- Skip to main content
- Accessibility help

Information
We use cookies to collect anonymous data to help us improve your site browsing experience.
Click 'Accept all cookies' to agree to all cookies that collect anonymous data. To only allow the cookies that make the site work, click 'Use essential cookies only.' Visit 'Set cookie preferences' to control specific cookies.
Your cookie preferences have been saved. You can change your cookie settings at any time.
Coronavirus (COVID-19) and society: what matters to people in Scotland?
Findings from an open free text survey taken to understand in greater detail how the pandemic has changed Scotland.
- This research has captured the diversity and complexity of people’s experiences.
- People’s experiences of the pandemic and their ability to stay safe has been impacted by a range of factors, including: their geographical environment, their financial situation, profession, their living situation and if they have any physical or mental health conditions.
- Even though the direct level of threat from COVID-19 has reduced (for some people), there is still concern about the longer term harm and disruption that COVID-19 has caused to people and communities, and worry about the threat of future waves of infection.
- This report captures a number of specific suggestions for support. For example, support for key workers, creating safer public environments, wide-scale financial support, greater awareness around the experiences of those who are at higher risk to COVID-19 and putting in place robust processes for learning and reflection on the impact of the pandemic.
- Public engagement in this open and unfiltered format is an essential part of making sense of people’s attitudes and behaviours within the context of their life.
Email: [email protected]
There is a problem
Thanks for your feedback
Your feedback helps us to improve this website. Do not give any personal information because we cannot reply to you directly.
- CBSE Class 10th
- CBSE Class 12th
- UP Board 10th
- UP Board 12th
- Bihar Board 10th
- Bihar Board 12th
- Top Schools in India
- Top Schools in Delhi
- Top Schools in Mumbai
- Top Schools in Chennai
- Top Schools in Hyderabad
- Top Schools in Kolkata
- Top Schools in Pune
- Top Schools in Bangalore
Products & Resources
- JEE Main Knockout April
- Free Sample Papers
- Free Ebooks
- NCERT Notes
- NCERT Syllabus
- NCERT Books
- RD Sharma Solutions
- Navodaya Vidyalaya Admission 2024-25
- NCERT Solutions
- NCERT Solutions for Class 12
- NCERT Solutions for Class 11
- NCERT solutions for Class 10
- NCERT solutions for Class 9
- NCERT solutions for Class 8
- NCERT Solutions for Class 7
- JEE Main 2024
- MHT CET 2024
- JEE Advanced 2024
- BITSAT 2024
- View All Engineering Exams
- Colleges Accepting B.Tech Applications
- Top Engineering Colleges in India
- Engineering Colleges in India
- Engineering Colleges in Tamil Nadu
- Engineering Colleges Accepting JEE Main
- Top IITs in India
- Top NITs in India
- Top IIITs in India
- JEE Main College Predictor
- JEE Main Rank Predictor
- MHT CET College Predictor
- AP EAMCET College Predictor
- GATE College Predictor
- KCET College Predictor
- JEE Advanced College Predictor
- View All College Predictors
- JEE Main Question Paper
- JEE Main Cutoff
- JEE Main Advanced Admit Card
- JEE Advanced Admit Card 2024
- Download E-Books and Sample Papers
- Compare Colleges
- B.Tech College Applications
- KCET Result
- MAH MBA CET Exam
- View All Management Exams
Colleges & Courses
- MBA College Admissions
- MBA Colleges in India
- Top IIMs Colleges in India
- Top Online MBA Colleges in India
- MBA Colleges Accepting XAT Score
- BBA Colleges in India
- XAT College Predictor 2024
- SNAP College Predictor
- NMAT College Predictor
- MAT College Predictor 2024
- CMAT College Predictor 2024
- CAT Percentile Predictor 2023
- CAT 2023 College Predictor
- CMAT 2024 Admit Card
- TS ICET 2024 Hall Ticket
- CMAT Result 2024
- MAH MBA CET Cutoff 2024
- Download Helpful Ebooks
- List of Popular Branches
- QnA - Get answers to your doubts
- IIM Fees Structure
- AIIMS Nursing
- Top Medical Colleges in India
- Top Medical Colleges in India accepting NEET Score
- Medical Colleges accepting NEET
- List of Medical Colleges in India
- List of AIIMS Colleges In India
- Medical Colleges in Maharashtra
- Medical Colleges in India Accepting NEET PG
- NEET College Predictor
- NEET PG College Predictor
- NEET MDS College Predictor
- NEET Rank Predictor
- DNB PDCET College Predictor
- NEET Admit Card 2024
- NEET PG Application Form 2024
- NEET Cut off
- NEET Online Preparation
- Download Helpful E-books
- Colleges Accepting Admissions
- Top Law Colleges in India
- Law College Accepting CLAT Score
- List of Law Colleges in India
- Top Law Colleges in Delhi
- Top NLUs Colleges in India
- Top Law Colleges in Chandigarh
- Top Law Collages in Lucknow
Predictors & E-Books
- CLAT College Predictor
- MHCET Law ( 5 Year L.L.B) College Predictor
- AILET College Predictor
- Sample Papers
- Compare Law Collages
- Careers360 Youtube Channel
- CLAT Syllabus 2025
- CLAT Previous Year Question Paper
- NID DAT Exam
- Pearl Academy Exam
Predictors & Articles
- NIFT College Predictor
- UCEED College Predictor
- NID DAT College Predictor
- NID DAT Syllabus 2025
- NID DAT 2025
- Design Colleges in India
- Top NIFT Colleges in India
- Fashion Design Colleges in India
- Top Interior Design Colleges in India
- Top Graphic Designing Colleges in India
- Fashion Design Colleges in Delhi
- Fashion Design Colleges in Mumbai
- Top Interior Design Colleges in Bangalore
- NIFT Result 2024
- NIFT Fees Structure
- NIFT Syllabus 2025
- Free Design E-books
- List of Branches
- Careers360 Youtube channel
- IPU CET BJMC
- JMI Mass Communication Entrance Exam
- IIMC Entrance Exam
- Media & Journalism colleges in Delhi
- Media & Journalism colleges in Bangalore
- Media & Journalism colleges in Mumbai
- List of Media & Journalism Colleges in India
- CA Intermediate
- CA Foundation
- CS Executive
- CS Professional
- Difference between CA and CS
- Difference between CA and CMA
- CA Full form
- CMA Full form
- CS Full form
- CA Salary In India
Top Courses & Careers
- Bachelor of Commerce (B.Com)
- Master of Commerce (M.Com)
- Company Secretary
- Cost Accountant
- Charted Accountant
- Credit Manager
- Financial Advisor
- Top Commerce Colleges in India
- Top Government Commerce Colleges in India
- Top Private Commerce Colleges in India
- Top M.Com Colleges in Mumbai
- Top B.Com Colleges in India
- IT Colleges in Tamil Nadu
- IT Colleges in Uttar Pradesh
- MCA Colleges in India
- BCA Colleges in India
Quick Links
- Information Technology Courses
- Programming Courses
- Web Development Courses
- Data Analytics Courses
- Big Data Analytics Courses
- RUHS Pharmacy Admission Test
- Top Pharmacy Colleges in India
- Pharmacy Colleges in Pune
- Pharmacy Colleges in Mumbai
- Colleges Accepting GPAT Score
- Pharmacy Colleges in Lucknow
- List of Pharmacy Colleges in Nagpur
- GPAT Result
- GPAT 2024 Admit Card
- GPAT Question Papers
- NCHMCT JEE 2024
- Mah BHMCT CET
- Top Hotel Management Colleges in Delhi
- Top Hotel Management Colleges in Hyderabad
- Top Hotel Management Colleges in Mumbai
- Top Hotel Management Colleges in Tamil Nadu
- Top Hotel Management Colleges in Maharashtra
- B.Sc Hotel Management
- Hotel Management
- Diploma in Hotel Management and Catering Technology
Diploma Colleges
- Top Diploma Colleges in Maharashtra
- UPSC IAS 2024
- SSC CGL 2024
- IBPS RRB 2024
- Previous Year Sample Papers
- Free Competition E-books
- Sarkari Result
- QnA- Get your doubts answered
- UPSC Previous Year Sample Papers
- CTET Previous Year Sample Papers
- SBI Clerk Previous Year Sample Papers
- NDA Previous Year Sample Papers
Upcoming Events
- NDA Application Form 2024
- UPSC IAS Application Form 2024
- CDS Application Form 2024
- CTET Admit card 2024
- HP TET Result 2023
- SSC GD Constable Admit Card 2024
- UPTET Notification 2024
- SBI Clerk Result 2024
Other Exams
- SSC CHSL 2024
- UP PCS 2024
- UGC NET 2024
- RRB NTPC 2024
- IBPS PO 2024
- IBPS Clerk 2024
- IBPS SO 2024
- Top University in USA
- Top University in Canada
- Top University in Ireland
- Top Universities in UK
- Top Universities in Australia
- Best MBA Colleges in Abroad
- Business Management Studies Colleges
Top Countries
- Study in USA
- Study in UK
- Study in Canada
- Study in Australia
- Study in Ireland
- Study in Germany
- Study in China
- Study in Europe
Student Visas
- Student Visa Canada
- Student Visa UK
- Student Visa USA
- Student Visa Australia
- Student Visa Germany
- Student Visa New Zealand
- Student Visa Ireland
- CUET PG 2024
- IGNOU B.Ed Admission 2024
- DU Admission 2024
- UP B.Ed JEE 2024
- LPU NEST 2024
- IIT JAM 2024
- IGNOU Online Admission 2024
- Universities in India
- Top Universities in India 2024
- Top Colleges in India
- Top Universities in Uttar Pradesh 2024
- Top Universities in Bihar
- Top Universities in Madhya Pradesh 2024
- Top Universities in Tamil Nadu 2024
- Central Universities in India
- CUET Exam City Intimation Slip 2024
- IGNOU Date Sheet
- CUET Mock Test 2024
- CUET Admit card 2024
- CUET Result 2024
- CUET Participating Universities 2024
- CUET Previous Year Question Paper
- CUET Syllabus 2024 for Science Students
- E-Books and Sample Papers
- CUET Exam Pattern 2024
- CUET Exam Date 2024
- CUET Cut Off 2024
- CUET Exam Analysis 2024
- IGNOU Exam Form 2024
- CUET 2024 Exam Live
- CUET Answer Key 2024
Engineering Preparation
- Knockout JEE Main 2024
- Test Series JEE Main 2024
- JEE Main 2024 Rank Booster
Medical Preparation
- Knockout NEET 2024
- Test Series NEET 2024
- Rank Booster NEET 2024
Online Courses
- JEE Main One Month Course
- NEET One Month Course
- IBSAT Free Mock Tests
- IIT JEE Foundation Course
- Knockout BITSAT 2024
- Career Guidance Tool
Top Streams
- IT & Software Certification Courses
- Engineering and Architecture Certification Courses
- Programming And Development Certification Courses
- Business and Management Certification Courses
- Marketing Certification Courses
- Health and Fitness Certification Courses
- Design Certification Courses
Specializations
- Digital Marketing Certification Courses
- Cyber Security Certification Courses
- Artificial Intelligence Certification Courses
- Business Analytics Certification Courses
- Data Science Certification Courses
- Cloud Computing Certification Courses
- Machine Learning Certification Courses
- View All Certification Courses
- UG Degree Courses
- PG Degree Courses
- Short Term Courses
- Free Courses
- Online Degrees and Diplomas
- Compare Courses
Top Providers
- Coursera Courses
- Udemy Courses
- Edx Courses
- Swayam Courses
- upGrad Courses
- Simplilearn Courses
- Great Learning Courses
Covid 19 Essay in English
Essay on Covid -19: In a very short amount of time, coronavirus has spread globally. It has had an enormous impact on people's lives, economy, and societies all around the world, affecting every country. Governments have had to take severe measures to try and contain the pandemic. The virus has altered our way of life in many ways, including its effects on our health and our economy. Here are a few sample essays on ‘CoronaVirus’.
100 Words Essay on Covid 19
200 words essay on covid 19, 500 words essay on covid 19.

COVID-19 or Corona Virus is a novel coronavirus that was first identified in 2019. It is similar to other coronaviruses, such as SARS-CoV and MERS-CoV, but it is more contagious and has caused more severe respiratory illness in people who have been infected. The novel coronavirus became a global pandemic in a very short period of time. It has affected lives, economies and societies across the world, leaving no country untouched. The virus has caused governments to take drastic measures to try and contain it. From health implications to economic and social ramifications, COVID-19 impacted every part of our lives. It has been more than 2 years since the pandemic hit and the world is still recovering from its effects.
Since the outbreak of COVID-19, the world has been impacted in a number of ways. For one, the global economy has taken a hit as businesses have been forced to close their doors. This has led to widespread job losses and an increase in poverty levels around the world. Additionally, countries have had to impose strict travel restrictions in an attempt to contain the virus, which has resulted in a decrease in tourism and international trade. Furthermore, the pandemic has put immense pressure on healthcare systems globally, as hospitals have been overwhelmed with patients suffering from the virus. Lastly, the outbreak has led to a general feeling of anxiety and uncertainty, as people are fearful of contracting the disease.
My Experience of COVID-19
I still remember how abruptly colleges and schools shut down in March 2020. I was a college student at that time and I was under the impression that everything would go back to normal in a few weeks. I could not have been more wrong. The situation only got worse every week and the government had to impose a lockdown. There were so many restrictions in place. For example, we had to wear face masks whenever we left the house, and we could only go out for essential errands. Restaurants and shops were only allowed to operate at take-out capacity, and many businesses were shut down.
In the current scenario, coronavirus is dominating all aspects of our lives. The coronavirus pandemic has wreaked havoc upon people’s lives, altering the way we live and work in a very short amount of time. It has revolutionised how we think about health care, education, and even social interaction. This virus has had long-term implications on our society, including its impact on mental health, economic stability, and global politics. But we as individuals can help to mitigate these effects by taking personal responsibility to protect themselves and those around them from infection.
Effects of CoronaVirus on Education
The outbreak of coronavirus has had a significant impact on education systems around the world. In China, where the virus originated, all schools and universities were closed for several weeks in an effort to contain the spread of the disease. Many other countries have followed suit, either closing schools altogether or suspending classes for a period of time.
This has resulted in a major disruption to the education of millions of students. Some have been able to continue their studies online, but many have not had access to the internet or have not been able to afford the costs associated with it. This has led to a widening of the digital divide between those who can afford to continue their education online and those who cannot.
The closure of schools has also had a negative impact on the mental health of many students. With no face-to-face contact with friends and teachers, some students have felt isolated and anxious. This has been compounded by the worry and uncertainty surrounding the virus itself.
The situation with coronavirus has improved and schools have been reopened but students are still catching up with the gap of 2 years that the pandemic created. In the meantime, governments and educational institutions are working together to find ways to support students and ensure that they are able to continue their education despite these difficult circumstances.
Effects of CoronaVirus on Economy
The outbreak of the coronavirus has had a significant impact on the global economy. The virus, which originated in China, has spread to over two hundred countries, resulting in widespread panic and a decrease in global trade. As a result of the outbreak, many businesses have been forced to close their doors, leading to a rise in unemployment. In addition, the stock market has taken a severe hit.
Effects of CoronaVirus on Health
The effects that coronavirus has on one's health are still being studied and researched as the virus continues to spread throughout the world. However, some of the potential effects on health that have been observed thus far include respiratory problems, fever, and coughing. In severe cases, pneumonia, kidney failure, and death can occur. It is important for people who think they may have been exposed to the virus to seek medical attention immediately so that they can be treated properly and avoid any serious complications. There is no specific cure or treatment for coronavirus at this time, but there are ways to help ease symptoms and prevent the virus from spreading.
Applications for Admissions are open.

Aakash iACST Scholarship Test 2024
Get up to 90% scholarship on NEET, JEE & Foundation courses

ALLEN Digital Scholarship Admission Test (ADSAT)
Register FREE for ALLEN Digital Scholarship Admission Test (ADSAT)

JEE Main Important Physics formulas
As per latest 2024 syllabus. Physics formulas, equations, & laws of class 11 & 12th chapters

PW JEE Coaching
Enrol in PW Vidyapeeth center for JEE coaching

PW NEET Coaching
Enrol in PW Vidyapeeth center for NEET coaching

JEE Main Important Chemistry formulas
As per latest 2024 syllabus. Chemistry formulas, equations, & laws of class 11 & 12th chapters
Download Careers360 App's
Regular exam updates, QnA, Predictors, College Applications & E-books now on your Mobile
Certifications
We Appeared in
How to Write About Coronavirus in a College Essay
Students can share how they navigated life during the coronavirus pandemic in a full-length essay or an optional supplement.
Writing About COVID-19 in College Essays

Getty Images
Experts say students should be honest and not limit themselves to merely their experiences with the pandemic.
The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no other. Both face unprecedented challenges and questions as they grapple with their respective futures amid the ongoing fallout of the pandemic.
Colleges must examine applicants without the aid of standardized test scores for many – a factor that prompted many schools to go test-optional for now . Even grades, a significant component of a college application, may be hard to interpret with some high schools adopting pass-fail classes last spring due to the pandemic. Major college admissions factors are suddenly skewed.
"I can't help but think other (admissions) factors are going to matter more," says Ethan Sawyer, founder of the College Essay Guy, a website that offers free and paid essay-writing resources.
College essays and letters of recommendation , Sawyer says, are likely to carry more weight than ever in this admissions cycle. And many essays will likely focus on how the pandemic shaped students' lives throughout an often tumultuous 2020.
But before writing a college essay focused on the coronavirus, students should explore whether it's the best topic for them.
Writing About COVID-19 for a College Application
Much of daily life has been colored by the coronavirus. Virtual learning is the norm at many colleges and high schools, many extracurriculars have vanished and social lives have stalled for students complying with measures to stop the spread of COVID-19.
"For some young people, the pandemic took away what they envisioned as their senior year," says Robert Alexander, dean of admissions, financial aid and enrollment management at the University of Rochester in New York. "Maybe that's a spot on a varsity athletic team or the lead role in the fall play. And it's OK for them to mourn what should have been and what they feel like they lost, but more important is how are they making the most of the opportunities they do have?"
That question, Alexander says, is what colleges want answered if students choose to address COVID-19 in their college essay.
But the question of whether a student should write about the coronavirus is tricky. The answer depends largely on the student.
"In general, I don't think students should write about COVID-19 in their main personal statement for their application," Robin Miller, master college admissions counselor at IvyWise, a college counseling company, wrote in an email.
"Certainly, there may be exceptions to this based on a student's individual experience, but since the personal essay is the main place in the application where the student can really allow their voice to be heard and share insight into who they are as an individual, there are likely many other topics they can choose to write about that are more distinctive and unique than COVID-19," Miller says.
Opinions among admissions experts vary on whether to write about the likely popular topic of the pandemic.
"If your essay communicates something positive, unique, and compelling about you in an interesting and eloquent way, go for it," Carolyn Pippen, principal college admissions counselor at IvyWise, wrote in an email. She adds that students shouldn't be dissuaded from writing about a topic merely because it's common, noting that "topics are bound to repeat, no matter how hard we try to avoid it."
Above all, she urges honesty.
"If your experience within the context of the pandemic has been truly unique, then write about that experience, and the standing out will take care of itself," Pippen says. "If your experience has been generally the same as most other students in your context, then trying to find a unique angle can easily cross the line into exploiting a tragedy, or at least appearing as though you have."
But focusing entirely on the pandemic can limit a student to a single story and narrow who they are in an application, Sawyer says. "There are so many wonderful possibilities for what you can say about yourself outside of your experience within the pandemic."
He notes that passions, strengths, career interests and personal identity are among the multitude of essay topic options available to applicants and encourages them to probe their values to help determine the topic that matters most to them – and write about it.
That doesn't mean the pandemic experience has to be ignored if applicants feel the need to write about it.
Writing About Coronavirus in Main and Supplemental Essays
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form.
To help students explain how the pandemic affected them, The Common App has added an optional section to address this topic. Applicants have 250 words to describe their pandemic experience and the personal and academic impact of COVID-19.
"That's not a trick question, and there's no right or wrong answer," Alexander says. Colleges want to know, he adds, how students navigated the pandemic, how they prioritized their time, what responsibilities they took on and what they learned along the way.
If students can distill all of the above information into 250 words, there's likely no need to write about it in a full-length college essay, experts say. And applicants whose lives were not heavily altered by the pandemic may even choose to skip the optional COVID-19 question.
"This space is best used to discuss hardship and/or significant challenges that the student and/or the student's family experienced as a result of COVID-19 and how they have responded to those difficulties," Miller notes. Using the section to acknowledge a lack of impact, she adds, "could be perceived as trite and lacking insight, despite the good intentions of the applicant."
To guard against this lack of awareness, Sawyer encourages students to tap someone they trust to review their writing , whether it's the 250-word Common App response or the full-length essay.
Experts tend to agree that the short-form approach to this as an essay topic works better, but there are exceptions. And if a student does have a coronavirus story that he or she feels must be told, Alexander encourages the writer to be authentic in the essay.
"My advice for an essay about COVID-19 is the same as my advice about an essay for any topic – and that is, don't write what you think we want to read or hear," Alexander says. "Write what really changed you and that story that now is yours and yours alone to tell."
Sawyer urges students to ask themselves, "What's the sentence that only I can write?" He also encourages students to remember that the pandemic is only a chapter of their lives and not the whole book.
Miller, who cautions against writing a full-length essay on the coronavirus, says that if students choose to do so they should have a conversation with their high school counselor about whether that's the right move. And if students choose to proceed with COVID-19 as a topic, she says they need to be clear, detailed and insightful about what they learned and how they adapted along the way.
"Approaching the essay in this manner will provide important balance while demonstrating personal growth and vulnerability," Miller says.
Pippen encourages students to remember that they are in an unprecedented time for college admissions.
"It is important to keep in mind with all of these (admission) factors that no colleges have ever had to consider them this way in the selection process, if at all," Pippen says. "They have had very little time to calibrate their evaluations of different application components within their offices, let alone across institutions. This means that colleges will all be handling the admissions process a little bit differently, and their approaches may even evolve over the course of the admissions cycle."
Searching for a college? Get our complete rankings of Best Colleges.
10 Ways to Discover College Essay Ideas

Tags: students , colleges , college admissions , college applications , college search , Coronavirus
2024 Best Colleges

Search for your perfect fit with the U.S. News rankings of colleges and universities.
College Admissions: Get a Step Ahead!
Sign up to receive the latest updates from U.S. News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
Ask an Alum: Making the Most Out of College
You May Also Like
Premedical programs: what to know.
Sarah Wood May 21, 2024

How Geography Affects College Admissions
Cole Claybourn May 21, 2024

Q&A: College Alumni Engagement
LaMont Jones, Jr. May 20, 2024

10 Destination West Coast College Towns
Cole Claybourn May 16, 2024

Scholarships for Lesser-Known Sports
Sarah Wood May 15, 2024

Should Students Submit Test Scores?
Sarah Wood May 13, 2024

Poll: Antisemitism a Problem on Campus
Lauren Camera May 13, 2024

Federal vs. Private Parent Student Loans
Erika Giovanetti May 9, 2024

14 Colleges With Great Food Options
Sarah Wood May 8, 2024

Colleges With Religious Affiliations
Anayat Durrani May 8, 2024

Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
by Alissa Wilkinson

The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
- The Vox guide to navigating the coronavirus crisis
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
- A syllabus for the end of the world
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
- What day is it today?
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
- Vox is starting a book club. Come read with us!
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
Most Popular
Massive invasive snakes are on the loose and spreading in puerto rico, the republican party's man inside the supreme court, why are whole-body deodorants suddenly everywhere, take a mental break with the newest vox crossword, the misleading, wasteful way we measure gas mileage, explained, today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
More in Culture

The video where Diddy attacks Cassie — and the allegations against him — explained

Is it ever okay to film strangers in public?

Sabrina Carpenter’s “Espresso,” the song of summer, explained

When TikTok therapy is more lucrative than seeing clients

You’re not imagining it — movies are getting longer

The controversy over Harrison Butker’s misogynistic commencement speech, explained

Why ICC arrest warrants matter, even if Israel and Hamas leaders evade them

Why the US built a pier to get aid into Gaza

Vanderpump Rules shows the limits of making money on reality TV

Bridgerton’s third season is more diverse — and even shallower — than ever

I Thought We’d Learned Nothing From the Pandemic. I Wasn’t Seeing the Full Picture

M y first home had a back door that opened to a concrete patio with a giant crack down the middle. When my sister and I played, I made sure to stay on the same side of the divide as her, just in case. The 1988 film The Land Before Time was one of the first movies I ever saw, and the image of the earth splintering into pieces planted its roots in my brain. I believed that, even in my own backyard, I could easily become the tiny Triceratops separated from her family, on the other side of the chasm, as everything crumbled into chaos.
Some 30 years later, I marvel at the eerie, unexpected ways that cartoonish nightmare came to life – not just for me and my family, but for all of us. The landscape was already covered in fissures well before COVID-19 made its way across the planet, but the pandemic applied pressure, and the cracks broke wide open, separating us from each other physically and ideologically. Under the weight of the crisis, we scattered and landed on such different patches of earth we could barely see each other’s faces, even when we squinted. We disagreed viciously with each other, about how to respond, but also about what was true.
Recently, someone asked me if we’ve learned anything from the pandemic, and my first thought was a flat no. Nothing. There was a time when I thought it would be the very thing to draw us together and catapult us – as a capital “S” Society – into a kinder future. It’s surreal to remember those early days when people rallied together, sewing masks for health care workers during critical shortages and gathering on balconies in cities from Dallas to New York City to clap and sing songs like “Yellow Submarine.” It felt like a giant lightning bolt shot across the sky, and for one breath, we all saw something that had been hidden in the dark – the inherent vulnerability in being human or maybe our inescapable connectedness .
More from TIME
Read More: The Family Time the Pandemic Stole
But it turns out, it was just a flash. The goodwill vanished as quickly as it appeared. A couple of years later, people feel lied to, abandoned, and all on their own. I’ve felt my own curiosity shrinking, my willingness to reach out waning , my ability to keep my hands open dwindling. I look out across the landscape and see selfishness and rage, burnt earth and so many dead bodies. Game over. We lost. And if we’ve already lost, why try?
Still, the question kept nagging me. I wondered, am I seeing the full picture? What happens when we focus not on the collective society but at one face, one story at a time? I’m not asking for a bow to minimize the suffering – a pretty flourish to put on top and make the whole thing “worth it.” Yuck. That’s not what we need. But I wondered about deep, quiet growth. The kind we feel in our bodies, relationships, homes, places of work, neighborhoods.
Like a walkie-talkie message sent to my allies on the ground, I posted a call on my Instagram. What do you see? What do you hear? What feels possible? Is there life out here? Sprouting up among the rubble? I heard human voices calling back – reports of life, personal and specific. I heard one story at a time – stories of grief and distrust, fury and disappointment. Also gratitude. Discovery. Determination.
Among the most prevalent were the stories of self-revelation. Almost as if machines were given the chance to live as humans, people described blossoming into fuller selves. They listened to their bodies’ cues, recognized their desires and comforts, tuned into their gut instincts, and honored the intuition they hadn’t realized belonged to them. Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. “The way I dress, the way I love, and the way I carry myself have both shrunk and expanded,” she shared. “I don’t love myself very well with an audience.” Without the daily ritual of trying to pass as “normal” in public, Tamar, a queer mom in the Netherlands, realized she’s autistic. “I think the pandemic helped me to recognize the mask,” she wrote. “Not that unmasking is easy now. But at least I know it’s there.” In a time of widespread suffering that none of us could solve on our own, many tended to our internal wounds and misalignments, large and small, and found clarity.
Read More: A Tool for Staying Grounded in This Era of Constant Uncertainty
I wonder if this flourishing of self-awareness is at least partially responsible for the life alterations people pursued. The pandemic broke open our personal notions of work and pushed us to reevaluate things like time and money. Lucy, a disabled writer in the U.K., made the hard decision to leave her job as a journalist covering Westminster to write freelance about her beloved disability community. “This work feels important in a way nothing else has ever felt,” she wrote. “I don’t think I’d have realized this was what I should be doing without the pandemic.” And she wasn’t alone – many people changed jobs , moved, learned new skills and hobbies, became politically engaged.
Perhaps more than any other shifts, people described a significant reassessment of their relationships. They set boundaries, said no, had challenging conversations. They also reconnected, fell in love, and learned to trust. Jeanne, a quilter in Indiana, got to know relatives she wouldn’t have connected with if lockdowns hadn’t prompted weekly family Zooms. “We are all over the map as regards to our belief systems,” she emphasized, “but it is possible to love people you don’t see eye to eye with on every issue.” Anna, an anti-violence advocate in Maine, learned she could trust her new marriage: “Life was not a honeymoon. But we still chose to turn to each other with kindness and curiosity.” So many bonds forged and broken, strengthened and strained.
Instead of relying on default relationships or institutional structures, widespread recalibrations allowed for going off script and fortifying smaller communities. Mara from Idyllwild, Calif., described the tangible plan for care enacted in her town. “We started a mutual-aid group at the beginning of the pandemic,” she wrote, “and it grew so quickly before we knew it we were feeding 400 of the 4000 residents.” She didn’t pretend the conditions were ideal. In fact, she expressed immense frustration with our collective response to the pandemic. Even so, the local group rallied and continues to offer assistance to their community with help from donations and volunteers (many of whom were originally on the receiving end of support). “I’ve learned that people thrive when they feel their connection to others,” she wrote. Clare, a teacher from the U.K., voiced similar conviction as she described a giant scarf she’s woven out of ribbons, each representing a single person. The scarf is “a collection of stories, moments and wisdom we are sharing with each other,” she wrote. It now stretches well over 1,000 feet.
A few hours into reading the comments, I lay back on my bed, phone held against my chest. The room was quiet, but my internal world was lighting up with firefly flickers. What felt different? Surely part of it was receiving personal accounts of deep-rooted growth. And also, there was something to the mere act of asking and listening. Maybe it connected me to humans before battle cries. Maybe it was the chance to be in conversation with others who were also trying to understand – what is happening to us? Underneath it all, an undeniable thread remained; I saw people peering into the mess and narrating their findings onto the shared frequency. Every comment was like a flare into the sky. I’m here! And if the sky is full of flares, we aren’t alone.
I recognized my own pandemic discoveries – some minor, others massive. Like washing off thick eyeliner and mascara every night is more effort than it’s worth; I can transform the mundane into the magical with a bedsheet, a movie projector, and twinkle lights; my paralyzed body can mother an infant in ways I’d never seen modeled for me. I remembered disappointing, bewildering conversations within my own family of origin and our imperfect attempts to remain close while also seeing things so differently. I realized that every time I get the weekly invite to my virtual “Find the Mumsies” call, with a tiny group of moms living hundreds of miles apart, I’m being welcomed into a pocket of unexpected community. Even though we’ve never been in one room all together, I’ve felt an uncommon kind of solace in their now-familiar faces.
Hope is a slippery thing. I desperately want to hold onto it, but everywhere I look there are real, weighty reasons to despair. The pandemic marks a stretch on the timeline that tangles with a teetering democracy, a deteriorating planet , the loss of human rights that once felt unshakable . When the world is falling apart Land Before Time style, it can feel trite, sniffing out the beauty – useless, firing off flares to anyone looking for signs of life. But, while I’m under no delusions that if we just keep trudging forward we’ll find our own oasis of waterfalls and grassy meadows glistening in the sunshine beneath a heavenly chorus, I wonder if trivializing small acts of beauty, connection, and hope actually cuts us off from resources essential to our survival. The group of abandoned dinosaurs were keeping each other alive and making each other laugh well before they made it to their fantasy ending.
Read More: How Ice Cream Became My Own Personal Act of Resistance
After the monarch butterfly went on the endangered-species list, my friend and fellow writer Hannah Soyer sent me wildflower seeds to plant in my yard. A simple act of big hope – that I will actually plant them, that they will grow, that a monarch butterfly will receive nourishment from whatever blossoms are able to push their way through the dirt. There are so many ways that could fail. But maybe the outcome wasn’t exactly the point. Maybe hope is the dogged insistence – the stubborn defiance – to continue cultivating moments of beauty regardless. There is value in the planting apart from the harvest.
I can’t point out a single collective lesson from the pandemic. It’s hard to see any great “we.” Still, I see the faces in my moms’ group, making pancakes for their kids and popping on between strings of meetings while we try to figure out how to raise these small people in this chaotic world. I think of my friends on Instagram tending to the selves they discovered when no one was watching and the scarf of ribbons stretching the length of more than three football fields. I remember my family of three, holding hands on the way up the ramp to the library. These bits of growth and rings of support might not be loud or right on the surface, but that’s not the same thing as nothing. If we only cared about the bottom-line defeats or sweeping successes of the big picture, we’d never plant flowers at all.
More Must-Reads from TIME
- The New Face of Doctor Who
- How Private Donors Shape Birth-Control Choices
- What Happens if Trump Is Convicted ? Your Questions, Answered
- Putin’s Enemies Are Struggling to Unite
- The Deadly Digital Frontiers at the Border
- Scientists Are Finding Out Just How Toxic Your Stuff Is
- The 31 Most Anticipated Movies of Summer 2024
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 76, Issue 2
- COVID-19 pandemic and its impact on social relationships and health
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-1512-4471 Emily Long 1 ,
- Susan Patterson 1 ,
- Karen Maxwell 1 ,
- Carolyn Blake 1 ,
- http://orcid.org/0000-0001-7342-4566 Raquel Bosó Pérez 1 ,
- Ruth Lewis 1 ,
- Mark McCann 1 ,
- Julie Riddell 1 ,
- Kathryn Skivington 1 ,
- Rachel Wilson-Lowe 1 ,
- http://orcid.org/0000-0002-4409-6601 Kirstin R Mitchell 2
- 1 MRC/CSO Social and Public Health Sciences Unit , University of Glasgow , Glasgow , UK
- 2 MRC/CSO Social and Public Health Sciences Unit, Institute of Health & Wellbeing , University of Glasgow , Glasgow , UK
- Correspondence to Dr Emily Long, MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, Glasgow G3 7HR, UK; emily.long{at}glasgow.ac.uk
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the nature of the public health response. We then introduce four distinct domains of social relationships: social networks, social support, social interaction and intimacy, highlighting the mechanisms through which the pandemic and associated public health response drastically altered social interactions in each domain. Throughout the essay, the lens of health inequalities, and perspective of relationships as interconnecting elements in a broader system, is used to explore the varying impact of these disruptions. The essay concludes by providing recommendations for longer term recovery ensuring that the social relational cost of COVID-19 is adequately considered in efforts to rebuild.
- inequalities
Data availability statement
Data sharing not applicable as no data sets generated and/or analysed for this study. Data sharing not applicable as no data sets generated or analysed for this essay.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/jech-2021-216690
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Infectious disease pandemics, including SARS and COVID-19, demand intrapersonal behaviour change and present highly complex challenges for public health. 1 A pandemic of an airborne infection, spread easily through social contact, assails human relationships by drastically altering the ways through which humans interact. In this essay, we draw on theories of social relationships to examine specific ways in which relational mechanisms key to health and well-being were disrupted by the COVID-19 pandemic. Relational mechanisms refer to the processes between people that lead to change in health outcomes.
At the time of writing, the future surrounding COVID-19 was uncertain. Vaccine programmes were being rolled out in countries that could afford them, but new and more contagious variants of the virus were also being discovered. The recovery journey looked long, with continued disruption to social relationships. The social cost of COVID-19 was only just beginning to emerge, but the mental health impact was already considerable, 2 3 and the inequality of the health burden stark. 4 Knowledge of the epidemiology of COVID-19 accrued rapidly, but evidence of the most effective policy responses remained uncertain.
The initial response to COVID-19 in the UK was reactive and aimed at reducing mortality, with little time to consider the social implications, including for interpersonal and community relationships. The terminology of ‘social distancing’ quickly became entrenched both in public and policy discourse. This equation of physical distance with social distance was regrettable, since only physical proximity causes viral transmission, whereas many forms of social proximity (eg, conversations while walking outdoors) are minimal risk, and are crucial to maintaining relationships supportive of health and well-being.
The aim of this essay is to explore four key relational mechanisms that were impacted by the pandemic and associated restrictions: social networks, social support, social interaction and intimacy. We use relational theories and emerging research on the effects of the COVID-19 pandemic response to make three key recommendations: one regarding public health responses; and two regarding social recovery. Our understanding of these mechanisms stems from a ‘systems’ perspective which casts social relationships as interdependent elements within a connected whole. 5
Social networks
Social networks characterise the individuals and social connections that compose a system (such as a workplace, community or society). Social relationships range from spouses and partners, to coworkers, friends and acquaintances. They vary across many dimensions, including, for example, frequency of contact and emotional closeness. Social networks can be understood both in terms of the individuals and relationships that compose the network, as well as the overall network structure (eg, how many of your friends know each other).
Social networks show a tendency towards homophily, or a phenomenon of associating with individuals who are similar to self. 6 This is particularly true for ‘core’ network ties (eg, close friends), while more distant, sometimes called ‘weak’ ties tend to show more diversity. During the height of COVID-19 restrictions, face-to-face interactions were often reduced to core network members, such as partners, family members or, potentially, live-in roommates; some ‘weak’ ties were lost, and interactions became more limited to those closest. Given that peripheral, weaker social ties provide a diversity of resources, opinions and support, 7 COVID-19 likely resulted in networks that were smaller and more homogenous.
Such changes were not inevitable nor necessarily enduring, since social networks are also adaptive and responsive to change, in that a disruption to usual ways of interacting can be replaced by new ways of engaging (eg, Zoom). Yet, important inequalities exist, wherein networks and individual relationships within networks are not equally able to adapt to such changes. For example, individuals with a large number of newly established relationships (eg, university students) may have struggled to transfer these relationships online, resulting in lost contacts and a heightened risk of social isolation. This is consistent with research suggesting that young adults were the most likely to report a worsening of relationships during COVID-19, whereas older adults were the least likely to report a change. 8
Lastly, social connections give rise to emergent properties of social systems, 9 where a community-level phenomenon develops that cannot be attributed to any one member or portion of the network. For example, local area-based networks emerged due to geographic restrictions (eg, stay-at-home orders), resulting in increases in neighbourly support and local volunteering. 10 In fact, research suggests that relationships with neighbours displayed the largest net gain in ratings of relationship quality compared with a range of relationship types (eg, partner, colleague, friend). 8 Much of this was built from spontaneous individual interactions within local communities, which together contributed to the ‘community spirit’ that many experienced. 11 COVID-19 restrictions thus impacted the personal social networks and the structure of the larger networks within the society.
Social support
Social support, referring to the psychological and material resources provided through social interaction, is a critical mechanism through which social relationships benefit health. In fact, social support has been shown to be one of the most important resilience factors in the aftermath of stressful events. 12 In the context of COVID-19, the usual ways in which individuals interact and obtain social support have been severely disrupted.
One such disruption has been to opportunities for spontaneous social interactions. For example, conversations with colleagues in a break room offer an opportunity for socialising beyond one’s core social network, and these peripheral conversations can provide a form of social support. 13 14 A chance conversation may lead to advice helpful to coping with situations or seeking formal help. Thus, the absence of these spontaneous interactions may mean the reduction of indirect support-seeking opportunities. While direct support-seeking behaviour is more effective at eliciting support, it also requires significantly more effort and may be perceived as forceful and burdensome. 15 The shift to homeworking and closure of community venues reduced the number of opportunities for these spontaneous interactions to occur, and has, second, focused them locally. Consequently, individuals whose core networks are located elsewhere, or who live in communities where spontaneous interaction is less likely, have less opportunity to benefit from spontaneous in-person supportive interactions.
However, alongside this disruption, new opportunities to interact and obtain social support have arisen. The surge in community social support during the initial lockdown mirrored that often seen in response to adverse events (eg, natural disasters 16 ). COVID-19 restrictions that confined individuals to their local area also compelled them to focus their in-person efforts locally. Commentators on the initial lockdown in the UK remarked on extraordinary acts of generosity between individuals who belonged to the same community but were unknown to each other. However, research on adverse events also tells us that such community support is not necessarily maintained in the longer term. 16
Meanwhile, online forms of social support are not bound by geography, thus enabling interactions and social support to be received from a wider network of people. Formal online social support spaces (eg, support groups) existed well before COVID-19, but have vastly increased since. While online interactions can increase perceived social support, it is unclear whether remote communication technologies provide an effective substitute from in-person interaction during periods of social distancing. 17 18 It makes intuitive sense that the usefulness of online social support will vary by the type of support offered, degree of social interaction and ‘online communication skills’ of those taking part. Youth workers, for instance, have struggled to keep vulnerable youth engaged in online youth clubs, 19 despite others finding a positive association between amount of digital technology used by individuals during lockdown and perceived social support. 20 Other research has found that more frequent face-to-face contact and phone/video contact both related to lower levels of depression during the time period of March to August 2020, but the negative effect of a lack of contact was greater for those with higher levels of usual sociability. 21 Relatedly, important inequalities in social support exist, such that individuals who occupy more socially disadvantaged positions in society (eg, low socioeconomic status, older people) tend to have less access to social support, 22 potentially exacerbated by COVID-19.
Social and interactional norms
Interactional norms are key relational mechanisms which build trust, belonging and identity within and across groups in a system. Individuals in groups and societies apply meaning by ‘approving, arranging and redefining’ symbols of interaction. 23 A handshake, for instance, is a powerful symbol of trust and equality. Depending on context, not shaking hands may symbolise a failure to extend friendship, or a failure to reach agreement. The norms governing these symbols represent shared values and identity; and mutual understanding of these symbols enables individuals to achieve orderly interactions, establish supportive relationship accountability and connect socially. 24 25
Physical distancing measures to contain the spread of COVID-19 radically altered these norms of interaction, particularly those used to convey trust, affinity, empathy and respect (eg, hugging, physical comforting). 26 As epidemic waves rose and fell, the work to negotiate these norms required intense cognitive effort; previously taken-for-granted interactions were re-examined, factoring in current restriction levels, own and (assumed) others’ vulnerability and tolerance of risk. This created awkwardness, and uncertainty, for example, around how to bring closure to an in-person interaction or convey warmth. The instability in scripted ways of interacting created particular strain for individuals who already struggled to encode and decode interactions with others (eg, those who are deaf or have autism spectrum disorder); difficulties often intensified by mask wearing. 27
Large social gatherings—for example, weddings, school assemblies, sporting events—also present key opportunities for affirming and assimilating interactional norms, building cohesion and shared identity and facilitating cooperation across social groups. 28 Online ‘equivalents’ do not easily support ‘social-bonding’ activities such as singing and dancing, and rarely enable chance/spontaneous one-on-one conversations with peripheral/weaker network ties (see the Social networks section) which can help strengthen bonds across a larger network. The loss of large gatherings to celebrate rites of passage (eg, bar mitzvah, weddings) has additional relational costs since these events are performed by and for communities to reinforce belonging, and to assist in transitioning to new phases of life. 29 The loss of interaction with diverse others via community and large group gatherings also reduces intergroup contact, which may then tend towards more prejudiced outgroup attitudes. While online interaction can go some way to mimicking these interaction norms, there are key differences. A sense of anonymity, and lack of in-person emotional cues, tends to support norms of polarisation and aggression in expressing differences of opinion online. And while online platforms have potential to provide intergroup contact, the tendency of much social media to form homogeneous ‘echo chambers’ can serve to further reduce intergroup contact. 30 31
Intimacy relates to the feeling of emotional connection and closeness with other human beings. Emotional connection, through romantic, friendship or familial relationships, fulfils a basic human need 32 and strongly benefits health, including reduced stress levels, improved mental health, lowered blood pressure and reduced risk of heart disease. 32 33 Intimacy can be fostered through familiarity, feeling understood and feeling accepted by close others. 34
Intimacy via companionship and closeness is fundamental to mental well-being. Positively, the COVID-19 pandemic has offered opportunities for individuals to (re)connect and (re)strengthen close relationships within their household via quality time together, following closure of many usual external social activities. Research suggests that the first full UK lockdown period led to a net gain in the quality of steady relationships at a population level, 35 but amplified existing inequalities in relationship quality. 35 36 For some in single-person households, the absence of a companion became more conspicuous, leading to feelings of loneliness and lower mental well-being. 37 38 Additional pandemic-related relational strain 39 40 resulted, for some, in the initiation or intensification of domestic abuse. 41 42
Physical touch is another key aspect of intimacy, a fundamental human need crucial in maintaining and developing intimacy within close relationships. 34 Restrictions on social interactions severely restricted the number and range of people with whom physical affection was possible. The reduction in opportunity to give and receive affectionate physical touch was not experienced equally. Many of those living alone found themselves completely without physical contact for extended periods. The deprivation of physical touch is evidenced to take a heavy emotional toll. 43 Even in future, once physical expressions of affection can resume, new levels of anxiety over germs may introduce hesitancy into previously fluent blending of physical and verbal intimate social connections. 44
The pandemic also led to shifts in practices and norms around sexual relationship building and maintenance, as individuals adapted and sought alternative ways of enacting sexual intimacy. This too is important, given that intimate sexual activity has known benefits for health. 45 46 Given that social restrictions hinged on reducing household mixing, possibilities for partnered sexual activity were primarily guided by living arrangements. While those in cohabiting relationships could potentially continue as before, those who were single or in non-cohabiting relationships generally had restricted opportunities to maintain their sexual relationships. Pornography consumption and digital partners were reported to increase since lockdown. 47 However, online interactions are qualitatively different from in-person interactions and do not provide the same opportunities for physical intimacy.
Recommendations and conclusions
In the sections above we have outlined the ways in which COVID-19 has impacted social relationships, showing how relational mechanisms key to health have been undermined. While some of the damage might well self-repair after the pandemic, there are opportunities inherent in deliberative efforts to build back in ways that facilitate greater resilience in social and community relationships. We conclude by making three recommendations: one regarding public health responses to the pandemic; and two regarding social recovery.
Recommendation 1: explicitly count the relational cost of public health policies to control the pandemic
Effective handling of a pandemic recognises that social, economic and health concerns are intricately interwoven. It is clear that future research and policy attention must focus on the social consequences. As described above, policies which restrict physical mixing across households carry heavy and unequal relational costs. These include for individuals (eg, loss of intimate touch), dyads (eg, loss of warmth, comfort), networks (eg, restricted access to support) and communities (eg, loss of cohesion and identity). Such costs—and their unequal impact—should not be ignored in short-term efforts to control an epidemic. Some public health responses—restrictions on international holiday travel and highly efficient test and trace systems—have relatively small relational costs and should be prioritised. At a national level, an earlier move to proportionate restrictions, and investment in effective test and trace systems, may help prevent escalation of spread to the point where a national lockdown or tight restrictions became an inevitability. Where policies with relational costs are unavoidable, close attention should be paid to the unequal relational impact for those whose personal circumstances differ from normative assumptions of two adult families. This includes consideration of whether expectations are fair (eg, for those who live alone), whether restrictions on social events are equitable across age group, religious/ethnic groupings and social class, and also to ensure that the language promoted by such policies (eg, households; families) is not exclusionary. 48 49 Forethought to unequal impacts on social relationships should thus be integral to the work of epidemic preparedness teams.
Recommendation 2: intelligently balance online and offline ways of relating
A key ingredient for well-being is ‘getting together’ in a physical sense. This is fundamental to a human need for intimate touch, physical comfort, reinforcing interactional norms and providing practical support. Emerging evidence suggests that online ways of relating cannot simply replace physical interactions. But online interaction has many benefits and for some it offers connections that did not exist previously. In particular, online platforms provide new forms of support for those unable to access offline services because of mobility issues (eg, older people) or because they are geographically isolated from their support community (eg, lesbian, gay, bisexual, transgender and queer (LGBTQ) youth). Ultimately, multiple forms of online and offline social interactions are required to meet the needs of varying groups of people (eg, LGBTQ, older people). Future research and practice should aim to establish ways of using offline and online support in complementary and even synergistic ways, rather than veering between them as social restrictions expand and contract. Intelligent balancing of online and offline ways of relating also pertains to future policies on home and flexible working. A decision to switch to wholesale or obligatory homeworking should consider the risk to relational ‘group properties’ of the workplace community and their impact on employees’ well-being, focusing in particular on unequal impacts (eg, new vs established employees). Intelligent blending of online and in-person working is required to achieve flexibility while also nurturing supportive networks at work. Intelligent balance also implies strategies to build digital literacy and minimise digital exclusion, as well as coproducing solutions with intended beneficiaries.
Recommendation 3: build stronger and sustainable localised communities
In balancing offline and online ways of interacting, there is opportunity to capitalise on the potential for more localised, coherent communities due to scaled-down travel, homeworking and local focus that will ideally continue after restrictions end. There are potential economic benefits after the pandemic, such as increased trade as home workers use local resources (eg, coffee shops), but also relational benefits from stronger relationships around the orbit of the home and neighbourhood. Experience from previous crises shows that community volunteer efforts generated early on will wane over time in the absence of deliberate work to maintain them. Adequately funded partnerships between local government, third sector and community groups are required to sustain community assets that began as a direct response to the pandemic. Such partnerships could work to secure green spaces and indoor (non-commercial) meeting spaces that promote community interaction. Green spaces in particular provide a triple benefit in encouraging physical activity and mental health, as well as facilitating social bonding. 50 In building local communities, small community networks—that allow for diversity and break down ingroup/outgroup views—may be more helpful than the concept of ‘support bubbles’, which are exclusionary and less sustainable in the longer term. Rigorously designed intervention and evaluation—taking a systems approach—will be crucial in ensuring scale-up and sustainability.
The dramatic change to social interaction necessitated by efforts to control the spread of COVID-19 created stark challenges but also opportunities. Our essay highlights opportunities for learning, both to ensure the equity and humanity of physical restrictions, and to sustain the salutogenic effects of social relationships going forward. The starting point for capitalising on this learning is recognition of the disruption to relational mechanisms as a key part of the socioeconomic and health impact of the pandemic. In recovery planning, a general rule is that what is good for decreasing health inequalities (such as expanding social protection and public services and pursuing green inclusive growth strategies) 4 will also benefit relationships and safeguard relational mechanisms for future generations. Putting this into action will require political will.
Ethics statements
Patient consent for publication.
Not required.
- Office for National Statistics (ONS)
- Ford T , et al
- Riordan R ,
- Ford J , et al
- Glonti K , et al
- McPherson JM ,
- Smith-Lovin L
- Granovetter MS
- Fancourt D et al
- Stadtfeld C
- Office for Civil Society
- Cook J et al
- Rodriguez-Llanes JM ,
- Guha-Sapir D
- Patulny R et al
- Granovetter M
- Winkeler M ,
- Filipp S-H ,
- Kaniasty K ,
- de Terte I ,
- Guilaran J , et al
- Wright KB ,
- Martin J et al
- Gabbiadini A ,
- Baldissarri C ,
- Durante F , et al
- Sommerlad A ,
- Marston L ,
- Huntley J , et al
- Turner RJ ,
- Bicchieri C
- Brennan G et al
- Watson-Jones RE ,
- Amichai-Hamburger Y ,
- McKenna KYA
- Page-Gould E ,
- Aron A , et al
- Pietromonaco PR ,
- Timmerman GM
- Bradbury-Jones C ,
- Mikocka-Walus A ,
- Klas A , et al
- Marshall L ,
- Steptoe A ,
- Stanley SM ,
- Campbell AM
- ↵ (ONS), O.f.N.S., Domestic abuse during the coronavirus (COVID-19) pandemic, England and Wales . Available: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/articles/domesticabuseduringthecoronaviruscovid19pandemicenglandandwales/november2020
- Rosenberg M ,
- Hensel D , et al
- Banerjee D ,
- Bruner DW , et al
- Bavel JJV ,
- Baicker K ,
- Boggio PS , et al
- van Barneveld K ,
- Quinlan M ,
- Kriesler P , et al
- Mitchell R ,
- de Vries S , et al
Twitter @karenmaxSPHSU, @Mark_McCann, @Rwilsonlowe, @KMitchinGlasgow
Contributors EL and KM led on the manuscript conceptualisation, review and editing. SP, KM, CB, RBP, RL, MM, JR, KS and RW-L contributed to drafting and revising the article. All authors assisted in revising the final draft.
Funding The research reported in this publication was supported by the Medical Research Council (MC_UU_00022/1, MC_UU_00022/3) and the Chief Scientist Office (SPHSU11, SPHSU14). EL is also supported by MRC Skills Development Fellowship Award (MR/S015078/1). KS and MM are also supported by a Medical Research Council Strategic Award (MC_PC_13027).
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Writing about COVID-19 in a college admission essay
by: Venkates Swaminathan | Updated: September 14, 2020
Print article

For students applying to college using the CommonApp, there are several different places where students and counselors can address the pandemic’s impact. The different sections have differing goals. You must understand how to use each section for its appropriate use.
The CommonApp COVID-19 question
First, the CommonApp this year has an additional question specifically about COVID-19 :
Community disruptions such as COVID-19 and natural disasters can have deep and long-lasting impacts. If you need it, this space is yours to describe those impacts. Colleges care about the effects on your health and well-being, safety, family circumstances, future plans, and education, including access to reliable technology and quiet study spaces. Please use this space to describe how these events have impacted you.
This question seeks to understand the adversity that students may have had to face due to the pandemic, the move to online education, or the shelter-in-place rules. You don’t have to answer this question if the impact on you wasn’t particularly severe. Some examples of things students should discuss include:
- The student or a family member had COVID-19 or suffered other illnesses due to confinement during the pandemic.
- The candidate had to deal with personal or family issues, such as abusive living situations or other safety concerns
- The student suffered from a lack of internet access and other online learning challenges.
- Students who dealt with problems registering for or taking standardized tests and AP exams.
Jeff Schiffman of the Tulane University admissions office has a blog about this section. He recommends students ask themselves several questions as they go about answering this section:
- Are my experiences different from others’?
- Are there noticeable changes on my transcript?
- Am I aware of my privilege?
- Am I specific? Am I explaining rather than complaining?
- Is this information being included elsewhere on my application?
If you do answer this section, be brief and to-the-point.
Counselor recommendations and school profiles
Second, counselors will, in their counselor forms and school profiles on the CommonApp, address how the school handled the pandemic and how it might have affected students, specifically as it relates to:
- Grading scales and policies
- Graduation requirements
- Instructional methods
- Schedules and course offerings
- Testing requirements
- Your academic calendar
- Other extenuating circumstances
Students don’t have to mention these matters in their application unless something unusual happened.
Writing about COVID-19 in your main essay
Write about your experiences during the pandemic in your main college essay if your experience is personal, relevant, and the most important thing to discuss in your college admission essay. That you had to stay home and study online isn’t sufficient, as millions of other students faced the same situation. But sometimes, it can be appropriate and helpful to write about something related to the pandemic in your essay. For example:
- One student developed a website for a local comic book store. The store might not have survived without the ability for people to order comic books online. The student had a long-standing relationship with the store, and it was an institution that created a community for students who otherwise felt left out.
- One student started a YouTube channel to help other students with academic subjects he was very familiar with and began tutoring others.
- Some students used their extra time that was the result of the stay-at-home orders to take online courses pursuing topics they are genuinely interested in or developing new interests, like a foreign language or music.
Experiences like this can be good topics for the CommonApp essay as long as they reflect something genuinely important about the student. For many students whose lives have been shaped by this pandemic, it can be a critical part of their college application.
Want more? Read 6 ways to improve a college essay , What the &%$! should I write about in my college essay , and Just how important is a college admissions essay? .
Homes Nearby
Homes for rent and sale near schools

How our schools are (and aren't) addressing race

The truth about homework in America

What should I write my college essay about?
What the #%@!& should I write about in my college essay?
Yes! Sign me up for updates relevant to my child's grade.
Please enter a valid email address
Thank you for signing up!
Server Issue: Please try again later. Sorry for the inconvenience
Persuasive Essay Guide
Persuasive Essay About Covid19
How to Write a Persuasive Essay About Covid19 | Examples & Tips
11 min read

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Persuasive Essay About Smoking - Making a Powerful Argument with Examples
Are you looking to write a persuasive essay about the Covid-19 pandemic?
Writing a compelling and informative essay about this global crisis can be challenging. It requires researching the latest information, understanding the facts, and presenting your argument persuasively.
But don’t worry! with some guidance from experts, you’ll be able to write an effective and persuasive essay about Covid-19.
In this blog post, we’ll outline the basics of writing a persuasive essay . We’ll provide clear examples, helpful tips, and essential information for crafting your own persuasive piece on Covid-19.
Read on to get started on your essay.
- 1. Steps to Write a Persuasive Essay About Covid-19
- 2. Examples of Persuasive Essay About Covid19
- 3. Examples of Persuasive Essay About Covid-19 Vaccine
- 4. Examples of Persuasive Essay About Covid-19 Integration
- 5. Examples of Argumentative Essay About Covid 19
- 6. Examples of Persuasive Speeches About Covid-19
- 7. Tips to Write a Persuasive Essay About Covid-19
- 8. Common Topics for a Persuasive Essay on COVID-19
Steps to Write a Persuasive Essay About Covid-19
Here are the steps to help you write a persuasive essay on this topic, along with an example essay:
Step 1: Choose a Specific Thesis Statement
Your thesis statement should clearly state your position on a specific aspect of COVID-19. It should be debatable and clear. For example:
Step 2: Research and Gather Information
Collect reliable and up-to-date information from reputable sources to support your thesis statement. This may include statistics, expert opinions, and scientific studies. For instance:
- COVID-19 vaccination effectiveness data
- Information on vaccine mandates in different countries
- Expert statements from health organizations like the WHO or CDC
Step 3: Outline Your Essay
Create a clear and organized outline to structure your essay. A persuasive essay typically follows this structure:
- Introduction
- Background Information
- Body Paragraphs (with supporting evidence)
- Counterarguments (addressing opposing views)
Step 4: Write the Introduction
In the introduction, grab your reader's attention and present your thesis statement. For example:
Step 5: Provide Background Information
Offer context and background information to help your readers understand the issue better. For instance:
Step 6: Develop Body Paragraphs
Each body paragraph should present a single point or piece of evidence that supports your thesis statement. Use clear topic sentences, evidence, and analysis. Here's an example:
Step 7: Address Counterarguments
Acknowledge opposing viewpoints and refute them with strong counterarguments. This demonstrates that you've considered different perspectives. For example:
Step 8: Write the Conclusion
Summarize your main points and restate your thesis statement in the conclusion. End with a strong call to action or thought-provoking statement. For instance:
Step 9: Revise and Proofread
Edit your essay for clarity, coherence, grammar, and spelling errors. Ensure that your argument flows logically.
Step 10: Cite Your Sources
Include proper citations and a bibliography page to give credit to your sources.
Remember to adjust your approach and arguments based on your target audience and the specific angle you want to take in your persuasive essay about COVID-19.
Paper Due? Why Suffer? That's our Job!
Examples of Persuasive Essay About Covid19
When writing a persuasive essay about the Covid-19 pandemic, it’s important to consider how you want to present your argument. To help you get started, here are some example essays for you to read:
Check out some more PDF examples below:
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
If you're in search of a compelling persuasive essay on business, don't miss out on our “ persuasive essay about business ” blog!
Examples of Persuasive Essay About Covid-19 Vaccine
Covid19 vaccines are one of the ways to prevent the spread of Covid-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your thoughts and persuading others.
A persuasive essay about the Covid-19 vaccine could consider the benefits of getting vaccinated as well as the potential side effects.
Below are some examples of persuasive essays on getting vaccinated for Covid-19.
Covid19 Vaccine Persuasive Essay
Persuasive Essay on Covid Vaccines
Interested in thought-provoking discussions on abortion? Read our persuasive essay about abortion blog to eplore arguments!
Examples of Persuasive Essay About Covid-19 Integration
Covid19 has drastically changed the way people interact in schools, markets, and workplaces. In short, it has affected all aspects of life. However, people have started to learn to live with Covid19.
Writing a persuasive essay about it shouldn't be stressful. Read the sample essay below to get idea for your own essay about Covid19 integration.
Persuasive Essay About Working From Home During Covid19
Searching for the topic of Online Education? Our persuasive essay about online education is a must-read.
Examples of Argumentative Essay About Covid 19
Covid-19 has been an ever-evolving issue, with new developments and discoveries being made on a daily basis.
Writing an argumentative essay about such an issue is both interesting and challenging. It allows you to evaluate different aspects of the pandemic, as well as consider potential solutions.
Here are some examples of argumentative essays on Covid19.
Argumentative Essay About Covid19 Sample
Argumentative Essay About Covid19 With Introduction Body and Conclusion
Looking for a persuasive take on the topic of smoking? You'll find it all related arguments in out Persuasive Essay About Smoking blog!
Examples of Persuasive Speeches About Covid-19
Do you need to prepare a speech about Covid19 and need examples? We have them for you!
Persuasive speeches about Covid-19 can provide the audience with valuable insights on how to best handle the pandemic. They can be used to advocate for specific changes in policies or simply raise awareness about the virus.
Check out some examples of persuasive speeches on Covid-19:
Persuasive Speech About Covid-19 Example
Persuasive Speech About Vaccine For Covid-19
You can also read persuasive essay examples on other topics to master your persuasive techniques!
Tips to Write a Persuasive Essay About Covid-19
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively.
Here are some tips to help you craft a compelling persuasive essay on this topic:
Choose a Specific Angle
Start by narrowing down your focus. COVID-19 is a broad topic, so selecting a specific aspect or issue related to it will make your essay more persuasive and manageable. For example, you could focus on vaccination, public health measures, the economic impact, or misinformation.
Provide Credible Sources
Support your arguments with credible sources such as scientific studies, government reports, and reputable news outlets. Reliable sources enhance the credibility of your essay.
Use Persuasive Language
Employ persuasive techniques, such as ethos (establishing credibility), pathos (appealing to emotions), and logos (using logic and evidence). Use vivid examples and anecdotes to make your points relatable.
Organize Your Essay
Structure your essay involves creating a persuasive essay outline and establishing a logical flow from one point to the next. Each paragraph should focus on a single point, and transitions between paragraphs should be smooth and logical.
Emphasize Benefits
Highlight the benefits of your proposed actions or viewpoints. Explain how your suggestions can improve public health, safety, or well-being. Make it clear why your audience should support your position.
Use Visuals -H3
Incorporate graphs, charts, and statistics when applicable. Visual aids can reinforce your arguments and make complex data more accessible to your readers.
Call to Action
End your essay with a strong call to action. Encourage your readers to take a specific step or consider your viewpoint. Make it clear what you want them to do or think after reading your essay.

Revise and Edit
Proofread your essay for grammar, spelling, and clarity. Make sure your arguments are well-structured and that your writing flows smoothly.
Seek Feedback
Have someone else read your essay to get feedback. They may offer valuable insights and help you identify areas where your persuasive techniques can be improved.
Tough Essay Due? Hire Tough Writers!
Common Topics for a Persuasive Essay on COVID-19
Here are some persuasive essay topics on COVID-19:
- The Importance of Vaccination Mandates for COVID-19 Control
- Balancing Public Health and Personal Freedom During a Pandemic
- The Economic Impact of Lockdowns vs. Public Health Benefits
- The Role of Misinformation in Fueling Vaccine Hesitancy
- Remote Learning vs. In-Person Education: What's Best for Students?
- The Ethics of Vaccine Distribution: Prioritizing Vulnerable Populations
- The Mental Health Crisis Amidst the COVID-19 Pandemic
- The Long-Term Effects of COVID-19 on Healthcare Systems
- Global Cooperation vs. Vaccine Nationalism in Fighting the Pandemic
- The Future of Telemedicine: Expanding Healthcare Access Post-COVID-19
In search of more inspiring topics for your next persuasive essay? Our persuasive essay topics blog has plenty of ideas!
To sum it up,
You have read good sample essays and got some helpful tips. You now have the tools you needed to write a persuasive essay about Covid-19. So don't let the doubts stop you, start writing!
If you need professional writing help, don't worry! We've got that for you as well.
MyPerfectWords.com is a professional persuasive essay writing service that can help you craft an excellent persuasive essay on Covid-19. Our experienced essay writer will create a well-structured, insightful paper in no time!
So don't hesitate and place your ' write my essay online ' request today!
Frequently Asked Questions
Are there any ethical considerations when writing a persuasive essay about covid-19.
Yes, there are ethical considerations when writing a persuasive essay about COVID-19. It's essential to ensure the information is accurate, not contribute to misinformation, and be sensitive to the pandemic's impact on individuals and communities. Additionally, respecting diverse viewpoints and emphasizing public health benefits can promote ethical communication.
What impact does COVID-19 have on society?
The impact of COVID-19 on society is far-reaching. It has led to job and economic losses, an increase in stress and mental health disorders, and changes in education systems. It has also had a negative effect on social interactions, as people have been asked to limit their contact with others.

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading


30,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- School Education /
Essay On Covid-19: 100, 200 and 300 Words

- Updated on
- Apr 30, 2024

COVID-19, also known as the Coronavirus, is a global pandemic that has affected people all around the world. It first emerged in a lab in Wuhan, China, in late 2019 and quickly spread to countries around the world. This virus was reportedly caused by SARS-CoV-2. Since then, it has spread rapidly to many countries, causing widespread illness and impacting our lives in numerous ways. This blog talks about the details of this virus and also drafts an essay on COVID-19 in 100, 200 and 300 words for students and professionals.
Table of Contents
- 1 Essay On COVID-19 in English 100 Words
- 2 Essay On COVID-19 in 200 Words
- 3 Essay On COVID-19 in 300 Words
- 4 Short Essay on Covid-19
Essay On COVID-19 in English 100 Words
COVID-19, also known as the coronavirus, is a global pandemic. It started in late 2019 and has affected people all around the world. The virus spreads very quickly through someone’s sneeze and respiratory issues.
COVID-19 has had a significant impact on our lives, with lockdowns, travel restrictions, and changes in daily routines. To prevent the spread of COVID-19, we should wear masks, practice social distancing, and wash our hands frequently.
People should follow social distancing and other safety guidelines and also learn the tricks to be safe stay healthy and work the whole challenging time.
Also Read: National Safe Motherhood Day 2023
Essay On COVID-19 in 200 Words
COVID-19 also known as coronavirus, became a global health crisis in early 2020 and impacted mankind around the world. This virus is said to have originated in Wuhan, China in late 2019. It belongs to the coronavirus family and causes flu-like symptoms. It impacted the healthcare systems, economies and the daily lives of people all over the world.
The most crucial aspect of COVID-19 is its highly spreadable nature. It is a communicable disease that spreads through various means such as coughs from infected persons, sneezes and communication. Due to its easy transmission leading to its outbreaks, there were many measures taken by the government from all over the world such as Lockdowns, Social Distancing, and wearing masks.
There are many changes throughout the economic systems, and also in daily routines. Other measures such as schools opting for Online schooling, Remote work options available and restrictions on travel throughout the country and internationally. Subsequently, to cure and top its outbreak, the government started its vaccine campaigns, and other preventive measures.
In conclusion, COVID-19 tested the patience and resilience of the mankind. This pandemic has taught people the importance of patience, effort and humbleness.
Also Read : Essay on My Best Friend
Essay On COVID-19 in 300 Words
COVID-19, also known as the coronavirus, is a serious and contagious disease that has affected people worldwide. It was first discovered in late 2019 in Cina and then got spread in the whole world. It had a major impact on people’s life, their school, work and daily lives.
COVID-19 is primarily transmitted from person to person through respiratory droplets produced and through sneezes, and coughs of an infected person. It can spread to thousands of people because of its highly contagious nature. To cure the widespread of this virus, there are thousands of steps taken by the people and the government.
Wearing masks is one of the essential precautions to prevent the virus from spreading. Social distancing is another vital practice, which involves maintaining a safe distance from others to minimize close contact.
Very frequent handwashing is also very important to stop the spread of this virus. Proper hand hygiene can help remove any potential virus particles from our hands, reducing the risk of infection.
In conclusion, the Coronavirus has changed people’s perspective on living. It has also changed people’s way of interacting and how to live. To deal with this virus, it is very important to follow the important guidelines such as masks, social distancing and techniques to wash your hands. Getting vaccinated is also very important to go back to normal life and cure this virus completely.
Also Read: Essay on Abortion in English in 650 Words
Short Essay on Covid-19
Please find below a sample of a short essay on Covid-19 for school students:
Also Read: Essay on Women’s Day in 200 and 500 words
to write an essay on COVID-19, understand your word limit and make sure to cover all the stages and symptoms of this disease. You need to highlight all the challenges and impacts of COVID-19. Do not forget to conclude your essay with positive precautionary measures.
Writing an essay on COVID-19 in 200 words requires you to cover all the challenges, impacts and precautions of this disease. You don’t need to describe all of these factors in brief, but make sure to add as many options as your word limit allows.
The full form for COVID-19 is Corona Virus Disease of 2019.
Related Reads
Hence, we hope that this blog has assisted you in comprehending with an essay on COVID-19. For more information on such interesting topics, visit our essay writing page and follow Leverage Edu.
Simran Popli
An avid writer and a creative person. With an experience of 1.5 years content writing, Simran has worked with different areas. From medical to working in a marketing agency with different clients to Ed-tech company, the journey has been diverse. Creative, vivacious and patient are the words that describe her personality.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
30,000+ students realised their study abroad dream with us. Take the first step today.

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out
- Open access
- Published: 04 February 2022
Analysis of the COVID-19 pandemic: lessons towards a more effective response to public health emergencies
- Yibeltal Assefa ORCID: orcid.org/0000-0003-2393-1492 1 ,
- Charles F. Gilks 1 ,
- Simon Reid 1 ,
- Remco van de Pas 2 ,
- Dereje Gedle Gete 1 &
- Wim Van Damme 2
Globalization and Health volume 18 , Article number: 10 ( 2022 ) Cite this article
39k Accesses
36 Citations
10 Altmetric
Metrics details
The pandemic of Coronavirus Disease 2019 (COVID-19) is a timely reminder of the nature and impact of Public Health Emergencies of International Concern. As of 12 January 2022, there were over 314 million cases and over 5.5 million deaths notified since the start of the pandemic. The COVID-19 pandemic takes variable shapes and forms, in terms of cases and deaths, in different regions and countries of the world. The objective of this study is to analyse the variable expression of COVID-19 pandemic so that lessons can be learned towards an effective public health emergency response.
We conducted a mixed-methods study to understand the heterogeneity of cases and deaths due to the COVID-19 pandemic. Correlation analysis and scatter plot were employed for the quantitative data. We used Spearman’s correlation analysis to determine relationship strength between cases and deaths and socio-economic and health systems. We organized qualitative information from the literature and conducted a thematic analysis to recognize patterns of cases and deaths and explain the findings from the quantitative data.
We have found that regions and countries with high human development index have higher cases and deaths per million population due to COVID-19. This is due to international connectedness and mobility of their population related to trade and tourism, and their vulnerability related to older populations and higher rates of non-communicable diseases. We have also identified that the burden of the pandemic is also variable among high- and middle-income countries due to differences in the governance of the pandemic, fragmentation of health systems, and socio-economic inequities.
The COVID-19 pandemic demonstrates that every country remains vulnerable to public health emergencies. The aspiration towards a healthier and safer society requires that countries develop and implement a coherent and context-specific national strategy, improve governance of public health emergencies, build the capacity of their (public) health systems, minimize fragmentation, and tackle upstream structural issues, including socio-economic inequities. This is possible through a primary health care approach, which ensures provision of universal and equitable promotive, preventive and curative services, through whole-of-government and whole-of-society approaches.
The pandemic of Coronavirus Disease 2019 (COVID-19) is a timely reminder of the nature and impact of emerging infectious diseases that become Public Health Emergency of International Concern (PHEIC) [ 1 ]. The COVID-19 pandemic takes variable shapes and forms in how it affects communities in different regions and countries [ 2 , 3 ]. As of 12 January, 2022, there were over 314 million cases and over 5.5 million deaths notified around the globe since the start of the pandemic. The number of cases per million population ranged from 7410 in Africa to 131,730 in Europe while the number of deaths per million population ranged from 110 in Oceania to 2740 in South America. Case-fatality rates (CFRs) ranged from 0.3% in Oceania to 2.9% in South America [ 4 , 5 ]. Regions and countries with high human development index (HDI), which is a composite index of life expectancy, education, and per capita income indicators [ 6 ], are affected by COVID-19 more than regions with low HDI. North America and Europe together account for 55 and 51% of cases and deaths, respectively. Regions with high HDI are affected by COVID-19 despite their high universal health coverage index (UHCI) and Global Health Security index (GHSI) [ 7 ].
This seems to be a paradox (against the established knowledge that countries with weak (public) health systems capacity will have worse health outcomes) in that the countries with higher UHCI and GHSI have experienced higher burdens of COVID-19 [ 7 ]. The paradox can partially be explained by variations in testing algorithms, capacity for testing, and reporting across different countries. Countries with high HDI have health systems with a high testing capacity; the average testing rate per million population is less than 32, 000 in Africa and 160,000 in Asia while it is more than 800, 000 in HICs (Europe and North America). This enables HICs to identify more confirmed cases that will ostensibly increase the number of reported cases [ 3 ]. Nevertheless, these are insufficient to explain the stark differences between countries with high HDI and those with low HDI. Many countries with high HDI have a high testing rate and a higher proportion of symptomatic and severe cases, which are also associated with higher deaths and CFRs [ 7 ]. On the other hand, there are countries with high HDI that sustain a lower level of the epidemic than others with a similar high HDI. It is, therefore, vital to analyse the heterogeneity of the COVID-19 pandemic and explain why some countries with high HDI, UHCI and GHSI have the highest burden of COVID-19 while others are able to suppress their epidemics and mitigate its impacts.
The objective of this study was to analyse the COVID-19 pandemic and understand its variable expression with the intention to learn lessons for an effective and sustainable response to public health emergencies. We hypothesised that high levels of HDI, UHCI and GHSI are essential but not sufficient to prevent and control COVID-19.
We conducted an explanatory mixed-methods study to understand and explain the heterogeneity of the pandemic around the world. The study integrated quantitative and qualitative secondary data. The following steps were included in the research process: (i) collecting and analysing quantitative epidemiological data, (ii) conducting literature review of qualitative secondary data and (iii) evaluating countries’ pandemic responses to explain the variability in the COVID-19 epidemiological outcomes. The study then illuminated specific factors that were vital towards an effective and sustainable epidemic response.
We used the publicly available secondary data sources from Johns Hopkins University ( https://coronavirus.jhu.edu/data/new-cases ) for COVID-19 and UNDP 2020 HDI report ( http://hdr.undp.org/en/2019-report ) for HDI, demographic and epidemiologic variables. These are open data sources which are regularly updated and utilized by researchers, policy makers and funders. We performed a correlation analysis of the COVID-19 pandemic. We determined the association between COVID-19 cases, severity, deaths and CFRs at the 0.01 and 0.05 levels (2-tailed). We used Spearman’s correlation analysis, as there is no normal distribution of the variables [ 8 ].
The UHCI is calculated as the geometric mean of the coverage of essential services based on 17 tracer indicators from: (1) reproductive, maternal, newborn and child health; (2) infectious diseases; (3) non-communicable diseases; and, (4) service capacity and access and health security [ 9 ]. The GHSI is a composite measure to assess a country’s capability to prevent, detect, and respond to epidemics and pandemics [ 10 ].
We then conducted a document review to explain the epidemic patterns in different countries. Secondary data was obtained from peer-reviewed journals, reputable online news outlets, government reports and publications by public health-related associations, such as the WHO. To explain the variability of COVID-19 across countries, a list of 14 indicators was established to systematically assess country’s preparedness, actual pandemic response, and overall socioeconomic and demographic profile in the context of COVID-19. The indicators used in this study include: 1) Universal Health Coverage Index, 2) public health capacity, 3) Global Health Security Index, 4) International Health Regulation, 5) leadership, governance and coordination of response, 6) community mobilization and engagement, 7) communication, 8) testing, quarantines and social distancing, 9) medical services at primary health care facilities and hospitals, 10) multisectoral actions, 11) social protection services, 12) absolute and relative poverty status, 13) demography, and 14) burden of communicable and non-communicable diseases. These indicators are based on our previous studies and recommendation from the World Health Organization [ 3 , 4 ]. We conducted thematic analysis and synthesis to identify the factors that may explain the heterogeneity of the pandemic.
Heterogeneity of COVID-19 cases and deaths around the world: what can explain it?
Table 1 indicates that the pandemic of COVID-19 is heterogeneous around regions of the world. Figure 1 also shows that there is a strong and significant correlation between HDI and globalisation (with an increase in trade and tourism as proxy indicators) and a corresponding strong and significant correlation with COVID-19 burden.
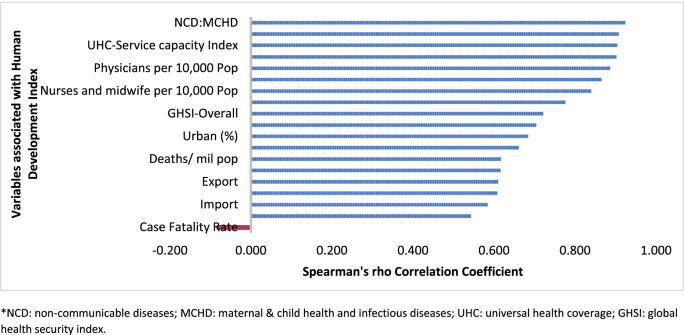
Human development index and its correlates associated with COVID-19 in 189 countries*
Globalisation and pandemics interact in various ways, including through international trade and mobility, which can lead to multiple waves of infections [ 11 ]. In at least the first waves of the pandemic, countries with high import and export of consumer goods, food products and tourism have high number of cases, severe cases, deaths and CFRs. Countries with high HDI are at a higher risk of importing (and exporting) COVID-19 due to high mobility linked to trade and tourism, which are drivers of the economy. These may have led to multiple introductions of COVID-19 into these countries before border closures.
The COVID-19 pandemic was first identified in China, which is central to the global network of trade, from where it spread to all parts of the world, especially those countries with strong links with China [ 12 ]. The epidemic then spread to Europe. There is very strong regional dimension to manufacturing and trading, which could be facilitate the spread of the virus. China is the heart of ‘Factory Asia’; Italy is in the heart of ‘Factory Europe’; the United States is the heart of ‘Factory North America’; and Brazil is the heart of ‘Factory Latin America’ [ 13 ]. These are the countries most affected by COVID-19 during the first wave of the pandemic [ 2 , 3 , 14 ].
It is also important to note that two-third of the countries currently reporting more than a million cases are middle-income countries (MICs), which are not only major emerging market economies but also regional political powers, including the BRICS countries (Brazil, Russia, India and South Africa) [ 3 , 15 ]. These countries participate in the global economy, with business travellers and tourists. They also have good domestic transportation networks that facilitate the internal spread of the virus. The strategies that helped these countries to become emerging markets also put them at greater risk for importing and spreading COVID-19 due to their connectivity to the rest of the world.
In addition, countries with high HDI may be more significantly impacted by COVID-19 due to the higher proportion of the elderly and higher rates of non-communicable diseases. Figure 1 shows that there is a strong and significant correlation between HDI and demographic transition (high proportion of old-age population) and epidemiologic transition (high proportion of the population with non-communicable diseases). Countries with a higher proportion of people older than 65 years and NCDs (compared to communicable diseases) have higher burden of COVID-19 [ 16 , 17 , 18 , 19 , 20 ]. Evidence has consistently shown a higher risk of severe COVID-19 in older individuals and those with underlying health conditions [ 21 , 22 , 23 , 24 , 25 ]. CFR is age-dependent; it is highest in persons aged ≥85 years (10 to 27%), followed by those among persons aged 65–84 years (3 to 11%), and those among persons aged 55-64 years (1 to 3%) [ 26 ].
On the other hand, regions and countries with low HDI have, to date, experienced less severe epidemics. For instance, as of January 12, 2022, the African region has recorded about 10.3 million cases and 233,000 deaths– far lower than other regions of the world (Table 1 ) [ 27 ]. These might be due to lower testing rates in Africa, where only 6.5% of the population has been tested for the virus [ 14 , 28 ], and a greater proportion of infections may remain asymptomatic [ 29 ]. Indeed, the results from sero-surveys in Africa show that more than 80% of people infected with the virus were asymptomatic compared to an estimated 40-50% asymptomatic infections in HICs [ 30 , 31 ]. Moreover, there is a weak vital registration system in the region indicating that reports might be underestimating and underreporting the disease burden [ 32 ]. However, does this fully explain the differences observed between Africa and Europe or the Americas?
Other possible factors that may explain the lower rates of cases and deaths in Africa include: (1) Africa is less internationally connected than other regions; (2) the imposition of early strict lockdowns in many African countries, at a time when case numbers were relatively small, limited the number of imported cases further [ 2 , 33 , 34 ]; (3) relatively poor road network has also limited the transmission of the virus to and in rural areas [ 35 ]; (4) a significant proportion of the population resides in rural areas while those in urban areas spend a lot of their time mostly outdoors; (5) only about 3% of Africans are over the age of 65 (so only a small proportion are at risk of severe COVID-19) [ 36 ]; (6) lower prevalence of NCDs, as disease burden in Africa comes from infectious causes, including coronaviruses, which may also have cross-immunity that may reduce the risk of developing symptomatic cases [ 37 ]; and (7) relative high temperature (a major source of vitamin D which influences COVID-19 infection and mortality) in the region may limit the spread of the virus [ 38 , 39 ]. We argue that a combination of all these factors might explain the lower COVID-19 burden in Africa.
The early and timely efforts by African leaders should not be underestimated. The African Union, African CDC, and WHO convened an emergency meeting of all African ministers of health to establish an African taskforce to develop and implement a coordinated continent-wide strategy focusing on: laboratory; surveillance; infection prevention and control; clinical treatment of people with severe COVID-19; risk communication; and supply chain management [ 40 ]. In April 2021, African Union and Africa CDC launched the Partnerships for African Vaccine Manufacturing (PAVM), framework to expanding Africa’s vaccine manufacturing capacity for health security [ 41 ].
Heterogeneity of the pandemic among countries with high HDI: what can explain it?
Figures 2 and 3 illustrate the variability of cases and deaths due to the COVID-19 pandemic across high-income countries (HICs). Contrary to the overall positive correlation between high HDI and cases, deaths and fatality rates due to COVID-19, there are outlier HICs, which have been able to control the epidemic. Several HICs, such as New Zealand, Australia, South Korea, Japan, Denmark, Iceland, and Norway, managed to contain their epidemics (Figs. 2 and 3 ) [ 15 , 42 , 43 ]. It is important to note that most of these countries (especially the island states) have far less cross-border mobility than other HICs.
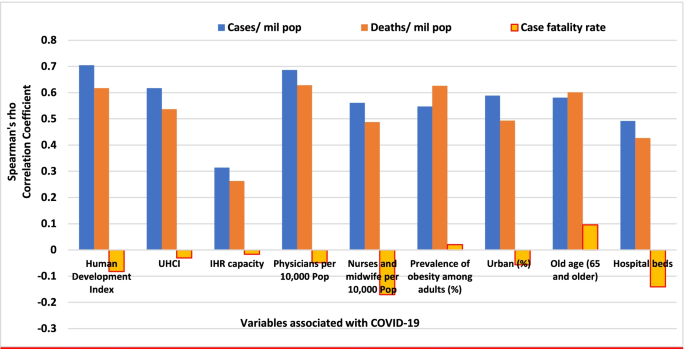
Scatter plot of COVID-19 cases per million population in countries with high human development index (> 0.70)
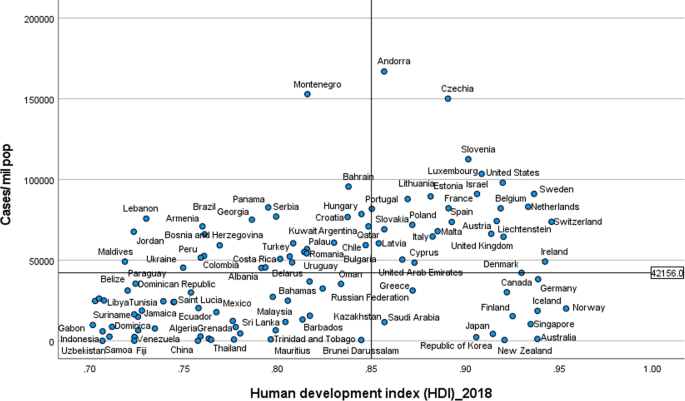
Scatter plot of COVID-19 deaths per million population in countries with high human development index (> 0.70)
HICs that have been successful at controlling their epidemics have similar characteristics, which are related to governance of the response [ 44 ], synergy between UHC and GHS, and existing relative socio-economic equity in the country. Governance and leadership is a crucial factor to explain the heterogeneity of the epidemic among countries with high HDI [ 45 ]. There has been substantial variation in the nature and timing of the public health responses implemented [ 46 ]. Adaptable and agile governments seem better able to respond to their epidemics [ 47 , 48 ]. Countries that have fared the best are the ones with good governance and public support [ 49 ]. Countries with an absence of coherent leadership and social trust have worse outcomes than countries with collective action, whether in a democracy or autocracy, and rapid mobilisation of resources [ 50 ]. The erosion of trust in the United States government has hurt the country’s ability to respond to the COVID-19 crisis [ 51 , 52 ]. The editors of the New England Journal of Medicine argued that the COVID-19 crisis has produced a test of leadership; but, the leaders in the United States had failed that test [ 47 ].
COVID-19 has exposed the fragility of health systems, not only in the public health and primary care, but also in acute and long-term care systems [ 49 ]. Fragmentation of health systems, defined here to mean inadequate synergy and/ or integration between GHS and UHC, is typical of countries most affected by the COVID-19 pandemic. Even though GHS and UHC agendas are convergent and interdependent, they tend to have different policies and practices [ 53 ]. The United States has the highest index for GHS preparedness; however, it has reported the world’s highest number of COVID-19 cases and deaths due to its greatly fragmented health system [ 54 , 55 ]. Countries with health systems and policies that are able to integrate International Health Regulations (IHR) core capacities with primary health care (PHC) services have been effective at mitigating the effects of COVID-19 [ 50 , 53 ]. Australia has been able to control its COVID-19 epidemic through a comprehensive primary care response, including protection of vulnerable people, provision of treatment and support services to affected people, continuity of regular healthcare services, protection and support of PHC workers and primary care services, and provision of mental health services to the community and the primary healthcare workforce [ 56 ]. Strict implementation of public health and social intervention together with UHC systems have ensured swift control of the epidemics in Singapore, South Korea, and Thailand [ 57 ].
The heterogeneity of cases and deaths, due to COVID-19, is also explained by differences in levels of socio-economic inequalities, which increase susceptibility to acquiring the infection and disease progression as well as worsening of health outcomes [ 58 ]. COVID-19 has been a stress test for public services and social protection systems. There is a higher burden of COVID-19 in Black, Asian and Minority Ethnic individuals due to socio-economic inequities in HICs [ 59 , 60 ]. Poor people are more likely to live in overcrowded accommodation, are more likely to have unstable work conditions and incomes, have comorbidities associated with poverty and precarious living conditions, and reduced access to health care [ 59 ].
The epidemiology of COVID-19 is also variable across MICs, with HDI between 0.70 and 0.85, around the world. Overall, the epidemic in MICs is exacerbated by the rapid demographic and epidemiologic transitions as well as high prevalence of obesity. While India and Brazil witnessed rapidly increasing rates of cases and deaths, China, Thailand, Vietnam have experienced a relatively lower disease burden [ 15 ]. This heterogeneity may be attributed to a number of factors, including governance, communication and service delivery. Thailand, China and Vietnam have implemented a national harmonized strategic response with decentralized implementation through provincial and district authorities [ 61 ]. Thailand increased its testing capacity from two to over 200 certified facilities that could process between 10,000 to 100,000 tests per day; moreover, over a million village health volunteers in Thailand supported primary health services [ 62 , 63 ]. China’s swift and decisive actions enabled the country to contain its epidemic though there was an initial delay in detecting the disease. China has been able to contain its epidemic through community-based measures, very high public cooperation and social mobilization, strategic lockdown and isolation, multi-sector action [ 64 ]. Overall, multi-level governance (effective and decisive leadership and accountability) of the response, together with coordination of public health and socio-economic services, and high levels of citizen adherence to personal protection, have enabled these countries to successfully contain their epidemics [ 61 , 65 , 66 ].
On the other hand, the Brazilian leadership was denounced for its failure to establish a national surveillance network early in the pandemic. In March 2020, the health minister was reported to have stated that mass testing was a waste of public funding, and to have advised against it [ 67 ]. This was considered as a sign of a collapse of public health leadership, characterized by ignorance, neoliberal authoritarianism [ 68 ]. There were also gaps in the public health capacity in different municipalities, which varied greatly, with a considerable number of Brazilian regions receiving less funding from the federal government due to political tension [ 69 ]. The epidemic has a disproportionate adverse burden on states and municipalities with high socio-economic vulnerability, exacerbated by the deep social and economic inequalities in Brazil [ 70 ].
India is another middle-income country with a high burden of COVID-19. It was one of the countries to institute strict measures in the early phase of the pandemic [ 71 , 72 ]. However, the government eased restrictions after the claim that India had beaten the pandemic, which lead to a rapid increase in disease incidence. Indeed, on 12 January 2022, India reported 36 million cumulative cases and almost 485,000 total deaths [ 15 ]. The second wave of the epidemic in India exposed weaknesses in governance and inadequacies in the country’s health and other social systems [ 73 ]. The nature of the Indian federation, which is highly centripetal, has prevented state and local governments from tailoring a policy response to suit local needs. A centralized one-size-fits-all strategy has been imposed despite high variations in resources, health systems capacity, and COVID-19 epidemics across states [ 74 ]. There were also loose social distancing and mask wearing, mass political rallies and religious events [ 75 ]. Rapid community transmission driven by high population density and multigenerational households has been a feature of the current wave in India [ 76 ]. In addition, several new variants of the virus, including the UK (B.1.1.7), the South Africa (20H/501Y or B.1.351), and Brazil (P.1), alongside a newly identified Indian variant (B.1.617), are circulating in India and have been implicated as factors in the second wave of the pandemic [ 75 , 76 ].
Heterogeneity of case-fatality rates around the world: what can explain it?
The pandemic is characterized by variable CFRs across regions and countries that are negatively associated with HDI (Fig. 1 ). The results presented in Fig. 4 show that the proportion of elderly population and rate of obesity are important factors which are positively associated with CFR. On the other hand, UHC, IHR capacity and other indicators of health systems capacity (health workforce density and hospital beds) are negatively associated with the CFR (Figs. 1 and 4 ).
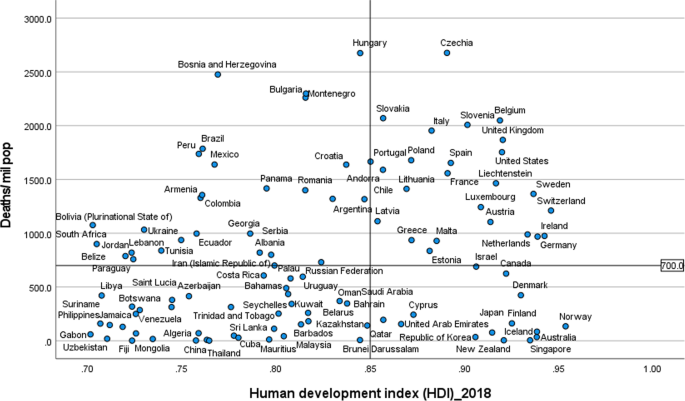
Correlates of COVID-19 cases, deaths and case-fatality rates in 189 countries
The evidence from several research indicates that heterogeneity can be explained by several factors, including differences in age-pyramid, socio-economic status, access to health services, or rates of undiagnosed infections. Differences in age-pyramid may explain some of the observed variation in epidemic severity and CFR between countries [ 77 ]. CFRs across countries look similar when taking age into account [ 78 ]. The elderly and other vulnerable populations in Africa and Asia are at a similar risk as populations in Europe and Americas [ 79 ]. Data from European countries suggest that as high as 57% of all deaths have happened in care homes and many deaths in the US have also occurred in nursing homes. On the other hand, in countries such as Mexico and India, individuals < 65 years contributed the majority of deaths [ 80 ].
Nevertheless, CFR also depends on the quality of hospital care, which can be used to judge the health system capacity, including the availability of healthcare workers, resources, and facilities, which affects outcomes [ 81 ]. The CFR can increase if there is a surge of infected patients, which adds to the strain on the health system [ 82 ]. COVID-19 fatality rates are affected by numerous health systems factors, including bed capacity, existence and capacity of intensive care unit (ICU), and critical care resources (such as oxygen and dexamethasone) in a hospital. Regions and countries with high HDI have a greater number of acute care facilities, ICU, and hospital bed capacities compared to lower HDI regions and countries [ 83 ]. Differences in health systems capacity could explain why North America and Europe, which have experienced much greater number of cases and deaths per million population, reported lower CFRs than the Southern American and the African regions, partly also due to limited testing capacity in these regions (Table 1 ) [ 84 , 85 , 86 ]. The higher CFR in Southern America can be explained by the relatively lower health systems surge capacity that could not adequately respond to the huge demand for health services [ 69 , 86 ]. The COVID-19 pandemic has highlighted existing health systems’ weaknesses, which are not able to effectively prepare for and respond to PHEs [ 87 ]. The high CFRs in the region are also exacerbated by the high social inequalities [ 69 ].
On the other hand, countries in Asia recorded lower CFRs (~ 1.4%) despite sharing many common risk factors (including overcrowding and poverty, weak health system capacity etc) with Africa. The Asian region shares many similar protective factors to the African region. They have been able to minimize their CFR by suppressing the transmission of the virus and flattening the epidemic curve of COVID-19 cases and deaths. Nevertheless, the epidemic in India is likely to be different because it has exceeded the health system capacity to respond and provide basic medical care and medical supplies such as oxygen [ 88 ]. Overall, many Asian countries were able to withstand the transmission of the virus and its effect due to swift action by governments in the early days of the pandemic despite the frequency of travel between China and neighbouring countries such as Hong Kong, Taiwan and Singapore [ 89 ]. This has helped them to contain the pandemic to ensure case numbers remain within their health systems capacity. These countries have benefited from their experience in the past in the prevention and control of epidemics [ 90 ].
There are a number of issues with the use of the CFR to compare the management of the pandemic between countries and regions [ 91 ], as it does not depict the true picture of the mortality burden of the pandemic. A major challenge with accurate calculation of the CFR is the denominator on number of identified cases, as asymptomatic infections and patients with mild symptoms are frequently left untested, and therefore omitted from CFR calculations. Testing might not be widely available, and proactive contact tracing and containment might not be employed, resulting in a smaller denominator, and skewing to a higher CFR [ 82 ]. It is, therefore, far more relevant to estimate infection fatality rate (IFR), the proportion of all infected individuals who have died due to the infection [ 91 ], which is central to understanding the public health impact of the pandemic and the required policies for its prevention and control [ 92 ].
Estimates of prevalence based on sero-surveys, which includes asymptomatic and mildly symptomatic infections, can be used to estimate IFR [ 93 ]. In a systematic review of 17 studies, seroprevalence rates ranged from 0.22% in Brazil to 53% in Argentina [ 94 ]. The review also identified that the seroprevalence estimate was higher than the cumulative reported case incidence, by a factor between 1.5 times in Germany to 717 times in Iran, in all but two studies (0.56 times in Brazil and 0.88 times in Denmark) [ 94 , 95 ]. The difference between seroprevalence and cumulative reported cases might be due to asymptomatic cases, atypical or pauci-symptomatic cases, or the lack of access to and uptake of testing [ 94 ]. There is only a modest gap between the estimated number of infections from seroprevalence surveys and the cumulative reported cases in regions with relatively thorough symptom-based testing. Much of the gap between reported cases and seroprevalence is likely to be due to undiagnosed symptomatic or asymptomatic infections [ 94 ].
Collateral effects of the COVID-19 pandemic
It is important to note that the pandemic has significant collateral effects on the provision of essential health services, in addition to the direct health effects [ 96 ]. Disruptions in the provision of essential health services, due to COVID-19, were reported by nearly all countries, though it is more so in lower-income than higher-income countries [ 97 , 98 ]. The biggest impact reported is on provision of day-to-day primary care to prevent and manage some of the most common health problems [ 99 ].
The causes of disruptions in service delivery were a mix of demand and supply factors [ 100 ]. Countries reported that just over one-third of services were disrupted due to health workforce-related reasons (the most common causes of service disruptions), supply chains, community mistrust and fears of becoming infected, and financial challenge s[ 101 ]. Cognizant of the disruptive effects of the pandemic, countries have reorganized their health system.
Countries with better response to COVID-19 have mobilized, trained and reallocated their health workforce in addition to hiring new staff, using volunteers and medical trainees and mobilizing retirees [ 102 ]. Several strategies have also been implemented to mitigate disruptions in service delivery and utilization, including: triaging to identify the most urgent patient needs, and postponing elective medical procedures; switching to alternative models of care, such as providing more home-based care and telemedicine [ 101 ].
This study identifies that the COVID-19 pandemic, in terms f cases and deaths, is heterogeneous around the world. This variability is explained by differences in vulnerability, preparedness, and response. It confirms that a high level of HDI, UHCI and GHSI are essential but not sufficient to control epidemics [ 103 ]. An effective response to public health emergencies requires a joint and reinforcing implementation of UHC, health emergency and disease control priorities [ 104 , 105 ], as well as good governance and social protection systems [ 106 ]. Important lessons have been learned to cope better with the COVID-19 pandemic and future emerging or re-emerging pandemics. Countries should strengthen health systems, minimize fragmentation of public health, primary care and secondary care, and improve coordination with other sectors. The pandemic has exposed the health effects of longstanding social inequities, which should be addressed through policies and actions to tackle vulnerability in living and working conditions [ 106 ].
The shift in the pandemic epicentre from high-income to MICs was observed in the second global wave of the pandemic. This is due to in part to the large-scale provision of vaccines in HICs [ 15 ] as well as the limitations in the response in LMICs, including inadequate testing, quarantine and isolation, contact tracing, and social distancing. The second wave of the pandemic in low- and middle-income countries spread more rapidly than the first wave and affected younger and healthier populations due to factors, including poor government decision making, citizen behaviour, and the emergence of highly transmissible SARS-CoV-2 variants [ 107 ]. It has become catastrophic in some MICs to prematurely relax key public health measures, such as mask wearing, physical distancing, and hand hygiene [ 108 ].
There is consensus that global vaccination is essential to ending the pandemic. Universal and equitable vaccine delivery, implemented with high volume, speed and quality, is vital for an effective and sustainable response to the current pandemic and future public health emergencies. There is, however, ongoing concern regarding access to COVID-19 vaccines in low-income countries [ 109 ]. Moreover, there is shortage of essential supplies, including oxygen, which has had a major impact on the prevention and control of the pandemic. It is, therefore, vital to transform (through good governance and financing mechanisms) the ACT-A platform to deliver vaccines, therapeutics, diagnostics, and other essential supplies [ 109 , 110 ]. The global health community has the responsibility to address these inequalities so that we can collectively end the pandemic [ 107 ].
The Omicron variant has a huge role in the current wave around the world despite high vaccine coverage [ 111 ]. Omicron appears to spread rapidly around the world ever since it was identified in November 2021 [ 112 ]. It becomes obvious that vaccination alone is inadequate for controlling the infection. This has changed our understanding of the COVID-19 pandemic endgame. The emergence of new variants of concern and their spread around the world has highlighted the importance of combination prevention, including high vaccination coverage in combination with other public health prevention measures [ 112 ].
Overall, the COVID-19 pandemic and the response to it emphasise valuable lessons towards an effective and sustainable response to public health emergencies. We argue that the PHC approach captures the different preparedness and response strategies required towards ensuring health security and UHC [ 113 ]. The PHC approach enables countries to progressively realize universal access to good-quality health services (including essential public health functions) and equity, empower people and communities, strengthen multi-sectoral policy and action for health, and enhance good governance [ 114 ]. These are essential in the prevention and control of public health emergencies, to suppress transmission, and reduce morbidity and mortality [ 115 ]. Access to high-quality primary care is at the foundation of any strong health system [ 116 ], which will, in turn, have effect on containing the epidemic, and reducing mortality and CFR [ 117 ]. Australia is a good example in this regard because it has implemented a comprehensive PHC approach in combination with border restrictions to ensure health system capacity is not exceeded [ 56 ]. The PHC approach will enable countries to develop and implement a context-specific health strategy, enhance governance, strengthen their (public) health systems, minimize segmentation and fragmentation, and tackle upstream structural issues, including discrimination and socio-economic inequities [ 118 ]. This is the type of public health approach (comprehensive, equity-focused and participatory) that will be effective and sustainable to tackle public health emergencies in the twenty-first century [ 119 , 120 ]. In addition, it is vital to transform the global and regional health systems, with a strong IHR and an empowered WHO at the apex [ 121 ]. We contend that this is the way towards a healthier and safer country, region and world.
The COVID-19 pandemic demonstrates that the world remains vulnerable to public health emergencies with significant health and other socio-economic impacts. The pandemic takes variable shapes and forms across regions and countries around the world. The pandemic has impacted countries with inadequate governance of the epidemic, fragmentation of their health systems and higher socio-economic inequities more than others. We argue that adequate response to public health emergencies requires that countries develop and implement a context-specific national strategy, enhance governance of public health emergency, build the capacity of their health systems, minimize fragmentation, and tackle socio-economic inequities. This is possible through a PHC approach that provides universal access to good-quality health services through empowered communities and multi-sectoral policy and action for health development. The pandemic has affected every corner of the world; it has demonstrated that “no country is safe unless other countries are safe”. This should be a call for a strong global health system based on the values of justice and capabilities for health.
Availability of data and materials
Data are available in a public, open access repository: Johns Hopkins University: https://coronavirus.jhu.edu/data/new-cases , and UNDP: http://hdr.undp.org/en/2019-report ; WHO: https://www.who.int/publications/m/item/weekly-epidemiological-update%2D%2D-22-december-2020
Abbreviations
Coronavirus Disease 2019
Case-fatality rates
Human development index
Universal health coverage index
Global Health Security index
High-income countries
Middle-income countries
El Zowalaty ME, Järhult JD. From SARS to COVID-19: A previously unknown SARS-CoV-2 virus of pandemic potential infecting humans–Call for a One Health approach. One Health. 2020;9:100124. https://doi.org/10.1016/j.onehlt.2020.100124 .
Van Damme W, Dahake R, Delamou A, Ingelbeen B, Wouters E, Vanham G, et al. The COVID-19 pandemic: diverse contexts; different epidemics—how and why? BMJ Glob Health. 2020;5(7):e003098.
Article PubMed Google Scholar
World Health Organization (WHO): Coronavirus disease ( COVID-19): situation report, 150. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200618-covid-19-sitrep-150.pdf .
Weekly epidemiological update - 22 December 2020 [ https://www.who.int/publications/m/item/weekly-epidemiological-update%2D%2D-22-december-2020 ].
Worldometer: COVID-19 coronavirus pandemic. 2020. https://www.worldometers.info/coronavirus/ .
Anand S, Sen A. Human Development Index: Methodology and Measurement. 1994. http://hdr.undp.org/en/content/human-development-index-methodology-and-measurement .
De Larochelambert Q, Marc A, Antero J, Le Bourg E, Toussaint J-F. Covid-19 mortality: a matter of vulnerability among nations facing limited margins of adaptation. Public Health. 2020;8. https://doi.org/10.3389/fpubh.2020.604339 .
de Winter JC, Gosling SD, Potter J. Comparing the Pearson and Spearman correlation coefficients across distributions and sample sizes: a tutorial using simulations and empirical data. Psychol Methods. 2016;21(3):273.
World Health Organization. Universal health coverage [ http://www.who.int/universal_health_coverage/en/ ].
Johns Hopkins Center for Health Security. Global Health Security Index [ https://www.ghsindex.org/ ].
Pol Antràs SJR. Esteban Rossi-Hansberg: how do globalisation and pandemics interact? Surprising insights from a new model. In: #LSEThinks | CEP | global development vol. 2020. London: London School of Economics; 2020.
Google Scholar
Cai P. Understanding China’s belt and road initiative; 2017.
Baldwin R, Tomiura E. Thinking ahead about the trade impact of COVID-19. Economics in the Time of COVID-19. 2020;59. https://repository.graduateinstitute.ch/record/298220?ln=en .
Organization WH: Coronavirus disease ( COVID-19): situation report, 182. 2020.
Johns Hopkins University: COVID-19 Map - Johns Hopkins Coronavirus Resource Center. In. Edited by Security JHUCfH; 2021. https://coronavirus.jhu.edu/map.html .
Wang T, Du Z, Zhu F, Cao Z, An Y, Gao Y, et al. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet. 2020;395(10228):e52.
Article CAS PubMed PubMed Central Google Scholar
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama. 2020;323(11):1061–9.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Hussain A, Bhowmik B, Do Vale Moreira NC. COVID-19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142. https://doi.org/10.1016/j.diabres.2020.108142 . Epub 2020 Apr 9.
Covid C, COVID C, COVID C, Chow N, Fleming-Dutra K, Gierke R, Hall A, et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–march 28, 2020. Morb Mortal Wkly Rep. 2020;69(13):382.
Group C-S. Characteristics of COVID-19 patients dying in Italy: report based on available data on March 20th, 2020. Rome: Instituto Superiore Di Sanita; 2020. https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_20_marzo_eng.pdf .
Guan W-j, Ni Z-y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
Article CAS PubMed Google Scholar
Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. Jama. 2020;323(16):1612–4.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area. JAMA. 2020;323(20):2052–9. https://doi.org/10.1001/jama.2020.6775 .
Covid C, Team R. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–march 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–6.
Article Google Scholar
Mbow M, Lell B, Jochems SP, Cisse B, Mboup S, Dewals BG, et al. COVID-19 in Africa: dampening the storm? Science. 2020;369(6504):624–6.
Kavanagh MM, Erondu NA, Tomori O, Dzau VJ, Okiro EA, Maleche A, et al. Access to lifesaving medical resources for African countries: COVID-19 testing and response, ethics, and politics. Lancet. 2020;395(10238):1735–8.
Nordling L. Africa's pandemic puzzle: why so few cases and deaths? In: American Association for the Advancement of Science; 2020.
Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173(5):362–7. https://doi.org/10.7326/M20-3012 . Epub 2020 Jun 3.
Nikolai LA, Meyer CG, Kremsner PG, Velavan TP. Asymptomatic SARS coronavirus 2 infection: invisible yet invincible. Int J Infect Dis. 2020;100:112–6. https://doi.org/10.1016/j.ijid.2020.08.076 . Epub 2020 Sep 3.
Rao C, Bradshaw D, Mathers CD. Improving death registration and statistics in developing countries: lessons from sub-Saharan Africa. Southern Afr J Demography. 2004:81–99.
Mehtar S, Preiser W, Lakhe NA, Bousso A, TamFum J-JM, Kallay O, et al. Limiting the spread of COVID-19 in Africa: one size mitigation strategies do not fit all countries. Lancet Glob Health. 2020;8(7):e881–3. Published online 2020 Apr 28. https://doi.org/10.1016/S2214-109X(20)30212-6 .
Nachega J, Seydi M, Zumla A. The late arrival of coronavirus disease 2019 (COVID-19) in Africa: mitigating pan-continental spread. Clin Infect Dis. 2020;71(15):875–8.
Gwilliam K, Foster V, Archondo-Callao R, Briceno-Garmendia C, Nogales A, Sethi K. Africa infrastructure country diagnostic: roads in sub-Saharan Africa: The World Bank; 2008.
Guengant J-P. Africa’s population: history, current status, and projections. In: Africa's Population: In Search of a Demographic Dividend: Springer; 2017. p. 11–31.
Collaborators GOD, Bernabe E, Marcenes W, Hernandez C, Bailey J, Abreu L, et al. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99(4):362–73.
Cambaza EM, Viegas GC, Cambaza C. Manuel a: potential impact of temperature and atmospheric pressure on the number of cases of COVID-19 in Mozambique, southern Africa. J Public Health Epidemiol. 2020;12(3):246–60.
Lawal Y. Africa’s low COVID-19 mortality rate: a paradox? Int J Infect Dis. 2021;102:118–22.
Nkengasong JN, Mankoula W. Looming threat of COVID-19 infection in Africa: act collectively, and fast. Lancet. 2020;395(10227):841–2.
African Union and Africa CDC. African union and Africa CDC launches partnerships for African vaccine manufacturing (PAVM), framework to achieve it and signs 2 MoUs: African Union and Africa CDC; 2021.
Forbes. What Do Countries With The Best Coronavirus Responses Have In Common? Women Leaders [ https://www.forbes.com/sites/avivahwittenbergcox/2020/04/13/what-do-countries-with-the-best-coronavirus-reponses-have-in-common-women-leaders/#603bd9433dec ].
University of Notre Dame. What can we learn from Austria’s response to COVID-19? [ https://keough.nd.edu/what-can-we-learn-from-austrias-response-to-covid-19/ ].
Stoller JK. Reflections on leadership in the time of COVID-19. BMJ Leader. 2020. https://doi.org/10.1136/leader-2020-000244 .
Houston Public Media. What 6 Of The 7 Countries With The Most COVID-19 Cases Have In Common [ https://www.npr.org/sections/goatsandsoda/2020/07/31/896879448/the-nations-with-the-most-to-lose-from-covid-19 ].
Hale T, Petherick A, Phillips T, Webster S. Variation in government responses to COVID-19. Blavatnik school of government working paper. 2020;31. https://en.unesco.org/inclusivepolicylab/sites/default/files/learning/document/2020/4/BSG-WP-2020-031-v3.0.pdf .
The Editors. Dying in a leadership vacuum. N Engl J Med. 2020;383(15):1479–80.
The Cable News Network. US and UK are bottom of the pile in rankings of governments' handling of coronavirus pandemic [ https://edition.cnn.com/2020/08/27/world/global-coronavirus-attitudes-pew-intl/index.html ].
Huston P, Campbell J, Russell G, Goodyear-Smith F, Phillips RL, van Weel C, et al. COVID-19 and primary care in six countries. BJGP Open. 2020;4(4):bjgpopen20X101128. https://doi.org/10.3399/bjgpopen20X101128 .
Goodyear-Smith F, Kinder K, Eden AR, Strydom S, Bazemore A, Phillips R, et al. Primary care perspectives on pandemic politics. Glob Public Health. 2021;16(8-9):1304–19. https://doi.org/10.1080/17441692.2021.1876751 . Epub 2021 Jan 24.
Rutledge PE. Trump, COVID-19, and the war on expertise. Am Rev Public Adm. 2020;50(6-7):505–11.
Ugarte DA, Cumberland WG, Flores L, Young SD. Public attitudes about COVID-19 in response to president trump's social media posts. JAMA Netw Open. 2021;4(2):e210101.
Article PubMed PubMed Central Google Scholar
Lal A, Erondu NA, Heymann DL, Gitahi G, Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet. 2021;397(10268):61–7. https://doi.org/10.1016/S0140-6736(20)32228-5 . Epub 2020 Dec 1.
Tromberg BJ, Schwetz TA, Pérez-Stable EJ, Hodes RJ, Woychik RP, Bright RA, et al. Rapid scaling up of Covid-19 diagnostic testing in the United States—the NIH RADx initiative. N Engl J Med. 2020;383(11):1071–7.
Marwaha J, Halamka J, Brat G. Lifesaving ventilators will sit unused without a national data-sharing effort; 2020.
Kidd MR. Five principles for pandemic preparedness: lessons from the Australian COVID-19 primary care response. Br J Gen Pract. 2020;70(696):316–7. https://doi.org/10.3399/bjgp20X710765 . Print 2020 Jul.
Hsu LY, Tan M-H. What Singapore can teach the US about responding to COVID-19. STAT News. 2020. https://www.statnews.com/2020/03/23/singapore-teach-united-states-about-covid-19-response/ .
Horton R. Offline: COVID-19 is not a pandemic. Lancet (London, England). 2020;396(10255):874.
Article CAS Google Scholar
Raisi-Estabragh Z, McCracken C, Bethell MS, Cooper J, Cooper C, Caulfield MJ, et al. Greater risk of severe COVID-19 in black, Asian and minority ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25 (OH)-vitamin D status: study of 1326 cases from the UK biobank. J Public Health. 2020;42(3):451–60.
Hamidianjahromi A. Why African Americans are a potential target for COVID-19 infection in the United States. J Med Internet Res. 2020;22(6):e19934.
Tangcharoensathien V, Bassett MT, Meng Q, Mills A. Are overwhelmed health systems an inevitable consequence of covid-19? Experiences from China, Thailand, and New York State. BMJ. 2021;372. https://doi.org/10.1136/bmj.n83 .
Organization WH: COVID-19 health system response monitor, Thailand. 2020.
Narkvichien M. Thailand’s 1 million village health volunteers-“unsung heroes”-are helping guard communities nationwide from COVID-19. Nonthaburi: World Health Organization; 2020.
Kupferschmidt K, Cohen J. Can China's COVID-19 strategy work elsewhere? In: American Association for the Advancement of Science; 2020.
Al Saidi AMO, Nur FA, Al-Mandhari AS, El Rabbat M, Hafeez A, Abubakar A. Decisive leadership is a necessity in the COVID-19 response. Lancet. 2020;396(10247):295–8.
Forman R, Atun R, McKee M, Mossialos E. 12 lessons learned from the management of the coronavirus pandemic. Health Policy. 2020;124(6):577–80. https://doi.org/10.1016/j.healthpol.2020.05.008 .
Barberia LG, Gómez EJ. Political and institutional perils of Brazil's COVID-19 crisis. Lancet. 2020;396(10248):367–8.
Ortega F, Orsini M. Governing COVID-19 without government in Brazil: ignorance, neoliberal authoritarianism, and the collapse of public health leadership. Global Public Health. 2020;15(9):1257–77.
Ezequiel GE, Jafet A, Hugo A, Pedro D, Ana Maria M, Carola OV, et al. The COVID-19 pandemic: a call to action for health systems in Latin America to strengthen quality of care. Int J Qual Health Care. 2021;33(1):mzaa062.
Rocha R, Atun R, Massuda A, Rache B, Spinola P, Nunes L, et al. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob Health. 2021;9(6):e782–92. https://doi.org/10.1016/S2214-109X(21)00081-4 . Epub 2021 Apr 12.
Lancet T. India under COVID-19 lockdown. Lancet (London, England). 2020;395(10233):1315.
Siddiqui AF, Wiederkehr M, Rozanova L, Flahault A. Situation of India in the COVID-19 pandemic: India’s initial pandemic experience. Int J Environ Res Public Health. 2020;17(23):8994.
Article CAS PubMed Central Google Scholar
Taneja P, Bali AS. India’s domestic and foreign policy responses to COVID-19. Round Table. 2021;110(1):46–61.
Choutagunta A, Manish G, Rajagopalan S. Battling COVID-19 with dysfunctional federalism: lessons from India. South Econ J. 2021;87(4):1267–99.
Mallapaty S. India's massive COVID surge puzzles scientists. Nature. 2021;592(7856):667–8.
Thiagarajan K. Why is India having a covid-19 surge? In: British Medical Journal Publishing Group; 2021.
Fisman DN, Greer AL, Tuite AR. Age is just a number: a critically important number for COVID-19 case fatality. Ann Intern Med. 2020;173(9):762–3.
Sudharsanan N, Didzun O, Bärnighausen T, Geldsetzer P. The contribution of the age distribution of cases to COVID-19 case fatality across countries: a 9-country demographic study. Ann Intern Med. 2020;173(9):714–20. https://doi.org/10.7326/M20-2973 . Epub 2020 Jul 22.
Think Global Health. The Myth of South Asian Exceptionalism. In: He Myth of South Asian Exceptionalism: South Asia's young population conceals the effects that COVID-19 has on its older and more vulnerable people. vol. 2020; 2020.
Ioannidis JP, Axfors C, Contopoulos-Ioannidis DG. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ Res. 2020;188:109890.
Kim D-H, Choe YJ, Jeong J-Y. Understanding and interpretation of case fatality rate of coronavirus disease 2019. J Korean Med Sci. 2020;35(12):e137. https://doi.org/10.3346/jkms.2020.35.e137 .
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7.
Sorci G, Faivre B, Morand S. Explaining among-country variation in COVID-19 case fatality rate. Sci Rep. 2020;10(1):1–11.
Sen-Crowe B, Sutherland M, McKenney M, Elkbuli A. A closer look into global hospital beds capacity and resource shortages during the COVID-19 pandemic. J Surg Res. 2021;260:56–63.
Li M, Zhang Z, Cao W, Liu Y, Du B, Chen C, et al. Identifying novel factors associated with COVID-19 transmission and fatality using the machine learning approach. Sci Total Environ. 2021;764:142810.
Undurraga EA, Chowell G, Mizumoto K. COVID-19 case fatality risk by age and gender in a high testing setting in Latin America: Chile, march–august 2020. Infect Dis Poverty. 2021;10(1):1–11.
Taylor L. How Latin America is fighting covid-19, for better and worse. BMJ. 2020;370:m3319. https://doi.org/10.1136/bmj.m3319 .
Bhuyan A. Covid-19: India looks to import oxygen as cases surge, overwhelming hospitals. In: British Medical Journal Publishing Group; 2021.
An BY, Tang S-Y. Lessons from COVID-19 responses in East Asia: institutional infrastructure and enduring policy instruments. Am Rev Public Adm. 2020;50(6-7):790–800.
Chen H, Shi L, Zhang Y, Wang X, Sun G. A cross-country core strategy comparison in China, Japan, Singapore and South Korea during the early COVID-19 pandemic. Glob Health. 2021;17(1):1–10.
Kahathuduwa CN, Dhanasekara CS, Chin S-H. Case fatality rate in COVID-19: a systematic review and meta-analysis. J Prev Med Hyg. 2021;62(2):E311–20. https://doi.org/10.15167/2421-4248/jpmh2021.62.2.1627 . eCollection 2021 Jun.
Meyerowitz-Katz G, Merone L. A systematic review and meta-analysis of published research data on COVID-19 infection-fatality rates. Int J Infect Dis. 2020.
Seoane B. A scaling approach to estimate the COVID-19 infection fatality ratio from incomplete data. PLoS One. 2021;16(2):e0246831. https://doi.org/10.1371/journal.pone.0246831 . eCollection 2021.
Byambasuren O, Dobler CC, Bell K, Rojas DP, Clark J, McLaws M-L, et al. Comparison of seroprevalence of SARS-CoV-2 infections with cumulative and imputed COVID-19 cases: systematic review. PLoS One. 2021;16(4):e0248946.
Shakiba M, Nazemipour M, Salari A, Mehrabian F, Nazari SSH, Rezvani SM, et al. Seroprevalence of SARS-CoV-2 in Guilan Province, Iran, April 2020. Emerg Infect Dis. 2021;27(2):636.
Blanchet K, Alwan A, Antoine C, Cros MJ, Feroz F, Guracha TA, et al. Protecting essential health services in low-income and middle-income countries and humanitarian settings while responding to the COVID-19 pandemic. BMJ Glob Health. 2020;5(10):e003675.
Thome J, Coogan AN, Fischer M, Tucha O, Faltraco F. Challenges for mental health services during the 2020 COVID-19 outbreak in Germany. Psychiatry Clin Neurosci. 2020;74(7):407. https://doi.org/10.1111/pcn.13019 . Epub 2020 May 26.
Riley T, Sully E, Ahmed Z, Biddlecom A. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low-and middle-income countries. Int Perspect Sex Reprod Health. 2020;46:73–6.
World Health Organization (WHO): Maintaining essential health services: operational guidance for the COVID-19 context: interim guidance, 1 June 2020. In.: World Health Organization; 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-essential_health_services-2020.2 .
World Health Organization (WHO): Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. In.: World Health Organization; 2020. https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-EHS_continuity-survey-2020.1 .
World Health Organization (WHO): Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 22 April 2021. In.: World Health Organization; 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1 .
Organization WH. COVID-19: operational guidance for maintaining essential health services during an outbreak: interim guidance, 25 march 2020: World Health Organization; 2020.
Chen Y-Y, Assefa Y. The heterogeneity of the COVID-19 pandemic and national responses: an explanatory mixed-methods study. BMC Public Health. 2021;21(1):1–15.
World Health Organization (WHO). Thirteenth general programme of work 2019–2023. The seventy-first world health assembly. Geneva (Switzerland): World Health Organization; 2018.
Mahjour J, Mirza Z, Rashidian A, Atta H, Hajjeh R, Thieren M, et al. " promote health, keep the world safe, serve the vulnerable" in the eastern Mediterranean region. East Mediterr Health J. 2018;24(4):323–4.
Rollston R, Galea S. COVID-19 and the social determinants of health. Am J Health Promot. 2020;34(6):687–9. https://doi.org/10.1177/0890117120930536b .
Nachega JB, Sam-Agudu NA, Masekela R, van der Zalm MM, Nsanzimana S, Condo J, et al. Addressing challenges to rolling out COVID-19 vaccines in African countries. Lancet Glob Health. 2021;9(6):e746–8. https://doi.org/10.1016/S2214-109X(21)00097-8 . Epub 2021 Mar 10.
Skegg D, Gluckman P, Boulton G, Hackmann H, Karim SSA, Piot P, et al. Future scenarios for the COVID-19 pandemic. Lancet. 2021;397(10276):777–8.
Nhamo G, Chikodzi D, Kunene HP, Mashula N. COVID-19 vaccines and treatments nationalism: challenges for low-income countries and the attainment of the SDGs. Global Public Health. 2021;16(3):319–39.
Figueroa JP, Bottazzi ME, Hotez P, Batista C, Ergonul O, Gilbert S, et al. Urgent needs of low-income and middle-income countries for COVID-19 vaccines and therapeutics. Lancet. 2021;397(10274):562–4.
He X, Hong W, Pan X, Lu G, Wei X. SARS-CoV-2 omicron variant: characteristics and prevention. Med Comm (2020). 2021;2(4):838–45. https://doi.org/10.1002/mco2.110 .
Karim SSA, Karim QA. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. 2021;398(10317):2126–8.
Sanders D, Nandi S, Labonté R, Vance C, Van Damme W. From primary health care to universal health coverage—one step forward and two steps back. Lancet. 2019;394(10199):619–21.
Hone T, Macinko J, Millett C. Revisiting Alma-Ata: what is the role of primary health care in achieving the sustainable development goals? Lancet. 2018;392(10156):1461–72.
Redwood-Campbell L, Abrahams J. Primary health care and disasters—the current state of the literature: what we know, gaps and next steps. Prehospital Disaster Med. 2011;26(3):184–91.
Bitton A, Ratcliffe HL, Veillard JH, Kress DH, Barkley S, Kimball M, et al. Primary health care as a foundation for strengthening health systems in low-and middle-income countries. J Gen Intern Med. 2017;32(5):566–71.
Dunlop C, Howe A, Li D, Allen LN. The coronavirus outbreak: the central role of primary care in emergency preparedness and response. BJGP Open. 2020;4(1):bjgpopen20X101041. https://doi.org/10.3399/bjgpopen20X101041 .
Assefa Y, Gilks CF, van de Pas R, Reid S, Gete DG, Van Damme W. Reimagining global health systems for the 21st century: lessons from the COVID-19 pandemic. BMJ Glob Health. 2021;6(4):e004882.
Loewenson R, Accoe K, Bajpai N, Buse K, Abi Deivanayagam T, London L, et al. Reclaiming comprehensive public health. BMJ Glob Health. 2020;5(9):e003886.
Rawaf S, Allen LN, Stigler FL, Kringos D, Quezada Yamamoto H, van Weel C, et al. Lessons on the COVID-19 pandemic, for and by primary care professionals worldwide. Eur J Gen Pract. 2020;26(1):129–33.
Gostin LO, Friedman EA. A retrospective and prospective analysis of the west African Ebola virus disease epidemic: robust national health systems at the foundation and an empowered WHO at the apex. Lancet. 2015;385(9980):1902–9.
Download references
Acknowledgements
Not applicable.
No funding was obtained for this study.
Author information
Authors and affiliations.
School of Public Health, the University of Queensland, Brisbane, Australia
Yibeltal Assefa, Charles F. Gilks, Simon Reid & Dereje Gedle Gete
Institute of Tropical Medicine, Antwerp, Belgium
Remco van de Pas & Wim Van Damme
You can also search for this author in PubMed Google Scholar
Contributions
YA conceived the idea of the research, collected and analysed the data, and prepared the first and subsequent drafts. DG participated in data collection and analysis. CFG, SR, RVDP, DG and WVD provided comments during subsequent drafts. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Yibeltal Assefa .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Assefa, Y., Gilks, C.F., Reid, S. et al. Analysis of the COVID-19 pandemic: lessons towards a more effective response to public health emergencies. Global Health 18 , 10 (2022). https://doi.org/10.1186/s12992-022-00805-9
Download citation
Received : 04 August 2021
Accepted : 14 January 2022
Published : 04 February 2022
DOI : https://doi.org/10.1186/s12992-022-00805-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Heterogeneity
Globalization and Health
ISSN: 1744-8603
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- First Online: 28 November 2023
Cite this chapter

- Tharun Dolla 4 ,
- Ganesh Devkar 5 &
- Boeing Laishram 6
Part of the book series: Contributions to Public Administration and Public Policy ((CPAPP))
69 Accesses
In December 2019, the Covid-19 pandemic has thrown life out of gear across the world. While writing this chapter, the world has experienced waves of Covid-19 infections, and threats of new virus mutations and deadlier infections still loom at large. As the infrastructure is an underlying fabric, like veins and blood in a human body, on which society and nation prospers, like human body, it too got disrupted owing to Covid-19. This disruption has forced the policy makers and stakeholders associated with the infrastructure delivery process to rethink the entire value chain of right from planning, design, construction to operation of created facility. The extent of “disruption” became a point of debate owing to perception about the “infrastructure” that it is created by keeping in mind the long horizon (of time) and it is expected to have resilience, adaptability, agility, and responsiveness built it in. Few stakeholders termed it as a “black swan event” and tried to discuss it under the cloud of “uncertainty” and “one of off” phenomena. However, many stakeholders kept themselves away from coining Covid-19 as “Unknown” event because human civilization has experienced pandemics in the past and opened healthy debates on how the infrastructure delivery process responded in the times of Covid-19 and what are the areas of improvements to be made in the process to deal with disruptions of similar nature. The infrastructure is shaped and delivered to the customers under the influence of and interaction with varied elements like infrastructure policies, laws and regulations, contractual agreement, design drivers, financing mechanisms, and community consultation process. As each country has a different set of elements in force, the quality and quantity of emergent infrastructure and the service delivered are different. The Covid-19 pandemic unearthed these facets of infrastructure, especially in the delivery of healthcare services. Even it may be apt to say that the Covid-19 pandemic opened the can of worms, and debates raged over the process followed for financial allocation of different infrastructure sectors, policy measures undertaken by the governments to address the infrastructure backlog, accessibility of infrastructure to poor and marginalized communities, measures to reduce carbon footprint of existing, and planned infrastructure. Among these issues, the policy makers and news media were keenly observing and scrutinizing the infrastructure which is created and delivered with Public-Private Partnership (PPP) model.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
https://infrascope.eiu.com/country-reports/
Author information
Authors and affiliations.
Department of Civil Engineering, Indian Institute of Technology Bombay, Mumbai, Maharashtra, India
Tharun Dolla
Faculty of Technology, CEPT University, Ahmedabad, Gujarat, India
Ganesh Devkar
Department of Civil Engineering, Indian Institute of Technology Guwahati, Guwahati, Assam, India
Boeing Laishram
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Tharun Dolla .
Editor information
Editors and affiliations, rights and permissions.
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Dolla, T., Devkar, G., Laishram, B. (2023). Conclusion. In: Dolla, T., Laishram, B., Devkar, G. (eds) Revisiting Public-Private Partnerships. Contributions to Public Administration and Public Policy. Springer, Cham. https://doi.org/10.1007/978-3-031-37015-1_16
Download citation
DOI : https://doi.org/10.1007/978-3-031-37015-1_16
Published : 28 November 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-37014-4
Online ISBN : 978-3-031-37015-1
eBook Packages : Economics and Finance Economics and Finance (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Seven short essays about life during the pandemic
The boston book festival's at home community writing project invites area residents to describe their experiences during this unprecedented time..

My alarm sounds at 8:15 a.m. I open my eyes and take a deep breath. I wiggle my toes and move my legs. I do this religiously every morning. Today, marks day 74 of staying at home.
My mornings are filled with reading biblical scripture, meditation, breathing in the scents of a hanging eucalyptus branch in the shower, and making tea before I log into my computer to work. After an hour-and-a-half Zoom meeting, I decided to take a long walk to the post office and grab a fresh bouquet of burnt orange ranunculus flowers. I embrace the warm sun beaming on my face. I feel joy. I feel at peace.
I enter my apartment and excessively wash my hands and face. I pour a glass of iced kombucha. I sit at my table and look at the text message on my phone. My coworker writes that she is thinking of me during this difficult time. She must be referring to the Amy Cooper incident. I learn shortly that she is not.
I Google Minneapolis and see his name: George Floyd. And just like that a simple and beautiful day transitions into a day of sorrow.
Nakia Hill, Boston
It was a wobbly, yet solemn little procession: three masked mourners and a canine. Beginning in Kenmore Square, at David and Sue Horner’s condo, it proceeded up Commonwealth Avenue Mall.
S. Sue Horner died on Good Friday, April 10, in the Year of the Virus. Sue did not die of the virus but her parting was hemmed by it: no gatherings to mark the passing of this splendid human being.
David devised a send-off nevertheless. On April 23rd, accompanied by his daughter and son-in-law, he set out for Old South Church. David led, bearing the urn. His daughter came next, holding her phone aloft, speaker on, through which her brother in Illinois played the bagpipes for the length of the procession, its soaring thrum infusing the Mall. Her husband came last with Melon, their golden retriever.
Advertisement
I unlocked the empty church and led the procession into the columbarium. David drew the urn from its velvet cover, revealing a golden vessel inset with incandescent tiles. We lifted the urn into the niche, prayed, recited Psalm 23, and shared some words.
It was far too small for the luminous “Dr. Sue”, but what we could manage in the Year of the Virus.
Nancy S. Taylor, Boston
On April 26, 2020, our household was a bustling home for four people. Our two sons, ages 18 and 22, have a lot of energy. We are among the lucky ones. I can work remotely. Our food and shelter are not at risk.
As I write this a week later, it is much quieter here.
On April 27, our older son, an EMT, transported a COVID-19 patient to the ER. He left home to protect my delicate health and became ill with the virus a week later.
On April 29, my husband’s 95-year-old father had a stroke. My husband left immediately to be with his 90-year-old mother near New York City and is now preparing for his father’s discharge from the hospital. Rehab people will come to the house; going to a facility would be too dangerous.
My husband just called me to describe today’s hospital visit. The doctors had warned that although his father had regained the ability to speak, he could only repeat what was said to him.
“It’s me,” said my husband.
“It’s me,” said my father-in-law.
“I love you,” said my husband.
“I love you,” said my father-in-law.
“Sooooooooo much,” said my father-in-law.
Lucia Thompson, Wayland
Would racism exist if we were blind?
I felt his eyes bore into me as I walked through the grocery store. At first, I thought nothing of it. With the angst in the air attributable to COVID, I understood the anxiety-provoking nature of feeling as though your 6-foot bubble had burst. So, I ignored him and maintained my distance. But he persisted, glaring at my face, squinting to see who I was underneath the mask. This time I looked back, when he yelled, in my mother tongue, for me to go back to my country.
In shock, I just laughed. How could he tell what I was under my mask? Or see anything through the sunglasses he was wearing inside? It baffled me. I laughed at the irony that he would use my own language against me, that he knew enough to guess where I was from in some version of culturally competent racism. I laughed because dealing with the truth behind that comment generated a sadness in me that was too much to handle. If not now, then when will we be together?
So I ask again, would racism exist if we were blind?
Faizah Shareef, Boston
My Family is “Out” There
But I am “in” here. Life is different now “in” Assisted Living since the deadly COVID-19 arrived. Now the staff, employees, and all 100 residents have our temperatures taken daily. Everyone else, including my family, is “out” there. People like the hairdresser are really missed — with long straight hair and masks, we don’t even recognize ourselves.
Since mid-March we are in quarantine “in” our rooms with meals served. Activities are practically non-existent. We can sit on the back patio 6 feet apart, wearing masks, do exercises there, chat, and walk nearby. Nothing inside. Hopefully June will improve.
My family is “out” there — somewhere! Most are working from home (or Montana). Hopefully an August wedding will happen, but unfortunately, I may still be “in” here.
From my window I wave to my son “out” there. Recently, when my daughter visited, I opened the window “in” my second-floor room and could see and hear her perfectly “out” there. Next time she will bring a chair so we can have an “in” and “out” conversation all day, or until we run out of words.
Barbara Anderson, Raynham
My boyfriend Marcial lives in Boston, and I live in New York City. We had been doing the long-distance thing pretty successfully until coronavirus hit. In mid-March, I was furloughed from my temp job, Marcial began working remotely, and New York started shutting down. I went to Boston to stay with Marcial.
We are opposites in many ways, but we share a love of food. The kitchen has been the center of quarantine life —and also quarantine problems.
Marcial and I have gone from eating out and cooking/grocery shopping for each other during our periodic visits to cooking/grocery shopping with each other all the time. We’ve argued over things like the proper way to make rice and what greens to buy for salad. Our habits are deeply rooted in our upbringing and individual cultures (Filipino immigrant and American-born Chinese, hence the strong rice opinions).
On top of the mundane issues, we’ve also dealt with a flooded kitchen (resulting in cockroaches) and a mandoline accident leading to an ER visit. Marcial and I have spent quarantine navigating how to handle the unexpected and how to integrate our lifestyles. We’ve been eating well along the way.
Melissa Lee, Waltham
It’s 3 a.m. and my dog Rikki just gave me a worried look. Up again?
“I can’t sleep,” I say. I flick the light, pick up “Non-Zero Probabilities.” But the words lay pinned to the page like swatted flies. I watch new “Killing Eve” episodes, play old Nathaniel Rateliff and The Night Sweats songs. Still night.
We are — what? — 12 agitated weeks into lockdown, and now this. The thing that got me was Chauvin’s sunglasses. Perched nonchalantly on his head, undisturbed, as if he were at a backyard BBQ. Or anywhere other than kneeling on George Floyd’s neck, on his life. And Floyd was a father, as we all now know, having seen his daughter Gianna on Stephen Jackson’s shoulders saying “Daddy changed the world.”
Precious child. I pray, safeguard her.
Rikki has her own bed. But she won’t leave me. A Goddess of Protection. She does that thing dogs do, hovers increasingly closely the more agitated I get. “I’m losing it,” I say. I know. And like those weighted gravity blankets meant to encourage sleep, she drapes her 70 pounds over me, covering my restless heart with safety.
As if daybreak, or a prayer, could bring peace today.
Kirstan Barnett, Watertown
Until June 30, send your essay (200 words or less) about life during COVID-19 via bostonbookfest.org . Some essays will be published on the festival’s blog and some will appear in The Boston Globe.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- JME Commentaries
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 49, Issue 3
- Vaccine mandates for healthcare workers beyond COVID-19
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-5163-3017 Alberto Giubilini 1 , 2 ,
- http://orcid.org/0000-0003-1691-6403 Julian Savulescu 1 , 2 , 3 ,
- Jonathan Pugh 1 ,
- http://orcid.org/0000-0003-3958-8633 Dominic Wilkinson 1 , 3 , 4
- 1 Oxford Uehiro Centre for Practical Ethics , University of Oxford , Oxford , UK
- 2 Wellcome Centre for Ethics and Humanities , University of Oxford , Oxford , UK
- 3 Murdoch Children's Research Institute , Melbourne , Victoria , Australia
- 4 Newborn Care , John Radcliffe Hospital , Oxford , UK
- Correspondence to Dr Alberto Giubilini, Philosophy, University of Oxford, Oxford Ox1 1PT, Oxfordshire, UK; alberto.giubilini{at}philosophy.ox.ac.uk
We provide ethical criteria to establish when vaccine mandates for healthcare workers are ethically justifiable. The relevant criteria are the utility of the vaccine for healthcare workers, the utility for patients (both in terms of prevention of transmission of infection and reduction in staff shortage), and the existence of less restrictive alternatives that can achieve comparable benefits. Healthcare workers have professional obligations to promote the interests of patients that entail exposure to greater risks or infringement of autonomy than ordinary members of the public. Thus, we argue that when vaccine mandates are justified on the basis of these criteria, they are not unfairly discriminatory and the level of coercion they involve is ethically acceptable—and indeed comparable to that already accepted in healthcare employment contracts. Such mandates might be justified even when general population mandates are not. Our conclusion is that, given current evidence, those ethical criteria justify mandates for influenza vaccination, but not COVID-19 vaccination, for healthcare workers. We extend our arguments to other vaccines.
- Health Personnel
Data availability statement
No data are available.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/medethics-2022-108229
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
During the COVID-19 pandemic, a number of countries introduced stringent measures designed to address vaccine hesitancy. Some countries implemented vaccine mandates in the general population, for example through some form of vaccine passports (eg, in many European countries) or outright fines for the unvaccinated in certain age groups (eg, in Italy). However, many countries, even those that did not have wider schemes or vaccine passports, made COVID-19 vaccination compulsory for healthcare workers (HCWs).
In England, the government initially planned to make COVID-19 vaccination compulsory for HCWs, starting from April 2022. It also launched a consultation on extending the same approach to influenza vaccination. The Department of Health and Social Care stated:
vaccination reduces the risk of infection, which in turn reduces the risk of transmission. The more staff who are vaccinated against flu and against COVID-19, the more likely it will be that vulnerable people in their care are protected; staff themselves will be protected and their colleagues will also be protected. 1
However, in January 2022, the UK Government reversed its decision: in the light of the milder Omicron variant (and because of worries about loss of staff), the mandate was no longer considered to be proportionate.
COVID-19 vaccination for HCWs is still mandated in many other countries, including in the European Union and the USA. In the USA, 6 states have mandated COVID-19 vaccination for HCWs as a condition of employment, 15 states have mandated either vaccination or testing, and 3 states have mandated either vaccination or testing and masking, although there are differences as to whether the mandate applies to state employees only and which specific healthcare settings it applies to. However, 13 states have banned vaccine mandates from employers. 1 The federal COVID-19 vaccine mandate applied to all workplaces was blocked by the Supreme Court, but allowed to go ahead for healthcare facilities receiving federal funding. 2 At the time of writing, in Australia all states have various forms of vaccine mandates for HCWs, as have all Canadian provinces except for, at the moment, Ontario and Quebec. Some European countries, including France and Italy, have made COVID-19 vaccination mandatory for HCWs.
State vaccine mandates for health professionals are a significant departure from prior policy in the UK and elsewhere. Despite well-documented problems of nosocomial transmission of vaccine-preventable illnesses (eg, influenza), 2 3 prior to the pandemic most countries did not require HCWs to be vaccinated. In the UK, approximately a quarter of HCWs do not receive the seasonal influenza vaccine. 4
The aim of this paper is to consider the implications of recent experience, policy and debate for future vaccine mandates. Should HCWs be required to have COVID-19 or annual influenza vaccine as a condition of employment? Should this be extended to include new vaccines against nosocomial infection that are released (eg, future norovirus vaccine 5 ), or vaccines against new pandemic threats? We will focus on HCWs, although many of the central issues overlap with questions for residential aged care workers. Recent debate and policies around COVID-19 vaccination for HCWs can be used to further discussion around such questions.
We will argue that, given the current situation in early 2022, COVID-19 vaccination should not be mandated for HCWs but influenza vaccination should. We will outline a framework under which vaccination should be mandatory, on the basis of empirically contingent factors: risks for HCWs, benefits for patients, and the effectiveness of less restrictive options. We will also argue that the level of coercion involved does not in itself make vaccine mandates ethically impermissible, but it must be proportionate to the benefits to patients. Importantly, while the principles we adopt would remain constant, the empirical facts and our level of knowledge may be different in the future, so the very same principles might yield different practical implications in different future scenarios.
Background on vaccine mandates for health or aged care workers
In healthcare settings, it is well established that vaccines significantly contribute to reducing various kinds of healthcare-associated infections, both viral and bacterial. For the latter, vaccines may have a secondary benefit for the problem of antimicrobial resistance by reducing the need for antibiotics.
The two main benefits of vaccination—illness and contagion prevention—are particularly relevant in the case of HCWs, although they provide different types of justification for vaccination requirements.
Preventing illness is obviously directly beneficial to the HCWs themselves. However, it also benefits the health system and the patients indirectly by reducing the risk of shortage of staff in healthcare settings, an ongoing problem during this pandemic. The probability of developing serious illness depends both on individual risk factors (age, underlying health conditions, obesity, previous infection) and degree of exposure. For instance, in the case of COVID-19, HCWs and other so-called ‘essential workers’ are at higher risk of severe illness than workers considered ‘non-essential’. 6 The direct benefit of immunity is evident, but the indirect benefit is even more widely enjoyed. Particularly where the requirement to isolate is based on positive tests rather on the presence of severe symptoms, the vaccine may be beneficial in preventing staff shortage even in those at low risk of serious illness.
In January 2022, several hospitals in the UK declared ‘critical incident’ status caused by isolation requirements of staff infected with the Omicron variant. In the week before Christmas 2021, the absence rate of National Health Service (NHS) staff was 8%, compared with a 5% average absence rate in winter months pre-COVID-19. 3 Influenza typically does not pose this problem to the same degree, since there typically is no routine testing for influenza and therefore no isolation requirement for staff. But in some influenza seasons staff shortages can happen as large numbers of staff fall ill and are unable to work. There is also the opposite problem of ‘presenteeism’, where staff with influenza or influenza-like illness attend work, thus increasing the risk of nosocomial infection. 7 Both problems could in principle be addressed by reducing the risk of infection in HCWs in the first place. With COVID-19, the widespread use of testing combined with isolation requirements and the presence of a highly transmissible variant like Omicron made the risk of staff shortages higher.
The second benefit of vaccination for HCWs is the potential reduction of serious harm to patients. Public Health England estimates that during the first wave of COVID-19 (beginning February to end of July 2020), 20%–25% of COVID-19 hospitalisations may have been nosocomial. 8 In Scotland, 30% of ‘COVID-19 deaths’, defined as deaths within 28 days of a positive COVID-19 test in 2020, were considered ‘definitive hospital onset’. 9 10 The real figures may be higher.
However, while COVID-19 infections have obviously attracted a lot of attention in the past 2 years, COVID-19 is by no means an exception. The lack of routine testing for influenza infection makes it difficult to estimate how many patients catch the influenza in hospitals or care homes every year. The number is not insignificant. For instance, genetic sequencing of influenza samples suggested 15% of patients hospitalised with influenza at London University College hospitals during the 2018–2019 influenza season had a nosocomial infection. 11
Vaccine mandates are typically controversial as they entail limitations of individual liberties for the sake of the collective good. There is a reasonable disagreement about the extent to which one person should be required to do things to prevent harm to others or even to contribute to collective goods from which they themselves benefit. 12 Different political and ethical sensitivities would weigh individual rights against the collective good in different ways.
However, when it comes to HCWs, liberty-based counterarguments are more difficult to apply. Quite simply, HCWs have an ethical and professional obligation not to harm patients, or to minimise the risk of harm to patients, which other people do not have. What such obligations include—and whether they include vaccination—depends in part on the standards of negligence, as determined by the majority of professional bodies’ opinions. Normally, they do include vaccination or equivalent safeguards. For instance, the Department of Health in the UK recommends health clearance for tuberculosis, hepatitis B and C, and HIV for new HCWs who will perform exposure-prone procedures. The reason is ‘not to prevent those infected with […] viruses from working in the NHS, but rather to restrict them from working in those clinical areas where their infection may pose a risk to patients in their care’. 13
This approach is typically reflected in the guidance about vaccination for healthcare staff by medical associations. In the UK, the code of Good Medical Practice states: ‘You should be immunised against common serious communicable diseases (unless otherwise contraindicated)’. 14 The reason offered is the prevention of passing diseases on to patients. Some Australian states, such as Victoria, also introduced vaccination requirements for healthcare staff before the COVID-19 pandemic. But the need to guarantee adequate healthcare by preventing staff shortage due to illness also features in medical codes. For instance, in September 2021, the American Medical Association called for mandatory COVID-19 vaccination of HCWs as it is ‘needed to sustain the health system into the future as we learn to live with COVID-19’ 4 .
Thus, a vaccine mandate for HCWs would be consistent with already existing professional requirements based on preventing harm to patients. However, a legally enforced mandate is different from a professional obligation and it requires additional justification. Not every professional obligation is also a legal requirement. In the next section, we provide three criteria that determine the ethical acceptability of vaccine mandates for HCWs: the criteria pertain to (1) risks of the vaccines, (2) benefits of the vaccines and (3) the availability of less restrictive alternatives to achieve comparable benefits. Criteria 1 and 2 are relevant to determining whether the risks of vaccination are proportionate to its benefits. Criteria 2 and 3 are relevant to determining whether the level of freedom restriction involved in a vaccine mandate is proportionate to its benefits.
Criteria for the acceptability of vaccine mandates for HCWs
Risk for hcws.
There is an ethical issue about the nature and magnitude of risks that HCWs should be expected or required to take on as a matter of contractual obligation, for the sake of their patients. It is already commonly accepted that HCWs should take on at least some additional health risk for the sake of their patients. This includes, for example, some additional risk of being exposed to infectious disease when they treat infected patients (eg, the risk of needlestick injury 15 ). The issue at stake is not if this is justified, but how much extra risk is justifiable by contractual and professional obligations. 16
If we define as supererogatory an action that goes beyond ‘the call of duty’, there is a higher bar for what makes a certain risk supererogatory for HCWs than for the rest of the population. There is a presumption that, barring any significant public health reason, individuals should be free to make their own risk assessment, also based on personal values, about any medical intervention. However, professional obligations more frequently trump individual freedoms.
Whether the risks are proportionate depends, in part, on the benefits we can expect to achieve. 5 In the case of vaccination, the benefits are measured in terms of the impact of vaccination on patients’ safety and healthcare delivery, which largely depends on the vaccine’s capacity to stop infections but also to prevent HCW staff shortage.
Given the special duties of healthcare professionals to prevent harm to patients, even a small reduction of risk in transmission might ground an ethical and a legal obligation to be vaccinated that does not apply to the general population.
When assessing the benefits of mandatory vaccination, two factors need to be considered: first, the magnitude of the public health threat; and second, whether the mandate can reasonably be expected to increase vaccine uptake in a way that actually translates into significant positive outcomes in terms of patients’ health. This depends in large part on how effective vaccines are at preventing infection and transmission.
Relative expected utility of a mandate compared with less restrictive options
Whether mandates are ethically justifiable, or even ethically required, depends in part on whether less restrictive options exist that can achieve the same goals.
One proposal is to adopt an intervention ladder on the model of the one the Nuffield Council on Bioethics 17 proposed for public health interventions more generally. On this proposal, a series of policies, from the least to the most restrictive, should be considered or implemented before the vaccine is made mandatory for HCWs. These are summarised in table 1 , which is about COVID-19 vaccines but can be extended to any other vaccination for HCWs and which also includes policies more restrictive than mandates. 18 Importantly, the table is only meant to present the options available and does not imply that they are all ethically justifiable (in particular, of course, forced vaccination).
- View inline
Possible vaccination policies for healthcare workers
However, the difference between less and more restrictive options can be a matter of probability of success. A vaccine mandate might not be strictly necessary, but nevertheless be more likely than a nudging policy or information campaign alone to yield the desired outcomes. In other words, applying a principle of least restrictive alternative often means assuming a risk.
A desire to seek the least restrictive alternative is the basis of the proposal for a ‘conditional mandate’. Such a mandate entails temporary redeployment of the HCW refusing the vaccine to non-clinical roles or, if this is not possible, paid leave, with the contract terminated only at the end of such period of leave if the HCW has not changed their mind and redeployment is still not an option. 18 This minimises the risk of reducing staff shortage while still achieving the goal of protecting patients.
However, the question is not simply one of using the ‘least restrictive alternative’. 17 The important question is whether the benefit associated with a more restrictive alternative is sufficiently great to justify the greater restriction.
COVID-19 vaccine mandates? Probably no
HCWs are at a higher risk of COVID-19 infection and death than the general population and COVID-19 has significant workforce implications, particularly without vaccination. 19 High infection rates among staff have other undesirable consequences, such as an increased fear in people of contracting COVID-19, which can prevent them from attending healthcare settings and lead to higher morbidity and mortality from other diseases because of late or missed diagnoses. 20
While these considerations weigh in favour of a COVID-19 vaccine mandate for HCWs, there seem to be, in the present context, stronger reasons against. We will see how COVID-19 vaccine mandates fare with regard to the three criteria identified above.
Risks for HCWs
COVID-19 vaccines are associated with non-trivial risks, and benefits may only marginally outweigh those risks for many HCWs, especially younger ones, given their relatively low risk of serious illness from COVID-19 and the known and unknown risks of the vaccine. For example, current adenovirus vaccines like the Oxford/AstraZeneca and the Johnson & Johnson vaccines come with a small risk of blood clots, which in 2021 led many countries, including the UK, the USA and Australia, to suspend the use of such vaccines for younger age groups. The Australian Government suspended the use of the AstraZeneca vaccine for people under 60 after having estimated a risk of blood clots of 3.1 cases per 100 000 people under 50 and 2.7 cases per 100 000 people aged 50–59 after one dose of the vaccine. 21 However, a risk of thrombocytopaenia and thrombosis is also present after contracting COVID-19, with a number of studies indicating that the risk (although still low) is higher after COVID-19 infection than after receiving adenovirus vaccines. 22
The mRNA vaccines come with risk of myocarditis. One study found that such risk, even if small in both cases, for people under 40 may be higher after the mRNA vaccines than after COVID-19 infection (with 15 excess cases per 1 million after two doses of the Moderna vaccine, lower for other vaccines, compared with 10 excess cases per 1 million after COVID-19 infection). 23 However, postvaccination myocarditis appears to be mostly mild (treated only with anti-inflammatories), 24 while COVID-19 (even in younger patients) is associated with increased risks of other severe complications. In the USA, the Centers for Disease Control and Prevention CDC estimate that in men aged 18–24 (the youngest age group likely to be working as HCWs and where the risk/benefit of vaccination is most finely balanced), 1 million mRNA COVID-19 vaccination doses would prevent 936 hospitalisations, 215 intensive care unit (ICU) admissions and 13 deaths, while simultaneously leading to 15–18 vaccine-associated myocarditis cases. (In women aged 18–24, mRNA COVID-19 vaccination would prevent 1127 hospitalisations, 93 ICU admissions and 13 deaths, while causing 4–5 myocarditis cases. 25
These considerations mean that the marginal benefit of vaccines, especially in young age groups, assuming it is present, is very small. Risks are not insignificant compared with the benefits. This by itself does not make COVID-19 vaccine mandates impermissible. However, it suggests that, at least for certain groups, the argument in favour of a vaccine mandate needs to rely in part on ethical obligations to act in the best interest of the patients or in the interest of the healthcare system, even when this entails some potential additional personal risk. The important question is whether these other benefits are sufficiently great.
As detailed above, COVID-19 has posed a public health threat of a significant magnitude. At earlier stages in the pandemic, the potential benefit of a vaccine mandate in terms of preventing serious illness in vulnerable patients was significant. However, it is less clear that still holds, even if we were to assume that a mandate would be extremely effective in increasing vaccine uptake.
First, current COVID-19 vaccines do not seem very effective at preventing transmission, especially with the highly transmissible Omicron variant, although there is some inconsistency across studies and some are more optimistic than others on the transmission-stopping effectiveness of vaccines. 26 Even with the less transmissible Delta variant, while vaccination reduced the risk of infection, the viral load (which is linked to risk of transmission) of double-vaccinated people who had breakthrough infection was similar to that of unvaccinated ones, suggesting that ‘both can efficiently transmit infection’. 27 This proved to be true also for asymptomatic individuals. 28 At the moment, the only way vaccines could have a significant effect at preventing transmission is by preventing people from getting infected in the first place. Yet vaccines do not appear to be very effective at doing that, although again some studies are slightly more optimistic than others. 26
As for preventing healthcare staff shortage, the benefit of the vaccine very much depends on the policy in place, particularly with regard to testing requirements. If the policy is that staff testing positive are required to stay home, then the vaccines’ benefits are probably negligible, given vaccines’ low effectiveness at preventing contagion. If there is no testing requirement for asymptomatic staff, then the benefit very much depends on vaccines’ effectiveness at preventing symptoms. A recent study has concluded that two doses of either the Pfizer/BioNTech or the Oxford/AstraZeneca vaccine provide limited protection against symptomatic disease caused by Omicron, and a ‘booster’ dose with an mRNA vaccine would increase protection substantially, but only for a short period of time, falling between 39% and 45% after 2 months. 29 Unless healthcare staff are required to get vaccinated every 2–3 months (which would compound the risks), it seems the benefit of vaccinating them, both in terms of reducing the risk of infecting patients and reducing staff shortages, would be very limited.
Second, the difference in risk of infection between vaccinated and unvaccinated HCWs has been reduced by significant exposure to the virus over the past 2 years. Prior infection with COVID-19 (sometimes called ‘natural immunity’) is comparable to vaccination in terms of effectiveness at reducing virus transmission of the Delta variant, with a benefit that lasts for at least 13 months. 30 It is likely that many HCWs have immunity to COVID-19 because of previous infection. Now, prior infection does not offer the same level of protection against Omicron as against Delta. One study estimates a protection through previous infection of 92% against Delta and 56% against Omicron. 31 A rapid analysis commissioned by the UK Government suggests that the rate of Omicron in those who had two vaccinations was 73.4 infections (per 10 000 person days), compared with 60.9 infections (per 10 000 person days) in those who were unvaccinated but had evidence of prior infection. 32 It is unclear at the moment for how long any ‘booster dose’ would have an effect on protecting individuals from infection—at the moment we have only observed its effect, which is significant (93%), over the period of a few weeks. 33 However, data from the Office for National Statistics in the UK indicate that in the first week of January 2022 ‘between 94.1% to 96.3% of the adult population would have tested positive for COVID-19 antibodies at or above a higher antibody threshold needed to provide protection from new COVID-19 infections for those who are vaccinated’. While it is difficult to exactly estimate the actual effect of natural immunity after a mass vaccination roll-out, it is quite telling that the percentage of the adult population who received three doses of the vaccine was estimated to be around only 70% when those data where gathered, 34 which suggests a significant contribution of natural immunity itself. A large study from Sweden found that it takes 767 people with natural immunity being vaccinated to prevent one reinfection during follow-up, and concluded that ‘[t]he risk of SARS-CoV-2 reinfection and COVID-19 hospitalisation in individuals who have recovered from a previous infection remained low for up to 20 months. Vaccination with an mRNA vaccine seemed to further decrease the risk, although the differences in absolute measures were small’. 35 If such data are confirmed, the marginal benefit of vaccination in terms of reduction of risk of transmission seems, at the moment, too small to justify a mandate.
Granted, natural immunity in a community might itself become more patchy when the disease is endemic and circulates more slowly. If natural immunity stops offering the level of protection it seems to offer now, the case for introducing vaccination requirements for HCWs in order to protect patients will become stronger.
Third, the severity of illness from COVID-19 has reduced, due to changes in the circulating form of the virus, high vaccine uptake in those at highest risk and increasingly more treatments becoming available.
If vaccines are not very effective at stopping transmission and hence do not prevent serious illness in patients, the infringement on individual freedom, as well as the imposition of vaccine risks on certain groups, might not be justified by the collective benefit. This will be even more likely where there are other, less restrictive ways to achieve a similar result.
Are there less restrictive policies?
There are other less restrictive ways of minimising the risk of HCWs infecting patients with COVID-19 which are arguably more effective than vaccines. Most obviously, these include regular testing of HCWs and use of personal protective equipment (PPE), in particular adequate masks. 36 Such alternatives come with their own costs. In particular, PPE can be cumbersome for clinicians to wear and could limit clinician–patient communication, which in some cases could result in worse patient care. That such measures are less restrictive does not mean that they are costless and, once again, the task is that of balancing the costs of different alternatives against each other.
Thus, at the moment the benefits of a mandate do not seem to justify the level of freedom infringement and the costs and risks imposed on the vaccinated. Some have also expressed concerns about the potential impact of a COVID-19 vaccine mandate for black and ethnic minority groups. 37 Within the NHS, the COVID-19 vaccine uptake in this community is lower than in other groups. 38 Some take this to mean that ‘they will be disproportionately impacted by the government’s policy’, 37 although it is worth noting that a vaccination requirement could also have an equalising effect in terms of health outcomes if it results in higher vaccine uptake among these communities. This is an issue that would require a separate discussion and we are not going to address in this article.
It is worth emphasising at this stage that we are putting forward claims about the ethical justification of a mandate, not about prudential considerations or ethical considerations for getting the vaccine. There can be strong ethical reasons for being vaccinated despite the small risk (eg, minimising the risk of needing scarce health resources in case one gets ill) and there can be good personal or prudential reasons for being vaccinated (eg, in the case of primary carers who would not be able to care for their dependants if they were severely ill for a prolonged time). Here we are only concerned with ethical and professional requirements as they pertain to HCWs.
Influenza vaccine mandates? Probably yes
Although the focus of public health policies over the last 2 years has been on COVID-19, influenza represents a significant public health threat. For example, in the 5 years before the COVID-19 pandemic in England, influenza caused on average more than 11 000 annual deaths, with over 22 000 deaths in the 2017 and 2018 season. 1 Most such deaths occur in people over 65 years, as a weaker immune system means that serious complications of influenza such as pneumonia are more likely and the immune response to the vaccine is poorer. 39 And of course, the elderly and those with significant comorbidities and/or a weak immune system are over-represented in hospitalised patients.
In the 2020–2021 season, 76.8% of front-line HCWs were vaccinated against influenza in England, with uptake in NHS Trusts ranging from 53.0% to 100%. 4 In the UK, there is no influenza vaccination requirement for HCWs as a state policy. This is in line with many other countries’ policy. For instance, in the USA no state requires influenza vaccination for HCWs as a condition of employment. Some states require employers to offer vaccination to their healthcare employees and some require them to report their employees’ vaccination status, but employees can be exempted for medical or religious reasons in some of these states and for any reason in the others. However, some individual organisations in the USA do require influenza vaccination as a condition of employment.
Influenza vaccines have been used for decades. Changes in the circulating strains causing seasonal influenza mean that protection does not last. The vaccine is modified each year, and both live attenuated and inactivated forms are used. Familiarity with the influenza vaccines means that they have a well-characterised safety profile. Side effects are usually mild and more serious side effects are rare. For example, there is a risk of postvaccine Guillain-Barre syndrome of one per million vaccine doses, although the risk of this is probably higher with influenza itself. 40
On the one hand, seasonal influenza, even in a bad year, causes considerably less serious illness and death than the COVID-19 pandemic (eg, 30 times fewer deaths based on a recent estimate compared with the 2009 influenza). 41 On the other hand, as we said above, the mean age at death for influenza is lower than with COVID-19, and the fact that it is endemic means that the total impact remains considerable. (When COVID-19 is endemic and everyone has been exposed, this difference will likely reduce, thanks to higher levels of natural immunity, unless the virus mutates significantly.)
A 2016 systematic review found that mandatory influenza vaccination for HCWs (including termination of employment for those who refuse the vaccine) was ‘by far the most effective single intervention’ at increasing vaccine uptake. 42 Effectiveness remains very high for cases of ‘soft mandates’. In such cases, declination statements explaining reasons for one’s refusal are sufficient grounds for exemption—a form of conscientious objection to vaccination. This seems confirmed by more recent evidence. In a 2020 study, monitoring the long-term effect of a mandate, the increase within a US institution was from 70% premandate to over 98% after the mandate, with the effect lasting over 10 years and a constant decrease over time in requests for exemptions. 43
Now, the effect of influenza vaccination in preventing symptomatic infection specifically in healthy adults might be very small. A systematic review suggested ‘healthy adults who receive inactivated parenteral influenza vaccine rather than no vaccine probably experience less influenza, from just over 2% to just under 1% (moderate-certainty evidence)’. 44 Yet the the Oxford Vaccine Group presents data suggesting that in the five influenza seasons preceding the pandemic, the influenza vaccine prevented 15%–52% of influenza cases across all population groups. 45
However, one problem is that individuals with asymptomatic influenza can transmit the virus, although the role of asymptomatic cases in virus transmission is uncertain. 46 A recent study in two South African communities across two influenza seasons has shown that asymptomatic cases of breakthrough infection transmitted infection to 6% of household contacts. 47 It is estimated that 30%–50% of influenza infections can be asymptomatic, 1 48 but there are significant challenges to studying influenza vaccine effectiveness against asymptomatic infection, in part because they are not captured by existing surveillance networks. However, to the extent that vaccination reduces the risk of infection, the reason to mandate the vaccine for HCWs in order to prevent harm to patients is strong.
Crucially though, we already have evidence suggesting that increasing vaccine uptake among HCWs translates into reduced risk of harm to patients. A meta-analysis 49 found a 4.4% reduction in all-cause mortality in hospitals that had increased HCW vaccine uptake by offering influenza vaccination to their staff. Estimates based on modelling indicate that 100% vaccination coverage of HCWs in acute care settings could result in a 43% reduction in the risk of infection in hospital patients and 60% reduction in nursing home patients. 50 It is worth noting, however, that a systematic review found ‘an absence of high quality evidence that vaccinating HCWs against influenza protects people aged 60 years or older in their care on influenza-specific outcomes’. 51 While this does not negate the previous claims, it certainly supports the need for high-quality evidence to support any future vaccine mandate.
Less restrictive measures can be beneficial. For example, simply offering vaccines on-site to HCWs has been shown to increase vaccine uptake. 52 However, as the evidence summarised above indicates, uptake is significantly higher with a mandate than with other measures. Other types of interventions such as increased awareness, educational initiatives and incentives were found individually to have little effect, although their cumulative effect was comparable to that of ‘soft mandates’. 42 A more recent meta-analysis further confirmed that interventions including multiple actions are more effective than single actions, finding small to moderate increases in uptake for non-mandatory actions and higher increase when these are accompanied by mandatory requirements (including formal opt-out declarations). 53
As mentioned above, influenza vaccines are not highly effective at protecting against symptomatic infection. Given this, it has been suggested that influenza vaccine mandates might not be worthwhile if the uptake baseline is already over 70%: it has been estimated that the same results in terms of expected reduced infection following a mandate could be achieved by a 2% reduction in ‘presenteeism’, or working while ill, 54 which would be a less restrictive measure. However, this line of objection assumes that achieving a 2% reduction in presenteeism could be achieved straightforwardly; yet this is far from obvious. Data suggest that 75% of HCWs who develop an infectious illness continue to work, 55 so even a 2% reduction in presenteeism represents a significant logistical challenge. 56 Aiming to reduce presenteeism could be a less restrictive way of potentially achieving a comparable benefit to a vaccine mandate, but it may also be less likely to succeed.
To summarise the argument, HCWs have a professional duty to minimise risk of harm to patients. For what we know at the moment, higher influenza vaccine uptake minimises risk of harm to patients, not just by reducing the risk of infection but also by reducing the risk of staff shortages. Vaccines are effective at reducing risk of infection and illness. Finally, influenza vaccine mandates increase vaccine uptake more than less severe measures (either by themselves or in addition to them).
The above analysis suggests that the relevant ethical criteria would justify mandating the influenza vaccine, but not the COVID-19 vaccine for HCWs at the present time, given the characteristics of current vaccines and the current dominant variant (see table 2 ). 6
Comparison between COVID-19 and flu vaccine
If this analysis is correct, the current situation, in which many states mandate the COVID-19 vaccine but do not mandate the influenza vaccine for HCWs, appears to be upside down. If vaccine mandates in HCWs are justified (and we believe that they can be), there is at the moment a stronger ethical case for mandating the influenza vaccine than the COVID-19 vaccine.
It is important to emphasise that we are mostly concerned here with the ethical reasons in support of such mandates. We have based our conclusion on those principles and the evidence currently available. The latter is of course subject to change and, if new evidence emerges that significantly affects the empirical landscape, the same ethical principles could very well support different conclusions.
Are vaccine mandates discriminatory and coercive?
We have assessed the ethical proportionality of a vaccine mandate—balancing risks, benefits and the restrictiveness. However, some might think that mandates in the form of conditions of employment are unjustifiable in principle, regardless of proportionality. In particular, vaccine mandates might be considered unfairly discriminatory and/or excessively coercive.
We will examine these two considerations separately.
In one sense, discrimination means, quite simply, treating different individuals differently. It is not ethically problematic in itself. In another, normative sense, discrimination is often used to mean ‘unfair discrimination’, that is, when individuals are treated differently on the basis of factors that should not be considered relevant. Thus, in the first, unproblematic sense, all conditions in employment contracts exclude from employment individuals who do not fulfil certain requirements. Vaccination requirements are in a sense not different from requirements to (for example) provide evidence of visa status, copies of qualifications, proof of address and police checks, and so on.
The relevant question is whether it is unfair to require vaccination. This would be the case if vaccination were an ethically irrelevant factor for employment, if vaccination status became a ‘protected characteristic’ that should not create any form of disadvantage in employment decisions (in the way, for example, disability and gender are), if individuals could not access vaccines (thus being excluded from jobs for factors beyond their control), or if the level of coercion involved were excessive.
Vaccination status is an ethically relevant factor when it significantly reduces the risk of infection and contagion. Such reduced risk allows HCWs to fulfil their professional responsibility to minimise the risk of harming patients and to benefit them, as well as healthcare systems’ responsibility to provide adequate healthcare by minimising the risks of shortage of staff.
At the moment, vaccination status is not a protected characteristic, although we do not exclude that it might qualify for this (eg, if vaccination status were taken to express one’s core ethical or religious beliefs). This is a question we are not addressing here. We will simply proceed on the assumption that it is not a protected characteristic, bearing in mind that this might well change.
It would be discriminatory to exclude HCWs if they were unable to access a vaccine (because of cost or availability) or because of a true medical exemption. However, in virtually all settings where a mandate might apply vaccines will be easily available (often at no cost) to HCWs. Those with true medical exemptions should be exempted from vaccination requirements, although in such cases alternative precautions should be adopted (eg, the use of masks and regular testing for asymptomatic infection, if available) if necessary to protect patients.
So the question that remains to be addressed is about the level of coercion involved in vaccine mandates for HCWs: are vaccine mandates coercive and, if so, is the level of coercion ethically acceptable?
All conditions in employment contracts ask future employees to choose between their job and whatever is required. For example, HCWs already agree to health and safety requirements such as washing of hands or wearing gloves and masks when providing (certain forms of) patient care. There is no serious question that an HCW who declined to wash hands (or wear masks/gloves) should not be eligible to provide direct patient care. If this is a form of coercion at all, it is an acceptable one. The problem seems to arise when requirements affect health and lifestyle choices which have broader implications affecting one’s life as a whole. In such cases, arguably the level of coercion is higher. Vaccine mandates fall in this category. However, whether they are excessively coercive depends in part on how one understands coercion.
On so-called non-normative accounts, coercion is what reduces the options available to someone by making them unreasonable, given the magnitude of the penalties for non-compliance or, on some accounts and more controversially, the incentives for compliance. 57 On such views, vaccine requirements of HCWs are coercive because they reduce the options available to those who refuse the vaccines. The degree of coercion involved will depend in part on the extent of the costs associated with giving up the option of a career as an HCW. However, on normative or ‘moralized accounts’, 58 coercion only occurs when threats of penalties remove options to which individuals have a right to, or in any case that have some particular moral value. In this sense, to the extent that alternative career paths are available, vaccine requirements for HCWs are not coercive: there is no right to become an HCW and there are plenty of professions (or perhaps specialisations within the healthcare profession) that do not require vaccination as a condition of employment. On this view, a vaccine mandate is no more coercive than any other condition of employment because someone can refuse the vaccine and choose another profession.
However, those who adopt non-normative accounts of coercion can claim that mandates are coercive, and they may note that the costs associated with giving up a career as an HCW are extensive. In particular, alternative career paths are not always easily available, as it presumably is not easy for someone to switch career after having been in the profession for some years. This sounds reasonable: the mandate might not be very coercive for someone who needs to decide whether to become a healthcare professional and knows that that option comes with a vaccination requirement, but it can be very coercive for someone who is already a professional (and entered the profession on the understanding that the vaccine they would rather not take was not mandated). Thus, one way to reduce this coercive pressure and strike a balance between individual freedom and patients’ interests is to make vaccination a condition of entry into the profession rather than mandating those already employed, and adopt a conditional mandate if at all possible for those already in the profession. This is because while someone can relatively easily choose a different career path when young and deciding whether to become a healthcare professional, it is way more difficult, or perhaps an unreasonable option, for someone in their 40s or 50s to switch career because of a new condition of employment that they never agreed to. Whether this level of coercion on someone already in the profession is ethically impermissible depends on whether it is reasonable to expect new health professionals to take future, as yet not developed, vaccines. If that is a reasonable expectation, then again the level of coercion does not seem different from the one posed by any other condition of employment that sets future expectations for employees.
In any case, even if a vaccine mandate places no more coercive pressure on an individual than other conditions of employment, some may regard it as more problematic because of the right it over-rides. Arguably, the right to bodily integrity or bodily autonomy (understood as a right to refuse physical interventions on the body) is a fundamental freedom. We might thus only be willing to accept a lower degree of coercive pressure when this right is at stake, compared with the degree of coercive pressure we accept when other lesser claims are at stake. To illustrate, those who take this view may see a vaccine mandate as problematically coercive where mask/glove/handwashing mandate for HCWs would not in so far as the former infringe upon the right to bodily integrity, but the latter would not. If this is the case, then the permissibility of a mandate will turn on the (1) extent of the coercive pressure that we are willing to accept with respect to interventions that interact with the right to bodily integrity, and (2) the degree of coercive pressure involved in a mandate. Our own view is that if different career choices are easily available (and that is a significant ‘if’), a vaccine mandate need not involve a degree of coercive pressure that would entail an infringement of the right to bodily integrity.
Ultimately, there is an ethical balance to be drawn between protecting patients (including their own right to not acquire serious but preventable nosocomial infections) and coercing some healthcare professionals into having a vaccine that they would prefer not to receive. The harm prevented should be great enough and the risks to professionals small enough to make the coercive pressure justified.
The analogy with conscientious objection
The balance between patient well-being and professional freedom involved in vaccine mandates for HCWs is similar in important respects to the case of conscientious objection in healthcare. The above suggestion of introducing a requirement as a condition of employment may also apply in this context. According to certain views, freedom of conscience is permissibly infringed upon when conscientious objection is ruled out by job contracts, as long as there is a reasonably available option to choose a different profession. This is because the right to freedom of conscience is a qualified one. It is legitimate to make employment subject to eligibility criteria that ensure that professional obligations are discharged. On such views, healthcare professionals do not have a right to conscientious objection where that would violate professional duties, including the duty of beneficence and non-maleficence. 59
Arguably, such view is questionable and indeed many would not agree. However, even those who think that this line is too strong and are in favour of some form of conscientious objection in healthcare tend to think that conscientious objection should be constrained, for example by requiring a duty of referral and a duty to provide the medical intervention in emergency cases. 60 This is because patients’ medical interest is taken to normally have priority over personal moral views of healthcare professionals.
Similarly, HCWs might be opposed to vaccines on personal moral or religious grounds. However, putting patients’ interests first means that professional and contractual obligations to avoid causing harm potentially trump those personal beliefs. It is not clear that the exemptions that allow health professionals to conscientiously object as long as a colleague is available to provide the contested service can be extended to non-vaccination for HCWs who have close patient contact. Every interaction means an increased risk of infection to the patient compared with a situation where the HCW is vaccinated.
Thus, a conditional mandate with redeployment to non-patient-facing roles (as per the proposal above) would appear to be the closest equivalent.
Conclusions: implications for vaccine mandates more generally
Recent debates and policy decisions relating to vaccine mandates for HCWs in the setting of the COVID-19 pandemic might be taken to set a clear precedent for future vaccines. In countries that have adopted such a mandate, the door might now be open for wider application. Given political and apparent ethical support for such mandates, it may be inevitable that countries like Australia, USA, and others will review their approach to influenza vaccination in the coming winters. Alternatively, countries that have taken the opposite approach might be seen to have foreclosed this option. For instance, UK’s former Health Secretary Jeremy Hunt expressed 7 his view that the scrapping of the COVID-19 vaccine mandate will make it hard to justify other vaccine mandates in the future.
However, in this paper we have suggested that while the ethical principles that support vaccine mandates for HCWs remain constant, circumstances and characteristics of viruses, diseases and vaccine differ. The same principles and criteria can justify mandates for certain vaccines and not for others. Here, we have argued that, given current evidence, they justify influenza vaccine mandates, but not COVID-19 vaccine mandate.
This might sound counterintuitive given that the COVID-19 pandemic has certainly caused substantially more deaths and morbidity than seasonal influenza. Current estimates suggest that it has caused 20 million excess deaths—substantially higher than annual influenza deaths (300 000–600 000). 61 However, for reasons that we have given above, the balance of risks and benefits suggests that an influenza vaccine mandate, but not a COVID-19 mandate, would currently be ethically proportionate. The same considerations would support mandates for HCWs for other vaccines that offer equivalent prevention of harm and at similar risk to individuals, such as hepatitis B.
Mandates should be introduced on a disease-specific and vaccine-specific basis. The problem must be a significant one, the vaccines must be safe and effective at preventing illness and/or transmission, mandatory measures must be superior to less coercive alternatives, and the costs in loss of liberty and risk to health professionals must be proportionate in professional terms to the benefits to patients. In box 1 , we provide a proposal for ethically assessing contractual vaccine mandates in healthcare.
A proposal for contractual vaccine mandates for healthcare workers ie
Employment contracts: the best way to minimise the degree of coercion while protecting patients and minimising the risk of staff shortage would be to include explicit clauses with vaccination requirements into new employment contracts or potentially at medical/nursing school entry.
Conditional mandate: for staff already employed, it would be preferable to use a conditional mandate where staff is redeployed to non-clinical roles until they are vaccinated, if at all possible, and for as long as it does not become disruptive of healthcare delivery or does not impose unfair burdens on vaccinated colleagues.
Selective mandate: mandates should be tailored to the specific risks that specific diseases pose. For example, hepatitis B vaccine mandates could be applied only to those involved in ‘exposure prone procedures’. Other mandates might apply only in settings where health professionals are in contact with patients at higher risk of serious illness.
Natural immunity exemption: natural immunity should be taken into account. Where it can reasonably be estimated to provide immunity comparable to or even superior to that provided by vaccines, vaccination should not be required as a condition of employment. This means that either healthcare workers with natural immunity should be exempted by any mandate that is otherwise ethically justified, or that the mandate should not be in place if natural immunity among healthcare workers is sufficient to protect patients.
In the case of new vaccines, mandates should be avoided at early stages, while risks are unclear, and be replaced by alternatives (such as testing and protecting personal equipment requirements) or other means to encourage uptake, such as some form of incentives (financial or non-financial). In those cases, contractual (conditional) vaccine mandates should only be considered if alternatives do not offer enough protection from nosocomial infection and there is sufficient evidence around their relative safety, bearing in mind that it is reasonable to expect HCWs to take on themselves some higher degree of risk for the sake of protecting patients than the general population.
Ethics statements
Patient consent for publication.
Not required.
- Department of Health and Social Care,
- Rudan I , et al
- Soldevila N , et al
- Esposito S ,
- Mutambudzi M ,
- Niedzwiedz C ,
- Macdonald EB , et al
- Tartari E ,
- Kenters N , et al
- ↵ Phe and LSHTM, the contribution of nosocomial infections to the first wave, 28 January 2021 . Available: https://www.gov.uk/government/publications/phe-and-lshtm-the-contribution-of-nosocomial-infections-to-the-first-wave-28-january-2021
- ↵ Public health Scotland, hospital onset COVID-19 mortality in Scotland 7 March to 31 December 2020 . Available: https://www.publichealthscotland.scot/media/7183/2021-02-24-covid19-hospitalonset-mortality-mar-dec-2020-summary.pdf
- McKeigue PM ,
- McAllister DA ,
- Caldwell D , et al
- Blackburn RM ,
- Frampton D ,
- Smith CM , et al
- Department of Health,
- ↵ General medical Council, good medical practice. domain 2: safety and quality2104 . Available: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice/domain-2----safety-and-quality
- Turbadkar D
- Giubilini A ,
- Savulescu J
- Nuffield Council on Bioethics
- Bradfield OM ,
- Giubilini A
- Nurmi E , et al
- Lazzerini M ,
- Apicella A , et al
- Hippisley-Cox J ,
- Mei XW , et al
- Handunnetthi L , et al
- Su JR , et al
- Gargano JW ,
- Wallace M ,
- Hadler SC , et al
- Stokel-Walker C
- Singanayagam A ,
- Dunning J , et al
- Acharya CB ,
- Mitchell AM , et al
- Andrews N ,
- Kirsebom F , et al
- Gordon SM ,
- Sheehan MM , et al
- Altarawneh HN ,
- Chemaitelly H ,
- Hasan MR , et al
- ↵ UK health security agency 2022. SARS-CoV-2 variants of concern and variants under investigation in England technical briefing 34 , 2022 . Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1050236/technical-briefing-34-14-january-2022.pdf
- ↵ ONS 2022, coronavirus (COVID-19) infection survey, antibody and vaccination data, UK . Available: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveyantibodyandvaccinationdatafortheuk/26january2022 [Accessed 8 Feb 2022 ].
- Nordström P ,
- Nordström A
- Andrejko KL ,
- Myers JF , et al
- Blackshaw BP
- Kadambari S ,
- Vanderslott S
- Reichert TA ,
- Simonsen L ,
- Sharma A , et al
- ↵ CDC Guillain-Barré syndrome and flu vaccine , 2015 . Available: https://www.cdc.gov/flu/prevent/guillainbarre.htm [Accessed 29 Mar 2022 ].
- Kopsachilis F ,
- Mouratidou E , et al
- Gemeinhart N ,
- Dunagan WC , et al
- Demicheli V ,
- Jefferson T ,
- Al-Ansary LA , et al
- Patrozou E ,
- Kleynhans J ,
- Moyes J , et al
- McMillan JA ,
- Serwint J , et al
- Lindley MC ,
- Allred N , et al
- van den Dool C ,
- Bonten MJM ,
- Hak E , et al
- Thomas RE ,
- Lasserson TJ , et al
- Chambers D ,
- Weingarten S ,
- Riedinger M ,
- Bolton LB , et al
- Wertheimer A
- Iuliano AD ,
- Roguski KM ,
- Chang HH , et al
Twitter @Neonatalethics
Contributors All authors contributed to the design of the paper and the formulation of the main arguments. AG wrote the first draft and JS, JP and DW did substantial editing of some sections. AG is the guarantor for the overall content of the paper.
Funding This study was funded by the UK Research and Innovation (AH/V013947/1), Department of Business and Innovation, Victoria State Government (Operational Infrastructure Support (OIS) Program), Wellcome Trust (203132/Z/16/Z, WT104848), and Australian Research Council (DP190101547).
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
↵ LeadingAge, 22 December 2021, Vaccine mandates by state: who is, who isn’t, and how?, at https://leadingage.org/workforce/vaccine-mandates-state-who-who-isnt-and-how .
↵ CNBC, 13 January 2022, Supreme Court blocks Biden Covid vaccine mandate for businesses, allows health care worker rule, at https://www.cnbc.com/2022/01/13/supreme-court-ruling-biden-covid-vaccine-mandates.html , accessed 3 February 2022.
↵ BBC, 4 January 2022, Covid: Hospital trusts declare critical incidents over staff shortages, at https://www.bbc.co.uk/news/uk-england-59866650 .
↵ AMA, AMA calls for mandatory vaccination for health care staff, GPNN 2, September 2021, at https://www.ama.com.au/gpnn/issue-21-number-34/articles/ama-calls-mandatory-vaccination-health-care-staff .
↵ We say ‘in part’ because there may be an upper limit on the level of risk that someone can be professionally or legally required to take, no matter how great the benefit. Above the limit, any additional risk of harm can no longer be ethically justified. The upper limit might be difficult to pin down in some non-arbitrary way. However, even if we have an idea of the threshold of justifiable risk HCWs can be exposed to for the sake of the patients, it remains true that whether the risk of harm is proportionate depends on the benefit that we can reasonably expect to result from it.
↵ Our analysis relates to current knowledge, vaccines and variants for COVID-19. Should a more virulent variant appear and more effective vaccines become available, those criteria might very well justify COVID-19 vaccine mandates in the future.
↵ See his point made in a Twitter thread at https://twitter.com/Jeremy_Hunt/status/1488220491374632963?ref_src=twsrc%5Etfw%7Ctwcamp%5Etweetembed%7Ctwterm%5E1488220491374632963%7Ctwgr%5E%7Ctwcon%5Es1_&ref_url=https%3A%2F%2Ftheconversation.com%2Fis-this-the-end-of-the-road-for-vaccine-mandates-in-healthcare-176310 .
Read the full text or download the PDF:
Other content recommended for you.
- Spoonful of honey or a gallon of vinegar? A conditional COVID-19 vaccination policy for front-line healthcare workers Owen M Bradfield et al., Journal of Medical Ethics, 2021
- Nudging towards COVID-19 and influenza vaccination uptake in medically at-risk children: EPIC study protocol of randomised controlled trials in Australian paediatric outpatient clinics Bing Wang et al., BMJ Open, 2024
- Influence of the COVID-19 pandemic and social media on the behaviour of pregnant and lactating women towards vaccination: a scoping review Larissa De Brabandere et al., BMJ Open, 2023
- Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review Mei Li et al., Postgraduate Medical Journal, 2021
- Exploring vaccine hesitancy in care home employees in North West England: a qualitative study Amelia Dennis et al., BMJ Open, 2022
- No Jab, No Job? Ethical Issues in Mandatory COVID-19 Vaccination of Healthcare Personnel Rachel Gur-Arie et al., BMJ Global Health, 2021
- Quantifying healthcare and welfare sector workers’ preferences around COVID-19 vaccination: a cross-sectional, single-profile discrete-choice experiment in France Carolina Díaz Luévano et al., BMJ Open, 2021
- Good reasons to vaccinate: mandatory or payment for risk? Julian Savulescu, Journal of Medical Ethics, 2020
- COVID-19 vaccine hesitancy and vaccine passports: a cross-sectional conjoint experiment in Japan Shohei Okamoto et al., BMJ Open, 2022
- Healthcare workers’ perceptions and attitudes towards the UK’s COVID-19 vaccination programme: a rapid qualitative appraisal Louisa Manby et al., BMJ Open, 2022
How COVID-19 Influenced Different Theories Essay
Introduction, the actor-network theory, food deserts, emotion management, intersection theory, neighborhood disadvantage.
The Corona pandemic has significantly disrupted people’s lives who were denied access to good food, causing death, health issues, and social and economic disruption. Food insecurity can be long-term or short-term and can be influenced by various factors, including an individual’s race, access to transportation, physical challenges, unemployment, and issues with purchasing food. COVID-19 has influenced the following theories; the Actor-Network Theory, food deserts, Emotion Management, Intersection Theory, and Neighborhood Disadvantage as they affect people’s social lives.
The actor-network concept is an advent to a social ideology that argues that everything in society and the natural world comprises ever-changing relationships. Human beings are considered as necessary as objects, ideas, processes, and other factors in creating social conditions. Innovation enables people to generate new information and direct their behavior in a specific direction. The actor-network theory views technologies and objects as an ever-changing network of individuals, their activities, and interactions. Humans are agents in these networks, but non-human entities are also considered actors. These things are made and used to replace actions that people usually have to do. The infection of the Coronavirus as an inhuman act fundamentally changes everything. Viruses and their adverse effects have disrupted the existence of almost everyone on the planet. Everyone has changed their actions to avoid getting infected and spreading the virus. Weddings have been postponed, vacations have been canceled, and traditions like proms and graduations have been canceled. Contagion destroys financial stability and puts an inexplicable strain on an organization. Apart from exacerbating political tensions, it has exposed the flaws and strengths of leadership.
Food deserts refer to urban areas whose residents live more than one or ten miles from a supermarket. Food deserts are often called communities that lack access to affordable and healthy food; food insecurity is worst in these food deserts. Most families living below the federal poverty level, whether in urban or rural areas, are more likely to struggle to find fresh food nearby. Many distant people in urban and rural communities are dying because of food deserts, food shortages, and COVID-19; children and women are particularly affected. The nutritional quality of food in food deserts and social determinants of food insecurity influence the transmission of COVID-19. The high levels of unemployment due to the epidemic may significantly impact the increased demand for food in food deserts. Diabetes and high blood pressure have increased among food-insecure people due to the availability of cheap, low-nutrient meals at local fast-food restaurants. Food insecurity often increases the risk of death from disease and many other adverse health issues. Improved laws and regulations must be enacted to help protect these communities without access to food.
Emotion management is a therapy that helps people understand, accept, manage, and express their emotions better. Doing so helps develop more reliable and helpful ways of dealing with the significant and harmful increases in reality. The COVID-19 pandemic and its effects have evolved into a global health crisis characterized by high unpredictability, high risk, complexity, and uncertainty. Like the COVID-19 pandemic, widespread disease outbreaks always harm physical and mental health. In line with this, an alarming increase in depression and anxiety, general malaise, sleep disturbances, and severe PTSD symptoms. Therefore, people’s emotional outcomes during COVID-19 may be affected by affective and emotion regulation strategies that alter the timing or intensity of emotional reactions. Although both adults and teenagers struggle with depression, young adults unequivocally loneliness worsens their emotional health during this pandemic. Children are also forced to use poor survival skills, such as playing alone and overinvesting in virtual entertainment. Lockdowns and development restrictions increase the potential to negatively affect people’s emotional health, with various groups of people often showing frustration and nervous reactions during the coronavirus lockdown.
Diversity refers to a concept in the social sciences that constructs how individuals face different forms of racism. This racism is based on their race, orientation, age, identity, physical ability, class, or other markers that may place them in the minority system. Although COVID-19 has disrupted modern social life, it is far from a great equalizer. Different social groups cope with other impacts of emergencies and face additional risks of infection. This indicates that disadvantaged communities face the most rapid death and spread of the virus, with minorities and immigrants facing a greater risk of disease than upper- and middle-class whites. Society is also struggling with measures of social exclusion and their adverse social and economic effects, which adversely affect the most vulnerable people in the community: ethnic minorities, children, low-income groups, and women. COVID-19 is a clear example of intersectionality: the individual and local effects on the openness of the Coronavirus are the results of different interrelated structures. The findings highlight the complex trade-offs between different factors related to race and location, including collective and financial imbalances that may exacerbate the absence of coronavirus deaths.
Neighborhood disadvantage pertains to the shortage of social and economic resources in a neighborhood and has been shown to affect health outcomes and personal characteristics but has so far not been recognized by social science research. Racism has been linked to disparities in financial status, leading to racial welfare biases. COVID-19 has disproportionately affected minorities in the United States. Hospitalizations and deaths have increased, reflecting health inequalities that already exist. The virus has killed more people in communities with high levels of socioeconomic disadvantage. The COVID-19 Inequality Index, which describes the exact nature of neighborhood disadvantage, serves as a map of this. Epidemiology dominated the initial discussion of COVID-19 disparities, which may explain why communities of color have higher death rates due to health disparities (Fritz et al. 840). Despite removing race and ethnicity from the direct measurements, black neighborhoods have the highest average inequality; a neighborhood loss returns the team to racial parity. White communities have lower levels of equality and this suggests that policymakers can target public health interventions using this index of neighborhood disadvantage.
From the above theories; race, class, and COVID-19 infections in New York are linked. Inequality is measured: in employment and transportation systems, access to food, social and economic conditions, and access to health services. Despite ongoing efforts to increase vaccinations, the United States death toll now exceeds half a million. To reduce the disproportionate load of Coronavirus and underscore the need to comprehensively address neighborhood disadvantage, an origin of widespread racial disparities in life. Through various types of rules and improvements implemented in the class, the health of the communities is affected by food laws. State, local, and federal governments are updating and revising food safety and food desert laws and policies. Countries have begun extensive programs to provide nutritious food to rural and urban communities.
Fritz, Bradley A., et al. “ Association of Race and Neighborhood Disadvantage with Patient Engagement in a Home-Based COVID-19 Remote Monitoring Program . Health & Place, vol. 68, 2021, pp. 838-846, Web.
- Food Desert Investigation and Analysis
- International Outbreak – Respiratory Syndrome Coronavirus
- Current COVID-19 Coronavirus Pandemic Agenda
- Genetics and Therapy for Pediatric Eye Diseases
- Internet-Based Incentives for Sedentary Adults
- Clinical Documentation and Treatment Planning Skills
- Organization and Display of Data in Healthcare
- Child Mild Measles Vaccination Study by Ward
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, May 18). How COVID-19 Influenced Different Theories. https://ivypanda.com/essays/how-covid-19-influenced-different-theories/
"How COVID-19 Influenced Different Theories." IvyPanda , 18 May 2024, ivypanda.com/essays/how-covid-19-influenced-different-theories/.
IvyPanda . (2024) 'How COVID-19 Influenced Different Theories'. 18 May.
IvyPanda . 2024. "How COVID-19 Influenced Different Theories." May 18, 2024. https://ivypanda.com/essays/how-covid-19-influenced-different-theories/.
1. IvyPanda . "How COVID-19 Influenced Different Theories." May 18, 2024. https://ivypanda.com/essays/how-covid-19-influenced-different-theories/.
Bibliography
IvyPanda . "How COVID-19 Influenced Different Theories." May 18, 2024. https://ivypanda.com/essays/how-covid-19-influenced-different-theories/.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

An Introduction to COVID-19
Simon james fong.
4 Department of Computer and Information Science, University of Macau, Taipa, Macau, China
Nilanjan Dey
5 Department of Information Technology, Techno International New Town, Kolkata, West Bengal India
Jyotismita Chaki
6 School of Information Technology and Engineering, Vellore Institute of Technology, Vellore, Tamil Nadu India
A novel coronavirus (CoV) named ‘2019-nCoV’ or ‘2019 novel coronavirus’ or ‘COVID-19’ by the World Health Organization (WHO) is in charge of the current outbreak of pneumonia that began at the beginning of December 2019 near in Wuhan City, Hubei Province, China [1–4]. COVID-19 is a pathogenic virus. From the phylogenetic analysis carried out with obtainable full genome sequences, bats occur to be the COVID-19 virus reservoir, but the intermediate host(s) has not been detected till now.
A Brief History of the Coronavirus Outbreak
A novel coronavirus (CoV) named ‘2019-nCoV’ or ‘2019 novel coronavirus’ or ‘COVID-19’ by the World Health Organization (WHO) is in charge of the current outbreak of pneumonia that began at the beginning of December 2019 near in Wuhan City, Hubei Province, China [ 1 – 4 ]. COVID-19 is a pathogenic virus. From the phylogenetic analysis carried out with obtainable full genome sequences, bats occur to be the COVID-19 virus reservoir, but the intermediate host(s) has not been detected till now. Though three major areas of work already are ongoing in China to advise our awareness of the pathogenic origin of the outbreak. These include early inquiries of cases with symptoms occurring near in Wuhan during December 2019, ecological sampling from the Huanan Wholesale Seafood Market as well as other area markets, and the collection of detailed reports of the point of origin and type of wildlife species marketed on the Huanan market and the destination of those animals after the market has been closed [ 5 – 8 ].
Coronaviruses mostly cause gastrointestinal and respiratory tract infections and are inherently categorized into four major types: Gammacoronavirus, Deltacoronavirus, Betacoronavirus and Alphacoronavirus [ 9 – 11 ]. The first two types mainly infect birds, while the last two mostly infect mammals. Six types of human CoVs have been formally recognized. These comprise HCoVHKU1, HCoV-OC43, Middle East Respiratory Syndrome coronavirus (MERS-CoV), Severe Acute Respiratory Syndrome coronavirus (SARS-CoV) which is the type of the Betacoronavirus, HCoV229E and HCoV-NL63, which are the member of the Alphacoronavirus. Coronaviruses did not draw global concern until the 2003 SARS pandemic [ 12 – 14 ], preceded by the 2012 MERS [ 15 – 17 ] and most recently by the COVID-19 outbreaks. SARS-CoV and MERS-CoV are known to be extremely pathogenic and spread from bats to palm civets or dromedary camels and eventually to humans.
COVID-19 is spread by dust particles and fomites while close unsafe touch between the infector and the infected individual. Airborne distribution has not been recorded for COVID-19 and is not known to be a significant transmission engine based on empirical evidence; although it can be imagined if such aerosol-generating practices are carried out in medical facilities. Faecal spreading has been seen in certain patients, and the active virus has been reported in a small number of clinical studies [ 18 – 20 ]. Furthermore, the faecal-oral route does not seem to be a COVID-19 transmission engine; its function and relevance for COVID-19 need to be identified.
For about 18,738,58 laboratory-confirmed cases recorded as of 2nd week of April 2020, the maximum number of cases (77.8%) was between 30 and 69 years of age. Among the recorded cases, 21.6% are farmers or employees by profession, 51.1% are male and 77.0% are Hubei.
However, there are already many concerns regarding the latest coronavirus. Although it seems to be transferred to humans by animals, it is important to recognize individual animals and other sources, the path of transmission, the incubation cycle, and the features of the susceptible community and the survival rate. Nonetheless, very little clinical knowledge on COVID-19 disease is currently accessible and details on age span, the animal origin of the virus, incubation time, outbreak curve, viral spectroscopy, dissemination pathogenesis, autopsy observations, and any clinical responses to antivirals are lacking among the serious cases.
How Different and Deadly COVID-19 is Compared to Plagues in History
COVID-19 has reached to more than 150 nations, including China, and has caused WHO to call the disease a worldwide pandemic. By the time of 2nd week of April 2020, this COVID-19 cases exceeded 18,738,58, although more than 1,160,45 deaths were recorded worldwide and United States of America became the global epicentre of coronavirus. More than one-third of the COVID-19 instances are outside of China. Past pandemics that have existed in the past decade or so, like bird flu, swine flu, and SARS, it is hard to find out the comparison between those pandemics and this coronavirus. Following is a guide to compare coronavirus with such diseases and recent pandemics that have reformed the world community.
Coronavirus Versus Seasonal Influenza
Influenza, or seasonal flu, occurs globally every year–usually between December and February. It is impossible to determine the number of reports per year because it is not a reportable infection (so no need to be recorded to municipality), so often patients with minor symptoms do not go to a physician. Recent figures placed the Rate of Case Fatality at 0.1% [ 21 – 23 ].
There are approximately 3–5 million reports of serious influenza a year, and about 250,000–500,000 deaths globally. In most developed nations, the majority of deaths arise in persons over 65 years of age. Moreover, it is unsafe for pregnant mothers, children under 59 months of age and individuals with serious illnesses.
The annual vaccination eliminates infection and severe risks in most developing countries but is nevertheless a recognized yet uncomfortable aspect of the season.
In contrast to the seasonal influenza, coronavirus is not so common, has led to fewer cases till now, has a higher rate of case fatality and has no antidote.
Coronavirus Versus Bird Flu (H5N1 and H7N9)
Several cases of bird flu have existed over the years, with the most severe in 2013 and 2016. This is usually from two separate strains—H5N1 and H7N9 [ 24 – 26 ].
The H7N9 outbreak in 2016 accounted for one-third of all confirmed human cases but remained confined relative to both coronavirus and other pandemics/outbreak cases. After the first outbreak, about 1,233 laboratory-confirmed reports of bird flu have occurred. The disease has a Rate of Case Fatality of 20–40%.
Although the percentage is very high, the blowout from individual to individual is restricted, which, in effect, has minimized the number of related deaths. It is also impossible to monitor as birds do not necessarily expire from sickness.
In contrast to the bird flu, coronavirus becomes more common, travels more quickly through human to human interaction, has an inferior cardiothoracic ratio, resulting in further total fatalities and spread from the initial source.
Coronavirus Versus Ebola Epidemic
The Ebola epidemic of 2013 was primarily centred in 10 nations, including Sierra Leone, Guinea and Liberia have the greatest effects, but the extremely high Case Fatality Rate of 40% has created this as a significant problem for health professionals nationwide [ 27 – 29 ].
Around 2013 and 2016, there were about 28,646 suspicious incidents and about 11,323 fatalities, although these are expected to be overlooked. Those who survived from the original epidemic may still become sick months or even years later, because the infection may stay inactive for prolonged periods. Thankfully, a vaccination was launched in December 2016 and is perceived to be effective.
In contrast to the Ebola, coronavirus is more common globally, has caused in fewer fatalities, has a lesser case fatality rate, has no reported problems during treatment and after recovery, does not have an appropriate vaccination.
Coronavirus Versus Camel Flu (MERS)
Camel flu is a misnomer–though camels have MERS antibodies and may have been included in the transmission of the disease; it was originally transmitted to humans through bats [ 30 – 32 ]. Like Ebola, it infected only a limited number of nations, i.e. about 27, but about 858 fatalities from about 2,494 laboratory-confirmed reports suggested that it was a significant threat if no steps were taken in place to control it.
In contrast to the camel flu, coronavirus is more common globally, has occurred more fatalities, has a lesser case fatality rate, and spreads more easily among humans.
Coronavirus Versus Swine Flu (H1N1)
Swine flu is the same form of influenza that wiped 1.7% of the world population in 1918. This was deemed a pandemic again in June 2009 an approximately-21% of the global population infected by this [ 33 – 35 ].
Thankfully, the case fatality rate is substantially lower than in the last pandemic, with 0.1%–0.5% of events ending in death. About 18,500 of these fatalities have been laboratory-confirmed, but statistics range as high as 151,700–575,400 worldwide. 50–80% of severe occurrences have been reported in individuals with chronic illnesses like asthma, obesity, cardiovascular diseases and diabetes.
In contrast to the swine flu, coronavirus is not so common, has caused fewer fatalities, has more case fatality rate, has a longer growth time and less impact on young people.
Coronavirus Versus Severe Acute Respiratory Syndrome (SARS)
SARS was discovered in 2003 as it spread from bats to humans resulted in about 774 fatalities. By May there were eventually about 8,100 reports across 17 countries, with a 15% case fatality rate. The number is estimated to be closer to 9.6% as confirmed cases are counted, with 0.9% cardiothoracic ratio for people aged 20–29, rising to 28% for people aged 70–79. Similar to coronavirus, SARS had bad results for males than females in all age categories [ 36 – 38 ].
Coronavirus is more common relative to SARS, which ended in more overall fatalities, lower case fatality rate, the even higher case fatality rate in older ages, and poorer results for males.
Coronavirus Versus Hong Kong Flu (H3N2)
The Hong Kong flu pandemic erupted on 13 July 1968, with 1–4 million deaths globally by 1969. It was one of the greatest flu pandemics of the twentieth century, but thankfully the case fatality rate was smaller than the epidemic of 1918, resulting in fewer fatalities overall. That may have been attributed to the fact that citizens had generated immunity owing to a previous epidemic in 1957 and to better medical treatment [ 39 ].
In contrast to the Hong Kong flu, coronavirus is not so common, has caused in fewer fatalities and has a higher case fatality rate.
Coronavirus Versus Spanish Flu (H1N1)
The 1918 Spanish flu pandemic was one of the greatest occurrences of recorded history. During the first year of the pandemic, lifespan in the US dropped by 12 years, with more civilians killed than HIV/AIDS in 24 h [ 40 – 42 ].
Regardless of the name, the epidemic did not necessarily arise in Spain; wartime censors in Germany, the United States, the United Kingdom and France blocked news of the disease, but Spain did not, creating the misleading perception that more cases and fatalities had occurred relative to its neighbours
This strain of H1N1 eventually affected more than 500 million men, or 27% of the world’s population at the moment, and had deaths of between 40 and 50 million. At the end of 1920, 1.7% of the world’s people had expired of this illness, including an exceptionally high death rate for young adults aged between 20 and 40 years.
In contrast to the Spanish flu, coronavirus is not so common, has caused in fewer fatalities, has a higher case fatality rate, is more harmful to older ages and is less risky for individuals aged 20–40 years.
Coronavirus Versus Common Cold (Typically Rhinovirus)
Common cold is the most common illness impacting people—Typically, a person suffers from 2–3 colds each year and the average kid will catch 6–8 during the similar time span. Although there are more than 200 cold-associated virus types, infections are uncommon and fatalities are very rare and typically arise mainly in extremely old, extremely young or immunosuppressed cases [ 43 , 44 ].
In contrast to the common cold, coronavirus is not so prevalent, causes more fatalities, has more case fatality rate, is less infectious and is less likely to impact small children.
Reviews of Online Portals and Social Media for Epidemic Information Dissemination
As COVID-19 started to propagate across the globe, the outbreak contributed to a significant change in the broad technology platforms. Where they once declined to engage in the affairs of their systems, except though the possible danger to public safety became obvious, the advent of a novel coronavirus placed them in a different interventionist way of thought. Big tech firms and social media are taking concrete steps to guide users to relevant, credible details on the virus [ 45 – 48 ]. And some of the measures they’re doing proactively. Below are a few of them.
Facebook started adding a box in the news feed that led users to the Centers for Disease Control website regarding COVID-19. It reflects a significant departure from the company’s normal strategy of placing items in the News Feed. The purpose of the update, after all, is personalization—Facebook tries to give the posts you’re going to care about, whether it is because you’re connected with a person or like a post. In the virus package, Facebook has placed a remarkable algorithmic thumb on the scale, potentially pushing millions of people to accurate, authenticated knowledge from a reputable source.
Similar initiatives have been adopted by Twitter. Searching for COVID-19 will carry you to a page highlighting the latest reports from public health groups and credible national news outlets. The search also allows for common misspellings. Twitter has stated that although Russian-style initiatives to cause discontent by large-scale intelligence operations have not yet been observed, a zero-tolerance approach to network exploitation and all other attempts to exploit their service at this crucial juncture will be expected. The problem has the attention of the organization. It also offers promotional support to public service agencies and other non-profit groups.
Google has made a step in making it better for those who choose to operate or research from home, offering specialized streaming services to all paying G Suite customers. Google also confirmed that free access to ‘advanced’ Hangouts Meet apps will be rolled out to both G Suite and G Suite for Education clients worldwide through 1st July. It ensures that companies can hold meetings of up to 250 people, broadcast live to up to about 100,000 users within a single network, and archive and export meetings to Google Drive. Usually, Google pays an additional $13 per person per month for these services in comparison to G Suite’s ‘enterprise’ membership, which adds up to a total of about $25 per client each month.
Microsoft took a similar move, introducing the software ‘Chat Device’ to help public health and protection in the coronavirus epidemic, which enables collaborative collaboration via video and text messaging. There’s an aspect of self-interest in this. Tech firms are offering out their goods free of charge during periods of emergency for the same purpose as newspapers are reducing their paywalls: it’s nice to draw more paying consumers.
Pinterest, which has introduced much of the anti-misinformation strategies that Facebook and Twitter are already embracing, is now restricting the search results for ‘coronavirus’, ‘COVID-19’ and similar words for ‘internationally recognized health organizations’.
Google-owned YouTube, traditionally the most conspiratorial website, has recently introduced a connection to the World Health Organization virus epidemic page to the top of the search results. In the early days of the epidemic, BuzzFeed found famous coronavirus conspiratorial videos on YouTube—especially in India, where one ‘explain’ with a false interpretation of the sources of the disease racketeered 13 million views before YouTube deleted it. Yet in the United States, conspiratorial posts regarding the illness have failed to gain only 1 million views.
That’s not to suggest that misinformation doesn’t propagate on digital platforms—just as it travels through the broader Internet, even though interaction with friends and relatives. When there’s a site that appears to be under-performing in the global epidemic, it’s Facebook-owned WhatsApp, where the Washington Post reported ‘a torrent of disinformation’ in places like Nigeria, Indonesia, Peru, Pakistan and Ireland. Given the encrypted existence of the app, it is difficult to measure the severity of the problem. Misinformation is also spread in WhatsApp communities, where participation is restricted to about 250 individuals. Knowledge of one category may be readily exchanged with another; however, there is a considerable amount of complexity of rotating several groups to peddle affected healing remedies or propagate false rumours.
Preventative Measures and Policies Enforced by the World Health Organization (WHO) and Different Countries
Coronavirus is already an ongoing epidemic, so it is necessary to take precautions to minimize both the risk of being sick and the transmission of the disease.
WHO Advice [ 49 ]
- Wash hands regularly with alcohol-based hand wash or soap and water.
- Preserve contact space (at least 1 m/3 feet between you and someone who sneezes or coughs).
- Don’t touch your nose, head and ears.
- Cover your nose and mouth as you sneeze or cough, preferably with your bent elbow or tissue.
- Try to find early medical attention if you have fatigue, cough and trouble breathing.
- Take preventive precautions if you are in or have recently go to places where coronavirus spreads.
The first person believed to have become sick because of the latest virus was near in Wuhan on 1 December 2019. A formal warning of the epidemic was released on 31 December. The World Health Organization was informed of the epidemic on the same day. Through 7 January, the Chinese Government addressed the avoidance and regulation of COVID-19. A curfew was declared on 23 January to prohibit flying in and out of Wuhan. Private usage of cars has been banned in the region. Chinese New Year (25 January) festivities have been cancelled in many locations [ 50 ].
On 26 January, the Communist Party and the Government adopted more steps to contain the COVID-19 epidemic, including safety warnings for travellers and improvements to national holidays. The leading party has agreed to prolong the Spring Festival holiday to control the outbreak. Universities and schools across the world have already been locked down. Many steps have been taken by the Hong Kong and Macau governments, in particular concerning schools and colleges. Remote job initiatives have been placed in effect in many regions of China. Several immigration limits have been enforced.
Certain counties and cities outside Hubei also implemented travel limits. Public transit has been changed and museums in China have been partially removed. Some experts challenged the quality of the number of cases announced by the Chinese Government, which constantly modified the way coronavirus cases were recorded.
Italy, a member state of the European Union and a popular tourist attraction, entered the list of coronavirus-affected nations on 30 January, when two positive cases in COVID-19 were identified among Chinese tourists. Italy has the largest number of coronavirus infections both in Europe and outside of China [ 51 ].
Infections, originally limited to northern Italy, gradually spread to all other areas. Many other nations in Asia, Europe and the Americas have tracked their local cases to Italy. Several Italian travellers were even infected with coronavirus-positive in foreign nations.
Late in Italy, the most impacted coronavirus cities and counties are Lombardia, accompanied by Veneto, Emilia-Romagna, Marche and Piedmonte. Milan, the second most populated city in Italy, is situated in Lombardy. Other regions in Italy with coronavirus comprised Campania, Toscana, Liguria, Lazio, Sicilia, Friuli Venezia Giulia, Umbria, Puglia, Trento, Abruzzo, Calabria, Molise, Valle d’Aosta, Sardegna, Bolzano and Basilicata.
Italy ranks 19th of the top 30 nations getting high-risk coronavirus airline passengers in China, as per WorldPop’s provisional study of the spread of COVID-19.
The Italian State has taken steps like the inspection and termination of large cultural activities during the early days of the coronavirus epidemic and has gradually declared the closing of educational establishments and airport hygiene/disinfection initiatives.
The Italian National Institute of Health suggested social distancing and agreed that the broader community of the country’s elderly is a problem. In the meantime, several other nations, including the US, have recommended that travel to Italy should be avoided temporarily, unless necessary.
The Italian government has declared the closing (quarantine) of the impacted areas in the northern region of the nation so as not to spread to the rest of the world. Italy has declared the immediate suspension of all to-and-fro air travel with China following coronavirus discovery by a Chinese tourist to Italy. Italian airlines, like Ryan Air, have begun introducing protective steps and have begun calling for the declaration forms to be submitted by passengers flying to Poland, Slovakia and Lithuania.
The Italian government first declined to permit fans to compete in sporting activities until early April to prevent the potential transmission of coronavirus. The step ensured players of health and stopped event cancellations because of coronavirus fears. Two days of the declaration, the government cancelled all athletic activities owing to the emergence of the outbreak asking for an emergency. Sports activities in Veneto, Lombardy and Emilia-Romagna, which recorded coronavirus-positive infections, were confirmed to be temporarily suspended. Schools and colleges in Italy have also been forced to shut down.
Iran announced the first recorded cases of SARS-CoV-2 infection on 19 February when, as per the Medical Education and Ministry of Health, two persons died later that day. The Ministry of Islamic Culture and Guidance has declared the cancellation of all concerts and other cultural activities for one week. The Medical Education and Ministry of Health has also declared the closing of universities, higher education colleges and schools in many cities and regions. The Department of Sports and Culture has taken action to suspend athletic activities, including football matches [ 52 ].
On 2 March 2020, the government revealed plans to train about 300,000 troops and volunteers to fight the outbreak of the epidemic, and also send robots and water cannons to clean the cities. The State also developed an initiative and a webpage to counter the epidemic. On 9 March 2020, nearly 70,000 inmates were immediately released from jail owing to the epidemic, presumably to prevent the further dissemination of the disease inside jails. The Revolutionary Guards declared a campaign on 13 March 2020 to clear highways, stores and public areas in Iran. President Hassan Rouhani stated on 26 February 2020 that there were no arrangements to quarantine areas impacted by the epidemic and only persons should be quarantined. The temples of Shia in Qom stayed open to pilgrims.
South Korea
On 20 January, South Korea announced its first occurrence. There was a large rise in cases on 20 February, possibly due to the meeting in Daegu of a progressive faith community recognized as the Shincheonji Church of Christ. Any citizens believed that the hospital was propagating the disease. As of 22 February, 1,261 of the 9,336 members of the church registered symptoms. A petition was distributed calling for the abolition of the church. More than 2,000 verified cases were registered on 28 February, increasing to 3,150 on 29 February [ 53 ].
Several educational establishments have been partially closing down, including hundreds of kindergartens in Daegu and many primary schools in Seoul. As of 18 February, several South Korean colleges had confirmed intentions to delay the launch of the spring semester. That included 155 institutions deciding to postpone the start of the semester by two weeks until 16 March, and 22 institutions deciding to delay the start of the semester by one week until 9 March. Also, on 23 February 2020, all primary schools, kindergartens, middle schools and secondary schools were declared to postpone the start of the semester from 2 March to 9 March.
South Korea’s economy is expected to expand by 1.9%, down from 2.1%. The State has given 136.7 billion won funding to local councils. The State has also coordinated the purchase of masks and other sanitary supplies. Entertainment Company SM Entertainment is confirmed to have contributed five hundred million won in attempts to fight the disease.
In the kpop industry, the widespread dissemination of coronavirus within South Korea has contributed to the cancellation or postponement of concerts and other programmes for kpop activities inside and outside South Korea. For instance, circumstances such as the cancellation of the remaining Asian dates and the European leg for the Seventeen’s Ode To You Tour on 9 February 2020 and the cancellation of all Seoul dates for the BTS Soul Tour Map. As of 15 March, a maximum of 136 countries and regions provided entry restrictions and/or expired visas for passengers from South Korea.
The overall reported cases of coronavirus rose significantly in France on 12 March. The areas with reported cases include Paris, Amiens, Bordeaux and Eastern Haute-Savoie. The first coronaviral death happened in France on 15 February, marking it the first death in Europe. The second death of a 60-year-old French national in Paris was announced on 26 February [ 54 ].
On February 28, fashion designer Agnès B. (not to be mistaken with Agnès Buzyn) cancelled fashion shows at the Paris Fashion Week, expected to continue until 3 March. On a subsequent day, the Paris half-marathon, planned for Sunday 1 March with 44,000 entrants, was postponed as one of a series of steps declared by Health Minister Olivier Véran.
On 13 March, the Ligue de Football Professional disbanded Ligue 1 and Ligue 2 (France’s tier two professional divisions) permanently due to safety threats.
Germany has a popular Regional Pandemic Strategy detailing the roles and activities of the health care system participants in the case of a significant outbreak. Epidemic surveillance is carried out by the federal government, like the Robert Koch Center, and by the German governments. The German States have their preparations for an outbreak. The regional strategy for the treatment of the current coronavirus epidemic was expanded by March 2020. Four primary goals are contained in this plan: (1) to minimize mortality and morbidity; (2) to guarantee the safety of sick persons; (3) to protect vital health services and (4) to offer concise and reliable reports to decision-makers, the media and the public [ 55 ].
The programme has three phases that may potentially overlap: (1) isolation (situation of individual cases and clusters), (2) safety (situation of further dissemination of pathogens and suspected causes of infection), (3) prevention (situation of widespread infection). So far, Germany has not set up border controls or common health condition tests at airports. Instead, while at the isolation stage-health officials are concentrating on recognizing contact individuals that are subject to specific quarantine and are tracked and checked. Specific quarantine is regulated by municipal health authorities. By doing so, the officials are seeking to hold the chains of infection small, contributing to decreased clusters. At the safety stage, the policy should shift to prevent susceptible individuals from being harmed by direct action. By the end of the day, the prevention process should aim to prevent cycles of acute treatment to retain emergency facilities.
United States
The very first case of coronavirus in the United States was identified in Washington on 21 January 2020 by an individual who flew to Wuhan and returned to the United States. The second case was recorded in Illinois by another individual who had travelled to Wuhan. Some of the regions with reported novel coronavirus infections in the US are California, Arizona, Connecticut, Illinois, Texas, Wisconsin and Washington [ 56 ].
As the epidemic increased, requests for domestic air travel decreased dramatically. By 4 March, U.S. carriers, like United Airlines and JetBlue Airways, started growing their domestic flight schedules, providing generous unpaid leave to workers and suspending recruits.
A significant number of universities and colleges cancelled classes and reopened dormitories in response to the epidemic, like Cornell University, Harvard University and the University of South Carolina.
On 3 March 2020, the Federal Reserve reduced its goal interest rate from 1.75% to 1.25%, the biggest emergency rate cut following the 2008 global financial crash, in combat the effect of the recession on the American economy. In February 2020, US businesses, including Apple Inc. and Microsoft, started to reduce sales projections due to supply chain delays in China caused by the COVID-19.
The pandemic, together with the subsequent financial market collapse, also contributed to greater criticism of the crisis in the United States. Researchers disagree about when a recession is likely to take effect, with others suggesting that it is not unavoidable, while some claim that the world might already be in recession. On 3 March, Federal Reserve Chairman Jerome Powell reported a 0.5% (50 basis point) interest rate cut from the coronavirus in the context of the evolving threats to economic growth.
When ‘social distance’ penetrated the national lexicon, disaster response officials promoted the cancellation of broad events to slow down the risk of infection. Technical conferences like E3 2020, Apple Inc.’s Worldwide Developers Conference (WWDC), Google I/O, Facebook F8, and Cloud Next and Microsoft’s MVP Conference have been either having replaced or cancelled in-person events with internet streaming events.
On February 29, the American Physical Society postponed its annual March gathering, planned for March 2–6 in Denver, Colorado, even though most of the more than 11,000 physicist attendees already had arrived and engaged in the pre-conference day activities. On March 6, the annual South to Southwest (SXSW) seminar and festival planned to take place from March 13–22 in Austin, Texas, was postponed after the city council announced a local disaster and forced conferences to be shut down for the first time in 34 years.
Four of North America’s major professional sports leagues—the National Hockey League (NHL), National Basketball Association (NBA), Major League Soccer (MLS) and Major League Baseball (MLB) —jointly declared on March 9 that they would all limit the media access to player accommodations (such as locker rooms) to control probable exposure.
Emergency Funding to Fight the COVID-19
COVID-19 pandemic has become a common international concern. Different countries are donating funds to fight against it [ 57 – 60 ]. Some of them are mentioned here.
China has allocated about 110.48 billion yuan ($15.93 billion) in coronavirus-related funding.
Foreign Minister Mohammad Javad Zarif said that Iran has requested the International Monetary Fund (IMF) of about $5 billion in emergency funding to help to tackle the coronavirus epidemic that has struck the Islamic Republic hard.
President Donald Trump approved the Emergency Supplementary Budget Bill to support the US response to a novel coronavirus epidemic. The budget plan would include about $8.3 billion in discretionary funding to local health authorities to promote vaccine research for production. Trump originally requested just about $2 billion to combat the epidemic, but Congress quadrupled the number in its version of the bill. Mr. Trump formally announced a national emergency that he claimed it will give states and territories access to up to about $50 billion in federal funding to tackle the spread of the coronavirus outbreak.
California politicians approved a plan to donate about $1 billion on the state’s emergency medical responses as it readies hospitals to fight an expected attack of patients because of the COVID-19 pandemic. The plans, drawn up rapidly in reaction to the dramatic rise in reported cases of the virus, would include the requisite funds to establish two new hospitals in California, with the assumption that the state may not have the resources to take care of the rise in patients. The bill calls for an immediate response of about $500 million from the State General Fund, with an additional about $500 million possible if requested.
India committed about $10 million to the COVID-19 Emergency Fund and said it was setting up a rapid response team of physicians for the South Asian Association for Regional Cooperation (Saarc) countries.
South Korea unveiled an economic stimulus package of about 11.7 trillion won ($9.8 billion) to soften the effects of the biggest coronavirus epidemic outside China as attempts to curb the disease exacerbate supply shortages and drain demand. Of the 11,7 trillion won expected, about 3.2 trillion won would cover up the budget shortfall, while an additional fiscal infusion of about 8.5 trillion won. An estimated 10.3 trillion won in government bonds will be sold this year to fund the extra expenditure. About 2.3 trillion won will be distributed to medical establishments and would support quarantine operations, with another 3.0 trillion won heading to small and medium-sized companies unable to pay salaries to their employees and child care supports.
The Swedish Parliament announced a set of initiatives costing more than 300 billion Swedish crowns ($30.94 billion) to help the economy in the view of the coronavirus pandemic. The plan contained steps like the central government paying the entire expense of the company’s sick leave during April and May, and also the high cost of compulsory redundancies owing to the crisis.
In consideration of the developing scenario, an updating of this strategy is planned to take place before the end of March and will recognize considerably greater funding demands for the country response, R&D and WHO itself.
Artificial Intelligence, Data Science and Technological Solutions Against COVID-19
These days, Artificial Intelligence (AI) takes a major role in health care. Throughout a worldwide pandemic such as the COVID-19, technology, artificial intelligence and data analytics have been crucial in helping communities cope successfully with the epidemic [ 61 – 65 ]. Through the aid of data mining and analytical modelling, medical practitioners are willing to learn more about several diseases.
Public Health Surveillance
The biggest risk of coronavirus is the level of spreading. That’s why policymakers are introducing steps like quarantines around the world because they can’t adequately monitor local outbreaks. One of the simplest measures to identify ill patients through the study of CCTV images that are still around us and to locate and separate individuals that have serious signs of the disease and who have touched and disinfected the related surfaces. Smartphone applications are often used to keep a watch on people’s activities and to assess whether or not they have come in touch with an infected human.
Remote Biosignal Measurement
Many of the signs such as temperature or heartbeat are very essential to overlook and rely entirely on the visual image that may be misleading. However, of course, we can’t prevent someone from checking their blood pressure, heart or temperature. Also, several advances in computer vision can predict pulse and blood pressure based on facial skin examination. Besides, there are several advances in computer vision that can predict pulse and blood pressure based on facial skin examination.
Access to public records has contributed to the development of dashboards that constantly track the virus. Several companies are designing large data dashboards. Face recognition and infrared temperature monitoring technologies have been mounted in all major cities. Chinese AI companies including Hanwang Technology and SenseTime have reported having established a special facial recognition system that can correctly identify people even though they are covered.
IoT and Wearables
Measurements like pulse are much more natural and easier to obtain from tracking gadgets like activity trackers and smartwatches that nearly everybody has already. Some work suggests that the study of cardiac activity and its variations from the standard will reveal early signs of influenza and, in this case, coronavirus.
Chatbots and Communication
Apart from public screening, people’s knowledge and self-assessment may also be used to track their health. If you can check your temperature and pulse every day and monitor your coughs time-to-time, you can even submit that to your record. If the symptoms are too serious, either an algorithm or a doctor remotely may prescribe a person to stay home, take several other preventive measures, or recommend a visit from the doctor.
Al Jazeera announced that China Mobile had sent text messages to state media departments, telling them about the citizens who had been affected. The communications contained all the specifics of the person’s travel history.
Tencent runs WeChat, and via it, citizens can use free online health consultation services. Chatbots have already become important connectivity platforms for transport and tourism service providers to keep passengers up-to-date with the current transport protocols and disturbances.
Social Media and Open Data
There are several people who post their health diary with total strangers via Facebook or Twitter. Such data becomes helpful for more general research about how far the epidemic has progressed. For consumer knowledge, we may even evaluate the social network group to attempt to predict what specific networks are at risk of being viral.
Canadian company BlueDot analyses far more than just social network data: for instance, global activities of more than four billion passengers on international flights per year; animal, human and insect population data; satellite environment data and relevant knowledge from health professionals and journalists, across 100,000 news posts per day covering 65 languages. This strategy was so successful that the corporation was able to alert clients about coronavirus until the World Health Organization and the Centers for Disease Control and Prevention notified the public.
Automated Diagnostics
COVID-19 has brought up another healthcare issue today: it will not scale when the number of patients increases exponentially (actually stressed doctors are always doing worse) and the rate of false-negative diagnosis remains very high. Machine learning therapies don’t get bored and scale simply by growing computing forces.
Baidu, the Chinese Internet company, has made the Lineatrfold algorithm accessible to the outbreak-fighting teams, according to the MIT Technology Review. Unlike HIV, Ebola and Influenza, COVID-19 has just one strand of RNA and it can mutate easily. The algorithm is also simpler than other algorithms that help to determine the nature of the virus. Baidu has also developed software to efficiently track large populations. It has also developed an Ai-powered infrared device that can detect a difference in the body temperature of a human. This is currently being used in Beijing’s Qinghe Railway Station to classify possibly contaminated travellers where up to 200 individuals may be checked in one minute without affecting traffic movement, reports the MIT Review.
Singapore-based Veredus Laboratories, a supplier of revolutionary molecular diagnostic tools, has currently announced the launch of the VereCoV detector package, a compact Lab-on-Chip device able to detect MERS-CoV, SARS-CoV and COVID-19, i.e. Wuhan Coronavirus, in a single study.
The VereCoV identification package is focused on VereChip technology, a Lab-on-Chip device that incorporates two important molecular biological systems, Polymerase Chain Reaction (PCR) and a microarray, which will be able to classify and distinguish within 2 h MERS-CoV, SARS-CoV and COVID-19 with high precision and responsiveness.
This is not just the medical activities of healthcare facilities that are being charged, but also the corporate and financial departments when they cope with the increase in patients. Ant Financials’ blockchain technology helps speed-up the collection of reports and decreases the number of face-to-face encounters with patients and medical personnel.
Companies like the Israeli company Sonovia are aiming to provide healthcare systems and others with face masks manufactured from their anti-pathogenic, anti-bacterial cloth that depends on metal-oxide nanoparticles.
Drug Development Research
Aside from identifying and stopping the transmission of pathogens, the need to develop vaccinations on a scale is also needed. One of the crucial things to make that possible is to consider the origin and essence of the virus. Google’s DeepMind, with their expertise in protein folding research, has rendered a jump in identifying the protein structure of the virus and making it open-source.
BenevolentAI uses AI technologies to develop medicines that will combat the most dangerous diseases in the world and is also working to promote attempts to cure coronavirus, the first time the organization has based its product on infectious diseases. Within weeks of the epidemic, it used its analytical capability to recommend new medicines that might be beneficial.
Robots are not vulnerable to the infection, and they are used to conduct other activities, like cooking meals in hospitals, doubling up as waiters in hotels, spraying disinfectants and washing, selling rice and hand sanitizers, robots are on the front lines all over to deter coronavirus spread. Robots also conduct diagnostics and thermal imaging in several hospitals. Shenzhen-based firm Multicopter uses robotics to move surgical samples. UVD robots from Blue Ocean Robotics use ultraviolet light to destroy viruses and bacteria separately. In China, Pudu Technology has introduced its robots, which are usually used in the cooking industry, to more than 40 hospitals throughout the region. According to the Reuters article, a tiny robot named Little Peanut is distributing food to passengers who have been on a flight from Singapore to Hangzhou, China, and are presently being quarantined in a hotel.
Colour Coding
Using its advanced and vast public service monitoring network, the Chinese government has collaborated with software companies Alibaba and Tencent to establish a colour-coded health ranking scheme that monitors millions of citizens every day. The mobile device was first introduced in Hangzhou with the cooperation of Alibaba. This applies three colours to people—red, green or yellow—based on their transportation and medical records. Tencent also developed related applications in the manufacturing centre of Shenzhen.
The decision of whether an individual will be quarantined or permitted in public spaces is dependent on the colour code. Citizens will sign into the system using pay wallet systems such as Alibaba’s Alipay and Ant’s wallet. Just those citizens who have been issued a green colour code will be permitted to use the QR code in public spaces at metro stations, workplaces, and other public areas. Checkpoints are in most public areas where the body temperature and the code of individual are tested. This programme is being used by more than 200 Chinese communities and will eventually be expanded nationwide.
In some of the seriously infected regions where people remain at risk of contracting the infection, drones are used to rescue. One of the easiest and quickest ways to bring emergency supplies where they need to go while on an epidemic of disease is by drone transportation. Drones carry all surgical instruments and patient samples. This saves time, improves the pace of distribution and reduces the chance of contamination of medical samples. Drones often operate QR code placards that can be checked to record health records. There are also agricultural drones distributing disinfectants in the farmland. Drones, operated by facial recognition, are often used to warn people not to leave their homes and to chide them for not using face masks. Terra Drone uses its unmanned drones to move patient samples and vaccination content at reduced risk between the Xinchang County Disease Control Center and the People’s Hospital. Drones are often used to monitor public areas, document non-compliance with quarantine laws and thermal imaging.
Autonomous Vehicles
At a period of considerable uncertainty to medical professionals and the danger to people-to-people communication, automated vehicles are proving to be of tremendous benefit in the transport of vital products, such as medications and foodstuffs. Apollo, the Baidu Autonomous Vehicle Project, has joined hands with the Neolix self-driving company to distribute food and supplies to a big hospital in Beijing. Baidu Apollo has also provided its micro-car packages and automated cloud driving systems accessible free of charge to virus-fighting organizations.
Idriverplus, a Chinese self-driving organization that runs electrical street cleaning vehicles, is also part of the project. The company’s signature trucks are used to clean hospitals.
This chapter provides an introduction to the coronavirus outbreak (COVID-19). A brief history of this virus along with the symptoms are reported in this chapter. Then the comparison between COVID-19 and other plagues like seasonal influenza, bird flu (H5N1 and H7N9), Ebola epidemic, camel flu (MERS), swine flu (H1N1), severe acute respiratory syndrome, Hong Kong flu (H3N2), Spanish flu and the common cold are included in this chapter. Reviews of online portal and social media like Facebook, Twitter, Google, Microsoft, Pinterest, YouTube and WhatsApp concerning COVID-19 are reported in this chapter. Also, the preventive measures and policies enforced by WHO and different countries such as China, Italy, Iran, South Korea, France, Germany and the United States for COVID-19 are included in this chapter. Emergency funding provided by different countries to fight the COVID-19 is mentioned in this chapter. Lastly, artificial intelligence, data science and technological solutions like public health surveillance, remote biosignal measurement, IoT and wearables, chatbots and communication, social media and open data, automated diagnostics, drug development research, robotics, colour coding, drones and autonomous vehicles are included in this chapter.

The risks of autoimmune- and inflammatory post-acute COVID-19 conditions: a network cohort study in six European countries, the US, and Korea
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Edward Burn
- ORCID record for Talita Duarte-Salles
- ORCID record for Daniel Prieto-Alhambra
- For correspondence: [email protected]
- ORCID record for Junqing Xie
- Info/History
- Supplementary material
- Preview PDF
Objectives We aimed to assess the risk of autoimmune- and inflammatory post-acute COVID-19 conditions.
Design Descriptive network cohort study.
Setting Electronic health records from UK and Dutch primary care, Norwegian linked health registry, hospital records of specialist centres in Spain, France, and Korea, and healthcare claims from Estonia and the US.
Participants We followed individuals between September 2020 and the latest available data from the day they fulfilled at least 365 days of prior observation (general population), additionally from day 91 after a SARS-Cov-2 negative test (comparator) or a COVID-19 record (exposed patients).
Main outcome measures We assessed postural orthostatic tachycardia syndrome (POTS) diagnoses/symptoms, myalgic encephalomyelitis / chronic fatigues syndrome (ME/CFS) diagnoses/symptoms, multi-inflammatory syndrome (MIS), and several autoimmune diseases. For contextualisation, we assessed any diabetes mellitus (DM).
Meta-analysed crude incidence rate ratios (IRR) of outcomes measures after COVID-19 versus negative testing yield the ratios of absolute risks. Furthermore, incidence rates (IR) of the outcomes in the general population describe the total disease burden.
Results We included 34’549’575 individuals of whom 2’521’812 had COVID-19, and 4’233’145 a first negative test. After COVID-19 compared to test negative patients, we observed IRRs of 1.24 (1.23-1.25), 1.22 (1.21-1.23), and 1.12 (1.04-1.21) for POTS symptoms, ME/CFS symptoms and diagnoses, respectively. In contrast, autoimmune diseases and DM did not yield higher rates after COVID-19. In individual general database populations, IRs of POTS and ME/CFS diagnoses were 17-1’477/100’000 person-years (pys) and 2-473/100’000 pys, respectively. IRs of MIS were lowest with IRs 0.4-16/100’000 pys, those of DM as a benchmark 8-86/100’000 pys. IRs largely depended on the care setting.
Conclusion In our unmatched comparison, we observed that, following COVID-19, POTS and ME/CFS yielded higher rates than after negative testing. In absolute terms, we observed POTS and ME/CFS diagnoses to have a similar disease burden as DM.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Observational research suggested positive associations between COVID-19 and so called post-acute COVID-19 conditions, whose spectrum is yet to be established
Basic research suggested pathways that link COVID-19 with autoimmune- and inflammatory diseases such as postural orthostatic tachycardia syndrome (POTS), myalgic encephalomyelitis / chronic fatigues syndrome (ME/CFS), multiple inflammatory syndrome (MIS), and autoimmune diseases
WHAT THIS STUDY ADDS
After COVID-19, the rates of POTS symptoms and ME/CFS symptoms/diagnoses was higher than those after negative testing
After COVID-19 versus negative testing, rates of ME/CFS diagnoses were increased in the working age group and rates of symptoms of POTS and ME/CFS were increased in children and elderly
Disease burdens of POTS and ME/CFS diagnoses in the general population were higher among women than among men and overall similar to that of diabetes mellitus
Competing Interest Statement
All authors have completed the ICMJE disclosure form at http://www.icmje.org/disclosure-of-interest/ and declare the following interests: DPAs research group has received research grants from the European Medicines Agency; the Innovative Medicines Initiative; Amgen, Chiesi, and UCB Biopharma; and consultancy or speaker fees from Astellas, Amgen, and UCB Biopharma. DDed and JOO are employees of the Medicines and Healthcare Products Regulatory Agency which provides the CPRD research service. KK is a consortia author in the US National Institutes of Health National COVID Cohort Collaborative (funding expired in 2022 with no renewal or active impact on any current work). RP has received receiving research grants paid to his institution from MSD, ViiV Healthcare, Gilead Sciences, and PharmaMar, and has participated in advisory boards for Gilead Sciences, Inc, Pfizer, Inc, Roche Therapeutics, MSD, GSK, ViiV Healthcare, Eli Lilly and Company, PharmaMar, and Atea Pharmaceuticals Inc.LM has received research grants from Grifols, consulting fees from Gilead Sciences and Merck, and honoraria from AstraZeneca, Gilead Sciences, GSK, and Pfizer.
Funding Statement
This research was partially funded by the European Health Data and Evidence Network (EHDEN) [grant number 806968], and the Oxford NIHR Biomedical Research Centre. The study funders had no role in the conceptualisation, design, data collection, analysis, decision to publish, or preparation of the manuscript. DPA receives funding from the UK National Institute for Health Research (NIHR) in the form of a senior research fellowship and the Oxford NIHR Biomedical Research Centre. KLG was supported by the Medical Research Council (grant number MR/W006731/1) and Bayer AG. LPC is funded by a Sara Borrell fellowship (CD23/00223) awarded by the Spanish Institute of Health Carlos III. CK and the institution he works for was supported by a government-wide R&D Fund project for infectious disease research (GFID), Republic of Korea (grant number: HG22C0024). RK was supported by the European Regional Development Fund (RITA 1/02-120) and the Estonian Research Council grant (PRG1844).
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
The protocol for this research was approved by the independent scientific advisory committee for Medicine and Healthcare products Regulatory Agency database research (protocol number 23_002603). Informed consent of individual patients was not required as anonymised information was obtained from medical records. Ethical approval for the Norwegian data in this study was obtained from The Regional Committee for Research Ethics (approval number 155294) and the Data Protection Officer at the University of Oslo (approval number 523275). Ethical approval for CORIVA data was obtained from the Research Ethics Committee of the University of Tartu (No. 351/M-8). Ethical approval for IMASIS was obtained by the Parc de Salut Mar Research Ethics Committee CEIm-Parc de Salut Mar (number 2021/9975). Ethical approval for IPCI was obtained by the Integrated Primary Care Information review board (registration number 9/2023). For CHUM, no ethical approval was required according to French law for this study. All patients admitted to the hospital are provided with general information about the collection and secondary use of their data, and an opt-out option is offered. PharMetrics Plus for Academics needed no approval for use of pseudoanonymised secondary data. Ethical approval for AUSOM was obtained by the Ajou University Medical Center Institutional Review Board (No. AJOUIRB-MDB-2021-694).
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
Patient level data cannot be shared without approval from data custodians owing to local information governance and data protection regulations. The analytical code is available at https://github.com/oxford-pharmacoepi/LongCovidStudyathon_W1 . The code for postprocessing and aggregated results are available at https://github.com/tiozab/immune_inflammatory_PACS/
View the discussion thread.
Supplementary Material
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
Subject Area
- Epidemiology
- Addiction Medicine (324)
- Allergy and Immunology (629)
- Anesthesia (166)
- Cardiovascular Medicine (2388)
- Dentistry and Oral Medicine (289)
- Dermatology (207)
- Emergency Medicine (380)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (840)
- Epidemiology (11783)
- Forensic Medicine (10)
- Gastroenterology (703)
- Genetic and Genomic Medicine (3758)
- Geriatric Medicine (350)
- Health Economics (636)
- Health Informatics (2402)
- Health Policy (935)
- Health Systems and Quality Improvement (902)
- Hematology (341)
- HIV/AIDS (782)
- Infectious Diseases (except HIV/AIDS) (13328)
- Intensive Care and Critical Care Medicine (769)
- Medical Education (366)
- Medical Ethics (105)
- Nephrology (400)
- Neurology (3515)
- Nursing (199)
- Nutrition (528)
- Obstetrics and Gynecology (676)
- Occupational and Environmental Health (665)
- Oncology (1827)
- Ophthalmology (538)
- Orthopedics (219)
- Otolaryngology (287)
- Pain Medicine (234)
- Palliative Medicine (66)
- Pathology (447)
- Pediatrics (1035)
- Pharmacology and Therapeutics (426)
- Primary Care Research (423)
- Psychiatry and Clinical Psychology (3185)
- Public and Global Health (6156)
- Radiology and Imaging (1283)
- Rehabilitation Medicine and Physical Therapy (750)
- Respiratory Medicine (830)
- Rheumatology (379)
- Sexual and Reproductive Health (372)
- Sports Medicine (324)
- Surgery (402)
- Toxicology (50)
- Transplantation (172)
- Urology (146)
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Healthy Habits
- Healthy and Safe Swimming
- How to Respond
- Healthy Swimming Communication Resources
- Aquatics Professionals Toolkit
- Pool Inspection Toolkit
- The Model Aquatic Health Code (MAHC): A Model Public Swimming Pool and Spa Code
Swimming and Your Health
- Water-based exercise offers physical and mental health benefits, including improved health for people with chronic illnesses like diabetes, heart disease, and arthritis.
- However, recreational water can also spread illness or cause injury, so it is important to know what to do to protect yourself and others.

Health benefits
Swimming can improve mood and people report enjoying water-based exercise more than exercising on land.
People are able to exercise longer in water without increased joint or muscle pain, which has been shown to be especially helpful for people with arthritis and osteoarthritis. Water-based exercise can help people with arthritis improve the use of their arthritic joints, decrease pain, and not worsen symptoms. People with rheumatoid arthritis have shown more health improvements after participating in hydrotherapy (exercising in warm water) than with other activities.
For people with fibromyalgia, swimming can decrease anxiety, and exercise therapy in warm water can decrease depression and improve mood. Parents of children with developmental disabilities find that recreational activities, such as swimming, improve family connections.
Water-based exercise can benefit older adults by improving their quality of life and decreasing disability. It can also improve or help maintain the bone health of post-menopausal women.
Staying healthy and safe while you swim
To stay healthy and safe while you swim, it is important to understand how to prevent illness and injury when you are in or around the water.
You can get swimming-related illnesses if you swallow, have contact with, or breathe in mists of water contaminated with germs. The most common swimming-related illnesses are diarrhea , skin rashes , swimmer's ear , pneumonia or flu-like illness , and irritation of the eyes or respiratory tract .
Learn more about what you can do to prevent these illnesses when you swim and how to protect yourself depending on where you go (pool, hot tub, splash pad, ocean, etc.)

Preventing Swimming-related Illnesses

Guidelines for Healthy and Safe Swimming
Keeping your pool and hot tub clean
Having pool or hot tub can be a fun way to be active or just relax. It is important to know what to do to reduce the risk of pool-related injury and illness, as well as how to clean your pool if it has been contaminated by poop, vomit, blood, or a dead animal.

Guidelines for Keeping Your Pool Safe and Healthy

Responding to Pool Contamination
- US Census Bureau. Statistical Abstract of the United States: 2012. Arts, Recreation, and Travel: Participation in Selected Sports Activities 2009. [XLS – 40 KB] ·
- U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans: Be active, healthy, and happy! In Chapter 2: Physical Activity Has Many Health Benefits. 2009.
- Westby MD. A health professional's guide to exercise prescription for people with arthritis: a review of aerobic fitness activities. Arthritis Rheum. 2001;45(6):501-11.
- Hall J, Skevington SM, Maddison PJ, Chapman K. A randomized and controlled trial of hydrotherapy in rheumatoid arthritis. Arthritis Care Res. 1996;9(3):206-15.
- Tomas-Carus P, Gusi N, Hakkinen A, Hakkinen K, Leal A, and Ortega-Alonso A. Eight months of physical training in warm water improves physical and mental health in women with fibromyalgia: a randomized controlled trial. J Rehabil Med. 2008;40(4):248-52.
- Broman G, Quintana M, Engardt M, Gullstrand L, Jansson E, and Kaijser L. Older women's cardiovascular responses to deep-water running. J Aging Phys Act. 2006;14(1):29-40.
- Cider A, Svealv BG, Tang MS, Schaufelberger M, and Andersson B. Immersion in warm water induces improvement in cardiac function in patients with chronic heart failure. Eur J Heart Fail. 2006;8(3):308-13.
- Bartels EM, Lund H, Hagen KB, Dagfinrud H, Christensen R, Danneskiold-Samsøe B. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2016;3:CD005523.
- Berger BG, and Owen DR. Mood alteration with yoga and swimming: aerobic exercise may not be necessary. Percept Mot Skills. 1992;75(3 Pt 2):1331-43.
- Gowans SE and deHueck A. Pool exercise for individuals with fibromyalgia. Curr Opin Rheumatol. 2007;19(2):168-73.
- Hartmann S and Bung P. Physical exercise during pregnancy—physiological considerations and recommendations. J Perinat Med. 1999;27(3):204-15.
- Mactavish JB and Schleien SJ. Re-injecting spontaneity and balance in family life: parents' perspectives on recreation in families that include children with developmental disability. J Intellect Disabil Res. 2004;48(Pt 2):123-41.
- Sato D, Kaneda K, Wakabayashi H, and Nomura T. The water exercise improves health-related quality of life of frail elderly people at day service facility. Qual Life Res. 2007;16:1577-85.
- Rotstein A, Harush M, and Vaisman N. The effect of water exercise program on bone density of postmenopausal Women. J Sports Med Phys Fitness. 2008;48(3):352-9.
Healthy Swimming
CDC’s Healthy Swimming website provides information on how to have healthy and safe swimming experiences while minimizing illness and injury.
For Everyone
Public health.

COMMENTS
27 June 2022. Directorate. Performance, Delivery and Resilience Directorate. Part of. Coronavirus (COVID-19) in Scotland. ISBN. 9781804356142. Findings from an open free text survey taken to understand in greater detail how the pandemic has changed Scotland. Supporting documents.
100 Words Essay on Covid 19. COVID-19 or Corona Virus is a novel coronavirus that was first identified in 2019. It is similar to other coronaviruses, such as SARS-CoV and MERS-CoV, but it is more contagious and has caused more severe respiratory illness in people who have been infected. The novel coronavirus became a global pandemic in a very ...
Writing About COVID-19 in College Essays. Experts say students should be honest and not limit themselves to merely their experiences with the pandemic. The global impact of COVID-19, the disease ...
The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good ...
The initial indication of a COVID-19 infection is coughing, fever, and short breath, and in the later stages, it can damage the kidney, cause pneumonia, and unexpected death (Mofijur et al., 2020). The vulnerability of the elderly (>80 years of age) is high, with a fatality rate of ~22% of cases infected by COVID-19 ( Abdullah et al., 2020 ).
Alex, a writer and fellow disabled parent, found the freedom to explore a fuller version of herself in the privacy the pandemic provided. "The way I dress, the way I love, and the way I carry ...
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the ...
Students working on college admission essays often struggle to figure out how to write about their experiences during the COVID-19 pandemic. For students applying to college using the CommonApp, there are several different places where students and counselors can address the pandemic's impact. The different sections have differing goals.
Abstract. In early December 2019, an outbreak of coronavirus disease 2019 (COVID-19), caused by a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), occurred in Wuhan City, Hubei Province, China. On January 30, 2020 the World Health Organization declared the outbreak as a Public Health Emergency of International Concern.
Thinking about COVID-19 and your introduction The personal and professional context of your thesis is likely to have changed as a result of COVID-19. The changes implied are immediate and short-term, but there will also be long term implications (for example, online teaching, the role of the state, levels of unemployment, return to deepened
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
Introduction. In December 2019, the 2019 novel coronavirus disease (COVID-19) caused by novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in China, followed by a rapid spread all over the world. On March 11, 2020, the World Health Organization (WHO) raised its pandemic alert. As of April 11, 2020, COVID-19 had caused ...
Conclusion: In conclusion, COVID-19 vaccination mandates are a crucial step toward controlling the pandemic, protecting public health, and preventing further loss of life. ... Covid19 has drastically changed the way people interact in schools, markets, and workplaces. In short, it has affected all aspects of life. ... Writing a persuasive essay ...
My COVID-19 Perspective Hi there, my name is Jack Gardner, a 5th year student at Purdue University. The ... Today, I am writing this short reflective essay to share my thoughts and experience during the worldwide COVID-19 Pandemic. I believe it is very beneficial to gain insight from multiple perspectives on the current situation.
Essay On Covid-19: 100, 200 and 300 Words. COVID-19, also known as the Coronavirus, is a global pandemic that has affected people all around the world. It first emerged in a lab in Wuhan, China, in late 2019 and quickly spread to countries around the world. This virus was reportedly caused by SARS-CoV-2. Since then, it has spread rapidly to ...
The pandemic of Coronavirus Disease 2019 (COVID-19) is a timely reminder of the nature and impact of Public Health Emergencies of International Concern. As of 12 January 2022, there were over 314 million cases and over 5.5 million deaths notified since the start of the pandemic. The COVID-19 pandemic takes variable shapes and forms, in terms of cases and deaths, in different regions and ...
In this final chapter we draw together some of the main themes emerging from the various chapters and reflect on what this tells us about being human in COVID-19 times. As outlined in the introduction, these essays have focused on three key issues during the pandemic that are fundamentally concerned with the experience, meaning and ...
1. Introduction. The coronavirus disease 2019 (COVID-19) pandemic has led to unprecedented changes in people's daily lives, with implications for mental health and well-being [1-4], both at the level of a given country's population, and when considering specific vulnerable groups [5-7].In order to mitigate the untoward impact of the pandemic (including lockdown) and support mental health ...
In December 2019, the Covid-19 pandemic has thrown life out of gear across the world. While writing this chapter, the world has experienced waves of Covid-19 infections, and threats of new virus mutations and deadlier infections still loom at large. ... Dolla, T., Devkar, G., Laishram, B. (2023). Conclusion. In: Dolla, T., Laishram, B., Devkar ...
Until June 30, send your essay (200 words or less) about life during COVID-19 via bostonbookfest.org. Some essays will be published on the festival's blog and some will appear in The Boston Globe.
Editor in Chief's Introduction to Essays on the Impact of COVID-19 on Work and Workers. On March 11, 2020, the World Health Organization declared that COVID-19 was a global pandemic, indicating significant global spread of an infectious disease ( World Health Organization, 2020 ). At that point, there were 118,000 confirmed cases of the ...
The COVID-19 pandemic has had a profound impact on individuals, societies, and economies worldwide. Its multifaceted nature presents a wealth of topics suitable for academic exploration. This essay provides guidance on developing engaging and insightful essay topics related to COVID-19, offering a comprehensive range of perspectives to choose from.
CDC's work during the COVID-19 pandemic included supporting emergency response, strengthening laboratory capacity, and improving global access to testing, diagnostics, and vaccines. CDC rapidly and effectively used existing global health programs such as the U.S. President's Emergency Plan for AIDS Relief (PEPFAR) and subject matter expertise ...
Introduction. During the COVID-19 pandemic, a number of countries introduced stringent measures designed to address vaccine hesitancy. Some countries implemented vaccine mandates in the general population, for example through some form of vaccine passports (eg, in many European countries) or outright fines for the unvaccinated in certain age groups (eg, in Italy).
Food insecurity can be long-term or short-term and can be influenced by various factors, including an individual's race, access to transportation, physical challenges, unemployment, and issues with purchasing food. COVID-19 has influenced the following theories; the Actor-Network Theory, food deserts, Emotion Management, Intersection Theory ...
Background As global travel resumed in COVID-19 endemicity, the potential of aircraft wastewater monitoring to provide early warning of disease trends for SARS-CoV-2 variants and other infectious diseases, particularly at international air travel hubs, was recognized. We therefore assessed and compared the feasibility of testing wastewater from inbound aircraft and airport terminals for 18 ...
A novel coronavirus (CoV) named '2019-nCoV' or '2019 novel coronavirus' or 'COVID-19' by the World Health Organization (WHO) is in charge of the current outbreak of pneumonia that began at the beginning of December 2019 near in Wuhan City, Hubei Province, China [1-4]. COVID-19 is a pathogenic virus. From the phylogenetic analysis ...
This paper examines emerging market and developing economy (EMDE) central bank interventions to maintain financial stability during the COVID-19 pandemic. Through empirical analysis and case study reviews, it identifies lessons for designing future programs to address challenges faced in EMDEs, including less-developed financial markets and lower levels of institutional credibility.
Objectives: We aimed to assess the risk of autoimmune- and inflammatory post-acute COVID-19 conditions. Design: Descriptive network cohort study. Setting: Electronic health records from UK and Dutch primary care, Norwegian linked health registry, hospital records of specialist centres in Spain, France, and Korea, and healthcare claims from Estonia and the US.
Health benefits. Swimming can improve mood and people report enjoying water-based exercise more than exercising on land. People are able to exercise longer in water without increased joint or muscle pain, which has been shown to be especially helpful for people with arthritis and osteoarthritis. Water-based exercise can help people with ...