Jump to navigation
We have changed our Terms of Use and Privacy Policy as of January 12th, 2021. By clicking Accept below, you acknowledge receipt of these new policies.
- US & Canada

Advanced Search

- América Latina: Español
- América Latina: Português
- Mission and goals
- Strategic partners
- Health Care Without Harm in Africa
- Global team
- Health Care Without Harm board
- Coronavirus resource center
- Climate and health news
- Subscribe to our newsletters
- About Global Green and Healty Hospitals
- Imagine a green and healthier world
- The Global Green and Healthy Hospitals agenda
- Climate Impact Checkup
- Climate change: an opportunity for action
- Our approach: mitigation, resilience and leadership
- Sustainable cooling
- Air pollution
- Why sustainable procurement
- Sustainable Health in Procurement Project (SHiPP)
- Sustainable Procurement Index for Health
- SDGs and procurement
- Impact of health care waste management
- What we are doing
- Health care waste and Sustainable Development Goals
- Projects and case studies
- Infectious waste
- Sharps waste
- Pharmaceutical waste
- Pathological and anatomical waste
- A fifteen years global campaign
- Mercury and environmental health
- Mercury free members
- Switching to alternatives
- Minamata Convention
- Model policies
- Chemicals and environmental health
- Chemicals in health care
- Plastic pollution
Why health care waste management
Each and every hospital, large and small, rural and urban, can have a positive impact on the public and environmental health of their community through sustainable health care waste management.
As the global health care system expands, reaching more people and offering ever more sophisticated treatments, a silent and largely neglected crisis is unfolding. The ever growing amount of waste that is generated by these lifesaving advances is not being treated properly, causing enormous suffering, pollution, unnecessary carbon emission, and waste of resources.

Incinerator in East Africa
Globally, health care waste management is underfunded and poorly implemented. The combined toxic infectious and other hazardous properties of medical waste represent a significant environmental and public health threat. Scientists (1) have estimated that over half of the world’s population is at risk from environmental, occupational, or public health threats deriving from improperly treated health care waste. As centers of healing whose priority is to first, do no harm, preventing these risks to their community and environment is imperative for health care facilities.
Unlike many other hazardous wastes, there is currently no international convention that directly covers medical waste management, so categorization systems vary from country to country. However, waste is usually categorized according to the risk it carries. The majority of medical waste – around 75 to 85 percent -- is similar to normal municipal waste, and of low risk unless burned. The remainder is composed of more hazardous types of medical wastes, including infectious and sharps wastes, chemical and radioactive wastes, and hospital wastewaters.
Burning medical waste releases many hazardous gases and compounds, including hydrochloric acid, dioxins and furans, as well as the toxic metals lead, cadmium, and mercury. It also releases large amounts of carbon dioxide, worsening climate change. The disposal of biodegradable waste produces greenhouse gas emissions, including methane, which has a bigger impact on the climate than any other gas than carbon dioxide (2). In many countries, the lack of recycling and disposal infrastructure means that waste- including a large percentage of plastic- is dumped, joining the millions of tonnes that annually pollute our lands and seas.
The good news is that solutions exist that can address these problems, and, in doing so, develop and popularise technologies, products and concepts that will help drive society forward to a zero waste, low carbon, toxics free, circular economy.
By reducing and segregating health care waste, health care facilities can reduce their operational costs, eliminate risks to their staff, enhance the local environment and improve community relations.
A large scale rotating autoclave
1. Harhay et al. 2009 Health care waste management: a neglected and growing public health problem worldwide. Tropical Medicine and International Health 14(11):1414-1417
2. IPCC 5th report Chapter 8, p677 https://www.ipcc.ch/pdf/assessment-report/ar5/wg1/WG1AR5_Chapter08_FINAL.pdf
Quick Links
Copyright © 2024 Health Care Without Harm
- Privacy Policy
- Terms of Use
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Guidelines and Guidance Library
- Core Practices
- Isolation Precautions Guideline
- Disinfection and Sterilization Guideline
- Environmental Infection Control Guidelines
- Hand Hygiene Guidelines
- Multidrug-resistant Organisms (MDRO) Management Guidelines
- Catheter-Associated Urinary Tract Infections (CAUTI) Prevention Guideline
- Tools and resources
- Evaluating Environmental Cleaning
I. Regulated Medical Waste
At a glance.
Guidelines for regulated medical waste from the Guidelines for Environmental Infection Control in Health-Care Facilities (2003).
1. Epidemiology
No epidemiologic evidence suggests that most of the solid- or liquid wastes from hospitals, other healthcare facilities, or clinical/research laboratories is any more infective than residential waste. Several studies have compared the microbial load and the diversity of microorganisms in residential wastes and wastes obtained from a variety of health-care settings. 1399–1402 Although hospital wastes had a greater number of different bacterial species compared with residential waste, wastes from residences were more heavily contaminated. 1397, 1398 Moreover, no epidemiologic evidence suggests that traditional waste-disposal practices of health-care facilities (whereby clinical and microbiological wastes were decontaminated on site before leaving the facility) have caused disease in either the health-care setting or the general community. 1400, 1401 This statement excludes, however, sharps injuries sustained during or immediately after the delivery of patient care before the sharp is "discarded." Therefore, identifying wastes for which handling and disposal precautions are indicated is largely a matter of judgment about the relative risk of disease transmission, because no reasonable standards on which to base these determinations have been developed. Aesthetic and emotional considerations (originating during the early years of the HIV epidemic) have, however, figured into the development of treatment and disposal policies, particularly for pathology and anatomy wastes and sharps. 1402–1405 Public concerns have resulted in the promulgation of federal, state, and local rules and regulations regarding medical waste management and disposal. 1406–1414
2. Categories of Medical Waste
Precisely defining medical waste on the basis of quantity and type of etiologic agents present is virtually impossible. The most practical approach to medical waste management is to identify wastes that represent a sufficient potential risk of causing infection during handling and disposal and for which some precautions likely are prudent. 2 Health-care facility medical wastes targeted for handling and disposal precautions include microbiology laboratory waste (e.g., microbiologic cultures and stocks of microorganisms), pathology and anatomy waste, blood specimens from clinics and laboratories, blood products, and other body-fluid specimens. 2 Moreover, the risk of either injury or infection from certain sharp items (e.g., needles and scalpel blades) contaminated with blood also must be considered. Although any item that has had contact with blood, exudates, or secretions may be potentially infective, treating all such waste as infective is neither practical nor necessary. Federal, state, and local guidelines and regulations specify the categories of medical waste that are subject to regulation and outline the requirements associated with treatment and disposal. The categorization of these wastes has generated the term "regulated medical waste." This term emphasizes the role of regulation in defining the actual material and as an alternative to "infectious waste," given the lack of evidence of this type of waste's infectivity. State regulations also address the degree or amount of contamination (e.g., blood-soaked gauze) that defines the discarded item as a regulated medical waste. The EPA's Manual for Infectious Waste Management identifies and categorizes other specific types of waste generated in health-care facilities with research laboratories that also require handling precautions. 1406
3. Management of Regulated Medical Waste in Health-Care Facilities
Ebola virus disease [august 2014] .
Medical wastes require careful disposal and containment before collection and consolidation for treatment. OSHA has dictated initial measures for discarding regulated medical-waste items. These measures are designed to protect the workers who generate medical wastes and who manage the wastes from point of generation to disposal. 967 A single, leak-resistant biohazard bag is usually adequate for containment of regulated medical wastes, provided the bag is sturdy and the waste can be discarded without contaminating the bag's exterior. The contamination or puncturing of the bag requires placement into a second biohazard bag. All bags should be securely closed for disposal. Puncture-resistant containers located at the point of use (e.g., sharps containers) are used as containment for discarded slides or tubes with small amounts of blood, scalpel blades, needles and syringes, and unused sterile sharps. 967 To prevent needlestick injuries, needles and other contaminated sharps should not be recapped, purposefully bent, or broken by hand. CDC has published general guidelines for handling sharps. 6, 1415 Health-care facilities may need additional precautions to prevent the production of aerosols during the handling of blood-contaminated items for certain rare diseases or conditions (e.g., Lassa fever and Ebola virus infection). 203 Transporting and storing regulated medical wastes within the health-care facility prior to terminal treatment is often necessary. Both federal and state regulations address the safe transport and storage of on- and off-site regulated medical wastes. 1406–1408 Health-care facilities are instructed to dispose medical wastes regularly to avoid accumulation. Medical wastes requiring storage should be kept in labeled, leak-proof, puncture-resistant containers under conditions that minimize or prevent foul odors. The storage area should be well ventilated and be inaccessible to pests. Any facility that generates regulated medical wastes should have a regulated medical waste management plan to ensure health and environmental safety as per federal, state, and local regulations.
Medical wastes require careful disposal and containment before collection and consolidation for treatment. OSHA has dictated initial measures for discarding regulated medical-waste items. These measures are designed to protect the workers who generate medical wastes and who manage the wastes from point of generation to disposal. 967 A single, leak-resistant biohazard bag is usually adequate for containment of regulated medical wastes, provided the bag is sturdy and the waste can be discarded without contaminating the bag's exterior. The contamination or puncturing of the bag requires placement into a second biohazard bag. All bags should be securely closed for disposal. Puncture-resistant containers located at the point of use (e.g., sharps containers) are used as containment for discarded slides or tubes with small amounts of blood, scalpel blades, needles and syringes, and unused sterile sharps. 967 To prevent needlestick injuries, needles and other contaminated sharps should not be recapped, purposefully bent, or broken by hand. CDC has published general guidelines for handling sharps. 6, 1415 Health-care facilities may need additional precautions to prevent the production of aerosols during the handling of blood-contaminated items for certain rare diseases or conditions (e.g., Lassa fever and Ebola virus infection). 203
Transporting and storing regulated medical wastes within the health-care facility prior to terminal treatment is often necessary. Both federal and state regulations address the safe transport and storage of on- and off-site regulated medical wastes. 1406–1408 Health-care facilities are instructed to dispose medical wastes regularly to avoid accumulation. Medical wastes requiring storage should be kept in labeled, leak-proof, puncture-resistant containers under conditions that minimize or prevent foul odors. The storage area should be well ventilated and be inaccessible to pests. Any facility that generates regulated medical wastes should have a regulated medical waste management plan to ensure health and environmental safety as per federal, state, and local regulations.
4. Treatment of Regulated Medical Waste
Regulated medical wastes are treated or decontaminated to reduce the microbial load in or on the waste and to render the by-products safe for further handling and disposal. From a microbiologic standpoint, waste need not be rendered "sterile" because the treated waste will not be deposited in a sterile site. In addition, waste need not be subjected to the same reprocessing standards as are surgical instruments. Historically, treatment methods involved steam-sterilization (i.e., autoclaving), incineration, or interment (for anatomy wastes). Alternative treatment methods developed in recent years include chemical disinfection, grinding/shredding/disinfection methods, energy-based technologies (e.g., microwave or radiowave treatments), and disinfection/encapsulation methods. 1409 State medical waste regulations specify appropriate treatment methods for each category of regulated medical waste.
Of all the categories comprising regulated medical waste, microbiologic wastes (e.g., untreated cultures, stocks, and amplified microbial populations) pose the greatest potential for infectious disease transmission, and sharps pose the greatest risk for injuries. Untreated stocks and cultures of microorganisms are subsets of the clinical laboratory or microbiologic waste stream. If the microorganism must be grown and amplified in culture to high concentration to permit work with the specimen, this item should be considered for on-site decontamination, preferably within the laboratory unit. Historically, this was accomplished effectively by either autoclaving (steam sterilization) or incineration. If steam sterilization in the health-care facility is used for waste treatment, exposure of the waste for up to 90 minutes at 250°F (121°C) in a autoclave (depending on the size of the load and type container) may be necessary to ensure an adequate decontamination cycle. 1416–1418 After steam sterilization, the residue can be safely handled and discarded with all other nonhazardous solid waste in accordance with state solid-waste disposal regulations. On-site incineration is another treatment option for microbiologic, pathologic, and anatomic waste, provided the incinerator is engineered to burn these wastes completely and stay within EPA emissions standards. 1410 Improper incineration of waste with high moisture and low energy content (e.g., pathology waste) can lead to emission problems. State medical-waste regulatory programs identify acceptable methods for inactivating amplified stocks and cultures of microorganisms, some of which may employ technology rather than steam sterilization or incineration.
Concerns have been raised about the ability of modern health-care facilities to inactivate microbiologic wastes on-site, given that many of these institutions have decommissioned their laboratory autoclaves. Current laboratory guidelines for working with infectious microorganisms at biosafety level (BSL) 3 recommend that all laboratory waste be decontaminated before disposal by an approved method, preferably within the laboratory. 1013 These same guidelines recommend that all materials removed from a BSL 4 laboratory (unless they are biological materials that are to remain viable) are to be decontaminated before they leave the laboratory. 1013 Recent federal regulations for laboratories that handle certain biological agents known as "select agents" (i.e., those that have the potential to pose a severe threat to public health and safety) require these agents (and those obtained from a clinical specimen intended for diagnostic, reference, or verification purposes) to be destroyed on-site before disposal. 1412 Although recommendations for laboratory waste disposal from BSL 1 or 2 laboratories (e.g., most health-care clinical and diagnostic laboratories) allow for these materials to be decontaminated off-site before disposal, on-site decontamination by a known effective method is preferred to reduce the potential of exposure during the handling of infectious material.
A recent outbreak of TB among workers in a regional medical-waste treatment facility in the United States demonstrated the hazards associated with aerosolized microbiologic wastes. 1419, 1420 The facility received diagnostic cultures of Mycobacterium tuberculosis from several different health-care facilities before these cultures were chemically disinfected; this facility treated this waste with a grinding/shredding process that generated aerosols from the material. 1419, 1420 Several operational deficiencies facilitated the release of aerosols and exposed workers to airborne M. tuberculosis . Among the suggested control measures was that health-care facilities perform on-site decontamination of laboratory waste containing live cultures of microorganisms before release of the waste to a waste management company. 1419, 1420 This measure is supported by recommendations found in the CDC/NIH guideline for laboratory workers. 1013 This outbreak demonstrates the need to avoid the use of any medical-waste treatment method or technology that can aerosolize pathogens from live cultures and stocks (especially those of airborne microorganisms) unless aerosols can be effectively contained and workers can be equipped with proper PPE. 1419–1421 Safe laboratory practices, including those addressing waste management, have been published. 1013, 1422
In an era when local, state, and federal health-care facilities and laboratories are developing bioterrorism response strategies and capabilities, the need to reinstate in-laboratory capacity to destroy cultures and stocks of microorganisms becomes a relevant issue. 1423 Recent federal regulations require health-care facility laboratories to maintain the capability of destroying discarded cultures and stocks on-site if these laboratories isolate from a clinical specimen any microorganism or toxin identified as a "select agent" from a clinical specimen (Table 27). 1412, 1413 As an alternative, isolated cultures of select agents can be transferred to a facility registered to accept these agents in accordance with federal regulations. 1412 State medical waste regulations can, however, complicate or completely prevent this transfer if these cultures are determined to be medical waste, because most states regulate the inter-facility transfer of untreated medical wastes.
Table 27. Microorganisms and biologicals identified as select agents A
Table 27 A. HHS Non-overlap select agents and toxins (42 CFR Part 73 §73.4) B
- Crimean-Congo hemorrhagic fever virus; Ebola viruses; Cercopithecine herpesvirus 1 (herpes B virus); Lassa fever virus; Marburg virus; monkeypox virus; South American hemorrhagic fever viruses (Junin, Machupo, Sabia, Flexal, Guanarito); tick-borne encephalitis complex (flavi) viruses (Central European tick-borne encephalitis, Far Eastern tick-borne encephalitis [Russian spring and summer encephalitis, Kyasnaur Forest disease, Omsk hemorrhagic fever]); variola major virus (smallpox virus); and variola minor virus (alastrim)
- Exclusions : C Vaccine strain of Junin virus (Candid. #1)
- Rickettsia prowazekii, R. rickettsii, Yersinia pestis
- Coccidioides posadasii
- Abrin; conotoxins; diacetoxyscirpenol; ricin; saxitoxin; Shiga-like ribosome inactivating proteins; tetrodotoxin
- Exclusions C : The following toxins (in purified form or in combinations of pure and impure forms) if the aggregate amount under the control of a principal investigator does not, at any time, exceed the amount specified: 100 mg of abrin; 100 mg of conotoxins; 1,000 mg of diacetoxyscirpenol; 100 mg of ricin; 100 mg of saxitoxin; 100 mg of Shiga-like ribosome inactivating proteins; or 100 mg of tetrodotoxin
- Select agent viral nucleic acids (synthetic or naturally-derived, contiguous or fragmented, in host chromosomes or in expression vectors) that can encode infectious and/or replication competent forms of any of the select agent viruses;
- Nucleic acids (synthetic or naturally-derived) that encode for the functional form(s) of any of the toxins listed in this table if the nucleic acids: are in a vector or host chromosome; can be expressed in vivo or in vitro ; or are in a vector or host chromosome and can be expressed in vivo or in vitro ;
- Viruses, bacteria, fungi, and toxins listed in this table that have been genetically modified.
Table 27 B. High consequence livestock pathogens and toxins/select agents (overlap agents) (42 CFR Part 73 §73.5 and USDA regulation 9 CFR Part 121) B
- Eastern equine encephalitis virus; Nipah and Hendra complex viruses; Rift Valley fever virus; Venezuelan equine encephalitis virus
- Exclusions: C MP-12 vaccine strain of Rift Valley fever virus; TC-83 vaccine strain of Venezuelan equine encephalitis virus
- Bacillus anthracis; Brucella abortus, B. melitensis, B. suis; Burkholderia mallei (formerly Pseudomonas mallei), B. pseudomallei (formerly P. pseudomallei); botulinum neurotoxin- producing species of Clostridium; Coxiella burnetii; Francisella tularensis
- Coccidioides immitis
- Botulinum neurotoxins; Clostridium perfringens epsilon toxin; Shigatoxin; staphylococcal enterotoxins; T-2 toxin
- Exclusions: C The following toxins (in purified form or in combinations of pure and impure forms) if the aggregate amount under the control of a principal investigator does not, at any time, exceed the amount specified: 0.5 mg of botulinum neurotoxins; 100 mg of Clostridium perfringens epsilon toxin; 100 mg of Shigatoxin; 5 mg of staphylococcal enterotoxins; or 1,000 mg of T-2 toxin
- Select agent viral nuclei acids (synthetic or naturally derived, contiguous or fragmented, in host chromosomes or in expression vectors) thatcan encode infectious and/or replication competent forms of any of the select agent viruses;
- Nucleic acids (synthetic or naturally derived) that encode for the functional form(s) of any of the toxins listed in this table if the nucleic acids: are in a vector or host chromosome; can be expressed in vivo or in vitro ; or are in a vector or host chromosome and can be expressed in vivo or in vitro ;
5. Discharging Blood, Fluids to Sanitary Sewers or Septic Tanks
The contents of all vessels that contain more than a few milliliters of blood remaining after laboratory procedures, suction fluids, or bulk blood can either be inactivated in accordance with state-approved treatment technologies or carefully poured down a utility sink drain or toilet. 1414 State regulations may dictate the maximum volume allowable for discharge of blood/body fluids to the sanitary sewer. No evidence indicates that bloodborne diseases have been transmitted from contact with raw or treated sewage. Many bloodborne pathogens, particularly bloodborne viruses, are not stable in the environment for long periods of time; 1425, 1426 therefore, the discharge of small quantities of blood and other body fluids to the sanitary sewer is considered a safe method of disposing of these waste materials. 1414 The following factors increase the likelihood that bloodborne pathogens will be inactivated in the disposal process:
- dilution of the discharged materials with water
- inactivation of pathogens resulting from exposure to cleaning chemicals, disinfectants, and other chemicals in raw sewage; and
- effectiveness of sewage treatment in inactivating any residual bloodborne pathogens that reach the treatment facility.
Small amounts of blood and other body fluids should not affect the functioning of a municipal sewer system. However, large quantities of these fluids, with their high protein content, might interfere with the biological oxygen demand (BOD) of the system. Local municipal sewage treatment restrictions may dictate that an alternative method of bulk fluid disposal be selected. State regulations may dictate what quantity constitutes a small amount of blood or body fluids.
Although concerns have been raised about the discharge of blood and other body fluids to a septic tank system, no evidence suggests that septic tanks have transmitted bloodborne infections. A properly functioning septic system is adequate for inactivating bloodborne pathogens. System manufacturers' instructions specify what materials may be discharged to the septic tank without jeopardizing its proper operation.
6. Medical Waste and CJD
Concerns also have been raised about the need for special handling and treatment procedures for wastes generated during the care of patients with CJD or other transmissible spongiform encephalopathies (TSEs). Prions, the agents that cause TSEs, have significant resistance to inactivation by a variety of physical, chemical, or gaseous methods. 1427 No epidemiologic evidence, however, links acquisition of CJD with medical-waste disposal practices. Although handling neurologic tissue for pathologic examination and autopsy materials with care, using barrier precautions, and following specific procedures for the autopsy are prudent measures, 1197 employing extraordinary measures once the materials are discarded is unnecessary. Regulated medical wastes generated during the care of the CJD patient can be managed using the same strategies as wastes generated during the care of other patients. After decontamination, these wastes may then be disposed in a sanitary landfill or discharged to the sanitary sewer, as appropriate.
- Material in this table is compiled from references 1412, 1413, 1424. Reference 1424 also contains lists of select agents that include plant pathogens and pathogens affecting livestock.
- 42 CFR 73 §§73.4 and 73.5 do not include any select agent or toxin that is in its naturally-occurring environment, provided it has not been intentionally introduced, cultivated, collected, or otherwise extracted from its natural source. These sections also do not include non-viable select agent organisms or nonfunctional toxins. This list of select agents is current as of 3 October 2003 and is subject to change pending the final adoption of 42 CFR Part 73.
- These table entries are listed in reference 1412 and 1413, but were not included in reference 1424.
Infection Control
CDC provides information on infection control and clinical safety to help reduce the risk of infections among healthcare workers, patients, and visitors.
For Everyone
Health care providers, public health.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Healthcare (Basel)

Healthcare Waste—A Serious Problem for Global Health
Edyta janik-karpinska.
1 Biohazard Prevention Centre, Faculty of Biology and Environmental Protection, University of Lodz, Pomorska 141/143, 90-236 Lodz, Poland
Rachele Brancaleoni
2 Bed Management Unit, Agostino Gemelli IRCCS University Hospital Foundation, Via della Pineta Sacchetti 217, 00168 Rome, Italy
Marcin Niemcewicz
Wiktor wojtas.
3 European Commission, Directorate-General Migration and Home Affairs, Rue du Luxembourg 46, 1000 Brussels, Belgium
Maurizio Foco
4 Emergency Surgery Department, Fondazione Policlinico Universitario A. Gemelli IRCCS, Pineta Sacchetti 217, 00168 Rome, Italy
Marcin Podogrocki
Michal bijak, associated data.
Not applicable.
Healthcare waste (HCW) is generated in different healthcare facilities (HCFs), such as hospitals, laboratories, veterinary clinics, research centres and nursing homes. It has been assessed that the majority of medical waste does not pose a risk to humans. It is estimated that 15% of the total amount of produced HCW is hazardous and can be infectious, toxic or radioactive. Hazardous waste is a special type of waste which, if not properly treated, can pose a risk to human health and to the environment. HCW contains potentially harmful microorganisms that can be spread among healthcare personnel, hospital patients and the general public, causing serious illnesses. Healthcare personnel are the specialists especially exposed to this risk. The most common medical procedure, which pose the highest risk, is injection (i.e, intramuscular, subcutaneous, intravenous, taking blood samples). The World Health Organization (WHO) estimates that around 16 billion injections are administered worldwide each year. However, if safety precautions are not followed, and needles and syringes are not properly disposed of, the risk of sharps injuries increases among medical staff, waste handlers and waste collectors. What is more, sharps injuries increase the risk of human immunodeficiency virus (HIV), hepatitis B and C viruses (HBV/HCV), tuberculosis (TB), diphtheria, malaria, syphilis, brucellosis and other transmissions. Disposing of medical waste in a landfill without segregation and processing will result in the entry of harmful microorganisms, chemicals or pharmaceuticals into soil and groundwater, causing their contamination. Open burning or incinerator malfunctioning will result in the emission of toxic substances, such as dioxins and furans, into the air. In order to reduce the negative impact of medical waste, waste management principles should be formulated. To minimize health risks, it is also important to build awareness among health professionals and the general public through various communication and educational methods. The aim of this paper is to present a general overwiev of medical waste, its categories, the principles of its management and the risks to human health and the environment resulting from inappropriate waste management.
1. Introduction
Healthcare facilities (HCFs) are the main healthcare waste producers. The most common term used to describe waste generated by HCFs is healthcare waste (HCW). There are several other terms such as medical waste, biomedical waste, clinical waste or health facility waste [ 1 ]. HCW is defined as all types of waste generated from HCFs, whether it is a hazardous or harmless material, and whether it is infectious or non-infectious in nature or a chemical [ 2 ]. It is estimated that HCWs constitute approx. 1–2% of total produced urban waste [ 3 ]. A total of 85% of the total amount of waste generated as a result of healthcare activities is non-hazardous. The remaining 15% are hazardous materials, which are infectious, radioactive or toxic ( Figure 1 ). The majority of HCW generators are hospitals, medical centers, laboratories, veterinary clinics, research centers, mortuaries, blood banks and nursing homes. High-income countries produce up to almost 11 kg of hazardous waste per hospital bed per day (kg/bed/day), while in low-income countries the production rate ranges up to 6 kg. However, in low-income countries, HCW is often not segregated into hazardous and non-hazardous waste, making the actual amount of produced hazardous waste much higher [ 4 , 5 ].

Standard waste composition in health facilities.
Economic conditions are an important factor in HCW management. In many industrialized countries, institutions that generate medical waste have a legal obligation to manage this type of waste. As a result, there are appropriate structures for handling each type of waste and the amount of hazardous waste generated is constantly monitored [ 6 ]. Problems in HCW management are more prevalent in developing countries that produce several hundred tons of waste daily. Studies performed in Ethiopia revealed that 35% of healthcare institutes collect and dispose of needles, syringes and other sharp objects in a way that puts healthcare personnel and the general public at a constantly increasing risk of exposure and injury [ 7 ]. These countries typically use HCW management methods such as landfilling, recycling, incineration or storage. Although HCW landfilling without pre-treatment is prohibited, it is the most common method of HCW disposal as it is a cheap and easy method. In practice, HCW is stored in open dumps in pits mixed with municipal waste and is then incinerated [ 8 , 9 ]. HCW can have a long-lasting effect on human health, both for the people handling, collecting and recycling the waste, and for the general public. The environment is also suffering from fresh water and soil contamination resulting from untreated medical waste pollution or by the process of surface waste burning [ 6 , 10 ].
The objective of this paper is to provide a general overview of medical waste issues, including their sources and categories, waste generation, the principles of waste management and the threat to human health and the environment resulting from improper waste management.
2. Categories and Sources of HCW
HCW and by-products are generated as a result of diagnosis, treatment, medical intervention or the immunization of human or animals [ 11 ]. They cover a wide range of materials and different categories as summarized in Table 1 [ 5 , 8 , 12 ].
Categories of healthcare waste.
HCW is generated in various types of healthcare units, such as hospitals, medical centers, private medical practices, veterinary clinics, clinical laboratories or pharmacies [ 13 ]. Depending on the source, different types of HCW are generated, and these are summarized in Table 2 [ 5 , 14 ].
Sources and examples of HCW.
3. HCW Production Rate
The HCW production rate in countries worldwide differs and depends on many factors. These factors include waste management methods, the type of healthcare facilities, and healthcare specializations, the amount of reusable equipment available in the facility and the number of patients treated daily [ 15 ]. However, registered HCW production is lower in developing countries than in developed countries. Detailed information on the HCW production rate in different continents and selected countries are presented in Table 3 .
Example of HCW production rate in various countries worldwide.
4. HCW Production Rate during Pandemic
The COVID-19 pandemic has been attracting global attention since December 2019, as has the area of HCW production. The World Health Organization (WHO), Centers for Disease Control and Prevention (CDC) and local governments have announced numerous guidelines, including good hygiene practices, social distancing and quarantines, in order to reduce the spread of a new coronavirus. In addition, medical personnel and the general public have been advised to use personal protective equipment (PPE), such as surgical or medical masks, non-medical face masks (including different forms of self-made or commercial masks made of fabric, cotton or other textile materials), face shields, gloves and aprons [ 37 ]. In many countries, it is recommended to wear masks in public places. According to the press conference of the Joint Prevention and Control Mechanism of China’s Council State, the daily amount of COVID-19-related HCW in China was around 468.9 tons [ 38 ]. At the peak of the pandemic, only in Wuhan, the waste generated reached approximately 240 tons of HCW per day, almost six times more than before the pandemic [ 39 ]. In Bangladesh, in April 2020, at least 14.5 thousand tons of HCW was generated across the country due to the COVID-19 pandemic. In Dhaka, an average of 206 tons of HCW per day is generated because of the pandemic [ 40 ]. In the USA, the estimated increase in HCW generation was reported to range from 5 million tons/year before the pandemic to 2.5 million tons/month during the pandemic. The drastic increase in the number of regions, countries and people infected with SARS-CoV-2 led to global problems related to proper HCW management [ 41 ].
5. HCW Management
The purpose of healthcare systems is to restore health and save patients’ lives, but sometimes adverse effects on the health of healthcare personnel and communities due to unsanitary methods of disposing of HCW is observed [ 42 ]. Poorly managed waste can cause long-term and undesirable risks to public health and is a potential source of re-infection, posing a significant threat to the environment. Therefore, the management of HCW requires special attention and should be considered a high priority [ 43 ]. The management of HCW is an integral part of national healthcare systems. Safe HCW management practices reflect on HCF service quality and cover all activities related to the generation, segregation, transportation, storage, treatment and disposal of waste [ 44 , 45 ]. Adequate management of medical waste in HCFs depends on the waste management team, good administration and organization, careful planning, legal frameworks, adequate funding and the full participation of trained personnel in this process [ 46 ]. Healthcare facilities managers are responsible for introducing and ensuring an appropriate waste management system, as well as supervising the compliance with appropriate procedures of all medical staff. Therefore, appropriate education and training systems must be available to all personnel responsible and engaged in both segregation and waste collection processes [ 47 , 48 , 49 ]. In line with WHO guidelines, waste segregation practices should be standardized across the country and included in national regulations for HCW management [ 5 ]. The key to the effective management of HCW is the segregation process at the point of waste generation. Segregation means the separation of various types of waste into different color-coded containers with liners at places where they are generated as a first step in HCW management [ 50 , 51 ]. According to WHO recommendations concerning segregation and collection, a general waste container should be black. Sharp, infectious and pathological waste containers should be marked yellow. Chemical and pharmaceutical waste container should have a brown color. It is also recommended that almost all waste categories should be collected at least once per day, or when three-quarters of the container is filled. The exceptions to this are pharmaceutical, chemical and radioactive waste, which can be collected on demand [ 52 , 53 ].
After segregation, waste is collected and transported outside the hospital or healthcare facility. The transportation of HCW is usually performed using dedicated trolleys and containers. The trolleys have to be cleaned and disinfected daily. Hazardous and non-hazardous waste has to always be transported separately [ 54 ]. The waste should be stored in designated rooms and appropriate safety and security measures should be taken. In general, non-hazardous, infectious and sharp, pathological, pharmaceutical, chemical and radiological waste should be stored separately in different places with different characteristics depending on the waste stored [ 53 ].
6. HCW Management during COVID-19 Pandemic
Since March 2020, the whole world has been focusing on the COVID-19 pandemic. It has been considered whether the spread of COVID-19 could also increase as a result of inadequate waste management. Performed studies indicated that the SARS-CoV-2 survival rate on different surface varied from 4 h on copper to up to 3 days on plastic and stainless steel [ 55 ]. The increase in waste generation during the pandemic, as well as the disposal of infected disposable masks and other PPE, has burdened waste management systems [ 56 , 57 , 58 ]. Therefore, ensuring the efficient, timely and harmless management of COVID-19 medical waste has also become a significant part of pandemic controlling [ 59 ]. In addition to introduced standards, such as proper identification, collection, segregation, storage, transport, processing and disposal, aspects such as disinfection, personnel protection and training have become part of effective HCW management [ 57 ]. It has been shown that fomites may not be as critical to the transmission of SARS-CoV-2 as initially suspected [ 60 ]. At this moment, there is no significant differences between overall COVID-19 HCW management and general pre-pandemic medical waste management [ 38 ].
7. Risk Related to HCW
HCW is potentially dangerous and a pollutant [ 43 ]. Everyone close to hazardous medical waste is potentially at risk, including those working in healthcare facilities, those handling medical waste or those exposed through careless actions. The main risk groups are physicians, nurses, healthcare support staff, patients, HCF visitors and support services workers, such as laundry workers, waste management and transportation staff and waste-disposal facility employees [ 61 ]. Globally, more than two million medical personnel are exposed to pathogens as a result of their daily work routines [ 1 ]. In conclusion, HCW poses a serious threat to human health and life especially in low- and middle-income countries. Globally, it is estimated that at least 5.2 million people worldwide die each year, including 4 million children, due to illnesses caused by unmanaged medical waste [ 40 ].
7.1. Infectious Waste and Sharps
Infectious waste is a variety of hazardous waste which, due to its pathogenic nature, pose a threat to human health. It should always be assumed that infectious waste may contain various pathogenic microorganisms [ 62 ]. HCW can transmit more than 30 dangerous blood-borne pathogens [ 1 ]. Pathogens in infectious waste that is not properly managed can enter the human body through damaged skin (rubbing, puncturing or cutting the skin), inhalation, mucous membranes or by ingestion [ 5 ]. Performed research indicates the presence of various pathogens in medical waste, as well as the possibility of their transmission routes. Therefore, it can be concluded that this type of waste poses a great potential risk to human health [ 63 , 64 , 65 ].
The greatest risk of transmission of blood-borne pathogens is caused by needle stick and sharp injuries (NSSIs) [ 66 ]. It is estimated that 600,000 to 800,000 needle stick injuries and other percutaneous injuries are reported annually in the U.S.A. In addition, around 100,000 NSSIs occur in the UK each year [ 67 ]. It has been estimated that up to 30% of hepatitis B, 1–3% of hepatitis C and 0.3% of HIV cases were caused by inappropriate HCW handling [ 68 ]. HBV is more contagious than other blood-borne viral pathogens and is approximately 100 times more contagious than HIV. Consequently, HBV poses the greatest occupational risk to non-immune healthcare personnel [ 69 ]. In addition, medical waste handlers are the group more vulnerable to HBV infection than other healthcare personnel, non-medical waste handlers or the general population [ 70 , 71 , 72 ]. The performed study showed that the prevalence of HBV and HCV was significantly higher in medical waste compared to non-clinical waste handlers. The authors clearly pointed out the reason for this situation. Poor waste management systems contributed to higher acute injuries incidences and splashes of blood and body fluids [ 73 ]. A. total of 70% of the world’s HIV-infected population comes from Sub-Saharan Africa, but only 4% of global occupational cases of HIV infection are reported from this region [ 67 ]. It is estimated that up to 5% of all HIV infections in Africa are due to unsafe injection administration, including exposure to sharps injuries during unsafe medical waste handling [ 74 ]. A study conducted in China showed low risk awareness among nurses concerning the risk of HIV infection and a lack of compliance with standard precautions in daily work [ 75 ]. Over 20 other infections can also be transmitted by NSSIs, including syphilis, herpes and malaria. While most NSSIs appear in developing countries, NSSIs are still reported in developed countries despite preventive measures taken, such as standard operating protocols and real-time injury-monitoring systems [ 35 , 76 , 77 , 78 ]. These injuries not only increase the possibility of negative health consequences, but also lead to mental stress, fear, tension and anxiety among healthcare personnel [ 79 ]. The implementation of safety protocols and compulsory training programs for healthcare professionals can reduce the prevalence of NSSIs and associated infections [ 80 , 81 ].
7.2. Chemical and Pharmaceutical Waste
Many chemicals and pharmaceuticals used in healthcare systems can be hazardous. They are usually found in small amounts in medical waste, while larger amounts can be found when unwanted or expired chemicals and pharmaceuticals are directed for disposal [ 5 ]. Chemical waste negatively affects human health and, in most cases, causes intoxication as a primary result of contact with them. Poisoning from the absorption of a chemical or pharmaceutical substance via the mucous membranes, the skin, inhalation or ingestion is the secondary result. Contact with corrosive, flammable or reactive chemicals (formaldehyde and other volatile substances) may cause injuries to the eyes, skin or mucous membranes of the respiratory tract and should be considered thirdly [ 82 ]. Pharmaceuticals enter the environment as a result of the improper handling of unused or expired pharmaceuticals, mainly disposed of into sewage systems. Pharmaceuticals have been reported in various places, such as groundwater, surface water and soil. The main groups of pharmaceuticals detected in environmental samples are antibiotics, hormones, non-steroidal anti-inflammatory drugs, beta blockers, lipid regulators and anti-depressant drugs [ 83 , 84 ]. The long-term presence of pharmaceuticals in the environment causes acute and chronic damage, behavioral changes, reproductive disorders and the inhibition of cell proliferation in animals [ 85 , 86 ]. The negative impact of pharmaceuticals on the environment is also evidenced by the development of antibiotic resistance in some bacterial strains, resulting in an accumulation of antibiotics in the environment. Therefore, it is essential to decontaminate chemical and pharmaceutical waste before placing them in landfills, as improper disposal will cause contact between environmental bacteria and antibiotics, which can lead to the evolution of antibiotic-resistant mechanisms among them [ 83 , 87 , 88 ].
7.3. Genotoxic Waste
The main routes of exposure to genotoxic waste are inhalation and skin absorption. However, ingestion and accidental injection or other sharps injuries are also possible. Exposure may also occur through contact with the patient’s body fluids and secretions (such as vomit, urine and feces) while undergoing chemotherapy [ 89 , 90 ]. Cytotoxic drugs or anticancer drugs are classified as dangerous medicaments. Acute exposure usually causes temporary symptoms, such as dizziness, headache, nausea and malaise. What is more, cytotoxic drugs possess strong irritating properties, and direct contact will lead to the appearance of local symptoms, such as rash, dermatitis, irritation of the skin, mucous membrane ulceration and irritation of the throat or eyes [ 91 ]. The side effects from prolonged or repeated exposure to cytotoxic drugs are significant and serious. An increased incidence of spontaneous abortions during pregnancy and malformations have been observed among children of females with a history of occupational exposure to anticancer medicaments [ 92 ]. Cytotoxic drugs are also not neutral to the environment, especially the aquatic environment [ 93 ]. Some cytotoxic drugs are not fully metabolized and are poorly biodegradable. They can also be resistant to conventional biological and chemical processes used in wastewater treatments and can challenge water-decontamination technology. While aquatic cytotoxic drug concentrations may stay below detection limits, they can reach alarming levels in fauna and flora through bioaccumulation and biomagnification processes. Therefore, their effect should be carefully investigated as unexpected delayed effects can be present in offspring [ 94 ]. Kovacs et al. demonstrated that long-term exposure of zebrafish to anticancer drugs impaired their DNA integrity and induced massive whole-transcriptome changes, which might affect entire zebrafish populations [ 95 ].
7.4. Radioactive Waste
The disease caused by radioactive waste depends on the type and extent of exposure. This can include headache, dizziness and vomiting, as well as much more serious problems. Radioactive waste is genotoxic and, if the radiation dose is high enough, it can also affect the genetic material. Inadequate handling of radiation diagnostic instruments can cause much more serious injuries, including tissue destruction, which in some cases requires the amputation of body parts. Extreme cases can be even fatal [ 5 , 96 ].
8. HCW Treatment and Safety Issues
The most common types of HCW treatments are steam-based treatments (autoclaving, microwave and frictional heat treatments), which are used to disinfect/sterilize highly infectious and sharp waste by subjecting them to moist heat and steam. Steam sterilization is used for sterilization instruments and for sharp and hazardous waste treatments. To reduce the volume of waste, steam sterilization can be combined with mechanical processes, such as mixing, grinding and shredding [ 53 ]. Incineration, the process of waste destruction by burning, removes hazardous materials, reduces their mass and volume and converts them into ashes. An incinerator that is not properly designed or operated, or is poorly maintained, emits toxic substances into the environment. If incinerators operate at low temperatures, they generate emissions containing dioxins and furans, which may cause health problems as they are carcinogenic [ 97 ]. Incinerators operating at 850–1100 °C and containing special gas-cleaning equipment can comply with international emission dioxin and furan standards. Dioxin-control technologies use activated carbon (AC) adsorption. Before flue gas flows into the dust-collection equipment, AC is injected to adsorb the dioxin and then is blocked by a bag filter [ 61 ]. The next method used is a chemical treatment process. It mostly relies on using disinfectants, ozone treatment and alkaline hydrolysis. Composting and vermicomposting (which uses earthworms to consume and recycle the organic waste) are successfully used to break down hospital kitchen waste, as well as other digestible organic and placental waste. Another example of a biological process is the natural decomposition of pathological waste through its burial. Non-hazardous waste should be recycled and regularly collected by the municipalities or transported by the facility to public landfills [ 53 ]. Inadequate HCW treatment can be dangerous for health. Incinerator control results in the release of small particulates that affect the functioning of the respiratory and cardiovascular systems. Volatile metals, such as mercury, lead, arsenic and cadmium, will damage the immune and neurological systems, as well as the kidneys, brain and lungs. The incineration of high-metal-content materials leads to the spread of toxic metals in the environment [ 98 , 99 ]. Various studies have shown adverse health effects in populations in the vicinity of incinerators, including cancer and reproductive dysfunction [ 100 , 101 , 102 ]. Ashes, as a result of the incineration of hazardous medical waste, are also hazardous. Bottom ash analyses of incinerated medical waste carried out in Tanzania indicate the hazardous nature of ash resulting from the presence of large amounts of heavy metals (iron, cadmium, lead, copper and manganese) [ 103 ]. Burying medical waste and depositing them in landfills is also dangerous. Medical waste is almost always contaminated with pathogens, and leaching toxic heavy metals and chemicals from solid medical waste into the soil occurs in poorly designed dump sites and landfills. The leachate can penetrate the soil and contaminate crops, surface and groundwater resources, posing a risk to human health by consuming water. To control the safety of these methods, hydro-geological conditions must be considered. Landfills should have restricted access, control scavenging, use a soil cover regularly, manage waste discharge, and control surface water and drainage [ 65 , 104 ]. An interesting solution is the possibility of thermal energy, fuel, and electric-power production from medical waste, and some studies concerning this issue have been conducted. One study showed that waste-disposable syringes treated with pyrolysis at 400–550 °C were used to produce liquid fuel. The produced pyrolysis oil had physical properties similar to that of a diesel or petrol mixture [ 105 ]. Fang et al. [ 106 ] showed that the pyrolysis of mixed medical waste, such as plastic, cotton and glass, at 500 °C can produce liquid fuel (pyrolysis oil). It can be refined by fractional condensation. In a different study, biogas from recycled medical cotton waste as a source of biogas recovery, using thermophilic bio-digestion conditions, was produced. It improved biogas yield by 92% [ 107 ]. These studies bring hope that in the future it will be possible to use medical waste to produce energy or fuel on a large scale.
9. Conclusions
Medical waste amounts have increased dramatically over the last 30 years, and health facilities around the world are producing more waste than ever before. The amount of HCW generation is rising with the increase in the world’s population, medical facilities’ multitude and with the widespread propensity to use disposable medical equipment. Due to the use of advanced technological practices and safety considerations, single-use equipment causes more waste generation [ 108 ]. Further problems include a lack of health risk awareness associated with HCW, insufficient training in proper waste management, inadequate human resources and the low priority given to this matter [ 8 ]. Studies in developing countries have shown evidence that medical waste is mixed and collectively combined with municipal waste or burned in the open air [ 8 , 96 ]. Such activities pose risks to public health and the environment. Medical waste can contain potentially harmful microorganisms that can infect healthcare professionals, patients and the general public. Potential risks include drug-resistant microorganisms that spread from HCFs into the environment. Another risk is the release of toxic compounds into the environment, such as heavy metals, dioxins and furans [ 5 , 109 ]. In order to reduce the risk associated with medical waste, it is necessary to focus on a few key aspects. Improved policies and procedures should be developed and implemented for the proper use of single-use or reusable items and the identification of recycling options. Activities may also include working with providers to make products available in materials that are more easily degraded, or that can be reused for secondary purposes. There are items that are not hazardous (such as clean packaging) and can be removed without unnecessary treatment prior to the final disposal. Another option is to minimize the impact by adjusting purchasing strategy and inventory control. This solution can also be implemented through the use of physical (steam treatment) instead of chemical disinfection, waste minimization by using less materials and finally by checking the expiration date of the products upon delivery and refuse to accept items with a short expiration date [ 5 , 110 ]. Major challenges related to the risk of HCW are misconceptions and a lack of education and awareness regarding which type of waste is hazardous and which is not. In particular, educating healthcare professionals on the proper segregation and disposal of different waste types would be very beneficial to waste reduction and proper infection control [ 111 , 112 ]. In summary, the risks of medical waste can be significantly reduced by implementing appropriate measures. This would result in fewer illnesses and accidental sharps injuries, but also less environmental pollution.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, M.B., R.B., W.W., M.F. and M.N.; supervision, M.B. and M.F.; writing—original draft preparation, E.J.-K., R.B., M.N. and M.P.; writing—review and editing, M.B., M.N. and W.W. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
10 Lessons and Tips from 2021 to Improve Medical Waste Management
- Knowledge Center

As we close out 2021, Daniels Health would like to take a moment to review 10 of the most useful tips and lessons we have shared this past year. Regardless of whether your medical facility is small or large, where it’s located, or how many patients you see a year, every healthcare provider should follow the rules when it comes to healthcare waste management practices. Here are our top ten tips to consider for compliance.
THE TEN LESSONS WE WILL COVER:
1 / Segregate your waste
2 / Know the difference betweem regulaed, infectious, and hazardous waste
3 / Avoid needlestick injuries
4 / Properly dispose of sharps
5 / Properly package and label waste streams
6 / Follow storage limitations and guidelines for medical waste
7 / Know your hazardous waste generator status
8 / Know the difference between bulk and trace chemotherapy waste
9 / Know your state’s approved disposal methods
10 / Know where to find the rules for your state
Tip #1 – Segregate your waste!
Always segregate medical waste at its point of origin. Knowledge of waste stream basics is the first step toward training your staff to properly dispose of medical waste in your hospital, clinic, outpatient surgical center, or dental office. Knowing the regulations of the federal government and your state will keep you compliant and safe, while protecting the environment.
Typically, medical waste is separated into eight different types: sharps, pathological/anatomical, pharmaceutical, biological (including blood and/or blood-related products), microbiological, isolation, and contaminated animal waste. Learn more about proper waste segregation here .
Tip #2 –Know the difference between regulated, infectious, and hazardous medical waste
A regulated medical waste is something that has the potential to be contaminated with a possible infectious material, such as blood or body fluids. In a nutshell, if a waste has blood that drips, pours, or flakes, even after it has dried, then it’s a regulated medical waste.
An infectious medical waste is defined as any waste product or organism typically generated in healthcare scenarios or health-related industries that is capable of producing infection or an infectious disease in humans. Check out our blog covering 10 Types of Infectious Waste .
A hazardous waste is a waste that exhibits certain characteristics. Such waste could be toxic or flammable. It might also have the capability of being reactive with another chemical. Finally, it can be corrosive in nature. A listing of hazardous waste and examples can be found here under the Code of Federal Regulations.
Tip #3 – Avoid Needlestick injuries
Injuries caused by sharps or needlestick accidents are considered a common healthcare industry hazard for nurses, doctors, and surgical staff. Unfortunately, injuries and infections can also occur within janitorial and housekeeping staff due to improper disposal practices.
On their website , the Occupational Safety and Health Administration (OSHA) stipulates that over five million healthcare industry workers – and ancillary occupations – continue to be at a risk for bloodborne pathogen exposure. Such exposures can include but are not limited to HIV, hepatitis B and C, and others. Properly dispose of sharps. (See Tip #4.)
Tip #4 – Properly dispose of sharps
A “sharp” can be anything that has an edge that can slash, poke, pierce, cut, or otherwise injure the skin. Sharps include not only needles, but broken glass, suture needles, broken or empty ampoules, trocars, butterflies, or culture slides or dishes, among others.
OSHA standards require that sharps containers must be closable, puncture resistant, and leak-proof on the sides and bottom. Maintain them in an upright position and do not overfill. The containers must be labeled and or color-coded according to 29 CFR 1910.1030(g)(1)(i), which states they should be red and clearly marked with the biohazard symbol. Learn more about safe disposal of sharps here .
Tip #5 – Properly package and label waste streams
In addition to federal guidelines on packing and labeling different types of healthcare waste, every state also has its own regulations regarding this topic. As such, every waste stream comes with its own rules for packaging and labeling for transportation. Shipping papers are required when medical waste is transported off-site for disposal or destruction. Such guidelines can be found in a state’s Administrative Codes or state-EPA rules for solid and hazardous waste.
Numerous agencies provide guidance for packaging and storage recommendations such as the EPA, OSHA, the Department of Transportation (DOT) and the Drug Enforcement Agency (DEA). For example, you can find federal guidelines for regulated medical waste in 49 CFR §173.197 – Regulated medical waste .
Check out our guide to proper labelling and color coding of various waste streams.
Tip #6 – Follow storage limitations and guidelines for medical waste
Storage time limitations depend on the type of waste, its volume, and temperature at which it’s stored. For example, in Arizona , biohazard medical waste cannot be stored longer than 90 days unless the waste generator receives approval with state agencies. In other cases, an infectious waste can be stored under refrigeration conditions for up to 30 days. Always check!
Tip #7 – Know your hazardous waste generator status
Do you know if your facility a large quantity generator or a small quantity generator of hazardous waste ? The EPA defines a waste generator status for any facility that produces hazardous waste based on the volume of such waste accumulated per month. Refer to Title 40 CFR Part 262 for additional details, but in a nutshell, generators can be defined as one of three categories:
- Very small quality generator (VSQG) – less than 220 pounds per month
- Small quantity generator (SQG) – more than 220 pounds per month but less than 2,200 pounds per month
- Large quantity generator (LQG) – more than 2,200 pounds per month
Be aware that states may have their own volume or weight recommendations.
Tip #8 – Know the difference between bulk and trace chemotherapy waste
Chemotherapy waste is typically defined as either trace chemotherapy waste or bulk chemotherapy waste. Chemotherapy wastes that are generally deemed trace often include IV tubing, IV bags, and vials, and are known as “ RCRA empty .” This type of listed waste is defined as a trace waste that can be managed as regulated medical waste but must also be properly contained and labeled. Trace chemotherapy waste containers should be yellow.
Bulk chemotherapy waste includes any type of container or bag that has held a chemotherapy agent and does not qualify under the RCRA empty rules. Bulk chemotherapy waste also includes sponges or other materials that might be used to clean up a spill or visibly contaminated personal protective equipment (PPE). Other types of bulk chemotherapy waste include full bottles, bags, or vials of U-listed chemotherapy drugs under RCRA hazardous waste regulations. Bulk chemo containers are often black.
Tip #9 – Know your state’s approved disposal methods
State and federal guidelines must be followed in order to remain compliant with your state’s medical waste disposal processes. In many cases, state guidelines are more detailed in context than federal regulations. Healthcare providers should be familiar with (read and review) guidelines provided by the Environmental Protection Agency (EPA) and the Resource Conservation and Recovery Act (RCRA) as well.
Tip #10 – Know where to find the rules for your state
In addition to federal guidelines, every state also has rules and regulations for healthcare waste management. Good places to start include the state government’s website. State Departments of Environmental Quality are also excellent sources for information, as are a state’s administrative codes or regulations. State Departments of Transportation are also good resources, as are a state’s Bureau of Waste Management.
Stay compliant.
Daniels Health is dedicated to the protection of healthcare providers through proper and compliant medical waste management and disposal practices. Such practices also protect state resources and environments. Turn to Daniels for resources, compliant products, and experienced services when it comes to your healthcare facility needs. Call a representative today to learn how you can ensure safe, compliant, cost-effective, and sustainable medical waste management processes.
Request a Consultation

Clinical Waste Educator
With 26 years experience working in healthcare, Amy has implemented sustainability initiatives for over 100 hospitals across the United States and brings unique practice and compliance expertise to healthcare waste management.
Let's Talk!
Your time is valuable, and we don't want to play hard to get. You can either phone us directly on the details listed on our contact page, or feel free to fill out this short form and one of our team members will get back to you as quickly as possible.
Request a quote
We would love to wow you with our service excellence. Fill in the form below to get in touch with one of our clinical superstars!
Search form
Environmental Impact of Medical Wastes Analytical Essay
Introduction.
Several incidents concerning medical waste being spotted on public and private beaches have drawn a lot of public attention on the issue of management of medical waste. One such incident happened back in June 1987, when in Indiana polis, twelve children were found playing with blood vials that they had picked from a bin placed outside an HMO medical office.
Two of these vials were infected with the AIDS virus (10). These issues and others raise concerns on how medical waste is handled, treated and disposed.
Medical waste can be defined as all the waste that is generated by health facilities and other sources such as funeral homes, research laboratories, doctor’s clinic funeral homes, nursing homes and veterinary facilities.
These wastes consists the hazardous (radioactive materials), infectious also referred to as red bag waste and any other waste generated within the facility (4). Medical waste although not voluminous, is infectious and toxic and leads to serious environmental pollution (1).
Background Information
According to Environmental protection Agency (EPA), hospitals generate around 3.2 million tons of medical wastes per annum. (10). 10 to 15 0percent of this medical waste generated is infectious. In most hospitals, the non infectious waste is land filled while the infectious one is incinerated.
Medical waste requires proper handling, disposal and treatment to minimize the environmental and health risks associated with it. Illegal or careless disposal of medical waste not only creates an aesthetic and health problem, but also increases public apprehension on the existing medical waste management methods.
Due to the liabilities and the safety related concerns, some municipals refuse or ban any medical waste from their incinerators and landfills. Various states have prohibited all un-sterilized infectious waste from the municipal landfills.
The states have also banned construction of commercial incinerators handling medical waste. These afro mentioned bans, have made it increasingly difficult for medical facilities and hospitals in the country to properly manage medical waste (3).
This situation is further complicated by the lack of clear and concise regulatory climate. These inconsistencies are present in the Federal guidelines laid down by the States with regards to the definition of medical waste and the management options available for handling, transporting, treating and disposing medical waste (5).
The current situation can only change if the Congress adopts bills relating to medical waste management. In the meantime, most states have been mandated to devise their own plans and programs of managing the medical waste generated. This means that there are a lot of variations between different states and local requirements.
This paper aims at looking at the disposal problems posed by medical waste for both the local government and hospitals, the methods used in disposing medical waste, the long term implications medical waste has on the environment and the conclusions drawn from the discussion (2).
Classification of Medical Wastes
Medical waste is heterogeneous in nature as it comprises a variety of materials ranging from general waste such as food, office waste and non-infectious waste from patients. It also includes infectious waste e.g. contaminated sharps and blood products, hazardous waste generated from pharmaceuticals, cytotoxic chemicals from chemotherapy, mercury as well as radioactive wastes.
Classifying infectious waste has proved difficult due to the variations resulting from different State regulations (10). These different classifications lead to inconsistency in storage, disposal and treatment practices across different states. The variations also influence the preferred treatment methods, cost of management and eventually, the possible environment and health hazards created by these wastes.
Around 10 to 15 percent of all medical waste is infectious but this percentage can differ from 3 to 90 percent, depending on the definition and procedure adopted (10). The state entities, EPA and Centers for Disease Control (CDC) have all tried to find the proper definition of infectious waste based on the characteristics of the waste.
According to EPA, infectious waste is any waste with the possibility of causing an infectious disease. EPA has broadened its category of infectious waste compared to CDC. This has led to the adoption of EPA instead of CDC guidelines, in hospitals and other areas that generate medical waste, helping in minimizing potential environmental and health risks (4).
Another concern is whether to classify infectious waste as hazardous which will increase the cost of managing it due the construction of special facilities. Such a move would improve the management of medical waste, but lead strict regulations and prosecution of illegal dumpers.
Some of the wastes recommended to be included in the infectious category are waste from dialysis, stocks and cultures with infectious agents, blood products and human blood, contaminated sharps, soiled dressings, surgical gloves sponges and other surgical waste (6).
Varied definition of infectious and hazardous medical waste has led to the public being exposed to this hazardous waste that poses a health risk. For example, the public was barred from accessing beaches in the East coast after bloody bandages, sutures and needles were found in the shores.
Infectious waste is sent to the incinerators, thus if the category was broadened as discussed above, such waste would not have ended up in the beaches (10).
Handling of Medical Waste
There are various occupational hazards associated with handling medical waste. Waste handlers and health workers are primarily exposed to this type of risk as they more than often handle this waste. Handling hospital waste include packing, storing and transporting it properly to avoid any contamination and littering as discussed below;
- Packaging- before packaging any medical waste, it must be sorted into different categories and packed accordingly. This is a time consuming activity and quite risky to the handler. Bulk waste is put in polythene bags and colors used in differentiating different categories of wastes. Infectious waste is placed in red bags and all the waste is securely closed in readiness for storage or transportation. Sharps are put in puncture proof containers due to their infectious capability and also due to their prick injuries (7).
- Storage- hospitals must designate special areas for storing the waste before it is transported or disposed. The area must be regularly disinfected and kept at the right temperature. According to EPA, storage areas must have the bio-hazard symbol and sufficient packaging to prevent vermin’s and rodents from accessing the area. The waste must also be stored for the shortest period possible, although EPA does not give the stipulated period, leading to a State disparity in specified temperatures and times. Lack of uniformity in regulating storage temperature and time can sometimes lead to increased rates of putrefaction and microbial growth (8).
- Transportation- EPA guidelines address the movement of infectious of waste on-site briefly, and provide limited information on how to move this waste off-site. Such recommendations involve using leak proof and rigid containers to move the waste and not using mechanical loading devices that can rapture packed waste. There are no guidelines on how to handle and transfer medical waste off-site. Although EPA, recommends that hazard labels be put on all medical waste in accordance to Federal, State and municipal regulations, the energy and transport department limit the use of this label, confusing commercial waste handlers (10).
Varied definition of infectious waste across different states complicates the matters and increases the likelihood of improper disposal and potential exposure to the public.
For example, if a state does not classify bloodied sutures and bandages as infectious waste, it can dispose this waste from another state in the municipal landfill. However, such waste can be washed by storm water to the beaches and pose a health risk (9).
Methods Used In Disposing Medical Waste
Incineration.
As hospitals generate a lot of waste, both non-infectious and infectious wastes are incinerated together. There is no data on the exact waste incinerated in hospitals or information on the number of current medical incinerators available.
Municipal incinerators burn a large volume of waste compared to hospital ones. However, hospital incinerators are situated in highly populated regions, leading to a greater probability of public exposure to toxic fumes and air pollutants.
These small incinerators emit higher levels of pollutants, although few risk assessments are carried out, making it impossible to evaluate the risks emanating from these incinerators in comparison to other sources e.g. the municipal incinerators (10).
Moreover, the short stacks in hospital incinerators might permit emissions from the incinerators to go into the hospitals via windows and air-conditioning ducts. Hospitals in US use three types of incinerators namely: rotary kiln models, multiple chamber air and controlled air.
Most medical waste incinerators are closed air, since they are associated with lower costs and lesser pollution. The advantage associated incinerators is that they can reduce large volumes of waste, sterilize it, and make it possible for it to be disposed traditionally through landfills. Secondly, modern incinerators harness the heat created during the process and use it to power generators within the facility (8).
Autoclaving uses steam sterilization in treating wastes before they are sent off to the landfills. Autoclaving is done in closed compartments, where pressure and heat are applied generating steam, within a given length of time so as to sterilize medical apparatus.
All microorganisms found in the medical waste are destroyed by the steam generated and then disposed off disposed in landfills. After autoclaving medical waste, it undergoes compaction through shredding so that it is not used for any other purposes and then later on disposed in the landfills.
However, autoclaving is not recommended for pathological waste due to the presence of low levels of radiation. The advantage of this method is that it can be used in processing 90 percent of medical waste and compaction reduces the volume of waste after (7).
Long term Environmental Implications of Medical Waste
Improper disposal of medical waste have far reaching environment impacts. Disposal of medical waste in oceans or other water bodies can lead to contamination of water by the pathogens found in this waste. Medical wastes such as soiled bandages or plastic gloves destroy the aesthetic appearance of the environment when they litter the beach or other places.
On the other hand, the disposal methods used in getting rid of the medical waste causes serious air pollution. According to a JAMA study carried out in 2009, the health sector accounts for 8 percent carbon emission (8). Most of the medical waste is plastic that produces furans and dioxins during combustion.
Most old medical incinerators have no equipment for controlling pollution. The incinerator ash generated from combusting contaminated waste may contain potentially toxic chemicals that will end up in the landfill and cause environmental pollution.
When autoclaving is used in disposal, the waste might not completely sterilized since the density and volume of material being sterilized determine the effectiveness of the process (7). There is a possibility of incomplete sterilization if the autoclave is overloaded and these pathogens will end up in the landfill, polluting the environment and posing a health risk to the public.
From the discussion above, it is clear that poor regulatory framework has hindered proper management of medical waste disposal. Medical waste is disposed through incineration and autoclaving, but both methods cause environmental pollution and pose a risk to the public health.
Incineration releases toxic gases, while in autoclaving there is the risk of incomplete sterilization, transferring pathogens to the landfills. It is important for medical facilities to adopt new technology in waste disposal to reduce the environmental pollution.
Landrum, VJ. Medical waste management and disposal. California:William Andrew; 1991.
NBCE. Medical, municipal and plastic waste management handbook. New Delhi: National Institute of Industrial Re; 2007.
Office of technology Assessment. Finding the Rx for managing medical wastes. Washington DC: Diane Publishing; 1990.
Friedman, M M and Rhinehart, E. Infection Control in Home Care. Sudbury: Jones & Bartlett Learning; 1999.
Hunt, DL and Fleming, D. Biological safety : principles and practices. Washington DC: ASM Press; 2000.
Bassey, BE, Benka-Coker, MO and Aluyi, HAS. Characterization and management of solid medical wastes in the Federal Capital Territory, Abuja Nigeria. Afri Health Sci. 2006 March; 6(1): 58–63.
Uzych, L. Medical waste management: regulatory issues and current legal requirements. J Environmental Health, 1990 May, 52 (3): 30-35.
Pyrek, KM. Infection control today. Phoenix Virgo publishing; 2010. Web.
Hossetti, BB. Prospects and Perspective of Solid Waste Management. Seborga: New Age International; 2006.
Federation of American scientists . Washington DC: The Association; c1988-2002. Group and Physicians Workshop: [about 3 screens]. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2019, April 1). Environmental Impact of Medical Wastes. https://ivypanda.com/essays/environmental-impact-of-medical-wastes/
"Environmental Impact of Medical Wastes." IvyPanda , 1 Apr. 2019, ivypanda.com/essays/environmental-impact-of-medical-wastes/.
IvyPanda . (2019) 'Environmental Impact of Medical Wastes'. 1 April.
IvyPanda . 2019. "Environmental Impact of Medical Wastes." April 1, 2019. https://ivypanda.com/essays/environmental-impact-of-medical-wastes/.
1. IvyPanda . "Environmental Impact of Medical Wastes." April 1, 2019. https://ivypanda.com/essays/environmental-impact-of-medical-wastes/.
Bibliography
IvyPanda . "Environmental Impact of Medical Wastes." April 1, 2019. https://ivypanda.com/essays/environmental-impact-of-medical-wastes/.
- Household Hazardous Waste Disposal Strategies
- Household Hazardous Waste in Different Countries
- Finance and Budgeting for EPA: Business and Economics
- Environmental Impacts and Solutions: Solid Waste
- Environmental Protection and Waste Management
- Managing Your School's Electronic Waste
- Sustainability and Waste Management in the Australian Construction Industry
- Waste Management Strategies in Australia

ESSAY SAUCE
FOR STUDENTS : ALL THE INGREDIENTS OF A GOOD ESSAY
Essay: Medical Waste Management
Essay details and download:.
- Subject area(s): Medicine essays
- Reading time: 21 minutes
- Price: Free download
- Published: 24 July 2019*
- File format: Text
- Words: 6,064 (approx)
- Number of pages: 25 (approx)
Text preview of this essay:
This page of the essay has 6,064 words. Download the full version above.
CHAPTER II REVIEW OF RELATED LITERATURE The value of medical waste management in the protection of public health and the environment cannot be denied (Thakur and Ramesh, 2015). One concern in the society nowadays is the inadequate treatment and improper disposal of medical wastes in various medical facilities due to the harmful effects of such wastes and its potential to transmit contagious diseases, which may harm humans and the environment. Medical care is vital for one’s wellness, being, and most importantly, to one’s life but, the wastes extracted from various medical services and activities pose potential risks to patients, doctors, people around the hospitals, and sanitation workers who administer in medial waste treatment and disposal (Sutha, 2018). As stated by Longe (2006), proper segregation, treatment, and disposal of medical waste, especially those that pose harm and infectious waste types is a key to achieving a safe and sound medical waste management therefore, a right step to health risk reduction. The ability of medical facilities to assess wastes based on their composition, type, and components can be of help in achieving a more sustainable way of medical waste management in the society. Furthermore, with the joint efforts of various medical staff and workers to administer in medical waste treatment, a greater possibility of decreased health hazards will come out as a result. MEDICAL WASTE IN GENERAL The World Health Organization (2007) states that, the waste produced by various health care activities includes a broad range of materials, such as used needles and syringes to soiled dressings, body parts, diagnostic samples, blood, chemicals, pharmaceuticals, medical devices and radioactive materials. Poor management of these medical wastes may potentially harm the health care workers, waste handlers, patients and the community to infection and other risk. It is also stated that it is important that all medical waste materials must be segregated, appropriately treated and disposed safely. In a study, the WHO also estimates the infection caused by injections using contaminated syringes and they found out that there were 21 million cases of hepatitis B virus by the year 2002, two million hepatitis C virus cases, and 260,000 HIV cases. According to United States Environmental Protection Agency (2017), medical waste or health care waste is defined as the subset of wastes that may be contaminated by blood, body fluids and other potential infectious materials. These potentially infectious materials are often called as regulated medical waste that can be found at any health care facilities including hospitals, medical research facilities and laboratories, blood banks and clinics. In addition, The Medical Waste Tracking Act of 1988 defines medical waste as “any solid waste that is generated in the diagnosis, treatment, or immunization of human beings or animals, in research pertaining there to, or in the production or testing of biologicals.” Another definition of medical waste given by Medical Waste Service (2018), medical waste is anything that is infectious or may cause infection. These wastes may contain body fluids and other contaminants. Sharps including needles, medical equipment and other broken glasses are also considered as medical waste. The waste may be produce during diagnosis, treatment, medical research and immunization. The World Health Organization (2017) categorized medical waste into eight distinct types. First are the infectious waste, these are waste hat may be infectious or that may cause infection. This may include excreta, swabs, equipment, tissues and lab cultures. Next are the sharps. This includes needles, broken glass, razors, and other medical equipment that may puncture the skin. The third category are compose of human tissue, body fluids, blood and other animal carcasses these are called Pathological waste. Fourth are the radioactive wastes. These waste are made up of unused radiotherapy liquid, and other supplies and equipment that may be contaminated with lab research liquid or radiotherapy liquid. Next are the pharmaceuticals these may include any expired, unused and contaminated drugs and vaccines, antibiotics and pills. Chemicals belongs to the sixth category in which it is composed of solvents, disinfectants, batteries and any heavy metals that are found in medical equipment. Mercury from thermometers may also be included in this category. Next are the genotoxic waste these waste are considered as the most hazardous and is mutagenic, carcinogenic or teratogenic. Cytotoxic drugs that are used in cancer treatment also fall into this category. The last are the general non-regulated medical waste or the non-hazardous waste. These are the harmless waste that contains no blood or bodily fluid, including papers, kitchen waste and other miscellaneous trash. According to Environmental Protection Agency (2017), medical waste can be identified into four categories the infectious, hazardous, radioactive, and general waste. First are the infectious wastes. These are waste that may cause harm to human being. This waste is associated or has something to do with medical equipment that is not properly disposed. In line with this category are the pathological wastes that contain pathogens and require methods to be treated. Next are the Hazardous waste that includes sharps or objects that may puncture the skin such as syringes, surgical equipment and glassware. Chemicals are also considered as hazardous waste and some infectious waste depending on how it is used. Old medicines and other chemotherapy agents are also sometimes considered as hazardous. Third are the radioactive wastes, these are waste that came from cancer therapies, nuclear medicine treatments and medical equipment that uses radioactive isotopes. Contaminated pathological waste also belongs to radioactive rather than infectious. The last category is general waste, which makes up at least 85% of medical waste. These are waste that is not different from household waste. EFFECTS OF MEDICAL WASTES According to Dr. Jeorge Emmanuel (2018), the burning of medical waste will result to a release of an unexpected high amount of extremely baleful pollutants such as Dioxins, a highly toxic compound for the environment. It is also known that these Dioxins will not only stay during our time but also to the lifespan of the future. If it were release due to incineration of medical wastes, the effects of dioxins include cancer, changes in the reproductive system of male and female and it affects the child development. Thus, Zafar S. (2016) added that medical waste like gloves, bandages and gauze that are used can affect the environment. Body fluids like blood can also be the cause to the contamination of habitat. These medical wastes, if not properly disposed, can pollute the air in which contaminated gases go airborne; water in which bodily fluids such as contaminated urines and blood contributes to the spread of diverse diseases; and even the soil wherein medical waste such as gloves and syringes that are thrown on the ground will not be decomposed when it goes underground, thus making the soil contaminated. Which then, affects all forms of life. Because of this, it can contribute to the growth of microorganisms such as bacteria and insects that carries different diseases that can lead to the transmission of diverse diseases. Akter N., Hussainz., Trankier J., and Parkpian P. (2002) proclaimed that not only the people of the outside of the hospital can be affected but also the people who work inside the facilities due to unethical practice. When hospital staffs were interviewed, they are suffering from different types of diseases due to the improper segregation and handling of medical wastes such as skin diseases or allergy, hepatitis and diarrhea. Moreover, Mastorakis N., Bulacia C., Oprea T., and Philippe D. (2010) summarized that diseases, which can be spread through contaminated syringes and medical wastes are skin infections such as rashes, a red spot on the skin that reacts to unpleasant happenings; ring worm, a disease that appears to be a ring-shaped mark on the skin; lastly, scabies wherein it is a disease that caused by small insects that may lead to itching and red spot on the skin. These infections are caused by bacteria and parasites, which can be found through unsanitary medical components and through doorknobs of hospital restrooms. Another disease caused by these equipment is viral hepatitis A and B. Hepatitis A is a viral liver disease that causes apical illness of the subject. On the other hand, viral hepatitis B Is an infection that affects the liver that causes chronic diseases which spread through blood and bodily fluids. Moreover, diarrhea, another disease that is caused by unsanitary components, is an illness when the body secretes liquid feces instead of the solid form. Cholera, on the other hand, is a serious disease that makes a person vomit and often leads to death. Lastly, typhoid, a communicable disease from contaminated food and water. According to Shikoska B., Shumanov G., Dimova C., and Vankovski V. (2016), medical wastes contain different types of disease or disease causing organisms that are completely transferable through the environment and the people in it. These type of wastes can be found usually in the hospital, private or public, clinics such as dental clinics and ENT clinics, nursing and residential care facilities and other medical equipment. It also covers the bodily fluids such as semen, blood, urine, mucus, and saliva. Nevertheless, Mathur P., Sangeeta P., and Shobhawat A. (2012), said that this will cause a huge increase at the amounts of rodents, insects and even worms. This will lead to the spread of different diseases such as typhoid, cholera, hepatitis, and aids. Furthermore, these wastes disposed around the hospitals may attract insects and even stray animals, which in the future will spread communicable diseases to the community. HOSPITAL SANITATION WORKERS AND ADMINISTRATION Sanitation workers play a vital role in a hospital. They are ensuring the safety and clean environment we rely on in hospitals. In addition, they are held liable for the proper conduct of all legal sanitation codes, which is highly expected, to local hospitals. Further, people who are suited for the job needs to be prepared for all circumstances as the duty relies on cleaning and maintaining the health facility that provides satisfaction to all their patients. Moreover, sanitation workers or personnel can be trained to sterilize medical equipment needed and disposal of used needles and those of which may impose a threat to all those near and even in the hospital itself. As Sanitation Worker, the responsibility of creating a healthy environment, keeping away potential harm to health such as medical wastes is a must. The level of responsibility in assuring the safety in terms of health around and in the hospital through the sanitation workers is at high (Murnaghan, 2018). In addition, Azam, et. al. (2008) have stated medical waste comprises of materials that involve threat to human health. Further, potential environmental hazard segregation also may impose a threat as recent studies have found out that it has been mixed with municipal solid wastes. In addition, the understanding of the medical waste composition can provide background and knowledge to facilities and patients which can step them out of ignorance that can help minimize or reduce its threat to humanity. But in the study conducted by Altrabshehb, et. al. (2006) in northern part of Jordan, the practice of medical waste management have less appropriate practice of disposal and handling of medical wastes. Also, guidelines or rules were not definite causing the personnel involved not to follow a systematic process in handling of such wastes. Thus, Abdulla et. al. (2007) that the need for training for personnel involved in medical waste management disposal in Jordan is a must for the study revealed that the threat to patients and other persons in the hospital is high for various medical waste types’ segregation is not properly conducted. Moreover, countries around the world have different medical waste management that needs to be discovered and needs to have solution. One of the example include the country of Brazil, in the study conducted by Da Silva, et. al. (2004), they have interviewed 91 health care facilities that may provide information about the segregation and disposal of medical wastes, ethical considerations were observed as the researchers did not disclose information about a certain health care facilities that which, the result implied that health care facilities do not comply with the Brazilian Legislation when it comes to proper waste management disposal. An average rate generation of 3.245 and 0.570 kg/bed-day were recorded when it comes to the total of infectious-biological wastes. In addition, the proper segregation of medical waste is a must factor in terms of choosing hospital have been thought of patients. In a study of medical waste management in Nanjing, China, about 77% of those being interviewed perceived proper waste segregation as a need when going to a certain hospital. A total of 15 hospitals, 200 patients and 3 disposal companies were involved in the study which then implies that there is insufficiency of public understanding of medical waste management as there are still remaining 20% unqualified staff in waste management of the hospitals. There are still a few percentage of which may impose a threat to the hospitals. Recommendations were suggested to those hospitals as their current situation can impose a hazard or risks and of that medical wastes can be properly disposed and threat to humanity may be minimized (Daweia, et. al., 2008). Askarian, et. al (2003) explains that hospital wastes impose hazard and can be considered as dangerous as it may contain pathogenic agents and which can cause effects and can threat the human health and the environment itself. Further, the inadequacy of rules to be followed as like in the country of Iran further provides more threat and harms everyone. In addition, the survey have resulted that the training for proper waste management was considered as ineffective and cannot aid to the need of the country. Also, the enabling the law to act upon the certain issue can be of help to aid to the need of the entire society of Fars Province, Iran. Moreover, sanitation personnel plays a vital role in maintaining the cleanliness of the hospital that of which implies that the formation and organization of sanitation team in hospitals provide an avenue to solve different problems with the regards to medical wastes. Furthermore, the inadequacy of employees training should as well be addressed which include on-the job trainings that can further enhance their skills which can improve the state of a certain medical facility or institution (Jiang, et. al., 2009). In addition, operational machines needs to aid as well with the need of treatment of medical waste. Qualified staff should be fully aware of the conditions prevalent in the hospital so that they can cope with the underlying needs of the hospital. Moreover, the knowledge, attitudes and practices of the personnel, which are in the field of medical waste greatly affect the proper treatment and disposal of medical wastes. Thus, hospitals should give adequate training and motivation, which should suffice the need to set up, standardized rules of medical wastes segregation with that of the hospitals (Chauhan and Sharma, 2007). Moreover, in the recent study conducted by Madhukumar and Ramesh (2012), it implies that the awareness of medical practitioners such as doctors and nurses regarding the medical wastes should be better and thus, they should be the key promoter of proper handling of as such. In addition, nurses and laboratory staff have found to have better ways of segregating and disposing off of medical wastes of the hospital in Bangalore. Lastly, the research have pointed out the massive need for training, as the study have found out that the lack of knowledge in terms of medical waste is highly observable for hospitals. Also, the focus on health care should not as well be neglected as which in connection to the study being presented by Barach, et. al. (2015) that accreditation of a certain hospital still relies on the safety measures and procurement of those practitioners who establish safety and reliability in a management of medical wastes. Moreover, the adoption of such a certain guidelines helps increase the way in which medical staff can evaluate accreditation of certain hospitals. In addition, accreditation of as certain hospital is still implemented for medical practitioners and sanitation workers still do their job of maintaining the cleanliness and sanitation of hospitals. Lastly, attitude as well can add up to the measures being determined. In a study being researched in Iran, it shows that the attitude of the personnel working can be associated with the way they work. Moreover, a dire need of education and increased awareness is suggested for it can still address and solve the issue of proper handling of services being rendered in a particular field like for example in is hospitals (Aminbaig, et. al., 2015). STRATEGIES IN DISPOSING MEDICAL WASTES Properly disposing medical wastes is important when it comes to sanitation procedures. If these wastes are not managed, it may cause various diseases to the living organisms. Many sanitation procedures have been implemented in different hospitals but their healthcare workers are not trained well. As a result, according to National Academy of Sciences (1989), before they hire healthcare workers, they make sure that they have the knowledge and they know the correct way on what are the sustainable ways on how those medical wastes can be managed. Disposing of medical waste materials especially the solid wastes should be put in sanitary landfills to secure the safety of people and the environment in terms of healthcare facilities. Another way of properly disposing medical waste is by means of incineration to lessen the amount of medical wastes of hospitals to prevent infections and contamination because many wastes especially those wastes coming from hospitals contains pathogens that can harm any people. Constructing ventilation exhausts is an effective way on how to protect microbiology laboratories from contracting with other bacteria. Contaminated wastes should be separated from non-contaminated one. Different working areas like rooms, laboratories and refrigerators should only be managed by the workers who have the knowledge on how these areas and equipment should be cleaned. According to Obid (2006), disposing medical wastes is still a major problem in most 0f the countries. Even though there are technologies used for disposing wastes, facilities should first have the knowledge on how to manipulate those kinds of technologies and machines. The sources of medical wastes include hospitals, healthcare centers, laboratories and clinics. The reasons why many of the healthcare facilities are not managing their medical wastes is because of the lack of sufficient funding. One of the ways on how should medical wastes can be managed is creating a specified landfill cell for the hazardous wastes. In some countries like Europe and United States of America, they constructed their own incinerators for preventing and to lessen the amount of wastes, but there is also a side effect to its people because of the gas emissions coming from the syringes, thermometers and amalgam that are rejected as medical wastes. There are also mercury and dioxin emissions. These treatments can be a solution in disposing hazardous medical wastes properly. To sum up, the different treatments on how wastes are being managed are by means of incineration, thermal treatment and disinfection, disinfecting materials through the use of microwaves and more. According to Mina (2012) in his book entitled, “Case Studies on Health Care Waste Management Practices of Selected Public and Private Hospitals in Metro Manila,” in order to minimize risks, hospital workers should segregate their wastes according to their types. Black container should only contain the non- infectious dry wastes, green is for non- infectious wets wastes, yellow is for the infectious and pathological wastes, yellow with black band is for the chemical wastes including the heavy metals, orange container is for the radioactive wastes and red container is for the sharp and pressurized containers. The way of disposing medical wastes are varied based from their types. For example, cytotoxic wastes must be collected in a leak- proof container, chemical wastes should be put in chemical- resistant containers and delivered to treatment facilities. Sharp equipment and wastes must be compiled together and the container must be puncture- proof and it is covered. Wastes that have heavy metals like mercury must be separated from other medical wastes. The aerosol containers should be collected together and should not be burnt or put into incinerators. Gases can be disposed through the use of vacuum lines direct outside the hospital. According to Revised Health Care Waste Management Manual in the year of 2005, storage areas should not be situated from food stores to prevent infections and the spreading of diseases. There should be water supply and drainage for wastes to prevent disinfection. Moreover, storage facilities should be restricted and has locks to prevent access by unauthorized people. If these things are being implemented in the hospitals, we can lessen the uncertainties that we might inherit. Medical wastes should be disposed, separated, sterilized and identified accordingly depending on their types. They are being disposed according to how they are being used. Just like the wastes that are hazardous, they should be put on safer places. In segregating medical wastes, hazardous ones should be put in red bags and those wastes having contact with blood should be the first one to dispose (medprodisposal.com, 2016) According to Curtis (1991), in his study entitled, “A Medical Waste Management Strategy,” it is essential to manage medical wastes properly because it may cause harm to the employees and to other people who are concerned with these kinds of wastes. Employees should be the one who will dispose medical wastes in a proper way. These medical wastes strategies are segregation, packing, in- house transport and storage of medical wastes to prevent infections and uncertainties. “Failure to effectively manage medical wastes puts patients, healthcare and sanitation workers at risk in having various diseases” (Floridahealth.gov,n.d., 2017). When an infection happened on a certain hospital, it means that there is a problem in their sanitation procedures. Some of its reasons is the lack of preparedness or they are unaware on the effect of not disposing medical wastes properly. Occupational Safety and Health Administration (OSHA) constructs rules to be followed to make sure that the safety of the healthcare workers is being prioritized while they are working. (Saber, 2017) Disposing medical wastes properly is the most essential thing that a hospital should do. If these wastes are not disposed properly, it will cause harm to their patients especially to the people around the vicinity of their hospitals. According to the United States Environmental Protection Agency (1988), there are three plans that should be implemented in all hospitals. First is to appraise information on the medical waste management, if they are implementing medical waste disposal practices. Secondly, is to determine the regulations that are connected in medical waste disposal and lastly is to stipulate applicable guidance, practices and education materials so that the facilities of the different hospitals will know the correct way in managing their medical wastes. MEDICAL WASTE MANAGEMENT IN A LEGAL PERSPECTIVE Medical Waste Management needs to be accompanied by laws and federal guidelines to be implemented properly. Medical facilities, hospitals, laboratories, clinics, and research centers are the leading producers of medical wastes and so; the stated establishments must abide the laws regarding the proper medical waste disposal to render quality services to the patients and ensure the safety of medical practitioners, the patients, and the people surrounding the vicinity of a particular medical facility. Currently, there are laws that strongly support the implementation of the proper medical waste disposal around the world. According to the published research of Aquino, A., Deriquito, J., and Festejo, M. (2013), the mismanagement of waste in general poses risks and potential hazards to the community and to the environment. Mismanagement of waste paved way for Republic Act (RA) 9003 or the Ecological Solid Waste Management of 2000 to be crafted and serve as a milestone for environmental legislation in the Philippines. The law was implemented to regulate the production of garbage around the country and to mitigate its effects to the environment. RA 9003 states the policy of the state in adopting a systematized, comprehensive and ecological solid waste management program that highly regards the public health’s protection and the environment. Thus, it also declares the proper segregation, collection, transport, storage, treatment and the disposal of any solid waste by the adoption and formulation of best environmental waste management practices. RA 9003 supports the recycling of solid wastes to mitigate the effects of poverty in the society. The Philippine Congress passed ecological Solid Waste Management on the 20th of December 2000 and was subsequently validated by the Office of the President on the 26th day of January 2001. The law comprises of seven chapters and sub-divided into 66 sections for an effective solid waste disposal in the Philippines. Along the same vein, there are also laws that truly support the correct practices on medical waste management besides RA 9003 or the so-called Ecological Solid Waste Management of 2000. Based on the South African Medical Journal (2014), the Constitution of the Republic of South Africa declares that everyone has the right to an environment that does not pose any harm to one’s health and well being. The illicit practice of improper waste dumping especially those that are hazardous may bring potential danger to the environment when pollutants interact to water sources and hugely cause the proliferation of infection and toxics, jeopardizing the environment and human health. To give effect to the Constitution, the safe disposal of hazardous waste is governed by legislation in South Africa. Cases of the illegal disposal of waste displays lack of awareness and practice in regard to the safe dumping of medical waste. As per the Hazardous Substances Act, waste can be classified as general of hazardous waste based on the potential harm it may bring. General waste is characterized as waste, which does not give ant potential harm to public health and the environment. On the other hand, hazardous waste, however, may bring adverse effect, even in low concentrations to the community and the environment (South African Medical Journal 2014). Stein, A. (2016), states that through the understanding of federal, state, and local medical waste management laws and regulations is key in the operation of an excellent medical business or facility. There are three federal acts in the United States of America that set the stage for today’s medical waste laws; these are Pharmaceutical Resource Conservation and Recovery Act, the Solid Waste Disposal Act of 1965, and the Medical Waste Tracking Act of 1988. In addition, some state regulated laws to monitor the production and disposal of medical waste. Over thirty years ago the Pharmaceutical Resource Conservation and Recovery Act or the RCRA was authorized to shield human well being and the environment from conceivably perilous waste disposal strategies. The RCRA amended the Solid Waste Disposal Act of 1965 and set national objectives for lessening the fraction of waste created. Furthermore, Solid Waste Disposal Act of 1965; known as one of the primary government endeavors to enhance waste disposal strategies has been implemented, the Solid Waste Disposal Act was passed in 1965. Within this act, the Hazardous and Solid Waste Amendment passed in 1984, including more stringent laws hazardous waste management. In addition, the Medical Waste Tracking Act of 1988 is also present in the implemented regulations with regards to proper medical waste disposal. The Medical Waste Tracking Act of 1988 was basically devised to monitor and regulate the treatment of biomedical waste and sharps waste from their production, transportation, and final resort or disposal. This particular law prompted congress to approve the bill to amend the Solid Waste Disposal Act (Stein A. 2016). All in all, laws and regulations regarding proper medical waste management must be implemented towards the state to supervise and monitor the production, release, and disposal of medical wastes. Through the laws and regulations being reinforced by the government, medical facilities will be able to render their service in a non-harmful way since they are knowledgeable about the guidelines posed by the state. Abiding the laws authorized by the government in accordance to medical waste management will ensure that every patient will receive services that are safe and under the provisions of the law. PAST STUDIES AND RESEARCHES REGARDING MEDICAL WASTES In all over the world, the management of hazardous wastes have received many attention due to its toxicity and infectious nature. It can affects not only human but also to the living things around the area. Hospitals and other healthcare facilities are responsible for the delivering the health care services to the patient. In the process of curing the disease of patient, healthcare waste is also produced. These menacing situation captured the attention of many researchers to study the different hospital wastes management. Many hospitals or health care facilities have faced financial difficulties and thus they have attempted to find cost-effective treatment and disposal methods of their medical wastes. In the past researches, medical waste was often mixed with municipal solid waste and disposed of in residential waste landfills or improper treatment facilities. In recent years, many efforts have been made by environmental regulatory agencies and waste generators to better manage the waste from healthcare facilities. Due to these problem, many alternative solution have been made like waste minimization and recycling, control of toxic air emissions at medical waste incinerators, and alternative treatment methods to incineration but these are regarded to be the major challenges in the future. Longe and Williams (2006), based on a study and investigations, three out of the four hospitals gave high priority to the segregation of wastes from infectious and sharp wastes by the use of color coding system in their waste containers. Improper labeling and the multiple uses of black plastic bags for storing both infectious and regulated wastes are mostly the conspicuous problem. In some cases, where hospitals achieved the commendable level of segregation, medical wastes are incessantly mixed together by the garbage collectors during collection or at the dumpsites as revealed in some surveys and past studies. According to Jang et.al (2005), majority of the healthcare facilities in Korea practiced the segregation of medical waste done at the point of generation. Human and animal tissues are placed in a red container either plastic, paper board or metal container, while pathological waste and discarded sharps are placed in yellow container. Placentas are commonly separated in a red container and then used for raw materials in pharmaceutical products. Recycling of any segregated wastes other than placentas is not currently being practiced on-site. All other wastes are placed in an orange container before shipment. All containers displayed and have a universal biohazard sign that is commonly used in many countries. As stated by Soncuya et.al (1997), it shows that there are no safe way even in managing all the hazardous medical wastes that are currently produced in Metro Manila. 13 hospitals in MM were discovered to have incinerators, yet most of them were unrestrained and do not meet the Philippine and International standards for incineration of infectious waste and for safe managing methods. Lee et.al (2003), revealed that hazardous hospital wastes are sometimes mixed with general medical wastes in the same container (black plastic bags) which should only contain non-infectious solid wastes. Past and recent studies revealed that majority of the hospitals is not observing pre-treatment procedures for their infectious waste and not applying the color-coded system required by MMDA Ordinance No. 16. According to Health Care Global (2014), every hospital should have a specific location for a temporary waste storage. The plans and ideas in these parts (waste storage) are usually included in the design and construction of the hospital. The storage area must be completely locked and must be separated from the supply rooms and food preparation areas. Waste should always be monitored and must be removed in a timely manner even inside the storage. All waste containers should be clearly labeled and hazardous and non-hazardous wastes should never be mixed. As asserted by Crean (2004), antiseptic wastes are usually disposed with some waste in sanitary landfill, or in some cases it is settled in to the sewer system. Ultimately, the expenses and regulation of these facilities have provoked organizations to hire contractors to collect, treat, and dispose of medical waste, and the percentage of medical organizations that perform their own treatment and disposal are anticipated to decrease. SYNTHESIS Medical waste management is one of the most common problem being faced among hospitals. There are different classifications and definitions being connected to medical wastes. World Health Organization (2017) classified eight distinct types of medical wastes that may pose threat when not being disposed and segregated properly. In addition, the United States Environmental Protection Agency (2017) also gave four types of as such that will also give a negative impact to the entire humanity. Medical wastes cover a broad aspect in which is needed to be chunked into pieces to fully understand effect it displays to the environment, as well as the people. Further, improper medical wastes segregation imply lasting effect to different sectors in the world we step in. In fact, burning of as such will release toxic gases such as dioxins that will not only be visible in our time but also for the next years to come. Unethical practices might also lead to harmful diseases (Emmanuel, 2018). Also, Zafar (2016) pointed out the effects in the environment when the used medical gloves and the like will not be disposed in the way it should be. In addition, spread of contagious diseases might as well be observed as the chemical properties these wastes contain might be releases as improper practice had been followed. Moreover, people in and outside the hospital facilities are greatly affected to these unethical standards being implied (Akter N., et. al., 2002). Lastly, different diseases such as with regards to skin diseases, widespread of communicable diseases through carriers such as rodents, and diseases causing organisms will increase in number as the practice continues (Mathur, et. al., 2012). Thus, with the studies and past researches it is clearly identifiable that sanitation workers play an essential role with regards to hospital administration. Sanitation workers must know the concepts and the way how to properly segregate wastes in accordance to the lawsuits being implemented by a certain place or by the laws in the hospital itself (Murnaghan, 2018). But with the researches being conducted, a very few knowledge with regards to medical wastes are observed to the people itself. Further, proper segregation was not observed to most of the hospitals giving a direct conclusion that the sanitation workers do not have a wide understanding and public knowledge on how to handle it. At the end, Madhukumar and Ramesh (2012) implies that trainings and seminars must be given to the workers. Thus, it briefly shows how the inadequacy of knowledge may also lead to diseases that which may lead to uncontrolled and cannot be solved epidemics of disease. Various ways on how to clean such wastes are being explained. Thus, a common result have explained that most of the countries still cannot properly manage to handle as such wastes. Despite the fact that technologies are present as of the moment, it cannot assure and guarantee a complete and accurate process of disposing wastes properly (Obid, 2006). The value of properly handling of such wastes constitutes to health care protection among people. According to National Academy of Sciences (1989), hiring someone who is knowledgeable and capable enough of handling medical wastes must be the standard when it comes to choosing workers. Furthermore, understanding the techniques of handling wastes properly will lead to good facility working. Further, different lawsuits have been created to protect the health of everyone, such law created contain objectives of promoting awareness to such wastes. Moreover, the implementation of laws that lets people become knowledgeable of the risks benefited most of the people for it contributed to new array of learning to everyone. Laws such as Ecological Solid Waste Management Act of 2000 of the Philippines and Foreign laws like Pharmaceutical Resource Conservation and Recovery Act (RCRA), Solid Waste Disposal Act of 1965, Medical Waste Tracking Act of 1988 was made into action. Lastly, the regulations being implemented helped not just to promote awareness but also to help people attain security among humanity. All in all, medical waste play a huge impact on the society. In addition, the past studies suggests that training and seminars must work out among the sanitation workers. Thus, in addition, medical wastes must be properly segregated to attain healthy environment in and outside of the hospital. Hospitals provide health care protection, it is just ironic that hospitals might also give diseases as stated in the study, and so, public understanding, awareness and accurate measurements to address the issue must be stated and thus, will be of help for the next years to come and also to the future researchers that will have interest on the studies
...(download the rest of the essay above)
About this essay:
If you use part of this page in your own work, you need to provide a citation, as follows:
Essay Sauce, Medical Waste Management . Available from:<https://www.essaysauce.com/medicine-essays/medical-waste-management/> [Accessed 20-05-24].
These Medicine essays have been submitted to us by students in order to help you with your studies.
* This essay may have been previously published on Essay.uk.com at an earlier date.
Essay Categories:
- Accounting essays
- Architecture essays
- Business essays
- Computer science essays
- Criminology essays
- Economics essays
- Education essays
- Engineering essays
- English language essays
- Environmental studies essays
- Essay examples
- Finance essays
- Geography essays
- Health essays
- History essays
- Hospitality and tourism essays
- Human rights essays
- Information technology essays
- International relations
- Leadership essays
- Linguistics essays
- Literature essays
- Management essays
- Marketing essays
- Mathematics essays
- Media essays
- Medicine essays
- Military essays
- Miscellaneous essays
- Music Essays
- Nursing essays
- Philosophy essays
- Photography and arts essays
- Politics essays
- Project management essays
- Psychology essays
- Religious studies and theology essays
- Sample essays
- Science essays
- Social work essays
- Sociology essays
- Sports essays
- Types of essay
- Zoology essays
4 Consumer Concerns Regarding the Impact of Medical Waste Management
Waste can have various impacts on individuals and communities, which underscores the importance of its proper management, particularly when dealing with medical waste. Recent insights and statistics from Stericycle's 2023 Healthcare Workplace Safety Trend Report (HWSTR) emphasize the significance of effective medical waste management, many of which reveal the direct concerns of consumers.
Consumers surveyed in the HWSTR report recognize the importance of effective medical waste management strategies. In total, 98% say it is at least somewhat critical. Forty-six percent say it is ‘extremely critical,’ and 22% say it is ‘the most critical factor’. Compared to healthcare professionals (HCPs), consumers are even more concerned about the impacts and risks of ineffective medical waste management and disposal.
The HWSTR report delves into four potential impacts of ineffective waste management and disposal that are top concerns for consumers: environmental impact, patient health and safety, HCPs safety, and community impacts.
1. Impact on the Environment
One estimate indicates that the average hospital produces approximately 29 pounds of waste per bed per day . Improper disposal of this waste has the potential to spread diseases to humans and animals, as discarded needles outside of their appropriate containers pose a risk of infections. Healthcare professionals and consumers surveyed in the HWSTR indicate that they are concerned about the environmental impact of ineffective medical waste management.
Improper waste segregation can negatively affect sustainability efforts and increase costs. Effective measures for managing medical waste not only reduce environmental impact but can also help organizations achieve sustainability and climate goals. As an industry leader, Stericycle understands the importance of compliantly managing the collection, transportation, treatment, and disposal of various types of medical wastes. Some of the different medical waste types may include:
- Regulated Medical Waste (RMW): Includes items saturated with human blood or other potentially infectious materials (OPIM).
- Trace Chemotherapy Waste: Includes empty chemo drug vials, syringes and hypodermic needles, spill kits, IV tubing and bags, contaminated gloves and gowns, materials from spill cleanups, or bodily fluids/waste.
- Pathological Waste: Human or animal body parts (exceptions apply, check the waste acceptance policy for details, organs, tissues, and surgical specimens (decanted of formaldehyde, formalin, or other preservatives).
- Sharps Waste: Needles, scalpels, blades, and pipettes that have come in contact with blood, body fluids, or microorganisms should be disposed of in a designated disposable sharps container.
- Pharmaceutical Waste: Includes unused, unwanted, or expired medications or supplements.
2. Risk to Patient Health and Safety
Patient safety is a paramount concern for healthcare facilities and professionals. According to the 2023 HWSTR, 90% of consumers surveyed said they agree that medical waste management is important to delivering the best possible patient care. Eighty-two percent of consumers responded that they are concerned about the risks medical waste management poses to patient health and safety. To create healthier and safer care environments, innovative approaches are required. Continuous communication, education, teamwork, and strict adherence to policies are vital.
3. Risk to Healthcare Professionals Safety
Healthcare professionals can face risks related to improper medical waste management. For example, a used sharp (such as a needle or syringe) disposed of in a regular trash can could lead to a needlestick injury. The HWSTR found that 81% of consumers surveyed are concerned about the risks of improper medical waste management on the health and safety of HCPs. Safety in medical waste segregation and disposal is essential for front-line healthcare workers and proper waste segregation can significantly reduce the risk of injury or exposure. Utilizing a closable, puncture-resistant, and appropriately labeled sharps container to dispose of used needles helps mitigate that risk of exposure.
Healthcare organizations can help avoid endangering workers by maintaining a robust medical waste segregation program. Proper medical waste management can also benefit patients and non-provider employees (such as Environmental Services staff). Organizations should train employees on the Occupational Safety and Health Administration (OSHA) Bloodborne Pathogens Standard , including job-related risks and how to prevent workplace exposures. Stericycle offers valuable resources, including Steri-Safe ® OSHA Compliance, which comprises comprehensive online training and resources designed to help healthcare facilities maintain OSHA compliance and create a safer workplace. These resources also assist staff in understanding how proper training and resources can significantly reduce the risks associated with medical waste management for healthcare professionals.
4. Impact on the Community: Opioid Epidemic
Improper disposal of pharmaceutical waste poses a significant risk to communities, particularly in the face of the ongoing opioid epidemic. The HWSTR reveals that both consumers and healthcare workers recognize the risk of drug diversion to the community. Stericycle Safe Community Solutions are available to address this issue. Stericycle helps support Drug Take Back Programs and works closely with hospital and retail pharmacies and other organizations to help enable the anonymous collection of unused drugs all year. Here are some ways we help dispose of unused consumer medications:
- MedDrop TM Medication Collection Kiosks: DEA-registered hospitals and retail pharmacies can encourage responsible drug collection with our MedDrop™ medication collection kiosks . Stericycle incinerates this collected material.
- Seal&Send TM Consumer Medication Mail Envelopes: For those who cannot access a drug-take back location, Stericycle offers Seal&Send™ Consumer Medication Mail Envelopes . These prepaid envelopes allow patients to send up to eight ounces of unused medication to Stericycle via USPS for incineration. Unlike drug collection kiosks, which can only be hosted by certain DEA registrants, any organization can purchase Seal&Send TM envelopes and provide them to patients, employees, students, and others.
Download our infographic for more consumer insights into medical waste management. Learn how Stericycle can help manage your facility’s medical waste .
Get the Info Sheet

You may also like...
What to Know About Proper Pharmaceutical Disposal Protocols

Guiding Through HIPAA: Five Strategies To Help Enhance Compliance

Considerations for Waste Determination

Enhancing Cybersecurity in Healthcare: The 405(d) Program's Role
Receive Stericycle’s latest content, including news and regulations on how you can maintain business compliance.
We have received your request and a representative will contact you shortly to discuss your business needs.
Submission Error - Please Refresh and Try Again
Please enter a valid value
To find out what personal data we collect and how we use it, please visit our Privacy Policy .
Contact us today for a free, no obligation quote.
Fill out the form or call 866-783-6275 to start protecting your business today.
This choice is required
Please enter a valid email address.
Please enter a valid 10 digit phone number.
Please enter a valid 5 or 9 digit ZIP code.
We have received your request and a representative will contact you shortly to discuss your business needs.
Advertisement

Medical solid waste management status in Zimbabwe
- Published: 12 January 2023
- Volume 25 , pages 717–732, ( 2023 )
Cite this article

- Shabani Takunda 1 &
- Jerie Steven 1
3825 Accesses
14 Citations
Explore all metrics
In Zimbabwe, management of medical solid waste is emerging as a visible dilemma. This is attributed to population explosion as well as outbreak of diseases and spread of already existing diseases which accelerate volume of medical solid waste generated by medical facilities. Consequently, the overarching objective of this paper was to review medical solid waste management status in Zimbabwe utilising published documents. The literature demonstrated that medical solid waste generated in Zimbabwe encompasses pathological, pharmaceutical, chemical, infectious, cytotoxic, sharps and general waste. Management approaches used by medical facilities are marred with inappropriateness as shown by storage, collection, conveyance and disposal of non-segregated waste. Verdicts of the study depict that open pit dumping, landfills, incineration, burying, open burning, ottoway pits and open dumpsites are discarding strategies used. However, these strategies pose water, air and soil pollution, therefore, impacting the ecosystem and humanity. Findings indicated that infectious diseases, respiratory diseases, gastro-intestinal problems and injuries emanate due to poor management of medical waste. The roots of unsafe management of medical solid waste include inadequate finance, weak enforcement of legislation, ignorance among health workers and waste workers as well as non-participatory approach in decision making. Zimbabwe is recommended to direct funds to medical solid waste, increase awareness of health workers through trainings and education and reinforcing enforcement of legislation linked to medical solid waste among others.
Similar content being viewed by others
Plastic Waste: Challenges and Opportunities to Mitigate Pollution and Effective Management
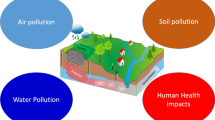
An overview of the environmental pollution and health effects associated with waste landfilling and open dumping
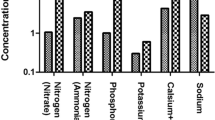
Wastewater Treatment and Reuse: a Review of its Applications and Health Implications
Avoid common mistakes on your manuscript.
Introduction
Medical solid waste is viewed as disposed waste generated from activities such as health protection, diagnosis, treatment, dental and scientific research [ 1 , 2 , 3 ]. However, this type of waste is also generated at household level during utilisation of dialysis, insulin injections and animal treatment in rural areas [ 4 , 5 ]. This implies that medical solid waste is confronting both rural and urban areas, hence demand attention. Medical solid waste generated in most continents like Africa consists of 85 percent non-hazardous and 15 percent hazardous waste [ 6 , 7 , 8 ]. In view of this, a large percentage of medical waste is similar to general municipal solid waste. Nevertheless, owing to insufficient separation medical solid waste turns into entirely hazardous waste [ 9 , 10 ]. Therefore, medical solid waste requires proper separation from generation to disposal sites to minimise quantity of hazardous waste. A view upheld by Vasistha et al . [ 4 ] is that proper management of medical solid waste is essential to protect the environment and uphold human health. Medical solid waste comprises of sharps, pathological, toxic medical chemicals, cytotoxic, medical radioactive, pharmaceutical, infectious and general waste [ 6 , 11 , 12 ]. Considering these various characteristics medical solid waste, its increase has potential to cause injuries, pricks and infectious diseases to people.
Currently, the globe is subjected to growth of medical solid waste quantities due to epidemic diseases like Covid-19 [ 10 , 13 ]. This was observed in India where medical solid waste volume raised from 0.5 kg to 4 kg per patient per day while in China it explode to 6 kg per bed per day [ 13 ]. Henceforth, besides increasing number of patients at medical facilities, diseases accelerate medical solid waste generation. Upsurge of medical solid waste is due to high hospitalisations and use of personal protective equipment such as masks, gloves and gowns [ 14 , 15 ]. Proliferation of medical solid waste means sustainable management to curb dire environmental impacts is vital. Medical solid waste is regarded as the 2nd perilous waste after radiation waste [ 2 , 3 , 16 ]. This means improper monitoring of the waste have potential to hinder achievement of sustainable development. Medical solid waste can impact water, soil, biodiversity, air and environmental aesthetic value negatively globally if improper management strategies are applied [ 8 , 17 ] and humanity is also affected [ 4 , 18 ]. Globally, at least 5.2 million human beings lost their lives annually due to diseases emanating from poorly managed medical solid waste [ 19 ]. Medical solid waste mismanagement is linked to nosocomial diseases, gastro-intestinal diseases, skin disorder [ 8 ] infectious diseases hepatitis B, C, HIV and AIDS [ 4 , 14 , 20 ]. In order to quell these health risks, health institutions must implement eco-friendly management strategies. However, in Africa apt management of solid waste including medical solid waste is difficult due to social, political, economic challenges and waste increase [ 21 ]. Consequently, a myriad of challenges need to be suppressed in order to achieve sustainable medical solid waste management.
Approximately, 67,740 health institutions are in Africa [ 7 ] and generate about 282,447 tonnes of medical solid waste yearly [ 8 ]. Nevertheless, medical solid waste generation trends may have increased due to Covid-19. These quantities call for vast financial, skilled personnel, effective planning and implementation of rigorous approaches. However, these necessities are inadequate in African countries [ 22 , 23 ]. Therefore, proper management is rare, presented by indiscriminate disposal of medical solid waste [ 1 , 20 ]. Bulky volume of medical solid waste is discarded in open pits, poorly constructed landfills, dumpsites as well as low standard incinerators without treatment [ 23 , 24 ]. This is indicated in Zimbabwe where solid waste including medical waste is monitored by incapacitated municipalities [ 25 , 26 ]. This revealed that committed government which supports municipalities is necessary to achieve proper medical solid waste management in African countries including Zimbabwe. Zimbabwean government is constructing health facilities to safeguard wellbeing of its citizens who are around 16.53 million as stated by Zimbabwe Statistics and World Bank in 2017. Consequently, the population facilitate high generation of medical solid waste by seeking assistance from health facilities. This concurs with Torkashvard [ 27 ] that growth of population upsurge quantity of solid waste, mainly medical solid waste. Zimbabwe is under threat of diseases associated with poor sanitation such as typhoid, cholera, malaria [ 10 , 12 , 14 ]. In addition, United Nations Development Program [ 28 ] revealed that over spilling of Covid-19 into Zimbabwe accelerate generation of medical solid waste since it escalates utilisation of personal protective equipment. Therefore, population growth and high disease prevalence are among the drivers of medical solid waste increase in the Zimbabwe.
However, solid waste explosion in Zimbabwe fails to correspond with the prevailing waste management systems [ 29 , 30 ]. Hence, medical solid waste is affecting the already overburdened solid waste management systems in Zimbabwe. This is because medical facilities in Zimbabwe generate a mixture of both hazardous and non-hazardous solid waste [ 31 , 32 ]. In the Zimbabwean context, improper management of medical solid waste is ascribed to fragmented weakly enforced solid waste policies and legislations [ 5 , 26 , 33 ]. Nonetheless, regardless of medical solid waste growth and existence of various management challenges in Zimbabwe its literature is limited compared to the quantity generated. This prospect drives the review to focus on medical solid waste management status in Zimbabwe as a general objective, although it will be guided by the following specific objectives: analyse the characteristics of medical solid waste generated, examine medical solid waste management approaches and assess potential environmental risks associated with the management approaches. Attention will also be given to proffering of an integrated sustainable model for medical solid waste management in Zimbabwe.
Zimbabwe is a landlocked nation occupying about 390,757 square kilometre area in Africa [ 33 ] between latitudes 15–23 0 S and longitudes 25–34 0 E [ 34 ]. Zimbabwe shares frontiers with Zambia, Mozambique, South Africa and Botswana [ 34 ]. Koppen–Geiger climate classification denotes that Zimbabwe experiences subtropical climate with hot wet summers and cool dry winters [ 33 , 35 ]. The country is divided into 5 regions basing on precipitation and temperature experienced in the area [ 36 , 37 ]. Zimbabwe received an average of about 670 mm of precipitation per annum whilst temperature is around 15 ℃ to 25 ℃ [ 38 ]. Zimbabwe Statistics and World Bank (2017) postulated that Zimbabwe’s population is approximately 16.53 million. Like any other country in Africa, people in Zimbabwe are affected by numerous types of diseases such as HIV and AIDS, tuberculosis and poor sanitation diseases such as cholera [ 39 , 40 ] and Covid-19 [ 28 ]. Consequently, they resort to medical facilities for assistance. The entire population is served by 214 medical facilities excluding smaller clinics [ 41 ], thus accelerating medical solid waste generation at the facilities. Medical solid waste increase adds burden to a country which is struggling with municipal solid waste [ 42 , 43 , 44 ]. This initiates the review to merely concentrate on medical solid waste management status in Zimbabwe.
Methodology
The study was grounded on already published literature on medical solid waste management. Similarly, general solid waste literature with aspects of medical solid waste was involved, since medical solid waste literature is limited in Zimbabwe. Articles published in English were reviewed to reach the goal of the review paper. In Zimbabwe, all types of solid waste management is regulated by the Environmental Management Act [Chapter 20:27], effluents and solid waste disposal regulations, 2007. Therefore, the literature published from 2007 to current date was reviewed during the study. However, Taru and Kuvarega [ 31 ]’s research was included since the research pave way for other researches linked to medical solid waste in Zimbabwe. The search was carried out utilising a combination of related key terms such as medical solid waste, clinical solid waste, healthcare solid waste and solid waste among others. However, medical solid waste management approaches and environmental health risks associated with the strategies were part of the keywords. Published articles, journals, abstracts, thesis, book chapters and books were retrieved from Google Scholar, Sage Publications, Springer, Science Direct, African Journals Online, Scopus, Web of Science Publications and Pubmed. Development of an integrated sustainable management model for medical solid waste management was based on the literature contextualised in Zimbabwe. Although it was guided by the Deming circle, a systematic review of published literature offers an understanding of medical solid waste management status and opportunity to proffer recommendations.
Types and characteristics of medical solid waste
In Zimbabwe, medical solid waste is produced by households, hospitals, clinics during patient treatment, diagnosis, caring and immunisation [ 31 ], in form of pathological, pharmaceuticals, sharps, radioactive, toxic chemical waste, infectious waste, cytotoxic waste and general waste [ 20 , 46 ]. Hence, medical solid waste generated by health institutions, households and elderly care facilities in Zimbabwe consists of hazardous and non-hazardous solid waste. This coincide with Ali et al. [ 9 ], Rahman et al . [ 45 ] , and WHO [ 54 ] that medical solid waste consist of 85 percent non-hazardous and 15 percent hazardous waste. This means Zimbabwe produces medical solid waste similar to other countries as demonstrated in Table 1 , hence need enhanced management approach.
Pathological waste produced consists of body parts, human tissues detached during surgery, operations and autopsy, placentas, and foetuses from stillbirths [ 46 , 54 ]. World Health Organisation [ 15 ] opines that pathological waste is infectious due to existence of virus and bacteria in human tissue samples. Therefore, proper handling of pathological waste should be mandatory among health workers in Zimbabwe to curb spread of infectious diseases. In Zimbabwe, expired drugs, contaminated drugs and their containers disposed in Zimbabwe are considered as pharmaceutical waste [ 47 , 48 ]. Nevertheless, pharmaceutical waste quantity is always low in Zimbabwe due to financial crisis which facilitates proper planning when purchasing and utilising drugs. Sharp waste includes needles, syringes, blades, broken glasses, knives, scalpels, infusion sets and pipettes [ 20 , 31 ]. Considering these categories of medical waste in Zimbabwe proper management is the only way forward to minimise health risks such as sharp injuries, cuts and pricks. Sharp waste may cause injuries, thus facilitating spread of diseases such as HIV and AIDS, and hepatitis B and C; hence, special care is recommended when dealing with medical sharp waste [ 49 , 50 ].
In the Zimbabwean context, infectious waste comprise of soiled dressings, surgical gloves, bandages, sponges as well as swabs contaminated by excreta, blood and fluids from patients with communicable and contagious diseases in isolation, surgical wards and theatre [ 20 , 31 ]. Currently, infectious waste explodes due to high use of personal protective equipment (gloves, gowns, masks, goggles, and boots) in Zimbabwean hospitals owing to Covid-19 outbreak [ 28 ]. As a result, stakeholders like Environmentalist and Health and Safety officers should co-ordinate to craft measures to protect both the environment and health workers from infectious waste. Utilisation of nuclear medicines, unsealed radionuclides and therapeutic procedures in Zimbabwe facilitate generation of radioactive waste [ 20 ]. Yves-Chartier [ 12 ] indicated that equipment (glassware, packages, absorbent paper) contaminated by radioactive substances during the diagnosis process are included as medical radioactive waste. This type has potential to cause genetic mutation and cancer to health workers in Zimbabwe, therefore, require close attention. Pressurised containers which include oxygen cylinders, aerosol and air fresheners containers are among medical solid waste. This simply means different methods are required to manage various types of solid waste from medical sector in Zimbabwe.
Jerie [ 51 ] revealed that medical toxic chemical waste consists of containers with remains of clinical chemicals, sterilant, disinfectants, reagents, solvents as well as heavy metals like mercury from batteries. Hence, medical facilities in Zimbabwe produce medical toxic chemical waste since chemical containers, broken clinical thermometers and blood pressure gauges with mercury are part of the waste. General medical solid waste is generated from administration offices such as papers, plastic containers, as well as food waste from the kitchen and visitors who brought food, flowers to their admitted relatives [ 20 , 31 ]. This suggests that medical facilities in Zimbabwe produce certain quantity of solid waste with similar characteristics to household waste, therefore, can be reused or recycled. Solid waste is considered non-hazardous if it is not mixed or get in contact with hazardous waste [ 49 , 50 ]. Therefore, improper segregation of medical waste in Zimbabwe hinders application of reuse and recycle strategies, since the waste became wholly hazardous. Zimbabwean hospitals generate cytotoxic drugs and their metabolites as part of cytotoxic waste. This clearly denotes that medical solid waste requires attention owing to existence of various categories of waste.
Medical solid waste management in Zimbabwe
In Zimbabwe, medical solid waste is managed as general municipal solid waste especially in urban areas. This is supported by Nhubu and Muzenda [ 52 ] and Nhubu et al . [ 53 ] definition of municipal solid waste which encompass medical solid waste is managed by or on behalf of municipalities.
Storage and segregation of medical solid waste
Studies by Tsiko and Togarepi [ 46 ] indicated that solid waste generated in hospital wards is put in small containers or boxes and they are emptied in large containers placed in the corridors. When the containers in the corridors are full with mixed medical solid waste, they are conveyed for storage site [ 31 ]. This suggests that medical solid waste storage in Zimbabwe is marred with confusion, since the storage process may expose humanity to health risks. As a result of continuous emptying of medical solid waste into containers placed in the corridors, their capacity will be exceeded resulting in spilling of waste to the floor [ 20 ]. Thus, exposing various groups of people to pricks, injuries, piercing and infections from poorly stored waste. Hence, there is need for medical facilities in Zimbabwe to have separate areas (rooms) for solid waste storage before conveyed from onsite to waste site.
Taru and Kuvarega [ 31 ] opined that in the Zimbabwean context, medical solid waste is stored indiscriminately since infectious waste and sharps are mixed with pathological waste. However, medical solid waste should be segregated in different colour-coded stiff containers with bin liners and lids during storage in a secured place [ 7 , 15 ]. Sharps are always stored in any container which is available and mixed up with other types of waste for instance pharmaceutical and infectious waste [ 20 ]. This goes against the view of World Health Organisation [ 54 ] and Zimbabwe Ministry of Health [ 55 ] that sharp waste should be stored in puncture proof containers which can be sealed when it is full. Taking into account the above, medical solid waste segregation is full of chaos since despite that medical solid waste is different it is indiscriminately stored and disposed. This coincide with Mangizvo and Chinamasa [ 20 ] that in Zimbabwe general solid waste generated is collected and disposed together with medical hazardous waste haphazardly. This suggests that segregation of medical solid waste should be done at initial stages of waste management chain like storage, to enable collection and disposal of segregated waste.
Collection and conveyance of medical solid waste
Tsiko and Togarepi [ 46 ] observed that collection and transportation is done utilising wheeled trolleys from points of generation (hospital departments and wards) to onsite areas of temporary storage. Medical solid waste is conveyed from areas of generation to final discarding areas, namely landfills, dumpsites and point of incineration by municipalities waste trucks [ 20 , 46 ]. Consequently, participation of medical solid waste generators in management of medical solid waste from cradle to grave is lagging behind in urban hospitals, since the burden shifted from medical sector to incapacitated municipalities. Municipalities collect medical solid waste to ensure that areas under their jurisdiction are not contaminated by solid waste as stipulated by the Urban Council Act (Chapter 15:09) [ 56 , 57 ]. However, the situation begs to differ in rural areas since medical waste generators manage medical solid waste from collection to disposal because they are not beneficiaries of the Act. This implies that legislations and Acts that cater for medical solid waste management in rural areas are prerequisite in the Zimbabwe.
In the Zimbabwean context, medical solid waste collection is inefficient owing to delays, due to shortage of capacity as a result of lack of dump trucks, finance and fuel. Collection rate of solid waste encompassing medical waste in Zimbabwe is approximately 60 percent [ 53 , 58 ]. This coincide with Haregu et al . [ 59 ] who revealed that collection of solid waste by municipalities in less industrialised countries is always less than 70 percent. Efficient collection of municipal solid waste in including medical solid waste in Zimbabwe is hindered by fuel, financial and transport deficit [ 53 , 60 ]. This shows that economic challenges in Zimbabwe crippled efficient collection and conveyance of medical solid waste, therefore, averting the ability to reach sustainable development goals. Solid waste in Zimbabwe should be collected at least twice per week due to climatic conditions in the country [ 26 , 61 ]. This means frequent collection of medical solid should be carried out in Zimbabwe, to avert odours from decomposing waste. However, in Zimbabwe, solid waste including medical solid waste is collected to areas of final disposal once a week or once a month due to fuels’ shortages [ 29 , 31 , 42 ]. This means collection of medical solid waste in Zimbabwe fail to conform to World Health Organisation guidelines. Postponement of medical solid waste collection gives pathological waste opportunity to decompose, hence exposing the environment and human health at risk. Heaping of uncollected waste is witnessed at medical facilities and households in Zimbabwe. As a result, scavenging domestic, wild and stray animals tear and open waste containers, hence exposing themselves to health problems. During deployment of waste trucks, no specific routes are followed; therefore, collection is done haphazardly [ 26 , 62 ]. Consequently, sometimes other suburbs and institutions are skipped; therefore, medical solid generated in those areas’ facilities will suffer since waste is not collected. Continuous accumulation of uncollected solid waste at onsite area creates conducive environment for breeding of cockroaches, rats and flies which speeds the spread of waste-related diseases [ 25 , 51 ]. This depicts that uncollected medical solid waste facilitates the occurrence of waste-related diseases; therefore, efficient collection rate is a mandatory. Nevertheless, municipalities argued that inadequate collection of solid waste including medical solid waste in Zimbabwe is ascribed to underfunding and limited co-operation of rate payers [ 26 ], although Zimbabwean residents conclude that funds misuse and misallocation by municipalities that exacerbate inefficiency collection of waste [ 53 ] and medical solid waste is not spared. This suggest that inappropriate collection of medical solid is a result of blame game between the city fathers and residents, hence they must work together to achieve efficient waste collection.
Disposal of medical solid waste
In Zimbabwe, about 90 percent of solid waste, including medical waste is disposed in indiscriminate state [ 26 , 58 ]. This revealed that sustainable alternatives such as recycle, reuse and prevention need to be applied in medical waste management in Zimbabwe, to minimise quantity of waste disposed. Approximately, 40 percent of solid waste encompassing medical solid waste is disposed in an illegally manner along road edges, in drains and open spaces [ 53 , 58 ]. This implies that a certain proportion of medical solid waste is also destined in undesignated disposal sites, thus exacerbating occurrence of environmental health problems. Taru and Kuvarega [ 31 ] revealed that medical solid waste disposal approaches utilised in Zimbabwe include open dumping, burying, open pits, and burning. This is pathetic since most the approaches used to dispose medical solid waste forms the base of solid waste management hierarchy. Makarichi et al . [ 57 ] pointed out that 37.6 percent of solid waste from different sources is burned through uncontrolled open burning at generation point in Zimbabwe. This point out that medical solid waste is also disposed through open burning which can be controlled or uncontrolled burning since it is capable to reduce quantity of waste as well as destroying pathogens, virus and bacteria.
In addition, Jerie and Musasa [ 46 ] asserted that incineration is highly utilised to dispose medical solid waste. Considering the mentioned approaches, it is clear that Zimbabwe is still utilising the least desired strategies to dispose medical solid waste; therefore, a road map to reach upper part of the waste management hierarchy is required. Strategies namely plasma, gasification as well as electro-thermal deactivation of medical waste can be used to treat and dispose medical solid waste in Zimbabwe, than solely relying on incineration. Ferreira and Veiga [ 63 ]; Rana and Ganguly [ 64 ] and Vasistha et al . [ 4 ] concur that medical facilities resort to incineration because it is capable to reduce the quantity of medical solid waste by about 80 percent, detoxification and destroy pathogens. In less developed nations, incineration is viewed as a golden approach, although utilisation of low standard incinerators result in spike of emissions in the atmosphere [ 9 , 17 ]. This is exemplified by Mangizvo and Chinamasa [ 20 ]’s studies in Kwekwe which demonstrate that the incinerator used for medical solid waste disposal was operating inadequately owing to collapse of furnace lining. In addition, overloaded non-segregated solid waste limits the efficiency of incinerators since non-combustible and wet waste is resistant to incineration [ 20 , 31 , 52 ]. Therefore, none ash residues of medical solid waste such as glasses, sharp waste and containers finds their way to disposal sites, exposing informal waste collectors to injuries.
Nyakatswau et al . [ 48 ] argued that solid waste in Zimbabwe is collected by municipality dump trucks to be discarded in official dumpsites despite difference of their origin, type or potential environmental effects. Hence, medical solid waste with its hazardous characteristics is also transported to dumpsites together with other general solid waste. This generally means policies and legislations which support segregation of medical solid waste at initial stages is required to achieve proper disposal. Approximately, 90 percent of solid waste generated in cities is conveyed to dumpsites for instance Pomona in Harare [ 52 , 58 ], this means medical solid waste is not spared. As evidenced by this a large volume of medical solid waste is disposed, therefore, recycling and reuse is rarely practised in Zimbabwe. This goes with Taru and Kuvarega [ 31 ] who postulated that medical solid waste generated by Parerenyatwa medical facilities is transported and discarded on dumpsites. Nevertheless, besides increasing environmental health risks, medical solid waste is partly speeding exhaustion of dumpsites which are already dying a slow death. This is demonstrated by the Pomona dumpsite which was projected to be closed in 2020, since solid waste was exceeding its capacity [ 52 ]. Consequently, Zimbabwe must not focus on collect and dispose approach when dealing with medical solid waste.
Moreover, medical solid waste generated by rural areas is discarded in open pits in Zimbabwe owing to its low costs. However, this approach can be a potential source of infection to public health and exacerbate cropping of different environmental problems if poorly managed [ 51 , 65 ]. In addition, openly discarded medical solid waste is exposed to blowing wind, thus accelerating rate of cross infection to the nearest residential areas. A view upheld by Jerie and Zulu [ 66 ] is that residential areas located less than 500 m from the dumpsites are vulnerable to problems associated with solid waste. Infectious medical solid waste is supposed to be treated utilising autoclaving system and chlorine to disinfect it before being disposal in Zimbabwe [ 20 ]. Nevertheless, these strategies cannot be applied frequently due to financial constraints; therefore, despite being a major emission generator, incineration remains the only option. This congruent with Tanyanyiwa [ 60 ] and Chapungu et al . [ 67 ] failure to adopt or utilise sustainable waste treatment or disposal in Zimbabwe that is attributed to limited finance.
Zimbabwe like other least industrialised nations, utilises landfilling as an alternative to dispose medical solid waste; however, the dilemma is they are operated like open dumpsites. In developing nations, approximately 50 percent of collected solid waste is discarded through poorly controlled landfills [ 59 , 68 ]. Landfills in Zimbabwe are like dumpsites since solid waste is non-compacted, not covered by soil and landfills lack leachate and gas control systems owing to limited funds and lack of experts [ 56 , 57 ]. This implies that pollutants from decomposed medical solid waste can potentially cause deleterious impacts to the environment. Municipality solid waste on dumpsites is always exposed to open burning [ 42 , 62 ]; therefore, medical solid waste is also burned at rural and urban health facilities. Therefore, medical solid waste is also destroyed through open combustion in Zimbabwe [ 20 , 31 ].
In rural hospitals, ottoway pits are also utilised to dispose pathological waste, but the problem is sharps and infectious waste mixed with pathological waste [ 20 ], hence finds their way into ottoway pits. This minimise effectiveness of ottoway pits as an alternative to dispose pathological waste. In addition, most of the times the ottoway pits are not lined, this gives the leachates from ottoway pits opportunity to pollute groundwater as well as soil. Unlined solid waste disposal sites produce leachates, acids and ions which contaminate soil and ground water [ 50 , 56 ]. In Zimbabwe rural medical facilities, burying of waste is usually practised [ 65 ]. From the above, it is not an exaggeration if one argues that most of the approaches utilised to dispose medical solid waste in Zimbabwe are far from the recommended standards to reach sustainability. Currently, disposal of solid waste including medical waste is problematic in Zimbabwe due to waste increase, sub-optimal infrastructure and absence adequate waste data [ 57 , 58 ]. However, Tanyanyiwa [ 60 ] and Nhubu and Muzenda [ 52 ] noted that disposal solid waste including medical waste is emerging as a problem due to Not In My Backyard syndrome. This principle increase difficulties to locate medical solid waste dumpsites since people are aware of environmental health risks associated with improperly monitored dumpsites.
Environmental health risks associated with medical solid waste management
Medical solid waste generated by health institutions may pose dire impacts to the environment, especially if the least desired discarding approaches are used [ 6 , 9 , 46 ]. This means flora and fauna as well as water sources, soil and air in Zimbabwe are at risk owing to improper medical solid waste management. According to Ali et al. [ 9 ], Askarian et al. [ 6 ] and Ansari et al. [ 49 ], non-treated medical solid waste release toxic pollutants and pathogens such as bacteria and viruses in the natural environment. Thus, exposing different fauna species with access to the dumpsites to viral and bacterial diseases. This is inevitable in Zimbabwe where most of the dumpsites are unsecured [ 46 ]. Inadequate incineration of medical solid waste with polyvinyl chloride results in air contamination by dispersing carbon monoxide, dioxide, nitrous oxide, furans and dioxins in the atmosphere [ 31 , 41 , 50 ]. This illustrates that improper management of medical solid waste is increasing human carbon footprint in Zimbabwe. This is the reason why medical facilities are regarded as the 5th emitter of greenhouses gases at global level, generating approximately 4.4 percent [ 7 , 9 , 49 ]. As a result, improper solid waste management including medical waste management in Zimbabwe accelerates climate change [ 52 , 58 ]; therefore, medical solid waste management cannot be neglected in Zimbabwe. Moreover, humans who inhale toxic gases from medical solid waste may suffer from chronic and acute respiratory diseases such as tuberculosis, coughing alongside cancer [ 6 , 49 , 51 ]. In Zimbabwe, less effective incinerators are utilised to dispose medical solid waste [ 20 , 31 ]. This implies that partially burnt solid waste such as sharps and bottles always finds their way to the dumpsites and speedy exhaustion of dumpsites. Therefore, in the Zimbabwean context methods such as granulation, shredding, crushing, pulverisation, grinding and crushing with potential to reduce volume of waste which is not suitable for incineration.
Medical facilities incinerate clinical thermometers, fluorescent tubes, blood pressure gauges and electrical gadgets which contain carcinogenic heavy metals such as mercury, cadmium, lead, copper and zinc [ 2 , 9 , 49 ]. Hence, human beings are vulnerable to neurological disorders, genetic mutation and blood pressure due to exposure to heavy metals. Disposed medical solid waste was found to generate copper, zinc, mercury, lead, cadmium and chromium [ 1 , 9 , 23 ]. However, the non-biodegradable characteristics of heavy metal increase its accumulation in the environment causing health problems to human beings [ 51 ]. This suggest that people who reside in proximity to medical solid waste incineration sites can be affected by various types of cancer such as colon cancer, since medical waste is a source of heavy metals. In addition, leachates containing heavy metals and pollutants from decomposed result in water pollution which later cause ulcers to people [ 27 , 51 ]. This implies that cost-effective as well as environmentally friendly strategies must be used to dispose medical waste to reduce quantity of heavy metals in the environment. Pollutants from medical waste and excessive radiation from incineration affect birth weight of unborn babies (foetuses) and catalyse occurrence of down syndromes [ 11 , 31 , 51 ]. This means medical solid waste incineration affects pregnant mothers, yet in rural areas of Zimbabwe, incineration is done at hospitals. Inefficiency solid waste collection in Zimbabwe is increasing ability of medical solid waste to cause dire impacts. This is because inadequate collection forces residents to turn to open burning [ 26 , 56 ] and this also infiltrate to medical facilities since they will be trying to reduce volume of uncollected waste. However, uncontrolled burning of medical solid waste produce smoke which act as nuisance to people and contaminates the air. Contaminated air causes eye irritation, bronchitis, dry cough, tuberculosis and asthma [ 51 , 68 ]. Hence, burning of medical solid waste has potential to diminish humanity’s wellbeing.
In Zimbabwe, medical solid waste is dumped in open pits which are improperly managed, thus increasing breading of diseases vectors and environmental pollution. Open pits and open dumping creates favourable breeding sites for mosquitoes, rats which cause malaria and rat-bite fever, respectively, alongside flies which transmit dysentery, typhoid and cholera [ 51 , 67 ]. Therefore, medical facilities, which are considered safe places, are now fuelling outbreak of diseases relating to poor solid waste management in Zimbabwe. Improper management of solid waste including medical solid waste also contributed to 2008–2009 outbreak which lead to death of approximately 3.500 people [ 39 , 69 ]. Furthermore, medical solid waste disposed in open pits are easily accessible by domestic dogs, goats, birds and cats, and this exacerbate cross infection to residential areas. Domestic animals like dogs always collect anything they pick to residential areas [ 20 ], thus increasing vulnerability of people to risks associated with medical solid waste namely infectious diseases. Decomposition of solid waste including medical waste on landfills and dumpsites generates leachates, acids and heavy metals which contaminate water and soil [ 52 , 57 ]. This advocates that decay of medical solid waste on landfills that pose dire impacts to water and soil quality; therefore, flora is not spared. Dissolved minerals from landfills and dumpsites cause water-borne diseases such as typhoid, cholera, and dysentery [ 70 ], as well as propelling growth of water hyacinth in water sources [ 26 , 58 ]. As a result of disposal of medical solid waste on poorly engineered landfills and dumpsites, water contamination is inevitable in Zimbabwe. Pomona, Chitungwiza and Golden Quarry dumpsites in Zimbabwe lack mechanisms that reduce infiltration of leachates to groundwater [ 57 ]; hence, ground water pollution is inevitable. Therefore, Zimbabwe as a country should put emphasis on constructing waste sites which impede free leachate movement.
Incineration of solid waste specifically medical solid waste produce ashes with high toxic heavy metals and organic contaminants with potential to pollute ground and surface water [ 53 , 71 , 72 ]. This revealed that it is vital for Zimbabwe medical sector to eliminate or reduce toxicity of incineration residues and ashes before disposing into landfills. Pollutants and heavy metals are absorbed by plant roots and trans-located to edible fruits and roots [ 73 ]. Given this, pollutants from medical solid waste find their way into the food chain since browsers and humans always survive from green plants and fruits. However, ingestion of fruits or roots containing pollutants increase occurrence of ulcers, cancer and diarrhoeal diseases [ 73 ]. A view upheld by Ansari et al . [ 49 ] is that impurities of medical solid waste in soil can pose various abdominal pains. Therefore, soil contaminated by medical solid waste pollutants can accelerate abdominal pains in Zimbabwe since geophagy is rampant. Landfills are known generators of irritating odours and methane gas, a greenhouse gas which accelerate global warming [ 70 ]. Henceforth, besides causing health problems, decomposed medical solid waste speeds up global warming, thus facilitating climate change. Mobile refuse trucks pollute the air since they utilise petrol or diesel which produce greenhouse gases [ 53 ], similarly medical solid waste refuse trucks produce toxic gases such as nitrous oxide, sulphur dioxide and hydrocarbon particles. Thus, increasing global warming and respiratory problems to people in the vicinity. Studies in Kwekwe show that open trucks which enable medical solid waste to fall were used to convey waste to incineration site [ 20 ]. Falling solid waste including medical solid waste result in land pollution [ 26 , 74 ], if it remain unpicked, visual pollution increases. Therefore, strict handling of medical solid waste and monitoring of dumpsites is required in Zimbabwe to avert appearance of medical waste as nuisance. Visual pollution diminishes aesthetic value of the environment [ 26 ], thus impacting tourism which a source of income in Zimbabwe. Therefore, apart from being an eyesore, medical solid waste hinders economic growth in Zimbabwe since it minimises inflow of tourist since they shun waste. This means utilisation of proper well-serviced vehicles is required when ferrying medical solid waste to minimise air pollution and land pollution.
Cuts, puncture, and injuries caused by disposed sharps such as needles and broken glasses cause easy penetration of fungi, virus and bacteria into human system [ 20 , 51 ]. Therefore, medical sharp waste has potential to increase spread of Hepatitis B, C, HIV and AIDS, Ebola and Covid-19 since they contain viruses from infected people. A view upheld by Ramteke and Sahu [ 13 ] and World Health Organisation [ 15 ] is that medical sharp results in injuries and cuts which increase transmission of Hepatitis B and C, HIV/AIDS and Covid-19. In 2018, HIV, hepatitis B and hepatitis C new infections caused by infected sharp waste like syringes was approximately 260,000, 21 million and 2 million, respectively [ 75 ]. In addition, medical solid waste contaminated by infectious saliva, blood and body fluids increase spread of infectious diseases [ 2 , 10 ]. This means in Zimbabwe, health workers, waste collectors, patients and public are under threat since they are always in contact with medical solid waste with various types of infectious waste such as sharp waste. In Zimbabwe, people are exposed to anthrax due to contact with medical waste generated during treatment of domestic animals. Children and scavengers who access dumpsites with medical waste without safety gear are also vulnerable to infectious diseases. Health workers and waste collectors in Zimbabwe took safety gear for granted and became more vulnerable to injuries and infections caused by medical sharp waste. This is supported by [ 76 , 77 ] that solid waste workers specifically informal workers (scavengers) are exposed to various waste-related injuries or diseases since they work without required personal protective equipment. In addition, sharp waste also contain biological pathogens which cause diseases like tetanus [ 50 , 51 ]. This means scavengers who look for valuable materials from dumpsites and children who use medical solid waste dumpsites as playgrounds are at risk of being infected by infectious diseases since they are always not vaccinated.
Competition of informal waste collectors and dogs to reach consumable, reusable and recyclable medical solid waste at the dumpsites expose human beings to injuries and being bitten. Jerie [ 51 ] postulated that human beings may be bitten by stray dogs during scavenging activities, hence became infected by rabies. Occupational risks like musculoskeletal disorders affect people who deal with lifting of objects such as loading and offloading of materials [ 43 , 51 ]. This implies that medical solid waste workers in Zimbabwe are affected by hands, wrist and shoulder injuries as well as upper, lower back pain alongside chest pain due to loading and offloading. Therefore, dealing with medical solid waste speeds lives of the waste workers to the grave unknowingly, hence strict legislation should be implemented to protect waste workers. In Kwekwe, Zimbabwe, medical solid waste collectors are always transported in the same truck with solid waste [ 20 ]. Consequently, the workers are exposed to infectious diseases which they also ferry to their families since they went home with their infected clothes. Open dumpsites are known as sources of spiders, scorpions, odours, houseflies, rats and cockroaches which can affect nearest residential areas [ 67 , 70 ]. Henceforth, attention in form of proper Environmental Impact Assessment is required when siting medical waste dumpsite. This is because households located less than 500 m from waste sites are under threat of problems that emanate from the sites [ 66 ]. This denotes that medical solid waste sites in rural areas pose numerous problems to people since they are located within the health premises. Njaya [ 78 ] observed that solid waste which rots quickly attract disease-transmitting organisms and vectors, thus impacting human health. Therefore, medical solid which consist of wet cotton wools, swabs, soiled bandages, pathological waste quickly decompose especially under high temperatures, hence generating odours, disease vectors.
Informal waste collectors inhale, ingest and absorb residues of chemicals such as fluorine, chlorine, deinking and cleaning detergents into their systems resulting in liver and kidney damage [ 51 , 79 ]. As a result, medical solid waste collectors’ health is affected since medical facilities are major homes of chemicals in Zimbabwe. Solid waste workers are exposed to health problems since they always contact medical toxic chemical and medical radioactive waste [ 19 , 43 , 46 ]. Therefore, activities involved in medical solid waste management in Zimbabwe from cradle to grave expose humanity to numerous health risks; however, the likelihood and severity differ. A view which correspond with Ghafuri [ 80 ] results obtained through Preliminary Hazard and Risk Analysis and Risk Assessment Matrix is that segregation of medical waste is a high risk activity, while collection, treatment alongside discarding are medium risk events. This is presented in Table 2 . Analysis goes on to demonstrate that pathological, infectious and sharp medical solid waste are considered as source of high risk [ 80 ] as shown in Table 2 . Considering findings in Table 2 , Zimbabwe’s health workers, waste collectors, community as well as the environment cannot escape risks associated with medical solid waste easily. Therefore, crafting of an integrated medical solid waste management model which capacitate co-ordination among different stakeholders pave way for Zimbabwe to reach sustainability.
Medical solid waste legislation and policies in Zimbabwe
Management of solid waste is a burning issue which was discussed at the Agenda 21 and the current Sustainable Development Goals. Consequently, Zimbabwe is giving attention to medical solid waste to achieve sustainability by 2030 [ 81 ]. In year 2012, Zimbabwe Ministry of Health and Child Care guided by the World Health Organisation protocols implemented guidelines for discarding pharmaceutical waste. However, the guidelines’ loophole is lack of waste reduction approaches and penalties imposed to those who fail to conform to the guidelines. Hence, medical waste in form of pharmaceutical waste remains a challenge in Zimbabwe. Zimbabwe’s Ministry of Health and Child Care informed medical facilities that they must acquire consent from the appropriate authority or manufacturer before discarding expired drugs [ 47 , 55 ]. The Ministry of Health and Child Care indicate the roadmap of monitoring medical solid waste generation to disposal, in the handbook entitled “Infection Prevention and Control Handbook, Written by Doctor Gwinji in 2013. In view of this, Ministry of Health and Child Care is eager to contain risks associated with medical solid waste, but due various challenges, their efforts remain in vain. In addition, Ministry of Health and Child Care handbook does not show how waste minimisation strategies can be applied.
Reviewing of worldwide conventions directed to medical solid waste management denote that Zimbabwe signed the Basel Convention, Stockholm Convention and Rotterdam Convention [ 28 ]. The country is a signatory of Bamako Convention as well as Minamata Convention. In addition, Basel convention which focus on trans-boundary movement and management of hazardous waste was ratified in 2012 by Zimbabwe. The Basel convention is centred on minimising dire impacts associated with hazardous waste including medical solid waste. Therefore, by being a signatory of this convention, Zimbabwe is willing to conform to sustainable management of medical solid waste. Moreover, in trying to deal with hazardous radioactive and chemical waste, Zimbabwe is part of countries who signed Bamako convention. Considering characteristics of medical solid waste, it is not excluded in the convention; therefore, Zimbabwe is following goals of Bamako convention to monitor the waste properly. However, despite being member of the conventions, failure of Zimbabwe to conform is ascribed to inadequate finance. There are also no clear objectives on how hazardous waste such as medical waste can be recycled or how resource recovery can be applied.
Zimbabwe signed and ratified the 2012 Stockholm convention. The convention encourages eradication or reduction of persistent organic pollutants through apt management of waste piles. Hence, medical solid waste is not spared since incineration and open burning is used to dispose waste in Zimbabwe. Under Article 5 and Annex C, members of the convention are required to avoid disposal methods that produce persistent organic pollutants mostly dibenzofurans and polychlorinated dibenzo-p-dioxins. Hence, Zimbabwe must fit in medical solid waste disposal strategies and structures that meet the demands of Stockholm convention. Moreover, Zimbabwe is guided by Minamata convention when dealing with materials that contain mercury. This implies that medical solid waste such as batteries, fluorescent lamps, dental amalgams and clinical thermometers are managed through requirements of the convention. This will enable the country to move towards sustainable development goals. Medical facilities produce containers with residues of chemicals such as detergents, reagents and other materials contaminated by chemicals [ 20 , 51 ]. Therefore, by being a member of Rotterdam convention, Zimbabwe is expected to deal with medical solid waste in a way that reduce detrimental impacts of chemical waste.
In the Zimbabwean context, specific Acts and Statutory Instruments related to medical solid waste does not exist. However, the legal framework for medical solid waste monitoring is grounded on the Environmental Management Act Chapter 20:27. The Act urges and encourages proper management of solid waste in Zimbabwe, and medical solid waste is not spared. However, the Act neglect aspects such as solid waste reduction, segregation as well as recovery approaches. Statutory Instrument 6 of 2007 on waste and solid waste and Statutory Instrument 268 of 2018 on hazardous waste offer regulations which encourage proper management of solid waste, including medical solid waste [ 82 ]. Although, statutory instrument fail to indicate clearly how various solid waste generators will be enforced to practise proper management of waste. The acts offers room for formulation of environmental quality standards and issues linked to environmental sustainability notably management of all types of solid waste. Nevertheless, it fails to consider vital issues like how integrated solid waste management can be achieved.
Environmental Management Act 20:27 criminalise pollution of the environment by individuals, formal and informal industries and medical facilities are not spared. Therefore, for medical facilities in Zimbabwe to be free from polluter paying principle, they must act according to requirements of Environmental Management Agency. Nevertheless, the fines imposed on medical facilities are very low; therefore, improper management of medical waste perpetuate. Zimbabwean Government [ 83 ] and De Gobbi [ 84 ] Environmental Management Agency Act 20:27 and 2013 Constitution of Zimbabwe Section 73 stipulates that every person has the right to a non-hazardous environment. Hence, if medical facilities fail to discard solid waste in an appropriate manner, they will contravene to the law. However, the problem is that environmental rights are centred on human beings while ignoring other environmental attributes affected by poorly disposed waste. Under Sections 55–56 of the Act institutions who produce polluting materials must conform to environmental quality standards. This suggests that health institutions are not spared since they generate solid waste which deform quality of the environment.
Zimbabwe also utilises Hazardous Substances Act Chapter 15:05, Statutory Instrument 10, of 2007 to monitor hospital solid waste [ 32 ]. The Act indicates that generators of hazardous waste are responsible for sustainable management of the waste. With this in mind, medical facilities in Zimbabwe are accountable for proper management of medical solid waste. Transportation of medical solid waste in Zimbabwe is guided by Hazardous Substances Act which stipulate that hazardous waste should be conveyed in specific vehicles. However, in Zimbabwe, multipurpose vehicles are used [ 20 ]. This is attributed to inadequate waste trucks as well as fuel. The major loophole of Hazardous Substances Act is that it is silent about the three Rs of solid waste management which are recycle, reuse and reduce. Hence, medical solid waste is mostly destined in disposal facilities. Urban Councils Act, Chapter 29:15 Statutory Instrument 68 of 2021 subsection 1 of section 4 shows that municipalities are responsible for offering waste collection services in urban areas [ 52 , 85 ]. This means medical facilities in urban areas benefit while rural health institutions deal with their own solid waste, although rural medical facilities produce medical solid waste with characteristics to waste from urban hospitals. In this view of this, an act directed to marginal areas must be crafted. In addition, Urban Council’s Act provides generators of medical waste in urban areas opportunity to be mere participants in management of their waste. Therefore, adding burden to already ill equipped municipalities, thus exacerbating mismanagement of medical waste. Nevertheless, the major weakness of the Act is failure to highlight the consequences a council will face if it failed provide waste services to areas in its jurisdiction. Moreover, it does not include solid waste management approaches a council should apply after collection; therefore, councils mostly relied on collection and disposal approach.
Zimbabwe also applies the Public Health Act Chapter 15:09, this act deals with the control of emission and disposal of waste to reduce outbreak of diseases. The Public Health Act Chapter 15:09 forms the basis for healthcare and environmental health service. The Act shows that individuals and organisations must utilise waste management approaches that reduce negative health impacts to the public for instance infectious diseases. This suggests that medical facilities have to conform to the requirements of Public Health Act, when disposing medical solid waste. Ineffectiveness of Public Health Act is ascribed to its failure to indicate clear standards and procedures in solid waste management. Consequently, adoption of proper management of medical solid waste remains at miniature stage. Environmental Management Act Chapter 20:27, Statutory Instrument 72 of 2009 is also vital for air pollution control. According to subsection 4, Section 63 of the Act, individuals, industries and institutions involved in activities which emit pollutants into the atmosphere are included. Hence, medical facilities who incinerate or burnt medical solid waste is not spared.
According to Statutory instrument 72, height of emitting chimney should be 50 m or taller than all the buildings at any institution. This guides health institutions when constructing chimneys of their incinerators. However, in Zimbabwe, hospitals always fail to conform the standard; hence, they are liable to heavy fines. The atmospheric pollution act gives Environmental Management Agency authority to inspect emission structures, this means hospital incinerators are also inspected. Emission samples are also tested using blue, green, yellow and red bands. If incinerator emissions are above the required colour bands, medical facilities will be susceptible to polluter pays principle. Although, the penalties and cost of remediation are unexceptionally very low. In addition, occupational health and safety legislation such as Statutory Instrument 68 of 1990 supported by the 1996 Factories and Works Act Chapter 14:08 protect employees including health workers against workplace injuries by promoting safe work environments [ 48 , 86 ]. This implies that medical solid waste generators, handlers and collectors are also protected since medical waste is hazardous. Factories and Works’ Act fail to address its objectives fully since it does not provide waste handling procedures and standards. In order to protect the general public, all organisations and individuals urged to discard or destroy pharmaceutical waste using strategies which are harmless to humans and their surroundings [ 48 , 55 ]. This advocates that in the Zimbabwe, medical facilities are supposed to monitor management of medical solid waste from cradle to grave. However, the situation begs to differ since municipalities are responsible for management of medical waste from collection to disposal.
Proposed integrated sustainable model for medical solid waste management
In the Zimbabwean context, medical solid waste mismanagement is omnipresent. This means there is need for a sustainable model to act as a pathway to achieve apt management of medical solid waste. As a result, an integrated sustainable model was crafted basing on the Deming OPDCA Circle of improvement. In the OPDCA abbreviation, O is for Observation, whereas P is planning, while D stands for Do, C represents Check and A is Act. OPDCA circle is considered as an effective strategy for improvement by [ 87 , 88 ]. This implies that to improve medical solid waste management, the OPDCA system must be adopted for proper decision making and enhancement of existing strategies. The proffered model in Fig. 1 demonstrates that different stakeholders for instance Ministry of Health Care, Environmental Management Agency, Hospital Environmental Health Departments as well as Local Authorities must observe the status of medical solid waste management through researches and site visits. This assist in figuring out the strength and loopholes of existing medical solid waste management approaches. Observations enable medical solid waste experts to know who is slacking and what is lacking in medical solid waste management. Unearthing of environmental health risks associated with the management approaches provide enough information to utilise during planning.
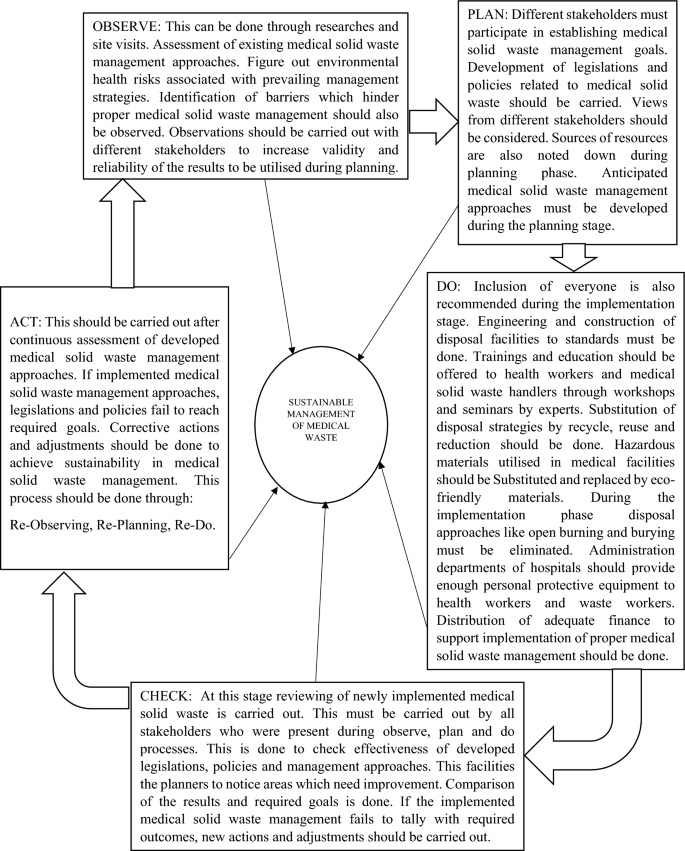
Conceptual model for sustainable medical solid waste management
Effective planning on medical solid waste management in Zimbabwe requires inclusion of different stakeholders. In order to establish real achievable goals towards medical solid waste management, various people from community to national level must be encompassed. A team comprising of people from different fields establish strategies and processes to be carried out to reach the required results. This suggests that numerous environmental experts, ministries, organisations as well as legal experts must be involved.
Ministry portfolios included in the framework are:
The Environment, Climate Change, Tourism and International Trade is included because medical solid waste can impact the environment, accelerate climate change. As well as minimise inflow of tourist from other countries since solid waste deform attractiveness of the environment. In addition, no single investor is attracted by an eye sore environment, thus affecting international trade. This implies that Minister of this Portfolio should be part of medical solid waste management planners. Furthermore, Finance and Economic Development Minister is one of the key stakeholders to facilitate the planning process. This is owing to the minister’s ability to do budgets and distribute finance to development processes in the country, including finance required to improve medical solid waste management. Minister of Health and Child Care must be encompassed in planning since the cadre is responsible for monitoring all the medical facilities in Zimbabwe. This means the minister is expected to have knowledge of existing medical solid waste management approaches. Challenges which hinder adoption of sustainable strategies at hospital level are also known by the minister and Hospital Environmental Department. Minister of Higher and Tertiary Education Science and Technology Development should be part of the planners. This is because the minister has power to deploy solid waste experts from universities to deal with medical solid waste issues. Ministry of Justice Legal and Parliamentary Affairs minister and his/her legal team assist Environmental management Agency to craft legislations and laws related to medical solid waste management.
The Local Authorities who deal with solid waste from collection to disposal in urban centres are governed by Minister of Local Government and Public Works. Solid waste budgets and by-laws crafted by Local Authorities are utilised after approval from the Local Government and Public Works minister. During the planning phase, health workers who are responsible for generation of medical solid and hospital cleaners must be involved. Similarly, the community people who are vulnerable environmental health risks that emanate from poorly managed medical solid waste should be present during planning. The reason is that National Social Security Authority is responsible protecting workers from workplace injuries. Planning enables financial and other resources desired in medical solid waste management to be put together before the implementation process. In addition, stakeholders involved in the planning stage should play a pivotal role in achieving sustainable management of medical solid waste. Those who are responsible for offering training and education to health workers must play their role for instance Hospital Environmental Health Departments. Enforcement of the developed medical solid waste legislations should be carried out by Environmental Management Agency. In order to achieve objectives highlighted during planning, finance directed to medical solid management should be pumped in. Engineering issues should be implemented effectively so that medical solid waste incinerators, landfills and ottoway pits are constructed to standards. This minimises contamination of air, water and soil which emerge as a result of poorly constructed disposal structures.
During the Do phase, supplied finance should be used to purchase environmental friendly resources to be used in hospitals. This implies that medical materials which are not eco-friendly are substituted to reach sustainability. Incineration should be substituted by processes like steaming which deactivate viruses and bacteria on medical solid waste. Elimination of disposal strategies which results in high environmental pollution and risks. This can be exemplified by eliminating uncontrolled open burning and burying of medical solid. Medical facility administrations should provide enough Personal Protective Equipment to health workers and waste workers to safeguard them from health problems associated with medical solid waste. Therefore, medical facilities administration departments must safeguard wellbeing of to reduce occurrence of injuries and health problems related to medical solid waste. At this stage, participation of every individual or group of people as well as applicability of developed strategies should be evaluated through checking.
Information gathered during the implementation phase is evaluated to compare the results with the anticipated outcomes. This suggests that Checking of effectiveness of planned and implemented medical solid waste management strategies is carried out. The Checking process facilitates to figure out the changes brought by newly implemented approaches as well as areas which need further improvement. This reviewing stage enable planners to check successfulness of newly initiated medical solid waste policies and legislations. If loopholes are discovered during reviewing of invented medical solid waste management strategies, new plans can be implemented. At this stage, if non-conformity or problems are noticed in terms of medical solid waste management, apt actions or adjustments are carried out. If the implemented medical solid waste management approaches fail to meet sustainability, the barriers are investigated. Therefore, re-observing of medical solid waste management from generation to disposal is done followed by altering issues noted during planning phase as shown in Fig. 1 .
Reviewed literature depicts that nature of medical solid waste generated in Zimbabwe encompasses pathological, sharps, pharmaceutical, chemical, radioactive, cytotoxic, infectious waste as well as general waste. Medical solid waste generation is driven by population increase which exacerbates the number of people to be dealt with at medical facilities. Moreover, outbreak and spread of various types of diseases such as HIV and AIDS, malaria, tuberculosis, Covid-19, typhoid alongside cholera increase the volumes of medical solid waste. Management of medical solid waste from point of generation to disposal shows ineffectiveness and inefficiency in Zimbabwe. This is exemplified by indiscriminate storage of sharps and other types of solid waste in single containers. Medical solid waste overloaded bins are stored in wards and corridors releasing odours to health workers, patients and visitors. Onsite conveyance of mixed medical waste is carried out using trolleys and wheel burrows while multipurpose trucks ferry medical solid waste together with general waste to offsite disposal sites. In Zimbabwe, inapt monitoring of medical solid waste is occurring owing to lack of resources, inadequate know how among those who deal with waste, non-existence of clear medical solid waste laws and policies coupled by low enforcement of environmental legislations.
Medical solid waste in Zimbabwe is transported using multipurpose vehicles and disposed in improperly engineered landfills, dumpsites, substandard incinerators as well as open burning. However, rural hospitals also utilise open pits and burying of medical solid waste in open spaces. Disposal approaches utilised compromise the quality of the environment by posing air, soil, water contamination and flora and fauna is impacted since the pollutants accumulate in the food chain. Leachates from dumpsites, ottoway pits and landfills contaminate soil and water, whereas odours and gases pollute the air. Medical solid waste affects humanity indirectly since polluted water result in gastro-intestinal problems while incineration and open burning accelerate occurrence of respiratory diseases. The study revealed that medical solid waste management system have potential to cause occupational risks for instance musculoskeletal problems like shoulder pain to those who load and offload the waste. Health workers are also vulnerable to injuries posed by sharp waste, if they handle waste without safety gear. Similarly, waste collectors, children and scavengers are under threat of injuries, pricks associated with sharp waste since they visit unsecured dumpsites. The review shows that sharp injuries expose people to different viral and bacterial diseases such as Hepatitis B, C, HIV and AIDS and tetanus. Hence, it is anticipated that the developed model may be used as a foundation to build sustainability in medical solid waste management.
Data availability statement
The data will be available from the authors on reasonable request.
Coker A, Sangodoyin A, Sridar M, Booth MC, Olomolayaiye C, Hammond A (2009) Medical waste management in Ibadan, Nigeria. Obstacles and prospects. Waste Manag 29(2):804–811
Article Google Scholar
Hossain MS, Santhanam A, Norulaini NAN, Omar AKM (2011) Clinical solid waste management practices and its impact on human health and environment-a review. WasteManag 31:754–766
Google Scholar
Rupani PF, Nilash M, Abumalloh RA, Asadi S, Samadi S, Wang S (2020) Corona virus pandemic (Covid-19) and its natural environmental impacts. Int J Environ Sci Technol 17:4655–4666
Vasistha P, Ganguly R, Gupta AK (2018) Biomedical waste generation and management in public sector hospital in Shimla City. Environmental pollution. Springer, Singapore, pp 225–232
Chapter Google Scholar
Dzawanda B, Moyo GA (2022) Challenges associated with household solid waste management (SWM) during COVID-19 lockdown period: a case of ward 12 Gweru City, Zimbabwe. Environ Monit Assess 194(7):1–15
Askarian M, Heidarpoor P, Assadian OA (2010) Total quality management approach to healthcare waste management in Namazi Hospital, Iran. Waste Manag 30(11):2321–2326
Udofia EA, Niragy J (2013) Healthcare waste in Africa: a silent Crisis? Glob Health Perspex 1(1):3–10
Udofia EA, Fobil JN, Gulis G (2015) Solid waste management in Africa. Afr J of Environ Sci Technol 9(3):244–254
Ali M, Wang W, Chaudhry N, Geng Y (2017) Hospital waste management in developing countries: a mini review. Waste Manag Res 34:87–90
Haji JJ, Subramanian A, Kumar P, Ramanathan K, Rajamani A (2020) State of personal protective equipment practice in lndian intensive care units amidst covid-19 pandemic: a nationwide survey. Ind J Crit Care Med 24:409–816
Rodriguez-Morales A (2013) Current topics in public health. InTech, Rijeka
Book Google Scholar
Yves Chartier JE, Pieper U, Prüss A, Rushbrook P, Stringer R, Townend W, Wilburn S, Zghondi R (2014) Safe management of wastes from health-care activities. World Health Organization (WHO)
Ramteke S, Sahu BL (2020) Novel coronavirus disease 2019 (Covid 19) pandemic: considerations for the biomedical waste sector in India. Case Stud Chem Environ Eng 2:100029
Wei G, Manyu L (2020) The hidden risks of medical waste and the COVID-19 pandemic. https://www.waste360.com/medical-waste/hidden-risks-medical-waste-and-covid-19-pandemic . Accessed 1 June 2022
World Health Organisation (2020b) Water, sanitation, hygiene, and waste management for the COVID-19 virus: in- terim guidance, World Health Organization. https://www.who.int/publications-de-tail/water-sanitation-hygiene-and-waste-management-for-covid-19
Das S, Lee SH, Kumar P, Kim KH, Lee SS (2019) Solid waste management: scope and the challenge of sustainability. J Clean Prod 228:658–678
Vivek JM, Singh R, Sutar RS, Asolekar SR (2019) Characterisation and disposal of ashes from biomedical waste incinerator. Advances in waste management. Springer, Singapore, pp 421–435
Mathur P, Patan S, Shobhawat AS (2012) Need of biomedical waste management system in hospitals-an emerging issue-a review. Curr World Environ 7(1):117
Star TD (2020) Poor medical waste management will increase infections. The Daily, Star. https://www.thedailystar.net./editorial/news
Mangizvo RV, Chinamasa R (2008) Solid medical waste management: the case of Kwekwe City in Midlands Province, Zimbabwe. J Sustain Dev Afr 10:3
Mulukuen A, Haimot G, Mesafint M (2013) Healthcare waste management practises among healthcare facilities of Gonder town, Northwest Ethiopia. Health Sci J 7(3):135–326
Omwoma S, Lalah JO, Kueppers S (2017) Technological tools for sustainable development in developing countries: the example of Africa, a review. Sustain Chem Pharm 6:67–81
Adelodun B, Ajibade FO, Ibrahim RG, Ighalo JO, Bakare HO, Kumar P, Choi KS (2021) Insights into hazardous solid waste generation during COVID-19 pandemic and sustainable management approaches for developing countries. J Mater Cycles Waste Manag 23(6):2077–2086
Saad SA (2013) Management of hospital solid waste in Khartoum state. Environ Monit Assess 185(10):8567–8582
Makwara E, Magudu S (2013) Gambling with people’s health and lives: urban solid waste management in Zimbabwe. Eur J Sustain Dev 2:67–98
Mandevere B (2015) An investigation into effectiveness of household solid waste management strategies in Harare, Zimbabwe. Published Dissertation. MSc in Environmental Management. Faculty of Environmental Management. University of South Africa, Pretoria, South Africa.
Torkashvard J, Pasari H, Jonidi-jafari A, Kermani M, Nasri O, Farzadkia M (2020) Medical waste management in Iran and comparison with neighbouring countries. Int J Environ Anal Chem 13:1–4
United Nations Development Programme (2020) Zimbabwe Country profile: healthcare waste management (HCWM) in the context of covid-19 September 2020. http://www.api.savinglivesustainably.org/documents/file/9b12951086321300c7d0721508217dd9/full/hash . Accessed 10 June 2022
Nhubu T, Muzenda E, Mbowa C, Agbenyuku E (2020) Sustainability context analysis of municipal solid waste management in Harare, Zimbabwe. Population 828:1–896
Nhubu T, Muzenda E, Muhamed B, Charles M (2021) Assessment of municipal solid waste transfer stations suitability in Harare, Zimbabwe. Adv Sci Technol Eng Syst J 6(2):1002–1012
Taru P, Kuvarega AT (2005) Solid medical waste management, the Case of Parirenyatwa Hospital, Zimbabwe. Rev Biomed 16(3):153–158
EMA (2007) Environmental management agency (hazardous waste management) regulations, 2007, statutory instrument (SI) 10 of 2007. Environmental Management Agency 2007, Harare, pp 1–68
Zimbabwe’s National Climate Change Response Strategy (2015). http://www4.unfccc.int/sites/nama/_layouts/UN/FCCC/NAMA/Download.aspx?ListName=NAMA&Id=165&FileName=Climate%20Change%20Response%20Strategy.pdf . Accessed 1 June 2022
World Bank Open Data (2021). https://data.worldbank.org . Accessed 18 May 2022
Bradley K, Ingham K (2020) Zimbabwe. Encyclopedia britannica. https://www.britannica.com/place/Zimbabwe .
Mugandani R, Wuta M, Makarau A, Chipindu B (2012) Re-classification of agro-ecological regions of Zimbabwe inconformity with climate variability and change. Afr Crop Sci J 20(2):361–369
Manyeruke C, Hamauswa S, Mhandara L (2013) The effects of climate change and variability on food security in Zimbabwe: a socio-economic and political analysis. Int J Humanit Soc Sci Vol. 3 No. 6. http://www.ijhssnet.com/journals/
Brazier A (2017) Climate change in Zimbabwe. A guide for planners and decision-makers. Konrad-Adenauer-Stiftung
Chirisa I, Nyamadzawo L, Bandauko E, Mutsindikwa N (2015) The 2008/2009 cholera outbreak in Harare, Zimbabwe: case of failure in urban environmental health and planning. Rev Environ Health 30(2):117–124
Chigudu S (2020) The political life of an epidemic: cholera, crisis, and citizenship in Zimbabwe. Cambridge University Press
Banya N (2018) Zimbabwe’s health delivery system. ZimFact. Retrieved 21 June 2022.
Nyatsanza T, Kudzai NS (2016) The usefulness of including women in household solid waste management. a case study of Dzivaresekwa high density suburb, Harare. Int J Soc Sci 21(3):92–108
Jerie S (2012) Occupational health and problems among workers in wood processing industries in Mutare, Zimbabwe. J Emerg Trends Econ Manag Sci 3(3):278–285
Sinthumule NI, Mkumbuzi SH (2019) Participation in community-based solid waste management in Nkulumane suburb, Bulawayo, Zimbabwe. Resources 8(1):30–46. https://doi.org/10.3390/resources8010030
Rahman MM, Bodrud-Doza M, Griffiths MD, Mamun MA (2020) Biomedical waste amid covid-19: perspectives from Bangladesh. Lancet Glob Health 8:E1262
Jerie S, Musasa T (2022) Solid waste management and the covid 19 pandemic lockdown in Zvishavane town, Zimbabwe. Ethiop J Environ Stud Manag 15(3):323–334
Medicines Control Authority of Zimbabwe (2020) Pharmacy guidelines for investigational medical products. Available at: https://www.mcaz.co.zw/index.php/downloads/category/15-guidelines?Download=319:pharmacy-guidelines-for-investigat-ional-medical-products .
Nyakatswau ST, Bangure D, Pierre G, Nyika H (2022) Disposal of medical waste: a legal perspective in Zimbabwe. Int J Community Med Public Health 9:2331–2333
Ansari M, Ehrampoush MH, Farzadkia M, Ahmadi O (2019) Dynamic assessment of economic and environmental performance index and generation, composition, environmental and human health risks of hospital solid waste in developing countries a state of that art of review. Environ Int 132(2019):105073
Kalogianndou K, Nikolakopoulou E, Komilis D (2018) Generation and composition of waste from medical histopathology laboratories. Waste Manag 79:435–442
Jerie S (2016) Occupational risks associated with solid waste management in the informal sector of Gweru, Zimbabwe. J Environ Public Health. https://doi.org/10.1155/902460
Nhubu T, Muzenda E (2019) Determination of the least impactful municipal solid waste management option in Harare, Zimbabwe. Processes 7:785–807
Nhubu T, Muzenda E, Mbohwa C (2019b) Impacts of waste management practices on waste resources in Harare. paper presented at the wastes: solutions, treatments and opportunities III: selected papers from the 5th international conference wastes 2019, Lisbon, Portugal, 4–6 September 2019.
World Health Organisation (2014) Safe management of wastes from healthcare activities, 2nd edn. Geneva, pp 5–6
Zimbabwe Ministry of Health (2013) National infection prevention and control guidelines. Ministry of Health and Child Care
Mahamba C (2015) Characterisation and management of non-formal solid waste management disposal sites in Harare, Zimbabwe. Published Dissertation. MSc in environmental management. Faculty of Environmental Management. University of South Africa, Pretoria, South Africa.
Makarichi L, Ka R, Jutidamrongphan W, Techato K (2018) Suitability of municipal solid waste in African cities for thermochemical wasteto-energy conversion: the case of Harare Metropolitan City, Zimbabwe. Waste Manag Res 37(1):83–94
Kwenda PR, Gareth L, Sibel E, Bas VR (2022) A mini-review on household solid waste management systems in low-income developing countries: a case study of urban Harare City, Zimbabwe. Waste Manag Res 40(2):139–153
Haregu TN, Ziraba AK, Aboderin I, Amugsi D, Muindi K, Mberu B (2017) An assessment of the evolution of Kenya’s solid waste management policies and their implementation in Nairobi and Mombasa: analysis of policies and practices. Environ Urban 29(2):515–532
Tanyanyiwa VI (2015) Not in my backyard (NIMBY)?: the accumulation of solid waste in the avenues area, Harare, Zimbabwe. Int J Innov Res Dev 4(2):122–128
Mandevere B, Jerie S (2018) Household solid waste management: how effective are the strategies used in Harare Zimbabwe. J Environ Waste Manag Recycl 2(1):29–35
Chikobvu D, Makarati F (2011) The challenges of solid waste disposal in rapidly urbanizing cities: a case of highfiel-d suburb in Harare, Zimbabwe. J Sustain Dev Afr 13:184–199
Ferreira AP, Veiga MM (2003) Hospital waste operational procedures: a case study in Brazil. Waste Manage Res 21(4):377–382
Rana R, Ganguly R, Kumar Gupta A (2017) Evaluation of solid waste management in satellite Towns of Mohali and Panchkula-India. J Solid Waste Technol Manag 43(4):280–294
Mafume N, Zendera W, Mutetwa M (2016) Challenges of solid waste management in Zimbabwe: a case study of Sakubva high density suburb. J Environ Waste Manag 3:142–155
Jerie S, Zulu S (2017) Site suitability analysis for solid waste landfill site location using geographic information systems and remote sensing. A case study of Banket Town Board. Zimbabwe. Rev Social 2:19–31
Chapungu L, Zinhiva H, Marange E (2015) Assessment of domestic solid waste management systems in rural district services centres: the case of Ngangu residential area in Chimanimani District, Zimbabwe. J Solid Waste Technol Manag 41:96–105
Munyai O, Nunu WN (2020) Health effects associated with proximity to waste collection points in Beitbridge Municipality, Zimbabwe. Waste Manage 105:501–510
Federation of Red Cross and Red Crescent (2010) Zimbabwe: cholera emergency appeal. Retrieved from: http://reliefweb.int/node/345114
Chanza N, Gundu-Jakarasi V (2020) Deciphering the climate change conundrum in Zimbabwe: an exposition. Global warming and climate change. IntechOpen
Heera S, Rajor A (2014) Bacterial treatment and metal characterization of biomedical waste ash. J Waste Manag. https://doi.org/10.1155/2014/956316
Luo H, Cheng Y, He D, Yang EH (2019) Review of leaching behavior of municipal solid waste incineration (MSWI) ash. Sci Total Environ 668:90–103
Shi P, Schulin R (2018) Erosion-induced losses of carbon, nitrogen, phosphorus and heavy metals from agricultural soils of contrasting organic matter management. Sci Total Environ 618:210–218. https://doi.org/10.1016/j.scitotenv.2017.11.060
Chatsiwa J (2015) Land pollution and population density: the case of Kwekwe City residential areas, Zimbabwe (Doctoral dissertation).
World Health Organisation (2018) Healthcare waste. Available at https.// www.who.int/news/room/factsheets/detail/healthcare waste. Accessed 15 July 2022.
Nyoni M (2020) Covid 19: the huge threat to Zimbabwe’s economy. Available at https://www.thestandard.co.zw/202.covid-19-huge-threatzimbabwes-economy .
Chikombe S (2017) Occupational safety and health hazards associated with solid waste management in Bindura, Zimbabwe. Masters Thesis. Midlands State University. Available at http://www.ir.msu.ac.zw:8080/jspui/bitstream/11408/2993/1/FINAL%20DISSERTATION%20SHUVAI%20C
Njaya T (2016) An evaluation of income disparities between male and female street vendors of Harare in Zimbabwe. J Study Soc Sci Humanit 2:106–114
Nemadire S, Mapurazi S, Nyamadzawo G (2017) Formalising informal solid waste recycling at the Pomona dumpsite in Harare, Zimbabwe. Nat Res Forum 41:176–178
Ghafuri Y, Shiri R, Jafari NA, Izanloo H (2020) Risk characterization and quantification of medical waste in Qom Province. J Environ Treat Tech 8(2):634–638
United Nations General Assembly (2015) Transforming our world: the 2030 agenda for sustainable development. United Nations; 2015. http://www.un.org/ga/ .
Zimbabwean Government (2018) Statutory instrument. 268 of 2018. Harare: government printer. Available at https://www.ema.co.zw/index.php/agency/downloads/file/Statutory%20Instruments/S.%20I.%20268%20of%202018%20Environmental%20Management%20Hazardous%20Sub.pdf . Accessed 7 July 2022.
Zimbabwean Government (2013) Constitution of Zimbabwe, No. 20 of 2013. Harare: Government Printer. Available at: https://www.parlzim.gov.zw/component/k2/download/1290_da9279a81557040d47c3a2c27012f6e . Accessed 1 July 2022. Management issues in Beitbridge border town: evidence from a participatory research.
de Gobbi M (2020) Environmental integrity and doing business in Zimbabwe challenges and engagement of sustainable enterprises. Proc Environ Sci 35:176–184. https://doi.org/10.1016/j.proenv.2016.07.073
Ministry of Local Government and Public Works (2021) Section 229 of the Urban Council Act Chapter 29:15
Zimbabwean Government (1996) Factories and works act (Chap 14:08). Government Printer. Available at: https://www.nssa.org.zw/uncategorized/factories-works-act-ensures-workers-safety/ . Accessed 1 July 2022.
Moen R, Norman C (2009) Evolution of the PDCA cycle (PDF). Westga.edu. Paper delivered to the Asian Network for Quality Conference in Tokyo on September 17, 2009. Retrieved 14 June 2022 .
Dubberly H (2008) [2004]. How do you design? A compendium of models. Dubberly.com. Retrieved 21 Dec 2017
Download references
Author information
Authors and affiliations.
Department of Geography, Environmental Sustainability and Resilience Building, Midlands State University, P. Bag 9055, Gweru, Zimbabwe
Shabani Takunda & Jerie Steven
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Shabani Takunda .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Takunda, S., Steven, J. Medical solid waste management status in Zimbabwe. J Mater Cycles Waste Manag 25 , 717–732 (2023). https://doi.org/10.1007/s10163-022-01578-4
Download citation
Received : 05 August 2022
Accepted : 13 December 2022
Published : 12 January 2023
Issue Date : March 2023
DOI : https://doi.org/10.1007/s10163-022-01578-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical solid waste
- Medical solid waste management practices
- Environmental health risks
- Find a journal
- Publish with us
- Track your research
Sustainable Medical Waste Management
Sustainable management of medical waste is one of the major concerns that the Ministry of Health of Viet Nam and hospitals are trying to deal with. Most medical wastes are unique and cannot be disposed of in the same manner as normal wastes. They are infectious and can also cause serious physical injuries if they are not properly disposed of.
The paper looks at the current strategies used by public hospitals in Viet Nam to manage medical wastes. It discusses the strategies used at the local level (public hospitals) to ensure that medical wastes do not pose any significant threat to the public. Issues such as waste segregation at the hospitals and different ways of disposing of different types of wastes are explored.
The study also looks at the level of awareness among doctors and nurses on sustainable management of medical wastes, based on the assertion made in the literature that one of the only ways of achieving success in sustainable medical waste efforts is to ensure that all doctor and nurses are involved and are empowered to dispose of medical wastes responsibly. The study finally looks at what can be done to promote sustainable medical waste management in Viet Nam. It provides several recommendations that could be implemented at the hospital level and at the national level to enhance sustainable waste management.
Introduction
The definition of sustainable development as “meeting the needs of the present without compromising the ability of future generations to meet their needs” was first put forth by Brundtland (1987) in the report ‘Our Common Future’. The report introduced the three fundamental components of sustainability as environment, economy and society and the need to balance the three of them in decision making, whilst also emphasising both intra-generational and inter-generational justice.
More recently, work around the planetary boundaries (Steffen et al. 2015) has reinforced the idea of environmental limits to growth, whilst the work of Raworth (2012) on “doughnut economics” has sought to reintegrate the importance of a ‘social floor’ to complement the concept of the ‘environmental ceiling’, aiming to generate both a “safe and just operating space for humanity.”
The pursuit of sustainable development is intimately connected to health issues. Much of the discussion has focused on the relationship between environmental pollution and public health. Early in the 1990s, Agenda 21 of the United Nations Conference on Environment and Development in Rio de Janeiro (UNCED 1992) defined reducing health risks from environmental pollution and hazards as one of the top concerns of the global community.
The Sustainable Development Commission (2010) emphasized the importance of “a focus on the environmental determinants of health and health inequalities, especially the effects of climate change”. More recently, health and well-being are perceived as integral to the achievement of Sustainable Development Goals launched in 2015, with Goal 3 explicitly aiming: to ensure healthy lives and promote the well-being for all at all ages.
There are multiple dimensions to the relationship between sustainable development and (public) health (Abdula, Qdais, & Rabi 2008). Besides the link between health and environmental quality, health care infrastructure itself has environmental impacts (Wilburn 2007). One could research carbon footprint, energy consumption, or water consumption of health care facilities, to name but a few areas (Abd El-Salam 2010).
This thesis focuses on one specific aspect: the current practices in the management of medical waste versus the required sustainable waste management paradigm. According to Pruss, Giroult, and Rushbrook (1999), poor medical waste management is linked with threats to the environment and human health.
Proper segregation, collection, storage treatment and disposal are important steps that take place at hospitals and under the scope of influence of health care workers (DARA 2010). Therefore, the daily practices of health care workers’ are important contributions to sustainable medical waste management and indeed to the sustainable development of a country’s health care system in general.
Much of the existing literature focuses on the medical waste management practices in the context of the developed world with a smaller number of articles exploring what sustainable medical waste management looks like in a developing country context (Ananth, Prashanthini, & Visvanathan 2010). This dissertation uses Viet Nam as the research context, based on a case study of the two major public hospitals, to identify the key actions for moving towards more sustainable medical waste management practice in the health care sector.
The purpose of this introductory chapter is to make the case for examining sustainable medical waste management in the Vietnamese health care context, with a specific focus on the role of healthcare workers, especially doctors and nurses.
Definition of Terms
Medical waste and classification.
The terms ‘clinical waste’, ‘medical waste’, ‘hospital waste’ and ‘health care waste’ are often used interchangeably in both academic studies and a policy/regulatory context.
Clinical waste is defined broadly by Controlled Waste Regulations (2012) as “any waste which consists wholly or partly of human or animal, drugs or other pharmaceutical products, swabs or dressings, syringes, needles or other sharp instruments; and any other waste arising from medical, nursing, dental, veterinary, pharmaceutical or similar practice, investigation, treatment, care, teaching or research, or the collection of blood for transfusion, being waste which may cause infection to any person coming into contact with it”.
Therefore, clinical waste can be divided into three broad groups of materials: a) any healthcare waste which poses a risk of infection; b) certain healthcare wastes which pose a chemical hazard; c) medicines and medicinally-contaminated waste containing a pharmaceutically-active agent (Dutta & Das 2010).
The World Health Organization (WHO) (2014) defined ‘health care waste’ as all waste generated within health-care facilities, research centres and laboratories related to medical procedures. Between 75% and 90% of the waste produced by health-care facilities is non-hazardous or general health-care waste, and only 10% to 25% of health-care waste has a hazard that requires careful management (AQI 2015).
The distinct categories of health-care waste are sharps, infectious waste, pathological waste, pharmaceutical (including cytotoxic) waste, hazardous chemical waste, radioactive waste and non-hazardous general waste (EPA 2009). Infectious waste can be further classified as wastes contaminated with blood or other body fluids, cultures and stocks, and waste from isolation wards. Hazardous chemical waste includes halogenated and non-halogenated solvents, disinfectants, toxic metals such as mercury, and other organic and inorganic chemicals.”
Directive 43 of the Ministry of Health of Viet Nam (2007) defines ‘medical waste’ as ‘materials in solid, liquid or gaseous form, discharged from medical establishments, including hazardous medical wastes and ordinary/general medical wastes’.
Hazardous waste is waste that contains “elements hazardous to human health and environment such as contagiousness, intoxication, radiation, flammability, explosiveness, corrosiveness or other hazardous characters if these wastes are not safely destroyed”. This is the definition that will be used in this study. Medical wastes are classified into 5 groups: a) infectious wastes; b) hazardous chemical wastes; c) radioactive wastes; d) pressure container; e) general (ordinary) wastes.
Management of medical waste
The process of medical waste management in hospitals includes several interrelated steps: segregation, collection, storage, transportation, treatment and disposal (Pruss, Giroult, & Rushbrook,1999).
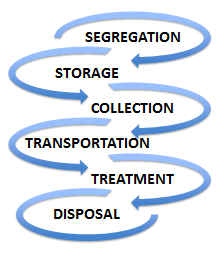
In these identified steps, segregation (to separate the waste into designated categories) is considered the most important step. Segregating potentially infectious material from clean waste at the point of generation may reduce both volume and cost (General Statistics Office of Viet Nam 2015). Improper segregation will lead to implications for public and environment health. Furthermore, infectious and hazardous wastes are subjected to special treatment (incineration, autoclave), which is very expensive before disposal. Autoclave, also known as steam sterilization, has been used for a long time in the medical sector.
Reduce, Reuse and Recycle
The 3Rs principle of reducing, recycling and recovery – also known as the ‘waste hierarchy’ – has been widely adopted since its articulation in 1995 (GFDRR 2011). The basic premise is that of reducing the amount of waste generated whenever and wherever possible. If a reduction is not practical, consideration should be given to re-use. Recovery is the final option if neither reduction nor reuse is practical (Jiang 2006). Currently, 3Rs has been accepted as Reduce, Reuse and Recycle.
Statement of the Problem
Viet Nam has experienced a dramatic increase in the amount of medical waste generated over the last 20 years, especially hazardous waste, due to the rise of complicated diseases in a growing population (International Conference on the Development of Biomedical Engineering 2015). When it comes to surveying Vietnamese medical waste collection, recycling, treatment and disposal, performance varies according to geography and type of healthcare facility.
Geographically, cities and urban centres with high populations tend to generate more wastes than rural and sparsely populated locations (Lye 2010). In terms of healthcare facilities, large referral hospitals tend to generate more medical wastes than small clinics, due to both handling more patients and also engaging in complex medical procedures that produce more wastes.
In terms of waste collection, according to the Ministry of Health of Viet Nam, in 2006, only 50 per cent of hospitals met the Ministry’s requirements around waste collection and segregation (Hoang 2009). According to a project by the Ministry of Health and the WHO (World Health Organization) in 2009 (MONRE 2011), it is estimated that more than 25% of medical waste can be recycled.
Most recycling activities, however, take place outside hospitals and under the management of contracted waste management companies. In 2003, a study by Cheremisinoff (2003) showed that only 5% of these wastes are recycled. The study attributes responsibility to various stakeholders, especially the government, for failing to come up with initiatives for recycling medical wastes.
In terms of waste treatment, current medical waste treatment facilities are not equipped with advanced technologies due to the limited state budget allocated. Whilst there is 71 per cent of public hospitals at the central level with wastewater treatment systems compared with 85 per cent in private hospitals, only 46 per cent have such facilities at the provincial level and 30 per cent at district level (Hoang 2009).
There is no single treatment or disposal method used for the various types of medical waste in Viet Nam (Kagonji & Manyele 2011). Common methods are incineration, landfilling, burning, autoclaving and chemical treatment (WHO 2014). Traditional waste treatment by incineration is still widely used for infectious medical waste. In Hanoi and Ho Chi Minh cities, hospitals have signed contracts with the third-party companies and medical waste is treated at centralized facilities using the incineration method (Hassan et al. 2008).
In other cities and provinces, hospitals are still using their incinerators. It is reported that the majority of hospital incinerators lack an air treatment system and the outdoor operating system also leads to environmental pollution (Hoang 2009). The Vietnamese Ministry of Natural Resources and the Environment (MONRE 2011) reported that only 50 per cent of the total incinerators in key cities are operating well, and as low as 20 per cent in other provinces.
Such issues have caused the Vietnamese MONRE to conclude that only 68 per cent of hazardous medical waste is properly treated, which presents a significant challenge for the goal of environment protection (MONRE 2011; p.92).
Furthermore, despite the efforts of the Government towards sustainable management of medical waste, multiple cases of poor handling, inappropriate treatment and disposal, and even waste being left completely untreated are still reported (Hutchins & White 2008). In 2015, a private hospital in Viet Nam was fined for illegally dumping 63 tons of untreated medical waste (Thanhnien NEWS 2015).
Recently, the largest and most prestigious public hospital in Viet Nam was blamed for wrong recycling activities of the hazardous waste, against the current regulations on medical waste management (Vietnamnet 2016). The Ministry of Health has come up with a legal and regulatory framework that guides how individual hospitals, both public and private, should manage their medical wastes.
Bolay, Hostettler, and Hazboun (2014), based on the study they conducted in Switzerland, say that the policies require hospitals to classify and segregate their wastes based on their impacts on the environment and ability to recycle them.
Bdour and Hadadin (2007), in their study conducted in Jordan, argue that policies also outline how hazardous medical wastes should be destroyed sustainably without posing any threat to the environment, people, plants, and animals. It is important to note that besides these government regulations, individual hospitals have their own internal medical waste management policies. However, their policies must conform to the policies set by the Ministry of Health.
Purpose of the Study
As the Literature Review will go on to explore, sustainable medical waste management involves, not only employing proper segregation, collection, transportation and disposal but also implementing the 3Rs of Reduce, Reuse and Recycle (Nihon 1999).
In a healthcare context, implementing ‘3Rs’ strategies needs to involve both the leadership provided by those in management positions and commitment to sustainable medical waste management amongst health care workers, especially doctors and nurses (Jiang 2006). This thesis argues that lack of such leadership and commitment could lead to increasing the amount of medical waste, non-compliant treatment, and therefore threats to the environment and public health.
Research Objectives and Questions
The following are the objectives of this study.
- To come up with effective sustainable waste management policies and practices that can be applied in Vietnamese hospitals
- To increase awareness among the stakeholders in the healthcare sector – specifically healthcare workers – on how to manage medical wastes using the 3Rs strategy.
- To achieve the above research objectives, the following questions were proposed to collect the relevant data.
- What are the current strategies used by the healthcare institutions in Viet Nam in managing medical wastes?
- What is the level of awareness among the stakeholders – specifically healthcare workers – on sustainable management of medical wastes?
- What are the barriers to implementing 3Rs strategies and what can be done to promote sustainable medical waste management in Viet Nam?
This research focused on two key public hospitals in two of the largest cities in Viet Nam based on population: one in Hanoi (in the North) and another in HoChiMinh city (in the South). Hanoi is the Vietnamese capital with a population of 7,096 million and HoChiMinh city has a population of 7,982 million, with the total population of the country as 90,700 million (General Statistics Office of Viet Nam 2015).

Significance of the Study
The recommendations from the study will be shared with those hospitals involved in the study, and the Ministry of Health of Viet Nam. It is hoped that the findings will enable the hospitals to address any identified gaps in daily practice in terms of implementing medical waste management policy. It is also hoped that, through examining the factors influencing the successful deployment of 3Rs strategy in other countries, this might be applied to the Vietnamese context to inform medical waste management, to contribute to the sustainable development of the country.
Literature Review
Sustainable medical waste management is an issue that has attracted the attention of many scholars and environmentalists who have conducted extensive research to find out the best approaches that can be used to manage different types of waste. The concept of sustainable medical waste management is becoming increasingly important in modern society.
As such, it has become necessary to develop better ways of managing these wastes (Blenkharn 2006). According to Sattler and Hall (2008), medical wastes are the most dangerous waste substances and if not disposed of properly, they may pose serious environmental problems. In Viet Nam, just like in many other countries around the world, medical wastes have increased significantly over the past three decades and managing these wastes is becoming an issue (Pariatamby & Tanaka 2013).
Substances such as syringe needles that were re-used after sterilization two decades ago are currently not re-usable because of fear of transfer of diseases such as Human Immunodeficiency Virus (HIV) (Birpinar, Bilgili, Erdogan 2009). The number of people seeking medical attention has also increased significantly due to the emergence of various lifestyle diseases (Ketlogetswe 2004). These are some of the reasons that have made it necessary for researchers to give serious attention to this topic.
As Visvanathan (2006) notes, for every research project, it is important to generate information that will enrich the existing bodies of knowledge. To ensure that the researcher does not duplicate the existing published information, the study first focused on a review of the literature before identifying key research questions and collecting the primary data. The review is important to understand what other scholars have found out in this topic and therefore identify potential research gaps that need further study.
Medical Waste Generation – A Geographical Overview
The health care industry is one of the largest producers of waste due to diagnostic, experimental activities and therapeutic methods (Diaz et al. 2008). As institutions that operate throughout the year, hospitals produce considerably large quantities of waste. The characteristics of medical waste are generally similar in all countries, but the amounts generated are different. This difference depends on variations in regulations and economic status between countries (Pruss, Giroult, &Rushbrook1999; Sakaguchi 2001).
Even within a country, generation of medical waste differs by geography, hospital level, and the departments in each hospital. It also depends on the types of health care service, the amount of disposable or reusable medical devices, and the regulations and policies governing medical waste management (Cesaro & Belgiorno 2015). For example, in a Vietnamese survey conducted in 24 hospitals, the intensive care unit, obstetric and surgical departments generated the largest amount of waste because of the nature of activities undertaken (Hoang 2009). The figure shown below is a comparison of medical waste generation from a global perspective.
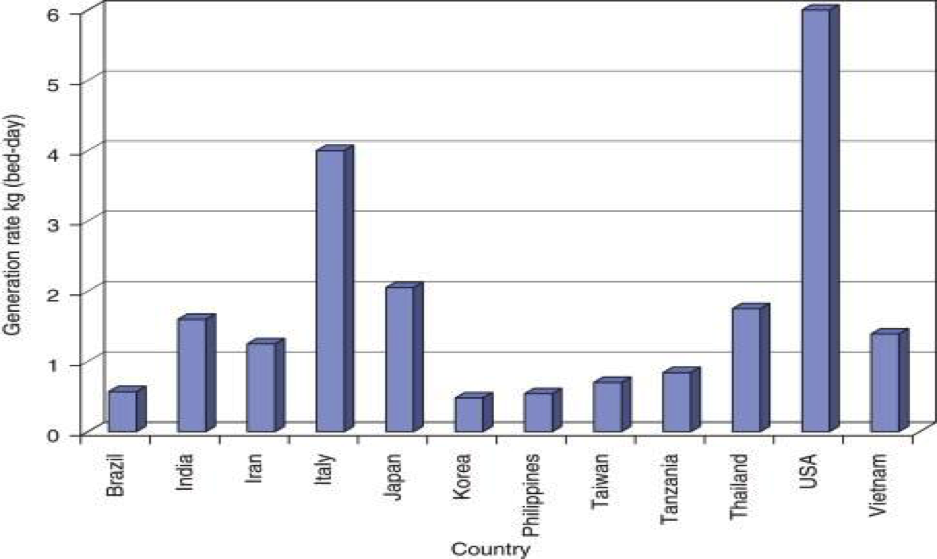
The information in the graph above shows that the developed countries produce the largest amount of medical wastes. The United States produces the highest amount of medical wastes in the world. As Sakaguchi (2001) notes, most Americans get regular medical check-up even in cases where they do not have a specific medical problem. Japan and Italy also produce significant amounts of medical wastes (Mbongwe, Mmereki, & Magashula 2008). China and India, because of the massive size of their population, also have a considerable amount of medical waste that need sustainable management.
The graph below provides further details in exploring medical waste generation in a section of Asian countries.
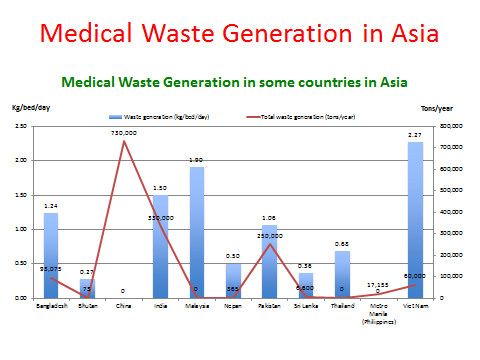
The graph above shows that different countries produce different amounts of medical wastes based on their population size and other demographic factors. According to Visvanathan (2006), across Asia, Viet Nam had the highest amount of waste generation (2.27kg/bed/day).
In 2011, Jang noted that Viet Nam is still one of the countries with a high generation rate of medical waste (higher than the Philippines, Taiwan, Korea, and Tanzania). This is attributed to several factors, including a growing population, increasing number of patients, changing lifestyle, and the increase of using disposal medical devices and access to medication, aligned with the growth of health care facilities annually (MONRE 2011; Mbongwe et al. 2008).
According to Sakaguchi (2001), in the late twentieth century, the government of Viet Nam focused on improving the healthcare system in the country. The increasing level of education in the country has also improved awareness about various diseases that has encouraged many people to take advantage of medical procedures to prevent these diseases. According to Le (2014), life expectancy in the country has improved significantly.
The Vietnamese Context
According to the Ministry of Health of Viet Nam, in October 2007, there were 1,087 hospitals with 140,000 beds in Viet Nam (1,023 public hospitals and 64 private hospitals) (Hoang 2009). In 2012, there were 1,250 hospitals (1,095 public hospitals and 155 private hospitals) (Ministry of Health 2013). The most recent figure from the Viet Nam Health and Environment Management Agency is 1411 hospitals nationwide (VIHEMA 2015a).
It is estimated that the daily amount of medical waste generated from Vietnamese hospitals alone is 450 tons of solid waste in 2015, comprising approximately 47 tons of hazardous solid waste (VIHEMA 2015b). It costs more than 500 billion Viet Nam dong (25 million USD)/year) to treat that waste and hospitals have to bear this cost without a separate fund allocated from the state budget.
The medical service fee charged does not cover the fee either (Mejia & Sattler 2009). This is a major challenge for the health care system in Viet Nam. Another issue is the number of patients served daily. It is obvious that a high number of patients served per day will lead to a higher amount of medical waste generated (Manyele & Lyasenga 2010). The World Bank estimates that it needs 500 million USD to develop the appropriate medical waste treatment system infrastructure (VIHEMA 2015b). The table below shows the amount of medical waste generated in Vietnamese hospitals.
Table 1: The amount of medical waste generated in Viet Nam (MONRE 2011)
Risks Associated with Medical Waste
Public injury and infection.
Bokhoree et al. (2014) indicate that whilst the amount of medical waste can be quite small versus the amount of total waste generated in a community, it poses more serious risks to human health in direct and indirect ways. Individuals like medical staff, patients, workers in waste disposal facilities and the general public are at risk of being injured or infected if exposed to infectious/hazardous waste, largely because physical injuries caused by discarded sharps may directly contribute to the transmission of microbial infectious agents.
According to the Pruss, Giroult, and Rushbrook (1999), human immunodeficiency virus (HIV), and hepatitis viruses B and C can be transmitted via healthcare waste. The WHO (2002) estimates that over the past ten years, there have been over 20 million infections of Hepatitis B, C and HIV globally associated with reuse of syringes and needles in the absence of sterilization. Additionally, the sale of recovered drugs also poses a risk to public health (WHO 2002).
Salkin (2004) confirms that health care waste contains hazardous components which pose physical, chemical, radiological and/or microbiological risks to occupational and public health, and needs to be treated properly before disposal. Furthermore, amongst the health care waste, hospital waste (10-25%) has a higher potential for injury, infection and environmental pollution, and when mixed with other waste sources, it can lead to the entire bulk of the waste becoming infectious (Bryman & Bell 2011).
Mato and Kassenga (1997) indicate that diarrhoea, leptospirosis, typhoid and cholera can be transmitted through untreated medical waste. The Viet Nam Health and Environment Management Agency and the Ministry of Health (VIHEMA 2015c) have pointed out that the number of broken thermometers (estimated by the UNDP) is 447,588 units /year. This leads to the release of 550kg of mercury/year to the environment (Moreira & Gunther 2013). The mercury poisoning following high-dose exposures leads to neurotoxicity.
Soil and groundwater contamination
There are also several indirect risks posed to the environment when dumping medical waste in uncontrolled areas. Studies have shown that the major effects of medical waste on the environment are water and air pollution (Hoang, 2009). This includes the contamination of soils, especially if the waste is non-biodegradable (Shah & Ranghieri 2012). Wastes that dissolve in water can contaminate groundwater, rendering such waters unfit for human and animal use (Hoang 2009). Foster (1996) argues that the real environmental impact is groundwater contamination, which affects drinking water supply.
Emissions from incineration
The two primary ways of treating medical waste are disposed to landfill (not applying to infectious medical waste) and incineration. Incineration, also known as thermal treatment, is defined by Le (2014, p. 56) as “a waste treatment process that involves the combustion of organic substances contained in waste materials.” The method is mainly used in treating combustible wastes that may pose a serious hazard if not properly disposed of (WHO 2014).
A proportion of medical waste is general waste and is incinerated together with the other wastes in the incinerators. Johnke (2000) confirms that the generation of climate-relevant emissions from the incineration of municipal waste is CO 2 (carbon dioxide), N 2 O (nitrous oxide), NOx (oxides of nitrogen), NH 3 (ammonia) and organic carbon. Abor (2007) points out that incineration of medical waste, in a South African context, has been associated with many health problems such as disruptive body hormones, the immune and reproductive systems, and cancer.
Dioxin – one of the most toxic substances if is inhaled or digested – can cause cancer through genetic change (EPA, 1997). Le (2014) indicated that incinerators which are used for burning industrial and medical wastes are responsible for dioxin emissions in Viet Nam. The EPA (1997) pointed out approximately 87% of mercury emissions come from combustion sources and if not managed properly may leak into the environment, a problem that is common in the developing countries such as Viet Nam (Carpenter & Hoppszallern 2010).
Given the above potential environmental and health impacts, it is clear that managing medical waste sustainably will reduce the number of pollutants that directly impact on climate change and public health in Viet Nam.
Medical Waste Management Policies and Regulations
Environmental protection became a legal obligation for the health care sector in general, and hospitals in particular (Richardson et al. 2012). Laws, policies, regulations and guidelines have been developed at international, national and hospital levels to establish a legal framework to protect human and environmental health against the risks from medical waste (Van 2015).
One of the common guidelines is colour-coded bins and bags to ensure correct segregation to prevent infection and injuries within and outside hospitals (Chaerul, Tanakab & Shekdarb 2007). The guidelines also provide information about medical waste substances that can be destroyed through incineration and those that require alternative waste management methods. The table below shows the legal documents underpinning medical waste management in Viet Nam.
Table 2: List of medical waste management policies and regulations (Viet Nam Laws)
Table 3: List of government programs on medical waste management (VIHEMA 2015a, p. 45)
It is worth noting that having policies and guidance in place is only part of the picture. Mato and Kassenga (1997) noted that even though a national standard for segregation (to ensure effective treatment) of hospital waste is in place, it is not applied adequately throughout the country. The issue is not a lack of legislation and policies but a lack of commitment to their implementation. The factors influencing this implementation of waste regulations and policies are explored further in the following sections.
Enablers/Drivers for Sustainable Practices in Medical Waste Management
This literature review explored the existing research around the enablers for sustainable medical waste management in a hospital context. Many authors when studying medical waste management have sought to identify the factors enabling the embedding of the 3Rs of Reduce, Reuse, and Recycle in hospital policy and practice around medical waste management (Cheng et al. 2009).
There are, of course, many different dimensions to this topic (Coker 2009). The available waste collection infrastructure, the capital available for investing in treatment infrastructure, and the particular medical products available to the procurement teams are all examples of material issues that will affect medical waste management (Strohschen 2009). This review focuses on the literature that specifically relates to the role of health care workers, and seeks to summarise the key themes emerging, as a basis for testing their application in a Vietnamese context.
Training and education at all levels
Chaerul et al. (2007) observed hospital waste management practices in Indonesia and pointed out that various issues (safety, public health, environmental conservation) are rarely considered by hospital management. The authors gave the example where infectious waste is mixed with municipal solid waste and disposed of in the landfill sites without any treatment before disposal.
Mato and Kassenga (1997) and Askarian, Vakili, and Kabir (2004) in their studies in Iran and Tanzania respectively identified that low awareness regarding the importance and benefit of sustainable hospital waste management was due to a range of actors, including staff unwillingness to participate, lack of motivation, limited training and education. Manyele and Lyasenga (2010) also pointed out the other factors contributed to such poor medical waste management is the involvement of individuals who lack medical knowledge when it comes to medical waste management.
Lee (2002) concluded that to increase recycling of wastes, education of workers and managers, and efforts of the entire hospital staff should be pursued. Tudor et al. (2008) confirmed that sustainable waste management programs should be targeted towards specific departments and involve staff throughout the entire process. There appeared to be a lack of consistency between the national guidance and local practices because the involved stakeholders are not taken through regular training, for example, the definitions of what constitutes clinical waste.
This leads to a situation where people develop their definition and sometimes create confusion when it comes to waste segregation. It shows how important training is and it relates to staff motivation. Richardson et al. (2012) suggested regular training for the nurses, doctors, janitors, and other medical staff who handle wastes in one way or the other. Regular training is meant to ensure that they understand the emerging trends in waste management (Strohschen 2009). The training can help staff have a better understanding of how to segregate clinical wastes.
Engagement and rewards
In the organisations where Richardson et al. (2012) conducted their study trying to understand the behaviour of non-staff stakeholders at a hospital regarding waste management, it was found out that effective and efficient waste segregation was rewarded. This was a good way to keep staff motivated to embrace the good practice, especially as existing staff could be shadowed by new ones and the good habits would be picked up (Kojima & Michida 2013).
Another suggestion emerging from the literature was that institutions could develop policies where each department is rated based on how effective they manage wastes and the department that comes at the top is given some form of reward as a sign that their commitment towards maintaining a clean medical environment is appreciated (Controlled Waste Regulations 2012). This can be done monthly. It was a good way to keep staff motivated to practice well. The approach will promote good practice in medical waste management.
Staff capacity
A study by Nichols et al. (2013) noted that a key factor affecting the ability of health care workers to carry out sustainable medical waste management was a heavy workload, leaving insufficient time “to do something massively different.” (p. 41). Manyele and Lyasenga (2010) argue that effective medical waste management is affected by the number of workers in health facilities.
In Viet Nam, according to the Joint Annual Health Review (2014), the number of health workers reached 7.5 doctors per 10,000 populations, although these are unequally distributed across regions and specialities. In Hanoi and Ho Chi Minh City, it could be 14 doctors per 10,000 population compared with 4-5 in far provinces (Joint Annual Health Review 2014). This imbalance can lead to the migration of patients to public hospitals in Hanoi and Ho Chi Minh City, which then leads to further overloading for the health workers there.
Working environment and infrastructure
Nichols et al. (2013) also noted that a key factor affecting the ability of health care workers to carry out sustainable medical waste management was the lack of space for recycling. When the environment lacks the right equipment such as waste segregation bins and medical waste incineration systems among others, then it may not be easy to manage wastes in an effective manner (Ozbek & Sanin 2004).
These two scholars argue that the management should always be supportive to the junior employees to create an environment where they can positively engage to find solutions to problems affecting their operations. Richardson (2012, p.16) argues that “individuals will change behaviour when it is easy for them to do so.” It means that the working environment should facilitate easy management as well as the removal of waste (Delving 2006). If not, the people who recycle at home may find it difficult to recycle at work.
Green champions
In their study in a county in the south-west of England, Nichols et al. (2013) found that participants identified the importance of understanding sustainability and waste management issues and this information being disseminated by ‘Green Champions’, driven by both environmental and financial points of view (Strohschen 2009).
Green Champions should include sufficient seniority to be respected and provide advice rather than disciplinary actions such as penalizing poor practice. As Kojima and Michida (2013) say, the aim should be to motivate the stakeholders, not through fear, but through a desire to have a sustainable environment that is appropriate for both the staff and patients.
The important role of nurses
Several studies point out the importance of nursing staff in promoting sustainable waste management. Harris et al. (2009) emphasised the important roles that nurses can play to make the hospital an environmentally sustainable setting. Nurses account for the largest number amongst the healthcare professionals in the health care sector and have the best opportunities to promote green initiatives (Nichols et al. 2013).
In daily work, nurses are interacting with the top hospital leaders and other stakeholders like patients, family and friends of the patients, and suppliers, providing them with opportunities to use the nursing process in education and policy efforts to promote going green (Dinkins & Sorrell 2007). Nurses can conduct orientation training for new staff regarding medical waste management and educate the patients. McDermott-Levy (2011) argues that nurses should become members of a hospital green team and influence product selection and appropriate product disposal.
Embedding in legislation, policy and practice
Nichols et al. (2013) concluded that legislation and regulation provide a driver and incentive for positive and sustainable changes in the management of medical waste. Studies have discussed the use of policy and practice interventions that can reduce the volume of wastes in the hospital.
A study by Almuneef and Memish (2003) conducted in Saudi Arabia has shown that a well-formulated waste management plan (written policy, mandatory in-service education, continuous waste audit and cooperation of all staffs) caused a 58% reduction in the amount of infectious waste incinerated which lead to more than 50% cost saving in fuel, labour, and spare parts.
In Richardson’s (2012) study, the participants shared their ideas of change, including ways to improve legislation, procurement, and interaction in terms of best practices. In terms of legislation, the legislators (Government, health care managers) should listen to the frontline staff to enhance receiving right feedbacks aimed at changing legislation (Clover 2009). This helps to ensure that the guidance on recycling of waste is taken into account at the clinical level.
The government of Viet Nam, through the Ministry of Health, Parliament, and other institutions, has developed policies and regulations that should be followed by various stakeholders in the healthcare sector to ensure that there is effective disposal of medical wastes.
According to Coker (2009), there should always be consistency between national guidance and local practices. A study by Richardson et al. (2012) focused on understanding current practices across public and private institutions managing healthcare waste in the U.K., found out that there appeared to be a lack of consistency between the national guidance and local practices because the involved stakeholders are not properly empowered.
Research Gaps
The literature reviewed provided a rich insight into the research topic, in particular identifying a range of potential drivers and enablers in embedding sustainable waste management in a medical context. Many of these studies, however, were conducted in a developed country context. Literature that specifically addresses sustainable medical waste management in Viet Nam are limited and disjointed (Le 2014). As such, further investigation is necessary for this area. Many of the studies above address the policies, plans, training, role-modelling and incentives and infrastructure that may encourage sustainable waste practice (Newswire 2016).
This study will aim, first of all, to examine the applicability of these strategies and practices in a Vietnamese context. Secondly, having identified various enablers and drivers, the research by Nichols et al. (2013) also suggests the need for further investigation about barriers to behavioural change.
This study will look at these barriers and how they might be overcome to foster an environment that is supportive of sustainable medical waste management at various levels. As McDermott-Levy (2011) notes, understanding the nature of change when introducing new policies is very important. In the analysis, the researcher will look at these changes that need to be put into consideration when coming up with new medical waste management.
Research Method
The methodology of this study was determined by the study aim. This chapter describes how the research was conducted including research design, subjects, data collection, limitations and ethical considerations.
Setting up the Study
The author initially contacted the Vice Director of the Viet Nam Health Environment Management Agency (VIHEMA), which is a unit within the Ministry of Health, to get his advice on which public hospitals performed well in medical waste management based on his expertise and supporting data. Following his consultation, the author selected two public hospitals with appropriate access for data collection. These were the ‘National Hospital of Tropical Diseases’ in Hanoi and ‘Thong Nhat hospital’ in Ho Chi Minh City. Both hospitals are under the management of the Ministry of Health.
The National Hospital of Tropical Diseases was developed from the infectious disease department of Bach Mai hospital which was established in1911. As such, it has inherited the Bach Mai’s waste treatment and disposal system. The hospital has 300 beds and 21 departments including 8 clinical departments and 7 subclinical departments. As of Nov 2014, there were 80 doctors and 203 nurses, amongst a total of 363 health care workers. The treatment methods for hazardous solid medical waste are the autoclave (steam sterilization) and micro-wave (sterilization process that is based on the microwave technology). The hospital is unusual in that it does not make use of an incinerator.
Thong Nhat hospital was established in1975. The hospital has 1,000 beds and 43 departments including 24 clinical departments and 10 subclinical departments. As of Nov 2014, there were 262 doctors and 565 nurses, amongst a total of 1,209 health care workers. Whilst it is responsible for collecting waste, the hospital does not treat hazardous waste inside the hospital. The third-party company collects it and is responsible for that treatment.
Research Design
The research design adopted was an exploratory investigation based on a qualitative approach. In the handbook of qualitative research, Denzin and Lincoln (2005, p.3) describe qualitative research as involving “an interpretive naturalistic approach to the world. This means that qualitative researchers study things in their natural settings, attempting to make sense of or interpret phenomena in terms of the meanings people bring to them.”
The qualitative approach was applied following a constructionist ontology and interpretivist epistemology. This recognises that the healthcare workers participating in the study would be constructing their own ‘reality’ of the situation based on their knowledge of the subject and their perception of what they had been doing towards sustainable medical waste management (Bell 2001). It also recognises that the researcher’s role is to interpret through those social constructions (Calabrese 2006).
Qualitative research is a research strategy that usually emphasizes words rather than quantification in the collection and analysis of data (Bryman & Bell 2011, p.386). In this research study, the qualitative approach consisted of twenty interviews with health care workers – doctors and nurses at different management levels – who were involved in medical waste management as a daily practice in two public hospitals in the two largest cities (Hanoi and Ho Chi Minh City) in Viet Nam.
The selection of these two hospitals is explained in section 3.1. The participants were interviewed to establish their current knowledge and awareness of the 3Rs approach to sustainable medical waste management, and the enablers and barriers to practice.
The data collection took place in two weeks of January 2016.The semi-structured interviews had a list of questions to be covered in venues agreed by the participants. An ‘interview guide’ (Goddard 2001) was used, which allows consistency of questioning in interviews whilst providing some freedom to build a better rapport with interviewees (Bouma 2000). Open-ended questions were used to enable the participants to justify their responses (Dunleavy 2003). The participants were briefed that the interviews would be coded to ensure anonymity, to encourage them to speak candidly. They all signed up to this process. Participants were identified in the analysis by a special number and hospital name (Gupta 2002).
Key question themes that were covered include the following:
- What is the level of awareness among the stakeholders on sustainable management of medical wastes?
- What are the barriers that currently exist in seeking to implement 3Rs strategies?
- What can be done to promote sustainable medical waste management in Viet Nam?
The interviews ranged from 20 minutes to 45 minutes. All the interviews were digitally audio-recorded and transcribed. Following the completion of all interviews, the author undertook a process of coding common themes in a spreadsheet, identifying categories from the data, and summarising key themes, using an inductive approach (Brause 2000). The findings were then analysed in light of the original literature review, and effort was made to understand and interpret the behaviour of healthcare workers regarding how they understand the importance of medical waste management, how they prioritise actions, what barriers they perceive, and how it is mobilised within hospitals.
The initial meeting in each hospital was with the Heads of the Nursing Department, during which the objectives of the study were explained. They were then requested to provide a list of doctors and nurses across the various hospital departments. The sampling strategy used in this research was a judgment-based sample approach based on the research question (Hakim 2000).
A snowballing approach was also used, identifying additional interviewees through recommendations from other interview respondents (Hinkel 2011). In both hospitals, hospital staff across different departments were approached, including both doctors and nurses in internal infectious and infection control departments, environmental specialists, and representatives from the management board (the Director or Vice Director of each hospital).
Twenty interviews were felt to represent a saturation point in the collection of data. Saturation is defined as “the point at which no new relevant information is forthcoming, even if more people are interviewed” (Galvin 2015, p.3) to ensure collected data was sufficient for analysis. Hospital documents (hospital guidelines and reports related to hospital waste management) were also analysed.
In this study, the sample included only two different groups of people who were interviewed. The first group of people were the doctors and the second group of people were nurses at the two hospitals that were identified. For the analysis, the researcher used TN to denote participants from the first hospital and ND to denote participants from the second hospital. The table below is a detailed identification of these participants based on their positions at the different hospitals.
Table 4: Sampled participants (developed by the author)
The classification system helped the researcher identify the participants in the study (Cramer 2003), whilst preserving the anonymity of the respondents. According to Andrzej and Buchaman (2007), it is ethical to conceal the identity of the respondents, especially if others can have access to the report. There are cases where people may be victimised because of their views which may contradict that of the majority (Creswell 2009).
In some studies, those in management positions have issued punitive measures if it is perceived that an employee has issued confidential information or maligned the image of the organisation. Protecting the identity of the respondents makes it almost impossible for them to be individually victimized (Anderson 2004). The codes also make it easy to classify the respondents and the responses based on the class in which the respondents fall. This way, it becomes easy to identify the pattern of response based on the area of expertise and experience of the respondent.
Limitations
According to Badenhorst (2007), when conducting a research project, several limitations may be encountered based on several factors that playoff in the course of planning, data collection, analysis, and presentation. It is important to highlight these limitations and where possible, state how they were dealt with in the study to promote the validity and reliability of the report.
In this study, the researcher encountered the following limitations.
When sampling the respondents, the researcher was at liberty to choose the participants for this study. This posed a potential challenge inherent in selecting a given group of respondents over others (Hoyle 2002). In particular, I gave more focus to the nurses over other respondents because of the personal belief that they are more responsible for medical waste management in healthcare institutions. I made an effort to eliminate or minimise the effect of personal biasness when selecting the samples by trying to pick the respondents in each of the two strata.
Personal position and its effect on interviewees
It was noted that my position as a Director at a pharmaceutical company could have influenced the response received from some of the respondents (Denzin & Lincoln 2011). Some of those interviewed requested to know my position before answering the questions. Most were satisfied with the assurance that their identity would remain anonymous, hence they appeared to answer the questions freely without seeming to attribute any importance to my personal views.
For one or two respondents, however, even after being assured of anonymity, there was a fear that they might be reported to the authorities. There was also the risk that such respondents provided answers to ‘please’ rather than sharing their honest views. It is important to note though that this problem was not common among all the respondents. Only a few of the respondents exhibited this behaviour.
Collecting data from only two hospitals
According to Barzun (2004), the problem of medical waste management varies from one institution to another and from one geographical setting to the other. There are cases where the problem is with the infrastructure, while in other cases the main problem is with the stakeholders involved.
The factors affecting private hospitals in terms of medical waste management may also be different from what is affecting public hospitals. In this research project, only two public hospitals were selected and consequently could not represent the entire population. Nonetheless, the study elicited insights for the chosen two contexts, which can then be tested for their applicability in other geographies or privately-owned institutions.
Primarily focusing on practitioners’ behaviour
Poor medical waste management is a problem that is caused by infrastructural, financial, and behavioural forces. When an institution lacks proper infrastructure to manage medical waste, then it may be impossible to safely and effectively dispose of these wastes. Financial considerations are also significant, in determining purchasing decisions, use of suppliers, and capital investment in equipment and infrastructure. There is the need to ensure that bills are paid and proper tools are purchased or replaced from time to time to enhance the efficiency of the system (Earl 2009).
In this paper, these two important factors were acknowledged as context, but the primary focus was placed on practitioners’ attitudes and behaviour towards medical waste management. Moreover, the research focused on healthcare workers, rather than the role of other functions within the hospital context, for example, procurement. The findings, therefore, should be examined in this light and would do well to consider other research looking at other dimensions of the system.
Relying on peoples’ reporting
This study largely relied on people’s reporting of their behaviour to understand the forces affecting the effective management of medical wastes. As Barthe (2010) says, sometimes people may deliberately hide the truth from a researcher for personal or organisational reasons. This is particularly common when interviewing people in managerial positions.
There is often the feeling that they are responsible for mistakes or shortcomings at the firm. To protect themselves, they might be tempted to cheat or provide half-truths. It may have been more appropriate for the researcher to observe the behaviour and attitude of the stakeholders in the sampled institutions without their knowledge. However, the amount of time available for the study could not permit the researcher to make such observations. The study had to rely on their reporting, assuming that their statement would be a fair reflection of their attitude and personal behaviour towards the issue under investigation.
Ethical considerations
The research study required the approval of the Viet Nam Health Environment Management Administration (VIHEMA), the Ministry of Health, and the hospitals’ Management Boards to research public hospitals. No patients were involved in the research.
The research was informed, designed and conducted in adherence to current principles applying for research involving human subjects, such as the right to withdraw and confidentiality, including demonstration of respect for all participants (Nurse and Midwifery Council 2008). A consent form was obtained, for each participant and, as explained earlier, all interview responses were coded for anonymity.
Findings and Analysis
The previous chapter has given a detailed analysis of the method that was used in collecting and analysing data. In this chapter, the focus will be on the analysis of the data and presentation of the findings. The study was designed to explore the level of knowledge and awareness of health care workers (doctors and nurses) about the 3Rs strategy in sustainable medical waste management, and to identify key drivers/enablers for implementing a 3Rs strategy in medical waste management in Vietnamese public hospitals, including quick wins and long-term objectives, and analysis of barriers.
The chapter outlines the findings from the qualitative interviews. These have been illustrated where appropriate by relevant quotes. As explained in the above chapter, the participants included 14 nurses and 6 doctors in different positions in the two hospitals. In the first part of the interview, the participants shared their view on current situation and factors influencing the good practices at their hospitals in terms of medical waste management. It is important to note that consideration of barriers is explored as part of exploring the enablers for change, because of the overlap in themes emerging.
Current situation
Based on the findings of this study, it is evident that in both hospitals where the primary data were collected, doctors and nurses are aware of improper medical waste management and its impact on humans and environment health. The awareness regarding this impact determines the attitude and practices in medical waste management among these medical staff. It is also evident that, the participants are satisfied with their organisation’s performance in medical waste management and understand the factors influencing good practices.
However, they showed their concerns about medical students, patients and their caregiver’s incorrect practice in medical waste disposal. As will be shown in this chapter, these participants felt that sustainable medical waste management needs attention of other relevant stakeholders, not just the medical staff alone. The respondents noted that irresponsible practices among the non-medical staff who visit hospitals regularly made the process of managing wastes more complex.
The respondents argued that recycling of some of the medical wastes may be one of the ways of enhancing sustainable waste management. To achieve success, these respondents emphasized on the need to embrace training and education for the medical staff, effective leadership among the administrators, proper supervisions at work, having adequate and modern medical waste management facilities in hospitals, and proper regulatory procedures. They also mentioned the need to promote knowledge about 3Rs principle among the medical staff.
Factors affecting good practices in medical waste management
Effective management of medical wastes is affected by a number of factors as was revealed in this study. The following are the factors that were identified.
All the respondents were unanimous about the relevance of leadership in effective management of medical wastes. They noted that leaders play a critical role in defining how wastes are managed within a healthcare facility. The director of the hospital is the person accountable for medical waste management within the hospital as defined by the Ministry of Health.
A number of participants confirmed that they are reminded regularly by their director about the need to pay attention and strictly adhere to the set guidelines when it comes to waste management. They also noted that the head of department and head of nurses often talk about waste management during hospital meetings and department meetings. In Thong Nhat Hospital, the director was praised as a leader who understands the need to have proper waste management system within his institution.
The interview results from the two hospitals show that it is very critical to engage all the stakeholders when trying to implement 3Rs strategy. The response shows that the support from management board is essential to encourage the implementation of medical waste management in hospitals.
“ The support of the management board is the foundation to build the background and to give the right orientation for developing all specialties from clinical to para-clinical and step by step standardise all activities and procedures” (ND2).
This claim was also supported by another participant who stated the following:
“ The management board must pay attention and prioritise the need for a ‘clean and hygienic’ hospital environment.” (TN2).
The participants also emphasised the need to ensure that all other healthcare workers are included in the entire process of strategy development and implementation. Those in management and non-management positions ought to work very closely to ensure that the desired success is achieved (TN2).
Training and education
The respondents unanimously confirmed that in order to reinforce the importance of the effective and efficient medical waste management, each hospital regularly conducts training and refresher training to promote awareness on health, safety, and environmental issues. Knowledge about handling and segregation of medical waste was noted to be very important during training processes.
The repeated training helps healthcare workers improve their knowledge of the risks caused by improper waste handling and segregation. This task is under the scope of the Infectious Control department in both hospitals. Hospital guidelines on medical waste management are summarised, printed, and posted on the wall in all departments of both hospitals.
Organising regular training on medical waste classification is a key action needed to achieve the required levels of best practice in hospitals. The analysis revealed that the targets for training should not be confined to hospital staffs that engage daily on medical waste management, but should be expanded to cover all the relevant categories such as caregivers and medical students.
“ The hospital has a continuous education program organised by the Infection Control Department. There is a Patient Committee that involves 1 – 2 patients of every specialty. Nurses will communicate with patients and their caregivers about the regulations right from the beginning” (TN3).
The statements from these respondents indicate that regular training is a very important enabler of this strategy. It empowers the stakeholders and makes them be aware of the environmental forces within their workplace. “The training should be repeated yearly in order to instil the habit” (TN9).
The response shows that it is important to ensure that the training is as detailed as possible to make the relevant stakeholders to understand what is expected of them. One respondent gave the following recommendation.
“ It is important to build capacity for nurses to ensure good practices and avoid repeated practices which lead to increasing the amount of waste” (TN4).
It is the responsibility of the management to build capacity and to promote best practices based on the industry standards. Nurses need regularly training to sharpen their skills and enable them understand emerging forces that affect their work.
“ Apprentice, caregivers, and visitors do not know what constitutes medical waste and its classification. Knowledge of medical waste management was also lacking” (TN5).
“ There are many cases of in-correct disposal of medical waste into the wrong recycle bin, especially by caregivers due to lack of knowledge” (TN10).
It is, therefore, important to come up with proper guideline for training these caregivers on strategies they should use in managing medical wastes. The limited knowledge of patients, caregivers, and medical students on what constitutes ‘medical waste’ is a major barrier for hospitals in reducing medical wastes. They tend to confuse normal waste and medical waste due to their limited of knowledge.
Supervision
The respondents confirmed that both the hospitals in which they work implement a regular supervision scheme, including ad-hoc and periodically checking for segregation of medical wastes. Across all departments, nurses are responsible for correct segregation of wastes into the bins. The head of nursing is also responsible for cross-checking between departments.
Their names and signatures appear on the bags when they are transported to the infectious department. When mistakes in segregation step are identified, the written minutes are recorded and shared in the hospital meetings to improve their performance and give warning to the other departments. Moreover, ad-hoc and regular supervision from the Ministry of Health and Department of Environment also takes place, which prepares the hospital for strict implementation.
The interviews conducted indicated that the role of regular follow up and back checks is critical to ensure there is compliance. Being compliant with the national standards is the first step towards ensuring that these hospitals embrace sustainable practices in waste management. Hospitals recognised the importance of supervision by an empowered team for periodical back checking. This is shown in the response shown below.
“ The Infection Control Department has monthly supervision and random checking without notice. There back checks within specialties, performed by nurses. The checks are often conducted without prior notice in order to test the efficiency of the system to give regular feedback” (ND5).
“ Thanks to training and regular checking, the knowledge of hospital employees about waste management has improved. Many hospitals are now applying ISO standards and do make regular notes when they discover a mistake” (ND6).
It became apparent that through regular supervision, it is possible to identify areas of weakness during the implementation process and to come up with measures to remedy such weaknesses.
Regulations and guidelines
One of the nurses stated that the strict regulations put in place by the Ministry of Health and clear guidelines from the hospitals governs the health care workers’ attitude and behaviour in medical waste management (ND3). These regulations are often updated regularly based on the changing trends. The interviewees confirmed that proper segregation and collection has now become a habit and is embedded in doctors and nurses’ practices (ND3).
There is neither a fine nor a reward scheme put in place so far in either hospital. In the National Hospital of Tropical Diseases, a written warning is mentioned in the hospital guidelines but not implemented yet. A verbal warning is common in both hospitals for the purpose of improving the attitude towards effective medical waste management.
All activities of hospitals on medical waste management are based on the current legal framework with decisions and guidelines of the Ministry of Health. Besides the MOH guidelines, the respondents stated that each hospital should also develop internal standard of practices (SOPs) for implementation based on each hospital’s unique situation. The following responses were obtained from the directors at the two institutions
“ Regulations and guidelines of MOH and Hospitals are available and clear for action” (TN10).
“ The specific hospital regulations are built up based on the Ministry of Health guidelines with direction for clear implementation” (ND7).
Their responses show that regulations and well-formulated plans can also act as enablers when implementing the strategy. They help the stakeholders to understand what is expected of them. These policies are ambitious and if implemented appropriately, they can truly bring about sustainable waste management not only at organisational level but also nationally. They can help deal with the problem of managing medical waste in Viet Nam.
Hospitals facilities
Across both hospitals, all interviewees stated that they believed their hospital was adequately equipped for segregation, collection and storage of medical wastes, with the exception of water waste treatment systems. Most of the respondents (18 out of the 20 participants) did not know about their hospital’s water waste treatment situation. It was only those working in the Infection Control Department who understood this issue.
The reason given among those working in Thong Nhat Hospital was that the hospital has a special way of doing this, which it has done for the 40 years that it has been operational. It was recognised that there is a need to invest in a new waste water treatment system which costs about $15 million, requiring state budget allocation and under consideration by the Ministry of Health. For the National Hospital of Tropical Diseases, as mentioned earlier in chapter 3, the hospital is using the same waste water treatment system with Bach Mai Hospital, which has a history of over 100 years and the participants working here refused to comment about this matter. Most of the bins are not properly labelled, which means that sorting becomes a major issue. These infrastructural challenges may have serious impact in sustainable medical waste management at organisational level.
Role of nurses
When analysing the interview results, the critical role of nurses at all levels was a repeated theme regarding good practices in medical waste management. Heads of nursing are the ones who motivate the hospital management and committee to initiate change management programs. They are responsible for the smooth running of the hospital in general and medical waste management in particular. They are also responsible for supervising the segregation and collection at the point of waste generation within the department.
They are members of Hospital Infectious Control Committee. The duty of the committee in both hospitals is to propose the revision of hospital guidelines in alignment with the Ministry of Health regulations. The committee is also expected to propose solutions to solve issues identified in daily practice, organise training, oversee communication programs, and undertake scientific study regarding control of infectious wastes in general and medical waste management in particular (MOH 2009).
Heads of nurses are responsible for training and educating new staff and medical students before they can come to work in the hospital. One respondent said, “At National Hospital of Tropical Diseases, all the new nurses and other staffs are taken through training before they can be assigned official duties,” (Van 2015, p. 12).
Analysis of the interview responses indicates that nurses are understood as the ones who should engage doctors, medical students, patients and their caregivers to ensure proper segregation and collection of waste. Before the waste is transported to the hospital’s storage area, in both institutions, they are responsible for checking to ensure proper segregation and identifying any mistakes.
Nurses are responsible for instructing patients and their caregivers on proper segregation of waste and following up their daily treatment until the treatment is completed. Given that nurses often have limited time to attend to patients, sometimes it may not be easy to ensure that these caregivers follow the instructions given.
In the hospitals, nurses participate in the Infection Control Committee of hospitals and are assigned to check and supervise the implementation of medical waste management in healthcare centres.
“ In hospitals, the head nurse is responsible for checking if the guidelines are effectively followed” (TN1).
“ The Infection Control department periodically checks the waste classification with what has been deposited. Nurse department also participates in the checking. The Head Nurse is responsible for checking at the Department” (TN4).
It was noted that nurses actually have many difficulties in the role of supervising the performance of medical waste management. Local nurses often find themselves faced with heavy workload compared to other regional countries, and it impacts on the effectiveness of their daily work of medical waste management.
“ Release workload for nurses: currently, a nurse takes care of 3 – 4 patients. The expectation is one nurse taking care of 1 – 2 patients” (TN7).
Together with the workload, some interviewees suggested that the mind set of physicians is also a challenge for nurses in the management and control of medical waste in hospitals, specifically around issues of respect: “ Physicians should coordinate with nurses. In developed countries, physicians respect nurses” (TN5) , with the implication that this was not the case in the Vietnamese context.
A further example given was around the attitude towards the use of specific medical materials:
“ Injections will increase contagious medical waste. It is necessary to reduce injections and replace it with oral drugs. We also need to change the mindset of physicians to reduce injections because they sometime prefer injections. Reducing injections also helps release workload of nurses” (TN5).
Awareness and Implementation of the 3Rs
It was noted that most of respondents understand and support the need to have effective medical waste management systems. Through sharing during the interviews, it seems there are many challenges in implementing the concept in the current condition of Viet Nam public hospital. People understand that reducing medical waste will help protect the environment. The plan is available in hospitals but the feasibility is still a question in the condition of overstretched hospitals.
All of hospital management board know and want to apply 3Rs concepts in the hospitals for both cost saving and environmental protection but the deployment in the hospitals is not enough and it may have the synchronised actions in the whole society. The consciousness on 3Rs should be well promoted in the society, instead of waiting for people to be hospitalised to be informed on how to manage medical wastes. Reducing medical waste is very important in enhancing management of medical waste.
“ All hospitals, not only in Viet Nam but also the world, would like to apply 3Rs but it is still a challenging to implement. Contagious waste will become normal waste after treatment and can be recycled. However, not everyone has the same understanding especially people in the society and environmental officers. Reducing and recycling will help hospitals reduce costs. However, hospitals do not have the permission to perform it themselves (It will be performed by professional third parties following the current regulations)” (ND4).
As noted in the above response, sometimes regulations may limit the capacity of individual hospitals to perform certain functions when it comes to management of medical wastes. In most of the cases, the major issue is often the feeling that these hospitals may not follow the right procedure in managing some medical waste which poses serious threat to the environment.
“ The plan to reduce medical waste is available but it is still on paper” (TN2).
“ Reducing solid medical waste is impossible because it depends on the number of patients, except shortening the treatment time for in-patients. It is very difficult to save water since it is required for the purpose of cleansing” (ND3).
Currently, hospitals have limited application of the concept by reuse of water bottles and glasses, and it is the most popular practice in the hospitals currently. It is important to promote knowledge on the issues of reuse based on the 3Rs strategy. The respondents gave suggestions on how to implement this strategy. One of the respondents stated.
“ To reduce medical waste, the plan is available but the implementation is not as easy as anticipated i.e. we cannot reduce plastic bags although it is accepted as a necessary action. Hospitals cannot immediately reduce medical wastes and the current focus is to just focus on how to better manage them” (TN1).
“ Hospital can reuse plastic and glasses bottles only” (TN3).
“ Glass materials can be reused, but it will need water and manpower to wash, and electricity to dry to sterilise” (TN8).
In the second part of the interviews, the participants were asked about what they understood by the term reduce, re-use, and recycle. Amongst 20 interviewees, there were only 3 persons- who belong to the Infection Control Department- who understanding this strategy as a way to minimise the impact on both financial benefit and human/environmental health. 12 people knew the term recycle because of recycling activities.
However, all of them doubted the feasibility of the deployment. For ‘reduce’, they said that they cannot reduce the number of patients but admitted that reducing of injection products and reducing the days of in-patient treatment by controlling cross-infection can reduce the amount of medical waste. For ‘reuse’, they argued that high demand of disposable medical devices which are safer than reused ones is creating the challenge for reusing.
The participants identified the barriers such as water, electricity, chemicals, time, and human resource needed for cleaning and disinfection in order to reuse those devices. They also noted that most of hospitals have inadequate staffing in terms of health care workers. The shortage puts a lot of pressure on the existing nurses, making it difficult for them to undertake some of the time consuming recycling processes. For ‘recycle’, most of recycling activities take place outside the hospital and out of the hospital’s control because of the existing policies.
That is the reason the cost benefit is not measured. The hospital only promotes the strategy to save water, electricity, and reduce cost of buying chemicals and other materials. These are consumables that these hospitals have full responsibility on. This could be a key area for supervision and control by a designated MOH team to significantly improve this area. The official data from both hospitals shows that one nurse has to serve 3-4 patients (1/3-4) whilst the ideal ratio should be 1/1 as is the case in the developed countries. This rate is even higher in the Intensive Care Unit department (1/4-5).
Healthcare Practices
In light of the challenges identified above regarding implementing the 3Rs, the responses obtained from the participants strongly indicated that specific healthcare practices embraced by workers can be enablers of implementing a 3Rs strategy. Some practices can hinder the implementation while others can enhance it. Policies and plans may be in place, but the reality is still far from the ideal because of some of the practices embedded within the hospitals studied.
Some interviewees identified specific healthcare practices, which could be reviewed to enhance sustainable waste management:
- Length of stay: “Reducing solid medical waste is sometimes not practical because it depends on the number of patients. The only option is to reduce their treatment duration in hospital” (ND3). The respondents also noted that it may not be easy to reduce the amount of water used in cleaning unless the days of patients’ visit can be reduced.
- Prescriptions: “Reducing medical waste by ‘accurate’ prescriptions being generated and avoiding injections will help reduce medical wastes” (TN4) and “using paper wrap for drugs instead of nylon wrap” (TN3).
- Treatment options: “Intravenous drug usage increases the amount of waste. It is needed to change doctors’ perception to increase oral drug usage. It also helps reduce workload for nurses” (TN5).
Nurses also ought to be careful when handling gloves because in most of the cases it may not be possible to recycle them, especially when handling different patients.
- Efficiency in routine procedures: “Improving the skill of nurses and avoiding repetitive operation are also solutions to reduce medical wastes” (TN4) and “[Reducing] in-patient time by using effective and efficient treatment” (ND2).
- Infection control: “Better management of hospital infections and controlling medical waste will help reduce cross-infection in hospital and shorten the duration of treatment of patients” (ND2).
- Certain technologies and procedures: Under the current practice and technologies used in cleaning medical equipment and facilities, specific volumes of water must be used. “It is very difficult to reduce waste water since there is a minimum volume for cleaning” (ND3).
The respondents also noted that procurement is another important issue as part of medical practices. The management is expected to have a procurement system that ensures that all drugs and any other medical consumables are delivered at the right time, in the right amount, and the right state to eliminate unnecessary wastages. Through effective procurement, the amount of medical wastes can be significantly reduced.
One respondent commented that it was important “ to plan well for purchasing drugs aimed at reducing cases of rampant expired drugs /chemicals” and “to have compensation scheme related to procurement” (TN11), whilst another suggested that “effective procurement practices will help to save cost of treatment as well as the volume of medical waste” (ND2).
The responses suggests that a time has come when stakeholders across both hospitals have to critically review the current practices with a view of being more dynamic and more focused on finding sustainable solutions to the current problem of managing medical wastes.
This chapter has provided an overview of the key themes emerging from the primary data collected from the respondents. Some of the findings support the information that was gathered during the review of literatures, whilst some findings highlight particular insights about the Vietnamese context on how medical wastes should be properly managed. Both primary and secondary sources are in agreement with the fact that it is important for healthcare organisations and the government to have effective ways of managing medical wastes.
Effective medical waste management requires a concerted effort from a number of stakeholders as shown in the above analysis. Nurses, doctors, hospital directors, caregivers, and patients all have a role to play in managing medical wastes. They must work very closely to ensure that policies and regulations regarding waste management is hospitals are followed effectively.
A number of drivers of effective waste management have been identified. Leadership, training and education, supervision, and regulations have been identified as very important drivers of effective medical waste management. Leadership helps in offering guidance and motivation when it comes to medical waste management. Training and education equips the hospital staff with the necessary skills they need in effective management of medical wastes.
Regulations outline what is expected of the staff when it comes to medical waste management. Other drivers include involvement of all stakeholders having proper regulations, and clearly outlining the role of nurses in medical waste managementThe government, medical staff, management of healthcare institutions, the patients, and the visitors all have their roles clearly defined in promoting effective medical waste management.
Conclusion and Recommendations
This study has clearly shown how important sustainable medical waste management is in Viet Nam. This study aimed to come up with effective sustainable waste management policies and practices that can be applied in Vietnamese hospitals. It was also important for the study to help increase awareness among the stakeholders in the healthcare sector on how to manage medical wastes using the 3Rs strategy. The study also focused on the barriers to effective medical waste management. In this chapter, conclusions and appropriate recommendations are given in the context of the findings of the study.
At a national level, the Ministry of Health in Viet Nam has clear guidelines in place for helping healthcare workers understand the relevance of medical waste management. The study reveals that the two hospitals studied are not fully compliant with national medical waste management policies that would help minimize risks to the environment and public health.
However, sustainable waste management arguably involves more than compliance with existing regulations, as existing regulations do not currently fully embrace the principles of 3Rs and the actions necessary for them to be implemented. Whilst healthcare workers are aware of these principles, there is evidence to suggest that they do not know exactly what they need to do to put them into practice.
Recommendations
Based on the findings from the above analysis, the following recommendations are suggested for promoting sustainable medical waste management. The recommendations, if followed properly, may help address some of the challenges that healthcare workers currently face in their efforts to manage medical wastes effectively. The recommendations target both health institutions (specifically the two hospitals examined) as well as the Ministry of Health.
For hospitals – promoting sustainable behaviour
A specific action plan aiming at reducing the waste and potential recycles (3Rs) should be in place. Potential 3Rs practices should be applied, such as:
- Proper procurement of products/devices that do not contain PVC plastic because of the challenges associated with managing plastic waste.
- Educate all health care workers, students, patients and their caregivers in regards to the urgent need to minimize the waste by strict segregation. These stakeholders should have proper knowledge on how to manage medical waste
- Developing proper infrastructure for sustainable medical waste management may also be critically important in these organisation
There is a need to find the actual cost of medical waste management in each hospital. It is also needed to have urgent studies in regards to the benefits of implementing 3Rs initiatives versus current activities. It will ease for behaviour change. In the analysis, the lack of cost-benefit analysis was identified as one of the barriers that limit the proper implementation of 3Rs initiatives. Most of these hospitals are yet to analyse the costs of implementing these strategies against the benefit they bring.
For the Ministry of Health: improve legislation, guidelines and policies
The ministry of health has to address several issues to ensure that there is the effective management of medical wastes within the country. The current regulations may need to be revised and set clear 3Rs strategy and guidance for hospitals in how to implement it successfully.
The study also found that sometimes the set policies by the ministry are not in tandem with the reality of the ground. The ministry should try and ensure that it consults the relevant stakeholders as much as possible every time it is planning on developing new policies. This way, the views of doctors and nurses will be taken into consideration. Doctors and nurses play a key role in the management of medical waste management amongst health care workers in hospitals because they have to segregate the waste before storing it in the correct bins at the point of generation, are facing daily the waste in healthcare service. Based on the information collected from the review of literature, the Ministry of Health in Viet Nam should encourage the industry to work with the government agencies together to develop standards for products and biodegradable materials used.
Recommendations for further study
This study is a source of information on medical waste management in Viet Nam. However, the result may not be applied to other hospitals. Thus, there is a need to do related research in more public hospitals in different geographies, and privately owned hospitals. Furthermore, it is needed to conduct further studies because there are issues that were not captured because of time constraints, such as water waste. Nonetheless, this study demonstrates the value of accessing the perspectives and ideas of healthcare workers, as an important step towards implementing sustainable waste management.
Bibliography
Abd El-Salam, M (2010) ‘Hospital waste management in El Beheira Governorate Egypt’, Journal of Environmental Management , vol. 91, no. 6, pp: 618-629.
Abdula, F, Qdais, A & Rabi, A 2008, ‘Site investigation on medical waste management practices in northern Jordan’ Journal of Waste Management’, vol. 28, no. 2, pp: 450-458
Abor, P 2007, ‘Medical Waste Management Practices in a Southern African Hospital’, J. Appl. Sci. Environ. Manage, vol. 1, no. 3, pp. 91–96.
Almuneef, M & Memish, Z 2003, ‘Effective medical waste management: It can be done’, American Journal of Infection Control, vol. 31, no. 3, pp. 188-192.
Ananth, A, Prashanthini, V & Visvanathan, C 2010 ‘Healthcare waste management in Asia’ Journal of Waste Management, vol. 30, no. pp. 145-161.
Anderson, P 2004, Research Methods in Human Resource Management, Chattered Institute of Personnel Management, London.
Andrzej, A & Buchaman, A 2007, Organizational Behavior , Prentice Hall, London.
AQI 2015, Air Pollution in the World: Real-time Air Quality Index(AQI) .
Askarian, M, Vakili, M & Kabir 2004, ‘Results of hospital waste in private hospitals in Far Provinces, Iran’, Waste Management , vol. 24, no. 6, pp. 347–352.
Badenhorst, C 2007, Research writing: breaking barriers , Van Schaik Publishers, Pretoria.
Bak, N 2004, Completing your thesis: a practical guide , Van Schaik, Pretoria.
Barthe, G 2010, Verification, Model Checking, and Abstract Interpretation , Springer, New York.
Barzun, J 2004, The modern researcher , Wadsworth, Belmont.
Bdour, A & Hadadin, N 2007, Assessment of medical wastes management practice: A case study of the northern part of Jordan .
Bell, P 2001, Evaluating, doing and writing research in psychology: a step-by-step guide for students , Sage, London.
Birpinar, M, Bilgili, S, Erdoğan, T 2009, ‘Medical waste management in Turkey: A case study of Istanbul.’ Journal of Waste Management , vol. 29, no. 4, pp: 445-448.
Blenkharn J 2006, ‘Standards of clinical waste management in UK hospitals’ Journal of Hospital Infection , vol. 62, no. 2, pp. 300–303.
Bokhoree, C, Beeharry, Y, Makoondlall-Chadee, T, Doobah, T & Soomary, N 2014, ‘Assessment of Environmental and Health Risks Associated with the Management of Medical Waste in Mauritius’, APCBEE Procedia , vol. 9, no. 3, pp. 36-41.
Bolay, J, Hostettler, S & Hazboun, E 2014, Technologies for sustainable development: A way to reduce poverty, Cengage, New York.
Bouma, G 2000, The research process , Oxford University Press, Oxford.
Brause, R 2000, Writing Your Doctoral Dissertation: Invisible Rules for Success , Falmer Press, London.
Brundtland G.H., (1987), Report of the World Commission on Environment and Development: Our Common Future . p.16
Bryman, A & Bell E 2011 , Business Research Method , Oxford University Press, Oxford.
Calabrese, R 2006, The elements of an effective dissertation and thesis: a step by step guide to getting it right the first time , Rowman & Littlefield, Lanham.
Carpenter, D & Hoppszallern S 2010, Green + Greener: Hospitals embrace environmentally sustainable practices, through laggards remain .
Cesaro, A & Belgiorno, V 2015, Medical waste generation and management in different sized facilities.
Chaerul M, Tanakab, M & Shekdarb, A 2007, A system dynamics approach for hospital waste management .
Cheng, Y, Sung, C, Yang, Y, Lo, H, Chung, T & Li C.,(2009)’Medical waste production at hospitals and associated factors.’ Waste Management , vol. 29, no. 1, pp 440-444.
Cheremisinoff, N 2003, Handbook of solid waste management and waste minimization technologies , Butterworth-Heinemann, Amsterdam.
Clarke J 2008, Clinical waste in developing countries .
Clover P 2009, ‘Safe management of healthcare waste guide’, London: Royal College of Nursing , vol. 33, no. 5, pp. 44-67.
Coker, A, Sangodoyin, A, Sridhar, M, Booth, C, Olomolaiye, P & Hammond F 2009, ‘Medical waste management in Ibadan, Nigeria: obstacles and prospects’. Journal of Waste Management , vol. 29, no. 3, pp: 804-811.
Controlled Waste Regulations 2012, Environmental Protection, England and Wales , 2016
COP21 Paris 2015, Sustainable Innovation Forum .
Cramer, D 2003, Advanced quantitative data analysis , Open University Press, Maidenhead.
Creswell, J 2009, Research design: qualitative, quantitative, and mixed methods approaches Sage, Thousand Oaks.
DARA 2010, Climate Vulnerability Monitor 2010 .
Delving, A 2006, Research methods: planning, conducting and presenting research , Wadsworth, Belmont.
Denzin, N & Lincoln Y 2011, The SAGE Handbook of Qualitative Research , Sage Publication Inc, New York.
Diaz, L, Eggerth, L, Enkhtsetseg, S & Savage, G 2008, ‘The characteristics of Healthcare waste’, Waste Management , vol. 28, no. 7, pp. 1219-1226.
Dinkins, C & Sorrell, J 2007, Ethics: The Expanding Circle of Environmental Ethics.
Dunleavy, P 2003, Authoring a PhD: how to plan, draft, write and finish a doctoral thesis or dissertation , Macmillan, New York.
Dutta, S & Das, A 2010, ‘Analytical perspective on waste management for environmental remediation’, Trends in Analytical Chemistry , vol. 29, no. 7, pp. 636-643.
Earl, B 2009, The practice of social research , Wadsworth, Belmont.
EPA 1997, Mercury Study Report to Congress .
EPA 2009, Economic Impacts of Revised MACT Standards for Hospital/Medical/Infectious Waste Incinerators .
Foster, D 1996, Groundwater Resources Beneath Rapidly Urbanising Cities – Implications and Priorities for Water Supply Management .
Galvin, R 2015, How many interviews are enough? Do qualitative interviews in building energy consumption research produce reliable knowledge?
General Statistics Office of Viet Nam 2015, Population and Employment .
GFDRR 2011, Vulnerability: Risk reduction and adaptation to Climate Change Viet Nam .
Goddard, W 2001, Research methodology: an introduction , Juta, Lansdowne.
Gupta, P 2002, Statistical Methods , Sultan Chand & Sons, New Delhi.
Hakim, C 2000, Research Design: Successful Designs for Social and Economic Research, Routledge, London.
Harris, N, Pisa, L, Talioaga, S, & Vezeau, T 2009, Hospitals Going Green: A Holistic View of the Issue and the Critical Role of the Nurse Leader .
Hassan, M, Ahmed, A, Rahman, A & Biswas, T 2008, Pattern of medical waste management: existing scenario in Dhaka City, Bangladesh .
Hinkel, E 2011, Handbook of Research in Second Language Teaching and Learning, Volume II , Routledge, New York.
Hoang, T 2009, Study on status and factors related to medical waste management in General Central hospital in Thai Nguyen province , Thai Nguyen University of Medicine and Pharmacy, Bangkok.
Hoffman, E 2001, Postgraduate research guidelines , Triangle Technikon, Vanderbijlpark.
Hoyle, R 2002, Research methods in social relations , Wadsworth, Fort Worth.
Hutchins, D & White, S 2008, Coming round to recycling .
International Conference on the Development of Biomedical Engineering, 2015, 5th International Conference on Biomedical Engineering in Viet Nam , McMillan, London.
International Conference on the Development of Biomedical Engineering 2015.
Jiang, S 2006, The practical implementation of the 3R’s of sustainable waste management in the Norfolk and Norwich university hospital .
Johnke, B 2000, Emissions from Waste Incineration .
Joint Annual Health Review 2014, Strengthening prevention and control of non-communication diseases.
Kagonji, S & Manyele, S 2011, Analysis of measured medical waste generation rate in Tanzania District hospitals using statistical methods .
Ketlogetswe, C 2004, Improved combustion process in medical waste incinerators for rural .
Kojima, M & Michida, E 2013, International trade in recyclable and hazardous waste in Asia , Edward Elgar, Cheltenham.
Kudoma, B 2013, An Evaluation of Clinical Waste Management in Garobone city Council Healthcare Facilities , University of South Africa, Cape Town.
Le, K 2014, Dioxin Contamination in Viet Nam: Emissions from industries and levels in the environment .
Lee, B 2002, Analysis of the recycling potential of medical plastic wastes .
Lye, L 2010, Sustainability matters: Environmental management in Asia , World Scientific, Singapore.
Manyele, S & Lyasenga, T 2010, Factor affecting medical waste management in low-level health facilities in Tanzania .
Mato, R & Kassenga, M. 1997, Critical review of industrial and medical waste practices in Dar es Salaam city .
Mbongwe, B, Mmereki, T & Magashula, A 2008, ‘Healthcare waste management: Current practices in selected healthcare facilities’, Waste Management , vol. 8, no. 1, pp. 226-233
McDermott-Levy R 2011, The nurse’s role on green teams: an environmental health opportunity.
Mejia, E & Sattler, B 2009, Starting a Health Care System Green Team .
Ministry of Health 2007, Directive No 43/2007/QD-BYT.
Ministry of Health 2013, Health Statistic Yearbook 2012 , McMillan, Hanoi.
MONRE 2011, The report on national environment – solid waste.
Moreira, A & Gunther W 2013, ‘Assessment of medical waste management and a primary health care centre in Sao Paulo, Brazil’, Journal of Waste Management , vol. 33, no. 6, pp. 162-167.
Newswire, P 2016, Doctors, Dentists and Nurses-Most trusted professionals to give advices, according to Harris Poll U.S. Adults.
Nguyen, T 2005, Solid Waste Management in Viet Nam .
Nichols, A, Grose, J, Bennallick, M & Richardson, J 2013, ‘Sustainable healthcare waste management: a qualitative investigation of its feasibility within a county in the south west of England , ’ Journal of Infection Prevention, vol. 14, no. 2, pp. 60.
Nihon, K 1999, The State of the environment in Asia , Institute of Southeast Asian Studies, Singapore.
Nurse and Midwifery Council 2008, The Code: Professional standards of practice and behavior for nurses and midwives .
Ozbek, M & Sanin, F 2004, A study of the dental solid waste produced in a school of dentistry in Turkey .
Pariatamby, A & Tanaka, M 2013, Municipal solid waste management in Asia and the Pacific Islands: Challenges and strategic solutions , McGrow Hill, New Delhi.
Pham, A & Eggleston, B 2015, Diabetes Prevalence and Risk Factors Amongst Vietnamese Adults: Finding from Community-Based Screening Programs .
Pruss, A, Giroult, E & Rushbrook, P 1999, Safe Management of Wastes from Health-Care Activities .
Public Health Association of HoChiMinh City 2014, Annual Conference against cancer in HCMC .
Raworth, K. 2012, A safe and just space for humanity . Can we live within the doughnut?, Oxfam Discussion Papers.
Richardson, J, Burton, R, Sewell, R, Spreckelsen, T & Montgomery, P 2012,
Docosahexaenoic Acid for Reading, Cognition and Behaviour in Children Aged 7–9 Years: A Randomized, Controlled Trial .
Sakaguchi, K 2001, ‘Hospital Waste Management in Japan and Viet Nam’, Japan Society of Waste Management Experts , vol. 37, no.1, pp. 2-3.
Salkin, F 2004 , Review of health impacts from microbial hazards in health care wastes .
Sattler, B & Hall, K 2008, Healthy Choices: Transforming Our Hospitals into Environmentally Healthy and Safe Places .
Shah, F & Ranghieri, F 2012, A workbook on planning for urban resilience in the face of disasters: Adapting experiences from Viet Nam’s cities to other cities , World Bank Washington.
Steffen, W 2013, The Great Acceleration: Towards Sustainability or Collapse? University of Cambridge, Unpublished.
Strohschen, G 2009, Handbook of blended shore education: Adult program development and delivery , Springer, New York.
Sustainable Development Commission 2010, Sustainable development: The key to tackling health inequalities . p.9
ThanhnienNEWS 2015, Vietnam hospital fined for dumping 63 tons of untreated medical waste.
Tudor T.L. et.al., 2008, Realising resource efficiency in the management of healthcare waste from the Cornwall National Health Service (NHS) in the UK .
UNCED, 1992, United Nations Conference on Environment and Development Rio de Janerio , Brazil, 3 to 14 June 1992: Agenda 21. p41
Van, S 2015, A Different Face of War: Memories of a Medical Service Corps Officer in Viet Nam , Wiley, Hoboken. Viet Nam Laws .
Vietnamnet 2016, Bach Mai hospital recycling medical waste .
VIHEMA 2015a, Workshop on the draft of Guidance on medical waste management for health care facilities generating less of medical waste .
VIHEMA 2015b, Medical Waste Management is still a burden to hospitals.
VIHEMA 2015c, The harm of mercury and its sources in the medical area .
Visvanathan, C 2006, Medical waste management issue in Asia .
WHO 2002, Injection Safety .
WHO 2014, Safe management of wastes from health-care activities .
Wilburn, S 2007, Overview and Summary: Environmental Health: Important Choices for a Greener World .

IMAGES
VIDEO
COMMENTS
Biomedical Waste Management Rules, 2016 (BMWM Rules, 2016) specify that every healthcare facility shall take all necessary steps to ensure that BMW is handled without any adverse effect on human and environmental health. This document contains six schedules, including the category of BMW, the color coding and type of containers, and labels for ...
Medical Waste Management and Disposal Plan Essay. The movement of hazardous medical waste needs to be carefully controlled from the point of generation to the point of final treatment. The approach described in the plan is a crucial first step in effectively managing hazardous medical waste. It evaluates the generation, collection ...
2.2. Medical Waste Management for a Sustainable Healthcare Environment. According to the WHO [ 7 ], 15% of all medical waste generated is hazardous. In high-income countries, 0.5 kg of hazardous medical waste is generated per hospital bed every day, whereas it is 0.2 kg in low-income countries.
The coronavirus (COVID-19) pandemic has created a global medical emergency. The unforeseen occurrence of a pandemic of this magnitude has resulted in overwhelming levels of medical waste and raises questions about management and disposal practices, and environmental impacts. The amount of medical waste generated from COVID-19 since the outbreak is estimated to be 2.6 million tons/day worldwide.
Many nations struggle with the collection, separation, and disposal of medical waste. However, extra caution is required to avoid the risk of injury, cross-contamination, and infection; thus, healthcare workers and individuals responsible for waste management must follow the mandatory safety procedures. In this review, a classification of the various types and categories of medical waste and ...
Please use one of the following formats to cite this article in your essay, paper or report: APA. Thomas, Liji. (2022, July 07). The Sustainable Management of Healthcare Waste.
Key facts. Of the total amount of waste generated by health-care activities, about 85% is general, non-hazardous waste. The remaining 15% is considered hazardous material that may be infectious, toxic or radioactive. Every year an estimated 16 billion injections are administered worldwide, but not all of the needles and syringes are properly ...
Globally, health care waste management is underfunded and poorly implemented. The combined toxic infectious and other hazardous properties of medical waste represent a significant environmental and public health threat. Scientists (1) have estimated that over half of the world's population is at risk from environmental, occupational, or ...
The compilation of 38 journal papers, 7 conference papers, 3 books, and 20 web pages offers valuable insights into medical waste management systems. The focus of the literature predominantly centers around the segregation stage, with a significant emphasis on digitalization for monitoring waste weight and bin status.
Medical waste disposal is an issue of considerable scale. As the world's top medical waste producing nation, the United States alone creates over 3.5 million tonnes of medical waste per year with an average disposal cost of $790 per tonne (Lee et al., 2004). Medical waste production in the developing world is rising quickly due to improved ...
1. INTRODUCTION. Medical waste is a subset of wastes generated at health care facilities, such as hospitals, physicians' offices, dental practices, blood banks, and veterinary hospitals/clinics, as well as medical research facilities and laboratories. Generally, medical waste is healthcare waste that that may be contaminated by blood, body ...
4. Treatment of Regulated Medical Waste. Regulated medical wastes are treated or decontaminated to reduce the microbial load in or on the waste and to render the by-products safe for further handling and disposal. From a microbiologic standpoint, waste need not be rendered "sterile" because the treated waste will not be deposited in a sterile site.
Healthcare waste (HCW) is generated in different healthcare facilities (HCFs), such as hospitals, laboratories, veterinary clinics, research centres and nursing homes. It has been assessed that the majority of medical waste does not pose a risk to humans. It is estimated that 15% of the total amount of produced HCW is hazardous and can be ...
T oday, biomedical. waste management has become one of major issue of concern in India taking into account the rate of growth of population and rapid urbanization. This. paper includes biomedical ...
Shipping papers are required when medical waste is transported off-site for disposal or destruction. Such guidelines can be found in a state's Administrative Codes or state-EPA rules for solid and hazardous waste. ... Call a representative today to learn how you can ensure safe, compliant, cost-effective, and sustainable medical waste ...
Background Information. According to Environmental protection Agency (EPA), hospitals generate around 3.2 million tons of medical wastes per annum. (10). 10 to 15 0percent of this medical waste generated is infectious. In most hospitals, the non infectious waste is land filled while the infectious one is incinerated.
This page of the essay has 6,064 words. Download the full version above. The value of medical waste management in the protection of public health and the environment cannot be denied (Thakur and Ramesh, 2015). One concern in the society nowadays is the inadequate treatment and improper disposal of medical wastes in various medical facilities ...
The HWSTR report delves into four potential impacts of ineffective waste management and disposal that are top concerns for consumers: environmental impact, patient health and safety, HCPs safety, and community impacts. 1. Impact on the Environment. One estimate indicates that the average hospital produces approximately 29 pounds of waste per ...
Inappropriate medical waste (MW) management practices have become one of the major concerns in developing countries. The objectives of this study are to appraise the procedures and techniques ...
Essay # 1. Introduction to Biomedical Waste Management: Hospitals and other health-care establishments have a 'duty of care' for the environment and for public health, and have particular responsibilities in relation to the waste they produce. Unfortunately, medical wastes are not given proper attention and these wastes are disposed of ...
The roots of unsafe management of medical solid waste include inadequate finance, weak enforcement of legislation, ignorance among health workers and waste workers as well as non-participatory approach in decision making. ... selected papers from the 5th international conference wastes 2019, Lisbon, Portugal, 4-6 September 2019. World Health ...
The process of medical waste management in hospitals includes several interrelated steps: segregation, collection, storage, transportation, treatment and disposal (Pruss, Giroult, & Rushbrook,1999). Figure 1: The process of medical waste management (Pruss, Giroult, & Rushbrook 1999) In these identified steps, segregation (to separate the waste ...
With the ever-increasing focus on sustainable development, recycling waste and renewable use of waste products has earned immense consideration from academics and policy makers. The serious pollution, complex types, and strong infectivity of medical waste have brought serious challenges to management. Although several researchers have addressed the issue by optimizing medical waste management ...
Efficient management of waste generated in healthcare systems is crucial to minimize its environmental impact and ensure public health. Sustainable medical waste management (MWM) systems require careful network design, which can be achieved through efficient optimization techniques. This work develops a mixed-integer linear programming (MILP) to formulate the problem, a two-step MILP (TSMILP ...