 2007–2017, were patient homicides, i.e. people in contact with mental health services in the 12 months prior to the offence [ 98 ].
A lack of confidence in discussing certain types of risks with service users was reported. For example, professionals expressed concern about approaching the topic of ‘risk to others’, and uncertainty in how to initiate discussions about suicide with service users. In mental health care, it is recognised that RA and RM practices focus on ‘dramatic risks’ that involve harm to self or others [ 37 ], however, these extreme harms relate to a minority of people in contact with mental health services [ 98 ]. Dixon [ 38 ] compared service users’ and professionals’ ratings of risk and found that service users identified more risks in relation to their vulnerability, such as self-neglect and suicide, than professionals did. In contrast, professionals identified more risks than service users in relation to risk of harm to others. A collaborative safety planning approach would broaden the focus on risk to include the service users perspectives and consideration of everyday risks that are common but less considered in the assessment and management of risk [ 37 ]. Changing the language of risk and basing discussions on safety-concerns offer an alternative way of involving service users’ in managing their own safety and opens discussion about risk [ 99 ].
In the current review, professionals questioned their ability to resolve disagreements with service users about risk to others. Consequently, conversations about risk with service users were described as difficult. A systematic review of services users’ perceptions of RM found that people’s desire for honesty and collaboration was fulfilled when they felt listened to, despite disagreements. Furthermore, some services users recognised disagreements as an authentic part of therapeutic relationships [ 43 ].
As found in the broader recovery-focused care-planning and coordination literature [ 75 ], high caseloads, staff shortages and a lack of resource were highlighted as factors that impede on practice. Professionals reported limited time or opportunity to support positive risk-taking or to meaningfully engage with service users. Also, insufficient training on RA and RM negatively impacted on professionals’ ability to talk openly about risk. In one of the included studies, a professional who had received RA training reported that it enabled him to face his fear in discussing risk openly with an individual who had previously damaged his office [ 16 ]. Higgins, Doyle [ 24 ] research findings indicate the need for training to enable professionals to adopt a collaborative RA and safety planning approach. They propose training delivered at undergraduate and postgraduate level that includes the skills necessary to engage service users and carers in the RA and safety planning process [ 24 ].
Professionals’ behaviours were guided by their perceived outcomes of implementing the SDM components in RA and RM. For some professionals, involving service users in RA and RM was not always a priority. Others, however, were motivated to involve service users for obligatory reasons, as well as to provide the service users with knowledge and understanding of risks and to collaborate in reducing risks. Similar to the findings of Kaminskiy, Senner [ 12 ] qualitative synthesis, this review found support from MHPs for the idea of implementing SDM or working in collaboration with service users. Professionals’ emphasised the importance in communicating risk with service users, promoting empowerment and demonstrating empathy. Some described adjusting their language to facilitate discussions about risk, while others expressed aspiration towards involving service users in future RA and RM practices, though it was recognised that aspiration may have not yet influenced practice.
Strengths and limitations
This is the first systematic review of evidence reporting MHPs’ experiences and attitudes towards SDM in RA and RM, which uses both the TDF and COM-B model to synthesise findings. The synthesis was informed by several psychological theories of behaviour change and empirical findings of included studies. However, this review is not without limitation. First, the review focused on MHPs’ experiences of SDM in RA and RM: thus, the service users’ perspective was not examined, however, a recent mixed-studies systematic review explored helpful RM practices from the service users’ viewpoint [ 43 ]. Secondly, despite conducting systematic searches, SDM is not a well-indexed term, and researchers have varying interpretations of the concept: therefore, our search strategy may have inadvertently missed relevant studies. To capture relevant studies in our searches, we used MeSH terms for SDM and included additional free text key terms related to the concept of SDM (e.g., service user involvement, patient-centred and recovery). Thirdly, it is important to note that the decision to conduct a qualitative systematic review was derived from the findings of a scoping search, which indicated that qualitative methods dominated this field of research. A quantitative survey study [ 24 ] was identified, however, but excluded on the review’s eligibility criteria. Although the key focus of Higgins, Doyle [ 24 ] study was to explore mental health nurses’ practices and confidence in RA and safety planning, there was a small amount of data relevant to the findings of this review (i.e. stakeholders’ involvement in the RA and RM process). Lastly, the wide variation in methods employed in qualitative research poses challenges in the assessment of quality and synthesis of findings for the purpose of a review [ 49 , 100 ]. Indeed, the present review included studies that differed significantly in design, data collection, and analysis method. Also, qualitative research is often criticised for lack of generalisability. Therefore, the strength of recommendation that can be made from the evidence included in this review is limited. Future reviews may wish to further develop the themes identified in this review by sourcing data from quantitative work.
The findings of this review indicate that there may be limited SDM in RA and RM with individuals with mental health problems. Langan and Lindow [ 42 ] reported this over 15 years ago, and despite policies endorsing SDM it, largely, is not happening. This review identifies some of the key issues that may be underpinning this lack of action and warrant further intervention and investigation.
Through the use of the TDF and COM-B model, this review explored MHPs’ perceived barriers and enablers to SDM in RA and RM. Key barriers were ‘power and best interest’ and ‘my professional role and responsibility’, whereas key enablers were ‘therapeutic relationship’ and ‘value collaboration’. These barriers, enablers and TDF domains matched COM-B components ‘opportunity’ and ‘motivation’.
The finding from the present study contributes to existing knowledge of SDM by providing insight into MHPs’ perceived barriers and enablers to implementing SDM in RA and RM. Consistent with a qualitative synthesis study that examined attitudes towards SDM in the broader field of mental health [ 12 ], a lack of capacity was identified as a barrier to SDM in RA and RM. Although justified in some situations, mental capacity fluctuates with time and research indicates that most psychiatric in-patients are capable of making key treatment decisions [ 101 ]. There are also methods that can be used to incorporate service users’ views, such as decision aids, advance directives and advocacy. Therefore, diminished capacity alone should not be reason to exclude the service user from the RA and RM process, as the service user may still be able to offer valuable insight into their perspective and experiences with risk that can inform the RM plan. The present study also highlights the importance of the therapeutic relationship in facilitating discussions about risk with service users, which corroborates findings from a previous systematic review of service users’ perspectives of RM [ 43 ]. Therefore, increasing professionals’ opportunity to develop the therapeutic relationship may influence their motivation to implement SDM in RA and RM.
The findings of this review highlight a complex range of social, cultural and environmental factors that together influence SDM in RA and RM. This information will be relevant to policymakers and practitioners and can also be used to develop targeted interventions aimed at changing practice in this challenging area. However, these findings are based on a small number of studies that are heterogeneous in aim and objective. Furthermore, none of the included studies directly investigated SDM in RA and RM with individuals with mental illness. Therefore, further extensive work is needed to better understand how best to implement SDM in RA and RM so that all parties feel comfortable. A qualitative study by the lead author, directly investigating the barriers and enablers to SDM in RA and RM, is currently underway and has been developed from the findings of this review. The benefits of implementing SDM in RA and RM planning is also insufficiently researched. It is important to build an evidence base on the impact, as well as the acceptability and feasibility of a collaborative approach.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
Shared Decision Making
Mental Health Professional
Risk Assessment
Risk Management
Department of Health
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
International prospective register of systematic reviews
Sample, Phenomenon of Interest, Design, Evaluation, Research type
Bielefeld Academic Search Engine
Theoretical Domains Framework
Capability, Opportunity, Motivation to Behaviour
United Kingdom
Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997;44(5):681–92. https://doi.org/10.1016/S0277-9536(96)00221-3 .
Article CAS PubMed Google Scholar
Stacey G, Felton A, Hui A, Stickley T, Houghton P, Diamond B, et al. Informed, involved and influential: three is of shared decision making. Ment Health Pract. 2015;19(4):31–5. https://doi.org/10.7748/mhp.19.4.31.s20 .
Article Google Scholar
Slade M. Implementing shared decision making in routine mental health care. World Psychiatry. 2017;16(2):146–53. https://doi.org/10.1002/wps.20412 .
Article PubMed PubMed Central Google Scholar
Coulter A, Collins A. Making shared decision-making a reality: no decision about me, without me. London: King's Fund; 2011.
Loh A, Simon D, Wills CE, Kriston L, Niebling W, Härter M. The effects of a shared decision-making intervention in primary care of depression: a cluster-randomized controlled trial. Patient Educ Couns. 2007;67(3):324–32. https://doi.org/10.1016/j.pec.2007.03.023 .
Article PubMed Google Scholar
Malm U, Ivarsson B, Allebeck P, Falloon I. Integrated care in schizophrenia: a 2-year randomized controlled study of two community-based treatment programs. Acta Psychiatr Scand. 2003;107(6):415–23. https://doi.org/10.1034/j.1600-0447.2003.00085.x .
Mott JM, Stanley MA, Street RL Jr, Grady RH, Teng EJ. Increasing engagement in evidence-based PTSD treatment through shared decision-making: a pilot study. Mil Med. 2014;179(2):143–9. https://doi.org/10.7205/MILMED-D-13-00363 .
Lovell K, Bee P, Brooks H, Cahoon P, Callaghan P, Carter L-A, et al. Embedding shared decision-making in the care of patients with severe and enduring mental health problems: the EQUIP pragmatic cluster randomised trial. PLoS One. 2018;13(8):e0201533. https://doi.org/10.1371/journal.pone.0201533 .
Article CAS PubMed PubMed Central Google Scholar
LeBlanc A, Herrin J, Williams MD, Inselman JW, Branda ME, Shah ND, et al. Shared decision making for antidepressants in primary care: a cluster randomized trial. JAMA Intern Med. 2015;175(11):1761–70. https://doi.org/10.1001/jamainternmed.2015.5214 .
Department of Health. Liberating the NHS: No decision about me, without me. London: Department of Health; 2012.
Härter M, Moumjid N, Cornuz J, Elwyn G, van der Weijden T. Shared decision making in 2017: international accomplishments in policy, research and implementation. Z Evid Fortbild Qual Gesundhwes. 2017;123:1–5.
Kaminskiy E, Senner S, Hamann J. Attitudes towards shared decision making in mental health: a qualitative synthesis. Ment Health Rev J. 2017;22(3):233–56. https://doi.org/10.1108/MHRJ-01-2017-0003 .
Langan J. Challenging assumptions about risk factors and the role of screening for violence risk in the field of mental health. Health Risk Soc. 2010;12(2):85–100. https://doi.org/10.1080/13698571003632429 .
Mahone IH, Farrell S, Hinton I, Johnson R, Moody D, Rifkin K, et al. Shared decision making in mental health treatment: qualitative findings from stakeholder focus groups. Arch Psychiatr Nurs. 2011;25(6):e27–36. https://doi.org/10.1016/j.apnu.2011.04.003 .
Boukouvalas E, El-Den S, Murphy AL, Salvador-Carulla L, O’Reilly CL. Exploring health care professionals’ knowledge of, attitudes towards, and confidence in caring for people at risk of suicide: a systematic review. Archives Suicide Res. 2019;24:1-31.
Langan J. Involving mental health service users considered to pose a risk to other people in risk assessment. J Ment Health. 2008;17(5):471–81. https://doi.org/10.1080/09638230701505848 .
Morgan JF. Giving up the culture of blame: risk assessment and risk management in psychiatric practice. London: Royal College of Psychiatrists; 2007.
Google Scholar
Royal College of Psychiatrists. Rethinking risk to others in mental health services. London: Royal College of Psychiatrists; 2008.
Sawyer A-M. Risk and new exclusions in community mental health practice. Aust Soc Work. 2008;61(4):327–41. https://doi.org/10.1080/03124070802428183 .
Coffey M, Cohen R, Faulkner A, Hannigan B, Simpson A, Barlow S. Ordinary risks and accepted fictions: how contrasting and competing priorities work in risk assessment and mental health care planning. Health Expect. 2017;20:471-83.
Dixon J. Balancing risk and recovery in mental health: an analysis of the way in which policy objectives around risk and recovery affect professional practice in England. Medicine, risk, discourse and power. London: Routledge; 2015. p. 120–40.
Kelly S, McKenna H. Risks to mental health patients discharged into the community. Health Risk Soc. 2004;6(4):377–85. https://doi.org/10.1080/13698570412331323252 .
Whitaker R. The case against antipsychotic drugs: a 50-year record of doing more harm than good. Med Hypotheses. 2004;62(1):5–13. https://doi.org/10.1016/S0306-9877(03)00293-7 .
Higgins A, Doyle L, Downes C, Morrissey J, Costello P, Brennan M, et al. There is more to risk and safety planning than dramatic risks: mental health nurses' risk assessment and safety-management practice. Int J Ment Health Nurs. 2016;25(2):159–70. https://doi.org/10.1111/inm.12180 .
Doyle M, Dolan M. Violence risk assessment: combining actuarial and clinical information to structure clinical judgements for the formulation and management of risk. J Psychiatr Ment Health Nurs. 2002;9(6):649–57 9p.
Godin P. You don't tick boxes on a form': a study of how community mental health nurses assess and manage risk. Health Risk Soc. 2004;6(4):347–60. https://doi.org/10.1080/13698570412331323234 .
Quinlivan L, Cooper J, Meehan D, Longson D, Potokar J, Hulme T, et al. Predictive accuracy of risk scales following self-harm: multicentre, prospective cohort study. Br J Psychiatry. 2017;210(6):429–36. https://doi.org/10.1192/bjp.bp.116.189993 .
Department of Health. Best Practice in Managing Risk: Principles and evidence for best practice in the assessment and management of risk to self and mental health services. 2007.
Higgins N, Watts D, Bindman J, Slade M, Thornicroft G. Assessing violence risk in general adult psychiatry. Psychiatr Bull. 2005;29(4):131–3. https://doi.org/10.1192/pb.29.4.131 .
MacCall CA. A review of approaches to forensic risk assessment in Australia and New Zealand. Psychiatry Psychol Law. 2003;10(1):221–6. https://doi.org/10.1375/pplt.2003.10.1.221 .
Bryan CJ, Rudd MD. Advances in the assessment of suicide risk. J Clin Psychol. 2006;62(2):185–200. https://doi.org/10.1002/jclp.20222 .
Fowler JC. Suicide risk assessment in clinical practice: pragmatic guidelines for imperfect assessments. Psychotherapy. 2012;49(1):81–90. https://doi.org/10.1037/a0026148 .
Higgins A, Morrissey J, Doyle L, Bailey J, Gill A. Best practice principles for risk assessment and safety planning for nurses working in mental health services; 2015.
Thornicroft G, Farrelly S, Szmukler G, Birchwood M, Waheed W, Flach C, et al. Clinical outcomes of joint crisis plans to reduce compulsory treatment for people with psychosis: a randomised controlled trial. Lancet. 2013;381(9878):1634–41. https://doi.org/10.1016/S0140-6736(13)60105-1 .
Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19(2):256–64. https://doi.org/10.1016/j.cbpra.2011.01.001 .
Ray I, Simpson AI. Shared risk formulation in forensic psychiatry. J Am Acad Psychiat Law. 2019;47(1):22–8. https://doi.org/10.29158/JAAPL.003813-19 .
Boardman J, Roberts G. Risk, safety and recovery. ImROC Briefing Paper. London: Centre for Mental Health and Mental Health Network; 2014.
Dixon J. Mentally disordered offenders' views of ‘their’risk assessment and management plans: perceptions of health risks. Health Risk Soc. 2012;14(7–8):667–80. https://doi.org/10.1080/13698575.2012.720965 .
Clancy L, Happell B, Moxham L. The language of risk: common understanding or diverse perspectives? Issues Mental Health Nurs. 2014;35(7):551–7. https://doi.org/10.3109/01612840.2014.880139 .
Markham S. Collaborative risk assessment in secure and forensic mental health settings in the UK. General Psychiatry. 2020;33(5). https://doi.org/10.1136/gpsych-2020-100291 .
Faulkner A. The right to take risks. J Adult Prot. 2012;14(6):287–96 10p.
Langan J, Lindow V. Living with risk: mental health service user involvement in risk assessment and management. Bristol: Policy Press; 2004.
Deering K, Pawson C, Summer N, Williams J. Patient perspectives of helpful risk management practices within mental health services. A mixed studies systematic review of primary research. J Psychiatr Ment Health Nurs. 2019;26(5-6):185-97.
Eidhammer G, Fluttert Frans AJ, Bjorkly S. User involvement in structured violence risk management within forensic mental health facilities -- a systematic literature review. J Clin Nurs. 2014;23(19–20):2716–24. https://doi.org/10.1111/jocn.12571 .
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9. https://doi.org/10.7326/0003-4819-151-4-200908180-00135 .
Cooke A, Smith D, Booth A. Beyond PICO the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–43. https://doi.org/10.1177/1049732312452938 .
Thomas J, Brunton J, Graziosi S. EPPI-Reviewer 4.0: software for research synthesis. EPPI-Centre Software. London: Social Science Research Unit. Institute of education, University of london; 2010.
QSR International Pty Ltd. Nvivo 11. 2016.
Dixon-Woods M, Shaw RL, Agarwal S, Smith JA. The problem of appraising qualitative research. BMJ Qual Saf. 2004;13(3):223–5. https://doi.org/10.1136/qshc.2003.008714 .
Article CAS Google Scholar
Shaw RL, Holland C, Pattison HM, Cooke R. Patients' perceptions and experiences of cardiovascular disease and diabetes prevention programmes: a systematic review and framework synthesis using the theoretical domains framework. Soc Sci Med. 2016;156:192–203. https://doi.org/10.1016/j.socscimed.2016.03.015 .
Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Safety Health Care. 2005;14(1):26–33. https://doi.org/10.1136/qshc.2004.011155 .
Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7(1):1.
Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):42. https://doi.org/10.1186/1748-5908-6-42 .
Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):77. https://doi.org/10.1186/s13012-017-0605-9 .
Roberts N, Lorencatto F, Manson J, Brundage SI, Jansen JO. What helps or hinders the transformation from a major tertiary center to a major trauma center? Identifying barriers and enablers using the Theoretical Domains Framework. Scand J Trauma Resusc Emerg Med. 2016;24(1):30.
Islam R, Tinmouth AT, Francis JJ, Brehaut JC, Born J, Stockton C, et al. A cross-country comparison of intensive care physicians’ beliefs about their transfusion behaviour: a qualitative study using the theoretical domains framework. Implement Sci. 2012;7(1):93. https://doi.org/10.1186/1748-5908-7-93 .
McBain H, Mulligan K, Lamontagne-Godwin F, Jones J, Haddad M, Flood C, et al. Implementation of recommended type 2 diabetes care for people with severe mental illness–a qualitative exploration with healthcare professionals. BMC Psychiat. 2016;16(1):222. https://doi.org/10.1186/s12888-016-0942-2 .
Birkimer JC, Brown JH. Back to basics: percentage agreement measures are adequate, but there are easier ways. J Appl Behav Anal. 1979;12(4):535–43. https://doi.org/10.1901/jaba.1979.12-535 .
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):1.
Forsberg N, Tai S, Awenat Y. Clinician perspectives on supporting adults with psychosis who wish to discontinue neuroleptic medication: qualitative analysis. Psychosis. 2018;10(4):239–50. https://doi.org/10.1080/17522439.2018.1534880 .
Nielsen LD, Gildberg FA, Bech P, Lange Dalgaard J, Munksgaard G, Hounsgaard L. Forensic mental health clinician's experiences with and assessment of alliance regarding the patient's readiness to be released from mechanical restraint. Int J Ment Health Nurs. 2018;27(1):116–25. https://doi.org/10.1111/inm.12300 .
Coffey M, Hannigan B, Barlow S, Cartwright M, Cohen R, Faulkner A, et al. Recovery-focused mental health care planning and co-ordination in acute inpatient mental health settings: a cross national comparative mixed methods study. BMC Psychiat. 2019;19(1):115. https://doi.org/10.1186/s12888-019-2094-7 .
Woods P. Risk assessment and management approaches on mental health units. J Psychiatr Ment Health Nurs. 2013;20(9):807–13 7p.
Nyman M, Hofvander B, Nilsson T, Wijk H. Mental health nurses’ experiences of risk assessments for care planning in forensic psychiatry. Int J Forensic Ment Health. 2020;19(2):103-13.
Rimondini M, Busch I, Mazzi M, Donisi V, Poli A, Bovolenta E, et al. Patient empowerment in risk management: a mixed-method study to explore mental health professionals’ perspective. BMC Health Serv Res. 2019;19(1):382. https://doi.org/10.1186/s12913-019-4215-x .
Felton A, Repper J, Avis M. Therapeutic relationships, risk, and mental health practice. Int J Ment Health Nurs. 2018;27(3):1137–48. https://doi.org/10.1111/inm.12430 .
Sun FK, Long A, Boore J, Tsao LI. A theory for the nursing care of patients at risk of suicide. J Adv Nurs. 2006;53(6):680–90. https://doi.org/10.1111/j.1365-2648.2006.03774.x .
Fletcher R. The process of constant observation: perspectives of staff and suicidal patients. J Psychiatr Ment Health Nurs. 1999;6(1):9–14. https://doi.org/10.1046/j.1365-2850.1999.00181.x .
Lees D, Procter N, Fassett D. Therapeutic engagement between consumers in suicidal crisis and mental health nurses. Int J Ment Health Nurs. 2014;23(4):306–15. https://doi.org/10.1111/inm.12061 .
Gunstone S. Risk assessment and management of patients whom self-neglect: a 'grey area' for mental health workers. J Psychiat Mental Health Nurs. 2003;10(3):287–96 10p.
Barnicot K, Insua-Summerhayes B, Plummer E, Hart A, Barker C, Priebe S. Staff and patient experiences of decision-making about continuous observation in psychiatric hospitals. Soc Psychiat Psychiatric Epidemiol. 2017;52(4):473-83.
Holley J, Chambers M, Gillard S. The impact of risk management practice upon the implementation of recovery-oriented care in community mental health services: a qualitative investigation. J Ment Health. 2016;25(4):315–22. https://doi.org/10.3109/09638237.2015.1124402 .
Nolan D, Quinn N. The context of risk management in mental health social work. Practice. 2012;24(3):175–88. https://doi.org/10.1080/09503153.2012.679257 .
Hagen J, Hjelmeland H, Knizek BL. Relational principles in the care of suicidal inpatients: experiences of therapists and mental health nurses. Issues Mental Health Nurs. 2017;38(2):99–106. https://doi.org/10.1080/01612840.2016.1246631 .
Simpson A, Hannigan B, Coffey M, Barlow S, Cohen R, Jones A, et al. Recovery-focused care planning and coordination in England and Wales: a cross-national mixed methods comparative case study. BMC Psychiat. 2016;16(1):147. https://doi.org/10.1186/s12888-016-0858-x .
Simpson A, Hannigan B, Coffey M, Jones A, Barlow S, Cohen R, et al. Cross-national comparative mixed-methods case study of recovery-focused mental health care planning and co-ordination: Collaborative Care Planning Project (COCAPP). Health Serv Deliv Res. 2016;4(5):1-190.
Insua-Summerhays B, Hart A, Plummer E, Priebe S, Barnicot K. Staff and patient perspectives on therapeutic engagement during one-to-one observation. J Psychiatr Ment Health Nurs. 2018;25(9–10):546–57. https://doi.org/10.1111/jpm.12497 .
Felton A, Repper J, Avis M. The construction of people with mental health problems as risk objects: findings of a case study inquiry. J Psychiatr Ment Health Nurs. 2018;25(9–10):558–68. https://doi.org/10.1111/jpm.12501 .
Hagen J, Hjelmeland H, Knizek BL. Connecting with suicidal patients in psychiatric wards: therapist challenges. Death Stud. 2017;41(6):360–7. https://doi.org/10.1080/07481187.2017.1284955 .
Hagen J, Knizek BL, Hjelmeland H. Mental health nurses' experiences of caring for suicidal patients in psychiatric wards: an emotional endeavor. Arch Psychiatr Nurs. 2017;31(1):31–7. https://doi.org/10.1016/j.apnu.2016.07.018 .
Awenat Y, Peters S, Shaw-Nunez E, Gooding P, Pratt D, Haddock G. Staff experiences and perceptions of working with in-patients who are suicidal: qualitative analysis. Br J Psychiatry. 2017;211(2):103–8. https://doi.org/10.1192/bjp.bp.116.191817 .
Vandewalle J, Beeckman D, Van Hecke A, Debyser B, Deproost E, Verhaeghe S. Contact and communication with patients experiencing suicidal ideation: a qualitative study of nurses’ perspectives. J Adv Nurs. 2019;75(11):2867–77. https://doi.org/10.1111/jan.14113 .
Vandewalle J, Beeckman D, Van Hecke A, Debyser B, Deproost E, Verhaeghe S. ‘Promoting and preserving safety and a life-oriented perspective’: a qualitative study of nurses’ interactions with patients experiencing suicidal ideation. Int J Ment Health Nurs. 2019;28(5):1122–34. https://doi.org/10.1111/inm.12623 .
Mental Health Division WDoH. Clinical risk assessment and management (CRAM) in Western Australian mental health services: policy and standards. Perth: Department of Health; 2008.
Simpson A. The impact of team processes on psychiatric case management. J Adv Nurs. 2007;60(4):409–18. https://doi.org/10.1111/j.1365-2648.2007.04402.x .
Beauchamp TL. The theory, method, and practice of Principlism. In: Sadler JZ, KWM F, Staden WV, editors. The Oxford Handbook of Psychiatric Ethics. Oxford: Oxford University Press; 2014.
Breeze J. Can paternalism be justified in mental health care? J Adv Nurs. 1998;28(2):260–5. https://doi.org/10.1046/j.1365-2648.1998.00786.x .
Felton A, Wright N, Stacey G. Therapeutic risk-taking: a justifiable choice. BJPsych Adv. 2017;23(2):81–8. https://doi.org/10.1192/apt.bp.115.015701 .
Department for Constitutional Affairs. Mental Capacity Act. London: HMSO; 2005.
Young AT, Green CA, Estroff SE. New endeavors, risk taking, and personal growth in the recovery process: findings from the STARS study. Psychiatr Serv. 2008;59(12):1430–6. https://doi.org/10.1176/ps.2008.59.12.1430 .
Manuel J, Crowe M. Clinical responsibility, accountability, and risk aversion in mental health nursing: a descriptive, qualitative study. Int J Ment Health Nurs. 2014;23(4):336–43. https://doi.org/10.1111/inm.12063 .
Wand T. Considering the culture of blame in mental health care and service delivery. Int J Ment Health Nurs. 2017;1(26):3–4.
Muir-Cochrane E, O'Kane D, Oster C. Fear and blame in mental health nurses’ accounts of restrictive practices: implications for the elimination of seclusion and restraint. Int J Ment Health Nurs. 2018;27(5):1511–21. https://doi.org/10.1111/inm.12451 .
Flewett T. Clinical risk management. Sydney: Churchill Livingstone; 2010.
Chen M, Lawrie S. Newspaper depictions of mental and physical health. BJPsych Bull. 2017;41(6):308–13. https://doi.org/10.1192/pb.bp.116.054775 .
Wahl OF. News media portrayal of mental illness: implications for public policy. Am Behav Sci. 2003;46(12):1594–600. https://doi.org/10.1177/0002764203254615 .
Stuart H. Media portrayal of mental illness and its treatments. CNS Drugs. 2006;20(2):99–106. https://doi.org/10.2165/00023210-200620020-00002 .
NCISH. The National Confidential Inquiry into suicide and safety in mental health. Annual report. England, Northern Ireland, Scotland and Wales: University of Manchester; 2019.
Jones M. Risk: a conversation worth having in mental health care? J Psychosocial Rehab Mental Health. 2020;7:97–101.
Hammersley M. Reflections on the methodological approach of systematic reviews. In: Zawacki-Richter O, Kerres M, Bedenlier S, Bond M, Buntins K, editors. Systematic reviews in educational research: methodology, perspectives and application. Wiesbaden: Springer Fachmedien Wiesbaden; 2020. p. 23–39. https://doi.org/10.1007/978-3-658-27602-7_2 .
Chapter Google Scholar
Okai D, Owen G, McGuire H, Singh S, Churchill R, Hotopf M. Mental capacity in psychiatric patients: systematic review. Br J Psychiatry. 2007;191(4):291–7. https://doi.org/10.1192/bjp.bp.106.035162 .
Download references
Acknowledgements
I would like to thank Dr. Afnan Aljaffary, and Dr. Una Foye for their support with appraising the quality of studies within this review.
This research was part of a PhD funded by City, University of London, and East London NHS Foundation Trust. Neither funding body had a role in the design of the study, data collection, analysis, interpretation of data or writing the manuscript.
Author information
Authors and affiliations.
Centre for Mental Health Research, School of Health Sciences, City University of London, Northampton Square, London, EC1V 0HB, UK
Nafiso Ahmed, Sally Barlow & Fareha Begum
School of Nursing, Midwifery and Allied Health, Buckinghamshire New University, 106 Oxford Rd, Uxbridge, UB8 1NA, UK
Lisa Reynolds
Centre for Health Services Research, School of Health Sciences, City University of London, Northampton Square, London, EC1V 0HB, UK
Nicholas Drey
Health Service and Population Research, David Goldberg Centre, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, De Crespigny Park, London, SE5 8AF, UK
Elizabeth Tuudah & Alan Simpson
South London and Maudsley NHS Foundation Trust, Maudsley Hospital, 111 Denmark Hill, London, SE5 8AZ, UK
Alan Simpson
Florence Nightingale Faculty of Nursing, Midwifery & Palliative Care, James Clerk Maxwell Building, King’s College London, 57 Waterloo Road, London, SE1 8WA, UK
You can also search for this author in PubMed Google Scholar
Contributions
NA contributed to the design of study, conducted the searches, screening, quality appraisal, data extraction, analysis, synthesis, drafted and edited the manuscript. AS contributed to the design of the study, supported screening, analysis, synthesis, and revised the manuscript. SB contributed to the design of the study, supported data extraction, screening and revised the manuscript. LR contributed to the design of the study, supported screening, and revised the manuscript. ND advised and revised the manuscript. FB supported title and abstract, and full text screening. ET contributed to the analysis and interpretation of data. All authors have read and approved the final version of the manuscript.
Corresponding author
Correspondence to Nafiso Ahmed .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., additional file 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ahmed, N., Barlow, S., Reynolds, L. et al. Mental health professionals’ perceived barriers and enablers to shared decision-making in risk assessment and risk management: a qualitative systematic review. BMC Psychiatry 21 , 594 (2021). https://doi.org/10.1186/s12888-021-03304-0
Download citation
Received : 07 July 2020
Accepted : 25 May 2021
Published : 25 November 2021
DOI : https://doi.org/10.1186/s12888-021-03304-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decision making
- Mental health
- Risk assessment
- Risk management
- Systematic review
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 04 February 2013
Clinical risk management in mental health: a qualitative study of main risks and related organizational management practices
- Matthias Briner 1 , 2 &
- Tanja Manser 3
BMC Health Services Research volume 13 , Article number: 44 ( 2013 ) Cite this article
24k Accesses
25 Citations
5 Altmetric
Metrics details
A scientific understanding of clinical risk management (CRM) in mental health care is essential for building safer health systems and for improving patient safety. While evidence on patient safety and CRM in physical health care has increased, there is limited research on these issues in mental health care. This qualitative study provides an overview of the most important clinical risks in mental health and related organizational management practices.
We conducted in-depth expert interviews with professionals responsible for CRM in psychiatric hospitals. Interviews were transcribed and analyzed applying qualitative content analysis to thematically sort the identified risks.
The main concerns for CRM in mental health are a) violence and self-destructive behavior (i.e. protecting patients and staff from other patients, and patients from themselves), b) treatment errors, especially in the process of therapy, and c) risks associated with mental illnesses (e.g. psychosis or depression). This study identified critical differences to CRM in hospitals for physical disorder and challenges specific to CRM in mental health. Firstly, many psychiatric patients do not believe that they are ill and are therefore in hospital against their will. Secondly, staff safety is a much more prominent theme for CRM in mental health care as it is directly related to the specifics of mental illnesses.
Conclusions
The current study contributes to the understanding of patient safety and raises awareness for CRM in mental health. The mental health specific overview of central risks and related organizational management practices offers a valuable basis for CRM development in mental health and an addition to CRM in general.
Peer Review reports
Understanding and improving patient safety is a growing concern, particularly following the publication of the Institute of Medicine reports “To err is human” [ 1 ], “Crossing the quality chasm” [ 2 ] and the NHS’s “Organisation with a memory” [ 3 ]. These reports highlight that between 3.7-16.6% of patients admitted to hospitals suffer an adverse event, at least half of which are preventable. Such adverse events can result in unnecessary injury or death as well as enormous economic costs. Despite being ostensibly concerned with patient safety and minimizing risks in health care, a systematic approach to patient safety or a systematic organizational management of clinical risks is difficult to implement and therefore, seldom seen [ 4 – 6 ].
Nevertheless, research and knowledge on patient safety, have increased rapidly and improved many aspects in acute medical health care settings [ 7 , 8 ]. However, in mental health care, there is a “lack of awareness of the issues as well as a shortage of research and information on the topic” [ 9 ], p. 39]. A comprehensive literature review highlights an inconsistency in basic patient safety concepts in mental health (e.g. defining and calculating adverse events), as well as a scarcity of high quality patient safety research in mental health [ 10 ]. Due to the resulting lack of patient safety principles specific to mental health care, concepts and strategies from acute medical health care settings are frequently adopted. This may be appropriate for some aspects, but mental health care differs from medical patient care in patient population and illnesses, as well as in historical and institutional contexts. There are also unique patient safety issues in mental health care that require further consideration [cf. [ 10 – 12 ], especially with regard to clinical risks. While medication related risks, such as medication mix-up or delivery of wrong dose, are found in acute medical care and mental health [e.g. [ 13 ], specific risks, such as suicide, violence and self-harm prevail in mental health [ 14 ]. To date, an overview of the spectrum of clinical risks found in mental health and the organizational risk management practices currently applied is lacking. Publications mostly discuss specific risks, such as violence, and do not offer an integrated view e.g. (for suicidal or violent patients, see [ 15 , 16 ]). Also, the traditional focus of the management of clinical risks in mental health care was located at the individual instead of the organizational level and was therefore narrowly “considered the business of predicting and preventing dangerousness” of patients [ 14 ], p. 3].
Furthermore, a systematic clinical risk management (CRM) can play a crucial role in enabling health care organizations to assess, manage, and contain risks related to patient safety and aims at reducing or eliminating harm to patients [ 8 , 17 ]. The more complex an organization, the greater the need for CRM. This is especially true for psychiatric hospitals, where the challenges to patient safety are varied and the connection between patient and staff safety is closer than in hospitals for medical complaints [e.g. [ 18 , 19 ].
To gain a systematic and comprehensive understanding of CRM in mental health, this study aims to provide an overview of clinical risks and related management practices in mental health. This is an important step in deepening our knowledge of patient safety and in supporting psychiatric hospitals to optimize their clinical risk management and to ultimately improve the health care system, for the mentally ill [ 13 ].
Sample, setting, and data collection
This study used semi-structured expert interviews to identify clinical risks in mental health care and organizational risk management practices. Expert interviews are a very useful instrument for innovative research taking into account the expert status of the interviewee; they allow for collecting the interviewees subjective experiences and interpretations regarding a predefined specialized topic [ 20 ]. The semi-structured form supports comparability between the interviews, yet allows for the inclusion of not anticipated, but important issues [ 21 ]. Interviewing persons with patient safety expertise in mental health care, therefore, is a valuable source of in-depth information that is urgently needed to expand research in this field where currently there is little research available [ 9 ].
The interviewees were selected following a national study on CRM in Switzerland in 2007/08 [see [ 4 , 17 ]. The sampling technique was purposive: all 11 experts were responsible for the coordination of CRM in their psychiatric hospital and had considerable knowledge and experience in the field of patient safety in mental health care. Eight of these experts had worked for more than five years in their respective institutions; six hospitals were public, five were private. Four hospitals had fewer than 100 beds (all private hospitals), two had 100–200 beds (all public), and five had over 200 beds (four public, one private). Participation was voluntary and did not affect respondents physically or mentally. All responses were de-identified. The research did not include any patients and is in line with the WMA Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects. Such research does not require ethics approval in Switzerland, as mere surveys in the sense of opinion surveys or interviews are not counted as research on humans (see http://www.vpf.ethz.ch/about/commissions/EK ).
Interviews were carried out by an experienced researcher (in most cases accompanied by an assistant) between June and September 2008 in the interviewees’ offices in the respective psychiatric hospital. In three interviews, additional personnel participated (nursing resp. medical head, responsible person for work safety). Interviews lasted between 80 and 160 minutes and were audio recorded.
The interview manual was developed as part of the project, “Clinical risk management in Swiss hospitals” [ 17 ]. It was based upon results from a literature review on CRM and was critically examined by an expert panel consisting of 11 patient safety experts (comprised of the persons in charge of patient safety and/or quality of five main Swiss healthcare institutions, the president of the Swiss Society for Quality Management in Health Care, the head of quality of a major reinsurance company, and four clinical experts with a proven record of accomplishment in patient safety. For details see [ 17 ]). The manual included exploratory questions on tasks, content and organization of CRM (e.g. “What is the meaning of CRM and patient safety in a psychiatric hospital?”), and questions on future developments pertaining to CRM (e.g. “What activities are planned in the next 12 months in the area of CRM/patient safety in your psychiatric hospital?”). It also comprised a structured review of the results of a 2007/2008 survey of CRM that is not part of the current study. The results from the survey are published in Briner, Manser and Kessler [ 4 ].
Data analysis
Interviews were transcribed verbatim and in their entirety, which is crucial for an explorative study, as protocols from memory or summaries reduce information in a methodologically uncontrolled way [ 22 ]. To achieve uniformity, the same researcher transcribed all the interviews. The transcripts were analyzed applying qualitative content analysis [ 23 ]. This method qualifies for semi-structured expert interviews as it is used for coding text with a predefined coding system which can be refined and completed with new themes emerging in the interviews [ 22 , 23 ]. Our initial coding system used categories which were defined following the literature review of CRM. It allows for organizing, sorting and retrieving the coded text passages. This technique for guiding the analysis of qualitative data relying on prior research had proven valuable in previous studies, for example, identifying and categorizing errors in mental health [ 13 ].
The coding was performed using the program MAXQDA2010 that was developed particularly for computer-assisted analysis of qualitative data. To begin the qualitative content analysis, two primary coders (MB and an assistant) coded the transcripts. The specific risks and related organizational risk management practices were assigned to the appropriate categories. Meaningful units (whole or part sentences) were defined as units of analysis. Results were compared between coders to deepen the understanding of the categories and to achieve consensus. The primary coders then reviewed all interviews a second time to refine, expand, bridge or eliminate categories for the purpose of fully describing risks and their organizational management. Inter-rater agreement was calculated to measure the extent different coders agreed upon which text passages were assigned to which categories [ 23 ]. Therefore, the spontaneously mentioned risks (risks that, at the beginning of each interview, were spontaneously mentioned to the question, “What is the meaning of CRM in a psychiatric hospital?”, were assigned to the respective categories by the three coders (MB and two assistants) independently. These spontaneously mentioned risks offer a heuristic [fast and frugal judgment, cf. [ 24 ] of frequent or obvious risks in mental health. Overall, an inter-rater agreement of 81% was reached. The remaining disagreements were discussed between the three coders until a consensus was reached. Where there was ambiguity, the coding system was adapted and refined accordingly. The two primary coders coded all interviews a third time using this refined coding system in order to reach a final assignment of text passages to categories. The results were further processed independently from the original text and codes were summarized thematically. The frequencies of risks mentioned across all interviews, as well as the spontaneously mentioned risks, were counted to indicate the relative importance of individual risk categories (see results and Table 1 ). Similar methods were also used by Brickell and McLean [ 9 ] for their qualitative analysis of expert perspectives on patient safety in mental health. As management of specific risks was often mentioned at the same time as the risk, it was coded simultaneously.
Focus group for reflecting interview results
Focus groups offer the possibility to deepen the understanding of results from qualitative studies [cf. [ 25 ]. Experts appraise, discuss and reflect upon the findings and thereby add content validity to a study [for the importance of content validity, see [ 26 ]. In our case, a focus group took place in August 2011. This comprised four renowned Swiss patient safety experts in mental health care. Each focus group participant was briefed on the study in advance and received a thematically organized tabular overview of the spontaneously mentioned risks found in all interviews (integrated in Table 1 , details see above) to prepare for the two-hour focus group session. Three experts were able to participate in the focus group (one was ill and gave written feedback). The three interview coders guided the discussion on the overview of risks in mental health. The discussion was recorded in writing and used to refine the overview of the main risk themes of CRM in mental health (Table 1 ).
Our results highlight specifics of CRM in mental health care and give an overview of risks in mental health. The most important organizational CRM practices are presented in conjunction with the corresponding risks, since the experts frequently mentioned them at the same time as the risk. Quotes were translated verbatim into English. The index number (e.g. I1, P3) indicates the interview and the paragraph where the quote was taken from.
Specifics of CRM in mental health care
It was highlighted throughout the interviews that CRM in mental health differs from CRM in medical health care in important aspects. A major difference lies in the characteristics of psychiatric patients, whose mental illnesses, such as psychosis or depression, entail specific clinical risks. Repeat admission patients are significant as they are characteristic to some kind of diagnoses. In addition, some patients do not believe that they are ill and therefore refuse treatment, whereas patients with an obvious physical injury, such as a broken leg, would not behave in that way. On the other hand, high-risk treatments such as surgery are not found in psychiatry. Therefore, clinical risks such as iatrogenic infections play a somewhat minor role. Overall, CRM in mental health was judged to be less advanced than in medical health care, but a rising awareness of the topic was noted. CRM was seen to support patient safety, but also to be important for staff and family safety: “Service provider and receiver should not be harmed. […] A patient should always leave the ward healthier than on admission” (I3, P17).
Overview of risks in mental health care
Figure 1 provides an overview of the most important risks in mental health. Blue (main categories) and yellow (sub categories) fields show risks that are specific to mental health. Dotted red lines show relations between different categories and dotted black lines show risks that affect staff safety, as well as patient safety. The full overview of the main risk themes of CRM in mental health care mentioned in the interviews and related organizational management practices is given in Table 1 .
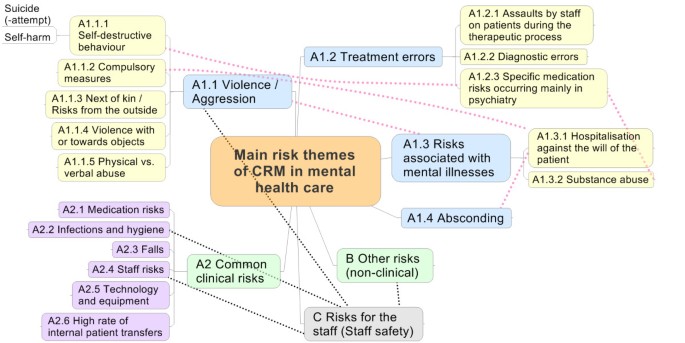
Overview of the main risk themes in mental health care.
The focus of this paper is clinical risks specific to mental health care (see A1.1-A1.4 in Figure 1 ). These were the clinical risks mentioned most frequently in the interviews (n=237), emphasizing their importance. All interviewees also mentioned clinical risks known from medical care that also appear in mental health care (A2, n=106). Additionally, all interviewees mentioned non-clinical risks that are mostly not specific for mental health care (B, n=47). All interviewees also referred explicitly to staff safety (C, n=38), highlighting the importance of this topic in mental health care.
Results from the focus group
The participants of the focus group for reflecting interview results agreed that a comprehensive and systematic overview of clinical risks in mental health care is lacking, and that a categorization of these risks is complex and challenging. Aggression and self-destructive behavior were approved as main themes in patient safety in mental health (A1.1). An alternate categorization of risks originating in the patient (peril to self or to others) and risks originating from treatment was outlined, but it was judged not to simplify the categorization.
A1) Clinical risks specific to mental health care
Violence and aggression (A1.1), treatment errors (especially errors in the process of therapy, A1.2), and risks associated with mental illnesses (A1.3) were the most important clinical risk themes specific to mental health care. An additional theme was leaving hospital against medical advice or absconding from the hospital (A1.4). A thorough admission interview was generally considered as an important measure for managing these risks. Other more specific measures are listed below in conjunction with the corresponding risks.
A1.1) Violence and aggression
The greatest focus was on violence/aggression (A1.1, n=141). This is in line with Flewett [ 14 ], who describes suicide, violence and self-harm as the most common risks. Violence against others was mentioned 42 times. This means physical (e.g. assault, breach) or verbal/psychological (e.g. threat) violence against fellow patients, staff or other persons (e.g. family members, next of kin). Training and education (aggression management training, fixation technics etc.) were recommended as possible measures against general violence as were violence risk assessments [e.g. prediction instruments such as the Brøset-Violence-Checklist, cf. [ 27 ].
Self-destructive behavior (A1.1.1) was mentioned most frequently (n=51), and was also the most frequent spontaneously stated risk. This category comprises suicide, attempted suicide and self-harming (e.g. cutting). All interview partners emphasized the importance of self-destructive behavior: one stated, “I have never seen a patient who could completely exclude suicide” (I5, P20). An assessment of suicidal tendency during admission and in subsequent interviews, no-suicide contracts and good anamnesis as well as architectural protection and intensive support and monitoring of endangered patients, were recommended as possible measures against self-destructive behavior. If something did happen, good follow-up care and debriefing for fellow patients, staff and next of kin is important. Therefore, many psychiatric hospitals developed standard procedures (e.g. procedures after (attempted) suicide).
Compulsory measures (A1.1.2) that are intended to be an activity to calm down violent patients were also seen as a risk (n=31). Compulsory measures are risky as they are usually applied against the will of the patient and sometimes require force to be administered. Training and education, and the use of standardized procedures, were recommended as CRM measures.
Other risks mentioned were violence from the outside (A1.1.3>, e.g. family of patients that threaten other patients or staff), violence with objects (A1.1.4, e.g. weapons) or towards objects (e.g. to destroy furniture etc.) and physical or verbal abuse (A1.1.5, e.g. death threat).
In sum, violence/aggression is linked closely to particular mental illnesses that increase the possibility for violent behavior. This topic is discussed more deeply in the section on risks associated with mental illnesses (see below, A1.3).
A1.2) Treatment errors (especially errors in the process of therapy)
The second focus regarding specific clinical risks in mental health care was on treatment errors, especially errors in the process of therapy (A1.2, n=49). Standard procedures for consultations, interdisciplinarity, sufficient staff, and anamnesis with pro-active risk assessment were generally mentioned as CRM measures. Three sub-categories could be identified. The first was assaults by staff on patients during the therapeutic process (A1.2.1, e.g. sexual contacts or abuse of power by the therapist). Suggested as possible measures were, special training, intervision (peer consulting) and supervision for staff, the recommendation to avoid one-to-one consultations, and the implementation of an ombudsman service that a patient can turn to.
The second sub-category was diagnostic errors (A1.2.2). This encompasses the misdiagnosis of a mental illness when it was a physical illness and the misdiagnosis of psychiatric illnesses [cf. [ 13 ]. This can result in incorrect treatment (therapy, medication) that can worsen the patient’s condition. Differential diagnoses are crucial to prevent diagnostic errors. Thus, many psychiatric hospitals use specific instruments to differentiate between physical and mental diagnoses.
The third sub-category concerns specific medication risks occurring mainly in psychiatry (A1.2.3). Here, side-effects of medication are most important (e.g. weight gain, loss of libido), as they are a primary reason for patients being non-compliant and not taking their medications. Another risk is apparent if patients accumulate medications for substance abuse or with the intention to commit suicide. Therefore, patients should be informed and educated about medications and their possible effects and side-effects, and patients’ needs should be clarified and taken into account. The distribution and intake of medication needs to be monitored rigorously.
The interviews showed that this very mental-health specific topic of errors in the process of therapy, especially in psychotherapy, is insufficiently discussed and still rather vague. Treatment errors are seldom recognized or if they are, it is often too late, as therapy deals with the psyche and not with the observable body. In mental health care it can even be that a patient is judged to be “resistant to therapy, something that would never be accepted for a knee injury” (I3, P70). Furthermore, there are often different ideas among the mental health care professionals of what the right therapy might be for which illnesses. In addition, sometimes it is “rather the environment and not the patient that needs treatment” (I6, P53).
A1.3) Risks associated with mental illnesses
The third focus regarding specific clinical risks in mental health care was on risks associated with mental illnesses (A1.3, n=37). This contains mentions of particular illnesses (e.g. addiction, acute psychosis, mania, depression, anxiety disorders, or personality disorders) that might increase the possibility for certain risks (e.g. violent behavior or suicide). Risks associated with schizophrenic/psychotic disorders were mentioned most frequently. Most private psychiatric hospitals in our sample select patients according to their mental illnesses as they are not obligated to accept all patients (in contrast to public hospitals). For example, patients with psychoses, addiction or major depression may not be accepted by a private hospital; thereby minimizing possible risks for the hospital. Overall, tools to assess the level of depression, suicidal tendencies, violence, etc. are most important to identify risks.
Most interviewees also mentioned that many psychiatric patients (“15-18%”, I11, P117) are in hospital against their will (A1.3.1). The patients might have an involuntary commitment or do not believe that they are ill, which can result in violence, compulsory measures (see above) or leaving hospital against medical advice. Another risk is substance abuse and its consequences (A1.3.2) if, for example, drugs and injection devices (e.g. syringes) are smuggled into the hospital. CRM practices mentioned are to require patients to sign a binding addiction contract and to search patients to prevent them from smuggling drugs into the hospital.
A1.4) Leaving hospital against medical advice (Absconding)
Six out of 11 interviewees mentioned leaving hospital against medical advice or absconding from the hospital as another specific risk in mental health care (A1.4, n=9). There are various reasons why a patient might want to escape from a psychiatric hospital. It can be a consequence of the mental illness (e.g. hearing imperative/bidding voices that command a patient to escape) or because a patient is hospitalized against his/her will (see above). An escape from treatment might have severe consequences (e.g. (attempted) suicide, assault). CRM measures mentioned were the internal transfer of endangered patients to a closed ward, a very close observation/support of the patient and, if the patient did escape, a search by police.
A2) Clinical risks in common with medical health care
All interviewees also mentioned clinical risks that are known in medical health care but are also important in mental health care (A2, n=106). They are described briefly as they are well documented in the literature and not the focus of this study. Medication risks were mentioned most frequently (A2.1, n=33): confusion of medication, incorrect dose, incorrect administration, etc. Some interviewees judged medication risks to be just as important as in medical health care, whereas others found them not to be as critical in mental health. Infections and hygiene (A2.2, n=26) were also mentioned, but were not considered as important as in medical health care. One reason for this being that psychiatric hospitals have no surgery. Falls (A2.3, n=12) were also a topic in some interviews, especially regarding geronto-psychiatry or in the context of withdrawal symptoms.
Risky organizational and technological conditions that influence patient safety were also mentioned. Staff risks (A2.4) were identified, including staff shortage, too many shift changes, and stress and workload often resulting in prolonged absences from work and high staff turnover. Some interviewees saw this as a problem specific to mental health care as staff absenteeism due to illness was judged as being much more common than in other domains, including medical health care. Regarding technology and equipment (A2.5), correct application and periodic maintenance were seen as being most important. A high rate of internal patient transfers (A2.6) was also seen as potentially risky as primary caregivers change, knowledge about the patient is lost and handovers must be organized.
B) Other risks (non-clinical)
All interviewees also mentioned non-clinical risks that are mostly not specific for mental health care (B, n=47). Economic, construction, infrastructural and fire risks were mentioned. These risks were not classified further because this was not the focus of this study. However, some risks, such as data protection (to protect patients from stigmatization), or risks relating to hospital image (to avoid negative press) were judged to be especially important for psychiatric hospitals.
C) Risks for the staff
Staff safety is an important topic in psychiatric hospitals and all interviewees explicitly referred to it (C, n=38). It is specific to mental health care insofar as staff face risks, such as aggression and violence, far more often than in medical health care. A prospective 1998 study in six psychiatric hospitals captured all obvious aggressive physical contacts over six months: 144 assaults on 170 members of staff were found [ 28 ]. “Working for 8 or more hours a day and being constantly conscious of the possibility of violence, I think, is almost unacceptable” (I2, P94). This can lead to work stress, burn-out and prolonged absenteeism from work due to illness (see above). “We have more than 25% drop-outs because of staff illnesses; this is a very high number” (I10, P55). Fellow staff members and patients suffer from such situations. Staff can also become a second victim [ 29 ] as (attempted) suicides, diagnostic errors, medication errors or performing compulsory measures can be enormously burdensome. Therefore, staff and patient safety are closely interrelated and affect each other, at least partially.
This study offers, for the first time, an overview of the main risk themes of CRM in mental health care and is independent of specific hospitals. The overview augments previous research, as it is systematic, exhaustive, and does not focus on selected risks. The result of counting the risks indicates which risks are common and important. Whereas medication errors are in the uppermost position of risks to patients in hospitals for physical disorder [cf. [ 1 , 8 ], CRM in mental health is first concerned with violence and self-harm. Self-destructive behavior (mainly suicide and attempted suicide) was mentioned the most, followed by violence/aggression from patients against others. In terms of CRM, this implies that the main goal, above all, is to protect patients and staff from other patients, as well as to protect patients from themselves [cf. [ 15 ]. Professional interventions can reduce violence in many cases. Important to achieving this are sensitization, education and training of staff as well as the use of preventive instruments to predict violence. If something is happening, de-escalation (to calm the patient), diversion, and engagement are recommended as proactive interventions [ 12 ]. The consideration between the surveillance of the patient and the possibility to allow the patient to move freely remains a particular problem. Permanent surveillance increases safety and prevents suicides, but the patient is literally imprisoned and the necessary staff resources for the hospital to achieve this are enormous [ 30 ]. Therefore, striking the right balance between safety and freedom is also one of the delicate challenges in mental health care.
The second main risk theme concerns treatment errors. In particular, errors in the process of therapy, notably in psychotherapy, are insufficiently discussed and still rather vague (see results above, A1.2) so need further investigation. Diagnostic errors were seldom mentioned and seem to be neglected and underestimated similarly as is the case in medical health care. Despite the fact that they account for about 15% of medical errors and are the leading cause of medical malpractice litigation (twice as many cases as medication errors), diagnostic errors receive little attention [cf. [ 31 , 32 ]. This is probably because they are hard to measure, there being little data of incidence available, and because it is sometimes difficult even for experts to agree on the right diagnosis. However, especially in mental health care, where an incorrect diagnosis can result in incorrect therapy and prolonged stays in the hospital (sometimes for years), sensitization of staff and taking diagnostic errors into account in CRM is essential.
The third specific risk theme was risks associated with mental illnesses, such as psychosis or depression. Furthermore, many psychiatric patients lack insight regarding their illness and do not themselves think that they are ill and are hospitalized against their will. Therefore, due to their illnesses, most patients in mental health care differ greatly from patients in medical health care. Staff safety is directly related to the specifics of mental illnesses and is, as shown, a central theme in mental health care. These are additional main reasons why CRM in mental health care needs specialized concepts and strategies that complement the knowledge from CRM in medical health care. Some clinical risks such as medication risks, infections, hygiene, and falls, are common to various specializations in health care, and would benefit from the application of similar CRM practices.
Limitations
A qualitative approach allows for the exploration of a subject where there is limited previous research. Although this approach proved to be valuable, the data were constrained by the number of participants available for interview. Therefore, the results may not be fully generalizable to all types of mental health hospitals (e.g. psychiatric units for geriatric or pediatric patients) and to other types of hospitals. Secondly, it is possible that the interviewees did not verbalize the full extent of their knowledge because of memory limitations and the fact that not all knowledge is conscious. These limitations are common in many qualitative studies [cf. [ 13 ]. However, the expert status and the diversity of the chosen interviewees guaranteed a thorough and expansive view of the subject.
Remarkably, interviewees only mentioned risks in inpatient psychiatry restrained to the period between admission and discharge of patients. The handovers from ambulatory to in-patient as well as the after-care were not discussed. For example, how does one ensure that a patient does not relapse promptly upon discharge only to be readmitted to the hospital? This situation mainly occurs if the ambulatory care setting is not clear, if a patient returns to his or her usual environment or if medications are discontinued.
The current study adds to the understanding of patient safety and raises awareness for clinical risks in mental health. It uses expert interviews as an empirically sound way of generating knowledge in an emerging field that suffers from a shortage of research activity and empirical evidence. The overview of the main risk themes of CRM in mental health care and the proposed organizational CRM practices offer a valuable basis for CRM in psychiatry and an addition to CRM in hospitals in general. Psychiatric hospitals can use the overview to review the completeness of their assessment and knowledge of risks. It can also be used to prioritize the risks that need to be addressed. The CRM practices mentioned in the interviews provide guidance on how to deal with these risks. These guidelines may also be supplemented with a further step, for example by using a quantitative survey to gather information on the probability of occurrence and severity of individual risks, and to collect information about the most effective and most feasible measures. Overall, research and knowledge of patient safety is growing. CRM offers an essential contribution as it aims to reduce harm to patients [ 8 ]. Studying CRM in particular settings, such as mental health care, is imperative in order to build safer health systems and to improve safety in general, but also for patients in mental health, whose illnesses render them extremely vulnerable.
Abbreviations
- Clinical risk management
P3: This index number indicates the interview and the paragraph where a quote was found.
Kohn LT, Corrigan JM, Donaldson MS: To err is human: building a safer health system. 1999, Washington, D.C.: National Academy Press
Google Scholar
Corrigan JM, Donaldson MS, Kohn LT, Maguire SK, Pike KC: Crossing the quality chasm: A new health system for the 21st century. 2001, Washington, D.C.: National Academy Press
Donaldson L: An organisation with a memory. Clin Med. 2002, 2 (5): 452-457.
Article Google Scholar
Briner M, Manser T, Kessler O: Clinical risk management in hospitals: strategy, central coordination and dialogue as key enablers. J Eval Clin Pract. 2013, in print
Leape LL, Berwick DM: Five years after To Err Is Human: What have we learned?. J Am Med Assoc. 2005, 293 (19): 2384-2390. 10.1001/jama.293.19.2384.
Article CAS Google Scholar
Clinical risk management: enhancing patient safety. Edited by: Vincent C. 2005, London: BMJ Books, 2nd
Chiozza ML, Plebani M: Clinical Governance: From clinical risk management to continuous quality improvement. Clin Chem Lab Med. 2006, 44 (6): 694-698.
Article CAS PubMed Google Scholar
Vincent C: Patient safety. 2010, Chichester: Wiley-Blackwell, 2nd
Book Google Scholar
Brickell TA, McLean C: Emerging issues and challenges for improving patient safety in mental health: a qualitative analysis of expert perspectives. J Patient Saf. 2011, 7 (1): 39-44. 10.1097/PTS.0b013e31820cd78e.
Article PubMed Google Scholar
Brickell TA, Nicholls TL, Procyshyn RM: Patient Safety and Mental Health. 2009, Edmonton, Alberta: Canadian Patient Safety Institute and Ontario Hospital Association, 58.
Callaly T, Arya D, Minas H: Quality, risk management and governance in mental health: an overview. Australas Psychiatry. 2005, 13 (1): 16-20.
Lipsedge M: Risk management in psychiatry. Clinical risk management: Enhancing patient safety. Edited by: Vincent C. 2001, London: BMJ Books, 219-240. 2nd
Cullen SW, Nath SB, Marcus SC: Toward understanding errors in inpatient psychiatry: a qualitative inquiry. Psychiatr Q. 2010, 81 (3): 197-205. 10.1007/s11126-010-9129-z.
Flewett T: Clinical risk management. An introductory text for mental health clinicans. 2010, Sydney: Elsevier Churchill Livingstone
Berman AL: Risk management with suicidal patients. J Clin Psychol. 2006, 62 (2): 171-184. 10.1002/jclp.20221.
Doyle M, Dolan M: Predicting community violence from patients discharged from mental health services. Br J Psychiatry. 2006, 189: 520-526. 10.1192/bjp.bp.105.021204.
Briner M, Kessler O, Pfeiffer Y, Wehner T, Manser T: Assessing hospitals' clinical risk management: Development of a monitoring instrument. BMC Health Serv Res. 2010, 10: 337-10.1186/1472-6963-10-337.
Article PubMed PubMed Central Google Scholar
Hahn S, Needham I, Abderhalden C, Duxbury JA, Halfens RJ: The effect of a training course on mental health nurses' attitudes on the reasons of patient aggression and its management. J Psychiatr Ment Health Nurs. 2006, 13 (2): 197-204. 10.1111/j.1365-2850.2006.00941.x.
Maden T: Treating violence: A guide to risk management in mental health. 2007, Oxford: Oxford University Press
Lamnek S: Qualitative Sozialforschung. [Qualitative social research]. 2010, Weinheim: Beltz, 5th
Langdridge D, Hagger-Johnson G: Introduction to research methods and data analysis in psychology. 2009, Edinburgh: Pearson Education, 2nd
Glaeser J, Laudel G: Experteninterviews und qualitative Inhaltsanalyse als Instrumente rekonstruierender Untersuchungen. [Expert interviews and qualitative content analysis as instruments of reconstructive research]. 2010, Wiesbaden: VS Verlag fuer Sozialwissenschaften, 4th
Mayring P: Qualitative Inhaltsanalyse. Grundlagen und Techniken. [Qualitative content analysis. Principles and procedures]. 2010, Weinheim: Beltz, 11th
Gigerenzer G, Todd PM: ABC Research Group: Simple heuristics that make us smart. 1999, New York: Oxford University Press
Morgan DL: Focus groups as qualitative research. 1997, Thousand Oaks etc: Sage Publications, 2nd
Rossiter JR: Content Validity of Measures of Abstract Constructs in Management and Organizational Research. Brit J Manage. 2008, 19 (4): 380-388. 10.1111/j.1467-8551.2008.00587.x.
Woods P, Almvik R: The Broset violence checklist (BVC). Acta Psychiatr Scand. 2002, 412: 103-105.
Richter D, Berger K: Patientenübergriffe auf Mitarbeiter: Eine prospektive Untersuchung der Häufigkeit, Situationen und Folgen. [Assaults from patients on staff. A prospective study of frequencies, situations and consequences]. Nervenarzt. 2001, 72: 693-699. 10.1007/s001150170048.
Wu AW: Medical error: The second victim: The doctor who makes the mistake needs help too. Br Med J. 2000, 320 (7237): 726-727. 10.1136/bmj.320.7237.726.
Simon RI: Patient Safety Versus Freedom of Movement: Coping With Uncertainty. The American Psychiatric Publishing textbook of suicide assessment and management. Edited by: Simon RI, Hales RE. 2006, Washington, DC: American Psychiatric Pub, 423-439.
Graber M: Diagnostic errors in medicine: a case of neglect. Jt Comm J Qual Patient Saf. 2005, 31 (2): 106-113.
PubMed Google Scholar
Phillips RL, Bartholomew LA, Dovey SM, Fryer GE, Miyoshi TJ, Green LA: Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care. 2004, 13 (2): 121-126. 10.1136/qshc.2003.008029.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1472-6963/13/44/prepub
Download references
Acknowledgements
This study was funded by the Foundation for Applied Psychology of Suzanne and Hans Biäsch (2008/15). Additional funding was provided by the Centre for Organizational and Occupational Sciences of the ETH Zurich and by the Swiss Commission for Technology and Innovation (KTI 8614.1 ESPP-ES).
We especially thank Lisa Liebke, Nina Albin, Ursina Pieth, Sandra De Pasquale and Fabian Probst for their assistance in the project “Clinical risks in mental health care”. We also thank Oliver Kessler, Theo Wehner and Yvonne Pfeiffer for their contributions to the project “Risk management in Swiss hospitals as social innovation”.
Author information
Authors and affiliations.
ETH Zurich, Centre for Organizational and Occupational Sciences, Weinbergstrasse 56/58, 8092, Zurich, Switzerland
Matthias Briner
Lucerne School of Business, Lucerne University of Applied Sciences and Arts, Zentralstrasse 9, 6002, Lucerne, Switzerland
Department of Psychology, University of Fribourg, Rue P.-A. de Faucigny 2, 1700, Fribourg, Switzerland
Tanja Manser
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Matthias Briner .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
MB and TM designed and executed the project. MB drafted the initial manuscript. TM revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Briner, M., Manser, T. Clinical risk management in mental health: a qualitative study of main risks and related organizational management practices. BMC Health Serv Res 13 , 44 (2013). https://doi.org/10.1186/1472-6963-13-44
Download citation
Received : 26 September 2012
Accepted : 28 January 2013
Published : 04 February 2013
DOI : https://doi.org/10.1186/1472-6963-13-44
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient safety
- Organizational risk management
- Mental health care
- Qualitative analysis
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Undergraduate Admissions
- Graduate Admissions
- Teacher Certification Options
- International Admissions Information
- Financial Aid & Scholarships
- Undergraduate Majors and Minors
- Master’s Programs
- Certificates of Advanced Study
- Doctoral Programs
- Online, Hybrid, and Flexible Programs
- Faculty and Academic Advising
- Career Services and Certification
- Undergraduate Peer Advisors
- Student Organizations
- Learning Communities
- For Families
- Study Abroad
- Field Placements & Internships
- Bridge to the City
- Spector/Warren Fellowship
- Orange Holmes Scholars
- Engaged BIPOC Scholar-Practitioner Program
- Research News
- Faculty Bookshelf
- Faculty Publications
- Grants & Awards
- Doctoral Dissertations
- Research Resources and Support
- Office of Professional Research and Development
- Atrocity Studies Annual Lecture
- Antiracist Algebra Coalition
- Ganders Lecture Series
- InquiryU@Solvay
- Intergroup Dialogue Program
- Otto’s Fall Reading Kickoff
- Psycho-Educational Teaching Laboratory
- The Study Council
- Writing Our Lives
- Center for Academic Achievement and Student Development
- Center on Disability and Inclusion
- Center for Experiential Pedagogy and Practice
- Latest News
- Upcoming Events
- Education Exchange
- Get Involved
- Advisory Board
- Tolley Medal
- Administration
- From the Dean
- Convocation
- Accreditation
- Request Info
- Grants & Awards
Suicide Risk: Case Studies and Vignettes
Identifying warning signs case study.
Taken from Patterson, C. W. (1981). Suicide. In Basic Psychopathology: A Programmed Text.
Instructions: Underline all words and phrases in the following case history that are related to INCREASED suicidal risk. Then answer the questions at the end of the exercise.
History of Present Illness
The client is a 65-year-old white male, divorced, living alone, admitted to the hospital in a near comatose condition yesterday because of an overdose of approximately thirty tablets of Valium, 5 mgm, combined with alcoholic intoxication. The client was given supportive care and is alert at the present time.
A heavy drinker, he has been unemployed from his janitorial job for the past three months because of his drinking. He acknowledges feeling increasingly depressed since being fired, and for the past two weeks has had insomnia, anorexia, and a ten pound weight loss. He indicates he wanted to die, had been thinking of suicide for the past week, planned the overdose, but had to “get drunk” because “I didn’t have the guts” [to kill myself]. He is unhappy that the attempt failed, states that, “nobody can help me” and he sees no way to help himself. He denies having any close relationships or caring how others would feel if he committed suicide (“who is there who cares?”). He views death as a “relief.” His use of alcohol has increased considerably in the past month. He denies having any hobbies or activities, “just drinking.”
Past Psychiatric History
Hospitalized in 1985 at Pleasantview Psychiatric Hospital for three months following a suicide attempt after his fourth wife left him. Treated with ECT, he did “pretty good, but only for about two years” thereafter.
Social History
An only child, his parents are deceased (father died by suicide when client was eight years old; mother died of “old age” two years ago). Raised in Boston, he moved to Los Angeles at twenty-one and has lived here since. Completed eighth grade (without any repeat) but quit to go to work (family needed money). Has never held a job longer than two years, usually quitting or being fired because of “my temper.” Usually worked as a laborer. Denies any physical problems other than feeling “tired all the time.” Currently living on Social Security income, he has no other financial resources. He received a bad conduct discharge from the army after three months for “disobeying an order and punching the officer.” He has had no legal problems other than several arrests in the past two years for public intoxication. Married and divorced four times, he has no children or close friends.
Mental Status Examination
65 y.o. W/M, short, thin, grey-haired, unkempt, with 2-3 day-old beard, lying passively in bed and avoiding eye contact. His speech was slow and he did not spontaneously offer information. Passively cooperative. Little movement of his extremities. His facial expression was sad and immobile.
Thought processes were logical and coherent, and no delusions or hallucinations were noted. Theme of talk centered around how hopeless the future was and his wishes to be dead. There were no thoughts about wishing to harm others.
Mood was one of depression. He was oriented to person, place, and time, and recent and remote memory was intact. He could perform simple calculations and his general fund of knowledge was fair. His intelligence was judged average.
Diagnostic Impression
- drug overdose (Valium and alcohol)
- Dysthymic Disorder (depression)
- Substance Use Disorder (alcohol)
Questions for Exercise
You have interviewed the client, obtained the above history, and now have to make some decisions about the client. He wants to leave the hospital.
- Is he a significant risk for suicide?
- discharging him as he wishes and with your concurrence?
- discharging him against medical advice (A.M.A.)?
- discharging him if he promises to see a therapist at a nearby mental health center within the next few days?
- holding him for purposes of getting his psychiatric in-client care even though he objects?
- Discuss briefly why you would not have chosen the other alternatives in question #2.
Identifying Warning Signs Case Study: Feedback/Answers
The client is a 65-year-old white male , divorced , living alone , admitted to the hospital in a near comatose condition yesterday because of an overdose of approximately thirty tablets of Valium, 5 mgm, combined with alcoholic intoxication. The client was given supportive care and is alert at the present time. A heavy drinker , he has been unemployed from his janitorial job for the past three months because of his drinking. He acknowledges feeling increasingly depressed since being fired, and for the past two weeks has had insomnia and a ten pound weight loss . He indicates he wanted to die, had been thinking of suicide for the past week, planned the overdose, but had to “get drunk” because “I didn’t have the guts” [to kill myself]. He is unhappy that the attempt failed , states that, “ nobody can help me ” and he sees no way to help himself. He denies having any close relationships or caring how others would feel if he committed suicide (“who is there who cares?”). He views death as a “relief.” His use of alcohol has increased considerably in the past month. He denies having any hobbies or activities , “just drinking.”
Hospitalized in 1985 at Pleasantview Psychiatric Hospital for three months following a suicide attempt after his fourth wife left him . Treated with ECT, he did “pretty good, but only for about two years” thereafter.
An only child, his parents are deceased ( father died by suicide when client was eight years old; mother died of “old age” two years ago). Raised in Boston, he moved to Los Angeles at twenty-one and has lived here since. Completed eighth grade (without any repeat) but quit to go to work (family needed money). Has never held a job longer than two years , usually quitting or being fired because of “ my temper .” Usually worked as a laborer. Denies any physical problems other than feeling “tired all the time.” Currently living on Social Security income, he has no other financial resources . He received a bad conduct discharge from the army after three months for “disobeying an order and punching the officer.” He has had no legal problems other than several arrests in the past two years for public intoxication. Married and divorced four times , he has no children or close friends .
65 y.o. W/M, short, thin, grey-haired, unkempt, with 2-3 day-old beard, lying passively in bed and avoiding eye contact. His speech was slow and he did not spontaneously offer information . Passively cooperative. Little movement of his extremities. His facial expression was sad and immobile. Thought processes were logical and coherent, and no delusions or hallucinations were noted. Theme of talk centered around how hopeless the future was and his wishes to be dead . There were no thoughts about wishing to harm others. Mood was one of depression . He was oriented to person, place, and time, and recent and remote memory was intact. He could perform simple calculations and his general fund of knowledge was fair. His intelligence was judged average.
- Is he a significant risk for suicide? Yes. The client presents a considerable suicidal risk, with respect to demographic characteristics, psychiatric diagnosis and mental status findings.
- Discuss briefly why you would not have chosen the other alternatives in question #2. The client appears to be actively suicidal at the present time,and may act upon his feelings. Nothing about his life has changed because of his attempt. He still is lonely, with limited social resources. He feels no remorse for his suicidal behavior and his future remains unaltered. He must be hospitalized until some therapeutic progress can be made.
Short-Term Suicide Risk Vignettes
*Case study vignettes taken from Maris, R. W., Berman, A. L., Maltsberger, J. T., & Yufit, R. I. (Eds), (1992). Assessment and prediction of suicide. New York: Guilford. And originally cited in Stelmachers, Z. T., & Sherman, R. E. (1990). Use of case vignettes in suicide risk assessment. Suicide and Life-Threatening Behavior, 20, 65-84.
The assessment of suicide risk is a complicated process. The following vignettes are provided to promote discussion of suicide risk factors, assessment procedures, and intervention strategies. The “answers” are not provided, rather students are encouraged to discuss cases with each other and faculty. Two examples of how discussions may be facilitated are provided.
37-year-old white female, self-referred. Stated plan is to drive her car off a bridge. Precipitant seems to be verbal abuse by her boss; after talking to her nightly for hours, he suddenly refused to talk to her. As a result, patient feels angry and hurt, threatened to kill herself. She is also angry at her mother, who will not let patient smoke or bring men to their home. Current alcohol level is .15; patient is confused, repetitive, and ataxic. History reveals a previous suicide attempt (overdose) 7 years ago, which resulted in hospitalization. After spending the night at CIC and sobering, patient denies further suicidal intent.
16-year-old Native American female, self-referred following an overdose of 12 aspirins. Precipitant: could not tolerate rumors at school that she and another girl are sharing the same boyfriend. Denies being suicidal at this time (“I won’t do it again; I learned my lesson”). Reports that she has always had difficulty expressing her feelings. In the interview, is quiet, guarded, and initially quite reluctant to talk. Diagnostic impression: adjustment disorder.
49-year-old white female brought by police on a transportation hold following threats to overdose on aspirin (initially telephoned CIC and was willing to give her address). Patient feels trapped and abused, can’t cope at home with her schizophrenic sister. Wants to be in the hospital and continues to feel like killing herself. Husband indicates that the patient has been threatening to shoot him and her daughter but probably has no gun. Recent arrest for disorderly conduct (threatened police with a butcher knife). History of aspirin overdose 3 years ago. In the interview, patient is cooperative; appears depressed, anxious, helpless, and hopeless. Appetite and sleep are down, and so is her self-esteem. Is described as “anhedonic.” Alcohol level: .12.
23-year-od white male, self-referred. Patient bought a gun 2 months ago to kill himself and claims to have the gun and four shells in his car (police found the gun but no shells). Patient reports having planned time and place for suicide several times in the past. States that he cannot live any more with his “emotional pain” since his wife left him3 years ago. This pain has increased during the last week, but the patient cannot pinpoint any precipitant. Patient has a history of chemical dependency, but has been sober for 20 months and currently goes to AA.
22-year-old black male referred to CIC from the Emergency Room on a transportation hold. He referred himself to the Emergency Room after making fairly deep cuts on his wrists requiring nine stitches. Current stress is recent breakup with his girlfriend and loss of job. Has developed depressive symptoms for the last 2 months, including social withdrawal, insomnia, anhedonia, and decreased appetite. Blames his sister for the breakup with girlfriend. Makes threats to sister (“I will slice up that bitch, she is dead when I get out”). Patient is an alcoholic who just completed court-ordered chemical dependency treatment lasting 3 weeks. He is also on parole for attempted rape. There is a history of previous suicide attempts and assaultive behavior, which led to the patient being jailed. In the interview, patient is vague regarding recent events and history. He denies intent to kill himself but admits to still being quite ambivalent about it. Diagnostic impression: antisocial personality.
19-year-old white male found by roommate in a “sluggish” state following the ingestion of 10 sleeping pills (Sominex) and one bottle of whiskey. Recently has been giving away his possessions and has written a suicide note. After being brought to the Emergency Room, declares that he will do it again. Blood alcohol level: .23. For the last 3 or 4 weeks there has been sleep and appetite disturbance, with a 15-pound weight loss and subjective feelings of depression. Diagnostic impression: adjustment disorder with depressed mood versus major depressive episode. Patient refused hospitalization.
30-year-old white male brought from his place of employment by a personnel representative. Patient has been thinking of suicide “all the time” because he “can’t cope.” Has a knot in his stomach; sleep and appetite are down (sleeps only 3 hours per night); and plans either to shoot himself, jump off a bridge, or drive recklessly. Precipitant: constant fighting with his wife leading to a recent breakup (there is a long history of mutual verbal/physical abuse). There is a history of a serious suicide attempt: patient jumped off a ledge and fractured both legs; the precipitant for that attempt was a previous divorce. There is a history of chemical dependency with two courses of treatment. There is no current problem with alcohol or drugs. Patient is tearful, shaking, frightened, feeling hopeless, and at high risk for impulsive acting out. He states that life isn’t worthwhile.
Vignette Discussion Examples
Vignette example 1.
Twenty-six year old white female phoned her counselor, stated that she might take pills, and then hung up and kept the phone off the hook. The counselor called the police and the patient was brought to the crisis intervention center on a transportation hold. Patient was angry, denied suicidal attempt, and refused evaluation; described as selectively mute, which means she wouldn’t answer any of the questions she didn’t like.
Facilitator: How high a risk is this person for committing suicide? Low, moderate or high? Student Answer 1: Maybe moderate because the person is warning somebody, basically a plea for help. Facilitator: Okay, so we have suicidal talk. That’s one of our red flags. What else? She said she might take pills, so we didn’t know if she does have the pills. So she has a plan. The plan would be to take pills, but we don’t know if we have means. Student Answer 2: High. She’s also angry. I don’t know if she’s angry often. Facilitator: A person in this situation who is really thinking about killing themselves tends not to deny it. They tend not to deny it. There are exceptions to everything, but most of the time, for some reason, this is one of the things where people tend to mostly tell you the truth. If you ask people, they tend to tell you the truth. It’s a very funny thing about suicide that way. That’s certainly not true about most things. If you ask people how much they drink…But, “Are you thinking about killing yourself?” “Well, yes.” If you ask a question, you tend to get a more or less accurate, straight answer. Student question: Is that because it doesn’t matter anymore? If they’re going to die anyway, who’s going to care about what anybody thinks or what happens? Facilitator: My hypothesis would be, when someone is at that point, they’re talking about real, true things. They’re not into play. This is where they are. If they’re really looking at it, then they’re just at that place. What’s to hide at that point? You don’t have anything to lose. It’s a state of mind. And then if you’re not in that place—it’s like, how close are you to the edge of that cliff? “I’m not there. I know where that is, and I’m not there.” “If you get there, will you tell me?” “Yeah, I’m not there.” So, people have a sense—if they’ve gotten that close, they know where that line is, and they know about where they stand in regard to it, because it’s a very hard-edged, true thing.
Twenty-three year old white male, self-referred. Patient bought a gun two months ago to kill himself and claims to have the gun and four shells in his car. Police found the gun but no shells. Patient reports having planned time and place for suicide several times in the past. States that he cannot live anymore with his emotional pain since his wife left him three years ago. This pain has increased during the last week, but the patient cannot pinpoint any precipitant. Patient has a history of chemical dependency but has been sober for 20 months and currently goes to AA.
Facilitator: How high a risk is this person for committing suicide? Low, moderate or high? On a scale from 0 to 7 (7 being very high). Student Answer 1: High. On a scale of 0 to 7? Student Answer: Six. Student Answer 2: I would say three. I think it would be lower because if he’s already bought the gun two months ago and he’s self-referring himself to get help, he wants to live. He has not made peace with whatever, and he’s more likely not give away his things, and he’s going to AA meetings. I think it’s lower than really an extreme…I would say a three or four. Student Answer 3: I would say a four or five, moderate. Student Answer 4: About a five..several times and hasn’t followed through, tells me he doesn’t really want to follow through with it. Facilitator: And there are no shells, right? So we can see some of the red flags are there, but some of them aren’t. He’s still sober… Student: He has a support group. Student: He’s not using, though he bought a gun—so that’s a concern. There is a lot there. Student: He may not have the shells so he doesn’t have the opportunity to. So does that make him more…? Student 2: Think I’ll change mine to a five. Facilitator: So the mean was 4.68, so 5 was the mode. If we’re saying this is a moderate risk, what things would we look for that would make this a high risk? Student: Take away AA. Student: If he falls off the wagon, he goes right to the top. Student: And if he finds the shells. Facilitator: Because it probably is not that hard to find shells. All these stores around here, you can get shells quicker than you can get a gun, so he’s only a five-minute purchase away from having lethal—in contrast to not having the gun. Student: Could there be a difference in the time? Let’s say his wife left him just four to six months ago rather than three years. Would that be something that would be more serious? Facilitator: Yes, or if his wife just left him. So, say his wife left him a month ago that would bump it up. So that’s unresolved. That’s taking a person that was worried and that’s pushing him higher. Student: It also raises the homicide rate. Facilitator: Yes, because these tend to be murder-suicides. How often have we seen that? Murder-suicide is a big deal. If she won’t be with me, she won’t be with anybody.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 09 May 2024
Predicting suicidality with small sets of interpretable reward behavior and survey variables
- Shamal Lalvani 1 ,
- Sumra Bari 2 na1 ,
- Nicole L. Vike 2 na1 ,
- Leandros Stefanopoulos ORCID: orcid.org/0000-0002-2682-5639 1 , 3 na1 ,
- Byoung-Woo Kim 2 na1 ,
- Martin Block 4 ,
- Nicos Maglaveras 3 ,
- Aggelos K. Katsaggelos 1 , 5 , 6 na2 &
- Hans C. Breiter 2 , 7 na2
Nature Mental Health ( 2024 ) Cite this article
747 Accesses
95 Altmetric
Metrics details
- Risk factors
- Translational research
The prediction of suicidal thought and behavior has met with mixed results. This study of 3,476 de-identified participants (4,019 before data exclusion) quantified the prediction of four suicidal thought and behavior (STB) variables using a short reward/aversion judgment task and a limited set of demographic and mental health surveys. The focus was to produce a simple, quick and objective framework for assessing STB that might be automatable, without the use of big data. A balanced random forest classifier performed better than a Gaussian mixture model and four standard machine learning classifiers for predicting passive suicide ideation, active suicide ideation, suicide planning and planning for safety. Accuracies ranged from 78% to 92% (optimal area under the curve between 0.80 and 0.95) without overfitting, and peak performance was observed for predicting suicide planning. The relative importance of features for prediction showed distinct weighting across judgment variables, contributing between 40% and 64% to prediction per Gini scores. Mediation/moderation analyses showed that depression, anxiety, loneliness and age variables moderated the judgment variables, indicating that the interaction of judgment with mental health and demographic indices is fundamental for the high-accuracy prediction of STB. These findings suggest the feasibility of an efficient and highly scalable system for suicide assessment, without requiring psychiatric records or neural measures. The findings suggest that STB might be understood within a cognitive framework for judgment with quantitative variables whose unique constellation separates passive and active suicidal thought (ideation) from suicide planning and planning for safety.
Similar content being viewed by others

Multidimensional variability in ecological assessments predicts two clusters of suicidal patients
Complex modeling with detailed temporal predictors does not improve health records-based suicide risk prediction
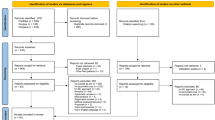
Machine learning and the prediction of suicide in psychiatric populations: a systematic review
Suicide rates in the United States increased by over 30% between 2000 and 2020 1 , and these rates were exacerbated by the COVID-19 pandemic 2 , 3 . Efforts predicting the potential for suicidal action are mixed, with some researchers being critical of prediction accuracy 4 , 5 . Recent research suggests that machine learning (ML) algorithms outperform traditional statistical approaches for the prediction of suicidal thought and behavior (STB) 6 , 7 . Furthermore, meta-analysis suggests that theories of suicide (for example, biosocial, biological, ideation and hopelessness theories 8 ) perform suboptimally when compared to ML algorithms in the prediction of suicidal ideation, suicidal attempt(s) and completed suicide 8 . Grounded by research suggesting that electronically delivered self-report questionnaires correlate significantly with clinical assessment for psychiatric conditions 9 , researchers have recently called for the development of a scalable detection platform for the prediction of STB 10 .Clinically related measures are predictive of STB, such as post traumatic stress disorder 11 and measures of anger 12 . Additionally, recent research suggests that social and behavioral measures play a key role in the prediction of STB, sometimes surpassing clinical variables in terms of predictive accuracy, such as when used in the context of social media behavior derived from natural language processing (NLP) analysis 10 , 13 and measures of social integration 14 . This is consistent with other literature suggesting that a clinically valid signal of psychiatric conditions may be available from social media behavior 15 . Although contextual risk factors are not typically studied in ML applications of STB 7 , predictive variables of STB are typically contextual 7 , 16 . For example, substance use and alcohol disorders play a greater risk in suicidal outcomes for veterans and service members than for the general population 16 .
Few ML studies have used emergency room (ER)-related questions to predict suicide risk, and no studies have applied small sets (for example, 20–30) of interpretable variables that can be easily acquired on digital devices to predict a set of suicidal thought and behavior variables with high accuracy (Supplementary Fig. 1 ). STB assessments in the ER generally ask about passive ideation as a framework for opening the topic to query, move to active ideation and planning for harm, and then assess the potential to plan for safety 17 . In the ML literature, passive and active suicidal ideation are often not segregated 18 , 19 , 20 , and intent for self-harm and past suicidal attempts tend to be targeted 21 , 22 , 23 rather than plans for suicide. However, truthful responses may be difficult to acquire regarding suicidal ideation and past suicide attempts due to cultural norms or other personal reasons 24 , 25 . Furthermore, no studies have predicted planning for safety, which is key for framing suicide risk 26 , and although it does not reduce suicidal ideation 27 , meta-analysis suggests it may reduce relative suicide risk by up to 57% (ref. 27 ), as well as reduce symptoms of depression, feelings of hopelessness and the incidence of hospitalization 28 , although there is a large heterogeneity of suicide planning intervention and study design 28 . No studies have assessed all four STB variables together (that is, passive ideation, active ideation, suicide planning, planning for safety).
Individuals with STB show alterations in reward/aversion judgment or preference 29 , such as heightened aversion to risk and loss 30 , lower focus on the negative consequences of decisions 31 , discounting of delayed rewards 32 , and higher bias to escape aversive situations 33 . In economic settings, preferences can be measured from forced choice data (typically through axioms of revealed preference 34 ). In the psychological literature, preferences can reflect ‘liking’ versus ‘wanting’ 35 , 36 , 37 , 38 , 39 , where the assessment of reward or aversion (that is, judgment) precedes an actual choice. Abnormalities in reward/aversion judgment have been linked to dopamine dysfunction in major depressive disorder, addiction, anxiety, chronic stress 40 , 41 and STB 41 . Reward/aversion judgment has been mathematically characterized by computational behavior variables reflecting biases 42 , 43 , like loss aversion 44 and risk aversion 45 . Recently, a broader set of 15 variables were found to model unique features of judgment from a picture-rating task that can be implemented on any cellphone or digital device 37 , 39 (Fig. 1 , Supplementary Fig. 2 and Table 1 ), and these are considered to reflect psychological ‘liking’ 35 , 37 , 39 , 46 , 47 . For the present study we hypothesized that this small set of judgment variables (as opposed to big data) would efficiently predict STB.
a , The value function in relative preference theory (RPT) resembles the value function in Kahneman and Tversky’s prospect theory (PT) 43 , albeit with very different variables. In both RPT and PT, functions follow a concave power-law function, and the avoidance curve tends to have a greater slope than the approach curve. The entropy H of ratings for each category is a function of the mean rating K for each stimulus category used in the rating task. b , The limit function in RPT corresponds to the variance–mean curve produced in Markowitz’s portfolio theory 105 , which shows the risk level an individual is willing to accept for a fixed reward. The variance of the picture rating of a category ( σ ) is plotted against the mean rating K for each category of images, producing a parabolic relationship in individuals. c , The tradeoff function in RPT characterizes an individual’s pattern of approach judgments versus avoidance judgments. The pattern/entropy of approach judgments ( H + ) is plotted against the pattern/entropy of avoidance judgments ( H − ) for each category of images used in the rating task.
This study tested whether these four STB variables could be predicted with 15 reward/aversion judgment variables (henceforth ‘judgment variables’, Fig. 1 ) derived from a short behavior task ( Methods ). We combined the behavior task with five other survey variables that were hypothesized to contextually frame the judgment variables, but only added minutes to the survey time. This framework was found to make highly accurate prediction using a small, interpretable variable set in lieu of the hundreds to thousands of variables used in traditional big data approaches. Mediation/moderation analyses further revealed that interactions between judgment and survey variables underpinned these high accuracies.
Given the current rates of STB, this approach using limited judgment and survey measures suggests a low-cost approach to STB assessment that could be administered to 85% of the world’s population with a personal digital device 48 . Use of variables that do not directly reference STB might also aide identification of at-risk individuals who might be hesitant to disclose self-harm. Ultimately, the power of psychological constructs depends on their capacity to make meaningful predictions, and not just their associations to neural measures.
Adults (ages 18–70 years) across the United States were surveyed in December 2021. High-quality data from 3,476 participants was drawn from (1) Patient Health Questionnaire 8 (PHQ8; absent the question on suicidality 49 ), (2) the State Trait Anxiety Inventory—State (STAI) 50 , (3) perceived loneliness (self-report), (4) prior attempts at self-harm in the past 1–12 months, (5) five demographic variables known to affect human neuroscience studies (age, ethnicity, education level, sex and handedness) 51 , 52 , 53 , 54 , (6) 15 judgment variables computationally derived from a simple picture-rating task 37 , 39 (Supplementary Figs. 3 and 4 and Table 1 ) and (7) four questions about passive ideation (STB1), active ideation (STB2), suicide planning (STB3) and planning for safety (STB4) on a five-point Likert scale (collectively referred to as STB variables) 17 , 55 ( Methods ). The predictive power of variables in (1) to (6) was tested using a balanced random forest (BRF) 56 approach (Supplementary Fig. 5 ) and Gaussian mixture models (GMMs) 57 (Supplementary Fig. 6 ) to discriminate between the low and high thresholds of the four STB variables. To provide a baseline against these analyses, we also performed the following four standard ML analyses: random forest (RF), logistic regression (LR), neural network (NN) and support vector machine (SVM) 58 . Given potential personal reluctance or cultural norms 59 , 60 against reporting past self-harm, variables from (1) to (3) and (5) and (6) were initially tested, followed by a minimal predictor set of (4) to (6). The full set of (1) to (6) was further tested. The relative importance of features used in prediction was evaluated using mutual information (MI) scoring (where a higher MI for a feature and predictor suggests predictive power) 61 and Gini score plots 62 . Mechanistic relationships between the top predictors were assessed using statistical mediation and moderation, where the four STB variables were dependent variables.
Prediction of STB variables
Given the higher sensitivity and specificity of BRF analyses, BRF outcomes are presented in the main text and the GMM results, along with the four standard ML results, are provided in Supplementary Tables 10–19 . In the following sections, ML results for judgment variables, PHQ8 score, STAI score and loneliness are described in the first paragraph, and the results for judgment variables, prior attempts and loneliness are described in the second paragraph. Results with inclusion of all predictors (judgment variables, PHQ8 score, STAI score, loneliness and prior attempts) are described in the third paragraph.
Passive suicidal ideation (STB1)
BRF prediction of STB1 (rated on a Likert scale of 1–5, where 1 = no suicidal ideation and 2–5 = increasing degrees of suicidal ideation; that is, threshold = 1) using judgment variables yielded higher accuracies with PHQ8, STAI and loneliness variables included (59.0–78.8%) (Supplementary Table 1a ). Sensitivities and specificities improved from 51.4% to 83.3% and from 61.0% to 77.7%, respectively. Adding demographics improved these metrics by less than 2%. Fusion of the PHQ8 score with judgment variables led to a consistent boost of ~18% for accuracy and 32% for sensitivity. Results with inclusion of judgment, PHQ8, STAI and loneliness features were similar (61.9–78.5%; Table 2a ) when the threshold for passive suicidal ideation was set to 2.
When judgment variables were fused with reports of prior suicide attempts and loneliness, predictive accuracy of STB1 at threshold = 1 was 78.4% and 78.1%, respectively. Sensitivity improved from 52.0% to 74.2% when loneliness was fused with judgment variables and prior attempts, whereas specificity showed a decrease from 85.4% to 79.1%. Prediction of STB1 at threshold = 2 when judgment variables were fused with reports of prior suicide attempts and loneliness was 83.4% and 80.4%, respectively, with similar sensitivities and specificities to threshold = 1.
Analysis with all predictors achieved maximum AUC scores of 0.905 for STB1 threshold = 1, and 0.907 when threshold = 2, achieving sensitivities of 84.8% and 85.1%, respectively.
Active suicidal ideation (STB2)
BRF prediction of STB2 (threshold = 1) using judgment variables yielded higher accuracies as PHQ8, STAI and loneliness variables were successively included (63.8–78.7%; Supplementary Table 1b ). Sensitivities and specificities improved from 56.0% to 86.1% and 65.1% to 77.5%, respectively. Further adding demographics improved these metrics by less than 1%. Fusion of the PHQ8 score with judgment variables boosted measures by 12% for accuracy and 28% for sensitivity. For threshold = 2, judgment variables yielded higher accuracies as PHQ8, STAI and loneliness features were successively included (62.7–78.0%; Table 2b ), with similar outcomes for sensitivity and specificity.
Prediction accuracy of STB2 (threshold = 1) when judgment variables were fused with reports of prior suicide attempts and loneliness was 86.4% and 84.7%, respectively. Sensitivity and specificity percentages were in the high 60–70s and 80–90s, respectively. Prediction of active suicidal ideation (threshold = 2) when judgment variables were fused with reports of prior suicide attempts and loneliness was 88.0% and 86.4%, respectively. Sensitivity and specificity percentages were in the 70s and high 80s, respectively.
Analysis with all predictor variables achieved maximum AUC scores of 0.935 at threshold = 1 and 0.931 at threshold = 2, achieving sensitivities in each case of 87.2% and 86.6%, respectively.
Suicide planning (STB3)
BRF prediction of STB3 (threshold = 1) using judgment variables yielded higher accuracies as PHQ8, STAI and loneliness variables were successively fused with them (64.4–79.4%; Supplementary Table 1c ). Sensitivities and specificities improved from 57.5% to 84.9% and 65.3% to 78.7%, respectively. Further adding demographics improved these metrics by less than 2%. Fusion of the PHQ8 score with judgment variables consistently boosted prediction by ~10% for accuracy and 20% for sensitivity. For threshold = 2, the judgment variables yielded higher accuracies as PHQ8, STAI and loneliness features were successively fused with them (66.8–79.7%; Table 2c ).
Prediction accuracy of STB3 (threshold = 1) when judgment variables were fused with reports of prior suicide attempts and loneliness variables was 92.2% and 90.8%, respectively. Sensitivities and specificities were in the high 70s and low 90s. Prediction of STB3 (threshold = 2) when judgment variables were fused with reports of prior suicide attempts and loneliness was 91.4% and 90.5%, respectively. Sensitivities and specificities were in the low 80s and low 90s, respectively.
Analysis with all predictor variables achieved maximum AUC scores of 0.953 with threshold = 1 and 0.948 for threshold = 2, achieving sensitivities of 86.4% and 88.7%, respectively.
Planning for safety (STB4)
BRF prediction of STB4 (threshold = 1) using judgment variables yielded higher accuracies as PHQ8, STAI and loneliness features were successively fused with them (59.4–73.8%; Supplementary Table 1d ). Further adding demographics improved these metrics by less than 2%. Sensitivities and specificities improved from 55.0% to 74.8% and 60.3% to 73.6%, respectively. Fusion of the PHQ8 score with judgment variables consistently boosted the prediction by ~14% for accuracy and 15% for sensitivity. For threshold = 2, the judgment variables also yielded higher accuracies as PHQ8, STAI and loneliness features were fused with them (71.7–79.9%; Table 2d ), with similar outcomes for other metrics.
Prediction accuracy of STB4 (threshold = 1) using judgment variables fused with prior suicide attempts and loneliness variables was 81.0% and 79.2%, respectively (Table 2d ). Sensitivity and specificity percentages were in the high 50s and mid 80s, respectively. Prediction of planning for safety (threshold = 2) when judgment features were fused with prior suicide attempts and loneliness was 77.7% and 61.9%, respectively (Table 2d ). Sensitivities and specificities were in the 50–60% range and 60–80% range, respectively.
Analysis with all predictor variables achieved maximum AUC scores of 0.837 at threshold = 1 and 0.831 at threshold = 2, while maintaining sensitivities of 73.1% and 74.1%, respectively.
Variable contributions to STB prediction
Distinct sets of judgment variables contributed to prediction of the four STB measures, as measured through normalized MI scoring (Fig. 2 and Supplementary Table 6a ). LA had zero MI for each STB measure. For passive suicidal ideation, no judgment variable predominated by MI value, and three had zero-value MIs. This profile was different for active suicidal ideation, where variables for aversion TP and tradeoff range had the highest MI. For suicide planning, the MI with the tradeoff range was far more than other judgment variables. For planning for safety, variables for aversion TP and reward TP were predominant. Despite the distinct patterns of MI for the 15 judgment variables among the four STB measures, regressions between these variables had consistent valences (except reward TP and total AR; Supplementary Table 6b ). On the basis of the valence between each judgment variable and STB measure, passive suicidal ideation and suicide planning shared the same patterns, and both differed from active suicidal ideation and planning for safety.
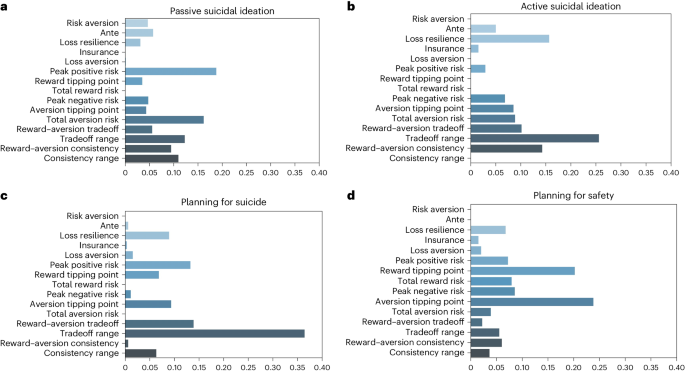
a – d , MI scoring of RPT features with respect to passive suicidal ideation ( a ), active suicidal ideation ( b ), planning for suicide ( c ) and having a plan for safety ( d ). Exact MI values are listed in Supplementary Table 6a . The MI between two variables informally expresses the amount of information gained about one variable by observation of another. In this context, this relates to the amount of information gained about STB variables by knowledge of the judgment variables. The length of the bars in the figures represents the MI ( x axis) of the RPT variables ( y axis). Longer bars indicate a higher MI between RPT variables and STB. This alludes to a larger predictive value. A MI score of zero implies that the two variables are independent, and therefore that prediction of one variable based on another is unlikely.
Gini score plots revealed that some survey variables were consistently highest in importance, but the full set of judgment variables were consistently grouped together (Fig. 3 and Supplementary Figs. 7 – 29 ). In all analyses, the grouped judgment variables produced summed Gini scores of 0.404 to 0.638—the highest summed Gini scores in 14 of the 24 analyses (Table 3 ). The 15 judgment variables were consistently more important than education, race, gender and handedness variables.
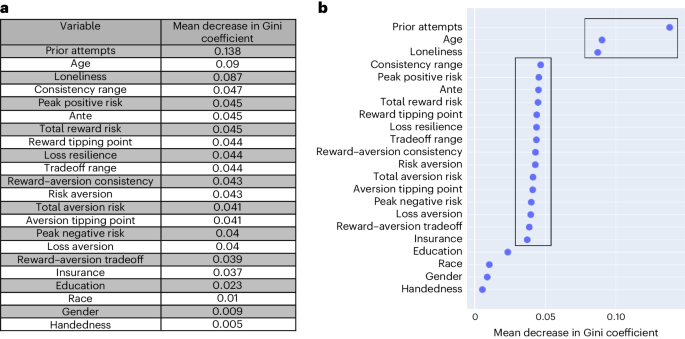
a , Gini importance values of the entire set of features used to predict planning for safety (STB4) at t = 2 using a BRF. The numerical values displayed are the mean decrease in Gini coefficient that occurs by removing each variable. The larger the mean decrease in Gini coefficient, the greater importance the feature has in the classifier. b , Visual display of the Gini importance values. Note that two boxes are shown. The highest box highlights the top variables in terms of Gini importance values, and the lower box represents the Gini importance values of the judgment variables.
The rank ordering of Gini scores for the survey variables was distinct for each STB measure, as it was for the 15 judgment variables. Despite this, STAI measures tended to have one of the top two Gini scores, and age was consistently one of the bottom of the five survey variables.
Mediation/moderation analysis
Mediation and moderation analyses followed published approaches 54 , 63 and were driven by the Gini score analyses 62 . The majority of judgment variables were involved in mediation/moderation relationships ( α = 0.05), excluding LA, total RR and reward TP for mediation, and excluding total RR and total AR for moderation (Supplementary Tables 2 – 4 ). Survey variables statistically mediated the relationship between 11 judgment variables and passive suicidal ideation, whereas they statistically moderated the relationship between eight judgment variables and passive suicidal ideation. For the other three STB measures, there was minimal mediation involving perceived loneliness, PHQ8 and STAI survey variables. Instead, there were salient moderation effects for these three survey measures with 12 of the 15 judgment variables (Supplementary Table 4 ).
Of the five survey variables, prior suicide attempts demonstrated mediation with four judgment variables to predict STB2–4 and moderated three judgment variables to predict STB1–2. Age showed mediation with six judgment variables, and moderation with one judgment variable (Supplementary Table 4 ).
This study sought a short, objective and automatable framework for predicting four STB measures using 15 variables for biases in reward/aversion judgment and a very limited set of demographic and mental health survey indices. Given that reward/aversion judgment is known to be affected by demographic and mental health indices, we fused demographics with the anxiety, depression and judgment variables for ML. This produced five primary results. (1) All four STB metrics were predicted with small sets of predictors within a range of 78–92% accuracy and 0.796–0.953 AUC; this compares favorably with the literature 4 , 19 , 20 , 21 , 23 , 64 , 65 , 66 , 67 , 68 , 69 , 70 . (2) Judgment variables and limited survey indices were most effective at predicting planning for suicide, producing accuracies in the upper range of what other studies have reported for suicide risk and suicide attempts (for example, AUC = 0.857 and 0.99, respectively, in the literature and 0.953 here) without using complex big data approaches (for example, 100+ variables or inclusion of neuroimaging) or retrospective data 19 , 20 , 64 , 65 , 66 , 67 , 68 , 69 , 70 . (3) Prediction of active suicidal ideation and planning for suicide was improved by the addition of one self-report measure of prior attempts of self-harm, similar to the addition of depression and other mental health indices. (4) Mediation/moderation analyses showed that depression, anxiety, loneliness and age variables had significant moderation effects on judgment variables, indicating that the interaction of mental health and contextual indices with judgment variables statistically predicted STB. (5) BRF prediction far outperformed GMM prediction and standard ML prediction (that is, RF, LR, NN and SVM prediction), particularly for the sensitivity index.
Collection of the limited set of variables used for prediction was more feasible and less time-consuming when compared to previous studies using larger datasets with hundreds to thousands of variables for prediction 19 , 20 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , and this task can be easily implemented on any digital device 37 , 38 , 39 . When the other mental health indices and demographics are included, data acquisition takes ~5 min to complete but has comparable prediction results to big data approaches 19 , 20 , 64 , 65 , 66 , 67 , 68 , 69 , 70 . Inclusion of the prior self-harm variable greatly improved the prediction of active suicidal ideation and planning for suicide, but did not improve prediction of passive suicidal ideation or planning for safety. This suggests that prior history might impact intention for harm, but not its inverse—the planning for self-preservation. Of the other mental health indices, the neurovegetative symptoms of depression in the PHQ8 most improved the predictive accuracy of the four STB variables, although by themselves each mental health index and age had higher Gini scores compared to the judgment variables. Loneliness is commonly considered a risk factor for STB 18 , and it was found to moderate the largest number of judgment variables in the prediction of STB variables. The addition of demographic variables was also not consistently beneficial for the prediction of STB, and competition between variables, leading to poorer prediction, cannot be ruled out 71 .
The sensitivity metric is important for evaluating the prediction efficacy of STB variables, particularly if intervention might be considered 4 , 19 , 20 , 21 , 23 , 64 , 65 , 66 , 67 , 68 , 69 , 70 . According to a review of studies since 2017 that reported a sensitivity metric for predicting suicidal ideation (Supplementary Table 5 ) 4 , 19 , 20 , 21 , 23 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , sensitivities ranged from 41% to 87%, with AUC scores ranging from 0.61 to 0.94, in line with our findings 4 , 19 , 21 , 64 , 65 . Higher AUC scores and sensitivities were typically provided for peer-reviewed work with large feature sets consisting of neuroimaging data, although none of these publications segregated passive and active ideation, as done commonly in clinical interviews 19 , 64 . Furthermore, a number of studies relied on anonymized electronic health records, and did not explicitly report the number of features used, which can vary per participant 4 , 21 , 23 , 65 , 67 . A similar range of sensitivities has been reported for the prediction of suicide attempt(s) (30.8–100%) with AUC scores ranging from 0.59 to 0.99 in cohorts of between 75 and 2,959,689 participants 4 , 19 , 20 , 21 , 23 , 65 , 66 . The prediction of suicidal attempt(s) appears to be more common in the literature than other STB outcomes, but has the caveat of being predominantly retrospective reporting 4 , 19 , 20 , 21 , 23 , 65 , 66 . In studies in the past five to six years providing sensitivity results, prediction of suicide risk provided similar sensitivities to suicidal ideation and suicidal attempt(s) (between 59% and 85.3%), and AUC scores of up to 0.857 (refs. 68 , 69 ). Finally, it must be noted that prediction of completed suicide reports showed much lower sensitivities (between 28% and 69%) and lower AUC scores (between 0.66 and 0.8) 21 , 70 . Relative to this literature, prior studies have not (1) segregated passive from active ideation in prediction of suicidal ideation 4 , 19 , 21 , 64 , 65 , (2) explicitly predicted planning for harm or (3) explicitly predicted planning for safety, all while achieving results in the upper range of what is reported for prediction of suicidal ideation, suicidal attempts and completed suicides (Supplementary Table 5 ) 4 , 19 , 20 , 21 , 23 , 64 , 65 , 66 , 67 , 68 , 69 , 70 .
The type of ML used for imbalanced data has become a topic of substantial research 72 , 73 , 74 , 75 . In this study, BRF prediction outperformed GMM prediction and four standard approaches to ML, consistent with the literature 76 . With BRF prediction, each STB variable further had a unique profile of judgment variables that contributed to their prediction, in that the MI metric of variable contribution was unique (Fig. 2 and Supplementary Table 6 ). The only exception was loss aversion (LA), which had no mutual information with any STB variable, and was not involved in any mediation/moderation relationship. The values for LA observed in this study were quite low, consistent with other work using picture ratings where there is no consequence for making a rating, unlike an operant keypress that changes view time 37 , 39 . Each of the four STB variables was best classified by a unique weighting of the 15 judgment variables, arguing that distinct aspects of reward/aversion judgment are important for each of the four STB metrics. This observation raises the hypothesis that unique constellations of judgment variables may underlie other forms of mental health conditions and behavior. Should further work show this for other mental health conditions (for example, depression, anxiety, substance use disorder), such findings would strongly support calls from the ML community to develop a standard model of mind 77 , albeit a model centered around processes for judgment and agency that focus on reward and aversion assessments by an organism.
Some limitations should be considered. First, the cohort was collected from the United States. As psychopathologies may differ across cultures 24 , 25 , cultural influences may result in different judgment variable groupings affecting prediction. Second, all variables were self-reported and not from clinical records, although it is not clear how a prospective study of STB with thousands of participants performing an experimental cognitive task could be run if there was a chance that breaking the blind would save lives. Third, the cohort was sampled during the COVID-19 pandemic, in which greater incidents of loneliness and suicidality were reported 2 , 3 , arguing for further work in the absence of a pandemic.

Conclusions
The current work found that 15 judgment variables and limited mental health and demographic information predicted four STB measures with sensitivities and specificities around 80% using a BRF approach that produced the highest sensitivities of the approaches used. There appear to be few studies that integrate quantitative judgment features, such as from a short behavioral task, to predict distinct STB measures. This work supports publications suggesting that social and behavioral measures play a key role in the prediction of STB, sometimes surpassing clinical variables in predictive accuracies 10 , 13 . Contextual risk factors are also not typically studied in ML applications of STB 7 , yet predictive variables of suicidality can be contextual 7 , 16 and the reported mediation/moderation results strongly support these reports. The current results contrast tendencies in the literature to either (1) use large feature sets for prediction (for example, hundreds to thousands of variables) 19 , 20 , 64 , 66 , 67 , 68 , 69 , 70 or (2) collect expensive clinical or biological measures for prediction 20 , 21 , 22 , 23 , 64 , 65 , 67 , 68 , 69 , 70 . The data needed for prediction in this study can readily be acquired by smart phones and other digital devices, which are currently available for 92% of the US population 78 and 85% of the world population 48 . The analysis does not require a supercomputer and thus can be scaled to populations for which big data and expensive clinical or biological measures are not available, meeting frameworks proposed by others for the development of a scalable detection platform for prediction of suicidality 10 . By combining multiple variables around STB, including assessments of planning for safety, this framework suggests a digital approach for early assessment and triage, which is particularly needed now 10 .
Going forward, future work might assess a broader set of features that can be extracted from the preference curves (that is the value, tradeoff and limit functions) besides the 15 used herein. Additionally, the analysis could be expanded to more deeply assess age and other demographic variables, such as between groups of adolescents and elderly participants. These age groups have different contextual risk factors 79 , 80 , 81 , 82 , making relevant contextual variables (retirement versus work status, insurance coverage, other medical illnesses, illness in peer group, familial social network and social media usage) potentially relevant variables. The study might also be followed up post pandemic to see if other variables become important as predictors or mediators/moderators. Given the current results, and the fact that every step of data collection, analysis and prediction can be automated, research groups with the requisite expertise might move forward with testing of such a system for populations at high risk (for example, higher education and the military) 83 , 84 .
Cohort recruitment
A third-party vendor, Gold Research Inc., recruited a population sample of adults across the United States (ages 18–70 years), with a final sample of 4,019 participants (see refs. 85 , 86 for the recruitment framework and procedures). To ensure adequate samples of participants with mental health conditions, Gold Research oversampled 15% of the sample for mental health conditions. Participant demographics were matched to the US Census Bureau at the time of sampling in December 2021. A total of 4,019 adults participated (mean age ± s.d. = 51.4 ± 14.9 years) (full demographics are provided in Supplementary Table 7 ), and, after applying data exclusion criteria, the data of 3,476 participants were retained. Informed consent was obtained for all participants, which included their primary participation in the study as well as the secondary usage of their anonymized, de-identified (that is, all identifying information removed by Gold Research Inc. before retrieval by the research group) data in secondary analyses. Informed consent was approved by the Institutional Review Board of Northwestern University (STU00213665 (ref. 55 )) and the University of Cincinnati (2023-0164), in accordance with the Declaration of Helsinki.
Reward/aversion judgment task
Participants completed a picture-rating task on their personal computers or cellphones. Each participant viewed a randomized sequence of 48 images, displayed one at a time. Images were from the International Affective Picture Set 87 , with eight images from each of the six picture categories sports, disasters, cute animals, aggressive animals, nature and adults in bathing suits. Participants were asked to rate each image on an integer scale from −3 (a strong disliking) to +3 (a strong liking), with zero being neutral (Supplementary Fig. 2 ). There was no time limit for making a picture rating, although participants were asked to rate the images as quickly as possible and to use their first impression. The next image was displayed once a rating was selected. The instructions shown to participants were as follows:
‘The next part of this survey involves looking at pictures and then responding how much you like or dislike the image. Please rate each image on a scale from −3 (Dislike Very Much) to +3 (Like Very Much). Zero (0) is neutral… meaning you have no feelings either way. The images are a set of photographs that have been used by scientists around the world for over 20 years.
It is important you rate each picture based on your initial emotional response. There are no right or wrong answers… just respond with your feelings and rate the pictures very quickly.
Please click ‘Next’ to begin . ’
See refs. 37 , 39 for further details.
Mental health indices and demographics
Demographics were acquired for five variables that have established relationships with neuroimaging 51 , 52 , 53 , 54 . Two published surveys were used in this study: (1) the Patient Health Questionnaire-9 (ref. 49 ), with the question about suicide removed and henceforth referred to as PHQ8, and (2) the State Trait Anxiety Inventory (STAI), where only state questions were used 50 . We further queried (1) perceived loneliness (self-report of a five-point Likert-like scale) and (2) the number of prior attempts at harming oneself in the past year. These variables (henceforth ‘survey variables’), along with the judgment variables (described below), were inputs for supervised ML prediction. We sought to predict four STB measures adopted from the Massachusetts General Hospital Subjective Question screener (MGH SQ) used in the Phenotype Genotype Project in Addiction and Mood Disorders 55 , 85 , 88 : (i) passive suicidal ideation, (ii) active suicidal ideation (STB1), (iii) planning for suicide and (iv) planning for safety. For the variables in (1), (2) and (i)–(iv), we used a five-point Likert scale: 1 being ‘Never’, 2 being ‘Rarely’, 3 being ‘Sometimes’, 4 being ‘Often’ and 5 being ‘Always’. Survey ratings for (i)–(iv) were answered by participants as relating to the past month. The MGH SQ has been used in multiple studies 38 , 89 , 90 , 91 , 92 , 93 , 94 and the four STB questions had been adapted to the MGH SQ from a clinical textbook on emergency psychiatry 17 .
Measurement of passive suicidality (‘Wishing to go to sleep and not wake up’) corresponded directly to the criteria of passive suicidality in the Columbia Suicide Severity Rating Scale (CSSRS) 95 and the Columbia Lighthouse Project for the Navy (CLPN) 96 , which measured passive suicidality as either wishing to be dead or wishing to go to sleep and not wake up. Active suicidality (‘Wanting to hurt yourself or take your own life’) also corresponded to measurements in the CSSRS and CLPN; however, it did not explicitly measure intent (for example, ‘Have you had any thoughts about how you might do this’). Planning for suicide (‘Having a plan to take your own life’) similarly corresponded to survey questions in the CSSRS (for example, ‘Have you thought about doing something to make yourself not alive anymore?’) and CLPN (for example, ‘Have you done anything, started to do anything, or prepared to do anything to end your own life?’). We note that planning for safety (‘Having a safety plan for not hurting yourself when these feelings arise’) is not specifically measured in the CSSRS or CLPN. However, it is a fundamental component of assessing suicide risk 17 , 26 .
Specific demographics collected were (1) age group, (2) gender at birth (that is, sex), (3) race/ethnicity, (4) highest education level completed and (5) handedness. Demographic categories and frequencies are listed in Supplementary Table 7 .
General data exclusion
The following quality assurance procedures were implemented as employed in other publications 37 , 39 , 55 , 85 . Participants meeting at least one of the following six criteria were omitted from the cohort: (1) participants with ten or more clinician-diagnosed illnesses, (2) participants that selected the same response for at least one section of the survey, (3) participants that rated all images in the behavioral task the same or with a variance of 1 (meaning only two of seven Likert points were used), (4) participants whose relative preference analysis yielded extreme outliers >3 Interquartile Ranges (IQRS) or incomplete measurements, (5) participants that had mismatching responses to years of education and education level in the survey, (6) participants that completed the questionnaire in less than 800 s (refs. 55 , 85 ). Data exclusion reduced the sample from 4,019 participants to 3,476 participants for analysis.
Reward/aversion judgment analysis
Computational behavior analysis used code published in refs. 38 , 39 . Ratings (Supplementary Fig. 2 ) were analyzed for each participant as schematized in Supplementary Fig. 3 , to produce relative preference theory (RPT) graphs (Fig. 1 ), which share a striking similarity to prospect theory and portfolio theory graphs 38 , 88 , 97 , yet use distinct variables. Procedures were performed in MATLAB as detailed elsewhere 38 , 88 , 97 ( Supplementary Methods ). Relative preference variables were extracted using MATLAB 7.1 with the following toolboxes: Curve Fitting Toolbox 1.1.4, Image Processing Toolbox 5.1, MATLAB Builder for Excel 1.2.5, Statistics Toolbox 5.1 and Symbolic Math Toolbox 3.1.3.
As described in Supplementary Fig. 3 , picture ratings produced an average magnitude ( K ), variance ( σ ) and pattern or information (that is, Shannon entropy ( H )) related to participants’ preference behavior. The variable K reflects the average (mean) of the positive ratings ( K + ) or negative ratings ( K − ) a participant made within each picture category. Similarly, the variance in positive ratings ( σ + ) or negative ratings ( σ − ), along with the Shannon entropy (that is, information 98 ) of positive ratings ( H + ) or negative ratings ( H − ) were computed for stimuli within each category. The Shannon entropy characterizes the degree of uncertainty across a set of responses 98 and is a core variable in information theory. Given it quantifies the pattern of judgments made to a set of stimuli, it could be considered a memory variable. These variables capture judgments about the magnitude (intensity of rating) and valence of judgment (positive versus negative or approach versus avoidance) to describe relative preferences (Fig. 1 ) 37 , 38 , 39 , 97 .
For the computation of H , data were screened for cases where K = 0 for a given category (that is, cases where the participant made all neutral ratings to neither approach nor to avoid any stimulus in the category). Computation of H for a given picture category requires that K > 0, because H computation results in an undefinable log 10 (0/0) when K = 0. In such cases, H was set to 0 for categories in which the participant rated ‘0’ for all the stimuli.
To fit the models to participants’ ratings, the data were further screened for inclusion/exclusion criteria as follows:
Valid entropy ( H ) calculations (as above)
Further exclusion of extreme outliers: loss aversion values > 200, resulting in N = 42 exclusions; positive quadratic area >100, resulting in N = 5 exclusions
Sufficient data points to fit the model with a computable R 2 (for example, at least three points for a nonlinear fit)
Coherence of model fits between individual and group data. This last criterion required that the curve direction for individual participant fits be consistent with the curve direction of the group-level statistical fits (and boundary envelopes).
Criteria (3) and (4) are necessary operational definitions for quality assurance given the potential for convergence failures with curve fitting. Overall, 3,476 of 4,019 participants met all quality assurance criteria for picture-rating data and survey data.
According to published procedures, six types of model fitting were performed for the rating data: group and individual models for the ( K , H ) data, ( K , σ ) data and ( H + , H − ) data. For the group data, we generated group-level data fits along with boundary envelopes (power-law fits and logarithmic fits for group ( K , H ) data), and quadratic fits for group ( K , σ ) data to guide the focus of statistical testing based on the power-law fits ( K , H ) and quadratic fits ( K , σ ) for individual data. Individual data then followed these fits based on logarithmic and simple power-law fits for individual ( K , H ) value functions, quadratic fits for individual ( K , σ ) limit functions, and radial fits for individual ( H + , H − ) tradeoff distributions 38 , 97 . For this study sample, participants’ ( K , H ) value functions were fit by concave-logarithmic or power-law functions (Supplementary Table 8 and Supplementary Fig. 4 ) with all R 2 values >0.80 and ranging from 0.84 to 0.96. For the limit functions, concave quadratic fits across participants’ ( K , σ ) data had goodness of fit assessed using the same metrics as for the ( K , H ) data (Supplementary Table 8 ), and the R 2 values varied from 0.85 to 0.94. Finally, radial functions were fit to test for tradeoff plots in the distribution of H − and H + values across categories within each participant, as shown in Supplementary Fig. 4 . Value (Supplementary Fig. 4a ), limit (Supplementary Fig. 4b ) and tradeoff (Supplementary Fig. 4c ) functions were plotted for 500 randomly sampled participants out of 3,476 whose data met all quality assurance criteria. The location and dispersion estimates of the R 2 , adjusted R 2 (accounting for degrees of freedom) and associated F -statistics for each participant’s model fit are provided in Supplementary Table 8 .
From these graphs, judgment variables (Supplementary Table 9 ) were derived for ML. At least 15 features can be mathematically derived from this framework that are psychologically interpretable and have been validated 37 , 39 as being discrete, recurrent and scalable by engineering criteria 38 , 97 . These 15 features are loss aversion, risk aversion, loss resilience, ante, insurance, peak positive risk, peak negative risk, reward tipping point, aversion tipping point, total reward risk, total aversion risk, reward–aversion tradeoff, tradeoff range, reward–aversion consistency and consistency range, as schematized in Fig. 1 and described in Table 1 . Loss aversion, risk aversion, loss resilience, ante and insurance are derived from the logarithmic or power-law fit of mean key presses ( K ) versus the entropy of key presses ( H ); this is referred to as the value function (Fig. 1a ). Peak positive risk, peak negative risk, reward tipping point, aversion tipping point, total reward risk and total aversion risk are derived from the quadratic fit of K versus the standard deviation of key presses ( σ ); this is referred to as the limit function (Fig. 1b ). Reward aversion tradeoff, tradeoff range, reward–aversion consistency, and consistency range are derived from the radial fit of the pattern of avoidance judgments ( H − ) versus the pattern of approach judgments ( H + ); this is referred to as the tradeoff function (Fig. 1c ). Each feature describes a quantitative component of a participant’s approach/avoidance or judgment/behavior (see Supplementary Methods for complete descriptions). Collectively, the 15 RPT features are referred to as ‘judgment variables’ herein.
Feature importance
Feature importance was assessed in two frameworks, one via an MI 61 assessment and the other via a Gini importance score 62 assessment. For this study, MI was computed between each of the 15 judgment variables and the four prediction outcomes of interest (passive suicidal ideation (STB1), active suicidal ideation (STB2), planning for suicide (STB3) and planning for safety (STB4)). The MI was used as a proxy for the dependence between the two random variables, with a larger mutual information between judgment variables and STB metrics suggesting higher importance of the feature in predicting STB. MI scores for the 15 judgment variables are expected to add to 1 for each of the STB measures tested. Note that the STB1–4 nomenclature is used only for figures and tables. Analyses were conducted using the package sklearn 99 to calculate the mutual information scores in Python.
Gini importance scores reflected the feature importance (that is, rank) as determined using the function model.feature_importances_ in Python, and the results were reported and plotted using matplotlib.
Machine learning
The sensitivity of a binary classifier measures its ability to accurately label a symptom-positive class 75 . Sensitivity plays an important role in STB prediction due to the relevance of correctly identifying STB-positive individuals for potential intervention. However, imbalanced datasets typically result in poor sensitivities when the positive class is substantially less in size compared to the negative class 75 . To enable prediction with high sensitivity, two classifiers with the reported ability to handle data imbalance 56 , 75 , 100 were compared to a set of standard classifiers. The BRF 56 and GMM 57 classifiers were thus chosen to predict the four STB measures, and compared to four standard classifiers (that is, random forest (RF), logistic regression (LR), neural network (NN) and support vector machine (SVM)) 58 . The ML analyses used the parameters detailed in the following (and referenced in ref. 39 ). Across the analyses, the code was implemented in Python 3.9 using the packages imblearn 0.0, sklearn 1.2.2, pandas 2.0.2 and pandas 2.0.2. Feature importance (Gini scores and MI scores) were obtained with sklearn 1.2.2. Figures related to variable importance were plotted with seaborn 0.12.2.
The classifiers used the following features: (1) PHQ8 (absent the question on suicidality), (2) STAI, (3) perceived loneliness (self-report), (4) prior attempts at self-harm in the past 1–12 months, (5) five demographic variables (age, ethnicity, education level, sex and handedness) and (6) 15 judgment variables computationally extracted from a simple picture-rating task. The predictive power of variables in (1)–(6) was tested using BRF, GMM and the four standard classifiers to discriminate between the low and high measures of the four STB variables. Each STB measure was partitioned as binary data in two different ways for its 1–5 Likert ratings: 1 versus 2–5 (threshold = 1), and 1,2 versus 3–5 (threshold = 2). In each case, the binary data were analyzed with BRF, GMM and the four standard classifiers. Given potential cultural norms against reporting past self-harm 59 , 60 , variables from (1)–(3), (5) and (6) were initially tested, followed by a minimal predictor set of (4)–(6). As a third framework, the full set of (1)–(6) was also tested. In the analysis of variables from (1)–(3), (5) and (6), judgment variables from (6) were first tested, then the other variables were added incrementally. The same was done with the other two analysis frameworks (that is, using just a minimal predictor set for (4)–(6), and using all variables).
BRF analysis
BRF (Supplementary Fig. 5 ) was implemented in Python with the package imblearn 100 with tenfold cross-validation. RF classifiers contain an ensemble of decision trees from which majority voting is performed to output a class label, and are typically trained by optimizing a Gini or information score 56 , 99 . In the BRF approach, an ensemble of 200 trees was constructed, where each bootstrap sample was randomly under-sampled to create a balanced dataset of both classes (that is, 50% of STB-positive and 50% of STB-negative data). Balancing was used for training only, and not for testing within cross-validation. No hyperparameter tuning was performed. Subsequent analysis was performed internally using the sklearn RF package through imblearn. Soft labels were used for majority voting, so that the majority vote was weighted on the probability of the sample belonging to the STB-positive class 56 , 99 , 100 . The BRF was trained using the Gini criterion, and no maximum tree depth was used, so nodes expanded until leaves were pure or contained at most one sample. The mean accuracy, sensitivity, specificity and AUC were reported.
GMM and standard classifiers
Analyses for GMM, RF, LR, NN and SVM classification were conducted with sklearn 99 in Python ( Supplementary Methods and Supplementary Fig. 6 ).
Unlike standard assessment of linear associations 101 , 102 , mediation assesses the causal pathway between variables and moderation assesses the interaction between such variables to predict a third variable 54 , 63 , 103 . Given the number of associations tested prior to mediation/moderation, and the potential for skewed distributions and outliers in human samples, we integrated Cook’s distance outlier analysis with mediation 54 , 63 , 103 to protect against false positives and increase the analytic power. Mediation/moderation analyses were conducted in R 4.2.0 with the libraries readxl 1.4.0, MASS 7.3-56 and stats 4.2.0. Mediation/moderation analyses used the code sequences detailed in refs. 54 , 63 .
Mediation analysis
Mediation models suggest that, instead of a direct causal relationship between the independent variable ( X ) and the dependent variable ( Y ), there is an intermediary variable ( M ) so that X influences M , which in turn influences Y . Mediation analyses were conducted for all combinations of STB variables as dependent variables, RPT features as independent variables, and prior attempts, age, loneliness, PHQ8 score and STAI score as mediators. The STB variables involved no thresholding. Beta coefficients and their standard error(s) terms from the following linear regression equations, followed the four-step process of ref. 104 , and were used from a regression to calculate Sobel P values and mediation effect percentages ( T eff ):
Step 1: Y = γ 1 + c ( X ) + ϵ 1
Step 2: M = γ 2 + a ( X ) + ϵ 2
Step 3: Y = γ 3 + c ′( X ) + b ( M ) + ϵ 3
Step 4: Sobel’s test was then used to test if c ′ was significantly lower than c using the following equation:
Using a standard two-tail z -score table, the Sobel P value was determined from the Sobel z -score, and the mediation effect percentage ( T eff ) was calculated using
For mediation to be considered significant, we required that all three regressions between X predicting Y (that is, P c ), X predicting M (that is, P a ), and M predicting Y (that is, P b' ) in Supplementary Table 3 show nominal significance with P < 0.05. Significant mediation further required the following: P Sobel < 0.05 and T eff > 50%, following previous publications 54 , 63 , 103 . Secondary mediation analysis was run by switching variables assigned to X and M to see if the mediation effects were directed. For secondary analysis if P Sobel > 0.05 and T eff < 50%, this added to the evidence of M lying in the causal pathway between X and Y .
Moderation analysis
Moderation models suggest that a moderator variable (Mo) controls the magnitude of the relationship between the independent variable ( X ) and the dependent variable ( Y ). Moderation analyses were conducted for all combinations of STB variables as dependent variables, RPT features as independent variables, and prior attempts, age, loneliness, PHQ8 score and STAI score as moderators. No thresholds were considered for the STB variables. The original data for STB variables, involving five categories of severity, were used. The moderation analyses involved fitting a logistic regression to the data, described by
The standard approach was used, where the moderation was deemed significant if the P value of the interaction term ( \({P}_{\rm{\beta }_{3}}\) ) and the P value of the overall model ( P overall ) were both less than or equal to 0.05 through likelihood ratio tests. The likelihood ratio test for the full model was implemented with the following null and alternative hypotheses:
The likelihood ratio test for the β 3 coefficient was implemented with the following null and alternative hypothesis, respectively:
where the restricted model is
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this Article.
Data availability
Data were de-identified before being provided to the investigators. Data are available in Microsoft Excel format and include relative preference variables, demographic metrics and survey variables inclusive of suicidal thought and behavior (STB) variables. The data may be accessed at https://osf.io/6e2d4/ . For questions concerning data availability, please contact the corresponding author.
Code availability
Computational behavior analysis used code published in refs. 37 , 38 . ML analyses used parameters as detailed in the Methods and referenced in ref. 39 . Mediation/moderation analyses used code sequences as detailed in refs. 54 , 63 .
Suicide Data and Statistics (Centers for Disease Control and Prevention & National Center for Health Statistics); https://www.cdc.gov/suicide/suicide-data-statistics.html
Farooq, S., Tunmore, J., Wajid Ali, M. & Ayub, M. Suicide, self-harm and suicidal ideation during COVID-19: a systematic review. Psychiatry Res. 306 , 114228 (2021).
Article PubMed PubMed Central Google Scholar
Hill, R. M. et al. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics 147 , e2020029280 (2021).
Article PubMed Google Scholar
McHugh, C. M., Corderoy, A., Ryan, C. J., Hickie, I. B. & Large, M. M. Association between suicidal ideation and suicide: meta-analyses of odds ratios, sensitivity, specificity and positive predictive value. BJPsych Open 5 , e18 (2019).
McHugh, C. M. & Large, M. M. Can machine-learning methods really help predict suicide? Curr. Opin. Psychiatry 33 , 369–374 (2020).
Linthicum, K. P., Schafer, K. M. & Ribeiro, J. D. Machine learning in suicide science: applications and ethics. Behav. Sci. Law 37 , 214–222 (2019).
Schafer, K. M. The Status of Suicidality Prediction Research : A Meta-Analysis . MSc thesis, Florida State Univ. (2019).
Schafer, K. M., Kennedy, G., Gallyer, A. & Resnik, P. A direct comparison of theory-driven and machine learning prediction of suicide: a meta-analysis. PLoS ONE 16 , e0249833 (2021).
Arrow, K. et al. Evaluating the use of online self-report questionnaires as clinically valid mental health monitoring tools in the clinical whitespace. Psychiatr. Q. 94 , 221–231 (2023).
Resnik, P., Foreman, A., Kuchuk, M., Musacchio Schafer, K. & Pinkham, B. Naturally occurring language as a source of evidence in suicide prevention. Suicide Life Threat Behav. 51 , 88–96 (2021).
Schafer, K. M., Clancy, K. J. & Joiner, T. An investigation into the bidirectional relationship between post-traumatic stress disorder and suicidal ideation: a nine year study. J. Anxiety Disord. 85 , 102510 (2022).
Schafer, K. M. et al. The relationship between anger and suicidal ideation: investigations in two samples. J. Clin. Psychol. 78 , 1866–1877 (2022).
Shing, H.-C., Resnik, P. & Oard, D. W. A prioritization model for suicidality risk assessment. In Proc. 58th Annual Meeting of the Association for Computational Linguistics (ed. Jurafsky, D. et al.) 8124–8137 (Association for Computational Linguistics, 2020).
Schafer, K. M., Wilson, E. & Joiner, T. Traumatic brain injury and suicidality among military veterans: the mediating role of social integration. J. Affect. Disord. 338 , 414–421 (2023).
Kelly, D. L. et al. Can language use in social media help in the treatment of severe mental illness? Curr. Res. Psychiatry 1 , 1–4 (2021).
PubMed PubMed Central Google Scholar
Schafer, K. M. et al. Suicidal ideation, suicide attempts and suicide death among Veterans and service members: a comprehensive meta-analysis of risk factors. Mil. Psychol. 34 , 129–146 (2022).
Hyman, S. & Tesar, G. Manual of Psychiatric Emergencies (Little Brown, 1994).
Bennardi, M. et al. Longitudinal relationships between positive affect, loneliness and suicide ideation: age-specific factors in a general population. Suicide Life Threat Behav. 49 , 90–103 (2019).
Chen, V. C.-H. et al. Convolutional neural network-based deep learning model for predicting differential suicidality in depressive patients using brain generalized q-sampling imaging. J. Clin. Psychiatry 82 , 19m13225 (2021).
Nordin, N., Zainol, Z., Mohd Noor, M. H. & Lai Fong, C. A comparative study of machine learning techniques for suicide attempts predictive model. Health Informatics J. 27 , 146045822198939 (2021).
Article Google Scholar
Bernert, R. A. et al. Artificial intelligence and suicide prevention: a systematic review of machine learning investigations. Int. J. Environ. Res. Public Health 17 , 5929 (2020).
Zalar, B., Kores Plesnicar, B., Zalar, I. & Mertik, M. Suicide and suicide attempt descriptors by multimethod approach. Psychiatr. Danub. 30 , 317–322 (2018).
Rozek, D. C. et al. Using machine learning to predict suicide attempts in military personnel. Psychiatry Res. 294 , 113515 (2020).
Kirmayer, L. J. The politics of diversity: pluralism, multiculturalism and mental health. Transcult. Psychiatry 56 , 1119–1138 (2019).
Bredström, A. Culture and context in mental health diagnosing: scrutinizing the DSM-5 revision. J. Med. Humanit. 40 , 347–363 (2019).
Moscardini, E. H. et al. Suicide safety planning: clinician training, comfort and safety plan utilization. Int. J. Environ. Res. Public Health 17 , 6444 (2020).
Nuij, C. et al. Safety planning-type interventions for suicide prevention: meta-analysis. Br. J. Psychiatry 219 , 419–426 (2021).
Ferguson, M., Rhodes, K., Loughhead, M., McIntyre, H. & Procter, N. The effectiveness of the safety planning intervention for adults experiencing suicide-related distress: a systematic review. Arch. Suicide Res. 26 , 1022–1045 (2022).
Takahashi, T. Neuroeconomics of suicide. NeuroEndocrinol. Lett. 32 , 400–404 (2011).
PubMed Google Scholar
Baek, K. et al. Heightened aversion to risk and loss in depressed patients with a suicide attempt history. Sci. Rep. 7 , 11228 (2017).
Hadlaczky, G. et al. Decision-making in suicidal behavior: the protective role of loss aversion. Front. Psychiatry 9 , 116 (2018).
Dombrovski, A. Y. et al. The temptation of suicide: striatal gray matter, discounting of delayed rewards and suicide attempts in late-life depression. Psychol. Med. 42 , 1203–1215 (2012).
Millner, A. J. et al. Suicidal thoughts and behaviors are associated with an increased decision-making bias for active responses to escape aversive states. J. Abnorm. Psychol. 128 , 106–118 (2019).
Mas-Collel, A., Whinston, M. & Greej, J. Microeconomic Theory (Oxford Univ. Press, 1995).
Dai, X., Brendl, C. M. & Ariely, D. Wanting, liking and preference construction. Emotion 10 , 324–334 (2010).
Lee, S. et al. The commonality of loss aversion across procedures and stimuli. PLoS ONE 10 , e0135216 (2015).
Azcona, E. A. et al. Discrete, recurrent and scalable patterns in human judgement underlie affective picture ratings. Preprint at https://arxiv.org/abs/2203.06448 (2022).
Kim, B. W. et al. Recurrent, robust and scalable patterns underlie human approach and avoidance. PLoS ONE 5 , e10613 (2010).
Vike, N. et al. Predicting COVID-19 vaccination uptake using a small and interpretable set of judgment and demographic variables: Cross-Sectional Cognitive Science Study. JMIR Public Health Surveill . https://doi.org/10.2196/47979 (2024).
Dillon, D. G. et al. Peril and pleasure: an RDoC-inspired examination of threat responses and reward processing in anxiety and depression. Depress. Anxiety 31 , 233–249 (2014).
Bogdan, R. & Pizzagalli, D. A. Acute stress reduces reward responsiveness: implications for depression. Biol. Psychiatry 60 , 1147–1154 (2006).
Tversky, A. & Kaheman, D. Judgment under uncertainty: heuristics and biases. Science 185 , 1124–1131 (1974).
Kahneman, D. & Tversky, A. Prospect theory: an analysis of decision under risk. Econometrica 47 , 263–292 (1970).
Chen, X., Voets, S., Jenkinson, N. & Galea, J. M. Dopamine-dependent loss aversion during effort-based decision-making. J. Neurosci. 40 , 661–670 (2020).
Wang, S., Krajbich, I., Adolphs, R. & Tsuchiya, N. The role of risk aversion in non-conscious decision making. Front. Psychol. 3 , 50 (2012).
Aharon, I. et al. Beautiful faces have variable reward value: fMRI and behavioral evidence. Neuron 32 , 537–551 (2001).
Montague, P. R. Free will. Curr. Biol. 18 , R584–R585 (2008).
Mobile Fact Sheet (Pew Research Center, 2021).
Spitzer, R. L. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA 282 , 1737–1744 (1999).
Spielberger, C. D., Gorsuch, R. L., Lushene, R., Vagg, P. R. & Jacobs, G. A. Manual for the State-Trait Anxiety Inventory (Consulting Psychologists Press, 1983).
HATTA, T. Handedness and the brain: a review of brain-imaging techniques. Magn. Reson. Med. Sci. 6 , 99–112 (2007).
Dotson, V. M. & Duarte, A. The importance of diversity in cognitive neuroscience. Ann. N. Y. Acad. Sci. 1464 , 181–191 (2020).
Kaczkurkin, A. N., Raznahan, A. & Satterthwaite, T. D. Sex differences in the developing brain: insights from multimodal neuroimaging. Neuropsychopharmacology 44 , 71–85 (2019).
Bari, S. et al. Integrating multi-omics with neuroimaging and behavior: a preliminary model of dysfunction in football athletes. Neuroimage Rep. 1 , 100032 (2021).
Woodward, S. F. et al. Anxiety, post-COVID-19 syndrome-related depression and suicidal thoughts and behaviors in COVID-19 survivors: cross-sectional study. JMIR Form. Res. 6 , e36656 (2022).
More, A. S. & Rana, D. P. Review of random forest classification techniques to resolve data imbalance. In Proc. 2017 1st International Conference on Intelligent Systems and Information Management ( ICISIM ) 72–78 (IEEE, 2017); https://doi.org/10.1109/ICISIM.2017.8122151
Hand, D. J., McLachlan, G. J. & Basford, K. E. Mixture models: inference and applications to clustering. Appl. Stat. 38 , 384–385 (1989).
Watt, J., Borhani, R. & Katsaggelos, A. Machine Learning Refined (Cambridge Univ. Press, 2020); https://doi.org/10.1017/9781108690935
Aggarwal, S., Borschmann, R. & Patton, G. C. Tackling stigma in self-harm and suicide in the young. Lancet Public Health 6 , e6–e7 (2021).
Oexle, N. et al. Mental illness stigma, secrecy and suicidal ideation. Epidemiol. Psychiatr. Sci. 26 , 53–60 (2017).
Duncan, T. E. On the calculation of mutual information. SIAM J. Appl. Math. 19 , 215–220 (1970).
Breiman, L., Friedman, J. H., Olshen, R. A. & Stone, C. J. Classification And Regression Trees (Routledge, 2017); https://doi.org/10.1201/9781315139470
Vike, N. L. et al. A preliminary model of football-related neural stress that integrates metabolomics with transcriptomics and virtual reality. iScience 25 , 103483 (2022).
Weng, J.-C. et al. An autoencoder and machine learning model to predict suicidal ideation with brain structural imaging. J. Clin. Med. 9 , 658 (2020).
Wilimitis, D. et al. Integration of face-to-face screening with real-time machine learning to predict risk of suicide among adults. JAMA Netw. Open 5 , e2212095 (2022).
Hettige, N. C. et al. Classification of suicide attempters in schizophrenia using sociocultural and clinical features: a machine learning approach. Gen. Hosp. Psychiatry 47 , 20–28 (2017).
Macalli, M. et al. A machine learning approach for predicting suicidal thoughts and behaviours among college students. Sci. Rep. 11 , 11363 (2021).
García de la Garza, Á., Blanco, C., Olfson, M. & Wall, M. M. Identification of suicide attempt risk factors in a national US survey using machine learning. JAMA Psychiatry 78 , 398–406 (2021).
Sawhney, R., Joshi, H., Gandhi, S., Jin, D. & Shah, R. R. Robust suicide risk assessment on social media via deep adversarial learning. J. Am. Med. Inform. Assoc. 28 , 1497–1506 (2021).
Kessler, R. C. et al. Predicting suicides after outpatient mental health visits in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Mol. Psychiatry 22 , 544–551 (2017).
Bolón-Canedo, V., Sánchez-Maroño, N. & Alonso-Betanzos, A. Feature Selection for High-Dimensional Data (Springer, 2015); https://doi.org/10.1007/978-3-319-21858-8
Kaur, H., Pannu, H. S. & Malhi, A. K. A systematic review on imbalanced data challenges in machine learning. ACM Comput. Surv. 52 , 1–36 (2020).
Google Scholar
Tran, T., Le, U. & Shi, Y. An effective up-sampling approach for breast cancer prediction with imbalanced data: a machine learning model-based comparative analysis. PLoS ONE 17 , e0269135 (2022).
Korkmaz, S. Deep learning-based imbalanced data classification for drug discovery. J. Chem. Inf. Model. 60 , 4180–4190 (2020).
He, H. & Ma, Y. Imbalanced Learning : Foundations , Algorithms and Applications (IEEE Press, 2013).
Fernandez-Delgado, M., Cernadas, E. & Barro, S. Do we need hundreds of classifiers to solve real world classification problems? J. Mach. Learn. Res. 15 , 3133–3181 (2014).
Laird, J. E., Lebiere, C. & Rosenbloom, P. S. A standard model of the mind: toward a common computational framework across artificial intelligence, cognitive science, neuroscience and robotics. AI Mag. 38 , 13–26 (2017).
Malone, L. Computer and Internet Use in the United States: 2018 (United States Census Bureau, 2021).
Wasserman, D., Carli, V., Iosue, M., Javed, A. & Herrman, H. Suicide prevention in childhood and adolescence: a narrative review of current knowledge on risk and protective factors and effectiveness of interventions. Asia Pac. Psychiatry 13 , e12452 (2021).
Ding, O. J. & Kennedy, G. J. Understanding vulnerability to late-life suicide. Curr. Psychiatry Rep. 23 , 58 (2021).
Raue, P. J., Ghesquiere, A. R. & Bruce, M. L. Suicide risk in primary care: identification and management in older adults. Curr. Psychiatry Rep. 16 , 466 (2014).
Becker, M. & Correll, C. U. Suicidality in childhood and adolescence. Dtsch. Arztebl. Int 117 , 261–267 (2020).
Bryan, C. J. & Rozek, D. C. Suicide prevention in the military: a mechanistic perspective. Curr. Opin. Psychol. 22 , 27–32 (2018).
Gonçalves, A., Sequeira, C., Duarte, J. & Freitas, P. Suicide ideation in higher education students: influence of social support. Aten. Primaria 46 , 88–91 (2014).
Bari, S. et al. The prevalence of psychotic symptoms, violent ideation, and disruptive behavior in a population with SARS-CoV-2 infection: preliminary study. JMIR Form. Res. 6 , e36444 (2022).
Vike, N. L. et al. The relationship between a history of high-risk and destructive behaviors and COVID-19 infection: preliminary study. JMIR Form. Res. 7 , e40821 (2023).
Lang, P., Bradley, M. & Cuthbert, B. International Affective Picture System ( IAPS ): Affective Ratings of Pictures and Instruction Manual . Technical Report A-8 (NIMH Center for the Study of Emotion and Attention, 2008).
Viswanathan, V. et al. A quantitative relationship between signal detection in attention and approach/avoidance behavior. Front. Psychol. 8 , 122 (2017).
Perlis, R. H. et al. Prevalence of incompletely penetrant Huntington’s disease alleles among individuals with major depressive disorder. Am. J. Psychiatry 167 , 574–579 (2010).
Perlis, R. H. Association of a polymorphism near CREB1 with differential aversion processing in the insula of healthy participants. Arch. Gen. Psychiatry 65 , 882–892 (2008).
Gasic, G. P. et al. BDNF, relative preference and reward circuitry responses to emotional communication. Am. J. Med. Genet. B Neuropsychiatr. Genet. 150B , 762–781 (2009).
Blood, A. J. et al. Microstructural abnormalities in subcortical reward circuitry of subjects with major depressive disorder. PLoS ONE 5 , e13945 (2010).
Makris, N. et al. Cortical thickness abnormalities in cocaine addiction—a reflection of both drug use and a pre-existing disposition to drug abuse? Neuron 60 , 174–188 (2008).
Viswanathan, V. et al. Age-related striatal BOLD changes without changes in behavioral loss aversion. Front. Hum. Neurosci. 9 , 176 (2015).
Posner, K. et al. The Columbia-suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am. J. Psychiatry 168 , 1266–1277 (2011).
Asking About Suicide is Vital for the Military and Veterans (Columbia Lighthouse Project, 2016); https://cssrs.columbia.edu/the-columbia-scale-c-ssrs/military/
Livengood, S. L. et al. Keypress-based musical preference is both individual and lawful. Front. Neurosci. 11 , 136 (2017).
Shannon, C. E. & Weaver, W. The Mathematical Theory of Communication (Univ. Illinois Press, 1949).
Pedregosa, F. et al. Scikit-learn: machine learning in Python. J. Mach. Learn. Res. 12 , 2825–2830 (2011).
Lemaitre, G., Nogueira, F. & Aridas, C. K. Imbalanced-learn: a Python toolbox to tackle the curse of imbalanced datasets in machine learning. J. Mach. Learn. Res. 18 , 1–5 (2017).
Hayes, A. F. Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun. Monogr. 76 , 408–420 (2009).
MacKinnon, D. P., Fairchild, A. J. & Fritz, M. S. Mediation analysis. Annu. Rev. Psychol. 58 , 593–614 (2007).
Chen, Y. et al. Brain perfusion mediates the relationship between miRNA levels and postural control. Cereb. Cortex Commun. 1 , tgaa078 (2020).
Baron, R. M. & Kenny, D. A. The moderator-mediator variable distinction in social psychological research: conceptual, strategic and statistical considerations. J. Pers. Soc. Psychol. 51 , 1173–1182 (1986).
Markowitz, H. Portfolio selection. J. Finance 7 , 77–91 (1952).
Download references
Acknowledgements
Funding for this work was provided in part to H.C.B. by the Office of Naval Research (ONR award no. N00014-21-1-2216) and to H.C.B. (contact primary investigator) and A.K.K. (subcontract primary investigator) (ONR award no. N00014-23-1-2396) and to H.C.B. from a Jim Goetz donation to the University of Cincinnati (UC), College of Engineering and Applied Science (CEAS). We also thank C. Ross, A. Braggs-Brown, T. Talavage, E. Nauman and M. Cahay at UC CEAS, who greatly impacted the transfer of research funding to UC, allowing this work to be completed. The opinions expressed herein are those of the authors and are not necessarily representative of those from their respective institutions.
Author information
These authors contributed equally: Sumra Bari, Nicole L. Vike, Leandros Stefanopoulos, Byoung-Woo Kim.
These authors jointly supervised this work: Aggelos K. Katsaggelos, Hans C. Breiter.
Authors and Affiliations
Department of Electrical and Computer Engineering, Northwestern University, Evanston, IL, USA
Shamal Lalvani, Leandros Stefanopoulos & Aggelos K. Katsaggelos
Departments of Computer Science & Biomedical Engineering, University of Cincinnati, Cincinnati, OH, USA
Sumra Bari, Nicole L. Vike, Byoung-Woo Kim & Hans C. Breiter
School of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece
Leandros Stefanopoulos & Nicos Maglaveras
Medill Integrated Marketing Communications, Northwestern University, Evanston, IL, USA
Martin Block
Department of Radiology, Northwestern University, Chicago, IL, USA
Aggelos K. Katsaggelos
Department of Computer Science, Northwestern University, Evanston, IL, USA
Laboratory of Neuroimaging and Genetics, Department of Psychiatry, Massachusetts General Hospital and Harvard School of Medicine, Boston, MA, USA
Hans C. Breiter
You can also search for this author in PubMed Google Scholar
Contributions
The study was conceived and designed by H.C.B., A.K.K. and S.L. Acquisition of the original data was performed by H.C.B., B.-W.K., N.L.V., S.B., S.L., L.S., M.B. and A.K.K. Coding of statistical tools was carried out by S.L., S.B. and B.-W.K. (with guidance from H.C.B. and A.K.K.). Data were analyzed by S.L., S.B. and B.-W.K. (with guidance from H.C.B. and A.K.K.). Data interpretation was carried out by S.L., H.C.B. and A.K.K. (with input from B.-W.K., N.L.V., S.B., L.S., M.B. and N.M.). Statistical assessments were performed by S.L., S.B. and B.-W.K. (with guidance from H.C.B. and A.K.K.). The original draft was written by S.L. and H.C.B. Figures were generated by S.L., L.S., B.-W.K. and H.C.B. Revision of the manuscript for content was performed by all authors. All authors approved the final version of the paper for submission.
Corresponding author
Correspondence to Hans C. Breiter .
Ethics declarations
Competing interests.
S.L., S.B., M.B., H.C.B., A.K., B.-W.K., L.S. and N.V. submitted a provisional patent “Systems and Methods Integrating Cognitive Science with Machine Learning for High Accuracy Prediction of Suicidal Thoughts and Behaviors”. The provisional application is led by University of Cincinnati (Office of Innovation) in conjunction with Northwestern University, Application # 63/551,326. The other authors declare no competing interests.
Inclusion and ethics statement
De-identified data were collected by a third-party vendor (Gold Research) to reflect the general population demographics in the United States at the time of collection (December 2021) and with oversampling by 15% for mental health conditions. All participants provided informed consent, which included their primary participation in the study as well as the secondary use of their anonymized, de-identified data (that is, all identifying information removed by Gold Research Inc. before retrieval by the research group) in secondary analyses. Informed consent was obtained for all participants, as approved by the Institutional Review Board of Northwestern University (NU; approval no. STU00213665) for initial project start and later also approved by the University of Cincinnati (UC) Institutional Review Board (approval no. 2023-0164) as some NU investigators moved to UC. All work was done in accordance with the Declaration of Helsinki.
Peer review
Peer review information.
Nature Mental Health thanks Katherine Schafer and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information.
A combined PDF containing the supplementary information.
Reporting Summary
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Lalvani, S., Bari, S., Vike, N.L. et al. Predicting suicidality with small sets of interpretable reward behavior and survey variables. Nat. Mental Health (2024). https://doi.org/10.1038/s44220-024-00229-x
Download citation
Received : 04 April 2023
Accepted : 06 March 2024
Published : 09 May 2024
DOI : https://doi.org/10.1038/s44220-024-00229-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
- NICE Guidance
- Conditions and diseases
- Mental health, behavioural and neurodevelopmental conditions
Common mental health problems: identification and pathways to care
Clinical guideline [CG123] Published: 25 May 2011
This guideline has been stood down. All of the recommendations are now covered in other NICE guidelines, or are out of date and no longer relevant to clinical practice.
For guidance on common mental health problems, see our guidelines on:
- Depression in adults
- Depression in adults with a chronic physical health problem
- Depression in children and young people
- Generalised anxiety disorder and panic disorder in adults
- Obsessive-compulsive disorder and body dysmorphic disorder
- Social anxiety disorder
Nursing assessment of mental health issues in the general clinical environment: A descriptive study
Affiliations.
- 1 School of Nursing and Midwifery, Edith Cowan University, Joondalup, Western Australia, Australia.
- 2 Joondalup Health Campus, Joondalup, Western Australia, Australia.
- PMID: 38738987
- DOI: 10.1111/jan.16214
Aims: To evaluate the effectiveness of a mental health screening form for early identification and care escalation of mental health issues in general settings. A secondary aim was to explore general nurses' use of the form and their confidence to discuss mental health issues with patients.
Methods: A cross-sectional design comprising a review of clinical records to determine use of the form, instances of missed care and escalation to the mental health team. The survey focused on nurses' confidence in general settings to engage in discussions with patients about mental health. Data were collected from April to December 2022. The Strengthening the Reporting of Observational Studies in Epidemiology Statement guided this study.
Results: Of 400 patient records, 397 were analysed; 293 (73.8%) of those had mental health screening by nurses. Age was a significant factor, with younger patients more likely to be screened although concerns were typically recognized in older patients. Of the 20 patients identified with mental health concerns, 9 (45%) were referred for further evaluation by the Clinical Liaison Team. While nurses were proactive in assessing physical risks, assessing risk factors that required deeper conversations with patients, including psychiatric history, was lacking. The survey highlighted fewer than half of the respondents (46%, n = 10) felt competent to engage in discussions about mental health; however, most (59%, n = 13) knew when to seek a mental health referral.
Conclusions: General nurses have a role in the early identification and referral of patients with mental health challenges. However, training is imperative to facilitate deeper patient interactions concerning mental health. Integrating mental health checks within general settings is crucial for early detection and intervention, aligning with global quality care standards.
Reporting method: STROBE guidelines.
Patient or public contribution: We received feedback that shaped the research protocol from a consumer representative.
Keywords: adult nursing; mental health; nurse roles; quantitative approaches; screening.
© 2024 The Authors. Journal of Advanced Nursing published by John Wiley & Sons Ltd.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Fam Physician
- v.60(11); 2014 Nov
Language: English | French
Screening for lifestyle and mental health risk factors in the waiting room
Dépister les facteurs de risque liés au mode de vie et à la santé mentale dans la salle d’attente.
To assess the feasibility and acceptability of administering the validated Case-finding Health Assessment Tool (CHAT) in Canadian family practice waiting rooms to identify risk factors for depression, anxiety, anger control, smoking, drinking, other drug use, gambling, exposure to abuse, and physical inactivity.
Cross-sectional survey.
One urban academic family practice and one inner-city community health centre in British Columbia.
Participants
Convenience sample of consecutive adult patients (19 years of age or older) and their attending family physicians.
Main outcome measures
Rates of completion; positive responses to and wanting help with identified lifestyle and mental health risk factors; rates of objections to any questions; and positive and negative comments about the CHAT by participating physicians and patients.
A total of 265 eligible adults presented in the waiting rooms over 5 full days and 3 half-days, 176 (66%) of whom enrolled in the study; 161 (91%) completed the CHAT, and 107 (66%) completed acceptability feedback forms. The prevalence of risk factors among patients in the academic and inner-city practice samples was different, with 20% and 63%, respectively, recording positive responses to both depression screening questions, 34% and 60% positive for anxiety, 11% and 71% currently smoking, 6% and 22% feeling they needed to cut down on alcohol, 1% and 48% having used recreational drugs in the past year, and 11% and 65% with problems controlling anger. While many requested help with reducing risk factors, such as smoking (20%) and mental health symptoms (25% to 27%), a total of 35% (57 of 161) wanted help with an identified issue that day. Patients and physicians found the CHAT acceptable, with no patients objecting to any question except the alcohol question (2 objected). Most comments were positive.
The CHAT allowed efficient identification of 9 risk factors, as well as identification of those wanting help. It could be used to screen all or targeted adult Canadian primary care patients in waiting rooms.
Résumé
Vérifier s’il est faisable et acceptable d’utiliser un outil déjà validé, le Case-finding Health Assessment Tool (CGAT) pour identifier les facteurs de risque pour la dépression, l’anxiété, la colère réprimée, le tabagisme, l’alcoolisme, la toxicomanie, le jeu, la présence de violence et la sédentarité.
Type d’étude
Enquête transversale.
Une clinique universitaire urbaine de médecine familiale et le centre de santé communautaire d’un centreville en Colombie-Britannique.
Un échantillon arbitraire de patients adultes consécutifs (âgés d’au moins 19 ans) et leurs médecins traitants.
Principaux paramètres à l’étude
Taux de réponses à l’enquête; réponses positives pour les facteurs de risque identifiés liés au mode de vie et à la santé mentale, et désir d’être aidé; taux d’opposition à toute question; et commentaires positifs ou négatifs au sujet du CHAT de la part des médecins et des patients participants.
Résultats
Sur les 265 adultes admissibles qui se sont présentés à la salle d’attente sur une période comprenant 5 jours complets et 3 demi-journées, 176 (66 %) ont accepté de participer; 161 d’entre eux (91 %) ont complété le CHAT et 107 (66 %) les formulaires de feedback sur l’acceptabilité. On observait une différence entre la clinique universitaire et celle du centre-ville pour ce qui est de la prévalence des facteurs de risque chez les patients, ces deux groupes rapportant respectivement 20 % et 63 % de réponses positives aux 2 questions pour le dépistage de la dépression, 34 % et 60 % pour l’anxiété, 11 % et 71 % pour le tabagisme actuel, 6 % et 22 % pour l’impression d’avoir à réduire l’alcool, 1 % et 48 % pour l’usage de drogues de rue au cours de l’année précédente, et 11 % et 65 % pour des difficultés à réprimer la colère. Alors que plusieurs souhaitaient être aidés pour réduire leurs facteurs de risque, comme le tabac (20 %) et certains symptômes de maladie mentale (25 % et 27 %), 57 des 161 participants (35 %) voulaient être aidés pour un problème identifié ce jour-là. Patients et médecins jugeaient le CHAT acceptable et, à part 2 patients qui se sont opposés à la question sur l’alcool, aucun autre n’a émis d’objection à propos des questions. La plupart des commentaires étaient positifs.
Le CHAT a permis d’identifier de façon efficace 9 facteurs de risque, en plus de révéler les patients qui désiraient être aidés. Utilisé en salle d’attente, cet outil pourrait servir au dépistage, sinon pour tous les patients des soins primaires au Canada, du moins pour certains groupes ciblés.
Physical and mental health and substance misuse are often interwoven. 1 Therefore, preventive care in family practice should involve identifying and addressing both lifestyle and mental health risk factors. However, many at-risk behaviour patterns and conditions are not identified in routine practice. 2 Mental health issues in particular are common in North America. 3 , 4 In Quebec, 25% of family practice consultations are for mental health problems, 5 and 10% of Canadians use services for their mental health annually, with family physicians being the most commonly consulted professionals. 3 However, only 40% of those with mental health problems seek professional help. 3 Further, identification of and subsequent intervention for modifiable risk factors such as smoking, problematic drinking, and physical inactivity can have a strong positive influence on many chronic conditions, such as heart disease, diabetes, chronic obstructive pulmonary disease, and lung cancer. 6
In Canada, 85% of those aged 12 and older reported having a regular medical doctor in 2009. 7 , 8 Family practice provides an ideal setting for identifying and addressing lifestyle and mental health risk factors. Routine screening for these potentially modifiable risk factors is likely to have much better coverage than opportunistic screening. 9 However, given visit time restraints, routine screening rates for individual items such as depression can be low. 10
The Case-finding Health Assessment Tool (CHAT) is a short, self-administered tool for lifestyle and mental health assessment of adult patients in family practice. The CHAT was developed by a multidisciplinary team (including family physicians, nurses, and psychologists) from the University of Auckland in New Zealand. The tool assesses for risky behaviour (smoking, drinking, other drug use, gambling, exposure to abuse, and physical inactivity) and mental health issues (depression, anxiety, and anger control) and can be administered in the waiting room in less than 5 minutes, before the physician visit. For each item, patients are asked if the issue is something they would like help with and, if the answer is yes, whether they want help that day. By combining substance use, other risky health behaviour including violence, and negative mood states, the CHAT recognizes the interrelationship of these domains and how intervening in one can have positive effects on another. The tool has undergone testing for acceptability (less than 1% of more than 2500 patients objected to any question), reliability, 11 – 13 and validity in New Zealand. The addition of the question about help increases test specificity (reducing false positives). 13 – 15 The multi-item nature also allows for assessment of comorbidities. 16 It has been assessed with white, Maori, and Pacific Island 11 and Asian peoples, 13 with high patient acceptability in each group. Effective brief interventions that can be delivered in family practice are available for each of the risk factor areas. 17 – 21 Before the CHAT is used and evaluated in the Canadian context, a study of the feasibility and acceptability of the CHAT content and process is required. The aim of this study was to assess the feasibility and acceptability of the CHAT, a brief validated lifestyle screening tool that can be administered in Canadian family practice waiting rooms. This paper presents the findings from this feasibility study.
Consecutive adult patients 19 years of age or older attending a family practice on the days of the study were invited to participate by a research assistant in the waiting room. Those who appeared obviously unwell as judged by any of the practice staff, or those unable to read or understand English or the contents of the study information were not invited. Those who had previously completed the CHAT were excluded. The study setting was 2 family practices in British Columbia. One practice is a university-affiliated practice providing care to patients of middle to high socioeconomic status in a teaching clinic environment with medical students, residents, and pharmacy students; the other is a block-funded inner-city health centre providing primary care for adults without medical coverage, many of whom suffer from mental health issues, addictions, or other chronic health problems. The study was carried out over 3 half-days and 3 full days at the first practice and over 2 full days at the second practice. Family physicians from the participating practices were also invited to provide feedback about the CHAT.
After providing informed consent, patients completed the CHAT in the waiting room, which took less than 5 minutes. The patient then brought the completed CHAT to the physician consultation. The physician had the opportunity to discuss the results with the patient and address any issues, if desired.
The measures of feasibility included the proportions of consecutive eligible patients who agreed to participate in the study and the questions completed. The rates of positive answers to each domain were also recorded. Acceptability of the CHAT to patients and physicians was assessed by the proportion of objections to questions in each domain and by open-ended questions on feedback forms. Feedback forms were filled out following completion of the CHAT form either before or after the physician visit.
Sample size calculations were not carried out, as this was a feasibility study; however, the investigators aimed to enrol 50 to 100 patients from each of the 2 practices. Numbers and percentages of each of the outcome measures and the open-ended question responses are presented.
The study was approved by the University of British Columbia Behavioural Research Ethics Board.
During the study period, 282 adults attended the practices; 265 (94%) patients were eligible to participate and 176 (66%) were enrolled ( Figure 1 ). The CHAT was completed by 161 (91%) enrolled patients before their consultations after they provided informed consent. Of those, 107 (66%) also completed the acceptability feedback form. Eight physicians were involved. There were also several residents in the academic practice, but they did not participate in the feedback.

Response rates
CHAT—Case-finding Health Assessment Tool.
The rates of positive responses to questions about mental health and lifestyle risk were very different in the 2 practices ( Table 1 ). Just 11% of the patients from the urban academic practice currently smoked, and only 1% reported ever having used nonprescription or recreational drugs. Corresponding rates in the inner-city community health centre were 71% and 48%, respectively. The identification of risk factors for depression and anxiety was high in both practices, with 60 of 161 (37%) answering yes to both depression screening questions and 42 of 161 (26%) requesting help for this. Overall, 9% (14 of 161) reported that there was someone in their lives they were afraid of; who wanted to hurt them; or who controlled them, preventing them from doing what they wanted. Only 2% reported problematic gambling. Table 2 presents the aspects of patients’ lives that caused them stress, with money and health being the most common stressors. There were high rates of some risk factors, and a number of people indicated that they would like help ( Table 3 ). The highest rates for requesting assistance were for smoking (20%), depression (26%), and anxiety (25%). Overall, 77 patients (48%) reported that they wanted help with at least 1 risk factor; however, only 57 individuals (35%) wanted help that day.
Positive responses to mental health and lifestyle screening questions of consecutive adult patients attending 2 family practices in British Columbia
Responses to the question about life stress
Respondents could select as many answers as applied to them.
Screened patients requesting assistance with identified risk factors
Of the 107 patients who completed the feedback form about the CHAT, 2 people (2%) objected to the alcohol questions. There were no objections identified to any other questions. Fifty-two participants (49%) wrote comments in response to the question, “What (if anything) did you like about the assessment form?” Participants commented that they thought the CHAT questions were simple, clear, thorough, relevant, and important; raised awareness of the issues; and showed concern. Seventeen participants wrote comments about what they did not like about it. Some thought the questions were too general; lacked flow; were not long enough; or should include other options such as sometimes , whether the issue was already being addressed, or room for comments. Some patients found the questions difficult to read and required their reading glasses. One respondent commented that the CHAT raised hopes of actually getting help. Another was concerned that his or her feelings of depression might have been an appropriate response rather than a “mental problem,” and one other thought the number of prescription drugs was also an issue that the CHAT should explore. Some thought that not much could be done about tobacco cessation or wanted more specific questions about the number of cigarettes smoked.
Eight physicians completed a feedback form about the CHAT, 7 of whom made positive comments. They liked that it facilitated discussion about potentially sensitive issues that otherwise might not have been talked about, and that patients had the option of “naming” an issue but indicating that they did not wish to discuss it now. Five made comments about possible disadvantages or suggestions for improvement, such as adding a place for the date, other screening tools, or the option being addressed for each issue. One thought it would not be useful for follow-up and another thought it too simple. The physicians did not think that patients would object to any questions. All physician respondents stated that they would use such a form, if available. Three thought they would screen all adult patients, one would use it opportunistically, and 4 said they would use another approach, such as targeted administration to new patients.
This study showed that it was feasible to screen for several mental health and lifestyle risk factors in the waiting room of 2 family physician practices with different patient profiles. There were high rates of adult patients at risk of depression and high rates of other risk factors identified, such as smoking, exessive alcohol consumption, and gambling, particularly in the inner-city practice; however, overall rates were similar to those found in previous studies in New Zealand. 12 The study also found that a portion of the patients with such risk factors were ready to make a behavioural change and indicated that they wanted help that day.
Overall there were 102 risk factors self-identified for which patients requested “help today” during 161 consultations (38 issues at 98 consultations in the urban academic practice and 64 issues at 63 consultations in the inner-city practice). If many of these issues were over and above the reason for the consultation, this might present an extra demand on time, either of the physician or of other health care providers. Even if patients were not ready to address the issues, the form provided information about risk factors that could be addressed sometime in the future. This information would also provide statistics about the practice prevalence of these risk factors if the CHAT form were used on all or randomly selected adult patients from the practice.
The CHAT was also found to be acceptable, with few objections to any of the questions. Participants liked the brevity and practicality of the CHAT and appreciated that the medical professionals cared. Participant comments suggested that the form also acted to increase awareness of the issues and provided an impetus for self-reflection, which in itself might represent an intervention. However, it is important to acknowledge the expectations of patients; as one patient stated, the CHAT might “rais[e] hopes on actually getting help.”
The physicians found the CHAT useful in bringing relevant issues forward and commented that it would be particularly useful for new patients. One physician suggested the addition of another screening tool for abuse.
Compared with the literature
The questions in the CHAT have been validated in consecutive patients. 22 The 2 depression questions in the CHAT have 96% sensitivity and 69% specificity 22 for diagnosing major depression, and 73% sensitivity and 98% specificity 23 for those who also request help. Rates were similar for the anxiety screening question. 22 , 23 Therefore, the rates of 26% and 25% of patients who requested help for depression and anxiety, respectively, in this study are consistent with the estimated prevalence of mental health conditions, such as depression and anxiety, seen both in the Canadian population 24 and among those visiting their family physicians. 3
It has become increasingly clear in recent years that addiction and mental health disorders often coexist, 25 and there has been a move from single-condition instruments toward screening tools that assess several mental health issues such as depression, anxiety, and somatisation 26 ; generalized distress 27 ; serious mental illness 28 ; and mental illness and trauma. 29 , 30 However, none of the other multi-item instruments is a generic primary care tool offering casefinding for both lifestyle factors and mental health issues. They deal with specific conditions such as substance abuse or mental distress, disease states like cancer or heart disease, or populations such as adolescents, the elderly, or pregnant women.
An electronic version of the CHAT, completed on tablet computers in waiting rooms, with results transmitted into the electronic medical records of family physicians at the point of care, has also been developed and is being trialed in New Zealand. 31 – 33 It incorporates a tree structure with added scored tools triggered where applicable: the Alcohol, Smoking and Substance Involvement Screening Test for smoking, alcohol, and other drug use 34 ; the Patient Health Questionnaire module for depression 35 ; and the Generalized Anxiety Disorder Assessment for anxiety. 36 It also incorporates 3 Alcohol Use Disorders Identification Test Consumption questions on alcohol. 37 For positive domains, the physician has electronic access to stepped-care clinical decision- support tools to guide decision making, including problem solving, goal setting, brief coaching, patient education, medications, and referrals.
Strengths and limitations
The main reason for non-participation was that patients were missed owing to a lack of time before the physician consultation. However, the exclusion of non-English-speaking patients, who might also be immigrants and have lower socioeconomic status, might have introduced a systematic bias. When used in practice, the screening tool alone would take less time without the study procedures, so a greater coverage is likely. In addition, the CHAT can be used annually, just for new patients, or only in those considered to be high risk, depending on the preference and profile of the practice. Of interest, there were few patients in either practice who declined to participate.
The study was a feasibility study within only 2 practices; thus “prevalence rates” of each risk factor are only relevant for the practices themselves and will not be representative of actual rates across family physician practices.
Mental health and lifestyle risk factors are often not detected or addressed during physician visits owing to time constraints. 2 The CHAT allowed efficient identification of 9 risk factors, as well as identification of those wanting help, and could be used in waiting rooms to screen all or targeted adult Canadian primary care patients (eg, patients new to the practice; those not seen for 2 years; antenatal patients; or those with pre-existing, long-term conditions, mental health issues, or substance misuse). The tool allows patients to prioritize the areas that they would like addressed and facilitates a conversation with their physicians for shared decision making. 32 Repeating the CHAT at a later date allows ease of tracking of patients’ progress over time.
In addition to time constraints, mental health and lifestyle risk factors are also often not detected either because patients do not know that these are concerns to bring to their physicians or because they might feel threatened if they are asked directly. Because sensitive questions are embedded in the CHAT, it increases the acceptability of such questions to patients. Physicians are also cautious about stigmatizing patients by direct questioning, and the CHAT brings the issues into the open and initiates the patient-physician conversation, reducing barriers for patients to seek and accept help.
EDITOR’S KEY POINTS
- Mental health and lifestyle risk factors are often not detected or addressed owing to time constraints. This study aimed to assess the feasibility and acceptability of administering the validated Case-finding Health Assessment Tool (CHAT) in Canadian family practice. The CHAT is a short, self-administered tool for lifestyle and mental health assessment of adult patients, which can be completed in the waiting room before the physician appointment.
- The CHAT allowed efficient identification of 9 risk factors, as well as identification of those wanting help. High rates of several of the risk factors were identified, and about a third of the patients with such risk factors were ready to make behavioural changes and indicated that they wanted help that day.
- The CHAT was also found to be acceptable, with few objections to any of the questions. Participants liked the brevity and practicality of the CHAT and appreciated that the medical professionals cared. Participant comments suggested that the form also acted to increase awareness of the issues and provided an impetus for self-reflection.
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
- Understanding Infant and Caregiver…
Understanding Infant and Caregiver Mental Health: What is the Impact of the COVID-19 Pandemic and Systemic Racism?
Date posted:.
Mental Health Awareness Month offers an opportunity to reflect on the importance of our health and well-being—including for the littlest amongst us. The first five years of life are a critically important period of physical, social, cultural, and emotional development in the lives of children and their families that sets the foundation for young children’s future health, development, and well-being. Importantly, all events that occur in the child’s life at this early stage are likely to have a significant impact as they develop.
Over the last several decades, we have learned that social determinants of health—including where children and families live, work, and play—are crucial in understanding how contexts impact health, and in the case of incredibly young children, their development.
Additionally, the well-being of young children depends heavily on the mental and physical health of their parents and caregivers. Thus, it is crucial to prioritize the mental well-being of these adults and the environments in which children are nurtured to address the challenges impacting infants, toddlers and preschoolers.
Amid this landscape of supports and challenges for families with young children, the past 4 years have been particularly difficult for many families with the rise of the COVID-19 pandemic and simultaneous increasing national awareness and discussion of long-standing racial inequities. Racism is a known social determinant of health which affects the mental health and well-being of families, particularly pregnant and postpartum individuals and their children.
As we have continued to wrestle with the COVID-19 pandemic, there have been increased efforts to better understand the impacts of this global event with racialized components on communities that have historically lacked access, services, and care. Our team’s Prenatal to Preschool (P2P) study , described below, is one such example of a project that originated during the pandemic with the explicit goal to better understand how this global crisis differentially impacted the mental health of families in our Philadelphia community.
Prenatal to Preschool (P2P): How are we understanding the mental health of very young children and their families?
P2P evaluates the simultaneous effects of the pandemic, stressors, and multiple forms of racism on mothers and their developing children, providing important insight into risk and resilience factors in early development and the peripartum period.
In the context of a major U.S. city, Philadelphia, like many others, is marked by pronounced neighborhood disparities, such that our group found it imperative for public health and policy efforts to better understand how known inequities impact the mental well-being of the city's thousands of very young children and their families. We are doing this by examining cross-cultural differences and experiences faced by Black and non-Latinx White families.
Our team began talking to families participating in the study when they were pregnant at the very beginning of the pandemic when the world shut down in April 2020. Over the last four years, as our global and local experiences of the pandemic changed, caregivers have answered questions about their health and well-being, as well as that of their growing child’s, and their partners in child-rearing. Questions have covered topics including depression, anxiety, parenting stress, social supports, experiences of multiple forms of racism, their child’s development, and COVID-related worries.
Our initial findings underscore the importance of supporting families with very young children in a variety of ways and amongst unprecedented challenges.
We hope that this project will set the foundation for future work to continue fostering diversity and equity in research, along with promoting the well-being of children and families impacted by the pandemic.
As the P2P families continue to participate as their children turn four, we will be able to look at the past four years with an additional goal to create individualized, culturally informed preventative interventions for all families. We aim to ensure that the work we are doing joins the work of so many others in achieving mental health equity for all young children and their families in our region and across the nation.
Latest Blog Posts

Recognizing Cross-sector Collaborations That Can Improve Financial Wellness and Educational Opportunities in 200 Words
Education pays. That truth underlies the role education plays in addressing poverty, and is part of why education has been acknowledged as a …
Utilizing Behavioral Health Research to Inform Policy: A Conversation with Dr. Rhonda Boyd
As the youth behavioral health crisis has grown in the past several years, members of PolicyLab’s Behavioral Health portfolio have continued to think…

Syringe Services Programs Are Critical for Adolescents and Young Adults: Research and Clinical Perspectives
As physicians who take care of young people with substance use disorders, we recognize the significance of harm reduction approaches in helping…
Check out our new Publications View Publications
Adolescent Health & Well-Being
Behavioral health, population health sciences, health equity, family & community health.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Talking with Your Healthcare Provider
- Birth Defects Statistics
- Birth Defects Resources
- Birth Defects Awareness Month
- Living with Down Syndrome
- Conversation Tips
- Growth Charts for Down Syndrome
- Accessing NBDPS and BD-STEPS Data
- Birth Defects Awareness Month Social Media Resources
- About Alcohol Use During Pregnancy
About Down Syndrome
- Down syndrome is a genetic condition where a person is born with an extra chromosome.
- This can affect how their brain and body develop.
- People diagnosed with Down syndrome can lead healthy lives with supportive care.

Down syndrome is a condition in which a person has an extra copy of chromosome 21. Chromosomes are small "packages" of genes in the body's cells, which determine how the body forms and functions.
When babies are growing, the extra chromosome changes how their body and brain develop. This can cause both physical and mental challenges.
People with Down syndrome often have developmental challenges, such as being slower to learn to speak than other children.
Distinct physical signs of Down syndrome are usually present at birth and become more apparent as the baby grows. They can include facial features, such as:
- A flattened face, especially the bridge of the nose
- Almond-shaped eyes that slant up
- A tongue that tends to stick out of the mouth
Other physical signs can include:
- A short neck
- Small ears, hands, and feet
- A single line across the palm of the hand (palmar crease)
- Small pinky fingers
- Poor muscle tone or loose joints
- Shorter-than-average height
Some people with Down syndrome have other medical problems as well. Common health problems include:
- Congenital heart defects
- Hearing loss
- Obstructive sleep apnea
Down syndrome is the most common chromosomal condition diagnosed in the United States. Each year, about 5,700 babies born in the US have Down syndrome. 1
There are three types of Down syndrome. The physical features and behaviors are similar for all three types.
With Trisomy 21, each cell in the body has three separate copies of chromosome 21. About 95% of people with Down syndrome have Trisomy 21.
Translocation Down syndrome
In this type, an extra part or a whole extra chromosome 21 is present. However, the extra chromosome is attached or "trans-located" to a different chromosome rather than being a separate chromosome 21. This type accounts for about 3% of people with Down syndrome.
Mosaic Down syndrome
Mosaic means mixture or combination. In this type, some cells have three copies of chromosome 21, but other cells have the typical two copies. People with mosaic Down syndrome may have fewer features of the condition. This type accounts for about 2% of people with Down syndrome.
Risk factors
We don't know for sure why Down syndrome occurs or how many different factors play a role. We do know that some things can affect your risk of having a baby with Down syndrome.
One factor is your age when you get pregnant. The risk of having a baby with Down syndrome increases with age, especially if you are 35 years or older when you get pregnant. 2 3 4
However, the majority of babies with Down syndrome are still born to mothers less than 35 years old. This is because there are many more births among younger women. 5 6
Regardless of age, parents who have one child with Down syndrome are at an increased risk of having another child with Down syndrome. 7
Screening and diagnosis
There are two types of tests available to detect Down syndrome during pregnancy: screening tests and diagnostic tests. A screening test can tell you if your pregnancy has a higher chance of being affected Down syndrome. Screening tests don't provide an absolute diagnosis.
Diagnostic tests can typically detect if a baby will have Down syndrome, but they carry more risk. Neither screening nor diagnostic tests can predict the full impact of Down syndrome on a baby.
The views of these organizations are their own and do not reflect the official position of CDC.
Down Syndrome Resource Foundation (DSRF) : The DSRF supports people living with Down syndrome and their families with individualized and leading-edge educational programs, health services, information resources, and rich social connections so each person can flourish in their own right.
GiGi's Playhouse : GiGi's Playhouse provides free educational, therapeutic-based, and career development programs for individuals with Down syndrome, their families, and the community, through a replicable playhouse model.
Global Down Syndrome Foundation : This foundation is dedicated to significantly improving the lives of people with Down syndrome through research, medical care, education and advocacy.
National Association for Down Syndrome : The National Association for Down Syndrome supports all persons with Down syndrome in achieving their full potential. They seek to help families, educate the public, address social issues and challenges, and facilitate active participation.
National Down Syndrome Society (NDSS) : NDSS seeks to increase awareness and acceptance of those with Down syndrome.
- Stallings, E. B., Isenburg, J. L., Rutkowski, R. E., Kirby, R. S., Nembhard, W.N., Sandidge, T., Villavicencio, S., Nguyen, H. H., McMahon, D. M., Nestoridi, E., Pabst, L. J., for the National Birth Defects Prevention Network. National population-based estimates for major birth defects, 2016–2020. Birth Defects Research. 2024 Jan;116(1), e2301.
- Allen EG, Freeman SB, Druschel C, et al. Maternal age and risk for trisomy 21 assessed by the origin of chromosome nondisjunction: a report from the Atlanta and National Down Syndrome Projects. Hum Genet. 2009 Feb;125(1):41-52.
- Ghosh S, Feingold E, Dey SK. Etiology of Down syndrome: Evidence for consistent association among altered meiotic recombination, nondisjunction, and maternal age across populations. Am J Med Genet A. 2009 Jul;149A(7):1415-20.
- Sherman SL, Allen EG, Bean LH, Freeman SB. Epidemiology of Down syndrome. Ment Retard Dev Disabil Res Rev. 2007;13(3):221-7.
- Olsen CL, Cross PK, Gensburg LJ, Hughes JP. The effects of prenatal diagnosis, population ageing, and changing fertility rates on the live birth prevalence of Down syndrome in New York State, 1983-1992. Prenat Diagn. 1996 Nov;16(11):991-1002.
- Adams MM, Erickson JD, Layde PM, Oakley GP. Down's syndrome. Recent trends in the United States. JAMA. 1981 Aug 14;246(7):758-60.
- Morris JK, Mutton DE, Alberman E. Recurrences of free trisomy 21: analysis of data from the National Down Syndrome Cytogenetic Register. Prenatal Diagnosis: Published in Affiliation With the International Society for Prenatal Diagnosis. 2005 Dec 15;25(12):1120-8.
Birth Defects
About one in every 33 babies is born with a birth defect. Although not all birth defects can be prevented, people can increase their chances of having a healthy baby by managing health conditions and adopting healthy behaviors before becoming pregnant.
For Everyone
Health care providers, public health.
Nitrate contamination in groundwater and its health risk assessment: a case study of Quanzhou, a typical coastal city in Southeast China
- Original Article
- Published: 13 May 2024
- Volume 83 , article number 331 , ( 2024 )
Cite this article

- Zhenghong Li 1 , 2 ,
- Jianfeng Li 1 , 2 ,
- Jin’ou Huang 3 &
- Yasong Li 1 , 2
Explore all metrics
Nitrate contamination has become an ecological and health issue in Quanzhou, a typical coastal city in Southeast China. Hydrogeological surveys reveal that NO 3 − is a major factor influencing the groundwater quality in Quanzhou City, Fujian Province, China. To protect public health, this study explored the geographical spatial distribution, contamination level, contamination sources, and noncancer risks of nitrates in the plain area of Quanzhou. Key findings are as follows: (1) The groundwater in Quanzhou’s plain area exhibits a high detection rate and over-limit ratio of NO 3 − –N of 99.3% and 57.86%, respectively. This result suggests that the groundwater in the area has been extensively contaminated by nitrates, with relatively severe nitrate contamination occurring in the Quanzhou Taiwanese Investment Zone, Jinjiang City, and Shishi City; (2) NO 3 − has become a major anion in groundwater in Quanzhou’s plain area, leading to significant geochemical changes in some groundwater. 26.4% of the groundwater samples exhibited a hydrochemical type of nitric acid (also referred to as NO 3 − type water), with X(NO 3 − ) ≥ 25%; (3) The primary nitrate contamination in groundwater in Quanzhou originates from the infiltration of domestic and industrial wastewater or landfill leachate; (4) 42.86%, 43.57%, and 67.14% of the samples posed health risks to adult males, adult females, and children, respectively when they were subjected to the prolonged exposure in a high-concentration nitrate environment. Additionally, the noncancer risks of nitrates principally stem from oral exposure for drinking water.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Groundwater nitrate contamination and associated health risk for the rural communities in an agricultural area of ningxia, northwest china.
Source identification and health risks of nitrate contamination in shallow groundwater: a case study in Subei Lake basin
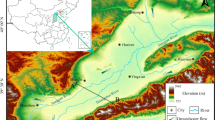
Poor groundwater quality and high potential health risks in the Datong Basin, northern China: research from published data
Data availability.
The data used to support the fndings of this study are available from the corresponding author upon request.
Abascal E, Gomez-Coma L, Ortiz I, Ortiz A (2022) Global diagnosis of nitrate pollution in groundwater and review of removal technologies. Sci Total Environ 810:152233
Article CAS Google Scholar
Abu-alnaeem M, Yusoff I, Ng T, Alias Y, Raksmey M (2018) Assessment of groundwater salinity and quality in Gaza coastal aquifer, Gaza Strip, Palestine: an integrated statistical, geostatistical and hydrogeochemical approaches study. Sci Total Environ 615:972–989
Bahadoran Z, Mirmiran P, Ghasemi A, Kabir A, Azizi F, Hadaegh F (2015) Is dietary nitrate/nitrite exposure a risk factor for development of thyroid abnormality? A systematic review and meta-analysis. Nitric Oxide 47:65–76
Banyikwa A (2023) Geochemistry and sources of fluoride and nitrate contamination of groundwater in six districts of the Dodoma region in Tanzania. Scient African 21:e01783
Bellettini A, Viero A, Neto A (2019) Hydrochemical and contamination evolution of Rio Bonito aquifer in the carboniferous region, Paraná Basin, Brazil. Environ Earth Sci 78:1–15
Google Scholar
Bian JM, Zhang ZZ, Han Y (2015) Spatial variability and health risk assessment of nitrogen pollution in groundwater in Songnen Plain. J Chongqing Univer 38(4):104–111 ( (in Chinese with English abstract) )
CAS Google Scholar
Bouderbala A (2019) The impact of climate change on groundwater resources in coastal aquifers: case of the alluvial aquifer of Mitidja in Algeria. Environ Earth Sci 78:1–13
Article Google Scholar
Canadian Council of Ministers of the Environment (CCME) (2014) Canadian environmental quality guidelines
Fujian Provincial Sports Bureau, China (2022) The fifth National Physical Fitness Monitoring Bulletin of Fujian Province. Fujian Province. (in Chinese)
Gallagher T, Gergel S (2017) Landscape indicators of groundwater nitrate concentrations: an approach for trans-border aquifer monitoring. Ecosphere 8(12):e02047. https://doi.org/10.1002/ecs2.2047
Gutierrez M, Biagioni R, Alarcon-Herrera M, Rivas-Lucero B (2018) An overview of nitrate sources and operating processes in arid and semiarid aquifer systems. Sci Total Environ 624:1513–1522
Heaton T, Stuart M, Sapiano M, Micallef Sultana M (2012) An isotope study of the sources of nitrate in Malta’s groundwater. J Hydrol 414–415:244–254
International Agency for Research on Cancer (IARC) (2022) Agents Classified by the IARC Monographs 1:132
Jiang WJ, Wang GC, Sheng YZ, Zhao D, Liu CL, Guo YH (2016) Enrichment and sources of nitrogen in groundwater in the Turpan-Hami area, Northwestern China. Expo Health 8:389–400
Kong XK, Zhang ZX, Wang P, Wang YY, Zhang ZJ, Han ZT, Ma LS (2022) Transformation of ammonium nitrogen and response characteristics of nitrifying functional genes in tannery sludge contaminated soil. J Groundwater Sci Eng 10(3):223–232
Lahjouj A, Hmaidi A, Bouhafa K (2020) Spatial and statistical assessment of nitrate contamination in groundwater: Case of Sais Basin, Morocco. J Groundwater Sci Eng 8(2):143–157
Li ZH, Zhang YL, Hu B, Wang LJ, Zhu YC, Li JF (2018) Driving action of human activities on NO 3 – -N pollution in confined groundwater of Togtoh County. Inner Mongolia Acta Geoscientica Sinica 39(3):358–364 ( (in Chinese with English abstract) )
Li Y, Kang FX, Zou AD (2019) Isotope analysis of nitrate pollution sources in groundwater of Dong’e geohydrological unit. J Groundwater Sci Eng 7(2):145–154
Li ZH, Li YS, Hao QC, Li JF, Zhu YC (2021) Characteristics, genesis and treatment measures of NO 3 type groundwater in Xiamen, Fujian Province. Geology in China 48(5): 1441–1452. 6 (in Chinese with English abstract)
Menció A, Mas-Pla J, Otero N, Regàs O, Boy-Roura M, Puig R, Bach J, Domènech C, Zamorano M, Brusi D, Folch A (2016) Nitrate pollution in groundwater; all right…, but nothing else? Sci Total Environ 539:241–251
Ministry of Ecology and Environmental PRC (2013) Chinese population Exposure Parameters Manual: Volume for children. Beijing, China Environmental Press (in Chinese).
Ministry of Ecology and Environmental PRC (2013) Chinese population Exposure Parameters Manual: Adult volume. Beijing, China Environmental Press ( in Chinese )
Monteny G (2001) The EU nitrates directive: a european approach to combat water pollution from agriculture. In Optimizing Nitrogen Management in Food and Energy Production and Environmental Pro tection: Proceedings of the 2nd International Nitrogen Conference on Science and Policy. The Scientific World 1(S2) 927–935
Musaed H, Al-Bassam A, Zaidi F, Alfaifi H, Ibrahim E (2020) Hydrochemical assessment of groundwater in mesozoic sedimentary aquifers in an arid region: a case study from Wadi Nisah in Central Saudi Arabia. Environ Earth Sci 79:1–12
National Health Commission, PRC, Standardization Administration, PRC (2022) Standards for dringing water quality. Beijing (in Chinese)
Panneerselvam B, Muniraj K, Duraisamy K, Pande C, Karuppannan S, Thomas M (2023) An integrated approach to explore the suitability of nitrate-contaminated groundwater for drinking purposes in a semiarid region of India. Environ Geochem Health 45:647–663
Papazotos P, Koumantakis I, Vasileiou E (2019) Hydrogeochemical assessment and suitability of groundwater in a typical Mediterranean coastal area: A case study of the Marathon basin, NE Attica, Greece. HydroResearch 2:49–59
Peixoto F, Cavalcante I, Gomes D (2020) Influence of land use and sanitation issues on water quality of an urban aquifer. Water Resour Manage 34:653–674
Pouye A, Cissé Faye S, Diédhiou M, Gaye C, Taylor R (2023) Nitrate contamination of urban groundwater and heavy rainfall: Observations from Dakar. Senegal Vadose Zone Jl 22:e20239
Rahman A, Mondal N, Tiwari K (2021) Anthropogenic nitrate in groundwater and its health risks in the view of background concentration in a semiarid area of Rajasthan. India. Scient Rep 11(1):1–13
Rezende D, Nishi L, Coldebella P, Mantovani D, Soares P, Carlos Valim Junior N, Vieira A, Bergamasco R (2019) Evaluation of the groundwater quality and hydrogeochemistry characterization using multivariate statistics methods: case study of a hydrographic basin in Brazil. Desalin Water Treat 161:203–215
Romanelli A, Soto D, Matiatos I, Martínez D, Esquius S (2020) A biological and nitrate isotopic assessment framework to understand eutrophication in aquatic ecosystems. Sci Total Environ 715:136909
Sheng DR, Wen XH, Feng Q, Wu J, Si JH, Wu M (2019) Groundwater nitrate pollution and human health risk assessment in the Zhangye Basin, Gansu. China J Desert Res 39(5):37–44 ( (in Chinese with English abstract) )
Stuart M, Gooddy D, Bloomfield J, Williams A (2011) A review of the impact of climate change on future nitrate concentrations in groundwater of the UK. Sci Total Environ 409(15):2859–2873
Sun XB, Guo CL, Zhang J, Sun JQ, Cui J, Liu MH (2023) Spatial-temporal difference between nitrate in groundwater and nitrogen in soil based on geostatistical analysis. J Groundwater Sci Eng 11:37–46
Tokazhanov G, Ramazanova E, Hamid S, Bae S, Lee W (2020) Advances in the catalytic reduction of nitrate by metallic catalysts for high efficiency and N 2 selectivity: A review. Chem Eng J 384:123252
United States Environment Protection Agency (U.S. EPA) (2022) Integrated risk information systerm
United States Environmental Protection Agency (U.S. EPA) (2017) Drinking water contaminants–standards and regulations
Verma A, Sharma A, Kumar R, Sharma P (2023) Nitrate contamination in groundwater and associated health risk assessment for Indo-Gangetic Plain. India Groundwater for Sustain Dev 23:100978
Vilmin L, Mogollon J, Beusen A, Bouwman A (2018) Forms and subannual variability of nitrogen and phosphorus loading to global river networks over the 20th century. Global Planet Change 163:67–85
Ward M, Jones R, Brender J, De Kok T, Weyer P, Nolan B, Villanueva C, Van Breda S (2018) Drinking water nitrate and human health: an updated review. Int J Environ Res Public Health 15(7):1557
WHO (2017) Guidelines for Drinking Water Quality: Fourth Edition Incorporating the First Addendum, fourthed. World Health Organization, Geneva
Yang M, Fei YH, Ju YW, Ma Z, Li HQ (2012) Health risk assessment of groundwater Pollution- a case study of typical city in North China Plain. J Earth Sci 23(3):335–348
Zakaria N, Gibrilla A, Owusu-Nimo O, Adomako D, Anornu G, Fianko J, Gyamfi C (2023) Quantifcation of nitrate contamination sources in groundwater from the Anayari catchment using major ions, stable isotopes, and Bayesian mixing model. Ghana Environ Earth Sci 82:381
Download references
Acknowledgements
This work was supported by the China Geological Survey project (Nos. DD20190303, DD20221773, DD20230459) and Zhejiang Provincial Geological Special Fund Project (No. 2023010)
Author information
Authors and affiliations.
Fujian Provincial Key Laboratory of Water Cycling and Eco-Geological Processes, Xiamen, 361000, China
Zhenghong Li, Jianfeng Li & Yasong Li
Institute of Hydrogeology and Environmental Geology, Chinese Academy of Geological Sciences, Shijiazhuang, 050061, China
Zhejiang Institute of Geosciences, Hangzhou, 310007, China
Jin’ou Huang
You can also search for this author in PubMed Google Scholar
Contributions
Writing-original draft, Zhenghong Li; Reviewing and editing, Jianfeng Li, Yasong Li; Methodology, Jianfeng Li, Yasong Li, Zhenghong Li, Jin’ou Huang; Investigation, data collection, Zhenghong Li, Jianfeng Li; Figures preparation, Zhenghong Li, Jin’ou Huang; All authors have read and agreed to the submitted version of the manuscript.
Corresponding author
Correspondence to Jianfeng Li .
Ethics declarations
Conflict of interest.
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Li, Z., Li, J., Huang, J. et al. Nitrate contamination in groundwater and its health risk assessment: a case study of Quanzhou, a typical coastal city in Southeast China. Environ Earth Sci 83 , 331 (2024). https://doi.org/10.1007/s12665-024-11608-z
Download citation
Received : 21 December 2023
Accepted : 18 April 2024
Published : 13 May 2024
DOI : https://doi.org/10.1007/s12665-024-11608-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Spatial distribution
- NO 3 − type water
- Hydrochemistry
- Risk assessment
- Southeast coast
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 10 May 2024
Short developmental milestone risk assessment tool to identify Duchenne muscular dystrophy in primary care
- Paula van Dommelen ORCID: orcid.org/0000-0001-5546-6244 1 ,
- Oisín van Dijk 2 ,
- Jeroen A. de Wilde 2 &
- Paul H. Verkerk 1
Orphanet Journal of Rare Diseases volume 19 , Article number: 192 ( 2024 ) Cite this article
222 Accesses
Metrics details
In patients without a family history, Duchenne muscular dystrophy (DMD) is typically diagnosed at around 4–5 years of age. It is important to diagnose DMD during infancy or toddler stage in order to have timely access to treatment, opportunities for reproductive options, prevention of potential fatal reactions to inhaled anesthetics, awareness of a child’s abilities needed for good parenting, and opportunities for enrolment in clinical trials.
We aimed to develop a short risk assessment tool based on developmental milestones that may contribute to the early detection of boys with DMD in primary care. As part of the case-control 4D-DMD study (Detection by Developmental Delay in Dutch boys with DMD), data on developmental milestones, symptoms and therapies for 76 boys with DMD and 12,414 boys from a control group were extracted from the health records of youth health care services and questionnaires. Multiple imputation, diagnostic validity and pooled backward logistic regression analyses with DMD (yes/no) as the dependent variable and attainment of 26 milestones until 36 months of age (yes/no) as the independent variable were performed. Descriptive statistics on symptoms and therapies were provided.
A tool with seven milestones assessed at specific ages between 12 and 36 months resulted in a sensitivity of 79% (95CI:67–88%), a specificity of 95.8% (95%CI:95.3–96.2), and a positive predictive value of 1:268 boys. Boys with DMD often had symptoms (e.g. 43% had calf muscle pseudohypertrophy) and were referred to therapy (e.g. 59% for physical therapy) before diagnosis.
This tool followed by the examination of other DMD-related symptoms could be used by youth health care professionals during day-to-day health assessments in the general population to flag children who require further action.
Conclusions
The majority of boys (79%) with DMD can be identified between 12 and 36 months of age with this tool. It increases the initial a priori risk of DMD from 1 in 5,000 to approximately 1 in 268 boys. We expect that other neuromuscular disorders and disabilities can also be found with this tool.
Worldwide, health care professionals often use monitoring tools to test the developmental skills of infants and toddlers [ 1 , 2 ]. An important goal of monitoring child development is the early identification of a wide range of disorders that impact child development. Typically, ‘red flags’ for milestone attainment are set at approximately the 90th percentile, i.e. with 90% of children attaining the milestone. However, if a child fails to attain a milestone, it is still uncertain if and to what extent the risk of a disorder is increased. For many disorders it is unknown how the monitoring tools can be optimally used to have a high sensitivity and specificity at field level.
One of such disorders is Duchenne muscular dystrophy (DMD). DMD is an inherited X-linked recessive neuromuscular disorder affecting approximately 1 in 5000 live male births [ 3 , 4 ]. DMD is typically diagnosed at around 4–5 years of age [ 5 , 6 , 7 ]. It is important to diagnose DMD during infancy or at the toddler stage in order to have timely access to treatment [ 8 , 9 ], opportunities for reproductive options, prevention of potential fatal reactions to inhaled anesthetics [ 10 ], awareness of a child’s abilities needed for good parenting, and opportunities for enrolment in clinical trials [ 11 ].
Previous studies have shown that more children with DMD fail to attain some developmental milestones compared to the general population [ 12 , 13 , 14 , 15 , 16 , 17 ]. Studies also recognized diagnostic delay despite parents noticing signs and symptoms in their child that are characteristic of DMD [ 5 ]. Several risk assessment tools were reported including developmental milestones for DMD [ 5 , 18 , 19 ]. These tools suggest performing a serum creatine kinase (CK) test if a child is unable to walk at 16–18 months [ 5 , 18 , 19 ], shows Gowers’ sign [ 19 ], or does not use at least ten recognizable words at 24 months of age [ 18 ]. However, the diagnostic validity of these tools was not assessed. Therefore, the tools do not indicate the increased risk of DMD given a developmental delay.
Our previous research investigated the diagnostic validity of a large number of individual milestones and showed that the milestones ‘walks well alone at 24 months’ and ‘walks smoothly at 36 months’ were most promising in detecting boys with DMD [ 17 ]. However, a tool that uses combinations of milestones may improve the diagnostic validity. Since there is a wide variation in the selection of milestones and the timing of their use worldwide, a short tool is needed to implement this in the primary care workflow to improve the early detection of DMD.
The aim of this study is to develop a short risk assessment tool based on developmental milestones for the early detection of DMD with acceptable diagnostic properties that can be easily applied during day-to-day health assessments in the general population.
Data collection
Within the 4D-DMD study (Detection by Developmental Delay in Dutch boys with DMD) with a case-control design, data were collected from: (1) health records of boys with DMD; characteristics, referrals to secondary and tertiary care, educational interventions, clinical descriptions typical of DMD, and developmental scores; (2) questionnaires completed by parents of boys with DMD; type of diagnosis, recall of developmental milestones, health care referrals, symptoms, concerns; and (3) health records of a control group of a general population of boys from the Youth Health Care (YHC) of The Hague (one boy with diagnosed DMD was excluded); characteristics, developmental scores, and referrals to other health professionals.
The diagnosis and date of diagnosis were obtained from the Dutch DMD patient registry. More information about the data collection within the 4D-DMD study is available in our previous research [ 17 ].
Developmental milestones
In the Netherlands, there is a well-organized YHC system, where 95% of all children are seen at regular visits [ 20 ]. Basic care within the Dutch YHC is supported by 35 evidence-based guidelines and validated screening tools [ 21 ], facilitating referrals as necessary. In the Netherlands, the Dutch Development Instrument (DDI) [ 22 ], a modification of the Gesell test, is used by YHC to assess the development of children. The DDI is mentioned in seven YHC guidelines, and among these, one guideline is dedicated to language development and one to motor development. However, none of these guidelines specifically address DMD. The DDI is a set of 75 developmental milestones that cover three domains of child development: (1) fine motor activity, adaptive behaviour, and personal/social behaviour; (2) communication; and (3) gross motor activity. The DDI is administered by trained YHC professionals at visits scheduled at the ages of 1, 2, 3, 6, 9, 12, 15, 18, 24, 30, 36, 42, and 48 months. For this study, we selected milestones up until 36 months of age. In many Dutch YHC services visits at 30 months are only scheduled for children considered at risk. Therefore, milestones registered during this visit were excluded. YHC professionals administer and register each milestone according to a uniform protocol. Two to seven specific milestones are registered in the health records at each visit. Some milestones may also be registered based on observations made by caregivers if the behaviour is not observed during the examination.
Statistical analysis
To develop the short risk assessment tool to identify boys with DMD that could easily be used in daily practice of primary care, we needed to determine which and to what extent the developmental milestones independently contribute to the risk of DMD. We applied the following six steps:
Pre-selection of data
Previous research within the 4D-DMD study showed that 26 milestones between 2 and 36 months were univariate significant at 0.01 level or lower between the DMD and control group [ 17 ]. For this study, we selected these 26 milestones to reduce the number of variables for the imputation in step 2, because the sample size in the DMD group does not allow a large number of variables.
From incomplete to complete data
Multiple imputation was applied in both groups (DMD, control) to predict missing data in the 26 milestones (see appendix for the observed and missing values) [ 23 ]. In total, 50 predictions were conducted to account for missing data uncertainty.
Models to obtain selection of milestones for the short risk assessment tool
We developed five age-dependent models for the early identification of DMD using milestones up until (1) 12 months, (2) 15 months, (3) 18 months, (4) 24 months, and (5) 36 months of age. For each prediction, logistic regression analyses were performed and afterwards pooled to test the impact of the milestones (independent variables) on group (DMD vs. control) outcome. Backward stepwise regression was applied on the pooled models till all remaining variables were significant at 0.05 level in the final model. We selected milestones that were statistically significantly associated with the outcome (DMD yes/no) in one or more of the final age-dependent models. Milestones that were not significant in all models (but significant in at least one model) were also taken into account, because these milestones may reduce the age of detection.
From model parameters to simple weighing factors
In order to create one practical tool that can be easily implemented in daily practice, we investigated whether simple weighting factors with integer numbers can be used instead of employing computer-intensive regression models. We tried several weighting factors (1 to 13) for each selected milestone from step 3 and calculated the sum score after weighting each milestone (with 1 point for a fail on a milestone and 0 points for a pass on a milestone or a when a milestone is not assessed) to achieve the highest predictive value. Note that a higher weight for a milestone implies a greater likelihood that the boy has DMD when the boy fails this milestone.
Predictive value of the cut-off values for the sum score
We then applied cut-off values for the sum score to calculate the sensitivity (% of referrals according to the tool within the DMD group) and specificity (% of non-referrals according to the tool within the control group), and the positive predictive value (PPV: how many boys with DMD are available within the referrals according to the tool assuming a prevalence of 1:5000 live male births). The negative predictive value (NPV: how many controls are available within the non-referrals according to the tool assuming a prevalence of 1:5000 live male births) was not calculated, because the prevalence of DMD is low and results in a NPV of almost 100%.
Selection of optimal cut-off values for the sum score
We obtained the most optimal weighting factors and cut-off value by choosing the highest sensitivity at a fixed specificity of approximately 95%. As a condition, the weighting factor for the milestone walks smoothly at 36 months was set at the highest cut-off value, because of the high risk of DMD. Also, up until 15 months of age, failures of at least two milestones were selected to reduce the number of false-positives at an early age.
All analyses were conducted in R Version 3.4.4 and SPSS Version 25.
The parents of 229 boys with DMD who met the inclusion criteria were invited to participate. In total, 87 boys with DMD and/or their parents gave written permission for retrieval of their health records. Retrieval was unsuccessful in ten cases: data were missing or not available for nine and one boy did not survive during retrieval of his records. In total, the health records of 76 boys with DMD were received. In addition, 71 parents of boys with DMD fully or partly completed the questionnaire.
Epidemiological and disease characteristics of boys with DMD and the general population are summarized in Table 1 . The proportions of boys with DMD (cases) and boys without DMD (controls) who failed the developmental milestones at each age in the observed (YHC and Questionnaire) and imputed data (YHC) are shown in the appendix .
A total of 570 referrals to 45 different healthcare providers or pedagogical interventions were extracted from the YHC records with a mean result of 7.5 referrals per boy with DMD. We combined data when data were available from both the YHC records and the Questionnaire (Q). A high number of undiagnosed boys with DMD were already referred to physiotherapy (26% aged 0-0.99y and 39% aged 1-3.99y, speech-language therapist (17%), Ear-Nose-Throat (ENT)-specialist (16%, YHC data) and preschool educational intervention (9%, YHC data). Symptoms that appeared often in DMD boys were pseudohypertrophy of the calf muscles (43%), falling more frequently compared to peers (27%, YHC data), stiff gait (19%, YHC data), a younger appearance than his chronological age (which may be related to behaviour and/or growth) (11%, YHC data). Between 0-3.99y, three in four parents of boys with DMD (77%, Q data) had concerns about their child’s developmental delay, mainly concerning their motor skills (85% out of concerned parents). Between 0-3.99y, approximately one in ten undiagnosed boys with DMD (11%, Q data) required surgery and were exposed to inhalational agents during surgery.
Table 2 shows the results from the five age-dependent pooled logistic regression models after stepwise backward regression on the developmental milestones. The footnote of Table 3 provides a detailed description of each milestone. Independent predictors of DMD were failing for ‘pulls up to standing position’, ‘reacts to a verbal request’, and ‘sits in stable position without support’ at 12 months, ‘crawls abdomen off the floor’ at 15 months, ‘walks alone’ at 18 months, ‘walks well’ at 24 months, and ‘walks smoothly’ at 36 months. Milestones before the age of 12 months were not statistically significant after adjustment for the milestones at 12 months of age. In total, seven milestones were independent predictors of DMD. As these models (with different weighing factors and an exponential component) are not easy to use in daily practice, we simplified the weighing factors (with integer numbers and a linear instead of an exponential component) in the next step of the analysis using these seven milestones.
Table 3 shows the results of the most optimal weighting factors and diagnostic value for the independent predictors of DMD. A higher sum score increased PPV and specificity, but decreased sensitivity. With this tool and a cut-off of 3 for the sum score, approximately eight out of ten boys may be identified by their development between 12 and 36 months of age and seven out of ten boys between 12 and 24 months of age. Further analyses on patients by mutation type revealed that the detection rate of the tool with a cut-off of 3 for the sum score was 73% in patients with a deletion in DMD-gene ( n = 40), 73% with an insertion in DMD-gene ( n = 12), 64% with a small or other mutation ( n = 12) and 88% in patients for whom the type of mutation was unknown.
The main finding of our study was that a combination of developmental milestones (six gross motor activity and one communication) assessed at specific ages may be a useful tool for primary care to identify boys at increased risk of DMD. Our study shows that the tool has the potential to detect eight in ten boys with DMD between 12 and 36 month of age. A sum score of ≥ 3 according to the tool increases the initial a priori risk of DMD from 1 in 5,000 to approximately 1 in 268 boys. Other findings of our study are that undiagnosed boys often had symptoms (e.g. 43% had calf muscle pseudohypertrophy) and were referred to therapy (e.g. 59% for physical therapy).
Important factors when choosing values for sensitivity and specificity of the tool include the prevalence and severity of the disease, the consequences of not detecting the disease, the importance of early detection and avoiding needless parental concern. In the recommendations on developmental screening tests from the American Academy of Pediatrics, sensitivity and specificity levels of 70–80% are considered acceptable [ 24 ]. In our study we selected higher specificity levels, because a low prevalence in combination with a relatively low specificity results in a low PPV. Therefore, we decided to develop a risk assessment tool instead of a screening tool, because the majority of disorders with a low prevalence cannot easily be found with factors others than blood or gene tests. However, in the case of developmental delay, other disorders that impact development may also be included in the prevalence. In total, 0.16% of all children have a neuromuscular disorder [ 25 ] and 5% have some type of moderate to severe disability [ 26 ]. We have, therefore, selected a minimum specificity of 95%. For many of these children, further investigation of the developmental delay may be helpful, because our previous research showed that disorders that impact development cannot always be regarded as isolated disorders [ 17 , 27 ].
With the present system, many boys with DMD are detected later than desired. Implementation of this tool in the Netherlands may improve this. Our tool is constructed in such a way that it can be easily implemented in other health care systems. Several of the milestones in the short risk assessment tool (not able to walk at 18 months [ 5 , 18 , 19 ]) and further specifications (weakness, toe walking, abnormal or clumsy gait, frequent falls [ 12 , 18 , 19 ]) were also mentioned in the literature. More risk factors were previously found in other studies such as Gowers’ sign, difficulty climbing stairs [ 5 , 12 , 19 ], painful legs or joints [ 18 ], and the presence of non-motor delay such as delayed speech and language acquisition [ 12 , 13 , 18 , 19 ], poor cognition or behaviour problems [ 28 ]. Moreover, growth failure and obesity were reported more often in boys with DMD [ 29 ].
Taken all this information into account, we have several recommendations for the early detection of DMD.
Recommendations for practical use of the tool
The tool with the seven milestones (see Table 3 ) could be used by YHC professionals during day-to-day health assessments in the general population to flag children who require further action. Further investigation into the presence of symptoms for neuromuscular disorders or disabilities is needed.
Our study found that several symptoms were often reported. The following questions may, therefore, be relevant to investigate if the child (in this case a boy) has a sum score ≥ 3 according to the tool:
A family history of neuromuscular disease?
Any presence of DMD-specific symptoms (calf muscle pseudohypertrophy, stiffy gait, falls more frequently compared to peers, appears to be younger than his chronological age)?
Attend therapy for his motor and/or speech delay (physical, speech-language)? Visited an ENT-specialist?
Parental concerns about their child’s motor (and speech) delay?
Failures on other milestones (shown in the Appendix )?
Literature shows that other questions may also be relevant [ 5 , 12 , 18 , 19 , 28 , 29 , 30 , 31 , 32 ].
Increased head circumference, failure to thrive, overweight?
Difficulty with stair climbing?
Difficulty with running?
Inability to jump?
Decreased endurance?
Weakness of the proximal muscles (has to use their hands and arms to “walk” up their own body from a squatting position: Gowers’ sign)?
Toe walking?
Inability to keep up with peers?
Painful legs or joints?
Cognitive delay?
Learning and attentional issues?
Behaviour issues?
Autism spectrum disorder?
We recommend YHC professionals to register information from these questions, as well as data from other health care providers involved with the child, in the electronic health records. When the investigation is complete, one may decide to wait and monitor the development closely or consider CK testing, because CK is extremely elevated (50- to 200-fold above normal levels [ 5 ]) in boys with DMD and it is a relatively cheap and fast test. Especially in the situation where there are concerns, either by the parents or by one or more health care providers, we recommend a CK test. High levels of CK prompts referral to a pediatric neurologist, with input from a geneticist or genetic counsellor, to prevent diagnostic delay [ 5 ]. However, even with normal levels of CK, referral to a pediatric neurologist or other specialists may be necessary to reduce diagnostic delay in other neuromuscular disorders or some other type of developmental disability such as cerebral palsy, non-syndromic intellectual developmental disorder and autism. In view of the current incurability, the progressive course and the always fatal outcome of DMD, the most important therapeutic task in the early course of DMD is the medical, psychosocial and genetic counselling of families.
The tool should not be promoted as a screening tool for DMD, due to its relatively low positive predictive value, the potential for yielding abnormal results for other conditions besides DMD, and to avoid stress among families. It is important to investigate the adoption and acceptability of the tool before proceeding with implementation. One of the aspects that requires attention is the naming of the tool without emphasizing the condition DMD.
Compared to newborn screening (NBS) where CK levels are evaluated in the first screen, an advantage of this approach would be that a smaller group undergoes testing, and avoids the potential problem of NBS of elevated CK levels being elevated in newborns due to birth trauma [ 33 ]. A disadvantage is that approximately two in ten boys with DMD cannot be identified by the tool, and the tool will lead to false-positive results, although some of these may have another disorder that impact development. Moreover, our study shows that approximately one in ten undiagnosed boys with DMD had an increased risk of detrimental consequences due to the exposure to inhalational agents during surgery before they were four years of age. To prevent such risks, and given advances in diagnostics and promising therapeutic approaches, the discussion on inclusion of DMD in NBS should be continued.
Strengths and limitations
A strength of our study is that milestones were determined during real-world regular day-to-day health assessments in the general population. This increases the generalizability of our tool for use in daily practice. Furthermore, YHC professionals were mainly blinded for the diagnosis because most of the data were registered before the diagnosis of DMD was made. A limitation is that the number of observations varied between milestones and visits. Although YHC in the Netherlands is highly standardized, parents do not always attend all visits when their child is between 1 and 36 months of age. Also, health care professionals do not always register all milestones during a visit, partly, we believe, attributable to time pressure in YHC practice. However, approximately the same attendance rates and the same registration method occurred for both the DMD and the control groups. Moreover, we applied multiple imputation to adjust for missing values. Another limitation is that we were unable to explore the likelihood of referral within the current YHC setting due to the potential for concerns to arise from various sources, including YHC, parents/caregivers, childcare facilities, general practitioners, or others.
Our short risk assessment tool, which was based on combinations of developmental milestones at specific ages, combined with symptoms and referrals to therapy could be helpful in identifying boys with DMD. This tool is quick and easy to implement. A major advantage would be that it could enable the majority of boys (79%) with DMD to be identified between 12 and 36 months of age, and 71% between 12 and 24 months. We expect that other neuromuscular disorders and disabilities can also be found with this tool. With preparation and investigation into its adoption and acceptability, this tool can be integrated into the workflow of primary care practices [ 34 ]. Using a validated risk assessment tool at regular, repeated intervals, in addition to physician surveillance at well-child visits, may improve early detection [ 30 ]. We recommend more research with new datasets to validate the tool.
Data availability
It is not possible to share research data publicly, because individual privacy could be compromised.
Sices L, Feudtner C, McLaughlin J, Drotar D, Williams M. How do primary care physicians identify young children with developmental delays? A national survey. J Dev Behav Pediatr. 2003;24:409–17.
Article PubMed Google Scholar
Fernald LCH, Prado E, Kariger P, Raikes A. A Toolkit for Measuring Early Childhood Development in Low and Middle-Income Countries. Washington, DC: World Bank; 2017. https://openknowledge.worldbank.org/handle/10986/29000 . License: CC BY 3.0 IGO. © World Bank.
Book Google Scholar
Ryder S, Leadley RM, Armstrong N, Westwood M, de Kock S, Butt T, et al. The burden, epidemiology, costs and treatment for Duchenne muscular dystrophy: an evidence review. Orphanet J Rare Dis. 2017;12:79.
Article CAS PubMed PubMed Central Google Scholar
Ellis JA, Vroom E, Muntoni F. 195th ENMC International Workshop: newborn screening for Duchenne muscular dystrophy 14–16th December, 2012, Naarden, The Netherlands. Neuromuscul Disord 2013;23:682–9.
Ciafaloni E, Fox DJ, Pandya S, Westfield CP, Puzhankara S, Romitti PA, et al. Delayed diagnosis in Duchenne muscular dystrophy: data from the muscular dystrophy surveillance, Tracking, and Research Network (MD STARnet). J Pediatr. 2009;155:380–5.
Article PubMed PubMed Central Google Scholar
van den Bergen JC, Ginjaar HB, van Essen AJ, Pangalila R, de Groot IJ, Wijkstra PJ, et al. Forty-five years of Duchenne muscular dystrophy in the Netherlands. J Neuromuscul Dis. 2014;1:99–109.
van Ruiten HJA, Straub V, Bushby K, Guglieri M. Improving recognition of Duchenne muscular dystrophy: a retrospective case note review. Arch Dis Child. 2014;99:1074–7.
Bushby K, Finkel R, Wong B, Barohn R, Campbell C, Comi GP, et al. Ataluren treatment of patients with nonsense mutation dystrophinopathy. Muscle Nerve. 2014;50:477–87.
Article CAS PubMed Google Scholar
European Medicines Agency. Translarna [Internet]. https://www.ema.europa.eu/en/medicines/human/EPAR/translarna . Accessed 15 December 2023.
Birnkrant DJ, Panitch HB, Benditt JO, Boitano LJ, Carter ER, Cwik VA, et al. American College of Chest Physicians consensus statement on the respiratory and related management of patients with Duchenne muscular dystrophy undergoing anesthesia or sedation. Chest. 2007;132:1977–86.
Wong SH, McClaren BJ, Dalton Archibald A, Weeks A, Langmaid T, Ryan MM, et al. A mixed methods study of age at diagnosis and diagnostic odyssey for Duchenne muscular dystrophy. Eur J Hum Genet. 2015;23:1294–300.
Parsons EP, Clarke AJ, Bradley DM. Developmental progress in Duchenne muscular dystrophy: lessons for earlier detection. Eur J Paediatr Neurol. 2004;8:145–53.
Cyrulnik SE, Fee RJ, De Vivo DC, Goldstein E, Hinton VJ. Delayed developmental language milestones in children with Duchenne’s muscular dystrophy. J Pediatr. 2007;150:474–8.
Connolly AM, Florence JM, Cradock MM, Malkus EC, Schierbecker JR, Siener CA, et al. Motor and cognitive assessment of infants and young boys with Duchenne muscular dystrophy: results from the muscular dystrophy Association DMD Clinical Research Network. Neuromuscul Disord. 2013;23:529–39.
Mirski KT, Crawford TO. Motor and cognitive delay in Duchenne muscular dystrophy: implication for early diagnosis. J Pediatr. 2014;165:1008–10.
Pane M, Scalise R, Berardinelli A, D’Angelo G, Ricotti V, Alfieri P, et al. Early neurodevelopmental assessment in Duchenne muscular dystrophy. Neuromuscul Disord. 2013;23:451–5.
van Dommelen P, van Dijk O, Wilde JA, Verkerk PH. Early developmental milestones in Duchenne muscular dystrophy. Dev Med Child Neurol. 2020;62:1198–204.
Mohamed K, Appleton R, Nicolaides P. Delayed diagnosis of Duchenne muscular dystrophy. Eur J Paediatr Neurol. 2000;4:219–23.
Noritz GH, Murphy NA, Neuromotor Screening Expert Panel. Motor delays: early identification and evaluation. Pediatrics. 2013;131:e2016–27.
Statistics Netherlands (CBS). Parents give child health centres a 7 out of 10 [Internet]. https://www.cbs.nl/en-gb/news/2014/44/parents-give-child-health-centres-a-7-out-of-10 . Accessed 15 December 2023.
Vanneste YTM, Lanting CI, Detmar SB. The preventive child and Youth Healthcare Service in the Netherlands: the state of the Art and challenges ahead. Int J Environ Res Public Health. 2022;19(14).
de Laurent MS, Brouwers-de Jong EA, Bijlsma-Schlösser JFM, Bulk-Bunschoten AMW, Pauwels JH, Steinbuch-Linstra I. Ontwikkelingsonderzoek in De Jeugdgezondheidszorg. Het Van Wiechenonderzoek–De Baecke-Fassaert Motoriektest. Assen: Van Gorcum; 2005.
Google Scholar
Van Buuren S, Chapman. & Hall/CRC Interdisciplinary Statistics) 2nd Edition. Chapman & Hall/CRC Interdisciplinary Statistics.
Council on Children With Disabilities, Section on Developmental Behavioral Pediatrics, Bright Futures Steering Committee MHI for CWSNPAC. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006;118:405–20.
Article Google Scholar
Deenen JC, Horlings CG, Verschuuren JJ, Verbeek AL, van Engelen BG. The Epidemiology of Neuromuscular disorders: a comprehensive overview of the literature. J Neuromuscul Dis. 2015;2:73–85.
Global Research on Developmental Disabilities Collaborators. Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Glob Health. 2018;6:e1100–21.
Diepeveen FB, van Dommelen P, Oudesluys-Murphy AM, Verkerk PH. Children with specific language impairment are more likely to reach motor milestones late. Child Care Health Dev. 2018;44:857–62.
Learning and Behavior in Duchenne Muscular. Dystrophy for parents and educators [Internet]. https://www.parentprojectmd.org/wp-content/uploads/2018/04/EdMatters_LearningAndBehavior.pdf . Accessed 15 December 2023.
Weber DR, Hadjiyannakis S, McMillan HJ, Noritz G, Ward LM. Obesity and Endocrine Management of the patient with Duchenne muscular dystrophy. Pediatrics. 2018;142(Suppl 2):S43–52.
D’Amico A, Catteruccia M, Baranello G, Politano L, Govoni A, Previtali SC, et al. Diagnosis of Duchenne Muscular Dystrophy in Italy in the last decade: critical issues and areas for improvements. Neuromuscul Disord. 2017;27(5):447–51.
Birnkrant DJ, Bushby K, Bann CM, Apkon SD, Blackwell A, Brumbaugh D, DMD Care Considerations Working Group, et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol. 2018;17(3):251–67.
Mercuri E, Pane M, Cicala G, Brogna C, Ciafaloni E. Detecting early signs in Duchenne muscular dystrophy: comprehensive review and diagnostic implications. Front Pediatr. 2023;11:1276144.
Mendell JR, Shilling C, Leslie ND, Flanigan KM, al-Dahhak R, Gastier-Foster J, et al. Evidence-based path to newborn screening for Duchenne muscular dystrophy. Ann Neurol. 2012;71:304–13.
Vitrikas K, Savard D, Bucaj M. Developmental Delay: when and how to screen. Am Fam Physician. 2017;96:36–43.
PubMed Google Scholar
Download references
Acknowledgements
This research project was funded by the Duchenne Parent Project. We thank the Duchenne Parent Project and Spierziekten Nederland for their help with inclusion of the participants. We thank Ieke Ginjaar for her help with retrieving the age at diagnosis for the boys with DMD. We thank our sounding board with the following members: Jos Hendriksen, Nathalie Goemans, Selma van der Harst, the parents of boys with DMD. We thank Bettie Carmiggelt for her help with the questionnaire. We thank the YHC of The Hague for providing their data for this study. We thank all YHC workers who retrieved the health records from our boys with DMD. We thank all parents and boys with DMD who participated in our study.
Columns 1–3, 6–7 from Table 1 and columns 1–5, 9–11 from the Appendix are adapted from ‘van Dommelen P, van Dijk O, Wilde JA, Verkerk PH. Early developmental milestones in Duchenne muscular dystrophy. Dev Med Child Neurol 2020;62: 1198–1204’.
This research project was funded by the Duchenne Parent Project.
Author information
Authors and affiliations.
Department of Child Health, The Netherlands Organization for Applied Scientific Research TNO, Leiden, The Netherlands
Paula van Dommelen & Paul H. Verkerk
Department of Public Health and Primary Care, Leiden University Medical Center, Leiden, The Netherlands
Oisín van Dijk & Jeroen A. de Wilde
You can also search for this author in PubMed Google Scholar
Contributions
PvD: substantial contributions to research design, the acquisition, analysis and interpretation of data, drafting the paper, approval of the submitted and final version. She had complete access to the study data that support the publication. OvD: substantial contributions to analysis and interpretation of data, drafting the paper, approval of the submitted and final version. He had complete access to the study data that support the publication. JAdW: substantial contributions to interpretation of data, revising the paper critically, approval of the submitted and final version. PHV: substantial contributions to research design, the acquisition, and interpretation of data, revising the paper critically, approval of the submitted and final version. He had complete access to the study data that support the publication.
Corresponding author
Correspondence to Paula van Dommelen .
Ethics declarations
Ethics approval and consent to participate.
This research protocol (registration number: 2017-001) was submitted to the Nederlandse Organisatie voor toegepast-natuurwetenschappelijk onderzoek (TNO) Institutional Review Board (IRB). The IRB approved this non-interventional research proposal. In its deliberations, the IRB considered the research design and privacy aspects, in addition to the ethical aspects and the burden and the risks to the research participants. If parents and/or children (depending on the age of the child) agreed to participate, they were asked to provide written consent for collection of their health records, their date of diagnosis, and for publication of the results. We obtained permission from the Youth Health Care of The Hague to extract anonymous data from the electronic health records of all children born between 2011 and 2013 (control group).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
van Dommelen, P., van Dijk, O., de Wilde, J.A. et al. Short developmental milestone risk assessment tool to identify Duchenne muscular dystrophy in primary care. Orphanet J Rare Dis 19 , 192 (2024). https://doi.org/10.1186/s13023-024-03208-8
Download citation
Received : 22 December 2023
Accepted : 05 May 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s13023-024-03208-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pediatrics; neuromuscular disorder
- Child Development
- Developmental Delay
- Early Childhood Development
- Motor skills
Orphanet Journal of Rare Diseases
ISSN: 1750-1172
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

COMMENTS
Case Study: High risk indicators. Jenny is 35 and lives with her husband and 9-year-old son. Though employed as a welfare officer, she has felt unable to work for over three months. A new manager joined her team six months ago, and has criticised her work performance on several occasions. Jenny has felt low since her mother died a year ago, to ...
Dr. SooJeong Youn: This case highlights the importance of attending to the intricate, multilevel, systemic factors that affect the mental health experience and clinical presentation of patients ...
Case vignette. In academic and practice guidance the notion of risk is often examined in a way that is somewhat removed from real-world clinical practice (Nathan Reference Nathan, Gabbay and Boyle 2021b).Key points raised in this article will be examined with reference to practice by using a case vignette that involves possible future harm.
Introduction. Mental health risk-assessments are a core aspect of nursing in mental health settings, and of invaluable assistance in the identification and mitigation (or prevention) of potential harm by a patient to self or others (Hautamäki, Citation 2018; Higgins et al., Citation 2016).This key decision-making process usually takes place in response to perceived indicators of risk, a ...
A guide for GPs. Background. Risk assessment of patients in general practice is a challenging area of clinical practice. Competing interests of managing patient wishes, consideration of duty to warn others and invoking the Mental Health Act while practising in a medicolegally accountable manner can be difficult. Objective.
In both forensic and general mental health care, a treatment or case management plan forms the transition between the assessment/diagnostic phase and the treatment phase. ... (2014). The HCR-20 Version 3: A case study in risk formulation. International ... Peterson-Badali, M., Skilling, T., & Haqanee, Z. (2015). Examining implementation of risk ...
employees whose work performance is affected by mental health symptoms.21 See the Case Study Reference Table (p.14) for a listing of case studies developed by other organizations that provide more information ... and multiple countries have mandated psychosocial risk assessment and prevention.17, 24-30 Several areas have been identified through ...
The aim of this integrative review was to review the literature on risk assessment in mental health practice to promote evidence-based care. Electronic databases were searched for articles available in English and published from 2013 to 2019. The findings from 12 articles evaluated the evidence for risk assessment tools utilised and discussed ...
Background Risk assessment and risk management are fundamental processes in the delivery of safe and effective mental health care, yet studies have shown that service users are often not directly involved or are unaware that an assessment has taken place. Shared decision-making in mental health systems is supported by research and advocated in policy. This systematic review (PROSPERO ...
Assessment processes need to be consistent across mental health services and include adequate training on how to assess, formulate, and manage suicide risk. An emphasis on patient and carer involvement is needed. In line with national guidance, risk assessment should not be seen as a way to predict future behaviour and should not be used as a means of allocating treatment.
Distribution of Risk and Need in the Mental Health Court Sample Risk Distribution: Overall, 27% of participants were re-arrested at one year, and 42% were re-arrested at two years. The COMPAS classified two-thirds (67%) of the sample as low risk for re-arrest, 20% as medium risk, and relatively few (13%) as high risk. On the
Introduction Understanding nurses' attitudes towards risk assessment could inform education and practice improvements. Aim/Question To explore mental health nurses' attitudes towards risk assessment. Method An integrative systematic review (PROSPERO: CRD42023398287). Multiple databases (PubMed, CINAHL, MEDLINE, EMBASE and PsycINFO) were searched for primary studies of mental health nurses ...
Scope of Mental Health Promotion and Prevention in the Current Situation. Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses (18, 36-42).There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe ...
Introduction. Aggression and violence in psychiatric wards remain a major problem [1, 2].The use of risk assessment tools in inpatient psychiatric settings may help to manage this problem [3, 4].Risk assessment tools are developed to monitor the possibility of aggressive behaviour in individual patients and allow the staff to anticipate problems and make decisions to adjust management ...
One study compared mental health nurse assessment with psychiatrist assessment (Murphy 2011). Please note that the included studies do not meet the inclusion criteria, in the sense that there were no studies that compared risk assessment (RA) plus risk formulation with RA alone or no RA, and no studies comparing RA alone with no RA.
A scientific understanding of clinical risk management (CRM) in mental health care is essential for building safer health systems and for improving patient safety. While evidence on patient safety and CRM in physical health care has increased, there is limited research on these issues in mental health care. This qualitative study provides an overview of the most important clinical risks in ...
Method This paper reports on a case study inquiry, using interviews with mental health professionals and observations in an acute ward and an assertive outreach team. Results Risk governed the practice of mental health professionals to such an extent it defined how service users were understood and treated.
Mental health risk-assessments are an important part of nursing in mental health settings, to protect patients or others from harm. Even so, nurses often have difficulty identifying patients posing a ... Using CCT, the aim of this study was to explore risk assess-ment of patients by nurses working in mental health settings. Table 1. CCt modes ...
Use of case vignettes in suicide risk assessment. Suicide and Life-Threatening Behavior, 20, 65-84. The assessment of suicide risk is a complicated process. The following vignettes are provided to promote discussion of suicide risk factors, assessment procedures, and intervention strategies. The "answers" are not provided, rather students ...
Previous research on risk assessments in mental health care has focused on the predictive validity of risk assessment ... Urheim, R., Rypdal, K., Palmstierna, T., & Mykletun, A. (2011). Patient autonomy versus risk management: A case study of change in a high security forensic psychiatric ward. International Journal of Forensic Mental Health ...
Kessler, R. C. et al. Predicting suicides after outpatient mental health visits in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Mol. Psychiatry 22 , 544-551 (2017).
For guidance on common mental health problems, see our guidelines on: Depression in adults. Depression in adults with a chronic physical health problem. Depression in children and young people. Generalised anxiety disorder and panic disorder in adults. Obsessive-compulsive disorder and body dysmorphic disorder. Social anxiety disorder.
Nursing assessment of mental health issues in the general clinical environment: A descriptive study J Adv Nurs. 2024 May 13. doi: 10.1111 ... assessing risk factors that required deeper conversations with patients, including psychiatric history, was lacking. The survey highlighted fewer than half of the respondents (46%, n = 10) felt competent ...
This study aimed to assess the feasibility and acceptability of administering the validated Case-finding Health Assessment Tool (CHAT) in Canadian family practice. The CHAT is a short, self-administered tool for lifestyle and mental health assessment of adult patients, which can be completed in the waiting room before the physician appointment.
Racism is a known social determinant of health which affects the mental health and well-being of families, particularly pregnant and postpartum individuals and their children.As we have continued to wrestle with the COVID-19 pandemic, there have been increased efforts to better understand the impacts of this global event with racialized ...
Some people with Down syndrome have other medical problems as well. Common health problems include: Congenital heart defects. Hearing loss. Obstructive sleep apnea. Down syndrome is the most common chromosomal condition diagnosed in the United States. Each year, about 5,700 babies born in the US have Down syndrome. 1
In order to achieve the goals of sustainable development, the integration of life cycle assessment (LCA) and health risk assessment (HRA) as complementary tools is an effective step towards comprehensive environmental management. As the need for electricity generation is growing increasingly, the integration of these tools can provide a broader perspective for decision-makers and policy-makers.
The long-awaited third edition of the HCR-20 violence risk assessment guide (Douglas, Hart, Webster, ... Caroline Logan Greater Manchester West Mental Health NHS Foundation Trust, Manchester, ... the process of risk formulation is described and illustrated with a case study—Paul. A brief report of the risk assessment, formulation and ...
Nitrate contamination has become an ecological and health issue in Quanzhou, a typical coastal city in Southeast China. Hydrogeological surveys reveal that NO3− is a major factor influencing the groundwater quality in Quanzhou City, Fujian Province, China. To protect public health, this study explored the geographical spatial distribution, contamination level, contamination sources, and ...
Data collection. Within the 4D-DMD study (Detection by Developmental Delay in Dutch boys with DMD) with a case-control design, data were collected from: (1) health records of boys with DMD; characteristics, referrals to secondary and tertiary care, educational interventions, clinical descriptions typical of DMD, and developmental scores; (2) questionnaires completed by parents of boys with DMD ...