
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What happens to your baby right after birth

What's a sunny-side up baby?

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Original Author(s): Minesh Mistry Last updated: 12th November 2018 Revisions: 7
- 1 Introduction
- 2 Preparation
- 3 General Inspection
- 4 Abdominal Inspection
- 5.1 Fundal Height
- 5.3 Presentation
- 5.4 Liquor Volume
- 5.5 Engagement
- 6 Fetal Auscultation
- 7 Completing the Examination
The obstetric examination is a type of abdominal examination performed in pregnancy.
It is unique in the fact that the clinician is simultaneously trying to assess the health of two individuals – the mother and the fetus.
In this article, we shall look at how to perform an obstetric examination in an OSCE-style setting.

Introduction
- Introduce yourself to the patient
- Wash your hands
- Explain to the patient what the examination involves and why it is necessary
- Obtain verbal consent
Preparation
- In the UK, this is performed at the booking appointment, and is not routinely recommended at subsequent visits
- Patient should have an empty bladder
- Cover above and below where appropriate
- Ask the patient to lie in the supine position with the head of the bed raised to 15 degrees
- Prepare your equipment: measuring tape, pinnard stethoscope or doppler transducer, ultrasound gel
General Inspection
- General wellbeing – at ease or distressed by physical pain.
- Hands – palpate the radial pulse.
- Head and neck – melasma, conjunctival pallor, jaundice, oedema.
- Legs and feet – calf swelling, oedema and varicose veins.
Abdominal Inspection
In the obstetric examination, inspect the abdomen for:
- Distension compatible with pregnancy
- Fetal movement (>24 weeks)
- Surgical scars – previous Caesarean section, laproscopic port scars
- Skin changes indicative of pregnancy – linea nigra (dark vertical line from umbilicus to the pubis), striae gravidarum (‘stretch marks’), striae albicans (old, silvery-white striae)
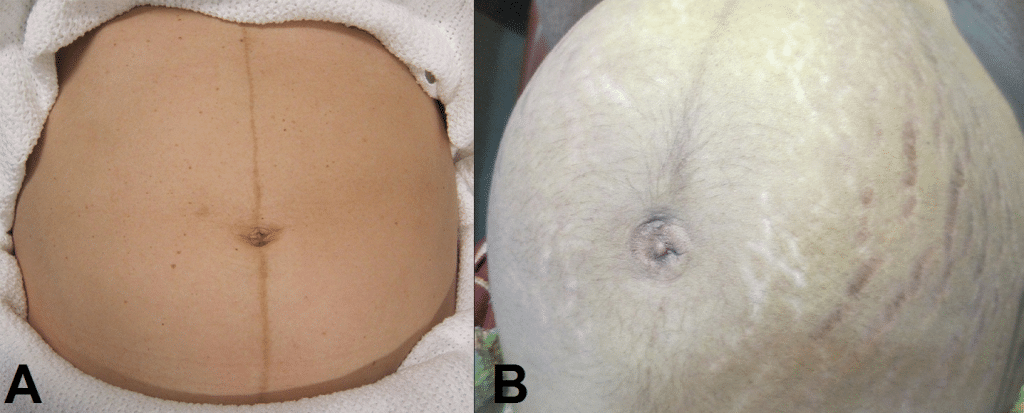
Fig 1 – Skin changes in pregnancy. A) Linea nigra. B) Striae gravidarum and albicans.
Ask the patient to comment on any tenderness and observe her facial and verbal responses throughout. Note any guarding.
Fundal Height
- Use the medial edge of the left hand to press down at the xiphisternum, working downwards to locate the fundus.
- Measure from here to the pubic symphysis in both cm and inches. Turn the measuring tape so that the numbers face the abdomen (to avoid bias in your measurements).
- Uterus should be palpable after 12 weeks, near the umbilicus at 20 weeks and near the xiphisternum at 36 weeks (these measurements are often slightly different if the woman is tall or short).
- The distance should be similar to gestational age in weeks (+/- 2 cm).
- Facing the patient’s head, place hands on either side of the top of the uterus and gently apply pressure
- Move the hands and palpate down the abdomen
- One side will feel fuller and firmer – this is the back. Fetal limbs may be palpable on the opposing side
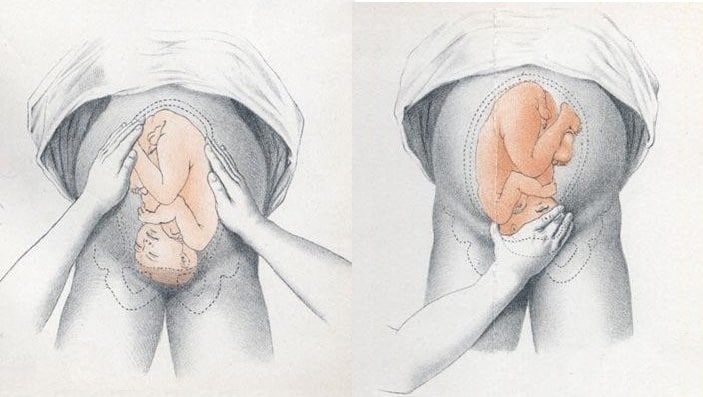
Fig 2 – Assessing fetal lie and presentation.
Presentation
- Palpate the lower uterus (below the umbilicus) to find the presenting part.
- Firm and round signifies cephalic, soft and/or non-round suggests breech. If breech presentation is suspected, the fetal head can be often be palpated in the upper uterus.
- Ballot head by pushing it gently from one side to the other.
Liquor Volume
- Palpate and ballot fluid to approximate volume to determine if there is oligohydraminos/polyhydramnios
- When assessing the lie, only feeling fetal parts on deep palpation suggests large amounts of fluid
- Fetal engagement refers to whether the presenting part has entered the bony pelvis
- Note how much of the head is palpable – if the entire head is palpable, the fetus is unengaged.
- Engagement is measured in 1/5s
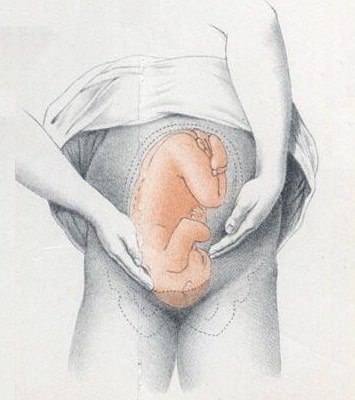
Fig 3 – Assessing fetal engagement.
Fetal Auscultation
- Hand-held Doppler machine >16 weeks (trying before this gestation often leads to anxiety if the heart cannot be auscultated).
- Pinard stethoscope over the anterior shoulder >28 weeks
- Feel the mother’s pulse at the same time
- Should be 110-160bpm (>24 weeks)
Completing the Examination
- Palpate the ankles for oedema and test for hyperreflexia (pre-eclampsia)
- Thank the patient and allow them to dress in private
- Summarise findings
- Blood pressure
- Urine dipstick
- Hands - palpate the radial pulse.
- Skin changes indicative of pregnancy - linea nigra (dark vertical line from umbilicus to the pubis), striae gravidarum ('stretch marks'), striae albicans (old, silvery-white striae)
- One side will feel fuller and firmer - this is the back. Fetal limbs may be palpable on the opposing side
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Leopold maneuvers.
Shervonne S. Superville ; Marco A. Siccardi .
Affiliations
Last Update: February 19, 2023 .
- Continuing Education Activity
The Leopold maneuvers are used to palpate the gravid uterus systematically. This method of abdominal palpation is of low cost, easy to perform, and non-invasive. It is used to determine the position, presentation, and engagement of the fetus in utero. This activity describes the four Leopold maneuvers and explains the method of systematic abdominal palpation used to assess fetal presentation and position in the third trimester of pregnancy.
- Describe the normal fetal presentation and position.
- Explain the four Leopold maneuvers.
- Summarize the clinical significance of abdominal palpation in the obstetric examination.
- Identify the importance of improving training in abdominal palpation to enhance the delivery of care for obstetric patients.
- Introduction
The Leopold maneuvers, named after the German obstetrician and gynecologist Christian Gerhard Leopold (1846–1911), are part of the physical examination of pregnant women. [1] [2] Four classical maneuvers are used to palpate the gravid uterus systematically. This method of abdominal palpation is of low cost, easy to perform, and non-invasive. It is used to determine the position, presentation, and engagement of the fetus in utero.
Fetal presentation refers to the fetal anatomic part proceeding first into the pelvic inlet. When the fetal head is approaching the pelvic inlet, it is referred to as a cephalic presentation. The commonest presentation is the vertex of the fetal head. Malpositions are abnormal positions of the vertex of the fetal head, using the occiput as the reference point, relative to the maternal pelvis. Malpresentations are all presentations of the fetus other than vertex, which includes the breech presentation, transverse and oblique lie. Spontaneous vaginal delivery is most common when a cephalic-presenting fetus is in the occiput anterior position. [3]
Malpresentation is estimated to occur in 5% of all deliveries and is an essential cause of the high cesarean delivery rate. [4] It is essential to detect non-cephalic presentations before the onset of labor to mitigate the maternal and neonatal risks associated with complicated vaginal delivery or cesarean section. Detection of malpresentation in late pregnancy allows for counseling on adequate care measures. The underutilized external cephalic version and intrapartum planning and consenting are choices that can be discussed. [5] [6] [7]
Accurate assessment of fetal presentation and position is crucial in guiding obstetric management. However, the accuracy of Leopold maneuvers varies depending on many factors, especially examiner experience. Therefore ultrasonographic examination remains the current gold standard investigation for ensuring the fetus is in the cephalic presentation during the third trimester of pregnancy. It is recommended for confirmation when any malpresentation is even slightly suspected. [8] [9]
- Indications
Palpation is the contact of the operator's fingers and hands with the body of the woman or child. It offers the possibility of collecting data on an area, structure, or function by touch. Uterine contractions, the size of the pregnant uterus, any uterine masses, and attitude, presentation, degree of commitment of the fetus, and any fetal-pelvic disproportions can be detected.
Abdominal palpation is accurate in identifying the presentation, mainly if performed by experienced healthcare professionals. If in doubt about the presentation part, obstetric ultrasound should be used to confirm the results of the palpation. Ultrasound can also rule out fetal abnormalities, low placenta, hyperextension of the baby's head, and the presence of the umbilical cord around the neck of the fetus. The palpation technique requires skill and delicacy. The entire palm and fingers are useful for detecting myometrial activity, fetal movements, or any neoformations (fibroids), or the degree of edema. Palpation can be superficial or deep (the superficial one must always precede the deep one since the latter can cause pain); avoid having long nails because they can cause discomfort or injury.
From a psychological point of view, palpation is to be considered a form of analog communication between the midwife and the woman. Therefore through this technique, the operator can transmit the feelings they have towards the patient.
- Contraindications
While the benefits of abdominal palpation are challenging to quantify, the risks have not been identified. Evaluation of presentation by abdominal palpation before 36 weeks is not always accurate. Routine evaluation of the presentation with abdominal palpation should not be offered before 36 weeks, due to any inaccuracies and inconvenience to the woman. The fetal presentation should be evaluated with the abdominal palpation at 36 weeks or later when the presentation can affect plans for childbirth.
Leopold maneuvers are complicated maneuvers to perform on obese women and women who have polyhydramnios. Palpation can sometimes be uncomfortable for the patient if no precautions are taken to ensure that she is well-positioned and relaxed.
- Preparation
The aim of Leopold maneuvers is to determine the fetal presentation and position by systematically palpating the gravid abdomen. The initial steps are described below:
- Explain the steps of the examination to the patient as this reduces anxiety and enhances cooperation
- Obtain consent
- The patient should be advised to void as an empty bladder promotes comfort and allows for more productive examination, and the distended bladder can obscure fetal contour
- Provision of privacy
- Prepare the equipment, such as measuring tape, Pinard stethoscope or Doppler transducer, and ultrasound gel
- Position the patient supine with the head of the bed raised to 15 degrees, and a small pillow or rolled towel placed on her right side
- Adequate exposure of the gravid abdomen from the xiphisternum to the pubic symphysis
- Inspect the gravid abdomen
- Technique or Treatment
The First Maneuver
The first maneuver also called the fundal grip, assesses the uterine fundus to determine its height and which fetal pole—that is, cephalic or podalic—occupies the fundus. The uterine contour is outlined by the examiner, placing both of his or her hands on each upper quadrant of the patient's abdomen facing the maternal xiphoid cartilage. The ulnar border of each hand is in contact with the abdominal wall, and the opposite fingers are touching each other. Using the fingertips, the fundus is gently palpated to identify which fetal part is present in the upper pole (fundus) of the uterus. The breach gives the sensation of a large, nodular mass, and its surface is uneven, non-ballotable, and not very mobile whereas the head feels hard and round with a smooth surface of uniform consistency, is very mobile and ballotable.
The first maneuver aims to determine the gestational age and the fetal lie.
Gestational age can be evaluated using fundal height or McDonald's rule. [1] The uterine fundus reaches:
- The public symphysis at the 12th week
- A point midway between the pubic symphysis and the transverse and the transverse umbilical plane at the 16th week
- The transverse umbilical plane at the 20th week
- Having crossed this line, it is assumed each transverse finger breath corresponds to two weeks
The Second Maneuver
The second maneuver, sometimes called the umbilical grip, involves palpation of the lateral uterine surfaces. Still facing the maternal xiphoid cartilage, both hands slide down from the uterine fundus towards the lateral uterine walls. The clinician's hands are placed flat and parallel to each other along the abdominal wall at the level of the umbilicus. It allows establishing if the fetus is in a longitudinal, transverse, or oblique situation, and to determine the position of the back and small parts.The operator places the two flat hands sideways to the uterus and tries to bring them closer to the midline. In the approach maneuvers, the operator's hands are one on the back of the fetus and one on the small parts, which give different tactile sensations.The approach is possible when the fetus is in a longitudinal position regardless of the type of presentation, while it is not possible when the situation is transverse or oblique. Furthermore, it is possible to understand from which side the fetal back is located.
If the identification of the fetal back proves to be difficult, the provider can perform the following maneuvers. A simple adjustment involves alternating two hand palpation of lateral uterine surfaces. By placing the right hand steady on one side of the abdomen while using the palm of the left hand, the right side of the gravid uterus is palpated gently. This is then repeated using the opposite side. Otherwise, the Budin maneuver, named after French obstetrician and gynecologist Pierre-Constant Budin 1846–1907, can be performed for the precise determination of the position of the fetal back. [2] The uterine fundus is pressed with force using one hand, which accentuates the curvature of the fetal back, allowing for easier palpation with the other hand. The fetal heart can be auscultated at this time, which can also provide information on fetal orientation. The heart is well perceived when the stethoscope or the doppler transducer is placed on the back of the fetus.
The Third Maneuver
The third maneuver was modified by Karel Pawlík (1849–1914), a Czech gynecologist and obstetrician, and is referred to as the Pawlik grips. This maneuver aids in the confirmation of fetal presentation.
The first Pawlík grip, sometimes called the first pelvic grip, helps to define which presenting part of the fetus is situated in hypogastrium. Using the thumb and fingers of the right hand close above the pubic symphysis, the presenting part is grasped at the lower portion of the abdomen and draws the thumb and finger near to clasp the lower uterine segment including its contents.
In the second Pawlík grip, the clinician carries on by sliding the hand upward to determine the cervical groove: if the mass moves, the presenting part is not engaged. Then lateral movements and ballottement are performed. The differentiation between head and breech is made as in the first maneuver. This maneuver also allows for an assessment of the fetal weight and the volume of amniotic fluid.
The Fourth Maneuver
This fourth maneuver resembles the first maneuver; however, the examiner faces towards the maternal pelvis. This maneuver involves the examiner placing the palms of both hands on either side of the lower abdomen, with the tips of the fingers facing downward toward the pelvic inlet. The fingertips of each hand are used to apply deep pressure from the outside to the inside and in a craniocaudal direction along the lower contour of the uterus towards the birth canal. It is possible to identify the characteristics of the part presented and confirm the findings detected with the third Leopold maneuver. The fingers of both hands move gently along the sides of the uterus towards the pubis. The side where there is resistance to the descent of the fingers towards the pubis is larger is where the forehead is located. If the head of the fetus is well flexed, it should be on the opposite side from the back of the fetus. If the head of the fetus is extended, however, the occiput is perceived and is on the same side of the spine. It is possible to evaluate the degree of descent of the presented part and to realize if there are gross disproportions between this and the pelvic inlet.
This maneuver identifies which presenting part is in the lower uterine pole. To perceive how much of the cephalic extremity, which we recognized to be at the lower pole, descends into the birth canal: if it is entirely external, then it has not confronted itself, if it is confronting itself or if it has ultimately descended. The fingers travel the upper contour of the cephalic end, around the neck of the fetus.
Completing the fourth maneuver with the so-called "fifth maneuver" of Leopold, or maneuver of Zagenmeister, also can allow the approximate distance between the presenting part and the maternal pelvis. In the cephalic presentation, the hand is placed flat on the pubic symphysis, and the palpation could delineate the fetal head portion that can be reached above the pelvic inlet. Using the rule of fifths, the distance between the base and vertex of the fetal head is divided into five equal parts. Each fifth corresponding to 2 cm or approximately one transverse fingerbreadth. If the fetal head accommodates two fingerbreadths above the pelvic brim, it is said to be engaged.
- Complications
A breech presentation occurs when the presenting part is either the buttocks and/or the feet. On examination, the head is felt in the upper uterine pole and the breech in the pelvic cavity. The fetal heart tones are auscultated higher than anticipated with a vertex presentation.
When the longest axis of the fetus is oriented transversely, the presenting part is typically the shoulder. In the transverse lie on palpation, neither the head nor the buttocks can be palpated in the lower uterine pole inlet, and the fetal head can be felt in the flank.
Occiput posterior position occurs when the fetal occiput is at or posterior to the sacroiliac joint. On examination, there is a lower abdomen flattened, fetal limbs are palpable anteriorly, and the fetal heart tones may be auscultated in the flank.
Brow presentation occurs with some extension of the fetal head. On palpation, the fetal occiput is higher than the sinciput, and more than half the fetal head is felt above the symphysis pubis.
Face presentation results from hyperextension of the fetal head. On palpation, the fold of the neck is felt as a deep indentation between the occiput and the back; however, in face presentation, this depression is limited.
- Clinical Significance
Few studies have compared the gold standard ultrasonography with clinical examination to detect non-cephalic presentation in the third trimester of pregnancy. These investigators found that abdominal palpation fails to detect a significant percentage of mal-presenting fetuses. [3]
Clinical examination was relatively sensitive in multiparous women and those with lower body mass indices. The specificity of clinical examination increased significantly as gestational age increased, and body mass index decreased. When abdominal palpation was evaluated as a screening tool for identifying malpresentation, it was found that false-positive diagnoses were a more frequent error because of the low prevalence of malpresentation in low-risk populations. [4]
Leopold maneuvers have been reported to be difficult in obese pregnant women and pregnancies complicated with polyhydramnios, fibroids, or anterior placental location. In clinical practice, the use of repeated procedures by a second examiner, pelvic examination, and rescheduling a return visit with a sequential abdominal examination can serve to improve the accuracy of abdominal palpation findings.
Leopold maneuvers can help mothers to perceive and visualize fetuses. Thus abdominal palpations can develop the maternal-fetal relationship, which plays an important role in a child's psychological, cognitive, and social development. [5] [6] [7]
- Enhancing Healthcare Team Outcomes
All healthcare providers should be competent with the methods to perform abdominal palpation of a gravid uterus and the significance of the findings. The findings observed should be documented and can be used to guide further obstetric management. Identifying pregnancies complicated by malpresentation and referral to appropriate facilities may lead to improved outcomes for both neonate and mother. [8]
Offering an external cephalic version (ECV) for breech presentation can contribute to the safe lowering of the primary cesarean delivery rate. [9] Training for existing or new staff who are moving to midwifery-obstetric care is necessary as experienced clinicians can be effective in using abdominal palpation as a screening tool for fetal malpresentation, particularly in settings where ultrasound may not be readily available. [4]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Leopold Maneuvers (A) , First Maneuver (B) Second Maneuver (C) Third Maneuver (D) Fourth Maneuver Illustrated by Junior Maloney
Disclosure: Shervonne Superville declares no relevant financial relationships with ineligible companies.
Disclosure: Marco Siccardi declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Superville SS, Siccardi MA. Leopold Maneuvers. [Updated 2023 Feb 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Stages of Labor. [StatPearls. 2024] Stages of Labor. Hutchison J, Mahdy H, Hutchison J. StatPearls. 2024 Jan
- Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. [Am J Obstet Gynecol MFM. 2020] Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. Bellussi F, Livi A, Cataneo I, Salsi G, Lenzi J, Pilu G. Am J Obstet Gynecol MFM. 2020 Nov; 2(4):100217. Epub 2020 Aug 18.
- Value of routine ultrasound examination at 35-37 weeks' gestation in diagnosis of non-cephalic presentation. [Ultrasound Obstet Gynecol. 2020] Value of routine ultrasound examination at 35-37 weeks' gestation in diagnosis of non-cephalic presentation. De Castro H, Ciobanu A, Formuso C, Akolekar R, Nicolaides KH. Ultrasound Obstet Gynecol. 2020 Feb; 55(2):248-256.
- Review Intrapartum ultrasound for the diagnosis of cephalic malpositions and malpresentations. [Am J Obstet Gynecol MFM. 2021] Review Intrapartum ultrasound for the diagnosis of cephalic malpositions and malpresentations. Gimovsky AC. Am J Obstet Gynecol MFM. 2021 Nov; 3(6S):100438. Epub 2021 Jul 22.
- Review Sonographic evaluation of the fetal head position and attitude during labor. [Am J Obstet Gynecol. 2022] Review Sonographic evaluation of the fetal head position and attitude during labor. Ghi T, Dall'Asta A. Am J Obstet Gynecol. 2022 Jul 6; . Epub 2022 Jul 6.
Recent Activity
- Leopold Maneuvers - StatPearls Leopold Maneuvers - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- MSD careers
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

Young Sheldon's Best Georgie & Mandy Episodes, Ranked
The following contains spoilers for Young Sheldon Season 7.
Although Young Sheldon ended on the tragic note of George Cooper's death , at least one couple made it out alive: Georgie Cooper and Mandy McAllister. The couple met in Season 5 and, after an unexpected pregnancy, got married in the final season of the series. The controversial nature of their age-inappropriate relationship didn't knock them down, however, as they're leading their own spinoff called Georgie & Mandy's First Marriage . Georgie and Mandy had their ups and downs throughout Young Sheldon , but in the end, they put away their differences to give the best life possible to their daughter CeeCee.
Their relationship changed the entire dynamic of Young Sheldon , so much so that the series temporarily put its titular character on the backburner. Georgie and Mandy's relationship quarrels came first as the Cooper and McAllister families melded, and family members had to deal with the societal fallout of the relationship. Before watching Georgie and Mandy's spinoff , fans will need to catch up with how they came to be Medford, Texas' newest it-couple. The best episodes are the ones where Georgie and Mandy hit big milestones and worked together as a couple, despite the backlash of others.
Mandy Meets George and Mary for the First Time
Season 5, episode 19, "a god-fearin' baptist and a hot trophy husband", young sheldon seasons 7, episodes 13 & 14 review: the two-part finale closes this chapter with a big bang.
The fact that Georgie got a woman pregnant shouldn't have been a surprise to the Cooper family. They always knew that Georgie would slip up and cause a teen pregnancy. But what disappointed his mother, Mary, the most was that she didn't even know who the girl was, or in this case, the 29-year-old woman.
In this episode, Georgie realizes he has a lot of growing up to do as he tells his parents of the pregnancy and introduces Mandy to them. Being a kid himself, he thinks it'll be a breeze to marry Mandy to be a good Christian. But to his surprise, Mandy is much more progressive and isn't down to marry a 17-year-old just because of religious beliefs.
Georgie and Mandy Disagree Over Mandy's New Venture
Season 6, episode 19, "a new weather girl and a stay-at-home coddler".
After giving birth to CeeCee, Mandy is ready to hit the job market again. But in 1990s Texas, Mandy faces some criticism for choosing a career and her child. "A New Weather Girl and a Stay-at-Home Coddler" tackles the outdated assumption that women must give up their careers to be a full-time mother, which even Georgie reinforces.
Resurrecting Mandy's career was long due for her, even before giving birth to CeeCee. Fortunately, Georgie comes to his senses and fully supports Mandy starting her career again by the end of the episode, reaffirming that he'll be a supportive partner for her. At least, until the unknown canon fallout that leads to Georgie and Mandy's divorce .
Georgie and Mandy Learn the Real Secret to a Healthy Relationship
Season 7, episode 10, "community service and the key to a happy marriage".
Georgie and Mandy didn't exactly grow up with a model of a healthy marriage. Georgie's parents -- Mary and George -- nearly caught themselves in infidelity scandals, while Mandy's parents -- Jim and Audrey -- have a toxic power dynamic. In this episode, the newlyweds learn that they need to form their own model for CeeCee.
Georgie takes Jim's advice to always agree with both Mandy and Audrey when the other isn't around to not cause conflicts. When Mandy catches on to Georgie's lies, they do what their parents could never dream of doing: talking it out. Who knew healthy communication could go a long way?
Mandy Reveals She's Pregnant With Georgie's Child
Season 5, episode 18, "babies, lies and a resplendent cannoli".
Mandy's pregnancy isn't the first scare Georgie has had. He once imagined a tedious life where he had to give up playing for Guns N' Roses when his ex-girlfriend thought she was pregnant. But with Mandy, it's the real deal. He quickly has to figure out how he's going to tell his parents the Cooper family is adding a new member .
Georgie consults with Connie's boyfriend, Dale, about how he should handle the situation. All Georgie can imagine are the worst-case scenarios of how George would react, like tearing up Dale's store. After witnessing Missy's failed attempt at babysitting, Georgie realizes he has to come clean to his dad.
Mandy Proposes After a Couple's Getaway
Season 6, episode 21, "a romantic getaway and a germanic meat-based diet".
Since getting Mandy pregnant and having CeeCee, Georgie has been begging Mandy to marry him. But Mandy was never thrilled about the age difference and the fact that Georgie is too immature for her. But nearing the end of Season 6, Mandy realizes that Georgie has put his teenage years behind him for the sake of Mandy and CeeCee.
The couple go on a romantic getaway to have a moment for themselves, but the entire affair is incredibly awkward. Georgie is receiving mixed messages from Mandy and thinks he's being tricked by her. When Mandy shockingly proposes to Georgie , he realizes that all his grand and minimal gestures to win her over have paid off.
Mandy and Georgie's Relationship Causes Controversy in Town
Season 5, episode 21, "white trash, holy rollers and punching people", young sheldon's george cooper actor had a secret cameo in series finale.
This episode doesn't hit any major milestones for Georgie and Mandy's relationship, but it shows the fallout that the pregnancy had on their small American Southern town. Gossip starts spreading as news gets out about their relationship, more importantly the fact that they'll have an illegitimate child.
As Medford becomes the central battleground for the Coopers vs. the church, Georgie almost shows the first signs of maturity when he shows up to Mandy's doctor's appointment. Even though a baby is usually a happy occasion, Young Sheldon shows that sometimes, it can cause immense strain in an extremely religious community when judgment rises.
Mary, Connie and Audrey Throw Mandy a Baby Shower
Season 6, episode 12, "a baby shower and a testosterone-rich banter".
"A Baby Shower and a Testosterone-Rich Banter" is the first time Mandy completes the Young Sheldon cast and truly feels like a part of the Cooper family. The women closest to Mandy throw her a baby shower, and she feels like a natural addition to characters that have been around since Season 1.
Mandy also comes to realize that Georgie may have been the one that got away. After he comes home from a date with his new girlfriend, Georgie gifts Mandy a locket with their baby's sonogram. To Mandy, it's scary to think that the father of her child is moving on while she feels stuck in the past.
Mandy Gives Birth to CeeCee
Season 6, episode 14, "a launch party and a whole human being".
Just as Sheldon is about to launch his database , Mandy launches her new baby. When Mandy goes into labor, Sheldon is the only one around to help. The situation forces Sheldon into an unsterile environment where he's clearly out of his depth, but thankfully, Mandy makes it to the hospital in time.
Despite Georgie's minor moment of doubt about being a father, he makes it to witness the birth of his daughter. Georgie reveals that they named her Constance (aka CeeCee) after Connie, who's been a big presence in both Georgie and Mandy's lives. With the birth of CeeCee juxtaposed against Mary and George's rocky marriage, Georgie and Mandy seem like the perfect couple all of a sudden.
Georgie and Mandy Have Their Meet-Cute in a Laundromat
Season 5, episode 11, "a lock-in, a weather girl and a disgusting habit".
Georgie and Mandy first met at the laundromat where Georgie is secretly working in the back-door gambling room. It's every person's idea of a meet-cute. Almost immediately, Georgie uses his charm to ask Mandy out on a date, which she's impressed by. The problem? Both Georgie and Mandy are lying about their age.
Georgie tells Mandy that he's 21 and continues to keep up the lie, even when Connie catches him in the act ordering alcohol at a restaurant. Lying is not the ideal way of starting a relationship, but it's certainly the Georgie Cooper-way. If there's anyone wondering why his spinoff is titled Georgie & Mandy's First Marriage and not Georgie & Mandy's Forever Marriage , look to this episode for the answer.
Georgie and Mandy Get Married in the Courthouse
Season 7, episode 7, "a proper wedding and skeletons in the closet", young sheldon ep addresses fan-favorite characters absence in final season.
Regardless of all the lying and the fact that a nearly 30-year-old person fell in love with a 17-year-old, Georgie and Mandy make it down the aisle. Just not in the traditional way that Mary and Audrey thought. Georgie and Mandy become fed up with their mothers fighting over CeeCee's religious upbringing, so they decide that their punishment needs to be harsh: both mothers aren't allowed to attend their spontaneous wedding.
But things don't go Georgie and Mandy's way, which turns out to be for the better. Everyone except for Sheldon shows up to their courthouse wedding to celebrate the happy occasion. The couple is gifted an all-inclusive trip to Dollywood for their honeymoon, which is every Southerner's dream destination.
All seven seasons of Young Sheldon are available to stream on Netflix, Max and Paramount+. Georgie and Mandy's First Marriage will premiere in fall 2024 on CBS.
Young Sheldon
Meet a child genius named Sheldon Cooper (already seen as an adult in The Big Bang Theory (2007)) and his family. Some unique challenges face Sheldon, who is socially impaired.
Release Date September 25, 2017
Cast Jim Parsons, Iain Armitage
Main Genre Sitcom
Genres Drama, Comedy
Rating TV-PG
Creator Chuck Lorre, Steven Molaro
Number of Episodes 127
Network CBS
Streaming Service(s) Fubo TV, Max, Hulu, Prime Video, Paramount+, Netflix


IMAGES
VIDEO
COMMENTS
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible. Variations in fetal presentation, position, or lie may occur when. The fetus is too large for the mother's pelvis (fetopelvic disproportion). The uterus is abnormally shaped or contains growths such as ...
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse. Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position. Abnormal fetal lie, presentation, or position may occur with. Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. ... In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than ...
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
The ideal fetal attitude is when the fetus has its: Chin tucked into its chest. Arms and legs drawn into the center of its chest. But, there can be times the fetal attitude is irregular. For example, its chin is tilted back instead of tucked. What is fetal lie? Fetal lie describes how the fetus's spine lines up with its birth parent's spine.
Abnormal Fetal Lie. If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation. ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen. It has an approximate success rate of 50% in primiparous women and 60% in multiparous women.
Lie. Facing the patient's head, place hands on either side of the top of the uterus and gently apply pressure. Move the hands and palpate down the abdomen. One side will feel fuller and firmer - this is the back. Fetal limbs may be palpable on the opposing side. Fig 2 - Assessing fetal lie and presentation.
The fetal presentation describes the fetal part that is lowest in the maternal abdomen. In case of labor, it is the lowest fetal part in the birth canal. Many fetal presentations are possible: Cephalic presentation: the fetal head is the lowest fetal part. This is by far the most common presentation at term of pregnancy and in labor.
It is best to detect abnormal fetal lie or presentation before delivery. During routine prenatal care, clinicians assess fetal lie and presentation with physical examination in the late third trimester. Ultrasonography can also be done. If breech presentation is detected, external cephalic version can sometimes move the fetus to vertex ...
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin.
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. In a frank breech, the fetus has flexion of both hips, and the legs are straight with the feet near the fetal face, in a pike position.
Determining fetal lie, position, presentation and attitude Follow the 4 steps of the Leopold Maneuver for abdominal palpation to determine fetal lie and presentation. Diagnose Count for 60 seconds to have the fetal heart rate bpm (beats per minute) or count for 15 seconds and multiply by 4.
Presentation. After the lie of the fetus is assessed, the clinician has to detail the fetus further by describing the lowermost structure of the fetus in the maternal pelvis. This is referred to as the fetal presentation. In a vertical (or longitudinal) lie, the fetal presentation can be either cephalic or breech. In the transverse lie, the ...
• Oblique lie: The fetal axis is diagonal to the uterine axis. • Transverse lie: The fetal longitudinal axis is perpendicular to the uterine axis. • Unstable lie: The fetal lie continues to change at or near term (usually from 37 weeks onwards). The lie varies between longitudinal, oblique, and transverse. Presentation. The fetal body ...
Fetal lie/presentation assessments are not included in the list of specific indications for examinations performed in these clinics. The data included a patient study identity code, date of examination, GA at examination, number of fetuses and fetal presentation. Examinations were performed between December 2004 and November 2011.
The commonest presentation is the vertex of the fetal head. Malpositions are abnormal positions of the vertex of the fetal head, using the occiput as the reference point, relative to the maternal pelvis. Malpresentations are all presentations of the fetus other than vertex, which includes the breech presentation, transverse and oblique lie.
The vertex presentation describes the orientation a fetus should be in for a safe vaginal delivery. It becomes important as you near your due date because it tells your pregnancy care provider how they may need to deliver your baby. Vertex means "crown of the head.". This means that the crown of the fetus's head is presenting towards the ...
The possibilities include a longitudinal lie, a transverse lie, and, on occasion, an oblique lie. Fetal presentation is a reference to the part of the fetus that is overlying the maternal pelvic inlet. The most common relationship between fetus and mother is the longitudinal lie, cephalic presentation. A breech fetus also is a longitudinal lie ...
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one ...
The most common fetal malpresentation in longitudinal lie is breech presentation which itself can be further subdivided into subtypes. Other malpresentations in longitudinal lie include face, brow and compound. The fetus in non-longitudinal lie may be oblique or transverse, with shoulder, arm or cord presentations.
Presentation of twins in Der Rosengarten ("The Rose Garden"), a standard medical text for midwives published in 1513. In obstetrics, the presentation of a fetus about to be born specifies which anatomical part of the fetus is leading, that is, is closest to the pelvic inlet of the birth canal. According to the leading part, this is identified as a cephalic, breech, or shoulder presentation.
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation, where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations ...
Season 6, Episode 12, "A Baby Shower and a Testosterone-Rich Banter" "A Baby Shower and a Testosterone-Rich Banter" is the first time Mandy completes the Young Sheldon cast and truly feels like a ...