An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley Open Access Collection


Looking through racism in the nurse–patient relationship from the lens of culturally congruent care: A scoping review
Mojtaba vaismoradi.
1 Faculty of Nursing and Health Sciences, Nord University, Bodø Norway
Cathrine Fredriksen Moe
Gøril ursin, kari ingstad, associated data.
Authors do not want to share the data.
This review aimed to identify the nature of racism in the nurse–patient relationship and summarize international research findings about it.
A scoping review of the international literature.
Data sources
The search process encompassed three main online databases of PubMed (including MEDLINE), Scopus and Embase, from 2009 until 2021.
Review methods
The scoping review was informed by the Levac et al.’s framework to map the research phenomenon and summarize current empirical research findings. Also, the review findings were reflected in the three‐dimensional puzzle model of culturally congruent care in the discussion section.
The search process led to retrieving 149 articles, of which 10 studies were entered into data analysis and reporting results. They had variations in the research methodology and the context of the nurse–patient relationship. The thematical analysis of the studies' findings led to the development of three categories as follows: bilateral ignition of racism, hidden and manifest consequences of racism and encountering strategies.
Racism threatens patients' and nurses' dignity in the healthcare system. There is a need to develop a framework of action based on the principles of culturally congruent care to eradicate racism from the nurse–patient relationship in the globalized context of healthcare.
Racism in the nurse–patient relationship has remained a relatively unexplored area of the nursing literature. It hinders efforts to meet patients' and families' needs and increases their dissatisfaction with nursing care. Also, racism from patients towards nurses causes emotional trauma and enhances job‐related stress among nurses. Further research should be conducted on this culturally variant phenomenon. Also, the participation of patients and nurses should be sought to prohibit racism in healthcare settings.
1. INTRODUCTION
According to the American Nurses Association, racism is defined as ‘assaults on the human spirit in the form of biases, prejudices and an ideology of superiority that persistently cause moral suffering and perpetuate injustices and inequities’ (American Nurses Association, 2021 ) (P.1). Neoliberalism across the globe has made that racism remains invisible in terms of restructuring social classes, producing race categories and racialization (Ahlberg et al., 2019 ). Racism as prejudice and discrimination based on individuals' race and skin colour is a common healthcare problem across the globe. Ever increasing demographics, globalization and cultural changes in the healthcare context have attracted the attention of policy makers and international authorities to this phenomenon (George et al., 2015 ).
1.1. Background
Racism is the main cause of the patient's harm. Those patients who experience racist discriminations often have poor healthcare outcomes and access to health care, and suffer from mental health issues (Stanley et al., 2019 ). Racism in its common form as implicit racial bias specially negative attitudes towards the patient of colour can be pervasively observed in the relationship between patients and healthcare providers leading to healthcare disparities (Hall et al., 2015 ; Sim et al., 2021 ). It can also hinder appropriate and adequate use of health care, following up screening programmes and preventive behaviours, adherence to the therapeutic regimen and trust in healthcare providers (Powell et al., 2019 ; Pugh et al., 2021 ; Rhee et al., 2019 ). Disparity due to racism leads to the development of new disabilities in patients or even can worsen the present one (Rogers et al., 2015 ).
Nurses are located at the forefront of patient advocacy and they are expected to address inequities in the provision of care to their clients. However, structural racism can be observed in nursing practice (Iheduru‐Anderson et al., 2021 ; Villarruel & Broome, 2020 ). The counter racism role of nurses across healthcare settings emphasizes the identification of discriminatory care, and the development of tolerance, respect and empathy models for other healthcare professionals (Willey et al., 2021 ).
Ethics is one part of the anti‐racism paradigm with solutions that prohibit racist attitudes and behaviours in health care (Ho, 2016 ). Racism violates ethical practice among healthcare professions specially among nurses who are committed to the provision of equitable care to patients as the main part of social solidarity (Hamed et al., 2020 ; Weitzel et al., 2020 ).
The international research mainly has addressed racism towards patients. The occurrence of racist behaviours from patients towards healthcare professionals should be also investigated to create an equitable environment that hinders racism from both sides. It has been stated that black, Asian and minority ethnic nurses receive a different treatment from patients as being racially stereotyped and are considered less powerful in comparison with white nurses (Brathwaite, 2018 ; Truitt & Snyder, 2019 ). Patients' prejudicial and discriminative behaviours in terms of rejecting suggested care, verbal abuse and even physical violence have been described by these nurses as very painful and disrespectful behaviours leading to moral distress and reduction in the quality of patient care (Chandrashekar & Jain, 2020 ; Keshet & Popper‐Giveon, 2018 ).
Racism in the healthcare system has a long history. The identification of the nature of racism and its manifestations helps develop appropriate strategies for its elimination from the healthcare system (Mateo & Williams, 2021 ). The development of actions to tackle racism and racial discriminations has been chosen as a high‐level event at the 76th session of the United Nations General Assembly (UNGA) in 2021 (World Health Organization, 2021 ). Nevertheless, our knowledge of the extent of racism in healthcare systems and how it can be detected and prevented has remained limited. A probable reason is that racism directly influences the identity and rationality of healthcare professionals, which hinders holding discussions on this phenomenon in public discourses (Hamed et al., 2020 ). Open discussions on the issue of racism within the nursing profession help identify the underlying causes of racism and eradicate it from the healthcare context (Iheduru‐Anderson et al., 2021 ).
Further research is needed to better define racial, ethnic and cultural factors contributing to racism in healthcare systems and develop strategies that minimize their impacts on patient care (Godlee, 2020 ; Paradies et al., 2014 ).
2. THE REVIEW
Previous reviews of the international literature have taken a general perspective towards racism in the multidisciplinary context of health care (Chen et al., 2021 ; Sim et al., 2021 ). None of them have investigated racism in the context of the nurse–patient relationship to articulate its characteristics. Therefore, this review of international literature was undertaken to identify the nature of racism in the context of the nurse–patient relationship and summarize international research findings about it.
2.2. Design
A scoping review was performed. It is a research method by which the breadth of evidence in a field is mapped and the nature of the research phenomenon is identified (Daudt et al., 2013 ). The findings of scoping reviews can inform planning for future research and policy making (Westphaln et al., 2021 ).
This scoping review was carried out based on the review framework suggested by Levac et al. ( 2010 ) consisting of the following steps: identification of the research question; literature search and retrieving relevant studies; selection of studies; charting; collating, summarizing data and reporting results; consultation (Levac et al., 2010 ). These review steps were described under subheadings suggested by the journal's author guidelines.
2.3. Search methods
The review question was identified as follows: ‘what is the nature of racism in the nurse–patient relationship?’ The review question was kept broad enough to identify all aspects of this phenomenon in various caring situations, but it focused on related incidents only within the relationship between nurses and patients. It was also formulated by PICO:
P (Population): patients and nurses; I (Interest): racism, and racist attitudes and behaviours in the nurse–patient relationship; Co (Context): all contexts in healthcare including short‐term, long‐term, acute healthcare settings, child, adult, physical and mental healthcare.
The authors designed the review protocol and agreed on its details (Supporting Information 1 ). They performed a pilot search on Google Scholar and some specialized databases to identify relevant search keywords and phrases. The search process initially was established using the development of keywords, Medical Subject Headings (MeSH), and thesauruses' entry term that were translated into databases. The Boolean method and truncations with the operators of AND/OR were used to create the search sentence, which was pilot‐tested to ensure of its adequacy for retrieving relevant studies and selection of the most relevant databases for conducting the search.
The search sentence included all variants of terms related to nurse, patient, racism (e.g. racial bias, racial prejudice, racial discrimination, covert racism, racial disparity) and relationship (e.g. communication and interaction) in the context of healthcare. After conducting a pilot search, three main online databases that covered the majority of the peer‐reviewed and scientific international literature on racism in the field of nursing consisting of PubMed (including MEDLINE), Scopus and Embase were chosen for conducting the search. A librarian was also consulted to ensure of the accuracy of the search process.
2.4. Search outcome
Retrieved studies should have met the following inclusion criteria to be included in the review: original and empirical studies (qualitative/quantitative/mixed methods); focused on the phenomenon of racism; the nurse–patient relationship; racism from patients towards nurses and from nurses towards patients; various healthcare contexts such as short‐term, long‐term, acute healthcare settings, child, adult, physical and mental healthcare; being published in English language in scientific peer‐reviewed journals.
The publication date was restricted as from 1 January 2009 until 31 October 2021 to comprehensively access relevant studies. Any article that did not provide empirical data (e.g. reviews, commentaries, letters, conference proceedings, books) and did not overlap the main domains of the review (i.e. nurse, patient, racism) was excluded. The search coverage was enhanced through conducting a manual search inside some reputed journals with the history of publishing relevant studies and cross‐referencing from selected studies' bibliographies and previous reviews. The EndNote software was used for data management.
2.5. Quality appraisal
Risk of Bias assessment and quality appraisal generally are not applicable to scoping reviews. Therefore, all relevant studies were included in the reporting of the review results.
2.6. Data abstraction
To prevent bias, the authors (MV, CFM, GU, KI) independently screened the titles and abstracts of retrieved studies. Also, they independently read the full texts of the studies to make decisions on their inclusion or exclusion based on the pre‐determined eligibility criteria. Discussions were held by the authors to reach agreements on the selection of articles and their inclusion in data analysis and reporting results.
An extraction table was used to chart data, facilitate data importing from the selected studies, and categorize their general characteristics based on the author's name, country, publication year, sample and setting and research design.
2.7. Synthesis
The analytic framework was developed by drawing tables to collate, summarize and compare the studies' findings in relation to the review phenomenon and present an overview of relevant literature's breadth (Levac et al., 2010 ). Also, the studies' findings were thematically analysed by comparing their similarities and differences to gain a more abstract and at a higher lever insight into racism in the nurse–patient relationship.
The consultation step is optional and aims at the provision of stakeholders' involvement by suggesting complementary references and giving insights beyond those found in the reviewed literature. The sensitivity of the research topic and the requirement to obtain ethical permissions for collecting data from nurses and patients hindered the authors to follow this step. Therefore, it was removed from the review process.
The review findings were reflected to the three‐dimensional puzzle model of culturally congruent care by Leininger and McFarland ( 2002 ) via the main aspects of the cultural competence puzzle at the healthcare provider's and patient's levels consisting of ‘cultural diversity’, ‘cultural awareness’, ‘cultural sensitivity’ and ‘cultural competence’ (Leininger & McFarland, 2002 ; Schim et al., 2007 ).
The reason for the selection of culture as the analytical framework in this review lies in its application as the point of reference to the concepts of race and ethnicity. Culture is a dynamic concept, broadly encompasses commonalities and diversities in people and communities, and pervasively influences all aspects of life and healthcare (Schim et al., 2007 ). This synergy can help heal racism in the healthcare system (Hassen et al., 2021 ).
The Preferred Reporting Items for Systematic reviews and Meta‐Analyses extension for Scoping Reviews (PRISMA‐ScR) was used to guide this review (Tricco et al., 2018 ).
3.1. Search results and selection of studies
In the search process, 149 studies were retrieved (Table 1 ). Duplicates and irrelevant studies were excluded during title screening and abstract reading via holding discussions between the authors. Therefore, 24 articles underwent full‐text reading and assessment, of which 10 studies were entered into data analysis and reporting results given the inclusion criteria (Figure 1 ).
Results of the different phases of the review

The process of search and inclusion of studies in the scoping review
3.2. Characteristics of selected studies
The general characteristics of the selected studies have been presented in Table 2 . They were published between 2009 and 2021 indicating the review coverage for more than one decade. Five studies were conducted in the United States (Benkert et al., 2009 ; Cottingham et al., 2018 ; Martin et al., 2016 ; Purtzer & Thomas, 2019 ; Wheeler et al., 2014 ), two in Norway (Debesay et al., 2014 , 2021 ), one each in the United Kingdom (Deacon, 2011 ), Australia (Lyles et al., 2011 ) and Canada (McFadden & Erikson, 2020 ).
List of final articles included in the research synthesis and reporting results
The studies mainly used the qualitative design (Cottingham et al., 2018 ; Deacon, 2011 ; Debesay et al., 2014 , 2021 ; Martin et al., 2016 ; McFadden & Erikson, 2020 ; Purtzer & Thomas, 2019 ; Wheeler et al., 2014 ), but two studies used the quantitative design (Benkert et al., 2009 ; Lyles et al., 2011 ). They were conducted in hospitals and community healthcare settings and were categorised based on their focuses as follows: patients' trust in nurses in relation to their racial identities (Benkert et al., 2009 ), nurses' confrontation with the racist expression by patients (Deacon, 2011 ), patient‐reported racial discrimination and communication with nurses (Lyles et al., 2011 ), perspectives of internationally educated nurses and American educated nurses about interactions with patients (Wheeler et al., 2014 ); nurses' experiences of home care provision to ethnic minority patients (Debesay et al., 2014 ); satisfaction of various racial groups of parents with neonatal nursing care (Martin et al., 2016 ); experiences of nurses of colour about negotiating with patients (Cottingham et al., 2018 ); health disparities during the nurse–patient relationship (Purtzer & Thomas, 2019 ); racializing mothers and breastfeeding (McFadden & Erikson, 2020 ); nurses' critical encounters with ethnic minority patients (Debesay et al., 2021 ).
3.3. Racism in the nurse–patient relationship
The thematic analysis of the studies' findings led to the development of three categories: bilateral ignition of racism, hidden and manifest consequences of racism and encountering strategies.
3.3.1. Bilateral ignition of racism
Pervasive racist perspectives and stereotypies among patients and nurses shaped their racist behaviours and negatively impacted the nurse–patient relationship.
Implicit bias among nurses towards racial and ethnic minorities was available in the form of having a general assumption about minorities, and was reflected through indirect negative racist expressions during the nurse–patient communication rather than direct impolite racist remarks (Debesay et al., 2021 ). From the macro‐perspective, power bias innated in the patient–nurse relationship. Considering patients in a weaker social position was the main cause of racist incidents (Debesay et al., 2021 ; Purtzer & Thomas, 2019 ).
Racism in institutional practice and policies also contributed to negative stereotypes. Ethnic minority patients who did not follow institutional guidelines were considered outsiders. They were labelled as clients who could not get integrated into social values, and were subject to racist remarks. Education in terms of hidden curricula and by learning from others when nurses worked in healthcare settings established racist stereotypes and attitudes towards patients (McFadden & Erikson, 2020 ; Purtzer & Thomas, 2019 ).
From a micro‐perspective, bias and stereotypical attitudes leading to racist behaviours rooted in nurses' personal perspectives towards ethnic minorities who had limited language proficiencies and substance dependencies, and suffered from mental illness (Debesay et al., 2021 ; Lyles et al., 2011 ; McFadden & Erikson, 2020 ; Purtzer & Thomas, 2019 ). Instead of assessing patients' cultural and ethnic backgrounds and investigating their cultural identities, nurses guessed on patients' cultural characteristics and needs based on their habits and last names to plan healthcare interventions (McFadden & Erikson, 2020 ). Failure to follow‐up nurses' health‐related advice, patients' socio‐economic factors and stereotypical attitudes developed by patients themselves towards their own physical and mental in‐capabilities enhanced racial distortions among nurses (McFadden & Erikson, 2020 ; Purtzer & Thomas, 2019 ).
On the other hand, patients' racism towards nurses was revealed in the experiences of nurses. Patients committed racial aggression when nurses were unable to meet their needs, which in some cases were unreasonable and beyond the defined nurse–patient relationship. Also, nurses' communication with accent triggered racist behaviours in patients (Cottingham et al., 2018 ; Debesay et al., 2021 ; Wheeler et al., 2014 ).
Nurses did not consider their position higher than patients in the nurse–patient interaction rounds. Nevertheless, some patients placed nurses at the lowest hierarchy of humanistic relationships and labelled them as subordinates. Patients' perspectives of nurses' ethnicity and cultural backgrounds determined the levels of nurses' competencies to provide care and receive respect. Nursing care was rejected by some patients, because of their personal orientations towards nurses' culture and ethnicity (Cottingham et al., 2018 ; Wheeler et al., 2014 ).
3.3.2. Hidden and manifest consequences of racism
Negative consequences of racism in the nurse–patient relationship were reported by both patients and nurses. Working in an environment in which stereotypical and racist attitudes influenced the nurse–patient relationship triggered the feeling of insecurity and uncertainty. Fear of making mistakes and crossing ethnic and cultural boundaries of minorities and the possibility of conflicts between patients' and families' beliefs, and nursing interventions enhanced work‐related stress among nurses (Debesay et al., 2014 , 2021 ). Nurses faced uncertainties with regard to how withhold their own personal prejudices and at the same time provide nursing care according to professional commitments (Debesay et al., 2021 ; Purtzer & Thomas, 2019 ).
Apparently, health disparities occurred given tensions between nurses and patients rooted in racist perspectives. They hindered nurses' efforts to provide appropriate care to patients and improve the nurse–patient relationship. When patients were not given opportunities to assert their cultural identities, they were discouraged to follow nurses' interventions and health‐related advice leading to more healthcare issues (Debesay et al., 2021 ; McFadden & Erikson, 2020 ; Purtzer & Thomas, 2019 ).
Patients mainly were dissatisfied with receiving support by nurses and complained about nurses' superior, cold and without sympathy communication style, inattention to their caring needs, not receiving suitable education, not spending enough time with patients and frequent nurses' turnover (Lyles et al., 2011 ; Martin et al., 2016 ; McFadden & Erikson, 2020 ).
A negative consequence of nurses' racist behaviours was the development of a negative perspective among patients towards the healthcare system. Racism was generalized to the whole healthcare system rather than taking it as a personal matter in the nurse–patient relationship (Benkert et al., 2009 ). Consequently, patients displayed disappointment or anger to all nurses and retaliated it, which damaged the sense of justice and pride even among those nurses who did their best to provide equitable care to patients (Debesay et al., 2021 ).
Those nurses who were subject to racist behaviours from patients experienced job‐related and emotional stress, which depleted their psychological resources and energy to deliver care. Assumption of incompetence due to racism led to emotional shift and encouraged nurses to retaliate. Therefore, instead of concentration on patient care, nurses focused on managing frustration and emotional trauma (Cottingham et al., 2018 ). Social isolation and disconnection, and leaving the nursing profession were some risky consequences of racist incidents (Cottingham et al., 2018 ; Wheeler et al., 2014 ).
3.3.3. Encountering strategies
Nurses and patients used strategies to avoid racism or at least minimize its impact on the nurse–patient relationship. Respect, trust and active participation in nursing care worked quite fine against stereotypical and racist behaviours. Compassionate care and respectful style of communication by nurses, friendliness, patience and taking care of patients' concerns and spending enough time for education were highlighted. These strategies could be all summarized into being patient‐centred (Lyles et al., 2011 ; Martin et al., 2016 ; Purtzer & Thomas, 2019 ).
Cultural mistrust as the outcome of racism could be avoided through the development of racial concordance in the nurse–patient relationship. The suggested strategy to achieve concordance was the provision of care by those nurses who had similar cultural and racial backgrounds to those of patients (Benkert et al., 2009 ; Lyles et al., 2011 ). Also, cultural understanding through the acknowledgment of patients' culture and learning about their values, ceremonies and traditions, integration of patients' values into nursing care and setting healthcare goals to preserve patients' cultural identity was required. Avoiding the creation of an unpleasant atmosphere in the nurse–patient relationship through not directly questioning patients' cultural characteristics, and balancing between care delivery and cultural rituals such as touching patients and undressing them helped prevent crossing cultural borders and creating the feeling of racism. Moreover, leading ethnic minority patients in healthcare journey and covering the gap between them and the requirements of the healthcare system were the main strategies for patient advocacy (Debesay et al., 2014 , 2021 ; McFadden & Erikson, 2020 ; Purtzer & Thomas, 2019 ).
When nurses faced racism from patients, they tried to avoid personalizing racist incidents and made jokes of them to control their anger and defend their own emotional well‐being. They considered such sorts of abuses one part of their daily work life that should be coped with (Cottingham et al., 2018 ; Deacon, 2011 ). Given the lack of policies in healthcare settings to manage racism, nurses coped with the situation and rationalized racist behaviours to reduce related emotional burdens. They tried to ignore racism and attributed it to patients' background diseases, age, previous negative life experiences and inability to take the responsibility of their own behaviours. As a confrontation strategy, some nurses reported the racist incident to authorities, used medications to calm patients, applied distraction techniques to patients, asked patients to refrain from being assaultive, and informed patients of their behaviours. In the worst case, some nurses decided to change their workplace (Cottingham et al., 2018 ; Deacon, 2011 ; Wheeler et al., 2014 ).
4. DISCUSSION
This scoping review of the international literature aimed to identify the nature of racism in the nurse–patient relationship and summarize international research findings about it. An overview of the breadth of the international literature on this phenomenon was presented consisting of three categories developed by the authors. Culture is intertwined with the phenomenon of racism and can critically influence the nurse–patient relationship (Crampton et al., 2003 ). Racism as an individual and systemic prejudice is imprinted in cultural artefacts and discourses (Salter et al., 2017 ). Racist perspectives, stereotypies and behaviours from patients and nurses can be attributed to cultural bias as the interpretation of situations and others' actions according to own set of personal perspectives, experiences and cultural standards.
Delivering unbiased and individualized care to culturally diverse patients is influenced by nurses' cultural competencies. Also, patients' personal attitudes and perspectives, and balancing the power between nurses and patients in healthcare situations are crucial to the development of an appropriate climate for patient care (Oxelmark et al., 2018 ; Vaismoradi et al., 2015 ). Accordingly, the findings of this review were discussed using the main aspects of the cultural competence puzzle consisting of cultural diversity, cultural awareness, cultural sensitivity and cultural competence as the elements of the three‐dimensional puzzle model of culturally congruent care at nurses' and patients' levels (Leininger & McFarland, 2002 ; Schim et al., 2007 ). The dimensions of this model have also the capacity to be the part of the patient's participation in the provision of culturally congruent care (Schim et al., 2007 ). Therefore, our discussion using this model covers racist behaviours from both patients and nurses. A summary of the review findings in connection to the culturally congruent care model has been presented in Figure 2 .

The review findings in connection to the culturally congruent care model
4.1. Cultural diversity
According to the review findings, racist behaviours in the nurse–patient relationship rooted in implicit and power biases demonstrating that the patient and the nurse had a low social position. Stereotypical attitudes were developed towards patients with limited language proficiencies, low socio‐economic conditions and different last names and cultural backgrounds.
Globalization is the cause of cultural diversities in health care. Similarities and differences between cultures in terms of race, ethnicity, nationality and ideology shape humanistic relationships in health care (Schim et al., 2007 ). The patient's and healthcare provider's cultural contexts are crucial in the development of the therapeutic relationship. The establishment of a constructive relationship between nurses and patients without the acknowledgment of their cultural diversities is impossible (Gopalkrishnan, 2018 ). Marginalization of ethnicities and minorities in the healthcare system should be avoided and instead their cultural diversities should be acknowledged and respected. All measures should be taken to avoid tensions when contacts between cultures occur. The assessment of cultural diversities is the cornerstone of planning for the provision of culturally congruent care through appropriate exposure to cultural differences and prevention of racism (Schim et al., 2007 ). Diversities in nurses' cultural backgrounds have been shown to be advantageous for the healthcare system in terms of improving the quality of patient care and healthcare economy (Gomez & Bernet, 2019 ).
4.2. Cultural awareness
In this review, education had an influence on the development of racism towards patients through hidden curricula and by learning at the workplace. Nurses felt uncertain about how to provide care that was congruent to patients' cultural backgrounds without having stress about crossing patients' cultural boundaries. Those nurses who faced racism from patients often were unable to manage the situation, were emotionally overloaded, and lost their concetration on the provision of care. Similarly, patients' racist behaviours towards nurses were attributed to a lack of understanding of nurses' cultural backgrounds.
Gaining knowledge about and recognition of other cultures help to identify the uniqueness of each culture and commonalities between the cultures. Cultural awareness aims at identifying similarities and differences between cultures in terms of religious rituals, routines, preferences and behaviours. It recognizes interpersonal comfort zones and customizes care to them, and suggest a method by which people can interact with others' cultures in the caring relationship leading to the delivery of culturally sensitive care (Schim et al., 2007 ).
Cultural awareness often happens in the process of informal nursing education because direct education may not be able to provide sufficient opportunities for nurses to become culturally aware (Hultsjö et al., 2019 ; Kaihlanen et al., 2019 ). Raising awareness about caring situations in which misinterpretations may occur help with the detection of underlying causes and finding a counteraction framework by which an equitable communication is made with patients and their satisfaction is preserved (Crawford et al., 2017 ; Tan & Li, 2016 ). Comparisons of cultures and discovery of common ethical values in the nursing profession help develop skills for the creation of dialogue between individuals' and facilitate integration to the global nursing context (Leung et al., 2020 ).
4.3. Cultural sensitivity
In this review, institutional practice and policies contributed to the development of negative stereotypes by which ethnic minority patients who did not follow institutional guidelines were subject to racist behaviours. Cultural sensitivity consists of individuals' attitudes towards others and themselves and understanding others' cultural characteristics. It motivates individuals to be cross‐cultural and acknowledges others' cultural heritages. Judging others' cultures based on own culture is against the principle of cultural sensitivity (Schim et al., 2007 ). Measures taken in healthcare systems to reduce bias and racism should encompass all types of inequalities among ethnic minorities (Sim et al., 2021 ). Improving cultural sensitivity enhances cultural intelligence and facilitates understanding the impact of culture on health and diseases. Therefore, the provision of intercultural healthcare based on understanding differences and similarities between cultures leads to the reduction of health inequalities and improvement of healthcare quality (Göl & Erkin, 2019 ; Yilmaz et al., 2017 ). Public and social media have important roles to tackle the problem of patients' racist behaviours towards nurses in care situations. They can debate healthcare policies, promote public health behaviours, educate patients and inform them of cultural norms in healthcare settings and engage them in the development of an environment that respects cultural diversities. Improving cultural sensitivity involves an increased focus on human rights. Individuals' equal worth and rights regardless of race, ethnicity, language and religion lay the foundation of human rights (United Nations, 2021 ).
4.4. Cultural competence
The findings of this review showed that patients could not assert their cultural identities and were dissatisfied with nurses' inappropriate communication style and lack of attention to their needs. Although there was no indication of training to nurses about culturally congruent care in our findings, the main focus of strategies to avoid racism by nurses was to acknowledge the patient culture, behave respectfully and provide compassionate care. This coping strategy supported nurses' personal well‐being and at the same time prevented the creation of negative stereotypes towards patients' cultural backgrounds. It is the demonstration of a series of behaviours and taking related actions indicating that healthcare professionals know how to acknowledge cultural diversities and are aware of and sensitive towards the patient's culture (Schim et al., 2007 ).
In the context of health care, it is to adapt care and comply skills to patients' needs. Being culturally competent facilitates culturally congruence care in the nurse–patient relationship. Cultural competence for ethnic minorities requires organizational support (Taylor, 2005 ) and it should include work at the system level (Sharifi et al., 2019 ). Cultural education and training have been emphasized as mitigating strategies that can reduce racism and bias, and enhance cope with cultural diversities. Cultural competence is an important strategy by which health inequities can be addressed (Horvat et al., 2014 ). It requires practising self‐reflexivity on routines that cause racism and bringing implicit bias to own conscious (Bradby et al., 2021 ; Medlock et al., 2017 ; Olukotun et al., 2018 ). Training about diversities and being exposed to cultural differences in practical placements can promote cultural competence and consequently interaction with culturally diverse patients (Levey, 2020 ; McLennon et al., 2019 ). Promoting cultural competence among healthcare providers prevents healthcare encounters and reduces shame and embarrassment among care receivers (Flynn et al., 2020 ).
4.5. Limitations and suggestions for future studies
This scoping review provided an overview of international knowledge about racism in the nurse–patient relationship in spite of retrieving a few empirical studies on this important phenomenon. More studies might have been published in languages other than English that could not be included in this review, and should be considered by future researchers. Racism in the nurse–patient relationship has remained a less explored area of nursing research specially regarding racism from patients towards nurses. Therefore, more studies about racism in the context of the nurse–patient relationship and in various healthcare contexts should be conducted to improve our knowledge of this culturally variant phenomenon and devise a general unified strategy for the eradication of racism from the nurse–patient relationship.
5. CONCLUSION
Racism threatens patients' and nurses' dignity in the healthcare system. It hinders efforts to meet patients' and families' needs and increases their dissatisfaction with nursing care leading to the loss of trust in nurses and reduction of quality of care. Also, racism from patients towards nurses causes emotional trauma and enhances job‐related stress among nurses leading to their turnover. Nurses often apply coping strategies to relieve the emotional pressure of racist incidents and protect their own emotional well‐being.
Racism in the globalized context of healthcare should be prevented and nurses' and patients' well‐being and dignity should be preserved. It needs the establishment of acts and legislations that prohibit racist behaviours and enforce their report to healthcare authorities to seek support and prosecute racist people. Also, there is a need to develop a framework of action based on the principles of culturally congruent care to eradicate racism from the nurse–patient relationship in the globalized context of healthcare.
The practical implications of the review findings based on the culturally congruent care model are as follows:
- Development of a practical guideline to help nurses and patients acknowledge cultural diversities and promote their awareness and sensitivity towards other cultures;
- Improvement of nurses' cultural competence through education and training about how to avoid racism during the provision of care to patients with different cultural backgrounds;
- Development of policies and practical strategies to ensure that patients are held responsible for racist behaviours that create a toxic environment for healthcare professionals;
- Comparing cultures and removing misperceptions about other cultures through communication and dialogue between nurses and patients;
- Rectification of institutional policies contributing to the creation of stereotypies about cultural minorities;
- Use of public and social media to inform patients of cultural norms in healthcare settings;
- Collaboration between associations supporting the human rights of nurses and patients for the development and implementation of zero‐tolerance and anti‐racism policies;
- Emphasis on the equal worth of people and human rights in healthcare settings;
- Cultural socialization of nurses through education and training about customizing care to patients' cultural backgrounds, demonstrating respect and providing compassionate care;
- Active screening and detection of stereotypes, implicit bias and racist attitudes among nurses through self‐reflexivity.
CONFLICT OF INTEREST
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
AUTHOR CONTRIBUTIONS
MV was involved in review design. MV, CFM, GU and KI were involved in data acquisition, analysis and interpretation for important intellectual content, drafting the manuscript and revising it for intellectual content and giving final approval of the version to be published in the journal.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.15267 .
Supporting information
Vaismoradi, M. , Fredriksen Moe, C. , Ursin, G. & Ingstad, K. (2022). Looking through racism in the nurse–patient relationship from the lens of culturally congruent care: A scoping review . Journal of Advanced Nursing , 78 , 2665–2677. 10.1111/jan.15267 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
The authors have received no financial support the research, authorship, and/or publication of this article.
DATA AVAILABILITY STATEMENT
- Ahlberg, B. M. , Hamed, S. , Thapar‐Björkert, S. , & Bradby, H. (2019). Invisibility of racism in the global neoliberal era: Implications for researching racism in healthcare [review] . Frontiers in Sociology , 4 ( 61 ). 10.3389/fsoc.2019.00061 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- American Nurses Association . (2021). National Commission to address racism in nursing: Defining racism . Retrieved November 5, 2021, from https://www.nursingworld.org/~49f737/globalassets/practiceandpolicy/workforce/commission‐to‐address‐racism/final‐defining‐racism‐june‐2021.pdf
- Benkert, R. , Hollie, B. , Nordstrom, C. K. , Wickson, B. , & Bins‐Emerick, L. (2009). Trust, mistrust, racial identity and patient satisfaction in urban African American primary care patients of nurse practitioners . Journal of Nursing Scholarship , 41 ( 2 ), 211–219. 10.1111/j.1547-5069.2009.01273.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradby, H. , Hamed, S. , Thapar‐Björkert, S. , & Ahlberg, B. M. (2021). Designing an education intervention for understanding racism in healthcare in Sweden: Development and implementation of anti‐racist strategies through shared knowledge production and evaluation . Scandinavian Journal of Public Health , 14034948211040963. 10.1177/14034948211040963 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brathwaite, B. (2018). Black, Asian and minority ethnic female nurses: Colonialism, power and racism . The British Journal of Nursing , 27 ( 5 ), 254–258. 10.12968/bjon.2018.27.5.254 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chandrashekar, P. , & Jain, S. H. (2020). Addressing patient bias and discrimination against clinicians of diverse backgrounds . Academic Medicine , 95 ( 12S ), S33–S43. 10.1097/acm.0000000000003682 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen, J. , Khazanchi, R. , Bearman, G. , & Marcelin, J. R. (2021). Racial/ethnic inequities in healthcare‐associated infections under the shadow of structural racism: Narrative review and call to action . Current Infectious Disease Reports , 23 ( 10 ), 17. 10.1007/s11908-021-00758-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cottingham, M. D. , Johnson, A. H. , & Erickson, R. J. (2018). “I can never be too comfortable”: Race, gender, and emotion at the hospital bedside . Qualitative Health Research , 28 ( 1 ), 145–158. 10.1177/1049732317737980 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crampton, P. , Dowell, A. , Parkin, C. , & Thompson, C. (2003). Combating effects of racism through a cultural immersion medical education program . Academic Medicine , 78 ( 6 ), 595–598. https://journals.lww.com/academicmedicine/Fulltext/2003/06000/Combating_Effects_of_Racism_Through_a_Cultural.8.aspx [ PubMed ] [ Google Scholar ]
- Crawford, T. , Candlin, S. , & Roger, P. (2017). New perspectives on understanding cultural diversity in nurse–patient communication . Collegian , 24 ( 1 ), 63–69. 10.1016/j.colegn.2015.09.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Daudt, H. M. , van Mossel, C. , & Scott, S. J. (2013). Enhancing the scoping study methodology: A large, inter‐professional team's experience with Arksey and O'Malley's framework . BMC Medical Research Methodology , 13 , 48. 10.1186/1471-2288-13-48 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Deacon, M. (2011). How should nurses deal with patients' personal racism? Learning from practice . Journal of Psychiatric and Mental Health Nursing , 18 ( 6 ), 493–500. 10.1111/j.1365-2850.2011.01696.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Debesay, J. , Harsløf, I. , Rechel, B. , & Vike, H. (2014). Facing diversity under institutional constraints: Challenging situations for community nurses when providing care to ethnic minority patients . Journal of Advanced Nursing , 70 ( 9 ), 2107–2116. 10.1111/jan.12369 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Debesay, J. , Kartzow, A. H. , & Fougner, M. (2021). Healthcare professionals' encounters with ethnic minority patients: The critical incident approach . Nursing Inquiry , e12421. 10.1111/nin.12421 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flynn, P. M. , Betancourt, H. , Emerson, N. D. , Nunez, E. I. , & Nance, C. M. (2020). Health professional cultural competence reduces the psychological and behavioral impact of negative healthcare encounters . Cultural Diversity & Ethnic Minority Psychology , 26 ( 3 ), 271–279. 10.1037/cdp0000295 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- George, R. , Thornicroft, G. , & Dogra, N. (2015). Exploration of cultural competency training in UK healthcare settings: A critical interpretive review of the literature . Diversity & Equality in Health and Care , 12 . 10.21767/2049-5471.100037 [ CrossRef ] [ Google Scholar ]
- Godlee, F. (2020). Racism: The other pandemic . British Medical Journal , 369 , m2303. 10.1136/bmj.m2303 [ CrossRef ] [ Google Scholar ]
- Gomez, L. E. , & Bernet, P. (2019). Diversity improves performance and outcomes . Journal of the National Medical Association , 111 ( 4 ), 383–392. 10.1016/j.jnma.2019.01.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gopalkrishnan, N. (2018). Cultural diversity and mental health: Considerations for policy and practice . Frontiers in Public Health , 6 , 179. 10.3389/fpubh.2018.00179 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Göl, İ. , & Erkin, Ö. (2019). Association between cultural intelligence and cultural sensitivity in nursing students: A cross‐sectional descriptive study . Collegian , 26 ( 4 ), 485–491. 10.1016/j.colegn.2018.12.007 [ CrossRef ] [ Google Scholar ]
- Hall, W. J. , Chapman, M. V. , Lee, K. M. , Merino, Y. M. , Thomas, T. W. , Payne, B. K. , Eng, E. , Day, S. H. , & Coyne‐Beasley, T. (2015). Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review . American Journal of Public Health , 105 ( 12 ), e60–e76. 10.2105/AJPH.2015.302903 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hamed, S. , Thapar‐Björkert, S. , Bradby, H. , & Ahlberg, B. M. (2020). Racism in European health care: Structural violence and beyond . Qualitative Health Research , 30 ( 11 ), 1662–1673. 10.1177/1049732320931430 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hassen, N. , Lofters, A. , Michael, S. , Mall, A. , Pinto, A. D. , & Rackal, J. (2021). Implementing anti‐racism interventions in healthcare settings: A scoping review . International Journal of Environmental Research and Public Health , 18 ( 6 ). 10.3390/ijerph18062993 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ho, A. (2016). Racism and bioethics: Are we part of the problem? The American Journal of Bioethics , 16 ( 4 ), 23–25. 10.1080/15265161.2016.1145293 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Horvat, L. , Horey, D. , Romios, P. , & Kis‐Rigo, J. (2014). Cultural competence education for health professionals . Cochrane Database of Systematic Reviews , ( 5 ), CD009405. 10.1002/14651858.CD009405.pub2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hultsjö, S. , Bachrach‐Lindström, M. , Safipour, J. , & Hadziabdic, E. (2019). "Cultural awareness requires more than theoretical education"—Nursing students' experiences . Nurse Education in Practice , 39 , 73–79. 10.1016/j.nepr.2019.07.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Iheduru‐Anderson, K. , Shingles, R. R. , & Akanegbu, C. (2021). Discourse of race and racism in nursing: An integrative review of literature . Public Health Nursing , 38 ( 1 ), 115–130. 10.1111/phn.12828 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaihlanen, A. M. , Hietapakka, L. , & Heponiemi, T. (2019). Increasing cultural awareness: Qualitative study of nurses' perceptions about cultural competence training . BMC Nursing , 18 , 38. 10.1186/s12912-019-0363-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Keshet, Y. , & Popper‐Giveon, A. (2018). Race‐based experiences of ethnic minority health professionals: Arab physicians and nurses in Israeli public healthcare organizations . Ethnicity & Health , 23 ( 4 ), 442–459. 10.1080/13557858.2017.1280131 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leininger, M. M. , & McFarland, M. F. (2002). Transcultural nursing: Concepts, theories, research and practice (3rd edition) . Journal of Transcultural Nursing , 13 ( 3 ), 261. 10.1177/104365960201300320 [ CrossRef ] [ Google Scholar ]
- Leung, D. Y. L. , Chan, E. A. , Wong, A. K. C. , Reisenhofer, S. , Stenberg, M. , Pui Sze, C. , Lai, K. H. , Cruz, E. , & Carlson, E. (2020). Advancing pedagogy of undergraduate nursing students' cultural awareness through internationalization webinars: A qualitative study . Nurse Education Today , 93 , 104514. 10.1016/j.nedt.2020.104514 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levac, D. , Colquhoun, H. , & O'Brien, K. K. (2010). Scoping studies: Advancing the methodology . Implementation Science , 5 , 69. 10.1186/1748-5908-5-69 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Levey, J. A. (2020). Teaching online graduate nursing students cultural diversity from an ethnic and nonethnic perspective . Journal of Transcultural Nursing , 31 ( 2 ), 202–208. 10.1177/1043659619868760 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lyles, C. R. , Karter, A. J. , Young, B. A. , Spigner, C. , Grembowski, D. , Schillinger, D. , & Adler, N. (2011). Provider factors and patient‐reported healthcare discrimination in the diabetes study of California (DISTANCE) . Patient Education and Counseling , 85 ( 3 ), e216–e224. 10.1016/j.pec.2011.04.031 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Martin, A. E. , D'Agostino, J. A. , Passarella, M. , & Lorch, S. A. (2016). Racial differences in parental satisfaction with neonatal intensive care unit nursing care . Journal of Perinatology , 36 ( 11 ), 1001–1007. 10.1038/jp.2016.142 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mateo, C. M. , & Williams, D. R. (2021). Racism: A fundamental driver of racial disparities in health‐care quality . Nature Reviews Disease Primers , 7 ( 1 ), 20. 10.1038/s41572-021-00258-1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McFadden, A. , & Erikson, S. L. (2020). How nurses come to race: Racialization in public health breastfeeding promotion . Advances in Nursing Science , 43 ( 1 ), E11–e24. 10.1097/ans.0000000000000288 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McLennon, S. M. , Rogers, T. L. , & Davis, A. (2019). Predictors of hospital Nurses' cultural competence: The value of diversity training . Journal of Continuing Education in Nursing , 50 ( 10 ), 469–474. 10.3928/00220124-20190917-09 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Medlock, M. , Weissman, A. , Wong, S. S. , Carlo, A. , Zeng, M. , Borba, C. , Curry, M. , & Shtasel, D. (2017). Racism as a unique social determinant of mental health: Development of a didactic curriculum for psychiatry residents . MedEdPORTAL , 13 . 10.15766/mep_2374-8265.10618 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Olukotun, O. , Mkandawire‐Vahlmu, L. , Kreuziger, S. B. , Dressel, A. , Wesp, L. , Sima, C. , Scheer, V. , Weitzel, J. , Washington, R. , Hess, A. , Kako, P. , & Stevens, P. (2018). Preparing culturally safe student nurses: An analysis of undergraduate cultural diversity course reflections . Journal of Professional Nursing , 34 ( 4 ), 245–252. 10.1016/j.profnurs.2017.11.011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oxelmark, L. , Ulin, K. , Chaboyer, W. , Bucknall, T. , & Ringdal, M. (2018). Registered Nurses' experiences of patient participation in hospital care: Supporting and hindering factors patient participation in care . Scandinavian Journal of Caring Sciences , 32 ( 2 ), 612–621. 10.1111/scs.12486 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Paradies, Y. , Truong, M. , & Priest, N. (2014). A systematic review of the extent and measurement of healthcare provider racism . Journal of General Internal Medicine , 29 ( 2 ), 364–387. 10.1007/s11606-013-2583-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Powell, W. , Richmond, J. , Mohottige, D. , Yen, I. , Joslyn, A. , & Corbie‐Smith, G. (2019). Medical mistrust, racism, and delays in preventive health screening among African‐American men . Behavioral Medicine , 45 ( 2 ), 102–117. 10.1080/08964289.2019.1585327 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pugh, M., Jr. , Perrin, P. B. , Rybarczyk, B. , & Tan, J. (2021). Racism, mental health, healthcare provider trust, and medication adherence among black patients in safety‐net primary care . Journal of Clinical Psychology in Medical Settings , 28 ( 1 ), 181–190. 10.1007/s10880-020-09702-y [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Purtzer, M. A. , & Thomas, J. J. (2019). Intentionality in reducing health disparities: Caring as connection . Public Health Nursing , 36 ( 3 ), 276–283. 10.1111/phn.12594 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rhee, T. G. , Marottoli, R. A. , Van Ness, P. H. , & Levy, B. R. (2019). Impact of perceived racism on healthcare access among older minority adults . American Journal of Preventive Medicine , 56 ( 4 ), 580–585. 10.1016/j.amepre.2018.10.010 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rogers, S. E. , Thrasher, A. D. , Miao, Y. , Boscardin, W. J. , & Smith, A. K. (2015). Discrimination in healthcare settings is associated with disability in older adults: Health and retirement study, 2008–2012 . Journal of General Internal Medicine , 30 ( 10 ), 1413–1420. 10.1007/s11606-015-3233-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Salter, P. S. , Adams, G. , & Perez, M. J. (2017). Racism in the structure of everyday worlds: A cultural‐psychological perspective . Current Directions in Psychological Science , 27 ( 3 ), 150–155. 10.1177/0963721417724239 [ CrossRef ] [ Google Scholar ]
- Schim, S. M. , Doorenbos, A. , Benkert, R. , & Miller, J. (2007). Culturally congruent care: Putting the puzzle together . Journal of Transcultural Nursing , 18 ( 2 ), 103–110. 10.1177/1043659606298613 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sharifi, N. , Adib‐Hajbaghery, M. , & Najafi, M. (2019). Cultural competence in nursing: A concept analysis . International Journal of Nursing Studies , 99 , 103386. 10.1016/j.ijnurstu.2019.103386 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sim, W. , Lim, W. H. , Ng, C. H. , Chin, Y. H. , Yaow, C. Y. L. , Cheong, C. W. Z. , Khoo, C. M. , Samarasekera, D. D. , Devi, M. K. , & Chong, C. S. (2021). The perspectives of health professionals and patients on racism in healthcare: A qualitative systematic review . PLoS One , 16 ( 8 ), e0255936. 10.1371/journal.pone.0255936 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stanley, J. , Harris, R. , Cormack, D. , Waa, A. , & Edwards, R. (2019). The impact of racism on the future health of adults: Protocol for a prospective cohort study . BMC Public Health , 19 ( 1 ), 346. 10.1186/s12889-019-6664-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tan, N. , & Li, S. (2016). Multiculturalism in healthcare: A review of current research into diversity found in the healthcare professional population and the patient population . International Journal of Medical Students , 4 ( 3 ), 112–119. 10.5195/ijms.2016.163 [ CrossRef ] [ Google Scholar ]
- Taylor, R. (2005). Addressing barriers to cultural competence . Journal for Nurses in Staff Development , 21 ( 4 ), 135‐142; quiz 143–144. 10.1097/00124645-200507000-00001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tricco, A. C. , Lillie, E. , Zarin, W. , O'Brien, K. K. , Colquhoun, H. , Levac, D. , Moher, D. , Peters, M. D. J. , Horsley, T. , Weeks, L. , Hempel, S. , Akl, E. A. , Chang, C. , McGowan, J. , Stewart, L. , Hartling, L. , Aldcroft, A. , Wilson, M. G. , Garritty, C. , … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA‐ScR): Checklist and explanation . Annals of Internal Medicine , 169 ( 7 ), 467–473. 10.7326/m18-0850 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Truitt, A. R. , & Snyder, C. R. (2019). Racialized experiences of black nursing professionals and certified nursing assistants in long‐term care settings . Journal of Transcultural Nursing , 31 ( 3 ), 312–318. 10.1177/1043659619863100 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- United Nations (UN) . (2021). Peace, dignity and equality on a healthy planet . Retrieved November 26, 2021, from . https://www.un.org/en/global‐issues/human‐rights
- Vaismoradi, M. , Jordan, S. , & Kangasniemi, M. (2015). Patient participation in patient safety and nursing input—A systematic review . Journal of Clinical Nursing , 24 ( 5–6 ), 627–639. 10.1111/jocn.12664 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Villarruel, A. M. , & Broome, M. E. (2020). Beyond the naming: Institutional racism in nursing . Nursing Outlook , 68 ( 4 ), 375–376. 10.1016/j.outlook.2020.06.009 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weitzel, J. , Luebke, J. , Wesp, L. , Graf, M. D. C. , Ruiz, A. , Dressel, A. , & Mkandawire‐Valhmu, L. (2020). The role of nurses as allies against racism and discrimination: An analysis of key resistance movements of our time . Advances in Nursing Science , 43 ( 2 ), 102–113. 10.1097/ans.0000000000000290 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Westphaln, K. K. , Regoeczi, W. , Masotya, M. , Vazquez‐Westphaln, B. , Lounsbury, K. , McDavid, L. , Lee, H. , Johnson, J. , & Ronis, S. D. (2021). From Arksey and O'Malley and beyond: Customizations to enhance a team‐based, mixed approach to scoping review methodology . Methods X , 8 , 101375. 10.1016/j.mex.2021.101375 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wheeler, R. M. , Foster, J. W. , & Hepburn, K. W. (2014). The experience of discrimination by US and internationally educated nurses in hospital practice in the USA: A qualitative study . Journal of Advanced Nursing , 70 ( 2 ), 350–359. 10.1111/jan.12197 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Willey, S. , Desmyth, K. , & Truong, M. (2021). Racism, healthcare access and health equity for people seeking asylum . Nursing Inquiry , 29 , e12440. 10.1111/nin.12440 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization . (2021). WHO at the high‐level session of the 76th UN General Assembly (UNGA) . Retrieved November 5, 2021, from . https://www.who.int/news‐room/events/detail/2021/09/14/default‐calendar/who‐at‐the‐high‐level‐session‐of‐the‐76th‐un‐general‐assembly‐(unga)
- Yilmaz, M. , Toksoy, S. , Direk, Z. D. , Bezirgan, S. , & Boylu, M. (2017). Cultural sensitivity among clinical nurses: A descriptive study . Journal of Nursing Scholarship , 49 ( 2 ), 153–161. 10.1111/jnu.12276 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Honor Society
- [ Member Login ]
- Search for: Search Button

National Commission to Address Racism in Nursing Releases Foundational Report
June 2, 2022

The National Commission to Address Racism in Nursing has issued a new foundational report that explores the impact of systemic racism on the nursing workforce and delivery of nursing care. The report closely examines the effects that racism has on nursing education, policy, research, and practice.
“These reports explore how racism shows up in our profession. We invite you to read each document with an open mind and heart, and with the empathy and thirst for knowledge that define excellence in nursing. How might this information influence you and your nursing practice? How might it be fuel for improving our profession, and the health, educational, and social systems in which we engage and work?”
OADN was invited to be an inaugural member of the Commission in January of 2021, and OADN members were asked to provide comments on the report’s initial draft in early 2022. OADN CEO Donna Meyer, MSN, RN, ANEF, FAADN, FAAN served as a commissioner for the report’s education workgroup, with Teaching and Learning in Nursing Editor-in-Chief Anna Valdez, Ph.D., RN, PHN, CEN, CNE, CFRN, FAEN, FAADN and OADN Board of Directors Member Jayson T. Valerio, DNP, RN serving as subject matter experts for the report’s education section.
Download The Full Report
The history of racism in nursing.
This report centers the experiences of nurses of color in U.S. history and how structural and systemic racism have hindered access to educational and professional opportunities as well as institutional power. The report also reviews some of the ways in which these nurses resisted, challenged, and achieved within the structures of racism.
Additionally, the report explains and critiques the central place that whiteness has occupied in histories of American nursing. More contextualized historical studies about the experiences of nurses of color and studies that explore the complicity of the nursing profession in perpetuating racism are needed.
Read this section
Contemporary Context
What does racism look like in the 21st Century? This essay examines power, privilege, and prejudice in nursing today. By looking at our history, we can understand the current inequities and discriminatory practices that hinder the progress of nurses of color.
Racism in nursing education has been prevalent since its beginning with roots in white supremacy. Today both students and faculty of color experience negative environments and limited opportunities.
Creating equitable and inclusive learning environments will lead to increased access and opportunities for students, faculty, and staff. This will eliminate many barriers and gaps that prevent success.
Due to the systemic nature of policies, they are a significant means by which racism within nursing is perpetuated.
A commitment must be made to eliminate racism in existing policy. Additionally, new policies that address past harms and advance the nursing profession are needed.
The impact of racism in the nurse’s work environment has significant implications on staff retention and physical and psychological safety. By viewing racism as a preventable harm, it is possible to see how it can be confronted through changes to structures, beliefs, policies, and practices.
This report also explores the ethical obligations to develop a culture where all staff and patients are treated fairly. Included are suggestions for how health care organizations can create an inclusive and civil culture.
Nursing research is overwhelmingly conducted by white nurse researchers. Research done with minoritized communities leaves impressions of exploitation and mistrust. Minority nurse researchers are key to address health disparities and inequities.
Current structures for research funding from healthcare institutions and governmental agencies are inequitable and must change. Bold funding decisions can level the field and lead to positive disruption.
PRESENTED BY:
- Julie Zerwic , PhD, FAHA, FAAN, Kelting Dean and Professor, College of Nursing, University of Iowa
- Kathy Dolter , PhD, RN Dean of Nursing, Kirkwood Community College
- Sarah Phipps , MSHSA, BSN, RN, Associate Executive Director, Idaho Board of Nursing
- Open access
- Published: 10 June 2022

Racism and antiracism in nursing education: confronting the problem of whiteness
- Sharissa Hantke 1 ,
- Verna St. Denis 1 &
- Holly Graham 1
BMC Nursing volume 21 , Article number: 146 ( 2022 ) Cite this article
6 Citations
4 Altmetric
Metrics details
Systemic racism in Canadian healthcare may be observed through racially inequitable outcomes, particularly for Indigenous people. Nursing approaches intending to respond to racism often focus on culture without critically addressing the roots of racist inequity directly. In contrast, the critical race theory approach used in this study identifies whiteness as the underlying problem; a system of racial hierarchy that accords value to white people while it devalues everyone else.
This qualitative study seeks to add depth to the understanding of how whiteness gets performed by nursing faculty and poses antiracism education as a necessary tool in addressing the systemic racism within Canadian healthcare. The methodology of poststructural discourse analysis is used to explore the research question: how do white nursing faculty draw on common discourses to produce themselves following introductory antiracism education?
Analysis of data reveals common patterns of innocent and superior white identity constructions including benevolence, neutrality, Knowing, and exceptionalism. While these patterns are established in other academic fields, the approaches and results of this study are not yet common in nursing literature.
Conclusions
The findings highlight the need for antiracism education at personal and policy levels beginning in nursing programs.
Peer Review reports
Racist health outcomes
The publicly funded Canadian healthcare system could be considered a point of national pride distinguishing us from the United States of America (USA) [ 1 ]. However, the outcomes of this system demonstrate that equal care and equal health are not made accessible for everyone. Indigenous people are frequently provided with substandard care, [ 2 , 3 ], and are subjected to disproportionate rates of poverty and illnesses including tuberculosis, human immunodeficiency virus (HIV), and diabetes [ 4 , 5 , 6 ]. The horrific death of Joyce Echaquan at the hands of Quebec nurses after they taunted her with anti-Indigenous stereotypes [ 3 ] has caused more nurses, managers, and nurse educators to recognize the widespread harms of racism within Canadian healthcare and the dire need for action. Despite national narratives of Canada as an accepting, diverse, multicultural country, our history demonstrates that from the early policies shaping the health of Canadians the healthcare system was created for, and continues to be for, the benefit of the white settler population and the simultaneous exclusion of Indigenous people, citizens of Colour, and immigrants of Colour [ 7 ]. A lack of public understanding of policies enacting racial exclusion enables white settler Canadians, including healthcare professionals, to participate in racist systems without seeing or understanding the racialized harms.
The racist violence of our system and its resulting harm, such as the numerous instances made evident in the In Plain Sight report [ 3 ], ought to be at the forefront of efforts to improve Canadian healthcare.
Why not focus on culture?
Nursing approaches attempting to respond to systemic racism in healthcare frequently focus on cultural learning, as in increasing one’s knowledge about ethnic minority cultures [ 8 , 9 ]. Healthcare could learn from what antiracist education scholar St. Denis [ 10 ] describes: “We started out a few decades ago in Aboriginal education believing that we could address the effects of racialization and colonization by affirming and validating the cultural traditions and heritage of Aboriginal peoples. There is increasing evidence that those efforts have limitations” (p. 178). Focusing on cultural education misdiagnoses the underlying problem, puts the onus for change onto the oppressed group, and absolves white people of responsibility for making changes [ 10 ]. Culturalist approaches within nursing reify discourses which other oppressed groups while either ignoring or inadequately focusing on race and racism [ 8 ]. Instead of focusing on learning about the Other, nursing needs anti-oppressive approaches which are critical of othering and approaches that seek to change students and society [ 11 ].
Sometimes cultural safety and cultural competence get conflated, as Curtis et al. [ 9 ] identify. While cultural competence more narrowly focuses on cross-cultural behaviours and acquiring knowledge about ethnic minority groups, cultural safety critically considers biases, stereotypes, power, and colonialism [ 9 ]. Bell [ 8 ] notes that “cultural safety and cultural humility pedagogies employ a more critical lens than previous iterations of culturally based approaches” (p. 3) such as cultural competence, transculturalism, and cultural sensitivity. Furthermore, Bell [ 8 ] argues that “cultural safety will not be possible to attain without explicit deconstruction of the white supremacist ideology that people in colonial and post-colonial states are socialized into so that people fundamentally understand and become accountable for their (our) oppressive and/or privileged behaviour” (p. 4).
To create an outcome of cultural safety for racially oppressed groups, we must address the racism underlying the harm. To address racism in the healthcare system, all healthcare workers, educators, and decision makers need the tools of antiracism education grounded in critical race theory and critical whiteness studies. We must work on understanding the attitudes and priorities of the healthcare system and how they enact harm so that instead of focusing on cultural learning as a solution to racist harm, we work to understand and address the underlying problem at the core of racialized health outcomes: whiteness.
Relevant nursing literature
Since Vaughan’s 1997 article [ 12 ] asks if there really is racism in nursing and answers with a definitive “yes”, very little nursing literature has explored racism in nursing, and less still has named whiteness as underlying racism. Prior to 2020, searching for nursing literature that critically addresses racism revealed few results. Exceptions include: Blanchet Garneau, Browne, and Varcoe [ 13 ] highlighting the need for antiracist pedagogy in nursing; Hilario, Browne, and McFadden [ 14 ] identify democratic racism in nursing—discourses that attempt to justify contradictions between Canadian values of tolerance and equity, and Canadian racism; Tang and Browne’s [ 15 ] study identify various ways that racist stereotypes impact Indigenous patients’ access to care; Scammell and Olumide [ 16 ] describe white nurses as “unwittingly” perpetuating racism; Van Herk, Smith, and Andrew [ 17 ] urgently suggest that intersectionality and critical pedagogy become part of nursing education and practice; and Walker’s dissertation [ 18 ] demonstrates the need for cultural safety training and delineating important differences between cultural competence and cultural safety.
How whiteness underpins racism
This study uses the term “whiteness” to point to the system of racial hierarchy that positions white racial identity at the top and thereby affords disproportionate power and privilege to people racialized as white at the expense of everyone not racialized as white [ 19 ]. The theoretical bases underpinning this research are Critical Race Theory (CRT) and Critical Whiteness Studies (CWS). Three particularly relevant shared tenets of these fields include (1) understanding racism as systemic and often invisible to white people [ 20 ]; (2) race and whiteness as socially constructed to serve white interests [ 21 , 22 , 23 ] as opposed to primarily biologically or genetically [ 24 ]; and (3) the necessity of directing the critical gaze away from those subjected to racism and toward those who are unduly privileged by racial dominance [ 20 , 25 ]. As such, this study understands racial categories as having been constructed in the eighteenth century to serve an exploitative agenda which still causes widespread health inequity [ 26 ]. Although the concept of races as biologically distinct categories is outdated and disproven, underlying biases based on these debunked ideas still get reified in science and health fields [ 8 , 27 ]. This study understands race to be immensely impactful because of its social construction and maintenance and therefore aims to keep a critical focus on how race and racism get produced.
Instead of recognizing racism as a primarily interpersonal phenomenon, this study urges readers to consider how systemic racism is constructed and maintained systemically through discourses. Of particular interest are discourses which function to position whiteness as superior and as innocent. Through identifying and analyzing the discursive resources [ 28 ] utilized by white settler nursing faculty, this study aims to highlight the need for personal antiracism learning for individual white nursing faculty, the need for inclusion of antiracism curriculum into nursing programs, and the need for an antiracism lens at the policy level of nursing programs.
Although this study examines Canadian healthcare and Canadian data, the findings may have relevance more broadly. The Canadian context has been shaped by colonization, and the resulting racial dynamics may have parallels wherever colonialism and European imperialism oppress Indigenous peoples with a “huge legacy of suffering and destruction” (p. 20) [ 29 ].
Researcher context and reflexivity
This research and the antiracism education preceding it were undertaken as part of Sharissa Hantke’s master’s thesis. Sharissa is a white settler cisgender woman and worked under the supervision of Indigenous scholar and antiracism education expert Dr. Verna St. Denis and Indigenous scholar, psychologist, and nursing faculty Dr. Holly Graham. Since Sharissa is a white settler critically studying how white nursing faculty perform whiteness, guidance and mentorship from Indigenous scholars was critical in mitigating the risks of perpetuating settler colonialism.
Study design
This study seeks to add depth to understanding how whiteness gets performed by nursing faculty and thereby to examine how the performance of whiteness functions to uphold racism within nursing education. The research question is therefore: how do white nursing faculty draw on common discourses to produce themselves following introductory antiracism education?
Following approval from the behavioural research ethics board, nursing faculty were recruited to a focus group interview to discuss their experience of a workshop introducing antiracism education. Such education is new to Saskatchewan nursing faculty, and the workshop sessions were made possible through funding from the Indigenous Research Chair of Canadian Institute of Health Research through the Dr. Graham’s wahkohtowin project. Although the entire workshop was 6 full days long, the training was offered in three two-day chunks, with four month breaks between. Due to time constraints, the 1.5 h focus group session was held after the first two-day workshop where participants had learned about race as a social construct, intersectionality, racism as systemic, history of racism in Canadian health care, debunking meritocracy, and exploring resistance to antiracist education. Recruitment occurred at the end of day two of the workshop session by inviting white nursing faculty to participate in the research study. Of the 24 registrants who met eligibility requirements for being white nursing faculty, three volunteered to participate in the focus group, and informed consent was obtained. These three white nursing faculty teach in different nursing programs, and their voluntary participation demonstrates their keenness to continue learning antiracism. These participants were provided with open ended reflection questions in advance which asked them about difficult/uncomfortable parts of the education, their anticipation of how the education may impact their teaching, and their next steps on their antiracism journey. The focus group interview was semi structured to allow for participants to respond to each other and build off each other’s responses in the group context. One strength of a focus group approach was that the conversation allowed participants to continue to learn from and to build relationships with each other. The focus group was facilitated by the primary author. These participants were at different points in their antiracism learning and this is reflected in the data which came from all three participants.
The focus group dialogue was transcribed and then discourses were identified consistent with critical race theory (CRT) literature [ 30 ]. Concept mapping was used to track discourses which connect to CRT. Data was interpreted from the poststructural discourse analysis perspective of language as not simply a means of neutrally describing reality—rather of discourses as doing particular things [ 28 ].
Wetherell [ 28 ] says that identities are “constituted as they are formulated in discourse” (p. 12). Focus group participants used their words to produce their own white nursing faculty identities in patterns consistent with literature in the field of Critical Whiteness Studies [ 21 , 31 , 32 , 33 , 34 ]. Critically examining how white people construct identity is imperative because of the connections to racialized health disparities.
Inequality is not first a fact of nature and then a topic of talk. Discourse is intimately involved in the construction and maintenance of inequality. Inequality is constructed and maintained when enough discursive resources can be mobilized to make colonial practices of land acquisition, for instance, legal, natural, normal, and ‘the way we do things.’ (p. 13) [ 28 ]
Therefore it is imperative to examine the sorts of discourses white nursing faculty employ so that we can learn how to identify deeply held beliefs which find their way into nursing practices and into policy, thereby producing racist outcomes (see Structural Determinism framework [ 35 ]). In seeking out these discourses, this research aims to gain more understanding of how white settlers contribute to racist harm and how to work toward both personal and policy level change.
As such, this study examines common, well-intentioned, and seemingly benign discursive maneuvers present in the focus group interview not for the purpose of critiquing the individuals who made the statements in the time they generously volunteered to the study, but rather to examine what these common statements and sentiments do in regards to race.
The data presented here reveal two aspects of whiteness so that white nurses and white nursing faculty can identify how whiteness functions. Those of us who inhabit whiteness find it difficult to identify [ 36 ] and thus whiteness must be “made strange” for white people to study it critically [ 37 ]. The seven pieces of data here each represents a commonplace example drawing upon discursive resources consistent with patterns of the performance of whiteness as established in CRT and CWS literature. Discursive maneuvers are presented here as they relate to two broad categories: innocence and superiority. Data were chosen for their commonplaceness; none of the discourses employed were unusual or surprising. Rather, they are oft-repeated, routine narratives [ 28 ] available to and employed by white settlers in Canada.
Tuck and Yang [ 38 ] identify that settler “moves to innocence” function to relieve guilt while abnegating responsibility for change. Employing discourses of innocence can redirect focus from the responsibility of addressing inequity to our own benevolence and good intentions. Innocence in this context can be understood as innocence from racism, where the definition of racism is limited to intentional interpersonal harm resulting from moral failing [ 32 ]. Scheurich and Young [ 39 ] point out that using this faulty definition of racism enables white university faculty to absolve themselves of personal responsibility. There is thus much to be accomplished in constructions of white innocence. The disadvantages racist policies and practices produce for Indigenous people in Canada relate directly to the advantages white settlers receive [ 40 ]. Rather than focus on Indigenous people as though they are the problem, this research highlights examples of discourses of innocence through which whiteness is produced.
This first piece of data is illustrative of innocent benevolence: “I just try to always remember that we ー I think we’re nice people and we’re coming from a good place and hopefully people understand that. That’s what I keep repeating to myself.” These sentences direct the focus onto the benevolent intentions of white people thereby precluding considering any harmful impact of one’s words or actions. The implication that nice white people must be innocent of racism serves to obscure the group members’ participation in racially unjust systems. Although the antiracism education may have destabilized white participants’ self-conception, rather than exploring a more complex identity such as “being an anti-racist racist” [ 41 ], the above statement insists on a nice, good, innocent understanding of self.
In addition to benevolence, white constructions of innocence may deploy neutrality through refusing to consider the racial power one holds. This second piece of data, a rhetorical strategy of neutrality is utilized to construct an innocent self. In reflecting upon what to do when someone makes a racist comment, one participant said, “you know sometimes even those comments, when people make those to you, do I [sic] stay neutral?” This sentence equates remaining silent as a sign of neutrality rather than seeing silence as a means of supporting or enabling the racist comment. Portraying the decision to be silent as somehow maintaining neutrality can function to grant the racist comment freedom to pass undisputed, or the silence can imply agreement. The phrasing of “staying neutral” reveals the speaker’s understanding of their white self as already neutral. Such rhetorical strategies of neutrality reinforce the construction of white innocence when white people speak as though our (Sharissa) whiteness does not position us with disproportionate power at the expense of Black people, Indigenous people, and people of Colour.
In a third data sample participants were asked to consider their next steps. The participant intended to tell their students that “you have to put your biases aside and treat every- do your best to treat everyone the same.” This statement once again seeks to construct white people as neutral and separable from their biases, ignoring white people’s deep socialization into white dominance [ 42 ]. The idealized notion of treating everyone the same is an example of meritocratic colourblind discourse. The meritocratic aspect of the statement functions to uphold the myth that all people start from the same place and therefore success is based solely on hard work and determination, as portrayed in McLean’s [ 43 ] impactful article that dispels the myth of meritocracy. Such a myth overlooks historical racial inequity produced by policies demonstrated in Fig. 1 . The colourblind aspect of the statement overlooks present day racial inequity by refusing to acknowledge difference [ 44 ]. This sentiment prioritizes sameness of treatment over the need to equitably address historical and present day racist harm. Through colourblind meritocratic discourses, the statement attempts to conceal sentiments which uphold the harmful status quo within seemingly open language.
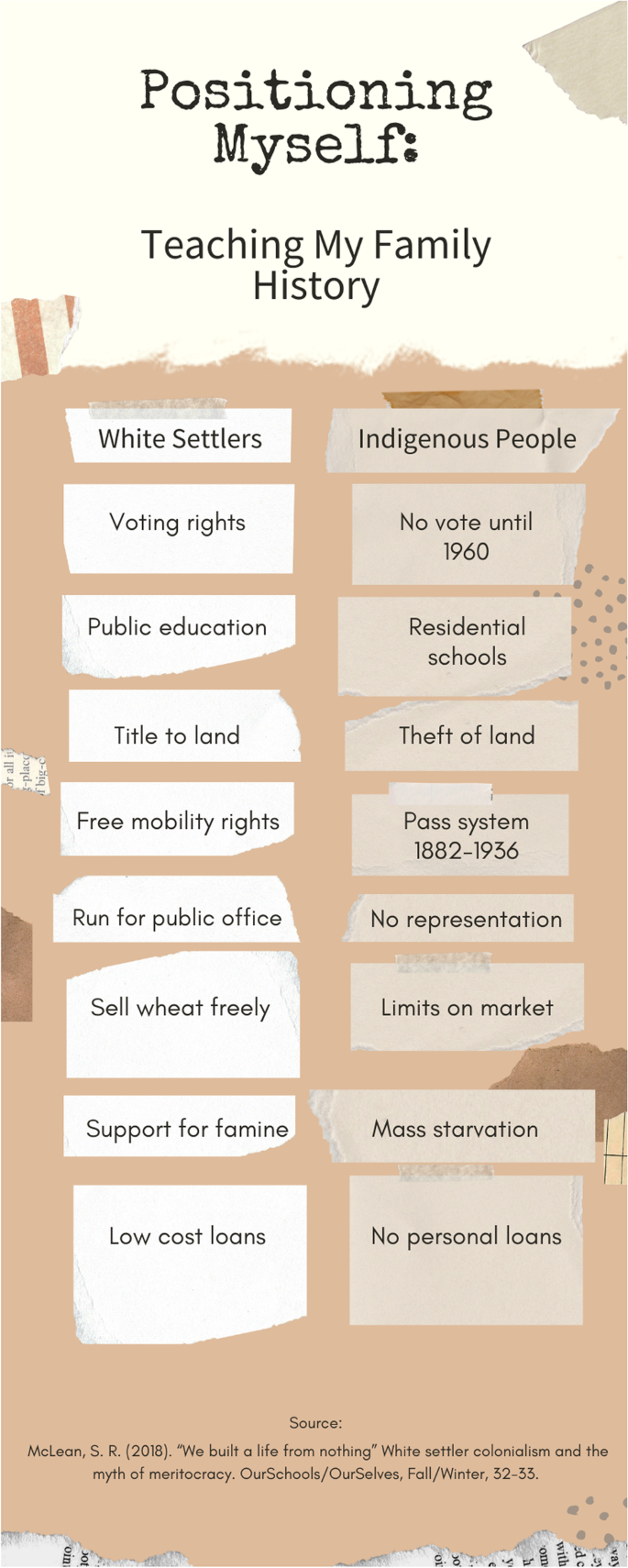
Positioning myself
Superiority
At the core of the construct of white racial identity is a deeply ingrained sense of superiority [ 45 ]. This section considers how identifying as a Knower and as exceptional are examples of a broader pattern of understanding the white self as superior. Superiority is a relative term; for superiority to be possible implies the necessity of inferiority as comparison. There are many ways that a sense of superiority can manifest, and the two demonstrated here were selected for their relevance among well-intentioned, open-minded white people who do not want to be (seen as) racist. Positioning oneself as a Knower can have the impact of seeming superior through authoritativeness. To be the one who knows is valued over being one who does not know, and thus this construction is desired as superior. Exceptionalism here means portraying oneself as somehow special, one of the “good ones,” and elevated above “those other” racist whites. Exceptionalism and being the Knower can go hand in hand, particularly when white people construct ourselves as exceptional by means of our antiracist knowledge.
The fourth piece of data is brief: “We know more than we think.” This was stated as the group articulated their intended next steps in antiracism. Neither the veracity nor the intention of this sentence will be examined here. Instead, we look at what the statement does . In context, it was being used to comfort the group of white nursing faculty by validating their knowledge. It constructs the group as those who already know and it could be an effort to avoid the discomfort of not knowing . Both the discomfort experienced in antiracist, anti-oppressive education, and the crisis that arises in this process, are necessary components of this education and ought not to be avoided [ 46 , 47 ].
Here is the fifth piece of data: “That’s what makes me angry, it makes me angry sometimes… the people that maybe really needed to be there don’t come to those things.” This statement refers to the participants’ colleagues who did not attend the antiracism education. By distinguishing the white focus group as those who showed up in contrast with those who actually needed the education, this statement positions the group members as exceptional. By creating a dichotomy of the racist ones who really need it and the good ones who showed up, the statement positions the workshop attendees and the keen focus group participants as not “really needing” antiracism education in contrast to those who did not join. Such positioning is at odds with participants’ descriptions of how much they learned during the sessions. How then, can they imply that they did not “really need” to be there? Additionally, emotions can be understood to do things [ 48 ] and we can understand the statement’s disclosure of anger to highlight and reinforce the white focus group participants’ sense of white exceptionality [ 49 , 50 , 51 ].
In a sixth data sample, the speaker constructs their self as both a Knower and as exceptional in their communications with students: “If I don’t have those [antiracist] conversations and show that they can happen and make mistakes with my students then they’re never going to have those conversations, right?” The statement demonstrates a prioritization of critical conversations, showing an understanding of how necessary antiracism work is. At the same time, the statement portrays the speaker as the one and only means by which their students would be exposed to antiracist conversations, therefore constructing their own exceptionalism as well as an identity as a lone white antiracist hero [ 52 ]. The statement also implies that the speaker is prepared and competent to have critical antiracist conversations, and is thus also constructing the speaker as an antiracist Knower.
In their 2005 article [ 53 ], Schick and St. Denis state, “this is the assumption of superiority that whiteness permits: what we have and who we are is what the world needs, whether it wants it or not” (p. 308). White nursing faculty, and nurses more generally must work to identify and uproot assumptions of superiority. Since these assumptions have been embedded from our (Sharissa) very early socialization into whiteness [ 42 ], identifying and unlearning them is an undertaking which will only be possible with deep and humble and ongoing reflection using the tools available in the scholarship of critical race theory and critical whiteness studies. One such tool white people can practice using is understanding our (Sharissa) complicity in systemic racism.
Having examined data which provides examples that function to construct white participants as innocent and superior, patterns which support the racist status quo, it is now time to consider one piece of data which does something different. When debriefing about feelings that arose during the antiracism education, one participant recognized an important moment, “For me I think it was just like oh my. I’m contributing to this.” This seventh data statement points to a moment of clarity which contrasts to the discourses of innocence and superiority mentioned above, and points toward a process of realizing complicity in the harmful systems which uphold the status quo. For white people who want to work toward a racially equitable future, it is necessary to not attempt to set oneself apart from “those racist whites” but instead to recognize the ongoing racist harm caused by participating in racist systems. Rather than focusing energy on defending individual goodness or innocence, white people need to be open to the deeply uncomfortable idea that despite intentions, they cause racist harm.
Reflecting upon one’s complicity in harmful systems is distinct from the emotions of guilt which may arise with this reflective work. Guilt might emerge in the process of learning about one’s personal complicity with whiteness, but guilt can stall out the antiracist efforts of white people, and is therefore a state to be worked through and learned from, not one to linger in. “While guilt is often a sign of a much-needed shift in consciousness, in itself it does nothing to motivate the responsibility necessary to actively dismantle entrenched systems of oppression” [ 54 ].
It is important that white people do not center their own feelings and self in antiracism work [ 49 ]. Learning about the complexities of the systems of racial oppression they participate in must be personal, but personal reflection is not the goal of antiracism work in and of itself. Antiracism work must seek to address racial injustice and work toward racial equity outcomes. As Kendi [ 55 ] emphasizes, unless policy change happens, antiracist change is not happening.
These data provide a snapshot of some discursive resources [ 28 ] which are available and utilized by highly educated, well-intentioned, open-minded white people. The analysis of the above statements demonstrates the use of poststructural discourse analysis by critically examining what each discourse accomplishes. Since beliefs and biases find their way into action, practices, and policies, they therefore cause harmful outcomes for oppressed groups [ 25 , 35 , 53 ]. The deeply socialized sense of superiority which shows up subtly (or not) in white people’s language has real world implications, resulting in the perpetuation of inequity and therefore if white people want to practice antiracism, they must work to identify and unlearn these deep beliefs.
It is necessary to excavate deeply embedded senses of superiority if white people want to address the crux of racial inequity. This deep and disruptive work will not be accomplished by cultural learning but through critical examination of unequal power and oppression through antiracist approaches.
Regarding the recommendations these findings point toward, it may be tempting to think that nursing programs could address the harms of whiteness by simply adding an antiracism course to our curriculum. While the addition of such content is desperately needed and will be an important step in equipping new generations of nurses with the tools of antiracism, it alone will not be enough. Nursing educators must first work to develop an antiracism lens through which they constantly teach and practice. We need major paradigm shifts, similar to the shifts to health promotion of the late twentieth century, to bring our programs into alignment with antiracist, anti-oppressive approaches. To prepare for such necessary policy changes, nursing program faculty, staff, and administration will need to be equipped with antiracist education. Therefore, this research urges as next steps the preparation of nursing faculty, staff, and administration with a solid grounding in antiracism education.
Specific changes and incremental steps are not provided in this article, and indeed require further efforts to determine. “Antiracist traditions provide us with useful critiques of existing situations, but tools developed to challenge racism will not always serve equally well to envision new racial possibilities. Critical tools are shaped to an important degree by the relations they are meant to disrupt” [ 49 ] (p. 21).
Strengths and limitations
Although the discourses considered in this paper are consistent with CRT and CWS literature, this study does not claim to be generalizable due to the small size and limited duration of the focus group. A significant limitation was the timing of the focus group session. The focus group happening after the first two-day educational workshop rather than after the third and final two-day workshop means that the discourses documented here emerged when the participants had only been introduced to very initial antiracism concepts. An advantage of the timing was that their discussion informed which content to prioritize in the following workshop days.
A strength of this research is that using poststructural discourse analysis to understand racism and whiteness is not yet common practice in nursing literature. Providing an example of the application of this methodology may demonstrate a tool which could be quite useful for nurses pursuing antiracist approaches.
The deeply rooted problem of racism in Canadian healthcare necessitates change at the foundational level. If we want to eliminate the racialized health outcomes evident in our system, we need to understand our colonial context which values whiteness. Since whiteness is a structure which devalues all who are not white, we must learn to identify how whiteness functions so that we can unlearn these ways and instead actively build and practice change which prioritizes equity. One aspect of identifying and unlearning whiteness is developing a capacity to identify the patterns of whiteness. Tools and theories that can inform and support this crucial work are available, particularly in the fields of CRT and CWS, and it is time for nursing to learn from them and integrate them into our education programs.
Availability of data and materials
The datasets analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Critical Race Theory
Critical Whiteness Studies
Forget EL. National identity and the challenge of health reform in Canada. Rev Soc Econ. 2002;60(3):359–75. https://doi.org/10.1080/0034676021000013368 .
Article Google Scholar
Allan B, Smylie J. First Peoples, second class treatment: The role of racism in the health and well-being of Indigenous peoples in Canada. Toronto: The Wellesley Institute. 2015. www.wellesleyinstitute.com/wp-content/uploads/2015/02/Summary-First-Peoples-Second-Class-Treatment-Final.pdf
Turpel-Lafond M. In Plain Sight: Addressing Indigenous-specific Racism and Discrimination in B.C. Health Care. Independent report prepared for the Government of British Columbia. 2020. https://engage.gov.bc.ca/app/uploads/sites/613/2020/11/In-Plain-Sight-Full-Report.pdf
Dyck R, Osgood N, Lin TH, Gao A, Stang MR. Epidemiology of diabetes mellitus among First Nations and non-First Nations adults. CMAJ. 2010;182(3):249–56. https://doi.org/10.1503/cmaj.090846 .
Article PubMed PubMed Central Google Scholar
Negin J, Aspin C, Gadsden T, Reading C. HIV among Indigenous peoples: a review of the literature on HIV-related behaviour since the beginning of the epidemic. AIDS Behav. 2019;19:1720–34. https://doi.org/10.1007/s10461-015-1023-0 .
Vachon J, Gallant V, Siu W. Tuberculosis in Canada, 2016. Can Commun Dis Rep. 2018;44(3–4):75–81. https://doi.org/10.14745/ccdr.v44i34a01 .
Article CAS PubMed PubMed Central Google Scholar
Thobani S. Exalted subjects: studies in the making of race and nation in Canada. Toronto: University of Toronto Press; 2007.
Google Scholar
Bell B. White dominance in nursing education: a target for anti-racist efforts. Nurs Inq, 2020;27(4); https://doi.org/10.1111/nin.12379
Curtis E, Jones R, Tipene-Leach D, et al. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. Int J Equity Health. 2019;18:174. https://doi.org/10.1186/s12939-019-1082-3 .
St. Denis V. Rethinking culture theory in Aboriginal education. In: Cannon MJ, Sunseri L, editors. Racism, Colonialism and Indigeneity in Canada. Oxford: Oxford University Press; 2011.
Kumashiro K. Toward a theory of anti-oppressive education. Rev Educ Res. 2000;70(1):25–53. https://doi.org/10.3102/00346543070001025 .
Vaughan J. Is there really racism in nursing? J Nurs Educ. 1997;36(3):135–9. https://doi.org/10.3928/0148-4834-19970301-09 .
Article CAS PubMed Google Scholar
Blanchet Garneau A, Browne AJ, Varcoe C. Drawing on antiracist approaches toward a critical anti discriminatory pedagogy for nursing. Nurs Inq. 2017;25(1):1–9.
Hilario CT, Browne AJ, McFadden A. The influence of democratic racism in nursing inquiry. Nurs Inq. 2018;25(1):1–7. https://doi.org/10.1111/nin.12213 .
Tang SY, Browne AJ. ‘Race’ matters: Racialization and egalitarian discourses involving Aboriginal people in the Canadian health care context. Ethn Health. 2008;13(2):109–27. https://doi.org/10.1080/13557850701830307 .
Article PubMed Google Scholar
Scammell JME, Olumide G. Racism and the mentor-student relationship: Nurse education through a white lens. Nurse Educ Today. 2012;32:545–50. https://doi.org/10.1016/j.nedt.2011.06.012 .
Van Herk KA, Smith D, Andrew C. Examining our privileges and oppressions: incorporating an intersectionality paradigm into nursing. Nurs Inq. 2011;18:29–39. https://doi.org/10.1111/j.1440-1800.2011.00539.x .
Walker P. Caring About Racism: Early Career Nurses’ Experiences with Aboriginal Cultural Safety (PhD dissertation). Department of Leadership: Higher and Adult Education, OISE/University of Toronto; 2017.
Alberta Civil Liberties Research Centre. (n.d.). Whiteness. https://www.aclrc.com/whiteness
McLean SR. Beyond the pale: Whiteness as innocence in education. Master’s thesis, University of Saskatchewan. www.academia.edu/download/31609645/Thesis.doc . 2007.
Lipsitz G. The possessive investment in whiteness: racialized social democracy and the “white” problem in American studies. Am Q. 1995;47(3):369–87.
Harris C. Whiteness as property. In: Martin Alcoff L, Mendita E, editors. Identities: race, class, gender, and nationality. Hoboken: Blackwell Publishing. 2003. p. 75–88.
Dyer R. White Screen. 1988;29(4):44–65. https://doi.org/10.1093/screen/29.4.44 .
Jupp JC, Berry TR, Lensmire TJ. Second-wave white teacher identity studies: a review of white teacher identity literatures from 2004 through 2014. Rev Educ Res. 2016;86(4):1151–91. https://doi.org/10.3102/0034654316629798 .
Gillies C. A critical race analysis of Métis teachers and racism in Saskatchewan schools. Unpublished doctoral dissertation. University of Saskatchewan, Saskatoon, Saskatchewan, Canada. 2018.
Tashiro CJ. The meaning of race in health care and research–part 1: the impact of history. Pediatr Nurs. 2005;31(3):208–10.
PubMed Google Scholar
Duster T. A post-genomic surprise. The molecular reinscription of race in science, law and medicine. Br J Sociol. 2015;66(1):1–27. https://doi.org/10.1111/1468-4446.12118 .
Wetherell M. Racism and the analysis of cultural resources in interviews. In: van den Berg H, Wetherell M, Houtkoop-Steenstra H, editors. Analyzing Race Talk. Cambridge University Press; 2003. p. 11–30.
Tuhiwai SL. Decolonizing methodologies: research and Indigenous peoples. London: Zed Press; 1999.
Gillies C. Seeing whiteness as property through Métis teachers’ K-12 stories of racism. Whiteness and Education. 2021.
Applebaum B. Critical Whiteness Studies. Oxford Research Encyclopedia of Education. 2016. https://www.oxfordre.com/education/view/ https://doi.org/10.1093/acrefore/9780190264093.001.0001/acrefore-9780190264093-e-5 .
DiAngelo R. White fragility: why it’s so hard for white people to talk about racism. Boston: Beacon Hill Press; 2018.
Lentin A. Beyond denial: ‘not racism’ as racist violence. Continuum. 2018;32(4):400–14. https://doi.org/10.1080/10304312.2018.1480309 .
Schick C. White women teachers accessing dominance. Discourse: Studies in the Cultural Politics of Education. 2000;21(3):299–309. https://doi.org/10.1080/713661167
Government of Alberta. Indigenous Learning Initiative. Engagement Summary Report: Indigenous Scholars; 2018.
Ahmed S. Declarations of whiteness: The non-performativity of anti-racism'. borderlands. 2006;5(3).
Dyer R. White. New York: Routledge. 1997
Tuck E, Yang KW. Decolonization is not a metaphor. Decolonization: Indigeneity, Education & Society. 2012;1(1):1–40.
Scheurich JJ, Young MD. Chapter 10. White racism among white faculty: From critical understanding to antiracist activism. In: Smith WA, Altbach PG, Lomotey K, editors. The Racial Crisis in American Higher Education. Albany: State of New York Press; 2002.
Harding L. What’s the harm? Examining the stereotyping of Indigenous peoples in health systems. Doctoral dissertation, Simon Fraser University. Summit Institutional Repository. 2018.
Leonardo Z, Zembylas M. Whiteness as technology of affect: Implications for educational praxis. Equity Excell Educ. 2013;46(1):150–65. https://doi.org/10.1080/10665684.2013.750539 .
Thandeka. Learning to Be White: Money, Race, and God in America. New York: The Continuum Publishing Company; 1999.
McLean SR. “We built a life from nothing” White settler colonialism and the myth of meritocracy. OurSchools/OurSelves. 2018;Fall/Winter:32–33.
Bonilla-Silva E. The linguistics of color blind racism: How to talk nasty about Blacks without sounding “racist.” Crit Sociol. 2002;28(1–2):41–64.
Schick C, St. Denis V. Troubling national discourses in anti-racist curricular planning. Can J Educ. 2005;28(3):295–317. https://doi.org/10.2307/4126472 .
Kumashiro K. Teaching and learning through desire, crisis, and difference: perverted reflections on anti-oppressive education. Radical Teacher. 2000. p. 58.
Ohito EO. Making the emperor’s new clothes visible in anti-racist teacher education: enacting a pedagogy of discomfort with white preservice teachers. Equity Excell Educ. 2016;49(4):454–67. https://doi.org/10.1080/10665684.2016.1226104 .
Ahmed S. Affective economies. Social Text. 2004;22(2):117–39.
Thompson A. Tiffany, friend of people of color: White investments in antiracism. Int J Qual Stud Educ. 2003;16(1):7–29. https://doi.org/10.1080/0951839032000033509 .
Lentin A. Racism in public or public racism: doing anti-racism in ‘post-racial’ times. Ethn Racial Stud. 2016;39(1):33–48. https://doi.org/10.1080/01419870.2016.1096409 .
Saad L. Me and white supremacy workbook: a 28-day challenge to combat racism, change the world, and become a good ancestor. Naperville: Sourcebooks; 2020.
Thompson A. Resisting the “Lone Hero” stance. In: Pollack M, editor. Everyday anti-racism: Getting real about race in school. New York: The New Press; 2008. p. 328–33.
St. Denis V, Schick C. What makes anti-racist pedagogy in teacher education difficult? Three popular ideological assumptions. Alta J Educ Res. 2003;XLIX(1):55–69.
Walia H. Decolonizing together. Briarpatch. 2012. https://briarpatchmagazine.com/articles/view/decolonizing-together Accessed 28 Feb 2022.
Kendi IX. How to be an Antiracist. New York: One World; 2019.
Download references
Acknowledgements
Special thanks to Dr. Manuela Valle-Castro for the support she provided in developing and delivering the antiracism content. Many thanks to the Anti-Racism Network for making this work possible.
This study was supported by Dr. Holly Graham, Indigenous Chair of Research in Nursing at the University of Saskatchewan. These funds come from Canadian Institutes of Health Research (CIHR), the Saskatchewan Health Research Foundation (SHRF), the Canadian Nurses Foundation (CNF), and the University of Saskatchewan.
Author information
Authors and affiliations.
University of Saskatchewan, Saskatoon, SK, Canada
Sharissa Hantke, Verna St. Denis & Holly Graham
You can also search for this author in PubMed Google Scholar
Contributions
HG guided the conception and design, and provided revisions to the article. SH collected and analyzed data and drafted the article. VSD supervised the collection and analysis of the data. HG, VSD, and SH approved the final version for publication.
Corresponding author
Correspondence to Sharissa Hantke .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from University of Saskatchewan Behavioural Research Ethics Board, approval no. 2028. All participants signed a written consent form before the focus group. Results were presented to all participants upon completion of analysis. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hantke, S., St. Denis, V. & Graham, H. Racism and antiracism in nursing education: confronting the problem of whiteness. BMC Nurs 21 , 146 (2022). https://doi.org/10.1186/s12912-022-00929-8
Download citation
Received : 02 March 2022
Accepted : 25 May 2022
Published : 10 June 2022
DOI : https://doi.org/10.1186/s12912-022-00929-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing education
- Critical race theory
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

- Latest Articles
- Clinical Practice
- ONS Leadership
- Get Involved

Nurses Have a Role and Responsibility in Ending Racism

- Share on Twitter
- Share on Facebook
- Share on Pinterest
- Share on LinkedIn
- Email Article
- Print Article
“ There’s no way you can extricate what’s been going on and the outcomes of the (COVID-19 coronavirus) from the basic racism and social injustice and inequities that have existed in this country for so many years,” American Academy of Nursing Living Legend Catherine Alicia Georges, EdD, RN, FAAN , said in a June 17, 2020, podcast. “ The chronicity of racism is the issue.”

Like most white people, I knew racial bias existed in the United States long before I learned of George Floyd’s murder , which sparked worldwide protests about systematic racism. In fact, through my graduate education and professional experiences as a nurse, I recognized that many of the nation’s social systems are unfair to minority populations. What I failed to realize was the extent to which our society is complicit in these issues.
We are amid a long-overdue, national awakening on systemic racism and social inequity, an awakening that minority communities have demanded for centuries. And as nurses, it is our responsibility to advocate for the most vulnerable members of society.
Today’s social climate gives me hope for the future of our profession and nation. This is an opportunity for nurses everywhere to leverage our knowledge and unique position to change the healthcare system from inside out. And here’s how we can do just that.
Acknowledge Our Nation’s Racist History
The first step to reform is looking internally.
Ask yourself: Does my race or gender afford me opportunities that are not afforded to others? Do I make assumptions about people because of how they look or who they love? Am I treating every person I interact with the way that I would want to be treated? We—and by “we,” I mean people who were granted certain privileges simply based on our race, gender, or sexuality—have a crucial responsibility to challenge ourselves with these questions.
Discrimination isn’t always overt or violent. It is systematically embedded in our society, from education to health care to government.
Review Reformative Resources
Educate yourself: Consult ONS Voice articles on cancer health disparities , such as race, gender, and sexuality, listen to Oncology Nursing Podcast episodes , and read ONS journal articles on social determinants of health.
Medium also offers an extensive list of books, articles, movies, documentaries, podcasts, and civic leaders to study. It includes antiracism resources for both adults and children, and many of the documentaries are available on Netflix.
These resources help us acknowledge the systematic inequality that’s existed throughout America’s history, and the microaggressions people of color face in everyday situations.
Leverage a Trust in Advocacy
Nursing is the most trusted profession , and we must lead by example. Nurses are integrated with all facets of society, from health care and education to public health and government. Our profession has a responsibility to be anti racist rather than “not racist .”
Equity and equality differ , although both are important in diminishing racism. As nurses we can acknowledge areas where we, our department, or our organization may be treating patients and colleagues unequally or inequitably.
Some racism may be intentional, but many times it is unintentional and has gone unnoticed for many years. Joining or starting a diversity and inclusion committee in your organization is a good first step to diminishing discrimination in the workplace.
Accept That You Will Make Mistakes
Acknowledging your own bias requires contradicting generations of legislation and social norms. Sometimes you will say or think the wrong thing, and that’s okay as long as you own your mistake, apologize, and, most importantly, learn from it. We can all do better. Harness that opportunity and use it to improve.
For me, becoming antiracist has been an evolutionary process and I have made many mistakes. No one is asking you to be perfect. Rather, be open to admitting that racism is embedded in this nation and now is the time to step up and change.
As we did with our LGBTQ friends and colleagues , we must stand behind the people of color in our lives, give them equal opportunity to navigate all facets of life, and leave discrimination of all forms in the past.
We always have an opportunity to make this country a better place for everyone, no matter their race, gender, or sexuality. And nurses can lead the way. The United States is a nation founded on “liberty and justice for all.” It’s time we act like it.
- Patient advocacy
- Oncology nurse influence
- Nurse empowerment
- Patient empowerment
Issue of Racism in Healthcare Essay
Introduction, ethical theories and principles.
Racism, rather than race, is a social determinant of health. Black and Latino populations are disproportionately affected by some diseases due to inequities in factors such as income, housing, and education that are sometimes driven by racism. Additionally, the beliefs held by healthcare professionals regarding race could be the reason why one person receives quality healthcare and another does not receive care at all. This paper explores the ethicality of racism in healthcare from various ethical theories and bioethical principles. It also explicates how the nursing profession and the law address this concern. Racism in healthcare is unethical because it denies equitable care to some populations.
The issue of racism in healthcare can be evaluated from various ethical theories, including utilitarianism and virtue ethics. According to the utilitarian ethical theory, an action is ethical if it brings happiness and maximizes utility for the greatest number of people (Häyry, 2020). The theory would be concerned about the ethicality of racism in healthcare because discrimination adversely affects some people’s health. For example, racism denies some people access to services and leads to poor health outcomes. The virtue ethics theory holds that an action is ethical if it reflects moral values such as honesty, empathy, kindness, integrity, and fairness. The theory would question whether racism in healthcare is ethical and whether it facilitates the provision of care in a manner that is centered on values such as compassion, fairness, and integrity.
Racism in healthcare can also be considered from the perspective of ethical principles. The bioethical principle of beneficence requires medical professionals to take actions with the intention of promoting the wellbeing of their patients (Avant & Swetz, 2020). Racist healthcare providers do not take actions that benefit their patients. For example, failing to prescribe necessary painkillers to a Black person because of the belief that Black people are more susceptible to painkiller addiction goes against the principle of beneficence.
Another bioethical principle is non-maleficence, which is a call for medical professionals to do no harm to their patients. Racism harms people in the form of late or no diagnosis, lower life expectancy, and harmful stereotypes. The principle of non-maleficence would argue against racism in healthcare. On the other hand, some people would argue that healthcare professionals do not intentionally harm their patients. For instance, many incidences of medical racism stem from implicit bias (Iheduru-Anderson et al., 2021). However, ignorance is not an excuse for harming a patient because nurses and other professionals have a duty not to harm their patients. Therefore, it is their responsibility to unlearn such unconscious bias that result in racism in healthcare.
Nursing Codes
The nursing profession, through various codes, advises nurses how to approach ethical concerns arising from racism in healthcare. The CNO consists of six main principles by which nurses should abide (College of Nurses of Ontario, 2019). The first principle requires nurses to treat patients with dignity. They should treat them with care, compassion, and respect for their identity. They should also disburse care that is free from judgment and discrimination. Additionally, nurses are advised not to impose their personal biases and beliefs on patients. Racism in healthcare goes against the first CNO principle because it defies all these values. The second principle promotes collaboration among nurses to address gaps in healthcare that impact health outcomes and patient care (College of Nurses of Ontario, 2019). Addressing racism in healthcare is one way nurses can put this principle into practice. Other principles require nurses to provide safe and competent care to gain and maintain patient trust. By dispensing equitable care regardless of a person’s race, nurses will increase trust in the healthcare system.
The Canadian Nurses Association (CNA) echoes the values and principles contained in the CNO. For instance, it emphasizes the importance of safe, competent, compassionate, and ethical care (Canadian Nurses Association, 2017). When nurses strive to provide this quality of care, they ensure that their practices are free from racism. Additionally, the Code advocates for justice in the provision of care (Canadian Nurses Association, 2017). Racism in healthcare denies due justice to people of certain races, such as Black and Latino people. Finally, the Code advocates for transparency and accountability in nursing practices. This means that nurses are responsible for unlearning implicit biases about race. The various codes that guide the nursing profession have principles that help nurses navigate ethical concerns concerning medical racism.
Social Justice and Legal Considerations
Social justice is a concept which asserts that people should have equal access to economic, political, and social services and opportunities. More precisely, “Social justice includes full and equal participation of individuals in all social institutions; fair, equitable distribution of material and nonmaterial goods” (Abbott, 2014). Racism is a social justice issue because it denies people fair and equitable access to a nonmaterial good, that is, healthcare. Healthcare is a social service, and in an ideal world, people should have fair access to it regardless of their race. When race is a factor that influences the quality of care a person receives, it goes against the concept of social justice.
There are many laws and statutes that pertain to racism in healthcare. For instance, one of the human rights according to the United Nations Universal Declaration of Human Rights is the right to no discrimination. Every person is entitled to their rights and freedoms without consideration for factors such as race, sex, color, religion, or political opinion (Tisdale & Symenuk¸ 2020). This implies that racism in healthcare violates the human right to fair treatment. Additionally, all persons have the right to social service, which includes basic necessities such as food, housing, clothing, security, and medical care. When people are provided with poor quality care or none at all, it violates their right to social services. Additionally, all provinces in Canada have human rights commissions that have codes that forbid discrimination (Tisdale & Symenuk¸ 2020). One such example is the Ontario’s Human Rights Code that provides for equal opportunities and protection from discrimination. The Nursing Act and the Regulated Health Professions Act, which regulate nursing in Ontario, do not have information regarding racism in nursing.
My Values, Values, and Religion
My practice as a nurse is based in values such as compassion, quality care, and justice. I aim to provide high-quality care to patients regardless of factors such as age, sex, or race. This means that racism in healthcare goes against my beliefs. I also believe in extending myself when providing care. This means that I go above and beyond to ensure patients are contented with the care they receive. If I were to treat patients differently based on their race, some patients would not be happy with my services. Additionally, in my culture, sick people are taken care of by the community until they feel better. Everyone is considered a valuable member of society who must be nursed back to health when they are sick. Therefore, racism in the provision of healthcare goes against my core values, beliefs, and culture.
Ethical Framework
To make a decision regarding my ethical concern, I would use the Oberle and Raffin model. First, I would assess the situation as well as relationships, beliefs, goals, and values (Canadian Nurses Association, 2017). Second, I would then evaluate potential actions. One option is to provide care to a patient without regard for their race while the other is to differentiate patients based on their race. Third, I would select an ethical action that maximizes good. The first option would ensure everyone receives equitable care and is the action that would maximize good. Fourth, I would evaluate whether I am acting ethically by analyzing whether my decision is according to the Code and professional standards. Finally, I would reflect on my action by considering whether I reported it through the appropriate channels. I would also assess how people were affected by my decision, whether I could have done anything differently, and whether the outcomes of my decision are acceptable.
Medical racism results in healthcare inequality that negatively impacts the health of certain populations. It leads to these people having poorer health outcomes and experiencing differential treatment due to stereotypes. From the perspectives of ethical theories such as utilitarianism and virtue ethics, racism in healthcare is unethical. It also goes against the bioethical principles of non-maleficence and beneficence. Consequently, there are nursing codes that have guidelines on this ethical concern. There are also laws and legislation against discrimination of persons. Aside from the professional codes and legal mandates, my personal beliefs and values are against providing subpar treatment to a person because they are of a certain race. Racism in healthcare is an ethical concern that all healthcare professionals should strive to eradicate.
Abbott, K. (2014) Social justice. In Michalos A.C. (ed) Encyclopedia of quality of life and well-being research . Springer, Dordrecht.
Avant, L. C., & Swetz, K. M. (2020). Revisiting beneficence: What is a ‘benefit’, and by what criteria? The American Journal of Bioethics, 20 (3), 75-77.
Canadian Nurses Association. (2017). Code of Ethics for registered nurses . Canadian Nurses Association. Web.
College of Nurses of Ontario. (2019). Practice standard: Code of conduct .
Häyry, M. (2021). Just better utilitarianism . Cambridge Quarterly of Healthcare Ethics, 30 (2), 343-367.
Iheduru-Anderson, K., Shingles, R. R., & Akanegbu, C. (2021). Discourse of race and racism in nursing: An integrative review of literature. Public Health Nursing, 38 (1), 115-130.
Tisdale, D., & Symenuk, P. M. (2020). Human rights and nursing codes of ethics in Canada 1953–2017 . Nursing Ethics, 27 (4), 1077-1088.
- Biomedical Technologies and Natural Family Planning
- Health Care Disparity and Principles of Biomedical Ethics
- Childhood Immunization Should Be Mandatory in Australia
- Facilitating Spiritual Care: Practicing Dignity
- Culturally Sensitive Spiritual Assessment
- Euthanasia in the Context of Christianity
- Biases and Executive Performance in Healthcare
- Christian Biblical Narrative and Decision-Making in Health Care
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, October 11). Issue of Racism in Healthcare. https://ivypanda.com/essays/issue-of-racism-in-healthcare/
"Issue of Racism in Healthcare." IvyPanda , 11 Oct. 2022, ivypanda.com/essays/issue-of-racism-in-healthcare/.
IvyPanda . (2022) 'Issue of Racism in Healthcare'. 11 October.
IvyPanda . 2022. "Issue of Racism in Healthcare." October 11, 2022. https://ivypanda.com/essays/issue-of-racism-in-healthcare/.
1. IvyPanda . "Issue of Racism in Healthcare." October 11, 2022. https://ivypanda.com/essays/issue-of-racism-in-healthcare/.
Bibliography
IvyPanda . "Issue of Racism in Healthcare." October 11, 2022. https://ivypanda.com/essays/issue-of-racism-in-healthcare/.

IMAGES
VIDEO
COMMENTS
Racism in the nurse-patient relationship has remained a relatively unexplored area of the nursing literature. It hinders efforts to meet patients' and families' needs and increases their dissatisfaction with nursing care. Also, racism from patients towards nurses causes emotional trauma and enhances job‐related stress among nurses.
Report #1 of 6 The History of Racism in Nursing: A Review of Existing Scholarship 3 Introduction 5 Nursing's Origin Story 8 Racism and War 11 Nursing and the Era of Enslavement 17 Nursing and Colonialism in the Indigenous United States 28 Nursing and American Imperialism Beyond the Continental U.S. 30 Intersections of Imperialism and Racism in Latino Nursing 33 Imperialist Legacy
The History of Racism in Nursing. This report centers the experiences of nurses of color in U.S. history and how structural and systemic racism have hindered access to educational and professional opportunities as well as institutional power. The report also reviews some of the ways in which these nurses resisted, challenged, and achieved ...
The Role of Nurses in Addressing Racism. Nurses are positioned to lead in addressing the underlying, interrelated complex of issues that link racism and health inequalities. Nursing must take stock, take stake, and take steps to pursue actions that confront institutional and interpersonal forms of racism. Nurses have a significant role to play ...
Racism has historically been entrenched in both nursing and nursing education in the United States, despite deliberate efforts to raise awareness about how racism can cause health disparities in ethnic minority patients. To date, approaches to racism in nursing have followed Leininger's Theory of Nursing, and have focused on teaching cultural competence skills.
In 2022, the American Nurses Association took the weighty step of beginning the conversation to address its role in perpetuating racism in nursing and established the National Commission to Address Racism in Nursing. A 2022 survey by the commission found that over 63% of nurses experience some form of racism in the workplace, with peers making ...
essay. This established form of essay reviews relevant published historical research that addresses issues central to examining the issue of racism in nursing. The research we review focuses primarily on issues of structural and systemic racism that have affected nursing: "forms of racism that are pervasively and deeply embedded in and throughout
Racism in the nurse-patient relationship has remained a relatively unexplored area of the nursing literature. It hinders efforts to meet patients' and families' needs and increases their dissatisfaction with nursing care. Also, racism from patients towards nurses causes emotional trauma and enhances job-related stress among nurses.
Confronting Racism in Nursing. Editor (s): Donnelly, Gloria F. PhD, RN, FAAN, FCPP, Editor in Chief. Author Information. The author has disclosed that she has no significant relationships with, or financial interest in, any commercial companies pertaining to this article. Holistic Nursing Practice: November/December 2020 - Volume 34 - Issue 6 ...
These papers covered data from 11 countries; the majority reported on data from the United Kingdom (10 papers) and the United States (8 papers). Most papers focused on nurses and auxiliary nurses (solely or among other professions) while two studies reported on nursing students (Ferns & Meerabeau, 2008; Zwane & Poggenpoel, 2000).
This. 31 established form of an essay reviews relevant published historical research that addresses. 32 issues central to examining the issue of racism in nursing. It moves forward in historical time to. 33 explain the evolution of relevant questions and issues.
This essay examines power, privilege, and prejudice in nursing today. By looking at our history, we can understand the current inequities and discriminatory practices that hinder the progress of nurses of color. Read this section. Education. Racism in nursing education has been prevalent since its beginning with roots in white supremacy.
Systemic racism in Canadian healthcare may be observed through racially inequitable outcomes, particularly for Indigenous people. Nursing approaches intending to respond to racism often focus on culture without critically addressing the roots of racist inequity directly. In contrast, the critical race theory approach used in this study identifies whiteness as the underlying problem; a system ...
Nursing is the most trusted profession, and we must lead by example. Nurses are integrated with all facets of society, from health care and education to public health and government. Our profession has a responsibility to be anti racist rather than "not racist.". Equity and equality differ, although both are important in diminishing racism.
This paper explores the ethicality of racism in healthcare from various ethical theories and bioethical principles. It also explicates how the nursing profession and the law address this concern. Racism in healthcare is unethical because it denies equitable care to some populations. We will write a custom essay on your topic.
In these past few weeks, we have seen and witnessed two symptoms of the same disease—the killing of George Floyd by a policeman and the disproportionate impact of COVID-19 on communities of color. Both are stark examples of the effects of structural racism, which refers to a system in which public policies, institutional practices, and other norms perpetuate racial group inequities, and is a ...
Health care organizations face challenges with the initiative to increase racial diversity within the nursing workforce. Despite efforts to diversify, the 2018 Bureau of Labor and Statistics showed that amongst 3.2 million registered nurses in the United States (U.S.), 75.5% are whites, 13.1 % are Black or African- American, 9% Asian and only 7 ...
Funding Opportunity. In January, 2024, the National Commission to Address Racism in Nursing awarded funds to ten organizations implementing evidence-based strategies to dismantle institutional, structural, and systemic racism in nursing. The funds were contributed by the American Nurses Association (ANA), as part of its journey of racial ...
Racism has been around for hundreds of years. There is no room for racism in nursing, although it does happen. The patients that nurses are treating are in a vulnerable state. They should be able to feel comfortable with their healthcare professional and should be able to trust them and the decisions they make regarding their care.
On January 25, 2021, leading nursing organizations launched the National Commission to Address Racism in Nursing (the Commission). The Commission examines the issue of racism within nursing nationwide focusing on the impact on nurses, patients, communities, and health care systems to motivate all nurses to confront individual and systemic ...